User login
Breaking a 10-year streak, the number of uninsured Americans rises
For the first time in a decade, the number of Americans without health insurance has risen – by about 2 million people in 2018 – according to the annual U.S. Census Bureau report released Sept. 10, 2019.
The Census found that 8.5% of the U.S. population went without medical insurance for all of 2018, up from 7.9% in 2017. By contrast, in 2013, before the Affordable Care Act took full effect, 13.3% were uninsured. It was the first year-to-year increase since 2008-09, Census officials said, adding that most of the drop in health coverage was related to a 0.7% decline in Medicaid participants. The number of people with private insurance remained steady and there was a 0.4% increase in those on Medicare.
Many of those losing coverage were noncitizens, a possible fallout from the Trump administration’s tough immigration policies and rhetoric. About 574,000 noncitizens lost coverage in 2018, a drop of about 2.3%, the report found.
“Uninsured noncitizens account for almost a third of the increase in uninsured, which may reflect the administration’s more aggressive stance on immigration,” said Joseph Antos, a health economist at the American Enterprise Institute.
The increase in the number of uninsured people in 2018 was remarkable because uninsured rates typically fall or hold steady when unemployment rates drop. The U.S. unemployment rate fell slightly from about 4.3% in 2017 to 4% in 2018.
The uninsured rate continued to vary by poverty status and whether a state expanded its Medicaid program under Obamacare. Texas (17.7%), Oklahoma (14.2%), Georgia (13.7%), and Florida (13%) had the highest uninsured rates in 2018, according to the report. None of those states have expanded Medicaid under Obamacare.
The percentage of uninsured children aged under 19 years increased by 0.6 percentage points from 2017 to 2018, to 5.5%.
“The Census data are clear – the uninsured rate for kids is up sharply and it’s due to a loss of public coverage – mostly Medicaid,” Joan Alker, executive director of Georgetown University Center for Children and Families, said in a statement.
“These children are not getting private coverage as the Trump administration has suggested but rather becoming uninsured,” she said. “This serious erosion of children’s health coverage is due in large part to the Trump administration’s actions that have made health care harder to access and have deterred families from enrolling their children.”
The share of Americans without medical insurance fell steadily since 2014 but then leveled off in 2017, the year Mr. Trump became president.
Health care advocates have complained that efforts by the Trump administration and Congress are jeopardizing insurance enrollment. They point to cuts in outreach programs that aim to tell consumers about their health care options under Obamacare and the elimination of the ACA’s tax penalty for people who don’t have health coverage.
Ms. Alker complained that the administration’s policies are causing the loss of children’s coverage. “In a period of continued economic and job growth, we shouldn’t be going backwards on health coverage,” said Judy Solomon, a senior fellow for the Center on Budget and Policy Priorities, a left-leaning think tank. “This backsliding almost certainly reflects, at least in part, Trump administration policies to weaken public health coverage.”
She attributed the drop to the Trump administration making it harder for families to enroll for coverage in Medicaid by curtailing outreach efforts, allowing states to ask for more paperwork and proposing a so-called public charge rule that would make it harder for legal immigrants to get permanent resident status if they have received certain kinds of public assistance – including Medicaid.
Tom Miller, a resident fellow at the American Enterprise Institute, a conservative think tank, said the drop in Medicaid coverage “is a positive.”
“When the economy grows Medicaid eventually drops,” he said.
One reason for the drop in health coverage is that middle-income families can’t afford the rising cost of insurance in the individual market, particularly if they don’t qualify for government subsidies, he added.
“On balance, this is some short-term noise,” he said of the uptick in the uninsured rate. “I would put more stake in it if happens for several years.”
Chris Pope, a senior fellow with the conservative Manhattan Institute, also said he considered the change “fairly small” and likely caused by increasing wages “pushing people above the income eligibility cutoff in Medicaid expansion states.”
But he suggested that next year would be a better indicator of how changes in the ACA are playing out. “I expect that the mandate repeal will make next year’s increase in the uninsured more significant.”
Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
For the first time in a decade, the number of Americans without health insurance has risen – by about 2 million people in 2018 – according to the annual U.S. Census Bureau report released Sept. 10, 2019.
The Census found that 8.5% of the U.S. population went without medical insurance for all of 2018, up from 7.9% in 2017. By contrast, in 2013, before the Affordable Care Act took full effect, 13.3% were uninsured. It was the first year-to-year increase since 2008-09, Census officials said, adding that most of the drop in health coverage was related to a 0.7% decline in Medicaid participants. The number of people with private insurance remained steady and there was a 0.4% increase in those on Medicare.
Many of those losing coverage were noncitizens, a possible fallout from the Trump administration’s tough immigration policies and rhetoric. About 574,000 noncitizens lost coverage in 2018, a drop of about 2.3%, the report found.
“Uninsured noncitizens account for almost a third of the increase in uninsured, which may reflect the administration’s more aggressive stance on immigration,” said Joseph Antos, a health economist at the American Enterprise Institute.
The increase in the number of uninsured people in 2018 was remarkable because uninsured rates typically fall or hold steady when unemployment rates drop. The U.S. unemployment rate fell slightly from about 4.3% in 2017 to 4% in 2018.
The uninsured rate continued to vary by poverty status and whether a state expanded its Medicaid program under Obamacare. Texas (17.7%), Oklahoma (14.2%), Georgia (13.7%), and Florida (13%) had the highest uninsured rates in 2018, according to the report. None of those states have expanded Medicaid under Obamacare.
The percentage of uninsured children aged under 19 years increased by 0.6 percentage points from 2017 to 2018, to 5.5%.
“The Census data are clear – the uninsured rate for kids is up sharply and it’s due to a loss of public coverage – mostly Medicaid,” Joan Alker, executive director of Georgetown University Center for Children and Families, said in a statement.
“These children are not getting private coverage as the Trump administration has suggested but rather becoming uninsured,” she said. “This serious erosion of children’s health coverage is due in large part to the Trump administration’s actions that have made health care harder to access and have deterred families from enrolling their children.”
The share of Americans without medical insurance fell steadily since 2014 but then leveled off in 2017, the year Mr. Trump became president.
Health care advocates have complained that efforts by the Trump administration and Congress are jeopardizing insurance enrollment. They point to cuts in outreach programs that aim to tell consumers about their health care options under Obamacare and the elimination of the ACA’s tax penalty for people who don’t have health coverage.
Ms. Alker complained that the administration’s policies are causing the loss of children’s coverage. “In a period of continued economic and job growth, we shouldn’t be going backwards on health coverage,” said Judy Solomon, a senior fellow for the Center on Budget and Policy Priorities, a left-leaning think tank. “This backsliding almost certainly reflects, at least in part, Trump administration policies to weaken public health coverage.”
She attributed the drop to the Trump administration making it harder for families to enroll for coverage in Medicaid by curtailing outreach efforts, allowing states to ask for more paperwork and proposing a so-called public charge rule that would make it harder for legal immigrants to get permanent resident status if they have received certain kinds of public assistance – including Medicaid.
Tom Miller, a resident fellow at the American Enterprise Institute, a conservative think tank, said the drop in Medicaid coverage “is a positive.”
“When the economy grows Medicaid eventually drops,” he said.
One reason for the drop in health coverage is that middle-income families can’t afford the rising cost of insurance in the individual market, particularly if they don’t qualify for government subsidies, he added.
“On balance, this is some short-term noise,” he said of the uptick in the uninsured rate. “I would put more stake in it if happens for several years.”
Chris Pope, a senior fellow with the conservative Manhattan Institute, also said he considered the change “fairly small” and likely caused by increasing wages “pushing people above the income eligibility cutoff in Medicaid expansion states.”
But he suggested that next year would be a better indicator of how changes in the ACA are playing out. “I expect that the mandate repeal will make next year’s increase in the uninsured more significant.”
Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
For the first time in a decade, the number of Americans without health insurance has risen – by about 2 million people in 2018 – according to the annual U.S. Census Bureau report released Sept. 10, 2019.
The Census found that 8.5% of the U.S. population went without medical insurance for all of 2018, up from 7.9% in 2017. By contrast, in 2013, before the Affordable Care Act took full effect, 13.3% were uninsured. It was the first year-to-year increase since 2008-09, Census officials said, adding that most of the drop in health coverage was related to a 0.7% decline in Medicaid participants. The number of people with private insurance remained steady and there was a 0.4% increase in those on Medicare.
Many of those losing coverage were noncitizens, a possible fallout from the Trump administration’s tough immigration policies and rhetoric. About 574,000 noncitizens lost coverage in 2018, a drop of about 2.3%, the report found.
“Uninsured noncitizens account for almost a third of the increase in uninsured, which may reflect the administration’s more aggressive stance on immigration,” said Joseph Antos, a health economist at the American Enterprise Institute.
The increase in the number of uninsured people in 2018 was remarkable because uninsured rates typically fall or hold steady when unemployment rates drop. The U.S. unemployment rate fell slightly from about 4.3% in 2017 to 4% in 2018.
The uninsured rate continued to vary by poverty status and whether a state expanded its Medicaid program under Obamacare. Texas (17.7%), Oklahoma (14.2%), Georgia (13.7%), and Florida (13%) had the highest uninsured rates in 2018, according to the report. None of those states have expanded Medicaid under Obamacare.
The percentage of uninsured children aged under 19 years increased by 0.6 percentage points from 2017 to 2018, to 5.5%.
“The Census data are clear – the uninsured rate for kids is up sharply and it’s due to a loss of public coverage – mostly Medicaid,” Joan Alker, executive director of Georgetown University Center for Children and Families, said in a statement.
“These children are not getting private coverage as the Trump administration has suggested but rather becoming uninsured,” she said. “This serious erosion of children’s health coverage is due in large part to the Trump administration’s actions that have made health care harder to access and have deterred families from enrolling their children.”
The share of Americans without medical insurance fell steadily since 2014 but then leveled off in 2017, the year Mr. Trump became president.
Health care advocates have complained that efforts by the Trump administration and Congress are jeopardizing insurance enrollment. They point to cuts in outreach programs that aim to tell consumers about their health care options under Obamacare and the elimination of the ACA’s tax penalty for people who don’t have health coverage.
Ms. Alker complained that the administration’s policies are causing the loss of children’s coverage. “In a period of continued economic and job growth, we shouldn’t be going backwards on health coverage,” said Judy Solomon, a senior fellow for the Center on Budget and Policy Priorities, a left-leaning think tank. “This backsliding almost certainly reflects, at least in part, Trump administration policies to weaken public health coverage.”
She attributed the drop to the Trump administration making it harder for families to enroll for coverage in Medicaid by curtailing outreach efforts, allowing states to ask for more paperwork and proposing a so-called public charge rule that would make it harder for legal immigrants to get permanent resident status if they have received certain kinds of public assistance – including Medicaid.
Tom Miller, a resident fellow at the American Enterprise Institute, a conservative think tank, said the drop in Medicaid coverage “is a positive.”
“When the economy grows Medicaid eventually drops,” he said.
One reason for the drop in health coverage is that middle-income families can’t afford the rising cost of insurance in the individual market, particularly if they don’t qualify for government subsidies, he added.
“On balance, this is some short-term noise,” he said of the uptick in the uninsured rate. “I would put more stake in it if happens for several years.”
Chris Pope, a senior fellow with the conservative Manhattan Institute, also said he considered the change “fairly small” and likely caused by increasing wages “pushing people above the income eligibility cutoff in Medicaid expansion states.”
But he suggested that next year would be a better indicator of how changes in the ACA are playing out. “I expect that the mandate repeal will make next year’s increase in the uninsured more significant.”
Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
CMS issues split decision on Arkansas Medicaid waiver
The Trump administration on March 5 approved Arkansas’ request for a Medicaid work requirement but deferred a decision on the state’s request to roll back its Medicaid expansion that has added 300,000 adults to the program.
Arkansas had sought to reduce the number of people eligible for Medicaid by allowing only those with incomes below the federal poverty level, or about $12,140 for an individual, to qualify. For the past 4 years, Arkansas Medicaid covered everyone with incomes under 138% of the poverty level, or about $16,750. The new policy would have cut the number of people eligible for Medicaid in the state by about 60,000 people.
Seema Verma, administrator of the Centers for Medicare & Medicaid Services, who announced the decision, has said her goal as head of the program was to grant states more flexibility in running their Medicaid programs than they’ve had before.
Arkansas follows Indiana and Kentucky this year in winning CMS’ approval for the work requirement. Arkansas plans to start the new requirement affecting adults under age 50 years by June, making it the first to do so.
Ms. Verma recused herself on CMS’ decisions involving Indiana and Kentucky because she used to consult with those state Medicaid agencies before joining the Trump administration in 2017. As a health care consultant, she also worked with Arkansas. But
CMS officials did not respond to questions about why she did not recuse herself again.
But a top Senate Democrat lambasted Ms. Verma’s decision.
“She pledged during her confirmation to recuse herself from working on many states’ Medicaid waivers to avoid conflicts of interest, including Arkansas, Sen. Ron Wyden (D-Ore.) said in a statement. “The Trump administration has simply made a mockery of the HHS ethics process.”
It is unclear why she deferred deciding on Arkansas’ request to scale back its Medicaid decision. Deferring a decision on rolling back expansion could be a way of rejecting the application but in a less politically harsh way. Arkansas was one of the few Southern states to expand Medicaid under the ACA, a decision that brought hundreds of millions of federal dollars into the state.
Nine other states have requests pending with CMS to enact a Medicaid work requirement.
In Arkansas, enrollees who don’t work or volunteer at least 80 hours a month could lose coverage as early as September. The work requirement exempts many people, such as those with opioid addiction and parents with dependent children.
Ms. Verma said the work requirement “is about helping people rise out of poverty to achieve the American dream.”
But advocates for the poor blasted the move, noting most Medicaid enrollees already work, go to school, or are taking care of sick relatives.
“The Trump administration’s approval of Arkansas’ harsh work requirement in Medicaid will likely set back the state’s considerable progress under the Affordable Care Act in increasing coverage and improving access to care, health and financial stability for low-income Arkansans,” said Judith Solomon, vice president for health policy at the left-leaning Center on Budget and Policy Priorities.
Arkansas officials said they need the work requirement because without it many enrollees won’t seek out work or job training. Since January 2017, fewer than 5% of Medicaid enrollees who were referred to the state Department of Workforce Services to help with job training followed through and accessed services.
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of the Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
The Trump administration on March 5 approved Arkansas’ request for a Medicaid work requirement but deferred a decision on the state’s request to roll back its Medicaid expansion that has added 300,000 adults to the program.
Arkansas had sought to reduce the number of people eligible for Medicaid by allowing only those with incomes below the federal poverty level, or about $12,140 for an individual, to qualify. For the past 4 years, Arkansas Medicaid covered everyone with incomes under 138% of the poverty level, or about $16,750. The new policy would have cut the number of people eligible for Medicaid in the state by about 60,000 people.
Seema Verma, administrator of the Centers for Medicare & Medicaid Services, who announced the decision, has said her goal as head of the program was to grant states more flexibility in running their Medicaid programs than they’ve had before.
Arkansas follows Indiana and Kentucky this year in winning CMS’ approval for the work requirement. Arkansas plans to start the new requirement affecting adults under age 50 years by June, making it the first to do so.
Ms. Verma recused herself on CMS’ decisions involving Indiana and Kentucky because she used to consult with those state Medicaid agencies before joining the Trump administration in 2017. As a health care consultant, she also worked with Arkansas. But
CMS officials did not respond to questions about why she did not recuse herself again.
But a top Senate Democrat lambasted Ms. Verma’s decision.
“She pledged during her confirmation to recuse herself from working on many states’ Medicaid waivers to avoid conflicts of interest, including Arkansas, Sen. Ron Wyden (D-Ore.) said in a statement. “The Trump administration has simply made a mockery of the HHS ethics process.”
It is unclear why she deferred deciding on Arkansas’ request to scale back its Medicaid decision. Deferring a decision on rolling back expansion could be a way of rejecting the application but in a less politically harsh way. Arkansas was one of the few Southern states to expand Medicaid under the ACA, a decision that brought hundreds of millions of federal dollars into the state.
Nine other states have requests pending with CMS to enact a Medicaid work requirement.
In Arkansas, enrollees who don’t work or volunteer at least 80 hours a month could lose coverage as early as September. The work requirement exempts many people, such as those with opioid addiction and parents with dependent children.
Ms. Verma said the work requirement “is about helping people rise out of poverty to achieve the American dream.”
But advocates for the poor blasted the move, noting most Medicaid enrollees already work, go to school, or are taking care of sick relatives.
“The Trump administration’s approval of Arkansas’ harsh work requirement in Medicaid will likely set back the state’s considerable progress under the Affordable Care Act in increasing coverage and improving access to care, health and financial stability for low-income Arkansans,” said Judith Solomon, vice president for health policy at the left-leaning Center on Budget and Policy Priorities.
