User login
Borderline personality disorder: Remember empathy and compassion
Oh, great!” a senior resident sardonically remarked with a smirk as they read up on the next patient in the clinic. “A borderline patient. Get ready for a rough one ... Ugh.”
Before ever stepping foot into the patient’s room, this resident had prematurely established and demonstrated an unfortunate dynamic for any student or trainee within earshot. This is an all-too-familiar occurrence when caring for individuals with borderline personality disorder (BPD), or any other patients deemed to be “difficult.” The patient, however, likely walked into the room with a traumatic past that they continue to suffer from, in addition to any other issues for which they were seeking care.
Consider what these patients have experienced
A typical profile of these resilient patients with BPD: They were born emotionally sensitive. They grew up in homes with caretakers who knowingly or unknowingly invalidated their complaints about having their feelings hurt, about being abused emotionally, sexually, or otherwise, or about their worries concerning their interactions with peers at school. These caretakers may have been frightening and unpredictable, randomly showing affection or arbitrarily punishing for any perceived misstep, which led these patients to develop (for their own safety’s sake) a hypersensitivity to the affect of others. Their wariness and distrust of their social surroundings may have led to a skeptical view of kindness from others. Over time, without any guidance from prior demonstrations of healthy coping skills or interpersonal outlets from their caregivers, the emotional pressure builds. This pressure finally erupts in the form of impulsivity, self-harm, desperation, and defensiveness—in other words, survival. This is often followed by these patients’ first experience with receiving some degree of appropriate response to their complaints—their first experience with feeling seen and heard by their caretakers. They learn that their needs are met only when they cry out in desperation.1-3
These patients typically bring these maladaptive coping skills with them into adulthood, which often leads to a series of intense, unhealthy, and short-lived interpersonal and professional connections. They desire healthy, lasting connections with others, but through no fault of their own are unable to appropriately manage the normal stressors therein.1 Often, these patients do not know of their eventual BPD diagnosis, or even reject it due to its ever-negative valence. For other patients, receiving a personality disorder diagnosis is incredibly validating because they are no longer alone regarding this type of suffering, and a doctor—a caretaker—is finally making sense of this tumultuous world.
The countertransference of frustration, anxiety, doubt, and annoyance we may feel when caring for patients with BPD pales in comparison to living in their shoes and carrying the weight of what they have had to endure before presenting to our care. As these resilient patients wait in the exam room for the chance to be heard, let this be a reminder to greet them with the patience, understanding, empathy, and compassion that physicians are known to embody.
Suggestions for working with ‘difficult’ patients
The following tips may be helpful for building rapport with patients with BPD or other “difficult” patients:
- validate their complaints, and the difficulties they cause
- be genuine and honest when discussing their complaints
- acknowledge your own mistakes and misunderstandings in their care
- don’t be defensive—accept criticism with an open mind
- practice listening with intent, and reflective listening
- set ground rules and stick to them (eg, time limits, prescribing expectations, patient-physician relationship boundaries)
- educate and support the patient and their loved ones.
1. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Association; 2013:947.
2. Porter C, Palmier-Claus J, Branitsky A, et al. Childhood adversity and borderline personality disorder: a meta-analysis. Acta Psychiatr Scand. 2020;141(1):6-20.
3. Sansone RA, Sansone LA. Emotional hyper-reactivity in borderline personality disorder. Psychiatry (Edgmont). 2010;7(9):16-20.
Oh, great!” a senior resident sardonically remarked with a smirk as they read up on the next patient in the clinic. “A borderline patient. Get ready for a rough one ... Ugh.”
Before ever stepping foot into the patient’s room, this resident had prematurely established and demonstrated an unfortunate dynamic for any student or trainee within earshot. This is an all-too-familiar occurrence when caring for individuals with borderline personality disorder (BPD), or any other patients deemed to be “difficult.” The patient, however, likely walked into the room with a traumatic past that they continue to suffer from, in addition to any other issues for which they were seeking care.
Consider what these patients have experienced
A typical profile of these resilient patients with BPD: They were born emotionally sensitive. They grew up in homes with caretakers who knowingly or unknowingly invalidated their complaints about having their feelings hurt, about being abused emotionally, sexually, or otherwise, or about their worries concerning their interactions with peers at school. These caretakers may have been frightening and unpredictable, randomly showing affection or arbitrarily punishing for any perceived misstep, which led these patients to develop (for their own safety’s sake) a hypersensitivity to the affect of others. Their wariness and distrust of their social surroundings may have led to a skeptical view of kindness from others. Over time, without any guidance from prior demonstrations of healthy coping skills or interpersonal outlets from their caregivers, the emotional pressure builds. This pressure finally erupts in the form of impulsivity, self-harm, desperation, and defensiveness—in other words, survival. This is often followed by these patients’ first experience with receiving some degree of appropriate response to their complaints—their first experience with feeling seen and heard by their caretakers. They learn that their needs are met only when they cry out in desperation.1-3
These patients typically bring these maladaptive coping skills with them into adulthood, which often leads to a series of intense, unhealthy, and short-lived interpersonal and professional connections. They desire healthy, lasting connections with others, but through no fault of their own are unable to appropriately manage the normal stressors therein.1 Often, these patients do not know of their eventual BPD diagnosis, or even reject it due to its ever-negative valence. For other patients, receiving a personality disorder diagnosis is incredibly validating because they are no longer alone regarding this type of suffering, and a doctor—a caretaker—is finally making sense of this tumultuous world.
The countertransference of frustration, anxiety, doubt, and annoyance we may feel when caring for patients with BPD pales in comparison to living in their shoes and carrying the weight of what they have had to endure before presenting to our care. As these resilient patients wait in the exam room for the chance to be heard, let this be a reminder to greet them with the patience, understanding, empathy, and compassion that physicians are known to embody.
Suggestions for working with ‘difficult’ patients
The following tips may be helpful for building rapport with patients with BPD or other “difficult” patients:
- validate their complaints, and the difficulties they cause
- be genuine and honest when discussing their complaints
- acknowledge your own mistakes and misunderstandings in their care
- don’t be defensive—accept criticism with an open mind
- practice listening with intent, and reflective listening
- set ground rules and stick to them (eg, time limits, prescribing expectations, patient-physician relationship boundaries)
- educate and support the patient and their loved ones.
Oh, great!” a senior resident sardonically remarked with a smirk as they read up on the next patient in the clinic. “A borderline patient. Get ready for a rough one ... Ugh.”
Before ever stepping foot into the patient’s room, this resident had prematurely established and demonstrated an unfortunate dynamic for any student or trainee within earshot. This is an all-too-familiar occurrence when caring for individuals with borderline personality disorder (BPD), or any other patients deemed to be “difficult.” The patient, however, likely walked into the room with a traumatic past that they continue to suffer from, in addition to any other issues for which they were seeking care.
Consider what these patients have experienced
A typical profile of these resilient patients with BPD: They were born emotionally sensitive. They grew up in homes with caretakers who knowingly or unknowingly invalidated their complaints about having their feelings hurt, about being abused emotionally, sexually, or otherwise, or about their worries concerning their interactions with peers at school. These caretakers may have been frightening and unpredictable, randomly showing affection or arbitrarily punishing for any perceived misstep, which led these patients to develop (for their own safety’s sake) a hypersensitivity to the affect of others. Their wariness and distrust of their social surroundings may have led to a skeptical view of kindness from others. Over time, without any guidance from prior demonstrations of healthy coping skills or interpersonal outlets from their caregivers, the emotional pressure builds. This pressure finally erupts in the form of impulsivity, self-harm, desperation, and defensiveness—in other words, survival. This is often followed by these patients’ first experience with receiving some degree of appropriate response to their complaints—their first experience with feeling seen and heard by their caretakers. They learn that their needs are met only when they cry out in desperation.1-3
These patients typically bring these maladaptive coping skills with them into adulthood, which often leads to a series of intense, unhealthy, and short-lived interpersonal and professional connections. They desire healthy, lasting connections with others, but through no fault of their own are unable to appropriately manage the normal stressors therein.1 Often, these patients do not know of their eventual BPD diagnosis, or even reject it due to its ever-negative valence. For other patients, receiving a personality disorder diagnosis is incredibly validating because they are no longer alone regarding this type of suffering, and a doctor—a caretaker—is finally making sense of this tumultuous world.
The countertransference of frustration, anxiety, doubt, and annoyance we may feel when caring for patients with BPD pales in comparison to living in their shoes and carrying the weight of what they have had to endure before presenting to our care. As these resilient patients wait in the exam room for the chance to be heard, let this be a reminder to greet them with the patience, understanding, empathy, and compassion that physicians are known to embody.
Suggestions for working with ‘difficult’ patients
The following tips may be helpful for building rapport with patients with BPD or other “difficult” patients:
- validate their complaints, and the difficulties they cause
- be genuine and honest when discussing their complaints
- acknowledge your own mistakes and misunderstandings in their care
- don’t be defensive—accept criticism with an open mind
- practice listening with intent, and reflective listening
- set ground rules and stick to them (eg, time limits, prescribing expectations, patient-physician relationship boundaries)
- educate and support the patient and their loved ones.
1. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Association; 2013:947.
2. Porter C, Palmier-Claus J, Branitsky A, et al. Childhood adversity and borderline personality disorder: a meta-analysis. Acta Psychiatr Scand. 2020;141(1):6-20.
3. Sansone RA, Sansone LA. Emotional hyper-reactivity in borderline personality disorder. Psychiatry (Edgmont). 2010;7(9):16-20.
1. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Association; 2013:947.
2. Porter C, Palmier-Claus J, Branitsky A, et al. Childhood adversity and borderline personality disorder: a meta-analysis. Acta Psychiatr Scand. 2020;141(1):6-20.
3. Sansone RA, Sansone LA. Emotional hyper-reactivity in borderline personality disorder. Psychiatry (Edgmont). 2010;7(9):16-20.
Borderline personality disorder: Is there an optimal therapy?
Schema is a form of psychotherapy that focuses on experiential approaches rather than on behavior change.
The findings from an international randomized controlled trial underscore the importance of offering both individual and group approaches to patients with BPD, study investigator Arnoud Arntz, PhD, professor in the department of clinical psychology at the University of Amsterdam, told this news organization.
“In the Netherlands, there’s a big push from mental health institutes to deliver treatments in group therapy [only] because people think it’s more cost-effective; but these findings question that idea,” Dr. Arntz said.
The findings were published online March 2 in JAMA Psychiatry.
Early childhood experiences
Patients with BPD exhibit extreme sensitivity to interpersonal slights, intense and volatile emotions, and impulsive behaviors. Many abuse drugs, self-harm, or attempt suicide.
Evidence-based guidelines recommend psychotherapy as the primary treatment for BPD.
Schema therapy uses techniques from traditional psychotherapy but focuses on an experiential strategy. It also delves into early childhood experiences, which is relevant because patients with BPD often experienced abuse or neglect early in life.
As well, with this approach, therapists take on a sort of parenting role with patients to try to meet needs “that were frustrated in childhood,” said Dr. Arntz.
Previous research has suggested both individual and group schema therapy help reduce BPD symptoms, but the effectiveness of combining these two approaches has been unclear.
The current study included 495 adult patients (mean age, 33.6 years; 86.2% women) enrolled at 15 sites in five countries: the Netherlands, England, Greece, Germany, and Australia. All participants had a Borderline Personality Disorder Severity Index IV (BPDSI-IV) score of more than 20.
The BPDSI-IV score ranges from 0 to 90, with a score of 15 being the cutoff for a BPD diagnosis.
Investigators randomly assigned participants to one of three arms: predominantly group schema therapy, combined individual and group schema therapy, and treatment as usual – which was the optimal psychological treatment available at the site.
The two schema therapy arms, whether group or individual, involved a similar number of sessions each week. However, the frequency was gradually reduced over the course of the study.
Improved severity
The primary outcome was change in BPD severity as assessed at baseline, 6 months, 12 months, 18 months, 24 months, and 36 months with the BPDSI-IV total score.
Researchers first compared both the group therapy and the combination therapy with treatment as usual and found that together, the two schema arms were superior for reducing total BPDSI-IV score, with a medium to large effect size (Cohen d, 0.73; 95% confidence interval, .29-1.18; P = .001).
The difference was significant at 1.5 years (mean difference, 2.38; 95% CI, .27-4.49; P = .03).
When the treatment arms were compared separately, the combination therapy was superior to both the group therapy (Cohen d, 0.84; 95% CI, .09-1.59; P = .03) and to treatment as usual (Cohen d, 1.14; 95% CI, .57-1.71; P < .001).
The effectiveness of the predominantly group therapy did not differ significantly from that of treatment as usual.
The difference in effectiveness of combined therapy compared with treatment as usual became significant at 1 year. It became significant at 2.5 years compared with predominantly group therapy.
Treatment retention
In both schema arms, session frequency was tapered to only once a month; and in year 3, no further treatment was offered. However, symptom improvement continued during years 2 and 3.
Dr. Arntz explained this could be because patients realized they could apply what they learned after therapy was discontinued, which boosted their self-confidence.
Treatment retention was greater with combined therapy compared to the other options.
There was also improvement in several secondary outcomes, including happiness and quality of life, in most patients. However, patterns of outcomes for societal and work functioning improved more for those in either arm that received schema therapy.
“Group therapy seems to offer something that is important for learning to cooperate with other people. At work, you often have to collaborate with people who are not necessarily your friends,” Dr. Arntz noted.
The number of suicide attempts declined over time, with the combination arm being significantly superior to treatment as usual. During the study period, three patients died from suicide: one from each treatment arm. Another death had an unknown cause.
Overall, the results suggest that group and individual sessions address different needs of patients, the investigators noted.
While patients may learn to get along with others in a group setting, they may be more comfortable discussing severe trauma or suicidal thoughts in one-on-one sessions with a therapist, they added.
Strengths, weaknesses
Commenting for this news organization, John M. Oldham, MD, Distinguished Emeritus Professor, Menninger Department of Psychiatry and Behavioral Sciences, Baylor College of Medicine, Houston, said the study had a number of strengths, including its size and “good, solid” methodology.
“This is another big study that demonstrates a well-established form of psychotherapy leads to effective improvement in patients with borderline,” said Dr. Oldham, who was not involved in the research.
However, he noted a number of study limitations. First, training for therapists to deliver schema therapy is not always readily available. In addition, schema therapists in the study “were pretty junior,” with some appearing to be “trained on the job,” he said.
Dr. Oldham noted that cost may be another deterrent to implementing this therapeutic approach. Only those with substantial financial resources could afford once-a-week group therapy and once-a-week individual therapy for 2 years, at least in the United States, he said.
Because patients had to be willing to undergo therapy for 2 years to be enrolled in the study, the results may not be generalizable to the entire BPD population, Dr. Oldham added. “Many borderline patients would turn around and walk out the door if asked to commit to that,” he said.
So the study population may be “better attuned and receptive to therapy” and less impaired compared to many patients with this condition, Dr. Oldham said.
He also said the study did not compare individual schema therapy alone with group schema alone.
Study sites were supported by the Netherlands Organization for Health Research and Development and the Netherlands Foundation for Mental Health Study; Else Kröner-Fresenius-Stiftung; Australian Rotary Health; Greek Society of Schema Therapy, First Department of Psychiatry of the Medical School of the University of Athens, and Institut für Verhaltenstherapie Ausbildung Hamburg; South London and Maudsley NHS Foundation Trust and the Research Center Experimental Psychopathology, Maastricht University and Bradford District Care NHS Foundation Trust. Dr. Arntz has received grants from the Netherlands Organization for Health Research and Development and the Netherlands Foundation for Mental Health. Dr. Oldham reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Schema is a form of psychotherapy that focuses on experiential approaches rather than on behavior change.
The findings from an international randomized controlled trial underscore the importance of offering both individual and group approaches to patients with BPD, study investigator Arnoud Arntz, PhD, professor in the department of clinical psychology at the University of Amsterdam, told this news organization.
“In the Netherlands, there’s a big push from mental health institutes to deliver treatments in group therapy [only] because people think it’s more cost-effective; but these findings question that idea,” Dr. Arntz said.
The findings were published online March 2 in JAMA Psychiatry.
Early childhood experiences
Patients with BPD exhibit extreme sensitivity to interpersonal slights, intense and volatile emotions, and impulsive behaviors. Many abuse drugs, self-harm, or attempt suicide.
Evidence-based guidelines recommend psychotherapy as the primary treatment for BPD.
Schema therapy uses techniques from traditional psychotherapy but focuses on an experiential strategy. It also delves into early childhood experiences, which is relevant because patients with BPD often experienced abuse or neglect early in life.
As well, with this approach, therapists take on a sort of parenting role with patients to try to meet needs “that were frustrated in childhood,” said Dr. Arntz.
Previous research has suggested both individual and group schema therapy help reduce BPD symptoms, but the effectiveness of combining these two approaches has been unclear.
The current study included 495 adult patients (mean age, 33.6 years; 86.2% women) enrolled at 15 sites in five countries: the Netherlands, England, Greece, Germany, and Australia. All participants had a Borderline Personality Disorder Severity Index IV (BPDSI-IV) score of more than 20.
The BPDSI-IV score ranges from 0 to 90, with a score of 15 being the cutoff for a BPD diagnosis.
Investigators randomly assigned participants to one of three arms: predominantly group schema therapy, combined individual and group schema therapy, and treatment as usual – which was the optimal psychological treatment available at the site.
The two schema therapy arms, whether group or individual, involved a similar number of sessions each week. However, the frequency was gradually reduced over the course of the study.
Improved severity
The primary outcome was change in BPD severity as assessed at baseline, 6 months, 12 months, 18 months, 24 months, and 36 months with the BPDSI-IV total score.
Researchers first compared both the group therapy and the combination therapy with treatment as usual and found that together, the two schema arms were superior for reducing total BPDSI-IV score, with a medium to large effect size (Cohen d, 0.73; 95% confidence interval, .29-1.18; P = .001).
The difference was significant at 1.5 years (mean difference, 2.38; 95% CI, .27-4.49; P = .03).
When the treatment arms were compared separately, the combination therapy was superior to both the group therapy (Cohen d, 0.84; 95% CI, .09-1.59; P = .03) and to treatment as usual (Cohen d, 1.14; 95% CI, .57-1.71; P < .001).
The effectiveness of the predominantly group therapy did not differ significantly from that of treatment as usual.
The difference in effectiveness of combined therapy compared with treatment as usual became significant at 1 year. It became significant at 2.5 years compared with predominantly group therapy.
Treatment retention
In both schema arms, session frequency was tapered to only once a month; and in year 3, no further treatment was offered. However, symptom improvement continued during years 2 and 3.
Dr. Arntz explained this could be because patients realized they could apply what they learned after therapy was discontinued, which boosted their self-confidence.
Treatment retention was greater with combined therapy compared to the other options.
There was also improvement in several secondary outcomes, including happiness and quality of life, in most patients. However, patterns of outcomes for societal and work functioning improved more for those in either arm that received schema therapy.
“Group therapy seems to offer something that is important for learning to cooperate with other people. At work, you often have to collaborate with people who are not necessarily your friends,” Dr. Arntz noted.
The number of suicide attempts declined over time, with the combination arm being significantly superior to treatment as usual. During the study period, three patients died from suicide: one from each treatment arm. Another death had an unknown cause.
Overall, the results suggest that group and individual sessions address different needs of patients, the investigators noted.
While patients may learn to get along with others in a group setting, they may be more comfortable discussing severe trauma or suicidal thoughts in one-on-one sessions with a therapist, they added.
Strengths, weaknesses
Commenting for this news organization, John M. Oldham, MD, Distinguished Emeritus Professor, Menninger Department of Psychiatry and Behavioral Sciences, Baylor College of Medicine, Houston, said the study had a number of strengths, including its size and “good, solid” methodology.
“This is another big study that demonstrates a well-established form of psychotherapy leads to effective improvement in patients with borderline,” said Dr. Oldham, who was not involved in the research.
However, he noted a number of study limitations. First, training for therapists to deliver schema therapy is not always readily available. In addition, schema therapists in the study “were pretty junior,” with some appearing to be “trained on the job,” he said.
Dr. Oldham noted that cost may be another deterrent to implementing this therapeutic approach. Only those with substantial financial resources could afford once-a-week group therapy and once-a-week individual therapy for 2 years, at least in the United States, he said.
Because patients had to be willing to undergo therapy for 2 years to be enrolled in the study, the results may not be generalizable to the entire BPD population, Dr. Oldham added. “Many borderline patients would turn around and walk out the door if asked to commit to that,” he said.
So the study population may be “better attuned and receptive to therapy” and less impaired compared to many patients with this condition, Dr. Oldham said.
He also said the study did not compare individual schema therapy alone with group schema alone.
Study sites were supported by the Netherlands Organization for Health Research and Development and the Netherlands Foundation for Mental Health Study; Else Kröner-Fresenius-Stiftung; Australian Rotary Health; Greek Society of Schema Therapy, First Department of Psychiatry of the Medical School of the University of Athens, and Institut für Verhaltenstherapie Ausbildung Hamburg; South London and Maudsley NHS Foundation Trust and the Research Center Experimental Psychopathology, Maastricht University and Bradford District Care NHS Foundation Trust. Dr. Arntz has received grants from the Netherlands Organization for Health Research and Development and the Netherlands Foundation for Mental Health. Dr. Oldham reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Schema is a form of psychotherapy that focuses on experiential approaches rather than on behavior change.
The findings from an international randomized controlled trial underscore the importance of offering both individual and group approaches to patients with BPD, study investigator Arnoud Arntz, PhD, professor in the department of clinical psychology at the University of Amsterdam, told this news organization.
“In the Netherlands, there’s a big push from mental health institutes to deliver treatments in group therapy [only] because people think it’s more cost-effective; but these findings question that idea,” Dr. Arntz said.
The findings were published online March 2 in JAMA Psychiatry.
Early childhood experiences
Patients with BPD exhibit extreme sensitivity to interpersonal slights, intense and volatile emotions, and impulsive behaviors. Many abuse drugs, self-harm, or attempt suicide.
Evidence-based guidelines recommend psychotherapy as the primary treatment for BPD.
Schema therapy uses techniques from traditional psychotherapy but focuses on an experiential strategy. It also delves into early childhood experiences, which is relevant because patients with BPD often experienced abuse or neglect early in life.
As well, with this approach, therapists take on a sort of parenting role with patients to try to meet needs “that were frustrated in childhood,” said Dr. Arntz.
Previous research has suggested both individual and group schema therapy help reduce BPD symptoms, but the effectiveness of combining these two approaches has been unclear.
The current study included 495 adult patients (mean age, 33.6 years; 86.2% women) enrolled at 15 sites in five countries: the Netherlands, England, Greece, Germany, and Australia. All participants had a Borderline Personality Disorder Severity Index IV (BPDSI-IV) score of more than 20.
The BPDSI-IV score ranges from 0 to 90, with a score of 15 being the cutoff for a BPD diagnosis.
Investigators randomly assigned participants to one of three arms: predominantly group schema therapy, combined individual and group schema therapy, and treatment as usual – which was the optimal psychological treatment available at the site.
The two schema therapy arms, whether group or individual, involved a similar number of sessions each week. However, the frequency was gradually reduced over the course of the study.
Improved severity
The primary outcome was change in BPD severity as assessed at baseline, 6 months, 12 months, 18 months, 24 months, and 36 months with the BPDSI-IV total score.
Researchers first compared both the group therapy and the combination therapy with treatment as usual and found that together, the two schema arms were superior for reducing total BPDSI-IV score, with a medium to large effect size (Cohen d, 0.73; 95% confidence interval, .29-1.18; P = .001).
The difference was significant at 1.5 years (mean difference, 2.38; 95% CI, .27-4.49; P = .03).
When the treatment arms were compared separately, the combination therapy was superior to both the group therapy (Cohen d, 0.84; 95% CI, .09-1.59; P = .03) and to treatment as usual (Cohen d, 1.14; 95% CI, .57-1.71; P < .001).
The effectiveness of the predominantly group therapy did not differ significantly from that of treatment as usual.
The difference in effectiveness of combined therapy compared with treatment as usual became significant at 1 year. It became significant at 2.5 years compared with predominantly group therapy.
Treatment retention
In both schema arms, session frequency was tapered to only once a month; and in year 3, no further treatment was offered. However, symptom improvement continued during years 2 and 3.
Dr. Arntz explained this could be because patients realized they could apply what they learned after therapy was discontinued, which boosted their self-confidence.
Treatment retention was greater with combined therapy compared to the other options.
There was also improvement in several secondary outcomes, including happiness and quality of life, in most patients. However, patterns of outcomes for societal and work functioning improved more for those in either arm that received schema therapy.
“Group therapy seems to offer something that is important for learning to cooperate with other people. At work, you often have to collaborate with people who are not necessarily your friends,” Dr. Arntz noted.
The number of suicide attempts declined over time, with the combination arm being significantly superior to treatment as usual. During the study period, three patients died from suicide: one from each treatment arm. Another death had an unknown cause.
Overall, the results suggest that group and individual sessions address different needs of patients, the investigators noted.
While patients may learn to get along with others in a group setting, they may be more comfortable discussing severe trauma or suicidal thoughts in one-on-one sessions with a therapist, they added.
Strengths, weaknesses
Commenting for this news organization, John M. Oldham, MD, Distinguished Emeritus Professor, Menninger Department of Psychiatry and Behavioral Sciences, Baylor College of Medicine, Houston, said the study had a number of strengths, including its size and “good, solid” methodology.
“This is another big study that demonstrates a well-established form of psychotherapy leads to effective improvement in patients with borderline,” said Dr. Oldham, who was not involved in the research.
However, he noted a number of study limitations. First, training for therapists to deliver schema therapy is not always readily available. In addition, schema therapists in the study “were pretty junior,” with some appearing to be “trained on the job,” he said.
Dr. Oldham noted that cost may be another deterrent to implementing this therapeutic approach. Only those with substantial financial resources could afford once-a-week group therapy and once-a-week individual therapy for 2 years, at least in the United States, he said.
Because patients had to be willing to undergo therapy for 2 years to be enrolled in the study, the results may not be generalizable to the entire BPD population, Dr. Oldham added. “Many borderline patients would turn around and walk out the door if asked to commit to that,” he said.
So the study population may be “better attuned and receptive to therapy” and less impaired compared to many patients with this condition, Dr. Oldham said.
He also said the study did not compare individual schema therapy alone with group schema alone.
Study sites were supported by the Netherlands Organization for Health Research and Development and the Netherlands Foundation for Mental Health Study; Else Kröner-Fresenius-Stiftung; Australian Rotary Health; Greek Society of Schema Therapy, First Department of Psychiatry of the Medical School of the University of Athens, and Institut für Verhaltenstherapie Ausbildung Hamburg; South London and Maudsley NHS Foundation Trust and the Research Center Experimental Psychopathology, Maastricht University and Bradford District Care NHS Foundation Trust. Dr. Arntz has received grants from the Netherlands Organization for Health Research and Development and the Netherlands Foundation for Mental Health. Dr. Oldham reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
DSM-5 update: What’s new?
Ahead of its official release on March 18, the new Diagnostic and Statistical Manual of Mental Disorders, which is in the form of a textbook, is already drawing some criticism.
It also includes symptom codes for suicidal behavior and nonsuicidal self-injury, clarifying modifications to criteria sets for more than 70 disorders, including autism spectrum disorder; changes in terminology for gender dysphoria; and a comprehensive review of the impact of racism and discrimination on the diagnosis and manifestations of mental disorders.
The Text Revision is a compilation of iterative changes that have been made online on a rolling basis since the DSM-5 was first published in 2013.
“The goal of the Text Revision was to allow a thorough revision of the text, not the criteria,” Paul Appelbaum, MD, chair of the APA’s DSM steering committee, told this news organization.
For the Text Revision, some 200 experts across a variety of APA working groups recommended changes to the text based on a comprehensive literature review, said Appelbaum, who is the Elizabeth K. Dollard Professor of Psychiatry, Medicine and Law, and director of the division of law, ethics and psychiatry at Columbia University, New York.
However, there’s not a lot that’s new, in part, because there have been few therapeutic advances.
Money maker?
Allen Frances, MD, chair of the DSM-4 task force and professor and chair emeritus of psychiatry at Duke University, Durham, N.C., said the APA is publishing the Text Revision “just to make money. They’re very anxious to do anything that will increase sales and having a revision forces some people, especially in institutions, to buy the book, even though it may not have anything substantive to add to the original.”
Dr. Frances told this news organization that when the APA published the first DSM in the late 1970s, “it became an instantaneous best-seller, to everyone’s surprise.”
The APA would not comment on how many of the $170 (list price) volumes it sells or how much those sales contribute to its budget.
Dr. Appelbaum acknowledged, “at any point in time, the canonical version is the online version.” However, it’s clear from DSM-5 sales “that many people still value having a hard copy of the DSM available to them.”
Prolonged grief: Timely or overkill?
Persistent complex bereavement disorder (PCBD) was listed as a “condition for further study” in DSM-5. After a 2019 workshop aimed at getting consensus for diagnosis criteria, the APA board approved the new prolonged grief disorder in October 2020, and the APA assembly approved the new disorder in November 2020.
Given the 950,000 deaths from COVID-19 over the past 2 years, inclusion of prolonged grief disorder in the DSM-5 may arrive at just the right time.
The diagnostic criteria for PCBD include:
- The development of a persistent grief response (longer than a year for adults and 6 months for children and adolescents) characterized by one or both of the following symptoms, which have been present most days to a clinically significant degree, and have occurred nearly every day for at least the last month: intense yearning/longing for the deceased person; preoccupation with thoughts or memories of the deceased person.
- Since the death, at least three symptoms present most days to a clinically significant degree, and occurring nearly every day for at least the last month, including identity disruption, marked sense of disbelief about the death, avoidance of reminders that the person is dead, intense emotional pain related to the death, difficulty reintegrating into one’s relationships and activities after the death, emotional numbness, feeling that life is meaningless as a result of the death, and intense loneliness as a result of the death.
- The disturbance causes clinically significant distress or impairment in social, occupational, or other important areas of functioning.
- The duration and severity of the bereavement reaction clearly exceed expected social, cultural, or religious norms for the individual’s culture and context.
- The symptoms are not better explained by another mental disorder, such as major depressive disorder (MDD) or PTSD, and are not attributable to the physiological effects of a substance or another medical condition.
Dr. Frances said he believes creating a new diagnosis pathologizes grief. In DSM-3 and DSM-4, an exception was made under the diagnosis of MDD for individuals who had recently lost a loved one. “We wanted to have at least an opportunity for people to grieve without being stigmatized, mislabeled, and overtreated with medication.”
DSM-5 removed the bereavement exclusion. After 2 weeks, people who are grieving and have particular symptoms could receive a diagnosis of MDD, said Dr. Frances. He believes the exclusion should have been broadened to cover anyone experiencing a major loss – such as a job loss or divorce. If someone is having prolonged symptoms that interfere with functioning, they should get an MDD diagnosis.
The new disorder “doesn’t solve anything, it just adds to the confusion and stigmatization, and it’s part of a kind of creeping medical imperialization of everyday life, where everything has to have a mental disorder label,” Dr. Frances said.
However, Dr. Appelbaum countered that “the criteria for prolonged grief disorder are constructed in such a way as to make every effort to exclude people who are going through a normal grieving process.”
“Part of the purpose of the data analyses was to ensure the criteria that were adopted would, in fact, effectively distinguish between what anybody goes through, say when someone close to you dies, and this unusual prolonged grieving process without end that affects a much smaller number of people but which really can be crippling for them,” he added.
The Text Revision adds new symptom codes for suicidal behavior and nonsuicidal self-injury, which appear in the chapter, “Other Conditions That May Be a Focus of Clinical Attention,” said Dr. Appelbaum.
“Both suicidal behavior and nonsuicidal self-injury seem pretty persuasively to fall into that category – something a clinician would want to know about, pay attention to, and factor into treatment planning, although they are behaviors that cross many diagnostic categories,” he added.
Codes also provide a systematic way of ascertaining the incidence and prevalence of such behaviors, said Dr. Appelbaum.
Changes to gender terminology
The Text Revision also tweaks some terminology with respect to transgender individuals. The term “desired gender” is now “experienced gender”, the term “cross-sex medical procedure” is now “gender-affirming medical procedure”, and the terms “natal male/natal female” are now “individual assigned male/female at birth”.
Dr. Frances said that the existence of gender dysphoria as a diagnosis has been a matter of controversy ever since it was first included.
“The transgender community has had mixed feelings on whether there should be anything at all in the manual,” he said. On one hand is the argument that gender dysphoria should be removed because it’s not really a psychiatric issue.
“We seriously considered eliminating it altogether in DSM-4,” said Dr. Frances.
However, an argument in favor of keeping it was that if the diagnosis was removed, it would mean that people could not receive treatment. “There’s no right argument for this dilemma,” he said.
Dr. Frances, who has been a frequent critic of DSM-5, said he believes the manual continues to miss opportunities to tighten criteria for many diagnoses, including ADHD and autism spectrum disorder.
“There’s a consistent pattern of taking behaviors and symptoms of behaviors that are on the border with normality and expanding the definition of mental disorder and reducing the realm of normality,” he said.
That has consequences, Dr. Frances added. “When someone gets a diagnosis that they need to get, it’s the beginning of a much better future. When someone gets a diagnosis that’s a mislabel that they don’t need, it has all harms and no benefits. It’s stigmatizing, leads to too much treatment, the wrong treatment, and it’s much more harmful than helpful.”
A version of this article first appeared on Medscape.com.
Ahead of its official release on March 18, the new Diagnostic and Statistical Manual of Mental Disorders, which is in the form of a textbook, is already drawing some criticism.
It also includes symptom codes for suicidal behavior and nonsuicidal self-injury, clarifying modifications to criteria sets for more than 70 disorders, including autism spectrum disorder; changes in terminology for gender dysphoria; and a comprehensive review of the impact of racism and discrimination on the diagnosis and manifestations of mental disorders.
The Text Revision is a compilation of iterative changes that have been made online on a rolling basis since the DSM-5 was first published in 2013.
“The goal of the Text Revision was to allow a thorough revision of the text, not the criteria,” Paul Appelbaum, MD, chair of the APA’s DSM steering committee, told this news organization.
For the Text Revision, some 200 experts across a variety of APA working groups recommended changes to the text based on a comprehensive literature review, said Appelbaum, who is the Elizabeth K. Dollard Professor of Psychiatry, Medicine and Law, and director of the division of law, ethics and psychiatry at Columbia University, New York.
However, there’s not a lot that’s new, in part, because there have been few therapeutic advances.
Money maker?
Allen Frances, MD, chair of the DSM-4 task force and professor and chair emeritus of psychiatry at Duke University, Durham, N.C., said the APA is publishing the Text Revision “just to make money. They’re very anxious to do anything that will increase sales and having a revision forces some people, especially in institutions, to buy the book, even though it may not have anything substantive to add to the original.”
Dr. Frances told this news organization that when the APA published the first DSM in the late 1970s, “it became an instantaneous best-seller, to everyone’s surprise.”
The APA would not comment on how many of the $170 (list price) volumes it sells or how much those sales contribute to its budget.
Dr. Appelbaum acknowledged, “at any point in time, the canonical version is the online version.” However, it’s clear from DSM-5 sales “that many people still value having a hard copy of the DSM available to them.”
Prolonged grief: Timely or overkill?
Persistent complex bereavement disorder (PCBD) was listed as a “condition for further study” in DSM-5. After a 2019 workshop aimed at getting consensus for diagnosis criteria, the APA board approved the new prolonged grief disorder in October 2020, and the APA assembly approved the new disorder in November 2020.
Given the 950,000 deaths from COVID-19 over the past 2 years, inclusion of prolonged grief disorder in the DSM-5 may arrive at just the right time.
The diagnostic criteria for PCBD include:
- The development of a persistent grief response (longer than a year for adults and 6 months for children and adolescents) characterized by one or both of the following symptoms, which have been present most days to a clinically significant degree, and have occurred nearly every day for at least the last month: intense yearning/longing for the deceased person; preoccupation with thoughts or memories of the deceased person.
- Since the death, at least three symptoms present most days to a clinically significant degree, and occurring nearly every day for at least the last month, including identity disruption, marked sense of disbelief about the death, avoidance of reminders that the person is dead, intense emotional pain related to the death, difficulty reintegrating into one’s relationships and activities after the death, emotional numbness, feeling that life is meaningless as a result of the death, and intense loneliness as a result of the death.
- The disturbance causes clinically significant distress or impairment in social, occupational, or other important areas of functioning.
- The duration and severity of the bereavement reaction clearly exceed expected social, cultural, or religious norms for the individual’s culture and context.
- The symptoms are not better explained by another mental disorder, such as major depressive disorder (MDD) or PTSD, and are not attributable to the physiological effects of a substance or another medical condition.
Dr. Frances said he believes creating a new diagnosis pathologizes grief. In DSM-3 and DSM-4, an exception was made under the diagnosis of MDD for individuals who had recently lost a loved one. “We wanted to have at least an opportunity for people to grieve without being stigmatized, mislabeled, and overtreated with medication.”
DSM-5 removed the bereavement exclusion. After 2 weeks, people who are grieving and have particular symptoms could receive a diagnosis of MDD, said Dr. Frances. He believes the exclusion should have been broadened to cover anyone experiencing a major loss – such as a job loss or divorce. If someone is having prolonged symptoms that interfere with functioning, they should get an MDD diagnosis.
The new disorder “doesn’t solve anything, it just adds to the confusion and stigmatization, and it’s part of a kind of creeping medical imperialization of everyday life, where everything has to have a mental disorder label,” Dr. Frances said.
However, Dr. Appelbaum countered that “the criteria for prolonged grief disorder are constructed in such a way as to make every effort to exclude people who are going through a normal grieving process.”
“Part of the purpose of the data analyses was to ensure the criteria that were adopted would, in fact, effectively distinguish between what anybody goes through, say when someone close to you dies, and this unusual prolonged grieving process without end that affects a much smaller number of people but which really can be crippling for them,” he added.
The Text Revision adds new symptom codes for suicidal behavior and nonsuicidal self-injury, which appear in the chapter, “Other Conditions That May Be a Focus of Clinical Attention,” said Dr. Appelbaum.
