User login
#Dermlife and the Burned-out Resident
Dermatologist Dr. Jeffrey Benabio quipped, “The phrase ‘dermatologist burnout’ may seem as oxymoronic as jumbo shrimp, yet both are real.”1 Indeed, dermatologists often self-report as among the happiest specialists both at work and home, according to the annual Medscape Physician Lifestyle and Happiness Report.2 Similarly, others in the medical field may perceive dermatologists as low-stress providers—well-groomed, well-rested rays of sunshine, getting out of work every day at 5:00
Burnout in Dermatology Residents
Burnout is a syndrome of emotional exhaustion, depersonalization, and a sense of reduced personal accomplishment that affects residents of all specialties3; however, there is a paucity of literature on burnout as it relates to dermatology. Although long work hours and schedule volatility have captured the focus of resident burnout conversations, a less discussed set of factors may contribute to dermatology resident burnout, such as increasing patient load, intensifying regulations, and an unrelenting pace of clinic. A recent survey study by Shoimer et al3 found that 61% of 116 participating Canadian dermatology residents cited examinations (including the board certifying examination) as their top stressor, followed by work (27%). Other stressors included family, relationships, finances, pressure from staff, research, and moving. More than 50% of dermatology residents surveyed experienced high levels of emotional exhaustion and depersonalization, while 40% demonstrated a low sense of personal accomplishment, all of which are determinants of the burnout syndrome.3
Comparison to Residents in Other Specialties
Although dermatology residents experience lower burnout rates than colleagues in other specialties, the absolute prevalence warrants attention. A recent study published in the Journal of the American Medical Association of 3588 second-year medical residents in the United States found that rates of burnout symptoms across clinical specialties ranged from 29.6% to 63.8%. The highest rates of burnout were found in urology (63.8%), neurology (61.6%), and ophthalmology (55.8%), but the lowest reported rate of burnout was demonstrated in dermatology (29.6%).4 Although dermatology ranked the lowest, that is still nearly a whopping 1 in 3 dermatology residents with burnout symptoms. The absolute prevalence should not be obscured by the ranking among other specialties.
Preventing Burnout
Several burnout prevention and coping strategies across specialties have been suggested.
Mindfulness and Self-awareness
A study by Chaukos et al5 found that mindfulness and self-awareness are resilience factors associated with resident burnout. Counseling is one strategy demonstrated to increase self-awareness. Mindfulness may be practiced through meditation or yoga. Regular meditation has been shown to improve mood and emotional stress.6 Similarly, yoga has been shown to yield physical, emotional, and psychological benefits to resdients.7
Work Factors
A supportive clinical faculty and receiving constructive monthly performance feedback have been negatively correlated with dermatology resident burnout.3 Other workplace interventions demonstrating utility in decreasing resident burnout include increasing staff awareness about burnout, increasing support for health professionals treating challenging populations, and ensuring a reasonable workload.6
Sleep
It has been demonstrated that sleeping less than 7 hours per night also is associated with resident burnout,7 yet it has been reported that 72% of dermatology residents fall into this category.3 Poor sleep quality has been shown to be a predictor of lower academic performance. It has been proposed that to minimize sleep deprivation and poor sleep quality, institutions should focus on programs that promote regular exercise, sleep hygiene, mindfulness, and time-out activities such as meditation.7
Social Support
Focusing on peers may foster the inner strength to endure suffering.1 Venting, laughing, and discussing care with colleagues has been demonstrated to decrease anxiety.6 Work-related social networks may be strengthened through attendance at conferences, lectures, and professional organizations.7 Additionally, social supports and spending quality time with family have been demonstrated as negative predictors of dermatology resident burnout.3
Physical Exercise
Exercise has been demonstrated to improve mood, anxiety, and depression, thereby decreasing resident burnout.6
Final Thoughts
Burnout among dermatology residents warrants awareness, as it does in other medical specialties. Awareness may facilitate identification and prevention, the latter of which is perhaps best summarized by the words of psychologist Dr. Christina Maslach: “If all of the knowledge and advice about how to beat burnout could be summed up in 1 word, that word would be balance—balance between giving and getting, balance between stress and calm, balance between work and home.”8
- Benabio J. Burnout. Dermatology News. November 14, 2017. https://www.mdedge.com/edermatologynews/article/152098/business-medicine/burnout. Accessed August 14, 2019.
- Martin KL. Medscape Physician Lifestyle & Happiness Report 2019. Medscape website. https://www.medscape.com/slideshow/2019-lifestyle-happiness-6011057. Published January 9, 2019. Accessed August 14, 2019.
- Shoimer I, Patten S, Mydlarski P. Burnout in dermatology residents: a Canadian perspective. Br J Dermatol. 2018;178:270-271.
- Dyrbye LN, Burke SE, Hardeman RR, et al. Association of clinical specialty with symptoms of burnout and career choice regret among us resident physicians. JAMA. 2018;320:1114-1130.
- Chaukos D, Chaed-Friedman E, Mehta D, et al. Risk and resilience factors associated with resident burnout. Acad Psychiatry. 2017;41:189-194.
- Ishak WW, Lederer S, Mandili C, et al. Burnout during residency training: a literature review. J Grad Med Educ. 2009;2:236-242.
- Tolentino J, Guo W, Ricca R, et al. What’s new in academic medicine: can we effectively address the burnout epidemic in healthcare? Int J Acad Med. 2017;3.
- Maslach C. Burnout: a multidimensional perspective. In: Schaufeli W, Maslach C, Marek T, eds. Professional Burnout: Recent Developments in Theory and Research. Washington, DC: Taylor and Francis; 1993:19-32.
Dermatologist Dr. Jeffrey Benabio quipped, “The phrase ‘dermatologist burnout’ may seem as oxymoronic as jumbo shrimp, yet both are real.”1 Indeed, dermatologists often self-report as among the happiest specialists both at work and home, according to the annual Medscape Physician Lifestyle and Happiness Report.2 Similarly, others in the medical field may perceive dermatologists as low-stress providers—well-groomed, well-rested rays of sunshine, getting out of work every day at 5:00
Burnout in Dermatology Residents
Burnout is a syndrome of emotional exhaustion, depersonalization, and a sense of reduced personal accomplishment that affects residents of all specialties3; however, there is a paucity of literature on burnout as it relates to dermatology. Although long work hours and schedule volatility have captured the focus of resident burnout conversations, a less discussed set of factors may contribute to dermatology resident burnout, such as increasing patient load, intensifying regulations, and an unrelenting pace of clinic. A recent survey study by Shoimer et al3 found that 61% of 116 participating Canadian dermatology residents cited examinations (including the board certifying examination) as their top stressor, followed by work (27%). Other stressors included family, relationships, finances, pressure from staff, research, and moving. More than 50% of dermatology residents surveyed experienced high levels of emotional exhaustion and depersonalization, while 40% demonstrated a low sense of personal accomplishment, all of which are determinants of the burnout syndrome.3
Comparison to Residents in Other Specialties
Although dermatology residents experience lower burnout rates than colleagues in other specialties, the absolute prevalence warrants attention. A recent study published in the Journal of the American Medical Association of 3588 second-year medical residents in the United States found that rates of burnout symptoms across clinical specialties ranged from 29.6% to 63.8%. The highest rates of burnout were found in urology (63.8%), neurology (61.6%), and ophthalmology (55.8%), but the lowest reported rate of burnout was demonstrated in dermatology (29.6%).4 Although dermatology ranked the lowest, that is still nearly a whopping 1 in 3 dermatology residents with burnout symptoms. The absolute prevalence should not be obscured by the ranking among other specialties.
Preventing Burnout
Several burnout prevention and coping strategies across specialties have been suggested.
Mindfulness and Self-awareness
A study by Chaukos et al5 found that mindfulness and self-awareness are resilience factors associated with resident burnout. Counseling is one strategy demonstrated to increase self-awareness. Mindfulness may be practiced through meditation or yoga. Regular meditation has been shown to improve mood and emotional stress.6 Similarly, yoga has been shown to yield physical, emotional, and psychological benefits to resdients.7
Work Factors
A supportive clinical faculty and receiving constructive monthly performance feedback have been negatively correlated with dermatology resident burnout.3 Other workplace interventions demonstrating utility in decreasing resident burnout include increasing staff awareness about burnout, increasing support for health professionals treating challenging populations, and ensuring a reasonable workload.6
Sleep
It has been demonstrated that sleeping less than 7 hours per night also is associated with resident burnout,7 yet it has been reported that 72% of dermatology residents fall into this category.3 Poor sleep quality has been shown to be a predictor of lower academic performance. It has been proposed that to minimize sleep deprivation and poor sleep quality, institutions should focus on programs that promote regular exercise, sleep hygiene, mindfulness, and time-out activities such as meditation.7
Social Support
Focusing on peers may foster the inner strength to endure suffering.1 Venting, laughing, and discussing care with colleagues has been demonstrated to decrease anxiety.6 Work-related social networks may be strengthened through attendance at conferences, lectures, and professional organizations.7 Additionally, social supports and spending quality time with family have been demonstrated as negative predictors of dermatology resident burnout.3
Physical Exercise
Exercise has been demonstrated to improve mood, anxiety, and depression, thereby decreasing resident burnout.6
Final Thoughts
Burnout among dermatology residents warrants awareness, as it does in other medical specialties. Awareness may facilitate identification and prevention, the latter of which is perhaps best summarized by the words of psychologist Dr. Christina Maslach: “If all of the knowledge and advice about how to beat burnout could be summed up in 1 word, that word would be balance—balance between giving and getting, balance between stress and calm, balance between work and home.”8
Dermatologist Dr. Jeffrey Benabio quipped, “The phrase ‘dermatologist burnout’ may seem as oxymoronic as jumbo shrimp, yet both are real.”1 Indeed, dermatologists often self-report as among the happiest specialists both at work and home, according to the annual Medscape Physician Lifestyle and Happiness Report.2 Similarly, others in the medical field may perceive dermatologists as low-stress providers—well-groomed, well-rested rays of sunshine, getting out of work every day at 5:00
Burnout in Dermatology Residents
Burnout is a syndrome of emotional exhaustion, depersonalization, and a sense of reduced personal accomplishment that affects residents of all specialties3; however, there is a paucity of literature on burnout as it relates to dermatology. Although long work hours and schedule volatility have captured the focus of resident burnout conversations, a less discussed set of factors may contribute to dermatology resident burnout, such as increasing patient load, intensifying regulations, and an unrelenting pace of clinic. A recent survey study by Shoimer et al3 found that 61% of 116 participating Canadian dermatology residents cited examinations (including the board certifying examination) as their top stressor, followed by work (27%). Other stressors included family, relationships, finances, pressure from staff, research, and moving. More than 50% of dermatology residents surveyed experienced high levels of emotional exhaustion and depersonalization, while 40% demonstrated a low sense of personal accomplishment, all of which are determinants of the burnout syndrome.3
Comparison to Residents in Other Specialties
Although dermatology residents experience lower burnout rates than colleagues in other specialties, the absolute prevalence warrants attention. A recent study published in the Journal of the American Medical Association of 3588 second-year medical residents in the United States found that rates of burnout symptoms across clinical specialties ranged from 29.6% to 63.8%. The highest rates of burnout were found in urology (63.8%), neurology (61.6%), and ophthalmology (55.8%), but the lowest reported rate of burnout was demonstrated in dermatology (29.6%).4 Although dermatology ranked the lowest, that is still nearly a whopping 1 in 3 dermatology residents with burnout symptoms. The absolute prevalence should not be obscured by the ranking among other specialties.
Preventing Burnout
Several burnout prevention and coping strategies across specialties have been suggested.
Mindfulness and Self-awareness
A study by Chaukos et al5 found that mindfulness and self-awareness are resilience factors associated with resident burnout. Counseling is one strategy demonstrated to increase self-awareness. Mindfulness may be practiced through meditation or yoga. Regular meditation has been shown to improve mood and emotional stress.6 Similarly, yoga has been shown to yield physical, emotional, and psychological benefits to resdients.7
Work Factors
A supportive clinical faculty and receiving constructive monthly performance feedback have been negatively correlated with dermatology resident burnout.3 Other workplace interventions demonstrating utility in decreasing resident burnout include increasing staff awareness about burnout, increasing support for health professionals treating challenging populations, and ensuring a reasonable workload.6
Sleep
It has been demonstrated that sleeping less than 7 hours per night also is associated with resident burnout,7 yet it has been reported that 72% of dermatology residents fall into this category.3 Poor sleep quality has been shown to be a predictor of lower academic performance. It has been proposed that to minimize sleep deprivation and poor sleep quality, institutions should focus on programs that promote regular exercise, sleep hygiene, mindfulness, and time-out activities such as meditation.7
Social Support
Focusing on peers may foster the inner strength to endure suffering.1 Venting, laughing, and discussing care with colleagues has been demonstrated to decrease anxiety.6 Work-related social networks may be strengthened through attendance at conferences, lectures, and professional organizations.7 Additionally, social supports and spending quality time with family have been demonstrated as negative predictors of dermatology resident burnout.3
Physical Exercise
Exercise has been demonstrated to improve mood, anxiety, and depression, thereby decreasing resident burnout.6
Final Thoughts
Burnout among dermatology residents warrants awareness, as it does in other medical specialties. Awareness may facilitate identification and prevention, the latter of which is perhaps best summarized by the words of psychologist Dr. Christina Maslach: “If all of the knowledge and advice about how to beat burnout could be summed up in 1 word, that word would be balance—balance between giving and getting, balance between stress and calm, balance between work and home.”8
- Benabio J. Burnout. Dermatology News. November 14, 2017. https://www.mdedge.com/edermatologynews/article/152098/business-medicine/burnout. Accessed August 14, 2019.
- Martin KL. Medscape Physician Lifestyle & Happiness Report 2019. Medscape website. https://www.medscape.com/slideshow/2019-lifestyle-happiness-6011057. Published January 9, 2019. Accessed August 14, 2019.
- Shoimer I, Patten S, Mydlarski P. Burnout in dermatology residents: a Canadian perspective. Br J Dermatol. 2018;178:270-271.
- Dyrbye LN, Burke SE, Hardeman RR, et al. Association of clinical specialty with symptoms of burnout and career choice regret among us resident physicians. JAMA. 2018;320:1114-1130.
- Chaukos D, Chaed-Friedman E, Mehta D, et al. Risk and resilience factors associated with resident burnout. Acad Psychiatry. 2017;41:189-194.
- Ishak WW, Lederer S, Mandili C, et al. Burnout during residency training: a literature review. J Grad Med Educ. 2009;2:236-242.
- Tolentino J, Guo W, Ricca R, et al. What’s new in academic medicine: can we effectively address the burnout epidemic in healthcare? Int J Acad Med. 2017;3.
- Maslach C. Burnout: a multidimensional perspective. In: Schaufeli W, Maslach C, Marek T, eds. Professional Burnout: Recent Developments in Theory and Research. Washington, DC: Taylor and Francis; 1993:19-32.
- Benabio J. Burnout. Dermatology News. November 14, 2017. https://www.mdedge.com/edermatologynews/article/152098/business-medicine/burnout. Accessed August 14, 2019.
- Martin KL. Medscape Physician Lifestyle & Happiness Report 2019. Medscape website. https://www.medscape.com/slideshow/2019-lifestyle-happiness-6011057. Published January 9, 2019. Accessed August 14, 2019.
- Shoimer I, Patten S, Mydlarski P. Burnout in dermatology residents: a Canadian perspective. Br J Dermatol. 2018;178:270-271.
- Dyrbye LN, Burke SE, Hardeman RR, et al. Association of clinical specialty with symptoms of burnout and career choice regret among us resident physicians. JAMA. 2018;320:1114-1130.
- Chaukos D, Chaed-Friedman E, Mehta D, et al. Risk and resilience factors associated with resident burnout. Acad Psychiatry. 2017;41:189-194.
- Ishak WW, Lederer S, Mandili C, et al. Burnout during residency training: a literature review. J Grad Med Educ. 2009;2:236-242.
- Tolentino J, Guo W, Ricca R, et al. What’s new in academic medicine: can we effectively address the burnout epidemic in healthcare? Int J Acad Med. 2017;3.
- Maslach C. Burnout: a multidimensional perspective. In: Schaufeli W, Maslach C, Marek T, eds. Professional Burnout: Recent Developments in Theory and Research. Washington, DC: Taylor and Francis; 1993:19-32.
Resident Pearl
- Reported techniques for preventing and coping with resident burnout include mindfulness and self-awareness, optimization of workplace factors, adequate sleep, social support, and physical exercise.
Challenges of Treating Primary Psychiatric Disease in Dermatology
Dermatology patients experience a high burden of mental health disturbance. Psychiatric disease is seen in an estimated 30% to 60% of our patients.1 It can be secondary to or comorbid with dermatologic disorders, or it can be the primary condition that is driving cutaneous disease. Patients with secondary or comorbid psychiatric disorders often are amenable to referral to a mental health provider or are already participating in some form of mental health treatment; however, patients with primary psychiatric disease who present to dermatology generally do not accept these referrals.2 Therefore, if these patients are to receive care anywhere in the health care system, it often must be in the department of dermatology.
What primary psychiatric conditions do we see in dermatology?
Common primary psychiatric conditions seen in dermatology include delusional infestation, obsessive-compulsive disorder and related disorders, and dermatitis artefacta.
Delusional Infestation
Also known as delusions of parasitosis or delusional parasitosis, delusional infestation presents as a fixed false belief that there is an organism or other foreign entity that is present in the skin and is the cause of cutaneous disruption. It often is an isolated delusion but can have a notable psychosocial impact. The term delusional infestation is sometimes preferred, as it is inclusive of delusions focused on any type of organism, not just parasites. It also encompasses delusions of infestation with nonliving matter such as fibers, also known as Morgellons disease.3
Obsessive-Compulsive Disorder and Related Disorders
This broad category includes several conditions encountered in dermatology. Body dysmorphic disorder (BDD), olfactory reference syndrome (ORS), excoriation disorder, and trichotillomania are some of the most common variants. In patients with BDD, skin and hair are the 2 most common preoccupations. It has been estimated that 12% of dermatology patients experience BDD. Unsurprisingly, it is more common in patients presenting to cosmetic dermatology, but general dermatology patients also are affected at a rate of 7%.2 Patients with ORS falsely believe they have body odor and/or halitosis. Excoriation disorder manifests as repetitive skin picking, either of normal skin or of lesions such as pimples and scabs. Trichotillomania presents as repeated hair pulling, and trichophagia (eating the pulled hair) also may be present.
Dermatitis Artefacta
Almost 1 in 4 patients who seek dermatologic evaluation for primarily psychiatric disorders have dermatitis artefacta, the presence of deliberately self-inflicted skin lesions.2 Patients with dermatitis artefacta have unconscious motives for their behavior and should be distinguished from malingering patients who have a conscious goal of secondary gain.
What treatments are available?
Antidepressants
Selective serotonin reuptake inhibitors are one of the first-line treatments for BDD and may be useful in ORS. In excoriation disorder and trichotillomania, selective serotonin reuptake inhibitors are the most commonly prescribed pharmacotherapy, but they have limited efficacy.2
Antipsychotics
The recommended treatment of delusional infestation is antipsychotic pharmacotherapy. Treatment with risperidone and olanzapine has been reported to achieve full or partial remission in more than two-thirds of cases.4 Aripiprazole, a newer antipsychotic, has fewer side effects and has been successful in several case reports.5-7
Cognitive Behavioral Therapy
Psychotherapy, most often in the form of cognitive behavioral therapy, has been reported as effective treatment of several psychocutaneous diseases. Cognitive behavioral therapy is considered first-line treatment of body-focused repetitive behavior disorders such as excoriation disorder and trichotillomania.2 It addresses maladaptive thought patterns to modify behavior.
Who treats patients with neurodermatoses?
If a patient presents to dermatology with a rash found to be related to an underlying thyroid disorder, the treatment plan likely would include referral to an endocrinologist. Similarly, patients with primary psychiatric conditions presenting to dermatology should ideally be referred to psychiatrists or psychotherapists, the providers most thoroughly trained and best equipped to treat them. The challenge in psychodermatology is that patients often are resistant to the assessment that the primary pathology is psychiatric. Patients may deny that they are “crazy” and see numerous providers in search of a dermatologist who “believes” them.8
Referral to mental health professionals almost always is refused by patients with primarily psychiatric neurodermatoses, which presents dermatologists with a dilemma. As the authors of the “Psychotropic Agents” chapter of Comprehensive Dermatologic Drug Therapy put it: “A dermatologist has two choices. The first is to try to ‘look the other way’ and pacify the patient by providing relatively benign, but minimally effective treatments. The other option is to try to directly address the psychological/psychiatric problems.” The chapter then provides a thorough guide for the use of psychotropic medications in the dermatology population, advocating for option 2: treatment by dermatologists.9
Should a dermatologist prescribe psychotropic drugs?
In Dermatology, the principle reference textbook in many dermatology training programs, it is stated that “[a]lthough less comprehensive than treatment delivered in collaboration with a psychiatrist, in the authors’ opinion, management of these issues by a dermatologist is better than no treatment at all.”10 Recent reviews in the dermatologic literature of psychiatric diseases and drugs in dermatology agree that dermatologists should feel comfortable with prescribing pharmacologic treatment.2,8,11 Performance of psychotherapy by dermatologists, on the other hand, is not recommended based on time constraints and lack of training.
Despite the apparent agreement in the texts and literature that pharmacotherapy of psychiatric neurodermatoses is within our scope of practice in dermatology, most dermatologists do not prescribe psychotropic agents. Dermatology residencies generally do not provide thorough training in psychopharmacotherapy.9 Unsurprisingly, a survey of 40 dermatologists at one academic institution found that only 11% felt comfortable prescribing an antidepressant and a mere 3% were comfortable prescribing an antipsychotic.12
Final Thoughts
The challenges involved in managing patients with primary psychiatric disease in dermatology are great and many patients are undertreated despite the availability of effective, evidence-based treatment options. We need to continue to work toward providing better access to these treatments in a way that maximizes the chance that our patients will accept our care.
- Korabel H, Dudek D, Jaworek A, et al. Psychodermatology: psychological and psychiatrical aspects of dermatology [in Polish]. Przegl Lek. 2008;65:244-248.
- Krooks JA, Weatherall AG, Holland PJ. Review of epidemiology, clinical presentation, diagnosis, and treatment of common primary psychiatric causes of cutaneous disease. J Dermatolog Treat. 2018;29:418-427.
- Bewley AP, Lepping P, Freundenmann RW, et al. Delusional parasitosis: time to call it delusional infestation. Br J Dermatol. 2018;163:1-2.
- Freudenmann RW, Lepping P. Second-generation antipsychotics in primary and secondary delusional parasitosis: outcome and efficacy. J Clin Psychopharmacol. 2008;28:500-508.
- Miyamoto S, Miyake N, Ogino S, et al. Successful treatment of delusional disorder with low-dose aripiprazole. Psychiatry Clin Neurosci. 2008;62:369.
- Ladizinski B, Busse KL, Bhutani T, et al. Aripiprazole as a viable alternative for treating delusions of parasitosis. J Drugs Dermatol. 2010;9:1531-1532.
- Huang WL, Chang LR. Aripiprazole in the treatment of delusional parasitosis with ocular and dermatologic presentations. J Clin Psychopharmacol. 2013;33:272-273.
- Campbell EH, Elston DM, Hawthorne JD, et al. Diagnosis and management of delusional parasitosis. J Am Acad Dermatol. 2019;80:1428-1434.
- Bhutani T, Lee CS, Koo JYM. Psychotropic agents. In: Wolverton SE, ed. Comprehensive Dermatologic Drug Therapy. 3rd ed. China: Elsevier Saunders; 2013:375-388.
- Duncan KO, Koo JYM. Psychocutaneous diseases. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. China: Elsevier; 2018:128-137.
- Shah B, Levenson JL. Use of psychotropic drugs in the dermatology patient: when to start and stop? Clin Dermatol. 2018;36:748-755.
- Gee SN, Zakhary L, Keuthen N, et al. A survey assessment of the recognition and treatment of psychocutaneous disorders in the outpatient dermatology setting: how prepared are we? J Am Acad Dermatol. 2013;68:47-52.
Dermatology patients experience a high burden of mental health disturbance. Psychiatric disease is seen in an estimated 30% to 60% of our patients.1 It can be secondary to or comorbid with dermatologic disorders, or it can be the primary condition that is driving cutaneous disease. Patients with secondary or comorbid psychiatric disorders often are amenable to referral to a mental health provider or are already participating in some form of mental health treatment; however, patients with primary psychiatric disease who present to dermatology generally do not accept these referrals.2 Therefore, if these patients are to receive care anywhere in the health care system, it often must be in the department of dermatology.
What primary psychiatric conditions do we see in dermatology?
Common primary psychiatric conditions seen in dermatology include delusional infestation, obsessive-compulsive disorder and related disorders, and dermatitis artefacta.
Delusional Infestation
Also known as delusions of parasitosis or delusional parasitosis, delusional infestation presents as a fixed false belief that there is an organism or other foreign entity that is present in the skin and is the cause of cutaneous disruption. It often is an isolated delusion but can have a notable psychosocial impact. The term delusional infestation is sometimes preferred, as it is inclusive of delusions focused on any type of organism, not just parasites. It also encompasses delusions of infestation with nonliving matter such as fibers, also known as Morgellons disease.3
Obsessive-Compulsive Disorder and Related Disorders
This broad category includes several conditions encountered in dermatology. Body dysmorphic disorder (BDD), olfactory reference syndrome (ORS), excoriation disorder, and trichotillomania are some of the most common variants. In patients with BDD, skin and hair are the 2 most common preoccupations. It has been estimated that 12% of dermatology patients experience BDD. Unsurprisingly, it is more common in patients presenting to cosmetic dermatology, but general dermatology patients also are affected at a rate of 7%.2 Patients with ORS falsely believe they have body odor and/or halitosis. Excoriation disorder manifests as repetitive skin picking, either of normal skin or of lesions such as pimples and scabs. Trichotillomania presents as repeated hair pulling, and trichophagia (eating the pulled hair) also may be present.
Dermatitis Artefacta
Almost 1 in 4 patients who seek dermatologic evaluation for primarily psychiatric disorders have dermatitis artefacta, the presence of deliberately self-inflicted skin lesions.2 Patients with dermatitis artefacta have unconscious motives for their behavior and should be distinguished from malingering patients who have a conscious goal of secondary gain.
What treatments are available?
Antidepressants
Selective serotonin reuptake inhibitors are one of the first-line treatments for BDD and may be useful in ORS. In excoriation disorder and trichotillomania, selective serotonin reuptake inhibitors are the most commonly prescribed pharmacotherapy, but they have limited efficacy.2
Antipsychotics
The recommended treatment of delusional infestation is antipsychotic pharmacotherapy. Treatment with risperidone and olanzapine has been reported to achieve full or partial remission in more than two-thirds of cases.4 Aripiprazole, a newer antipsychotic, has fewer side effects and has been successful in several case reports.5-7
Cognitive Behavioral Therapy
Psychotherapy, most often in the form of cognitive behavioral therapy, has been reported as effective treatment of several psychocutaneous diseases. Cognitive behavioral therapy is considered first-line treatment of body-focused repetitive behavior disorders such as excoriation disorder and trichotillomania.2 It addresses maladaptive thought patterns to modify behavior.
Who treats patients with neurodermatoses?
If a patient presents to dermatology with a rash found to be related to an underlying thyroid disorder, the treatment plan likely would include referral to an endocrinologist. Similarly, patients with primary psychiatric conditions presenting to dermatology should ideally be referred to psychiatrists or psychotherapists, the providers most thoroughly trained and best equipped to treat them. The challenge in psychodermatology is that patients often are resistant to the assessment that the primary pathology is psychiatric. Patients may deny that they are “crazy” and see numerous providers in search of a dermatologist who “believes” them.8
Referral to mental health professionals almost always is refused by patients with primarily psychiatric neurodermatoses, which presents dermatologists with a dilemma. As the authors of the “Psychotropic Agents” chapter of Comprehensive Dermatologic Drug Therapy put it: “A dermatologist has two choices. The first is to try to ‘look the other way’ and pacify the patient by providing relatively benign, but minimally effective treatments. The other option is to try to directly address the psychological/psychiatric problems.” The chapter then provides a thorough guide for the use of psychotropic medications in the dermatology population, advocating for option 2: treatment by dermatologists.9
Should a dermatologist prescribe psychotropic drugs?
In Dermatology, the principle reference textbook in many dermatology training programs, it is stated that “[a]lthough less comprehensive than treatment delivered in collaboration with a psychiatrist, in the authors’ opinion, management of these issues by a dermatologist is better than no treatment at all.”10 Recent reviews in the dermatologic literature of psychiatric diseases and drugs in dermatology agree that dermatologists should feel comfortable with prescribing pharmacologic treatment.2,8,11 Performance of psychotherapy by dermatologists, on the other hand, is not recommended based on time constraints and lack of training.
Despite the apparent agreement in the texts and literature that pharmacotherapy of psychiatric neurodermatoses is within our scope of practice in dermatology, most dermatologists do not prescribe psychotropic agents. Dermatology residencies generally do not provide thorough training in psychopharmacotherapy.9 Unsurprisingly, a survey of 40 dermatologists at one academic institution found that only 11% felt comfortable prescribing an antidepressant and a mere 3% were comfortable prescribing an antipsychotic.12
Final Thoughts
The challenges involved in managing patients with primary psychiatric disease in dermatology are great and many patients are undertreated despite the availability of effective, evidence-based treatment options. We need to continue to work toward providing better access to these treatments in a way that maximizes the chance that our patients will accept our care.
