User login
Residency programs need greater focus on BPD treatment
Borderline personality disorder (BPD) has suffered from underdiagnosis, in part because not enough clinicians know how to handle patients with BPD. “They don’t have the tools to know how to manage these situations effectively,” Lois W. Choi-Kain, MEd, MD, director of the Gunderson Personality Disorders Institute, McLean Hospital, Belmont, Mass., said in an interview.
As a result, the clinician avoids the BPD patient, who feels demeaned and never finds the capacity to get better.
Psychiatry training in residency tends to emphasize biomedical treatments and does not focus enough on learning psychotherapy and other psychosocial treatments, according to Eric M. Plakun, MD, DLFAPA, FACPsych, medical director/CEO of the Austen Riggs Center in Stockbridge, Mass.
“This is where I see the need for a greater psychotherapy teaching focus in residency, along with teaching of general principles for working with patients with BPD,” said Dr. Plakun.
In his last phase of his career, BPD pioneer John G. Gunderson, MD, worked with Dr. Choi-Kain to train clinicians on general psychiatric management (GPM), which employs a sensitive, nonattacking approach to diffuse and calm situations with BPD patients.
As interest grows in combining GPM with manual treatments, GPM alone offers a more accessible approach for therapist and patient, said Dr. Choi-Kain, who has been trying to promote its use and do research on its techniques.
“It’s trying to boil it down to make it simple,” she said. As much as evidence-based, manualized approaches have advanced the field, they’re just not that widely available, she said.
Orchestrating treatments such as dialectical behavior therapy and mentalization-based therapy takes a lot of specialization, noted Dr. Choi-Kain. “And because of the amount of work that it involves for both the clinician and the patient, it decreases the capacity that clinicians and systems have to offer treatment to a wider number of patients.”
Learning a manualized treatment for BPD is asking a lot from residents, agreed Dr. Plakun. “Those who want more immersion in treating these patients can pursue further training in residency electives, in postresidency graduate medical education programs or through psychoanalytic training.”
Borderline personality disorder (BPD) has suffered from underdiagnosis, in part because not enough clinicians know how to handle patients with BPD. “They don’t have the tools to know how to manage these situations effectively,” Lois W. Choi-Kain, MEd, MD, director of the Gunderson Personality Disorders Institute, McLean Hospital, Belmont, Mass., said in an interview.
As a result, the clinician avoids the BPD patient, who feels demeaned and never finds the capacity to get better.
Psychiatry training in residency tends to emphasize biomedical treatments and does not focus enough on learning psychotherapy and other psychosocial treatments, according to Eric M. Plakun, MD, DLFAPA, FACPsych, medical director/CEO of the Austen Riggs Center in Stockbridge, Mass.
“This is where I see the need for a greater psychotherapy teaching focus in residency, along with teaching of general principles for working with patients with BPD,” said Dr. Plakun.
In his last phase of his career, BPD pioneer John G. Gunderson, MD, worked with Dr. Choi-Kain to train clinicians on general psychiatric management (GPM), which employs a sensitive, nonattacking approach to diffuse and calm situations with BPD patients.
As interest grows in combining GPM with manual treatments, GPM alone offers a more accessible approach for therapist and patient, said Dr. Choi-Kain, who has been trying to promote its use and do research on its techniques.
“It’s trying to boil it down to make it simple,” she said. As much as evidence-based, manualized approaches have advanced the field, they’re just not that widely available, she said.
Orchestrating treatments such as dialectical behavior therapy and mentalization-based therapy takes a lot of specialization, noted Dr. Choi-Kain. “And because of the amount of work that it involves for both the clinician and the patient, it decreases the capacity that clinicians and systems have to offer treatment to a wider number of patients.”
Learning a manualized treatment for BPD is asking a lot from residents, agreed Dr. Plakun. “Those who want more immersion in treating these patients can pursue further training in residency electives, in postresidency graduate medical education programs or through psychoanalytic training.”
Borderline personality disorder (BPD) has suffered from underdiagnosis, in part because not enough clinicians know how to handle patients with BPD. “They don’t have the tools to know how to manage these situations effectively,” Lois W. Choi-Kain, MEd, MD, director of the Gunderson Personality Disorders Institute, McLean Hospital, Belmont, Mass., said in an interview.
As a result, the clinician avoids the BPD patient, who feels demeaned and never finds the capacity to get better.
Psychiatry training in residency tends to emphasize biomedical treatments and does not focus enough on learning psychotherapy and other psychosocial treatments, according to Eric M. Plakun, MD, DLFAPA, FACPsych, medical director/CEO of the Austen Riggs Center in Stockbridge, Mass.
“This is where I see the need for a greater psychotherapy teaching focus in residency, along with teaching of general principles for working with patients with BPD,” said Dr. Plakun.
In his last phase of his career, BPD pioneer John G. Gunderson, MD, worked with Dr. Choi-Kain to train clinicians on general psychiatric management (GPM), which employs a sensitive, nonattacking approach to diffuse and calm situations with BPD patients.
As interest grows in combining GPM with manual treatments, GPM alone offers a more accessible approach for therapist and patient, said Dr. Choi-Kain, who has been trying to promote its use and do research on its techniques.
“It’s trying to boil it down to make it simple,” she said. As much as evidence-based, manualized approaches have advanced the field, they’re just not that widely available, she said.
Orchestrating treatments such as dialectical behavior therapy and mentalization-based therapy takes a lot of specialization, noted Dr. Choi-Kain. “And because of the amount of work that it involves for both the clinician and the patient, it decreases the capacity that clinicians and systems have to offer treatment to a wider number of patients.”
Learning a manualized treatment for BPD is asking a lot from residents, agreed Dr. Plakun. “Those who want more immersion in treating these patients can pursue further training in residency electives, in postresidency graduate medical education programs or through psychoanalytic training.”
A new name for BPD?
Michael A. Cummings, MD, has never liked the term “borderline personality disorder” (BPD). In his view, it’s a misnomer and needs to be changed.
“What is it bordering on? It’s not bordering on something, it’s a disorder on its own,” said Dr. Cummings of the department of psychiatry at the University of California, Riverside, and a psychopharmacology consultant with the California Department of State Hospitals’ Psychopharmacology Resource Network.
BPD grew out of the concept that patients were bordering on something, perhaps becoming bipolar. “In many ways, I don’t think it is even a personality disorder. It appears to be an inherent temperament that evolves into an inability to regulate mood.”
In his view, this puts it in the category of a mood dysregulation disorder.
Changing the label would not necessarily improve treatment, he added. However, transitioning from a pejorative to a more neutral label could make it easier for people to say, “this is just a type of mood disorder. It’s not necessarily easy, but it’s workable,” said Dr. Cummings.
Others in the field contend that the term fits the condition. BPD “describes how it encompasses a lot of complex psychological difficulties, undermining functioning of patients in a specific way,” said Lois W. Choi-Kain, MD, MEd, director of the Gunderson Personality Disorders Institute, McLean Hospital, Belmont, Mass. The disorder was identified because of its relationship with other known psychiatric disorders, said Dr. Choi-Kain. “There’s an element of BPD that borders on mood disorders because moods are so unstable with BPD. It also borders on trauma-related disorders. It borders on psychotic disorders because there’s sometimes stress-induced experiences of losing contact with realistic thinking.”
If anything needs to change, it’s the attitude toward the disorder, not the name. “I don’t think the term itself is pejorative. But I think that associations with the term have been very stigmatizing. For a long time, there was an attitude that these patients could not be treated or had negative therapeutic reactions.”
Data suggest that these patients are highly prevalent in clinical settings. “And I interpret that as them seeking the care that they need rather than resisting care or not responding to care,” said Dr. Choi-Kain.
Michael A. Cummings, MD, has never liked the term “borderline personality disorder” (BPD). In his view, it’s a misnomer and needs to be changed.
“What is it bordering on? It’s not bordering on something, it’s a disorder on its own,” said Dr. Cummings of the department of psychiatry at the University of California, Riverside, and a psychopharmacology consultant with the California Department of State Hospitals’ Psychopharmacology Resource Network.
BPD grew out of the concept that patients were bordering on something, perhaps becoming bipolar. “In many ways, I don’t think it is even a personality disorder. It appears to be an inherent temperament that evolves into an inability to regulate mood.”
In his view, this puts it in the category of a mood dysregulation disorder.
Changing the label would not necessarily improve treatment, he added. However, transitioning from a pejorative to a more neutral label could make it easier for people to say, “this is just a type of mood disorder. It’s not necessarily easy, but it’s workable,” said Dr. Cummings.
Others in the field contend that the term fits the condition. BPD “describes how it encompasses a lot of complex psychological difficulties, undermining functioning of patients in a specific way,” said Lois W. Choi-Kain, MD, MEd, director of the Gunderson Personality Disorders Institute, McLean Hospital, Belmont, Mass. The disorder was identified because of its relationship with other known psychiatric disorders, said Dr. Choi-Kain. “There’s an element of BPD that borders on mood disorders because moods are so unstable with BPD. It also borders on trauma-related disorders. It borders on psychotic disorders because there’s sometimes stress-induced experiences of losing contact with realistic thinking.”
If anything needs to change, it’s the attitude toward the disorder, not the name. “I don’t think the term itself is pejorative. But I think that associations with the term have been very stigmatizing. For a long time, there was an attitude that these patients could not be treated or had negative therapeutic reactions.”
Data suggest that these patients are highly prevalent in clinical settings. “And I interpret that as them seeking the care that they need rather than resisting care or not responding to care,” said Dr. Choi-Kain.
Michael A. Cummings, MD, has never liked the term “borderline personality disorder” (BPD). In his view, it’s a misnomer and needs to be changed.
“What is it bordering on? It’s not bordering on something, it’s a disorder on its own,” said Dr. Cummings of the department of psychiatry at the University of California, Riverside, and a psychopharmacology consultant with the California Department of State Hospitals’ Psychopharmacology Resource Network.
BPD grew out of the concept that patients were bordering on something, perhaps becoming bipolar. “In many ways, I don’t think it is even a personality disorder. It appears to be an inherent temperament that evolves into an inability to regulate mood.”
In his view, this puts it in the category of a mood dysregulation disorder.
Changing the label would not necessarily improve treatment, he added. However, transitioning from a pejorative to a more neutral label could make it easier for people to say, “this is just a type of mood disorder. It’s not necessarily easy, but it’s workable,” said Dr. Cummings.
Others in the field contend that the term fits the condition. BPD “describes how it encompasses a lot of complex psychological difficulties, undermining functioning of patients in a specific way,” said Lois W. Choi-Kain, MD, MEd, director of the Gunderson Personality Disorders Institute, McLean Hospital, Belmont, Mass. The disorder was identified because of its relationship with other known psychiatric disorders, said Dr. Choi-Kain. “There’s an element of BPD that borders on mood disorders because moods are so unstable with BPD. It also borders on trauma-related disorders. It borders on psychotic disorders because there’s sometimes stress-induced experiences of losing contact with realistic thinking.”
If anything needs to change, it’s the attitude toward the disorder, not the name. “I don’t think the term itself is pejorative. But I think that associations with the term have been very stigmatizing. For a long time, there was an attitude that these patients could not be treated or had negative therapeutic reactions.”
Data suggest that these patients are highly prevalent in clinical settings. “And I interpret that as them seeking the care that they need rather than resisting care or not responding to care,” said Dr. Choi-Kain.
