User login
Hospital readmissions penalties now in 5th year
With the Hospital Readmissions Reduction Program (HRRP) in its 5th year, what has been the impact on hospitals and on hospitalists?
First of all, a lot of penalties have been paid by hospitals. According to an analysis by Kaiser Health News,1 the Centers for Medicare and Medicaid Services will withhold $528 million from 2,597 hospitals in the current fiscal year, Oct. 1, 2016 to Sept. 30, 2017, for readmissions for six diagnoses that occurred between July 2012 and June 2015. The number of penalized hospitals is down slightly from 2,665 the year before, but the total annual withhold will go up by $108 million.
HRRP exacts Medicare payment penalties from hospitals that have rates of readmissions – within 30 days of discharge – that are higher than expected, based on national rates and the health of their patient population. The maximum penalty is now up to 3% of a hospital’s Medicare reimbursement. Hospitals are being penalized an average of 0.73% of their annual Medicare reimbursement, and cumulative HRRP penalties will reach nearly $1.9 billion by the end of the fiscal year, Kaiser Health News reports.2
“Basically, we chose to introduce the idea of measuring readmissions because we felt it represented an adverse outcome for many people that was being ignored; that risk could be reduced; and improvements would yield benefits for people as well as save money for the health care system,” he told The Hospitalist.
“More than anything, HRRP has sharpened the focus on considering the episode of care from the patient’s perspective – rather than just focusing on venues of care like the hospitalization alone,” Dr. Krumholz said. “The focus on readmission forced many of us in the health professions to consider what the experience was like to leave the acute setting – how information flowed, what kind of concerns people had, the degree to which they understood what had happened to them, the extent to which they were prepared for the next steps.”
Once the patient leaves the hospital, there are myriad factors that will influence their likelihood of returning, notes researcher Karen Joynt, MD, MPH, of the Department of Health Policy and Management at Harvard’s School of Public Health, Boston. “The proportion of patients readmitted to the hospital because of gross error is low, but sometimes we’re too optimistic about our patients’ ability to manage postdischarge,” she said.
“We all know we can do better at providing softer landings, and anyone who’s ever been a hospital patient or a family member of one knows that leaving the hospital is incredibly tumultuous. I experienced that with my own parents, and it’s frightening, even if everything is done right. It’s still a very vulnerable time.”
HRRP has fundamentally changed the conversation about hospital care, Dr. Joynt said. “I think we need to change the conversation even more and talk more about how to prevent admissions in the first place. As a clinician, I think we need to be more innovative, recognizing that the ways we’ll make a real difference probably has more to do with what happens outside of the hospital. My personal hope is that new alternate payment models like accountable care organizations will lead to more creative partnerships with other providers.”
What have we learned about readmissions in 5 years?
A lot of recently published research about readmissions has documented modest decreases in overall readmissions nationally, from over 21% to under 18% between 2007 and 2014, although most of the reduction occurred in the first couple of years after HRRP was announced and it has since largely leveled off.
Other research has tried to explore the relationship between readmissions rates and other outcomes that might matter more to patients or that might be better proxies for the quality of the hospital experience. Is readmission rate a true measure of quality, or just a utilization measure? Research has also tried to document what works: what are the best strategies for preventing avoidable readmissions by improving the discharge process, care transitions, and the coordination of care postdischarge in the community – although no silver bullet has yet been identified.
A recent effort to inject more equity into the penalties program, contained in the wide-ranging 21st Century Cures Act signed into law by President Obama in December 2016, requires Medicare to account for patients’ socio-economic backgrounds when it calculates reductions in its payments to hospitals under HRRP. The law directs the government to change the way pay for performance is applied to safety net hospitals by setting different penalty thresholds for hospitals based on the proportion of their patients who are dually eligible for Medicare and Medicaid.
It remains to be seen how this will be implemented and with what impact. But some critics have continued to question whether hospitals should be held accountable for readmissions, whether 30 days is the correct time frame for that accountability, and whether some hospitals might be simply taking the penalty hit rather than investing in the hard work of care transitions.
Impact on working hospitalists
One expert, Ashish Jha, MD, MPH, director of Harvard’s Global Health Institute, wants to see hospitalists get more engaged in the conversation about how to improve hospital care overall.
Experts say there aren’t metrics available that could allocate penalties to individual hospitalists for their performance in readmissions prevention. But hospitals, clearly, are paying attention, and hospitalist groups may find that part of their negotiation of quality and performance incentives with the hospital includes readmissions.
“There are so many other variables that go into transitions of care, and it would be unreasonable to try to hold the individual doctor responsible for all of them,” he said. But accountability can be passed on to the hospitalist group. “My hospital contracts with a national hospitalist company and our agreement has quality measures that we review with them. We ask them to focus on readmissions.”
Dr. Harte said that when patients are discharged from the hospital, they go from an environment where everything is taken care of for them, to total responsibility for their self-care. Yet we are asking ever more from patients in terms of self-management.
“We need to focus on the human side of the experience. The hospital is a place to be avoided wherever possible,” he said. Yet some readmissions are largely unpreventable. Hospitalists should focus on the patient’s greatest risk of preventable readmission. “Is it health literacy? Is it transportation?”
Readmissions at the front lines
Preetham Talari, MD, FACP, FHM, hospitalist at University of Kentucky HealthCare in Lexington, has an interest in health care safety, quality improvement, and value. He has led the university’s site participation in Project BOOST, the Society of Hospital Medicine’s national mentored quality improvement initiative for care transitions. Dr. Talari also led a quality initiative at the university called the Interprofessional Teamwork Innovation Model to systematize teamwork, first piloted on a 30-bed hospitalist unit where he is medical director.
“Readmissions are not just about doctors, they are more about patient factors, socioeconomic factors, where they live,” Dr. Talari said. “Those are harder to impact, but in my experience, it comes down to thinking about the patient’s needs before discharge – really from the time of admission: What are all the things we can do in the hospital to make sure the patient is safely transitioned home?”
According to Dr. Talari, complex issues like readmissions don’t depend on just one, two, or three factors. “But we do the interventions believing that it will improve processes and outcomes, and then add another intervention and another,” he said. “All of these interventions will add up like a jigsaw puzzle to achieve a final, sustainable outcome. One thing I believe is hospitalists should be leading these efforts.”
Better interventions, better infrastructure
Leora Horwitz, MD, MHS, director of the Center for Healthcare Innovation and Delivery Science at New York University School of Public Health, says the biggest change she has seen resulting from readmissions penalties is that transitions of care are now understood to be both important and the responsibility of front line hospitalists. “That was not true 5 or 10 years ago. We used to spend hours admitting patients to the hospital and then 5 minutes on their discharge.”
“We’ve also learned that the infrastructure can be built better. Historically, hospital discharge summaries have been abysmal. But we can automate the importation of pending labs into the electronic health record. These are things you can change for everybody by changing your template. Sit down in a room together every afternoon to talk about what will happen to the patients when they go home. That’s become standard at our hospital. That was never done before.”
Evidence for improved outcomes is mixed, Dr. Horwitz noted. However, she pointed out, is there any evidence that readmissions penalties have produced adverse outcomes? Did they increase mortality, or length of stay? “So far the evidence suggests that they did not,” she said.
“I think it’s generally likely that the work we have done has resulted in better care. Thousands of people haven’t had to go back to the hospital, and that’s a good thing.”
Recent research on readmissions penalties
A survey by Yale researchers, published in JAMA in December 2016, found that hospitals financially penalized under HRRP reduced their readmissions rates at a higher rate than nonpenalized hospitals, “which implies that penalties can improve quality and readmission performance for hospitals with the most room for improvement,” coauthor Kumar Dharmarajan, MD, MBA, said in a statement.4 The hospitals responded to external pressures – in other words, financial penalties worked. But most of the reduction happened in the 2 years before actual penalties went into effect, which suggests that further improvement will not be easy, the authors note.
A survey of the attitudes of hospital leaders on the HRRP found that it has had a major impact on their efforts to reduce readmissions rates, although the failure to take sociodemographic factors into account was a major complaint for these leaders.5 Most said the penalties were too large, but 42.5% believed HRRP was likely to improve quality.
Some have questioned whether readmissions penalties were just encouraging hospitals to reduce their rates by keeping returning patients in observation units rather than formally readmitting them. Zuckerman et al. in the New England Journal of Medicine found no evidence that changes in observation unit stays accounted for the documented decrease in readmissions.6
But according to Papanicolas et al. in Health Affairs, patient hospital experience has improved only modestly under hospital value-based purchasing for U.S. hospitals, with no evidence that the program has had a beneficial effect on overall patient experience.7 Another study from Harvard by Figueroa et al. found that evidence is lacking that hospital value-based purchasing leads to lower mortality rates.8
“Patients and caregivers tell us: Hey, you people are the experts. You’ve taken care of lots of people with my medical condition before. You should know what my needs are going to be postdischarge and help me anticipate them,” he said.
References
1. Rau J. Medicare’s Readmission Penalties Hit New High. Kaiser Health News. 2016 Aug 2.
2. Boccuti C, Casillas G. Aiming for Fewer Hospital U-turns: The Medicare Hospital Readmission Reduction Program. Kaiser Health News, 2016 Sep 30.
3. Keenan PS, Normand SLT, Lin Z, et al. An administrative claims measure suitable for profiling hospital performance on the basis of 30-day all-cause readmission rates among patients with heart failure. Circ Cardiovasc Qual Outcomes. 2008;1:29-37.
4. Desai NR, Ross JS, Kwon JY, et al. Association between hospital penalty status under the Hospital Readmission Reduction Program and readmission rates for target and nontarget conditions. JAMA. 2016 Dec 27;316(24):2647-56.
5. Joynt KE, Figueroa JF, Orav EJ, Jha AK. Opinions on the Hospital Readmissions Reduction Program: Results of a national survey of hospital leaders. Am J Manag Care. 2016 Aug 1;222(8):e287-94.
6. Zuckerman RB, Sheingold SH, Orav EJ, et al. Readmissions, observation, and the Hospital Readmissions Reduction Program. N Engl J Med. 2016 Apr 21;374(16):1543-51.
7. Papanicolas I, Figueroa JF, Orav EJ, Jha AK. Patient hospital experience improved modestly, but no evidence Medicare incentives promoted meaningful gain. Health Aff (Millwood). 2017 Jan;36(1):133-40.
8. Figueroa JF, Tsugawa Y, Zheng J, et al. Association between the value-based purchasing pay for performance program and patient mortality in US hospitals: observational study. BMJ. 2016;353:i2214.
With the Hospital Readmissions Reduction Program (HRRP) in its 5th year, what has been the impact on hospitals and on hospitalists?
First of all, a lot of penalties have been paid by hospitals. According to an analysis by Kaiser Health News,1 the Centers for Medicare and Medicaid Services will withhold $528 million from 2,597 hospitals in the current fiscal year, Oct. 1, 2016 to Sept. 30, 2017, for readmissions for six diagnoses that occurred between July 2012 and June 2015. The number of penalized hospitals is down slightly from 2,665 the year before, but the total annual withhold will go up by $108 million.
HRRP exacts Medicare payment penalties from hospitals that have rates of readmissions – within 30 days of discharge – that are higher than expected, based on national rates and the health of their patient population. The maximum penalty is now up to 3% of a hospital’s Medicare reimbursement. Hospitals are being penalized an average of 0.73% of their annual Medicare reimbursement, and cumulative HRRP penalties will reach nearly $1.9 billion by the end of the fiscal year, Kaiser Health News reports.2
“Basically, we chose to introduce the idea of measuring readmissions because we felt it represented an adverse outcome for many people that was being ignored; that risk could be reduced; and improvements would yield benefits for people as well as save money for the health care system,” he told The Hospitalist.
“More than anything, HRRP has sharpened the focus on considering the episode of care from the patient’s perspective – rather than just focusing on venues of care like the hospitalization alone,” Dr. Krumholz said. “The focus on readmission forced many of us in the health professions to consider what the experience was like to leave the acute setting – how information flowed, what kind of concerns people had, the degree to which they understood what had happened to them, the extent to which they were prepared for the next steps.”
Once the patient leaves the hospital, there are myriad factors that will influence their likelihood of returning, notes researcher Karen Joynt, MD, MPH, of the Department of Health Policy and Management at Harvard’s School of Public Health, Boston. “The proportion of patients readmitted to the hospital because of gross error is low, but sometimes we’re too optimistic about our patients’ ability to manage postdischarge,” she said.
“We all know we can do better at providing softer landings, and anyone who’s ever been a hospital patient or a family member of one knows that leaving the hospital is incredibly tumultuous. I experienced that with my own parents, and it’s frightening, even if everything is done right. It’s still a very vulnerable time.”
HRRP has fundamentally changed the conversation about hospital care, Dr. Joynt said. “I think we need to change the conversation even more and talk more about how to prevent admissions in the first place. As a clinician, I think we need to be more innovative, recognizing that the ways we’ll make a real difference probably has more to do with what happens outside of the hospital. My personal hope is that new alternate payment models like accountable care organizations will lead to more creative partnerships with other providers.”
What have we learned about readmissions in 5 years?
A lot of recently published research about readmissions has documented modest decreases in overall readmissions nationally, from over 21% to under 18% between 2007 and 2014, although most of the reduction occurred in the first couple of years after HRRP was announced and it has since largely leveled off.
Other research has tried to explore the relationship between readmissions rates and other outcomes that might matter more to patients or that might be better proxies for the quality of the hospital experience. Is readmission rate a true measure of quality, or just a utilization measure? Research has also tried to document what works: what are the best strategies for preventing avoidable readmissions by improving the discharge process, care transitions, and the coordination of care postdischarge in the community – although no silver bullet has yet been identified.
A recent effort to inject more equity into the penalties program, contained in the wide-ranging 21st Century Cures Act signed into law by President Obama in December 2016, requires Medicare to account for patients’ socio-economic backgrounds when it calculates reductions in its payments to hospitals under HRRP. The law directs the government to change the way pay for performance is applied to safety net hospitals by setting different penalty thresholds for hospitals based on the proportion of their patients who are dually eligible for Medicare and Medicaid.
It remains to be seen how this will be implemented and with what impact. But some critics have continued to question whether hospitals should be held accountable for readmissions, whether 30 days is the correct time frame for that accountability, and whether some hospitals might be simply taking the penalty hit rather than investing in the hard work of care transitions.
Impact on working hospitalists
One expert, Ashish Jha, MD, MPH, director of Harvard’s Global Health Institute, wants to see hospitalists get more engaged in the conversation about how to improve hospital care overall.
Experts say there aren’t metrics available that could allocate penalties to individual hospitalists for their performance in readmissions prevention. But hospitals, clearly, are paying attention, and hospitalist groups may find that part of their negotiation of quality and performance incentives with the hospital includes readmissions.
“There are so many other variables that go into transitions of care, and it would be unreasonable to try to hold the individual doctor responsible for all of them,” he said. But accountability can be passed on to the hospitalist group. “My hospital contracts with a national hospitalist company and our agreement has quality measures that we review with them. We ask them to focus on readmissions.”
Dr. Harte said that when patients are discharged from the hospital, they go from an environment where everything is taken care of for them, to total responsibility for their self-care. Yet we are asking ever more from patients in terms of self-management.
“We need to focus on the human side of the experience. The hospital is a place to be avoided wherever possible,” he said. Yet some readmissions are largely unpreventable. Hospitalists should focus on the patient’s greatest risk of preventable readmission. “Is it health literacy? Is it transportation?”
Readmissions at the front lines
Preetham Talari, MD, FACP, FHM, hospitalist at University of Kentucky HealthCare in Lexington, has an interest in health care safety, quality improvement, and value. He has led the university’s site participation in Project BOOST, the Society of Hospital Medicine’s national mentored quality improvement initiative for care transitions. Dr. Talari also led a quality initiative at the university called the Interprofessional Teamwork Innovation Model to systematize teamwork, first piloted on a 30-bed hospitalist unit where he is medical director.
“Readmissions are not just about doctors, they are more about patient factors, socioeconomic factors, where they live,” Dr. Talari said. “Those are harder to impact, but in my experience, it comes down to thinking about the patient’s needs before discharge – really from the time of admission: What are all the things we can do in the hospital to make sure the patient is safely transitioned home?”
According to Dr. Talari, complex issues like readmissions don’t depend on just one, two, or three factors. “But we do the interventions believing that it will improve processes and outcomes, and then add another intervention and another,” he said. “All of these interventions will add up like a jigsaw puzzle to achieve a final, sustainable outcome. One thing I believe is hospitalists should be leading these efforts.”
Better interventions, better infrastructure
Leora Horwitz, MD, MHS, director of the Center for Healthcare Innovation and Delivery Science at New York University School of Public Health, says the biggest change she has seen resulting from readmissions penalties is that transitions of care are now understood to be both important and the responsibility of front line hospitalists. “That was not true 5 or 10 years ago. We used to spend hours admitting patients to the hospital and then 5 minutes on their discharge.”
“We’ve also learned that the infrastructure can be built better. Historically, hospital discharge summaries have been abysmal. But we can automate the importation of pending labs into the electronic health record. These are things you can change for everybody by changing your template. Sit down in a room together every afternoon to talk about what will happen to the patients when they go home. That’s become standard at our hospital. That was never done before.”
Evidence for improved outcomes is mixed, Dr. Horwitz noted. However, she pointed out, is there any evidence that readmissions penalties have produced adverse outcomes? Did they increase mortality, or length of stay? “So far the evidence suggests that they did not,” she said.
“I think it’s generally likely that the work we have done has resulted in better care. Thousands of people haven’t had to go back to the hospital, and that’s a good thing.”
