User login
Postop delirium linked to greater long-term cognitive decline
Patients with postoperative delirium have significantly worse preoperative short-term cognitive performance and significantly greater long-term cognitive decline, compared with patients without delirium, according to Sharon K. Inouye, MD, and her associates.
In a prospective cohort study of 560 patients aged 70 years and older, 134 patients were selected for the delirium group and 426 for the nondelirium group. The delirium group had a significantly greater decline (–1.03 points) at 1 month, compared with those without delirium (P = .003). After cognitive function had recovered at 2 months, there were no significant differences between groups (P = 0.99). After 2 months, both groups decline on average; however, the delirium group declined significantly more (–1.07) in adjusted mean scores at 36 months (P =.02).
From baseline to 36 months, there was a significant change for the delirium group (–1.30, P less than .01) and no significant change for the group without delirium (–0.23, P = .30). Researchers noted that the effect of delirium remains undiminished after consecutive rehospitalizations, intercurrent illnesses, and major postoperative complications were controlled for.
The patients underwent major noncardiac surgery, such as total hip or knee replacement, open abdominal aortic aneurysm repair, colectomy, and lower-extremity arterial bypass.
“This study provides a novel presentation of the biphasic relationship of delirium and cognitive trajectory, both its well-recognized acute effects but also long-term effects,” the researchers wrote. “Our results suggest that after a period of initial recovery, patients with delirium experience a substantially accelerated trajectory of cognitive aging.”
Read the full study in Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association (doi:10.1016/j.jalz.2016.03.005).
Patients with postoperative delirium have significantly worse preoperative short-term cognitive performance and significantly greater long-term cognitive decline, compared with patients without delirium, according to Sharon K. Inouye, MD, and her associates.
In a prospective cohort study of 560 patients aged 70 years and older, 134 patients were selected for the delirium group and 426 for the nondelirium group. The delirium group had a significantly greater decline (–1.03 points) at 1 month, compared with those without delirium (P = .003). After cognitive function had recovered at 2 months, there were no significant differences between groups (P = 0.99). After 2 months, both groups decline on average; however, the delirium group declined significantly more (–1.07) in adjusted mean scores at 36 months (P =.02).
From baseline to 36 months, there was a significant change for the delirium group (–1.30, P less than .01) and no significant change for the group without delirium (–0.23, P = .30). Researchers noted that the effect of delirium remains undiminished after consecutive rehospitalizations, intercurrent illnesses, and major postoperative complications were controlled for.
The patients underwent major noncardiac surgery, such as total hip or knee replacement, open abdominal aortic aneurysm repair, colectomy, and lower-extremity arterial bypass.
“This study provides a novel presentation of the biphasic relationship of delirium and cognitive trajectory, both its well-recognized acute effects but also long-term effects,” the researchers wrote. “Our results suggest that after a period of initial recovery, patients with delirium experience a substantially accelerated trajectory of cognitive aging.”
Read the full study in Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association (doi:10.1016/j.jalz.2016.03.005).
Patients with postoperative delirium have significantly worse preoperative short-term cognitive performance and significantly greater long-term cognitive decline, compared with patients without delirium, according to Sharon K. Inouye, MD, and her associates.
In a prospective cohort study of 560 patients aged 70 years and older, 134 patients were selected for the delirium group and 426 for the nondelirium group. The delirium group had a significantly greater decline (–1.03 points) at 1 month, compared with those without delirium (P = .003). After cognitive function had recovered at 2 months, there were no significant differences between groups (P = 0.99). After 2 months, both groups decline on average; however, the delirium group declined significantly more (–1.07) in adjusted mean scores at 36 months (P =.02).
From baseline to 36 months, there was a significant change for the delirium group (–1.30, P less than .01) and no significant change for the group without delirium (–0.23, P = .30). Researchers noted that the effect of delirium remains undiminished after consecutive rehospitalizations, intercurrent illnesses, and major postoperative complications were controlled for.
The patients underwent major noncardiac surgery, such as total hip or knee replacement, open abdominal aortic aneurysm repair, colectomy, and lower-extremity arterial bypass.
“This study provides a novel presentation of the biphasic relationship of delirium and cognitive trajectory, both its well-recognized acute effects but also long-term effects,” the researchers wrote. “Our results suggest that after a period of initial recovery, patients with delirium experience a substantially accelerated trajectory of cognitive aging.”
Read the full study in Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association (doi:10.1016/j.jalz.2016.03.005).
FROM ALZHEIMER’S & DEMENTIA
The ‘guilty’ associates of silent thoracic aneurysm fingered
NEW YORK – Aortic aneurysm ranks as one of the top 20 causes of death in the United States. Most of these aneurysms are clinically silent until they rupture, but Yale cardiovascular surgeon John A. Elefteriades, MD, has developed a clinical paradigm that identifies eight markers that physicians can use to detect the disease before it strikes.
Dr. Elefteriades calls his paradigm “Guilt by Association.” It is based on an article he published online last year in the journal Open Heart (2015;2:e000169).
“What we need is for our colleagues in affiliated disciplines to recognize the importance of these offenders in indicating the presence of thoracic aortic aneurysm,” he said, reporting on the paradigm at the meeting sponsored by the American Association for Thoracic Surgery. He noted that studies from Japan of people who had died from out-of-hospital cardiac arrest found that 8% of them had a type A aortic dissection (Am J Cardiol 2016;117:1826-30).
He outlined eight “associates” of thoracic aortic aneurysm (TAA): intracranial aneurysm; bovine aortic arch; abdominal aortic aneurysm; simple renal cysts; bicuspid aortic valve; family history; positive thumb-palm test; and temporal arteritis and other autoimmune disorders.
A patient with TAA has a 10% likelihood of harboring an intracranial aneurysm (Am J Cardiol 2010;105:417-20). “It’s even more common in the descending, compared to the ascending group in examples that we’ve identified,” Dr. Elefteriades said. Particularly vulnerable are patients over age 70 and those with an intracranial aneurysm larger than 4 mm: the former has a 9% chance of harboring a TAA, the latter a 6% chance, he said.
The bovine arch had been thought to be benign, but, Dr. Elefteriades said, “We don’t think it is.”
Bovine arch refers to a group of congenital aortic arch vessels with an aberrant origin of the left common carotid artery. “We recently looked at this as a marker for thoracic aortic disease, and please note that 20% of our TAA patients have a bovine arch,” he said. “This is much higher than in the general population.”
Abdominal aortic aneurysm has long been associated with TAA, he said. “When these aneurysms are identified by ultrasound, it’s important that the thoracic aorta be checked as well,” he said.
“This is a message for internists and our vascular colleagues.”
Simple renal cysts have been found in patients with TAA at a “much higher” rate than the general population, as high as 57% of those with descending aortic aneurysms vs. 11%-13.7% of the general population, Dr. Elefteriades said (J. Am. Heart Assoc. 2016;5:e002248). Simple renal cysts are detected by abdominal CT scan. “It’s just a matter of a few more slices with the CT scan to get the entirety of the thoracic aorta evaluated,” he said.
“We encourage our radiology colleagues to do this when a renal cyst is detected.”
Bicuspid aortic valve mandates “support from our cardiac colleagues when they find one of these to let the patient know he has to be monitored lifelong for later development of this aneurysm,” Dr. Elefteriades said.
Family history of TAA has been known as a strong predictor, but genetic studies have provided clarity on the association (Arch Surg. 1999;134:361‐7). “If the proband has a thoracic aortic aneurysm, there’s 21% likelihood there’s a family member who is affected with an aneurysm somewhere in the body,” he said.
Location of aneurysms in family members is also important, Dr. Elefteriades said. “If the proband has a ascending aortic aneurysm, the kindred also have an ascending aortic aneurysm; but if the proband has a descending aneurysm, the likelihood is that the kindred will have an abdominal aortic aneurysm,” he said. “To identify silent disease, it’s very important we check siblings and children, and now, of course, we’re using whole-exome sequencing.” So far, Dr. Elefteriades has obtained whole-exome sequencing in 200 patients.
The thumb-palm test involves the patient touching the thumb to the palm; the thumb crossing the edge of the flat palm is an indicator of connective tissue disease. “It doesn’t cost anything,” Dr. Elefteriades said. “It is a very simple thing for internists to do to identify those connective tissue diseases.”
Temporal arteritis has become increasingly common in elderly women. “They have a markedly increased likelihood of having a thoracic aortic aneurysm – about 8% in some studies,’ Dr. Elefteriades said. “So we want our neurology colleagues to be aware of this and to look for thoracic aortic aneurysm.”
Dr. Elefteriades disclosed he has received consulting fees from Baxter, Covidien, Datascope, and CryoLife, and a research grant from Medtronic.
NEW YORK – Aortic aneurysm ranks as one of the top 20 causes of death in the United States. Most of these aneurysms are clinically silent until they rupture, but Yale cardiovascular surgeon John A. Elefteriades, MD, has developed a clinical paradigm that identifies eight markers that physicians can use to detect the disease before it strikes.
Dr. Elefteriades calls his paradigm “Guilt by Association.” It is based on an article he published online last year in the journal Open Heart (2015;2:e000169).
“What we need is for our colleagues in affiliated disciplines to recognize the importance of these offenders in indicating the presence of thoracic aortic aneurysm,” he said, reporting on the paradigm at the meeting sponsored by the American Association for Thoracic Surgery. He noted that studies from Japan of people who had died from out-of-hospital cardiac arrest found that 8% of them had a type A aortic dissection (Am J Cardiol 2016;117:1826-30).
He outlined eight “associates” of thoracic aortic aneurysm (TAA): intracranial aneurysm; bovine aortic arch; abdominal aortic aneurysm; simple renal cysts; bicuspid aortic valve; family history; positive thumb-palm test; and temporal arteritis and other autoimmune disorders.
A patient with TAA has a 10% likelihood of harboring an intracranial aneurysm (Am J Cardiol 2010;105:417-20). “It’s even more common in the descending, compared to the ascending group in examples that we’ve identified,” Dr. Elefteriades said. Particularly vulnerable are patients over age 70 and those with an intracranial aneurysm larger than 4 mm: the former has a 9% chance of harboring a TAA, the latter a 6% chance, he said.
The bovine arch had been thought to be benign, but, Dr. Elefteriades said, “We don’t think it is.”
Bovine arch refers to a group of congenital aortic arch vessels with an aberrant origin of the left common carotid artery. “We recently looked at this as a marker for thoracic aortic disease, and please note that 20% of our TAA patients have a bovine arch,” he said. “This is much higher than in the general population.”
Abdominal aortic aneurysm has long been associated with TAA, he said. “When these aneurysms are identified by ultrasound, it’s important that the thoracic aorta be checked as well,” he said.
“This is a message for internists and our vascular colleagues.”
Simple renal cysts have been found in patients with TAA at a “much higher” rate than the general population, as high as 57% of those with descending aortic aneurysms vs. 11%-13.7% of the general population, Dr. Elefteriades said (J. Am. Heart Assoc. 2016;5:e002248). Simple renal cysts are detected by abdominal CT scan. “It’s just a matter of a few more slices with the CT scan to get the entirety of the thoracic aorta evaluated,” he said.
“We encourage our radiology colleagues to do this when a renal cyst is detected.”
Bicuspid aortic valve mandates “support from our cardiac colleagues when they find one of these to let the patient know he has to be monitored lifelong for later development of this aneurysm,” Dr. Elefteriades said.
Family history of TAA has been known as a strong predictor, but genetic studies have provided clarity on the association (Arch Surg. 1999;134:361‐7). “If the proband has a thoracic aortic aneurysm, there’s 21% likelihood there’s a family member who is affected with an aneurysm somewhere in the body,” he said.
Location of aneurysms in family members is also important, Dr. Elefteriades said. “If the proband has a ascending aortic aneurysm, the kindred also have an ascending aortic aneurysm; but if the proband has a descending aneurysm, the likelihood is that the kindred will have an abdominal aortic aneurysm,” he said. “To identify silent disease, it’s very important we check siblings and children, and now, of course, we’re using whole-exome sequencing.” So far, Dr. Elefteriades has obtained whole-exome sequencing in 200 patients.
The thumb-palm test involves the patient touching the thumb to the palm; the thumb crossing the edge of the flat palm is an indicator of connective tissue disease. “It doesn’t cost anything,” Dr. Elefteriades said. “It is a very simple thing for internists to do to identify those connective tissue diseases.”
Temporal arteritis has become increasingly common in elderly women. “They have a markedly increased likelihood of having a thoracic aortic aneurysm – about 8% in some studies,’ Dr. Elefteriades said. “So we want our neurology colleagues to be aware of this and to look for thoracic aortic aneurysm.”
Dr. Elefteriades disclosed he has received consulting fees from Baxter, Covidien, Datascope, and CryoLife, and a research grant from Medtronic.
NEW YORK – Aortic aneurysm ranks as one of the top 20 causes of death in the United States. Most of these aneurysms are clinically silent until they rupture, but Yale cardiovascular surgeon John A. Elefteriades, MD, has developed a clinical paradigm that identifies eight markers that physicians can use to detect the disease before it strikes.
Dr. Elefteriades calls his paradigm “Guilt by Association.” It is based on an article he published online last year in the journal Open Heart (2015;2:e000169).