Dermatology patients experience a high burden of mental health disturbance. Psychiatric disease is seen in an estimated 30% to 60% of our patients.1 It can be secondary to or comorbid with dermatologic disorders, or it can be the primary condition that is driving cutaneous disease. Patients with secondary or comorbid psychiatric disorders often are amenable to referral to a mental health provider or are already participating in some form of mental health treatment; however, patients with primary psychiatric disease who present to dermatology generally do not accept these referrals.2 Therefore, if these patients are to receive care anywhere in the health care system, it often must be in the department of dermatology.
What primary psychiatric conditions do we see in dermatology?
Common primary psychiatric conditions seen in dermatology include delusional infestation, obsessive-compulsive disorder and related disorders, and dermatitis artefacta.
Delusional Infestation
Also known as delusions of parasitosis or delusional parasitosis, delusional infestation presents as a fixed false belief that there is an organism or other foreign entity that is present in the skin and is the cause of cutaneous disruption. It often is an isolated delusion but can have a notable psychosocial impact. The term delusional infestation is sometimes preferred, as it is inclusive of delusions focused on any type of organism, not just parasites. It also encompasses delusions of infestation with nonliving matter such as fibers, also known as Morgellons disease.3
Obsessive-Compulsive Disorder and Related Disorders
This broad category includes several conditions encountered in dermatology. Body dysmorphic disorder (BDD), olfactory reference syndrome (ORS), excoriation disorder, and trichotillomania are some of the most common variants. In patients with BDD, skin and hair are the 2 most common preoccupations. It has been estimated that 12% of dermatology patients experience BDD. Unsurprisingly, it is more common in patients presenting to cosmetic dermatology, but general dermatology patients also are affected at a rate of 7%.2 Patients with ORS falsely believe they have body odor and/or halitosis. Excoriation disorder manifests as repetitive skin picking, either of normal skin or of lesions such as pimples and scabs. Trichotillomania presents as repeated hair pulling, and trichophagia (eating the pulled hair) also may be present.
Dermatitis Artefacta
Almost 1 in 4 patients who seek dermatologic evaluation for primarily psychiatric disorders have dermatitis artefacta, the presence of deliberately self-inflicted skin lesions.2 Patients with dermatitis artefacta have unconscious motives for their behavior and should be distinguished from malingering patients who have a conscious goal of secondary gain.
What treatments are available?
Antidepressants
Selective serotonin reuptake inhibitors are one of the first-line treatments for BDD and may be useful in ORS. In excoriation disorder and trichotillomania, selective serotonin reuptake inhibitors are the most commonly prescribed pharmacotherapy, but they have limited efficacy.2
Antipsychotics
The recommended treatment of delusional infestation is antipsychotic pharmacotherapy. Treatment with risperidone and olanzapine has been reported to achieve full or partial remission in more than two-thirds of cases.4 Aripiprazole, a newer antipsychotic, has fewer side effects and has been successful in several case reports.5-7
Cognitive Behavioral Therapy
Psychotherapy, most often in the form of cognitive behavioral therapy, has been reported as effective treatment of several psychocutaneous diseases. Cognitive behavioral therapy is considered first-line treatment of body-focused repetitive behavior disorders such as excoriation disorder and trichotillomania.2 It addresses maladaptive thought patterns to modify behavior.
Who treats patients with neurodermatoses?
If a patient presents to dermatology with a rash found to be related to an underlying thyroid disorder, the treatment plan likely would include referral to an endocrinologist. Similarly, patients with primary psychiatric conditions presenting to dermatology should ideally be referred to psychiatrists or psychotherapists, the providers most thoroughly trained and best equipped to treat them. The challenge in psychodermatology is that patients often are resistant to the assessment that the primary pathology is psychiatric. Patients may deny that they are “crazy” and see numerous providers in search of a dermatologist who “believes” them.8
Referral to mental health professionals almost always is refused by patients with primarily psychiatric neurodermatoses, which presents dermatologists with a dilemma. As the authors of the “Psychotropic Agents” chapter of Comprehensive Dermatologic Drug Therapy put it: “A dermatologist has two choices. The first is to try to ‘look the other way’ and pacify the patient by providing relatively benign, but minimally effective treatments. The other option is to try to directly address the psychological/psychiatric problems.” The chapter then provides a thorough guide for the use of psychotropic medications in the dermatology population, advocating for option 2: treatment by dermatologists.9
Should a dermatologist prescribe psychotropic drugs?
In Dermatology, the principle reference textbook in many dermatology training programs, it is stated that “[a]lthough less comprehensive than treatment delivered in collaboration with a psychiatrist, in the authors’ opinion, management of these issues by a dermatologist is better than no treatment at all.”10 Recent reviews in the dermatologic literature of psychiatric diseases and drugs in dermatology agree that dermatologists should feel comfortable with prescribing pharmacologic treatment.2,8,11 Performance of psychotherapy by dermatologists, on the other hand, is not recommended based on time constraints and lack of training.
Despite the apparent agreement in the texts and literature that pharmacotherapy of psychiatric neurodermatoses is within our scope of practice in dermatology, most dermatologists do not prescribe psychotropic agents. Dermatology residencies generally do not provide thorough training in psychopharmacotherapy.9 Unsurprisingly, a survey of 40 dermatologists at one academic institution found that only 11% felt comfortable prescribing an antidepressant and a mere 3% were comfortable prescribing an antipsychotic.12
Final Thoughts
The challenges involved in managing patients with primary psychiatric disease in dermatology are great and many patients are undertreated despite the availability of effective, evidence-based treatment options. We need to continue to work toward providing better access to these treatments in a way that maximizes the chance that our patients will accept our care.
- Korabel H, Dudek D, Jaworek A, et al. Psychodermatology: psychological and psychiatrical aspects of dermatology [in Polish]. Przegl Lek. 2008;65:244-248.
- Krooks JA, Weatherall AG, Holland PJ. Review of epidemiology, clinical presentation, diagnosis, and treatment of common primary psychiatric causes of cutaneous disease. J Dermatolog Treat. 2018;29:418-427.
- Bewley AP, Lepping P, Freundenmann RW, et al. Delusional parasitosis: time to call it delusional infestation. Br J Dermatol. 2018;163:1-2.
- Freudenmann RW, Lepping P. Second-generation antipsychotics in primary and secondary delusional parasitosis: outcome and efficacy. J Clin Psychopharmacol. 2008;28:500-508.
- Miyamoto S, Miyake N, Ogino S, et al. Successful treatment of delusional disorder with low-dose aripiprazole. Psychiatry Clin Neurosci. 2008;62:369.
- Ladizinski B, Busse KL, Bhutani T, et al. Aripiprazole as a viable alternative for treating delusions of parasitosis. J Drugs Dermatol. 2010;9:1531-1532.
- Huang WL, Chang LR. Aripiprazole in the treatment of delusional parasitosis with ocular and dermatologic presentations. J Clin Psychopharmacol. 2013;33:272-273.
- Campbell EH, Elston DM, Hawthorne JD, et al. Diagnosis and management of delusional parasitosis. J Am Acad Dermatol. 2019;80:1428-1434.
- Bhutani T, Lee CS, Koo JYM. Psychotropic agents. In: Wolverton SE, ed. Comprehensive Dermatologic Drug Therapy. 3rd ed. China: Elsevier Saunders; 2013:375-388.
- Duncan KO, Koo JYM. Psychocutaneous diseases. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. China: Elsevier; 2018:128-137.
- Shah B, Levenson JL. Use of psychotropic drugs in the dermatology patient: when to start and stop? Clin Dermatol. 2018;36:748-755.
- Gee SN, Zakhary L, Keuthen N, et al. A survey assessment of the recognition and treatment of psychocutaneous disorders in the outpatient dermatology setting: how prepared are we? J Am Acad Dermatol. 2013;68:47-52.
- Korabel H, Dudek D, Jaworek A, et al. Psychodermatology: psychological and psychiatrical aspects of dermatology [in Polish]. Przegl Lek. 2008;65:244-248.
- Krooks JA, Weatherall AG, Holland PJ. Review of epidemiology, clinical presentation, diagnosis, and treatment of common primary psychiatric causes of cutaneous disease. J Dermatolog Treat. 2018;29:418-427.
- Bewley AP, Lepping P, Freundenmann RW, et al. Delusional parasitosis: time to call it delusional infestation. Br J Dermatol. 2018;163:1-2.
- Freudenmann RW, Lepping P. Second-generation antipsychotics in primary and secondary delusional parasitosis: outcome and efficacy. J Clin Psychopharmacol. 2008;28:500-508.
- Miyamoto S, Miyake N, Ogino S, et al. Successful treatment of delusional disorder with low-dose aripiprazole. Psychiatry Clin Neurosci. 2008;62:369.
- Ladizinski B, Busse KL, Bhutani T, et al. Aripiprazole as a viable alternative for treating delusions of parasitosis. J Drugs Dermatol. 2010;9:1531-1532.
- Huang WL, Chang LR. Aripiprazole in the treatment of delusional parasitosis with ocular and dermatologic presentations. J Clin Psychopharmacol. 2013;33:272-273.
- Campbell EH, Elston DM, Hawthorne JD, et al. Diagnosis and management of delusional parasitosis. J Am Acad Dermatol. 2019;80:1428-1434.
- Bhutani T, Lee CS, Koo JYM. Psychotropic agents. In: Wolverton SE, ed. Comprehensive Dermatologic Drug Therapy. 3rd ed. China: Elsevier Saunders; 2013:375-388.
- Duncan KO, Koo JYM. Psychocutaneous diseases. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. China: Elsevier; 2018:128-137.
- Shah B, Levenson JL. Use of psychotropic drugs in the dermatology patient: when to start and stop? Clin Dermatol. 2018;36:748-755.
- Gee SN, Zakhary L, Keuthen N, et al. A survey assessment of the recognition and treatment of psychocutaneous disorders in the outpatient dermatology setting: how prepared are we? J Am Acad Dermatol. 2013;68:47-52.
Resident Pearl
- Patients often present to dermatology with primary psychologic disorders such as delusional infestation or trichotillomania. Treatment of such conditions with antidepressants and antipsychotics can be highly effective and is within our scope of practice. Increased emphasis on psychopharmacotherapy in dermatology training would increase access to appropriate care for this patient population.
The ABCs of COCs: A Guide for Dermatology Residents on Combined Oral Contraceptives
The American Academy of Dermatology confers combined oral contraceptives (COCs) a strength A recommendation for the treatment of acne based on level I evidence, and 4 COCs are approved for the treatment of acne by the US Food and Drug Administration (FDA).1 Furthermore, when dermatologists prescribe isotretinoin and thalidomide to women of reproductive potential, the iPLEDGE and THALOMID Risk Evaluation and Mitigation Strategy (REMS) programs require 2 concurrent methods of contraception, one of which may be a COC. In addition, COCs have several potential off-label indications in dermatology including idiopathic hirsutism, female pattern hair loss, hidradenitis suppurativa, and autoimmune progesterone dermatitis.
Despite this evidence and opportunity, research suggests that dermatologists underprescribe COCs. The National Ambulatory Medical Care Survey found that between 1993 and 2008, dermatologists in the United States prescribed COCs to only 2.03% of women presenting for acne treatment, which was less often than obstetricians/gynecologists (36.03%) and internists (10.76%).2 More recently, in a survey of 130 US dermatologists conducted from 2014 to 2015, only 55.4% reported prescribing COCs. This survey also found that only 45.8% of dermatologists who prescribed COCs felt very comfortable counseling on how to begin taking them, only 48.6% felt very comfortable counseling patients on side effects, and only 22.2% felt very comfortable managing side effects.3
In light of these data, this article reviews the basics of COCs for dermatology residents, from assessing patient eligibility and selecting a COC to counseling on use and managing risks and side effects. Because there are different approaches to prescribing COCs, readers are encouraged to integrate the information in this article with what they have learned from other sources.
Assess Patient Eligibility
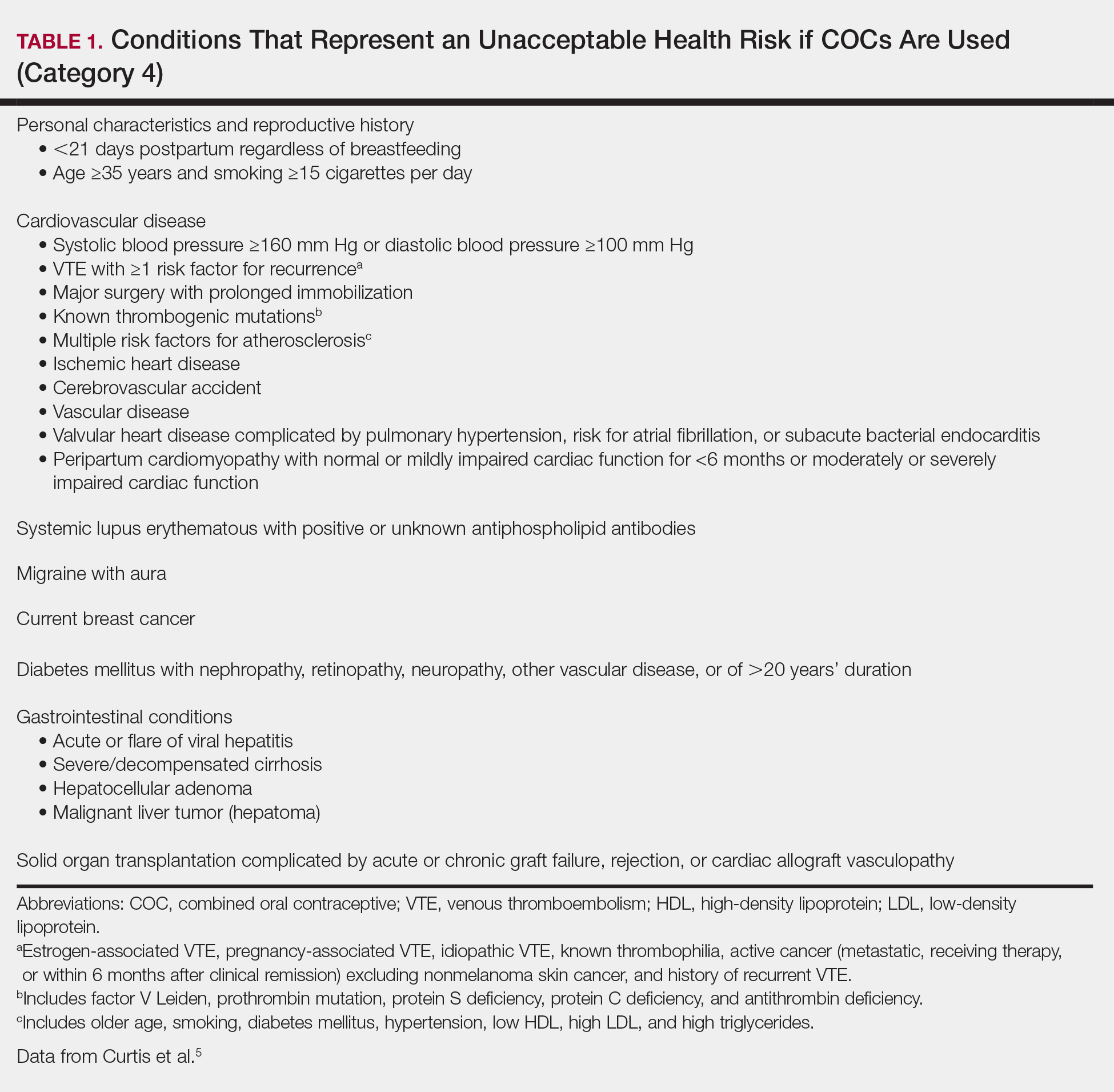
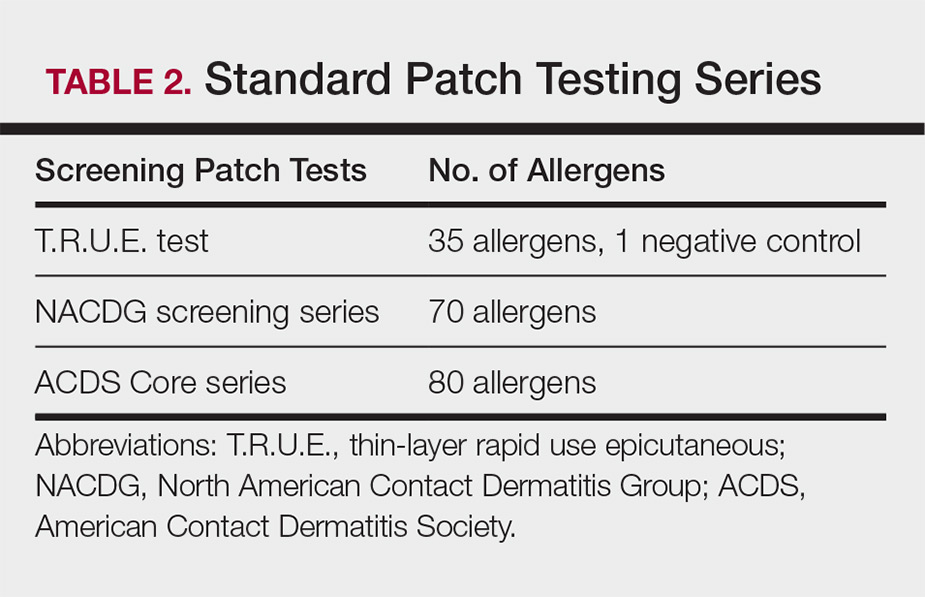
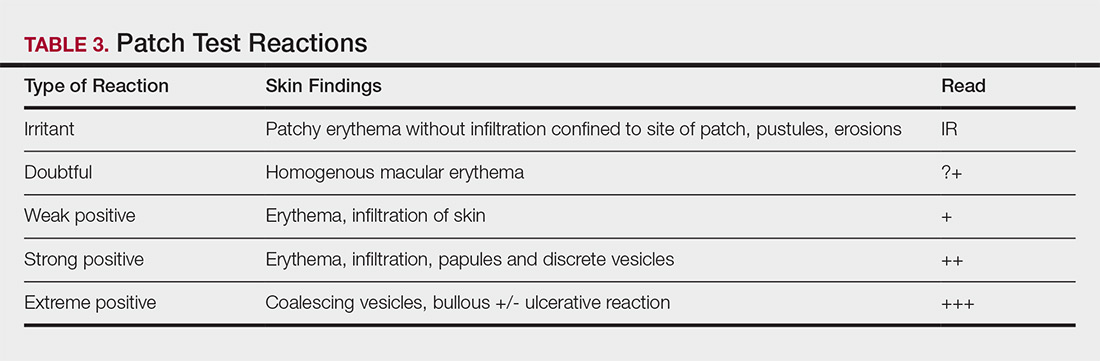
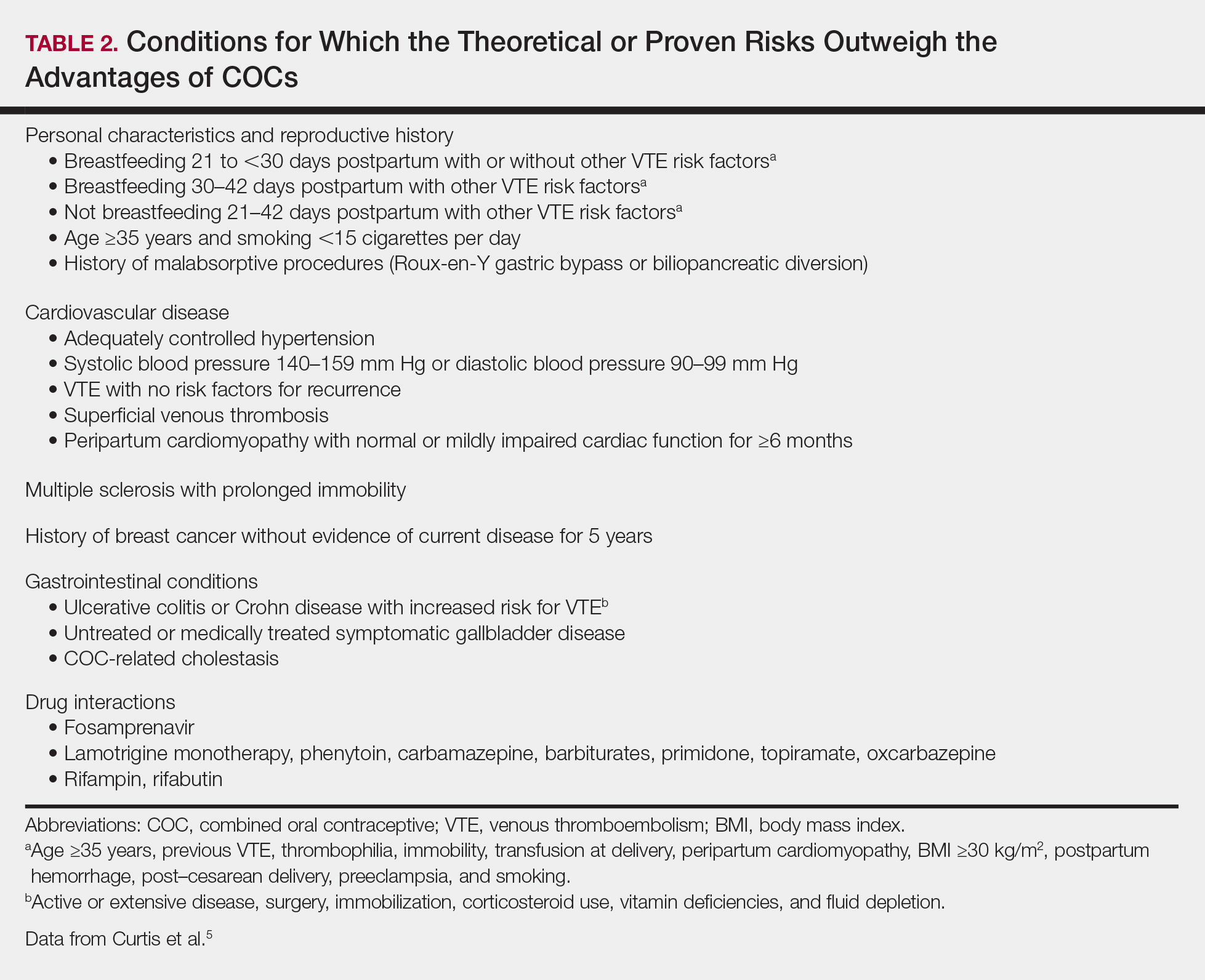
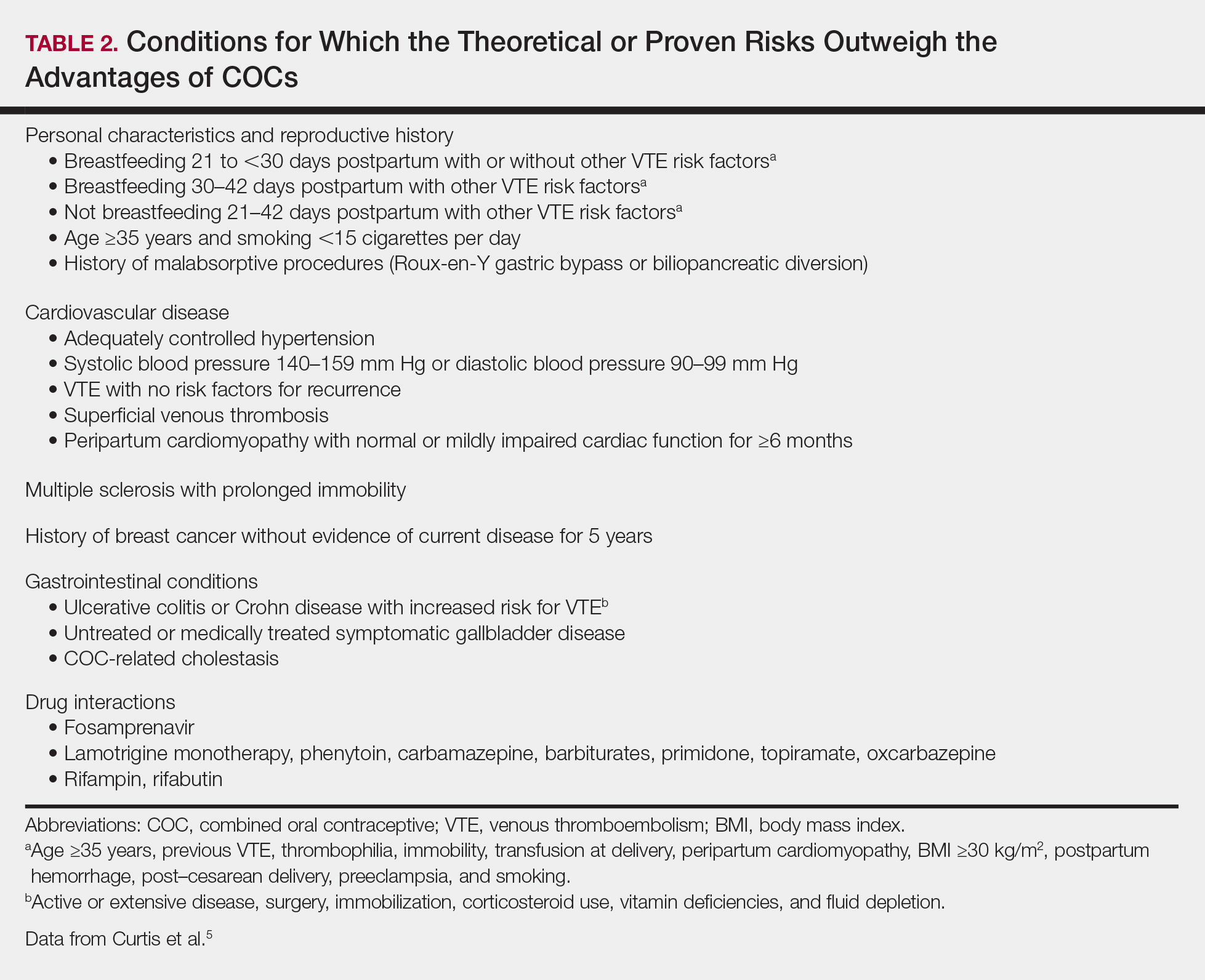
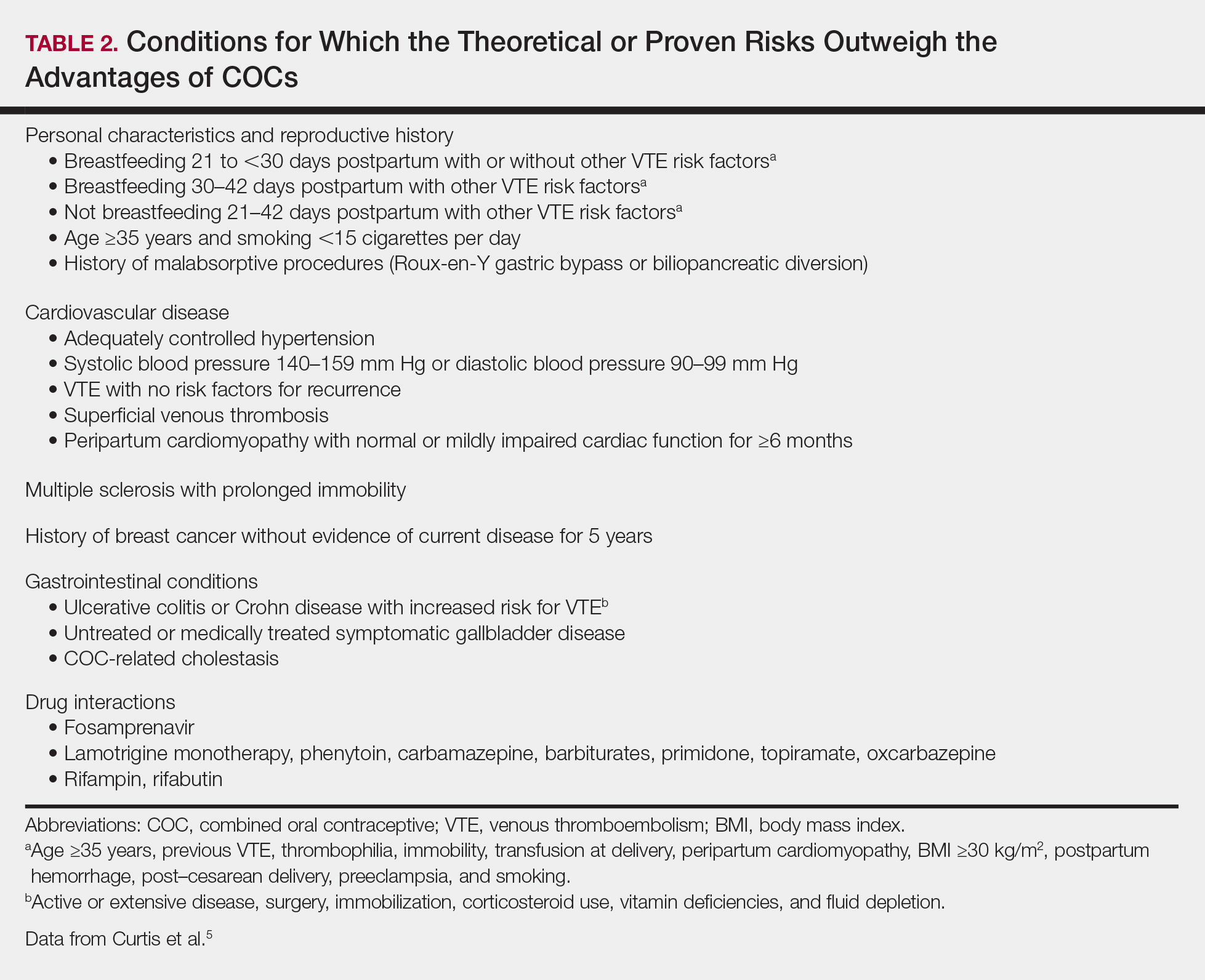
In general, patients should be at least 14 years of age and have waited 2 years after menarche to start COCs. They can be taken until menopause.1,4 Contraindications can be screened for by taking a medical history and measuring a baseline blood pressure (Tables 1 and 2).5 In addition, pregnancy should be excluded with a urine or serum pregnancy test or criteria provided in Box 2 of the 2016 US Selected Practice Recommendations for Contraceptive Use from the Centers for Disease Control and Prevention (CDC).4 Although important for women’s overall health, a pelvic examination is not required to start COCs according to the CDC and the American Academy of Dermatology.1,4
Select the COC
Combined oral contraceptives combine estrogen, usually in the form of ethinyl estradiol, with a progestin. Data suggest that all COCs effectively treat acne, but 4 are specifically FDA approved for acne: ethinyl estradiol–norethindrone acetate–ferrous fumarate, ethinyl estradiol–norgestimate, ethinyl estradiol–drospirenone, and ethinyl estradiol–drospirenone–levomefolate.1 Ethinyl estradiol–desogestrel and ethinyl estradiol–drospirenone are 2 go-to COCs for some of the attending physicians at my residency program. All COCs are FDA approved for contraception. When selecting a COC, one approach is to start with the patient’s drug formulary, then consider the following characteristics.