Recent research on readmissions penalties
A survey by Yale researchers, published in JAMA in December 2016, found that hospitals financially penalized under HRRP reduced their readmissions rates at a higher rate than nonpenalized hospitals, “which implies that penalties can improve quality and readmission performance for hospitals with the most room for improvement,” coauthor Kumar Dharmarajan, MD, MBA, said in a statement.4 The hospitals responded to external pressures – in other words, financial penalties worked. But most of the reduction happened in the 2 years before actual penalties went into effect, which suggests that further improvement will not be easy, the authors note.
A survey of the attitudes of hospital leaders on the HRRP found that it has had a major impact on their efforts to reduce readmissions rates, although the failure to take sociodemographic factors into account was a major complaint for these leaders.5 Most said the penalties were too large, but 42.5% believed HRRP was likely to improve quality.
Some have questioned whether readmissions penalties were just encouraging hospitals to reduce their rates by keeping returning patients in observation units rather than formally readmitting them. Zuckerman et al. in the New England Journal of Medicine found no evidence that changes in observation unit stays accounted for the documented decrease in readmissions.6
But according to Papanicolas et al. in Health Affairs, patient hospital experience has improved only modestly under hospital value-based purchasing for U.S. hospitals, with no evidence that the program has had a beneficial effect on overall patient experience.7 Another study from Harvard by Figueroa et al. found that evidence is lacking that hospital value-based purchasing leads to lower mortality rates.8
“Patients and caregivers tell us: Hey, you people are the experts. You’ve taken care of lots of people with my medical condition before. You should know what my needs are going to be postdischarge and help me anticipate them,” he said.
References
1. Rau J. Medicare’s Readmission Penalties Hit New High. Kaiser Health News. 2016 Aug 2.
2. Boccuti C, Casillas G. Aiming for Fewer Hospital U-turns: The Medicare Hospital Readmission Reduction Program. Kaiser Health News, 2016 Sep 30.
3. Keenan PS, Normand SLT, Lin Z, et al. An administrative claims measure suitable for profiling hospital performance on the basis of 30-day all-cause readmission rates among patients with heart failure. Circ Cardiovasc Qual Outcomes. 2008;1:29-37.
4. Desai NR, Ross JS, Kwon JY, et al. Association between hospital penalty status under the Hospital Readmission Reduction Program and readmission rates for target and nontarget conditions. JAMA. 2016 Dec 27;316(24):2647-56.
5. Joynt KE, Figueroa JF, Orav EJ, Jha AK. Opinions on the Hospital Readmissions Reduction Program: Results of a national survey of hospital leaders. Am J Manag Care. 2016 Aug 1;222(8):e287-94.
6. Zuckerman RB, Sheingold SH, Orav EJ, et al. Readmissions, observation, and the Hospital Readmissions Reduction Program. N Engl J Med. 2016 Apr 21;374(16):1543-51.
7. Papanicolas I, Figueroa JF, Orav EJ, Jha AK. Patient hospital experience improved modestly, but no evidence Medicare incentives promoted meaningful gain. Health Aff (Millwood). 2017 Jan;36(1):133-40.
8. Figueroa JF, Tsugawa Y, Zheng J, et al. Association between the value-based purchasing pay for performance program and patient mortality in US hospitals: observational study. BMJ. 2016;353:i2214.
With the Hospital Readmissions Reduction Program (HRRP) in its 5th year, what has been the impact on hospitals and on hospitalists?
First of all, a lot of penalties have been paid by hospitals. According to an analysis by Kaiser Health News,1 the Centers for Medicare and Medicaid Services will withhold $528 million from 2,597 hospitals in the current fiscal year, Oct. 1, 2016 to Sept. 30, 2017, for readmissions for six diagnoses that occurred between July 2012 and June 2015. The number of penalized hospitals is down slightly from 2,665 the year before, but the total annual withhold will go up by $108 million.
HRRP exacts Medicare payment penalties from hospitals that have rates of readmissions – within 30 days of discharge – that are higher than expected, based on national rates and the health of their patient population. The maximum penalty is now up to 3% of a hospital’s Medicare reimbursement. Hospitals are being penalized an average of 0.73% of their annual Medicare reimbursement, and cumulative HRRP penalties will reach nearly $1.9 billion by the end of the fiscal year, Kaiser Health News reports.2
“Basically, we chose to introduce the idea of measuring readmissions because we felt it represented an adverse outcome for many people that was being ignored; that risk could be reduced; and improvements would yield benefits for people as well as save money for the health care system,” he told The Hospitalist.
“More than anything, HRRP has sharpened the focus on considering the episode of care from the patient’s perspective – rather than just focusing on venues of care like the hospitalization alone,” Dr. Krumholz said. “The focus on readmission forced many of us in the health professions to consider what the experience was like to leave the acute setting – how information flowed, what kind of concerns people had, the degree to which they understood what had happened to them, the extent to which they were prepared for the next steps.”
Once the patient leaves the hospital, there are myriad factors that will influence their likelihood of returning, notes researcher Karen Joynt, MD, MPH, of the Department of Health Policy and Management at Harvard’s School of Public Health, Boston. “The proportion of patients readmitted to the hospital because of gross error is low, but sometimes we’re too optimistic about our patients’ ability to manage postdischarge,” she said.
“We all know we can do better at providing softer landings, and anyone who’s ever been a hospital patient or a family member of one knows that leaving the hospital is incredibly tumultuous. I experienced that with my own parents, and it’s frightening, even if everything is done right. It’s still a very vulnerable time.”
HRRP has fundamentally changed the conversation about hospital care, Dr. Joynt said. “I think we need to change the conversation even more and talk more about how to prevent admissions in the first place. As a clinician, I think we need to be more innovative, recognizing that the ways we’ll make a real difference probably has more to do with what happens outside of the hospital. My personal hope is that new alternate payment models like accountable care organizations will lead to more creative partnerships with other providers.”
What have we learned about readmissions in 5 years?
A lot of recently published research about readmissions has documented modest decreases in overall readmissions nationally, from over 21% to under 18% between 2007 and 2014, although most of the reduction occurred in the first couple of years after HRRP was announced and it has since largely leveled off.
Other research has tried to explore the relationship between readmissions rates and other outcomes that might matter more to patients or that might be better proxies for the quality of the hospital experience. Is readmission rate a true measure of quality, or just a utilization measure? Research has also tried to document what works: what are the best strategies for preventing avoidable readmissions by improving the discharge process, care transitions, and the coordination of care postdischarge in the community – although no silver bullet has yet been identified.
A recent effort to inject more equity into the penalties program, contained in the wide-ranging 21st Century Cures Act signed into law by President Obama in December 2016, requires Medicare to account for patients’ socio-economic backgrounds when it calculates reductions in its payments to hospitals under HRRP. The law directs the government to change the way pay for performance is applied to safety net hospitals by setting different penalty thresholds for hospitals based on the proportion of their patients who are dually eligible for Medicare and Medicaid.
It remains to be seen how this will be implemented and with what impact. But some critics have continued to question whether hospitals should be held accountable for readmissions, whether 30 days is the correct time frame for that accountability, and whether some hospitals might be simply taking the penalty hit rather than investing in the hard work of care transitions.
Impact on working hospitalists
One expert, Ashish Jha, MD, MPH, director of Harvard’s Global Health Institute, wants to see hospitalists get more engaged in the conversation about how to improve hospital care overall.
Experts say there aren’t metrics available that could allocate penalties to individual hospitalists for their performance in readmissions prevention. But hospitals, clearly, are paying attention, and hospitalist groups may find that part of their negotiation of quality and performance incentives with the hospital includes readmissions.
“There are so many other variables that go into transitions of care, and it would be unreasonable to try to hold the individual doctor responsible for all of them,” he said. But accountability can be passed on to the hospitalist group. “My hospital contracts with a national hospitalist company and our agreement has quality measures that we review with them. We ask them to focus on readmissions.”
Dr. Harte said that when patients are discharged from the hospital, they go from an environment where everything is taken care of for them, to total responsibility for their self-care. Yet we are asking ever more from patients in terms of self-management.
“We need to focus on the human side of the experience. The hospital is a place to be avoided wherever possible,” he said. Yet some readmissions are largely unpreventable. Hospitalists should focus on the patient’s greatest risk of preventable readmission. “Is it health literacy? Is it transportation?”
Readmissions at the front lines
Preetham Talari, MD, FACP, FHM, hospitalist at University of Kentucky HealthCare in Lexington, has an interest in health care safety, quality improvement, and value. He has led the university’s site participation in Project BOOST, the Society of Hospital Medicine’s national mentored quality improvement initiative for care transitions. Dr. Talari also led a quality initiative at the university called the Interprofessional Teamwork Innovation Model to systematize teamwork, first piloted on a 30-bed hospitalist unit where he is medical director.
“Readmissions are not just about doctors, they are more about patient factors, socioeconomic factors, where they live,” Dr. Talari said. “Those are harder to impact, but in my experience, it comes down to thinking about the patient’s needs before discharge – really from the time of admission: What are all the things we can do in the hospital to make sure the patient is safely transitioned home?”
According to Dr. Talari, complex issues like readmissions don’t depend on just one, two, or three factors. “But we do the interventions believing that it will improve processes and outcomes, and then add another intervention and another,” he said. “All of these interventions will add up like a jigsaw puzzle to achieve a final, sustainable outcome. One thing I believe is hospitalists should be leading these efforts.”
Better interventions, better infrastructure
Leora Horwitz, MD, MHS, director of the Center for Healthcare Innovation and Delivery Science at New York University School of Public Health, says the biggest change she has seen resulting from readmissions penalties is that transitions of care are now understood to be both important and the responsibility of front line hospitalists. “That was not true 5 or 10 years ago. We used to spend hours admitting patients to the hospital and then 5 minutes on their discharge.”
“We’ve also learned that the infrastructure can be built better. Historically, hospital discharge summaries have been abysmal. But we can automate the importation of pending labs into the electronic health record. These are things you can change for everybody by changing your template. Sit down in a room together every afternoon to talk about what will happen to the patients when they go home. That’s become standard at our hospital. That was never done before.”
Evidence for improved outcomes is mixed, Dr. Horwitz noted. However, she pointed out, is there any evidence that readmissions penalties have produced adverse outcomes? Did they increase mortality, or length of stay? “So far the evidence suggests that they did not,” she said.
“I think it’s generally likely that the work we have done has resulted in better care. Thousands of people haven’t had to go back to the hospital, and that’s a good thing.”
Recent research on readmissions penalties
A survey by Yale researchers, published in JAMA in December 2016, found that hospitals financially penalized under HRRP reduced their readmissions rates at a higher rate than nonpenalized hospitals, “which implies that penalties can improve quality and readmission performance for hospitals with the most room for improvement,” coauthor Kumar Dharmarajan, MD, MBA, said in a statement.4 The hospitals responded to external pressures – in other words, financial penalties worked. But most of the reduction happened in the 2 years before actual penalties went into effect, which suggests that further improvement will not be easy, the authors note.
A survey of the attitudes of hospital leaders on the HRRP found that it has had a major impact on their efforts to reduce readmissions rates, although the failure to take sociodemographic factors into account was a major complaint for these leaders.5 Most said the penalties were too large, but 42.5% believed HRRP was likely to improve quality.
Some have questioned whether readmissions penalties were just encouraging hospitals to reduce their rates by keeping returning patients in observation units rather than formally readmitting them. Zuckerman et al. in the New England Journal of Medicine found no evidence that changes in observation unit stays accounted for the documented decrease in readmissions.6
But according to Papanicolas et al. in Health Affairs, patient hospital experience has improved only modestly under hospital value-based purchasing for U.S. hospitals, with no evidence that the program has had a beneficial effect on overall patient experience.7 Another study from Harvard by Figueroa et al. found that evidence is lacking that hospital value-based purchasing leads to lower mortality rates.8
“Patients and caregivers tell us: Hey, you people are the experts. You’ve taken care of lots of people with my medical condition before. You should know what my needs are going to be postdischarge and help me anticipate them,” he said.
References
1. Rau J. Medicare’s Readmission Penalties Hit New High. Kaiser Health News. 2016 Aug 2.
2. Boccuti C, Casillas G. Aiming for Fewer Hospital U-turns: The Medicare Hospital Readmission Reduction Program. Kaiser Health News, 2016 Sep 30.
3. Keenan PS, Normand SLT, Lin Z, et al. An administrative claims measure suitable for profiling hospital performance on the basis of 30-day all-cause readmission rates among patients with heart failure. Circ Cardiovasc Qual Outcomes. 2008;1:29-37.
4. Desai NR, Ross JS, Kwon JY, et al. Association between hospital penalty status under the Hospital Readmission Reduction Program and readmission rates for target and nontarget conditions. JAMA. 2016 Dec 27;316(24):2647-56.
5. Joynt KE, Figueroa JF, Orav EJ, Jha AK. Opinions on the Hospital Readmissions Reduction Program: Results of a national survey of hospital leaders. Am J Manag Care. 2016 Aug 1;222(8):e287-94.
6. Zuckerman RB, Sheingold SH, Orav EJ, et al. Readmissions, observation, and the Hospital Readmissions Reduction Program. N Engl J Med. 2016 Apr 21;374(16):1543-51.
7. Papanicolas I, Figueroa JF, Orav EJ, Jha AK. Patient hospital experience improved modestly, but no evidence Medicare incentives promoted meaningful gain. Health Aff (Millwood). 2017 Jan;36(1):133-40.
8. Figueroa JF, Tsugawa Y, Zheng J, et al. Association between the value-based purchasing pay for performance program and patient mortality in US hospitals: observational study. BMJ. 2016;353:i2214.
How hospitalists can help reduce readmissions
Hospital readmissions are frequent, harmful, and costly. Consider the fact that 18% of Medicare patients can expect to be readmitted within 30 days at a cost of more than $17 billion.1 Recent changes in health care policy aimed at reducing readmission have substantially increased attention to this major health care issue.2
The Affordable Care Act has mandated that the Centers for Medicare & Medicaid Services reduce payment to hospitals with higher-than-expected 30-day readmissions, with its Hospital Readmissions Reduction Program. This has driven rapid growth in the study of patients rehospitalized within 30 days of discharge.3 So what are some strategies that have either been proven to reduce readmissions or show promise in doing so? 
An ounce of prevention
In studying inpatient and outpatient physicians’ perspectives regarding factors contributing to readmission,4 Shoshana Herzig, MD, MPH, assistant professor of medicine, Harvard Medical School, and director of Hospital Medicine Research, Beth Israel Deaconess Medical Center and Harvard Medical School, Boston, and her colleagues identified some potential preventive strategies.
The most commonly endorsed strategy to prevent readmissions by both primary care physicians and hospitalists surveyed involved improving self-management plans at discharge. “This refers to actions such as providing patient-centered discharge instructions (that is, making sure they are written in language that patients can understand) or asking transition coaches to help facilitate a successful transition,” Dr. Herzig said. “This finding is consistent with the fact that the factor most commonly identified as contributing to readmissions was insufficient patient understanding or ability to self-manage. Combined, these findings suggest that strategies to enhance patient understanding of their illness, care plan, and what to expect after hospital discharge, are likely to be important components of successful readmission reduction programs.”
Provisioning of resources to patients to help them manage their care after discharge is also recommended. For example, engaging nurses or pharmacists who can help with issues that arise after discharge may help keep patients out of the hospital.
“Hospitalists should be aware of what resources are available to help patients manage their care,” Dr. Herzig said. For example, if a patient needs periodic blood pressure monitoring, the hospitalist can tell the patient about free blood pressure checkpoints or suggest a home-automated blood pressure monitor.
The study also showed that improved coordination of care between inpatient and outpatient providers, such as sharing medical records, could reduce readmission rates. “This allows for better inpatient care and increased ability for primary care physicians to react appropriately to issues arising after discharge,” Dr. Herzig said. “In the absence of a shared system, hospitalists should complete discharge summaries in a timely fashion and ensure that they’re promptly transmitted to primary care physicians.”
Dr. Herzig said it’s important to note that hospitalists and primary care physicians had different appraisals of reasons for readmission. Therefore, when designing readmission reduction programs or determining specific services to prevent a readmission for a given patient, it is important for hospitalists to obtain input from primary care physicians to ensure that they address all of the potential contributors to readmission for a given patient.
Interviewing patients regarding readmissions
After involved clinicians and independent physician reviewers performed extensive case reviews of more than 700 readmitted patients,6 Ashley Busuttil, MD, FHM, associate section chief, Hospital Medicine, University of California, Los Angeles Department of Medicine; and executive medical director, Medicine Services, UCLA Department of Medicine, and Erin Dowling, MD, assistant clinical professor, General Internal Medicine, Hospitalist Services, UCLA Medical Center, Santa Monica, Calif., and their colleagues were unable to identify which readmissions could have easily been prevented, and found that readmission causality varied extensively.
Through interviews with patients, the researchers determined that patients were more likely to think that their readmission was preventable if they felt unready for discharge during their initial hospitalization. This was despite the fact that patients met what clinicians would consider “ready” by objective, provider-centric criteria: they were medically stable, they had in-home support services, they had follow-up arranged, and so forth. As such, they wanted to put effort into educating and preparing patients for what home will look and feel like posthospitalization to address their feelings of unreadiness.
To that end, the researchers created an enhanced transition initiative that included showing an educational video near the time of admission and a patient-centered discharge checklist to help patients identify questions they might have after discharge. The discharge checklist asks patients to put themselves in the position of being at home and working through scenarios they may face so they will know how to deal with them. For example, if you have pain, who should you call? What should you do if you run out of medication?
