User login
Recognize early window of opportunity in hidradenitis suppurativa
MADRID – Antonio Martorell, MD, said at the annual congress of the European Academy of Dermatology and Venereology.
This distinction is critical in recognizing a window of opportunity in the management of hidradenitis suppurativa (HS): The period early in the disease course when medical therapy alone can be life-changing.
“The window of opportunity is an old concept in gastroenterology, but it’s a new idea in dermatology: It’s the moment in which the patient can have the best results with medical control of inflammation, before progression to tissue scarring has occurred,” explained Dr. Martorell, a dermatologist at the Hospital of Manises in Valencia, Spain, and coauthor of recent HS treatment recommendations by an international expert panel (J Eur Acad Dermatol Venereol. 2019 Jan;33[1]:19-31).
Symptoms in patients with HS can be caused by either dynamic or static lesions. Dynamic lesions arise directly from acute inflammation that can be treated with antibiotics and immunomodulatory therapy. Static lesions are associated with tissue scarring secondary to inflammatory activity and generally benefit only from surgery.
Dynamic lesions consist of nodules, abscesses, and some but not all fistulae. Although the traditional view among dermatologists has been that fistulae simply don’t respond to medical therapy and must be treated surgically, Dr. Martorell and coinvestigators have recently demonstrated in a retrospective study of 117 fistulae in 40 patients that ultrasound was useful in distinguishing four fistular subtypes, two of which responded reasonably well to medical management.
What the investigators call Type A or dermal fistulae are by definition not connected to tunnels. In Dr. Martorell’s study, they had a 95% complete resolution rate after 6 months of various medications. Dermoepidermal fistulae tunnel through the dermis to the epidermis; they had a 65% complete resolution rate. In contrast, Type C or complex fistulae, identified by the ultrasound finding of multiple tunnels extending through the dermis into underlying fat tissue, had no significant response to medical management. Neither did Type D fistulae, which are essentially Type C lesions with scarring (Dermatol Surg. 2019 Oct;45[10]:1237-44).
Thus, ultrasound can have an important impact on patient management and the decision to opt for a combined medical/surgical approach.
“It’s important to apply the HS severity scores and complete the clinical exam, but it’s also important to use ultrasound or another imaging technique,” Dr. Martorell concluded.
MADRID – Antonio Martorell, MD, said at the annual congress of the European Academy of Dermatology and Venereology.
This distinction is critical in recognizing a window of opportunity in the management of hidradenitis suppurativa (HS): The period early in the disease course when medical therapy alone can be life-changing.
“The window of opportunity is an old concept in gastroenterology, but it’s a new idea in dermatology: It’s the moment in which the patient can have the best results with medical control of inflammation, before progression to tissue scarring has occurred,” explained Dr. Martorell, a dermatologist at the Hospital of Manises in Valencia, Spain, and coauthor of recent HS treatment recommendations by an international expert panel (J Eur Acad Dermatol Venereol. 2019 Jan;33[1]:19-31).
Symptoms in patients with HS can be caused by either dynamic or static lesions. Dynamic lesions arise directly from acute inflammation that can be treated with antibiotics and immunomodulatory therapy. Static lesions are associated with tissue scarring secondary to inflammatory activity and generally benefit only from surgery.
Dynamic lesions consist of nodules, abscesses, and some but not all fistulae. Although the traditional view among dermatologists has been that fistulae simply don’t respond to medical therapy and must be treated surgically, Dr. Martorell and coinvestigators have recently demonstrated in a retrospective study of 117 fistulae in 40 patients that ultrasound was useful in distinguishing four fistular subtypes, two of which responded reasonably well to medical management.
What the investigators call Type A or dermal fistulae are by definition not connected to tunnels. In Dr. Martorell’s study, they had a 95% complete resolution rate after 6 months of various medications. Dermoepidermal fistulae tunnel through the dermis to the epidermis; they had a 65% complete resolution rate. In contrast, Type C or complex fistulae, identified by the ultrasound finding of multiple tunnels extending through the dermis into underlying fat tissue, had no significant response to medical management. Neither did Type D fistulae, which are essentially Type C lesions with scarring (Dermatol Surg. 2019 Oct;45[10]:1237-44).
Thus, ultrasound can have an important impact on patient management and the decision to opt for a combined medical/surgical approach.
“It’s important to apply the HS severity scores and complete the clinical exam, but it’s also important to use ultrasound or another imaging technique,” Dr. Martorell concluded.
MADRID – Antonio Martorell, MD, said at the annual congress of the European Academy of Dermatology and Venereology.
This distinction is critical in recognizing a window of opportunity in the management of hidradenitis suppurativa (HS): The period early in the disease course when medical therapy alone can be life-changing.
“The window of opportunity is an old concept in gastroenterology, but it’s a new idea in dermatology: It’s the moment in which the patient can have the best results with medical control of inflammation, before progression to tissue scarring has occurred,” explained Dr. Martorell, a dermatologist at the Hospital of Manises in Valencia, Spain, and coauthor of recent HS treatment recommendations by an international expert panel (J Eur Acad Dermatol Venereol. 2019 Jan;33[1]:19-31).
Symptoms in patients with HS can be caused by either dynamic or static lesions. Dynamic lesions arise directly from acute inflammation that can be treated with antibiotics and immunomodulatory therapy. Static lesions are associated with tissue scarring secondary to inflammatory activity and generally benefit only from surgery.
Dynamic lesions consist of nodules, abscesses, and some but not all fistulae. Although the traditional view among dermatologists has been that fistulae simply don’t respond to medical therapy and must be treated surgically, Dr. Martorell and coinvestigators have recently demonstrated in a retrospective study of 117 fistulae in 40 patients that ultrasound was useful in distinguishing four fistular subtypes, two of which responded reasonably well to medical management.
What the investigators call Type A or dermal fistulae are by definition not connected to tunnels. In Dr. Martorell’s study, they had a 95% complete resolution rate after 6 months of various medications. Dermoepidermal fistulae tunnel through the dermis to the epidermis; they had a 65% complete resolution rate. In contrast, Type C or complex fistulae, identified by the ultrasound finding of multiple tunnels extending through the dermis into underlying fat tissue, had no significant response to medical management. Neither did Type D fistulae, which are essentially Type C lesions with scarring (Dermatol Surg. 2019 Oct;45[10]:1237-44).
Thus, ultrasound can have an important impact on patient management and the decision to opt for a combined medical/surgical approach.
“It’s important to apply the HS severity scores and complete the clinical exam, but it’s also important to use ultrasound or another imaging technique,” Dr. Martorell concluded.
EXPERT ANALYSIS FROM THE EADV CONGRESS
Bimekizumab elevates psoriasis therapy
MADRID – Renowned dermatologic clinical trialist Kim A. Papp, MD, PhD, is known to pick his words carefully, and the word he uses to describe the quality of life improvement documented in psoriasis patients treated with the novel investigational humanized monoclonal antibody bimekizumab is “phenomenal.”
Dr. Papp was lead investigator in the previously reported phase 2b multicenter BE ABLE 1 trial, in which 250 patients with moderate to severe chronic plaque psoriasis were randomized double-blind to various doses of bimekizumab or placebo every 4 weeks for 12 weeks (J Am Acad Dermatol. 2018 Aug;79[2]:277-86.e10. doi: 10.1016/j.jaad.2018.03.037). He was also lead investigator in the 48-week phase 2b BE ABLE 2 extension study. He presented the 60-week quality-of-life BE ABLE 2 results for the first time at the annual congress of the European Academy of Dermatology and Venereology.
“Small numbers, but the results are nonetheless very compelling,” said Dr. Papp, president and founder of Probity Medical Research in Waterloo, Ont.
Bimekizumab is unique in that it selectively neutralizes both interleukin-17A and -17F, two closely related proinflammatory cytokines which, when upregulated, synergize with other proinflammatory cytokines to drive psoriasis and other immune-mediated inflammatory diseases. In contrast, secukinumab (Cosentyx) and ixekizumab (Taltz) specifically inhibit only IL-17A, and brodalumab (Siliq) targets the IL-17 receptor A. The bimekizumab clinical trials program – a work in progress – aims to demonstrate that dual neutralization of IL-17A and -17F provides a more complete therapeutic approach in psoriasis, with greater efficacy and fewer safety concerns than with current biologics, the dermatologist explained.
In BE ABLE 1, the primary endpoint of at least a 90% reduction in Psoriasis Area and Severity Index (PASI90) response was achieved at week 12 in 46%-79% of patients randomized to bimekizumab in dose-dependent fashion. Those PASI90 responses were maintained with additional treatment out to week 60 in BE ABLE 2 in 80%-100% of patients.
Dr. Papp’s focus at EADV 2019 was on the quality-of-life improvement achieved in bimekizumab-treated patients, a benefit not captured by PASI scores. For this purpose, he and coinvestigators turned to the Dermatology Life Quality Index (DLQI), measured in structured fashion every 4 weeks out to week 60.
“We often forget that even though we’re looking at the patient from the outside, what’s really important is how well they respond to our treatments internally. The DLQI is not a perfect tool, but it’s the best tool we have available. It gives us a fairly good survey of the various domains that affect patients’ day-to-day living,” he said.
In BE ABLE 1, the proportion of week-12 PASI90 responders achieving a DLQI of 0 or 1 – indicative of essentially no disease impact on quality of life – increased rapidly up until week 8. At week 12, 70%-100% of the PASI90 responders in the various treatment arms had a DLQI of 0 or 1. This quality-of-life improvement, like the PASI90 response, proved durable: When the week-12 PASI90 responders were assessed at week 60 in BE ABLE 2, 76%-93% of them had a DLQI of 0 or 1.
The improvements in quality of life correlated with clinical response. BE ABLE enrollees had an average PASI score of 19 at baseline. Overall, 79% of those with an absolute PASI score of 0 at week 12 had a DLQI of 0 or 1 at that time, as did 95% of those with a PASI of 0 at week 60. A PASI of 1 was associated with a 77% likelihood of a DLQI of 0 or 1 at week 12 and an 82% rate at week 60. In contrast, patients with an absolute PASI of 2-4 at week 12 had a 46% rate of DLQI 0/1, and those with a PASI 2-4 at week 60 had a 50% chance of having a DLQI of 0/1.
Phase 3 clinical trials of bimekizumab totaling several thousand psoriasis patients are ongoing.
The BE ABLE trials were sponsored by UCB Pharma. Dr. Papp reported serving as a consultant to and/or recipient of research grants from UCB and dozens of other pharmaceutical companies.
SOURCE: Papp KA. EADV 2019 Abstract FC02.02.
MADRID – Renowned dermatologic clinical trialist Kim A. Papp, MD, PhD, is known to pick his words carefully, and the word he uses to describe the quality of life improvement documented in psoriasis patients treated with the novel investigational humanized monoclonal antibody bimekizumab is “phenomenal.”
Dr. Papp was lead investigator in the previously reported phase 2b multicenter BE ABLE 1 trial, in which 250 patients with moderate to severe chronic plaque psoriasis were randomized double-blind to various doses of bimekizumab or placebo every 4 weeks for 12 weeks (J Am Acad Dermatol. 2018 Aug;79[2]:277-86.e10. doi: 10.1016/j.jaad.2018.03.037). He was also lead investigator in the 48-week phase 2b BE ABLE 2 extension study. He presented the 60-week quality-of-life BE ABLE 2 results for the first time at the annual congress of the European Academy of Dermatology and Venereology.
“Small numbers, but the results are nonetheless very compelling,” said Dr. Papp, president and founder of Probity Medical Research in Waterloo, Ont.
Bimekizumab is unique in that it selectively neutralizes both interleukin-17A and -17F, two closely related proinflammatory cytokines which, when upregulated, synergize with other proinflammatory cytokines to drive psoriasis and other immune-mediated inflammatory diseases. In contrast, secukinumab (Cosentyx) and ixekizumab (Taltz) specifically inhibit only IL-17A, and brodalumab (Siliq) targets the IL-17 receptor A. The bimekizumab clinical trials program – a work in progress – aims to demonstrate that dual neutralization of IL-17A and -17F provides a more complete therapeutic approach in psoriasis, with greater efficacy and fewer safety concerns than with current biologics, the dermatologist explained.
In BE ABLE 1, the primary endpoint of at least a 90% reduction in Psoriasis Area and Severity Index (PASI90) response was achieved at week 12 in 46%-79% of patients randomized to bimekizumab in dose-dependent fashion. Those PASI90 responses were maintained with additional treatment out to week 60 in BE ABLE 2 in 80%-100% of patients.
Dr. Papp’s focus at EADV 2019 was on the quality-of-life improvement achieved in bimekizumab-treated patients, a benefit not captured by PASI scores. For this purpose, he and coinvestigators turned to the Dermatology Life Quality Index (DLQI), measured in structured fashion every 4 weeks out to week 60.
“We often forget that even though we’re looking at the patient from the outside, what’s really important is how well they respond to our treatments internally. The DLQI is not a perfect tool, but it’s the best tool we have available. It gives us a fairly good survey of the various domains that affect patients’ day-to-day living,” he said.
In BE ABLE 1, the proportion of week-12 PASI90 responders achieving a DLQI of 0 or 1 – indicative of essentially no disease impact on quality of life – increased rapidly up until week 8. At week 12, 70%-100% of the PASI90 responders in the various treatment arms had a DLQI of 0 or 1. This quality-of-life improvement, like the PASI90 response, proved durable: When the week-12 PASI90 responders were assessed at week 60 in BE ABLE 2, 76%-93% of them had a DLQI of 0 or 1.
The improvements in quality of life correlated with clinical response. BE ABLE enrollees had an average PASI score of 19 at baseline. Overall, 79% of those with an absolute PASI score of 0 at week 12 had a DLQI of 0 or 1 at that time, as did 95% of those with a PASI of 0 at week 60. A PASI of 1 was associated with a 77% likelihood of a DLQI of 0 or 1 at week 12 and an 82% rate at week 60. In contrast, patients with an absolute PASI of 2-4 at week 12 had a 46% rate of DLQI 0/1, and those with a PASI 2-4 at week 60 had a 50% chance of having a DLQI of 0/1.
Phase 3 clinical trials of bimekizumab totaling several thousand psoriasis patients are ongoing.
The BE ABLE trials were sponsored by UCB Pharma. Dr. Papp reported serving as a consultant to and/or recipient of research grants from UCB and dozens of other pharmaceutical companies.
SOURCE: Papp KA. EADV 2019 Abstract FC02.02.
MADRID – Renowned dermatologic clinical trialist Kim A. Papp, MD, PhD, is known to pick his words carefully, and the word he uses to describe the quality of life improvement documented in psoriasis patients treated with the novel investigational humanized monoclonal antibody bimekizumab is “phenomenal.”
Dr. Papp was lead investigator in the previously reported phase 2b multicenter BE ABLE 1 trial, in which 250 patients with moderate to severe chronic plaque psoriasis were randomized double-blind to various doses of bimekizumab or placebo every 4 weeks for 12 weeks (J Am Acad Dermatol. 2018 Aug;79[2]:277-86.e10. doi: 10.1016/j.jaad.2018.03.037). He was also lead investigator in the 48-week phase 2b BE ABLE 2 extension study. He presented the 60-week quality-of-life BE ABLE 2 results for the first time at the annual congress of the European Academy of Dermatology and Venereology.
“Small numbers, but the results are nonetheless very compelling,” said Dr. Papp, president and founder of Probity Medical Research in Waterloo, Ont.
Bimekizumab is unique in that it selectively neutralizes both interleukin-17A and -17F, two closely related proinflammatory cytokines which, when upregulated, synergize with other proinflammatory cytokines to drive psoriasis and other immune-mediated inflammatory diseases. In contrast, secukinumab (Cosentyx) and ixekizumab (Taltz) specifically inhibit only IL-17A, and brodalumab (Siliq) targets the IL-17 receptor A. The bimekizumab clinical trials program – a work in progress – aims to demonstrate that dual neutralization of IL-17A and -17F provides a more complete therapeutic approach in psoriasis, with greater efficacy and fewer safety concerns than with current biologics, the dermatologist explained.
In BE ABLE 1, the primary endpoint of at least a 90% reduction in Psoriasis Area and Severity Index (PASI90) response was achieved at week 12 in 46%-79% of patients randomized to bimekizumab in dose-dependent fashion. Those PASI90 responses were maintained with additional treatment out to week 60 in BE ABLE 2 in 80%-100% of patients.