Monophasic vs Multiphasic
All the hormonally active pills in a monophasic formulation contain the same dose of estrogen and progestin; however, these doses change per pill in a multiphasic formulation, which requires that patients take the pills in a specific order. Given this greater complexity and the fact that multiphasic formulations often are more expensive and lack evidence of superiority, a 2011 Cochrane review recommended monophasic formulations as first line.6 In addition, monophasic formulations are preferred for autoimmune progesterone dermatitis because of the stable progestin dose.
Hormone-Free Interval
Some COCs include placebo pills during which hormone withdrawal symptoms such as bleeding, pelvic pain, mood changes, and headache may occur. If a patient is concerned about these symptoms, choose a COC with no or fewer placebo pills, or have the patient skip the hormone-free interval altogether and start the next pack early7; in this case, the prescription should be written with instructions to allow the patient to get earlier refills from the pharmacy.
Estrogen Dose
To minimize estrogen-related side effects, the lowest possible dose of ethinyl estradiol that is effective and tolerable should be prescribed7,8; 20 μg of ethinyl estradiol generally is the lowest dose available, but it may be associated with more frequent breakthrough bleeding.9 The International Planned Parenthood Federation recommends starting with COCs that contain 30 to 35 μg of estrogen.10 Synthesizing this information, one option is to start with 20 μg of ethinyl estradiol and increase the dose if breakthrough bleeding persists after 3 cycles.
Progestin Type
First-generation progestins (eg, norethindrone), second-generation progestins (eg, norgestrel, levonorgestrel), and third-generation progestins (eg, norgestimate, desogestrel) are derived from testosterone and therefore are variably androgenic; second-generation progestins are the most androgenic, and third-generation progestins are the least. On the other hand, drospirenone, the fourth-generation progestin available in the United States, is derived from 17α-spironolactone and thus is mildly antiandrogenic (3 mg of drospirenone is considered equivalent to 25 mg of spironolactone).
Although COCs with less androgenic progestins should theoretically treat acne better, a 2012 Cochrane review of COCs and acne concluded that “differences in the comparative effectiveness of COCs containing varying progestin types and dosages were less clear, and data were limited for any particular comparison.”11 As a result, regardless of the progestin, all COCs are believed to have a net antiandrogenic effect due to their estrogen component.1
Counsel on Use
Combined oral contraceptives can be started on any day of the menstrual cycle, including the day the prescription is given. If a patient begins a COC within 5 days of the first day of her most recent period, backup contraception is not needed.4 If she begins the COC more than 5 days after the first day of her most recent period, she needs to use backup contraception or abstain from sexual intercourse for the next 7 days.4 In general, at least 3 months of therapy are required to evaluate the effectiveness of COCs for acne.1
Manage Risks and Side Effects
Breakthrough Bleeding
The most common side effect of breakthrough bleeding can be minimized by taking COCs at approximately the same time every day and avoiding missed pills. If breakthrough bleeding does not stop after 3 cycles, consider increasing the estrogen dose to 30 to 35 μg and/or referring to an obstetrician/gynecologist to rule out other etiologies of bleeding.7,8
Nausea, Headache, Bloating, and Breast Tenderness
These symptoms typically resolve after the first 3 months. To minimize nausea, patients should take COCs in the early evening and eat breakfast the next morning.7,8 For headaches that occur during the hormone-free interval, consider skipping the placebo pills and starting the next pack early. Switching the progestin to drospirenone, which has a mild diuretic effect, can help with bloating as well as breast tenderness.7 For persistent symptoms, consider a lower estrogen dose.7,8
Changes in Libido
In a systemic review including 8422 COC users, 64% reported no change in libido, 22% reported an increase, and 15% reported a decrease.12
Weight Gain
Although patients may be concerned that COCs cause weight gain, a 2014 Cochrane review concluded that “available evidence is insufficient to determine the effect of combination contraceptives on weight, but no large effect is evident.”13 If weight gain does occur, anecdotal evidence suggests it tends to be not more than 5 pounds. If weight gain is an issue, consider a less androgenic progestin.8
Venous Thromboembolism
Use the 3-6-9-12 model to contextualize venous thromboembolism (VTE) risk: a woman’s annual VTE risk is 3 per 10,000 women at baseline, 6 per 10,000 women with nondrospirenone COCs, 9 per 10,000 women with drospirenone-containing COCs, and 12 per 10,000 women when pregnant.14 Patients should be counseled on the signs and symptoms of VTE such as unilateral or bilateral leg or arm swelling, pain, warmth, redness, and/or shortness of breath. The British Society for Haematology recommends maintaining mobility as a reasonable precaution when traveling for more than 3 hours.15
Cardiovascular Disease
A 2015 Cochrane review found that the risk for myocardial infarction or ischemic stroke is increased 1.6‐fold in COC users.16 Despite this increased relative risk, the increased absolute annual risk of myocardial infarction in nonsmoking women remains low: increased from 0.83 to 3.53 per 10,000,000 women younger than 35 years and from 9.45 to 40.4 per 10,000,000 women 35 years and older.17
Breast Cancer and Cervical Cancer
Data are mixed on the effect of COCs on the risk for breast cancer and cervical cancer.1 According to the CDC, COC use for 5 or more years might increase the risk of cervical carcinoma in situ and invasive cervical carcinoma in women with persistent human papillomavirus infection.5 Regardless of COC use, women should undergo age-appropriate screening for breast cancer and cervical cancer.
Melasma
Melasma is an estrogen-mediated side effect of COCs.8 A study from 1967 found that 29% of COC users (N=212) developed melasma; however, they were taking COCs with much higher ethinyl estradiol doses (50–100 μg) than typically used today.18 Nevertheless, as part of an overall skin care regimen, photoprotection should be encouraged with a broad-spectrum, water-resistant sunscreen that has a sun protection factor of at least 30. In addition, sunscreens with iron oxides have been shown to better prevent melasma relapse by protecting against the shorter wavelengths of visible light.19
- Zaenglein AL, Pathy AL, Schlosser BJ, et al. Guidelines of care for the management of acne vulgaris. J Am Acad Dermatol. 2016;74:945-973.e933.
- Landis ET, Levender MM, Davis SA, et al. Isotretinoin and oral contraceptive use in female acne patients varies by physician specialty: analysis of data from the National Ambulatory Medical Care Survey. J Dermatolog Treat. 2012;23:272-277.
- Fitzpatrick L, Mauer E, Chen CL. Oral contraceptives for acne treatment: US dermatologists’ knowledge, comfort, and prescribing practices. Cutis. 2017;99:195-201.
- Curtis KM, Jatlaoui TC, Tepper NK, et al. U.S. Selected Practice Recommendations for Contraceptive Use, 2016. MMWR Recomm Rep. 2016;65:1-66.
- Curtis KM, Tepper NK, Jatlaoui TC, et al. U.S. Medical Eligibility Criteria for Contraceptive Use, 2016. MMWR Recomm Rep. 2016;65:1-103.
- Van Vliet HA, Grimes DA, Lopez LM, et al. Triphasic versus monophasic oral contraceptives for contraception. Cochrane Database Syst Rev. 2011:CD003553.
- Stewart M, Black K. Choosing a combined oral contraceptive pill. Aust Prescr. 2015;38:6-11.
- McKinney K. Understanding the options: a guide to oral contraceptives. https://www.cecentral.com/assets/2097/022%20Oral%20Contraceptives%2010-26-09.pdf. Published November 5, 2009. Accessed June 20, 2019.
- Gallo MF, Nanda K, Grimes DA, et al. 20 microg versus >20 microg estrogen combined oral contraceptives for contraception. Cochrane Database Syst Rev. 2013:CD003989.
- Terki F, Malhotra U. Medical and Service Delivery Guidelines for Sexual and Reproductive Health Services. London, United Kingdom: International Planned Parenthood Federation; 2004.
- Arowojolu AO, Gallo MF, Lopez LM, et al. Combined oral contraceptive pills for treatment of acne. Cochrane Database Syst Rev. 2012:CD004425.
- Pastor Z, Holla K, Chmel R. The influence of combined oral contraceptives on female sexual desire: a systematic review. Eur J Contracept Reprod Health Care. 2013;18:27-43.
- Gallo MF, Lopez LM, Grimes DA, et al. Combination contraceptives: effects on weight. Cochrane Database Syst Rev. 2014:CD003987.
- Birth control pills for acne: tips from Julie Harper at the Summer AAD. Cutis. https://www.mdedge.com/dermatology/article/144550/acne/birth-control-pills-acne-tips-julie-harper-summer-aad. Published August 14, 2017. Accessed June 24, 2019.
- Watson HG, Baglin TP. Guidelines on travel-related venous thrombosis. Br J Haematol. 2011;152:31-34.
- Roach RE, Helmerhorst FM, Lijfering WM, et al. Combined oral contraceptives: the risk of myocardial infarction and ischemic stroke. Cochrane Database Syst Rev. 2015:CD011054.
- Acute myocardial infarction and combined oral contraceptives: results of an international multicentre case-control study. WHO Collaborative Study of Cardiovascular Disease and Steroid Hormone Contraception. Lancet. 1997;349:1202-1209.
- Resnik S. Melasma induced by oral contraceptive drugs. JAMA. 1967;199:601-605.
- Boukari F, Jourdan E, Fontas E, et al. Prevention of melasma relapses with sunscreen combining protection against UV and short wavelengths of visible light: a prospective randomized comparative trial. J Am Acad Dermatol. 2015;72:189-190.e181.
The American Academy of Dermatology confers combined oral contraceptives (COCs) a strength A recommendation for the treatment of acne based on level I evidence, and 4 COCs are approved for the treatment of acne by the US Food and Drug Administration (FDA).1 Furthermore, when dermatologists prescribe isotretinoin and thalidomide to women of reproductive potential, the iPLEDGE and THALOMID Risk Evaluation and Mitigation Strategy (REMS) programs require 2 concurrent methods of contraception, one of which may be a COC. In addition, COCs have several potential off-label indications in dermatology including idiopathic hirsutism, female pattern hair loss, hidradenitis suppurativa, and autoimmune progesterone dermatitis.
Despite this evidence and opportunity, research suggests that dermatologists underprescribe COCs. The National Ambulatory Medical Care Survey found that between 1993 and 2008, dermatologists in the United States prescribed COCs to only 2.03% of women presenting for acne treatment, which was less often than obstetricians/gynecologists (36.03%) and internists (10.76%).2 More recently, in a survey of 130 US dermatologists conducted from 2014 to 2015, only 55.4% reported prescribing COCs. This survey also found that only 45.8% of dermatologists who prescribed COCs felt very comfortable counseling on how to begin taking them, only 48.6% felt very comfortable counseling patients on side effects, and only 22.2% felt very comfortable managing side effects.3
In light of these data, this article reviews the basics of COCs for dermatology residents, from assessing patient eligibility and selecting a COC to counseling on use and managing risks and side effects. Because there are different approaches to prescribing COCs, readers are encouraged to integrate the information in this article with what they have learned from other sources.
Assess Patient Eligibility
In general, patients should be at least 14 years of age and have waited 2 years after menarche to start COCs. They can be taken until menopause.1,4 Contraindications can be screened for by taking a medical history and measuring a baseline blood pressure (Tables 1 and 2).5 In addition, pregnancy should be excluded with a urine or serum pregnancy test or criteria provided in Box 2 of the 2016 US Selected Practice Recommendations for Contraceptive Use from the Centers for Disease Control and Prevention (CDC).4 Although important for women’s overall health, a pelvic examination is not required to start COCs according to the CDC and the American Academy of Dermatology.1,4
Select the COC
Combined oral contraceptives combine estrogen, usually in the form of ethinyl estradiol, with a progestin. Data suggest that all COCs effectively treat acne, but 4 are specifically FDA approved for acne: ethinyl estradiol–norethindrone acetate–ferrous fumarate, ethinyl estradiol–norgestimate, ethinyl estradiol–drospirenone, and ethinyl estradiol–drospirenone–levomefolate.1 Ethinyl estradiol–desogestrel and ethinyl estradiol–drospirenone are 2 go-to COCs for some of the attending physicians at my residency program. All COCs are FDA approved for contraception. When selecting a COC, one approach is to start with the patient’s drug formulary, then consider the following characteristics.
Monophasic vs Multiphasic
All the hormonally active pills in a monophasic formulation contain the same dose of estrogen and progestin; however, these doses change per pill in a multiphasic formulation, which requires that patients take the pills in a specific order. Given this greater complexity and the fact that multiphasic formulations often are more expensive and lack evidence of superiority, a 2011 Cochrane review recommended monophasic formulations as first line.6 In addition, monophasic formulations are preferred for autoimmune progesterone dermatitis because of the stable progestin dose.
Hormone-Free Interval
Some COCs include placebo pills during which hormone withdrawal symptoms such as bleeding, pelvic pain, mood changes, and headache may occur. If a patient is concerned about these symptoms, choose a COC with no or fewer placebo pills, or have the patient skip the hormone-free interval altogether and start the next pack early7; in this case, the prescription should be written with instructions to allow the patient to get earlier refills from the pharmacy.
Estrogen Dose
To minimize estrogen-related side effects, the lowest possible dose of ethinyl estradiol that is effective and tolerable should be prescribed7,8; 20 μg of ethinyl estradiol generally is the lowest dose available, but it may be associated with more frequent breakthrough bleeding.9 The International Planned Parenthood Federation recommends starting with COCs that contain 30 to 35 μg of estrogen.10 Synthesizing this information, one option is to start with 20 μg of ethinyl estradiol and increase the dose if breakthrough bleeding persists after 3 cycles.
Progestin Type
First-generation progestins (eg, norethindrone), second-generation progestins (eg, norgestrel, levonorgestrel), and third-generation progestins (eg, norgestimate, desogestrel) are derived from testosterone and therefore are variably androgenic; second-generation progestins are the most androgenic, and third-generation progestins are the least. On the other hand, drospirenone, the fourth-generation progestin available in the United States, is derived from 17α-spironolactone and thus is mildly antiandrogenic (3 mg of drospirenone is considered equivalent to 25 mg of spironolactone).
Although COCs with less androgenic progestins should theoretically treat acne better, a 2012 Cochrane review of COCs and acne concluded that “differences in the comparative effectiveness of COCs containing varying progestin types and dosages were less clear, and data were limited for any particular comparison.”11 As a result, regardless of the progestin, all COCs are believed to have a net antiandrogenic effect due to their estrogen component.1
Counsel on Use
Combined oral contraceptives can be started on any day of the menstrual cycle, including the day the prescription is given. If a patient begins a COC within 5 days of the first day of her most recent period, backup contraception is not needed.4 If she begins the COC more than 5 days after the first day of her most recent period, she needs to use backup contraception or abstain from sexual intercourse for the next 7 days.4 In general, at least 3 months of therapy are required to evaluate the effectiveness of COCs for acne.1
Manage Risks and Side Effects
Breakthrough Bleeding
The most common side effect of breakthrough bleeding can be minimized by taking COCs at approximately the same time every day and avoiding missed pills. If breakthrough bleeding does not stop after 3 cycles, consider increasing the estrogen dose to 30 to 35 μg and/or referring to an obstetrician/gynecologist to rule out other etiologies of bleeding.7,8
Nausea, Headache, Bloating, and Breast Tenderness
These symptoms typically resolve after the first 3 months. To minimize nausea, patients should take COCs in the early evening and eat breakfast the next morning.7,8 For headaches that occur during the hormone-free interval, consider skipping the placebo pills and starting the next pack early. Switching the progestin to drospirenone, which has a mild diuretic effect, can help with bloating as well as breast tenderness.7 For persistent symptoms, consider a lower estrogen dose.7,8
Changes in Libido
In a systemic review including 8422 COC users, 64% reported no change in libido, 22% reported an increase, and 15% reported a decrease.12
Weight Gain
Although patients may be concerned that COCs cause weight gain, a 2014 Cochrane review concluded that “available evidence is insufficient to determine the effect of combination contraceptives on weight, but no large effect is evident.”13 If weight gain does occur, anecdotal evidence suggests it tends to be not more than 5 pounds. If weight gain is an issue, consider a less androgenic progestin.8
Venous Thromboembolism
Use the 3-6-9-12 model to contextualize venous thromboembolism (VTE) risk: a woman’s annual VTE risk is 3 per 10,000 women at baseline, 6 per 10,000 women with nondrospirenone COCs, 9 per 10,000 women with drospirenone-containing COCs, and 12 per 10,000 women when pregnant.14 Patients should be counseled on the signs and symptoms of VTE such as unilateral or bilateral leg or arm swelling, pain, warmth, redness, and/or shortness of breath. The British Society for Haematology recommends maintaining mobility as a reasonable precaution when traveling for more than 3 hours.15
Cardiovascular Disease
A 2015 Cochrane review found that the risk for myocardial infarction or ischemic stroke is increased 1.6‐fold in COC users.16 Despite this increased relative risk, the increased absolute annual risk of myocardial infarction in nonsmoking women remains low: increased from 0.83 to 3.53 per 10,000,000 women younger than 35 years and from 9.45 to 40.4 per 10,000,000 women 35 years and older.17
Breast Cancer and Cervical Cancer
Data are mixed on the effect of COCs on the risk for breast cancer and cervical cancer.1 According to the CDC, COC use for 5 or more years might increase the risk of cervical carcinoma in situ and invasive cervical carcinoma in women with persistent human papillomavirus infection.5 Regardless of COC use, women should undergo age-appropriate screening for breast cancer and cervical cancer.
Melasma
Melasma is an estrogen-mediated side effect of COCs.8 A study from 1967 found that 29% of COC users (N=212) developed melasma; however, they were taking COCs with much higher ethinyl estradiol doses (50–100 μg) than typically used today.18 Nevertheless, as part of an overall skin care regimen, photoprotection should be encouraged with a broad-spectrum, water-resistant sunscreen that has a sun protection factor of at least 30. In addition, sunscreens with iron oxides have been shown to better prevent melasma relapse by protecting against the shorter wavelengths of visible light.19
The American Academy of Dermatology confers combined oral contraceptives (COCs) a strength A recommendation for the treatment of acne based on level I evidence, and 4 COCs are approved for the treatment of acne by the US Food and Drug Administration (FDA).1 Furthermore, when dermatologists prescribe isotretinoin and thalidomide to women of reproductive potential, the iPLEDGE and THALOMID Risk Evaluation and Mitigation Strategy (REMS) programs require 2 concurrent methods of contraception, one of which may be a COC. In addition, COCs have several potential off-label indications in dermatology including idiopathic hirsutism, female pattern hair loss, hidradenitis suppurativa, and autoimmune progesterone dermatitis.
Despite this evidence and opportunity, research suggests that dermatologists underprescribe COCs. The National Ambulatory Medical Care Survey found that between 1993 and 2008, dermatologists in the United States prescribed COCs to only 2.03% of women presenting for acne treatment, which was less often than obstetricians/gynecologists (36.03%) and internists (10.76%).2 More recently, in a survey of 130 US dermatologists conducted from 2014 to 2015, only 55.4% reported prescribing COCs. This survey also found that only 45.8% of dermatologists who prescribed COCs felt very comfortable counseling on how to begin taking them, only 48.6% felt very comfortable counseling patients on side effects, and only 22.2% felt very comfortable managing side effects.3
In light of these data, this article reviews the basics of COCs for dermatology residents, from assessing patient eligibility and selecting a COC to counseling on use and managing risks and side effects. Because there are different approaches to prescribing COCs, readers are encouraged to integrate the information in this article with what they have learned from other sources.
Assess Patient Eligibility
In general, patients should be at least 14 years of age and have waited 2 years after menarche to start COCs. They can be taken until menopause.1,4 Contraindications can be screened for by taking a medical history and measuring a baseline blood pressure (Tables 1 and 2).5 In addition, pregnancy should be excluded with a urine or serum pregnancy test or criteria provided in Box 2 of the 2016 US Selected Practice Recommendations for Contraceptive Use from the Centers for Disease Control and Prevention (CDC).4 Although important for women’s overall health, a pelvic examination is not required to start COCs according to the CDC and the American Academy of Dermatology.1,4
Select the COC
Combined oral contraceptives combine estrogen, usually in the form of ethinyl estradiol, with a progestin. Data suggest that all COCs effectively treat acne, but 4 are specifically FDA approved for acne: ethinyl estradiol–norethindrone acetate–ferrous fumarate, ethinyl estradiol–norgestimate, ethinyl estradiol–drospirenone, and ethinyl estradiol–drospirenone–levomefolate.1 Ethinyl estradiol–desogestrel and ethinyl estradiol–drospirenone are 2 go-to COCs for some of the attending physicians at my residency program. All COCs are FDA approved for contraception. When selecting a COC, one approach is to start with the patient’s drug formulary, then consider the following characteristics.
Monophasic vs Multiphasic
All the hormonally active pills in a monophasic formulation contain the same dose of estrogen and progestin; however, these doses change per pill in a multiphasic formulation, which requires that patients take the pills in a specific order. Given this greater complexity and the fact that multiphasic formulations often are more expensive and lack evidence of superiority, a 2011 Cochrane review recommended monophasic formulations as first line.6 In addition, monophasic formulations are preferred for autoimmune progesterone dermatitis because of the stable progestin dose.
Hormone-Free Interval
Some COCs include placebo pills during which hormone withdrawal symptoms such as bleeding, pelvic pain, mood changes, and headache may occur. If a patient is concerned about these symptoms, choose a COC with no or fewer placebo pills, or have the patient skip the hormone-free interval altogether and start the next pack early7; in this case, the prescription should be written with instructions to allow the patient to get earlier refills from the pharmacy.
Estrogen Dose
To minimize estrogen-related side effects, the lowest possible dose of ethinyl estradiol that is effective and tolerable should be prescribed7,8; 20 μg of ethinyl estradiol generally is the lowest dose available, but it may be associated with more frequent breakthrough bleeding.9 The International Planned Parenthood Federation recommends starting with COCs that contain 30 to 35 μg of estrogen.10 Synthesizing this information, one option is to start with 20 μg of ethinyl estradiol and increase the dose if breakthrough bleeding persists after 3 cycles.
Progestin Type
First-generation progestins (eg, norethindrone), second-generation progestins (eg, norgestrel, levonorgestrel), and third-generation progestins (eg, norgestimate, desogestrel) are derived from testosterone and therefore are variably androgenic; second-generation progestins are the most androgenic, and third-generation progestins are the least. On the other hand, drospirenone, the fourth-generation progestin available in the United States, is derived from 17α-spironolactone and thus is mildly antiandrogenic (3 mg of drospirenone is considered equivalent to 25 mg of spironolactone).
Although COCs with less androgenic progestins should theoretically treat acne better, a 2012 Cochrane review of COCs and acne concluded that “differences in the comparative effectiveness of COCs containing varying progestin types and dosages were less clear, and data were limited for any particular comparison.”11 As a result, regardless of the progestin, all COCs are believed to have a net antiandrogenic effect due to their estrogen component.1
Counsel on Use
Combined oral contraceptives can be started on any day of the menstrual cycle, including the day the prescription is given. If a patient begins a COC within 5 days of the first day of her most recent period, backup contraception is not needed.4 If she begins the COC more than 5 days after the first day of her most recent period, she needs to use backup contraception or abstain from sexual intercourse for the next 7 days.4 In general, at least 3 months of therapy are required to evaluate the effectiveness of COCs for acne.1
Manage Risks and Side Effects
Breakthrough Bleeding
The most common side effect of breakthrough bleeding can be minimized by taking COCs at approximately the same time every day and avoiding missed pills. If breakthrough bleeding does not stop after 3 cycles, consider increasing the estrogen dose to 30 to 35 μg and/or referring to an obstetrician/gynecologist to rule out other etiologies of bleeding.7,8
Nausea, Headache, Bloating, and Breast Tenderness
These symptoms typically resolve after the first 3 months. To minimize nausea, patients should take COCs in the early evening and eat breakfast the next morning.7,8 For headaches that occur during the hormone-free interval, consider skipping the placebo pills and starting the next pack early. Switching the progestin to drospirenone, which has a mild diuretic effect, can help with bloating as well as breast tenderness.7 For persistent symptoms, consider a lower estrogen dose.7,8
Changes in Libido
In a systemic review including 8422 COC users, 64% reported no change in libido, 22% reported an increase, and 15% reported a decrease.12
Weight Gain
Although patients may be concerned that COCs cause weight gain, a 2014 Cochrane review concluded that “available evidence is insufficient to determine the effect of combination contraceptives on weight, but no large effect is evident.”13 If weight gain does occur, anecdotal evidence suggests it tends to be not more than 5 pounds. If weight gain is an issue, consider a less androgenic progestin.8
Venous Thromboembolism
Use the 3-6-9-12 model to contextualize venous thromboembolism (VTE) risk: a woman’s annual VTE risk is 3 per 10,000 women at baseline, 6 per 10,000 women with nondrospirenone COCs, 9 per 10,000 women with drospirenone-containing COCs, and 12 per 10,000 women when pregnant.14 Patients should be counseled on the signs and symptoms of VTE such as unilateral or bilateral leg or arm swelling, pain, warmth, redness, and/or shortness of breath. The British Society for Haematology recommends maintaining mobility as a reasonable precaution when traveling for more than 3 hours.15
Cardiovascular Disease
A 2015 Cochrane review found that the risk for myocardial infarction or ischemic stroke is increased 1.6‐fold in COC users.16 Despite this increased relative risk, the increased absolute annual risk of myocardial infarction in nonsmoking women remains low: increased from 0.83 to 3.53 per 10,000,000 women younger than 35 years and from 9.45 to 40.4 per 10,000,000 women 35 years and older.17
Breast Cancer and Cervical Cancer
Data are mixed on the effect of COCs on the risk for breast cancer and cervical cancer.1 According to the CDC, COC use for 5 or more years might increase the risk of cervical carcinoma in situ and invasive cervical carcinoma in women with persistent human papillomavirus infection.5 Regardless of COC use, women should undergo age-appropriate screening for breast cancer and cervical cancer.
Melasma
Melasma is an estrogen-mediated side effect of COCs.8 A study from 1967 found that 29% of COC users (N=212) developed melasma; however, they were taking COCs with much higher ethinyl estradiol doses (50–100 μg) than typically used today.18 Nevertheless, as part of an overall skin care regimen, photoprotection should be encouraged with a broad-spectrum, water-resistant sunscreen that has a sun protection factor of at least 30. In addition, sunscreens with iron oxides have been shown to better prevent melasma relapse by protecting against the shorter wavelengths of visible light.19
- Zaenglein AL, Pathy AL, Schlosser BJ, et al. Guidelines of care for the management of acne vulgaris. J Am Acad Dermatol. 2016;74:945-973.e933.
- Landis ET, Levender MM, Davis SA, et al. Isotretinoin and oral contraceptive use in female acne patients varies by physician specialty: analysis of data from the National Ambulatory Medical Care Survey. J Dermatolog Treat. 2012;23:272-277.
- Fitzpatrick L, Mauer E, Chen CL. Oral contraceptives for acne treatment: US dermatologists’ knowledge, comfort, and prescribing practices. Cutis. 2017;99:195-201.
- Curtis KM, Jatlaoui TC, Tepper NK, et al. U.S. Selected Practice Recommendations for Contraceptive Use, 2016. MMWR Recomm Rep. 2016;65:1-66.
- Curtis KM, Tepper NK, Jatlaoui TC, et al. U.S. Medical Eligibility Criteria for Contraceptive Use, 2016. MMWR Recomm Rep. 2016;65:1-103.
- Van Vliet HA, Grimes DA, Lopez LM, et al. Triphasic versus monophasic oral contraceptives for contraception. Cochrane Database Syst Rev. 2011:CD003553.
- Stewart M, Black K. Choosing a combined oral contraceptive pill. Aust Prescr. 2015;38:6-11.
