User login
Long COVID could spell kidney troubles down the line
Physicians caring for COVID-19 survivors should routinely check kidney function, which is often damaged by the SARS-CoV-2 virus months after both severe and milder cases, new research indicates.
The largest study to date with the longest follow-up of COVID-19-related kidney outcomes also found that every type of kidney problem, including end-stage kidney disease (ESKD), was far more common in COVID-19 survivors who were admitted to the ICU or experienced acute kidney injury (AKI) while hospitalized.
Researchers analyzed U.S. Veterans Health Administration data from more than 1.7 million patients, including more than 89,000 who tested positive for COVID-19, for the study, which was published online Sept. 1, 2021, in the Journal of the American Society of Nephrology.
The risk of kidney problems “is more robust or pronounced in people who have had severe infection, but present in even asymptomatic and mild disease, which shouldn’t be discounted. Those people represent the majority of those with COVID-19,” said senior author Ziyad Al-Aly, MD, of the Veteran Affairs St. Louis Health Care System.
“That’s why the results are important, because even in people with mild disease to start with, the risk of kidney problems is not trivial,” he told this news organization. “It’s smaller than in people who were in the ICU, but it’s not ... zero.”
Experts aren’t yet certain how COVID-19 can damage the kidneys, hypothesizing that several factors may be at play. The virus may directly infect kidney cells rich in ACE2 receptors, which are key to infection, said nephrologist F. Perry Wilson, MD, of Yale University, New Haven, Conn., and a member of Medscape’s advisory board.
Kidneys might also be particularly vulnerable to the inflammatory cascade or blood clotting often seen in COVID-19, Dr. Al-Aly and Wilson both suggested.
COVID-19 survivors more likely to have kidney damage than controls
“A lot of health systems either have or are establishing post-COVID care clinics, which we think should definitely incorporate a kidney component,” Dr. Al-Aly advised. “They should check patients’ blood and urine for kidney problems.”
This is particularly important because “kidney problems, for the most part, are painless and silent,” he added.
“Realizing 2 years down the road that someone has ESKD, where they need dialysis or a kidney transplant, is what we don’t want. We don’t want this to be unrecognized, uncared for, unattended to,” he said.
Dr. Al-Aly and colleagues evaluated VA health system records, including data from 89,216 patients who tested positive for COVID-19 between March 2020 and March 2021, as well as 1.7 million controls who did not have COVID-19. Over a median follow-up of about 5.5 months, participants’ estimated glomerular filtration rate and serum creatinine levels were tracked to assess kidney health and outcomes according to infection severity.
Results were striking, with COVID-19 survivors about one-third more likely than controls to have kidney damage or significant declines in kidney function between 1 and 6 months after infection. More than 4,700 COVID-19 survivors had lost at least 30% of their kidney function within a year, and these patients were 25% more likely to reach that level of decline than controls.
Additionally, COVID-19 survivors were nearly twice as likely to experience AKI and almost three times as likely to be diagnosed with ESKD as controls.
If your patient had COVID-19, ‘it’s reasonable to check kidney function’
“This information tells us that if your patient was sick with COVID-19 and comes for follow-up visits, it’s reasonable to check their kidney function,” Dr. Wilson, who was not involved with the research, told this news organization.
“Even for patients who were not hospitalized, if they were laid low or dehydrated ... it should be part of the post-COVID care package,” he said.
If just a fraction of the millions of COVID-19 survivors in the United States develop long-term kidney problems, the ripple effect on American health care could be substantial, Dr. Wilson and Dr. Al-Aly agreed.
“We’re still living in a pandemic, so it’s hard to tell the total impact,” Dr. Al-Aly said. “But this ultimately will contribute to a rise in burden of kidney disease. This and other long COVID manifestations are going to alter the landscape of clinical care and health care in the United States for a decade or more.”
Because renal problems can limit a patient’s treatment options for other major diseases, including diabetes and cancer, COVID-related kidney damage can ultimately impact survivability.
“There are a lot of medications you can’t use in people with advanced kidney problems,” Dr. Al-Aly said.
The main study limitation was that patients were mostly older White men (median age, 68 years), although more than 9,000 women were included in the VA data, Dr. Al-Aly noted. Additionally, controls were more likely to be younger, Black, living in long-term care, and have higher rates of chronic health conditions and medication use.
The experts agreed that ongoing research tracking kidney outcomes is crucial for years to come.
“We also need to be following a cohort of these patients as part of a research protocol where they come in every 6 months for a standard set of lab tests to really understand what’s going on with their kidneys,” Dr. Wilson said.
“Lastly – and a much tougher sell – is we need biopsies. It’s very hard to infer what’s going on in complex disease with the kidneys without biopsy tissue,” he added.
The study was funded by the American Society of Nephrology and the Department of Veterans Affairs. Dr. Al-Aly and Dr. Wilson reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Physicians caring for COVID-19 survivors should routinely check kidney function, which is often damaged by the SARS-CoV-2 virus months after both severe and milder cases, new research indicates.
The largest study to date with the longest follow-up of COVID-19-related kidney outcomes also found that every type of kidney problem, including end-stage kidney disease (ESKD), was far more common in COVID-19 survivors who were admitted to the ICU or experienced acute kidney injury (AKI) while hospitalized.
Researchers analyzed U.S. Veterans Health Administration data from more than 1.7 million patients, including more than 89,000 who tested positive for COVID-19, for the study, which was published online Sept. 1, 2021, in the Journal of the American Society of Nephrology.
The risk of kidney problems “is more robust or pronounced in people who have had severe infection, but present in even asymptomatic and mild disease, which shouldn’t be discounted. Those people represent the majority of those with COVID-19,” said senior author Ziyad Al-Aly, MD, of the Veteran Affairs St. Louis Health Care System.
“That’s why the results are important, because even in people with mild disease to start with, the risk of kidney problems is not trivial,” he told this news organization. “It’s smaller than in people who were in the ICU, but it’s not ... zero.”
Experts aren’t yet certain how COVID-19 can damage the kidneys, hypothesizing that several factors may be at play. The virus may directly infect kidney cells rich in ACE2 receptors, which are key to infection, said nephrologist F. Perry Wilson, MD, of Yale University, New Haven, Conn., and a member of Medscape’s advisory board.
Kidneys might also be particularly vulnerable to the inflammatory cascade or blood clotting often seen in COVID-19, Dr. Al-Aly and Wilson both suggested.
COVID-19 survivors more likely to have kidney damage than controls
“A lot of health systems either have or are establishing post-COVID care clinics, which we think should definitely incorporate a kidney component,” Dr. Al-Aly advised. “They should check patients’ blood and urine for kidney problems.”
This is particularly important because “kidney problems, for the most part, are painless and silent,” he added.
“Realizing 2 years down the road that someone has ESKD, where they need dialysis or a kidney transplant, is what we don’t want. We don’t want this to be unrecognized, uncared for, unattended to,” he said.
Dr. Al-Aly and colleagues evaluated VA health system records, including data from 89,216 patients who tested positive for COVID-19 between March 2020 and March 2021, as well as 1.7 million controls who did not have COVID-19. Over a median follow-up of about 5.5 months, participants’ estimated glomerular filtration rate and serum creatinine levels were tracked to assess kidney health and outcomes according to infection severity.
Results were striking, with COVID-19 survivors about one-third more likely than controls to have kidney damage or significant declines in kidney function between 1 and 6 months after infection. More than 4,700 COVID-19 survivors had lost at least 30% of their kidney function within a year, and these patients were 25% more likely to reach that level of decline than controls.
Additionally, COVID-19 survivors were nearly twice as likely to experience AKI and almost three times as likely to be diagnosed with ESKD as controls.
If your patient had COVID-19, ‘it’s reasonable to check kidney function’
“This information tells us that if your patient was sick with COVID-19 and comes for follow-up visits, it’s reasonable to check their kidney function,” Dr. Wilson, who was not involved with the research, told this news organization.
“Even for patients who were not hospitalized, if they were laid low or dehydrated ... it should be part of the post-COVID care package,” he said.
If just a fraction of the millions of COVID-19 survivors in the United States develop long-term kidney problems, the ripple effect on American health care could be substantial, Dr. Wilson and Dr. Al-Aly agreed.
“We’re still living in a pandemic, so it’s hard to tell the total impact,” Dr. Al-Aly said. “But this ultimately will contribute to a rise in burden of kidney disease. This and other long COVID manifestations are going to alter the landscape of clinical care and health care in the United States for a decade or more.”
Because renal problems can limit a patient’s treatment options for other major diseases, including diabetes and cancer, COVID-related kidney damage can ultimately impact survivability.
“There are a lot of medications you can’t use in people with advanced kidney problems,” Dr. Al-Aly said.
The main study limitation was that patients were mostly older White men (median age, 68 years), although more than 9,000 women were included in the VA data, Dr. Al-Aly noted. Additionally, controls were more likely to be younger, Black, living in long-term care, and have higher rates of chronic health conditions and medication use.
The experts agreed that ongoing research tracking kidney outcomes is crucial for years to come.
“We also need to be following a cohort of these patients as part of a research protocol where they come in every 6 months for a standard set of lab tests to really understand what’s going on with their kidneys,” Dr. Wilson said.
“Lastly – and a much tougher sell – is we need biopsies. It’s very hard to infer what’s going on in complex disease with the kidneys without biopsy tissue,” he added.
The study was funded by the American Society of Nephrology and the Department of Veterans Affairs. Dr. Al-Aly and Dr. Wilson reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Physicians caring for COVID-19 survivors should routinely check kidney function, which is often damaged by the SARS-CoV-2 virus months after both severe and milder cases, new research indicates.
The largest study to date with the longest follow-up of COVID-19-related kidney outcomes also found that every type of kidney problem, including end-stage kidney disease (ESKD), was far more common in COVID-19 survivors who were admitted to the ICU or experienced acute kidney injury (AKI) while hospitalized.
Researchers analyzed U.S. Veterans Health Administration data from more than 1.7 million patients, including more than 89,000 who tested positive for COVID-19, for the study, which was published online Sept. 1, 2021, in the Journal of the American Society of Nephrology.
The risk of kidney problems “is more robust or pronounced in people who have had severe infection, but present in even asymptomatic and mild disease, which shouldn’t be discounted. Those people represent the majority of those with COVID-19,” said senior author Ziyad Al-Aly, MD, of the Veteran Affairs St. Louis Health Care System.
“That’s why the results are important, because even in people with mild disease to start with, the risk of kidney problems is not trivial,” he told this news organization. “It’s smaller than in people who were in the ICU, but it’s not ... zero.”
Experts aren’t yet certain how COVID-19 can damage the kidneys, hypothesizing that several factors may be at play. The virus may directly infect kidney cells rich in ACE2 receptors, which are key to infection, said nephrologist F. Perry Wilson, MD, of Yale University, New Haven, Conn., and a member of Medscape’s advisory board.
Kidneys might also be particularly vulnerable to the inflammatory cascade or blood clotting often seen in COVID-19, Dr. Al-Aly and Wilson both suggested.
COVID-19 survivors more likely to have kidney damage than controls
“A lot of health systems either have or are establishing post-COVID care clinics, which we think should definitely incorporate a kidney component,” Dr. Al-Aly advised. “They should check patients’ blood and urine for kidney problems.”
This is particularly important because “kidney problems, for the most part, are painless and silent,” he added.
“Realizing 2 years down the road that someone has ESKD, where they need dialysis or a kidney transplant, is what we don’t want. We don’t want this to be unrecognized, uncared for, unattended to,” he said.
Dr. Al-Aly and colleagues evaluated VA health system records, including data from 89,216 patients who tested positive for COVID-19 between March 2020 and March 2021, as well as 1.7 million controls who did not have COVID-19. Over a median follow-up of about 5.5 months, participants’ estimated glomerular filtration rate and serum creatinine levels were tracked to assess kidney health and outcomes according to infection severity.
Results were striking, with COVID-19 survivors about one-third more likely than controls to have kidney damage or significant declines in kidney function between 1 and 6 months after infection. More than 4,700 COVID-19 survivors had lost at least 30% of their kidney function within a year, and these patients were 25% more likely to reach that level of decline than controls.
Additionally, COVID-19 survivors were nearly twice as likely to experience AKI and almost three times as likely to be diagnosed with ESKD as controls.
If your patient had COVID-19, ‘it’s reasonable to check kidney function’
“This information tells us that if your patient was sick with COVID-19 and comes for follow-up visits, it’s reasonable to check their kidney function,” Dr. Wilson, who was not involved with the research, told this news organization.
“Even for patients who were not hospitalized, if they were laid low or dehydrated ... it should be part of the post-COVID care package,” he said.
If just a fraction of the millions of COVID-19 survivors in the United States develop long-term kidney problems, the ripple effect on American health care could be substantial, Dr. Wilson and Dr. Al-Aly agreed.
“We’re still living in a pandemic, so it’s hard to tell the total impact,” Dr. Al-Aly said. “But this ultimately will contribute to a rise in burden of kidney disease. This and other long COVID manifestations are going to alter the landscape of clinical care and health care in the United States for a decade or more.”
Because renal problems can limit a patient’s treatment options for other major diseases, including diabetes and cancer, COVID-related kidney damage can ultimately impact survivability.
“There are a lot of medications you can’t use in people with advanced kidney problems,” Dr. Al-Aly said.
The main study limitation was that patients were mostly older White men (median age, 68 years), although more than 9,000 women were included in the VA data, Dr. Al-Aly noted. Additionally, controls were more likely to be younger, Black, living in long-term care, and have higher rates of chronic health conditions and medication use.
The experts agreed that ongoing research tracking kidney outcomes is crucial for years to come.
“We also need to be following a cohort of these patients as part of a research protocol where they come in every 6 months for a standard set of lab tests to really understand what’s going on with their kidneys,” Dr. Wilson said.
“Lastly – and a much tougher sell – is we need biopsies. It’s very hard to infer what’s going on in complex disease with the kidneys without biopsy tissue,” he added.
The study was funded by the American Society of Nephrology and the Department of Veterans Affairs. Dr. Al-Aly and Dr. Wilson reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Medical education must takes broader view of disabilities
“All physicians, regardless of specialty, will work with patients with disabilities,” Corrie Harris, MD, of the University of Louisville (Ky.), said in a plenary session presentation at the 2021 virtual Pediatric Hospital Medicine conference.
Disabilities vary in their visibility, from cognitive and sensory impairments that are not immediately obvious to an obvious physical disability, she said.
One in four adults and one in six children in the United States has a disability, said Dr. Harris. The prevalence of disability increases with age, but occurs across the lifespan, and will likely increase in the future with greater improvements in health care overall.
Dr. Harris reviewed the current conceptual model that forms the basis for the World Health Organization definition of functioning disability. This “functional model” defines disability as caused by interactions between health conditions and the environment, and the response is to “prioritize function to meet patient goals,” Dr. Harris said at the meeting, sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, and the Academic Pediatric Association.
This model is based on collaboration between health care providers and their patients with disabilities, and training is important to help providers make this collaboration successful, said Dr. Harris. Without training, physicians may be ineffective in communicating with patients with disabilities by not speaking directly to the patient, not speaking in a way the patient can understand clearly, and not providing accessible patient education materials. Physicians also tend to minimize the extent of the patient’s expertise in their own condition based on their lived experiences, and tend to underestimate the abilities of patients with disabilities.
However, direct experience with disabled patients and an understanding of the health disparities they endure can help physicians look at these patients “through a more intersectional lens,” that also takes into account social determinants of health, Dr. Harris said. “I have found that people with disabilities are the best teachers about disability, because they have expertise that comes from their lived experience.”
Patients are the best teachers
Several initiatives are helping physicians to bridge this gap in understanding and reduce disparities in care. One such program is FRAME: Faces Redefining the Art of Medical Education. FRAME is a web-based film library designed to present medical information to health care providers in training, clinicians, families, and communities in a dignified and humanizing way. FRAME was developed in part by fashion photographer Rick Guidotti, who was inspired after meeting a young woman with albinism to create Positive Exposure, an ongoing project featuring children and adolescents with various disabilities.
FRAME films are “short films presenting all the basic hallmark characteristics of a certain genetic condition, but presented by somebody living with that condition,” said Mr. Guidotti in his presentation during the session.
The National Curriculum Initiative in Developmental Medicine (NCIDM) is designed to incorporate care for individuals with disabilities into medical education. NCIDM is a project created by the American Academy of Developmental Medicine and Dentistry (AADMD).
“The need for this program is that there is no U.S. requirement for medical schools to teach about intellectual and developmental disabilities,” Priya Chandan, MD, also of the University of Louisville, said in her presentation during the session. “Approximately 81% of graduating medical students have no training in caring for adults with disabilities,” said Dr. Chandan, who serves as director of the NCIDM.
The current NCIDM was created as a 5-year partnership between the AADMD and Special Olympics, supported in part by the Centers for Disease Control and Prevention, Dr. Chandan said. The purpose was to provide training to medical students in the field of developmental medicine, meaning the care of individuals with intellectual/developmental disabilities (IDD) across the lifespan. The AADMD has expanded to 26 medical schools in the United States and will reach approximately 4,000 medical students by the conclusion of the current initiative.
