User login
American Academy of Pediatrics (AAP): 2017 National Conference and Exhibition
New AAP policy recommends flu vaccination regardless of egg allergy
CHICAGO – The American Academy of Pediatrics has released a new policy statement that in part suggests that physicians can administer influenza vaccine to children and teenagers with egg allergies without any special precautions beyond those that apply to other vaccines.
This is some “egg-citing news,” said Mary Ann Jackson, MD. “In 28 studies with 4,315 egg allergic subjects, 656 of whom had severe allergies, there were no serious allergic reactions.” In other words, there was no respiratory distress or hypotension observed after participants received the influenza vaccine in these studies, she added.
Officially, the policy statement from the academy’s Committee on Infectious Diseases reads: “All children with egg allergy of any severity can receive influenza vaccine without any additional precautions beyond those recommended for any vaccine. Special precautions for egg-allergic recipients of IIV [inactivated influenza vaccine] are not warranted, as the rate of anaphylaxis after IIV administration is no greater in egg-allergic than non–egg-allergic recipients or from other universally recommended vaccines. Standard vaccination practice for all vaccines in children should include the ability to respond to rare acute hypersensitivity reactions.” The full policy statement was published online in the journal Pediatrics (2017 Sep. 6; doi: 10.1542/peds.2017-2550.)
This new policy “makes your life so much easier … and allows you to continue to recommend the vaccine strongly,” said Dr. Jackson, division director of infectious diseases at Children’s Mercy Hospital and professor of pediatrics at the University of Missouri at Kansas City.
Other reasons to recommend flu vaccination
Dr. Jackson also gave an overview of influenza epidemiology and why ongoing education of patients and families remains essential. “It’s almost flu season now. It’s inevitable – like RSV [respiratory syncytial virus] is inevitable – but when the seasons starts is unknown,” she said. “How severe and long the season will be is also unpredictable.” Which viruses are spread and whether there is a good match between circulating virus and the vaccine are additional unknowns each year.
Patient and family education are important for these reasons, and because “it’s the most likely vaccine to be opted out of by the otherwise fully immunized,” she noted.
The lowest covered population are individuals between 18 years and 49 years, Dr. Jackson said. “My young adult son did not think he needed to worry about flu for himself; he said he was healthy and well. But it’s a bummer when your mom is an ID doctor who likes vaccines, because I made it happen for him.”
Dr. Jackson had no relevant financial disclosures.
CHICAGO – The American Academy of Pediatrics has released a new policy statement that in part suggests that physicians can administer influenza vaccine to children and teenagers with egg allergies without any special precautions beyond those that apply to other vaccines.
This is some “egg-citing news,” said Mary Ann Jackson, MD. “In 28 studies with 4,315 egg allergic subjects, 656 of whom had severe allergies, there were no serious allergic reactions.” In other words, there was no respiratory distress or hypotension observed after participants received the influenza vaccine in these studies, she added.
Officially, the policy statement from the academy’s Committee on Infectious Diseases reads: “All children with egg allergy of any severity can receive influenza vaccine without any additional precautions beyond those recommended for any vaccine. Special precautions for egg-allergic recipients of IIV [inactivated influenza vaccine] are not warranted, as the rate of anaphylaxis after IIV administration is no greater in egg-allergic than non–egg-allergic recipients or from other universally recommended vaccines. Standard vaccination practice for all vaccines in children should include the ability to respond to rare acute hypersensitivity reactions.” The full policy statement was published online in the journal Pediatrics (2017 Sep. 6; doi: 10.1542/peds.2017-2550.)
This new policy “makes your life so much easier … and allows you to continue to recommend the vaccine strongly,” said Dr. Jackson, division director of infectious diseases at Children’s Mercy Hospital and professor of pediatrics at the University of Missouri at Kansas City.
Other reasons to recommend flu vaccination
Dr. Jackson also gave an overview of influenza epidemiology and why ongoing education of patients and families remains essential. “It’s almost flu season now. It’s inevitable – like RSV [respiratory syncytial virus] is inevitable – but when the seasons starts is unknown,” she said. “How severe and long the season will be is also unpredictable.” Which viruses are spread and whether there is a good match between circulating virus and the vaccine are additional unknowns each year.
Patient and family education are important for these reasons, and because “it’s the most likely vaccine to be opted out of by the otherwise fully immunized,” she noted.
The lowest covered population are individuals between 18 years and 49 years, Dr. Jackson said. “My young adult son did not think he needed to worry about flu for himself; he said he was healthy and well. But it’s a bummer when your mom is an ID doctor who likes vaccines, because I made it happen for him.”
Dr. Jackson had no relevant financial disclosures.
CHICAGO – The American Academy of Pediatrics has released a new policy statement that in part suggests that physicians can administer influenza vaccine to children and teenagers with egg allergies without any special precautions beyond those that apply to other vaccines.
This is some “egg-citing news,” said Mary Ann Jackson, MD. “In 28 studies with 4,315 egg allergic subjects, 656 of whom had severe allergies, there were no serious allergic reactions.” In other words, there was no respiratory distress or hypotension observed after participants received the influenza vaccine in these studies, she added.
Officially, the policy statement from the academy’s Committee on Infectious Diseases reads: “All children with egg allergy of any severity can receive influenza vaccine without any additional precautions beyond those recommended for any vaccine. Special precautions for egg-allergic recipients of IIV [inactivated influenza vaccine] are not warranted, as the rate of anaphylaxis after IIV administration is no greater in egg-allergic than non–egg-allergic recipients or from other universally recommended vaccines. Standard vaccination practice for all vaccines in children should include the ability to respond to rare acute hypersensitivity reactions.” The full policy statement was published online in the journal Pediatrics (2017 Sep. 6; doi: 10.1542/peds.2017-2550.)
This new policy “makes your life so much easier … and allows you to continue to recommend the vaccine strongly,” said Dr. Jackson, division director of infectious diseases at Children’s Mercy Hospital and professor of pediatrics at the University of Missouri at Kansas City.
Other reasons to recommend flu vaccination
Dr. Jackson also gave an overview of influenza epidemiology and why ongoing education of patients and families remains essential. “It’s almost flu season now. It’s inevitable – like RSV [respiratory syncytial virus] is inevitable – but when the seasons starts is unknown,” she said. “How severe and long the season will be is also unpredictable.” Which viruses are spread and whether there is a good match between circulating virus and the vaccine are additional unknowns each year.
Patient and family education are important for these reasons, and because “it’s the most likely vaccine to be opted out of by the otherwise fully immunized,” she noted.
The lowest covered population are individuals between 18 years and 49 years, Dr. Jackson said. “My young adult son did not think he needed to worry about flu for himself; he said he was healthy and well. But it’s a bummer when your mom is an ID doctor who likes vaccines, because I made it happen for him.”
Dr. Jackson had no relevant financial disclosures.
AT AAP 2017
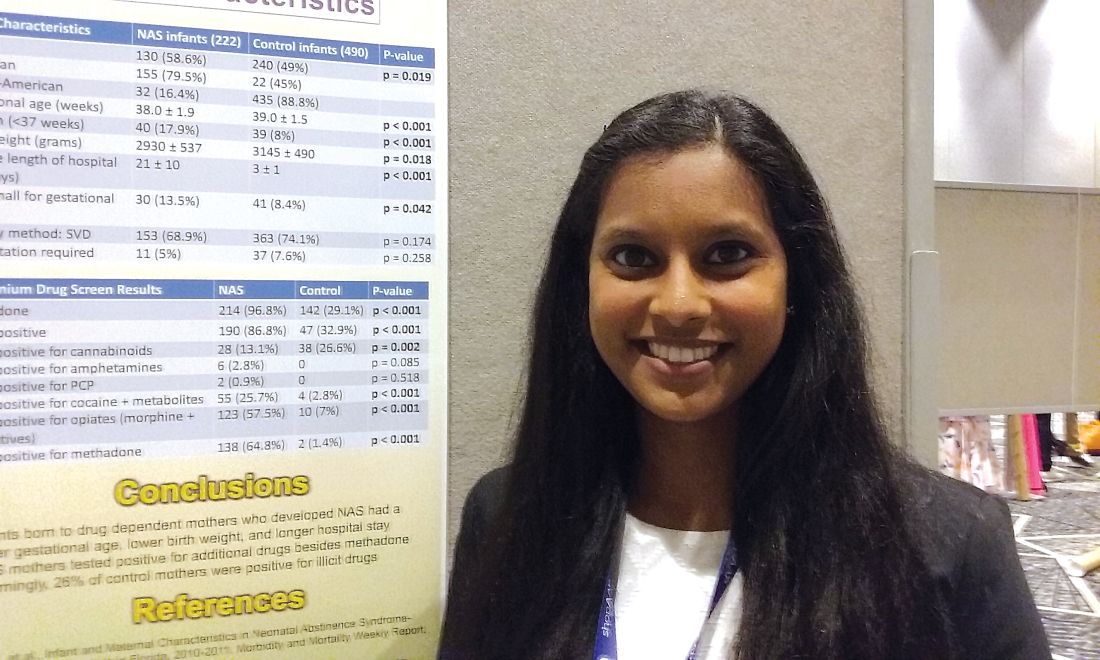
One in four ‘control’ mothers in NAS study tests positive for drug use
CHICAGO – A study that compares babies who develop neonatal abstinence syndrome (NAS) with a control group of healthy newborns found largely what researchers expected to see – lower gestational ages, lower birth weights, and substance use in 100% of the mothers in the affected group. It’s when they looked at the control group of healthy newborns and their mothers that they got a surprise.
“Something that was very alarming in our study is [that] one in four of the control mothers was also positive for illicit drugs. That is something we definitely didn’t expect,” said Pallavi Karunakaran MD, a pediatric resident at Children’s Hospital of Michigan in Detroit.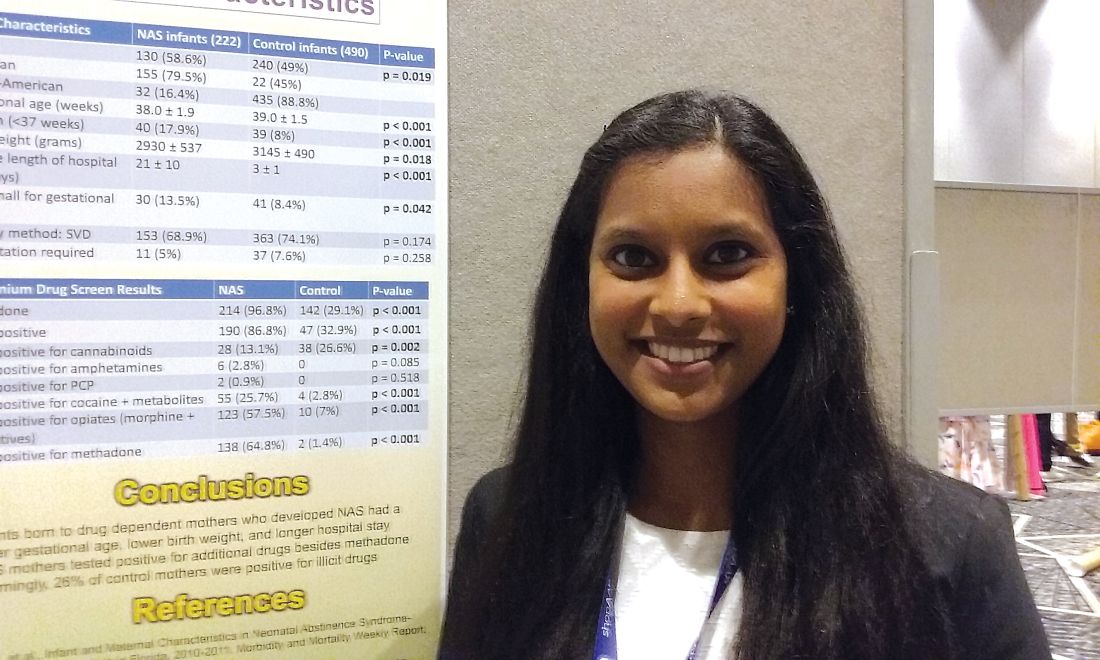
The investigators also looked at maternal characteristics in both groups, with data available on 198 mothers whose babies developed the syndrome and 490 controls. “Interestingly enough, we expected that the mothers of the NAS babies would have some kind of drug use, [but] a lot of the NAS cohort mothers tested positive for additional drugs, other than methadone, which is usually how babies end up developing neonatal abstinence syndrome,” Dr. Karunakaran said at the annual meeting of the American Academy of Pediatrics. Drug use in mothers of affected babies included opioids among 81% (including methadone for 70%); heroin, 42%; cocaine, 29%; marijuana, 26%; benzodiazepines, 18%; buprenorphine, 6%; and barbiturates, 2%.
