User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
Apixaban cuts stroke but ups bleeding in subclinical AFib: ARTESIA
in the ARTESIA study.
The results appear to contrast somewhat with the recently reported NOAH-AFNET 6 trial, which failed to show a reduction in stroke with the anticoagulant edoxaban versus placebo in a similar patient group, but that trial was stopped early and so was underpowered.
However, the lead investigators of both trials say the studies actually show consistent results – both found a lower rate of stroke than expected in this population, but the confidence intervals for stroke reduction with anticoagulation overlap, suggesting there is likely some effect, albeit less than that in clinical AFib.
The big question is whether the reduction in stroke with anticoagulation outweighs the increase in major bleeding.
A new meta-analysis of the two trials showed that “oral anticoagulation with edoxaban or apixaban reduces the risk of ischemic stroke by approximately one-third and increases major bleeding by roughly double.”
In absolute numbers, there were three fewer ischemic strokes per 1,000 patient-years with anticoagulation in the two trials combined, at the cost of seven more major bleeds.
The lead investigators of the two trials have somewhat different opinions on how these findings may translate into clinical practice.
Jeff Healey, MD, Population Health Research Institute, McMaster University, Hamilton, Ont., lead investigator of the ARTESIA trial, believes that the risks and benefits need to be assessed in individual patients, but there should be some patient groups that will benefit from anticoagulation treatment.
“In patients with pacemakers or implantable loop recorders with continuous monitoring, subclinical AF[ib] is detected in about one third of patients, so this is extremely common,” he said in an interview. “The question is whether this is just a normal feature of getting older or is this like AF[ib] that we see in the clinic which increases stroke risk, and I think we can conclude from ARTESIA that this subclinical AF[ib] is associated with an increased risk of stroke, although that is lower than the risk with clinical AF[ib], and that it can be reduced by anticoagulation.”
Until recently it hasn’t been possible to quantify the risk associated with subclinical AFib, he noted. “But now we have a rich dataset to use to see if we can tease out some specifics on this. Future analyses of this dataset will help define patients where the benefits outweigh the risks of bleeding. For now, I think we can look at the data in a qualitative way and consider the totality of risk factors in each patient – their bleeding risk, stroke risk, how much AF[ib] they have, and make a decision as to whether to give anticoagulation or not.”
But Paulus Kirchhof, MD, University Heart and Vascular Center Hamburg (Germany), lead investigator of the NOAH-AFNET 6 trial said: “Both trials showed the stroke rate is low in these patients – about 1% per year – and that anticoagulation can reduce it a bit further at the expense of increasing major bleeding. I don’t believe the AF[ib] episodes picked up on these devices constitute a sufficient stroke risk to warrant anticoagulation, given the bleeding risk.”
Dr. Kirchhof suggests an alternate approach of performing further traditional AFib monitoring on these patients.
“I think going forward in my practice, when we come across this device-detected AF[ib], we will do further investigations with an established method for detecting AF[ib] involving surface ECG monitoring – maybe a 3-day or 7-day Holter. If that shows AF[ib], then we will be on firm ground to start anticoagulation. If that doesn’t show AF[ib], we will probably not use anticoagulation.”
The ARTESIA trial and the meta-analysis of the two trials were both presented at the annual scientific sessions of the American Heart Association. Both studies were also simultaneously published online – ARTESIA in the New England Journal of Medicine and the meta-analysis in Circulation.
ARTESIA
For the ARTESIA study, 4012 patients with device-detected AFib and other clinical risk factors for stroke were randomly assigned to treatment with apixaban (5 mg twice daily) or aspirin (81 mg daily).
After a mean follow-up of 3.5 years, the primary endpoint – stroke or systemic embolism – occurred in 55 patients in the apixaban group (0.78% per patient-year), compared with 86 patients in the aspirin group (1.24% per patient-year), giving a hazard ratio of 0.63 (95% confidence interval, 0.45-0.88; P = .007).
“The risk of stroke or systemic embolism was lower by 37% with apixaban than with aspirin, and the risk of disabling or fatal stroke was lower by 49%,” Dr. Healey reported.
In the “on-treatment” population, the rate of major bleeding was 1.71% per patient-year in the apixaban group and 0.94% per patient-year in the aspirin group (HR, 1.80; 95% CI, 1.26-2.57; P = .001).
Fatal bleeding occurred in five patients in the apixaban group and eight patients in the aspirin group. Symptomatic intracranial hemorrhage occurred in 12 patients with apixaban and 15 patients with aspirin.
One of the main findings of the trial is the lower-than-expected risk of ischemic stroke in this population – about 1% per year in the aspirin group, which was reduced to 0.64% per year in the apixaban group.
The authors noted that “simply counting strokes as compared with bleeding events might suggest a neutral overall effect. With apixaban as compared with aspirin, 31 fewer cases of stroke or systemic embolism were seen in the intention-to-treat analysis, as compared with 39 more major bleeding events in the on-treatment analysis.”
However, they pointed out that strokes involve permanent loss of brain tissue, whereas major bleeding is usually reversible, with most patients having complete recovery, which was the case in this study.
“Thus, on the basis of the considerably greater severity of the stroke events prevented than the bleeding events caused, we believe that these findings favor consideration of the use of oral anticoagulation for patients with risk factors for stroke in whom subclinical atrial fibrillation develops,” they concluded.
First well-powered trial addressing this question
Discussing the ARTESIA trial at an AHA press conference, Christine Albert, MD, Cedars-Sinai Medical Center, Los Angeles, said: “I want to emphasize how important this trial is.”
She explained that current guidelines do not recommend any treatment for patients with device-detected AFib that is not shown on ECG, even though it is known this confers some excess risk of stroke.
“ARTESIA is the first well-powered, long-term trial looking at this question,” she said. “It found a clear reduction in the risk of stroke/systemic embolism with apixaban vs aspirin, but there was also a significant amount of bleeding – about an 80% increase. The question is whether the benefit on stroke is worth it given the bleeding risk.”
Dr. Albert highlighted the low absolute risk of stroke in this study population of around 1.2%, pointing out that even with the 37% relative reduction with anticoagulation, stroke is only reduced in absolute terms by 0.4%.
“We are going to have to take this back to committees and guidelines and look at the balance between the benefit on stroke and the increase in bleeding,” she concluded.
Noting that observational studies have shown that the duration of AFib impacts the risk of stroke, Dr. Albert suggested that patients with longer-duration AFib may benefit from anticoagulation to a greater extent; and given that the bleeding seen in ARTESIA was mainly GI bleeding, it might be possible to screen out patients at high risk of GI bleeding.
She also pointed out that a lot of patients discontinued anticoagulation treatment in both ARTESIA and NOAH-AFNET 6, showing that this is not an easy strategy for elderly patients.
In an editorial accompanying publication of the ARTESIA trial, Emma Svennberg, MD, Karolinska Institute, Stockholm, also concluded that, “going forward, we must balance the increased bleeding risks with the risk for disabling strokes,” and that “future substudies and meta-analyses may provide further insights regarding treatment benefits in specific subgroups.”
NOAH-AFNET 6: New subgroup analysis
The previously reported NOAH-AFNET 6 study randomly assigned 2,538 patients with subclinical AFib and additional risk factors for stroke to anticoagulation with edoxaban or placebo. The trial was stopped early, so it was underpowered – but it found no difference between groups in the incidence of the composite endpoint of stroke, systemic embolism, or death from cardiovascular causes or in the incidence of stroke, although there was higher risk of major bleeding.
Again, there was a low rate of stroke in this trial with just 49 strokes in total in the whole study. The NOAH-AFNET-6 investigators concluded that these patients should not receive anticoagulation because the risk of bleeding outweighed any potential benefits.
A new subanalysis of the 259 patients who had durations of subclinical AFib of 24 hours or longer in the NOAH-AFNET 6 trial was presented at the AHA meeting, and simultaneously published online in the European Heart Journal.
This showed that the rate of stroke also appeared low in patients with these long durations of subclinical AFib, and that there was no interaction between the duration of subclinical AFib and the efficacy and safety of oral anticoagulation.
But with such a low number of events in the study as a whole and in the long duration subclinical AFib subgroup (in which there were just two strokes in each treatment group), this analysis was unlikely to show a difference, Dr. Kirchhof commented.
The subgroup analysis did, however, show that patients experiencing subclinical AFib durations of 24 hours or more were more likely to develop clinical AFib over time than those with shorter durations, suggesting the need for regular ECGs in these patients.
Dr. Kirchhof said better methods are needed to detect patients with subclinical AFib at high risk of stroke. “I don’t think our clinical stroke risk factor scores such as CHA2DS2-VASc are sufficient to detect high-risk patients. Patients in both NOAH-AFNET 6 and ARTESIA had a median CHA2DS2-VASc score of 4, but they had a stroke rate of just 1% per year,” he noted.
The meta-analysis of the two trials showed that the results from both are consistent, with an overall reduction in ischemic stroke with oral anticoagulation (relative risk, 0.68). Oral anticoagulation also reduced a composite of cardiovascular death, all-cause stroke, peripheral arterial embolism, myocardial infarction, or pulmonary embolism (RR, 0.85).
There was no significant difference in cardiovascular death (RR, 0.95) or all-cause mortality (RR, 1.08), but anticoagulation significantly increased major bleeding (RR, 1.62).
Aspirin use complicates results
Dr. Healey said further analyses of the ARTESIA data will try to tease out the effect of concomitant aspirin use in the trial.
He explained that patients in this trial were allowed to take a single antiplatelet agent on top of study therapy.
“It is difficult to work out the exact use of antiplatelet therapy as it changed throughout the study,” he said. “About two-thirds were taking antiplatelet agents at the time of enrollment into the trial, but this decreased throughout the study. Many clinicians stopped open-label antiplatelet therapy during the trial when new evidence came out to suggest that there was no added benefit of adding aspirin on top of anticoagulants.
“We need to look carefully as to what impact that may have had,” Dr. Healey added. “We know from other studies that adding an antiplatelet on top of an anticoagulant doesn’t do much to thromboembolic events, but it approximately doubles the risk of major bleeding.”
In contrast, the NOAH-AFNET trial did not allow aspirin use in the anticoagulation group and aspirin was taken by around half the patients in the placebo group who had an indication for its use.
The authors of the meta-analysis pointed out that the omission of aspirin in nearly half of the control patients in NOAH-AFNET 6 and the early termination of the trial may have led to a slightly higher estimate for excess major bleeding with anticoagulation.
The ARTESIA study was supported by the Canadian Institutes for Health Research, the Bristol Myers Squibb-Pfizer Alliance, the Heart and Stroke Foundation of Canada, the Canadian Stroke Prevention Intervention Network, Hamilton Health Sciences, the Advancing Clinical Trials Network and the Population Health Research Institute. Dr. Healey reported research grants and speaking fees from BMS/Pfizer Alliance, Servier, Novartis, Boston Scientific, Medtronic; and acts as a consultant to Bayer, Servier and Boston Scientific. The NOAH-AFNET 6 trial was an investigator-initiated trial funded by the German Center for Cardiovascular Research and Daiichi Sankyo Europe. Dr. Kirchhof reported research support from several drug and device companies active in AFib. He is also listed as an inventor on two patents held by the University of Hamburg on AFib therapy and AFib markers.
A version of this article first appeared on Medscape.com.
in the ARTESIA study.
The results appear to contrast somewhat with the recently reported NOAH-AFNET 6 trial, which failed to show a reduction in stroke with the anticoagulant edoxaban versus placebo in a similar patient group, but that trial was stopped early and so was underpowered.
However, the lead investigators of both trials say the studies actually show consistent results – both found a lower rate of stroke than expected in this population, but the confidence intervals for stroke reduction with anticoagulation overlap, suggesting there is likely some effect, albeit less than that in clinical AFib.
The big question is whether the reduction in stroke with anticoagulation outweighs the increase in major bleeding.
A new meta-analysis of the two trials showed that “oral anticoagulation with edoxaban or apixaban reduces the risk of ischemic stroke by approximately one-third and increases major bleeding by roughly double.”
In absolute numbers, there were three fewer ischemic strokes per 1,000 patient-years with anticoagulation in the two trials combined, at the cost of seven more major bleeds.
The lead investigators of the two trials have somewhat different opinions on how these findings may translate into clinical practice.
Jeff Healey, MD, Population Health Research Institute, McMaster University, Hamilton, Ont., lead investigator of the ARTESIA trial, believes that the risks and benefits need to be assessed in individual patients, but there should be some patient groups that will benefit from anticoagulation treatment.
“In patients with pacemakers or implantable loop recorders with continuous monitoring, subclinical AF[ib] is detected in about one third of patients, so this is extremely common,” he said in an interview. “The question is whether this is just a normal feature of getting older or is this like AF[ib] that we see in the clinic which increases stroke risk, and I think we can conclude from ARTESIA that this subclinical AF[ib] is associated with an increased risk of stroke, although that is lower than the risk with clinical AF[ib], and that it can be reduced by anticoagulation.”
Until recently it hasn’t been possible to quantify the risk associated with subclinical AFib, he noted. “But now we have a rich dataset to use to see if we can tease out some specifics on this. Future analyses of this dataset will help define patients where the benefits outweigh the risks of bleeding. For now, I think we can look at the data in a qualitative way and consider the totality of risk factors in each patient – their bleeding risk, stroke risk, how much AF[ib] they have, and make a decision as to whether to give anticoagulation or not.”
But Paulus Kirchhof, MD, University Heart and Vascular Center Hamburg (Germany), lead investigator of the NOAH-AFNET 6 trial said: “Both trials showed the stroke rate is low in these patients – about 1% per year – and that anticoagulation can reduce it a bit further at the expense of increasing major bleeding. I don’t believe the AF[ib] episodes picked up on these devices constitute a sufficient stroke risk to warrant anticoagulation, given the bleeding risk.”
Dr. Kirchhof suggests an alternate approach of performing further traditional AFib monitoring on these patients.
“I think going forward in my practice, when we come across this device-detected AF[ib], we will do further investigations with an established method for detecting AF[ib] involving surface ECG monitoring – maybe a 3-day or 7-day Holter. If that shows AF[ib], then we will be on firm ground to start anticoagulation. If that doesn’t show AF[ib], we will probably not use anticoagulation.”
The ARTESIA trial and the meta-analysis of the two trials were both presented at the annual scientific sessions of the American Heart Association. Both studies were also simultaneously published online – ARTESIA in the New England Journal of Medicine and the meta-analysis in Circulation.
ARTESIA
For the ARTESIA study, 4012 patients with device-detected AFib and other clinical risk factors for stroke were randomly assigned to treatment with apixaban (5 mg twice daily) or aspirin (81 mg daily).
After a mean follow-up of 3.5 years, the primary endpoint – stroke or systemic embolism – occurred in 55 patients in the apixaban group (0.78% per patient-year), compared with 86 patients in the aspirin group (1.24% per patient-year), giving a hazard ratio of 0.63 (95% confidence interval, 0.45-0.88; P = .007).
“The risk of stroke or systemic embolism was lower by 37% with apixaban than with aspirin, and the risk of disabling or fatal stroke was lower by 49%,” Dr. Healey reported.
In the “on-treatment” population, the rate of major bleeding was 1.71% per patient-year in the apixaban group and 0.94% per patient-year in the aspirin group (HR, 1.80; 95% CI, 1.26-2.57; P = .001).
Fatal bleeding occurred in five patients in the apixaban group and eight patients in the aspirin group. Symptomatic intracranial hemorrhage occurred in 12 patients with apixaban and 15 patients with aspirin.
One of the main findings of the trial is the lower-than-expected risk of ischemic stroke in this population – about 1% per year in the aspirin group, which was reduced to 0.64% per year in the apixaban group.
The authors noted that “simply counting strokes as compared with bleeding events might suggest a neutral overall effect. With apixaban as compared with aspirin, 31 fewer cases of stroke or systemic embolism were seen in the intention-to-treat analysis, as compared with 39 more major bleeding events in the on-treatment analysis.”
However, they pointed out that strokes involve permanent loss of brain tissue, whereas major bleeding is usually reversible, with most patients having complete recovery, which was the case in this study.
“Thus, on the basis of the considerably greater severity of the stroke events prevented than the bleeding events caused, we believe that these findings favor consideration of the use of oral anticoagulation for patients with risk factors for stroke in whom subclinical atrial fibrillation develops,” they concluded.
First well-powered trial addressing this question
Discussing the ARTESIA trial at an AHA press conference, Christine Albert, MD, Cedars-Sinai Medical Center, Los Angeles, said: “I want to emphasize how important this trial is.”
She explained that current guidelines do not recommend any treatment for patients with device-detected AFib that is not shown on ECG, even though it is known this confers some excess risk of stroke.
“ARTESIA is the first well-powered, long-term trial looking at this question,” she said. “It found a clear reduction in the risk of stroke/systemic embolism with apixaban vs aspirin, but there was also a significant amount of bleeding – about an 80% increase. The question is whether the benefit on stroke is worth it given the bleeding risk.”
Dr. Albert highlighted the low absolute risk of stroke in this study population of around 1.2%, pointing out that even with the 37% relative reduction with anticoagulation, stroke is only reduced in absolute terms by 0.4%.
“We are going to have to take this back to committees and guidelines and look at the balance between the benefit on stroke and the increase in bleeding,” she concluded.
Noting that observational studies have shown that the duration of AFib impacts the risk of stroke, Dr. Albert suggested that patients with longer-duration AFib may benefit from anticoagulation to a greater extent; and given that the bleeding seen in ARTESIA was mainly GI bleeding, it might be possible to screen out patients at high risk of GI bleeding.
She also pointed out that a lot of patients discontinued anticoagulation treatment in both ARTESIA and NOAH-AFNET 6, showing that this is not an easy strategy for elderly patients.
