User login
Bone marrow transplantation for epidermolysis bullosa continues to evolve
CHICAGO – Bone marrow transplantation is evolving as a promising treatment for patients with the most severe forms of epidermolysis bullosa.
“Is this a cure? It’s not,” Dr. Jakub Tolar, MD, PhD, said at the World Congress of Pediatric Dermatology. “It is, however, a path toward understanding how we can treat this grave disorder in a systemic way.”
The University of Minnesota BMT Team has also observed a correlation between the engraftment in the blood and engraftment in the skin. “We have skin engraftment as high as 50%, which is good,” Dr. Tolar said. “The more donor cells engrafted in the skin, the more types of collagen you express.”
The clinicians have also been able to reduce the amount of chemotherapy and radiation patients require prior to transplant, for the BMT to work and skin to heal. “We were able to make it so that the last 11 patients are surviving and having benefit from the transplant, with the exception of one,” Dr. Tolar said. “How does this work? We still don’t entirely know. This is not a shot in the dark, however, this is the continuation of a very long process where we were first able to show that bone marrow transplant is an efficient stem cell therapy for leukemia, and about 20 years ago for the lysosomal enzyme deficiencies.” Their hunt for the cell that travels from the bone marrow to skin and produces type 7 collagen is continuing. “What haunts me is that BMT, which works in recessive dystrophic EB, works only in some types of junctional EB, those with alpha-3 chain deficiency of laminin 322.” he continued. “There has been no benefit to bone marrow transplantation for children with mutations of beta-3 chain of laminin 322, so we have closed enrollment for this one form of junctional EB. Survival in this group was 40%. Other types of junctional EB continue to be eligible for the study.”
Dr. Tolar recommended keratinocyte-driven or thymic epithelium cell type–driven therapy for patients with mutations of beta-3. “The deficiency of thymic function seems to be key in the inability to benefit from BMT in this form of junctional EB,” he said. “We have seen children who have engrafted, their skin got better, and then they died of infection many months after transplant. When we look at the immune profile and the thymic epithelial cells, they are both deficient – very abnormal.”
Despite current challenges, Dr. Tolar expressed optimism about the future of BMT in EB patients. “We have the same approach that we have in cancer care: deep empathy for all patients, radical international collaboration, and rapid laboratory and clinical prototyping,” he said. “It’s time to move from two-dimensional science to three-dimensional science; we need to study all aspects of EB simultaneously, from gene to cell to tissue to individual to patient population, and to understand the properties of the whole EB pathobiology that emerge at each level of biological complexity. By connecting information from these layers of disease network, we can better understand EB and create comb
Dr. Tolar reported having no financial disclosures.
CHICAGO – Bone marrow transplantation is evolving as a promising treatment for patients with the most severe forms of epidermolysis bullosa.
“Is this a cure? It’s not,” Dr. Jakub Tolar, MD, PhD, said at the World Congress of Pediatric Dermatology. “It is, however, a path toward understanding how we can treat this grave disorder in a systemic way.”
The University of Minnesota BMT Team has also observed a correlation between the engraftment in the blood and engraftment in the skin. “We have skin engraftment as high as 50%, which is good,” Dr. Tolar said. “The more donor cells engrafted in the skin, the more types of collagen you express.”
The clinicians have also been able to reduce the amount of chemotherapy and radiation patients require prior to transplant, for the BMT to work and skin to heal. “We were able to make it so that the last 11 patients are surviving and having benefit from the transplant, with the exception of one,” Dr. Tolar said. “How does this work? We still don’t entirely know. This is not a shot in the dark, however, this is the continuation of a very long process where we were first able to show that bone marrow transplant is an efficient stem cell therapy for leukemia, and about 20 years ago for the lysosomal enzyme deficiencies.” Their hunt for the cell that travels from the bone marrow to skin and produces type 7 collagen is continuing. “What haunts me is that BMT, which works in recessive dystrophic EB, works only in some types of junctional EB, those with alpha-3 chain deficiency of laminin 322.” he continued. “There has been no benefit to bone marrow transplantation for children with mutations of beta-3 chain of laminin 322, so we have closed enrollment for this one form of junctional EB. Survival in this group was 40%. Other types of junctional EB continue to be eligible for the study.”
Dr. Tolar recommended keratinocyte-driven or thymic epithelium cell type–driven therapy for patients with mutations of beta-3. “The deficiency of thymic function seems to be key in the inability to benefit from BMT in this form of junctional EB,” he said. “We have seen children who have engrafted, their skin got better, and then they died of infection many months after transplant. When we look at the immune profile and the thymic epithelial cells, they are both deficient – very abnormal.”
Despite current challenges, Dr. Tolar expressed optimism about the future of BMT in EB patients. “We have the same approach that we have in cancer care: deep empathy for all patients, radical international collaboration, and rapid laboratory and clinical prototyping,” he said. “It’s time to move from two-dimensional science to three-dimensional science; we need to study all aspects of EB simultaneously, from gene to cell to tissue to individual to patient population, and to understand the properties of the whole EB pathobiology that emerge at each level of biological complexity. By connecting information from these layers of disease network, we can better understand EB and create comb
Dr. Tolar reported having no financial disclosures.
CHICAGO – Bone marrow transplantation is evolving as a promising treatment for patients with the most severe forms of epidermolysis bullosa.
“Is this a cure? It’s not,” Dr. Jakub Tolar, MD, PhD, said at the World Congress of Pediatric Dermatology. “It is, however, a path toward understanding how we can treat this grave disorder in a systemic way.”
The University of Minnesota BMT Team has also observed a correlation between the engraftment in the blood and engraftment in the skin. “We have skin engraftment as high as 50%, which is good,” Dr. Tolar said. “The more donor cells engrafted in the skin, the more types of collagen you express.”
The clinicians have also been able to reduce the amount of chemotherapy and radiation patients require prior to transplant, for the BMT to work and skin to heal. “We were able to make it so that the last 11 patients are surviving and having benefit from the transplant, with the exception of one,” Dr. Tolar said. “How does this work? We still don’t entirely know. This is not a shot in the dark, however, this is the continuation of a very long process where we were first able to show that bone marrow transplant is an efficient stem cell therapy for leukemia, and about 20 years ago for the lysosomal enzyme deficiencies.” Their hunt for the cell that travels from the bone marrow to skin and produces type 7 collagen is continuing. “What haunts me is that BMT, which works in recessive dystrophic EB, works only in some types of junctional EB, those with alpha-3 chain deficiency of laminin 322.” he continued. “There has been no benefit to bone marrow transplantation for children with mutations of beta-3 chain of laminin 322, so we have closed enrollment for this one form of junctional EB. Survival in this group was 40%. Other types of junctional EB continue to be eligible for the study.”
Dr. Tolar recommended keratinocyte-driven or thymic epithelium cell type–driven therapy for patients with mutations of beta-3. “The deficiency of thymic function seems to be key in the inability to benefit from BMT in this form of junctional EB,” he said. “We have seen children who have engrafted, their skin got better, and then they died of infection many months after transplant. When we look at the immune profile and the thymic epithelial cells, they are both deficient – very abnormal.”
Despite current challenges, Dr. Tolar expressed optimism about the future of BMT in EB patients. “We have the same approach that we have in cancer care: deep empathy for all patients, radical international collaboration, and rapid laboratory and clinical prototyping,” he said. “It’s time to move from two-dimensional science to three-dimensional science; we need to study all aspects of EB simultaneously, from gene to cell to tissue to individual to patient population, and to understand the properties of the whole EB pathobiology that emerge at each level of biological complexity. By connecting information from these layers of disease network, we can better understand EB and create comb
Dr. Tolar reported having no financial disclosures.
AT WCPD 2017
Lasers still play a role in treatment of dermatologic conditions in children
CHICAGO – Multiple laser and light options are available to treat children with infantile hemangiomas, port wine birthmarks, and angiofibromas, according to Kristen M. Kelly, MD.
“Combination treatments with procedures and medications can improve treatment in many cases,” Dr. Kelly said at the World Congress of Pediatric Dermatology.
Dr. Kelly, professor of dermatology and surgery at the University of California, Irvine, said that the use of lasers and other light sources for infantile hemangiomas has dramatically decreased since propranolol, timolol, and other beta-blockers have become available. Most children are candidates for beta-blocker therapy, she said, but for those who are not, the pulsed dye laser (PDL) may be a good option. She also considers using the PDL for ulcerated lesions. “Of course concern comes up, because lasers can sometimes cause ulcerations, so you have to be aware of that,” she said.
“For the more proliferative phase of infantile hemangiomas, I’ll use a larger spot size: 10-12 mm, and short pulse durations: 0.45 to 1.5 milliseconds, and low energies,” Dr. Kelly said. “I would start with an energy of 5 or 5.5 J/cm2. I may creep that up a little with time, but I don’t feel that you need to use very high energies. For lesions that are starting to involute, you could consider higher energies.”
Consider the combination of PDL and propranolol for patients who have a superficial component, for ulcerated lesions, or for rapidly progressing lesions that are not responding to your treatment. “You can also use the combination of PDL and timolol,” she said. “Starting treatment can avoid the need for reconstruction later.”
Dr. Kelly then discussed her approach to treating port wine birthmarks. She almost exclusively uses the PDL and the 755-nm Alexandrite lasers for these lesions. “For some of the resistant lesions, I’ll consider some of the combined treatments, like the combined 1064/532 nm system,” she said. “If I have really young patients, I use the PDL almost exclusively. I find the Alexandrite laser useful when I have thicker lesions that have hypertrophied.”
For optimal effect, she recommends treating lesions as early as possible and increasing chromophore target by placing patients with facial lesions in the Trendelenburg position during treatment sessions. Her preferred PDL parameters are a wavelength of 585 nm or 595 nm with a pulse duration of 0.45 to 1.5 milliseconds for the vast majority of lesions. “I try to vary the pulse duration over time, so if I’m getting a great result with 0.45 milliseconds, I’ll do that a couple of times,” Dr. Kelly said. “Once I feel I’ve reached a plateau, I might change to 1.5 milliseconds, or consider doing a second pass.”
Whenever possible she uses larger spot sizes and chooses the level of energy based on the type of lesion she’s treating. “I think it’s important to look for an endpoint,” she said. “I like to see deep purpura but I don’t like to see gray, because I feel that’s where you’re going to get epidermal injury or [there is] the chance for scarring and dyspigmentation, which can be permanent in some patients.”
Patients with port wine birthmarks require 3-15 treatments or more, typically 4 weeks apart. “Some people do 2- or 3-week intervals; that’s something to consider,” Dr. Kelly said. “In a darker-skinned patient with hyperpigmentation, I will use longer intervals, especially on an extremity that may take a little longer to heal.”
Alternative treatments are being studied, including the use of lasers in combination with antiangiogenic agents. “Rapamycin has been looked at most extensively, and it’s been shown to have a significant benefit,” she said.
According to Dr. Kelly, a new device for treating port wine birthmarks is being developed that combines pulse dye laser, Nd:YAG, and radiofrequency. “The potential advantage of this is that when we use the PDL alone, we probably cannot get very deep into those vessels,” she said. “The combination of the PDL and radiofrequency may allow us to more completely coagulate these vessels and get better response.”
Dr. Kelly closed her presentation by discussing angiofibromas, disfiguring skin lesions that are associated with tuberous sclerosis and have a fairly rapid recurrence. Topical and/or oral rapamycin are treatment options, but so are laser and light sources. She cited approaches published by Roy Geronemus MD, of the Laser and Skin Surgery Center of New York, and his associates, which included PDL treatment with a 10-mm spot size delivered at 7.5 J/cm2 with a pulse duration of 1.5 ms, and dynamic cooling spray duration of 30 ms (Lasers Surg Med 2013;45:555-7). This was followed by ablative fractional resurfacing with a 15-mm spot size at 70 mJ per pulse and 40% coverage. Other treatment options for angiofibromas include pinpoint electrosurgery to papular, fibrotic lesions and topical rapamycin ointment twice a day.
Dr. Kelly disclosed having drugs or devices donated by Light Sciences Oncology, Solta Medical, Cynosure, Syneron Candela, and Novartis. She is a consultant for MundiPharma, Allergan, and Syneron Candela, and has received research funding from the American Society of Laser Medicine and Surgery, the National Institutes of Health, the Sturge-Weber Foundation, and the UC Irvine Institute of Clinical and Translational Science.
CHICAGO – Multiple laser and light options are available to treat children with infantile hemangiomas, port wine birthmarks, and angiofibromas, according to Kristen M. Kelly, MD.
“Combination treatments with procedures and medications can improve treatment in many cases,” Dr. Kelly said at the World Congress of Pediatric Dermatology.
Dr. Kelly, professor of dermatology and surgery at the University of California, Irvine, said that the use of lasers and other light sources for infantile hemangiomas has dramatically decreased since propranolol, timolol, and other beta-blockers have become available. Most children are candidates for beta-blocker therapy, she said, but for those who are not, the pulsed dye laser (PDL) may be a good option. She also considers using the PDL for ulcerated lesions. “Of course concern comes up, because lasers can sometimes cause ulcerations, so you have to be aware of that,” she said.
“For the more proliferative phase of infantile hemangiomas, I’ll use a larger spot size: 10-12 mm, and short pulse durations: 0.45 to 1.5 milliseconds, and low energies,” Dr. Kelly said. “I would start with an energy of 5 or 5.5 J/cm2. I may creep that up a little with time, but I don’t feel that you need to use very high energies. For lesions that are starting to involute, you could consider higher energies.”
Consider the combination of PDL and propranolol for patients who have a superficial component, for ulcerated lesions, or for rapidly progressing lesions that are not responding to your treatment. “You can also use the combination of PDL and timolol,” she said. “Starting treatment can avoid the need for reconstruction later.”
Dr. Kelly then discussed her approach to treating port wine birthmarks. She almost exclusively uses the PDL and the 755-nm Alexandrite lasers for these lesions. “For some of the resistant lesions, I’ll consider some of the combined treatments, like the combined 1064/532 nm system,” she said. “If I have really young patients, I use the PDL almost exclusively. I find the Alexandrite laser useful when I have thicker lesions that have hypertrophied.”
For optimal effect, she recommends treating lesions as early as possible and increasing chromophore target by placing patients with facial lesions in the Trendelenburg position during treatment sessions. Her preferred PDL parameters are a wavelength of 585 nm or 595 nm with a pulse duration of 0.45 to 1.5 milliseconds for the vast majority of lesions. “I try to vary the pulse duration over time, so if I’m getting a great result with 0.45 milliseconds, I’ll do that a couple of times,” Dr. Kelly said. “Once I feel I’ve reached a plateau, I might change to 1.5 milliseconds, or consider doing a second pass.”
Whenever possible she uses larger spot sizes and chooses the level of energy based on the type of lesion she’s treating. “I think it’s important to look for an endpoint,” she said. “I like to see deep purpura but I don’t like to see gray, because I feel that’s where you’re going to get epidermal injury or [there is] the chance for scarring and dyspigmentation, which can be permanent in some patients.”
Patients with port wine birthmarks require 3-15 treatments or more, typically 4 weeks apart. “Some people do 2- or 3-week intervals; that’s something to consider,” Dr. Kelly said. “In a darker-skinned patient with hyperpigmentation, I will use longer intervals, especially on an extremity that may take a little longer to heal.”
Alternative treatments are being studied, including the use of lasers in combination with antiangiogenic agents. “Rapamycin has been looked at most extensively, and it’s been shown to have a significant benefit,” she said.
According to Dr. Kelly, a new device for treating port wine birthmarks is being developed that combines pulse dye laser, Nd:YAG, and radiofrequency. “The potential advantage of this is that when we use the PDL alone, we probably cannot get very deep into those vessels,” she said. “The combination of the PDL and radiofrequency may allow us to more completely coagulate these vessels and get better response.”
