User login
Vancomycin loading boost yields better C. diff outcomes
SAN FRANCISCO – A heightened loading dose of vancomycin may lead to faster recovery and greater efficacy in Clostridium difficile infections, according to the results of a quasi-experimental study presented at an annual scientific meeting on infectious diseases.
The study looked at a loading dose of 500 mg of vancomycin delivered four times per day for the first 48 hours, followed by a step down to 125 mg every 6 hours. It came on the heels of an attempted randomized, clinical trial that was inconclusive because of insufficient recruitment. Still, the results were promising enough to convince the Yale New Haven Hospital to make it standard practice in C. difficile patients.
Samad Tirmizi, PharmD, an infectious disease pharmacist at Stony Brook University (N.Y.), shares the results of a comparison of outcomes before and after the initiation of this treatment protocol in a video interview.
The approach grew out of concerns that vancomycin may not achieve sufficient concentrations in the colon early in treatment. A pharmacokinetics study published in 2010 suggested that a high initial loading led to higher fecal vancomycin levels, even in patients with increased stool frequency (BMC Infect Dis. 2010 Dec 30;10:363).
SOURCE: Tirmizi S et al. IDWeek 2018, Abstract 1980.
SAN FRANCISCO – A heightened loading dose of vancomycin may lead to faster recovery and greater efficacy in Clostridium difficile infections, according to the results of a quasi-experimental study presented at an annual scientific meeting on infectious diseases.
The study looked at a loading dose of 500 mg of vancomycin delivered four times per day for the first 48 hours, followed by a step down to 125 mg every 6 hours. It came on the heels of an attempted randomized, clinical trial that was inconclusive because of insufficient recruitment. Still, the results were promising enough to convince the Yale New Haven Hospital to make it standard practice in C. difficile patients.
Samad Tirmizi, PharmD, an infectious disease pharmacist at Stony Brook University (N.Y.), shares the results of a comparison of outcomes before and after the initiation of this treatment protocol in a video interview.
The approach grew out of concerns that vancomycin may not achieve sufficient concentrations in the colon early in treatment. A pharmacokinetics study published in 2010 suggested that a high initial loading led to higher fecal vancomycin levels, even in patients with increased stool frequency (BMC Infect Dis. 2010 Dec 30;10:363).
SOURCE: Tirmizi S et al. IDWeek 2018, Abstract 1980.
SAN FRANCISCO – A heightened loading dose of vancomycin may lead to faster recovery and greater efficacy in Clostridium difficile infections, according to the results of a quasi-experimental study presented at an annual scientific meeting on infectious diseases.
The study looked at a loading dose of 500 mg of vancomycin delivered four times per day for the first 48 hours, followed by a step down to 125 mg every 6 hours. It came on the heels of an attempted randomized, clinical trial that was inconclusive because of insufficient recruitment. Still, the results were promising enough to convince the Yale New Haven Hospital to make it standard practice in C. difficile patients.
Samad Tirmizi, PharmD, an infectious disease pharmacist at Stony Brook University (N.Y.), shares the results of a comparison of outcomes before and after the initiation of this treatment protocol in a video interview.
The approach grew out of concerns that vancomycin may not achieve sufficient concentrations in the colon early in treatment. A pharmacokinetics study published in 2010 suggested that a high initial loading led to higher fecal vancomycin levels, even in patients with increased stool frequency (BMC Infect Dis. 2010 Dec 30;10:363).
SOURCE: Tirmizi S et al. IDWeek 2018, Abstract 1980.
REPORTING FROM IDWEEK 2018
Discharge trends for septic shock survivors remain steady
SAN ANTONIO – While septic shock mortality has decreased since the Surviving Sepsis Campaign guidelines were introduced, discharge trends for survivors have not changed significantly over time, a recent analysis suggests.
The percentage of survivors discharged to subacute rehab or long-term facilities did not change appreciably over time, according to the 10-year retrospective analysis, presented at the annual meeting of the American College of Chest Physicians.
However, average length of stay did significantly trend downward over the decade analyzed, while total charge per septic shock admission significantly increased, according to investigator Di Pan, DO, Icahn School of Medicine at Mount Sinai, New York, and his colleagues.
This is one of few studies looking at outcomes in survivors of septic shock, as most analyses have primarily focused on mortality outcomes, the investigators said.
Their analysis was based on the 2004 to 2014 National (Nationwide) Inpatient Sample databases and included patients with a primary diagnosis of septic shock at discharge.
Out of nearly 1.8 million patients with septic shock in that cohort, about 1 million survived, according to data Dr. Pan and colleagues provided in an abstract of the presentation.
In-hospital mortality decreased from 51.7% in 2004 to 39.3% in 2014 (P less than .001), the investigators reported.
The proportion of survivors discharged to subacute rehab or long-term acute care facilities was 61.9% in 2004, and similarly, 62.4% in 2014 (P = .1), while the percentage discharged home was 17.1% in 2004 and 15.1% in 2014 (P = 0.55).
However, there was a small but statistically significant downtick in mean length of stay, from 12.6 days in 2004 to 11.05 days in 2014, the investigators said. Meanwhile, total hospitalization charges surged from $105,776 in 2004 to $134,394 over the same time period.
The first edition of the Surviving Sepsis Campaign guidelines for management of severe sepsis and septic shock was published in March 2004 in Critical Care Medicine.
Future studies and clinical trials should look beyond mortality outcomes to additionally evaluate morbidity outcomes in septic shock survivors, Dr. Pan and coauthors said in their report.
The researchers had no relationships to disclose relevant to the presented study.
SOURCE: Pan D et al. CHEST 2018. doi: 10.1016/j.chest.2018.08.339.
SAN ANTONIO – While septic shock mortality has decreased since the Surviving Sepsis Campaign guidelines were introduced, discharge trends for survivors have not changed significantly over time, a recent analysis suggests.
The percentage of survivors discharged to subacute rehab or long-term facilities did not change appreciably over time, according to the 10-year retrospective analysis, presented at the annual meeting of the American College of Chest Physicians.
However, average length of stay did significantly trend downward over the decade analyzed, while total charge per septic shock admission significantly increased, according to investigator Di Pan, DO, Icahn School of Medicine at Mount Sinai, New York, and his colleagues.
This is one of few studies looking at outcomes in survivors of septic shock, as most analyses have primarily focused on mortality outcomes, the investigators said.
Their analysis was based on the 2004 to 2014 National (Nationwide) Inpatient Sample databases and included patients with a primary diagnosis of septic shock at discharge.
Out of nearly 1.8 million patients with septic shock in that cohort, about 1 million survived, according to data Dr. Pan and colleagues provided in an abstract of the presentation.
In-hospital mortality decreased from 51.7% in 2004 to 39.3% in 2014 (P less than .001), the investigators reported.
The proportion of survivors discharged to subacute rehab or long-term acute care facilities was 61.9% in 2004, and similarly, 62.4% in 2014 (P = .1), while the percentage discharged home was 17.1% in 2004 and 15.1% in 2014 (P = 0.55).
However, there was a small but statistically significant downtick in mean length of stay, from 12.6 days in 2004 to 11.05 days in 2014, the investigators said. Meanwhile, total hospitalization charges surged from $105,776 in 2004 to $134,394 over the same time period.
The first edition of the Surviving Sepsis Campaign guidelines for management of severe sepsis and septic shock was published in March 2004 in Critical Care Medicine.
Future studies and clinical trials should look beyond mortality outcomes to additionally evaluate morbidity outcomes in septic shock survivors, Dr. Pan and coauthors said in their report.
The researchers had no relationships to disclose relevant to the presented study.
SOURCE: Pan D et al. CHEST 2018. doi: 10.1016/j.chest.2018.08.339.
SAN ANTONIO – While septic shock mortality has decreased since the Surviving Sepsis Campaign guidelines were introduced, discharge trends for survivors have not changed significantly over time, a recent analysis suggests.
The percentage of survivors discharged to subacute rehab or long-term facilities did not change appreciably over time, according to the 10-year retrospective analysis, presented at the annual meeting of the American College of Chest Physicians.
However, average length of stay did significantly trend downward over the decade analyzed, while total charge per septic shock admission significantly increased, according to investigator Di Pan, DO, Icahn School of Medicine at Mount Sinai, New York, and his colleagues.
This is one of few studies looking at outcomes in survivors of septic shock, as most analyses have primarily focused on mortality outcomes, the investigators said.
Their analysis was based on the 2004 to 2014 National (Nationwide) Inpatient Sample databases and included patients with a primary diagnosis of septic shock at discharge.
Out of nearly 1.8 million patients with septic shock in that cohort, about 1 million survived, according to data Dr. Pan and colleagues provided in an abstract of the presentation.
In-hospital mortality decreased from 51.7% in 2004 to 39.3% in 2014 (P less than .001), the investigators reported.
The proportion of survivors discharged to subacute rehab or long-term acute care facilities was 61.9% in 2004, and similarly, 62.4% in 2014 (P = .1), while the percentage discharged home was 17.1% in 2004 and 15.1% in 2014 (P = 0.55).
However, there was a small but statistically significant downtick in mean length of stay, from 12.6 days in 2004 to 11.05 days in 2014, the investigators said. Meanwhile, total hospitalization charges surged from $105,776 in 2004 to $134,394 over the same time period.
The first edition of the Surviving Sepsis Campaign guidelines for management of severe sepsis and septic shock was published in March 2004 in Critical Care Medicine.
Future studies and clinical trials should look beyond mortality outcomes to additionally evaluate morbidity outcomes in septic shock survivors, Dr. Pan and coauthors said in their report.
The researchers had no relationships to disclose relevant to the presented study.
SOURCE: Pan D et al. CHEST 2018. doi: 10.1016/j.chest.2018.08.339.
REPORTING FROM CHEST 2018
Key clinical point: While septic shock mortality has decreased over time, discharge trends for survivors have remained steady.
Major finding: In-hospital mortality dropped from about 52% to 39% over the 2004-2014 period, while discharges to subacute rehab or long-term facilities stayed around 62%.
Study details: Retrospective analysis of nearly 1.8 million patients with septic shock, of whom about 1 million survived.
Disclosures: The authors had no relationships to disclose relevant to the presented study.
Source: Pan D et al. CHEST 2018.