“Both suicidal behavior and nonsuicidal self-injury seem pretty persuasively to fall into that category – something a clinician would want to know about, pay attention to, and factor into treatment planning, although they are behaviors that cross many diagnostic categories,” he added.
Codes also provide a systematic way of ascertaining the incidence and prevalence of such behaviors, said Dr. Appelbaum.
Changes to gender terminology
The Text Revision also tweaks some terminology with respect to transgender individuals. The term “desired gender” is now “experienced gender”, the term “cross-sex medical procedure” is now “gender-affirming medical procedure”, and the terms “natal male/natal female” are now “individual assigned male/female at birth”.
Dr. Frances said that the existence of gender dysphoria as a diagnosis has been a matter of controversy ever since it was first included.
“The transgender community has had mixed feelings on whether there should be anything at all in the manual,” he said. On one hand is the argument that gender dysphoria should be removed because it’s not really a psychiatric issue.
“We seriously considered eliminating it altogether in DSM-4,” said Dr. Frances.
However, an argument in favor of keeping it was that if the diagnosis was removed, it would mean that people could not receive treatment. “There’s no right argument for this dilemma,” he said.
Dr. Frances, who has been a frequent critic of DSM-5, said he believes the manual continues to miss opportunities to tighten criteria for many diagnoses, including ADHD and autism spectrum disorder.
“There’s a consistent pattern of taking behaviors and symptoms of behaviors that are on the border with normality and expanding the definition of mental disorder and reducing the realm of normality,” he said.
That has consequences, Dr. Frances added. “When someone gets a diagnosis that they need to get, it’s the beginning of a much better future. When someone gets a diagnosis that’s a mislabel that they don’t need, it has all harms and no benefits. It’s stigmatizing, leads to too much treatment, the wrong treatment, and it’s much more harmful than helpful.”
A version of this article first appeared on Medscape.com.
Ahead of its official release on March 18, the new Diagnostic and Statistical Manual of Mental Disorders, which is in the form of a textbook, is already drawing some criticism.
It also includes symptom codes for suicidal behavior and nonsuicidal self-injury, clarifying modifications to criteria sets for more than 70 disorders, including autism spectrum disorder; changes in terminology for gender dysphoria; and a comprehensive review of the impact of racism and discrimination on the diagnosis and manifestations of mental disorders.
The Text Revision is a compilation of iterative changes that have been made online on a rolling basis since the DSM-5 was first published in 2013.
“The goal of the Text Revision was to allow a thorough revision of the text, not the criteria,” Paul Appelbaum, MD, chair of the APA’s DSM steering committee, told this news organization.
For the Text Revision, some 200 experts across a variety of APA working groups recommended changes to the text based on a comprehensive literature review, said Appelbaum, who is the Elizabeth K. Dollard Professor of Psychiatry, Medicine and Law, and director of the division of law, ethics and psychiatry at Columbia University, New York.
However, there’s not a lot that’s new, in part, because there have been few therapeutic advances.
Money maker?
Allen Frances, MD, chair of the DSM-4 task force and professor and chair emeritus of psychiatry at Duke University, Durham, N.C., said the APA is publishing the Text Revision “just to make money. They’re very anxious to do anything that will increase sales and having a revision forces some people, especially in institutions, to buy the book, even though it may not have anything substantive to add to the original.”
Dr. Frances told this news organization that when the APA published the first DSM in the late 1970s, “it became an instantaneous best-seller, to everyone’s surprise.”
The APA would not comment on how many of the $170 (list price) volumes it sells or how much those sales contribute to its budget.
Dr. Appelbaum acknowledged, “at any point in time, the canonical version is the online version.” However, it’s clear from DSM-5 sales “that many people still value having a hard copy of the DSM available to them.”
Prolonged grief: Timely or overkill?
Persistent complex bereavement disorder (PCBD) was listed as a “condition for further study” in DSM-5. After a 2019 workshop aimed at getting consensus for diagnosis criteria, the APA board approved the new prolonged grief disorder in October 2020, and the APA assembly approved the new disorder in November 2020.
Given the 950,000 deaths from COVID-19 over the past 2 years, inclusion of prolonged grief disorder in the DSM-5 may arrive at just the right time.
The diagnostic criteria for PCBD include:
- The development of a persistent grief response (longer than a year for adults and 6 months for children and adolescents) characterized by one or both of the following symptoms, which have been present most days to a clinically significant degree, and have occurred nearly every day for at least the last month: intense yearning/longing for the deceased person; preoccupation with thoughts or memories of the deceased person.
- Since the death, at least three symptoms present most days to a clinically significant degree, and occurring nearly every day for at least the last month, including identity disruption, marked sense of disbelief about the death, avoidance of reminders that the person is dead, intense emotional pain related to the death, difficulty reintegrating into one’s relationships and activities after the death, emotional numbness, feeling that life is meaningless as a result of the death, and intense loneliness as a result of the death.
- The disturbance causes clinically significant distress or impairment in social, occupational, or other important areas of functioning.
- The duration and severity of the bereavement reaction clearly exceed expected social, cultural, or religious norms for the individual’s culture and context.
- The symptoms are not better explained by another mental disorder, such as major depressive disorder (MDD) or PTSD, and are not attributable to the physiological effects of a substance or another medical condition.
Dr. Frances said he believes creating a new diagnosis pathologizes grief. In DSM-3 and DSM-4, an exception was made under the diagnosis of MDD for individuals who had recently lost a loved one. “We wanted to have at least an opportunity for people to grieve without being stigmatized, mislabeled, and overtreated with medication.”
DSM-5 removed the bereavement exclusion. After 2 weeks, people who are grieving and have particular symptoms could receive a diagnosis of MDD, said Dr. Frances. He believes the exclusion should have been broadened to cover anyone experiencing a major loss – such as a job loss or divorce. If someone is having prolonged symptoms that interfere with functioning, they should get an MDD diagnosis.
The new disorder “doesn’t solve anything, it just adds to the confusion and stigmatization, and it’s part of a kind of creeping medical imperialization of everyday life, where everything has to have a mental disorder label,” Dr. Frances said.
However, Dr. Appelbaum countered that “the criteria for prolonged grief disorder are constructed in such a way as to make every effort to exclude people who are going through a normal grieving process.”
“Part of the purpose of the data analyses was to ensure the criteria that were adopted would, in fact, effectively distinguish between what anybody goes through, say when someone close to you dies, and this unusual prolonged grieving process without end that affects a much smaller number of people but which really can be crippling for them,” he added.
The Text Revision adds new symptom codes for suicidal behavior and nonsuicidal self-injury, which appear in the chapter, “Other Conditions That May Be a Focus of Clinical Attention,” said Dr. Appelbaum.
“Both suicidal behavior and nonsuicidal self-injury seem pretty persuasively to fall into that category – something a clinician would want to know about, pay attention to, and factor into treatment planning, although they are behaviors that cross many diagnostic categories,” he added.
Codes also provide a systematic way of ascertaining the incidence and prevalence of such behaviors, said Dr. Appelbaum.
Changes to gender terminology
The Text Revision also tweaks some terminology with respect to transgender individuals. The term “desired gender” is now “experienced gender”, the term “cross-sex medical procedure” is now “gender-affirming medical procedure”, and the terms “natal male/natal female” are now “individual assigned male/female at birth”.
Dr. Frances said that the existence of gender dysphoria as a diagnosis has been a matter of controversy ever since it was first included.
“The transgender community has had mixed feelings on whether there should be anything at all in the manual,” he said. On one hand is the argument that gender dysphoria should be removed because it’s not really a psychiatric issue.
“We seriously considered eliminating it altogether in DSM-4,” said Dr. Frances.
However, an argument in favor of keeping it was that if the diagnosis was removed, it would mean that people could not receive treatment. “There’s no right argument for this dilemma,” he said.
Dr. Frances, who has been a frequent critic of DSM-5, said he believes the manual continues to miss opportunities to tighten criteria for many diagnoses, including ADHD and autism spectrum disorder.
“There’s a consistent pattern of taking behaviors and symptoms of behaviors that are on the border with normality and expanding the definition of mental disorder and reducing the realm of normality,” he said.
That has consequences, Dr. Frances added. “When someone gets a diagnosis that they need to get, it’s the beginning of a much better future. When someone gets a diagnosis that’s a mislabel that they don’t need, it has all harms and no benefits. It’s stigmatizing, leads to too much treatment, the wrong treatment, and it’s much more harmful than helpful.”
A version of this article first appeared on Medscape.com.
Differentiating pediatric schizotypal disorder from schizophrenia and autism
Schizotypal disorder is a complex condition that is characterized by cognitive-perceptual impairments, oddness, disorganization, and interpersonal difficulties. It often is unrecognized or underdiagnosed. In DSM-5, schizotypal disorder is categorized a personality disorder, but it is also considered part of the schizophrenia spectrum disorders.1 The diagnostic criteria for schizotypal disorder are outlined in the Table.1,2
Although schizotypal disorder has a lifetime prevalence of approximately 4% in the general population of the United States,2 it can present during childhood or adolescence and may be overlooked in the differential diagnosis for psychotic symptoms in pediatric patients.3 Schizotypal disorder of childhood (SDC) can present with significant overlap with several pediatric diagnoses, including schizophrenia spectrum disorders and autism spectrum disorder (ASD), all of which may include psychotic symptoms and difficulties in interpersonal relationships. This overlap, combined with the lack of awareness of schizotypal disorder, can pose a diagnostic challenge. Better recognition of SDC could result in earlier and more effective treatment. In this article, we provide tips for differentiating SDC from childhood-onset schizophrenia and from ASD.
Differentiating SDC from schizophrenia
SDC may be mistaken for childhood-onset schizophrenia due to its perceptual disturbances (which may be interpreted as visual or auditory hallucinations), bizarre fantasies (which may be mistaken for overt delusions), paranoia, and odd behavior. Two ways to distinguish SDC from childhood schizophrenia are by clinical course and by severity of negative psychotic symptoms.
SDC tends to have an overall stable clinical course,4 with patients experiencing periods of time when they exhibit a more normal mental status complemented by fluctuations in symptom severity, which are exacerbated by stressors and followed by a return to baseline.3 SDC psychotic symptoms are predominantly positive, and patients typically do not demonstrate negative features beyond social difficulties. Childhood-onset schizophrenia is typically progressive and disabling, with worsening severity over time, and is much more likely to incorporate prominent negative symptoms.3
Differentiating SDC from ASD
SDC also demonstrates considerable diagnostic overlap with ASD, especially with regards to inappropriate affect; odd thinking, behavior, and speech; and social difficulties. Further complicating the diagnosis, ASD and SDC are comorbid in approximately 40% of ASD cases.3,5 The Melbourne Assessment of Schizotypy in Kids demonstrates validity in diagnosing schizotypal disorder in patients with comorbid ASD.5,6 For clinicians without easy access to advanced testing, 2 ways to distinguish SDC from ASD are the content of the odd behavior and thoughts, and the patient’s reaction to social deficits.
In SDC, odd behavior and thoughts most often revolve around daydreaming and a focus on “elaborate inner fantasies.”3,6 Unlike in ASD, in patients with SDC, behaviors don’t typically involve stereotyped mannerisms, the patient is unlikely to have rigid interests (apart from their fantasies), and there is not a particular focus on detail in the external world.3,6 Notably, imaginary companions are common in SDC; children with ASD are less likely to have an imaginary companion compared with children with SDC or those with no psychiatric diagnosis.6 Patients with SDC have social difficulties (often due to social anxiety stemming from their paranoia) but usually seek out interaction and are bothered by alienation, while patients with ASD may have less interest in social engagement.6
1. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. 5th ed. American Psychiatric Association; 2013.
2. Pulay AJ, Stinson FS, Dawson DA, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV schizotypal personality disorder: results from the wave 2 national epidemiologic survey on alcohol and related conditions. Prim Care Companion J Clin Psychiatry. 2009;11(2):53-67. doi:10.4088/pcc.08m00679
3. Tonge BJ, Testa R, Díaz-Arteche C, et al. Schizotypal disorder in children—a neglected diagnosis. Schizophrenia Bulletin Open. 2020;1(1):sgaa048. doi:10.1093/schizbullopen/sgaa048
4. Asarnow JR. Childhood-onset schizotypal disorder: a follow-up study and comparison with childhood-onset schizophrenia. J Child Adolesc Psychopharmacol. 2005;15(3):395-402.
5. Jones HP, Testa RR, Ross N, et al. The Melbourne Assessment of Schizotypy in Kids: a useful measure of childhood schizotypal personality disorder. Biomed Res Int. 2015;2015:635732. doi:10.1155/2015/635732
6. Poletti M, Raballo A. Childhood schizotypal features vs. high-functioning autism spectrum disorder: developmental overlaps and phenomenological differences. Schizophr Res. 2020;223:53-58. doi:10.1016/j.schres.2020.09.027
Schizotypal disorder is a complex condition that is characterized by cognitive-perceptual impairments, oddness, disorganization, and interpersonal difficulties. It often is unrecognized or underdiagnosed. In DSM-5, schizotypal disorder is categorized a personality disorder, but it is also considered part of the schizophrenia spectrum disorders.1 The diagnostic criteria for schizotypal disorder are outlined in the Table.1,2
Although schizotypal disorder has a lifetime prevalence of approximately 4% in the general population of the United States,2 it can present during childhood or adolescence and may be overlooked in the differential diagnosis for psychotic symptoms in pediatric patients.3 Schizotypal disorder of childhood (SDC) can present with significant overlap with several pediatric diagnoses, including schizophrenia spectrum disorders and autism spectrum disorder (ASD), all of which may include psychotic symptoms and difficulties in interpersonal relationships. This overlap, combined with the lack of awareness of schizotypal disorder, can pose a diagnostic challenge. Better recognition of SDC could result in earlier and more effective treatment. In this article, we provide tips for differentiating SDC from childhood-onset schizophrenia and from ASD.
Differentiating SDC from schizophrenia
SDC may be mistaken for childhood-onset schizophrenia due to its perceptual disturbances (which may be interpreted as visual or auditory hallucinations), bizarre fantasies (which may be mistaken for overt delusions), paranoia, and odd behavior. Two ways to distinguish SDC from childhood schizophrenia are by clinical course and by severity of negative psychotic symptoms.
SDC tends to have an overall stable clinical course,4 with patients experiencing periods of time when they exhibit a more normal mental status complemented by fluctuations in symptom severity, which are exacerbated by stressors and followed by a return to baseline.3 SDC psychotic symptoms are predominantly positive, and patients typically do not demonstrate negative features beyond social difficulties. Childhood-onset schizophrenia is typically progressive and disabling, with worsening severity over time, and is much more likely to incorporate prominent negative symptoms.3
Differentiating SDC from ASD
SDC also demonstrates considerable diagnostic overlap with ASD, especially with regards to inappropriate affect; odd thinking, behavior, and speech; and social difficulties. Further complicating the diagnosis, ASD and SDC are comorbid in approximately 40% of ASD cases.3,5 The Melbourne Assessment of Schizotypy in Kids demonstrates validity in diagnosing schizotypal disorder in patients with comorbid ASD.5,6 For clinicians without easy access to advanced testing, 2 ways to distinguish SDC from ASD are the content of the odd behavior and thoughts, and the patient’s reaction to social deficits.
In SDC, odd behavior and thoughts most often revolve around daydreaming and a focus on “elaborate inner fantasies.”3,6 Unlike in ASD, in patients with SDC, behaviors don’t typically involve stereotyped mannerisms, the patient is unlikely to have rigid interests (apart from their fantasies), and there is not a particular focus on detail in the external world.3,6 Notably, imaginary companions are common in SDC; children with ASD are less likely to have an imaginary companion compared with children with SDC or those with no psychiatric diagnosis.6 Patients with SDC have social difficulties (often due to social anxiety stemming from their paranoia) but usually seek out interaction and are bothered by alienation, while patients with ASD may have less interest in social engagement.6
Schizotypal disorder is a complex condition that is characterized by cognitive-perceptual impairments, oddness, disorganization, and interpersonal difficulties. It often is unrecognized or underdiagnosed. In DSM-5, schizotypal disorder is categorized a personality disorder, but it is also considered part of the schizophrenia spectrum disorders.1 The diagnostic criteria for schizotypal disorder are outlined in the Table.1,2
Although schizotypal disorder has a lifetime prevalence of approximately 4% in the general population of the United States,2 it can present during childhood or adolescence and may be overlooked in the differential diagnosis for psychotic symptoms in pediatric patients.3 Schizotypal disorder of childhood (SDC) can present with significant overlap with several pediatric diagnoses, including schizophrenia spectrum disorders and autism spectrum disorder (ASD), all of which may include psychotic symptoms and difficulties in interpersonal relationships. This overlap, combined with the lack of awareness of schizotypal disorder, can pose a diagnostic challenge. Better recognition of SDC could result in earlier and more effective treatment. In this article, we provide tips for differentiating SDC from childhood-onset schizophrenia and from ASD.
Differentiating SDC from schizophrenia
SDC may be mistaken for childhood-onset schizophrenia due to its perceptual disturbances (which may be interpreted as visual or auditory hallucinations), bizarre fantasies (which may be mistaken for overt delusions), paranoia, and odd behavior. Two ways to distinguish SDC from childhood schizophrenia are by clinical course and by severity of negative psychotic symptoms.
SDC tends to have an overall stable clinical course,4 with patients experiencing periods of time when they exhibit a more normal mental status complemented by fluctuations in symptom severity, which are exacerbated by stressors and followed by a return to baseline.3 SDC psychotic symptoms are predominantly positive, and patients typically do not demonstrate negative features beyond social difficulties. Childhood-onset schizophrenia is typically progressive and disabling, with worsening severity over time, and is much more likely to incorporate prominent negative symptoms.3
Differentiating SDC from ASD
SDC also demonstrates considerable diagnostic overlap with ASD, especially with regards to inappropriate affect; odd thinking, behavior, and speech; and social difficulties. Further complicating the diagnosis, ASD and SDC are comorbid in approximately 40% of ASD cases.3,5 The Melbourne Assessment of Schizotypy in Kids demonstrates validity in diagnosing schizotypal disorder in patients with comorbid ASD.5,6 For clinicians without easy access to advanced testing, 2 ways to distinguish SDC from ASD are the content of the odd behavior and thoughts, and the patient’s reaction to social deficits.
In SDC, odd behavior and thoughts most often revolve around daydreaming and a focus on “elaborate inner fantasies.”3,6 Unlike in ASD, in patients with SDC, behaviors don’t typically involve stereotyped mannerisms, the patient is unlikely to have rigid interests (apart from their fantasies), and there is not a particular focus on detail in the external world.3,6 Notably, imaginary companions are common in SDC; children with ASD are less likely to have an imaginary companion compared with children with SDC or those with no psychiatric diagnosis.6 Patients with SDC have social difficulties (often due to social anxiety stemming from their paranoia) but usually seek out interaction and are bothered by alienation, while patients with ASD may have less interest in social engagement.6
1. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. 5th ed. American Psychiatric Association; 2013.
2. Pulay AJ, Stinson FS, Dawson DA, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV schizotypal personality disorder: results from the wave 2 national epidemiologic survey on alcohol and related conditions. Prim Care Companion J Clin Psychiatry. 2009;11(2):53-67. doi:10.4088/pcc.08m00679
3. Tonge BJ, Testa R, Díaz-Arteche C, et al. Schizotypal disorder in children—a neglected diagnosis. Schizophrenia Bulletin Open. 2020;1(1):sgaa048. doi:10.1093/schizbullopen/sgaa048
4. Asarnow JR. Childhood-onset schizotypal disorder: a follow-up study and comparison with childhood-onset schizophrenia. J Child Adolesc Psychopharmacol. 2005;15(3):395-402.
5. Jones HP, Testa RR, Ross N, et al. The Melbourne Assessment of Schizotypy in Kids: a useful measure of childhood schizotypal personality disorder. Biomed Res Int. 2015;2015:635732. doi:10.1155/2015/635732
6. Poletti M, Raballo A. Childhood schizotypal features vs. high-functioning autism spectrum disorder: developmental overlaps and phenomenological differences. Schizophr Res. 2020;223:53-58. doi:10.1016/j.schres.2020.09.027
1. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. 5th ed. American Psychiatric Association; 2013.
2. Pulay AJ, Stinson FS, Dawson DA, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV schizotypal personality disorder: results from the wave 2 national epidemiologic survey on alcohol and related conditions. Prim Care Companion J Clin Psychiatry. 2009;11(2):53-67. doi:10.4088/pcc.08m00679
3. Tonge BJ, Testa R, Díaz-Arteche C, et al. Schizotypal disorder in children—a neglected diagnosis. Schizophrenia Bulletin Open. 2020;1(1):sgaa048. doi:10.1093/schizbullopen/sgaa048
4. Asarnow JR. Childhood-onset schizotypal disorder: a follow-up study and comparison with childhood-onset schizophrenia. J Child Adolesc Psychopharmacol. 2005;15(3):395-402.
5. Jones HP, Testa RR, Ross N, et al. The Melbourne Assessment of Schizotypy in Kids: a useful measure of childhood schizotypal personality disorder. Biomed Res Int. 2015;2015:635732. doi:10.1155/2015/635732
6. Poletti M, Raballo A. Childhood schizotypal features vs. high-functioning autism spectrum disorder: developmental overlaps and phenomenological differences. Schizophr Res. 2020;223:53-58. doi:10.1016/j.schres.2020.09.027
Borderline personality disorder: 6 studies of psychosocial interventions
SECOND OF 2 PARTS
Borderline personality disorder (BPD) is associated with serious impairment in psychosocial functioning.1 It is characterized by an ongoing pattern of mood instability, cognitive distortions, problems with self-image, and impulsive behavior that often results in problems in relationships. As a result, patients with BPD tend to utilize more mental health services than patients with other personality disorders or major depressive disorder.2
Some clinicians believe BPD is difficult to treat. While historically there has been little consensus on the best treatments for this disorder, current options include both pharmacologic and psychological interventions. In Part 1 of this 2-part article, we focused on 6 studies that evaluated biological interventions.3 Here in Part 2, we focus on findings from 6 recent randomized controlled trials (RCTs) of psychosocial interventions for BPD
1. Zanarini MC, Conkey LC, Temes CM, et al. Randomized controlled trial of web-based psychoeducation for women with borderline personality disorder. J Clin Psychiatry. 2018;79(3):16m11153. doi: 10.4088/JCP.16m11153
Research has shown that BPD is a treatable illness with a more favorable prognosis than previously believed. Despite this, patients often experience difficulty accessing the most up-to-date information on BPD, which can impede their treatment. A 2008 study by Zanarini et al10 of younger female patients with BPD demonstrated that immediate, in-person psychoeducation improved impulsivity and relationships. Widespread implementation of this program proved problematic, however, due to cost and personnel constraints. To resolve this issue, researchers developed an internet-based version of the program. In a 2018 follow-up study, Zanarini et al4 examined the effect of this internet-based psychoeducation program on symptoms of BPD.
Continue to: Study design...
Study design
- Women (age 18 to 30) who met DSM-IV and Diagnostic Interview for Borderlines–Revised criteria for BPD were randomized to an internet-based psychoeducation treatment group (n = 40) or a control group (n = 40).
- Ten outcomes concerning symptom severity and psychosocial functioning were assessed during weeks 1 to 12 (acute phase) and at months 6, 9, and 12 (maintenance phase) using the self-report version of the Zanarini Rating Scale for BPD (ZAN-BPD), the Borderline Evaluation of Severity over Time, the Sheehan Disability Scale, the Clinically Useful Depression Outcome Scale, the Clinically Useful Anxiety Outcome Scale, and Weissman’s Social Adjustment Scale (SAS).
Outcomes
- In the acute phase, treatment group participants experienced statistically significant improvements in all 10 outcomes. Control group participants demonstrated similar results, achieving statistically significant improvements in 7 of 10 outcomes.
- Compared to the control group, the treatment group experienced a more significant reduction in impulsivity and improvement in psychosocial functioning as measured by the ZAN-BPD and SAS.
- In the maintenance phase, treatment group participants achieved statistically significant improvements in 9 of 10 outcomes, whereas control group participants demonstrated statistically significant improvements in only 3 of 10 outcomes.
- Compared to the control group, the treatment group also demonstrated a significantly greater improvement in all 4 sector scores and the total score of the ZAN-BP
Conclusions/limitations
- In patients with BPD, internet-based psychoeducation reduced symptom severity and improved psychosocial functioning, with effects lasting 1 year. Treatment group participants experienced clinically significant improvements in all outcomes measured during the acute phase of the study; most improvements were maintained over 1 year.
- While the control group initially saw similar improvements in most measurements, these improvements were not maintained as effectively over 1 year.
- Limitations include a female-only population, the restricted age range of participants, and recruitment exclusively from volunteers.
2. McMain SF, Guimond T, Barnhart R, et al. A randomized trial of brief dialectical behaviour therapy skills training in suicidal patients suffering from borderline disorder. Acta Psychiatr Scand. 2017;135(2):138-148.
Standard dialectical behavior therapy (DBT) is an effective treatment for BPD; however, access is often limited by shortages of clinicians and resources. Therefore, it has become increasingly common for clinical settings to offer patients only the skills training component of DBT, which requires fewer resources. While several clinical trials examining brief DBT skills–only treatment for BPD have shown promising results, it is unclear how effective this intervention is at reducing suicidal or nonsuicidal self-injury (NSSI) episodes. McMain et al5 explored the effectiveness of brief DBT skills–only adjunctive treatment on the rates of suicidal and NSSI episodes in patients with BPD.
Study design
- In this 2-arm, single-blind, prospective controlled trial, 84 adults who met DSM-IV criteria for BPD were randomized to a 20-week DBT skills training group (DBT group) or an active waitlist (WL group). No restrictions on additional psychosocial or pharmacologic treatments were imposed on either group.
- The primary outcome was the frequency of suicidal and NSSI episodes as measured by the Lifetime Suicide Attempt Self-Injury Interview and the Deliberate Self-Harm Inventory (DSHI). Measurements occurred at baseline, 10 weeks, 20 weeks, and 3 months posttreatment (32 weeks).
- Secondary outcomes included changes in health care utilization, BPD symptoms, and coping. These were assessed using the Treatment History Interview-2, Borderline Symptom List-23, State-Trait Anger Expression Inventory, Symptom Checklist-90-revised (SCL-90-R), Barratt Impulsiveness Scale-11, Beck Depression Inventory (BDI)-II, Social Adjustment Scale Self-report, Difficulties in Emotion Regulation Scale, Distress Tolerance Scale, and Kentucky Inventory of Mindfulness Scale.
Outcomes
- At Week 32, compared to the WL group, the DBT group showed statistically significant greater reductions in the frequency of suicidal and NSSI episodes as measured by the LSASI but not by the DSHI. The DBT group experienced statistically significant improvements in distress tolerance and emotion regulation over the WL group at all points, but no difference on mindfulness. The DBT group achieved greater reductions in anger over time as compared to the WL group.
- At Week 20, compared to the WL group, the DBT group showed significant improvements in social adjustment, symptom distress, and borderline symptoms. There were no significant group differences on impulsivity. Between-group differences in the number of hospital admissions favored the DBT group at 10 and 20 weeks, but not at 32 weeks. There was no statistically significant difference between the groups with respect to the number of emergency department visits.
- Analyses of group differences in clinical improvement as measured by the SCL-90-R revealed statistically reliable and clinically significant changes in the DBT group over the WL group at 20 weeks, but not at 32 weeks.
Conclusions/limitations
- Brief DBT skills training reduced suicidal and NSSI episodes in patients with BPD. Participants in the DBT group also demonstrated greater improvement in anger, distress tolerance, and emotion regulation compared to the control group. These results were evident 3 months after treatment. However, any gains in health care utilization, social adjustment, symptom distress, and borderline symptoms diminished or did not differ from waitlist participants at Week 32. At that time, participants in the DBT group demonstrated a similar level of symptomatology as the WL group.
- Limitations include the use of an active waitlist control group, allowance of concurrent treatments, the absence of an active therapeutic comparator group, use of self-report measures, use of an instrument with unknown psychometric properties, and a relatively short 3-month follow-up period.
3. Bozzatello P, Bellino S. Combined therapy with interpersonal psychotherapy adapted for borderline personality disorder: a two-years follow-up. Psychiatry Res. 2016;240:151-156.
Psychotherapeutic options for treating BPD include DBT, mentalization-based treatment, schema-focused therapy, transference-based psychotherapy, and systems training for emotional predictability and problem solving. More recently, interpersonal therapy also has been adapted for BPD (IPT-BPD). However, thus far no trials have investigated the long-term effects of this therapy on BPD. In 2010, Bellino et al11 published a 32-week RCT examining the effect of IPT-BPD on BPD. They concluded that IPT-BPD plus fluoxetine was superior to fluoxetine alone in improving symptoms and quality of life. The present study by Bozzatello et al6 examined whether the benefits of IPT-BPD plus fluoxetine demonstrated in the 2010 study persisted over a 24-month follow-up.
Continue to: Study design...
Study design
- In the 2010 study by Bellino et al,11 55 outpatients who met DSM-IV criteria for BPD were randomized to receive IPT-BPD plus fluoxetine (combined therapy) or fluoxetine alone for 32 weeks. Forty-four participants completed a 24-month follow-up study (n = 22 for IPT-BPD plus fluoxetine, n = 22 for fluoxetine only).
- Clinical assessments were performed at 6, 12, and 24 months, and used the same instruments as the original study, including the Clinical Global Impression Scale–Severity item, Hamilton Depression Rating Scale, Hamilton Anxiety Rating Scale (HARS), Social and Occupational Functioning Assessment, Satisfaction Profile (SAT-P), and the Borderline Personality Disorder Severity Index (BPDSI).
Outcomes
- While the original study demonstrated that combined therapy had a clinically significant effect over fluoxetine alone on both HARS score and the BPDSI item “affective instability” at 32 weeks, this advantage was maintained only at the 6-month assessment.
- The improvements that the combined therapy provided over fluoxetine monotherapy on the BPDSI items of “impulsivity” and “interpersonal relationships” as well as the SAT-P factors of social and psychological functioning at 32 weeks were preserved at 24 months. No additional improvements were seen.
Conclusions/limitations
- The improvements in impulsivity, interpersonal functioning, social functioning, and psychological functioning at 32 weeks seen with IPT-BPD plus fluoxetine compared with fluoxetine alone persisted for 2 years after completing therapy; no further improvements were seen.
- The improvements to anxiety and affective instability that combined therapy demonstrated over fluoxetine monotherapy at 32 weeks were not maintained at 24 months.
- Limitations include a small sample size, exclusion of psychiatric comorbidities, and a lack of assessment of session or medication adherence.
4. Antonsen BT, Kvarstein EH, Urnes Ø, et al. Favourable outcome of long-term combined psychotherapy for patients with borderline personality disorder: six-year follow-up of a randomized study. Psychother Res. 2017;27(1):51-63.
While many studies have demonstrated the benefits of psychotherapy for treating personality disorders, there is limited research of how different levels of psychotherapy may impact treatment outcomes. An RCT called the Ullevål Personality Project (UPP)12 compared an intensive combined treatment program (CP) with outpatient individual psychotherapy (OIP) in patients with personality disorders. The CP program consisted of short-term day-hospital treatment followed by outpatient combined group and individual psychotherapy. The outcomes this RCT evaluated included suicide attempts, suicidal thoughts, self-injury, psychosocial functioning, symptom distress, and interpersonal and personality problems. A 6-year follow-up concluded there were no differences in outcomes between the 2 treatment groups. However, in this RCT, Antonsen et al7 examined whether CP produced statistically significant benefits over OIP in a subset of patients with BPD.
Study design
- In the UPP trial,12 117 patients who met DSM-IV criteria for personality disorders (excluding antisocial and schizotypal personality disorder) were randomized to receive 18 weeks of day hospital psychotherapy followed by CP or OIP. Fifty-two participants in the UPP were diagnosed with BPD, and 34 of these participants completed the 6-year follow-up investigation.
- Symptom distress, psychosocial functioning, interpersonal problems, quality of life, personality functioning, and self-harm/suicidal thoughts/suicide attempts were assessed at baseline, 8 months, 18 months, 3 years, and 6 years using the SCL-90-R Global Severity Index (GSI), BDI, Global Assessment of Functioning (GAF), Work and Social Adjustment Scale (WSAS), Quality of Life 10-point scale (QOL), Circumplex of Interpersonal Problems (CIP), and the 60-item short form of the Severity Indices of Personality Problems (SIPP-118) questionnaire.
Outcomes
- Compared to the OIP group, the CP group demonstrated statistically significant reductions in symptom distress at Year 6 as measured by the SCL-90-R GSI. Between Years 3 and 6, the CP group continued to show improvements in psychosocial functioning as demonstrated by improvements in GAF and WSAS scores. The OIP group’s scores worsened during this time. Compared to the OIP group, participants in the CP group also had significantly better outcomes on the SIPP-118 domains of self-control and identity integration.
- There were no significant differences between groups on the proportion of participants who engaged in self-harm or experienced suicidal thoughts or attempts. There were no significant differences in outcomes between the treatment groups on the CIP, BDI, or QOL.
- Participants in CP group tended to use fewer psychotropic medications than those in the OIP group over time, but this difference was not statistically significant. The 2 groups did not differ in use of health care services over the last year.
- Avoidant personality disorder (AVPD) did not have a significant moderator effect on GAF score. Comorbid AVPD was a negative predictor of GAF score, independent of the group.
Conclusions/limitations
- Both groups experienced a remission rate of 90% at 6-year follow-up. Compared with the OIP group, participants in the CP group experienced significantly greater reductions in symptom distress and improvements in self-control and identity integration at 6 years. Between Years 3 and 6, participants in the CP group experienced significant improvements in psychosocial functioning compared with OIP group participants. The 2 groups did not differ on other outcomes, including the CIP, BDI, QOL, suicidal thoughts, suicidal attempts, self-harm, and health care utilization.
- Despite statistically significant differences in GAF scores favoring the CP group over the OIP group during Years 3 to 6, GAF scores did not differ significantly in the final year, which suggests that symptomatic remission does not equal functional improvement.
- Limitations include a lack of control for intensity or length of treatment in statistical analyses, small sample size, lack of correction for multiple testing, lack of an a priori power analysis, missing data and potential violation of the missing at random assumption, use of therapists’ preferred treatment method/practice, and a lack of control for other treatments.
5. Bateman A, Constantinou MP, Fonagy P, et al. Eight-year prospective follow-up of mentalization-based treatment versus structured clinical management for people with borderline personality disorder. Personal Disord. 2021;12(4):291-299.
The efficacy of various psychotherapies for symptoms of BPD has been well established. However, there is limited evidence that these effects persist over time. In 2009, Bateman et al13 conducted an 18-month RCT comparing the effectiveness of outpatient mentalization-based treatment (MBT) against structured clinical management (SCM) for patients with BPD. Both groups experienced substantial improvements, but patients assigned to MBT demonstrated greater improvement in clinically significant problems, including suicide attempts and hospitalizations. In a 2021 follow-up to this study, Bateman et al8 investigated whether the MBT group’s gains in the primary outcomes (absence of severe self-harm, suicide attempts, and inpatient admissions in the previous 12 months), social functioning, vocational engagement, and mental health service usage were maintained throughout an 8-year follow-up period.
Continue to: Study design...
Study design
- In the 2009 trial, Bateman et al13 randomized adult participants who met DSM-IV criteria for BPD and had a suicide attempt or episode of life-threatening self-harm in the past 6 months to receive 18 months of MBT or SCM. The primary outcome was crisis events, defined as a composite of suicidal and severe self-injurious behaviors and hospitalizations. The 2021 Bateman et al8 study expanded this investigation by collecting additional data on a yearly basis for 8 years.
- Of the 134 original participants, 98 agreed to complete the follow-up. Due to attrition, the follow-up period was limited to 8 years. At each yearly visit, researchers collected information on the primary outcome, the absence of severe self-harm, suicide attempts, and inpatient admissions in the previous 12 months.
- Secondary measures were collected mainly through a modified version of the Client Service Receipt Inventory and included critical incidents, psychiatric and medical hospital and community services, employment and other personally meaningful activity, psychoactive medication, and other mental health treatments.
Outcomes
- The number of participants who met diagnostic criteria for BPD at the 1-year follow-up was significantly lower in the MBT group compared with the SCM group. To improve participant retention, this outcome was not evaluated at later visits.
- The number of participants who achieved the primary recovery criteria of the original trial (absence of severe self-harm, suicide attempts, and inpatient admissions in the previous 12 months) and remained well throughout the entire follow-up period was significantly higher in the MBT group compared with the SCM group. The average number of years during which participants failed to meet recovery criteria was significantly greater in the SCM group compared with the MBT group.
- When controlling for age, treatment group was a significant predictor of recovery during the follow-up period. Overall, significantly fewer participants in the MBT group experienced critical incidents during the follow-up period.
- The SCM group used crisis mental health services for a significantly greater number of follow-up years than the MBT group, although the likelihood of ever using crisis services did not statistically differ between the groups. Both groups had similar use of outpatient mental health services, primary care services, and nonmental health medical services. Compared to the SCM group, the MBT group had significantly fewer professional support service visits and significantly fewer outpatient psychiatrist visits.
- MBT group participants spent more time in education, were less likely to be unemployed, and were less likely to use social care interventions than SCM group participants. Although those in the MBT group spent more months engaged in purposeful activity, there was no significant difference between the groups in the proportion of participants who did not engage in purposeful activity.
- The MBT group spent fewer months receiving psychotherapeutic medication compared with the SCM group. The variables that yielded significant 2-way interactions were eating disorder, substance use disorder, and physical abuse, suggesting greater benefit from MBT with these concurrent diagnoses. Younger age was associated with better outcomes.
Conclusions/limitations
- This study demonstrated that patients with BPD significantly benefited from specialized therapies such as MBT.
- At the 1 follow-up visit, the number of participants who met diagnostic criteria for BPD was significantly lower in the MBT group compared with the SCM group.
- The number of participants who had achieved the primary recovery criteria and remained well during the 8-year follow-up period was significantly higher in the MBT group compared to the SCM group.