Trust is key in treating borderline personality disorder
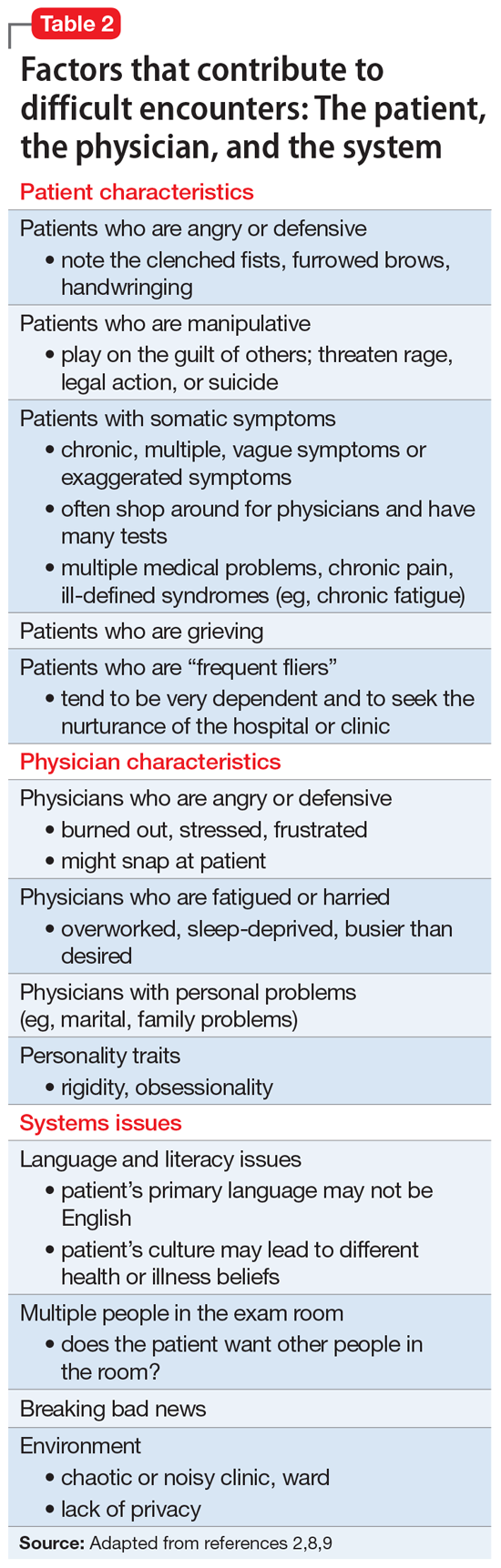
Difficulties associated with treating borderline personality disorder (BPD) make for an uneasy alliance between patient and clinician. Deep-seated anxiety and trust issues often lead to patients skipping visits or raging at those who treat them, leaving clinicians frustrated and ready to give up or relying on a pill to make the patient better.
John M. Oldham, MD, MS, recalls one patient he almost lost, a woman who was struggling with aggressive behavior. Initially cooperative and punctual, the patient gradually became distrustful, grilling Dr. Oldham on his training and credentials. “As the questions continued, she slipped from being very cooperative to being enraged and attacking me,” said Dr. Oldham, Distinguished Emeritus Professor in the Menninger department of psychiatry and behavioral sciences at Baylor College in Houston.
Dr. Oldham eventually drew her back in by earning her trust. “There’s no magic to this,” he acknowledged. “You try to be as alert and informed and vigilant for anything you say that produces a negative or concerning reaction in the patient.”
This interactive approach to BPD treatment has been gaining traction in a profession that often looks to medications to alleviate specific symptoms. It’s so effective that it sometimes even surprises the patient, Dr. Oldham noted. “When you approach them like this, they can begin to settle down,” which was the case with the female patient he once treated.
About 1.4% of the U.S. population has BPD, according to the National Institute of Mental Health. Conceptualized by the late John G. Gunderson, MD, BPD initially was seen as floating on the borderline between psychosis and neurosis. Clinicians now understand that this isn’t the case. The patients need, as Dr. Gunderson once pointed out, constant vigilance because of attachment issues and childhood trauma.
A stable therapeutic alliance between patient and physician, sometimes in combination with evidence-based therapies, is a formula for success, some experts say.
A misunderstood condition
Although there is some degree of heritable risk, BPD patients are often the product of an invalidating environment in childhood. “As kids, we’re guided and nurtured by caring adults to provide models of reasonable, trustworthy behavior. If those role models are missing or just so inconsistent and unpredictable, the patient doesn’t end up with a sturdy self-image. Instead, they’re adrift, trying to figure out who will be helpful and be a meaningful, trustworthy companion and adviser,” Dr. Oldham said.
Emotional or affective instability and impulsivity, sometimes impulsive aggression, often characterize their condition. “Brain-imaging studies have revealed that certain nerve pathways that are necessary to regulate emotions are impoverished in patients with BPD,” Dr. Oldham said.
An analogy is a car going too fast, with a runaway engine that’s running too hot – and the brakes don’t work, he added.
“People think these patients are trying to create big drama, that they’re putting on a big show. That’s not accurate,” he continued. These patients don’t have the ability to stop the trigger that leads to their emotional storms. They also don’t have the ability to regulate themselves. “We may say, it’s a beautiful day outside, but I still have to go to work. Someone with BPD may say: It’s a beautiful day; I’m going to the beach,” Dr. Oldham explained.
A person with BPD might sound coherent when arguing with someone else. But their words are driven by the storm they can’t turn off.
This can lead to their own efforts to turn off the intensity. They might become self-injurious or push other people away. It’s one of the ironies of this condition because BPD patients desperately want to trust others but are scared to do so. “They look for any little signal – that someone else will hurt, disappoint, or leave them. Eventually their relationships unravel,” Dr. Oldham saod.
For some, suicide is sometimes a final solution.
Those traits make it difficult for a therapist to connect with a patient. “This is a very difficult group of people to treat and to establish treatment,” said Michael A. Cummings, MD, of the department of psychiatry at University of California, Riverside, and a psychopharmacology consultant with the California Department of State Hospitals’ Psychopharmacology Resource Network.
BPD patients tend to idealize people who are attempting to help them. When they become frustrated or disappointed in some way, “they then devalue the caregiver or the treatment and not infrequently, fall out of treatment,” Dr. Cummings said. It can be a very taxing experience, particularly for younger, less experienced therapists.
Medication only goes so far
Psychiatrists tend to look at BPD patients as receptor sites for molecules, assessing symptoms they can prescribe for, Eric M. Plakun, MD, DLFAPA, FACPsych, medical director/CEO of the Austen Riggs Center in Stockbridge, Mass., said in an interview.
Yet, BPD is not a molecular problem, principally. It’s an interpersonal disorder. When BPD is a co-occurring disorder, as is often the case, the depressive, anxiety, or other disorder can mask the BPD, he added, citing his 2018 paper on tensions in psychiatry between the biomedical and biopsychosocial models (Psychiatr Clin North Am. 2018 Jun;41[2]:237-48).
In one longitudinal study (J Pers Disord. 2005 Oct;19[5]:487-504), the presence of BPD strongly predicted the persistence of depression. BPD comorbid with depression is often a recipe for treatment-resistant depression, which results in higher costs, more utilization of resources, and higher suicide rates. Too often, psychiatrists diagnose the depression but miss the BPD. They keep trying molecular approaches with prescription drugs – even though it’s really the interpersonal issues of BPD that need to be addressed, said Dr. Plakun, who is a member of the Group for the Advancement of Psychiatry’s Psychotherapy Committee, and founder and past leader of the American Psychiatric Association’s Psychotherapy Caucus.
Medication can be helpful as a short-term adjunctive therapy. Long term, it’s not a sustainable approach, said Dr. Oldham. “If a patient is in a particularly stressful period, in the middle of a stormy breakup or having a depressive episode or talking about suicide, a time-limited course of an antidepressant may be helpful,” he said. They could also benefit from an anxiety-related drug or medication to help them sleep.
What you don’t want is for the patient to start relying on medications to help them feel better. The problem is, many are suffering so much that they’ll go to their primary care doctor and say, “I’m suffering from anxiety,” and get an antianxiety drug. Or they’re depressed or in pain and end up with a cocktail of medications. “And that’s just going to make matters worse,” Dr. Oldham said.
Psychotherapy as a first-line approach
APA practice guidelines and others worldwide have all come to the same conclusion about BPD. , who chaired an APA committee that developed an evidence-based practice guideline for patients with BPD.
Psychotherapy keeps the patient from firing you, he asserted. “Because of the lack of trust, they push away. They’re very scared, and this fear also applies to therapist. The goal is to help the patient learn to trust you. To do that, you need to develop a strong therapeutic alliance.”
In crafting the APA’s practice guideline, Dr. Oldham and his colleagues studied a variety of approaches, including mentalization-based therapy (MBT) and dialectical behavior therapy (DBT), which was developed by Marsha Linehan, PhD. Since then, other approaches have demonstrated efficacy in randomized clinical trials, including schema-based therapy (SBT), cognitive-behavioral therapy (CBT), and transference-focused psychotherapy (TFP).
Those treatments might complement the broader goal of establishing a strong alliance with the patient, Dr. Oldham said. Manualized approaches can help prepackage a program that allows clinicians and patients to look at their problems in an objective, nonpejorative way, Lois W. Choi-Kain, MD, MEd, director of the Gunderson Personality Disorders Institute at McLean Hospital in Belmont, Mass., said in an interview. DBT, for example, focuses on emotion dysregulation. MBT addresses how the patient sees themselves through others and their interactions with others. “It destigmatizes a problem as a clinical entity rather than an interpersonal problem between the patient and the clinician,” Dr. Choi-Kain said.
The choice of approach depends on several factors: the patient’s needs and preferences, and the therapist’s skills and experience, said Dr. Oldham. Some patients don’t do well with DBT because it involves a lot of homework and didactic work. Others do better with TFP because they want to understand what drives their behavior.
Dr. Cummings recalled how one of his patients used TFP to look inward and heal.
He first met the patient when she was in her early 30s. “She had made some progress, but I remember she was still struggling mightily with relationship issues and with identifying her role in relationships,” he said. The patient was becoming increasingly aware that she was going to end up alone and didn’t want that as an outcome.
Adapting to a TFP model, “she worked very hard trying to understand herself as she related to other people, understanding her own emotional volatility, and some of her proneness to behavioral problems,” Dr. Cummings said. The patient also had to learn how to negotiate her relationships to the point where she didn’t end up destroying them and alienating people.
Customizing the treatment
Physicians can choose from one of these manualized forms of treatment to see what’s appropriate and what works for the patient. “You can individualize the treatment, borrowing from these approaches and shaping it based on what your patient needs,” Dr. Oldham recommended.
Recently, the field of psychiatry has seen the benefits of combining manualized, evidence-based approaches with general psychiatric management (GPM), a method conceived by Dr. Gunderson. GPM “reflects a sensitive understanding of mental illness, offering ‘non attacking’ or collaborative work with the patient and a sensitive recognition of appropriate interventions or corrections to help the patient stay in treatment,” said Dr. Oldham.
It aims to conceptualize BPD in a clinically objective way, medicalizing the disorder so it’s something that the patient has, rather than something he or she is, explained Dr. Choi-Kain, who worked with Dr. Gunderson to train clinicians on using this approach. Using a framework that’s compatible with good medical practices, the clinician tries to define the problem together with the patient, “really assessing whether or not the treatment works, setting goals, managing safety, and trying to promote functioning, something we need to pay more attention to with BPD,” she said.
For these patients, the goal is to have positive, corrective experiences in the real world, reinforcing their hopes and what they’re capable of, and an interface with the world that makes them feel like contributors, she said.
Cycle of rupture and repair
Many people with BPD struggle with the desire to find and feel love, but also deal with their rage and hate. Hence, therapists must prepare themselves for the experience of sometimes being hated, said Dr. Plakun. The patient needs to feel they’re in a safe enough space to express those feelings, activating a cycle of “rupture and repair,” he continued.
The key in working with these patients is to avoid any language that will make them feel attacked or criticized, said Dr. Oldham.
A patient may get furious and say “I don’t know what you’re talking about. I didn’t say that.” When in truth, the psychiatrist is flat accurate about what the patient said. Instead of arguing with the patient, a physician can back up and say: “Help me understand what you’re feeling right now. What did I say that made you feel that you couldn’t trust me? Help me understand you. I may have made a mistake,” he advised.