Arkansas officials said they need the work requirement because without it many enrollees won’t seek out work or job training. Since January 2017, fewer than 5% of Medicaid enrollees who were referred to the state Department of Workforce Services to help with job training followed through and accessed services.
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of the Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
The Trump administration on March 5 approved Arkansas’ request for a Medicaid work requirement but deferred a decision on the state’s request to roll back its Medicaid expansion that has added 300,000 adults to the program.
Arkansas had sought to reduce the number of people eligible for Medicaid by allowing only those with incomes below the federal poverty level, or about $12,140 for an individual, to qualify. For the past 4 years, Arkansas Medicaid covered everyone with incomes under 138% of the poverty level, or about $16,750. The new policy would have cut the number of people eligible for Medicaid in the state by about 60,000 people.
Seema Verma, administrator of the Centers for Medicare & Medicaid Services, who announced the decision, has said her goal as head of the program was to grant states more flexibility in running their Medicaid programs than they’ve had before.
Arkansas follows Indiana and Kentucky this year in winning CMS’ approval for the work requirement. Arkansas plans to start the new requirement affecting adults under age 50 years by June, making it the first to do so.
Ms. Verma recused herself on CMS’ decisions involving Indiana and Kentucky because she used to consult with those state Medicaid agencies before joining the Trump administration in 2017. As a health care consultant, she also worked with Arkansas. But
CMS officials did not respond to questions about why she did not recuse herself again.
But a top Senate Democrat lambasted Ms. Verma’s decision.
“She pledged during her confirmation to recuse herself from working on many states’ Medicaid waivers to avoid conflicts of interest, including Arkansas, Sen. Ron Wyden (D-Ore.) said in a statement. “The Trump administration has simply made a mockery of the HHS ethics process.”
It is unclear why she deferred deciding on Arkansas’ request to scale back its Medicaid decision. Deferring a decision on rolling back expansion could be a way of rejecting the application but in a less politically harsh way. Arkansas was one of the few Southern states to expand Medicaid under the ACA, a decision that brought hundreds of millions of federal dollars into the state.
Nine other states have requests pending with CMS to enact a Medicaid work requirement.
In Arkansas, enrollees who don’t work or volunteer at least 80 hours a month could lose coverage as early as September. The work requirement exempts many people, such as those with opioid addiction and parents with dependent children.
Ms. Verma said the work requirement “is about helping people rise out of poverty to achieve the American dream.”
But advocates for the poor blasted the move, noting most Medicaid enrollees already work, go to school, or are taking care of sick relatives.
“The Trump administration’s approval of Arkansas’ harsh work requirement in Medicaid will likely set back the state’s considerable progress under the Affordable Care Act in increasing coverage and improving access to care, health and financial stability for low-income Arkansans,” said Judith Solomon, vice president for health policy at the left-leaning Center on Budget and Policy Priorities.
Arkansas officials said they need the work requirement because without it many enrollees won’t seek out work or job training. Since January 2017, fewer than 5% of Medicaid enrollees who were referred to the state Department of Workforce Services to help with job training followed through and accessed services.
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of the Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
Indiana gets Medicaid waiver that could slice enrollment
Indiana is the second state to win federal approval to add a work requirement for adult Medicaid recipients who gained coverage under the Affordable Care Act, but a less debated “lockout” provision in its new plan could lead to tens of thousands of enrollees losing coverage.
The federal approval was announced Feb. 2 by Health & Human Services Secretary Alex Azar in Indianapolis.
Medicaid participants who fail to submit their paperwork in a timely manner showing that they still qualify for the program will be blocked from enrollment for 3 months, according to the updated rules.
Since November 2015, more than 91,000 enrollees in Indiana were kicked off Medicaid for failing to complete the eligibility redetermination process, according to state records. The process requires applicants to show proof of income and family size, among other things, to see if they still qualify for the coverage. Until now, these enrollees could simply reapply anytime. Although many of those people likely were no longer eligible, state officials estimate about half of those who failed to comply with its reenrollment rules were still qualified.
Indiana’s Medicaid expansion began in February 2015, providing coverage to 240,000 people who were previously uninsured, helping drop the state’s uninsured rate from 14% in 2013 to 8% last year. The HHS approval extends the program, which was expiring this month, through 2020.
The new lockout builds on one already in place for Indiana residents who failed to pay monthly premiums and had annual incomes above the federal poverty level, or about $12,200 for an individual. They are barred for 6 months from coverage. During the first 2 years of the experiment, about 10,000 Indiana Medicaid enrollees were subject to the lockout for failing to pay the premium for 2 months in a row, according to state data.
In addition, more than 25,000 enrollees were dropped from the program after they failed to make the payments, although half of them found another source of coverage, usually through their jobs.
Another 46,000 were blocked from coverage because they failed to make the initial payment.
“The ‘lockout” is one of the worst policies to hit Medicaid in a long time,” said Joan Alker, executive director of the Georgetown University Center for Children and Families, in Washington. “Forcing people to remain uninsured for months because they missed a paperwork deadline or missed a premium payment is too high a price to pay. From a health policy perspective, it makes no sense because during that period, chronic health conditions such as hypertension or diabetes are just likely to worsen.”
Indiana’s Medicaid expansion is being closely watched in part because it was spearheaded by then-governor Mike Pence, who is now vice president, and his top health consultant, Seema Verma, who now heads the federal Centers for Medicare & Medicaid Services.
The expansion, known as Healthy Indiana, enabled nondisabled adults access to Medicaid. It has elicited criticism from patient advocates for complex and onerous rules that require these poor adults to make payments ranging from $1 to $27 per month into health savings accounts or risk losing their vision and dental benefits or even all their coverage, depending on their income level.
Indiana Medicaid officials said they added the newest lockout provision in an effort to prompt enrollees to get their paperwork submitted in time. The state initially requested a 6-month lockout.
“Enforcement may encourage better compliance,” the state officials wrote in their waiver application to CMS in July.
The new rule will lead to a 1% cut in Medicaid enrollment in the first year, state officials said. It will also lead to a $15 million reduction in Medicaid costs in 2018 and about $32 million in savings in 2019, the state estimated.
The number of Medicaid enrollees losing coverage for failing to comply with redetermining their eligibility has varied dramatically each quarter from a peak of 19,197 from February 2016 to April 2017 to 1,165 from November 2015 to January 2016, state reports show. In the latest state report, 12,470 enrollees lost coverage from August to October 2017.
The Kentucky Medicaid waiver approved by the Trump administration in January included a similar lockout provision for both failing to pay the monthly premiums or providing paperwork on time. Penalties there are 6 months for both measures. But the provision was overshadowed because of the attention to the first federal approval for a Medicaid work requirement.
Like Kentucky, Indiana’s Medicaid waiver’s work requirements, which mandate adult enrollees to work an average of 20 hours a month, go into effect in 2019. But Indiana’s waiver is more lenient. It exempts people aged 60 years and older and its work-hour requirements are gradually phased in over 18 months. For example, enrollees need to work only 5 hours per week until their 10th month on the program.
Most Medicaid adult enrollees do work, go to school, or are too sick to work, studies show.
Indiana also has a long list of exemptions and alternatives to employment. This includes attending school or job training, volunteering or caring for a dependent child or disabled parent. Nurses, doctors and physician assistants can give enrollees an exemption due to illness or injury.
Three patient advocacy groups have filed suit in federal court seeking to block the work requirements.
Robin Rudowitz, associate director for the Kaiser Family Foundation’s Program on Medicaid and the Uninsured, said it’s difficult to gauge whether work requirements or renewal lockouts will have more of an impact on coverage. She noted both provisions apply to most demonstration beneficiaries. (KHN is an editorially independent program of the foundation).
“Any documentation requirement could lead to increased complexity in terms of states administering the requirements and individuals complying,” she said, adding that it could result “in potentially eligible people falling off of coverage.”
Kaiser Health News (KHN) is a national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation which is not affiliated with Kaiser Permanente.
Indiana is the second state to win federal approval to add a work requirement for adult Medicaid recipients who gained coverage under the Affordable Care Act, but a less debated “lockout” provision in its new plan could lead to tens of thousands of enrollees losing coverage.
The federal approval was announced Feb. 2 by Health & Human Services Secretary Alex Azar in Indianapolis.
Medicaid participants who fail to submit their paperwork in a timely manner showing that they still qualify for the program will be blocked from enrollment for 3 months, according to the updated rules.
Since November 2015, more than 91,000 enrollees in Indiana were kicked off Medicaid for failing to complete the eligibility redetermination process, according to state records. The process requires applicants to show proof of income and family size, among other things, to see if they still qualify for the coverage. Until now, these enrollees could simply reapply anytime. Although many of those people likely were no longer eligible, state officials estimate about half of those who failed to comply with its reenrollment rules were still qualified.
Indiana’s Medicaid expansion began in February 2015, providing coverage to 240,000 people who were previously uninsured, helping drop the state’s uninsured rate from 14% in 2013 to 8% last year. The HHS approval extends the program, which was expiring this month, through 2020.
The new lockout builds on one already in place for Indiana residents who failed to pay monthly premiums and had annual incomes above the federal poverty level, or about $12,200 for an individual. They are barred for 6 months from coverage. During the first 2 years of the experiment, about 10,000 Indiana Medicaid enrollees were subject to the lockout for failing to pay the premium for 2 months in a row, according to state data.
In addition, more than 25,000 enrollees were dropped from the program after they failed to make the payments, although half of them found another source of coverage, usually through their jobs.
Another 46,000 were blocked from coverage because they failed to make the initial payment.
“The ‘lockout” is one of the worst policies to hit Medicaid in a long time,” said Joan Alker, executive director of the Georgetown University Center for Children and Families, in Washington. “Forcing people to remain uninsured for months because they missed a paperwork deadline or missed a premium payment is too high a price to pay. From a health policy perspective, it makes no sense because during that period, chronic health conditions such as hypertension or diabetes are just likely to worsen.”
Indiana’s Medicaid expansion is being closely watched in part because it was spearheaded by then-governor Mike Pence, who is now vice president, and his top health consultant, Seema Verma, who now heads the federal Centers for Medicare & Medicaid Services.
The expansion, known as Healthy Indiana, enabled nondisabled adults access to Medicaid. It has elicited criticism from patient advocates for complex and onerous rules that require these poor adults to make payments ranging from $1 to $27 per month into health savings accounts or risk losing their vision and dental benefits or even all their coverage, depending on their income level.
Indiana Medicaid officials said they added the newest lockout provision in an effort to prompt enrollees to get their paperwork submitted in time. The state initially requested a 6-month lockout.
“Enforcement may encourage better compliance,” the state officials wrote in their waiver application to CMS in July.
The new rule will lead to a 1% cut in Medicaid enrollment in the first year, state officials said. It will also lead to a $15 million reduction in Medicaid costs in 2018 and about $32 million in savings in 2019, the state estimated.
The number of Medicaid enrollees losing coverage for failing to comply with redetermining their eligibility has varied dramatically each quarter from a peak of 19,197 from February 2016 to April 2017 to 1,165 from November 2015 to January 2016, state reports show. In the latest state report, 12,470 enrollees lost coverage from August to October 2017.
The Kentucky Medicaid waiver approved by the Trump administration in January included a similar lockout provision for both failing to pay the monthly premiums or providing paperwork on time. Penalties there are 6 months for both measures. But the provision was overshadowed because of the attention to the first federal approval for a Medicaid work requirement.
Like Kentucky, Indiana’s Medicaid waiver’s work requirements, which mandate adult enrollees to work an average of 20 hours a month, go into effect in 2019. But Indiana’s waiver is more lenient. It exempts people aged 60 years and older and its work-hour requirements are gradually phased in over 18 months. For example, enrollees need to work only 5 hours per week until their 10th month on the program.
Most Medicaid adult enrollees do work, go to school, or are too sick to work, studies show.
Indiana also has a long list of exemptions and alternatives to employment. This includes attending school or job training, volunteering or caring for a dependent child or disabled parent. Nurses, doctors and physician assistants can give enrollees an exemption due to illness or injury.
Three patient advocacy groups have filed suit in federal court seeking to block the work requirements.
Robin Rudowitz, associate director for the Kaiser Family Foundation’s Program on Medicaid and the Uninsured, said it’s difficult to gauge whether work requirements or renewal lockouts will have more of an impact on coverage. She noted both provisions apply to most demonstration beneficiaries. (KHN is an editorially independent program of the foundation).
“Any documentation requirement could lead to increased complexity in terms of states administering the requirements and individuals complying,” she said, adding that it could result “in potentially eligible people falling off of coverage.”
Kaiser Health News (KHN) is a national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation which is not affiliated with Kaiser Permanente.
Indiana is the second state to win federal approval to add a work requirement for adult Medicaid recipients who gained coverage under the Affordable Care Act, but a less debated “lockout” provision in its new plan could lead to tens of thousands of enrollees losing coverage.
The federal approval was announced Feb. 2 by Health & Human Services Secretary Alex Azar in Indianapolis.
Medicaid participants who fail to submit their paperwork in a timely manner showing that they still qualify for the program will be blocked from enrollment for 3 months, according to the updated rules.
Since November 2015, more than 91,000 enrollees in Indiana were kicked off Medicaid for failing to complete the eligibility redetermination process, according to state records. The process requires applicants to show proof of income and family size, among other things, to see if they still qualify for the coverage. Until now, these enrollees could simply reapply anytime. Although many of those people likely were no longer eligible, state officials estimate about half of those who failed to comply with its reenrollment rules were still qualified.
Indiana’s Medicaid expansion began in February 2015, providing coverage to 240,000 people who were previously uninsured, helping drop the state’s uninsured rate from 14% in 2013 to 8% last year. The HHS approval extends the program, which was expiring this month, through 2020.
The new lockout builds on one already in place for Indiana residents who failed to pay monthly premiums and had annual incomes above the federal poverty level, or about $12,200 for an individual. They are barred for 6 months from coverage. During the first 2 years of the experiment, about 10,000 Indiana Medicaid enrollees were subject to the lockout for failing to pay the premium for 2 months in a row, according to state data.
In addition, more than 25,000 enrollees were dropped from the program after they failed to make the payments, although half of them found another source of coverage, usually through their jobs.
Another 46,000 were blocked from coverage because they failed to make the initial payment.
“The ‘lockout” is one of the worst policies to hit Medicaid in a long time,” said Joan Alker, executive director of the Georgetown University Center for Children and Families, in Washington. “Forcing people to remain uninsured for months because they missed a paperwork deadline or missed a premium payment is too high a price to pay. From a health policy perspective, it makes no sense because during that period, chronic health conditions such as hypertension or diabetes are just likely to worsen.”
Indiana’s Medicaid expansion is being closely watched in part because it was spearheaded by then-governor Mike Pence, who is now vice president, and his top health consultant, Seema Verma, who now heads the federal Centers for Medicare & Medicaid Services.
The expansion, known as Healthy Indiana, enabled nondisabled adults access to Medicaid. It has elicited criticism from patient advocates for complex and onerous rules that require these poor adults to make payments ranging from $1 to $27 per month into health savings accounts or risk losing their vision and dental benefits or even all their coverage, depending on their income level.
Indiana Medicaid officials said they added the newest lockout provision in an effort to prompt enrollees to get their paperwork submitted in time. The state initially requested a 6-month lockout.
“Enforcement may encourage better compliance,” the state officials wrote in their waiver application to CMS in July.
The new rule will lead to a 1% cut in Medicaid enrollment in the first year, state officials said. It will also lead to a $15 million reduction in Medicaid costs in 2018 and about $32 million in savings in 2019, the state estimated.
The number of Medicaid enrollees losing coverage for failing to comply with redetermining their eligibility has varied dramatically each quarter from a peak of 19,197 from February 2016 to April 2017 to 1,165 from November 2015 to January 2016, state reports show. In the latest state report, 12,470 enrollees lost coverage from August to October 2017.
The Kentucky Medicaid waiver approved by the Trump administration in January included a similar lockout provision for both failing to pay the monthly premiums or providing paperwork on time. Penalties there are 6 months for both measures. But the provision was overshadowed because of the attention to the first federal approval for a Medicaid work requirement.
Like Kentucky, Indiana’s Medicaid waiver’s work requirements, which mandate adult enrollees to work an average of 20 hours a month, go into effect in 2019. But Indiana’s waiver is more lenient. It exempts people aged 60 years and older and its work-hour requirements are gradually phased in over 18 months. For example, enrollees need to work only 5 hours per week until their 10th month on the program.
Most Medicaid adult enrollees do work, go to school, or are too sick to work, studies show.
Indiana also has a long list of exemptions and alternatives to employment. This includes attending school or job training, volunteering or caring for a dependent child or disabled parent. Nurses, doctors and physician assistants can give enrollees an exemption due to illness or injury.