- McKinney K. Understanding the options: a guide to oral contraceptives. https://www.cecentral.com/assets/2097/022%20Oral%20Contraceptives%2010-26-09.pdf. Published November 5, 2009. Accessed June 20, 2019.
- Gallo MF, Nanda K, Grimes DA, et al. 20 microg versus >20 microg estrogen combined oral contraceptives for contraception. Cochrane Database Syst Rev. 2013:CD003989.
- Terki F, Malhotra U. Medical and Service Delivery Guidelines for Sexual and Reproductive Health Services. London, United Kingdom: International Planned Parenthood Federation; 2004.
- Arowojolu AO, Gallo MF, Lopez LM, et al. Combined oral contraceptive pills for treatment of acne. Cochrane Database Syst Rev. 2012:CD004425.
- Pastor Z, Holla K, Chmel R. The influence of combined oral contraceptives on female sexual desire: a systematic review. Eur J Contracept Reprod Health Care. 2013;18:27-43.
- Gallo MF, Lopez LM, Grimes DA, et al. Combination contraceptives: effects on weight. Cochrane Database Syst Rev. 2014:CD003987.
- Birth control pills for acne: tips from Julie Harper at the Summer AAD. Cutis. https://www.mdedge.com/dermatology/article/144550/acne/birth-control-pills-acne-tips-julie-harper-summer-aad. Published August 14, 2017. Accessed June 24, 2019.
- Watson HG, Baglin TP. Guidelines on travel-related venous thrombosis. Br J Haematol. 2011;152:31-34.
- Roach RE, Helmerhorst FM, Lijfering WM, et al. Combined oral contraceptives: the risk of myocardial infarction and ischemic stroke. Cochrane Database Syst Rev. 2015:CD011054.
- Acute myocardial infarction and combined oral contraceptives: results of an international multicentre case-control study. WHO Collaborative Study of Cardiovascular Disease and Steroid Hormone Contraception. Lancet. 1997;349:1202-1209.
- Resnik S. Melasma induced by oral contraceptive drugs. JAMA. 1967;199:601-605.
- Boukari F, Jourdan E, Fontas E, et al. Prevention of melasma relapses with sunscreen combining protection against UV and short wavelengths of visible light: a prospective randomized comparative trial. J Am Acad Dermatol. 2015;72:189-190.e181.
- Zaenglein AL, Pathy AL, Schlosser BJ, et al. Guidelines of care for the management of acne vulgaris. J Am Acad Dermatol. 2016;74:945-973.e933.
- Landis ET, Levender MM, Davis SA, et al. Isotretinoin and oral contraceptive use in female acne patients varies by physician specialty: analysis of data from the National Ambulatory Medical Care Survey. J Dermatolog Treat. 2012;23:272-277.
- Fitzpatrick L, Mauer E, Chen CL. Oral contraceptives for acne treatment: US dermatologists’ knowledge, comfort, and prescribing practices. Cutis. 2017;99:195-201.
- Curtis KM, Jatlaoui TC, Tepper NK, et al. U.S. Selected Practice Recommendations for Contraceptive Use, 2016. MMWR Recomm Rep. 2016;65:1-66.
- Curtis KM, Tepper NK, Jatlaoui TC, et al. U.S. Medical Eligibility Criteria for Contraceptive Use, 2016. MMWR Recomm Rep. 2016;65:1-103.
- Van Vliet HA, Grimes DA, Lopez LM, et al. Triphasic versus monophasic oral contraceptives for contraception. Cochrane Database Syst Rev. 2011:CD003553.
- Stewart M, Black K. Choosing a combined oral contraceptive pill. Aust Prescr. 2015;38:6-11.
- McKinney K. Understanding the options: a guide to oral contraceptives. https://www.cecentral.com/assets/2097/022%20Oral%20Contraceptives%2010-26-09.pdf. Published November 5, 2009. Accessed June 20, 2019.
- Gallo MF, Nanda K, Grimes DA, et al. 20 microg versus >20 microg estrogen combined oral contraceptives for contraception. Cochrane Database Syst Rev. 2013:CD003989.
- Terki F, Malhotra U. Medical and Service Delivery Guidelines for Sexual and Reproductive Health Services. London, United Kingdom: International Planned Parenthood Federation; 2004.
- Arowojolu AO, Gallo MF, Lopez LM, et al. Combined oral contraceptive pills for treatment of acne. Cochrane Database Syst Rev. 2012:CD004425.
- Pastor Z, Holla K, Chmel R. The influence of combined oral contraceptives on female sexual desire: a systematic review. Eur J Contracept Reprod Health Care. 2013;18:27-43.
- Gallo MF, Lopez LM, Grimes DA, et al. Combination contraceptives: effects on weight. Cochrane Database Syst Rev. 2014:CD003987.
- Birth control pills for acne: tips from Julie Harper at the Summer AAD. Cutis. https://www.mdedge.com/dermatology/article/144550/acne/birth-control-pills-acne-tips-julie-harper-summer-aad. Published August 14, 2017. Accessed June 24, 2019.
- Watson HG, Baglin TP. Guidelines on travel-related venous thrombosis. Br J Haematol. 2011;152:31-34.
- Roach RE, Helmerhorst FM, Lijfering WM, et al. Combined oral contraceptives: the risk of myocardial infarction and ischemic stroke. Cochrane Database Syst Rev. 2015:CD011054.
- Acute myocardial infarction and combined oral contraceptives: results of an international multicentre case-control study. WHO Collaborative Study of Cardiovascular Disease and Steroid Hormone Contraception. Lancet. 1997;349:1202-1209.
- Resnik S. Melasma induced by oral contraceptive drugs. JAMA. 1967;199:601-605.
- Boukari F, Jourdan E, Fontas E, et al. Prevention of melasma relapses with sunscreen combining protection against UV and short wavelengths of visible light: a prospective randomized comparative trial. J Am Acad Dermatol. 2015;72:189-190.e181.
Resident Pearls
- Screen for contraindications to combined oral contraceptives (COCs) by taking a medical history, measuring a baseline blood pressure, and excluding pregnancy. A baseline pelvic examination is unnecessary.
- Characteristics to consider when selecting a COC include the formulation, hormone-free interval, estrogen dose, and progestin type.
- Combined oral contraceptives can be initiated on any day of the menstrual cycle, with the need for backup contraception based on the number of days since the first day of the patient’s most recent period.
- Management of risks and side effects includes simple lifestyle changes, skipping the hormone-free interval, switching the COC, and referring to an obstetrician/gynecologist.
Surgical Dermatoethics for the Trainee
It is an uncomfortable and unavoidable reality as physicians that for every procedure we learn, there must be a first time we perform it. As with any type of skill, it takes practice to become proficient. The unique challenge in medicine is that the practice involves performing procedures on real patients. We cannot avoid the hands-on nature of the training process; we can, however, approach its ethical challenges mindfully. Herein, I will discuss some of the ethical considerations in providing care as a trainee and identify potential barriers to best practices, particularly as they relate to procedural dermatology.
Tell Patients You Are in Training
In every patient encounter, we must introduce ourselves as a trainee. The principle of right to the truth dictates that we are transparent about our level of training and do not misrepresent ourselves to our patients. A statement released by the American Medical Association (AMA) Council on Ethical and Judicial Affairs asserts that “[p]atients should be informed of the identity and training status of individuals involved in their care.”1
Although straightforward in theory, this mandate is not always simple in practice. With patients unfamiliar with the health care system, it could be more onerous to clearly communicate training status than simply introducing oneself as a resident. A study conducted in the emergency department at Vanderbilt University Hospital (Nashville, Tennessee) found that many patients and their family members (N=430) did not understand the various roles and responsibilities of physicians in the teaching hospital setting. For example, 30% believed an attending physician requires supervision by a resident, and an additional 17% of those surveyed were not sure.2 The AMA requests we “refrain from using terms that may be confusing when describing the training status of the students,”1 which evidently is audience specific. Thus, as with any type of patient education, a thorough introduction may require assessment of understanding.
Disclosure of Experience Level With a Particular Procedure
There is a clear professional expectation that we disclose to patients that we are in training; however, a universal standard does not exist for disclosure of our exact level of experience in a particular procedure. Do we need to tell patients if it is our first time performing a given procedure? What if it is our tenth? Multiple studies have found that patients want specifics. In one study of bariatric surgery patients (N=108), 93% felt that they should always be informed if it was the first time a trainee was performing a particular procedure.3 A study conducted in the emergency department setting (N=202) also found that the majority of patients thought they should be informed if a resident was performing a procedure for the first time, but the distribution differed by procedure (66% for suturing vs 82% for lumbar puncture).4
Despite these findings, this degree of specificity is not always discussed with patients and perhaps does not need to be. LaRosa and Grant-Kels5 analyzed a hypothetical scenario in which a dermatology resident is to perform his first excision under attending supervision and concluded that broad disclosure of training status would suffice in the given scenario, as it would not be necessary to state that it was his first time performing an excision. It is unclear if the same conclusion could be drawn for all procedures and levels of experience. Outcome data would help inform the analysis, but the available data are from other specialties including general surgery, gynecology, and urology. Some studies demonstrate an increased risk of adverse outcomes with trainee involvement in procedures such as bariatric surgery and emergency general surgery, but the data are mixed and may not be generalizable to dermatologic procedures.6-8
The appropriate level of detail to disclose regarding a physician’s experience may need to be assessed on a case-by-case basis, and the principles of informed consent can help. Informed consent requires understanding of the diagnosis, the treatment options including nonintervention, and the risks and benefits of each alternative. In obtaining informed consent, we must disclose “any facts which are necessary to form the basis of an intelligent consent by the patient to the proposed treatment.”9 Providers must determine what aspects of a trainee’s experience level are relevant to the risk-benefit analysis in a given set of circumstances. Surely, there is a large degree of subjectivity in this determination as data are limited, but information deemed relevant must be shared. Information that is inconsequential, on the other hand, may be omitted. It could even be argued that more detailed information, especially if it may cause anxiety, would be detrimental to share. For example, we would not list the chemical name of every preservative in every vaccine we recommend for children if there is no evidence of inflicting harm. If the information has not been shown to have clinical impact or affect safety concerns, the anxiety may be undue.
Withholding Information Can Violate Ethical Principles
We must be careful not to withhold details of our experience level with a particular procedure for the wrong reasons. It would be wrong, for example, to withhold information simply to avoid causing anxiety, which could be seen as an invocation of therapeutic privilege, a controversial practice of withholding important information that poses a psychological threat to the patient. A classic example is the physician who defers disclosure of a terminal diagnosis to preserve hope. Although therapeutic privilege theoretically promotes the principle of beneficence, it violates the principles of autonomy and right to truth and therefore generally is regarded as unethically paternalistic in modern medical ethics.9
Patients Can Refuse Trainee Participation
It also is unethical to withhold information to obtain consent and avoid refusal of our care. Refusal of trainee participation is not uncommon. In the aforementioned study of bariatric surgery patients, 92.4% supported their procedure being performed at a teaching hospital, but only 56% would consent to a resident assisting staff during the procedure. A mere 33% of those patients would consent to a resident primarily performing with staff assisting.3 Although the proportion of patients who refuse certainly depends on the type of procedure among other factors, it is a reality in any teaching environment. The training paradigm in medicine depends on being able to practice procedures with supervision before we are independent providers. If patients refuse our care, our training suffers. However, the AMA maintains that “[p]atients are free to choose from whom they receive treatment,”1 and we must respect this aspect of patient autonomy.
Final Thoughts
When it comes to the performance of procedures, there are a few basic principles to keep in mind to provide ethical care to our patients while we are in training. Although we must accept that a crucial part of learning dermatologic procedures is hands on with real patients, we also need to come prepared having learned what we can through reading and practice with cadavers or skin substitutes. Procedures we execute as residents should be performed with adequate supervision, and as we progress through residency, we should be given increased autonomy and graded responsibility to prepare us for independent practice at graduation. Although it is the responsibility of the attending physician to provide appropriate oversight for the resident’s level of training, we should feel empowered to ask for help and have the humility to know when we need it.
- Medical student involvement in patient care: report of the council on ethical and judicial affairs. Virtual Mentor. 2001;3. doi:10.1001/virtualmentor.2001.3.3.code1-0103.
- Santen S, Hemphill RR, Prough E, et al. Do patients understand their physician’s level of training? a survey of emergency department patients. Acad Med. 2004;79:139-143.
- McClellan JM, Nelson D, Porta CR, et al. Bariatric surgery patient perceptions and willingness to consent to resident participation. Surg Obes Relat Dis. 2016;12:1065-1071.
- Santen SA, Hemphill RR, McDonald MF, et al. Patients’ willingness to allow residents to learn to practice medical procedures. Acad Med. 2004;79:144-147.
- LaRosa C, Grant-Kels JM. See one, do one, teach one: the ethical dilemma of residents performing their first procedure on patients. J Am Acad Dermatol. 2016;75:845-848.
- Can MF. The trainee effect on early postoperative surgical outcomes: reflects the effect of resident involvement or hospital capacity to overcome complications? J Invest Surg. 2017;31:67-68.
- Goldberg I, Yang J, Park J, et al. Surgical trainee impact on bariatric surgery safety [published online November 13, 2018]. Surg Endosc. doi:10.1007/s00464-018-6587-0.
- Kasotakis G, Lakha A, Sarkar B, et al. Trainee participation is associated with adverse outcomes in emergency general surgery: an analysis of the National Surgical Quality Improvement Program database. Ann Surg. 2014;3:483-490.
- Richard C, Lajeunesse Y, Lussier MT. Therapeutic privilege: between the ethics of lying and the practice of truth. J Med Ethics. 2010;36:353-357.
It is an uncomfortable and unavoidable reality as physicians that for every procedure we learn, there must be a first time we perform it. As with any type of skill, it takes practice to become proficient. The unique challenge in medicine is that the practice involves performing procedures on real patients. We cannot avoid the hands-on nature of the training process; we can, however, approach its ethical challenges mindfully. Herein, I will discuss some of the ethical considerations in providing care as a trainee and identify potential barriers to best practices, particularly as they relate to procedural dermatology.
Tell Patients You Are in Training
In every patient encounter, we must introduce ourselves as a trainee. The principle of right to the truth dictates that we are transparent about our level of training and do not misrepresent ourselves to our patients. A statement released by the American Medical Association (AMA) Council on Ethical and Judicial Affairs asserts that “[p]atients should be informed of the identity and training status of individuals involved in their care.”1
Although straightforward in theory, this mandate is not always simple in practice. With patients unfamiliar with the health care system, it could be more onerous to clearly communicate training status than simply introducing oneself as a resident. A study conducted in the emergency department at Vanderbilt University Hospital (Nashville, Tennessee) found that many patients and their family members (N=430) did not understand the various roles and responsibilities of physicians in the teaching hospital setting. For example, 30% believed an attending physician requires supervision by a resident, and an additional 17% of those surveyed were not sure.2 The AMA requests we “refrain from using terms that may be confusing when describing the training status of the students,”1 which evidently is audience specific. Thus, as with any type of patient education, a thorough introduction may require assessment of understanding.
Disclosure of Experience Level With a Particular Procedure
There is a clear professional expectation that we disclose to patients that we are in training; however, a universal standard does not exist for disclosure of our exact level of experience in a particular procedure. Do we need to tell patients if it is our first time performing a given procedure? What if it is our tenth? Multiple studies have found that patients want specifics. In one study of bariatric surgery patients (N=108), 93% felt that they should always be informed if it was the first time a trainee was performing a particular procedure.3 A study conducted in the emergency department setting (N=202) also found that the majority of patients thought they should be informed if a resident was performing a procedure for the first time, but the distribution differed by procedure (66% for suturing vs 82% for lumbar puncture).4
Despite these findings, this degree of specificity is not always discussed with patients and perhaps does not need to be. LaRosa and Grant-Kels5 analyzed a hypothetical scenario in which a dermatology resident is to perform his first excision under attending supervision and concluded that broad disclosure of training status would suffice in the given scenario, as it would not be necessary to state that it was his first time performing an excision. It is unclear if the same conclusion could be drawn for all procedures and levels of experience. Outcome data would help inform the analysis, but the available data are from other specialties including general surgery, gynecology, and urology. Some studies demonstrate an increased risk of adverse outcomes with trainee involvement in procedures such as bariatric surgery and emergency general surgery, but the data are mixed and may not be generalizable to dermatologic procedures.6-8
The appropriate level of detail to disclose regarding a physician’s experience may need to be assessed on a case-by-case basis, and the principles of informed consent can help. Informed consent requires understanding of the diagnosis, the treatment options including nonintervention, and the risks and benefits of each alternative. In obtaining informed consent, we must disclose “any facts which are necessary to form the basis of an intelligent consent by the patient to the proposed treatment.”9 Providers must determine what aspects of a trainee’s experience level are relevant to the risk-benefit analysis in a given set of circumstances. Surely, there is a large degree of subjectivity in this determination as data are limited, but information deemed relevant must be shared. Information that is inconsequential, on the other hand, may be omitted. It could even be argued that more detailed information, especially if it may cause anxiety, would be detrimental to share. For example, we would not list the chemical name of every preservative in every vaccine we recommend for children if there is no evidence of inflicting harm. If the information has not been shown to have clinical impact or affect safety concerns, the anxiety may be undue.
Withholding Information Can Violate Ethical Principles
We must be careful not to withhold details of our experience level with a particular procedure for the wrong reasons. It would be wrong, for example, to withhold information simply to avoid causing anxiety, which could be seen as an invocation of therapeutic privilege, a controversial practice of withholding important information that poses a psychological threat to the patient. A classic example is the physician who defers disclosure of a terminal diagnosis to preserve hope. Although therapeutic privilege theoretically promotes the principle of beneficence, it violates the principles of autonomy and right to truth and therefore generally is regarded as unethically paternalistic in modern medical ethics.9
Patients Can Refuse Trainee Participation
It also is unethical to withhold information to obtain consent and avoid refusal of our care. Refusal of trainee participation is not uncommon. In the aforementioned study of bariatric surgery patients, 92.4% supported their procedure being performed at a teaching hospital, but only 56% would consent to a resident assisting staff during the procedure. A mere 33% of those patients would consent to a resident primarily performing with staff assisting.3 Although the proportion of patients who refuse certainly depends on the type of procedure among other factors, it is a reality in any teaching environment. The training paradigm in medicine depends on being able to practice procedures with supervision before we are independent providers. If patients refuse our care, our training suffers. However, the AMA maintains that “[p]atients are free to choose from whom they receive treatment,”1 and we must respect this aspect of patient autonomy.
Final Thoughts
When it comes to the performance of procedures, there are a few basic principles to keep in mind to provide ethical care to our patients while we are in training. Although we must accept that a crucial part of learning dermatologic procedures is hands on with real patients, we also need to come prepared having learned what we can through reading and practice with cadavers or skin substitutes. Procedures we execute as residents should be performed with adequate supervision, and as we progress through residency, we should be given increased autonomy and graded responsibility to prepare us for independent practice at graduation. Although it is the responsibility of the attending physician to provide appropriate oversight for the resident’s level of training, we should feel empowered to ask for help and have the humility to know when we need it.
It is an uncomfortable and unavoidable reality as physicians that for every procedure we learn, there must be a first time we perform it. As with any type of skill, it takes practice to become proficient. The unique challenge in medicine is that the practice involves performing procedures on real patients. We cannot avoid the hands-on nature of the training process; we can, however, approach its ethical challenges mindfully. Herein, I will discuss some of the ethical considerations in providing care as a trainee and identify potential barriers to best practices, particularly as they relate to procedural dermatology.
Tell Patients You Are in Training
In every patient encounter, we must introduce ourselves as a trainee. The principle of right to the truth dictates that we are transparent about our level of training and do not misrepresent ourselves to our patients. A statement released by the American Medical Association (AMA) Council on Ethical and Judicial Affairs asserts that “[p]atients should be informed of the identity and training status of individuals involved in their care.”1
Although straightforward in theory, this mandate is not always simple in practice. With patients unfamiliar with the health care system, it could be more onerous to clearly communicate training status than simply introducing oneself as a resident. A study conducted in the emergency department at Vanderbilt University Hospital (Nashville, Tennessee) found that many patients and their family members (N=430) did not understand the various roles and responsibilities of physicians in the teaching hospital setting. For example, 30% believed an attending physician requires supervision by a resident, and an additional 17% of those surveyed were not sure.2 The AMA requests we “refrain from using terms that may be confusing when describing the training status of the students,”1 which evidently is audience specific. Thus, as with any type of patient education, a thorough introduction may require assessment of understanding.
Disclosure of Experience Level With a Particular Procedure
There is a clear professional expectation that we disclose to patients that we are in training; however, a universal standard does not exist for disclosure of our exact level of experience in a particular procedure. Do we need to tell patients if it is our first time performing a given procedure? What if it is our tenth? Multiple studies have found that patients want specifics. In one study of bariatric surgery patients (N=108), 93% felt that they should always be informed if it was the first time a trainee was performing a particular procedure.3 A study conducted in the emergency department setting (N=202) also found that the majority of patients thought they should be informed if a resident was performing a procedure for the first time, but the distribution differed by procedure (66% for suturing vs 82% for lumbar puncture).4
Despite these findings, this degree of specificity is not always discussed with patients and perhaps does not need to be. LaRosa and Grant-Kels5 analyzed a hypothetical scenario in which a dermatology resident is to perform his first excision under attending supervision and concluded that broad disclosure of training status would suffice in the given scenario, as it would not be necessary to state that it was his first time performing an excision. It is unclear if the same conclusion could be drawn for all procedures and levels of experience. Outcome data would help inform the analysis, but the available data are from other specialties including general surgery, gynecology, and urology. Some studies demonstrate an increased risk of adverse outcomes with trainee involvement in procedures such as bariatric surgery and emergency general surgery, but the data are mixed and may not be generalizable to dermatologic procedures.6-8
The appropriate level of detail to disclose regarding a physician’s experience may need to be assessed on a case-by-case basis, and the principles of informed consent can help. Informed consent requires understanding of the diagnosis, the treatment options including nonintervention, and the risks and benefits of each alternative. In obtaining informed consent, we must disclose “any facts which are necessary to form the basis of an intelligent consent by the patient to the proposed treatment.”9 Providers must determine what aspects of a trainee’s experience level are relevant to the risk-benefit analysis in a given set of circumstances. Surely, there is a large degree of subjectivity in this determination as data are limited, but information deemed relevant must be shared. Information that is inconsequential, on the other hand, may be omitted. It could even be argued that more detailed information, especially if it may cause anxiety, would be detrimental to share. For example, we would not list the chemical name of every preservative in every vaccine we recommend for children if there is no evidence of inflicting harm. If the information has not been shown to have clinical impact or affect safety concerns, the anxiety may be undue.
Withholding Information Can Violate Ethical Principles
We must be careful not to withhold details of our experience level with a particular procedure for the wrong reasons. It would be wrong, for example, to withhold information simply to avoid causing anxiety, which could be seen as an invocation of therapeutic privilege, a controversial practice of withholding important information that poses a psychological threat to the patient. A classic example is the physician who defers disclosure of a terminal diagnosis to preserve hope. Although therapeutic privilege theoretically promotes the principle of beneficence, it violates the principles of autonomy and right to truth and therefore generally is regarded as unethically paternalistic in modern medical ethics.9
Patients Can Refuse Trainee Participation
It also is unethical to withhold information to obtain consent and avoid refusal of our care. Refusal of trainee participation is not uncommon. In the aforementioned study of bariatric surgery patients, 92.4% supported their procedure being performed at a teaching hospital, but only 56% would consent to a resident assisting staff during the procedure. A mere 33% of those patients would consent to a resident primarily performing with staff assisting.3 Although the proportion of patients who refuse certainly depends on the type of procedure among other factors, it is a reality in any teaching environment. The training paradigm in medicine depends on being able to practice procedures with supervision before we are independent providers. If patients refuse our care, our training suffers. However, the AMA maintains that “[p]atients are free to choose from whom they receive treatment,”1 and we must respect this aspect of patient autonomy.
Final Thoughts
When it comes to the performance of procedures, there are a few basic principles to keep in mind to provide ethical care to our patients while we are in training. Although we must accept that a crucial part of learning dermatologic procedures is hands on with real patients, we also need to come prepared having learned what we can through reading and practice with cadavers or skin substitutes. Procedures we execute as residents should be performed with adequate supervision, and as we progress through residency, we should be given increased autonomy and graded responsibility to prepare us for independent practice at graduation. Although it is the responsibility of the attending physician to provide appropriate oversight for the resident’s level of training, we should feel empowered to ask for help and have the humility to know when we need it.
- Medical student involvement in patient care: report of the council on ethical and judicial affairs. Virtual Mentor. 2001;3. doi:10.1001/virtualmentor.2001.3.3.code1-0103.
- Santen S, Hemphill RR, Prough E, et al. Do patients understand their physician’s level of training? a survey of emergency department patients. Acad Med. 2004;79:139-143.
- McClellan JM, Nelson D, Porta CR, et al. Bariatric surgery patient perceptions and willingness to consent to resident participation. Surg Obes Relat Dis. 2016;12:1065-1071.
- Santen SA, Hemphill RR, McDonald MF, et al. Patients’ willingness to allow residents to learn to practice medical procedures. Acad Med. 2004;79:144-147.
- LaRosa C, Grant-Kels JM. See one, do one, teach one: the ethical dilemma of residents performing their first procedure on patients. J Am Acad Dermatol. 2016;75:845-848.
- Can MF. The trainee effect on early postoperative surgical outcomes: reflects the effect of resident involvement or hospital capacity to overcome complications? J Invest Surg. 2017;31:67-68.
- Goldberg I, Yang J, Park J, et al. Surgical trainee impact on bariatric surgery safety [published online November 13, 2018]. Surg Endosc. doi:10.1007/s00464-018-6587-0.
- Kasotakis G, Lakha A, Sarkar B, et al. Trainee participation is associated with adverse outcomes in emergency general surgery: an analysis of the National Surgical Quality Improvement Program database. Ann Surg. 2014;3:483-490.
- Richard C, Lajeunesse Y, Lussier MT. Therapeutic privilege: between the ethics of lying and the practice of truth. J Med Ethics. 2010;36:353-357.
- Medical student involvement in patient care: report of the council on ethical and judicial affairs. Virtual Mentor. 2001;3. doi:10.1001/virtualmentor.2001.3.3.code1-0103.
- Santen S, Hemphill RR, Prough E, et al. Do patients understand their physician’s level of training? a survey of emergency department patients. Acad Med. 2004;79:139-143.
- McClellan JM, Nelson D, Porta CR, et al. Bariatric surgery patient perceptions and willingness to consent to resident participation. Surg Obes Relat Dis. 2016;12:1065-1071.
- Santen SA, Hemphill RR, McDonald MF, et al. Patients’ willingness to allow residents to learn to practice medical procedures. Acad Med. 2004;79:144-147.
- LaRosa C, Grant-Kels JM. See one, do one, teach one: the ethical dilemma of residents performing their first procedure on patients. J Am Acad Dermatol. 2016;75:845-848.
- Can MF. The trainee effect on early postoperative surgical outcomes: reflects the effect of resident involvement or hospital capacity to overcome complications? J Invest Surg. 2017;31:67-68.
- Goldberg I, Yang J, Park J, et al. Surgical trainee impact on bariatric surgery safety [published online November 13, 2018]. Surg Endosc. doi:10.1007/s00464-018-6587-0.
- Kasotakis G, Lakha A, Sarkar B, et al. Trainee participation is associated with adverse outcomes in emergency general surgery: an analysis of the National Surgical Quality Improvement Program database. Ann Surg. 2014;3:483-490.
- Richard C, Lajeunesse Y, Lussier MT. Therapeutic privilege: between the ethics of lying and the practice of truth. J Med Ethics. 2010;36:353-357.
Resident Pearl
- As residents, we must gain experience performing procedures on real patients to enter independent practice as proficient dermatologists. It is important to be mindful of the ethical challenges inherent to the hands-on training process and to understand the ethical principles that guide best practices.
The Evolution of the Micrographic Surgery and Dermatologic Oncology Fellowship
Originating in 1968, the dermatologic surgery fellowship is as young as many dermatologists in practice today. Not surprisingly, the blossoming fellowship has undergone its fair share of both growth and growing pains over the last 5 decades.