Dr. Kelly closed her presentation by discussing angiofibromas, disfiguring skin lesions that are associated with tuberous sclerosis and have a fairly rapid recurrence. Topical and/or oral rapamycin are treatment options, but so are laser and light sources. She cited approaches published by Roy Geronemus MD, of the Laser and Skin Surgery Center of New York, and his associates, which included PDL treatment with a 10-mm spot size delivered at 7.5 J/cm2 with a pulse duration of 1.5 ms, and dynamic cooling spray duration of 30 ms (Lasers Surg Med 2013;45:555-7). This was followed by ablative fractional resurfacing with a 15-mm spot size at 70 mJ per pulse and 40% coverage. Other treatment options for angiofibromas include pinpoint electrosurgery to papular, fibrotic lesions and topical rapamycin ointment twice a day.
Dr. Kelly disclosed having drugs or devices donated by Light Sciences Oncology, Solta Medical, Cynosure, Syneron Candela, and Novartis. She is a consultant for MundiPharma, Allergan, and Syneron Candela, and has received research funding from the American Society of Laser Medicine and Surgery, the National Institutes of Health, the Sturge-Weber Foundation, and the UC Irvine Institute of Clinical and Translational Science.
CHICAGO – Multiple laser and light options are available to treat children with infantile hemangiomas, port wine birthmarks, and angiofibromas, according to Kristen M. Kelly, MD.
“Combination treatments with procedures and medications can improve treatment in many cases,” Dr. Kelly said at the World Congress of Pediatric Dermatology.
Dr. Kelly, professor of dermatology and surgery at the University of California, Irvine, said that the use of lasers and other light sources for infantile hemangiomas has dramatically decreased since propranolol, timolol, and other beta-blockers have become available. Most children are candidates for beta-blocker therapy, she said, but for those who are not, the pulsed dye laser (PDL) may be a good option. She also considers using the PDL for ulcerated lesions. “Of course concern comes up, because lasers can sometimes cause ulcerations, so you have to be aware of that,” she said.
“For the more proliferative phase of infantile hemangiomas, I’ll use a larger spot size: 10-12 mm, and short pulse durations: 0.45 to 1.5 milliseconds, and low energies,” Dr. Kelly said. “I would start with an energy of 5 or 5.5 J/cm2. I may creep that up a little with time, but I don’t feel that you need to use very high energies. For lesions that are starting to involute, you could consider higher energies.”
Consider the combination of PDL and propranolol for patients who have a superficial component, for ulcerated lesions, or for rapidly progressing lesions that are not responding to your treatment. “You can also use the combination of PDL and timolol,” she said. “Starting treatment can avoid the need for reconstruction later.”
Dr. Kelly then discussed her approach to treating port wine birthmarks. She almost exclusively uses the PDL and the 755-nm Alexandrite lasers for these lesions. “For some of the resistant lesions, I’ll consider some of the combined treatments, like the combined 1064/532 nm system,” she said. “If I have really young patients, I use the PDL almost exclusively. I find the Alexandrite laser useful when I have thicker lesions that have hypertrophied.”
For optimal effect, she recommends treating lesions as early as possible and increasing chromophore target by placing patients with facial lesions in the Trendelenburg position during treatment sessions. Her preferred PDL parameters are a wavelength of 585 nm or 595 nm with a pulse duration of 0.45 to 1.5 milliseconds for the vast majority of lesions. “I try to vary the pulse duration over time, so if I’m getting a great result with 0.45 milliseconds, I’ll do that a couple of times,” Dr. Kelly said. “Once I feel I’ve reached a plateau, I might change to 1.5 milliseconds, or consider doing a second pass.”
Whenever possible she uses larger spot sizes and chooses the level of energy based on the type of lesion she’s treating. “I think it’s important to look for an endpoint,” she said. “I like to see deep purpura but I don’t like to see gray, because I feel that’s where you’re going to get epidermal injury or [there is] the chance for scarring and dyspigmentation, which can be permanent in some patients.”
Patients with port wine birthmarks require 3-15 treatments or more, typically 4 weeks apart. “Some people do 2- or 3-week intervals; that’s something to consider,” Dr. Kelly said. “In a darker-skinned patient with hyperpigmentation, I will use longer intervals, especially on an extremity that may take a little longer to heal.”
Alternative treatments are being studied, including the use of lasers in combination with antiangiogenic agents. “Rapamycin has been looked at most extensively, and it’s been shown to have a significant benefit,” she said.
According to Dr. Kelly, a new device for treating port wine birthmarks is being developed that combines pulse dye laser, Nd:YAG, and radiofrequency. “The potential advantage of this is that when we use the PDL alone, we probably cannot get very deep into those vessels,” she said. “The combination of the PDL and radiofrequency may allow us to more completely coagulate these vessels and get better response.”
Dr. Kelly closed her presentation by discussing angiofibromas, disfiguring skin lesions that are associated with tuberous sclerosis and have a fairly rapid recurrence. Topical and/or oral rapamycin are treatment options, but so are laser and light sources. She cited approaches published by Roy Geronemus MD, of the Laser and Skin Surgery Center of New York, and his associates, which included PDL treatment with a 10-mm spot size delivered at 7.5 J/cm2 with a pulse duration of 1.5 ms, and dynamic cooling spray duration of 30 ms (Lasers Surg Med 2013;45:555-7). This was followed by ablative fractional resurfacing with a 15-mm spot size at 70 mJ per pulse and 40% coverage. Other treatment options for angiofibromas include pinpoint electrosurgery to papular, fibrotic lesions and topical rapamycin ointment twice a day.
Dr. Kelly disclosed having drugs or devices donated by Light Sciences Oncology, Solta Medical, Cynosure, Syneron Candela, and Novartis. She is a consultant for MundiPharma, Allergan, and Syneron Candela, and has received research funding from the American Society of Laser Medicine and Surgery, the National Institutes of Health, the Sturge-Weber Foundation, and the UC Irvine Institute of Clinical and Translational Science.
AT WCPD 2017
Tips for managing dermatology procedures in kids
CHICAGO – True complications in pediatric dermatologic surgery probably aren’t that frequent, but no solid data on the topic exist in the medical literature.
“An appropriate and thorough perioperative evaluation and planning may limit complications,” Harper N. Price, MD, said at the World Congress of Pediatric Dermatology.
The first step is to make the child comfortable in the office or operating room (OR) setting; this can include approaching children slowly unless you know them well. “Sit at their level, because coming up very fast and being over ... them is intimidating,” she advised. “Make sure you include the child in the conversation you’re having; it elicits more trust and belief in what’s going to happen. You want to explain what’s going to happen in a friendly manner. I think sometimes we have residents who are new to pediatrics that come in and say, ‘We’re going to cut this out,’ and the next thing you know, the child’s in tears. Describe what the procedure is going to be like in words that they can understand, and whatever you do, do not lie about what’s going to happen.”
Dr. Price also makes it a point to cover surgical trays before they’re wheeled in. “They don’t need to see needles and sharp objects,” she said. “Even afterward, bloody gauze can be scary to kids.” Positioning the patient properly also is important. “We’ll wrap young children up in a swaddle,” she said. “In my opinion, you should not be forcefully restraining an older child. They need to cooperate and it needs to be a safe procedure, otherwise, you should consider doing it in the operating room. I never enlist a parent to hold or restrain a child.”
One key to managing pain during dermatologic procedures in children comes down to anticipation: What kinds of distractions might the child need? What preoperative analgesia will be required? What postoperative pain medications should be used? “We know that certain procedures in children might be more painful, such as nail procedures, ablative laser procedures, and large excisions with extensive undermining,” Dr. Price said. “Pain is subjective and differs from child to child in the way it’s experienced, so you need to consider the child’s age, coping style, and temperament, and what their history of pain is like. We know that inadequate pain control in children has a negative impact and a negative implication on their future health care interventions, as well as their reactions to further pain.”
Parental involvement can sometimes help. “I like a parent to stay in the room if I’m doing a procedure in the office, as long as they agree to stay seated,” she said. “It may make your office staff more anxious, and it may make parents more anxious, too, so it’s something to think about.” There is some evidence that having a parent present during an in-office procedure increases parental satisfaction as well.
In an effort to minimize pain and anxiety before in-office procedures, Dr. Price and her associates at Phoenix Children’s Hospital often use instant ice packs. “They get cold really fast, they’re cheap, and you don’t have to run to a refrigerator to get ice,” she said. Other beneficial measures include topical anesthetics and breathing techniques, such as having the child blow on a pinwheel, blow bubbles, or perform diaphragmatic breathing. Using distractions – stuffed animals, picture books, or video games on a tablet – can also help. “If the child is going to the OR, using preoperative midazolam can help relax the child, especially if they’re having repeated procedures,” Dr. Price said. Oral sucrose solution in infants, especially in young infants, provides about 5-8 minutes of temporary analgesia and can be placed on their pacifier or their tongue, she added, noting that ethyl chloride spray can also be helpful prior to injections.
During the procedure itself, counter-stimulatory methods can be helpful; this can include handheld devices that use a combination of vibration, ice, and distraction methods. “Buffer your lidocaine and don’t inject cold lidocaine; that hurts a lot more,” she recommended. “Inject slowly; inject deep. If you have a painful procedure and you’re in an OR setting where you give Marcaine [bupivacaine], put that in at the end of the procedure for short-term postoperative pain relief.” After the procedure, it’s better not to apologize for causing pain or if the procedure didn’t go well. “Give positive incentives like stickers and stuffed animals, and use a dressing wrap with bright colors,” she said. “We often doctor up stuffed animals in the OR so when [the children] wake up, they have something fun to look at.”
Postoperatively, the best way to prevent pain is to recommend limited physical activity. “Children become active quickly after a procedure, and then they hurt,” Dr. Price said. “For extremity wounds, consider ice and elevation. I like bulky dressings to prevent trauma, to remind the families that they’ve had a procedure done. They can usually keep them on for several days.”
Surgical site infections are uncommon, but if they do occur, it’s usually between postoperative days 4 and 10. “The biggest indicator of an infection in my opinion is pain,” she said. “If they’re having a lot of pain, I would be concerned. Causes may be the presence of bacteria on the skin or mucosa or improper wound care at home.”
The risk factors for surgical site infections in children are not well defined in dermatologic surgery, Dr. Price added, “but we know that if you’re going to be operating in the diaper area, that’s a place where you’re going to have a high risk of infection. Preoperative hair removal – if you shave the scalp before surgery creating small nicks – could [introduce] bacteria. And it’s likely that the overall health of the patient may impact their risk of infection. You want to know the difference between normal wound healing and an infection. Culture it. If you’re worried, you may want to start empiric antibiotics. If you have a severe infection, something with necrosis, fluctuance, or dehiscence, you might want to consider partially opening that wound and letting it drain and heal in by secondary intention.”
Measures to prevent postoperative infections include perioperative counseling to restrict excessive activity to prevent trauma, bleeding, and dehiscence; use of bulky dressings, and explicit wound care instructions. “My nurse calls [the patient’s family] the day after a procedure, and I usually have them come in for a wound check, even if there are no sutures to remove, just to make sure things look OK,” she said.
Suture reactions are another potential complication of dermatologic surgery in children. The incidence is unknown, but suture reactions usually occur around 6 weeks postoperatively and tend to happen more often in older children. “Excessive reactions, while uncommon, can lead to an increased risk of dehiscence, infection, and delayed healing,” Dr. Price said. Small caliber monofilament sutures are less reactive than large caliber, multifilament sutures, she added, while synthetic and nonabsorbable sutures are less reactive than natural materials such as silk and surgical gut. Dr. Price favors using poliglecaprone, polyglactin 910, and polypropylene.
Tips for minimizing suture reactions include the following: Use the smallest caliber suture appropriate for the wound; avoid buried sutures too close to the surface of the skin; use a smaller caliber suture at the end of excisions, where there tends to be less tension; and keep knots small and flat at the apexes of excision. “Manage suture reactions with reassurance,” she said. “The nice thing is that these often heal fine without any delay. When possible, remove the offending suture material. A lot of times, I’ll use sterile forceps. At home, I’ll have [parents] massage the area with warm compresses to try to extrude the suture. But, if you wait long enough, it usually comes out.”
Dr. Price reported having no financial disclosures.
dbrunk@frontlinemedcom.com
CHICAGO – True complications in pediatric dermatologic surgery probably aren’t that frequent, but no solid data on the topic exist in the medical literature.
“An appropriate and thorough perioperative evaluation and planning may limit complications,” Harper N. Price, MD, said at the World Congress of Pediatric Dermatology.
The first step is to make the child comfortable in the office or operating room (OR) setting; this can include approaching children slowly unless you know them well. “Sit at their level, because coming up very fast and being over ... them is intimidating,” she advised. “Make sure you include the child in the conversation you’re having; it elicits more trust and belief in what’s going to happen. You want to explain what’s going to happen in a friendly manner. I think sometimes we have residents who are new to pediatrics that come in and say, ‘We’re going to cut this out,’ and the next thing you know, the child’s in tears. Describe what the procedure is going to be like in words that they can understand, and whatever you do, do not lie about what’s going to happen.”
Dr. Price also makes it a point to cover surgical trays before they’re wheeled in. “They don’t need to see needles and sharp objects,” she said. “Even afterward, bloody gauze can be scary to kids.” Positioning the patient properly also is important. “We’ll wrap young children up in a swaddle,” she said. “In my opinion, you should not be forcefully restraining an older child. They need to cooperate and it needs to be a safe procedure, otherwise, you should consider doing it in the operating room. I never enlist a parent to hold or restrain a child.”
One key to managing pain during dermatologic procedures in children comes down to anticipation: What kinds of distractions might the child need? What preoperative analgesia will be required? What postoperative pain medications should be used? “We know that certain procedures in children might be more painful, such as nail procedures, ablative laser procedures, and large excisions with extensive undermining,” Dr. Price said. “Pain is subjective and differs from child to child in the way it’s experienced, so you need to consider the child’s age, coping style, and temperament, and what their history of pain is like. We know that inadequate pain control in children has a negative impact and a negative implication on their future health care interventions, as well as their reactions to further pain.”
Parental involvement can sometimes help. “I like a parent to stay in the room if I’m doing a procedure in the office, as long as they agree to stay seated,” she said. “It may make your office staff more anxious, and it may make parents more anxious, too, so it’s something to think about.” There is some evidence that having a parent present during an in-office procedure increases parental satisfaction as well.
In an effort to minimize pain and anxiety before in-office procedures, Dr. Price and her associates at Phoenix Children’s Hospital often use instant ice packs. “They get cold really fast, they’re cheap, and you don’t have to run to a refrigerator to get ice,” she said. Other beneficial measures include topical anesthetics and breathing techniques, such as having the child blow on a pinwheel, blow bubbles, or perform diaphragmatic breathing. Using distractions – stuffed animals, picture books, or video games on a tablet – can also help. “If the child is going to the OR, using preoperative midazolam can help relax the child, especially if they’re having repeated procedures,” Dr. Price said. Oral sucrose solution in infants, especially in young infants, provides about 5-8 minutes of temporary analgesia and can be placed on their pacifier or their tongue, she added, noting that ethyl chloride spray can also be helpful prior to injections.
During the procedure itself, counter-stimulatory methods can be helpful; this can include handheld devices that use a combination of vibration, ice, and distraction methods. “Buffer your lidocaine and don’t inject cold lidocaine; that hurts a lot more,” she recommended. “Inject slowly; inject deep. If you have a painful procedure and you’re in an OR setting where you give Marcaine [bupivacaine], put that in at the end of the procedure for short-term postoperative pain relief.” After the procedure, it’s better not to apologize for causing pain or if the procedure didn’t go well. “Give positive incentives like stickers and stuffed animals, and use a dressing wrap with bright colors,” she said. “We often doctor up stuffed animals in the OR so when [the children] wake up, they have something fun to look at.”
Postoperatively, the best way to prevent pain is to recommend limited physical activity. “Children become active quickly after a procedure, and then they hurt,” Dr. Price said. “For extremity wounds, consider ice and elevation. I like bulky dressings to prevent trauma, to remind the families that they’ve had a procedure done. They can usually keep them on for several days.”
