User login
Progress stalling on malaria elimination
In its final report on the E-2020 initiative, the World Health Organization touted its progress on its goal of eliminating malaria throughout the world. But critics are charging that progress has stalled.
The E-2020 initiative supported the efforts of 21 countries in eliminating malaria. In a remarkable achievement, especially during the COVID-19 pandemic, eight E-2020 member countries reported zero cases of malaria in 2020. The WHO’s next target is the elimination of malaria in 20 of those countries by 2025.
While applauding these successes, in an interview with this news organization, Sir Nicholas J. White, FRS, professor of tropical medicine, Mahidol University, Salaya, Thailand, and Oxford (England) University, also put those successes in perspective. For one thing, the original 2020 goal was the elimination of malaria in 10 countries. Prof. White acknowledged that there had been very “substantial reductions in global morbidity and mortality” from 2000 to 2015, but he pointed out that those advances have not been sustained.
Prof. White added, “There has never been a really good, detailed inquiry as to why progress has stalled” in the high-burden countries.
Prof. White also provided important historical context, explaining that “100 years ago, malaria was pretty much a global disease. There were few places in the world which did not have malaria. You had malaria up to the Arctic Circle. You had malaria in the United States, particularly in the Tennessee Valley in the southeastern part of the United States. The Centers for Disease Control was formed specifically to counter malaria and malaria interfering with the building of the Erie and Ottawa canals.”
Kim Lindblade, PhD, malaria elimination team lead of the WHO’s Global Malaria Program, addressed those concerns with this news organization. “It’s not completely clear why [progress] has stalled,” she said. “There are lots of potential reasons for it, including stagnating funding.”
Dr. Lindblade added that high-burden countries are “facing big challenges. [Since 2015] there’s this stagnation. We’re fighting against population growth, and countries need to get back on track to continue to decrease their malaria burden. So that’s the big focus right now, to reorganize efforts to help countries achieve the goals of the World Health Assembly.”
Asked how these countries might approach the problem differently, Dr. Lindblade said that in the recent past, there was “almost a one-size-fits-all strategy. Now we’re looking much more carefully at conditions at the district level or provincial level and saying, What is it that this particular district or province needs? … It’s becoming much more tailored to the environment and to the specific epidemiological situation. … and I think that’s gotten a lot of people very excited.”
Because of travel restrictions and lockdowns because of COVID-19, the number of imported cases of malaria has declined. That’s the good news. But the pandemic has made elimination more difficult in other ways. For example, the delivery of insecticide-treated bed nets has been delayed in some areas, as has targeted indoor spraying. People in many areas have put off seeking medical care. Diagnostic capabilities have been reduced because of health care personnel having been diverted to address the COVID-19 crisis.
Still, some of the successes in eliminating malaria have been striking. Iran, for example, reduced its cases from about 98,000 in 1991 to 12,000 just 10 years later. Since then, Iran has established rapid response teams equipped with insecticide-impregnated nets, rapid diagnostic tests, and antimalarials. A network of more than 3,700 community health volunteers has been trained and deployed throughout the country.
A key element of Iran’s success – and that of some of the other countries – is the political will to tackle malaria. This translates to funding. Notably, the most successful countries provide free primary health care to everyone, regardless of their legal or residency status. Volunteer migrant workers are trained to diagnose malaria and to educate fellow migrants about the disease and prevention strategies.
Malaysia and China are examples of two countries at risk of importing malaria through their many people who work abroad in malaria-endemic regions. They have had to increase their surveillance.
Although Malaysia has eliminated most malaria species – those transmitted through people – they still have problems with the malaria parasite hosted by monkeys.
The WHO report stresses the lessons learned through their E-2020 program. Two key criteria are political commitment and associated funding. Next are surveillance and efforts to reach everyone, even in geographically remote or marginalized communities. Close surveillance also enables strategies to be modified to local needs.
Countries need to cooperate, especially along border areas and in regard to communications. The WHO stressed the need for countries to have an integrated response in their approach to malaria, including accurate surveillance, diagnostic testing, treatment, and robust education in preventive measures.
Although these successes were not as evident in some high-burden countries, Prof. White applauded their perseverance, noting, “It’s quite difficult to sustain the political momentum. … That endgame to keep the motivation, keep the support, to getting rid of something is hard.”
Prof. White and Dr. Lindberg have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In its final report on the E-2020 initiative, the World Health Organization touted its progress on its goal of eliminating malaria throughout the world. But critics are charging that progress has stalled.
The E-2020 initiative supported the efforts of 21 countries in eliminating malaria. In a remarkable achievement, especially during the COVID-19 pandemic, eight E-2020 member countries reported zero cases of malaria in 2020. The WHO’s next target is the elimination of malaria in 20 of those countries by 2025.
While applauding these successes, in an interview with this news organization, Sir Nicholas J. White, FRS, professor of tropical medicine, Mahidol University, Salaya, Thailand, and Oxford (England) University, also put those successes in perspective. For one thing, the original 2020 goal was the elimination of malaria in 10 countries. Prof. White acknowledged that there had been very “substantial reductions in global morbidity and mortality” from 2000 to 2015, but he pointed out that those advances have not been sustained.
Prof. White added, “There has never been a really good, detailed inquiry as to why progress has stalled” in the high-burden countries.
Prof. White also provided important historical context, explaining that “100 years ago, malaria was pretty much a global disease. There were few places in the world which did not have malaria. You had malaria up to the Arctic Circle. You had malaria in the United States, particularly in the Tennessee Valley in the southeastern part of the United States. The Centers for Disease Control was formed specifically to counter malaria and malaria interfering with the building of the Erie and Ottawa canals.”
Kim Lindblade, PhD, malaria elimination team lead of the WHO’s Global Malaria Program, addressed those concerns with this news organization. “It’s not completely clear why [progress] has stalled,” she said. “There are lots of potential reasons for it, including stagnating funding.”
Dr. Lindblade added that high-burden countries are “facing big challenges. [Since 2015] there’s this stagnation. We’re fighting against population growth, and countries need to get back on track to continue to decrease their malaria burden. So that’s the big focus right now, to reorganize efforts to help countries achieve the goals of the World Health Assembly.”
Asked how these countries might approach the problem differently, Dr. Lindblade said that in the recent past, there was “almost a one-size-fits-all strategy. Now we’re looking much more carefully at conditions at the district level or provincial level and saying, What is it that this particular district or province needs? … It’s becoming much more tailored to the environment and to the specific epidemiological situation. … and I think that’s gotten a lot of people very excited.”
Because of travel restrictions and lockdowns because of COVID-19, the number of imported cases of malaria has declined. That’s the good news. But the pandemic has made elimination more difficult in other ways. For example, the delivery of insecticide-treated bed nets has been delayed in some areas, as has targeted indoor spraying. People in many areas have put off seeking medical care. Diagnostic capabilities have been reduced because of health care personnel having been diverted to address the COVID-19 crisis.
Still, some of the successes in eliminating malaria have been striking. Iran, for example, reduced its cases from about 98,000 in 1991 to 12,000 just 10 years later. Since then, Iran has established rapid response teams equipped with insecticide-impregnated nets, rapid diagnostic tests, and antimalarials. A network of more than 3,700 community health volunteers has been trained and deployed throughout the country.
A key element of Iran’s success – and that of some of the other countries – is the political will to tackle malaria. This translates to funding. Notably, the most successful countries provide free primary health care to everyone, regardless of their legal or residency status. Volunteer migrant workers are trained to diagnose malaria and to educate fellow migrants about the disease and prevention strategies.
Malaysia and China are examples of two countries at risk of importing malaria through their many people who work abroad in malaria-endemic regions. They have had to increase their surveillance.
Although Malaysia has eliminated most malaria species – those transmitted through people – they still have problems with the malaria parasite hosted by monkeys.
The WHO report stresses the lessons learned through their E-2020 program. Two key criteria are political commitment and associated funding. Next are surveillance and efforts to reach everyone, even in geographically remote or marginalized communities. Close surveillance also enables strategies to be modified to local needs.
Countries need to cooperate, especially along border areas and in regard to communications. The WHO stressed the need for countries to have an integrated response in their approach to malaria, including accurate surveillance, diagnostic testing, treatment, and robust education in preventive measures.
Although these successes were not as evident in some high-burden countries, Prof. White applauded their perseverance, noting, “It’s quite difficult to sustain the political momentum. … That endgame to keep the motivation, keep the support, to getting rid of something is hard.”
Prof. White and Dr. Lindberg have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In its final report on the E-2020 initiative, the World Health Organization touted its progress on its goal of eliminating malaria throughout the world. But critics are charging that progress has stalled.
The E-2020 initiative supported the efforts of 21 countries in eliminating malaria. In a remarkable achievement, especially during the COVID-19 pandemic, eight E-2020 member countries reported zero cases of malaria in 2020. The WHO’s next target is the elimination of malaria in 20 of those countries by 2025.
While applauding these successes, in an interview with this news organization, Sir Nicholas J. White, FRS, professor of tropical medicine, Mahidol University, Salaya, Thailand, and Oxford (England) University, also put those successes in perspective. For one thing, the original 2020 goal was the elimination of malaria in 10 countries. Prof. White acknowledged that there had been very “substantial reductions in global morbidity and mortality” from 2000 to 2015, but he pointed out that those advances have not been sustained.
Prof. White added, “There has never been a really good, detailed inquiry as to why progress has stalled” in the high-burden countries.
Prof. White also provided important historical context, explaining that “100 years ago, malaria was pretty much a global disease. There were few places in the world which did not have malaria. You had malaria up to the Arctic Circle. You had malaria in the United States, particularly in the Tennessee Valley in the southeastern part of the United States. The Centers for Disease Control was formed specifically to counter malaria and malaria interfering with the building of the Erie and Ottawa canals.”
Kim Lindblade, PhD, malaria elimination team lead of the WHO’s Global Malaria Program, addressed those concerns with this news organization. “It’s not completely clear why [progress] has stalled,” she said. “There are lots of potential reasons for it, including stagnating funding.”
Dr. Lindblade added that high-burden countries are “facing big challenges. [Since 2015] there’s this stagnation. We’re fighting against population growth, and countries need to get back on track to continue to decrease their malaria burden. So that’s the big focus right now, to reorganize efforts to help countries achieve the goals of the World Health Assembly.”
Asked how these countries might approach the problem differently, Dr. Lindblade said that in the recent past, there was “almost a one-size-fits-all strategy. Now we’re looking much more carefully at conditions at the district level or provincial level and saying, What is it that this particular district or province needs? … It’s becoming much more tailored to the environment and to the specific epidemiological situation. … and I think that’s gotten a lot of people very excited.”
Because of travel restrictions and lockdowns because of COVID-19, the number of imported cases of malaria has declined. That’s the good news. But the pandemic has made elimination more difficult in other ways. For example, the delivery of insecticide-treated bed nets has been delayed in some areas, as has targeted indoor spraying. People in many areas have put off seeking medical care. Diagnostic capabilities have been reduced because of health care personnel having been diverted to address the COVID-19 crisis.
Still, some of the successes in eliminating malaria have been striking. Iran, for example, reduced its cases from about 98,000 in 1991 to 12,000 just 10 years later. Since then, Iran has established rapid response teams equipped with insecticide-impregnated nets, rapid diagnostic tests, and antimalarials. A network of more than 3,700 community health volunteers has been trained and deployed throughout the country.
A key element of Iran’s success – and that of some of the other countries – is the political will to tackle malaria. This translates to funding. Notably, the most successful countries provide free primary health care to everyone, regardless of their legal or residency status. Volunteer migrant workers are trained to diagnose malaria and to educate fellow migrants about the disease and prevention strategies.
Malaysia and China are examples of two countries at risk of importing malaria through their many people who work abroad in malaria-endemic regions. They have had to increase their surveillance.
Although Malaysia has eliminated most malaria species – those transmitted through people – they still have problems with the malaria parasite hosted by monkeys.
The WHO report stresses the lessons learned through their E-2020 program. Two key criteria are political commitment and associated funding. Next are surveillance and efforts to reach everyone, even in geographically remote or marginalized communities. Close surveillance also enables strategies to be modified to local needs.
Countries need to cooperate, especially along border areas and in regard to communications. The WHO stressed the need for countries to have an integrated response in their approach to malaria, including accurate surveillance, diagnostic testing, treatment, and robust education in preventive measures.
Although these successes were not as evident in some high-burden countries, Prof. White applauded their perseverance, noting, “It’s quite difficult to sustain the political momentum. … That endgame to keep the motivation, keep the support, to getting rid of something is hard.”
Prof. White and Dr. Lindberg have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Malaria resistant to artemisinin emerging in Africa
A new study shows disturbing evidence that malaria is becoming resistant to artemisinin, a drug critical for treatment in Africa. Although artemisinin resistance has long plagued the Mekong Delta, it is relatively new to Africa.