A Brief History
The first dermatologic surgery fellowship was born in 1968 when Dr. Perry Robins established a program at the New York University Medical Center for training in chemosurgery.1 The fellowship quickly underwent notable change with the rising popularity of the fresh tissue technique, which was first performed by Dr. Fred Mohs in 1953 and made popular following publication of a series of landmark articles on the technique by Drs. Sam Stegman and Theodore Tromovitch in the late 1960s and early 1970s. The fellowship correspondingly saw a rise in fresh tissue technique training, accompanied by a decline in chemosurgery training. In 1974, Dr. Daniel Jones coined the term micrographic surgery to describe the favored technique, and at the 1985 annual meeting of the American College of Chemosurgery, the name of the technique was changed to Mohs micrographic surgery.1
By 1995, the fellowship was officially named Procedural Dermatology, and programs were exclusively accredited by the American College of Mohs Surgery (ACMS). A 1-year Procedural Dermatology fellowship gained accreditation by the Accreditation Council for Graduate Medical Education (ACGME) in 2003.2 Beginning in July 2013, all fellowship programs in the United States fell under the governance of the ACGME; however, the ACMS has remained the sponsor of the matching process.3 In 2014, the ACGME changed the name of the fellowship to Micrographic Surgery and Dermatologic Oncology (MSDO).2 Fellowship training today is centered on the core elements of cutaneous oncologic surgery, cutaneous reconstructive surgery, and dermatologic oncology; however, the scope of training in technologies and techniques offered has continued to broaden.4 Many programs now offer additional training in cosmetic and other procedural dermatology. To date, there are 76 accredited MSDO fellowship training programs in the United States and more than 1500 fellowship-trained micrographic surgeons.2,4
Trends in Program and Match Statistics
As the role of dermatologic surgery within the field of dermatology continues to expand, the MSDO fellowship has become increasingly popular over the last decade. From 2005 to 2018, applicants participating in the fellowship match increased by 34%.3 Despite the fellowship’s growing popularity, programs participating in the match have remained largely stable from 2005 to 2018, with 50 positions offered in 2005 and 58 in 2018. The match rate has correspondingly decreased from 66.2% in 2005 to 61.1% in 2018.3
Changes in the Match Process
The fellowship match is processed by the SF Match and sponsored by the ACMS. Over the last decade, programs have increasingly opted for exemptions from participation in the SF Match. In 2005, there were 8 match exemptions. In 2018, there were 20.4 Despite the increasing popularity of match exemptions, in October 2018 the ACMS Board of Directors approved a new policy that eliminated match exemptions, with the exception of applicants on active military duty and international (non-Canadian) applicants. All other applicants applying for a fellowship position for the 2020-2021 academic year must participate in the match.4 This new policy attempts to ensure a fair match process, especially for applicants who have trained at a program without an affiliated MSDO fellowship.
The Road to Board Certification
Further growth during the fellowship’s mid-adult years centered on the long-contested debate on subspecialty board certification. In 2009, an American Society for Dermatologic Surgery membership survey demonstrated an overwhelming majority in opposition. In 2014, the debate resurfaced. At the 2016 American Society for Dermatologic Surgery annual meeting, former American Academy of Dermatology presidents Brett Coldiron, MD, and Darrell S. Rigel, MD, MS, conveyed opposing positions, after which an audience survey demonstrated a 69% opposition rate. Proponents continued to argue that board certification would decrease divisiveness in the specialty, create a better brand, help to obtain a Medicare specialty designation that could help prevent exclusion of Mohs surgeons from insurance networks, give allopathic dermatologists the same opportunity for certification as osteopathic counterparts, and demonstrate competence to the public. Those in opposition argued that the term dermatologic oncology erroneously suggests general dermatologists are not experts in the treatment of skin cancers, practices may be restricted by carriers misusing the new credential, and subspecialty certification would actually create division among practicing dermatologists.5
Following years of debate, the American Board of Dermatology’s proposal to offer subspecialty certification in Micrographic Dermatologic Surgery was submitted to the American Board of Medical Specialties and approved on October 26, 2018. The name of the new subspecialty (Micrographic Dermatologic Surgery) is different than that of the fellowship (Micrographic Surgery and Dermatologic Oncology), a decision reached in response to diplomats indicating discomfort with the term oncology potentially misleading the public that general dermatologists do not treat skin cancer. Per the American Board of Dermatology official website, the first certification examination likely will take place in about 2 years. A maintenance of certification examination for the subspecialty will be required every 10 years.6
Final Thoughts
During its short history, the MSDO fellowship has undergone a notable evolution in recognition, popularity among residents, match process, and board certification, which attests to its adaptability over time and growing prominence.
- Robins P, Ebede TL, Hale EK. The evolution of Mohs micrographic surgery. Skin Cancer Foundation website. https://www.skincancer.org/skin-cancer-information/mohs-surgery/evolution-of-mohs. Updated July 13, 2016. Accessed April 17, 2019.
- Micrographic surgery and dermatologic oncology. American Board of Dermatology website. https://www.abderm.org/residents-and-fellows/fellowship-training/micrographic-surgery-and-dermatologic-oncology.aspx. Accessed April 9, 2019.
- Micrographic Surgery and Dermatologic Oncology Fellowship. San Francisco Match website. https://sfmatch.org/SpecialtyInsideAll.aspx?id=10&typ=1&name=Micrographic%20Surgery%20and%20Dermatologic%20Oncology. Accessed April 9, 2019.
- ACMS fellowship training. American College of Mohs Surgery website. https://www.mohscollege.org/fellowship-training. Accessed April 9, 2019.
- Should the ABD offer a Mohs surgery sub-certification? Dermatology World. April 26, 2017. https://www.aad.org/dw/dw-weekly/should-the-abd-offer-a-mohs-surgery-sub-certification. Accessed April 9, 2019.
- ABD Micrographic Dermatologic Surgery (MDS) subspecialty certification. American Board of Dermatology website. https://www.abderm.org/residents-and-fellows/fellowship-training/micrographic-dermatologic-surgery-mds-questions-and-answers-1.aspx. Accessed April 9, 2019.
Originating in 1968, the dermatologic surgery fellowship is as young as many dermatologists in practice today. Not surprisingly, the blossoming fellowship has undergone its fair share of both growth and growing pains over the last 5 decades.
A Brief History
The first dermatologic surgery fellowship was born in 1968 when Dr. Perry Robins established a program at the New York University Medical Center for training in chemosurgery.1 The fellowship quickly underwent notable change with the rising popularity of the fresh tissue technique, which was first performed by Dr. Fred Mohs in 1953 and made popular following publication of a series of landmark articles on the technique by Drs. Sam Stegman and Theodore Tromovitch in the late 1960s and early 1970s. The fellowship correspondingly saw a rise in fresh tissue technique training, accompanied by a decline in chemosurgery training. In 1974, Dr. Daniel Jones coined the term micrographic surgery to describe the favored technique, and at the 1985 annual meeting of the American College of Chemosurgery, the name of the technique was changed to Mohs micrographic surgery.1
By 1995, the fellowship was officially named Procedural Dermatology, and programs were exclusively accredited by the American College of Mohs Surgery (ACMS). A 1-year Procedural Dermatology fellowship gained accreditation by the Accreditation Council for Graduate Medical Education (ACGME) in 2003.2 Beginning in July 2013, all fellowship programs in the United States fell under the governance of the ACGME; however, the ACMS has remained the sponsor of the matching process.3 In 2014, the ACGME changed the name of the fellowship to Micrographic Surgery and Dermatologic Oncology (MSDO).2 Fellowship training today is centered on the core elements of cutaneous oncologic surgery, cutaneous reconstructive surgery, and dermatologic oncology; however, the scope of training in technologies and techniques offered has continued to broaden.4 Many programs now offer additional training in cosmetic and other procedural dermatology. To date, there are 76 accredited MSDO fellowship training programs in the United States and more than 1500 fellowship-trained micrographic surgeons.2,4
Trends in Program and Match Statistics
As the role of dermatologic surgery within the field of dermatology continues to expand, the MSDO fellowship has become increasingly popular over the last decade. From 2005 to 2018, applicants participating in the fellowship match increased by 34%.3 Despite the fellowship’s growing popularity, programs participating in the match have remained largely stable from 2005 to 2018, with 50 positions offered in 2005 and 58 in 2018. The match rate has correspondingly decreased from 66.2% in 2005 to 61.1% in 2018.3
Changes in the Match Process
The fellowship match is processed by the SF Match and sponsored by the ACMS. Over the last decade, programs have increasingly opted for exemptions from participation in the SF Match. In 2005, there were 8 match exemptions. In 2018, there were 20.4 Despite the increasing popularity of match exemptions, in October 2018 the ACMS Board of Directors approved a new policy that eliminated match exemptions, with the exception of applicants on active military duty and international (non-Canadian) applicants. All other applicants applying for a fellowship position for the 2020-2021 academic year must participate in the match.4 This new policy attempts to ensure a fair match process, especially for applicants who have trained at a program without an affiliated MSDO fellowship.
The Road to Board Certification
Further growth during the fellowship’s mid-adult years centered on the long-contested debate on subspecialty board certification. In 2009, an American Society for Dermatologic Surgery membership survey demonstrated an overwhelming majority in opposition. In 2014, the debate resurfaced. At the 2016 American Society for Dermatologic Surgery annual meeting, former American Academy of Dermatology presidents Brett Coldiron, MD, and Darrell S. Rigel, MD, MS, conveyed opposing positions, after which an audience survey demonstrated a 69% opposition rate. Proponents continued to argue that board certification would decrease divisiveness in the specialty, create a better brand, help to obtain a Medicare specialty designation that could help prevent exclusion of Mohs surgeons from insurance networks, give allopathic dermatologists the same opportunity for certification as osteopathic counterparts, and demonstrate competence to the public. Those in opposition argued that the term dermatologic oncology erroneously suggests general dermatologists are not experts in the treatment of skin cancers, practices may be restricted by carriers misusing the new credential, and subspecialty certification would actually create division among practicing dermatologists.5
Following years of debate, the American Board of Dermatology’s proposal to offer subspecialty certification in Micrographic Dermatologic Surgery was submitted to the American Board of Medical Specialties and approved on October 26, 2018. The name of the new subspecialty (Micrographic Dermatologic Surgery) is different than that of the fellowship (Micrographic Surgery and Dermatologic Oncology), a decision reached in response to diplomats indicating discomfort with the term oncology potentially misleading the public that general dermatologists do not treat skin cancer. Per the American Board of Dermatology official website, the first certification examination likely will take place in about 2 years. A maintenance of certification examination for the subspecialty will be required every 10 years.6
Final Thoughts
During its short history, the MSDO fellowship has undergone a notable evolution in recognition, popularity among residents, match process, and board certification, which attests to its adaptability over time and growing prominence.
Originating in 1968, the dermatologic surgery fellowship is as young as many dermatologists in practice today. Not surprisingly, the blossoming fellowship has undergone its fair share of both growth and growing pains over the last 5 decades.
A Brief History
The first dermatologic surgery fellowship was born in 1968 when Dr. Perry Robins established a program at the New York University Medical Center for training in chemosurgery.1 The fellowship quickly underwent notable change with the rising popularity of the fresh tissue technique, which was first performed by Dr. Fred Mohs in 1953 and made popular following publication of a series of landmark articles on the technique by Drs. Sam Stegman and Theodore Tromovitch in the late 1960s and early 1970s. The fellowship correspondingly saw a rise in fresh tissue technique training, accompanied by a decline in chemosurgery training. In 1974, Dr. Daniel Jones coined the term micrographic surgery to describe the favored technique, and at the 1985 annual meeting of the American College of Chemosurgery, the name of the technique was changed to Mohs micrographic surgery.1
By 1995, the fellowship was officially named Procedural Dermatology, and programs were exclusively accredited by the American College of Mohs Surgery (ACMS). A 1-year Procedural Dermatology fellowship gained accreditation by the Accreditation Council for Graduate Medical Education (ACGME) in 2003.2 Beginning in July 2013, all fellowship programs in the United States fell under the governance of the ACGME; however, the ACMS has remained the sponsor of the matching process.3 In 2014, the ACGME changed the name of the fellowship to Micrographic Surgery and Dermatologic Oncology (MSDO).2 Fellowship training today is centered on the core elements of cutaneous oncologic surgery, cutaneous reconstructive surgery, and dermatologic oncology; however, the scope of training in technologies and techniques offered has continued to broaden.4 Many programs now offer additional training in cosmetic and other procedural dermatology. To date, there are 76 accredited MSDO fellowship training programs in the United States and more than 1500 fellowship-trained micrographic surgeons.2,4
Trends in Program and Match Statistics
As the role of dermatologic surgery within the field of dermatology continues to expand, the MSDO fellowship has become increasingly popular over the last decade. From 2005 to 2018, applicants participating in the fellowship match increased by 34%.3 Despite the fellowship’s growing popularity, programs participating in the match have remained largely stable from 2005 to 2018, with 50 positions offered in 2005 and 58 in 2018. The match rate has correspondingly decreased from 66.2% in 2005 to 61.1% in 2018.3
Changes in the Match Process
The fellowship match is processed by the SF Match and sponsored by the ACMS. Over the last decade, programs have increasingly opted for exemptions from participation in the SF Match. In 2005, there were 8 match exemptions. In 2018, there were 20.4 Despite the increasing popularity of match exemptions, in October 2018 the ACMS Board of Directors approved a new policy that eliminated match exemptions, with the exception of applicants on active military duty and international (non-Canadian) applicants. All other applicants applying for a fellowship position for the 2020-2021 academic year must participate in the match.4 This new policy attempts to ensure a fair match process, especially for applicants who have trained at a program without an affiliated MSDO fellowship.
The Road to Board Certification
Further growth during the fellowship’s mid-adult years centered on the long-contested debate on subspecialty board certification. In 2009, an American Society for Dermatologic Surgery membership survey demonstrated an overwhelming majority in opposition. In 2014, the debate resurfaced. At the 2016 American Society for Dermatologic Surgery annual meeting, former American Academy of Dermatology presidents Brett Coldiron, MD, and Darrell S. Rigel, MD, MS, conveyed opposing positions, after which an audience survey demonstrated a 69% opposition rate. Proponents continued to argue that board certification would decrease divisiveness in the specialty, create a better brand, help to obtain a Medicare specialty designation that could help prevent exclusion of Mohs surgeons from insurance networks, give allopathic dermatologists the same opportunity for certification as osteopathic counterparts, and demonstrate competence to the public. Those in opposition argued that the term dermatologic oncology erroneously suggests general dermatologists are not experts in the treatment of skin cancers, practices may be restricted by carriers misusing the new credential, and subspecialty certification would actually create division among practicing dermatologists.5
Following years of debate, the American Board of Dermatology’s proposal to offer subspecialty certification in Micrographic Dermatologic Surgery was submitted to the American Board of Medical Specialties and approved on October 26, 2018. The name of the new subspecialty (Micrographic Dermatologic Surgery) is different than that of the fellowship (Micrographic Surgery and Dermatologic Oncology), a decision reached in response to diplomats indicating discomfort with the term oncology potentially misleading the public that general dermatologists do not treat skin cancer. Per the American Board of Dermatology official website, the first certification examination likely will take place in about 2 years. A maintenance of certification examination for the subspecialty will be required every 10 years.6
Final Thoughts
During its short history, the MSDO fellowship has undergone a notable evolution in recognition, popularity among residents, match process, and board certification, which attests to its adaptability over time and growing prominence.
- Robins P, Ebede TL, Hale EK. The evolution of Mohs micrographic surgery. Skin Cancer Foundation website. https://www.skincancer.org/skin-cancer-information/mohs-surgery/evolution-of-mohs. Updated July 13, 2016. Accessed April 17, 2019.
- Micrographic surgery and dermatologic oncology. American Board of Dermatology website. https://www.abderm.org/residents-and-fellows/fellowship-training/micrographic-surgery-and-dermatologic-oncology.aspx. Accessed April 9, 2019.
- Micrographic Surgery and Dermatologic Oncology Fellowship. San Francisco Match website. https://sfmatch.org/SpecialtyInsideAll.aspx?id=10&typ=1&name=Micrographic%20Surgery%20and%20Dermatologic%20Oncology. Accessed April 9, 2019.
- ACMS fellowship training. American College of Mohs Surgery website. https://www.mohscollege.org/fellowship-training. Accessed April 9, 2019.
- Should the ABD offer a Mohs surgery sub-certification? Dermatology World. April 26, 2017. https://www.aad.org/dw/dw-weekly/should-the-abd-offer-a-mohs-surgery-sub-certification. Accessed April 9, 2019.
- ABD Micrographic Dermatologic Surgery (MDS) subspecialty certification. American Board of Dermatology website. https://www.abderm.org/residents-and-fellows/fellowship-training/micrographic-dermatologic-surgery-mds-questions-and-answers-1.aspx. Accessed April 9, 2019.
- Robins P, Ebede TL, Hale EK. The evolution of Mohs micrographic surgery. Skin Cancer Foundation website. https://www.skincancer.org/skin-cancer-information/mohs-surgery/evolution-of-mohs. Updated July 13, 2016. Accessed April 17, 2019.
- Micrographic surgery and dermatologic oncology. American Board of Dermatology website. https://www.abderm.org/residents-and-fellows/fellowship-training/micrographic-surgery-and-dermatologic-oncology.aspx. Accessed April 9, 2019.
- Micrographic Surgery and Dermatologic Oncology Fellowship. San Francisco Match website. https://sfmatch.org/SpecialtyInsideAll.aspx?id=10&typ=1&name=Micrographic%20Surgery%20and%20Dermatologic%20Oncology. Accessed April 9, 2019.
- ACMS fellowship training. American College of Mohs Surgery website. https://www.mohscollege.org/fellowship-training. Accessed April 9, 2019.
- Should the ABD offer a Mohs surgery sub-certification? Dermatology World. April 26, 2017. https://www.aad.org/dw/dw-weekly/should-the-abd-offer-a-mohs-surgery-sub-certification. Accessed April 9, 2019.
- ABD Micrographic Dermatologic Surgery (MDS) subspecialty certification. American Board of Dermatology website. https://www.abderm.org/residents-and-fellows/fellowship-training/micrographic-dermatologic-surgery-mds-questions-and-answers-1.aspx. Accessed April 9, 2019.
Resident Pearl
- Residents should be aware of recent changes to the Micrographic Surgery and Dermatologic Oncology fellowship: the elimination of fellowship match exemptions for most applicants for the upcoming 2019-2020 academic year, the American Board of Medical Specialties approval of subspecialty certification in Micrographic Dermatologic Surgery, and the likelihood of the first subspecialty certification examination in the next 2 years.
Supercharge Your On-Call Bag: 4 Must-Have Items for Dermatology Residents
It is no secret that a well-stocked on-call bag is one of the keys to providing inpatient care as a dermatology resident. Beyond the basic items that should never be left at home, there are some lesser-known tools that I have learned about from my book- and street-smart attendings and co-residents in the Department of Dermatology at the State University of New York Downstate Medical Center (referred to here as Downstate). Here are our top 4 items to pack the next time you are on call. (Bonus: you will find them helpful in clinic, too.)
Item 1: WoundSeal Powder
The most valuable player in my on-call bag, WoundSeal Powder (Biolife) is an over-the-counter hemostatic agent that I learned about from Daniel M. Siegel, MD, MS, a Mohs surgeon at Downstate and former president of the American Academy of Dermatology. The powder consists of a hydrophilic polymer and potassium ferrate.1 When poured over a bleeding wound and pressed in place (eg, with a sterile cotton-tipped swab), the hydrophilic polymer absorbs plasma while the iron in potassium ferrate agglomerates blood solids. The result is a scablike seal that is safe to leave in place until the wound has healed.1
Since Dr. Siegel introduced WoundSeal to Downstate about a decade ago, it has become our department’s go-to hemostatic agent for most punch biopsies performed in the inpatient setting. In our experience, achieving hemostasis in the hospital usually is easier, safer, and faster with WoundSeal than suture. Furthermore, using WoundSeal eliminates the need for patients to follow up for suture removal. From a practical perspective, WoundSeal works best when the biopsy defect is positioned parallel to the ground so the powder can be poured directly over and into the defect. From a cosmetic perspective, we have found that WoundSeal and suture have similar outcomes when used for punch biopsies up to 4 mm in size on the trunk and extremities in both adult and pediatric patients. Working with other dermatology attendings such as Sharon A. Glick, MD; Eve Lowenstein, MD, PhD; and Jeannette Jakus, MD, MBA, I also have found WoundSeal helpful when taking care of suture-phobic children or patients with lesions that are less amenable to suture, such as an ulcer or indurated plaque.
Item 2: Purple Surgical Marker
Another tip I have learned from Drs. Siegel and Jakus: If you are ever in a bind for a topical antibacterial or antifungal agent, look no further than a sterile purple surgical marker. These markers are a surprising source of gentian violet, the same purple dye that is the basis of Gram staining and sold as an over-the-counter antiseptic in 1% to 2% concentrations. Purple surgical markers, on the other hand, are 2.5% to 10% gentian violet.2
Gentian violet has been shown to have antibacterial, antifungal, antiviral, antihelminthic, and antitrypanosomal properties, but its efficacy has been mostly demonstrated against Streptococcus, methicillin-sensitive and methicillin-resistant Staphylococcus aureus, and Candida.3 Given the dermatologic relevance of these organisms, gentian violet is a favorite among attendings at my residency program; it is not uncommon to remove a patient’s dressing and uncover an iatrogenically purple wound. Best of all, pediatric patients are invariably amused when they see someone drawing on their skin with a purple marker.
When using a sterile surgical marker to apply gentian violet to the skin, we use either the marker tip or the ink core, which Dr. Siegel taught me can be easily accessed by snapping most plastic markers in half.
Item 3: Handheld Blacklight
The Wood lamp is a useful tool in the diagnosis of various infectious diseases and pigmentary disorders,4 but it is not always practical to use when on call, as standard ones are relatively large and corded, so they must be plugged into an electric outlet to work. You can therefore imagine the gratitude I have for my co-residents Miriam Lieberman, MD; Jaime Alexander, MD; Nicole Weiler, MD; and Alessandra Haskin, MD, for introducing me to the most convenient Wood lamp: the handheld blacklight. For less than $10, this gadget combines the diagnostic power of UV light with the portability of a pocket-sized, battery-powered flashlight. You will never want to use another Wood lamp again.
Item 4: Normal Saline Flush
Normal saline can be used for more than storing specimens for frozen section or tissue culture; it also can substitute for Michel solution when storing specimens for direct immunofluorescence (DIF) studies. I learned this tip from Edward Heilman, MD, a dermatopathologist at Downstate. For the last 20 years, Dr. Heilman has been successfully storing DIF specimens in refrigerated normal saline for up to 24 hours when Michel solution is unavailable, after which the specimen is processed or transferred to Michel solution for further storage while being transported to an immunofluorescence laboratory.
In 2004, Vodegel et al5 formally studied this technique in 25 patients with autoimmune skin diseases such as pemphigus and pemphigoid. (Thanks to Dr. Lieberman for telling me about this study.) The experiment involved taking 4 punch biopsies from each patient and placing them in either normal saline at −80°C for 24 or 48 hours, room temperature Michel solution for 48 hours, or liquid nitrogen for up to 2 weeks before being processed for DIF and analyzed by a blinded interpreter. Interestingly, specimens stored in normal saline for 24 hours were the most diagnostic, with a conclusive diagnosis reached in 21 of 25 specimens (84%). This result was attributed to the statistically significant reduction (P<.01) in background fluorescence with normal saline compared to Michel solution and liquid nitrogen, which in turn allowed for easier detection of diagnostic immunoreactants. Similar to Dr. Heilman, the authors cautioned against placing DIF specimens in normal saline for more than 24 hours; in their experience, the risk for an artefactual split developing at the dermoepidermal junction increases with this practice.5
- Biolife. How WoundSeal works. WoundSeal website. http://woundseal.com/how-it-works. Accessed March 7, 2019.
- Viscot Medical, LLC. Safety data sheet. http://www.viscot.com/download/MSDS%20Gentian%20Violet%20Ink.pdf. Published September 11, 2014. Accessed March 7, 2019.
- Maley AM, Arbiser JL. Gentian violet: a 19th century drug re-emerges in the 21st century. Exp Dermatol. 2013;22:775-780.
- Klatte JL, van der Beek N, Kemperman PM. 100 years of Wood’s lamp revised. J Eur Acad Dermatol Venereol. 2015;29:842-847.
- Vodegel RM, de Jong MC, Meijer HJ, et al. Enhanced diagnostic immunofluorescence using biopsies transported in saline. BMC Dermatol. 2004;4:10.
It is no secret that a well-stocked on-call bag is one of the keys to providing inpatient care as a dermatology resident. Beyond the basic items that should never be left at home, there are some lesser-known tools that I have learned about from my book- and street-smart attendings and co-residents in the Department of Dermatology at the State University of New York Downstate Medical Center (referred to here as Downstate). Here are our top 4 items to pack the next time you are on call. (Bonus: you will find them helpful in clinic, too.)
Item 1: WoundSeal Powder
The most valuable player in my on-call bag, WoundSeal Powder (Biolife) is an over-the-counter hemostatic agent that I learned about from Daniel M. Siegel, MD, MS, a Mohs surgeon at Downstate and former president of the American Academy of Dermatology. The powder consists of a hydrophilic polymer and potassium ferrate.1 When poured over a bleeding wound and pressed in place (eg, with a sterile cotton-tipped swab), the hydrophilic polymer absorbs plasma while the iron in potassium ferrate agglomerates blood solids. The result is a scablike seal that is safe to leave in place until the wound has healed.1
Since Dr. Siegel introduced WoundSeal to Downstate about a decade ago, it has become our department’s go-to hemostatic agent for most punch biopsies performed in the inpatient setting. In our experience, achieving hemostasis in the hospital usually is easier, safer, and faster with WoundSeal than suture. Furthermore, using WoundSeal eliminates the need for patients to follow up for suture removal. From a practical perspective, WoundSeal works best when the biopsy defect is positioned parallel to the ground so the powder can be poured directly over and into the defect. From a cosmetic perspective, we have found that WoundSeal and suture have similar outcomes when used for punch biopsies up to 4 mm in size on the trunk and extremities in both adult and pediatric patients. Working with other dermatology attendings such as Sharon A. Glick, MD; Eve Lowenstein, MD, PhD; and Jeannette Jakus, MD, MBA, I also have found WoundSeal helpful when taking care of suture-phobic children or patients with lesions that are less amenable to suture, such as an ulcer or indurated plaque.
Item 2: Purple Surgical Marker
Another tip I have learned from Drs. Siegel and Jakus: If you are ever in a bind for a topical antibacterial or antifungal agent, look no further than a sterile purple surgical marker. These markers are a surprising source of gentian violet, the same purple dye that is the basis of Gram staining and sold as an over-the-counter antiseptic in 1% to 2% concentrations. Purple surgical markers, on the other hand, are 2.5% to 10% gentian violet.2
Gentian violet has been shown to have antibacterial, antifungal, antiviral, antihelminthic, and antitrypanosomal properties, but its efficacy has been mostly demonstrated against Streptococcus, methicillin-sensitive and methicillin-resistant Staphylococcus aureus, and Candida.3 Given the dermatologic relevance of these organisms, gentian violet is a favorite among attendings at my residency program; it is not uncommon to remove a patient’s dressing and uncover an iatrogenically purple wound. Best of all, pediatric patients are invariably amused when they see someone drawing on their skin with a purple marker.
When using a sterile surgical marker to apply gentian violet to the skin, we use either the marker tip or the ink core, which Dr. Siegel taught me can be easily accessed by snapping most plastic markers in half.
Item 3: Handheld Blacklight
The Wood lamp is a useful tool in the diagnosis of various infectious diseases and pigmentary disorders,4 but it is not always practical to use when on call, as standard ones are relatively large and corded, so they must be plugged into an electric outlet to work. You can therefore imagine the gratitude I have for my co-residents Miriam Lieberman, MD; Jaime Alexander, MD; Nicole Weiler, MD; and Alessandra Haskin, MD, for introducing me to the most convenient Wood lamp: the handheld blacklight. For less than $10, this gadget combines the diagnostic power of UV light with the portability of a pocket-sized, battery-powered flashlight. You will never want to use another Wood lamp again.
Item 4: Normal Saline Flush
Normal saline can be used for more than storing specimens for frozen section or tissue culture; it also can substitute for Michel solution when storing specimens for direct immunofluorescence (DIF) studies. I learned this tip from Edward Heilman, MD, a dermatopathologist at Downstate. For the last 20 years, Dr. Heilman has been successfully storing DIF specimens in refrigerated normal saline for up to 24 hours when Michel solution is unavailable, after which the specimen is processed or transferred to Michel solution for further storage while being transported to an immunofluorescence laboratory.
In 2004, Vodegel et al5 formally studied this technique in 25 patients with autoimmune skin diseases such as pemphigus and pemphigoid. (Thanks to Dr. Lieberman for telling me about this study.) The experiment involved taking 4 punch biopsies from each patient and placing them in either normal saline at −80°C for 24 or 48 hours, room temperature Michel solution for 48 hours, or liquid nitrogen for up to 2 weeks before being processed for DIF and analyzed by a blinded interpreter. Interestingly, specimens stored in normal saline for 24 hours were the most diagnostic, with a conclusive diagnosis reached in 21 of 25 specimens (84%). This result was attributed to the statistically significant reduction (P<.01) in background fluorescence with normal saline compared to Michel solution and liquid nitrogen, which in turn allowed for easier detection of diagnostic immunoreactants. Similar to Dr. Heilman, the authors cautioned against placing DIF specimens in normal saline for more than 24 hours; in their experience, the risk for an artefactual split developing at the dermoepidermal junction increases with this practice.5
It is no secret that a well-stocked on-call bag is one of the keys to providing inpatient care as a dermatology resident. Beyond the basic items that should never be left at home, there are some lesser-known tools that I have learned about from my book- and street-smart attendings and co-residents in the Department of Dermatology at the State University of New York Downstate Medical Center (referred to here as Downstate). Here are our top 4 items to pack the next time you are on call. (Bonus: you will find them helpful in clinic, too.)