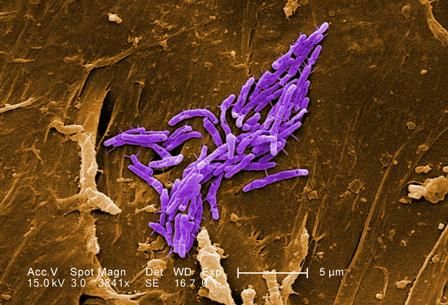
NYC outbreak of Candida auris linked to 45% mortality
Mortality within 90 days of infection was 45% among 51 patients diagnosed with antibiotic-resistant Candida auris infections in a multihospital outbreak in New York City from 2012 to 2017.
Transmission is ongoing in health care facilities, primarily among patients with extensive health care exposures, according to a report published in Emerging Infectious Diseases.
“Intensive infection prevention and control efforts continue; the goals are delaying endemicity, preventing outbreaks within facilities, reducing transmission and geographic spread, and blunting the effect of C. auris in New York and the rest of the United States,” Eleanor Adams, MD, of the New York Health Department, and her colleagues wrote. “Among medically fragile patients in NYC who had a history of extensive contact with health care facilities, clinicians should include C. auris in the differential diagnosis for patients with symptoms compatible with bloodstream infection.”
In the intensive case-patient analysis conducted by the New York State Health Department, 21 cases were from seven hospitals in Brooklyn, 16 were from three hospitals and one private medical office in Queens, 12 were from five hospitals and one long-term acute care hospital in Manhattan, and 1 was from a hospital in the Bronx. The remaining clinical case was identified in a western New York hospital in a patient who had recently been admitted to an involved Brooklyn hospital.
Among these patients, 31 (61%) had resided in long-term care facilities immediately before being admitted to the hospital in which their infection was diagnosed, and 19 of these 31 resided in skilled nursing facilities with ventilator beds; 1 (2%) resided in a long-term acute care hospital; 5 (10%) had been transferred from another hospital; and 4 (8%) had traveled internationally within 5 years before diagnosis, according to the investigators.
Isolates from 50 patients (98%) were resistant to fluconazole and 13 (25%) were resistant to fluconazole and amphotericin B. No initial isolates were resistant to echinocandins, although subsequent isolates obtained from 3 persons who had received an echinocandin acquired resistance to it, according to the researchers. Whole-genome sequencing performed at The Centers for Disease Control and Prevention indicated that 50 of 51 isolates belonged to a South Asia clade; the remaining isolate was the only one susceptible to fluconazole.
The work was supported by the CDC. No disclosures were reported.
SOURCE: Adams E et al. Emerg Infect Dis. 2018 Sep 12; 24(10); ID: 18-0649.
Mortality within 90 days of infection was 45% among 51 patients diagnosed with antibiotic-resistant Candida auris infections in a multihospital outbreak in New York City from 2012 to 2017.
Transmission is ongoing in health care facilities, primarily among patients with extensive health care exposures, according to a report published in Emerging Infectious Diseases.
“Intensive infection prevention and control efforts continue; the goals are delaying endemicity, preventing outbreaks within facilities, reducing transmission and geographic spread, and blunting the effect of C. auris in New York and the rest of the United States,” Eleanor Adams, MD, of the New York Health Department, and her colleagues wrote. “Among medically fragile patients in NYC who had a history of extensive contact with health care facilities, clinicians should include C. auris in the differential diagnosis for patients with symptoms compatible with bloodstream infection.”
In the intensive case-patient analysis conducted by the New York State Health Department, 21 cases were from seven hospitals in Brooklyn, 16 were from three hospitals and one private medical office in Queens, 12 were from five hospitals and one long-term acute care hospital in Manhattan, and 1 was from a hospital in the Bronx. The remaining clinical case was identified in a western New York hospital in a patient who had recently been admitted to an involved Brooklyn hospital.
Among these patients, 31 (61%) had resided in long-term care facilities immediately before being admitted to the hospital in which their infection was diagnosed, and 19 of these 31 resided in skilled nursing facilities with ventilator beds; 1 (2%) resided in a long-term acute care hospital; 5 (10%) had been transferred from another hospital; and 4 (8%) had traveled internationally within 5 years before diagnosis, according to the investigators.
Isolates from 50 patients (98%) were resistant to fluconazole and 13 (25%) were resistant to fluconazole and amphotericin B. No initial isolates were resistant to echinocandins, although subsequent isolates obtained from 3 persons who had received an echinocandin acquired resistance to it, according to the researchers. Whole-genome sequencing performed at The Centers for Disease Control and Prevention indicated that 50 of 51 isolates belonged to a South Asia clade; the remaining isolate was the only one susceptible to fluconazole.
The work was supported by the CDC. No disclosures were reported.
SOURCE: Adams E et al. Emerg Infect Dis. 2018 Sep 12; 24(10); ID: 18-0649.
Mortality within 90 days of infection was 45% among 51 patients diagnosed with antibiotic-resistant Candida auris infections in a multihospital outbreak in New York City from 2012 to 2017.
Transmission is ongoing in health care facilities, primarily among patients with extensive health care exposures, according to a report published in Emerging Infectious Diseases.
“Intensive infection prevention and control efforts continue; the goals are delaying endemicity, preventing outbreaks within facilities, reducing transmission and geographic spread, and blunting the effect of C. auris in New York and the rest of the United States,” Eleanor Adams, MD, of the New York Health Department, and her colleagues wrote. “Among medically fragile patients in NYC who had a history of extensive contact with health care facilities, clinicians should include C. auris in the differential diagnosis for patients with symptoms compatible with bloodstream infection.”
In the intensive case-patient analysis conducted by the New York State Health Department, 21 cases were from seven hospitals in Brooklyn, 16 were from three hospitals and one private medical office in Queens, 12 were from five hospitals and one long-term acute care hospital in Manhattan, and 1 was from a hospital in the Bronx. The remaining clinical case was identified in a western New York hospital in a patient who had recently been admitted to an involved Brooklyn hospital.
Among these patients, 31 (61%) had resided in long-term care facilities immediately before being admitted to the hospital in which their infection was diagnosed, and 19 of these 31 resided in skilled nursing facilities with ventilator beds; 1 (2%) resided in a long-term acute care hospital; 5 (10%) had been transferred from another hospital; and 4 (8%) had traveled internationally within 5 years before diagnosis, according to the investigators.
Isolates from 50 patients (98%) were resistant to fluconazole and 13 (25%) were resistant to fluconazole and amphotericin B. No initial isolates were resistant to echinocandins, although subsequent isolates obtained from 3 persons who had received an echinocandin acquired resistance to it, according to the researchers. Whole-genome sequencing performed at The Centers for Disease Control and Prevention indicated that 50 of 51 isolates belonged to a South Asia clade; the remaining isolate was the only one susceptible to fluconazole.
The work was supported by the CDC. No disclosures were reported.
SOURCE: Adams E et al. Emerg Infect Dis. 2018 Sep 12; 24(10); ID: 18-0649.
FROM EMERGING INFECTIOUS DISEASES
Review protocols, follow reprocessing guidelines to cut device-related HAIs
ATLANTA – Ongoing vigilance regarding the role of and transmission of antimicrobial-resistant pathogen is needed, according to Isaac Benowitz, MD, of the Centers for Disease Control and Prevention’s Division of Healthcare Quality Promotion (DHQP).
A review of records from the DHQP, which investigates and responds to infections and related adverse events in health care settings upon invitation, showed that in 2017 environmental pathogens were most often the triggers for these investigations, said Dr. Benowitz, a medical epidemiologist.
He reviewed internal records for consultations with state and local health departments involving medical devices and collected data on health care setting, pathogen, investigation findings including possible exposure or transmission, and public health actions.
Of 285 consultations, 48 involved a specific medical device or general medical device reprocessing, he said, noting that most of those 48 were in an acute care hospital (63%) or clinic (19%).
“The most frequent pathogens noted in these consultations were nontuberculous mycobacteria at 21%, Candida species ... at 10%, and Burkholderia species ... at 8%,” he said, noting that a wide variety of devices were implicated.
In the inpatient setting these devices included ventilators, dialysis machines, breast pumps, central lines, and respiratory therapy equipment. In the outpatient setting they included glucometers and opthalmic equipment.
“In many settings we saw issues with endoscopes, including duodenoscopes, but also bronchoscopes,” he added.
Actions taken as part of the investigations included medical device recalls, improved infection control and reprocessing procedures, and patient notification, education, guidance, testing, and treatment.
In some cases there was disciplinary action or oversight for health care professionals, he added.
Investigations identified medical devices contaminated in manufacturing, incorrect reprocessing of endoscopes or ventilators, and inappropriate medical device use or reuse, he said.
A number of lessons can be learned from these and other investigations, he added.
“First, devices can be reservoirs and transmission vectors for health care–associated infections. Second, health care facilities, health care facility staff, and public health partners should take opportunities to review protocols and the practices within those protocol,” he said. “These are opportunities to strengthen infection control practices even in the absence of documented transmission.”
In fact, in most of the investigations he discussed, transmission was rarely confirmed to be associated with a medical device. This was largely because of a lack of “epidemiological rigor,” but associations between health care–associated infections and medical devices “are still quite meaningful and often actionable,” he said.
Dr. Benowitz stressed the importance of engaging public health partners to discuss findings and actions, explaining that “what may look like a single-facility issue may have a very different perspective when you realize that there’s a similar issue at another facility elsewhere.”
“For all devices, it’s important to ensure adherence to the device reprocessing guidelines, “ he added, noting that these include a combination of facility protocols, manufacturer instructions for use, and guidance from organizations like the Food and Drug Administration and the CDC.
Dr. Benowitz reported having no disclosures.
sworcester@mdedge.com
SOURCE: Benowitz I et al. ICEID 2018, Oral Abstract Presentation E2.
ATLANTA – Ongoing vigilance regarding the role of and transmission of antimicrobial-resistant pathogen is needed, according to Isaac Benowitz, MD, of the Centers for Disease Control and Prevention’s Division of Healthcare Quality Promotion (DHQP).
A review of records from the DHQP, which investigates and responds to infections and related adverse events in health care settings upon invitation, showed that in 2017 environmental pathogens were most often the triggers for these investigations, said Dr. Benowitz, a medical epidemiologist.
He reviewed internal records for consultations with state and local health departments involving medical devices and collected data on health care setting, pathogen, investigation findings including possible exposure or transmission, and public health actions.
Of 285 consultations, 48 involved a specific medical device or general medical device reprocessing, he said, noting that most of those 48 were in an acute care hospital (63%) or clinic (19%).