- Limitations include increasing attrition over time, possible allegiance effects and unmasking of research assistants, lack of self-report questionnaires, and the potentially erroneous conclusion that increased use of services equates to poorer treatment response and greater need for support.
6. Klein JP, Hauer-von Mauschwitz A, Berger T, et al. Effectiveness and safety of the adjunctive use of an internet-based self-management intervention for borderline personality disorder in addition to care as usual: results from a randomised controlled trial. BMJ Open. 2021;11(9):e047771.
Fewer than 1 in 4 patients with BPD have access to effective psychotherapies. The use of internet-based self-management interventions (SMIs) developed from evidence-based psychotherapies can help close this treatment gap. Although the efficacy of SMIs for several mental disorders has been demonstrated in multiple meta-analyses, results for BPD are mixed. In this study, Klein et al9 examined the effectiveness and safety of the adjunctive use of an SMI based on schema therapy in addition to care as usual (CAU) in patients with BPD.
Study design
- In a 12-month, rater-blind, controlled parallel group trial, adults who had a total BPDSI score ≥15 and either a diagnosis of BPD according to DSM-IV criteria or a probable diagnosis of BPD (if they had also received a BPD diagnosis from their treating physician) were randomized to an internet-based SMI based on schema therapy called priovi (n = 103) or CAU (n = 101). Participants could complete the SMI content in approximately 6 months but were recommended to use the intervention for the entire year.
- Participation in psychotherapy and psychiatric treatment, including pharmacotherapy, was permitted. At baseline, 74% of participants were receiving psychotherapy and 88% were receiving psychiatric treatment.
- The primary outcome was change in BPDSI score at 12 months. The primary safety outcome was the number of serious adverse events at 12 months. Secondary outcomes included BPD severity, depressive symptoms, anxiety symptoms, quality of life, uncontrolled internet use, negative treatment effects, and satisfaction with the intervention. Most assessments were measured at baseline, 3 months, 6 months, 9 months, and 12 months.
Outcomes
- Large reductions in the severity of BPD symptoms as measured by change in BPDSI score was observed in both groups. Although the average reduction in BPDSI score was greater in the SMI group, this difference was not statistically significant from the CAU group.
- There was no statistically significant difference in the number of serious adverse events between groups at any time.
Conclusions/limitations
- Treatment with SMI did not result in improved outcomes over CAU. Although the average reduction in BPDSI score was greater in the SMI group compared to the CAU group, this difference was not statistically significant.
- The authors cautioned that the smaller-than-expected between-groups effect size must be interpreted against the background of an unexpectedly large effect in the CAU group. In fact, the CAU group pre/post effect was comparable to the pre/post effect of intensive specialized DBT treatment groups in previous RCTs.
- The authors also suggested that the high percentage of participants who received psychotherapy did not allow for an additional benefit from SMI.
- Limitations include recruitment method, lack of systematic assessment of accidental unblinding, high exclusion rate due to failure of the participant or treating clinician to provide confirmation of diagnosis, and the use of a serious adverse events assessment that is not psychometrically validated.
Bottom Line
Evidence from randomized controlled trials suggests that internet-based psychoeducation, brief dialectical behavior therapy skills-only treatment, interpersonal therapy, a program that combines day treatment with individual and group psychotherapy, and mentalization-based treatment can improve symptoms and quality of life for patients with borderline personality disorder.
1. Skodol AE, Gunderson JG, McGlashan TM, et al. Functional impairment in patients with schizotypal, borderline, avoidant, or obsessive-compulsive personality disorder. Am J Psychiatry. 2002;159(2):276-83.
2. Bender DS, Dolan RT, Skodol AE, et al. Treatment utilization by patients with personality disorders. Am J Psychiatry. 2001;158(2):295-302.
3. Saeed SA, Kallis AC. Borderline personality disorder: 6 studies of biological interventions. Current Psychiatry. 2021;20(11):26-30,34-36.
4. Zanarini MC, Conkey LC, Temes CM, et al. Randomized controlled trial of web-based psychoeducation for women with borderline personality disorder. J Clin Psychiatry. 2018;79(3):16m11153. doi:10.4088/JCP.16m11153
5. McMain SF, Guimond T, Barnhart R, et al. A randomized trial of brief dialectical behaviour therapy skills training in suicidal patients suffering from borderline disorder. Acta Psychiatr Scand. 2017;135(2):138-148. doi:10.1111/acps.12664
6. Bozzatello P, Bellino S. Combined therapy with interpersonal psychotherapy adapted for borderline personality disorder: a two-years follow-up. Psychiatry Res. 2016;240:151-156. doi:10.1016/j.psychres.2016.04.014
7. Antonsen BT, Kvarstein EH, Urnes Ø, et al. Favourable outcome of long-term combined psychotherapy for patients with borderline personality disorder: six-year follow-up of a randomized study. Psychother Res. 2017;27(1):51-63. doi:10.1080/10503307.2015.1072283
8. Bateman A, Constantinou MP, Fonagy P, et al. Eight-year prospective follow-up of mentalization-based treatment versus structured clinical management for people with borderline personality disorder. Personal Disord. 2021;12(4):291-299. doi:10.1037/per0000422
9. Klein JP, Hauer-von Mauschwitz A, Berger T, et al. Effectiveness and safety of the adjunctive use of an internet-based self-management intervention for borderline personality disorder in addition to care as usual: results from a randomised controlled trial. BMJ Open. 2021;11(9):e047771. doi:10.1136/bmjopen-2020-047771
10. Zanarini MC, Frankenburg FR. A preliminary, randomized trial of psychoeducation for women with borderline personality disorder. J Pers Disord. 2008;22(3):284-290.
11. Bellino S, Rinaldi C, Bogetto F. Adaptation of interpersonal psychotherapy to borderline personality disorder: a comparison of combined therapy and single pharmacotherapy. Can J Psychiatry. 2010;55(2):74-81.
12. Arnevik E, Wilberg T, Urnes Ø, et al. Psychotherapy for personality disorders: short-term day hospital psychotherapy versus outpatient individual therapy – a randomized controlled study. Eur Psychiatry. 2009,24(2):71-78. doi:10.1016/j.eurpsy.2008.09.004
13. Bateman A, Fonagy P. Randomized controlled trial of outpatient mentalization-based treatment versus structured clinical management for borderline personality disorder. Am J Psychiatry. 2009;166(12):1355-1364.
SECOND OF 2 PARTS
Borderline personality disorder (BPD) is associated with serious impairment in psychosocial functioning.1 It is characterized by an ongoing pattern of mood instability, cognitive distortions, problems with self-image, and impulsive behavior that often results in problems in relationships. As a result, patients with BPD tend to utilize more mental health services than patients with other personality disorders or major depressive disorder.2
Some clinicians believe BPD is difficult to treat. While historically there has been little consensus on the best treatments for this disorder, current options include both pharmacologic and psychological interventions. In Part 1 of this 2-part article, we focused on 6 studies that evaluated biological interventions.3 Here in Part 2, we focus on findings from 6 recent randomized controlled trials (RCTs) of psychosocial interventions for BPD
1. Zanarini MC, Conkey LC, Temes CM, et al. Randomized controlled trial of web-based psychoeducation for women with borderline personality disorder. J Clin Psychiatry. 2018;79(3):16m11153. doi: 10.4088/JCP.16m11153
Research has shown that BPD is a treatable illness with a more favorable prognosis than previously believed. Despite this, patients often experience difficulty accessing the most up-to-date information on BPD, which can impede their treatment. A 2008 study by Zanarini et al10 of younger female patients with BPD demonstrated that immediate, in-person psychoeducation improved impulsivity and relationships. Widespread implementation of this program proved problematic, however, due to cost and personnel constraints. To resolve this issue, researchers developed an internet-based version of the program. In a 2018 follow-up study, Zanarini et al4 examined the effect of this internet-based psychoeducation program on symptoms of BPD.
Continue to: Study design...
Study design
- Women (age 18 to 30) who met DSM-IV and Diagnostic Interview for Borderlines–Revised criteria for BPD were randomized to an internet-based psychoeducation treatment group (n = 40) or a control group (n = 40).
- Ten outcomes concerning symptom severity and psychosocial functioning were assessed during weeks 1 to 12 (acute phase) and at months 6, 9, and 12 (maintenance phase) using the self-report version of the Zanarini Rating Scale for BPD (ZAN-BPD), the Borderline Evaluation of Severity over Time, the Sheehan Disability Scale, the Clinically Useful Depression Outcome Scale, the Clinically Useful Anxiety Outcome Scale, and Weissman’s Social Adjustment Scale (SAS).
Outcomes
- In the acute phase, treatment group participants experienced statistically significant improvements in all 10 outcomes. Control group participants demonstrated similar results, achieving statistically significant improvements in 7 of 10 outcomes.
- Compared to the control group, the treatment group experienced a more significant reduction in impulsivity and improvement in psychosocial functioning as measured by the ZAN-BPD and SAS.
- In the maintenance phase, treatment group participants achieved statistically significant improvements in 9 of 10 outcomes, whereas control group participants demonstrated statistically significant improvements in only 3 of 10 outcomes.
- Compared to the control group, the treatment group also demonstrated a significantly greater improvement in all 4 sector scores and the total score of the ZAN-BP
Conclusions/limitations
- In patients with BPD, internet-based psychoeducation reduced symptom severity and improved psychosocial functioning, with effects lasting 1 year. Treatment group participants experienced clinically significant improvements in all outcomes measured during the acute phase of the study; most improvements were maintained over 1 year.
- While the control group initially saw similar improvements in most measurements, these improvements were not maintained as effectively over 1 year.
- Limitations include a female-only population, the restricted age range of participants, and recruitment exclusively from volunteers.
2. McMain SF, Guimond T, Barnhart R, et al. A randomized trial of brief dialectical behaviour therapy skills training in suicidal patients suffering from borderline disorder. Acta Psychiatr Scand. 2017;135(2):138-148.
Standard dialectical behavior therapy (DBT) is an effective treatment for BPD; however, access is often limited by shortages of clinicians and resources. Therefore, it has become increasingly common for clinical settings to offer patients only the skills training component of DBT, which requires fewer resources. While several clinical trials examining brief DBT skills–only treatment for BPD have shown promising results, it is unclear how effective this intervention is at reducing suicidal or nonsuicidal self-injury (NSSI) episodes. McMain et al5 explored the effectiveness of brief DBT skills–only adjunctive treatment on the rates of suicidal and NSSI episodes in patients with BPD.
Study design
- In this 2-arm, single-blind, prospective controlled trial, 84 adults who met DSM-IV criteria for BPD were randomized to a 20-week DBT skills training group (DBT group) or an active waitlist (WL group). No restrictions on additional psychosocial or pharmacologic treatments were imposed on either group.
- The primary outcome was the frequency of suicidal and NSSI episodes as measured by the Lifetime Suicide Attempt Self-Injury Interview and the Deliberate Self-Harm Inventory (DSHI). Measurements occurred at baseline, 10 weeks, 20 weeks, and 3 months posttreatment (32 weeks).
- Secondary outcomes included changes in health care utilization, BPD symptoms, and coping. These were assessed using the Treatment History Interview-2, Borderline Symptom List-23, State-Trait Anger Expression Inventory, Symptom Checklist-90-revised (SCL-90-R), Barratt Impulsiveness Scale-11, Beck Depression Inventory (BDI)-II, Social Adjustment Scale Self-report, Difficulties in Emotion Regulation Scale, Distress Tolerance Scale, and Kentucky Inventory of Mindfulness Scale.
Outcomes
- At Week 32, compared to the WL group, the DBT group showed statistically significant greater reductions in the frequency of suicidal and NSSI episodes as measured by the LSASI but not by the DSHI. The DBT group experienced statistically significant improvements in distress tolerance and emotion regulation over the WL group at all points, but no difference on mindfulness. The DBT group achieved greater reductions in anger over time as compared to the WL group.
- At Week 20, compared to the WL group, the DBT group showed significant improvements in social adjustment, symptom distress, and borderline symptoms. There were no significant group differences on impulsivity. Between-group differences in the number of hospital admissions favored the DBT group at 10 and 20 weeks, but not at 32 weeks. There was no statistically significant difference between the groups with respect to the number of emergency department visits.
- Analyses of group differences in clinical improvement as measured by the SCL-90-R revealed statistically reliable and clinically significant changes in the DBT group over the WL group at 20 weeks, but not at 32 weeks.
Conclusions/limitations
- Brief DBT skills training reduced suicidal and NSSI episodes in patients with BPD. Participants in the DBT group also demonstrated greater improvement in anger, distress tolerance, and emotion regulation compared to the control group. These results were evident 3 months after treatment. However, any gains in health care utilization, social adjustment, symptom distress, and borderline symptoms diminished or did not differ from waitlist participants at Week 32. At that time, participants in the DBT group demonstrated a similar level of symptomatology as the WL group.
- Limitations include the use of an active waitlist control group, allowance of concurrent treatments, the absence of an active therapeutic comparator group, use of self-report measures, use of an instrument with unknown psychometric properties, and a relatively short 3-month follow-up period.
3. Bozzatello P, Bellino S. Combined therapy with interpersonal psychotherapy adapted for borderline personality disorder: a two-years follow-up. Psychiatry Res. 2016;240:151-156.
Psychotherapeutic options for treating BPD include DBT, mentalization-based treatment, schema-focused therapy, transference-based psychotherapy, and systems training for emotional predictability and problem solving. More recently, interpersonal therapy also has been adapted for BPD (IPT-BPD). However, thus far no trials have investigated the long-term effects of this therapy on BPD. In 2010, Bellino et al11 published a 32-week RCT examining the effect of IPT-BPD on BPD. They concluded that IPT-BPD plus fluoxetine was superior to fluoxetine alone in improving symptoms and quality of life. The present study by Bozzatello et al6 examined whether the benefits of IPT-BPD plus fluoxetine demonstrated in the 2010 study persisted over a 24-month follow-up.
Continue to: Study design...
Study design
- In the 2010 study by Bellino et al,11 55 outpatients who met DSM-IV criteria for BPD were randomized to receive IPT-BPD plus fluoxetine (combined therapy) or fluoxetine alone for 32 weeks. Forty-four participants completed a 24-month follow-up study (n = 22 for IPT-BPD plus fluoxetine, n = 22 for fluoxetine only).
- Clinical assessments were performed at 6, 12, and 24 months, and used the same instruments as the original study, including the Clinical Global Impression Scale–Severity item, Hamilton Depression Rating Scale, Hamilton Anxiety Rating Scale (HARS), Social and Occupational Functioning Assessment, Satisfaction Profile (SAT-P), and the Borderline Personality Disorder Severity Index (BPDSI).
Outcomes
- While the original study demonstrated that combined therapy had a clinically significant effect over fluoxetine alone on both HARS score and the BPDSI item “affective instability” at 32 weeks, this advantage was maintained only at the 6-month assessment.
- The improvements that the combined therapy provided over fluoxetine monotherapy on the BPDSI items of “impulsivity” and “interpersonal relationships” as well as the SAT-P factors of social and psychological functioning at 32 weeks were preserved at 24 months. No additional improvements were seen.
Conclusions/limitations
- The improvements in impulsivity, interpersonal functioning, social functioning, and psychological functioning at 32 weeks seen with IPT-BPD plus fluoxetine compared with fluoxetine alone persisted for 2 years after completing therapy; no further improvements were seen.
- The improvements to anxiety and affective instability that combined therapy demonstrated over fluoxetine monotherapy at 32 weeks were not maintained at 24 months.
- Limitations include a small sample size, exclusion of psychiatric comorbidities, and a lack of assessment of session or medication adherence.
4. Antonsen BT, Kvarstein EH, Urnes Ø, et al. Favourable outcome of long-term combined psychotherapy for patients with borderline personality disorder: six-year follow-up of a randomized study. Psychother Res. 2017;27(1):51-63.
While many studies have demonstrated the benefits of psychotherapy for treating personality disorders, there is limited research of how different levels of psychotherapy may impact treatment outcomes. An RCT called the Ullevål Personality Project (UPP)12 compared an intensive combined treatment program (CP) with outpatient individual psychotherapy (OIP) in patients with personality disorders. The CP program consisted of short-term day-hospital treatment followed by outpatient combined group and individual psychotherapy. The outcomes this RCT evaluated included suicide attempts, suicidal thoughts, self-injury, psychosocial functioning, symptom distress, and interpersonal and personality problems. A 6-year follow-up concluded there were no differences in outcomes between the 2 treatment groups. However, in this RCT, Antonsen et al7 examined whether CP produced statistically significant benefits over OIP in a subset of patients with BPD.
Study design
- In the UPP trial,12 117 patients who met DSM-IV criteria for personality disorders (excluding antisocial and schizotypal personality disorder) were randomized to receive 18 weeks of day hospital psychotherapy followed by CP or OIP. Fifty-two participants in the UPP were diagnosed with BPD, and 34 of these participants completed the 6-year follow-up investigation.
- Symptom distress, psychosocial functioning, interpersonal problems, quality of life, personality functioning, and self-harm/suicidal thoughts/suicide attempts were assessed at baseline, 8 months, 18 months, 3 years, and 6 years using the SCL-90-R Global Severity Index (GSI), BDI, Global Assessment of Functioning (GAF), Work and Social Adjustment Scale (WSAS), Quality of Life 10-point scale (QOL), Circumplex of Interpersonal Problems (CIP), and the 60-item short form of the Severity Indices of Personality Problems (SIPP-118) questionnaire.
Outcomes
- Compared to the OIP group, the CP group demonstrated statistically significant reductions in symptom distress at Year 6 as measured by the SCL-90-R GSI. Between Years 3 and 6, the CP group continued to show improvements in psychosocial functioning as demonstrated by improvements in GAF and WSAS scores. The OIP group’s scores worsened during this time. Compared to the OIP group, participants in the CP group also had significantly better outcomes on the SIPP-118 domains of self-control and identity integration.
- There were no significant differences between groups on the proportion of participants who engaged in self-harm or experienced suicidal thoughts or attempts. There were no significant differences in outcomes between the treatment groups on the CIP, BDI, or QOL.
- Participants in CP group tended to use fewer psychotropic medications than those in the OIP group over time, but this difference was not statistically significant. The 2 groups did not differ in use of health care services over the last year.
- Avoidant personality disorder (AVPD) did not have a significant moderator effect on GAF score. Comorbid AVPD was a negative predictor of GAF score, independent of the group.
Conclusions/limitations
- Both groups experienced a remission rate of 90% at 6-year follow-up. Compared with the OIP group, participants in the CP group experienced significantly greater reductions in symptom distress and improvements in self-control and identity integration at 6 years. Between Years 3 and 6, participants in the CP group experienced significant improvements in psychosocial functioning compared with OIP group participants. The 2 groups did not differ on other outcomes, including the CIP, BDI, QOL, suicidal thoughts, suicidal attempts, self-harm, and health care utilization.
- Despite statistically significant differences in GAF scores favoring the CP group over the OIP group during Years 3 to 6, GAF scores did not differ significantly in the final year, which suggests that symptomatic remission does not equal functional improvement.
- Limitations include a lack of control for intensity or length of treatment in statistical analyses, small sample size, lack of correction for multiple testing, lack of an a priori power analysis, missing data and potential violation of the missing at random assumption, use of therapists’ preferred treatment method/practice, and a lack of control for other treatments.
5. Bateman A, Constantinou MP, Fonagy P, et al. Eight-year prospective follow-up of mentalization-based treatment versus structured clinical management for people with borderline personality disorder. Personal Disord. 2021;12(4):291-299.
The efficacy of various psychotherapies for symptoms of BPD has been well established. However, there is limited evidence that these effects persist over time. In 2009, Bateman et al13 conducted an 18-month RCT comparing the effectiveness of outpatient mentalization-based treatment (MBT) against structured clinical management (SCM) for patients with BPD. Both groups experienced substantial improvements, but patients assigned to MBT demonstrated greater improvement in clinically significant problems, including suicide attempts and hospitalizations. In a 2021 follow-up to this study, Bateman et al8 investigated whether the MBT group’s gains in the primary outcomes (absence of severe self-harm, suicide attempts, and inpatient admissions in the previous 12 months), social functioning, vocational engagement, and mental health service usage were maintained throughout an 8-year follow-up period.
Continue to: Study design...
Study design
- In the 2009 trial, Bateman et al13 randomized adult participants who met DSM-IV criteria for BPD and had a suicide attempt or episode of life-threatening self-harm in the past 6 months to receive 18 months of MBT or SCM. The primary outcome was crisis events, defined as a composite of suicidal and severe self-injurious behaviors and hospitalizations. The 2021 Bateman et al8 study expanded this investigation by collecting additional data on a yearly basis for 8 years.
- Of the 134 original participants, 98 agreed to complete the follow-up. Due to attrition, the follow-up period was limited to 8 years. At each yearly visit, researchers collected information on the primary outcome, the absence of severe self-harm, suicide attempts, and inpatient admissions in the previous 12 months.
- Secondary measures were collected mainly through a modified version of the Client Service Receipt Inventory and included critical incidents, psychiatric and medical hospital and community services, employment and other personally meaningful activity, psychoactive medication, and other mental health treatments.
Outcomes
- The number of participants who met diagnostic criteria for BPD at the 1-year follow-up was significantly lower in the MBT group compared with the SCM group. To improve participant retention, this outcome was not evaluated at later visits.
- The number of participants who achieved the primary recovery criteria of the original trial (absence of severe self-harm, suicide attempts, and inpatient admissions in the previous 12 months) and remained well throughout the entire follow-up period was significantly higher in the MBT group compared with the SCM group. The average number of years during which participants failed to meet recovery criteria was significantly greater in the SCM group compared with the MBT group.
- When controlling for age, treatment group was a significant predictor of recovery during the follow-up period. Overall, significantly fewer participants in the MBT group experienced critical incidents during the follow-up period.
- The SCM group used crisis mental health services for a significantly greater number of follow-up years than the MBT group, although the likelihood of ever using crisis services did not statistically differ between the groups. Both groups had similar use of outpatient mental health services, primary care services, and nonmental health medical services. Compared to the SCM group, the MBT group had significantly fewer professional support service visits and significantly fewer outpatient psychiatrist visits.
- MBT group participants spent more time in education, were less likely to be unemployed, and were less likely to use social care interventions than SCM group participants. Although those in the MBT group spent more months engaged in purposeful activity, there was no significant difference between the groups in the proportion of participants who did not engage in purposeful activity.
- The MBT group spent fewer months receiving psychotherapeutic medication compared with the SCM group. The variables that yielded significant 2-way interactions were eating disorder, substance use disorder, and physical abuse, suggesting greater benefit from MBT with these concurrent diagnoses. Younger age was associated with better outcomes.
Conclusions/limitations
- This study demonstrated that patients with BPD significantly benefited from specialized therapies such as MBT.
- At the 1 follow-up visit, the number of participants who met diagnostic criteria for BPD was significantly lower in the MBT group compared with the SCM group.
- The number of participants who had achieved the primary recovery criteria and remained well during the 8-year follow-up period was significantly higher in the MBT group compared to the SCM group.
- Limitations include increasing attrition over time, possible allegiance effects and unmasking of research assistants, lack of self-report questionnaires, and the potentially erroneous conclusion that increased use of services equates to poorer treatment response and greater need for support.
6. Klein JP, Hauer-von Mauschwitz A, Berger T, et al. Effectiveness and safety of the adjunctive use of an internet-based self-management intervention for borderline personality disorder in addition to care as usual: results from a randomised controlled trial. BMJ Open. 2021;11(9):e047771.
Fewer than 1 in 4 patients with BPD have access to effective psychotherapies. The use of internet-based self-management interventions (SMIs) developed from evidence-based psychotherapies can help close this treatment gap. Although the efficacy of SMIs for several mental disorders has been demonstrated in multiple meta-analyses, results for BPD are mixed. In this study, Klein et al9 examined the effectiveness and safety of the adjunctive use of an SMI based on schema therapy in addition to care as usual (CAU) in patients with BPD.
Study design
- In a 12-month, rater-blind, controlled parallel group trial, adults who had a total BPDSI score ≥15 and either a diagnosis of BPD according to DSM-IV criteria or a probable diagnosis of BPD (if they had also received a BPD diagnosis from their treating physician) were randomized to an internet-based SMI based on schema therapy called priovi (n = 103) or CAU (n = 101). Participants could complete the SMI content in approximately 6 months but were recommended to use the intervention for the entire year.
- Participation in psychotherapy and psychiatric treatment, including pharmacotherapy, was permitted. At baseline, 74% of participants were receiving psychotherapy and 88% were receiving psychiatric treatment.
- The primary outcome was change in BPDSI score at 12 months. The primary safety outcome was the number of serious adverse events at 12 months. Secondary outcomes included BPD severity, depressive symptoms, anxiety symptoms, quality of life, uncontrolled internet use, negative treatment effects, and satisfaction with the intervention. Most assessments were measured at baseline, 3 months, 6 months, 9 months, and 12 months.
Outcomes
- Large reductions in the severity of BPD symptoms as measured by change in BPDSI score was observed in both groups. Although the average reduction in BPDSI score was greater in the SMI group, this difference was not statistically significant from the CAU group.
- There was no statistically significant difference in the number of serious adverse events between groups at any time.
Conclusions/limitations
- Treatment with SMI did not result in improved outcomes over CAU. Although the average reduction in BPDSI score was greater in the SMI group compared to the CAU group, this difference was not statistically significant.
- The authors cautioned that the smaller-than-expected between-groups effect size must be interpreted against the background of an unexpectedly large effect in the CAU group. In fact, the CAU group pre/post effect was comparable to the pre/post effect of intensive specialized DBT treatment groups in previous RCTs.
- The authors also suggested that the high percentage of participants who received psychotherapy did not allow for an additional benefit from SMI.
- Limitations include recruitment method, lack of systematic assessment of accidental unblinding, high exclusion rate due to failure of the participant or treating clinician to provide confirmation of diagnosis, and the use of a serious adverse events assessment that is not psychometrically validated.
Bottom Line
Evidence from randomized controlled trials suggests that internet-based psychoeducation, brief dialectical behavior therapy skills-only treatment, interpersonal therapy, a program that combines day treatment with individual and group psychotherapy, and mentalization-based treatment can improve symptoms and quality of life for patients with borderline personality disorder.
SECOND OF 2 PARTS
Borderline personality disorder (BPD) is associated with serious impairment in psychosocial functioning.1 It is characterized by an ongoing pattern of mood instability, cognitive distortions, problems with self-image, and impulsive behavior that often results in problems in relationships. As a result, patients with BPD tend to utilize more mental health services than patients with other personality disorders or major depressive disorder.2
Some clinicians believe BPD is difficult to treat. While historically there has been little consensus on the best treatments for this disorder, current options include both pharmacologic and psychological interventions. In Part 1 of this 2-part article, we focused on 6 studies that evaluated biological interventions.3 Here in Part 2, we focus on findings from 6 recent randomized controlled trials (RCTs) of psychosocial interventions for BPD
1. Zanarini MC, Conkey LC, Temes CM, et al. Randomized controlled trial of web-based psychoeducation for women with borderline personality disorder. J Clin Psychiatry. 2018;79(3):16m11153. doi: 10.4088/JCP.16m11153
Research has shown that BPD is a treatable illness with a more favorable prognosis than previously believed. Despite this, patients often experience difficulty accessing the most up-to-date information on BPD, which can impede their treatment. A 2008 study by Zanarini et al10 of younger female patients with BPD demonstrated that immediate, in-person psychoeducation improved impulsivity and relationships. Widespread implementation of this program proved problematic, however, due to cost and personnel constraints. To resolve this issue, researchers developed an internet-based version of the program. In a 2018 follow-up study, Zanarini et al4 examined the effect of this internet-based psychoeducation program on symptoms of BPD.
Continue to: Study design...
Study design
- Women (age 18 to 30) who met DSM-IV and Diagnostic Interview for Borderlines–Revised criteria for BPD were randomized to an internet-based psychoeducation treatment group (n = 40) or a control group (n = 40).
- Ten outcomes concerning symptom severity and psychosocial functioning were assessed during weeks 1 to 12 (acute phase) and at months 6, 9, and 12 (maintenance phase) using the self-report version of the Zanarini Rating Scale for BPD (ZAN-BPD), the Borderline Evaluation of Severity over Time, the Sheehan Disability Scale, the Clinically Useful Depression Outcome Scale, the Clinically Useful Anxiety Outcome Scale, and Weissman’s Social Adjustment Scale (SAS).
Outcomes
- In the acute phase, treatment group participants experienced statistically significant improvements in all 10 outcomes. Control group participants demonstrated similar results, achieving statistically significant improvements in 7 of 10 outcomes.
- Compared to the control group, the treatment group experienced a more significant reduction in impulsivity and improvement in psychosocial functioning as measured by the ZAN-BPD and SAS.
- In the maintenance phase, treatment group participants achieved statistically significant improvements in 9 of 10 outcomes, whereas control group participants demonstrated statistically significant improvements in only 3 of 10 outcomes.
- Compared to the control group, the treatment group also demonstrated a significantly greater improvement in all 4 sector scores and the total score of the ZAN-BP
Conclusions/limitations
- In patients with BPD, internet-based psychoeducation reduced symptom severity and improved psychosocial functioning, with effects lasting 1 year. Treatment group participants experienced clinically significant improvements in all outcomes measured during the acute phase of the study; most improvements were maintained over 1 year.
- While the control group initially saw similar improvements in most measurements, these improvements were not maintained as effectively over 1 year.
- Limitations include a female-only population, the restricted age range of participants, and recruitment exclusively from volunteers.
2. McMain SF, Guimond T, Barnhart R, et al. A randomized trial of brief dialectical behaviour therapy skills training in suicidal patients suffering from borderline disorder. Acta Psychiatr Scand. 2017;135(2):138-148.
Standard dialectical behavior therapy (DBT) is an effective treatment for BPD; however, access is often limited by shortages of clinicians and resources. Therefore, it has become increasingly common for clinical settings to offer patients only the skills training component of DBT, which requires fewer resources. While several clinical trials examining brief DBT skills–only treatment for BPD have shown promising results, it is unclear how effective this intervention is at reducing suicidal or nonsuicidal self-injury (NSSI) episodes. McMain et al5 explored the effectiveness of brief DBT skills–only adjunctive treatment on the rates of suicidal and NSSI episodes in patients with BPD.
Study design
- In this 2-arm, single-blind, prospective controlled trial, 84 adults who met DSM-IV criteria for BPD were randomized to a 20-week DBT skills training group (DBT group) or an active waitlist (WL group). No restrictions on additional psychosocial or pharmacologic treatments were imposed on either group.
- The primary outcome was the frequency of suicidal and NSSI episodes as measured by the Lifetime Suicide Attempt Self-Injury Interview and the Deliberate Self-Harm Inventory (DSHI). Measurements occurred at baseline, 10 weeks, 20 weeks, and 3 months posttreatment (32 weeks).
- Secondary outcomes included changes in health care utilization, BPD symptoms, and coping. These were assessed using the Treatment History Interview-2, Borderline Symptom List-23, State-Trait Anger Expression Inventory, Symptom Checklist-90-revised (SCL-90-R), Barratt Impulsiveness Scale-11, Beck Depression Inventory (BDI)-II, Social Adjustment Scale Self-report, Difficulties in Emotion Regulation Scale, Distress Tolerance Scale, and Kentucky Inventory of Mindfulness Scale.
Outcomes
- At Week 32, compared to the WL group, the DBT group showed statistically significant greater reductions in the frequency of suicidal and NSSI episodes as measured by the LSASI but not by the DSHI. The DBT group experienced statistically significant improvements in distress tolerance and emotion regulation over the WL group at all points, but no difference on mindfulness. The DBT group achieved greater reductions in anger over time as compared to the WL group.
- At Week 20, compared to the WL group, the DBT group showed significant improvements in social adjustment, symptom distress, and borderline symptoms. There were no significant group differences on impulsivity. Between-group differences in the number of hospital admissions favored the DBT group at 10 and 20 weeks, but not at 32 weeks. There was no statistically significant difference between the groups with respect to the number of emergency department visits.
- Analyses of group differences in clinical improvement as measured by the SCL-90-R revealed statistically reliable and clinically significant changes in the DBT group over the WL group at 20 weeks, but not at 32 weeks.
Conclusions/limitations
- Brief DBT skills training reduced suicidal and NSSI episodes in patients with BPD. Participants in the DBT group also demonstrated greater improvement in anger, distress tolerance, and emotion regulation compared to the control group. These results were evident 3 months after treatment. However, any gains in health care utilization, social adjustment, symptom distress, and borderline symptoms diminished or did not differ from waitlist participants at Week 32. At that time, participants in the DBT group demonstrated a similar level of symptomatology as the WL group.
- Limitations include the use of an active waitlist control group, allowance of concurrent treatments, the absence of an active therapeutic comparator group, use of self-report measures, use of an instrument with unknown psychometric properties, and a relatively short 3-month follow-up period.
3. Bozzatello P, Bellino S. Combined therapy with interpersonal psychotherapy adapted for borderline personality disorder: a two-years follow-up. Psychiatry Res. 2016;240:151-156.
Psychotherapeutic options for treating BPD include DBT, mentalization-based treatment, schema-focused therapy, transference-based psychotherapy, and systems training for emotional predictability and problem solving. More recently, interpersonal therapy also has been adapted for BPD (IPT-BPD). However, thus far no trials have investigated the long-term effects of this therapy on BPD. In 2010, Bellino et al11 published a 32-week RCT examining the effect of IPT-BPD on BPD. They concluded that IPT-BPD plus fluoxetine was superior to fluoxetine alone in improving symptoms and quality of life. The present study by Bozzatello et al6 examined whether the benefits of IPT-BPD plus fluoxetine demonstrated in the 2010 study persisted over a 24-month follow-up.
Continue to: Study design...
Study design
- In the 2010 study by Bellino et al,11 55 outpatients who met DSM-IV criteria for BPD were randomized to receive IPT-BPD plus fluoxetine (combined therapy) or fluoxetine alone for 32 weeks. Forty-four participants completed a 24-month follow-up study (n = 22 for IPT-BPD plus fluoxetine, n = 22 for fluoxetine only).
- Clinical assessments were performed at 6, 12, and 24 months, and used the same instruments as the original study, including the Clinical Global Impression Scale–Severity item, Hamilton Depression Rating Scale, Hamilton Anxiety Rating Scale (HARS), Social and Occupational Functioning Assessment, Satisfaction Profile (SAT-P), and the Borderline Personality Disorder Severity Index (BPDSI).
Outcomes
- While the original study demonstrated that combined therapy had a clinically significant effect over fluoxetine alone on both HARS score and the BPDSI item “affective instability” at 32 weeks, this advantage was maintained only at the 6-month assessment.
- The improvements that the combined therapy provided over fluoxetine monotherapy on the BPDSI items of “impulsivity” and “interpersonal relationships” as well as the SAT-P factors of social and psychological functioning at 32 weeks were preserved at 24 months. No additional improvements were seen.
Conclusions/limitations
- The improvements in impulsivity, interpersonal functioning, social functioning, and psychological functioning at 32 weeks seen with IPT-BPD plus fluoxetine compared with fluoxetine alone persisted for 2 years after completing therapy; no further improvements were seen.
- The improvements to anxiety and affective instability that combined therapy demonstrated over fluoxetine monotherapy at 32 weeks were not maintained at 24 months.
- Limitations include a small sample size, exclusion of psychiatric comorbidities, and a lack of assessment of session or medication adherence.
4. Antonsen BT, Kvarstein EH, Urnes Ø, et al. Favourable outcome of long-term combined psychotherapy for patients with borderline personality disorder: six-year follow-up of a randomized study. Psychother Res. 2017;27(1):51-63.
While many studies have demonstrated the benefits of psychotherapy for treating personality disorders, there is limited research of how different levels of psychotherapy may impact treatment outcomes. An RCT called the Ullevål Personality Project (UPP)12 compared an intensive combined treatment program (CP) with outpatient individual psychotherapy (OIP) in patients with personality disorders. The CP program consisted of short-term day-hospital treatment followed by outpatient combined group and individual psychotherapy. The outcomes this RCT evaluated included suicide attempts, suicidal thoughts, self-injury, psychosocial functioning, symptom distress, and interpersonal and personality problems. A 6-year follow-up concluded there were no differences in outcomes between the 2 treatment groups. However, in this RCT, Antonsen et al7 examined whether CP produced statistically significant benefits over OIP in a subset of patients with BPD.
Study design
- In the UPP trial,12 117 patients who met DSM-IV criteria for personality disorders (excluding antisocial and schizotypal personality disorder) were randomized to receive 18 weeks of day hospital psychotherapy followed by CP or OIP. Fifty-two participants in the UPP were diagnosed with BPD, and 34 of these participants completed the 6-year follow-up investigation.
- Symptom distress, psychosocial functioning, interpersonal problems, quality of life, personality functioning, and self-harm/suicidal thoughts/suicide attempts were assessed at baseline, 8 months, 18 months, 3 years, and 6 years using the SCL-90-R Global Severity Index (GSI), BDI, Global Assessment of Functioning (GAF), Work and Social Adjustment Scale (WSAS), Quality of Life 10-point scale (QOL), Circumplex of Interpersonal Problems (CIP), and the 60-item short form of the Severity Indices of Personality Problems (SIPP-118) questionnaire.
Outcomes
- Compared to the OIP group, the CP group demonstrated statistically significant reductions in symptom distress at Year 6 as measured by the SCL-90-R GSI. Between Years 3 and 6, the CP group continued to show improvements in psychosocial functioning as demonstrated by improvements in GAF and WSAS scores. The OIP group’s scores worsened during this time. Compared to the OIP group, participants in the CP group also had significantly better outcomes on the SIPP-118 domains of self-control and identity integration.
- There were no significant differences between groups on the proportion of participants who engaged in self-harm or experienced suicidal thoughts or attempts. There were no significant differences in outcomes between the treatment groups on the CIP, BDI, or QOL.
- Participants in CP group tended to use fewer psychotropic medications than those in the OIP group over time, but this difference was not statistically significant. The 2 groups did not differ in use of health care services over the last year.