“What we need is for our colleagues in affiliated disciplines to recognize the importance of these offenders in indicating the presence of thoracic aortic aneurysm,” he said, reporting on the paradigm at the meeting sponsored by the American Association for Thoracic Surgery. He noted that studies from Japan of people who had died from out-of-hospital cardiac arrest found that 8% of them had a type A aortic dissection (Am J Cardiol 2016;117:1826-30).
He outlined eight “associates” of thoracic aortic aneurysm (TAA): intracranial aneurysm; bovine aortic arch; abdominal aortic aneurysm; simple renal cysts; bicuspid aortic valve; family history; positive thumb-palm test; and temporal arteritis and other autoimmune disorders.
A patient with TAA has a 10% likelihood of harboring an intracranial aneurysm (Am J Cardiol 2010;105:417-20). “It’s even more common in the descending, compared to the ascending group in examples that we’ve identified,” Dr. Elefteriades said. Particularly vulnerable are patients over age 70 and those with an intracranial aneurysm larger than 4 mm: the former has a 9% chance of harboring a TAA, the latter a 6% chance, he said.
The bovine arch had been thought to be benign, but, Dr. Elefteriades said, “We don’t think it is.”
Bovine arch refers to a group of congenital aortic arch vessels with an aberrant origin of the left common carotid artery. “We recently looked at this as a marker for thoracic aortic disease, and please note that 20% of our TAA patients have a bovine arch,” he said. “This is much higher than in the general population.”
Abdominal aortic aneurysm has long been associated with TAA, he said. “When these aneurysms are identified by ultrasound, it’s important that the thoracic aorta be checked as well,” he said.
“This is a message for internists and our vascular colleagues.”
Simple renal cysts have been found in patients with TAA at a “much higher” rate than the general population, as high as 57% of those with descending aortic aneurysms vs. 11%-13.7% of the general population, Dr. Elefteriades said (J. Am. Heart Assoc. 2016;5:e002248). Simple renal cysts are detected by abdominal CT scan. “It’s just a matter of a few more slices with the CT scan to get the entirety of the thoracic aorta evaluated,” he said.
“We encourage our radiology colleagues to do this when a renal cyst is detected.”
Bicuspid aortic valve mandates “support from our cardiac colleagues when they find one of these to let the patient know he has to be monitored lifelong for later development of this aneurysm,” Dr. Elefteriades said.
Family history of TAA has been known as a strong predictor, but genetic studies have provided clarity on the association (Arch Surg. 1999;134:361‐7). “If the proband has a thoracic aortic aneurysm, there’s 21% likelihood there’s a family member who is affected with an aneurysm somewhere in the body,” he said.
Location of aneurysms in family members is also important, Dr. Elefteriades said. “If the proband has a ascending aortic aneurysm, the kindred also have an ascending aortic aneurysm; but if the proband has a descending aneurysm, the likelihood is that the kindred will have an abdominal aortic aneurysm,” he said. “To identify silent disease, it’s very important we check siblings and children, and now, of course, we’re using whole-exome sequencing.” So far, Dr. Elefteriades has obtained whole-exome sequencing in 200 patients.
The thumb-palm test involves the patient touching the thumb to the palm; the thumb crossing the edge of the flat palm is an indicator of connective tissue disease. “It doesn’t cost anything,” Dr. Elefteriades said. “It is a very simple thing for internists to do to identify those connective tissue diseases.”
Temporal arteritis has become increasingly common in elderly women. “They have a markedly increased likelihood of having a thoracic aortic aneurysm – about 8% in some studies,’ Dr. Elefteriades said. “So we want our neurology colleagues to be aware of this and to look for thoracic aortic aneurysm.”
Dr. Elefteriades disclosed he has received consulting fees from Baxter, Covidien, Datascope, and CryoLife, and a research grant from Medtronic.
EXPERT ANALYSIS FROM AATS AORTIC SYMPOSIUM 2016
Key clinical point: Eight markers may detect silent thoracic aneurysms before rupture.
Major finding: The eight “associates” of TAA include intracranial aneurysm; bovine aortic arch; abdominal aortic aneurysm; simple renal cysts; and bicuspid aortic valve.
Data source: The “Guilt by Association” paradigm was based upon a review of the literature by Dr. Elefteriades and his own published reports.
Disclosures: Dr. Elefteriades disclosed he has received consulting fees from Baxter, Covidien, Datascope, and CryoLife, and a research grant from Medtroni
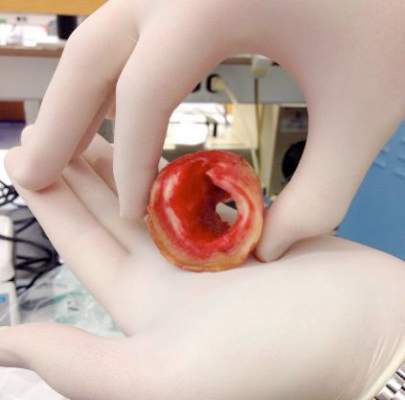
Bioabsorbable percutaneous device fully closes large femoral arteriotomies
PARIS – A new bioabsorbable sutureless device provides operators with a safe, simple, and dependable option for fully percutaneous closure of the large, 12-24 French femoral arteriotomies created for transcatheter aortic valve replacement or endovascular abdominal aortic aneurysm repair, Arne Schwindt, MD, reported at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
He presented the 12-month follow-up results of the FRONTIER II study of the Vivasure PerQseal device. The device recently received European marketing approval on the strength of FRONTIER II but remains investigational in the United States.
The PerQseal device is deployed in less than 1 minute at the end of the primary procedure and achieves immediate hemostasis. It’s a simple three-step deployment process with essentially no learning curve, as evidenced by the fact that in FRONTIER II, the technical success rate starting from no experience was 97%, explained Dr. Schwindt of St. Franziskus Hospital in Muenster, Germany.
The large femoral arteriotomies created for TAVR or endovascular abdominal aortic aneurysm repair have typically required surgical cut down and sutured repair with a 3- to 5-cm incision. Vascular complications have been common. Indeed, the literature shows this method entails on average a 14.7% rate of major vascular complications up to 3 months post procedure, so that was the bar set in FRONTIER II: In order for the PerQseal to be deemed noninferior to surgical cut down and sutured repair, the rate of major complications directly related to the novel device at 3 months follow-up could be no greater than 14.7%. The current Valve Academic Research Consortium (VARC) 2 definition of major complications was used.
In fact, the vascular complication rate proved to be zero. Moreover, at 12 months of follow-up, no cases of groin fibrosis or scarring had been observed, Dr. Schwindt reported.
FRONTIER II was a single-arm, prospective, multicenter European study of 58 patients who received the PerQseal device for 66 closures. They were evaluated at discharge and 1, 3, and 12 months post procedure by Doppler ultrasound, with uniformly unremarkable findings.
PerQseal features a synthetic low-profile implant with over-the-wire delivery. The implant is loaded into a sheath, released by pulling back on the sheath, then pulled up against the arteriotomy from the inside. Blood pressure molds the device to the arterial wall and seals it. The device is fully absorbed in 180 days.
Session co-chair Dr. Ted E. Feldman was favorably impressed.
“This is really terrific. It’s very nice to see we’re finally making progress with large-bore closure devices,” commented Dr. Feldman, professor of medicine at Northwestern University, Chicago.
Dr. Schwindt reported receiving a research grant from Vivasure, which sponsored the FRONTIER II study. In addition, he serves as a consultant to a half dozen medical device companies.
PARIS – A new bioabsorbable sutureless device provides operators with a safe, simple, and dependable option for fully percutaneous closure of the large, 12-24 French femoral arteriotomies created for transcatheter aortic valve replacement or endovascular abdominal aortic aneurysm repair, Arne Schwindt, MD, reported at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
He presented the 12-month follow-up results of the FRONTIER II study of the Vivasure PerQseal device. The device recently received European marketing approval on the strength of FRONTIER II but remains investigational in the United States.
The PerQseal device is deployed in less than 1 minute at the end of the primary procedure and achieves immediate hemostasis. It’s a simple three-step deployment process with essentially no learning curve, as evidenced by the fact that in FRONTIER II, the technical success rate starting from no experience was 97%, explained Dr. Schwindt of St. Franziskus Hospital in Muenster, Germany.
The large femoral arteriotomies created for TAVR or endovascular abdominal aortic aneurysm repair have typically required surgical cut down and sutured repair with a 3- to 5-cm incision. Vascular complications have been common. Indeed, the literature shows this method entails on average a 14.7% rate of major vascular complications up to 3 months post procedure, so that was the bar set in FRONTIER II: In order for the PerQseal to be deemed noninferior to surgical cut down and sutured repair, the rate of major complications directly related to the novel device at 3 months follow-up could be no greater than 14.7%. The current Valve Academic Research Consortium (VARC) 2 definition of major complications was used.
In fact, the vascular complication rate proved to be zero. Moreover, at 12 months of follow-up, no cases of groin fibrosis or scarring had been observed, Dr. Schwindt reported.
FRONTIER II was a single-arm, prospective, multicenter European study of 58 patients who received the PerQseal device for 66 closures. They were evaluated at discharge and 1, 3, and 12 months post procedure by Doppler ultrasound, with uniformly unremarkable findings.
PerQseal features a synthetic low-profile implant with over-the-wire delivery. The implant is loaded into a sheath, released by pulling back on the sheath, then pulled up against the arteriotomy from the inside. Blood pressure molds the device to the arterial wall and seals it. The device is fully absorbed in 180 days.
Session co-chair Dr. Ted E. Feldman was favorably impressed.
“This is really terrific. It’s very nice to see we’re finally making progress with large-bore closure devices,” commented Dr. Feldman, professor of medicine at Northwestern University, Chicago.
Dr. Schwindt reported receiving a research grant from Vivasure, which sponsored the FRONTIER II study. In addition, he serves as a consultant to a half dozen medical device companies.
PARIS – A new bioabsorbable sutureless device provides operators with a safe, simple, and dependable option for fully percutaneous closure of the large, 12-24 French femoral arteriotomies created for transcatheter aortic valve replacement or endovascular abdominal aortic aneurysm repair, Arne Schwindt, MD, reported at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
He presented the 12-month follow-up results of the FRONTIER II study of the Vivasure PerQseal device. The device recently received European marketing approval on the strength of FRONTIER II but remains investigational in the United States.
The PerQseal device is deployed in less than 1 minute at the end of the primary procedure and achieves immediate hemostasis. It’s a simple three-step deployment process with essentially no learning curve, as evidenced by the fact that in FRONTIER II, the technical success rate starting from no experience was 97%, explained Dr. Schwindt of St. Franziskus Hospital in Muenster, Germany.
The large femoral arteriotomies created for TAVR or endovascular abdominal aortic aneurysm repair have typically required surgical cut down and sutured repair with a 3- to 5-cm incision. Vascular complications have been common. Indeed, the literature shows this method entails on average a 14.7% rate of major vascular complications up to 3 months post procedure, so that was the bar set in FRONTIER II: In order for the PerQseal to be deemed noninferior to surgical cut down and sutured repair, the rate of major complications directly related to the novel device at 3 months follow-up could be no greater than 14.7%. The current Valve Academic Research Consortium (VARC) 2 definition of major complications was used.
In fact, the vascular complication rate proved to be zero. Moreover, at 12 months of follow-up, no cases of groin fibrosis or scarring had been observed, Dr. Schwindt reported.
FRONTIER II was a single-arm, prospective, multicenter European study of 58 patients who received the PerQseal device for 66 closures. They were evaluated at discharge and 1, 3, and 12 months post procedure by Doppler ultrasound, with uniformly unremarkable findings.
PerQseal features a synthetic low-profile implant with over-the-wire delivery. The implant is loaded into a sheath, released by pulling back on the sheath, then pulled up against the arteriotomy from the inside. Blood pressure molds the device to the arterial wall and seals it. The device is fully absorbed in 180 days.
Session co-chair Dr. Ted E. Feldman was favorably impressed.
“This is really terrific. It’s very nice to see we’re finally making progress with large-bore closure devices,” commented Dr. Feldman, professor of medicine at Northwestern University, Chicago.
Dr. Schwindt reported receiving a research grant from Vivasure, which sponsored the FRONTIER II study. In addition, he serves as a consultant to a half dozen medical device companies.
AT EUROPCR 2016
Key clinical point: The PerQseal device provides a simpler alternative to existing closure methods.
Major finding: No major vascular complications were seen during structured follow-up of recipients of the novel bioabsorbable fully percutaneous PerQseal device for closure of large-bore femoral arteriotomies.
Data source: FRONTIER II was a prospective, single-arm, 12-month multicenter study including 58 patients who underwent closure of 66 large femoral arteriotomies using the PerQseal device.
Disclosures: The presenter reported receiving a research grant from Vivasure, which sponsored the FRONTIER II study.