Dr. Papp’s focus at EADV 2019 was on the quality-of-life improvement achieved in bimekizumab-treated patients, a benefit not captured by PASI scores. For this purpose, he and coinvestigators turned to the Dermatology Life Quality Index (DLQI), measured in structured fashion every 4 weeks out to week 60.
“We often forget that even though we’re looking at the patient from the outside, what’s really important is how well they respond to our treatments internally. The DLQI is not a perfect tool, but it’s the best tool we have available. It gives us a fairly good survey of the various domains that affect patients’ day-to-day living,” he said.
In BE ABLE 1, the proportion of week-12 PASI90 responders achieving a DLQI of 0 or 1 – indicative of essentially no disease impact on quality of life – increased rapidly up until week 8. At week 12, 70%-100% of the PASI90 responders in the various treatment arms had a DLQI of 0 or 1. This quality-of-life improvement, like the PASI90 response, proved durable: When the week-12 PASI90 responders were assessed at week 60 in BE ABLE 2, 76%-93% of them had a DLQI of 0 or 1.
The improvements in quality of life correlated with clinical response. BE ABLE enrollees had an average PASI score of 19 at baseline. Overall, 79% of those with an absolute PASI score of 0 at week 12 had a DLQI of 0 or 1 at that time, as did 95% of those with a PASI of 0 at week 60. A PASI of 1 was associated with a 77% likelihood of a DLQI of 0 or 1 at week 12 and an 82% rate at week 60. In contrast, patients with an absolute PASI of 2-4 at week 12 had a 46% rate of DLQI 0/1, and those with a PASI 2-4 at week 60 had a 50% chance of having a DLQI of 0/1.
Phase 3 clinical trials of bimekizumab totaling several thousand psoriasis patients are ongoing.
The BE ABLE trials were sponsored by UCB Pharma. Dr. Papp reported serving as a consultant to and/or recipient of research grants from UCB and dozens of other pharmaceutical companies.
SOURCE: Papp KA. EADV 2019 Abstract FC02.02.
REPORTING FROM THE EADV CONGRESS
Experts in Europe issue guidance on atopic dermatitis in pregnancy
MADRID – European atopic dermatitis experts have issued formal guidance on a seriously neglected topic: treatment of the disease during pregnancy, breastfeeding, and in men planning to father children.
The impetus for the project was clear: “,” Christian Vestergaard, MD, PhD, declared at a meeting of the European Task Force on Atopic Dermatitis held in conjunction with the annual congress of the European Academy of Dermatology and Venereology.
He presented highlights of the task force’s position paper on the topic, for which he served as first author. The group’s recommendations are based on expert opinion, since randomized clinical trial literature in this area is nonexistent because of ethical concerns. But the task force, comprising a who’s who in European dermatology, drew on a wealth of collective clinical experience in this area.
“We have all of Europe involved in doing this position statement. It’s meant as what we think is proper treatment and what we can say about the different drugs,” explained Dr. Vestergaard, a dermatologist at the University of Aarhus (Denmark).
Most nonobstetricians are intimidated by atopic dermatitis (AD) in pregnancy, and are concerned about the potential for treatment-related harm to the fetus. As a consequence, they are reluctant to recommend anything beyond weak class I topical corticosteroids and emollients. That’s clearly insufficient in light of the vast scope of need, he asserted. After all, AD affects 15%-20% of all children and persists or reappears in adulthood in one out of five of them. Half of those adults are women, many of whom will at some point wish to become pregnant. And many men with AD will eventually want to father children.
A key message from the task force is that untreated AD in pregnancy potentially places the mother and fetus at risk of serious complications, including Staphylococcus aureus infection and eczema herpeticum.
“If you take one thing away from our position paper, it’s that you can use class II or III topical corticosteroids in pregnant women as first-line therapy,” Dr. Vestergaard said.
This stance contradicts a longstanding widely held concern that topical steroids in pregnancy might increase the risk of facial cleft in the offspring, a worry that has been convincingly debunked in a Cochrane systematic review of 14 studies including more than 1.6 million pregnancies. The report concluded there was no association between topical corticosteroids of any potency with preterm delivery, birth defects, or low Apgar scores (Cochrane Database Syst Rev. 2015 Oct 26. doi: 10.1002/14651858.CD007346.pub3).
The task force recommends that if class II or III topical corticosteroid use in pregnancy exceeds 200 g/month, it’s worth considering add-on UV therapy, with narrow band UVB-311 nm as the regimen of choice; it can be used liberally. UV therapy with psoralens is not advised because of a theoretical risk of mutagenicity.
Product labeling for the topical calcineurin inhibitors declares that the agents should not be used during pregnancy. However, the European task force position paper takes issue with that and declares that topical tacrolimus (Protopic) can be considered an off-label first-line therapy in pregnant women with an insufficient response to liberal use of emollients. The same holds true for breastfeeding patients with AD. Just as when topical corticosteroids are used in the nipple area, topical tacrolimus should be applied after nursing, and the nipple area should be gently cleaned before nursing.
The rationale behind recommending topical tacrolimus as a first-line treatment is that systemic absorption of the drug is trivial. Plus, observational studies of oral tacrolimus in pregnant women who have received a solid organ transplant have shown no increase in congenital malformations.
The task force recommends against the use of topical pimecrolimus (Elidel) or crisaborole (Eucrisa) in pregnancy or lactation due to lack of clinical experience in these settings, Dr. Vestergaard continued.
The task force position is that chlorhexidine and other topical antiseptics – with the notable exception of triclosan – can be used in pregnancy to prevent recurrent skin infections. Aminoglycosides should be avoided, but topical fusidic acid is a reasonable antibiotic for treatment of small areas of clinically infected atopic dermatitis in pregnancy.
Systemic therapies
If disease control is insufficient with topical therapy, it’s appropriate to engage in shared decision-making with the patient regarding systemic treatment. She needs to understand up front that the worldwide overall background stillbirth rate in the general population is about 3%, and that severe congenital malformations are present in up to 6% of all live births.
“You need to inform them that they can have systemic therapy and give birth to a child with congenital defects which have nothing to do with the medication,” noted Dr. Vestergaard.
That said, the task force recommends cyclosporine as the off-label, first-line systemic therapy in pregnancy and lactation when long-term treatment is required. This guidance is based largely upon reassuring evidence in solid organ transplant recipients.
The recommended second-line therapy is systemic corticosteroids, but it’s a qualified recommendation. Dr. Vestergaard and colleagues find that systemic corticosteroid therapy is only rarely needed in pregnant AD patients, and the task force recommendation is to limit the use to less than 2-3 weeks and no more than 0.5 mg/kg per day of prednisone. Dexamethasone is not recommended.
Azathioprine should not be started in pregnancy, according to the task force, but when no other options are available, it may be continued in women already on the drug, albeit at half of the prepregnancy dose.
Dupilumab (Dupixent) is to be avoided in pregnant women with AD until more clinical experience becomes available.
Treatment of prospective fathers with AD
The European task force recommends that topical therapies can be prescribed in prospective fathers without any special concerns. The same is true for systemic corticosteroids. Methotrexate should be halted 3 months before planned pregnancy, as is the case for mycophenolate mofetil (CellCept). Azathioprine is recommended when other options have failed. Cyclosporine is deemed a reasonable option in the treatment of men with severe AD at the time of conception if other treatments have failed; of note, neither the Food and Drug Administration nor the European regulatory agency have issued contraindications for the use of the drug in men who wish to become fathers.
Mycophenolate mofetil carries a theoretical risk of teratogenicity. The European task force recommends that men should use condoms while on the drug and for at least 90 days afterward.
Unplanned pregnancy in women on systemic therapy
The recommended course of action is to immediately stop systemic therapy, intensify appropriate topical therapy in anticipation of worsening AD, and refer the patient to an obstetrician and a teratology information center for an individualized risk assessment. Methotrexate and mycophenolate mofetil are known teratogens.
The full 16-page task force position paper was published shortly before EADV 2019 (J Eur Acad Dermatol Venereol. 2019 Sep;33[9]:1644-59).
The report was developed without commercial sponsorship. Dr. Vestergaard indicated he has received research grants from and/or serves as a consultant to eight pharmaceutical companies.
Jenny Murase, MD, is with the department of dermatology, University of California, San Francisco, and is the director of medical consultative dermatology at the Palo Alto Foundation Medical Group, Mountain View, Calif. She has served on advisory boards for Dermira, Sanofi, and UCB; performed dermatologic consulting for UpToDate and Ferndale, and given nonbranded lectures for disease state management awareness for Regeneron and UCB.
Jenny Murase, MD, is with the department of dermatology, University of California, San Francisco, and is the director of medical consultative dermatology at the Palo Alto Foundation Medical Group, Mountain View, Calif. She has served on advisory boards for Dermira, Sanofi, and UCB; performed dermatologic consulting for UpToDate and Ferndale, and given nonbranded lectures for disease state management awareness for Regeneron and UCB.
Jenny Murase, MD, is with the department of dermatology, University of California, San Francisco, and is the director of medical consultative dermatology at the Palo Alto Foundation Medical Group, Mountain View, Calif. She has served on advisory boards for Dermira, Sanofi, and UCB; performed dermatologic consulting for UpToDate and Ferndale, and given nonbranded lectures for disease state management awareness for Regeneron and UCB.
MADRID – European atopic dermatitis experts have issued formal guidance on a seriously neglected topic: treatment of the disease during pregnancy, breastfeeding, and in men planning to father children.
The impetus for the project was clear: “,” Christian Vestergaard, MD, PhD, declared at a meeting of the European Task Force on Atopic Dermatitis held in conjunction with the annual congress of the European Academy of Dermatology and Venereology.
He presented highlights of the task force’s position paper on the topic, for which he served as first author. The group’s recommendations are based on expert opinion, since randomized clinical trial literature in this area is nonexistent because of ethical concerns. But the task force, comprising a who’s who in European dermatology, drew on a wealth of collective clinical experience in this area.
“We have all of Europe involved in doing this position statement. It’s meant as what we think is proper treatment and what we can say about the different drugs,” explained Dr. Vestergaard, a dermatologist at the University of Aarhus (Denmark).
Most nonobstetricians are intimidated by atopic dermatitis (AD) in pregnancy, and are concerned about the potential for treatment-related harm to the fetus. As a consequence, they are reluctant to recommend anything beyond weak class I topical corticosteroids and emollients. That’s clearly insufficient in light of the vast scope of need, he asserted. After all, AD affects 15%-20% of all children and persists or reappears in adulthood in one out of five of them. Half of those adults are women, many of whom will at some point wish to become pregnant. And many men with AD will eventually want to father children.
A key message from the task force is that untreated AD in pregnancy potentially places the mother and fetus at risk of serious complications, including Staphylococcus aureus infection and eczema herpeticum.
“If you take one thing away from our position paper, it’s that you can use class II or III topical corticosteroids in pregnant women as first-line therapy,” Dr. Vestergaard said.
This stance contradicts a longstanding widely held concern that topical steroids in pregnancy might increase the risk of facial cleft in the offspring, a worry that has been convincingly debunked in a Cochrane systematic review of 14 studies including more than 1.6 million pregnancies. The report concluded there was no association between topical corticosteroids of any potency with preterm delivery, birth defects, or low Apgar scores (Cochrane Database Syst Rev. 2015 Oct 26. doi: 10.1002/14651858.CD007346.pub3).
The task force recommends that if class II or III topical corticosteroid use in pregnancy exceeds 200 g/month, it’s worth considering add-on UV therapy, with narrow band UVB-311 nm as the regimen of choice; it can be used liberally. UV therapy with psoralens is not advised because of a theoretical risk of mutagenicity.
Product labeling for the topical calcineurin inhibitors declares that the agents should not be used during pregnancy. However, the European task force position paper takes issue with that and declares that topical tacrolimus (Protopic) can be considered an off-label first-line therapy in pregnant women with an insufficient response to liberal use of emollients. The same holds true for breastfeeding patients with AD. Just as when topical corticosteroids are used in the nipple area, topical tacrolimus should be applied after nursing, and the nipple area should be gently cleaned before nursing.
The rationale behind recommending topical tacrolimus as a first-line treatment is that systemic absorption of the drug is trivial. Plus, observational studies of oral tacrolimus in pregnant women who have received a solid organ transplant have shown no increase in congenital malformations.
The task force recommends against the use of topical pimecrolimus (Elidel) or crisaborole (Eucrisa) in pregnancy or lactation due to lack of clinical experience in these settings, Dr. Vestergaard continued.
The task force position is that chlorhexidine and other topical antiseptics – with the notable exception of triclosan – can be used in pregnancy to prevent recurrent skin infections. Aminoglycosides should be avoided, but topical fusidic acid is a reasonable antibiotic for treatment of small areas of clinically infected atopic dermatitis in pregnancy.
Systemic therapies
If disease control is insufficient with topical therapy, it’s appropriate to engage in shared decision-making with the patient regarding systemic treatment. She needs to understand up front that the worldwide overall background stillbirth rate in the general population is about 3%, and that severe congenital malformations are present in up to 6% of all live births.
“You need to inform them that they can have systemic therapy and give birth to a child with congenital defects which have nothing to do with the medication,” noted Dr. Vestergaard.
That said, the task force recommends cyclosporine as the off-label, first-line systemic therapy in pregnancy and lactation when long-term treatment is required. This guidance is based largely upon reassuring evidence in solid organ transplant recipients.
The recommended second-line therapy is systemic corticosteroids, but it’s a qualified recommendation. Dr. Vestergaard and colleagues find that systemic corticosteroid therapy is only rarely needed in pregnant AD patients, and the task force recommendation is to limit the use to less than 2-3 weeks and no more than 0.5 mg/kg per day of prednisone. Dexamethasone is not recommended.
Azathioprine should not be started in pregnancy, according to the task force, but when no other options are available, it may be continued in women already on the drug, albeit at half of the prepregnancy dose.
Dupilumab (Dupixent) is to be avoided in pregnant women with AD until more clinical experience becomes available.
Treatment of prospective fathers with AD
The European task force recommends that topical therapies can be prescribed in prospective fathers without any special concerns. The same is true for systemic corticosteroids. Methotrexate should be halted 3 months before planned pregnancy, as is the case for mycophenolate mofetil (CellCept). Azathioprine is recommended when other options have failed. Cyclosporine is deemed a reasonable option in the treatment of men with severe AD at the time of conception if other treatments have failed; of note, neither the Food and Drug Administration nor the European regulatory agency have issued contraindications for the use of the drug in men who wish to become fathers.
Mycophenolate mofetil carries a theoretical risk of teratogenicity. The European task force recommends that men should use condoms while on the drug and for at least 90 days afterward.
Unplanned pregnancy in women on systemic therapy
The recommended course of action is to immediately stop systemic therapy, intensify appropriate topical therapy in anticipation of worsening AD, and refer the patient to an obstetrician and a teratology information center for an individualized risk assessment. Methotrexate and mycophenolate mofetil are known teratogens.
The full 16-page task force position paper was published shortly before EADV 2019 (J Eur Acad Dermatol Venereol. 2019 Sep;33[9]:1644-59).
The report was developed without commercial sponsorship. Dr. Vestergaard indicated he has received research grants from and/or serves as a consultant to eight pharmaceutical companies.
MADRID – European atopic dermatitis experts have issued formal guidance on a seriously neglected topic: treatment of the disease during pregnancy, breastfeeding, and in men planning to father children.
The impetus for the project was clear: “,” Christian Vestergaard, MD, PhD, declared at a meeting of the European Task Force on Atopic Dermatitis held in conjunction with the annual congress of the European Academy of Dermatology and Venereology.
He presented highlights of the task force’s position paper on the topic, for which he served as first author. The group’s recommendations are based on expert opinion, since randomized clinical trial literature in this area is nonexistent because of ethical concerns. But the task force, comprising a who’s who in European dermatology, drew on a wealth of collective clinical experience in this area.
“We have all of Europe involved in doing this position statement. It’s meant as what we think is proper treatment and what we can say about the different drugs,” explained Dr. Vestergaard, a dermatologist at the University of Aarhus (Denmark).
Most nonobstetricians are intimidated by atopic dermatitis (AD) in pregnancy, and are concerned about the potential for treatment-related harm to the fetus. As a consequence, they are reluctant to recommend anything beyond weak class I topical corticosteroids and emollients. That’s clearly insufficient in light of the vast scope of need, he asserted. After all, AD affects 15%-20% of all children and persists or reappears in adulthood in one out of five of them. Half of those adults are women, many of whom will at some point wish to become pregnant. And many men with AD will eventually want to father children.
A key message from the task force is that untreated AD in pregnancy potentially places the mother and fetus at risk of serious complications, including Staphylococcus aureus infection and eczema herpeticum.