“The most frequent pathogens noted in these consultations were nontuberculous mycobacteria at 21%, Candida species ... at 10%, and Burkholderia species ... at 8%,” he said, noting that a wide variety of devices were implicated.
In the inpatient setting these devices included ventilators, dialysis machines, breast pumps, central lines, and respiratory therapy equipment. In the outpatient setting they included glucometers and opthalmic equipment.
“In many settings we saw issues with endoscopes, including duodenoscopes, but also bronchoscopes,” he added.
Actions taken as part of the investigations included medical device recalls, improved infection control and reprocessing procedures, and patient notification, education, guidance, testing, and treatment.
In some cases there was disciplinary action or oversight for health care professionals, he added.
Investigations identified medical devices contaminated in manufacturing, incorrect reprocessing of endoscopes or ventilators, and inappropriate medical device use or reuse, he said.
A number of lessons can be learned from these and other investigations, he added.
“First, devices can be reservoirs and transmission vectors for health care–associated infections. Second, health care facilities, health care facility staff, and public health partners should take opportunities to review protocols and the practices within those protocol,” he said. “These are opportunities to strengthen infection control practices even in the absence of documented transmission.”
In fact, in most of the investigations he discussed, transmission was rarely confirmed to be associated with a medical device. This was largely because of a lack of “epidemiological rigor,” but associations between health care–associated infections and medical devices “are still quite meaningful and often actionable,” he said.
Dr. Benowitz stressed the importance of engaging public health partners to discuss findings and actions, explaining that “what may look like a single-facility issue may have a very different perspective when you realize that there’s a similar issue at another facility elsewhere.”
“For all devices, it’s important to ensure adherence to the device reprocessing guidelines, “ he added, noting that these include a combination of facility protocols, manufacturer instructions for use, and guidance from organizations like the Food and Drug Administration and the CDC.
Dr. Benowitz reported having no disclosures.
sworcester@mdedge.com
SOURCE: Benowitz I et al. ICEID 2018, Oral Abstract Presentation E2.
ATLANTA – Ongoing vigilance regarding the role of and transmission of antimicrobial-resistant pathogen is needed, according to Isaac Benowitz, MD, of the Centers for Disease Control and Prevention’s Division of Healthcare Quality Promotion (DHQP).
A review of records from the DHQP, which investigates and responds to infections and related adverse events in health care settings upon invitation, showed that in 2017 environmental pathogens were most often the triggers for these investigations, said Dr. Benowitz, a medical epidemiologist.
He reviewed internal records for consultations with state and local health departments involving medical devices and collected data on health care setting, pathogen, investigation findings including possible exposure or transmission, and public health actions.
Of 285 consultations, 48 involved a specific medical device or general medical device reprocessing, he said, noting that most of those 48 were in an acute care hospital (63%) or clinic (19%).
“The most frequent pathogens noted in these consultations were nontuberculous mycobacteria at 21%, Candida species ... at 10%, and Burkholderia species ... at 8%,” he said, noting that a wide variety of devices were implicated.
In the inpatient setting these devices included ventilators, dialysis machines, breast pumps, central lines, and respiratory therapy equipment. In the outpatient setting they included glucometers and opthalmic equipment.
“In many settings we saw issues with endoscopes, including duodenoscopes, but also bronchoscopes,” he added.
Actions taken as part of the investigations included medical device recalls, improved infection control and reprocessing procedures, and patient notification, education, guidance, testing, and treatment.
In some cases there was disciplinary action or oversight for health care professionals, he added.
Investigations identified medical devices contaminated in manufacturing, incorrect reprocessing of endoscopes or ventilators, and inappropriate medical device use or reuse, he said.
A number of lessons can be learned from these and other investigations, he added.
“First, devices can be reservoirs and transmission vectors for health care–associated infections. Second, health care facilities, health care facility staff, and public health partners should take opportunities to review protocols and the practices within those protocol,” he said. “These are opportunities to strengthen infection control practices even in the absence of documented transmission.”
In fact, in most of the investigations he discussed, transmission was rarely confirmed to be associated with a medical device. This was largely because of a lack of “epidemiological rigor,” but associations between health care–associated infections and medical devices “are still quite meaningful and often actionable,” he said.
Dr. Benowitz stressed the importance of engaging public health partners to discuss findings and actions, explaining that “what may look like a single-facility issue may have a very different perspective when you realize that there’s a similar issue at another facility elsewhere.”
“For all devices, it’s important to ensure adherence to the device reprocessing guidelines, “ he added, noting that these include a combination of facility protocols, manufacturer instructions for use, and guidance from organizations like the Food and Drug Administration and the CDC.
Dr. Benowitz reported having no disclosures.
sworcester@mdedge.com
SOURCE: Benowitz I et al. ICEID 2018, Oral Abstract Presentation E2.
REPORTING FROM ICEID 2018
Key clinical point: Medical devices can be reservoirs and transmission vectors for health care–associated infections.
Major finding: Of 285 consultations, 48 involved medical devices or device reprocessing.
Study details: A review of records from 285 consultations
Disclosures: Dr. Benowitz reported having no disclosures
Source: Benowitz I et al. ICEID 2018, Oral Abstract Presentation E2.
United Kingdom experience provides important lessons for controlling C. auris outbreaks
ATLANTA – The persistence and transmission of Candida auris in health care settings appears to be dependent on environmental survival, underscoring the need for careful investigation of the environment – and, in particular, multiuse patient equipment.
That’s the key lesson from one of the largest outbreaks of the emerging, multidrug-resistant pathogen to date, David Eyre, DPhil, said at the International Conference on Emerging Infectious Diseases.
“Our experience at Oxford began with a Public Health England alert, which closely followed a similar alert from the [Centers for Disease Control and Prevention] in the summer of 2016,” Dr. Eyre of the University of Oxford (England) said during an update on the epidemiology of the outbreak and the successful, multipronged effort to control it.
The outbreak, which occurred in the neurosciences intensive care unit of Oxford University Hospitals beginning in early 2015, was detected in 2016 when a cluster of C. auris infections was identified and traced to the unit. An intensive patient and environmental screening program was established, isolation protocols were used for patients who tested positive, enhanced cleaning processes were initiated, and equipment was removed and replaced with single-use equipment when possible.
“We also worked quite closely with our staff to raise awareness,” he said, adding that colonized patients who were undergoing a surgical procedure received single-dose antifungal prophylaxis prior to the procedure.
A case-control study was conducted, and after the researchers used multivariate logistic regression to control for length of stay, patient physiology, and biomarkers, exposure to multiuse skin surface axillary temperature monitoring was shown to be one of the strongest independent predictors of C. auris colonization and infection (odds ratio 6.80), he said, adding that antifungal exposure was also a significant risk factor, but only 5% of patients had received antifungals.
The axillary probes were then removed from the environment. As of April 2017 (when the probes were removed), 66 patients had been colonized or infected, and an additional 10 cases occurred after the probes were removed, with the last case occurring in November 2017.
Seven of the 76 cases involved invasive infection, and 1 patient died several months after hospital discharge, Dr. Eyre said.
The patient screening processes allowed for estimation of colonization time (approximately 2 months), and also allowed for whole-genome sequencing of 79 samples from 43 patients, 6 environmental isolates, and 2 isolates from regional surveillance, Dr. Eyre said.
All outbreak sequences formed a single genetic cluster within the C. auris South African clade, and were found to have been introduced to Oxford around 2012 or 2013, with about six mutations per year, or “roughly 12 million base pairs in total,” he said, adding that both patients and temperature probes were colonized with multiple strains, and there was “close mixing” between the two.
This pattern changed following removal of the temperature probes, but it took some time.
“However, from November [2017] onward – so that’s now 291 days ... we’ve not had another new patient isolate, and that’s not only no invasive infection, but also no colonization despite continuing the screening program,” he said.
According to the CDC, C. auris is “an emerging fungus that presents a serious global health threat” because of its often multidrug-resistant nature, difficulty identifying the pathogen using standard laboratory methods, and the risk for misidentification in labs without specific technology, which could lead to inappropriate management.
“It has caused outbreaks in health care settings. For this reason, it is important to quickly identify C. auris in a hospitalized patient so that health care facilities can take special precautions to stop its spread,” a CDC page on C. auris states. “CDC encourages all U.S. laboratory staff who identify C. auris to notify their state or local public health authorities and CDC at candidaauris@cdc.gov.”
Dr. Eyre reported having no disclosures.
SOURCE: Eyre D et al. ICEID 2018 Oral Abstract Presentation.
ATLANTA – The persistence and transmission of Candida auris in health care settings appears to be dependent on environmental survival, underscoring the need for careful investigation of the environment – and, in particular, multiuse patient equipment.
That’s the key lesson from one of the largest outbreaks of the emerging, multidrug-resistant pathogen to date, David Eyre, DPhil, said at the International Conference on Emerging Infectious Diseases.
“Our experience at Oxford began with a Public Health England alert, which closely followed a similar alert from the [Centers for Disease Control and Prevention] in the summer of 2016,” Dr. Eyre of the University of Oxford (England) said during an update on the epidemiology of the outbreak and the successful, multipronged effort to control it.
The outbreak, which occurred in the neurosciences intensive care unit of Oxford University Hospitals beginning in early 2015, was detected in 2016 when a cluster of C. auris infections was identified and traced to the unit. An intensive patient and environmental screening program was established, isolation protocols were used for patients who tested positive, enhanced cleaning processes were initiated, and equipment was removed and replaced with single-use equipment when possible.
“We also worked quite closely with our staff to raise awareness,” he said, adding that colonized patients who were undergoing a surgical procedure received single-dose antifungal prophylaxis prior to the procedure.
A case-control study was conducted, and after the researchers used multivariate logistic regression to control for length of stay, patient physiology, and biomarkers, exposure to multiuse skin surface axillary temperature monitoring was shown to be one of the strongest independent predictors of C. auris colonization and infection (odds ratio 6.80), he said, adding that antifungal exposure was also a significant risk factor, but only 5% of patients had received antifungals.
The axillary probes were then removed from the environment. As of April 2017 (when the probes were removed), 66 patients had been colonized or infected, and an additional 10 cases occurred after the probes were removed, with the last case occurring in November 2017.
Seven of the 76 cases involved invasive infection, and 1 patient died several months after hospital discharge, Dr. Eyre said.
The patient screening processes allowed for estimation of colonization time (approximately 2 months), and also allowed for whole-genome sequencing of 79 samples from 43 patients, 6 environmental isolates, and 2 isolates from regional surveillance, Dr. Eyre said.
