User login
Conference News Roundup—Association of Academic Physiatrists
Electrical Stimulation Device Improves Motor Function
A person with a spinal cord injury can improve his or her ability to grip and move household objects by using an electrical stimulation device controlled by his or her thoughts, according to researchers. The study suggests that this new technology could one day enhance quality of life among people with disabilities and allow them to live more independently.
People with tetraplegia lose upper-limb strength and dexterity, which has a severe impact on their independence and quality of life. New technology that connects a person’s brain to an implanted functional electrical stimulation orthotics device on the hands could restore manual dexterity and grip strength, thus allowing him or her to perform simple daily tasks like holding a toothbrush without help.
“Individuals with cervical spinal cord injury identify recovery of the use of their hands as the single most impactful way that neurotechnology could change their lives,” said Marcie Bockbrader, MD, PhD, Assistant Professor of Physical Medicine and Rehabilitation at the Ohio State University Wexner Medical Center in Columbus. “Giving a person back [his or her] hands reduces dependence on others. It makes it possible to do the little things—like cutting food or opening a door—that are so essential to being able to take care of oneself.”
To test how well this thought-controlled brain–computer interface system works in real life to improve hand strength and dexterity, Dr. Bockbrader and her research team surgically implanted one of these devices into the hand of a 26-year-old man with C5-level, nonspastic tetraplegia following a spinal cord injury. He practiced using the device three times per week for four hours each session for more than 1,000 days. The research team administered standardized tests of upper-limb motor ability and functional participation to see how well the system improved his grip strength, quickness, and other basic skills.
Using this device improved the man’s upper-limb motor ability dramatically, according to several standardized tests. He improved his ability to grip and manipulate basic objects, and showed that he could perform ordinary tasks with his hands at the speed and dexterity levels of healthy individuals. He could move objects of different sizes and weights. With practice, he improved his ability to manipulate smaller household objects like a toothbrush or hairbrush. He also demonstrated that he could imagine different hand positions to proportionally adjust and control different hand movements.
“Our study demonstrated that patients with tetraplegia might be able to restore some of their skilled hand function with an implanted device that allows them to control movements with their own thoughts,” said Dr. Bockbrader. “Although this technology must be refined and tested before it can go from the laboratory to the public, it may one day offer people with disabilities a way to live and work more independently, and enable them to perform daily tasks.”
Concussion Recovery Varies Among Children
Not all children follow the same path to concussion recovery, nor do they have the same predictors for returning to normal activity, investigators reported. Their study also suggests that younger children should be considered separately from high-school students.
“Concussions are common among children, yet the literature is limited with regard to understanding trajectory of recovery after concussion, particularly in children with non-sports-related injuries and for younger children,” said Kaitlyn Chin, a second-year medical student at University of New England College of Osteopathic Medicine in Biddeford, Maine. “We were particularly interested in understanding how activity levels during recovery from concussion influence time to full recovery, to be able to identify modifiable factors to help guide concussion care. Previous studies have noted differences in the amount of time it takes children to recover from a concussion, and our team recently initiated a study to see if we can identify predictors associated with the amount of time between injury and when a child is medically cleared to return to activities which place the child at risk for reinjury.”
Ms. Chin’s team at Kennedy Krieger Institute in Baltimore reviewed the medical records of 178 children who were treated for concussions at an academically affiliated, rehabilitation-based clinic. The children had been medically cleared to return to play between September 2015 and February 2017. The children included in the study ranged in age from 6 to 17. A slight majority was younger than 14. Each child’s first visit to the clinic was within 60 days of his or her concussion.
The researchers reviewed each child’s record, noting when they had been approved to return to play. Then they looked at several other factors for each child, including sex, cause of the concussion (ie, sports or non-sports-related), number of symptoms, school attendance, and exercise status at the initial visit to the clinic. Finally, they considered these factors when the children were placed into two categories—children under 14 and children over 14—to examine potential differences related to age.
Ms. Chin’s team found that the number of symptoms affected how quickly all children were cleared to return to play. Fewer symptoms were associated with a faster return to play. For older children, male sex and higher level of exercise during recovery were associated with a faster return to play. For younger children, higher levels of exercise and school participation (eg, attending class and completing homework and tests) were associated with faster return to play.
Overall, this study shows that elementary and middle-school-aged children should be considered separately from high-school-aged students when considering risk factors for prolonged recovery from a concussion. Furthermore, Ms. Chin’s team found that school participation and exercise were not harmful and did not prolong recovery.
“Our study adds to the literature supporting that return to cognitive and safe physical activities while a child is still recovering from concussion does not prolong time to recovery,” said Ms. Chin. “Every child is different, and recovery is different for each concussion. [Therefore], a concussion recovery plan should be tailored for each child, and parents should seek help from the child’s pediatrician or other medical professionals for guiding care after a concussion.”
Medicine May Not Affect Concussion Recovery
Medications commonly prescribed to reduce symptoms of concussion may not affect recovery, said investigators. Sports medicine physicians commonly treat patients with concussion, so researchers in Utah investigated how some widely prescribed treatments might affect patients’ recovery.
“We really do not have much other than rest and gentle exercise to combat symptoms of concussion,” said Venessa Lee, MD, a physical medicine and rehabilitation resident at University of Utah Health in Salt Lake City. “Medications are commonly prescribed to help with symptoms, but there is little evidence that they help more than just time and rest.”
Although FDA has not approved any medication to treat concussion, physicians may prescribe medications like gabapentin or tricyclic antidepressants (TCAs) to help reduce symptoms during recovery. To examine whether these drugs benefit patients, Dr. Lee and her research team looked at 277 patients who had been diagnosed with concussion at a local academic sports medicine practice. At each of their visits to the clinic during recovery, patients reported their postconcussion symptoms. The research team used a score sheet to measure their symptoms, and they tracked scores of patients who had more than one visit to the clinic for as long as one year.
Patients were separated into three groups for the study: those not prescribed any medication, those prescribed gabapentin, and those prescribed one of two TCAs, amitriptyline or nortriptyline. Based on self-reported information, investigators gave each patient a score for two factors of postconcussion recovery: headaches and a combination of 22 symptoms, including headaches. Each score was on a scale of 0 to 6.
After they adjusted scores for gender and age, Dr. Lee’s team found that headache and combined symptoms scores decreased significantly within days after the first clinic visit for all three groups of patients—those who had taken no medications, those who had been prescribed gabapentin, and those who had been prescribed a TCA. Patients who had been prescribed any of the medications had significantly higher scores for headaches and overall postconcussion symptoms to begin with, but no one type of medication had any better or worse effect over the duration of the study.
“Patients’ symptoms improve with time after a concussion,” said Dr. Lee. “When we looked at [patients who received] gabapentin and TCAs, their symptoms improved over time as well, but similar to those that did not receive a medication.”
Based on this study, neither gabapentin nor TCAs appear to provide any additional benefit for postconcussion recovery. With this information, patients may be able to avoid taking unnecessary medications as they recover from concussions. Patients should speak with a physician about their symptoms after a concussion, said Dr. Lee.
“Though the two medications we studied did not show a profound improvement in our analysis, this was a retrospective study … which has many drawbacks and limitations. We need to do more research to really find the best method for improving postconcussive symptoms.”
Ballet Helps Children with Musculoskeletal and Neurologic Conditions
Adaptive ballet classes provide functional improvement and social interactions for children with musculoskeletal and neurologic conditions, according to researchers. This type of arts-based adaptive therapy is a promising expansion to successful adaptive sports therapies, said the investigators.
“While great strides have been made in adaptive sports, there are still relatively few opportunities in the arts for people with disabilities,” said Sarah Stauder, MD, a physician at the Medical College of Wisconsin in Milwaukee. “Because of this [scarcity], we wanted to evaluate the effect of adaptive ballet on the physical, emotional, social, and academic function of children with physical impairments. The program is a collaboration between a children’s hospital and a metropolitan ballet company that brings together professional dancers, pediatric doctors, physical and occupational therapists, and children with physical disabilities for a series of dance classes.”
The goal of the study was to see whether a weekly, 45-mintute ballet class with 15 minutes of ballet education over five consecutive weeks would improve the children’s balance, physical functions, social skills, and overall quality of life. Eighteen children (17 girls) from ages 5 to 14, took part in the class. Assessments of each child were performed before and after the series of classes using the Pediatric Quality of Life Inventory, the PEDI-CAT survey, and the Pediatric Balance Scale. Finally, a questionnaire was used to assess each child’s success in achieving individual goals set for the class.
At the end of the five weeks, 94% of participants reached their individual goals for the ballet program. PEDI-CAT scores improved after completion of the program, and the program was most beneficial to participants who had lower functioning and quality of life at the beginning of the program. Finally, the researchers noticed an average improvement in balance among the participants.
“Adaptive programs like the one studied here give children the opportunity to participate in activities they otherwise would have no way to do,” said Dr. Stauder. “More specifically, these dance classes instilled a sense of pride and confidence in the children while improving their physical functioning and quality of life. Our study should open the door to more arts-based therapy for children. It is an effective and enjoyable way for patients to get the therapy they need. When kids are active in an activity that interests them, they naturally make greater strides, and we were able to see this in their day-to-day function.”
Genetic Risk Score Predicts TBI Outcomes
A genetic risk score could help predict a patient’s quality of life after a traumatic brain injury (TBI), said researchers. One day, physicians could have a simple method to forecast a patient’s recovery and personalize therapy to maximize quality of life.
“Gene pathways can influence all of our biologic functions and risk for many health outcomes,” said Mark Linsenmeyer, MD, a resident physician at the University of Pittsburgh Medical Center. “Each person has a unique inherited genetic code. By studying one gene pathway in a large group of people with the same disease or health problem, we hope to unlock clues to why some people have different outcomes than others. This knowledge may be used to help physicians make the best treatment choice for each person.”
Dr. Linsenmeyer and colleagues set out to investigate how genes that affect the brain’s dopamine pathways could predict recovery in people with moderate-to-severe TBI. The team recruited 94 adults with TBI from a level-1 trauma center. They focused on the following five genes in the dopamine pathways: COMT rs4680, VMAT2 rs363226, DRD2 rs6279, ANKK1 Taq1a, and MAOA VNTR. They defined which risk genotypes were associated with lower average scores on surveys filled out by patients with TBI to describe their overall quality of life at six and 12 months after their injuries.
The researchers analyzed how individual variants of each of these five genes could affect patients’ quality of life, and then generated a weighted gene risk score as a measure to reflect cumulative risk represented by all genotypes included in the score. Based on available literature about dopamine pathway genetics, they predicted that their gene risk score calculation tool should be specific to a patient’s sex.
Before they calculated gene risk scores, the research team noticed that only COMT could significantly predict quality of life for a subset of patients six months after their injuries. After generating sex-specific gene risk scores, they found that variants of all five genes on the dopamine pathway could meaningfully contribute to a gene risk score that was highly predictive of quality of life after six months for patients of both sexes with TBI, and also predictive of quality of life after one year for women.
Electrical Stimulation Device Improves Motor Function
A person with a spinal cord injury can improve his or her ability to grip and move household objects by using an electrical stimulation device controlled by his or her thoughts, according to researchers. The study suggests that this new technology could one day enhance quality of life among people with disabilities and allow them to live more independently.
People with tetraplegia lose upper-limb strength and dexterity, which has a severe impact on their independence and quality of life. New technology that connects a person’s brain to an implanted functional electrical stimulation orthotics device on the hands could restore manual dexterity and grip strength, thus allowing him or her to perform simple daily tasks like holding a toothbrush without help.
“Individuals with cervical spinal cord injury identify recovery of the use of their hands as the single most impactful way that neurotechnology could change their lives,” said Marcie Bockbrader, MD, PhD, Assistant Professor of Physical Medicine and Rehabilitation at the Ohio State University Wexner Medical Center in Columbus. “Giving a person back [his or her] hands reduces dependence on others. It makes it possible to do the little things—like cutting food or opening a door—that are so essential to being able to take care of oneself.”
To test how well this thought-controlled brain–computer interface system works in real life to improve hand strength and dexterity, Dr. Bockbrader and her research team surgically implanted one of these devices into the hand of a 26-year-old man with C5-level, nonspastic tetraplegia following a spinal cord injury. He practiced using the device three times per week for four hours each session for more than 1,000 days. The research team administered standardized tests of upper-limb motor ability and functional participation to see how well the system improved his grip strength, quickness, and other basic skills.
Using this device improved the man’s upper-limb motor ability dramatically, according to several standardized tests. He improved his ability to grip and manipulate basic objects, and showed that he could perform ordinary tasks with his hands at the speed and dexterity levels of healthy individuals. He could move objects of different sizes and weights. With practice, he improved his ability to manipulate smaller household objects like a toothbrush or hairbrush. He also demonstrated that he could imagine different hand positions to proportionally adjust and control different hand movements.
“Our study demonstrated that patients with tetraplegia might be able to restore some of their skilled hand function with an implanted device that allows them to control movements with their own thoughts,” said Dr. Bockbrader. “Although this technology must be refined and tested before it can go from the laboratory to the public, it may one day offer people with disabilities a way to live and work more independently, and enable them to perform daily tasks.”
Concussion Recovery Varies Among Children
Not all children follow the same path to concussion recovery, nor do they have the same predictors for returning to normal activity, investigators reported. Their study also suggests that younger children should be considered separately from high-school students.
“Concussions are common among children, yet the literature is limited with regard to understanding trajectory of recovery after concussion, particularly in children with non-sports-related injuries and for younger children,” said Kaitlyn Chin, a second-year medical student at University of New England College of Osteopathic Medicine in Biddeford, Maine. “We were particularly interested in understanding how activity levels during recovery from concussion influence time to full recovery, to be able to identify modifiable factors to help guide concussion care. Previous studies have noted differences in the amount of time it takes children to recover from a concussion, and our team recently initiated a study to see if we can identify predictors associated with the amount of time between injury and when a child is medically cleared to return to activities which place the child at risk for reinjury.”
Ms. Chin’s team at Kennedy Krieger Institute in Baltimore reviewed the medical records of 178 children who were treated for concussions at an academically affiliated, rehabilitation-based clinic. The children had been medically cleared to return to play between September 2015 and February 2017. The children included in the study ranged in age from 6 to 17. A slight majority was younger than 14. Each child’s first visit to the clinic was within 60 days of his or her concussion.
The researchers reviewed each child’s record, noting when they had been approved to return to play. Then they looked at several other factors for each child, including sex, cause of the concussion (ie, sports or non-sports-related), number of symptoms, school attendance, and exercise status at the initial visit to the clinic. Finally, they considered these factors when the children were placed into two categories—children under 14 and children over 14—to examine potential differences related to age.
Ms. Chin’s team found that the number of symptoms affected how quickly all children were cleared to return to play. Fewer symptoms were associated with a faster return to play. For older children, male sex and higher level of exercise during recovery were associated with a faster return to play. For younger children, higher levels of exercise and school participation (eg, attending class and completing homework and tests) were associated with faster return to play.
Overall, this study shows that elementary and middle-school-aged children should be considered separately from high-school-aged students when considering risk factors for prolonged recovery from a concussion. Furthermore, Ms. Chin’s team found that school participation and exercise were not harmful and did not prolong recovery.
“Our study adds to the literature supporting that return to cognitive and safe physical activities while a child is still recovering from concussion does not prolong time to recovery,” said Ms. Chin. “Every child is different, and recovery is different for each concussion. [Therefore], a concussion recovery plan should be tailored for each child, and parents should seek help from the child’s pediatrician or other medical professionals for guiding care after a concussion.”
Medicine May Not Affect Concussion Recovery
Medications commonly prescribed to reduce symptoms of concussion may not affect recovery, said investigators. Sports medicine physicians commonly treat patients with concussion, so researchers in Utah investigated how some widely prescribed treatments might affect patients’ recovery.
“We really do not have much other than rest and gentle exercise to combat symptoms of concussion,” said Venessa Lee, MD, a physical medicine and rehabilitation resident at University of Utah Health in Salt Lake City. “Medications are commonly prescribed to help with symptoms, but there is little evidence that they help more than just time and rest.”
Although FDA has not approved any medication to treat concussion, physicians may prescribe medications like gabapentin or tricyclic antidepressants (TCAs) to help reduce symptoms during recovery. To examine whether these drugs benefit patients, Dr. Lee and her research team looked at 277 patients who had been diagnosed with concussion at a local academic sports medicine practice. At each of their visits to the clinic during recovery, patients reported their postconcussion symptoms. The research team used a score sheet to measure their symptoms, and they tracked scores of patients who had more than one visit to the clinic for as long as one year.
Patients were separated into three groups for the study: those not prescribed any medication, those prescribed gabapentin, and those prescribed one of two TCAs, amitriptyline or nortriptyline. Based on self-reported information, investigators gave each patient a score for two factors of postconcussion recovery: headaches and a combination of 22 symptoms, including headaches. Each score was on a scale of 0 to 6.
After they adjusted scores for gender and age, Dr. Lee’s team found that headache and combined symptoms scores decreased significantly within days after the first clinic visit for all three groups of patients—those who had taken no medications, those who had been prescribed gabapentin, and those who had been prescribed a TCA. Patients who had been prescribed any of the medications had significantly higher scores for headaches and overall postconcussion symptoms to begin with, but no one type of medication had any better or worse effect over the duration of the study.