Three patient advocacy groups have filed suit in federal court seeking to block the work requirements.
Robin Rudowitz, associate director for the Kaiser Family Foundation’s Program on Medicaid and the Uninsured, said it’s difficult to gauge whether work requirements or renewal lockouts will have more of an impact on coverage. She noted both provisions apply to most demonstration beneficiaries. (KHN is an editorially independent program of the foundation).
“Any documentation requirement could lead to increased complexity in terms of states administering the requirements and individuals complying,” she said, adding that it could result “in potentially eligible people falling off of coverage.”
Kaiser Health News (KHN) is a national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation which is not affiliated with Kaiser Permanente.
Trump administration clears way to require work for some Medicaid enrollees
The Trump administration early on Jan. 11 initiated a pivotal change in the Medicaid program, announcing that
The announcement came in a 10-page memo with detailed directions about how states can reshape the federal-state health program for low-income people.
The document says who should be excluded from the new work requirements – including children and people being treated for opioid abuse – and offers suggestions as to what counts as “work.” Besides employment, it can include job training, volunteering, or caring for a close relative.
“Medicaid needs to be more flexible so that states can best address the needs of this population,” Seema Verma, administrator of the Centers for Medicare & Medicaid Services, said in a press release. “Our fundamental goal is to make a positive and lasting difference in the health and wellness of our beneficiaries.”
Adding a work requirement to Medicaid would mark one of the biggest changes to the program since its inception in 1966. It is likely to prompt a lawsuit from patient advocacy groups, which claim the requirement is inconsistent with Medicaid’s objectives and would require an act of Congress.
Republicans have been pushing for the change since the Affordable Care Act added millions of so called “able-bodied” adults to Medicaid. It allowed states to provide coverage to anyone earning up to 138% of the federal poverty level (about $16,600 for an individual).
The Obama administration turned down several state requests to add a work requirement.
Ten states have applied for a federal waiver to add a work requirement – Arizona, Arkansas, Indiana, Kansas, Kentucky, Maine, New Hampshire, North Carolina, Utah and Wisconsin. Officials in several other states have said they are interested in the idea.
An HHS official, who spoke on the condition of anonymity because the official had not been authorized to discuss the developments, said the agency may approve Kentucky’s request as early asJan. 12. Gov. Matt Bevin, a Republican, first sought to add such a provision in 2016. The current request would require able-bodied adults without dependents to work at least 20 hours a week.
Kentucky, which has some of the poorest counties in the country, has seen its Medicaid enrollment double in the past 3 years after the state expanded eligibility under the ACA.
While more than 74 million people are enrolled in Medicaid, only a small fraction would be affected by the work requirement. That’s because children – who make up nearly half of Medicaid enrollees – are excluded. So are the more than 10 million people on Medicaid because they have a disability.
More than 4 in 10 adults with Medicaid coverage already work full time, and most others either go to school, take care of a relative, or are too sick to work.
Still, critics fear a work requirement could have a chilling effect on people signing up for Medicaid or make it harder for people to get coverage.
But work requirements have strong public backing. About 70% of Americans say they support states imposing a work requirement on non-disabled adults, according to a Kaiser Family Foundation poll last year.
The Trump administration, along with many Republican leaders in Congress, has long supported such a move. The failed efforts in the House to replace Obamacare included a work requirement for Medicaid.
In its guidance to states, CMS said they should consider how some communities have high unemployment rates and whether enrollees need to care for young children and elderly families.
CMS also advised states to make work requirements for Medicaid similar than those used with food stamps to “reduce the burden on both states and beneficiaries.”
“This new guidance paves the way for states to demonstrate how their ideas will improve the health of Medicaid beneficiaries, as well as potentially improve their economic well-being,” Brian Neale, CMS deputy administrator and director for the Center for Medicaid and CHIP Services, said in the press release.
Ms. Verma, who has said she doesn’t think Medicaid should become a way of life for people who are not disabled, said the new guidance shows how the administration is trying to give states more flexibility in running Medicaid.
“Our policy guidance was in response to states that asked us for the flexibility they need to improve their programs and to help people in achieving greater well-being and self-sufficiency,” she said.
Ms. Verma, who worked with Kentucky and Indiana on their work requirement waivers as a health consultant before joining the Trump administration, recused herself from the decision on those states’ waiver requests.
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of the Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
The Trump administration early on Jan. 11 initiated a pivotal change in the Medicaid program, announcing that
The announcement came in a 10-page memo with detailed directions about how states can reshape the federal-state health program for low-income people.
The document says who should be excluded from the new work requirements – including children and people being treated for opioid abuse – and offers suggestions as to what counts as “work.” Besides employment, it can include job training, volunteering, or caring for a close relative.
“Medicaid needs to be more flexible so that states can best address the needs of this population,” Seema Verma, administrator of the Centers for Medicare & Medicaid Services, said in a press release. “Our fundamental goal is to make a positive and lasting difference in the health and wellness of our beneficiaries.”
Adding a work requirement to Medicaid would mark one of the biggest changes to the program since its inception in 1966. It is likely to prompt a lawsuit from patient advocacy groups, which claim the requirement is inconsistent with Medicaid’s objectives and would require an act of Congress.
Republicans have been pushing for the change since the Affordable Care Act added millions of so called “able-bodied” adults to Medicaid. It allowed states to provide coverage to anyone earning up to 138% of the federal poverty level (about $16,600 for an individual).
The Obama administration turned down several state requests to add a work requirement.
Ten states have applied for a federal waiver to add a work requirement – Arizona, Arkansas, Indiana, Kansas, Kentucky, Maine, New Hampshire, North Carolina, Utah and Wisconsin. Officials in several other states have said they are interested in the idea.
An HHS official, who spoke on the condition of anonymity because the official had not been authorized to discuss the developments, said the agency may approve Kentucky’s request as early asJan. 12. Gov. Matt Bevin, a Republican, first sought to add such a provision in 2016. The current request would require able-bodied adults without dependents to work at least 20 hours a week.
Kentucky, which has some of the poorest counties in the country, has seen its Medicaid enrollment double in the past 3 years after the state expanded eligibility under the ACA.
While more than 74 million people are enrolled in Medicaid, only a small fraction would be affected by the work requirement. That’s because children – who make up nearly half of Medicaid enrollees – are excluded. So are the more than 10 million people on Medicaid because they have a disability.
More than 4 in 10 adults with Medicaid coverage already work full time, and most others either go to school, take care of a relative, or are too sick to work.
Still, critics fear a work requirement could have a chilling effect on people signing up for Medicaid or make it harder for people to get coverage.
But work requirements have strong public backing. About 70% of Americans say they support states imposing a work requirement on non-disabled adults, according to a Kaiser Family Foundation poll last year.
The Trump administration, along with many Republican leaders in Congress, has long supported such a move. The failed efforts in the House to replace Obamacare included a work requirement for Medicaid.
In its guidance to states, CMS said they should consider how some communities have high unemployment rates and whether enrollees need to care for young children and elderly families.
CMS also advised states to make work requirements for Medicaid similar than those used with food stamps to “reduce the burden on both states and beneficiaries.”
“This new guidance paves the way for states to demonstrate how their ideas will improve the health of Medicaid beneficiaries, as well as potentially improve their economic well-being,” Brian Neale, CMS deputy administrator and director for the Center for Medicaid and CHIP Services, said in the press release.
Ms. Verma, who has said she doesn’t think Medicaid should become a way of life for people who are not disabled, said the new guidance shows how the administration is trying to give states more flexibility in running Medicaid.
“Our policy guidance was in response to states that asked us for the flexibility they need to improve their programs and to help people in achieving greater well-being and self-sufficiency,” she said.
Ms. Verma, who worked with Kentucky and Indiana on their work requirement waivers as a health consultant before joining the Trump administration, recused herself from the decision on those states’ waiver requests.
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of the Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
The Trump administration early on Jan. 11 initiated a pivotal change in the Medicaid program, announcing that
The announcement came in a 10-page memo with detailed directions about how states can reshape the federal-state health program for low-income people.
The document says who should be excluded from the new work requirements – including children and people being treated for opioid abuse – and offers suggestions as to what counts as “work.” Besides employment, it can include job training, volunteering, or caring for a close relative.
“Medicaid needs to be more flexible so that states can best address the needs of this population,” Seema Verma, administrator of the Centers for Medicare & Medicaid Services, said in a press release. “Our fundamental goal is to make a positive and lasting difference in the health and wellness of our beneficiaries.”
Adding a work requirement to Medicaid would mark one of the biggest changes to the program since its inception in 1966. It is likely to prompt a lawsuit from patient advocacy groups, which claim the requirement is inconsistent with Medicaid’s objectives and would require an act of Congress.
Republicans have been pushing for the change since the Affordable Care Act added millions of so called “able-bodied” adults to Medicaid. It allowed states to provide coverage to anyone earning up to 138% of the federal poverty level (about $16,600 for an individual).
The Obama administration turned down several state requests to add a work requirement.
Ten states have applied for a federal waiver to add a work requirement – Arizona, Arkansas, Indiana, Kansas, Kentucky, Maine, New Hampshire, North Carolina, Utah and Wisconsin. Officials in several other states have said they are interested in the idea.
An HHS official, who spoke on the condition of anonymity because the official had not been authorized to discuss the developments, said the agency may approve Kentucky’s request as early asJan. 12. Gov. Matt Bevin, a Republican, first sought to add such a provision in 2016. The current request would require able-bodied adults without dependents to work at least 20 hours a week.
Kentucky, which has some of the poorest counties in the country, has seen its Medicaid enrollment double in the past 3 years after the state expanded eligibility under the ACA.
While more than 74 million people are enrolled in Medicaid, only a small fraction would be affected by the work requirement. That’s because children – who make up nearly half of Medicaid enrollees – are excluded. So are the more than 10 million people on Medicaid because they have a disability.
More than 4 in 10 adults with Medicaid coverage already work full time, and most others either go to school, take care of a relative, or are too sick to work.
Still, critics fear a work requirement could have a chilling effect on people signing up for Medicaid or make it harder for people to get coverage.
But work requirements have strong public backing. About 70% of Americans say they support states imposing a work requirement on non-disabled adults, according to a Kaiser Family Foundation poll last year.
The Trump administration, along with many Republican leaders in Congress, has long supported such a move. The failed efforts in the House to replace Obamacare included a work requirement for Medicaid.
In its guidance to states, CMS said they should consider how some communities have high unemployment rates and whether enrollees need to care for young children and elderly families.
CMS also advised states to make work requirements for Medicaid similar than those used with food stamps to “reduce the burden on both states and beneficiaries.”
“This new guidance paves the way for states to demonstrate how their ideas will improve the health of Medicaid beneficiaries, as well as potentially improve their economic well-being,” Brian Neale, CMS deputy administrator and director for the Center for Medicaid and CHIP Services, said in the press release.
Ms. Verma, who has said she doesn’t think Medicaid should become a way of life for people who are not disabled, said the new guidance shows how the administration is trying to give states more flexibility in running Medicaid.
“Our policy guidance was in response to states that asked us for the flexibility they need to improve their programs and to help people in achieving greater well-being and self-sufficiency,” she said.
Ms. Verma, who worked with Kentucky and Indiana on their work requirement waivers as a health consultant before joining the Trump administration, recused herself from the decision on those states’ waiver requests.
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of the Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
Running on empty: CHIP funding could run out Jan. 19 for some states
Some states are facing a mid-January loss of funding for their Children’s Health Insurance Program (CHIP) despite spending approved by Congress in late December that was expected to keep the program running for 3 months, federal health officials said Jan. 5.
The $2.85 billion was supposed to fund states’ CHIP programs through March 31. But some states will start running out of money after Jan. 19, according to the Centers for Medicare & Medicaid Services. The CMS did not say which states are likely to be affected first.
The latest estimates for when federal funding runs out could cause states to soon freeze enrollment and alert parents that the program could soon shut down.
The CHIP program provides health coverage to 9 million children from lower-income households that make too much money to qualify for Medicaid. Its federal authorization ended Oct. 1, and states were then forced to use unspent funds to carry them over while the House and Senate try to agree on a way to continue funding.
Congress extended funding on Dec. 21 and touted that states would have money to last while Congress worked on a long-term funding solution. But the CMS said on Jan. 5 it could only guarantee that the appropriation will be enough to fund all states through Jan. 19.
The CMS said the agency is in discussions with states to help deal with the funding shortfall.
“The funding … should carry all the states through January 19th based upon best estimates of state expenditures to date,” said CMS spokesman Johnathan Monroe. “However, due to a number of variables relating to state expenditure rates and reporting, we are unable to say with certainty whether there is enough funding for every state to continue its CHIP program through March 31, 2018.”
“States need to know whether they will need to find additional funding for children covered under the Medicaid CHIP program at a much lower federal matching rate, send letters to families, and re-program their eligibility systems,” said Lisa Dubay, a senior fellow at the Urban Institute. “Of course, the implications for families with CHIP-eligible children cannot be understated: Parents are worried that their children will lose coverage. And they should be.”
Although the program enjoys bipartisan support on Capitol Hill, the Republican-controlled House and Senate have for months been unable to agree on how to continue funding CHIP, which began in 1997.
The House plan includes a controversial funding provision – opposed by Democrats -– that takes millions of dollars from the Affordable Care Act’s Prevention and Public Health Fund and increases Medicare premiums for some higher-earning beneficiaries.
The Senate Finance Committee reached an agreement to extend the program for 5 years but did not unite around a plan on funding.
Before the CHIP funding extension on Dec. 21, Alabama said it would freeze enrollment Jan. 1 and shut down the program Jan. 31. Colorado, Connecticut, and Virginia sent letters to CHIP families warning that the program could soon end.
After the funding extension, Alabama put a hold on shutting down CHIP.
“Some states will begin exhausting all available funding earlier than others,” a CMS official said Jan. 5. “But the exact timing of when states will exhaust their funding is a moving target.”
Bruce Lesley, president of First Focus, a child advocacy group, said Congress should have known its short-term funding plan was not enough.
“The math never worked on the patch, as it only bought a few weeks,” he said. “Congress must get this finalized before Jan. 19.”
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of the Kaiser Family Foundation that is not affiliated with Kaiser Permanente. KHN’s coverage of children’s health care issues is supported in part by the Heising-Simons Foundation.
Some states are facing a mid-January loss of funding for their Children’s Health Insurance Program (CHIP) despite spending approved by Congress in late December that was expected to keep the program running for 3 months, federal health officials said Jan. 5.
The $2.85 billion was supposed to fund states’ CHIP programs through March 31. But some states will start running out of money after Jan. 19, according to the Centers for Medicare & Medicaid Services. The CMS did not say which states are likely to be affected first.
The latest estimates for when federal funding runs out could cause states to soon freeze enrollment and alert parents that the program could soon shut down.
The CHIP program provides health coverage to 9 million children from lower-income households that make too much money to qualify for Medicaid. Its federal authorization ended Oct. 1, and states were then forced to use unspent funds to carry them over while the House and Senate try to agree on a way to continue funding.
Congress extended funding on Dec. 21 and touted that states would have money to last while Congress worked on a long-term funding solution. But the CMS said on Jan. 5 it could only guarantee that the appropriation will be enough to fund all states through Jan. 19.
The CMS said the agency is in discussions with states to help deal with the funding shortfall.
“The funding … should carry all the states through January 19th based upon best estimates of state expenditures to date,” said CMS spokesman Johnathan Monroe. “However, due to a number of variables relating to state expenditure rates and reporting, we are unable to say with certainty whether there is enough funding for every state to continue its CHIP program through March 31, 2018.”
“States need to know whether they will need to find additional funding for children covered under the Medicaid CHIP program at a much lower federal matching rate, send letters to families, and re-program their eligibility systems,” said Lisa Dubay, a senior fellow at the Urban Institute. “Of course, the implications for families with CHIP-eligible children cannot be understated: Parents are worried that their children will lose coverage. And they should be.”
Although the program enjoys bipartisan support on Capitol Hill, the Republican-controlled House and Senate have for months been unable to agree on how to continue funding CHIP, which began in 1997.
The House plan includes a controversial funding provision – opposed by Democrats -– that takes millions of dollars from the Affordable Care Act’s Prevention and Public Health Fund and increases Medicare premiums for some higher-earning beneficiaries.
The Senate Finance Committee reached an agreement to extend the program for 5 years but did not unite around a plan on funding.
Before the CHIP funding extension on Dec. 21, Alabama said it would freeze enrollment Jan. 1 and shut down the program Jan. 31. Colorado, Connecticut, and Virginia sent letters to CHIP families warning that the program could soon end.
After the funding extension, Alabama put a hold on shutting down CHIP.
“Some states will begin exhausting all available funding earlier than others,” a CMS official said Jan. 5. “But the exact timing of when states will exhaust their funding is a moving target.”
Bruce Lesley, president of First Focus, a child advocacy group, said Congress should have known its short-term funding plan was not enough.