“If you take one thing away from our position paper, it’s that you can use class II or III topical corticosteroids in pregnant women as first-line therapy,” Dr. Vestergaard said.
This stance contradicts a longstanding widely held concern that topical steroids in pregnancy might increase the risk of facial cleft in the offspring, a worry that has been convincingly debunked in a Cochrane systematic review of 14 studies including more than 1.6 million pregnancies. The report concluded there was no association between topical corticosteroids of any potency with preterm delivery, birth defects, or low Apgar scores (Cochrane Database Syst Rev. 2015 Oct 26. doi: 10.1002/14651858.CD007346.pub3).
The task force recommends that if class II or III topical corticosteroid use in pregnancy exceeds 200 g/month, it’s worth considering add-on UV therapy, with narrow band UVB-311 nm as the regimen of choice; it can be used liberally. UV therapy with psoralens is not advised because of a theoretical risk of mutagenicity.
Product labeling for the topical calcineurin inhibitors declares that the agents should not be used during pregnancy. However, the European task force position paper takes issue with that and declares that topical tacrolimus (Protopic) can be considered an off-label first-line therapy in pregnant women with an insufficient response to liberal use of emollients. The same holds true for breastfeeding patients with AD. Just as when topical corticosteroids are used in the nipple area, topical tacrolimus should be applied after nursing, and the nipple area should be gently cleaned before nursing.
The rationale behind recommending topical tacrolimus as a first-line treatment is that systemic absorption of the drug is trivial. Plus, observational studies of oral tacrolimus in pregnant women who have received a solid organ transplant have shown no increase in congenital malformations.
The task force recommends against the use of topical pimecrolimus (Elidel) or crisaborole (Eucrisa) in pregnancy or lactation due to lack of clinical experience in these settings, Dr. Vestergaard continued.
The task force position is that chlorhexidine and other topical antiseptics – with the notable exception of triclosan – can be used in pregnancy to prevent recurrent skin infections. Aminoglycosides should be avoided, but topical fusidic acid is a reasonable antibiotic for treatment of small areas of clinically infected atopic dermatitis in pregnancy.
Systemic therapies
If disease control is insufficient with topical therapy, it’s appropriate to engage in shared decision-making with the patient regarding systemic treatment. She needs to understand up front that the worldwide overall background stillbirth rate in the general population is about 3%, and that severe congenital malformations are present in up to 6% of all live births.
“You need to inform them that they can have systemic therapy and give birth to a child with congenital defects which have nothing to do with the medication,” noted Dr. Vestergaard.
That said, the task force recommends cyclosporine as the off-label, first-line systemic therapy in pregnancy and lactation when long-term treatment is required. This guidance is based largely upon reassuring evidence in solid organ transplant recipients.
The recommended second-line therapy is systemic corticosteroids, but it’s a qualified recommendation. Dr. Vestergaard and colleagues find that systemic corticosteroid therapy is only rarely needed in pregnant AD patients, and the task force recommendation is to limit the use to less than 2-3 weeks and no more than 0.5 mg/kg per day of prednisone. Dexamethasone is not recommended.
Azathioprine should not be started in pregnancy, according to the task force, but when no other options are available, it may be continued in women already on the drug, albeit at half of the prepregnancy dose.
Dupilumab (Dupixent) is to be avoided in pregnant women with AD until more clinical experience becomes available.
Treatment of prospective fathers with AD
The European task force recommends that topical therapies can be prescribed in prospective fathers without any special concerns. The same is true for systemic corticosteroids. Methotrexate should be halted 3 months before planned pregnancy, as is the case for mycophenolate mofetil (CellCept). Azathioprine is recommended when other options have failed. Cyclosporine is deemed a reasonable option in the treatment of men with severe AD at the time of conception if other treatments have failed; of note, neither the Food and Drug Administration nor the European regulatory agency have issued contraindications for the use of the drug in men who wish to become fathers.
Mycophenolate mofetil carries a theoretical risk of teratogenicity. The European task force recommends that men should use condoms while on the drug and for at least 90 days afterward.
Unplanned pregnancy in women on systemic therapy
The recommended course of action is to immediately stop systemic therapy, intensify appropriate topical therapy in anticipation of worsening AD, and refer the patient to an obstetrician and a teratology information center for an individualized risk assessment. Methotrexate and mycophenolate mofetil are known teratogens.
The full 16-page task force position paper was published shortly before EADV 2019 (J Eur Acad Dermatol Venereol. 2019 Sep;33[9]:1644-59).
The report was developed without commercial sponsorship. Dr. Vestergaard indicated he has received research grants from and/or serves as a consultant to eight pharmaceutical companies.
REPORTING FROM THE EADV CONGRESS
Dupilumab-induced head and neck erythema described in atopic dermatitis patients
MADRID – A growing recognition that from their background skin disease emerged as a hot topic of discussion at a meeting of the European Task Force on Atopic Dermatitis held in conjunction with the annual congress of the European Academy of Dermatology and Venereology.
“During treatment with dupilumab, we saw something that is really different from the classic eczema that patients experienced prior to dupilumab, with no or minimal scaling, itch, or burning sensation. We do not believe this is a delayed effect of dupilumab on that specific region. We think this is a dupilumab-induced entity that we’re looking at. You should take home, in my opinion, that this is a common side effect that’s underreported in daily practice at this moment, and it’s not reported in clinical trials at all,” said Linde de Wijs, MD, of the department of dermatology, Erasmus University Medical Center in Rotterdam, the Netherlands.
She presented a detailed case series of seven affected patients which included histologic examination of lesional skin biopsies. The biopsies were characterized by a perivascular lymphohistiocytic infiltrate, an increase in ectatic capillaries in the papillary dermis, and a notable dearth of spongiosis, eosinophils, and neutrophils. Four patients had bulbous elongated rete ridges evocative of a psoriasiform dermatitis. The overall histologic picture was suggestive of a drug-induced skin reaction.
A striking finding was that, even though AD patients typically place high importance on achieving total clearing of disease on the head and neck, these seven closely studied patients nonetheless rated their treatment satisfaction as 9 out of a possible 10 points. Dr. de Wijs interpreted this as testimony to dupilumab’s potent efficacy and comparatively acceptable safety profile, especially the apparent side effect’s absence of scaling and itch.
“Remember, these are patients with really severe atopic dermatitis who’ve been treated with a lot of immunosuppressants prior to dupilumab,” she said.
Once the investigators began to suspect the existence of a novel dupilumab-induced skin reaction, they conducted a retrospective chart review of more than 150 patients treated with dupilumab (Dupixent) and determined that roughly 30% had developed this distinctive sharply demarcated patchy erythema on the head and neck characterized by absence of itch. The sequence involved clearance of the AD in response to dupilumab, followed by gradual development of the head and neck erythema 10-39 weeks after the start of treatment.
The erythema proved treatment refractory. Dr. de Wijs and her colleagues tried topical corticosteroids, including potent ones, as well as topical tacrolimus, antifungals, antibiotics, emollients, oral steroids, and antihistamines, to no avail. Patch testing to investigate allergic contact dermatitis as a possible etiology was unremarkable.
She hypothesized that, since dupilumab blocks the key signaling pathways for Th2 T-cell differentiation by targeting the interleukin-4 receptor alpha, it’s possible that the biologic promotes a shift towards activation of the Th17 pathway, which might explain the observed histologic findings.
The fact that this erythema wasn’t reported in the major randomized clinical trials of dupilumab underscores the enormous value of clinical practice registries, she said.
“We are not the only ones observing this phenomenon,” noted Dr. de Wijs, citing recently published reports by other investigators (J Am Acad Dermatol. 2020 Jan;82[1]:230-2; JAMA Dermatol. 2019 Jul 1;155[7]:850-2).
Indeed, her talk was immediately followed by a presentation by Sebastien Barbarot, MD, PhD, who reported on a French national retrospective study of head and neck dermatitis arising in patients on dupilumab that was conducted by the French Atopic Dermatitis Network using the organization’s GREAT database. Among 1,000 adult patients with AD treated with the biologic at 29 French centers, 10 developed a de novo head and neck dermatitis, and 32 others experienced more than 50% worsening of eczema signs on the head and neck from baseline beginning about 2 months after starting on dupilumab.
This 4.2% incidence is probably an underestimate, since dermatologists weren’t aware of the phenomenon and didn’t specifically ask patients about it, observed Dr. Barbarot, a dermatologist at the University of Nantes (France).
Among the key findings: No differences in clinical characteristics were found between the de novo and exacerbation groups, nearly half of affected patients had concomitant conjunctivitis, and seven patients discontinued dupilumab because of an intolerable burning sensation on the head/neck.
“I think this condition is quite different from rosacea,” Dr. Barbarot emphasized.
French dermatologists generally turned to topical corticosteroids or topical tacrolimus to treat the face and neck dermatitis, with mixed results; 22 of the 42 patients showed improvement and 8 worsened.
Marjolein de Bruin-Weller, MD, PhD, a dermatologist at Utrecht (the Netherlands) University and head of the Dutch National Eczema Expertise Center, said she and her colleagues have also encountered this dupilumab-related head and neck erythema and are convinced that a subset of affected patients have Malassezia-induced dermatitis with neutrophils present on lesional biopsies. “It responds very well to treatment. I think it’s very important to try itraconazole because sometimes it works,” she said.
Dr. de Wijs replied that she and her coworkers tried 2 weeks of itraconazole in several patients, with no effect. And none of their seven biopsied patients had an increase in neutrophils.
“It might be a very heterogenous polyform entity that we’re now observing,” she commented. Dr. de Bruin-Weller concurred.
Dr. Barbarot said he’d be interested in a formal study of antifungal therapy in patients with dupilumab-related head and neck dermatitis. Mechanistically, it seems plausible that dupilumab-induced activation of the TH17 pathway might lead to proliferation of Malassezia fungus.
Dr. de Wijs and Dr. Barbarot reported having no financial conflicts regarding their respective studies, which were conducted free of commercial sponsorship.
MADRID – A growing recognition that from their background skin disease emerged as a hot topic of discussion at a meeting of the European Task Force on Atopic Dermatitis held in conjunction with the annual congress of the European Academy of Dermatology and Venereology.
“During treatment with dupilumab, we saw something that is really different from the classic eczema that patients experienced prior to dupilumab, with no or minimal scaling, itch, or burning sensation. We do not believe this is a delayed effect of dupilumab on that specific region. We think this is a dupilumab-induced entity that we’re looking at. You should take home, in my opinion, that this is a common side effect that’s underreported in daily practice at this moment, and it’s not reported in clinical trials at all,” said Linde de Wijs, MD, of the department of dermatology, Erasmus University Medical Center in Rotterdam, the Netherlands.
She presented a detailed case series of seven affected patients which included histologic examination of lesional skin biopsies. The biopsies were characterized by a perivascular lymphohistiocytic infiltrate, an increase in ectatic capillaries in the papillary dermis, and a notable dearth of spongiosis, eosinophils, and neutrophils. Four patients had bulbous elongated rete ridges evocative of a psoriasiform dermatitis. The overall histologic picture was suggestive of a drug-induced skin reaction.
A striking finding was that, even though AD patients typically place high importance on achieving total clearing of disease on the head and neck, these seven closely studied patients nonetheless rated their treatment satisfaction as 9 out of a possible 10 points. Dr. de Wijs interpreted this as testimony to dupilumab’s potent efficacy and comparatively acceptable safety profile, especially the apparent side effect’s absence of scaling and itch.
“Remember, these are patients with really severe atopic dermatitis who’ve been treated with a lot of immunosuppressants prior to dupilumab,” she said.
Once the investigators began to suspect the existence of a novel dupilumab-induced skin reaction, they conducted a retrospective chart review of more than 150 patients treated with dupilumab (Dupixent) and determined that roughly 30% had developed this distinctive sharply demarcated patchy erythema on the head and neck characterized by absence of itch. The sequence involved clearance of the AD in response to dupilumab, followed by gradual development of the head and neck erythema 10-39 weeks after the start of treatment.
The erythema proved treatment refractory. Dr. de Wijs and her colleagues tried topical corticosteroids, including potent ones, as well as topical tacrolimus, antifungals, antibiotics, emollients, oral steroids, and antihistamines, to no avail. Patch testing to investigate allergic contact dermatitis as a possible etiology was unremarkable.
She hypothesized that, since dupilumab blocks the key signaling pathways for Th2 T-cell differentiation by targeting the interleukin-4 receptor alpha, it’s possible that the biologic promotes a shift towards activation of the Th17 pathway, which might explain the observed histologic findings.
The fact that this erythema wasn’t reported in the major randomized clinical trials of dupilumab underscores the enormous value of clinical practice registries, she said.
“We are not the only ones observing this phenomenon,” noted Dr. de Wijs, citing recently published reports by other investigators (J Am Acad Dermatol. 2020 Jan;82[1]:230-2; JAMA Dermatol. 2019 Jul 1;155[7]:850-2).
Indeed, her talk was immediately followed by a presentation by Sebastien Barbarot, MD, PhD, who reported on a French national retrospective study of head and neck dermatitis arising in patients on dupilumab that was conducted by the French Atopic Dermatitis Network using the organization’s GREAT database. Among 1,000 adult patients with AD treated with the biologic at 29 French centers, 10 developed a de novo head and neck dermatitis, and 32 others experienced more than 50% worsening of eczema signs on the head and neck from baseline beginning about 2 months after starting on dupilumab.
This 4.2% incidence is probably an underestimate, since dermatologists weren’t aware of the phenomenon and didn’t specifically ask patients about it, observed Dr. Barbarot, a dermatologist at the University of Nantes (France).
Among the key findings: No differences in clinical characteristics were found between the de novo and exacerbation groups, nearly half of affected patients had concomitant conjunctivitis, and seven patients discontinued dupilumab because of an intolerable burning sensation on the head/neck.
“I think this condition is quite different from rosacea,” Dr. Barbarot emphasized.
French dermatologists generally turned to topical corticosteroids or topical tacrolimus to treat the face and neck dermatitis, with mixed results; 22 of the 42 patients showed improvement and 8 worsened.
Marjolein de Bruin-Weller, MD, PhD, a dermatologist at Utrecht (the Netherlands) University and head of the Dutch National Eczema Expertise Center, said she and her colleagues have also encountered this dupilumab-related head and neck erythema and are convinced that a subset of affected patients have Malassezia-induced dermatitis with neutrophils present on lesional biopsies. “It responds very well to treatment. I think it’s very important to try itraconazole because sometimes it works,” she said.
Dr. de Wijs replied that she and her coworkers tried 2 weeks of itraconazole in several patients, with no effect. And none of their seven biopsied patients had an increase in neutrophils.
“It might be a very heterogenous polyform entity that we’re now observing,” she commented. Dr. de Bruin-Weller concurred.
Dr. Barbarot said he’d be interested in a formal study of antifungal therapy in patients with dupilumab-related head and neck dermatitis. Mechanistically, it seems plausible that dupilumab-induced activation of the TH17 pathway might lead to proliferation of Malassezia fungus.
Dr. de Wijs and Dr. Barbarot reported having no financial conflicts regarding their respective studies, which were conducted free of commercial sponsorship.
MADRID – A growing recognition that from their background skin disease emerged as a hot topic of discussion at a meeting of the European Task Force on Atopic Dermatitis held in conjunction with the annual congress of the European Academy of Dermatology and Venereology.
“During treatment with dupilumab, we saw something that is really different from the classic eczema that patients experienced prior to dupilumab, with no or minimal scaling, itch, or burning sensation. We do not believe this is a delayed effect of dupilumab on that specific region. We think this is a dupilumab-induced entity that we’re looking at. You should take home, in my opinion, that this is a common side effect that’s underreported in daily practice at this moment, and it’s not reported in clinical trials at all,” said Linde de Wijs, MD, of the department of dermatology, Erasmus University Medical Center in Rotterdam, the Netherlands.
She presented a detailed case series of seven affected patients which included histologic examination of lesional skin biopsies. The biopsies were characterized by a perivascular lymphohistiocytic infiltrate, an increase in ectatic capillaries in the papillary dermis, and a notable dearth of spongiosis, eosinophils, and neutrophils. Four patients had bulbous elongated rete ridges evocative of a psoriasiform dermatitis. The overall histologic picture was suggestive of a drug-induced skin reaction.
A striking finding was that, even though AD patients typically place high importance on achieving total clearing of disease on the head and neck, these seven closely studied patients nonetheless rated their treatment satisfaction as 9 out of a possible 10 points. Dr. de Wijs interpreted this as testimony to dupilumab’s potent efficacy and comparatively acceptable safety profile, especially the apparent side effect’s absence of scaling and itch.