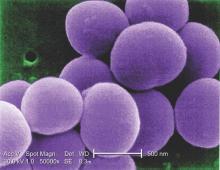
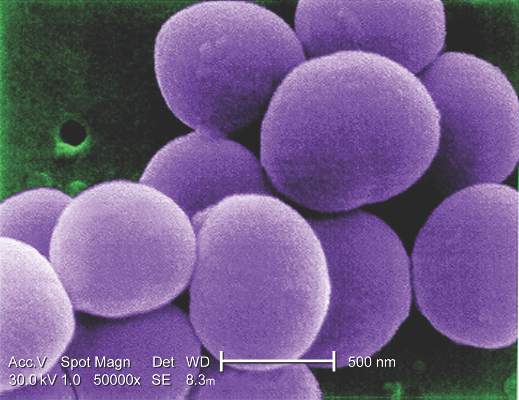
Additional antibiotics needed when implanting cryopreserved human aortic grafts
Infections of aortic prosthetic grafts can be a devastating complication, and while cryopreserved human allografts (CHA) can continue to possess antibacterial activity even after 5 years or more in storage, cardiac surgeons may want to apply additional antibiotic agents during implantation to boost bacterial resistance, investigators from Germany reported in the May issue of the Journal of Thoracic and Cardiovascular Surgery (2016;151:1251-9).
The researchers compared three different antibiotic regimens used in processing CHA aortic tissue and valves to determine the impact each can have on long-term bacterial resistance.
“Antibiotic combinations applied during CHA processing have a significant influence on their infection resistance,” said Dr. Viola Steffen of Hannover (Germany) Medical School and her colleagues. The average storage time of CHAs was 8.5 years, with the longest having been stored for 10 years.
The study involved microbiologic tests in vitro of three different antibiotic regimens used in processing CHA: gentamicin-piperacillin-vancomycin-metronidazole-amphotericin B (group A); gentamicin-piperacillin-flucloxacillin-metronidazole-amphotericin B (group B); and meropenem-vancomycin-tobramycin-colistin-amphotericin B (group C). The combinations are used to counteract Staphylococcus epidermidis and Staphylococcus aureus.
The study exposed pieces of 10 CHAs to different microbes and determined that regimen groups B and C were more effective than group A in eradicating gram-positive organisms. Specifically, group C was most resistant to Escherichia coli, whereas group B was most effective against Pseudomonas aeruginosa. Aortic tissue showed significantly less contamination with staphylococcal bacteria than valve grafts, the study reported.
Dr. Steffen and her colleagues said that tissue banks use antibiotic protocols during CHA processing, but they differ substantially. “Our results support the hypothesis that infection resistance of CHAs depends on the antibiotic pretreatment during processing and their residual activity,” they said.
The study had four key findings:
• The infection resistance of aortic wall and valve tissue differed significantly.
• In aortic wall specimens, group A specimens exhibited increased adherence of S. epidermidis, with vancomycin in group A and flucloxacillin in group B being the only differentiating agents between the two.
• Cryopreserved aortic vessels had a propensity toward reduced infection resistance against P. aeruginosa.
• Morphologic changes occurred in the microorganisms, especially rod-shaped E. coli, indicating that regional antibiotic release alters bacterial growth without eliminating all adherent bacteria.
Dr. Steffen and her colleagues noted that while previous studies determined that residual concentrations of antibiotics used in processing CHA heart valves and blood vessels are still present after they are prepared for implantation, they neither measured the antibacterial affect, clarified the period of cryopreservation nor differentiated between valve and vessel tissue (PLoS One. 2014;9:e112679; Transfus Med Hemother. 2011;38:379-86).
The Hannover researchers found that only a few gram-positive microorganisms adhered to aortic wall specimens, although they found “extensive adherence” of S. epidermidis in group A specimens. Valves, however, “were completely colonized” with both strains of staphylococcal bacteria, although the severity of contamination varied depending on the regimen used.
The findings raise some questions about the antibiotic properties of CHAs. “Because their infection resistance depends on the antibiotic combination selected during processing, further investigations concerning this treatment are necessary to improve the antimicrobial activity against frequent and highly virulent infection-causing bacteria,” Dr. Steffen and her colleagues said.
Dr. Steffen and her coauthors had no financial relationships to disclose.
Infections of aortic prosthetic grafts can be a devastating complication, and while cryopreserved human allografts (CHA) can continue to possess antibacterial activity even after 5 years or more in storage, cardiac surgeons may want to apply additional antibiotic agents during implantation to boost bacterial resistance, investigators from Germany reported in the May issue of the Journal of Thoracic and Cardiovascular Surgery (2016;151:1251-9).
The researchers compared three different antibiotic regimens used in processing CHA aortic tissue and valves to determine the impact each can have on long-term bacterial resistance.
“Antibiotic combinations applied during CHA processing have a significant influence on their infection resistance,” said Dr. Viola Steffen of Hannover (Germany) Medical School and her colleagues. The average storage time of CHAs was 8.5 years, with the longest having been stored for 10 years.
The study involved microbiologic tests in vitro of three different antibiotic regimens used in processing CHA: gentamicin-piperacillin-vancomycin-metronidazole-amphotericin B (group A); gentamicin-piperacillin-flucloxacillin-metronidazole-amphotericin B (group B); and meropenem-vancomycin-tobramycin-colistin-amphotericin B (group C). The combinations are used to counteract Staphylococcus epidermidis and Staphylococcus aureus.
The study exposed pieces of 10 CHAs to different microbes and determined that regimen groups B and C were more effective than group A in eradicating gram-positive organisms. Specifically, group C was most resistant to Escherichia coli, whereas group B was most effective against Pseudomonas aeruginosa. Aortic tissue showed significantly less contamination with staphylococcal bacteria than valve grafts, the study reported.
Dr. Steffen and her colleagues said that tissue banks use antibiotic protocols during CHA processing, but they differ substantially. “Our results support the hypothesis that infection resistance of CHAs depends on the antibiotic pretreatment during processing and their residual activity,” they said.
The study had four key findings:
• The infection resistance of aortic wall and valve tissue differed significantly.
• In aortic wall specimens, group A specimens exhibited increased adherence of S. epidermidis, with vancomycin in group A and flucloxacillin in group B being the only differentiating agents between the two.
• Cryopreserved aortic vessels had a propensity toward reduced infection resistance against P. aeruginosa.
• Morphologic changes occurred in the microorganisms, especially rod-shaped E. coli, indicating that regional antibiotic release alters bacterial growth without eliminating all adherent bacteria.
Dr. Steffen and her colleagues noted that while previous studies determined that residual concentrations of antibiotics used in processing CHA heart valves and blood vessels are still present after they are prepared for implantation, they neither measured the antibacterial affect, clarified the period of cryopreservation nor differentiated between valve and vessel tissue (PLoS One. 2014;9:e112679; Transfus Med Hemother. 2011;38:379-86).
The Hannover researchers found that only a few gram-positive microorganisms adhered to aortic wall specimens, although they found “extensive adherence” of S. epidermidis in group A specimens. Valves, however, “were completely colonized” with both strains of staphylococcal bacteria, although the severity of contamination varied depending on the regimen used.
The findings raise some questions about the antibiotic properties of CHAs. “Because their infection resistance depends on the antibiotic combination selected during processing, further investigations concerning this treatment are necessary to improve the antimicrobial activity against frequent and highly virulent infection-causing bacteria,” Dr. Steffen and her colleagues said.
Dr. Steffen and her coauthors had no financial relationships to disclose.
Infections of aortic prosthetic grafts can be a devastating complication, and while cryopreserved human allografts (CHA) can continue to possess antibacterial activity even after 5 years or more in storage, cardiac surgeons may want to apply additional antibiotic agents during implantation to boost bacterial resistance, investigators from Germany reported in the May issue of the Journal of Thoracic and Cardiovascular Surgery (2016;151:1251-9).
The researchers compared three different antibiotic regimens used in processing CHA aortic tissue and valves to determine the impact each can have on long-term bacterial resistance.
“Antibiotic combinations applied during CHA processing have a significant influence on their infection resistance,” said Dr. Viola Steffen of Hannover (Germany) Medical School and her colleagues. The average storage time of CHAs was 8.5 years, with the longest having been stored for 10 years.
The study involved microbiologic tests in vitro of three different antibiotic regimens used in processing CHA: gentamicin-piperacillin-vancomycin-metronidazole-amphotericin B (group A); gentamicin-piperacillin-flucloxacillin-metronidazole-amphotericin B (group B); and meropenem-vancomycin-tobramycin-colistin-amphotericin B (group C). The combinations are used to counteract Staphylococcus epidermidis and Staphylococcus aureus.
The study exposed pieces of 10 CHAs to different microbes and determined that regimen groups B and C were more effective than group A in eradicating gram-positive organisms. Specifically, group C was most resistant to Escherichia coli, whereas group B was most effective against Pseudomonas aeruginosa. Aortic tissue showed significantly less contamination with staphylococcal bacteria than valve grafts, the study reported.
Dr. Steffen and her colleagues said that tissue banks use antibiotic protocols during CHA processing, but they differ substantially. “Our results support the hypothesis that infection resistance of CHAs depends on the antibiotic pretreatment during processing and their residual activity,” they said.
The study had four key findings:
• The infection resistance of aortic wall and valve tissue differed significantly.
• In aortic wall specimens, group A specimens exhibited increased adherence of S. epidermidis, with vancomycin in group A and flucloxacillin in group B being the only differentiating agents between the two.
• Cryopreserved aortic vessels had a propensity toward reduced infection resistance against P. aeruginosa.
• Morphologic changes occurred in the microorganisms, especially rod-shaped E. coli, indicating that regional antibiotic release alters bacterial growth without eliminating all adherent bacteria.
Dr. Steffen and her colleagues noted that while previous studies determined that residual concentrations of antibiotics used in processing CHA heart valves and blood vessels are still present after they are prepared for implantation, they neither measured the antibacterial affect, clarified the period of cryopreservation nor differentiated between valve and vessel tissue (PLoS One. 2014;9:e112679; Transfus Med Hemother. 2011;38:379-86).
The Hannover researchers found that only a few gram-positive microorganisms adhered to aortic wall specimens, although they found “extensive adherence” of S. epidermidis in group A specimens. Valves, however, “were completely colonized” with both strains of staphylococcal bacteria, although the severity of contamination varied depending on the regimen used.
The findings raise some questions about the antibiotic properties of CHAs. “Because their infection resistance depends on the antibiotic combination selected during processing, further investigations concerning this treatment are necessary to improve the antimicrobial activity against frequent and highly virulent infection-causing bacteria,” Dr. Steffen and her colleagues said.
Dr. Steffen and her coauthors had no financial relationships to disclose.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: The infection resistance of cryopreserved human allografts (CHAs) depends on antibiotic pretreatment during processing.
Major finding: Cardiac surgeons can recommend CHAs to patients either with active destructive infections or at high risk of reinfection, but they may want to apply additional antibiotic agents during implantation to enhance bacterial resistance.
Data source: Pieces of 10 CHAs were microbiologically tested in vitro and exposed to bacterial contamination and the number of attached bacteria quantified.
Disclosures: Dr. Steffen and her coauthors had no financial relationships to disclose.
General surgeons getting less vascular training
Vascular surgery fellow case logs reflect an increase in endovascular interventions, but general surgery residents may be missing out on training opportunities, according to a study of national case data.
In addition, general surgery residents saw a decrease in open vascular surgery cases, which was not reflected among the vascular surgery fellows, according to Dr. Rose C. Pedersen and colleagues in the department of surgery, Kaiser Permanente Los Angeles Medical Center. The report was published online in Annals of Vascular Surgery (doi: 10.1016/j.avsg.2016.02.008).
The paper was originally presented at the 2105 annual meeting of the Southern California Vascular Society. The study reports findings of a review of the Accreditation Council for Graduate Medical Education national case log reports from 2001 to 2012.
During that period, the number of general surgery residents increased from 1,021 to 1,098, while the number of vascular surgery fellows increased from 96 to 121. The total number of vascular cases logged by the vascular fellows significantly increased by 161%, from an average of 298 cases to 762 cases over the time period assessed. During that same period, vascular cases done by general surgery residents significantly decreased by 40%, from an average of 186 to 116 cases.
In terms of open cases. vascular fellows saw a significant 43% decrease in open abdominal aortic aneurysm (AAA) cases, going from 26 to 15, and a slight but significant increase in carotid endarterectomy cases logged (44 to 49). Hemodialysis access and major amputations also both increased significantly. A decreases in open surgery for peripheral obstructive disease was small and not significant.
General surgery residents saw decreases in all open surgery areas over the time period: AAA cases fell significantly by 78% (9 cases to 2 cases); carotid endarterectomies decreased significantly from 23 to 12 cases; and surgery for peripheral obstructive disease fell significantly from 21 to 8). Hemodialysis access cases and major amputations both decreased as well, but not significantly.
Endovascular cases increased from 2001 to 2012 for both vascular fellows and general surgery residents. Vascular fellows saw endovascular AAA repair significantly increase from an average of 17 to 46 cases, while those for general surgery residents rosed from roughly 1 to 3 cases. Similarly, endovascular interventions for peripheral obstructive disease significantly increased for vascular fellows from 17 to 85, and from 1.3 to 4 for general surgery residents.
“The contemporary management of abdominal aortic aneurysmal diseases and peripheral obstructive diseases has been particularly changed by endovascular therapies that have been adopted into the training experience of vascular surgery fellows, but not those of general surgery residents. Open surgery experience has decreased overall for general surgery residents in all major categories, a change not seen in vascular fellows,” the researchers concluded.
The authors reported no relevant disclosures.