Surgical site infections are uncommon, but if they do occur, it’s usually between postoperative days 4 and 10. “The biggest indicator of an infection in my opinion is pain,” she said. “If they’re having a lot of pain, I would be concerned. Causes may be the presence of bacteria on the skin or mucosa or improper wound care at home.”
The risk factors for surgical site infections in children are not well defined in dermatologic surgery, Dr. Price added, “but we know that if you’re going to be operating in the diaper area, that’s a place where you’re going to have a high risk of infection. Preoperative hair removal – if you shave the scalp before surgery creating small nicks – could [introduce] bacteria. And it’s likely that the overall health of the patient may impact their risk of infection. You want to know the difference between normal wound healing and an infection. Culture it. If you’re worried, you may want to start empiric antibiotics. If you have a severe infection, something with necrosis, fluctuance, or dehiscence, you might want to consider partially opening that wound and letting it drain and heal in by secondary intention.”
Measures to prevent postoperative infections include perioperative counseling to restrict excessive activity to prevent trauma, bleeding, and dehiscence; use of bulky dressings, and explicit wound care instructions. “My nurse calls [the patient’s family] the day after a procedure, and I usually have them come in for a wound check, even if there are no sutures to remove, just to make sure things look OK,” she said.
Suture reactions are another potential complication of dermatologic surgery in children. The incidence is unknown, but suture reactions usually occur around 6 weeks postoperatively and tend to happen more often in older children. “Excessive reactions, while uncommon, can lead to an increased risk of dehiscence, infection, and delayed healing,” Dr. Price said. Small caliber monofilament sutures are less reactive than large caliber, multifilament sutures, she added, while synthetic and nonabsorbable sutures are less reactive than natural materials such as silk and surgical gut. Dr. Price favors using poliglecaprone, polyglactin 910, and polypropylene.
Tips for minimizing suture reactions include the following: Use the smallest caliber suture appropriate for the wound; avoid buried sutures too close to the surface of the skin; use a smaller caliber suture at the end of excisions, where there tends to be less tension; and keep knots small and flat at the apexes of excision. “Manage suture reactions with reassurance,” she said. “The nice thing is that these often heal fine without any delay. When possible, remove the offending suture material. A lot of times, I’ll use sterile forceps. At home, I’ll have [parents] massage the area with warm compresses to try to extrude the suture. But, if you wait long enough, it usually comes out.”
Dr. Price reported having no financial disclosures.
dbrunk@frontlinemedcom.com
CHICAGO – True complications in pediatric dermatologic surgery probably aren’t that frequent, but no solid data on the topic exist in the medical literature.
“An appropriate and thorough perioperative evaluation and planning may limit complications,” Harper N. Price, MD, said at the World Congress of Pediatric Dermatology.
The first step is to make the child comfortable in the office or operating room (OR) setting; this can include approaching children slowly unless you know them well. “Sit at their level, because coming up very fast and being over ... them is intimidating,” she advised. “Make sure you include the child in the conversation you’re having; it elicits more trust and belief in what’s going to happen. You want to explain what’s going to happen in a friendly manner. I think sometimes we have residents who are new to pediatrics that come in and say, ‘We’re going to cut this out,’ and the next thing you know, the child’s in tears. Describe what the procedure is going to be like in words that they can understand, and whatever you do, do not lie about what’s going to happen.”
Dr. Price also makes it a point to cover surgical trays before they’re wheeled in. “They don’t need to see needles and sharp objects,” she said. “Even afterward, bloody gauze can be scary to kids.” Positioning the patient properly also is important. “We’ll wrap young children up in a swaddle,” she said. “In my opinion, you should not be forcefully restraining an older child. They need to cooperate and it needs to be a safe procedure, otherwise, you should consider doing it in the operating room. I never enlist a parent to hold or restrain a child.”
One key to managing pain during dermatologic procedures in children comes down to anticipation: What kinds of distractions might the child need? What preoperative analgesia will be required? What postoperative pain medications should be used? “We know that certain procedures in children might be more painful, such as nail procedures, ablative laser procedures, and large excisions with extensive undermining,” Dr. Price said. “Pain is subjective and differs from child to child in the way it’s experienced, so you need to consider the child’s age, coping style, and temperament, and what their history of pain is like. We know that inadequate pain control in children has a negative impact and a negative implication on their future health care interventions, as well as their reactions to further pain.”
Parental involvement can sometimes help. “I like a parent to stay in the room if I’m doing a procedure in the office, as long as they agree to stay seated,” she said. “It may make your office staff more anxious, and it may make parents more anxious, too, so it’s something to think about.” There is some evidence that having a parent present during an in-office procedure increases parental satisfaction as well.
In an effort to minimize pain and anxiety before in-office procedures, Dr. Price and her associates at Phoenix Children’s Hospital often use instant ice packs. “They get cold really fast, they’re cheap, and you don’t have to run to a refrigerator to get ice,” she said. Other beneficial measures include topical anesthetics and breathing techniques, such as having the child blow on a pinwheel, blow bubbles, or perform diaphragmatic breathing. Using distractions – stuffed animals, picture books, or video games on a tablet – can also help. “If the child is going to the OR, using preoperative midazolam can help relax the child, especially if they’re having repeated procedures,” Dr. Price said. Oral sucrose solution in infants, especially in young infants, provides about 5-8 minutes of temporary analgesia and can be placed on their pacifier or their tongue, she added, noting that ethyl chloride spray can also be helpful prior to injections.
During the procedure itself, counter-stimulatory methods can be helpful; this can include handheld devices that use a combination of vibration, ice, and distraction methods. “Buffer your lidocaine and don’t inject cold lidocaine; that hurts a lot more,” she recommended. “Inject slowly; inject deep. If you have a painful procedure and you’re in an OR setting where you give Marcaine [bupivacaine], put that in at the end of the procedure for short-term postoperative pain relief.” After the procedure, it’s better not to apologize for causing pain or if the procedure didn’t go well. “Give positive incentives like stickers and stuffed animals, and use a dressing wrap with bright colors,” she said. “We often doctor up stuffed animals in the OR so when [the children] wake up, they have something fun to look at.”
Postoperatively, the best way to prevent pain is to recommend limited physical activity. “Children become active quickly after a procedure, and then they hurt,” Dr. Price said. “For extremity wounds, consider ice and elevation. I like bulky dressings to prevent trauma, to remind the families that they’ve had a procedure done. They can usually keep them on for several days.”
Surgical site infections are uncommon, but if they do occur, it’s usually between postoperative days 4 and 10. “The biggest indicator of an infection in my opinion is pain,” she said. “If they’re having a lot of pain, I would be concerned. Causes may be the presence of bacteria on the skin or mucosa or improper wound care at home.”
The risk factors for surgical site infections in children are not well defined in dermatologic surgery, Dr. Price added, “but we know that if you’re going to be operating in the diaper area, that’s a place where you’re going to have a high risk of infection. Preoperative hair removal – if you shave the scalp before surgery creating small nicks – could [introduce] bacteria. And it’s likely that the overall health of the patient may impact their risk of infection. You want to know the difference between normal wound healing and an infection. Culture it. If you’re worried, you may want to start empiric antibiotics. If you have a severe infection, something with necrosis, fluctuance, or dehiscence, you might want to consider partially opening that wound and letting it drain and heal in by secondary intention.”
Measures to prevent postoperative infections include perioperative counseling to restrict excessive activity to prevent trauma, bleeding, and dehiscence; use of bulky dressings, and explicit wound care instructions. “My nurse calls [the patient’s family] the day after a procedure, and I usually have them come in for a wound check, even if there are no sutures to remove, just to make sure things look OK,” she said.
Suture reactions are another potential complication of dermatologic surgery in children. The incidence is unknown, but suture reactions usually occur around 6 weeks postoperatively and tend to happen more often in older children. “Excessive reactions, while uncommon, can lead to an increased risk of dehiscence, infection, and delayed healing,” Dr. Price said. Small caliber monofilament sutures are less reactive than large caliber, multifilament sutures, she added, while synthetic and nonabsorbable sutures are less reactive than natural materials such as silk and surgical gut. Dr. Price favors using poliglecaprone, polyglactin 910, and polypropylene.
Tips for minimizing suture reactions include the following: Use the smallest caliber suture appropriate for the wound; avoid buried sutures too close to the surface of the skin; use a smaller caliber suture at the end of excisions, where there tends to be less tension; and keep knots small and flat at the apexes of excision. “Manage suture reactions with reassurance,” she said. “The nice thing is that these often heal fine without any delay. When possible, remove the offending suture material. A lot of times, I’ll use sterile forceps. At home, I’ll have [parents] massage the area with warm compresses to try to extrude the suture. But, if you wait long enough, it usually comes out.”
Dr. Price reported having no financial disclosures.
dbrunk@frontlinemedcom.com
AT WCPD 2017
Clues to drug adulteration may lie skin deep
CHICAGO – Sometimes, the skin can provide the first clues that a patient has been exposed to a drug product that has been adulterated or an over-the-counter product illegally sold in this country that contains a prescription medication, according to pediatric dermatologist Scott Norton, MD.
Speaking at the World Congress of Pediatric Dermatology, he reviewed some of the reactions associated with exposure to counterfeit drugs, contraband drugs, as well as products, misrepresented as drugs that do not include any active pharmaceutical ingredients. The worldwide market for these products is a “hugely profitable industry,” and the scope of the problem should not be underestimated, said Dr. Norton, chief of dermatology at Children’s National Health System, Washington.
It’s particularly important to have a high index of suspicion for such products given an increasingly mobile worldwide population. Today, patients and their family members who travel out of the country – and even local shopkeepers – may bring in these sorts of products from outside the United States, many of which would require a prescription in the United States.
In the United States, there have been several reports of a mysterious fixed drug eruption in patients reported to have taken Baczol, a cold and flu remedy available over the counter in El Salvador for upper respiratory infections. Two of the ingredients listed on the Baczol label are sulfamethoxazole and trimethoprim, two prescription antibiotics. After determining that two Salvadoran American children with a suspected fixed drug eruption had taken a Baczol product, Dr. Norton, with the aid of medical students, was able to find Baczol containing trimethoprim-sulfamethoxazole for sale over the counter in more than one-third of the shops visited in the greater Washington area (MMWR Morb Mortal Wkly Rep. 2013 Nov 22;62[46]:914-6). Eventually, the Food and Drug Administration issued a consumer alert regarding certain Baczol products containing these ingredients, but Dr. Norton said he is still concerned about the possibility for more grave hypersensitivity reactions to these sulfa antibiotics in the Salvadoran product.
Sometimes, said Dr. Norton, the problem lies in the lack of an expected ingredient. He and his team at Children’s National Health System helped solve a medical mystery involving a skin ailment in very premature infants with cholestasis. An interdisciplinary team was convened after the neonatal intensive care unit at the hospital saw its third infant with severe blistering and erosions in an acral, perianal, and perioral pattern that did not respond to empiric treatment for herpes simplex virus and staphylococcal infection – a pattern reminiscent of zinc deficiency dermatitis. Dietitians reported that there was a nationwide shortage of sterile injectable zinc, so total parenteral nutrition was being formulated without zinc. All three of the premature infants were receiving total parenteral nutrition and were so premature that they had insufficient zinc stores. The problem was identified and corrected (MMWR 2014 Jan. 17;63[02];35-7).
A more pervasive issue, which has global significance, pertains to counterfeit vaccines prepared with absolutely no vaccine components, often made in China or Nigeria with high-quality and sophisticated packaging, said Dr. Norton.
Keeping a lid on counterfeit drugs is challenging since there are so many potential entry points into the supply chain, Dr. Norton pointed out. Weak points include mislabeled raw ingredients, packaging, storage, transportation, repackaging, and distribution. The proliferation of online pharmacies also makes regulation more difficult.
There is some international cooperation to detect and combat drug counterfeiting and adulteration: For example, Interpol, the International Coalition of Medicines Regulatory Authorities, the Pharmaceutical Security Institute, and even the United Nations are developing cooperative strategies to combat the problem.
In the meantime, he emphasized that physicians must maintain a high index of suspicion and keep in mind that the first signs of adulterated drugs or prescription drugs available OTC may appear on the skin.
Dr. Norton reported no conflicts of interest.
koakes@frontlinemedcom.com
On Twitter @karioakes
CHICAGO – Sometimes, the skin can provide the first clues that a patient has been exposed to a drug product that has been adulterated or an over-the-counter product illegally sold in this country that contains a prescription medication, according to pediatric dermatologist Scott Norton, MD.
Speaking at the World Congress of Pediatric Dermatology, he reviewed some of the reactions associated with exposure to counterfeit drugs, contraband drugs, as well as products, misrepresented as drugs that do not include any active pharmaceutical ingredients. The worldwide market for these products is a “hugely profitable industry,” and the scope of the problem should not be underestimated, said Dr. Norton, chief of dermatology at Children’s National Health System, Washington.
It’s particularly important to have a high index of suspicion for such products given an increasingly mobile worldwide population. Today, patients and their family members who travel out of the country – and even local shopkeepers – may bring in these sorts of products from outside the United States, many of which would require a prescription in the United States.
In the United States, there have been several reports of a mysterious fixed drug eruption in patients reported to have taken Baczol, a cold and flu remedy available over the counter in El Salvador for upper respiratory infections. Two of the ingredients listed on the Baczol label are sulfamethoxazole and trimethoprim, two prescription antibiotics. After determining that two Salvadoran American children with a suspected fixed drug eruption had taken a Baczol product, Dr. Norton, with the aid of medical students, was able to find Baczol containing trimethoprim-sulfamethoxazole for sale over the counter in more than one-third of the shops visited in the greater Washington area (MMWR Morb Mortal Wkly Rep. 2013 Nov 22;62[46]:914-6). Eventually, the Food and Drug Administration issued a consumer alert regarding certain Baczol products containing these ingredients, but Dr. Norton said he is still concerned about the possibility for more grave hypersensitivity reactions to these sulfa antibiotics in the Salvadoran product.
Sometimes, said Dr. Norton, the problem lies in the lack of an expected ingredient. He and his team at Children’s National Health System helped solve a medical mystery involving a skin ailment in very premature infants with cholestasis. An interdisciplinary team was convened after the neonatal intensive care unit at the hospital saw its third infant with severe blistering and erosions in an acral, perianal, and perioral pattern that did not respond to empiric treatment for herpes simplex virus and staphylococcal infection – a pattern reminiscent of zinc deficiency dermatitis. Dietitians reported that there was a nationwide shortage of sterile injectable zinc, so total parenteral nutrition was being formulated without zinc. All three of the premature infants were receiving total parenteral nutrition and were so premature that they had insufficient zinc stores. The problem was identified and corrected (MMWR 2014 Jan. 17;63[02];35-7).
A more pervasive issue, which has global significance, pertains to counterfeit vaccines prepared with absolutely no vaccine components, often made in China or Nigeria with high-quality and sophisticated packaging, said Dr. Norton.
Keeping a lid on counterfeit drugs is challenging since there are so many potential entry points into the supply chain, Dr. Norton pointed out. Weak points include mislabeled raw ingredients, packaging, storage, transportation, repackaging, and distribution. The proliferation of online pharmacies also makes regulation more difficult.
There is some international cooperation to detect and combat drug counterfeiting and adulteration: For example, Interpol, the International Coalition of Medicines Regulatory Authorities, the Pharmaceutical Security Institute, and even the United Nations are developing cooperative strategies to combat the problem.
In the meantime, he emphasized that physicians must maintain a high index of suspicion and keep in mind that the first signs of adulterated drugs or prescription drugs available OTC may appear on the skin.
Dr. Norton reported no conflicts of interest.
koakes@frontlinemedcom.com
On Twitter @karioakes
CHICAGO – Sometimes, the skin can provide the first clues that a patient has been exposed to a drug product that has been adulterated or an over-the-counter product illegally sold in this country that contains a prescription medication, according to pediatric dermatologist Scott Norton, MD.