“Patients’ symptoms improve with time after a concussion,” said Dr. Lee. “When we looked at [patients who received] gabapentin and TCAs, their symptoms improved over time as well, but similar to those that did not receive a medication.”
Based on this study, neither gabapentin nor TCAs appear to provide any additional benefit for postconcussion recovery. With this information, patients may be able to avoid taking unnecessary medications as they recover from concussions. Patients should speak with a physician about their symptoms after a concussion, said Dr. Lee.
“Though the two medications we studied did not show a profound improvement in our analysis, this was a retrospective study … which has many drawbacks and limitations. We need to do more research to really find the best method for improving postconcussive symptoms.”
Ballet Helps Children with Musculoskeletal and Neurologic Conditions
Adaptive ballet classes provide functional improvement and social interactions for children with musculoskeletal and neurologic conditions, according to researchers. This type of arts-based adaptive therapy is a promising expansion to successful adaptive sports therapies, said the investigators.
“While great strides have been made in adaptive sports, there are still relatively few opportunities in the arts for people with disabilities,” said Sarah Stauder, MD, a physician at the Medical College of Wisconsin in Milwaukee. “Because of this [scarcity], we wanted to evaluate the effect of adaptive ballet on the physical, emotional, social, and academic function of children with physical impairments. The program is a collaboration between a children’s hospital and a metropolitan ballet company that brings together professional dancers, pediatric doctors, physical and occupational therapists, and children with physical disabilities for a series of dance classes.”
The goal of the study was to see whether a weekly, 45-mintute ballet class with 15 minutes of ballet education over five consecutive weeks would improve the children’s balance, physical functions, social skills, and overall quality of life. Eighteen children (17 girls) from ages 5 to 14, took part in the class. Assessments of each child were performed before and after the series of classes using the Pediatric Quality of Life Inventory, the PEDI-CAT survey, and the Pediatric Balance Scale. Finally, a questionnaire was used to assess each child’s success in achieving individual goals set for the class.
At the end of the five weeks, 94% of participants reached their individual goals for the ballet program. PEDI-CAT scores improved after completion of the program, and the program was most beneficial to participants who had lower functioning and quality of life at the beginning of the program. Finally, the researchers noticed an average improvement in balance among the participants.
“Adaptive programs like the one studied here give children the opportunity to participate in activities they otherwise would have no way to do,” said Dr. Stauder. “More specifically, these dance classes instilled a sense of pride and confidence in the children while improving their physical functioning and quality of life. Our study should open the door to more arts-based therapy for children. It is an effective and enjoyable way for patients to get the therapy they need. When kids are active in an activity that interests them, they naturally make greater strides, and we were able to see this in their day-to-day function.”
Genetic Risk Score Predicts TBI Outcomes
A genetic risk score could help predict a patient’s quality of life after a traumatic brain injury (TBI), said researchers. One day, physicians could have a simple method to forecast a patient’s recovery and personalize therapy to maximize quality of life.
“Gene pathways can influence all of our biologic functions and risk for many health outcomes,” said Mark Linsenmeyer, MD, a resident physician at the University of Pittsburgh Medical Center. “Each person has a unique inherited genetic code. By studying one gene pathway in a large group of people with the same disease or health problem, we hope to unlock clues to why some people have different outcomes than others. This knowledge may be used to help physicians make the best treatment choice for each person.”
Dr. Linsenmeyer and colleagues set out to investigate how genes that affect the brain’s dopamine pathways could predict recovery in people with moderate-to-severe TBI. The team recruited 94 adults with TBI from a level-1 trauma center. They focused on the following five genes in the dopamine pathways: COMT rs4680, VMAT2 rs363226, DRD2 rs6279, ANKK1 Taq1a, and MAOA VNTR. They defined which risk genotypes were associated with lower average scores on surveys filled out by patients with TBI to describe their overall quality of life at six and 12 months after their injuries.
The researchers analyzed how individual variants of each of these five genes could affect patients’ quality of life, and then generated a weighted gene risk score as a measure to reflect cumulative risk represented by all genotypes included in the score. Based on available literature about dopamine pathway genetics, they predicted that their gene risk score calculation tool should be specific to a patient’s sex.
Before they calculated gene risk scores, the research team noticed that only COMT could significantly predict quality of life for a subset of patients six months after their injuries. After generating sex-specific gene risk scores, they found that variants of all five genes on the dopamine pathway could meaningfully contribute to a gene risk score that was highly predictive of quality of life after six months for patients of both sexes with TBI, and also predictive of quality of life after one year for women.
Electrical Stimulation Device Improves Motor Function
A person with a spinal cord injury can improve his or her ability to grip and move household objects by using an electrical stimulation device controlled by his or her thoughts, according to researchers. The study suggests that this new technology could one day enhance quality of life among people with disabilities and allow them to live more independently.
People with tetraplegia lose upper-limb strength and dexterity, which has a severe impact on their independence and quality of life. New technology that connects a person’s brain to an implanted functional electrical stimulation orthotics device on the hands could restore manual dexterity and grip strength, thus allowing him or her to perform simple daily tasks like holding a toothbrush without help.
“Individuals with cervical spinal cord injury identify recovery of the use of their hands as the single most impactful way that neurotechnology could change their lives,” said Marcie Bockbrader, MD, PhD, Assistant Professor of Physical Medicine and Rehabilitation at the Ohio State University Wexner Medical Center in Columbus. “Giving a person back [his or her] hands reduces dependence on others. It makes it possible to do the little things—like cutting food or opening a door—that are so essential to being able to take care of oneself.”
To test how well this thought-controlled brain–computer interface system works in real life to improve hand strength and dexterity, Dr. Bockbrader and her research team surgically implanted one of these devices into the hand of a 26-year-old man with C5-level, nonspastic tetraplegia following a spinal cord injury. He practiced using the device three times per week for four hours each session for more than 1,000 days. The research team administered standardized tests of upper-limb motor ability and functional participation to see how well the system improved his grip strength, quickness, and other basic skills.
Using this device improved the man’s upper-limb motor ability dramatically, according to several standardized tests. He improved his ability to grip and manipulate basic objects, and showed that he could perform ordinary tasks with his hands at the speed and dexterity levels of healthy individuals. He could move objects of different sizes and weights. With practice, he improved his ability to manipulate smaller household objects like a toothbrush or hairbrush. He also demonstrated that he could imagine different hand positions to proportionally adjust and control different hand movements.
“Our study demonstrated that patients with tetraplegia might be able to restore some of their skilled hand function with an implanted device that allows them to control movements with their own thoughts,” said Dr. Bockbrader. “Although this technology must be refined and tested before it can go from the laboratory to the public, it may one day offer people with disabilities a way to live and work more independently, and enable them to perform daily tasks.”
Concussion Recovery Varies Among Children
Not all children follow the same path to concussion recovery, nor do they have the same predictors for returning to normal activity, investigators reported. Their study also suggests that younger children should be considered separately from high-school students.
“Concussions are common among children, yet the literature is limited with regard to understanding trajectory of recovery after concussion, particularly in children with non-sports-related injuries and for younger children,” said Kaitlyn Chin, a second-year medical student at University of New England College of Osteopathic Medicine in Biddeford, Maine. “We were particularly interested in understanding how activity levels during recovery from concussion influence time to full recovery, to be able to identify modifiable factors to help guide concussion care. Previous studies have noted differences in the amount of time it takes children to recover from a concussion, and our team recently initiated a study to see if we can identify predictors associated with the amount of time between injury and when a child is medically cleared to return to activities which place the child at risk for reinjury.”
Ms. Chin’s team at Kennedy Krieger Institute in Baltimore reviewed the medical records of 178 children who were treated for concussions at an academically affiliated, rehabilitation-based clinic. The children had been medically cleared to return to play between September 2015 and February 2017. The children included in the study ranged in age from 6 to 17. A slight majority was younger than 14. Each child’s first visit to the clinic was within 60 days of his or her concussion.
The researchers reviewed each child’s record, noting when they had been approved to return to play. Then they looked at several other factors for each child, including sex, cause of the concussion (ie, sports or non-sports-related), number of symptoms, school attendance, and exercise status at the initial visit to the clinic. Finally, they considered these factors when the children were placed into two categories—children under 14 and children over 14—to examine potential differences related to age.
Ms. Chin’s team found that the number of symptoms affected how quickly all children were cleared to return to play. Fewer symptoms were associated with a faster return to play. For older children, male sex and higher level of exercise during recovery were associated with a faster return to play. For younger children, higher levels of exercise and school participation (eg, attending class and completing homework and tests) were associated with faster return to play.
Overall, this study shows that elementary and middle-school-aged children should be considered separately from high-school-aged students when considering risk factors for prolonged recovery from a concussion. Furthermore, Ms. Chin’s team found that school participation and exercise were not harmful and did not prolong recovery.
“Our study adds to the literature supporting that return to cognitive and safe physical activities while a child is still recovering from concussion does not prolong time to recovery,” said Ms. Chin. “Every child is different, and recovery is different for each concussion. [Therefore], a concussion recovery plan should be tailored for each child, and parents should seek help from the child’s pediatrician or other medical professionals for guiding care after a concussion.”
Medicine May Not Affect Concussion Recovery
Medications commonly prescribed to reduce symptoms of concussion may not affect recovery, said investigators. Sports medicine physicians commonly treat patients with concussion, so researchers in Utah investigated how some widely prescribed treatments might affect patients’ recovery.
“We really do not have much other than rest and gentle exercise to combat symptoms of concussion,” said Venessa Lee, MD, a physical medicine and rehabilitation resident at University of Utah Health in Salt Lake City. “Medications are commonly prescribed to help with symptoms, but there is little evidence that they help more than just time and rest.”
Although FDA has not approved any medication to treat concussion, physicians may prescribe medications like gabapentin or tricyclic antidepressants (TCAs) to help reduce symptoms during recovery. To examine whether these drugs benefit patients, Dr. Lee and her research team looked at 277 patients who had been diagnosed with concussion at a local academic sports medicine practice. At each of their visits to the clinic during recovery, patients reported their postconcussion symptoms. The research team used a score sheet to measure their symptoms, and they tracked scores of patients who had more than one visit to the clinic for as long as one year.
Patients were separated into three groups for the study: those not prescribed any medication, those prescribed gabapentin, and those prescribed one of two TCAs, amitriptyline or nortriptyline. Based on self-reported information, investigators gave each patient a score for two factors of postconcussion recovery: headaches and a combination of 22 symptoms, including headaches. Each score was on a scale of 0 to 6.
After they adjusted scores for gender and age, Dr. Lee’s team found that headache and combined symptoms scores decreased significantly within days after the first clinic visit for all three groups of patients—those who had taken no medications, those who had been prescribed gabapentin, and those who had been prescribed a TCA. Patients who had been prescribed any of the medications had significantly higher scores for headaches and overall postconcussion symptoms to begin with, but no one type of medication had any better or worse effect over the duration of the study.
“Patients’ symptoms improve with time after a concussion,” said Dr. Lee. “When we looked at [patients who received] gabapentin and TCAs, their symptoms improved over time as well, but similar to those that did not receive a medication.”
Based on this study, neither gabapentin nor TCAs appear to provide any additional benefit for postconcussion recovery. With this information, patients may be able to avoid taking unnecessary medications as they recover from concussions. Patients should speak with a physician about their symptoms after a concussion, said Dr. Lee.
“Though the two medications we studied did not show a profound improvement in our analysis, this was a retrospective study … which has many drawbacks and limitations. We need to do more research to really find the best method for improving postconcussive symptoms.”
Ballet Helps Children with Musculoskeletal and Neurologic Conditions
Adaptive ballet classes provide functional improvement and social interactions for children with musculoskeletal and neurologic conditions, according to researchers. This type of arts-based adaptive therapy is a promising expansion to successful adaptive sports therapies, said the investigators.
“While great strides have been made in adaptive sports, there are still relatively few opportunities in the arts for people with disabilities,” said Sarah Stauder, MD, a physician at the Medical College of Wisconsin in Milwaukee. “Because of this [scarcity], we wanted to evaluate the effect of adaptive ballet on the physical, emotional, social, and academic function of children with physical impairments. The program is a collaboration between a children’s hospital and a metropolitan ballet company that brings together professional dancers, pediatric doctors, physical and occupational therapists, and children with physical disabilities for a series of dance classes.”
The goal of the study was to see whether a weekly, 45-mintute ballet class with 15 minutes of ballet education over five consecutive weeks would improve the children’s balance, physical functions, social skills, and overall quality of life. Eighteen children (17 girls) from ages 5 to 14, took part in the class. Assessments of each child were performed before and after the series of classes using the Pediatric Quality of Life Inventory, the PEDI-CAT survey, and the Pediatric Balance Scale. Finally, a questionnaire was used to assess each child’s success in achieving individual goals set for the class.
At the end of the five weeks, 94% of participants reached their individual goals for the ballet program. PEDI-CAT scores improved after completion of the program, and the program was most beneficial to participants who had lower functioning and quality of life at the beginning of the program. Finally, the researchers noticed an average improvement in balance among the participants.
“Adaptive programs like the one studied here give children the opportunity to participate in activities they otherwise would have no way to do,” said Dr. Stauder. “More specifically, these dance classes instilled a sense of pride and confidence in the children while improving their physical functioning and quality of life. Our study should open the door to more arts-based therapy for children. It is an effective and enjoyable way for patients to get the therapy they need. When kids are active in an activity that interests them, they naturally make greater strides, and we were able to see this in their day-to-day function.”
Genetic Risk Score Predicts TBI Outcomes
A genetic risk score could help predict a patient’s quality of life after a traumatic brain injury (TBI), said researchers. One day, physicians could have a simple method to forecast a patient’s recovery and personalize therapy to maximize quality of life.
“Gene pathways can influence all of our biologic functions and risk for many health outcomes,” said Mark Linsenmeyer, MD, a resident physician at the University of Pittsburgh Medical Center. “Each person has a unique inherited genetic code. By studying one gene pathway in a large group of people with the same disease or health problem, we hope to unlock clues to why some people have different outcomes than others. This knowledge may be used to help physicians make the best treatment choice for each person.”
Dr. Linsenmeyer and colleagues set out to investigate how genes that affect the brain’s dopamine pathways could predict recovery in people with moderate-to-severe TBI. The team recruited 94 adults with TBI from a level-1 trauma center. They focused on the following five genes in the dopamine pathways: COMT rs4680, VMAT2 rs363226, DRD2 rs6279, ANKK1 Taq1a, and MAOA VNTR. They defined which risk genotypes were associated with lower average scores on surveys filled out by patients with TBI to describe their overall quality of life at six and 12 months after their injuries.
The researchers analyzed how individual variants of each of these five genes could affect patients’ quality of life, and then generated a weighted gene risk score as a measure to reflect cumulative risk represented by all genotypes included in the score. Based on available literature about dopamine pathway genetics, they predicted that their gene risk score calculation tool should be specific to a patient’s sex.
Before they calculated gene risk scores, the research team noticed that only COMT could significantly predict quality of life for a subset of patients six months after their injuries. After generating sex-specific gene risk scores, they found that variants of all five genes on the dopamine pathway could meaningfully contribute to a gene risk score that was highly predictive of quality of life after six months for patients of both sexes with TBI, and also predictive of quality of life after one year for women.
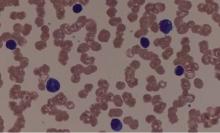
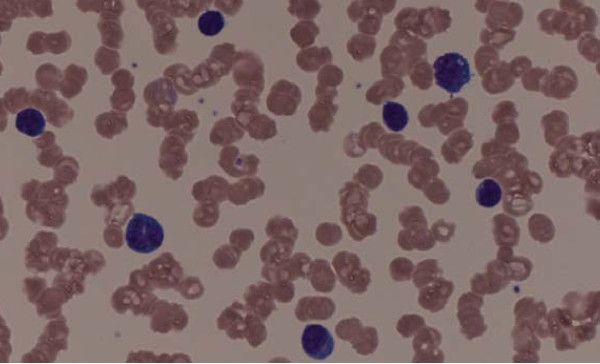
Mogamulizumab active in HTLV-1–associated myelopathy
Mogamulizumab reduced the number of HTLV-1–infected cells and levels of inflammatory markers in patients with HTLV-1–associated myelopathy–tropical spastic paraparesis (HAM-TSP) in a recently reported phase 1-2a study.
Treatment with the anti-CCR4 monoclonal antibody also reduced spasticity and motor disability in some patients with HAM-TSP, according to results published in the New England Journal of Medicine.
Rash was the main side effect of treatment, but the 21-patient trial was “too small and too short to evaluate the clinical safety of mogamulizumab,” said lead author Tomoo Sato, MD, PhD, of the Department of Rare Diseases Research, St. Marianna University, Kawasaki, Japan, and colleagues.
HAM-TSP is a chronic, progressive, and debilitating neuroinflammatory disorder primarily seen in equatorial regions, according to the National Institute of Neurological Disorders and Stroke.
HTVL-1 infects primarily CCR4+ T cells, and mogamulizumab is an anti-CCR4 antibody that targets those affected cells, according to Dr. Sato and colleagues.
Current treatment for HAM-TSP is typically focused on suppressing inflammation with glucocorticoid or interferon-alpha rather than attacking infected cells and reducing proviral load.
The current investigator-initiated study included 21 patients with glucocorticoid-refractory HAM-TSP. In phase 1 of the study, patients received a single intravenous infusion of mogamulizumab and were observed for 85 days. Of those patients, 19 continued to phase 2a and received infusions at 8- or 12-week intervals for a total of 24 weeks.