Trust is a key ingredient in an alliance-based intervention for suicidal patients with BPD that Dr. Plakun has frequently written about. A bond he had with a deeply suicidal patient helped her overcome her grief and come to terms with an abusive childhood.
“She had a horrible history of abuse and had BPD and bipolar disorder. Even controlled with medications her life was still awful. She contemplated suicide relentlessly.” Working through her history of sexual abuse, the patient discovered that much of what she and clinicians thought of as a depressive illness was in fact intense grief about the irreparable damage that had taken place during childhood.
Through their work she was able to mourn, and her depression and BPD improved.
Developing a trusting relationship with the patient isn’t a starting point; it’s the goal, he emphasized.
“You don’t prescribe trust to someone. It’s earned.” Through the shared journey of therapy, as the patient suffers from inevitable injuries and ruptures and as the therapist reveals his or her imperfections, opportunities arise to nonjudgmentally examine and repair ruptures. This lead to gains in trust, he said.
It’s not just about genes
Many in the psychiatric and psychological communities tend to develop a very nihilistic view of BPD patients, observed Dr. Cummings. “They’ll say: ‘Oh, well, it’s hopeless. There’s nothing that can be done.’ That isn’t true,” he said.
Epidemiologic studies of these individuals have shown that many of these patients no longer meet the diagnostic criteria for BPD by the time they reach middle age. This means they get better over time, noted Dr. Cummings.
Dr. Plakun’s hope is that the field will evolve in a direction that recognizes the importance of psychosocial treatments like psychotherapy, in addition to biomedical treatments. The drive to medicate still exists, which can contribute to underdiagnosis and undertreatment of BPD, he said. “Although there are manualized, evidence-based treatments, few clinicians learn even one of these for BPD, not to mention those for other disorders.”
In 1996, Francis S. Collins, MD, PhD, the current director of the National Institutes of Health, predicted that the decoding of the human genome would transform treatment of medical and mental disorders [and] “that we would discover the ways in which genes equal disease,” said Dr. Plakun. What the science has since shown, is genes by environmental interaction lead to disease and health.
Nature and nurture both matter. “And I don’t think we’re paying enough attention to the nurture side,” Dr. Plakun said.
The solution is a return to a biopsychosocial model, recognizing that psychotherapy is an essential part of treatment of BPD and other conditions, and an essential clinician skill, he said.
Dr. Oldham is coeditor of the “Textbook of Personality Disorders”, 3rd edition (Washington: American Psychiatric Association Publishing, 2021).Dr. Choi-Kain is coeditor with Dr. Gunderson of “Applications of Good Psychiatric Management for Borderline Personality Disorder: A Practical Guide” (Washington: American Psychiatric Association Publishing, 2019).
Dr. Cummings and Dr. Plakun had no disclosures.
Difficulties associated with treating borderline personality disorder (BPD) make for an uneasy alliance between patient and clinician. Deep-seated anxiety and trust issues often lead to patients skipping visits or raging at those who treat them, leaving clinicians frustrated and ready to give up or relying on a pill to make the patient better.
John M. Oldham, MD, MS, recalls one patient he almost lost, a woman who was struggling with aggressive behavior. Initially cooperative and punctual, the patient gradually became distrustful, grilling Dr. Oldham on his training and credentials. “As the questions continued, she slipped from being very cooperative to being enraged and attacking me,” said Dr. Oldham, Distinguished Emeritus Professor in the Menninger department of psychiatry and behavioral sciences at Baylor College in Houston.
Dr. Oldham eventually drew her back in by earning her trust. “There’s no magic to this,” he acknowledged. “You try to be as alert and informed and vigilant for anything you say that produces a negative or concerning reaction in the patient.”
This interactive approach to BPD treatment has been gaining traction in a profession that often looks to medications to alleviate specific symptoms. It’s so effective that it sometimes even surprises the patient, Dr. Oldham noted. “When you approach them like this, they can begin to settle down,” which was the case with the female patient he once treated.
About 1.4% of the U.S. population has BPD, according to the National Institute of Mental Health. Conceptualized by the late John G. Gunderson, MD, BPD initially was seen as floating on the borderline between psychosis and neurosis. Clinicians now understand that this isn’t the case. The patients need, as Dr. Gunderson once pointed out, constant vigilance because of attachment issues and childhood trauma.
A stable therapeutic alliance between patient and physician, sometimes in combination with evidence-based therapies, is a formula for success, some experts say.
A misunderstood condition
Although there is some degree of heritable risk, BPD patients are often the product of an invalidating environment in childhood. “As kids, we’re guided and nurtured by caring adults to provide models of reasonable, trustworthy behavior. If those role models are missing or just so inconsistent and unpredictable, the patient doesn’t end up with a sturdy self-image. Instead, they’re adrift, trying to figure out who will be helpful and be a meaningful, trustworthy companion and adviser,” Dr. Oldham said.
Emotional or affective instability and impulsivity, sometimes impulsive aggression, often characterize their condition. “Brain-imaging studies have revealed that certain nerve pathways that are necessary to regulate emotions are impoverished in patients with BPD,” Dr. Oldham said.
An analogy is a car going too fast, with a runaway engine that’s running too hot – and the brakes don’t work, he added.
“People think these patients are trying to create big drama, that they’re putting on a big show. That’s not accurate,” he continued. These patients don’t have the ability to stop the trigger that leads to their emotional storms. They also don’t have the ability to regulate themselves. “We may say, it’s a beautiful day outside, but I still have to go to work. Someone with BPD may say: It’s a beautiful day; I’m going to the beach,” Dr. Oldham explained.
A person with BPD might sound coherent when arguing with someone else. But their words are driven by the storm they can’t turn off.
This can lead to their own efforts to turn off the intensity. They might become self-injurious or push other people away. It’s one of the ironies of this condition because BPD patients desperately want to trust others but are scared to do so. “They look for any little signal – that someone else will hurt, disappoint, or leave them. Eventually their relationships unravel,” Dr. Oldham saod.
For some, suicide is sometimes a final solution.
Those traits make it difficult for a therapist to connect with a patient. “This is a very difficult group of people to treat and to establish treatment,” said Michael A. Cummings, MD, of the department of psychiatry at University of California, Riverside, and a psychopharmacology consultant with the California Department of State Hospitals’ Psychopharmacology Resource Network.
BPD patients tend to idealize people who are attempting to help them. When they become frustrated or disappointed in some way, “they then devalue the caregiver or the treatment and not infrequently, fall out of treatment,” Dr. Cummings said. It can be a very taxing experience, particularly for younger, less experienced therapists.
Medication only goes so far
Psychiatrists tend to look at BPD patients as receptor sites for molecules, assessing symptoms they can prescribe for, Eric M. Plakun, MD, DLFAPA, FACPsych, medical director/CEO of the Austen Riggs Center in Stockbridge, Mass., said in an interview.
Yet, BPD is not a molecular problem, principally. It’s an interpersonal disorder. When BPD is a co-occurring disorder, as is often the case, the depressive, anxiety, or other disorder can mask the BPD, he added, citing his 2018 paper on tensions in psychiatry between the biomedical and biopsychosocial models (Psychiatr Clin North Am. 2018 Jun;41[2]:237-48).
In one longitudinal study (J Pers Disord. 2005 Oct;19[5]:487-504), the presence of BPD strongly predicted the persistence of depression. BPD comorbid with depression is often a recipe for treatment-resistant depression, which results in higher costs, more utilization of resources, and higher suicide rates. Too often, psychiatrists diagnose the depression but miss the BPD. They keep trying molecular approaches with prescription drugs – even though it’s really the interpersonal issues of BPD that need to be addressed, said Dr. Plakun, who is a member of the Group for the Advancement of Psychiatry’s Psychotherapy Committee, and founder and past leader of the American Psychiatric Association’s Psychotherapy Caucus.
Medication can be helpful as a short-term adjunctive therapy. Long term, it’s not a sustainable approach, said Dr. Oldham. “If a patient is in a particularly stressful period, in the middle of a stormy breakup or having a depressive episode or talking about suicide, a time-limited course of an antidepressant may be helpful,” he said. They could also benefit from an anxiety-related drug or medication to help them sleep.
What you don’t want is for the patient to start relying on medications to help them feel better. The problem is, many are suffering so much that they’ll go to their primary care doctor and say, “I’m suffering from anxiety,” and get an antianxiety drug. Or they’re depressed or in pain and end up with a cocktail of medications. “And that’s just going to make matters worse,” Dr. Oldham said.
Psychotherapy as a first-line approach
APA practice guidelines and others worldwide have all come to the same conclusion about BPD. , who chaired an APA committee that developed an evidence-based practice guideline for patients with BPD.
Psychotherapy keeps the patient from firing you, he asserted. “Because of the lack of trust, they push away. They’re very scared, and this fear also applies to therapist. The goal is to help the patient learn to trust you. To do that, you need to develop a strong therapeutic alliance.”
In crafting the APA’s practice guideline, Dr. Oldham and his colleagues studied a variety of approaches, including mentalization-based therapy (MBT) and dialectical behavior therapy (DBT), which was developed by Marsha Linehan, PhD. Since then, other approaches have demonstrated efficacy in randomized clinical trials, including schema-based therapy (SBT), cognitive-behavioral therapy (CBT), and transference-focused psychotherapy (TFP).
Those treatments might complement the broader goal of establishing a strong alliance with the patient, Dr. Oldham said. Manualized approaches can help prepackage a program that allows clinicians and patients to look at their problems in an objective, nonpejorative way, Lois W. Choi-Kain, MD, MEd, director of the Gunderson Personality Disorders Institute at McLean Hospital in Belmont, Mass., said in an interview. DBT, for example, focuses on emotion dysregulation. MBT addresses how the patient sees themselves through others and their interactions with others. “It destigmatizes a problem as a clinical entity rather than an interpersonal problem between the patient and the clinician,” Dr. Choi-Kain said.
The choice of approach depends on several factors: the patient’s needs and preferences, and the therapist’s skills and experience, said Dr. Oldham. Some patients don’t do well with DBT because it involves a lot of homework and didactic work. Others do better with TFP because they want to understand what drives their behavior.
Dr. Cummings recalled how one of his patients used TFP to look inward and heal.
He first met the patient when she was in her early 30s. “She had made some progress, but I remember she was still struggling mightily with relationship issues and with identifying her role in relationships,” he said. The patient was becoming increasingly aware that she was going to end up alone and didn’t want that as an outcome.
Adapting to a TFP model, “she worked very hard trying to understand herself as she related to other people, understanding her own emotional volatility, and some of her proneness to behavioral problems,” Dr. Cummings said. The patient also had to learn how to negotiate her relationships to the point where she didn’t end up destroying them and alienating people.
Customizing the treatment
Physicians can choose from one of these manualized forms of treatment to see what’s appropriate and what works for the patient. “You can individualize the treatment, borrowing from these approaches and shaping it based on what your patient needs,” Dr. Oldham recommended.
Recently, the field of psychiatry has seen the benefits of combining manualized, evidence-based approaches with general psychiatric management (GPM), a method conceived by Dr. Gunderson. GPM “reflects a sensitive understanding of mental illness, offering ‘non attacking’ or collaborative work with the patient and a sensitive recognition of appropriate interventions or corrections to help the patient stay in treatment,” said Dr. Oldham.
It aims to conceptualize BPD in a clinically objective way, medicalizing the disorder so it’s something that the patient has, rather than something he or she is, explained Dr. Choi-Kain, who worked with Dr. Gunderson to train clinicians on using this approach. Using a framework that’s compatible with good medical practices, the clinician tries to define the problem together with the patient, “really assessing whether or not the treatment works, setting goals, managing safety, and trying to promote functioning, something we need to pay more attention to with BPD,” she said.
For these patients, the goal is to have positive, corrective experiences in the real world, reinforcing their hopes and what they’re capable of, and an interface with the world that makes them feel like contributors, she said.
