User login
MD-IQ only
Multidisciplinary management of endometriosis-associated pain
Andrea Rapkin, MD, is Board Certified by the American College of Obstetricians and Gynecologists (of which she is also a fellow). After obtaining her MD, she completed her residency in OBGYN at UCLA then joined the faculty at UCLA and is a Professor of Obstetrics and Gynecology. She was one of the first Obstetrician-Gynecologists to adapt the multidisciplinary pain management approach to the evaluation and treatment of women with pelvic and vulvar pain.
You are the founder and director of a clinic focused on a multidisciplinary pain management approach to the evaluation and treatment of women with pelvic and vulvar pain. How did you identify such a clinic as a therapeutic need for patients?
Dr. Rapkin: The short answer is that a significant proportion of women were not experiencing pain relief or had incomplete relief with traditional medical or surgical therapy. At the time, we also identified various red flags for traditional treatment failures. These red flags included the following: pain of greater than 6 months duration, pain out of proportion to pathology found on examination, multiple visceral and somatic complaints, and psychosocial abnormalities. We now understand more about the neurobiology underpinning these red flags.
With the widespread availability of laparoscopy in the late 70s and early 80s, many studies investigated the relationship between endometriosis lesions and pain. The general consensus is that there is no relationship between the location or severity of the endometriosis lesions or the disease stage (American Society for Reproductive Medicine staging) with type of symptoms, symptom severity, treatment response, recurrence, or even prognosis. In fact, pain recurrence after adequate surgical treatment is unrelated to the presence of endometriosis lesions found at the time of repeat laparoscopy. This lack of association between pain and presence of visible disease was supported by a recent New England Journal of Medicine article by Zondervan and colleagues demonstrating that up to 30% of women with chronic pelvic pain, present after excision of endometriotic lesions, become unresponsive to conventional treatment.
The neurobiological responses in an individual with chronic pain are more complicated than those seen in the setting of acute pain. Chronic pain may be triggered or maintained by an inflammatory process such as endometriosis but, over time, altered neural processing and psychosocial maladaptation can occur. The altered processing consists of both peripheral and central sensitization which change the way sensory information from the pelvic viscera and surrounding somatic structures in the periphery is transmitted and interpreted in the central nervous system (spinal cord and brain). Visceral pelvic pain can emanate from the uterus, ovaries and fallopian tubes, the urinary bladder, and the bowel, while the somatic sources include the surrounding abdominal wall, low back and pelvic floor muscles, and fascia, and bones. Signal amplification or peripheral sensitization in the pelvic region in women with endometriosis starts with localized inflammation, neovascularization, invasion and innervation of endometriotic implants. As the pelvic organs share thoracolumbar and sacral autonomic neural pathways, inflammation or dysfunction in one organ or tissue, such as the uterus, over time can sensitize or lead to dysfunction in other pelvic organs, such as the bladder or bowel (called viscero-visceral cross sensitization). Finally, somatic structures sharing intervention with the pelvic viscera, such as the fascia and muscles of the lower abdomen, pelvic floor lower back also become sources of pain because of a process called viscero-somatic sensitization. Women who have endometriosis are therefore more likely to experience IBS, bladder pain syndrome/interstitial cystitis and vulvodynia, and up to 80% of individuals can develop myofascial pain related to trigger points and muscle dysfunction. Up to 50% of women with bladder pain have endometriosis. Those with endometriosis or bladder pain are 2.5 times more likely to also have IBS.
Over time, other visceral and somatic structures innervated by higher levels of the spinal cord can be affected, leading to more widespread pain. Central sensitization manifests as an amplification of pain in the spinal cord and brain. The presence of more than two chronic “unexplained” pain conditions, such as chronic pelvic pain, vulvodynia, myofascial pain, headache, etc suggest the presence of central sensitization. Anxiety, depression, and maladaptive coping strategies often ensue. Functional MRI studies have documented altered central processing in the brain in many chronic pain states including endometriosis. Interdisciplinary therapy including physical therapy, mental health, and pain management/anesthesiology is more effective compared with medical and or surgical therapy alone for endometriosis-related pain in the setting of peripheral and central sensitization.
What should clinicians look for, or what stands out to them, to confirm the endometriosis diagnosis when pain is the presenting symptom?
Dr. Rapkin: There are no pathognomonic symptoms or biomarkers for endometriosis; however, the following historical features have been shown to be linked with a greater likelihood of finding endometriosis:
- persistent dysmenorrhea (menstrual pain) despite NSAID and hormonal treatment
- cyclical pain that is premenstrual and menstrual that progresses to chronic pain or is accompanied by abnormal or heavy menstrual bleeding
- deep dyspareunia
- dyschezia (pain with bowel movements), and sometimes bloating.
An individual with menstrual pain since menarche can have up to a 5% increased risk of endometriosis. Endometriosis in a first-degree relative elevates the risk for endometriosis by 7% to 10%.
Given the complexity of chronic pain, it is important not to assume endometriosis is the only source of pain. All the pelvic visceral and somatic structures should be evaluated. A thorough history addresses all the patient’s symptoms, including vaginal, gastrointestinal and genitourinary. Aggravating factors such as menstrual cycle, bowel and bladder functioning, physical activity, sexual intercourse and stress should be queried. In addition, assessment of mood, anxiety or depression, sleep disturbance and effect of pain on daily functioning are relevant as is history of abuse or trauma (physical, sexual or emotional). This history can be lengthy, so a detailed pain questionnaire is helpful. (See the pelvicpain.org website for a user-friendly pain questionnaire).
With the previously mentioned risk factors in mind, and after a thorough history has been obtained, a pain-localizing exam should be conducted including the abdominal wall, pelvic floor, and then the bimanual and rectovaginal exams for the abdominal wall myofascial/neuropathic pain assessment for which Carnett’s test can be very useful—tender points on the abdominal wall are palpitated and the patient is asked to give a numerical rating of the pain (1-10/10) and marked with a pen. The patient is then asked to either perform a bilateral straight leg raise or an abdominal crunch, and the areas are re-palpitated. If the marked areas are more painful to palpation during the abdominal crunch or the bilateral straight leg raise, it suggests an abdominal wall pain (myofascial or neuropathic) or component of the pain. Similarly, pelvic floor muscles should be assessed after the abdominal wall exam is completed. This is best accomplished with a unit-digital exam with palpation of pelvic muscles for tenderness and hypertonia on exam. These myofascial findings are often present in the setting of endometriosis, but they can be primary-unrelated to presence or absence of endometriosis.
What are your focused disciplines for approaching endometriosis-associated pain? How do you recommend these clinicians or specialists come together to effectively manage a patient’s conditions?
Dr. Rapkin: The gynecologist or primary care provider can address the chronic inflammatory, estrogen-dependent aspect of endometriosis. Begin with nonsteroidal, anti-inflammatory medication and combined estrogen-progestin or high-dose progestin-alone hormonal therapy to lower estrogenic stimulation of lesions and decidualize those progestin-sensitive lesions. For menstrual cycle related pain (luteal periovulatory or menstrual phase) cyclical exacerbation of other chronic pain conditions, early intervention is recommended. Adequately dosed preemptive nonsteroidal inflammatory agents and, if not tolerated or effective, begin combined hormonal contraceptives or intrauterine or higher dose progestins menstrual suppression, with either continuous monophasic hormonal contraceptives or progestins, is very important for pain that is cyclical or exacerbated in a cyclical fashion. Progestins can be administered orally, such as norethindrone acetate; intramuscularly or subdermally (depot medroxyprogesterone acetate or etonogestrel implant); or intrauterine (which does not lower estrogen levels but can be therapeutic for suppression of menses and local treatment of endometriosis). Failure of hormonal therapy and management of other co-occurring pain conditions warrants trial of a second-line medical therapy such as gonadotropin-releasing hormone antagonist or agonist or surgery for definitive diagnosis and surgical ablation or excision of endometriosis lesions.
I would suggest that gynecologists who treat women with endometriosis and chronic pain try to build a team in their geographic area. Relevant specialists for an interdisciplinary approach include:
- Pelvic floor physical therapist to evaluate and address myofascial dysfunction and pain and voiding abnormalities, such as urinary urgency or frequency and constipation
- Gastroenterologist for evaluation and treatment of irritable bowel or functional abdominal pain and bloating syndrome or inflammatory bowel disease. Urologist or urogynecologist to assess and treat bladder pain syndrome/interstitial cystitis
- Primary care evaluation for diffuse myofascial pain, fibromyalgia, arthralgias, and other inflammatory conditions, and for management of headache and migraine. Rheumatology and neurology specialists may be needed
- Mental health providers for treatment of anxiety, depression, or PTSD and to address stress management, coping skills and provide cognitive behavioral therapy
- Interventional pain management specialist such as physical medicine and rehabilitation (PM and R), pain anesthiologist, neurologist or interventional radiologist to provide relevant nerve blocks, trigger point injections, or botulinum toxin injection.
- Gynecologists experienced in the management of chronic pelvic pain also provide nerve blocks, trigger point and botulinum toxin injections.
Andrea Rapkin, MD, is Board Certified by the American College of Obstetricians and Gynecologists (of which she is also a fellow). After obtaining her MD, she completed her residency in OBGYN at UCLA then joined the faculty at UCLA and is a Professor of Obstetrics and Gynecology. She was one of the first Obstetrician-Gynecologists to adapt the multidisciplinary pain management approach to the evaluation and treatment of women with pelvic and vulvar pain.
You are the founder and director of a clinic focused on a multidisciplinary pain management approach to the evaluation and treatment of women with pelvic and vulvar pain. How did you identify such a clinic as a therapeutic need for patients?
Dr. Rapkin: The short answer is that a significant proportion of women were not experiencing pain relief or had incomplete relief with traditional medical or surgical therapy. At the time, we also identified various red flags for traditional treatment failures. These red flags included the following: pain of greater than 6 months duration, pain out of proportion to pathology found on examination, multiple visceral and somatic complaints, and psychosocial abnormalities. We now understand more about the neurobiology underpinning these red flags.
With the widespread availability of laparoscopy in the late 70s and early 80s, many studies investigated the relationship between endometriosis lesions and pain. The general consensus is that there is no relationship between the location or severity of the endometriosis lesions or the disease stage (American Society for Reproductive Medicine staging) with type of symptoms, symptom severity, treatment response, recurrence, or even prognosis. In fact, pain recurrence after adequate surgical treatment is unrelated to the presence of endometriosis lesions found at the time of repeat laparoscopy. This lack of association between pain and presence of visible disease was supported by a recent New England Journal of Medicine article by Zondervan and colleagues demonstrating that up to 30% of women with chronic pelvic pain, present after excision of endometriotic lesions, become unresponsive to conventional treatment.
The neurobiological responses in an individual with chronic pain are more complicated than those seen in the setting of acute pain. Chronic pain may be triggered or maintained by an inflammatory process such as endometriosis but, over time, altered neural processing and psychosocial maladaptation can occur. The altered processing consists of both peripheral and central sensitization which change the way sensory information from the pelvic viscera and surrounding somatic structures in the periphery is transmitted and interpreted in the central nervous system (spinal cord and brain). Visceral pelvic pain can emanate from the uterus, ovaries and fallopian tubes, the urinary bladder, and the bowel, while the somatic sources include the surrounding abdominal wall, low back and pelvic floor muscles, and fascia, and bones. Signal amplification or peripheral sensitization in the pelvic region in women with endometriosis starts with localized inflammation, neovascularization, invasion and innervation of endometriotic implants. As the pelvic organs share thoracolumbar and sacral autonomic neural pathways, inflammation or dysfunction in one organ or tissue, such as the uterus, over time can sensitize or lead to dysfunction in other pelvic organs, such as the bladder or bowel (called viscero-visceral cross sensitization). Finally, somatic structures sharing intervention with the pelvic viscera, such as the fascia and muscles of the lower abdomen, pelvic floor lower back also become sources of pain because of a process called viscero-somatic sensitization. Women who have endometriosis are therefore more likely to experience IBS, bladder pain syndrome/interstitial cystitis and vulvodynia, and up to 80% of individuals can develop myofascial pain related to trigger points and muscle dysfunction. Up to 50% of women with bladder pain have endometriosis. Those with endometriosis or bladder pain are 2.5 times more likely to also have IBS.
Over time, other visceral and somatic structures innervated by higher levels of the spinal cord can be affected, leading to more widespread pain. Central sensitization manifests as an amplification of pain in the spinal cord and brain. The presence of more than two chronic “unexplained” pain conditions, such as chronic pelvic pain, vulvodynia, myofascial pain, headache, etc suggest the presence of central sensitization. Anxiety, depression, and maladaptive coping strategies often ensue. Functional MRI studies have documented altered central processing in the brain in many chronic pain states including endometriosis. Interdisciplinary therapy including physical therapy, mental health, and pain management/anesthesiology is more effective compared with medical and or surgical therapy alone for endometriosis-related pain in the setting of peripheral and central sensitization.
What should clinicians look for, or what stands out to them, to confirm the endometriosis diagnosis when pain is the presenting symptom?
Dr. Rapkin: There are no pathognomonic symptoms or biomarkers for endometriosis; however, the following historical features have been shown to be linked with a greater likelihood of finding endometriosis:
- persistent dysmenorrhea (menstrual pain) despite NSAID and hormonal treatment
- cyclical pain that is premenstrual and menstrual that progresses to chronic pain or is accompanied by abnormal or heavy menstrual bleeding
- deep dyspareunia
- dyschezia (pain with bowel movements), and sometimes bloating.
An individual with menstrual pain since menarche can have up to a 5% increased risk of endometriosis. Endometriosis in a first-degree relative elevates the risk for endometriosis by 7% to 10%.
Given the complexity of chronic pain, it is important not to assume endometriosis is the only source of pain. All the pelvic visceral and somatic structures should be evaluated. A thorough history addresses all the patient’s symptoms, including vaginal, gastrointestinal and genitourinary. Aggravating factors such as menstrual cycle, bowel and bladder functioning, physical activity, sexual intercourse and stress should be queried. In addition, assessment of mood, anxiety or depression, sleep disturbance and effect of pain on daily functioning are relevant as is history of abuse or trauma (physical, sexual or emotional). This history can be lengthy, so a detailed pain questionnaire is helpful. (See the pelvicpain.org website for a user-friendly pain questionnaire).
With the previously mentioned risk factors in mind, and after a thorough history has been obtained, a pain-localizing exam should be conducted including the abdominal wall, pelvic floor, and then the bimanual and rectovaginal exams for the abdominal wall myofascial/neuropathic pain assessment for which Carnett’s test can be very useful—tender points on the abdominal wall are palpitated and the patient is asked to give a numerical rating of the pain (1-10/10) and marked with a pen. The patient is then asked to either perform a bilateral straight leg raise or an abdominal crunch, and the areas are re-palpitated. If the marked areas are more painful to palpation during the abdominal crunch or the bilateral straight leg raise, it suggests an abdominal wall pain (myofascial or neuropathic) or component of the pain. Similarly, pelvic floor muscles should be assessed after the abdominal wall exam is completed. This is best accomplished with a unit-digital exam with palpation of pelvic muscles for tenderness and hypertonia on exam. These myofascial findings are often present in the setting of endometriosis, but they can be primary-unrelated to presence or absence of endometriosis.
What are your focused disciplines for approaching endometriosis-associated pain? How do you recommend these clinicians or specialists come together to effectively manage a patient’s conditions?
Dr. Rapkin: The gynecologist or primary care provider can address the chronic inflammatory, estrogen-dependent aspect of endometriosis. Begin with nonsteroidal, anti-inflammatory medication and combined estrogen-progestin or high-dose progestin-alone hormonal therapy to lower estrogenic stimulation of lesions and decidualize those progestin-sensitive lesions. For menstrual cycle related pain (luteal periovulatory or menstrual phase) cyclical exacerbation of other chronic pain conditions, early intervention is recommended. Adequately dosed preemptive nonsteroidal inflammatory agents and, if not tolerated or effective, begin combined hormonal contraceptives or intrauterine or higher dose progestins menstrual suppression, with either continuous monophasic hormonal contraceptives or progestins, is very important for pain that is cyclical or exacerbated in a cyclical fashion. Progestins can be administered orally, such as norethindrone acetate; intramuscularly or subdermally (depot medroxyprogesterone acetate or etonogestrel implant); or intrauterine (which does not lower estrogen levels but can be therapeutic for suppression of menses and local treatment of endometriosis). Failure of hormonal therapy and management of other co-occurring pain conditions warrants trial of a second-line medical therapy such as gonadotropin-releasing hormone antagonist or agonist or surgery for definitive diagnosis and surgical ablation or excision of endometriosis lesions.
I would suggest that gynecologists who treat women with endometriosis and chronic pain try to build a team in their geographic area. Relevant specialists for an interdisciplinary approach include:
- Pelvic floor physical therapist to evaluate and address myofascial dysfunction and pain and voiding abnormalities, such as urinary urgency or frequency and constipation
- Gastroenterologist for evaluation and treatment of irritable bowel or functional abdominal pain and bloating syndrome or inflammatory bowel disease. Urologist or urogynecologist to assess and treat bladder pain syndrome/interstitial cystitis
- Primary care evaluation for diffuse myofascial pain, fibromyalgia, arthralgias, and other inflammatory conditions, and for management of headache and migraine. Rheumatology and neurology specialists may be needed
- Mental health providers for treatment of anxiety, depression, or PTSD and to address stress management, coping skills and provide cognitive behavioral therapy
- Interventional pain management specialist such as physical medicine and rehabilitation (PM and R), pain anesthiologist, neurologist or interventional radiologist to provide relevant nerve blocks, trigger point injections, or botulinum toxin injection.
- Gynecologists experienced in the management of chronic pelvic pain also provide nerve blocks, trigger point and botulinum toxin injections.
Andrea Rapkin, MD, is Board Certified by the American College of Obstetricians and Gynecologists (of which she is also a fellow). After obtaining her MD, she completed her residency in OBGYN at UCLA then joined the faculty at UCLA and is a Professor of Obstetrics and Gynecology. She was one of the first Obstetrician-Gynecologists to adapt the multidisciplinary pain management approach to the evaluation and treatment of women with pelvic and vulvar pain.
You are the founder and director of a clinic focused on a multidisciplinary pain management approach to the evaluation and treatment of women with pelvic and vulvar pain. How did you identify such a clinic as a therapeutic need for patients?
Dr. Rapkin: The short answer is that a significant proportion of women were not experiencing pain relief or had incomplete relief with traditional medical or surgical therapy. At the time, we also identified various red flags for traditional treatment failures. These red flags included the following: pain of greater than 6 months duration, pain out of proportion to pathology found on examination, multiple visceral and somatic complaints, and psychosocial abnormalities. We now understand more about the neurobiology underpinning these red flags.
With the widespread availability of laparoscopy in the late 70s and early 80s, many studies investigated the relationship between endometriosis lesions and pain. The general consensus is that there is no relationship between the location or severity of the endometriosis lesions or the disease stage (American Society for Reproductive Medicine staging) with type of symptoms, symptom severity, treatment response, recurrence, or even prognosis. In fact, pain recurrence after adequate surgical treatment is unrelated to the presence of endometriosis lesions found at the time of repeat laparoscopy. This lack of association between pain and presence of visible disease was supported by a recent New England Journal of Medicine article by Zondervan and colleagues demonstrating that up to 30% of women with chronic pelvic pain, present after excision of endometriotic lesions, become unresponsive to conventional treatment.
The neurobiological responses in an individual with chronic pain are more complicated than those seen in the setting of acute pain. Chronic pain may be triggered or maintained by an inflammatory process such as endometriosis but, over time, altered neural processing and psychosocial maladaptation can occur. The altered processing consists of both peripheral and central sensitization which change the way sensory information from the pelvic viscera and surrounding somatic structures in the periphery is transmitted and interpreted in the central nervous system (spinal cord and brain). Visceral pelvic pain can emanate from the uterus, ovaries and fallopian tubes, the urinary bladder, and the bowel, while the somatic sources include the surrounding abdominal wall, low back and pelvic floor muscles, and fascia, and bones. Signal amplification or peripheral sensitization in the pelvic region in women with endometriosis starts with localized inflammation, neovascularization, invasion and innervation of endometriotic implants. As the pelvic organs share thoracolumbar and sacral autonomic neural pathways, inflammation or dysfunction in one organ or tissue, such as the uterus, over time can sensitize or lead to dysfunction in other pelvic organs, such as the bladder or bowel (called viscero-visceral cross sensitization). Finally, somatic structures sharing intervention with the pelvic viscera, such as the fascia and muscles of the lower abdomen, pelvic floor lower back also become sources of pain because of a process called viscero-somatic sensitization. Women who have endometriosis are therefore more likely to experience IBS, bladder pain syndrome/interstitial cystitis and vulvodynia, and up to 80% of individuals can develop myofascial pain related to trigger points and muscle dysfunction. Up to 50% of women with bladder pain have endometriosis. Those with endometriosis or bladder pain are 2.5 times more likely to also have IBS.
Over time, other visceral and somatic structures innervated by higher levels of the spinal cord can be affected, leading to more widespread pain. Central sensitization manifests as an amplification of pain in the spinal cord and brain. The presence of more than two chronic “unexplained” pain conditions, such as chronic pelvic pain, vulvodynia, myofascial pain, headache, etc suggest the presence of central sensitization. Anxiety, depression, and maladaptive coping strategies often ensue. Functional MRI studies have documented altered central processing in the brain in many chronic pain states including endometriosis. Interdisciplinary therapy including physical therapy, mental health, and pain management/anesthesiology is more effective compared with medical and or surgical therapy alone for endometriosis-related pain in the setting of peripheral and central sensitization.
What should clinicians look for, or what stands out to them, to confirm the endometriosis diagnosis when pain is the presenting symptom?
Dr. Rapkin: There are no pathognomonic symptoms or biomarkers for endometriosis; however, the following historical features have been shown to be linked with a greater likelihood of finding endometriosis:
- persistent dysmenorrhea (menstrual pain) despite NSAID and hormonal treatment
- cyclical pain that is premenstrual and menstrual that progresses to chronic pain or is accompanied by abnormal or heavy menstrual bleeding
- deep dyspareunia
- dyschezia (pain with bowel movements), and sometimes bloating.
An individual with menstrual pain since menarche can have up to a 5% increased risk of endometriosis. Endometriosis in a first-degree relative elevates the risk for endometriosis by 7% to 10%.
Given the complexity of chronic pain, it is important not to assume endometriosis is the only source of pain. All the pelvic visceral and somatic structures should be evaluated. A thorough history addresses all the patient’s symptoms, including vaginal, gastrointestinal and genitourinary. Aggravating factors such as menstrual cycle, bowel and bladder functioning, physical activity, sexual intercourse and stress should be queried. In addition, assessment of mood, anxiety or depression, sleep disturbance and effect of pain on daily functioning are relevant as is history of abuse or trauma (physical, sexual or emotional). This history can be lengthy, so a detailed pain questionnaire is helpful. (See the pelvicpain.org website for a user-friendly pain questionnaire).
With the previously mentioned risk factors in mind, and after a thorough history has been obtained, a pain-localizing exam should be conducted including the abdominal wall, pelvic floor, and then the bimanual and rectovaginal exams for the abdominal wall myofascial/neuropathic pain assessment for which Carnett’s test can be very useful—tender points on the abdominal wall are palpitated and the patient is asked to give a numerical rating of the pain (1-10/10) and marked with a pen. The patient is then asked to either perform a bilateral straight leg raise or an abdominal crunch, and the areas are re-palpitated. If the marked areas are more painful to palpation during the abdominal crunch or the bilateral straight leg raise, it suggests an abdominal wall pain (myofascial or neuropathic) or component of the pain. Similarly, pelvic floor muscles should be assessed after the abdominal wall exam is completed. This is best accomplished with a unit-digital exam with palpation of pelvic muscles for tenderness and hypertonia on exam. These myofascial findings are often present in the setting of endometriosis, but they can be primary-unrelated to presence or absence of endometriosis.
What are your focused disciplines for approaching endometriosis-associated pain? How do you recommend these clinicians or specialists come together to effectively manage a patient’s conditions?
Dr. Rapkin: The gynecologist or primary care provider can address the chronic inflammatory, estrogen-dependent aspect of endometriosis. Begin with nonsteroidal, anti-inflammatory medication and combined estrogen-progestin or high-dose progestin-alone hormonal therapy to lower estrogenic stimulation of lesions and decidualize those progestin-sensitive lesions. For menstrual cycle related pain (luteal periovulatory or menstrual phase) cyclical exacerbation of other chronic pain conditions, early intervention is recommended. Adequately dosed preemptive nonsteroidal inflammatory agents and, if not tolerated or effective, begin combined hormonal contraceptives or intrauterine or higher dose progestins menstrual suppression, with either continuous monophasic hormonal contraceptives or progestins, is very important for pain that is cyclical or exacerbated in a cyclical fashion. Progestins can be administered orally, such as norethindrone acetate; intramuscularly or subdermally (depot medroxyprogesterone acetate or etonogestrel implant); or intrauterine (which does not lower estrogen levels but can be therapeutic for suppression of menses and local treatment of endometriosis). Failure of hormonal therapy and management of other co-occurring pain conditions warrants trial of a second-line medical therapy such as gonadotropin-releasing hormone antagonist or agonist or surgery for definitive diagnosis and surgical ablation or excision of endometriosis lesions.