All outbreak sequences formed a single genetic cluster within the C. auris South African clade, and were found to have been introduced to Oxford around 2012 or 2013, with about six mutations per year, or “roughly 12 million base pairs in total,” he said, adding that both patients and temperature probes were colonized with multiple strains, and there was “close mixing” between the two.
This pattern changed following removal of the temperature probes, but it took some time.
“However, from November [2017] onward – so that’s now 291 days ... we’ve not had another new patient isolate, and that’s not only no invasive infection, but also no colonization despite continuing the screening program,” he said.
According to the CDC, C. auris is “an emerging fungus that presents a serious global health threat” because of its often multidrug-resistant nature, difficulty identifying the pathogen using standard laboratory methods, and the risk for misidentification in labs without specific technology, which could lead to inappropriate management.
“It has caused outbreaks in health care settings. For this reason, it is important to quickly identify C. auris in a hospitalized patient so that health care facilities can take special precautions to stop its spread,” a CDC page on C. auris states. “CDC encourages all U.S. laboratory staff who identify C. auris to notify their state or local public health authorities and CDC at candidaauris@cdc.gov.”
Dr. Eyre reported having no disclosures.
SOURCE: Eyre D et al. ICEID 2018 Oral Abstract Presentation.
ATLANTA – The persistence and transmission of Candida auris in health care settings appears to be dependent on environmental survival, underscoring the need for careful investigation of the environment – and, in particular, multiuse patient equipment.
That’s the key lesson from one of the largest outbreaks of the emerging, multidrug-resistant pathogen to date, David Eyre, DPhil, said at the International Conference on Emerging Infectious Diseases.
“Our experience at Oxford began with a Public Health England alert, which closely followed a similar alert from the [Centers for Disease Control and Prevention] in the summer of 2016,” Dr. Eyre of the University of Oxford (England) said during an update on the epidemiology of the outbreak and the successful, multipronged effort to control it.
The outbreak, which occurred in the neurosciences intensive care unit of Oxford University Hospitals beginning in early 2015, was detected in 2016 when a cluster of C. auris infections was identified and traced to the unit. An intensive patient and environmental screening program was established, isolation protocols were used for patients who tested positive, enhanced cleaning processes were initiated, and equipment was removed and replaced with single-use equipment when possible.
“We also worked quite closely with our staff to raise awareness,” he said, adding that colonized patients who were undergoing a surgical procedure received single-dose antifungal prophylaxis prior to the procedure.
A case-control study was conducted, and after the researchers used multivariate logistic regression to control for length of stay, patient physiology, and biomarkers, exposure to multiuse skin surface axillary temperature monitoring was shown to be one of the strongest independent predictors of C. auris colonization and infection (odds ratio 6.80), he said, adding that antifungal exposure was also a significant risk factor, but only 5% of patients had received antifungals.
The axillary probes were then removed from the environment. As of April 2017 (when the probes were removed), 66 patients had been colonized or infected, and an additional 10 cases occurred after the probes were removed, with the last case occurring in November 2017.
Seven of the 76 cases involved invasive infection, and 1 patient died several months after hospital discharge, Dr. Eyre said.
The patient screening processes allowed for estimation of colonization time (approximately 2 months), and also allowed for whole-genome sequencing of 79 samples from 43 patients, 6 environmental isolates, and 2 isolates from regional surveillance, Dr. Eyre said.
All outbreak sequences formed a single genetic cluster within the C. auris South African clade, and were found to have been introduced to Oxford around 2012 or 2013, with about six mutations per year, or “roughly 12 million base pairs in total,” he said, adding that both patients and temperature probes were colonized with multiple strains, and there was “close mixing” between the two.
This pattern changed following removal of the temperature probes, but it took some time.
“However, from November [2017] onward – so that’s now 291 days ... we’ve not had another new patient isolate, and that’s not only no invasive infection, but also no colonization despite continuing the screening program,” he said.
According to the CDC, C. auris is “an emerging fungus that presents a serious global health threat” because of its often multidrug-resistant nature, difficulty identifying the pathogen using standard laboratory methods, and the risk for misidentification in labs without specific technology, which could lead to inappropriate management.
“It has caused outbreaks in health care settings. For this reason, it is important to quickly identify C. auris in a hospitalized patient so that health care facilities can take special precautions to stop its spread,” a CDC page on C. auris states. “CDC encourages all U.S. laboratory staff who identify C. auris to notify their state or local public health authorities and CDC at candidaauris@cdc.gov.”
Dr. Eyre reported having no disclosures.
SOURCE: Eyre D et al. ICEID 2018 Oral Abstract Presentation.
REPORTING FROM ICEID 2018
Key clinical point:
Major finding: Ten additional cases occurred in the 7 months after the axillary probes were removed from the environment.
Study details: A review of the epidemiology and control of a C. auris outbreak affecting 76 patients.
Disclosures: Dr. Eyre reported having no disclosures.
Source: Eyre D et al. ICEID 2018 Oral Abstract Presentation.
Patient transfers between hospitals contribute substantially to CDI burden
ATLANTA – Patient sharing among hospital facilities contributed substantially to the overall Clostridium difficile infection rate, an analysis of interhospital contamination effects showed.
In fact, 7.6% of all Clostridium difficile infection (CDI) cases at the nearly 400 California hospitals included in the study were directly attributable to the patient-sharing network, Daniel Sewell, PhD, reported at the International Conference on Emerging Infectious Diseases.
“The methods that we employed allowed us to estimate the expected increase in CDI cases due to transfers as a function of the CDI rate at the hospital from which those patients were brought. These transfer patients were responsible for about 3.06 times the number of CDI cases as a normal patient,” said Dr. Sewell, a biostatistician at the University of Iowa, Iowa City.
The findings, which underscored the importance of regional (rather than local) efforts to minimize the spread of health care–associated infections, are based on an analysis of 27,200,873 hospital admissions and 532,320 same-day patient transfers identified from the Healthcare Cost and Utilization Project California State Inpatient Database for 2005-2011.
Transfer networks based on the monthly average number of patients discharged from one hospital and admitted to another on the same day were constructed, and the monthly average number of CDI cases per hospital were considered, along with hospital-level characteristics such as patient length of stay, age, and number of diagnoses. Network autocorrelation models that help eliminate bias were then used to assess the contamination effects between hospitals, he explained.
This led to development of an equation that can be used to determine the expected number of CDI cases in a hospital as a function of the number of transfers coming in and the contamination level of the source hospitals. The ability to calculate the expected number of CDI cases in this fashion is an important factor for the success of regional versus local intervention efforts, which are increasingly thought to be important for reducing health care–associated infections.
“If we want to design a coordinated or regional approach, we’ve got to have a much better understanding of the role that patient transfers have in these diseases,” Dr. Sewell said.
As most hospitals included in the study had a low CDI rate and a low transfer rate, the CDIs attributable to transfers represent a minority of cases, but they are a substantial minority, he said, noting that the main concern is with the “perfect storm” of high CDI rate plus high transfer rate.
The methodological approach used in this study to estimate CDI rates can be used for any health care–associated infection of interest, he added.
Dr. Sewell reported that he had no disclosures.
ATLANTA – Patient sharing among hospital facilities contributed substantially to the overall Clostridium difficile infection rate, an analysis of interhospital contamination effects showed.
In fact, 7.6% of all Clostridium difficile infection (CDI) cases at the nearly 400 California hospitals included in the study were directly attributable to the patient-sharing network, Daniel Sewell, PhD, reported at the International Conference on Emerging Infectious Diseases.
“The methods that we employed allowed us to estimate the expected increase in CDI cases due to transfers as a function of the CDI rate at the hospital from which those patients were brought. These transfer patients were responsible for about 3.06 times the number of CDI cases as a normal patient,” said Dr. Sewell, a biostatistician at the University of Iowa, Iowa City.
The findings, which underscored the importance of regional (rather than local) efforts to minimize the spread of health care–associated infections, are based on an analysis of 27,200,873 hospital admissions and 532,320 same-day patient transfers identified from the Healthcare Cost and Utilization Project California State Inpatient Database for 2005-2011.
Transfer networks based on the monthly average number of patients discharged from one hospital and admitted to another on the same day were constructed, and the monthly average number of CDI cases per hospital were considered, along with hospital-level characteristics such as patient length of stay, age, and number of diagnoses. Network autocorrelation models that help eliminate bias were then used to assess the contamination effects between hospitals, he explained.
This led to development of an equation that can be used to determine the expected number of CDI cases in a hospital as a function of the number of transfers coming in and the contamination level of the source hospitals. The ability to calculate the expected number of CDI cases in this fashion is an important factor for the success of regional versus local intervention efforts, which are increasingly thought to be important for reducing health care–associated infections.
“If we want to design a coordinated or regional approach, we’ve got to have a much better understanding of the role that patient transfers have in these diseases,” Dr. Sewell said.
As most hospitals included in the study had a low CDI rate and a low transfer rate, the CDIs attributable to transfers represent a minority of cases, but they are a substantial minority, he said, noting that the main concern is with the “perfect storm” of high CDI rate plus high transfer rate.
The methodological approach used in this study to estimate CDI rates can be used for any health care–associated infection of interest, he added.
Dr. Sewell reported that he had no disclosures.
ATLANTA – Patient sharing among hospital facilities contributed substantially to the overall Clostridium difficile infection rate, an analysis of interhospital contamination effects showed.
In fact, 7.6% of all Clostridium difficile infection (CDI) cases at the nearly 400 California hospitals included in the study were directly attributable to the patient-sharing network, Daniel Sewell, PhD, reported at the International Conference on Emerging Infectious Diseases.
“The methods that we employed allowed us to estimate the expected increase in CDI cases due to transfers as a function of the CDI rate at the hospital from which those patients were brought. These transfer patients were responsible for about 3.06 times the number of CDI cases as a normal patient,” said Dr. Sewell, a biostatistician at the University of Iowa, Iowa City.
The findings, which underscored the importance of regional (rather than local) efforts to minimize the spread of health care–associated infections, are based on an analysis of 27,200,873 hospital admissions and 532,320 same-day patient transfers identified from the Healthcare Cost and Utilization Project California State Inpatient Database for 2005-2011.
Transfer networks based on the monthly average number of patients discharged from one hospital and admitted to another on the same day were constructed, and the monthly average number of CDI cases per hospital were considered, along with hospital-level characteristics such as patient length of stay, age, and number of diagnoses. Network autocorrelation models that help eliminate bias were then used to assess the contamination effects between hospitals, he explained.