Dr. Dowling believes that the hospitalist will, over time, become essential to assessing patient readiness. “As we learn more about how patients approach discharge, hospitalists’ understanding of patient needs beyond straightforward medical care will be crucial to having smoother transitions of care,” she said.
The researchers also explored pain control. As a health system, UCLA Medical Center has formed a multidisciplinary task force to optimize its approach to pain control. “If we can address comfort – for both patients at high risk of readmission and those that aren’t – we hope we can improve symptom control overall,” Dr. Busuttil said. “It’s not uncommon for patients to feel inadequate symptom control at discharge. While this is likely only one component of all the readmission pieces, a patient who feels that their symptoms are not controlled is likely to feel less ready for discharge. Increasing patient readiness, perhaps by increasing symptom control and improving communication regarding symptom management expectations, is a task that the hospitalist is well positioned to address.”
The researchers also wanted to find out why patients may not use available outpatient resources, and assessed them for decisional conflict – a measure of certainty with decision making – when selecting from multiple options for accessing medical care if they were home postdischarge and began to feel ill again. “Patients with decisional conflict were more likely to state that they would go the emergency room rather than call their primary medical physician or visit an urgent care center,” Dr. Busuttil said.
The health system continues to screen patients for decisional conflict. “When positive, we provide bedside education on when to seek medical care through primary care, urgent care, or the emergency department,” Dr. Busuttil said. “We also provide patients with information on how to access each of these resources.”
While a prior discharge plan may have seemed ideal on paper, time and time again it’s not logistically possible for certain patients. “By having this knowledge gleaned from patient interviews, hospitalists are able to provide feedback to health systems regarding different options of outpatient care that may work for the different patient populations they serve,” Dr. Dowling said.
To understand why one particular patient population is being readmitted requires taking the time to understand that population, Dr. Dowling noted. “While many validated risk stratification tools are available, they may only serve as general guides,” she said. “To impact the population you serve, you must first understand the readmission process as it looks to them.”
Employing the HOSPITAL score
In another effort to reduce hospital readmissions, Jacques Donzé, MD, MSc, associate physician, Bern University Hospital, Switzerland, and research associate, Brigham and Women’s Hospital, Boston, and his colleagues used the HOSPITAL score to identify patients at high risk of 30-day potentially avoidable readmission.
To most efficiently reduce hospital readmissions, hospitals need to target complex and intensive discharge interventions for patients at high risk of potentially avoidable readmission who are more likely to benefit.2 “However, prior research indicates that clinical health care providers are not able to accurately identify which patients are at high risk for readmission,” Dr. Donzé said.
Dr. Donzé believes that several factors may influence the performance of a prediction model, such as the initial selection of the potential predictors, the quality of the derivation method, including readily available predictors commonly available, and including reliable factors that aren’t subject to subjective evaluation. “All of these factors can play a role in the performance and generalizability of the HOSPITAL score,” he said.
When a patient is identified as high risk to be readmitted, hospitalists can take certain actions to prevent readmission. “Interventions are more likely to be effective when they include several components,” Dr. Donzé said. “These include follow-up phone calls and/or home visits, review of the patient’s medication list, patient education, and sending a discharge summary to the patient’s primary care physician in a timely manner. For now, enough evidence for a specific effective multimodal intervention to be generalizable to the majority of patients is lacking.”
Currently, the HOSPITAL score has been validated in approximately 180,000 patients in 14 hospitals across five countries and three continents – always showing good performance and generalizability. The HOSPITAL score includes seven variables readily available before hospital discharge, is easy to use, and is the most widely validated prediction model for readmission, Dr. Donzé said.
Before being implemented into practice, a score should ideally reach the highest level of validation, that is, show its clinical impact. “We expect that the score will not only be able to accurately predict high-risk patients, but using the score will also impact patient care by reducing readmissions when coupled with an appropriate intervention,” Dr. Donzé said.
In summary, research has shown that a variety of methods can be used to reduce hospital readmissions, including studying inpatient and outpatient physicians’ perspectives regarding factors contributing to readmission; interviewing patients regarding readmissions; and identifying patients at high risk of readmission using the HOSPITAL score.
Many researchers are continuing their studies in these areas.
Karen Appold is a medical writer in Pennsylvania.
Using hospitalist reflections as a means to reduce readmissions
Readmission studies and the development of readmission scoring systems and prediction tools rely on data from a large number of patients, typically extracted from administrative databases.
To complement this data, Deanne Kashiwagi, MD, consultant, Hospital Internal Medicine, Mayo Clinic, Rochester, Minn., and her colleagues asked hospitalists to reflect upon the readmissions of patients for whom they cared to add insight into the culture of patient care transitions within the health system.
“We felt there was some value in considering these nuances of the local care environment, which may not be represented in studies drawing from large databases, as potential targets for readmission efforts,” she said.
Dr. Kashiwagi believes that including elements of local practice and culture was the strength of their work. “Groups interested in replicating this reflective process should consider including factors specific to their practices that may contribute to readmission,” she said.
Asking hospitalists to perform reviews has led to implementing changes. Physicians were prompted to schedule earlier follow-up appointments and nurse practitioners and physician assistants have worked to improve the quality of their discharge summaries. The exercise also engaged hospitalists to suggest system changes that might contribute to decreased readmissions, such as a geriatrician-run service (which was recently begun) to provide multidisciplinary acute geriatric care for hospitalized older adults.
“Although large-scale studies are clearly important, readmission review at a more granular level may have merit as well,” Dr. Kashiwagi said, noting that such reviews identify local practice factors that groups may quickly act upon to help decrease readmissions. “Hospitalists readily engaged in this reflective exercise, which yielded actionable information to decrease readmissions.”
In commenting on why a different similar study7 didn’t mimic the results of Mayo Clinic’s study, Dr. Kashiwagi said there were some differences in methodology that may explain the difference in readmission rates. “First, this group excluded patients on dialysis, which in our study was a common comorbidity of our readmitted patients,” she said. “It is also notable that the chart review tool was different. Perhaps there is less representation of local factors, unique to that hospitalist group and their practice culture, than on our review form. These investigators also discussed their readmissions at routine intervals. Additionally, their preintervention readmission rate was lower than Mayo Clinic’s group, and although the readmission rate trended downward postintervention, it did not reach statistical significance.”
References
1. Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360(14):1418-28.
2. Donzé JD, Williams MV, Robinson EJ, et al. International validity of the HOSPITAL Score to predict 30-day potentially avoidable hospital readmissions. JAMA Intern Med. 2016 Apr;176(4):496-502.
3. Kashiwagi DT, Burton MC, Hakim FA, et al. Reflective practice: a tool for readmission reduction. Am J Med Qual. 2016 May;31(3):265-71.
4. Herzig SJ, Schnipper JL, Doctoroff L, et al. Physician perspectives on factors contributing to readmissions and potential prevention strategies: a multicenter survey. J Gen Intern Med. 2016 Nov;31(11):1287-93. Epub 2016 Jun 9.
5. Allaudeen N, Schnipper JL, Orav EJ, et al. Inability of providers to predict unplanned readmissions. J Gen Intern Med. 2011 Jul;26(7):771-6.
6. Busuttil A, Howard-Anderson J, Dowling EP, et al. Building a comprehensive patient-centered readmission reduction program [abstract]. J Hosp Med. 2016;11(suppl 1).
7. Rana V, Thapa B, Saini SC, et al. Self-reflection as a tool to increase hospitalist participation in readmission quality improvement. Qual Manag Health Care. 2016 Oct/Dec;25(4):219-24.
Hospital readmissions are frequent, harmful, and costly. Consider the fact that 18% of Medicare patients can expect to be readmitted within 30 days at a cost of more than $17 billion.1 Recent changes in health care policy aimed at reducing readmission have substantially increased attention to this major health care issue.2
The Affordable Care Act has mandated that the Centers for Medicare & Medicaid Services reduce payment to hospitals with higher-than-expected 30-day readmissions, with its Hospital Readmissions Reduction Program. This has driven rapid growth in the study of patients rehospitalized within 30 days of discharge.3 So what are some strategies that have either been proven to reduce readmissions or show promise in doing so? 
An ounce of prevention
In studying inpatient and outpatient physicians’ perspectives regarding factors contributing to readmission,4 Shoshana Herzig, MD, MPH, assistant professor of medicine, Harvard Medical School, and director of Hospital Medicine Research, Beth Israel Deaconess Medical Center and Harvard Medical School, Boston, and her colleagues identified some potential preventive strategies.
The most commonly endorsed strategy to prevent readmissions by both primary care physicians and hospitalists surveyed involved improving self-management plans at discharge. “This refers to actions such as providing patient-centered discharge instructions (that is, making sure they are written in language that patients can understand) or asking transition coaches to help facilitate a successful transition,” Dr. Herzig said. “This finding is consistent with the fact that the factor most commonly identified as contributing to readmissions was insufficient patient understanding or ability to self-manage. Combined, these findings suggest that strategies to enhance patient understanding of their illness, care plan, and what to expect after hospital discharge, are likely to be important components of successful readmission reduction programs.”
Provisioning of resources to patients to help them manage their care after discharge is also recommended. For example, engaging nurses or pharmacists who can help with issues that arise after discharge may help keep patients out of the hospital.
“Hospitalists should be aware of what resources are available to help patients manage their care,” Dr. Herzig said. For example, if a patient needs periodic blood pressure monitoring, the hospitalist can tell the patient about free blood pressure checkpoints or suggest a home-automated blood pressure monitor.
The study also showed that improved coordination of care between inpatient and outpatient providers, such as sharing medical records, could reduce readmission rates. “This allows for better inpatient care and increased ability for primary care physicians to react appropriately to issues arising after discharge,” Dr. Herzig said. “In the absence of a shared system, hospitalists should complete discharge summaries in a timely fashion and ensure that they’re promptly transmitted to primary care physicians.”
Dr. Herzig said it’s important to note that hospitalists and primary care physicians had different appraisals of reasons for readmission. Therefore, when designing readmission reduction programs or determining specific services to prevent a readmission for a given patient, it is important for hospitalists to obtain input from primary care physicians to ensure that they address all of the potential contributors to readmission for a given patient.
Interviewing patients regarding readmissions
After involved clinicians and independent physician reviewers performed extensive case reviews of more than 700 readmitted patients,6 Ashley Busuttil, MD, FHM, associate section chief, Hospital Medicine, University of California, Los Angeles Department of Medicine; and executive medical director, Medicine Services, UCLA Department of Medicine, and Erin Dowling, MD, assistant clinical professor, General Internal Medicine, Hospitalist Services, UCLA Medical Center, Santa Monica, Calif., and their colleagues were unable to identify which readmissions could have easily been prevented, and found that readmission causality varied extensively.
Through interviews with patients, the researchers determined that patients were more likely to think that their readmission was preventable if they felt unready for discharge during their initial hospitalization. This was despite the fact that patients met what clinicians would consider “ready” by objective, provider-centric criteria: they were medically stable, they had in-home support services, they had follow-up arranged, and so forth. As such, they wanted to put effort into educating and preparing patients for what home will look and feel like posthospitalization to address their feelings of unreadiness.
To that end, the researchers created an enhanced transition initiative that included showing an educational video near the time of admission and a patient-centered discharge checklist to help patients identify questions they might have after discharge. The discharge checklist asks patients to put themselves in the position of being at home and working through scenarios they may face so they will know how to deal with them. For example, if you have pain, who should you call? What should you do if you run out of medication?
Dr. Dowling believes that the hospitalist will, over time, become essential to assessing patient readiness. “As we learn more about how patients approach discharge, hospitalists’ understanding of patient needs beyond straightforward medical care will be crucial to having smoother transitions of care,” she said.
The researchers also explored pain control. As a health system, UCLA Medical Center has formed a multidisciplinary task force to optimize its approach to pain control. “If we can address comfort – for both patients at high risk of readmission and those that aren’t – we hope we can improve symptom control overall,” Dr. Busuttil said. “It’s not uncommon for patients to feel inadequate symptom control at discharge. While this is likely only one component of all the readmission pieces, a patient who feels that their symptoms are not controlled is likely to feel less ready for discharge. Increasing patient readiness, perhaps by increasing symptom control and improving communication regarding symptom management expectations, is a task that the hospitalist is well positioned to address.”
The researchers also wanted to find out why patients may not use available outpatient resources, and assessed them for decisional conflict – a measure of certainty with decision making – when selecting from multiple options for accessing medical care if they were home postdischarge and began to feel ill again. “Patients with decisional conflict were more likely to state that they would go the emergency room rather than call their primary medical physician or visit an urgent care center,” Dr. Busuttil said.
The health system continues to screen patients for decisional conflict. “When positive, we provide bedside education on when to seek medical care through primary care, urgent care, or the emergency department,” Dr. Busuttil said. “We also provide patients with information on how to access each of these resources.”
While a prior discharge plan may have seemed ideal on paper, time and time again it’s not logistically possible for certain patients. “By having this knowledge gleaned from patient interviews, hospitalists are able to provide feedback to health systems regarding different options of outpatient care that may work for the different patient populations they serve,” Dr. Dowling said.
To understand why one particular patient population is being readmitted requires taking the time to understand that population, Dr. Dowling noted. “While many validated risk stratification tools are available, they may only serve as general guides,” she said. “To impact the population you serve, you must first understand the readmission process as it looks to them.”
Employing the HOSPITAL score
In another effort to reduce hospital readmissions, Jacques Donzé, MD, MSc, associate physician, Bern University Hospital, Switzerland, and research associate, Brigham and Women’s Hospital, Boston, and his colleagues used the HOSPITAL score to identify patients at high risk of 30-day potentially avoidable readmission.
To most efficiently reduce hospital readmissions, hospitals need to target complex and intensive discharge interventions for patients at high risk of potentially avoidable readmission who are more likely to benefit.2 “However, prior research indicates that clinical health care providers are not able to accurately identify which patients are at high risk for readmission,” Dr. Donzé said.
Dr. Donzé believes that several factors may influence the performance of a prediction model, such as the initial selection of the potential predictors, the quality of the derivation method, including readily available predictors commonly available, and including reliable factors that aren’t subject to subjective evaluation. “All of these factors can play a role in the performance and generalizability of the HOSPITAL score,” he said.
When a patient is identified as high risk to be readmitted, hospitalists can take certain actions to prevent readmission. “Interventions are more likely to be effective when they include several components,” Dr. Donzé said. “These include follow-up phone calls and/or home visits, review of the patient’s medication list, patient education, and sending a discharge summary to the patient’s primary care physician in a timely manner. For now, enough evidence for a specific effective multimodal intervention to be generalizable to the majority of patients is lacking.”
Currently, the HOSPITAL score has been validated in approximately 180,000 patients in 14 hospitals across five countries and three continents – always showing good performance and generalizability. The HOSPITAL score includes seven variables readily available before hospital discharge, is easy to use, and is the most widely validated prediction model for readmission, Dr. Donzé said.
Before being implemented into practice, a score should ideally reach the highest level of validation, that is, show its clinical impact. “We expect that the score will not only be able to accurately predict high-risk patients, but using the score will also impact patient care by reducing readmissions when coupled with an appropriate intervention,” Dr. Donzé said.
In summary, research has shown that a variety of methods can be used to reduce hospital readmissions, including studying inpatient and outpatient physicians’ perspectives regarding factors contributing to readmission; interviewing patients regarding readmissions; and identifying patients at high risk of readmission using the HOSPITAL score.
Many researchers are continuing their studies in these areas.
Karen Appold is a medical writer in Pennsylvania.
Using hospitalist reflections as a means to reduce readmissions
Readmission studies and the development of readmission scoring systems and prediction tools rely on data from a large number of patients, typically extracted from administrative databases.
To complement this data, Deanne Kashiwagi, MD, consultant, Hospital Internal Medicine, Mayo Clinic, Rochester, Minn., and her colleagues asked hospitalists to reflect upon the readmissions of patients for whom they cared to add insight into the culture of patient care transitions within the health system.
“We felt there was some value in considering these nuances of the local care environment, which may not be represented in studies drawing from large databases, as potential targets for readmission efforts,” she said.
Dr. Kashiwagi believes that including elements of local practice and culture was the strength of their work. “Groups interested in replicating this reflective process should consider including factors specific to their practices that may contribute to readmission,” she said.
Asking hospitalists to perform reviews has led to implementing changes. Physicians were prompted to schedule earlier follow-up appointments and nurse practitioners and physician assistants have worked to improve the quality of their discharge summaries. The exercise also engaged hospitalists to suggest system changes that might contribute to decreased readmissions, such as a geriatrician-run service (which was recently begun) to provide multidisciplinary acute geriatric care for hospitalized older adults.
“Although large-scale studies are clearly important, readmission review at a more granular level may have merit as well,” Dr. Kashiwagi said, noting that such reviews identify local practice factors that groups may quickly act upon to help decrease readmissions. “Hospitalists readily engaged in this reflective exercise, which yielded actionable information to decrease readmissions.”
In commenting on why a different similar study7 didn’t mimic the results of Mayo Clinic’s study, Dr. Kashiwagi said there were some differences in methodology that may explain the difference in readmission rates. “First, this group excluded patients on dialysis, which in our study was a common comorbidity of our readmitted patients,” she said. “It is also notable that the chart review tool was different. Perhaps there is less representation of local factors, unique to that hospitalist group and their practice culture, than on our review form. These investigators also discussed their readmissions at routine intervals. Additionally, their preintervention readmission rate was lower than Mayo Clinic’s group, and although the readmission rate trended downward postintervention, it did not reach statistical significance.”
References
1. Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360(14):1418-28.
2. Donzé JD, Williams MV, Robinson EJ, et al. International validity of the HOSPITAL Score to predict 30-day potentially avoidable hospital readmissions. JAMA Intern Med. 2016 Apr;176(4):496-502.