“The math never worked on the patch, as it only bought a few weeks,” he said. “Congress must get this finalized before Jan. 19.”
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of the Kaiser Family Foundation that is not affiliated with Kaiser Permanente. KHN’s coverage of children’s health care issues is supported in part by the Heising-Simons Foundation.
Some states are facing a mid-January loss of funding for their Children’s Health Insurance Program (CHIP) despite spending approved by Congress in late December that was expected to keep the program running for 3 months, federal health officials said Jan. 5.
The $2.85 billion was supposed to fund states’ CHIP programs through March 31. But some states will start running out of money after Jan. 19, according to the Centers for Medicare & Medicaid Services. The CMS did not say which states are likely to be affected first.
The latest estimates for when federal funding runs out could cause states to soon freeze enrollment and alert parents that the program could soon shut down.
The CHIP program provides health coverage to 9 million children from lower-income households that make too much money to qualify for Medicaid. Its federal authorization ended Oct. 1, and states were then forced to use unspent funds to carry them over while the House and Senate try to agree on a way to continue funding.
Congress extended funding on Dec. 21 and touted that states would have money to last while Congress worked on a long-term funding solution. But the CMS said on Jan. 5 it could only guarantee that the appropriation will be enough to fund all states through Jan. 19.
The CMS said the agency is in discussions with states to help deal with the funding shortfall.
“The funding … should carry all the states through January 19th based upon best estimates of state expenditures to date,” said CMS spokesman Johnathan Monroe. “However, due to a number of variables relating to state expenditure rates and reporting, we are unable to say with certainty whether there is enough funding for every state to continue its CHIP program through March 31, 2018.”
“States need to know whether they will need to find additional funding for children covered under the Medicaid CHIP program at a much lower federal matching rate, send letters to families, and re-program their eligibility systems,” said Lisa Dubay, a senior fellow at the Urban Institute. “Of course, the implications for families with CHIP-eligible children cannot be understated: Parents are worried that their children will lose coverage. And they should be.”
Although the program enjoys bipartisan support on Capitol Hill, the Republican-controlled House and Senate have for months been unable to agree on how to continue funding CHIP, which began in 1997.
The House plan includes a controversial funding provision – opposed by Democrats -– that takes millions of dollars from the Affordable Care Act’s Prevention and Public Health Fund and increases Medicare premiums for some higher-earning beneficiaries.
The Senate Finance Committee reached an agreement to extend the program for 5 years but did not unite around a plan on funding.
Before the CHIP funding extension on Dec. 21, Alabama said it would freeze enrollment Jan. 1 and shut down the program Jan. 31. Colorado, Connecticut, and Virginia sent letters to CHIP families warning that the program could soon end.
After the funding extension, Alabama put a hold on shutting down CHIP.
“Some states will begin exhausting all available funding earlier than others,” a CMS official said Jan. 5. “But the exact timing of when states will exhaust their funding is a moving target.”
Bruce Lesley, president of First Focus, a child advocacy group, said Congress should have known its short-term funding plan was not enough.
“The math never worked on the patch, as it only bought a few weeks,” he said. “Congress must get this finalized before Jan. 19.”
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of the Kaiser Family Foundation that is not affiliated with Kaiser Permanente. KHN’s coverage of children’s health care issues is supported in part by the Heising-Simons Foundation.
With CHIP in limbo, here are five takeaways on the congressional impasse
Two months past its deadline, Congress has yet to fund the Children’s Health Insurance Program, leaving several states scrambling for cash.
Lawmakers grappling with the failed repeal of the Affordable Care Act allowed authorization of the program to lapse on Sept. 30. Although CHIP has always had broad bipartisan support, the House and Senate cannot agree on how to continue federal funding. And the Trump administration has been mostly silent on the issue.
CHIP benefits 9 million children nationwide and 370,000 pregnant women a year. It helps lower- and middle-income families who otherwise earn too much to be eligible for Medicaid. Like Medicaid, CHIP is paid for with state and federal funds, but the federal government covers close to 90% of the cost.
To keep the program going, states with unspent federal CHIP money have seen their excess sent to a handful of states running low on funds. But that is a bureaucratic Band-Aid; some large states are warning families they may not be able to rely on CHIP for much longer.
All told, the CMS has given out $1.2 billion in redistribution dollars since October. To keep the program going would cost the federal government $8.5 billion over 5 years, the Congressional Budget Office estimates.
Dec. 2 marked the 25th anniversary of Pennsylvania approving the original CHIP program, which served as a model for the national law, established in 1997. Since then, CHIP has been left in the fiscal lurch only once before. In 2007, CHIP went several weeks without funding authorization from Congress.
Here’s a quick look at what the shortfall may mean to daily life.
1. Are any kids hurting because Congress has failed to fund CHIP?
No. But states such as California will run out of money within weeks. That state alone accounts for nearly 15% of all children benefiting from CHIP. Without federal money, state programs could freeze enrollment or suspend operation.
2. What are states doing since Congress missed the deadline?
Most states are doing little except looking for other unspent federal funds or asking the federal government to send some unspent funds from other states. But some, such as Colorado, are sending warning letters to beneficiaries to tell them that the program could soon end and to look for alternatives. This could mean exploring the ACA marketplace for coverage or researching if a child qualifies for Medicaid.
Colorado said it has only enough CHIP funding to last through January and then the program, without federal dollars, will end.
Arizona officials announced Nov. 30 that it will use Medicaid funding to fill in the shortage of CHIP dollars to extend the life of its CHIP program.
Virginia officials plan to send out a similar notice to parents of CHIP members by early December.
Minnesota is keeping CHIP alive by paying the federal share with state funds.
In Oregon, Democratic Gov. Kate Brown recently said that she is ready to spend $35 million in state funds to keep CHIP running through December.
Nevada announced on Nov. 30 it had been approved for extra funding from the Centers for Medicare & Medicaid Services – nearly $5.7 million – which could keep CHIP alive through December and possibly January.
California, which leads the nation in CHIP enrollment, has received the lion’s share of CMS redistribution funds since October: nearly $692 million.
“Approximately 98% of the 1.3 million population now covered using CHIP funding would continue to receive coverage under the Medicaid program because of a legal obligation to cover them through September 2019,” said California Medicaid/CHIP spokesman Tony Cava. “If CHIP is not reauthorized, the governor and Legislature would need to deliberate on how best to address the population no longer eligible for federal CHIP funding.”
3. When is Congress likely to act?
Not sure. CHIP reauthorization could be included in an appropriations bill that Congress must pass to fund the government into 2018. (Congress now has funded the government through Dec. 8.) A “continuing resolution” bill would have to be approved by then to avert a government shutdown.
4. If CHIP is so popular among Republicans and Democrats, what’s the problem?
There is little debate about its worth and value, but the momentum on CHIP was lost amid disagreements over the Affordable Care Act. The House did extend authorization with a vote – mostly along party lines – on Nov. 3. The Senate itself has yet to vote. The Senate Finance Committee on Oct. 3 approved a bipartisan bill to extend the program for 5 years.
The sticking point is not whether to keep CHIP running but how to raise the cash needed. The House agreed to charge higher premiums to wealthier Medicare beneficiaries, cut money from the ACA’s preventive health fund and shorten the grace period for ACA enrollees who fail to make monthly premium payments.
Like the House bill, the Senate committee bill eliminated an ACA provision to increase CHIP matching funds – to states – by 23%. The increased funding would continue through fiscal year 2019 and fall to 11.5 percent in fiscal year 2020. It would be cut entirely in the following fiscal year.
5. How does CHIP differ based on where you live?
CHIP income eligibility levels vary by state. About 90% of children who qualify are from families earning 200% of poverty or less ($40,840 for a family of three). CHIP covers children up to age 19. But states have the option to cover pregnant women, and 18 states plus the District of Columbia do so.
Some states call CHIP by different names. For example, it is known as Hoosier Healthwise in Indiana, PeachCare for Kids in Georgia and KidsCare in Arizona.
KHN’s coverage of children’s health care issues is supported in part by the Heising-Simons Foundation. Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of the Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
Two months past its deadline, Congress has yet to fund the Children’s Health Insurance Program, leaving several states scrambling for cash.
Lawmakers grappling with the failed repeal of the Affordable Care Act allowed authorization of the program to lapse on Sept. 30. Although CHIP has always had broad bipartisan support, the House and Senate cannot agree on how to continue federal funding. And the Trump administration has been mostly silent on the issue.
CHIP benefits 9 million children nationwide and 370,000 pregnant women a year. It helps lower- and middle-income families who otherwise earn too much to be eligible for Medicaid. Like Medicaid, CHIP is paid for with state and federal funds, but the federal government covers close to 90% of the cost.
To keep the program going, states with unspent federal CHIP money have seen their excess sent to a handful of states running low on funds. But that is a bureaucratic Band-Aid; some large states are warning families they may not be able to rely on CHIP for much longer.
All told, the CMS has given out $1.2 billion in redistribution dollars since October. To keep the program going would cost the federal government $8.5 billion over 5 years, the Congressional Budget Office estimates.
Dec. 2 marked the 25th anniversary of Pennsylvania approving the original CHIP program, which served as a model for the national law, established in 1997. Since then, CHIP has been left in the fiscal lurch only once before. In 2007, CHIP went several weeks without funding authorization from Congress.
Here’s a quick look at what the shortfall may mean to daily life.
1. Are any kids hurting because Congress has failed to fund CHIP?
No. But states such as California will run out of money within weeks. That state alone accounts for nearly 15% of all children benefiting from CHIP. Without federal money, state programs could freeze enrollment or suspend operation.
2. What are states doing since Congress missed the deadline?
Most states are doing little except looking for other unspent federal funds or asking the federal government to send some unspent funds from other states. But some, such as Colorado, are sending warning letters to beneficiaries to tell them that the program could soon end and to look for alternatives. This could mean exploring the ACA marketplace for coverage or researching if a child qualifies for Medicaid.
Colorado said it has only enough CHIP funding to last through January and then the program, without federal dollars, will end.
Arizona officials announced Nov. 30 that it will use Medicaid funding to fill in the shortage of CHIP dollars to extend the life of its CHIP program.
Virginia officials plan to send out a similar notice to parents of CHIP members by early December.
Minnesota is keeping CHIP alive by paying the federal share with state funds.
In Oregon, Democratic Gov. Kate Brown recently said that she is ready to spend $35 million in state funds to keep CHIP running through December.
Nevada announced on Nov. 30 it had been approved for extra funding from the Centers for Medicare & Medicaid Services – nearly $5.7 million – which could keep CHIP alive through December and possibly January.
California, which leads the nation in CHIP enrollment, has received the lion’s share of CMS redistribution funds since October: nearly $692 million.
“Approximately 98% of the 1.3 million population now covered using CHIP funding would continue to receive coverage under the Medicaid program because of a legal obligation to cover them through September 2019,” said California Medicaid/CHIP spokesman Tony Cava. “If CHIP is not reauthorized, the governor and Legislature would need to deliberate on how best to address the population no longer eligible for federal CHIP funding.”
3. When is Congress likely to act?
Not sure. CHIP reauthorization could be included in an appropriations bill that Congress must pass to fund the government into 2018. (Congress now has funded the government through Dec. 8.) A “continuing resolution” bill would have to be approved by then to avert a government shutdown.
4. If CHIP is so popular among Republicans and Democrats, what’s the problem?
There is little debate about its worth and value, but the momentum on CHIP was lost amid disagreements over the Affordable Care Act. The House did extend authorization with a vote – mostly along party lines – on Nov. 3. The Senate itself has yet to vote. The Senate Finance Committee on Oct. 3 approved a bipartisan bill to extend the program for 5 years.
The sticking point is not whether to keep CHIP running but how to raise the cash needed. The House agreed to charge higher premiums to wealthier Medicare beneficiaries, cut money from the ACA’s preventive health fund and shorten the grace period for ACA enrollees who fail to make monthly premium payments.
Like the House bill, the Senate committee bill eliminated an ACA provision to increase CHIP matching funds – to states – by 23%. The increased funding would continue through fiscal year 2019 and fall to 11.5 percent in fiscal year 2020. It would be cut entirely in the following fiscal year.
5. How does CHIP differ based on where you live?
CHIP income eligibility levels vary by state. About 90% of children who qualify are from families earning 200% of poverty or less ($40,840 for a family of three). CHIP covers children up to age 19. But states have the option to cover pregnant women, and 18 states plus the District of Columbia do so.
Some states call CHIP by different names. For example, it is known as Hoosier Healthwise in Indiana, PeachCare for Kids in Georgia and KidsCare in Arizona.
KHN’s coverage of children’s health care issues is supported in part by the Heising-Simons Foundation. Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of the Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
Two months past its deadline, Congress has yet to fund the Children’s Health Insurance Program, leaving several states scrambling for cash.
Lawmakers grappling with the failed repeal of the Affordable Care Act allowed authorization of the program to lapse on Sept. 30. Although CHIP has always had broad bipartisan support, the House and Senate cannot agree on how to continue federal funding. And the Trump administration has been mostly silent on the issue.
CHIP benefits 9 million children nationwide and 370,000 pregnant women a year. It helps lower- and middle-income families who otherwise earn too much to be eligible for Medicaid. Like Medicaid, CHIP is paid for with state and federal funds, but the federal government covers close to 90% of the cost.
To keep the program going, states with unspent federal CHIP money have seen their excess sent to a handful of states running low on funds. But that is a bureaucratic Band-Aid; some large states are warning families they may not be able to rely on CHIP for much longer.
All told, the CMS has given out $1.2 billion in redistribution dollars since October. To keep the program going would cost the federal government $8.5 billion over 5 years, the Congressional Budget Office estimates.
Dec. 2 marked the 25th anniversary of Pennsylvania approving the original CHIP program, which served as a model for the national law, established in 1997. Since then, CHIP has been left in the fiscal lurch only once before. In 2007, CHIP went several weeks without funding authorization from Congress.
Here’s a quick look at what the shortfall may mean to daily life.
1. Are any kids hurting because Congress has failed to fund CHIP?
No. But states such as California will run out of money within weeks. That state alone accounts for nearly 15% of all children benefiting from CHIP. Without federal money, state programs could freeze enrollment or suspend operation.
2. What are states doing since Congress missed the deadline?
Most states are doing little except looking for other unspent federal funds or asking the federal government to send some unspent funds from other states. But some, such as Colorado, are sending warning letters to beneficiaries to tell them that the program could soon end and to look for alternatives. This could mean exploring the ACA marketplace for coverage or researching if a child qualifies for Medicaid.
Colorado said it has only enough CHIP funding to last through January and then the program, without federal dollars, will end.
Arizona officials announced Nov. 30 that it will use Medicaid funding to fill in the shortage of CHIP dollars to extend the life of its CHIP program.
Virginia officials plan to send out a similar notice to parents of CHIP members by early December.
Minnesota is keeping CHIP alive by paying the federal share with state funds.
In Oregon, Democratic Gov. Kate Brown recently said that she is ready to spend $35 million in state funds to keep CHIP running through December.
Nevada announced on Nov. 30 it had been approved for extra funding from the Centers for Medicare & Medicaid Services – nearly $5.7 million – which could keep CHIP alive through December and possibly January.
California, which leads the nation in CHIP enrollment, has received the lion’s share of CMS redistribution funds since October: nearly $692 million.
“Approximately 98% of the 1.3 million population now covered using CHIP funding would continue to receive coverage under the Medicaid program because of a legal obligation to cover them through September 2019,” said California Medicaid/CHIP spokesman Tony Cava. “If CHIP is not reauthorized, the governor and Legislature would need to deliberate on how best to address the population no longer eligible for federal CHIP funding.”
3. When is Congress likely to act?
Not sure. CHIP reauthorization could be included in an appropriations bill that Congress must pass to fund the government into 2018. (Congress now has funded the government through Dec. 8.) A “continuing resolution” bill would have to be approved by then to avert a government shutdown.
4. If CHIP is so popular among Republicans and Democrats, what’s the problem?
There is little debate about its worth and value, but the momentum on CHIP was lost amid disagreements over the Affordable Care Act. The House did extend authorization with a vote – mostly along party lines – on Nov. 3. The Senate itself has yet to vote. The Senate Finance Committee on Oct. 3 approved a bipartisan bill to extend the program for 5 years.
The sticking point is not whether to keep CHIP running but how to raise the cash needed. The House agreed to charge higher premiums to wealthier Medicare beneficiaries, cut money from the ACA’s preventive health fund and shorten the grace period for ACA enrollees who fail to make monthly premium payments.
Like the House bill, the Senate committee bill eliminated an ACA provision to increase CHIP matching funds – to states – by 23%. The increased funding would continue through fiscal year 2019 and fall to 11.5 percent in fiscal year 2020. It would be cut entirely in the following fiscal year.