Speaking at the World Congress of Pediatric Dermatology, he reviewed some of the reactions associated with exposure to counterfeit drugs, contraband drugs, as well as products, misrepresented as drugs that do not include any active pharmaceutical ingredients. The worldwide market for these products is a “hugely profitable industry,” and the scope of the problem should not be underestimated, said Dr. Norton, chief of dermatology at Children’s National Health System, Washington.
It’s particularly important to have a high index of suspicion for such products given an increasingly mobile worldwide population. Today, patients and their family members who travel out of the country – and even local shopkeepers – may bring in these sorts of products from outside the United States, many of which would require a prescription in the United States.
In the United States, there have been several reports of a mysterious fixed drug eruption in patients reported to have taken Baczol, a cold and flu remedy available over the counter in El Salvador for upper respiratory infections. Two of the ingredients listed on the Baczol label are sulfamethoxazole and trimethoprim, two prescription antibiotics. After determining that two Salvadoran American children with a suspected fixed drug eruption had taken a Baczol product, Dr. Norton, with the aid of medical students, was able to find Baczol containing trimethoprim-sulfamethoxazole for sale over the counter in more than one-third of the shops visited in the greater Washington area (MMWR Morb Mortal Wkly Rep. 2013 Nov 22;62[46]:914-6). Eventually, the Food and Drug Administration issued a consumer alert regarding certain Baczol products containing these ingredients, but Dr. Norton said he is still concerned about the possibility for more grave hypersensitivity reactions to these sulfa antibiotics in the Salvadoran product.
Sometimes, said Dr. Norton, the problem lies in the lack of an expected ingredient. He and his team at Children’s National Health System helped solve a medical mystery involving a skin ailment in very premature infants with cholestasis. An interdisciplinary team was convened after the neonatal intensive care unit at the hospital saw its third infant with severe blistering and erosions in an acral, perianal, and perioral pattern that did not respond to empiric treatment for herpes simplex virus and staphylococcal infection – a pattern reminiscent of zinc deficiency dermatitis. Dietitians reported that there was a nationwide shortage of sterile injectable zinc, so total parenteral nutrition was being formulated without zinc. All three of the premature infants were receiving total parenteral nutrition and were so premature that they had insufficient zinc stores. The problem was identified and corrected (MMWR 2014 Jan. 17;63[02];35-7).
A more pervasive issue, which has global significance, pertains to counterfeit vaccines prepared with absolutely no vaccine components, often made in China or Nigeria with high-quality and sophisticated packaging, said Dr. Norton.
Keeping a lid on counterfeit drugs is challenging since there are so many potential entry points into the supply chain, Dr. Norton pointed out. Weak points include mislabeled raw ingredients, packaging, storage, transportation, repackaging, and distribution. The proliferation of online pharmacies also makes regulation more difficult.
There is some international cooperation to detect and combat drug counterfeiting and adulteration: For example, Interpol, the International Coalition of Medicines Regulatory Authorities, the Pharmaceutical Security Institute, and even the United Nations are developing cooperative strategies to combat the problem.
In the meantime, he emphasized that physicians must maintain a high index of suspicion and keep in mind that the first signs of adulterated drugs or prescription drugs available OTC may appear on the skin.
Dr. Norton reported no conflicts of interest.
koakes@frontlinemedcom.com
On Twitter @karioakes
EXPERT ANALYSIS FROM WCPD 2017
Many aspects to caring for epidermolysis bullosa patients
CHICAGO – Ask patients with recessive dystrophic epidermolysis bullosa (EB) to name their most bothersome symptom, and they’re likely to say itch, followed closely by pain, according to Jemima Mellerio, MD.
“We don’t really understand a lot about the mechanism of itch in patients with this disease, which is one of the reasons why we don’t have good treatments,” Prof. Mellerio said at the World Congress of Pediatric Dermatology.
A key resource for patients with EB and clinicians who care for them is Debra International, a network of national groups working on behalf of people with EB, which is undertaking a longterm initiative to develop clinical practice guidelines for the disorder. “This has been going on for about five years and is gathering momentum,” Prof. Mellerio said. “In the EB literature, there is very little that is good quality, evidence-based medicine.” Links to existing guidelines can be accessed DEBRA website.
She shared clinical tips for managing various aspects of EB, including pain, which was the subject of a recent 23-page clinical practice guideline (BMC Med. 2014;12:178). “It’s important to take a proper history: What kind of pain is it and when do they get it?” she commented. “Is there anything that is triggering it?” Basic treatment principles are to start with simple options like acetaminophen/NSAIDs and add in weak opiates as appropriate. Go a bit stronger if necessary, titrating to get the desired effect. “If you have specialist pain services, that can be extremely useful in some of the more complex cases,” she said.
Many EB patients are plagued by neuropathic pain that burns and stings. “For these cases, you might try tricyclic antidepressants or anticonvulsants like gabapentin and pregabalin,” she noted. Anxiolytics such as midazolam can be used to reduce anxiety during procedures, bathing, and dressings. A wide range of pain formulations exist to meet patient needs or preferences, including oral tablets or suspensions, lozenges, intranasal preparations, transdermal patches and intramuscular and intravenous injections.
Topical measures for isolated, painful wounds include ibuprofen-impregnated dressings such as Biatain Ibu and topical morphine gel. “You can get this made up by using morphine sulfate and mixing it in a hydrogel,” Prof. Mellerio said. “You apply that when you have a limited number of painful wounds, so you don’t get the systemic effects from having morphine but you get the local beneficial effects.” [This approach was described in Arch Dis Child. 2004;89:679-81.] Adding salt to a bath can also ameliorate pain for patients. She recommends adding 90g of salt to 10L bath water for a 0.9% solution, which translates into about 800g salt for a half-full tub of water.
Basic skin care is another challenge for EB patients. For those with extremely fragile skin, Prof. Mellerio recommends applying a primary layer of a soft silicone or lipidocolloid dressing under a secondary dressing layer. “There’s a whole range of soft silicone foam dressings or polymeric membrane, which is a nice soft dressing that can go over a primary dressing or directly on the skin if fragility is not a problem,” she said. “Really, it comes down to patient and carer choice as to what to use. It depends on many factors including site, exudate, pain, and dressing size. The frequency of wound changes will also vary. So, if you’ve got an infected, more heavily exuding wound, the dressing changes will be more frequent.”
Critical colonization and infection are significant problems for EB patients and are ideally managed with topical antimicrobials such as hydrogen peroxide cream, enzymatic antimicrobials, polyhexamethylene biguanide, and medical grade honey. “Topical antibiotics such as mupirocin can also be used, but there are problems with resistance if you’re using it long-term and potential for sensitization,” Prof. Mellerio said. “Other options include antimicrobial dressings such as polymeric membrane, polyhexamethylene biguanide, and silver. With silver dressings, there is the potential to absorb silver, so, if you’re a child and you have a lot of wounds on your skin, you can absorb silver at significant levels, which could be a problem.”
If patients don’t respond to topical measures, consider using oral antibiotics for 10-14 days, she said. Swab first for sensitivity and to look for Streptococcal carriage “because you can get a lot of problems like renal damage,” and use IV antibiotics only for severe infections, she said. “Best Practice Guidelines for Skin and Wound Care in Epidermolysis Bullosa,” supported by an award from the Urgo Foundation and produced by Wounds International/Wounds UK, are available.
Prof. Mellerio noted that EB can also adversely affect oral health and lead to the formation of painful blisters, scarring, microstomia, and ankyloglossia, which “can contribute to difficulties eating and speaking and make it hard to keep the teeth clean.” Analgesics can be helpful, as can an NSAID mouthwash or spray or mucoprotectants like Episil that coat the surface of lesions. “Alcohol-free chlorhexidine washes and fluoride mouth washes can help, as can high fluoride toothpaste and trying to limit the consumption of sugary foods and snacks,” she said. “You can adapt things like toothbrushes with a grip, which means that it’s a bit easier for somebody with EB to be able to keep their teeth clean.”
Keeping bones strong is also a concern, since osteopenia and osteoporosis are common in EB. “We’ve seen vertebral crush fractures in children as young as five years old,” Prof. Mellerio said. “Optimize calcium and vitamin D and mobility, which is important in helping people accrue their bone mineral density throughout life. Sometimes we have to use bisphosphonate therapies, but there isn’t a great deal in the literature to support what the best way of doing this is.”
Prof. Mellerio reported having no financial disclosures.
CHICAGO – Ask patients with recessive dystrophic epidermolysis bullosa (EB) to name their most bothersome symptom, and they’re likely to say itch, followed closely by pain, according to Jemima Mellerio, MD.
“We don’t really understand a lot about the mechanism of itch in patients with this disease, which is one of the reasons why we don’t have good treatments,” Prof. Mellerio said at the World Congress of Pediatric Dermatology.
A key resource for patients with EB and clinicians who care for them is Debra International, a network of national groups working on behalf of people with EB, which is undertaking a longterm initiative to develop clinical practice guidelines for the disorder. “This has been going on for about five years and is gathering momentum,” Prof. Mellerio said. “In the EB literature, there is very little that is good quality, evidence-based medicine.” Links to existing guidelines can be accessed DEBRA website.
She shared clinical tips for managing various aspects of EB, including pain, which was the subject of a recent 23-page clinical practice guideline (BMC Med. 2014;12:178). “It’s important to take a proper history: What kind of pain is it and when do they get it?” she commented. “Is there anything that is triggering it?” Basic treatment principles are to start with simple options like acetaminophen/NSAIDs and add in weak opiates as appropriate. Go a bit stronger if necessary, titrating to get the desired effect. “If you have specialist pain services, that can be extremely useful in some of the more complex cases,” she said.
Many EB patients are plagued by neuropathic pain that burns and stings. “For these cases, you might try tricyclic antidepressants or anticonvulsants like gabapentin and pregabalin,” she noted. Anxiolytics such as midazolam can be used to reduce anxiety during procedures, bathing, and dressings. A wide range of pain formulations exist to meet patient needs or preferences, including oral tablets or suspensions, lozenges, intranasal preparations, transdermal patches and intramuscular and intravenous injections.
Topical measures for isolated, painful wounds include ibuprofen-impregnated dressings such as Biatain Ibu and topical morphine gel. “You can get this made up by using morphine sulfate and mixing it in a hydrogel,” Prof. Mellerio said. “You apply that when you have a limited number of painful wounds, so you don’t get the systemic effects from having morphine but you get the local beneficial effects.” [This approach was described in Arch Dis Child. 2004;89:679-81.] Adding salt to a bath can also ameliorate pain for patients. She recommends adding 90g of salt to 10L bath water for a 0.9% solution, which translates into about 800g salt for a half-full tub of water.
Basic skin care is another challenge for EB patients. For those with extremely fragile skin, Prof. Mellerio recommends applying a primary layer of a soft silicone or lipidocolloid dressing under a secondary dressing layer. “There’s a whole range of soft silicone foam dressings or polymeric membrane, which is a nice soft dressing that can go over a primary dressing or directly on the skin if fragility is not a problem,” she said. “Really, it comes down to patient and carer choice as to what to use. It depends on many factors including site, exudate, pain, and dressing size. The frequency of wound changes will also vary. So, if you’ve got an infected, more heavily exuding wound, the dressing changes will be more frequent.”
Critical colonization and infection are significant problems for EB patients and are ideally managed with topical antimicrobials such as hydrogen peroxide cream, enzymatic antimicrobials, polyhexamethylene biguanide, and medical grade honey. “Topical antibiotics such as mupirocin can also be used, but there are problems with resistance if you’re using it long-term and potential for sensitization,” Prof. Mellerio said. “Other options include antimicrobial dressings such as polymeric membrane, polyhexamethylene biguanide, and silver. With silver dressings, there is the potential to absorb silver, so, if you’re a child and you have a lot of wounds on your skin, you can absorb silver at significant levels, which could be a problem.”
If patients don’t respond to topical measures, consider using oral antibiotics for 10-14 days, she said. Swab first for sensitivity and to look for Streptococcal carriage “because you can get a lot of problems like renal damage,” and use IV antibiotics only for severe infections, she said. “Best Practice Guidelines for Skin and Wound Care in Epidermolysis Bullosa,” supported by an award from the Urgo Foundation and produced by Wounds International/Wounds UK, are available.
Prof. Mellerio noted that EB can also adversely affect oral health and lead to the formation of painful blisters, scarring, microstomia, and ankyloglossia, which “can contribute to difficulties eating and speaking and make it hard to keep the teeth clean.” Analgesics can be helpful, as can an NSAID mouthwash or spray or mucoprotectants like Episil that coat the surface of lesions. “Alcohol-free chlorhexidine washes and fluoride mouth washes can help, as can high fluoride toothpaste and trying to limit the consumption of sugary foods and snacks,” she said. “You can adapt things like toothbrushes with a grip, which means that it’s a bit easier for somebody with EB to be able to keep their teeth clean.”
Keeping bones strong is also a concern, since osteopenia and osteoporosis are common in EB. “We’ve seen vertebral crush fractures in children as young as five years old,” Prof. Mellerio said. “Optimize calcium and vitamin D and mobility, which is important in helping people accrue their bone mineral density throughout life. Sometimes we have to use bisphosphonate therapies, but there isn’t a great deal in the literature to support what the best way of doing this is.”
Prof. Mellerio reported having no financial disclosures.
CHICAGO – Ask patients with recessive dystrophic epidermolysis bullosa (EB) to name their most bothersome symptom, and they’re likely to say itch, followed closely by pain, according to Jemima Mellerio, MD.
“We don’t really understand a lot about the mechanism of itch in patients with this disease, which is one of the reasons why we don’t have good treatments,” Prof. Mellerio said at the World Congress of Pediatric Dermatology.
A key resource for patients with EB and clinicians who care for them is Debra International, a network of national groups working on behalf of people with EB, which is undertaking a longterm initiative to develop clinical practice guidelines for the disorder. “This has been going on for about five years and is gathering momentum,” Prof. Mellerio said. “In the EB literature, there is very little that is good quality, evidence-based medicine.” Links to existing guidelines can be accessed DEBRA website.
She shared clinical tips for managing various aspects of EB, including pain, which was the subject of a recent 23-page clinical practice guideline (BMC Med. 2014;12:178). “It’s important to take a proper history: What kind of pain is it and when do they get it?” she commented. “Is there anything that is triggering it?” Basic treatment principles are to start with simple options like acetaminophen/NSAIDs and add in weak opiates as appropriate. Go a bit stronger if necessary, titrating to get the desired effect. “If you have specialist pain services, that can be extremely useful in some of the more complex cases,” she said.
Many EB patients are plagued by neuropathic pain that burns and stings. “For these cases, you might try tricyclic antidepressants or anticonvulsants like gabapentin and pregabalin,” she noted. Anxiolytics such as midazolam can be used to reduce anxiety during procedures, bathing, and dressings. A wide range of pain formulations exist to meet patient needs or preferences, including oral tablets or suspensions, lozenges, intranasal preparations, transdermal patches and intramuscular and intravenous injections.
Topical measures for isolated, painful wounds include ibuprofen-impregnated dressings such as Biatain Ibu and topical morphine gel. “You can get this made up by using morphine sulfate and mixing it in a hydrogel,” Prof. Mellerio said. “You apply that when you have a limited number of painful wounds, so you don’t get the systemic effects from having morphine but you get the local beneficial effects.” [This approach was described in Arch Dis Child. 2004;89:679-81.] Adding salt to a bath can also ameliorate pain for patients. She recommends adding 90g of salt to 10L bath water for a 0.9% solution, which translates into about 800g salt for a half-full tub of water.