In a study published online April 14 in The Lancet Infectious Diseases, researchers found that the typical 3-day course of treatment did not totally eradicate Plasmodium falciparum, the parasite that causes malaria. A delayed clearance of the parasite was shown and found to be associated with a genetic mutation called Pfkelch13 R561H.
P. falciparum isolates with this mutation were found in 7.5% of infected children in one area of Rwanda. Further genomic studies showed that this mutation was locally acquired and did not emerge from Southeast Asia. This is well illustrated in a genomic tree published in Nature Medicine in August, 2020. That study reported data collected from adults from 2013 to 2015.
The delay in reporting the mutation was due, in part, to the burdensome process of whole-genome sequencing and transfection studies, Pascal Ringwald, MD, PhD, coordinator of the Global Malaria Programme at WHO, and coauthor of the Nature Medicine study, said in an interview. In transfection studies, the mutation is inserted into parasites and the resultant effect is observed.
Aline Uwimana, MD, of Rwanda Biomedical Centre. is the lead author on both studies.
Meera Venkatesan, PhD, chief of the Case Management, Monitoring and Evaluation Branch, President’s Malaria Initiative, USAID, noted that the Lancet Infectious Diseases study was a therapeutic efficacy study (TES) on samples from children from 2018. In an interview, Dr. Venkatesan explained that the study is noteworthy because it demonstrated the clinical significance of this mutation with delayed parasite clearance. She did note that although there was a lag in publication of the initial reports of artemisinin resistance mutations, that information – and its implications – was promptly shared with the global malaria research community, as are other findings of public health importance.
Although most of the children got better, this “partial resistance” emerged while patients were taking artemether–lumefantrine. This is a type of artemisinin-based combination therapy (ACT) with two drugs intended to stall the emergence of resistance.
The delayed clearance will be a problem because it can contribute to the selection and spread of the partially resistant malaria parasite.
To slow the spread of artemisinin resistance, Dr. Ringwald emphasized the need to add a gametocidal drug to block the transmission to humans. “You give a single dose of primaquine, which will help stop the spread,” he said in an interview. “Continuing surveillance and mapping. These are priorities.”
So are following national guidelines and banning the use of artemisinin monotherapy. Dr. Ringwald stressed two additional priorities: the need for accurate diagnosis of malaria, and the need to use “good-quality drugs and to avoid substandard or fake medicines” by not purchasing drugs on the street.
Unscrupulous individuals are also selling artemisia preparations to treat or prevent COVID-19, when it has no such activity. Similarly, artemisia teas are sold as herbal remedies and nutraceuticals.
Philippe Guérin, MD, director of the Worldwide Antimalarial Resistance Network (WWARN), listed the same recommendations, focusing a bit more on accurate detection of malaria and treatment with a multidrug regimen plus primaquine. You need “to have different first-line treatment (different ACTs) to avoid drug pressure” and resistance to the partner drug emerging, he said in an interview.
Such multiple first-line treatments rely on artemisinin in combination with various drugs, but this can cause some logistical challenges. Resistance is so problematic that the MORU (Mahidol Oxford Tropical Medicine Research Unit) Tropical Health Network in Bangkok is studying triple drug combinations, adding amodiaquine or mefloquine to an artemisinin-based combination.
Dr. Guérin emphasized two other problems regarding the monitoring of malaria resistance in Africa (although not specifically Rwanda). One is the inability to do adequate surveillance in active conflict zones and areas of instability. The other is that COVID-19 is causing resources to be taken away from malaria and redirected to the more immediate crisis. By having to focus on the immediate viral pandemic, public-health authorities are missing the chance to address other critically important infectious diseases with large burdens – specifically malaria, TB, and HIV – which might have greater impacts on future generations.
Dr. Guérin noted that although we now have solid evidence of artemisinin resistance in Rwanda, and isolated cases in other African countries, we have little idea of the magnitude of the problem because testing is not widespread throughout parts of the continent.
What would widespread P. falciparum malaria resistance in Africa mean? Children are the most vulnerable to malaria, and account for two-thirds of the deaths. One study suggests there could be 78 million more cases over a 5-year period, along with far more deaths. Hence, there is a heightened urgency to implement the outlined strategies to prevent a looming catastrophe.
The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A new study shows disturbing evidence that malaria is becoming resistant to artemisinin, a drug critical for treatment in Africa. Although artemisinin resistance has long plagued the Mekong Delta, it is relatively new to Africa.
In a study published online April 14 in The Lancet Infectious Diseases, researchers found that the typical 3-day course of treatment did not totally eradicate Plasmodium falciparum, the parasite that causes malaria. A delayed clearance of the parasite was shown and found to be associated with a genetic mutation called Pfkelch13 R561H.
P. falciparum isolates with this mutation were found in 7.5% of infected children in one area of Rwanda. Further genomic studies showed that this mutation was locally acquired and did not emerge from Southeast Asia. This is well illustrated in a genomic tree published in Nature Medicine in August, 2020. That study reported data collected from adults from 2013 to 2015.
The delay in reporting the mutation was due, in part, to the burdensome process of whole-genome sequencing and transfection studies, Pascal Ringwald, MD, PhD, coordinator of the Global Malaria Programme at WHO, and coauthor of the Nature Medicine study, said in an interview. In transfection studies, the mutation is inserted into parasites and the resultant effect is observed.
Aline Uwimana, MD, of Rwanda Biomedical Centre. is the lead author on both studies.
Meera Venkatesan, PhD, chief of the Case Management, Monitoring and Evaluation Branch, President’s Malaria Initiative, USAID, noted that the Lancet Infectious Diseases study was a therapeutic efficacy study (TES) on samples from children from 2018. In an interview, Dr. Venkatesan explained that the study is noteworthy because it demonstrated the clinical significance of this mutation with delayed parasite clearance. She did note that although there was a lag in publication of the initial reports of artemisinin resistance mutations, that information – and its implications – was promptly shared with the global malaria research community, as are other findings of public health importance.
Although most of the children got better, this “partial resistance” emerged while patients were taking artemether–lumefantrine. This is a type of artemisinin-based combination therapy (ACT) with two drugs intended to stall the emergence of resistance.
The delayed clearance will be a problem because it can contribute to the selection and spread of the partially resistant malaria parasite.
To slow the spread of artemisinin resistance, Dr. Ringwald emphasized the need to add a gametocidal drug to block the transmission to humans. “You give a single dose of primaquine, which will help stop the spread,” he said in an interview. “Continuing surveillance and mapping. These are priorities.”
So are following national guidelines and banning the use of artemisinin monotherapy. Dr. Ringwald stressed two additional priorities: the need for accurate diagnosis of malaria, and the need to use “good-quality drugs and to avoid substandard or fake medicines” by not purchasing drugs on the street.
Unscrupulous individuals are also selling artemisia preparations to treat or prevent COVID-19, when it has no such activity. Similarly, artemisia teas are sold as herbal remedies and nutraceuticals.
Philippe Guérin, MD, director of the Worldwide Antimalarial Resistance Network (WWARN), listed the same recommendations, focusing a bit more on accurate detection of malaria and treatment with a multidrug regimen plus primaquine. You need “to have different first-line treatment (different ACTs) to avoid drug pressure” and resistance to the partner drug emerging, he said in an interview.
Such multiple first-line treatments rely on artemisinin in combination with various drugs, but this can cause some logistical challenges. Resistance is so problematic that the MORU (Mahidol Oxford Tropical Medicine Research Unit) Tropical Health Network in Bangkok is studying triple drug combinations, adding amodiaquine or mefloquine to an artemisinin-based combination.
Dr. Guérin emphasized two other problems regarding the monitoring of malaria resistance in Africa (although not specifically Rwanda). One is the inability to do adequate surveillance in active conflict zones and areas of instability. The other is that COVID-19 is causing resources to be taken away from malaria and redirected to the more immediate crisis. By having to focus on the immediate viral pandemic, public-health authorities are missing the chance to address other critically important infectious diseases with large burdens – specifically malaria, TB, and HIV – which might have greater impacts on future generations.
Dr. Guérin noted that although we now have solid evidence of artemisinin resistance in Rwanda, and isolated cases in other African countries, we have little idea of the magnitude of the problem because testing is not widespread throughout parts of the continent.
What would widespread P. falciparum malaria resistance in Africa mean? Children are the most vulnerable to malaria, and account for two-thirds of the deaths. One study suggests there could be 78 million more cases over a 5-year period, along with far more deaths. Hence, there is a heightened urgency to implement the outlined strategies to prevent a looming catastrophe.
The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A new study shows disturbing evidence that malaria is becoming resistant to artemisinin, a drug critical for treatment in Africa. Although artemisinin resistance has long plagued the Mekong Delta, it is relatively new to Africa.
In a study published online April 14 in The Lancet Infectious Diseases, researchers found that the typical 3-day course of treatment did not totally eradicate Plasmodium falciparum, the parasite that causes malaria. A delayed clearance of the parasite was shown and found to be associated with a genetic mutation called Pfkelch13 R561H.
P. falciparum isolates with this mutation were found in 7.5% of infected children in one area of Rwanda. Further genomic studies showed that this mutation was locally acquired and did not emerge from Southeast Asia. This is well illustrated in a genomic tree published in Nature Medicine in August, 2020. That study reported data collected from adults from 2013 to 2015.
The delay in reporting the mutation was due, in part, to the burdensome process of whole-genome sequencing and transfection studies, Pascal Ringwald, MD, PhD, coordinator of the Global Malaria Programme at WHO, and coauthor of the Nature Medicine study, said in an interview. In transfection studies, the mutation is inserted into parasites and the resultant effect is observed.
Aline Uwimana, MD, of Rwanda Biomedical Centre. is the lead author on both studies.
Meera Venkatesan, PhD, chief of the Case Management, Monitoring and Evaluation Branch, President’s Malaria Initiative, USAID, noted that the Lancet Infectious Diseases study was a therapeutic efficacy study (TES) on samples from children from 2018. In an interview, Dr. Venkatesan explained that the study is noteworthy because it demonstrated the clinical significance of this mutation with delayed parasite clearance. She did note that although there was a lag in publication of the initial reports of artemisinin resistance mutations, that information – and its implications – was promptly shared with the global malaria research community, as are other findings of public health importance.
Although most of the children got better, this “partial resistance” emerged while patients were taking artemether–lumefantrine. This is a type of artemisinin-based combination therapy (ACT) with two drugs intended to stall the emergence of resistance.
The delayed clearance will be a problem because it can contribute to the selection and spread of the partially resistant malaria parasite.
To slow the spread of artemisinin resistance, Dr. Ringwald emphasized the need to add a gametocidal drug to block the transmission to humans. “You give a single dose of primaquine, which will help stop the spread,” he said in an interview. “Continuing surveillance and mapping. These are priorities.”
So are following national guidelines and banning the use of artemisinin monotherapy. Dr. Ringwald stressed two additional priorities: the need for accurate diagnosis of malaria, and the need to use “good-quality drugs and to avoid substandard or fake medicines” by not purchasing drugs on the street.
Unscrupulous individuals are also selling artemisia preparations to treat or prevent COVID-19, when it has no such activity. Similarly, artemisia teas are sold as herbal remedies and nutraceuticals.
Philippe Guérin, MD, director of the Worldwide Antimalarial Resistance Network (WWARN), listed the same recommendations, focusing a bit more on accurate detection of malaria and treatment with a multidrug regimen plus primaquine. You need “to have different first-line treatment (different ACTs) to avoid drug pressure” and resistance to the partner drug emerging, he said in an interview.
Such multiple first-line treatments rely on artemisinin in combination with various drugs, but this can cause some logistical challenges. Resistance is so problematic that the MORU (Mahidol Oxford Tropical Medicine Research Unit) Tropical Health Network in Bangkok is studying triple drug combinations, adding amodiaquine or mefloquine to an artemisinin-based combination.
Dr. Guérin emphasized two other problems regarding the monitoring of malaria resistance in Africa (although not specifically Rwanda). One is the inability to do adequate surveillance in active conflict zones and areas of instability. The other is that COVID-19 is causing resources to be taken away from malaria and redirected to the more immediate crisis. By having to focus on the immediate viral pandemic, public-health authorities are missing the chance to address other critically important infectious diseases with large burdens – specifically malaria, TB, and HIV – which might have greater impacts on future generations.
Dr. Guérin noted that although we now have solid evidence of artemisinin resistance in Rwanda, and isolated cases in other African countries, we have little idea of the magnitude of the problem because testing is not widespread throughout parts of the continent.