5. How does CHIP differ based on where you live?
CHIP income eligibility levels vary by state. About 90% of children who qualify are from families earning 200% of poverty or less ($40,840 for a family of three). CHIP covers children up to age 19. But states have the option to cover pregnant women, and 18 states plus the District of Columbia do so.
Some states call CHIP by different names. For example, it is known as Hoosier Healthwise in Indiana, PeachCare for Kids in Georgia and KidsCare in Arizona.
KHN’s coverage of children’s health care issues is supported in part by the Heising-Simons Foundation. Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of the Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
Five takeaways from Congress’ failure to extend funding for children’s coverage
Congress finally seems ready to take action on the Children’s Health Insurance Program after funding lapsed Sept. 30.
Before the deadline, lawmakers were busy grappling with the failed repeal of the Affordable Care Act.
CHIP covers 9 million children nationwide. But until Congress renews CHIP, states are cut off from additional federal funding that helps lower- and middle-income families.
CHIP, which has enjoyed broad bipartisan support, helps lower- and middle-income families that otherwise earn too much to be eligible for Medicaid. Besides children, it covers 370,000 pregnant women a year. Like Medicaid, CHIP is traditionally paid for with state and federal funds, but the federal government covers most of the cost.
Though current authorization for spending has expired, states can use some of their unspent federal CHIP money. Still, several states are expected to run out of money before the end of 2017, and most of the rest will run out by next summer. CHIP has been in this fix only one other time since it was established in 1997. In 2007, CHIP went weeks without funding authorization from Congress.
Here’s a quick look at what may lie ahead for the program.
1. Will children lose coverage because Congress missed the deadline?
They could eventually, but not immediately. A few states facing the most immediate threat – including California and Arizona – have enough funding to last only until the end of the year.
No states have yet announced plans to freeze enrollment or alert families about any potential end in coverage. But if Congress fails to renew funding quickly, some states may begin taking steps to unwind the program in the next few weeks.
2. What are states doing in reaction to Congress missing the deadline?
Most states are doing little except reaching into their unspent federal funds.
However, Minnesota was among those most imperiled because it had spent all its funds. State officials said Tuesday that the federal Centers for Medicare & Medicaid Services (CMS) was giving Minnesota $3.6 million from unspent national funds to cover CHIP this month.
Emily Piper, commissioner of the Minnesota Department of Human Services, reported in a newspaper commentary in September that her state’s funds would be exhausted by the end of that month.
Even without the last-minute infusion of funding from CMS, most of the children covered by CHIP would have continued to receive care under the state’s Medicaid program, but Minnesota would get fewer federal dollars for each child, according to Piper’s commentary. However, she added, those most at risk are the 1,700 pregnant women covered by CHIP, because they wouldn’t be eligible for Medicaid.
Utah has notified CMS that it plans to discontinue its CHIP program by the end of the year unless it receives more federal money. About 19,000 children are in the state’s CHIP program, state officials say. So far, though, the state said it is not moving to suspend service or enrollment or alert enrollees about any possible changes.
Nevada officials said if funding is not extended it might have to freeze enrollment on Nov. 1 and end coverage by Nov. 30.
California, which has 1.3 million children covered by CHIP, has the highest enrollment of any state running out of funding this year. But, so far, it’s continuing business as usual.
“We estimate that we have available CHIP funding at least through December 2017,” said Tony Cava, spokesman for California Department of Health Services. “Our CHIP program is open for enrollment and continues to operate normally.”
Oregon said it has enough CHIP funding to last through October for its program that covers 98,000 children.
3. When is Congress likely to act?
The Senate Finance and the House Energy and Commerce committees have scheduled votes Wednesday on legislation to extend CHIP funding. If both approve their individual bills, floor votes could come quickly, and then both houses would need to resolve any differences.
Senate Finance Committee Chairman Orrin Hatch (R-Utah) and the committee’s ranking Democrat, Sen. Ron Wyden of Oregon, announced an agreement in mid-September to renew CHIP funding. Under the proposed deal, federal CHIP funding would drop by 23 percentage points starting in by 2020, returning to its pre-Affordable Care Act levels. The agreement would extend the life of the CHIP program through 2022.
Hatch and Wyden did not provide any details on how they would pay for the CHIP extension.
The House Energy and Commerce Committee posted its bill just before midnight Monday. It mirrors the Senate Finance plan by extending funding for CHIP for five years and gradually phasing down the 23-percentage-point funding increase provided under Affordable Care Act over the next two years.
4. If CHIP is so popular among Republicans and Democrats, why hasn’t Congress renewed the program yet?
The funding renewal was not a priority among Republican leaders, who have spent most of this year trying to replace the Affordable Care Act and dramatically overhaul the Medicaid program. Some in Congress also thought the Sept. 30 deadline was squishy since states could extend their existing funds beyond that.
5. Who benefits from CHIP?
While CHIP income eligibility levels vary by state, about 90 percent of children covered are in families earning 200 percent of poverty or less ($40,840 for a family of three). CHIP covers children up to age 19. States have the option to cover pregnant women, and 18 plus the District of Columbia do so.
The program is known by different names in different states such as Hoosier Healthwise in Indiana and PeachCare for Kids in Georgia.
For families that move out of Medicaid as their incomes rise, CHIP is an affordable option that ensures continued coverage for their children. Many states operate their CHIP programs as part of Medicaid.
KHN’s coverage of children’s health care issues is supported in part by a grant from The Heising-Simons Foundation.
Kaiser Health News is a national health policy news service that is part of the nonpartisan Henry J. Kaiser Family Foundation.
Congress finally seems ready to take action on the Children’s Health Insurance Program after funding lapsed Sept. 30.
Before the deadline, lawmakers were busy grappling with the failed repeal of the Affordable Care Act.
CHIP covers 9 million children nationwide. But until Congress renews CHIP, states are cut off from additional federal funding that helps lower- and middle-income families.
CHIP, which has enjoyed broad bipartisan support, helps lower- and middle-income families that otherwise earn too much to be eligible for Medicaid. Besides children, it covers 370,000 pregnant women a year. Like Medicaid, CHIP is traditionally paid for with state and federal funds, but the federal government covers most of the cost.
Though current authorization for spending has expired, states can use some of their unspent federal CHIP money. Still, several states are expected to run out of money before the end of 2017, and most of the rest will run out by next summer. CHIP has been in this fix only one other time since it was established in 1997. In 2007, CHIP went weeks without funding authorization from Congress.
Here’s a quick look at what may lie ahead for the program.
1. Will children lose coverage because Congress missed the deadline?
They could eventually, but not immediately. A few states facing the most immediate threat – including California and Arizona – have enough funding to last only until the end of the year.
No states have yet announced plans to freeze enrollment or alert families about any potential end in coverage. But if Congress fails to renew funding quickly, some states may begin taking steps to unwind the program in the next few weeks.
2. What are states doing in reaction to Congress missing the deadline?
Most states are doing little except reaching into their unspent federal funds.
However, Minnesota was among those most imperiled because it had spent all its funds. State officials said Tuesday that the federal Centers for Medicare & Medicaid Services (CMS) was giving Minnesota $3.6 million from unspent national funds to cover CHIP this month.
Emily Piper, commissioner of the Minnesota Department of Human Services, reported in a newspaper commentary in September that her state’s funds would be exhausted by the end of that month.
Even without the last-minute infusion of funding from CMS, most of the children covered by CHIP would have continued to receive care under the state’s Medicaid program, but Minnesota would get fewer federal dollars for each child, according to Piper’s commentary. However, she added, those most at risk are the 1,700 pregnant women covered by CHIP, because they wouldn’t be eligible for Medicaid.
Utah has notified CMS that it plans to discontinue its CHIP program by the end of the year unless it receives more federal money. About 19,000 children are in the state’s CHIP program, state officials say. So far, though, the state said it is not moving to suspend service or enrollment or alert enrollees about any possible changes.
Nevada officials said if funding is not extended it might have to freeze enrollment on Nov. 1 and end coverage by Nov. 30.
California, which has 1.3 million children covered by CHIP, has the highest enrollment of any state running out of funding this year. But, so far, it’s continuing business as usual.
“We estimate that we have available CHIP funding at least through December 2017,” said Tony Cava, spokesman for California Department of Health Services. “Our CHIP program is open for enrollment and continues to operate normally.”
Oregon said it has enough CHIP funding to last through October for its program that covers 98,000 children.
3. When is Congress likely to act?
The Senate Finance and the House Energy and Commerce committees have scheduled votes Wednesday on legislation to extend CHIP funding. If both approve their individual bills, floor votes could come quickly, and then both houses would need to resolve any differences.
Senate Finance Committee Chairman Orrin Hatch (R-Utah) and the committee’s ranking Democrat, Sen. Ron Wyden of Oregon, announced an agreement in mid-September to renew CHIP funding. Under the proposed deal, federal CHIP funding would drop by 23 percentage points starting in by 2020, returning to its pre-Affordable Care Act levels. The agreement would extend the life of the CHIP program through 2022.
Hatch and Wyden did not provide any details on how they would pay for the CHIP extension.
The House Energy and Commerce Committee posted its bill just before midnight Monday. It mirrors the Senate Finance plan by extending funding for CHIP for five years and gradually phasing down the 23-percentage-point funding increase provided under Affordable Care Act over the next two years.
4. If CHIP is so popular among Republicans and Democrats, why hasn’t Congress renewed the program yet?
The funding renewal was not a priority among Republican leaders, who have spent most of this year trying to replace the Affordable Care Act and dramatically overhaul the Medicaid program. Some in Congress also thought the Sept. 30 deadline was squishy since states could extend their existing funds beyond that.
5. Who benefits from CHIP?
While CHIP income eligibility levels vary by state, about 90 percent of children covered are in families earning 200 percent of poverty or less ($40,840 for a family of three). CHIP covers children up to age 19. States have the option to cover pregnant women, and 18 plus the District of Columbia do so.
The program is known by different names in different states such as Hoosier Healthwise in Indiana and PeachCare for Kids in Georgia.
For families that move out of Medicaid as their incomes rise, CHIP is an affordable option that ensures continued coverage for their children. Many states operate their CHIP programs as part of Medicaid.
KHN’s coverage of children’s health care issues is supported in part by a grant from The Heising-Simons Foundation.
Kaiser Health News is a national health policy news service that is part of the nonpartisan Henry J. Kaiser Family Foundation.
Congress finally seems ready to take action on the Children’s Health Insurance Program after funding lapsed Sept. 30.
Before the deadline, lawmakers were busy grappling with the failed repeal of the Affordable Care Act.
CHIP covers 9 million children nationwide. But until Congress renews CHIP, states are cut off from additional federal funding that helps lower- and middle-income families.
CHIP, which has enjoyed broad bipartisan support, helps lower- and middle-income families that otherwise earn too much to be eligible for Medicaid. Besides children, it covers 370,000 pregnant women a year. Like Medicaid, CHIP is traditionally paid for with state and federal funds, but the federal government covers most of the cost.
Though current authorization for spending has expired, states can use some of their unspent federal CHIP money. Still, several states are expected to run out of money before the end of 2017, and most of the rest will run out by next summer. CHIP has been in this fix only one other time since it was established in 1997. In 2007, CHIP went weeks without funding authorization from Congress.
Here’s a quick look at what may lie ahead for the program.
1. Will children lose coverage because Congress missed the deadline?
They could eventually, but not immediately. A few states facing the most immediate threat – including California and Arizona – have enough funding to last only until the end of the year.
No states have yet announced plans to freeze enrollment or alert families about any potential end in coverage. But if Congress fails to renew funding quickly, some states may begin taking steps to unwind the program in the next few weeks.
2. What are states doing in reaction to Congress missing the deadline?
Most states are doing little except reaching into their unspent federal funds.
However, Minnesota was among those most imperiled because it had spent all its funds. State officials said Tuesday that the federal Centers for Medicare & Medicaid Services (CMS) was giving Minnesota $3.6 million from unspent national funds to cover CHIP this month.
Emily Piper, commissioner of the Minnesota Department of Human Services, reported in a newspaper commentary in September that her state’s funds would be exhausted by the end of that month.
Even without the last-minute infusion of funding from CMS, most of the children covered by CHIP would have continued to receive care under the state’s Medicaid program, but Minnesota would get fewer federal dollars for each child, according to Piper’s commentary. However, she added, those most at risk are the 1,700 pregnant women covered by CHIP, because they wouldn’t be eligible for Medicaid.
Utah has notified CMS that it plans to discontinue its CHIP program by the end of the year unless it receives more federal money. About 19,000 children are in the state’s CHIP program, state officials say. So far, though, the state said it is not moving to suspend service or enrollment or alert enrollees about any possible changes.
Nevada officials said if funding is not extended it might have to freeze enrollment on Nov. 1 and end coverage by Nov. 30.
California, which has 1.3 million children covered by CHIP, has the highest enrollment of any state running out of funding this year. But, so far, it’s continuing business as usual.
“We estimate that we have available CHIP funding at least through December 2017,” said Tony Cava, spokesman for California Department of Health Services. “Our CHIP program is open for enrollment and continues to operate normally.”
Oregon said it has enough CHIP funding to last through October for its program that covers 98,000 children.
3. When is Congress likely to act?
The Senate Finance and the House Energy and Commerce committees have scheduled votes Wednesday on legislation to extend CHIP funding. If both approve their individual bills, floor votes could come quickly, and then both houses would need to resolve any differences.
Senate Finance Committee Chairman Orrin Hatch (R-Utah) and the committee’s ranking Democrat, Sen. Ron Wyden of Oregon, announced an agreement in mid-September to renew CHIP funding. Under the proposed deal, federal CHIP funding would drop by 23 percentage points starting in by 2020, returning to its pre-Affordable Care Act levels. The agreement would extend the life of the CHIP program through 2022.
Hatch and Wyden did not provide any details on how they would pay for the CHIP extension.
The House Energy and Commerce Committee posted its bill just before midnight Monday. It mirrors the Senate Finance plan by extending funding for CHIP for five years and gradually phasing down the 23-percentage-point funding increase provided under Affordable Care Act over the next two years.
4. If CHIP is so popular among Republicans and Democrats, why hasn’t Congress renewed the program yet?
The funding renewal was not a priority among Republican leaders, who have spent most of this year trying to replace the Affordable Care Act and dramatically overhaul the Medicaid program. Some in Congress also thought the Sept. 30 deadline was squishy since states could extend their existing funds beyond that.
5. Who benefits from CHIP?
While CHIP income eligibility levels vary by state, about 90 percent of children covered are in families earning 200 percent of poverty or less ($40,840 for a family of three). CHIP covers children up to age 19. States have the option to cover pregnant women, and 18 plus the District of Columbia do so.
The program is known by different names in different states such as Hoosier Healthwise in Indiana and PeachCare for Kids in Georgia.
For families that move out of Medicaid as their incomes rise, CHIP is an affordable option that ensures continued coverage for their children. Many states operate their CHIP programs as part of Medicaid.
KHN’s coverage of children’s health care issues is supported in part by a grant from The Heising-Simons Foundation.
Kaiser Health News is a national health policy news service that is part of the nonpartisan Henry J. Kaiser Family Foundation.
21 Medicare health plans warned to fix provider directory errors
Federal officials this month warned 21 Medicare Advantage insurers with high rates of errors in their online network directories that they could face heavy fines or have to stop enrolling people if the problems are not fixed by Feb. 6.
Among the plans that were cited are Blue Cross Blue Shield of Michigan, Highmark of Pennsylvania, SCAN Health Plan of California as well as some regional plans owned by national carriers such as UnitedHealthcare and Humana.
The action follows the government’s first in-depth review of the accuracy of Medicare Advantage provider directories, which consumers and advocates have complained about for years. More than 17 million Americans, or nearly a third of Medicare beneficiaries, get coverage through private Medicare Advantage plans.