“Remember, these are patients with really severe atopic dermatitis who’ve been treated with a lot of immunosuppressants prior to dupilumab,” she said.
Once the investigators began to suspect the existence of a novel dupilumab-induced skin reaction, they conducted a retrospective chart review of more than 150 patients treated with dupilumab (Dupixent) and determined that roughly 30% had developed this distinctive sharply demarcated patchy erythema on the head and neck characterized by absence of itch. The sequence involved clearance of the AD in response to dupilumab, followed by gradual development of the head and neck erythema 10-39 weeks after the start of treatment.
The erythema proved treatment refractory. Dr. de Wijs and her colleagues tried topical corticosteroids, including potent ones, as well as topical tacrolimus, antifungals, antibiotics, emollients, oral steroids, and antihistamines, to no avail. Patch testing to investigate allergic contact dermatitis as a possible etiology was unremarkable.
She hypothesized that, since dupilumab blocks the key signaling pathways for Th2 T-cell differentiation by targeting the interleukin-4 receptor alpha, it’s possible that the biologic promotes a shift towards activation of the Th17 pathway, which might explain the observed histologic findings.
The fact that this erythema wasn’t reported in the major randomized clinical trials of dupilumab underscores the enormous value of clinical practice registries, she said.
“We are not the only ones observing this phenomenon,” noted Dr. de Wijs, citing recently published reports by other investigators (J Am Acad Dermatol. 2020 Jan;82[1]:230-2; JAMA Dermatol. 2019 Jul 1;155[7]:850-2).
Indeed, her talk was immediately followed by a presentation by Sebastien Barbarot, MD, PhD, who reported on a French national retrospective study of head and neck dermatitis arising in patients on dupilumab that was conducted by the French Atopic Dermatitis Network using the organization’s GREAT database. Among 1,000 adult patients with AD treated with the biologic at 29 French centers, 10 developed a de novo head and neck dermatitis, and 32 others experienced more than 50% worsening of eczema signs on the head and neck from baseline beginning about 2 months after starting on dupilumab.
This 4.2% incidence is probably an underestimate, since dermatologists weren’t aware of the phenomenon and didn’t specifically ask patients about it, observed Dr. Barbarot, a dermatologist at the University of Nantes (France).
Among the key findings: No differences in clinical characteristics were found between the de novo and exacerbation groups, nearly half of affected patients had concomitant conjunctivitis, and seven patients discontinued dupilumab because of an intolerable burning sensation on the head/neck.
“I think this condition is quite different from rosacea,” Dr. Barbarot emphasized.
French dermatologists generally turned to topical corticosteroids or topical tacrolimus to treat the face and neck dermatitis, with mixed results; 22 of the 42 patients showed improvement and 8 worsened.
Marjolein de Bruin-Weller, MD, PhD, a dermatologist at Utrecht (the Netherlands) University and head of the Dutch National Eczema Expertise Center, said she and her colleagues have also encountered this dupilumab-related head and neck erythema and are convinced that a subset of affected patients have Malassezia-induced dermatitis with neutrophils present on lesional biopsies. “It responds very well to treatment. I think it’s very important to try itraconazole because sometimes it works,” she said.
Dr. de Wijs replied that she and her coworkers tried 2 weeks of itraconazole in several patients, with no effect. And none of their seven biopsied patients had an increase in neutrophils.
“It might be a very heterogenous polyform entity that we’re now observing,” she commented. Dr. de Bruin-Weller concurred.
Dr. Barbarot said he’d be interested in a formal study of antifungal therapy in patients with dupilumab-related head and neck dermatitis. Mechanistically, it seems plausible that dupilumab-induced activation of the TH17 pathway might lead to proliferation of Malassezia fungus.
Dr. de Wijs and Dr. Barbarot reported having no financial conflicts regarding their respective studies, which were conducted free of commercial sponsorship.
REPORTING FROM THE EADV CONGRESS
Adult atopic dermatitis brings increased osteoporosis risk
MADRID – – even if they’ve never taken systemic corticosteroids, according to a large observational Danish national registry study.
A key study finding was that these elevated risks were concentrated in the patients who used potent or superpotent topical corticosteroids. Adult AD patients who used mild- or moderate-potency topical steroids were not at significantly increased risk. Neither were patients on topical calcineurin inhibitors, Jacob P. Thyssen, MD, PhD, reported at a meeting of the European Task Force on Atopic Dermatitis held in conjunction with the annual congress of the European Academy of Dermatology and Venereology.
“The absolute risk is low, but it’s real,” commented Dr. Thyssen, professor of dermatology at the University of Copenhagen.
His advice to colleagues: “Dermatologists should consider alternative treatments in the chronic excessive users of topical corticosteroids, or use them in combination with prophylactic treatment to preserve bone homeostasis in such patients.”
He presented the results of a retrospective case-control study of 10,636 Danish adults with AD and 87,989 matched controls. At baseline in this study, which featured a maximum of 20 years of follow-up starting in 1997, participants had no history of osteoporosis.
Dr. Thyssen expressed the absolute risk of being diagnosed with osteoporosis in the study as follows: If 10,000 adult AD patients were followed for 1 year, on average 23.5 of them would be diagnosed with osteoporosis, a rate more than double the 10.3 per 10,000 in the general population. Moreover, on average, 42.6 out of 10,000 adult AD patients would incur a major osteoporotic fracture during a year of follow-up, compared with 32.3 individuals in the general population.
In the subgroup of patients who never used systemic corticosteroids, the risk of being diagnosed with osteoporosis was 12.8 per 10,000 per year, significantly higher than the 7.4 per 10,000 rate in the general population. Similarly, the 1-year rate of major osteoporotic fractures was 33.1 per 10,000 among the AD group and 29.6 in matched controls.
In a Cox regression analysis adjusted for age, sex, socioeconomic status, body mass index, asthma, and the use of a variety of medications thought to potentially have a negative effect upon bone metabolism, the risk of osteoporosis in the entire group of 10,636 adult AD patients was 51% greater than in matched controls, and their risk of major osteoporotic fractures was 18% greater. In the subgroup of AD patients who never used systemic steroids, the risks of osteoporosis and major osteoporotic fractures were 82% and 14% greater than in controls. The medications adjusted for in the regression analysis included proton pump inhibitors, thiazide diuretics, H2 receptor blockers, statins, cyclosporine, hormone therapy, contraceptives, and psychotropic medications.
Scoring Atopic Dermatitis (SCORAD) ratings were available on roughly 4,000 of the adult AD patients. In an analysis of this large subgroup, disease severity as reflected in SCORAD scores did not explain the increased osteoporosis and fracture risks. However, the use of potent or superpotent topical corticosteroids did. Patients who used potent topical steroids had a statistically significant 16% increased risk of being diagnosed with osteoporosis than nonusers, as well as a 7% increased risk of major osteoporotic fractures. Patients who applied superpotent topical steroids had 42% and 18% increased risks of those two adverse outcomes.
In contrast, neither the use of topical calcineurin inhibitors nor mild- or mid-potency topical steroids was associated with increased risk of bone events in a Cox regression analysis adjusted for potential confounders.
A relationship between the use of high-potency topical corticosteroids and adverse bone events is biologically plausible, according to Dr. Thyssen. He and his coinvestigators have previously documented a 100%-400% increased rate of chemical penetration through atopic skin, which is notoriously barrier damaged.
“We find it very likely that, if you put topical steroids on atopic skin in high amounts and for a very long time, you may have systemic effects,” he said.
A great many adult AD patients do exactly that. When Dr. Thyssen and coworkers analyzed Danish national prescription drug registry data for their patient cohort, they found that roughly one-third of the elderly subgroup had filled prescriptions totaling greater than 2 kg of mometasone or other similar-potency steroids over the previous 10 years.
“So we know that a significant proportion of our atopic dermatitis patients are really high users of topical corticosteroids,” the dermatologist noted.
Dr. Thyssen’s national osteoporosis and fracture study was funded with a government research grant. He reported serving as an advisor to and/or recipient of research grants from AbbVie, Pfizer, Leo Pharma, Eli Lilly, Regeneron, Sanofi Genzyme, and Union Therapeutics.
MADRID – – even if they’ve never taken systemic corticosteroids, according to a large observational Danish national registry study.
A key study finding was that these elevated risks were concentrated in the patients who used potent or superpotent topical corticosteroids. Adult AD patients who used mild- or moderate-potency topical steroids were not at significantly increased risk. Neither were patients on topical calcineurin inhibitors, Jacob P. Thyssen, MD, PhD, reported at a meeting of the European Task Force on Atopic Dermatitis held in conjunction with the annual congress of the European Academy of Dermatology and Venereology.
“The absolute risk is low, but it’s real,” commented Dr. Thyssen, professor of dermatology at the University of Copenhagen.
His advice to colleagues: “Dermatologists should consider alternative treatments in the chronic excessive users of topical corticosteroids, or use them in combination with prophylactic treatment to preserve bone homeostasis in such patients.”
He presented the results of a retrospective case-control study of 10,636 Danish adults with AD and 87,989 matched controls. At baseline in this study, which featured a maximum of 20 years of follow-up starting in 1997, participants had no history of osteoporosis.
Dr. Thyssen expressed the absolute risk of being diagnosed with osteoporosis in the study as follows: If 10,000 adult AD patients were followed for 1 year, on average 23.5 of them would be diagnosed with osteoporosis, a rate more than double the 10.3 per 10,000 in the general population. Moreover, on average, 42.6 out of 10,000 adult AD patients would incur a major osteoporotic fracture during a year of follow-up, compared with 32.3 individuals in the general population.
In the subgroup of patients who never used systemic corticosteroids, the risk of being diagnosed with osteoporosis was 12.8 per 10,000 per year, significantly higher than the 7.4 per 10,000 rate in the general population. Similarly, the 1-year rate of major osteoporotic fractures was 33.1 per 10,000 among the AD group and 29.6 in matched controls.
In a Cox regression analysis adjusted for age, sex, socioeconomic status, body mass index, asthma, and the use of a variety of medications thought to potentially have a negative effect upon bone metabolism, the risk of osteoporosis in the entire group of 10,636 adult AD patients was 51% greater than in matched controls, and their risk of major osteoporotic fractures was 18% greater. In the subgroup of AD patients who never used systemic steroids, the risks of osteoporosis and major osteoporotic fractures were 82% and 14% greater than in controls. The medications adjusted for in the regression analysis included proton pump inhibitors, thiazide diuretics, H2 receptor blockers, statins, cyclosporine, hormone therapy, contraceptives, and psychotropic medications.
Scoring Atopic Dermatitis (SCORAD) ratings were available on roughly 4,000 of the adult AD patients. In an analysis of this large subgroup, disease severity as reflected in SCORAD scores did not explain the increased osteoporosis and fracture risks. However, the use of potent or superpotent topical corticosteroids did. Patients who used potent topical steroids had a statistically significant 16% increased risk of being diagnosed with osteoporosis than nonusers, as well as a 7% increased risk of major osteoporotic fractures. Patients who applied superpotent topical steroids had 42% and 18% increased risks of those two adverse outcomes.
In contrast, neither the use of topical calcineurin inhibitors nor mild- or mid-potency topical steroids was associated with increased risk of bone events in a Cox regression analysis adjusted for potential confounders.
A relationship between the use of high-potency topical corticosteroids and adverse bone events is biologically plausible, according to Dr. Thyssen. He and his coinvestigators have previously documented a 100%-400% increased rate of chemical penetration through atopic skin, which is notoriously barrier damaged.
“We find it very likely that, if you put topical steroids on atopic skin in high amounts and for a very long time, you may have systemic effects,” he said.
A great many adult AD patients do exactly that. When Dr. Thyssen and coworkers analyzed Danish national prescription drug registry data for their patient cohort, they found that roughly one-third of the elderly subgroup had filled prescriptions totaling greater than 2 kg of mometasone or other similar-potency steroids over the previous 10 years.
“So we know that a significant proportion of our atopic dermatitis patients are really high users of topical corticosteroids,” the dermatologist noted.
Dr. Thyssen’s national osteoporosis and fracture study was funded with a government research grant. He reported serving as an advisor to and/or recipient of research grants from AbbVie, Pfizer, Leo Pharma, Eli Lilly, Regeneron, Sanofi Genzyme, and Union Therapeutics.
MADRID – – even if they’ve never taken systemic corticosteroids, according to a large observational Danish national registry study.
A key study finding was that these elevated risks were concentrated in the patients who used potent or superpotent topical corticosteroids. Adult AD patients who used mild- or moderate-potency topical steroids were not at significantly increased risk. Neither were patients on topical calcineurin inhibitors, Jacob P. Thyssen, MD, PhD, reported at a meeting of the European Task Force on Atopic Dermatitis held in conjunction with the annual congress of the European Academy of Dermatology and Venereology.
“The absolute risk is low, but it’s real,” commented Dr. Thyssen, professor of dermatology at the University of Copenhagen.
His advice to colleagues: “Dermatologists should consider alternative treatments in the chronic excessive users of topical corticosteroids, or use them in combination with prophylactic treatment to preserve bone homeostasis in such patients.”
He presented the results of a retrospective case-control study of 10,636 Danish adults with AD and 87,989 matched controls. At baseline in this study, which featured a maximum of 20 years of follow-up starting in 1997, participants had no history of osteoporosis.
Dr. Thyssen expressed the absolute risk of being diagnosed with osteoporosis in the study as follows: If 10,000 adult AD patients were followed for 1 year, on average 23.5 of them would be diagnosed with osteoporosis, a rate more than double the 10.3 per 10,000 in the general population. Moreover, on average, 42.6 out of 10,000 adult AD patients would incur a major osteoporotic fracture during a year of follow-up, compared with 32.3 individuals in the general population.
In the subgroup of patients who never used systemic corticosteroids, the risk of being diagnosed with osteoporosis was 12.8 per 10,000 per year, significantly higher than the 7.4 per 10,000 rate in the general population. Similarly, the 1-year rate of major osteoporotic fractures was 33.1 per 10,000 among the AD group and 29.6 in matched controls.
In a Cox regression analysis adjusted for age, sex, socioeconomic status, body mass index, asthma, and the use of a variety of medications thought to potentially have a negative effect upon bone metabolism, the risk of osteoporosis in the entire group of 10,636 adult AD patients was 51% greater than in matched controls, and their risk of major osteoporotic fractures was 18% greater. In the subgroup of AD patients who never used systemic steroids, the risks of osteoporosis and major osteoporotic fractures were 82% and 14% greater than in controls. The medications adjusted for in the regression analysis included proton pump inhibitors, thiazide diuretics, H2 receptor blockers, statins, cyclosporine, hormone therapy, contraceptives, and psychotropic medications.
Scoring Atopic Dermatitis (SCORAD) ratings were available on roughly 4,000 of the adult AD patients. In an analysis of this large subgroup, disease severity as reflected in SCORAD scores did not explain the increased osteoporosis and fracture risks. However, the use of potent or superpotent topical corticosteroids did. Patients who used potent topical steroids had a statistically significant 16% increased risk of being diagnosed with osteoporosis than nonusers, as well as a 7% increased risk of major osteoporotic fractures. Patients who applied superpotent topical steroids had 42% and 18% increased risks of those two adverse outcomes.
In contrast, neither the use of topical calcineurin inhibitors nor mild- or mid-potency topical steroids was associated with increased risk of bone events in a Cox regression analysis adjusted for potential confounders.
A relationship between the use of high-potency topical corticosteroids and adverse bone events is biologically plausible, according to Dr. Thyssen. He and his coinvestigators have previously documented a 100%-400% increased rate of chemical penetration through atopic skin, which is notoriously barrier damaged.
“We find it very likely that, if you put topical steroids on atopic skin in high amounts and for a very long time, you may have systemic effects,” he said.
A great many adult AD patients do exactly that. When Dr. Thyssen and coworkers analyzed Danish national prescription drug registry data for their patient cohort, they found that roughly one-third of the elderly subgroup had filled prescriptions totaling greater than 2 kg of mometasone or other similar-potency steroids over the previous 10 years.
“So we know that a significant proportion of our atopic dermatitis patients are really high users of topical corticosteroids,” the dermatologist noted.
Dr. Thyssen’s national osteoporosis and fracture study was funded with a government research grant. He reported serving as an advisor to and/or recipient of research grants from AbbVie, Pfizer, Leo Pharma, Eli Lilly, Regeneron, Sanofi Genzyme, and Union Therapeutics.