Basic skin care is another challenge for EB patients. For those with extremely fragile skin, Prof. Mellerio recommends applying a primary layer of a soft silicone or lipidocolloid dressing under a secondary dressing layer. “There’s a whole range of soft silicone foam dressings or polymeric membrane, which is a nice soft dressing that can go over a primary dressing or directly on the skin if fragility is not a problem,” she said. “Really, it comes down to patient and carer choice as to what to use. It depends on many factors including site, exudate, pain, and dressing size. The frequency of wound changes will also vary. So, if you’ve got an infected, more heavily exuding wound, the dressing changes will be more frequent.”
Critical colonization and infection are significant problems for EB patients and are ideally managed with topical antimicrobials such as hydrogen peroxide cream, enzymatic antimicrobials, polyhexamethylene biguanide, and medical grade honey. “Topical antibiotics such as mupirocin can also be used, but there are problems with resistance if you’re using it long-term and potential for sensitization,” Prof. Mellerio said. “Other options include antimicrobial dressings such as polymeric membrane, polyhexamethylene biguanide, and silver. With silver dressings, there is the potential to absorb silver, so, if you’re a child and you have a lot of wounds on your skin, you can absorb silver at significant levels, which could be a problem.”
If patients don’t respond to topical measures, consider using oral antibiotics for 10-14 days, she said. Swab first for sensitivity and to look for Streptococcal carriage “because you can get a lot of problems like renal damage,” and use IV antibiotics only for severe infections, she said. “Best Practice Guidelines for Skin and Wound Care in Epidermolysis Bullosa,” supported by an award from the Urgo Foundation and produced by Wounds International/Wounds UK, are available.
Prof. Mellerio noted that EB can also adversely affect oral health and lead to the formation of painful blisters, scarring, microstomia, and ankyloglossia, which “can contribute to difficulties eating and speaking and make it hard to keep the teeth clean.” Analgesics can be helpful, as can an NSAID mouthwash or spray or mucoprotectants like Episil that coat the surface of lesions. “Alcohol-free chlorhexidine washes and fluoride mouth washes can help, as can high fluoride toothpaste and trying to limit the consumption of sugary foods and snacks,” she said. “You can adapt things like toothbrushes with a grip, which means that it’s a bit easier for somebody with EB to be able to keep their teeth clean.”
Keeping bones strong is also a concern, since osteopenia and osteoporosis are common in EB. “We’ve seen vertebral crush fractures in children as young as five years old,” Prof. Mellerio said. “Optimize calcium and vitamin D and mobility, which is important in helping people accrue their bone mineral density throughout life. Sometimes we have to use bisphosphonate therapies, but there isn’t a great deal in the literature to support what the best way of doing this is.”
Prof. Mellerio reported having no financial disclosures.
AT WCPD 2017
Supportive care alone linked to worse outcomes in mucocutaneous reactions
CHICAGO – , compared with other treatment modalities, a systematic review suggested.
Although rare in the pediatric population – with an incidence of approximately 1 case in 2 million – Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN) are both life-threatening mucocutaneous reactions.
Because reliable and validated data in the management of these conditions are lacking, he and his associates performed a systematic review to evaluate the effectiveness of reported treatment modalities using specific outcome measures.
“This study is unique in that it aims to not only capture more commonly employed interventions such as supportive care, surgical debridement, intravenous immunoglobulin [IVIG], and corticosteroids but also newer modalities that coincide with our improved understanding of the pathogenesis of the disease, such as the use of cyclosporine and biologics,” said Mr. Mansour, a third-year medical student at the University of Toronto.
The researchers systematically reviewed English and non-English articles using EMBASE, MEDLINE, the Cochrane Central Register of Controlled Trials, the Cochrane Database of Systematic Reviews, the Database of Abstracts of Reviews of Effects, the NHS Economic Evaluation Database, and the Health Technology Assessment Database. They excluded nonpediatric cases and those in which specific treatment modalities and outcome measures of interest were missing. In all, 302 articles were included in the study – 197 that examined mortality and 105 that examined time for arrest of progression of blistering, re-epithelialization, and length of hospital stay.
The main treatment modalities included supportive care alone, IVIG, corticosteroids, cyclosporine, surgical debridement, and biologics. The average time for arrest of progression of blistering was 8.4 days for supportive care, 4 days for IVIG, 6 days for corticosteroids, 2.5 days for cyclosporine, and 1 for infliximab. No data were available for time to arrest of progression for surgical debridement alone.
The average time for re-epithelialization was 24 days for supportive care, 18 days for surgical debridement, 8.7 days for IVIG, 12.2 days for corticosteroids, 10.6 days for cyclosporine, and 13 days for infliximab. Average length of hospital stay varied from 15.6 days for supportive care, 24.3 days for surgical debridement, 17.4 days for IVIG, 11.5 for corticosteroids, 15.5 for cyclosporine, and 26.3 for biologics.
The overall mortality was 4.6% among those who received supportive care alone, 8.3% among those who received IVIG, 4.5% among those who received corticosteroids, and 0.9% among those who received IVIG plus corticosteroids. Specifically, the rates of mortality for SJS and TEN cases treated with supportive care alone were 2% for SJS cases and 15.3% for TEN cases, respectively. The rates for other treatment modalities were 3.1% and 11% for IVIG, 1.7% and 9.3% for corticosteroids, and 0% and 2.1% for IVIG plus corticosteroids.
“While it was not surprising that mortality rates in pediatric SJS and TEN are low, the rates were slightly higher than anticipated,” Mr. Mansour said. “In addition, our data show that, although mortality is not influenced by certain therapeutic interventions in SJS patients, it may play a role in the management of the more severe disease, TEN.”
He acknowledged certain limitations of the study, including the fact that many of the data were derived from small-cohort retrospective studies and isolated case reports, giving rise to data heterogeneity and publication bias. “In addition, the mortality data we gathered may not necessarily represent patient survival, as many studies had variable follow-up duration,” he said. “Lastly, the additive effect of combination treatment and variable dosing was not captured in the present analysis, and further statistical analysis is required for re-epithelialization–based outcome measures and length of stay to ascertain significance.”
Mr. Mansour reported having no financial disclosures.
CHICAGO – , compared with other treatment modalities, a systematic review suggested.
Although rare in the pediatric population – with an incidence of approximately 1 case in 2 million – Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN) are both life-threatening mucocutaneous reactions.
Because reliable and validated data in the management of these conditions are lacking, he and his associates performed a systematic review to evaluate the effectiveness of reported treatment modalities using specific outcome measures.
“This study is unique in that it aims to not only capture more commonly employed interventions such as supportive care, surgical debridement, intravenous immunoglobulin [IVIG], and corticosteroids but also newer modalities that coincide with our improved understanding of the pathogenesis of the disease, such as the use of cyclosporine and biologics,” said Mr. Mansour, a third-year medical student at the University of Toronto.
The researchers systematically reviewed English and non-English articles using EMBASE, MEDLINE, the Cochrane Central Register of Controlled Trials, the Cochrane Database of Systematic Reviews, the Database of Abstracts of Reviews of Effects, the NHS Economic Evaluation Database, and the Health Technology Assessment Database. They excluded nonpediatric cases and those in which specific treatment modalities and outcome measures of interest were missing. In all, 302 articles were included in the study – 197 that examined mortality and 105 that examined time for arrest of progression of blistering, re-epithelialization, and length of hospital stay.
The main treatment modalities included supportive care alone, IVIG, corticosteroids, cyclosporine, surgical debridement, and biologics. The average time for arrest of progression of blistering was 8.4 days for supportive care, 4 days for IVIG, 6 days for corticosteroids, 2.5 days for cyclosporine, and 1 for infliximab. No data were available for time to arrest of progression for surgical debridement alone.
The average time for re-epithelialization was 24 days for supportive care, 18 days for surgical debridement, 8.7 days for IVIG, 12.2 days for corticosteroids, 10.6 days for cyclosporine, and 13 days for infliximab. Average length of hospital stay varied from 15.6 days for supportive care, 24.3 days for surgical debridement, 17.4 days for IVIG, 11.5 for corticosteroids, 15.5 for cyclosporine, and 26.3 for biologics.
The overall mortality was 4.6% among those who received supportive care alone, 8.3% among those who received IVIG, 4.5% among those who received corticosteroids, and 0.9% among those who received IVIG plus corticosteroids. Specifically, the rates of mortality for SJS and TEN cases treated with supportive care alone were 2% for SJS cases and 15.3% for TEN cases, respectively. The rates for other treatment modalities were 3.1% and 11% for IVIG, 1.7% and 9.3% for corticosteroids, and 0% and 2.1% for IVIG plus corticosteroids.
“While it was not surprising that mortality rates in pediatric SJS and TEN are low, the rates were slightly higher than anticipated,” Mr. Mansour said. “In addition, our data show that, although mortality is not influenced by certain therapeutic interventions in SJS patients, it may play a role in the management of the more severe disease, TEN.”
He acknowledged certain limitations of the study, including the fact that many of the data were derived from small-cohort retrospective studies and isolated case reports, giving rise to data heterogeneity and publication bias. “In addition, the mortality data we gathered may not necessarily represent patient survival, as many studies had variable follow-up duration,” he said. “Lastly, the additive effect of combination treatment and variable dosing was not captured in the present analysis, and further statistical analysis is required for re-epithelialization–based outcome measures and length of stay to ascertain significance.”
Mr. Mansour reported having no financial disclosures.
CHICAGO – , compared with other treatment modalities, a systematic review suggested.
Although rare in the pediatric population – with an incidence of approximately 1 case in 2 million – Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN) are both life-threatening mucocutaneous reactions.
Because reliable and validated data in the management of these conditions are lacking, he and his associates performed a systematic review to evaluate the effectiveness of reported treatment modalities using specific outcome measures.
“This study is unique in that it aims to not only capture more commonly employed interventions such as supportive care, surgical debridement, intravenous immunoglobulin [IVIG], and corticosteroids but also newer modalities that coincide with our improved understanding of the pathogenesis of the disease, such as the use of cyclosporine and biologics,” said Mr. Mansour, a third-year medical student at the University of Toronto.
The researchers systematically reviewed English and non-English articles using EMBASE, MEDLINE, the Cochrane Central Register of Controlled Trials, the Cochrane Database of Systematic Reviews, the Database of Abstracts of Reviews of Effects, the NHS Economic Evaluation Database, and the Health Technology Assessment Database. They excluded nonpediatric cases and those in which specific treatment modalities and outcome measures of interest were missing. In all, 302 articles were included in the study – 197 that examined mortality and 105 that examined time for arrest of progression of blistering, re-epithelialization, and length of hospital stay.
The main treatment modalities included supportive care alone, IVIG, corticosteroids, cyclosporine, surgical debridement, and biologics. The average time for arrest of progression of blistering was 8.4 days for supportive care, 4 days for IVIG, 6 days for corticosteroids, 2.5 days for cyclosporine, and 1 for infliximab. No data were available for time to arrest of progression for surgical debridement alone.
The average time for re-epithelialization was 24 days for supportive care, 18 days for surgical debridement, 8.7 days for IVIG, 12.2 days for corticosteroids, 10.6 days for cyclosporine, and 13 days for infliximab. Average length of hospital stay varied from 15.6 days for supportive care, 24.3 days for surgical debridement, 17.4 days for IVIG, 11.5 for corticosteroids, 15.5 for cyclosporine, and 26.3 for biologics.
The overall mortality was 4.6% among those who received supportive care alone, 8.3% among those who received IVIG, 4.5% among those who received corticosteroids, and 0.9% among those who received IVIG plus corticosteroids. Specifically, the rates of mortality for SJS and TEN cases treated with supportive care alone were 2% for SJS cases and 15.3% for TEN cases, respectively. The rates for other treatment modalities were 3.1% and 11% for IVIG, 1.7% and 9.3% for corticosteroids, and 0% and 2.1% for IVIG plus corticosteroids.
“While it was not surprising that mortality rates in pediatric SJS and TEN are low, the rates were slightly higher than anticipated,” Mr. Mansour said. “In addition, our data show that, although mortality is not influenced by certain therapeutic interventions in SJS patients, it may play a role in the management of the more severe disease, TEN.”
He acknowledged certain limitations of the study, including the fact that many of the data were derived from small-cohort retrospective studies and isolated case reports, giving rise to data heterogeneity and publication bias. “In addition, the mortality data we gathered may not necessarily represent patient survival, as many studies had variable follow-up duration,” he said. “Lastly, the additive effect of combination treatment and variable dosing was not captured in the present analysis, and further statistical analysis is required for re-epithelialization–based outcome measures and length of stay to ascertain significance.”
Mr. Mansour reported having no financial disclosures.
AT WCPD 2017
Key clinical point: Reliable and validated data informing the best treatment intervention for Stevens-Johnson Syndrome (SJS) and Toxic Epidermal Necrolysis (TEN) are lacking.
Major finding: The overall mortality was 4.6% among those who received supportive care alone, 8.3% among those who received IVIG, 4.5% among those who received corticosteroids, and 0.9% among those who received IVIG plus corticosteroids.
Data source: A systematic review of 302 studies that evaluated the effectiveness of reported treatment modalities for SJS/TEN using specific outcome measures.
Disclosures: Mr. Mansour reported having no financial disclosures.
Children with psoriasis face multitude of comorbidities
CHICAGO – Children with psoriasis face a multitude of potential problems and comorbidities, ranging from anxiety and depression to obesity and metabolic disease, so early and proactive identification is key.
“These children are more likely to engage in high-risk behavior such as use of alcohol, tobacco, and drugs – a trend that continues into adult ages,” Kelly M. Cordoro, MD, said at the World Congress for Pediatric Dermatology. “They also have a higher association with inflammatory bowel disease, among other conditions. Those of us who care for pediatric psoriasis patients are on the front lines of recognition of these potential comorbidities, which allow for, ideally, prevention and certainly, early intervention.”
Obesity ranks as the most well understood comorbidity of psoriasis in children. Study after study has demonstrated this association. In addition, obese children with psoriasis may also harbor components of the metabolic syndrome – hypertension, dyslipidemia, and diabetes. “They’re not as much at risk for metabolic syndrome in the absence of obesity, but there’s still a small signal,” Dr. Cordoro said. “We ask ourselves this question as clinicians: Are these pediatric patients at risk for cardiovascular and cerebrovascular disease as they get older? In other words, what is the health of a 6-year-old, obese child with severe psoriasis, who may also have other components of the metabolic syndrome, going to be like when he is 35 or 40? Are these the children who go on to have cardiovascular events as documented in adult studies of psoriasis?”
To date, several studies have identified a clear link between psoriasis and obesity, and between psoriasis and hypertension, diabetes, and dyslipidemia in certain populations. “There is a dose-response effect,” Dr. Cordoro said. “The more severe the psoriasis, the more likely the patient is to be obese, and vice versa.” In one study, researchers analyzed 409 psoriasis patients up to age 17 years in nine countries (JAMA Dermatol. 2013;149:166-76). They concluded that globally, children with psoriasis have excess adiposity and increased central adiposity regardless of psoriasis severity. The researchers used multiple measures of adiposity, not just body mass index, but also waist circumference and waist-to-height ratio. “Waist circumference and waist-to-height ratio are surrogates for central and visceral adiposity,” said Dr. Cordoro, who was involved with the study. “And central adiposity may be a more sensitive indicator of metabolic disease and cardiovascular risk than BMI [body mass index] alone.”
Another study demonstrated that high adiposity preceded psoriasis by up to 2 years in 93% of overweight or obese psoriatic children (JAMA Dermatol. 2014;150:573-4).
In a more recent analysis, researchers evaluated lipid function in 44 psoriatic children (J Invest Dermatol. 2016;136[1]:67-73). Compared with age-matched controls, children with psoriasis were found to have higher waist-to-hip ratio, higher insulin resistance, and 27% were obese. “There was no difference in fasting lipid levels but the blood profiles had atherogenic markers that are worrisome for ongoing risk for atherosclerosis, cardiovascular disease, and cerebrovascular disease,” Dr. Cordoro said.