Item 1: WoundSeal Powder
The most valuable player in my on-call bag, WoundSeal Powder (Biolife) is an over-the-counter hemostatic agent that I learned about from Daniel M. Siegel, MD, MS, a Mohs surgeon at Downstate and former president of the American Academy of Dermatology. The powder consists of a hydrophilic polymer and potassium ferrate.1 When poured over a bleeding wound and pressed in place (eg, with a sterile cotton-tipped swab), the hydrophilic polymer absorbs plasma while the iron in potassium ferrate agglomerates blood solids. The result is a scablike seal that is safe to leave in place until the wound has healed.1
Since Dr. Siegel introduced WoundSeal to Downstate about a decade ago, it has become our department’s go-to hemostatic agent for most punch biopsies performed in the inpatient setting. In our experience, achieving hemostasis in the hospital usually is easier, safer, and faster with WoundSeal than suture. Furthermore, using WoundSeal eliminates the need for patients to follow up for suture removal. From a practical perspective, WoundSeal works best when the biopsy defect is positioned parallel to the ground so the powder can be poured directly over and into the defect. From a cosmetic perspective, we have found that WoundSeal and suture have similar outcomes when used for punch biopsies up to 4 mm in size on the trunk and extremities in both adult and pediatric patients. Working with other dermatology attendings such as Sharon A. Glick, MD; Eve Lowenstein, MD, PhD; and Jeannette Jakus, MD, MBA, I also have found WoundSeal helpful when taking care of suture-phobic children or patients with lesions that are less amenable to suture, such as an ulcer or indurated plaque.
Item 2: Purple Surgical Marker
Another tip I have learned from Drs. Siegel and Jakus: If you are ever in a bind for a topical antibacterial or antifungal agent, look no further than a sterile purple surgical marker. These markers are a surprising source of gentian violet, the same purple dye that is the basis of Gram staining and sold as an over-the-counter antiseptic in 1% to 2% concentrations. Purple surgical markers, on the other hand, are 2.5% to 10% gentian violet.2
Gentian violet has been shown to have antibacterial, antifungal, antiviral, antihelminthic, and antitrypanosomal properties, but its efficacy has been mostly demonstrated against Streptococcus, methicillin-sensitive and methicillin-resistant Staphylococcus aureus, and Candida.3 Given the dermatologic relevance of these organisms, gentian violet is a favorite among attendings at my residency program; it is not uncommon to remove a patient’s dressing and uncover an iatrogenically purple wound. Best of all, pediatric patients are invariably amused when they see someone drawing on their skin with a purple marker.
When using a sterile surgical marker to apply gentian violet to the skin, we use either the marker tip or the ink core, which Dr. Siegel taught me can be easily accessed by snapping most plastic markers in half.
Item 3: Handheld Blacklight
The Wood lamp is a useful tool in the diagnosis of various infectious diseases and pigmentary disorders,4 but it is not always practical to use when on call, as standard ones are relatively large and corded, so they must be plugged into an electric outlet to work. You can therefore imagine the gratitude I have for my co-residents Miriam Lieberman, MD; Jaime Alexander, MD; Nicole Weiler, MD; and Alessandra Haskin, MD, for introducing me to the most convenient Wood lamp: the handheld blacklight. For less than $10, this gadget combines the diagnostic power of UV light with the portability of a pocket-sized, battery-powered flashlight. You will never want to use another Wood lamp again.
Item 4: Normal Saline Flush
Normal saline can be used for more than storing specimens for frozen section or tissue culture; it also can substitute for Michel solution when storing specimens for direct immunofluorescence (DIF) studies. I learned this tip from Edward Heilman, MD, a dermatopathologist at Downstate. For the last 20 years, Dr. Heilman has been successfully storing DIF specimens in refrigerated normal saline for up to 24 hours when Michel solution is unavailable, after which the specimen is processed or transferred to Michel solution for further storage while being transported to an immunofluorescence laboratory.
In 2004, Vodegel et al5 formally studied this technique in 25 patients with autoimmune skin diseases such as pemphigus and pemphigoid. (Thanks to Dr. Lieberman for telling me about this study.) The experiment involved taking 4 punch biopsies from each patient and placing them in either normal saline at −80°C for 24 or 48 hours, room temperature Michel solution for 48 hours, or liquid nitrogen for up to 2 weeks before being processed for DIF and analyzed by a blinded interpreter. Interestingly, specimens stored in normal saline for 24 hours were the most diagnostic, with a conclusive diagnosis reached in 21 of 25 specimens (84%). This result was attributed to the statistically significant reduction (P<.01) in background fluorescence with normal saline compared to Michel solution and liquid nitrogen, which in turn allowed for easier detection of diagnostic immunoreactants. Similar to Dr. Heilman, the authors cautioned against placing DIF specimens in normal saline for more than 24 hours; in their experience, the risk for an artefactual split developing at the dermoepidermal junction increases with this practice.5
- Biolife. How WoundSeal works. WoundSeal website. http://woundseal.com/how-it-works. Accessed March 7, 2019.
- Viscot Medical, LLC. Safety data sheet. http://www.viscot.com/download/MSDS%20Gentian%20Violet%20Ink.pdf. Published September 11, 2014. Accessed March 7, 2019.
- Maley AM, Arbiser JL. Gentian violet: a 19th century drug re-emerges in the 21st century. Exp Dermatol. 2013;22:775-780.
- Klatte JL, van der Beek N, Kemperman PM. 100 years of Wood’s lamp revised. J Eur Acad Dermatol Venereol. 2015;29:842-847.
- Vodegel RM, de Jong MC, Meijer HJ, et al. Enhanced diagnostic immunofluorescence using biopsies transported in saline. BMC Dermatol. 2004;4:10.
- Biolife. How WoundSeal works. WoundSeal website. http://woundseal.com/how-it-works. Accessed March 7, 2019.
- Viscot Medical, LLC. Safety data sheet. http://www.viscot.com/download/MSDS%20Gentian%20Violet%20Ink.pdf. Published September 11, 2014. Accessed March 7, 2019.
- Maley AM, Arbiser JL. Gentian violet: a 19th century drug re-emerges in the 21st century. Exp Dermatol. 2013;22:775-780.
- Klatte JL, van der Beek N, Kemperman PM. 100 years of Wood’s lamp revised. J Eur Acad Dermatol Venereol. 2015;29:842-847.
- Vodegel RM, de Jong MC, Meijer HJ, et al. Enhanced diagnostic immunofluorescence using biopsies transported in saline. BMC Dermatol. 2004;4:10.
Resident Pearl
- The following unconventional items will come in handy the next time you are on call (or in clinic) and need an alternative to a suture, topical antimicrobial, Wood lamp, or Michel solution.
Miscommunication With Dermatology Patients: Are We Speaking the Same Language?
I was a third-year medical student, dutifully reviewing discharge instructions with a patient and her family. The patient’s adult daughter asked, “What about that diet you put her on?” As they looked at me quizzically, I looked back equally confused, until it clicked: We needed to talk about the word diet. In everyday conversation, diet generally is understood to mean restriction of food to lose weight, which is what the family hoped would be prescribed for their obese family member. I needed to tell them that I was sorry for the misunderstanding. If they overheard us “ordering a diet,” we simply meant providing trays of hospital food.
We become so familiar with the language of our profession that we do not remember it may be foreign to our patients. In dermatology, we are aware that our specialty is full of esoteric jargon and complex concepts that need to be carefully explained to our patients in simpler terms. But since that incident in medical school, I have been interested in the more insidious potential misunderstandings that can arise from words as seemingly simple as diet. There are many examples in dermatology, particularly in the way we prescribe topical therapy and use trade names.
Topical Therapy
Instructions for systemic medications may be as simple as “take 1 pill twice daily.” Prescriptions for topical medications can be written with an equally simple patient signature such as “apply twice daily to affected area,” but the simplicity is deceptive. The direction to “apply” may seem intuitive to the prescriber, but we do not always specify the amount. Sunscreen, for example, is notoriously underapplied when the actual amount of product needed for protection is not demonstrated.1 One study of new dermatology patients given a prescription for a new topical medication found that the majority of patients underdosed.2
Determination of an “affected area,” regardless of whether the site is indicated, can be even less straightforward. In acne treatment, the affected area is the whole region prone to acne breakouts, whereas in psoriasis it may be discrete psoriatic plaques. We may believe our explanations are perfectly clear, but we have all seen patients spot treating their acne or psoriasis patients covering entire territories of normal skin with topical steroids, despite our education. One study of eczema action plans found that there was considerable variability in the way different providers described disease flares that require treatment. For example, redness was only used as a descriptor of an eczema flare in 68.2% of eczema action plans studied.3 Ensuring our patients understand our criteria for skin requiring topical treatment may mean the difference between treatment success and failure and also may help to avoid unnecessary side effects.
Adherence to topical medication regimens is poor, and inadequate patient education is only one factor.4,5 One study found that more than one-third of new prescriptions for topical medications were never even filled.6 However, improving our communication about application of topical drugs is one way we must address the complicated issue of adherence.
Trade Names
In dermatology, we often use trade names to refer to our medications, even if we do not intend to reference the brand name of the drug specifically. We may tell a patient to use Lidex (Medicis Pharmaceutical Corporation) for her hands but then send an escript to her pharmacy for fluocinonide. Trade names are designed to roll off the tongue, in contrast to the unwieldy, clumsily long generic names assigned to many of our medications.
Substituting trade names may facilitate more natural conversation to promote patient understanding in some cases; however, there are pitfalls associated with this habit. First, we may be doing our patients a disservice if we do not clarify when it would be acceptable to substitute with the generic when the medication is available over-the-counter. If we decide to treat with Rogaine (Johnson & Johnson Consumer Inc) but do not suggest the option of purchasing the generic minoxidil, the patient could be unnecessarily overpaying for a brand name by following our instructions.
Conversely, there are scenarios in which the use of a brand name is actually not specific enough. A patient once told me she was using Differin (Galderma Laboratories, LP) as discussed at her prior visit, but she revealed she was washing it off after application. I initially assumed she misunderstood that adapalene was a gel to be applied and left on. After additional questioning, however, it became clear that she purchased the Differin gentle cleanser, a nonmedicated facial wash, rather than the retinoid we had intended for her. I had not considered that Differin would market an entire line of skin care products but now realize we must be cautious using Differin and adapalene interchangeably. Other examples include popular over-the-counter antihistamine brands such as Allegra (Chattem, a Sanofi company) or Benadryl (Johnson & Johnson Consumer Inc) that market multiple products with different active ingredients.
Final Thoughts
The smooth transfer of information between physician and patient is key to a healthy therapeutic relationship. In residency and throughout our careers, we will continue to develop and refine our communication skills to best serve our patients. We should pay particular attention to the unexpected and surprising ways in which we fail to adequately communicate, make note of these patterns, and share with our colleagues so that we can all learn from our collective experiences.
- Schneider, J. The teaspoon rule of applying sunscreen. Arch Dermatol. 2002;138:838-839.
- Storm A, Benfeldt E, Andersen SE, et al. A prospective study of patient adherence to topical treatments: 95% of patients underdose. J Am Acad Dermatol. 2008;59:975-980.
- Stringer T, Yin HS, Gittler J, et al. The readability, suitability, and content features of eczema action plans in the United States. Pediatr Dermatol. 2018;35:800-807.
- Hougeir FG, Cook-Bolden FE, Rodriguez D, et al. Critical considerations on optimizing topical corticosteroid therapy. J Clin Aesthet Dermatol. 2015;8(suppl 1):S2-S14.
- Savary J, Ortonne JP, Aractingi S. The right dose in the right place: an overview of current prescription, instruction and application modalities for topical psoriasis treatments. J Eur Acad Dermatol Venereol. 2005;19:14-17.
- Storm A, Anderson SE, Benfeldt E, et al. One in 3 prescriptions are never redeemed: primary nonadherence in an outpatient clinic. J Am Acad Dermatol. 2008;59:27-33.
I was a third-year medical student, dutifully reviewing discharge instructions with a patient and her family. The patient’s adult daughter asked, “What about that diet you put her on?” As they looked at me quizzically, I looked back equally confused, until it clicked: We needed to talk about the word diet. In everyday conversation, diet generally is understood to mean restriction of food to lose weight, which is what the family hoped would be prescribed for their obese family member. I needed to tell them that I was sorry for the misunderstanding. If they overheard us “ordering a diet,” we simply meant providing trays of hospital food.
We become so familiar with the language of our profession that we do not remember it may be foreign to our patients. In dermatology, we are aware that our specialty is full of esoteric jargon and complex concepts that need to be carefully explained to our patients in simpler terms. But since that incident in medical school, I have been interested in the more insidious potential misunderstandings that can arise from words as seemingly simple as diet. There are many examples in dermatology, particularly in the way we prescribe topical therapy and use trade names.
Topical Therapy
Instructions for systemic medications may be as simple as “take 1 pill twice daily.” Prescriptions for topical medications can be written with an equally simple patient signature such as “apply twice daily to affected area,” but the simplicity is deceptive. The direction to “apply” may seem intuitive to the prescriber, but we do not always specify the amount. Sunscreen, for example, is notoriously underapplied when the actual amount of product needed for protection is not demonstrated.1 One study of new dermatology patients given a prescription for a new topical medication found that the majority of patients underdosed.2
Determination of an “affected area,” regardless of whether the site is indicated, can be even less straightforward. In acne treatment, the affected area is the whole region prone to acne breakouts, whereas in psoriasis it may be discrete psoriatic plaques. We may believe our explanations are perfectly clear, but we have all seen patients spot treating their acne or psoriasis patients covering entire territories of normal skin with topical steroids, despite our education. One study of eczema action plans found that there was considerable variability in the way different providers described disease flares that require treatment. For example, redness was only used as a descriptor of an eczema flare in 68.2% of eczema action plans studied.3 Ensuring our patients understand our criteria for skin requiring topical treatment may mean the difference between treatment success and failure and also may help to avoid unnecessary side effects.
Adherence to topical medication regimens is poor, and inadequate patient education is only one factor.4,5 One study found that more than one-third of new prescriptions for topical medications were never even filled.6 However, improving our communication about application of topical drugs is one way we must address the complicated issue of adherence.
Trade Names
In dermatology, we often use trade names to refer to our medications, even if we do not intend to reference the brand name of the drug specifically. We may tell a patient to use Lidex (Medicis Pharmaceutical Corporation) for her hands but then send an escript to her pharmacy for fluocinonide. Trade names are designed to roll off the tongue, in contrast to the unwieldy, clumsily long generic names assigned to many of our medications.
Substituting trade names may facilitate more natural conversation to promote patient understanding in some cases; however, there are pitfalls associated with this habit. First, we may be doing our patients a disservice if we do not clarify when it would be acceptable to substitute with the generic when the medication is available over-the-counter. If we decide to treat with Rogaine (Johnson & Johnson Consumer Inc) but do not suggest the option of purchasing the generic minoxidil, the patient could be unnecessarily overpaying for a brand name by following our instructions.
Conversely, there are scenarios in which the use of a brand name is actually not specific enough. A patient once told me she was using Differin (Galderma Laboratories, LP) as discussed at her prior visit, but she revealed she was washing it off after application. I initially assumed she misunderstood that adapalene was a gel to be applied and left on. After additional questioning, however, it became clear that she purchased the Differin gentle cleanser, a nonmedicated facial wash, rather than the retinoid we had intended for her. I had not considered that Differin would market an entire line of skin care products but now realize we must be cautious using Differin and adapalene interchangeably. Other examples include popular over-the-counter antihistamine brands such as Allegra (Chattem, a Sanofi company) or Benadryl (Johnson & Johnson Consumer Inc) that market multiple products with different active ingredients.
Final Thoughts
The smooth transfer of information between physician and patient is key to a healthy therapeutic relationship. In residency and throughout our careers, we will continue to develop and refine our communication skills to best serve our patients. We should pay particular attention to the unexpected and surprising ways in which we fail to adequately communicate, make note of these patterns, and share with our colleagues so that we can all learn from our collective experiences.
I was a third-year medical student, dutifully reviewing discharge instructions with a patient and her family. The patient’s adult daughter asked, “What about that diet you put her on?” As they looked at me quizzically, I looked back equally confused, until it clicked: We needed to talk about the word diet. In everyday conversation, diet generally is understood to mean restriction of food to lose weight, which is what the family hoped would be prescribed for their obese family member. I needed to tell them that I was sorry for the misunderstanding. If they overheard us “ordering a diet,” we simply meant providing trays of hospital food.
We become so familiar with the language of our profession that we do not remember it may be foreign to our patients. In dermatology, we are aware that our specialty is full of esoteric jargon and complex concepts that need to be carefully explained to our patients in simpler terms. But since that incident in medical school, I have been interested in the more insidious potential misunderstandings that can arise from words as seemingly simple as diet. There are many examples in dermatology, particularly in the way we prescribe topical therapy and use trade names.
Topical Therapy
Instructions for systemic medications may be as simple as “take 1 pill twice daily.” Prescriptions for topical medications can be written with an equally simple patient signature such as “apply twice daily to affected area,” but the simplicity is deceptive. The direction to “apply” may seem intuitive to the prescriber, but we do not always specify the amount. Sunscreen, for example, is notoriously underapplied when the actual amount of product needed for protection is not demonstrated.1 One study of new dermatology patients given a prescription for a new topical medication found that the majority of patients underdosed.2
Determination of an “affected area,” regardless of whether the site is indicated, can be even less straightforward. In acne treatment, the affected area is the whole region prone to acne breakouts, whereas in psoriasis it may be discrete psoriatic plaques. We may believe our explanations are perfectly clear, but we have all seen patients spot treating their acne or psoriasis patients covering entire territories of normal skin with topical steroids, despite our education. One study of eczema action plans found that there was considerable variability in the way different providers described disease flares that require treatment. For example, redness was only used as a descriptor of an eczema flare in 68.2% of eczema action plans studied.3 Ensuring our patients understand our criteria for skin requiring topical treatment may mean the difference between treatment success and failure and also may help to avoid unnecessary side effects.
Adherence to topical medication regimens is poor, and inadequate patient education is only one factor.4,5 One study found that more than one-third of new prescriptions for topical medications were never even filled.6 However, improving our communication about application of topical drugs is one way we must address the complicated issue of adherence.
Trade Names
In dermatology, we often use trade names to refer to our medications, even if we do not intend to reference the brand name of the drug specifically. We may tell a patient to use Lidex (Medicis Pharmaceutical Corporation) for her hands but then send an escript to her pharmacy for fluocinonide. Trade names are designed to roll off the tongue, in contrast to the unwieldy, clumsily long generic names assigned to many of our medications.
Substituting trade names may facilitate more natural conversation to promote patient understanding in some cases; however, there are pitfalls associated with this habit. First, we may be doing our patients a disservice if we do not clarify when it would be acceptable to substitute with the generic when the medication is available over-the-counter. If we decide to treat with Rogaine (Johnson & Johnson Consumer Inc) but do not suggest the option of purchasing the generic minoxidil, the patient could be unnecessarily overpaying for a brand name by following our instructions.
Conversely, there are scenarios in which the use of a brand name is actually not specific enough. A patient once told me she was using Differin (Galderma Laboratories, LP) as discussed at her prior visit, but she revealed she was washing it off after application. I initially assumed she misunderstood that adapalene was a gel to be applied and left on. After additional questioning, however, it became clear that she purchased the Differin gentle cleanser, a nonmedicated facial wash, rather than the retinoid we had intended for her. I had not considered that Differin would market an entire line of skin care products but now realize we must be cautious using Differin and adapalene interchangeably. Other examples include popular over-the-counter antihistamine brands such as Allegra (Chattem, a Sanofi company) or Benadryl (Johnson & Johnson Consumer Inc) that market multiple products with different active ingredients.
Final Thoughts
The smooth transfer of information between physician and patient is key to a healthy therapeutic relationship. In residency and throughout our careers, we will continue to develop and refine our communication skills to best serve our patients. We should pay particular attention to the unexpected and surprising ways in which we fail to adequately communicate, make note of these patterns, and share with our colleagues so that we can all learn from our collective experiences.
- Schneider, J. The teaspoon rule of applying sunscreen. Arch Dermatol. 2002;138:838-839.
- Storm A, Benfeldt E, Andersen SE, et al. A prospective study of patient adherence to topical treatments: 95% of patients underdose. J Am Acad Dermatol. 2008;59:975-980.
- Stringer T, Yin HS, Gittler J, et al. The readability, suitability, and content features of eczema action plans in the United States. Pediatr Dermatol. 2018;35:800-807.
- Hougeir FG, Cook-Bolden FE, Rodriguez D, et al. Critical considerations on optimizing topical corticosteroid therapy. J Clin Aesthet Dermatol. 2015;8(suppl 1):S2-S14.
- Savary J, Ortonne JP, Aractingi S. The right dose in the right place: an overview of current prescription, instruction and application modalities for topical psoriasis treatments. J Eur Acad Dermatol Venereol. 2005;19:14-17.
- Storm A, Anderson SE, Benfeldt E, et al. One in 3 prescriptions are never redeemed: primary nonadherence in an outpatient clinic. J Am Acad Dermatol. 2008;59:27-33.
- Schneider, J. The teaspoon rule of applying sunscreen. Arch Dermatol. 2002;138:838-839.
- Storm A, Benfeldt E, Andersen SE, et al. A prospective study of patient adherence to topical treatments: 95% of patients underdose. J Am Acad Dermatol. 2008;59:975-980.
- Stringer T, Yin HS, Gittler J, et al. The readability, suitability, and content features of eczema action plans in the United States. Pediatr Dermatol. 2018;35:800-807.
- Hougeir FG, Cook-Bolden FE, Rodriguez D, et al. Critical considerations on optimizing topical corticosteroid therapy. J Clin Aesthet Dermatol. 2015;8(suppl 1):S2-S14.
- Savary J, Ortonne JP, Aractingi S. The right dose in the right place: an overview of current prescription, instruction and application modalities for topical psoriasis treatments. J Eur Acad Dermatol Venereol. 2005;19:14-17.
- Storm A, Anderson SE, Benfeldt E, et al. One in 3 prescriptions are never redeemed: primary nonadherence in an outpatient clinic. J Am Acad Dermatol. 2008;59:27-33.
Resident Pearl
- It is not just the esoteric jargon and complex pathophysiologic concepts in dermatology that can challenge effective communication with our patients. We face potential for misunderstanding even in situations that may seem straightforward. Vigilance in avoiding ambiguity in all our exchanges with patients can help foster therapeutic relationships and optimize patient care.
Survey: Barriers discourage diverse students from dermatology career
A .
Yssra S. Soliman of the division of dermatology, in the department of medicine, Albert Einstein College of Medicine, New York, and colleagues surveyed 155 students from 28 different medical schools between January and April 2018 about barriers to applying for a dermatology residency. Of total participants, 43% expressed an interest in applying for a dermatology residency. Of the 155 survey respondents, 58% were nonwhite.
Students of ethnic minorities and students with lower incomes cited lack of diversity in dermatology as a top barrier to applying for a dermatology residency, according to a research letter published in JAMA Dermatology.Other primary barriers reported by students of color were negative perceptions of minority students by residencies, such as lower performance expectations; socioeconomic factors, such as lack of loan forgiveness; and a lack of mentors. (Minorities in the study were defined as nonwhite students and lower-income students were defined as those with annual household incomes below $40,000.)
Study authors wrote that the results highlight the need to recruit and mentor students of all backgrounds. Furthermore, efforts should be made to increase minority students’ exposure to dermatology through curriculum, providing research opportunities, and reducing the cost of visiting electives by providing stipends, they concluded.
The survey results are not surprising, said Susan C. Taylor, MD, cofounder of the Skin of Color Center at St. Luke’s-Roosevelt Hospital in New York and a Philadelphia-based dermatologist. “I think that [the survey] is accurate and reflects the most common barriers for minority students,” Dr. Taylor said in an interview.
While recent progress has been made in discussing the subject of diversity in dermatology and identifying ways to improve, there has been little change in the actual numbers of diverse dermatologists, she noted.
Dermatology remains the least diverse medical field, after orthopedics. Blacks for example, compose 13% of the U.S. population and Hispanics compose 16% of the population, but each group represents less than 5% of dermatologists, according to the JAMA Dermatology article. At the same time, data show that race-concordant visits are longer and have higher ratings of patient satisfaction. In addition, minority physicians are more likely to care for patients of their own race or ethnic group, practice in underserved areas, care for poor patients and those with Medicaid, and treat patients who report poor health status, studies have found.
Amit Pandya, MD, chair of the American Academy of Dermatology membership committee, said that, while the response rate for the JAMA Dermatology survey was small, the results add important new information about the views of medical students regarding a career in dermatology.
“More research in a larger population of students is needed to learn more about the barriers to matching in dermatology, particularly for students from an under-represented minority background,” Dr. Pandya, professor of dermatology at the University of Texas Southwestern Medical Center, Dallas, said in an interview.
He added that AAD is making marked efforts to improve diversity in dermatology through its diversity committee. AAD diversity initiatives include an intersociety Work Group on Diversity in Dermatology, a diversity mentorship program for medical students, sponsorship of Nth Dimension bioskill workshops, and the Diversity Champion program, which promotes mentorship, volunteerism, and educational activities for students underrepresented in medicine.
It’s too early to tell if the efforts are working, Dr. Pandya said. It will take a few years to see if the efforts result in more minority applicants being interviewed or accepted to a dermatology residency program.
The AAD will hold a Diversity Champion conference in September in Chicago, which is open to “diversity champions” from dermatology residency programs across the United States. The conference is sponsored by the AAD, Association of Professors of Dermatology, Women’s Dermatologic Society, Skin of Color Society, and Society of Investigative Dermatology.
“It will be an annual conference with the goal of improving diversity in our field,” said Dr. Pandya, conference cochair.
SOURCE: Soliman YS et al. JAMA Dermatol. 2019 Jan 9. doi: 10.1001/jamadermatol.2018.4813.
A .
Yssra S. Soliman of the division of dermatology, in the department of medicine, Albert Einstein College of Medicine, New York, and colleagues surveyed 155 students from 28 different medical schools between January and April 2018 about barriers to applying for a dermatology residency. Of total participants, 43% expressed an interest in applying for a dermatology residency. Of the 155 survey respondents, 58% were nonwhite.
Students of ethnic minorities and students with lower incomes cited lack of diversity in dermatology as a top barrier to applying for a dermatology residency, according to a research letter published in JAMA Dermatology.Other primary barriers reported by students of color were negative perceptions of minority students by residencies, such as lower performance expectations; socioeconomic factors, such as lack of loan forgiveness; and a lack of mentors. (Minorities in the study were defined as nonwhite students and lower-income students were defined as those with annual household incomes below $40,000.)
Study authors wrote that the results highlight the need to recruit and mentor students of all backgrounds. Furthermore, efforts should be made to increase minority students’ exposure to dermatology through curriculum, providing research opportunities, and reducing the cost of visiting electives by providing stipends, they concluded.
The survey results are not surprising, said Susan C. Taylor, MD, cofounder of the Skin of Color Center at St. Luke’s-Roosevelt Hospital in New York and a Philadelphia-based dermatologist. “I think that [the survey] is accurate and reflects the most common barriers for minority students,” Dr. Taylor said in an interview.
While recent progress has been made in discussing the subject of diversity in dermatology and identifying ways to improve, there has been little change in the actual numbers of diverse dermatologists, she noted.
Dermatology remains the least diverse medical field, after orthopedics. Blacks for example, compose 13% of the U.S. population and Hispanics compose 16% of the population, but each group represents less than 5% of dermatologists, according to the JAMA Dermatology article. At the same time, data show that race-concordant visits are longer and have higher ratings of patient satisfaction. In addition, minority physicians are more likely to care for patients of their own race or ethnic group, practice in underserved areas, care for poor patients and those with Medicaid, and treat patients who report poor health status, studies have found.
Amit Pandya, MD, chair of the American Academy of Dermatology membership committee, said that, while the response rate for the JAMA Dermatology survey was small, the results add important new information about the views of medical students regarding a career in dermatology.
“More research in a larger population of students is needed to learn more about the barriers to matching in dermatology, particularly for students from an under-represented minority background,” Dr. Pandya, professor of dermatology at the University of Texas Southwestern Medical Center, Dallas, said in an interview.
He added that AAD is making marked efforts to improve diversity in dermatology through its diversity committee. AAD diversity initiatives include an intersociety Work Group on Diversity in Dermatology, a diversity mentorship program for medical students, sponsorship of Nth Dimension bioskill workshops, and the Diversity Champion program, which promotes mentorship, volunteerism, and educational activities for students underrepresented in medicine.
It’s too early to tell if the efforts are working, Dr. Pandya said. It will take a few years to see if the efforts result in more minority applicants being interviewed or accepted to a dermatology residency program.
The AAD will hold a Diversity Champion conference in September in Chicago, which is open to “diversity champions” from dermatology residency programs across the United States. The conference is sponsored by the AAD, Association of Professors of Dermatology, Women’s Dermatologic Society, Skin of Color Society, and Society of Investigative Dermatology.
“It will be an annual conference with the goal of improving diversity in our field,” said Dr. Pandya, conference cochair.
SOURCE: Soliman YS et al. JAMA Dermatol. 2019 Jan 9. doi: 10.1001/jamadermatol.2018.4813.
A .
Yssra S. Soliman of the division of dermatology, in the department of medicine, Albert Einstein College of Medicine, New York, and colleagues surveyed 155 students from 28 different medical schools between January and April 2018 about barriers to applying for a dermatology residency. Of total participants, 43% expressed an interest in applying for a dermatology residency. Of the 155 survey respondents, 58% were nonwhite.
Students of ethnic minorities and students with lower incomes cited lack of diversity in dermatology as a top barrier to applying for a dermatology residency, according to a research letter published in JAMA Dermatology.Other primary barriers reported by students of color were negative perceptions of minority students by residencies, such as lower performance expectations; socioeconomic factors, such as lack of loan forgiveness; and a lack of mentors. (Minorities in the study were defined as nonwhite students and lower-income students were defined as those with annual household incomes below $40,000.)