One challenge in medical education is getting past the idea that people living with disabilities need to be fixed, said Dr. Chandan. The NCIDM approach reflects Mr. Guidotti’s approach in both the FRAME initiatives and his Positive Exposure foundation, with a focus on treating people as people, and letting individuals with disabilities represent themselves.
Dr. Chandan described the NCIDM curriculum as allowing for flexible teaching methodologies and materials, as long as they meet the NCIDM-created learning goals and objectives. The curriculum also includes standardized evaluations. Each NCIDM program in a participating medical school includes a faculty champion, and the curriculum supports meeting people with IDD not only inside medical settings, but also outside in the community.
NCIDM embraces the idea of community-engaged scholarship, which Dr. Chandan defined as “a form of scholarship that directly benefits the community and is consistent with university and unit missions.” This method combined teaching and conducting research while providing a service to the community.
The next steps for the current NCIDM initiative are to complete collection of data and course evaluations from participating schools by early 2022, followed by continued dissemination and collaboration through AADMD.
Overall, the content of the curriculum explores how and where IDD fits into clinical care, Dr. Chandan said, who also emphasized the implications of communication. “How we think affects how we communicate,” she added. Be mindful of the language used to talk to and about patients with disabilities, both to colleagues and to learners.
When talking to the patient, find something in common, beyond the diagnosis, said Dr. Chandan. Remember that some disabilities are visible and some are not. “Treat people with respect, because you won’t know what their functional level is just by looking,” she concluded.
The presenters had no financial conflicts to disclose.
“All physicians, regardless of specialty, will work with patients with disabilities,” Corrie Harris, MD, of the University of Louisville (Ky.), said in a plenary session presentation at the 2021 virtual Pediatric Hospital Medicine conference.
Disabilities vary in their visibility, from cognitive and sensory impairments that are not immediately obvious to an obvious physical disability, she said.
One in four adults and one in six children in the United States has a disability, said Dr. Harris. The prevalence of disability increases with age, but occurs across the lifespan, and will likely increase in the future with greater improvements in health care overall.
Dr. Harris reviewed the current conceptual model that forms the basis for the World Health Organization definition of functioning disability. This “functional model” defines disability as caused by interactions between health conditions and the environment, and the response is to “prioritize function to meet patient goals,” Dr. Harris said at the meeting, sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, and the Academic Pediatric Association.
This model is based on collaboration between health care providers and their patients with disabilities, and training is important to help providers make this collaboration successful, said Dr. Harris. Without training, physicians may be ineffective in communicating with patients with disabilities by not speaking directly to the patient, not speaking in a way the patient can understand clearly, and not providing accessible patient education materials. Physicians also tend to minimize the extent of the patient’s expertise in their own condition based on their lived experiences, and tend to underestimate the abilities of patients with disabilities.
However, direct experience with disabled patients and an understanding of the health disparities they endure can help physicians look at these patients “through a more intersectional lens,” that also takes into account social determinants of health, Dr. Harris said. “I have found that people with disabilities are the best teachers about disability, because they have expertise that comes from their lived experience.”
Patients are the best teachers
Several initiatives are helping physicians to bridge this gap in understanding and reduce disparities in care. One such program is FRAME: Faces Redefining the Art of Medical Education. FRAME is a web-based film library designed to present medical information to health care providers in training, clinicians, families, and communities in a dignified and humanizing way. FRAME was developed in part by fashion photographer Rick Guidotti, who was inspired after meeting a young woman with albinism to create Positive Exposure, an ongoing project featuring children and adolescents with various disabilities.
FRAME films are “short films presenting all the basic hallmark characteristics of a certain genetic condition, but presented by somebody living with that condition,” said Mr. Guidotti in his presentation during the session.
The National Curriculum Initiative in Developmental Medicine (NCIDM) is designed to incorporate care for individuals with disabilities into medical education. NCIDM is a project created by the American Academy of Developmental Medicine and Dentistry (AADMD).
“The need for this program is that there is no U.S. requirement for medical schools to teach about intellectual and developmental disabilities,” Priya Chandan, MD, also of the University of Louisville, said in her presentation during the session. “Approximately 81% of graduating medical students have no training in caring for adults with disabilities,” said Dr. Chandan, who serves as director of the NCIDM.
The current NCIDM was created as a 5-year partnership between the AADMD and Special Olympics, supported in part by the Centers for Disease Control and Prevention, Dr. Chandan said. The purpose was to provide training to medical students in the field of developmental medicine, meaning the care of individuals with intellectual/developmental disabilities (IDD) across the lifespan. The AADMD has expanded to 26 medical schools in the United States and will reach approximately 4,000 medical students by the conclusion of the current initiative.
One challenge in medical education is getting past the idea that people living with disabilities need to be fixed, said Dr. Chandan. The NCIDM approach reflects Mr. Guidotti’s approach in both the FRAME initiatives and his Positive Exposure foundation, with a focus on treating people as people, and letting individuals with disabilities represent themselves.
Dr. Chandan described the NCIDM curriculum as allowing for flexible teaching methodologies and materials, as long as they meet the NCIDM-created learning goals and objectives. The curriculum also includes standardized evaluations. Each NCIDM program in a participating medical school includes a faculty champion, and the curriculum supports meeting people with IDD not only inside medical settings, but also outside in the community.
NCIDM embraces the idea of community-engaged scholarship, which Dr. Chandan defined as “a form of scholarship that directly benefits the community and is consistent with university and unit missions.” This method combined teaching and conducting research while providing a service to the community.
The next steps for the current NCIDM initiative are to complete collection of data and course evaluations from participating schools by early 2022, followed by continued dissemination and collaboration through AADMD.
Overall, the content of the curriculum explores how and where IDD fits into clinical care, Dr. Chandan said, who also emphasized the implications of communication. “How we think affects how we communicate,” she added. Be mindful of the language used to talk to and about patients with disabilities, both to colleagues and to learners.
When talking to the patient, find something in common, beyond the diagnosis, said Dr. Chandan. Remember that some disabilities are visible and some are not. “Treat people with respect, because you won’t know what their functional level is just by looking,” she concluded.
The presenters had no financial conflicts to disclose.
“All physicians, regardless of specialty, will work with patients with disabilities,” Corrie Harris, MD, of the University of Louisville (Ky.), said in a plenary session presentation at the 2021 virtual Pediatric Hospital Medicine conference.
Disabilities vary in their visibility, from cognitive and sensory impairments that are not immediately obvious to an obvious physical disability, she said.
One in four adults and one in six children in the United States has a disability, said Dr. Harris. The prevalence of disability increases with age, but occurs across the lifespan, and will likely increase in the future with greater improvements in health care overall.
Dr. Harris reviewed the current conceptual model that forms the basis for the World Health Organization definition of functioning disability. This “functional model” defines disability as caused by interactions between health conditions and the environment, and the response is to “prioritize function to meet patient goals,” Dr. Harris said at the meeting, sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, and the Academic Pediatric Association.
This model is based on collaboration between health care providers and their patients with disabilities, and training is important to help providers make this collaboration successful, said Dr. Harris. Without training, physicians may be ineffective in communicating with patients with disabilities by not speaking directly to the patient, not speaking in a way the patient can understand clearly, and not providing accessible patient education materials. Physicians also tend to minimize the extent of the patient’s expertise in their own condition based on their lived experiences, and tend to underestimate the abilities of patients with disabilities.
However, direct experience with disabled patients and an understanding of the health disparities they endure can help physicians look at these patients “through a more intersectional lens,” that also takes into account social determinants of health, Dr. Harris said. “I have found that people with disabilities are the best teachers about disability, because they have expertise that comes from their lived experience.”
Patients are the best teachers
Several initiatives are helping physicians to bridge this gap in understanding and reduce disparities in care. One such program is FRAME: Faces Redefining the Art of Medical Education. FRAME is a web-based film library designed to present medical information to health care providers in training, clinicians, families, and communities in a dignified and humanizing way. FRAME was developed in part by fashion photographer Rick Guidotti, who was inspired after meeting a young woman with albinism to create Positive Exposure, an ongoing project featuring children and adolescents with various disabilities.
FRAME films are “short films presenting all the basic hallmark characteristics of a certain genetic condition, but presented by somebody living with that condition,” said Mr. Guidotti in his presentation during the session.
The National Curriculum Initiative in Developmental Medicine (NCIDM) is designed to incorporate care for individuals with disabilities into medical education. NCIDM is a project created by the American Academy of Developmental Medicine and Dentistry (AADMD).
“The need for this program is that there is no U.S. requirement for medical schools to teach about intellectual and developmental disabilities,” Priya Chandan, MD, also of the University of Louisville, said in her presentation during the session. “Approximately 81% of graduating medical students have no training in caring for adults with disabilities,” said Dr. Chandan, who serves as director of the NCIDM.
The current NCIDM was created as a 5-year partnership between the AADMD and Special Olympics, supported in part by the Centers for Disease Control and Prevention, Dr. Chandan said. The purpose was to provide training to medical students in the field of developmental medicine, meaning the care of individuals with intellectual/developmental disabilities (IDD) across the lifespan. The AADMD has expanded to 26 medical schools in the United States and will reach approximately 4,000 medical students by the conclusion of the current initiative.
One challenge in medical education is getting past the idea that people living with disabilities need to be fixed, said Dr. Chandan. The NCIDM approach reflects Mr. Guidotti’s approach in both the FRAME initiatives and his Positive Exposure foundation, with a focus on treating people as people, and letting individuals with disabilities represent themselves.
Dr. Chandan described the NCIDM curriculum as allowing for flexible teaching methodologies and materials, as long as they meet the NCIDM-created learning goals and objectives. The curriculum also includes standardized evaluations. Each NCIDM program in a participating medical school includes a faculty champion, and the curriculum supports meeting people with IDD not only inside medical settings, but also outside in the community.
NCIDM embraces the idea of community-engaged scholarship, which Dr. Chandan defined as “a form of scholarship that directly benefits the community and is consistent with university and unit missions.” This method combined teaching and conducting research while providing a service to the community.
The next steps for the current NCIDM initiative are to complete collection of data and course evaluations from participating schools by early 2022, followed by continued dissemination and collaboration through AADMD.
Overall, the content of the curriculum explores how and where IDD fits into clinical care, Dr. Chandan said, who also emphasized the implications of communication. “How we think affects how we communicate,” she added. Be mindful of the language used to talk to and about patients with disabilities, both to colleagues and to learners.
When talking to the patient, find something in common, beyond the diagnosis, said Dr. Chandan. Remember that some disabilities are visible and some are not. “Treat people with respect, because you won’t know what their functional level is just by looking,” she concluded.
The presenters had no financial conflicts to disclose.
FROM PHM 2021
Choosing Wisely campaign targets waste and overuse in hospital pediatrics
“Health care spending and health care waste is a huge problem in the U.S., including for children,” Vivian Lee, MD, of Children’s Hospital, Los Angeles, said in a presentation at the 2021 virtual Pediatric Hospital Medicine conference.
Data from a 2019 study suggested that approximately 25% of health care spending in the United States qualifies as “wasteful spending,” in categories such as overtesting, and unnecessary hospitalization, Dr. Lee said. “It is essential for physicians in hospitals to be stewards of high-value care,” she emphasized.
To combat wasteful spending and control health care costs, the Choosing Wisely campaign was created in 2012 as an initiative from the American Board of Internal Medicine Foundation. An ongoing goal of the campaign is to raise awareness among physicians and patients about potential areas of low-value services and overuse. The overall campaign includes clinician-driven recommendations from multiple medical organizations.
The PHM produced its first set of five recommendations in 2012, Dr. Lee said. These recommendations, titled “Five Things Physicians and Patients Should Question,” have been updated for 2021. The updated recommendations were created as a partnership among the Academic Pediatric Association, the American Academy of Pediatrics, and the Society of Hospital Medicine. A joint committee reviewed the latest evidence, and the updates were approved by the societies and published by the ABIM in January 2021.
“We think these recommendations truly reflect an exciting and evolving landscape for pediatric hospitalists,” Dr. Lee said. “There is a greater focus on opportunities to transition out of the hospital sooner, or avoid hospitalization altogether. There is an emphasis on antibiotic stewardship and a growing recognition of the impact that overuse may have on our vulnerable neonatal population,” she said. Several members of the Choosing Wisely panel presented the recommendations during the virtual presentation.
Revised recommendations
The new “Five Things Physicians and Patients Should Question” are as follows:
1. Do not prescribe IV antibiotics for predetermined durations for patients hospitalized with infections such as pyelonephritis, osteomyelitis, and complicated pneumonia. Consider early transition to oral antibiotics.
Many antibiotic doses used in clinical practice are preset durations that are not based on high-quality evidence, said Mike Tchou, MD, of Children’s Hospital of Colorado in Aurora. However, studies now show that earlier transition to enteral antibiotics can improve a range of outcomes including neonatal UTIs, osteomyelitis, and complicated pneumonia, he said. Considering early transition based on a patient’s response can decrease adverse events, pain, length of stay, and health care costs, he explained.
2. Do not continue hospitalization in well-appearing febrile infants once bacterial cultures (i.e., blood, cerebrospinal, and/or urine) have been confirmed negative for 24-36 hours, if adequate outpatient follow-up can be assured.
Recent data indicate that continuing hospitalization beyond 24-36 hours of confirmed negative bacterial cultures does not improve clinical outcomes for well-appearing infants admitted for concern of serious bacterial infection, said Paula Soung, MD, of Children’s Wisconsin in Milwaukee. In fact, “blood culture yield is highest in the first 12-36 hours after incubation with multiple studies demonstrating > 90% of pathogen cultures being positive by 24 hours,” Dr. Soung said. “If adequate outpatient follow-up can be assured, discharging well-appearing febrile infants at 24-36 hours after confirming cultures are negative has many positive outcomes,” she said.
3. Do not initiate phototherapy in term or late preterm well-appearing infants with neonatal hyperbilirubinemia if their bilirubin is below levels at which the AAP guidelines recommend treatment.
In making this recommendation, “we considered that the risk of kernicterus and cerebral palsy is extremely low in otherwise healthy term and late preterm newborns,” said Allison Holmes, MD, of Children’s Hospital at Dartmouth-Hitchcock, Manchester, N.H. “Subthreshold phototherapy leads to unnecessary hospitalization and its associated costs and harms,” and data show that kernicterus generally occurs close to 40 mg/dL and occurs most often in infants with hemolysis, she added.
The evidence for the recommendations included data showing that, among other factors, 8.6 of 100,000 babies have a bilirubin greater than 30 mg/dL, said Dr. Holmes. Risks of using subthreshold phototherapy include increased length of stay, increased readmissions, and increased costs, as well as decreased breastfeeding, bonding with parents, and increased parental anxiety. “Adding prolonged hospitalization for an intervention that might not be necessary can be stressful for parents,” she said.
4. Do not use broad-spectrum antibiotics such as ceftriaxone for children hospitalized with uncomplicated community-acquired pneumonia. Use narrow-spectrum antibiotics such as penicillin, ampicillin, or amoxicillin.
Michelle Lossius, MD, of the Shands Hospital for Children at the University of Florida, Gainesville, noted that the recommendations reflect IDSA guidelines from 2011 advising the use of ampicillin or penicillin for this population of children. More recent studies with large populations support the ability of narrow-spectrum antibiotics to limit the development of resistant organisms while achieving the same or better outcomes for children hospitalized with CAP, she said.
5. Do not start IV antibiotic therapy on well-appearing newborn infants with isolated risk factors for sepsis such as maternal chorioamnionitis, prolonged rupture of membranes, or untreated group-B streptococcal colonization. Use clinical tools such as an evidence-based sepsis risk calculator to guide management.
“This recommendation combines other recommendations,” said Prabi Rajbhandari, MD, of Akron (Ohio) Children’s Hospital. The evidence is ample, as the Centers for Disease Control and Prevention recommends the use of sepsis calculators to guide clinical management in sepsis patients, she said.
Data comparing periods before and after the adoption of a sepsis risk calculator showed a significant reduction in the use of blood cultures and antibiotics, she noted. Other risks of jumping to IV antibiotics include increased hospital stay, increased parental anxiety, and decreased parental bonding, Dr. Rajbhandari added.
Next steps include how to prioritize implementation, as well as deimplementation of outdated practices, said Francisco Alvarez, MD, of Lucile Packard Children’s Hospital, Palo Alto, Calif. “A lot of our practices were started without good evidence for why they should be done,” he said. Other steps include value improvement research; use of dashboards and benchmarking; involving other stakeholders including patients, families, and other health care providers; and addressing racial disparities, he concluded.
The presenters had no financial conflicts to disclose. The conference was sponsored by the Academic Pediatric Association, the American Academy of Pediatrics, and the Society of Hospital Medicine.
“Health care spending and health care waste is a huge problem in the U.S., including for children,” Vivian Lee, MD, of Children’s Hospital, Los Angeles, said in a presentation at the 2021 virtual Pediatric Hospital Medicine conference.
Data from a 2019 study suggested that approximately 25% of health care spending in the United States qualifies as “wasteful spending,” in categories such as overtesting, and unnecessary hospitalization, Dr. Lee said. “It is essential for physicians in hospitals to be stewards of high-value care,” she emphasized.