Research among adults has demonstrated that psoriasis confers an independent risk of atherosclerosis, MI, stroke, and early cardiovascular-related mortality, the so-called “psoriatic march.” Theoretically, Dr. Cordoro said, severe psoriasis sets up a state of chronic systemic inflammation, which leads to insulin resistance, which predisposes affected individuals to endothelial dysfunction, and eventually can lead to atherosclerosis. “When atherosclerosis becomes unstable, now you’ve gone from having severe psoriasis into a situation where the chronic inflammation may have predisposed you to having a thrombotic event such as a heart attack or stroke,” she said. “Obesity replicates that same pattern. What does this all mean? Is this real or is this just a theory? We don’t know, but it’s certainly biologically plausible. It’s not been proven with long-term prospective studies, which we need.”
Dr. Cordoro went on to discuss the importance of assessing young psoriasis patients for psychiatric and emotional comorbidities, including anxiety, depression, and eating disorders. “These kids can become socially isolated, which can lead to more downstream effects: more anxiety, more depression, sometimes overeating and obesity,” she said. “It’s not only that the patient has situational anxiety or depression, the notion that ‘My skin looks terrible. I’m really depressed about it;’ it’s more than that. It turns out that the same inflammatory milieu in psoriasis lesions can be replicated in the brain inflammatory milieu in patients with depression and other psychiatric disorders. That’s fascinating to recognize that these comorbidities can be intrinsic. There’s a biological basis and not just a downstream effect.”
She advises clinicians who care for children with psoriasis to keep potential comorbidities in mind, and to make sure families understand that there can be psychiatric, emotional, and physical consequences to undertreated disease. “We do not yet know how to risk stratify these patients. At the very least, you want to identify overweight or obese children with moderate to severe disease for early intervention,” Dr. Cordoro said. “Weight loss and lifestyle interventions are the hardest goals to accomplish but are really critical. Prevention is the best strategy. We can help ourselves and help our patients by referring to obesity and nutrition experts who can not only help the child but get the entire family involved.”
In a consensus statement published online in JAMA Dermatology, a multidisciplinary panel of experts including Dr. Cordoro offer an evidence- and consensus-based approach to screening children with psoriasis, based on a review of 153 manuscripts in the medical literature. The panel recommends that all psoriasis patients 2-21 years of age should undergo annual measurements of blood pressure and BMI, and screenings for arthritis and mood disorders. “These don’t have to be formal mood disorder screens,” Dr. Cordoro said. “They can be informal questioning about anxiety and depression, like ‘How is your psoriasis impacting you? How do you feel about your psoriasis? What do you say when people ask you about your psoriasis?’ It’s also important to ask overweight patients what they’re doing to keep their weight in check. Oftentimes when you ask a question about mood or impact of disease or stigma or bullying, the child will be completely silent and either stay silent or start crying or start telling you their stories. It’s really important to ask, because it validates that their concerns are more than just about vanity but about their overall health, and that is a critical difference.”
Dr. Cordoro disclosed that she is a consultant for Pfizer and Valeant.
CHICAGO – Children with psoriasis face a multitude of potential problems and comorbidities, ranging from anxiety and depression to obesity and metabolic disease, so early and proactive identification is key.
“These children are more likely to engage in high-risk behavior such as use of alcohol, tobacco, and drugs – a trend that continues into adult ages,” Kelly M. Cordoro, MD, said at the World Congress for Pediatric Dermatology. “They also have a higher association with inflammatory bowel disease, among other conditions. Those of us who care for pediatric psoriasis patients are on the front lines of recognition of these potential comorbidities, which allow for, ideally, prevention and certainly, early intervention.”
Obesity ranks as the most well understood comorbidity of psoriasis in children. Study after study has demonstrated this association. In addition, obese children with psoriasis may also harbor components of the metabolic syndrome – hypertension, dyslipidemia, and diabetes. “They’re not as much at risk for metabolic syndrome in the absence of obesity, but there’s still a small signal,” Dr. Cordoro said. “We ask ourselves this question as clinicians: Are these pediatric patients at risk for cardiovascular and cerebrovascular disease as they get older? In other words, what is the health of a 6-year-old, obese child with severe psoriasis, who may also have other components of the metabolic syndrome, going to be like when he is 35 or 40? Are these the children who go on to have cardiovascular events as documented in adult studies of psoriasis?”
To date, several studies have identified a clear link between psoriasis and obesity, and between psoriasis and hypertension, diabetes, and dyslipidemia in certain populations. “There is a dose-response effect,” Dr. Cordoro said. “The more severe the psoriasis, the more likely the patient is to be obese, and vice versa.” In one study, researchers analyzed 409 psoriasis patients up to age 17 years in nine countries (JAMA Dermatol. 2013;149:166-76). They concluded that globally, children with psoriasis have excess adiposity and increased central adiposity regardless of psoriasis severity. The researchers used multiple measures of adiposity, not just body mass index, but also waist circumference and waist-to-height ratio. “Waist circumference and waist-to-height ratio are surrogates for central and visceral adiposity,” said Dr. Cordoro, who was involved with the study. “And central adiposity may be a more sensitive indicator of metabolic disease and cardiovascular risk than BMI [body mass index] alone.”
Another study demonstrated that high adiposity preceded psoriasis by up to 2 years in 93% of overweight or obese psoriatic children (JAMA Dermatol. 2014;150:573-4).
In a more recent analysis, researchers evaluated lipid function in 44 psoriatic children (J Invest Dermatol. 2016;136[1]:67-73). Compared with age-matched controls, children with psoriasis were found to have higher waist-to-hip ratio, higher insulin resistance, and 27% were obese. “There was no difference in fasting lipid levels but the blood profiles had atherogenic markers that are worrisome for ongoing risk for atherosclerosis, cardiovascular disease, and cerebrovascular disease,” Dr. Cordoro said.
Research among adults has demonstrated that psoriasis confers an independent risk of atherosclerosis, MI, stroke, and early cardiovascular-related mortality, the so-called “psoriatic march.” Theoretically, Dr. Cordoro said, severe psoriasis sets up a state of chronic systemic inflammation, which leads to insulin resistance, which predisposes affected individuals to endothelial dysfunction, and eventually can lead to atherosclerosis. “When atherosclerosis becomes unstable, now you’ve gone from having severe psoriasis into a situation where the chronic inflammation may have predisposed you to having a thrombotic event such as a heart attack or stroke,” she said. “Obesity replicates that same pattern. What does this all mean? Is this real or is this just a theory? We don’t know, but it’s certainly biologically plausible. It’s not been proven with long-term prospective studies, which we need.”
Dr. Cordoro went on to discuss the importance of assessing young psoriasis patients for psychiatric and emotional comorbidities, including anxiety, depression, and eating disorders. “These kids can become socially isolated, which can lead to more downstream effects: more anxiety, more depression, sometimes overeating and obesity,” she said. “It’s not only that the patient has situational anxiety or depression, the notion that ‘My skin looks terrible. I’m really depressed about it;’ it’s more than that. It turns out that the same inflammatory milieu in psoriasis lesions can be replicated in the brain inflammatory milieu in patients with depression and other psychiatric disorders. That’s fascinating to recognize that these comorbidities can be intrinsic. There’s a biological basis and not just a downstream effect.”
She advises clinicians who care for children with psoriasis to keep potential comorbidities in mind, and to make sure families understand that there can be psychiatric, emotional, and physical consequences to undertreated disease. “We do not yet know how to risk stratify these patients. At the very least, you want to identify overweight or obese children with moderate to severe disease for early intervention,” Dr. Cordoro said. “Weight loss and lifestyle interventions are the hardest goals to accomplish but are really critical. Prevention is the best strategy. We can help ourselves and help our patients by referring to obesity and nutrition experts who can not only help the child but get the entire family involved.”
In a consensus statement published online in JAMA Dermatology, a multidisciplinary panel of experts including Dr. Cordoro offer an evidence- and consensus-based approach to screening children with psoriasis, based on a review of 153 manuscripts in the medical literature. The panel recommends that all psoriasis patients 2-21 years of age should undergo annual measurements of blood pressure and BMI, and screenings for arthritis and mood disorders. “These don’t have to be formal mood disorder screens,” Dr. Cordoro said. “They can be informal questioning about anxiety and depression, like ‘How is your psoriasis impacting you? How do you feel about your psoriasis? What do you say when people ask you about your psoriasis?’ It’s also important to ask overweight patients what they’re doing to keep their weight in check. Oftentimes when you ask a question about mood or impact of disease or stigma or bullying, the child will be completely silent and either stay silent or start crying or start telling you their stories. It’s really important to ask, because it validates that their concerns are more than just about vanity but about their overall health, and that is a critical difference.”
Dr. Cordoro disclosed that she is a consultant for Pfizer and Valeant.
CHICAGO – Children with psoriasis face a multitude of potential problems and comorbidities, ranging from anxiety and depression to obesity and metabolic disease, so early and proactive identification is key.
“These children are more likely to engage in high-risk behavior such as use of alcohol, tobacco, and drugs – a trend that continues into adult ages,” Kelly M. Cordoro, MD, said at the World Congress for Pediatric Dermatology. “They also have a higher association with inflammatory bowel disease, among other conditions. Those of us who care for pediatric psoriasis patients are on the front lines of recognition of these potential comorbidities, which allow for, ideally, prevention and certainly, early intervention.”
Obesity ranks as the most well understood comorbidity of psoriasis in children. Study after study has demonstrated this association. In addition, obese children with psoriasis may also harbor components of the metabolic syndrome – hypertension, dyslipidemia, and diabetes. “They’re not as much at risk for metabolic syndrome in the absence of obesity, but there’s still a small signal,” Dr. Cordoro said. “We ask ourselves this question as clinicians: Are these pediatric patients at risk for cardiovascular and cerebrovascular disease as they get older? In other words, what is the health of a 6-year-old, obese child with severe psoriasis, who may also have other components of the metabolic syndrome, going to be like when he is 35 or 40? Are these the children who go on to have cardiovascular events as documented in adult studies of psoriasis?”
To date, several studies have identified a clear link between psoriasis and obesity, and between psoriasis and hypertension, diabetes, and dyslipidemia in certain populations. “There is a dose-response effect,” Dr. Cordoro said. “The more severe the psoriasis, the more likely the patient is to be obese, and vice versa.” In one study, researchers analyzed 409 psoriasis patients up to age 17 years in nine countries (JAMA Dermatol. 2013;149:166-76). They concluded that globally, children with psoriasis have excess adiposity and increased central adiposity regardless of psoriasis severity. The researchers used multiple measures of adiposity, not just body mass index, but also waist circumference and waist-to-height ratio. “Waist circumference and waist-to-height ratio are surrogates for central and visceral adiposity,” said Dr. Cordoro, who was involved with the study. “And central adiposity may be a more sensitive indicator of metabolic disease and cardiovascular risk than BMI [body mass index] alone.”
Another study demonstrated that high adiposity preceded psoriasis by up to 2 years in 93% of overweight or obese psoriatic children (JAMA Dermatol. 2014;150:573-4).
In a more recent analysis, researchers evaluated lipid function in 44 psoriatic children (J Invest Dermatol. 2016;136[1]:67-73). Compared with age-matched controls, children with psoriasis were found to have higher waist-to-hip ratio, higher insulin resistance, and 27% were obese. “There was no difference in fasting lipid levels but the blood profiles had atherogenic markers that are worrisome for ongoing risk for atherosclerosis, cardiovascular disease, and cerebrovascular disease,” Dr. Cordoro said.
Research among adults has demonstrated that psoriasis confers an independent risk of atherosclerosis, MI, stroke, and early cardiovascular-related mortality, the so-called “psoriatic march.” Theoretically, Dr. Cordoro said, severe psoriasis sets up a state of chronic systemic inflammation, which leads to insulin resistance, which predisposes affected individuals to endothelial dysfunction, and eventually can lead to atherosclerosis. “When atherosclerosis becomes unstable, now you’ve gone from having severe psoriasis into a situation where the chronic inflammation may have predisposed you to having a thrombotic event such as a heart attack or stroke,” she said. “Obesity replicates that same pattern. What does this all mean? Is this real or is this just a theory? We don’t know, but it’s certainly biologically plausible. It’s not been proven with long-term prospective studies, which we need.”
Dr. Cordoro went on to discuss the importance of assessing young psoriasis patients for psychiatric and emotional comorbidities, including anxiety, depression, and eating disorders. “These kids can become socially isolated, which can lead to more downstream effects: more anxiety, more depression, sometimes overeating and obesity,” she said. “It’s not only that the patient has situational anxiety or depression, the notion that ‘My skin looks terrible. I’m really depressed about it;’ it’s more than that. It turns out that the same inflammatory milieu in psoriasis lesions can be replicated in the brain inflammatory milieu in patients with depression and other psychiatric disorders. That’s fascinating to recognize that these comorbidities can be intrinsic. There’s a biological basis and not just a downstream effect.”
She advises clinicians who care for children with psoriasis to keep potential comorbidities in mind, and to make sure families understand that there can be psychiatric, emotional, and physical consequences to undertreated disease. “We do not yet know how to risk stratify these patients. At the very least, you want to identify overweight or obese children with moderate to severe disease for early intervention,” Dr. Cordoro said. “Weight loss and lifestyle interventions are the hardest goals to accomplish but are really critical. Prevention is the best strategy. We can help ourselves and help our patients by referring to obesity and nutrition experts who can not only help the child but get the entire family involved.”
In a consensus statement published online in JAMA Dermatology, a multidisciplinary panel of experts including Dr. Cordoro offer an evidence- and consensus-based approach to screening children with psoriasis, based on a review of 153 manuscripts in the medical literature. The panel recommends that all psoriasis patients 2-21 years of age should undergo annual measurements of blood pressure and BMI, and screenings for arthritis and mood disorders. “These don’t have to be formal mood disorder screens,” Dr. Cordoro said. “They can be informal questioning about anxiety and depression, like ‘How is your psoriasis impacting you? How do you feel about your psoriasis? What do you say when people ask you about your psoriasis?’ It’s also important to ask overweight patients what they’re doing to keep their weight in check. Oftentimes when you ask a question about mood or impact of disease or stigma or bullying, the child will be completely silent and either stay silent or start crying or start telling you their stories. It’s really important to ask, because it validates that their concerns are more than just about vanity but about their overall health, and that is a critical difference.”
Dr. Cordoro disclosed that she is a consultant for Pfizer and Valeant.
AT WCPD 2017
How to get through the tough talks about alopecia areata
CHICAGO – If you can’t set the temptation to hurry aside and take the time to listen, things may not go well, said Neil Prose, MD.
With the caveat that Janus kinase inhibitors show promise, Dr. Prose said that “most children who are destined to lose their hair will probably do so despite all of our best efforts.” Figuring out how to engage children and parents and frame a positive conversation about alopecia can present a real challenge, especially in the context of a busy practice, said Dr. Prose, professor of dermatology and medical director of Patterson Place Pediatric Dermatology at Duke University, Durham, N.C.
“These are very culturally-specific suggestions, but see which ones work for you,” said Dr. Prose, speaking to an international audience at the World Congress of Pediatric Dermatology.
Dr. Prose depicted two opposing images. In one, he said, the patient and you are sitting on opposite sides of the table, with the prospect of hair loss looming between them. By contrast, “imagine what it would take to be on the same side of the table, looking at the problem together,” he said.
There are many barriers that stand in the way of getting you and the patient on the same side of the issue of dealing with severe alopecia areata. The high emotional content of the discussion can be big factor, not just for the patient and family members, but also for you.
“We are often dealing with patient disappointment and, frankly, with our own sense of personal failure” when there isn’t always a good set of options, said Dr. Prose. Other specific aspects of severe pediatric alopecia areata that make the conversation difficult include the high degree of uncertainty that any particular treatment will succeed and a knowledge of how to give patients and family members hope without raising expectations unrealistically.
Coming back to the important first steps of not rushing the visit and being sure to listen, Dr. Prose said that, for him, the process begins before he enters the room, when he takes a moment to clear his mind. “It starts for me just before I open the door to the examining room. As human beings, we are infinitely distractible. It’s very hard for us to simply pay attention.”