- Avoidant personality disorder (AVPD) did not have a significant moderator effect on GAF score. Comorbid AVPD was a negative predictor of GAF score, independent of the group.
Conclusions/limitations
- Both groups experienced a remission rate of 90% at 6-year follow-up. Compared with the OIP group, participants in the CP group experienced significantly greater reductions in symptom distress and improvements in self-control and identity integration at 6 years. Between Years 3 and 6, participants in the CP group experienced significant improvements in psychosocial functioning compared with OIP group participants. The 2 groups did not differ on other outcomes, including the CIP, BDI, QOL, suicidal thoughts, suicidal attempts, self-harm, and health care utilization.
- Despite statistically significant differences in GAF scores favoring the CP group over the OIP group during Years 3 to 6, GAF scores did not differ significantly in the final year, which suggests that symptomatic remission does not equal functional improvement.
- Limitations include a lack of control for intensity or length of treatment in statistical analyses, small sample size, lack of correction for multiple testing, lack of an a priori power analysis, missing data and potential violation of the missing at random assumption, use of therapists’ preferred treatment method/practice, and a lack of control for other treatments.
5. Bateman A, Constantinou MP, Fonagy P, et al. Eight-year prospective follow-up of mentalization-based treatment versus structured clinical management for people with borderline personality disorder. Personal Disord. 2021;12(4):291-299.
The efficacy of various psychotherapies for symptoms of BPD has been well established. However, there is limited evidence that these effects persist over time. In 2009, Bateman et al13 conducted an 18-month RCT comparing the effectiveness of outpatient mentalization-based treatment (MBT) against structured clinical management (SCM) for patients with BPD. Both groups experienced substantial improvements, but patients assigned to MBT demonstrated greater improvement in clinically significant problems, including suicide attempts and hospitalizations. In a 2021 follow-up to this study, Bateman et al8 investigated whether the MBT group’s gains in the primary outcomes (absence of severe self-harm, suicide attempts, and inpatient admissions in the previous 12 months), social functioning, vocational engagement, and mental health service usage were maintained throughout an 8-year follow-up period.
Continue to: Study design...
Study design
- In the 2009 trial, Bateman et al13 randomized adult participants who met DSM-IV criteria for BPD and had a suicide attempt or episode of life-threatening self-harm in the past 6 months to receive 18 months of MBT or SCM. The primary outcome was crisis events, defined as a composite of suicidal and severe self-injurious behaviors and hospitalizations. The 2021 Bateman et al8 study expanded this investigation by collecting additional data on a yearly basis for 8 years.
- Of the 134 original participants, 98 agreed to complete the follow-up. Due to attrition, the follow-up period was limited to 8 years. At each yearly visit, researchers collected information on the primary outcome, the absence of severe self-harm, suicide attempts, and inpatient admissions in the previous 12 months.
- Secondary measures were collected mainly through a modified version of the Client Service Receipt Inventory and included critical incidents, psychiatric and medical hospital and community services, employment and other personally meaningful activity, psychoactive medication, and other mental health treatments.
Outcomes
- The number of participants who met diagnostic criteria for BPD at the 1-year follow-up was significantly lower in the MBT group compared with the SCM group. To improve participant retention, this outcome was not evaluated at later visits.
- The number of participants who achieved the primary recovery criteria of the original trial (absence of severe self-harm, suicide attempts, and inpatient admissions in the previous 12 months) and remained well throughout the entire follow-up period was significantly higher in the MBT group compared with the SCM group. The average number of years during which participants failed to meet recovery criteria was significantly greater in the SCM group compared with the MBT group.
- When controlling for age, treatment group was a significant predictor of recovery during the follow-up period. Overall, significantly fewer participants in the MBT group experienced critical incidents during the follow-up period.
- The SCM group used crisis mental health services for a significantly greater number of follow-up years than the MBT group, although the likelihood of ever using crisis services did not statistically differ between the groups. Both groups had similar use of outpatient mental health services, primary care services, and nonmental health medical services. Compared to the SCM group, the MBT group had significantly fewer professional support service visits and significantly fewer outpatient psychiatrist visits.
- MBT group participants spent more time in education, were less likely to be unemployed, and were less likely to use social care interventions than SCM group participants. Although those in the MBT group spent more months engaged in purposeful activity, there was no significant difference between the groups in the proportion of participants who did not engage in purposeful activity.
- The MBT group spent fewer months receiving psychotherapeutic medication compared with the SCM group. The variables that yielded significant 2-way interactions were eating disorder, substance use disorder, and physical abuse, suggesting greater benefit from MBT with these concurrent diagnoses. Younger age was associated with better outcomes.
Conclusions/limitations
- This study demonstrated that patients with BPD significantly benefited from specialized therapies such as MBT.
- At the 1 follow-up visit, the number of participants who met diagnostic criteria for BPD was significantly lower in the MBT group compared with the SCM group.
- The number of participants who had achieved the primary recovery criteria and remained well during the 8-year follow-up period was significantly higher in the MBT group compared to the SCM group.
- Limitations include increasing attrition over time, possible allegiance effects and unmasking of research assistants, lack of self-report questionnaires, and the potentially erroneous conclusion that increased use of services equates to poorer treatment response and greater need for support.
6. Klein JP, Hauer-von Mauschwitz A, Berger T, et al. Effectiveness and safety of the adjunctive use of an internet-based self-management intervention for borderline personality disorder in addition to care as usual: results from a randomised controlled trial. BMJ Open. 2021;11(9):e047771.
Fewer than 1 in 4 patients with BPD have access to effective psychotherapies. The use of internet-based self-management interventions (SMIs) developed from evidence-based psychotherapies can help close this treatment gap. Although the efficacy of SMIs for several mental disorders has been demonstrated in multiple meta-analyses, results for BPD are mixed. In this study, Klein et al9 examined the effectiveness and safety of the adjunctive use of an SMI based on schema therapy in addition to care as usual (CAU) in patients with BPD.
Study design
- In a 12-month, rater-blind, controlled parallel group trial, adults who had a total BPDSI score ≥15 and either a diagnosis of BPD according to DSM-IV criteria or a probable diagnosis of BPD (if they had also received a BPD diagnosis from their treating physician) were randomized to an internet-based SMI based on schema therapy called priovi (n = 103) or CAU (n = 101). Participants could complete the SMI content in approximately 6 months but were recommended to use the intervention for the entire year.
- Participation in psychotherapy and psychiatric treatment, including pharmacotherapy, was permitted. At baseline, 74% of participants were receiving psychotherapy and 88% were receiving psychiatric treatment.
- The primary outcome was change in BPDSI score at 12 months. The primary safety outcome was the number of serious adverse events at 12 months. Secondary outcomes included BPD severity, depressive symptoms, anxiety symptoms, quality of life, uncontrolled internet use, negative treatment effects, and satisfaction with the intervention. Most assessments were measured at baseline, 3 months, 6 months, 9 months, and 12 months.
Outcomes
- Large reductions in the severity of BPD symptoms as measured by change in BPDSI score was observed in both groups. Although the average reduction in BPDSI score was greater in the SMI group, this difference was not statistically significant from the CAU group.
- There was no statistically significant difference in the number of serious adverse events between groups at any time.
Conclusions/limitations
- Treatment with SMI did not result in improved outcomes over CAU. Although the average reduction in BPDSI score was greater in the SMI group compared to the CAU group, this difference was not statistically significant.
- The authors cautioned that the smaller-than-expected between-groups effect size must be interpreted against the background of an unexpectedly large effect in the CAU group. In fact, the CAU group pre/post effect was comparable to the pre/post effect of intensive specialized DBT treatment groups in previous RCTs.
- The authors also suggested that the high percentage of participants who received psychotherapy did not allow for an additional benefit from SMI.
- Limitations include recruitment method, lack of systematic assessment of accidental unblinding, high exclusion rate due to failure of the participant or treating clinician to provide confirmation of diagnosis, and the use of a serious adverse events assessment that is not psychometrically validated.
Bottom Line
Evidence from randomized controlled trials suggests that internet-based psychoeducation, brief dialectical behavior therapy skills-only treatment, interpersonal therapy, a program that combines day treatment with individual and group psychotherapy, and mentalization-based treatment can improve symptoms and quality of life for patients with borderline personality disorder.
1. Skodol AE, Gunderson JG, McGlashan TM, et al. Functional impairment in patients with schizotypal, borderline, avoidant, or obsessive-compulsive personality disorder. Am J Psychiatry. 2002;159(2):276-83.
2. Bender DS, Dolan RT, Skodol AE, et al. Treatment utilization by patients with personality disorders. Am J Psychiatry. 2001;158(2):295-302.
3. Saeed SA, Kallis AC. Borderline personality disorder: 6 studies of biological interventions. Current Psychiatry. 2021;20(11):26-30,34-36.
4. Zanarini MC, Conkey LC, Temes CM, et al. Randomized controlled trial of web-based psychoeducation for women with borderline personality disorder. J Clin Psychiatry. 2018;79(3):16m11153. doi:10.4088/JCP.16m11153
5. McMain SF, Guimond T, Barnhart R, et al. A randomized trial of brief dialectical behaviour therapy skills training in suicidal patients suffering from borderline disorder. Acta Psychiatr Scand. 2017;135(2):138-148. doi:10.1111/acps.12664
6. Bozzatello P, Bellino S. Combined therapy with interpersonal psychotherapy adapted for borderline personality disorder: a two-years follow-up. Psychiatry Res. 2016;240:151-156. doi:10.1016/j.psychres.2016.04.014
7. Antonsen BT, Kvarstein EH, Urnes Ø, et al. Favourable outcome of long-term combined psychotherapy for patients with borderline personality disorder: six-year follow-up of a randomized study. Psychother Res. 2017;27(1):51-63. doi:10.1080/10503307.2015.1072283
8. Bateman A, Constantinou MP, Fonagy P, et al. Eight-year prospective follow-up of mentalization-based treatment versus structured clinical management for people with borderline personality disorder. Personal Disord. 2021;12(4):291-299. doi:10.1037/per0000422
9. Klein JP, Hauer-von Mauschwitz A, Berger T, et al. Effectiveness and safety of the adjunctive use of an internet-based self-management intervention for borderline personality disorder in addition to care as usual: results from a randomised controlled trial. BMJ Open. 2021;11(9):e047771. doi:10.1136/bmjopen-2020-047771
10. Zanarini MC, Frankenburg FR. A preliminary, randomized trial of psychoeducation for women with borderline personality disorder. J Pers Disord. 2008;22(3):284-290.
11. Bellino S, Rinaldi C, Bogetto F. Adaptation of interpersonal psychotherapy to borderline personality disorder: a comparison of combined therapy and single pharmacotherapy. Can J Psychiatry. 2010;55(2):74-81.
12. Arnevik E, Wilberg T, Urnes Ø, et al. Psychotherapy for personality disorders: short-term day hospital psychotherapy versus outpatient individual therapy – a randomized controlled study. Eur Psychiatry. 2009,24(2):71-78. doi:10.1016/j.eurpsy.2008.09.004
13. Bateman A, Fonagy P. Randomized controlled trial of outpatient mentalization-based treatment versus structured clinical management for borderline personality disorder. Am J Psychiatry. 2009;166(12):1355-1364.
1. Skodol AE, Gunderson JG, McGlashan TM, et al. Functional impairment in patients with schizotypal, borderline, avoidant, or obsessive-compulsive personality disorder. Am J Psychiatry. 2002;159(2):276-83.
2. Bender DS, Dolan RT, Skodol AE, et al. Treatment utilization by patients with personality disorders. Am J Psychiatry. 2001;158(2):295-302.
3. Saeed SA, Kallis AC. Borderline personality disorder: 6 studies of biological interventions. Current Psychiatry. 2021;20(11):26-30,34-36.
4. Zanarini MC, Conkey LC, Temes CM, et al. Randomized controlled trial of web-based psychoeducation for women with borderline personality disorder. J Clin Psychiatry. 2018;79(3):16m11153. doi:10.4088/JCP.16m11153
5. McMain SF, Guimond T, Barnhart R, et al. A randomized trial of brief dialectical behaviour therapy skills training in suicidal patients suffering from borderline disorder. Acta Psychiatr Scand. 2017;135(2):138-148. doi:10.1111/acps.12664
6. Bozzatello P, Bellino S. Combined therapy with interpersonal psychotherapy adapted for borderline personality disorder: a two-years follow-up. Psychiatry Res. 2016;240:151-156. doi:10.1016/j.psychres.2016.04.014
7. Antonsen BT, Kvarstein EH, Urnes Ø, et al. Favourable outcome of long-term combined psychotherapy for patients with borderline personality disorder: six-year follow-up of a randomized study. Psychother Res. 2017;27(1):51-63. doi:10.1080/10503307.2015.1072283
8. Bateman A, Constantinou MP, Fonagy P, et al. Eight-year prospective follow-up of mentalization-based treatment versus structured clinical management for people with borderline personality disorder. Personal Disord. 2021;12(4):291-299. doi:10.1037/per0000422
9. Klein JP, Hauer-von Mauschwitz A, Berger T, et al. Effectiveness and safety of the adjunctive use of an internet-based self-management intervention for borderline personality disorder in addition to care as usual: results from a randomised controlled trial. BMJ Open. 2021;11(9):e047771. doi:10.1136/bmjopen-2020-047771
10. Zanarini MC, Frankenburg FR. A preliminary, randomized trial of psychoeducation for women with borderline personality disorder. J Pers Disord. 2008;22(3):284-290.
11. Bellino S, Rinaldi C, Bogetto F. Adaptation of interpersonal psychotherapy to borderline personality disorder: a comparison of combined therapy and single pharmacotherapy. Can J Psychiatry. 2010;55(2):74-81.
12. Arnevik E, Wilberg T, Urnes Ø, et al. Psychotherapy for personality disorders: short-term day hospital psychotherapy versus outpatient individual therapy – a randomized controlled study. Eur Psychiatry. 2009,24(2):71-78. doi:10.1016/j.eurpsy.2008.09.004
13. Bateman A, Fonagy P. Randomized controlled trial of outpatient mentalization-based treatment versus structured clinical management for borderline personality disorder. Am J Psychiatry. 2009;166(12):1355-1364.
Depressed and awkward: Is it more than that?
CASE Treatment-resistant MDD
Ms. P, age 21, presents to the outpatient clinic. She has diagnoses of treatment-resistant major depressive disorder (MDD) and schizoid personality disorder (SPD). Ms. P was diagnosed with MDD 3 years ago after reporting symptoms of prevailing sadness for approximately 8 years, described as feelings of worthlessness, anhedonia, social withdrawal, and decreased hygiene and self-care behaviors, as well as suicidal ideation and self-harm. SPD was diagnosed 1 year earlier based on her “odd” behaviors and disheveled appearance following observation and in collateral with her family. Her odd behaviors are described as spending most of her time alone, preferring solitary activities, and having little contact with people other than her parents.
Ms. P reports that she was previously treated with citalopram, 20 mg/d, bupropion, 150 mg/d, aripiprazole, 3.75 mg/d, topiramate, 100 mg twice daily, and melatonin, 9 mg/d at bedtime, but discontinued follow-up appointments and medications after no significant improvement in symptoms.
[polldaddy:11027942]
The authors’ observations
The term “schizoid” first made its debut in the medical community to describe the prodromal social withdrawal and isolation observed in schizophrenia.1 The use of schizoid to describe a personality type first occurred in DSM-III in 1980.2 SPD is a Cluster A personality disorder that groups personalities characterized by common traits that are “odd” or “eccentric” and may resemble the positive and/or negative symptoms of schizophrenia.3,4 Relatively uncommon in clinical settings, SPD includes individuals who do not desire or enjoy close relationships. Those afflicted with SPD will be described as isolated, aloof, and detached from social relationships with others, even immediate family members. Individuals with SPD may appear indifferent to criticism and praise, and may take pleasure in only a few activities. They may exhibit a general absence of affective range, which contributes to their characterization as flat, blunted, or emotionally vacant. SPD is more commonly diagnosed in males and may be present in childhood and adolescence. These children are typified by solitariness, poor peer relationships, and underachievement in school. SPD impacts 3.1% to 4.9% of the United States population and approximately 1% of community populations.5,6
EVALUATION Persistent depressive symptoms
Ms. P is accompanied by her parents for the examination. She reports a chronic, persistent sad mood, hopelessness, anergia, insomnia, anhedonia, and decreased concentration and appetite. She says she experiences episodes of intense worry, along with tension, restlessness, feelings of being on the edge, irritability, and difficulty relaxing. Socially, she is withdrawn, preferring to stay alone in her room most of the day watching YouTube or trying to write stories. She has 2 friends with whom she does not interact with in person, but rather through digital means. Ms. P has never enjoyed attending school and feels “nervous” when she is around people. She has difficulty expressing her thoughts and often looks to her parents for help. Her parents add that getting Ms. P to attend school was a struggle, which resulted in periods of home schooling throughout high school.
The treating team prescribes citalopram, 10 mg/d, and aripiprazole, 2 mg/d. On subsequent follow-up visits, Ms. P’s depression improves with an increase in citalopram to 40 mg/d. Psychotherapy is added to her treatment plan to help address the persistent social deficits, odd behavior, and anxieties.
Continue to: Evaluation Psychological assessment...
EVALUATION Psychological assessment
At her psychotherapy intake appointment with the clinical neuropsychologist, Ms. P is dressed in purple from head to toe and sits clutching her purse and looking at the ground. She is overweight with clean, fitting clothing. Ms. P takes a secondary role during most of the interview, allowing her parents to answer most questions. When asked why she is starting therapy, Ms. P replies, “Well, I’ve been using the bathroom a lot.” She describes a feeling of comfort and calmness while in the restroom. Suddenly, she asks her parents to exit the exam room for a moment. Once they leave, she leans in and whispers, “Have you ever heard of self-sabotage? I think that’s what I’m doing.”
Her mood is euthymic, with a blunted affect. She scores 2 on the Patient Health Questionnaire-9 (PHQ-9) and 10 on the Generalized Anxiety Disorder 7-item scale (GAD-7), which indicates the positive impact of medication on her depressive symptoms but continuing moderate anxious distress. She endorses fear of the night, insomnia, and suicidal ideation. She reports an unusual “constant itching sensation,” resulting in hours of repetitive excoriation. Physical examination reveals several significant scars and scabs covering her bilateral upper and lower extremities. Her vocational history is brief; she had held 2 entry-level customer service positions that lasted <1 year. She was fired due to excessive bathroom use.
As the interview progresses, the intake clinician’s background in neuropsychological assessment facilitates screening for possible developmental disorders. Given the nature of the referral and psychotherapy intake, a full neuropsychological assessment is not conducted. The clinician emphasizes verbal abstraction and theory of mind. Ms. P’s IQ was estimated to be average by Wide Range Achievement Test 4 word reading and interview questions about her academic history. Questions are abstracted from the Autism Diagnostic Observation Schedule, Module 4, to assess for conversation ability, emotional insight, awareness and expression, relationships, and areas of functioning in daily living. Developmental history questions, such as those found on the Adaptive Behavior Assessment System, 3rd edition, help guide developmental information provided by parents in the areas of communication, emotion and eye-gaze, gestures, sensory function, language, social functioning, hygiene behavior, and specific interests.
Ms. P’s mother describes a normal pregnancy and delivery; however, she states that Ms. P was “born with problems,” including difficulty with rooting and sucking, and required gastrointestinal intubation until age 3. Cyclical vomiting followed normal food consumption. Ambulation, language acquisition, toilet training, and hygiene behavior were delayed. Ms. P experienced improvements with early intervention in intensive physical and occupational therapy.
Ms. P’s hygiene is well below average, and she requires cueing from her parents. She attended general education until she reached high school, when she began special education. She was sensitive to sensory stimulation from infancy, with sensory sensitivity to textures. Ms. P continues to report sensory sensitivity and lapses in hygiene.
She has difficulty establishing and maintaining relationships with her peers, and prefers solitary activities. Ms. P has no history of romantic relationships, although she does desire one. When asked about her understanding of various relationships, Ms. P’s responses are stereotyped, such as “I know someone is my friend because they are nice to me” and “People get married because they love each other.” She struggles to offer greater insight into the nuances that form lasting relationships and bonds. Ms. P struggles to imitate and describe the physical and internal cues of several basic emotions (eg, fear, joy, anger).
Her conversational and social skills are assessed by asking her to engage in a conversation with the examiner as if meeting for the first time. Her speech is reciprocal, aprosodic, and delayed. The conversation is one-sided, and the examiner fills in several awkward pauses. Ms. P’s gaze at times is intense and prolonged, especially when responding to questions. She tends to use descriptive statements (eg, “I like your purple pen, I like your shirt”) to engage in conversation, rather than gathering more information through reflective statements, questions, or expressing a shared interest.
Ms. P’s verbal abstraction is screened using questions from the Wechsler Adult Intelligence Scale, 4th edition Similarities subtest, to which she provides several responses within normal limits. Her understanding of colloquial speech is assessed by asking her the meaning of common phrases (eg, “Get knocked down 9 times, get up 10,” “Jack and Jill are 2 peas in a pod”). On many occasions, she is able to limit her response to 1 word, (eg, “resiliency”), demonstrating intact ability to decipher idioms.
[polldaddy:11027971]
The authors’ observations
Upon reflection of Ms. P’s clinical presentation and history of developmental delays, social deficits, sensory sensitivity since infancy, and repetitive behaviors (all which continue to impact her), the clinical team concluded that the diagnosis of autism spectrum disorder (ASD) helps explain the patient’s “odd” behaviors, more so than SPD.
ASD is a heterogenous, complex neuropsychiatric disorder characterized by a persistent deficit in social reciprocity, verbal, and nonverbal communication, and includes a pattern of restricted, repetitive and/or stereotyped behaviors and/or interests.5 The term “autismus” is Greek meaning “self,” and was first used to classify the qualities of “morbid self-admiration” observed in prodromal schizophrenia.7
To properly distinguish these disorders, keep in mind that patients with ASD have repetitive and restricted patterns of behaviors or interests that are not found in SPD, and experience deficits in forming, maintaining, and understanding relationships since they lack those skills, while patients with SPD are more prone to desire solitary activities and limited relationships.5,9
There has been an increased interest in determining why for some patients the diagnosis of ASD is delayed until they reach adulthood. Limited or no access to the patient’s childhood caregiver to obtain a developmental history, as well as generational differences on what constitutes typical childhood behavior, could contribute to a delayed diagnosis of ASD until adulthood. Some patients develop camouflaging strategies that allow them to navigate social expectations to a limited degree, such as learning stock phrases, imitating gestures, and telling anecdotes. Another factor to consider is that co-occurring psychiatric disorders may take center stage when patients present for mental health services.10 Fusar-Poli et al11 investigated the characteristics of patients who received a diagnosis of ASD in adulthood. They found that the median time from the initial clinical evaluation to diagnosis of ASD in adulthood was 11 years. In adults identified with ASD, their cognitive abilities ranged from average to above average, and they required less support. Additionally, they also had higher rates of being previously diagnosed with psychotic disorders and personality disorders.11
It is important to keep in mind that the wide spectrum of autism as currently defined by DSM-5 and its overlap of symptoms with other psychiatric disorders can make the diagnosis challenging for both child and adolescent psychiatrists and adult psychiatrists and might help explain why severe cases of ASD are more readily identified earlier than milder cases of ASD.10
Ms. P’s case is also an example of how women are more likely than men to be overlooked when evaluated for ASD. According to DSM-5, the estimated gender ratio for ASD is believed to be 4:1 (male:female).5 However, upon systematic review and meta-analysis, Loomes et al12 found that the gender ratio may be closer to 3:1 (male:female). These authors suggested that diagnostic bias and a failure of passive case ascertainment to estimate gender ratios as stated by DSM-5 in identifying ASD might explain the lower gender ratio.12 A growing body of evidence suggests that ASD is different in males and females. A 2019 qualitative study by Milner et al13 found that female participants reported using masking and camouflaging strategies to appear neurotypical. Compensatory behaviors were found to be linked to a delay in diagnosis and support for ASD.13
Cognitive ability as measured by IQ has also been found to be a factor in receiving a diagnosis of ASD. In a 2010 secondary analysis of a population-based study of the prevalence of ASD, Giarelli et al14found that girls with cognitive impairments as measured by IQ were less likely to be diagnosed with ASD than boys with cognitive impairment, despite meeting the criteria for ASD. Females tend to exhibit fewer repetitive behaviors than males, and tend to be more likely to show accompanying intellectual disability, which suggests that females with ASD may go unrecognized when they exhibit average intelligence with less impairment of behavior and subtler manifestation of social and communication deficits.15 Consequently, females tend to receive this diagnosis later than males.
Continue to: Treatment...
TREATMENT Adding CBT
At an interdisciplinary session several weeks later that includes Ms. P and her parents, the treatment team discusses the revised diagnoses of ASD and MDD, a treatment recommendation for cognitive-behavioral therapy (CBT), and continued use of medication. At this session, Ms. P discloses that she has not been consistent with her medication regimen since her last appointment, which helps explain the increase in her PHQ-9 score from 2 to 14 and GAD-7 score
[polldaddy:11027990]
The authors’ observations
CBT can be helpful in improving medication adherence, developing coping skills, and modifying maladaptive behaviors.
OUTCOME Improvement with psychotherapy
Ms. P and family agree with the team’s recommendations. The aims of Ms. P’s psychotherapy are to maintain medication compliance; implement behavioral modification, vocational rehabilitation, and community engagement; develop social skills; increase functional independence; and develop coping skills for depression and anxiety.
Bottom Line
The prevalence of schizoid personality disorder (SPD) is low, and its symptoms overlap with those of autism spectrum disorder. Therefore, before diagnosing SPD in an adult patient, it is important to obtain a detailed developmental history and include an interdisciplinary team to assess for autism spectrum disorder.
1. Fariba K, Gupta V. Schizoid personality disorder. StatPearls Publishing. Updated June 9, 2021. Accessed January 6, 2021. https://www.ncbi.nlm.nih.gov/books/NBK559234/
2. Diagnostic and Statistical Manual of Mental Disorders: DSM-III. 3rd ed rev. American Psychiatric Association; 1987.
3. Esterberg ML, Goulding SM, Walker EF. Cluster A personality disorders: schizotypal, schizoid and paranoid personality disorders in childhood and adolescence. J Psychopathol Behav Assess. 2010;32(4):515-528. doi:10.1007/s10862-010-9183-8
4. Kalus O, Bernstein DP, Siever LJ. Schizoid personality disorder: a review of current status and implications for DSM-IV. Journal of Personality Disorders. 1993;7(1), 43-52.
5. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. 5th ed. American Psychiatric Association; 2013.
6. Eaton NR, Greene AL. Personality disorders: community prevalence and socio-demographic correlates. Curr Opin Psychol. 2018;21:28-32. doi:10.1016/j.copsyc.2017.09.001
7. Vatano
8. Ritsner MS. Handbook of Schizophrenia Spectrum Disorders, Volume I: Conceptual Issues and Neurobiological Advances. Springer; 2011.
9. Cook ML, Zhang Y, Constantino JN. On the continuity between autistic and schizoid personality disorder trait burden: a prospective study in adolescence. J Nerv Ment Dis. 2020;208(2):94-100. doi:10.1097/NMD.0000000000001105
10. Lai MC, Baron-Cohen S. Identifying the lost generation of adults with autism spectrum conditions. Lancet Psychiatry. 2015;2(11):1013-1027. doi:10.1016/S2215-0366(15)00277-1
11. Fusar-Poli L, Brondino N, Politi P, et al. Missed diagnoses and misdiagnoses of adults with autism spectrum disorder. Eur Arch Psychiatry Clin Neurosci. 2020;10.1007/s00406-020-01189-2. doi:10.1007/s00406-020-01189-w
12. Loomes R, Hull L, Mandy WPL. What is the male-to-female ratio in autism spectrum disorder? A systematic review and meta-analysis. J Am Acad Child Adolesc Psychiatry. 2017;56(6):466-474. doi:10.1016/j.jaac.2017.03.013
13. Milner V, McIntosh H, Colvert E, et al. A qualitative exploration of the female experience of autism spectrum disorder (ASD). J Autism Dev Disord. 2019;49(6):2389-2402. doi:10.1007/s10803-019-03906-4
14. Giarelli E, Wiggins LD, Rice CE, et al. Sex differences in the evaluation and diagnosis of autism spectrum disorders among children. Disabil Health J. 2010;3(2):107-116. doi:10.1016/j.dhjo.2009.07.001
15. Frazier TW, Georgiades S, Bishop SL, et al. Behavioral and cognitive characteristics of females and males with autism in the Simons Simplex Collection. J Am Acad Child Adolesc Psychiatry. 2014;53(3):329-40.e403. doi:10.1016/j.jaac.2013.12.004
16. Julius RJ, Novitsky MA Jr, et al. Medication adherence: a review of the literature and implications for clinical practice. J Psychiatr Pract. 2009;15(1):34-44. doi:10.1097/01.pra.0000344917.43780.77
17. Spain D, Sin J, Chalder T, et al. Cognitive behaviour therapy for adults with autism spectrum disorders and psychiatric co-morbidity: a review. Research in Autism Spectrum Disorders. 2015;9, 151-162. https://doi.org/10.1016/j.rasd.2014.10.019
18. Bishop-Fitzpatrick L, Minshew NJ, Eack SM. A systematic review of psychosocial interventions for adults with autism spectrum disorders. J Autism Dev Disord. 2013;43(3):687-694. doi:10.1007/s10803-012-1615-8
CASE Treatment-resistant MDD
Ms. P, age 21, presents to the outpatient clinic. She has diagnoses of treatment-resistant major depressive disorder (MDD) and schizoid personality disorder (SPD). Ms. P was diagnosed with MDD 3 years ago after reporting symptoms of prevailing sadness for approximately 8 years, described as feelings of worthlessness, anhedonia, social withdrawal, and decreased hygiene and self-care behaviors, as well as suicidal ideation and self-harm. SPD was diagnosed 1 year earlier based on her “odd” behaviors and disheveled appearance following observation and in collateral with her family. Her odd behaviors are described as spending most of her time alone, preferring solitary activities, and having little contact with people other than her parents.
Ms. P reports that she was previously treated with citalopram, 20 mg/d, bupropion, 150 mg/d, aripiprazole, 3.75 mg/d, topiramate, 100 mg twice daily, and melatonin, 9 mg/d at bedtime, but discontinued follow-up appointments and medications after no significant improvement in symptoms.
[polldaddy:11027942]
The authors’ observations
The term “schizoid” first made its debut in the medical community to describe the prodromal social withdrawal and isolation observed in schizophrenia.1 The use of schizoid to describe a personality type first occurred in DSM-III in 1980.2 SPD is a Cluster A personality disorder that groups personalities characterized by common traits that are “odd” or “eccentric” and may resemble the positive and/or negative symptoms of schizophrenia.3,4 Relatively uncommon in clinical settings, SPD includes individuals who do not desire or enjoy close relationships. Those afflicted with SPD will be described as isolated, aloof, and detached from social relationships with others, even immediate family members. Individuals with SPD may appear indifferent to criticism and praise, and may take pleasure in only a few activities. They may exhibit a general absence of affective range, which contributes to their characterization as flat, blunted, or emotionally vacant. SPD is more commonly diagnosed in males and may be present in childhood and adolescence. These children are typified by solitariness, poor peer relationships, and underachievement in school. SPD impacts 3.1% to 4.9% of the United States population and approximately 1% of community populations.5,6
EVALUATION Persistent depressive symptoms
Ms. P is accompanied by her parents for the examination. She reports a chronic, persistent sad mood, hopelessness, anergia, insomnia, anhedonia, and decreased concentration and appetite. She says she experiences episodes of intense worry, along with tension, restlessness, feelings of being on the edge, irritability, and difficulty relaxing. Socially, she is withdrawn, preferring to stay alone in her room most of the day watching YouTube or trying to write stories. She has 2 friends with whom she does not interact with in person, but rather through digital means. Ms. P has never enjoyed attending school and feels “nervous” when she is around people. She has difficulty expressing her thoughts and often looks to her parents for help. Her parents add that getting Ms. P to attend school was a struggle, which resulted in periods of home schooling throughout high school.
The treating team prescribes citalopram, 10 mg/d, and aripiprazole, 2 mg/d. On subsequent follow-up visits, Ms. P’s depression improves with an increase in citalopram to 40 mg/d. Psychotherapy is added to her treatment plan to help address the persistent social deficits, odd behavior, and anxieties.
Continue to: Evaluation Psychological assessment...
EVALUATION Psychological assessment
At her psychotherapy intake appointment with the clinical neuropsychologist, Ms. P is dressed in purple from head to toe and sits clutching her purse and looking at the ground. She is overweight with clean, fitting clothing. Ms. P takes a secondary role during most of the interview, allowing her parents to answer most questions. When asked why she is starting therapy, Ms. P replies, “Well, I’ve been using the bathroom a lot.” She describes a feeling of comfort and calmness while in the restroom. Suddenly, she asks her parents to exit the exam room for a moment. Once they leave, she leans in and whispers, “Have you ever heard of self-sabotage? I think that’s what I’m doing.”
Her mood is euthymic, with a blunted affect. She scores 2 on the Patient Health Questionnaire-9 (PHQ-9) and 10 on the Generalized Anxiety Disorder 7-item scale (GAD-7), which indicates the positive impact of medication on her depressive symptoms but continuing moderate anxious distress. She endorses fear of the night, insomnia, and suicidal ideation. She reports an unusual “constant itching sensation,” resulting in hours of repetitive excoriation. Physical examination reveals several significant scars and scabs covering her bilateral upper and lower extremities. Her vocational history is brief; she had held 2 entry-level customer service positions that lasted <1 year. She was fired due to excessive bathroom use.
As the interview progresses, the intake clinician’s background in neuropsychological assessment facilitates screening for possible developmental disorders. Given the nature of the referral and psychotherapy intake, a full neuropsychological assessment is not conducted. The clinician emphasizes verbal abstraction and theory of mind. Ms. P’s IQ was estimated to be average by Wide Range Achievement Test 4 word reading and interview questions about her academic history. Questions are abstracted from the Autism Diagnostic Observation Schedule, Module 4, to assess for conversation ability, emotional insight, awareness and expression, relationships, and areas of functioning in daily living. Developmental history questions, such as those found on the Adaptive Behavior Assessment System, 3rd edition, help guide developmental information provided by parents in the areas of communication, emotion and eye-gaze, gestures, sensory function, language, social functioning, hygiene behavior, and specific interests.
Ms. P’s mother describes a normal pregnancy and delivery; however, she states that Ms. P was “born with problems,” including difficulty with rooting and sucking, and required gastrointestinal intubation until age 3. Cyclical vomiting followed normal food consumption. Ambulation, language acquisition, toilet training, and hygiene behavior were delayed. Ms. P experienced improvements with early intervention in intensive physical and occupational therapy.
Ms. P’s hygiene is well below average, and she requires cueing from her parents. She attended general education until she reached high school, when she began special education. She was sensitive to sensory stimulation from infancy, with sensory sensitivity to textures. Ms. P continues to report sensory sensitivity and lapses in hygiene.
She has difficulty establishing and maintaining relationships with her peers, and prefers solitary activities. Ms. P has no history of romantic relationships, although she does desire one. When asked about her understanding of various relationships, Ms. P’s responses are stereotyped, such as “I know someone is my friend because they are nice to me” and “People get married because they love each other.” She struggles to offer greater insight into the nuances that form lasting relationships and bonds. Ms. P struggles to imitate and describe the physical and internal cues of several basic emotions (eg, fear, joy, anger).
Her conversational and social skills are assessed by asking her to engage in a conversation with the examiner as if meeting for the first time. Her speech is reciprocal, aprosodic, and delayed. The conversation is one-sided, and the examiner fills in several awkward pauses. Ms. P’s gaze at times is intense and prolonged, especially when responding to questions. She tends to use descriptive statements (eg, “I like your purple pen, I like your shirt”) to engage in conversation, rather than gathering more information through reflective statements, questions, or expressing a shared interest.
Ms. P’s verbal abstraction is screened using questions from the Wechsler Adult Intelligence Scale, 4th edition Similarities subtest, to which she provides several responses within normal limits. Her understanding of colloquial speech is assessed by asking her the meaning of common phrases (eg, “Get knocked down 9 times, get up 10,” “Jack and Jill are 2 peas in a pod”). On many occasions, she is able to limit her response to 1 word, (eg, “resiliency”), demonstrating intact ability to decipher idioms.
[polldaddy:11027971]
The authors’ observations
Upon reflection of Ms. P’s clinical presentation and history of developmental delays, social deficits, sensory sensitivity since infancy, and repetitive behaviors (all which continue to impact her), the clinical team concluded that the diagnosis of autism spectrum disorder (ASD) helps explain the patient’s “odd” behaviors, more so than SPD.