To combat wasteful spending and control health care costs, the Choosing Wisely campaign was created in 2012 as an initiative from the American Board of Internal Medicine Foundation. An ongoing goal of the campaign is to raise awareness among physicians and patients about potential areas of low-value services and overuse. The overall campaign includes clinician-driven recommendations from multiple medical organizations.
The PHM produced its first set of five recommendations in 2012, Dr. Lee said. These recommendations, titled “Five Things Physicians and Patients Should Question,” have been updated for 2021. The updated recommendations were created as a partnership among the Academic Pediatric Association, the American Academy of Pediatrics, and the Society of Hospital Medicine. A joint committee reviewed the latest evidence, and the updates were approved by the societies and published by the ABIM in January 2021.
“We think these recommendations truly reflect an exciting and evolving landscape for pediatric hospitalists,” Dr. Lee said. “There is a greater focus on opportunities to transition out of the hospital sooner, or avoid hospitalization altogether. There is an emphasis on antibiotic stewardship and a growing recognition of the impact that overuse may have on our vulnerable neonatal population,” she said. Several members of the Choosing Wisely panel presented the recommendations during the virtual presentation.
Revised recommendations
The new “Five Things Physicians and Patients Should Question” are as follows:
1. Do not prescribe IV antibiotics for predetermined durations for patients hospitalized with infections such as pyelonephritis, osteomyelitis, and complicated pneumonia. Consider early transition to oral antibiotics.
Many antibiotic doses used in clinical practice are preset durations that are not based on high-quality evidence, said Mike Tchou, MD, of Children’s Hospital of Colorado in Aurora. However, studies now show that earlier transition to enteral antibiotics can improve a range of outcomes including neonatal UTIs, osteomyelitis, and complicated pneumonia, he said. Considering early transition based on a patient’s response can decrease adverse events, pain, length of stay, and health care costs, he explained.
2. Do not continue hospitalization in well-appearing febrile infants once bacterial cultures (i.e., blood, cerebrospinal, and/or urine) have been confirmed negative for 24-36 hours, if adequate outpatient follow-up can be assured.
Recent data indicate that continuing hospitalization beyond 24-36 hours of confirmed negative bacterial cultures does not improve clinical outcomes for well-appearing infants admitted for concern of serious bacterial infection, said Paula Soung, MD, of Children’s Wisconsin in Milwaukee. In fact, “blood culture yield is highest in the first 12-36 hours after incubation with multiple studies demonstrating > 90% of pathogen cultures being positive by 24 hours,” Dr. Soung said. “If adequate outpatient follow-up can be assured, discharging well-appearing febrile infants at 24-36 hours after confirming cultures are negative has many positive outcomes,” she said.
3. Do not initiate phototherapy in term or late preterm well-appearing infants with neonatal hyperbilirubinemia if their bilirubin is below levels at which the AAP guidelines recommend treatment.
In making this recommendation, “we considered that the risk of kernicterus and cerebral palsy is extremely low in otherwise healthy term and late preterm newborns,” said Allison Holmes, MD, of Children’s Hospital at Dartmouth-Hitchcock, Manchester, N.H. “Subthreshold phototherapy leads to unnecessary hospitalization and its associated costs and harms,” and data show that kernicterus generally occurs close to 40 mg/dL and occurs most often in infants with hemolysis, she added.
The evidence for the recommendations included data showing that, among other factors, 8.6 of 100,000 babies have a bilirubin greater than 30 mg/dL, said Dr. Holmes. Risks of using subthreshold phototherapy include increased length of stay, increased readmissions, and increased costs, as well as decreased breastfeeding, bonding with parents, and increased parental anxiety. “Adding prolonged hospitalization for an intervention that might not be necessary can be stressful for parents,” she said.
4. Do not use broad-spectrum antibiotics such as ceftriaxone for children hospitalized with uncomplicated community-acquired pneumonia. Use narrow-spectrum antibiotics such as penicillin, ampicillin, or amoxicillin.
Michelle Lossius, MD, of the Shands Hospital for Children at the University of Florida, Gainesville, noted that the recommendations reflect IDSA guidelines from 2011 advising the use of ampicillin or penicillin for this population of children. More recent studies with large populations support the ability of narrow-spectrum antibiotics to limit the development of resistant organisms while achieving the same or better outcomes for children hospitalized with CAP, she said.
5. Do not start IV antibiotic therapy on well-appearing newborn infants with isolated risk factors for sepsis such as maternal chorioamnionitis, prolonged rupture of membranes, or untreated group-B streptococcal colonization. Use clinical tools such as an evidence-based sepsis risk calculator to guide management.
“This recommendation combines other recommendations,” said Prabi Rajbhandari, MD, of Akron (Ohio) Children’s Hospital. The evidence is ample, as the Centers for Disease Control and Prevention recommends the use of sepsis calculators to guide clinical management in sepsis patients, she said.
Data comparing periods before and after the adoption of a sepsis risk calculator showed a significant reduction in the use of blood cultures and antibiotics, she noted. Other risks of jumping to IV antibiotics include increased hospital stay, increased parental anxiety, and decreased parental bonding, Dr. Rajbhandari added.
Next steps include how to prioritize implementation, as well as deimplementation of outdated practices, said Francisco Alvarez, MD, of Lucile Packard Children’s Hospital, Palo Alto, Calif. “A lot of our practices were started without good evidence for why they should be done,” he said. Other steps include value improvement research; use of dashboards and benchmarking; involving other stakeholders including patients, families, and other health care providers; and addressing racial disparities, he concluded.
The presenters had no financial conflicts to disclose. The conference was sponsored by the Academic Pediatric Association, the American Academy of Pediatrics, and the Society of Hospital Medicine.
“Health care spending and health care waste is a huge problem in the U.S., including for children,” Vivian Lee, MD, of Children’s Hospital, Los Angeles, said in a presentation at the 2021 virtual Pediatric Hospital Medicine conference.
Data from a 2019 study suggested that approximately 25% of health care spending in the United States qualifies as “wasteful spending,” in categories such as overtesting, and unnecessary hospitalization, Dr. Lee said. “It is essential for physicians in hospitals to be stewards of high-value care,” she emphasized.
To combat wasteful spending and control health care costs, the Choosing Wisely campaign was created in 2012 as an initiative from the American Board of Internal Medicine Foundation. An ongoing goal of the campaign is to raise awareness among physicians and patients about potential areas of low-value services and overuse. The overall campaign includes clinician-driven recommendations from multiple medical organizations.
The PHM produced its first set of five recommendations in 2012, Dr. Lee said. These recommendations, titled “Five Things Physicians and Patients Should Question,” have been updated for 2021. The updated recommendations were created as a partnership among the Academic Pediatric Association, the American Academy of Pediatrics, and the Society of Hospital Medicine. A joint committee reviewed the latest evidence, and the updates were approved by the societies and published by the ABIM in January 2021.
“We think these recommendations truly reflect an exciting and evolving landscape for pediatric hospitalists,” Dr. Lee said. “There is a greater focus on opportunities to transition out of the hospital sooner, or avoid hospitalization altogether. There is an emphasis on antibiotic stewardship and a growing recognition of the impact that overuse may have on our vulnerable neonatal population,” she said. Several members of the Choosing Wisely panel presented the recommendations during the virtual presentation.
Revised recommendations
The new “Five Things Physicians and Patients Should Question” are as follows:
1. Do not prescribe IV antibiotics for predetermined durations for patients hospitalized with infections such as pyelonephritis, osteomyelitis, and complicated pneumonia. Consider early transition to oral antibiotics.
Many antibiotic doses used in clinical practice are preset durations that are not based on high-quality evidence, said Mike Tchou, MD, of Children’s Hospital of Colorado in Aurora. However, studies now show that earlier transition to enteral antibiotics can improve a range of outcomes including neonatal UTIs, osteomyelitis, and complicated pneumonia, he said. Considering early transition based on a patient’s response can decrease adverse events, pain, length of stay, and health care costs, he explained.
2. Do not continue hospitalization in well-appearing febrile infants once bacterial cultures (i.e., blood, cerebrospinal, and/or urine) have been confirmed negative for 24-36 hours, if adequate outpatient follow-up can be assured.
Recent data indicate that continuing hospitalization beyond 24-36 hours of confirmed negative bacterial cultures does not improve clinical outcomes for well-appearing infants admitted for concern of serious bacterial infection, said Paula Soung, MD, of Children’s Wisconsin in Milwaukee. In fact, “blood culture yield is highest in the first 12-36 hours after incubation with multiple studies demonstrating > 90% of pathogen cultures being positive by 24 hours,” Dr. Soung said. “If adequate outpatient follow-up can be assured, discharging well-appearing febrile infants at 24-36 hours after confirming cultures are negative has many positive outcomes,” she said.
3. Do not initiate phototherapy in term or late preterm well-appearing infants with neonatal hyperbilirubinemia if their bilirubin is below levels at which the AAP guidelines recommend treatment.
In making this recommendation, “we considered that the risk of kernicterus and cerebral palsy is extremely low in otherwise healthy term and late preterm newborns,” said Allison Holmes, MD, of Children’s Hospital at Dartmouth-Hitchcock, Manchester, N.H. “Subthreshold phototherapy leads to unnecessary hospitalization and its associated costs and harms,” and data show that kernicterus generally occurs close to 40 mg/dL and occurs most often in infants with hemolysis, she added.
The evidence for the recommendations included data showing that, among other factors, 8.6 of 100,000 babies have a bilirubin greater than 30 mg/dL, said Dr. Holmes. Risks of using subthreshold phototherapy include increased length of stay, increased readmissions, and increased costs, as well as decreased breastfeeding, bonding with parents, and increased parental anxiety. “Adding prolonged hospitalization for an intervention that might not be necessary can be stressful for parents,” she said.
4. Do not use broad-spectrum antibiotics such as ceftriaxone for children hospitalized with uncomplicated community-acquired pneumonia. Use narrow-spectrum antibiotics such as penicillin, ampicillin, or amoxicillin.
Michelle Lossius, MD, of the Shands Hospital for Children at the University of Florida, Gainesville, noted that the recommendations reflect IDSA guidelines from 2011 advising the use of ampicillin or penicillin for this population of children. More recent studies with large populations support the ability of narrow-spectrum antibiotics to limit the development of resistant organisms while achieving the same or better outcomes for children hospitalized with CAP, she said.
5. Do not start IV antibiotic therapy on well-appearing newborn infants with isolated risk factors for sepsis such as maternal chorioamnionitis, prolonged rupture of membranes, or untreated group-B streptococcal colonization. Use clinical tools such as an evidence-based sepsis risk calculator to guide management.
“This recommendation combines other recommendations,” said Prabi Rajbhandari, MD, of Akron (Ohio) Children’s Hospital. The evidence is ample, as the Centers for Disease Control and Prevention recommends the use of sepsis calculators to guide clinical management in sepsis patients, she said.
Data comparing periods before and after the adoption of a sepsis risk calculator showed a significant reduction in the use of blood cultures and antibiotics, she noted. Other risks of jumping to IV antibiotics include increased hospital stay, increased parental anxiety, and decreased parental bonding, Dr. Rajbhandari added.
Next steps include how to prioritize implementation, as well as deimplementation of outdated practices, said Francisco Alvarez, MD, of Lucile Packard Children’s Hospital, Palo Alto, Calif. “A lot of our practices were started without good evidence for why they should be done,” he said. Other steps include value improvement research; use of dashboards and benchmarking; involving other stakeholders including patients, families, and other health care providers; and addressing racial disparities, he concluded.
The presenters had no financial conflicts to disclose. The conference was sponsored by the Academic Pediatric Association, the American Academy of Pediatrics, and the Society of Hospital Medicine.
FROM PHM 2021
United States reaches 5 million cases of child COVID
Cases of child COVID-19 set a new 1-week record and the total number of children infected during the pandemic passed 5 million, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
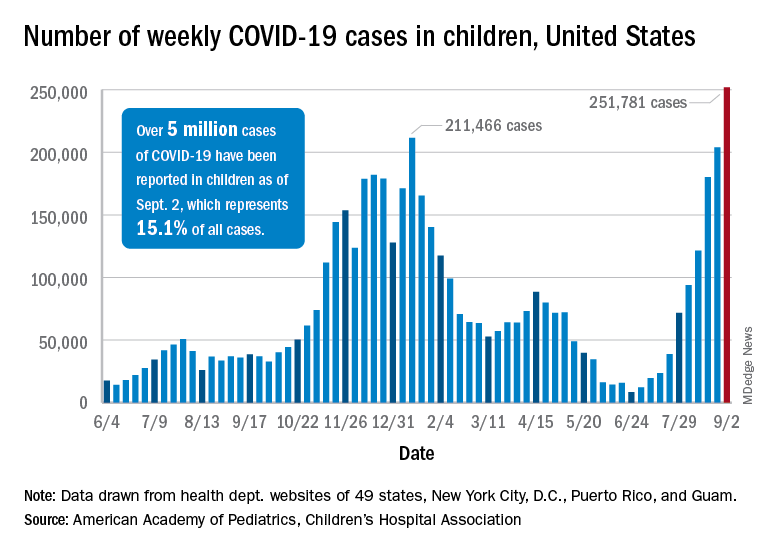
The nearly 282,000 new cases reported in the United States during the week ending Sept. 2 broke the record of 211,000 set in mid-January and brought the cumulative count to 5,049,465 children with COVID-19 since the pandemic began, the AAP and the CHA said in their weekly COVID report.
Hospitalizations in children aged 0-17 years have also reached record levels in recent days. The highest daily admission rate since the pandemic began, 0.51 per 100,000 population, was recorded on Sept. 2, less than 2 months after the nation saw its lowest child COVID admission rate for 1 day: 0.07 per 100,000 on July 4. That’s an increase of 629%, according to data from the Centers for Disease Control and Prevention.
Vaccinations in children, however, did not follow suit. New vaccinations in children aged 12-17 years dropped by 4.5% for the week ending Sept. 6, compared with the week before. Initiations were actually up almost 12% for children aged 16-17, but that was not enough to overcome the continued decline among 12- to 15-year-olds, the CDC said on its COVID Data Tracker.
Despite the decline in new vaccinations, those younger children passed a noteworthy group milestone: 50.9% of all 12- to 15-year-olds now have received at least one dose, with 38.6% having completed the regimen. The 16- to 17-year-olds got an earlier start and have reached 58.9% coverage for one dose and 47.6% for two, the CDC said.
A total of 12.2 million children aged 12-17 years had received at least one dose of COVID vaccine as of Sept. 6, of whom almost 9.5 million are fully vaccinated, based on the CDC data.
At the state level, Vermont has the highest rates for vaccine initiation (75%) and full vaccination (65%), with Massachusetts (75%/62%) and Connecticut (73%/59%) just behind. The other end of the scale is occupied by Wyoming (28% initiation/19% full vaccination), Alabama (32%/19%), and North Dakota (32%/23%), the AAP said in a separate report.
In a recent letter to the Food and Drug Administration, AAP President Lee Savio Beers, MD, said that the “Delta variant is surging at extremely alarming rates in every region of America. This surge is seriously impacting all populations, including children.” Dr. Beers urged the FDA to work “aggressively toward authorizing safe and effective COVID-19 vaccines for children under age 12 as soon as possible.”
Cases of child COVID-19 set a new 1-week record and the total number of children infected during the pandemic passed 5 million, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
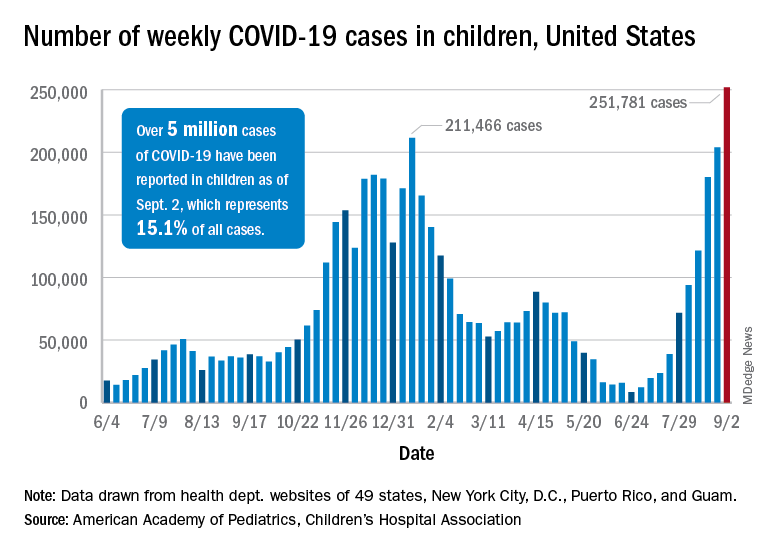
The nearly 282,000 new cases reported in the United States during the week ending Sept. 2 broke the record of 211,000 set in mid-January and brought the cumulative count to 5,049,465 children with COVID-19 since the pandemic began, the AAP and the CHA said in their weekly COVID report.
Hospitalizations in children aged 0-17 years have also reached record levels in recent days. The highest daily admission rate since the pandemic began, 0.51 per 100,000 population, was recorded on Sept. 2, less than 2 months after the nation saw its lowest child COVID admission rate for 1 day: 0.07 per 100,000 on July 4. That’s an increase of 629%, according to data from the Centers for Disease Control and Prevention.