In an editorial accompanying publication of the ARTESIA trial, Emma Svennberg, MD, Karolinska Institute, Stockholm, also concluded that, “going forward, we must balance the increased bleeding risks with the risk for disabling strokes,” and that “future substudies and meta-analyses may provide further insights regarding treatment benefits in specific subgroups.”
NOAH-AFNET 6: New subgroup analysis
The previously reported NOAH-AFNET 6 study randomly assigned 2,538 patients with subclinical AFib and additional risk factors for stroke to anticoagulation with edoxaban or placebo. The trial was stopped early, so it was underpowered – but it found no difference between groups in the incidence of the composite endpoint of stroke, systemic embolism, or death from cardiovascular causes or in the incidence of stroke, although there was higher risk of major bleeding.
Again, there was a low rate of stroke in this trial with just 49 strokes in total in the whole study. The NOAH-AFNET-6 investigators concluded that these patients should not receive anticoagulation because the risk of bleeding outweighed any potential benefits.
A new subanalysis of the 259 patients who had durations of subclinical AFib of 24 hours or longer in the NOAH-AFNET 6 trial was presented at the AHA meeting, and simultaneously published online in the European Heart Journal.
This showed that the rate of stroke also appeared low in patients with these long durations of subclinical AFib, and that there was no interaction between the duration of subclinical AFib and the efficacy and safety of oral anticoagulation.
But with such a low number of events in the study as a whole and in the long duration subclinical AFib subgroup (in which there were just two strokes in each treatment group), this analysis was unlikely to show a difference, Dr. Kirchhof commented.
The subgroup analysis did, however, show that patients experiencing subclinical AFib durations of 24 hours or more were more likely to develop clinical AFib over time than those with shorter durations, suggesting the need for regular ECGs in these patients.
Dr. Kirchhof said better methods are needed to detect patients with subclinical AFib at high risk of stroke. “I don’t think our clinical stroke risk factor scores such as CHA2DS2-VASc are sufficient to detect high-risk patients. Patients in both NOAH-AFNET 6 and ARTESIA had a median CHA2DS2-VASc score of 4, but they had a stroke rate of just 1% per year,” he noted.
The meta-analysis of the two trials showed that the results from both are consistent, with an overall reduction in ischemic stroke with oral anticoagulation (relative risk, 0.68). Oral anticoagulation also reduced a composite of cardiovascular death, all-cause stroke, peripheral arterial embolism, myocardial infarction, or pulmonary embolism (RR, 0.85).
There was no significant difference in cardiovascular death (RR, 0.95) or all-cause mortality (RR, 1.08), but anticoagulation significantly increased major bleeding (RR, 1.62).
Aspirin use complicates results
Dr. Healey said further analyses of the ARTESIA data will try to tease out the effect of concomitant aspirin use in the trial.
He explained that patients in this trial were allowed to take a single antiplatelet agent on top of study therapy.
“It is difficult to work out the exact use of antiplatelet therapy as it changed throughout the study,” he said. “About two-thirds were taking antiplatelet agents at the time of enrollment into the trial, but this decreased throughout the study. Many clinicians stopped open-label antiplatelet therapy during the trial when new evidence came out to suggest that there was no added benefit of adding aspirin on top of anticoagulants.
“We need to look carefully as to what impact that may have had,” Dr. Healey added. “We know from other studies that adding an antiplatelet on top of an anticoagulant doesn’t do much to thromboembolic events, but it approximately doubles the risk of major bleeding.”
In contrast, the NOAH-AFNET trial did not allow aspirin use in the anticoagulation group and aspirin was taken by around half the patients in the placebo group who had an indication for its use.
The authors of the meta-analysis pointed out that the omission of aspirin in nearly half of the control patients in NOAH-AFNET 6 and the early termination of the trial may have led to a slightly higher estimate for excess major bleeding with anticoagulation.
The ARTESIA study was supported by the Canadian Institutes for Health Research, the Bristol Myers Squibb-Pfizer Alliance, the Heart and Stroke Foundation of Canada, the Canadian Stroke Prevention Intervention Network, Hamilton Health Sciences, the Advancing Clinical Trials Network and the Population Health Research Institute. Dr. Healey reported research grants and speaking fees from BMS/Pfizer Alliance, Servier, Novartis, Boston Scientific, Medtronic; and acts as a consultant to Bayer, Servier and Boston Scientific. The NOAH-AFNET 6 trial was an investigator-initiated trial funded by the German Center for Cardiovascular Research and Daiichi Sankyo Europe. Dr. Kirchhof reported research support from several drug and device companies active in AFib. He is also listed as an inventor on two patents held by the University of Hamburg on AFib therapy and AFib markers.
A version of this article first appeared on Medscape.com.
in the ARTESIA study.
The results appear to contrast somewhat with the recently reported NOAH-AFNET 6 trial, which failed to show a reduction in stroke with the anticoagulant edoxaban versus placebo in a similar patient group, but that trial was stopped early and so was underpowered.
However, the lead investigators of both trials say the studies actually show consistent results – both found a lower rate of stroke than expected in this population, but the confidence intervals for stroke reduction with anticoagulation overlap, suggesting there is likely some effect, albeit less than that in clinical AFib.
The big question is whether the reduction in stroke with anticoagulation outweighs the increase in major bleeding.
A new meta-analysis of the two trials showed that “oral anticoagulation with edoxaban or apixaban reduces the risk of ischemic stroke by approximately one-third and increases major bleeding by roughly double.”
In absolute numbers, there were three fewer ischemic strokes per 1,000 patient-years with anticoagulation in the two trials combined, at the cost of seven more major bleeds.
The lead investigators of the two trials have somewhat different opinions on how these findings may translate into clinical practice.
Jeff Healey, MD, Population Health Research Institute, McMaster University, Hamilton, Ont., lead investigator of the ARTESIA trial, believes that the risks and benefits need to be assessed in individual patients, but there should be some patient groups that will benefit from anticoagulation treatment.
“In patients with pacemakers or implantable loop recorders with continuous monitoring, subclinical AF[ib] is detected in about one third of patients, so this is extremely common,” he said in an interview. “The question is whether this is just a normal feature of getting older or is this like AF[ib] that we see in the clinic which increases stroke risk, and I think we can conclude from ARTESIA that this subclinical AF[ib] is associated with an increased risk of stroke, although that is lower than the risk with clinical AF[ib], and that it can be reduced by anticoagulation.”
Until recently it hasn’t been possible to quantify the risk associated with subclinical AFib, he noted. “But now we have a rich dataset to use to see if we can tease out some specifics on this. Future analyses of this dataset will help define patients where the benefits outweigh the risks of bleeding. For now, I think we can look at the data in a qualitative way and consider the totality of risk factors in each patient – their bleeding risk, stroke risk, how much AF[ib] they have, and make a decision as to whether to give anticoagulation or not.”
But Paulus Kirchhof, MD, University Heart and Vascular Center Hamburg (Germany), lead investigator of the NOAH-AFNET 6 trial said: “Both trials showed the stroke rate is low in these patients – about 1% per year – and that anticoagulation can reduce it a bit further at the expense of increasing major bleeding. I don’t believe the AF[ib] episodes picked up on these devices constitute a sufficient stroke risk to warrant anticoagulation, given the bleeding risk.”
Dr. Kirchhof suggests an alternate approach of performing further traditional AFib monitoring on these patients.
“I think going forward in my practice, when we come across this device-detected AF[ib], we will do further investigations with an established method for detecting AF[ib] involving surface ECG monitoring – maybe a 3-day or 7-day Holter. If that shows AF[ib], then we will be on firm ground to start anticoagulation. If that doesn’t show AF[ib], we will probably not use anticoagulation.”
The ARTESIA trial and the meta-analysis of the two trials were both presented at the annual scientific sessions of the American Heart Association. Both studies were also simultaneously published online – ARTESIA in the New England Journal of Medicine and the meta-analysis in Circulation.
ARTESIA
For the ARTESIA study, 4012 patients with device-detected AFib and other clinical risk factors for stroke were randomly assigned to treatment with apixaban (5 mg twice daily) or aspirin (81 mg daily).
After a mean follow-up of 3.5 years, the primary endpoint – stroke or systemic embolism – occurred in 55 patients in the apixaban group (0.78% per patient-year), compared with 86 patients in the aspirin group (1.24% per patient-year), giving a hazard ratio of 0.63 (95% confidence interval, 0.45-0.88; P = .007).
“The risk of stroke or systemic embolism was lower by 37% with apixaban than with aspirin, and the risk of disabling or fatal stroke was lower by 49%,” Dr. Healey reported.
In the “on-treatment” population, the rate of major bleeding was 1.71% per patient-year in the apixaban group and 0.94% per patient-year in the aspirin group (HR, 1.80; 95% CI, 1.26-2.57; P = .001).
Fatal bleeding occurred in five patients in the apixaban group and eight patients in the aspirin group. Symptomatic intracranial hemorrhage occurred in 12 patients with apixaban and 15 patients with aspirin.
One of the main findings of the trial is the lower-than-expected risk of ischemic stroke in this population – about 1% per year in the aspirin group, which was reduced to 0.64% per year in the apixaban group.
The authors noted that “simply counting strokes as compared with bleeding events might suggest a neutral overall effect. With apixaban as compared with aspirin, 31 fewer cases of stroke or systemic embolism were seen in the intention-to-treat analysis, as compared with 39 more major bleeding events in the on-treatment analysis.”
However, they pointed out that strokes involve permanent loss of brain tissue, whereas major bleeding is usually reversible, with most patients having complete recovery, which was the case in this study.
“Thus, on the basis of the considerably greater severity of the stroke events prevented than the bleeding events caused, we believe that these findings favor consideration of the use of oral anticoagulation for patients with risk factors for stroke in whom subclinical atrial fibrillation develops,” they concluded.
First well-powered trial addressing this question
Discussing the ARTESIA trial at an AHA press conference, Christine Albert, MD, Cedars-Sinai Medical Center, Los Angeles, said: “I want to emphasize how important this trial is.”
She explained that current guidelines do not recommend any treatment for patients with device-detected AFib that is not shown on ECG, even though it is known this confers some excess risk of stroke.
“ARTESIA is the first well-powered, long-term trial looking at this question,” she said. “It found a clear reduction in the risk of stroke/systemic embolism with apixaban vs aspirin, but there was also a significant amount of bleeding – about an 80% increase. The question is whether the benefit on stroke is worth it given the bleeding risk.”
Dr. Albert highlighted the low absolute risk of stroke in this study population of around 1.2%, pointing out that even with the 37% relative reduction with anticoagulation, stroke is only reduced in absolute terms by 0.4%.
“We are going to have to take this back to committees and guidelines and look at the balance between the benefit on stroke and the increase in bleeding,” she concluded.
Noting that observational studies have shown that the duration of AFib impacts the risk of stroke, Dr. Albert suggested that patients with longer-duration AFib may benefit from anticoagulation to a greater extent; and given that the bleeding seen in ARTESIA was mainly GI bleeding, it might be possible to screen out patients at high risk of GI bleeding.
She also pointed out that a lot of patients discontinued anticoagulation treatment in both ARTESIA and NOAH-AFNET 6, showing that this is not an easy strategy for elderly patients.
In an editorial accompanying publication of the ARTESIA trial, Emma Svennberg, MD, Karolinska Institute, Stockholm, also concluded that, “going forward, we must balance the increased bleeding risks with the risk for disabling strokes,” and that “future substudies and meta-analyses may provide further insights regarding treatment benefits in specific subgroups.”
NOAH-AFNET 6: New subgroup analysis
The previously reported NOAH-AFNET 6 study randomly assigned 2,538 patients with subclinical AFib and additional risk factors for stroke to anticoagulation with edoxaban or placebo. The trial was stopped early, so it was underpowered – but it found no difference between groups in the incidence of the composite endpoint of stroke, systemic embolism, or death from cardiovascular causes or in the incidence of stroke, although there was higher risk of major bleeding.
Again, there was a low rate of stroke in this trial with just 49 strokes in total in the whole study. The NOAH-AFNET-6 investigators concluded that these patients should not receive anticoagulation because the risk of bleeding outweighed any potential benefits.
A new subanalysis of the 259 patients who had durations of subclinical AFib of 24 hours or longer in the NOAH-AFNET 6 trial was presented at the AHA meeting, and simultaneously published online in the European Heart Journal.
This showed that the rate of stroke also appeared low in patients with these long durations of subclinical AFib, and that there was no interaction between the duration of subclinical AFib and the efficacy and safety of oral anticoagulation.
But with such a low number of events in the study as a whole and in the long duration subclinical AFib subgroup (in which there were just two strokes in each treatment group), this analysis was unlikely to show a difference, Dr. Kirchhof commented.
The subgroup analysis did, however, show that patients experiencing subclinical AFib durations of 24 hours or more were more likely to develop clinical AFib over time than those with shorter durations, suggesting the need for regular ECGs in these patients.
Dr. Kirchhof said better methods are needed to detect patients with subclinical AFib at high risk of stroke. “I don’t think our clinical stroke risk factor scores such as CHA2DS2-VASc are sufficient to detect high-risk patients. Patients in both NOAH-AFNET 6 and ARTESIA had a median CHA2DS2-VASc score of 4, but they had a stroke rate of just 1% per year,” he noted.
The meta-analysis of the two trials showed that the results from both are consistent, with an overall reduction in ischemic stroke with oral anticoagulation (relative risk, 0.68). Oral anticoagulation also reduced a composite of cardiovascular death, all-cause stroke, peripheral arterial embolism, myocardial infarction, or pulmonary embolism (RR, 0.85).
There was no significant difference in cardiovascular death (RR, 0.95) or all-cause mortality (RR, 1.08), but anticoagulation significantly increased major bleeding (RR, 1.62).
Aspirin use complicates results
Dr. Healey said further analyses of the ARTESIA data will try to tease out the effect of concomitant aspirin use in the trial.
He explained that patients in this trial were allowed to take a single antiplatelet agent on top of study therapy.
“It is difficult to work out the exact use of antiplatelet therapy as it changed throughout the study,” he said. “About two-thirds were taking antiplatelet agents at the time of enrollment into the trial, but this decreased throughout the study. Many clinicians stopped open-label antiplatelet therapy during the trial when new evidence came out to suggest that there was no added benefit of adding aspirin on top of anticoagulants.
“We need to look carefully as to what impact that may have had,” Dr. Healey added. “We know from other studies that adding an antiplatelet on top of an anticoagulant doesn’t do much to thromboembolic events, but it approximately doubles the risk of major bleeding.”
In contrast, the NOAH-AFNET trial did not allow aspirin use in the anticoagulation group and aspirin was taken by around half the patients in the placebo group who had an indication for its use.
The authors of the meta-analysis pointed out that the omission of aspirin in nearly half of the control patients in NOAH-AFNET 6 and the early termination of the trial may have led to a slightly higher estimate for excess major bleeding with anticoagulation.
The ARTESIA study was supported by the Canadian Institutes for Health Research, the Bristol Myers Squibb-Pfizer Alliance, the Heart and Stroke Foundation of Canada, the Canadian Stroke Prevention Intervention Network, Hamilton Health Sciences, the Advancing Clinical Trials Network and the Population Health Research Institute. Dr. Healey reported research grants and speaking fees from BMS/Pfizer Alliance, Servier, Novartis, Boston Scientific, Medtronic; and acts as a consultant to Bayer, Servier and Boston Scientific. The NOAH-AFNET 6 trial was an investigator-initiated trial funded by the German Center for Cardiovascular Research and Daiichi Sankyo Europe. Dr. Kirchhof reported research support from several drug and device companies active in AFib. He is also listed as an inventor on two patents held by the University of Hamburg on AFib therapy and AFib markers.
A version of this article first appeared on Medscape.com.
FROM AHA 2023
Impressive bleeding profile with factor XI inhibitor in AFib: AZALEA
; the risk of stroke was moderate to high.
The trial was stopped earlier this year because of an “overwhelming” reduction in bleeding with abelacimab in comparison to rivaroxaban. Abelacimab is a monoclonal antibody given by subcutaneous injection once a month.
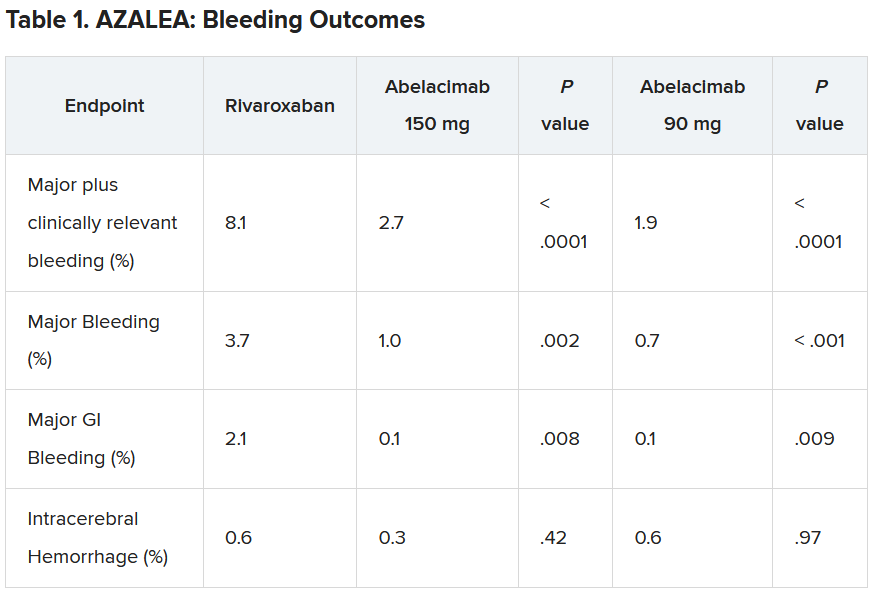
“Details of the bleeding results have now shown that the 150-mg dose of abelacimab, which is the dose being carried forward to phase 3 trials, was associated with a 67% reduction in major or clinically relevant nonmajor bleeding, the primary endpoint of the study.”