Vascular surgical practice has evolved with the introduction of minimally invasive technology and advancement of endovascular techniques, and as such, the training of the vascular surgical specialist too has evolved. This article highlights the effect of these technological advancements on the vascular surgical fellowship training experience and points out the effect of this embracing of endovascular techniques by academic centers in their general surgery trainee vascular surgical experience. Open operative case numbers are declining and endovascular case numbers are increasing significantly.
As traditionally performed open procedures are being substituted for endovascular repairs, the open operative experience for vascular surgery trainees is declining or staying stable at the expense of the general surgery resident experience. Open cases (open aneurysm repairs, aortofemoral artery bypasses, visceral artery bypasses, carotid endarterectomies), because they are performed infrequently now, have become fellow cases.
 |
Dr. Erica L. Mitchell |
Endovascular cases, which have increased over 300%-400%, too are essentially fellow cases (or in 0+5 programs, which are not discussed in this manuscript, vascular surgery resident cases) because the endovascular skill set does not appear to translate or transfer (and therefore is not considered relevant to the general surgery resident planning on a fellowship or career in the traditional surgical specialties) into open and laparoscopic skills desired by general surgery trainees.
Unfortunately, this open to endovascular operative experience shift will only increase with the introduction and early adoption (in academic centers) of complex endovascular techniques for the management of complex obstructive and aneurysmal arterial disease. A review of case log data for 0+5 and 5+2 residents completing programs in 2014-2015 reveals the operative experience and continued decline in open operative case numbers and increases in endovascular case numbers.
Vascular surgery training programs and their faculties have a responsibility to make sure the operative experience of general surgery residents is a worthwhile one. We, the faculty, need to keep encouraging general surgery residents to come to the operating room, even if they are not the primary surgeons. To make this worthwhile for them (because residents will not come to the operating room if there is nothing to be gained for themselves), we have to let them participate in the case somehow. One of the most critical aspects of a vascular surgical procedure is the operative exposure.
Having the general surgery residents participate in the vascular exposure is not only formative to their understanding of surgical anatomy, and applicable to all aspects of surgical practice, it is also critical to trainee development of decision making, judgment, and situational awareness. These exposures can and should be logged, using the e-code, to receive ACGME case log credit for vascular surgical procedures. E-codes, additionally, allow more than one resident to take credit for an arterial exposure and repair. We must also encourage trainees to come to the angio suite, while these cases, on the outset do not seem relevant to general surgery training, they do provide the learner with a greater appreciation of the complexity of vascular anatomy.
Importantly, as long as we continue to train vascular surgery specialists via the traditional 5+2 paradigm, we must keep general surgery residents, rotating through our services, interested and engaged in the management of vascular diseases. The simplest way to engage them is to make them feel relevant and to make them feel relevant they have to participate, both inside and outside of the operating room. It is, after all, our duty as surgical educators and advocates for our specialty to train the next generation of vascular surgical specialists!
Dr. Erica L. Mitchell is professor of surgery, program director for vascular surgery, and vice-chair of quality, department of surgery, Oregon Health & Science University, Portland. She is an associate medical editor of Vascular Specialist.
Vascular surgical practice has evolved with the introduction of minimally invasive technology and advancement of endovascular techniques, and as such, the training of the vascular surgical specialist too has evolved. This article highlights the effect of these technological advancements on the vascular surgical fellowship training experience and points out the effect of this embracing of endovascular techniques by academic centers in their general surgery trainee vascular surgical experience. Open operative case numbers are declining and endovascular case numbers are increasing significantly.
As traditionally performed open procedures are being substituted for endovascular repairs, the open operative experience for vascular surgery trainees is declining or staying stable at the expense of the general surgery resident experience. Open cases (open aneurysm repairs, aortofemoral artery bypasses, visceral artery bypasses, carotid endarterectomies), because they are performed infrequently now, have become fellow cases.
 |
Dr. Erica L. Mitchell |
Endovascular cases, which have increased over 300%-400%, too are essentially fellow cases (or in 0+5 programs, which are not discussed in this manuscript, vascular surgery resident cases) because the endovascular skill set does not appear to translate or transfer (and therefore is not considered relevant to the general surgery resident planning on a fellowship or career in the traditional surgical specialties) into open and laparoscopic skills desired by general surgery trainees.
Unfortunately, this open to endovascular operative experience shift will only increase with the introduction and early adoption (in academic centers) of complex endovascular techniques for the management of complex obstructive and aneurysmal arterial disease. A review of case log data for 0+5 and 5+2 residents completing programs in 2014-2015 reveals the operative experience and continued decline in open operative case numbers and increases in endovascular case numbers.
Vascular surgery training programs and their faculties have a responsibility to make sure the operative experience of general surgery residents is a worthwhile one. We, the faculty, need to keep encouraging general surgery residents to come to the operating room, even if they are not the primary surgeons. To make this worthwhile for them (because residents will not come to the operating room if there is nothing to be gained for themselves), we have to let them participate in the case somehow. One of the most critical aspects of a vascular surgical procedure is the operative exposure.
Having the general surgery residents participate in the vascular exposure is not only formative to their understanding of surgical anatomy, and applicable to all aspects of surgical practice, it is also critical to trainee development of decision making, judgment, and situational awareness. These exposures can and should be logged, using the e-code, to receive ACGME case log credit for vascular surgical procedures. E-codes, additionally, allow more than one resident to take credit for an arterial exposure and repair. We must also encourage trainees to come to the angio suite, while these cases, on the outset do not seem relevant to general surgery training, they do provide the learner with a greater appreciation of the complexity of vascular anatomy.
Importantly, as long as we continue to train vascular surgery specialists via the traditional 5+2 paradigm, we must keep general surgery residents, rotating through our services, interested and engaged in the management of vascular diseases. The simplest way to engage them is to make them feel relevant and to make them feel relevant they have to participate, both inside and outside of the operating room. It is, after all, our duty as surgical educators and advocates for our specialty to train the next generation of vascular surgical specialists!
Dr. Erica L. Mitchell is professor of surgery, program director for vascular surgery, and vice-chair of quality, department of surgery, Oregon Health & Science University, Portland. She is an associate medical editor of Vascular Specialist.
Vascular surgical practice has evolved with the introduction of minimally invasive technology and advancement of endovascular techniques, and as such, the training of the vascular surgical specialist too has evolved. This article highlights the effect of these technological advancements on the vascular surgical fellowship training experience and points out the effect of this embracing of endovascular techniques by academic centers in their general surgery trainee vascular surgical experience. Open operative case numbers are declining and endovascular case numbers are increasing significantly.
As traditionally performed open procedures are being substituted for endovascular repairs, the open operative experience for vascular surgery trainees is declining or staying stable at the expense of the general surgery resident experience. Open cases (open aneurysm repairs, aortofemoral artery bypasses, visceral artery bypasses, carotid endarterectomies), because they are performed infrequently now, have become fellow cases.
 |
Dr. Erica L. Mitchell |
Endovascular cases, which have increased over 300%-400%, too are essentially fellow cases (or in 0+5 programs, which are not discussed in this manuscript, vascular surgery resident cases) because the endovascular skill set does not appear to translate or transfer (and therefore is not considered relevant to the general surgery resident planning on a fellowship or career in the traditional surgical specialties) into open and laparoscopic skills desired by general surgery trainees.
Unfortunately, this open to endovascular operative experience shift will only increase with the introduction and early adoption (in academic centers) of complex endovascular techniques for the management of complex obstructive and aneurysmal arterial disease. A review of case log data for 0+5 and 5+2 residents completing programs in 2014-2015 reveals the operative experience and continued decline in open operative case numbers and increases in endovascular case numbers.
Vascular surgery training programs and their faculties have a responsibility to make sure the operative experience of general surgery residents is a worthwhile one. We, the faculty, need to keep encouraging general surgery residents to come to the operating room, even if they are not the primary surgeons. To make this worthwhile for them (because residents will not come to the operating room if there is nothing to be gained for themselves), we have to let them participate in the case somehow. One of the most critical aspects of a vascular surgical procedure is the operative exposure.
Having the general surgery residents participate in the vascular exposure is not only formative to their understanding of surgical anatomy, and applicable to all aspects of surgical practice, it is also critical to trainee development of decision making, judgment, and situational awareness. These exposures can and should be logged, using the e-code, to receive ACGME case log credit for vascular surgical procedures. E-codes, additionally, allow more than one resident to take credit for an arterial exposure and repair. We must also encourage trainees to come to the angio suite, while these cases, on the outset do not seem relevant to general surgery training, they do provide the learner with a greater appreciation of the complexity of vascular anatomy.
Importantly, as long as we continue to train vascular surgery specialists via the traditional 5+2 paradigm, we must keep general surgery residents, rotating through our services, interested and engaged in the management of vascular diseases. The simplest way to engage them is to make them feel relevant and to make them feel relevant they have to participate, both inside and outside of the operating room. It is, after all, our duty as surgical educators and advocates for our specialty to train the next generation of vascular surgical specialists!
Dr. Erica L. Mitchell is professor of surgery, program director for vascular surgery, and vice-chair of quality, department of surgery, Oregon Health & Science University, Portland. She is an associate medical editor of Vascular Specialist.
Vascular surgery fellow case logs reflect an increase in endovascular interventions, but general surgery residents may be missing out on training opportunities, according to a study of national case data.
In addition, general surgery residents saw a decrease in open vascular surgery cases, which was not reflected among the vascular surgery fellows, according to Dr. Rose C. Pedersen and colleagues in the department of surgery, Kaiser Permanente Los Angeles Medical Center. The report was published online in Annals of Vascular Surgery (doi: 10.1016/j.avsg.2016.02.008).
The paper was originally presented at the 2105 annual meeting of the Southern California Vascular Society. The study reports findings of a review of the Accreditation Council for Graduate Medical Education national case log reports from 2001 to 2012.
During that period, the number of general surgery residents increased from 1,021 to 1,098, while the number of vascular surgery fellows increased from 96 to 121. The total number of vascular cases logged by the vascular fellows significantly increased by 161%, from an average of 298 cases to 762 cases over the time period assessed. During that same period, vascular cases done by general surgery residents significantly decreased by 40%, from an average of 186 to 116 cases.
In terms of open cases. vascular fellows saw a significant 43% decrease in open abdominal aortic aneurysm (AAA) cases, going from 26 to 15, and a slight but significant increase in carotid endarterectomy cases logged (44 to 49). Hemodialysis access and major amputations also both increased significantly. A decreases in open surgery for peripheral obstructive disease was small and not significant.
General surgery residents saw decreases in all open surgery areas over the time period: AAA cases fell significantly by 78% (9 cases to 2 cases); carotid endarterectomies decreased significantly from 23 to 12 cases; and surgery for peripheral obstructive disease fell significantly from 21 to 8). Hemodialysis access cases and major amputations both decreased as well, but not significantly.
Endovascular cases increased from 2001 to 2012 for both vascular fellows and general surgery residents. Vascular fellows saw endovascular AAA repair significantly increase from an average of 17 to 46 cases, while those for general surgery residents rosed from roughly 1 to 3 cases. Similarly, endovascular interventions for peripheral obstructive disease significantly increased for vascular fellows from 17 to 85, and from 1.3 to 4 for general surgery residents.
“The contemporary management of abdominal aortic aneurysmal diseases and peripheral obstructive diseases has been particularly changed by endovascular therapies that have been adopted into the training experience of vascular surgery fellows, but not those of general surgery residents. Open surgery experience has decreased overall for general surgery residents in all major categories, a change not seen in vascular fellows,” the researchers concluded.
The authors reported no relevant disclosures.
Vascular surgery fellow case logs reflect an increase in endovascular interventions, but general surgery residents may be missing out on training opportunities, according to a study of national case data.
In addition, general surgery residents saw a decrease in open vascular surgery cases, which was not reflected among the vascular surgery fellows, according to Dr. Rose C. Pedersen and colleagues in the department of surgery, Kaiser Permanente Los Angeles Medical Center. The report was published online in Annals of Vascular Surgery (doi: 10.1016/j.avsg.2016.02.008).
The paper was originally presented at the 2105 annual meeting of the Southern California Vascular Society. The study reports findings of a review of the Accreditation Council for Graduate Medical Education national case log reports from 2001 to 2012.
During that period, the number of general surgery residents increased from 1,021 to 1,098, while the number of vascular surgery fellows increased from 96 to 121. The total number of vascular cases logged by the vascular fellows significantly increased by 161%, from an average of 298 cases to 762 cases over the time period assessed. During that same period, vascular cases done by general surgery residents significantly decreased by 40%, from an average of 186 to 116 cases.
In terms of open cases. vascular fellows saw a significant 43% decrease in open abdominal aortic aneurysm (AAA) cases, going from 26 to 15, and a slight but significant increase in carotid endarterectomy cases logged (44 to 49). Hemodialysis access and major amputations also both increased significantly. A decreases in open surgery for peripheral obstructive disease was small and not significant.
General surgery residents saw decreases in all open surgery areas over the time period: AAA cases fell significantly by 78% (9 cases to 2 cases); carotid endarterectomies decreased significantly from 23 to 12 cases; and surgery for peripheral obstructive disease fell significantly from 21 to 8). Hemodialysis access cases and major amputations both decreased as well, but not significantly.