REPORTING FROM EADV 2019
Which children are at greatest risk for atopic dermatitis?
MADRID – A parental history of asthma or allergic rhinitis significantly increases the risk that a child will develop atopic dermatitis, and that risk doubles if a parent has a history of atopic dermatitis rather than another atopic disease, Nina H. Ravn reported at a meeting of the European Task Force on Atopic Dermatitis held in conjunction with the annual congress of the European Academy of Dermatology and Venereology.
She presented a comprehensive meta-analysis of 149 published studies addressing the risk of developing atopic dermatitis according to parental history of atopic disease. The studies included more than 656,000 participants. The picture that emerged from the meta-analysis was one of a stepwise increase in the risk of pediatric atopic dermatitis according to the type and number of parental atopic diseases present.
“This is something that hopefully can be useful when you talk with parents or parents-to-be with atopic diseases and they want to know how their disease might affect their child,” explained Ms. Ravn of the University of Copenhagen.
It’s also information that clinicians will find helpful in appropriately targeting primary prevention interventions if and when methods of proven efficacy become available. That’s a likely prospect, as this is now an extremely active field of research, she noted.
The meta-analysis showed that a parental history of atopic dermatitis was associated with a 3.3-fold greater risk of atopic dermatitis in the offspring than in families without a parental history of atopy. A parental history of asthma was associated with a 1.56-fold increased risk, while allergic rhinitis in a parent was linked to a 1.68-fold increased risk.
“It does matter what type of atopic disease the parents have,” she observed. “Those with a parental history of asthma or allergic rhinitis can be considered as being at more of an intermediate risk level, while those with a parental history of atopic dermatitis are a particularly high risk group.”
Of note, the risk of pediatric atopic dermatitis was the same regardless of whether the father or mother was the one with a history of atopic disease. If one parent had a history of an atopic disease, the pediatric risk was increased 1.3-fold compared to when the parental history was negative. If both parents had a history of atopic illness, the risk jumped to 2.08-fold. And if one parent had a history of more than one form of atopic disease, the pediatric risk of atopic dermatitis was increased 2.32-fold.
“An interesting result that was new to me what that fathers’ and mothers’ contribution to risk is equal,” said session cochair Andreas Wollenberg, MD, professor of dermatology at Ludwig Maximilian University of Munich. “For the past 2 decades we were always taught that the mother would have a greater impact on that risk.”
“I was also surprised by our findings,” Ms. Ravn replied. “But when we pooled all the data there really was no difference, nor in any of our subanalyses.”
She reported having no financial conflicts regarding her study.
SOURCE: Ravn NH. THE EADV CONGRESS.
MADRID – A parental history of asthma or allergic rhinitis significantly increases the risk that a child will develop atopic dermatitis, and that risk doubles if a parent has a history of atopic dermatitis rather than another atopic disease, Nina H. Ravn reported at a meeting of the European Task Force on Atopic Dermatitis held in conjunction with the annual congress of the European Academy of Dermatology and Venereology.
She presented a comprehensive meta-analysis of 149 published studies addressing the risk of developing atopic dermatitis according to parental history of atopic disease. The studies included more than 656,000 participants. The picture that emerged from the meta-analysis was one of a stepwise increase in the risk of pediatric atopic dermatitis according to the type and number of parental atopic diseases present.
“This is something that hopefully can be useful when you talk with parents or parents-to-be with atopic diseases and they want to know how their disease might affect their child,” explained Ms. Ravn of the University of Copenhagen.
It’s also information that clinicians will find helpful in appropriately targeting primary prevention interventions if and when methods of proven efficacy become available. That’s a likely prospect, as this is now an extremely active field of research, she noted.
The meta-analysis showed that a parental history of atopic dermatitis was associated with a 3.3-fold greater risk of atopic dermatitis in the offspring than in families without a parental history of atopy. A parental history of asthma was associated with a 1.56-fold increased risk, while allergic rhinitis in a parent was linked to a 1.68-fold increased risk.
“It does matter what type of atopic disease the parents have,” she observed. “Those with a parental history of asthma or allergic rhinitis can be considered as being at more of an intermediate risk level, while those with a parental history of atopic dermatitis are a particularly high risk group.”
Of note, the risk of pediatric atopic dermatitis was the same regardless of whether the father or mother was the one with a history of atopic disease. If one parent had a history of an atopic disease, the pediatric risk was increased 1.3-fold compared to when the parental history was negative. If both parents had a history of atopic illness, the risk jumped to 2.08-fold. And if one parent had a history of more than one form of atopic disease, the pediatric risk of atopic dermatitis was increased 2.32-fold.
“An interesting result that was new to me what that fathers’ and mothers’ contribution to risk is equal,” said session cochair Andreas Wollenberg, MD, professor of dermatology at Ludwig Maximilian University of Munich. “For the past 2 decades we were always taught that the mother would have a greater impact on that risk.”
“I was also surprised by our findings,” Ms. Ravn replied. “But when we pooled all the data there really was no difference, nor in any of our subanalyses.”
She reported having no financial conflicts regarding her study.
SOURCE: Ravn NH. THE EADV CONGRESS.
MADRID – A parental history of asthma or allergic rhinitis significantly increases the risk that a child will develop atopic dermatitis, and that risk doubles if a parent has a history of atopic dermatitis rather than another atopic disease, Nina H. Ravn reported at a meeting of the European Task Force on Atopic Dermatitis held in conjunction with the annual congress of the European Academy of Dermatology and Venereology.
She presented a comprehensive meta-analysis of 149 published studies addressing the risk of developing atopic dermatitis according to parental history of atopic disease. The studies included more than 656,000 participants. The picture that emerged from the meta-analysis was one of a stepwise increase in the risk of pediatric atopic dermatitis according to the type and number of parental atopic diseases present.
“This is something that hopefully can be useful when you talk with parents or parents-to-be with atopic diseases and they want to know how their disease might affect their child,” explained Ms. Ravn of the University of Copenhagen.
It’s also information that clinicians will find helpful in appropriately targeting primary prevention interventions if and when methods of proven efficacy become available. That’s a likely prospect, as this is now an extremely active field of research, she noted.
The meta-analysis showed that a parental history of atopic dermatitis was associated with a 3.3-fold greater risk of atopic dermatitis in the offspring than in families without a parental history of atopy. A parental history of asthma was associated with a 1.56-fold increased risk, while allergic rhinitis in a parent was linked to a 1.68-fold increased risk.
“It does matter what type of atopic disease the parents have,” she observed. “Those with a parental history of asthma or allergic rhinitis can be considered as being at more of an intermediate risk level, while those with a parental history of atopic dermatitis are a particularly high risk group.”
Of note, the risk of pediatric atopic dermatitis was the same regardless of whether the father or mother was the one with a history of atopic disease. If one parent had a history of an atopic disease, the pediatric risk was increased 1.3-fold compared to when the parental history was negative. If both parents had a history of atopic illness, the risk jumped to 2.08-fold. And if one parent had a history of more than one form of atopic disease, the pediatric risk of atopic dermatitis was increased 2.32-fold.
“An interesting result that was new to me what that fathers’ and mothers’ contribution to risk is equal,” said session cochair Andreas Wollenberg, MD, professor of dermatology at Ludwig Maximilian University of Munich. “For the past 2 decades we were always taught that the mother would have a greater impact on that risk.”
“I was also surprised by our findings,” Ms. Ravn replied. “But when we pooled all the data there really was no difference, nor in any of our subanalyses.”
She reported having no financial conflicts regarding her study.
SOURCE: Ravn NH. THE EADV CONGRESS.
REPORTING FROM The EADV CONGRESS
Key clinical point: Pediatric atopic dermatitis risk varies according to type of parental history of atopic disease.
Major finding: A parental history of atopic dermatitis is associated with a 3.3-fold increased risk of atopic dermatitis in the child, twice the risk associated with parental asthma or allergic rhinitis.
Study details: This was a systematic review and meta-analysis of 149 published studies with 656,711 participants.
Disclosures: The presenter reported having no financial conflicts regarding the study, conducted free of commercial support.
Source: Ravn NH. The EADV Congress.
Oral BTK inhibitor shows continued promise for pemphigus
MADRID – A novel Dedee F. Murrell, MD, said at the annual congress of the European Academy of Dermatology and Venereology.
“In pemphigus, we have a considerable unmet medical need. We could do with a treatment that has rapid onset, is steroid sparing or avoiding, safe for chronic administration, avoids chronic B cell depletion – which is an issue with rituxumab – is efficacious in both newly diagnosed as well as in our commonly relapsing patients, and is convenient to administer,” observed Dr. Murrell, professor of dermatology at the University of New South Wales in Sydney.
In the phase 2 BELIEVE trial, the BTK inhibitor known for now only as PRN1008 appeared to check all the boxes. However, definitive evidence of the drug’s efficacy and safety must await the results of the ongoing, double-bind, placebo-controlled, pivotal phase 3 PEGASUS trial, which is enrolling a planned 120 patients with pemphigus vulgaris or foliaceus in 19 countries.
Pemphigus is driven by autoantibodies against desmogleins 1 and 3. Even in contemporary practice, this blistering disease has roughly a 5% mortality rate. Current management of the disease with high-dose corticosteroids at 1 mg/kg per day or more with or without rituximab (Rituxan) is challenging because of the associated pronounced toxicities. And even when rituximab is utilized, patients need to be on high-dose steroids for at least 3-6 months before a rituximab response is achieved, Dr. Murrell said.
PRN1008 has three mechanisms of action targeting the drivers of pemphigus and other immune-mediated diseases, she explained. The drug blocks inflammatory B cells, neutrophils, and macrophages; eliminates downstream signalling by antidesmoglein autoantibodies; and prevents production of new autoantibodies. The drug has a double lock-and-key mechanism which makes it highly specific for its target, so treated patients are much less likely to experience bruising, diarrhea, and other off-target effects than is the case with other tyrosine kinase inhibitors.
“Also, PRN1008 is reversible. It comes off its target receptor after about 12 hours, at which point serum levels become low. So if any side effects do develop, the patient can recover quickly, unlike with rituximab, which involves ongoing inhibition of B cells for a long period of time,” the dermatologist noted.
BELIEVE was a phase 2 dose-ranging study of 27 patients with pemphigus treated open-label with PRN1008 for 12 weeks. The primary endpoint was control of disease activity, meaning no new lesions while established lesions showed some evidence of healing on no more than 0.5 mg/kg per day of prednisone. This outcome was achieved in 27% of participants at 2 weeks, 54% at 4 weeks, and 73% at 12 weeks. Autoantibody levels dropped by a mean of 65% at 12 weeks, with a median 70% reduction in Pemphigus Disease Activity Index scores while patients were on an average of just 12 mg of prednisone per day.
Phase 2b of BELIEVE included a separate group of 15 patients on PRN1008 for 24 weeks. Nine achieved a Pemphigus Disease Activity Index score of 0 or 1. Six patients had a complete response, meaning an absence of both new and established lesions while on no or a very low dose of prednisone. Another five patients were unable to achieve a complete response, and the jury was still out on another four still on treatment.
The side effect profile was benign in comparison with that of current standard therapies, she said. It consisted of a handful of cases of mild, transient nausea, headache, or upper abdominal pain and a few Grade 1 infections. There have been no severe treatment-related adverse events in BELIEVE participants.
Patients enrolled in the ongoing phase 3 PEGASUS trial start with a short course of high-dose corticosteroids, followed by double-blind randomization to PRN1008 at 400 mg twice a day or placebo, with a corticosteroid taper. The primary endpoint is durable complete remission at week 37, defined as no lesions being present for at least the previous 8 weeks while on no more than 5 mg/day of prednisone.
Secondary endpoints include cumulative corticosteroid dose through 36 weeks and patient-reported quality of life measures assessed out to 61 weeks. The trial is scheduled for completion in the spring of 2022.
Dr. Murrell reported serving as a consultant to the study sponsor, Principia Biopharma, as well as numerous other pharmaceutical companies.
MADRID – A novel Dedee F. Murrell, MD, said at the annual congress of the European Academy of Dermatology and Venereology.
“In pemphigus, we have a considerable unmet medical need. We could do with a treatment that has rapid onset, is steroid sparing or avoiding, safe for chronic administration, avoids chronic B cell depletion – which is an issue with rituxumab – is efficacious in both newly diagnosed as well as in our commonly relapsing patients, and is convenient to administer,” observed Dr. Murrell, professor of dermatology at the University of New South Wales in Sydney.
In the phase 2 BELIEVE trial, the BTK inhibitor known for now only as PRN1008 appeared to check all the boxes. However, definitive evidence of the drug’s efficacy and safety must await the results of the ongoing, double-bind, placebo-controlled, pivotal phase 3 PEGASUS trial, which is enrolling a planned 120 patients with pemphigus vulgaris or foliaceus in 19 countries.
Pemphigus is driven by autoantibodies against desmogleins 1 and 3. Even in contemporary practice, this blistering disease has roughly a 5% mortality rate. Current management of the disease with high-dose corticosteroids at 1 mg/kg per day or more with or without rituximab (Rituxan) is challenging because of the associated pronounced toxicities. And even when rituximab is utilized, patients need to be on high-dose steroids for at least 3-6 months before a rituximab response is achieved, Dr. Murrell said.
PRN1008 has three mechanisms of action targeting the drivers of pemphigus and other immune-mediated diseases, she explained. The drug blocks inflammatory B cells, neutrophils, and macrophages; eliminates downstream signalling by antidesmoglein autoantibodies; and prevents production of new autoantibodies. The drug has a double lock-and-key mechanism which makes it highly specific for its target, so treated patients are much less likely to experience bruising, diarrhea, and other off-target effects than is the case with other tyrosine kinase inhibitors.
“Also, PRN1008 is reversible. It comes off its target receptor after about 12 hours, at which point serum levels become low. So if any side effects do develop, the patient can recover quickly, unlike with rituximab, which involves ongoing inhibition of B cells for a long period of time,” the dermatologist noted.
BELIEVE was a phase 2 dose-ranging study of 27 patients with pemphigus treated open-label with PRN1008 for 12 weeks. The primary endpoint was control of disease activity, meaning no new lesions while established lesions showed some evidence of healing on no more than 0.5 mg/kg per day of prednisone. This outcome was achieved in 27% of participants at 2 weeks, 54% at 4 weeks, and 73% at 12 weeks. Autoantibody levels dropped by a mean of 65% at 12 weeks, with a median 70% reduction in Pemphigus Disease Activity Index scores while patients were on an average of just 12 mg of prednisone per day.
Phase 2b of BELIEVE included a separate group of 15 patients on PRN1008 for 24 weeks. Nine achieved a Pemphigus Disease Activity Index score of 0 or 1. Six patients had a complete response, meaning an absence of both new and established lesions while on no or a very low dose of prednisone. Another five patients were unable to achieve a complete response, and the jury was still out on another four still on treatment.
The side effect profile was benign in comparison with that of current standard therapies, she said. It consisted of a handful of cases of mild, transient nausea, headache, or upper abdominal pain and a few Grade 1 infections. There have been no severe treatment-related adverse events in BELIEVE participants.
Patients enrolled in the ongoing phase 3 PEGASUS trial start with a short course of high-dose corticosteroids, followed by double-blind randomization to PRN1008 at 400 mg twice a day or placebo, with a corticosteroid taper. The primary endpoint is durable complete remission at week 37, defined as no lesions being present for at least the previous 8 weeks while on no more than 5 mg/day of prednisone.
Secondary endpoints include cumulative corticosteroid dose through 36 weeks and patient-reported quality of life measures assessed out to 61 weeks. The trial is scheduled for completion in the spring of 2022.
Dr. Murrell reported serving as a consultant to the study sponsor, Principia Biopharma, as well as numerous other pharmaceutical companies.
MADRID – A novel Dedee F. Murrell, MD, said at the annual congress of the European Academy of Dermatology and Venereology.
“In pemphigus, we have a considerable unmet medical need. We could do with a treatment that has rapid onset, is steroid sparing or avoiding, safe for chronic administration, avoids chronic B cell depletion – which is an issue with rituxumab – is efficacious in both newly diagnosed as well as in our commonly relapsing patients, and is convenient to administer,” observed Dr. Murrell, professor of dermatology at the University of New South Wales in Sydney.
In the phase 2 BELIEVE trial, the BTK inhibitor known for now only as PRN1008 appeared to check all the boxes. However, definitive evidence of the drug’s efficacy and safety must await the results of the ongoing, double-bind, placebo-controlled, pivotal phase 3 PEGASUS trial, which is enrolling a planned 120 patients with pemphigus vulgaris or foliaceus in 19 countries.