I would suggest that gynecologists who treat women with endometriosis and chronic pain try to build a team in their geographic area. Relevant specialists for an interdisciplinary approach include:
- Pelvic floor physical therapist to evaluate and address myofascial dysfunction and pain and voiding abnormalities, such as urinary urgency or frequency and constipation
- Gastroenterologist for evaluation and treatment of irritable bowel or functional abdominal pain and bloating syndrome or inflammatory bowel disease. Urologist or urogynecologist to assess and treat bladder pain syndrome/interstitial cystitis
- Primary care evaluation for diffuse myofascial pain, fibromyalgia, arthralgias, and other inflammatory conditions, and for management of headache and migraine. Rheumatology and neurology specialists may be needed
- Mental health providers for treatment of anxiety, depression, or PTSD and to address stress management, coping skills and provide cognitive behavioral therapy
- Interventional pain management specialist such as physical medicine and rehabilitation (PM and R), pain anesthiologist, neurologist or interventional radiologist to provide relevant nerve blocks, trigger point injections, or botulinum toxin injection.
- Gynecologists experienced in the management of chronic pelvic pain also provide nerve blocks, trigger point and botulinum toxin injections.
Step-wise medical therapy is cost effective for endometriosis
For patients with endometriosis-related dysmenorrhea, it is cost effective to use medical therapy before surgery, according to investigators.
A stepwise strategy involving two medications, then surgery, was associated with the lowest cost per quality-adjusted life-years (QALYs), reported lead author, Jacqueline A. Bohn, MD, of Oregon Health & Science University, Portland, and colleagues.
“In 2009, the medical costs associated with endometriosis in the United States were estimated at $69.4 billion annually,” the investigators wrote in Obstetrics and Gynecology. “Despite the recognized cost burden of this disease, cost-effectiveness data on the various treatment strategies is limited. Previous studies have investigated the direct and indirect costs regarding endometriosis; however, there are no prior studies that evaluate the cost-effectiveness of a stepwise regimen to guide management.”
To fill this knowledge gap, Dr. Bohn and colleagues created a cost-effectiveness model comparing four treatment strategies:
NSAIDs, then surgery
NSAIDs, then short-acting reversible contraceptives or long-acting reversible contraceptives (LARCs), then surgery
NSAIDs, then a short-acting reversible contraceptive or a LARC, then a LARC or gonadotropin-releasing hormone (GnRH) modulator, then surgery
Surgery alone
The analysis, which compared costs, QALYs, and incremental cost-effectiveness ratios, involved a theoretical cohort of 4,817,894 women aged 18-45 years, representing the estimated number of reproductive-age women in the United States with endometriosis-related dysmenorrhea. Costs were determined from published literature and inflated to 2019 dollars. Medical treatments were theoretically given for 6 months each, and the cost of laparoscopic surgery incorporated 12 months of postoperative care.
Of the four strategies, the two-medication approach was most cost effective, with a cost per QALY of $1,158. This was followed closely by the three-medication regimen, at $1,158, the single-medication regimen, at $2,108, and finally, surgery alone, at $4,338.
“We found that, although cost effective, requiring trial of a third medication offered little comparative advantage before proceeding directly to surgery after the second therapy fails,” the investigators wrote. “Yet, for the woman who is anxious about surgical intervention, or when a prolonged wait for a surgical specialist occurs, trial of a GnRH modulator may be worthwhile.”
Compared with surgery alone, each regimen starting with medical therapy remained below the standard willingness-to-pay threshold of $100,000 per QALY; however, the investigators recommend against trying more than three medications.
“Delaying surgical management in a woman with pain refractory to more than three medications may decrease quality of life and further increase cost,” they wrote.
To make surgery alone the most cost-effective option, surgery success would need to exceed 83%, Dr. Bohn and colleagues concluded.
According to Hugh Taylor, MD, of Yale University, New Haven, Conn., it’s unlikely that this surgery success threshold will be met, since surgery alone typically leads to recurrence.
“We know there’s a very high relapse rate after surgery,” Dr. Taylor said in an interview. “Even if the surgery may be initially successful, there’s roughly a 50% recurrence rate after about 2 years. So, finding the right medical therapy will give you more chance for long-term success.”
Dr. Taylor said it’s “really nice” that Dr. Bohn and colleagues conducted a sequential analysis because the findings support the most common approach in real-world practice.
“It confirms that starting with a medical therapy prior to surgery is an appropriate, successful treatment for endometriosis, which is something that many, many people in the community do, but we haven’t had a real trial to show that,” he said.
Dr. Taylor offered two areas of improvement for similar studies in the future: First, he suggested separating LARCs from oral contraceptives because LARCs may be less effective for some patients with endometriosis; and second, he suggested that limiting the third medication to a GnRH antagonist would be more applicable to real-world practice than using the broader category of GnRH modulators.
Although the three-medication approach involving a GnRH modulator was slightly more expensive than the two-medication approach, Dr. Taylor said the costs were so similar that a three-medication approach is “still reasonable,” particularly because it could spare patients from surgery.
Dr. Taylor also speculated that trying a GnRH antagonist could become more cost effective soon. Although only one GnRH antagonist is currently on the market, he noted that a second agent is poised for Food and Drug Administration approval, while a third is in the pipeline, and this competition may decrease drug prices.
The investigators disclosed support from the National Institutes of Health, Arnold Ventures, the World Health Organization, Merck, and others. Dr. Taylor reported that Yale University receives funding for endometriosis biomarker research from AbbVie.
For patients with endometriosis-related dysmenorrhea, it is cost effective to use medical therapy before surgery, according to investigators.
A stepwise strategy involving two medications, then surgery, was associated with the lowest cost per quality-adjusted life-years (QALYs), reported lead author, Jacqueline A. Bohn, MD, of Oregon Health & Science University, Portland, and colleagues.
“In 2009, the medical costs associated with endometriosis in the United States were estimated at $69.4 billion annually,” the investigators wrote in Obstetrics and Gynecology. “Despite the recognized cost burden of this disease, cost-effectiveness data on the various treatment strategies is limited. Previous studies have investigated the direct and indirect costs regarding endometriosis; however, there are no prior studies that evaluate the cost-effectiveness of a stepwise regimen to guide management.”
To fill this knowledge gap, Dr. Bohn and colleagues created a cost-effectiveness model comparing four treatment strategies:
NSAIDs, then surgery
NSAIDs, then short-acting reversible contraceptives or long-acting reversible contraceptives (LARCs), then surgery
NSAIDs, then a short-acting reversible contraceptive or a LARC, then a LARC or gonadotropin-releasing hormone (GnRH) modulator, then surgery
Surgery alone
The analysis, which compared costs, QALYs, and incremental cost-effectiveness ratios, involved a theoretical cohort of 4,817,894 women aged 18-45 years, representing the estimated number of reproductive-age women in the United States with endometriosis-related dysmenorrhea. Costs were determined from published literature and inflated to 2019 dollars. Medical treatments were theoretically given for 6 months each, and the cost of laparoscopic surgery incorporated 12 months of postoperative care.
Of the four strategies, the two-medication approach was most cost effective, with a cost per QALY of $1,158. This was followed closely by the three-medication regimen, at $1,158, the single-medication regimen, at $2,108, and finally, surgery alone, at $4,338.
“We found that, although cost effective, requiring trial of a third medication offered little comparative advantage before proceeding directly to surgery after the second therapy fails,” the investigators wrote. “Yet, for the woman who is anxious about surgical intervention, or when a prolonged wait for a surgical specialist occurs, trial of a GnRH modulator may be worthwhile.”
Compared with surgery alone, each regimen starting with medical therapy remained below the standard willingness-to-pay threshold of $100,000 per QALY; however, the investigators recommend against trying more than three medications.
“Delaying surgical management in a woman with pain refractory to more than three medications may decrease quality of life and further increase cost,” they wrote.
To make surgery alone the most cost-effective option, surgery success would need to exceed 83%, Dr. Bohn and colleagues concluded.
According to Hugh Taylor, MD, of Yale University, New Haven, Conn., it’s unlikely that this surgery success threshold will be met, since surgery alone typically leads to recurrence.
“We know there’s a very high relapse rate after surgery,” Dr. Taylor said in an interview. “Even if the surgery may be initially successful, there’s roughly a 50% recurrence rate after about 2 years. So, finding the right medical therapy will give you more chance for long-term success.”
Dr. Taylor said it’s “really nice” that Dr. Bohn and colleagues conducted a sequential analysis because the findings support the most common approach in real-world practice.
“It confirms that starting with a medical therapy prior to surgery is an appropriate, successful treatment for endometriosis, which is something that many, many people in the community do, but we haven’t had a real trial to show that,” he said.
Dr. Taylor offered two areas of improvement for similar studies in the future: First, he suggested separating LARCs from oral contraceptives because LARCs may be less effective for some patients with endometriosis; and second, he suggested that limiting the third medication to a GnRH antagonist would be more applicable to real-world practice than using the broader category of GnRH modulators.
Although the three-medication approach involving a GnRH modulator was slightly more expensive than the two-medication approach, Dr. Taylor said the costs were so similar that a three-medication approach is “still reasonable,” particularly because it could spare patients from surgery.
Dr. Taylor also speculated that trying a GnRH antagonist could become more cost effective soon. Although only one GnRH antagonist is currently on the market, he noted that a second agent is poised for Food and Drug Administration approval, while a third is in the pipeline, and this competition may decrease drug prices.
The investigators disclosed support from the National Institutes of Health, Arnold Ventures, the World Health Organization, Merck, and others. Dr. Taylor reported that Yale University receives funding for endometriosis biomarker research from AbbVie.
For patients with endometriosis-related dysmenorrhea, it is cost effective to use medical therapy before surgery, according to investigators.
A stepwise strategy involving two medications, then surgery, was associated with the lowest cost per quality-adjusted life-years (QALYs), reported lead author, Jacqueline A. Bohn, MD, of Oregon Health & Science University, Portland, and colleagues.
“In 2009, the medical costs associated with endometriosis in the United States were estimated at $69.4 billion annually,” the investigators wrote in Obstetrics and Gynecology. “Despite the recognized cost burden of this disease, cost-effectiveness data on the various treatment strategies is limited. Previous studies have investigated the direct and indirect costs regarding endometriosis; however, there are no prior studies that evaluate the cost-effectiveness of a stepwise regimen to guide management.”
To fill this knowledge gap, Dr. Bohn and colleagues created a cost-effectiveness model comparing four treatment strategies:
NSAIDs, then surgery
NSAIDs, then short-acting reversible contraceptives or long-acting reversible contraceptives (LARCs), then surgery
NSAIDs, then a short-acting reversible contraceptive or a LARC, then a LARC or gonadotropin-releasing hormone (GnRH) modulator, then surgery
Surgery alone
The analysis, which compared costs, QALYs, and incremental cost-effectiveness ratios, involved a theoretical cohort of 4,817,894 women aged 18-45 years, representing the estimated number of reproductive-age women in the United States with endometriosis-related dysmenorrhea. Costs were determined from published literature and inflated to 2019 dollars. Medical treatments were theoretically given for 6 months each, and the cost of laparoscopic surgery incorporated 12 months of postoperative care.
Of the four strategies, the two-medication approach was most cost effective, with a cost per QALY of $1,158. This was followed closely by the three-medication regimen, at $1,158, the single-medication regimen, at $2,108, and finally, surgery alone, at $4,338.
“We found that, although cost effective, requiring trial of a third medication offered little comparative advantage before proceeding directly to surgery after the second therapy fails,” the investigators wrote. “Yet, for the woman who is anxious about surgical intervention, or when a prolonged wait for a surgical specialist occurs, trial of a GnRH modulator may be worthwhile.”
Compared with surgery alone, each regimen starting with medical therapy remained below the standard willingness-to-pay threshold of $100,000 per QALY; however, the investigators recommend against trying more than three medications.
“Delaying surgical management in a woman with pain refractory to more than three medications may decrease quality of life and further increase cost,” they wrote.
To make surgery alone the most cost-effective option, surgery success would need to exceed 83%, Dr. Bohn and colleagues concluded.
According to Hugh Taylor, MD, of Yale University, New Haven, Conn., it’s unlikely that this surgery success threshold will be met, since surgery alone typically leads to recurrence.
“We know there’s a very high relapse rate after surgery,” Dr. Taylor said in an interview. “Even if the surgery may be initially successful, there’s roughly a 50% recurrence rate after about 2 years. So, finding the right medical therapy will give you more chance for long-term success.”
Dr. Taylor said it’s “really nice” that Dr. Bohn and colleagues conducted a sequential analysis because the findings support the most common approach in real-world practice.
“It confirms that starting with a medical therapy prior to surgery is an appropriate, successful treatment for endometriosis, which is something that many, many people in the community do, but we haven’t had a real trial to show that,” he said.
Dr. Taylor offered two areas of improvement for similar studies in the future: First, he suggested separating LARCs from oral contraceptives because LARCs may be less effective for some patients with endometriosis; and second, he suggested that limiting the third medication to a GnRH antagonist would be more applicable to real-world practice than using the broader category of GnRH modulators.
Although the three-medication approach involving a GnRH modulator was slightly more expensive than the two-medication approach, Dr. Taylor said the costs were so similar that a three-medication approach is “still reasonable,” particularly because it could spare patients from surgery.
Dr. Taylor also speculated that trying a GnRH antagonist could become more cost effective soon. Although only one GnRH antagonist is currently on the market, he noted that a second agent is poised for Food and Drug Administration approval, while a third is in the pipeline, and this competition may decrease drug prices.
The investigators disclosed support from the National Institutes of Health, Arnold Ventures, the World Health Organization, Merck, and others. Dr. Taylor reported that Yale University receives funding for endometriosis biomarker research from AbbVie.
FROM OBSTETRICS & GYNECOLOGY
Sacral nerve root endometriosis

Additional videos from SGS are available here, including these recent offerings:

Additional videos from SGS are available here, including these recent offerings:

Additional videos from SGS are available here, including these recent offerings:
3 cases of hormone therapy optimized to match the patient problem
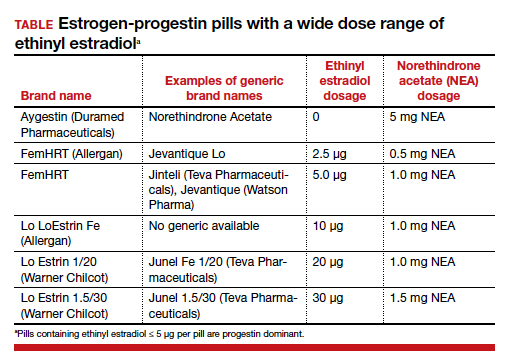
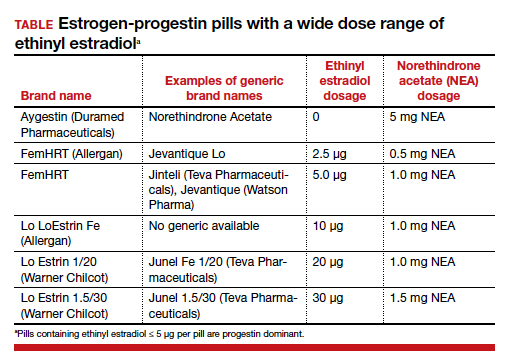
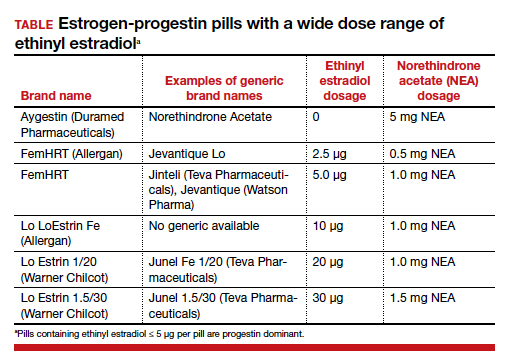
There are dozens of medications containing combinations of estrogen and progestin. I am often confused by the bewildering proliferation of generic brand names used to describe the same estrogen-progestin (E-P) regimen. For example, the combination medication containing ethinyl estradiol 20 µg plus norethindrone acetate (NEA) 1 mg is available under at least 5 different names: Lo Estrin 1/20 (Warner Chilcot), Junel 1/20 (Teva Pharmaceuticals), Microgestin Fe 1/20 (Mayne Pharma), Gildess 1/20 (Qualitest Pharmaceuticals), and Larin 1/20 (Novast Laboratories). To reduce the confusion, it is often useful to select a single preferred estrogen and progestin and use the dose combinations that are available to treat a wide range of gynecology problems (TABLE). In this editorial I focus on using various dose combinations of ethinyl estradiol and NEA to treat 3 common gynecologic problems.
CASE 1 Polycystic ovary syndrome
A 19-year-old woman reports 4 spontaneous menses in the past year and bothersome facial hair and acne. Her total testosterone concentration is at the upper limit of normal (0.46 ng/mL) and her sex hormone binding globulin (SHBG) concentration is at the lower limit of normal (35 nM). For treatment of the patient’s menstrual disorder, what is an optimal E-P combination?
Prioritize the use of an estrogen-dominant medication
Based on the Rotterdam criteria this woman has polycystic ovary syndrome (PCOS).1 In women with PCOS, luteinizing hormone (LH) secretion is increased, stimulating excessive ovarian production of testosterone.2 In addition, many women with PCOS have decreased hepatic secretion of SHBG, a binding protein that prevents testosterone from entering cells, resulting in excessive bioavailable testosterone.3 The Endocrine Society recommends that women with PCOS who have menstrual dysfunction or hirsutism be treated initially with a combination E-P hormone medication.1 Combination E-P medications suppress pituitary secretion of LH, thereby reducing ovarian production of testosterone, and ethinyl estradiol increases hepatic secretion of SHBG, reducing bioavailable testosterone. These two goals are best accomplished with an oral E-P hormone medication containing ethinyl estradiol doses of 20 µg to 30 µg per pill. An E-P hormone medication containing pills with an ethinyl estradiol dose ≤ 10 µg-daily may stimulate less hepatic production of SHBG than a pill with an ethinyl estradiol dose of 20 µg or 30 µg daily.4,5 In addition, E-P pills containing levonorgestrel suppress SHBG hormone secretion compared with E-P pills with other progestins.6 Therefore, levonorgestrel-containing E-P pills should not be prioritized for use in women with PCOS because the estrogen-induced increase in SHBG will be blunted by levonorgestrel.
CASE 2 Moderate to severe pelvic pain caused by endometriosis
A 25-year-old woman (G0) with severe dysmenorrhea had a laparoscopy showing endometriosis lesions in the cul-de-sac and a peritoneal window near the left uterosacral ligament. Biopsy showed endometriosis. Postoperatively, the patient was treated with an E-P pill containing 30 µg ethinyl estradiol and 0.15 mg desogestrel per pill using a continuous-dosing protocol. During the year following the laparoscopy, her pelvic pain symptoms gradually increased until they became severe, preventing her from performing daily activities on multiple days per month. She was prescribed elagolix but her insurance did not approve the treatment. What alternative treatment would you prescribe?
Continue to: Use progestin-dominant pills to treat pelvic pain...
Use progestin-dominant pills to treat pelvic pain
Cellular activity in endometriosis lesions is stimulated by estradiol and inhibited by a high concentration of androgenic progestins or androgens. This simplified endocrine paradigm explains the effectiveness of hormonal treatments that suppress ovarian estradiol production, including leuprolide, elagolix, medroxyprogesterone acetate, and NEA. For the woman in the above case, I would advocate for elagolix treatment but, following the insurance denial of the prescription, an alternative treatment for moderate or severe pelvic pain caused by endometriosis would be a progestin-dominant hormone medication (for example, NEA 5 mg daily). Norethindrone acetate 5 mg daily may be associated with bothersome adverse effects including weight gain (16% of patients; mean weight gain, 3.1 kg), acne (10%), mood lability (9%), hot flashes (8%), depression (6%), scalp hair loss (4%), headache (4%), nausea (3%), and deepening of the voice (1%).7
I sometimes see women with moderate to severe pelvic pain caused by endometriosis being treated with norethindrone 0.35 mg daily. This dose of norethindrone is suboptimal for pain treatment because it does not reliably suppress ovarian production of estradiol. In addition, the cells in endometriosis lesions are often resistant to the effects of progesterone, requiring higher dosages to produce secretory or decidual changes. In most situations, I recommend against the use of norethindrone 0.35 mg daily for the treatment of pelvic pain caused by endometriosis.
Patients commonly ask if NEA 5 mg daily has contraceptive efficacy. Although it is not approved at this dosage by the US Food and Drug Administration as a contraceptive,8 norethindrone 0.35 mg daily is approved as a progestin-only contraceptive.9 Norethindrone acetate is rapidly and completely deacetylated to norethindrone and the disposition of oral NEA is indistinguishable from that of norethindrone (which is the FDA-approved dosage mentioned above). Since norethindrone 0.35 mg daily is approved as a contraceptive, it is highly likely that NEA 5 mg daily has contraceptive efficacy, especially if there is good adherence with the daily medication.
CASE 3 Perimenopausal AUB
A 45-year-old woman reports varying menstrual cycle lengths from 24 to 60 days with very heavy menses in some cycles. Pelvic ultrasonography shows no abnormality. Endometrial biopsy shows a proliferative endometrium. Her serum progesterone level, obtained 1 week before the onset of menses, is < 3 ng/mL. She has no past history of heavy menses, easy bruising, excessive bleeding with procedures, or a family history of bleeding problems. She also reports occasional hot flashes that wake her from sleep.
Use an estrogen step-down regimen to manage postmenopause transition
This patient is likely in the perimenopause transition, and the abnormal uterine bleeding (AUB) is caused, in part, by oligo- or anovulation. Perimenopausal women with AUB may have cycles characterized by above normal ovarian estradiol production and below normal progesterone production, or frank anovulation.10 Elevated ovarian estrogen and low progesterone production sets the stage for heavy bleeding in the perimenopause, regardless of the presence of uterine pathology such as fibroids.
For perimenopausal women, one option for treatment of AUB due to anovulation is to prescribe an estrogen step-down regimen. For the 45-year-old woman in this case, initiating treatment with an E-P pill containing ethinyl estradiol 10 µg and NEA 1 mg will likely control the AUB and her occasional hot flash.11 As the woman ages, the ethinyl estradiol dose can be decreased to pills containing 5 µg and then 2.5 µg, covering the transition into postmenopause. Once the woman is in the postmenopause, treatment with transdermal estradiol and oral micronized progesterone is an option to treat menopausal vasomotor symptoms.
Optimize estrogen and progestin treatment for your patients
Many gynecologic problems are effectively treated by estrogen and/or progestin steroids. The dose of estrogen and progestin should be tailored to the specific problem. For PCOS, the estrogen dose selected should be sufficient to safely stimulate hepatic SHBG production. For endometriosis, if a GnRH antagonist is not available to the patient, a high-dose progestin, such as NEA 5 mg, may be an effective treatment. During the perimenopause transition in a woman with AUB, a treatment plan using a sequential E-P step-down program might control symptoms and help smoothly glide the patient into the postmenopause. ●
- Legro RS, Arslanian SA, Ehrmann DA, et al. Diagnosis and treatment of polycystic ovary syndrome: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2013;98:4565-4592. doi: 10.1210/jc.2013-2350.
- Rosenfield RL, Ehrmann DA. The pathogenesis of polycystic ovary syndrome (PCOS): the hypothesis of PCOS as functional ovarian hyperandrogenism revisited. Endocr Rev. 2016;37:467-520. doi: 10.1210/er.2015-1104.
- Zhu JL, Chen Z, Feng WJ, et al. Sex hormone-binding globulin and polycystic ovary syndrome. Clin Chim Acta. 2019;499:142-148. doi: 10.1016/j.cca.2019.09.010.
- Oner G, Muderris II. A prospective randomized trial comparing low-dose ethinyl estradiol and drospirenone 24/4 combined oral contraceptive vs. ethinyl estradiol and drospirenone 21/7 combined oral contraceptive in the treatment of hirsutism. Contraception. 2011;84:508-511. doi: 10.1016/j.contraception.2011.03.002.
- Boyd RA, Zegarac EA, Posvar EL, et al. Minimal androgenic activity of a new oral contraceptive containing norethindrone acetate and graduated doses of ethinyl estradiol. Contraception. 2001;63:71-76. doi: 10.1016/s0010-7824(01)00179-2.
- Thorneycroft IH, Stanczyk FZ, Bradshaw KD, et al. Effect of low-dose oral contraceptives on androgenic markers and acne. Contraception. 1999;60:255-262. doi: 10.1016/s0010-7824(99)00093-1.
- Kaser DJ, Missmer SA, Berry KF, et al. Use of norethindrone acetate alone for postoperative suppression of endometriosis symptoms. J Pediatr Adolesc Gynecol. 2012;25:105-108. doi: 10.1016/j.jpag.2011.09.013.
- Aygestin [package insert]. Pomona, NY: Duramed Pharmaceuticals; 2007.
- Camila [package insert]. Greenville, NC; Mayne Pharma; 2018.
- Santoro N, Brown JR, Adel T, et al. Characterization of reproductive hormonal dynamics in the perimenopause. J Clin Endocrinol Metab. 1996;81:1495-1501. doi: 10.1210/jcem.81.4.8636357.
- Speroff L, Symons J, Kempfert N, et al; FemHrt Study Investigators. The effect of varying low-dose combinations of norethindrone acetate and ethinyl estradiol (Femhrt) on the frequency and intensity of vasomotor symptoms. Menopause. 2000;7:383-390. doi: 10.1097/00042192-200011000-00003.