Treatment resulted in a reduction of 64.9% (95% confidence interval, 51.7-78.1) in proviral load in peripheral-blood mononuclear cells by day 15 postinfusion. Reductions in inflammatory markers at day 29 were also reported, including a 37.3% decrease in CXCL10 levels and a 21.0% decrease in neopterin levels.
In all, 79% of patients had a reduction in spasticity, and 32% had decreased motor disability after treatment.
“The clinical effects appeared very quickly, long before any changes in the markers of inflammation in the central nervous system,” the investigators said.
Grade 1 or 2 rash was seen in 48% of patients, while lymphopenia and leukopenia were seen in 33% of patients each.
A phase 2 study is ongoing to evaluate the long-term safety and efficacy of mogamulizumab in patients with HAM-TSP.
The study was supported by the Japan Agency for Medical Research and Development and by the Ministry of Health, Labor, and Welfare. Two of the coauthors reported patents related to treating HTLV-I–related myelopathy.
SOURCE: Sato T et al. N Engl J Med. 2018;378:529-38.
Mogamulizumab reduced the number of HTLV-1–infected cells and levels of inflammatory markers in patients with HTLV-1–associated myelopathy–tropical spastic paraparesis (HAM-TSP) in a recently reported phase 1-2a study.
Treatment with the anti-CCR4 monoclonal antibody also reduced spasticity and motor disability in some patients with HAM-TSP, according to results published in the New England Journal of Medicine.
Rash was the main side effect of treatment, but the 21-patient trial was “too small and too short to evaluate the clinical safety of mogamulizumab,” said lead author Tomoo Sato, MD, PhD, of the Department of Rare Diseases Research, St. Marianna University, Kawasaki, Japan, and colleagues.
HAM-TSP is a chronic, progressive, and debilitating neuroinflammatory disorder primarily seen in equatorial regions, according to the National Institute of Neurological Disorders and Stroke.
HTVL-1 infects primarily CCR4+ T cells, and mogamulizumab is an anti-CCR4 antibody that targets those affected cells, according to Dr. Sato and colleagues.
Current treatment for HAM-TSP is typically focused on suppressing inflammation with glucocorticoid or interferon-alpha rather than attacking infected cells and reducing proviral load.
The current investigator-initiated study included 21 patients with glucocorticoid-refractory HAM-TSP. In phase 1 of the study, patients received a single intravenous infusion of mogamulizumab and were observed for 85 days. Of those patients, 19 continued to phase 2a and received infusions at 8- or 12-week intervals for a total of 24 weeks.
Treatment resulted in a reduction of 64.9% (95% confidence interval, 51.7-78.1) in proviral load in peripheral-blood mononuclear cells by day 15 postinfusion. Reductions in inflammatory markers at day 29 were also reported, including a 37.3% decrease in CXCL10 levels and a 21.0% decrease in neopterin levels.
In all, 79% of patients had a reduction in spasticity, and 32% had decreased motor disability after treatment.
“The clinical effects appeared very quickly, long before any changes in the markers of inflammation in the central nervous system,” the investigators said.
Grade 1 or 2 rash was seen in 48% of patients, while lymphopenia and leukopenia were seen in 33% of patients each.
A phase 2 study is ongoing to evaluate the long-term safety and efficacy of mogamulizumab in patients with HAM-TSP.
The study was supported by the Japan Agency for Medical Research and Development and by the Ministry of Health, Labor, and Welfare. Two of the coauthors reported patents related to treating HTLV-I–related myelopathy.
SOURCE: Sato T et al. N Engl J Med. 2018;378:529-38.
Mogamulizumab reduced the number of HTLV-1–infected cells and levels of inflammatory markers in patients with HTLV-1–associated myelopathy–tropical spastic paraparesis (HAM-TSP) in a recently reported phase 1-2a study.
Treatment with the anti-CCR4 monoclonal antibody also reduced spasticity and motor disability in some patients with HAM-TSP, according to results published in the New England Journal of Medicine.
Rash was the main side effect of treatment, but the 21-patient trial was “too small and too short to evaluate the clinical safety of mogamulizumab,” said lead author Tomoo Sato, MD, PhD, of the Department of Rare Diseases Research, St. Marianna University, Kawasaki, Japan, and colleagues.
HAM-TSP is a chronic, progressive, and debilitating neuroinflammatory disorder primarily seen in equatorial regions, according to the National Institute of Neurological Disorders and Stroke.
HTVL-1 infects primarily CCR4+ T cells, and mogamulizumab is an anti-CCR4 antibody that targets those affected cells, according to Dr. Sato and colleagues.
Current treatment for HAM-TSP is typically focused on suppressing inflammation with glucocorticoid or interferon-alpha rather than attacking infected cells and reducing proviral load.
The current investigator-initiated study included 21 patients with glucocorticoid-refractory HAM-TSP. In phase 1 of the study, patients received a single intravenous infusion of mogamulizumab and were observed for 85 days. Of those patients, 19 continued to phase 2a and received infusions at 8- or 12-week intervals for a total of 24 weeks.
Treatment resulted in a reduction of 64.9% (95% confidence interval, 51.7-78.1) in proviral load in peripheral-blood mononuclear cells by day 15 postinfusion. Reductions in inflammatory markers at day 29 were also reported, including a 37.3% decrease in CXCL10 levels and a 21.0% decrease in neopterin levels.
In all, 79% of patients had a reduction in spasticity, and 32% had decreased motor disability after treatment.
“The clinical effects appeared very quickly, long before any changes in the markers of inflammation in the central nervous system,” the investigators said.
Grade 1 or 2 rash was seen in 48% of patients, while lymphopenia and leukopenia were seen in 33% of patients each.
A phase 2 study is ongoing to evaluate the long-term safety and efficacy of mogamulizumab in patients with HAM-TSP.
The study was supported by the Japan Agency for Medical Research and Development and by the Ministry of Health, Labor, and Welfare. Two of the coauthors reported patents related to treating HTLV-I–related myelopathy.
SOURCE: Sato T et al. N Engl J Med. 2018;378:529-38.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point:
Major finding: Investigators reported a 64.9% reduction in proviral load by day 15 postinfusion and reductions in inflammatory markers by day 29.
Study details: An investigator-initiated, uncontrolled phase 1-2a study of mogamulizumab in 21 patients with glucocorticoid-refractory HAM-TSP.
Disclosures: The study was supported by the Japan Agency for Medical Research and Development and by the Ministry of Health, Labor, and Welfare. Two of the coauthors reported patents related to treating HTLV-I–related myelopathy.
Source: Sato T et al. N Engl J Med. 2018;378:529-38.
C7 Nerve Transfer May Reduce Spastic Arm Paralysis
Patients with spastic arm paralysis who receive a contralateral C7 nerve graft from their nonparalyzed side to their paralyzed side may have greater improvement in arm function and reduction in spasticity after a year, compared with patients who undergo rehabilitation alone, according to research published January 4 in the New England Journal of Medicine.
The researchers randomly assigned 36 patients who had had unilateral arm paralysis for at least five years to either surgical C7 nerve transfer plus rehabilitation or rehabilitation alone. Participants in the surgery group had an average increase of 17.7 points on the Fugl-Meyer score, while those in the rehabilitation-only group had an average increase of 2.6 points.
To evaluate spasticity, the researchers used the Modified Ashworth Scale, which is scored from 0 to 5. A higher score indicates greater spasticity. Patients who received surgery had improvement from baseline in all five areas measured, and none worsened. The smallest difference between the two groups was in thumb extension. On this measure, 15 surgery patients had a one- or two-unit improvement and three had no change, while seven controls had a one- or two-unit improvement, seven had no improvement, and four had a one-unit worsening. At one year, 16 (89%) patients in the surgery group were able to accomplish three or more of the functional tasks that researchers gave them, whereas none of the controls could do so.
“The majority of clinical improvements coincided with physiologic evidence of connectivity between the hemisphere on the side of the donor nerve and the paralyzed arm,” said lead author Mou-Xiong Zheng, MD, PhD, a hand surgeon at Huashan Hospital at Fudan University in Shanghai, and colleagues.
A Modification to a Previous Surgical Method
Damage to the contralateral cerebral hemisphere after stroke arises from interruption of the inhibitory activity of upper motor neurons. This interruption causes spasticity, along with hand weakness and loss of fractionated fine motor control. In previous studies, researchers have observed activity in the cerebral hemisphere on the same side of paralysis during stroke recovery, but Dr. Zheng and coauthors asserted that connections between the hand and that part of the brain are “sparse,” thus limiting the body’s ability to compensate for spasticity and functional loss.
The latest findings are consistent with those of earlier studies, including one by Dr. Zheng’s coauthors that suggested that the paralyzed hand could be connected to the unaffected hemisphere by transferring a cervical spine nerve from the nonparalyzed side. Researchers previously found this treatment effective for injuries of the brachial plexus. Of the five nerves of the brachial plexus, Dr. Zheng and coauthors chose the C7 nerve because it accounts for about 20% of the nerve fibers in the brachial bundle. Severing the nerve typically results in transient weakness and numbness in the arm or leg on the same side. When they evaluated the hand on the side of the donor graft, the researchers found no significant changes in power, tactile threshold, or two-point discrimination as a result of surgery.
The authors’ surgical approach was a modification of the C7 nerve transfer method that Dr. Zheng and coauthors had previously reported. The operation involved making an incision at the superior aspect of the sternum, mobilizing the donor C7 nerve on the nonparalyzed side, and routing it between the spinal column and esophagus. Then, an anastomosis was performed directly with the C7 nerve on the paralyzed side.
Rehabilitation therapy for the surgery group and controls was identical. Rehabilitation sessions took place four times weekly for 12 months at a single facility, although surgery patients wore an immobilizing cast after their operations.
The nature of the study population (ie, men of various ages with various causes of the underlying cerebral lesions) makes it difficult to draw general conclusions from the findings, Dr. Zheng and coauthors noted. “A larger cohort, followed for a longer period, would be necessary to determine whether cervical nerve transfer results in safe, consistent, and long-term improvements in the function of an arm that is chronically paralyzed as a result of a cerebral lesion,” the authors concluded.
Results Need Clarification
The results that Dr. Zheng and coauthors reported “are exciting, but need clarification and confirmation,” said Robert J. Spinner, MD, Chair of the Department of Neurologic Surgery; Alexander Y. Shin, MD, Consultant in the Department of Orthopedic Surgery; and Allen T. Bishop, MD, Consultant in the Department of Orthopedic Surgery; all at the Mayo Clinic in Rochester, Minnesota, in an accompanying editorial.
Among the questions Dr. Spinner and coauthors raised about the study are whether distal muscles can functionally reinnervate in a year, and whether C7 neurotomy on the paralyzed side led to improvements in spasticity and function. “The C7 neurotomy itself, associated with an immediate reduction in spasticity, represents a major advance for some patients with brain injury who have poor function and spasticity,” they noted. Improvement of the damaged motor cortex, which ongoing physical therapy may enhance, may also contribute to a reduction in spasticity.
Dr. Spinner and coauthors also cited a previous trial by some of Dr. Zheng’s colleagues in which 49% of patients with brachial plexus injury had motor recovery within seven years. “The presence of physiological connectivity observed in the trials does not necessarily equate with functional recovery,” the authors stated.
Future studies of surgical C7 nerve transfer in patients with one-sided arm paralysis should include patients who have C7 neurotomy without nerve transfer, said Dr. Spinner and colleagues. They also noted that because Dr. Zheng and colleagues perform a relatively high volume of these operations, their results might not be easy to reproduce elsewhere.
“Factors other than technical ones, including differences in BMI and limb length across different populations, may lead to different surgical outcomes,” said Dr. Spinner and coauthors. Future research should focus on ways to enhance or speed up nerve regeneration, improve plasticity, and maximize rehabilitation, they added.
—Richard Mark Kirkner
Suggested Reading
Spinner RJ, Shin AY, Bishop AT. Rewiring to regain function in patients with spastic hemiplegia. N Engl J Med. 2018;378(1):83-84.
Zheng MX, Hua XY, Feng JT, et al. Trial of contralateral seventh cervical nerve transfer for spastic arm paralysis. N Engl J Med. 2018;378(1):22-34.
Patients with spastic arm paralysis who receive a contralateral C7 nerve graft from their nonparalyzed side to their paralyzed side may have greater improvement in arm function and reduction in spasticity after a year, compared with patients who undergo rehabilitation alone, according to research published January 4 in the New England Journal of Medicine.
The researchers randomly assigned 36 patients who had had unilateral arm paralysis for at least five years to either surgical C7 nerve transfer plus rehabilitation or rehabilitation alone. Participants in the surgery group had an average increase of 17.7 points on the Fugl-Meyer score, while those in the rehabilitation-only group had an average increase of 2.6 points.
To evaluate spasticity, the researchers used the Modified Ashworth Scale, which is scored from 0 to 5. A higher score indicates greater spasticity. Patients who received surgery had improvement from baseline in all five areas measured, and none worsened. The smallest difference between the two groups was in thumb extension. On this measure, 15 surgery patients had a one- or two-unit improvement and three had no change, while seven controls had a one- or two-unit improvement, seven had no improvement, and four had a one-unit worsening. At one year, 16 (89%) patients in the surgery group were able to accomplish three or more of the functional tasks that researchers gave them, whereas none of the controls could do so.
“The majority of clinical improvements coincided with physiologic evidence of connectivity between the hemisphere on the side of the donor nerve and the paralyzed arm,” said lead author Mou-Xiong Zheng, MD, PhD, a hand surgeon at Huashan Hospital at Fudan University in Shanghai, and colleagues.
A Modification to a Previous Surgical Method
Damage to the contralateral cerebral hemisphere after stroke arises from interruption of the inhibitory activity of upper motor neurons. This interruption causes spasticity, along with hand weakness and loss of fractionated fine motor control. In previous studies, researchers have observed activity in the cerebral hemisphere on the same side of paralysis during stroke recovery, but Dr. Zheng and coauthors asserted that connections between the hand and that part of the brain are “sparse,” thus limiting the body’s ability to compensate for spasticity and functional loss.
The latest findings are consistent with those of earlier studies, including one by Dr. Zheng’s coauthors that suggested that the paralyzed hand could be connected to the unaffected hemisphere by transferring a cervical spine nerve from the nonparalyzed side. Researchers previously found this treatment effective for injuries of the brachial plexus. Of the five nerves of the brachial plexus, Dr. Zheng and coauthors chose the C7 nerve because it accounts for about 20% of the nerve fibers in the brachial bundle. Severing the nerve typically results in transient weakness and numbness in the arm or leg on the same side. When they evaluated the hand on the side of the donor graft, the researchers found no significant changes in power, tactile threshold, or two-point discrimination as a result of surgery.
The authors’ surgical approach was a modification of the C7 nerve transfer method that Dr. Zheng and coauthors had previously reported. The operation involved making an incision at the superior aspect of the sternum, mobilizing the donor C7 nerve on the nonparalyzed side, and routing it between the spinal column and esophagus. Then, an anastomosis was performed directly with the C7 nerve on the paralyzed side.
Rehabilitation therapy for the surgery group and controls was identical. Rehabilitation sessions took place four times weekly for 12 months at a single facility, although surgery patients wore an immobilizing cast after their operations.
The nature of the study population (ie, men of various ages with various causes of the underlying cerebral lesions) makes it difficult to draw general conclusions from the findings, Dr. Zheng and coauthors noted. “A larger cohort, followed for a longer period, would be necessary to determine whether cervical nerve transfer results in safe, consistent, and long-term improvements in the function of an arm that is chronically paralyzed as a result of a cerebral lesion,” the authors concluded.
Results Need Clarification
The results that Dr. Zheng and coauthors reported “are exciting, but need clarification and confirmation,” said Robert J. Spinner, MD, Chair of the Department of Neurologic Surgery; Alexander Y. Shin, MD, Consultant in the Department of Orthopedic Surgery; and Allen T. Bishop, MD, Consultant in the Department of Orthopedic Surgery; all at the Mayo Clinic in Rochester, Minnesota, in an accompanying editorial.
Among the questions Dr. Spinner and coauthors raised about the study are whether distal muscles can functionally reinnervate in a year, and whether C7 neurotomy on the paralyzed side led to improvements in spasticity and function. “The C7 neurotomy itself, associated with an immediate reduction in spasticity, represents a major advance for some patients with brain injury who have poor function and spasticity,” they noted. Improvement of the damaged motor cortex, which ongoing physical therapy may enhance, may also contribute to a reduction in spasticity.
Dr. Spinner and coauthors also cited a previous trial by some of Dr. Zheng’s colleagues in which 49% of patients with brachial plexus injury had motor recovery within seven years. “The presence of physiological connectivity observed in the trials does not necessarily equate with functional recovery,” the authors stated.
Future studies of surgical C7 nerve transfer in patients with one-sided arm paralysis should include patients who have C7 neurotomy without nerve transfer, said Dr. Spinner and colleagues. They also noted that because Dr. Zheng and colleagues perform a relatively high volume of these operations, their results might not be easy to reproduce elsewhere.
“Factors other than technical ones, including differences in BMI and limb length across different populations, may lead to different surgical outcomes,” said Dr. Spinner and coauthors. Future research should focus on ways to enhance or speed up nerve regeneration, improve plasticity, and maximize rehabilitation, they added.