Endovascular cases increased from 2001 to 2012 for both vascular fellows and general surgery residents. Vascular fellows saw endovascular AAA repair significantly increase from an average of 17 to 46 cases, while those for general surgery residents rosed from roughly 1 to 3 cases. Similarly, endovascular interventions for peripheral obstructive disease significantly increased for vascular fellows from 17 to 85, and from 1.3 to 4 for general surgery residents.
“The contemporary management of abdominal aortic aneurysmal diseases and peripheral obstructive diseases has been particularly changed by endovascular therapies that have been adopted into the training experience of vascular surgery fellows, but not those of general surgery residents. Open surgery experience has decreased overall for general surgery residents in all major categories, a change not seen in vascular fellows,” the researchers concluded.
The authors reported no relevant disclosures.
FROM ANNALS OF VASCULAR SURGERY
Cold turkey better for smoking cessation
Quitting smoking abruptly rather than gradually leads to higher abstinence rates both at 4 weeks and 6 months, a report published online March 14 shows.
Worldwide guidelines for smoking cessation generally recommend abrupt cessation over a gradual reduction in smoking, based on data from observational studies. However a recent review of 10 randomized trials concluded that quitting “cold turkey” produces only slightly higher quit rates, said Nicola Lindson-Hawley, Ph.D., of the department of primary care health services, University of Oxford (England), and her associates.
They compared the two approaches in a noninferiority trial involving 697 adults treated at 31 primary care practices in England during a 2.5-year period. The study participants smoked at least 15 cigarettes per day and had an end-expiratory carbon monoxide concentration of at least 15 parts per million. The average age was 49 years, and the study population was evenly divided between men and women. Their mean score on the Fagerström Test for Cigarette Dependence was 6, indicating a high degree of dependence.
These participants were randomly assigned either to stop smoking abruptly on a quit date 2 weeks from baseline (355 patients) or to stop gradually, by reducing their cigarette use by half at 1 week from baseline, by half again during the second week, and completely by a quit date 2 weeks from baseline. The latter group was given a choice of three structured reduction programs to follow before the quit date, as well as nicotine patches and a choice of short-acting nicotine replacement products (gum, lozenges, nasal sprays, sublingual tablets, inhalators, or mouth sprays). The abrupt-cessation group received only the nicotine patches just before the quit day. Both groups received identical behavioral counseling, nicotine patches, and nicotine replacement products after the quit date.
The primary outcome measure, abstinence at 4 weeks, was achieved by 49% of the abrupt-cessation group, compared with only 39.2% of the gradual-cessation group (relative risk, 0.80). Thus, gradual cessation did not prove to be noninferior to abrupt cessation. The secondary outcome measure of abstinence at 6 months also was superior for the abrupt-cessation group (22%) over the gradual-cessation group (15.5%), Dr. Lindson-Hawley and her associates reported (Ann Intern Med. 2016 Mar 15. doi: 10.7326/M14-2805).
Most of the between-group difference was attributed to the fact that fewer participants in the gradual-cessation group actually attempted to quit on their quit date (61.4% vs. 71.0%). Relapse rates were similar between the two study groups at 4 weeks (36.2% vs. 31.0%) and at 6 months (74.8% vs. 69.1%).
“These results imply that, in clinical practice, we should encourage persons to stop smoking abruptly and not gradually,” Dr. Lindson-Hawley and her associates wrote. “However, gradual cessation programs could still be worthwhile if they increase the number of persons who try to quit or take up support and medication while trying.”
The study was supported by the British Heart Foundation, Cancer Research United Kingdom, the Economic and Social Research Council, the Medical Research Council, and the National Institute for Health Research. Dr. Lindson-Hawley reported having no relevant financial disclosures; two of her associates reported ties to Pfizer, GlaxoSmithKline, and McNeil.
The trial by Nicola Lindson-Hawley, Ph.D., is well designed and suggests that “setting a quit date and quitting abruptly increases long-term cessation rates in smokers who want to quit,” Dr. Gabriela S. Ferreira and Dr. Michael B. Steinberg wrote in an accompanying editorial. However, a gradual approach to smoking cessation still may be useful for some smokers, so that method shouldn’t be entirely abandoned just yet.
Many smokers try several times to quit abruptly but are not successful. They may not wish to set another abrupt quit date for fear of “failing” yet again. However, they may instead respond well to gradually reducing their smoking, with the eventual goal of reducing it all the way to zero.
These findings raise important questions about how clinicians should approach patients who smoke and are ready to quit, they wrote.
Dr. Ferreira and Dr. Steinberg are at the Robert Wood Johnson Medical School in New Brunswick. Dr. Ferreira reported having no relevant financial disclosures; Dr. Steinberg reported receiving personal fees from Arena Pharmaceuticals, Major League Baseball, and Pfizer outside of this work. Their remarks (Ann Intern Med. 2016 Mar 15. doi: 10.7326/M16-0362) accompanied Dr. Lindson-Hawley’s report.
The trial by Nicola Lindson-Hawley, Ph.D., is well designed and suggests that “setting a quit date and quitting abruptly increases long-term cessation rates in smokers who want to quit,” Dr. Gabriela S. Ferreira and Dr. Michael B. Steinberg wrote in an accompanying editorial. However, a gradual approach to smoking cessation still may be useful for some smokers, so that method shouldn’t be entirely abandoned just yet.
Many smokers try several times to quit abruptly but are not successful. They may not wish to set another abrupt quit date for fear of “failing” yet again. However, they may instead respond well to gradually reducing their smoking, with the eventual goal of reducing it all the way to zero.
These findings raise important questions about how clinicians should approach patients who smoke and are ready to quit, they wrote.
Dr. Ferreira and Dr. Steinberg are at the Robert Wood Johnson Medical School in New Brunswick. Dr. Ferreira reported having no relevant financial disclosures; Dr. Steinberg reported receiving personal fees from Arena Pharmaceuticals, Major League Baseball, and Pfizer outside of this work. Their remarks (Ann Intern Med. 2016 Mar 15. doi: 10.7326/M16-0362) accompanied Dr. Lindson-Hawley’s report.
The trial by Nicola Lindson-Hawley, Ph.D., is well designed and suggests that “setting a quit date and quitting abruptly increases long-term cessation rates in smokers who want to quit,” Dr. Gabriela S. Ferreira and Dr. Michael B. Steinberg wrote in an accompanying editorial. However, a gradual approach to smoking cessation still may be useful for some smokers, so that method shouldn’t be entirely abandoned just yet.
Many smokers try several times to quit abruptly but are not successful. They may not wish to set another abrupt quit date for fear of “failing” yet again. However, they may instead respond well to gradually reducing their smoking, with the eventual goal of reducing it all the way to zero.
These findings raise important questions about how clinicians should approach patients who smoke and are ready to quit, they wrote.
Dr. Ferreira and Dr. Steinberg are at the Robert Wood Johnson Medical School in New Brunswick. Dr. Ferreira reported having no relevant financial disclosures; Dr. Steinberg reported receiving personal fees from Arena Pharmaceuticals, Major League Baseball, and Pfizer outside of this work. Their remarks (Ann Intern Med. 2016 Mar 15. doi: 10.7326/M16-0362) accompanied Dr. Lindson-Hawley’s report.
Quitting smoking abruptly rather than gradually leads to higher abstinence rates both at 4 weeks and 6 months, a report published online March 14 shows.
Worldwide guidelines for smoking cessation generally recommend abrupt cessation over a gradual reduction in smoking, based on data from observational studies. However a recent review of 10 randomized trials concluded that quitting “cold turkey” produces only slightly higher quit rates, said Nicola Lindson-Hawley, Ph.D., of the department of primary care health services, University of Oxford (England), and her associates.
They compared the two approaches in a noninferiority trial involving 697 adults treated at 31 primary care practices in England during a 2.5-year period. The study participants smoked at least 15 cigarettes per day and had an end-expiratory carbon monoxide concentration of at least 15 parts per million. The average age was 49 years, and the study population was evenly divided between men and women. Their mean score on the Fagerström Test for Cigarette Dependence was 6, indicating a high degree of dependence.
These participants were randomly assigned either to stop smoking abruptly on a quit date 2 weeks from baseline (355 patients) or to stop gradually, by reducing their cigarette use by half at 1 week from baseline, by half again during the second week, and completely by a quit date 2 weeks from baseline. The latter group was given a choice of three structured reduction programs to follow before the quit date, as well as nicotine patches and a choice of short-acting nicotine replacement products (gum, lozenges, nasal sprays, sublingual tablets, inhalators, or mouth sprays). The abrupt-cessation group received only the nicotine patches just before the quit day. Both groups received identical behavioral counseling, nicotine patches, and nicotine replacement products after the quit date.
The primary outcome measure, abstinence at 4 weeks, was achieved by 49% of the abrupt-cessation group, compared with only 39.2% of the gradual-cessation group (relative risk, 0.80). Thus, gradual cessation did not prove to be noninferior to abrupt cessation. The secondary outcome measure of abstinence at 6 months also was superior for the abrupt-cessation group (22%) over the gradual-cessation group (15.5%), Dr. Lindson-Hawley and her associates reported (Ann Intern Med. 2016 Mar 15. doi: 10.7326/M14-2805).
Most of the between-group difference was attributed to the fact that fewer participants in the gradual-cessation group actually attempted to quit on their quit date (61.4% vs. 71.0%). Relapse rates were similar between the two study groups at 4 weeks (36.2% vs. 31.0%) and at 6 months (74.8% vs. 69.1%).
“These results imply that, in clinical practice, we should encourage persons to stop smoking abruptly and not gradually,” Dr. Lindson-Hawley and her associates wrote. “However, gradual cessation programs could still be worthwhile if they increase the number of persons who try to quit or take up support and medication while trying.”
The study was supported by the British Heart Foundation, Cancer Research United Kingdom, the Economic and Social Research Council, the Medical Research Council, and the National Institute for Health Research. Dr. Lindson-Hawley reported having no relevant financial disclosures; two of her associates reported ties to Pfizer, GlaxoSmithKline, and McNeil.
Quitting smoking abruptly rather than gradually leads to higher abstinence rates both at 4 weeks and 6 months, a report published online March 14 shows.
Worldwide guidelines for smoking cessation generally recommend abrupt cessation over a gradual reduction in smoking, based on data from observational studies. However a recent review of 10 randomized trials concluded that quitting “cold turkey” produces only slightly higher quit rates, said Nicola Lindson-Hawley, Ph.D., of the department of primary care health services, University of Oxford (England), and her associates.
They compared the two approaches in a noninferiority trial involving 697 adults treated at 31 primary care practices in England during a 2.5-year period. The study participants smoked at least 15 cigarettes per day and had an end-expiratory carbon monoxide concentration of at least 15 parts per million. The average age was 49 years, and the study population was evenly divided between men and women. Their mean score on the Fagerström Test for Cigarette Dependence was 6, indicating a high degree of dependence.
These participants were randomly assigned either to stop smoking abruptly on a quit date 2 weeks from baseline (355 patients) or to stop gradually, by reducing their cigarette use by half at 1 week from baseline, by half again during the second week, and completely by a quit date 2 weeks from baseline. The latter group was given a choice of three structured reduction programs to follow before the quit date, as well as nicotine patches and a choice of short-acting nicotine replacement products (gum, lozenges, nasal sprays, sublingual tablets, inhalators, or mouth sprays). The abrupt-cessation group received only the nicotine patches just before the quit day. Both groups received identical behavioral counseling, nicotine patches, and nicotine replacement products after the quit date.
The primary outcome measure, abstinence at 4 weeks, was achieved by 49% of the abrupt-cessation group, compared with only 39.2% of the gradual-cessation group (relative risk, 0.80). Thus, gradual cessation did not prove to be noninferior to abrupt cessation. The secondary outcome measure of abstinence at 6 months also was superior for the abrupt-cessation group (22%) over the gradual-cessation group (15.5%), Dr. Lindson-Hawley and her associates reported (Ann Intern Med. 2016 Mar 15. doi: 10.7326/M14-2805).
Most of the between-group difference was attributed to the fact that fewer participants in the gradual-cessation group actually attempted to quit on their quit date (61.4% vs. 71.0%). Relapse rates were similar between the two study groups at 4 weeks (36.2% vs. 31.0%) and at 6 months (74.8% vs. 69.1%).
“These results imply that, in clinical practice, we should encourage persons to stop smoking abruptly and not gradually,” Dr. Lindson-Hawley and her associates wrote. “However, gradual cessation programs could still be worthwhile if they increase the number of persons who try to quit or take up support and medication while trying.”
The study was supported by the British Heart Foundation, Cancer Research United Kingdom, the Economic and Social Research Council, the Medical Research Council, and the National Institute for Health Research. Dr. Lindson-Hawley reported having no relevant financial disclosures; two of her associates reported ties to Pfizer, GlaxoSmithKline, and McNeil.
FROM THE ANNALS OF INTERNAL MEDICINE
Key clinical point: Quitting cigarette smoking abruptly rather than gradually leads to higher abstinence rates in the short and long term.
Major finding: The primary outcome measure, abstinence at 4 weeks, was achieved by 49% of the abrupt-cessation group, compared with only 39.2% of the gradual-cessation group (RR, 0.80).
Data source: A randomized, controlled noninferiority study involving 697 smokers at 31 primary care practices in England.