In addition, major bleeding was reduced by 74%, and major gastrointestinal bleeding was reduced by 93%.
“We are seeing really profound reductions in bleeding with this agent vs. a NOAC [novel oral anticoagulant],” lead AZALEA investigator Christian Ruff, MD, professor of medicine at Brigham and Women’s Hospital, Boston, said in an interview.
“Major bleeding – effectively the type of bleeding that results in hospitalization – is reduced by more than two-thirds, and major GI bleeding – which is the most common type of bleeding experienced by AF patients on anticoagulants – is almost eliminated. This gives us real hope that we have finally found an anticoagulant that is remarkably safe and will allow us to use anticoagulation in our most vulnerable patients,” he said.
Dr. Ruff presented the full results from the AZALEA trial at the American Heart Association scientific sessions.
He noted that AFib is one of the most common medical conditions in the world and that it confers an increased risk of stroke. Anticoagulants reduce this risk very effectively, and while the NOACS, such as apixaban and rivaroxaban, are safer than warfarin, significant bleeding still occurs, and “shockingly,” he said, between 30% and 60% of patients are not prescribed an anticoagulant or discontinue treatment because of bleeding concerns.
“Clearly, we need safer anticoagulants to protect these patients. Factor XI inhibitors, of which abelacimab is one, have emerged as the most promising agents, as they are thought to provide precision anticoagulation,” Dr. Ruff said.
He explained that factor XI appears to be involved in the formation of thrombus, which blocks arteries and causes strokes and myocardial infarction (thrombosis), but not in the healing process of blood vessels after injury (hemostasis). So, it is believed that inhibiting factor XI should reduce thrombotic events without causing excess bleeding.
AZALEA, which is the largest and longest trial of a factor XI inhibitor to date, enrolled 1,287 adults with AF who were at moderate to high risk of stroke.
They were randomly assigned to receive one of three treatments: oral rivaroxaban 20 mg daily; abelacimab 90 mg; or abelacimab 150 mg. Abelacimab was given monthly by injection.
Both doses of abelacimab inhibited factor XI almost completely; 97% inhibition was achieved with the 90-mg dose, and 99% inhibition was achieved with the 150-mg dose.
Results showed that after a median follow-up of 1.8 years, there was a clear reduction in all bleeding endpoints with both doses of abelacimab, compared with rivaroxaban.
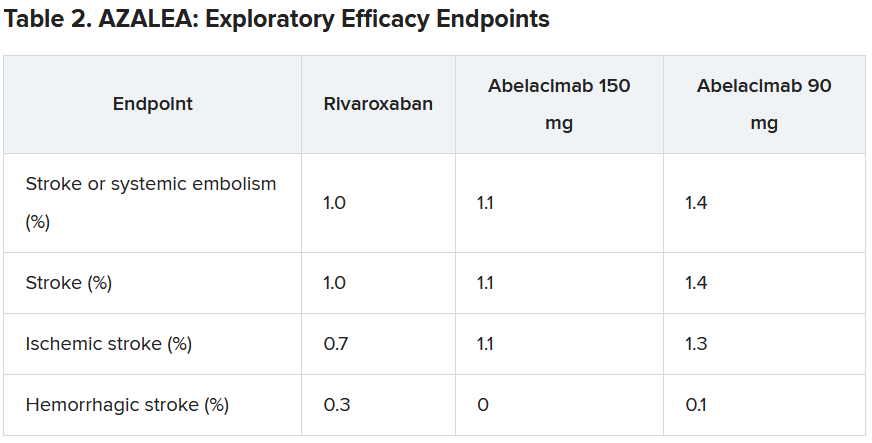
Dr. Ruff explained that the trial was powered to detect differences in bleeding, not stroke, but the investigators approached this in an exploratory way.
“As expected, the numbers were low, with just 25 strokes (23 ischemic strokes) across all three groups in the trial. So, because of this very low rate, we are really not able to compare how abelacimab compares with rivaroxaban in reducing stroke,” he commented.
He did, however, suggest that the low stroke rate in the study was encouraging.
“If we look at the same population without anticoagulation, the stroke rate would be about 7% per year. And we see here in this trial that in all three arms, the stroke rate was just above 1% per year. I think this shows that all the patients in the trial were getting highly effective anticoagulation,” he said.
“But what this trial doesn’t answer – because the numbers are so low – is exactly how effective factor XI inhibition with abelacimab is, compared to NOACs in reducing stroke rates. That requires dedicated phase 3 trials.”
Dr. Ruff pointed out that there are some reassuring data from phase 2 trials in venous thromboembolism (VTE), in which the 150-mg dose of abelacimab was associated with an 80% reduction in VTE, compared with enoxaparin. “Historically in the development of anticoagulants, efficacy in VTE has translated into efficacy in stroke prevention, so that is very encouraging,” he commented.
“So, I think our results along with the VTE results are encouraging, but the precision regarding the relative efficacy compared to NOACs is still an open question that needs to be clarified in phase 3 trials,” he concluded.
Several phase 3 trials are now underway with abelacimab and two other small-molecule orally available factor XI inhibitors, milvexian (BMS/Janssen) and asundexian (Bayer).
The designated discussant of the AZALEA study at the AHA meeting, Manesh Patel. MD, Duke University, Durham, N.C., described the results as “an important step forward.”
“This trial, with the prior data in this field, show that factor XI inhibition as a target is biologically possible (studies showing > 95% inhibition), significantly less bleeding than NOACS. We await the phase 3 studies, but having significantly less bleeding and similar or less stroke would be a substantial step forward for the field,” he said.
John Alexander, MD, also from Duke University, said: “There were clinically important reductions in bleeding with both doses of abelacimab, compared with rivaroxaban. This is consistent to what we’ve seen with comparisons between other factor XI inhibitors and other factor Xa inhibitors.”
On the exploratory efficacy results, Dr. Alexander agreed with Dr. Ruff that it was not possible to get any idea of how abelacimab compared with rivaroxaban in reducing stroke. “The hazard ratio and confidence intervals comparing abelacimab and rivaroxaban include substantial lower rates, no difference, and substantially higher rates,” he noted.
“We need to wait for the results of phase 3 trials, with abelacimab and other factor XI inhibitors, to understand how well factor XI inhibition prevents stroke and systemic embolism in patients with atrial fibrillation,” Dr. Alexander added. “These trials are ongoing.”
Dr. Ruff concluded: “Assuming the data from ongoing phase 3 trials confirm the benefit of factor XI inhibitors for stroke prevention in people with AF, it will really be transformative for the field of cardiology.
“Our first mission in treating people with AF is to prevent stroke, and our ability to do this with a remarkably safe anticoagulant such as abelacimab would be an incredible advance,” he concluded.
Dr. Ruff receives research funding from Anthos for abelacimab trials, is on an AF executive committee for BMS/Janssen (milvexian), and has been on an advisory board for Bayer (asundexian). Dr. Patel has received grants from and acts as an advisor to Bayer and Janssen. Dr. Alexander receives research funding from Bayer.
A version of this article first appeared on Medscape.com.
; the risk of stroke was moderate to high.
The trial was stopped earlier this year because of an “overwhelming” reduction in bleeding with abelacimab in comparison to rivaroxaban. Abelacimab is a monoclonal antibody given by subcutaneous injection once a month.
“Details of the bleeding results have now shown that the 150-mg dose of abelacimab, which is the dose being carried forward to phase 3 trials, was associated with a 67% reduction in major or clinically relevant nonmajor bleeding, the primary endpoint of the study.”
In addition, major bleeding was reduced by 74%, and major gastrointestinal bleeding was reduced by 93%.
“We are seeing really profound reductions in bleeding with this agent vs. a NOAC [novel oral anticoagulant],” lead AZALEA investigator Christian Ruff, MD, professor of medicine at Brigham and Women’s Hospital, Boston, said in an interview.
“Major bleeding – effectively the type of bleeding that results in hospitalization – is reduced by more than two-thirds, and major GI bleeding – which is the most common type of bleeding experienced by AF patients on anticoagulants – is almost eliminated. This gives us real hope that we have finally found an anticoagulant that is remarkably safe and will allow us to use anticoagulation in our most vulnerable patients,” he said.
Dr. Ruff presented the full results from the AZALEA trial at the American Heart Association scientific sessions.
He noted that AFib is one of the most common medical conditions in the world and that it confers an increased risk of stroke. Anticoagulants reduce this risk very effectively, and while the NOACS, such as apixaban and rivaroxaban, are safer than warfarin, significant bleeding still occurs, and “shockingly,” he said, between 30% and 60% of patients are not prescribed an anticoagulant or discontinue treatment because of bleeding concerns.
“Clearly, we need safer anticoagulants to protect these patients. Factor XI inhibitors, of which abelacimab is one, have emerged as the most promising agents, as they are thought to provide precision anticoagulation,” Dr. Ruff said.
He explained that factor XI appears to be involved in the formation of thrombus, which blocks arteries and causes strokes and myocardial infarction (thrombosis), but not in the healing process of blood vessels after injury (hemostasis). So, it is believed that inhibiting factor XI should reduce thrombotic events without causing excess bleeding.
AZALEA, which is the largest and longest trial of a factor XI inhibitor to date, enrolled 1,287 adults with AF who were at moderate to high risk of stroke.
They were randomly assigned to receive one of three treatments: oral rivaroxaban 20 mg daily; abelacimab 90 mg; or abelacimab 150 mg. Abelacimab was given monthly by injection.
Both doses of abelacimab inhibited factor XI almost completely; 97% inhibition was achieved with the 90-mg dose, and 99% inhibition was achieved with the 150-mg dose.
Results showed that after a median follow-up of 1.8 years, there was a clear reduction in all bleeding endpoints with both doses of abelacimab, compared with rivaroxaban.
Dr. Ruff explained that the trial was powered to detect differences in bleeding, not stroke, but the investigators approached this in an exploratory way.
“As expected, the numbers were low, with just 25 strokes (23 ischemic strokes) across all three groups in the trial. So, because of this very low rate, we are really not able to compare how abelacimab compares with rivaroxaban in reducing stroke,” he commented.
He did, however, suggest that the low stroke rate in the study was encouraging.
“If we look at the same population without anticoagulation, the stroke rate would be about 7% per year. And we see here in this trial that in all three arms, the stroke rate was just above 1% per year. I think this shows that all the patients in the trial were getting highly effective anticoagulation,” he said.
“But what this trial doesn’t answer – because the numbers are so low – is exactly how effective factor XI inhibition with abelacimab is, compared to NOACs in reducing stroke rates. That requires dedicated phase 3 trials.”
Dr. Ruff pointed out that there are some reassuring data from phase 2 trials in venous thromboembolism (VTE), in which the 150-mg dose of abelacimab was associated with an 80% reduction in VTE, compared with enoxaparin. “Historically in the development of anticoagulants, efficacy in VTE has translated into efficacy in stroke prevention, so that is very encouraging,” he commented.
“So, I think our results along with the VTE results are encouraging, but the precision regarding the relative efficacy compared to NOACs is still an open question that needs to be clarified in phase 3 trials,” he concluded.
Several phase 3 trials are now underway with abelacimab and two other small-molecule orally available factor XI inhibitors, milvexian (BMS/Janssen) and asundexian (Bayer).
The designated discussant of the AZALEA study at the AHA meeting, Manesh Patel. MD, Duke University, Durham, N.C., described the results as “an important step forward.”
“This trial, with the prior data in this field, show that factor XI inhibition as a target is biologically possible (studies showing > 95% inhibition), significantly less bleeding than NOACS. We await the phase 3 studies, but having significantly less bleeding and similar or less stroke would be a substantial step forward for the field,” he said.
John Alexander, MD, also from Duke University, said: “There were clinically important reductions in bleeding with both doses of abelacimab, compared with rivaroxaban. This is consistent to what we’ve seen with comparisons between other factor XI inhibitors and other factor Xa inhibitors.”
On the exploratory efficacy results, Dr. Alexander agreed with Dr. Ruff that it was not possible to get any idea of how abelacimab compared with rivaroxaban in reducing stroke. “The hazard ratio and confidence intervals comparing abelacimab and rivaroxaban include substantial lower rates, no difference, and substantially higher rates,” he noted.
“We need to wait for the results of phase 3 trials, with abelacimab and other factor XI inhibitors, to understand how well factor XI inhibition prevents stroke and systemic embolism in patients with atrial fibrillation,” Dr. Alexander added. “These trials are ongoing.”
Dr. Ruff concluded: “Assuming the data from ongoing phase 3 trials confirm the benefit of factor XI inhibitors for stroke prevention in people with AF, it will really be transformative for the field of cardiology.
“Our first mission in treating people with AF is to prevent stroke, and our ability to do this with a remarkably safe anticoagulant such as abelacimab would be an incredible advance,” he concluded.
Dr. Ruff receives research funding from Anthos for abelacimab trials, is on an AF executive committee for BMS/Janssen (milvexian), and has been on an advisory board for Bayer (asundexian). Dr. Patel has received grants from and acts as an advisor to Bayer and Janssen. Dr. Alexander receives research funding from Bayer.
A version of this article first appeared on Medscape.com.
; the risk of stroke was moderate to high.
The trial was stopped earlier this year because of an “overwhelming” reduction in bleeding with abelacimab in comparison to rivaroxaban. Abelacimab is a monoclonal antibody given by subcutaneous injection once a month.
“Details of the bleeding results have now shown that the 150-mg dose of abelacimab, which is the dose being carried forward to phase 3 trials, was associated with a 67% reduction in major or clinically relevant nonmajor bleeding, the primary endpoint of the study.”
In addition, major bleeding was reduced by 74%, and major gastrointestinal bleeding was reduced by 93%.
“We are seeing really profound reductions in bleeding with this agent vs. a NOAC [novel oral anticoagulant],” lead AZALEA investigator Christian Ruff, MD, professor of medicine at Brigham and Women’s Hospital, Boston, said in an interview.
“Major bleeding – effectively the type of bleeding that results in hospitalization – is reduced by more than two-thirds, and major GI bleeding – which is the most common type of bleeding experienced by AF patients on anticoagulants – is almost eliminated. This gives us real hope that we have finally found an anticoagulant that is remarkably safe and will allow us to use anticoagulation in our most vulnerable patients,” he said.
Dr. Ruff presented the full results from the AZALEA trial at the American Heart Association scientific sessions.
He noted that AFib is one of the most common medical conditions in the world and that it confers an increased risk of stroke. Anticoagulants reduce this risk very effectively, and while the NOACS, such as apixaban and rivaroxaban, are safer than warfarin, significant bleeding still occurs, and “shockingly,” he said, between 30% and 60% of patients are not prescribed an anticoagulant or discontinue treatment because of bleeding concerns.
“Clearly, we need safer anticoagulants to protect these patients. Factor XI inhibitors, of which abelacimab is one, have emerged as the most promising agents, as they are thought to provide precision anticoagulation,” Dr. Ruff said.
He explained that factor XI appears to be involved in the formation of thrombus, which blocks arteries and causes strokes and myocardial infarction (thrombosis), but not in the healing process of blood vessels after injury (hemostasis). So, it is believed that inhibiting factor XI should reduce thrombotic events without causing excess bleeding.
AZALEA, which is the largest and longest trial of a factor XI inhibitor to date, enrolled 1,287 adults with AF who were at moderate to high risk of stroke.
They were randomly assigned to receive one of three treatments: oral rivaroxaban 20 mg daily; abelacimab 90 mg; or abelacimab 150 mg. Abelacimab was given monthly by injection.
Both doses of abelacimab inhibited factor XI almost completely; 97% inhibition was achieved with the 90-mg dose, and 99% inhibition was achieved with the 150-mg dose.
Results showed that after a median follow-up of 1.8 years, there was a clear reduction in all bleeding endpoints with both doses of abelacimab, compared with rivaroxaban.
Dr. Ruff explained that the trial was powered to detect differences in bleeding, not stroke, but the investigators approached this in an exploratory way.
“As expected, the numbers were low, with just 25 strokes (23 ischemic strokes) across all three groups in the trial. So, because of this very low rate, we are really not able to compare how abelacimab compares with rivaroxaban in reducing stroke,” he commented.
He did, however, suggest that the low stroke rate in the study was encouraging.
“If we look at the same population without anticoagulation, the stroke rate would be about 7% per year. And we see here in this trial that in all three arms, the stroke rate was just above 1% per year. I think this shows that all the patients in the trial were getting highly effective anticoagulation,” he said.
“But what this trial doesn’t answer – because the numbers are so low – is exactly how effective factor XI inhibition with abelacimab is, compared to NOACs in reducing stroke rates. That requires dedicated phase 3 trials.”
Dr. Ruff pointed out that there are some reassuring data from phase 2 trials in venous thromboembolism (VTE), in which the 150-mg dose of abelacimab was associated with an 80% reduction in VTE, compared with enoxaparin. “Historically in the development of anticoagulants, efficacy in VTE has translated into efficacy in stroke prevention, so that is very encouraging,” he commented.
“So, I think our results along with the VTE results are encouraging, but the precision regarding the relative efficacy compared to NOACs is still an open question that needs to be clarified in phase 3 trials,” he concluded.
Several phase 3 trials are now underway with abelacimab and two other small-molecule orally available factor XI inhibitors, milvexian (BMS/Janssen) and asundexian (Bayer).
The designated discussant of the AZALEA study at the AHA meeting, Manesh Patel. MD, Duke University, Durham, N.C., described the results as “an important step forward.”