Cycle of rupture and repair
Many people with BPD struggle with the desire to find and feel love, but also deal with their rage and hate. Hence, therapists must prepare themselves for the experience of sometimes being hated, said Dr. Plakun. The patient needs to feel they’re in a safe enough space to express those feelings, activating a cycle of “rupture and repair,” he continued.
The key in working with these patients is to avoid any language that will make them feel attacked or criticized, said Dr. Oldham.
A patient may get furious and say “I don’t know what you’re talking about. I didn’t say that.” When in truth, the psychiatrist is flat accurate about what the patient said. Instead of arguing with the patient, a physician can back up and say: “Help me understand what you’re feeling right now. What did I say that made you feel that you couldn’t trust me? Help me understand you. I may have made a mistake,” he advised.
Trust is a key ingredient in an alliance-based intervention for suicidal patients with BPD that Dr. Plakun has frequently written about. A bond he had with a deeply suicidal patient helped her overcome her grief and come to terms with an abusive childhood.
“She had a horrible history of abuse and had BPD and bipolar disorder. Even controlled with medications her life was still awful. She contemplated suicide relentlessly.” Working through her history of sexual abuse, the patient discovered that much of what she and clinicians thought of as a depressive illness was in fact intense grief about the irreparable damage that had taken place during childhood.
Through their work she was able to mourn, and her depression and BPD improved.
Developing a trusting relationship with the patient isn’t a starting point; it’s the goal, he emphasized.
“You don’t prescribe trust to someone. It’s earned.” Through the shared journey of therapy, as the patient suffers from inevitable injuries and ruptures and as the therapist reveals his or her imperfections, opportunities arise to nonjudgmentally examine and repair ruptures. This lead to gains in trust, he said.
It’s not just about genes
Many in the psychiatric and psychological communities tend to develop a very nihilistic view of BPD patients, observed Dr. Cummings. “They’ll say: ‘Oh, well, it’s hopeless. There’s nothing that can be done.’ That isn’t true,” he said.
Epidemiologic studies of these individuals have shown that many of these patients no longer meet the diagnostic criteria for BPD by the time they reach middle age. This means they get better over time, noted Dr. Cummings.
Dr. Plakun’s hope is that the field will evolve in a direction that recognizes the importance of psychosocial treatments like psychotherapy, in addition to biomedical treatments. The drive to medicate still exists, which can contribute to underdiagnosis and undertreatment of BPD, he said. “Although there are manualized, evidence-based treatments, few clinicians learn even one of these for BPD, not to mention those for other disorders.”
In 1996, Francis S. Collins, MD, PhD, the current director of the National Institutes of Health, predicted that the decoding of the human genome would transform treatment of medical and mental disorders [and] “that we would discover the ways in which genes equal disease,” said Dr. Plakun. What the science has since shown, is genes by environmental interaction lead to disease and health.
Nature and nurture both matter. “And I don’t think we’re paying enough attention to the nurture side,” Dr. Plakun said.
The solution is a return to a biopsychosocial model, recognizing that psychotherapy is an essential part of treatment of BPD and other conditions, and an essential clinician skill, he said.
Dr. Oldham is coeditor of the “Textbook of Personality Disorders”, 3rd edition (Washington: American Psychiatric Association Publishing, 2021).Dr. Choi-Kain is coeditor with Dr. Gunderson of “Applications of Good Psychiatric Management for Borderline Personality Disorder: A Practical Guide” (Washington: American Psychiatric Association Publishing, 2019).
Dr. Cummings and Dr. Plakun had no disclosures.
Difficulties associated with treating borderline personality disorder (BPD) make for an uneasy alliance between patient and clinician. Deep-seated anxiety and trust issues often lead to patients skipping visits or raging at those who treat them, leaving clinicians frustrated and ready to give up or relying on a pill to make the patient better.
John M. Oldham, MD, MS, recalls one patient he almost lost, a woman who was struggling with aggressive behavior. Initially cooperative and punctual, the patient gradually became distrustful, grilling Dr. Oldham on his training and credentials. “As the questions continued, she slipped from being very cooperative to being enraged and attacking me,” said Dr. Oldham, Distinguished Emeritus Professor in the Menninger department of psychiatry and behavioral sciences at Baylor College in Houston.
Dr. Oldham eventually drew her back in by earning her trust. “There’s no magic to this,” he acknowledged. “You try to be as alert and informed and vigilant for anything you say that produces a negative or concerning reaction in the patient.”
This interactive approach to BPD treatment has been gaining traction in a profession that often looks to medications to alleviate specific symptoms. It’s so effective that it sometimes even surprises the patient, Dr. Oldham noted. “When you approach them like this, they can begin to settle down,” which was the case with the female patient he once treated.
About 1.4% of the U.S. population has BPD, according to the National Institute of Mental Health. Conceptualized by the late John G. Gunderson, MD, BPD initially was seen as floating on the borderline between psychosis and neurosis. Clinicians now understand that this isn’t the case. The patients need, as Dr. Gunderson once pointed out, constant vigilance because of attachment issues and childhood trauma.
A stable therapeutic alliance between patient and physician, sometimes in combination with evidence-based therapies, is a formula for success, some experts say.
A misunderstood condition
Although there is some degree of heritable risk, BPD patients are often the product of an invalidating environment in childhood. “As kids, we’re guided and nurtured by caring adults to provide models of reasonable, trustworthy behavior. If those role models are missing or just so inconsistent and unpredictable, the patient doesn’t end up with a sturdy self-image. Instead, they’re adrift, trying to figure out who will be helpful and be a meaningful, trustworthy companion and adviser,” Dr. Oldham said.
Emotional or affective instability and impulsivity, sometimes impulsive aggression, often characterize their condition. “Brain-imaging studies have revealed that certain nerve pathways that are necessary to regulate emotions are impoverished in patients with BPD,” Dr. Oldham said.
An analogy is a car going too fast, with a runaway engine that’s running too hot – and the brakes don’t work, he added.
“People think these patients are trying to create big drama, that they’re putting on a big show. That’s not accurate,” he continued. These patients don’t have the ability to stop the trigger that leads to their emotional storms. They also don’t have the ability to regulate themselves. “We may say, it’s a beautiful day outside, but I still have to go to work. Someone with BPD may say: It’s a beautiful day; I’m going to the beach,” Dr. Oldham explained.
A person with BPD might sound coherent when arguing with someone else. But their words are driven by the storm they can’t turn off.
This can lead to their own efforts to turn off the intensity. They might become self-injurious or push other people away. It’s one of the ironies of this condition because BPD patients desperately want to trust others but are scared to do so. “They look for any little signal – that someone else will hurt, disappoint, or leave them. Eventually their relationships unravel,” Dr. Oldham saod.
For some, suicide is sometimes a final solution.
Those traits make it difficult for a therapist to connect with a patient. “This is a very difficult group of people to treat and to establish treatment,” said Michael A. Cummings, MD, of the department of psychiatry at University of California, Riverside, and a psychopharmacology consultant with the California Department of State Hospitals’ Psychopharmacology Resource Network.
BPD patients tend to idealize people who are attempting to help them. When they become frustrated or disappointed in some way, “they then devalue the caregiver or the treatment and not infrequently, fall out of treatment,” Dr. Cummings said. It can be a very taxing experience, particularly for younger, less experienced therapists.
Medication only goes so far
Psychiatrists tend to look at BPD patients as receptor sites for molecules, assessing symptoms they can prescribe for, Eric M. Plakun, MD, DLFAPA, FACPsych, medical director/CEO of the Austen Riggs Center in Stockbridge, Mass., said in an interview.
Yet, BPD is not a molecular problem, principally. It’s an interpersonal disorder. When BPD is a co-occurring disorder, as is often the case, the depressive, anxiety, or other disorder can mask the BPD, he added, citing his 2018 paper on tensions in psychiatry between the biomedical and biopsychosocial models (Psychiatr Clin North Am. 2018 Jun;41[2]:237-48).
In one longitudinal study (J Pers Disord. 2005 Oct;19[5]:487-504), the presence of BPD strongly predicted the persistence of depression. BPD comorbid with depression is often a recipe for treatment-resistant depression, which results in higher costs, more utilization of resources, and higher suicide rates. Too often, psychiatrists diagnose the depression but miss the BPD. They keep trying molecular approaches with prescription drugs – even though it’s really the interpersonal issues of BPD that need to be addressed, said Dr. Plakun, who is a member of the Group for the Advancement of Psychiatry’s Psychotherapy Committee, and founder and past leader of the American Psychiatric Association’s Psychotherapy Caucus.
Medication can be helpful as a short-term adjunctive therapy. Long term, it’s not a sustainable approach, said Dr. Oldham. “If a patient is in a particularly stressful period, in the middle of a stormy breakup or having a depressive episode or talking about suicide, a time-limited course of an antidepressant may be helpful,” he said. They could also benefit from an anxiety-related drug or medication to help them sleep.
What you don’t want is for the patient to start relying on medications to help them feel better. The problem is, many are suffering so much that they’ll go to their primary care doctor and say, “I’m suffering from anxiety,” and get an antianxiety drug. Or they’re depressed or in pain and end up with a cocktail of medications. “And that’s just going to make matters worse,” Dr. Oldham said.
Psychotherapy as a first-line approach
APA practice guidelines and others worldwide have all come to the same conclusion about BPD. , who chaired an APA committee that developed an evidence-based practice guideline for patients with BPD.
Psychotherapy keeps the patient from firing you, he asserted. “Because of the lack of trust, they push away. They’re very scared, and this fear also applies to therapist. The goal is to help the patient learn to trust you. To do that, you need to develop a strong therapeutic alliance.”
In crafting the APA’s practice guideline, Dr. Oldham and his colleagues studied a variety of approaches, including mentalization-based therapy (MBT) and dialectical behavior therapy (DBT), which was developed by Marsha Linehan, PhD. Since then, other approaches have demonstrated efficacy in randomized clinical trials, including schema-based therapy (SBT), cognitive-behavioral therapy (CBT), and transference-focused psychotherapy (TFP).
Those treatments might complement the broader goal of establishing a strong alliance with the patient, Dr. Oldham said. Manualized approaches can help prepackage a program that allows clinicians and patients to look at their problems in an objective, nonpejorative way, Lois W. Choi-Kain, MD, MEd, director of the Gunderson Personality Disorders Institute at McLean Hospital in Belmont, Mass., said in an interview. DBT, for example, focuses on emotion dysregulation. MBT addresses how the patient sees themselves through others and their interactions with others. “It destigmatizes a problem as a clinical entity rather than an interpersonal problem between the patient and the clinician,” Dr. Choi-Kain said.
The choice of approach depends on several factors: the patient’s needs and preferences, and the therapist’s skills and experience, said Dr. Oldham. Some patients don’t do well with DBT because it involves a lot of homework and didactic work. Others do better with TFP because they want to understand what drives their behavior.
Dr. Cummings recalled how one of his patients used TFP to look inward and heal.
He first met the patient when she was in her early 30s. “She had made some progress, but I remember she was still struggling mightily with relationship issues and with identifying her role in relationships,” he said. The patient was becoming increasingly aware that she was going to end up alone and didn’t want that as an outcome.
Adapting to a TFP model, “she worked very hard trying to understand herself as she related to other people, understanding her own emotional volatility, and some of her proneness to behavioral problems,” Dr. Cummings said. The patient also had to learn how to negotiate her relationships to the point where she didn’t end up destroying them and alienating people.
Customizing the treatment
Physicians can choose from one of these manualized forms of treatment to see what’s appropriate and what works for the patient. “You can individualize the treatment, borrowing from these approaches and shaping it based on what your patient needs,” Dr. Oldham recommended.
Recently, the field of psychiatry has seen the benefits of combining manualized, evidence-based approaches with general psychiatric management (GPM), a method conceived by Dr. Gunderson. GPM “reflects a sensitive understanding of mental illness, offering ‘non attacking’ or collaborative work with the patient and a sensitive recognition of appropriate interventions or corrections to help the patient stay in treatment,” said Dr. Oldham.