ASD is a heterogenous, complex neuropsychiatric disorder characterized by a persistent deficit in social reciprocity, verbal, and nonverbal communication, and includes a pattern of restricted, repetitive and/or stereotyped behaviors and/or interests.5 The term “autismus” is Greek meaning “self,” and was first used to classify the qualities of “morbid self-admiration” observed in prodromal schizophrenia.7
To properly distinguish these disorders, keep in mind that patients with ASD have repetitive and restricted patterns of behaviors or interests that are not found in SPD, and experience deficits in forming, maintaining, and understanding relationships since they lack those skills, while patients with SPD are more prone to desire solitary activities and limited relationships.5,9
There has been an increased interest in determining why for some patients the diagnosis of ASD is delayed until they reach adulthood. Limited or no access to the patient’s childhood caregiver to obtain a developmental history, as well as generational differences on what constitutes typical childhood behavior, could contribute to a delayed diagnosis of ASD until adulthood. Some patients develop camouflaging strategies that allow them to navigate social expectations to a limited degree, such as learning stock phrases, imitating gestures, and telling anecdotes. Another factor to consider is that co-occurring psychiatric disorders may take center stage when patients present for mental health services.10 Fusar-Poli et al11 investigated the characteristics of patients who received a diagnosis of ASD in adulthood. They found that the median time from the initial clinical evaluation to diagnosis of ASD in adulthood was 11 years. In adults identified with ASD, their cognitive abilities ranged from average to above average, and they required less support. Additionally, they also had higher rates of being previously diagnosed with psychotic disorders and personality disorders.11
It is important to keep in mind that the wide spectrum of autism as currently defined by DSM-5 and its overlap of symptoms with other psychiatric disorders can make the diagnosis challenging for both child and adolescent psychiatrists and adult psychiatrists and might help explain why severe cases of ASD are more readily identified earlier than milder cases of ASD.10
Ms. P’s case is also an example of how women are more likely than men to be overlooked when evaluated for ASD. According to DSM-5, the estimated gender ratio for ASD is believed to be 4:1 (male:female).5 However, upon systematic review and meta-analysis, Loomes et al12 found that the gender ratio may be closer to 3:1 (male:female). These authors suggested that diagnostic bias and a failure of passive case ascertainment to estimate gender ratios as stated by DSM-5 in identifying ASD might explain the lower gender ratio.12 A growing body of evidence suggests that ASD is different in males and females. A 2019 qualitative study by Milner et al13 found that female participants reported using masking and camouflaging strategies to appear neurotypical. Compensatory behaviors were found to be linked to a delay in diagnosis and support for ASD.13
Cognitive ability as measured by IQ has also been found to be a factor in receiving a diagnosis of ASD. In a 2010 secondary analysis of a population-based study of the prevalence of ASD, Giarelli et al14found that girls with cognitive impairments as measured by IQ were less likely to be diagnosed with ASD than boys with cognitive impairment, despite meeting the criteria for ASD. Females tend to exhibit fewer repetitive behaviors than males, and tend to be more likely to show accompanying intellectual disability, which suggests that females with ASD may go unrecognized when they exhibit average intelligence with less impairment of behavior and subtler manifestation of social and communication deficits.15 Consequently, females tend to receive this diagnosis later than males.
Continue to: Treatment...
TREATMENT Adding CBT
At an interdisciplinary session several weeks later that includes Ms. P and her parents, the treatment team discusses the revised diagnoses of ASD and MDD, a treatment recommendation for cognitive-behavioral therapy (CBT), and continued use of medication. At this session, Ms. P discloses that she has not been consistent with her medication regimen since her last appointment, which helps explain the increase in her PHQ-9 score from 2 to 14 and GAD-7 score
[polldaddy:11027990]
The authors’ observations
CBT can be helpful in improving medication adherence, developing coping skills, and modifying maladaptive behaviors.
OUTCOME Improvement with psychotherapy
Ms. P and family agree with the team’s recommendations. The aims of Ms. P’s psychotherapy are to maintain medication compliance; implement behavioral modification, vocational rehabilitation, and community engagement; develop social skills; increase functional independence; and develop coping skills for depression and anxiety.
Bottom Line
The prevalence of schizoid personality disorder (SPD) is low, and its symptoms overlap with those of autism spectrum disorder. Therefore, before diagnosing SPD in an adult patient, it is important to obtain a detailed developmental history and include an interdisciplinary team to assess for autism spectrum disorder.
CASE Treatment-resistant MDD
Ms. P, age 21, presents to the outpatient clinic. She has diagnoses of treatment-resistant major depressive disorder (MDD) and schizoid personality disorder (SPD). Ms. P was diagnosed with MDD 3 years ago after reporting symptoms of prevailing sadness for approximately 8 years, described as feelings of worthlessness, anhedonia, social withdrawal, and decreased hygiene and self-care behaviors, as well as suicidal ideation and self-harm. SPD was diagnosed 1 year earlier based on her “odd” behaviors and disheveled appearance following observation and in collateral with her family. Her odd behaviors are described as spending most of her time alone, preferring solitary activities, and having little contact with people other than her parents.
Ms. P reports that she was previously treated with citalopram, 20 mg/d, bupropion, 150 mg/d, aripiprazole, 3.75 mg/d, topiramate, 100 mg twice daily, and melatonin, 9 mg/d at bedtime, but discontinued follow-up appointments and medications after no significant improvement in symptoms.
[polldaddy:11027942]
The authors’ observations
The term “schizoid” first made its debut in the medical community to describe the prodromal social withdrawal and isolation observed in schizophrenia.1 The use of schizoid to describe a personality type first occurred in DSM-III in 1980.2 SPD is a Cluster A personality disorder that groups personalities characterized by common traits that are “odd” or “eccentric” and may resemble the positive and/or negative symptoms of schizophrenia.3,4 Relatively uncommon in clinical settings, SPD includes individuals who do not desire or enjoy close relationships. Those afflicted with SPD will be described as isolated, aloof, and detached from social relationships with others, even immediate family members. Individuals with SPD may appear indifferent to criticism and praise, and may take pleasure in only a few activities. They may exhibit a general absence of affective range, which contributes to their characterization as flat, blunted, or emotionally vacant. SPD is more commonly diagnosed in males and may be present in childhood and adolescence. These children are typified by solitariness, poor peer relationships, and underachievement in school. SPD impacts 3.1% to 4.9% of the United States population and approximately 1% of community populations.5,6
EVALUATION Persistent depressive symptoms
Ms. P is accompanied by her parents for the examination. She reports a chronic, persistent sad mood, hopelessness, anergia, insomnia, anhedonia, and decreased concentration and appetite. She says she experiences episodes of intense worry, along with tension, restlessness, feelings of being on the edge, irritability, and difficulty relaxing. Socially, she is withdrawn, preferring to stay alone in her room most of the day watching YouTube or trying to write stories. She has 2 friends with whom she does not interact with in person, but rather through digital means. Ms. P has never enjoyed attending school and feels “nervous” when she is around people. She has difficulty expressing her thoughts and often looks to her parents for help. Her parents add that getting Ms. P to attend school was a struggle, which resulted in periods of home schooling throughout high school.
The treating team prescribes citalopram, 10 mg/d, and aripiprazole, 2 mg/d. On subsequent follow-up visits, Ms. P’s depression improves with an increase in citalopram to 40 mg/d. Psychotherapy is added to her treatment plan to help address the persistent social deficits, odd behavior, and anxieties.
Continue to: Evaluation Psychological assessment...
EVALUATION Psychological assessment
At her psychotherapy intake appointment with the clinical neuropsychologist, Ms. P is dressed in purple from head to toe and sits clutching her purse and looking at the ground. She is overweight with clean, fitting clothing. Ms. P takes a secondary role during most of the interview, allowing her parents to answer most questions. When asked why she is starting therapy, Ms. P replies, “Well, I’ve been using the bathroom a lot.” She describes a feeling of comfort and calmness while in the restroom. Suddenly, she asks her parents to exit the exam room for a moment. Once they leave, she leans in and whispers, “Have you ever heard of self-sabotage? I think that’s what I’m doing.”
Her mood is euthymic, with a blunted affect. She scores 2 on the Patient Health Questionnaire-9 (PHQ-9) and 10 on the Generalized Anxiety Disorder 7-item scale (GAD-7), which indicates the positive impact of medication on her depressive symptoms but continuing moderate anxious distress. She endorses fear of the night, insomnia, and suicidal ideation. She reports an unusual “constant itching sensation,” resulting in hours of repetitive excoriation. Physical examination reveals several significant scars and scabs covering her bilateral upper and lower extremities. Her vocational history is brief; she had held 2 entry-level customer service positions that lasted <1 year. She was fired due to excessive bathroom use.
As the interview progresses, the intake clinician’s background in neuropsychological assessment facilitates screening for possible developmental disorders. Given the nature of the referral and psychotherapy intake, a full neuropsychological assessment is not conducted. The clinician emphasizes verbal abstraction and theory of mind. Ms. P’s IQ was estimated to be average by Wide Range Achievement Test 4 word reading and interview questions about her academic history. Questions are abstracted from the Autism Diagnostic Observation Schedule, Module 4, to assess for conversation ability, emotional insight, awareness and expression, relationships, and areas of functioning in daily living. Developmental history questions, such as those found on the Adaptive Behavior Assessment System, 3rd edition, help guide developmental information provided by parents in the areas of communication, emotion and eye-gaze, gestures, sensory function, language, social functioning, hygiene behavior, and specific interests.
Ms. P’s mother describes a normal pregnancy and delivery; however, she states that Ms. P was “born with problems,” including difficulty with rooting and sucking, and required gastrointestinal intubation until age 3. Cyclical vomiting followed normal food consumption. Ambulation, language acquisition, toilet training, and hygiene behavior were delayed. Ms. P experienced improvements with early intervention in intensive physical and occupational therapy.
Ms. P’s hygiene is well below average, and she requires cueing from her parents. She attended general education until she reached high school, when she began special education. She was sensitive to sensory stimulation from infancy, with sensory sensitivity to textures. Ms. P continues to report sensory sensitivity and lapses in hygiene.
She has difficulty establishing and maintaining relationships with her peers, and prefers solitary activities. Ms. P has no history of romantic relationships, although she does desire one. When asked about her understanding of various relationships, Ms. P’s responses are stereotyped, such as “I know someone is my friend because they are nice to me” and “People get married because they love each other.” She struggles to offer greater insight into the nuances that form lasting relationships and bonds. Ms. P struggles to imitate and describe the physical and internal cues of several basic emotions (eg, fear, joy, anger).
Her conversational and social skills are assessed by asking her to engage in a conversation with the examiner as if meeting for the first time. Her speech is reciprocal, aprosodic, and delayed. The conversation is one-sided, and the examiner fills in several awkward pauses. Ms. P’s gaze at times is intense and prolonged, especially when responding to questions. She tends to use descriptive statements (eg, “I like your purple pen, I like your shirt”) to engage in conversation, rather than gathering more information through reflective statements, questions, or expressing a shared interest.
Ms. P’s verbal abstraction is screened using questions from the Wechsler Adult Intelligence Scale, 4th edition Similarities subtest, to which she provides several responses within normal limits. Her understanding of colloquial speech is assessed by asking her the meaning of common phrases (eg, “Get knocked down 9 times, get up 10,” “Jack and Jill are 2 peas in a pod”). On many occasions, she is able to limit her response to 1 word, (eg, “resiliency”), demonstrating intact ability to decipher idioms.
[polldaddy:11027971]
The authors’ observations
Upon reflection of Ms. P’s clinical presentation and history of developmental delays, social deficits, sensory sensitivity since infancy, and repetitive behaviors (all which continue to impact her), the clinical team concluded that the diagnosis of autism spectrum disorder (ASD) helps explain the patient’s “odd” behaviors, more so than SPD.
ASD is a heterogenous, complex neuropsychiatric disorder characterized by a persistent deficit in social reciprocity, verbal, and nonverbal communication, and includes a pattern of restricted, repetitive and/or stereotyped behaviors and/or interests.5 The term “autismus” is Greek meaning “self,” and was first used to classify the qualities of “morbid self-admiration” observed in prodromal schizophrenia.7
To properly distinguish these disorders, keep in mind that patients with ASD have repetitive and restricted patterns of behaviors or interests that are not found in SPD, and experience deficits in forming, maintaining, and understanding relationships since they lack those skills, while patients with SPD are more prone to desire solitary activities and limited relationships.5,9
There has been an increased interest in determining why for some patients the diagnosis of ASD is delayed until they reach adulthood. Limited or no access to the patient’s childhood caregiver to obtain a developmental history, as well as generational differences on what constitutes typical childhood behavior, could contribute to a delayed diagnosis of ASD until adulthood. Some patients develop camouflaging strategies that allow them to navigate social expectations to a limited degree, such as learning stock phrases, imitating gestures, and telling anecdotes. Another factor to consider is that co-occurring psychiatric disorders may take center stage when patients present for mental health services.10 Fusar-Poli et al11 investigated the characteristics of patients who received a diagnosis of ASD in adulthood. They found that the median time from the initial clinical evaluation to diagnosis of ASD in adulthood was 11 years. In adults identified with ASD, their cognitive abilities ranged from average to above average, and they required less support. Additionally, they also had higher rates of being previously diagnosed with psychotic disorders and personality disorders.11
It is important to keep in mind that the wide spectrum of autism as currently defined by DSM-5 and its overlap of symptoms with other psychiatric disorders can make the diagnosis challenging for both child and adolescent psychiatrists and adult psychiatrists and might help explain why severe cases of ASD are more readily identified earlier than milder cases of ASD.10
Ms. P’s case is also an example of how women are more likely than men to be overlooked when evaluated for ASD. According to DSM-5, the estimated gender ratio for ASD is believed to be 4:1 (male:female).5 However, upon systematic review and meta-analysis, Loomes et al12 found that the gender ratio may be closer to 3:1 (male:female). These authors suggested that diagnostic bias and a failure of passive case ascertainment to estimate gender ratios as stated by DSM-5 in identifying ASD might explain the lower gender ratio.12 A growing body of evidence suggests that ASD is different in males and females. A 2019 qualitative study by Milner et al13 found that female participants reported using masking and camouflaging strategies to appear neurotypical. Compensatory behaviors were found to be linked to a delay in diagnosis and support for ASD.13
Cognitive ability as measured by IQ has also been found to be a factor in receiving a diagnosis of ASD. In a 2010 secondary analysis of a population-based study of the prevalence of ASD, Giarelli et al14found that girls with cognitive impairments as measured by IQ were less likely to be diagnosed with ASD than boys with cognitive impairment, despite meeting the criteria for ASD. Females tend to exhibit fewer repetitive behaviors than males, and tend to be more likely to show accompanying intellectual disability, which suggests that females with ASD may go unrecognized when they exhibit average intelligence with less impairment of behavior and subtler manifestation of social and communication deficits.15 Consequently, females tend to receive this diagnosis later than males.
Continue to: Treatment...
TREATMENT Adding CBT
At an interdisciplinary session several weeks later that includes Ms. P and her parents, the treatment team discusses the revised diagnoses of ASD and MDD, a treatment recommendation for cognitive-behavioral therapy (CBT), and continued use of medication. At this session, Ms. P discloses that she has not been consistent with her medication regimen since her last appointment, which helps explain the increase in her PHQ-9 score from 2 to 14 and GAD-7 score
[polldaddy:11027990]
The authors’ observations
CBT can be helpful in improving medication adherence, developing coping skills, and modifying maladaptive behaviors.
OUTCOME Improvement with psychotherapy
Ms. P and family agree with the team’s recommendations. The aims of Ms. P’s psychotherapy are to maintain medication compliance; implement behavioral modification, vocational rehabilitation, and community engagement; develop social skills; increase functional independence; and develop coping skills for depression and anxiety.
Bottom Line
The prevalence of schizoid personality disorder (SPD) is low, and its symptoms overlap with those of autism spectrum disorder. Therefore, before diagnosing SPD in an adult patient, it is important to obtain a detailed developmental history and include an interdisciplinary team to assess for autism spectrum disorder.
1. Fariba K, Gupta V. Schizoid personality disorder. StatPearls Publishing. Updated June 9, 2021. Accessed January 6, 2021. https://www.ncbi.nlm.nih.gov/books/NBK559234/
2. Diagnostic and Statistical Manual of Mental Disorders: DSM-III. 3rd ed rev. American Psychiatric Association; 1987.
3. Esterberg ML, Goulding SM, Walker EF. Cluster A personality disorders: schizotypal, schizoid and paranoid personality disorders in childhood and adolescence. J Psychopathol Behav Assess. 2010;32(4):515-528. doi:10.1007/s10862-010-9183-8
4. Kalus O, Bernstein DP, Siever LJ. Schizoid personality disorder: a review of current status and implications for DSM-IV. Journal of Personality Disorders. 1993;7(1), 43-52.
5. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. 5th ed. American Psychiatric Association; 2013.
6. Eaton NR, Greene AL. Personality disorders: community prevalence and socio-demographic correlates. Curr Opin Psychol. 2018;21:28-32. doi:10.1016/j.copsyc.2017.09.001
7. Vatano
8. Ritsner MS. Handbook of Schizophrenia Spectrum Disorders, Volume I: Conceptual Issues and Neurobiological Advances. Springer; 2011.
9. Cook ML, Zhang Y, Constantino JN. On the continuity between autistic and schizoid personality disorder trait burden: a prospective study in adolescence. J Nerv Ment Dis. 2020;208(2):94-100. doi:10.1097/NMD.0000000000001105
10. Lai MC, Baron-Cohen S. Identifying the lost generation of adults with autism spectrum conditions. Lancet Psychiatry. 2015;2(11):1013-1027. doi:10.1016/S2215-0366(15)00277-1
11. Fusar-Poli L, Brondino N, Politi P, et al. Missed diagnoses and misdiagnoses of adults with autism spectrum disorder. Eur Arch Psychiatry Clin Neurosci. 2020;10.1007/s00406-020-01189-2. doi:10.1007/s00406-020-01189-w
12. Loomes R, Hull L, Mandy WPL. What is the male-to-female ratio in autism spectrum disorder? A systematic review and meta-analysis. J Am Acad Child Adolesc Psychiatry. 2017;56(6):466-474. doi:10.1016/j.jaac.2017.03.013
13. Milner V, McIntosh H, Colvert E, et al. A qualitative exploration of the female experience of autism spectrum disorder (ASD). J Autism Dev Disord. 2019;49(6):2389-2402. doi:10.1007/s10803-019-03906-4
14. Giarelli E, Wiggins LD, Rice CE, et al. Sex differences in the evaluation and diagnosis of autism spectrum disorders among children. Disabil Health J. 2010;3(2):107-116. doi:10.1016/j.dhjo.2009.07.001
15. Frazier TW, Georgiades S, Bishop SL, et al. Behavioral and cognitive characteristics of females and males with autism in the Simons Simplex Collection. J Am Acad Child Adolesc Psychiatry. 2014;53(3):329-40.e403. doi:10.1016/j.jaac.2013.12.004
16. Julius RJ, Novitsky MA Jr, et al. Medication adherence: a review of the literature and implications for clinical practice. J Psychiatr Pract. 2009;15(1):34-44. doi:10.1097/01.pra.0000344917.43780.77
17. Spain D, Sin J, Chalder T, et al. Cognitive behaviour therapy for adults with autism spectrum disorders and psychiatric co-morbidity: a review. Research in Autism Spectrum Disorders. 2015;9, 151-162. https://doi.org/10.1016/j.rasd.2014.10.019
18. Bishop-Fitzpatrick L, Minshew NJ, Eack SM. A systematic review of psychosocial interventions for adults with autism spectrum disorders. J Autism Dev Disord. 2013;43(3):687-694. doi:10.1007/s10803-012-1615-8
1. Fariba K, Gupta V. Schizoid personality disorder. StatPearls Publishing. Updated June 9, 2021. Accessed January 6, 2021. https://www.ncbi.nlm.nih.gov/books/NBK559234/
2. Diagnostic and Statistical Manual of Mental Disorders: DSM-III. 3rd ed rev. American Psychiatric Association; 1987.
3. Esterberg ML, Goulding SM, Walker EF. Cluster A personality disorders: schizotypal, schizoid and paranoid personality disorders in childhood and adolescence. J Psychopathol Behav Assess. 2010;32(4):515-528. doi:10.1007/s10862-010-9183-8
4. Kalus O, Bernstein DP, Siever LJ. Schizoid personality disorder: a review of current status and implications for DSM-IV. Journal of Personality Disorders. 1993;7(1), 43-52.
5. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. 5th ed. American Psychiatric Association; 2013.
6. Eaton NR, Greene AL. Personality disorders: community prevalence and socio-demographic correlates. Curr Opin Psychol. 2018;21:28-32. doi:10.1016/j.copsyc.2017.09.001
7. Vatano
8. Ritsner MS. Handbook of Schizophrenia Spectrum Disorders, Volume I: Conceptual Issues and Neurobiological Advances. Springer; 2011.
9. Cook ML, Zhang Y, Constantino JN. On the continuity between autistic and schizoid personality disorder trait burden: a prospective study in adolescence. J Nerv Ment Dis. 2020;208(2):94-100. doi:10.1097/NMD.0000000000001105
10. Lai MC, Baron-Cohen S. Identifying the lost generation of adults with autism spectrum conditions. Lancet Psychiatry. 2015;2(11):1013-1027. doi:10.1016/S2215-0366(15)00277-1
11. Fusar-Poli L, Brondino N, Politi P, et al. Missed diagnoses and misdiagnoses of adults with autism spectrum disorder. Eur Arch Psychiatry Clin Neurosci. 2020;10.1007/s00406-020-01189-2. doi:10.1007/s00406-020-01189-w
12. Loomes R, Hull L, Mandy WPL. What is the male-to-female ratio in autism spectrum disorder? A systematic review and meta-analysis. J Am Acad Child Adolesc Psychiatry. 2017;56(6):466-474. doi:10.1016/j.jaac.2017.03.013
13. Milner V, McIntosh H, Colvert E, et al. A qualitative exploration of the female experience of autism spectrum disorder (ASD). J Autism Dev Disord. 2019;49(6):2389-2402. doi:10.1007/s10803-019-03906-4
14. Giarelli E, Wiggins LD, Rice CE, et al. Sex differences in the evaluation and diagnosis of autism spectrum disorders among children. Disabil Health J. 2010;3(2):107-116. doi:10.1016/j.dhjo.2009.07.001
15. Frazier TW, Georgiades S, Bishop SL, et al. Behavioral and cognitive characteristics of females and males with autism in the Simons Simplex Collection. J Am Acad Child Adolesc Psychiatry. 2014;53(3):329-40.e403. doi:10.1016/j.jaac.2013.12.004
16. Julius RJ, Novitsky MA Jr, et al. Medication adherence: a review of the literature and implications for clinical practice. J Psychiatr Pract. 2009;15(1):34-44. doi:10.1097/01.pra.0000344917.43780.77
17. Spain D, Sin J, Chalder T, et al. Cognitive behaviour therapy for adults with autism spectrum disorders and psychiatric co-morbidity: a review. Research in Autism Spectrum Disorders. 2015;9, 151-162. https://doi.org/10.1016/j.rasd.2014.10.019
18. Bishop-Fitzpatrick L, Minshew NJ, Eack SM. A systematic review of psychosocial interventions for adults with autism spectrum disorders. J Autism Dev Disord. 2013;43(3):687-694. doi:10.1007/s10803-012-1615-8
Identifying and preventing IPV: Are clinicians doing enough?
Violence against women remains a global dilemma in need of attention. Physical violence in particular, is the most prevalent type of violence across all genders, races, and nationalities.
The Centers for Disease Control and Prevention says more than 43 million women and 38 million men report experiencing psychological aggression by an intimate partner in their lifetime. Meanwhile, 11 million women and 5 million men report enduring sexual or physical violence and intimate partner violence (IPV), and/or stalking by an intimate partner during their lifetimes, according to the CDC.1
Women who have endured this kind of violence might present differently from men. Some studies, for example, show a more significant association between mutual violence, depression, and substance use among women than men.2 Studies on the phenomenon of IPV victims/survivors becoming perpetrators of abuse are limited, but that this happens in some cases.
Having a psychiatric disorder is associated with a higher likelihood of being physically violent with a partner.3,4 One recent study of 250 female psychiatric patients who were married and had no history of drug abuse found that almost 68% reported psychological abuse, 52% reported sexual abuse, 38% social abuse, 37% reported economic abuse, and 25% reported physical abuse.5
Given those statistics and trends, it is incumbent upon clinicians – including those in primary care, psychiatry, and emergency medicine – to learn to quickly identify IPV survivors, and to use available prognostic tools to monitor perpetrators and survivors.
COVID pandemic’s influence
Isolation tied to the COVID-19 pandemic has been linked to increased IPV. A study conducted by researchers at the University of California, Davis, suggested that extra stress experienced during the COVID-19 pandemic caused by income loss, and the inability to pay for housing and food exacerbated the prevalence of IPV early during the pandemic.6
That study, where researchers collected in surveys of nearly 400 adults in the beginning in April 2020 for 10 weeks, showed that more services and communication are needed so that frontline health care and food bank workers, for example, in addition to social workers, doctors, and therapists, can spot the signs and ask clients questions about potential IPV. They could then link survivors to pertinent assistance and resources.
Furthermore, multiple factors probably have played a pivotal role in increasing the prevalence of IPV during the COVID-19 pandemic. For instance, disruption to usual health and social services as well as diminished access to support systems, such as shelters, and charity helplines negatively affected the reporting of domestic violence.
Long before the pandemic, over the past decade, international and national bodies have played a crucial role in terms of improving the awareness and response to domestic violence.7,8 In addition, several policies have been introduced in countries around the globe emphasizing the need to inquire routinely about domestic violence. Nevertheless, mental health services often fail to adequately address domestic violence in clinical encounters. A systematic review of domestic violence assessment screening performed in a variety of health care settings found that evidence was insufficient to conclude that routine inquiry improved morbidity and mortality among victims of IPV.9 So the question becomes: How can we get our patients to tell us about these experiences so we can intervene?
Gender differences in perpetuating IPV
Several studies have found that abuse can result in various mental illnesses, such as depression, PTSD, anxiety, and suicidal ideation. Again, men have a disproportionately higher rate of perpetrating IPV, compared with women. This theory has been a source of debate in the academic community for years, but recent research has confirmed that women do perpetuate violence against their partners to some extent.10,11
Some members of the LGBTQ+ community also report experiencing violence from partners, so as clinicians, we also need to raise our awareness about the existence of violence among same-sex couples. In fact, a team of Italian researchers report more than 50% of gay men and almost 75% of lesbian women reported that they had been psychologically abused by a partner.12 More research into this area is needed.
Our role as health care professionals
The U.S. Preventive Services Task Force advises that all clinic visits include regular IPV screening.13 But these screenings are all too rare. In fact, a meta-analysis of 19 trials of more than 1,600 participants showed only 9%-40% of doctors routinely test for IPV.14 That research clearly shows how important it is for all clinicians to execute IPV screening. However, numerous challenges toward screening exist, including personal discomfort, limited time during appointments, insufficient resources, and inadequate training.
One ongoing debate revolves around which clinician should screen for IPV. Should the psychiatrist carry out this role – or perhaps the primary care physician, nurse, or social worker? These issues become even more fraught when clinicians worry about offending the patient – especially if the clinician is a male.15
The bottom line is that physicians should inquire about intimate partner violence, because research indicates that women are more likely to reveal abuse when prompted. In addition, during physician appointments, they can use the physician-patient therapeutic connection to conduct a domestic violence evaluation, give resources to victims, and provide ongoing care. Patients who exhibit treatment resistance, persistent pain, depression, sleeplessness, and headaches should prompt psychiatrists to conduct additional investigations into the likelihood of intimate partner violence and domestic abuse.
W also should be attentive when counseling patients about domestic violence when suggesting life-changing events such as pregnancy, employment loss, separation, or divorce. Similar to the recommendations of the USPSTF that all women and men should be screened for IPV, it is suggested that physicians be conscious of facilitating a conversation and not being overtly judgmental while observing body cues. Using the statements such as “we have been hearing a lot of violence in our community lately” could be a segue to introduce the subject.
Asking the question of whether you are being hit rather than being abused has allowed more women to open up more about domestic violence. While physicians are aware that most victims might recant and often go back to their abusers, victims need to be counseled that the abuse might intensify and lead to death.
For women who perpetuate IPV and survivors of IPV, safety is the priority. Physicians should provide safety options and be the facilitators. Studies have shown that fewer victims get the referral to the supporting agencies when IPV is indicated, which puts their safety at risk. In women who commit IPV, clinicians should assess the role of the individual in an IPV disclosure. There are various treatment modalities, whether the violence is performed through self-defense, bidirectionally, or because of aggression.
With the advancement of technology, web-based training on how to ask for IPV, documentation, acknowledgment, and structured referral increase physicians’ confidence when faced with an IPV disclosure than none.16 Treatment modalities should include medication reconciliation and cognitive-behavioral therapy – focusing on emotion regulation.
Using instruments such as the danger assessment tool can help physicians intervene early, reducing the risk of domestic violence and IPV recurrence instead of using clinical assessment alone.17 Physicians should convey empathy, validate victims, and help, especially when abuse is reported.
Also, it is important to evaluate survivors’ safety. Counseling can help people rebuild their self-esteem. Structured referrals for psychiatric help and support services are needed to help survivors on the long road to recovery.
Training all physicians, regardless of specialty, is essential to improve prompt IPV identification and bring awareness to resources available to survivors when IPV is disclosed. Although we described an association between IPV victims becoming possible perpetrators of IPV, more long-term studies are required to show the various processes that influence IPV perpetration rates, especially by survivors.
We would also like international and national regulatory bodies to increase the awareness of IPV and adequately address IPV with special emphasis on how mental health services should assess, identify, and respond to services for people who are survivors and perpetrators of IPV.
Dr. Kumari, Dr. Otite, Dr. Afzal, Dr. Alcera, and Dr. Doumas are affiliated with Hackensack Meridian Health at Ocean Medical Center, Brick, N.J. They have no conflicts of interest.
References
1. Centers for Disease Control and Prevention. Preventing intimate partner violence. 2020 Oct 9.
2. Yu R et al. PLOS Med. 16(12):e1002995. doi: 10.1371/journal.pmed.1002995.
3. Oram S et al. Epidemiol Psychiatr Sci. 2014 Dec;23(4):361-76.
4. Munro OE and Sellbom M. Pers Ment Health. 2020 Mar 11. doi: 10.1002/pmh.1480.
5. Sahraian A et al. Asian J Psychiatry. 2020 Jun. doi: 10.1016/j.ajp.2020.102062.
6. Nikos-Rose K. “COVID-19 Isolation Linked to Increased Domestic Violence, Researchers Suggest.” 2021 Feb 24. University of California, Davis.
7. World Health Organization. “Responding to intimate partner violence and sexual violence against women.” WHO clinical policy guidelines. 2013.
8. National Institute for Health and Care Excellence. “Domestic violence and abuse: Multi-agency working.” PH50. 2014 Feb 26.
9. Feder GS et al. Arch Intern Med. 2006;166(1):22-37.
10. Gondolf EW. Violence Against Women. 2014 Dec;20(12)1539-46.
11. Hamberger LK and Larsen SE. J Fam Violence. 2015;30(6):699-717.
12. Rollè L et al. Front Psychol. 21 Aug 2018. doi: 10.3389/fpsyg.2018.01506.
13. Paterno MT and Draughon JE. J Midwif Women Health. 2016;61(31):370-5.
14. Kalra N et al. Cochrane Database Syst Rev. 2021 May 31;5(5)CD012423.
15. Larsen SE and Hamberger LK. J Fam Viol. 2015;30:1007-30.
16. Kalra N et al. Cochrane Database Syst Rev. 2017 Feb;2017(2):CD012423.
17. Campbell JC et al. J Interpers Violence. 2009;24(4):653-74.
Violence against women remains a global dilemma in need of attention. Physical violence in particular, is the most prevalent type of violence across all genders, races, and nationalities.
The Centers for Disease Control and Prevention says more than 43 million women and 38 million men report experiencing psychological aggression by an intimate partner in their lifetime. Meanwhile, 11 million women and 5 million men report enduring sexual or physical violence and intimate partner violence (IPV), and/or stalking by an intimate partner during their lifetimes, according to the CDC.1
Women who have endured this kind of violence might present differently from men. Some studies, for example, show a more significant association between mutual violence, depression, and substance use among women than men.2 Studies on the phenomenon of IPV victims/survivors becoming perpetrators of abuse are limited, but that this happens in some cases.
Having a psychiatric disorder is associated with a higher likelihood of being physically violent with a partner.3,4 One recent study of 250 female psychiatric patients who were married and had no history of drug abuse found that almost 68% reported psychological abuse, 52% reported sexual abuse, 38% social abuse, 37% reported economic abuse, and 25% reported physical abuse.5
Given those statistics and trends, it is incumbent upon clinicians – including those in primary care, psychiatry, and emergency medicine – to learn to quickly identify IPV survivors, and to use available prognostic tools to monitor perpetrators and survivors.
COVID pandemic’s influence
Isolation tied to the COVID-19 pandemic has been linked to increased IPV. A study conducted by researchers at the University of California, Davis, suggested that extra stress experienced during the COVID-19 pandemic caused by income loss, and the inability to pay for housing and food exacerbated the prevalence of IPV early during the pandemic.6
That study, where researchers collected in surveys of nearly 400 adults in the beginning in April 2020 for 10 weeks, showed that more services and communication are needed so that frontline health care and food bank workers, for example, in addition to social workers, doctors, and therapists, can spot the signs and ask clients questions about potential IPV. They could then link survivors to pertinent assistance and resources.
Furthermore, multiple factors probably have played a pivotal role in increasing the prevalence of IPV during the COVID-19 pandemic. For instance, disruption to usual health and social services as well as diminished access to support systems, such as shelters, and charity helplines negatively affected the reporting of domestic violence.
Long before the pandemic, over the past decade, international and national bodies have played a crucial role in terms of improving the awareness and response to domestic violence.7,8 In addition, several policies have been introduced in countries around the globe emphasizing the need to inquire routinely about domestic violence. Nevertheless, mental health services often fail to adequately address domestic violence in clinical encounters. A systematic review of domestic violence assessment screening performed in a variety of health care settings found that evidence was insufficient to conclude that routine inquiry improved morbidity and mortality among victims of IPV.9 So the question becomes: How can we get our patients to tell us about these experiences so we can intervene?
Gender differences in perpetuating IPV
Several studies have found that abuse can result in various mental illnesses, such as depression, PTSD, anxiety, and suicidal ideation. Again, men have a disproportionately higher rate of perpetrating IPV, compared with women. This theory has been a source of debate in the academic community for years, but recent research has confirmed that women do perpetuate violence against their partners to some extent.10,11
Some members of the LGBTQ+ community also report experiencing violence from partners, so as clinicians, we also need to raise our awareness about the existence of violence among same-sex couples. In fact, a team of Italian researchers report more than 50% of gay men and almost 75% of lesbian women reported that they had been psychologically abused by a partner.12 More research into this area is needed.
Our role as health care professionals
The U.S. Preventive Services Task Force advises that all clinic visits include regular IPV screening.13 But these screenings are all too rare. In fact, a meta-analysis of 19 trials of more than 1,600 participants showed only 9%-40% of doctors routinely test for IPV.14 That research clearly shows how important it is for all clinicians to execute IPV screening. However, numerous challenges toward screening exist, including personal discomfort, limited time during appointments, insufficient resources, and inadequate training.
One ongoing debate revolves around which clinician should screen for IPV. Should the psychiatrist carry out this role – or perhaps the primary care physician, nurse, or social worker? These issues become even more fraught when clinicians worry about offending the patient – especially if the clinician is a male.15
The bottom line is that physicians should inquire about intimate partner violence, because research indicates that women are more likely to reveal abuse when prompted. In addition, during physician appointments, they can use the physician-patient therapeutic connection to conduct a domestic violence evaluation, give resources to victims, and provide ongoing care. Patients who exhibit treatment resistance, persistent pain, depression, sleeplessness, and headaches should prompt psychiatrists to conduct additional investigations into the likelihood of intimate partner violence and domestic abuse.
W also should be attentive when counseling patients about domestic violence when suggesting life-changing events such as pregnancy, employment loss, separation, or divorce. Similar to the recommendations of the USPSTF that all women and men should be screened for IPV, it is suggested that physicians be conscious of facilitating a conversation and not being overtly judgmental while observing body cues. Using the statements such as “we have been hearing a lot of violence in our community lately” could be a segue to introduce the subject.
Asking the question of whether you are being hit rather than being abused has allowed more women to open up more about domestic violence. While physicians are aware that most victims might recant and often go back to their abusers, victims need to be counseled that the abuse might intensify and lead to death.
For women who perpetuate IPV and survivors of IPV, safety is the priority. Physicians should provide safety options and be the facilitators. Studies have shown that fewer victims get the referral to the supporting agencies when IPV is indicated, which puts their safety at risk. In women who commit IPV, clinicians should assess the role of the individual in an IPV disclosure. There are various treatment modalities, whether the violence is performed through self-defense, bidirectionally, or because of aggression.
With the advancement of technology, web-based training on how to ask for IPV, documentation, acknowledgment, and structured referral increase physicians’ confidence when faced with an IPV disclosure than none.16 Treatment modalities should include medication reconciliation and cognitive-behavioral therapy – focusing on emotion regulation.
Using instruments such as the danger assessment tool can help physicians intervene early, reducing the risk of domestic violence and IPV recurrence instead of using clinical assessment alone.17 Physicians should convey empathy, validate victims, and help, especially when abuse is reported.
Also, it is important to evaluate survivors’ safety. Counseling can help people rebuild their self-esteem. Structured referrals for psychiatric help and support services are needed to help survivors on the long road to recovery.
Training all physicians, regardless of specialty, is essential to improve prompt IPV identification and bring awareness to resources available to survivors when IPV is disclosed. Although we described an association between IPV victims becoming possible perpetrators of IPV, more long-term studies are required to show the various processes that influence IPV perpetration rates, especially by survivors.
We would also like international and national regulatory bodies to increase the awareness of IPV and adequately address IPV with special emphasis on how mental health services should assess, identify, and respond to services for people who are survivors and perpetrators of IPV.
Dr. Kumari, Dr. Otite, Dr. Afzal, Dr. Alcera, and Dr. Doumas are affiliated with Hackensack Meridian Health at Ocean Medical Center, Brick, N.J. They have no conflicts of interest.
References
1. Centers for Disease Control and Prevention. Preventing intimate partner violence. 2020 Oct 9.
2. Yu R et al. PLOS Med. 16(12):e1002995. doi: 10.1371/journal.pmed.1002995.
3. Oram S et al. Epidemiol Psychiatr Sci. 2014 Dec;23(4):361-76.
4. Munro OE and Sellbom M. Pers Ment Health. 2020 Mar 11. doi: 10.1002/pmh.1480.
5. Sahraian A et al. Asian J Psychiatry. 2020 Jun. doi: 10.1016/j.ajp.2020.102062.
6. Nikos-Rose K. “COVID-19 Isolation Linked to Increased Domestic Violence, Researchers Suggest.” 2021 Feb 24. University of California, Davis.
7. World Health Organization. “Responding to intimate partner violence and sexual violence against women.” WHO clinical policy guidelines. 2013.
8. National Institute for Health and Care Excellence. “Domestic violence and abuse: Multi-agency working.” PH50. 2014 Feb 26.