—Richard Mark Kirkner
Suggested Reading
Spinner RJ, Shin AY, Bishop AT. Rewiring to regain function in patients with spastic hemiplegia. N Engl J Med. 2018;378(1):83-84.
Zheng MX, Hua XY, Feng JT, et al. Trial of contralateral seventh cervical nerve transfer for spastic arm paralysis. N Engl J Med. 2018;378(1):22-34.
Patients with spastic arm paralysis who receive a contralateral C7 nerve graft from their nonparalyzed side to their paralyzed side may have greater improvement in arm function and reduction in spasticity after a year, compared with patients who undergo rehabilitation alone, according to research published January 4 in the New England Journal of Medicine.
The researchers randomly assigned 36 patients who had had unilateral arm paralysis for at least five years to either surgical C7 nerve transfer plus rehabilitation or rehabilitation alone. Participants in the surgery group had an average increase of 17.7 points on the Fugl-Meyer score, while those in the rehabilitation-only group had an average increase of 2.6 points.
To evaluate spasticity, the researchers used the Modified Ashworth Scale, which is scored from 0 to 5. A higher score indicates greater spasticity. Patients who received surgery had improvement from baseline in all five areas measured, and none worsened. The smallest difference between the two groups was in thumb extension. On this measure, 15 surgery patients had a one- or two-unit improvement and three had no change, while seven controls had a one- or two-unit improvement, seven had no improvement, and four had a one-unit worsening. At one year, 16 (89%) patients in the surgery group were able to accomplish three or more of the functional tasks that researchers gave them, whereas none of the controls could do so.
“The majority of clinical improvements coincided with physiologic evidence of connectivity between the hemisphere on the side of the donor nerve and the paralyzed arm,” said lead author Mou-Xiong Zheng, MD, PhD, a hand surgeon at Huashan Hospital at Fudan University in Shanghai, and colleagues.
A Modification to a Previous Surgical Method
Damage to the contralateral cerebral hemisphere after stroke arises from interruption of the inhibitory activity of upper motor neurons. This interruption causes spasticity, along with hand weakness and loss of fractionated fine motor control. In previous studies, researchers have observed activity in the cerebral hemisphere on the same side of paralysis during stroke recovery, but Dr. Zheng and coauthors asserted that connections between the hand and that part of the brain are “sparse,” thus limiting the body’s ability to compensate for spasticity and functional loss.
The latest findings are consistent with those of earlier studies, including one by Dr. Zheng’s coauthors that suggested that the paralyzed hand could be connected to the unaffected hemisphere by transferring a cervical spine nerve from the nonparalyzed side. Researchers previously found this treatment effective for injuries of the brachial plexus. Of the five nerves of the brachial plexus, Dr. Zheng and coauthors chose the C7 nerve because it accounts for about 20% of the nerve fibers in the brachial bundle. Severing the nerve typically results in transient weakness and numbness in the arm or leg on the same side. When they evaluated the hand on the side of the donor graft, the researchers found no significant changes in power, tactile threshold, or two-point discrimination as a result of surgery.
The authors’ surgical approach was a modification of the C7 nerve transfer method that Dr. Zheng and coauthors had previously reported. The operation involved making an incision at the superior aspect of the sternum, mobilizing the donor C7 nerve on the nonparalyzed side, and routing it between the spinal column and esophagus. Then, an anastomosis was performed directly with the C7 nerve on the paralyzed side.
Rehabilitation therapy for the surgery group and controls was identical. Rehabilitation sessions took place four times weekly for 12 months at a single facility, although surgery patients wore an immobilizing cast after their operations.
The nature of the study population (ie, men of various ages with various causes of the underlying cerebral lesions) makes it difficult to draw general conclusions from the findings, Dr. Zheng and coauthors noted. “A larger cohort, followed for a longer period, would be necessary to determine whether cervical nerve transfer results in safe, consistent, and long-term improvements in the function of an arm that is chronically paralyzed as a result of a cerebral lesion,” the authors concluded.
Results Need Clarification
The results that Dr. Zheng and coauthors reported “are exciting, but need clarification and confirmation,” said Robert J. Spinner, MD, Chair of the Department of Neurologic Surgery; Alexander Y. Shin, MD, Consultant in the Department of Orthopedic Surgery; and Allen T. Bishop, MD, Consultant in the Department of Orthopedic Surgery; all at the Mayo Clinic in Rochester, Minnesota, in an accompanying editorial.
Among the questions Dr. Spinner and coauthors raised about the study are whether distal muscles can functionally reinnervate in a year, and whether C7 neurotomy on the paralyzed side led to improvements in spasticity and function. “The C7 neurotomy itself, associated with an immediate reduction in spasticity, represents a major advance for some patients with brain injury who have poor function and spasticity,” they noted. Improvement of the damaged motor cortex, which ongoing physical therapy may enhance, may also contribute to a reduction in spasticity.
Dr. Spinner and coauthors also cited a previous trial by some of Dr. Zheng’s colleagues in which 49% of patients with brachial plexus injury had motor recovery within seven years. “The presence of physiological connectivity observed in the trials does not necessarily equate with functional recovery,” the authors stated.
Future studies of surgical C7 nerve transfer in patients with one-sided arm paralysis should include patients who have C7 neurotomy without nerve transfer, said Dr. Spinner and colleagues. They also noted that because Dr. Zheng and colleagues perform a relatively high volume of these operations, their results might not be easy to reproduce elsewhere.
“Factors other than technical ones, including differences in BMI and limb length across different populations, may lead to different surgical outcomes,” said Dr. Spinner and coauthors. Future research should focus on ways to enhance or speed up nerve regeneration, improve plasticity, and maximize rehabilitation, they added.
—Richard Mark Kirkner
Suggested Reading
Spinner RJ, Shin AY, Bishop AT. Rewiring to regain function in patients with spastic hemiplegia. N Engl J Med. 2018;378(1):83-84.
Zheng MX, Hua XY, Feng JT, et al. Trial of contralateral seventh cervical nerve transfer for spastic arm paralysis. N Engl J Med. 2018;378(1):22-34.
Genetic Screens Yield Potential Therapies for Neurodegenerative Diseases
SAN DIEGO—Cross-species genetic screens are helping researchers find molecules that modulate the proteins that cause adult neurodegenerative disease, according to a lecture delivered at the 142nd Annual Meeting of the American Neurological Association. Such screening thus reveals potential therapeutic targets and augments scientific understanding of the biology of these proteins.
The research raises the possibility that clinicians will be able to delay or prevent neurodegenerative disease in the future through the early administration of molecules that target these proteins. “We need to identify those at risk and begin the therapy … before the symptoms develop, just like you would treat somebody with statins if they have high cholesterol before they have a heart attack,” said Huda Y. Zoghbi, MD, an investigator with the Howard Hughes Medical Institute; Professor of Pediatrics, Molecular and Human Genetics, Neuroscience, and Neurology at Baylor College of Medicine; and Director of the Jan and Dan Duncan Neurological Research Institute in Houston.
Research Into a Rare Disorder
Studying the rare disorder spinocerebellar ataxia type 1 (SCA1) has yielded information that could be applicable to more common neurodegenerative diseases, said Dr. Zoghbi. SCA1 is characterized by a loss of Purkinje cells and brainstem neurons that impairs balance and coordination and increases the risk of premature death. In 1993, Dr. Zoghbi; Harry Orr, PhD, Professor and Tulloch Chair in Genetics at the University of Minnesota in Minneapolis; and colleagues discovered that a CAG repeat expansion in ATXN1 causes SCA1 by producing an abnormally long version of the ataxin-1 protein. They also found that neurodegeneration results if levels of normal ataxin-1 are increased by 20% or 30%. The brain thus is highly sensitive to ataxin-1 levels, said Dr. Zoghbi.
Borrowing a technique from cancer research, the investigators performed genetic screening using fruit fly and human cells to find targets that would reduce ataxin-1 levels when inhibited. They found approximately 30 relevant genes in each organism, and about 12 were common to both organisms. All of the shared genes operate in the mitogen-activated protein (MAP) kinase pathway, and inhibiting each gene lowered ataxin-1 in cells and flies.
Inhibiting Enzymes
The researchers also observed that the enzymes MSK1 and MSK2 intervene in the pathway and promote ataxin-1 accumulation. Inhibiting MSK1 produced clinical improvement in SCA1 mouse models, and inhibiting MSK1 and MSK2 together produced still more improvement. A small molecule that inhibited MSK1 therefore could help patients with SCA1, said Dr. Zoghbi.
Inhibiting enzymes such as MSK1 and MSK2 for years at a time could raise safety concerns, however. The investigators thus decided to look for other modulators of ataxin-1, on the theory that targeting modulators that function in different pathways could reduce the amount of inhibition required and decrease the risk of adverse events.
Further screening revealed that PKA1 appeared to modulate ataxin-1 by a mechanism similar to that of MSK1. An animal study indicated that inhibiting MSK1 and inhibiting PKA1 produced equivalent reductions on ataxin-1, but that inhibiting both in tandem yielded a greater reduction. The investigators then found that the PAK1 enzyme promoted ataxin-1 accumulation through a pathway different from that of MSK1 and PKA1. Inhibiting PAK1 reduced ataxin-1 levels, and inhibiting PAK1 and MSK1 simultaneously had a still greater effect.
Targeting Tauopathies
Their research into kinases and enzymes prompted Dr. Zoghbi and colleagues to consider whole genome screening as a method of targeting proteins that cause neurodegenerative diseases other than SCA1. Overexpression of tau, for example, causes neurodegeneration, regardless of whether the overexpression results from a mutation in tau-encoding genes. “Tau is a true culprit in dementias, and we thought that if we could find something to lower it, we could help patients with these disorders,” said Dr. Zoghbi.
Another genetic screen suggested that the enzyme Nuak1 stabilizes tau by phosphorylating it at Ser356. The investigators observed that inhibiting Nuak1 reduced tau levels and suppressed neurodegeneration in human cells and in fruit flies. Tau accumulation decreases fruit flies’ climbing ability, and inhibiting Nuak1 improved this ability in flies with tau accumulation.
In a subsequent mouse study, Dr. Zoghbi and colleagues found that inhibiting Nuak1 significantly reduced levels of phosphorylated tau and provided smaller reductions in total tau and endogenous tau. They also observed that mice with tauopathy took longer than wild-type mice to complete a water maze task. Inhibiting Nuak1 in mice with tauopathy improved their performance on this task. Nuak1 inhibition also restored synaptic plasticity in these mice to a level similar to that of wild-type mice. Finally, Nuak1 inhibition reduced tau tangle pathology and increased survival. Dr. Zoghbi and colleagues are now searching for small-molecule Nuak1 inhibitors that could provide protection against tauopathy.
In Search of More Targets
The investigators next looked for genes that influence tau. Successive levels of genetic screening identified 59 genes that “robustly lower tau levels,” said Dr. Zoghbi. She and her colleagues prioritized 12 of the genes for investigation.
They used adenoassociated viral vectors to deliver therapies that can knock out mouse genes for as long as a year. With this technique, the investigators confirmed that all of the initial 12 genes decreased tau levels. In principle, this strategy could enable researchers to scan the whole genome for genes that modulate tau, said Dr. Zoghbi.
—Erik Greb
Suggested Reading
Lasagna-Reeves CA, de Haro M, Hao S, et al. Reduction of Nuak1 decreases tau and reverses phenotypes in a tauopathy mouse model. Neuron. 2016; 92(2):407-418.
Park J, Al-Ramahi I, Tan Q, et al. RAS-MAPK-MSK1 pathway modulates ataxin 1 protein levels and toxicity in SCA1. Nature. 2013;498(7454):325-331.
Rousseaux MW, de Haro M, Lasagna-Reeves CA, et al. TRIM28 regulates the nuclear accumulation and toxicity of both alpha-synuclein and tau. Elife. 2016 Oct 25;5. pii: e19809
SAN DIEGO—Cross-species genetic screens are helping researchers find molecules that modulate the proteins that cause adult neurodegenerative disease, according to a lecture delivered at the 142nd Annual Meeting of the American Neurological Association. Such screening thus reveals potential therapeutic targets and augments scientific understanding of the biology of these proteins.
The research raises the possibility that clinicians will be able to delay or prevent neurodegenerative disease in the future through the early administration of molecules that target these proteins. “We need to identify those at risk and begin the therapy … before the symptoms develop, just like you would treat somebody with statins if they have high cholesterol before they have a heart attack,” said Huda Y. Zoghbi, MD, an investigator with the Howard Hughes Medical Institute; Professor of Pediatrics, Molecular and Human Genetics, Neuroscience, and Neurology at Baylor College of Medicine; and Director of the Jan and Dan Duncan Neurological Research Institute in Houston.
Research Into a Rare Disorder
Studying the rare disorder spinocerebellar ataxia type 1 (SCA1) has yielded information that could be applicable to more common neurodegenerative diseases, said Dr. Zoghbi. SCA1 is characterized by a loss of Purkinje cells and brainstem neurons that impairs balance and coordination and increases the risk of premature death. In 1993, Dr. Zoghbi; Harry Orr, PhD, Professor and Tulloch Chair in Genetics at the University of Minnesota in Minneapolis; and colleagues discovered that a CAG repeat expansion in ATXN1 causes SCA1 by producing an abnormally long version of the ataxin-1 protein. They also found that neurodegeneration results if levels of normal ataxin-1 are increased by 20% or 30%. The brain thus is highly sensitive to ataxin-1 levels, said Dr. Zoghbi.
Borrowing a technique from cancer research, the investigators performed genetic screening using fruit fly and human cells to find targets that would reduce ataxin-1 levels when inhibited. They found approximately 30 relevant genes in each organism, and about 12 were common to both organisms. All of the shared genes operate in the mitogen-activated protein (MAP) kinase pathway, and inhibiting each gene lowered ataxin-1 in cells and flies.
Inhibiting Enzymes
The researchers also observed that the enzymes MSK1 and MSK2 intervene in the pathway and promote ataxin-1 accumulation. Inhibiting MSK1 produced clinical improvement in SCA1 mouse models, and inhibiting MSK1 and MSK2 together produced still more improvement. A small molecule that inhibited MSK1 therefore could help patients with SCA1, said Dr. Zoghbi.
Inhibiting enzymes such as MSK1 and MSK2 for years at a time could raise safety concerns, however. The investigators thus decided to look for other modulators of ataxin-1, on the theory that targeting modulators that function in different pathways could reduce the amount of inhibition required and decrease the risk of adverse events.
Further screening revealed that PKA1 appeared to modulate ataxin-1 by a mechanism similar to that of MSK1. An animal study indicated that inhibiting MSK1 and inhibiting PKA1 produced equivalent reductions on ataxin-1, but that inhibiting both in tandem yielded a greater reduction. The investigators then found that the PAK1 enzyme promoted ataxin-1 accumulation through a pathway different from that of MSK1 and PKA1. Inhibiting PAK1 reduced ataxin-1 levels, and inhibiting PAK1 and MSK1 simultaneously had a still greater effect.
Targeting Tauopathies
Their research into kinases and enzymes prompted Dr. Zoghbi and colleagues to consider whole genome screening as a method of targeting proteins that cause neurodegenerative diseases other than SCA1. Overexpression of tau, for example, causes neurodegeneration, regardless of whether the overexpression results from a mutation in tau-encoding genes. “Tau is a true culprit in dementias, and we thought that if we could find something to lower it, we could help patients with these disorders,” said Dr. Zoghbi.
Another genetic screen suggested that the enzyme Nuak1 stabilizes tau by phosphorylating it at Ser356. The investigators observed that inhibiting Nuak1 reduced tau levels and suppressed neurodegeneration in human cells and in fruit flies. Tau accumulation decreases fruit flies’ climbing ability, and inhibiting Nuak1 improved this ability in flies with tau accumulation.
In a subsequent mouse study, Dr. Zoghbi and colleagues found that inhibiting Nuak1 significantly reduced levels of phosphorylated tau and provided smaller reductions in total tau and endogenous tau. They also observed that mice with tauopathy took longer than wild-type mice to complete a water maze task. Inhibiting Nuak1 in mice with tauopathy improved their performance on this task. Nuak1 inhibition also restored synaptic plasticity in these mice to a level similar to that of wild-type mice. Finally, Nuak1 inhibition reduced tau tangle pathology and increased survival. Dr. Zoghbi and colleagues are now searching for small-molecule Nuak1 inhibitors that could provide protection against tauopathy.
In Search of More Targets
The investigators next looked for genes that influence tau. Successive levels of genetic screening identified 59 genes that “robustly lower tau levels,” said Dr. Zoghbi. She and her colleagues prioritized 12 of the genes for investigation.
They used adenoassociated viral vectors to deliver therapies that can knock out mouse genes for as long as a year. With this technique, the investigators confirmed that all of the initial 12 genes decreased tau levels. In principle, this strategy could enable researchers to scan the whole genome for genes that modulate tau, said Dr. Zoghbi.
—Erik Greb
Suggested Reading
Lasagna-Reeves CA, de Haro M, Hao S, et al. Reduction of Nuak1 decreases tau and reverses phenotypes in a tauopathy mouse model. Neuron. 2016; 92(2):407-418.
Park J, Al-Ramahi I, Tan Q, et al. RAS-MAPK-MSK1 pathway modulates ataxin 1 protein levels and toxicity in SCA1. Nature. 2013;498(7454):325-331.