Vaccinations in children, however, did not follow suit. New vaccinations in children aged 12-17 years dropped by 4.5% for the week ending Sept. 6, compared with the week before. Initiations were actually up almost 12% for children aged 16-17, but that was not enough to overcome the continued decline among 12- to 15-year-olds, the CDC said on its COVID Data Tracker.
Despite the decline in new vaccinations, those younger children passed a noteworthy group milestone: 50.9% of all 12- to 15-year-olds now have received at least one dose, with 38.6% having completed the regimen. The 16- to 17-year-olds got an earlier start and have reached 58.9% coverage for one dose and 47.6% for two, the CDC said.
A total of 12.2 million children aged 12-17 years had received at least one dose of COVID vaccine as of Sept. 6, of whom almost 9.5 million are fully vaccinated, based on the CDC data.
At the state level, Vermont has the highest rates for vaccine initiation (75%) and full vaccination (65%), with Massachusetts (75%/62%) and Connecticut (73%/59%) just behind. The other end of the scale is occupied by Wyoming (28% initiation/19% full vaccination), Alabama (32%/19%), and North Dakota (32%/23%), the AAP said in a separate report.
In a recent letter to the Food and Drug Administration, AAP President Lee Savio Beers, MD, said that the “Delta variant is surging at extremely alarming rates in every region of America. This surge is seriously impacting all populations, including children.” Dr. Beers urged the FDA to work “aggressively toward authorizing safe and effective COVID-19 vaccines for children under age 12 as soon as possible.”
Cases of child COVID-19 set a new 1-week record and the total number of children infected during the pandemic passed 5 million, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
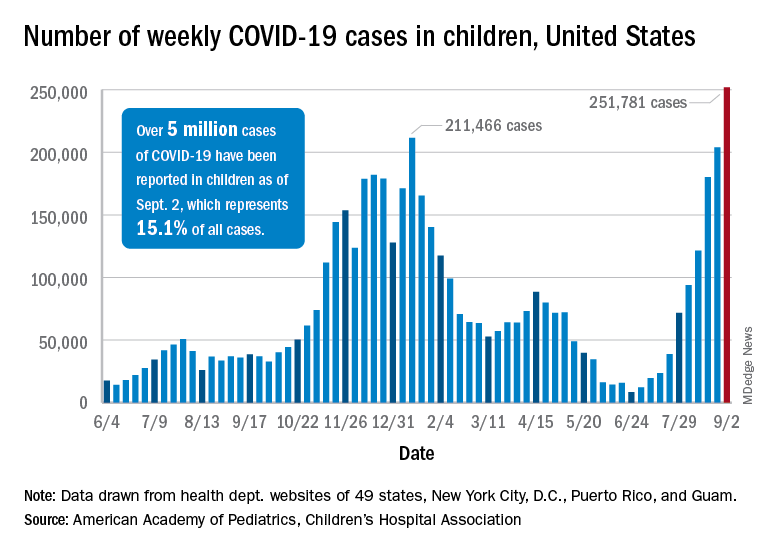
The nearly 282,000 new cases reported in the United States during the week ending Sept. 2 broke the record of 211,000 set in mid-January and brought the cumulative count to 5,049,465 children with COVID-19 since the pandemic began, the AAP and the CHA said in their weekly COVID report.
Hospitalizations in children aged 0-17 years have also reached record levels in recent days. The highest daily admission rate since the pandemic began, 0.51 per 100,000 population, was recorded on Sept. 2, less than 2 months after the nation saw its lowest child COVID admission rate for 1 day: 0.07 per 100,000 on July 4. That’s an increase of 629%, according to data from the Centers for Disease Control and Prevention.
Vaccinations in children, however, did not follow suit. New vaccinations in children aged 12-17 years dropped by 4.5% for the week ending Sept. 6, compared with the week before. Initiations were actually up almost 12% for children aged 16-17, but that was not enough to overcome the continued decline among 12- to 15-year-olds, the CDC said on its COVID Data Tracker.
Despite the decline in new vaccinations, those younger children passed a noteworthy group milestone: 50.9% of all 12- to 15-year-olds now have received at least one dose, with 38.6% having completed the regimen. The 16- to 17-year-olds got an earlier start and have reached 58.9% coverage for one dose and 47.6% for two, the CDC said.
A total of 12.2 million children aged 12-17 years had received at least one dose of COVID vaccine as of Sept. 6, of whom almost 9.5 million are fully vaccinated, based on the CDC data.
At the state level, Vermont has the highest rates for vaccine initiation (75%) and full vaccination (65%), with Massachusetts (75%/62%) and Connecticut (73%/59%) just behind. The other end of the scale is occupied by Wyoming (28% initiation/19% full vaccination), Alabama (32%/19%), and North Dakota (32%/23%), the AAP said in a separate report.
In a recent letter to the Food and Drug Administration, AAP President Lee Savio Beers, MD, said that the “Delta variant is surging at extremely alarming rates in every region of America. This surge is seriously impacting all populations, including children.” Dr. Beers urged the FDA to work “aggressively toward authorizing safe and effective COVID-19 vaccines for children under age 12 as soon as possible.”
COVID-19 continues to complicate children’s mental health care
The COVID-19 pandemic continues to impact child and adolescent mental health, and clinicians are learning as they go to develop strategies that address the challenges of providing both medical and mental health care to young patients, including those who test positive for COVID-19, according to Hani Talebi, PhD, director of pediatric psychology, and Jorge Ganem, MD, FAAP, director of pediatric hospital medicine, both of the University of Texas at Austin and Dell Children’s Medical Center.
In a presentation at the 2021 virtual Pediatric Hospital Medicine conference, Dr. Talebi and Dr. Ganem shared their experiences in identifying the impact of the pandemic on mental health services in a freestanding hospital, and synthesizing inpatient mental health care and medical care outside of a dedicated mental health unit.
Mental health is a significant pediatric issue; approximately one in five children have a diagnosable mental or behavioral health problem, but nearly two-thirds get little or no help, Dr. Talebi said. “COVID-19 has only exacerbated these mental health challenges,” he said.
He noted that beginning in April 2020, the proportion of children’s mental health-related emergency department visits increased and remained elevated through the spring, summer, and fall of 2020, as families fearful of COVID-19 avoided regular hospital visits.
Data suggest that up to 50% of all adolescent psychiatric crises that led to inpatient admissions were related in some way to COVID-19, Dr. Talebi said. In addition, “individuals with a recent diagnosis of a mental health disorder are at increased risk for COVID-19 infection,” and the risk is even higher among women and African Americans, he said.
The past year significantly impacted the mental wellbeing of parents and children, Dr. Talebi said. He cited a June 2020 study in Pediatrics in which 27% of parents reported worsening mental health for themselves, and 14% reported worsening behavioral health for their children. Ongoing issues including food insecurity, loss of regular child care, and an overall “very disorienting experience in the day-to-day” compromised the mental health of families, Dr. Talebi emphasized. Children isolated at home were not meeting developmental milestones that organically occur when socializing with peers, parents didn’t know how to handle some of their children’s issues without support from schools, and many people were struggling with other preexisting health conditions, he said.
This confluence of factors helped drive a surge in emergency department visits, meaning longer wait times and concerns about meeting urgent medical and mental health needs while maintaining safety, he added.
Parents and children waited longer to seek care, and community hospitals such as Dell Children’s Medical Center were faced with children in the emergency department with crisis-level mental health issues, along with children already waiting in the ED to address medical emergencies. All these patients had to be tested for COVID-19 and managed accordingly, Dr. Talebi noted.
Dr. Talebi emphasized the need for clinically robust care of the children who were in isolation for 10 days on the medical unit, waiting to test negative. New protocols were created for social workers to conduct daily safety checks, and to develop regular schedules for screening, “so they are having an experience on the medical floors similar to what they would have in a mental health unit,” he said.
Dr. Ganem reflected on the logistical challenges of managing mental health care while observing COVID-19 safety protocols. “COVID-19 added a new wrinkle of isolation,” he said. As institutional guidelines on testing and isolation evolved, negative COVID-19 tests were required for admission to the mental health units both in the hospital and throughout the region. Patients who tested positive had to be quarantined for 10 days, at which time they could be admitted to a mental health unit if necessary, he said.
Dr. Ganem shared details of some strategies adopted by Dell Children’s. He explained that the COVID-19 psychiatry patient workflow started with an ED evaluation, followed by medical clearance and consideration for admission.
“There was significant coordination between the social worker in the emergency department and the psychiatry social worker,” he said.
Key elements of the treatment plan for children with positive COVID-19 tests included an “interprofessional huddle” to coordinate the plan of care, goals for admission, and goals for safety, Dr. Ganem said.
Patients who required admission were expected to have an initial length of stay of 72 hours, and those who tested positive for COVID-19 were admitted to a medical unit with COVID-19 isolation, he said.
Once a patient is admitted, an RN activates a suicide prevention pathway, and an interprofessional team meets to determine what patients need for safe and effective discharge, said Dr. Ganem. He cited the SAFE-T protocol (Suicide Assessment Five-step Evaluation and Triage) as one of the tools used to determine safe discharge criteria. Considerations on the SAFE-T list include family support, an established outpatient therapist and psychiatrist, no suicide attempts prior to the current admission, or a low lethality attempt, and access to partial hospitalization or intensive outpatient programs.
Patients who could not be discharged because of suicidality or inadequate support or concerns about safety at home were considered for inpatient admission. Patients with COVID-19–positive tests who had continued need for inpatient mental health services could be transferred to an inpatient mental health unit after a 10-day quarantine.
Overall, “this has been a continuum of lessons learned, with some things we know now that we didn’t know in April or May of 2020,” Dr. Ganem said. Early in the pandemic, the focus was on minimizing risk, securing personal protective equipment, and determining who provided services in a patient’s room. “We developed new paradigms on the fly,” he said, including the use of virtual visits, which included securing and cleaning devices, as well as learning how to use them in this setting,” he said.
More recently, the emphasis has been on providing services to patients before they need to visit the hospital, rather than automatically admitting any patients with suicidal ideation and a positive COVID-19 test, Dr. Ganem said.
Dr. Talebi and Dr. Ganem had no financial conflicts to disclose. The conference was sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, and the Academic Pediatric Association.
The COVID-19 pandemic continues to impact child and adolescent mental health, and clinicians are learning as they go to develop strategies that address the challenges of providing both medical and mental health care to young patients, including those who test positive for COVID-19, according to Hani Talebi, PhD, director of pediatric psychology, and Jorge Ganem, MD, FAAP, director of pediatric hospital medicine, both of the University of Texas at Austin and Dell Children’s Medical Center.
In a presentation at the 2021 virtual Pediatric Hospital Medicine conference, Dr. Talebi and Dr. Ganem shared their experiences in identifying the impact of the pandemic on mental health services in a freestanding hospital, and synthesizing inpatient mental health care and medical care outside of a dedicated mental health unit.
Mental health is a significant pediatric issue; approximately one in five children have a diagnosable mental or behavioral health problem, but nearly two-thirds get little or no help, Dr. Talebi said. “COVID-19 has only exacerbated these mental health challenges,” he said.
He noted that beginning in April 2020, the proportion of children’s mental health-related emergency department visits increased and remained elevated through the spring, summer, and fall of 2020, as families fearful of COVID-19 avoided regular hospital visits.
Data suggest that up to 50% of all adolescent psychiatric crises that led to inpatient admissions were related in some way to COVID-19, Dr. Talebi said. In addition, “individuals with a recent diagnosis of a mental health disorder are at increased risk for COVID-19 infection,” and the risk is even higher among women and African Americans, he said.
The past year significantly impacted the mental wellbeing of parents and children, Dr. Talebi said. He cited a June 2020 study in Pediatrics in which 27% of parents reported worsening mental health for themselves, and 14% reported worsening behavioral health for their children. Ongoing issues including food insecurity, loss of regular child care, and an overall “very disorienting experience in the day-to-day” compromised the mental health of families, Dr. Talebi emphasized. Children isolated at home were not meeting developmental milestones that organically occur when socializing with peers, parents didn’t know how to handle some of their children’s issues without support from schools, and many people were struggling with other preexisting health conditions, he said.
This confluence of factors helped drive a surge in emergency department visits, meaning longer wait times and concerns about meeting urgent medical and mental health needs while maintaining safety, he added.
Parents and children waited longer to seek care, and community hospitals such as Dell Children’s Medical Center were faced with children in the emergency department with crisis-level mental health issues, along with children already waiting in the ED to address medical emergencies. All these patients had to be tested for COVID-19 and managed accordingly, Dr. Talebi noted.
Dr. Talebi emphasized the need for clinically robust care of the children who were in isolation for 10 days on the medical unit, waiting to test negative. New protocols were created for social workers to conduct daily safety checks, and to develop regular schedules for screening, “so they are having an experience on the medical floors similar to what they would have in a mental health unit,” he said.
Dr. Ganem reflected on the logistical challenges of managing mental health care while observing COVID-19 safety protocols. “COVID-19 added a new wrinkle of isolation,” he said. As institutional guidelines on testing and isolation evolved, negative COVID-19 tests were required for admission to the mental health units both in the hospital and throughout the region. Patients who tested positive had to be quarantined for 10 days, at which time they could be admitted to a mental health unit if necessary, he said.
Dr. Ganem shared details of some strategies adopted by Dell Children’s. He explained that the COVID-19 psychiatry patient workflow started with an ED evaluation, followed by medical clearance and consideration for admission.
“There was significant coordination between the social worker in the emergency department and the psychiatry social worker,” he said.
Key elements of the treatment plan for children with positive COVID-19 tests included an “interprofessional huddle” to coordinate the plan of care, goals for admission, and goals for safety, Dr. Ganem said.
Patients who required admission were expected to have an initial length of stay of 72 hours, and those who tested positive for COVID-19 were admitted to a medical unit with COVID-19 isolation, he said.
Once a patient is admitted, an RN activates a suicide prevention pathway, and an interprofessional team meets to determine what patients need for safe and effective discharge, said Dr. Ganem. He cited the SAFE-T protocol (Suicide Assessment Five-step Evaluation and Triage) as one of the tools used to determine safe discharge criteria. Considerations on the SAFE-T list include family support, an established outpatient therapist and psychiatrist, no suicide attempts prior to the current admission, or a low lethality attempt, and access to partial hospitalization or intensive outpatient programs.
Patients who could not be discharged because of suicidality or inadequate support or concerns about safety at home were considered for inpatient admission. Patients with COVID-19–positive tests who had continued need for inpatient mental health services could be transferred to an inpatient mental health unit after a 10-day quarantine.
Overall, “this has been a continuum of lessons learned, with some things we know now that we didn’t know in April or May of 2020,” Dr. Ganem said. Early in the pandemic, the focus was on minimizing risk, securing personal protective equipment, and determining who provided services in a patient’s room. “We developed new paradigms on the fly,” he said, including the use of virtual visits, which included securing and cleaning devices, as well as learning how to use them in this setting,” he said.
More recently, the emphasis has been on providing services to patients before they need to visit the hospital, rather than automatically admitting any patients with suicidal ideation and a positive COVID-19 test, Dr. Ganem said.
Dr. Talebi and Dr. Ganem had no financial conflicts to disclose. The conference was sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, and the Academic Pediatric Association.
The COVID-19 pandemic continues to impact child and adolescent mental health, and clinicians are learning as they go to develop strategies that address the challenges of providing both medical and mental health care to young patients, including those who test positive for COVID-19, according to Hani Talebi, PhD, director of pediatric psychology, and Jorge Ganem, MD, FAAP, director of pediatric hospital medicine, both of the University of Texas at Austin and Dell Children’s Medical Center.
In a presentation at the 2021 virtual Pediatric Hospital Medicine conference, Dr. Talebi and Dr. Ganem shared their experiences in identifying the impact of the pandemic on mental health services in a freestanding hospital, and synthesizing inpatient mental health care and medical care outside of a dedicated mental health unit.
Mental health is a significant pediatric issue; approximately one in five children have a diagnosable mental or behavioral health problem, but nearly two-thirds get little or no help, Dr. Talebi said. “COVID-19 has only exacerbated these mental health challenges,” he said.
He noted that beginning in April 2020, the proportion of children’s mental health-related emergency department visits increased and remained elevated through the spring, summer, and fall of 2020, as families fearful of COVID-19 avoided regular hospital visits.
Data suggest that up to 50% of all adolescent psychiatric crises that led to inpatient admissions were related in some way to COVID-19, Dr. Talebi said. In addition, “individuals with a recent diagnosis of a mental health disorder are at increased risk for COVID-19 infection,” and the risk is even higher among women and African Americans, he said.
The past year significantly impacted the mental wellbeing of parents and children, Dr. Talebi said. He cited a June 2020 study in Pediatrics in which 27% of parents reported worsening mental health for themselves, and 14% reported worsening behavioral health for their children. Ongoing issues including food insecurity, loss of regular child care, and an overall “very disorienting experience in the day-to-day” compromised the mental health of families, Dr. Talebi emphasized. Children isolated at home were not meeting developmental milestones that organically occur when socializing with peers, parents didn’t know how to handle some of their children’s issues without support from schools, and many people were struggling with other preexisting health conditions, he said.
This confluence of factors helped drive a surge in emergency department visits, meaning longer wait times and concerns about meeting urgent medical and mental health needs while maintaining safety, he added.