Among the control group mothers, drug use included marijuana among 20.4%; opioids, 1.8%; cocaine, 1.2%; benzodiazepines, 0.6%; heroin, 0.2%; and barbiturates, 0.2%.
Mean gestational age for affected infants was 38 weeks versus 39 weeks in controls, a significant difference (P less than .001). Mean birth weight for affected infants was 2,930 grams versus 3,145 grams in controls (P = .018). The average length of hospital stay was 21 days for infants who developed NAS, compared with 3 days among control infants (P less than .001). Mean Apgar scores were not significantly different between groups.
“The next step in terms of taking care of our population – is we’re trying to see how we can catch those one in four control mothers who are having well babies because we want to make sure we’re also taking care of them while they’re pregnant,” Dr. Karunakaran said. “If they’re involved in drug use, we want to get them the right resources and the right doctors they may need.”
Dr. Karunakaran had no relevant financial disclosures.
CHICAGO – A study that compares babies who develop neonatal abstinence syndrome (NAS) with a control group of healthy newborns found largely what researchers expected to see – lower gestational ages, lower birth weights, and substance use in 100% of the mothers in the affected group. It’s when they looked at the control group of healthy newborns and their mothers that they got a surprise.
“Something that was very alarming in our study is [that] one in four of the control mothers was also positive for illicit drugs. That is something we definitely didn’t expect,” said Pallavi Karunakaran MD, a pediatric resident at Children’s Hospital of Michigan in Detroit.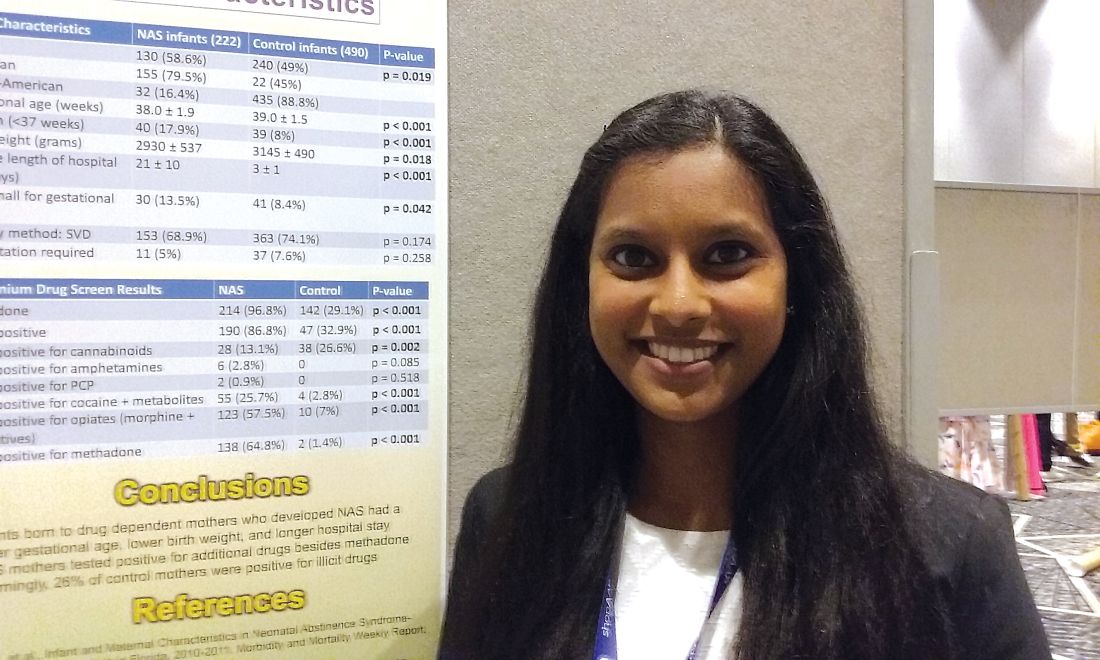
The investigators also looked at maternal characteristics in both groups, with data available on 198 mothers whose babies developed the syndrome and 490 controls. “Interestingly enough, we expected that the mothers of the NAS babies would have some kind of drug use, [but] a lot of the NAS cohort mothers tested positive for additional drugs, other than methadone, which is usually how babies end up developing neonatal abstinence syndrome,” Dr. Karunakaran said at the annual meeting of the American Academy of Pediatrics. Drug use in mothers of affected babies included opioids among 81% (including methadone for 70%); heroin, 42%; cocaine, 29%; marijuana, 26%; benzodiazepines, 18%; buprenorphine, 6%; and barbiturates, 2%.
Among the control group mothers, drug use included marijuana among 20.4%; opioids, 1.8%; cocaine, 1.2%; benzodiazepines, 0.6%; heroin, 0.2%; and barbiturates, 0.2%.
Mean gestational age for affected infants was 38 weeks versus 39 weeks in controls, a significant difference (P less than .001). Mean birth weight for affected infants was 2,930 grams versus 3,145 grams in controls (P = .018). The average length of hospital stay was 21 days for infants who developed NAS, compared with 3 days among control infants (P less than .001). Mean Apgar scores were not significantly different between groups.
“The next step in terms of taking care of our population – is we’re trying to see how we can catch those one in four control mothers who are having well babies because we want to make sure we’re also taking care of them while they’re pregnant,” Dr. Karunakaran said. “If they’re involved in drug use, we want to get them the right resources and the right doctors they may need.”
Dr. Karunakaran had no relevant financial disclosures.
CHICAGO – A study that compares babies who develop neonatal abstinence syndrome (NAS) with a control group of healthy newborns found largely what researchers expected to see – lower gestational ages, lower birth weights, and substance use in 100% of the mothers in the affected group. It’s when they looked at the control group of healthy newborns and their mothers that they got a surprise.
“Something that was very alarming in our study is [that] one in four of the control mothers was also positive for illicit drugs. That is something we definitely didn’t expect,” said Pallavi Karunakaran MD, a pediatric resident at Children’s Hospital of Michigan in Detroit.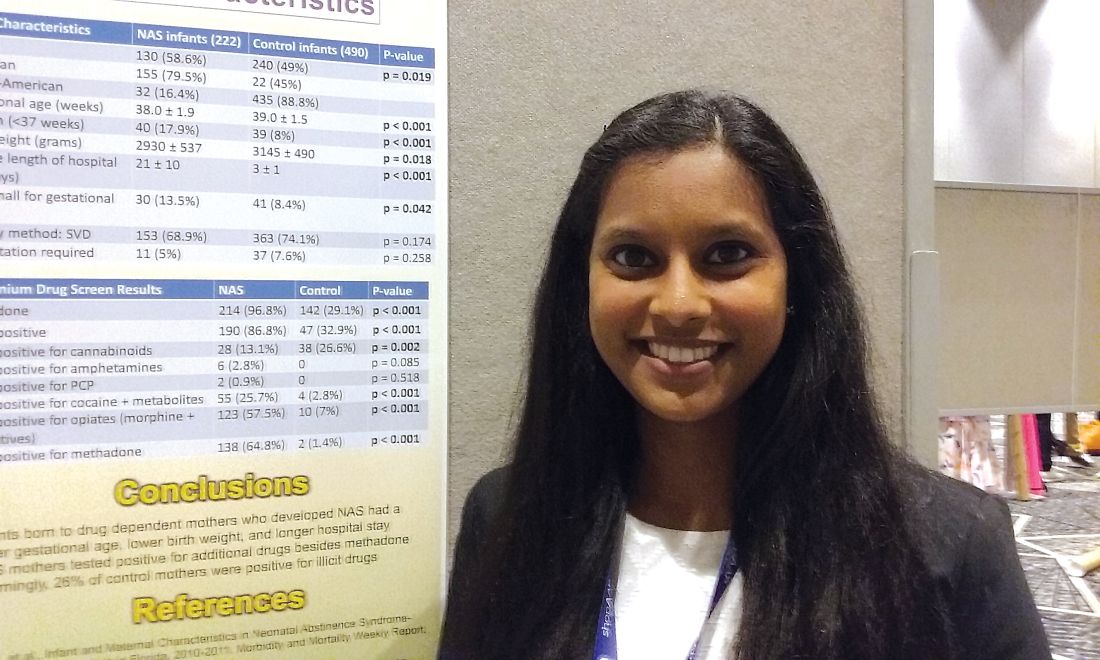
The investigators also looked at maternal characteristics in both groups, with data available on 198 mothers whose babies developed the syndrome and 490 controls. “Interestingly enough, we expected that the mothers of the NAS babies would have some kind of drug use, [but] a lot of the NAS cohort mothers tested positive for additional drugs, other than methadone, which is usually how babies end up developing neonatal abstinence syndrome,” Dr. Karunakaran said at the annual meeting of the American Academy of Pediatrics. Drug use in mothers of affected babies included opioids among 81% (including methadone for 70%); heroin, 42%; cocaine, 29%; marijuana, 26%; benzodiazepines, 18%; buprenorphine, 6%; and barbiturates, 2%.
Among the control group mothers, drug use included marijuana among 20.4%; opioids, 1.8%; cocaine, 1.2%; benzodiazepines, 0.6%; heroin, 0.2%; and barbiturates, 0.2%.
Mean gestational age for affected infants was 38 weeks versus 39 weeks in controls, a significant difference (P less than .001). Mean birth weight for affected infants was 2,930 grams versus 3,145 grams in controls (P = .018). The average length of hospital stay was 21 days for infants who developed NAS, compared with 3 days among control infants (P less than .001). Mean Apgar scores were not significantly different between groups.
“The next step in terms of taking care of our population – is we’re trying to see how we can catch those one in four control mothers who are having well babies because we want to make sure we’re also taking care of them while they’re pregnant,” Dr. Karunakaran said. “If they’re involved in drug use, we want to get them the right resources and the right doctors they may need.”
Dr. Karunakaran had no relevant financial disclosures.
AT AAP 2017
Key clinical point: Investigators studied mothers whose babies developed NAS and were surprised when almost 25% of women in the control group also tested positive for illicit drug use.
Major finding: Among the control mothers, drug use included marijuana 20.4%, opioids 1.8%, cocaine 1.2%, benzodiazepines 0.6%, heroin 0.2%, and barbiturates 0.2%.
Data source: Chart review of 222 infants who developed neonatal abstinence syndrome, compared with 490 controls.
Disclosures: Dr. Karunakaran had no relevant financial disclosures.
Make teen suicide screenings a part of everyday practice
CHICAGO – at the annual meeting of the American Academy of Pediatrics.
An estimated 2 million teenagers, aged 15-19 years, have attempted suicide within the past year, based on data from the Centers for Disease Control and Prevention. According to the CDC’s 1991-2015 High School Youth Risk Behavior Survey data, nearly a third of students (30%) have felt so sad or helpless nearly daily for at least 2 weeks that they stopped doing their normal activities, and 18% had seriously considered suicide within the past year. One in seven (15%) had made a plan for attempting suicide, 9% had attempted suicide at least once, and 3% attempted suicide that required medical treatment. About twice as many females as males had considered, planned, and/or attempted suicide.
“The offspring of suicide attempters have a sixfold higher risk of suicide than their peers whose parents have not attempted suicide,” Dr. Cody said. Other major risk factors include a history of being bullied, a history of abuse, and a history of substance abuse, particularly alcohol and opioids.
Once you identify a patient at risk for suicide, Dr. Cody advised that you should follow a suicide assessment management protocol, such as the one developed by Angela Stanley, PsyD, of the Medical College of Wisconsin and the Children’s Hospital of Wisconsin, both in Milwaukee. Doctors should identify the teen’s intensity of suicidal ideation, ask how far they are in their plans, ascertain their access to means, create a safety plan, refer the patient for mental health care, and follow up frequently.