The Centers for Medicare & Medicaid Services in October reported some of the results of the audit, but they had not released names or statistics from the individual plans.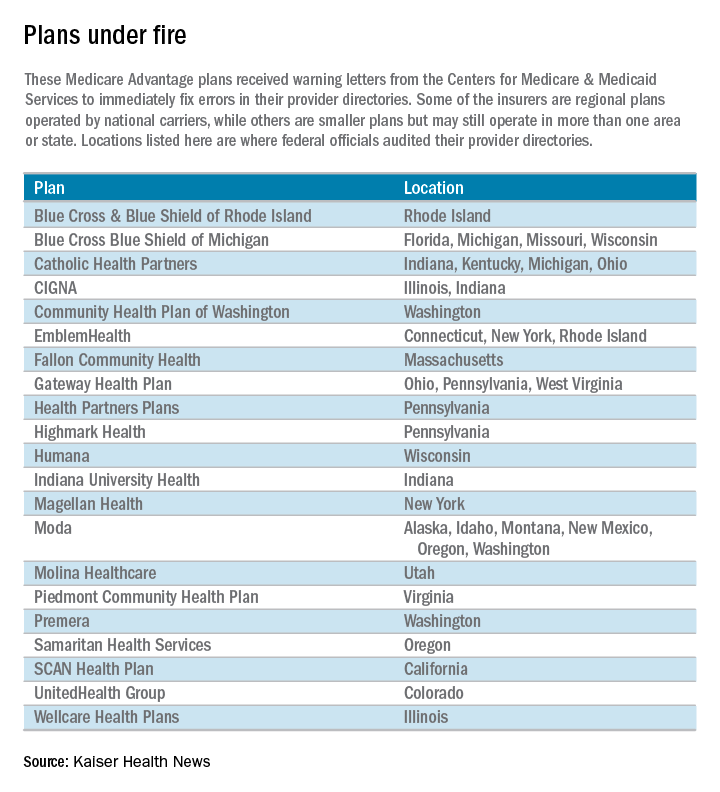
“Because Medicare Advantage members rely on provider directories to locate an in-network provider, these inaccuracies pose a significant access-to-care barrier,” Medicare officials wrote in a report outlining the problems.
Unlike traditional Medicare, the private Medicare plans typically restrict beneficiaries to a network of doctors and hospitals.
Piedmont Community Health Plan, a small Medicare plan with about 5,200 members in southwest Virginia, had the highest rate of inaccuracies among the 54 insurers examined. Officials found errors in the listings of 87 of 108 doctors checked in Piedmont’s directory, according to the report. Most of the errors involved providing the wrong locations for doctors and doctors who should not have been listed. Piedmont officials did not return calls for comment.
Piedmont and two other plans with the highest error rates – a WellCare plan in Illinois and Emblem Health’s ConnectiCare subsidiary – were required by Medicare to submit specific business plans detailing how they intend to address the issue.
The individual plans receiving warning letters cover more than 1.4 million beneficiaries. Most operate in numerous states, although CMS generally limited its review to a specific state or geographic area.
The federal review focused on primary care doctors, cardiologists, ophthalmologists, and oncologists. It involved individual calls to check on the listings for 108 doctors in each health plan. “We encountered several instances where a call to a provider’s office resulted in determining that the provider had been retired or deceased for a long period of time, sometimes years,” the report said.
Almost half of the 5,832 doctors listed had incorrect information, including wrong addresses and wrong phone numbers. Most health plans had inaccurate information for 30%-60% of their providers’ offices, the report said. The report blamed the insurers for failing to do enough to keep their directories accurate.
“We saw a general lack of internal audit and testing of directory accuracy among many” Medicare Advantage organizations, the report said.
CMS’ survey found the most error-prone listings involved doctors with multiple offices that did not serve health plan members at each location.
The health plans were sent the warning letters Jan. 6 and given 30 days to fix the mistakes or face possible fines or sanctions, which could include suspending marketing and enrollment. CMS officials said the report was not issued before the annual open enrollment period – which ended Dec. 7 – because of the need to allow the health plans to review the findings before the report was made public.
Medicare Advantage members have until Feb. 14 to disenroll and join traditional Medicare but after that they are locked into their plan for the rest of the year. Seniors may be able to request permission to change plans on a case-by-case basis by calling 800-MEDICARE.
Another 32 companies with less serious mistakes also received letters saying their directories did not comply with a rule that took effect last year requiring plans to contact doctors and other providers every 3 months and to update their online directories in “real time.”
ConnectiCare spokeswoman Kimberly Kann acknowledged the difficulties. “Keeping these directories up to date is a two-way street and we are working with doctors and other medical professionals to continue providing quality service,” she said.
WellCare spokeswoman Crystal Warwell Walker said the Tampa, Fla.–based company took the survey results seriously. “We modified our data gathering techniques and online reporting options to ensure that when more than one address is listed for a provider, that provider is practicing at that location on a routine basis and access to care is not compromised,” she said.
CMS is continuing its investigation of provider directories this year and expects to examine all 300 companies by end of 2018.
Kaiser Health News is a national health policy news service that is part of the nonpartisan Henry J. Kaiser Family Foundation.
Federal officials this month warned 21 Medicare Advantage insurers with high rates of errors in their online network directories that they could face heavy fines or have to stop enrolling people if the problems are not fixed by Feb. 6.
Among the plans that were cited are Blue Cross Blue Shield of Michigan, Highmark of Pennsylvania, SCAN Health Plan of California as well as some regional plans owned by national carriers such as UnitedHealthcare and Humana.
The action follows the government’s first in-depth review of the accuracy of Medicare Advantage provider directories, which consumers and advocates have complained about for years. More than 17 million Americans, or nearly a third of Medicare beneficiaries, get coverage through private Medicare Advantage plans.
The Centers for Medicare & Medicaid Services in October reported some of the results of the audit, but they had not released names or statistics from the individual plans.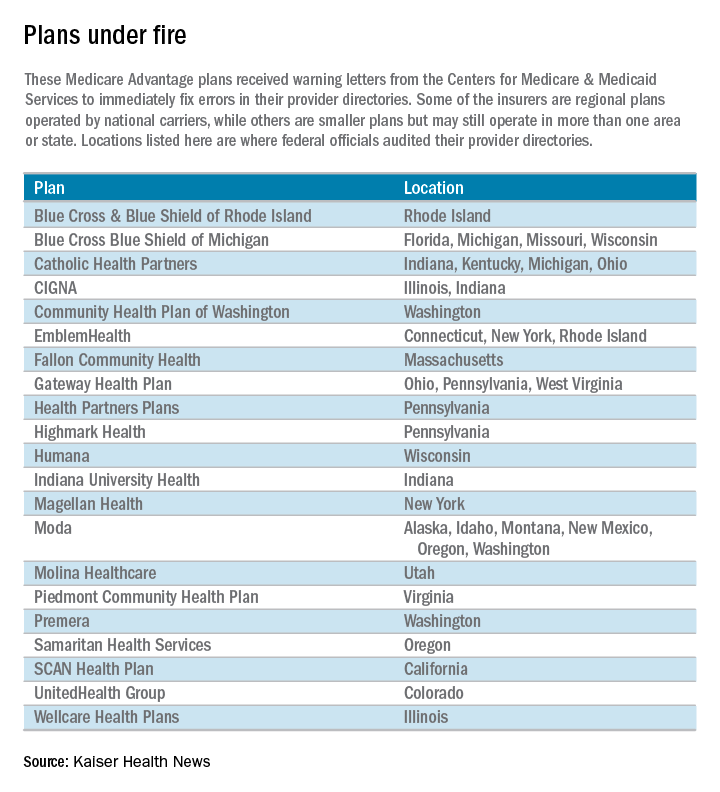
“Because Medicare Advantage members rely on provider directories to locate an in-network provider, these inaccuracies pose a significant access-to-care barrier,” Medicare officials wrote in a report outlining the problems.
Unlike traditional Medicare, the private Medicare plans typically restrict beneficiaries to a network of doctors and hospitals.
Piedmont Community Health Plan, a small Medicare plan with about 5,200 members in southwest Virginia, had the highest rate of inaccuracies among the 54 insurers examined. Officials found errors in the listings of 87 of 108 doctors checked in Piedmont’s directory, according to the report. Most of the errors involved providing the wrong locations for doctors and doctors who should not have been listed. Piedmont officials did not return calls for comment.
Piedmont and two other plans with the highest error rates – a WellCare plan in Illinois and Emblem Health’s ConnectiCare subsidiary – were required by Medicare to submit specific business plans detailing how they intend to address the issue.
The individual plans receiving warning letters cover more than 1.4 million beneficiaries. Most operate in numerous states, although CMS generally limited its review to a specific state or geographic area.
The federal review focused on primary care doctors, cardiologists, ophthalmologists, and oncologists. It involved individual calls to check on the listings for 108 doctors in each health plan. “We encountered several instances where a call to a provider’s office resulted in determining that the provider had been retired or deceased for a long period of time, sometimes years,” the report said.
Almost half of the 5,832 doctors listed had incorrect information, including wrong addresses and wrong phone numbers. Most health plans had inaccurate information for 30%-60% of their providers’ offices, the report said. The report blamed the insurers for failing to do enough to keep their directories accurate.
“We saw a general lack of internal audit and testing of directory accuracy among many” Medicare Advantage organizations, the report said.
CMS’ survey found the most error-prone listings involved doctors with multiple offices that did not serve health plan members at each location.
The health plans were sent the warning letters Jan. 6 and given 30 days to fix the mistakes or face possible fines or sanctions, which could include suspending marketing and enrollment. CMS officials said the report was not issued before the annual open enrollment period – which ended Dec. 7 – because of the need to allow the health plans to review the findings before the report was made public.
Medicare Advantage members have until Feb. 14 to disenroll and join traditional Medicare but after that they are locked into their plan for the rest of the year. Seniors may be able to request permission to change plans on a case-by-case basis by calling 800-MEDICARE.
Another 32 companies with less serious mistakes also received letters saying their directories did not comply with a rule that took effect last year requiring plans to contact doctors and other providers every 3 months and to update their online directories in “real time.”
ConnectiCare spokeswoman Kimberly Kann acknowledged the difficulties. “Keeping these directories up to date is a two-way street and we are working with doctors and other medical professionals to continue providing quality service,” she said.
WellCare spokeswoman Crystal Warwell Walker said the Tampa, Fla.–based company took the survey results seriously. “We modified our data gathering techniques and online reporting options to ensure that when more than one address is listed for a provider, that provider is practicing at that location on a routine basis and access to care is not compromised,” she said.
CMS is continuing its investigation of provider directories this year and expects to examine all 300 companies by end of 2018.
Kaiser Health News is a national health policy news service that is part of the nonpartisan Henry J. Kaiser Family Foundation.
Federal officials this month warned 21 Medicare Advantage insurers with high rates of errors in their online network directories that they could face heavy fines or have to stop enrolling people if the problems are not fixed by Feb. 6.
Among the plans that were cited are Blue Cross Blue Shield of Michigan, Highmark of Pennsylvania, SCAN Health Plan of California as well as some regional plans owned by national carriers such as UnitedHealthcare and Humana.
The action follows the government’s first in-depth review of the accuracy of Medicare Advantage provider directories, which consumers and advocates have complained about for years. More than 17 million Americans, or nearly a third of Medicare beneficiaries, get coverage through private Medicare Advantage plans.
The Centers for Medicare & Medicaid Services in October reported some of the results of the audit, but they had not released names or statistics from the individual plans.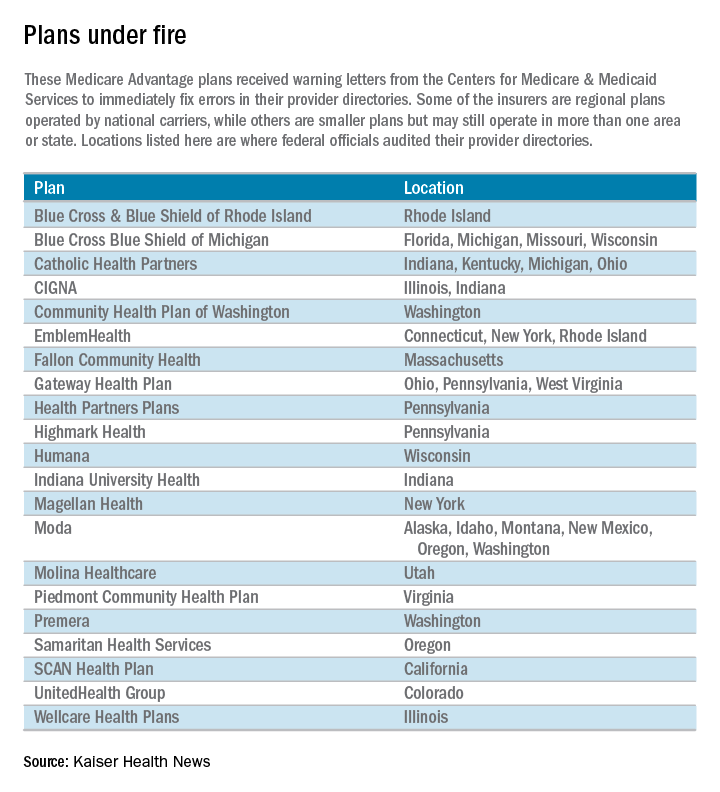
“Because Medicare Advantage members rely on provider directories to locate an in-network provider, these inaccuracies pose a significant access-to-care barrier,” Medicare officials wrote in a report outlining the problems.
Unlike traditional Medicare, the private Medicare plans typically restrict beneficiaries to a network of doctors and hospitals.
Piedmont Community Health Plan, a small Medicare plan with about 5,200 members in southwest Virginia, had the highest rate of inaccuracies among the 54 insurers examined. Officials found errors in the listings of 87 of 108 doctors checked in Piedmont’s directory, according to the report. Most of the errors involved providing the wrong locations for doctors and doctors who should not have been listed. Piedmont officials did not return calls for comment.
Piedmont and two other plans with the highest error rates – a WellCare plan in Illinois and Emblem Health’s ConnectiCare subsidiary – were required by Medicare to submit specific business plans detailing how they intend to address the issue.
The individual plans receiving warning letters cover more than 1.4 million beneficiaries. Most operate in numerous states, although CMS generally limited its review to a specific state or geographic area.
The federal review focused on primary care doctors, cardiologists, ophthalmologists, and oncologists. It involved individual calls to check on the listings for 108 doctors in each health plan. “We encountered several instances where a call to a provider’s office resulted in determining that the provider had been retired or deceased for a long period of time, sometimes years,” the report said.
Almost half of the 5,832 doctors listed had incorrect information, including wrong addresses and wrong phone numbers. Most health plans had inaccurate information for 30%-60% of their providers’ offices, the report said. The report blamed the insurers for failing to do enough to keep their directories accurate.
“We saw a general lack of internal audit and testing of directory accuracy among many” Medicare Advantage organizations, the report said.
CMS’ survey found the most error-prone listings involved doctors with multiple offices that did not serve health plan members at each location.
The health plans were sent the warning letters Jan. 6 and given 30 days to fix the mistakes or face possible fines or sanctions, which could include suspending marketing and enrollment. CMS officials said the report was not issued before the annual open enrollment period – which ended Dec. 7 – because of the need to allow the health plans to review the findings before the report was made public.
Medicare Advantage members have until Feb. 14 to disenroll and join traditional Medicare but after that they are locked into their plan for the rest of the year. Seniors may be able to request permission to change plans on a case-by-case basis by calling 800-MEDICARE.
Another 32 companies with less serious mistakes also received letters saying their directories did not comply with a rule that took effect last year requiring plans to contact doctors and other providers every 3 months and to update their online directories in “real time.”
ConnectiCare spokeswoman Kimberly Kann acknowledged the difficulties. “Keeping these directories up to date is a two-way street and we are working with doctors and other medical professionals to continue providing quality service,” she said.
WellCare spokeswoman Crystal Warwell Walker said the Tampa, Fla.–based company took the survey results seriously. “We modified our data gathering techniques and online reporting options to ensure that when more than one address is listed for a provider, that provider is practicing at that location on a routine basis and access to care is not compromised,” she said.
CMS is continuing its investigation of provider directories this year and expects to examine all 300 companies by end of 2018.
Kaiser Health News is a national health policy news service that is part of the nonpartisan Henry J. Kaiser Family Foundation.
VA Treats Patients’ Impatience With Clinical Pharmacists
MADISON, WIS.— Something astonishing has happened in the past year to outpatient treatment at the Veterans Affairs hospital here.
Vets regularly get next-day and even same-day appointments for primary care now, no longer waiting a month or more to see a doctor as many once did.
The reason is they don’t all see doctors. Clinical pharmacists — whose special training permits them to prescribe drugs, order lab tests, make referrals to specialists and do physical examinations — are handling more patients’ chronic care needs. That frees physicians to concentrate on new patients and others with complex needs.
A quarter of primary care appointments at the Madison hospital are now handled by clinical pharmacists since they were integrated in patient care teams in 2015. Several VA hospitals — in El Paso, Texas, and Kansas City, Mo., among them — have followed Madison’s approach and more than 36 others are considering it, according to hospital officials.
“It’s made a tremendous positive impact in improving access,” said Dr. Jean Montgomery, chief of primary care services at the Madison hospital.
That’s critical for the VA, the focus of a national scandal in 2014 after news reports revealed the Phoenix VA hospital had booked primary care appointments months in advance, schedulers falsified wait times to make them look shorter and dozens had died awaiting care. Further investigations uncovered similar problems at other VA facilities. More than two years later, tens of thousands of vets are still waiting a month or two for an appointment, according to the latest data from the VA.
The Obama administration has allowed some veterans to seek care in the private sector if they choose, but VA wait times remain long and more action is needed, theGeneral Accountability Office reported in April.
Expanding clinical pharmacists’ role is a solution.