3. Kashiwagi DT, Burton MC, Hakim FA, et al. Reflective practice: a tool for readmission reduction. Am J Med Qual. 2016 May;31(3):265-71.
4. Herzig SJ, Schnipper JL, Doctoroff L, et al. Physician perspectives on factors contributing to readmissions and potential prevention strategies: a multicenter survey. J Gen Intern Med. 2016 Nov;31(11):1287-93. Epub 2016 Jun 9.
5. Allaudeen N, Schnipper JL, Orav EJ, et al. Inability of providers to predict unplanned readmissions. J Gen Intern Med. 2011 Jul;26(7):771-6.
6. Busuttil A, Howard-Anderson J, Dowling EP, et al. Building a comprehensive patient-centered readmission reduction program [abstract]. J Hosp Med. 2016;11(suppl 1).
7. Rana V, Thapa B, Saini SC, et al. Self-reflection as a tool to increase hospitalist participation in readmission quality improvement. Qual Manag Health Care. 2016 Oct/Dec;25(4):219-24.
Hospital readmissions are frequent, harmful, and costly. Consider the fact that 18% of Medicare patients can expect to be readmitted within 30 days at a cost of more than $17 billion.1 Recent changes in health care policy aimed at reducing readmission have substantially increased attention to this major health care issue.2
The Affordable Care Act has mandated that the Centers for Medicare & Medicaid Services reduce payment to hospitals with higher-than-expected 30-day readmissions, with its Hospital Readmissions Reduction Program. This has driven rapid growth in the study of patients rehospitalized within 30 days of discharge.3 So what are some strategies that have either been proven to reduce readmissions or show promise in doing so? 
An ounce of prevention
In studying inpatient and outpatient physicians’ perspectives regarding factors contributing to readmission,4 Shoshana Herzig, MD, MPH, assistant professor of medicine, Harvard Medical School, and director of Hospital Medicine Research, Beth Israel Deaconess Medical Center and Harvard Medical School, Boston, and her colleagues identified some potential preventive strategies.
The most commonly endorsed strategy to prevent readmissions by both primary care physicians and hospitalists surveyed involved improving self-management plans at discharge. “This refers to actions such as providing patient-centered discharge instructions (that is, making sure they are written in language that patients can understand) or asking transition coaches to help facilitate a successful transition,” Dr. Herzig said. “This finding is consistent with the fact that the factor most commonly identified as contributing to readmissions was insufficient patient understanding or ability to self-manage. Combined, these findings suggest that strategies to enhance patient understanding of their illness, care plan, and what to expect after hospital discharge, are likely to be important components of successful readmission reduction programs.”
Provisioning of resources to patients to help them manage their care after discharge is also recommended. For example, engaging nurses or pharmacists who can help with issues that arise after discharge may help keep patients out of the hospital.
“Hospitalists should be aware of what resources are available to help patients manage their care,” Dr. Herzig said. For example, if a patient needs periodic blood pressure monitoring, the hospitalist can tell the patient about free blood pressure checkpoints or suggest a home-automated blood pressure monitor.
The study also showed that improved coordination of care between inpatient and outpatient providers, such as sharing medical records, could reduce readmission rates. “This allows for better inpatient care and increased ability for primary care physicians to react appropriately to issues arising after discharge,” Dr. Herzig said. “In the absence of a shared system, hospitalists should complete discharge summaries in a timely fashion and ensure that they’re promptly transmitted to primary care physicians.”
Dr. Herzig said it’s important to note that hospitalists and primary care physicians had different appraisals of reasons for readmission. Therefore, when designing readmission reduction programs or determining specific services to prevent a readmission for a given patient, it is important for hospitalists to obtain input from primary care physicians to ensure that they address all of the potential contributors to readmission for a given patient.
Interviewing patients regarding readmissions
After involved clinicians and independent physician reviewers performed extensive case reviews of more than 700 readmitted patients,6 Ashley Busuttil, MD, FHM, associate section chief, Hospital Medicine, University of California, Los Angeles Department of Medicine; and executive medical director, Medicine Services, UCLA Department of Medicine, and Erin Dowling, MD, assistant clinical professor, General Internal Medicine, Hospitalist Services, UCLA Medical Center, Santa Monica, Calif., and their colleagues were unable to identify which readmissions could have easily been prevented, and found that readmission causality varied extensively.
Through interviews with patients, the researchers determined that patients were more likely to think that their readmission was preventable if they felt unready for discharge during their initial hospitalization. This was despite the fact that patients met what clinicians would consider “ready” by objective, provider-centric criteria: they were medically stable, they had in-home support services, they had follow-up arranged, and so forth. As such, they wanted to put effort into educating and preparing patients for what home will look and feel like posthospitalization to address their feelings of unreadiness.
To that end, the researchers created an enhanced transition initiative that included showing an educational video near the time of admission and a patient-centered discharge checklist to help patients identify questions they might have after discharge. The discharge checklist asks patients to put themselves in the position of being at home and working through scenarios they may face so they will know how to deal with them. For example, if you have pain, who should you call? What should you do if you run out of medication?
Dr. Dowling believes that the hospitalist will, over time, become essential to assessing patient readiness. “As we learn more about how patients approach discharge, hospitalists’ understanding of patient needs beyond straightforward medical care will be crucial to having smoother transitions of care,” she said.
The researchers also explored pain control. As a health system, UCLA Medical Center has formed a multidisciplinary task force to optimize its approach to pain control. “If we can address comfort – for both patients at high risk of readmission and those that aren’t – we hope we can improve symptom control overall,” Dr. Busuttil said. “It’s not uncommon for patients to feel inadequate symptom control at discharge. While this is likely only one component of all the readmission pieces, a patient who feels that their symptoms are not controlled is likely to feel less ready for discharge. Increasing patient readiness, perhaps by increasing symptom control and improving communication regarding symptom management expectations, is a task that the hospitalist is well positioned to address.”
The researchers also wanted to find out why patients may not use available outpatient resources, and assessed them for decisional conflict – a measure of certainty with decision making – when selecting from multiple options for accessing medical care if they were home postdischarge and began to feel ill again. “Patients with decisional conflict were more likely to state that they would go the emergency room rather than call their primary medical physician or visit an urgent care center,” Dr. Busuttil said.
The health system continues to screen patients for decisional conflict. “When positive, we provide bedside education on when to seek medical care through primary care, urgent care, or the emergency department,” Dr. Busuttil said. “We also provide patients with information on how to access each of these resources.”
While a prior discharge plan may have seemed ideal on paper, time and time again it’s not logistically possible for certain patients. “By having this knowledge gleaned from patient interviews, hospitalists are able to provide feedback to health systems regarding different options of outpatient care that may work for the different patient populations they serve,” Dr. Dowling said.
To understand why one particular patient population is being readmitted requires taking the time to understand that population, Dr. Dowling noted. “While many validated risk stratification tools are available, they may only serve as general guides,” she said. “To impact the population you serve, you must first understand the readmission process as it looks to them.”
Employing the HOSPITAL score
In another effort to reduce hospital readmissions, Jacques Donzé, MD, MSc, associate physician, Bern University Hospital, Switzerland, and research associate, Brigham and Women’s Hospital, Boston, and his colleagues used the HOSPITAL score to identify patients at high risk of 30-day potentially avoidable readmission.
To most efficiently reduce hospital readmissions, hospitals need to target complex and intensive discharge interventions for patients at high risk of potentially avoidable readmission who are more likely to benefit.2 “However, prior research indicates that clinical health care providers are not able to accurately identify which patients are at high risk for readmission,” Dr. Donzé said.
Dr. Donzé believes that several factors may influence the performance of a prediction model, such as the initial selection of the potential predictors, the quality of the derivation method, including readily available predictors commonly available, and including reliable factors that aren’t subject to subjective evaluation. “All of these factors can play a role in the performance and generalizability of the HOSPITAL score,” he said.
When a patient is identified as high risk to be readmitted, hospitalists can take certain actions to prevent readmission. “Interventions are more likely to be effective when they include several components,” Dr. Donzé said. “These include follow-up phone calls and/or home visits, review of the patient’s medication list, patient education, and sending a discharge summary to the patient’s primary care physician in a timely manner. For now, enough evidence for a specific effective multimodal intervention to be generalizable to the majority of patients is lacking.”
Currently, the HOSPITAL score has been validated in approximately 180,000 patients in 14 hospitals across five countries and three continents – always showing good performance and generalizability. The HOSPITAL score includes seven variables readily available before hospital discharge, is easy to use, and is the most widely validated prediction model for readmission, Dr. Donzé said.
Before being implemented into practice, a score should ideally reach the highest level of validation, that is, show its clinical impact. “We expect that the score will not only be able to accurately predict high-risk patients, but using the score will also impact patient care by reducing readmissions when coupled with an appropriate intervention,” Dr. Donzé said.
In summary, research has shown that a variety of methods can be used to reduce hospital readmissions, including studying inpatient and outpatient physicians’ perspectives regarding factors contributing to readmission; interviewing patients regarding readmissions; and identifying patients at high risk of readmission using the HOSPITAL score.
Many researchers are continuing their studies in these areas.
Karen Appold is a medical writer in Pennsylvania.
Using hospitalist reflections as a means to reduce readmissions
Readmission studies and the development of readmission scoring systems and prediction tools rely on data from a large number of patients, typically extracted from administrative databases.
To complement this data, Deanne Kashiwagi, MD, consultant, Hospital Internal Medicine, Mayo Clinic, Rochester, Minn., and her colleagues asked hospitalists to reflect upon the readmissions of patients for whom they cared to add insight into the culture of patient care transitions within the health system.
“We felt there was some value in considering these nuances of the local care environment, which may not be represented in studies drawing from large databases, as potential targets for readmission efforts,” she said.
Dr. Kashiwagi believes that including elements of local practice and culture was the strength of their work. “Groups interested in replicating this reflective process should consider including factors specific to their practices that may contribute to readmission,” she said.
Asking hospitalists to perform reviews has led to implementing changes. Physicians were prompted to schedule earlier follow-up appointments and nurse practitioners and physician assistants have worked to improve the quality of their discharge summaries. The exercise also engaged hospitalists to suggest system changes that might contribute to decreased readmissions, such as a geriatrician-run service (which was recently begun) to provide multidisciplinary acute geriatric care for hospitalized older adults.
“Although large-scale studies are clearly important, readmission review at a more granular level may have merit as well,” Dr. Kashiwagi said, noting that such reviews identify local practice factors that groups may quickly act upon to help decrease readmissions. “Hospitalists readily engaged in this reflective exercise, which yielded actionable information to decrease readmissions.”
In commenting on why a different similar study7 didn’t mimic the results of Mayo Clinic’s study, Dr. Kashiwagi said there were some differences in methodology that may explain the difference in readmission rates. “First, this group excluded patients on dialysis, which in our study was a common comorbidity of our readmitted patients,” she said. “It is also notable that the chart review tool was different. Perhaps there is less representation of local factors, unique to that hospitalist group and their practice culture, than on our review form. These investigators also discussed their readmissions at routine intervals. Additionally, their preintervention readmission rate was lower than Mayo Clinic’s group, and although the readmission rate trended downward postintervention, it did not reach statistical significance.”
References
1. Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360(14):1418-28.
2. Donzé JD, Williams MV, Robinson EJ, et al. International validity of the HOSPITAL Score to predict 30-day potentially avoidable hospital readmissions. JAMA Intern Med. 2016 Apr;176(4):496-502.
3. Kashiwagi DT, Burton MC, Hakim FA, et al. Reflective practice: a tool for readmission reduction. Am J Med Qual. 2016 May;31(3):265-71.
4. Herzig SJ, Schnipper JL, Doctoroff L, et al. Physician perspectives on factors contributing to readmissions and potential prevention strategies: a multicenter survey. J Gen Intern Med. 2016 Nov;31(11):1287-93. Epub 2016 Jun 9.
5. Allaudeen N, Schnipper JL, Orav EJ, et al. Inability of providers to predict unplanned readmissions. J Gen Intern Med. 2011 Jul;26(7):771-6.
6. Busuttil A, Howard-Anderson J, Dowling EP, et al. Building a comprehensive patient-centered readmission reduction program [abstract]. J Hosp Med. 2016;11(suppl 1).
7. Rana V, Thapa B, Saini SC, et al. Self-reflection as a tool to increase hospitalist participation in readmission quality improvement. Qual Manag Health Care. 2016 Oct/Dec;25(4):219-24.
Hospital value-based purchasing is largely ineffective
Over the last 5 years, I’ve periodically devoted this column to providing updates to the Hospital Value-Based Purchasing program. HVBP launched in 2013 as a 5-year mixed upside/downside incentive program with mandatory participation for all U.S. acute care hospitals (critical access, acute inpatient rehabilitation, and long-term acute care hospitals are exempt). The program initially included process and patient experience measures. It later added measures for mortality, efficiency, and patient safety.
For the 2017 version of HVBP, the measures are allocated as follows: eight for patient experience, seven for patient safety (1 of which is a roll up of 11 claims-based measures), three for process, and three for mortality. HVBP uses a budget-neutral funding approach with some winners and some losers but overall net zero spending on the program. It initially put hospitals at risk for 1% of their Medicare inpatient payments (in 2013), with a progressive increase to 2% by this year. HVBP has used a complex approach to determining incentives and penalties, rewarding either improvement or achievement, depending on the baseline performance of the hospital.
Has HVBP improved quality? Two studies looking at the early period of HVBP failed to show improvements in process or patient experience measures and demonstrated no change in mortality for heart failure, pneumonia, or heart attack.1,2 Now that the program is in its 5th and final year, thanks to a recent study by Ryan et al., we have an idea if HVBP is associated with longer-term improvements in quality.3
In the study, Ryan et al. compared hospitals participating in HVBP with critical access hospitals, which are exempt from the program. The study yielded some disappointing, if not surprising, results. Improvements in process and patient experience measures for HVBP hospitals were no greater than those for the control group. HVBP was not associated with a significant reduction in mortality for heart failure or heart attack, but was associated with a mortality reduction for pneumonia. In sum, HVBP was not associated with improvements in process or patient experience, and was not associated with lower mortality, except in pneumonia.
As a program designed to incentivize better quality, where did HVBP go wrong? I believe HVBP simply had too many measures for the cognitive bandwidth of an individual or a team looking to improve quality. The total measure count for 2017 is 21! I submit that a hospitalist working to improve quality can keep top-of-mind one or two measures, possibly three at most. While others have postulated that the amount of dollars at risk are too small, I don’t think that’s the problem. Instead, my sense is that hospitalists and other members of the hospital team have quality improvement in their DNA and, regardless of the size of the financial incentives, will work to improve it as long as they have the right tools. Chief among these are good performance data and the time to focus on a finite number of projects.
What lessons can inform better design in the future? As of January 2017, the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) – representing the biggest change in reimbursement in a generation – progressively exposes doctors and other professionals to upside/downside incentives for quality, resource utilization, use of a certified electronic health record (hospitalists are exempt as they already use the hospital’s EHR), and practice improvement activities.
It would be wise to learn from the shortcomings of HVBP. Namely, if MACRA keeps on its course to incentivize physicians using a complicated formula based on four domains and many more subdomains, it will repeat the mistakes of HVBP and – while creating more administrative burden – likely improve quality very little, if at all. Instead, MACRA should delineate a simple measure set representing improvement activities that physicians and teams can incorporate into their regular work flow without more time taken away from patient care.
The reality is that complicated pay-for-performance programs divert limited available resources away from meaningful improvement activities in order to comply with onerous reporting requirements. As we gain a more nuanced understanding of how these programs work, policy makers should pay attention to the elements of “low-value” and “high-value” incentive systems and apply the “less is more” ethos of high-value care to the next generation of pay-for-performance programs.
Dr. Whitcomb is chief medical officer at Remedy Partners in Darien, Conn., and a cofounder and past president of SHM.
References
1. Ryan AM, Burgess JF, Pesko MF, Borden WB, Dimick JB. “The early effects of Medicare’s mandatory hospital pay-for-performance program” Health Serv Res. 2015;50:81-97.
2. Figueroa JF, Tsugawa Y, Zheng J, Orav EJ, Jha AK. “Association between the Value-Based Purchasing pay for performance program and patient mortality in US hospitals: observational study” BMJ. 2016;353:i2214.
3. Ryan AM, Krinsky S, Maurer KA, Dimick JB. “Changes in Hospital Quality Associated with Hospital Value-Based Purchasing” N Engl J Med. 2017;376:2358-66.
Over the last 5 years, I’ve periodically devoted this column to providing updates to the Hospital Value-Based Purchasing program. HVBP launched in 2013 as a 5-year mixed upside/downside incentive program with mandatory participation for all U.S. acute care hospitals (critical access, acute inpatient rehabilitation, and long-term acute care hospitals are exempt). The program initially included process and patient experience measures. It later added measures for mortality, efficiency, and patient safety.
For the 2017 version of HVBP, the measures are allocated as follows: eight for patient experience, seven for patient safety (1 of which is a roll up of 11 claims-based measures), three for process, and three for mortality. HVBP uses a budget-neutral funding approach with some winners and some losers but overall net zero spending on the program. It initially put hospitals at risk for 1% of their Medicare inpatient payments (in 2013), with a progressive increase to 2% by this year. HVBP has used a complex approach to determining incentives and penalties, rewarding either improvement or achievement, depending on the baseline performance of the hospital.