9. Feder GS et al. Arch Intern Med. 2006;166(1):22-37.
10. Gondolf EW. Violence Against Women. 2014 Dec;20(12)1539-46.
11. Hamberger LK and Larsen SE. J Fam Violence. 2015;30(6):699-717.
12. Rollè L et al. Front Psychol. 21 Aug 2018. doi: 10.3389/fpsyg.2018.01506.
13. Paterno MT and Draughon JE. J Midwif Women Health. 2016;61(31):370-5.
14. Kalra N et al. Cochrane Database Syst Rev. 2021 May 31;5(5)CD012423.
15. Larsen SE and Hamberger LK. J Fam Viol. 2015;30:1007-30.
16. Kalra N et al. Cochrane Database Syst Rev. 2017 Feb;2017(2):CD012423.
17. Campbell JC et al. J Interpers Violence. 2009;24(4):653-74.
Violence against women remains a global dilemma in need of attention. Physical violence in particular, is the most prevalent type of violence across all genders, races, and nationalities.
The Centers for Disease Control and Prevention says more than 43 million women and 38 million men report experiencing psychological aggression by an intimate partner in their lifetime. Meanwhile, 11 million women and 5 million men report enduring sexual or physical violence and intimate partner violence (IPV), and/or stalking by an intimate partner during their lifetimes, according to the CDC.1
Women who have endured this kind of violence might present differently from men. Some studies, for example, show a more significant association between mutual violence, depression, and substance use among women than men.2 Studies on the phenomenon of IPV victims/survivors becoming perpetrators of abuse are limited, but that this happens in some cases.
Having a psychiatric disorder is associated with a higher likelihood of being physically violent with a partner.3,4 One recent study of 250 female psychiatric patients who were married and had no history of drug abuse found that almost 68% reported psychological abuse, 52% reported sexual abuse, 38% social abuse, 37% reported economic abuse, and 25% reported physical abuse.5
Given those statistics and trends, it is incumbent upon clinicians – including those in primary care, psychiatry, and emergency medicine – to learn to quickly identify IPV survivors, and to use available prognostic tools to monitor perpetrators and survivors.
COVID pandemic’s influence
Isolation tied to the COVID-19 pandemic has been linked to increased IPV. A study conducted by researchers at the University of California, Davis, suggested that extra stress experienced during the COVID-19 pandemic caused by income loss, and the inability to pay for housing and food exacerbated the prevalence of IPV early during the pandemic.6
That study, where researchers collected in surveys of nearly 400 adults in the beginning in April 2020 for 10 weeks, showed that more services and communication are needed so that frontline health care and food bank workers, for example, in addition to social workers, doctors, and therapists, can spot the signs and ask clients questions about potential IPV. They could then link survivors to pertinent assistance and resources.
Furthermore, multiple factors probably have played a pivotal role in increasing the prevalence of IPV during the COVID-19 pandemic. For instance, disruption to usual health and social services as well as diminished access to support systems, such as shelters, and charity helplines negatively affected the reporting of domestic violence.
Long before the pandemic, over the past decade, international and national bodies have played a crucial role in terms of improving the awareness and response to domestic violence.7,8 In addition, several policies have been introduced in countries around the globe emphasizing the need to inquire routinely about domestic violence. Nevertheless, mental health services often fail to adequately address domestic violence in clinical encounters. A systematic review of domestic violence assessment screening performed in a variety of health care settings found that evidence was insufficient to conclude that routine inquiry improved morbidity and mortality among victims of IPV.9 So the question becomes: How can we get our patients to tell us about these experiences so we can intervene?
Gender differences in perpetuating IPV
Several studies have found that abuse can result in various mental illnesses, such as depression, PTSD, anxiety, and suicidal ideation. Again, men have a disproportionately higher rate of perpetrating IPV, compared with women. This theory has been a source of debate in the academic community for years, but recent research has confirmed that women do perpetuate violence against their partners to some extent.10,11
Some members of the LGBTQ+ community also report experiencing violence from partners, so as clinicians, we also need to raise our awareness about the existence of violence among same-sex couples. In fact, a team of Italian researchers report more than 50% of gay men and almost 75% of lesbian women reported that they had been psychologically abused by a partner.12 More research into this area is needed.
Our role as health care professionals
The U.S. Preventive Services Task Force advises that all clinic visits include regular IPV screening.13 But these screenings are all too rare. In fact, a meta-analysis of 19 trials of more than 1,600 participants showed only 9%-40% of doctors routinely test for IPV.14 That research clearly shows how important it is for all clinicians to execute IPV screening. However, numerous challenges toward screening exist, including personal discomfort, limited time during appointments, insufficient resources, and inadequate training.
One ongoing debate revolves around which clinician should screen for IPV. Should the psychiatrist carry out this role – or perhaps the primary care physician, nurse, or social worker? These issues become even more fraught when clinicians worry about offending the patient – especially if the clinician is a male.15
The bottom line is that physicians should inquire about intimate partner violence, because research indicates that women are more likely to reveal abuse when prompted. In addition, during physician appointments, they can use the physician-patient therapeutic connection to conduct a domestic violence evaluation, give resources to victims, and provide ongoing care. Patients who exhibit treatment resistance, persistent pain, depression, sleeplessness, and headaches should prompt psychiatrists to conduct additional investigations into the likelihood of intimate partner violence and domestic abuse.
W also should be attentive when counseling patients about domestic violence when suggesting life-changing events such as pregnancy, employment loss, separation, or divorce. Similar to the recommendations of the USPSTF that all women and men should be screened for IPV, it is suggested that physicians be conscious of facilitating a conversation and not being overtly judgmental while observing body cues. Using the statements such as “we have been hearing a lot of violence in our community lately” could be a segue to introduce the subject.
Asking the question of whether you are being hit rather than being abused has allowed more women to open up more about domestic violence. While physicians are aware that most victims might recant and often go back to their abusers, victims need to be counseled that the abuse might intensify and lead to death.
For women who perpetuate IPV and survivors of IPV, safety is the priority. Physicians should provide safety options and be the facilitators. Studies have shown that fewer victims get the referral to the supporting agencies when IPV is indicated, which puts their safety at risk. In women who commit IPV, clinicians should assess the role of the individual in an IPV disclosure. There are various treatment modalities, whether the violence is performed through self-defense, bidirectionally, or because of aggression.
With the advancement of technology, web-based training on how to ask for IPV, documentation, acknowledgment, and structured referral increase physicians’ confidence when faced with an IPV disclosure than none.16 Treatment modalities should include medication reconciliation and cognitive-behavioral therapy – focusing on emotion regulation.
Using instruments such as the danger assessment tool can help physicians intervene early, reducing the risk of domestic violence and IPV recurrence instead of using clinical assessment alone.17 Physicians should convey empathy, validate victims, and help, especially when abuse is reported.
Also, it is important to evaluate survivors’ safety. Counseling can help people rebuild their self-esteem. Structured referrals for psychiatric help and support services are needed to help survivors on the long road to recovery.
Training all physicians, regardless of specialty, is essential to improve prompt IPV identification and bring awareness to resources available to survivors when IPV is disclosed. Although we described an association between IPV victims becoming possible perpetrators of IPV, more long-term studies are required to show the various processes that influence IPV perpetration rates, especially by survivors.
We would also like international and national regulatory bodies to increase the awareness of IPV and adequately address IPV with special emphasis on how mental health services should assess, identify, and respond to services for people who are survivors and perpetrators of IPV.
Dr. Kumari, Dr. Otite, Dr. Afzal, Dr. Alcera, and Dr. Doumas are affiliated with Hackensack Meridian Health at Ocean Medical Center, Brick, N.J. They have no conflicts of interest.
References
1. Centers for Disease Control and Prevention. Preventing intimate partner violence. 2020 Oct 9.
2. Yu R et al. PLOS Med. 16(12):e1002995. doi: 10.1371/journal.pmed.1002995.
3. Oram S et al. Epidemiol Psychiatr Sci. 2014 Dec;23(4):361-76.
4. Munro OE and Sellbom M. Pers Ment Health. 2020 Mar 11. doi: 10.1002/pmh.1480.
5. Sahraian A et al. Asian J Psychiatry. 2020 Jun. doi: 10.1016/j.ajp.2020.102062.
6. Nikos-Rose K. “COVID-19 Isolation Linked to Increased Domestic Violence, Researchers Suggest.” 2021 Feb 24. University of California, Davis.
7. World Health Organization. “Responding to intimate partner violence and sexual violence against women.” WHO clinical policy guidelines. 2013.
8. National Institute for Health and Care Excellence. “Domestic violence and abuse: Multi-agency working.” PH50. 2014 Feb 26.
9. Feder GS et al. Arch Intern Med. 2006;166(1):22-37.
10. Gondolf EW. Violence Against Women. 2014 Dec;20(12)1539-46.
11. Hamberger LK and Larsen SE. J Fam Violence. 2015;30(6):699-717.
12. Rollè L et al. Front Psychol. 21 Aug 2018. doi: 10.3389/fpsyg.2018.01506.
13. Paterno MT and Draughon JE. J Midwif Women Health. 2016;61(31):370-5.
14. Kalra N et al. Cochrane Database Syst Rev. 2021 May 31;5(5)CD012423.
15. Larsen SE and Hamberger LK. J Fam Viol. 2015;30:1007-30.
16. Kalra N et al. Cochrane Database Syst Rev. 2017 Feb;2017(2):CD012423.
17. Campbell JC et al. J Interpers Violence. 2009;24(4):653-74.
Effective alternatives to psychotherapy for borderline personality disorder
Early interventions that focus on clinical case management and psychiatric care, and not necessarily on individual psychotherapy, are effective for young patients with borderline personality disorder (BPD), new research suggests.
Findings from the Monitoring Outcomes of Borderline Personality Disorder in Youth (MOBY) trial also showed improved psychosocial functioning and reduced suicide ideation with these therapies.
The results suggest that, contrary to common belief, psychotherapy is not the only effective approach for early BPD, lead author Andrew M. Chanen, PhD, director of clinical programs and services and head of personality disorder research at Orygen, Melbourne, told this news organization.
“We can say that early diagnosis and early treatment is effective, and the treatment doesn’t need to involve individual psychotherapy but does need to involve clinical case management and psychiatric care,” said Dr. Chanen, a professorial fellow at the Centre for Youth Mental Health, University of Melbourne.
The findings were published online in JAMA Psychiatry.
Extreme sensitivity
Patients with BPD have “extreme sensitivity to interpersonal slights” and often exhibit intense and volatile emotions and impulsive behavior, Dr. Chanen noted. Many will self-harm, abuse drugs, or attempt suicide; the suicide rate among patients with BPD is 8%-10%.
The condition is typically diagnosed in puberty or early adulthood, affecting about 3% of young people and a little more than 1% of adults.
Because of their aggression and interpersonal difficulties, patients with BPD are often discriminated against by health professionals and end up not getting treated, said Dr. Chanen.
Those who are treated often receive individual psychotherapy, such as dialectical behavior therapy (DBT). That type of therapy, which teaches healthy ways to cope with stress and regulate emotions, is very effective, Dr. Chanen said.
The MOBY trial examined three treatment approaches: the Helping Young People Early (HYPE) model, HYPE combined with weekly “befriending,” and a general youth mental health service (YMHS) model combined with befriending.
A key element of HYPE is cognitive analytic therapy, a psychotherapy program focused on understanding problematic self-management and interpersonal relationship patterns. The model includes clinical case management, such as attending to housing, vocational and educational issues, other mental health needs, and physical health needs.
In the second model, the psychotherapy of the HYPE program was replaced with befriending, which involves chatting with a patient about neutral topics such as sports and avoiding emotionally loaded topics such as interpersonal problems.
For YMHS plus befriending, experts trained in treating young people, but not specialized in treating BPD, were involved in managing patients.
‘High satisfaction’
Researchers randomly assigned 139 participants aged 15-25 years (80.6% women; mean age, 19.1 years) with BPD to one of the treatment arms. Of these, 128 (92.1%) were included in the intent-to-treat analysis.
The primary endpoint was psychosocial functioning, as measured by the Inventory of Interpersonal Problems Circumplex Version and the Social Adjustment Scale–Self-Report. Secondary endpoints included suicidal ideation, suicide attempts, nonsuicidal self-injury, depression, substance use, and treatment satisfaction.
The investigators reported group averages, but the study’s noninferiority design did not allow for determining if one treatment had superior efficacy.
All groups improved significantly on the primary endpoint. At 12 months, there was a mean 28.91-point (23.8%) drop in interpersonal problems and a mean 0.55-point (19.3%) drop in social adjustment scores.
For secondary outcomes, mean improvements at 12 months ranged from 40.7% (17.64 points) on the depression scale to 52.7% (6.22 points) for suicide ideation.
“The only area where the treatment didn’t really have an impact was substance use,” said Dr. Chanen. “Satisfaction was high for all three interventions throughout the study, and it’s hard to improve on high satisfaction.”
‘Turns things upside down’
That patients across all groups had marked and sustained improvements “in ways you wouldn’t expect for BPD” supports the conclusion that the interventions had a true effect, Dr. Chanen said.
he added.
They also imply there are effective alternatives to psychotherapy, which many individuals in the field insist is the only way to treat BPD. “This study turns things upside down and says actually it’s not. It’s the basics of treatment that are important,” Dr. Chanen said.
When a patient presents at the emergency department following a severe overdose, “it’s a reflex” for clinicians to refer that person to a psychotherapy program. “The problem is, these programs are not plentiful enough to be able to service the needs of this group,” Dr. Chanen noted.
On the other hand, the skills for clinical case management and psychiatric care “are available throughout the mental health systems,” he added.
The researchers are planning another analysis to determine whether age and sex predict better outcomes in these patients with BPD.
Unique contribution
Commenting for this news organization, John M. Oldham, MD, distinguished emeritus professor, Baylor College of Medicine, Houston, said a “unique and important contribution” of the study is the focus on early intervention.
“The general standard approach in psychiatry and the diagnostic world has been to not even consider anything until after somebody is 18 years of age, which is a mistake because these kids can become quite impaired earlier than that,” he said.
Dr. Oldham, who was not involved with the research, chaired the American Psychiatric Association workgroup that developed the 2001 evidence-based practice guideline for treating BPD, which recommended psychotherapy as the primary treatment. The guideline was last updated in 2005 – and another update is currently being developed, he noted.
There is an emerging trend toward “good psychiatric management” that focuses on level of functioning rather than on a specific strategy requiring a certificate of training that “not many people out there have,” said Dr. Oldham.
“You’re not going to make much headway with these kids if you’re going to be searching around for a DBT-certified therapist. What you need is to bring them in, get them to trust you, and in a sense be a kind of overall behavioral medicine navigator for them,” he added.
Dr. Oldham noted that, although the primary study outcome improved between 19% and 24%, “that means three-quarters of the people didn’t improve.”
He also pointed out this was only a 1-year trial. “Sometimes treatment for people with a personality disorder such as borderline takes a lot longer than that,” Dr. Oldham concluded.
The trial was funded by the National Health and Medical Research Council. Dr. Chanen reports receiving grants from the Australian government’s National Health and Medical Research Council during the conduct of the study and other support from the Helping Young People Early (HYPE) translational program outside the submitted work. He and another investigator cofounded and lead the HYPE clinical program, a government-funded program with continuous support, and the HYPE translational program, a not-for-profit training program. Dr. Oldham reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Early interventions that focus on clinical case management and psychiatric care, and not necessarily on individual psychotherapy, are effective for young patients with borderline personality disorder (BPD), new research suggests.
Findings from the Monitoring Outcomes of Borderline Personality Disorder in Youth (MOBY) trial also showed improved psychosocial functioning and reduced suicide ideation with these therapies.
The results suggest that, contrary to common belief, psychotherapy is not the only effective approach for early BPD, lead author Andrew M. Chanen, PhD, director of clinical programs and services and head of personality disorder research at Orygen, Melbourne, told this news organization.
“We can say that early diagnosis and early treatment is effective, and the treatment doesn’t need to involve individual psychotherapy but does need to involve clinical case management and psychiatric care,” said Dr. Chanen, a professorial fellow at the Centre for Youth Mental Health, University of Melbourne.
The findings were published online in JAMA Psychiatry.
Extreme sensitivity
Patients with BPD have “extreme sensitivity to interpersonal slights” and often exhibit intense and volatile emotions and impulsive behavior, Dr. Chanen noted. Many will self-harm, abuse drugs, or attempt suicide; the suicide rate among patients with BPD is 8%-10%.
The condition is typically diagnosed in puberty or early adulthood, affecting about 3% of young people and a little more than 1% of adults.
Because of their aggression and interpersonal difficulties, patients with BPD are often discriminated against by health professionals and end up not getting treated, said Dr. Chanen.
Those who are treated often receive individual psychotherapy, such as dialectical behavior therapy (DBT). That type of therapy, which teaches healthy ways to cope with stress and regulate emotions, is very effective, Dr. Chanen said.
The MOBY trial examined three treatment approaches: the Helping Young People Early (HYPE) model, HYPE combined with weekly “befriending,” and a general youth mental health service (YMHS) model combined with befriending.
A key element of HYPE is cognitive analytic therapy, a psychotherapy program focused on understanding problematic self-management and interpersonal relationship patterns. The model includes clinical case management, such as attending to housing, vocational and educational issues, other mental health needs, and physical health needs.
In the second model, the psychotherapy of the HYPE program was replaced with befriending, which involves chatting with a patient about neutral topics such as sports and avoiding emotionally loaded topics such as interpersonal problems.
For YMHS plus befriending, experts trained in treating young people, but not specialized in treating BPD, were involved in managing patients.
‘High satisfaction’
Researchers randomly assigned 139 participants aged 15-25 years (80.6% women; mean age, 19.1 years) with BPD to one of the treatment arms. Of these, 128 (92.1%) were included in the intent-to-treat analysis.
The primary endpoint was psychosocial functioning, as measured by the Inventory of Interpersonal Problems Circumplex Version and the Social Adjustment Scale–Self-Report. Secondary endpoints included suicidal ideation, suicide attempts, nonsuicidal self-injury, depression, substance use, and treatment satisfaction.
The investigators reported group averages, but the study’s noninferiority design did not allow for determining if one treatment had superior efficacy.
All groups improved significantly on the primary endpoint. At 12 months, there was a mean 28.91-point (23.8%) drop in interpersonal problems and a mean 0.55-point (19.3%) drop in social adjustment scores.
For secondary outcomes, mean improvements at 12 months ranged from 40.7% (17.64 points) on the depression scale to 52.7% (6.22 points) for suicide ideation.
“The only area where the treatment didn’t really have an impact was substance use,” said Dr. Chanen. “Satisfaction was high for all three interventions throughout the study, and it’s hard to improve on high satisfaction.”
‘Turns things upside down’
That patients across all groups had marked and sustained improvements “in ways you wouldn’t expect for BPD” supports the conclusion that the interventions had a true effect, Dr. Chanen said.
he added.
They also imply there are effective alternatives to psychotherapy, which many individuals in the field insist is the only way to treat BPD. “This study turns things upside down and says actually it’s not. It’s the basics of treatment that are important,” Dr. Chanen said.
When a patient presents at the emergency department following a severe overdose, “it’s a reflex” for clinicians to refer that person to a psychotherapy program. “The problem is, these programs are not plentiful enough to be able to service the needs of this group,” Dr. Chanen noted.
On the other hand, the skills for clinical case management and psychiatric care “are available throughout the mental health systems,” he added.
The researchers are planning another analysis to determine whether age and sex predict better outcomes in these patients with BPD.
Unique contribution
Commenting for this news organization, John M. Oldham, MD, distinguished emeritus professor, Baylor College of Medicine, Houston, said a “unique and important contribution” of the study is the focus on early intervention.
“The general standard approach in psychiatry and the diagnostic world has been to not even consider anything until after somebody is 18 years of age, which is a mistake because these kids can become quite impaired earlier than that,” he said.
Dr. Oldham, who was not involved with the research, chaired the American Psychiatric Association workgroup that developed the 2001 evidence-based practice guideline for treating BPD, which recommended psychotherapy as the primary treatment. The guideline was last updated in 2005 – and another update is currently being developed, he noted.
There is an emerging trend toward “good psychiatric management” that focuses on level of functioning rather than on a specific strategy requiring a certificate of training that “not many people out there have,” said Dr. Oldham.
“You’re not going to make much headway with these kids if you’re going to be searching around for a DBT-certified therapist. What you need is to bring them in, get them to trust you, and in a sense be a kind of overall behavioral medicine navigator for them,” he added.
Dr. Oldham noted that, although the primary study outcome improved between 19% and 24%, “that means three-quarters of the people didn’t improve.”
He also pointed out this was only a 1-year trial. “Sometimes treatment for people with a personality disorder such as borderline takes a lot longer than that,” Dr. Oldham concluded.
The trial was funded by the National Health and Medical Research Council. Dr. Chanen reports receiving grants from the Australian government’s National Health and Medical Research Council during the conduct of the study and other support from the Helping Young People Early (HYPE) translational program outside the submitted work. He and another investigator cofounded and lead the HYPE clinical program, a government-funded program with continuous support, and the HYPE translational program, a not-for-profit training program. Dr. Oldham reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Early interventions that focus on clinical case management and psychiatric care, and not necessarily on individual psychotherapy, are effective for young patients with borderline personality disorder (BPD), new research suggests.
Findings from the Monitoring Outcomes of Borderline Personality Disorder in Youth (MOBY) trial also showed improved psychosocial functioning and reduced suicide ideation with these therapies.
The results suggest that, contrary to common belief, psychotherapy is not the only effective approach for early BPD, lead author Andrew M. Chanen, PhD, director of clinical programs and services and head of personality disorder research at Orygen, Melbourne, told this news organization.
“We can say that early diagnosis and early treatment is effective, and the treatment doesn’t need to involve individual psychotherapy but does need to involve clinical case management and psychiatric care,” said Dr. Chanen, a professorial fellow at the Centre for Youth Mental Health, University of Melbourne.
The findings were published online in JAMA Psychiatry.
Extreme sensitivity
Patients with BPD have “extreme sensitivity to interpersonal slights” and often exhibit intense and volatile emotions and impulsive behavior, Dr. Chanen noted. Many will self-harm, abuse drugs, or attempt suicide; the suicide rate among patients with BPD is 8%-10%.
The condition is typically diagnosed in puberty or early adulthood, affecting about 3% of young people and a little more than 1% of adults.
Because of their aggression and interpersonal difficulties, patients with BPD are often discriminated against by health professionals and end up not getting treated, said Dr. Chanen.
Those who are treated often receive individual psychotherapy, such as dialectical behavior therapy (DBT). That type of therapy, which teaches healthy ways to cope with stress and regulate emotions, is very effective, Dr. Chanen said.
The MOBY trial examined three treatment approaches: the Helping Young People Early (HYPE) model, HYPE combined with weekly “befriending,” and a general youth mental health service (YMHS) model combined with befriending.
A key element of HYPE is cognitive analytic therapy, a psychotherapy program focused on understanding problematic self-management and interpersonal relationship patterns. The model includes clinical case management, such as attending to housing, vocational and educational issues, other mental health needs, and physical health needs.
In the second model, the psychotherapy of the HYPE program was replaced with befriending, which involves chatting with a patient about neutral topics such as sports and avoiding emotionally loaded topics such as interpersonal problems.
For YMHS plus befriending, experts trained in treating young people, but not specialized in treating BPD, were involved in managing patients.
‘High satisfaction’
Researchers randomly assigned 139 participants aged 15-25 years (80.6% women; mean age, 19.1 years) with BPD to one of the treatment arms. Of these, 128 (92.1%) were included in the intent-to-treat analysis.
The primary endpoint was psychosocial functioning, as measured by the Inventory of Interpersonal Problems Circumplex Version and the Social Adjustment Scale–Self-Report. Secondary endpoints included suicidal ideation, suicide attempts, nonsuicidal self-injury, depression, substance use, and treatment satisfaction.
The investigators reported group averages, but the study’s noninferiority design did not allow for determining if one treatment had superior efficacy.
All groups improved significantly on the primary endpoint. At 12 months, there was a mean 28.91-point (23.8%) drop in interpersonal problems and a mean 0.55-point (19.3%) drop in social adjustment scores.
For secondary outcomes, mean improvements at 12 months ranged from 40.7% (17.64 points) on the depression scale to 52.7% (6.22 points) for suicide ideation.
“The only area where the treatment didn’t really have an impact was substance use,” said Dr. Chanen. “Satisfaction was high for all three interventions throughout the study, and it’s hard to improve on high satisfaction.”
‘Turns things upside down’
That patients across all groups had marked and sustained improvements “in ways you wouldn’t expect for BPD” supports the conclusion that the interventions had a true effect, Dr. Chanen said.
he added.
They also imply there are effective alternatives to psychotherapy, which many individuals in the field insist is the only way to treat BPD. “This study turns things upside down and says actually it’s not. It’s the basics of treatment that are important,” Dr. Chanen said.
When a patient presents at the emergency department following a severe overdose, “it’s a reflex” for clinicians to refer that person to a psychotherapy program. “The problem is, these programs are not plentiful enough to be able to service the needs of this group,” Dr. Chanen noted.
On the other hand, the skills for clinical case management and psychiatric care “are available throughout the mental health systems,” he added.
The researchers are planning another analysis to determine whether age and sex predict better outcomes in these patients with BPD.
Unique contribution
Commenting for this news organization, John M. Oldham, MD, distinguished emeritus professor, Baylor College of Medicine, Houston, said a “unique and important contribution” of the study is the focus on early intervention.
“The general standard approach in psychiatry and the diagnostic world has been to not even consider anything until after somebody is 18 years of age, which is a mistake because these kids can become quite impaired earlier than that,” he said.
Dr. Oldham, who was not involved with the research, chaired the American Psychiatric Association workgroup that developed the 2001 evidence-based practice guideline for treating BPD, which recommended psychotherapy as the primary treatment. The guideline was last updated in 2005 – and another update is currently being developed, he noted.
There is an emerging trend toward “good psychiatric management” that focuses on level of functioning rather than on a specific strategy requiring a certificate of training that “not many people out there have,” said Dr. Oldham.
“You’re not going to make much headway with these kids if you’re going to be searching around for a DBT-certified therapist. What you need is to bring them in, get them to trust you, and in a sense be a kind of overall behavioral medicine navigator for them,” he added.
Dr. Oldham noted that, although the primary study outcome improved between 19% and 24%, “that means three-quarters of the people didn’t improve.”
He also pointed out this was only a 1-year trial. “Sometimes treatment for people with a personality disorder such as borderline takes a lot longer than that,” Dr. Oldham concluded.
The trial was funded by the National Health and Medical Research Council. Dr. Chanen reports receiving grants from the Australian government’s National Health and Medical Research Council during the conduct of the study and other support from the Helping Young People Early (HYPE) translational program outside the submitted work. He and another investigator cofounded and lead the HYPE clinical program, a government-funded program with continuous support, and the HYPE translational program, a not-for-profit training program. Dr. Oldham reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA PSYCHIATRY
Telehealth safe, effective for a challenging psychiatric disorder
Telehealth is safe and effective for the treatment of borderline personality disorder (BPD) and may even have an edge over in-person treatment, new research suggests.
Investigators compared BPD outcomes with therapy delivered in person and via telemedicine and found comparable reductions in depression, anxiety, and anger symptoms as well as improved overall well-being and mental health.
The results also suggest a telehealth advantage with significantly better patient attendance vs. patients treated in-person.
“We found a large effect size of treatment in both groups, as well as comparable levels of satisfaction with treatment, symptom reduction, and improved functioning, coping ability, positive mental health, and general well-being,” study investigator Mark Zimmerman, MD, professor of psychiatry and human behavior, Brown University, Providence, R.I., said in an interview.
The study was published online Nov. 8 in the Journal of Personality Disorders.
‘No other option’
Most previous research investigating telehealth has occurred in outpatient, individual treatment settings and has not examined telehealth-delivered group therapy or partial hospitalization, the authors noted.
“Until the pandemic, we were delivering care in person, but when the pandemic began, because of public safety recommendations, we knew that we could no longer continue doing so,” said Dr. Zimmerman, director of the outpatient division at the partial hospital program (PHP), Rhode Island Hospital.
“In switching to a telehealth platform, we were concerned about patient safety and acceptability of delivering care in that manner, especially with patients with BPD, which is associated with impulsive behavior, self-harm, and suicidal behavior, among other problems,” he said. However “we had no other option” than to utilize a telehealth delivery mode, since the alternative was to shut down the program.
The investigators were “interested in whether or not virtual treatment in an acute intensive setting, such as a PHP, would be as safe, acceptable, and effective as in-person treatment.”
The study was part of the ongoing work of the Rhode Island Methods to Improve Diagnostic Assessment and Services.
Additional safety measures
Treatment, consisting of an Acceptance and Commitment Therapy (ACT) treatment model – including intake assessments, individual therapy, psychiatric visits, and group therapy – was delivered by a multidisciplinary team via Zoom.
Dr. Zimmerman noted that the team implemented additional safety precautions, including having patients check in at the beginning of each day to indicate their location, not seeing patients who were out of state, and making sure all patients had a contact person.
In addition, beyond the therapist leading the group, another therapist was always available, overseeing groups and meeting one-on-one (virtually) with participants if they had been triggered by the group process and were highly distressed.
Patients were asked to complete a number of questionnaires, including the Clinically Useful Patient Satisfaction Scale (CUPSS) at the end of their intake session. The primary outcome measure was the Remission from Depression Questionnaire (RDQ-M).
The study was conducted between May 1 and Dec. 15 of 2020 and included 64 patients with BPD who were treated for the first time in the Rhode Island Hospital PHP. They were compared to 117 patients who participated in the in-person program during the same months in 2019.
Participant characteristics were similar – for example, three-quarters of the participants in both groups were female, and the mean age was 34 years.
‘Sea change’
Most patients in the telehealth and in-person groups reported being “very” or “extremely” satisfied with the initial evaluation (90% vs. 85.3%, c2 = 0.74) and were hopeful that they would get better (85.8% vs. 82.1%, c2 = 0.45).
(c2 = 4.62), and “under both telehealth and in-person treatment conditions, the patients significantly improved from admission to discharge on each of the RDQ-M subscales, with large effect sizes found for most of the subscales,” the authors reported.
There were significant differences between the groups in the average number of days of attendance and number of days missed.
A nonsignificantly higher proportion of patients completed the telehealth program, vs. the in-person program (68.8% vs. 59%, c2 = 1.69).
In both programs, transfer to inpatient care and dissatisfaction-related withdrawal from the program were low (both < 2%). Notably, no patients attempted or completed suicide during treatment.
Virtual treatment is more convenient than in-person treatment, Dr. Zimmerman noted. “Some patients – generally those with medical or transportation issues – told us they otherwise would not have been able to participate [in the program] if treatment had been in person.”
He added, “My prediction is that 5 years from now, two-thirds to three-quarters of outpatient visits will be virtual because that is what the patients prefer – and although there will certainly be individuals who prefer in-person care, I think we’ve witnessed a sea change in how behavioral health care will be delivered.”
‘Game changer’
In an interview, Monica Carsky, PhD, clinical assistant professor of psychology in psychiatry and a senior fellow at the Personality Disorders Institute, Weill Cornell Medical College, New York, said the study has “a lot of valuable detail about how to set up a virtual PHP, which could guide any group wanting to try this.”
Dr. Carsky, who was not involved with the study, called it “a very important contribution to the research literature on efficacious treatment of BPD,” although it is not a randomized controlled trial.
“Adding more individual attention to the virtual group (e.g., having a co-host in the groups) seems as though it may be an important factor in dealing with the limitations of virtual treatment,” she noted.
However, she continued, “a limitation is that outcome assessment relied on self-administered questionnaires and did not include clinician rating scales, so the response may have been subject to the effects of social desirability bias.”
Donald W. Black, MD, associate chief of staff for mental health at the Iowa City Veterans Administration Hospital, said in an interview that the pandemic has been a “game changer, as we have had to quickly adapt mental health programs to a virtual format.
“For the most part, they have been remarkably successful for a variety of conditions, and Zimmerman and colleagues now show this for BPD families,” said Dr. Black, who was not associated with the research.
No study funding was listed. The study authors, Dr. Carsky, and Dr. Black have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Telehealth is safe and effective for the treatment of borderline personality disorder (BPD) and may even have an edge over in-person treatment, new research suggests.
Investigators compared BPD outcomes with therapy delivered in person and via telemedicine and found comparable reductions in depression, anxiety, and anger symptoms as well as improved overall well-being and mental health.
The results also suggest a telehealth advantage with significantly better patient attendance vs. patients treated in-person.
“We found a large effect size of treatment in both groups, as well as comparable levels of satisfaction with treatment, symptom reduction, and improved functioning, coping ability, positive mental health, and general well-being,” study investigator Mark Zimmerman, MD, professor of psychiatry and human behavior, Brown University, Providence, R.I., said in an interview.
The study was published online Nov. 8 in the Journal of Personality Disorders.
‘No other option’
Most previous research investigating telehealth has occurred in outpatient, individual treatment settings and has not examined telehealth-delivered group therapy or partial hospitalization, the authors noted.
“Until the pandemic, we were delivering care in person, but when the pandemic began, because of public safety recommendations, we knew that we could no longer continue doing so,” said Dr. Zimmerman, director of the outpatient division at the partial hospital program (PHP), Rhode Island Hospital.
“In switching to a telehealth platform, we were concerned about patient safety and acceptability of delivering care in that manner, especially with patients with BPD, which is associated with impulsive behavior, self-harm, and suicidal behavior, among other problems,” he said. However “we had no other option” than to utilize a telehealth delivery mode, since the alternative was to shut down the program.
The investigators were “interested in whether or not virtual treatment in an acute intensive setting, such as a PHP, would be as safe, acceptable, and effective as in-person treatment.”
The study was part of the ongoing work of the Rhode Island Methods to Improve Diagnostic Assessment and Services.
Additional safety measures
Treatment, consisting of an Acceptance and Commitment Therapy (ACT) treatment model – including intake assessments, individual therapy, psychiatric visits, and group therapy – was delivered by a multidisciplinary team via Zoom.
Dr. Zimmerman noted that the team implemented additional safety precautions, including having patients check in at the beginning of each day to indicate their location, not seeing patients who were out of state, and making sure all patients had a contact person.
In addition, beyond the therapist leading the group, another therapist was always available, overseeing groups and meeting one-on-one (virtually) with participants if they had been triggered by the group process and were highly distressed.
Patients were asked to complete a number of questionnaires, including the Clinically Useful Patient Satisfaction Scale (CUPSS) at the end of their intake session. The primary outcome measure was the Remission from Depression Questionnaire (RDQ-M).
The study was conducted between May 1 and Dec. 15 of 2020 and included 64 patients with BPD who were treated for the first time in the Rhode Island Hospital PHP. They were compared to 117 patients who participated in the in-person program during the same months in 2019.
Participant characteristics were similar – for example, three-quarters of the participants in both groups were female, and the mean age was 34 years.
‘Sea change’
Most patients in the telehealth and in-person groups reported being “very” or “extremely” satisfied with the initial evaluation (90% vs. 85.3%, c2 = 0.74) and were hopeful that they would get better (85.8% vs. 82.1%, c2 = 0.45).
(c2 = 4.62), and “under both telehealth and in-person treatment conditions, the patients significantly improved from admission to discharge on each of the RDQ-M subscales, with large effect sizes found for most of the subscales,” the authors reported.
There were significant differences between the groups in the average number of days of attendance and number of days missed.
A nonsignificantly higher proportion of patients completed the telehealth program, vs. the in-person program (68.8% vs. 59%, c2 = 1.69).
In both programs, transfer to inpatient care and dissatisfaction-related withdrawal from the program were low (both < 2%). Notably, no patients attempted or completed suicide during treatment.
Virtual treatment is more convenient than in-person treatment, Dr. Zimmerman noted. “Some patients – generally those with medical or transportation issues – told us they otherwise would not have been able to participate [in the program] if treatment had been in person.”
He added, “My prediction is that 5 years from now, two-thirds to three-quarters of outpatient visits will be virtual because that is what the patients prefer – and although there will certainly be individuals who prefer in-person care, I think we’ve witnessed a sea change in how behavioral health care will be delivered.”
‘Game changer’
In an interview, Monica Carsky, PhD, clinical assistant professor of psychology in psychiatry and a senior fellow at the Personality Disorders Institute, Weill Cornell Medical College, New York, said the study has “a lot of valuable detail about how to set up a virtual PHP, which could guide any group wanting to try this.”
Dr. Carsky, who was not involved with the study, called it “a very important contribution to the research literature on efficacious treatment of BPD,” although it is not a randomized controlled trial.
“Adding more individual attention to the virtual group (e.g., having a co-host in the groups) seems as though it may be an important factor in dealing with the limitations of virtual treatment,” she noted.
However, she continued, “a limitation is that outcome assessment relied on self-administered questionnaires and did not include clinician rating scales, so the response may have been subject to the effects of social desirability bias.”
Donald W. Black, MD, associate chief of staff for mental health at the Iowa City Veterans Administration Hospital, said in an interview that the pandemic has been a “game changer, as we have had to quickly adapt mental health programs to a virtual format.
“For the most part, they have been remarkably successful for a variety of conditions, and Zimmerman and colleagues now show this for BPD families,” said Dr. Black, who was not associated with the research.
No study funding was listed. The study authors, Dr. Carsky, and Dr. Black have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Telehealth is safe and effective for the treatment of borderline personality disorder (BPD) and may even have an edge over in-person treatment, new research suggests.
Investigators compared BPD outcomes with therapy delivered in person and via telemedicine and found comparable reductions in depression, anxiety, and anger symptoms as well as improved overall well-being and mental health.
The results also suggest a telehealth advantage with significantly better patient attendance vs. patients treated in-person.
“We found a large effect size of treatment in both groups, as well as comparable levels of satisfaction with treatment, symptom reduction, and improved functioning, coping ability, positive mental health, and general well-being,” study investigator Mark Zimmerman, MD, professor of psychiatry and human behavior, Brown University, Providence, R.I., said in an interview.
The study was published online Nov. 8 in the Journal of Personality Disorders.