It aims to conceptualize BPD in a clinically objective way, medicalizing the disorder so it’s something that the patient has, rather than something he or she is, explained Dr. Choi-Kain, who worked with Dr. Gunderson to train clinicians on using this approach. Using a framework that’s compatible with good medical practices, the clinician tries to define the problem together with the patient, “really assessing whether or not the treatment works, setting goals, managing safety, and trying to promote functioning, something we need to pay more attention to with BPD,” she said.
For these patients, the goal is to have positive, corrective experiences in the real world, reinforcing their hopes and what they’re capable of, and an interface with the world that makes them feel like contributors, she said.
Cycle of rupture and repair
Many people with BPD struggle with the desire to find and feel love, but also deal with their rage and hate. Hence, therapists must prepare themselves for the experience of sometimes being hated, said Dr. Plakun. The patient needs to feel they’re in a safe enough space to express those feelings, activating a cycle of “rupture and repair,” he continued.
The key in working with these patients is to avoid any language that will make them feel attacked or criticized, said Dr. Oldham.
A patient may get furious and say “I don’t know what you’re talking about. I didn’t say that.” When in truth, the psychiatrist is flat accurate about what the patient said. Instead of arguing with the patient, a physician can back up and say: “Help me understand what you’re feeling right now. What did I say that made you feel that you couldn’t trust me? Help me understand you. I may have made a mistake,” he advised.
Trust is a key ingredient in an alliance-based intervention for suicidal patients with BPD that Dr. Plakun has frequently written about. A bond he had with a deeply suicidal patient helped her overcome her grief and come to terms with an abusive childhood.
“She had a horrible history of abuse and had BPD and bipolar disorder. Even controlled with medications her life was still awful. She contemplated suicide relentlessly.” Working through her history of sexual abuse, the patient discovered that much of what she and clinicians thought of as a depressive illness was in fact intense grief about the irreparable damage that had taken place during childhood.
Through their work she was able to mourn, and her depression and BPD improved.
Developing a trusting relationship with the patient isn’t a starting point; it’s the goal, he emphasized.
“You don’t prescribe trust to someone. It’s earned.” Through the shared journey of therapy, as the patient suffers from inevitable injuries and ruptures and as the therapist reveals his or her imperfections, opportunities arise to nonjudgmentally examine and repair ruptures. This lead to gains in trust, he said.
It’s not just about genes
Many in the psychiatric and psychological communities tend to develop a very nihilistic view of BPD patients, observed Dr. Cummings. “They’ll say: ‘Oh, well, it’s hopeless. There’s nothing that can be done.’ That isn’t true,” he said.
Epidemiologic studies of these individuals have shown that many of these patients no longer meet the diagnostic criteria for BPD by the time they reach middle age. This means they get better over time, noted Dr. Cummings.
Dr. Plakun’s hope is that the field will evolve in a direction that recognizes the importance of psychosocial treatments like psychotherapy, in addition to biomedical treatments. The drive to medicate still exists, which can contribute to underdiagnosis and undertreatment of BPD, he said. “Although there are manualized, evidence-based treatments, few clinicians learn even one of these for BPD, not to mention those for other disorders.”
In 1996, Francis S. Collins, MD, PhD, the current director of the National Institutes of Health, predicted that the decoding of the human genome would transform treatment of medical and mental disorders [and] “that we would discover the ways in which genes equal disease,” said Dr. Plakun. What the science has since shown, is genes by environmental interaction lead to disease and health.
Nature and nurture both matter. “And I don’t think we’re paying enough attention to the nurture side,” Dr. Plakun said.
The solution is a return to a biopsychosocial model, recognizing that psychotherapy is an essential part of treatment of BPD and other conditions, and an essential clinician skill, he said.
Dr. Oldham is coeditor of the “Textbook of Personality Disorders”, 3rd edition (Washington: American Psychiatric Association Publishing, 2021).Dr. Choi-Kain is coeditor with Dr. Gunderson of “Applications of Good Psychiatric Management for Borderline Personality Disorder: A Practical Guide” (Washington: American Psychiatric Association Publishing, 2019).
Dr. Cummings and Dr. Plakun had no disclosures.
PUFAs a promising add-on for borderline personality disorder
Marine omega-3 fatty acids may be a promising add-on therapy for improving symptoms of borderline personality disorder (BPD), new research suggests.
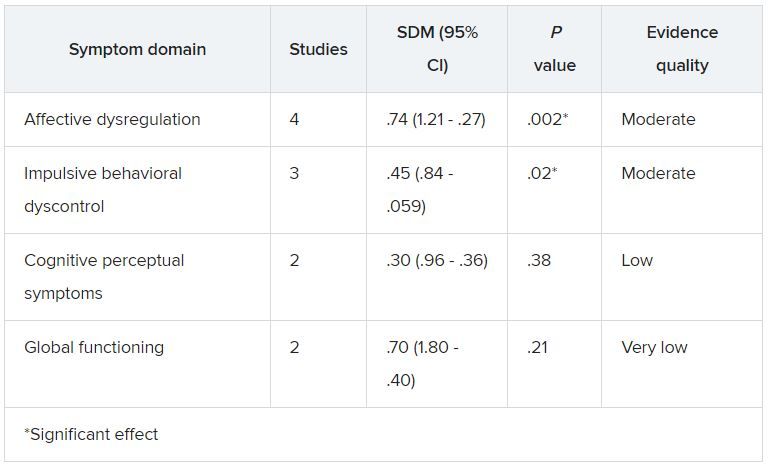
A meta-analysis of four randomized controlled trials showed that adjunctive omega-3 fatty polyunsaturated fatty acids (PUFAs) significantly reduced overall BPD symptom severity, particularly affect dysregulation and impulsive behavior.
“Given the mechanisms of action and beneficial side effect profile, this [analysis] suggests that omega-3 fatty acids could be considered as add-on treatment” for patients with BPD, senior author Roel J. T. Mocking MD, PhD, resident in psychiatry and postdoctoral researcher at Academisch Medisch Centrum, Amsterdam, said in an interview.
The findings were published online in the Journal of Clinical Psychiatry.
Urgent need
“There are several effective treatments, but not all patients respond sufficiently,” which points to an urgent need for additional treatment options, Dr. Mocking said.
He noted that, although “several prior studies showed promising effects of omega-3 fatty acids” for patients with BPD, those studies were relatively small, which precluded more definitive overall conclusions.
The investigators wanted to combine results of the earlier studies to provide a combined estimate of overall effectiveness of the use of omega-3 fatty acids for patients with BP, with the intention of “guiding clinicians and individuals suffering from borderline personality disorder to decide on whether they should add omega-3 fatty acids to their treatment.”
The analyzed four studies that had a total of 137 patients. Three of the studies included patients diagnosed with BPD; one included individuals with recurrent self-harm, most of whom were also diagnosed with BPD.
Omega-3 fatty acids were used as monotherapy in one study. In the other studies, they were used as add-on therapy to other agents, such as antidepressants, benzodiazepines, and/or valproic acid. None of the studies included patients who were taking antipsychotics.
The type of omega-3 PUFAs were derived from marine rather than plant sources.
Three studies compared omega-3 fatty acids with placebo. One study compared valproic acid monotherapy with valproic acid plus omega-3 fatty acids and did not include a placebo group.
Significant symptom reduction
Random-effects meta-analyses showed an “overall significant decreasing effect” of omega-3 fatty acids on overall BPD symptom severity (standardized difference in means, 0.54; 95% CI, 0.91-0.17; P = .004) in the omega-3 group compared with the control group, with a medium effect size.
The investigators added that there was “no relevant heterogeneity” (P = .45).
Although heterogeneity was “more pronounced” in the affective dysregulation symptom domain, it did not reach statistical significance, the researchers noted.
The impulsive behavioral dyscontrol and cognitive perceptual symptom domains had “no relevant heterogeneity.” On the other hand, there was “substantial heterogeneity” in the global functioning symptom group.
Omega-3 fatty acids “have multiple bioactive roles in the brain. For example, they form essential components of the membrane of brain cells and thereby influence the structure and functioning of the brain. They also have an effect on inflammation levels in the brain,” Dr. Mocking said.
“Because we cannot synthesize these omega-3 fatty acids ourselves, we are dependent on our diet. The main dietary source of omega-3 fatty acids is fatty fish. However, since the industrial revolution, we eat less and less fatty fish, risking deficiency of omega-3 fatty acids causing brain dysfunction,” he added.
Dr. Mocking noted that
This “suggests that they could be combined to increase overall effectiveness,” he said.
Important benefit
Commenting on the study, Roger McIntyre, MD, professor of psychiatry and pharmacology, University of Toronto, and head of the mood disorders psychopharmacology unit, said that the benefit of omega-3 “on impulsivity and mood symptoms is especially important, as these are some of the most debilitating aspects of BPD and lead to service utilization, such as ER, primary care, and specialty care.”
In addition, “impulsivity often presages suicidality,” he noted.
Dr. McIntyre, who is also chair and executive director of the Brain and Cognition Discovery Foundation in Toronto and was not involved with the study, called the effect size “quite reasonable.”
“The mechanistic story is very strong around anti-inflammatory effect, which particularly implied mood and cognition. In other words, inflammation is highly associated with mood and cognitive difficulties,” he said.
However, Dr. McIntyre also pointed to several significant challenges, including “quality assurance on the purchase of the product of fish oil, as it is not sufficiently regulated.” It is also unclear which individuals are more likely to benefit from it.
For example, major depressive disorder data have shown that “fish oils are not as effective as we hoped but are especially effective in people with baseline elevation of inflammatory markers,” Dr. McIntyre said.
“In other words, is there a way to identify a biomarkers/biosignature or phenomenology that’s more likely to identify a subgroup of people with BPD who might benefit benefiting from omega-3?” he asked.
Dr. Mocking and the other investigators reported no relevant financial relationships. Dr. McIntyre has received research grant support from CIHR/GACD/Chinese National Natural Research Foundation and speaker/consultation fees from Lundbeck, Janssen, Purdue, Pfizer, Otsuka, Allergan, Takeda, Neurocrine, Sunovion, Eisai, Minerva, Intra-Cellular, and AbbVie. Dr. McIntyre is also CEO of AltMed.
A version of this article first appeared on Medscape.com.
Marine omega-3 fatty acids may be a promising add-on therapy for improving symptoms of borderline personality disorder (BPD), new research suggests.
A meta-analysis of four randomized controlled trials showed that adjunctive omega-3 fatty polyunsaturated fatty acids (PUFAs) significantly reduced overall BPD symptom severity, particularly affect dysregulation and impulsive behavior.
“Given the mechanisms of action and beneficial side effect profile, this [analysis] suggests that omega-3 fatty acids could be considered as add-on treatment” for patients with BPD, senior author Roel J. T. Mocking MD, PhD, resident in psychiatry and postdoctoral researcher at Academisch Medisch Centrum, Amsterdam, said in an interview.
The findings were published online in the Journal of Clinical Psychiatry.
Urgent need
“There are several effective treatments, but not all patients respond sufficiently,” which points to an urgent need for additional treatment options, Dr. Mocking said.
He noted that, although “several prior studies showed promising effects of omega-3 fatty acids” for patients with BPD, those studies were relatively small, which precluded more definitive overall conclusions.
The investigators wanted to combine results of the earlier studies to provide a combined estimate of overall effectiveness of the use of omega-3 fatty acids for patients with BP, with the intention of “guiding clinicians and individuals suffering from borderline personality disorder to decide on whether they should add omega-3 fatty acids to their treatment.”
The analyzed four studies that had a total of 137 patients. Three of the studies included patients diagnosed with BPD; one included individuals with recurrent self-harm, most of whom were also diagnosed with BPD.