Study authors wrote that the results highlight the need to recruit and mentor students of all backgrounds. Furthermore, efforts should be made to increase minority students’ exposure to dermatology through curriculum, providing research opportunities, and reducing the cost of visiting electives by providing stipends, they concluded.
The survey results are not surprising, said Susan C. Taylor, MD, cofounder of the Skin of Color Center at St. Luke’s-Roosevelt Hospital in New York and a Philadelphia-based dermatologist. “I think that [the survey] is accurate and reflects the most common barriers for minority students,” Dr. Taylor said in an interview.
While recent progress has been made in discussing the subject of diversity in dermatology and identifying ways to improve, there has been little change in the actual numbers of diverse dermatologists, she noted.
Dermatology remains the least diverse medical field, after orthopedics. Blacks for example, compose 13% of the U.S. population and Hispanics compose 16% of the population, but each group represents less than 5% of dermatologists, according to the JAMA Dermatology article. At the same time, data show that race-concordant visits are longer and have higher ratings of patient satisfaction. In addition, minority physicians are more likely to care for patients of their own race or ethnic group, practice in underserved areas, care for poor patients and those with Medicaid, and treat patients who report poor health status, studies have found.
Amit Pandya, MD, chair of the American Academy of Dermatology membership committee, said that, while the response rate for the JAMA Dermatology survey was small, the results add important new information about the views of medical students regarding a career in dermatology.
“More research in a larger population of students is needed to learn more about the barriers to matching in dermatology, particularly for students from an under-represented minority background,” Dr. Pandya, professor of dermatology at the University of Texas Southwestern Medical Center, Dallas, said in an interview.
He added that AAD is making marked efforts to improve diversity in dermatology through its diversity committee. AAD diversity initiatives include an intersociety Work Group on Diversity in Dermatology, a diversity mentorship program for medical students, sponsorship of Nth Dimension bioskill workshops, and the Diversity Champion program, which promotes mentorship, volunteerism, and educational activities for students underrepresented in medicine.
It’s too early to tell if the efforts are working, Dr. Pandya said. It will take a few years to see if the efforts result in more minority applicants being interviewed or accepted to a dermatology residency program.
The AAD will hold a Diversity Champion conference in September in Chicago, which is open to “diversity champions” from dermatology residency programs across the United States. The conference is sponsored by the AAD, Association of Professors of Dermatology, Women’s Dermatologic Society, Skin of Color Society, and Society of Investigative Dermatology.
“It will be an annual conference with the goal of improving diversity in our field,” said Dr. Pandya, conference cochair.
SOURCE: Soliman YS et al. JAMA Dermatol. 2019 Jan 9. doi: 10.1001/jamadermatol.2018.4813.
Emerging Roles of Social Media in Dermatology
As the residents on the podium ran through case presentations at the Texas Dermatological Society meeting this past fall (September 21-22, 2018; Galveston, Texas), I discretely surveyed the room. To no surprise, perhaps half of the attendees at some point during the hour-long presentation glanced down at their smartphones, and 2018 statistics suggest that approximately 74% of these Internet glances were made by engagers of social media sites.1 My FOMO (fear of missing out) kicked in. What was everyone looking at? I opened Instagram on my smartphone and plastered at the top of my home page were Texas Dermatological Society–related “stories” posted by other dermatology residents from across the state, one story featuring the very presentation I was attending. I peeked 2 rows ahead to find the social media “influencer” I have been following on Instagram for months in real life for the first time.
It is not just the younger population glued to their social media accounts. In fact, Facebook boasted a more than 80% increase in users 55 years and older between 2011 and 2014 and a 41% increase in users aged 35 to 54 years.2 In total, there were 3.2 billion social media users globally in 2018.3 With such a large portion of the population engaged in social media, it is no wonder that it has become a rapidly emerging presence within the field of dermatology.
#Ad
Social media has become a powerful marketing tool for the practicing dermatologist. In a recent survey, 41% of social media users reported that social media influenced their choice of a particular physician, facility, or medical practice.4 Corresponding to this behavior, dermatology practices also have used social media to educate patients on services offered, acquire new patients, engage existing patients, create brand loyalty, become a trusted source of medical information in a sea of digital misinformation, and facilitate positive word-of-mouth opportunities.5 In fact, 53% of physician practices in the United States operate a Facebook page.6 For these physicians, marketing through social media carries the advantages of low cost and rapid transmission of information to a wide audience.7 Furthermore, the development of business insights and statistics by some social media platforms, such as those available to users on business profiles on Instagram, enables practices and marketers to target their audiences and optimize reach.
#DermLife
The role of social media in dermatology extends far beyond marketing. Lifestyle blogs centered on daily life as a medical provider, even within the field of dermatology, are gaining popularity. Dermatology-centered lifestyle blogs often incorporate the root derm in their handle, enabling other users to identify the account holder and interact in meaningful ways. According to a post from one popular Instagram influencer Dr. Audrey Sue Cruz (@dr.audreyxsue), such profiles may serve to prevent burnout, provide a creative outlet, share life as a resident, develop a supportive community, provide mentorship, and spread inspiration.
#Hashtag
Another interesting utility of social media is the use of standardized hashtags to facilitate scientific and clinical dialogue among medical professionals. Standardization of hashtag ontology on Twitter and Instagram has been adopted by the urology and gastroenterology fields to filter out “noise” by individuals not intending to join academic discussion.8 In dermatology, standardized hashtags have not been adopted, to my knowledge; however, a search for esoteric dermatologic terms such as #dermatopathology or #mohssurgery directs users to specialty-specific discussions.
#DontFryDay
Another role of social media in dermatology is dissemination of information. One notable example is the reach on Twitter of the “Don’t Fry Day” campaign, an annual campaign by the National Council on Skin Cancer Prevention to promote sun safety awareness and sun protection behaviors. In a recent study by Nguyen et al,9 the hashtag #DontFryDay was tracked on Twitter to assess the reach of the campaign. They found that this campaign had an impressive reach of approximately 1200 contributors, resulting in more than 16.5 million impressions; 18 celebrities and verified individuals accounted for 8,735,549 impressions.9
Despite the large potential for dissemination of information on social media, in 2014 none of the top 10 dermatologic journals or professional dermatologic organizations maintained an Instagram account. Only one of the top 10 patient advocate groups related to dermatology conditions—the Melanoma Research Foundation—was found on Instagram as of 2014.10 Furthermore, none of the top 10 most popular dermatology journals, professional dermatology organizations, or dermatology-related patient advocate groups could be found on Tumblr as of 2014.11 Although some of the aforementioned organizations have since adopted social media accounts, such as Cutis and Dermatology News (@mdedgederm) on Instagram in 2018, these social media platforms remain largely untapped outlets for dissemination of information to the public by reputable sources.
#VerifyHealthcare
Although social media has offered many advantages to the field of dermatology, it also has brought about unique challenges such as blind authorship, lack of source citation, and presentation of opinion as fact.7 To compound the challenge, 90% of millennials aged 18 to 24 years reportedly trust health care information shared by others on social media.12 Do we, as dermatologists, have a duty to take to social media to provide reputable health information? In an effort to address this emerging problem, popular Instagram influencer Dr. Austin Chiang (@austinchiangmd) initiated the #VerifyHealthcare movement, which called for physicians active on social media to practice transparency by providing users with their credentials.13 The goal of the movement is to help users differentiate medical information disseminated by trained medical professionals from misinformation by disreputable sources.
Final Thoughts
Despite its shortcomings, the emerging roles of social media in dermatology have proven to be a prominent force here to stay, providing new and innovative opportunities to dermatologists for social networking, dissemination of health information, motivation and inspiration, and marketing.
- Warden C. 30 statistics on social media and healthcare. Referral MD website. https://getreferralmd.com/2017/01/30-facts-statistics-on-social-media-and-healthcare/. Accessed January 16, 2019.
- Saul DJ. 3 million teens leave Facebook in 3 years: the Facebook demographic report. ISL website. https://isl.co/2014/01/3-million-teens-leave-facebook-in-3-years-the-2014-facebook-demographic-report/. Published January 15, 2014. Accessed January 9, 2019.
- Chaffey D. Global social media research summary 2018. Smart Insights website. https://www.smartinsights.com/social-media-marketing/social-media-strategy/new-global-social-media-research/. Published November 23, 2018. Accessed January 3, 2019.
- Ottenhoff M. Infographic: rising use of social and mobile in healthcare. The Spark Report. December 17, 2012. http://thesparkreport.com/infographic-social-mobile-healthcare/. Accessed January 9, 2019.
- Benabio J. The value of social media for dermatologists. Cutis. 2013;91:269-270.
- The healthcare social media shakeup. CDW Healthcare website. http://www.cdwcommunit.com/resources/infographic/social-media/. Accessed January 9, 2019.
- Vance K, Howe W, Dellavelle RP. Social internet sites as a source of public health information. Dermatol Clin. 2009;27:133-136.
- Chang AL, Vartabedian B, Spiegel B. Harnessing the hashtag: a standard approach to GI dialogue on social media. Am J Gastroeneterol. 2016;111:1082-1084.
- Nguyen JL, Heckman C, Perna F. Analysis of the Twitter “Don’t Fry Day” campaign. JAMA Dermatol. 2018;154:961-962.
- Karimkhani C, Connett J, Boyars L, et al. Dermatology on Instagram. Dermatol Online J. 2014;20. pii:13030/qt71g178w9.
- Correnti C, Boyars L, Karimkhani C, et al. Dermatology on Tumblr. Dermatol Online J. 2014;20:22642.
- Honigman B. 24 outstanding statistics on how social media has impacted healthcare. Referral MD website. https://getreferralmd.com/2013/09/healthcare-social-media-statistics. Accessed January 16, 2019.
- Oliver E. #VerifyHealthcare campaign seeks to increase social media transparency—5 insights. Becker’s GI & Endoscopy website. https://www.beckersasc.com/gastroenterology-and-endoscopy/verifyhealthcare-campaign-seeks-to-increase-social-media-transparency-5-insights.html. Published September 24, 2018. Accessed January 16, 2019.
As the residents on the podium ran through case presentations at the Texas Dermatological Society meeting this past fall (September 21-22, 2018; Galveston, Texas), I discretely surveyed the room. To no surprise, perhaps half of the attendees at some point during the hour-long presentation glanced down at their smartphones, and 2018 statistics suggest that approximately 74% of these Internet glances were made by engagers of social media sites.1 My FOMO (fear of missing out) kicked in. What was everyone looking at? I opened Instagram on my smartphone and plastered at the top of my home page were Texas Dermatological Society–related “stories” posted by other dermatology residents from across the state, one story featuring the very presentation I was attending. I peeked 2 rows ahead to find the social media “influencer” I have been following on Instagram for months in real life for the first time.
It is not just the younger population glued to their social media accounts. In fact, Facebook boasted a more than 80% increase in users 55 years and older between 2011 and 2014 and a 41% increase in users aged 35 to 54 years.2 In total, there were 3.2 billion social media users globally in 2018.3 With such a large portion of the population engaged in social media, it is no wonder that it has become a rapidly emerging presence within the field of dermatology.
#Ad
Social media has become a powerful marketing tool for the practicing dermatologist. In a recent survey, 41% of social media users reported that social media influenced their choice of a particular physician, facility, or medical practice.4 Corresponding to this behavior, dermatology practices also have used social media to educate patients on services offered, acquire new patients, engage existing patients, create brand loyalty, become a trusted source of medical information in a sea of digital misinformation, and facilitate positive word-of-mouth opportunities.5 In fact, 53% of physician practices in the United States operate a Facebook page.6 For these physicians, marketing through social media carries the advantages of low cost and rapid transmission of information to a wide audience.7 Furthermore, the development of business insights and statistics by some social media platforms, such as those available to users on business profiles on Instagram, enables practices and marketers to target their audiences and optimize reach.
#DermLife
The role of social media in dermatology extends far beyond marketing. Lifestyle blogs centered on daily life as a medical provider, even within the field of dermatology, are gaining popularity. Dermatology-centered lifestyle blogs often incorporate the root derm in their handle, enabling other users to identify the account holder and interact in meaningful ways. According to a post from one popular Instagram influencer Dr. Audrey Sue Cruz (@dr.audreyxsue), such profiles may serve to prevent burnout, provide a creative outlet, share life as a resident, develop a supportive community, provide mentorship, and spread inspiration.
#Hashtag
Another interesting utility of social media is the use of standardized hashtags to facilitate scientific and clinical dialogue among medical professionals. Standardization of hashtag ontology on Twitter and Instagram has been adopted by the urology and gastroenterology fields to filter out “noise” by individuals not intending to join academic discussion.8 In dermatology, standardized hashtags have not been adopted, to my knowledge; however, a search for esoteric dermatologic terms such as #dermatopathology or #mohssurgery directs users to specialty-specific discussions.
#DontFryDay
Another role of social media in dermatology is dissemination of information. One notable example is the reach on Twitter of the “Don’t Fry Day” campaign, an annual campaign by the National Council on Skin Cancer Prevention to promote sun safety awareness and sun protection behaviors. In a recent study by Nguyen et al,9 the hashtag #DontFryDay was tracked on Twitter to assess the reach of the campaign. They found that this campaign had an impressive reach of approximately 1200 contributors, resulting in more than 16.5 million impressions; 18 celebrities and verified individuals accounted for 8,735,549 impressions.9
Despite the large potential for dissemination of information on social media, in 2014 none of the top 10 dermatologic journals or professional dermatologic organizations maintained an Instagram account. Only one of the top 10 patient advocate groups related to dermatology conditions—the Melanoma Research Foundation—was found on Instagram as of 2014.10 Furthermore, none of the top 10 most popular dermatology journals, professional dermatology organizations, or dermatology-related patient advocate groups could be found on Tumblr as of 2014.11 Although some of the aforementioned organizations have since adopted social media accounts, such as Cutis and Dermatology News (@mdedgederm) on Instagram in 2018, these social media platforms remain largely untapped outlets for dissemination of information to the public by reputable sources.
#VerifyHealthcare
Although social media has offered many advantages to the field of dermatology, it also has brought about unique challenges such as blind authorship, lack of source citation, and presentation of opinion as fact.7 To compound the challenge, 90% of millennials aged 18 to 24 years reportedly trust health care information shared by others on social media.12 Do we, as dermatologists, have a duty to take to social media to provide reputable health information? In an effort to address this emerging problem, popular Instagram influencer Dr. Austin Chiang (@austinchiangmd) initiated the #VerifyHealthcare movement, which called for physicians active on social media to practice transparency by providing users with their credentials.13 The goal of the movement is to help users differentiate medical information disseminated by trained medical professionals from misinformation by disreputable sources.
Final Thoughts
Despite its shortcomings, the emerging roles of social media in dermatology have proven to be a prominent force here to stay, providing new and innovative opportunities to dermatologists for social networking, dissemination of health information, motivation and inspiration, and marketing.
As the residents on the podium ran through case presentations at the Texas Dermatological Society meeting this past fall (September 21-22, 2018; Galveston, Texas), I discretely surveyed the room. To no surprise, perhaps half of the attendees at some point during the hour-long presentation glanced down at their smartphones, and 2018 statistics suggest that approximately 74% of these Internet glances were made by engagers of social media sites.1 My FOMO (fear of missing out) kicked in. What was everyone looking at? I opened Instagram on my smartphone and plastered at the top of my home page were Texas Dermatological Society–related “stories” posted by other dermatology residents from across the state, one story featuring the very presentation I was attending. I peeked 2 rows ahead to find the social media “influencer” I have been following on Instagram for months in real life for the first time.
It is not just the younger population glued to their social media accounts. In fact, Facebook boasted a more than 80% increase in users 55 years and older between 2011 and 2014 and a 41% increase in users aged 35 to 54 years.2 In total, there were 3.2 billion social media users globally in 2018.3 With such a large portion of the population engaged in social media, it is no wonder that it has become a rapidly emerging presence within the field of dermatology.
#Ad
Social media has become a powerful marketing tool for the practicing dermatologist. In a recent survey, 41% of social media users reported that social media influenced their choice of a particular physician, facility, or medical practice.4 Corresponding to this behavior, dermatology practices also have used social media to educate patients on services offered, acquire new patients, engage existing patients, create brand loyalty, become a trusted source of medical information in a sea of digital misinformation, and facilitate positive word-of-mouth opportunities.5 In fact, 53% of physician practices in the United States operate a Facebook page.6 For these physicians, marketing through social media carries the advantages of low cost and rapid transmission of information to a wide audience.7 Furthermore, the development of business insights and statistics by some social media platforms, such as those available to users on business profiles on Instagram, enables practices and marketers to target their audiences and optimize reach.
#DermLife
The role of social media in dermatology extends far beyond marketing. Lifestyle blogs centered on daily life as a medical provider, even within the field of dermatology, are gaining popularity. Dermatology-centered lifestyle blogs often incorporate the root derm in their handle, enabling other users to identify the account holder and interact in meaningful ways. According to a post from one popular Instagram influencer Dr. Audrey Sue Cruz (@dr.audreyxsue), such profiles may serve to prevent burnout, provide a creative outlet, share life as a resident, develop a supportive community, provide mentorship, and spread inspiration.
#Hashtag
Another interesting utility of social media is the use of standardized hashtags to facilitate scientific and clinical dialogue among medical professionals. Standardization of hashtag ontology on Twitter and Instagram has been adopted by the urology and gastroenterology fields to filter out “noise” by individuals not intending to join academic discussion.8 In dermatology, standardized hashtags have not been adopted, to my knowledge; however, a search for esoteric dermatologic terms such as #dermatopathology or #mohssurgery directs users to specialty-specific discussions.
#DontFryDay
Another role of social media in dermatology is dissemination of information. One notable example is the reach on Twitter of the “Don’t Fry Day” campaign, an annual campaign by the National Council on Skin Cancer Prevention to promote sun safety awareness and sun protection behaviors. In a recent study by Nguyen et al,9 the hashtag #DontFryDay was tracked on Twitter to assess the reach of the campaign. They found that this campaign had an impressive reach of approximately 1200 contributors, resulting in more than 16.5 million impressions; 18 celebrities and verified individuals accounted for 8,735,549 impressions.9
Despite the large potential for dissemination of information on social media, in 2014 none of the top 10 dermatologic journals or professional dermatologic organizations maintained an Instagram account. Only one of the top 10 patient advocate groups related to dermatology conditions—the Melanoma Research Foundation—was found on Instagram as of 2014.10 Furthermore, none of the top 10 most popular dermatology journals, professional dermatology organizations, or dermatology-related patient advocate groups could be found on Tumblr as of 2014.11 Although some of the aforementioned organizations have since adopted social media accounts, such as Cutis and Dermatology News (@mdedgederm) on Instagram in 2018, these social media platforms remain largely untapped outlets for dissemination of information to the public by reputable sources.
#VerifyHealthcare
Although social media has offered many advantages to the field of dermatology, it also has brought about unique challenges such as blind authorship, lack of source citation, and presentation of opinion as fact.7 To compound the challenge, 90% of millennials aged 18 to 24 years reportedly trust health care information shared by others on social media.12 Do we, as dermatologists, have a duty to take to social media to provide reputable health information? In an effort to address this emerging problem, popular Instagram influencer Dr. Austin Chiang (@austinchiangmd) initiated the #VerifyHealthcare movement, which called for physicians active on social media to practice transparency by providing users with their credentials.13 The goal of the movement is to help users differentiate medical information disseminated by trained medical professionals from misinformation by disreputable sources.
Final Thoughts
Despite its shortcomings, the emerging roles of social media in dermatology have proven to be a prominent force here to stay, providing new and innovative opportunities to dermatologists for social networking, dissemination of health information, motivation and inspiration, and marketing.
- Warden C. 30 statistics on social media and healthcare. Referral MD website. https://getreferralmd.com/2017/01/30-facts-statistics-on-social-media-and-healthcare/. Accessed January 16, 2019.
- Saul DJ. 3 million teens leave Facebook in 3 years: the Facebook demographic report. ISL website. https://isl.co/2014/01/3-million-teens-leave-facebook-in-3-years-the-2014-facebook-demographic-report/. Published January 15, 2014. Accessed January 9, 2019.
- Chaffey D. Global social media research summary 2018. Smart Insights website. https://www.smartinsights.com/social-media-marketing/social-media-strategy/new-global-social-media-research/. Published November 23, 2018. Accessed January 3, 2019.
- Ottenhoff M. Infographic: rising use of social and mobile in healthcare. The Spark Report. December 17, 2012. http://thesparkreport.com/infographic-social-mobile-healthcare/. Accessed January 9, 2019.
- Benabio J. The value of social media for dermatologists. Cutis. 2013;91:269-270.
- The healthcare social media shakeup. CDW Healthcare website. http://www.cdwcommunit.com/resources/infographic/social-media/. Accessed January 9, 2019.
- Vance K, Howe W, Dellavelle RP. Social internet sites as a source of public health information. Dermatol Clin. 2009;27:133-136.
- Chang AL, Vartabedian B, Spiegel B. Harnessing the hashtag: a standard approach to GI dialogue on social media. Am J Gastroeneterol. 2016;111:1082-1084.
- Nguyen JL, Heckman C, Perna F. Analysis of the Twitter “Don’t Fry Day” campaign. JAMA Dermatol. 2018;154:961-962.
- Karimkhani C, Connett J, Boyars L, et al. Dermatology on Instagram. Dermatol Online J. 2014;20. pii:13030/qt71g178w9.
- Correnti C, Boyars L, Karimkhani C, et al. Dermatology on Tumblr. Dermatol Online J. 2014;20:22642.
- Honigman B. 24 outstanding statistics on how social media has impacted healthcare. Referral MD website. https://getreferralmd.com/2013/09/healthcare-social-media-statistics. Accessed January 16, 2019.
- Oliver E. #VerifyHealthcare campaign seeks to increase social media transparency—5 insights. Becker’s GI & Endoscopy website. https://www.beckersasc.com/gastroenterology-and-endoscopy/verifyhealthcare-campaign-seeks-to-increase-social-media-transparency-5-insights.html. Published September 24, 2018. Accessed January 16, 2019.
- Warden C. 30 statistics on social media and healthcare. Referral MD website. https://getreferralmd.com/2017/01/30-facts-statistics-on-social-media-and-healthcare/. Accessed January 16, 2019.
- Saul DJ. 3 million teens leave Facebook in 3 years: the Facebook demographic report. ISL website. https://isl.co/2014/01/3-million-teens-leave-facebook-in-3-years-the-2014-facebook-demographic-report/. Published January 15, 2014. Accessed January 9, 2019.
- Chaffey D. Global social media research summary 2018. Smart Insights website. https://www.smartinsights.com/social-media-marketing/social-media-strategy/new-global-social-media-research/. Published November 23, 2018. Accessed January 3, 2019.
- Ottenhoff M. Infographic: rising use of social and mobile in healthcare. The Spark Report. December 17, 2012. http://thesparkreport.com/infographic-social-mobile-healthcare/. Accessed January 9, 2019.
- Benabio J. The value of social media for dermatologists. Cutis. 2013;91:269-270.
- The healthcare social media shakeup. CDW Healthcare website. http://www.cdwcommunit.com/resources/infographic/social-media/. Accessed January 9, 2019.
- Vance K, Howe W, Dellavelle RP. Social internet sites as a source of public health information. Dermatol Clin. 2009;27:133-136.
- Chang AL, Vartabedian B, Spiegel B. Harnessing the hashtag: a standard approach to GI dialogue on social media. Am J Gastroeneterol. 2016;111:1082-1084.
- Nguyen JL, Heckman C, Perna F. Analysis of the Twitter “Don’t Fry Day” campaign. JAMA Dermatol. 2018;154:961-962.
- Karimkhani C, Connett J, Boyars L, et al. Dermatology on Instagram. Dermatol Online J. 2014;20. pii:13030/qt71g178w9.
- Correnti C, Boyars L, Karimkhani C, et al. Dermatology on Tumblr. Dermatol Online J. 2014;20:22642.
- Honigman B. 24 outstanding statistics on how social media has impacted healthcare. Referral MD website. https://getreferralmd.com/2013/09/healthcare-social-media-statistics. Accessed January 16, 2019.
- Oliver E. #VerifyHealthcare campaign seeks to increase social media transparency—5 insights. Becker’s GI & Endoscopy website. https://www.beckersasc.com/gastroenterology-and-endoscopy/verifyhealthcare-campaign-seeks-to-increase-social-media-transparency-5-insights.html. Published September 24, 2018. Accessed January 16, 2019.
Resident Pearl
- The emerging presence of social media in dermatology provides opportunities for dermatologists to participate in dissemination and consumption of reliable health information, marketing, social networking among colleagues, and motivation and inspiration. It has been proposed that participation may serve to prevent resident burnout.
Allergy Testing in Dermatology and Beyond
Allergy testing typically refers to evaluation of a patient for suspected type I or type IV hypersensitivity.1,2 The possibility of type I hypersensitivity is raised in patients presenting with food allergies, allergic rhinitis, asthma, and immediate adverse reactions to medications, whereas type IV hypersensitivity is suspected in patients with eczematous eruptions, delayed adverse cutaneous reactions to medications, and failure of metallic implants (eg, metal joint replacements, cardiac stents) in conjunction with overlying skin rashes (Table 1).1-5 Type II (eg, pemphigus vulgaris) and type III (eg, IgA vasculitis) hypersensitivities are not evaluated with screening allergy tests.
Type I Sensitization
Type I hypersensitivity is an immediate hypersensitivity mediated predominantly by IgE activation of mast cells in the skin as well as the respiratory and gastric mucosa.1 Sensitization of an individual patient occurs when antigen-presenting cells induce a helper T cell (TH2) cytokine response leading to B-cell class switching and allergen-specific IgE production. Upon repeat exposure to the allergen, circulating antibodies then bind to high-affinity receptors on mast cells and basophils and initiate an allergic inflammatory response, leading to a clinical presentation of allergic rhinitis, urticaria, or immediate drug reactions. Confirming type I sensitization may be performed via serologic (in vitro) or skin testing (in vivo).5,6
Serologic Testing (In Vitro)
Serologic testing is a blood test that detects circulating IgE levels against specific allergens.5 The first such test, the radioallergosorbent test, was introduced in the 1970s but is not quantitative and is no longer used. Although common, it is inaccurate to describe current serum IgE (s-IgE) testing as radioallergosorbent testing. There are several US Food and Drug Administration-approved s-IgE assays in common use, and these tests may be helpful in elucidating relevant allergens and for tailoring therapy appropriately, which may consist of avoidance of certain foods or environmental agents and/or allergen immunotherapy.
Skin Testing (In Vivo)
Skin testing can be performed percutaneously (eg, percutaneous skin testing) or intradermally (eg, intradermal testing).6 Percutaneous skin testing is performed by placing a drop of allergen extract on the skin, after which a lancet is used to lightly scratch the skin; intradermal testing is performed by injecting a small amount of allergen extract into the dermis. In both cases, the skin is evaluated after 15 to 20 minutes for the presence and size of a cutaneous wheal. Medications with antihistaminergic activity must be discontinued prior to testing. Both s-IgE and skin testing assess for type I hypersensitivity, and factors such as extensive rash, concern for anaphylaxis, or inability to discontinue antihistamines may favor s-IgE testing versus skin testing. False-positive results can occur with both tests, and for this reason, test results should always be interpreted in conjunction with clinical examination and patient history to determine relevant allergies.
Type IV Sensitization
Type IV hypersensitivity is a delayed hypersensitivity mediated primarily by lymphocytes.2 Sensitization occurs when haptens bind to host proteins and are presented by epidermal and dermal dendritic cells to T lymphocytes in the skin. These lymphocytes then migrate to regional lymph nodes where antigen-specific T lymphocytes are produced and home back to the skin. Upon reexposure to the allergen, these memory T lymphocytes become activated and incite a delayed allergic response. Confirming type IV hypersensitivity primarily is accomplished via patch testing, though other testing modalities exist.
Skin Biopsy
Biopsy is sometimes performed in the workup of an individual presenting with allergic contact dermatitis (ACD) and typically will show spongiosis with normal stratum corneum and epidermal thickness in the setting of acute ACD and mild to marked acanthosis and parakeratosis in chronic ACD.7 The findings, however, are nonspecific and the differential of these histopathologic findings encompasses nummular dermatitis, atopic dermatitis, irritant contact dermatitis, and dyshidrotic eczema, among others. The presence of eosinophils and Langerhans cell microabscesses may provide supportive evidence for ACD over the other spongiotic dermatitides.7,8
Patch Testing
Patch testing is the gold standard in diagnosing type IV hypersensitivities resulting in a clinical presentation of ACD. Hundreds of allergens are commercially available for patch testing, and more commonly tested allergens fall into one of several categories, such as cosmetic preservatives, rubbers, metals, textiles, fragrances, adhesives, antibiotics, plants, and even corticosteroids. Of note, a common misconception is that ACD must result from new exposures; however, patients may develop ACD secondary to an exposure or product they have been using for many years without a problem.