There are dozens of medications containing combinations of estrogen and progestin. I am often confused by the bewildering proliferation of generic brand names used to describe the same estrogen-progestin (E-P) regimen. For example, the combination medication containing ethinyl estradiol 20 µg plus norethindrone acetate (NEA) 1 mg is available under at least 5 different names: Lo Estrin 1/20 (Warner Chilcot), Junel 1/20 (Teva Pharmaceuticals), Microgestin Fe 1/20 (Mayne Pharma), Gildess 1/20 (Qualitest Pharmaceuticals), and Larin 1/20 (Novast Laboratories). To reduce the confusion, it is often useful to select a single preferred estrogen and progestin and use the dose combinations that are available to treat a wide range of gynecology problems (TABLE). In this editorial I focus on using various dose combinations of ethinyl estradiol and NEA to treat 3 common gynecologic problems.
CASE 1 Polycystic ovary syndrome
A 19-year-old woman reports 4 spontaneous menses in the past year and bothersome facial hair and acne. Her total testosterone concentration is at the upper limit of normal (0.46 ng/mL) and her sex hormone binding globulin (SHBG) concentration is at the lower limit of normal (35 nM). For treatment of the patient’s menstrual disorder, what is an optimal E-P combination?
Prioritize the use of an estrogen-dominant medication
Based on the Rotterdam criteria this woman has polycystic ovary syndrome (PCOS).1 In women with PCOS, luteinizing hormone (LH) secretion is increased, stimulating excessive ovarian production of testosterone.2 In addition, many women with PCOS have decreased hepatic secretion of SHBG, a binding protein that prevents testosterone from entering cells, resulting in excessive bioavailable testosterone.3 The Endocrine Society recommends that women with PCOS who have menstrual dysfunction or hirsutism be treated initially with a combination E-P hormone medication.1 Combination E-P medications suppress pituitary secretion of LH, thereby reducing ovarian production of testosterone, and ethinyl estradiol increases hepatic secretion of SHBG, reducing bioavailable testosterone. These two goals are best accomplished with an oral E-P hormone medication containing ethinyl estradiol doses of 20 µg to 30 µg per pill. An E-P hormone medication containing pills with an ethinyl estradiol dose ≤ 10 µg-daily may stimulate less hepatic production of SHBG than a pill with an ethinyl estradiol dose of 20 µg or 30 µg daily.4,5 In addition, E-P pills containing levonorgestrel suppress SHBG hormone secretion compared with E-P pills with other progestins.6 Therefore, levonorgestrel-containing E-P pills should not be prioritized for use in women with PCOS because the estrogen-induced increase in SHBG will be blunted by levonorgestrel.
CASE 2 Moderate to severe pelvic pain caused by endometriosis
A 25-year-old woman (G0) with severe dysmenorrhea had a laparoscopy showing endometriosis lesions in the cul-de-sac and a peritoneal window near the left uterosacral ligament. Biopsy showed endometriosis. Postoperatively, the patient was treated with an E-P pill containing 30 µg ethinyl estradiol and 0.15 mg desogestrel per pill using a continuous-dosing protocol. During the year following the laparoscopy, her pelvic pain symptoms gradually increased until they became severe, preventing her from performing daily activities on multiple days per month. She was prescribed elagolix but her insurance did not approve the treatment. What alternative treatment would you prescribe?
Continue to: Use progestin-dominant pills to treat pelvic pain...
Use progestin-dominant pills to treat pelvic pain
Cellular activity in endometriosis lesions is stimulated by estradiol and inhibited by a high concentration of androgenic progestins or androgens. This simplified endocrine paradigm explains the effectiveness of hormonal treatments that suppress ovarian estradiol production, including leuprolide, elagolix, medroxyprogesterone acetate, and NEA. For the woman in the above case, I would advocate for elagolix treatment but, following the insurance denial of the prescription, an alternative treatment for moderate or severe pelvic pain caused by endometriosis would be a progestin-dominant hormone medication (for example, NEA 5 mg daily). Norethindrone acetate 5 mg daily may be associated with bothersome adverse effects including weight gain (16% of patients; mean weight gain, 3.1 kg), acne (10%), mood lability (9%), hot flashes (8%), depression (6%), scalp hair loss (4%), headache (4%), nausea (3%), and deepening of the voice (1%).7
I sometimes see women with moderate to severe pelvic pain caused by endometriosis being treated with norethindrone 0.35 mg daily. This dose of norethindrone is suboptimal for pain treatment because it does not reliably suppress ovarian production of estradiol. In addition, the cells in endometriosis lesions are often resistant to the effects of progesterone, requiring higher dosages to produce secretory or decidual changes. In most situations, I recommend against the use of norethindrone 0.35 mg daily for the treatment of pelvic pain caused by endometriosis.
Patients commonly ask if NEA 5 mg daily has contraceptive efficacy. Although it is not approved at this dosage by the US Food and Drug Administration as a contraceptive,8 norethindrone 0.35 mg daily is approved as a progestin-only contraceptive.9 Norethindrone acetate is rapidly and completely deacetylated to norethindrone and the disposition of oral NEA is indistinguishable from that of norethindrone (which is the FDA-approved dosage mentioned above). Since norethindrone 0.35 mg daily is approved as a contraceptive, it is highly likely that NEA 5 mg daily has contraceptive efficacy, especially if there is good adherence with the daily medication.
CASE 3 Perimenopausal AUB
A 45-year-old woman reports varying menstrual cycle lengths from 24 to 60 days with very heavy menses in some cycles. Pelvic ultrasonography shows no abnormality. Endometrial biopsy shows a proliferative endometrium. Her serum progesterone level, obtained 1 week before the onset of menses, is < 3 ng/mL. She has no past history of heavy menses, easy bruising, excessive bleeding with procedures, or a family history of bleeding problems. She also reports occasional hot flashes that wake her from sleep.
Use an estrogen step-down regimen to manage postmenopause transition
This patient is likely in the perimenopause transition, and the abnormal uterine bleeding (AUB) is caused, in part, by oligo- or anovulation. Perimenopausal women with AUB may have cycles characterized by above normal ovarian estradiol production and below normal progesterone production, or frank anovulation.10 Elevated ovarian estrogen and low progesterone production sets the stage for heavy bleeding in the perimenopause, regardless of the presence of uterine pathology such as fibroids.
For perimenopausal women, one option for treatment of AUB due to anovulation is to prescribe an estrogen step-down regimen. For the 45-year-old woman in this case, initiating treatment with an E-P pill containing ethinyl estradiol 10 µg and NEA 1 mg will likely control the AUB and her occasional hot flash.11 As the woman ages, the ethinyl estradiol dose can be decreased to pills containing 5 µg and then 2.5 µg, covering the transition into postmenopause. Once the woman is in the postmenopause, treatment with transdermal estradiol and oral micronized progesterone is an option to treat menopausal vasomotor symptoms.
Optimize estrogen and progestin treatment for your patients
Many gynecologic problems are effectively treated by estrogen and/or progestin steroids. The dose of estrogen and progestin should be tailored to the specific problem. For PCOS, the estrogen dose selected should be sufficient to safely stimulate hepatic SHBG production. For endometriosis, if a GnRH antagonist is not available to the patient, a high-dose progestin, such as NEA 5 mg, may be an effective treatment. During the perimenopause transition in a woman with AUB, a treatment plan using a sequential E-P step-down program might control symptoms and help smoothly glide the patient into the postmenopause. ●
There are dozens of medications containing combinations of estrogen and progestin. I am often confused by the bewildering proliferation of generic brand names used to describe the same estrogen-progestin (E-P) regimen. For example, the combination medication containing ethinyl estradiol 20 µg plus norethindrone acetate (NEA) 1 mg is available under at least 5 different names: Lo Estrin 1/20 (Warner Chilcot), Junel 1/20 (Teva Pharmaceuticals), Microgestin Fe 1/20 (Mayne Pharma), Gildess 1/20 (Qualitest Pharmaceuticals), and Larin 1/20 (Novast Laboratories). To reduce the confusion, it is often useful to select a single preferred estrogen and progestin and use the dose combinations that are available to treat a wide range of gynecology problems (TABLE). In this editorial I focus on using various dose combinations of ethinyl estradiol and NEA to treat 3 common gynecologic problems.
CASE 1 Polycystic ovary syndrome
A 19-year-old woman reports 4 spontaneous menses in the past year and bothersome facial hair and acne. Her total testosterone concentration is at the upper limit of normal (0.46 ng/mL) and her sex hormone binding globulin (SHBG) concentration is at the lower limit of normal (35 nM). For treatment of the patient’s menstrual disorder, what is an optimal E-P combination?
Prioritize the use of an estrogen-dominant medication
Based on the Rotterdam criteria this woman has polycystic ovary syndrome (PCOS).1 In women with PCOS, luteinizing hormone (LH) secretion is increased, stimulating excessive ovarian production of testosterone.2 In addition, many women with PCOS have decreased hepatic secretion of SHBG, a binding protein that prevents testosterone from entering cells, resulting in excessive bioavailable testosterone.3 The Endocrine Society recommends that women with PCOS who have menstrual dysfunction or hirsutism be treated initially with a combination E-P hormone medication.1 Combination E-P medications suppress pituitary secretion of LH, thereby reducing ovarian production of testosterone, and ethinyl estradiol increases hepatic secretion of SHBG, reducing bioavailable testosterone. These two goals are best accomplished with an oral E-P hormone medication containing ethinyl estradiol doses of 20 µg to 30 µg per pill. An E-P hormone medication containing pills with an ethinyl estradiol dose ≤ 10 µg-daily may stimulate less hepatic production of SHBG than a pill with an ethinyl estradiol dose of 20 µg or 30 µg daily.4,5 In addition, E-P pills containing levonorgestrel suppress SHBG hormone secretion compared with E-P pills with other progestins.6 Therefore, levonorgestrel-containing E-P pills should not be prioritized for use in women with PCOS because the estrogen-induced increase in SHBG will be blunted by levonorgestrel.
CASE 2 Moderate to severe pelvic pain caused by endometriosis
A 25-year-old woman (G0) with severe dysmenorrhea had a laparoscopy showing endometriosis lesions in the cul-de-sac and a peritoneal window near the left uterosacral ligament. Biopsy showed endometriosis. Postoperatively, the patient was treated with an E-P pill containing 30 µg ethinyl estradiol and 0.15 mg desogestrel per pill using a continuous-dosing protocol. During the year following the laparoscopy, her pelvic pain symptoms gradually increased until they became severe, preventing her from performing daily activities on multiple days per month. She was prescribed elagolix but her insurance did not approve the treatment. What alternative treatment would you prescribe?
Continue to: Use progestin-dominant pills to treat pelvic pain...
Use progestin-dominant pills to treat pelvic pain
Cellular activity in endometriosis lesions is stimulated by estradiol and inhibited by a high concentration of androgenic progestins or androgens. This simplified endocrine paradigm explains the effectiveness of hormonal treatments that suppress ovarian estradiol production, including leuprolide, elagolix, medroxyprogesterone acetate, and NEA. For the woman in the above case, I would advocate for elagolix treatment but, following the insurance denial of the prescription, an alternative treatment for moderate or severe pelvic pain caused by endometriosis would be a progestin-dominant hormone medication (for example, NEA 5 mg daily). Norethindrone acetate 5 mg daily may be associated with bothersome adverse effects including weight gain (16% of patients; mean weight gain, 3.1 kg), acne (10%), mood lability (9%), hot flashes (8%), depression (6%), scalp hair loss (4%), headache (4%), nausea (3%), and deepening of the voice (1%).7
I sometimes see women with moderate to severe pelvic pain caused by endometriosis being treated with norethindrone 0.35 mg daily. This dose of norethindrone is suboptimal for pain treatment because it does not reliably suppress ovarian production of estradiol. In addition, the cells in endometriosis lesions are often resistant to the effects of progesterone, requiring higher dosages to produce secretory or decidual changes. In most situations, I recommend against the use of norethindrone 0.35 mg daily for the treatment of pelvic pain caused by endometriosis.
Patients commonly ask if NEA 5 mg daily has contraceptive efficacy. Although it is not approved at this dosage by the US Food and Drug Administration as a contraceptive,8 norethindrone 0.35 mg daily is approved as a progestin-only contraceptive.9 Norethindrone acetate is rapidly and completely deacetylated to norethindrone and the disposition of oral NEA is indistinguishable from that of norethindrone (which is the FDA-approved dosage mentioned above). Since norethindrone 0.35 mg daily is approved as a contraceptive, it is highly likely that NEA 5 mg daily has contraceptive efficacy, especially if there is good adherence with the daily medication.
CASE 3 Perimenopausal AUB
A 45-year-old woman reports varying menstrual cycle lengths from 24 to 60 days with very heavy menses in some cycles. Pelvic ultrasonography shows no abnormality. Endometrial biopsy shows a proliferative endometrium. Her serum progesterone level, obtained 1 week before the onset of menses, is < 3 ng/mL. She has no past history of heavy menses, easy bruising, excessive bleeding with procedures, or a family history of bleeding problems. She also reports occasional hot flashes that wake her from sleep.
Use an estrogen step-down regimen to manage postmenopause transition
This patient is likely in the perimenopause transition, and the abnormal uterine bleeding (AUB) is caused, in part, by oligo- or anovulation. Perimenopausal women with AUB may have cycles characterized by above normal ovarian estradiol production and below normal progesterone production, or frank anovulation.10 Elevated ovarian estrogen and low progesterone production sets the stage for heavy bleeding in the perimenopause, regardless of the presence of uterine pathology such as fibroids.
For perimenopausal women, one option for treatment of AUB due to anovulation is to prescribe an estrogen step-down regimen. For the 45-year-old woman in this case, initiating treatment with an E-P pill containing ethinyl estradiol 10 µg and NEA 1 mg will likely control the AUB and her occasional hot flash.11 As the woman ages, the ethinyl estradiol dose can be decreased to pills containing 5 µg and then 2.5 µg, covering the transition into postmenopause. Once the woman is in the postmenopause, treatment with transdermal estradiol and oral micronized progesterone is an option to treat menopausal vasomotor symptoms.
Optimize estrogen and progestin treatment for your patients
Many gynecologic problems are effectively treated by estrogen and/or progestin steroids. The dose of estrogen and progestin should be tailored to the specific problem. For PCOS, the estrogen dose selected should be sufficient to safely stimulate hepatic SHBG production. For endometriosis, if a GnRH antagonist is not available to the patient, a high-dose progestin, such as NEA 5 mg, may be an effective treatment. During the perimenopause transition in a woman with AUB, a treatment plan using a sequential E-P step-down program might control symptoms and help smoothly glide the patient into the postmenopause. ●
- Legro RS, Arslanian SA, Ehrmann DA, et al. Diagnosis and treatment of polycystic ovary syndrome: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2013;98:4565-4592. doi: 10.1210/jc.2013-2350.
- Rosenfield RL, Ehrmann DA. The pathogenesis of polycystic ovary syndrome (PCOS): the hypothesis of PCOS as functional ovarian hyperandrogenism revisited. Endocr Rev. 2016;37:467-520. doi: 10.1210/er.2015-1104.
- Zhu JL, Chen Z, Feng WJ, et al. Sex hormone-binding globulin and polycystic ovary syndrome. Clin Chim Acta. 2019;499:142-148. doi: 10.1016/j.cca.2019.09.010.
- Oner G, Muderris II. A prospective randomized trial comparing low-dose ethinyl estradiol and drospirenone 24/4 combined oral contraceptive vs. ethinyl estradiol and drospirenone 21/7 combined oral contraceptive in the treatment of hirsutism. Contraception. 2011;84:508-511. doi: 10.1016/j.contraception.2011.03.002.
- Boyd RA, Zegarac EA, Posvar EL, et al. Minimal androgenic activity of a new oral contraceptive containing norethindrone acetate and graduated doses of ethinyl estradiol. Contraception. 2001;63:71-76. doi: 10.1016/s0010-7824(01)00179-2.
- Thorneycroft IH, Stanczyk FZ, Bradshaw KD, et al. Effect of low-dose oral contraceptives on androgenic markers and acne. Contraception. 1999;60:255-262. doi: 10.1016/s0010-7824(99)00093-1.
- Kaser DJ, Missmer SA, Berry KF, et al. Use of norethindrone acetate alone for postoperative suppression of endometriosis symptoms. J Pediatr Adolesc Gynecol. 2012;25:105-108. doi: 10.1016/j.jpag.2011.09.013.
- Aygestin [package insert]. Pomona, NY: Duramed Pharmaceuticals; 2007.
- Camila [package insert]. Greenville, NC; Mayne Pharma; 2018.
- Santoro N, Brown JR, Adel T, et al. Characterization of reproductive hormonal dynamics in the perimenopause. J Clin Endocrinol Metab. 1996;81:1495-1501. doi: 10.1210/jcem.81.4.8636357.
- Speroff L, Symons J, Kempfert N, et al; FemHrt Study Investigators. The effect of varying low-dose combinations of norethindrone acetate and ethinyl estradiol (Femhrt) on the frequency and intensity of vasomotor symptoms. Menopause. 2000;7:383-390. doi: 10.1097/00042192-200011000-00003.
- Legro RS, Arslanian SA, Ehrmann DA, et al. Diagnosis and treatment of polycystic ovary syndrome: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2013;98:4565-4592. doi: 10.1210/jc.2013-2350.
- Rosenfield RL, Ehrmann DA. The pathogenesis of polycystic ovary syndrome (PCOS): the hypothesis of PCOS as functional ovarian hyperandrogenism revisited. Endocr Rev. 2016;37:467-520. doi: 10.1210/er.2015-1104.
- Zhu JL, Chen Z, Feng WJ, et al. Sex hormone-binding globulin and polycystic ovary syndrome. Clin Chim Acta. 2019;499:142-148. doi: 10.1016/j.cca.2019.09.010.
- Oner G, Muderris II. A prospective randomized trial comparing low-dose ethinyl estradiol and drospirenone 24/4 combined oral contraceptive vs. ethinyl estradiol and drospirenone 21/7 combined oral contraceptive in the treatment of hirsutism. Contraception. 2011;84:508-511. doi: 10.1016/j.contraception.2011.03.002.
- Boyd RA, Zegarac EA, Posvar EL, et al. Minimal androgenic activity of a new oral contraceptive containing norethindrone acetate and graduated doses of ethinyl estradiol. Contraception. 2001;63:71-76. doi: 10.1016/s0010-7824(01)00179-2.
- Thorneycroft IH, Stanczyk FZ, Bradshaw KD, et al. Effect of low-dose oral contraceptives on androgenic markers and acne. Contraception. 1999;60:255-262. doi: 10.1016/s0010-7824(99)00093-1.
- Kaser DJ, Missmer SA, Berry KF, et al. Use of norethindrone acetate alone for postoperative suppression of endometriosis symptoms. J Pediatr Adolesc Gynecol. 2012;25:105-108. doi: 10.1016/j.jpag.2011.09.013.
- Aygestin [package insert]. Pomona, NY: Duramed Pharmaceuticals; 2007.
- Camila [package insert]. Greenville, NC; Mayne Pharma; 2018.
- Santoro N, Brown JR, Adel T, et al. Characterization of reproductive hormonal dynamics in the perimenopause. J Clin Endocrinol Metab. 1996;81:1495-1501. doi: 10.1210/jcem.81.4.8636357.
- Speroff L, Symons J, Kempfert N, et al; FemHrt Study Investigators. The effect of varying low-dose combinations of norethindrone acetate and ethinyl estradiol (Femhrt) on the frequency and intensity of vasomotor symptoms. Menopause. 2000;7:383-390. doi: 10.1097/00042192-200011000-00003.
Diaphragmatic endometriosis diagnosed many years after symptom onset
Diaphragmatic endometriosis is often diagnosed several years after the start of symptoms – mainly moderate to severe pain – and this is potentially because of general lack of awareness of diaphragmatic endometriosis among the general population and medical professionals.
Findings of the international survey that explored the diagnosis and treatment of diaphragmatic endometriosis were presented at this year’s Royal College of Obstetricians and Gynecologists 2021 Virtual World Congress by medical student Rachel Piccus, MSc, based at the University of Birmingham (England). Robert Sutcliffe, MD, consultant in hepatobiliary and pancreatic surgery, at Queen Elizabeth Hospital Birmingham was senior author. Results were also published in the May 2021 issue of the European Journal of Obstetrics and Gynaecology and Reproductive Biology.
The study found that it took an average of five visits to a primary physician before referral to a gynecologist.
“Late diagnosis could also be due to the idea that diaphragmatic endometriosis symptoms often present before pelvic symptoms and therefore the site of pain is considered atypical for pelvic endometriosis,” Ms. Piccus said, adding that “clinicians are screening for cyclical pain, which is typical of endometriosis, but our study has shown that pain can in fact be more frequent – daily and weekly.”
These significant diagnostic delays, seen from the time of the initial primary care and gynecology consultation has the potential to significantly affect quality of life as seen in pelvic endometriosis, said Ms. Piccus. “These delays are partly due to a lack of awareness among gynecologists, but could also be due to pelvic laparoscopy being insufficient to examine the diaphragm behind the liver.”
Justin Clark, MD, consultant gynaecologist, Birmingham (England) Women’s and Children Hospital, moderated the session and agreed that the study highlights the need for greater awareness of this variant of endometriosis. “Whilst endometriosis affecting the diaphragm, subdiaphragm, and thorax is rare, the condition causes substantial morbidity.”
“Greater knowledge of thoracic endometriosis amongst clinicians in both primary and secondary care is needed to ensure accurate and timely diagnosis,” he added.
Diaphragmatic endometriosis is estimated to affect 1%-1.5% of all endometriosis patients and presents as cyclical pain in the chest, abdomen, and shoulder tip, as well as other respiratory symptoms such as catamenial pneumothorax and difficulty breathing.
“Cross-sectional imaging has shown low sensitivity so upper abdominal laparoscopy is the gold standard; however, this has implications for diagnostic delay because a strong clinical suspicion is required to refer for this invasive procedure,” explained Ms. Piccus referring to one of the reasons underpinning the need for the study.
When successfully diagnosed, treatment requires excision or ablation surgery and studies show symptomatic relief in 75%-100% of cases.
To gauge the extent of delayed diagnosis as well as treatment outcomes from a patient perspective, Ms. Piccus circulated an anonymous online survey among women with a previous history of surgery for diaphragmatic endometriosis.
Diaphragmatic endometriosis pain – daily and weekly as well as cyclical
A total of 137 participants responded to the survey, with a median age of 34 years (range, 19-53). Median age of diaphragmatic endometriosis onset was 27 years (range, 11-50), and importantly, diaphragmatic endometriosis symptoms started before pelvic symptoms in 90 respondents (66%).
The dominant symptom was pain. A total of 38% reported cyclical pain (related to endometrial shedding during menstruation), 15% weekly pain, and 47% daily pain, both of which were worse during the menstrual cycle. Furthermore, 14% reported other symptoms including catamenial pneumothorax, difficulty breathing, and hemoptysis.
“Whilst this cyclical pain is typical of endometriosis, we see that diagnostic delays may be due to misdiagnosis because clinicians are screening for this cyclical pain whilst our study has shown that pain can in fact be more frequent, being daily and weekly,” noted Ms. Piccus. Moderate to severe pain was reported in 67% of respondents and moderate in 31%, only 2% reported pain as mild.
Location of pain comprised moderate to severe pain in the upper abdomen (68%), chest (64%) and shoulder (54%). Pain was right-sided in 54%, left-sided in 11% and bilateral in 35%. Upper back and neck were also reported as sites of pain.
Indirectly providing a measure of the lack of awareness of diaphragmatic endometriosis on behalf of primary care, 122 participants reported initially visiting their primary care physician for help and 65 were given a diagnosis – in only 14 cases was that diaphragmatic endometriosis. There were a range of other gynecologic (e.g. ovarian cyst, two), respiratory (spontaneous pneumothorax, seven), gastrointestinal (gastritis/reflux, eight), musculoskeletal (six), and psychological (anxiety/stress, four) diagnoses.
A median of 5 primary care consultations (range, 1-100) were required before referral to a gynecologist, with 30% seeing a primary care physician over 10 times. A further 14 patients self-referred to gynecologist.
“These findings have implications for diagnostic delay, added Ms. Piccus. “While the majority of respondents were diagnosed less than a year from the first GP visit, the median delay was 2 years, with 31% diagnosed after 5 or more years. One took 23 years for an initial diagnosis.”
Most cases were diagnosed at the time of surgery – 93%, with 52% at pelvic laparoscopy, 35% upper abdominal laparoscopy, with 30% requiring two or more laparoscopies before they were diagnosed with diaphragmatic endometriosis. A total of 7% were diagnosed via cross-sectional imaging prior to surgery.
Treatment outcomes for diaphragmatic endometriosis
Reflecting the literature, surgery to remove the endometriosis lesions was mainly laparoscopic with 47% abdominal excisions, and 29% abdominal ablations; 6% received open abdominal procedures, and 18% received open thoracotomy or video-assisted thoracoscopic surgery.
The survey asked about postoperative symptoms 6 months after surgery and at the time of survey. Symptoms at 6 months post surgery had completely resolved in 18%, shown significant improvement in 48%, and no improvement in 20%. Worsening of symptoms was seen in 14%. Long-term pain was reported by 21% as severe, 27% as moderate, 35% as mild, and 17% had no symptoms.