Rousseaux MW, de Haro M, Lasagna-Reeves CA, et al. TRIM28 regulates the nuclear accumulation and toxicity of both alpha-synuclein and tau. Elife. 2016 Oct 25;5. pii: e19809
SAN DIEGO—Cross-species genetic screens are helping researchers find molecules that modulate the proteins that cause adult neurodegenerative disease, according to a lecture delivered at the 142nd Annual Meeting of the American Neurological Association. Such screening thus reveals potential therapeutic targets and augments scientific understanding of the biology of these proteins.
The research raises the possibility that clinicians will be able to delay or prevent neurodegenerative disease in the future through the early administration of molecules that target these proteins. “We need to identify those at risk and begin the therapy … before the symptoms develop, just like you would treat somebody with statins if they have high cholesterol before they have a heart attack,” said Huda Y. Zoghbi, MD, an investigator with the Howard Hughes Medical Institute; Professor of Pediatrics, Molecular and Human Genetics, Neuroscience, and Neurology at Baylor College of Medicine; and Director of the Jan and Dan Duncan Neurological Research Institute in Houston.
Research Into a Rare Disorder
Studying the rare disorder spinocerebellar ataxia type 1 (SCA1) has yielded information that could be applicable to more common neurodegenerative diseases, said Dr. Zoghbi. SCA1 is characterized by a loss of Purkinje cells and brainstem neurons that impairs balance and coordination and increases the risk of premature death. In 1993, Dr. Zoghbi; Harry Orr, PhD, Professor and Tulloch Chair in Genetics at the University of Minnesota in Minneapolis; and colleagues discovered that a CAG repeat expansion in ATXN1 causes SCA1 by producing an abnormally long version of the ataxin-1 protein. They also found that neurodegeneration results if levels of normal ataxin-1 are increased by 20% or 30%. The brain thus is highly sensitive to ataxin-1 levels, said Dr. Zoghbi.
Borrowing a technique from cancer research, the investigators performed genetic screening using fruit fly and human cells to find targets that would reduce ataxin-1 levels when inhibited. They found approximately 30 relevant genes in each organism, and about 12 were common to both organisms. All of the shared genes operate in the mitogen-activated protein (MAP) kinase pathway, and inhibiting each gene lowered ataxin-1 in cells and flies.
Inhibiting Enzymes
The researchers also observed that the enzymes MSK1 and MSK2 intervene in the pathway and promote ataxin-1 accumulation. Inhibiting MSK1 produced clinical improvement in SCA1 mouse models, and inhibiting MSK1 and MSK2 together produced still more improvement. A small molecule that inhibited MSK1 therefore could help patients with SCA1, said Dr. Zoghbi.
Inhibiting enzymes such as MSK1 and MSK2 for years at a time could raise safety concerns, however. The investigators thus decided to look for other modulators of ataxin-1, on the theory that targeting modulators that function in different pathways could reduce the amount of inhibition required and decrease the risk of adverse events.
Further screening revealed that PKA1 appeared to modulate ataxin-1 by a mechanism similar to that of MSK1. An animal study indicated that inhibiting MSK1 and inhibiting PKA1 produced equivalent reductions on ataxin-1, but that inhibiting both in tandem yielded a greater reduction. The investigators then found that the PAK1 enzyme promoted ataxin-1 accumulation through a pathway different from that of MSK1 and PKA1. Inhibiting PAK1 reduced ataxin-1 levels, and inhibiting PAK1 and MSK1 simultaneously had a still greater effect.
Targeting Tauopathies
Their research into kinases and enzymes prompted Dr. Zoghbi and colleagues to consider whole genome screening as a method of targeting proteins that cause neurodegenerative diseases other than SCA1. Overexpression of tau, for example, causes neurodegeneration, regardless of whether the overexpression results from a mutation in tau-encoding genes. “Tau is a true culprit in dementias, and we thought that if we could find something to lower it, we could help patients with these disorders,” said Dr. Zoghbi.
Another genetic screen suggested that the enzyme Nuak1 stabilizes tau by phosphorylating it at Ser356. The investigators observed that inhibiting Nuak1 reduced tau levels and suppressed neurodegeneration in human cells and in fruit flies. Tau accumulation decreases fruit flies’ climbing ability, and inhibiting Nuak1 improved this ability in flies with tau accumulation.
In a subsequent mouse study, Dr. Zoghbi and colleagues found that inhibiting Nuak1 significantly reduced levels of phosphorylated tau and provided smaller reductions in total tau and endogenous tau. They also observed that mice with tauopathy took longer than wild-type mice to complete a water maze task. Inhibiting Nuak1 in mice with tauopathy improved their performance on this task. Nuak1 inhibition also restored synaptic plasticity in these mice to a level similar to that of wild-type mice. Finally, Nuak1 inhibition reduced tau tangle pathology and increased survival. Dr. Zoghbi and colleagues are now searching for small-molecule Nuak1 inhibitors that could provide protection against tauopathy.
In Search of More Targets
The investigators next looked for genes that influence tau. Successive levels of genetic screening identified 59 genes that “robustly lower tau levels,” said Dr. Zoghbi. She and her colleagues prioritized 12 of the genes for investigation.
They used adenoassociated viral vectors to deliver therapies that can knock out mouse genes for as long as a year. With this technique, the investigators confirmed that all of the initial 12 genes decreased tau levels. In principle, this strategy could enable researchers to scan the whole genome for genes that modulate tau, said Dr. Zoghbi.
—Erik Greb
Suggested Reading
Lasagna-Reeves CA, de Haro M, Hao S, et al. Reduction of Nuak1 decreases tau and reverses phenotypes in a tauopathy mouse model. Neuron. 2016; 92(2):407-418.
Park J, Al-Ramahi I, Tan Q, et al. RAS-MAPK-MSK1 pathway modulates ataxin 1 protein levels and toxicity in SCA1. Nature. 2013;498(7454):325-331.
Rousseaux MW, de Haro M, Lasagna-Reeves CA, et al. TRIM28 regulates the nuclear accumulation and toxicity of both alpha-synuclein and tau. Elife. 2016 Oct 25;5. pii: e19809
FDA cites manufacturer of autologous stem cells for regulatory, manufacturing missteps
for manufacturing processes that may compromise its safety and for failing to toe the regulatory line in marketing.
American CryoStem received an FDA warning letter Jan. 3 demanding that the company comply with best-manufacturing processes and obtain an investigational new drug application if it wishes to continue marketing ATCELL for its currently advertised clinical indications and administration routes. These include intravenous, intrathecal, or aerosol inhalation of the product for anoxic brain injury, Parkinson’s disease, amyotrophic lateral sclerosis, stroke, and multiple sclerosis.
“Please be advised that, to lawfully market a drug that is a biological product, a valid biologics license must be in effect,” noted the letter. “Such licenses are issued only after a showing that the product is safe, pure, and potent. While in the development stage, such products may be distributed for clinical use in humans only if the sponsor has an investigational new drug application (IND) in effect as specified by FDA regulations. ATCELL is not the subject of an approved biologics license application nor is there an IND in effect. Based on this information, we have determined that your actions have violated the Food, Drug, and Cosmetic Act and the Public Health Service Act.”
FDA inspectors conducted a site inspection of American CryoStem in Eatontown, N.J., last summer, during which they “documented evidence of significant deviations from current good manufacturing practice.” The agency then provided the company a chance to respond to these issues. The new warning letter discussed each complaint, noting that some were inadequately addressed, and demanded that the company take action within 15 working days or face potential legal process, including seizure and/or injunction.
American CryoStem is one of the first companies to experience increased scrutiny under FDA’s new commitment to regulate the rapid growth and development of regenerative medicine products, which include novel cellular therapies, with the aim of ensuring their safety and effectiveness.
The new policy is designed to support the potential of cellular rejuvenation medicine, while protecting patients from “unscrupulous actors” who might endanger public health with untested products, according to FDA Commissioner Scott Gottlieb, MD. As enthusiasm for stem cell treatments surges, so are reports of adverse events. The New England Journal of Medicine recently reported on three patients with age-related macular degeneration who were blinded by intravitreal injection of autologous adipose-derived stem cells (N Engl J Med. 2017;376:1047-53).
Under the new policy, cell- and tissue-based products could be exempt from FDA premarket review only if they are removed from and implanted back into the same patient in their original form, or if the products are “minimally manipulated.” ATCELL fulfills neither qualification, the FDA warning letter said.
“You process adipose tissue ... to isolate cellular components of adipose tissue, commonly referred to as stromal vascular fraction [SVF]. Such processing is more than minimal manipulation because [it alters] the original relevant characteristics of the [tissue] relating to its utility for reconstruction, repair, or replacement. Then you process the SVF by expanding it in cell culture to manufacture ATCELL. Such expansion also is more than minimal manipulation because it alters the original relevant characteristics of the tissue.”
Furthermore, the letter noted, at least one of the components used in the clonal expansion process is investigational and not intended for human use. The manufacturer of that component, which was not named, “indicates the following: ‘Unless otherwise stated in our catalog or other company documentation accompanying the product(s), our products are intended for research use only and are not to be used for any other purpose, which includes but is not limited to, unauthorized commercial uses, in vitro diagnostic uses, ex vivo or in vivo therapeutic uses or any type of consumption or application to human and animals.”
The FDA also took exception with several equipment and lab safety issues. ATCELL was being created in areas that had no clean space designation – a serious concern, the letter said.
“American CryoStem’s unvalidated processes, inadequately controlled environment, lack of control of components used in production, and lack of sufficient and validated product testing ... pose a significant risk that ATCELL may be contaminated with microorganisms or have other serious product quality defects ... Because the product is administered to humans by various higher risk routes of administration, including intravenously, intrathecally, and by aerosol inhalation, if contaminated, its use could cause a range of adverse events, from infections to death.”
FDA also expressed concerns over a lack of consistent quality control testing of each batch and questioned whether the company’s method of shipping ATCELL to clinicians had been adequately validated.
Finally, the agency raised concerns that ATCELL, while it is labeled as being for research purposes only, may harm patients indirectly by preventing them from seeking timely treatment with proven therapies.
“ATCELL is intended to treat a variety of serious or life-threatening diseases or conditions, all of which are non-homologous uses,” the warning letter noted. “Such uses raise potential significant safety concerns because there is less basis on which to predict the product’s behavior in the recipient, and use of these unapproved products may cause users to delay or discontinue medical treatments that have been found safe and effective.”
SOURCE: FDA warning letter
for manufacturing processes that may compromise its safety and for failing to toe the regulatory line in marketing.
American CryoStem received an FDA warning letter Jan. 3 demanding that the company comply with best-manufacturing processes and obtain an investigational new drug application if it wishes to continue marketing ATCELL for its currently advertised clinical indications and administration routes. These include intravenous, intrathecal, or aerosol inhalation of the product for anoxic brain injury, Parkinson’s disease, amyotrophic lateral sclerosis, stroke, and multiple sclerosis.
“Please be advised that, to lawfully market a drug that is a biological product, a valid biologics license must be in effect,” noted the letter. “Such licenses are issued only after a showing that the product is safe, pure, and potent. While in the development stage, such products may be distributed for clinical use in humans only if the sponsor has an investigational new drug application (IND) in effect as specified by FDA regulations. ATCELL is not the subject of an approved biologics license application nor is there an IND in effect. Based on this information, we have determined that your actions have violated the Food, Drug, and Cosmetic Act and the Public Health Service Act.”
FDA inspectors conducted a site inspection of American CryoStem in Eatontown, N.J., last summer, during which they “documented evidence of significant deviations from current good manufacturing practice.” The agency then provided the company a chance to respond to these issues. The new warning letter discussed each complaint, noting that some were inadequately addressed, and demanded that the company take action within 15 working days or face potential legal process, including seizure and/or injunction.
American CryoStem is one of the first companies to experience increased scrutiny under FDA’s new commitment to regulate the rapid growth and development of regenerative medicine products, which include novel cellular therapies, with the aim of ensuring their safety and effectiveness.
The new policy is designed to support the potential of cellular rejuvenation medicine, while protecting patients from “unscrupulous actors” who might endanger public health with untested products, according to FDA Commissioner Scott Gottlieb, MD. As enthusiasm for stem cell treatments surges, so are reports of adverse events. The New England Journal of Medicine recently reported on three patients with age-related macular degeneration who were blinded by intravitreal injection of autologous adipose-derived stem cells (N Engl J Med. 2017;376:1047-53).
Under the new policy, cell- and tissue-based products could be exempt from FDA premarket review only if they are removed from and implanted back into the same patient in their original form, or if the products are “minimally manipulated.” ATCELL fulfills neither qualification, the FDA warning letter said.
“You process adipose tissue ... to isolate cellular components of adipose tissue, commonly referred to as stromal vascular fraction [SVF]. Such processing is more than minimal manipulation because [it alters] the original relevant characteristics of the [tissue] relating to its utility for reconstruction, repair, or replacement. Then you process the SVF by expanding it in cell culture to manufacture ATCELL. Such expansion also is more than minimal manipulation because it alters the original relevant characteristics of the tissue.”
Furthermore, the letter noted, at least one of the components used in the clonal expansion process is investigational and not intended for human use. The manufacturer of that component, which was not named, “indicates the following: ‘Unless otherwise stated in our catalog or other company documentation accompanying the product(s), our products are intended for research use only and are not to be used for any other purpose, which includes but is not limited to, unauthorized commercial uses, in vitro diagnostic uses, ex vivo or in vivo therapeutic uses or any type of consumption or application to human and animals.”
The FDA also took exception with several equipment and lab safety issues. ATCELL was being created in areas that had no clean space designation – a serious concern, the letter said.
“American CryoStem’s unvalidated processes, inadequately controlled environment, lack of control of components used in production, and lack of sufficient and validated product testing ... pose a significant risk that ATCELL may be contaminated with microorganisms or have other serious product quality defects ... Because the product is administered to humans by various higher risk routes of administration, including intravenously, intrathecally, and by aerosol inhalation, if contaminated, its use could cause a range of adverse events, from infections to death.”
FDA also expressed concerns over a lack of consistent quality control testing of each batch and questioned whether the company’s method of shipping ATCELL to clinicians had been adequately validated.
Finally, the agency raised concerns that ATCELL, while it is labeled as being for research purposes only, may harm patients indirectly by preventing them from seeking timely treatment with proven therapies.
“ATCELL is intended to treat a variety of serious or life-threatening diseases or conditions, all of which are non-homologous uses,” the warning letter noted. “Such uses raise potential significant safety concerns because there is less basis on which to predict the product’s behavior in the recipient, and use of these unapproved products may cause users to delay or discontinue medical treatments that have been found safe and effective.”
SOURCE: FDA warning letter
for manufacturing processes that may compromise its safety and for failing to toe the regulatory line in marketing.
American CryoStem received an FDA warning letter Jan. 3 demanding that the company comply with best-manufacturing processes and obtain an investigational new drug application if it wishes to continue marketing ATCELL for its currently advertised clinical indications and administration routes. These include intravenous, intrathecal, or aerosol inhalation of the product for anoxic brain injury, Parkinson’s disease, amyotrophic lateral sclerosis, stroke, and multiple sclerosis.
“Please be advised that, to lawfully market a drug that is a biological product, a valid biologics license must be in effect,” noted the letter. “Such licenses are issued only after a showing that the product is safe, pure, and potent. While in the development stage, such products may be distributed for clinical use in humans only if the sponsor has an investigational new drug application (IND) in effect as specified by FDA regulations. ATCELL is not the subject of an approved biologics license application nor is there an IND in effect. Based on this information, we have determined that your actions have violated the Food, Drug, and Cosmetic Act and the Public Health Service Act.”
FDA inspectors conducted a site inspection of American CryoStem in Eatontown, N.J., last summer, during which they “documented evidence of significant deviations from current good manufacturing practice.” The agency then provided the company a chance to respond to these issues. The new warning letter discussed each complaint, noting that some were inadequately addressed, and demanded that the company take action within 15 working days or face potential legal process, including seizure and/or injunction.
American CryoStem is one of the first companies to experience increased scrutiny under FDA’s new commitment to regulate the rapid growth and development of regenerative medicine products, which include novel cellular therapies, with the aim of ensuring their safety and effectiveness.
The new policy is designed to support the potential of cellular rejuvenation medicine, while protecting patients from “unscrupulous actors” who might endanger public health with untested products, according to FDA Commissioner Scott Gottlieb, MD. As enthusiasm for stem cell treatments surges, so are reports of adverse events. The New England Journal of Medicine recently reported on three patients with age-related macular degeneration who were blinded by intravitreal injection of autologous adipose-derived stem cells (N Engl J Med. 2017;376:1047-53).
Under the new policy, cell- and tissue-based products could be exempt from FDA premarket review only if they are removed from and implanted back into the same patient in their original form, or if the products are “minimally manipulated.” ATCELL fulfills neither qualification, the FDA warning letter said.
“You process adipose tissue ... to isolate cellular components of adipose tissue, commonly referred to as stromal vascular fraction [SVF]. Such processing is more than minimal manipulation because [it alters] the original relevant characteristics of the [tissue] relating to its utility for reconstruction, repair, or replacement. Then you process the SVF by expanding it in cell culture to manufacture ATCELL. Such expansion also is more than minimal manipulation because it alters the original relevant characteristics of the tissue.”