Pemphigus is driven by autoantibodies against desmogleins 1 and 3. Even in contemporary practice, this blistering disease has roughly a 5% mortality rate. Current management of the disease with high-dose corticosteroids at 1 mg/kg per day or more with or without rituximab (Rituxan) is challenging because of the associated pronounced toxicities. And even when rituximab is utilized, patients need to be on high-dose steroids for at least 3-6 months before a rituximab response is achieved, Dr. Murrell said.
PRN1008 has three mechanisms of action targeting the drivers of pemphigus and other immune-mediated diseases, she explained. The drug blocks inflammatory B cells, neutrophils, and macrophages; eliminates downstream signalling by antidesmoglein autoantibodies; and prevents production of new autoantibodies. The drug has a double lock-and-key mechanism which makes it highly specific for its target, so treated patients are much less likely to experience bruising, diarrhea, and other off-target effects than is the case with other tyrosine kinase inhibitors.
“Also, PRN1008 is reversible. It comes off its target receptor after about 12 hours, at which point serum levels become low. So if any side effects do develop, the patient can recover quickly, unlike with rituximab, which involves ongoing inhibition of B cells for a long period of time,” the dermatologist noted.
BELIEVE was a phase 2 dose-ranging study of 27 patients with pemphigus treated open-label with PRN1008 for 12 weeks. The primary endpoint was control of disease activity, meaning no new lesions while established lesions showed some evidence of healing on no more than 0.5 mg/kg per day of prednisone. This outcome was achieved in 27% of participants at 2 weeks, 54% at 4 weeks, and 73% at 12 weeks. Autoantibody levels dropped by a mean of 65% at 12 weeks, with a median 70% reduction in Pemphigus Disease Activity Index scores while patients were on an average of just 12 mg of prednisone per day.
Phase 2b of BELIEVE included a separate group of 15 patients on PRN1008 for 24 weeks. Nine achieved a Pemphigus Disease Activity Index score of 0 or 1. Six patients had a complete response, meaning an absence of both new and established lesions while on no or a very low dose of prednisone. Another five patients were unable to achieve a complete response, and the jury was still out on another four still on treatment.
The side effect profile was benign in comparison with that of current standard therapies, she said. It consisted of a handful of cases of mild, transient nausea, headache, or upper abdominal pain and a few Grade 1 infections. There have been no severe treatment-related adverse events in BELIEVE participants.
Patients enrolled in the ongoing phase 3 PEGASUS trial start with a short course of high-dose corticosteroids, followed by double-blind randomization to PRN1008 at 400 mg twice a day or placebo, with a corticosteroid taper. The primary endpoint is durable complete remission at week 37, defined as no lesions being present for at least the previous 8 weeks while on no more than 5 mg/day of prednisone.
Secondary endpoints include cumulative corticosteroid dose through 36 weeks and patient-reported quality of life measures assessed out to 61 weeks. The trial is scheduled for completion in the spring of 2022.
Dr. Murrell reported serving as a consultant to the study sponsor, Principia Biopharma, as well as numerous other pharmaceutical companies.
REPORTING FROM THE EADV CONGRESS
Certolizumab safety profile varies widely across indications
MADRID – , Andrew Blauvelt, MD, reported at the annual congress of the European Academy of Dermatology and Venereology.
He presented a comprehensive analysis of safety data from all 49 clinical trials of the tumor necrosis factor inhibitor for its approved indications. The data set included 11,317 patients who received certolizumab for a collective 21,695 person-years in 27 trials in rheumatoid arthritis patients, 5 in psoriasis, 15 for Crohn’s disease, and one trial each for axial spondyloarthritis and psoriatic arthritis.
“It’s not real-world data, but it is a large group of patients [studied] over many years,” noted Dr. Blauvelt, a dermatologist and president of the Oregon Medical Research Center, Portland.
As a renowned authority on psoriasis, he was part of a multidisciplinary expert panel commissioned by UCB to analyze serious adverse events in the complete clinical trials experience involving the company’s tumor necrosis factor inhibitor certolizumab (Cimzia). The panel included experts from rheumatology, gastroenterology, epidemiology, and other disciplines.
The key takeaway: “When you think about the serious side effects of the drug, you have to think about what the indication is, whether the patients are on systemic corticosteroids, and whether they’re heavy or not,” Dr. Blauvelt said.
Take, for example, the risk of serious infections requiring treatment with intravenous antibiotics. The incidence rates ranged from a low of 1.5 per 100 patient-years in psoriasis patients on certolizumab to a high of 5.97 in those with Crohn’s disease, with rates of 3.44 cases per 100 patient-years among rheumatoid arthritis patients and 1.64-1.67 in those with psoriatic arthritis and ankylosing spondylitis, respectively. Patients with Crohn’s disease were 2.22-fold more likely than were those with rheumatoid arthritis to experience a serious infection during their clinical trial experience on certolizumab. In contrast, psoriasis patients had a 52% relative risk reduction and those with psoriatic arthritis were 31% less likely to develop a serious infection compared with those with rheumatoid arthritis.
The explanation for these highly variable serious infection rates lies in part on the huge differences in the concurrent use of systemic corticosteroids with certolizumab across indications. A mere 3.3% of psoriasis patients were also on steroids, compared with 46.2% of rheumatoid arthritis patients, 50.8% of those with ankylosing spondylitis, and about 25% of the Crohn’s disease and psoriatic arthritis patients, he noted.
Advanced age was independently associated with increased risk of serious infections. Patients aged 65 or older were 1.68-fold more likely to experience this event than were those under age 45. And patients whose disease duration was 10 years or more at baseline had a 1.36-fold increased serious infection risk compared with those who had less than a 1-year-long disease history, independent of which disease they had.
The prevalence of baseline obesity varied by indication. The mean body mass index was 30.1 kg/m2 in the psoriasis patients, 29.8 kg/m2 in those with psoriatic arthritis, lowest at 24 kg/m2 in Crohn’s disease patients, and a bit over 27 kg/m2 in those with rheumatoid arthritis or ankylosing spondylitis.
Obesity alone was not an independent risk factor for serious infection in certolizumab-treated patients; however, the combination of a BMI of 30 kg/m2 or more plus systemic corticosteroid use was associated with a greater risk than with steroids alone.
Based upon a multivariate regression analysis adjusted for age, sex, indication, disease duration, use of methotrexate, and prior use of other TNF inhibitors, the investigators calculated that in patients with Crohn’s disease 16.6% of serious infections in patients on certolizumab were attributable to systemic corticosteroid use.
Risks of major adverse cardiovascular events and cancer on certolizumab
The risk of major adverse cardiovascular events (MACE) while on certolizumab ranged from a high of 0.62 MACE events per 100 patient-years in the rheumatoid arthritis population to a low of 0.1 per 100 patient-years in patients treated for Crohn’s disease or ankylosing spondylitis. Psoriasis and psoriatic arthritis patients had MACE rates of 0.27 and 0.54, respectively.
Obesity was independently associated with increased risk of an acute MI and other MACEs. So was advanced age. No surprises there. The investigators calculated that 16.7% of MACEs in patients on certolizumab were attributable to obesity and another 20.9% were attributable to use of systemic corticosteroids.
The incidence rate for all malignancies, including nonmelanoma skin cancer, ranged from a low of 0.46 cases per 100 patient-years in the psoriatic arthritis cohort on certolizumab to a high of 0.93 in those with rheumatoid arthritis, with rates of 0.68, 0.73, and 0.51 in patients with psoriasis, Crohn’s disease, and ankylosing spondylitis, respectively.
Neither systemic corticosteroids, obesity, disease duration, or prior exposure to a TNF inhibitor was linked to increased risk of cancer in patients on certolizumab. The standout risk factor was age: Patients who were 65 or older at baseline were 11.4-fold more likely to develop cancer during participation in their clinical trial than were those younger than 45. Those who were 45 to 65 years old were 4.3-fold more likely to be diagnosed with a malignancy than were those younger than age 45.
Of note, concomitant use of methotrexate was associated with a statistically significant 28% reduction in malignancy risk.
Dr. Blauvelt reported serving as a consultant to and receiving research funding from UCB, the study sponsor, as well as more than two dozen other pharmaceutical companies.
SOURCE: Blauvelt A. EADV Congress, Abstract FC04.06.
MADRID – , Andrew Blauvelt, MD, reported at the annual congress of the European Academy of Dermatology and Venereology.
He presented a comprehensive analysis of safety data from all 49 clinical trials of the tumor necrosis factor inhibitor for its approved indications. The data set included 11,317 patients who received certolizumab for a collective 21,695 person-years in 27 trials in rheumatoid arthritis patients, 5 in psoriasis, 15 for Crohn’s disease, and one trial each for axial spondyloarthritis and psoriatic arthritis.
“It’s not real-world data, but it is a large group of patients [studied] over many years,” noted Dr. Blauvelt, a dermatologist and president of the Oregon Medical Research Center, Portland.
As a renowned authority on psoriasis, he was part of a multidisciplinary expert panel commissioned by UCB to analyze serious adverse events in the complete clinical trials experience involving the company’s tumor necrosis factor inhibitor certolizumab (Cimzia). The panel included experts from rheumatology, gastroenterology, epidemiology, and other disciplines.
The key takeaway: “When you think about the serious side effects of the drug, you have to think about what the indication is, whether the patients are on systemic corticosteroids, and whether they’re heavy or not,” Dr. Blauvelt said.
Take, for example, the risk of serious infections requiring treatment with intravenous antibiotics. The incidence rates ranged from a low of 1.5 per 100 patient-years in psoriasis patients on certolizumab to a high of 5.97 in those with Crohn’s disease, with rates of 3.44 cases per 100 patient-years among rheumatoid arthritis patients and 1.64-1.67 in those with psoriatic arthritis and ankylosing spondylitis, respectively. Patients with Crohn’s disease were 2.22-fold more likely than were those with rheumatoid arthritis to experience a serious infection during their clinical trial experience on certolizumab. In contrast, psoriasis patients had a 52% relative risk reduction and those with psoriatic arthritis were 31% less likely to develop a serious infection compared with those with rheumatoid arthritis.
The explanation for these highly variable serious infection rates lies in part on the huge differences in the concurrent use of systemic corticosteroids with certolizumab across indications. A mere 3.3% of psoriasis patients were also on steroids, compared with 46.2% of rheumatoid arthritis patients, 50.8% of those with ankylosing spondylitis, and about 25% of the Crohn’s disease and psoriatic arthritis patients, he noted.
Advanced age was independently associated with increased risk of serious infections. Patients aged 65 or older were 1.68-fold more likely to experience this event than were those under age 45. And patients whose disease duration was 10 years or more at baseline had a 1.36-fold increased serious infection risk compared with those who had less than a 1-year-long disease history, independent of which disease they had.
The prevalence of baseline obesity varied by indication. The mean body mass index was 30.1 kg/m2 in the psoriasis patients, 29.8 kg/m2 in those with psoriatic arthritis, lowest at 24 kg/m2 in Crohn’s disease patients, and a bit over 27 kg/m2 in those with rheumatoid arthritis or ankylosing spondylitis.
Obesity alone was not an independent risk factor for serious infection in certolizumab-treated patients; however, the combination of a BMI of 30 kg/m2 or more plus systemic corticosteroid use was associated with a greater risk than with steroids alone.
Based upon a multivariate regression analysis adjusted for age, sex, indication, disease duration, use of methotrexate, and prior use of other TNF inhibitors, the investigators calculated that in patients with Crohn’s disease 16.6% of serious infections in patients on certolizumab were attributable to systemic corticosteroid use.
Risks of major adverse cardiovascular events and cancer on certolizumab
The risk of major adverse cardiovascular events (MACE) while on certolizumab ranged from a high of 0.62 MACE events per 100 patient-years in the rheumatoid arthritis population to a low of 0.1 per 100 patient-years in patients treated for Crohn’s disease or ankylosing spondylitis. Psoriasis and psoriatic arthritis patients had MACE rates of 0.27 and 0.54, respectively.
Obesity was independently associated with increased risk of an acute MI and other MACEs. So was advanced age. No surprises there. The investigators calculated that 16.7% of MACEs in patients on certolizumab were attributable to obesity and another 20.9% were attributable to use of systemic corticosteroids.
The incidence rate for all malignancies, including nonmelanoma skin cancer, ranged from a low of 0.46 cases per 100 patient-years in the psoriatic arthritis cohort on certolizumab to a high of 0.93 in those with rheumatoid arthritis, with rates of 0.68, 0.73, and 0.51 in patients with psoriasis, Crohn’s disease, and ankylosing spondylitis, respectively.
Neither systemic corticosteroids, obesity, disease duration, or prior exposure to a TNF inhibitor was linked to increased risk of cancer in patients on certolizumab. The standout risk factor was age: Patients who were 65 or older at baseline were 11.4-fold more likely to develop cancer during participation in their clinical trial than were those younger than 45. Those who were 45 to 65 years old were 4.3-fold more likely to be diagnosed with a malignancy than were those younger than age 45.
Of note, concomitant use of methotrexate was associated with a statistically significant 28% reduction in malignancy risk.
Dr. Blauvelt reported serving as a consultant to and receiving research funding from UCB, the study sponsor, as well as more than two dozen other pharmaceutical companies.
SOURCE: Blauvelt A. EADV Congress, Abstract FC04.06.
MADRID – , Andrew Blauvelt, MD, reported at the annual congress of the European Academy of Dermatology and Venereology.
He presented a comprehensive analysis of safety data from all 49 clinical trials of the tumor necrosis factor inhibitor for its approved indications. The data set included 11,317 patients who received certolizumab for a collective 21,695 person-years in 27 trials in rheumatoid arthritis patients, 5 in psoriasis, 15 for Crohn’s disease, and one trial each for axial spondyloarthritis and psoriatic arthritis.
“It’s not real-world data, but it is a large group of patients [studied] over many years,” noted Dr. Blauvelt, a dermatologist and president of the Oregon Medical Research Center, Portland.
As a renowned authority on psoriasis, he was part of a multidisciplinary expert panel commissioned by UCB to analyze serious adverse events in the complete clinical trials experience involving the company’s tumor necrosis factor inhibitor certolizumab (Cimzia). The panel included experts from rheumatology, gastroenterology, epidemiology, and other disciplines.
The key takeaway: “When you think about the serious side effects of the drug, you have to think about what the indication is, whether the patients are on systemic corticosteroids, and whether they’re heavy or not,” Dr. Blauvelt said.
Take, for example, the risk of serious infections requiring treatment with intravenous antibiotics. The incidence rates ranged from a low of 1.5 per 100 patient-years in psoriasis patients on certolizumab to a high of 5.97 in those with Crohn’s disease, with rates of 3.44 cases per 100 patient-years among rheumatoid arthritis patients and 1.64-1.67 in those with psoriatic arthritis and ankylosing spondylitis, respectively. Patients with Crohn’s disease were 2.22-fold more likely than were those with rheumatoid arthritis to experience a serious infection during their clinical trial experience on certolizumab. In contrast, psoriasis patients had a 52% relative risk reduction and those with psoriatic arthritis were 31% less likely to develop a serious infection compared with those with rheumatoid arthritis.
The explanation for these highly variable serious infection rates lies in part on the huge differences in the concurrent use of systemic corticosteroids with certolizumab across indications. A mere 3.3% of psoriasis patients were also on steroids, compared with 46.2% of rheumatoid arthritis patients, 50.8% of those with ankylosing spondylitis, and about 25% of the Crohn’s disease and psoriatic arthritis patients, he noted.
Advanced age was independently associated with increased risk of serious infections. Patients aged 65 or older were 1.68-fold more likely to experience this event than were those under age 45. And patients whose disease duration was 10 years or more at baseline had a 1.36-fold increased serious infection risk compared with those who had less than a 1-year-long disease history, independent of which disease they had.
The prevalence of baseline obesity varied by indication. The mean body mass index was 30.1 kg/m2 in the psoriasis patients, 29.8 kg/m2 in those with psoriatic arthritis, lowest at 24 kg/m2 in Crohn’s disease patients, and a bit over 27 kg/m2 in those with rheumatoid arthritis or ankylosing spondylitis.
Obesity alone was not an independent risk factor for serious infection in certolizumab-treated patients; however, the combination of a BMI of 30 kg/m2 or more plus systemic corticosteroid use was associated with a greater risk than with steroids alone.