Parents and children waited longer to seek care, and community hospitals such as Dell Children’s Medical Center were faced with children in the emergency department with crisis-level mental health issues, along with children already waiting in the ED to address medical emergencies. All these patients had to be tested for COVID-19 and managed accordingly, Dr. Talebi noted.
Dr. Talebi emphasized the need for clinically robust care of the children who were in isolation for 10 days on the medical unit, waiting to test negative. New protocols were created for social workers to conduct daily safety checks, and to develop regular schedules for screening, “so they are having an experience on the medical floors similar to what they would have in a mental health unit,” he said.
Dr. Ganem reflected on the logistical challenges of managing mental health care while observing COVID-19 safety protocols. “COVID-19 added a new wrinkle of isolation,” he said. As institutional guidelines on testing and isolation evolved, negative COVID-19 tests were required for admission to the mental health units both in the hospital and throughout the region. Patients who tested positive had to be quarantined for 10 days, at which time they could be admitted to a mental health unit if necessary, he said.
Dr. Ganem shared details of some strategies adopted by Dell Children’s. He explained that the COVID-19 psychiatry patient workflow started with an ED evaluation, followed by medical clearance and consideration for admission.
“There was significant coordination between the social worker in the emergency department and the psychiatry social worker,” he said.
Key elements of the treatment plan for children with positive COVID-19 tests included an “interprofessional huddle” to coordinate the plan of care, goals for admission, and goals for safety, Dr. Ganem said.
Patients who required admission were expected to have an initial length of stay of 72 hours, and those who tested positive for COVID-19 were admitted to a medical unit with COVID-19 isolation, he said.
Once a patient is admitted, an RN activates a suicide prevention pathway, and an interprofessional team meets to determine what patients need for safe and effective discharge, said Dr. Ganem. He cited the SAFE-T protocol (Suicide Assessment Five-step Evaluation and Triage) as one of the tools used to determine safe discharge criteria. Considerations on the SAFE-T list include family support, an established outpatient therapist and psychiatrist, no suicide attempts prior to the current admission, or a low lethality attempt, and access to partial hospitalization or intensive outpatient programs.
Patients who could not be discharged because of suicidality or inadequate support or concerns about safety at home were considered for inpatient admission. Patients with COVID-19–positive tests who had continued need for inpatient mental health services could be transferred to an inpatient mental health unit after a 10-day quarantine.
Overall, “this has been a continuum of lessons learned, with some things we know now that we didn’t know in April or May of 2020,” Dr. Ganem said. Early in the pandemic, the focus was on minimizing risk, securing personal protective equipment, and determining who provided services in a patient’s room. “We developed new paradigms on the fly,” he said, including the use of virtual visits, which included securing and cleaning devices, as well as learning how to use them in this setting,” he said.
More recently, the emphasis has been on providing services to patients before they need to visit the hospital, rather than automatically admitting any patients with suicidal ideation and a positive COVID-19 test, Dr. Ganem said.
Dr. Talebi and Dr. Ganem had no financial conflicts to disclose. The conference was sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, and the Academic Pediatric Association.
FROM PHM 2021
Anakinra improved survival in hospitalized COVID-19 patients
Hospitalized COVID-19 patients at increased risk for respiratory failure showed significant improvement after treatment with anakinra, compared with placebo, based on data from a phase 3, randomized trial of nearly 600 patients who also received standard of care treatment.
Anakinra, a recombinant interleukin (IL)-1 receptor antagonist that blocks activity for both IL-1 alpha and beta, showed a 70% decrease in the risk of progression to severe respiratory failure in a prior open-label, phase 2, proof-of-concept study, wrote Evdoxia Kyriazopoulou, MD, PhD, of National and Kapodistrian University of Athens, and colleagues.
Previous research has shown that soluble urokinase plasminogen activator receptor (suPAR) serum levels can signal increased risk of progression to severe disease and respiratory failure in COVID-19 patients, they noted.
Supported by these early findings, “the SAVE-MORE study (suPAR-guided anakinra treatment for validation of the risk and early management of severe respiratory failure by COVID-19) is a pivotal, confirmatory, phase 3, double-blind, randomized controlled trial that evaluated the efficacy and safety of early initiation of anakinra treatment in hospitalized patients with moderate or severe COVID-19,” the researchers said.
In the SAVE-MORE study published Sept. 3 in Nature Medicine, the researchers identified 594 adults with COVID-19 who were hospitalized at 37 centers in Greece and Italy and at risk of progressing to respiratory failure based on plasma suPAR levels of at least 6 ng/mL.
The primary objective was to assess the impact of early anakinra treatment on the clinical status of COVID-19 patients at risk for severe disease according to the 11-point, ordinal World Health Organization Clinical Progression Scale (WHO-CPS) at 28 days after starting treatment. All patients received standard of care, which consisted of regular monitoring of physical signs, oximetry, and anticoagulation. Patients with severe disease by the WHO definition were also received 6 mg of dexamethasone intravenously daily for 10 days. A total of 405 were randomized to anakinra and 189 to placebo. Approximately 92% of the study participants had severe pneumonia according to the WHO classification for COVID-19. The average age of the patients was 62 years, 58% were male, and the average body mass index was 29.5 kg/m2.
At 28 days, 204 (50.4%) of the anakinra-treated patients had fully recovered, with no detectable viral RNA, compared with 50 (26.5%) of the placebo-treated patients (P < .0001). In addition, significantly fewer patients in the anakinra group had died by 28 days (13 patients, 3.2%), compared with patients in the placebo group (13 patients, 6.9%).
The median decrease in WHO-CPS scores from baseline to 28 days was 4 points in the anakinra group and 3 points in the placebo group, a statistically significant difference (P < .0001).
“Overall, the unadjusted proportional odds of having a worse score on the 11-point WHO-CPS at day 28 with anakinra was 0.36 versus placebo,” and this number remained the same in adjusted analysis, the researchers wrote.
All five secondary endpoints on the WHO-CPS showed significant benefits of anakinra, compared with placebo. These included an absolute decrease of WHO-CPS at day 28 and day 14 from baseline; an absolute decrease of Sequential Organ Failure Assessment scores at day 7 from baseline; and a significantly shorter mean time to both hospital and ICU discharge (1 day and 4 days, respectively) with anakinra versus placebo.
Follow-up laboratory data showed a significant increase in absolute lymphocyte count at 7 days, a significant decrease in circulating IL-6 levels at 4 and 7 days, and significantly decreased plasma C-reactive protein (CRP) levels at 7 days.
Serious treatment-emergent adverse events were reported in 16% with anakinra and in 21.7% with placebo; the most common of these events were infections (8.4% with anakinra and 15.9% with placebo). The next most common serious treatment-emergent adverse events were ventilator-associated pneumonia, septic shock and multiple organ dysfunction, bloodstream infections, and pulmonary embolism. The most common nonserious treatment-emergent adverse events were an increase of liver function tests and hyperglycemia (similar in anakinra and placebo groups) and nonserious anemia (lower in the anakinra group).
The study findings were limited by several factors, including the lack of patients with critical COVID-19 disease and the challenge of application of suPAR in all hospital settings, the researchers noted. However, “the results validate the findings of the previous SAVE open-label phase 2 trial,” they said. The results suggest “that suPAR should be measured upon admission of all patients with COVID-19 who do not need oxygen or who need nasal or mask oxygen, and that, if suPAR levels are 6 ng/mL or higher, anakinra treatment might be a suitable therapy,” they concluded.
Cytokine storm syndrome remains a treatment challenge
“Many who die from COVID-19 suffer hyperinflammation with features of cytokine storm syndrome (CSS) and associated acute respiratory distress syndrome,” wrote Randy Q. Cron, MD, and W. Winn Chatham, MD, of the University of Alabama at Birmingham, and Roberto Caricchio, MD, of Temple University, Philadelphia, in an accompanying editorial. They noted that the SAVE-MORE trial results contrast with another recent randomized trial of canakinumab, which failed to show notable benefits, compared with placebo, in treating hospitalized patients with COVID-19 pneumonia.
“There are some key differences between these trials, one being that anakinra blocks signaling of both IL-1 alpha and IL-1 beta, whereas canakinumab binds only IL-1 beta,” the editorialists explained. “SARS-CoV-2–infected endothelium may be a particularly important source of IL-1 alpha that is not targeted by canakinumab,” they noted.
Additional studies have examined IL-6 inhibition to treat COVID-19 patients, but data have been inconsistent, the editorialists said.
“One thing that is clearly emerging from this pandemic is that the CSS associated with COVID-19 is relatively unique, with only modestly elevated levels of IL-6, CRP, and ferritin, for example,” they noted. However, the SAVE-MORE study suggests that more targeted approaches, such as anakinra, “may allow earlier introduction of anticytokine treatment” and support the use of IL-1 blockade with anakinra for cases of severe COVID-19 pneumonia.
Predicting risk for severe disease
“One of the major challenges in the management of patients with COVID-19 is identifying patients at risk of severe disease who would warrant early intervention with anti-inflammatory therapy,” said Salim Hayek, MD, medical director of the University of Michigan’s Frankel Cardiovascular Center Clinics, in an interview. “We and others had found that soluble urokinase plasminogen activator receptor (suPAR) levels are the strongest predictor of severe disease amongst biomarkers of inflammation,” he said. “In this study, patients with high suPAR levels derived benefit from anakinra, compared to those with placebo. This study is a great example of how suPAR levels could be used to identify high-risk patients that would benefit from therapies targeting inflammation,” Dr. Hayek emphasized.
“The findings are in line with the hypothesis that patients with the highest degrees of inflammation would benefit the best from targeting the hyperinflammatory cascade using anakinra or other interleukin antagonists,” Dr. Hayek said. “Given suPAR levels are the best predictors of high-risk disease, it is not surprising to see that patients with high levels benefit from targeting inflammation,” he noted.
The take-home message for clinicians at this time is that anakinra effectively improves outcomes in COVID-19 patients with high suPAR levels, Dr. Hayek said. “SuPAR can be measured easily at the point of care. Thus, a targeted strategy using suPAR to identify patients who would benefit from anakinra appears to be viable,” he explained.
However, “Whether anakinra is effective in patients with lower suPAR levels (<6 ng/mL) is unclear and was not answered by this study,” he said. “We eagerly await results of other trials to make that determination. Whether suPAR levels can also help guide the use of other therapies for COVID-19 should be explored and would enhance the personalization of treatment for COVID-19 according to the underlying inflammatory state,” he added.
The SAVE-MORE study was funded by the Hellenic Institute for the Study of Sepsis and Sobi, which manufactures anakinra. Some of the study authors reported financial relationships with Sobi and other pharmaceutical companies.
Dr. Cron disclosed serving as a consultant to Sobi, Novartis, Pfizer, and Sironax. Dr. Cron and Dr. Chatham disclosed having received grant support from Sobi for investigator-initiated clinical trials, and Dr. Caricchio disclosed serving as a consultant to GlaxoSmithKline, Johnson & Johnson, Aurinia, and Bristol-Myers Squibb. Dr. Hayek had no relevant financial conflicts to disclose.
Hospitalized COVID-19 patients at increased risk for respiratory failure showed significant improvement after treatment with anakinra, compared with placebo, based on data from a phase 3, randomized trial of nearly 600 patients who also received standard of care treatment.
Anakinra, a recombinant interleukin (IL)-1 receptor antagonist that blocks activity for both IL-1 alpha and beta, showed a 70% decrease in the risk of progression to severe respiratory failure in a prior open-label, phase 2, proof-of-concept study, wrote Evdoxia Kyriazopoulou, MD, PhD, of National and Kapodistrian University of Athens, and colleagues.
Previous research has shown that soluble urokinase plasminogen activator receptor (suPAR) serum levels can signal increased risk of progression to severe disease and respiratory failure in COVID-19 patients, they noted.
Supported by these early findings, “the SAVE-MORE study (suPAR-guided anakinra treatment for validation of the risk and early management of severe respiratory failure by COVID-19) is a pivotal, confirmatory, phase 3, double-blind, randomized controlled trial that evaluated the efficacy and safety of early initiation of anakinra treatment in hospitalized patients with moderate or severe COVID-19,” the researchers said.
In the SAVE-MORE study published Sept. 3 in Nature Medicine, the researchers identified 594 adults with COVID-19 who were hospitalized at 37 centers in Greece and Italy and at risk of progressing to respiratory failure based on plasma suPAR levels of at least 6 ng/mL.
The primary objective was to assess the impact of early anakinra treatment on the clinical status of COVID-19 patients at risk for severe disease according to the 11-point, ordinal World Health Organization Clinical Progression Scale (WHO-CPS) at 28 days after starting treatment. All patients received standard of care, which consisted of regular monitoring of physical signs, oximetry, and anticoagulation. Patients with severe disease by the WHO definition were also received 6 mg of dexamethasone intravenously daily for 10 days. A total of 405 were randomized to anakinra and 189 to placebo. Approximately 92% of the study participants had severe pneumonia according to the WHO classification for COVID-19. The average age of the patients was 62 years, 58% were male, and the average body mass index was 29.5 kg/m2.
At 28 days, 204 (50.4%) of the anakinra-treated patients had fully recovered, with no detectable viral RNA, compared with 50 (26.5%) of the placebo-treated patients (P < .0001). In addition, significantly fewer patients in the anakinra group had died by 28 days (13 patients, 3.2%), compared with patients in the placebo group (13 patients, 6.9%).
The median decrease in WHO-CPS scores from baseline to 28 days was 4 points in the anakinra group and 3 points in the placebo group, a statistically significant difference (P < .0001).
“Overall, the unadjusted proportional odds of having a worse score on the 11-point WHO-CPS at day 28 with anakinra was 0.36 versus placebo,” and this number remained the same in adjusted analysis, the researchers wrote.
All five secondary endpoints on the WHO-CPS showed significant benefits of anakinra, compared with placebo. These included an absolute decrease of WHO-CPS at day 28 and day 14 from baseline; an absolute decrease of Sequential Organ Failure Assessment scores at day 7 from baseline; and a significantly shorter mean time to both hospital and ICU discharge (1 day and 4 days, respectively) with anakinra versus placebo.
Follow-up laboratory data showed a significant increase in absolute lymphocyte count at 7 days, a significant decrease in circulating IL-6 levels at 4 and 7 days, and significantly decreased plasma C-reactive protein (CRP) levels at 7 days.
Serious treatment-emergent adverse events were reported in 16% with anakinra and in 21.7% with placebo; the most common of these events were infections (8.4% with anakinra and 15.9% with placebo). The next most common serious treatment-emergent adverse events were ventilator-associated pneumonia, septic shock and multiple organ dysfunction, bloodstream infections, and pulmonary embolism. The most common nonserious treatment-emergent adverse events were an increase of liver function tests and hyperglycemia (similar in anakinra and placebo groups) and nonserious anemia (lower in the anakinra group).
The study findings were limited by several factors, including the lack of patients with critical COVID-19 disease and the challenge of application of suPAR in all hospital settings, the researchers noted. However, “the results validate the findings of the previous SAVE open-label phase 2 trial,” they said. The results suggest “that suPAR should be measured upon admission of all patients with COVID-19 who do not need oxygen or who need nasal or mask oxygen, and that, if suPAR levels are 6 ng/mL or higher, anakinra treatment might be a suitable therapy,” they concluded.
Cytokine storm syndrome remains a treatment challenge
“Many who die from COVID-19 suffer hyperinflammation with features of cytokine storm syndrome (CSS) and associated acute respiratory distress syndrome,” wrote Randy Q. Cron, MD, and W. Winn Chatham, MD, of the University of Alabama at Birmingham, and Roberto Caricchio, MD, of Temple University, Philadelphia, in an accompanying editorial. They noted that the SAVE-MORE trial results contrast with another recent randomized trial of canakinumab, which failed to show notable benefits, compared with placebo, in treating hospitalized patients with COVID-19 pneumonia.
“There are some key differences between these trials, one being that anakinra blocks signaling of both IL-1 alpha and IL-1 beta, whereas canakinumab binds only IL-1 beta,” the editorialists explained. “SARS-CoV-2–infected endothelium may be a particularly important source of IL-1 alpha that is not targeted by canakinumab,” they noted.
Additional studies have examined IL-6 inhibition to treat COVID-19 patients, but data have been inconsistent, the editorialists said.
“One thing that is clearly emerging from this pandemic is that the CSS associated with COVID-19 is relatively unique, with only modestly elevated levels of IL-6, CRP, and ferritin, for example,” they noted. However, the SAVE-MORE study suggests that more targeted approaches, such as anakinra, “may allow earlier introduction of anticytokine treatment” and support the use of IL-1 blockade with anakinra for cases of severe COVID-19 pneumonia.
Predicting risk for severe disease
“One of the major challenges in the management of patients with COVID-19 is identifying patients at risk of severe disease who would warrant early intervention with anti-inflammatory therapy,” said Salim Hayek, MD, medical director of the University of Michigan’s Frankel Cardiovascular Center Clinics, in an interview. “We and others had found that soluble urokinase plasminogen activator receptor (suPAR) levels are the strongest predictor of severe disease amongst biomarkers of inflammation,” he said. “In this study, patients with high suPAR levels derived benefit from anakinra, compared to those with placebo. This study is a great example of how suPAR levels could be used to identify high-risk patients that would benefit from therapies targeting inflammation,” Dr. Hayek emphasized.