Yet, this is vitally important, he said, because families need to be heard. Citing the oft-quoted statistic that, on average, a physician interrupts a patient in the first 17 seconds of the office visit, Dr. Prose said, “Many of us are ‘explainaholics,’ ’’ spending precious visit time talking about what the physician thinks is important.
Still, it’s important to validate parents’ concerns and to alleviate guilt. “Patients’ families sometimes feel guilty because they are so upset and worried – and it’s not cancer,” said Dr. Prose. Potential impacts on quality of life are still huge, and all parents want the best for their children, he pointed out.
One way he likes to begin a follow-up visit is simply to ask, “So, how’s everyone doing?” This opens the door to allow the child and the family to talk about what’s important to them. These may be symptom-related, but social issues also may be what’s looming largest.
In order to decipher how hair loss is affecting a particular child, Dr. Prose said he likes to say, “I need to understand how this is affecting you, so we can decide together where to go from here.” This gives the family control in setting the agenda and begins the process of bringing you to the same side of the table.
Specific prompts that can help you understand how alopecia is affecting a child can include asking about how things are going at school, what the child’s friends know about his or her alopecia, whether there is mocking or bullying occurring, and how the patient, family, and teachers are addressing the global picture.
Parents can be asked whether they are noticing changes in behavior, and it’s a good idea to check in on how parents are coping as well, said Dr. Prose.
To ensure that families feel they’re being heard, and to make sure you are understanding correctly, it’s useful to mirror what’s been said, beginning with a phrase like, “So, what you’re saying is …” Putting a name to the emotions that emerge during the visit also can be useful, using phrases like, “I can imagine that this has been disappointing,” or “It feels like everyone is very worried.”
But, said Dr. Prose, don’t forget about opportunities to praise patients and their families when they’ve come through a tough time well. This validation is important, he said.
When treatment isn’t working, a first place to start is to acknowledge that you, along with the family, wish that things were turning out differently. Then, said Dr. Prose, it can be really important to reappraise treatment goals. After taking the emotional temperature of the room, it may be appropriate to ask, “Is it time to talk about not doing any more treatments?” This question can be put within the framework that hair may or may not regrow spontaneously anyway and that new treatments are emerging that may help in future.
When giving advice or talking about difficult issues, it can be helpful to ask permission, said Dr. Prose. He likes to begin with, “Would it be okay if I ...?” Then, he said, the door can be opened to give advice about school issues, to ask about difficult treatment decisions, or even to share tips learned from other families’ coping methods.
Don’t forget, said Dr. Prose, to refer patients to high-quality information and online support resources, such as the National Alopecia Areata Foundation. The Internet is full of inaccurate and scary information, and patients and families need help with this navigation, he said.
The very last question Dr. Prose asks during a visit is “What other questions do you have?” The question is always framed exactly like this, he said, because it assumes there will be more questions, and it gives families permission to ask more. Although most of the time there aren’t any further questions, Dr. Prose said, “Do not ask the question with your hand on the doorknob!”
Dr. Prose had no relevant financial disclosures.
koakes@frontlinemedcom.com
On Twitter @karioakes
CHICAGO – If you can’t set the temptation to hurry aside and take the time to listen, things may not go well, said Neil Prose, MD.
With the caveat that Janus kinase inhibitors show promise, Dr. Prose said that “most children who are destined to lose their hair will probably do so despite all of our best efforts.” Figuring out how to engage children and parents and frame a positive conversation about alopecia can present a real challenge, especially in the context of a busy practice, said Dr. Prose, professor of dermatology and medical director of Patterson Place Pediatric Dermatology at Duke University, Durham, N.C.
“These are very culturally-specific suggestions, but see which ones work for you,” said Dr. Prose, speaking to an international audience at the World Congress of Pediatric Dermatology.
Dr. Prose depicted two opposing images. In one, he said, the patient and you are sitting on opposite sides of the table, with the prospect of hair loss looming between them. By contrast, “imagine what it would take to be on the same side of the table, looking at the problem together,” he said.
There are many barriers that stand in the way of getting you and the patient on the same side of the issue of dealing with severe alopecia areata. The high emotional content of the discussion can be big factor, not just for the patient and family members, but also for you.
“We are often dealing with patient disappointment and, frankly, with our own sense of personal failure” when there isn’t always a good set of options, said Dr. Prose. Other specific aspects of severe pediatric alopecia areata that make the conversation difficult include the high degree of uncertainty that any particular treatment will succeed and a knowledge of how to give patients and family members hope without raising expectations unrealistically.
Coming back to the important first steps of not rushing the visit and being sure to listen, Dr. Prose said that, for him, the process begins before he enters the room, when he takes a moment to clear his mind. “It starts for me just before I open the door to the examining room. As human beings, we are infinitely distractible. It’s very hard for us to simply pay attention.”
Yet, this is vitally important, he said, because families need to be heard. Citing the oft-quoted statistic that, on average, a physician interrupts a patient in the first 17 seconds of the office visit, Dr. Prose said, “Many of us are ‘explainaholics,’ ’’ spending precious visit time talking about what the physician thinks is important.
Still, it’s important to validate parents’ concerns and to alleviate guilt. “Patients’ families sometimes feel guilty because they are so upset and worried – and it’s not cancer,” said Dr. Prose. Potential impacts on quality of life are still huge, and all parents want the best for their children, he pointed out.
One way he likes to begin a follow-up visit is simply to ask, “So, how’s everyone doing?” This opens the door to allow the child and the family to talk about what’s important to them. These may be symptom-related, but social issues also may be what’s looming largest.
In order to decipher how hair loss is affecting a particular child, Dr. Prose said he likes to say, “I need to understand how this is affecting you, so we can decide together where to go from here.” This gives the family control in setting the agenda and begins the process of bringing you to the same side of the table.
Specific prompts that can help you understand how alopecia is affecting a child can include asking about how things are going at school, what the child’s friends know about his or her alopecia, whether there is mocking or bullying occurring, and how the patient, family, and teachers are addressing the global picture.
Parents can be asked whether they are noticing changes in behavior, and it’s a good idea to check in on how parents are coping as well, said Dr. Prose.
To ensure that families feel they’re being heard, and to make sure you are understanding correctly, it’s useful to mirror what’s been said, beginning with a phrase like, “So, what you’re saying is …” Putting a name to the emotions that emerge during the visit also can be useful, using phrases like, “I can imagine that this has been disappointing,” or “It feels like everyone is very worried.”
But, said Dr. Prose, don’t forget about opportunities to praise patients and their families when they’ve come through a tough time well. This validation is important, he said.
When treatment isn’t working, a first place to start is to acknowledge that you, along with the family, wish that things were turning out differently. Then, said Dr. Prose, it can be really important to reappraise treatment goals. After taking the emotional temperature of the room, it may be appropriate to ask, “Is it time to talk about not doing any more treatments?” This question can be put within the framework that hair may or may not regrow spontaneously anyway and that new treatments are emerging that may help in future.
When giving advice or talking about difficult issues, it can be helpful to ask permission, said Dr. Prose. He likes to begin with, “Would it be okay if I ...?” Then, he said, the door can be opened to give advice about school issues, to ask about difficult treatment decisions, or even to share tips learned from other families’ coping methods.
Don’t forget, said Dr. Prose, to refer patients to high-quality information and online support resources, such as the National Alopecia Areata Foundation. The Internet is full of inaccurate and scary information, and patients and families need help with this navigation, he said.
The very last question Dr. Prose asks during a visit is “What other questions do you have?” The question is always framed exactly like this, he said, because it assumes there will be more questions, and it gives families permission to ask more. Although most of the time there aren’t any further questions, Dr. Prose said, “Do not ask the question with your hand on the doorknob!”
Dr. Prose had no relevant financial disclosures.
koakes@frontlinemedcom.com
On Twitter @karioakes
CHICAGO – If you can’t set the temptation to hurry aside and take the time to listen, things may not go well, said Neil Prose, MD.
With the caveat that Janus kinase inhibitors show promise, Dr. Prose said that “most children who are destined to lose their hair will probably do so despite all of our best efforts.” Figuring out how to engage children and parents and frame a positive conversation about alopecia can present a real challenge, especially in the context of a busy practice, said Dr. Prose, professor of dermatology and medical director of Patterson Place Pediatric Dermatology at Duke University, Durham, N.C.
“These are very culturally-specific suggestions, but see which ones work for you,” said Dr. Prose, speaking to an international audience at the World Congress of Pediatric Dermatology.
Dr. Prose depicted two opposing images. In one, he said, the patient and you are sitting on opposite sides of the table, with the prospect of hair loss looming between them. By contrast, “imagine what it would take to be on the same side of the table, looking at the problem together,” he said.
There are many barriers that stand in the way of getting you and the patient on the same side of the issue of dealing with severe alopecia areata. The high emotional content of the discussion can be big factor, not just for the patient and family members, but also for you.
“We are often dealing with patient disappointment and, frankly, with our own sense of personal failure” when there isn’t always a good set of options, said Dr. Prose. Other specific aspects of severe pediatric alopecia areata that make the conversation difficult include the high degree of uncertainty that any particular treatment will succeed and a knowledge of how to give patients and family members hope without raising expectations unrealistically.
Coming back to the important first steps of not rushing the visit and being sure to listen, Dr. Prose said that, for him, the process begins before he enters the room, when he takes a moment to clear his mind. “It starts for me just before I open the door to the examining room. As human beings, we are infinitely distractible. It’s very hard for us to simply pay attention.”
Yet, this is vitally important, he said, because families need to be heard. Citing the oft-quoted statistic that, on average, a physician interrupts a patient in the first 17 seconds of the office visit, Dr. Prose said, “Many of us are ‘explainaholics,’ ’’ spending precious visit time talking about what the physician thinks is important.
Still, it’s important to validate parents’ concerns and to alleviate guilt. “Patients’ families sometimes feel guilty because they are so upset and worried – and it’s not cancer,” said Dr. Prose. Potential impacts on quality of life are still huge, and all parents want the best for their children, he pointed out.
One way he likes to begin a follow-up visit is simply to ask, “So, how’s everyone doing?” This opens the door to allow the child and the family to talk about what’s important to them. These may be symptom-related, but social issues also may be what’s looming largest.
In order to decipher how hair loss is affecting a particular child, Dr. Prose said he likes to say, “I need to understand how this is affecting you, so we can decide together where to go from here.” This gives the family control in setting the agenda and begins the process of bringing you to the same side of the table.
Specific prompts that can help you understand how alopecia is affecting a child can include asking about how things are going at school, what the child’s friends know about his or her alopecia, whether there is mocking or bullying occurring, and how the patient, family, and teachers are addressing the global picture.
Parents can be asked whether they are noticing changes in behavior, and it’s a good idea to check in on how parents are coping as well, said Dr. Prose.
To ensure that families feel they’re being heard, and to make sure you are understanding correctly, it’s useful to mirror what’s been said, beginning with a phrase like, “So, what you’re saying is …” Putting a name to the emotions that emerge during the visit also can be useful, using phrases like, “I can imagine that this has been disappointing,” or “It feels like everyone is very worried.”
But, said Dr. Prose, don’t forget about opportunities to praise patients and their families when they’ve come through a tough time well. This validation is important, he said.
When treatment isn’t working, a first place to start is to acknowledge that you, along with the family, wish that things were turning out differently. Then, said Dr. Prose, it can be really important to reappraise treatment goals. After taking the emotional temperature of the room, it may be appropriate to ask, “Is it time to talk about not doing any more treatments?” This question can be put within the framework that hair may or may not regrow spontaneously anyway and that new treatments are emerging that may help in future.
When giving advice or talking about difficult issues, it can be helpful to ask permission, said Dr. Prose. He likes to begin with, “Would it be okay if I ...?” Then, he said, the door can be opened to give advice about school issues, to ask about difficult treatment decisions, or even to share tips learned from other families’ coping methods.
Don’t forget, said Dr. Prose, to refer patients to high-quality information and online support resources, such as the National Alopecia Areata Foundation. The Internet is full of inaccurate and scary information, and patients and families need help with this navigation, he said.
The very last question Dr. Prose asks during a visit is “What other questions do you have?” The question is always framed exactly like this, he said, because it assumes there will be more questions, and it gives families permission to ask more. Although most of the time there aren’t any further questions, Dr. Prose said, “Do not ask the question with your hand on the doorknob!”
Dr. Prose had no relevant financial disclosures.
koakes@frontlinemedcom.com
On Twitter @karioakes
EXPERT ANALYSIS FROM WCPD 2017
Study spotlights pediatric dermatology workplace trends
CHICAGO – Geographic maldistribution of trained pediatric dermatologists and long wait times for new-patient appointments are two key hurdles impacting patient access to pediatric dermatology care, according to a survey of workforce trends.
“There are large areas of the country that don’t have any pediatric dermatologists, which influences how we can train dermatologists, pediatricians, and medical students who want to do pediatric dermatology,” study author Brea Prindaville, MD, said in an interview at the World Congress for Pediatric Dermatology. “We’re trying to keep an eye on how that’s going, and how we can improve not only the geographic distribution, but also the numbers that we have in the workforce.”
In a project spearheaded by the Society for Pediatric Dermatology (SPD) workforce committee, Dr. Prindaville of Children’s Mercy-Kansas City (Mo.) and her associates emailed a nine-question survey to the 484 SPD members in the United States to determine practice location, number and types of patients seen, wait times, and association with advance practice providers between November and December of 2016. In all, 146 surveys were completed, for a response rate of 30%. Of these, 75% were from board-certified pediatric dermatologists. The majority of survey respondents were practicing in and around large cities, while 60% of all respondents and 68% of board-certified respondents were practicing full-time, seeing pediatric patients exclusively. An additional 30% were practicing part-time or also seeing adults. Board-certified pediatric dermatologists saw an average of 80 pediatric patients per week.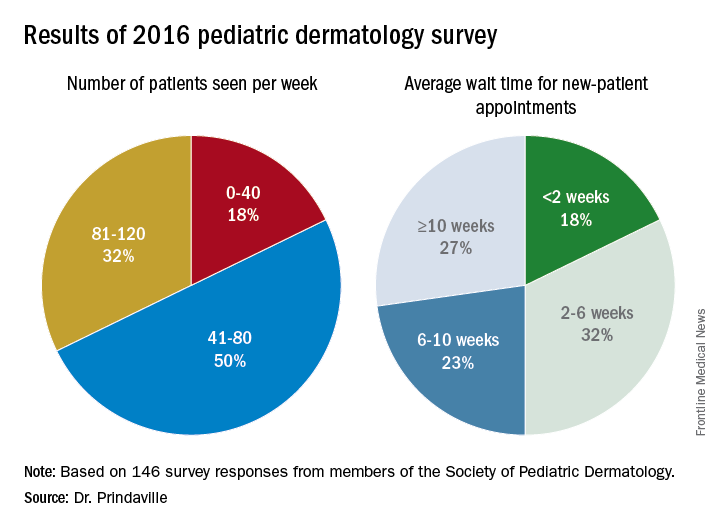
Only 10% of survey respondents did not accept Medicaid, and about 50% of patients seen by board-certified pediatric dermatologists were insured by Medicaid. In addition, about half of respondents worked with one to three advanced practice providers.
Dr. Prindaville, who helped conduct the study during her pediatric dermatology fellowship at the University of Massachusetts, Worcester, acknowledged certain limitations of the analysis, including its low response rate, the limited number of survey questions, and the question design. Going forward, she and her associates hope to keep a pulse on workplace trends by surveying SPD members annually, perhaps with membership renewal.
The survey was supported by the SPD. Dr. Prindaville reported having no relevant financial disclosures.
CHICAGO – Geographic maldistribution of trained pediatric dermatologists and long wait times for new-patient appointments are two key hurdles impacting patient access to pediatric dermatology care, according to a survey of workforce trends.