“This trial, with the prior data in this field, show that factor XI inhibition as a target is biologically possible (studies showing > 95% inhibition), significantly less bleeding than NOACS. We await the phase 3 studies, but having significantly less bleeding and similar or less stroke would be a substantial step forward for the field,” he said.
John Alexander, MD, also from Duke University, said: “There were clinically important reductions in bleeding with both doses of abelacimab, compared with rivaroxaban. This is consistent to what we’ve seen with comparisons between other factor XI inhibitors and other factor Xa inhibitors.”
On the exploratory efficacy results, Dr. Alexander agreed with Dr. Ruff that it was not possible to get any idea of how abelacimab compared with rivaroxaban in reducing stroke. “The hazard ratio and confidence intervals comparing abelacimab and rivaroxaban include substantial lower rates, no difference, and substantially higher rates,” he noted.
“We need to wait for the results of phase 3 trials, with abelacimab and other factor XI inhibitors, to understand how well factor XI inhibition prevents stroke and systemic embolism in patients with atrial fibrillation,” Dr. Alexander added. “These trials are ongoing.”
Dr. Ruff concluded: “Assuming the data from ongoing phase 3 trials confirm the benefit of factor XI inhibitors for stroke prevention in people with AF, it will really be transformative for the field of cardiology.
“Our first mission in treating people with AF is to prevent stroke, and our ability to do this with a remarkably safe anticoagulant such as abelacimab would be an incredible advance,” he concluded.
Dr. Ruff receives research funding from Anthos for abelacimab trials, is on an AF executive committee for BMS/Janssen (milvexian), and has been on an advisory board for Bayer (asundexian). Dr. Patel has received grants from and acts as an advisor to Bayer and Janssen. Dr. Alexander receives research funding from Bayer.
A version of this article first appeared on Medscape.com.
FROM AHA 2023
Atrial fibrillation linked to dementia, especially when diagnosed before age 65 years
TOPLINE:
Adults with atrial fibrillation (AFib) are at increased risk for dementia, especially when AFib occurs before age 65 years, new research shows. Investigators note the findings highlight the importance of monitoring cognitive function in adults with AF.
METHODOLOGY:
- This prospective, population-based cohort study leveraged data from 433,746 UK Biobank participants (55% women), including 30,601 with AFib, who were followed for a median of 12.6 years
- Incident cases of dementia were determined through linkage from multiple databases.
- Cox proportional hazards models and propensity score matching were used to estimate the association between age at onset of AFib and incident dementia.
TAKEAWAY:
- During follow-up, new-onset dementia occurred in 5,898 participants (2,546 with Alzheimer’s disease [AD] and 1,211 with vascular dementia [VD]), of which, 1,031 had AFib (350 with AD; 320 with VD).
- Compared with participants without AFib, those with AFib had a 42% higher risk for all-cause dementia (adjusted hazard ratio, 1.42; P < .001) and more than double the risk for VD (aHR, 2.06; P < .001), but no significantly higher risk for AD.
- Younger age at AFib onset was associated with higher risks for all-cause dementia, AD and VD, with aHRs per 10-year decrease of 1.23, 1.27, and 1.35, respectively (P < .001 for all).
- After propensity score matching, AFib onset before age 65 years had the highest risk for all-cause dementia (aHR, 1.82; P < .001), followed by AF onset at age 65-74 years (aHR, 1.47; P < .001). Similar results were seen in AD and VD.
IN PRACTICE:
“The findings indicate that careful monitoring of cognitive function for patients with a younger [AFib] onset age, particularly those diagnosed with [AFib] before age 65 years, is important to attenuate the risk of subsequent dementia,” the authors write.
SOURCE:
The study, with first author Wenya Zhang, with the Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, was published online in JAMA Network Open.
LIMITATIONS:
Because the study was observational, a cause-effect relationship cannot be established. Despite the adjustment for many underlying confounders, residual unidentified confounders may still exist. The vast majority of participants were White. The analyses did not consider the potential impact of effective treatment of AFib on dementia risk.
DISCLOSURES:
The study had no commercial funding. The authors have declared no conflicts of interest.
A version of this article appeared on Medscape.com.
TOPLINE:
Adults with atrial fibrillation (AFib) are at increased risk for dementia, especially when AFib occurs before age 65 years, new research shows. Investigators note the findings highlight the importance of monitoring cognitive function in adults with AF.
METHODOLOGY:
- This prospective, population-based cohort study leveraged data from 433,746 UK Biobank participants (55% women), including 30,601 with AFib, who were followed for a median of 12.6 years
- Incident cases of dementia were determined through linkage from multiple databases.
- Cox proportional hazards models and propensity score matching were used to estimate the association between age at onset of AFib and incident dementia.
TAKEAWAY:
- During follow-up, new-onset dementia occurred in 5,898 participants (2,546 with Alzheimer’s disease [AD] and 1,211 with vascular dementia [VD]), of which, 1,031 had AFib (350 with AD; 320 with VD).
- Compared with participants without AFib, those with AFib had a 42% higher risk for all-cause dementia (adjusted hazard ratio, 1.42; P < .001) and more than double the risk for VD (aHR, 2.06; P < .001), but no significantly higher risk for AD.
- Younger age at AFib onset was associated with higher risks for all-cause dementia, AD and VD, with aHRs per 10-year decrease of 1.23, 1.27, and 1.35, respectively (P < .001 for all).
- After propensity score matching, AFib onset before age 65 years had the highest risk for all-cause dementia (aHR, 1.82; P < .001), followed by AF onset at age 65-74 years (aHR, 1.47; P < .001). Similar results were seen in AD and VD.
IN PRACTICE:
“The findings indicate that careful monitoring of cognitive function for patients with a younger [AFib] onset age, particularly those diagnosed with [AFib] before age 65 years, is important to attenuate the risk of subsequent dementia,” the authors write.
SOURCE:
The study, with first author Wenya Zhang, with the Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, was published online in JAMA Network Open.
LIMITATIONS:
Because the study was observational, a cause-effect relationship cannot be established. Despite the adjustment for many underlying confounders, residual unidentified confounders may still exist. The vast majority of participants were White. The analyses did not consider the potential impact of effective treatment of AFib on dementia risk.
DISCLOSURES:
The study had no commercial funding. The authors have declared no conflicts of interest.
A version of this article appeared on Medscape.com.
TOPLINE:
Adults with atrial fibrillation (AFib) are at increased risk for dementia, especially when AFib occurs before age 65 years, new research shows. Investigators note the findings highlight the importance of monitoring cognitive function in adults with AF.
METHODOLOGY:
- This prospective, population-based cohort study leveraged data from 433,746 UK Biobank participants (55% women), including 30,601 with AFib, who were followed for a median of 12.6 years
- Incident cases of dementia were determined through linkage from multiple databases.
- Cox proportional hazards models and propensity score matching were used to estimate the association between age at onset of AFib and incident dementia.
TAKEAWAY:
- During follow-up, new-onset dementia occurred in 5,898 participants (2,546 with Alzheimer’s disease [AD] and 1,211 with vascular dementia [VD]), of which, 1,031 had AFib (350 with AD; 320 with VD).
- Compared with participants without AFib, those with AFib had a 42% higher risk for all-cause dementia (adjusted hazard ratio, 1.42; P < .001) and more than double the risk for VD (aHR, 2.06; P < .001), but no significantly higher risk for AD.
- Younger age at AFib onset was associated with higher risks for all-cause dementia, AD and VD, with aHRs per 10-year decrease of 1.23, 1.27, and 1.35, respectively (P < .001 for all).
- After propensity score matching, AFib onset before age 65 years had the highest risk for all-cause dementia (aHR, 1.82; P < .001), followed by AF onset at age 65-74 years (aHR, 1.47; P < .001). Similar results were seen in AD and VD.
IN PRACTICE:
“The findings indicate that careful monitoring of cognitive function for patients with a younger [AFib] onset age, particularly those diagnosed with [AFib] before age 65 years, is important to attenuate the risk of subsequent dementia,” the authors write.
SOURCE:
The study, with first author Wenya Zhang, with the Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, was published online in JAMA Network Open.
LIMITATIONS:
Because the study was observational, a cause-effect relationship cannot be established. Despite the adjustment for many underlying confounders, residual unidentified confounders may still exist. The vast majority of participants were White. The analyses did not consider the potential impact of effective treatment of AFib on dementia risk.
DISCLOSURES:
The study had no commercial funding. The authors have declared no conflicts of interest.
A version of this article appeared on Medscape.com.
Blood pressure lowering reduces dementia risk
Results of a trial using an intensive, 4-year program aimed at blood pressure lowering showed that intervention reduced not only blood pressure, but also significantly reduced the risk of total dementia over that period.
and cognitive impairment no dementia (CIND), a secondary outcome, was also significantly reduced by 16%.
“Blood pressure reduction is effective in reducing the risk of dementia in patients with hypertension,” concluded Jiang He, MD, PhD, professor of epidemiology and medicine and director of Tulane University’s Translational Science Institute, New Orleans. “This proven, effective intervention should be widely scaled up to reduce the global burden of dementia.”
He presented these results from the China Rural Hypertension Control Project (CRHCP) at the annual scientific sessions of the American Heart Association.
Target organ damage
Keith Ferdinand, MD, also from Tulane University, commented on the findings during a press conference at the meeting, noting that the result “opens our opportunity to recognize that the target organ damage of hypertension also now includes dementia.”
The researchers were able to “rigorously lower blood pressure from 157 to 127.6 in the intervention, 155 to 147 in the controls – 22 mg Hg – and if you look at the P values for all the various outcomes, they were very robust,” Dr. Ferdinand said.
Another interesting feature about the strategy used in this trial is that “this was true team-based care,” he pointed out. The trained interventionists in the study, called village doctors, collaborated with primary care physicians and initiated medications. “They stayed on a simple treatment protocol, and they were able to assist patients to ensure they had free medications, health coaching for lifestyle, home blood pressure measurement, and ensuring adherence.”
So, Dr. Ferdinand added, “one of the questions is whether this is a model we can use in other places around the globe, in places with low resources, and in the United States in disadvantaged populations.”
Public health priority
It’s estimated that the global number of those living with dementia will increase from 57.4 million in 2019 to 152.8 million by 2050, Dr. He said. “In the absence of curative treatment, the primary prevention of dementia through risk factor reduction, such as blood pressure lowering, becomes a public health priority.”
Previous randomized trials have lacked sample size and duration but have reported a nonsignificant reduction in dementia associated with antihypertensive treatment in patients with hypertension or a history of stroke, Dr. He noted.
This new trial aimed to test the effectiveness of intensive BP intervention to reduce the risk of all-cause dementia and cognitive impairment over a 48-month intervention period versus usual care.
It was an open-label, blinded-endpoint, cluster-randomized trial, and included 33,995 individual patients from 325 villages in China, aged 40 years and older, with untreated hypertension. The villages were randomly assigned to an intervention group or usual care, stratified by province, county, and township.
Patients were eligible if they had mean untreated systolic BP greater than 140 mm Hg and/or diastolic BP greater than 90 mm Hg or mean treated systolic BP of greater than 130 and/or diastolic greater than 80 mm Hg. Patients with a history of cardiovascular disease, chronic kidney disease, or diabetes and a mean systolic BP greater than 130 mm Hg and/or diastolic BP greater than 80 mm Hg from six measures on two different days were also eligible.
All were enrolled in the China New Rural Cooperative Medical Scheme, which covers 99% of rural residents for health care services, Dr. He noted.
The intervention was a simple stepped-care protocol for hypertension treatment, aimed at achieving a target systolic BP of less than 130 mm Hg and diastolic of less than 80 mm Hg.
Village doctors started and titrated antihypertensive treatment based on a protocol and were able to deliver discounted and free medications to patients. They also did health coaching on lifestyle modification and adherence to medication, and instructed patients on home BP monitoring.
Patients were provided training, supervision, and consultation by primary care physicians and hypertension specialists.
At the month 48 follow-up visit, the participants were assessed by neurologists who were blinded to randomization assignments. Neurologists did a variety of tests and assessments including collecting data on the patient’s medical and psychiatric history and risk factors for dementia, as well as neurologic assessment using the Mini-Mental State Examination, the Functional Activities Questionnaire, and the Quick Dementia Rating System.
The primary outcome was all-cause dementia, defined according to recommendations from the National Institute on Aging–Alzheimer’s Association work groups on diagnostic guidelines for Alzheimer’s disease.
Secondary outcomes included CIND, a composite outcome of dementia or CIND, and a composite of dementia or deaths.
The final diagnosis of all-cause dementia or CIND was made by an expert adjudication panel blinded to the intervention assignment.
At 48 months, 91.3% of patients completed the follow-up for clinical outcomes. Participants were an average of 63 years of age, 61% were female, and 23% had less than a primary school education, Dr. He noted.
The net group differences in systolic and diastolic BP reduction were 22 and 9.3 mm Hg, respectively (P < .0001).
Significant differences were also seen between the groups in the primary outcome of all-cause dementia, as well as secondary outcomes of CIND, dementia or cognitive impairment, or dementia or deaths.
Serious adverse events were more common in the usual care group, and there was no difference between groups in the occurrence of falls or syncope.
The effect was consistent across subgroups, Dr. He said, including age, sex, education, cigarette smoking, body mass index, systolic BP, and fasting plasma glucose at baseline.
First definitive evidence
Invited discussant for the trial, Daniel W. Jones, MD, University of Mississippi Medical Center, Jackson, and past president of the AHA, pointed out that previous results from CRHCP on cardiovascular outcomes, reported earlier in 2023 in The Lancet, showed that, similar to results of the large SPRINT trial, lowering systolic BP to a goal of less than 130 mm Hg reduced a composite endpoint of MI, stroke, heart failure requiring hospitalization, and cardiovascular disease death over the 36-month follow-up.
The SPRINT findings also suggested a possible reduction in dementia, Dr. Jones said.
Now, in these new CRHCP results, “there was a clear benefit for intensive BP control in reducing risk for dementia and cognitive dysfunction,” he said. “This is, importantly, the first definitive evidence of dementia risk reduction demonstrated in a randomized controlled clinical trial. This outcome supports observational data that shows a strong relationship between BP and dementia.”
Since it is the first of its kind though, replication of the results will be important, he noted.
The study also showed that the intervention, using minimally trained village doctors, sustained BP control for 48 months. “This model could be used in any setting with modifications, including in the United States,” Dr. Jones said.
The study was supported by the Ministry of Science and Technology of China; U.S. investigators did not receive financial support from this study. The researchers and Dr. Jones disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Results of a trial using an intensive, 4-year program aimed at blood pressure lowering showed that intervention reduced not only blood pressure, but also significantly reduced the risk of total dementia over that period.
and cognitive impairment no dementia (CIND), a secondary outcome, was also significantly reduced by 16%.
“Blood pressure reduction is effective in reducing the risk of dementia in patients with hypertension,” concluded Jiang He, MD, PhD, professor of epidemiology and medicine and director of Tulane University’s Translational Science Institute, New Orleans. “This proven, effective intervention should be widely scaled up to reduce the global burden of dementia.”
He presented these results from the China Rural Hypertension Control Project (CRHCP) at the annual scientific sessions of the American Heart Association.
Target organ damage
Keith Ferdinand, MD, also from Tulane University, commented on the findings during a press conference at the meeting, noting that the result “opens our opportunity to recognize that the target organ damage of hypertension also now includes dementia.”
The researchers were able to “rigorously lower blood pressure from 157 to 127.6 in the intervention, 155 to 147 in the controls – 22 mg Hg – and if you look at the P values for all the various outcomes, they were very robust,” Dr. Ferdinand said.
Another interesting feature about the strategy used in this trial is that “this was true team-based care,” he pointed out. The trained interventionists in the study, called village doctors, collaborated with primary care physicians and initiated medications. “They stayed on a simple treatment protocol, and they were able to assist patients to ensure they had free medications, health coaching for lifestyle, home blood pressure measurement, and ensuring adherence.”
So, Dr. Ferdinand added, “one of the questions is whether this is a model we can use in other places around the globe, in places with low resources, and in the United States in disadvantaged populations.”
Public health priority
It’s estimated that the global number of those living with dementia will increase from 57.4 million in 2019 to 152.8 million by 2050, Dr. He said. “In the absence of curative treatment, the primary prevention of dementia through risk factor reduction, such as blood pressure lowering, becomes a public health priority.”
Previous randomized trials have lacked sample size and duration but have reported a nonsignificant reduction in dementia associated with antihypertensive treatment in patients with hypertension or a history of stroke, Dr. He noted.
This new trial aimed to test the effectiveness of intensive BP intervention to reduce the risk of all-cause dementia and cognitive impairment over a 48-month intervention period versus usual care.
It was an open-label, blinded-endpoint, cluster-randomized trial, and included 33,995 individual patients from 325 villages in China, aged 40 years and older, with untreated hypertension. The villages were randomly assigned to an intervention group or usual care, stratified by province, county, and township.
Patients were eligible if they had mean untreated systolic BP greater than 140 mm Hg and/or diastolic BP greater than 90 mm Hg or mean treated systolic BP of greater than 130 and/or diastolic greater than 80 mm Hg. Patients with a history of cardiovascular disease, chronic kidney disease, or diabetes and a mean systolic BP greater than 130 mm Hg and/or diastolic BP greater than 80 mm Hg from six measures on two different days were also eligible.
All were enrolled in the China New Rural Cooperative Medical Scheme, which covers 99% of rural residents for health care services, Dr. He noted.
The intervention was a simple stepped-care protocol for hypertension treatment, aimed at achieving a target systolic BP of less than 130 mm Hg and diastolic of less than 80 mm Hg.