What would widespread P. falciparum malaria resistance in Africa mean? Children are the most vulnerable to malaria, and account for two-thirds of the deaths. One study suggests there could be 78 million more cases over a 5-year period, along with far more deaths. Hence, there is a heightened urgency to implement the outlined strategies to prevent a looming catastrophe.
The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Global Ebola vaccine stockpile established
The International Coordinating Group (ICG) on Vaccine Provision announced the establishment of a global Ebola vaccine stockpile initiative.
The ICG, which was established in 1997, is made up of the World Health Organization, the United Nations Children’s Fund, the International Federation of Red Cross and Red Crescent Societies, and Médecins Sans Frontières.
The stockpile was created in order to make the single-dose Ebola vaccine (rVSV∆G-ZEBOV-GP, live; trade name Everbo) rapidly available at the start of the next Ebola outbreak anywhere in the world. The vaccine was developed and is marketed by Merck Sharp & Dohme, with financial support from the United States.
The stockpile, which is maintained in Switzerland and managed by UNICEF, is designed to be readily deployed to other countries whenever there is an outbreak. The ICG will be the decision-making body for the vaccine’s allocation and release, as is also the case with previously created stockpiles of cholera, meningitis, and yellow fever vaccines.
“The decision to allocate the vaccine will be made within 48 hours of receiving a request from a country; vaccines will be made available together with ultra-cold chain packaging by the manufacturer for shipment to countries within 48 hours of the decision. The targeted overall delivery time from the stockpile to countries is 7 days,” according to the WHO press release.
Currently 6,890 doses are available for outbreak response, with further quantities to be delivered into the stockpile throughout 2021 and beyond. Initial use of the vaccine will be directed to health care and frontline workers. It is expected that it will take 2-3 years to reach the Strategic Advisory Group of Experts on Immunization–recommended level of 500,000 doses for the stockpile of Ebola vaccines.
The International Coordinating Group (ICG) on Vaccine Provision announced the establishment of a global Ebola vaccine stockpile initiative.
The ICG, which was established in 1997, is made up of the World Health Organization, the United Nations Children’s Fund, the International Federation of Red Cross and Red Crescent Societies, and Médecins Sans Frontières.
The stockpile was created in order to make the single-dose Ebola vaccine (rVSV∆G-ZEBOV-GP, live; trade name Everbo) rapidly available at the start of the next Ebola outbreak anywhere in the world. The vaccine was developed and is marketed by Merck Sharp & Dohme, with financial support from the United States.
The stockpile, which is maintained in Switzerland and managed by UNICEF, is designed to be readily deployed to other countries whenever there is an outbreak. The ICG will be the decision-making body for the vaccine’s allocation and release, as is also the case with previously created stockpiles of cholera, meningitis, and yellow fever vaccines.
“The decision to allocate the vaccine will be made within 48 hours of receiving a request from a country; vaccines will be made available together with ultra-cold chain packaging by the manufacturer for shipment to countries within 48 hours of the decision. The targeted overall delivery time from the stockpile to countries is 7 days,” according to the WHO press release.
Currently 6,890 doses are available for outbreak response, with further quantities to be delivered into the stockpile throughout 2021 and beyond. Initial use of the vaccine will be directed to health care and frontline workers. It is expected that it will take 2-3 years to reach the Strategic Advisory Group of Experts on Immunization–recommended level of 500,000 doses for the stockpile of Ebola vaccines.
The International Coordinating Group (ICG) on Vaccine Provision announced the establishment of a global Ebola vaccine stockpile initiative.
The ICG, which was established in 1997, is made up of the World Health Organization, the United Nations Children’s Fund, the International Federation of Red Cross and Red Crescent Societies, and Médecins Sans Frontières.
The stockpile was created in order to make the single-dose Ebola vaccine (rVSV∆G-ZEBOV-GP, live; trade name Everbo) rapidly available at the start of the next Ebola outbreak anywhere in the world. The vaccine was developed and is marketed by Merck Sharp & Dohme, with financial support from the United States.
The stockpile, which is maintained in Switzerland and managed by UNICEF, is designed to be readily deployed to other countries whenever there is an outbreak. The ICG will be the decision-making body for the vaccine’s allocation and release, as is also the case with previously created stockpiles of cholera, meningitis, and yellow fever vaccines.
“The decision to allocate the vaccine will be made within 48 hours of receiving a request from a country; vaccines will be made available together with ultra-cold chain packaging by the manufacturer for shipment to countries within 48 hours of the decision. The targeted overall delivery time from the stockpile to countries is 7 days,” according to the WHO press release.
Currently 6,890 doses are available for outbreak response, with further quantities to be delivered into the stockpile throughout 2021 and beyond. Initial use of the vaccine will be directed to health care and frontline workers. It is expected that it will take 2-3 years to reach the Strategic Advisory Group of Experts on Immunization–recommended level of 500,000 doses for the stockpile of Ebola vaccines.
Organoid model unveils response to Shiga toxin
The study explored new territory in Shiga toxin research, enabled by the use of human intestinal organoids (HIOs), reported lead author Suman Pradhan, PhD, of the University of Cincinnati, and colleagues.
Each year, Shiga toxin–producing Escherichia coli infections cause approximately 3 million cases of bloody diarrheal disease, with about 4,000 of those patients developing the life-threatening complication of hemolytic uremic syndrome (HUS), the investigators wrote in Cellular and Molecular Gastroenterology and Hepatology.
But little is known about the underlying biological processes driving Shiga-induced disease.
“Developing effective interventions for disease resulting from Shiga toxin is exacerbated by a lack of tractable model systems,” the investigators wrote. “Mice do not develop the symptoms characteristic of HUS, and the murine intestinal tract is resistant to Shiga toxin.”
To overcome this obstacle, Dr. Pradhan and colleagues turned to HIOs, which are grown in culture by directing differentiation of pluripotent stem cells. HIOs represent the small bowel, complete with a lumen surrounded by epithelial and mesenchymal layers that include typical cell types, such as goblet cells and myofibroblasts. The model is made more realistic by transplantation into mice, where it grows under the kidney capsule to form crypts, structured villi, and proliferating progenitor zones. And HIOs grown with neuronal precursors develop an enteric nervous system, complete with functional peristalsis.
For the present study, the investigators evaluated the effect of Shiga toxin on HIOs both in culture and after transplantation into mice.
First, they demonstrated that HIOs in culture expressed glycolipid Gb3, the Shiga toxin receptor. “Reports regarding expression of glycolipid Gb3 ... on human intestine have been inconsistent,” the investigators noted. “For negative reports, the inability to detect Gb3 could be owing to technical limitations.”
Next, Dr. Pradhan and colleagues showed that HIOs were susceptible to Shiga toxin whether it be delivered lumenally or basolaterally, which respectively represent intestinal exposure and exposure via circulating toxin or after breakdown of the epithelial barrier. Leakage from the lumen was observed with both Shiga toxin 1 (Stx1) and 2 (Stx2). Subsequent testing involved only Stx2, as this form is more relevant to human disease.
In addition to lumenal leakage, Stx2 exposure caused significant transcriptional up-regulation of multiple gene families, including those involved in cellular transport and metabolic processes. Increased expression also was observed for epithelial structural proteins, lineage-specific proteins, factors involved in mucus layer formation and stabilization, and cytokines interleukin-18 and CCL15.
In both epithelial and mesenchymal layers, transcriptional changes were accompanied by cellular necrosis and apoptosis, and, to a greater degree with interstitial exposure, cellular proliferation.
With lumenal exposure, mesenchymal necrosis was observed before loss of epithelial barrier function, indicating toxin access to mesenchymal cells. This phenomenon was explained by transcytosis, which the investigators observed in two-dimensional monolayers of enteroids grown in Transwells.
“[Shiga toxin] was transferred from the apical to the basolateral surface in the absence of loss of epithelial barrier function,” the investigators wrote, noting that this finding explains how Shiga toxin can quickly access the circulatory system, and from there damage the kidneys and brain, as seen in cases of HUS.
Mice with transplanted HIOs, and those receiving HIOs with an enteric nervous system (HIO + ENS), lost weight when organoids were injected with 10 ng of Stx2. Mice with HIO + ENS transplants developed more severe responses, prompting closer analysis.
Postmortem histologic examination of HIO + ENS transplants revealed epithelial damage and blood accumulation in the mesenchyme and villi. Additional staining showed signs of apoptosis and mesenchymal-epithelial transition.
Dr. Pradham and colleagues suggested that their findings could inform therapeutic research.
“If preventing cellular death is to be an effective intervention, it is likely that both necrosis and apoptosis need to be targeted,” the investigators wrote.
More generally, the study supports the use of HIOs as a disease model for future investigations.
“The advent of stem cell–derived human tissue models, both in vitro and in vivo, has a tremendous potential to increase our understanding of Shiga toxin disease and lead to development of therapeutic interventions,” the investigators concluded.
The study was funded by the National Institutes of Health, the Center for Clinical and Translational Science, the National Institute of Diabetes and Digestive and Kidney Diseases, and others. The investigators disclosed no conflicts of interest.
SOURCE: Pradhan S et al. Cell Mol Gastroenterol Hepatol. 2020 Mar 5. doi: 10.1016/j.jcmgh.2020.02.006.
Limited therapies exist to mitigate the life-threatening sequelae of Shiga toxin (Stx)–producing Escherichia coli (STEC) infections. Stx continues to be a leading cause of hemolytic uremic syndrome and can devastate the kidneys, central nervous system, and other vital organs. Conflicting results from animal models and cell lines have left important questions unanswered, slowing therapy development. This study by Pradhan et al. takes advantage of the human intestinal organoid system to provide insight to questions pertinent to understanding Stx mechanism of action. Importantly, the authors find that intestinal epithelial cells (IECs) are a direct target of Stx and express the Stx receptor, Gb3, a point that had not been previously well established. They further confirm that IECs efficiently transport Stx from the apical to basolateral surface, before barrier integrity is compromised. This likely allows Stx to rapidly access circulation and other affected organs to cause disease.
Nicole Maloney Belle, MD, PhD, is an instructor of medicine, division of gastroenterology and hepatology, at the University of Pennsylvania, Philadelphia. She has no conflicts.
Limited therapies exist to mitigate the life-threatening sequelae of Shiga toxin (Stx)–producing Escherichia coli (STEC) infections. Stx continues to be a leading cause of hemolytic uremic syndrome and can devastate the kidneys, central nervous system, and other vital organs. Conflicting results from animal models and cell lines have left important questions unanswered, slowing therapy development. This study by Pradhan et al. takes advantage of the human intestinal organoid system to provide insight to questions pertinent to understanding Stx mechanism of action. Importantly, the authors find that intestinal epithelial cells (IECs) are a direct target of Stx and express the Stx receptor, Gb3, a point that had not been previously well established. They further confirm that IECs efficiently transport Stx from the apical to basolateral surface, before barrier integrity is compromised. This likely allows Stx to rapidly access circulation and other affected organs to cause disease.
Nicole Maloney Belle, MD, PhD, is an instructor of medicine, division of gastroenterology and hepatology, at the University of Pennsylvania, Philadelphia. She has no conflicts.
Limited therapies exist to mitigate the life-threatening sequelae of Shiga toxin (Stx)–producing Escherichia coli (STEC) infections. Stx continues to be a leading cause of hemolytic uremic syndrome and can devastate the kidneys, central nervous system, and other vital organs. Conflicting results from animal models and cell lines have left important questions unanswered, slowing therapy development. This study by Pradhan et al. takes advantage of the human intestinal organoid system to provide insight to questions pertinent to understanding Stx mechanism of action. Importantly, the authors find that intestinal epithelial cells (IECs) are a direct target of Stx and express the Stx receptor, Gb3, a point that had not been previously well established. They further confirm that IECs efficiently transport Stx from the apical to basolateral surface, before barrier integrity is compromised. This likely allows Stx to rapidly access circulation and other affected organs to cause disease.
Nicole Maloney Belle, MD, PhD, is an instructor of medicine, division of gastroenterology and hepatology, at the University of Pennsylvania, Philadelphia. She has no conflicts.
The study explored new territory in Shiga toxin research, enabled by the use of human intestinal organoids (HIOs), reported lead author Suman Pradhan, PhD, of the University of Cincinnati, and colleagues.
Each year, Shiga toxin–producing Escherichia coli infections cause approximately 3 million cases of bloody diarrheal disease, with about 4,000 of those patients developing the life-threatening complication of hemolytic uremic syndrome (HUS), the investigators wrote in Cellular and Molecular Gastroenterology and Hepatology.
But little is known about the underlying biological processes driving Shiga-induced disease.
“Developing effective interventions for disease resulting from Shiga toxin is exacerbated by a lack of tractable model systems,” the investigators wrote. “Mice do not develop the symptoms characteristic of HUS, and the murine intestinal tract is resistant to Shiga toxin.”