This led to development of an equation that can be used to determine the expected number of CDI cases in a hospital as a function of the number of transfers coming in and the contamination level of the source hospitals. The ability to calculate the expected number of CDI cases in this fashion is an important factor for the success of regional versus local intervention efforts, which are increasingly thought to be important for reducing health care–associated infections.
“If we want to design a coordinated or regional approach, we’ve got to have a much better understanding of the role that patient transfers have in these diseases,” Dr. Sewell said.
As most hospitals included in the study had a low CDI rate and a low transfer rate, the CDIs attributable to transfers represent a minority of cases, but they are a substantial minority, he said, noting that the main concern is with the “perfect storm” of high CDI rate plus high transfer rate.
The methodological approach used in this study to estimate CDI rates can be used for any health care–associated infection of interest, he added.
Dr. Sewell reported that he had no disclosures.
REPORTING FROM ICEID 2018
Key clinical point: Patient sharing among hospitals contributes substantially to Clostridium difficile infection (CDI) rates.
Major finding: Patient transfers account for 7.6% of the overall CDI burden.
Study details: A statistical analysis to estimate interhospital CDI transmissions.
Disclosures: Dr. Sewell reported that he had no disclosures.
Hand hygiene linked to reduced ICU health care–associated infections
A hospital-wide infection control program (ICP) was found to be associated with reduced health care-associated severe sepsis/septic shock or death in the ICU, but it was not clear whether this decrease was a consequence of the ICP or because of a concomitant improvement in HAI case management, according to a the results of a prospective analysis.
In addition, there was no significant decrease in overall HAIs seen despite implementation of the program, according to the report published online in Clinical Microbiology and Infection (doi: 10.1016/j.cmi.2018.07.010), according to Stefan Hagel, MD, of the Institute for Infectious Diseases and Infection Control, Jena (Germany) University Hospital, and his colleagues.
They assessed two surveillance periods (September 2011 to August 2012 and May 2013 to August 2014). The ICP started in October 2012, and included hand-hygiene promotion and bundle implementation for common HAIs.
The data were analyzed by segmented mixed-effects Poisson regression and multi-state models and reported as adjusted incidence rate ratios (aIRR) and 50 adjusted hazard ratios (aHR) with 95% confidence intervals (CI).
In the first period, 62,154 patients were under surveillance, with 1,568 HAIs identified in 1,170 patients (4.3/100 admissions) and 2,336 HAIs identified in 1,711 patients (4.9/100 admissions) in the second surveillance period. No differences were found in the overall HAI incidence rates between the periods in the general wards and ICUs. There was only a slight decline in the incidence rate of HAIs in the ICUs (aIRR 0.98 [0.97, 1.00] per 1-week increment), compared with the general wards (aIRR 1.01 [1.00, 1.02]).
However, a reduction in severe HAIs (aIRR 0.13 [0.05, 0.32]) and a lower probability of HAI-associated in-hospital deaths (aHR 0.56 [0.31, 0.99]) were observed in the second period in the ICUs.
In attempting to explain the variance seen between the results for general wards and the ICU, an analysis of alcohol-based handrub solution consumption as a marker of hand-hygiene behavior indicated that a remarkable increase in consumption occurred in the ICUs while a less pronounced increase occurred in the general wards. “This finding might explain the observed decline in the HAI incidence after starting the campaign in the ICUs, which was not observed on the general wards.” Dr. Hagel and his colleagues suggested.
The authors discussed how several confounding factors that influenced the incidence of HAIs needed to be considered. As a consequence of the improvement in HAI management, the number of collected blood culture sets nearly doubled hospital-wide from 13,126 to 25,805 per year between 2011 and 2014, which likely undermined the study objective, they stated. The increase in cultures may have impacted the number of overall HAIs found.
“Although the primary aim of the study of reducing the overall incidence of HAIs was not achieved, the study demonstrated a decline of severe HAIs in patients in ICUs in the second surveillance period. Whether this result was a consequence of the ICP or a general improvement in HAI management remains unclear,” the researchers concluded.
The authors reported that they had no conflicts of interest.
SOURCE: Hagel S et al. Clin Microbiol Infect. doi: 10.1016/j.cmi.2018.07.010].
A hospital-wide infection control program (ICP) was found to be associated with reduced health care-associated severe sepsis/septic shock or death in the ICU, but it was not clear whether this decrease was a consequence of the ICP or because of a concomitant improvement in HAI case management, according to a the results of a prospective analysis.
In addition, there was no significant decrease in overall HAIs seen despite implementation of the program, according to the report published online in Clinical Microbiology and Infection (doi: 10.1016/j.cmi.2018.07.010), according to Stefan Hagel, MD, of the Institute for Infectious Diseases and Infection Control, Jena (Germany) University Hospital, and his colleagues.
They assessed two surveillance periods (September 2011 to August 2012 and May 2013 to August 2014). The ICP started in October 2012, and included hand-hygiene promotion and bundle implementation for common HAIs.
The data were analyzed by segmented mixed-effects Poisson regression and multi-state models and reported as adjusted incidence rate ratios (aIRR) and 50 adjusted hazard ratios (aHR) with 95% confidence intervals (CI).
In the first period, 62,154 patients were under surveillance, with 1,568 HAIs identified in 1,170 patients (4.3/100 admissions) and 2,336 HAIs identified in 1,711 patients (4.9/100 admissions) in the second surveillance period. No differences were found in the overall HAI incidence rates between the periods in the general wards and ICUs. There was only a slight decline in the incidence rate of HAIs in the ICUs (aIRR 0.98 [0.97, 1.00] per 1-week increment), compared with the general wards (aIRR 1.01 [1.00, 1.02]).
However, a reduction in severe HAIs (aIRR 0.13 [0.05, 0.32]) and a lower probability of HAI-associated in-hospital deaths (aHR 0.56 [0.31, 0.99]) were observed in the second period in the ICUs.
In attempting to explain the variance seen between the results for general wards and the ICU, an analysis of alcohol-based handrub solution consumption as a marker of hand-hygiene behavior indicated that a remarkable increase in consumption occurred in the ICUs while a less pronounced increase occurred in the general wards. “This finding might explain the observed decline in the HAI incidence after starting the campaign in the ICUs, which was not observed on the general wards.” Dr. Hagel and his colleagues suggested.
The authors discussed how several confounding factors that influenced the incidence of HAIs needed to be considered. As a consequence of the improvement in HAI management, the number of collected blood culture sets nearly doubled hospital-wide from 13,126 to 25,805 per year between 2011 and 2014, which likely undermined the study objective, they stated. The increase in cultures may have impacted the number of overall HAIs found.
“Although the primary aim of the study of reducing the overall incidence of HAIs was not achieved, the study demonstrated a decline of severe HAIs in patients in ICUs in the second surveillance period. Whether this result was a consequence of the ICP or a general improvement in HAI management remains unclear,” the researchers concluded.
The authors reported that they had no conflicts of interest.
SOURCE: Hagel S et al. Clin Microbiol Infect. doi: 10.1016/j.cmi.2018.07.010].
A hospital-wide infection control program (ICP) was found to be associated with reduced health care-associated severe sepsis/septic shock or death in the ICU, but it was not clear whether this decrease was a consequence of the ICP or because of a concomitant improvement in HAI case management, according to a the results of a prospective analysis.
In addition, there was no significant decrease in overall HAIs seen despite implementation of the program, according to the report published online in Clinical Microbiology and Infection (doi: 10.1016/j.cmi.2018.07.010), according to Stefan Hagel, MD, of the Institute for Infectious Diseases and Infection Control, Jena (Germany) University Hospital, and his colleagues.
They assessed two surveillance periods (September 2011 to August 2012 and May 2013 to August 2014). The ICP started in October 2012, and included hand-hygiene promotion and bundle implementation for common HAIs.
The data were analyzed by segmented mixed-effects Poisson regression and multi-state models and reported as adjusted incidence rate ratios (aIRR) and 50 adjusted hazard ratios (aHR) with 95% confidence intervals (CI).
In the first period, 62,154 patients were under surveillance, with 1,568 HAIs identified in 1,170 patients (4.3/100 admissions) and 2,336 HAIs identified in 1,711 patients (4.9/100 admissions) in the second surveillance period. No differences were found in the overall HAI incidence rates between the periods in the general wards and ICUs. There was only a slight decline in the incidence rate of HAIs in the ICUs (aIRR 0.98 [0.97, 1.00] per 1-week increment), compared with the general wards (aIRR 1.01 [1.00, 1.02]).
However, a reduction in severe HAIs (aIRR 0.13 [0.05, 0.32]) and a lower probability of HAI-associated in-hospital deaths (aHR 0.56 [0.31, 0.99]) were observed in the second period in the ICUs.
In attempting to explain the variance seen between the results for general wards and the ICU, an analysis of alcohol-based handrub solution consumption as a marker of hand-hygiene behavior indicated that a remarkable increase in consumption occurred in the ICUs while a less pronounced increase occurred in the general wards. “This finding might explain the observed decline in the HAI incidence after starting the campaign in the ICUs, which was not observed on the general wards.” Dr. Hagel and his colleagues suggested.
The authors discussed how several confounding factors that influenced the incidence of HAIs needed to be considered. As a consequence of the improvement in HAI management, the number of collected blood culture sets nearly doubled hospital-wide from 13,126 to 25,805 per year between 2011 and 2014, which likely undermined the study objective, they stated. The increase in cultures may have impacted the number of overall HAIs found.
“Although the primary aim of the study of reducing the overall incidence of HAIs was not achieved, the study demonstrated a decline of severe HAIs in patients in ICUs in the second surveillance period. Whether this result was a consequence of the ICP or a general improvement in HAI management remains unclear,” the researchers concluded.
The authors reported that they had no conflicts of interest.
SOURCE: Hagel S et al. Clin Microbiol Infect. doi: 10.1016/j.cmi.2018.07.010].
FROM CLINICAL MICROBIOLOGY AND INFECTION
Key clinical point: Hand hygiene was the key factor associated with a decrease in severe HAIs.
Major finding: A reduction in severe HAIs (aIRR 0.13) and a lower probability of HAI-associated in-hospital deaths (aHR 0.56]) were observed.
Study details: A prospective database analysis of more nearly 65,000 hospitalized patients.
Disclosures: The authors reported that they had no conflicts of interest.
Source: Hagel S et al. Clin Microbiol Infect. doi: 10.1016/j.cmi.2018.07.010.