Has HVBP improved quality? Two studies looking at the early period of HVBP failed to show improvements in process or patient experience measures and demonstrated no change in mortality for heart failure, pneumonia, or heart attack.1,2 Now that the program is in its 5th and final year, thanks to a recent study by Ryan et al., we have an idea if HVBP is associated with longer-term improvements in quality.3
In the study, Ryan et al. compared hospitals participating in HVBP with critical access hospitals, which are exempt from the program. The study yielded some disappointing, if not surprising, results. Improvements in process and patient experience measures for HVBP hospitals were no greater than those for the control group. HVBP was not associated with a significant reduction in mortality for heart failure or heart attack, but was associated with a mortality reduction for pneumonia. In sum, HVBP was not associated with improvements in process or patient experience, and was not associated with lower mortality, except in pneumonia.
As a program designed to incentivize better quality, where did HVBP go wrong? I believe HVBP simply had too many measures for the cognitive bandwidth of an individual or a team looking to improve quality. The total measure count for 2017 is 21! I submit that a hospitalist working to improve quality can keep top-of-mind one or two measures, possibly three at most. While others have postulated that the amount of dollars at risk are too small, I don’t think that’s the problem. Instead, my sense is that hospitalists and other members of the hospital team have quality improvement in their DNA and, regardless of the size of the financial incentives, will work to improve it as long as they have the right tools. Chief among these are good performance data and the time to focus on a finite number of projects.
What lessons can inform better design in the future? As of January 2017, the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) – representing the biggest change in reimbursement in a generation – progressively exposes doctors and other professionals to upside/downside incentives for quality, resource utilization, use of a certified electronic health record (hospitalists are exempt as they already use the hospital’s EHR), and practice improvement activities.
It would be wise to learn from the shortcomings of HVBP. Namely, if MACRA keeps on its course to incentivize physicians using a complicated formula based on four domains and many more subdomains, it will repeat the mistakes of HVBP and – while creating more administrative burden – likely improve quality very little, if at all. Instead, MACRA should delineate a simple measure set representing improvement activities that physicians and teams can incorporate into their regular work flow without more time taken away from patient care.
The reality is that complicated pay-for-performance programs divert limited available resources away from meaningful improvement activities in order to comply with onerous reporting requirements. As we gain a more nuanced understanding of how these programs work, policy makers should pay attention to the elements of “low-value” and “high-value” incentive systems and apply the “less is more” ethos of high-value care to the next generation of pay-for-performance programs.
Dr. Whitcomb is chief medical officer at Remedy Partners in Darien, Conn., and a cofounder and past president of SHM.
References
1. Ryan AM, Burgess JF, Pesko MF, Borden WB, Dimick JB. “The early effects of Medicare’s mandatory hospital pay-for-performance program” Health Serv Res. 2015;50:81-97.
2. Figueroa JF, Tsugawa Y, Zheng J, Orav EJ, Jha AK. “Association between the Value-Based Purchasing pay for performance program and patient mortality in US hospitals: observational study” BMJ. 2016;353:i2214.
3. Ryan AM, Krinsky S, Maurer KA, Dimick JB. “Changes in Hospital Quality Associated with Hospital Value-Based Purchasing” N Engl J Med. 2017;376:2358-66.
Over the last 5 years, I’ve periodically devoted this column to providing updates to the Hospital Value-Based Purchasing program. HVBP launched in 2013 as a 5-year mixed upside/downside incentive program with mandatory participation for all U.S. acute care hospitals (critical access, acute inpatient rehabilitation, and long-term acute care hospitals are exempt). The program initially included process and patient experience measures. It later added measures for mortality, efficiency, and patient safety.
For the 2017 version of HVBP, the measures are allocated as follows: eight for patient experience, seven for patient safety (1 of which is a roll up of 11 claims-based measures), three for process, and three for mortality. HVBP uses a budget-neutral funding approach with some winners and some losers but overall net zero spending on the program. It initially put hospitals at risk for 1% of their Medicare inpatient payments (in 2013), with a progressive increase to 2% by this year. HVBP has used a complex approach to determining incentives and penalties, rewarding either improvement or achievement, depending on the baseline performance of the hospital.
Has HVBP improved quality? Two studies looking at the early period of HVBP failed to show improvements in process or patient experience measures and demonstrated no change in mortality for heart failure, pneumonia, or heart attack.1,2 Now that the program is in its 5th and final year, thanks to a recent study by Ryan et al., we have an idea if HVBP is associated with longer-term improvements in quality.3
In the study, Ryan et al. compared hospitals participating in HVBP with critical access hospitals, which are exempt from the program. The study yielded some disappointing, if not surprising, results. Improvements in process and patient experience measures for HVBP hospitals were no greater than those for the control group. HVBP was not associated with a significant reduction in mortality for heart failure or heart attack, but was associated with a mortality reduction for pneumonia. In sum, HVBP was not associated with improvements in process or patient experience, and was not associated with lower mortality, except in pneumonia.
As a program designed to incentivize better quality, where did HVBP go wrong? I believe HVBP simply had too many measures for the cognitive bandwidth of an individual or a team looking to improve quality. The total measure count for 2017 is 21! I submit that a hospitalist working to improve quality can keep top-of-mind one or two measures, possibly three at most. While others have postulated that the amount of dollars at risk are too small, I don’t think that’s the problem. Instead, my sense is that hospitalists and other members of the hospital team have quality improvement in their DNA and, regardless of the size of the financial incentives, will work to improve it as long as they have the right tools. Chief among these are good performance data and the time to focus on a finite number of projects.
What lessons can inform better design in the future? As of January 2017, the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) – representing the biggest change in reimbursement in a generation – progressively exposes doctors and other professionals to upside/downside incentives for quality, resource utilization, use of a certified electronic health record (hospitalists are exempt as they already use the hospital’s EHR), and practice improvement activities.
It would be wise to learn from the shortcomings of HVBP. Namely, if MACRA keeps on its course to incentivize physicians using a complicated formula based on four domains and many more subdomains, it will repeat the mistakes of HVBP and – while creating more administrative burden – likely improve quality very little, if at all. Instead, MACRA should delineate a simple measure set representing improvement activities that physicians and teams can incorporate into their regular work flow without more time taken away from patient care.
The reality is that complicated pay-for-performance programs divert limited available resources away from meaningful improvement activities in order to comply with onerous reporting requirements. As we gain a more nuanced understanding of how these programs work, policy makers should pay attention to the elements of “low-value” and “high-value” incentive systems and apply the “less is more” ethos of high-value care to the next generation of pay-for-performance programs.
Dr. Whitcomb is chief medical officer at Remedy Partners in Darien, Conn., and a cofounder and past president of SHM.
References
1. Ryan AM, Burgess JF, Pesko MF, Borden WB, Dimick JB. “The early effects of Medicare’s mandatory hospital pay-for-performance program” Health Serv Res. 2015;50:81-97.
2. Figueroa JF, Tsugawa Y, Zheng J, Orav EJ, Jha AK. “Association between the Value-Based Purchasing pay for performance program and patient mortality in US hospitals: observational study” BMJ. 2016;353:i2214.
3. Ryan AM, Krinsky S, Maurer KA, Dimick JB. “Changes in Hospital Quality Associated with Hospital Value-Based Purchasing” N Engl J Med. 2017;376:2358-66.
Sneak Peek: The Hospital Leader blog - Aug. 2017 “A Conversation with Dr. Eric Howell”
Quality improvement became a foundational theme for SHM early in the growth of hospitalists. It’s not a coincidence that many of our leaders, such as Bob Wachter, Win Whitcomb, Greg Maynard, and Mark Williams are QI leaders as well. As hospitalists, we were and are best positioned to impact quality in the hospital.
Eric Howell, MD, of Johns Hopkins Bayview Medical Center in Baltimore serves as the senior physician advisor for SHM’s Center for Quality Improvement, while Jenna Goldstein runs the day-to-day aspects at SHM headquarters. A few months ago, Dr. Howell and I discussed how he started in QI, the role of SHM’s Center, and how hospitalists can receive effective QI training. The following Q&A is edited for conciseness and clarity.
You’ve been a leader in QI for many years; how did you get started in QI?
I trained as an electrical engineer before I went to medical school, which helped me when I went to residency.
When I was a chief at Hopkins Bayview in 1999, there were a number of systems-related issues, including throughput from the emergency department. I became involved with QI because I looked at these systems, thinking they could be better if I used the lens of an engineer. The hospital was very interested in reducing costs, and the physicians, including myself, were interested in making things safer. I was successful because I didn’t just focus on QI but on both sides of the value equation. In the early 2000s, I started to do more and more re-engineering and system improvement projects, and I found them very rewarding. As I showed some success, I was asked to do more.
What you are describing is hands-on training, learning by doing. It seems a lot of your QI training was hands on, as opposed to structured coursework. Was there formal training or is getting your hands dirty in a project the best way to start learning QI?
There is no replacement for actually doing it.
My training was in leadership, which is an integral part of QI. It’s pretty hard to get people to change for quality if you can’t lead them through that change. Initially, I did a lot of work to improve my leadership potential. As faculty, we taught teaching skills, which is a part of leadership. I spent time teaching residents best practices. That’s why I became involved early on with SHM’s Leadership Academy from its start in 2005. I also read a lot of books and still read often to improve my weaknesses. I have my own physicians go through Lean Six Sigma training and get their green belt or black belt.
That said, there is no substitute for doing it and, as they say, “bruising your knuckles” in QI.
Read the full post at hospitalleader.org.
Also on The Hospital Leader…
- From SXSW to SHM: Our Tour to Promote Value Conversations Between Doctors & Patients by Chris Moriates, MD
- It’s Time for a Buzz Cut by Tracy Cardin, ACNP-NC, SFHM
- The Essentials of QI Leadership: A Conversation with Dr. Eric Howell, Part 2 by Jordan Messler, MD, SFHM
Quality improvement became a foundational theme for SHM early in the growth of hospitalists. It’s not a coincidence that many of our leaders, such as Bob Wachter, Win Whitcomb, Greg Maynard, and Mark Williams are QI leaders as well. As hospitalists, we were and are best positioned to impact quality in the hospital.
Eric Howell, MD, of Johns Hopkins Bayview Medical Center in Baltimore serves as the senior physician advisor for SHM’s Center for Quality Improvement, while Jenna Goldstein runs the day-to-day aspects at SHM headquarters. A few months ago, Dr. Howell and I discussed how he started in QI, the role of SHM’s Center, and how hospitalists can receive effective QI training. The following Q&A is edited for conciseness and clarity.
You’ve been a leader in QI for many years; how did you get started in QI?
I trained as an electrical engineer before I went to medical school, which helped me when I went to residency.
When I was a chief at Hopkins Bayview in 1999, there were a number of systems-related issues, including throughput from the emergency department. I became involved with QI because I looked at these systems, thinking they could be better if I used the lens of an engineer. The hospital was very interested in reducing costs, and the physicians, including myself, were interested in making things safer. I was successful because I didn’t just focus on QI but on both sides of the value equation. In the early 2000s, I started to do more and more re-engineering and system improvement projects, and I found them very rewarding. As I showed some success, I was asked to do more.
What you are describing is hands-on training, learning by doing. It seems a lot of your QI training was hands on, as opposed to structured coursework. Was there formal training or is getting your hands dirty in a project the best way to start learning QI?
There is no replacement for actually doing it.
My training was in leadership, which is an integral part of QI. It’s pretty hard to get people to change for quality if you can’t lead them through that change. Initially, I did a lot of work to improve my leadership potential. As faculty, we taught teaching skills, which is a part of leadership. I spent time teaching residents best practices. That’s why I became involved early on with SHM’s Leadership Academy from its start in 2005. I also read a lot of books and still read often to improve my weaknesses. I have my own physicians go through Lean Six Sigma training and get their green belt or black belt.
That said, there is no substitute for doing it and, as they say, “bruising your knuckles” in QI.
Read the full post at hospitalleader.org.
Also on The Hospital Leader…
- From SXSW to SHM: Our Tour to Promote Value Conversations Between Doctors & Patients by Chris Moriates, MD
- It’s Time for a Buzz Cut by Tracy Cardin, ACNP-NC, SFHM
- The Essentials of QI Leadership: A Conversation with Dr. Eric Howell, Part 2 by Jordan Messler, MD, SFHM
Quality improvement became a foundational theme for SHM early in the growth of hospitalists. It’s not a coincidence that many of our leaders, such as Bob Wachter, Win Whitcomb, Greg Maynard, and Mark Williams are QI leaders as well. As hospitalists, we were and are best positioned to impact quality in the hospital.
Eric Howell, MD, of Johns Hopkins Bayview Medical Center in Baltimore serves as the senior physician advisor for SHM’s Center for Quality Improvement, while Jenna Goldstein runs the day-to-day aspects at SHM headquarters. A few months ago, Dr. Howell and I discussed how he started in QI, the role of SHM’s Center, and how hospitalists can receive effective QI training. The following Q&A is edited for conciseness and clarity.
You’ve been a leader in QI for many years; how did you get started in QI?
I trained as an electrical engineer before I went to medical school, which helped me when I went to residency.
When I was a chief at Hopkins Bayview in 1999, there were a number of systems-related issues, including throughput from the emergency department. I became involved with QI because I looked at these systems, thinking they could be better if I used the lens of an engineer. The hospital was very interested in reducing costs, and the physicians, including myself, were interested in making things safer. I was successful because I didn’t just focus on QI but on both sides of the value equation. In the early 2000s, I started to do more and more re-engineering and system improvement projects, and I found them very rewarding. As I showed some success, I was asked to do more.
What you are describing is hands-on training, learning by doing. It seems a lot of your QI training was hands on, as opposed to structured coursework. Was there formal training or is getting your hands dirty in a project the best way to start learning QI?
There is no replacement for actually doing it.
My training was in leadership, which is an integral part of QI. It’s pretty hard to get people to change for quality if you can’t lead them through that change. Initially, I did a lot of work to improve my leadership potential. As faculty, we taught teaching skills, which is a part of leadership. I spent time teaching residents best practices. That’s why I became involved early on with SHM’s Leadership Academy from its start in 2005. I also read a lot of books and still read often to improve my weaknesses. I have my own physicians go through Lean Six Sigma training and get their green belt or black belt.
That said, there is no substitute for doing it and, as they say, “bruising your knuckles” in QI.
Read the full post at hospitalleader.org.
Also on The Hospital Leader…
- From SXSW to SHM: Our Tour to Promote Value Conversations Between Doctors & Patients by Chris Moriates, MD
- It’s Time for a Buzz Cut by Tracy Cardin, ACNP-NC, SFHM
- The Essentials of QI Leadership: A Conversation with Dr. Eric Howell, Part 2 by Jordan Messler, MD, SFHM
Sneak Peek: Journal of Hospital Medicine – August 2017
BACKGROUND: There is increasing recognition that patients have critical insights into care experiences, including about breakdowns in care. Harnessing patient perspectives for hospital improvement requires an in-depth understanding of the types of breakdowns patients identify and the impact of these events.
RESULTS: Of 979 interviewees, 386 (39.4%) believed they had experienced at least one breakdown in care. The most common reported breakdowns involved information exchange (n = 158; 16.1%), medications (n = 120; 12.3%), delays in admission (n = 90; 9.2%), team communication (n = 65; 6.6%), providers’ manner (n = 62; 6.3%), and discharge (n = 56; 5.7%). Of the 386 interviewees who reported a breakdown, 140 (36.3%) perceived associated harm. Patient-perceived harms included physical (e.g., pain), emotional (e.g., distress, worry), damage to relationship with providers, need for additional care or prolonged hospital stay, and life disruption. We found higher rates of reporting breakdowns among younger (less than 60 years old) patients (45.4% vs. 34.5%; P less than .001), those with at least some college education (46.8% vs 32.7%; P less than .001), and those with another person (family or friend) present during the interview or interviewed in lieu of the patient (53.4% vs 37.8%; P = .002).
CONCLUSIONS: When asked directly, almost 4 out of 10 hospitalized patients reported a breakdown in their care. Patient-perceived breakdowns in care are frequently associated with perceived harm, illustrating the importance of detecting and addressing these events.
Also in JHM
Excess readmission vs. excess penalties: Maximum readmission penalties as a function of socioeconomics and geography
AUTHORS: Chris M. Caracciolo, MPH, Devin M. Parker, MS, Emily Marshall, MS, Jeremiah R. Brown, PhD, MS
Impact of a safety huddle-based intervention on monitor alarm rates in low-acuity pediatric intensive care unit patientsAUTHORS: Maya Dewan, MD, MPH, Heather Wolfe, MD, MSHP, Richard Lin, MD, Eileen Ware, RN, Michelle Weiss, RN, Lihai Song, MS, Matthew MacMurchy, BA, Daniela Davis, MD, MSCE, Christopher P. Bonafide MD MSCE
Perspectives of clinicians at skilled nursing facilities on 30-day hospital readmissions: A qualitative studyAUTHORS: Bennett W. Clark, MD, Katelyn Baron, MSIOP, Kathleen Tynan-McKiernan, RN, MSN, Meredith Campbell Britton, LMSW, Karl E. Minges, PhD, Sarwat I. Chaudhry, MD
Use of postacute facility care in children hospitalized with acute respiratory illnessAUTHORS: Jay G. Berry, MD, MPH, Karen M. Wilson, MD, MPH, FAAP, Helene Dumas, PT, MS, Edwin Simpser, MD, Jane O’Brien, MD, Kathleen Whitford, PNP, Rachna May, MD, Vineeta Mittal, MD, Nancy Murphy, MD, David Steinhorn, MD, Rishi Agrawal, MD, MPH, Kris Rehm, MD, Michelle Marks, DO, FAAP, SFHM, Christine Traul, MD, Michael Dribbon, PhD, Christopher J. Haines, DO, MBA, FAAP, FACEP, Matt Hall, PhD
A contemporary assessment of mechanical complication rates and trainee perceptions of central venous catheter insertionAUTHORS: Lauren Heidemann, MD, Niket Nathani, MD, Rommel Sagana, MD, Vineet Chopra, MD, MSc, Michael Heung, MD, MS
For more articles and subscription information, visit www.journalofhospitalmedicine.com.