Based upon a multivariate regression analysis adjusted for age, sex, indication, disease duration, use of methotrexate, and prior use of other TNF inhibitors, the investigators calculated that in patients with Crohn’s disease 16.6% of serious infections in patients on certolizumab were attributable to systemic corticosteroid use.
Risks of major adverse cardiovascular events and cancer on certolizumab
The risk of major adverse cardiovascular events (MACE) while on certolizumab ranged from a high of 0.62 MACE events per 100 patient-years in the rheumatoid arthritis population to a low of 0.1 per 100 patient-years in patients treated for Crohn’s disease or ankylosing spondylitis. Psoriasis and psoriatic arthritis patients had MACE rates of 0.27 and 0.54, respectively.
Obesity was independently associated with increased risk of an acute MI and other MACEs. So was advanced age. No surprises there. The investigators calculated that 16.7% of MACEs in patients on certolizumab were attributable to obesity and another 20.9% were attributable to use of systemic corticosteroids.
The incidence rate for all malignancies, including nonmelanoma skin cancer, ranged from a low of 0.46 cases per 100 patient-years in the psoriatic arthritis cohort on certolizumab to a high of 0.93 in those with rheumatoid arthritis, with rates of 0.68, 0.73, and 0.51 in patients with psoriasis, Crohn’s disease, and ankylosing spondylitis, respectively.
Neither systemic corticosteroids, obesity, disease duration, or prior exposure to a TNF inhibitor was linked to increased risk of cancer in patients on certolizumab. The standout risk factor was age: Patients who were 65 or older at baseline were 11.4-fold more likely to develop cancer during participation in their clinical trial than were those younger than 45. Those who were 45 to 65 years old were 4.3-fold more likely to be diagnosed with a malignancy than were those younger than age 45.
Of note, concomitant use of methotrexate was associated with a statistically significant 28% reduction in malignancy risk.
Dr. Blauvelt reported serving as a consultant to and receiving research funding from UCB, the study sponsor, as well as more than two dozen other pharmaceutical companies.
SOURCE: Blauvelt A. EADV Congress, Abstract FC04.06.
REPORTING FROM THE EADV CONGRESS
Oral baricitinib performs well in phase 3 for atopic dermatitis
MADRID – Adding the oral Janus kinase (JAK) inhibitor baricitinib to standard atopic dermatitis therapy with low- and midpotency topical corticosteroids markedly improved disease severity and key patient-reported outcomes, compared with topical corticosteroids alone, in the phase 3, randomized, double-blind BREEZE-AD7 trial, Kristian Reich, MD, reported at the annual congress of the European Academy of Dermatology and Venereology.
in the phase 3 BREEZE-AD1 and -AD2 trials. But BREEZE-AD7 further advances the field because it’s the first phase 3 study testing the efficacy of a JAK inhibitor in combination with low- and midpotency topical steroids.
“I think this study is important because it looks into the situation that’s more like what happens in the real world, which is, as with dupilumab and other drugs, we use the systemic agent in combination with topical therapies and, in particular, with topical corticosteroids,” commented Dr. Reich, professor of dermatology at University Medical Center, Hamburg, and medical director at SCIderm, a scientific research company.
“This is what I think we can expect from existing and upcoming systemic therapies in atopic dermatitis: We will use them in combination with topical corticosteroids, and hopefully this will allow patients to dramatically reduce the concomitant use of topical corticosteroids, as shown here in BREEZE-AD7,” he added.
BREEZE-AD7 was a 16-week study that included 329 adults with moderate or severe atopic dermatitis who were randomized to low- and midpotency topical corticosteroids plus either baricitinib at 2 mg once daily, baricitinib at 4 mg once daily, or placebo. The group’s mean baseline Eczema Area and Severity Index (EASI) score was 29. Overall, 45% of participants had a baseline Investigator’s Global Assessment (IGA) of disease severity of 4 on a 0-4 scale.
The primary endpoint was achievement of an IGA of 0 or 1, meaning clear or almost clear, along with at least a 2-point IGA improvement from baseline at week 16. This was accomplished in 30.6% of those on 4 mg/day of baricitinib, 23.9% of patients in the 2-mg group, and 14.7% of controls.
The 4-mg dose of baricitinib was statistically superior to placebo; the 2-mg dose was not. However, Dr. Reich indicated he was untroubled by this because the primary endpoint was set at a high bar, and both doses of baricitinib proved to be significantly better than topical steroids plus placebo in terms of EASI 75 response rates, as well as reductions in itch, skin pain, and sleep problems, which aren’t captured in EASI scores (see graphic).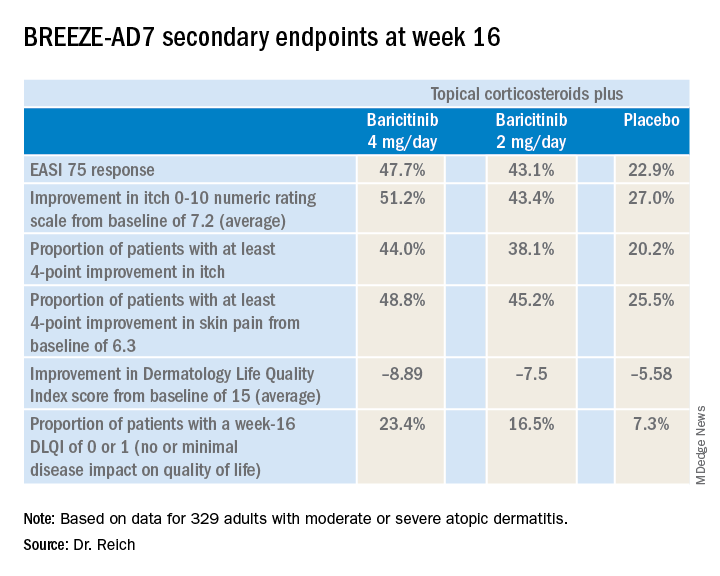
“One of my big learnings from this year’s EADV is that we have to rethink the dimensions of atopic dermatitis. I think we have underestimated the relevance of important symptoms such as itch, the impact atopic dermatitis has on pain, and the effect it has on sleeping problems,” the dermatologist said. “My feeling is that baricitinib is strongest in reducing itch, improving sleep, and reducing pain, but it also has good effects on the clinical signs of atopic dermatitis.”
The baricitinib-treated patients’ rapidity of improvement in the various endpoints was particularly impressive. Both doses of the JAK 1/2 inhibitor showed significant separation from the control group in the first week, and the majority of improvement occurred by week 4.
A key finding was that patients on baricitinib at 2 mg/day and 4 mg/day used a mean total of 162 g and 137 g of midpotency topical steroids, respectively, during the 16 weeks, compared with 225 g in the control group. The higher-dose baricitinib group was topical corticosteroid-free on 33% of study days, compared with 25% of days for the baricitinib 2 mg patients and 17% of days for controls.
In terms of safety, there was a case of pulmonary embolism in the higher-dose baricitinib group and an opportunistic toxoplasmosis eye infection in the control population. The frequency of oral herpes and herpes simplex virus infections was 2.8% in controls, 4.6% in the baricitinib 2-mg group, and 6.3% in the 4-mg group. There was also a signal of a dose-dependent increased risk of new-onset acne, with rates of 0.9% in controls and patients on baricitinib 2 mg, climbing to 3.6% with baricitinib 4 mg.
“In phase 2 results with upadacitinib [another oral JAK inhibitor], we saw that more than 10% of patients in the highest-dose group developed what was classified as acne. I cannot explain this, but it’s something we will monitor in the future,” Dr. Reich promised.
A fuller picture of baricitinib’s safety profile in the setting of atopic dermatitis clearly requires larger and longer-term studies, he added.
Baricitinib at the 2 mg daily dose is already marketed as Olumiant for the treatment of rheumatoid arthritis, with labeling that includes a boxed warning about serious infections, malignancy, and thrombosis. The Food and Drug Administration did not approve the 4-mg dose after determining that its higher safety hazard outweighed the efficacy advantage over the lower dose.
The BREEZE-AD7 study was sponsored by Eli Lilly. Dr. Reich reported serving as an adviser to, paid speaker for, and recipient of research grants from that pharmaceutical company and more than two dozen others.
MADRID – Adding the oral Janus kinase (JAK) inhibitor baricitinib to standard atopic dermatitis therapy with low- and midpotency topical corticosteroids markedly improved disease severity and key patient-reported outcomes, compared with topical corticosteroids alone, in the phase 3, randomized, double-blind BREEZE-AD7 trial, Kristian Reich, MD, reported at the annual congress of the European Academy of Dermatology and Venereology.
in the phase 3 BREEZE-AD1 and -AD2 trials. But BREEZE-AD7 further advances the field because it’s the first phase 3 study testing the efficacy of a JAK inhibitor in combination with low- and midpotency topical steroids.
“I think this study is important because it looks into the situation that’s more like what happens in the real world, which is, as with dupilumab and other drugs, we use the systemic agent in combination with topical therapies and, in particular, with topical corticosteroids,” commented Dr. Reich, professor of dermatology at University Medical Center, Hamburg, and medical director at SCIderm, a scientific research company.
“This is what I think we can expect from existing and upcoming systemic therapies in atopic dermatitis: We will use them in combination with topical corticosteroids, and hopefully this will allow patients to dramatically reduce the concomitant use of topical corticosteroids, as shown here in BREEZE-AD7,” he added.
BREEZE-AD7 was a 16-week study that included 329 adults with moderate or severe atopic dermatitis who were randomized to low- and midpotency topical corticosteroids plus either baricitinib at 2 mg once daily, baricitinib at 4 mg once daily, or placebo. The group’s mean baseline Eczema Area and Severity Index (EASI) score was 29. Overall, 45% of participants had a baseline Investigator’s Global Assessment (IGA) of disease severity of 4 on a 0-4 scale.
The primary endpoint was achievement of an IGA of 0 or 1, meaning clear or almost clear, along with at least a 2-point IGA improvement from baseline at week 16. This was accomplished in 30.6% of those on 4 mg/day of baricitinib, 23.9% of patients in the 2-mg group, and 14.7% of controls.
The 4-mg dose of baricitinib was statistically superior to placebo; the 2-mg dose was not. However, Dr. Reich indicated he was untroubled by this because the primary endpoint was set at a high bar, and both doses of baricitinib proved to be significantly better than topical steroids plus placebo in terms of EASI 75 response rates, as well as reductions in itch, skin pain, and sleep problems, which aren’t captured in EASI scores (see graphic).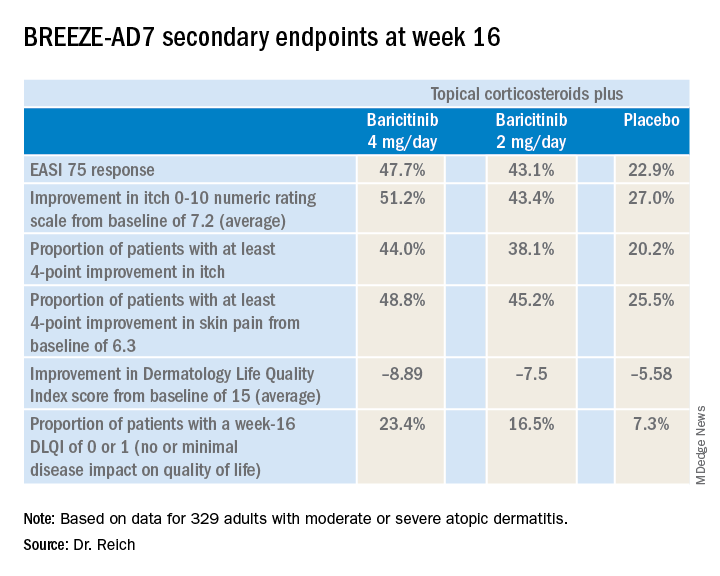
“One of my big learnings from this year’s EADV is that we have to rethink the dimensions of atopic dermatitis. I think we have underestimated the relevance of important symptoms such as itch, the impact atopic dermatitis has on pain, and the effect it has on sleeping problems,” the dermatologist said. “My feeling is that baricitinib is strongest in reducing itch, improving sleep, and reducing pain, but it also has good effects on the clinical signs of atopic dermatitis.”
The baricitinib-treated patients’ rapidity of improvement in the various endpoints was particularly impressive. Both doses of the JAK 1/2 inhibitor showed significant separation from the control group in the first week, and the majority of improvement occurred by week 4.
A key finding was that patients on baricitinib at 2 mg/day and 4 mg/day used a mean total of 162 g and 137 g of midpotency topical steroids, respectively, during the 16 weeks, compared with 225 g in the control group. The higher-dose baricitinib group was topical corticosteroid-free on 33% of study days, compared with 25% of days for the baricitinib 2 mg patients and 17% of days for controls.
In terms of safety, there was a case of pulmonary embolism in the higher-dose baricitinib group and an opportunistic toxoplasmosis eye infection in the control population. The frequency of oral herpes and herpes simplex virus infections was 2.8% in controls, 4.6% in the baricitinib 2-mg group, and 6.3% in the 4-mg group. There was also a signal of a dose-dependent increased risk of new-onset acne, with rates of 0.9% in controls and patients on baricitinib 2 mg, climbing to 3.6% with baricitinib 4 mg.
“In phase 2 results with upadacitinib [another oral JAK inhibitor], we saw that more than 10% of patients in the highest-dose group developed what was classified as acne. I cannot explain this, but it’s something we will monitor in the future,” Dr. Reich promised.
A fuller picture of baricitinib’s safety profile in the setting of atopic dermatitis clearly requires larger and longer-term studies, he added.
Baricitinib at the 2 mg daily dose is already marketed as Olumiant for the treatment of rheumatoid arthritis, with labeling that includes a boxed warning about serious infections, malignancy, and thrombosis. The Food and Drug Administration did not approve the 4-mg dose after determining that its higher safety hazard outweighed the efficacy advantage over the lower dose.
The BREEZE-AD7 study was sponsored by Eli Lilly. Dr. Reich reported serving as an adviser to, paid speaker for, and recipient of research grants from that pharmaceutical company and more than two dozen others.
MADRID – Adding the oral Janus kinase (JAK) inhibitor baricitinib to standard atopic dermatitis therapy with low- and midpotency topical corticosteroids markedly improved disease severity and key patient-reported outcomes, compared with topical corticosteroids alone, in the phase 3, randomized, double-blind BREEZE-AD7 trial, Kristian Reich, MD, reported at the annual congress of the European Academy of Dermatology and Venereology.
in the phase 3 BREEZE-AD1 and -AD2 trials. But BREEZE-AD7 further advances the field because it’s the first phase 3 study testing the efficacy of a JAK inhibitor in combination with low- and midpotency topical steroids.
“I think this study is important because it looks into the situation that’s more like what happens in the real world, which is, as with dupilumab and other drugs, we use the systemic agent in combination with topical therapies and, in particular, with topical corticosteroids,” commented Dr. Reich, professor of dermatology at University Medical Center, Hamburg, and medical director at SCIderm, a scientific research company.
“This is what I think we can expect from existing and upcoming systemic therapies in atopic dermatitis: We will use them in combination with topical corticosteroids, and hopefully this will allow patients to dramatically reduce the concomitant use of topical corticosteroids, as shown here in BREEZE-AD7,” he added.
BREEZE-AD7 was a 16-week study that included 329 adults with moderate or severe atopic dermatitis who were randomized to low- and midpotency topical corticosteroids plus either baricitinib at 2 mg once daily, baricitinib at 4 mg once daily, or placebo. The group’s mean baseline Eczema Area and Severity Index (EASI) score was 29. Overall, 45% of participants had a baseline Investigator’s Global Assessment (IGA) of disease severity of 4 on a 0-4 scale.
The primary endpoint was achievement of an IGA of 0 or 1, meaning clear or almost clear, along with at least a 2-point IGA improvement from baseline at week 16. This was accomplished in 30.6% of those on 4 mg/day of baricitinib, 23.9% of patients in the 2-mg group, and 14.7% of controls.