Fewer groin infections with closed incision negative pressure therapy after vascular surgery
Closed incision negative pressure therapy (ciNPT) was found to reduce surgical site infections (SSI) in vascular surgery, according to the results of a prospective, randomized, industry-sponsored trial of patients who underwent vascular surgery for peripheral artery disease (PAD) published online in the European Journal of Vascular and Endovascular Surgery.
The investigator-initiated Reduction of Groin Wound Infections After Vascular Surgery by Using an Incision Management System trial (NCT02395159) included 204 patients who underwent vascular surgery involving longitudinal groin incision to treat the lower extremity or the iliac arteries between July 2015 and May 2017 at two study centers.
The primary endpoint was the occurrence of SSI assessed by the Szilagyi classification (grades I-III). The mean patient age was nearly 67 years and 70% were men. In terms of PAD staging, 52% were stage 2B, 28% were stage 3, and 19% were stage 4. Among the patients, 45% had a previous groin incision and 42% had diabetes.
All patients underwent similar preoperative treatment: hair shaving and preparation with Poly Alcohol (Antiseptica, Pulheim, Germany) and Braunoderm (Braun, Melsungen, Germany). At 30 minutes preincision, patients received intravenous antibiotic treatment (1.5 g cefuroxime or 600 mg clindamycin, if allergic to penicillin). After closure, the incision and surrounding skin area was cleaned and dried using sterile gauze. In the control group, a sterile adhesive wound dressing was applied to the wound, which was changed daily. In the treatment group, ciNPT was applied under sterile conditions in the operating room using the Prevena device, which exerts a continuous negative pressure of 125 mm Hg on the closed incision during the time of application. The device was removed at 5-7 days postoperatively, and no further wound dressings were used in the treatment group unless an SSI occurred.
The control group experienced more frequent SSIs (33.3%) than the intervention group (13.2%) (P =.0015). This difference was based on an increased rate of Szilagyi grade I SSI in the control group (24.6% vs. 8.1%, P = .0012), according to Alexander Gombert, MD, of the University Hospital Aachen (Germany), and his colleagues. The absolute risk difference based on the Szilagyi classification was –20.1 per 100 (95% confidence interval, –31.9 to –8.2).
In addition, there was a statistically significantly lower rate of SSI when using ciNPT within the subgroups at greater risk of infection, compared with controls: PAD stage greater than or equal to 3 (P less than .001), body mass index greater than 25 kg/m2 (P less than .001), and previous groin incision (P = .016).
There were no statistical differences between the two groups in Szilagyi grade II and III SSIs (which occurred in 5.8% of all procedures).
No potentially device-related complications were observed in the trial and there were no failures of the device seen.
“The use of ciNPT rather than standard wound dressing after groin incision as access for vascular surgery was associated with a reduced rate of superficial SSI classified by Szilagyi, suggesting that ciNPT may be useful for reducing the SSI rate among high-risk patients,” the researchers concluded.
The trial was funded by Acelity. Dr. Gombert received travel grants from Acelity.
SOURCE: Gombert A et al. Eur J Vasc Surg. 2018 Jul 2. doi: 10.1016/j.ejvs.2018.05.018.
Closed incision negative pressure therapy (ciNPT) was found to reduce surgical site infections (SSI) in vascular surgery, according to the results of a prospective, randomized, industry-sponsored trial of patients who underwent vascular surgery for peripheral artery disease (PAD) published online in the European Journal of Vascular and Endovascular Surgery.
The investigator-initiated Reduction of Groin Wound Infections After Vascular Surgery by Using an Incision Management System trial (NCT02395159) included 204 patients who underwent vascular surgery involving longitudinal groin incision to treat the lower extremity or the iliac arteries between July 2015 and May 2017 at two study centers.
The primary endpoint was the occurrence of SSI assessed by the Szilagyi classification (grades I-III). The mean patient age was nearly 67 years and 70% were men. In terms of PAD staging, 52% were stage 2B, 28% were stage 3, and 19% were stage 4. Among the patients, 45% had a previous groin incision and 42% had diabetes.
All patients underwent similar preoperative treatment: hair shaving and preparation with Poly Alcohol (Antiseptica, Pulheim, Germany) and Braunoderm (Braun, Melsungen, Germany). At 30 minutes preincision, patients received intravenous antibiotic treatment (1.5 g cefuroxime or 600 mg clindamycin, if allergic to penicillin). After closure, the incision and surrounding skin area was cleaned and dried using sterile gauze. In the control group, a sterile adhesive wound dressing was applied to the wound, which was changed daily. In the treatment group, ciNPT was applied under sterile conditions in the operating room using the Prevena device, which exerts a continuous negative pressure of 125 mm Hg on the closed incision during the time of application. The device was removed at 5-7 days postoperatively, and no further wound dressings were used in the treatment group unless an SSI occurred.
The control group experienced more frequent SSIs (33.3%) than the intervention group (13.2%) (P =.0015). This difference was based on an increased rate of Szilagyi grade I SSI in the control group (24.6% vs. 8.1%, P = .0012), according to Alexander Gombert, MD, of the University Hospital Aachen (Germany), and his colleagues. The absolute risk difference based on the Szilagyi classification was –20.1 per 100 (95% confidence interval, –31.9 to –8.2).
In addition, there was a statistically significantly lower rate of SSI when using ciNPT within the subgroups at greater risk of infection, compared with controls: PAD stage greater than or equal to 3 (P less than .001), body mass index greater than 25 kg/m2 (P less than .001), and previous groin incision (P = .016).
There were no statistical differences between the two groups in Szilagyi grade II and III SSIs (which occurred in 5.8% of all procedures).
No potentially device-related complications were observed in the trial and there were no failures of the device seen.
“The use of ciNPT rather than standard wound dressing after groin incision as access for vascular surgery was associated with a reduced rate of superficial SSI classified by Szilagyi, suggesting that ciNPT may be useful for reducing the SSI rate among high-risk patients,” the researchers concluded.
The trial was funded by Acelity. Dr. Gombert received travel grants from Acelity.
SOURCE: Gombert A et al. Eur J Vasc Surg. 2018 Jul 2. doi: 10.1016/j.ejvs.2018.05.018.
Closed incision negative pressure therapy (ciNPT) was found to reduce surgical site infections (SSI) in vascular surgery, according to the results of a prospective, randomized, industry-sponsored trial of patients who underwent vascular surgery for peripheral artery disease (PAD) published online in the European Journal of Vascular and Endovascular Surgery.
The investigator-initiated Reduction of Groin Wound Infections After Vascular Surgery by Using an Incision Management System trial (NCT02395159) included 204 patients who underwent vascular surgery involving longitudinal groin incision to treat the lower extremity or the iliac arteries between July 2015 and May 2017 at two study centers.
The primary endpoint was the occurrence of SSI assessed by the Szilagyi classification (grades I-III). The mean patient age was nearly 67 years and 70% were men. In terms of PAD staging, 52% were stage 2B, 28% were stage 3, and 19% were stage 4. Among the patients, 45% had a previous groin incision and 42% had diabetes.
All patients underwent similar preoperative treatment: hair shaving and preparation with Poly Alcohol (Antiseptica, Pulheim, Germany) and Braunoderm (Braun, Melsungen, Germany). At 30 minutes preincision, patients received intravenous antibiotic treatment (1.5 g cefuroxime or 600 mg clindamycin, if allergic to penicillin). After closure, the incision and surrounding skin area was cleaned and dried using sterile gauze. In the control group, a sterile adhesive wound dressing was applied to the wound, which was changed daily. In the treatment group, ciNPT was applied under sterile conditions in the operating room using the Prevena device, which exerts a continuous negative pressure of 125 mm Hg on the closed incision during the time of application. The device was removed at 5-7 days postoperatively, and no further wound dressings were used in the treatment group unless an SSI occurred.
The control group experienced more frequent SSIs (33.3%) than the intervention group (13.2%) (P =.0015). This difference was based on an increased rate of Szilagyi grade I SSI in the control group (24.6% vs. 8.1%, P = .0012), according to Alexander Gombert, MD, of the University Hospital Aachen (Germany), and his colleagues. The absolute risk difference based on the Szilagyi classification was –20.1 per 100 (95% confidence interval, –31.9 to –8.2).
In addition, there was a statistically significantly lower rate of SSI when using ciNPT within the subgroups at greater risk of infection, compared with controls: PAD stage greater than or equal to 3 (P less than .001), body mass index greater than 25 kg/m2 (P less than .001), and previous groin incision (P = .016).
There were no statistical differences between the two groups in Szilagyi grade II and III SSIs (which occurred in 5.8% of all procedures).
No potentially device-related complications were observed in the trial and there were no failures of the device seen.
“The use of ciNPT rather than standard wound dressing after groin incision as access for vascular surgery was associated with a reduced rate of superficial SSI classified by Szilagyi, suggesting that ciNPT may be useful for reducing the SSI rate among high-risk patients,” the researchers concluded.
The trial was funded by Acelity. Dr. Gombert received travel grants from Acelity.
SOURCE: Gombert A et al. Eur J Vasc Surg. 2018 Jul 2. doi: 10.1016/j.ejvs.2018.05.018.
FROM THE EUROPEAN JOURNAL OF VASCULAR AND ENDOVASCULAR SURGERY
Key clinical point: Closed incision negative pressure therapy lessened the incidence of groin infection after vascular surgery.
Major finding: The control group experienced more frequent surgical site infections (33.3%) than the intervention group (13.2%) (P =.0015).
Study details: A randomized, controlled trial of 204 patients with peripheral artery disease who underwent vascular surgery.
Disclosures: The trial was funded by Acelity. Dr. Gombert received travel grants from Acelity.
Source: Gombert A et al. Eur J Vasc Surg. 2018 Jul 2. doi: 10.1016/j.ejvs.2018.05.018.
Timely culture reports lower LOS for neonatal fever
ATLANTA – An adjustment in the culture reporting schedule at Texas Children’s Hospital, Houston, helped reduce the average length of stay for neonatal fever from 48 to 43 hours, without increasing readmissions for serious bacterial infections, according to a review presented at the Pediatric Hospital Medicine meeting.
Investigators there were working to meet the goals of the Reducing Excessive Variability in Infant Sepsis Evaluation project (REVISE), a national collaboration aimed at improving care. One of the goals is to reduce the length of stay (LOS) for neonatal fever to fewer than 30 hours for low-risk infants and fewer than 42 hours among high-risk infants.