BACKGROUND: There is increasing recognition that patients have critical insights into care experiences, including about breakdowns in care. Harnessing patient perspectives for hospital improvement requires an in-depth understanding of the types of breakdowns patients identify and the impact of these events.
RESULTS: Of 979 interviewees, 386 (39.4%) believed they had experienced at least one breakdown in care. The most common reported breakdowns involved information exchange (n = 158; 16.1%), medications (n = 120; 12.3%), delays in admission (n = 90; 9.2%), team communication (n = 65; 6.6%), providers’ manner (n = 62; 6.3%), and discharge (n = 56; 5.7%). Of the 386 interviewees who reported a breakdown, 140 (36.3%) perceived associated harm. Patient-perceived harms included physical (e.g., pain), emotional (e.g., distress, worry), damage to relationship with providers, need for additional care or prolonged hospital stay, and life disruption. We found higher rates of reporting breakdowns among younger (less than 60 years old) patients (45.4% vs. 34.5%; P less than .001), those with at least some college education (46.8% vs 32.7%; P less than .001), and those with another person (family or friend) present during the interview or interviewed in lieu of the patient (53.4% vs 37.8%; P = .002).
CONCLUSIONS: When asked directly, almost 4 out of 10 hospitalized patients reported a breakdown in their care. Patient-perceived breakdowns in care are frequently associated with perceived harm, illustrating the importance of detecting and addressing these events.
Also in JHM
Excess readmission vs. excess penalties: Maximum readmission penalties as a function of socioeconomics and geography
AUTHORS: Chris M. Caracciolo, MPH, Devin M. Parker, MS, Emily Marshall, MS, Jeremiah R. Brown, PhD, MS
Impact of a safety huddle-based intervention on monitor alarm rates in low-acuity pediatric intensive care unit patientsAUTHORS: Maya Dewan, MD, MPH, Heather Wolfe, MD, MSHP, Richard Lin, MD, Eileen Ware, RN, Michelle Weiss, RN, Lihai Song, MS, Matthew MacMurchy, BA, Daniela Davis, MD, MSCE, Christopher P. Bonafide MD MSCE
Perspectives of clinicians at skilled nursing facilities on 30-day hospital readmissions: A qualitative studyAUTHORS: Bennett W. Clark, MD, Katelyn Baron, MSIOP, Kathleen Tynan-McKiernan, RN, MSN, Meredith Campbell Britton, LMSW, Karl E. Minges, PhD, Sarwat I. Chaudhry, MD
Use of postacute facility care in children hospitalized with acute respiratory illnessAUTHORS: Jay G. Berry, MD, MPH, Karen M. Wilson, MD, MPH, FAAP, Helene Dumas, PT, MS, Edwin Simpser, MD, Jane O’Brien, MD, Kathleen Whitford, PNP, Rachna May, MD, Vineeta Mittal, MD, Nancy Murphy, MD, David Steinhorn, MD, Rishi Agrawal, MD, MPH, Kris Rehm, MD, Michelle Marks, DO, FAAP, SFHM, Christine Traul, MD, Michael Dribbon, PhD, Christopher J. Haines, DO, MBA, FAAP, FACEP, Matt Hall, PhD
A contemporary assessment of mechanical complication rates and trainee perceptions of central venous catheter insertionAUTHORS: Lauren Heidemann, MD, Niket Nathani, MD, Rommel Sagana, MD, Vineet Chopra, MD, MSc, Michael Heung, MD, MS
For more articles and subscription information, visit www.journalofhospitalmedicine.com.
BACKGROUND: There is increasing recognition that patients have critical insights into care experiences, including about breakdowns in care. Harnessing patient perspectives for hospital improvement requires an in-depth understanding of the types of breakdowns patients identify and the impact of these events.
RESULTS: Of 979 interviewees, 386 (39.4%) believed they had experienced at least one breakdown in care. The most common reported breakdowns involved information exchange (n = 158; 16.1%), medications (n = 120; 12.3%), delays in admission (n = 90; 9.2%), team communication (n = 65; 6.6%), providers’ manner (n = 62; 6.3%), and discharge (n = 56; 5.7%). Of the 386 interviewees who reported a breakdown, 140 (36.3%) perceived associated harm. Patient-perceived harms included physical (e.g., pain), emotional (e.g., distress, worry), damage to relationship with providers, need for additional care or prolonged hospital stay, and life disruption. We found higher rates of reporting breakdowns among younger (less than 60 years old) patients (45.4% vs. 34.5%; P less than .001), those with at least some college education (46.8% vs 32.7%; P less than .001), and those with another person (family or friend) present during the interview or interviewed in lieu of the patient (53.4% vs 37.8%; P = .002).
CONCLUSIONS: When asked directly, almost 4 out of 10 hospitalized patients reported a breakdown in their care. Patient-perceived breakdowns in care are frequently associated with perceived harm, illustrating the importance of detecting and addressing these events.
Also in JHM
Excess readmission vs. excess penalties: Maximum readmission penalties as a function of socioeconomics and geography
AUTHORS: Chris M. Caracciolo, MPH, Devin M. Parker, MS, Emily Marshall, MS, Jeremiah R. Brown, PhD, MS
Impact of a safety huddle-based intervention on monitor alarm rates in low-acuity pediatric intensive care unit patientsAUTHORS: Maya Dewan, MD, MPH, Heather Wolfe, MD, MSHP, Richard Lin, MD, Eileen Ware, RN, Michelle Weiss, RN, Lihai Song, MS, Matthew MacMurchy, BA, Daniela Davis, MD, MSCE, Christopher P. Bonafide MD MSCE
Perspectives of clinicians at skilled nursing facilities on 30-day hospital readmissions: A qualitative studyAUTHORS: Bennett W. Clark, MD, Katelyn Baron, MSIOP, Kathleen Tynan-McKiernan, RN, MSN, Meredith Campbell Britton, LMSW, Karl E. Minges, PhD, Sarwat I. Chaudhry, MD
Use of postacute facility care in children hospitalized with acute respiratory illnessAUTHORS: Jay G. Berry, MD, MPH, Karen M. Wilson, MD, MPH, FAAP, Helene Dumas, PT, MS, Edwin Simpser, MD, Jane O’Brien, MD, Kathleen Whitford, PNP, Rachna May, MD, Vineeta Mittal, MD, Nancy Murphy, MD, David Steinhorn, MD, Rishi Agrawal, MD, MPH, Kris Rehm, MD, Michelle Marks, DO, FAAP, SFHM, Christine Traul, MD, Michael Dribbon, PhD, Christopher J. Haines, DO, MBA, FAAP, FACEP, Matt Hall, PhD
A contemporary assessment of mechanical complication rates and trainee perceptions of central venous catheter insertionAUTHORS: Lauren Heidemann, MD, Niket Nathani, MD, Rommel Sagana, MD, Vineet Chopra, MD, MSc, Michael Heung, MD, MS
For more articles and subscription information, visit www.journalofhospitalmedicine.com.
Standardized infection ratio for CLABSI almost halved since 2009
The standardized infection ratio (SIR) for central line–associated bloodstream infections dropped 42% from 2009 to 2014, according to the Agency for Healthcare Research and Quality.
For acute care hospitalizations, the SIR for central line–associated bloodstream infections (CLABSIs) fell from 0.854 in 2009 to 0.495 in 2014. Over that same time period, the SIR for surgical site infections involving Surgical Care Improvement Project procedures decreased from 0.981 to 0.827 – almost 16%, the AHRQ said in its annual National Healthcare Quality and Disparities Report.
From 2010 to 2014, the SIR for catheter-associated urinary tract infections increased 6.7% from 0.937 to 1.000, but that change was not significant. For laboratory-identified hospital-onset Clostridium difficile infection, the SIR dropped from 0.963 to 0.924 – about 4% – from 2012 to 2014, the AHRQ reported using data from the National Center for Emerging and Zoonotic Infectious Diseases and the National Healthcare Safety Network.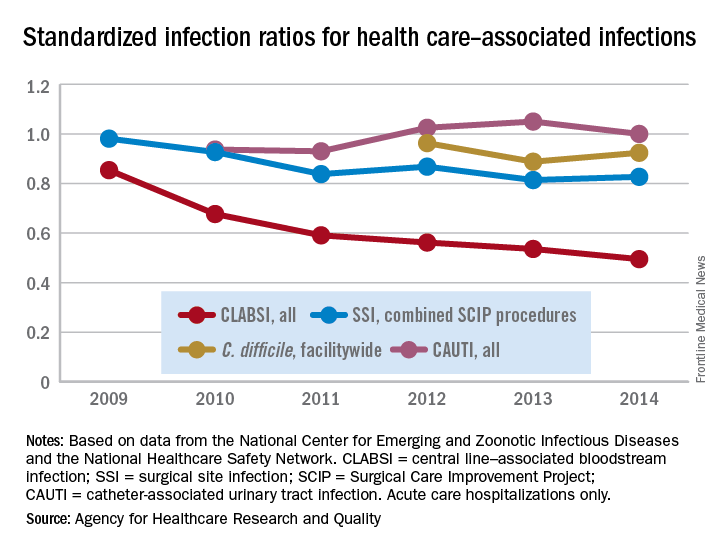
The standardized infection ratio (SIR) for central line–associated bloodstream infections dropped 42% from 2009 to 2014, according to the Agency for Healthcare Research and Quality.
For acute care hospitalizations, the SIR for central line–associated bloodstream infections (CLABSIs) fell from 0.854 in 2009 to 0.495 in 2014. Over that same time period, the SIR for surgical site infections involving Surgical Care Improvement Project procedures decreased from 0.981 to 0.827 – almost 16%, the AHRQ said in its annual National Healthcare Quality and Disparities Report.
From 2010 to 2014, the SIR for catheter-associated urinary tract infections increased 6.7% from 0.937 to 1.000, but that change was not significant. For laboratory-identified hospital-onset Clostridium difficile infection, the SIR dropped from 0.963 to 0.924 – about 4% – from 2012 to 2014, the AHRQ reported using data from the National Center for Emerging and Zoonotic Infectious Diseases and the National Healthcare Safety Network.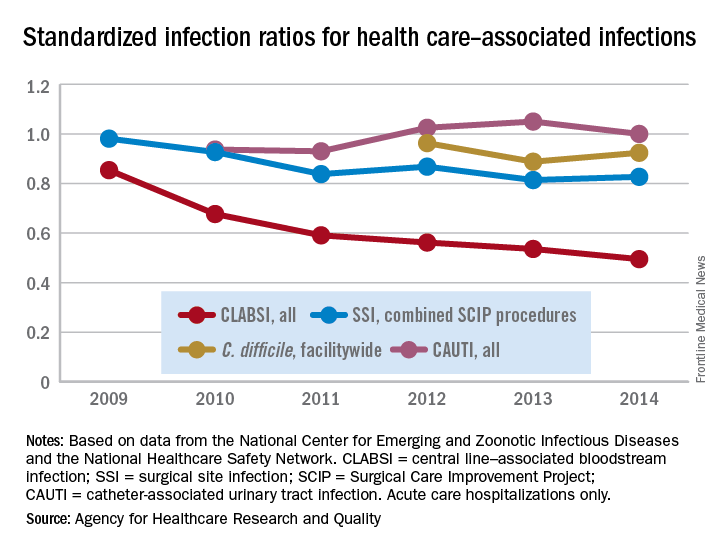
The standardized infection ratio (SIR) for central line–associated bloodstream infections dropped 42% from 2009 to 2014, according to the Agency for Healthcare Research and Quality.
For acute care hospitalizations, the SIR for central line–associated bloodstream infections (CLABSIs) fell from 0.854 in 2009 to 0.495 in 2014. Over that same time period, the SIR for surgical site infections involving Surgical Care Improvement Project procedures decreased from 0.981 to 0.827 – almost 16%, the AHRQ said in its annual National Healthcare Quality and Disparities Report.
From 2010 to 2014, the SIR for catheter-associated urinary tract infections increased 6.7% from 0.937 to 1.000, but that change was not significant. For laboratory-identified hospital-onset Clostridium difficile infection, the SIR dropped from 0.963 to 0.924 – about 4% – from 2012 to 2014, the AHRQ reported using data from the National Center for Emerging and Zoonotic Infectious Diseases and the National Healthcare Safety Network.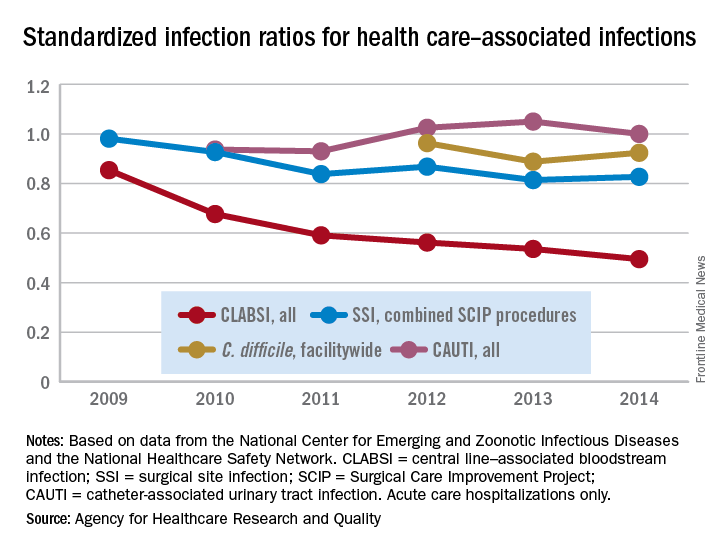
QI enthusiast to QI leader: Luci Leykum, MD
Editor’s Note: This ongoing series highlights the professional pathways of quality improvement leaders. This month features the story of Luci Leykum, MD, division chief, general and hospital medicine at the University of Texas Health Science Center, San Antonio.
Luci Leykum, MD, MBA, MSc, FACP, SFHM, became familiar with inpatient medicine at age 9 years, when her grandfather contracted non-AB hepatitis from a postoperative blood transfusion. In the ensuing years, Dr. Leykum visited her grandfather during his frequent hospitalizations, keeping a close watch on the physicians charged with his care.
“It was when HIV and what we now think is hep C were just emerging, and there was a lot to figure out,” Dr. Leykum recalled of these formative experiences. Her interests in problem-solving, human relationships, and physiology led to enrollment years later as a medical student at Columbia University’s College of Physicians and Surgeons, where her keen observation skills led to a life-changing, “how did we get here?” moment.
Shortly before Dr. Leykum entered residency in 1999, New York Hospital and Columbia Presbyterian Hospital announced that they were merging. The timing was ideal for someone with Dr. Leykum’s acumen in business and medicine, and, as a resident, she began working with the chief medical officer for quality at the new, combined health system to identify quality improvement opportunities.
From there, the projects began pouring in: tracking phone hold times for residents; updating policies to reduce staff exposure to blood-borne pathogens and other infectious diseases; and monitoring flow through the hospitalization process. “In the progression of a few years, I was able to see important aspects of how the system came together,” said Dr. Leykum, “and how decisions were made around standards and metrics for the system as a whole and for its multiple individual hospital facilities.”
In 2004, two years out of residency, Dr. Leykum relocated to San Antonio to accept a clinician investigator position with the South Texas Veterans Health Care System/University of Texas Health Science Center San Antonio (UTHSCSA). Research, she said, has allowed her to delve deeper into the underlying mechanisms that impact systems of health care. She sees the complementary sides of quality improvement and research.
“Through our quality improvement initiatives, we can evaluate and improve specific aspects of care, in specific contexts or systems,” Dr. Leykum explained. “In our research projects, we look for new insights that can be more broadly applied across contexts. With funding, you are able to look at things with a scope, depth, or time horizon beyond what you typically have with a QI project.”
Since joining the UTHSCSA/VA system, Dr. Leykum has participated in more than 15 externally funded studies, 6 as principal investigator. She joined SHM’s research committee in 2009, serving as chair for 6 years, and is currently working with the committee to implement the Improving Hospital Outcomes through Patient Engagement (i-HOPE) Study.
I-HOPE, funded through the Patient-Centered Outcomes Research Institute, is a project to develop a patient- and stakeholder-partnered research agenda to improve the care of hospitalized patients. Dr. Leykum is also involved in implementing a collaborative care model at University Health System, a patient-partnered, interprofessional model that “focuses on improving interconnections, relationships, and sense making,” in the hospital system, she explained. “It was motivated strongly by our desire to improve our partnerships with patients and other providers in the hospital as a strategy to improve care.”
In addition to the many professional responsibilities she manages as division chief of general and hospital medicine at UTHSCSA – a position she has held for hospital medicine since 2006 and for the combined division since 2016 – Dr. Leykum continues to play an integral role in multiple academic and research initiatives for SHM.
She encourages anyone considering a concentration in QI and research to seek opportunities to actively learn these skills and, more importantly, let other people know their interests.
“The value of talking with colleagues at other places is so high,” she said. “When you actively reach out, you find that most people are happy to share their knowledge. Networking is one of the best parts of the SHM annual meeting – there’s an energy and excitement in learning about what others are doing. Wander into the poster and special interest sessions and see what people are working on, get email addresses, and participate on committees.”
Editor’s Note: This ongoing series highlights the professional pathways of quality improvement leaders. This month features the story of Luci Leykum, MD, division chief, general and hospital medicine at the University of Texas Health Science Center, San Antonio.