Village doctors started and titrated antihypertensive treatment based on a protocol and were able to deliver discounted and free medications to patients. They also did health coaching on lifestyle modification and adherence to medication, and instructed patients on home BP monitoring.
Patients were provided training, supervision, and consultation by primary care physicians and hypertension specialists.
At the month 48 follow-up visit, the participants were assessed by neurologists who were blinded to randomization assignments. Neurologists did a variety of tests and assessments including collecting data on the patient’s medical and psychiatric history and risk factors for dementia, as well as neurologic assessment using the Mini-Mental State Examination, the Functional Activities Questionnaire, and the Quick Dementia Rating System.
The primary outcome was all-cause dementia, defined according to recommendations from the National Institute on Aging–Alzheimer’s Association work groups on diagnostic guidelines for Alzheimer’s disease.
Secondary outcomes included CIND, a composite outcome of dementia or CIND, and a composite of dementia or deaths.
The final diagnosis of all-cause dementia or CIND was made by an expert adjudication panel blinded to the intervention assignment.
At 48 months, 91.3% of patients completed the follow-up for clinical outcomes. Participants were an average of 63 years of age, 61% were female, and 23% had less than a primary school education, Dr. He noted.
The net group differences in systolic and diastolic BP reduction were 22 and 9.3 mm Hg, respectively (P < .0001).
Significant differences were also seen between the groups in the primary outcome of all-cause dementia, as well as secondary outcomes of CIND, dementia or cognitive impairment, or dementia or deaths.
Serious adverse events were more common in the usual care group, and there was no difference between groups in the occurrence of falls or syncope.
The effect was consistent across subgroups, Dr. He said, including age, sex, education, cigarette smoking, body mass index, systolic BP, and fasting plasma glucose at baseline.
First definitive evidence
Invited discussant for the trial, Daniel W. Jones, MD, University of Mississippi Medical Center, Jackson, and past president of the AHA, pointed out that previous results from CRHCP on cardiovascular outcomes, reported earlier in 2023 in The Lancet, showed that, similar to results of the large SPRINT trial, lowering systolic BP to a goal of less than 130 mm Hg reduced a composite endpoint of MI, stroke, heart failure requiring hospitalization, and cardiovascular disease death over the 36-month follow-up.
The SPRINT findings also suggested a possible reduction in dementia, Dr. Jones said.
Now, in these new CRHCP results, “there was a clear benefit for intensive BP control in reducing risk for dementia and cognitive dysfunction,” he said. “This is, importantly, the first definitive evidence of dementia risk reduction demonstrated in a randomized controlled clinical trial. This outcome supports observational data that shows a strong relationship between BP and dementia.”
Since it is the first of its kind though, replication of the results will be important, he noted.
The study also showed that the intervention, using minimally trained village doctors, sustained BP control for 48 months. “This model could be used in any setting with modifications, including in the United States,” Dr. Jones said.
The study was supported by the Ministry of Science and Technology of China; U.S. investigators did not receive financial support from this study. The researchers and Dr. Jones disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Results of a trial using an intensive, 4-year program aimed at blood pressure lowering showed that intervention reduced not only blood pressure, but also significantly reduced the risk of total dementia over that period.
and cognitive impairment no dementia (CIND), a secondary outcome, was also significantly reduced by 16%.
“Blood pressure reduction is effective in reducing the risk of dementia in patients with hypertension,” concluded Jiang He, MD, PhD, professor of epidemiology and medicine and director of Tulane University’s Translational Science Institute, New Orleans. “This proven, effective intervention should be widely scaled up to reduce the global burden of dementia.”
He presented these results from the China Rural Hypertension Control Project (CRHCP) at the annual scientific sessions of the American Heart Association.
Target organ damage
Keith Ferdinand, MD, also from Tulane University, commented on the findings during a press conference at the meeting, noting that the result “opens our opportunity to recognize that the target organ damage of hypertension also now includes dementia.”
The researchers were able to “rigorously lower blood pressure from 157 to 127.6 in the intervention, 155 to 147 in the controls – 22 mg Hg – and if you look at the P values for all the various outcomes, they were very robust,” Dr. Ferdinand said.
Another interesting feature about the strategy used in this trial is that “this was true team-based care,” he pointed out. The trained interventionists in the study, called village doctors, collaborated with primary care physicians and initiated medications. “They stayed on a simple treatment protocol, and they were able to assist patients to ensure they had free medications, health coaching for lifestyle, home blood pressure measurement, and ensuring adherence.”
So, Dr. Ferdinand added, “one of the questions is whether this is a model we can use in other places around the globe, in places with low resources, and in the United States in disadvantaged populations.”
Public health priority
It’s estimated that the global number of those living with dementia will increase from 57.4 million in 2019 to 152.8 million by 2050, Dr. He said. “In the absence of curative treatment, the primary prevention of dementia through risk factor reduction, such as blood pressure lowering, becomes a public health priority.”
Previous randomized trials have lacked sample size and duration but have reported a nonsignificant reduction in dementia associated with antihypertensive treatment in patients with hypertension or a history of stroke, Dr. He noted.
This new trial aimed to test the effectiveness of intensive BP intervention to reduce the risk of all-cause dementia and cognitive impairment over a 48-month intervention period versus usual care.
It was an open-label, blinded-endpoint, cluster-randomized trial, and included 33,995 individual patients from 325 villages in China, aged 40 years and older, with untreated hypertension. The villages were randomly assigned to an intervention group or usual care, stratified by province, county, and township.
Patients were eligible if they had mean untreated systolic BP greater than 140 mm Hg and/or diastolic BP greater than 90 mm Hg or mean treated systolic BP of greater than 130 and/or diastolic greater than 80 mm Hg. Patients with a history of cardiovascular disease, chronic kidney disease, or diabetes and a mean systolic BP greater than 130 mm Hg and/or diastolic BP greater than 80 mm Hg from six measures on two different days were also eligible.
All were enrolled in the China New Rural Cooperative Medical Scheme, which covers 99% of rural residents for health care services, Dr. He noted.
The intervention was a simple stepped-care protocol for hypertension treatment, aimed at achieving a target systolic BP of less than 130 mm Hg and diastolic of less than 80 mm Hg.
Village doctors started and titrated antihypertensive treatment based on a protocol and were able to deliver discounted and free medications to patients. They also did health coaching on lifestyle modification and adherence to medication, and instructed patients on home BP monitoring.
Patients were provided training, supervision, and consultation by primary care physicians and hypertension specialists.
At the month 48 follow-up visit, the participants were assessed by neurologists who were blinded to randomization assignments. Neurologists did a variety of tests and assessments including collecting data on the patient’s medical and psychiatric history and risk factors for dementia, as well as neurologic assessment using the Mini-Mental State Examination, the Functional Activities Questionnaire, and the Quick Dementia Rating System.
The primary outcome was all-cause dementia, defined according to recommendations from the National Institute on Aging–Alzheimer’s Association work groups on diagnostic guidelines for Alzheimer’s disease.
Secondary outcomes included CIND, a composite outcome of dementia or CIND, and a composite of dementia or deaths.
The final diagnosis of all-cause dementia or CIND was made by an expert adjudication panel blinded to the intervention assignment.
At 48 months, 91.3% of patients completed the follow-up for clinical outcomes. Participants were an average of 63 years of age, 61% were female, and 23% had less than a primary school education, Dr. He noted.
The net group differences in systolic and diastolic BP reduction were 22 and 9.3 mm Hg, respectively (P < .0001).
Significant differences were also seen between the groups in the primary outcome of all-cause dementia, as well as secondary outcomes of CIND, dementia or cognitive impairment, or dementia or deaths.
Serious adverse events were more common in the usual care group, and there was no difference between groups in the occurrence of falls or syncope.
The effect was consistent across subgroups, Dr. He said, including age, sex, education, cigarette smoking, body mass index, systolic BP, and fasting plasma glucose at baseline.
First definitive evidence
Invited discussant for the trial, Daniel W. Jones, MD, University of Mississippi Medical Center, Jackson, and past president of the AHA, pointed out that previous results from CRHCP on cardiovascular outcomes, reported earlier in 2023 in The Lancet, showed that, similar to results of the large SPRINT trial, lowering systolic BP to a goal of less than 130 mm Hg reduced a composite endpoint of MI, stroke, heart failure requiring hospitalization, and cardiovascular disease death over the 36-month follow-up.
The SPRINT findings also suggested a possible reduction in dementia, Dr. Jones said.
Now, in these new CRHCP results, “there was a clear benefit for intensive BP control in reducing risk for dementia and cognitive dysfunction,” he said. “This is, importantly, the first definitive evidence of dementia risk reduction demonstrated in a randomized controlled clinical trial. This outcome supports observational data that shows a strong relationship between BP and dementia.”
Since it is the first of its kind though, replication of the results will be important, he noted.
The study also showed that the intervention, using minimally trained village doctors, sustained BP control for 48 months. “This model could be used in any setting with modifications, including in the United States,” Dr. Jones said.
The study was supported by the Ministry of Science and Technology of China; U.S. investigators did not receive financial support from this study. The researchers and Dr. Jones disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
FROM AHA 2023
Alpha-gal syndrome: Red meat is ‘just the beginning,’ expert says
ANAHEIM, CALIF. – allergist and immunologist Scott P. Commins, MD, PhD, told attendees at the annual meeting of the American College of Allergy, Asthma, and Immunology (ACAAI) annual meeting.
Dr. Commins, associate chief for allergy and immunology at the University of North Carolina at Chapel Hill, has made alpha-gal, a potentially fatal allergy, which, in the United States is tied to the bite of the Lone Star tick, his primary research focus.
Beyond red meat, “there are some people who are allergic to all things mammal,” he explained. Dairy products from mammals, medical devices made from mammalian products, vaccines and medicines that contain gelatin, and even commercial products such as perfumes and cosmetics may be behind an AGS reaction.
“The derived products from pigs and cows really find their way into a lot of our day-to-day products,” he said. “I try to keep an open mind about these exposures.”
Physicians should also be aware that “this can happen to kids,” said Dr. Commins. “It looks very similar to adults’ [AGS]. They can end up in the emergency department.”
He also had clinical advice about food challenges for AGS. He explained that there’s more alpha-gal in beef than in other red meats (including pork, venison, and lamb) with the exception of pork kidney. Pork kidney, he said, “has the most alpha-gal that we can find in the lab.”
Dr. Commins said he has stopped using beef for AGS food challenges and has switched to pork sausage patties with a high fat content microwaved in the clinic because they have less alpha-gal in general and he views them as safer.
Long delay in symptom onset
AGS symptoms typically take 2-6 hours to appear after eating red meat or being exposed to mammalian products, but Dr. Commins related a story about a patient he sent home who had very mild symptoms (some lower back itching) after he had spent the day at the clinic after a pork sausage food challenge for AGS.
The patient had returned home. Eight hours after the food challenge, his wife sent Dr. Commins a picture of her husband’s back, which was riddled with welts and was itching badly.
“I learned that if you’re going to do these food challenges, if there is a hint of symptoms at the clinic at 6 hours, keep them in the clinic, because it may really take that long to evolve,” Dr. Commins said.
One of the early signs he’s discovered is palmar erythema (redness and swelling of the hands).
Research has shown that AGS has been heavily concentrated in the Southeast, where Lone Star tick populations are clustered, but research has shown that from 2017 to 2022, it moved up the East Coast to the central United States and Upper Midwest.
“We are seeing increasing diagnoses of AGS in places that are not, perhaps, where we first thought this allergy existed,” said Dr. Commins. “Stay aware,” he cautioned.
The allergy is not exclusive to the United States, he noted. In Europe and Australia, for example, AGS is not thought to be tied to the Lone Star tick, which doesn’t inhabit those regions.
“It is a global phenomenon,” Dr. Commins said.
In August, the CDC alerted physicians to emerging cases of alpha-gal allergy after an article in Morbidity and Mortality Weekly Report indicated that health care providers have little knowledge about the allergy. Of the 1,500 health care providers surveyed, 42% had never heard of the syndrome, and another 35% were not confident in diagnosing or managing affected patients.
Matthew Lau, MD, an allergist with Kaiser Permanente in Honolulu who listened to Dr. Commins’ talk, told this news organization, “It’s important to raise awareness in primary care particularly, he said, as “allergists see only a fraction of the [AGS] patients.”
Allergists can help raise awareness
“Allergists have a role to alert the general community” and to drive more referrals, he said. That includes emergency departments, where physicians commonly see anaphylaxis.
Dr. Lau said he expects the incidence of AGS to increase, because global warming will likely lengthen warmer seasons and cause the geographic distribution to change.
Jay Lieberman, MD, a pediatric allergist at Le Bonheur Children’s Hospital in Memphis, Tenn., told this news organization, “There’s still a lot of confusion, and hearing from an expert like Dr. Commins helps tease out the not-obvious things about patients who are having more mild symptoms,” such as from allergy to dairy or medicines or vaccines that contain gelatin.
As a pediatric allergist, Dr. Lieberman said he sees less alpha-gal than his colleagues, but, he said, “On the adult side in Tennessee, it’s rampant.”
Dr. Commins, Dr. Lieberman, and Dr. Lau report no relevant financial relationships.
A version of this article appeared on Medscape.com.
ANAHEIM, CALIF. – allergist and immunologist Scott P. Commins, MD, PhD, told attendees at the annual meeting of the American College of Allergy, Asthma, and Immunology (ACAAI) annual meeting.
Dr. Commins, associate chief for allergy and immunology at the University of North Carolina at Chapel Hill, has made alpha-gal, a potentially fatal allergy, which, in the United States is tied to the bite of the Lone Star tick, his primary research focus.
Beyond red meat, “there are some people who are allergic to all things mammal,” he explained. Dairy products from mammals, medical devices made from mammalian products, vaccines and medicines that contain gelatin, and even commercial products such as perfumes and cosmetics may be behind an AGS reaction.
“The derived products from pigs and cows really find their way into a lot of our day-to-day products,” he said. “I try to keep an open mind about these exposures.”
Physicians should also be aware that “this can happen to kids,” said Dr. Commins. “It looks very similar to adults’ [AGS]. They can end up in the emergency department.”
He also had clinical advice about food challenges for AGS. He explained that there’s more alpha-gal in beef than in other red meats (including pork, venison, and lamb) with the exception of pork kidney. Pork kidney, he said, “has the most alpha-gal that we can find in the lab.”
Dr. Commins said he has stopped using beef for AGS food challenges and has switched to pork sausage patties with a high fat content microwaved in the clinic because they have less alpha-gal in general and he views them as safer.
Long delay in symptom onset
AGS symptoms typically take 2-6 hours to appear after eating red meat or being exposed to mammalian products, but Dr. Commins related a story about a patient he sent home who had very mild symptoms (some lower back itching) after he had spent the day at the clinic after a pork sausage food challenge for AGS.
The patient had returned home. Eight hours after the food challenge, his wife sent Dr. Commins a picture of her husband’s back, which was riddled with welts and was itching badly.
“I learned that if you’re going to do these food challenges, if there is a hint of symptoms at the clinic at 6 hours, keep them in the clinic, because it may really take that long to evolve,” Dr. Commins said.
One of the early signs he’s discovered is palmar erythema (redness and swelling of the hands).
Research has shown that AGS has been heavily concentrated in the Southeast, where Lone Star tick populations are clustered, but research has shown that from 2017 to 2022, it moved up the East Coast to the central United States and Upper Midwest.
“We are seeing increasing diagnoses of AGS in places that are not, perhaps, where we first thought this allergy existed,” said Dr. Commins. “Stay aware,” he cautioned.
The allergy is not exclusive to the United States, he noted. In Europe and Australia, for example, AGS is not thought to be tied to the Lone Star tick, which doesn’t inhabit those regions.
“It is a global phenomenon,” Dr. Commins said.
In August, the CDC alerted physicians to emerging cases of alpha-gal allergy after an article in Morbidity and Mortality Weekly Report indicated that health care providers have little knowledge about the allergy. Of the 1,500 health care providers surveyed, 42% had never heard of the syndrome, and another 35% were not confident in diagnosing or managing affected patients.
Matthew Lau, MD, an allergist with Kaiser Permanente in Honolulu who listened to Dr. Commins’ talk, told this news organization, “It’s important to raise awareness in primary care particularly, he said, as “allergists see only a fraction of the [AGS] patients.”
Allergists can help raise awareness
“Allergists have a role to alert the general community” and to drive more referrals, he said. That includes emergency departments, where physicians commonly see anaphylaxis.
Dr. Lau said he expects the incidence of AGS to increase, because global warming will likely lengthen warmer seasons and cause the geographic distribution to change.
Jay Lieberman, MD, a pediatric allergist at Le Bonheur Children’s Hospital in Memphis, Tenn., told this news organization, “There’s still a lot of confusion, and hearing from an expert like Dr. Commins helps tease out the not-obvious things about patients who are having more mild symptoms,” such as from allergy to dairy or medicines or vaccines that contain gelatin.
As a pediatric allergist, Dr. Lieberman said he sees less alpha-gal than his colleagues, but, he said, “On the adult side in Tennessee, it’s rampant.”
Dr. Commins, Dr. Lieberman, and Dr. Lau report no relevant financial relationships.
A version of this article appeared on Medscape.com.
ANAHEIM, CALIF. – allergist and immunologist Scott P. Commins, MD, PhD, told attendees at the annual meeting of the American College of Allergy, Asthma, and Immunology (ACAAI) annual meeting.
Dr. Commins, associate chief for allergy and immunology at the University of North Carolina at Chapel Hill, has made alpha-gal, a potentially fatal allergy, which, in the United States is tied to the bite of the Lone Star tick, his primary research focus.
Beyond red meat, “there are some people who are allergic to all things mammal,” he explained. Dairy products from mammals, medical devices made from mammalian products, vaccines and medicines that contain gelatin, and even commercial products such as perfumes and cosmetics may be behind an AGS reaction.