To overcome this obstacle, Dr. Pradhan and colleagues turned to HIOs, which are grown in culture by directing differentiation of pluripotent stem cells. HIOs represent the small bowel, complete with a lumen surrounded by epithelial and mesenchymal layers that include typical cell types, such as goblet cells and myofibroblasts. The model is made more realistic by transplantation into mice, where it grows under the kidney capsule to form crypts, structured villi, and proliferating progenitor zones. And HIOs grown with neuronal precursors develop an enteric nervous system, complete with functional peristalsis.
For the present study, the investigators evaluated the effect of Shiga toxin on HIOs both in culture and after transplantation into mice.
First, they demonstrated that HIOs in culture expressed glycolipid Gb3, the Shiga toxin receptor. “Reports regarding expression of glycolipid Gb3 ... on human intestine have been inconsistent,” the investigators noted. “For negative reports, the inability to detect Gb3 could be owing to technical limitations.”
Next, Dr. Pradhan and colleagues showed that HIOs were susceptible to Shiga toxin whether it be delivered lumenally or basolaterally, which respectively represent intestinal exposure and exposure via circulating toxin or after breakdown of the epithelial barrier. Leakage from the lumen was observed with both Shiga toxin 1 (Stx1) and 2 (Stx2). Subsequent testing involved only Stx2, as this form is more relevant to human disease.
In addition to lumenal leakage, Stx2 exposure caused significant transcriptional up-regulation of multiple gene families, including those involved in cellular transport and metabolic processes. Increased expression also was observed for epithelial structural proteins, lineage-specific proteins, factors involved in mucus layer formation and stabilization, and cytokines interleukin-18 and CCL15.
In both epithelial and mesenchymal layers, transcriptional changes were accompanied by cellular necrosis and apoptosis, and, to a greater degree with interstitial exposure, cellular proliferation.
With lumenal exposure, mesenchymal necrosis was observed before loss of epithelial barrier function, indicating toxin access to mesenchymal cells. This phenomenon was explained by transcytosis, which the investigators observed in two-dimensional monolayers of enteroids grown in Transwells.
“[Shiga toxin] was transferred from the apical to the basolateral surface in the absence of loss of epithelial barrier function,” the investigators wrote, noting that this finding explains how Shiga toxin can quickly access the circulatory system, and from there damage the kidneys and brain, as seen in cases of HUS.
Mice with transplanted HIOs, and those receiving HIOs with an enteric nervous system (HIO + ENS), lost weight when organoids were injected with 10 ng of Stx2. Mice with HIO + ENS transplants developed more severe responses, prompting closer analysis.
Postmortem histologic examination of HIO + ENS transplants revealed epithelial damage and blood accumulation in the mesenchyme and villi. Additional staining showed signs of apoptosis and mesenchymal-epithelial transition.
Dr. Pradham and colleagues suggested that their findings could inform therapeutic research.
“If preventing cellular death is to be an effective intervention, it is likely that both necrosis and apoptosis need to be targeted,” the investigators wrote.
More generally, the study supports the use of HIOs as a disease model for future investigations.
“The advent of stem cell–derived human tissue models, both in vitro and in vivo, has a tremendous potential to increase our understanding of Shiga toxin disease and lead to development of therapeutic interventions,” the investigators concluded.
The study was funded by the National Institutes of Health, the Center for Clinical and Translational Science, the National Institute of Diabetes and Digestive and Kidney Diseases, and others. The investigators disclosed no conflicts of interest.
SOURCE: Pradhan S et al. Cell Mol Gastroenterol Hepatol. 2020 Mar 5. doi: 10.1016/j.jcmgh.2020.02.006.
The study explored new territory in Shiga toxin research, enabled by the use of human intestinal organoids (HIOs), reported lead author Suman Pradhan, PhD, of the University of Cincinnati, and colleagues.
Each year, Shiga toxin–producing Escherichia coli infections cause approximately 3 million cases of bloody diarrheal disease, with about 4,000 of those patients developing the life-threatening complication of hemolytic uremic syndrome (HUS), the investigators wrote in Cellular and Molecular Gastroenterology and Hepatology.
But little is known about the underlying biological processes driving Shiga-induced disease.
“Developing effective interventions for disease resulting from Shiga toxin is exacerbated by a lack of tractable model systems,” the investigators wrote. “Mice do not develop the symptoms characteristic of HUS, and the murine intestinal tract is resistant to Shiga toxin.”
To overcome this obstacle, Dr. Pradhan and colleagues turned to HIOs, which are grown in culture by directing differentiation of pluripotent stem cells. HIOs represent the small bowel, complete with a lumen surrounded by epithelial and mesenchymal layers that include typical cell types, such as goblet cells and myofibroblasts. The model is made more realistic by transplantation into mice, where it grows under the kidney capsule to form crypts, structured villi, and proliferating progenitor zones. And HIOs grown with neuronal precursors develop an enteric nervous system, complete with functional peristalsis.
For the present study, the investigators evaluated the effect of Shiga toxin on HIOs both in culture and after transplantation into mice.
First, they demonstrated that HIOs in culture expressed glycolipid Gb3, the Shiga toxin receptor. “Reports regarding expression of glycolipid Gb3 ... on human intestine have been inconsistent,” the investigators noted. “For negative reports, the inability to detect Gb3 could be owing to technical limitations.”
Next, Dr. Pradhan and colleagues showed that HIOs were susceptible to Shiga toxin whether it be delivered lumenally or basolaterally, which respectively represent intestinal exposure and exposure via circulating toxin or after breakdown of the epithelial barrier. Leakage from the lumen was observed with both Shiga toxin 1 (Stx1) and 2 (Stx2). Subsequent testing involved only Stx2, as this form is more relevant to human disease.
In addition to lumenal leakage, Stx2 exposure caused significant transcriptional up-regulation of multiple gene families, including those involved in cellular transport and metabolic processes. Increased expression also was observed for epithelial structural proteins, lineage-specific proteins, factors involved in mucus layer formation and stabilization, and cytokines interleukin-18 and CCL15.
In both epithelial and mesenchymal layers, transcriptional changes were accompanied by cellular necrosis and apoptosis, and, to a greater degree with interstitial exposure, cellular proliferation.
With lumenal exposure, mesenchymal necrosis was observed before loss of epithelial barrier function, indicating toxin access to mesenchymal cells. This phenomenon was explained by transcytosis, which the investigators observed in two-dimensional monolayers of enteroids grown in Transwells.
“[Shiga toxin] was transferred from the apical to the basolateral surface in the absence of loss of epithelial barrier function,” the investigators wrote, noting that this finding explains how Shiga toxin can quickly access the circulatory system, and from there damage the kidneys and brain, as seen in cases of HUS.
Mice with transplanted HIOs, and those receiving HIOs with an enteric nervous system (HIO + ENS), lost weight when organoids were injected with 10 ng of Stx2. Mice with HIO + ENS transplants developed more severe responses, prompting closer analysis.
Postmortem histologic examination of HIO + ENS transplants revealed epithelial damage and blood accumulation in the mesenchyme and villi. Additional staining showed signs of apoptosis and mesenchymal-epithelial transition.
Dr. Pradham and colleagues suggested that their findings could inform therapeutic research.
“If preventing cellular death is to be an effective intervention, it is likely that both necrosis and apoptosis need to be targeted,” the investigators wrote.
More generally, the study supports the use of HIOs as a disease model for future investigations.
“The advent of stem cell–derived human tissue models, both in vitro and in vivo, has a tremendous potential to increase our understanding of Shiga toxin disease and lead to development of therapeutic interventions,” the investigators concluded.
The study was funded by the National Institutes of Health, the Center for Clinical and Translational Science, the National Institute of Diabetes and Digestive and Kidney Diseases, and others. The investigators disclosed no conflicts of interest.
SOURCE: Pradhan S et al. Cell Mol Gastroenterol Hepatol. 2020 Mar 5. doi: 10.1016/j.jcmgh.2020.02.006.
FROM CELLULAR AND MOLECULAR GASTROENTEROLOGY AND HEPATOLOGY
Upcoming vaccine may offset surge in polio subtypes
Although wild poliovirus type 3 has not been detected globally for 7 years, the number of wild type 1 cases increased from 33 in 2018 to 173 in 2019. In response, a modified oral vaccine is being developed, according to Stephen Cochi, MD, of the Centers for Disease Control and Prevention’s Center for Global Health.
Several factors, including a Taliban ban on house-to-house vaccination in Afghanistan and a delay of large-scale vaccinations in Pakistan contributed to the surge in polio infections, Dr. Cochi said in a presentation at the February meeting of the CDC’s Advisory Committee on Immunization Practices (ACIP).
In addition, circulating vaccine-derived polioviruses (cVDPV) outbreaks have occurred in multiple countries including sub-Saharan Africa, China, Pakistan, and the Philippines. These outbreaks threaten the success of the bivalent oral polio vaccine introduced in April 2016 in 155 countries, Dr. Cochi said.
Outbreaks tend to occur just outside targeted areas for campaigns, caused by decreasing population immunity, he said.
The novel OPV2 (nOPV2) is a genetic modification of the existing OPV2 vaccine designed to improve genetic stability, Dr. Cochi explained. The modifications would “decrease the risk of seeding new cVDPVs and the risk of vaccine-associated paralytic poliomyelitis (VAPP),” he said.
The Emergency Use Listing (EUL) was developed by the World Health Organization in response to the Ebola virus outbreak in 2014-2016 and is the fastest way to obtain regulatory review and approval of drug products, said Dr. Cochi.
A pilot plant has been established in Indonesia, and upon EUL approval, 4-8 million doses of the nOPV2 should be available for use in the second quarter of 2020, he concluded.
Dr. Cochi had no relevant financial conflicts to disclose.
Although wild poliovirus type 3 has not been detected globally for 7 years, the number of wild type 1 cases increased from 33 in 2018 to 173 in 2019. In response, a modified oral vaccine is being developed, according to Stephen Cochi, MD, of the Centers for Disease Control and Prevention’s Center for Global Health.
Several factors, including a Taliban ban on house-to-house vaccination in Afghanistan and a delay of large-scale vaccinations in Pakistan contributed to the surge in polio infections, Dr. Cochi said in a presentation at the February meeting of the CDC’s Advisory Committee on Immunization Practices (ACIP).
In addition, circulating vaccine-derived polioviruses (cVDPV) outbreaks have occurred in multiple countries including sub-Saharan Africa, China, Pakistan, and the Philippines. These outbreaks threaten the success of the bivalent oral polio vaccine introduced in April 2016 in 155 countries, Dr. Cochi said.
Outbreaks tend to occur just outside targeted areas for campaigns, caused by decreasing population immunity, he said.
The novel OPV2 (nOPV2) is a genetic modification of the existing OPV2 vaccine designed to improve genetic stability, Dr. Cochi explained. The modifications would “decrease the risk of seeding new cVDPVs and the risk of vaccine-associated paralytic poliomyelitis (VAPP),” he said.
The Emergency Use Listing (EUL) was developed by the World Health Organization in response to the Ebola virus outbreak in 2014-2016 and is the fastest way to obtain regulatory review and approval of drug products, said Dr. Cochi.
A pilot plant has been established in Indonesia, and upon EUL approval, 4-8 million doses of the nOPV2 should be available for use in the second quarter of 2020, he concluded.
Dr. Cochi had no relevant financial conflicts to disclose.
Although wild poliovirus type 3 has not been detected globally for 7 years, the number of wild type 1 cases increased from 33 in 2018 to 173 in 2019. In response, a modified oral vaccine is being developed, according to Stephen Cochi, MD, of the Centers for Disease Control and Prevention’s Center for Global Health.
Several factors, including a Taliban ban on house-to-house vaccination in Afghanistan and a delay of large-scale vaccinations in Pakistan contributed to the surge in polio infections, Dr. Cochi said in a presentation at the February meeting of the CDC’s Advisory Committee on Immunization Practices (ACIP).
In addition, circulating vaccine-derived polioviruses (cVDPV) outbreaks have occurred in multiple countries including sub-Saharan Africa, China, Pakistan, and the Philippines. These outbreaks threaten the success of the bivalent oral polio vaccine introduced in April 2016 in 155 countries, Dr. Cochi said.
Outbreaks tend to occur just outside targeted areas for campaigns, caused by decreasing population immunity, he said.
The novel OPV2 (nOPV2) is a genetic modification of the existing OPV2 vaccine designed to improve genetic stability, Dr. Cochi explained. The modifications would “decrease the risk of seeding new cVDPVs and the risk of vaccine-associated paralytic poliomyelitis (VAPP),” he said.