Dr. Cody emphasized that “suicide contracts” and “safety plans” are different things. Suicide pacts are agreements not to hurt oneself, whereas safety plans include concrete, collaborative, proactive steps a person will take if experiencing suicidal thoughts.
“There is no evidence that contracts prevent suicide, but a lot of research shows that safety or crisis plans are much more effective at preventing a person from committing suicide,” Dr. Cody stated.
The first step of screening is asking a patient directly whether they have ever wished they were dead or had thoughts about killing themselves.
“Some pediatricians are afraid to ask the questions because they’re afraid they’re going to put the idea of suicide in the child’s head, but there is no evidence that screening puts kids at risk,” Dr. Cody said. The other reason you may feel uneasy asking about self-harm is not knowing what to do if a teen says that she is feeling suicidal. That’s where an assessment protocol helps.
If a patient has considered suicide more than a month prior, it shouldn’t be ignored, although the situation may require less urgency but further follow-up. For those with more recent suicidal ideation but without a plan or intent, Dr. Cody recommends following up within 2 weeks because the adolescent’s situation may change.
For those with suicidal ideation and a plan, you should ask three questions:
- What ways of killing yourself have you thought about?
- How likely is it you will follow through on your plan?
- When you think about killing yourself, what stops you?
These questions can help you determine risk acuity: The more specific, realistic, available, and lethal a plan is, the more acute the risk. You then should ask questions to try to determine how likely the teen is to follow through, such as asking about his future plans, his connectedness with others, and his religious beliefs.
Asking about a plan helps determine how much access the patient has to a lethal, realistic means. Firearms are responsible for 52% of teen suicides, followed by hanging/suffocation (25%) and poisoning (16%).
“This is why it’s a really important part of social history to screen for guns in the house,” Dr. Cody told attendees. “I know it’s been really controversial, but it’s something that’s really important, especially if you have an adolescent in the house that’s having suicidal ideation.”
Teens with suicidal ideation and a plan but no intent require a safety plan along with follow-up within 1 week. Those with a plan and intent, or those with no intent but an unwillingness agree to a safety plan, should be immediately hospitalized, Dr. Cody said.
These suicide screenings should occur at annual well-child visits, Dr. Cody said, but they also should be done at acute visits; basically, any time you see your preteen and adolescent patients. Ideally, these should take place during alone time, without any parents present.
You also should share resources with your patients, including the National Suicide Prevention Lifeline at 1-800-273-8255 and the Crisis TextLine at 741741.
Dr. Cody reported having no disclosures, and no external funding was used for the presentation.
CHICAGO – at the annual meeting of the American Academy of Pediatrics.
An estimated 2 million teenagers, aged 15-19 years, have attempted suicide within the past year, based on data from the Centers for Disease Control and Prevention. According to the CDC’s 1991-2015 High School Youth Risk Behavior Survey data, nearly a third of students (30%) have felt so sad or helpless nearly daily for at least 2 weeks that they stopped doing their normal activities, and 18% had seriously considered suicide within the past year. One in seven (15%) had made a plan for attempting suicide, 9% had attempted suicide at least once, and 3% attempted suicide that required medical treatment. About twice as many females as males had considered, planned, and/or attempted suicide.
“The offspring of suicide attempters have a sixfold higher risk of suicide than their peers whose parents have not attempted suicide,” Dr. Cody said. Other major risk factors include a history of being bullied, a history of abuse, and a history of substance abuse, particularly alcohol and opioids.
Once you identify a patient at risk for suicide, Dr. Cody advised that you should follow a suicide assessment management protocol, such as the one developed by Angela Stanley, PsyD, of the Medical College of Wisconsin and the Children’s Hospital of Wisconsin, both in Milwaukee. Doctors should identify the teen’s intensity of suicidal ideation, ask how far they are in their plans, ascertain their access to means, create a safety plan, refer the patient for mental health care, and follow up frequently.
Dr. Cody emphasized that “suicide contracts” and “safety plans” are different things. Suicide pacts are agreements not to hurt oneself, whereas safety plans include concrete, collaborative, proactive steps a person will take if experiencing suicidal thoughts.
“There is no evidence that contracts prevent suicide, but a lot of research shows that safety or crisis plans are much more effective at preventing a person from committing suicide,” Dr. Cody stated.
The first step of screening is asking a patient directly whether they have ever wished they were dead or had thoughts about killing themselves.
“Some pediatricians are afraid to ask the questions because they’re afraid they’re going to put the idea of suicide in the child’s head, but there is no evidence that screening puts kids at risk,” Dr. Cody said. The other reason you may feel uneasy asking about self-harm is not knowing what to do if a teen says that she is feeling suicidal. That’s where an assessment protocol helps.
If a patient has considered suicide more than a month prior, it shouldn’t be ignored, although the situation may require less urgency but further follow-up. For those with more recent suicidal ideation but without a plan or intent, Dr. Cody recommends following up within 2 weeks because the adolescent’s situation may change.
For those with suicidal ideation and a plan, you should ask three questions:
- What ways of killing yourself have you thought about?
- How likely is it you will follow through on your plan?
- When you think about killing yourself, what stops you?
These questions can help you determine risk acuity: The more specific, realistic, available, and lethal a plan is, the more acute the risk. You then should ask questions to try to determine how likely the teen is to follow through, such as asking about his future plans, his connectedness with others, and his religious beliefs.
Asking about a plan helps determine how much access the patient has to a lethal, realistic means. Firearms are responsible for 52% of teen suicides, followed by hanging/suffocation (25%) and poisoning (16%).
“This is why it’s a really important part of social history to screen for guns in the house,” Dr. Cody told attendees. “I know it’s been really controversial, but it’s something that’s really important, especially if you have an adolescent in the house that’s having suicidal ideation.”
Teens with suicidal ideation and a plan but no intent require a safety plan along with follow-up within 1 week. Those with a plan and intent, or those with no intent but an unwillingness agree to a safety plan, should be immediately hospitalized, Dr. Cody said.
These suicide screenings should occur at annual well-child visits, Dr. Cody said, but they also should be done at acute visits; basically, any time you see your preteen and adolescent patients. Ideally, these should take place during alone time, without any parents present.
You also should share resources with your patients, including the National Suicide Prevention Lifeline at 1-800-273-8255 and the Crisis TextLine at 741741.
Dr. Cody reported having no disclosures, and no external funding was used for the presentation.
CHICAGO – at the annual meeting of the American Academy of Pediatrics.
An estimated 2 million teenagers, aged 15-19 years, have attempted suicide within the past year, based on data from the Centers for Disease Control and Prevention. According to the CDC’s 1991-2015 High School Youth Risk Behavior Survey data, nearly a third of students (30%) have felt so sad or helpless nearly daily for at least 2 weeks that they stopped doing their normal activities, and 18% had seriously considered suicide within the past year. One in seven (15%) had made a plan for attempting suicide, 9% had attempted suicide at least once, and 3% attempted suicide that required medical treatment. About twice as many females as males had considered, planned, and/or attempted suicide.
“The offspring of suicide attempters have a sixfold higher risk of suicide than their peers whose parents have not attempted suicide,” Dr. Cody said. Other major risk factors include a history of being bullied, a history of abuse, and a history of substance abuse, particularly alcohol and opioids.
Once you identify a patient at risk for suicide, Dr. Cody advised that you should follow a suicide assessment management protocol, such as the one developed by Angela Stanley, PsyD, of the Medical College of Wisconsin and the Children’s Hospital of Wisconsin, both in Milwaukee. Doctors should identify the teen’s intensity of suicidal ideation, ask how far they are in their plans, ascertain their access to means, create a safety plan, refer the patient for mental health care, and follow up frequently.
Dr. Cody emphasized that “suicide contracts” and “safety plans” are different things. Suicide pacts are agreements not to hurt oneself, whereas safety plans include concrete, collaborative, proactive steps a person will take if experiencing suicidal thoughts.
“There is no evidence that contracts prevent suicide, but a lot of research shows that safety or crisis plans are much more effective at preventing a person from committing suicide,” Dr. Cody stated.
The first step of screening is asking a patient directly whether they have ever wished they were dead or had thoughts about killing themselves.
“Some pediatricians are afraid to ask the questions because they’re afraid they’re going to put the idea of suicide in the child’s head, but there is no evidence that screening puts kids at risk,” Dr. Cody said. The other reason you may feel uneasy asking about self-harm is not knowing what to do if a teen says that she is feeling suicidal. That’s where an assessment protocol helps.
If a patient has considered suicide more than a month prior, it shouldn’t be ignored, although the situation may require less urgency but further follow-up. For those with more recent suicidal ideation but without a plan or intent, Dr. Cody recommends following up within 2 weeks because the adolescent’s situation may change.
For those with suicidal ideation and a plan, you should ask three questions:
- What ways of killing yourself have you thought about?
- How likely is it you will follow through on your plan?
- When you think about killing yourself, what stops you?
These questions can help you determine risk acuity: The more specific, realistic, available, and lethal a plan is, the more acute the risk. You then should ask questions to try to determine how likely the teen is to follow through, such as asking about his future plans, his connectedness with others, and his religious beliefs.
Asking about a plan helps determine how much access the patient has to a lethal, realistic means. Firearms are responsible for 52% of teen suicides, followed by hanging/suffocation (25%) and poisoning (16%).
“This is why it’s a really important part of social history to screen for guns in the house,” Dr. Cody told attendees. “I know it’s been really controversial, but it’s something that’s really important, especially if you have an adolescent in the house that’s having suicidal ideation.”
Teens with suicidal ideation and a plan but no intent require a safety plan along with follow-up within 1 week. Those with a plan and intent, or those with no intent but an unwillingness agree to a safety plan, should be immediately hospitalized, Dr. Cody said.
These suicide screenings should occur at annual well-child visits, Dr. Cody said, but they also should be done at acute visits; basically, any time you see your preteen and adolescent patients. Ideally, these should take place during alone time, without any parents present.
You also should share resources with your patients, including the National Suicide Prevention Lifeline at 1-800-273-8255 and the Crisis TextLine at 741741.
Dr. Cody reported having no disclosures, and no external funding was used for the presentation.
EXPERT ANALYSIS FROM AAP 2017
When is it really recurrent strep throat?
CHICAGO – When a child is sitting in your exam room with recurrent strep pharyngitis, the first question to ask yourself is “Is it real?”
According to pediatric infectious disease specialist John Bradley, MD, the answer to that question comes with careful attention to the history and clinical presentation, but titers and viral polymerase chain reaction tests can also help clarify the diagnosis.
Although that involves some detective work and perhaps some legwork by the provider or the office staff, it’s worth the effort, especially in an era of increased concerns about antimicrobial stewardship, said Dr. Bradley during an antimicrobial update session at the annual meeting of the American Academy of Pediatrics.
“Are the episodes really documented by you in your office?” asked Dr. Bradley. If so, the job is easier. If not, it’s important to differentiate whether documentation of the strep infection was done by culture, whether it was done by an extremely sensitive rapid test, or whether any testing has been done at all, said Dr. Bradley, chief of the division of infectious diseases at the University of California, San Diego.
Somehow, said Dr. Bradley, it’s still true that all group A streptococci are susceptible to penicillin, but penicillin does not always work. There’s about a 10% failure rate for reasons that are not completely understood. Perhaps some individuals have other oropharyngeal flora that produce beta-lactamases, thereby negating penicillin’s efficacy against the strep, he added.
One very good clue as to whether the child has recurrent strep is the appearance of the throat, said Dr. Bradley. A viral illness also can produce a very red posterior oropharynx, so – unless there’s frank pus – it’s unlikely to be strep pharyngitis.
Some patients will, in fact, have recurrent strep, but some patients who might even have positive rapid strep tests may actually be carriers.
So, “what the heck is the carrier state?” asked Dr. Bradley. Although a rapid strep test will occasionally be positive, he explained, the culture is only weakly positive, with growth that’s usually less than 1+. The child who’s a carrier is not symptomatic, will not have an elevated antistreptolysin O titer, and is not contagious. Also, the child will not respond to penicillin treatment.
How can clinicians differentiate recurrent strep from a child with frequent viral illnesses who’s a carrier?