“The derived products from pigs and cows really find their way into a lot of our day-to-day products,” he said. “I try to keep an open mind about these exposures.”
Physicians should also be aware that “this can happen to kids,” said Dr. Commins. “It looks very similar to adults’ [AGS]. They can end up in the emergency department.”
He also had clinical advice about food challenges for AGS. He explained that there’s more alpha-gal in beef than in other red meats (including pork, venison, and lamb) with the exception of pork kidney. Pork kidney, he said, “has the most alpha-gal that we can find in the lab.”
Dr. Commins said he has stopped using beef for AGS food challenges and has switched to pork sausage patties with a high fat content microwaved in the clinic because they have less alpha-gal in general and he views them as safer.
Long delay in symptom onset
AGS symptoms typically take 2-6 hours to appear after eating red meat or being exposed to mammalian products, but Dr. Commins related a story about a patient he sent home who had very mild symptoms (some lower back itching) after he had spent the day at the clinic after a pork sausage food challenge for AGS.
The patient had returned home. Eight hours after the food challenge, his wife sent Dr. Commins a picture of her husband’s back, which was riddled with welts and was itching badly.
“I learned that if you’re going to do these food challenges, if there is a hint of symptoms at the clinic at 6 hours, keep them in the clinic, because it may really take that long to evolve,” Dr. Commins said.
One of the early signs he’s discovered is palmar erythema (redness and swelling of the hands).
Research has shown that AGS has been heavily concentrated in the Southeast, where Lone Star tick populations are clustered, but research has shown that from 2017 to 2022, it moved up the East Coast to the central United States and Upper Midwest.
“We are seeing increasing diagnoses of AGS in places that are not, perhaps, where we first thought this allergy existed,” said Dr. Commins. “Stay aware,” he cautioned.
The allergy is not exclusive to the United States, he noted. In Europe and Australia, for example, AGS is not thought to be tied to the Lone Star tick, which doesn’t inhabit those regions.
“It is a global phenomenon,” Dr. Commins said.
In August, the CDC alerted physicians to emerging cases of alpha-gal allergy after an article in Morbidity and Mortality Weekly Report indicated that health care providers have little knowledge about the allergy. Of the 1,500 health care providers surveyed, 42% had never heard of the syndrome, and another 35% were not confident in diagnosing or managing affected patients.
Matthew Lau, MD, an allergist with Kaiser Permanente in Honolulu who listened to Dr. Commins’ talk, told this news organization, “It’s important to raise awareness in primary care particularly, he said, as “allergists see only a fraction of the [AGS] patients.”
Allergists can help raise awareness
“Allergists have a role to alert the general community” and to drive more referrals, he said. That includes emergency departments, where physicians commonly see anaphylaxis.
Dr. Lau said he expects the incidence of AGS to increase, because global warming will likely lengthen warmer seasons and cause the geographic distribution to change.
Jay Lieberman, MD, a pediatric allergist at Le Bonheur Children’s Hospital in Memphis, Tenn., told this news organization, “There’s still a lot of confusion, and hearing from an expert like Dr. Commins helps tease out the not-obvious things about patients who are having more mild symptoms,” such as from allergy to dairy or medicines or vaccines that contain gelatin.
As a pediatric allergist, Dr. Lieberman said he sees less alpha-gal than his colleagues, but, he said, “On the adult side in Tennessee, it’s rampant.”
Dr. Commins, Dr. Lieberman, and Dr. Lau report no relevant financial relationships.
A version of this article appeared on Medscape.com.
Salt intake associated with increased type 2 diabetes risk
TOPLINE:
, even after adjustment for confounding factors.
METHODOLOGY:
- Researchers identified 402,982 participants in the UK Biobank from March 2006 to October 2010 who had completed a questionnaire about the frequency with which they added salt to food and who did not have diabetes, chronic kidney disease, cancer, or cardiovascular disease at baseline.
- Urine samples were collected at baseline, sodium and potassium levels were measured, and 24-hour sodium excretion was estimated.
- Investigators followed participants from baseline to diagnosis of diabetes, death, or the censoring date (May 23, 2021), whichever occurred first. Information on T2D events were collected through medical history linkage to data on hospital admissions, questionnaire, and the death register.
TAKEAWAY:
- During a mean follow-up of 11.9 years, 13,120 incident cases of T2D were documented.
- Compared with people who reported “never/rarely” adding salt to food, the sex- and age-adjusted hazard ratios (HRs) for developing T2D were 1.20, 1.32, and 1.86 for those who reported “sometimes,” “usually,” and “always” adding salt, respectively (P-trend < .001).
- After further adjustment for the Townsend deprivation index, education level, income, smoking, drinking, physical activity, and high cholesterol, the association was attenuated but remained significant, with HRs of 1.11, 1.18, and 1.28 for “sometimes,” “usually,” and “always” responses, respectively (P-trend < .001).
- After full adjustment, there was also a dose-dependent relationship across quintiles of urinary sodium and higher T2D risk, with HRs of 1 (reference), 1.12, 1.17, 1.28, and 1.34 for quintiles 2-5, respectively (P-trend < .001).
- Body fat percentage and body fat mass significantly mediated the association of adding salt with T2D, by estimated effects of 37.9% and 39.9%, respectively (both P < .001).
IN PRACTICE:
“These findings provide support that reduction of adding salt to foods may act as a potential behavioral intervention approach for preventing T2D. Future clinical trials are needed to further validate our findings,” the authors wrote.
SOURCE:
The study by Xuan Wang, MD, PhD, department of epidemiology, School of Public Health and Tropical Medicine, Tulane University, New Orleans, and colleagues was published in the November 2023 issue of Mayo Clinic Proceedings.
LIMITATIONS:
The researchers could not completely exclude the possibility that high frequency of adding salt to foods is a marker for an unhealthy lifestyle. Self-reported frequency of adding salt to food might be subject to information bias and did not provide quantitative information on total sodium intake. In addition, participants were mainly of European descent, making application of the findings to other ethnic groups unclear; the observational design meant researchers could not rule out residual confounding; and information on addition of salt to food was available only at baseline, so potential changes in salt consumption during follow-up could not be considered.
DISCLOSURES:
The study was supported by grants from the National Heart, Lung, and Blood Institute; the National Institute of Diabetes and Digestive and Kidney Diseases; the Fogarty International Center; and Tulane Research Centers of Excellence Awards. The authors reported no potential competing interests.
A version of this article appeared on Medscape.com.
TOPLINE:
, even after adjustment for confounding factors.
METHODOLOGY:
- Researchers identified 402,982 participants in the UK Biobank from March 2006 to October 2010 who had completed a questionnaire about the frequency with which they added salt to food and who did not have diabetes, chronic kidney disease, cancer, or cardiovascular disease at baseline.
- Urine samples were collected at baseline, sodium and potassium levels were measured, and 24-hour sodium excretion was estimated.
- Investigators followed participants from baseline to diagnosis of diabetes, death, or the censoring date (May 23, 2021), whichever occurred first. Information on T2D events were collected through medical history linkage to data on hospital admissions, questionnaire, and the death register.
TAKEAWAY:
- During a mean follow-up of 11.9 years, 13,120 incident cases of T2D were documented.
- Compared with people who reported “never/rarely” adding salt to food, the sex- and age-adjusted hazard ratios (HRs) for developing T2D were 1.20, 1.32, and 1.86 for those who reported “sometimes,” “usually,” and “always” adding salt, respectively (P-trend < .001).
- After further adjustment for the Townsend deprivation index, education level, income, smoking, drinking, physical activity, and high cholesterol, the association was attenuated but remained significant, with HRs of 1.11, 1.18, and 1.28 for “sometimes,” “usually,” and “always” responses, respectively (P-trend < .001).
- After full adjustment, there was also a dose-dependent relationship across quintiles of urinary sodium and higher T2D risk, with HRs of 1 (reference), 1.12, 1.17, 1.28, and 1.34 for quintiles 2-5, respectively (P-trend < .001).
- Body fat percentage and body fat mass significantly mediated the association of adding salt with T2D, by estimated effects of 37.9% and 39.9%, respectively (both P < .001).
IN PRACTICE:
“These findings provide support that reduction of adding salt to foods may act as a potential behavioral intervention approach for preventing T2D. Future clinical trials are needed to further validate our findings,” the authors wrote.
SOURCE:
The study by Xuan Wang, MD, PhD, department of epidemiology, School of Public Health and Tropical Medicine, Tulane University, New Orleans, and colleagues was published in the November 2023 issue of Mayo Clinic Proceedings.
LIMITATIONS:
The researchers could not completely exclude the possibility that high frequency of adding salt to foods is a marker for an unhealthy lifestyle. Self-reported frequency of adding salt to food might be subject to information bias and did not provide quantitative information on total sodium intake. In addition, participants were mainly of European descent, making application of the findings to other ethnic groups unclear; the observational design meant researchers could not rule out residual confounding; and information on addition of salt to food was available only at baseline, so potential changes in salt consumption during follow-up could not be considered.
DISCLOSURES:
The study was supported by grants from the National Heart, Lung, and Blood Institute; the National Institute of Diabetes and Digestive and Kidney Diseases; the Fogarty International Center; and Tulane Research Centers of Excellence Awards. The authors reported no potential competing interests.
A version of this article appeared on Medscape.com.
TOPLINE:
, even after adjustment for confounding factors.
METHODOLOGY:
- Researchers identified 402,982 participants in the UK Biobank from March 2006 to October 2010 who had completed a questionnaire about the frequency with which they added salt to food and who did not have diabetes, chronic kidney disease, cancer, or cardiovascular disease at baseline.
- Urine samples were collected at baseline, sodium and potassium levels were measured, and 24-hour sodium excretion was estimated.
- Investigators followed participants from baseline to diagnosis of diabetes, death, or the censoring date (May 23, 2021), whichever occurred first. Information on T2D events were collected through medical history linkage to data on hospital admissions, questionnaire, and the death register.
TAKEAWAY:
- During a mean follow-up of 11.9 years, 13,120 incident cases of T2D were documented.
- Compared with people who reported “never/rarely” adding salt to food, the sex- and age-adjusted hazard ratios (HRs) for developing T2D were 1.20, 1.32, and 1.86 for those who reported “sometimes,” “usually,” and “always” adding salt, respectively (P-trend < .001).
- After further adjustment for the Townsend deprivation index, education level, income, smoking, drinking, physical activity, and high cholesterol, the association was attenuated but remained significant, with HRs of 1.11, 1.18, and 1.28 for “sometimes,” “usually,” and “always” responses, respectively (P-trend < .001).
- After full adjustment, there was also a dose-dependent relationship across quintiles of urinary sodium and higher T2D risk, with HRs of 1 (reference), 1.12, 1.17, 1.28, and 1.34 for quintiles 2-5, respectively (P-trend < .001).
- Body fat percentage and body fat mass significantly mediated the association of adding salt with T2D, by estimated effects of 37.9% and 39.9%, respectively (both P < .001).
IN PRACTICE:
“These findings provide support that reduction of adding salt to foods may act as a potential behavioral intervention approach for preventing T2D. Future clinical trials are needed to further validate our findings,” the authors wrote.
SOURCE:
The study by Xuan Wang, MD, PhD, department of epidemiology, School of Public Health and Tropical Medicine, Tulane University, New Orleans, and colleagues was published in the November 2023 issue of Mayo Clinic Proceedings.
LIMITATIONS:
The researchers could not completely exclude the possibility that high frequency of adding salt to foods is a marker for an unhealthy lifestyle. Self-reported frequency of adding salt to food might be subject to information bias and did not provide quantitative information on total sodium intake. In addition, participants were mainly of European descent, making application of the findings to other ethnic groups unclear; the observational design meant researchers could not rule out residual confounding; and information on addition of salt to food was available only at baseline, so potential changes in salt consumption during follow-up could not be considered.
DISCLOSURES:
The study was supported by grants from the National Heart, Lung, and Blood Institute; the National Institute of Diabetes and Digestive and Kidney Diseases; the Fogarty International Center; and Tulane Research Centers of Excellence Awards. The authors reported no potential competing interests.
A version of this article appeared on Medscape.com.
AAD updates guidelines for managing AD with phototherapy and systemic therapies
.
The guidelines cover approved and off-label uses of systemic therapies and phototherapy, including new treatments that have become available since the last guidelines were published almost a decade ago. These include biologics and oral Janus kinase (JAK) inhibitors, as well as older oral or injectable immunomodulators and antimetabolites, oral antibiotics, antihistamines, and phosphodiesterase-4 inhibitors. The guidelines rate the existing evidence as “strong” for dupilumab, tralokinumab, abrocitinib, baricitinib, and upadacitinib. They also conditionally recommend phototherapy, as well as cyclosporine, methotrexate, azathioprine, and mycophenolate, but recommend against the use of systemic corticosteroids.
The guidelines update the AAD’s 2014 recommendations for managing AD in adults with phototherapy and systemic therapies. “At that time, prednisone – universally agreed to be the least appropriate chronic therapy for AD – was the only Food and Drug Administration–approved agent,” Robert Sidbury, MD, MPH, who cochaired a 14-member multidisciplinary work group that assembled the guidelines, told this news organization. “This was the driver.”
The latest guidelines were published online in the Journal of the American Academy of Dermatology.
Broad evidence review
Dr. Sidbury, chief of the division of dermatology at Seattle Children’s Hospital, guidelines cochair Dawn M. R. Davis, MD, a dermatologist at the Mayo Clinic, Rochester, Minn., and colleagues conducted a systematic evidence review of phototherapy such as narrowband and broadband UVB and systemic therapies, including biologics such as dupilumab and tralokinumab, JAK inhibitors such as upadacitinib and abrocitinib, and immunosuppressants such as methotrexate and azathioprine.
Next, the work group applied the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) approach for assessing the certainty of the evidence and formulating and grading clinical recommendations based on relevant randomized trials in the medical literature.
Recommendations, future studies
Of the 11 evidence-based recommendations of therapies for adults with AD refractory to topical medications, the work group ranks 5 as “strong” based on the evidence and the rest as “conditional.” “Strong” implies the benefits clearly outweigh risks and burdens, they apply to most patients in most circumstances, and they fall under good clinical practice. “Conditional” means the benefits and risks are closely balanced for most patients, “but the appropriate action may different depending on the patient or other stakeholder values,” the authors wrote.
In their remarks about phototherapy, the work group noted that most published literature on the topic “reports on the efficacy and safety of narrow band UVB. Wherever possible, use a light source that minimizes the potential for harm under the supervision of a qualified clinician.”
In their remarks about cyclosporine, they noted that evidence suggests an initial dose of 3 mg/kg per day to 5 mg/kg per day is effective, but that the Food and Drug Administration has not approved cyclosporine for use in AD. “The FDA has approved limited-term use (up to 1 year) in psoriasis,” they wrote. “Comorbidities or drug interactions that may exacerbate toxicity make this intervention inappropriate for select patients.” The work group noted that significant research gaps remain in phototherapy, especially trials that compare different phototherapy modalities and those that compare phototherapy with other AD treatment strategies.
“Larger clinical trials would also be helpful for cyclosporine, methotrexate, azathioprine, and mycophenolate to improve the certainty of evidence for those medications,” they added. “Furthermore, formal cost-effectiveness analyses comparing older to newer treatments are needed.”
They recommended the inclusion of active comparator arms in randomized, controlled trials as new systemic therapies continue to be developed and tested.
The work group ranked the level of evidence they reviewed for the therapies from very low to moderate. No therapy was judged to have high evidence. They also cited the short duration of most randomized controlled trials of phototherapy.
Using the guidelines in clinical care
According to Dr. Davis, the topic of which agent if any should be considered “first line” generated robust discussion among the work group members.
“When there are not robust head-to-head trials – and there are not – it is often opinion that governs this decision, and opinion should not, when possible, govern a guideline,” Dr. Davis said. “Accordingly, we determined based upon the evidence agents – plural – that deserve to be considered ‘first line’ but not a single agent.”
In her opinion, the top three considerations regarding use of systemic therapy for AD relate to patient selection and shared decision making. One, standard therapy has failed. Two, diagnosis is assured. And three, “steroid phobia should be considered,” and patients should be “fully informed of risks and benefits of both treating and not treating,” she said.
Dr. Sidbury reported that he serves as an advisory board member for Pfizer, a principal investigator for Regeneron, an investigator for Brickell Biotech and Galderma USA, and a consultant for Galderma Global and Micreos. Dr. Davis reported having no relevant disclosures. Other work group members reported having financial disclosures with many pharmaceutical companies. The study was supported by internal funds from the American Academy of Dermatology.
.
The guidelines cover approved and off-label uses of systemic therapies and phototherapy, including new treatments that have become available since the last guidelines were published almost a decade ago. These include biologics and oral Janus kinase (JAK) inhibitors, as well as older oral or injectable immunomodulators and antimetabolites, oral antibiotics, antihistamines, and phosphodiesterase-4 inhibitors. The guidelines rate the existing evidence as “strong” for dupilumab, tralokinumab, abrocitinib, baricitinib, and upadacitinib. They also conditionally recommend phototherapy, as well as cyclosporine, methotrexate, azathioprine, and mycophenolate, but recommend against the use of systemic corticosteroids.
The guidelines update the AAD’s 2014 recommendations for managing AD in adults with phototherapy and systemic therapies. “At that time, prednisone – universally agreed to be the least appropriate chronic therapy for AD – was the only Food and Drug Administration–approved agent,” Robert Sidbury, MD, MPH, who cochaired a 14-member multidisciplinary work group that assembled the guidelines, told this news organization. “This was the driver.”
The latest guidelines were published online in the Journal of the American Academy of Dermatology.