The Emergency Use Listing (EUL) was developed by the World Health Organization in response to the Ebola virus outbreak in 2014-2016 and is the fastest way to obtain regulatory review and approval of drug products, said Dr. Cochi.
A pilot plant has been established in Indonesia, and upon EUL approval, 4-8 million doses of the nOPV2 should be available for use in the second quarter of 2020, he concluded.
Dr. Cochi had no relevant financial conflicts to disclose.
FROM AN ACIP MEETING
ACIP advocates pre-exposure Ebola vaccination for high-risk groups
Vaccination against the Ebola virus is recommended for first responders, health care personnel, and laboratory workers deemed at high risk of exposure, according to the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices (ACIP).
The committee voted unanimously to recommended pre-exposure vaccination with the rVSVdeltaG-ZEBOV-GP vaccine for adults aged 18 years and older who are at potential risk of exposure to the Ebola species Zaire ebolavirus because they fall into any of the following three categories:
- They are responding to an outbreak of Ebola virus disease.
- They are working as health care personnel at a federally designated Ebola Treatment Center in the United States.
- The are working in laboratories or are other staff members at biosafety-level 4 facilities in the United States.
Mary Choi, MD, of the CDC’s National Center for Emerging and Zoonotic Infectious Diseases (NCEZID) presented data on the safety and effectiveness of the vaccine and the work group considerations in recommending vaccination in the three target populations.
In clinical trials, the most commonly reported adverse events associated with the vaccine were arthritis and arthralgia, Dr. Choi said, but the duration of those cases was limited to months and did not persist long term.
Pre-exposure vaccination for health care personnel, laboratory workers, and support staff would provide an additional layer of protection, she explained, in addition to existing safeguards such as personal protective equipment and engineering controls at the facility. The work group’s research showed that most of the target population believed that the desirable effects of that protection outweigh potentially undesirable effects, Dr. Choi noted.
Some committee members expressed concerns about vaccination of pregnant women. But the recommendations are presented as “population based, not shared decision making,” said Sharon E. Frey, MD, of Saint Louis University in St. Louis, Missouri.
Several members noted that pregnant women should not be automatically included or excluded from vaccination if they fall into a high-risk population. And the committee agreed that additional guidance in the policy note will help assess risk and that organizations will determine the risk for their employees and whether to offer the vaccine.
The FDA approved the currently available U.S. vaccine for Ebola in 2019. Merck manufactures that vaccine.
The ACIP members had no relevant financial conflicts to disclose.
Vaccination against the Ebola virus is recommended for first responders, health care personnel, and laboratory workers deemed at high risk of exposure, according to the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices (ACIP).
The committee voted unanimously to recommended pre-exposure vaccination with the rVSVdeltaG-ZEBOV-GP vaccine for adults aged 18 years and older who are at potential risk of exposure to the Ebola species Zaire ebolavirus because they fall into any of the following three categories:
- They are responding to an outbreak of Ebola virus disease.
- They are working as health care personnel at a federally designated Ebola Treatment Center in the United States.
- The are working in laboratories or are other staff members at biosafety-level 4 facilities in the United States.
Mary Choi, MD, of the CDC’s National Center for Emerging and Zoonotic Infectious Diseases (NCEZID) presented data on the safety and effectiveness of the vaccine and the work group considerations in recommending vaccination in the three target populations.
In clinical trials, the most commonly reported adverse events associated with the vaccine were arthritis and arthralgia, Dr. Choi said, but the duration of those cases was limited to months and did not persist long term.
Pre-exposure vaccination for health care personnel, laboratory workers, and support staff would provide an additional layer of protection, she explained, in addition to existing safeguards such as personal protective equipment and engineering controls at the facility. The work group’s research showed that most of the target population believed that the desirable effects of that protection outweigh potentially undesirable effects, Dr. Choi noted.
Some committee members expressed concerns about vaccination of pregnant women. But the recommendations are presented as “population based, not shared decision making,” said Sharon E. Frey, MD, of Saint Louis University in St. Louis, Missouri.
Several members noted that pregnant women should not be automatically included or excluded from vaccination if they fall into a high-risk population. And the committee agreed that additional guidance in the policy note will help assess risk and that organizations will determine the risk for their employees and whether to offer the vaccine.
The FDA approved the currently available U.S. vaccine for Ebola in 2019. Merck manufactures that vaccine.
The ACIP members had no relevant financial conflicts to disclose.
Vaccination against the Ebola virus is recommended for first responders, health care personnel, and laboratory workers deemed at high risk of exposure, according to the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices (ACIP).
The committee voted unanimously to recommended pre-exposure vaccination with the rVSVdeltaG-ZEBOV-GP vaccine for adults aged 18 years and older who are at potential risk of exposure to the Ebola species Zaire ebolavirus because they fall into any of the following three categories:
- They are responding to an outbreak of Ebola virus disease.
- They are working as health care personnel at a federally designated Ebola Treatment Center in the United States.
- The are working in laboratories or are other staff members at biosafety-level 4 facilities in the United States.
Mary Choi, MD, of the CDC’s National Center for Emerging and Zoonotic Infectious Diseases (NCEZID) presented data on the safety and effectiveness of the vaccine and the work group considerations in recommending vaccination in the three target populations.
In clinical trials, the most commonly reported adverse events associated with the vaccine were arthritis and arthralgia, Dr. Choi said, but the duration of those cases was limited to months and did not persist long term.
Pre-exposure vaccination for health care personnel, laboratory workers, and support staff would provide an additional layer of protection, she explained, in addition to existing safeguards such as personal protective equipment and engineering controls at the facility. The work group’s research showed that most of the target population believed that the desirable effects of that protection outweigh potentially undesirable effects, Dr. Choi noted.
Some committee members expressed concerns about vaccination of pregnant women. But the recommendations are presented as “population based, not shared decision making,” said Sharon E. Frey, MD, of Saint Louis University in St. Louis, Missouri.
Several members noted that pregnant women should not be automatically included or excluded from vaccination if they fall into a high-risk population. And the committee agreed that additional guidance in the policy note will help assess risk and that organizations will determine the risk for their employees and whether to offer the vaccine.
The FDA approved the currently available U.S. vaccine for Ebola in 2019. Merck manufactures that vaccine.
The ACIP members had no relevant financial conflicts to disclose.
As novel coronavirus outbreak evolves, critical care providers need to be prepared
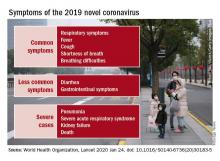
ORLANDO – While the impact of the 2019 novel coronavirus outbreak on hospitals outside of China remains to be determined, there are several practical points critical care professionals need to know to be prepared in the face of this dynamic and rapidly evolving outbreak, speakers said at the Critical Care Congress sponsored by the Society of Critical Care Medicine.
“Priorities for us in our hospitals are early detection, infection prevention, staff safety, and obviously, taking care of sick people,” said Ryan C. Maves, MD, of the Naval Medical Center San Diego in a special session on the 2019 Novel Coronavirus outbreak.*
Approximately 72,000 cases of coronavirus disease 2019 (COVID-19) had been reported as of Feb. 17, 2020, the day of Dr. Maves’ talk, according to statistics from Johns Hopkins Center for Science and Engineering in Baltimore. A total of 1,775 deaths had been recorded, nearly all of which were in Hubei Province, the central point of the outbreak. In the United States, the number of cases stood at 15, with no deaths reported.
While the dynamics of the 2019 novel coronavirus are still being learned, the estimated range of spread for droplet transmission is 2 meters, according to Dr. Maves. The duration of environmental persistence is not yet known, but he said that other coronaviruses persist in low-humidity conditions for up to 4 days.
The number of secondary cases that arise from a primary infection, or R0, is estimated to be between 1.5 and 3, though it can change as exposure evolves; by comparison, the R0 for H1N1 influenza has been reported as 1.5, while measles is 12-18, indicating that it is “very contagious,” said Dr. Maves. Severe acute respiratory syndrome had an initial R0 of about 3.5, which he said declined rapidly to 0.7 as environmental and policy controls were put into place.
Critical care professionals need to know how to identify patients at risk of having COVID-19 and determine whether they need further work-up, according to Dr. Maves, who highlighted recent criteria released by the Centers for Disease Control and Prevention.
The highest-risk category, he said, are individuals exposed to a laboratory-confirmed coronavirus case, which along with fever or signs and symptoms of a lower respiratory illness would be sufficient to classify them as a “person of interest” requiring further evaluation for disease. A history of travel from Hubei Province plus fever and signs/symptoms of lower respiratory illness would also meet criteria for evaluation, according to the CDC, while travel to mainland China would also meet the threshold, if those symptoms required hospitalization.
The CDC also published a step-wise flowchart to evaluate patients who may have been exposed to the 2019 novel coronavirus. According to that flowchart, if an individual has traveled to China or had close contact with someone infected with the 2019 Novel Coronavirus within 14 days of symptoms, and that individual has fever or symptoms of lower respiratory illness such as cough or shortness of breath, then providers should isolate that individual and assess clinical status, in addition to contacting the local health department.
Laura E. Evans, MD, MS, FCCM, of New York University, said she might recommend providers “flip the script” on that CDC algorithm when it comes to identifying patients who may have been exposed.
“I think perhaps what we should be doing at sites of entry is not talking about travel as the first question, but rather fever or symptoms of lower respiratory illnesses as the first question, and use that as the opportunity to implement risk mitigation at that stage,” Dr. Evans said in a presentation on preparing for COVID-19.
Even with “substantial uncertainty” about the potential impact of the 2019 Novel Coronavirus, a significant influx of seriously ill patients would put strain the U.S. health care delivery system, she added.
“None of us have tons of extra capacity in our emergency departments, inpatient units, or ICUs, and I think we need to be prepared for that,” she added. “We need to know what our process is for ‘identify, isolate, and inform,’ and we need to be testing that now.”
Dr. Maves and Dr. Evans both reported that they had no financial conflicts of interest to report. Dr. Maves indicated that the views expressed in his presentation did not necessarily reflect the official policy or position of the Department of the Navy, Department of Defense, or the United States government.
*Correction, 2/19/20: An earlier version of this article misstated the location of the naval center.
ORLANDO – While the impact of the 2019 novel coronavirus outbreak on hospitals outside of China remains to be determined, there are several practical points critical care professionals need to know to be prepared in the face of this dynamic and rapidly evolving outbreak, speakers said at the Critical Care Congress sponsored by the Society of Critical Care Medicine.
“Priorities for us in our hospitals are early detection, infection prevention, staff safety, and obviously, taking care of sick people,” said Ryan C. Maves, MD, of the Naval Medical Center San Diego in a special session on the 2019 Novel Coronavirus outbreak.*
Approximately 72,000 cases of coronavirus disease 2019 (COVID-19) had been reported as of Feb. 17, 2020, the day of Dr. Maves’ talk, according to statistics from Johns Hopkins Center for Science and Engineering in Baltimore. A total of 1,775 deaths had been recorded, nearly all of which were in Hubei Province, the central point of the outbreak. In the United States, the number of cases stood at 15, with no deaths reported.
While the dynamics of the 2019 novel coronavirus are still being learned, the estimated range of spread for droplet transmission is 2 meters, according to Dr. Maves. The duration of environmental persistence is not yet known, but he said that other coronaviruses persist in low-humidity conditions for up to 4 days.
The number of secondary cases that arise from a primary infection, or R0, is estimated to be between 1.5 and 3, though it can change as exposure evolves; by comparison, the R0 for H1N1 influenza has been reported as 1.5, while measles is 12-18, indicating that it is “very contagious,” said Dr. Maves. Severe acute respiratory syndrome had an initial R0 of about 3.5, which he said declined rapidly to 0.7 as environmental and policy controls were put into place.
Critical care professionals need to know how to identify patients at risk of having COVID-19 and determine whether they need further work-up, according to Dr. Maves, who highlighted recent criteria released by the Centers for Disease Control and Prevention.
The highest-risk category, he said, are individuals exposed to a laboratory-confirmed coronavirus case, which along with fever or signs and symptoms of a lower respiratory illness would be sufficient to classify them as a “person of interest” requiring further evaluation for disease. A history of travel from Hubei Province plus fever and signs/symptoms of lower respiratory illness would also meet criteria for evaluation, according to the CDC, while travel to mainland China would also meet the threshold, if those symptoms required hospitalization.
The CDC also published a step-wise flowchart to evaluate patients who may have been exposed to the 2019 novel coronavirus. According to that flowchart, if an individual has traveled to China or had close contact with someone infected with the 2019 Novel Coronavirus within 14 days of symptoms, and that individual has fever or symptoms of lower respiratory illness such as cough or shortness of breath, then providers should isolate that individual and assess clinical status, in addition to contacting the local health department.