Omega-3 fatty acids were used as monotherapy in one study. In the other studies, they were used as add-on therapy to other agents, such as antidepressants, benzodiazepines, and/or valproic acid. None of the studies included patients who were taking antipsychotics.
The type of omega-3 PUFAs were derived from marine rather than plant sources.
Three studies compared omega-3 fatty acids with placebo. One study compared valproic acid monotherapy with valproic acid plus omega-3 fatty acids and did not include a placebo group.
Significant symptom reduction
Random-effects meta-analyses showed an “overall significant decreasing effect” of omega-3 fatty acids on overall BPD symptom severity (standardized difference in means, 0.54; 95% CI, 0.91-0.17; P = .004) in the omega-3 group compared with the control group, with a medium effect size.
The investigators added that there was “no relevant heterogeneity” (P = .45).
Although heterogeneity was “more pronounced” in the affective dysregulation symptom domain, it did not reach statistical significance, the researchers noted.
The impulsive behavioral dyscontrol and cognitive perceptual symptom domains had “no relevant heterogeneity.” On the other hand, there was “substantial heterogeneity” in the global functioning symptom group.
Omega-3 fatty acids “have multiple bioactive roles in the brain. For example, they form essential components of the membrane of brain cells and thereby influence the structure and functioning of the brain. They also have an effect on inflammation levels in the brain,” Dr. Mocking said.
“Because we cannot synthesize these omega-3 fatty acids ourselves, we are dependent on our diet. The main dietary source of omega-3 fatty acids is fatty fish. However, since the industrial revolution, we eat less and less fatty fish, risking deficiency of omega-3 fatty acids causing brain dysfunction,” he added.
Dr. Mocking noted that
This “suggests that they could be combined to increase overall effectiveness,” he said.
Important benefit
Commenting on the study, Roger McIntyre, MD, professor of psychiatry and pharmacology, University of Toronto, and head of the mood disorders psychopharmacology unit, said that the benefit of omega-3 “on impulsivity and mood symptoms is especially important, as these are some of the most debilitating aspects of BPD and lead to service utilization, such as ER, primary care, and specialty care.”
In addition, “impulsivity often presages suicidality,” he noted.
Dr. McIntyre, who is also chair and executive director of the Brain and Cognition Discovery Foundation in Toronto and was not involved with the study, called the effect size “quite reasonable.”
“The mechanistic story is very strong around anti-inflammatory effect, which particularly implied mood and cognition. In other words, inflammation is highly associated with mood and cognitive difficulties,” he said.
However, Dr. McIntyre also pointed to several significant challenges, including “quality assurance on the purchase of the product of fish oil, as it is not sufficiently regulated.” It is also unclear which individuals are more likely to benefit from it.
For example, major depressive disorder data have shown that “fish oils are not as effective as we hoped but are especially effective in people with baseline elevation of inflammatory markers,” Dr. McIntyre said.
“In other words, is there a way to identify a biomarkers/biosignature or phenomenology that’s more likely to identify a subgroup of people with BPD who might benefit benefiting from omega-3?” he asked.
Dr. Mocking and the other investigators reported no relevant financial relationships. Dr. McIntyre has received research grant support from CIHR/GACD/Chinese National Natural Research Foundation and speaker/consultation fees from Lundbeck, Janssen, Purdue, Pfizer, Otsuka, Allergan, Takeda, Neurocrine, Sunovion, Eisai, Minerva, Intra-Cellular, and AbbVie. Dr. McIntyre is also CEO of AltMed.
A version of this article first appeared on Medscape.com.
Marine omega-3 fatty acids may be a promising add-on therapy for improving symptoms of borderline personality disorder (BPD), new research suggests.
A meta-analysis of four randomized controlled trials showed that adjunctive omega-3 fatty polyunsaturated fatty acids (PUFAs) significantly reduced overall BPD symptom severity, particularly affect dysregulation and impulsive behavior.
“Given the mechanisms of action and beneficial side effect profile, this [analysis] suggests that omega-3 fatty acids could be considered as add-on treatment” for patients with BPD, senior author Roel J. T. Mocking MD, PhD, resident in psychiatry and postdoctoral researcher at Academisch Medisch Centrum, Amsterdam, said in an interview.
The findings were published online in the Journal of Clinical Psychiatry.
Urgent need
“There are several effective treatments, but not all patients respond sufficiently,” which points to an urgent need for additional treatment options, Dr. Mocking said.
He noted that, although “several prior studies showed promising effects of omega-3 fatty acids” for patients with BPD, those studies were relatively small, which precluded more definitive overall conclusions.
The investigators wanted to combine results of the earlier studies to provide a combined estimate of overall effectiveness of the use of omega-3 fatty acids for patients with BP, with the intention of “guiding clinicians and individuals suffering from borderline personality disorder to decide on whether they should add omega-3 fatty acids to their treatment.”
The analyzed four studies that had a total of 137 patients. Three of the studies included patients diagnosed with BPD; one included individuals with recurrent self-harm, most of whom were also diagnosed with BPD.
Omega-3 fatty acids were used as monotherapy in one study. In the other studies, they were used as add-on therapy to other agents, such as antidepressants, benzodiazepines, and/or valproic acid. None of the studies included patients who were taking antipsychotics.
The type of omega-3 PUFAs were derived from marine rather than plant sources.
Three studies compared omega-3 fatty acids with placebo. One study compared valproic acid monotherapy with valproic acid plus omega-3 fatty acids and did not include a placebo group.
Significant symptom reduction
Random-effects meta-analyses showed an “overall significant decreasing effect” of omega-3 fatty acids on overall BPD symptom severity (standardized difference in means, 0.54; 95% CI, 0.91-0.17; P = .004) in the omega-3 group compared with the control group, with a medium effect size.
The investigators added that there was “no relevant heterogeneity” (P = .45).
Although heterogeneity was “more pronounced” in the affective dysregulation symptom domain, it did not reach statistical significance, the researchers noted.
The impulsive behavioral dyscontrol and cognitive perceptual symptom domains had “no relevant heterogeneity.” On the other hand, there was “substantial heterogeneity” in the global functioning symptom group.
Omega-3 fatty acids “have multiple bioactive roles in the brain. For example, they form essential components of the membrane of brain cells and thereby influence the structure and functioning of the brain. They also have an effect on inflammation levels in the brain,” Dr. Mocking said.
“Because we cannot synthesize these omega-3 fatty acids ourselves, we are dependent on our diet. The main dietary source of omega-3 fatty acids is fatty fish. However, since the industrial revolution, we eat less and less fatty fish, risking deficiency of omega-3 fatty acids causing brain dysfunction,” he added.
Dr. Mocking noted that
This “suggests that they could be combined to increase overall effectiveness,” he said.
Important benefit
Commenting on the study, Roger McIntyre, MD, professor of psychiatry and pharmacology, University of Toronto, and head of the mood disorders psychopharmacology unit, said that the benefit of omega-3 “on impulsivity and mood symptoms is especially important, as these are some of the most debilitating aspects of BPD and lead to service utilization, such as ER, primary care, and specialty care.”
In addition, “impulsivity often presages suicidality,” he noted.
Dr. McIntyre, who is also chair and executive director of the Brain and Cognition Discovery Foundation in Toronto and was not involved with the study, called the effect size “quite reasonable.”
“The mechanistic story is very strong around anti-inflammatory effect, which particularly implied mood and cognition. In other words, inflammation is highly associated with mood and cognitive difficulties,” he said.
However, Dr. McIntyre also pointed to several significant challenges, including “quality assurance on the purchase of the product of fish oil, as it is not sufficiently regulated.” It is also unclear which individuals are more likely to benefit from it.
For example, major depressive disorder data have shown that “fish oils are not as effective as we hoped but are especially effective in people with baseline elevation of inflammatory markers,” Dr. McIntyre said.
“In other words, is there a way to identify a biomarkers/biosignature or phenomenology that’s more likely to identify a subgroup of people with BPD who might benefit benefiting from omega-3?” he asked.
Dr. Mocking and the other investigators reported no relevant financial relationships. Dr. McIntyre has received research grant support from CIHR/GACD/Chinese National Natural Research Foundation and speaker/consultation fees from Lundbeck, Janssen, Purdue, Pfizer, Otsuka, Allergan, Takeda, Neurocrine, Sunovion, Eisai, Minerva, Intra-Cellular, and AbbVie. Dr. McIntyre is also CEO of AltMed.
A version of this article first appeared on Medscape.com.
Psychiatric genomics has a diversity problem
In combing the genome, scientists can use genetic clues to determine a person’s risk for psychiatric disease and even identify new drug targets. But the benefits of these discoveries will be limited to people of European descent.
Nearly 90% of participants in genome-wide association studies (GWASs), which search for gene variants linked to disease, are of European ancestry. This Eurocentric focus threatens to widen existing disparities in racial and ethnic mental health.
“If you develop certain interventions based on only a single population profile, then you’ll be leaving out the rest of the populations in the world,” says Solomon Teferra, MD, PhD, associate professor of psychiatry at Addis Ababa University, Ethiopia. In a growing trend, psychiatric researchers are diverging from the field’s European bias and are working to correct the imbalance in DNA databases.
The significant downsides of genomics’ one-track mind
One obstacle hindering therapeutic advances in psychiatry is a shallow understanding of the mechanisms of disorders. “The biggest problem in terms of advancing research for mental health conditions is that we don’t understand the underlying biology,” says Laramie Duncan, PhD, assistant professor of psychiatry and behavioral sciences at Stanford (Calif.) University. “Genetics is one of the best ways to systematically look for new clues about the underlying biology.”
At the advent of genomic research, scientists thought it best to study DNA from people of a single ancestry from one continent. “Researchers for a long time held the idea that it was going to be too complicated to include multiple ancestries in the first rounds of genetic analyses,” says Dr. Duncan.
Studying DNA from someone with ancestors from multiple parts of the world wasn’t compatible with methods used in the early days of GWASs. “Individual parts of a person’s DNA can be linked back to one region of the world or another, and most of our methods essentially assume that all of a person’s DNA came from one region of the world,” says Dr. Duncan.
Because many genes are usually involved in psychiatric disorders, scientists need large numbers of participants to detect uncommon, influential variants. Early research was concentrated in North America and Europe so that scientists could readily collect samples from people of European ancestry.
“It then went out of hand because it became routine practice to use only this one group, essentially White, European ancestry people,” says Karoline Kuchenbaecker, PhD, associate professor of psychiatry at University College London.
Yet findings from one population won’t necessarily translate to others. “And that’s exactly what has been shown,” says Dr. Teferra. Polygenic risk scores developed for schizophrenia from European samples, for example, perform poorly among people of African ancestry, although among Europeans, they are strongly effective at differentiating European individuals with and those without schizophrenia. Moreover, drugs that target a gene identified from studies in European populations may be harmful to other groups.
Studies drawn from a diverse pool of participants would benefit a wider swath of humanity. They would also allow scientists to discover small areas of overlap in genomes of different populations, which would help them close in on the true biology of diseases and ensure that “we’re all benefiting from more diverse data in genetics and psychiatric genetics,” says Dr. Kuchenbaecker.
New efforts aim at filling the gaps
, not African, Latin American, or Indigenous ancestry.
Efforts to increase representation of persons of African ancestry have largely focused on African Americans; fewer efforts have extended to the African continent, home to the most genetically diverse populations. Even fewer have focused on mental health. “The little that was being done was on a very small scale,” says Karestan Koenen, PhD, a professor at Harvard School of Public Health, Boston.
With this in mind, researchers from institutions in Kenya, Uganda, South Africa, and Ethiopia partnered with researchers at the Broad Institute of the Massachusetts Institute of Technology and Harvard to conduct the largest GWAS of psychiatric disorders in Africa. Dr. Koenen leads the project, Neuropsychiatric Genetics of African Populations–Psychosis (NeuroGAP-Psychosis), which will analyze DNA from over 35,000 people of African ancestry in each of these four countries. Investigators will compare the half of participants who have no history of psychosis with the half with schizophrenia or bipolar disorder in the hopes of identifying the genetic determinants of psychosis.