Broad evidence review
Dr. Sidbury, chief of the division of dermatology at Seattle Children’s Hospital, guidelines cochair Dawn M. R. Davis, MD, a dermatologist at the Mayo Clinic, Rochester, Minn., and colleagues conducted a systematic evidence review of phototherapy such as narrowband and broadband UVB and systemic therapies, including biologics such as dupilumab and tralokinumab, JAK inhibitors such as upadacitinib and abrocitinib, and immunosuppressants such as methotrexate and azathioprine.
Next, the work group applied the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) approach for assessing the certainty of the evidence and formulating and grading clinical recommendations based on relevant randomized trials in the medical literature.
Recommendations, future studies
Of the 11 evidence-based recommendations of therapies for adults with AD refractory to topical medications, the work group ranks 5 as “strong” based on the evidence and the rest as “conditional.” “Strong” implies the benefits clearly outweigh risks and burdens, they apply to most patients in most circumstances, and they fall under good clinical practice. “Conditional” means the benefits and risks are closely balanced for most patients, “but the appropriate action may different depending on the patient or other stakeholder values,” the authors wrote.
In their remarks about phototherapy, the work group noted that most published literature on the topic “reports on the efficacy and safety of narrow band UVB. Wherever possible, use a light source that minimizes the potential for harm under the supervision of a qualified clinician.”
In their remarks about cyclosporine, they noted that evidence suggests an initial dose of 3 mg/kg per day to 5 mg/kg per day is effective, but that the Food and Drug Administration has not approved cyclosporine for use in AD. “The FDA has approved limited-term use (up to 1 year) in psoriasis,” they wrote. “Comorbidities or drug interactions that may exacerbate toxicity make this intervention inappropriate for select patients.” The work group noted that significant research gaps remain in phototherapy, especially trials that compare different phototherapy modalities and those that compare phototherapy with other AD treatment strategies.
“Larger clinical trials would also be helpful for cyclosporine, methotrexate, azathioprine, and mycophenolate to improve the certainty of evidence for those medications,” they added. “Furthermore, formal cost-effectiveness analyses comparing older to newer treatments are needed.”
They recommended the inclusion of active comparator arms in randomized, controlled trials as new systemic therapies continue to be developed and tested.
The work group ranked the level of evidence they reviewed for the therapies from very low to moderate. No therapy was judged to have high evidence. They also cited the short duration of most randomized controlled trials of phototherapy.
Using the guidelines in clinical care
According to Dr. Davis, the topic of which agent if any should be considered “first line” generated robust discussion among the work group members.
“When there are not robust head-to-head trials – and there are not – it is often opinion that governs this decision, and opinion should not, when possible, govern a guideline,” Dr. Davis said. “Accordingly, we determined based upon the evidence agents – plural – that deserve to be considered ‘first line’ but not a single agent.”
In her opinion, the top three considerations regarding use of systemic therapy for AD relate to patient selection and shared decision making. One, standard therapy has failed. Two, diagnosis is assured. And three, “steroid phobia should be considered,” and patients should be “fully informed of risks and benefits of both treating and not treating,” she said.
Dr. Sidbury reported that he serves as an advisory board member for Pfizer, a principal investigator for Regeneron, an investigator for Brickell Biotech and Galderma USA, and a consultant for Galderma Global and Micreos. Dr. Davis reported having no relevant disclosures. Other work group members reported having financial disclosures with many pharmaceutical companies. The study was supported by internal funds from the American Academy of Dermatology.
.
The guidelines cover approved and off-label uses of systemic therapies and phototherapy, including new treatments that have become available since the last guidelines were published almost a decade ago. These include biologics and oral Janus kinase (JAK) inhibitors, as well as older oral or injectable immunomodulators and antimetabolites, oral antibiotics, antihistamines, and phosphodiesterase-4 inhibitors. The guidelines rate the existing evidence as “strong” for dupilumab, tralokinumab, abrocitinib, baricitinib, and upadacitinib. They also conditionally recommend phototherapy, as well as cyclosporine, methotrexate, azathioprine, and mycophenolate, but recommend against the use of systemic corticosteroids.
The guidelines update the AAD’s 2014 recommendations for managing AD in adults with phototherapy and systemic therapies. “At that time, prednisone – universally agreed to be the least appropriate chronic therapy for AD – was the only Food and Drug Administration–approved agent,” Robert Sidbury, MD, MPH, who cochaired a 14-member multidisciplinary work group that assembled the guidelines, told this news organization. “This was the driver.”
The latest guidelines were published online in the Journal of the American Academy of Dermatology.
Broad evidence review
Dr. Sidbury, chief of the division of dermatology at Seattle Children’s Hospital, guidelines cochair Dawn M. R. Davis, MD, a dermatologist at the Mayo Clinic, Rochester, Minn., and colleagues conducted a systematic evidence review of phototherapy such as narrowband and broadband UVB and systemic therapies, including biologics such as dupilumab and tralokinumab, JAK inhibitors such as upadacitinib and abrocitinib, and immunosuppressants such as methotrexate and azathioprine.
Next, the work group applied the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) approach for assessing the certainty of the evidence and formulating and grading clinical recommendations based on relevant randomized trials in the medical literature.
Recommendations, future studies
Of the 11 evidence-based recommendations of therapies for adults with AD refractory to topical medications, the work group ranks 5 as “strong” based on the evidence and the rest as “conditional.” “Strong” implies the benefits clearly outweigh risks and burdens, they apply to most patients in most circumstances, and they fall under good clinical practice. “Conditional” means the benefits and risks are closely balanced for most patients, “but the appropriate action may different depending on the patient or other stakeholder values,” the authors wrote.
In their remarks about phototherapy, the work group noted that most published literature on the topic “reports on the efficacy and safety of narrow band UVB. Wherever possible, use a light source that minimizes the potential for harm under the supervision of a qualified clinician.”
In their remarks about cyclosporine, they noted that evidence suggests an initial dose of 3 mg/kg per day to 5 mg/kg per day is effective, but that the Food and Drug Administration has not approved cyclosporine for use in AD. “The FDA has approved limited-term use (up to 1 year) in psoriasis,” they wrote. “Comorbidities or drug interactions that may exacerbate toxicity make this intervention inappropriate for select patients.” The work group noted that significant research gaps remain in phototherapy, especially trials that compare different phototherapy modalities and those that compare phototherapy with other AD treatment strategies.
“Larger clinical trials would also be helpful for cyclosporine, methotrexate, azathioprine, and mycophenolate to improve the certainty of evidence for those medications,” they added. “Furthermore, formal cost-effectiveness analyses comparing older to newer treatments are needed.”
They recommended the inclusion of active comparator arms in randomized, controlled trials as new systemic therapies continue to be developed and tested.
The work group ranked the level of evidence they reviewed for the therapies from very low to moderate. No therapy was judged to have high evidence. They also cited the short duration of most randomized controlled trials of phototherapy.
Using the guidelines in clinical care
According to Dr. Davis, the topic of which agent if any should be considered “first line” generated robust discussion among the work group members.
“When there are not robust head-to-head trials – and there are not – it is often opinion that governs this decision, and opinion should not, when possible, govern a guideline,” Dr. Davis said. “Accordingly, we determined based upon the evidence agents – plural – that deserve to be considered ‘first line’ but not a single agent.”
In her opinion, the top three considerations regarding use of systemic therapy for AD relate to patient selection and shared decision making. One, standard therapy has failed. Two, diagnosis is assured. And three, “steroid phobia should be considered,” and patients should be “fully informed of risks and benefits of both treating and not treating,” she said.
Dr. Sidbury reported that he serves as an advisory board member for Pfizer, a principal investigator for Regeneron, an investigator for Brickell Biotech and Galderma USA, and a consultant for Galderma Global and Micreos. Dr. Davis reported having no relevant disclosures. Other work group members reported having financial disclosures with many pharmaceutical companies. The study was supported by internal funds from the American Academy of Dermatology.
FROM JAMA DERMATOLOGY
The easy way to talk about penises
This transcript has been edited for clarity.
I mean it. Penis problems are very common and are an early sign that patients could have a cardiac event. Think about it: Clogging the arteries of the heart is called a heart attack; clogging the arteries to the penis is a penis attack, or as doctors like to call it, erectile dysfunction.
The arteries to the penis are only 1 mm in diameter. They develop plaque and clog the circulation long before the 3-mm cardiac arteries. So, it’s very important for primary care doctors to talk to their patients about erection health. And I’ll be honest: It’s easier to talk to patients about how lifestyle is affecting their penis health than it is to discuss how lifestyle affects longevity or prevents cancer. I get a lot of men to quit smoking because I tell them what it’s doing to their penises.
It can be challenging for doctors and patients to talk about penises. It doesn’t come naturally for many of us. If a 20-year-old comes in to my office with his 85-year-old grandfather and they both say their penises aren’t working, how do you figure out what’s going on? Do they even have the same thing wrong with them?
Here’s a fun and helpful tool that I use in my office. It’s called the Erection Hardness Score. It was developed around the time that Viagra came out, in 1998. It’s been game-changing for me to get patients more comfortable talking about their erection issues.
I tell them it’s a 4-number scale. A “1” is no erection at all. A “2” is when it gets harder and larger, but it’s not going to penetrate. A “3” will penetrate, but it’s pretty wobbly. A “4” is that perfect cucumber–porn star erection that everyone is seeking. I have the patient tell me a story. They may say, “When I wake up in the morning, I’m at a 2. When I stimulate myself, I can get up to a 3. When I’m with my partner, sometimes I can get up to a 4.”
This is really helpful because they can talk in numbers. And after I give them treatments such as lifestyle changes, sex therapy, testosterone, a PDE5 inhibitor such as Viagra or Cialis, or an injection, they can come back and tell me how the story has changed. I have an objective measure that shows me how the treatment is affecting their erections. Not only do I feel more confident having those objective measures, but my patients feel more confident in the care that they’re getting, and they feel more comfortable talking to me about the changes. So, I encourage all of you to bring that EHS tool into your office. Show it to patients and get them more comfortable talking about erections.
Dr. Rubin is assistant clinical professor, department of urology, Georgetown University, Washington. She disclosed financial relationships with Absorption Pharmaceuticals, GlaxoSmithKline, and Endo Pharmaceuticals; has served as a speaker for Sprout; and has received research grant from Maternal Medical.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
I mean it. Penis problems are very common and are an early sign that patients could have a cardiac event. Think about it: Clogging the arteries of the heart is called a heart attack; clogging the arteries to the penis is a penis attack, or as doctors like to call it, erectile dysfunction.
The arteries to the penis are only 1 mm in diameter. They develop plaque and clog the circulation long before the 3-mm cardiac arteries. So, it’s very important for primary care doctors to talk to their patients about erection health. And I’ll be honest: It’s easier to talk to patients about how lifestyle is affecting their penis health than it is to discuss how lifestyle affects longevity or prevents cancer. I get a lot of men to quit smoking because I tell them what it’s doing to their penises.
It can be challenging for doctors and patients to talk about penises. It doesn’t come naturally for many of us. If a 20-year-old comes in to my office with his 85-year-old grandfather and they both say their penises aren’t working, how do you figure out what’s going on? Do they even have the same thing wrong with them?
Here’s a fun and helpful tool that I use in my office. It’s called the Erection Hardness Score. It was developed around the time that Viagra came out, in 1998. It’s been game-changing for me to get patients more comfortable talking about their erection issues.
I tell them it’s a 4-number scale. A “1” is no erection at all. A “2” is when it gets harder and larger, but it’s not going to penetrate. A “3” will penetrate, but it’s pretty wobbly. A “4” is that perfect cucumber–porn star erection that everyone is seeking. I have the patient tell me a story. They may say, “When I wake up in the morning, I’m at a 2. When I stimulate myself, I can get up to a 3. When I’m with my partner, sometimes I can get up to a 4.”
This is really helpful because they can talk in numbers. And after I give them treatments such as lifestyle changes, sex therapy, testosterone, a PDE5 inhibitor such as Viagra or Cialis, or an injection, they can come back and tell me how the story has changed. I have an objective measure that shows me how the treatment is affecting their erections. Not only do I feel more confident having those objective measures, but my patients feel more confident in the care that they’re getting, and they feel more comfortable talking to me about the changes. So, I encourage all of you to bring that EHS tool into your office. Show it to patients and get them more comfortable talking about erections.
Dr. Rubin is assistant clinical professor, department of urology, Georgetown University, Washington. She disclosed financial relationships with Absorption Pharmaceuticals, GlaxoSmithKline, and Endo Pharmaceuticals; has served as a speaker for Sprout; and has received research grant from Maternal Medical.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
I mean it. Penis problems are very common and are an early sign that patients could have a cardiac event. Think about it: Clogging the arteries of the heart is called a heart attack; clogging the arteries to the penis is a penis attack, or as doctors like to call it, erectile dysfunction.
The arteries to the penis are only 1 mm in diameter. They develop plaque and clog the circulation long before the 3-mm cardiac arteries. So, it’s very important for primary care doctors to talk to their patients about erection health. And I’ll be honest: It’s easier to talk to patients about how lifestyle is affecting their penis health than it is to discuss how lifestyle affects longevity or prevents cancer. I get a lot of men to quit smoking because I tell them what it’s doing to their penises.
It can be challenging for doctors and patients to talk about penises. It doesn’t come naturally for many of us. If a 20-year-old comes in to my office with his 85-year-old grandfather and they both say their penises aren’t working, how do you figure out what’s going on? Do they even have the same thing wrong with them?
Here’s a fun and helpful tool that I use in my office. It’s called the Erection Hardness Score. It was developed around the time that Viagra came out, in 1998. It’s been game-changing for me to get patients more comfortable talking about their erection issues.
I tell them it’s a 4-number scale. A “1” is no erection at all. A “2” is when it gets harder and larger, but it’s not going to penetrate. A “3” will penetrate, but it’s pretty wobbly. A “4” is that perfect cucumber–porn star erection that everyone is seeking. I have the patient tell me a story. They may say, “When I wake up in the morning, I’m at a 2. When I stimulate myself, I can get up to a 3. When I’m with my partner, sometimes I can get up to a 4.”
This is really helpful because they can talk in numbers. And after I give them treatments such as lifestyle changes, sex therapy, testosterone, a PDE5 inhibitor such as Viagra or Cialis, or an injection, they can come back and tell me how the story has changed. I have an objective measure that shows me how the treatment is affecting their erections. Not only do I feel more confident having those objective measures, but my patients feel more confident in the care that they’re getting, and they feel more comfortable talking to me about the changes. So, I encourage all of you to bring that EHS tool into your office. Show it to patients and get them more comfortable talking about erections.
Dr. Rubin is assistant clinical professor, department of urology, Georgetown University, Washington. She disclosed financial relationships with Absorption Pharmaceuticals, GlaxoSmithKline, and Endo Pharmaceuticals; has served as a speaker for Sprout; and has received research grant from Maternal Medical.
A version of this article appeared on Medscape.com.
CPPD nomenclature is sore subject for gout group
LA JOLLA, CALIF. – Twelve years ago, an international task force of the European Alliance of Associations for Rheumatology (EULAR) released recommendations regarding nomenclature in calcium pyrophosphate deposition disease (CPPD), aiming to standardize the way the condition is described. “Pseudogout” was out, and “acute CPP crystal arthritis” was in, and a confusing array of multi-named phenotypes gained specific labels.
Since 2011, the nomenclature guidelines have been cited hundreds of times, but a new report finds that the medical literature mostly hasn’t followed the recommendations. The findings were released at the annual research symposium of the Gout, Hyperuricemia, and Crystal Associated Disease Network (G-CAN), which is taking another stab at overhauling CPPD nomenclature.
“The objective is to uniform and standardize the labels of the disease, the disease elements, and the clinical states,” rheumatologist Charlotte Jauffret, MD, of the Catholic University of Lille (France), said in a presentation. CPPD is a widely underdiagnosed disease that’s worth the same efforts to standardize nomenclature as occurred in gout, she said.
As Dr. Jauffret explained, CPPD has a diversity of phenotypes in asymptomatic, acute, and chronic forms that pose challenges to diagnosis. “The same terms are used to depict different concepts, and some disease elements are depicted through different names,” she said.
Among other suggestions, the 2011 EULAR recommendations suggested that rheumatologists use the terms chronic CPP crystal inflammatory arthritis instead of “pseudo-rheumatoid arthritis,” osteoarthritis with CPPD, instead of “pseudo-osteoarthritis,” and severe joint degeneration instead of “pseudo-neuropathic joint disease.”
Later reports noted that terms such as CPPD and chondrocalcinosis are still wrongly used interchangeably and called for an international consensus on nomenclature, Dr. Jauffret said.
For the new report, Dr. Jauffret and colleagues examined 985 articles from 2000-2022. The guidelines were often not followed even after the release of the recommendations.
For example, 49% of relevant papers used the label “pseudogout” before 2011, and 43% did afterward. A total of 34% of relevant papers described CPPD as chondrocalcinosis prior to 2011, and 22% did afterward.
G-CAN’s next steps are to reach consensus on terminology through online and in-person meetings in 2024, Dr. Jauffret said.
Use of correct gout nomenclature labels improved
In a related presentation, rheumatologist Ellen Prendergast, MBChB, of Dunedin Hospital in New Zealand, reported the results of a newly published review of gout studies before and after G-CAN released consensus recommendations for gout nomenclature in 2019. “There has been improvement in the agreed labels in some areas, but there remains quite significant variability,” she said.
The review examined American College of Rheumatology and EULAR annual meeting abstracts: 596 from 2016-2017 and 392 from 2020-2021. Dr. Prendergast said researchers focused on abstracts instead of published studies in order to gain the most up-to-date understanding of nomenclature.