Laura E. Evans, MD, MS, FCCM, of New York University, said she might recommend providers “flip the script” on that CDC algorithm when it comes to identifying patients who may have been exposed.
“I think perhaps what we should be doing at sites of entry is not talking about travel as the first question, but rather fever or symptoms of lower respiratory illnesses as the first question, and use that as the opportunity to implement risk mitigation at that stage,” Dr. Evans said in a presentation on preparing for COVID-19.
Even with “substantial uncertainty” about the potential impact of the 2019 Novel Coronavirus, a significant influx of seriously ill patients would put strain the U.S. health care delivery system, she added.
“None of us have tons of extra capacity in our emergency departments, inpatient units, or ICUs, and I think we need to be prepared for that,” she added. “We need to know what our process is for ‘identify, isolate, and inform,’ and we need to be testing that now.”
Dr. Maves and Dr. Evans both reported that they had no financial conflicts of interest to report. Dr. Maves indicated that the views expressed in his presentation did not necessarily reflect the official policy or position of the Department of the Navy, Department of Defense, or the United States government.
*Correction, 2/19/20: An earlier version of this article misstated the location of the naval center.
ORLANDO – While the impact of the 2019 novel coronavirus outbreak on hospitals outside of China remains to be determined, there are several practical points critical care professionals need to know to be prepared in the face of this dynamic and rapidly evolving outbreak, speakers said at the Critical Care Congress sponsored by the Society of Critical Care Medicine.
“Priorities for us in our hospitals are early detection, infection prevention, staff safety, and obviously, taking care of sick people,” said Ryan C. Maves, MD, of the Naval Medical Center San Diego in a special session on the 2019 Novel Coronavirus outbreak.*
Approximately 72,000 cases of coronavirus disease 2019 (COVID-19) had been reported as of Feb. 17, 2020, the day of Dr. Maves’ talk, according to statistics from Johns Hopkins Center for Science and Engineering in Baltimore. A total of 1,775 deaths had been recorded, nearly all of which were in Hubei Province, the central point of the outbreak. In the United States, the number of cases stood at 15, with no deaths reported.
While the dynamics of the 2019 novel coronavirus are still being learned, the estimated range of spread for droplet transmission is 2 meters, according to Dr. Maves. The duration of environmental persistence is not yet known, but he said that other coronaviruses persist in low-humidity conditions for up to 4 days.
The number of secondary cases that arise from a primary infection, or R0, is estimated to be between 1.5 and 3, though it can change as exposure evolves; by comparison, the R0 for H1N1 influenza has been reported as 1.5, while measles is 12-18, indicating that it is “very contagious,” said Dr. Maves. Severe acute respiratory syndrome had an initial R0 of about 3.5, which he said declined rapidly to 0.7 as environmental and policy controls were put into place.
Critical care professionals need to know how to identify patients at risk of having COVID-19 and determine whether they need further work-up, according to Dr. Maves, who highlighted recent criteria released by the Centers for Disease Control and Prevention.
The highest-risk category, he said, are individuals exposed to a laboratory-confirmed coronavirus case, which along with fever or signs and symptoms of a lower respiratory illness would be sufficient to classify them as a “person of interest” requiring further evaluation for disease. A history of travel from Hubei Province plus fever and signs/symptoms of lower respiratory illness would also meet criteria for evaluation, according to the CDC, while travel to mainland China would also meet the threshold, if those symptoms required hospitalization.
The CDC also published a step-wise flowchart to evaluate patients who may have been exposed to the 2019 novel coronavirus. According to that flowchart, if an individual has traveled to China or had close contact with someone infected with the 2019 Novel Coronavirus within 14 days of symptoms, and that individual has fever or symptoms of lower respiratory illness such as cough or shortness of breath, then providers should isolate that individual and assess clinical status, in addition to contacting the local health department.
Laura E. Evans, MD, MS, FCCM, of New York University, said she might recommend providers “flip the script” on that CDC algorithm when it comes to identifying patients who may have been exposed.
“I think perhaps what we should be doing at sites of entry is not talking about travel as the first question, but rather fever or symptoms of lower respiratory illnesses as the first question, and use that as the opportunity to implement risk mitigation at that stage,” Dr. Evans said in a presentation on preparing for COVID-19.
Even with “substantial uncertainty” about the potential impact of the 2019 Novel Coronavirus, a significant influx of seriously ill patients would put strain the U.S. health care delivery system, she added.
“None of us have tons of extra capacity in our emergency departments, inpatient units, or ICUs, and I think we need to be prepared for that,” she added. “We need to know what our process is for ‘identify, isolate, and inform,’ and we need to be testing that now.”
Dr. Maves and Dr. Evans both reported that they had no financial conflicts of interest to report. Dr. Maves indicated that the views expressed in his presentation did not necessarily reflect the official policy or position of the Department of the Navy, Department of Defense, or the United States government.
*Correction, 2/19/20: An earlier version of this article misstated the location of the naval center.
EXPERT ANALYSIS FROM CCC49
Wuhan coronavirus cluster suggests human-to-human spread
A Chinese man became ill from a novel coronavirus (2019-nCoV) 4 days after arriving in Vietnam to visit his 27-year-old son. Three days later the healthy young man was also stricken, according to a report published online Jan. 28 in the New England Journal of Medicine.
“This family cluster of 2019-nCoV infection that occurred outside China arouses concern regarding human-to-human transmission,” the authors wrote.
The father, age 65 years and with multiple comorbidities including hypertension, type 2 diabetes, coronary heart disease with stent placement, and lung cancer, flew to Hanoi with his wife on January 13; they traveled from the Wuchang district in Wuhan, China, where outbreaks of 2019-nCoV have been occurring.
On Jan. 17, the older man and his wife met their adult son in Ho Chi Minh City, Vietnam, and shared a hotel room with him for 3 days. The father developed a fever that same day and the son developed a dry cough, fever, diarrhea, and vomiting on Jan. 20. Both men went to a hospital ED on Jan. 22.
The authors say the timing of the son’s symptoms suggests the incubation period may have been 3 days or fewer.
Upon admission to the hospital, the father reported that he had not visited a “wet market” where live and dead animals are sold while he was in Wuhan. Throat swabs were positive for 2019-nCoV on real-time reverse-transcription–polymerase-chain-reaction assays.
The man was placed in isolation and “treated empirically with antiviral agents, broad-spectrum antibiotics, and supportive therapies,” wrote Lan T. Phan, PhD, from the Pasteur Institute Ho Chi Minh City and coauthors.
On admission, chest radiographs revealed an infiltrate in the upper lobe of his left lung; he developed worsening dyspnea with hypoxemia on Jan. 25 and required supplemental oxygen at 5 L/min by nasal cannula. Chest radiographs showed a progressive infiltrate and consolidation. His fever resolved on that day and he has progressively improved.
The man’s son had a fever of 39° C (102.2° F) when the two men arrived at the hospital on Jan. 22; hospital staff isolated the son, and chest radiographs and other laboratory tests were normal with the exception of an increased C-reactive protein level.
The son’s throat swab was positive for 2019-nCoV and he is believed to have been exposed from his father; however, the strains have not been ascertained.
“This family had traveled to four cities across Vietnam using various forms of transportation, including planes, trains, and taxis,” the authors wrote. A total of 28 close contacts were identified, none of whom have developed respiratory symptoms. The older man’s wife has been healthy as well.
The authors have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
A Chinese man became ill from a novel coronavirus (2019-nCoV) 4 days after arriving in Vietnam to visit his 27-year-old son. Three days later the healthy young man was also stricken, according to a report published online Jan. 28 in the New England Journal of Medicine.
“This family cluster of 2019-nCoV infection that occurred outside China arouses concern regarding human-to-human transmission,” the authors wrote.
The father, age 65 years and with multiple comorbidities including hypertension, type 2 diabetes, coronary heart disease with stent placement, and lung cancer, flew to Hanoi with his wife on January 13; they traveled from the Wuchang district in Wuhan, China, where outbreaks of 2019-nCoV have been occurring.
On Jan. 17, the older man and his wife met their adult son in Ho Chi Minh City, Vietnam, and shared a hotel room with him for 3 days. The father developed a fever that same day and the son developed a dry cough, fever, diarrhea, and vomiting on Jan. 20. Both men went to a hospital ED on Jan. 22.
The authors say the timing of the son’s symptoms suggests the incubation period may have been 3 days or fewer.
Upon admission to the hospital, the father reported that he had not visited a “wet market” where live and dead animals are sold while he was in Wuhan. Throat swabs were positive for 2019-nCoV on real-time reverse-transcription–polymerase-chain-reaction assays.
The man was placed in isolation and “treated empirically with antiviral agents, broad-spectrum antibiotics, and supportive therapies,” wrote Lan T. Phan, PhD, from the Pasteur Institute Ho Chi Minh City and coauthors.
On admission, chest radiographs revealed an infiltrate in the upper lobe of his left lung; he developed worsening dyspnea with hypoxemia on Jan. 25 and required supplemental oxygen at 5 L/min by nasal cannula. Chest radiographs showed a progressive infiltrate and consolidation. His fever resolved on that day and he has progressively improved.
The man’s son had a fever of 39° C (102.2° F) when the two men arrived at the hospital on Jan. 22; hospital staff isolated the son, and chest radiographs and other laboratory tests were normal with the exception of an increased C-reactive protein level.
The son’s throat swab was positive for 2019-nCoV and he is believed to have been exposed from his father; however, the strains have not been ascertained.
“This family had traveled to four cities across Vietnam using various forms of transportation, including planes, trains, and taxis,” the authors wrote. A total of 28 close contacts were identified, none of whom have developed respiratory symptoms. The older man’s wife has been healthy as well.
The authors have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
A Chinese man became ill from a novel coronavirus (2019-nCoV) 4 days after arriving in Vietnam to visit his 27-year-old son. Three days later the healthy young man was also stricken, according to a report published online Jan. 28 in the New England Journal of Medicine.
“This family cluster of 2019-nCoV infection that occurred outside China arouses concern regarding human-to-human transmission,” the authors wrote.
The father, age 65 years and with multiple comorbidities including hypertension, type 2 diabetes, coronary heart disease with stent placement, and lung cancer, flew to Hanoi with his wife on January 13; they traveled from the Wuchang district in Wuhan, China, where outbreaks of 2019-nCoV have been occurring.
On Jan. 17, the older man and his wife met their adult son in Ho Chi Minh City, Vietnam, and shared a hotel room with him for 3 days. The father developed a fever that same day and the son developed a dry cough, fever, diarrhea, and vomiting on Jan. 20. Both men went to a hospital ED on Jan. 22.
The authors say the timing of the son’s symptoms suggests the incubation period may have been 3 days or fewer.
Upon admission to the hospital, the father reported that he had not visited a “wet market” where live and dead animals are sold while he was in Wuhan. Throat swabs were positive for 2019-nCoV on real-time reverse-transcription–polymerase-chain-reaction assays.
The man was placed in isolation and “treated empirically with antiviral agents, broad-spectrum antibiotics, and supportive therapies,” wrote Lan T. Phan, PhD, from the Pasteur Institute Ho Chi Minh City and coauthors.
On admission, chest radiographs revealed an infiltrate in the upper lobe of his left lung; he developed worsening dyspnea with hypoxemia on Jan. 25 and required supplemental oxygen at 5 L/min by nasal cannula. Chest radiographs showed a progressive infiltrate and consolidation. His fever resolved on that day and he has progressively improved.
The man’s son had a fever of 39° C (102.2° F) when the two men arrived at the hospital on Jan. 22; hospital staff isolated the son, and chest radiographs and other laboratory tests were normal with the exception of an increased C-reactive protein level.
The son’s throat swab was positive for 2019-nCoV and he is believed to have been exposed from his father; however, the strains have not been ascertained.
“This family had traveled to four cities across Vietnam using various forms of transportation, including planes, trains, and taxis,” the authors wrote. A total of 28 close contacts were identified, none of whom have developed respiratory symptoms. The older man’s wife has been healthy as well.
The authors have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Wuhan virus: What clinicians need to know
As the Wuhan coronavirus story unfolds, , according to infectious disease experts.

“We are asking that of everyone with fever and respiratory symptoms who comes to our clinics, hospital, or emergency room. It’s a powerful screening tool,” said William Schaffner, MD, professor of preventive medicine and infectious diseases at Vanderbilt University Medical Center, Nashville, Tenn.
In addition to fever, common signs of infection include cough, shortness of breath, and breathing difficulties. Some patients have had diarrhea, vomiting, and other gastrointestinal symptoms. In more severe cases, infection can cause pneumonia, severe acute respiratory syndrome, kidney failure, and death. The incubation period appears to be up to 2 weeks, according to the World Health Organization (WHO).