“For the standard case of ‘recurrent strep,’ please get cultures and document the density of group A strep to rule out the carrier state,” said Dr. Bradley. Having parents text pictures of the throat during an episode – for which his facility has a secure portal – can save families an office visit. A negative antistreptolysin O titer can help rule out a recurrent infection, he added.
When a child is having recurrent bouts of pharyngitis, but the clinical picture isn’t clearly consistent with strep, physicians can consider submitting multiplex viral polymerase chain reaction tests. “This can give the family an alternative diagnosis” and reassure parents that it’s safe to hold off on antibiotics, noted Dr. Bradley.
Culturing between episodes of pharyngitis, when the patient is asymptomatic, can also help determine whether a child is a carrier. Sometimes, it makes sense to culture the whole family, and there have also been reports of family pets being Group A strep reservoirs, said Dr. Bradley.
For recurrent infection, choose a broad spectrum agent that will knock back both Group A strep and the oral flora that may be producing beta-lactamases or adhesion molecules that negate penicillin’s efficacy. One logical choice is clindamycin for 10 days, although some strains are resistant. Another good choice is amoxicillin/clavulanate for 10 days or 10 days of a cephalosporin. Penicillin can still be used if it’s augmented by oral rifampin during the last 4 days of the 10-day course.
Long-term prophylaxis can also be considered for stubborn recurrences, he noted.
Dr. Bradley reported no relevant conflicts of interest.
CHICAGO – When a child is sitting in your exam room with recurrent strep pharyngitis, the first question to ask yourself is “Is it real?”
According to pediatric infectious disease specialist John Bradley, MD, the answer to that question comes with careful attention to the history and clinical presentation, but titers and viral polymerase chain reaction tests can also help clarify the diagnosis.
Although that involves some detective work and perhaps some legwork by the provider or the office staff, it’s worth the effort, especially in an era of increased concerns about antimicrobial stewardship, said Dr. Bradley during an antimicrobial update session at the annual meeting of the American Academy of Pediatrics.
“Are the episodes really documented by you in your office?” asked Dr. Bradley. If so, the job is easier. If not, it’s important to differentiate whether documentation of the strep infection was done by culture, whether it was done by an extremely sensitive rapid test, or whether any testing has been done at all, said Dr. Bradley, chief of the division of infectious diseases at the University of California, San Diego.
Somehow, said Dr. Bradley, it’s still true that all group A streptococci are susceptible to penicillin, but penicillin does not always work. There’s about a 10% failure rate for reasons that are not completely understood. Perhaps some individuals have other oropharyngeal flora that produce beta-lactamases, thereby negating penicillin’s efficacy against the strep, he added.
One very good clue as to whether the child has recurrent strep is the appearance of the throat, said Dr. Bradley. A viral illness also can produce a very red posterior oropharynx, so – unless there’s frank pus – it’s unlikely to be strep pharyngitis.
Some patients will, in fact, have recurrent strep, but some patients who might even have positive rapid strep tests may actually be carriers.
So, “what the heck is the carrier state?” asked Dr. Bradley. Although a rapid strep test will occasionally be positive, he explained, the culture is only weakly positive, with growth that’s usually less than 1+. The child who’s a carrier is not symptomatic, will not have an elevated antistreptolysin O titer, and is not contagious. Also, the child will not respond to penicillin treatment.
How can clinicians differentiate recurrent strep from a child with frequent viral illnesses who’s a carrier?
“For the standard case of ‘recurrent strep,’ please get cultures and document the density of group A strep to rule out the carrier state,” said Dr. Bradley. Having parents text pictures of the throat during an episode – for which his facility has a secure portal – can save families an office visit. A negative antistreptolysin O titer can help rule out a recurrent infection, he added.
When a child is having recurrent bouts of pharyngitis, but the clinical picture isn’t clearly consistent with strep, physicians can consider submitting multiplex viral polymerase chain reaction tests. “This can give the family an alternative diagnosis” and reassure parents that it’s safe to hold off on antibiotics, noted Dr. Bradley.
Culturing between episodes of pharyngitis, when the patient is asymptomatic, can also help determine whether a child is a carrier. Sometimes, it makes sense to culture the whole family, and there have also been reports of family pets being Group A strep reservoirs, said Dr. Bradley.
For recurrent infection, choose a broad spectrum agent that will knock back both Group A strep and the oral flora that may be producing beta-lactamases or adhesion molecules that negate penicillin’s efficacy. One logical choice is clindamycin for 10 days, although some strains are resistant. Another good choice is amoxicillin/clavulanate for 10 days or 10 days of a cephalosporin. Penicillin can still be used if it’s augmented by oral rifampin during the last 4 days of the 10-day course.
Long-term prophylaxis can also be considered for stubborn recurrences, he noted.
Dr. Bradley reported no relevant conflicts of interest.
CHICAGO – When a child is sitting in your exam room with recurrent strep pharyngitis, the first question to ask yourself is “Is it real?”
According to pediatric infectious disease specialist John Bradley, MD, the answer to that question comes with careful attention to the history and clinical presentation, but titers and viral polymerase chain reaction tests can also help clarify the diagnosis.
Although that involves some detective work and perhaps some legwork by the provider or the office staff, it’s worth the effort, especially in an era of increased concerns about antimicrobial stewardship, said Dr. Bradley during an antimicrobial update session at the annual meeting of the American Academy of Pediatrics.
“Are the episodes really documented by you in your office?” asked Dr. Bradley. If so, the job is easier. If not, it’s important to differentiate whether documentation of the strep infection was done by culture, whether it was done by an extremely sensitive rapid test, or whether any testing has been done at all, said Dr. Bradley, chief of the division of infectious diseases at the University of California, San Diego.
Somehow, said Dr. Bradley, it’s still true that all group A streptococci are susceptible to penicillin, but penicillin does not always work. There’s about a 10% failure rate for reasons that are not completely understood. Perhaps some individuals have other oropharyngeal flora that produce beta-lactamases, thereby negating penicillin’s efficacy against the strep, he added.
One very good clue as to whether the child has recurrent strep is the appearance of the throat, said Dr. Bradley. A viral illness also can produce a very red posterior oropharynx, so – unless there’s frank pus – it’s unlikely to be strep pharyngitis.
Some patients will, in fact, have recurrent strep, but some patients who might even have positive rapid strep tests may actually be carriers.
So, “what the heck is the carrier state?” asked Dr. Bradley. Although a rapid strep test will occasionally be positive, he explained, the culture is only weakly positive, with growth that’s usually less than 1+. The child who’s a carrier is not symptomatic, will not have an elevated antistreptolysin O titer, and is not contagious. Also, the child will not respond to penicillin treatment.
How can clinicians differentiate recurrent strep from a child with frequent viral illnesses who’s a carrier?
“For the standard case of ‘recurrent strep,’ please get cultures and document the density of group A strep to rule out the carrier state,” said Dr. Bradley. Having parents text pictures of the throat during an episode – for which his facility has a secure portal – can save families an office visit. A negative antistreptolysin O titer can help rule out a recurrent infection, he added.
When a child is having recurrent bouts of pharyngitis, but the clinical picture isn’t clearly consistent with strep, physicians can consider submitting multiplex viral polymerase chain reaction tests. “This can give the family an alternative diagnosis” and reassure parents that it’s safe to hold off on antibiotics, noted Dr. Bradley.
Culturing between episodes of pharyngitis, when the patient is asymptomatic, can also help determine whether a child is a carrier. Sometimes, it makes sense to culture the whole family, and there have also been reports of family pets being Group A strep reservoirs, said Dr. Bradley.
For recurrent infection, choose a broad spectrum agent that will knock back both Group A strep and the oral flora that may be producing beta-lactamases or adhesion molecules that negate penicillin’s efficacy. One logical choice is clindamycin for 10 days, although some strains are resistant. Another good choice is amoxicillin/clavulanate for 10 days or 10 days of a cephalosporin. Penicillin can still be used if it’s augmented by oral rifampin during the last 4 days of the 10-day course.
Long-term prophylaxis can also be considered for stubborn recurrences, he noted.
Dr. Bradley reported no relevant conflicts of interest.
EXPERT ANALYSIS FROM AAP 2017
Teens smoking more pot than cigarettes
CHICAGO – The challenge of addressing marijuana use by children and teens is increasing with its wider availability; 29 states have now legalized cannabis for medical use, and 8 of them plus the District of Columbia have legalized recreational marijuana use.
“Past-month marijuana use is now higher than past-month use of cigarettes” based on teens’ responses to surveys from the National Institute on Drug Abuse (NIDA), Karen M. Wilson, MD, said at the annual meeting of the American Academy of Pediatrics.
Dr. Wilson emphasized the importance of discussing drug use and attitudes about drug use with young teens, as well as educating them about risks.
Recent research suggests the brain does not fully mature until the mid-20s, and marijuana has been shown to impair working memory, cognitive flexibility, learning, attention, and verbal functions. Marijuana may alter the developing brain in ways that cannot be repaired in those who halt use at an older age, said Dr. Wilson, division chief of general pediatrics and vice-chair for clinical and translational research at the Icahn School of Medicine at Mount Sinai, New York. Marijuana use becomes an addictive behavior in 9% of users, and this addictive behavior is more likely to persist in those who begin to use marijuana at a young age.
“Whether it’s alcohol or marijuana or tobacco, even if they’re only using it on the weekends,” the behavior can progress to addictive behavior, she said. Discussions should determine how much cannabis is used, how often, and why it is used.
“Kids may be self-medicating if they have depression, anxiety, or chronic pain,” Dr. Wilson said. “That could be something you could provide a more appropriate pharmacological intervention for.”
Motivational interviewing – a collaborative, person-centered form of guiding to elicit and strengthen motivation for change – can be the impetus for discussion about whether young patients can try quitting for a short time to show they can do it.
One challenge of discouraging and reducing teens’ marijuana use is the increasing diversity of products and consumption methods. From candy and baked goods to electronic “vaping” products and dissolvable strips similar to breath mints, it’s difficult to keep up. Dr. Wilson showed an image of a new product that looks exactly like a medical inhaler.
Couse of marijuana with tobacco also presents challenges since researchers have little data on how dual use may affect the ability to quit using either drug. “Joints,” rolled in paper, contain only marijuana, but a “blunt” is marijuana rolled in a tobacco leaf, and “spliffs” contain both marijuana and tobacco. Both blunts and spliffs, therefore, include nicotine which is addictive.
Other inhaled substances that can potentially damage the lungs include “lung juice,” a herbal product marketed to “clean out” the lungs. “We should encourage teens to get clean lungs by not inhaling things that aren’t good for you.”
Dr. Wilson reported having no disclosures, and no external funding was used for the presentation.
CHICAGO – The challenge of addressing marijuana use by children and teens is increasing with its wider availability; 29 states have now legalized cannabis for medical use, and 8 of them plus the District of Columbia have legalized recreational marijuana use.
“Past-month marijuana use is now higher than past-month use of cigarettes” based on teens’ responses to surveys from the National Institute on Drug Abuse (NIDA), Karen M. Wilson, MD, said at the annual meeting of the American Academy of Pediatrics.
Dr. Wilson emphasized the importance of discussing drug use and attitudes about drug use with young teens, as well as educating them about risks.
Recent research suggests the brain does not fully mature until the mid-20s, and marijuana has been shown to impair working memory, cognitive flexibility, learning, attention, and verbal functions. Marijuana may alter the developing brain in ways that cannot be repaired in those who halt use at an older age, said Dr. Wilson, division chief of general pediatrics and vice-chair for clinical and translational research at the Icahn School of Medicine at Mount Sinai, New York. Marijuana use becomes an addictive behavior in 9% of users, and this addictive behavior is more likely to persist in those who begin to use marijuana at a young age.
“Whether it’s alcohol or marijuana or tobacco, even if they’re only using it on the weekends,” the behavior can progress to addictive behavior, she said. Discussions should determine how much cannabis is used, how often, and why it is used.
“Kids may be self-medicating if they have depression, anxiety, or chronic pain,” Dr. Wilson said. “That could be something you could provide a more appropriate pharmacological intervention for.”
Motivational interviewing – a collaborative, person-centered form of guiding to elicit and strengthen motivation for change – can be the impetus for discussion about whether young patients can try quitting for a short time to show they can do it.