‘No other option’
Most previous research investigating telehealth has occurred in outpatient, individual treatment settings and has not examined telehealth-delivered group therapy or partial hospitalization, the authors noted.
“Until the pandemic, we were delivering care in person, but when the pandemic began, because of public safety recommendations, we knew that we could no longer continue doing so,” said Dr. Zimmerman, director of the outpatient division at the partial hospital program (PHP), Rhode Island Hospital.
“In switching to a telehealth platform, we were concerned about patient safety and acceptability of delivering care in that manner, especially with patients with BPD, which is associated with impulsive behavior, self-harm, and suicidal behavior, among other problems,” he said. However “we had no other option” than to utilize a telehealth delivery mode, since the alternative was to shut down the program.
The investigators were “interested in whether or not virtual treatment in an acute intensive setting, such as a PHP, would be as safe, acceptable, and effective as in-person treatment.”
The study was part of the ongoing work of the Rhode Island Methods to Improve Diagnostic Assessment and Services.
Additional safety measures
Treatment, consisting of an Acceptance and Commitment Therapy (ACT) treatment model – including intake assessments, individual therapy, psychiatric visits, and group therapy – was delivered by a multidisciplinary team via Zoom.
Dr. Zimmerman noted that the team implemented additional safety precautions, including having patients check in at the beginning of each day to indicate their location, not seeing patients who were out of state, and making sure all patients had a contact person.
In addition, beyond the therapist leading the group, another therapist was always available, overseeing groups and meeting one-on-one (virtually) with participants if they had been triggered by the group process and were highly distressed.
Patients were asked to complete a number of questionnaires, including the Clinically Useful Patient Satisfaction Scale (CUPSS) at the end of their intake session. The primary outcome measure was the Remission from Depression Questionnaire (RDQ-M).
The study was conducted between May 1 and Dec. 15 of 2020 and included 64 patients with BPD who were treated for the first time in the Rhode Island Hospital PHP. They were compared to 117 patients who participated in the in-person program during the same months in 2019.
Participant characteristics were similar – for example, three-quarters of the participants in both groups were female, and the mean age was 34 years.
‘Sea change’
Most patients in the telehealth and in-person groups reported being “very” or “extremely” satisfied with the initial evaluation (90% vs. 85.3%, c2 = 0.74) and were hopeful that they would get better (85.8% vs. 82.1%, c2 = 0.45).
(c2 = 4.62), and “under both telehealth and in-person treatment conditions, the patients significantly improved from admission to discharge on each of the RDQ-M subscales, with large effect sizes found for most of the subscales,” the authors reported.
There were significant differences between the groups in the average number of days of attendance and number of days missed.
A nonsignificantly higher proportion of patients completed the telehealth program, vs. the in-person program (68.8% vs. 59%, c2 = 1.69).
In both programs, transfer to inpatient care and dissatisfaction-related withdrawal from the program were low (both < 2%). Notably, no patients attempted or completed suicide during treatment.
Virtual treatment is more convenient than in-person treatment, Dr. Zimmerman noted. “Some patients – generally those with medical or transportation issues – told us they otherwise would not have been able to participate [in the program] if treatment had been in person.”
He added, “My prediction is that 5 years from now, two-thirds to three-quarters of outpatient visits will be virtual because that is what the patients prefer – and although there will certainly be individuals who prefer in-person care, I think we’ve witnessed a sea change in how behavioral health care will be delivered.”
‘Game changer’
In an interview, Monica Carsky, PhD, clinical assistant professor of psychology in psychiatry and a senior fellow at the Personality Disorders Institute, Weill Cornell Medical College, New York, said the study has “a lot of valuable detail about how to set up a virtual PHP, which could guide any group wanting to try this.”
Dr. Carsky, who was not involved with the study, called it “a very important contribution to the research literature on efficacious treatment of BPD,” although it is not a randomized controlled trial.
“Adding more individual attention to the virtual group (e.g., having a co-host in the groups) seems as though it may be an important factor in dealing with the limitations of virtual treatment,” she noted.
However, she continued, “a limitation is that outcome assessment relied on self-administered questionnaires and did not include clinician rating scales, so the response may have been subject to the effects of social desirability bias.”
Donald W. Black, MD, associate chief of staff for mental health at the Iowa City Veterans Administration Hospital, said in an interview that the pandemic has been a “game changer, as we have had to quickly adapt mental health programs to a virtual format.
“For the most part, they have been remarkably successful for a variety of conditions, and Zimmerman and colleagues now show this for BPD families,” said Dr. Black, who was not associated with the research.
No study funding was listed. The study authors, Dr. Carsky, and Dr. Black have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF PERSONALITY DISORDERS
Borderline personality disorder: 6 studies of biological interventions
FIRST OF 2 PARTS
Borderline personality disorder (BPD) is marked by an ongoing pattern of mood instability, cognitive distortions, problems with self-image, and impulsive behavior, often resulting in problems in relationships. BPD is associated with serious impairment in psychosocial functioning.1 Patients with BPD tend to use more mental health services than patients with other personality disorders or those with major depressive disorder (MDD).2 However, there has been little consensus on the best treatment(s) for this serious and debilitating disorder, and some clinicians view BPD as difficult to treat.
Current treatments for BPD include psychological and pharmacological interventions. Neuromodulation techniques, such as repetitive transcranial magnetic stimulation, may also positively affect BPD symptomatology. In recent years, there have been some promising findings in the treatment of BPD. In this 2-part article, we focus on current (within the last 5 years) findings from randomized controlled trials (RCTs) of BPD treatments. Here in Part 1, we focus on 6 studies that evaluated biological interventions (Table,3-8). In Part 2, we will focus on RCTs that investigated psychological interventions.
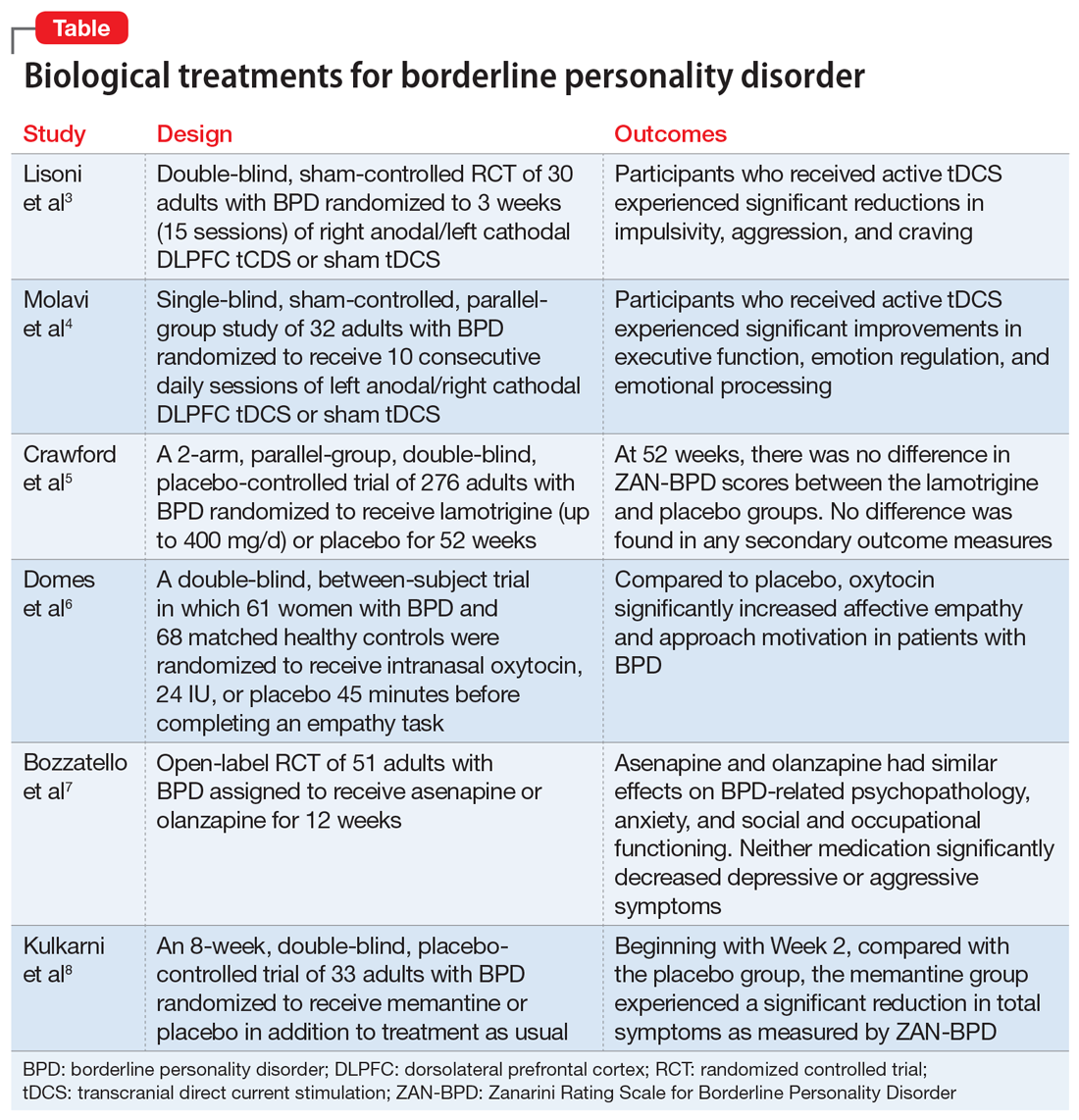
1. Lisoni J, Miotto P, Barlati S, et al. Change in core symptoms of borderline personality disorder by tDCS: a pilot study. Psychiatry Res. 2020;291:113261. doi: 10.1016/j.psychres.2020.113261
Impulsivity has been described as the core feature of BPD that best explains its behavioral, cognitive, and clinical manifestations. Studies have repeatedly demonstrated the role of the prefrontal cortex in modulating impulsivity. Dysfunction of the
Continue to: Study design...
Study design
- In a double-blind, sham-controlled trial, adults who met DSM-IV-TR criteria for BPD were randomized to 3 weeks (15 sessions) of right anodal/left cathodal DLPFC tCDS (n = 15) or sham tDCS (n = 15). This study included patients with comorbid psychiatric disorders, including substance use disorders. Discontinuation or alteration of existing medications was not allowed.
- The presence, severity, and change over time of BPD core symptoms was assessed at baseline and after 3 weeks using several clinical scales, self-questionnaires, and neuropsychological tests, including the Barratt Impulsiveness Scale-11 (BIS-11), Buss-Perry Aggression Questionnaire (BP-AQ), Difficulties in Emotion Regulation Scale (DERS), Hamilton Depression Rating Scale (HAM-D), Beck Depression Inventory (BDI), Hamilton Anxiety Rating Scale (HAM-A), Irritability-Depression Anxiety Scale (IDA), Visual Analog Scales (VAS), and Iowa Gambling Task.
Outcomes
- Participants in the active tDCS group experienced significant reductions in impulsivity, aggression, and craving as measured by the BIS-11, BP-AQ, and VAS.
- Compared to the sham group, the active tDCS group had greater reductions in HAM-D and BDI scores.
- HAM-A and IDA scores were improved in both groups, although the active tDCS group showed greater reductions in IDA scores compared with the sham group.
- As measured by DERS, active tDCS did not improve affective dysregulation more than sham tDCS.
Conclusions/limitations
- Bilateral tDCS targeting the right DLPFC with anodal stimulation is a safe, well-tolerated technique that may modulate core dimensions of BPD, including impulsivity, aggression, and craving.
- Excitatory anodal stimulation of the right DLFPC coupled with inhibitory cathodal stimulation on the left DLPFC may be an effective montage for targeting impulsivity in patients with BPD.
- Study limitations include a small sample size, use of targeted questionnaires only, inclusion of patients with BPD who also had certain comorbid psychiatric disorders, lack of analysis of the contributions of medications, lack of functional neuroimaging, and lack of a follow-up phase.
2. Molavi P, Aziziaram S, Basharpoor S, et al. Repeated transcranial direct current stimulation of dorsolateral-prefrontal cortex improves executive functions, cognitive reappraisal emotion regulation, and control over emotional processing in borderline personality disorder: a randomized, sham-controlled, parallel-group study. J Affect Disord. 2020;274:93-102. doi: 10.1016/j.jad.2020.05.007
Emotional dysregulation is considered a core feature of BPD psychopathology and is closely associated with executive dysfunction and cognitive control. Manifestations of executive dysfunction include aggressiveness, impulsive decision-making, disinhibition, and self-destructive behaviors. Neuroimaging of patients with BPD has shown enhanced activity in the insula, posterior cingulate cortex, and amygdala, with reduced activity in the medial PFC, subgenual anterior cingulate cortex, and DLPFC. Molavi et al4 postulated that increasing DLPFC activation with left anodal tDCS would result in improved executive functioning and emotion dysregulation in patients with BPD.
Study design
- In this single-blind, sham-controlled, parallel-group study, adults who met DSM-5 criteria for BPD were randomized to receive 10 consecutive daily sessions of left anodal/right cathodal DLPFC tDCS (n = 16) or sham tDCS (n = 16).
- The effect of tDCS on executive dysfunction, emotion dysregulation, and emotional processing was measured using the Executive Skills Questionnaire for Adults (ESQ), Emotion Regulation Questionnaire (ERQ), and Emotional Processing Scale (EPS). Measurements occurred at baseline and after 10 sessions of active or sham tDCS.
Outcomes
- Participants who received active tDCS experienced significant improvements in ESQ overall score and most of the executive function domains measured by the ESQ.
- Those in the active tDCS group also experienced significant improvement in emotion regulation as measured by the cognitive reappraisal subscale (but not the expressive suppression subscale) of the ERQ after the intervention.
- Overall emotional processing as measured by the EPS was significantly improved in the active tDCS group following the intervention.
Conclusions/limitations
- Repeated bilateral left anodal/right cathodal tDCS stimulation of the DLPFC significantly improved executive functioning and aspects of emotion regulation and emotional processing in patients with BPD. This improvement was presumed to be the result of increased activity of left DLPFC.
- Study limitations include a single-blind design, lack of follow-up to assess durability and stability of response over time, reliance on self-report measures, lack of functional neuroimaging, and limited focality of tDCS.
3. Crawford MJ, Sanatinia R, Barrett B, et al; LABILE study team. The clinical effectiveness and cost-effectiveness of lamotrigine in borderline personality disorder: a randomized placebo-controlled trial. Am J Psychiatry. 2018;175(8):756-764. doi: 10.1176/appi.ajp.2018.17091006
One of the hallmark symptoms of BPD is mood dysregulation. Current treatment guidelines recommend the use of mood stabilizers for BPD despite limited quality evidence of effectiveness and a lack of FDA-approved medications with this indication. In this RCT, Crawford et al5 examined whether lamotrigine is a clinically effective and cost-effective treatment for people with BPD.
Continue to: Study design...
Study design
- In this 2-arm, parallel-group, double-blind, placebo-controlled trial, 276 adults who met DSM-IV criteria for BPD were randomized to receive lamotrigine (up to 400 mg/d) or placebo for 52 weeks.
- The primary outcome was the score on the Zanarini Rating Scale for Borderline Personality Disorder (ZAN-BPD) at 52 weeks. Secondary outcomes included depressive symptoms, deliberate self-harm, social functioning, health-related quality of life, resource use and costs, treatment adverse effects, and adverse events. These were assessed using the BDI; Acts of Deliberate Self-Harm Inventory; Social Functioning Questionnaire; Alcohol, Smoking, and Substance Involvement Screening Test; and the EQ-5D-3L.
Outcomes
- Mean ZAN-BPD score decreased at 12 weeks in both groups, after which time the score remained stable.
- There was no difference in ZAN-BPD scores at 52 weeks between treatment arms. No difference was found in any secondary outcome measures.
- Difference in costs between groups was not significant.
Conclusions/limitations
- There was no evidence that lamotrigine led to clinical improvements in BPD symptomatology, social functioning, health-related quality of life, or substance use.
- Lamotrigine is neither clinically effective nor a cost-effective use of resources in the treatment of BPD.
- Limitations include a low level of adherence.
4. Domes G, Ower N, von Dawans B, et al. Effects of intranasal oxytocin administration on empathy and approach motivation in women with borderline personality disorder: a randomized controlled trial. Transl Psychiatry. 2019;9(1):328. doi: 10.1038/s41398-019-0658-4
A core feature of BPD is impairment in empathy; adequate empathy is required for intact social functioning. Oxytocin is a neuropeptide that helps regulate complex social cognition and behavior. Prior research has found that oxytocin administration enhances emotion regulation and empathy. Women with BPD have been observed to have lower levels of oxytocin. Domes et al6 conducted an RCT to see if oxytocin could have a beneficial effect on social approach and social cognition in women with BPD.
Study design
- In a double-blind, placebo-controlled, between-subject trial, 61 women who met DSM-IV criteria for BPD and 68 matched healthy controls were randomized to receive intranasal oxytocin, 24 IU, or placebo 45 minutes before completing an empathy task.
- An extended version of the Multifaceted Empathy Test was used to assess empathy and approach motivation.
Outcomes
- For cognitive empathy, patients with BPD exhibited significantly lower overall performance compared to controls. There was no effect of oxytocin on this performance in either group.
- Patients with BPD had significantly lower affective empathy compared with controls. After oxytocin administration, patients with BPD had significantly higher affective empathy than those with BPD who received placebo, reaching the level of healthy controls who received placebo.
- For positive stimuli, patients with BPD showed lower affective empathy than controls. Oxytocin treatment increased affective empathy in both groups.
- For negative stimuli, oxytocin increased affective empathy more in patients with BPD than in controls.
- Patients with BPD demonstrated less approach motivation than controls. Oxytocin increased approach motivation more in patients with BPD than in controls. For approach motivation toward positive stimuli, oxytocin had a significant effect on patients with BPD.
Continue to: Conclusions/limitations...
Conclusions/limitations
- Patients with BPD showed reduced cognitive and affective empathy and less approach behavior motivation than healthy controls.
- Patients with BPD who received oxytocin attained a level of affective empathy and approach motivation similar to that of healthy controls who received placebo. For positive stimuli, both groups exhibited comparable improvements from oxytocin. For negative stimuli, patients with BPD patients showed significant improvement with oxytocin, whereas healthy controls received no such benefit.
- Limitations include the use of self-report scales, lack of a control group, and inclusion of patients using psychotherapeutic medications. The study lacks generalizability because only women were included; the effect of exogenous oxytocin on men may differ.
5. Bozzatello P, Rocca P, Uscinska M, et al. Efficacy and tolerability of asenapine compared with olanzapine in borderline personality disorder: an open-label randomized controlled trial. CNS Drugs. 2017;31(9):809-819. doi: 10.1007/s40263-017-0458-4
The last decade has seen a noticeable shift in clinical practice from the use of antidepressants to mood stabilizers and second-generation antipsychotics (SGAs) in the treatment of BPD. Studies have demonstrated therapeutic effects of antipsychotic drugs across a wide range of BPD symptoms. Among SGAs, olanzapine is the most extensively studied across case reports, open-label studies, and RCTs of patients with BPD. In an RCT, Bozzatello et al7 compared the efficacy and tolerability of asenapine to olanzapine.
Study design
- In this open-label RCT, adults who met DSM-5 criteria for BPD were assigned to receive asenapine (n = 25) or olanzapine (n = 26) for 12 weeks.
- Study measurements included the Clinical Global Impression Scale, Severity item, HAM-D, HAM-A, Social and Occupational Functioning Assessment Scale, Borderline Personality Disorder Severity Index (BPDSI), BIS-11, Modified Overt Aggression Scale, and Dosage Record Treatment Emergent Symptom Scale.
Outcomes
- Asenapine and olanzapine had similar effects on BPD-related psychopathology, anxiety, and social and occupational functioning.
- Neither medication significantly decreased depressive or aggressive symptoms.
- Asenapine was superior to olanzapine in reducing the affective instability score of the BPDSI.
- Akathisia and restlessness/anxiety were more common with asenapine, and somnolence and fatigue were more common with olanzapine.
Conclusions/limitations
- The overall efficacy of asenapine was not different from olanzapine, and both medications were well-tolerated.
- Neither medication led to an improvement in depression or aggression, but asenapine was superior to olanzapine in reducing the severity of affective instability.
- Limitations include an open-label design, lack of placebo group, small sample size, high drop-out rate, exclusion of participants with co-occurring MDD and substance abuse/dependence, lack of data on prior pharmacotherapies and psychotherapies, and lack of power to detect a difference on the dissociation/paranoid ideation item of BPDSI.
6. Kulkarni J, Thomas N, Hudaib AR, et al. Effect of the glutamate NMDA receptor antagonist memantine as adjunctive treatment in borderline personality disorder: an exploratory, randomised, double-blind, placebo-controlled trial. CNS Drugs. 2018;32(2):179-187. doi: 10.1007/s40263-018-0506-8
It has been hypothesized that glutamate dysregulation and excitotoxicity are crucial to the development of the cognitive disturbances that underlie BPD. As such, glutamate modulators such as memantine hold promise for the treatment of BPD. In this RCT, Kulkarni et al8 examined the efficacy and tolerability of memantine compared with treatment as usual in patients with BPD.
Continue to: Study design...
Study design
- In an 8-week, double-blind, placebo-controlled trial, adults diagnosed with BPD according to the Diagnostic Interview for Borderline Patients were randomized to receive memantine (n = 17) or placebo (n = 16) in addition to treatment as usual. Treatment as usual included the use of antidepressants, mood stabilizers, and antipsychotics as well as psychotherapy and other psychosocial interventions.
- Patients were initiated on placebo or memantine, 10 mg/d. Memantine was increased to 20 mg/d after 7 days.
- ZAN-BPD score was the primary outcome and was measured at baseline and 2, 4, 6, and 8 weeks. An adverse effects questionnaire was administered every 2 weeks to assess tolerability.
Outcomes
- During the first 2 weeks of treatment, there were no significant improvements in ZAN-BPD score in the memantine group compared with the placebo group.
- Beginning with Week 2, compared with the placebo group, the memantine group experienced a significant reduction in total symptoms as measured by ZAN-BPD.
- There were no statistically significant differences in adverse events between groups.
Conclusions/limitations
- Memantine appears to be a well-tolerated treatment option for patients with BPD and merits further study.
- Limitations include a small sample size, and an inability to reach plateau of ZAN-BPD total score in either group. Also, there is considerable individual variability in memantine steady-state plasma concentrations, but plasma levels were not measured in this study.
Bottom Line
Findings from small randomized controlled trials suggest that transcranial direct current stimulation, oxytocin, asenapine, olanzapine, and memantine may have beneficial effects on some core symptoms of borderline personality disorder. These findings need to be replicated in larger studies.
1. Skodol AE, Gunderson JG, McGlashan TM, et al. Functional impairment in patients with schizotypal, borderline, avoidant, or obsessive-compulsive personality disorder. Am J Psychiatry. 2002; 159:276-283.
2. Bender DS, Dolan RT, Skodol AE, et al. Treatment utilization by patients with personality disorders. Am J Psychiatry. 2001;158:295-302.
3. Lisoni J, Miotto P, Barlati S, et al. Change in core symptoms of borderline personality disorder by tDCS: a pilot study. Psychiatry Res. 2020;291:113261. doi: 10.1016/j.psychres.2020.113261
4. Molavi P, Aziziaram S, Basharpoor S, et al. Repeated transcranial direct current stimulation of dorsolateral-prefrontal cortex improves executive functions, cognitive reappraisal emotion regulation, and control over emotional processing in borderline personality disorder: a randomized, sham-controlled, parallel-group study. J Affect Disord. 2020;274:93-102. doi: 10.1016/j.jad.2020.05.007
5. Crawford MJ, Sanatinia R, Barrett B, et al; LABILE study team. The clinical effectiveness and cost-effectiveness of lamotrigine in borderline personality disorder: a randomized placebo-controlled trial. Am J Psychiatry. 2018;175(8):756-764. doi: 10.1176/appi.ajp.2018.17091006
6. Domes G, Ower N, von Dawans B, et al. Effects of intranasal oxytocin administration on empathy and approach motivation in women with borderline personality disorder: a randomized controlled trial. Transl Psychiatry. 2019;9(1):328. doi: 10.1038/s41398-019-0658-4
7. Bozzatello P, Rocca P, Uscinska M, et al. Efficacy and tolerability of asenapine compared with olanzapine in borderline personality disorder: an open-label randomized controlled trial. CNS Drugs. 2017;31(9):809-819. doi: 10.1007/s40263-017-0458-4
8. Kulkarni J, Thomas N, Hudaib AR, et al. Effect of the glutamate NMDA receptor antagonist memantine as adjunctive treatment in borderline personality disorder: an exploratory, randomised, double-blind, placebo-controlled trial. CNS Drugs. 2018;32(2):179-187. doi: 10.1007/s40263-018-0506-8
FIRST OF 2 PARTS
Borderline personality disorder (BPD) is marked by an ongoing pattern of mood instability, cognitive distortions, problems with self-image, and impulsive behavior, often resulting in problems in relationships. BPD is associated with serious impairment in psychosocial functioning.1 Patients with BPD tend to use more mental health services than patients with other personality disorders or those with major depressive disorder (MDD).2 However, there has been little consensus on the best treatment(s) for this serious and debilitating disorder, and some clinicians view BPD as difficult to treat.
Current treatments for BPD include psychological and pharmacological interventions. Neuromodulation techniques, such as repetitive transcranial magnetic stimulation, may also positively affect BPD symptomatology. In recent years, there have been some promising findings in the treatment of BPD. In this 2-part article, we focus on current (within the last 5 years) findings from randomized controlled trials (RCTs) of BPD treatments. Here in Part 1, we focus on 6 studies that evaluated biological interventions (Table,3-8). In Part 2, we will focus on RCTs that investigated psychological interventions.
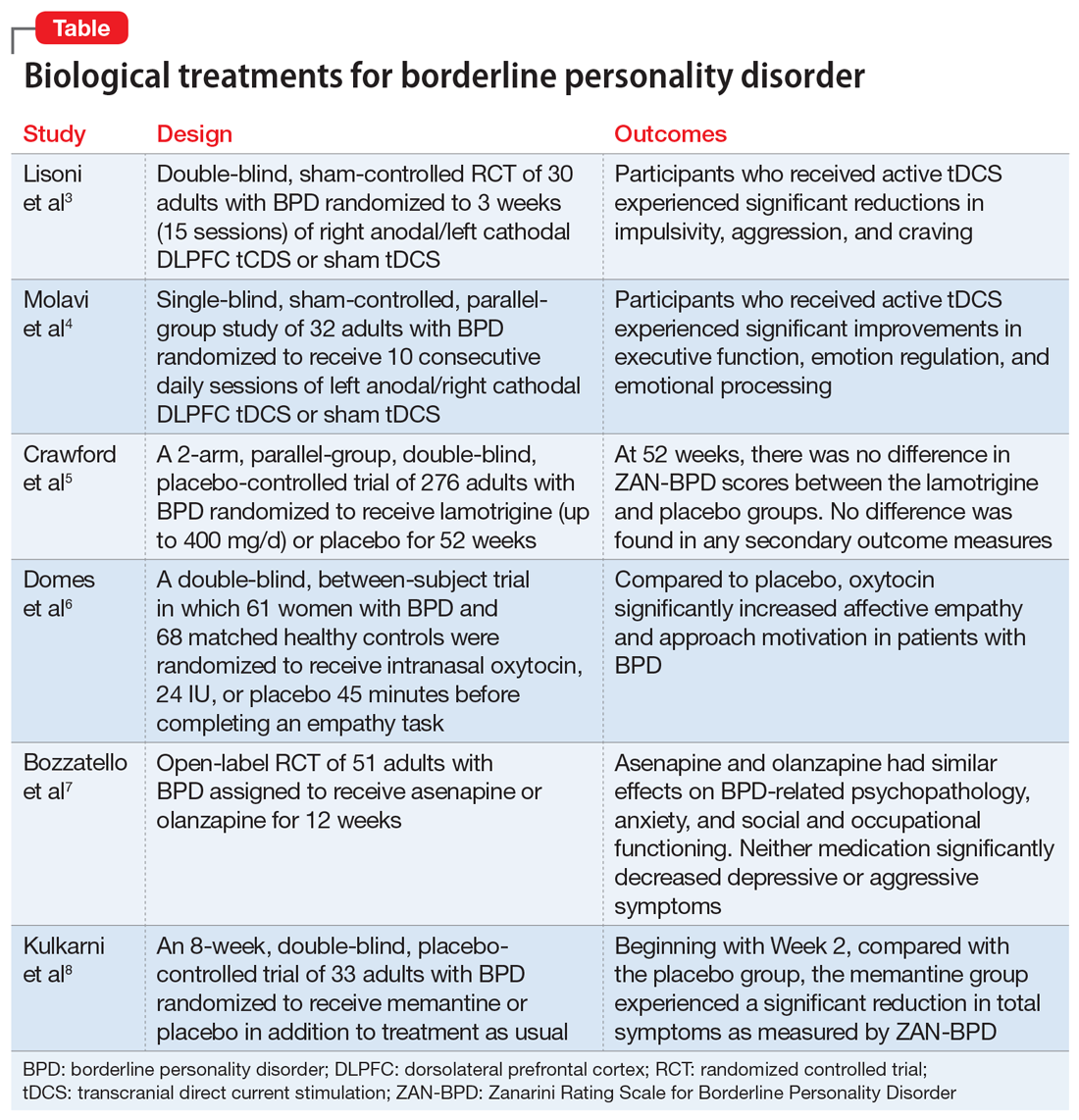
1. Lisoni J, Miotto P, Barlati S, et al. Change in core symptoms of borderline personality disorder by tDCS: a pilot study. Psychiatry Res. 2020;291:113261. doi: 10.1016/j.psychres.2020.113261
Impulsivity has been described as the core feature of BPD that best explains its behavioral, cognitive, and clinical manifestations. Studies have repeatedly demonstrated the role of the prefrontal cortex in modulating impulsivity. Dysfunction of the
Continue to: Study design...
Study design
- In a double-blind, sham-controlled trial, adults who met DSM-IV-TR criteria for BPD were randomized to 3 weeks (15 sessions) of right anodal/left cathodal DLPFC tCDS (n = 15) or sham tDCS (n = 15). This study included patients with comorbid psychiatric disorders, including substance use disorders. Discontinuation or alteration of existing medications was not allowed.
- The presence, severity, and change over time of BPD core symptoms was assessed at baseline and after 3 weeks using several clinical scales, self-questionnaires, and neuropsychological tests, including the Barratt Impulsiveness Scale-11 (BIS-11), Buss-Perry Aggression Questionnaire (BP-AQ), Difficulties in Emotion Regulation Scale (DERS), Hamilton Depression Rating Scale (HAM-D), Beck Depression Inventory (BDI), Hamilton Anxiety Rating Scale (HAM-A), Irritability-Depression Anxiety Scale (IDA), Visual Analog Scales (VAS), and Iowa Gambling Task.
Outcomes
- Participants in the active tDCS group experienced significant reductions in impulsivity, aggression, and craving as measured by the BIS-11, BP-AQ, and VAS.
- Compared to the sham group, the active tDCS group had greater reductions in HAM-D and BDI scores.
- HAM-A and IDA scores were improved in both groups, although the active tDCS group showed greater reductions in IDA scores compared with the sham group.
- As measured by DERS, active tDCS did not improve affective dysregulation more than sham tDCS.
Conclusions/limitations
- Bilateral tDCS targeting the right DLPFC with anodal stimulation is a safe, well-tolerated technique that may modulate core dimensions of BPD, including impulsivity, aggression, and craving.
- Excitatory anodal stimulation of the right DLFPC coupled with inhibitory cathodal stimulation on the left DLPFC may be an effective montage for targeting impulsivity in patients with BPD.
- Study limitations include a small sample size, use of targeted questionnaires only, inclusion of patients with BPD who also had certain comorbid psychiatric disorders, lack of analysis of the contributions of medications, lack of functional neuroimaging, and lack of a follow-up phase.
2. Molavi P, Aziziaram S, Basharpoor S, et al. Repeated transcranial direct current stimulation of dorsolateral-prefrontal cortex improves executive functions, cognitive reappraisal emotion regulation, and control over emotional processing in borderline personality disorder: a randomized, sham-controlled, parallel-group study. J Affect Disord. 2020;274:93-102. doi: 10.1016/j.jad.2020.05.007
Emotional dysregulation is considered a core feature of BPD psychopathology and is closely associated with executive dysfunction and cognitive control. Manifestations of executive dysfunction include aggressiveness, impulsive decision-making, disinhibition, and self-destructive behaviors. Neuroimaging of patients with BPD has shown enhanced activity in the insula, posterior cingulate cortex, and amygdala, with reduced activity in the medial PFC, subgenual anterior cingulate cortex, and DLPFC. Molavi et al4 postulated that increasing DLPFC activation with left anodal tDCS would result in improved executive functioning and emotion dysregulation in patients with BPD.
Study design
- In this single-blind, sham-controlled, parallel-group study, adults who met DSM-5 criteria for BPD were randomized to receive 10 consecutive daily sessions of left anodal/right cathodal DLPFC tDCS (n = 16) or sham tDCS (n = 16).
- The effect of tDCS on executive dysfunction, emotion dysregulation, and emotional processing was measured using the Executive Skills Questionnaire for Adults (ESQ), Emotion Regulation Questionnaire (ERQ), and Emotional Processing Scale (EPS). Measurements occurred at baseline and after 10 sessions of active or sham tDCS.
Outcomes
- Participants who received active tDCS experienced significant improvements in ESQ overall score and most of the executive function domains measured by the ESQ.
- Those in the active tDCS group also experienced significant improvement in emotion regulation as measured by the cognitive reappraisal subscale (but not the expressive suppression subscale) of the ERQ after the intervention.
- Overall emotional processing as measured by the EPS was significantly improved in the active tDCS group following the intervention.
Conclusions/limitations
- Repeated bilateral left anodal/right cathodal tDCS stimulation of the DLPFC significantly improved executive functioning and aspects of emotion regulation and emotional processing in patients with BPD. This improvement was presumed to be the result of increased activity of left DLPFC.
- Study limitations include a single-blind design, lack of follow-up to assess durability and stability of response over time, reliance on self-report measures, lack of functional neuroimaging, and limited focality of tDCS.
3. Crawford MJ, Sanatinia R, Barrett B, et al; LABILE study team. The clinical effectiveness and cost-effectiveness of lamotrigine in borderline personality disorder: a randomized placebo-controlled trial. Am J Psychiatry. 2018;175(8):756-764. doi: 10.1176/appi.ajp.2018.17091006
One of the hallmark symptoms of BPD is mood dysregulation. Current treatment guidelines recommend the use of mood stabilizers for BPD despite limited quality evidence of effectiveness and a lack of FDA-approved medications with this indication. In this RCT, Crawford et al5 examined whether lamotrigine is a clinically effective and cost-effective treatment for people with BPD.
Continue to: Study design...
Study design
- In this 2-arm, parallel-group, double-blind, placebo-controlled trial, 276 adults who met DSM-IV criteria for BPD were randomized to receive lamotrigine (up to 400 mg/d) or placebo for 52 weeks.
- The primary outcome was the score on the Zanarini Rating Scale for Borderline Personality Disorder (ZAN-BPD) at 52 weeks. Secondary outcomes included depressive symptoms, deliberate self-harm, social functioning, health-related quality of life, resource use and costs, treatment adverse effects, and adverse events. These were assessed using the BDI; Acts of Deliberate Self-Harm Inventory; Social Functioning Questionnaire; Alcohol, Smoking, and Substance Involvement Screening Test; and the EQ-5D-3L.
Outcomes
- Mean ZAN-BPD score decreased at 12 weeks in both groups, after which time the score remained stable.
- There was no difference in ZAN-BPD scores at 52 weeks between treatment arms. No difference was found in any secondary outcome measures.
- Difference in costs between groups was not significant.
Conclusions/limitations
- There was no evidence that lamotrigine led to clinical improvements in BPD symptomatology, social functioning, health-related quality of life, or substance use.
- Lamotrigine is neither clinically effective nor a cost-effective use of resources in the treatment of BPD.
- Limitations include a low level of adherence.
4. Domes G, Ower N, von Dawans B, et al. Effects of intranasal oxytocin administration on empathy and approach motivation in women with borderline personality disorder: a randomized controlled trial. Transl Psychiatry. 2019;9(1):328. doi: 10.1038/s41398-019-0658-4
A core feature of BPD is impairment in empathy; adequate empathy is required for intact social functioning. Oxytocin is a neuropeptide that helps regulate complex social cognition and behavior. Prior research has found that oxytocin administration enhances emotion regulation and empathy. Women with BPD have been observed to have lower levels of oxytocin. Domes et al6 conducted an RCT to see if oxytocin could have a beneficial effect on social approach and social cognition in women with BPD.
Study design
- In a double-blind, placebo-controlled, between-subject trial, 61 women who met DSM-IV criteria for BPD and 68 matched healthy controls were randomized to receive intranasal oxytocin, 24 IU, or placebo 45 minutes before completing an empathy task.
- An extended version of the Multifaceted Empathy Test was used to assess empathy and approach motivation.
Outcomes
- For cognitive empathy, patients with BPD exhibited significantly lower overall performance compared to controls. There was no effect of oxytocin on this performance in either group.
- Patients with BPD had significantly lower affective empathy compared with controls. After oxytocin administration, patients with BPD had significantly higher affective empathy than those with BPD who received placebo, reaching the level of healthy controls who received placebo.
- For positive stimuli, patients with BPD showed lower affective empathy than controls. Oxytocin treatment increased affective empathy in both groups.
- For negative stimuli, oxytocin increased affective empathy more in patients with BPD than in controls.
- Patients with BPD demonstrated less approach motivation than controls. Oxytocin increased approach motivation more in patients with BPD than in controls. For approach motivation toward positive stimuli, oxytocin had a significant effect on patients with BPD.
Continue to: Conclusions/limitations...
Conclusions/limitations
- Patients with BPD showed reduced cognitive and affective empathy and less approach behavior motivation than healthy controls.