If patients exhibit symptoms and either they or a close contact has returned from China recently, take standard airborne precautions and send specimens – a serum sample, oral and nasal pharyngeal swabs, and lower respiratory tract specimens if available – to the local health department, which will forward them to the Centers for Disease Control and Prevention (CDC) for testing. Turnaround time is 24-48 hours.
The 2019 Novel Coronavirus (2019-nCoV), identified as the cause of an outbreak of respiratory illness first detected in December in association with a live animal market in Wuhan, China, has been implicated in almost 2,000 cases and 56 deaths in that country. Cases have been reported in 13 countries besides China. Five cases of 2019-nCoV infection have been confirmed in the United States, all in people recently returned from Wuhan. As the virus spreads in China, however, it’s almost certain more cases will show up in the United States. Travel history is key, Dr. Schaffner and others said.
Plan and rehearse
The first step to prepare is to use the CDC’s Interim Guidance for Healthcare Professionals to make a written plan specific to your practice to respond to a potential case. The plan must include notifying the local health department, the CDC liaison for testing, and tracking down patient contacts.
“It’s not good enough to just download CDC’s guidance; use it to make your own local plan and know what to do 24/7,” said Daniel Lucey, MD, an infectious disease expert at Georgetown University Medical Center, Washington, D.C.
“Know who is on call at the health department on weekends and nights,” he said. Know where the patient is going to be isolated; figure out what to do if there’s more than one, and tests come back positive. Have masks on hand, and rehearse the response. “Make a coronavirus team, and absolutely have the nurses involved,” as well as other providers who may come into contact with a case, he added.
“You want to be able to do as well as your counterparts in Washington state and Chicago,” where the first two U.S. cases emerged. “They were prepared. They knew what to do,” Dr. Lucey said.
Those first two U.S. patients – a man in Everett, Wash., and a Chicago woman – developed symptoms after returning from Wuhan, a city of 11 million just over 400 miles inland from the port city of Shanghai. On Jan. 26 three more cases were confirmed by the CDC, two in California and one in Arizona, and each had recently traveled to Wuhan. All five patients remain hospitalized, and there’s no evidence they spread the infection further. There is also no evidence of human-to-human transmission of other cases exported from China to any other countries, according to the WHO.
WHO declined to declare a global health emergency – a Public Health Emergency of International Concern, in its parlance – on Jan. 23. The step would have triggered travel and trade restrictions in member states, including the United States. For now, at least, the group said it wasn’t warranted at this point.
Fatality rates
The focus right now is China. The outbreak has spread beyond Wuhan to other parts of the country, and there’s evidence of fourth-generation spread.
Transportation into and out of Wuhan and other cities has been curtailed, Lunar New Year festivals have been canceled, and the Shanghai Disneyland has been closed, among other measures taken by Chinese officials.
The government could be taking drastic measures in part to prevent the public criticism it took in the early 2000’s for the delayed response and lack of transparency during the global outbreak of another wildlife market coronavirus epidemic, severe acute respiratory syndrome (SARS). In a press conference Jan. 22, WHO officials commended the government’s containment efforts but did not say they recommended them.
According to WHO, serious cases in China have mostly been in people over 40 years old with significant comorbidities and have skewed towards men. Spread seems to be limited to family members, health care providers, and other close contacts, probably by respiratory droplets. If that pattern holds, WHO officials said, the outbreak is containable.
The fatality rate appears to be around 3%, a good deal lower than the 10% reported for SARS and much lower than the nearly 40% reported for Middle East respiratory syndrome (MERS), another recent coronavirus mutation from the animal trade.
The Wuhan virus fatality rate might drop as milder cases are detected and added to the denominator. “It definitely appears to be less severe than SARS and MERS,” said Amesh Adalja, MD, an infectious disease physician in Pittsburgh and emerging infectious disease researcher at Johns Hopkins University, Baltimore.
SARS: Lessons learned
In general, the world is much better equipped for coronavirus outbreaks than when SARS, in particular, emerged in 2003.
WHO officials in their press conference lauded China for it openness with the current outbreak, and for isolating and sequencing the virus immediately, which gave the world a diagnostic test in the first days of the outbreak, something that wasn’t available for SARS. China and other countries also are cooperating and working closely to contain the Wuhan virus.
“What we know today might change tomorrow, so we have to keep tuned in to new information, but we learned a lot from SARS,” Dr. Shaffner said. Overall, it’s likely “the impact on the United States of this new coronavirus is going to be trivial,” he predicted.
Dr. Lucey, however, recalled that the SARS outbreak in Toronto in 2003 started with one missed case. A woman returned asymptomatic from Hong Kong and spread the infection to her family members before she died. Her cause of death wasn’t immediately recognized, nor was the reason her family members were sick, since they hadn’t been to Hong Kong recently.
The infection ultimately spread to more than 200 people, about half of them health care workers. A few people died.
If a virus is sufficiently contagious, “it just takes one. You don’t want to be the one who misses that first patient,” Dr. Lucey said.
Currently, there are no antivirals or vaccines for coronaviruses; researchers are working on both, but for now, care is supportive.
This article was updated with new case numbers on 1/26/20.
As the Wuhan coronavirus story unfolds, , according to infectious disease experts.

“We are asking that of everyone with fever and respiratory symptoms who comes to our clinics, hospital, or emergency room. It’s a powerful screening tool,” said William Schaffner, MD, professor of preventive medicine and infectious diseases at Vanderbilt University Medical Center, Nashville, Tenn.
In addition to fever, common signs of infection include cough, shortness of breath, and breathing difficulties. Some patients have had diarrhea, vomiting, and other gastrointestinal symptoms. In more severe cases, infection can cause pneumonia, severe acute respiratory syndrome, kidney failure, and death. The incubation period appears to be up to 2 weeks, according to the World Health Organization (WHO).
If patients exhibit symptoms and either they or a close contact has returned from China recently, take standard airborne precautions and send specimens – a serum sample, oral and nasal pharyngeal swabs, and lower respiratory tract specimens if available – to the local health department, which will forward them to the Centers for Disease Control and Prevention (CDC) for testing. Turnaround time is 24-48 hours.
The 2019 Novel Coronavirus (2019-nCoV), identified as the cause of an outbreak of respiratory illness first detected in December in association with a live animal market in Wuhan, China, has been implicated in almost 2,000 cases and 56 deaths in that country. Cases have been reported in 13 countries besides China. Five cases of 2019-nCoV infection have been confirmed in the United States, all in people recently returned from Wuhan. As the virus spreads in China, however, it’s almost certain more cases will show up in the United States. Travel history is key, Dr. Schaffner and others said.
Plan and rehearse
The first step to prepare is to use the CDC’s Interim Guidance for Healthcare Professionals to make a written plan specific to your practice to respond to a potential case. The plan must include notifying the local health department, the CDC liaison for testing, and tracking down patient contacts.
“It’s not good enough to just download CDC’s guidance; use it to make your own local plan and know what to do 24/7,” said Daniel Lucey, MD, an infectious disease expert at Georgetown University Medical Center, Washington, D.C.
“Know who is on call at the health department on weekends and nights,” he said. Know where the patient is going to be isolated; figure out what to do if there’s more than one, and tests come back positive. Have masks on hand, and rehearse the response. “Make a coronavirus team, and absolutely have the nurses involved,” as well as other providers who may come into contact with a case, he added.
“You want to be able to do as well as your counterparts in Washington state and Chicago,” where the first two U.S. cases emerged. “They were prepared. They knew what to do,” Dr. Lucey said.
Those first two U.S. patients – a man in Everett, Wash., and a Chicago woman – developed symptoms after returning from Wuhan, a city of 11 million just over 400 miles inland from the port city of Shanghai. On Jan. 26 three more cases were confirmed by the CDC, two in California and one in Arizona, and each had recently traveled to Wuhan. All five patients remain hospitalized, and there’s no evidence they spread the infection further. There is also no evidence of human-to-human transmission of other cases exported from China to any other countries, according to the WHO.
WHO declined to declare a global health emergency – a Public Health Emergency of International Concern, in its parlance – on Jan. 23. The step would have triggered travel and trade restrictions in member states, including the United States. For now, at least, the group said it wasn’t warranted at this point.
Fatality rates
The focus right now is China. The outbreak has spread beyond Wuhan to other parts of the country, and there’s evidence of fourth-generation spread.
Transportation into and out of Wuhan and other cities has been curtailed, Lunar New Year festivals have been canceled, and the Shanghai Disneyland has been closed, among other measures taken by Chinese officials.
The government could be taking drastic measures in part to prevent the public criticism it took in the early 2000’s for the delayed response and lack of transparency during the global outbreak of another wildlife market coronavirus epidemic, severe acute respiratory syndrome (SARS). In a press conference Jan. 22, WHO officials commended the government’s containment efforts but did not say they recommended them.
According to WHO, serious cases in China have mostly been in people over 40 years old with significant comorbidities and have skewed towards men. Spread seems to be limited to family members, health care providers, and other close contacts, probably by respiratory droplets. If that pattern holds, WHO officials said, the outbreak is containable.
The fatality rate appears to be around 3%, a good deal lower than the 10% reported for SARS and much lower than the nearly 40% reported for Middle East respiratory syndrome (MERS), another recent coronavirus mutation from the animal trade.
The Wuhan virus fatality rate might drop as milder cases are detected and added to the denominator. “It definitely appears to be less severe than SARS and MERS,” said Amesh Adalja, MD, an infectious disease physician in Pittsburgh and emerging infectious disease researcher at Johns Hopkins University, Baltimore.
SARS: Lessons learned
In general, the world is much better equipped for coronavirus outbreaks than when SARS, in particular, emerged in 2003.
WHO officials in their press conference lauded China for it openness with the current outbreak, and for isolating and sequencing the virus immediately, which gave the world a diagnostic test in the first days of the outbreak, something that wasn’t available for SARS. China and other countries also are cooperating and working closely to contain the Wuhan virus.
“What we know today might change tomorrow, so we have to keep tuned in to new information, but we learned a lot from SARS,” Dr. Shaffner said. Overall, it’s likely “the impact on the United States of this new coronavirus is going to be trivial,” he predicted.
Dr. Lucey, however, recalled that the SARS outbreak in Toronto in 2003 started with one missed case. A woman returned asymptomatic from Hong Kong and spread the infection to her family members before she died. Her cause of death wasn’t immediately recognized, nor was the reason her family members were sick, since they hadn’t been to Hong Kong recently.
The infection ultimately spread to more than 200 people, about half of them health care workers. A few people died.
If a virus is sufficiently contagious, “it just takes one. You don’t want to be the one who misses that first patient,” Dr. Lucey said.
Currently, there are no antivirals or vaccines for coronaviruses; researchers are working on both, but for now, care is supportive.
This article was updated with new case numbers on 1/26/20.
As the Wuhan coronavirus story unfolds, , according to infectious disease experts.

“We are asking that of everyone with fever and respiratory symptoms who comes to our clinics, hospital, or emergency room. It’s a powerful screening tool,” said William Schaffner, MD, professor of preventive medicine and infectious diseases at Vanderbilt University Medical Center, Nashville, Tenn.
In addition to fever, common signs of infection include cough, shortness of breath, and breathing difficulties. Some patients have had diarrhea, vomiting, and other gastrointestinal symptoms. In more severe cases, infection can cause pneumonia, severe acute respiratory syndrome, kidney failure, and death. The incubation period appears to be up to 2 weeks, according to the World Health Organization (WHO).
If patients exhibit symptoms and either they or a close contact has returned from China recently, take standard airborne precautions and send specimens – a serum sample, oral and nasal pharyngeal swabs, and lower respiratory tract specimens if available – to the local health department, which will forward them to the Centers for Disease Control and Prevention (CDC) for testing. Turnaround time is 24-48 hours.
The 2019 Novel Coronavirus (2019-nCoV), identified as the cause of an outbreak of respiratory illness first detected in December in association with a live animal market in Wuhan, China, has been implicated in almost 2,000 cases and 56 deaths in that country. Cases have been reported in 13 countries besides China. Five cases of 2019-nCoV infection have been confirmed in the United States, all in people recently returned from Wuhan. As the virus spreads in China, however, it’s almost certain more cases will show up in the United States. Travel history is key, Dr. Schaffner and others said.
Plan and rehearse
The first step to prepare is to use the CDC’s Interim Guidance for Healthcare Professionals to make a written plan specific to your practice to respond to a potential case. The plan must include notifying the local health department, the CDC liaison for testing, and tracking down patient contacts.
“It’s not good enough to just download CDC’s guidance; use it to make your own local plan and know what to do 24/7,” said Daniel Lucey, MD, an infectious disease expert at Georgetown University Medical Center, Washington, D.C.