One challenge of discouraging and reducing teens’ marijuana use is the increasing diversity of products and consumption methods. From candy and baked goods to electronic “vaping” products and dissolvable strips similar to breath mints, it’s difficult to keep up. Dr. Wilson showed an image of a new product that looks exactly like a medical inhaler.
Couse of marijuana with tobacco also presents challenges since researchers have little data on how dual use may affect the ability to quit using either drug. “Joints,” rolled in paper, contain only marijuana, but a “blunt” is marijuana rolled in a tobacco leaf, and “spliffs” contain both marijuana and tobacco. Both blunts and spliffs, therefore, include nicotine which is addictive.
Other inhaled substances that can potentially damage the lungs include “lung juice,” a herbal product marketed to “clean out” the lungs. “We should encourage teens to get clean lungs by not inhaling things that aren’t good for you.”
Dr. Wilson reported having no disclosures, and no external funding was used for the presentation.
CHICAGO – The challenge of addressing marijuana use by children and teens is increasing with its wider availability; 29 states have now legalized cannabis for medical use, and 8 of them plus the District of Columbia have legalized recreational marijuana use.
“Past-month marijuana use is now higher than past-month use of cigarettes” based on teens’ responses to surveys from the National Institute on Drug Abuse (NIDA), Karen M. Wilson, MD, said at the annual meeting of the American Academy of Pediatrics.
Dr. Wilson emphasized the importance of discussing drug use and attitudes about drug use with young teens, as well as educating them about risks.
Recent research suggests the brain does not fully mature until the mid-20s, and marijuana has been shown to impair working memory, cognitive flexibility, learning, attention, and verbal functions. Marijuana may alter the developing brain in ways that cannot be repaired in those who halt use at an older age, said Dr. Wilson, division chief of general pediatrics and vice-chair for clinical and translational research at the Icahn School of Medicine at Mount Sinai, New York. Marijuana use becomes an addictive behavior in 9% of users, and this addictive behavior is more likely to persist in those who begin to use marijuana at a young age.
“Whether it’s alcohol or marijuana or tobacco, even if they’re only using it on the weekends,” the behavior can progress to addictive behavior, she said. Discussions should determine how much cannabis is used, how often, and why it is used.
“Kids may be self-medicating if they have depression, anxiety, or chronic pain,” Dr. Wilson said. “That could be something you could provide a more appropriate pharmacological intervention for.”
Motivational interviewing – a collaborative, person-centered form of guiding to elicit and strengthen motivation for change – can be the impetus for discussion about whether young patients can try quitting for a short time to show they can do it.
One challenge of discouraging and reducing teens’ marijuana use is the increasing diversity of products and consumption methods. From candy and baked goods to electronic “vaping” products and dissolvable strips similar to breath mints, it’s difficult to keep up. Dr. Wilson showed an image of a new product that looks exactly like a medical inhaler.
Couse of marijuana with tobacco also presents challenges since researchers have little data on how dual use may affect the ability to quit using either drug. “Joints,” rolled in paper, contain only marijuana, but a “blunt” is marijuana rolled in a tobacco leaf, and “spliffs” contain both marijuana and tobacco. Both blunts and spliffs, therefore, include nicotine which is addictive.
Other inhaled substances that can potentially damage the lungs include “lung juice,” a herbal product marketed to “clean out” the lungs. “We should encourage teens to get clean lungs by not inhaling things that aren’t good for you.”
Dr. Wilson reported having no disclosures, and no external funding was used for the presentation.
EXPERT ANALYSIS FROM AAP 2017
Female physicians can face breastfeeding challenges at work
CHICAGO – Physician mothers who breastfeed and wish to pump milk during work hours can face many of the same challenges as other working mothers, as well as some issues unique to the profession, a new survey revealed.
“Although physician mothers have high rates of intention to breastfeed while they are pregnant, and initiation of breastfeeding at birth, we unfortunately have low rates of continuing to breastfeed and even meeting the [6 month] recommendations for exclusive breastfeeding,” Rebecca Cantu, MD, MPH said at the annual meeting of the American Academy of Pediatrics.
Dr. Cantu and her colleagues surveyed providers affiliated with the University of Arkansas for Medical Sciences in Little Rock in 2016. The 3-item, Web-based survey was anonymous and assessed role [trainee (medical student, resident physician, fellow) or faculty physician], breastfeeding experience, and perceived barriers to successful breastfeeding.
Common barriers identified
Of the 223 responses, 38% were from medical students, 31% from faculty, 24% from residents, and 7% from fellows. Of the 97 physicians who had breastfed at some point, 97% identified at least one barrier they felt inhibited their breastfeeding goals, said Dr. Cantu, a pediatric hospitalist at Arkansas Children’s Hospital in Little Rock. The survey revealed a total 397 barriers, for an average of 3.7 per person. Being faced with barriers could lead to early unintentional weaning and other consequences like mastitis, decreased milk supply, or anxiety, she added.
“We did find trainees identified a significantly higher median number of barriers, five, versus three for faculty [P less than .01],” Dr. Cantu said. Only one respondent said she faced no barriers.
Lack of time and place to pump breast milk, an unpredictable schedule, short maternity leave, and long working hours were among the most common barriers cited.
“For physicians, we don’t have time. I don’t have a protected lunch break. I’m a hospitalist rounding for hours in the morning,” Dr. Cantu said. “Also, residents don’t always feel comfortable asking for time to leave, and we don’t have people identified to cover our patients. So, depending on the institution, there can be many areas that need to be addressed.”
“The last place I worked had many lactation rooms scattered throughout the hospital, some for physicians only,” she said. “Where I work now we have one room for breastfeeding with two chairs for the entire medical center. So space is a problem.”
A little over half (56%) of respondents had never breastfed. Another 30% had previously breastfed and weaned and 14% were currently breastfeeding at the time of the survey. Of those who had never breastfed, 87% indicated that they planned to at some point in the future. “This emphasizes that the current problem is something we need to continue to work on. We need to address these barriers, and find ways to decrease the impact these barriers have on breastfeeding physicians.”
Future research will investigate association between these barriers and breastfeeding duration and other outcomes, Dr. Cantu said.
Potential solutions
“Policy can play a role here. Plenty of studies have shown that supporting physicians who breastfeed is associated with better patient outcomes, and institutions that support breastfeeding can have a financial benefit,” she said, adding, “If the hospitals cannot even support breastfeeding mothers, how do we expect other places to?”
During the Q&A after Dr. Cantu’s presentation, a meeting attendee suggested using a Freemie pump.* It’s a smaller and more discreet pump that can be used “at an airport, restaurant or while charting in the emergency department.” Dr. Cantu agreed that Freemie pumps could help.
Dr. Cantu also recommended the Dr. Milk support group website and Facebook pages. “I refer a lot of trainees there because you can post a question and get tons of peer advice and support, and find out what’s worked for other people.:
Dr. Cantu had no relevant financial disclosures.
* This article was updated on 1/11/18.
CHICAGO – Physician mothers who breastfeed and wish to pump milk during work hours can face many of the same challenges as other working mothers, as well as some issues unique to the profession, a new survey revealed.
“Although physician mothers have high rates of intention to breastfeed while they are pregnant, and initiation of breastfeeding at birth, we unfortunately have low rates of continuing to breastfeed and even meeting the [6 month] recommendations for exclusive breastfeeding,” Rebecca Cantu, MD, MPH said at the annual meeting of the American Academy of Pediatrics.
Dr. Cantu and her colleagues surveyed providers affiliated with the University of Arkansas for Medical Sciences in Little Rock in 2016. The 3-item, Web-based survey was anonymous and assessed role [trainee (medical student, resident physician, fellow) or faculty physician], breastfeeding experience, and perceived barriers to successful breastfeeding.
Common barriers identified
Of the 223 responses, 38% were from medical students, 31% from faculty, 24% from residents, and 7% from fellows. Of the 97 physicians who had breastfed at some point, 97% identified at least one barrier they felt inhibited their breastfeeding goals, said Dr. Cantu, a pediatric hospitalist at Arkansas Children’s Hospital in Little Rock. The survey revealed a total 397 barriers, for an average of 3.7 per person. Being faced with barriers could lead to early unintentional weaning and other consequences like mastitis, decreased milk supply, or anxiety, she added.
“We did find trainees identified a significantly higher median number of barriers, five, versus three for faculty [P less than .01],” Dr. Cantu said. Only one respondent said she faced no barriers.
Lack of time and place to pump breast milk, an unpredictable schedule, short maternity leave, and long working hours were among the most common barriers cited.
“For physicians, we don’t have time. I don’t have a protected lunch break. I’m a hospitalist rounding for hours in the morning,” Dr. Cantu said. “Also, residents don’t always feel comfortable asking for time to leave, and we don’t have people identified to cover our patients. So, depending on the institution, there can be many areas that need to be addressed.”
“The last place I worked had many lactation rooms scattered throughout the hospital, some for physicians only,” she said. “Where I work now we have one room for breastfeeding with two chairs for the entire medical center. So space is a problem.”
A little over half (56%) of respondents had never breastfed. Another 30% had previously breastfed and weaned and 14% were currently breastfeeding at the time of the survey. Of those who had never breastfed, 87% indicated that they planned to at some point in the future. “This emphasizes that the current problem is something we need to continue to work on. We need to address these barriers, and find ways to decrease the impact these barriers have on breastfeeding physicians.”
Future research will investigate association between these barriers and breastfeeding duration and other outcomes, Dr. Cantu said.
Potential solutions
“Policy can play a role here. Plenty of studies have shown that supporting physicians who breastfeed is associated with better patient outcomes, and institutions that support breastfeeding can have a financial benefit,” she said, adding, “If the hospitals cannot even support breastfeeding mothers, how do we expect other places to?”
During the Q&A after Dr. Cantu’s presentation, a meeting attendee suggested using a Freemie pump.* It’s a smaller and more discreet pump that can be used “at an airport, restaurant or while charting in the emergency department.” Dr. Cantu agreed that Freemie pumps could help.
Dr. Cantu also recommended the Dr. Milk support group website and Facebook pages. “I refer a lot of trainees there because you can post a question and get tons of peer advice and support, and find out what’s worked for other people.:
Dr. Cantu had no relevant financial disclosures.
* This article was updated on 1/11/18.
CHICAGO – Physician mothers who breastfeed and wish to pump milk during work hours can face many of the same challenges as other working mothers, as well as some issues unique to the profession, a new survey revealed.
“Although physician mothers have high rates of intention to breastfeed while they are pregnant, and initiation of breastfeeding at birth, we unfortunately have low rates of continuing to breastfeed and even meeting the [6 month] recommendations for exclusive breastfeeding,” Rebecca Cantu, MD, MPH said at the annual meeting of the American Academy of Pediatrics.
Dr. Cantu and her colleagues surveyed providers affiliated with the University of Arkansas for Medical Sciences in Little Rock in 2016. The 3-item, Web-based survey was anonymous and assessed role [trainee (medical student, resident physician, fellow) or faculty physician], breastfeeding experience, and perceived barriers to successful breastfeeding.
Common barriers identified
Of the 223 responses, 38% were from medical students, 31% from faculty, 24% from residents, and 7% from fellows. Of the 97 physicians who had breastfed at some point, 97% identified at least one barrier they felt inhibited their breastfeeding goals, said Dr. Cantu, a pediatric hospitalist at Arkansas Children’s Hospital in Little Rock. The survey revealed a total 397 barriers, for an average of 3.7 per person. Being faced with barriers could lead to early unintentional weaning and other consequences like mastitis, decreased milk supply, or anxiety, she added.
“We did find trainees identified a significantly higher median number of barriers, five, versus three for faculty [P less than .01],” Dr. Cantu said. Only one respondent said she faced no barriers.
Lack of time and place to pump breast milk, an unpredictable schedule, short maternity leave, and long working hours were among the most common barriers cited.
“For physicians, we don’t have time. I don’t have a protected lunch break. I’m a hospitalist rounding for hours in the morning,” Dr. Cantu said. “Also, residents don’t always feel comfortable asking for time to leave, and we don’t have people identified to cover our patients. So, depending on the institution, there can be many areas that need to be addressed.”
“The last place I worked had many lactation rooms scattered throughout the hospital, some for physicians only,” she said. “Where I work now we have one room for breastfeeding with two chairs for the entire medical center. So space is a problem.”