Furthermore, the letter noted, at least one of the components used in the clonal expansion process is investigational and not intended for human use. The manufacturer of that component, which was not named, “indicates the following: ‘Unless otherwise stated in our catalog or other company documentation accompanying the product(s), our products are intended for research use only and are not to be used for any other purpose, which includes but is not limited to, unauthorized commercial uses, in vitro diagnostic uses, ex vivo or in vivo therapeutic uses or any type of consumption or application to human and animals.”
The FDA also took exception with several equipment and lab safety issues. ATCELL was being created in areas that had no clean space designation – a serious concern, the letter said.
“American CryoStem’s unvalidated processes, inadequately controlled environment, lack of control of components used in production, and lack of sufficient and validated product testing ... pose a significant risk that ATCELL may be contaminated with microorganisms or have other serious product quality defects ... Because the product is administered to humans by various higher risk routes of administration, including intravenously, intrathecally, and by aerosol inhalation, if contaminated, its use could cause a range of adverse events, from infections to death.”
FDA also expressed concerns over a lack of consistent quality control testing of each batch and questioned whether the company’s method of shipping ATCELL to clinicians had been adequately validated.
Finally, the agency raised concerns that ATCELL, while it is labeled as being for research purposes only, may harm patients indirectly by preventing them from seeking timely treatment with proven therapies.
“ATCELL is intended to treat a variety of serious or life-threatening diseases or conditions, all of which are non-homologous uses,” the warning letter noted. “Such uses raise potential significant safety concerns because there is less basis on which to predict the product’s behavior in the recipient, and use of these unapproved products may cause users to delay or discontinue medical treatments that have been found safe and effective.”
SOURCE: FDA warning letter
Conference News Roundup—American Heart Association
Does Cholesterol Testing Reduce Risk of Recurrent Stroke?
When a patient has a heart attack or stroke, it is critical for his or her clinician to perform a follow-up cholesterol test, according to a study conducted at the Intermountain Medical Center Heart Institute in Salt Lake City. This additional measure is significantly associated with reduced risk of having another serious cardiovascular episode.
Investigators found that patients who do not follow up with their doctor by getting a low-density lipoprotein (LDL) cholesterol test after a heart attack or stroke are significantly more likely to have a recurrence. They also found a significant and clinically meaningful difference in major adverse outcomes—including death, heart attack, stroke, and a vascular bypass or an angioplasty—based on whether or not a patient has a follow-up measurement of his or her LDL cholesterol.
“It is clear that anyone with a previous heart problem caused by clogged arteries should be taking a cholesterol-lowering medication,” said Kirk U. Knowlton, MD, Director of Cardiovascular Research at the Intermountain Medical Center Heart Institute.
The study of more than 60,000 patients with known heart disease, cerebrovascular disease, or peripheral artery disease, including patients with stroke and heart attack, showed that the major adverse clinical event rate was lower in patients who took cholesterol-lowering statins and in those who did not take them if their LDL was measured.
“The large difference is surprising. The risk of dying after three years with no LDL follow-up is 21% versus 5.9% for patients who have an LDL follow-up,” said Dr. Knowlton.
Researchers reviewed Intermountain Healthcare’s enterprise data warehouse to identify all adults who came to one of Intermountain’s 22 hospitals for the first time with a heart attack or stroke. These data included patients with coronary artery disease, cerebrovascular disease, and peripheral arterial disease admitted between January 1, 1999, and December 31, 2013.
Investigators observed patients who survived and were followed for three years or more or until their death. Patient demographics, history, prescribed medications, and whether LDL was measured was analyzed.
The study compared 62,070 patients in the database who met the study criteria. The mean age was 66, and 65% of patients were male. Of those who met the criteria, 69.3% had coronary artery disease, 18.6% had cerebrovascular disease, and 12.1% had peripheral arterial disease when they came to the hospital with their first heart attack or stroke.
Researchers found that the risk of a patient having a secondary event or dying decreased in patients who had a follow-up LDL test before a subsequent adverse outcome or before the end of their follow-up.
Coffee Is Associated With Lower Risk of Heart Failure and Stroke
Drinking coffee may be associated with a decreased risk of heart failure or stroke, according to researchers.
Investigators used machine learning to analyze data from the long-running Framingham Heart Study, which includes information about what people eat and their cardiovascular health. They found that every additional cup of coffee consumed per week was associated with a 7% decreased risk of heart failure and an 8% reduced risk of stroke, compared with non-coffee drinkers.
The researchers further investigated the machine learning results using traditional analysis in two studies with similar sets of data: the Cardiovascular Heart Study and the Atherosclerosis Risk In Communities Study. The association between drinking coffee and a decreased risk of heart failure and stroke was observed consistently in all three studies.
Another potential risk factor identified by machine-learning analysis was red meat consumption. The association between red meat consumption and heart failure or stroke was less clear, however. Eating red meat was associated with decreased risk of heart failure and stroke in the Framingham Heart Study, but validating the finding in comparable studies is more challenging due to differences in the definitions of red meat between studies, said the researchers. Further investigation to better determine how red meat consumption affects risk for heart failure and stroke is ongoing.
The researchers also built a predictive model using known risk factors from the Framingham Risk Score such as blood pressure, age, and other patient characteristics associated with cardiovascular disease. “By including coffee in the model, the prediction accuracy increased by 4%. Machine learning may be a useful addition to the way we look at data and may help us to find new ways to lower the risk of heart failure and strokes,” said David Kao, MD, Assistant Professor of Medicine in the Division of Cardiology at the University of Colorado School of Medicine in Aurora.
Statins May Improve Stroke Outcome
Patients with a prior history of heart attack or stroke have better outcomes when cholesterol-lowering medications are used after they are discharged from the hospital, according to researchers.
Prior surveys in hospitals found that statins are not being used consistently in patients who have been admitted to the hospital following a heart attack or stroke. Researchers also found that when the medication is prescribed, dosing is likely not as high as it should be to provide optimal benefits.
Researchers examined more than 62,000 records of patients from the Intermountain Healthcare system between 1999 and 2013 who survived an initial atherosclerotic cardiovascular disease event, such as a heart attack or stroke. They were then followed for three years or until death to identify the effectiveness of statin use prescribed at the time of their discharge.
“Patients who were prescribed a statin medication following an initial heart attack or stroke reduced their risk of a future adverse event such as a future heart attack, stroke, revascularization, or death by almost 25%—the rate dropped from 34% to 26%,” said Jeffrey L. Anderson, MD, a cardiovascular researcher at the Intermountain Medical Center Heart Institute. “The patients who were discharged on what is considered a high-intensity dose of a statin saw a 21% reduction in their risk,” compared with those discharged on a low-intensity statin dose.”
Investigators found that 30% of patients in the study who were discharged from the hospital following a heart attack or stroke were not prescribed a statin. This factor led to worse outcomes for those patients.
Researchers also found that only 13% of patients were given a high-intensity dose of statins, but noted that patients on those higher doses experienced fewer heart attacks or strokes. For patients younger than age 76, a high-intensity statin is indicated, according to American Heart Association guidelines. Only 17.7% of these patients were discharged on a high-intensity dose, however.
Does Cholesterol Testing Reduce Risk of Recurrent Stroke?
When a patient has a heart attack or stroke, it is critical for his or her clinician to perform a follow-up cholesterol test, according to a study conducted at the Intermountain Medical Center Heart Institute in Salt Lake City. This additional measure is significantly associated with reduced risk of having another serious cardiovascular episode.
Investigators found that patients who do not follow up with their doctor by getting a low-density lipoprotein (LDL) cholesterol test after a heart attack or stroke are significantly more likely to have a recurrence. They also found a significant and clinically meaningful difference in major adverse outcomes—including death, heart attack, stroke, and a vascular bypass or an angioplasty—based on whether or not a patient has a follow-up measurement of his or her LDL cholesterol.
“It is clear that anyone with a previous heart problem caused by clogged arteries should be taking a cholesterol-lowering medication,” said Kirk U. Knowlton, MD, Director of Cardiovascular Research at the Intermountain Medical Center Heart Institute.
The study of more than 60,000 patients with known heart disease, cerebrovascular disease, or peripheral artery disease, including patients with stroke and heart attack, showed that the major adverse clinical event rate was lower in patients who took cholesterol-lowering statins and in those who did not take them if their LDL was measured.
“The large difference is surprising. The risk of dying after three years with no LDL follow-up is 21% versus 5.9% for patients who have an LDL follow-up,” said Dr. Knowlton.
Researchers reviewed Intermountain Healthcare’s enterprise data warehouse to identify all adults who came to one of Intermountain’s 22 hospitals for the first time with a heart attack or stroke. These data included patients with coronary artery disease, cerebrovascular disease, and peripheral arterial disease admitted between January 1, 1999, and December 31, 2013.
Investigators observed patients who survived and were followed for three years or more or until their death. Patient demographics, history, prescribed medications, and whether LDL was measured was analyzed.
The study compared 62,070 patients in the database who met the study criteria. The mean age was 66, and 65% of patients were male. Of those who met the criteria, 69.3% had coronary artery disease, 18.6% had cerebrovascular disease, and 12.1% had peripheral arterial disease when they came to the hospital with their first heart attack or stroke.
Researchers found that the risk of a patient having a secondary event or dying decreased in patients who had a follow-up LDL test before a subsequent adverse outcome or before the end of their follow-up.
Coffee Is Associated With Lower Risk of Heart Failure and Stroke
Drinking coffee may be associated with a decreased risk of heart failure or stroke, according to researchers.
Investigators used machine learning to analyze data from the long-running Framingham Heart Study, which includes information about what people eat and their cardiovascular health. They found that every additional cup of coffee consumed per week was associated with a 7% decreased risk of heart failure and an 8% reduced risk of stroke, compared with non-coffee drinkers.
The researchers further investigated the machine learning results using traditional analysis in two studies with similar sets of data: the Cardiovascular Heart Study and the Atherosclerosis Risk In Communities Study. The association between drinking coffee and a decreased risk of heart failure and stroke was observed consistently in all three studies.
Another potential risk factor identified by machine-learning analysis was red meat consumption. The association between red meat consumption and heart failure or stroke was less clear, however. Eating red meat was associated with decreased risk of heart failure and stroke in the Framingham Heart Study, but validating the finding in comparable studies is more challenging due to differences in the definitions of red meat between studies, said the researchers. Further investigation to better determine how red meat consumption affects risk for heart failure and stroke is ongoing.
The researchers also built a predictive model using known risk factors from the Framingham Risk Score such as blood pressure, age, and other patient characteristics associated with cardiovascular disease. “By including coffee in the model, the prediction accuracy increased by 4%. Machine learning may be a useful addition to the way we look at data and may help us to find new ways to lower the risk of heart failure and strokes,” said David Kao, MD, Assistant Professor of Medicine in the Division of Cardiology at the University of Colorado School of Medicine in Aurora.
Statins May Improve Stroke Outcome
Patients with a prior history of heart attack or stroke have better outcomes when cholesterol-lowering medications are used after they are discharged from the hospital, according to researchers.
Prior surveys in hospitals found that statins are not being used consistently in patients who have been admitted to the hospital following a heart attack or stroke. Researchers also found that when the medication is prescribed, dosing is likely not as high as it should be to provide optimal benefits.
Researchers examined more than 62,000 records of patients from the Intermountain Healthcare system between 1999 and 2013 who survived an initial atherosclerotic cardiovascular disease event, such as a heart attack or stroke. They were then followed for three years or until death to identify the effectiveness of statin use prescribed at the time of their discharge.
“Patients who were prescribed a statin medication following an initial heart attack or stroke reduced their risk of a future adverse event such as a future heart attack, stroke, revascularization, or death by almost 25%—the rate dropped from 34% to 26%,” said Jeffrey L. Anderson, MD, a cardiovascular researcher at the Intermountain Medical Center Heart Institute. “The patients who were discharged on what is considered a high-intensity dose of a statin saw a 21% reduction in their risk,” compared with those discharged on a low-intensity statin dose.”
Investigators found that 30% of patients in the study who were discharged from the hospital following a heart attack or stroke were not prescribed a statin. This factor led to worse outcomes for those patients.
Researchers also found that only 13% of patients were given a high-intensity dose of statins, but noted that patients on those higher doses experienced fewer heart attacks or strokes. For patients younger than age 76, a high-intensity statin is indicated, according to American Heart Association guidelines. Only 17.7% of these patients were discharged on a high-intensity dose, however.
Does Cholesterol Testing Reduce Risk of Recurrent Stroke?
When a patient has a heart attack or stroke, it is critical for his or her clinician to perform a follow-up cholesterol test, according to a study conducted at the Intermountain Medical Center Heart Institute in Salt Lake City. This additional measure is significantly associated with reduced risk of having another serious cardiovascular episode.
Investigators found that patients who do not follow up with their doctor by getting a low-density lipoprotein (LDL) cholesterol test after a heart attack or stroke are significantly more likely to have a recurrence. They also found a significant and clinically meaningful difference in major adverse outcomes—including death, heart attack, stroke, and a vascular bypass or an angioplasty—based on whether or not a patient has a follow-up measurement of his or her LDL cholesterol.
“It is clear that anyone with a previous heart problem caused by clogged arteries should be taking a cholesterol-lowering medication,” said Kirk U. Knowlton, MD, Director of Cardiovascular Research at the Intermountain Medical Center Heart Institute.
The study of more than 60,000 patients with known heart disease, cerebrovascular disease, or peripheral artery disease, including patients with stroke and heart attack, showed that the major adverse clinical event rate was lower in patients who took cholesterol-lowering statins and in those who did not take them if their LDL was measured.
“The large difference is surprising. The risk of dying after three years with no LDL follow-up is 21% versus 5.9% for patients who have an LDL follow-up,” said Dr. Knowlton.
Researchers reviewed Intermountain Healthcare’s enterprise data warehouse to identify all adults who came to one of Intermountain’s 22 hospitals for the first time with a heart attack or stroke. These data included patients with coronary artery disease, cerebrovascular disease, and peripheral arterial disease admitted between January 1, 1999, and December 31, 2013.
Investigators observed patients who survived and were followed for three years or more or until their death. Patient demographics, history, prescribed medications, and whether LDL was measured was analyzed.
The study compared 62,070 patients in the database who met the study criteria. The mean age was 66, and 65% of patients were male. Of those who met the criteria, 69.3% had coronary artery disease, 18.6% had cerebrovascular disease, and 12.1% had peripheral arterial disease when they came to the hospital with their first heart attack or stroke.
Researchers found that the risk of a patient having a secondary event or dying decreased in patients who had a follow-up LDL test before a subsequent adverse outcome or before the end of their follow-up.
Coffee Is Associated With Lower Risk of Heart Failure and Stroke
Drinking coffee may be associated with a decreased risk of heart failure or stroke, according to researchers.
Investigators used machine learning to analyze data from the long-running Framingham Heart Study, which includes information about what people eat and their cardiovascular health. They found that every additional cup of coffee consumed per week was associated with a 7% decreased risk of heart failure and an 8% reduced risk of stroke, compared with non-coffee drinkers.
The researchers further investigated the machine learning results using traditional analysis in two studies with similar sets of data: the Cardiovascular Heart Study and the Atherosclerosis Risk In Communities Study. The association between drinking coffee and a decreased risk of heart failure and stroke was observed consistently in all three studies.
Another potential risk factor identified by machine-learning analysis was red meat consumption. The association between red meat consumption and heart failure or stroke was less clear, however. Eating red meat was associated with decreased risk of heart failure and stroke in the Framingham Heart Study, but validating the finding in comparable studies is more challenging due to differences in the definitions of red meat between studies, said the researchers. Further investigation to better determine how red meat consumption affects risk for heart failure and stroke is ongoing.
The researchers also built a predictive model using known risk factors from the Framingham Risk Score such as blood pressure, age, and other patient characteristics associated with cardiovascular disease. “By including coffee in the model, the prediction accuracy increased by 4%. Machine learning may be a useful addition to the way we look at data and may help us to find new ways to lower the risk of heart failure and strokes,” said David Kao, MD, Assistant Professor of Medicine in the Division of Cardiology at the University of Colorado School of Medicine in Aurora.
Statins May Improve Stroke Outcome
Patients with a prior history of heart attack or stroke have better outcomes when cholesterol-lowering medications are used after they are discharged from the hospital, according to researchers.
Prior surveys in hospitals found that statins are not being used consistently in patients who have been admitted to the hospital following a heart attack or stroke. Researchers also found that when the medication is prescribed, dosing is likely not as high as it should be to provide optimal benefits.
Researchers examined more than 62,000 records of patients from the Intermountain Healthcare system between 1999 and 2013 who survived an initial atherosclerotic cardiovascular disease event, such as a heart attack or stroke. They were then followed for three years or until death to identify the effectiveness of statin use prescribed at the time of their discharge.
“Patients who were prescribed a statin medication following an initial heart attack or stroke reduced their risk of a future adverse event such as a future heart attack, stroke, revascularization, or death by almost 25%—the rate dropped from 34% to 26%,” said Jeffrey L. Anderson, MD, a cardiovascular researcher at the Intermountain Medical Center Heart Institute. “The patients who were discharged on what is considered a high-intensity dose of a statin saw a 21% reduction in their risk,” compared with those discharged on a low-intensity statin dose.”
Investigators found that 30% of patients in the study who were discharged from the hospital following a heart attack or stroke were not prescribed a statin. This factor led to worse outcomes for those patients.