Further findings included that 23% underwent additional procedures to treat their diaphragmatic endometriosis, and that there was no significant difference between excision and ablation, nor between age of onset of symptoms or length of diagnostic delay.
“Surgical treatment to remove these extra pelvic deposits of endometriosis will depend upon the type and distribution of thoracic endometriosis and a variety of surgical specialties may need to be involved including gynecologists, cardiothoracic, and upper gastrointestinal/liver surgeons,” Dr. Clark said.
He added that familiar hormonal medical treatments for more typical pelvic endometriosis should also be considered for primary and maintenance treatment. “These data suggest a high symptomatic recurrence rate after surgical treatment and so medical treatments should be considered to try and minimize the risks of endometriosis symptoms returning.”
Dr. Clark also pointed out that multidisciplinary clinical teams should be established in specialized centers to plan surgical and medical management to enhance clinical outcomes and collect data to better understand this enigmatic condition.
Ms. Piccus and Dr. Clark have no relevant conflicts of interest.
Diaphragmatic endometriosis is often diagnosed several years after the start of symptoms – mainly moderate to severe pain – and this is potentially because of general lack of awareness of diaphragmatic endometriosis among the general population and medical professionals.
Findings of the international survey that explored the diagnosis and treatment of diaphragmatic endometriosis were presented at this year’s Royal College of Obstetricians and Gynecologists 2021 Virtual World Congress by medical student Rachel Piccus, MSc, based at the University of Birmingham (England). Robert Sutcliffe, MD, consultant in hepatobiliary and pancreatic surgery, at Queen Elizabeth Hospital Birmingham was senior author. Results were also published in the May 2021 issue of the European Journal of Obstetrics and Gynaecology and Reproductive Biology.
The study found that it took an average of five visits to a primary physician before referral to a gynecologist.
“Late diagnosis could also be due to the idea that diaphragmatic endometriosis symptoms often present before pelvic symptoms and therefore the site of pain is considered atypical for pelvic endometriosis,” Ms. Piccus said, adding that “clinicians are screening for cyclical pain, which is typical of endometriosis, but our study has shown that pain can in fact be more frequent – daily and weekly.”
These significant diagnostic delays, seen from the time of the initial primary care and gynecology consultation has the potential to significantly affect quality of life as seen in pelvic endometriosis, said Ms. Piccus. “These delays are partly due to a lack of awareness among gynecologists, but could also be due to pelvic laparoscopy being insufficient to examine the diaphragm behind the liver.”
Justin Clark, MD, consultant gynaecologist, Birmingham (England) Women’s and Children Hospital, moderated the session and agreed that the study highlights the need for greater awareness of this variant of endometriosis. “Whilst endometriosis affecting the diaphragm, subdiaphragm, and thorax is rare, the condition causes substantial morbidity.”
“Greater knowledge of thoracic endometriosis amongst clinicians in both primary and secondary care is needed to ensure accurate and timely diagnosis,” he added.
Diaphragmatic endometriosis is estimated to affect 1%-1.5% of all endometriosis patients and presents as cyclical pain in the chest, abdomen, and shoulder tip, as well as other respiratory symptoms such as catamenial pneumothorax and difficulty breathing.
“Cross-sectional imaging has shown low sensitivity so upper abdominal laparoscopy is the gold standard; however, this has implications for diagnostic delay because a strong clinical suspicion is required to refer for this invasive procedure,” explained Ms. Piccus referring to one of the reasons underpinning the need for the study.
When successfully diagnosed, treatment requires excision or ablation surgery and studies show symptomatic relief in 75%-100% of cases.
To gauge the extent of delayed diagnosis as well as treatment outcomes from a patient perspective, Ms. Piccus circulated an anonymous online survey among women with a previous history of surgery for diaphragmatic endometriosis.
Diaphragmatic endometriosis pain – daily and weekly as well as cyclical
A total of 137 participants responded to the survey, with a median age of 34 years (range, 19-53). Median age of diaphragmatic endometriosis onset was 27 years (range, 11-50), and importantly, diaphragmatic endometriosis symptoms started before pelvic symptoms in 90 respondents (66%).
The dominant symptom was pain. A total of 38% reported cyclical pain (related to endometrial shedding during menstruation), 15% weekly pain, and 47% daily pain, both of which were worse during the menstrual cycle. Furthermore, 14% reported other symptoms including catamenial pneumothorax, difficulty breathing, and hemoptysis.
“Whilst this cyclical pain is typical of endometriosis, we see that diagnostic delays may be due to misdiagnosis because clinicians are screening for this cyclical pain whilst our study has shown that pain can in fact be more frequent, being daily and weekly,” noted Ms. Piccus. Moderate to severe pain was reported in 67% of respondents and moderate in 31%, only 2% reported pain as mild.
Location of pain comprised moderate to severe pain in the upper abdomen (68%), chest (64%) and shoulder (54%). Pain was right-sided in 54%, left-sided in 11% and bilateral in 35%. Upper back and neck were also reported as sites of pain.
Indirectly providing a measure of the lack of awareness of diaphragmatic endometriosis on behalf of primary care, 122 participants reported initially visiting their primary care physician for help and 65 were given a diagnosis – in only 14 cases was that diaphragmatic endometriosis. There were a range of other gynecologic (e.g. ovarian cyst, two), respiratory (spontaneous pneumothorax, seven), gastrointestinal (gastritis/reflux, eight), musculoskeletal (six), and psychological (anxiety/stress, four) diagnoses.
A median of 5 primary care consultations (range, 1-100) were required before referral to a gynecologist, with 30% seeing a primary care physician over 10 times. A further 14 patients self-referred to gynecologist.
“These findings have implications for diagnostic delay, added Ms. Piccus. “While the majority of respondents were diagnosed less than a year from the first GP visit, the median delay was 2 years, with 31% diagnosed after 5 or more years. One took 23 years for an initial diagnosis.”
Most cases were diagnosed at the time of surgery – 93%, with 52% at pelvic laparoscopy, 35% upper abdominal laparoscopy, with 30% requiring two or more laparoscopies before they were diagnosed with diaphragmatic endometriosis. A total of 7% were diagnosed via cross-sectional imaging prior to surgery.
Treatment outcomes for diaphragmatic endometriosis
Reflecting the literature, surgery to remove the endometriosis lesions was mainly laparoscopic with 47% abdominal excisions, and 29% abdominal ablations; 6% received open abdominal procedures, and 18% received open thoracotomy or video-assisted thoracoscopic surgery.
The survey asked about postoperative symptoms 6 months after surgery and at the time of survey. Symptoms at 6 months post surgery had completely resolved in 18%, shown significant improvement in 48%, and no improvement in 20%. Worsening of symptoms was seen in 14%. Long-term pain was reported by 21% as severe, 27% as moderate, 35% as mild, and 17% had no symptoms.
Further findings included that 23% underwent additional procedures to treat their diaphragmatic endometriosis, and that there was no significant difference between excision and ablation, nor between age of onset of symptoms or length of diagnostic delay.
“Surgical treatment to remove these extra pelvic deposits of endometriosis will depend upon the type and distribution of thoracic endometriosis and a variety of surgical specialties may need to be involved including gynecologists, cardiothoracic, and upper gastrointestinal/liver surgeons,” Dr. Clark said.
He added that familiar hormonal medical treatments for more typical pelvic endometriosis should also be considered for primary and maintenance treatment. “These data suggest a high symptomatic recurrence rate after surgical treatment and so medical treatments should be considered to try and minimize the risks of endometriosis symptoms returning.”
Dr. Clark also pointed out that multidisciplinary clinical teams should be established in specialized centers to plan surgical and medical management to enhance clinical outcomes and collect data to better understand this enigmatic condition.
Ms. Piccus and Dr. Clark have no relevant conflicts of interest.
Diaphragmatic endometriosis is often diagnosed several years after the start of symptoms – mainly moderate to severe pain – and this is potentially because of general lack of awareness of diaphragmatic endometriosis among the general population and medical professionals.
Findings of the international survey that explored the diagnosis and treatment of diaphragmatic endometriosis were presented at this year’s Royal College of Obstetricians and Gynecologists 2021 Virtual World Congress by medical student Rachel Piccus, MSc, based at the University of Birmingham (England). Robert Sutcliffe, MD, consultant in hepatobiliary and pancreatic surgery, at Queen Elizabeth Hospital Birmingham was senior author. Results were also published in the May 2021 issue of the European Journal of Obstetrics and Gynaecology and Reproductive Biology.
The study found that it took an average of five visits to a primary physician before referral to a gynecologist.
“Late diagnosis could also be due to the idea that diaphragmatic endometriosis symptoms often present before pelvic symptoms and therefore the site of pain is considered atypical for pelvic endometriosis,” Ms. Piccus said, adding that “clinicians are screening for cyclical pain, which is typical of endometriosis, but our study has shown that pain can in fact be more frequent – daily and weekly.”
These significant diagnostic delays, seen from the time of the initial primary care and gynecology consultation has the potential to significantly affect quality of life as seen in pelvic endometriosis, said Ms. Piccus. “These delays are partly due to a lack of awareness among gynecologists, but could also be due to pelvic laparoscopy being insufficient to examine the diaphragm behind the liver.”
Justin Clark, MD, consultant gynaecologist, Birmingham (England) Women’s and Children Hospital, moderated the session and agreed that the study highlights the need for greater awareness of this variant of endometriosis. “Whilst endometriosis affecting the diaphragm, subdiaphragm, and thorax is rare, the condition causes substantial morbidity.”
“Greater knowledge of thoracic endometriosis amongst clinicians in both primary and secondary care is needed to ensure accurate and timely diagnosis,” he added.
Diaphragmatic endometriosis is estimated to affect 1%-1.5% of all endometriosis patients and presents as cyclical pain in the chest, abdomen, and shoulder tip, as well as other respiratory symptoms such as catamenial pneumothorax and difficulty breathing.
“Cross-sectional imaging has shown low sensitivity so upper abdominal laparoscopy is the gold standard; however, this has implications for diagnostic delay because a strong clinical suspicion is required to refer for this invasive procedure,” explained Ms. Piccus referring to one of the reasons underpinning the need for the study.
When successfully diagnosed, treatment requires excision or ablation surgery and studies show symptomatic relief in 75%-100% of cases.
To gauge the extent of delayed diagnosis as well as treatment outcomes from a patient perspective, Ms. Piccus circulated an anonymous online survey among women with a previous history of surgery for diaphragmatic endometriosis.
Diaphragmatic endometriosis pain – daily and weekly as well as cyclical
A total of 137 participants responded to the survey, with a median age of 34 years (range, 19-53). Median age of diaphragmatic endometriosis onset was 27 years (range, 11-50), and importantly, diaphragmatic endometriosis symptoms started before pelvic symptoms in 90 respondents (66%).
The dominant symptom was pain. A total of 38% reported cyclical pain (related to endometrial shedding during menstruation), 15% weekly pain, and 47% daily pain, both of which were worse during the menstrual cycle. Furthermore, 14% reported other symptoms including catamenial pneumothorax, difficulty breathing, and hemoptysis.
“Whilst this cyclical pain is typical of endometriosis, we see that diagnostic delays may be due to misdiagnosis because clinicians are screening for this cyclical pain whilst our study has shown that pain can in fact be more frequent, being daily and weekly,” noted Ms. Piccus. Moderate to severe pain was reported in 67% of respondents and moderate in 31%, only 2% reported pain as mild.
Location of pain comprised moderate to severe pain in the upper abdomen (68%), chest (64%) and shoulder (54%). Pain was right-sided in 54%, left-sided in 11% and bilateral in 35%. Upper back and neck were also reported as sites of pain.
Indirectly providing a measure of the lack of awareness of diaphragmatic endometriosis on behalf of primary care, 122 participants reported initially visiting their primary care physician for help and 65 were given a diagnosis – in only 14 cases was that diaphragmatic endometriosis. There were a range of other gynecologic (e.g. ovarian cyst, two), respiratory (spontaneous pneumothorax, seven), gastrointestinal (gastritis/reflux, eight), musculoskeletal (six), and psychological (anxiety/stress, four) diagnoses.
A median of 5 primary care consultations (range, 1-100) were required before referral to a gynecologist, with 30% seeing a primary care physician over 10 times. A further 14 patients self-referred to gynecologist.
“These findings have implications for diagnostic delay, added Ms. Piccus. “While the majority of respondents were diagnosed less than a year from the first GP visit, the median delay was 2 years, with 31% diagnosed after 5 or more years. One took 23 years for an initial diagnosis.”
Most cases were diagnosed at the time of surgery – 93%, with 52% at pelvic laparoscopy, 35% upper abdominal laparoscopy, with 30% requiring two or more laparoscopies before they were diagnosed with diaphragmatic endometriosis. A total of 7% were diagnosed via cross-sectional imaging prior to surgery.
Treatment outcomes for diaphragmatic endometriosis
Reflecting the literature, surgery to remove the endometriosis lesions was mainly laparoscopic with 47% abdominal excisions, and 29% abdominal ablations; 6% received open abdominal procedures, and 18% received open thoracotomy or video-assisted thoracoscopic surgery.
The survey asked about postoperative symptoms 6 months after surgery and at the time of survey. Symptoms at 6 months post surgery had completely resolved in 18%, shown significant improvement in 48%, and no improvement in 20%. Worsening of symptoms was seen in 14%. Long-term pain was reported by 21% as severe, 27% as moderate, 35% as mild, and 17% had no symptoms.
Further findings included that 23% underwent additional procedures to treat their diaphragmatic endometriosis, and that there was no significant difference between excision and ablation, nor between age of onset of symptoms or length of diagnostic delay.
“Surgical treatment to remove these extra pelvic deposits of endometriosis will depend upon the type and distribution of thoracic endometriosis and a variety of surgical specialties may need to be involved including gynecologists, cardiothoracic, and upper gastrointestinal/liver surgeons,” Dr. Clark said.
He added that familiar hormonal medical treatments for more typical pelvic endometriosis should also be considered for primary and maintenance treatment. “These data suggest a high symptomatic recurrence rate after surgical treatment and so medical treatments should be considered to try and minimize the risks of endometriosis symptoms returning.”
Dr. Clark also pointed out that multidisciplinary clinical teams should be established in specialized centers to plan surgical and medical management to enhance clinical outcomes and collect data to better understand this enigmatic condition.
Ms. Piccus and Dr. Clark have no relevant conflicts of interest.
Managing deep infiltrating endometriosis
Deep endometriosis, including bowel endometriosis, happens in more than 10% of all women with endometriosis. Because it can be debilitating and difficult to diagnose, how is it identified?
Dr. Kho: Diagnosing deep infiltrating endometriosis (DIE) is one of the biggest challenges in the field. Currently, the gold standard is still histologic confirmation of endometriosis lesions, but I think the paradigm is shifting significantly. Advanced centers are now moving towards the use of imaging to visualize suspected endometriosis better. In skilled hands, ultrasonography and MRI can accurately detect DIE. The advantage of visualizing suspected deep endometriosis before surgery is that we can offer better counseling to patients and offer medical or surgical treatments or a combination of both. When the patient chooses surgery, we can be better prepared with a multidisciplinary team to remove the lesions completely.
The treatment of deep endometriosis can be challenging because it does not always respond to medical therapy, such as oral contraceptive pills or GnRH agonists. What treatment options have shown effectiveness?
Dr. Kho: It should be understood that we need to manage the symptoms and not the lesions. Just because there are endometriosis lesions identified does NOT mean that they need to be removed. The decision should be based on what the treatment goals are. A good discussion with the patient is important to determine what the treatment objectives are. Are we managing pain? Are we surgically treating infertility? Are we treating something else, such as bowel obstruction or blood in the urine? These questions and their answers should be first and foremost in the clinician’s mind.
Different medical treatment therapies are available and have been shown to be effective in managing endometriosis symptoms without having to immediately resort to surgery as with certain cases of suspected DIE. These medical management options include combined estrogen and progesterone contraceptive formulations, progesterone-only formulations, and GnRH agonists and antagonists. Patients should be counseled about the different options and their associated risks. Often, patients need to switch from one form to another when side effects encumber them.
If imaging or an exam reveals incidental findings of suspected deep endometriosis, it does not mean that treatment is required because some patients can be without symptoms or have no issues. But when the indication for pain or desire to achieve a pregnancy is clear, and the decision is to proceed with treatment, there are some guidelines:
- If the pain is severe and affects the patient’s daily quality of life, for example, with large, deep lesions, surgical excision appears to be effective in improving the patient’s quality of life.
- If infertility is the main indication, then other factors need to be considered. Has she had previous surgeries? What is her age? What is her ovarian reserve? What is the condition of the tubes? Is the use of artificial reproductive technology, or ART, an option for the couple? What is her cancer risk?
- Lastly, what is the extent of the lesion(s)? Both medical and surgical approaches for treatment carry risks. For surgery, complications can be severe with long-term consequences. Therefore, it is important to discuss all of this in detail with the patient.
When we understand what the main goal of the treatment is for endometriosis—such as either to treat pain or to achieve pregnancy, or both—we can tailor our surgical approach to achieve the goal(s). For example, in a patient who wants to achieve a pregnancy in the future, we may opt to do only what is necessary to remove endometriosis and relieve pain without impairing the patient’s fertility potential and overall quality of life.
Post-operatively, if the patient does not desire to become pregnant, medications to suppress the ovaries are an option to reduce the chance of disease recurrence.
What pearls can you provide when it comes to surgical techniques available and benefits for short- and long-term risks and limitations?
Dr. Kho: The surgeon should tailor his or her level of radicality to excise endometriosis to achieve the treatment goals that are mutually agreed on with the patient. For the surgeon bringing the patient into surgery, go in prepared. I strongly believe in preoperative imaging to provide the best mapping of the disease and in having other specialists or surgeons available—whether it be a urologist, a colorectal surgeon, a thoracic surgeon, a vascular surgeon, or an orthopedic surgeon (if needed)—depending on where the lesions are located.
Because we know that the best surgical outcomes come from surgeons with the highest volume, providers should be willing to refer patients with advanced disease to centers that specialize in the treatment of endometriosis. Many providers with this expertise undergo additional training to advance their skills. Advanced centers in endometriosis also provide patients with a multidisciplinary team to provide the best care.
What is the most optimal setup for a multidisciplinary team treating deep infiltrating endometriosis?
Dr. Kho: You will find that advanced centers for endometriosis will have in place a multidisciplinary team that includes a pain specialist, a surgical specialist, a pain psychologist, physical therapy, urologist, colorectal surgeon, and other sub-specialty surgeons to be able to look at the patients from all the different aspects. Often a reproductive endocrinologist or REI specialist would also be part of the group.
At our center, we have what we call a “benign tumor board,” where we discuss complex cases with representatives from different areas. This allows us to discuss the case, review what is known in the literature, and collectively develop a treatment plan.
Is there anything that was not covered in this discussion that you would like to mention?
Dr. Kho: Something that should be mentioned is that ovarian endometriosis is often associated with advanced endometriosis, often Stage 3 or 4. Clinicians should be aware that when imaging suggests the presence of ovarian endometriosis, studies show that the disease is isolated in the ovary in only 15% of cases—meaning that there is an 85% chance that endometriosis is present elsewhere in the pelvis. Therefore, the surgeon should be prepared for more extensive dissection when they bring the patient into surgery.
Deep endometriosis, including bowel endometriosis, happens in more than 10% of all women with endometriosis. Because it can be debilitating and difficult to diagnose, how is it identified?
Dr. Kho: Diagnosing deep infiltrating endometriosis (DIE) is one of the biggest challenges in the field. Currently, the gold standard is still histologic confirmation of endometriosis lesions, but I think the paradigm is shifting significantly. Advanced centers are now moving towards the use of imaging to visualize suspected endometriosis better. In skilled hands, ultrasonography and MRI can accurately detect DIE. The advantage of visualizing suspected deep endometriosis before surgery is that we can offer better counseling to patients and offer medical or surgical treatments or a combination of both. When the patient chooses surgery, we can be better prepared with a multidisciplinary team to remove the lesions completely.
The treatment of deep endometriosis can be challenging because it does not always respond to medical therapy, such as oral contraceptive pills or GnRH agonists. What treatment options have shown effectiveness?
Dr. Kho: It should be understood that we need to manage the symptoms and not the lesions. Just because there are endometriosis lesions identified does NOT mean that they need to be removed. The decision should be based on what the treatment goals are. A good discussion with the patient is important to determine what the treatment objectives are. Are we managing pain? Are we surgically treating infertility? Are we treating something else, such as bowel obstruction or blood in the urine? These questions and their answers should be first and foremost in the clinician’s mind.
Different medical treatment therapies are available and have been shown to be effective in managing endometriosis symptoms without having to immediately resort to surgery as with certain cases of suspected DIE. These medical management options include combined estrogen and progesterone contraceptive formulations, progesterone-only formulations, and GnRH agonists and antagonists. Patients should be counseled about the different options and their associated risks. Often, patients need to switch from one form to another when side effects encumber them.
If imaging or an exam reveals incidental findings of suspected deep endometriosis, it does not mean that treatment is required because some patients can be without symptoms or have no issues. But when the indication for pain or desire to achieve a pregnancy is clear, and the decision is to proceed with treatment, there are some guidelines:
- If the pain is severe and affects the patient’s daily quality of life, for example, with large, deep lesions, surgical excision appears to be effective in improving the patient’s quality of life.
- If infertility is the main indication, then other factors need to be considered. Has she had previous surgeries? What is her age? What is her ovarian reserve? What is the condition of the tubes? Is the use of artificial reproductive technology, or ART, an option for the couple? What is her cancer risk?
- Lastly, what is the extent of the lesion(s)? Both medical and surgical approaches for treatment carry risks. For surgery, complications can be severe with long-term consequences. Therefore, it is important to discuss all of this in detail with the patient.
When we understand what the main goal of the treatment is for endometriosis—such as either to treat pain or to achieve pregnancy, or both—we can tailor our surgical approach to achieve the goal(s). For example, in a patient who wants to achieve a pregnancy in the future, we may opt to do only what is necessary to remove endometriosis and relieve pain without impairing the patient’s fertility potential and overall quality of life.
Post-operatively, if the patient does not desire to become pregnant, medications to suppress the ovaries are an option to reduce the chance of disease recurrence.
What pearls can you provide when it comes to surgical techniques available and benefits for short- and long-term risks and limitations?
Dr. Kho: The surgeon should tailor his or her level of radicality to excise endometriosis to achieve the treatment goals that are mutually agreed on with the patient. For the surgeon bringing the patient into surgery, go in prepared. I strongly believe in preoperative imaging to provide the best mapping of the disease and in having other specialists or surgeons available—whether it be a urologist, a colorectal surgeon, a thoracic surgeon, a vascular surgeon, or an orthopedic surgeon (if needed)—depending on where the lesions are located.
Because we know that the best surgical outcomes come from surgeons with the highest volume, providers should be willing to refer patients with advanced disease to centers that specialize in the treatment of endometriosis. Many providers with this expertise undergo additional training to advance their skills. Advanced centers in endometriosis also provide patients with a multidisciplinary team to provide the best care.
What is the most optimal setup for a multidisciplinary team treating deep infiltrating endometriosis?
Dr. Kho: You will find that advanced centers for endometriosis will have in place a multidisciplinary team that includes a pain specialist, a surgical specialist, a pain psychologist, physical therapy, urologist, colorectal surgeon, and other sub-specialty surgeons to be able to look at the patients from all the different aspects. Often a reproductive endocrinologist or REI specialist would also be part of the group.
At our center, we have what we call a “benign tumor board,” where we discuss complex cases with representatives from different areas. This allows us to discuss the case, review what is known in the literature, and collectively develop a treatment plan.
Is there anything that was not covered in this discussion that you would like to mention?
Dr. Kho: Something that should be mentioned is that ovarian endometriosis is often associated with advanced endometriosis, often Stage 3 or 4. Clinicians should be aware that when imaging suggests the presence of ovarian endometriosis, studies show that the disease is isolated in the ovary in only 15% of cases—meaning that there is an 85% chance that endometriosis is present elsewhere in the pelvis. Therefore, the surgeon should be prepared for more extensive dissection when they bring the patient into surgery.
Deep endometriosis, including bowel endometriosis, happens in more than 10% of all women with endometriosis. Because it can be debilitating and difficult to diagnose, how is it identified?
Dr. Kho: Diagnosing deep infiltrating endometriosis (DIE) is one of the biggest challenges in the field. Currently, the gold standard is still histologic confirmation of endometriosis lesions, but I think the paradigm is shifting significantly. Advanced centers are now moving towards the use of imaging to visualize suspected endometriosis better. In skilled hands, ultrasonography and MRI can accurately detect DIE. The advantage of visualizing suspected deep endometriosis before surgery is that we can offer better counseling to patients and offer medical or surgical treatments or a combination of both. When the patient chooses surgery, we can be better prepared with a multidisciplinary team to remove the lesions completely.
The treatment of deep endometriosis can be challenging because it does not always respond to medical therapy, such as oral contraceptive pills or GnRH agonists. What treatment options have shown effectiveness?
Dr. Kho: It should be understood that we need to manage the symptoms and not the lesions. Just because there are endometriosis lesions identified does NOT mean that they need to be removed. The decision should be based on what the treatment goals are. A good discussion with the patient is important to determine what the treatment objectives are. Are we managing pain? Are we surgically treating infertility? Are we treating something else, such as bowel obstruction or blood in the urine? These questions and their answers should be first and foremost in the clinician’s mind.