A little over half (56%) of respondents had never breastfed. Another 30% had previously breastfed and weaned and 14% were currently breastfeeding at the time of the survey. Of those who had never breastfed, 87% indicated that they planned to at some point in the future. “This emphasizes that the current problem is something we need to continue to work on. We need to address these barriers, and find ways to decrease the impact these barriers have on breastfeeding physicians.”
Future research will investigate association between these barriers and breastfeeding duration and other outcomes, Dr. Cantu said.
Potential solutions
“Policy can play a role here. Plenty of studies have shown that supporting physicians who breastfeed is associated with better patient outcomes, and institutions that support breastfeeding can have a financial benefit,” she said, adding, “If the hospitals cannot even support breastfeeding mothers, how do we expect other places to?”
During the Q&A after Dr. Cantu’s presentation, a meeting attendee suggested using a Freemie pump.* It’s a smaller and more discreet pump that can be used “at an airport, restaurant or while charting in the emergency department.” Dr. Cantu agreed that Freemie pumps could help.
Dr. Cantu also recommended the Dr. Milk support group website and Facebook pages. “I refer a lot of trainees there because you can post a question and get tons of peer advice and support, and find out what’s worked for other people.:
Dr. Cantu had no relevant financial disclosures.
* This article was updated on 1/11/18.
AT AAP 2017
Key clinical point: .
Major finding: Of 97 physicians who had ever breastfed, 97% perceived at least one barrier at work that inhibited meeting their breastfeeding goals.
Data source: Survey responses from 223 physicians and medical students affiliated with the University of Arkansas.
Disclosures: Dr. Cantu had no relevant financial disclosures.
Subtle hearing loss after concussion could impair learning
CHICAGO – Children who experience concussion can develop deficits in auditory processing that could impair long-term academic performance and carry implications for return-to-play strategies, according to a study.
Investigators assessed 40 children aged 8-15 years, half of whom experienced concussion. The postconcussion group of 20 children had slower and smaller neural responses to speech, compared with 20 control children, on the noninvasive frequency-following response measure.
“The ability to hear in noise following concussion is impaired in the pediatric population, based on our results, which suggests it might pose additional challenges for classroom learning,” Ms. Thompson said. The study also suggests that auditory function should be considered part of acute and long-term assessment of children post concussion.
Importantly, all participants in the study had normal hearing. “It’s important to know these are very subtle auditory deficits that only emerge if you’re looking for them,” Ms. Thompson said at the annual meeting of the American Academy of Pediatrics.
Children in the concussion group were recruited from the concussion clinic at the Ann and Robert H. Lurie Children’s Hospital of Chicago. Patients were assessed an average of 27 days post injury, with most still symptomatic. The children in the control group had been treated for musculoskeletal injuries. The concussed and control groups were matched for sex and gender.
“We think that these results have implications beyond the classroom,” Ms. Thompson said. “Auditory deficits might increase risk of reinjury if sports are being played in loud, noisy gymnasiums or crowded soccer fields. So this is important to consider with return-to-play strategies.” She added, “There is hope. Auditory processing is a malleable skill, and it can be a useful target for rehabilitation and recovery.”
Ms. Thompson had no relevant financial disclosures. The study was supported by the Knowles Hearing Center.
CHICAGO – Children who experience concussion can develop deficits in auditory processing that could impair long-term academic performance and carry implications for return-to-play strategies, according to a study.
Investigators assessed 40 children aged 8-15 years, half of whom experienced concussion. The postconcussion group of 20 children had slower and smaller neural responses to speech, compared with 20 control children, on the noninvasive frequency-following response measure.
“The ability to hear in noise following concussion is impaired in the pediatric population, based on our results, which suggests it might pose additional challenges for classroom learning,” Ms. Thompson said. The study also suggests that auditory function should be considered part of acute and long-term assessment of children post concussion.
Importantly, all participants in the study had normal hearing. “It’s important to know these are very subtle auditory deficits that only emerge if you’re looking for them,” Ms. Thompson said at the annual meeting of the American Academy of Pediatrics.
Children in the concussion group were recruited from the concussion clinic at the Ann and Robert H. Lurie Children’s Hospital of Chicago. Patients were assessed an average of 27 days post injury, with most still symptomatic. The children in the control group had been treated for musculoskeletal injuries. The concussed and control groups were matched for sex and gender.
“We think that these results have implications beyond the classroom,” Ms. Thompson said. “Auditory deficits might increase risk of reinjury if sports are being played in loud, noisy gymnasiums or crowded soccer fields. So this is important to consider with return-to-play strategies.” She added, “There is hope. Auditory processing is a malleable skill, and it can be a useful target for rehabilitation and recovery.”
Ms. Thompson had no relevant financial disclosures. The study was supported by the Knowles Hearing Center.
CHICAGO – Children who experience concussion can develop deficits in auditory processing that could impair long-term academic performance and carry implications for return-to-play strategies, according to a study.
Investigators assessed 40 children aged 8-15 years, half of whom experienced concussion. The postconcussion group of 20 children had slower and smaller neural responses to speech, compared with 20 control children, on the noninvasive frequency-following response measure.
“The ability to hear in noise following concussion is impaired in the pediatric population, based on our results, which suggests it might pose additional challenges for classroom learning,” Ms. Thompson said. The study also suggests that auditory function should be considered part of acute and long-term assessment of children post concussion.
Importantly, all participants in the study had normal hearing. “It’s important to know these are very subtle auditory deficits that only emerge if you’re looking for them,” Ms. Thompson said at the annual meeting of the American Academy of Pediatrics.
Children in the concussion group were recruited from the concussion clinic at the Ann and Robert H. Lurie Children’s Hospital of Chicago. Patients were assessed an average of 27 days post injury, with most still symptomatic. The children in the control group had been treated for musculoskeletal injuries. The concussed and control groups were matched for sex and gender.
“We think that these results have implications beyond the classroom,” Ms. Thompson said. “Auditory deficits might increase risk of reinjury if sports are being played in loud, noisy gymnasiums or crowded soccer fields. So this is important to consider with return-to-play strategies.” She added, “There is hope. Auditory processing is a malleable skill, and it can be a useful target for rehabilitation and recovery.”
Ms. Thompson had no relevant financial disclosures. The study was supported by the Knowles Hearing Center.
AT AAP 2017
Key clinical point:
Major finding: Children with concussion symptoms performed significantly poorer on the Hearing in Noise Test, compared with nonconcussed peers (P = .001).
Data source: Study of 40 children in a sports medicine tertiary clinic: half experienced concussion and half served as controls.
Disclosures: Ms. Thompson had no relevant financial disclosures. The study was supported by the Knowles Hearing Center.
Tattooing and piercing are no longer taboo, but health concerns persist
Educate adolescents about the potential medical complications and social consequences of tattooing and body piercing as their popularity rises, an American Academy of Pediatrics clinical report recommends.
The most common complications post tattooing are bacterial and viral infections, and inflammation at the site of the tattoo. Rarely, more serious complications can arise in the form of endocarditis, gangrene, and amputations. Postprocedure care is important in preventing most complications: “Reputable tattoo parlors and piercing salons should provide a long list of do’s and don’ts on how to care for the area that was worked on, and what signs might indicate a problem,” Cora C. Breuner, MD, chairperson of the AAP Committee on Adolescence and coauthor of the report, said in a press statement. The clinical report was presented at the AAP annual meeting in Chicago and simultaneously published in the journal Pediatrics (2017 Sep 18. doi: 10.1542/peds.2017-1962).
Data concerning adolescent tattooing and piercing vary by source and age, but there is a distinct trend of adolescents getting or having an interest in body modification. In samples of adolescents attending clinics at ages 12-22 years, 10%-23% had tattoos and 27%-42% had body piercing (other than the earlobe); rates were higher among girls vs. boys and among older vs. young adolescents. “Of students with current piercings, high-ear cartilage (53%) was the most common visible piercing, followed by navel (38%), tongue (13%), and nipple and genital (9%) piercings” according to the report.
A concern that many adolescents and young adults may not consider is how tattoos affect society’s perception of tattooed and pierced people. A 2008 study found that 29% of people surveyed thought tattooed people were more likely to engage in deviant behavior; this belief had decreased to 24% by 2012 , according to a Harris Poll.
While society at large may appear more accepting of tattooed individuals, employers may be less open to hiring them. According to an executive career coach, “37% of human resource managers cite tattoos as the third physical attribute likely to limit career potential” with non-ear piercings in the top two barriers to career advancement (Am J Nurs. 2012;112[5]:15). In a 2014 survey of 2,675 people, 76% thought that tattoos and/or piercings had hurt their chances of getting a job, and 39% thought employees with tattoos and/or body piercings reflect poorly on their employers. Also, 42% of those surveyed felt visible tattoos are inappropriate at work, with 55% felt the same about body piercings.
“In most cases, teens just enjoy the look of the tattoo or piercing, but we do advise them to talk any decision over with their parents or another adult first,” David Levine, MD, coauthor of the AAP report, said in a press statement. “They may not realize how expensive it is to remove a tattoo, or how a piercing on your tongue might result in a chipped tooth.”
Laser removal of tattoos can range from $49 to $300 per square inch of treatment area, according to the report.
Some tips from the report
- You should advise adolescent patients to assess sanitary and hygienic practices of the tattoo parlors and tattoo artists, including: “use of new, disposable gloves; removal of the new needle and equipment from a sealed, sterile container; and the use of fresh, unused ink poured into a new, disposable container with each new client.”
- You should advise adolescents with tattoos to come to the office if there are signs and symptoms of infection .
- Lesions that appear to grow and/or change within a tattoo suggest a neoplasm.
- You should familiarize yourself with local laws and regulations related to tattooing so you can inform patients and parents.
- Counsel adolescents about the implications of visible tattoos on jobs.
- Use antibiotic agents with good coverage against Pseudomonas and Staphylococcus species (such as fluoroquinolones) to treat piercing-associated infections of the auricular cartilage.
- Recommend removing all jewelry during contact sports. If jewelry interferes with mouth guards or protective equipment, it should be removed before play. Have patients remove nipple jewelry prior to breastfeeding.
The authors have no relevant financial disclosures.
Educate adolescents about the potential medical complications and social consequences of tattooing and body piercing as their popularity rises, an American Academy of Pediatrics clinical report recommends.
The most common complications post tattooing are bacterial and viral infections, and inflammation at the site of the tattoo. Rarely, more serious complications can arise in the form of endocarditis, gangrene, and amputations. Postprocedure care is important in preventing most complications: “Reputable tattoo parlors and piercing salons should provide a long list of do’s and don’ts on how to care for the area that was worked on, and what signs might indicate a problem,” Cora C. Breuner, MD, chairperson of the AAP Committee on Adolescence and coauthor of the report, said in a press statement. The clinical report was presented at the AAP annual meeting in Chicago and simultaneously published in the journal Pediatrics (2017 Sep 18. doi: 10.1542/peds.2017-1962).
Data concerning adolescent tattooing and piercing vary by source and age, but there is a distinct trend of adolescents getting or having an interest in body modification. In samples of adolescents attending clinics at ages 12-22 years, 10%-23% had tattoos and 27%-42% had body piercing (other than the earlobe); rates were higher among girls vs. boys and among older vs. young adolescents. “Of students with current piercings, high-ear cartilage (53%) was the most common visible piercing, followed by navel (38%), tongue (13%), and nipple and genital (9%) piercings” according to the report.
A concern that many adolescents and young adults may not consider is how tattoos affect society’s perception of tattooed and pierced people. A 2008 study found that 29% of people surveyed thought tattooed people were more likely to engage in deviant behavior; this belief had decreased to 24% by 2012 , according to a Harris Poll.
While society at large may appear more accepting of tattooed individuals, employers may be less open to hiring them. According to an executive career coach, “37% of human resource managers cite tattoos as the third physical attribute likely to limit career potential” with non-ear piercings in the top two barriers to career advancement (Am J Nurs. 2012;112[5]:15). In a 2014 survey of 2,675 people, 76% thought that tattoos and/or piercings had hurt their chances of getting a job, and 39% thought employees with tattoos and/or body piercings reflect poorly on their employers. Also, 42% of those surveyed felt visible tattoos are inappropriate at work, with 55% felt the same about body piercings.