“There are large areas of the country that don’t have any pediatric dermatologists, which influences how we can train dermatologists, pediatricians, and medical students who want to do pediatric dermatology,” study author Brea Prindaville, MD, said in an interview at the World Congress for Pediatric Dermatology. “We’re trying to keep an eye on how that’s going, and how we can improve not only the geographic distribution, but also the numbers that we have in the workforce.”
In a project spearheaded by the Society for Pediatric Dermatology (SPD) workforce committee, Dr. Prindaville of Children’s Mercy-Kansas City (Mo.) and her associates emailed a nine-question survey to the 484 SPD members in the United States to determine practice location, number and types of patients seen, wait times, and association with advance practice providers between November and December of 2016. In all, 146 surveys were completed, for a response rate of 30%. Of these, 75% were from board-certified pediatric dermatologists. The majority of survey respondents were practicing in and around large cities, while 60% of all respondents and 68% of board-certified respondents were practicing full-time, seeing pediatric patients exclusively. An additional 30% were practicing part-time or also seeing adults. Board-certified pediatric dermatologists saw an average of 80 pediatric patients per week.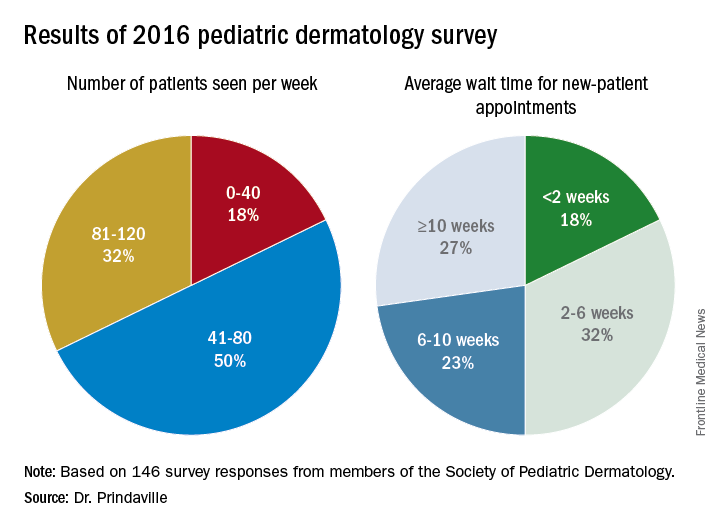
Only 10% of survey respondents did not accept Medicaid, and about 50% of patients seen by board-certified pediatric dermatologists were insured by Medicaid. In addition, about half of respondents worked with one to three advanced practice providers.
Dr. Prindaville, who helped conduct the study during her pediatric dermatology fellowship at the University of Massachusetts, Worcester, acknowledged certain limitations of the analysis, including its low response rate, the limited number of survey questions, and the question design. Going forward, she and her associates hope to keep a pulse on workplace trends by surveying SPD members annually, perhaps with membership renewal.
The survey was supported by the SPD. Dr. Prindaville reported having no relevant financial disclosures.
CHICAGO – Geographic maldistribution of trained pediatric dermatologists and long wait times for new-patient appointments are two key hurdles impacting patient access to pediatric dermatology care, according to a survey of workforce trends.
“There are large areas of the country that don’t have any pediatric dermatologists, which influences how we can train dermatologists, pediatricians, and medical students who want to do pediatric dermatology,” study author Brea Prindaville, MD, said in an interview at the World Congress for Pediatric Dermatology. “We’re trying to keep an eye on how that’s going, and how we can improve not only the geographic distribution, but also the numbers that we have in the workforce.”
In a project spearheaded by the Society for Pediatric Dermatology (SPD) workforce committee, Dr. Prindaville of Children’s Mercy-Kansas City (Mo.) and her associates emailed a nine-question survey to the 484 SPD members in the United States to determine practice location, number and types of patients seen, wait times, and association with advance practice providers between November and December of 2016. In all, 146 surveys were completed, for a response rate of 30%. Of these, 75% were from board-certified pediatric dermatologists. The majority of survey respondents were practicing in and around large cities, while 60% of all respondents and 68% of board-certified respondents were practicing full-time, seeing pediatric patients exclusively. An additional 30% were practicing part-time or also seeing adults. Board-certified pediatric dermatologists saw an average of 80 pediatric patients per week.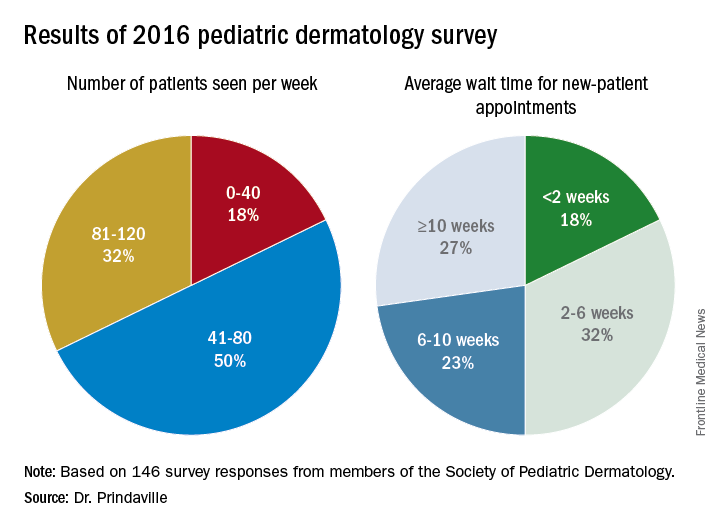
Only 10% of survey respondents did not accept Medicaid, and about 50% of patients seen by board-certified pediatric dermatologists were insured by Medicaid. In addition, about half of respondents worked with one to three advanced practice providers.
Dr. Prindaville, who helped conduct the study during her pediatric dermatology fellowship at the University of Massachusetts, Worcester, acknowledged certain limitations of the analysis, including its low response rate, the limited number of survey questions, and the question design. Going forward, she and her associates hope to keep a pulse on workplace trends by surveying SPD members annually, perhaps with membership renewal.
The survey was supported by the SPD. Dr. Prindaville reported having no relevant financial disclosures.
AT WCPD 2017
Key clinical point:
Major finding: The majority of survey respondents were practicing in and around large cities, and the average wait time for a new-patient appointment for all respondents was about 6 weeks.
Data source: Online survey completed by 146 Society for Pediatric Dermatology (SPD) members in the United States.
Disclosures: The survey was supported by the SPD. Dr. Prindaville reported having no relevant financial disclosures.
Standardization lacking in pediatric trials of atopic dermatitis
CHICAGO – There is considerable variability and poor documentation of severity assessments used for inclusion criteria and baseline severity evaluations in randomized, controlled pediatric atopic dermatitis (AD) trials, results from a systematic review showed.
“It is important for clinicians and investigators to recognize that these differences may limit our ability to reproduce trials, interpret individual studies, and compare results between studies of similar target populations for severity,” lead study author Rishi Chopra, MS, said in an interview in advance of the World Congress of Pediatric Dermatology. “Moreover, this heterogeneity should be considered when retroactively pooling results for meta-analyses of pediatric atopic dermatitis randomized, controlled trials.”
In an effort to evaluate the documentation and characterize the severity assessments used in inclusion criteria and baseline evaluations for randomized, controlled trials of pediatric AD internationally, the researchers performed a systematic review of relevant studies contained in the Cochrane Library, Embase, LILACS, GREAT, MEDLINE, and Scopus databases during 2007-2016. Inclusion criteria were RCT with a pharmacological intervention and any comparison with a control group, children, and males or females. In all, 89 studies met the inclusion/exclusion criteria. Most (70.8%) were studies of pediatric populations aged 0-17 years, and almost 17% were studies of infants aged 0-1 years. The most common target populations were mild-moderate AD (31.5%), moderate-severe AD (18.0%), or undefined (36.0%).
Mr. Chopra and his associates found that the most commonly used severity indices were Scoring AD (SCORAD) in 29.2%, Body Surface Area (BSA) in 16.9%, and global assessments in 13.4%, while the most common assessments of baseline severity were SCORAD in 43.8%, global assessments in 20.2%, Eczema Area and Severity Index in 17.9%, BSA in 14.6%, and visual itch in 13.5%. Only 85.4% of studies recorded the severity assessments used for recruiting the predefined target population and only 76.4% of studies documented baseline severity.
There was considerable heterogeneity across studies, as 16 unique assessments were used as inclusion criteria and 34 assessments were used to evaluate baseline severity. “In addition, even within an individual study, there was substantial discordance in their use as only 71.2% of studies used the same assessments for inclusion and documenting baseline disease severity,” Mr. Chopra said. “Altogether, this multidimensional lack of documentation and heterogeneity of inclusion criteria and baseline severity assessments limits our ability to assess whether the recruitment methods for patients were adequate and confirm whether the intended target population for severity was successfully enrolled.”
He acknowledged certain limitations of the study, including the fact that it may not be generalizable to nonpharmacological interventional trials or noninterventional studies. “In addition, we could only conduct an analysis for studies that provided adequate documentation of inclusion criteria and baseline severity,” Mr. Chopra said. “Thus, those studies that did not provide this information were left out. Nevertheless, across all studies, the uniformity and concordance between assessments likely are even more negatively impacted. It should also be noted that lack of documentation of assessments for inclusion criteria and baseline severity does not imply lack of their utilization. Finally, it is important to acknowledge that AD’s diverse phenotype and relapsing and remitting course may result in the unavoidable heterogeneity of severity assessment use. This may actually help to capture a broader range of disease and improve the external validity of results.”
He reported having no financial disclosures.
CHICAGO – There is considerable variability and poor documentation of severity assessments used for inclusion criteria and baseline severity evaluations in randomized, controlled pediatric atopic dermatitis (AD) trials, results from a systematic review showed.
“It is important for clinicians and investigators to recognize that these differences may limit our ability to reproduce trials, interpret individual studies, and compare results between studies of similar target populations for severity,” lead study author Rishi Chopra, MS, said in an interview in advance of the World Congress of Pediatric Dermatology. “Moreover, this heterogeneity should be considered when retroactively pooling results for meta-analyses of pediatric atopic dermatitis randomized, controlled trials.”
In an effort to evaluate the documentation and characterize the severity assessments used in inclusion criteria and baseline evaluations for randomized, controlled trials of pediatric AD internationally, the researchers performed a systematic review of relevant studies contained in the Cochrane Library, Embase, LILACS, GREAT, MEDLINE, and Scopus databases during 2007-2016. Inclusion criteria were RCT with a pharmacological intervention and any comparison with a control group, children, and males or females. In all, 89 studies met the inclusion/exclusion criteria. Most (70.8%) were studies of pediatric populations aged 0-17 years, and almost 17% were studies of infants aged 0-1 years. The most common target populations were mild-moderate AD (31.5%), moderate-severe AD (18.0%), or undefined (36.0%).
Mr. Chopra and his associates found that the most commonly used severity indices were Scoring AD (SCORAD) in 29.2%, Body Surface Area (BSA) in 16.9%, and global assessments in 13.4%, while the most common assessments of baseline severity were SCORAD in 43.8%, global assessments in 20.2%, Eczema Area and Severity Index in 17.9%, BSA in 14.6%, and visual itch in 13.5%. Only 85.4% of studies recorded the severity assessments used for recruiting the predefined target population and only 76.4% of studies documented baseline severity.
There was considerable heterogeneity across studies, as 16 unique assessments were used as inclusion criteria and 34 assessments were used to evaluate baseline severity. “In addition, even within an individual study, there was substantial discordance in their use as only 71.2% of studies used the same assessments for inclusion and documenting baseline disease severity,” Mr. Chopra said. “Altogether, this multidimensional lack of documentation and heterogeneity of inclusion criteria and baseline severity assessments limits our ability to assess whether the recruitment methods for patients were adequate and confirm whether the intended target population for severity was successfully enrolled.”
He acknowledged certain limitations of the study, including the fact that it may not be generalizable to nonpharmacological interventional trials or noninterventional studies. “In addition, we could only conduct an analysis for studies that provided adequate documentation of inclusion criteria and baseline severity,” Mr. Chopra said. “Thus, those studies that did not provide this information were left out. Nevertheless, across all studies, the uniformity and concordance between assessments likely are even more negatively impacted. It should also be noted that lack of documentation of assessments for inclusion criteria and baseline severity does not imply lack of their utilization. Finally, it is important to acknowledge that AD’s diverse phenotype and relapsing and remitting course may result in the unavoidable heterogeneity of severity assessment use. This may actually help to capture a broader range of disease and improve the external validity of results.”
He reported having no financial disclosures.
CHICAGO – There is considerable variability and poor documentation of severity assessments used for inclusion criteria and baseline severity evaluations in randomized, controlled pediatric atopic dermatitis (AD) trials, results from a systematic review showed.
“It is important for clinicians and investigators to recognize that these differences may limit our ability to reproduce trials, interpret individual studies, and compare results between studies of similar target populations for severity,” lead study author Rishi Chopra, MS, said in an interview in advance of the World Congress of Pediatric Dermatology. “Moreover, this heterogeneity should be considered when retroactively pooling results for meta-analyses of pediatric atopic dermatitis randomized, controlled trials.”
In an effort to evaluate the documentation and characterize the severity assessments used in inclusion criteria and baseline evaluations for randomized, controlled trials of pediatric AD internationally, the researchers performed a systematic review of relevant studies contained in the Cochrane Library, Embase, LILACS, GREAT, MEDLINE, and Scopus databases during 2007-2016. Inclusion criteria were RCT with a pharmacological intervention and any comparison with a control group, children, and males or females. In all, 89 studies met the inclusion/exclusion criteria. Most (70.8%) were studies of pediatric populations aged 0-17 years, and almost 17% were studies of infants aged 0-1 years. The most common target populations were mild-moderate AD (31.5%), moderate-severe AD (18.0%), or undefined (36.0%).
Mr. Chopra and his associates found that the most commonly used severity indices were Scoring AD (SCORAD) in 29.2%, Body Surface Area (BSA) in 16.9%, and global assessments in 13.4%, while the most common assessments of baseline severity were SCORAD in 43.8%, global assessments in 20.2%, Eczema Area and Severity Index in 17.9%, BSA in 14.6%, and visual itch in 13.5%. Only 85.4% of studies recorded the severity assessments used for recruiting the predefined target population and only 76.4% of studies documented baseline severity.
There was considerable heterogeneity across studies, as 16 unique assessments were used as inclusion criteria and 34 assessments were used to evaluate baseline severity. “In addition, even within an individual study, there was substantial discordance in their use as only 71.2% of studies used the same assessments for inclusion and documenting baseline disease severity,” Mr. Chopra said. “Altogether, this multidimensional lack of documentation and heterogeneity of inclusion criteria and baseline severity assessments limits our ability to assess whether the recruitment methods for patients were adequate and confirm whether the intended target population for severity was successfully enrolled.”
He acknowledged certain limitations of the study, including the fact that it may not be generalizable to nonpharmacological interventional trials or noninterventional studies. “In addition, we could only conduct an analysis for studies that provided adequate documentation of inclusion criteria and baseline severity,” Mr. Chopra said. “Thus, those studies that did not provide this information were left out. Nevertheless, across all studies, the uniformity and concordance between assessments likely are even more negatively impacted. It should also be noted that lack of documentation of assessments for inclusion criteria and baseline severity does not imply lack of their utilization. Finally, it is important to acknowledge that AD’s diverse phenotype and relapsing and remitting course may result in the unavoidable heterogeneity of severity assessment use. This may actually help to capture a broader range of disease and improve the external validity of results.”
He reported having no financial disclosures.
AT WCPD 2017
Key clinical point:
Major finding: Only 85.4% of studies recorded the severity assessments used for recruiting the predefined target population, and only 76.4% of studies documented baseline severity.
Data source: A systematic review of 89 pediatric atopic dermatitis randomized, controlled trials published during 2007-2016.
Disclosures: Mr. Chopra reported having no financial disclosures.