- Patients with BPD who received oxytocin attained a level of affective empathy and approach motivation similar to that of healthy controls who received placebo. For positive stimuli, both groups exhibited comparable improvements from oxytocin. For negative stimuli, patients with BPD patients showed significant improvement with oxytocin, whereas healthy controls received no such benefit.
- Limitations include the use of self-report scales, lack of a control group, and inclusion of patients using psychotherapeutic medications. The study lacks generalizability because only women were included; the effect of exogenous oxytocin on men may differ.
5. Bozzatello P, Rocca P, Uscinska M, et al. Efficacy and tolerability of asenapine compared with olanzapine in borderline personality disorder: an open-label randomized controlled trial. CNS Drugs. 2017;31(9):809-819. doi: 10.1007/s40263-017-0458-4
The last decade has seen a noticeable shift in clinical practice from the use of antidepressants to mood stabilizers and second-generation antipsychotics (SGAs) in the treatment of BPD. Studies have demonstrated therapeutic effects of antipsychotic drugs across a wide range of BPD symptoms. Among SGAs, olanzapine is the most extensively studied across case reports, open-label studies, and RCTs of patients with BPD. In an RCT, Bozzatello et al7 compared the efficacy and tolerability of asenapine to olanzapine.
Study design
- In this open-label RCT, adults who met DSM-5 criteria for BPD were assigned to receive asenapine (n = 25) or olanzapine (n = 26) for 12 weeks.
- Study measurements included the Clinical Global Impression Scale, Severity item, HAM-D, HAM-A, Social and Occupational Functioning Assessment Scale, Borderline Personality Disorder Severity Index (BPDSI), BIS-11, Modified Overt Aggression Scale, and Dosage Record Treatment Emergent Symptom Scale.
Outcomes
- Asenapine and olanzapine had similar effects on BPD-related psychopathology, anxiety, and social and occupational functioning.
- Neither medication significantly decreased depressive or aggressive symptoms.
- Asenapine was superior to olanzapine in reducing the affective instability score of the BPDSI.
- Akathisia and restlessness/anxiety were more common with asenapine, and somnolence and fatigue were more common with olanzapine.
Conclusions/limitations
- The overall efficacy of asenapine was not different from olanzapine, and both medications were well-tolerated.
- Neither medication led to an improvement in depression or aggression, but asenapine was superior to olanzapine in reducing the severity of affective instability.
- Limitations include an open-label design, lack of placebo group, small sample size, high drop-out rate, exclusion of participants with co-occurring MDD and substance abuse/dependence, lack of data on prior pharmacotherapies and psychotherapies, and lack of power to detect a difference on the dissociation/paranoid ideation item of BPDSI.
6. Kulkarni J, Thomas N, Hudaib AR, et al. Effect of the glutamate NMDA receptor antagonist memantine as adjunctive treatment in borderline personality disorder: an exploratory, randomised, double-blind, placebo-controlled trial. CNS Drugs. 2018;32(2):179-187. doi: 10.1007/s40263-018-0506-8
It has been hypothesized that glutamate dysregulation and excitotoxicity are crucial to the development of the cognitive disturbances that underlie BPD. As such, glutamate modulators such as memantine hold promise for the treatment of BPD. In this RCT, Kulkarni et al8 examined the efficacy and tolerability of memantine compared with treatment as usual in patients with BPD.
Continue to: Study design...
Study design
- In an 8-week, double-blind, placebo-controlled trial, adults diagnosed with BPD according to the Diagnostic Interview for Borderline Patients were randomized to receive memantine (n = 17) or placebo (n = 16) in addition to treatment as usual. Treatment as usual included the use of antidepressants, mood stabilizers, and antipsychotics as well as psychotherapy and other psychosocial interventions.
- Patients were initiated on placebo or memantine, 10 mg/d. Memantine was increased to 20 mg/d after 7 days.
- ZAN-BPD score was the primary outcome and was measured at baseline and 2, 4, 6, and 8 weeks. An adverse effects questionnaire was administered every 2 weeks to assess tolerability.
Outcomes
- During the first 2 weeks of treatment, there were no significant improvements in ZAN-BPD score in the memantine group compared with the placebo group.
- Beginning with Week 2, compared with the placebo group, the memantine group experienced a significant reduction in total symptoms as measured by ZAN-BPD.
- There were no statistically significant differences in adverse events between groups.
Conclusions/limitations
- Memantine appears to be a well-tolerated treatment option for patients with BPD and merits further study.
- Limitations include a small sample size, and an inability to reach plateau of ZAN-BPD total score in either group. Also, there is considerable individual variability in memantine steady-state plasma concentrations, but plasma levels were not measured in this study.
Bottom Line
Findings from small randomized controlled trials suggest that transcranial direct current stimulation, oxytocin, asenapine, olanzapine, and memantine may have beneficial effects on some core symptoms of borderline personality disorder. These findings need to be replicated in larger studies.
FIRST OF 2 PARTS
Borderline personality disorder (BPD) is marked by an ongoing pattern of mood instability, cognitive distortions, problems with self-image, and impulsive behavior, often resulting in problems in relationships. BPD is associated with serious impairment in psychosocial functioning.1 Patients with BPD tend to use more mental health services than patients with other personality disorders or those with major depressive disorder (MDD).2 However, there has been little consensus on the best treatment(s) for this serious and debilitating disorder, and some clinicians view BPD as difficult to treat.
Current treatments for BPD include psychological and pharmacological interventions. Neuromodulation techniques, such as repetitive transcranial magnetic stimulation, may also positively affect BPD symptomatology. In recent years, there have been some promising findings in the treatment of BPD. In this 2-part article, we focus on current (within the last 5 years) findings from randomized controlled trials (RCTs) of BPD treatments. Here in Part 1, we focus on 6 studies that evaluated biological interventions (Table,3-8). In Part 2, we will focus on RCTs that investigated psychological interventions.
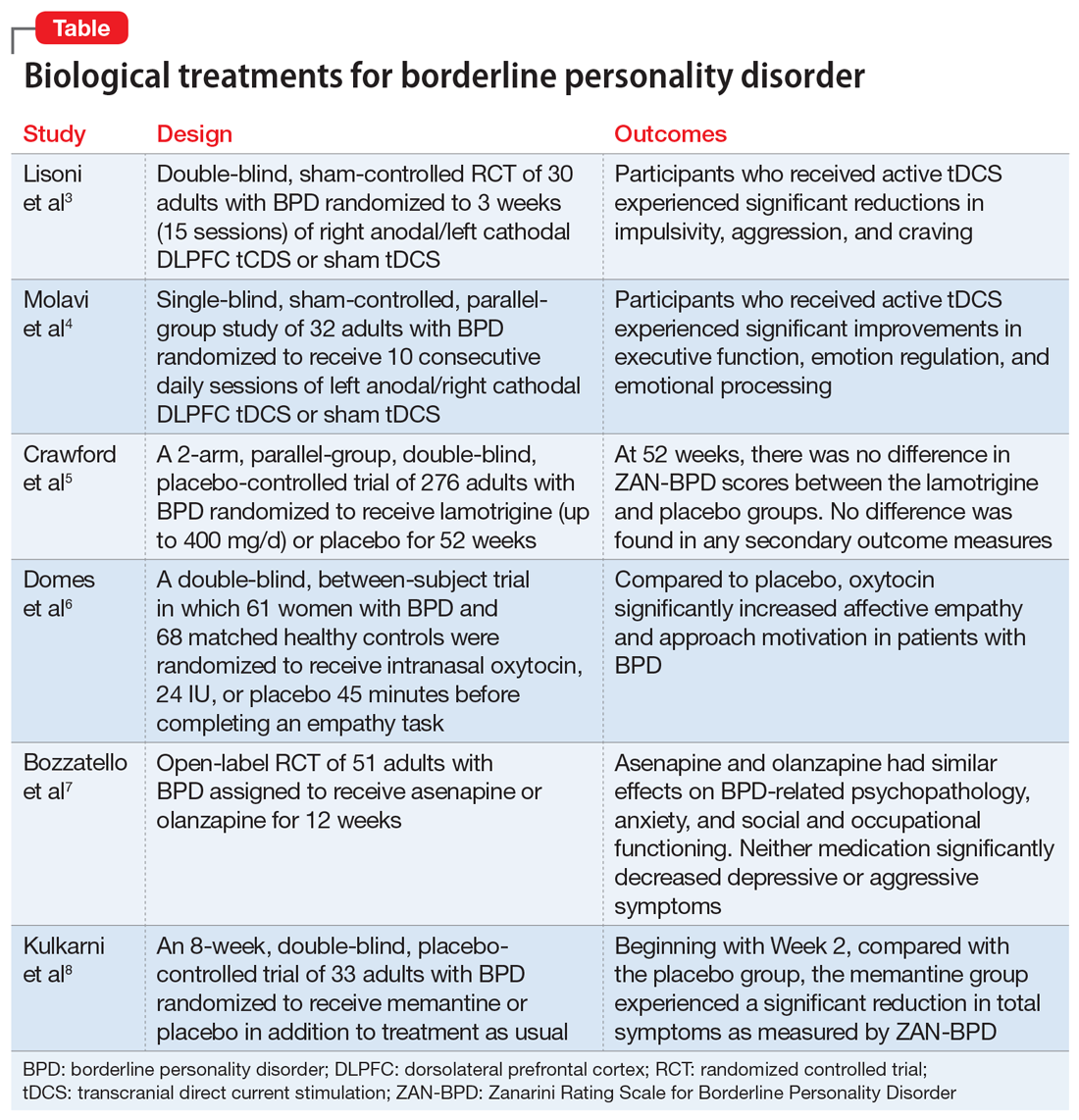
1. Lisoni J, Miotto P, Barlati S, et al. Change in core symptoms of borderline personality disorder by tDCS: a pilot study. Psychiatry Res. 2020;291:113261. doi: 10.1016/j.psychres.2020.113261
Impulsivity has been described as the core feature of BPD that best explains its behavioral, cognitive, and clinical manifestations. Studies have repeatedly demonstrated the role of the prefrontal cortex in modulating impulsivity. Dysfunction of the
Continue to: Study design...
Study design
- In a double-blind, sham-controlled trial, adults who met DSM-IV-TR criteria for BPD were randomized to 3 weeks (15 sessions) of right anodal/left cathodal DLPFC tCDS (n = 15) or sham tDCS (n = 15). This study included patients with comorbid psychiatric disorders, including substance use disorders. Discontinuation or alteration of existing medications was not allowed.
- The presence, severity, and change over time of BPD core symptoms was assessed at baseline and after 3 weeks using several clinical scales, self-questionnaires, and neuropsychological tests, including the Barratt Impulsiveness Scale-11 (BIS-11), Buss-Perry Aggression Questionnaire (BP-AQ), Difficulties in Emotion Regulation Scale (DERS), Hamilton Depression Rating Scale (HAM-D), Beck Depression Inventory (BDI), Hamilton Anxiety Rating Scale (HAM-A), Irritability-Depression Anxiety Scale (IDA), Visual Analog Scales (VAS), and Iowa Gambling Task.
Outcomes
- Participants in the active tDCS group experienced significant reductions in impulsivity, aggression, and craving as measured by the BIS-11, BP-AQ, and VAS.
- Compared to the sham group, the active tDCS group had greater reductions in HAM-D and BDI scores.
- HAM-A and IDA scores were improved in both groups, although the active tDCS group showed greater reductions in IDA scores compared with the sham group.
- As measured by DERS, active tDCS did not improve affective dysregulation more than sham tDCS.
Conclusions/limitations
- Bilateral tDCS targeting the right DLPFC with anodal stimulation is a safe, well-tolerated technique that may modulate core dimensions of BPD, including impulsivity, aggression, and craving.
- Excitatory anodal stimulation of the right DLFPC coupled with inhibitory cathodal stimulation on the left DLPFC may be an effective montage for targeting impulsivity in patients with BPD.
- Study limitations include a small sample size, use of targeted questionnaires only, inclusion of patients with BPD who also had certain comorbid psychiatric disorders, lack of analysis of the contributions of medications, lack of functional neuroimaging, and lack of a follow-up phase.
2. Molavi P, Aziziaram S, Basharpoor S, et al. Repeated transcranial direct current stimulation of dorsolateral-prefrontal cortex improves executive functions, cognitive reappraisal emotion regulation, and control over emotional processing in borderline personality disorder: a randomized, sham-controlled, parallel-group study. J Affect Disord. 2020;274:93-102. doi: 10.1016/j.jad.2020.05.007
Emotional dysregulation is considered a core feature of BPD psychopathology and is closely associated with executive dysfunction and cognitive control. Manifestations of executive dysfunction include aggressiveness, impulsive decision-making, disinhibition, and self-destructive behaviors. Neuroimaging of patients with BPD has shown enhanced activity in the insula, posterior cingulate cortex, and amygdala, with reduced activity in the medial PFC, subgenual anterior cingulate cortex, and DLPFC. Molavi et al4 postulated that increasing DLPFC activation with left anodal tDCS would result in improved executive functioning and emotion dysregulation in patients with BPD.
Study design
- In this single-blind, sham-controlled, parallel-group study, adults who met DSM-5 criteria for BPD were randomized to receive 10 consecutive daily sessions of left anodal/right cathodal DLPFC tDCS (n = 16) or sham tDCS (n = 16).
- The effect of tDCS on executive dysfunction, emotion dysregulation, and emotional processing was measured using the Executive Skills Questionnaire for Adults (ESQ), Emotion Regulation Questionnaire (ERQ), and Emotional Processing Scale (EPS). Measurements occurred at baseline and after 10 sessions of active or sham tDCS.
Outcomes
- Participants who received active tDCS experienced significant improvements in ESQ overall score and most of the executive function domains measured by the ESQ.
- Those in the active tDCS group also experienced significant improvement in emotion regulation as measured by the cognitive reappraisal subscale (but not the expressive suppression subscale) of the ERQ after the intervention.
- Overall emotional processing as measured by the EPS was significantly improved in the active tDCS group following the intervention.
Conclusions/limitations
- Repeated bilateral left anodal/right cathodal tDCS stimulation of the DLPFC significantly improved executive functioning and aspects of emotion regulation and emotional processing in patients with BPD. This improvement was presumed to be the result of increased activity of left DLPFC.
- Study limitations include a single-blind design, lack of follow-up to assess durability and stability of response over time, reliance on self-report measures, lack of functional neuroimaging, and limited focality of tDCS.
3. Crawford MJ, Sanatinia R, Barrett B, et al; LABILE study team. The clinical effectiveness and cost-effectiveness of lamotrigine in borderline personality disorder: a randomized placebo-controlled trial. Am J Psychiatry. 2018;175(8):756-764. doi: 10.1176/appi.ajp.2018.17091006
One of the hallmark symptoms of BPD is mood dysregulation. Current treatment guidelines recommend the use of mood stabilizers for BPD despite limited quality evidence of effectiveness and a lack of FDA-approved medications with this indication. In this RCT, Crawford et al5 examined whether lamotrigine is a clinically effective and cost-effective treatment for people with BPD.
Continue to: Study design...
Study design
- In this 2-arm, parallel-group, double-blind, placebo-controlled trial, 276 adults who met DSM-IV criteria for BPD were randomized to receive lamotrigine (up to 400 mg/d) or placebo for 52 weeks.
- The primary outcome was the score on the Zanarini Rating Scale for Borderline Personality Disorder (ZAN-BPD) at 52 weeks. Secondary outcomes included depressive symptoms, deliberate self-harm, social functioning, health-related quality of life, resource use and costs, treatment adverse effects, and adverse events. These were assessed using the BDI; Acts of Deliberate Self-Harm Inventory; Social Functioning Questionnaire; Alcohol, Smoking, and Substance Involvement Screening Test; and the EQ-5D-3L.
Outcomes
- Mean ZAN-BPD score decreased at 12 weeks in both groups, after which time the score remained stable.
- There was no difference in ZAN-BPD scores at 52 weeks between treatment arms. No difference was found in any secondary outcome measures.
- Difference in costs between groups was not significant.
Conclusions/limitations
- There was no evidence that lamotrigine led to clinical improvements in BPD symptomatology, social functioning, health-related quality of life, or substance use.
- Lamotrigine is neither clinically effective nor a cost-effective use of resources in the treatment of BPD.
- Limitations include a low level of adherence.
4. Domes G, Ower N, von Dawans B, et al. Effects of intranasal oxytocin administration on empathy and approach motivation in women with borderline personality disorder: a randomized controlled trial. Transl Psychiatry. 2019;9(1):328. doi: 10.1038/s41398-019-0658-4
A core feature of BPD is impairment in empathy; adequate empathy is required for intact social functioning. Oxytocin is a neuropeptide that helps regulate complex social cognition and behavior. Prior research has found that oxytocin administration enhances emotion regulation and empathy. Women with BPD have been observed to have lower levels of oxytocin. Domes et al6 conducted an RCT to see if oxytocin could have a beneficial effect on social approach and social cognition in women with BPD.
Study design
- In a double-blind, placebo-controlled, between-subject trial, 61 women who met DSM-IV criteria for BPD and 68 matched healthy controls were randomized to receive intranasal oxytocin, 24 IU, or placebo 45 minutes before completing an empathy task.
- An extended version of the Multifaceted Empathy Test was used to assess empathy and approach motivation.
Outcomes
- For cognitive empathy, patients with BPD exhibited significantly lower overall performance compared to controls. There was no effect of oxytocin on this performance in either group.
- Patients with BPD had significantly lower affective empathy compared with controls. After oxytocin administration, patients with BPD had significantly higher affective empathy than those with BPD who received placebo, reaching the level of healthy controls who received placebo.
- For positive stimuli, patients with BPD showed lower affective empathy than controls. Oxytocin treatment increased affective empathy in both groups.
- For negative stimuli, oxytocin increased affective empathy more in patients with BPD than in controls.
- Patients with BPD demonstrated less approach motivation than controls. Oxytocin increased approach motivation more in patients with BPD than in controls. For approach motivation toward positive stimuli, oxytocin had a significant effect on patients with BPD.
Continue to: Conclusions/limitations...
Conclusions/limitations
- Patients with BPD showed reduced cognitive and affective empathy and less approach behavior motivation than healthy controls.
- Patients with BPD who received oxytocin attained a level of affective empathy and approach motivation similar to that of healthy controls who received placebo. For positive stimuli, both groups exhibited comparable improvements from oxytocin. For negative stimuli, patients with BPD patients showed significant improvement with oxytocin, whereas healthy controls received no such benefit.
- Limitations include the use of self-report scales, lack of a control group, and inclusion of patients using psychotherapeutic medications. The study lacks generalizability because only women were included; the effect of exogenous oxytocin on men may differ.
5. Bozzatello P, Rocca P, Uscinska M, et al. Efficacy and tolerability of asenapine compared with olanzapine in borderline personality disorder: an open-label randomized controlled trial. CNS Drugs. 2017;31(9):809-819. doi: 10.1007/s40263-017-0458-4
The last decade has seen a noticeable shift in clinical practice from the use of antidepressants to mood stabilizers and second-generation antipsychotics (SGAs) in the treatment of BPD. Studies have demonstrated therapeutic effects of antipsychotic drugs across a wide range of BPD symptoms. Among SGAs, olanzapine is the most extensively studied across case reports, open-label studies, and RCTs of patients with BPD. In an RCT, Bozzatello et al7 compared the efficacy and tolerability of asenapine to olanzapine.
Study design
- In this open-label RCT, adults who met DSM-5 criteria for BPD were assigned to receive asenapine (n = 25) or olanzapine (n = 26) for 12 weeks.
- Study measurements included the Clinical Global Impression Scale, Severity item, HAM-D, HAM-A, Social and Occupational Functioning Assessment Scale, Borderline Personality Disorder Severity Index (BPDSI), BIS-11, Modified Overt Aggression Scale, and Dosage Record Treatment Emergent Symptom Scale.
Outcomes
- Asenapine and olanzapine had similar effects on BPD-related psychopathology, anxiety, and social and occupational functioning.
- Neither medication significantly decreased depressive or aggressive symptoms.
- Asenapine was superior to olanzapine in reducing the affective instability score of the BPDSI.
- Akathisia and restlessness/anxiety were more common with asenapine, and somnolence and fatigue were more common with olanzapine.
Conclusions/limitations
- The overall efficacy of asenapine was not different from olanzapine, and both medications were well-tolerated.
- Neither medication led to an improvement in depression or aggression, but asenapine was superior to olanzapine in reducing the severity of affective instability.
- Limitations include an open-label design, lack of placebo group, small sample size, high drop-out rate, exclusion of participants with co-occurring MDD and substance abuse/dependence, lack of data on prior pharmacotherapies and psychotherapies, and lack of power to detect a difference on the dissociation/paranoid ideation item of BPDSI.
6. Kulkarni J, Thomas N, Hudaib AR, et al. Effect of the glutamate NMDA receptor antagonist memantine as adjunctive treatment in borderline personality disorder: an exploratory, randomised, double-blind, placebo-controlled trial. CNS Drugs. 2018;32(2):179-187. doi: 10.1007/s40263-018-0506-8
It has been hypothesized that glutamate dysregulation and excitotoxicity are crucial to the development of the cognitive disturbances that underlie BPD. As such, glutamate modulators such as memantine hold promise for the treatment of BPD. In this RCT, Kulkarni et al8 examined the efficacy and tolerability of memantine compared with treatment as usual in patients with BPD.
Continue to: Study design...
Study design
- In an 8-week, double-blind, placebo-controlled trial, adults diagnosed with BPD according to the Diagnostic Interview for Borderline Patients were randomized to receive memantine (n = 17) or placebo (n = 16) in addition to treatment as usual. Treatment as usual included the use of antidepressants, mood stabilizers, and antipsychotics as well as psychotherapy and other psychosocial interventions.
- Patients were initiated on placebo or memantine, 10 mg/d. Memantine was increased to 20 mg/d after 7 days.
- ZAN-BPD score was the primary outcome and was measured at baseline and 2, 4, 6, and 8 weeks. An adverse effects questionnaire was administered every 2 weeks to assess tolerability.
Outcomes
- During the first 2 weeks of treatment, there were no significant improvements in ZAN-BPD score in the memantine group compared with the placebo group.
- Beginning with Week 2, compared with the placebo group, the memantine group experienced a significant reduction in total symptoms as measured by ZAN-BPD.
- There were no statistically significant differences in adverse events between groups.
Conclusions/limitations
- Memantine appears to be a well-tolerated treatment option for patients with BPD and merits further study.
- Limitations include a small sample size, and an inability to reach plateau of ZAN-BPD total score in either group. Also, there is considerable individual variability in memantine steady-state plasma concentrations, but plasma levels were not measured in this study.
Bottom Line
Findings from small randomized controlled trials suggest that transcranial direct current stimulation, oxytocin, asenapine, olanzapine, and memantine may have beneficial effects on some core symptoms of borderline personality disorder. These findings need to be replicated in larger studies.
1. Skodol AE, Gunderson JG, McGlashan TM, et al. Functional impairment in patients with schizotypal, borderline, avoidant, or obsessive-compulsive personality disorder. Am J Psychiatry. 2002; 159:276-283.
2. Bender DS, Dolan RT, Skodol AE, et al. Treatment utilization by patients with personality disorders. Am J Psychiatry. 2001;158:295-302.
3. Lisoni J, Miotto P, Barlati S, et al. Change in core symptoms of borderline personality disorder by tDCS: a pilot study. Psychiatry Res. 2020;291:113261. doi: 10.1016/j.psychres.2020.113261
4. Molavi P, Aziziaram S, Basharpoor S, et al. Repeated transcranial direct current stimulation of dorsolateral-prefrontal cortex improves executive functions, cognitive reappraisal emotion regulation, and control over emotional processing in borderline personality disorder: a randomized, sham-controlled, parallel-group study. J Affect Disord. 2020;274:93-102. doi: 10.1016/j.jad.2020.05.007
5. Crawford MJ, Sanatinia R, Barrett B, et al; LABILE study team. The clinical effectiveness and cost-effectiveness of lamotrigine in borderline personality disorder: a randomized placebo-controlled trial. Am J Psychiatry. 2018;175(8):756-764. doi: 10.1176/appi.ajp.2018.17091006
6. Domes G, Ower N, von Dawans B, et al. Effects of intranasal oxytocin administration on empathy and approach motivation in women with borderline personality disorder: a randomized controlled trial. Transl Psychiatry. 2019;9(1):328. doi: 10.1038/s41398-019-0658-4
7. Bozzatello P, Rocca P, Uscinska M, et al. Efficacy and tolerability of asenapine compared with olanzapine in borderline personality disorder: an open-label randomized controlled trial. CNS Drugs. 2017;31(9):809-819. doi: 10.1007/s40263-017-0458-4
8. Kulkarni J, Thomas N, Hudaib AR, et al. Effect of the glutamate NMDA receptor antagonist memantine as adjunctive treatment in borderline personality disorder: an exploratory, randomised, double-blind, placebo-controlled trial. CNS Drugs. 2018;32(2):179-187. doi: 10.1007/s40263-018-0506-8
1. Skodol AE, Gunderson JG, McGlashan TM, et al. Functional impairment in patients with schizotypal, borderline, avoidant, or obsessive-compulsive personality disorder. Am J Psychiatry. 2002; 159:276-283.
2. Bender DS, Dolan RT, Skodol AE, et al. Treatment utilization by patients with personality disorders. Am J Psychiatry. 2001;158:295-302.
3. Lisoni J, Miotto P, Barlati S, et al. Change in core symptoms of borderline personality disorder by tDCS: a pilot study. Psychiatry Res. 2020;291:113261. doi: 10.1016/j.psychres.2020.113261
4. Molavi P, Aziziaram S, Basharpoor S, et al. Repeated transcranial direct current stimulation of dorsolateral-prefrontal cortex improves executive functions, cognitive reappraisal emotion regulation, and control over emotional processing in borderline personality disorder: a randomized, sham-controlled, parallel-group study. J Affect Disord. 2020;274:93-102. doi: 10.1016/j.jad.2020.05.007
5. Crawford MJ, Sanatinia R, Barrett B, et al; LABILE study team. The clinical effectiveness and cost-effectiveness of lamotrigine in borderline personality disorder: a randomized placebo-controlled trial. Am J Psychiatry. 2018;175(8):756-764. doi: 10.1176/appi.ajp.2018.17091006
6. Domes G, Ower N, von Dawans B, et al. Effects of intranasal oxytocin administration on empathy and approach motivation in women with borderline personality disorder: a randomized controlled trial. Transl Psychiatry. 2019;9(1):328. doi: 10.1038/s41398-019-0658-4
7. Bozzatello P, Rocca P, Uscinska M, et al. Efficacy and tolerability of asenapine compared with olanzapine in borderline personality disorder: an open-label randomized controlled trial. CNS Drugs. 2017;31(9):809-819. doi: 10.1007/s40263-017-0458-4
8. Kulkarni J, Thomas N, Hudaib AR, et al. Effect of the glutamate NMDA receptor antagonist memantine as adjunctive treatment in borderline personality disorder: an exploratory, randomised, double-blind, placebo-controlled trial. CNS Drugs. 2018;32(2):179-187. doi: 10.1007/s40263-018-0506-8






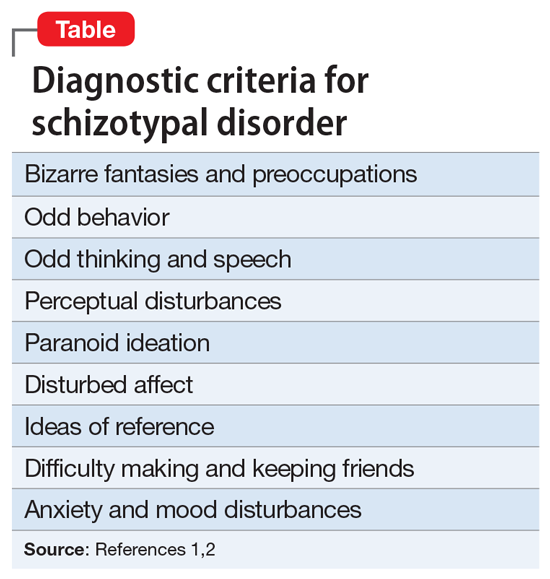
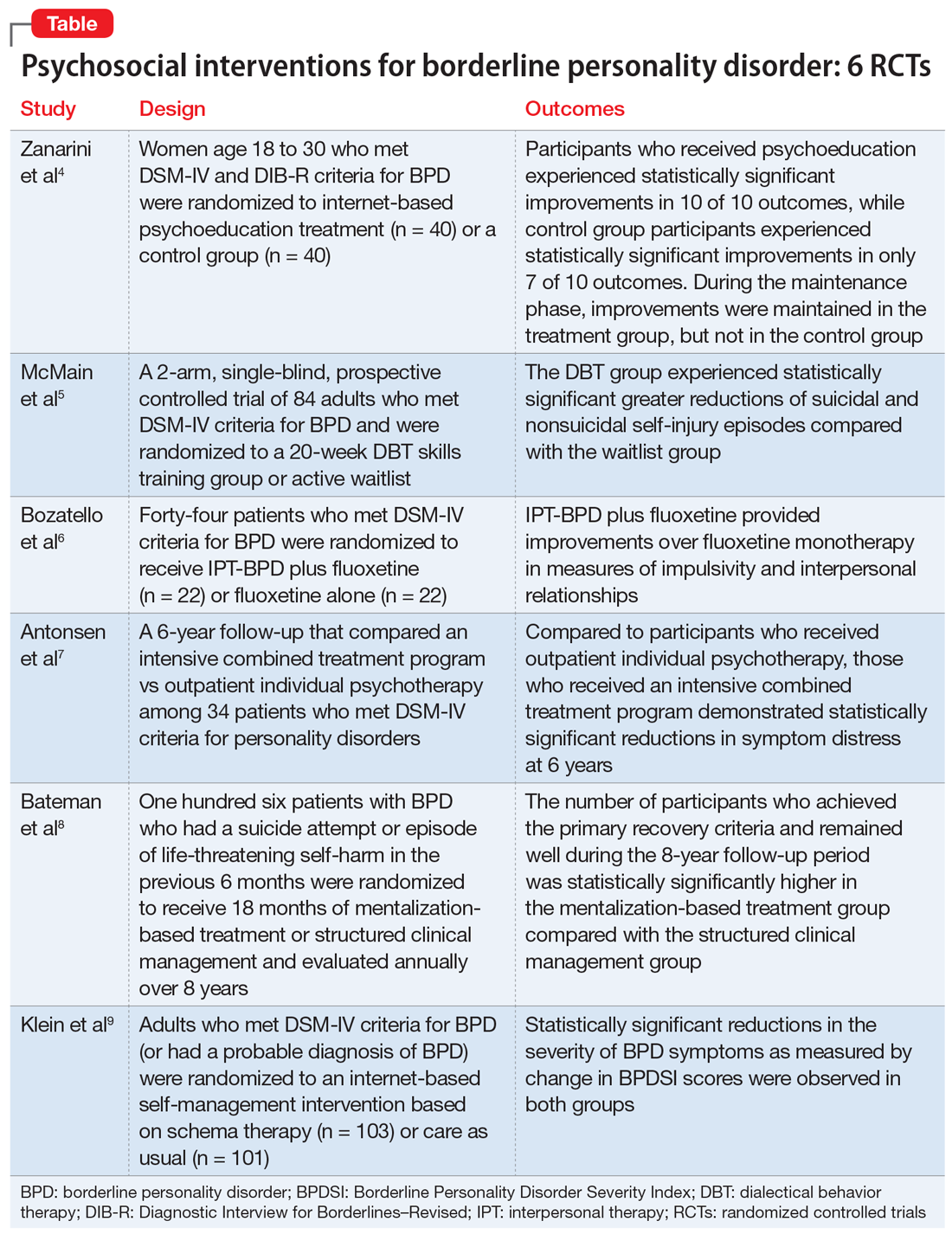
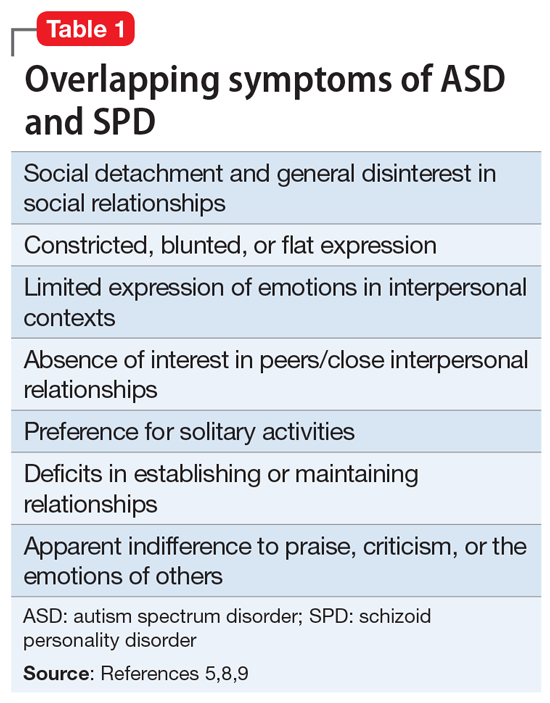
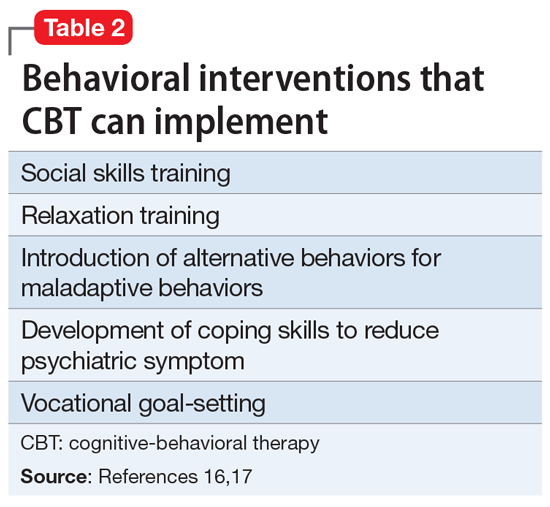






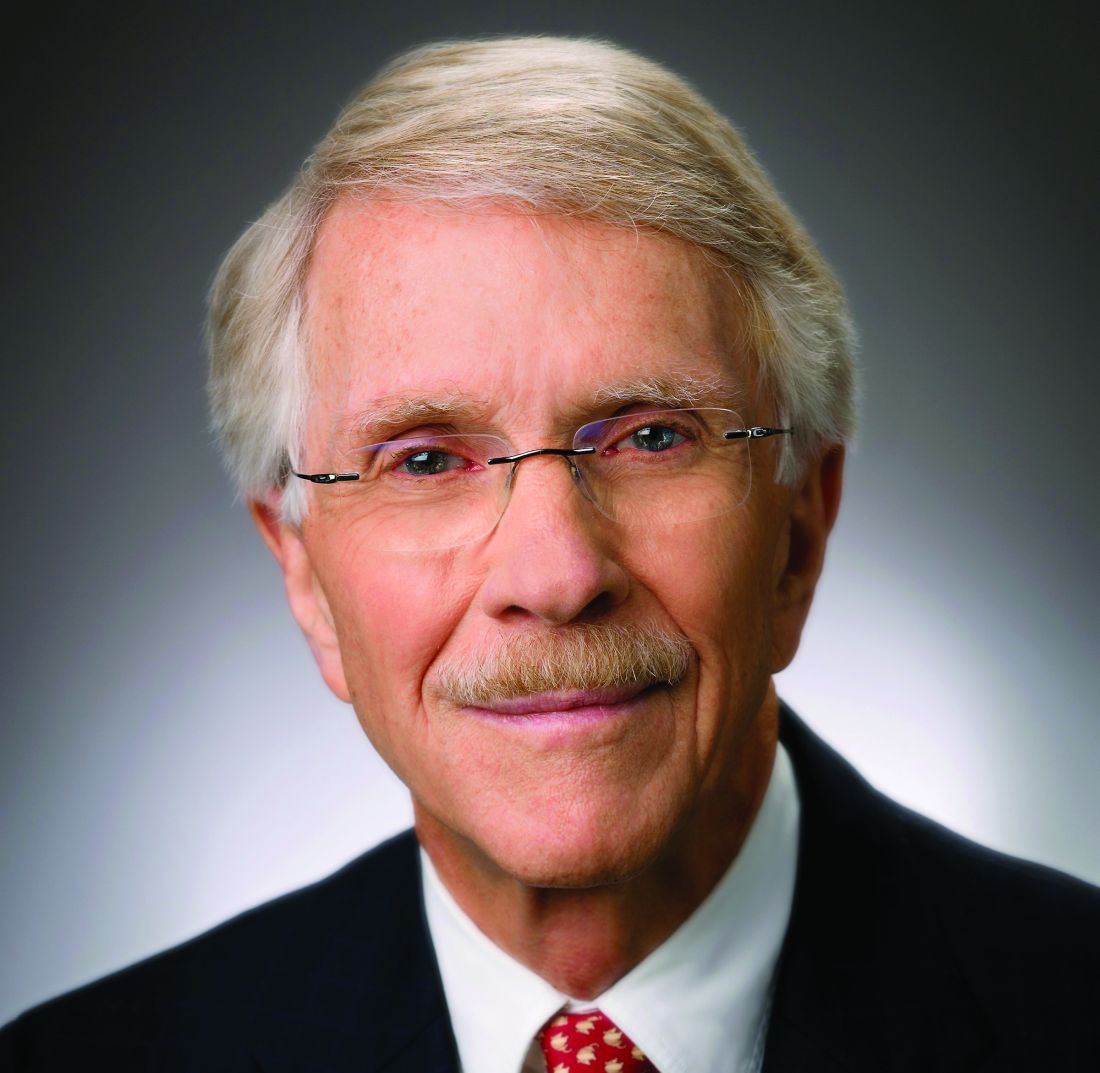

![&quot;For the most part, [virtual formats] have been remarkably successful for a variety of conditions, and Zimmerman and colleagues now show this for BPD families,&quot; said Dr. Donald W. Black, who was not associated with the research.](https://cdn.mdedge.com/files/s3fs-public/styles/medium/public/Black_Donald_IA_web.jpg?itok=ZS25deq_)