Disclosures: This study was supported by the British Heart Foundation, Cancer Research United Kingdom, the Economic and Social Research Council, the Medical Research Council, and the National Institute for Health Research. Dr. Lindson-Hawley reported having no relevant financial disclosures; two of her associates reported ties to Pfizer, GlaxoSmithKline, and McNeil.
Recent active asthma raises AAA rupture risk
Patients aged 50 and older with recent active asthma are at elevated risk of abdominal aortic aneurysm and aneurysm rupture, according to new research.
A common inflammatory pathway between asthma and AAA, first observed nearly a decade ago in mice, is thought to be responsible.
The new findings, published online Feb. 11 in Arteriosclerosis, Thrombosis, and Vascular Biology (Arterioscler Thromb Vasc Biol. 2016. doi: 10.1161/ATVBAHA.115.306497) support the association in humans.
In a news release accompanying the findings, lead study author Guo-Ping Shi, ScD, of Brigham and Women’s Hospital and Harvard Medical School, Boston, said that the findings had clear clinical implications for older patients with a recent asthma diagnosis. Such patients, particularly older men, “should be checked for signs” of abdominal aortic aneurysm, Dr. Shi said.*
For their research, Dr. Shi, along with colleagues at Zhengzhou (China) University, used data from a large Danish population-based cohort of nearly 16,000 patients (81% men) with AAA between 1996 and 2012, of which about 4,500 patients had rupture. They also looked at data from a comparison cohort of patients with and without AAA from a slightly larger population-based vascular screening trial of men in Denmark.
The investigators showed that hospital diagnosis of asthma within the previous year (n = 514) was associated with significantly higher risk of hospital admission with AAA rupture (n = 146) both before and after adjustment for AAA comorbidities (adjusted odds ratio 1.51-2.06). Higher risk of rupture also was seen for patients filling prescriptions for bronchodilators within the previous 3 months (aOR = 1.10-1.31), and for patients prescribed anti-asthma drugs (aOR OR = 1.09-1.48), which were seen as indicative of an outpatient asthma diagnosis.
“A hospital diagnosis of asthma or a recently filled prescription of an anti-asthmatic drug is associated with an increased risk of admission with rAAA compared with admission with intact AAA, both before and after adjusting for AAA comorbidities and relevant medications,” the researchers wrote in their analysis.
Moreover, “an asthma diagnosis or the use of bronchodilators or other anti-asthmatic drug prescriptions closer to the date of admission with AAA correlated directly with a higher risk of aortic rupture. The results remained robust after adjusting for a wide range of relevant possible confounders,” the researchers wrote.
In the cohort of patients from the vascular screening study, which included age-matched controls without AAA, asthma (measured by recent anti-asthmatic medication use) was seen associated with a significantly elevated risk of AAA before (OR = 1.45) and after adjustment for smoking (OR = 1.45) or other risk factors (OR = 1.46). This does not refer to rupture but just AAA.
Dr. Shi and colleagues noted that the AAA cohort lacked sufficient information on cigarette smoking, a known risk factor for AAA and AAA rupture, to preclude the possibility of confounding; however, the second all-male cohort did have extensive data on smoking, “and the risk of AAA among patients with asthma remained 45% higher than that of patients with nonasthma” even after adjustment.
The researchers hypothesized that an inflammatory response characterized by elevated immunoglobulin E may be the link between AAA pathogenesis and asthma, and that other allergic inflammatory diseases, including atopic dermatitis, allergic rhinitis, and some ocular allergic diseases, could potentially carry risks for AAA formation and rupture. Dr. Shi and colleagues previously investigated the IgE and aneurysm link in animal studies.
“The results have implications for the development of much needed advances in the prevention, screening criteria, and treatment of AAA, common conditions for which we currently lack sufficiently effective approaches,” the investigators wrote.
The Chinese, Danish, and U.S. governments sponsored the study. The investigators disclosed no conflicts of interest.
*CORRECTION 8/12/2020: Dr. Shi's credential was misstated in the original version on this article and has been corrected to ScD.
Patients aged 50 and older with recent active asthma are at elevated risk of abdominal aortic aneurysm and aneurysm rupture, according to new research.
A common inflammatory pathway between asthma and AAA, first observed nearly a decade ago in mice, is thought to be responsible.
The new findings, published online Feb. 11 in Arteriosclerosis, Thrombosis, and Vascular Biology (Arterioscler Thromb Vasc Biol. 2016. doi: 10.1161/ATVBAHA.115.306497) support the association in humans.
In a news release accompanying the findings, lead study author Guo-Ping Shi, ScD, of Brigham and Women’s Hospital and Harvard Medical School, Boston, said that the findings had clear clinical implications for older patients with a recent asthma diagnosis. Such patients, particularly older men, “should be checked for signs” of abdominal aortic aneurysm, Dr. Shi said.*
For their research, Dr. Shi, along with colleagues at Zhengzhou (China) University, used data from a large Danish population-based cohort of nearly 16,000 patients (81% men) with AAA between 1996 and 2012, of which about 4,500 patients had rupture. They also looked at data from a comparison cohort of patients with and without AAA from a slightly larger population-based vascular screening trial of men in Denmark.
The investigators showed that hospital diagnosis of asthma within the previous year (n = 514) was associated with significantly higher risk of hospital admission with AAA rupture (n = 146) both before and after adjustment for AAA comorbidities (adjusted odds ratio 1.51-2.06). Higher risk of rupture also was seen for patients filling prescriptions for bronchodilators within the previous 3 months (aOR = 1.10-1.31), and for patients prescribed anti-asthma drugs (aOR OR = 1.09-1.48), which were seen as indicative of an outpatient asthma diagnosis.
“A hospital diagnosis of asthma or a recently filled prescription of an anti-asthmatic drug is associated with an increased risk of admission with rAAA compared with admission with intact AAA, both before and after adjusting for AAA comorbidities and relevant medications,” the researchers wrote in their analysis.
Moreover, “an asthma diagnosis or the use of bronchodilators or other anti-asthmatic drug prescriptions closer to the date of admission with AAA correlated directly with a higher risk of aortic rupture. The results remained robust after adjusting for a wide range of relevant possible confounders,” the researchers wrote.
In the cohort of patients from the vascular screening study, which included age-matched controls without AAA, asthma (measured by recent anti-asthmatic medication use) was seen associated with a significantly elevated risk of AAA before (OR = 1.45) and after adjustment for smoking (OR = 1.45) or other risk factors (OR = 1.46). This does not refer to rupture but just AAA.
Dr. Shi and colleagues noted that the AAA cohort lacked sufficient information on cigarette smoking, a known risk factor for AAA and AAA rupture, to preclude the possibility of confounding; however, the second all-male cohort did have extensive data on smoking, “and the risk of AAA among patients with asthma remained 45% higher than that of patients with nonasthma” even after adjustment.
The researchers hypothesized that an inflammatory response characterized by elevated immunoglobulin E may be the link between AAA pathogenesis and asthma, and that other allergic inflammatory diseases, including atopic dermatitis, allergic rhinitis, and some ocular allergic diseases, could potentially carry risks for AAA formation and rupture. Dr. Shi and colleagues previously investigated the IgE and aneurysm link in animal studies.
“The results have implications for the development of much needed advances in the prevention, screening criteria, and treatment of AAA, common conditions for which we currently lack sufficiently effective approaches,” the investigators wrote.
The Chinese, Danish, and U.S. governments sponsored the study. The investigators disclosed no conflicts of interest.
*CORRECTION 8/12/2020: Dr. Shi's credential was misstated in the original version on this article and has been corrected to ScD.
Patients aged 50 and older with recent active asthma are at elevated risk of abdominal aortic aneurysm and aneurysm rupture, according to new research.
A common inflammatory pathway between asthma and AAA, first observed nearly a decade ago in mice, is thought to be responsible.
The new findings, published online Feb. 11 in Arteriosclerosis, Thrombosis, and Vascular Biology (Arterioscler Thromb Vasc Biol. 2016. doi: 10.1161/ATVBAHA.115.306497) support the association in humans.
In a news release accompanying the findings, lead study author Guo-Ping Shi, ScD, of Brigham and Women’s Hospital and Harvard Medical School, Boston, said that the findings had clear clinical implications for older patients with a recent asthma diagnosis. Such patients, particularly older men, “should be checked for signs” of abdominal aortic aneurysm, Dr. Shi said.*
For their research, Dr. Shi, along with colleagues at Zhengzhou (China) University, used data from a large Danish population-based cohort of nearly 16,000 patients (81% men) with AAA between 1996 and 2012, of which about 4,500 patients had rupture. They also looked at data from a comparison cohort of patients with and without AAA from a slightly larger population-based vascular screening trial of men in Denmark.
The investigators showed that hospital diagnosis of asthma within the previous year (n = 514) was associated with significantly higher risk of hospital admission with AAA rupture (n = 146) both before and after adjustment for AAA comorbidities (adjusted odds ratio 1.51-2.06). Higher risk of rupture also was seen for patients filling prescriptions for bronchodilators within the previous 3 months (aOR = 1.10-1.31), and for patients prescribed anti-asthma drugs (aOR OR = 1.09-1.48), which were seen as indicative of an outpatient asthma diagnosis.
“A hospital diagnosis of asthma or a recently filled prescription of an anti-asthmatic drug is associated with an increased risk of admission with rAAA compared with admission with intact AAA, both before and after adjusting for AAA comorbidities and relevant medications,” the researchers wrote in their analysis.
Moreover, “an asthma diagnosis or the use of bronchodilators or other anti-asthmatic drug prescriptions closer to the date of admission with AAA correlated directly with a higher risk of aortic rupture. The results remained robust after adjusting for a wide range of relevant possible confounders,” the researchers wrote.
In the cohort of patients from the vascular screening study, which included age-matched controls without AAA, asthma (measured by recent anti-asthmatic medication use) was seen associated with a significantly elevated risk of AAA before (OR = 1.45) and after adjustment for smoking (OR = 1.45) or other risk factors (OR = 1.46). This does not refer to rupture but just AAA.
Dr. Shi and colleagues noted that the AAA cohort lacked sufficient information on cigarette smoking, a known risk factor for AAA and AAA rupture, to preclude the possibility of confounding; however, the second all-male cohort did have extensive data on smoking, “and the risk of AAA among patients with asthma remained 45% higher than that of patients with nonasthma” even after adjustment.
The researchers hypothesized that an inflammatory response characterized by elevated immunoglobulin E may be the link between AAA pathogenesis and asthma, and that other allergic inflammatory diseases, including atopic dermatitis, allergic rhinitis, and some ocular allergic diseases, could potentially carry risks for AAA formation and rupture. Dr. Shi and colleagues previously investigated the IgE and aneurysm link in animal studies.
“The results have implications for the development of much needed advances in the prevention, screening criteria, and treatment of AAA, common conditions for which we currently lack sufficiently effective approaches,” the investigators wrote.
The Chinese, Danish, and U.S. governments sponsored the study. The investigators disclosed no conflicts of interest.
*CORRECTION 8/12/2020: Dr. Shi's credential was misstated in the original version on this article and has been corrected to ScD.
FROM ARTERIOSCLEROSIS, THROMBOSIS, AND VASCULAR BIOLOGY
Key clinical point: Older patients with a recent asthma diagnosis, particularly men, should be checked for abdominal aortic aneurysms.
Major finding: People over 50 with recent active asthma and abdominal aortic aneurysm saw a more than 50% greater risk of rupture compared with patients without asthma.
Data source: Two large cohorts from Denmark of AAA patients 50 and older (n = 15,942) and men 65 and older with and without AAA (n = 18,749), with information on asthma diagnosis and rupture.
Disclosures: The Chinese, Danish, and U.S. governments sponsored the study. The investigators disclosed no conflicts of interest.
Aortic aneurysms pose unique challenges in transplant recipients
CHICAGO – Surgeons can expect to see more abdominal organ transplant recipients presenting with aortic aneurysms, as transplant survival rates increase along with the age of organ donors and recipients.
“The consensus is that abdominal aortic aneurysms (AAAs) have a more aggressive course post-transplant and within that context, probably need to be managed more aggressively,” Dr. Michael J. Englesbe of the University of Michigan, Ann Arbor said at the annual Northwestern Vascular Symposium.
Some 270,000 Americans are living with a functioning liver or kidney graft, and their average age has risen from 47 years to 57 years over the last decade.
Though the data isn’t great, it’s hypothesized that the immunosuppression prerequisite for successful organ transplantation promotes the progression of atherosclerosis and aneurysm growth in transplant patients, he said.
New-onset diabetes, hyperlipidemia, and hypertension are all common post-transplant due to immunosuppression therapy. Aortic aneurysms are also reported to rupture at smaller sizes in transplant recipients.
Intriguingly, the opposite effect has been observed in experimental animal models, where immunosuppression with calcineurin inhibitors and mammalian target of rapamycin (mTOR) inhibitors has been shown to stabilize atherosclerotic lesions and inhibit aneurysm expansion.
The reason for this disparity is unclear, but immunosuppressants likely augment other cardiovascular comorbidities such as hypertension and atherosclerosis and this may trump their anti-inflammatory effects and lead to worse aneurysm disease and faster expansion in humans, Dr. Englesbe speculated in an interview.