“Then any potential intervention or therapeutics that will be developed will also be useful for Africans,” says Dr. Teferra, a NeuroGAP principal investigator. Because of the tremendous degree of genetic diversity among people on the continent, however, findings still might not translate to all African populations.
But correcting equity problems in genomics isn’t as simple as recruiting people with non-European backgrounds, especially if those people are unfamiliar with research or have been subject to scientific exploitation. “Special care needs to be taken to, first of all, provide information that’s appropriate [to participants], but also motivate people to take part and then find ways to keep these communities involved and understand what they’re interested in,” says Dr. Kuchenbaecker, who is not involved with NeuroGAP.
For NeuroGAP, the team needed to work with ethical committees at all of the institutions involved, ensure research materials were appropriate for each community’s cultural context, and gain the trust of local communities.
“One of the biggest criticisms within the scientific world is that people from more endowed countries just fly in, bully everyone, collect the data, and leave, with no credit to the local scientists or communities,” says NeuroGAP principal investigator Lukoye Atwoli, MMed, PhD, professor of psychiatry and dean of the Medical College, East Africa, at the Aga Khan University, Nairobi, Kenya. “That is one of the biggest pitfalls we had to grapple with.”
To address that concern, NeuroGAP is training local researchers and is providing them with requested resources so they can carry out similar studies in the future. “We will be looking to address a real need in the academic community and in clinical service delivery,” says Dr. Atwoli.
Dr. Kuchenbaecker says that NeuroGAP demonstrates features necessary for projects seeking to improve equity in psychiatric genomics. “What they’re doing right is recruiting really large numbers, recruiting from different African countries, and involving African investigators,” she says.
In the Americas, Janitza Montalvo-Ortiz, PhD, assistant professor in the Division of Genetics, department of psychiatry, Yale University, New Haven, Conn., and her colleagues are expanding psychiatric genomics projects in Latin America. She co-founded the Latin American Genomics Consortium in 2019, a network of scientists supporting psychiatric genomic research in the region. The consortium also involves the Neuropsychiatric Genetics in Mexican Populations project, which is similar to NeuroGAP and is also led by Dr. Koenan.
The study of Latin American populations is complicated, because genes in these populations reflect Indigenous American, European, and African ancestries. Even when investigators sampled DNA from Latin American individuals, that data often went unused. “Now with new methods emerging to allow us to properly analyze admixed populations in GWAS studies, we’re making efforts to compile different datasets scattered across different large-scale cohorts,” says Dr. Montalvo-Ortiz. “Our ultimate goal is to conduct the first large-scale LatinX GWAS of psychiatry,” she says.
With these projects, researchers hope that new psychiatric research will produce clinical advances for people historically left on the sidelines of genomic studies. By involving their communities in genomic research, “whatever is going to be developed will also benefit our community,” says Dr. Teferra. “We will not be left out.”
A version of this article first appeared on Medscape.com.
In combing the genome, scientists can use genetic clues to determine a person’s risk for psychiatric disease and even identify new drug targets. But the benefits of these discoveries will be limited to people of European descent.
Nearly 90% of participants in genome-wide association studies (GWASs), which search for gene variants linked to disease, are of European ancestry. This Eurocentric focus threatens to widen existing disparities in racial and ethnic mental health.
“If you develop certain interventions based on only a single population profile, then you’ll be leaving out the rest of the populations in the world,” says Solomon Teferra, MD, PhD, associate professor of psychiatry at Addis Ababa University, Ethiopia. In a growing trend, psychiatric researchers are diverging from the field’s European bias and are working to correct the imbalance in DNA databases.
The significant downsides of genomics’ one-track mind
One obstacle hindering therapeutic advances in psychiatry is a shallow understanding of the mechanisms of disorders. “The biggest problem in terms of advancing research for mental health conditions is that we don’t understand the underlying biology,” says Laramie Duncan, PhD, assistant professor of psychiatry and behavioral sciences at Stanford (Calif.) University. “Genetics is one of the best ways to systematically look for new clues about the underlying biology.”
At the advent of genomic research, scientists thought it best to study DNA from people of a single ancestry from one continent. “Researchers for a long time held the idea that it was going to be too complicated to include multiple ancestries in the first rounds of genetic analyses,” says Dr. Duncan.
Studying DNA from someone with ancestors from multiple parts of the world wasn’t compatible with methods used in the early days of GWASs. “Individual parts of a person’s DNA can be linked back to one region of the world or another, and most of our methods essentially assume that all of a person’s DNA came from one region of the world,” says Dr. Duncan.
Because many genes are usually involved in psychiatric disorders, scientists need large numbers of participants to detect uncommon, influential variants. Early research was concentrated in North America and Europe so that scientists could readily collect samples from people of European ancestry.
“It then went out of hand because it became routine practice to use only this one group, essentially White, European ancestry people,” says Karoline Kuchenbaecker, PhD, associate professor of psychiatry at University College London.
Yet findings from one population won’t necessarily translate to others. “And that’s exactly what has been shown,” says Dr. Teferra. Polygenic risk scores developed for schizophrenia from European samples, for example, perform poorly among people of African ancestry, although among Europeans, they are strongly effective at differentiating European individuals with and those without schizophrenia. Moreover, drugs that target a gene identified from studies in European populations may be harmful to other groups.
Studies drawn from a diverse pool of participants would benefit a wider swath of humanity. They would also allow scientists to discover small areas of overlap in genomes of different populations, which would help them close in on the true biology of diseases and ensure that “we’re all benefiting from more diverse data in genetics and psychiatric genetics,” says Dr. Kuchenbaecker.
New efforts aim at filling the gaps
, not African, Latin American, or Indigenous ancestry.
Efforts to increase representation of persons of African ancestry have largely focused on African Americans; fewer efforts have extended to the African continent, home to the most genetically diverse populations. Even fewer have focused on mental health. “The little that was being done was on a very small scale,” says Karestan Koenen, PhD, a professor at Harvard School of Public Health, Boston.
With this in mind, researchers from institutions in Kenya, Uganda, South Africa, and Ethiopia partnered with researchers at the Broad Institute of the Massachusetts Institute of Technology and Harvard to conduct the largest GWAS of psychiatric disorders in Africa. Dr. Koenen leads the project, Neuropsychiatric Genetics of African Populations–Psychosis (NeuroGAP-Psychosis), which will analyze DNA from over 35,000 people of African ancestry in each of these four countries. Investigators will compare the half of participants who have no history of psychosis with the half with schizophrenia or bipolar disorder in the hopes of identifying the genetic determinants of psychosis.
“Then any potential intervention or therapeutics that will be developed will also be useful for Africans,” says Dr. Teferra, a NeuroGAP principal investigator. Because of the tremendous degree of genetic diversity among people on the continent, however, findings still might not translate to all African populations.
But correcting equity problems in genomics isn’t as simple as recruiting people with non-European backgrounds, especially if those people are unfamiliar with research or have been subject to scientific exploitation. “Special care needs to be taken to, first of all, provide information that’s appropriate [to participants], but also motivate people to take part and then find ways to keep these communities involved and understand what they’re interested in,” says Dr. Kuchenbaecker, who is not involved with NeuroGAP.
For NeuroGAP, the team needed to work with ethical committees at all of the institutions involved, ensure research materials were appropriate for each community’s cultural context, and gain the trust of local communities.
“One of the biggest criticisms within the scientific world is that people from more endowed countries just fly in, bully everyone, collect the data, and leave, with no credit to the local scientists or communities,” says NeuroGAP principal investigator Lukoye Atwoli, MMed, PhD, professor of psychiatry and dean of the Medical College, East Africa, at the Aga Khan University, Nairobi, Kenya. “That is one of the biggest pitfalls we had to grapple with.”
To address that concern, NeuroGAP is training local researchers and is providing them with requested resources so they can carry out similar studies in the future. “We will be looking to address a real need in the academic community and in clinical service delivery,” says Dr. Atwoli.
Dr. Kuchenbaecker says that NeuroGAP demonstrates features necessary for projects seeking to improve equity in psychiatric genomics. “What they’re doing right is recruiting really large numbers, recruiting from different African countries, and involving African investigators,” she says.
In the Americas, Janitza Montalvo-Ortiz, PhD, assistant professor in the Division of Genetics, department of psychiatry, Yale University, New Haven, Conn., and her colleagues are expanding psychiatric genomics projects in Latin America. She co-founded the Latin American Genomics Consortium in 2019, a network of scientists supporting psychiatric genomic research in the region. The consortium also involves the Neuropsychiatric Genetics in Mexican Populations project, which is similar to NeuroGAP and is also led by Dr. Koenan.
The study of Latin American populations is complicated, because genes in these populations reflect Indigenous American, European, and African ancestries. Even when investigators sampled DNA from Latin American individuals, that data often went unused. “Now with new methods emerging to allow us to properly analyze admixed populations in GWAS studies, we’re making efforts to compile different datasets scattered across different large-scale cohorts,” says Dr. Montalvo-Ortiz. “Our ultimate goal is to conduct the first large-scale LatinX GWAS of psychiatry,” she says.
With these projects, researchers hope that new psychiatric research will produce clinical advances for people historically left on the sidelines of genomic studies. By involving their communities in genomic research, “whatever is going to be developed will also benefit our community,” says Dr. Teferra. “We will not be left out.”
A version of this article first appeared on Medscape.com.
In combing the genome, scientists can use genetic clues to determine a person’s risk for psychiatric disease and even identify new drug targets. But the benefits of these discoveries will be limited to people of European descent.
Nearly 90% of participants in genome-wide association studies (GWASs), which search for gene variants linked to disease, are of European ancestry. This Eurocentric focus threatens to widen existing disparities in racial and ethnic mental health.
“If you develop certain interventions based on only a single population profile, then you’ll be leaving out the rest of the populations in the world,” says Solomon Teferra, MD, PhD, associate professor of psychiatry at Addis Ababa University, Ethiopia. In a growing trend, psychiatric researchers are diverging from the field’s European bias and are working to correct the imbalance in DNA databases.
The significant downsides of genomics’ one-track mind
One obstacle hindering therapeutic advances in psychiatry is a shallow understanding of the mechanisms of disorders. “The biggest problem in terms of advancing research for mental health conditions is that we don’t understand the underlying biology,” says Laramie Duncan, PhD, assistant professor of psychiatry and behavioral sciences at Stanford (Calif.) University. “Genetics is one of the best ways to systematically look for new clues about the underlying biology.”
At the advent of genomic research, scientists thought it best to study DNA from people of a single ancestry from one continent. “Researchers for a long time held the idea that it was going to be too complicated to include multiple ancestries in the first rounds of genetic analyses,” says Dr. Duncan.
Studying DNA from someone with ancestors from multiple parts of the world wasn’t compatible with methods used in the early days of GWASs. “Individual parts of a person’s DNA can be linked back to one region of the world or another, and most of our methods essentially assume that all of a person’s DNA came from one region of the world,” says Dr. Duncan.
Because many genes are usually involved in psychiatric disorders, scientists need large numbers of participants to detect uncommon, influential variants. Early research was concentrated in North America and Europe so that scientists could readily collect samples from people of European ancestry.
“It then went out of hand because it became routine practice to use only this one group, essentially White, European ancestry people,” says Karoline Kuchenbaecker, PhD, associate professor of psychiatry at University College London.
Yet findings from one population won’t necessarily translate to others. “And that’s exactly what has been shown,” says Dr. Teferra. Polygenic risk scores developed for schizophrenia from European samples, for example, perform poorly among people of African ancestry, although among Europeans, they are strongly effective at differentiating European individuals with and those without schizophrenia. Moreover, drugs that target a gene identified from studies in European populations may be harmful to other groups.
Studies drawn from a diverse pool of participants would benefit a wider swath of humanity. They would also allow scientists to discover small areas of overlap in genomes of different populations, which would help them close in on the true biology of diseases and ensure that “we’re all benefiting from more diverse data in genetics and psychiatric genetics,” says Dr. Kuchenbaecker.