Luci Leykum, MD, MBA, MSc, FACP, SFHM, became familiar with inpatient medicine at age 9 years, when her grandfather contracted non-AB hepatitis from a postoperative blood transfusion. In the ensuing years, Dr. Leykum visited her grandfather during his frequent hospitalizations, keeping a close watch on the physicians charged with his care.
“It was when HIV and what we now think is hep C were just emerging, and there was a lot to figure out,” Dr. Leykum recalled of these formative experiences. Her interests in problem-solving, human relationships, and physiology led to enrollment years later as a medical student at Columbia University’s College of Physicians and Surgeons, where her keen observation skills led to a life-changing, “how did we get here?” moment.
Shortly before Dr. Leykum entered residency in 1999, New York Hospital and Columbia Presbyterian Hospital announced that they were merging. The timing was ideal for someone with Dr. Leykum’s acumen in business and medicine, and, as a resident, she began working with the chief medical officer for quality at the new, combined health system to identify quality improvement opportunities.
From there, the projects began pouring in: tracking phone hold times for residents; updating policies to reduce staff exposure to blood-borne pathogens and other infectious diseases; and monitoring flow through the hospitalization process. “In the progression of a few years, I was able to see important aspects of how the system came together,” said Dr. Leykum, “and how decisions were made around standards and metrics for the system as a whole and for its multiple individual hospital facilities.”
In 2004, two years out of residency, Dr. Leykum relocated to San Antonio to accept a clinician investigator position with the South Texas Veterans Health Care System/University of Texas Health Science Center San Antonio (UTHSCSA). Research, she said, has allowed her to delve deeper into the underlying mechanisms that impact systems of health care. She sees the complementary sides of quality improvement and research.
“Through our quality improvement initiatives, we can evaluate and improve specific aspects of care, in specific contexts or systems,” Dr. Leykum explained. “In our research projects, we look for new insights that can be more broadly applied across contexts. With funding, you are able to look at things with a scope, depth, or time horizon beyond what you typically have with a QI project.”
Since joining the UTHSCSA/VA system, Dr. Leykum has participated in more than 15 externally funded studies, 6 as principal investigator. She joined SHM’s research committee in 2009, serving as chair for 6 years, and is currently working with the committee to implement the Improving Hospital Outcomes through Patient Engagement (i-HOPE) Study.
I-HOPE, funded through the Patient-Centered Outcomes Research Institute, is a project to develop a patient- and stakeholder-partnered research agenda to improve the care of hospitalized patients. Dr. Leykum is also involved in implementing a collaborative care model at University Health System, a patient-partnered, interprofessional model that “focuses on improving interconnections, relationships, and sense making,” in the hospital system, she explained. “It was motivated strongly by our desire to improve our partnerships with patients and other providers in the hospital as a strategy to improve care.”
In addition to the many professional responsibilities she manages as division chief of general and hospital medicine at UTHSCSA – a position she has held for hospital medicine since 2006 and for the combined division since 2016 – Dr. Leykum continues to play an integral role in multiple academic and research initiatives for SHM.
She encourages anyone considering a concentration in QI and research to seek opportunities to actively learn these skills and, more importantly, let other people know their interests.
“The value of talking with colleagues at other places is so high,” she said. “When you actively reach out, you find that most people are happy to share their knowledge. Networking is one of the best parts of the SHM annual meeting – there’s an energy and excitement in learning about what others are doing. Wander into the poster and special interest sessions and see what people are working on, get email addresses, and participate on committees.”
Editor’s Note: This ongoing series highlights the professional pathways of quality improvement leaders. This month features the story of Luci Leykum, MD, division chief, general and hospital medicine at the University of Texas Health Science Center, San Antonio.
Luci Leykum, MD, MBA, MSc, FACP, SFHM, became familiar with inpatient medicine at age 9 years, when her grandfather contracted non-AB hepatitis from a postoperative blood transfusion. In the ensuing years, Dr. Leykum visited her grandfather during his frequent hospitalizations, keeping a close watch on the physicians charged with his care.
“It was when HIV and what we now think is hep C were just emerging, and there was a lot to figure out,” Dr. Leykum recalled of these formative experiences. Her interests in problem-solving, human relationships, and physiology led to enrollment years later as a medical student at Columbia University’s College of Physicians and Surgeons, where her keen observation skills led to a life-changing, “how did we get here?” moment.
Shortly before Dr. Leykum entered residency in 1999, New York Hospital and Columbia Presbyterian Hospital announced that they were merging. The timing was ideal for someone with Dr. Leykum’s acumen in business and medicine, and, as a resident, she began working with the chief medical officer for quality at the new, combined health system to identify quality improvement opportunities.
From there, the projects began pouring in: tracking phone hold times for residents; updating policies to reduce staff exposure to blood-borne pathogens and other infectious diseases; and monitoring flow through the hospitalization process. “In the progression of a few years, I was able to see important aspects of how the system came together,” said Dr. Leykum, “and how decisions were made around standards and metrics for the system as a whole and for its multiple individual hospital facilities.”
In 2004, two years out of residency, Dr. Leykum relocated to San Antonio to accept a clinician investigator position with the South Texas Veterans Health Care System/University of Texas Health Science Center San Antonio (UTHSCSA). Research, she said, has allowed her to delve deeper into the underlying mechanisms that impact systems of health care. She sees the complementary sides of quality improvement and research.
“Through our quality improvement initiatives, we can evaluate and improve specific aspects of care, in specific contexts or systems,” Dr. Leykum explained. “In our research projects, we look for new insights that can be more broadly applied across contexts. With funding, you are able to look at things with a scope, depth, or time horizon beyond what you typically have with a QI project.”
Since joining the UTHSCSA/VA system, Dr. Leykum has participated in more than 15 externally funded studies, 6 as principal investigator. She joined SHM’s research committee in 2009, serving as chair for 6 years, and is currently working with the committee to implement the Improving Hospital Outcomes through Patient Engagement (i-HOPE) Study.
I-HOPE, funded through the Patient-Centered Outcomes Research Institute, is a project to develop a patient- and stakeholder-partnered research agenda to improve the care of hospitalized patients. Dr. Leykum is also involved in implementing a collaborative care model at University Health System, a patient-partnered, interprofessional model that “focuses on improving interconnections, relationships, and sense making,” in the hospital system, she explained. “It was motivated strongly by our desire to improve our partnerships with patients and other providers in the hospital as a strategy to improve care.”
In addition to the many professional responsibilities she manages as division chief of general and hospital medicine at UTHSCSA – a position she has held for hospital medicine since 2006 and for the combined division since 2016 – Dr. Leykum continues to play an integral role in multiple academic and research initiatives for SHM.
She encourages anyone considering a concentration in QI and research to seek opportunities to actively learn these skills and, more importantly, let other people know their interests.
“The value of talking with colleagues at other places is so high,” she said. “When you actively reach out, you find that most people are happy to share their knowledge. Networking is one of the best parts of the SHM annual meeting – there’s an energy and excitement in learning about what others are doing. Wander into the poster and special interest sessions and see what people are working on, get email addresses, and participate on committees.”
When families participate in rounds, errors decrease
NASHVILLE, TENN. – When families are actively included in pediatric hospital rounds, preventable adverse events drop 38% and families report better hospital experiences, with no negative impact on rounds duration or teaching, according to a prospective investigation on inpatient pediatric units of seven North American hospitals.
“We always talk about how parents know their children better than anyone else; empowering the family to know what we are looking for can have downstream safety implications,” she said. In the study, families often caught problems before medical staff, such as IV infiltrations. They also reported delays in diagnoses and conflicting information, among other things, Dr. Khan explained at the Pediatric Hospital Medicine meeting.
There’s not much data on family-centered rounds in pediatric medicine, so Dr. Khan and her team decided to investigate. They modified the I-PASS resident handoff model (illness severity; patient summary; action list; situation awareness and contingency planning; and synthesis by receiver) to be more family friendly.
Families were given a short form before rounds that asked if their child was better, worse, or about the same as the day before, and what questions and items they wanted to address. There was also space for them to take notes during the presentation about what had changed overnight, what still needed to be done, and what to look out for.
Families were given the opportunity to speak first during rounds, and medical staff used plain language: “has a fever” instead of “febrile,” for instance. At the end of the presentation, families were asked to read back their take-aways.
The investigators compared baseline data from the 3 months before implementation with data for the 3 months afterward. The study included more than 1,500 patients and more than 300 rounds in both the pre- and postimplementation arms. The children were general inpatients; surgery and ICU patients were excluded.
Harmful errors/preventable AEs dropped from 20.7/1,000 patients days to 12.9/1,000 after implementation, a 38% reduction (P = .01). There was also a reduction in overall AEs from 34 to 18.5/1,000 patient-days (P = .002).
Compared with baseline data, after implementation, families were more likely to report that they understood the medical plan and what was said on rounds. They also were more likely to report that nurses had addressed their concerns and made them feel like an important member of the team.
Direct observation of pre- and postimplementation rounds showed that family and nursing engagement improved and families more often got written updates. There were no statistically significant differences in rounds duration or decreases in teaching.
“Congratulations. This is very impressive work, and also the right thing to do,” an audience member said after Dr. Khan’s presentation at the meeting, sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, and the Academic Pediatric Association.
The work was funded by the Patient-Centered Outcomes Research Institute and the Agency for Healthcare Research and Quality. Dr. Khan had no disclosures.
NASHVILLE, TENN. – When families are actively included in pediatric hospital rounds, preventable adverse events drop 38% and families report better hospital experiences, with no negative impact on rounds duration or teaching, according to a prospective investigation on inpatient pediatric units of seven North American hospitals.
“We always talk about how parents know their children better than anyone else; empowering the family to know what we are looking for can have downstream safety implications,” she said. In the study, families often caught problems before medical staff, such as IV infiltrations. They also reported delays in diagnoses and conflicting information, among other things, Dr. Khan explained at the Pediatric Hospital Medicine meeting.
There’s not much data on family-centered rounds in pediatric medicine, so Dr. Khan and her team decided to investigate. They modified the I-PASS resident handoff model (illness severity; patient summary; action list; situation awareness and contingency planning; and synthesis by receiver) to be more family friendly.
Families were given a short form before rounds that asked if their child was better, worse, or about the same as the day before, and what questions and items they wanted to address. There was also space for them to take notes during the presentation about what had changed overnight, what still needed to be done, and what to look out for.
Families were given the opportunity to speak first during rounds, and medical staff used plain language: “has a fever” instead of “febrile,” for instance. At the end of the presentation, families were asked to read back their take-aways.
The investigators compared baseline data from the 3 months before implementation with data for the 3 months afterward. The study included more than 1,500 patients and more than 300 rounds in both the pre- and postimplementation arms. The children were general inpatients; surgery and ICU patients were excluded.
Harmful errors/preventable AEs dropped from 20.7/1,000 patients days to 12.9/1,000 after implementation, a 38% reduction (P = .01). There was also a reduction in overall AEs from 34 to 18.5/1,000 patient-days (P = .002).
Compared with baseline data, after implementation, families were more likely to report that they understood the medical plan and what was said on rounds. They also were more likely to report that nurses had addressed their concerns and made them feel like an important member of the team.
Direct observation of pre- and postimplementation rounds showed that family and nursing engagement improved and families more often got written updates. There were no statistically significant differences in rounds duration or decreases in teaching.
“Congratulations. This is very impressive work, and also the right thing to do,” an audience member said after Dr. Khan’s presentation at the meeting, sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, and the Academic Pediatric Association.
The work was funded by the Patient-Centered Outcomes Research Institute and the Agency for Healthcare Research and Quality. Dr. Khan had no disclosures.
NASHVILLE, TENN. – When families are actively included in pediatric hospital rounds, preventable adverse events drop 38% and families report better hospital experiences, with no negative impact on rounds duration or teaching, according to a prospective investigation on inpatient pediatric units of seven North American hospitals.
“We always talk about how parents know their children better than anyone else; empowering the family to know what we are looking for can have downstream safety implications,” she said. In the study, families often caught problems before medical staff, such as IV infiltrations. They also reported delays in diagnoses and conflicting information, among other things, Dr. Khan explained at the Pediatric Hospital Medicine meeting.
There’s not much data on family-centered rounds in pediatric medicine, so Dr. Khan and her team decided to investigate. They modified the I-PASS resident handoff model (illness severity; patient summary; action list; situation awareness and contingency planning; and synthesis by receiver) to be more family friendly.
Families were given a short form before rounds that asked if their child was better, worse, or about the same as the day before, and what questions and items they wanted to address. There was also space for them to take notes during the presentation about what had changed overnight, what still needed to be done, and what to look out for.
Families were given the opportunity to speak first during rounds, and medical staff used plain language: “has a fever” instead of “febrile,” for instance. At the end of the presentation, families were asked to read back their take-aways.
The investigators compared baseline data from the 3 months before implementation with data for the 3 months afterward. The study included more than 1,500 patients and more than 300 rounds in both the pre- and postimplementation arms. The children were general inpatients; surgery and ICU patients were excluded.
Harmful errors/preventable AEs dropped from 20.7/1,000 patients days to 12.9/1,000 after implementation, a 38% reduction (P = .01). There was also a reduction in overall AEs from 34 to 18.5/1,000 patient-days (P = .002).
Compared with baseline data, after implementation, families were more likely to report that they understood the medical plan and what was said on rounds. They also were more likely to report that nurses had addressed their concerns and made them feel like an important member of the team.
Direct observation of pre- and postimplementation rounds showed that family and nursing engagement improved and families more often got written updates. There were no statistically significant differences in rounds duration or decreases in teaching.
“Congratulations. This is very impressive work, and also the right thing to do,” an audience member said after Dr. Khan’s presentation at the meeting, sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, and the Academic Pediatric Association.
The work was funded by the Patient-Centered Outcomes Research Institute and the Agency for Healthcare Research and Quality. Dr. Khan had no disclosures.
AT PHM 2017
Key clinical point:
Major finding: Harmful errors/preventable AEs dropped from 20.7/1,000 patients days to 12.9 after implementation of a program to engage families in pediatric rounds, a 38% reduction (P = .01).
Data source: More than 600 pediatric inpatient rounds at seven North American hospitals.
Disclosures: The work was funded by the Patient-Centered Outcomes Research Institute and the Agency for Healthcare Research and Quality. The lead investigator had no disclosures.
Future Hospitalist: Top 10 tips for carrying out a successful quality improvement project
Editor’s Note: This column is a quarterly feature written by members of the Physicians in Training Committee. It aims to encourage and educate students, residents, and early career hospitalists.
One of the biggest challenges early career hospitalists, residents and medical students face in launching their first quality improvement (QI) project is knowing how and where to get started. QI can be highly rewarding, but it can also take valuable time and resources without guarantees of sustainable improvement. In this article, we outline 10 key factors to consider when starting a new project.
1. Frame your project so that it aligns with your hospital’s current goals
Choose a project with your hospital’s goals in mind. Securing resources such as health IT, financial, or staffing support will prove difficult unless you get buy-in from hospital leadership. If your project does not directly address hospital goals, frame the purpose to demonstrate that it still fits with leadership priorities. For example, though improving handoffs from daytime to nighttime providers may not be a specific goal, leadership should appreciate that this project is expected to improve patient safety.
2. Be SMART about goals
Many QI projects fail because the scope of the initial project is too large, unrealistic, or vague. Creating a clear and focused aim statement and keeping it “SMART” (Specific, Measurable, Achievable, Realistic, and Timely) will bring structure to the project.1 “We will reduce Congestive Heart Failure readmissions on 5 medicine units at our hospital by 2.5% in 6 months” is an example of a SMART aim statement.
3. Involve the right people from the start
QI project disasters often start with the wrong team. Select members based on who is needed and not who is available. It is critical to include representatives or “champions” from each area that will be affected. People will buy into a new methodology much more quickly if they were engaged in its development or know that respected members in their area were involved.
4. Use a simple, systematic approach to guide improvement work
Various QI models exist and each offers a systematic approach for assessing and improving care services. The Model for Improvement developed by the Associates in Process Improvement2 is a simple and powerful framework for quality improvement that asks three questions: (1) What are we trying to accomplish? (2) How will we know a change is an improvement? (3) What changes can we make that will result in improvement? The model incorporates Plan-Do-Study-Act (PDSA) cycles to test changes on a small scale.
5. Good projects start with good background data
6. Choose interventions that are high impact, low effort
People will more easily change if the change itself is easy. So consider the question “does this intervention add significant work?” The best interventions change a process without causing undue burden to the clinicians and staff involved.
7. If you can’t measure it, you can’t improve it
After implementation, collect enough data to know whether the changes made improved the process. Study outcome, process, and balancing measures. If possible, use data already being collected by your institution. While it is critical to have quantitative measures, qualitative data such as surveys and observations can also enrich understanding.
Example: Increasing early discharges in medical unit.
Outcome measure – This is the desired outcome that the project aims to improve. This may be the percentage of discharges before noon (DBN) or the average discharge time.
Process measure – This is a measure of a specific change made to improve the outcome metric. The discharge orders may need to be placed earlier in the electronic medical record to improve DBN. This average discharge order time is an example of a process measure.
Balance measure – This metric evaluates whether the intended outcome is leading to unintended consequences. For example, tracking the readmission rate is an important balance measure to assess whether improved DBN is associated with rushed discharges and possible unsafe transitions.