As for when aneurysms should be fixed, kidney transplant candidates should undergo AAA repair prior to transplantation since the risk of renal complications after aneurysm repair puts the allograft at risk, Dr. Englesbe advised. Either an open or endovascular approach can be used.
In liver transplant candidates, elective AAA repair should be avoided if possible and is contraindicated if any signs of hepatic decompensation are present such as muscle wasting, ascites, platelet count less than 50 x 109/L, or encephalopathy. For well-compensated cirrhotic patients, endovascular repair is best.
One of the most important considerations for any solid-organ transplant patient undergoing aneurysm repair is perioperative management of immunosuppression, Dr. Englesbe stressed.
Transplant patients are maintained on oral calcineurin inhibitors such as cyclosporine and tacrolimus (Prograf) throughout the perioperative period to prevent organ rejection, but these drugs have nephrotoxic effects. About 10% of recipients, typically the sicker patients, will be switched to mTOR inhibitors such as everolimus (Afinitor) and sirolumus (Rapamune) as a kidney-sparing alternative.
“Part of the mechanism of these [mTOR] drugs is that they really affect fibroblast functioning, so patients that are on these medications, their wound will fall apart and they will invariably get a hernia,” Dr. Englesbe said. “You have to stop them upwards of about 6 weeks before surgical intervention, and I think this is also true for many endografts.”
He highlighted a case in which an mTOR inhibitor was started three months after liver transplant due to renal dysfunction in a patient who was fully healed, but within three weeks, “her wound fell apart, completely fell apart.” She developed several seromas underneath her incision, one of which became infected and took months to close.
“The transplant professionals – your nephrologists, your cardiologists – aren’t going to know this fact, but as a transplant surgeon it’s usually the first question we’re going to ask with respect to any post-transplant patient we’re going to operate on, so it’s something to keep in mind,” Dr. Englesbe said.
Another take-home message was the importance of maintaining kidney function in kidney recipients presenting with aortic aneurysm, as mortality in these patients is about 10-fold higher once the kidney fails, he said. A recent study reported that AAAs are significantly more common in kidney than liver transplant recipients (29.6% vs. 11.4%; P = .02), despite a similar prevalence for any aneurysm (4%) in both groups (J Vasc Surg. 2014 Mar;59;594-8).
When kidney recipients present, preoperative imaging of the aorta from the aneurysm to the kidney allograft is mandatory, he said. Endovascular repair is preferred, whenever possible.
The renal graft is typically sewn to the external iliac artery 3 cm to 10 cm from the bifurcation of the external and internal iliac arteries. Because of this, repair is challenging when aneurysmal disease involves the iliac artery, Dr. Englesbe observed. Aneurysmal dilation is less common in the external iliac, but stenting an iliac aneurysm can still compromise inflow to the transplanted kidney.
Several surgical techniques including axillofemoral bypass, aortofemoral shunt, or extracorporeal circuit have been reported to preserve renal function during open AAA repair in renal transplant recipients. These techniques are not without their own risk of complications and should be avoided in patients with low creatinine, but are appropriate in patients with marginal or impaired renal function, according to Dr. Englesbe, who reported having no relevant disclosures.
CHICAGO – Surgeons can expect to see more abdominal organ transplant recipients presenting with aortic aneurysms, as transplant survival rates increase along with the age of organ donors and recipients.
“The consensus is that abdominal aortic aneurysms (AAAs) have a more aggressive course post-transplant and within that context, probably need to be managed more aggressively,” Dr. Michael J. Englesbe of the University of Michigan, Ann Arbor said at the annual Northwestern Vascular Symposium.
Some 270,000 Americans are living with a functioning liver or kidney graft, and their average age has risen from 47 years to 57 years over the last decade.
Though the data isn’t great, it’s hypothesized that the immunosuppression prerequisite for successful organ transplantation promotes the progression of atherosclerosis and aneurysm growth in transplant patients, he said.
New-onset diabetes, hyperlipidemia, and hypertension are all common post-transplant due to immunosuppression therapy. Aortic aneurysms are also reported to rupture at smaller sizes in transplant recipients.
Intriguingly, the opposite effect has been observed in experimental animal models, where immunosuppression with calcineurin inhibitors and mammalian target of rapamycin (mTOR) inhibitors has been shown to stabilize atherosclerotic lesions and inhibit aneurysm expansion.
The reason for this disparity is unclear, but immunosuppressants likely augment other cardiovascular comorbidities such as hypertension and atherosclerosis and this may trump their anti-inflammatory effects and lead to worse aneurysm disease and faster expansion in humans, Dr. Englesbe speculated in an interview.
As for when aneurysms should be fixed, kidney transplant candidates should undergo AAA repair prior to transplantation since the risk of renal complications after aneurysm repair puts the allograft at risk, Dr. Englesbe advised. Either an open or endovascular approach can be used.
In liver transplant candidates, elective AAA repair should be avoided if possible and is contraindicated if any signs of hepatic decompensation are present such as muscle wasting, ascites, platelet count less than 50 x 109/L, or encephalopathy. For well-compensated cirrhotic patients, endovascular repair is best.
One of the most important considerations for any solid-organ transplant patient undergoing aneurysm repair is perioperative management of immunosuppression, Dr. Englesbe stressed.
Transplant patients are maintained on oral calcineurin inhibitors such as cyclosporine and tacrolimus (Prograf) throughout the perioperative period to prevent organ rejection, but these drugs have nephrotoxic effects. About 10% of recipients, typically the sicker patients, will be switched to mTOR inhibitors such as everolimus (Afinitor) and sirolumus (Rapamune) as a kidney-sparing alternative.
“Part of the mechanism of these [mTOR] drugs is that they really affect fibroblast functioning, so patients that are on these medications, their wound will fall apart and they will invariably get a hernia,” Dr. Englesbe said. “You have to stop them upwards of about 6 weeks before surgical intervention, and I think this is also true for many endografts.”
He highlighted a case in which an mTOR inhibitor was started three months after liver transplant due to renal dysfunction in a patient who was fully healed, but within three weeks, “her wound fell apart, completely fell apart.” She developed several seromas underneath her incision, one of which became infected and took months to close.
“The transplant professionals – your nephrologists, your cardiologists – aren’t going to know this fact, but as a transplant surgeon it’s usually the first question we’re going to ask with respect to any post-transplant patient we’re going to operate on, so it’s something to keep in mind,” Dr. Englesbe said.
Another take-home message was the importance of maintaining kidney function in kidney recipients presenting with aortic aneurysm, as mortality in these patients is about 10-fold higher once the kidney fails, he said. A recent study reported that AAAs are significantly more common in kidney than liver transplant recipients (29.6% vs. 11.4%; P = .02), despite a similar prevalence for any aneurysm (4%) in both groups (J Vasc Surg. 2014 Mar;59;594-8).
When kidney recipients present, preoperative imaging of the aorta from the aneurysm to the kidney allograft is mandatory, he said. Endovascular repair is preferred, whenever possible.
The renal graft is typically sewn to the external iliac artery 3 cm to 10 cm from the bifurcation of the external and internal iliac arteries. Because of this, repair is challenging when aneurysmal disease involves the iliac artery, Dr. Englesbe observed. Aneurysmal dilation is less common in the external iliac, but stenting an iliac aneurysm can still compromise inflow to the transplanted kidney.
Several surgical techniques including axillofemoral bypass, aortofemoral shunt, or extracorporeal circuit have been reported to preserve renal function during open AAA repair in renal transplant recipients. These techniques are not without their own risk of complications and should be avoided in patients with low creatinine, but are appropriate in patients with marginal or impaired renal function, according to Dr. Englesbe, who reported having no relevant disclosures.
CHICAGO – Surgeons can expect to see more abdominal organ transplant recipients presenting with aortic aneurysms, as transplant survival rates increase along with the age of organ donors and recipients.
“The consensus is that abdominal aortic aneurysms (AAAs) have a more aggressive course post-transplant and within that context, probably need to be managed more aggressively,” Dr. Michael J. Englesbe of the University of Michigan, Ann Arbor said at the annual Northwestern Vascular Symposium.
Some 270,000 Americans are living with a functioning liver or kidney graft, and their average age has risen from 47 years to 57 years over the last decade.
Though the data isn’t great, it’s hypothesized that the immunosuppression prerequisite for successful organ transplantation promotes the progression of atherosclerosis and aneurysm growth in transplant patients, he said.
New-onset diabetes, hyperlipidemia, and hypertension are all common post-transplant due to immunosuppression therapy. Aortic aneurysms are also reported to rupture at smaller sizes in transplant recipients.
Intriguingly, the opposite effect has been observed in experimental animal models, where immunosuppression with calcineurin inhibitors and mammalian target of rapamycin (mTOR) inhibitors has been shown to stabilize atherosclerotic lesions and inhibit aneurysm expansion.
The reason for this disparity is unclear, but immunosuppressants likely augment other cardiovascular comorbidities such as hypertension and atherosclerosis and this may trump their anti-inflammatory effects and lead to worse aneurysm disease and faster expansion in humans, Dr. Englesbe speculated in an interview.
As for when aneurysms should be fixed, kidney transplant candidates should undergo AAA repair prior to transplantation since the risk of renal complications after aneurysm repair puts the allograft at risk, Dr. Englesbe advised. Either an open or endovascular approach can be used.
In liver transplant candidates, elective AAA repair should be avoided if possible and is contraindicated if any signs of hepatic decompensation are present such as muscle wasting, ascites, platelet count less than 50 x 109/L, or encephalopathy. For well-compensated cirrhotic patients, endovascular repair is best.
One of the most important considerations for any solid-organ transplant patient undergoing aneurysm repair is perioperative management of immunosuppression, Dr. Englesbe stressed.
Transplant patients are maintained on oral calcineurin inhibitors such as cyclosporine and tacrolimus (Prograf) throughout the perioperative period to prevent organ rejection, but these drugs have nephrotoxic effects. About 10% of recipients, typically the sicker patients, will be switched to mTOR inhibitors such as everolimus (Afinitor) and sirolumus (Rapamune) as a kidney-sparing alternative.
“Part of the mechanism of these [mTOR] drugs is that they really affect fibroblast functioning, so patients that are on these medications, their wound will fall apart and they will invariably get a hernia,” Dr. Englesbe said. “You have to stop them upwards of about 6 weeks before surgical intervention, and I think this is also true for many endografts.”
He highlighted a case in which an mTOR inhibitor was started three months after liver transplant due to renal dysfunction in a patient who was fully healed, but within three weeks, “her wound fell apart, completely fell apart.” She developed several seromas underneath her incision, one of which became infected and took months to close.
“The transplant professionals – your nephrologists, your cardiologists – aren’t going to know this fact, but as a transplant surgeon it’s usually the first question we’re going to ask with respect to any post-transplant patient we’re going to operate on, so it’s something to keep in mind,” Dr. Englesbe said.
Another take-home message was the importance of maintaining kidney function in kidney recipients presenting with aortic aneurysm, as mortality in these patients is about 10-fold higher once the kidney fails, he said. A recent study reported that AAAs are significantly more common in kidney than liver transplant recipients (29.6% vs. 11.4%; P = .02), despite a similar prevalence for any aneurysm (4%) in both groups (J Vasc Surg. 2014 Mar;59;594-8).
When kidney recipients present, preoperative imaging of the aorta from the aneurysm to the kidney allograft is mandatory, he said. Endovascular repair is preferred, whenever possible.
The renal graft is typically sewn to the external iliac artery 3 cm to 10 cm from the bifurcation of the external and internal iliac arteries. Because of this, repair is challenging when aneurysmal disease involves the iliac artery, Dr. Englesbe observed. Aneurysmal dilation is less common in the external iliac, but stenting an iliac aneurysm can still compromise inflow to the transplanted kidney.
Several surgical techniques including axillofemoral bypass, aortofemoral shunt, or extracorporeal circuit have been reported to preserve renal function during open AAA repair in renal transplant recipients. These techniques are not without their own risk of complications and should be avoided in patients with low creatinine, but are appropriate in patients with marginal or impaired renal function, according to Dr. Englesbe, who reported having no relevant disclosures.
EXPERT ANALYSIS FROM THE NORTHWESTERN VASCULAR SYMPOSIUM
Tocilizumab effective in giant cell arteritis
SAN FRANCISCO – Mounting evidence supports the use of tocilizumab in giant cell arteritis (GCA), and a new study supports use of the drug for induction and maintenance therapy in patients with newly diagnosed or relapsed GCA in the context of rapidly tapered glucocorticoid therapy.
“This is the first randomized controlled trial to prove efficacy of tocilizumab in induction and maintenance of remission in GCA. Tocilizumab reached the primary and secondary endpoints in our trial compared with placebo. After 12 months of therapy, more serious adverse events were observed in the placebo group,” said lead author Dr. Sabine Adler, University Hospital, Bern, Switzerland. Dr. Adler presented results of this late-breaking abstract at a special session during the annual meeting of the American College of Rheumatology.
A recent small open-label trial showed that tocilizumab was effective in patients with refractory GCA and unacceptable side effects on glucocorticoid (GC) therapy (Sem Arthr Rheum. Dec. 26, 2014. DOI:10.1016/j.semarthrit.2014.12.005). The present study was of newly diagnosed patients or those who had relapsed.