Researchers also found that only 13% of patients were given a high-intensity dose of statins, but noted that patients on those higher doses experienced fewer heart attacks or strokes. For patients younger than age 76, a high-intensity statin is indicated, according to American Heart Association guidelines. Only 17.7% of these patients were discharged on a high-intensity dose, however.
Cardiosphere-derived cells may reverse Duchenne heart scarring
ANAHEIM, CALIF. – One-time infusion of cardiosphere-derived cells into the three major coronary arteries seemed to prevent and perhaps even reverse cardiac scarring, as well as improve arm function, in the open-label phase 1-2 HOPE-Duchenne trial of 25 boys with advanced Duchenne muscular dystrophy.
“Decreased scarring is really a big deal because this is counter to the natural history of Duchenne, where all the scars progress, senior investigator Ronald G. Victor, MD, said at the American Heart Association scientific sessions. “It was gratifying to see that the changes in scar coincided with improved regional systolic wall thickening, particularly in the inferior wall of the left ventricle, which is the very area disproportionately affected early and thus severely in Duchenne.”
Glucocorticoids are the only thing that help to date, prolonging ambulation by about 3 years, but with Cushingoid features and other well-known side effects.
Cardiosphere-derived cells (CDCs) – cardiac progenitor cells – have shown some promise for heart failure. They don’t seem to engraft and grow, but rather to release extracellular vesicles packed with proteins, RNA, and other bioactive molecules. “They act as a role model to get endogenous cells to do the right thing. That’s what we think,” Dr. Victor said.
The HOPE-Duchenne trial [Halt Cardiomyopathy Progression in Duchenne] randomized 12 boys with Duchenne to usual care and 13 others to usual care plus a single infusion of 75 million CDCs divided equally among the left anterior descending, circumflex, and right coronary arteries. The cells were derived from donated heart muscle. The specific CDC preparation tested was “CAP-1002” from Capricor Therapeutics, the study’s sponsor.
The boys were aged 12-22 years, with a mean age of 17.8 years. They had left ventricle scarring in at least four MRI segments; their mean left ventricle ejection fraction was just below 50%; 68% were wheel-chair bound, and all were on stable steroid regimens.
At 12 months, cardiac scarring had increased about 5% in the control group, but decreased by about 7% in the treatment arm, although with no change ejection fraction improvement (P = .03).
Skeletal muscle was assessed by mid-level and distal performance of upper limb scoring, a measure of arm function developed specifically for Duchenne. “For patients who have lost ambulation, the ability to use a joystick to drive a scooter, the ability to feed themselves and use a computer and cellphone are absolutely key to quality of life,” he said.
At 12 months, performance of upper limb scores were largely unchanged in the control group, but improved in about half of the treated boys. “A couple were quite dramatic,” Dr. Victor said. The differences were statistically significant (P = .007) when limited to subjects who started with scores below 55 points, with 58 points meaning normal function.
On the safety side, nothing unusual happened in the control arm, except a femur fracture.
One boy in the treatment arm went into ventricular fibrillation during the diagnostic angiogram. Five had periprocedural atrial fibrillation. All 13 had periprocedural troponin elevations, versus two boys in the control group over the entire course of the study. Dr. Victor didn’t report any deaths, but safety concerns are probably why Capricor is shifting to intravenous infusion for the next trial, HOPE-2.
Dr. Victor noted that troponin leaks “wax and wane” over time in Duchenne, so the transient increases in the treatment arm “were superimposed on a baseline of abnormal cardiac enzymes.”
The Food and Drug Administration has green-lighted the company’s HOPE-2 trial to start enrollment in early 2018, with a larger number of patients and intravenous CDC delivery at 3 month intervals.
Several investigators were Capricor employees. Others were consultants or reported ownership interests. Dr. Victor was the principal investigator at Cedars-Sinai, and was on the trial’s steering committee. The University of Florida, Gainesville, and Cincinnati Children’s Hospital Medical Center, Ohio, were the other two study sites.
SOURCE: Ronald Victor, MD; 2017 AHA Scientific Sessions abstract number S1177
This is a tough disease, and therapies are desperately needed.
The HOPE-Duchenne data look pretty good, and everything seems to be moving in the same direction, but 13 people treated for even 12 months doesn’t really tell us much about safety.
The pipeline for this disease is filling up, but a lot of therapies are aimed at younger patients with the hopes of keeping them functional for as long as possible. I’m glad to see a treatment aimed at more advanced disease.
In general, when the choice is made to enter a clinical trial, it may mean you can’t enter another clinical trial, and these people are in a desperate situation. We need to sort out what should be tested, not just what can be tested.
Robert M. Califf, MD, is professor of cardiology at Duke University, Durham, N.C. He was the study discussant, and wasn’t involved in the work.
This is a tough disease, and therapies are desperately needed.
The HOPE-Duchenne data look pretty good, and everything seems to be moving in the same direction, but 13 people treated for even 12 months doesn’t really tell us much about safety.
The pipeline for this disease is filling up, but a lot of therapies are aimed at younger patients with the hopes of keeping them functional for as long as possible. I’m glad to see a treatment aimed at more advanced disease.
In general, when the choice is made to enter a clinical trial, it may mean you can’t enter another clinical trial, and these people are in a desperate situation. We need to sort out what should be tested, not just what can be tested.
Robert M. Califf, MD, is professor of cardiology at Duke University, Durham, N.C. He was the study discussant, and wasn’t involved in the work.
This is a tough disease, and therapies are desperately needed.
The HOPE-Duchenne data look pretty good, and everything seems to be moving in the same direction, but 13 people treated for even 12 months doesn’t really tell us much about safety.
The pipeline for this disease is filling up, but a lot of therapies are aimed at younger patients with the hopes of keeping them functional for as long as possible. I’m glad to see a treatment aimed at more advanced disease.
In general, when the choice is made to enter a clinical trial, it may mean you can’t enter another clinical trial, and these people are in a desperate situation. We need to sort out what should be tested, not just what can be tested.
Robert M. Califf, MD, is professor of cardiology at Duke University, Durham, N.C. He was the study discussant, and wasn’t involved in the work.
ANAHEIM, CALIF. – One-time infusion of cardiosphere-derived cells into the three major coronary arteries seemed to prevent and perhaps even reverse cardiac scarring, as well as improve arm function, in the open-label phase 1-2 HOPE-Duchenne trial of 25 boys with advanced Duchenne muscular dystrophy.
“Decreased scarring is really a big deal because this is counter to the natural history of Duchenne, where all the scars progress, senior investigator Ronald G. Victor, MD, said at the American Heart Association scientific sessions. “It was gratifying to see that the changes in scar coincided with improved regional systolic wall thickening, particularly in the inferior wall of the left ventricle, which is the very area disproportionately affected early and thus severely in Duchenne.”
Glucocorticoids are the only thing that help to date, prolonging ambulation by about 3 years, but with Cushingoid features and other well-known side effects.
Cardiosphere-derived cells (CDCs) – cardiac progenitor cells – have shown some promise for heart failure. They don’t seem to engraft and grow, but rather to release extracellular vesicles packed with proteins, RNA, and other bioactive molecules. “They act as a role model to get endogenous cells to do the right thing. That’s what we think,” Dr. Victor said.
The HOPE-Duchenne trial [Halt Cardiomyopathy Progression in Duchenne] randomized 12 boys with Duchenne to usual care and 13 others to usual care plus a single infusion of 75 million CDCs divided equally among the left anterior descending, circumflex, and right coronary arteries. The cells were derived from donated heart muscle. The specific CDC preparation tested was “CAP-1002” from Capricor Therapeutics, the study’s sponsor.
The boys were aged 12-22 years, with a mean age of 17.8 years. They had left ventricle scarring in at least four MRI segments; their mean left ventricle ejection fraction was just below 50%; 68% were wheel-chair bound, and all were on stable steroid regimens.
At 12 months, cardiac scarring had increased about 5% in the control group, but decreased by about 7% in the treatment arm, although with no change ejection fraction improvement (P = .03).
Skeletal muscle was assessed by mid-level and distal performance of upper limb scoring, a measure of arm function developed specifically for Duchenne. “For patients who have lost ambulation, the ability to use a joystick to drive a scooter, the ability to feed themselves and use a computer and cellphone are absolutely key to quality of life,” he said.
At 12 months, performance of upper limb scores were largely unchanged in the control group, but improved in about half of the treated boys. “A couple were quite dramatic,” Dr. Victor said. The differences were statistically significant (P = .007) when limited to subjects who started with scores below 55 points, with 58 points meaning normal function.
On the safety side, nothing unusual happened in the control arm, except a femur fracture.
One boy in the treatment arm went into ventricular fibrillation during the diagnostic angiogram. Five had periprocedural atrial fibrillation. All 13 had periprocedural troponin elevations, versus two boys in the control group over the entire course of the study. Dr. Victor didn’t report any deaths, but safety concerns are probably why Capricor is shifting to intravenous infusion for the next trial, HOPE-2.
Dr. Victor noted that troponin leaks “wax and wane” over time in Duchenne, so the transient increases in the treatment arm “were superimposed on a baseline of abnormal cardiac enzymes.”
The Food and Drug Administration has green-lighted the company’s HOPE-2 trial to start enrollment in early 2018, with a larger number of patients and intravenous CDC delivery at 3 month intervals.
Several investigators were Capricor employees. Others were consultants or reported ownership interests. Dr. Victor was the principal investigator at Cedars-Sinai, and was on the trial’s steering committee. The University of Florida, Gainesville, and Cincinnati Children’s Hospital Medical Center, Ohio, were the other two study sites.
SOURCE: Ronald Victor, MD; 2017 AHA Scientific Sessions abstract number S1177
ANAHEIM, CALIF. – One-time infusion of cardiosphere-derived cells into the three major coronary arteries seemed to prevent and perhaps even reverse cardiac scarring, as well as improve arm function, in the open-label phase 1-2 HOPE-Duchenne trial of 25 boys with advanced Duchenne muscular dystrophy.
“Decreased scarring is really a big deal because this is counter to the natural history of Duchenne, where all the scars progress, senior investigator Ronald G. Victor, MD, said at the American Heart Association scientific sessions. “It was gratifying to see that the changes in scar coincided with improved regional systolic wall thickening, particularly in the inferior wall of the left ventricle, which is the very area disproportionately affected early and thus severely in Duchenne.”
Glucocorticoids are the only thing that help to date, prolonging ambulation by about 3 years, but with Cushingoid features and other well-known side effects.
Cardiosphere-derived cells (CDCs) – cardiac progenitor cells – have shown some promise for heart failure. They don’t seem to engraft and grow, but rather to release extracellular vesicles packed with proteins, RNA, and other bioactive molecules. “They act as a role model to get endogenous cells to do the right thing. That’s what we think,” Dr. Victor said.
The HOPE-Duchenne trial [Halt Cardiomyopathy Progression in Duchenne] randomized 12 boys with Duchenne to usual care and 13 others to usual care plus a single infusion of 75 million CDCs divided equally among the left anterior descending, circumflex, and right coronary arteries. The cells were derived from donated heart muscle. The specific CDC preparation tested was “CAP-1002” from Capricor Therapeutics, the study’s sponsor.
The boys were aged 12-22 years, with a mean age of 17.8 years. They had left ventricle scarring in at least four MRI segments; their mean left ventricle ejection fraction was just below 50%; 68% were wheel-chair bound, and all were on stable steroid regimens.
At 12 months, cardiac scarring had increased about 5% in the control group, but decreased by about 7% in the treatment arm, although with no change ejection fraction improvement (P = .03).
Skeletal muscle was assessed by mid-level and distal performance of upper limb scoring, a measure of arm function developed specifically for Duchenne. “For patients who have lost ambulation, the ability to use a joystick to drive a scooter, the ability to feed themselves and use a computer and cellphone are absolutely key to quality of life,” he said.
At 12 months, performance of upper limb scores were largely unchanged in the control group, but improved in about half of the treated boys. “A couple were quite dramatic,” Dr. Victor said. The differences were statistically significant (P = .007) when limited to subjects who started with scores below 55 points, with 58 points meaning normal function.
On the safety side, nothing unusual happened in the control arm, except a femur fracture.
One boy in the treatment arm went into ventricular fibrillation during the diagnostic angiogram. Five had periprocedural atrial fibrillation. All 13 had periprocedural troponin elevations, versus two boys in the control group over the entire course of the study. Dr. Victor didn’t report any deaths, but safety concerns are probably why Capricor is shifting to intravenous infusion for the next trial, HOPE-2.
Dr. Victor noted that troponin leaks “wax and wane” over time in Duchenne, so the transient increases in the treatment arm “were superimposed on a baseline of abnormal cardiac enzymes.”
The Food and Drug Administration has green-lighted the company’s HOPE-2 trial to start enrollment in early 2018, with a larger number of patients and intravenous CDC delivery at 3 month intervals.
Several investigators were Capricor employees. Others were consultants or reported ownership interests. Dr. Victor was the principal investigator at Cedars-Sinai, and was on the trial’s steering committee. The University of Florida, Gainesville, and Cincinnati Children’s Hospital Medical Center, Ohio, were the other two study sites.
SOURCE: Ronald Victor, MD; 2017 AHA Scientific Sessions abstract number S1177
REPORTING FROM THE AHA SCIENTIFIC SESSIONS
Key clinical point: One-time infusion of cardiosphere-derived cells (CDCs) into the three major coronary arteries seemed to prevent and perhaps even reverse cardiac scarring, as well as improve arm function, in boys with advanced Duchenne muscular dystrophy.
Major finding: At 12 months, cardiac scarring increased about 5% in the control group, but decreased about 7% in the treatment arm, although with no change in ejection fraction (P = .03).
Study details: HOPE-Duchenne, an open-label, phase 1-2 trial involving 25 boys
Disclosures: The study was funded by Capricor Therapeutics, makers of the CDC preparation tested. Several investigators were Capricor employees. Others were consultants or reported ownership interests. The senior investigator and presenter was on the trial’s steering committee.
Source: Victor R, et al. 2017 AHA Scientific Sessions abstract number S1177.
Rare neurological complication linked to Waldenstrom disease
Bilateral facial nerve palsy has been associated with underlying Waldenstrom disease in only one other known published case report, which was published in 2014. In a more recent case report published in the Journal of Clinical Neuroscience, Gabriel Torrealba-Acosta, MD, and colleagues in the department of neurology at Massachusetts General Hospital, Boston, described a second case involving a 67-year-old Hispanic man with a history of Waldenstrom disease who presented with subacute onset of bilateral facial weakness.
The patient, who had longstanding painful neuropathy, had presented to urgent care with a new-onset left facial nerve palsy, was then diagnosed with left Bell’s palsy, and began treatment with valacyclovir and prednisone.
The left-sided facial weakness gradually progressed to total paralysis of the left lower face and inability to close the left eye, and 2 weeks later, he developed right facial weakness that ran a similar course. The patient had a complicated clinical course that included symptomatic acute-on-chronic subdural hematoma, among other complications; eventually the patient’s symptoms stabilized and cranial neuropathies gradually improved, according to the report.
Bilateral facial nerve palsy is an extremely rare condition, occurring in just 0.3%-2% of all facial nerve palsy cases, according to the authors. By contrast, unilateral facial nerve palsy (or Bell’s palsy) is far more common, but it still occurs in only 25 patients per 100,000 population, they said.
Most cases of bilateral facial nerve palsy are caused by underlying Guillain-Barré syndrome, though some are congenital, related to trauma, or caused by etiologies that are metabolic, immunologic, or neoplastic in nature. While various types of neurological disturbances – from ischemic and hemorrhagic events to meningoencephalitis – have been documented to occur in up to a quarter of patients with Waldenstrom disease.
“Given the large differential that comprises the assessment of a bilateral facial nerve palsy, it warrants for an extensive work-up, and Waldenstrom’s macroglobulinemia should be sought as an additional possible etiology,” the authors wrote.
Dr. Torrealba-Acosta and coauthors reported having no financial disclosures.
SOURCE: Torrealba-Acosta G et al. J Clin Neurosci. 2017. doi: 10.1016/j.jocn.2017.10.081.
Bilateral facial nerve palsy has been associated with underlying Waldenstrom disease in only one other known published case report, which was published in 2014. In a more recent case report published in the Journal of Clinical Neuroscience, Gabriel Torrealba-Acosta, MD, and colleagues in the department of neurology at Massachusetts General Hospital, Boston, described a second case involving a 67-year-old Hispanic man with a history of Waldenstrom disease who presented with subacute onset of bilateral facial weakness.
The patient, who had longstanding painful neuropathy, had presented to urgent care with a new-onset left facial nerve palsy, was then diagnosed with left Bell’s palsy, and began treatment with valacyclovir and prednisone.
The left-sided facial weakness gradually progressed to total paralysis of the left lower face and inability to close the left eye, and 2 weeks later, he developed right facial weakness that ran a similar course. The patient had a complicated clinical course that included symptomatic acute-on-chronic subdural hematoma, among other complications; eventually the patient’s symptoms stabilized and cranial neuropathies gradually improved, according to the report.
Bilateral facial nerve palsy is an extremely rare condition, occurring in just 0.3%-2% of all facial nerve palsy cases, according to the authors. By contrast, unilateral facial nerve palsy (or Bell’s palsy) is far more common, but it still occurs in only 25 patients per 100,000 population, they said.
Most cases of bilateral facial nerve palsy are caused by underlying Guillain-Barré syndrome, though some are congenital, related to trauma, or caused by etiologies that are metabolic, immunologic, or neoplastic in nature. While various types of neurological disturbances – from ischemic and hemorrhagic events to meningoencephalitis – have been documented to occur in up to a quarter of patients with Waldenstrom disease.