8. Communicate project goals and progress
9. Manage resistance to change
“People responsible for planning and implementing change often forget that while the first task of change management is to understand the destination and how to get there, the first task of transition management is to convince people to leave home.” – William Bridges
Inertia is powerful. We may consider our continuous performance improvement initiative as “the next big thing” but others may not share this enthusiasm. We therefore need to build a compelling reason for others to become engaged and accept major changes to work flow. Different strategies may be needed depending on your audience. Though for some, data and a rational analysis will be persuasive, for others the emotional argument will be the most motivating. Share personal anecdotes and use patient stories. In addition, let providers know “what’s in it for them.” Some may have a personal interest in your project or may need QI experience for career advancement; others might be motivated by the possibilities for scholarship arising from this work.
10. Make the work count twice
Consider QI as a scholarly initiative from the start to bring rigor to the project at all phases. Describe the project in an abstract or manuscript once improvements have been made. Publication is a great way to boost team morale and help make a business case for future improvement work. The Standards for Quality Improvement Reporting Excellence (SQUIRE) guidelines provide an excellent framework for designing and writing up an improvement project.4 The guidelines focus on why the project was started, what was done, what was found, and what the findings mean.
Driving change is challenging, and it is tempting to jump ahead to “fixing the problem.” But implementing a successful QI project requires intelligent direction, strategic planning, and skillful execution. It is our hope that following the above tips will help you develop the best possible ideas and approach implementation in a systematic way, ultimately leading to meaningful change.
Dr. Reyna is assistant professor in the division of hospital medicine and unit medical director at Mount Sinai Medical Center in New York City. She is a Certified Clinical Microsystems Coach. Dr. Burger is associate professor and associate program director, internal medicine residency, at Mount Sinai Beth Israel. He is on the faculty for the SGIM Annual Meeting Precourse on QI and is head of the high value care committee at the department of medicine at Mount Sinai Beth Israel. Dr. Cho is assistant professor and director of quality and safety in the division of hospital medicine at Mount Sinai. He is a senior fellow at the Lown Institute.
References
1. MacLeod L. Making SMART goals smarter. Physician Exec. 2012 Mar-Apr;38(2):68-70, 72.
2. Langley GL, Moen R, Nolan KM, Nolan TW, Norman CL, Provost LP. The Improvement Guide: A Practical Approach to Enhancing Organizational Performance (2nd edition). San Francisco: Jossey-Bass Publishers; 2009.
3. Nelson EC, Batalden PB, Godfrey MM. Quality By Design: A Clinical Microsystems Approach. San Francisco, California: Jossey-Bass; 2007.
4. Ogrinc G, Davies L, Goodman D et.al. SQUIRE 2.0 (Standards for Quality Improvement Reporting Excellence): revised publication guidelines from a detailed consensus process. BMJ Qual Saf. 2015 Sep 14.
Editor’s Note: This column is a quarterly feature written by members of the Physicians in Training Committee. It aims to encourage and educate students, residents, and early career hospitalists.
One of the biggest challenges early career hospitalists, residents and medical students face in launching their first quality improvement (QI) project is knowing how and where to get started. QI can be highly rewarding, but it can also take valuable time and resources without guarantees of sustainable improvement. In this article, we outline 10 key factors to consider when starting a new project.
1. Frame your project so that it aligns with your hospital’s current goals
Choose a project with your hospital’s goals in mind. Securing resources such as health IT, financial, or staffing support will prove difficult unless you get buy-in from hospital leadership. If your project does not directly address hospital goals, frame the purpose to demonstrate that it still fits with leadership priorities. For example, though improving handoffs from daytime to nighttime providers may not be a specific goal, leadership should appreciate that this project is expected to improve patient safety.
2. Be SMART about goals
Many QI projects fail because the scope of the initial project is too large, unrealistic, or vague. Creating a clear and focused aim statement and keeping it “SMART” (Specific, Measurable, Achievable, Realistic, and Timely) will bring structure to the project.1 “We will reduce Congestive Heart Failure readmissions on 5 medicine units at our hospital by 2.5% in 6 months” is an example of a SMART aim statement.
3. Involve the right people from the start
QI project disasters often start with the wrong team. Select members based on who is needed and not who is available. It is critical to include representatives or “champions” from each area that will be affected. People will buy into a new methodology much more quickly if they were engaged in its development or know that respected members in their area were involved.
4. Use a simple, systematic approach to guide improvement work
Various QI models exist and each offers a systematic approach for assessing and improving care services. The Model for Improvement developed by the Associates in Process Improvement2 is a simple and powerful framework for quality improvement that asks three questions: (1) What are we trying to accomplish? (2) How will we know a change is an improvement? (3) What changes can we make that will result in improvement? The model incorporates Plan-Do-Study-Act (PDSA) cycles to test changes on a small scale.
5. Good projects start with good background data
6. Choose interventions that are high impact, low effort
People will more easily change if the change itself is easy. So consider the question “does this intervention add significant work?” The best interventions change a process without causing undue burden to the clinicians and staff involved.
7. If you can’t measure it, you can’t improve it
After implementation, collect enough data to know whether the changes made improved the process. Study outcome, process, and balancing measures. If possible, use data already being collected by your institution. While it is critical to have quantitative measures, qualitative data such as surveys and observations can also enrich understanding.
Example: Increasing early discharges in medical unit.
Outcome measure – This is the desired outcome that the project aims to improve. This may be the percentage of discharges before noon (DBN) or the average discharge time.
Process measure – This is a measure of a specific change made to improve the outcome metric. The discharge orders may need to be placed earlier in the electronic medical record to improve DBN. This average discharge order time is an example of a process measure.
Balance measure – This metric evaluates whether the intended outcome is leading to unintended consequences. For example, tracking the readmission rate is an important balance measure to assess whether improved DBN is associated with rushed discharges and possible unsafe transitions.
8. Communicate project goals and progress
9. Manage resistance to change
“People responsible for planning and implementing change often forget that while the first task of change management is to understand the destination and how to get there, the first task of transition management is to convince people to leave home.” – William Bridges
Inertia is powerful. We may consider our continuous performance improvement initiative as “the next big thing” but others may not share this enthusiasm. We therefore need to build a compelling reason for others to become engaged and accept major changes to work flow. Different strategies may be needed depending on your audience. Though for some, data and a rational analysis will be persuasive, for others the emotional argument will be the most motivating. Share personal anecdotes and use patient stories. In addition, let providers know “what’s in it for them.” Some may have a personal interest in your project or may need QI experience for career advancement; others might be motivated by the possibilities for scholarship arising from this work.
10. Make the work count twice
Consider QI as a scholarly initiative from the start to bring rigor to the project at all phases. Describe the project in an abstract or manuscript once improvements have been made. Publication is a great way to boost team morale and help make a business case for future improvement work. The Standards for Quality Improvement Reporting Excellence (SQUIRE) guidelines provide an excellent framework for designing and writing up an improvement project.4 The guidelines focus on why the project was started, what was done, what was found, and what the findings mean.
Driving change is challenging, and it is tempting to jump ahead to “fixing the problem.” But implementing a successful QI project requires intelligent direction, strategic planning, and skillful execution. It is our hope that following the above tips will help you develop the best possible ideas and approach implementation in a systematic way, ultimately leading to meaningful change.
Dr. Reyna is assistant professor in the division of hospital medicine and unit medical director at Mount Sinai Medical Center in New York City. She is a Certified Clinical Microsystems Coach. Dr. Burger is associate professor and associate program director, internal medicine residency, at Mount Sinai Beth Israel. He is on the faculty for the SGIM Annual Meeting Precourse on QI and is head of the high value care committee at the department of medicine at Mount Sinai Beth Israel. Dr. Cho is assistant professor and director of quality and safety in the division of hospital medicine at Mount Sinai. He is a senior fellow at the Lown Institute.
References
1. MacLeod L. Making SMART goals smarter. Physician Exec. 2012 Mar-Apr;38(2):68-70, 72.
2. Langley GL, Moen R, Nolan KM, Nolan TW, Norman CL, Provost LP. The Improvement Guide: A Practical Approach to Enhancing Organizational Performance (2nd edition). San Francisco: Jossey-Bass Publishers; 2009.
3. Nelson EC, Batalden PB, Godfrey MM. Quality By Design: A Clinical Microsystems Approach. San Francisco, California: Jossey-Bass; 2007.
4. Ogrinc G, Davies L, Goodman D et.al. SQUIRE 2.0 (Standards for Quality Improvement Reporting Excellence): revised publication guidelines from a detailed consensus process. BMJ Qual Saf. 2015 Sep 14.
Editor’s Note: This column is a quarterly feature written by members of the Physicians in Training Committee. It aims to encourage and educate students, residents, and early career hospitalists.
One of the biggest challenges early career hospitalists, residents and medical students face in launching their first quality improvement (QI) project is knowing how and where to get started. QI can be highly rewarding, but it can also take valuable time and resources without guarantees of sustainable improvement. In this article, we outline 10 key factors to consider when starting a new project.
1. Frame your project so that it aligns with your hospital’s current goals
Choose a project with your hospital’s goals in mind. Securing resources such as health IT, financial, or staffing support will prove difficult unless you get buy-in from hospital leadership. If your project does not directly address hospital goals, frame the purpose to demonstrate that it still fits with leadership priorities. For example, though improving handoffs from daytime to nighttime providers may not be a specific goal, leadership should appreciate that this project is expected to improve patient safety.
2. Be SMART about goals
Many QI projects fail because the scope of the initial project is too large, unrealistic, or vague. Creating a clear and focused aim statement and keeping it “SMART” (Specific, Measurable, Achievable, Realistic, and Timely) will bring structure to the project.1 “We will reduce Congestive Heart Failure readmissions on 5 medicine units at our hospital by 2.5% in 6 months” is an example of a SMART aim statement.
3. Involve the right people from the start
QI project disasters often start with the wrong team. Select members based on who is needed and not who is available. It is critical to include representatives or “champions” from each area that will be affected. People will buy into a new methodology much more quickly if they were engaged in its development or know that respected members in their area were involved.
4. Use a simple, systematic approach to guide improvement work
Various QI models exist and each offers a systematic approach for assessing and improving care services. The Model for Improvement developed by the Associates in Process Improvement2 is a simple and powerful framework for quality improvement that asks three questions: (1) What are we trying to accomplish? (2) How will we know a change is an improvement? (3) What changes can we make that will result in improvement? The model incorporates Plan-Do-Study-Act (PDSA) cycles to test changes on a small scale.
5. Good projects start with good background data
6. Choose interventions that are high impact, low effort
People will more easily change if the change itself is easy. So consider the question “does this intervention add significant work?” The best interventions change a process without causing undue burden to the clinicians and staff involved.
7. If you can’t measure it, you can’t improve it
After implementation, collect enough data to know whether the changes made improved the process. Study outcome, process, and balancing measures. If possible, use data already being collected by your institution. While it is critical to have quantitative measures, qualitative data such as surveys and observations can also enrich understanding.
Example: Increasing early discharges in medical unit.
Outcome measure – This is the desired outcome that the project aims to improve. This may be the percentage of discharges before noon (DBN) or the average discharge time.
Process measure – This is a measure of a specific change made to improve the outcome metric. The discharge orders may need to be placed earlier in the electronic medical record to improve DBN. This average discharge order time is an example of a process measure.
Balance measure – This metric evaluates whether the intended outcome is leading to unintended consequences. For example, tracking the readmission rate is an important balance measure to assess whether improved DBN is associated with rushed discharges and possible unsafe transitions.
8. Communicate project goals and progress
9. Manage resistance to change
“People responsible for planning and implementing change often forget that while the first task of change management is to understand the destination and how to get there, the first task of transition management is to convince people to leave home.” – William Bridges
Inertia is powerful. We may consider our continuous performance improvement initiative as “the next big thing” but others may not share this enthusiasm. We therefore need to build a compelling reason for others to become engaged and accept major changes to work flow. Different strategies may be needed depending on your audience. Though for some, data and a rational analysis will be persuasive, for others the emotional argument will be the most motivating. Share personal anecdotes and use patient stories. In addition, let providers know “what’s in it for them.” Some may have a personal interest in your project or may need QI experience for career advancement; others might be motivated by the possibilities for scholarship arising from this work.
10. Make the work count twice
Consider QI as a scholarly initiative from the start to bring rigor to the project at all phases. Describe the project in an abstract or manuscript once improvements have been made. Publication is a great way to boost team morale and help make a business case for future improvement work. The Standards for Quality Improvement Reporting Excellence (SQUIRE) guidelines provide an excellent framework for designing and writing up an improvement project.4 The guidelines focus on why the project was started, what was done, what was found, and what the findings mean.
Driving change is challenging, and it is tempting to jump ahead to “fixing the problem.” But implementing a successful QI project requires intelligent direction, strategic planning, and skillful execution. It is our hope that following the above tips will help you develop the best possible ideas and approach implementation in a systematic way, ultimately leading to meaningful change.
Dr. Reyna is assistant professor in the division of hospital medicine and unit medical director at Mount Sinai Medical Center in New York City. She is a Certified Clinical Microsystems Coach. Dr. Burger is associate professor and associate program director, internal medicine residency, at Mount Sinai Beth Israel. He is on the faculty for the SGIM Annual Meeting Precourse on QI and is head of the high value care committee at the department of medicine at Mount Sinai Beth Israel. Dr. Cho is assistant professor and director of quality and safety in the division of hospital medicine at Mount Sinai. He is a senior fellow at the Lown Institute.
References
1. MacLeod L. Making SMART goals smarter. Physician Exec. 2012 Mar-Apr;38(2):68-70, 72.
2. Langley GL, Moen R, Nolan KM, Nolan TW, Norman CL, Provost LP. The Improvement Guide: A Practical Approach to Enhancing Organizational Performance (2nd edition). San Francisco: Jossey-Bass Publishers; 2009.
3. Nelson EC, Batalden PB, Godfrey MM. Quality By Design: A Clinical Microsystems Approach. San Francisco, California: Jossey-Bass; 2007.
4. Ogrinc G, Davies L, Goodman D et.al. SQUIRE 2.0 (Standards for Quality Improvement Reporting Excellence): revised publication guidelines from a detailed consensus process. BMJ Qual Saf. 2015 Sep 14.
Award for best hospital goes to … the Mayo Clinic
For the second consecutive year, the Mayo Clinic was named the top hospital in the country by U.S. News & World Report.
Also for the second consecutive year, the Cleveland Clinic is ranked second, while Johns Hopkins Hospital in Baltimore and Massachusetts General Hospital in Boston finished third and fourth – switching their places from last year’s ranking – and UCSF Medical Center in San Francisco is fifth after ranking seventh last year, according to the 2017-2018 Best Hospitals ranking.
The Mayo Clinic is nationally ranked in 15 of the 16 specialties included in the overall process, which started with 4,658 community inpatient hospitals and finished with 152 ranking nationally in at least one specialty and 20 earning Honor Roll status with high rankings in multiple specialties. The specialties used in the ranking process include 12 that are data driven – cancer; cardiology and heart surgery; diabetes and endocrinology; otolaryngology; gastroenterology and gastrointestinal surgery; geriatrics; gynecology; nephrology; neurology and neurosurgery; orthopedics; pulmonology; and urology – and four rated by reputation only – ophthalmology; psychiatry; rehabilitation; and rheumatology.
The research organization RTI International conducted the physician survey and produced the Best Hospitals methodology and national rankings under contract with U.S. News. The launch of this year’s edition of Best Hospitals is sponsored by Fidelity Investments.
For the second consecutive year, the Mayo Clinic was named the top hospital in the country by U.S. News & World Report.
Also for the second consecutive year, the Cleveland Clinic is ranked second, while Johns Hopkins Hospital in Baltimore and Massachusetts General Hospital in Boston finished third and fourth – switching their places from last year’s ranking – and UCSF Medical Center in San Francisco is fifth after ranking seventh last year, according to the 2017-2018 Best Hospitals ranking.
The Mayo Clinic is nationally ranked in 15 of the 16 specialties included in the overall process, which started with 4,658 community inpatient hospitals and finished with 152 ranking nationally in at least one specialty and 20 earning Honor Roll status with high rankings in multiple specialties. The specialties used in the ranking process include 12 that are data driven – cancer; cardiology and heart surgery; diabetes and endocrinology; otolaryngology; gastroenterology and gastrointestinal surgery; geriatrics; gynecology; nephrology; neurology and neurosurgery; orthopedics; pulmonology; and urology – and four rated by reputation only – ophthalmology; psychiatry; rehabilitation; and rheumatology.
The research organization RTI International conducted the physician survey and produced the Best Hospitals methodology and national rankings under contract with U.S. News. The launch of this year’s edition of Best Hospitals is sponsored by Fidelity Investments.
For the second consecutive year, the Mayo Clinic was named the top hospital in the country by U.S. News & World Report.
Also for the second consecutive year, the Cleveland Clinic is ranked second, while Johns Hopkins Hospital in Baltimore and Massachusetts General Hospital in Boston finished third and fourth – switching their places from last year’s ranking – and UCSF Medical Center in San Francisco is fifth after ranking seventh last year, according to the 2017-2018 Best Hospitals ranking.
The Mayo Clinic is nationally ranked in 15 of the 16 specialties included in the overall process, which started with 4,658 community inpatient hospitals and finished with 152 ranking nationally in at least one specialty and 20 earning Honor Roll status with high rankings in multiple specialties. The specialties used in the ranking process include 12 that are data driven – cancer; cardiology and heart surgery; diabetes and endocrinology; otolaryngology; gastroenterology and gastrointestinal surgery; geriatrics; gynecology; nephrology; neurology and neurosurgery; orthopedics; pulmonology; and urology – and four rated by reputation only – ophthalmology; psychiatry; rehabilitation; and rheumatology.
The research organization RTI International conducted the physician survey and produced the Best Hospitals methodology and national rankings under contract with U.S. News. The launch of this year’s edition of Best Hospitals is sponsored by Fidelity Investments.