They receive two more years of education than regular pharmacists and they can handle many primary care needs for patients, particularly after physicians have diagnosed their conditions.
The VA has had them for more than 20 years, but their growing involvement in patient care is more recent. This year it employs 3,185 clinical pharmacists with authority to prescribe medications, order lab tests and perform physical assessments — nearly a 50 percent increase since 2011.
“It’s having a significant impact on reducing wait times and our office is trying to expand more of them nationally to increase access,” said Heather Ourth, national clinical program manager for VA Pharmacy Benefits Management Services.
In 2015, VA clinical pharmacists wrote 1.9 million prescriptions for chronic diseases, according to a report co-authored by Ourth and published in September in the American Journal of Health-System Pharmacy.
A goal is to increase the use of clinical pharmacists to help patients with mental health needs and pain management.
“This helps open up appointment slots for physicians to meet patients with acute care needs,” Ourth said.
Clinical pharmacists’ authority is determined at each VA hospital based on their training and knowledge.
The Madison VA allowed clinical pharmacists to take over management of patients with chronic diseases such as diabetes and high blood pressure, participate in weekly meetings with doctors and other members of patients’ care teams and handle patients’ calls about medications.
They typically see five patients in their office each day, usually for 30 minutes each, and they talk to another 10 by telephone, said Ellina Seckel, the clinical pharmacist who led the changes at the hospital.
Many issues involve adjusting medication dosages such as insulin, which do not require a face-to-face visit. When Seckel sees patients, she often helps them lower the number of drugs they take because they may cause unnecessary complications.
Expanding clinical pharmacists’ role in primary care has cut readmission rates and helped more patients keep their diabetes under control, Seckel said.
VA hospital officials in both Madison and El Paso said they faced challenges initially in persuading doctors to delegate some duties to qualified pharmacists.
“Some physicians feel like it’s a turf war and don’t want to refer their patients because they feel the clinical pharmacist is trying to practice medicine,” said Lanre’ Obisesan, a clinical pharmacist and assistant chief of pharmacy at the El Paso VA.
Even so, the El Paso VA’s average wait time fell from two months to two weeks, he said, after it added several clinical pharmacists and gave them independence to help patients. About 30 percent of the VA patients in El Paso have used clinical pharmacists, Obisesan said.
That share will rise. The hospital now has one clinical pharmacist for every six physicians, but it aims to add more pharmacists to reduce the ratio to 1 to 3.
The Madison VA is close to that ratio now after adding four clinical pharmacist positions in the past year.
Patients there can choose whether to see a doctor or a pharmacist. With approval from primary care physicians, pharmacists took over 27 percent of the follow-up appointments for patients with chronic illnesses, Seckel said.
That shift yields benefits for both doctors and patients, said Montgomery, the head of primary care services at the Madison VA.
Many VA doctors only have time to deal with patients’ acute care issues, such as knee or back pain, with little time to focus on a patient’s multiple chronic illnesses and often a dozen or more medications they may be taking for them.
“The more we can have members of the team to do routine things that do not require a physician’s time the better the quality of the visit and the better patient outcomes,” he said.
Patients seem to like what the hospital is doing.
Stephen Howard Foster saw a clinical pharmacist recently who told him he could stop taking one heartburn medication and switched him to another medicine to reduce side effects. He said he was comfortable with the pharmacist advising him without first consulting his physician and he saved time.
“This is a good idea rather than put up with normal delays,” said Foster, 51.
Another Madison VA patient, Mike Fonger, 71, saw clinical pharmacist Anita Kashyap recently to get a blood pressure check, lab test results, a review of his medications and to change an ointment he was taking for back and shoulder pain. Kashyap also helped him ease the side effects from the cholesterol-lowering drug he takes by cutting his dosage in half.
“I like the extra attention I get here,” Fonger said.
This story was produced by Kaiser Health News, which publishes California Healthline, a service of the California Health Care Foundation.
MADISON, WIS.— Something astonishing has happened in the past year to outpatient treatment at the Veterans Affairs hospital here.
Vets regularly get next-day and even same-day appointments for primary care now, no longer waiting a month or more to see a doctor as many once did.
The reason is they don’t all see doctors. Clinical pharmacists — whose special training permits them to prescribe drugs, order lab tests, make referrals to specialists and do physical examinations — are handling more patients’ chronic care needs. That frees physicians to concentrate on new patients and others with complex needs.
A quarter of primary care appointments at the Madison hospital are now handled by clinical pharmacists since they were integrated in patient care teams in 2015. Several VA hospitals — in El Paso, Texas, and Kansas City, Mo., among them — have followed Madison’s approach and more than 36 others are considering it, according to hospital officials.
“It’s made a tremendous positive impact in improving access,” said Dr. Jean Montgomery, chief of primary care services at the Madison hospital.
That’s critical for the VA, the focus of a national scandal in 2014 after news reports revealed the Phoenix VA hospital had booked primary care appointments months in advance, schedulers falsified wait times to make them look shorter and dozens had died awaiting care. Further investigations uncovered similar problems at other VA facilities. More than two years later, tens of thousands of vets are still waiting a month or two for an appointment, according to the latest data from the VA.
The Obama administration has allowed some veterans to seek care in the private sector if they choose, but VA wait times remain long and more action is needed, theGeneral Accountability Office reported in April.
Expanding clinical pharmacists’ role is a solution.
They receive two more years of education than regular pharmacists and they can handle many primary care needs for patients, particularly after physicians have diagnosed their conditions.
The VA has had them for more than 20 years, but their growing involvement in patient care is more recent. This year it employs 3,185 clinical pharmacists with authority to prescribe medications, order lab tests and perform physical assessments — nearly a 50 percent increase since 2011.
“It’s having a significant impact on reducing wait times and our office is trying to expand more of them nationally to increase access,” said Heather Ourth, national clinical program manager for VA Pharmacy Benefits Management Services.
In 2015, VA clinical pharmacists wrote 1.9 million prescriptions for chronic diseases, according to a report co-authored by Ourth and published in September in the American Journal of Health-System Pharmacy.
A goal is to increase the use of clinical pharmacists to help patients with mental health needs and pain management.
“This helps open up appointment slots for physicians to meet patients with acute care needs,” Ourth said.
Clinical pharmacists’ authority is determined at each VA hospital based on their training and knowledge.
The Madison VA allowed clinical pharmacists to take over management of patients with chronic diseases such as diabetes and high blood pressure, participate in weekly meetings with doctors and other members of patients’ care teams and handle patients’ calls about medications.
They typically see five patients in their office each day, usually for 30 minutes each, and they talk to another 10 by telephone, said Ellina Seckel, the clinical pharmacist who led the changes at the hospital.
Many issues involve adjusting medication dosages such as insulin, which do not require a face-to-face visit. When Seckel sees patients, she often helps them lower the number of drugs they take because they may cause unnecessary complications.
Expanding clinical pharmacists’ role in primary care has cut readmission rates and helped more patients keep their diabetes under control, Seckel said.
VA hospital officials in both Madison and El Paso said they faced challenges initially in persuading doctors to delegate some duties to qualified pharmacists.
“Some physicians feel like it’s a turf war and don’t want to refer their patients because they feel the clinical pharmacist is trying to practice medicine,” said Lanre’ Obisesan, a clinical pharmacist and assistant chief of pharmacy at the El Paso VA.
Even so, the El Paso VA’s average wait time fell from two months to two weeks, he said, after it added several clinical pharmacists and gave them independence to help patients. About 30 percent of the VA patients in El Paso have used clinical pharmacists, Obisesan said.
That share will rise. The hospital now has one clinical pharmacist for every six physicians, but it aims to add more pharmacists to reduce the ratio to 1 to 3.
The Madison VA is close to that ratio now after adding four clinical pharmacist positions in the past year.
Patients there can choose whether to see a doctor or a pharmacist. With approval from primary care physicians, pharmacists took over 27 percent of the follow-up appointments for patients with chronic illnesses, Seckel said.
That shift yields benefits for both doctors and patients, said Montgomery, the head of primary care services at the Madison VA.
Many VA doctors only have time to deal with patients’ acute care issues, such as knee or back pain, with little time to focus on a patient’s multiple chronic illnesses and often a dozen or more medications they may be taking for them.
“The more we can have members of the team to do routine things that do not require a physician’s time the better the quality of the visit and the better patient outcomes,” he said.
Patients seem to like what the hospital is doing.
Stephen Howard Foster saw a clinical pharmacist recently who told him he could stop taking one heartburn medication and switched him to another medicine to reduce side effects. He said he was comfortable with the pharmacist advising him without first consulting his physician and he saved time.
“This is a good idea rather than put up with normal delays,” said Foster, 51.
Another Madison VA patient, Mike Fonger, 71, saw clinical pharmacist Anita Kashyap recently to get a blood pressure check, lab test results, a review of his medications and to change an ointment he was taking for back and shoulder pain. Kashyap also helped him ease the side effects from the cholesterol-lowering drug he takes by cutting his dosage in half.
“I like the extra attention I get here,” Fonger said.
This story was produced by Kaiser Health News, which publishes California Healthline, a service of the California Health Care Foundation.
MADISON, WIS.— Something astonishing has happened in the past year to outpatient treatment at the Veterans Affairs hospital here.
Vets regularly get next-day and even same-day appointments for primary care now, no longer waiting a month or more to see a doctor as many once did.
The reason is they don’t all see doctors. Clinical pharmacists — whose special training permits them to prescribe drugs, order lab tests, make referrals to specialists and do physical examinations — are handling more patients’ chronic care needs. That frees physicians to concentrate on new patients and others with complex needs.
A quarter of primary care appointments at the Madison hospital are now handled by clinical pharmacists since they were integrated in patient care teams in 2015. Several VA hospitals — in El Paso, Texas, and Kansas City, Mo., among them — have followed Madison’s approach and more than 36 others are considering it, according to hospital officials.
“It’s made a tremendous positive impact in improving access,” said Dr. Jean Montgomery, chief of primary care services at the Madison hospital.
That’s critical for the VA, the focus of a national scandal in 2014 after news reports revealed the Phoenix VA hospital had booked primary care appointments months in advance, schedulers falsified wait times to make them look shorter and dozens had died awaiting care. Further investigations uncovered similar problems at other VA facilities. More than two years later, tens of thousands of vets are still waiting a month or two for an appointment, according to the latest data from the VA.
The Obama administration has allowed some veterans to seek care in the private sector if they choose, but VA wait times remain long and more action is needed, theGeneral Accountability Office reported in April.
Expanding clinical pharmacists’ role is a solution.
They receive two more years of education than regular pharmacists and they can handle many primary care needs for patients, particularly after physicians have diagnosed their conditions.
The VA has had them for more than 20 years, but their growing involvement in patient care is more recent. This year it employs 3,185 clinical pharmacists with authority to prescribe medications, order lab tests and perform physical assessments — nearly a 50 percent increase since 2011.
“It’s having a significant impact on reducing wait times and our office is trying to expand more of them nationally to increase access,” said Heather Ourth, national clinical program manager for VA Pharmacy Benefits Management Services.
In 2015, VA clinical pharmacists wrote 1.9 million prescriptions for chronic diseases, according to a report co-authored by Ourth and published in September in the American Journal of Health-System Pharmacy.
A goal is to increase the use of clinical pharmacists to help patients with mental health needs and pain management.
“This helps open up appointment slots for physicians to meet patients with acute care needs,” Ourth said.
Clinical pharmacists’ authority is determined at each VA hospital based on their training and knowledge.
The Madison VA allowed clinical pharmacists to take over management of patients with chronic diseases such as diabetes and high blood pressure, participate in weekly meetings with doctors and other members of patients’ care teams and handle patients’ calls about medications.
They typically see five patients in their office each day, usually for 30 minutes each, and they talk to another 10 by telephone, said Ellina Seckel, the clinical pharmacist who led the changes at the hospital.
Many issues involve adjusting medication dosages such as insulin, which do not require a face-to-face visit. When Seckel sees patients, she often helps them lower the number of drugs they take because they may cause unnecessary complications.
Expanding clinical pharmacists’ role in primary care has cut readmission rates and helped more patients keep their diabetes under control, Seckel said.
VA hospital officials in both Madison and El Paso said they faced challenges initially in persuading doctors to delegate some duties to qualified pharmacists.
“Some physicians feel like it’s a turf war and don’t want to refer their patients because they feel the clinical pharmacist is trying to practice medicine,” said Lanre’ Obisesan, a clinical pharmacist and assistant chief of pharmacy at the El Paso VA.
Even so, the El Paso VA’s average wait time fell from two months to two weeks, he said, after it added several clinical pharmacists and gave them independence to help patients. About 30 percent of the VA patients in El Paso have used clinical pharmacists, Obisesan said.
That share will rise. The hospital now has one clinical pharmacist for every six physicians, but it aims to add more pharmacists to reduce the ratio to 1 to 3.
The Madison VA is close to that ratio now after adding four clinical pharmacist positions in the past year.
Patients there can choose whether to see a doctor or a pharmacist. With approval from primary care physicians, pharmacists took over 27 percent of the follow-up appointments for patients with chronic illnesses, Seckel said.
That shift yields benefits for both doctors and patients, said Montgomery, the head of primary care services at the Madison VA.
Many VA doctors only have time to deal with patients’ acute care issues, such as knee or back pain, with little time to focus on a patient’s multiple chronic illnesses and often a dozen or more medications they may be taking for them.
“The more we can have members of the team to do routine things that do not require a physician’s time the better the quality of the visit and the better patient outcomes,” he said.
Patients seem to like what the hospital is doing.
Stephen Howard Foster saw a clinical pharmacist recently who told him he could stop taking one heartburn medication and switched him to another medicine to reduce side effects. He said he was comfortable with the pharmacist advising him without first consulting his physician and he saved time.
“This is a good idea rather than put up with normal delays,” said Foster, 51.
Another Madison VA patient, Mike Fonger, 71, saw clinical pharmacist Anita Kashyap recently to get a blood pressure check, lab test results, a review of his medications and to change an ointment he was taking for back and shoulder pain. Kashyap also helped him ease the side effects from the cholesterol-lowering drug he takes by cutting his dosage in half.
“I like the extra attention I get here,” Fonger said.
This story was produced by Kaiser Health News, which publishes California Healthline, a service of the California Health Care Foundation.
Obamacare marketplace shakeout rocks Arizona, Southeast
Some of the Affordable Care Act’s insurance marketplaces are in turmoil as the fourth open enrollment season approaches this fall, but what’s ahead for consumers very much depends on where they live.
Competition on these exchanges will be diminished next year when three of the nation’s largest health insurers – Aetna, UnitedHealthcare and Humana – will sell individual plans in many fewer markets. So too will several Blue Cross and Blue Shield plans in various states. That’s on top of the 16 nonprofit co-ops that have closed since January 2015.
The announcements, however, apply generally only to the individual market. The much larger market of employer-sponsored insurance is not part of the health law exchanges.
Aetna’s exit announcement Aug. 15 that blamed financial losses on its marketplace plans gave Obamacare opponents who have from the start predicted the ACA’s failure a fresh chance to proclaim “I told you so.”
That story line got more complicated Aug. 17 after the Huffington Post reported that Aetna CEO Mark Bertolini sent a letter to the Department of Justice (DOJ) on July 5 threatening to withdraw from the Obamacare marketplaces if the DOJ sued to block his company’s planned merger with Humana. The DOJ did just that a couple weeks later.
But most marketplace consumers won’t see any ill effects from insurers’ withdrawals, according to ACA advocates and independent experts.
“The effect on consumers is going to be mixed around the country,” said Katherine Hempstead, PhD, a senior adviser at the nonpartisan Robert Wood Johnson Foundation. “Most of these marketplaces are not dependent on” the large national carriers.
Many major metropolitan areas, such as those in California, New York, and Texas, will still have several insurers for individual health insurance consumers to choose from. In Texas, all major metro areas – including Austin, Dallas, Houston, and San Antonio – will have at least three insurers after Aetna and UnitedHealthcare exit.
That’s true also for most urban exchange customers living in the Northwest, the Midwest, and New England.
Most hurt will be marketplace consumers in Arizona, North and South Carolina, Georgia, and parts of Florida, where only one or two insurers will be left when open enrollment season begins Nov. 15.
Remaining insurers might raise their monthly premiums as a result, but more than eight in 10 consumers on the marketplaces who get government subsidies would be insulated. Subsidies increase as premiums rise.
Still, health experts worry that with less competition, insurers may tighten their provider networks and give these consumers fewer choices of hospitals and doctors. That trend started several years ago, and some states have responded with regulations requiring insurers to provide customers with reasonable access to doctors and hospitals in each county where they sell plans.
Nearly 13 million people signed up for Obamacare marketplace policies for 2016. Aetna, UnitedHealthcare, and Humana have 2 million members in total, but their exit from certain states is predicted to affect between 1 million and 1.5 million people who will have to choose new carriers.