The traditional standard is to keep children in the hospital for 48 hours to rule out sepsis, but that thinking has begun to change amid evidence that blood cultures generally do not need that long to turn positive, among other findings, said investigator Huay-Ying Lo, MD, a pediatrician at Texas Children’s.
“At our institution,” which admits more than 200 NF cases annually, “we have order sets for neonatal fever, and we’re actually doing pretty well” meeting most of the REVISE goals, “so we decided to focus on reducing length of stay,” she said at the meeting.
Evidence of the safety and cost savings of earlier discharge was presented to providers, and weekly emails reminded them of the early discharge goal and updated them on the current average LOS for NF.
Dr. Lo and her team also brainstormed with providers to identify problems. “One of the barriers they consistently mentioned was the timing of cultures being reported out from the microbiology lab. A lot of time, people were just waiting for the report to say no growth for 36 hours or whatever it was going to be,” she said.
That led to talks with the microbiology department. Blood cultures were already automated, so there wasn’t much that needed to be done. Urine cultures were read manually three to four times a day after the initial incubation period. However, after an initial Gram stain, CSF cultures were read manually only one or two times a day – whenever somebody had time. The hours were random, and sometimes results were not reported until the evening, which meant the child had to spend another night in the hospital.
The lab director agreed that it was a problem, and standardized procedures to read cultures twice a day, at 7 a.m. and 2 p.m. “The times we agreed upon; 7 a.m. works really well for morning discharge, and at 2 p.m., the day team is still there and can get kids out that day,” Dr. Lo explained.
. Among infants 7-60 days old admitted with NF – excluding ill-appearing children and those with comorbidities that increased the risk of infections – the mean LOS fell from 48 hours among 144 infants treated before the intervention, to 43 hours among 157 treated afterward (P = .001), and “we didn’t have any more readmission for serious bacterial infections,” Dr. Lo said.
“We want to reduce it further. If we get to 42 hours, we’ll be pretty happy.” Updating discharge criteria, and letting providers know how their LOS’s compare with their peers’ might help. “I’m sure some people are more conservative and some a little more liberal,” she said.
There was no industry funding for the work, and the investigators had no disclosures. The meeting was sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, and the Academic Pediatric Association.
ATLANTA – An adjustment in the culture reporting schedule at Texas Children’s Hospital, Houston, helped reduce the average length of stay for neonatal fever from 48 to 43 hours, without increasing readmissions for serious bacterial infections, according to a review presented at the Pediatric Hospital Medicine meeting.
Investigators there were working to meet the goals of the Reducing Excessive Variability in Infant Sepsis Evaluation project (REVISE), a national collaboration aimed at improving care. One of the goals is to reduce the length of stay (LOS) for neonatal fever to fewer than 30 hours for low-risk infants and fewer than 42 hours among high-risk infants.
The traditional standard is to keep children in the hospital for 48 hours to rule out sepsis, but that thinking has begun to change amid evidence that blood cultures generally do not need that long to turn positive, among other findings, said investigator Huay-Ying Lo, MD, a pediatrician at Texas Children’s.
“At our institution,” which admits more than 200 NF cases annually, “we have order sets for neonatal fever, and we’re actually doing pretty well” meeting most of the REVISE goals, “so we decided to focus on reducing length of stay,” she said at the meeting.
Evidence of the safety and cost savings of earlier discharge was presented to providers, and weekly emails reminded them of the early discharge goal and updated them on the current average LOS for NF.
Dr. Lo and her team also brainstormed with providers to identify problems. “One of the barriers they consistently mentioned was the timing of cultures being reported out from the microbiology lab. A lot of time, people were just waiting for the report to say no growth for 36 hours or whatever it was going to be,” she said.
That led to talks with the microbiology department. Blood cultures were already automated, so there wasn’t much that needed to be done. Urine cultures were read manually three to four times a day after the initial incubation period. However, after an initial Gram stain, CSF cultures were read manually only one or two times a day – whenever somebody had time. The hours were random, and sometimes results were not reported until the evening, which meant the child had to spend another night in the hospital.
The lab director agreed that it was a problem, and standardized procedures to read cultures twice a day, at 7 a.m. and 2 p.m. “The times we agreed upon; 7 a.m. works really well for morning discharge, and at 2 p.m., the day team is still there and can get kids out that day,” Dr. Lo explained.
. Among infants 7-60 days old admitted with NF – excluding ill-appearing children and those with comorbidities that increased the risk of infections – the mean LOS fell from 48 hours among 144 infants treated before the intervention, to 43 hours among 157 treated afterward (P = .001), and “we didn’t have any more readmission for serious bacterial infections,” Dr. Lo said.
“We want to reduce it further. If we get to 42 hours, we’ll be pretty happy.” Updating discharge criteria, and letting providers know how their LOS’s compare with their peers’ might help. “I’m sure some people are more conservative and some a little more liberal,” she said.
There was no industry funding for the work, and the investigators had no disclosures. The meeting was sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, and the Academic Pediatric Association.
ATLANTA – An adjustment in the culture reporting schedule at Texas Children’s Hospital, Houston, helped reduce the average length of stay for neonatal fever from 48 to 43 hours, without increasing readmissions for serious bacterial infections, according to a review presented at the Pediatric Hospital Medicine meeting.
Investigators there were working to meet the goals of the Reducing Excessive Variability in Infant Sepsis Evaluation project (REVISE), a national collaboration aimed at improving care. One of the goals is to reduce the length of stay (LOS) for neonatal fever to fewer than 30 hours for low-risk infants and fewer than 42 hours among high-risk infants.
The traditional standard is to keep children in the hospital for 48 hours to rule out sepsis, but that thinking has begun to change amid evidence that blood cultures generally do not need that long to turn positive, among other findings, said investigator Huay-Ying Lo, MD, a pediatrician at Texas Children’s.
“At our institution,” which admits more than 200 NF cases annually, “we have order sets for neonatal fever, and we’re actually doing pretty well” meeting most of the REVISE goals, “so we decided to focus on reducing length of stay,” she said at the meeting.
Evidence of the safety and cost savings of earlier discharge was presented to providers, and weekly emails reminded them of the early discharge goal and updated them on the current average LOS for NF.
Dr. Lo and her team also brainstormed with providers to identify problems. “One of the barriers they consistently mentioned was the timing of cultures being reported out from the microbiology lab. A lot of time, people were just waiting for the report to say no growth for 36 hours or whatever it was going to be,” she said.
That led to talks with the microbiology department. Blood cultures were already automated, so there wasn’t much that needed to be done. Urine cultures were read manually three to four times a day after the initial incubation period. However, after an initial Gram stain, CSF cultures were read manually only one or two times a day – whenever somebody had time. The hours were random, and sometimes results were not reported until the evening, which meant the child had to spend another night in the hospital.
The lab director agreed that it was a problem, and standardized procedures to read cultures twice a day, at 7 a.m. and 2 p.m. “The times we agreed upon; 7 a.m. works really well for morning discharge, and at 2 p.m., the day team is still there and can get kids out that day,” Dr. Lo explained.
. Among infants 7-60 days old admitted with NF – excluding ill-appearing children and those with comorbidities that increased the risk of infections – the mean LOS fell from 48 hours among 144 infants treated before the intervention, to 43 hours among 157 treated afterward (P = .001), and “we didn’t have any more readmission for serious bacterial infections,” Dr. Lo said.
“We want to reduce it further. If we get to 42 hours, we’ll be pretty happy.” Updating discharge criteria, and letting providers know how their LOS’s compare with their peers’ might help. “I’m sure some people are more conservative and some a little more liberal,” she said.
There was no industry funding for the work, and the investigators had no disclosures. The meeting was sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, and the Academic Pediatric Association.
REPORTING FROM PHM 2018
Key clinical point: An adjustment in the culture reporting schedule at Texas Children’s Hospital, Houston, helped reduce the average length of stay for neonatal fever, without increasing readmissions for serious bacterial infections.
Major finding: The mean length of stay fell from 48 hours among 144 infants treated before the intervention, to 43 hours among 157 treated afterward (P = .001).
Study details: Pre/post analysis of quality improvement project.
Disclosures: There was no industry funding for the work, and the investigators had no disclosures.
Primary cirrhotic prophylaxis of bacterial peritonitis falls short
WASHINGTON –
The mortality rate during follow-up of cirrhotic patients hospitalized while on primary prophylaxis against spontaneous bacterial peritonitis (SBP) was 19%, compared with a 9% death rate among cirrhotic patients hospitalized while on secondary prophylaxis, Jasmohan S. Bajaj, MD, said at the annual Digestive Disease Week®.
Although the findings raised questions about the value of primary prophylaxis with an antibiotic in cirrhotic patients for preventing a first episode of SBP, secondary prophylaxis remains an important precaution.
“There is clear benefit from secondary prophylaxis; please use it. The data supporting it are robust,” said Dr. Bajaj, a hepatologist at Virginia Commonwealth University, Richmond. In contrast, the evidence supporting benefits from primary prophylaxis is weaker, he said. The findings were also counterintuitive, because patients who experience repeat episodes of SBP might be expected to fare worse than those hit by SBP just once.
Dr. Bajaj also acknowledged the substantial confounding that distinguishes patients with cirrhosis receiving primary or secondary prophylaxis, and the difficulty of fully adjusting for all this confounding by statistical analyses. “There is selective bias for secondary prevention, and there is no way to correct for this,” he explained. Patients who need secondary prophylaxis have “weathered the storm” of a first episode of SBP, which might have exerted selection pressure, and might have triggered important immunologic changes, Dr. Bajaj suggested.
The findings also raised concerns about the appropriateness of existing antibiotic prophylaxis for SBP. The patients included in the study all received similar regimens regardless of whether they were on primary or secondary prophylaxis. Three-quarters of primary prophylaxis patients received a fluoroquinolone, as did 81% on secondary prophylaxis. All other patients received trimethoprim-sulfamethoxazole. These regimens are aimed at preventing gram-negative infections; however, an increasing number of SBP episodes are caused by either gram-positive pathogens or strains of gram-negative bacteria or fungi resistant to standard antibiotics.
Clinicians “absolutely” need to rethink their approach to both primary and secondary prophylaxis, Dr. Bajaj said. “As fast as treatment evolves, bacteria evolve 20 times faster. We need to find ways to prevent infections without antibiotic prophylaxis, whatever that might be.”