“In most cases, teens just enjoy the look of the tattoo or piercing, but we do advise them to talk any decision over with their parents or another adult first,” David Levine, MD, coauthor of the AAP report, said in a press statement. “They may not realize how expensive it is to remove a tattoo, or how a piercing on your tongue might result in a chipped tooth.”
Laser removal of tattoos can range from $49 to $300 per square inch of treatment area, according to the report.
Some tips from the report
- You should advise adolescent patients to assess sanitary and hygienic practices of the tattoo parlors and tattoo artists, including: “use of new, disposable gloves; removal of the new needle and equipment from a sealed, sterile container; and the use of fresh, unused ink poured into a new, disposable container with each new client.”
- You should advise adolescents with tattoos to come to the office if there are signs and symptoms of infection .
- Lesions that appear to grow and/or change within a tattoo suggest a neoplasm.
- You should familiarize yourself with local laws and regulations related to tattooing so you can inform patients and parents.
- Counsel adolescents about the implications of visible tattoos on jobs.
- Use antibiotic agents with good coverage against Pseudomonas and Staphylococcus species (such as fluoroquinolones) to treat piercing-associated infections of the auricular cartilage.
- Recommend removing all jewelry during contact sports. If jewelry interferes with mouth guards or protective equipment, it should be removed before play. Have patients remove nipple jewelry prior to breastfeeding.
The authors have no relevant financial disclosures.
Educate adolescents about the potential medical complications and social consequences of tattooing and body piercing as their popularity rises, an American Academy of Pediatrics clinical report recommends.
The most common complications post tattooing are bacterial and viral infections, and inflammation at the site of the tattoo. Rarely, more serious complications can arise in the form of endocarditis, gangrene, and amputations. Postprocedure care is important in preventing most complications: “Reputable tattoo parlors and piercing salons should provide a long list of do’s and don’ts on how to care for the area that was worked on, and what signs might indicate a problem,” Cora C. Breuner, MD, chairperson of the AAP Committee on Adolescence and coauthor of the report, said in a press statement. The clinical report was presented at the AAP annual meeting in Chicago and simultaneously published in the journal Pediatrics (2017 Sep 18. doi: 10.1542/peds.2017-1962).
Data concerning adolescent tattooing and piercing vary by source and age, but there is a distinct trend of adolescents getting or having an interest in body modification. In samples of adolescents attending clinics at ages 12-22 years, 10%-23% had tattoos and 27%-42% had body piercing (other than the earlobe); rates were higher among girls vs. boys and among older vs. young adolescents. “Of students with current piercings, high-ear cartilage (53%) was the most common visible piercing, followed by navel (38%), tongue (13%), and nipple and genital (9%) piercings” according to the report.
A concern that many adolescents and young adults may not consider is how tattoos affect society’s perception of tattooed and pierced people. A 2008 study found that 29% of people surveyed thought tattooed people were more likely to engage in deviant behavior; this belief had decreased to 24% by 2012 , according to a Harris Poll.
While society at large may appear more accepting of tattooed individuals, employers may be less open to hiring them. According to an executive career coach, “37% of human resource managers cite tattoos as the third physical attribute likely to limit career potential” with non-ear piercings in the top two barriers to career advancement (Am J Nurs. 2012;112[5]:15). In a 2014 survey of 2,675 people, 76% thought that tattoos and/or piercings had hurt their chances of getting a job, and 39% thought employees with tattoos and/or body piercings reflect poorly on their employers. Also, 42% of those surveyed felt visible tattoos are inappropriate at work, with 55% felt the same about body piercings.
“In most cases, teens just enjoy the look of the tattoo or piercing, but we do advise them to talk any decision over with their parents or another adult first,” David Levine, MD, coauthor of the AAP report, said in a press statement. “They may not realize how expensive it is to remove a tattoo, or how a piercing on your tongue might result in a chipped tooth.”
Laser removal of tattoos can range from $49 to $300 per square inch of treatment area, according to the report.
Some tips from the report
- You should advise adolescent patients to assess sanitary and hygienic practices of the tattoo parlors and tattoo artists, including: “use of new, disposable gloves; removal of the new needle and equipment from a sealed, sterile container; and the use of fresh, unused ink poured into a new, disposable container with each new client.”
- You should advise adolescents with tattoos to come to the office if there are signs and symptoms of infection .
- Lesions that appear to grow and/or change within a tattoo suggest a neoplasm.
- You should familiarize yourself with local laws and regulations related to tattooing so you can inform patients and parents.
- Counsel adolescents about the implications of visible tattoos on jobs.
- Use antibiotic agents with good coverage against Pseudomonas and Staphylococcus species (such as fluoroquinolones) to treat piercing-associated infections of the auricular cartilage.
- Recommend removing all jewelry during contact sports. If jewelry interferes with mouth guards or protective equipment, it should be removed before play. Have patients remove nipple jewelry prior to breastfeeding.
The authors have no relevant financial disclosures.
FROM AAP 2017
How can pediatricians help prevent preschool expulsions?
CHICAGO –
Young African American boys are particularly at risk, said Claire Lerner, a senior parenting specialist with the nonprofit organization Zero to Three in Washington.
Speaking at the annual meeting of the American Academy of Pediatrics, Ms. Lerner cited data from 2005 showing that 10.4% of prekindergarten (preK) teachers had expelled at least one child for behavior problems during the previous year, yielding a preK expulsion rate of 6.7 per 1,000 students. This contrasts with a K-12 expulsion rate of 2.1 per 1,000 students.
“What I would say to you is that if a parent, or school, or caregiver comes to you and says, ‘The teacher’s concerned about X,’ don’t dismiss it. I cannot tell you how many times parents have come to me and said, ‘Well, the pediatrician says he’s totally fine. He’s just two.’”
This is not to blame pediatricians, said Ms. Lerner. Rather, “it’s to help you remember that teachers are smart, and they’re with these kids in a natural environment all day long. ...You are seeing such a random, finite, artificial experience in that room that you don’t see what’s going on in the classroom.” The child’s interactions with other children -- usually the impetus for disciplinary action -- will not necessarily be apparent in the pediatrician’s office.
Often, said Ms. Lerner, the child in question isn’t picking up on verbal and physical clues from other children, leading to behavior that’s seen as inappropriate or aggressive by other children -- and by staff. “A lot of these kids have motor planning problems, meaning they don’t know how to take their idea and execute it, so they’re the ones who are knocking down towers, and in kids’ faces. ...Those are the things that I’m talking about that are very unlikely to be picked up in a pediatric well-child visit,” she said.
“The evidence tells us that gender and race matter” in preschool suspensions and expulsions, said Ms. Lerner, noting that black preschool children are 3.6 times as likely as white children to be given an out-of-school suspension.
Black boys, she said, are 19% of male preschool attendees but make up 45% of the preschool children who receive out-of-school suspensions. Black girls make up 20% of female preschool attendees, but 54% of preschool girls who receive out-of-school suspensions are black.
In public preschools, 78% of those suspended are boys, though they make up just 54% of the attendees.
Aside from the home and work disruption caused by these suspensions, Ms. Lerner said that later outcomes are much worse for young students who are expelled or suspended, stacking the deck further against success. Rates of dropping out of high school, grade retention, and incarceration may be up to 10 times higher for these children.
Many school-related factors, including a higher child-teacher ratio and a longer school day, are associated with higher rates of preschool expulsion. Also, teachers who report more job stress are more likely to mete out suspensions or expulsions. By contrast, the availability of behavioral consultations reduces the risk of expulsion.
Within the realistic constraints of a busy pediatric practice, what can a physician do?
At the very least, said Ms. Lerner, pay attention when a parent comes to you and says, “My child’s getting in trouble in the classroom, and I’m afraid he’s going to get kicked out.” At that point, she said, the pediatrician should get in touch with the school. An approach that can be used in communicating with the school is to say, “We’re not seeing that, but we want to learn more,” said Ms. Lerner.
Just the fact that a pediatrician or his or her team members would reach out to the teacher for collaboration helps the teacher and school or daycare center realize that the family is taking the concerns seriously, said Ms. Lerner. “I will tell you that even just that phone call changes what happens for that kid,” she said.
Facilitating appropriate behavioral and mental health evaluations allows those professionals to become part of the problem-solving team for the child, school, and family.
Physicians can also help children and families by being familiar with the Americans with Disabilities Act safeguards for children with an Individualized Education Program (IEP) or a 504 Plan and making sure that families know about these protections.
Within the larger context of the school district and the community, a pediatrician’s voice can be a powerful advocacy tool to lobby against zero tolerance policies, and for stronger prevention and outreach strategies to help avoid out-of-school suspensions and expulsions for the very young. “There are things you can do -- starting tomorrow -- that will change the course for these children,” said Ms. Lerner.
Ms. Lerner is employed by Zero to Three. She reported no conflicts of interest.
CHICAGO –
Young African American boys are particularly at risk, said Claire Lerner, a senior parenting specialist with the nonprofit organization Zero to Three in Washington.
Speaking at the annual meeting of the American Academy of Pediatrics, Ms. Lerner cited data from 2005 showing that 10.4% of prekindergarten (preK) teachers had expelled at least one child for behavior problems during the previous year, yielding a preK expulsion rate of 6.7 per 1,000 students. This contrasts with a K-12 expulsion rate of 2.1 per 1,000 students.
“What I would say to you is that if a parent, or school, or caregiver comes to you and says, ‘The teacher’s concerned about X,’ don’t dismiss it. I cannot tell you how many times parents have come to me and said, ‘Well, the pediatrician says he’s totally fine. He’s just two.’”
This is not to blame pediatricians, said Ms. Lerner. Rather, “it’s to help you remember that teachers are smart, and they’re with these kids in a natural environment all day long. ...You are seeing such a random, finite, artificial experience in that room that you don’t see what’s going on in the classroom.” The child’s interactions with other children -- usually the impetus for disciplinary action -- will not necessarily be apparent in the pediatrician’s office.
Often, said Ms. Lerner, the child in question isn’t picking up on verbal and physical clues from other children, leading to behavior that’s seen as inappropriate or aggressive by other children -- and by staff. “A lot of these kids have motor planning problems, meaning they don’t know how to take their idea and execute it, so they’re the ones who are knocking down towers, and in kids’ faces. ...Those are the things that I’m talking about that are very unlikely to be picked up in a pediatric well-child visit,” she said.
“The evidence tells us that gender and race matter” in preschool suspensions and expulsions, said Ms. Lerner, noting that black preschool children are 3.6 times as likely as white children to be given an out-of-school suspension.
Black boys, she said, are 19% of male preschool attendees but make up 45% of the preschool children who receive out-of-school suspensions. Black girls make up 20% of female preschool attendees, but 54% of preschool girls who receive out-of-school suspensions are black.
In public preschools, 78% of those suspended are boys, though they make up just 54% of the attendees.
Aside from the home and work disruption caused by these suspensions, Ms. Lerner said that later outcomes are much worse for young students who are expelled or suspended, stacking the deck further against success. Rates of dropping out of high school, grade retention, and incarceration may be up to 10 times higher for these children.
Many school-related factors, including a higher child-teacher ratio and a longer school day, are associated with higher rates of preschool expulsion. Also, teachers who report more job stress are more likely to mete out suspensions or expulsions. By contrast, the availability of behavioral consultations reduces the risk of expulsion.
Within the realistic constraints of a busy pediatric practice, what can a physician do?
At the very least, said Ms. Lerner, pay attention when a parent comes to you and says, “My child’s getting in trouble in the classroom, and I’m afraid he’s going to get kicked out.” At that point, she said, the pediatrician should get in touch with the school. An approach that can be used in communicating with the school is to say, “We’re not seeing that, but we want to learn more,” said Ms. Lerner.
Just the fact that a pediatrician or his or her team members would reach out to the teacher for collaboration helps the teacher and school or daycare center realize that the family is taking the concerns seriously, said Ms. Lerner. “I will tell you that even just that phone call changes what happens for that kid,” she said.
Facilitating appropriate behavioral and mental health evaluations allows those professionals to become part of the problem-solving team for the child, school, and family.
Physicians can also help children and families by being familiar with the Americans with Disabilities Act safeguards for children with an Individualized Education Program (IEP) or a 504 Plan and making sure that families know about these protections.