“Know who is on call at the health department on weekends and nights,” he said. Know where the patient is going to be isolated; figure out what to do if there’s more than one, and tests come back positive. Have masks on hand, and rehearse the response. “Make a coronavirus team, and absolutely have the nurses involved,” as well as other providers who may come into contact with a case, he added.
“You want to be able to do as well as your counterparts in Washington state and Chicago,” where the first two U.S. cases emerged. “They were prepared. They knew what to do,” Dr. Lucey said.
Those first two U.S. patients – a man in Everett, Wash., and a Chicago woman – developed symptoms after returning from Wuhan, a city of 11 million just over 400 miles inland from the port city of Shanghai. On Jan. 26 three more cases were confirmed by the CDC, two in California and one in Arizona, and each had recently traveled to Wuhan. All five patients remain hospitalized, and there’s no evidence they spread the infection further. There is also no evidence of human-to-human transmission of other cases exported from China to any other countries, according to the WHO.
WHO declined to declare a global health emergency – a Public Health Emergency of International Concern, in its parlance – on Jan. 23. The step would have triggered travel and trade restrictions in member states, including the United States. For now, at least, the group said it wasn’t warranted at this point.
Fatality rates
The focus right now is China. The outbreak has spread beyond Wuhan to other parts of the country, and there’s evidence of fourth-generation spread.
Transportation into and out of Wuhan and other cities has been curtailed, Lunar New Year festivals have been canceled, and the Shanghai Disneyland has been closed, among other measures taken by Chinese officials.
The government could be taking drastic measures in part to prevent the public criticism it took in the early 2000’s for the delayed response and lack of transparency during the global outbreak of another wildlife market coronavirus epidemic, severe acute respiratory syndrome (SARS). In a press conference Jan. 22, WHO officials commended the government’s containment efforts but did not say they recommended them.
According to WHO, serious cases in China have mostly been in people over 40 years old with significant comorbidities and have skewed towards men. Spread seems to be limited to family members, health care providers, and other close contacts, probably by respiratory droplets. If that pattern holds, WHO officials said, the outbreak is containable.
The fatality rate appears to be around 3%, a good deal lower than the 10% reported for SARS and much lower than the nearly 40% reported for Middle East respiratory syndrome (MERS), another recent coronavirus mutation from the animal trade.
The Wuhan virus fatality rate might drop as milder cases are detected and added to the denominator. “It definitely appears to be less severe than SARS and MERS,” said Amesh Adalja, MD, an infectious disease physician in Pittsburgh and emerging infectious disease researcher at Johns Hopkins University, Baltimore.
SARS: Lessons learned
In general, the world is much better equipped for coronavirus outbreaks than when SARS, in particular, emerged in 2003.
WHO officials in their press conference lauded China for it openness with the current outbreak, and for isolating and sequencing the virus immediately, which gave the world a diagnostic test in the first days of the outbreak, something that wasn’t available for SARS. China and other countries also are cooperating and working closely to contain the Wuhan virus.
“What we know today might change tomorrow, so we have to keep tuned in to new information, but we learned a lot from SARS,” Dr. Shaffner said. Overall, it’s likely “the impact on the United States of this new coronavirus is going to be trivial,” he predicted.
Dr. Lucey, however, recalled that the SARS outbreak in Toronto in 2003 started with one missed case. A woman returned asymptomatic from Hong Kong and spread the infection to her family members before she died. Her cause of death wasn’t immediately recognized, nor was the reason her family members were sick, since they hadn’t been to Hong Kong recently.
The infection ultimately spread to more than 200 people, about half of them health care workers. A few people died.
If a virus is sufficiently contagious, “it just takes one. You don’t want to be the one who misses that first patient,” Dr. Lucey said.
Currently, there are no antivirals or vaccines for coronaviruses; researchers are working on both, but for now, care is supportive.
This article was updated with new case numbers on 1/26/20.
Exogenous boosting against shingles not as robust as thought
Exposure to children with chickenpox reduces the incidence of shingles in adults 33% over 2 years, and 27% out to 20 years, according to British investigators.
Being exposed to children with illness due to varicella infection acts as an “exogenous booster” in adults who had chickenpox themselves as children, making shingles less likely, they explained in a BMJ article.
Although that’s good news, it’s been reported previously that exposure to children with chickenpox confers complete protection against shingles in adults for years afterward.
The finding matters in the United Kingdom because varicella vaccine is not part of the pediatric immunization schedule. The United States is the only country that mandates two shots as a requirement for children to attend school.
The United Kingdom, however, is reconsidering its policy. In the past, the exogenous booster idea has been one of the arguments used against mandating the vaccine for children; the concern is that preventing chickenpox in children – and subsequent reexposure to herpes zoster in adults – would kick off a costly wave of shingles in adults.
The study results “are themselves unable to justify for or against specific vaccination schedules, but they do suggest that revised mathematical models are required to estimate the impact of varicella vaccination, with the updated assumption that exogenous boosting is incomplete and only reduces the risk of zoster by about 30%,” noted the investigators, led by Harriet Forbes of the London School of Hygiene and Tropical Medicine.
The researchers identified 9,604 adults with a shingles diagnosis during 1997-2018 who at some point lived with a child who had chickenpox. Data came from the U.K. Clinical Practice Research Datalink, a general practice database.
They then looked at the incidence of shingles within 20 years of exposure to the sick child and compared it with the incidence before exposure and after 20 years, by which time the exogenous booster is thought to wear off. It was a self-controlled case series analysis, “a relatively novel epidemiological study design where individuals act as their own controls. Comparisons are made within individuals rather than between individuals as in a cohort or case control study,” Ms. Forbes and colleagues explained.
After adjustment for age, calendar time, and season, they found that in the 2 years after household exposure to a child with varicella, adults were 33% less likely to develop zoster (incidence ratio 0.67, 95% confidence interval 0.62-0.73), and 27% less likely from 10 to 20 years (IR 0.73, CI 0.62-0.87). The boosting effect appeared to be stronger in men.
“Exogenous boosting provides some protection from the risk of herpes zoster, but not complete immunity, as assumed by previous cost effectiveness estimates of varicella immunization,” the researchers said.
More than two-thirds of the adults with shingles were women, which fits with previous reports. Median age of exposure to a child with varicella was 38 years.
Ms. Forbes and colleagues noted that “the study design required patients with zoster to be living with a child with varicella, therefore the study cohort is younger than a general population with zoster. ... However, when we restricted our analysis to adults aged 50 and older at exposure to varicella, a similar pattern of association was observed, with no evidence of effect modification by age. This suggests that although the median age of our study cohort ... was low, the findings can be generalized to older people.”
There was no external funding for the work, and the lead investigator had no relevant financial disclosures. One investigator reported research grants from GSK and Merck, both makers of chickenpox and shingles vaccines.
SOURCE: Forbes H et al. BMJ. 2020 Jan 22;368:l6987.
Exposure to children with chickenpox reduces the incidence of shingles in adults 33% over 2 years, and 27% out to 20 years, according to British investigators.
Being exposed to children with illness due to varicella infection acts as an “exogenous booster” in adults who had chickenpox themselves as children, making shingles less likely, they explained in a BMJ article.
Although that’s good news, it’s been reported previously that exposure to children with chickenpox confers complete protection against shingles in adults for years afterward.
The finding matters in the United Kingdom because varicella vaccine is not part of the pediatric immunization schedule. The United States is the only country that mandates two shots as a requirement for children to attend school.
The United Kingdom, however, is reconsidering its policy. In the past, the exogenous booster idea has been one of the arguments used against mandating the vaccine for children; the concern is that preventing chickenpox in children – and subsequent reexposure to herpes zoster in adults – would kick off a costly wave of shingles in adults.
The study results “are themselves unable to justify for or against specific vaccination schedules, but they do suggest that revised mathematical models are required to estimate the impact of varicella vaccination, with the updated assumption that exogenous boosting is incomplete and only reduces the risk of zoster by about 30%,” noted the investigators, led by Harriet Forbes of the London School of Hygiene and Tropical Medicine.
The researchers identified 9,604 adults with a shingles diagnosis during 1997-2018 who at some point lived with a child who had chickenpox. Data came from the U.K. Clinical Practice Research Datalink, a general practice database.
They then looked at the incidence of shingles within 20 years of exposure to the sick child and compared it with the incidence before exposure and after 20 years, by which time the exogenous booster is thought to wear off. It was a self-controlled case series analysis, “a relatively novel epidemiological study design where individuals act as their own controls. Comparisons are made within individuals rather than between individuals as in a cohort or case control study,” Ms. Forbes and colleagues explained.
After adjustment for age, calendar time, and season, they found that in the 2 years after household exposure to a child with varicella, adults were 33% less likely to develop zoster (incidence ratio 0.67, 95% confidence interval 0.62-0.73), and 27% less likely from 10 to 20 years (IR 0.73, CI 0.62-0.87). The boosting effect appeared to be stronger in men.
“Exogenous boosting provides some protection from the risk of herpes zoster, but not complete immunity, as assumed by previous cost effectiveness estimates of varicella immunization,” the researchers said.
More than two-thirds of the adults with shingles were women, which fits with previous reports. Median age of exposure to a child with varicella was 38 years.
Ms. Forbes and colleagues noted that “the study design required patients with zoster to be living with a child with varicella, therefore the study cohort is younger than a general population with zoster. ... However, when we restricted our analysis to adults aged 50 and older at exposure to varicella, a similar pattern of association was observed, with no evidence of effect modification by age. This suggests that although the median age of our study cohort ... was low, the findings can be generalized to older people.”
There was no external funding for the work, and the lead investigator had no relevant financial disclosures. One investigator reported research grants from GSK and Merck, both makers of chickenpox and shingles vaccines.
SOURCE: Forbes H et al. BMJ. 2020 Jan 22;368:l6987.
Exposure to children with chickenpox reduces the incidence of shingles in adults 33% over 2 years, and 27% out to 20 years, according to British investigators.
Being exposed to children with illness due to varicella infection acts as an “exogenous booster” in adults who had chickenpox themselves as children, making shingles less likely, they explained in a BMJ article.
Although that’s good news, it’s been reported previously that exposure to children with chickenpox confers complete protection against shingles in adults for years afterward.
The finding matters in the United Kingdom because varicella vaccine is not part of the pediatric immunization schedule. The United States is the only country that mandates two shots as a requirement for children to attend school.
The United Kingdom, however, is reconsidering its policy. In the past, the exogenous booster idea has been one of the arguments used against mandating the vaccine for children; the concern is that preventing chickenpox in children – and subsequent reexposure to herpes zoster in adults – would kick off a costly wave of shingles in adults.
The study results “are themselves unable to justify for or against specific vaccination schedules, but they do suggest that revised mathematical models are required to estimate the impact of varicella vaccination, with the updated assumption that exogenous boosting is incomplete and only reduces the risk of zoster by about 30%,” noted the investigators, led by Harriet Forbes of the London School of Hygiene and Tropical Medicine.
The researchers identified 9,604 adults with a shingles diagnosis during 1997-2018 who at some point lived with a child who had chickenpox. Data came from the U.K. Clinical Practice Research Datalink, a general practice database.
They then looked at the incidence of shingles within 20 years of exposure to the sick child and compared it with the incidence before exposure and after 20 years, by which time the exogenous booster is thought to wear off. It was a self-controlled case series analysis, “a relatively novel epidemiological study design where individuals act as their own controls. Comparisons are made within individuals rather than between individuals as in a cohort or case control study,” Ms. Forbes and colleagues explained.
After adjustment for age, calendar time, and season, they found that in the 2 years after household exposure to a child with varicella, adults were 33% less likely to develop zoster (incidence ratio 0.67, 95% confidence interval 0.62-0.73), and 27% less likely from 10 to 20 years (IR 0.73, CI 0.62-0.87). The boosting effect appeared to be stronger in men.
“Exogenous boosting provides some protection from the risk of herpes zoster, but not complete immunity, as assumed by previous cost effectiveness estimates of varicella immunization,” the researchers said.
More than two-thirds of the adults with shingles were women, which fits with previous reports. Median age of exposure to a child with varicella was 38 years.
Ms. Forbes and colleagues noted that “the study design required patients with zoster to be living with a child with varicella, therefore the study cohort is younger than a general population with zoster. ... However, when we restricted our analysis to adults aged 50 and older at exposure to varicella, a similar pattern of association was observed, with no evidence of effect modification by age. This suggests that although the median age of our study cohort ... was low, the findings can be generalized to older people.”
There was no external funding for the work, and the lead investigator had no relevant financial disclosures. One investigator reported research grants from GSK and Merck, both makers of chickenpox and shingles vaccines.
SOURCE: Forbes H et al. BMJ. 2020 Jan 22;368:l6987.
FROM BMJ