“The findings are in line with the hypothesis that patients with the highest degrees of inflammation would benefit the best from targeting the hyperinflammatory cascade using anakinra or other interleukin antagonists,” Dr. Hayek said. “Given suPAR levels are the best predictors of high-risk disease, it is not surprising to see that patients with high levels benefit from targeting inflammation,” he noted.
The take-home message for clinicians at this time is that anakinra effectively improves outcomes in COVID-19 patients with high suPAR levels, Dr. Hayek said. “SuPAR can be measured easily at the point of care. Thus, a targeted strategy using suPAR to identify patients who would benefit from anakinra appears to be viable,” he explained.
However, “Whether anakinra is effective in patients with lower suPAR levels (<6 ng/mL) is unclear and was not answered by this study,” he said. “We eagerly await results of other trials to make that determination. Whether suPAR levels can also help guide the use of other therapies for COVID-19 should be explored and would enhance the personalization of treatment for COVID-19 according to the underlying inflammatory state,” he added.
The SAVE-MORE study was funded by the Hellenic Institute for the Study of Sepsis and Sobi, which manufactures anakinra. Some of the study authors reported financial relationships with Sobi and other pharmaceutical companies.
Dr. Cron disclosed serving as a consultant to Sobi, Novartis, Pfizer, and Sironax. Dr. Cron and Dr. Chatham disclosed having received grant support from Sobi for investigator-initiated clinical trials, and Dr. Caricchio disclosed serving as a consultant to GlaxoSmithKline, Johnson & Johnson, Aurinia, and Bristol-Myers Squibb. Dr. Hayek had no relevant financial conflicts to disclose.
Hospitalized COVID-19 patients at increased risk for respiratory failure showed significant improvement after treatment with anakinra, compared with placebo, based on data from a phase 3, randomized trial of nearly 600 patients who also received standard of care treatment.
Anakinra, a recombinant interleukin (IL)-1 receptor antagonist that blocks activity for both IL-1 alpha and beta, showed a 70% decrease in the risk of progression to severe respiratory failure in a prior open-label, phase 2, proof-of-concept study, wrote Evdoxia Kyriazopoulou, MD, PhD, of National and Kapodistrian University of Athens, and colleagues.
Previous research has shown that soluble urokinase plasminogen activator receptor (suPAR) serum levels can signal increased risk of progression to severe disease and respiratory failure in COVID-19 patients, they noted.
Supported by these early findings, “the SAVE-MORE study (suPAR-guided anakinra treatment for validation of the risk and early management of severe respiratory failure by COVID-19) is a pivotal, confirmatory, phase 3, double-blind, randomized controlled trial that evaluated the efficacy and safety of early initiation of anakinra treatment in hospitalized patients with moderate or severe COVID-19,” the researchers said.
In the SAVE-MORE study published Sept. 3 in Nature Medicine, the researchers identified 594 adults with COVID-19 who were hospitalized at 37 centers in Greece and Italy and at risk of progressing to respiratory failure based on plasma suPAR levels of at least 6 ng/mL.
The primary objective was to assess the impact of early anakinra treatment on the clinical status of COVID-19 patients at risk for severe disease according to the 11-point, ordinal World Health Organization Clinical Progression Scale (WHO-CPS) at 28 days after starting treatment. All patients received standard of care, which consisted of regular monitoring of physical signs, oximetry, and anticoagulation. Patients with severe disease by the WHO definition were also received 6 mg of dexamethasone intravenously daily for 10 days. A total of 405 were randomized to anakinra and 189 to placebo. Approximately 92% of the study participants had severe pneumonia according to the WHO classification for COVID-19. The average age of the patients was 62 years, 58% were male, and the average body mass index was 29.5 kg/m2.
At 28 days, 204 (50.4%) of the anakinra-treated patients had fully recovered, with no detectable viral RNA, compared with 50 (26.5%) of the placebo-treated patients (P < .0001). In addition, significantly fewer patients in the anakinra group had died by 28 days (13 patients, 3.2%), compared with patients in the placebo group (13 patients, 6.9%).
The median decrease in WHO-CPS scores from baseline to 28 days was 4 points in the anakinra group and 3 points in the placebo group, a statistically significant difference (P < .0001).
“Overall, the unadjusted proportional odds of having a worse score on the 11-point WHO-CPS at day 28 with anakinra was 0.36 versus placebo,” and this number remained the same in adjusted analysis, the researchers wrote.
All five secondary endpoints on the WHO-CPS showed significant benefits of anakinra, compared with placebo. These included an absolute decrease of WHO-CPS at day 28 and day 14 from baseline; an absolute decrease of Sequential Organ Failure Assessment scores at day 7 from baseline; and a significantly shorter mean time to both hospital and ICU discharge (1 day and 4 days, respectively) with anakinra versus placebo.
Follow-up laboratory data showed a significant increase in absolute lymphocyte count at 7 days, a significant decrease in circulating IL-6 levels at 4 and 7 days, and significantly decreased plasma C-reactive protein (CRP) levels at 7 days.
Serious treatment-emergent adverse events were reported in 16% with anakinra and in 21.7% with placebo; the most common of these events were infections (8.4% with anakinra and 15.9% with placebo). The next most common serious treatment-emergent adverse events were ventilator-associated pneumonia, septic shock and multiple organ dysfunction, bloodstream infections, and pulmonary embolism. The most common nonserious treatment-emergent adverse events were an increase of liver function tests and hyperglycemia (similar in anakinra and placebo groups) and nonserious anemia (lower in the anakinra group).
The study findings were limited by several factors, including the lack of patients with critical COVID-19 disease and the challenge of application of suPAR in all hospital settings, the researchers noted. However, “the results validate the findings of the previous SAVE open-label phase 2 trial,” they said. The results suggest “that suPAR should be measured upon admission of all patients with COVID-19 who do not need oxygen or who need nasal or mask oxygen, and that, if suPAR levels are 6 ng/mL or higher, anakinra treatment might be a suitable therapy,” they concluded.
Cytokine storm syndrome remains a treatment challenge
“Many who die from COVID-19 suffer hyperinflammation with features of cytokine storm syndrome (CSS) and associated acute respiratory distress syndrome,” wrote Randy Q. Cron, MD, and W. Winn Chatham, MD, of the University of Alabama at Birmingham, and Roberto Caricchio, MD, of Temple University, Philadelphia, in an accompanying editorial. They noted that the SAVE-MORE trial results contrast with another recent randomized trial of canakinumab, which failed to show notable benefits, compared with placebo, in treating hospitalized patients with COVID-19 pneumonia.
“There are some key differences between these trials, one being that anakinra blocks signaling of both IL-1 alpha and IL-1 beta, whereas canakinumab binds only IL-1 beta,” the editorialists explained. “SARS-CoV-2–infected endothelium may be a particularly important source of IL-1 alpha that is not targeted by canakinumab,” they noted.
Additional studies have examined IL-6 inhibition to treat COVID-19 patients, but data have been inconsistent, the editorialists said.
“One thing that is clearly emerging from this pandemic is that the CSS associated with COVID-19 is relatively unique, with only modestly elevated levels of IL-6, CRP, and ferritin, for example,” they noted. However, the SAVE-MORE study suggests that more targeted approaches, such as anakinra, “may allow earlier introduction of anticytokine treatment” and support the use of IL-1 blockade with anakinra for cases of severe COVID-19 pneumonia.
Predicting risk for severe disease
“One of the major challenges in the management of patients with COVID-19 is identifying patients at risk of severe disease who would warrant early intervention with anti-inflammatory therapy,” said Salim Hayek, MD, medical director of the University of Michigan’s Frankel Cardiovascular Center Clinics, in an interview. “We and others had found that soluble urokinase plasminogen activator receptor (suPAR) levels are the strongest predictor of severe disease amongst biomarkers of inflammation,” he said. “In this study, patients with high suPAR levels derived benefit from anakinra, compared to those with placebo. This study is a great example of how suPAR levels could be used to identify high-risk patients that would benefit from therapies targeting inflammation,” Dr. Hayek emphasized.
“The findings are in line with the hypothesis that patients with the highest degrees of inflammation would benefit the best from targeting the hyperinflammatory cascade using anakinra or other interleukin antagonists,” Dr. Hayek said. “Given suPAR levels are the best predictors of high-risk disease, it is not surprising to see that patients with high levels benefit from targeting inflammation,” he noted.
The take-home message for clinicians at this time is that anakinra effectively improves outcomes in COVID-19 patients with high suPAR levels, Dr. Hayek said. “SuPAR can be measured easily at the point of care. Thus, a targeted strategy using suPAR to identify patients who would benefit from anakinra appears to be viable,” he explained.
However, “Whether anakinra is effective in patients with lower suPAR levels (<6 ng/mL) is unclear and was not answered by this study,” he said. “We eagerly await results of other trials to make that determination. Whether suPAR levels can also help guide the use of other therapies for COVID-19 should be explored and would enhance the personalization of treatment for COVID-19 according to the underlying inflammatory state,” he added.
The SAVE-MORE study was funded by the Hellenic Institute for the Study of Sepsis and Sobi, which manufactures anakinra. Some of the study authors reported financial relationships with Sobi and other pharmaceutical companies.
Dr. Cron disclosed serving as a consultant to Sobi, Novartis, Pfizer, and Sironax. Dr. Cron and Dr. Chatham disclosed having received grant support from Sobi for investigator-initiated clinical trials, and Dr. Caricchio disclosed serving as a consultant to GlaxoSmithKline, Johnson & Johnson, Aurinia, and Bristol-Myers Squibb. Dr. Hayek had no relevant financial conflicts to disclose.
FROM NATURE MEDICINE
Health care–associated infections spiked in 2020 in U.S. hospitals
Several health care-associated infections in U.S. hospitals spiked in 2020 compared to the previous year, according to a Centers for Disease Control and Prevention analysis published Sept. 2 in Infection Control and Hospital Epidemiology. Soaring hospitalization rates, sicker patients who required more frequent and intense care, and staffing and supply shortages caused by the COVID-19 pandemic are thought to have contributed to this increase.
This is the first increase in health care–associated infections since 2015.
These findings “are a reflection of the enormous stress that COVID has placed on our health care system,” Arjun Srinivasan, MD (Capt, USPHS), the associate director of the CDC’s Health care-Associated Infection Prevention Programs, Atlanta, told this news organization. He was not an author of the article, but he supervised the research. “We don’t want anyone to read this report and think that it represents a failure of the individual provider or a failure of health care providers in this country in their care of COVID patients,” he said. He noted that health care professionals have provided “tremendously good care to patients under extremely difficult circumstances.”
“People don’t fail – systems fail – and that’s what happened here,” he said. “Our systems that we need to have in place to prevent health care–associated infection simply were not as strong as they needed to be to survive this challenge.”
In the study, researchers used data reported to the National Healthcare Safety Network, the CDC’s tracking system for health care–associated infections. The team compared national standard infection ratios – calculated by dividing the number of reported infections by the number of predicted infections – between 2019 and 2020 for six routinely tracked events:
- Central line–associated bloodstream infections.
- Catheter-associated urinary tract infections (CAUTIs).
- Ventilator-associated events (VAEs).
- Infections associated with colon surgery and abdominal hysterectomy.
- Clostridioides difficile infections.
- Methicillin-resistant Staphylococcus aureus (MRSA) infections.
Infections were estimated using regression models created with baseline data from 2015.
“The new report highlights the need for health care facilities to strengthen their infection prevention programs and support them with adequate resources so that they can handle emerging threats to public health, while at the same time ensuring that gains made in combating HAIs [health care–associated infections] are not lost,” said the Association for Professionals in Infection Control and Epidemiology in a statement.
The analysis revealed significant national increases in central line–associated bloodstream infections, CAUTIs, VAEs, and MRSA infections in 2020 compared to 2019. Among all infection types, the greatest increase was in central-line infections, which were 46% to 47% higher in the third quarter and fourth quarter (Q4) of 2020 relative to the same periods the previous year. VAEs rose by 45%, MRSA infections increased by 34%, and CAUTIs increased by 19% in Q4 of 2020 compared to 2019.
The influx of sicker patients in hospitals throughout 2020 led to more frequent and longer use of medical devices such as catheters and ventilators. The use of these devices increases risk for infection, David P. Calfee, MD, chief medical epidemiologist at the New York–Presbyterian/Weill Cornell Medical Center, said in an interview. He is an editor of Infection Control and Hospital Epidemiology and was not involved with the study. Shortages in personal protective equipment and crowded intensive care units could also have affected how care was delivered, he said. These factors could have led to “reductions in the ability to provide some of the types of care that are needed to optimally reduce the risk of infection.”
There was either no change or decreases in infections associated with colon surgery or abdominal hysterectomy, likely because there were fewer elective surgeries performed, said Dr. Srinivasan. C. difficile–associated infections also decreased throughout 2020 compared to the previous year. Common practices to prevent the spread of COVID-19 in hospitals, such as environmental cleaning, use of personal protective equipment, and patient isolation, likely helped to curb the spread of C. difficile. Although these mitigating procedures do help protect against MRSA infection, many other factors, notably, the use of medical devices such as ventilators and catheters, can increase the risk for MRSA infection, Dr. Srinivasan added.
Although more research is needed to identify the reasons for these spikes in infection, the findings help quantify the scope of these increases across the United States, Dr. Calfee said. The data allow hospitals and health care professionals to “look back at what we did and then think forward in terms of what we can do different in the future,” he added, “so that these stresses to the system have less of an impact on how we are able to provide care.”
Dr. Srinivasan and Dr. Calfee report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Several health care-associated infections in U.S. hospitals spiked in 2020 compared to the previous year, according to a Centers for Disease Control and Prevention analysis published Sept. 2 in Infection Control and Hospital Epidemiology. Soaring hospitalization rates, sicker patients who required more frequent and intense care, and staffing and supply shortages caused by the COVID-19 pandemic are thought to have contributed to this increase.
This is the first increase in health care–associated infections since 2015.
These findings “are a reflection of the enormous stress that COVID has placed on our health care system,” Arjun Srinivasan, MD (Capt, USPHS), the associate director of the CDC’s Health care-Associated Infection Prevention Programs, Atlanta, told this news organization. He was not an author of the article, but he supervised the research. “We don’t want anyone to read this report and think that it represents a failure of the individual provider or a failure of health care providers in this country in their care of COVID patients,” he said. He noted that health care professionals have provided “tremendously good care to patients under extremely difficult circumstances.”
“People don’t fail – systems fail – and that’s what happened here,” he said. “Our systems that we need to have in place to prevent health care–associated infection simply were not as strong as they needed to be to survive this challenge.”
In the study, researchers used data reported to the National Healthcare Safety Network, the CDC’s tracking system for health care–associated infections. The team compared national standard infection ratios – calculated by dividing the number of reported infections by the number of predicted infections – between 2019 and 2020 for six routinely tracked events:
- Central line–associated bloodstream infections.
- Catheter-associated urinary tract infections (CAUTIs).
- Ventilator-associated events (VAEs).
- Infections associated with colon surgery and abdominal hysterectomy.
- Clostridioides difficile infections.
- Methicillin-resistant Staphylococcus aureus (MRSA) infections.
Infections were estimated using regression models created with baseline data from 2015.
“The new report highlights the need for health care facilities to strengthen their infection prevention programs and support them with adequate resources so that they can handle emerging threats to public health, while at the same time ensuring that gains made in combating HAIs [health care–associated infections] are not lost,” said the Association for Professionals in Infection Control and Epidemiology in a statement.
The analysis revealed significant national increases in central line–associated bloodstream infections, CAUTIs, VAEs, and MRSA infections in 2020 compared to 2019. Among all infection types, the greatest increase was in central-line infections, which were 46% to 47% higher in the third quarter and fourth quarter (Q4) of 2020 relative to the same periods the previous year. VAEs rose by 45%, MRSA infections increased by 34%, and CAUTIs increased by 19% in Q4 of 2020 compared to 2019.
The influx of sicker patients in hospitals throughout 2020 led to more frequent and longer use of medical devices such as catheters and ventilators. The use of these devices increases risk for infection, David P. Calfee, MD, chief medical epidemiologist at the New York–Presbyterian/Weill Cornell Medical Center, said in an interview. He is an editor of Infection Control and Hospital Epidemiology and was not involved with the study. Shortages in personal protective equipment and crowded intensive care units could also have affected how care was delivered, he said. These factors could have led to “reductions in the ability to provide some of the types of care that are needed to optimally reduce the risk of infection.”
There was either no change or decreases in infections associated with colon surgery or abdominal hysterectomy, likely because there were fewer elective surgeries performed, said Dr. Srinivasan. C. difficile–associated infections also decreased throughout 2020 compared to the previous year. Common practices to prevent the spread of COVID-19 in hospitals, such as environmental cleaning, use of personal protective equipment, and patient isolation, likely helped to curb the spread of C. difficile. Although these mitigating procedures do help protect against MRSA infection, many other factors, notably, the use of medical devices such as ventilators and catheters, can increase the risk for MRSA infection, Dr. Srinivasan added.