Different medical treatment therapies are available and have been shown to be effective in managing endometriosis symptoms without having to immediately resort to surgery as with certain cases of suspected DIE. These medical management options include combined estrogen and progesterone contraceptive formulations, progesterone-only formulations, and GnRH agonists and antagonists. Patients should be counseled about the different options and their associated risks. Often, patients need to switch from one form to another when side effects encumber them.
If imaging or an exam reveals incidental findings of suspected deep endometriosis, it does not mean that treatment is required because some patients can be without symptoms or have no issues. But when the indication for pain or desire to achieve a pregnancy is clear, and the decision is to proceed with treatment, there are some guidelines:
- If the pain is severe and affects the patient’s daily quality of life, for example, with large, deep lesions, surgical excision appears to be effective in improving the patient’s quality of life.
- If infertility is the main indication, then other factors need to be considered. Has she had previous surgeries? What is her age? What is her ovarian reserve? What is the condition of the tubes? Is the use of artificial reproductive technology, or ART, an option for the couple? What is her cancer risk?
- Lastly, what is the extent of the lesion(s)? Both medical and surgical approaches for treatment carry risks. For surgery, complications can be severe with long-term consequences. Therefore, it is important to discuss all of this in detail with the patient.
When we understand what the main goal of the treatment is for endometriosis—such as either to treat pain or to achieve pregnancy, or both—we can tailor our surgical approach to achieve the goal(s). For example, in a patient who wants to achieve a pregnancy in the future, we may opt to do only what is necessary to remove endometriosis and relieve pain without impairing the patient’s fertility potential and overall quality of life.
Post-operatively, if the patient does not desire to become pregnant, medications to suppress the ovaries are an option to reduce the chance of disease recurrence.
What pearls can you provide when it comes to surgical techniques available and benefits for short- and long-term risks and limitations?
Dr. Kho: The surgeon should tailor his or her level of radicality to excise endometriosis to achieve the treatment goals that are mutually agreed on with the patient. For the surgeon bringing the patient into surgery, go in prepared. I strongly believe in preoperative imaging to provide the best mapping of the disease and in having other specialists or surgeons available—whether it be a urologist, a colorectal surgeon, a thoracic surgeon, a vascular surgeon, or an orthopedic surgeon (if needed)—depending on where the lesions are located.
Because we know that the best surgical outcomes come from surgeons with the highest volume, providers should be willing to refer patients with advanced disease to centers that specialize in the treatment of endometriosis. Many providers with this expertise undergo additional training to advance their skills. Advanced centers in endometriosis also provide patients with a multidisciplinary team to provide the best care.
What is the most optimal setup for a multidisciplinary team treating deep infiltrating endometriosis?
Dr. Kho: You will find that advanced centers for endometriosis will have in place a multidisciplinary team that includes a pain specialist, a surgical specialist, a pain psychologist, physical therapy, urologist, colorectal surgeon, and other sub-specialty surgeons to be able to look at the patients from all the different aspects. Often a reproductive endocrinologist or REI specialist would also be part of the group.
At our center, we have what we call a “benign tumor board,” where we discuss complex cases with representatives from different areas. This allows us to discuss the case, review what is known in the literature, and collectively develop a treatment plan.
Is there anything that was not covered in this discussion that you would like to mention?
Dr. Kho: Something that should be mentioned is that ovarian endometriosis is often associated with advanced endometriosis, often Stage 3 or 4. Clinicians should be aware that when imaging suggests the presence of ovarian endometriosis, studies show that the disease is isolated in the ovary in only 15% of cases—meaning that there is an 85% chance that endometriosis is present elsewhere in the pelvis. Therefore, the surgeon should be prepared for more extensive dissection when they bring the patient into surgery.
Lesions in pelvis may be ‘tip of the iceberg’ in endometriosis
Recognizing the systemic effects of endometriosis may help doctors better understand the experiences of patients with the disease and guide the approach to diagnosis and treatment, according to the president of the American Society for Reproductive Medicine (ASRM).
, Hugh S. Taylor, MD, said at the 2021 virtual meeting of the American College of Obstetricians and Gynecologists.
Its systemic manifestations may explain why women with endometriosis tend to have a lower body mass index, compared with women without the disease, Dr. Taylor said.
“Stem cells, microRNAs, and generalized inflammation are some of the mechanisms that mediate these long-range effects on distant organ systems,” he said.
Studies have indicated that lesions in the pelvis do not fully explain the disease, and investigators continue to elucidate how “endometriosis that we see in the pelvis is really just the tip of the iceberg,” said Dr. Taylor, chair of obstetrics, gynecology, and reproductive sciences at Yale University, New Haven, Conn.
Pain, including dysmenorrhea, pelvic pain, and dyspareunia, “can be just as bad with ... stage 1 disease as it can be with stage 4 disease,” he said.
Some patients may not have pain, but have infertility. Other women are asymptomatic, and doctors find endometriosis incidentally.
One common definition of endometriosis – ectopic endometrial glands and stroma predominantly caused by retrograde menstruation – “probably overly simplifies this complex disease,” said Dr. Taylor, who reviewed the current understanding of endometriosis in an article in The Lancet. “The lesions in the pelvis are important. We see them. We treat them. But endometriosis has ... effects throughout the body.”
Dr. Taylor’s research group has shown that stem cells are a potential source of endometriosis. “There are cells from the endometriosis that can be found traveling in the circulation,” but their effects are unclear, he said.
Levels of several microRNAs may be increased or decreased in women with endometriosis, and these altered levels may induce the production of inflammatory cytokines. They also may serve as the basis of a blood test for endometriosis that could be ready for clinical use soon, Dr. Taylor said.
In a mouse model of endometriosis, the disease changes the electrophysiology of the brain and behavior. “We see changes in anxiety induced by endometriosis. We see changes in pain sensitivity induced by endometriosis. And we also see an increase in depression induced by endometriosis in this animal model,” Dr. Taylor said.
Although surgical therapy treats local disease, medical therapy may be needed to treat the systemic manifestations.
During a question-and-answer period after the presentation, Marcelle I. Cedars, MD, asked whether analgesic and hormonal management may be sufficient when a woman has suspected or laparoscopically diagnosed endometriosis and pain is the primary complaint.
“Given the understanding of endometriosis, how would you suggest approaching treatment?” asked Dr. Cedars, president elect of the ASRM and director of the division of reproductive endocrinology and infertility at the University of California, San Francisco.
Analgesic and hormonal therapies remain “the best treatments we have,” Dr. Taylor said. He starts treatment with an oral contraceptive and a nonsteroidal anti-inflammatory medication – “not only for pain relief but to tamp some of the inflammation associated with endometriosis,” he said. If an oral contraceptive does not work, a gonadotropin-releasing hormone antagonist typically is the next step.
Dr. Taylor has disclosed ties to Dot Lab and AbbVie. Dr. Cedars had no disclosures.
Recognizing the systemic effects of endometriosis may help doctors better understand the experiences of patients with the disease and guide the approach to diagnosis and treatment, according to the president of the American Society for Reproductive Medicine (ASRM).
, Hugh S. Taylor, MD, said at the 2021 virtual meeting of the American College of Obstetricians and Gynecologists.
Its systemic manifestations may explain why women with endometriosis tend to have a lower body mass index, compared with women without the disease, Dr. Taylor said.
“Stem cells, microRNAs, and generalized inflammation are some of the mechanisms that mediate these long-range effects on distant organ systems,” he said.
Studies have indicated that lesions in the pelvis do not fully explain the disease, and investigators continue to elucidate how “endometriosis that we see in the pelvis is really just the tip of the iceberg,” said Dr. Taylor, chair of obstetrics, gynecology, and reproductive sciences at Yale University, New Haven, Conn.
Pain, including dysmenorrhea, pelvic pain, and dyspareunia, “can be just as bad with ... stage 1 disease as it can be with stage 4 disease,” he said.
Some patients may not have pain, but have infertility. Other women are asymptomatic, and doctors find endometriosis incidentally.
One common definition of endometriosis – ectopic endometrial glands and stroma predominantly caused by retrograde menstruation – “probably overly simplifies this complex disease,” said Dr. Taylor, who reviewed the current understanding of endometriosis in an article in The Lancet. “The lesions in the pelvis are important. We see them. We treat them. But endometriosis has ... effects throughout the body.”
Dr. Taylor’s research group has shown that stem cells are a potential source of endometriosis. “There are cells from the endometriosis that can be found traveling in the circulation,” but their effects are unclear, he said.
Levels of several microRNAs may be increased or decreased in women with endometriosis, and these altered levels may induce the production of inflammatory cytokines. They also may serve as the basis of a blood test for endometriosis that could be ready for clinical use soon, Dr. Taylor said.
In a mouse model of endometriosis, the disease changes the electrophysiology of the brain and behavior. “We see changes in anxiety induced by endometriosis. We see changes in pain sensitivity induced by endometriosis. And we also see an increase in depression induced by endometriosis in this animal model,” Dr. Taylor said.
Although surgical therapy treats local disease, medical therapy may be needed to treat the systemic manifestations.
During a question-and-answer period after the presentation, Marcelle I. Cedars, MD, asked whether analgesic and hormonal management may be sufficient when a woman has suspected or laparoscopically diagnosed endometriosis and pain is the primary complaint.
“Given the understanding of endometriosis, how would you suggest approaching treatment?” asked Dr. Cedars, president elect of the ASRM and director of the division of reproductive endocrinology and infertility at the University of California, San Francisco.
Analgesic and hormonal therapies remain “the best treatments we have,” Dr. Taylor said. He starts treatment with an oral contraceptive and a nonsteroidal anti-inflammatory medication – “not only for pain relief but to tamp some of the inflammation associated with endometriosis,” he said. If an oral contraceptive does not work, a gonadotropin-releasing hormone antagonist typically is the next step.
Dr. Taylor has disclosed ties to Dot Lab and AbbVie. Dr. Cedars had no disclosures.
Recognizing the systemic effects of endometriosis may help doctors better understand the experiences of patients with the disease and guide the approach to diagnosis and treatment, according to the president of the American Society for Reproductive Medicine (ASRM).
, Hugh S. Taylor, MD, said at the 2021 virtual meeting of the American College of Obstetricians and Gynecologists.
Its systemic manifestations may explain why women with endometriosis tend to have a lower body mass index, compared with women without the disease, Dr. Taylor said.
“Stem cells, microRNAs, and generalized inflammation are some of the mechanisms that mediate these long-range effects on distant organ systems,” he said.
Studies have indicated that lesions in the pelvis do not fully explain the disease, and investigators continue to elucidate how “endometriosis that we see in the pelvis is really just the tip of the iceberg,” said Dr. Taylor, chair of obstetrics, gynecology, and reproductive sciences at Yale University, New Haven, Conn.
Pain, including dysmenorrhea, pelvic pain, and dyspareunia, “can be just as bad with ... stage 1 disease as it can be with stage 4 disease,” he said.
Some patients may not have pain, but have infertility. Other women are asymptomatic, and doctors find endometriosis incidentally.
One common definition of endometriosis – ectopic endometrial glands and stroma predominantly caused by retrograde menstruation – “probably overly simplifies this complex disease,” said Dr. Taylor, who reviewed the current understanding of endometriosis in an article in The Lancet. “The lesions in the pelvis are important. We see them. We treat them. But endometriosis has ... effects throughout the body.”
Dr. Taylor’s research group has shown that stem cells are a potential source of endometriosis. “There are cells from the endometriosis that can be found traveling in the circulation,” but their effects are unclear, he said.
Levels of several microRNAs may be increased or decreased in women with endometriosis, and these altered levels may induce the production of inflammatory cytokines. They also may serve as the basis of a blood test for endometriosis that could be ready for clinical use soon, Dr. Taylor said.
In a mouse model of endometriosis, the disease changes the electrophysiology of the brain and behavior. “We see changes in anxiety induced by endometriosis. We see changes in pain sensitivity induced by endometriosis. And we also see an increase in depression induced by endometriosis in this animal model,” Dr. Taylor said.
Although surgical therapy treats local disease, medical therapy may be needed to treat the systemic manifestations.
During a question-and-answer period after the presentation, Marcelle I. Cedars, MD, asked whether analgesic and hormonal management may be sufficient when a woman has suspected or laparoscopically diagnosed endometriosis and pain is the primary complaint.
“Given the understanding of endometriosis, how would you suggest approaching treatment?” asked Dr. Cedars, president elect of the ASRM and director of the division of reproductive endocrinology and infertility at the University of California, San Francisco.
Analgesic and hormonal therapies remain “the best treatments we have,” Dr. Taylor said. He starts treatment with an oral contraceptive and a nonsteroidal anti-inflammatory medication – “not only for pain relief but to tamp some of the inflammation associated with endometriosis,” he said. If an oral contraceptive does not work, a gonadotropin-releasing hormone antagonist typically is the next step.
Dr. Taylor has disclosed ties to Dot Lab and AbbVie. Dr. Cedars had no disclosures.
FROM ACOG 2021
Can a once-daily oral formulation treat symptoms of uterine fibroids without causing hot flashes or bone loss?
Al-Hendy A, Lukes AS, Poindexter AN 3rd, et al. Treatment of uterine fibroid symptoms with relugolix combination therapy. N Engl J Med. 2021;384:630-642. doi: 10.1056/NEJMoa2008283
Expert Commentary
By age 50, approximately 70% of White women and 80% of Black women will have uterine fibroids.1 Of these, about 25% will have symptoms—most often including heavy menstrual bleeding,2 and associated pain the second most common symptom.3 First-line treatment has traditionally been hormonal contraceptives. Injectable gonadotropin-releasing hormone (GnRH) antagonist like leuprolide acetate have been commonly employed, although their actual approved indication is “for concomitant use with iron therapy for preoperative hematologic improvement of patients with anemia caused by uterine leiomyomata (fibroids).”4 Recently, an oral GnRH antagonist, elagolix, combined with estrogen and progestogen, was approved for treatment of uterine fibroids for up to 24 months. However, it is dosed twice per day because of its short half-life and results in a loss of bone mineral density at 1 year.5,6
Details of the studies
Al-Hendy and colleagues report on two double-blind 24-week phase 3 trials involving women with heavy menstrual bleeding associated with fibroids. There were just under 400 women in each trial. There was a 1:1:1 randomization to: placebo, once-daily oral relugolix 40 mg with 1 mg estradiol and 0.5 mg norethindrone acetate, or oral relugolix by itself for 12 weeks followed by the combination for 12 weeks (referred to as the “delayed relugolix combination therapy” arm).
Results. The primary end point was the percentage of patients who had a volume of menstrual blood loss less than 80 mL and a ≥50% reduction in blood loss volume as measured by the alkaline hematin method. The baseline blood loss in these studies ranged from approximately 210–250 mL. Secondary end points included amenorrhea, volume of menstrual blood loss, distress from bleeding and pelvic discomfort, anemia, pain, uterine volume, and the largest fibroid volume.
In trials one and two, 73% and 71% of patients in the relugolix combination groups, respectively, achieved the primary endpoint, compared with 19% and 15% in the placebo groups (P <.001). In addition, all secondary endpoints except largest fibroid volume were significantly improved versus placebo. Adverse events, including any change in bone mineral density, were no different between the combination and placebo groups. The delayed combination groups did have more hot flashes and diminished bone density compared with both the placebo and combination groups.
Strengths and weaknesses
The studies appropriately enrolled women with a mean age of 41–42 years and a mean BMI >30 kg/m2, and more than 50% were African American. Thus, the samples are adequately representative of the type of population most likely to have fibroids and associated symptoms. The results showed the advantages of built-in “add back therapy” with estrogen plus progestogen, as the vasomotor symptoms and bone loss that treatment with a GnRH antagonist alone produces were reduced.
Although the trials were only conducted for 24 weeks, efficacy was seen as early as 4 weeks, and was clearly maintained throughout the full trials—and there is no scientific reason to assume it would not be maintained indefinitely. However, one cannot make a similar assumption about long-term safety. As another GnRH antagonist, with a shorter half-life requiring twice-daily-dosing with add back therapy, has been approved for use for 2 years, it is likely that the once-daily formulation of combination relugolix will be approved for this timeframe as well. Still, with patients’ mean age of 41–42 years, what will clinicians do after 2-year treatment? Clearly, study of long-term safety would be valuable. ●
Fibroids are extremely common in clinical practice, with their associated symptoms depending greatly on size and location. In many patients, symptoms are serious enough to be the most common indication for hysterectomy. In the past, combination oral contraceptives, injectable leuprolide acetate, and more recently, a GnRH antagonist given twice daily with estrogen/progestogen add-back have been utilized. The formulation described in Al-Hendy and colleagues’ study, which is dosed once per day and appears to not increase vasomotor symptoms or diminish bone mass, may provide a very nice “tool” in the clinician’s toolbox to either avoid any surgery in some patients (likely those aged closer to menopause) or optimize other patients preoperatively in terms of reversing anemia and reducing uterine volume, thus making any planned surgical procedure safer.
STEVEN R. GOLDSTEIN, MD, NCMP, CCD
- Wise LA, Laughlin-Tommaso SK. Epidemiology of uterine fibroids: from menarche to menopause. Clin Obstet Gynecol. 2016;59:2-24.
- Borah BJ, Nicholson WK, Bradley L, et al. The impact of uterine leiomyomas: a national survey of affected women. Am J Obstet Gynecol. 2013;209:319.e1-319.e20.
- David M, Pitz CM, Mihaylova A, et al. Myoma-associated pain frequency and intensity: a retrospective evaluation of 1548 myoma patients. Eur J Obstet Gynecol Reprod Biol. 2016;199:137-140.
- Lupron Depot [package insert]. North Chicago, IL: AbbVie Inc.; 2018.
- Schlaff WD, Ackerman RT, Al-Hendy A, et al. Elagolix for heavy menstrual bleeding in women with uterine fibroids. N Engl J Med. 2020;382:328-340.
- Oriahnn [package insert]. North Chicago, IL: AbbVie Inc.; 2020.
Al-Hendy A, Lukes AS, Poindexter AN 3rd, et al. Treatment of uterine fibroid symptoms with relugolix combination therapy. N Engl J Med. 2021;384:630-642. doi: 10.1056/NEJMoa2008283
Expert Commentary
By age 50, approximately 70% of White women and 80% of Black women will have uterine fibroids.1 Of these, about 25% will have symptoms—most often including heavy menstrual bleeding,2 and associated pain the second most common symptom.3 First-line treatment has traditionally been hormonal contraceptives. Injectable gonadotropin-releasing hormone (GnRH) antagonist like leuprolide acetate have been commonly employed, although their actual approved indication is “for concomitant use with iron therapy for preoperative hematologic improvement of patients with anemia caused by uterine leiomyomata (fibroids).”4 Recently, an oral GnRH antagonist, elagolix, combined with estrogen and progestogen, was approved for treatment of uterine fibroids for up to 24 months. However, it is dosed twice per day because of its short half-life and results in a loss of bone mineral density at 1 year.5,6
Details of the studies
Al-Hendy and colleagues report on two double-blind 24-week phase 3 trials involving women with heavy menstrual bleeding associated with fibroids. There were just under 400 women in each trial. There was a 1:1:1 randomization to: placebo, once-daily oral relugolix 40 mg with 1 mg estradiol and 0.5 mg norethindrone acetate, or oral relugolix by itself for 12 weeks followed by the combination for 12 weeks (referred to as the “delayed relugolix combination therapy” arm).
Results. The primary end point was the percentage of patients who had a volume of menstrual blood loss less than 80 mL and a ≥50% reduction in blood loss volume as measured by the alkaline hematin method. The baseline blood loss in these studies ranged from approximately 210–250 mL. Secondary end points included amenorrhea, volume of menstrual blood loss, distress from bleeding and pelvic discomfort, anemia, pain, uterine volume, and the largest fibroid volume.
In trials one and two, 73% and 71% of patients in the relugolix combination groups, respectively, achieved the primary endpoint, compared with 19% and 15% in the placebo groups (P <.001). In addition, all secondary endpoints except largest fibroid volume were significantly improved versus placebo. Adverse events, including any change in bone mineral density, were no different between the combination and placebo groups. The delayed combination groups did have more hot flashes and diminished bone density compared with both the placebo and combination groups.
Strengths and weaknesses
The studies appropriately enrolled women with a mean age of 41–42 years and a mean BMI >30 kg/m2, and more than 50% were African American. Thus, the samples are adequately representative of the type of population most likely to have fibroids and associated symptoms. The results showed the advantages of built-in “add back therapy” with estrogen plus progestogen, as the vasomotor symptoms and bone loss that treatment with a GnRH antagonist alone produces were reduced.
Although the trials were only conducted for 24 weeks, efficacy was seen as early as 4 weeks, and was clearly maintained throughout the full trials—and there is no scientific reason to assume it would not be maintained indefinitely. However, one cannot make a similar assumption about long-term safety. As another GnRH antagonist, with a shorter half-life requiring twice-daily-dosing with add back therapy, has been approved for use for 2 years, it is likely that the once-daily formulation of combination relugolix will be approved for this timeframe as well. Still, with patients’ mean age of 41–42 years, what will clinicians do after 2-year treatment? Clearly, study of long-term safety would be valuable. ●
Fibroids are extremely common in clinical practice, with their associated symptoms depending greatly on size and location. In many patients, symptoms are serious enough to be the most common indication for hysterectomy. In the past, combination oral contraceptives, injectable leuprolide acetate, and more recently, a GnRH antagonist given twice daily with estrogen/progestogen add-back have been utilized. The formulation described in Al-Hendy and colleagues’ study, which is dosed once per day and appears to not increase vasomotor symptoms or diminish bone mass, may provide a very nice “tool” in the clinician’s toolbox to either avoid any surgery in some patients (likely those aged closer to menopause) or optimize other patients preoperatively in terms of reversing anemia and reducing uterine volume, thus making any planned surgical procedure safer.
STEVEN R. GOLDSTEIN, MD, NCMP, CCD
Al-Hendy A, Lukes AS, Poindexter AN 3rd, et al. Treatment of uterine fibroid symptoms with relugolix combination therapy. N Engl J Med. 2021;384:630-642. doi: 10.1056/NEJMoa2008283
Expert Commentary
By age 50, approximately 70% of White women and 80% of Black women will have uterine fibroids.1 Of these, about 25% will have symptoms—most often including heavy menstrual bleeding,2 and associated pain the second most common symptom.3 First-line treatment has traditionally been hormonal contraceptives. Injectable gonadotropin-releasing hormone (GnRH) antagonist like leuprolide acetate have been commonly employed, although their actual approved indication is “for concomitant use with iron therapy for preoperative hematologic improvement of patients with anemia caused by uterine leiomyomata (fibroids).”4 Recently, an oral GnRH antagonist, elagolix, combined with estrogen and progestogen, was approved for treatment of uterine fibroids for up to 24 months. However, it is dosed twice per day because of its short half-life and results in a loss of bone mineral density at 1 year.5,6
Details of the studies
Al-Hendy and colleagues report on two double-blind 24-week phase 3 trials involving women with heavy menstrual bleeding associated with fibroids. There were just under 400 women in each trial. There was a 1:1:1 randomization to: placebo, once-daily oral relugolix 40 mg with 1 mg estradiol and 0.5 mg norethindrone acetate, or oral relugolix by itself for 12 weeks followed by the combination for 12 weeks (referred to as the “delayed relugolix combination therapy” arm).
Results. The primary end point was the percentage of patients who had a volume of menstrual blood loss less than 80 mL and a ≥50% reduction in blood loss volume as measured by the alkaline hematin method. The baseline blood loss in these studies ranged from approximately 210–250 mL. Secondary end points included amenorrhea, volume of menstrual blood loss, distress from bleeding and pelvic discomfort, anemia, pain, uterine volume, and the largest fibroid volume.
In trials one and two, 73% and 71% of patients in the relugolix combination groups, respectively, achieved the primary endpoint, compared with 19% and 15% in the placebo groups (P <.001). In addition, all secondary endpoints except largest fibroid volume were significantly improved versus placebo. Adverse events, including any change in bone mineral density, were no different between the combination and placebo groups. The delayed combination groups did have more hot flashes and diminished bone density compared with both the placebo and combination groups.
Strengths and weaknesses
The studies appropriately enrolled women with a mean age of 41–42 years and a mean BMI >30 kg/m2, and more than 50% were African American. Thus, the samples are adequately representative of the type of population most likely to have fibroids and associated symptoms. The results showed the advantages of built-in “add back therapy” with estrogen plus progestogen, as the vasomotor symptoms and bone loss that treatment with a GnRH antagonist alone produces were reduced.
Although the trials were only conducted for 24 weeks, efficacy was seen as early as 4 weeks, and was clearly maintained throughout the full trials—and there is no scientific reason to assume it would not be maintained indefinitely. However, one cannot make a similar assumption about long-term safety. As another GnRH antagonist, with a shorter half-life requiring twice-daily-dosing with add back therapy, has been approved for use for 2 years, it is likely that the once-daily formulation of combination relugolix will be approved for this timeframe as well. Still, with patients’ mean age of 41–42 years, what will clinicians do after 2-year treatment? Clearly, study of long-term safety would be valuable. ●
Fibroids are extremely common in clinical practice, with their associated symptoms depending greatly on size and location. In many patients, symptoms are serious enough to be the most common indication for hysterectomy. In the past, combination oral contraceptives, injectable leuprolide acetate, and more recently, a GnRH antagonist given twice daily with estrogen/progestogen add-back have been utilized. The formulation described in Al-Hendy and colleagues’ study, which is dosed once per day and appears to not increase vasomotor symptoms or diminish bone mass, may provide a very nice “tool” in the clinician’s toolbox to either avoid any surgery in some patients (likely those aged closer to menopause) or optimize other patients preoperatively in terms of reversing anemia and reducing uterine volume, thus making any planned surgical procedure safer.