“Given the large differential that comprises the assessment of a bilateral facial nerve palsy, it warrants for an extensive work-up, and Waldenstrom’s macroglobulinemia should be sought as an additional possible etiology,” the authors wrote.
Dr. Torrealba-Acosta and coauthors reported having no financial disclosures.
SOURCE: Torrealba-Acosta G et al. J Clin Neurosci. 2017. doi: 10.1016/j.jocn.2017.10.081.
Bilateral facial nerve palsy has been associated with underlying Waldenstrom disease in only one other known published case report, which was published in 2014. In a more recent case report published in the Journal of Clinical Neuroscience, Gabriel Torrealba-Acosta, MD, and colleagues in the department of neurology at Massachusetts General Hospital, Boston, described a second case involving a 67-year-old Hispanic man with a history of Waldenstrom disease who presented with subacute onset of bilateral facial weakness.
The patient, who had longstanding painful neuropathy, had presented to urgent care with a new-onset left facial nerve palsy, was then diagnosed with left Bell’s palsy, and began treatment with valacyclovir and prednisone.
The left-sided facial weakness gradually progressed to total paralysis of the left lower face and inability to close the left eye, and 2 weeks later, he developed right facial weakness that ran a similar course. The patient had a complicated clinical course that included symptomatic acute-on-chronic subdural hematoma, among other complications; eventually the patient’s symptoms stabilized and cranial neuropathies gradually improved, according to the report.
Bilateral facial nerve palsy is an extremely rare condition, occurring in just 0.3%-2% of all facial nerve palsy cases, according to the authors. By contrast, unilateral facial nerve palsy (or Bell’s palsy) is far more common, but it still occurs in only 25 patients per 100,000 population, they said.
Most cases of bilateral facial nerve palsy are caused by underlying Guillain-Barré syndrome, though some are congenital, related to trauma, or caused by etiologies that are metabolic, immunologic, or neoplastic in nature. While various types of neurological disturbances – from ischemic and hemorrhagic events to meningoencephalitis – have been documented to occur in up to a quarter of patients with Waldenstrom disease.
“Given the large differential that comprises the assessment of a bilateral facial nerve palsy, it warrants for an extensive work-up, and Waldenstrom’s macroglobulinemia should be sought as an additional possible etiology,” the authors wrote.
Dr. Torrealba-Acosta and coauthors reported having no financial disclosures.
SOURCE: Torrealba-Acosta G et al. J Clin Neurosci. 2017. doi: 10.1016/j.jocn.2017.10.081.
FROM THE JOURNAL OF CLINICAL NEUROSCIENCE
Edaravone: Costs versus benefits
On May 5, 2017, the Food and Drug Administration approved edaravone (Radicava) for the treatment of patients with amyotrophic lateral sclerosis (ALS). Developed by Mitsubishi Tanabe Pharma Corporation, edaravone is the first FDA-approved treatment for ALS since the approval of riluzole (Rilutek) in 1995. Edaravone was originally developed as an acute stroke treatment and then later studied in two separate trials in Japan to assess its efficacy in treating ALS.
Edaravone is administered intravenously and the standard dose of 60 mg takes about 1 hour to complete. The initial treatment cycle consists of once-daily dosing for 2 weeks, followed by a 2-week drug-free period. After the initial cycle, subsequent cycles consist of once-daily dosing for 10 days out of the next 2 weeks, followed by a 2-week drug-free period. The question of how long patients should take edaravone has not been resolved. The FDA did not define a limit to the duration of treatment. Some insurance companies have limited authorization to 6 months as that was the duration of treatment that showed benefit in the study. However, an open-label, 24-week extension of the second study showed that the change in ALSFRS-R was linear throughout the study. This suggests that the treatment benefit in patients with short duration of illness may continue for an additional 24 weeks. Thus, patients who have duration of illness of less than 2 years at presentation may benefit from 12 months of treatment.
The rigorous treatment schedule and IV administration of edaravone create additional concerns for ALS patients. Many patients will need to have a port placed. Patients with impaired mobility will need assistance with transportation to an infusion center. The time involved with taking all of these IV infusions will be considerable. Our experience at the Mayo Clinic reflects differing patient opinions. Some ALS patients with short duration of illness who clearly meet the criteria are not willing to commit to this form of therapy even if insurance will cover it. In contrast, some patients with advanced disease who do not meet the eligibility criteria have expressed the wish to try it.
To have access to edaravone in the United States, ALS patients must first complete an enrollment form and register with a Mitsubishi Tanabe subsidiary called Searchlight. Searchlight creates a Searchlight patient ID and conducts a benefit investigation to determine if the patient’s insurance will cover edaravone treatment. If the patient’s insurance approves edaravone, arrangements are made to ship the drug to the site or company that will perform the infusions. Insurance companies have taken different approaches to the approval of edaravone for ALS patients. Some insurers require that the patient meets the eligibility requirements of the Japanese study that showed benefit (duration of illness less than 2 years from symptom onset and forced vital capacity of at least 80% predicted). These strict criteria will exclude many patients. Other insurers have required only the diagnosis of ALS and the physician’s order. The cost of edaravone is estimated to be around $145,500 per year. The actual out-of-pocket cost to patients will vary depending on their specific insurance plans. In-home infusion of edaravone is another option patients can consider. Patients can pay the separate charges for in-home infusion if their insurance plans do not cover this.
The costs of edaravone are substantial. Beyond the expenses for the medication and infusion services, the patient faces the burden of committing time to frequent IV infusions and potential complications associated with having a port placed. Many ALS patients have decided against pursuing edaravone, suggesting that the perceived costs exceed the perceived benefits. Many ALS patients have started edaravone treatment with the belief that slowing of progression is worth the costs. It is too soon to know if those who have started edaravone will remain committed to the treatment for 6-12 months. Despite the differing approaches to edaravone treatment, it can be agreed upon that it is good to have a new treatment for ALS and that we must continue working to find therapies effective in substantially slowing or stopping the progression of ALS.
Ms. Chang is a research intern, and Dr. Ross is a professor of neurology and director of the ALS Clinic, at Mayo Clinic Arizona in Scottsdale. Dr. Ross reported serving as the Mayo Clinic Arizona site primary investigator for the ALS investigational drug NP001.
On May 5, 2017, the Food and Drug Administration approved edaravone (Radicava) for the treatment of patients with amyotrophic lateral sclerosis (ALS). Developed by Mitsubishi Tanabe Pharma Corporation, edaravone is the first FDA-approved treatment for ALS since the approval of riluzole (Rilutek) in 1995. Edaravone was originally developed as an acute stroke treatment and then later studied in two separate trials in Japan to assess its efficacy in treating ALS.
Edaravone is administered intravenously and the standard dose of 60 mg takes about 1 hour to complete. The initial treatment cycle consists of once-daily dosing for 2 weeks, followed by a 2-week drug-free period. After the initial cycle, subsequent cycles consist of once-daily dosing for 10 days out of the next 2 weeks, followed by a 2-week drug-free period. The question of how long patients should take edaravone has not been resolved. The FDA did not define a limit to the duration of treatment. Some insurance companies have limited authorization to 6 months as that was the duration of treatment that showed benefit in the study. However, an open-label, 24-week extension of the second study showed that the change in ALSFRS-R was linear throughout the study. This suggests that the treatment benefit in patients with short duration of illness may continue for an additional 24 weeks. Thus, patients who have duration of illness of less than 2 years at presentation may benefit from 12 months of treatment.
The rigorous treatment schedule and IV administration of edaravone create additional concerns for ALS patients. Many patients will need to have a port placed. Patients with impaired mobility will need assistance with transportation to an infusion center. The time involved with taking all of these IV infusions will be considerable. Our experience at the Mayo Clinic reflects differing patient opinions. Some ALS patients with short duration of illness who clearly meet the criteria are not willing to commit to this form of therapy even if insurance will cover it. In contrast, some patients with advanced disease who do not meet the eligibility criteria have expressed the wish to try it.
To have access to edaravone in the United States, ALS patients must first complete an enrollment form and register with a Mitsubishi Tanabe subsidiary called Searchlight. Searchlight creates a Searchlight patient ID and conducts a benefit investigation to determine if the patient’s insurance will cover edaravone treatment. If the patient’s insurance approves edaravone, arrangements are made to ship the drug to the site or company that will perform the infusions. Insurance companies have taken different approaches to the approval of edaravone for ALS patients. Some insurers require that the patient meets the eligibility requirements of the Japanese study that showed benefit (duration of illness less than 2 years from symptom onset and forced vital capacity of at least 80% predicted). These strict criteria will exclude many patients. Other insurers have required only the diagnosis of ALS and the physician’s order. The cost of edaravone is estimated to be around $145,500 per year. The actual out-of-pocket cost to patients will vary depending on their specific insurance plans. In-home infusion of edaravone is another option patients can consider. Patients can pay the separate charges for in-home infusion if their insurance plans do not cover this.
The costs of edaravone are substantial. Beyond the expenses for the medication and infusion services, the patient faces the burden of committing time to frequent IV infusions and potential complications associated with having a port placed. Many ALS patients have decided against pursuing edaravone, suggesting that the perceived costs exceed the perceived benefits. Many ALS patients have started edaravone treatment with the belief that slowing of progression is worth the costs. It is too soon to know if those who have started edaravone will remain committed to the treatment for 6-12 months. Despite the differing approaches to edaravone treatment, it can be agreed upon that it is good to have a new treatment for ALS and that we must continue working to find therapies effective in substantially slowing or stopping the progression of ALS.
Ms. Chang is a research intern, and Dr. Ross is a professor of neurology and director of the ALS Clinic, at Mayo Clinic Arizona in Scottsdale. Dr. Ross reported serving as the Mayo Clinic Arizona site primary investigator for the ALS investigational drug NP001.
On May 5, 2017, the Food and Drug Administration approved edaravone (Radicava) for the treatment of patients with amyotrophic lateral sclerosis (ALS). Developed by Mitsubishi Tanabe Pharma Corporation, edaravone is the first FDA-approved treatment for ALS since the approval of riluzole (Rilutek) in 1995. Edaravone was originally developed as an acute stroke treatment and then later studied in two separate trials in Japan to assess its efficacy in treating ALS.
Edaravone is administered intravenously and the standard dose of 60 mg takes about 1 hour to complete. The initial treatment cycle consists of once-daily dosing for 2 weeks, followed by a 2-week drug-free period. After the initial cycle, subsequent cycles consist of once-daily dosing for 10 days out of the next 2 weeks, followed by a 2-week drug-free period. The question of how long patients should take edaravone has not been resolved. The FDA did not define a limit to the duration of treatment. Some insurance companies have limited authorization to 6 months as that was the duration of treatment that showed benefit in the study. However, an open-label, 24-week extension of the second study showed that the change in ALSFRS-R was linear throughout the study. This suggests that the treatment benefit in patients with short duration of illness may continue for an additional 24 weeks. Thus, patients who have duration of illness of less than 2 years at presentation may benefit from 12 months of treatment.
The rigorous treatment schedule and IV administration of edaravone create additional concerns for ALS patients. Many patients will need to have a port placed. Patients with impaired mobility will need assistance with transportation to an infusion center. The time involved with taking all of these IV infusions will be considerable. Our experience at the Mayo Clinic reflects differing patient opinions. Some ALS patients with short duration of illness who clearly meet the criteria are not willing to commit to this form of therapy even if insurance will cover it. In contrast, some patients with advanced disease who do not meet the eligibility criteria have expressed the wish to try it.
To have access to edaravone in the United States, ALS patients must first complete an enrollment form and register with a Mitsubishi Tanabe subsidiary called Searchlight. Searchlight creates a Searchlight patient ID and conducts a benefit investigation to determine if the patient’s insurance will cover edaravone treatment. If the patient’s insurance approves edaravone, arrangements are made to ship the drug to the site or company that will perform the infusions. Insurance companies have taken different approaches to the approval of edaravone for ALS patients. Some insurers require that the patient meets the eligibility requirements of the Japanese study that showed benefit (duration of illness less than 2 years from symptom onset and forced vital capacity of at least 80% predicted). These strict criteria will exclude many patients. Other insurers have required only the diagnosis of ALS and the physician’s order. The cost of edaravone is estimated to be around $145,500 per year. The actual out-of-pocket cost to patients will vary depending on their specific insurance plans. In-home infusion of edaravone is another option patients can consider. Patients can pay the separate charges for in-home infusion if their insurance plans do not cover this.
The costs of edaravone are substantial. Beyond the expenses for the medication and infusion services, the patient faces the burden of committing time to frequent IV infusions and potential complications associated with having a port placed. Many ALS patients have decided against pursuing edaravone, suggesting that the perceived costs exceed the perceived benefits. Many ALS patients have started edaravone treatment with the belief that slowing of progression is worth the costs. It is too soon to know if those who have started edaravone will remain committed to the treatment for 6-12 months. Despite the differing approaches to edaravone treatment, it can be agreed upon that it is good to have a new treatment for ALS and that we must continue working to find therapies effective in substantially slowing or stopping the progression of ALS.
Ms. Chang is a research intern, and Dr. Ross is a professor of neurology and director of the ALS Clinic, at Mayo Clinic Arizona in Scottsdale. Dr. Ross reported serving as the Mayo Clinic Arizona site primary investigator for the ALS investigational drug NP001.
Further evidence supports link between Zika and GBS
Newly identified risk factors add to the growing evidence of a causal association between Zika virus and Guillain-Barré Syndrome (GBS), according to a case-control study.
In a study conducted in Puerto Rico, GBS diagnosis was confirmed in 39 of 47 (83%) patients with clinical suspicion of the syndrome from nine hospitals from April 2016 to December 2016. They were compared with 78 control patients to identify GBS risk factors. Three risk factors were identified, Emilio Dirlikov, PhD, of the division of scientific education and professional development for the Centers for Disease Control and Prevention in San Juan, Puerto Rico, and his coauthors said in a research letter to JAMA (2017;318[15]:1498).
“During Zika virus outbreaks, clinical suspicion should be elevated to improve GBS patient prognosis through prompt diagnosis and treatment,” Dr. Dirlikov and his coauthors wrote. This was a small study. “The pathophysiology of Zika virus infection and risk factors for developing GBS require further investigation. Clinical trials of the Zika virus vaccine should monitor for GBS,” they said.
The study was supported with a grant from the National Institutes of Health. Carlos A. Luciano, MD, also reported grant funding from the University of Puerto Rico Medical Sciences, San Juan. No other authors reported any financial disclosures.
Newly identified risk factors add to the growing evidence of a causal association between Zika virus and Guillain-Barré Syndrome (GBS), according to a case-control study.
In a study conducted in Puerto Rico, GBS diagnosis was confirmed in 39 of 47 (83%) patients with clinical suspicion of the syndrome from nine hospitals from April 2016 to December 2016. They were compared with 78 control patients to identify GBS risk factors. Three risk factors were identified, Emilio Dirlikov, PhD, of the division of scientific education and professional development for the Centers for Disease Control and Prevention in San Juan, Puerto Rico, and his coauthors said in a research letter to JAMA (2017;318[15]:1498).
“During Zika virus outbreaks, clinical suspicion should be elevated to improve GBS patient prognosis through prompt diagnosis and treatment,” Dr. Dirlikov and his coauthors wrote. This was a small study. “The pathophysiology of Zika virus infection and risk factors for developing GBS require further investigation. Clinical trials of the Zika virus vaccine should monitor for GBS,” they said.
The study was supported with a grant from the National Institutes of Health. Carlos A. Luciano, MD, also reported grant funding from the University of Puerto Rico Medical Sciences, San Juan. No other authors reported any financial disclosures.
Newly identified risk factors add to the growing evidence of a causal association between Zika virus and Guillain-Barré Syndrome (GBS), according to a case-control study.
In a study conducted in Puerto Rico, GBS diagnosis was confirmed in 39 of 47 (83%) patients with clinical suspicion of the syndrome from nine hospitals from April 2016 to December 2016. They were compared with 78 control patients to identify GBS risk factors. Three risk factors were identified, Emilio Dirlikov, PhD, of the division of scientific education and professional development for the Centers for Disease Control and Prevention in San Juan, Puerto Rico, and his coauthors said in a research letter to JAMA (2017;318[15]:1498).
“During Zika virus outbreaks, clinical suspicion should be elevated to improve GBS patient prognosis through prompt diagnosis and treatment,” Dr. Dirlikov and his coauthors wrote. This was a small study. “The pathophysiology of Zika virus infection and risk factors for developing GBS require further investigation. Clinical trials of the Zika virus vaccine should monitor for GBS,” they said.
The study was supported with a grant from the National Institutes of Health. Carlos A. Luciano, MD, also reported grant funding from the University of Puerto Rico Medical Sciences, San Juan. No other authors reported any financial disclosures.
FROM JAMA
Key clinical point:
Major finding: Case patients saw higher rates of acute illness within the previous 2 months (82%), acute Zika virus infection (23%), and any laboratory evidence of Zika virus infection (69%), compared with controls.
Data source: A case-control study of 39 patients with GBS and 78 controls.
Disclosures: The study was supported with a grant from the National Institutes of Health. Carlos A. Luciano, MD, also reported grant funding from the University of Puerto Rico Medical Sciences, San Juan. No other authors reported any financial disclosures.