GCA is characterized by destructive inflammation in the walls of medium and large arteries. GC treatment has been the mainstay of therapy, controlling symptoms and reducing the risk of dreaded complications such as blindness, stroke, and claudication. But many patients require prolonged treatment, and cumulative doses of GC lead to substantial toxicity and morbidity. Thus, a better treatment is needed.
IL-6, the target of tocilizumab, is one of the cytokines involved in the pathogenesis of GCA. It is elevated in the serum and tissue of affected patients, Dr. Adler explained.
Dr. Adler and colleagues conducted a single-center, randomized, placebo-controlled trial evaluating tocilizumab in 30 patients with newly diagnosed or recurrent GCA. Patients were randomized in a 2:1 ratio to receive tocilizumab 8 mg/kg IV plus oral GC or IV placebo and oral GC. Infusions were given every 4 weeks for 1 year, over which time GC dose was slowly tapered to 0 mg in all patients. Some patients underwent angiography to rule out or define aortic involvement. Most patients in the trial had new onset GCA, she said.
The primary endpoint was complete remission at week 12 with GC dose of 0.1 mg/kg/day. Complete remission was defined as the absence of clinical signs and symptoms of GCA plus negative values for C-reactive protein (CRP) and erythrocyte sedimentation rate. At 12 weeks, the complete response rate was 85% for tocilizumab versus 40% for placebo, a significant difference. At the end of the trial, 85% and 20%, respectively, had not had a relapse; this difference was significant.
Placebo patients received a higher cumulative dose of GC, she continued.
There were 7 serious adverse events reported in the tocilizumab arm and 5 in the placebo arm; 1 death occurred in the placebo arm due to myocardial infarction.
“A closer look at serious adverse events reveals few cardiovascular problems,” Dr. Adler continued. Back pain and psychosis were reported as reasons for hospitalization.
During the question and answer session, an audience member noted that it was difficult to understand how a short-term treatment is effective in a chronic disease. “Probably patients will relapse when they stop the medication, so we are not on the ‘green’ side yet,” she replied. Dr. Adler noted that it could be possible that a reduced dose of tocilizumab could be effective but have fewer side effects, but that has not been studied.
Tocilizumab was provided by Roche for this investigator-initiated trial. Dr. Adler reported no financial disclosures.
SAN FRANCISCO – Mounting evidence supports the use of tocilizumab in giant cell arteritis (GCA), and a new study supports use of the drug for induction and maintenance therapy in patients with newly diagnosed or relapsed GCA in the context of rapidly tapered glucocorticoid therapy.
“This is the first randomized controlled trial to prove efficacy of tocilizumab in induction and maintenance of remission in GCA. Tocilizumab reached the primary and secondary endpoints in our trial compared with placebo. After 12 months of therapy, more serious adverse events were observed in the placebo group,” said lead author Dr. Sabine Adler, University Hospital, Bern, Switzerland. Dr. Adler presented results of this late-breaking abstract at a special session during the annual meeting of the American College of Rheumatology.
A recent small open-label trial showed that tocilizumab was effective in patients with refractory GCA and unacceptable side effects on glucocorticoid (GC) therapy (Sem Arthr Rheum. Dec. 26, 2014. DOI:10.1016/j.semarthrit.2014.12.005). The present study was of newly diagnosed patients or those who had relapsed.
GCA is characterized by destructive inflammation in the walls of medium and large arteries. GC treatment has been the mainstay of therapy, controlling symptoms and reducing the risk of dreaded complications such as blindness, stroke, and claudication. But many patients require prolonged treatment, and cumulative doses of GC lead to substantial toxicity and morbidity. Thus, a better treatment is needed.
IL-6, the target of tocilizumab, is one of the cytokines involved in the pathogenesis of GCA. It is elevated in the serum and tissue of affected patients, Dr. Adler explained.
Dr. Adler and colleagues conducted a single-center, randomized, placebo-controlled trial evaluating tocilizumab in 30 patients with newly diagnosed or recurrent GCA. Patients were randomized in a 2:1 ratio to receive tocilizumab 8 mg/kg IV plus oral GC or IV placebo and oral GC. Infusions were given every 4 weeks for 1 year, over which time GC dose was slowly tapered to 0 mg in all patients. Some patients underwent angiography to rule out or define aortic involvement. Most patients in the trial had new onset GCA, she said.
The primary endpoint was complete remission at week 12 with GC dose of 0.1 mg/kg/day. Complete remission was defined as the absence of clinical signs and symptoms of GCA plus negative values for C-reactive protein (CRP) and erythrocyte sedimentation rate. At 12 weeks, the complete response rate was 85% for tocilizumab versus 40% for placebo, a significant difference. At the end of the trial, 85% and 20%, respectively, had not had a relapse; this difference was significant.
Placebo patients received a higher cumulative dose of GC, she continued.
There were 7 serious adverse events reported in the tocilizumab arm and 5 in the placebo arm; 1 death occurred in the placebo arm due to myocardial infarction.
“A closer look at serious adverse events reveals few cardiovascular problems,” Dr. Adler continued. Back pain and psychosis were reported as reasons for hospitalization.
During the question and answer session, an audience member noted that it was difficult to understand how a short-term treatment is effective in a chronic disease. “Probably patients will relapse when they stop the medication, so we are not on the ‘green’ side yet,” she replied. Dr. Adler noted that it could be possible that a reduced dose of tocilizumab could be effective but have fewer side effects, but that has not been studied.
Tocilizumab was provided by Roche for this investigator-initiated trial. Dr. Adler reported no financial disclosures.
SAN FRANCISCO – Mounting evidence supports the use of tocilizumab in giant cell arteritis (GCA), and a new study supports use of the drug for induction and maintenance therapy in patients with newly diagnosed or relapsed GCA in the context of rapidly tapered glucocorticoid therapy.
“This is the first randomized controlled trial to prove efficacy of tocilizumab in induction and maintenance of remission in GCA. Tocilizumab reached the primary and secondary endpoints in our trial compared with placebo. After 12 months of therapy, more serious adverse events were observed in the placebo group,” said lead author Dr. Sabine Adler, University Hospital, Bern, Switzerland. Dr. Adler presented results of this late-breaking abstract at a special session during the annual meeting of the American College of Rheumatology.
A recent small open-label trial showed that tocilizumab was effective in patients with refractory GCA and unacceptable side effects on glucocorticoid (GC) therapy (Sem Arthr Rheum. Dec. 26, 2014. DOI:10.1016/j.semarthrit.2014.12.005). The present study was of newly diagnosed patients or those who had relapsed.
GCA is characterized by destructive inflammation in the walls of medium and large arteries. GC treatment has been the mainstay of therapy, controlling symptoms and reducing the risk of dreaded complications such as blindness, stroke, and claudication. But many patients require prolonged treatment, and cumulative doses of GC lead to substantial toxicity and morbidity. Thus, a better treatment is needed.
IL-6, the target of tocilizumab, is one of the cytokines involved in the pathogenesis of GCA. It is elevated in the serum and tissue of affected patients, Dr. Adler explained.
Dr. Adler and colleagues conducted a single-center, randomized, placebo-controlled trial evaluating tocilizumab in 30 patients with newly diagnosed or recurrent GCA. Patients were randomized in a 2:1 ratio to receive tocilizumab 8 mg/kg IV plus oral GC or IV placebo and oral GC. Infusions were given every 4 weeks for 1 year, over which time GC dose was slowly tapered to 0 mg in all patients. Some patients underwent angiography to rule out or define aortic involvement. Most patients in the trial had new onset GCA, she said.
The primary endpoint was complete remission at week 12 with GC dose of 0.1 mg/kg/day. Complete remission was defined as the absence of clinical signs and symptoms of GCA plus negative values for C-reactive protein (CRP) and erythrocyte sedimentation rate. At 12 weeks, the complete response rate was 85% for tocilizumab versus 40% for placebo, a significant difference. At the end of the trial, 85% and 20%, respectively, had not had a relapse; this difference was significant.
Placebo patients received a higher cumulative dose of GC, she continued.
There were 7 serious adverse events reported in the tocilizumab arm and 5 in the placebo arm; 1 death occurred in the placebo arm due to myocardial infarction.
“A closer look at serious adverse events reveals few cardiovascular problems,” Dr. Adler continued. Back pain and psychosis were reported as reasons for hospitalization.
During the question and answer session, an audience member noted that it was difficult to understand how a short-term treatment is effective in a chronic disease. “Probably patients will relapse when they stop the medication, so we are not on the ‘green’ side yet,” she replied. Dr. Adler noted that it could be possible that a reduced dose of tocilizumab could be effective but have fewer side effects, but that has not been studied.
Tocilizumab was provided by Roche for this investigator-initiated trial. Dr. Adler reported no financial disclosures.
AT THE ACR ANNUAL MEETING
Key clinical point: Tocilizumab was effective in newly diagnosed and recurrent giant cell arteritis.
Major finding: At week 12, 85% of the tocilizumab-treated patients were in complete remission versus 40% of placebo patients.
Data source: Single-center, randomized, double-blind trial of 30 patients.
Disclosures: Tocilizumab was provided by Roche for this investigator-initiated trial. Dr. Adler reported no financial disclosures.
Low incidence of DVT reported after percutaneous EVAR
Completely percutaneous endovascular aortic aneurysm repair (PEVAR) has become more common, using the suture-mediated “preclose” technique. The rate of periprocedural, iatrogenic, acute deep vein thrombosis (DVT), hitherto unknown, was found to be low for this approach, according to a study reported by Dr. Courtney E. Morgan and her colleagues at the Northwestern University, Chicago.
The researchers assessed 52 consecutive patients (44 men) with a mean age of 73 years, who underwent PEVAR at their center. Only 6% had a prior history of DVT (J Vasc Surg. 2015 Aug; 62:351-4).
Acute DVT was seen in four patients on postoperative day 1. These four DVTs comprised one femoropopliteal, and three calf DVTs. Three of these patients had associated risk factors: history of DVT (two patients); active smokers (one patient); and obesity (body mass index greater than 30 kg/m2 in all three patients).
At 2 weeks postoperatively, 75% of the DVTs had resolved.
“We found an overall rate of proximal DVT of 4% after PEVAR, which increased to 13% when calf-vein DVTs were included. Most patients with postoperative DVT had preexisting risk factors, which suggests that routine duplex ultrasound screening after PEVAR is not necessary unless there exist preclinical risk factors or postprocedural clinical indications suggestive of DVT,” the authors concluded.
Two of the researchers have received funding and/or served as speakers/consultants for device companies involved in EVAR.
Read the full study online in the Journal of Vascular Surgery.
Completely percutaneous endovascular aortic aneurysm repair (PEVAR) has become more common, using the suture-mediated “preclose” technique. The rate of periprocedural, iatrogenic, acute deep vein thrombosis (DVT), hitherto unknown, was found to be low for this approach, according to a study reported by Dr. Courtney E. Morgan and her colleagues at the Northwestern University, Chicago.
The researchers assessed 52 consecutive patients (44 men) with a mean age of 73 years, who underwent PEVAR at their center. Only 6% had a prior history of DVT (J Vasc Surg. 2015 Aug; 62:351-4).
Acute DVT was seen in four patients on postoperative day 1. These four DVTs comprised one femoropopliteal, and three calf DVTs. Three of these patients had associated risk factors: history of DVT (two patients); active smokers (one patient); and obesity (body mass index greater than 30 kg/m2 in all three patients).
At 2 weeks postoperatively, 75% of the DVTs had resolved.
“We found an overall rate of proximal DVT of 4% after PEVAR, which increased to 13% when calf-vein DVTs were included. Most patients with postoperative DVT had preexisting risk factors, which suggests that routine duplex ultrasound screening after PEVAR is not necessary unless there exist preclinical risk factors or postprocedural clinical indications suggestive of DVT,” the authors concluded.
Two of the researchers have received funding and/or served as speakers/consultants for device companies involved in EVAR.
Read the full study online in the Journal of Vascular Surgery.
Completely percutaneous endovascular aortic aneurysm repair (PEVAR) has become more common, using the suture-mediated “preclose” technique. The rate of periprocedural, iatrogenic, acute deep vein thrombosis (DVT), hitherto unknown, was found to be low for this approach, according to a study reported by Dr. Courtney E. Morgan and her colleagues at the Northwestern University, Chicago.
The researchers assessed 52 consecutive patients (44 men) with a mean age of 73 years, who underwent PEVAR at their center. Only 6% had a prior history of DVT (J Vasc Surg. 2015 Aug; 62:351-4).
Acute DVT was seen in four patients on postoperative day 1. These four DVTs comprised one femoropopliteal, and three calf DVTs. Three of these patients had associated risk factors: history of DVT (two patients); active smokers (one patient); and obesity (body mass index greater than 30 kg/m2 in all three patients).
At 2 weeks postoperatively, 75% of the DVTs had resolved.
“We found an overall rate of proximal DVT of 4% after PEVAR, which increased to 13% when calf-vein DVTs were included. Most patients with postoperative DVT had preexisting risk factors, which suggests that routine duplex ultrasound screening after PEVAR is not necessary unless there exist preclinical risk factors or postprocedural clinical indications suggestive of DVT,” the authors concluded.
Two of the researchers have received funding and/or served as speakers/consultants for device companies involved in EVAR.
Read the full study online in the Journal of Vascular Surgery.
FROM THE JOURNAL OF VASCULAR SURGERY