The 4-mg dose of baricitinib was statistically superior to placebo; the 2-mg dose was not. However, Dr. Reich indicated he was untroubled by this because the primary endpoint was set at a high bar, and both doses of baricitinib proved to be significantly better than topical steroids plus placebo in terms of EASI 75 response rates, as well as reductions in itch, skin pain, and sleep problems, which aren’t captured in EASI scores (see graphic).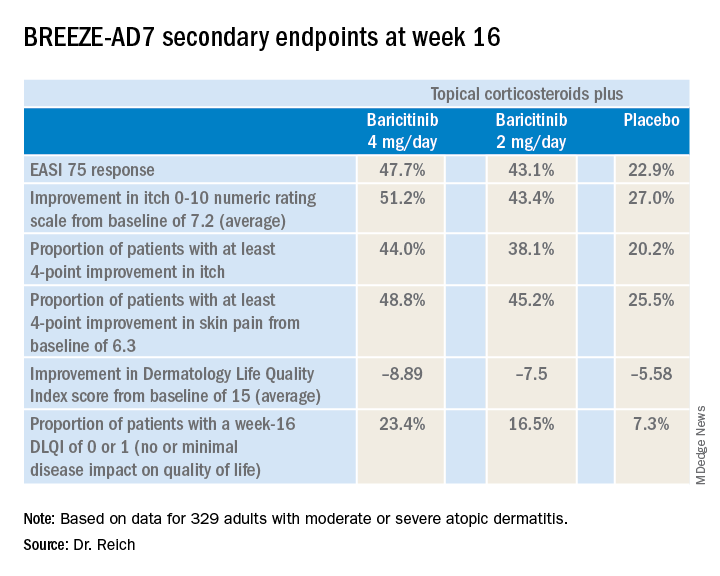
“One of my big learnings from this year’s EADV is that we have to rethink the dimensions of atopic dermatitis. I think we have underestimated the relevance of important symptoms such as itch, the impact atopic dermatitis has on pain, and the effect it has on sleeping problems,” the dermatologist said. “My feeling is that baricitinib is strongest in reducing itch, improving sleep, and reducing pain, but it also has good effects on the clinical signs of atopic dermatitis.”
The baricitinib-treated patients’ rapidity of improvement in the various endpoints was particularly impressive. Both doses of the JAK 1/2 inhibitor showed significant separation from the control group in the first week, and the majority of improvement occurred by week 4.
A key finding was that patients on baricitinib at 2 mg/day and 4 mg/day used a mean total of 162 g and 137 g of midpotency topical steroids, respectively, during the 16 weeks, compared with 225 g in the control group. The higher-dose baricitinib group was topical corticosteroid-free on 33% of study days, compared with 25% of days for the baricitinib 2 mg patients and 17% of days for controls.
In terms of safety, there was a case of pulmonary embolism in the higher-dose baricitinib group and an opportunistic toxoplasmosis eye infection in the control population. The frequency of oral herpes and herpes simplex virus infections was 2.8% in controls, 4.6% in the baricitinib 2-mg group, and 6.3% in the 4-mg group. There was also a signal of a dose-dependent increased risk of new-onset acne, with rates of 0.9% in controls and patients on baricitinib 2 mg, climbing to 3.6% with baricitinib 4 mg.
“In phase 2 results with upadacitinib [another oral JAK inhibitor], we saw that more than 10% of patients in the highest-dose group developed what was classified as acne. I cannot explain this, but it’s something we will monitor in the future,” Dr. Reich promised.
A fuller picture of baricitinib’s safety profile in the setting of atopic dermatitis clearly requires larger and longer-term studies, he added.
Baricitinib at the 2 mg daily dose is already marketed as Olumiant for the treatment of rheumatoid arthritis, with labeling that includes a boxed warning about serious infections, malignancy, and thrombosis. The Food and Drug Administration did not approve the 4-mg dose after determining that its higher safety hazard outweighed the efficacy advantage over the lower dose.
The BREEZE-AD7 study was sponsored by Eli Lilly. Dr. Reich reported serving as an adviser to, paid speaker for, and recipient of research grants from that pharmaceutical company and more than two dozen others.
REPORTING FROM EADV CONGRESS
Key clinical point: The Janus kinase 1/2 inhibitor baricitinib shows promise as a novel oral treatment for moderate or severe atopic dermatitis.
Major finding: Among atopic dermatitis patients on concomitant topical corticosteroids, a 75% improvement on Eczema Area and Severity Index at 16 weeks was achieved in 48% of those on baricitinib at 4 mg/day, 43% with baricitinib at 2 mg/day, and 23% on placebo.
Study details: BREEZE-AD7 was a phase 3, multicenter, 16-week, double-blind, three-arm study including 329 adults with moderate or severe atopic dermatitis.
Disclosures: The BREEZE-AD7 study was sponsored by Eli Lilly. The presenter reported serving as an adviser to, paid speaker for, and/or recipient of research grants from that pharmaceutical company and more than two dozen others.
Source: Reich K. EADV Congress, late breaker.
IL-1 alpha is a new target in atopic dermatitis
MADRID – on the basis of an encouraging phase 2, proof-of-concept study involving bermekimab, an investigational monoclonal antibody directed at that cytokine.
The mechanism of benefit is unclear, although there are a number of plausible possibilities, all orbiting around the notion that AD is not only a Th2 immunity–mediated disease, but that Th1 immunity plays a role, too.
“The ultimate proof, as you will see, is that it works,” Alice B. Gottlieb, MD, PhD, observed in presenting the phase 2 study findings at the annual congress of the European Academy of Dermatology and Venereology.
Bermekimab is a monoclonal antibody cloned from human peripheral B lymphocytes. Sources of its target – IL-1 alpha – that are of therapeutic relevance include neutrophils, keratinocytes, platelets, and monocytes.
The study included 10 adults with moderate to severe AD who received a single subcutaneous injection of 200 mg of bermekimab and 28 who received 400 mg weekly for 8 weeks. Lumping together the various outcome measures employed in the study, the 400-mg dose was three times more effective than the 200-mg dose, a finding explainable by the 240% higher serum levels at 400 mg, according to Dr. Gottlieb, medical director of Mount Sinai Beth Israel Dermatology in the department of dermatology at the Icahn School of Medicine at Mount Sinai, New York.
This was a small, uncontrolled, proof-of-concept study; at this early stage, results painted a favorable picture of efficacy and safety. For example, scores on the Eczema Area and Severity Index dropped by a mean of 65% from baseline at week 4 of bermekimab at 400 mg/week and by 80% at week 8. Scoring Atopic Dermatitis scores dropped by about 55% at week 4 and by nearly 70% at 8 weeks. Scores on the 0-4 Investigator Global Assessment improved by 1.2 points at week 4 and 1.4 points by week 8. Dermatology Life Quality Index scores improved by a mean of 70% by week 8, at which point 61% of patients had a DLQI of 0-1, indicating that AD had no or only a slight impact on quality of life. Scores on the Hospital Anxiety and Depression Scale improved by about 45% at 4 weeks and 65% at 8 weeks.
At baseline, most patients rated their pain as 7 out of 10. By week 8, pain scores had dropped by an average of 80%, and 80% of patients experienced a 4-point drop or greater. Similarly, 80% of patients had at least a 4-point drop in their self-rated worst itch scores on a 0-10 scale. The greatest improvement in both pain and itch scores occurred in the first 4 weeks, after which further improvement continued, albeit at a slower rate.
Adverse events consisted of grade 2 wheezing in two patients, grade 1 nausea in two patients, and a 3% rate of mild injection-site reactions.
An audience member rose to comment: “This is really interesting data, and it goes against everything that we think about atopic dermatitis. But we know from allergic contact dermatitis that IL-1 is a very early signal coming out of keratinocytes. It almost makes you wonder whether that’s not a primary problem in atopic dermatitis that we haven’t realized – that the keratinocytes are under stress because of damage to the skin barrier or other functions, and by alleviating that stress by blocking IL-1, you block the progression into what we previously thought was an Th2-mediated disease, atopic dermatitis.”
“I was thinking that, too – that the keratinocytes could be playing a role in atopic dermatitis through IL-1,” Dr. Gottlieb replied.
She noted that her Mount Sinai colleague Emma Guttman-Yassky, MD, PhD, and coinvestigators have demonstrated that a monoclonal antibody that blocks IL-17C is effective in treating AD, and that IL-17C causes keratinocytes to release proinflammatory IL-1 alpha. High levels of IL-1 alpha have been shown to drive leukocyte recruitment into the skin, promote breakdown of the skin barrier through production of matrix metalloproteinase, stimulate itch by a direct effect on nerves, and cause leaky vascular endothelium.
A phase 2 study of bermekimab for treatment of AD enrolled the first patient in mid-November. In addition, Dr. Gottlieb has led a positive phase 2 study of the monoclonal antibody in patients with hidradenitis suppurativa, with a phase 3 trial in the works.
She reported receiving research funding from and serving as a consultant without personal compensation to XBiotech, which sponsored the AD and hidradenitis suppurativa studies. She has similar financial relationships with numerous pharmaceutical companies developing psoriasis medications.
MADRID – on the basis of an encouraging phase 2, proof-of-concept study involving bermekimab, an investigational monoclonal antibody directed at that cytokine.
The mechanism of benefit is unclear, although there are a number of plausible possibilities, all orbiting around the notion that AD is not only a Th2 immunity–mediated disease, but that Th1 immunity plays a role, too.
“The ultimate proof, as you will see, is that it works,” Alice B. Gottlieb, MD, PhD, observed in presenting the phase 2 study findings at the annual congress of the European Academy of Dermatology and Venereology.
Bermekimab is a monoclonal antibody cloned from human peripheral B lymphocytes. Sources of its target – IL-1 alpha – that are of therapeutic relevance include neutrophils, keratinocytes, platelets, and monocytes.
The study included 10 adults with moderate to severe AD who received a single subcutaneous injection of 200 mg of bermekimab and 28 who received 400 mg weekly for 8 weeks. Lumping together the various outcome measures employed in the study, the 400-mg dose was three times more effective than the 200-mg dose, a finding explainable by the 240% higher serum levels at 400 mg, according to Dr. Gottlieb, medical director of Mount Sinai Beth Israel Dermatology in the department of dermatology at the Icahn School of Medicine at Mount Sinai, New York.
This was a small, uncontrolled, proof-of-concept study; at this early stage, results painted a favorable picture of efficacy and safety. For example, scores on the Eczema Area and Severity Index dropped by a mean of 65% from baseline at week 4 of bermekimab at 400 mg/week and by 80% at week 8. Scoring Atopic Dermatitis scores dropped by about 55% at week 4 and by nearly 70% at 8 weeks. Scores on the 0-4 Investigator Global Assessment improved by 1.2 points at week 4 and 1.4 points by week 8. Dermatology Life Quality Index scores improved by a mean of 70% by week 8, at which point 61% of patients had a DLQI of 0-1, indicating that AD had no or only a slight impact on quality of life. Scores on the Hospital Anxiety and Depression Scale improved by about 45% at 4 weeks and 65% at 8 weeks.
At baseline, most patients rated their pain as 7 out of 10. By week 8, pain scores had dropped by an average of 80%, and 80% of patients experienced a 4-point drop or greater. Similarly, 80% of patients had at least a 4-point drop in their self-rated worst itch scores on a 0-10 scale. The greatest improvement in both pain and itch scores occurred in the first 4 weeks, after which further improvement continued, albeit at a slower rate.
Adverse events consisted of grade 2 wheezing in two patients, grade 1 nausea in two patients, and a 3% rate of mild injection-site reactions.
An audience member rose to comment: “This is really interesting data, and it goes against everything that we think about atopic dermatitis. But we know from allergic contact dermatitis that IL-1 is a very early signal coming out of keratinocytes. It almost makes you wonder whether that’s not a primary problem in atopic dermatitis that we haven’t realized – that the keratinocytes are under stress because of damage to the skin barrier or other functions, and by alleviating that stress by blocking IL-1, you block the progression into what we previously thought was an Th2-mediated disease, atopic dermatitis.”
“I was thinking that, too – that the keratinocytes could be playing a role in atopic dermatitis through IL-1,” Dr. Gottlieb replied.
She noted that her Mount Sinai colleague Emma Guttman-Yassky, MD, PhD, and coinvestigators have demonstrated that a monoclonal antibody that blocks IL-17C is effective in treating AD, and that IL-17C causes keratinocytes to release proinflammatory IL-1 alpha. High levels of IL-1 alpha have been shown to drive leukocyte recruitment into the skin, promote breakdown of the skin barrier through production of matrix metalloproteinase, stimulate itch by a direct effect on nerves, and cause leaky vascular endothelium.
A phase 2 study of bermekimab for treatment of AD enrolled the first patient in mid-November. In addition, Dr. Gottlieb has led a positive phase 2 study of the monoclonal antibody in patients with hidradenitis suppurativa, with a phase 3 trial in the works.
She reported receiving research funding from and serving as a consultant without personal compensation to XBiotech, which sponsored the AD and hidradenitis suppurativa studies. She has similar financial relationships with numerous pharmaceutical companies developing psoriasis medications.
MADRID – on the basis of an encouraging phase 2, proof-of-concept study involving bermekimab, an investigational monoclonal antibody directed at that cytokine.
The mechanism of benefit is unclear, although there are a number of plausible possibilities, all orbiting around the notion that AD is not only a Th2 immunity–mediated disease, but that Th1 immunity plays a role, too.
“The ultimate proof, as you will see, is that it works,” Alice B. Gottlieb, MD, PhD, observed in presenting the phase 2 study findings at the annual congress of the European Academy of Dermatology and Venereology.
Bermekimab is a monoclonal antibody cloned from human peripheral B lymphocytes. Sources of its target – IL-1 alpha – that are of therapeutic relevance include neutrophils, keratinocytes, platelets, and monocytes.
The study included 10 adults with moderate to severe AD who received a single subcutaneous injection of 200 mg of bermekimab and 28 who received 400 mg weekly for 8 weeks. Lumping together the various outcome measures employed in the study, the 400-mg dose was three times more effective than the 200-mg dose, a finding explainable by the 240% higher serum levels at 400 mg, according to Dr. Gottlieb, medical director of Mount Sinai Beth Israel Dermatology in the department of dermatology at the Icahn School of Medicine at Mount Sinai, New York.
This was a small, uncontrolled, proof-of-concept study; at this early stage, results painted a favorable picture of efficacy and safety. For example, scores on the Eczema Area and Severity Index dropped by a mean of 65% from baseline at week 4 of bermekimab at 400 mg/week and by 80% at week 8. Scoring Atopic Dermatitis scores dropped by about 55% at week 4 and by nearly 70% at 8 weeks. Scores on the 0-4 Investigator Global Assessment improved by 1.2 points at week 4 and 1.4 points by week 8. Dermatology Life Quality Index scores improved by a mean of 70% by week 8, at which point 61% of patients had a DLQI of 0-1, indicating that AD had no or only a slight impact on quality of life. Scores on the Hospital Anxiety and Depression Scale improved by about 45% at 4 weeks and 65% at 8 weeks.
At baseline, most patients rated their pain as 7 out of 10. By week 8, pain scores had dropped by an average of 80%, and 80% of patients experienced a 4-point drop or greater. Similarly, 80% of patients had at least a 4-point drop in their self-rated worst itch scores on a 0-10 scale. The greatest improvement in both pain and itch scores occurred in the first 4 weeks, after which further improvement continued, albeit at a slower rate.
Adverse events consisted of grade 2 wheezing in two patients, grade 1 nausea in two patients, and a 3% rate of mild injection-site reactions.
An audience member rose to comment: “This is really interesting data, and it goes against everything that we think about atopic dermatitis. But we know from allergic contact dermatitis that IL-1 is a very early signal coming out of keratinocytes. It almost makes you wonder whether that’s not a primary problem in atopic dermatitis that we haven’t realized – that the keratinocytes are under stress because of damage to the skin barrier or other functions, and by alleviating that stress by blocking IL-1, you block the progression into what we previously thought was an Th2-mediated disease, atopic dermatitis.”
“I was thinking that, too – that the keratinocytes could be playing a role in atopic dermatitis through IL-1,” Dr. Gottlieb replied.
She noted that her Mount Sinai colleague Emma Guttman-Yassky, MD, PhD, and coinvestigators have demonstrated that a monoclonal antibody that blocks IL-17C is effective in treating AD, and that IL-17C causes keratinocytes to release proinflammatory IL-1 alpha. High levels of IL-1 alpha have been shown to drive leukocyte recruitment into the skin, promote breakdown of the skin barrier through production of matrix metalloproteinase, stimulate itch by a direct effect on nerves, and cause leaky vascular endothelium.
A phase 2 study of bermekimab for treatment of AD enrolled the first patient in mid-November. In addition, Dr. Gottlieb has led a positive phase 2 study of the monoclonal antibody in patients with hidradenitis suppurativa, with a phase 3 trial in the works.
She reported receiving research funding from and serving as a consultant without personal compensation to XBiotech, which sponsored the AD and hidradenitis suppurativa studies. She has similar financial relationships with numerous pharmaceutical companies developing psoriasis medications.
REPORTING FROM EADV 2019