STEVEN R. GOLDSTEIN, MD, NCMP, CCD
- Wise LA, Laughlin-Tommaso SK. Epidemiology of uterine fibroids: from menarche to menopause. Clin Obstet Gynecol. 2016;59:2-24.
- Borah BJ, Nicholson WK, Bradley L, et al. The impact of uterine leiomyomas: a national survey of affected women. Am J Obstet Gynecol. 2013;209:319.e1-319.e20.
- David M, Pitz CM, Mihaylova A, et al. Myoma-associated pain frequency and intensity: a retrospective evaluation of 1548 myoma patients. Eur J Obstet Gynecol Reprod Biol. 2016;199:137-140.
- Lupron Depot [package insert]. North Chicago, IL: AbbVie Inc.; 2018.
- Schlaff WD, Ackerman RT, Al-Hendy A, et al. Elagolix for heavy menstrual bleeding in women with uterine fibroids. N Engl J Med. 2020;382:328-340.
- Oriahnn [package insert]. North Chicago, IL: AbbVie Inc.; 2020.
- Wise LA, Laughlin-Tommaso SK. Epidemiology of uterine fibroids: from menarche to menopause. Clin Obstet Gynecol. 2016;59:2-24.
- Borah BJ, Nicholson WK, Bradley L, et al. The impact of uterine leiomyomas: a national survey of affected women. Am J Obstet Gynecol. 2013;209:319.e1-319.e20.
- David M, Pitz CM, Mihaylova A, et al. Myoma-associated pain frequency and intensity: a retrospective evaluation of 1548 myoma patients. Eur J Obstet Gynecol Reprod Biol. 2016;199:137-140.
- Lupron Depot [package insert]. North Chicago, IL: AbbVie Inc.; 2018.
- Schlaff WD, Ackerman RT, Al-Hendy A, et al. Elagolix for heavy menstrual bleeding in women with uterine fibroids. N Engl J Med. 2020;382:328-340.
- Oriahnn [package insert]. North Chicago, IL: AbbVie Inc.; 2020.
Optimize your treatment of endometriosis by using an FDA-approved hormonal medication
Women with endometriosis often present for medical care for one or more of the following health issues: pelvic pain, infertility, and/or an adnexal cyst (endometrioma). For women with moderate or severe pelvic pain and laparoscopically diagnosed endometriosis, hormone therapy is often necessary to achieve maximal long-term reduction in pain and optimize health. I focus on opportunities to optimize hormonal treatment of endometriosis in this editorial.
When plan A is not working, move expeditiously to plan B
Cyclic or continuous combination estrogen-progestin contraceptives are commonly prescribed to treat pelvic pain caused by endometriosis. Although endometriosis pain may initially improve with estrogen-progestin contraceptives, many women on this medication will eventually report that they have worsening pelvic pain that adversely impacts their daily activities. Surprisingly, clinicians often continue to prescribe estrogen-progestin contraceptives even after the patient reports that the treatment is not effective, and their pain continues to be bothersome.
Patients benefit when they have access to the full range of hormone treatments that have been approved by the FDA for the treatment of moderate to severe pelvic pain caused by endometriosis (TABLE). In the situation where an estrogen-progestin contraceptive is no longer effective at reducing the pelvic pain, I will often offer the patient the option of norethindrone acetate (NEA) or elagolix treatment. My experience is that stopping the estrogen-progestin contraceptive and starting NEA or elagolix will result in a significant decrease in pain symptoms and improvement in the patient’s quality of life.

Other FDA-approved options to treat pelvic pain caused by endometriosis include depot medroxyprogesterone acetate injectable suspension, depot leuprolide acetate, goserelin implant, and danazol. I do not routinely prescribe depot medroxyprogesterone acetate because some patients report new onset or worsening symptoms of depression on the medication. I prescribe depot-leuprolide acetate less often than in the past, because many patients report moderate to severe hypoestrogenic symptoms on this medication. In women taking depot-leuprolide acetate, moderate to severe vasomotor symptoms can be improved by prescribing NEA pills, but the alternative of norethindrone monotherapy is less expensive. I seldom use goserelin or danazol in my practice. The needle required to place the goserelin implant has a diameter of approximately 1.7 mm (16 gauge) or 2.1 mm (14 gauge), for the 3.6 mg and 10 mg doses, respectively. The large diameter of the needle can cause pain and bruising at the implant site. As a comparison, the progestin subdermal implant needle is approximately 2.1 mm in diameter. Danazol is associated with weight gain, and most women prefer to avoid this side effect.
Continue to: Norethindrone acetate...
Norethindrone acetate
NEA 5 mg daily is approved by the FDA to treat endometriosis.1 NEA was approved at a time when large controlled clinical trials were not routinely required for a medicine to be approved. The data to support NEA treatment of pelvic pain caused by endometriosis is based on cohort studies. In a study of 194 women, median age 21 years with moderate to severe pelvic pain and surgically proven endometriosis, the effect of NEA on pelvic pain was explored.2 The initial dose of NEA was 5 mg daily. If the patient did not achieve a reduction in pelvic pain and amenorrhea on the NEA dose of 5 mg daily, the dose was increased by 2.5 mg every 2 weeks, up to a maximum of 15 mg, until amenorrhea and/or a decrease in pelvic pain was achieved. Ninety-five percent of the women in this cohort had previously been treated with an estrogen-progestin contraceptive or a GnRH antagonist and had discontinued those medications because of inadequate control of pelvic pain or because of side effects of the medication.
In this large cohort, 65% of women reported significant improvement in pelvic pain, with a median pain score of 5 before treatment and 0 following NEA treatment. About 55% of the women reported no side effects. The most commonly reported side effects were weight gain (16%; mean weight gain, 3.1 kg), acne (10%), mood lability (9%), hot flashes (8%), depression (6%), scalp hair loss (4%), headache (4%), nausea (3%), and deepening of the voice (1%). (In this study women could report more than one side effect.)
In another cohort study of 52 women with pelvic pain and surgically confirmed endometriosis, NEA treatment resulted in pain relief in 94% of the women.3 Breakthrough bleeding was a common side effect, reported by 58% of participants. The investigators concluded that NEA treatment was a “cost-effective alternative with relatively mild side effects in the treatment of symptomatic endometriosis.” A conclusion which I endorse.
NEA has been reported to effectively treat ovarian endometriomas and rectovaginal endometriosis.4,5 In a cohort of 18 women who had previously had the surgical resection of an ovarian endometriosis cyst and had postoperative recurrence of pelvic pain and ovarian endometriosis, treatment was initiated with an escalating NEA regimen.4 Treatment was initiated with NEA 5 mg daily, with the dosage increased every 2 weeks by 2.5 mg until amenorrhea was established. Most women achieved amenorrhea with NEA 5 mg daily, and 89% had reduced pelvic pain. The investigators reported complete regression of the endometriosis cyst(s) in 74% of the women. In my experience, NEA does not result in complete regression of endometriosis cysts, but it does cause a reduction in cyst diameter and total volume.
In a retrospective cohort study, 61 women with pelvic pain and rectovaginal endometriosis had 5 years of treatment with NEA 2.5 mg or 5.0 mg daily.5 NEA treatment resulted in a decrease in dysmenorrhea, deep dyspareunia, and dyschezia. The most common side effects attributed to NEA treatment were weight gain (30%), vaginal bleeding (23%), decreased libido (11%), headache (9%), bloating or swelling (8%), depression (7%), and acne (5%). In women who had sequential imaging studies, NEA treatment resulted in a decrease in rectovaginal lesion volume, stable disease volume, or an increase in lesion volume in 56%, 32%, and 12% of the women, respectively. The investigators concluded that for women with rectovaginal endometriosis, NEA treatment is a low-cost option for long-term treatment.
In my practice, I do not prescribe NEA at doses greater than 5 mg daily. There are case reports that NEA at a dose of ≥10 mg daily is associated with the development of a hepatic adenoma,6 elevated liver transaminase concentration,7 and jaundice.8 If NEA 5 mg daily is not effective in controlling pelvic pain caused by endometriosis, I stop the NEA and start a GnRH analogue, most often elagolix.
NEA 5 mg is not FDA approved as a contraceptive. However, norethindrone 0.35 mg daily, also known as the “mini-pill”, is approved as a progestin-only contraceptive.9 NEA is rapidly and completely deacetylated to norethindrone, and the disposition of oral NEA is indistinguishable from that of norethindrone.1 Since norethindrone 0.35 mg daily is approved as a contraceptive, it is highly likely that NEA 5 mg has contraceptive properties if taken daily.
Continue to: Elagolix...
Elagolix
Elagolix is FDA approved for the treatment of pelvic pain caused by endometriosis. I reviewed the key studies resulting in FDA approval in the November 2018 issue of
In the Elaris Endometriosis-I study, 872 women with endometriosis and pelvic pain were randomly assigned to treatment with 1 of 2 doses of elagolix (high-dose [200 mg twice daily] and low-dose [150 mg once daily]) or placebo.11 After 3 months of therapy, a clinically meaningful reduction in dysmenorrhea pain was reported by 76%, 46%, and 20% of the women in the high-dose elagolix, low-dose elagolix, and placebo groups, respectively (P<.001 for comparisons of elagolix to placebo). After 3 months of therapy, a clinically meaningful reduction in nonmenstrual pain or decreased or stable use of rescue analgesics was reported by 55%, 50%, and 37% of the women in the high-dose elagolix, low-dose elagolix, and placebo groups, respectively (P<.01 low-dose elagolix vs placebo and P<.001 high-dose elagolix vs placebo).
Hot flashes that were severe enough to be reported as an adverse event by the study participants were reported by 42%, 24%, and 7% of the women in the high-dose elagolix, low-dose elagolix, and placebo groups. Bone density was measured at baseline and after 6 months of treatment. Lumbar bone density changes were -2.61%, -0.32%, and +0.47% and hip femoral neck bone density changes were -1.89%, -0.39%, and +0.02% in the high-dose elagolix, low-dose elagolix, and placebo groups, respectively.
Another large clinical trial of elagolix for the treatment of pelvic pain caused by endometriosis, Elaris EM-II, involving 817 women, produced results very similar to those reported in Elaris EM-I. The elagolix continuation studies, Elaris EM-III and -IV, demonstrated efficacy and safety of elagolix through 12 months of treatment.12
In my 2018 review,10 I noted that elagolix dose adjustment can be utilized to attempt to achieve maximal pain relief with minimal vasomotor symptoms. Elagolix at 200 mg twice daily produces a mean estradiol concentration of 12 pg/mL, whereas elagolix at 150 mg daily resulted in a mean estradiol concentration of 41 pg/mL.13 The estrogen threshold hypothesis posits that in women with endometriosis a stable estradiol concentration of 20 to 30 pg/mL is often associated with decreased pain and fewer vasomotor events.14 To achieve the target estradiol range of 20 to 30 pg/mL, I often initiate elagolix treatment with 200 mg twice daily. This enables a rapid onset of amenorrhea and a reduction in pelvic pain. Once amenorrhea has been achieved and a decrease in pelvic pain has occurred, I adjust the dose downward to 200 mg twice daily on even calendar days of each month and 200 mg once daily on odd calendar days each month. Some women will have continued pain relief and amenorrhea when the dose is further decreased to 200 mg once daily. If bothersome bleeding recurs and/or pain symptoms increase in severity, the dose can be increased to 200 mg twice daily or an alternating regimen of 200 mg twice daily and 200 mg once daily, every 2 days. An alternative to dose adjustment is to combine elagolix with NEA, which can reduce the severity of hot flashes and reduce bone loss caused by hypoestrogenism.15,16
Health insurers and pharmacy benefits managers may require a prior authorization before approving and dispensing elagolix. The prior authorization process can be burdensome for clinicians, consuming limited healthcare resources, contributing to burnout and frustrating patients.17 Elagolix is less expensive than depot-leuprolide acetate and nafarelin nasal spray and somewhat more expensive than a goserelin implant.18,19
Elagolix is not approved as a contraceptive. In the Elaris EM-I and -II trials women were advised to use 2 forms of contraception, although pregnancies did occur. There were 6 pregnancies among 475 women taking elagolix 150 mg daily and 2 pregnancies among 477 women taking elagolix 200 mg twice daily.20 Women taking elagolix should be advised to use a contraceptive, but not an estrogen-progestin contraceptive.
Continue to: Do not use opioids to treat chronic pelvic pain caused by endometriosis...
Do not use opioids to treat chronic pelvic pain caused by endometriosis
One of the greatest public health tragedies of our era is the opioid misuse epidemic. Hundreds of thousands of deaths have been caused by opioid misuse. The Centers for Disease Control and Prevention reported that for the 12-month period ending in May 2020, there were 81,000 opioid-related deaths, the greatest number ever reported in a 12-month period.21 Many authorities believe that in the United States opioid medications have been over-prescribed, contributing to the opioid misuse epidemic. There is little evidence that chronic pelvic pain is optimally managed by chronic treatment with an opioid.22,23 Prescribing opioids to vulnerable individuals to treat chronic pelvic pain may result in opioid dependency and adversely affect the patient’s health. It is best to pledge not to prescribe an opioid medication for a woman with chronic pelvic pain caused by endometriosis. In situations when pelvic pain is difficult to control with hormonal therapy and nonopioid pain medications, referral to a specialty pain practice may be warranted.
Post–conservative surgery hormone treatment reduces pelvic pain recurrence
In a meta-analysis of 14 studies that reported on endometriosis recurrence rates following conservative surgery, recurrence (defined as recurrent pelvic pain or an imaging study showing recurrent endometriosis) was significantly reduced with the use of hormone treatment compared with expectant management or placebo treatment.24 The postoperative relative risk of endometriosis recurrence was reduced by 83% with progestin treatment, 64% with estrogen-progestin contraceptive treatment, and 38% with GnRH analogue treatment. Overall, the number of patients that needed to be treated to prevent one endometriosis recurrence was 10, assuming a recurrence rate of 25% in the placebo treatment or expectant management groups.
For women with pelvic pain caused by endometriosis who develop a recurrence of pelvic pain while on postoperative hormone treatment, it is important for the prescribing clinician to be flexible and consider changing the hormone regimen. For example, if a postoperative patient is treated with a continuous estrogen-progestin contraceptive and develops recurrent pain, I will stop the contraceptive and initiate treatment with either NEA or elagolix.
Capitalize on opportunities to improve the medical care of women with endometriosis
Early diagnosis of endometriosis can be facilitated by recognizing that the condition is a common cause of moderate to severe dysmenorrhea. In 5 studies involving 1,187 women, the mean length of time from onset of pelvic pain symptoms to diagnosis of endometriosis was 8.6 years.25 If a woman with pelvic pain caused by endometriosis has not had sufficient pain relief with one brand of continuous estrogen-progestin contraceptive, it is best not to prescribe an alternative brand but rather to switch to a progestin-only treatment or a GnRH antagonist. If plan A is not working, move expeditiously to plan B. ●
- Aygestin [package insert]. Barr Laboratories: Pomona, NY; 2007.
- Kaser DJ, Missmer SA, Berry KF, et al. Use of norethindrone acetate alone for postoperative suppression of endometriosis symptoms. J Pediatr Adolesc Gynecol. 2012;25:105-108.
- Muneyyirci-Delale O, Karacan M. Effect of norethindrone acetate in the treatment of symptomatic endometriosis. Int J Fertil Womens Med. 1998;43:24-27.
- Muneyyirci-Delale O, Anopa J, Charles C, et al. Medical management of recurrent endometrioma with long-term norethindrone acetate. Int J Women Health. 2012;4:149-154.
- Morotti M, Venturini PL, Biscaldi E, et al. Efficacy and acceptability of long-term norethindrone acetate for the treatment of rectovaginal endometriosis. Eur J Obstet Gynecol Repro Biol. 2017;213:4-10.
- Brady PC, Missmer SA, Laufer MR. Hepatic adenomas in adolescents and young women with endometriosis treated with norethindrone acetate. J Pediatr Adolesc Gynecol. 2017;30:422-424.
- Choudhary NS, Bodh V, Chaudhari S, et al. Norethisterone related drug induced liver injury: a series of 3 cases. J Clin Exp Hepatol. 2017;7:266- 268.
- Perez-Mera RA, Shields CE. Jaundice associated with norethindrone acetate therapy. N Engl J Med. 1962;267:1137-1138.
- Camila [package insert]. Mayne Pharma Inc: Greenville, NC; 2018.
- Barbieri RL. Elagolix: a new treatment for pelvic pain caused by endometriosis. OBG Manag. 2018;30:10,12-14, 20.
- Taylor HS, Giudice LC, Lessey BA, et al. Treatment of endometriosis-associated pain with elagolix, an oral GnRH antagonist. N Engl J Med. 2017;377:28-40.
- Surrey E, Taylor HS, Giudice L, et al. Long-term outcomes of elagolix in women with endometriosis: results from two extension studies. Obstet Gynecol. 2018;132:147-160.
- Orilissa [package insert]. AbbVie Inc; North Chicago, IL; 2018.
- Barbieri RL. Hormonal treatment of endometriosis: the estrogen threshold hypothesis. Am J Obstet Gynecol. 1992;166:740-745.
- Hornstein MD, Surrey ES, Weisberg GW, et al. Leuprolide acetate depot and hormonal add-back in endometriosis: a 12-month study. Lupron Add-Back Study Group. Obstet Gynecol. 1998;91:16-24.
- Gallagher JS, Missmer SA, Hornstein MD, et al. Long-term effects of gonadotropin-releasing hormone agonists and add-back in adolescent endometriosis. J Pediatr Adolesc Gynecol. 2018;31:376- 381.
- Miller A, Shor R, Waites T, et al. Prior authorization reform for better patient care. J Am Coll Cardiol. 2018;71:1937-1939.
- Depot-leuprolide acetate. Good Rx website. https://www.goodrx.com/. Accessed January 22, 2021.
- Goserelin. Good Rx website. https://www .goodrx.com/. Accessed January 22, 2021
- Taylor HS, Giudice LC, Lessey BA, et al. Treatment of endometriosis-associated pain with elagolix, an oral GnRH antagonist. N Engl J Med. 2017;377:28-40.
- Centers for Disease Control and Prevention. Overdose deaths accelerating during COVID19. https://www.cdc.gov/media/releases/2020 /p1218-overdose-deaths-covid-19.html. Reviewed December 18, 2020. Accessed March 24, 2021.
- Till SR, As-Sanie S. 3 cases of chronic pelvic pain with nonsurgical, nonopioid therapies. OBG Manag. 2018;30:41-48.
- Steele A. Opioid use and depression in chronic pelvic pain. Obstet Gynecol Clin North Am. 2014;41:491-501.
- Zakhari A, Delpero E, McKeown S, et al. Endometriosis recurrence following post-operative hormonal suppression: a systematic review and meta-analysis. Hum Reprod Update. 2021;27:96- 107.
- Barbieri RL. Why are there delays in the diagnosis of endometriosis? OBG Manag. 2017;29:8, 10-11, 16.
Women with endometriosis often present for medical care for one or more of the following health issues: pelvic pain, infertility, and/or an adnexal cyst (endometrioma). For women with moderate or severe pelvic pain and laparoscopically diagnosed endometriosis, hormone therapy is often necessary to achieve maximal long-term reduction in pain and optimize health. I focus on opportunities to optimize hormonal treatment of endometriosis in this editorial.
When plan A is not working, move expeditiously to plan B
Cyclic or continuous combination estrogen-progestin contraceptives are commonly prescribed to treat pelvic pain caused by endometriosis. Although endometriosis pain may initially improve with estrogen-progestin contraceptives, many women on this medication will eventually report that they have worsening pelvic pain that adversely impacts their daily activities. Surprisingly, clinicians often continue to prescribe estrogen-progestin contraceptives even after the patient reports that the treatment is not effective, and their pain continues to be bothersome.
Patients benefit when they have access to the full range of hormone treatments that have been approved by the FDA for the treatment of moderate to severe pelvic pain caused by endometriosis (TABLE). In the situation where an estrogen-progestin contraceptive is no longer effective at reducing the pelvic pain, I will often offer the patient the option of norethindrone acetate (NEA) or elagolix treatment. My experience is that stopping the estrogen-progestin contraceptive and starting NEA or elagolix will result in a significant decrease in pain symptoms and improvement in the patient’s quality of life.

Other FDA-approved options to treat pelvic pain caused by endometriosis include depot medroxyprogesterone acetate injectable suspension, depot leuprolide acetate, goserelin implant, and danazol. I do not routinely prescribe depot medroxyprogesterone acetate because some patients report new onset or worsening symptoms of depression on the medication. I prescribe depot-leuprolide acetate less often than in the past, because many patients report moderate to severe hypoestrogenic symptoms on this medication. In women taking depot-leuprolide acetate, moderate to severe vasomotor symptoms can be improved by prescribing NEA pills, but the alternative of norethindrone monotherapy is less expensive. I seldom use goserelin or danazol in my practice. The needle required to place the goserelin implant has a diameter of approximately 1.7 mm (16 gauge) or 2.1 mm (14 gauge), for the 3.6 mg and 10 mg doses, respectively. The large diameter of the needle can cause pain and bruising at the implant site. As a comparison, the progestin subdermal implant needle is approximately 2.1 mm in diameter. Danazol is associated with weight gain, and most women prefer to avoid this side effect.
Continue to: Norethindrone acetate...
Norethindrone acetate
NEA 5 mg daily is approved by the FDA to treat endometriosis.1 NEA was approved at a time when large controlled clinical trials were not routinely required for a medicine to be approved. The data to support NEA treatment of pelvic pain caused by endometriosis is based on cohort studies. In a study of 194 women, median age 21 years with moderate to severe pelvic pain and surgically proven endometriosis, the effect of NEA on pelvic pain was explored.2 The initial dose of NEA was 5 mg daily. If the patient did not achieve a reduction in pelvic pain and amenorrhea on the NEA dose of 5 mg daily, the dose was increased by 2.5 mg every 2 weeks, up to a maximum of 15 mg, until amenorrhea and/or a decrease in pelvic pain was achieved. Ninety-five percent of the women in this cohort had previously been treated with an estrogen-progestin contraceptive or a GnRH antagonist and had discontinued those medications because of inadequate control of pelvic pain or because of side effects of the medication.
In this large cohort, 65% of women reported significant improvement in pelvic pain, with a median pain score of 5 before treatment and 0 following NEA treatment. About 55% of the women reported no side effects. The most commonly reported side effects were weight gain (16%; mean weight gain, 3.1 kg), acne (10%), mood lability (9%), hot flashes (8%), depression (6%), scalp hair loss (4%), headache (4%), nausea (3%), and deepening of the voice (1%). (In this study women could report more than one side effect.)
In another cohort study of 52 women with pelvic pain and surgically confirmed endometriosis, NEA treatment resulted in pain relief in 94% of the women.3 Breakthrough bleeding was a common side effect, reported by 58% of participants. The investigators concluded that NEA treatment was a “cost-effective alternative with relatively mild side effects in the treatment of symptomatic endometriosis.” A conclusion which I endorse.
NEA has been reported to effectively treat ovarian endometriomas and rectovaginal endometriosis.4,5 In a cohort of 18 women who had previously had the surgical resection of an ovarian endometriosis cyst and had postoperative recurrence of pelvic pain and ovarian endometriosis, treatment was initiated with an escalating NEA regimen.4 Treatment was initiated with NEA 5 mg daily, with the dosage increased every 2 weeks by 2.5 mg until amenorrhea was established. Most women achieved amenorrhea with NEA 5 mg daily, and 89% had reduced pelvic pain. The investigators reported complete regression of the endometriosis cyst(s) in 74% of the women. In my experience, NEA does not result in complete regression of endometriosis cysts, but it does cause a reduction in cyst diameter and total volume.
In a retrospective cohort study, 61 women with pelvic pain and rectovaginal endometriosis had 5 years of treatment with NEA 2.5 mg or 5.0 mg daily.5 NEA treatment resulted in a decrease in dysmenorrhea, deep dyspareunia, and dyschezia. The most common side effects attributed to NEA treatment were weight gain (30%), vaginal bleeding (23%), decreased libido (11%), headache (9%), bloating or swelling (8%), depression (7%), and acne (5%). In women who had sequential imaging studies, NEA treatment resulted in a decrease in rectovaginal lesion volume, stable disease volume, or an increase in lesion volume in 56%, 32%, and 12% of the women, respectively. The investigators concluded that for women with rectovaginal endometriosis, NEA treatment is a low-cost option for long-term treatment.
In my practice, I do not prescribe NEA at doses greater than 5 mg daily. There are case reports that NEA at a dose of ≥10 mg daily is associated with the development of a hepatic adenoma,6 elevated liver transaminase concentration,7 and jaundice.8 If NEA 5 mg daily is not effective in controlling pelvic pain caused by endometriosis, I stop the NEA and start a GnRH analogue, most often elagolix.