While changing plans can force people to find new doctors, it’s also the best way for consumers get the best deals on coverage.
Aetna will exit 11 of 15 states where it sells plans on the exchanges. UnitedHealthcare has said it will quit 22 of 34 states, and Humana will leave 4 of the 15 states where it operates.
In late May, the Kaiser Family Foundation estimated the number of rural counties at risk of having one insurer on the exchanges would triple in 2017. That was before Humana and Aetna detailed their plans. (KHN is an editorially independent project of the foundation.)
Now, “we could be looking at about one in four counties in the U.S. with just one exchange insurer next year, though this could change between now and open enrollment in November,” said Cynthia Cox, associate director for the Kaiser Family Foundation Program for the Study of Health Reform and Private Insurance.
Overshadowed by the big insurers’ withdrawals is the prospect that other carriers will enter markets the three giants are leaving. Smaller insurers Molina and Centene have said they’re doing fine on the exchanges. And Cigna, a larger insurer, has said it will move into some North Carolina counties for 2017.
North Carolina will be left with just one or two plans in most of the state after it loses UnitedHealthcare and Aetna plans. Health insurance experts say three insurers are needed for a healthy competitive market.
“We’ve had a very robust enrollment under the ACA and hope consumers will still see benefits of having coverage even if they have fewer options,” said Ciara Zachary, health policy analyst for the North Carolina Justice Center’s Health Access Coalition.
Rural Americans had few health insurers to choose from even before Obamacare, but some suburban and urban parts of the Southeast will be in the same fix next year. In southeast Florida, consumers in counties near Naples and Fort Myers will have only one marketplace insurer – Florida Blue – next year, unless other insurers step in.
“There are some headwinds, but it’s not a question of whether the market will stabilize but how quickly and how well,” said Dr. Hempstead.
Strong winds are already blowing toward Arizona’s Pinal County, southeast of Phoenix, health care advocates say. Nearly 10,000 people enrolled in Obamacare marketplace policies this year and about 85% received a federal subsidy.
In 2017, Pinal stands to lose its only two insurers – UnitedHealthcare and Blue Cross and Blue Shield of Arizona.
“Clearly this is a big concern for consumers,” said Allen Gjersvig, director of navigator and enrollment services for the Arizona Alliance for Community Health Centers. He said he is hopeful, but not confident, that another insurer will step in.
Neighboring Maricopa County, which includes Phoenix, is expected to have just two relatively small insurers left on its marketplace next year. Mr. Gjersvig said that he questions whether those two – Cigna and Phoenix Health Plan – will have enough doctors and hospitals under contract to handle their new members after larger rival Blue Cross and Blue Shield of Arizona gives up its 40,000 customers.
At least a dozen other counties in Arizona will be left with just one health insurer, he said.
Arizona had eight insurers operating in various parts of the state this year, but four are leaving entirely – Aetna, UnitedHealthcare, Humana, and Health Choice. Two more, Blue Cross Blue Shield and Health Net, are scaling back their participation.
Despite the problems with the marketplaces, Mr. Gjersvig said thousands of people have gained coverage through them and he is confident they will survive.
“We do not see this as a death knell for the marketplace,” he said.
Tammie King, an insurance agent in Columbia, S.C., is less sure how insurer departures will affect consumers in the Palmetto State. Pullouts by UnitedHealthcare and Aetna mean only one carrier in the state in 2017 – Blue Cross and Blue Shield of South Carolina.
That’s a concern in Columbia, S.C., because the Blue Cross plan does not include one of the biggest hospitals, Lexington Medical Center, and its affiliated physicians, she said.
“People will be left unable to see the doctors they are now using,” she added.
Ms. King said she worried the Blue Cross plan will use its monopoly power to further reduce the number of doctors and hospitals in its network and limit its choice of prescription drugs. “You can’t blame them because … they have to do something to control costs,” she said.
This story appears courtesy of Kaiser Health News, a national health policy news service that is part of the nonpartisan Henry J. Kaiser Family Foundation.
Some of the Affordable Care Act’s insurance marketplaces are in turmoil as the fourth open enrollment season approaches this fall, but what’s ahead for consumers very much depends on where they live.
Competition on these exchanges will be diminished next year when three of the nation’s largest health insurers – Aetna, UnitedHealthcare and Humana – will sell individual plans in many fewer markets. So too will several Blue Cross and Blue Shield plans in various states. That’s on top of the 16 nonprofit co-ops that have closed since January 2015.
The announcements, however, apply generally only to the individual market. The much larger market of employer-sponsored insurance is not part of the health law exchanges.
Aetna’s exit announcement Aug. 15 that blamed financial losses on its marketplace plans gave Obamacare opponents who have from the start predicted the ACA’s failure a fresh chance to proclaim “I told you so.”
That story line got more complicated Aug. 17 after the Huffington Post reported that Aetna CEO Mark Bertolini sent a letter to the Department of Justice (DOJ) on July 5 threatening to withdraw from the Obamacare marketplaces if the DOJ sued to block his company’s planned merger with Humana. The DOJ did just that a couple weeks later.
But most marketplace consumers won’t see any ill effects from insurers’ withdrawals, according to ACA advocates and independent experts.
“The effect on consumers is going to be mixed around the country,” said Katherine Hempstead, PhD, a senior adviser at the nonpartisan Robert Wood Johnson Foundation. “Most of these marketplaces are not dependent on” the large national carriers.
Many major metropolitan areas, such as those in California, New York, and Texas, will still have several insurers for individual health insurance consumers to choose from. In Texas, all major metro areas – including Austin, Dallas, Houston, and San Antonio – will have at least three insurers after Aetna and UnitedHealthcare exit.
That’s true also for most urban exchange customers living in the Northwest, the Midwest, and New England.
Most hurt will be marketplace consumers in Arizona, North and South Carolina, Georgia, and parts of Florida, where only one or two insurers will be left when open enrollment season begins Nov. 15.
Remaining insurers might raise their monthly premiums as a result, but more than eight in 10 consumers on the marketplaces who get government subsidies would be insulated. Subsidies increase as premiums rise.
Still, health experts worry that with less competition, insurers may tighten their provider networks and give these consumers fewer choices of hospitals and doctors. That trend started several years ago, and some states have responded with regulations requiring insurers to provide customers with reasonable access to doctors and hospitals in each county where they sell plans.
Nearly 13 million people signed up for Obamacare marketplace policies for 2016. Aetna, UnitedHealthcare, and Humana have 2 million members in total, but their exit from certain states is predicted to affect between 1 million and 1.5 million people who will have to choose new carriers.
While changing plans can force people to find new doctors, it’s also the best way for consumers get the best deals on coverage.
Aetna will exit 11 of 15 states where it sells plans on the exchanges. UnitedHealthcare has said it will quit 22 of 34 states, and Humana will leave 4 of the 15 states where it operates.
In late May, the Kaiser Family Foundation estimated the number of rural counties at risk of having one insurer on the exchanges would triple in 2017. That was before Humana and Aetna detailed their plans. (KHN is an editorially independent project of the foundation.)
Now, “we could be looking at about one in four counties in the U.S. with just one exchange insurer next year, though this could change between now and open enrollment in November,” said Cynthia Cox, associate director for the Kaiser Family Foundation Program for the Study of Health Reform and Private Insurance.
Overshadowed by the big insurers’ withdrawals is the prospect that other carriers will enter markets the three giants are leaving. Smaller insurers Molina and Centene have said they’re doing fine on the exchanges. And Cigna, a larger insurer, has said it will move into some North Carolina counties for 2017.
North Carolina will be left with just one or two plans in most of the state after it loses UnitedHealthcare and Aetna plans. Health insurance experts say three insurers are needed for a healthy competitive market.
“We’ve had a very robust enrollment under the ACA and hope consumers will still see benefits of having coverage even if they have fewer options,” said Ciara Zachary, health policy analyst for the North Carolina Justice Center’s Health Access Coalition.
Rural Americans had few health insurers to choose from even before Obamacare, but some suburban and urban parts of the Southeast will be in the same fix next year. In southeast Florida, consumers in counties near Naples and Fort Myers will have only one marketplace insurer – Florida Blue – next year, unless other insurers step in.
“There are some headwinds, but it’s not a question of whether the market will stabilize but how quickly and how well,” said Dr. Hempstead.
Strong winds are already blowing toward Arizona’s Pinal County, southeast of Phoenix, health care advocates say. Nearly 10,000 people enrolled in Obamacare marketplace policies this year and about 85% received a federal subsidy.
In 2017, Pinal stands to lose its only two insurers – UnitedHealthcare and Blue Cross and Blue Shield of Arizona.
“Clearly this is a big concern for consumers,” said Allen Gjersvig, director of navigator and enrollment services for the Arizona Alliance for Community Health Centers. He said he is hopeful, but not confident, that another insurer will step in.
Neighboring Maricopa County, which includes Phoenix, is expected to have just two relatively small insurers left on its marketplace next year. Mr. Gjersvig said that he questions whether those two – Cigna and Phoenix Health Plan – will have enough doctors and hospitals under contract to handle their new members after larger rival Blue Cross and Blue Shield of Arizona gives up its 40,000 customers.
At least a dozen other counties in Arizona will be left with just one health insurer, he said.
Arizona had eight insurers operating in various parts of the state this year, but four are leaving entirely – Aetna, UnitedHealthcare, Humana, and Health Choice. Two more, Blue Cross Blue Shield and Health Net, are scaling back their participation.
Despite the problems with the marketplaces, Mr. Gjersvig said thousands of people have gained coverage through them and he is confident they will survive.
“We do not see this as a death knell for the marketplace,” he said.
Tammie King, an insurance agent in Columbia, S.C., is less sure how insurer departures will affect consumers in the Palmetto State. Pullouts by UnitedHealthcare and Aetna mean only one carrier in the state in 2017 – Blue Cross and Blue Shield of South Carolina.
That’s a concern in Columbia, S.C., because the Blue Cross plan does not include one of the biggest hospitals, Lexington Medical Center, and its affiliated physicians, she said.
“People will be left unable to see the doctors they are now using,” she added.
Ms. King said she worried the Blue Cross plan will use its monopoly power to further reduce the number of doctors and hospitals in its network and limit its choice of prescription drugs. “You can’t blame them because … they have to do something to control costs,” she said.
This story appears courtesy of Kaiser Health News, a national health policy news service that is part of the nonpartisan Henry J. Kaiser Family Foundation.
Some of the Affordable Care Act’s insurance marketplaces are in turmoil as the fourth open enrollment season approaches this fall, but what’s ahead for consumers very much depends on where they live.
Competition on these exchanges will be diminished next year when three of the nation’s largest health insurers – Aetna, UnitedHealthcare and Humana – will sell individual plans in many fewer markets. So too will several Blue Cross and Blue Shield plans in various states. That’s on top of the 16 nonprofit co-ops that have closed since January 2015.
The announcements, however, apply generally only to the individual market. The much larger market of employer-sponsored insurance is not part of the health law exchanges.
Aetna’s exit announcement Aug. 15 that blamed financial losses on its marketplace plans gave Obamacare opponents who have from the start predicted the ACA’s failure a fresh chance to proclaim “I told you so.”
That story line got more complicated Aug. 17 after the Huffington Post reported that Aetna CEO Mark Bertolini sent a letter to the Department of Justice (DOJ) on July 5 threatening to withdraw from the Obamacare marketplaces if the DOJ sued to block his company’s planned merger with Humana. The DOJ did just that a couple weeks later.
But most marketplace consumers won’t see any ill effects from insurers’ withdrawals, according to ACA advocates and independent experts.
“The effect on consumers is going to be mixed around the country,” said Katherine Hempstead, PhD, a senior adviser at the nonpartisan Robert Wood Johnson Foundation. “Most of these marketplaces are not dependent on” the large national carriers.
Many major metropolitan areas, such as those in California, New York, and Texas, will still have several insurers for individual health insurance consumers to choose from. In Texas, all major metro areas – including Austin, Dallas, Houston, and San Antonio – will have at least three insurers after Aetna and UnitedHealthcare exit.
That’s true also for most urban exchange customers living in the Northwest, the Midwest, and New England.
Most hurt will be marketplace consumers in Arizona, North and South Carolina, Georgia, and parts of Florida, where only one or two insurers will be left when open enrollment season begins Nov. 15.
Remaining insurers might raise their monthly premiums as a result, but more than eight in 10 consumers on the marketplaces who get government subsidies would be insulated. Subsidies increase as premiums rise.
Still, health experts worry that with less competition, insurers may tighten their provider networks and give these consumers fewer choices of hospitals and doctors. That trend started several years ago, and some states have responded with regulations requiring insurers to provide customers with reasonable access to doctors and hospitals in each county where they sell plans.
Nearly 13 million people signed up for Obamacare marketplace policies for 2016. Aetna, UnitedHealthcare, and Humana have 2 million members in total, but their exit from certain states is predicted to affect between 1 million and 1.5 million people who will have to choose new carriers.
While changing plans can force people to find new doctors, it’s also the best way for consumers get the best deals on coverage.
Aetna will exit 11 of 15 states where it sells plans on the exchanges. UnitedHealthcare has said it will quit 22 of 34 states, and Humana will leave 4 of the 15 states where it operates.
In late May, the Kaiser Family Foundation estimated the number of rural counties at risk of having one insurer on the exchanges would triple in 2017. That was before Humana and Aetna detailed their plans. (KHN is an editorially independent project of the foundation.)
Now, “we could be looking at about one in four counties in the U.S. with just one exchange insurer next year, though this could change between now and open enrollment in November,” said Cynthia Cox, associate director for the Kaiser Family Foundation Program for the Study of Health Reform and Private Insurance.
Overshadowed by the big insurers’ withdrawals is the prospect that other carriers will enter markets the three giants are leaving. Smaller insurers Molina and Centene have said they’re doing fine on the exchanges. And Cigna, a larger insurer, has said it will move into some North Carolina counties for 2017.
North Carolina will be left with just one or two plans in most of the state after it loses UnitedHealthcare and Aetna plans. Health insurance experts say three insurers are needed for a healthy competitive market.
“We’ve had a very robust enrollment under the ACA and hope consumers will still see benefits of having coverage even if they have fewer options,” said Ciara Zachary, health policy analyst for the North Carolina Justice Center’s Health Access Coalition.
Rural Americans had few health insurers to choose from even before Obamacare, but some suburban and urban parts of the Southeast will be in the same fix next year. In southeast Florida, consumers in counties near Naples and Fort Myers will have only one marketplace insurer – Florida Blue – next year, unless other insurers step in.
“There are some headwinds, but it’s not a question of whether the market will stabilize but how quickly and how well,” said Dr. Hempstead.
Strong winds are already blowing toward Arizona’s Pinal County, southeast of Phoenix, health care advocates say. Nearly 10,000 people enrolled in Obamacare marketplace policies this year and about 85% received a federal subsidy.
In 2017, Pinal stands to lose its only two insurers – UnitedHealthcare and Blue Cross and Blue Shield of Arizona.
“Clearly this is a big concern for consumers,” said Allen Gjersvig, director of navigator and enrollment services for the Arizona Alliance for Community Health Centers. He said he is hopeful, but not confident, that another insurer will step in.
Neighboring Maricopa County, which includes Phoenix, is expected to have just two relatively small insurers left on its marketplace next year. Mr. Gjersvig said that he questions whether those two – Cigna and Phoenix Health Plan – will have enough doctors and hospitals under contract to handle their new members after larger rival Blue Cross and Blue Shield of Arizona gives up its 40,000 customers.
At least a dozen other counties in Arizona will be left with just one health insurer, he said.
Arizona had eight insurers operating in various parts of the state this year, but four are leaving entirely – Aetna, UnitedHealthcare, Humana, and Health Choice. Two more, Blue Cross Blue Shield and Health Net, are scaling back their participation.
Despite the problems with the marketplaces, Mr. Gjersvig said thousands of people have gained coverage through them and he is confident they will survive.
“We do not see this as a death knell for the marketplace,” he said.
Tammie King, an insurance agent in Columbia, S.C., is less sure how insurer departures will affect consumers in the Palmetto State. Pullouts by UnitedHealthcare and Aetna mean only one carrier in the state in 2017 – Blue Cross and Blue Shield of South Carolina.
That’s a concern in Columbia, S.C., because the Blue Cross plan does not include one of the biggest hospitals, Lexington Medical Center, and its affiliated physicians, she said.
“People will be left unable to see the doctors they are now using,” she added.
Ms. King said she worried the Blue Cross plan will use its monopoly power to further reduce the number of doctors and hospitals in its network and limit its choice of prescription drugs. “You can’t blame them because … they have to do something to control costs,” she said.
This story appears courtesy of Kaiser Health News, a national health policy news service that is part of the nonpartisan Henry J. Kaiser Family Foundation.