Within the larger context of the school district and the community, a pediatrician’s voice can be a powerful advocacy tool to lobby against zero tolerance policies, and for stronger prevention and outreach strategies to help avoid out-of-school suspensions and expulsions for the very young. “There are things you can do -- starting tomorrow -- that will change the course for these children,” said Ms. Lerner.
Ms. Lerner is employed by Zero to Three. She reported no conflicts of interest.
CHICAGO –
Young African American boys are particularly at risk, said Claire Lerner, a senior parenting specialist with the nonprofit organization Zero to Three in Washington.
Speaking at the annual meeting of the American Academy of Pediatrics, Ms. Lerner cited data from 2005 showing that 10.4% of prekindergarten (preK) teachers had expelled at least one child for behavior problems during the previous year, yielding a preK expulsion rate of 6.7 per 1,000 students. This contrasts with a K-12 expulsion rate of 2.1 per 1,000 students.
“What I would say to you is that if a parent, or school, or caregiver comes to you and says, ‘The teacher’s concerned about X,’ don’t dismiss it. I cannot tell you how many times parents have come to me and said, ‘Well, the pediatrician says he’s totally fine. He’s just two.’”
This is not to blame pediatricians, said Ms. Lerner. Rather, “it’s to help you remember that teachers are smart, and they’re with these kids in a natural environment all day long. ...You are seeing such a random, finite, artificial experience in that room that you don’t see what’s going on in the classroom.” The child’s interactions with other children -- usually the impetus for disciplinary action -- will not necessarily be apparent in the pediatrician’s office.
Often, said Ms. Lerner, the child in question isn’t picking up on verbal and physical clues from other children, leading to behavior that’s seen as inappropriate or aggressive by other children -- and by staff. “A lot of these kids have motor planning problems, meaning they don’t know how to take their idea and execute it, so they’re the ones who are knocking down towers, and in kids’ faces. ...Those are the things that I’m talking about that are very unlikely to be picked up in a pediatric well-child visit,” she said.
“The evidence tells us that gender and race matter” in preschool suspensions and expulsions, said Ms. Lerner, noting that black preschool children are 3.6 times as likely as white children to be given an out-of-school suspension.
Black boys, she said, are 19% of male preschool attendees but make up 45% of the preschool children who receive out-of-school suspensions. Black girls make up 20% of female preschool attendees, but 54% of preschool girls who receive out-of-school suspensions are black.
In public preschools, 78% of those suspended are boys, though they make up just 54% of the attendees.
Aside from the home and work disruption caused by these suspensions, Ms. Lerner said that later outcomes are much worse for young students who are expelled or suspended, stacking the deck further against success. Rates of dropping out of high school, grade retention, and incarceration may be up to 10 times higher for these children.
Many school-related factors, including a higher child-teacher ratio and a longer school day, are associated with higher rates of preschool expulsion. Also, teachers who report more job stress are more likely to mete out suspensions or expulsions. By contrast, the availability of behavioral consultations reduces the risk of expulsion.
Within the realistic constraints of a busy pediatric practice, what can a physician do?
At the very least, said Ms. Lerner, pay attention when a parent comes to you and says, “My child’s getting in trouble in the classroom, and I’m afraid he’s going to get kicked out.” At that point, she said, the pediatrician should get in touch with the school. An approach that can be used in communicating with the school is to say, “We’re not seeing that, but we want to learn more,” said Ms. Lerner.
Just the fact that a pediatrician or his or her team members would reach out to the teacher for collaboration helps the teacher and school or daycare center realize that the family is taking the concerns seriously, said Ms. Lerner. “I will tell you that even just that phone call changes what happens for that kid,” she said.
Facilitating appropriate behavioral and mental health evaluations allows those professionals to become part of the problem-solving team for the child, school, and family.
Physicians can also help children and families by being familiar with the Americans with Disabilities Act safeguards for children with an Individualized Education Program (IEP) or a 504 Plan and making sure that families know about these protections.
Within the larger context of the school district and the community, a pediatrician’s voice can be a powerful advocacy tool to lobby against zero tolerance policies, and for stronger prevention and outreach strategies to help avoid out-of-school suspensions and expulsions for the very young. “There are things you can do -- starting tomorrow -- that will change the course for these children,” said Ms. Lerner.
Ms. Lerner is employed by Zero to Three. She reported no conflicts of interest.
EXPERT ANALYSIS FROM AAP 2017
Soccer-playing girls 5 times more likely to return to same-day play after concussion
CHICAGO – , according to a study presented at the annual meeting of the American Academy of Pediatrics.
Records from 87 soccer players aged 7-18 years (median, 14 years) were examined in a retrospective review of patients seen over a 2-year period by a single physician at a pediatric sports medicine center. Of these, two thirds (n = 58) were girls.
The soccer players included children participating in recreational, club, and school-sponsored soccer, said senior author Shane M. Miller, MD, in an interview. All patients were assessed according to a standardized concussion protocol that involved a neurologic exam and validated concussion evaluation testing, including the ImPACT and the Sports Concussion Assessment Tool (SCAT) tests.
As soccer has grown in popularity as a youth sport, so has the number of reported concussions. “The incidence of reported concussions has increased 1,600% from 1990 to 2014,” wrote Dr. Miller and his coauthors in the abstract accompanying the presentation. Dr. Miller said that girls are 1.5 times more likely than boys to sustain a concussion while playing soccer.
While seeing the patients who were the subject of the study, Dr. Miller realized that most of the soccer players had not come out of play for evaluation after the head impact. Rather, they had continued to play, only later reporting concussion symptoms to coaches, trainers, or parents.
“The athletes may have chosen not to say anything because they didn’t want to come out of the game,” said Dr. Miller, a sports medicine physician at Texas Scottish Rite Hospital for Children, Dallas.
“I was surprised by the significant degree of difference” between male and female soccer players, said Dr. Miller. The study was not designed to get at the reason for the discrepancy, so Dr. Miller could not say with certainty whether awareness of concussion symptoms is significantly lower for female athletes, or whether the athletic culture more strongly encourages minimization of symptoms for girls than boys. In any case, he said, there is room for education of players, coaches, and families to raise awareness of the importance to recognize and report concussion, and then remove the affected athlete from play,
Dr. Miller said that future research directions include collaboration with other facilities to conduct prospective research using a concussion registry. This will allow more robust statistical analysis, and help ascertain the degree of regional variation in pediatric sports concussion management.
“Current education efforts may not be enough to help athletes, parents, and coaches identify concussion symptoms, know the guidelines for immediate removal from play, and understand the risks of returning to play after an injury. More research is needed on how to better spread this message intended to protect the health of young athletes…” Aaron Zynda, the study’s first author and clinical research coordinator at Texas Scottish Rite, said in a press release accompanying the abstract. “Concussion recognition and identification is a team effort,” he said.
Neither Mr. Zynda nor Dr. Miller had any relevant conflicts of interest.
koakes@frontlinemedcom.com
CHICAGO – , according to a study presented at the annual meeting of the American Academy of Pediatrics.
Records from 87 soccer players aged 7-18 years (median, 14 years) were examined in a retrospective review of patients seen over a 2-year period by a single physician at a pediatric sports medicine center. Of these, two thirds (n = 58) were girls.
The soccer players included children participating in recreational, club, and school-sponsored soccer, said senior author Shane M. Miller, MD, in an interview. All patients were assessed according to a standardized concussion protocol that involved a neurologic exam and validated concussion evaluation testing, including the ImPACT and the Sports Concussion Assessment Tool (SCAT) tests.
As soccer has grown in popularity as a youth sport, so has the number of reported concussions. “The incidence of reported concussions has increased 1,600% from 1990 to 2014,” wrote Dr. Miller and his coauthors in the abstract accompanying the presentation. Dr. Miller said that girls are 1.5 times more likely than boys to sustain a concussion while playing soccer.
While seeing the patients who were the subject of the study, Dr. Miller realized that most of the soccer players had not come out of play for evaluation after the head impact. Rather, they had continued to play, only later reporting concussion symptoms to coaches, trainers, or parents.
“The athletes may have chosen not to say anything because they didn’t want to come out of the game,” said Dr. Miller, a sports medicine physician at Texas Scottish Rite Hospital for Children, Dallas.
“I was surprised by the significant degree of difference” between male and female soccer players, said Dr. Miller. The study was not designed to get at the reason for the discrepancy, so Dr. Miller could not say with certainty whether awareness of concussion symptoms is significantly lower for female athletes, or whether the athletic culture more strongly encourages minimization of symptoms for girls than boys. In any case, he said, there is room for education of players, coaches, and families to raise awareness of the importance to recognize and report concussion, and then remove the affected athlete from play,
Dr. Miller said that future research directions include collaboration with other facilities to conduct prospective research using a concussion registry. This will allow more robust statistical analysis, and help ascertain the degree of regional variation in pediatric sports concussion management.
“Current education efforts may not be enough to help athletes, parents, and coaches identify concussion symptoms, know the guidelines for immediate removal from play, and understand the risks of returning to play after an injury. More research is needed on how to better spread this message intended to protect the health of young athletes…” Aaron Zynda, the study’s first author and clinical research coordinator at Texas Scottish Rite, said in a press release accompanying the abstract. “Concussion recognition and identification is a team effort,” he said.
Neither Mr. Zynda nor Dr. Miller had any relevant conflicts of interest.
koakes@frontlinemedcom.com
CHICAGO – , according to a study presented at the annual meeting of the American Academy of Pediatrics.
Records from 87 soccer players aged 7-18 years (median, 14 years) were examined in a retrospective review of patients seen over a 2-year period by a single physician at a pediatric sports medicine center. Of these, two thirds (n = 58) were girls.
The soccer players included children participating in recreational, club, and school-sponsored soccer, said senior author Shane M. Miller, MD, in an interview. All patients were assessed according to a standardized concussion protocol that involved a neurologic exam and validated concussion evaluation testing, including the ImPACT and the Sports Concussion Assessment Tool (SCAT) tests.
As soccer has grown in popularity as a youth sport, so has the number of reported concussions. “The incidence of reported concussions has increased 1,600% from 1990 to 2014,” wrote Dr. Miller and his coauthors in the abstract accompanying the presentation. Dr. Miller said that girls are 1.5 times more likely than boys to sustain a concussion while playing soccer.
While seeing the patients who were the subject of the study, Dr. Miller realized that most of the soccer players had not come out of play for evaluation after the head impact. Rather, they had continued to play, only later reporting concussion symptoms to coaches, trainers, or parents.
“The athletes may have chosen not to say anything because they didn’t want to come out of the game,” said Dr. Miller, a sports medicine physician at Texas Scottish Rite Hospital for Children, Dallas.
“I was surprised by the significant degree of difference” between male and female soccer players, said Dr. Miller. The study was not designed to get at the reason for the discrepancy, so Dr. Miller could not say with certainty whether awareness of concussion symptoms is significantly lower for female athletes, or whether the athletic culture more strongly encourages minimization of symptoms for girls than boys. In any case, he said, there is room for education of players, coaches, and families to raise awareness of the importance to recognize and report concussion, and then remove the affected athlete from play,
Dr. Miller said that future research directions include collaboration with other facilities to conduct prospective research using a concussion registry. This will allow more robust statistical analysis, and help ascertain the degree of regional variation in pediatric sports concussion management.
“Current education efforts may not be enough to help athletes, parents, and coaches identify concussion symptoms, know the guidelines for immediate removal from play, and understand the risks of returning to play after an injury. More research is needed on how to better spread this message intended to protect the health of young athletes…” Aaron Zynda, the study’s first author and clinical research coordinator at Texas Scottish Rite, said in a press release accompanying the abstract. “Concussion recognition and identification is a team effort,” he said.
Neither Mr. Zynda nor Dr. Miller had any relevant conflicts of interest.
koakes@frontlinemedcom.com
At AAP 2017
Key clinical point: Girls who played soccer were five times as likely as boys to return to play on the same day of concussion.
Major finding: Thirty of 58 girls with concussion returned to same-day play, compared with 5 of 29 boys.
Study details: Retrospective single-site study of 87 soccer players with concussion, median age 14 years.
Disclosures: None of the study authors had relevant conflicts of interest.