Although more research is needed to identify the reasons for these spikes in infection, the findings help quantify the scope of these increases across the United States, Dr. Calfee said. The data allow hospitals and health care professionals to “look back at what we did and then think forward in terms of what we can do different in the future,” he added, “so that these stresses to the system have less of an impact on how we are able to provide care.”
Dr. Srinivasan and Dr. Calfee report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Several health care-associated infections in U.S. hospitals spiked in 2020 compared to the previous year, according to a Centers for Disease Control and Prevention analysis published Sept. 2 in Infection Control and Hospital Epidemiology. Soaring hospitalization rates, sicker patients who required more frequent and intense care, and staffing and supply shortages caused by the COVID-19 pandemic are thought to have contributed to this increase.
This is the first increase in health care–associated infections since 2015.
These findings “are a reflection of the enormous stress that COVID has placed on our health care system,” Arjun Srinivasan, MD (Capt, USPHS), the associate director of the CDC’s Health care-Associated Infection Prevention Programs, Atlanta, told this news organization. He was not an author of the article, but he supervised the research. “We don’t want anyone to read this report and think that it represents a failure of the individual provider or a failure of health care providers in this country in their care of COVID patients,” he said. He noted that health care professionals have provided “tremendously good care to patients under extremely difficult circumstances.”
“People don’t fail – systems fail – and that’s what happened here,” he said. “Our systems that we need to have in place to prevent health care–associated infection simply were not as strong as they needed to be to survive this challenge.”
In the study, researchers used data reported to the National Healthcare Safety Network, the CDC’s tracking system for health care–associated infections. The team compared national standard infection ratios – calculated by dividing the number of reported infections by the number of predicted infections – between 2019 and 2020 for six routinely tracked events:
- Central line–associated bloodstream infections.
- Catheter-associated urinary tract infections (CAUTIs).
- Ventilator-associated events (VAEs).
- Infections associated with colon surgery and abdominal hysterectomy.
- Clostridioides difficile infections.
- Methicillin-resistant Staphylococcus aureus (MRSA) infections.
Infections were estimated using regression models created with baseline data from 2015.
“The new report highlights the need for health care facilities to strengthen their infection prevention programs and support them with adequate resources so that they can handle emerging threats to public health, while at the same time ensuring that gains made in combating HAIs [health care–associated infections] are not lost,” said the Association for Professionals in Infection Control and Epidemiology in a statement.
The analysis revealed significant national increases in central line–associated bloodstream infections, CAUTIs, VAEs, and MRSA infections in 2020 compared to 2019. Among all infection types, the greatest increase was in central-line infections, which were 46% to 47% higher in the third quarter and fourth quarter (Q4) of 2020 relative to the same periods the previous year. VAEs rose by 45%, MRSA infections increased by 34%, and CAUTIs increased by 19% in Q4 of 2020 compared to 2019.
The influx of sicker patients in hospitals throughout 2020 led to more frequent and longer use of medical devices such as catheters and ventilators. The use of these devices increases risk for infection, David P. Calfee, MD, chief medical epidemiologist at the New York–Presbyterian/Weill Cornell Medical Center, said in an interview. He is an editor of Infection Control and Hospital Epidemiology and was not involved with the study. Shortages in personal protective equipment and crowded intensive care units could also have affected how care was delivered, he said. These factors could have led to “reductions in the ability to provide some of the types of care that are needed to optimally reduce the risk of infection.”
There was either no change or decreases in infections associated with colon surgery or abdominal hysterectomy, likely because there were fewer elective surgeries performed, said Dr. Srinivasan. C. difficile–associated infections also decreased throughout 2020 compared to the previous year. Common practices to prevent the spread of COVID-19 in hospitals, such as environmental cleaning, use of personal protective equipment, and patient isolation, likely helped to curb the spread of C. difficile. Although these mitigating procedures do help protect against MRSA infection, many other factors, notably, the use of medical devices such as ventilators and catheters, can increase the risk for MRSA infection, Dr. Srinivasan added.
Although more research is needed to identify the reasons for these spikes in infection, the findings help quantify the scope of these increases across the United States, Dr. Calfee said. The data allow hospitals and health care professionals to “look back at what we did and then think forward in terms of what we can do different in the future,” he added, “so that these stresses to the system have less of an impact on how we are able to provide care.”
Dr. Srinivasan and Dr. Calfee report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Beta-blocker reduces lung inflammation in critical COVID-19
In a small study, intravenous administration of the beta-blocker metoprolol to critically ill COVID-19 patients with acute respiratory distress syndrome (ARDS) safely blunted lung inflammation associated with the disease.
Metoprolol administration also resulted in better oxygenation and fewer days on intensive mechanical ventilation and in the ICU, compared with no treatment.
These data suggest that metoprolol repurposing for the treatment of ARDS in COVID-19 patients is a safe and inexpensive strategy with the potential to improve outcomes, the researchers said.
“Metoprolol repurposing for the treatment of ARDS associated with COVID-19 is a safe and cheap intervention that can help to alleviate the massive personal and health care burden associated with the pandemic,” they concluded.
The results, from the MADRID-COVID pilot trial from Agustin Clemente-Moragon, BSc, Centro National de Investigaciones Cardiovasculares, Madrid, and colleagues, were published online Aug. 30, 2021, in the Journal of the American College of Cardiology.
In previous work, the researchers showed that metoprolol, but not other clinically available intravenous beta-blockers, abrogates neutrophil-driven exacerbated inflammation, neutrophil-platelet interaction, and formation of neutrophil extracellular traps in a mouse model of acute lung injury.
These results prompted the current pilot trial in 20 patients, ages 18-80 years, with COVID-19–associated ARDS.
Randomization was stratified by age (59 and younger vs. 60 and older), history of hypertension (yes or no), and circulating neutrophil counts (<6,000 vs. ≥6,000). Bronchoalveolar lavage (BAL) fluid and blood samples were obtained from patients at randomization and 24 hours after the third metoprolol dose in the treatment group, and on day 4 in controls.
Because of the cardiovascular effects of metoprolol, patients were monitored invasively and by echocardiography, the authors noted.
As expected, metoprolol significantly reduced heart rate (P < .01) and systolic blood pressure (P < .05), although both remained within the physiological range. Echocardiography showed no deterioration of cardiac function after metoprolol treatment.
To assess the ability of metoprolol to address neutrophil-mediated exacerbated lung inflammation, the researchers analyzed leukocyte populations in BAL samples by flow cytometry at baseline and on day 4.
At baseline, the metoprolol and control groups showed no differences in BAL neutrophil content. But on day 4, after 3 days of treatment with metoprolol, neutrophil content was significantly lower in the metoprolol group (median, 14.3 neutrophils/mcL) than in the control group (median, 397 neutrophils/mcL).
Metoprolol-treated patients also had lower total inflammatory-cell content and lower monocyte/macrophage content. Lymphocytes did not differ between the groups.
The investigators also explored the impact of metoprolol on the chemokine, monocyte chemoattractant protein–1 (MCP-1), as it has been shown to promote pulmonary fibrosis in late-stage ARDS.
They found that MCP-1 was significantly attenuated after 3 days of metoprolol treatment. At baseline, the median MCP-1 level was 298 pg/mL; on day 4 after metoprolol, it was 203 pg/mL (P = .009).
MCP-1 levels remained unchanged in control patients.
An elegant study
In an accompanying editorial, Mourad H. Senussi, MD, assistant professor at Baylor College of Medicine, Houston, wrote: “Although the study has a small sample size, we commend the authors, who attempt to shed light on the important pathophysiological underpinnings that help establish biological plausibility for this inexpensive, safe, and widely available medication.”
In an interview with this news organization, Dr. Senussi added that metoprolol is not itself something primarily used to treat COVID-19 per se. “Rather, the drug blunts the sympathetic-host response. There is a fine balance between that sympathetic surge that is helpful to the body, and then a sympathetic surge that if left unchecked, can lead to significant damage. And so, I think this study really shows that medications like metoprolol can help blunt that initial sympathetic effect.”
A larger study is “absolutely” warranted, he added, “this is a drug that is readily available, safe, and inexpensive. The study design here was simple and most importantly, showed biological plausibility.”
Dr. Senussi also noted that, although the benefit was noted in COVID-19 patients, the study sets the groundwork for further research in the use of beta-blockade in the critically ill. “Further studies are needed to elucidate and identify where along the inflammatory spectrum these critically ill patients lie, which patients would benefit from beta-blockers, and at what time point during their hospital stay.”
The MADRID-COVID authors and Dr. Senussi disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a small study, intravenous administration of the beta-blocker metoprolol to critically ill COVID-19 patients with acute respiratory distress syndrome (ARDS) safely blunted lung inflammation associated with the disease.
Metoprolol administration also resulted in better oxygenation and fewer days on intensive mechanical ventilation and in the ICU, compared with no treatment.
These data suggest that metoprolol repurposing for the treatment of ARDS in COVID-19 patients is a safe and inexpensive strategy with the potential to improve outcomes, the researchers said.
“Metoprolol repurposing for the treatment of ARDS associated with COVID-19 is a safe and cheap intervention that can help to alleviate the massive personal and health care burden associated with the pandemic,” they concluded.
The results, from the MADRID-COVID pilot trial from Agustin Clemente-Moragon, BSc, Centro National de Investigaciones Cardiovasculares, Madrid, and colleagues, were published online Aug. 30, 2021, in the Journal of the American College of Cardiology.
In previous work, the researchers showed that metoprolol, but not other clinically available intravenous beta-blockers, abrogates neutrophil-driven exacerbated inflammation, neutrophil-platelet interaction, and formation of neutrophil extracellular traps in a mouse model of acute lung injury.
These results prompted the current pilot trial in 20 patients, ages 18-80 years, with COVID-19–associated ARDS.
Randomization was stratified by age (59 and younger vs. 60 and older), history of hypertension (yes or no), and circulating neutrophil counts (<6,000 vs. ≥6,000). Bronchoalveolar lavage (BAL) fluid and blood samples were obtained from patients at randomization and 24 hours after the third metoprolol dose in the treatment group, and on day 4 in controls.
Because of the cardiovascular effects of metoprolol, patients were monitored invasively and by echocardiography, the authors noted.
As expected, metoprolol significantly reduced heart rate (P < .01) and systolic blood pressure (P < .05), although both remained within the physiological range. Echocardiography showed no deterioration of cardiac function after metoprolol treatment.
To assess the ability of metoprolol to address neutrophil-mediated exacerbated lung inflammation, the researchers analyzed leukocyte populations in BAL samples by flow cytometry at baseline and on day 4.
At baseline, the metoprolol and control groups showed no differences in BAL neutrophil content. But on day 4, after 3 days of treatment with metoprolol, neutrophil content was significantly lower in the metoprolol group (median, 14.3 neutrophils/mcL) than in the control group (median, 397 neutrophils/mcL).
Metoprolol-treated patients also had lower total inflammatory-cell content and lower monocyte/macrophage content. Lymphocytes did not differ between the groups.
The investigators also explored the impact of metoprolol on the chemokine, monocyte chemoattractant protein–1 (MCP-1), as it has been shown to promote pulmonary fibrosis in late-stage ARDS.
They found that MCP-1 was significantly attenuated after 3 days of metoprolol treatment. At baseline, the median MCP-1 level was 298 pg/mL; on day 4 after metoprolol, it was 203 pg/mL (P = .009).
MCP-1 levels remained unchanged in control patients.
An elegant study
In an accompanying editorial, Mourad H. Senussi, MD, assistant professor at Baylor College of Medicine, Houston, wrote: “Although the study has a small sample size, we commend the authors, who attempt to shed light on the important pathophysiological underpinnings that help establish biological plausibility for this inexpensive, safe, and widely available medication.”
In an interview with this news organization, Dr. Senussi added that metoprolol is not itself something primarily used to treat COVID-19 per se. “Rather, the drug blunts the sympathetic-host response. There is a fine balance between that sympathetic surge that is helpful to the body, and then a sympathetic surge that if left unchecked, can lead to significant damage. And so, I think this study really shows that medications like metoprolol can help blunt that initial sympathetic effect.”
A larger study is “absolutely” warranted, he added, “this is a drug that is readily available, safe, and inexpensive. The study design here was simple and most importantly, showed biological plausibility.”
Dr. Senussi also noted that, although the benefit was noted in COVID-19 patients, the study sets the groundwork for further research in the use of beta-blockade in the critically ill. “Further studies are needed to elucidate and identify where along the inflammatory spectrum these critically ill patients lie, which patients would benefit from beta-blockers, and at what time point during their hospital stay.”
The MADRID-COVID authors and Dr. Senussi disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a small study, intravenous administration of the beta-blocker metoprolol to critically ill COVID-19 patients with acute respiratory distress syndrome (ARDS) safely blunted lung inflammation associated with the disease.
Metoprolol administration also resulted in better oxygenation and fewer days on intensive mechanical ventilation and in the ICU, compared with no treatment.
These data suggest that metoprolol repurposing for the treatment of ARDS in COVID-19 patients is a safe and inexpensive strategy with the potential to improve outcomes, the researchers said.
“Metoprolol repurposing for the treatment of ARDS associated with COVID-19 is a safe and cheap intervention that can help to alleviate the massive personal and health care burden associated with the pandemic,” they concluded.
The results, from the MADRID-COVID pilot trial from Agustin Clemente-Moragon, BSc, Centro National de Investigaciones Cardiovasculares, Madrid, and colleagues, were published online Aug. 30, 2021, in the Journal of the American College of Cardiology.
In previous work, the researchers showed that metoprolol, but not other clinically available intravenous beta-blockers, abrogates neutrophil-driven exacerbated inflammation, neutrophil-platelet interaction, and formation of neutrophil extracellular traps in a mouse model of acute lung injury.
These results prompted the current pilot trial in 20 patients, ages 18-80 years, with COVID-19–associated ARDS.
Randomization was stratified by age (59 and younger vs. 60 and older), history of hypertension (yes or no), and circulating neutrophil counts (<6,000 vs. ≥6,000). Bronchoalveolar lavage (BAL) fluid and blood samples were obtained from patients at randomization and 24 hours after the third metoprolol dose in the treatment group, and on day 4 in controls.
Because of the cardiovascular effects of metoprolol, patients were monitored invasively and by echocardiography, the authors noted.
As expected, metoprolol significantly reduced heart rate (P < .01) and systolic blood pressure (P < .05), although both remained within the physiological range. Echocardiography showed no deterioration of cardiac function after metoprolol treatment.
To assess the ability of metoprolol to address neutrophil-mediated exacerbated lung inflammation, the researchers analyzed leukocyte populations in BAL samples by flow cytometry at baseline and on day 4.
At baseline, the metoprolol and control groups showed no differences in BAL neutrophil content. But on day 4, after 3 days of treatment with metoprolol, neutrophil content was significantly lower in the metoprolol group (median, 14.3 neutrophils/mcL) than in the control group (median, 397 neutrophils/mcL).
Metoprolol-treated patients also had lower total inflammatory-cell content and lower monocyte/macrophage content. Lymphocytes did not differ between the groups.
The investigators also explored the impact of metoprolol on the chemokine, monocyte chemoattractant protein–1 (MCP-1), as it has been shown to promote pulmonary fibrosis in late-stage ARDS.
They found that MCP-1 was significantly attenuated after 3 days of metoprolol treatment. At baseline, the median MCP-1 level was 298 pg/mL; on day 4 after metoprolol, it was 203 pg/mL (P = .009).
MCP-1 levels remained unchanged in control patients.
An elegant study
In an accompanying editorial, Mourad H. Senussi, MD, assistant professor at Baylor College of Medicine, Houston, wrote: “Although the study has a small sample size, we commend the authors, who attempt to shed light on the important pathophysiological underpinnings that help establish biological plausibility for this inexpensive, safe, and widely available medication.”
In an interview with this news organization, Dr. Senussi added that metoprolol is not itself something primarily used to treat COVID-19 per se. “Rather, the drug blunts the sympathetic-host response. There is a fine balance between that sympathetic surge that is helpful to the body, and then a sympathetic surge that if left unchecked, can lead to significant damage. And so, I think this study really shows that medications like metoprolol can help blunt that initial sympathetic effect.”
A larger study is “absolutely” warranted, he added, “this is a drug that is readily available, safe, and inexpensive. The study design here was simple and most importantly, showed biological plausibility.”
Dr. Senussi also noted that, although the benefit was noted in COVID-19 patients, the study sets the groundwork for further research in the use of beta-blockade in the critically ill. “Further studies are needed to elucidate and identify where along the inflammatory spectrum these critically ill patients lie, which patients would benefit from beta-blockers, and at what time point during their hospital stay.”
The MADRID-COVID authors and Dr. Senussi disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
‘Lopioid protocol’ – low-dose opioids – proposed for fracture surgery
In a paper presented at the annual meeting of the American Academy of Orthopaedic Surgeons, researchers from NYU reported on the implementation of their multimodal strategy, dubbed the “lopioid protocol.”
According to the 2019 National Survey on Drug Use and Health, orthopedic surgeons are the third-highest opioid prescribers in the United States.
Kennneth A. Egol, MD, vice chair of the department of orthopedic surgery at NYU, who is the first author of the study, was motivated to help create the protocol following misconceptions that orthopedic surgeons were helping to fuel the opioid epidemic.