NEA 5 mg is not FDA approved as a contraceptive. However, norethindrone 0.35 mg daily, also known as the “mini-pill”, is approved as a progestin-only contraceptive.9 NEA is rapidly and completely deacetylated to norethindrone, and the disposition of oral NEA is indistinguishable from that of norethindrone.1 Since norethindrone 0.35 mg daily is approved as a contraceptive, it is highly likely that NEA 5 mg has contraceptive properties if taken daily.
Continue to: Elagolix...
Elagolix
Elagolix is FDA approved for the treatment of pelvic pain caused by endometriosis. I reviewed the key studies resulting in FDA approval in the November 2018 issue of
In the Elaris Endometriosis-I study, 872 women with endometriosis and pelvic pain were randomly assigned to treatment with 1 of 2 doses of elagolix (high-dose [200 mg twice daily] and low-dose [150 mg once daily]) or placebo.11 After 3 months of therapy, a clinically meaningful reduction in dysmenorrhea pain was reported by 76%, 46%, and 20% of the women in the high-dose elagolix, low-dose elagolix, and placebo groups, respectively (P<.001 for comparisons of elagolix to placebo). After 3 months of therapy, a clinically meaningful reduction in nonmenstrual pain or decreased or stable use of rescue analgesics was reported by 55%, 50%, and 37% of the women in the high-dose elagolix, low-dose elagolix, and placebo groups, respectively (P<.01 low-dose elagolix vs placebo and P<.001 high-dose elagolix vs placebo).
Hot flashes that were severe enough to be reported as an adverse event by the study participants were reported by 42%, 24%, and 7% of the women in the high-dose elagolix, low-dose elagolix, and placebo groups. Bone density was measured at baseline and after 6 months of treatment. Lumbar bone density changes were -2.61%, -0.32%, and +0.47% and hip femoral neck bone density changes were -1.89%, -0.39%, and +0.02% in the high-dose elagolix, low-dose elagolix, and placebo groups, respectively.
Another large clinical trial of elagolix for the treatment of pelvic pain caused by endometriosis, Elaris EM-II, involving 817 women, produced results very similar to those reported in Elaris EM-I. The elagolix continuation studies, Elaris EM-III and -IV, demonstrated efficacy and safety of elagolix through 12 months of treatment.12
In my 2018 review,10 I noted that elagolix dose adjustment can be utilized to attempt to achieve maximal pain relief with minimal vasomotor symptoms. Elagolix at 200 mg twice daily produces a mean estradiol concentration of 12 pg/mL, whereas elagolix at 150 mg daily resulted in a mean estradiol concentration of 41 pg/mL.13 The estrogen threshold hypothesis posits that in women with endometriosis a stable estradiol concentration of 20 to 30 pg/mL is often associated with decreased pain and fewer vasomotor events.14 To achieve the target estradiol range of 20 to 30 pg/mL, I often initiate elagolix treatment with 200 mg twice daily. This enables a rapid onset of amenorrhea and a reduction in pelvic pain. Once amenorrhea has been achieved and a decrease in pelvic pain has occurred, I adjust the dose downward to 200 mg twice daily on even calendar days of each month and 200 mg once daily on odd calendar days each month. Some women will have continued pain relief and amenorrhea when the dose is further decreased to 200 mg once daily. If bothersome bleeding recurs and/or pain symptoms increase in severity, the dose can be increased to 200 mg twice daily or an alternating regimen of 200 mg twice daily and 200 mg once daily, every 2 days. An alternative to dose adjustment is to combine elagolix with NEA, which can reduce the severity of hot flashes and reduce bone loss caused by hypoestrogenism.15,16
Health insurers and pharmacy benefits managers may require a prior authorization before approving and dispensing elagolix. The prior authorization process can be burdensome for clinicians, consuming limited healthcare resources, contributing to burnout and frustrating patients.17 Elagolix is less expensive than depot-leuprolide acetate and nafarelin nasal spray and somewhat more expensive than a goserelin implant.18,19
Elagolix is not approved as a contraceptive. In the Elaris EM-I and -II trials women were advised to use 2 forms of contraception, although pregnancies did occur. There were 6 pregnancies among 475 women taking elagolix 150 mg daily and 2 pregnancies among 477 women taking elagolix 200 mg twice daily.20 Women taking elagolix should be advised to use a contraceptive, but not an estrogen-progestin contraceptive.
Continue to: Do not use opioids to treat chronic pelvic pain caused by endometriosis...
Do not use opioids to treat chronic pelvic pain caused by endometriosis
One of the greatest public health tragedies of our era is the opioid misuse epidemic. Hundreds of thousands of deaths have been caused by opioid misuse. The Centers for Disease Control and Prevention reported that for the 12-month period ending in May 2020, there were 81,000 opioid-related deaths, the greatest number ever reported in a 12-month period.21 Many authorities believe that in the United States opioid medications have been over-prescribed, contributing to the opioid misuse epidemic. There is little evidence that chronic pelvic pain is optimally managed by chronic treatment with an opioid.22,23 Prescribing opioids to vulnerable individuals to treat chronic pelvic pain may result in opioid dependency and adversely affect the patient’s health. It is best to pledge not to prescribe an opioid medication for a woman with chronic pelvic pain caused by endometriosis. In situations when pelvic pain is difficult to control with hormonal therapy and nonopioid pain medications, referral to a specialty pain practice may be warranted.
Post–conservative surgery hormone treatment reduces pelvic pain recurrence
In a meta-analysis of 14 studies that reported on endometriosis recurrence rates following conservative surgery, recurrence (defined as recurrent pelvic pain or an imaging study showing recurrent endometriosis) was significantly reduced with the use of hormone treatment compared with expectant management or placebo treatment.24 The postoperative relative risk of endometriosis recurrence was reduced by 83% with progestin treatment, 64% with estrogen-progestin contraceptive treatment, and 38% with GnRH analogue treatment. Overall, the number of patients that needed to be treated to prevent one endometriosis recurrence was 10, assuming a recurrence rate of 25% in the placebo treatment or expectant management groups.
For women with pelvic pain caused by endometriosis who develop a recurrence of pelvic pain while on postoperative hormone treatment, it is important for the prescribing clinician to be flexible and consider changing the hormone regimen. For example, if a postoperative patient is treated with a continuous estrogen-progestin contraceptive and develops recurrent pain, I will stop the contraceptive and initiate treatment with either NEA or elagolix.
Capitalize on opportunities to improve the medical care of women with endometriosis
Early diagnosis of endometriosis can be facilitated by recognizing that the condition is a common cause of moderate to severe dysmenorrhea. In 5 studies involving 1,187 women, the mean length of time from onset of pelvic pain symptoms to diagnosis of endometriosis was 8.6 years.25 If a woman with pelvic pain caused by endometriosis has not had sufficient pain relief with one brand of continuous estrogen-progestin contraceptive, it is best not to prescribe an alternative brand but rather to switch to a progestin-only treatment or a GnRH antagonist. If plan A is not working, move expeditiously to plan B. ●
Women with endometriosis often present for medical care for one or more of the following health issues: pelvic pain, infertility, and/or an adnexal cyst (endometrioma). For women with moderate or severe pelvic pain and laparoscopically diagnosed endometriosis, hormone therapy is often necessary to achieve maximal long-term reduction in pain and optimize health. I focus on opportunities to optimize hormonal treatment of endometriosis in this editorial.
When plan A is not working, move expeditiously to plan B
Cyclic or continuous combination estrogen-progestin contraceptives are commonly prescribed to treat pelvic pain caused by endometriosis. Although endometriosis pain may initially improve with estrogen-progestin contraceptives, many women on this medication will eventually report that they have worsening pelvic pain that adversely impacts their daily activities. Surprisingly, clinicians often continue to prescribe estrogen-progestin contraceptives even after the patient reports that the treatment is not effective, and their pain continues to be bothersome.
Patients benefit when they have access to the full range of hormone treatments that have been approved by the FDA for the treatment of moderate to severe pelvic pain caused by endometriosis (TABLE). In the situation where an estrogen-progestin contraceptive is no longer effective at reducing the pelvic pain, I will often offer the patient the option of norethindrone acetate (NEA) or elagolix treatment. My experience is that stopping the estrogen-progestin contraceptive and starting NEA or elagolix will result in a significant decrease in pain symptoms and improvement in the patient’s quality of life.

Other FDA-approved options to treat pelvic pain caused by endometriosis include depot medroxyprogesterone acetate injectable suspension, depot leuprolide acetate, goserelin implant, and danazol. I do not routinely prescribe depot medroxyprogesterone acetate because some patients report new onset or worsening symptoms of depression on the medication. I prescribe depot-leuprolide acetate less often than in the past, because many patients report moderate to severe hypoestrogenic symptoms on this medication. In women taking depot-leuprolide acetate, moderate to severe vasomotor symptoms can be improved by prescribing NEA pills, but the alternative of norethindrone monotherapy is less expensive. I seldom use goserelin or danazol in my practice. The needle required to place the goserelin implant has a diameter of approximately 1.7 mm (16 gauge) or 2.1 mm (14 gauge), for the 3.6 mg and 10 mg doses, respectively. The large diameter of the needle can cause pain and bruising at the implant site. As a comparison, the progestin subdermal implant needle is approximately 2.1 mm in diameter. Danazol is associated with weight gain, and most women prefer to avoid this side effect.
Continue to: Norethindrone acetate...
Norethindrone acetate
NEA 5 mg daily is approved by the FDA to treat endometriosis.1 NEA was approved at a time when large controlled clinical trials were not routinely required for a medicine to be approved. The data to support NEA treatment of pelvic pain caused by endometriosis is based on cohort studies. In a study of 194 women, median age 21 years with moderate to severe pelvic pain and surgically proven endometriosis, the effect of NEA on pelvic pain was explored.2 The initial dose of NEA was 5 mg daily. If the patient did not achieve a reduction in pelvic pain and amenorrhea on the NEA dose of 5 mg daily, the dose was increased by 2.5 mg every 2 weeks, up to a maximum of 15 mg, until amenorrhea and/or a decrease in pelvic pain was achieved. Ninety-five percent of the women in this cohort had previously been treated with an estrogen-progestin contraceptive or a GnRH antagonist and had discontinued those medications because of inadequate control of pelvic pain or because of side effects of the medication.
In this large cohort, 65% of women reported significant improvement in pelvic pain, with a median pain score of 5 before treatment and 0 following NEA treatment. About 55% of the women reported no side effects. The most commonly reported side effects were weight gain (16%; mean weight gain, 3.1 kg), acne (10%), mood lability (9%), hot flashes (8%), depression (6%), scalp hair loss (4%), headache (4%), nausea (3%), and deepening of the voice (1%). (In this study women could report more than one side effect.)
In another cohort study of 52 women with pelvic pain and surgically confirmed endometriosis, NEA treatment resulted in pain relief in 94% of the women.3 Breakthrough bleeding was a common side effect, reported by 58% of participants. The investigators concluded that NEA treatment was a “cost-effective alternative with relatively mild side effects in the treatment of symptomatic endometriosis.” A conclusion which I endorse.
NEA has been reported to effectively treat ovarian endometriomas and rectovaginal endometriosis.4,5 In a cohort of 18 women who had previously had the surgical resection of an ovarian endometriosis cyst and had postoperative recurrence of pelvic pain and ovarian endometriosis, treatment was initiated with an escalating NEA regimen.4 Treatment was initiated with NEA 5 mg daily, with the dosage increased every 2 weeks by 2.5 mg until amenorrhea was established. Most women achieved amenorrhea with NEA 5 mg daily, and 89% had reduced pelvic pain. The investigators reported complete regression of the endometriosis cyst(s) in 74% of the women. In my experience, NEA does not result in complete regression of endometriosis cysts, but it does cause a reduction in cyst diameter and total volume.
In a retrospective cohort study, 61 women with pelvic pain and rectovaginal endometriosis had 5 years of treatment with NEA 2.5 mg or 5.0 mg daily.5 NEA treatment resulted in a decrease in dysmenorrhea, deep dyspareunia, and dyschezia. The most common side effects attributed to NEA treatment were weight gain (30%), vaginal bleeding (23%), decreased libido (11%), headache (9%), bloating or swelling (8%), depression (7%), and acne (5%). In women who had sequential imaging studies, NEA treatment resulted in a decrease in rectovaginal lesion volume, stable disease volume, or an increase in lesion volume in 56%, 32%, and 12% of the women, respectively. The investigators concluded that for women with rectovaginal endometriosis, NEA treatment is a low-cost option for long-term treatment.
In my practice, I do not prescribe NEA at doses greater than 5 mg daily. There are case reports that NEA at a dose of ≥10 mg daily is associated with the development of a hepatic adenoma,6 elevated liver transaminase concentration,7 and jaundice.8 If NEA 5 mg daily is not effective in controlling pelvic pain caused by endometriosis, I stop the NEA and start a GnRH analogue, most often elagolix.
NEA 5 mg is not FDA approved as a contraceptive. However, norethindrone 0.35 mg daily, also known as the “mini-pill”, is approved as a progestin-only contraceptive.9 NEA is rapidly and completely deacetylated to norethindrone, and the disposition of oral NEA is indistinguishable from that of norethindrone.1 Since norethindrone 0.35 mg daily is approved as a contraceptive, it is highly likely that NEA 5 mg has contraceptive properties if taken daily.
Continue to: Elagolix...
Elagolix
Elagolix is FDA approved for the treatment of pelvic pain caused by endometriosis. I reviewed the key studies resulting in FDA approval in the November 2018 issue of
In the Elaris Endometriosis-I study, 872 women with endometriosis and pelvic pain were randomly assigned to treatment with 1 of 2 doses of elagolix (high-dose [200 mg twice daily] and low-dose [150 mg once daily]) or placebo.11 After 3 months of therapy, a clinically meaningful reduction in dysmenorrhea pain was reported by 76%, 46%, and 20% of the women in the high-dose elagolix, low-dose elagolix, and placebo groups, respectively (P<.001 for comparisons of elagolix to placebo). After 3 months of therapy, a clinically meaningful reduction in nonmenstrual pain or decreased or stable use of rescue analgesics was reported by 55%, 50%, and 37% of the women in the high-dose elagolix, low-dose elagolix, and placebo groups, respectively (P<.01 low-dose elagolix vs placebo and P<.001 high-dose elagolix vs placebo).
Hot flashes that were severe enough to be reported as an adverse event by the study participants were reported by 42%, 24%, and 7% of the women in the high-dose elagolix, low-dose elagolix, and placebo groups. Bone density was measured at baseline and after 6 months of treatment. Lumbar bone density changes were -2.61%, -0.32%, and +0.47% and hip femoral neck bone density changes were -1.89%, -0.39%, and +0.02% in the high-dose elagolix, low-dose elagolix, and placebo groups, respectively.
Another large clinical trial of elagolix for the treatment of pelvic pain caused by endometriosis, Elaris EM-II, involving 817 women, produced results very similar to those reported in Elaris EM-I. The elagolix continuation studies, Elaris EM-III and -IV, demonstrated efficacy and safety of elagolix through 12 months of treatment.12
In my 2018 review,10 I noted that elagolix dose adjustment can be utilized to attempt to achieve maximal pain relief with minimal vasomotor symptoms. Elagolix at 200 mg twice daily produces a mean estradiol concentration of 12 pg/mL, whereas elagolix at 150 mg daily resulted in a mean estradiol concentration of 41 pg/mL.13 The estrogen threshold hypothesis posits that in women with endometriosis a stable estradiol concentration of 20 to 30 pg/mL is often associated with decreased pain and fewer vasomotor events.14 To achieve the target estradiol range of 20 to 30 pg/mL, I often initiate elagolix treatment with 200 mg twice daily. This enables a rapid onset of amenorrhea and a reduction in pelvic pain. Once amenorrhea has been achieved and a decrease in pelvic pain has occurred, I adjust the dose downward to 200 mg twice daily on even calendar days of each month and 200 mg once daily on odd calendar days each month. Some women will have continued pain relief and amenorrhea when the dose is further decreased to 200 mg once daily. If bothersome bleeding recurs and/or pain symptoms increase in severity, the dose can be increased to 200 mg twice daily or an alternating regimen of 200 mg twice daily and 200 mg once daily, every 2 days. An alternative to dose adjustment is to combine elagolix with NEA, which can reduce the severity of hot flashes and reduce bone loss caused by hypoestrogenism.15,16
Health insurers and pharmacy benefits managers may require a prior authorization before approving and dispensing elagolix. The prior authorization process can be burdensome for clinicians, consuming limited healthcare resources, contributing to burnout and frustrating patients.17 Elagolix is less expensive than depot-leuprolide acetate and nafarelin nasal spray and somewhat more expensive than a goserelin implant.18,19
Elagolix is not approved as a contraceptive. In the Elaris EM-I and -II trials women were advised to use 2 forms of contraception, although pregnancies did occur. There were 6 pregnancies among 475 women taking elagolix 150 mg daily and 2 pregnancies among 477 women taking elagolix 200 mg twice daily.20 Women taking elagolix should be advised to use a contraceptive, but not an estrogen-progestin contraceptive.
Continue to: Do not use opioids to treat chronic pelvic pain caused by endometriosis...
Do not use opioids to treat chronic pelvic pain caused by endometriosis
One of the greatest public health tragedies of our era is the opioid misuse epidemic. Hundreds of thousands of deaths have been caused by opioid misuse. The Centers for Disease Control and Prevention reported that for the 12-month period ending in May 2020, there were 81,000 opioid-related deaths, the greatest number ever reported in a 12-month period.21 Many authorities believe that in the United States opioid medications have been over-prescribed, contributing to the opioid misuse epidemic. There is little evidence that chronic pelvic pain is optimally managed by chronic treatment with an opioid.22,23 Prescribing opioids to vulnerable individuals to treat chronic pelvic pain may result in opioid dependency and adversely affect the patient’s health. It is best to pledge not to prescribe an opioid medication for a woman with chronic pelvic pain caused by endometriosis. In situations when pelvic pain is difficult to control with hormonal therapy and nonopioid pain medications, referral to a specialty pain practice may be warranted.
Post–conservative surgery hormone treatment reduces pelvic pain recurrence
In a meta-analysis of 14 studies that reported on endometriosis recurrence rates following conservative surgery, recurrence (defined as recurrent pelvic pain or an imaging study showing recurrent endometriosis) was significantly reduced with the use of hormone treatment compared with expectant management or placebo treatment.24 The postoperative relative risk of endometriosis recurrence was reduced by 83% with progestin treatment, 64% with estrogen-progestin contraceptive treatment, and 38% with GnRH analogue treatment. Overall, the number of patients that needed to be treated to prevent one endometriosis recurrence was 10, assuming a recurrence rate of 25% in the placebo treatment or expectant management groups.
For women with pelvic pain caused by endometriosis who develop a recurrence of pelvic pain while on postoperative hormone treatment, it is important for the prescribing clinician to be flexible and consider changing the hormone regimen. For example, if a postoperative patient is treated with a continuous estrogen-progestin contraceptive and develops recurrent pain, I will stop the contraceptive and initiate treatment with either NEA or elagolix.
Capitalize on opportunities to improve the medical care of women with endometriosis
Early diagnosis of endometriosis can be facilitated by recognizing that the condition is a common cause of moderate to severe dysmenorrhea. In 5 studies involving 1,187 women, the mean length of time from onset of pelvic pain symptoms to diagnosis of endometriosis was 8.6 years.25 If a woman with pelvic pain caused by endometriosis has not had sufficient pain relief with one brand of continuous estrogen-progestin contraceptive, it is best not to prescribe an alternative brand but rather to switch to a progestin-only treatment or a GnRH antagonist. If plan A is not working, move expeditiously to plan B. ●
- Aygestin [package insert]. Barr Laboratories: Pomona, NY; 2007.
- Kaser DJ, Missmer SA, Berry KF, et al. Use of norethindrone acetate alone for postoperative suppression of endometriosis symptoms. J Pediatr Adolesc Gynecol. 2012;25:105-108.
- Muneyyirci-Delale O, Karacan M. Effect of norethindrone acetate in the treatment of symptomatic endometriosis. Int J Fertil Womens Med. 1998;43:24-27.
- Muneyyirci-Delale O, Anopa J, Charles C, et al. Medical management of recurrent endometrioma with long-term norethindrone acetate. Int J Women Health. 2012;4:149-154.
- Morotti M, Venturini PL, Biscaldi E, et al. Efficacy and acceptability of long-term norethindrone acetate for the treatment of rectovaginal endometriosis. Eur J Obstet Gynecol Repro Biol. 2017;213:4-10.
- Brady PC, Missmer SA, Laufer MR. Hepatic adenomas in adolescents and young women with endometriosis treated with norethindrone acetate. J Pediatr Adolesc Gynecol. 2017;30:422-424.
- Choudhary NS, Bodh V, Chaudhari S, et al. Norethisterone related drug induced liver injury: a series of 3 cases. J Clin Exp Hepatol. 2017;7:266- 268.
- Perez-Mera RA, Shields CE. Jaundice associated with norethindrone acetate therapy. N Engl J Med. 1962;267:1137-1138.
- Camila [package insert]. Mayne Pharma Inc: Greenville, NC; 2018.
- Barbieri RL. Elagolix: a new treatment for pelvic pain caused by endometriosis. OBG Manag. 2018;30:10,12-14, 20.
- Taylor HS, Giudice LC, Lessey BA, et al. Treatment of endometriosis-associated pain with elagolix, an oral GnRH antagonist. N Engl J Med. 2017;377:28-40.
- Surrey E, Taylor HS, Giudice L, et al. Long-term outcomes of elagolix in women with endometriosis: results from two extension studies. Obstet Gynecol. 2018;132:147-160.
- Orilissa [package insert]. AbbVie Inc; North Chicago, IL; 2018.
- Barbieri RL. Hormonal treatment of endometriosis: the estrogen threshold hypothesis. Am J Obstet Gynecol. 1992;166:740-745.
- Hornstein MD, Surrey ES, Weisberg GW, et al. Leuprolide acetate depot and hormonal add-back in endometriosis: a 12-month study. Lupron Add-Back Study Group. Obstet Gynecol. 1998;91:16-24.
- Gallagher JS, Missmer SA, Hornstein MD, et al. Long-term effects of gonadotropin-releasing hormone agonists and add-back in adolescent endometriosis. J Pediatr Adolesc Gynecol. 2018;31:376- 381.
- Miller A, Shor R, Waites T, et al. Prior authorization reform for better patient care. J Am Coll Cardiol. 2018;71:1937-1939.
- Depot-leuprolide acetate. Good Rx website. https://www.goodrx.com/. Accessed January 22, 2021.
- Goserelin. Good Rx website. https://www .goodrx.com/. Accessed January 22, 2021
- Taylor HS, Giudice LC, Lessey BA, et al. Treatment of endometriosis-associated pain with elagolix, an oral GnRH antagonist. N Engl J Med. 2017;377:28-40.
- Centers for Disease Control and Prevention. Overdose deaths accelerating during COVID19. https://www.cdc.gov/media/releases/2020 /p1218-overdose-deaths-covid-19.html. Reviewed December 18, 2020. Accessed March 24, 2021.
- Till SR, As-Sanie S. 3 cases of chronic pelvic pain with nonsurgical, nonopioid therapies. OBG Manag. 2018;30:41-48.
- Steele A. Opioid use and depression in chronic pelvic pain. Obstet Gynecol Clin North Am. 2014;41:491-501.
- Zakhari A, Delpero E, McKeown S, et al. Endometriosis recurrence following post-operative hormonal suppression: a systematic review and meta-analysis. Hum Reprod Update. 2021;27:96- 107.
- Barbieri RL. Why are there delays in the diagnosis of endometriosis? OBG Manag. 2017;29:8, 10-11, 16.
- Aygestin [package insert]. Barr Laboratories: Pomona, NY; 2007.
- Kaser DJ, Missmer SA, Berry KF, et al. Use of norethindrone acetate alone for postoperative suppression of endometriosis symptoms. J Pediatr Adolesc Gynecol. 2012;25:105-108.
- Muneyyirci-Delale O, Karacan M. Effect of norethindrone acetate in the treatment of symptomatic endometriosis. Int J Fertil Womens Med. 1998;43:24-27.
- Muneyyirci-Delale O, Anopa J, Charles C, et al. Medical management of recurrent endometrioma with long-term norethindrone acetate. Int J Women Health. 2012;4:149-154.
- Morotti M, Venturini PL, Biscaldi E, et al. Efficacy and acceptability of long-term norethindrone acetate for the treatment of rectovaginal endometriosis. Eur J Obstet Gynecol Repro Biol. 2017;213:4-10.
- Brady PC, Missmer SA, Laufer MR. Hepatic adenomas in adolescents and young women with endometriosis treated with norethindrone acetate. J Pediatr Adolesc Gynecol. 2017;30:422-424.
- Choudhary NS, Bodh V, Chaudhari S, et al. Norethisterone related drug induced liver injury: a series of 3 cases. J Clin Exp Hepatol. 2017;7:266- 268.
- Perez-Mera RA, Shields CE. Jaundice associated with norethindrone acetate therapy. N Engl J Med. 1962;267:1137-1138.
- Camila [package insert]. Mayne Pharma Inc: Greenville, NC; 2018.
- Barbieri RL. Elagolix: a new treatment for pelvic pain caused by endometriosis. OBG Manag. 2018;30:10,12-14, 20.
- Taylor HS, Giudice LC, Lessey BA, et al. Treatment of endometriosis-associated pain with elagolix, an oral GnRH antagonist. N Engl J Med. 2017;377:28-40.