The study used data collected prospectively from patients with cirrhosis at any of 12 U.S. and 2 Canadian centers that belonged to the North American Consortium for the Study of End-Stage Liver Disease. Among 2,731 cirrhotic patients admitted nonelectively, 492 (18%) were on antibiotic prophylaxis at the time of their admission, 305 for primary prophylaxis and 187 for secondary prophylaxis. Dr. Bajaj and his associates used both the baseline model for end-stage liver disease score and serum albumin level of each patient to focus on a group of 154 primary prophylaxis and 154 secondary prophylaxis patients who were similar by these two criteria. Despite this matching, the two subgroups showed statistically significant differences at the time of their index hospitalization for several important clinical measures.
The secondary prophylaxis patients were significantly more likely to have been hospitalized within the previous 6 months, significantly more likely to be on treatment for hepatic encephalopathy at the time of their index admission, and significantly less likely to have systemic inflammatory response syndrome on admission.
Also, at the time of admission, secondary prophylaxis patients were significantly more likely to have an infection of any type at a rate of 40%, compared with 24% among those on primary prophylaxis, as well as a significantly higher rate of SBP at 16%, compared with a 9% rate among the primary prophylaxis patients. During hospitalization, nosocomial SBP occurred significantly more often among the secondary prophylaxis patients at a rate of 6%, compared with a 0.5% rate among those on primary prophylaxis.
Despite these between-group differences, the average duration of hospitalization, and the average incidence of acute-on-chronic liver failure during follow-up out to 30 days post discharge was similar in the two subgroups. And the patients on secondary prophylaxis showed better outcomes by two important parameters: mortality during hospitalization and 30 days post discharge; and the incidence of ICU admission during hospitalization, which was significantly greater for primary prophylaxis patients at 31%, compared with 21% among the secondary prophylaxis patients, Dr. Bajaj reported.
Dr. Bajaj has been a consultant for Norgine and Salix Pharmaceuticals and has received research support from Grifols and Salix Pharmaceuticals.
WASHINGTON –
The mortality rate during follow-up of cirrhotic patients hospitalized while on primary prophylaxis against spontaneous bacterial peritonitis (SBP) was 19%, compared with a 9% death rate among cirrhotic patients hospitalized while on secondary prophylaxis, Jasmohan S. Bajaj, MD, said at the annual Digestive Disease Week®.
Although the findings raised questions about the value of primary prophylaxis with an antibiotic in cirrhotic patients for preventing a first episode of SBP, secondary prophylaxis remains an important precaution.
“There is clear benefit from secondary prophylaxis; please use it. The data supporting it are robust,” said Dr. Bajaj, a hepatologist at Virginia Commonwealth University, Richmond. In contrast, the evidence supporting benefits from primary prophylaxis is weaker, he said. The findings were also counterintuitive, because patients who experience repeat episodes of SBP might be expected to fare worse than those hit by SBP just once.
Dr. Bajaj also acknowledged the substantial confounding that distinguishes patients with cirrhosis receiving primary or secondary prophylaxis, and the difficulty of fully adjusting for all this confounding by statistical analyses. “There is selective bias for secondary prevention, and there is no way to correct for this,” he explained. Patients who need secondary prophylaxis have “weathered the storm” of a first episode of SBP, which might have exerted selection pressure, and might have triggered important immunologic changes, Dr. Bajaj suggested.
The findings also raised concerns about the appropriateness of existing antibiotic prophylaxis for SBP. The patients included in the study all received similar regimens regardless of whether they were on primary or secondary prophylaxis. Three-quarters of primary prophylaxis patients received a fluoroquinolone, as did 81% on secondary prophylaxis. All other patients received trimethoprim-sulfamethoxazole. These regimens are aimed at preventing gram-negative infections; however, an increasing number of SBP episodes are caused by either gram-positive pathogens or strains of gram-negative bacteria or fungi resistant to standard antibiotics.
Clinicians “absolutely” need to rethink their approach to both primary and secondary prophylaxis, Dr. Bajaj said. “As fast as treatment evolves, bacteria evolve 20 times faster. We need to find ways to prevent infections without antibiotic prophylaxis, whatever that might be.”
The study used data collected prospectively from patients with cirrhosis at any of 12 U.S. and 2 Canadian centers that belonged to the North American Consortium for the Study of End-Stage Liver Disease. Among 2,731 cirrhotic patients admitted nonelectively, 492 (18%) were on antibiotic prophylaxis at the time of their admission, 305 for primary prophylaxis and 187 for secondary prophylaxis. Dr. Bajaj and his associates used both the baseline model for end-stage liver disease score and serum albumin level of each patient to focus on a group of 154 primary prophylaxis and 154 secondary prophylaxis patients who were similar by these two criteria. Despite this matching, the two subgroups showed statistically significant differences at the time of their index hospitalization for several important clinical measures.
The secondary prophylaxis patients were significantly more likely to have been hospitalized within the previous 6 months, significantly more likely to be on treatment for hepatic encephalopathy at the time of their index admission, and significantly less likely to have systemic inflammatory response syndrome on admission.
Also, at the time of admission, secondary prophylaxis patients were significantly more likely to have an infection of any type at a rate of 40%, compared with 24% among those on primary prophylaxis, as well as a significantly higher rate of SBP at 16%, compared with a 9% rate among the primary prophylaxis patients. During hospitalization, nosocomial SBP occurred significantly more often among the secondary prophylaxis patients at a rate of 6%, compared with a 0.5% rate among those on primary prophylaxis.
Despite these between-group differences, the average duration of hospitalization, and the average incidence of acute-on-chronic liver failure during follow-up out to 30 days post discharge was similar in the two subgroups. And the patients on secondary prophylaxis showed better outcomes by two important parameters: mortality during hospitalization and 30 days post discharge; and the incidence of ICU admission during hospitalization, which was significantly greater for primary prophylaxis patients at 31%, compared with 21% among the secondary prophylaxis patients, Dr. Bajaj reported.
Dr. Bajaj has been a consultant for Norgine and Salix Pharmaceuticals and has received research support from Grifols and Salix Pharmaceuticals.
WASHINGTON –
The mortality rate during follow-up of cirrhotic patients hospitalized while on primary prophylaxis against spontaneous bacterial peritonitis (SBP) was 19%, compared with a 9% death rate among cirrhotic patients hospitalized while on secondary prophylaxis, Jasmohan S. Bajaj, MD, said at the annual Digestive Disease Week®.
Although the findings raised questions about the value of primary prophylaxis with an antibiotic in cirrhotic patients for preventing a first episode of SBP, secondary prophylaxis remains an important precaution.
“There is clear benefit from secondary prophylaxis; please use it. The data supporting it are robust,” said Dr. Bajaj, a hepatologist at Virginia Commonwealth University, Richmond. In contrast, the evidence supporting benefits from primary prophylaxis is weaker, he said. The findings were also counterintuitive, because patients who experience repeat episodes of SBP might be expected to fare worse than those hit by SBP just once.
Dr. Bajaj also acknowledged the substantial confounding that distinguishes patients with cirrhosis receiving primary or secondary prophylaxis, and the difficulty of fully adjusting for all this confounding by statistical analyses. “There is selective bias for secondary prevention, and there is no way to correct for this,” he explained. Patients who need secondary prophylaxis have “weathered the storm” of a first episode of SBP, which might have exerted selection pressure, and might have triggered important immunologic changes, Dr. Bajaj suggested.
The findings also raised concerns about the appropriateness of existing antibiotic prophylaxis for SBP. The patients included in the study all received similar regimens regardless of whether they were on primary or secondary prophylaxis. Three-quarters of primary prophylaxis patients received a fluoroquinolone, as did 81% on secondary prophylaxis. All other patients received trimethoprim-sulfamethoxazole. These regimens are aimed at preventing gram-negative infections; however, an increasing number of SBP episodes are caused by either gram-positive pathogens or strains of gram-negative bacteria or fungi resistant to standard antibiotics.
Clinicians “absolutely” need to rethink their approach to both primary and secondary prophylaxis, Dr. Bajaj said. “As fast as treatment evolves, bacteria evolve 20 times faster. We need to find ways to prevent infections without antibiotic prophylaxis, whatever that might be.”
The study used data collected prospectively from patients with cirrhosis at any of 12 U.S. and 2 Canadian centers that belonged to the North American Consortium for the Study of End-Stage Liver Disease. Among 2,731 cirrhotic patients admitted nonelectively, 492 (18%) were on antibiotic prophylaxis at the time of their admission, 305 for primary prophylaxis and 187 for secondary prophylaxis. Dr. Bajaj and his associates used both the baseline model for end-stage liver disease score and serum albumin level of each patient to focus on a group of 154 primary prophylaxis and 154 secondary prophylaxis patients who were similar by these two criteria. Despite this matching, the two subgroups showed statistically significant differences at the time of their index hospitalization for several important clinical measures.
The secondary prophylaxis patients were significantly more likely to have been hospitalized within the previous 6 months, significantly more likely to be on treatment for hepatic encephalopathy at the time of their index admission, and significantly less likely to have systemic inflammatory response syndrome on admission.
Also, at the time of admission, secondary prophylaxis patients were significantly more likely to have an infection of any type at a rate of 40%, compared with 24% among those on primary prophylaxis, as well as a significantly higher rate of SBP at 16%, compared with a 9% rate among the primary prophylaxis patients. During hospitalization, nosocomial SBP occurred significantly more often among the secondary prophylaxis patients at a rate of 6%, compared with a 0.5% rate among those on primary prophylaxis.
Despite these between-group differences, the average duration of hospitalization, and the average incidence of acute-on-chronic liver failure during follow-up out to 30 days post discharge was similar in the two subgroups. And the patients on secondary prophylaxis showed better outcomes by two important parameters: mortality during hospitalization and 30 days post discharge; and the incidence of ICU admission during hospitalization, which was significantly greater for primary prophylaxis patients at 31%, compared with 21% among the secondary prophylaxis patients, Dr. Bajaj reported.
Dr. Bajaj has been a consultant for Norgine and Salix Pharmaceuticals and has received research support from Grifols and Salix Pharmaceuticals.
REPORTING FROM DDW 2018
Key clinical point: Antibiotic prophylaxis for bacterial peritonitis showed limitations, especially for primary prophylaxis.
Major finding: Mortality was 19% among primary prophylaxis patients and 9% among secondary prophylaxis patients during hospitalization and 30 days following.
Study details: An analysis of data from 308 cirrhotic patients on antibiotic prophylaxis at 14 North American centers.
Disclosures: Dr. Bajaj has been a consultant for Norgine and Salix Pharmaceuticals and has received research support from Grifols and Salix Pharmaceuticals.