Three commonly used screening series are the thin-layer rapid use epicutaneous (T.R.U.E.) test (SmartPractice), North American Contact Dermatitis Group screening series, and American Contact Dermatitis Society Core 80 allergen series, which have some variation in the type and number of allergens included (Table 2). The T.R.U.E. test will miss a notable number of clinically relevant allergens in comparison to the North American Contact Dermatitis Group and American Contact Dermatitis Society Core series, and it may be of particularly low utility in identifying fragrance or preservative ACD.9
Allergens are placed on the back in chambers in a petrolatum or aqueous medium. The patches remain affixed for 48 hours, during which time the patient is asked to refrain from showering or exercising to prevent loss of patches. The patient's skin is then evaluated for reactions to allergens on 2 separate occasions: at the time of patch removal 48 hours after initial placement, then the areas of patches are marked for delayed readings at day 4 to day 7 after initial patch placement. Results are scored based on the degree of the inflammatory reaction (Table 3). Delayed readings beyond day 7 may be necessary for metals, specific preservatives (eg, dodecyl gallate, propolis), and neomycin.10
There is a wide spectrum of cutaneous disease that should prompt consideration of patch testing, including well-circumscribed eczematous dermatitis (eg, recurrent lip, hand, and foot dermatitis); patchy or diffuse eczema, especially if recently worsened and/or unresponsive to topical steroids; lichenoid eruptions, particularly of mucosal surfaces; mucous membrane eruptions (eg, stomatitis, vulvitis); and eczematous presentations that raise concern for airborne (photodistributed) or systemic contact dermatitis.11-13 Although further studies of efficacy and safety are ongoing, patch testing also may be useful in the diagnosis of nonimmediate cutaneous adverse drug reactions, especially fixed drug eruptions, acute generalized exanthematous pustulosis, systemic contact dermatitis from medications, and drug-induced hypersensitivity syndrome.3 Lastly, patients with type IV hypersensitivity to metals, adhesives, or antibiotics used in metallic orthopedic or cardiac implants may experience implant failure, regional contact dermatitis, or both, and benefit from patch testing prior to implant replacement to assess for potential allergens. Of the joints that fail, it is estimated that up to 5% are due to metal hypersensitivity.4
Throughout patch testing, patients may continue to manage their skin condition with oral antihistamines and topical steroids, though application to the site at which the patches are applied should be avoided throughout patch testing and during the week prior. According to expert consensus, immunosuppressive medications that are less likely to impact patch testing and therefore may be continued include low-dose methotrexate, oral prednisone less than 10 mg daily, biologic therapy, and low-dose cyclosporine (<2 mg/kg daily). Therapeutic interventions that are more likely to impact patch testing and should be avoided include phototherapy or extensive sun exposure within a week prior to testing, oral prednisone more than 10 mg daily, intramuscular triamcinolone within the preceding month, and high-dose cyclosporine (>2 mg/kg daily).14
An important component to successful patch testing is posttest patient counseling. Providers can create a safe list of products for patients by logging onto the American Contact Dermatitis Society website and accessing the Contact Allergen Management Program (CAMP).15 All relevant allergens found on patch testing may be selected and patient-specific identification codes generated. Once these codes are entered into the CAMP app on the patient's cellular device, a personalized, regularly updated list of safe products appears for many categories of products, including shampoos, sunscreens, moisturizers, cosmetic products, and laundry or dish detergents, among others. Of note, this app is not helpful for avoidance in patients with textile allergies. Patients should be counseled that improvement occurs with avoidance, which usually occurs within weeks but may slowly occur over time in some cases.
Lymphocyte Transformation Test (In Vitro)
The lymphocyte transformation test is an experimental in vitro test for type IV hypersensitivity. This serologic test utilizes allergens to stimulate memory T lymphocytes in vitro and measures the degree of response to the allergen. Although this test has generated excitement, particularly for the potential to safely evaluate for severe adverse cutaneous drug reactions, it currently is not the standard of care and is not utilized in the United States.16
Conclusion
Dermatologists play a vital role in the workup of suspected type IV hypersensitivities. Patch testing is an important but underutilized tool in the arsenal of allergy testing and may be indicated in a wide variety of cutaneous presentations, adverse reactions to medications, and implanted device failures. Identification and avoidance of a culprit allergen has the potential to lead to complete resolution of disease and notable improvement in quality of life for patients.
Acknowledgments
The author thanks Nina Botto, MD (San Francisco, California), for her mentorship in the arena of ACD as well as the Women's Dermatologic Society for the support they provided through the mentorship program.
- Oettgen H, Broide DH. Introduction to the mechanisms of allergic disease. In: Holgate ST, Church MK, Broide DH, et al, eds. Allergy. 4th ed. Philadelphia, PA: Elsevier Saunders; 2012:1-32.
- Werfel T, Kapp A. Atopic dermatitis and allergic contact dermatitis. In: Holgate ST, Church MK, Broide DH, et al, eds. Allergy. 4th ed. Philadelphia, PA: Elsevier Saunders; 2012:263-286.
- Zinn A, Gayam S, Chelliah MP, et al. Patch testing for nonimmediate cutaneous adverse drug reactions. J Am Acad Dermatol. 2018;78:421-423.
- Thyssen JP, Menne T, Schalock PC, et al. Pragmatic approach to the clinical work-up of patients with putative allergic disease to metallic orthopaedic implants before and after surgery. Br J Dermatol. 2011;164:473-478.
- Cox L. Overview of serological-specific IgE antibody testing in children. Curr Allergy Asthma Rep. 2011;11:447-453.
- Dolen WK. Skin testing and immunoassays for allergen-specific IgE. Clin Rev Allergy Immunol. 2001;21:229-239.
- Keeling BH, Gavino AC, Gavino AC. Skin biopsy, the allergists' tool: how to interpret a report. Curr Allergy Asthma Rep. 2015;15:62.
- Rosa G, Fernandez AP, Vij A, et al. Langerhans cell collections, but not eosinophils, are clues to a diagnosis of allergic contact dermatitis in appropriate skin biopsies. J Cutan Pathol. 2016;43:498-504.
- DeKoven JG, Warshaw EM, Belsito DV. North American Contact Dermatitis Group patch test results 2013-2014. Dermatitis. 2017;28:33-46.
- Davis MD, Bhate K, Rohlinger AL, et al. Delayed patch test reading after 5 days: the Mayo Clinic experience. J Am Acad Dermatol. 2008;59:225-233.
- Rajagopalan R, Anderson RT. The profile of a patient with contact dermatitis and a suspicion of contact allergy (history, physical characteristics, and dermatology-specific quality of life). Am J Contact Dermat. 1997;8:26-31.
- Huygens S, Goossens A. An update on airborne contact dermatitis. Contact Dermatitis. 2001;44:1-6.
- Salam TN, Fowler JF. Balsam-related systemic contact dermatitis. J Am Acad Dermatol. 2001;45:377-381.
- Fowler JF, Maibach HI, Zirwas M, et al. Effects of immunomodulatory agents on patch testing: expert opinion 2012. Dermatitis. 2012;23:301-303.
- ACDS CAMP. American Contact Dermatitis Society website. https://www.contactderm.org/i4a/pages/index.cfm?pageid=3489. Accessed November 14, 2018.
- Popple A, Williams J, Maxwell G, et al. The lymphocyte transformation test in allergic contact dermatitis: new opportunities. J Immunotoxicol. 2016;13:84-91.
Allergy testing typically refers to evaluation of a patient for suspected type I or type IV hypersensitivity.1,2 The possibility of type I hypersensitivity is raised in patients presenting with food allergies, allergic rhinitis, asthma, and immediate adverse reactions to medications, whereas type IV hypersensitivity is suspected in patients with eczematous eruptions, delayed adverse cutaneous reactions to medications, and failure of metallic implants (eg, metal joint replacements, cardiac stents) in conjunction with overlying skin rashes (Table 1).1-5 Type II (eg, pemphigus vulgaris) and type III (eg, IgA vasculitis) hypersensitivities are not evaluated with screening allergy tests.
Type I Sensitization
Type I hypersensitivity is an immediate hypersensitivity mediated predominantly by IgE activation of mast cells in the skin as well as the respiratory and gastric mucosa.1 Sensitization of an individual patient occurs when antigen-presenting cells induce a helper T cell (TH2) cytokine response leading to B-cell class switching and allergen-specific IgE production. Upon repeat exposure to the allergen, circulating antibodies then bind to high-affinity receptors on mast cells and basophils and initiate an allergic inflammatory response, leading to a clinical presentation of allergic rhinitis, urticaria, or immediate drug reactions. Confirming type I sensitization may be performed via serologic (in vitro) or skin testing (in vivo).5,6
Serologic Testing (In Vitro)
Serologic testing is a blood test that detects circulating IgE levels against specific allergens.5 The first such test, the radioallergosorbent test, was introduced in the 1970s but is not quantitative and is no longer used. Although common, it is inaccurate to describe current serum IgE (s-IgE) testing as radioallergosorbent testing. There are several US Food and Drug Administration-approved s-IgE assays in common use, and these tests may be helpful in elucidating relevant allergens and for tailoring therapy appropriately, which may consist of avoidance of certain foods or environmental agents and/or allergen immunotherapy.
Skin Testing (In Vivo)
Skin testing can be performed percutaneously (eg, percutaneous skin testing) or intradermally (eg, intradermal testing).6 Percutaneous skin testing is performed by placing a drop of allergen extract on the skin, after which a lancet is used to lightly scratch the skin; intradermal testing is performed by injecting a small amount of allergen extract into the dermis. In both cases, the skin is evaluated after 15 to 20 minutes for the presence and size of a cutaneous wheal. Medications with antihistaminergic activity must be discontinued prior to testing. Both s-IgE and skin testing assess for type I hypersensitivity, and factors such as extensive rash, concern for anaphylaxis, or inability to discontinue antihistamines may favor s-IgE testing versus skin testing. False-positive results can occur with both tests, and for this reason, test results should always be interpreted in conjunction with clinical examination and patient history to determine relevant allergies.
Type IV Sensitization
Type IV hypersensitivity is a delayed hypersensitivity mediated primarily by lymphocytes.2 Sensitization occurs when haptens bind to host proteins and are presented by epidermal and dermal dendritic cells to T lymphocytes in the skin. These lymphocytes then migrate to regional lymph nodes where antigen-specific T lymphocytes are produced and home back to the skin. Upon reexposure to the allergen, these memory T lymphocytes become activated and incite a delayed allergic response. Confirming type IV hypersensitivity primarily is accomplished via patch testing, though other testing modalities exist.
Skin Biopsy
Biopsy is sometimes performed in the workup of an individual presenting with allergic contact dermatitis (ACD) and typically will show spongiosis with normal stratum corneum and epidermal thickness in the setting of acute ACD and mild to marked acanthosis and parakeratosis in chronic ACD.7 The findings, however, are nonspecific and the differential of these histopathologic findings encompasses nummular dermatitis, atopic dermatitis, irritant contact dermatitis, and dyshidrotic eczema, among others. The presence of eosinophils and Langerhans cell microabscesses may provide supportive evidence for ACD over the other spongiotic dermatitides.7,8
Patch Testing
Patch testing is the gold standard in diagnosing type IV hypersensitivities resulting in a clinical presentation of ACD. Hundreds of allergens are commercially available for patch testing, and more commonly tested allergens fall into one of several categories, such as cosmetic preservatives, rubbers, metals, textiles, fragrances, adhesives, antibiotics, plants, and even corticosteroids. Of note, a common misconception is that ACD must result from new exposures; however, patients may develop ACD secondary to an exposure or product they have been using for many years without a problem.
Three commonly used screening series are the thin-layer rapid use epicutaneous (T.R.U.E.) test (SmartPractice), North American Contact Dermatitis Group screening series, and American Contact Dermatitis Society Core 80 allergen series, which have some variation in the type and number of allergens included (Table 2). The T.R.U.E. test will miss a notable number of clinically relevant allergens in comparison to the North American Contact Dermatitis Group and American Contact Dermatitis Society Core series, and it may be of particularly low utility in identifying fragrance or preservative ACD.9
Allergens are placed on the back in chambers in a petrolatum or aqueous medium. The patches remain affixed for 48 hours, during which time the patient is asked to refrain from showering or exercising to prevent loss of patches. The patient's skin is then evaluated for reactions to allergens on 2 separate occasions: at the time of patch removal 48 hours after initial placement, then the areas of patches are marked for delayed readings at day 4 to day 7 after initial patch placement. Results are scored based on the degree of the inflammatory reaction (Table 3). Delayed readings beyond day 7 may be necessary for metals, specific preservatives (eg, dodecyl gallate, propolis), and neomycin.10
There is a wide spectrum of cutaneous disease that should prompt consideration of patch testing, including well-circumscribed eczematous dermatitis (eg, recurrent lip, hand, and foot dermatitis); patchy or diffuse eczema, especially if recently worsened and/or unresponsive to topical steroids; lichenoid eruptions, particularly of mucosal surfaces; mucous membrane eruptions (eg, stomatitis, vulvitis); and eczematous presentations that raise concern for airborne (photodistributed) or systemic contact dermatitis.11-13 Although further studies of efficacy and safety are ongoing, patch testing also may be useful in the diagnosis of nonimmediate cutaneous adverse drug reactions, especially fixed drug eruptions, acute generalized exanthematous pustulosis, systemic contact dermatitis from medications, and drug-induced hypersensitivity syndrome.3 Lastly, patients with type IV hypersensitivity to metals, adhesives, or antibiotics used in metallic orthopedic or cardiac implants may experience implant failure, regional contact dermatitis, or both, and benefit from patch testing prior to implant replacement to assess for potential allergens. Of the joints that fail, it is estimated that up to 5% are due to metal hypersensitivity.4
Throughout patch testing, patients may continue to manage their skin condition with oral antihistamines and topical steroids, though application to the site at which the patches are applied should be avoided throughout patch testing and during the week prior. According to expert consensus, immunosuppressive medications that are less likely to impact patch testing and therefore may be continued include low-dose methotrexate, oral prednisone less than 10 mg daily, biologic therapy, and low-dose cyclosporine (<2 mg/kg daily). Therapeutic interventions that are more likely to impact patch testing and should be avoided include phototherapy or extensive sun exposure within a week prior to testing, oral prednisone more than 10 mg daily, intramuscular triamcinolone within the preceding month, and high-dose cyclosporine (>2 mg/kg daily).14
An important component to successful patch testing is posttest patient counseling. Providers can create a safe list of products for patients by logging onto the American Contact Dermatitis Society website and accessing the Contact Allergen Management Program (CAMP).15 All relevant allergens found on patch testing may be selected and patient-specific identification codes generated. Once these codes are entered into the CAMP app on the patient's cellular device, a personalized, regularly updated list of safe products appears for many categories of products, including shampoos, sunscreens, moisturizers, cosmetic products, and laundry or dish detergents, among others. Of note, this app is not helpful for avoidance in patients with textile allergies. Patients should be counseled that improvement occurs with avoidance, which usually occurs within weeks but may slowly occur over time in some cases.
Lymphocyte Transformation Test (In Vitro)
The lymphocyte transformation test is an experimental in vitro test for type IV hypersensitivity. This serologic test utilizes allergens to stimulate memory T lymphocytes in vitro and measures the degree of response to the allergen. Although this test has generated excitement, particularly for the potential to safely evaluate for severe adverse cutaneous drug reactions, it currently is not the standard of care and is not utilized in the United States.16
Conclusion
Dermatologists play a vital role in the workup of suspected type IV hypersensitivities. Patch testing is an important but underutilized tool in the arsenal of allergy testing and may be indicated in a wide variety of cutaneous presentations, adverse reactions to medications, and implanted device failures. Identification and avoidance of a culprit allergen has the potential to lead to complete resolution of disease and notable improvement in quality of life for patients.
Acknowledgments
The author thanks Nina Botto, MD (San Francisco, California), for her mentorship in the arena of ACD as well as the Women's Dermatologic Society for the support they provided through the mentorship program.
Allergy testing typically refers to evaluation of a patient for suspected type I or type IV hypersensitivity.1,2 The possibility of type I hypersensitivity is raised in patients presenting with food allergies, allergic rhinitis, asthma, and immediate adverse reactions to medications, whereas type IV hypersensitivity is suspected in patients with eczematous eruptions, delayed adverse cutaneous reactions to medications, and failure of metallic implants (eg, metal joint replacements, cardiac stents) in conjunction with overlying skin rashes (Table 1).1-5 Type II (eg, pemphigus vulgaris) and type III (eg, IgA vasculitis) hypersensitivities are not evaluated with screening allergy tests.
Type I Sensitization
Type I hypersensitivity is an immediate hypersensitivity mediated predominantly by IgE activation of mast cells in the skin as well as the respiratory and gastric mucosa.1 Sensitization of an individual patient occurs when antigen-presenting cells induce a helper T cell (TH2) cytokine response leading to B-cell class switching and allergen-specific IgE production. Upon repeat exposure to the allergen, circulating antibodies then bind to high-affinity receptors on mast cells and basophils and initiate an allergic inflammatory response, leading to a clinical presentation of allergic rhinitis, urticaria, or immediate drug reactions. Confirming type I sensitization may be performed via serologic (in vitro) or skin testing (in vivo).5,6
Serologic Testing (In Vitro)
Serologic testing is a blood test that detects circulating IgE levels against specific allergens.5 The first such test, the radioallergosorbent test, was introduced in the 1970s but is not quantitative and is no longer used. Although common, it is inaccurate to describe current serum IgE (s-IgE) testing as radioallergosorbent testing. There are several US Food and Drug Administration-approved s-IgE assays in common use, and these tests may be helpful in elucidating relevant allergens and for tailoring therapy appropriately, which may consist of avoidance of certain foods or environmental agents and/or allergen immunotherapy.
Skin Testing (In Vivo)
Skin testing can be performed percutaneously (eg, percutaneous skin testing) or intradermally (eg, intradermal testing).6 Percutaneous skin testing is performed by placing a drop of allergen extract on the skin, after which a lancet is used to lightly scratch the skin; intradermal testing is performed by injecting a small amount of allergen extract into the dermis. In both cases, the skin is evaluated after 15 to 20 minutes for the presence and size of a cutaneous wheal. Medications with antihistaminergic activity must be discontinued prior to testing. Both s-IgE and skin testing assess for type I hypersensitivity, and factors such as extensive rash, concern for anaphylaxis, or inability to discontinue antihistamines may favor s-IgE testing versus skin testing. False-positive results can occur with both tests, and for this reason, test results should always be interpreted in conjunction with clinical examination and patient history to determine relevant allergies.
Type IV Sensitization
Type IV hypersensitivity is a delayed hypersensitivity mediated primarily by lymphocytes.2 Sensitization occurs when haptens bind to host proteins and are presented by epidermal and dermal dendritic cells to T lymphocytes in the skin. These lymphocytes then migrate to regional lymph nodes where antigen-specific T lymphocytes are produced and home back to the skin. Upon reexposure to the allergen, these memory T lymphocytes become activated and incite a delayed allergic response. Confirming type IV hypersensitivity primarily is accomplished via patch testing, though other testing modalities exist.
Skin Biopsy
Biopsy is sometimes performed in the workup of an individual presenting with allergic contact dermatitis (ACD) and typically will show spongiosis with normal stratum corneum and epidermal thickness in the setting of acute ACD and mild to marked acanthosis and parakeratosis in chronic ACD.7 The findings, however, are nonspecific and the differential of these histopathologic findings encompasses nummular dermatitis, atopic dermatitis, irritant contact dermatitis, and dyshidrotic eczema, among others. The presence of eosinophils and Langerhans cell microabscesses may provide supportive evidence for ACD over the other spongiotic dermatitides.7,8
Patch Testing
Patch testing is the gold standard in diagnosing type IV hypersensitivities resulting in a clinical presentation of ACD. Hundreds of allergens are commercially available for patch testing, and more commonly tested allergens fall into one of several categories, such as cosmetic preservatives, rubbers, metals, textiles, fragrances, adhesives, antibiotics, plants, and even corticosteroids. Of note, a common misconception is that ACD must result from new exposures; however, patients may develop ACD secondary to an exposure or product they have been using for many years without a problem.
Three commonly used screening series are the thin-layer rapid use epicutaneous (T.R.U.E.) test (SmartPractice), North American Contact Dermatitis Group screening series, and American Contact Dermatitis Society Core 80 allergen series, which have some variation in the type and number of allergens included (Table 2). The T.R.U.E. test will miss a notable number of clinically relevant allergens in comparison to the North American Contact Dermatitis Group and American Contact Dermatitis Society Core series, and it may be of particularly low utility in identifying fragrance or preservative ACD.9
Allergens are placed on the back in chambers in a petrolatum or aqueous medium. The patches remain affixed for 48 hours, during which time the patient is asked to refrain from showering or exercising to prevent loss of patches. The patient's skin is then evaluated for reactions to allergens on 2 separate occasions: at the time of patch removal 48 hours after initial placement, then the areas of patches are marked for delayed readings at day 4 to day 7 after initial patch placement. Results are scored based on the degree of the inflammatory reaction (Table 3). Delayed readings beyond day 7 may be necessary for metals, specific preservatives (eg, dodecyl gallate, propolis), and neomycin.10
There is a wide spectrum of cutaneous disease that should prompt consideration of patch testing, including well-circumscribed eczematous dermatitis (eg, recurrent lip, hand, and foot dermatitis); patchy or diffuse eczema, especially if recently worsened and/or unresponsive to topical steroids; lichenoid eruptions, particularly of mucosal surfaces; mucous membrane eruptions (eg, stomatitis, vulvitis); and eczematous presentations that raise concern for airborne (photodistributed) or systemic contact dermatitis.11-13 Although further studies of efficacy and safety are ongoing, patch testing also may be useful in the diagnosis of nonimmediate cutaneous adverse drug reactions, especially fixed drug eruptions, acute generalized exanthematous pustulosis, systemic contact dermatitis from medications, and drug-induced hypersensitivity syndrome.3 Lastly, patients with type IV hypersensitivity to metals, adhesives, or antibiotics used in metallic orthopedic or cardiac implants may experience implant failure, regional contact dermatitis, or both, and benefit from patch testing prior to implant replacement to assess for potential allergens. Of the joints that fail, it is estimated that up to 5% are due to metal hypersensitivity.4
Throughout patch testing, patients may continue to manage their skin condition with oral antihistamines and topical steroids, though application to the site at which the patches are applied should be avoided throughout patch testing and during the week prior. According to expert consensus, immunosuppressive medications that are less likely to impact patch testing and therefore may be continued include low-dose methotrexate, oral prednisone less than 10 mg daily, biologic therapy, and low-dose cyclosporine (<2 mg/kg daily). Therapeutic interventions that are more likely to impact patch testing and should be avoided include phototherapy or extensive sun exposure within a week prior to testing, oral prednisone more than 10 mg daily, intramuscular triamcinolone within the preceding month, and high-dose cyclosporine (>2 mg/kg daily).14
An important component to successful patch testing is posttest patient counseling. Providers can create a safe list of products for patients by logging onto the American Contact Dermatitis Society website and accessing the Contact Allergen Management Program (CAMP).15 All relevant allergens found on patch testing may be selected and patient-specific identification codes generated. Once these codes are entered into the CAMP app on the patient's cellular device, a personalized, regularly updated list of safe products appears for many categories of products, including shampoos, sunscreens, moisturizers, cosmetic products, and laundry or dish detergents, among others. Of note, this app is not helpful for avoidance in patients with textile allergies. Patients should be counseled that improvement occurs with avoidance, which usually occurs within weeks but may slowly occur over time in some cases.
Lymphocyte Transformation Test (In Vitro)
The lymphocyte transformation test is an experimental in vitro test for type IV hypersensitivity. This serologic test utilizes allergens to stimulate memory T lymphocytes in vitro and measures the degree of response to the allergen. Although this test has generated excitement, particularly for the potential to safely evaluate for severe adverse cutaneous drug reactions, it currently is not the standard of care and is not utilized in the United States.16
Conclusion
Dermatologists play a vital role in the workup of suspected type IV hypersensitivities. Patch testing is an important but underutilized tool in the arsenal of allergy testing and may be indicated in a wide variety of cutaneous presentations, adverse reactions to medications, and implanted device failures. Identification and avoidance of a culprit allergen has the potential to lead to complete resolution of disease and notable improvement in quality of life for patients.
Acknowledgments
The author thanks Nina Botto, MD (San Francisco, California), for her mentorship in the arena of ACD as well as the Women's Dermatologic Society for the support they provided through the mentorship program.
- Oettgen H, Broide DH. Introduction to the mechanisms of allergic disease. In: Holgate ST, Church MK, Broide DH, et al, eds. Allergy. 4th ed. Philadelphia, PA: Elsevier Saunders; 2012:1-32.
- Werfel T, Kapp A. Atopic dermatitis and allergic contact dermatitis. In: Holgate ST, Church MK, Broide DH, et al, eds. Allergy. 4th ed. Philadelphia, PA: Elsevier Saunders; 2012:263-286.
- Zinn A, Gayam S, Chelliah MP, et al. Patch testing for nonimmediate cutaneous adverse drug reactions. J Am Acad Dermatol. 2018;78:421-423.
- Thyssen JP, Menne T, Schalock PC, et al. Pragmatic approach to the clinical work-up of patients with putative allergic disease to metallic orthopaedic implants before and after surgery. Br J Dermatol. 2011;164:473-478.
- Cox L. Overview of serological-specific IgE antibody testing in children. Curr Allergy Asthma Rep. 2011;11:447-453.
- Dolen WK. Skin testing and immunoassays for allergen-specific IgE. Clin Rev Allergy Immunol. 2001;21:229-239.
- Keeling BH, Gavino AC, Gavino AC. Skin biopsy, the allergists' tool: how to interpret a report. Curr Allergy Asthma Rep. 2015;15:62.
- Rosa G, Fernandez AP, Vij A, et al. Langerhans cell collections, but not eosinophils, are clues to a diagnosis of allergic contact dermatitis in appropriate skin biopsies. J Cutan Pathol. 2016;43:498-504.
- DeKoven JG, Warshaw EM, Belsito DV. North American Contact Dermatitis Group patch test results 2013-2014. Dermatitis. 2017;28:33-46.
- Davis MD, Bhate K, Rohlinger AL, et al. Delayed patch test reading after 5 days: the Mayo Clinic experience. J Am Acad Dermatol. 2008;59:225-233.
- Rajagopalan R, Anderson RT. The profile of a patient with contact dermatitis and a suspicion of contact allergy (history, physical characteristics, and dermatology-specific quality of life). Am J Contact Dermat. 1997;8:26-31.
- Huygens S, Goossens A. An update on airborne contact dermatitis. Contact Dermatitis. 2001;44:1-6.
- Salam TN, Fowler JF. Balsam-related systemic contact dermatitis. J Am Acad Dermatol. 2001;45:377-381.
- Fowler JF, Maibach HI, Zirwas M, et al. Effects of immunomodulatory agents on patch testing: expert opinion 2012. Dermatitis. 2012;23:301-303.
- ACDS CAMP. American Contact Dermatitis Society website. https://www.contactderm.org/i4a/pages/index.cfm?pageid=3489. Accessed November 14, 2018.
- Popple A, Williams J, Maxwell G, et al. The lymphocyte transformation test in allergic contact dermatitis: new opportunities. J Immunotoxicol. 2016;13:84-91.
- Oettgen H, Broide DH. Introduction to the mechanisms of allergic disease. In: Holgate ST, Church MK, Broide DH, et al, eds. Allergy. 4th ed. Philadelphia, PA: Elsevier Saunders; 2012:1-32.
- Werfel T, Kapp A. Atopic dermatitis and allergic contact dermatitis. In: Holgate ST, Church MK, Broide DH, et al, eds. Allergy. 4th ed. Philadelphia, PA: Elsevier Saunders; 2012:263-286.
- Zinn A, Gayam S, Chelliah MP, et al. Patch testing for nonimmediate cutaneous adverse drug reactions. J Am Acad Dermatol. 2018;78:421-423.
- Thyssen JP, Menne T, Schalock PC, et al. Pragmatic approach to the clinical work-up of patients with putative allergic disease to metallic orthopaedic implants before and after surgery. Br J Dermatol. 2011;164:473-478.
- Cox L. Overview of serological-specific IgE antibody testing in children. Curr Allergy Asthma Rep. 2011;11:447-453.
- Dolen WK. Skin testing and immunoassays for allergen-specific IgE. Clin Rev Allergy Immunol. 2001;21:229-239.
- Keeling BH, Gavino AC, Gavino AC. Skin biopsy, the allergists' tool: how to interpret a report. Curr Allergy Asthma Rep. 2015;15:62.
- Rosa G, Fernandez AP, Vij A, et al. Langerhans cell collections, but not eosinophils, are clues to a diagnosis of allergic contact dermatitis in appropriate skin biopsies. J Cutan Pathol. 2016;43:498-504.
- DeKoven JG, Warshaw EM, Belsito DV. North American Contact Dermatitis Group patch test results 2013-2014. Dermatitis. 2017;28:33-46.
- Davis MD, Bhate K, Rohlinger AL, et al. Delayed patch test reading after 5 days: the Mayo Clinic experience. J Am Acad Dermatol. 2008;59:225-233.
- Rajagopalan R, Anderson RT. The profile of a patient with contact dermatitis and a suspicion of contact allergy (history, physical characteristics, and dermatology-specific quality of life). Am J Contact Dermat. 1997;8:26-31.
- Huygens S, Goossens A. An update on airborne contact dermatitis. Contact Dermatitis. 2001;44:1-6.
- Salam TN, Fowler JF. Balsam-related systemic contact dermatitis. J Am Acad Dermatol. 2001;45:377-381.
- Fowler JF, Maibach HI, Zirwas M, et al. Effects of immunomodulatory agents on patch testing: expert opinion 2012. Dermatitis. 2012;23:301-303.
- ACDS CAMP. American Contact Dermatitis Society website. https://www.contactderm.org/i4a/pages/index.cfm?pageid=3489. Accessed November 14, 2018.
- Popple A, Williams J, Maxwell G, et al. The lymphocyte transformation test in allergic contact dermatitis: new opportunities. J Immunotoxicol. 2016;13:84-91.