- Surrey E, Taylor HS, Giudice L, et al. Long-term outcomes of elagolix in women with endometriosis: results from two extension studies. Obstet Gynecol. 2018;132:147-160.
- Orilissa [package insert]. AbbVie Inc; North Chicago, IL; 2018.
- Barbieri RL. Hormonal treatment of endometriosis: the estrogen threshold hypothesis. Am J Obstet Gynecol. 1992;166:740-745.
- Hornstein MD, Surrey ES, Weisberg GW, et al. Leuprolide acetate depot and hormonal add-back in endometriosis: a 12-month study. Lupron Add-Back Study Group. Obstet Gynecol. 1998;91:16-24.
- Gallagher JS, Missmer SA, Hornstein MD, et al. Long-term effects of gonadotropin-releasing hormone agonists and add-back in adolescent endometriosis. J Pediatr Adolesc Gynecol. 2018;31:376- 381.
- Miller A, Shor R, Waites T, et al. Prior authorization reform for better patient care. J Am Coll Cardiol. 2018;71:1937-1939.
- Depot-leuprolide acetate. Good Rx website. https://www.goodrx.com/. Accessed January 22, 2021.
- Goserelin. Good Rx website. https://www .goodrx.com/. Accessed January 22, 2021
- Taylor HS, Giudice LC, Lessey BA, et al. Treatment of endometriosis-associated pain with elagolix, an oral GnRH antagonist. N Engl J Med. 2017;377:28-40.
- Centers for Disease Control and Prevention. Overdose deaths accelerating during COVID19. https://www.cdc.gov/media/releases/2020 /p1218-overdose-deaths-covid-19.html. Reviewed December 18, 2020. Accessed March 24, 2021.
- Till SR, As-Sanie S. 3 cases of chronic pelvic pain with nonsurgical, nonopioid therapies. OBG Manag. 2018;30:41-48.
- Steele A. Opioid use and depression in chronic pelvic pain. Obstet Gynecol Clin North Am. 2014;41:491-501.
- Zakhari A, Delpero E, McKeown S, et al. Endometriosis recurrence following post-operative hormonal suppression: a systematic review and meta-analysis. Hum Reprod Update. 2021;27:96- 107.
- Barbieri RL. Why are there delays in the diagnosis of endometriosis? OBG Manag. 2017;29:8, 10-11, 16.
Using (dynamic) ultrasound to make an earlier diagnosis of endometriosis
Can you provide some background on endometriosis and the importance of early diagnosis?
Dr. Goldstein: Endometriosis is an inflammatory condition, characterized by endometrial tissue at sites outside the uterus—this definition comes from the World Endometriosis Society.
Endometriosis is said to affect about 10% of women of reproductive age, and if you look at a group, a subset of women with pelvic pain or infertility, the numbers rise to the range of 35% to 50%. It can present in a multitude of locations, mainly in the pelvis, although occasionally even in places like the lung. When it occurs in the uterus, it is known as adenomyosis; when it occurs inside the ovary, it can cause an endometrioma (or what is sometimes referred to as chocolate cyst of the ovary), but you can see endometriotic implants anywhere in the peritoneum—along the urinary tract, rectum, uterosacral ligaments, rectovaginal septum, and even the vaginal wall occasionally.
What I am really interested in is an earlier diagnosis of superficial endometriosis, and it should be apparent to the reader why this is important—the quality of life from pain from endometriosis can be debilitating. It can be a source of infertility, a source of menstrual irregularities, and a source of not only quality of life but also economic consequences. Many women can also undergo as much as a 7-year delay in diagnosis, so the need for a timely diagnosis and initiation of treatment is extremely important.
What is the role of ultrasound in endometriosis diagnostics?
Dr. Goldstein: In an article that I authored 31 years ago, I wrote that there was a difference between an ultrasound examination by referral and examining one’s patients with ultrasound. I coined a phrase: the “ultrasound-enhanced bimanual exam.” I believed that this term should become a routine part of the overall gynecologic exam. I wanted people to think about the bimanual that we had done for at least half a century, which, in my opinion, consists of 2 components:
- An objective component: Is this uterus normal? Is it enlarged or irregular in contour, suggesting maybe fibroids? Is an ovary enlarged? If so, does it feel cystic or solid?
- A subjective component: Does this patient have tenderness through the pelvis. Is there normal mobility of the pelvic organs?
Part of the thesis was that the objective portion could be replaced by an image that could be produced in seconds, dependent on the operator’s training and availability of equipment. The subjective portion, however, depended on the experience and, often, nuance of the examiner. Lately, I have been seeking to expand that thesis by having the imager use examination as part of their overall imaging—this is the concept of dynamic imaging.
Can you expand on the concept of dynamic ultrasound in this setting?
Dr. Goldstein: Presently, most imagers take a multitude of pictures, what I would call 2-dimensional snapshots, to illustrate anatomy. This is usually done by a sonographer, or a technician, who collects the images for viewing by the physician, who then often does so without holding the transducer. Increasing utilization of remote tools like teleradiology only makes this more likely, and for a minority of people who may use video clips instead of still images, they are still simply representations of anatomy. The guidelines for pelvic ultrasound are the underpinning of the expectation of those who are scanning the female pelvis. With dynamic imaging, the operator uses their other hand on the abdomen as well as some motion with the probe to see if they can elicit pain with the vaginal probe, checking for mobility, asking the patient to bear down. Whether you are a sonographer, a radiologist, or an ObGyn, dynamic imaging can bring the examination process into the imager’s hands.
Can you tell us more about the indications for pelvic sonography for endometriosis and what data can you give to support this?
Dr. Goldstein: There is a document titled “Ultrasound Examination of the Female Pelvis,” that was originally developed by the American Institute of Ultrasound in Medicine (AIUM). In this document, there are about 19 different indications for pelvic sonography (in no defined order), and it is interesting that the first indication listed is evaluation of pelvic pain. Well, I would ask you, how do you evaluate pelvic pain with a series of anatomic images? If you have a classic ovarian endometrioma, or you have a classic hydrosalpinx, you can surmise that these are the source of the pain that the patient is reporting. But how do you properly evaluate pain with just an anatomic image? Thus, the need to use dynamic assessment.
There was a concept first introduced by my colleague, Dr. Ilan Timor, known as the sliding organ sign, that was mainly used to determine if 2 structures were adherent or separate. This involved use of the abdominal hand, liberal use of the probe moving in and out, and under real-time vision, examining the patient with the ultrasound transducer; this is the concept of dynamic ultrasound. This practice can be expanded to verify if there is pelvic tenderness and can be a significant part of the nonlaparoscopic, presumptive diagnosis of endometriosis, even when there is no ovarian endometrioma.
To support this theory, I would point you toward a classic article by E Okaro and colleagues in the British Journal of OB-GYN. This study took 120 consecutive women with chronic pelvic pain who were scheduled for laparoscopy, but performed a transvaginal ultrasound prior, and they looked for anatomic abnormalities and divided this into hard markers and soft markers. Hard markers were obvious endometriomas and hydrosalpinges, while soft markers included things like reduced ovarian mobility, site-specific pelvic tenderness, and presence of loculated peritoneal fluid in the pelvis. These were typical of chronic pelvic pain patients that ranged from late teens to almost menopausal, as the average age was about 30 years old.
Patients had experienced pain for anywhere from 6 months to 12 years, but the average was about 4 years. At laparoscopy, 58% of these patients had pelvic pathology, and 42% had a normal pelvis. Of the 58% with pathology, the overwhelming majority—about 51 of 70 women—had endometriosis alone, and another 7 had endometriosis with adhesions. A normal ultrasound, based on the absence of hard markers, was found in 96 of 120 women. Thus, 24 of the 120 women had an abnormal scan based on the presence of these hard markers. At laparoscopy, all 24 women had abnormal laparoscopies. Of those 96 women who would have had a normal ultrasound, based on the anatomic absence of some pathology, 53% had an abnormal scan based on the presence of these soft markers while the remaining women had no soft- or hard-markers suggesting any pelvic pathology. At laparoscopy, 73% of the patients with soft markers had pelvic pathology and 27% had a normal laparoscopy. Of 45 patients who had a normal, transvaginal ultrasound, 9 were found to have small evidence of endometriosis without discrete endometriomas at laparoscopy.
To summarize the study data, 100% of patients with hard markers and chronic pelvic pain had abnormal anatomy at laparoscopy, but 73% of patients who had soft markers but otherwise would have been interpreted as normal anatomic findings had evidence of pelvic pathology. Such an approach, if used, could lead to a reduction in the number of unnecessary laparoscopies.
What it really boils down to is, if you have 100 women with chronic pelvic pain, are you willing to treat 100 patients without laparoscopy, knowing that 73 are going to have a positive laparoscopy and will require treatment anyway? You would treat 27% with a pharmaceutical agent that may provide relief of their pain, or may not, depending on what the true etiology was. I would be willing to do so, as a positive predictive value of 73% makes doing that worthwhile, and I believe a majority of clinicians would agree.
Do you have any other tips or ways to improve the reader’s understanding of transvaginal ultrasound?
Dr. Goldstein: Pelvic organs have mobility. If a premenopausal woman is examined in lithotomy position, if the ovaries are freely mobile, by gravity, they are going to go lateral to the uterus and are seen immediately adjacent to the iliac vessels. But remember, iliac vessels are retroperitoneal as they are outside the peritoneal cavity. If you were to turn that patient onto all fours, so that the ovaries are freely mobile, they are going to move somewhat toward the anterior abdominal wall. When an ovary is seen in a nonanatomic position, it could be normal or it could be held up by a loop of bowel, but it may indicate adhesions. This is where this sliding organ sign and liberal use of the other hand on the lower abdomen can be extremely important. The reader should also understand that our ability to localize ovaries on ultrasound depends on the amount of folliculogenesis. Follicles are black circles that are sonolucent, because they contain fluid, so they make it easy to localize ovaries, but also their anatomic position relative to the iliac vessels. However, there is a caveat—which is, sometimes an ovary might look like it is behind the uterus and not in its normal anatomic location. When dynamic imaging is used, you are able to cajole that ovary to move lateral and sit on top of the iliac vessels, which can enable you make the proper diagnosis.
Can you provide some background on endometriosis and the importance of early diagnosis?
Dr. Goldstein: Endometriosis is an inflammatory condition, characterized by endometrial tissue at sites outside the uterus—this definition comes from the World Endometriosis Society.
Endometriosis is said to affect about 10% of women of reproductive age, and if you look at a group, a subset of women with pelvic pain or infertility, the numbers rise to the range of 35% to 50%. It can present in a multitude of locations, mainly in the pelvis, although occasionally even in places like the lung. When it occurs in the uterus, it is known as adenomyosis; when it occurs inside the ovary, it can cause an endometrioma (or what is sometimes referred to as chocolate cyst of the ovary), but you can see endometriotic implants anywhere in the peritoneum—along the urinary tract, rectum, uterosacral ligaments, rectovaginal septum, and even the vaginal wall occasionally.
What I am really interested in is an earlier diagnosis of superficial endometriosis, and it should be apparent to the reader why this is important—the quality of life from pain from endometriosis can be debilitating. It can be a source of infertility, a source of menstrual irregularities, and a source of not only quality of life but also economic consequences. Many women can also undergo as much as a 7-year delay in diagnosis, so the need for a timely diagnosis and initiation of treatment is extremely important.
What is the role of ultrasound in endometriosis diagnostics?
Dr. Goldstein: In an article that I authored 31 years ago, I wrote that there was a difference between an ultrasound examination by referral and examining one’s patients with ultrasound. I coined a phrase: the “ultrasound-enhanced bimanual exam.” I believed that this term should become a routine part of the overall gynecologic exam. I wanted people to think about the bimanual that we had done for at least half a century, which, in my opinion, consists of 2 components:
- An objective component: Is this uterus normal? Is it enlarged or irregular in contour, suggesting maybe fibroids? Is an ovary enlarged? If so, does it feel cystic or solid?
- A subjective component: Does this patient have tenderness through the pelvis. Is there normal mobility of the pelvic organs?
Part of the thesis was that the objective portion could be replaced by an image that could be produced in seconds, dependent on the operator’s training and availability of equipment. The subjective portion, however, depended on the experience and, often, nuance of the examiner. Lately, I have been seeking to expand that thesis by having the imager use examination as part of their overall imaging—this is the concept of dynamic imaging.
Can you expand on the concept of dynamic ultrasound in this setting?
Dr. Goldstein: Presently, most imagers take a multitude of pictures, what I would call 2-dimensional snapshots, to illustrate anatomy. This is usually done by a sonographer, or a technician, who collects the images for viewing by the physician, who then often does so without holding the transducer. Increasing utilization of remote tools like teleradiology only makes this more likely, and for a minority of people who may use video clips instead of still images, they are still simply representations of anatomy. The guidelines for pelvic ultrasound are the underpinning of the expectation of those who are scanning the female pelvis. With dynamic imaging, the operator uses their other hand on the abdomen as well as some motion with the probe to see if they can elicit pain with the vaginal probe, checking for mobility, asking the patient to bear down. Whether you are a sonographer, a radiologist, or an ObGyn, dynamic imaging can bring the examination process into the imager’s hands.
Can you tell us more about the indications for pelvic sonography for endometriosis and what data can you give to support this?
Dr. Goldstein: There is a document titled “Ultrasound Examination of the Female Pelvis,” that was originally developed by the American Institute of Ultrasound in Medicine (AIUM). In this document, there are about 19 different indications for pelvic sonography (in no defined order), and it is interesting that the first indication listed is evaluation of pelvic pain. Well, I would ask you, how do you evaluate pelvic pain with a series of anatomic images? If you have a classic ovarian endometrioma, or you have a classic hydrosalpinx, you can surmise that these are the source of the pain that the patient is reporting. But how do you properly evaluate pain with just an anatomic image? Thus, the need to use dynamic assessment.
There was a concept first introduced by my colleague, Dr. Ilan Timor, known as the sliding organ sign, that was mainly used to determine if 2 structures were adherent or separate. This involved use of the abdominal hand, liberal use of the probe moving in and out, and under real-time vision, examining the patient with the ultrasound transducer; this is the concept of dynamic ultrasound. This practice can be expanded to verify if there is pelvic tenderness and can be a significant part of the nonlaparoscopic, presumptive diagnosis of endometriosis, even when there is no ovarian endometrioma.
To support this theory, I would point you toward a classic article by E Okaro and colleagues in the British Journal of OB-GYN. This study took 120 consecutive women with chronic pelvic pain who were scheduled for laparoscopy, but performed a transvaginal ultrasound prior, and they looked for anatomic abnormalities and divided this into hard markers and soft markers. Hard markers were obvious endometriomas and hydrosalpinges, while soft markers included things like reduced ovarian mobility, site-specific pelvic tenderness, and presence of loculated peritoneal fluid in the pelvis. These were typical of chronic pelvic pain patients that ranged from late teens to almost menopausal, as the average age was about 30 years old.
Patients had experienced pain for anywhere from 6 months to 12 years, but the average was about 4 years. At laparoscopy, 58% of these patients had pelvic pathology, and 42% had a normal pelvis. Of the 58% with pathology, the overwhelming majority—about 51 of 70 women—had endometriosis alone, and another 7 had endometriosis with adhesions. A normal ultrasound, based on the absence of hard markers, was found in 96 of 120 women. Thus, 24 of the 120 women had an abnormal scan based on the presence of these hard markers. At laparoscopy, all 24 women had abnormal laparoscopies. Of those 96 women who would have had a normal ultrasound, based on the anatomic absence of some pathology, 53% had an abnormal scan based on the presence of these soft markers while the remaining women had no soft- or hard-markers suggesting any pelvic pathology. At laparoscopy, 73% of the patients with soft markers had pelvic pathology and 27% had a normal laparoscopy. Of 45 patients who had a normal, transvaginal ultrasound, 9 were found to have small evidence of endometriosis without discrete endometriomas at laparoscopy.
To summarize the study data, 100% of patients with hard markers and chronic pelvic pain had abnormal anatomy at laparoscopy, but 73% of patients who had soft markers but otherwise would have been interpreted as normal anatomic findings had evidence of pelvic pathology. Such an approach, if used, could lead to a reduction in the number of unnecessary laparoscopies.
What it really boils down to is, if you have 100 women with chronic pelvic pain, are you willing to treat 100 patients without laparoscopy, knowing that 73 are going to have a positive laparoscopy and will require treatment anyway? You would treat 27% with a pharmaceutical agent that may provide relief of their pain, or may not, depending on what the true etiology was. I would be willing to do so, as a positive predictive value of 73% makes doing that worthwhile, and I believe a majority of clinicians would agree.
Do you have any other tips or ways to improve the reader’s understanding of transvaginal ultrasound?
Dr. Goldstein: Pelvic organs have mobility. If a premenopausal woman is examined in lithotomy position, if the ovaries are freely mobile, by gravity, they are going to go lateral to the uterus and are seen immediately adjacent to the iliac vessels. But remember, iliac vessels are retroperitoneal as they are outside the peritoneal cavity. If you were to turn that patient onto all fours, so that the ovaries are freely mobile, they are going to move somewhat toward the anterior abdominal wall. When an ovary is seen in a nonanatomic position, it could be normal or it could be held up by a loop of bowel, but it may indicate adhesions. This is where this sliding organ sign and liberal use of the other hand on the lower abdomen can be extremely important. The reader should also understand that our ability to localize ovaries on ultrasound depends on the amount of folliculogenesis. Follicles are black circles that are sonolucent, because they contain fluid, so they make it easy to localize ovaries, but also their anatomic position relative to the iliac vessels. However, there is a caveat—which is, sometimes an ovary might look like it is behind the uterus and not in its normal anatomic location. When dynamic imaging is used, you are able to cajole that ovary to move lateral and sit on top of the iliac vessels, which can enable you make the proper diagnosis.
Can you provide some background on endometriosis and the importance of early diagnosis?
Dr. Goldstein: Endometriosis is an inflammatory condition, characterized by endometrial tissue at sites outside the uterus—this definition comes from the World Endometriosis Society.
Endometriosis is said to affect about 10% of women of reproductive age, and if you look at a group, a subset of women with pelvic pain or infertility, the numbers rise to the range of 35% to 50%. It can present in a multitude of locations, mainly in the pelvis, although occasionally even in places like the lung. When it occurs in the uterus, it is known as adenomyosis; when it occurs inside the ovary, it can cause an endometrioma (or what is sometimes referred to as chocolate cyst of the ovary), but you can see endometriotic implants anywhere in the peritoneum—along the urinary tract, rectum, uterosacral ligaments, rectovaginal septum, and even the vaginal wall occasionally.
What I am really interested in is an earlier diagnosis of superficial endometriosis, and it should be apparent to the reader why this is important—the quality of life from pain from endometriosis can be debilitating. It can be a source of infertility, a source of menstrual irregularities, and a source of not only quality of life but also economic consequences. Many women can also undergo as much as a 7-year delay in diagnosis, so the need for a timely diagnosis and initiation of treatment is extremely important.
What is the role of ultrasound in endometriosis diagnostics?
Dr. Goldstein: In an article that I authored 31 years ago, I wrote that there was a difference between an ultrasound examination by referral and examining one’s patients with ultrasound. I coined a phrase: the “ultrasound-enhanced bimanual exam.” I believed that this term should become a routine part of the overall gynecologic exam. I wanted people to think about the bimanual that we had done for at least half a century, which, in my opinion, consists of 2 components:
- An objective component: Is this uterus normal? Is it enlarged or irregular in contour, suggesting maybe fibroids? Is an ovary enlarged? If so, does it feel cystic or solid?
- A subjective component: Does this patient have tenderness through the pelvis. Is there normal mobility of the pelvic organs?
Part of the thesis was that the objective portion could be replaced by an image that could be produced in seconds, dependent on the operator’s training and availability of equipment. The subjective portion, however, depended on the experience and, often, nuance of the examiner. Lately, I have been seeking to expand that thesis by having the imager use examination as part of their overall imaging—this is the concept of dynamic imaging.
Can you expand on the concept of dynamic ultrasound in this setting?
Dr. Goldstein: Presently, most imagers take a multitude of pictures, what I would call 2-dimensional snapshots, to illustrate anatomy. This is usually done by a sonographer, or a technician, who collects the images for viewing by the physician, who then often does so without holding the transducer. Increasing utilization of remote tools like teleradiology only makes this more likely, and for a minority of people who may use video clips instead of still images, they are still simply representations of anatomy. The guidelines for pelvic ultrasound are the underpinning of the expectation of those who are scanning the female pelvis. With dynamic imaging, the operator uses their other hand on the abdomen as well as some motion with the probe to see if they can elicit pain with the vaginal probe, checking for mobility, asking the patient to bear down. Whether you are a sonographer, a radiologist, or an ObGyn, dynamic imaging can bring the examination process into the imager’s hands.
Can you tell us more about the indications for pelvic sonography for endometriosis and what data can you give to support this?
Dr. Goldstein: There is a document titled “Ultrasound Examination of the Female Pelvis,” that was originally developed by the American Institute of Ultrasound in Medicine (AIUM). In this document, there are about 19 different indications for pelvic sonography (in no defined order), and it is interesting that the first indication listed is evaluation of pelvic pain. Well, I would ask you, how do you evaluate pelvic pain with a series of anatomic images? If you have a classic ovarian endometrioma, or you have a classic hydrosalpinx, you can surmise that these are the source of the pain that the patient is reporting. But how do you properly evaluate pain with just an anatomic image? Thus, the need to use dynamic assessment.
There was a concept first introduced by my colleague, Dr. Ilan Timor, known as the sliding organ sign, that was mainly used to determine if 2 structures were adherent or separate. This involved use of the abdominal hand, liberal use of the probe moving in and out, and under real-time vision, examining the patient with the ultrasound transducer; this is the concept of dynamic ultrasound. This practice can be expanded to verify if there is pelvic tenderness and can be a significant part of the nonlaparoscopic, presumptive diagnosis of endometriosis, even when there is no ovarian endometrioma.
To support this theory, I would point you toward a classic article by E Okaro and colleagues in the British Journal of OB-GYN. This study took 120 consecutive women with chronic pelvic pain who were scheduled for laparoscopy, but performed a transvaginal ultrasound prior, and they looked for anatomic abnormalities and divided this into hard markers and soft markers. Hard markers were obvious endometriomas and hydrosalpinges, while soft markers included things like reduced ovarian mobility, site-specific pelvic tenderness, and presence of loculated peritoneal fluid in the pelvis. These were typical of chronic pelvic pain patients that ranged from late teens to almost menopausal, as the average age was about 30 years old.
Patients had experienced pain for anywhere from 6 months to 12 years, but the average was about 4 years. At laparoscopy, 58% of these patients had pelvic pathology, and 42% had a normal pelvis. Of the 58% with pathology, the overwhelming majority—about 51 of 70 women—had endometriosis alone, and another 7 had endometriosis with adhesions. A normal ultrasound, based on the absence of hard markers, was found in 96 of 120 women. Thus, 24 of the 120 women had an abnormal scan based on the presence of these hard markers. At laparoscopy, all 24 women had abnormal laparoscopies. Of those 96 women who would have had a normal ultrasound, based on the anatomic absence of some pathology, 53% had an abnormal scan based on the presence of these soft markers while the remaining women had no soft- or hard-markers suggesting any pelvic pathology. At laparoscopy, 73% of the patients with soft markers had pelvic pathology and 27% had a normal laparoscopy. Of 45 patients who had a normal, transvaginal ultrasound, 9 were found to have small evidence of endometriosis without discrete endometriomas at laparoscopy.
To summarize the study data, 100% of patients with hard markers and chronic pelvic pain had abnormal anatomy at laparoscopy, but 73% of patients who had soft markers but otherwise would have been interpreted as normal anatomic findings had evidence of pelvic pathology. Such an approach, if used, could lead to a reduction in the number of unnecessary laparoscopies.
What it really boils down to is, if you have 100 women with chronic pelvic pain, are you willing to treat 100 patients without laparoscopy, knowing that 73 are going to have a positive laparoscopy and will require treatment anyway? You would treat 27% with a pharmaceutical agent that may provide relief of their pain, or may not, depending on what the true etiology was. I would be willing to do so, as a positive predictive value of 73% makes doing that worthwhile, and I believe a majority of clinicians would agree.
Do you have any other tips or ways to improve the reader’s understanding of transvaginal ultrasound?
Dr. Goldstein: Pelvic organs have mobility. If a premenopausal woman is examined in lithotomy position, if the ovaries are freely mobile, by gravity, they are going to go lateral to the uterus and are seen immediately adjacent to the iliac vessels. But remember, iliac vessels are retroperitoneal as they are outside the peritoneal cavity. If you were to turn that patient onto all fours, so that the ovaries are freely mobile, they are going to move somewhat toward the anterior abdominal wall. When an ovary is seen in a nonanatomic position, it could be normal or it could be held up by a loop of bowel, but it may indicate adhesions. This is where this sliding organ sign and liberal use of the other hand on the lower abdomen can be extremely important. The reader should also understand that our ability to localize ovaries on ultrasound depends on the amount of folliculogenesis. Follicles are black circles that are sonolucent, because they contain fluid, so they make it easy to localize ovaries, but also their anatomic position relative to the iliac vessels. However, there is a caveat—which is, sometimes an ovary might look like it is behind the uterus and not in its normal anatomic location. When dynamic imaging is used, you are able to cajole that ovary to move lateral and sit on top of the iliac vessels, which can enable you make the proper diagnosis.