“Use of the agreed labels ‘urate’ and ‘gout flare’ increased between the two periods. There were 219 of 383 (57.2%) abstracts with the agreed label ‘urate’ in 2016-2017, compared with 164 of 232 (70.7%) in 2020-2021 (P = .001),” the researchers reported. “There were 60 of 175 (34.3%) abstracts with the agreed label ‘gout flare’ in 2016-2017, compared with 57 of 109 (52.3%) in 2020-2021 (P = .003).”
And the use of the term “chronic gout,” which the guidelines recommend against, fell from 29 of 596 (4.9%) abstracts in 2016-2017 to 8 of 392 (2.0%) abstracts in 2020-2021 (P = .02).
One author of the gout nomenclature study reports various consulting fees, speaker fees, or grants outside the submitted work. The other authors of the two studies report no disclosures.
LA JOLLA, CALIF. – Twelve years ago, an international task force of the European Alliance of Associations for Rheumatology (EULAR) released recommendations regarding nomenclature in calcium pyrophosphate deposition disease (CPPD), aiming to standardize the way the condition is described. “Pseudogout” was out, and “acute CPP crystal arthritis” was in, and a confusing array of multi-named phenotypes gained specific labels.
Since 2011, the nomenclature guidelines have been cited hundreds of times, but a new report finds that the medical literature mostly hasn’t followed the recommendations. The findings were released at the annual research symposium of the Gout, Hyperuricemia, and Crystal Associated Disease Network (G-CAN), which is taking another stab at overhauling CPPD nomenclature.
“The objective is to uniform and standardize the labels of the disease, the disease elements, and the clinical states,” rheumatologist Charlotte Jauffret, MD, of the Catholic University of Lille (France), said in a presentation. CPPD is a widely underdiagnosed disease that’s worth the same efforts to standardize nomenclature as occurred in gout, she said.
As Dr. Jauffret explained, CPPD has a diversity of phenotypes in asymptomatic, acute, and chronic forms that pose challenges to diagnosis. “The same terms are used to depict different concepts, and some disease elements are depicted through different names,” she said.
Among other suggestions, the 2011 EULAR recommendations suggested that rheumatologists use the terms chronic CPP crystal inflammatory arthritis instead of “pseudo-rheumatoid arthritis,” osteoarthritis with CPPD, instead of “pseudo-osteoarthritis,” and severe joint degeneration instead of “pseudo-neuropathic joint disease.”
Later reports noted that terms such as CPPD and chondrocalcinosis are still wrongly used interchangeably and called for an international consensus on nomenclature, Dr. Jauffret said.
For the new report, Dr. Jauffret and colleagues examined 985 articles from 2000-2022. The guidelines were often not followed even after the release of the recommendations.
For example, 49% of relevant papers used the label “pseudogout” before 2011, and 43% did afterward. A total of 34% of relevant papers described CPPD as chondrocalcinosis prior to 2011, and 22% did afterward.
G-CAN’s next steps are to reach consensus on terminology through online and in-person meetings in 2024, Dr. Jauffret said.
Use of correct gout nomenclature labels improved
In a related presentation, rheumatologist Ellen Prendergast, MBChB, of Dunedin Hospital in New Zealand, reported the results of a newly published review of gout studies before and after G-CAN released consensus recommendations for gout nomenclature in 2019. “There has been improvement in the agreed labels in some areas, but there remains quite significant variability,” she said.
The review examined American College of Rheumatology and EULAR annual meeting abstracts: 596 from 2016-2017 and 392 from 2020-2021. Dr. Prendergast said researchers focused on abstracts instead of published studies in order to gain the most up-to-date understanding of nomenclature.
“Use of the agreed labels ‘urate’ and ‘gout flare’ increased between the two periods. There were 219 of 383 (57.2%) abstracts with the agreed label ‘urate’ in 2016-2017, compared with 164 of 232 (70.7%) in 2020-2021 (P = .001),” the researchers reported. “There were 60 of 175 (34.3%) abstracts with the agreed label ‘gout flare’ in 2016-2017, compared with 57 of 109 (52.3%) in 2020-2021 (P = .003).”
And the use of the term “chronic gout,” which the guidelines recommend against, fell from 29 of 596 (4.9%) abstracts in 2016-2017 to 8 of 392 (2.0%) abstracts in 2020-2021 (P = .02).
One author of the gout nomenclature study reports various consulting fees, speaker fees, or grants outside the submitted work. The other authors of the two studies report no disclosures.
LA JOLLA, CALIF. – Twelve years ago, an international task force of the European Alliance of Associations for Rheumatology (EULAR) released recommendations regarding nomenclature in calcium pyrophosphate deposition disease (CPPD), aiming to standardize the way the condition is described. “Pseudogout” was out, and “acute CPP crystal arthritis” was in, and a confusing array of multi-named phenotypes gained specific labels.
Since 2011, the nomenclature guidelines have been cited hundreds of times, but a new report finds that the medical literature mostly hasn’t followed the recommendations. The findings were released at the annual research symposium of the Gout, Hyperuricemia, and Crystal Associated Disease Network (G-CAN), which is taking another stab at overhauling CPPD nomenclature.
“The objective is to uniform and standardize the labels of the disease, the disease elements, and the clinical states,” rheumatologist Charlotte Jauffret, MD, of the Catholic University of Lille (France), said in a presentation. CPPD is a widely underdiagnosed disease that’s worth the same efforts to standardize nomenclature as occurred in gout, she said.
As Dr. Jauffret explained, CPPD has a diversity of phenotypes in asymptomatic, acute, and chronic forms that pose challenges to diagnosis. “The same terms are used to depict different concepts, and some disease elements are depicted through different names,” she said.
Among other suggestions, the 2011 EULAR recommendations suggested that rheumatologists use the terms chronic CPP crystal inflammatory arthritis instead of “pseudo-rheumatoid arthritis,” osteoarthritis with CPPD, instead of “pseudo-osteoarthritis,” and severe joint degeneration instead of “pseudo-neuropathic joint disease.”
Later reports noted that terms such as CPPD and chondrocalcinosis are still wrongly used interchangeably and called for an international consensus on nomenclature, Dr. Jauffret said.
For the new report, Dr. Jauffret and colleagues examined 985 articles from 2000-2022. The guidelines were often not followed even after the release of the recommendations.
For example, 49% of relevant papers used the label “pseudogout” before 2011, and 43% did afterward. A total of 34% of relevant papers described CPPD as chondrocalcinosis prior to 2011, and 22% did afterward.
G-CAN’s next steps are to reach consensus on terminology through online and in-person meetings in 2024, Dr. Jauffret said.
Use of correct gout nomenclature labels improved
In a related presentation, rheumatologist Ellen Prendergast, MBChB, of Dunedin Hospital in New Zealand, reported the results of a newly published review of gout studies before and after G-CAN released consensus recommendations for gout nomenclature in 2019. “There has been improvement in the agreed labels in some areas, but there remains quite significant variability,” she said.
The review examined American College of Rheumatology and EULAR annual meeting abstracts: 596 from 2016-2017 and 392 from 2020-2021. Dr. Prendergast said researchers focused on abstracts instead of published studies in order to gain the most up-to-date understanding of nomenclature.
“Use of the agreed labels ‘urate’ and ‘gout flare’ increased between the two periods. There were 219 of 383 (57.2%) abstracts with the agreed label ‘urate’ in 2016-2017, compared with 164 of 232 (70.7%) in 2020-2021 (P = .001),” the researchers reported. “There were 60 of 175 (34.3%) abstracts with the agreed label ‘gout flare’ in 2016-2017, compared with 57 of 109 (52.3%) in 2020-2021 (P = .003).”
And the use of the term “chronic gout,” which the guidelines recommend against, fell from 29 of 596 (4.9%) abstracts in 2016-2017 to 8 of 392 (2.0%) abstracts in 2020-2021 (P = .02).
One author of the gout nomenclature study reports various consulting fees, speaker fees, or grants outside the submitted work. The other authors of the two studies report no disclosures.
At G-CAN 2023
Long COVID and mental illness: New guidance
The consensus guidance statement on the assessment and treatment of mental health symptoms in patients with post-acute sequelae of SARS-CoV-2 infection (PASC), also known as long COVID, was published online in Physical Medicine and Rehabilitation, the journal of the American Academy of Physical Medicine and Rehabilitation (AAPM&R).
The statement was developed by a task force that included experts from physical medicine, neurology, neuropsychiatry, neuropsychology, rehabilitation psychology, and primary care. It is the eighth guidance statement on long COVID published by AAPM&R).
“Many of our patients have reported experiences in which their symptoms of long COVID have been dismissed either by loved ones in the community, or also amongst health care providers, and they’ve been told their symptoms are in their head or due to a mental health condition, but that’s simply not true,” Abby L. Cheng, MD, a physiatrist at Barnes Jewish Hospital in St. Louis and a coauthor of the new guidance, said in a press briefing.
“Long COVID is real, and mental health conditions do not cause long COVID,” Dr. Cheng added.
Millions of Americans affected
Anxiety and depression have been reported as the second and third most common symptoms of long COVID, according to the guidance statement.
There is some evidence that the body’s inflammatory response – specifically, circulating cytokines – may contribute to the worsening of mental health symptoms or may bring on new symptoms of anxiety or depression, said Dr. Cheng. Cytokines may also affect levels of brain chemicals, such as serotonin, she said.
Researchers are also exploring whether the persistence of virus in the body, miniature blood clots in the body and brain, and changes to the gut microbiome affect the mental health of people with long COVID.
Some mental health symptoms – such as fatigue, brain fog, sleep disturbances, and tachycardia – can mimic long COVID symptoms, said Dr. Cheng.
The treatment is the same for someone with or without long COVID who has anxiety, depression, posttraumatic stress disorder, or other mental health conditions and includes treatment of coexisting medical conditions, supportive therapy and cognitive-behavioral therapy, and pharmacologic interventions, she said.
“Group therapy may have a particular role in the long COVID population because it really provides that social connection and awareness of additional resources in addition to validation of their experiences,” Dr. Cheng said.
The guidance suggests that primary care practitioners – if it’s within their comfort zone and they have the training – can be the first line for managing mental health symptoms.
But for patients whose symptoms are interfering with functioning and their ability to interact with the community, the guidance urges primary care clinicians to refer the patient to a specialist.
“It leaves the door open to them to practice within their scope but also gives guidance as to how, why, and who should be referred to the next level of care,” said Dr. Cheng.
Coauthor Monica Verduzco-Gutierrez, MD, chair of rehabilitation medicine at UT Health San Antonio, Texas, said that although fewer people are now getting long COVID, “it’s still an impactful number.”
The Centers for Disease Control and Prevention recently estimated that about 7% of American adults (18 million) and 1.3% of children had experienced long COVID.
Dr. Gutierrez said that it’s an evolving number, as some patients who have a second or third or fourth SARS-CoV-2 infection experience exacerbations of previous bouts of long COVID or develop long COVID for the first time.
“We are still getting new patients on a regular basis with long COVID,” said AAPM&R President Steven R. Flanagan, MD, a physical medicine specialist.
“This is a problem that really is not going away. It is still real and still ever-present,” said Dr. Flanagan, chair of rehabilitation medicine at NYU Langone Health.
A version of this article first appeared on Medscape.com.
The consensus guidance statement on the assessment and treatment of mental health symptoms in patients with post-acute sequelae of SARS-CoV-2 infection (PASC), also known as long COVID, was published online in Physical Medicine and Rehabilitation, the journal of the American Academy of Physical Medicine and Rehabilitation (AAPM&R).
The statement was developed by a task force that included experts from physical medicine, neurology, neuropsychiatry, neuropsychology, rehabilitation psychology, and primary care. It is the eighth guidance statement on long COVID published by AAPM&R).
“Many of our patients have reported experiences in which their symptoms of long COVID have been dismissed either by loved ones in the community, or also amongst health care providers, and they’ve been told their symptoms are in their head or due to a mental health condition, but that’s simply not true,” Abby L. Cheng, MD, a physiatrist at Barnes Jewish Hospital in St. Louis and a coauthor of the new guidance, said in a press briefing.
“Long COVID is real, and mental health conditions do not cause long COVID,” Dr. Cheng added.
Millions of Americans affected
Anxiety and depression have been reported as the second and third most common symptoms of long COVID, according to the guidance statement.
There is some evidence that the body’s inflammatory response – specifically, circulating cytokines – may contribute to the worsening of mental health symptoms or may bring on new symptoms of anxiety or depression, said Dr. Cheng. Cytokines may also affect levels of brain chemicals, such as serotonin, she said.
Researchers are also exploring whether the persistence of virus in the body, miniature blood clots in the body and brain, and changes to the gut microbiome affect the mental health of people with long COVID.
Some mental health symptoms – such as fatigue, brain fog, sleep disturbances, and tachycardia – can mimic long COVID symptoms, said Dr. Cheng.
The treatment is the same for someone with or without long COVID who has anxiety, depression, posttraumatic stress disorder, or other mental health conditions and includes treatment of coexisting medical conditions, supportive therapy and cognitive-behavioral therapy, and pharmacologic interventions, she said.
“Group therapy may have a particular role in the long COVID population because it really provides that social connection and awareness of additional resources in addition to validation of their experiences,” Dr. Cheng said.
The guidance suggests that primary care practitioners – if it’s within their comfort zone and they have the training – can be the first line for managing mental health symptoms.
But for patients whose symptoms are interfering with functioning and their ability to interact with the community, the guidance urges primary care clinicians to refer the patient to a specialist.
“It leaves the door open to them to practice within their scope but also gives guidance as to how, why, and who should be referred to the next level of care,” said Dr. Cheng.
Coauthor Monica Verduzco-Gutierrez, MD, chair of rehabilitation medicine at UT Health San Antonio, Texas, said that although fewer people are now getting long COVID, “it’s still an impactful number.”
The Centers for Disease Control and Prevention recently estimated that about 7% of American adults (18 million) and 1.3% of children had experienced long COVID.
Dr. Gutierrez said that it’s an evolving number, as some patients who have a second or third or fourth SARS-CoV-2 infection experience exacerbations of previous bouts of long COVID or develop long COVID for the first time.
“We are still getting new patients on a regular basis with long COVID,” said AAPM&R President Steven R. Flanagan, MD, a physical medicine specialist.
“This is a problem that really is not going away. It is still real and still ever-present,” said Dr. Flanagan, chair of rehabilitation medicine at NYU Langone Health.
A version of this article first appeared on Medscape.com.
The consensus guidance statement on the assessment and treatment of mental health symptoms in patients with post-acute sequelae of SARS-CoV-2 infection (PASC), also known as long COVID, was published online in Physical Medicine and Rehabilitation, the journal of the American Academy of Physical Medicine and Rehabilitation (AAPM&R).
The statement was developed by a task force that included experts from physical medicine, neurology, neuropsychiatry, neuropsychology, rehabilitation psychology, and primary care. It is the eighth guidance statement on long COVID published by AAPM&R).
“Many of our patients have reported experiences in which their symptoms of long COVID have been dismissed either by loved ones in the community, or also amongst health care providers, and they’ve been told their symptoms are in their head or due to a mental health condition, but that’s simply not true,” Abby L. Cheng, MD, a physiatrist at Barnes Jewish Hospital in St. Louis and a coauthor of the new guidance, said in a press briefing.
“Long COVID is real, and mental health conditions do not cause long COVID,” Dr. Cheng added.
Millions of Americans affected
Anxiety and depression have been reported as the second and third most common symptoms of long COVID, according to the guidance statement.
There is some evidence that the body’s inflammatory response – specifically, circulating cytokines – may contribute to the worsening of mental health symptoms or may bring on new symptoms of anxiety or depression, said Dr. Cheng. Cytokines may also affect levels of brain chemicals, such as serotonin, she said.
Researchers are also exploring whether the persistence of virus in the body, miniature blood clots in the body and brain, and changes to the gut microbiome affect the mental health of people with long COVID.
Some mental health symptoms – such as fatigue, brain fog, sleep disturbances, and tachycardia – can mimic long COVID symptoms, said Dr. Cheng.
The treatment is the same for someone with or without long COVID who has anxiety, depression, posttraumatic stress disorder, or other mental health conditions and includes treatment of coexisting medical conditions, supportive therapy and cognitive-behavioral therapy, and pharmacologic interventions, she said.
“Group therapy may have a particular role in the long COVID population because it really provides that social connection and awareness of additional resources in addition to validation of their experiences,” Dr. Cheng said.
The guidance suggests that primary care practitioners – if it’s within their comfort zone and they have the training – can be the first line for managing mental health symptoms.
But for patients whose symptoms are interfering with functioning and their ability to interact with the community, the guidance urges primary care clinicians to refer the patient to a specialist.
“It leaves the door open to them to practice within their scope but also gives guidance as to how, why, and who should be referred to the next level of care,” said Dr. Cheng.
Coauthor Monica Verduzco-Gutierrez, MD, chair of rehabilitation medicine at UT Health San Antonio, Texas, said that although fewer people are now getting long COVID, “it’s still an impactful number.”
The Centers for Disease Control and Prevention recently estimated that about 7% of American adults (18 million) and 1.3% of children had experienced long COVID.
Dr. Gutierrez said that it’s an evolving number, as some patients who have a second or third or fourth SARS-CoV-2 infection experience exacerbations of previous bouts of long COVID or develop long COVID for the first time.
“We are still getting new patients on a regular basis with long COVID,” said AAPM&R President Steven R. Flanagan, MD, a physical medicine specialist.
“This is a problem that really is not going away. It is still real and still ever-present,” said Dr. Flanagan, chair of rehabilitation medicine at NYU Langone Health.
A version of this article first appeared on Medscape.com.
FROM PHYSICAL MEDICINE AND REHABILITATION