Dr. Egol pointed to the year 1995, when pain became the fifth vital sign after body temperature, pulse rate, respiratory rate, and blood pressure.
Since then, in light of the opioid epidemic, the focus of physicians has shifted away from prescribing strong pain medication and reducing pain scores to zero to instead reducing pain to a manageable level.
Reducing opioid prescriptions can be challenging when patients are prescribed an anti-inflammatory and they subsequently ask their physician for a “pain pill.” Patients sometimes don’t understand that inflammation is what causes pain.
It can also be difficult to convince patients that medications that they can buy over the counter can adequately control their pain, as confirmed in numerous studies.
Multimodal pain therapy aims to reduce the need for opioids by supplementing their use with other oral medications and, at times, long-lasting regional nerve blocks.
Anti-inflammatories act at the site of injury or surgery where inflammation is occurring. Nerves then carry the pain signal to the brain. These signals can be dampened by medications such as gabapentin that act on the nerves themselves. The pain signal is received in the brain, where opioids act by binding to receptors in the brain.
The so-called lopioid protocol does not eliminate opioids completely but rather uses “safer” opioids, such as tramadol, in lieu of stronger narcotics.
The protocol began at NYU on Jan. 1, 2019. It consists in the prescribing of tramadol, meloxicam, gabapentin, and acetaminophen.
The study presented at the AAOS meeting demonstrated statistically significant reductions in visual analogue pain scores at discharge and subsequent medication refills for the 931 patients in the lopioid group, compared with a group of 848 patients who received narcotic prescriptions containing oxycodone from the year prior to the protocol initiation.
Educating patients on the rationale for the prescription combination can help to allay their fears. Dr. Egol thinks it’s important for physicians to explain the dangers of opioids to patients. He said in an interview that he also believes surgeons need to “give [patients] an understanding of why we are pursuing these protocols. They also need to know we will not ignore their pain and concerns.”
Brannon Orton, MD, is an orthopedic surgeon at Confluence Health, in Moses Lake, Wash. He sees a large number of trauma patients and thinks NYU is doing a good job of addressing a difficult problem in orthopedics – especially in the field of trauma.
He said in an interview: “Managing narcotics postoperatively can be challenging due to the fact that many people come into these fractures with a history of narcotic use.” Not only are they used to turning to opioids for pain relief, but they also may have built up a tolerance to them.
Although he hasn’t been using the lopioid protocol specifically, he has been following a multimodal approach regarding the postoperative use of narcotics. Of the study by Dr. Egol and colleagues, he said, “I think their paper presents an effective way of decreasing use of oral narcotics and still adequately managing patients’ pain postoperatively.” Dr. Orton’s own practice utilizes tramadol, acetaminophen, and ibuprofen after fracture surgery.
From Dr. Orton’s perspective, a significant challenge in implementing the lopioid protocol in practice is simply sticking to the plan. “It can become difficult when patients are pressuring staff or physicians for more narcotics. However, I feel that if everybody is on the same page with the plan, then it can be very doable.”
Dr. Egol and NYU try to limit narcotic prescriptions beginning with the patient’s initial visit to the ED. The ED physicians at his institution only “prescribe small amounts of narcotics. Our ED people really limit the amount of opioids prescribed.”
Dr. Egol recommends that all practitioners begin with nonnarcotic medication, even if treating a fracture nonoperatively. “Start low and go higher. I always try to start with NSAIDs and Tylenol,” he said.
Dr. Egol and Dr. Orton reported no relevant financial disclosures.
A version of this article first appeared on Medscape.com.
In a paper presented at the annual meeting of the American Academy of Orthopaedic Surgeons, researchers from NYU reported on the implementation of their multimodal strategy, dubbed the “lopioid protocol.”
According to the 2019 National Survey on Drug Use and Health, orthopedic surgeons are the third-highest opioid prescribers in the United States.
Kennneth A. Egol, MD, vice chair of the department of orthopedic surgery at NYU, who is the first author of the study, was motivated to help create the protocol following misconceptions that orthopedic surgeons were helping to fuel the opioid epidemic.
Dr. Egol pointed to the year 1995, when pain became the fifth vital sign after body temperature, pulse rate, respiratory rate, and blood pressure.
Since then, in light of the opioid epidemic, the focus of physicians has shifted away from prescribing strong pain medication and reducing pain scores to zero to instead reducing pain to a manageable level.
Reducing opioid prescriptions can be challenging when patients are prescribed an anti-inflammatory and they subsequently ask their physician for a “pain pill.” Patients sometimes don’t understand that inflammation is what causes pain.
It can also be difficult to convince patients that medications that they can buy over the counter can adequately control their pain, as confirmed in numerous studies.
Multimodal pain therapy aims to reduce the need for opioids by supplementing their use with other oral medications and, at times, long-lasting regional nerve blocks.
Anti-inflammatories act at the site of injury or surgery where inflammation is occurring. Nerves then carry the pain signal to the brain. These signals can be dampened by medications such as gabapentin that act on the nerves themselves. The pain signal is received in the brain, where opioids act by binding to receptors in the brain.
The so-called lopioid protocol does not eliminate opioids completely but rather uses “safer” opioids, such as tramadol, in lieu of stronger narcotics.
The protocol began at NYU on Jan. 1, 2019. It consists in the prescribing of tramadol, meloxicam, gabapentin, and acetaminophen.
The study presented at the AAOS meeting demonstrated statistically significant reductions in visual analogue pain scores at discharge and subsequent medication refills for the 931 patients in the lopioid group, compared with a group of 848 patients who received narcotic prescriptions containing oxycodone from the year prior to the protocol initiation.
Educating patients on the rationale for the prescription combination can help to allay their fears. Dr. Egol thinks it’s important for physicians to explain the dangers of opioids to patients. He said in an interview that he also believes surgeons need to “give [patients] an understanding of why we are pursuing these protocols. They also need to know we will not ignore their pain and concerns.”
Brannon Orton, MD, is an orthopedic surgeon at Confluence Health, in Moses Lake, Wash. He sees a large number of trauma patients and thinks NYU is doing a good job of addressing a difficult problem in orthopedics – especially in the field of trauma.
He said in an interview: “Managing narcotics postoperatively can be challenging due to the fact that many people come into these fractures with a history of narcotic use.” Not only are they used to turning to opioids for pain relief, but they also may have built up a tolerance to them.
Although he hasn’t been using the lopioid protocol specifically, he has been following a multimodal approach regarding the postoperative use of narcotics. Of the study by Dr. Egol and colleagues, he said, “I think their paper presents an effective way of decreasing use of oral narcotics and still adequately managing patients’ pain postoperatively.” Dr. Orton’s own practice utilizes tramadol, acetaminophen, and ibuprofen after fracture surgery.
From Dr. Orton’s perspective, a significant challenge in implementing the lopioid protocol in practice is simply sticking to the plan. “It can become difficult when patients are pressuring staff or physicians for more narcotics. However, I feel that if everybody is on the same page with the plan, then it can be very doable.”
Dr. Egol and NYU try to limit narcotic prescriptions beginning with the patient’s initial visit to the ED. The ED physicians at his institution only “prescribe small amounts of narcotics. Our ED people really limit the amount of opioids prescribed.”
Dr. Egol recommends that all practitioners begin with nonnarcotic medication, even if treating a fracture nonoperatively. “Start low and go higher. I always try to start with NSAIDs and Tylenol,” he said.
Dr. Egol and Dr. Orton reported no relevant financial disclosures.
A version of this article first appeared on Medscape.com.
In a paper presented at the annual meeting of the American Academy of Orthopaedic Surgeons, researchers from NYU reported on the implementation of their multimodal strategy, dubbed the “lopioid protocol.”
According to the 2019 National Survey on Drug Use and Health, orthopedic surgeons are the third-highest opioid prescribers in the United States.
Kennneth A. Egol, MD, vice chair of the department of orthopedic surgery at NYU, who is the first author of the study, was motivated to help create the protocol following misconceptions that orthopedic surgeons were helping to fuel the opioid epidemic.
Dr. Egol pointed to the year 1995, when pain became the fifth vital sign after body temperature, pulse rate, respiratory rate, and blood pressure.
Since then, in light of the opioid epidemic, the focus of physicians has shifted away from prescribing strong pain medication and reducing pain scores to zero to instead reducing pain to a manageable level.
Reducing opioid prescriptions can be challenging when patients are prescribed an anti-inflammatory and they subsequently ask their physician for a “pain pill.” Patients sometimes don’t understand that inflammation is what causes pain.
It can also be difficult to convince patients that medications that they can buy over the counter can adequately control their pain, as confirmed in numerous studies.
Multimodal pain therapy aims to reduce the need for opioids by supplementing their use with other oral medications and, at times, long-lasting regional nerve blocks.
Anti-inflammatories act at the site of injury or surgery where inflammation is occurring. Nerves then carry the pain signal to the brain. These signals can be dampened by medications such as gabapentin that act on the nerves themselves. The pain signal is received in the brain, where opioids act by binding to receptors in the brain.
The so-called lopioid protocol does not eliminate opioids completely but rather uses “safer” opioids, such as tramadol, in lieu of stronger narcotics.
The protocol began at NYU on Jan. 1, 2019. It consists in the prescribing of tramadol, meloxicam, gabapentin, and acetaminophen.
The study presented at the AAOS meeting demonstrated statistically significant reductions in visual analogue pain scores at discharge and subsequent medication refills for the 931 patients in the lopioid group, compared with a group of 848 patients who received narcotic prescriptions containing oxycodone from the year prior to the protocol initiation.
Educating patients on the rationale for the prescription combination can help to allay their fears. Dr. Egol thinks it’s important for physicians to explain the dangers of opioids to patients. He said in an interview that he also believes surgeons need to “give [patients] an understanding of why we are pursuing these protocols. They also need to know we will not ignore their pain and concerns.”
Brannon Orton, MD, is an orthopedic surgeon at Confluence Health, in Moses Lake, Wash. He sees a large number of trauma patients and thinks NYU is doing a good job of addressing a difficult problem in orthopedics – especially in the field of trauma.
He said in an interview: “Managing narcotics postoperatively can be challenging due to the fact that many people come into these fractures with a history of narcotic use.” Not only are they used to turning to opioids for pain relief, but they also may have built up a tolerance to them.
Although he hasn’t been using the lopioid protocol specifically, he has been following a multimodal approach regarding the postoperative use of narcotics. Of the study by Dr. Egol and colleagues, he said, “I think their paper presents an effective way of decreasing use of oral narcotics and still adequately managing patients’ pain postoperatively.” Dr. Orton’s own practice utilizes tramadol, acetaminophen, and ibuprofen after fracture surgery.
From Dr. Orton’s perspective, a significant challenge in implementing the lopioid protocol in practice is simply sticking to the plan. “It can become difficult when patients are pressuring staff or physicians for more narcotics. However, I feel that if everybody is on the same page with the plan, then it can be very doable.”
Dr. Egol and NYU try to limit narcotic prescriptions beginning with the patient’s initial visit to the ED. The ED physicians at his institution only “prescribe small amounts of narcotics. Our ED people really limit the amount of opioids prescribed.”
Dr. Egol recommends that all practitioners begin with nonnarcotic medication, even if treating a fracture nonoperatively. “Start low and go higher. I always try to start with NSAIDs and Tylenol,” he said.
Dr. Egol and Dr. Orton reported no relevant financial disclosures.
A version of this article first appeared on Medscape.com.
WHO tracking new COVID-19 variant called Mu
The variant, also known as B.1.621, was first identified in Colombia in January. It has now been detected in 43 countries and was added to the WHO’s “variant of interest” list Aug. 30.
“The Mu variant has a constellation of mutations that indicate potential properties of immune escape,” the WHO wrote in its weekly COVID-19 update on Aug 31.
Preliminary data suggests that the Mu variant may be able to evade antibodies at levels similar to the Beta variant, the WHO wrote, though more studies are needed. The Beta variant, also known as B.1.351, was first detected in South Africa and has shown some ability to evade vaccines.
As of Aug. 29, the global prevalence of the Mu variant appears to be less than 0.1%. But its prevalence in South America has “consistently increased,” the WHO wrote, now making up 39% of cases in Colombia and 13% of cases in Ecuador.
More than 4,700 cases of the Mu variant have been identified worldwide through genomic sequencing, according to Outbreak.info, an open-source database operated by Scripps Research. The United States has identified 2,011 of these cases, with 348 in California. As of Sept. 2, only one state -- Nebraska -- had not yet reported a Mu case.
“At the moment, it looks like there’s genuine cause for concern in USA, Central America, and South America, but as we saw with Delta, a potent variant can traverse the globe in the blink of an eye,” Danny Altmann, PhD, an immunologist at Imperial College London, told The Telegraph.
The WHO is monitoring nine variants with genetic mutations that could make them more transmissible, lead to more severe disease, and help them evade vaccines. The Delta variant, which is now a dominant form of the virus in the United States and worldwide, has led to a surge in cases and hospitalizations this summer.
In its report, the WHO said it would monitor the Mu variant for changes, “particularly with the co-circulation of the Delta variant.”
“Mu looks potentially good at immune evasion,” Dr. Altmann told The Telegraph. “For my taste, it’s a stark reminder that this isn’t by any means over. On a planet of 4.4 million-plus new infections per week, there are new variants popping up all the time, and little reason to feel complacent.”
A version of this article first appeared on WebMD.com.
The variant, also known as B.1.621, was first identified in Colombia in January. It has now been detected in 43 countries and was added to the WHO’s “variant of interest” list Aug. 30.
“The Mu variant has a constellation of mutations that indicate potential properties of immune escape,” the WHO wrote in its weekly COVID-19 update on Aug 31.
Preliminary data suggests that the Mu variant may be able to evade antibodies at levels similar to the Beta variant, the WHO wrote, though more studies are needed. The Beta variant, also known as B.1.351, was first detected in South Africa and has shown some ability to evade vaccines.
As of Aug. 29, the global prevalence of the Mu variant appears to be less than 0.1%. But its prevalence in South America has “consistently increased,” the WHO wrote, now making up 39% of cases in Colombia and 13% of cases in Ecuador.
More than 4,700 cases of the Mu variant have been identified worldwide through genomic sequencing, according to Outbreak.info, an open-source database operated by Scripps Research. The United States has identified 2,011 of these cases, with 348 in California. As of Sept. 2, only one state -- Nebraska -- had not yet reported a Mu case.
“At the moment, it looks like there’s genuine cause for concern in USA, Central America, and South America, but as we saw with Delta, a potent variant can traverse the globe in the blink of an eye,” Danny Altmann, PhD, an immunologist at Imperial College London, told The Telegraph.
The WHO is monitoring nine variants with genetic mutations that could make them more transmissible, lead to more severe disease, and help them evade vaccines. The Delta variant, which is now a dominant form of the virus in the United States and worldwide, has led to a surge in cases and hospitalizations this summer.
In its report, the WHO said it would monitor the Mu variant for changes, “particularly with the co-circulation of the Delta variant.”
“Mu looks potentially good at immune evasion,” Dr. Altmann told The Telegraph. “For my taste, it’s a stark reminder that this isn’t by any means over. On a planet of 4.4 million-plus new infections per week, there are new variants popping up all the time, and little reason to feel complacent.”
A version of this article first appeared on WebMD.com.
The variant, also known as B.1.621, was first identified in Colombia in January. It has now been detected in 43 countries and was added to the WHO’s “variant of interest” list Aug. 30.
“The Mu variant has a constellation of mutations that indicate potential properties of immune escape,” the WHO wrote in its weekly COVID-19 update on Aug 31.
Preliminary data suggests that the Mu variant may be able to evade antibodies at levels similar to the Beta variant, the WHO wrote, though more studies are needed. The Beta variant, also known as B.1.351, was first detected in South Africa and has shown some ability to evade vaccines.
As of Aug. 29, the global prevalence of the Mu variant appears to be less than 0.1%. But its prevalence in South America has “consistently increased,” the WHO wrote, now making up 39% of cases in Colombia and 13% of cases in Ecuador.
More than 4,700 cases of the Mu variant have been identified worldwide through genomic sequencing, according to Outbreak.info, an open-source database operated by Scripps Research. The United States has identified 2,011 of these cases, with 348 in California. As of Sept. 2, only one state -- Nebraska -- had not yet reported a Mu case.
“At the moment, it looks like there’s genuine cause for concern in USA, Central America, and South America, but as we saw with Delta, a potent variant can traverse the globe in the blink of an eye,” Danny Altmann, PhD, an immunologist at Imperial College London, told The Telegraph.
The WHO is monitoring nine variants with genetic mutations that could make them more transmissible, lead to more severe disease, and help them evade vaccines. The Delta variant, which is now a dominant form of the virus in the United States and worldwide, has led to a surge in cases and hospitalizations this summer.
In its report, the WHO said it would monitor the Mu variant for changes, “particularly with the co-circulation of the Delta variant.”
“Mu looks potentially good at immune evasion,” Dr. Altmann told The Telegraph. “For my taste, it’s a stark reminder that this isn’t by any means over. On a planet of 4.4 million-plus new infections per week, there are new variants popping up all the time, and little reason to feel complacent.”
A version of this article first appeared on WebMD.com.