New efforts aim at filling the gaps
, not African, Latin American, or Indigenous ancestry.
Efforts to increase representation of persons of African ancestry have largely focused on African Americans; fewer efforts have extended to the African continent, home to the most genetically diverse populations. Even fewer have focused on mental health. “The little that was being done was on a very small scale,” says Karestan Koenen, PhD, a professor at Harvard School of Public Health, Boston.
With this in mind, researchers from institutions in Kenya, Uganda, South Africa, and Ethiopia partnered with researchers at the Broad Institute of the Massachusetts Institute of Technology and Harvard to conduct the largest GWAS of psychiatric disorders in Africa. Dr. Koenen leads the project, Neuropsychiatric Genetics of African Populations–Psychosis (NeuroGAP-Psychosis), which will analyze DNA from over 35,000 people of African ancestry in each of these four countries. Investigators will compare the half of participants who have no history of psychosis with the half with schizophrenia or bipolar disorder in the hopes of identifying the genetic determinants of psychosis.
“Then any potential intervention or therapeutics that will be developed will also be useful for Africans,” says Dr. Teferra, a NeuroGAP principal investigator. Because of the tremendous degree of genetic diversity among people on the continent, however, findings still might not translate to all African populations.
But correcting equity problems in genomics isn’t as simple as recruiting people with non-European backgrounds, especially if those people are unfamiliar with research or have been subject to scientific exploitation. “Special care needs to be taken to, first of all, provide information that’s appropriate [to participants], but also motivate people to take part and then find ways to keep these communities involved and understand what they’re interested in,” says Dr. Kuchenbaecker, who is not involved with NeuroGAP.
For NeuroGAP, the team needed to work with ethical committees at all of the institutions involved, ensure research materials were appropriate for each community’s cultural context, and gain the trust of local communities.
“One of the biggest criticisms within the scientific world is that people from more endowed countries just fly in, bully everyone, collect the data, and leave, with no credit to the local scientists or communities,” says NeuroGAP principal investigator Lukoye Atwoli, MMed, PhD, professor of psychiatry and dean of the Medical College, East Africa, at the Aga Khan University, Nairobi, Kenya. “That is one of the biggest pitfalls we had to grapple with.”
To address that concern, NeuroGAP is training local researchers and is providing them with requested resources so they can carry out similar studies in the future. “We will be looking to address a real need in the academic community and in clinical service delivery,” says Dr. Atwoli.
Dr. Kuchenbaecker says that NeuroGAP demonstrates features necessary for projects seeking to improve equity in psychiatric genomics. “What they’re doing right is recruiting really large numbers, recruiting from different African countries, and involving African investigators,” she says.
In the Americas, Janitza Montalvo-Ortiz, PhD, assistant professor in the Division of Genetics, department of psychiatry, Yale University, New Haven, Conn., and her colleagues are expanding psychiatric genomics projects in Latin America. She co-founded the Latin American Genomics Consortium in 2019, a network of scientists supporting psychiatric genomic research in the region. The consortium also involves the Neuropsychiatric Genetics in Mexican Populations project, which is similar to NeuroGAP and is also led by Dr. Koenan.
The study of Latin American populations is complicated, because genes in these populations reflect Indigenous American, European, and African ancestries. Even when investigators sampled DNA from Latin American individuals, that data often went unused. “Now with new methods emerging to allow us to properly analyze admixed populations in GWAS studies, we’re making efforts to compile different datasets scattered across different large-scale cohorts,” says Dr. Montalvo-Ortiz. “Our ultimate goal is to conduct the first large-scale LatinX GWAS of psychiatry,” she says.
With these projects, researchers hope that new psychiatric research will produce clinical advances for people historically left on the sidelines of genomic studies. By involving their communities in genomic research, “whatever is going to be developed will also benefit our community,” says Dr. Teferra. “We will not be left out.”
A version of this article first appeared on Medscape.com.
Managing ‘difficult’ patient encounters
“I did not like those patients… They made me angry and I found myself irritated to experience them as they seemed so distant from myself and from all that is human. This is an astonishing intolerance which brands me a poor psychiatrist.”
Sigmund Freud, Letter to István Hollós (1928)
While Freud was referring to psychotic patients,1 his evident frustration shows that difficult and challenging patients have vexed even the best of us. All physicians and other clinicians will experience patient encounters that lead to anger or frustration, or even challenge their sense of equanimity and professional identity. In short, difficult and challenging patient interactions are unavoidable, regardless of the physician’s discipline.2-5 At times, physicians might struggle with demanding, unpleasant, ungrateful, and possibly dangerous patients, while sometimes the struggle is with the patient’s family members. No physician is immune to the problem, which makes it crucial to learn to anticipate and manage difficult patient interactions, skills which are generally not taught in medical schools or residency programs.
One prospective study of clinic patients found that up to 15% of patient encounters are deemed “difficult.”6 Common scenarios include patients (or their relatives) who seek certain tests after researching symptoms online, threats of legal or social media action in response to feeling that the physician is not listening to them, demands for a second opinion after disagreeing with the physician’s diagnosis, and mistrust of doctors after presenting with symptoms and not receiving a diagnosis. It is also common to care for patients who focus on negative outcomes or fail to adhere to treatment recommendations. These encounters can make physicians feel stressed out, disrespected, abused, or even fearful if threatened. Some physicians may come to feel they are trapped in a hostile work environment with little support from their supervisors or administrators. Patients often have a complaint office or department to turn to, but there is no equivalent for physicians, who are expected to soldier on regardless.
This article highlights a model that describes poor physician-patient encounters, factors contributing to these issues, how to manage these difficult interactions, and what to do if the relationship cannot be remediated.
Describing the ‘difficult’ patient
In a landmark 1978 paper, Groves7 provided one of the first descriptions of “difficult” patients. His colorful observations continue to provide useful insights. Groves emphasized that most medical texts ignore the issue of difficult patients and provide little or no guidance—which is still true 43 years later. He observed that physicians cannot avoid occasional negative feelings toward some patients. Further, Groves suggested that countertransference is often at the root of hateful reactions, a process he defines as “conscious or unconscious unbidden and unwanted hostile or sexual feelings toward the patient.”7Table 17 outlines how Groves divided “hateful” patients into several categories, and how physicians might respond to such patients.
A model for understanding difficult patient encounters
Adams and Murray2 created a model to help explain interactions with difficult or challenging patients that consists of 3 elements: the patient, the physician, and the system (ie, situation or environment). Hull and Broquet8 and Hardavella et al9 later adapted the model and described its components (Table 22,8,9).
Continue to: When considering...
When considering difficult interactions, it is important to be aware that all 3 components could interact, or merely 1 or 2 could come into play, but all should be explored as possible contributing factors.
Patient factors
The patient’s role in initiating or maintaining a problematic interaction should be explored. While some physicians are tempted to conclude that a personality disorder underlies difficult interactions, research shows a more complex picture. First, not all difficult patients have a psychiatric disorder, let alone a personality disorder. Jackson and Kroenke6 reported that among 74 difficult patients in an ambulatory clinic, 29% had a depressive disorder or anxiety disorder, with 11% experiencing 2 or more disorders. Major depressive disorder was present in 8.4% patients, other depressive disorders in 17.4%, panic disorder in 1.4%, and other anxiety disorders in 14.2%.6 These researchers found that difficult patient interactions were associated with the presence of a psychiatric disorder, especially depressive or anxiety disorders, and multiple physical symptoms.
Importantly, difficult patients are not unique to psychiatry, and are found in all medical disciplines and every type of practice situation. Some problematic patients have a substance use disorder, and their difficulty might stem from intoxication, withdrawal, or drug-seeking behaviors. Psychotic disorders can be the source of difficult interactions, typically resulting from the patient’s symptoms (ie, hallucinations, delusions, or bizarre behavior). Physicians tend to be forgiving toward these patients because they understand the extent of the individual’s illness. The same is true for a patient with dementia, who might be disruptive and loud, yet clearly is not in control of their behavior.
Koekkoek et al5 reviewed 94 articles that focused on difficult patients seen in mental health settings. Most patients were male (60% to 68%), and most were age 26 to 32 years. Diagnoses of psychotic disorders and personality disorders were the most frequent, while mood and other disorders were less common. In 1 of the studies reviewed, 6% of psychiatric inpatients were considered difficult. Koekkoek et al5 proposed that there are 3 groups of difficult patients:
- care avoiders: patients with psychosis who lack insight
- care seekers: patients who are chronically ill who have trouble maintaining a steady relationship with their caregivers
- care claimers: patients who do not require long-term care, but need housing, medication, or a “declaration of incompetence.”
Physician factors
Physicians are frequent contributors to bad interactions with their patients.2,7,8 They can become angry or defensive because of burnout, stress, or frustration, which might lead them to snap or otherwise respond inappropriately to their patients. Many physicians are overworked, sleep-deprived, or busier than they would prefer. Personal problems can be preoccupying and contribute to a physician being ill-tempered or distracted (eg, marital or family problems). Some physicians are simply poor communicators and might not understand the need to adapt their communication style to their patient, instead using medical jargon the patient does not understand. Ideally, physicians should modify their language to suit the patient’s level of education, degree of medical sophistication, and cultural background.
Continue to: A physician's personality traits...
A physician’s personality traits could clash with those of the patient, particularly if the physician is especially rigid or obsessional. Rather than “going with the flow,” the overly rigid physician might become impatient with patients who fail to understand diagnostic assessments or treatment recommendations. Inefficient physicians might not be able to keep up with the daily schedule, which could fuel impatience and perhaps even lead them to think that the patient is taking too much of their valuable time. Some might not know how to convey empathy, for example when giving bad news (“The tests show you have cancer…”). Others fail to make consistent eye contact with patients without understanding its importance to communication, a problem made worse by the use of electronic medical record systems (EMRs).
Systems issues
Systems issues also contribute to suboptimal physician-patient interactions, and some issues can be attributed to administrative problems. Examples of systems issues include:
- when a patient has difficulty making an appointment and is forced to listen to a confusing menu of choices
- a busy clinic that can only offer a patient an appointment 6 months away
- crowded or noisy waiting rooms
- language barriers for patients whose primary langage is not English. Not having access to an interpreter can exacerbate their frustration
- the use of EMRs is a growing threat to positive physician-patient interactions, yet their influence is often ignored. Widely disliked by physicians,10 EMRs are required in all but the smallest independent practice settings. Many busy physicians focus their attention on the computer, giving the patient the impression that the physician is not listening to them. Many patients conclude that they are less important than the process.
The consequences of difficult interactions
Following a bad interaction, dissatisfied patients are more likely to leave the clinic or hospital and ignore medical advice. These patients might then show up in crowded emergency departments, which may lead to poor use of health care resources. For physicians, challenging situations sap their emotional energy, cause demoralization, and interfere with their sense of job fulfillment. In extreme cases, such feelings might lead the physician to dislike and even avoid the patient.
How to manage challenging situations
Taking the following steps can help physicians work through challenging situations with their patients.
Diagnose the problem. First, recognize the difficult situation, analyze it, and identify how the patient, the physician, and the system are contributing to a bad physician-patient interaction. Diagnosing the interactional difficulty should precede the diagnosis and management of the patient’s disease. Physicians should acknowledge their own contribution through their attitude or actions. Finally, determine if there are system issues that are contributing to the problem, or if it is the clinic or inpatient setting itself (eg, noisy inpatient unit).
Continue to: Maintain your cool
Maintain your cool. With any difficult interaction, a physician’s first obligation is to remain calm and professional, while modeling appropriate behavior. If the patient is angry or emotionally intense, talking over them or interrupting them only makes the situation worse. Try to see the interaction from the patient’s perspective. Both parties should work together to find a common ground.
Collaborate, respect boundaries, and empathize. One study of a group of 100 family physicians found that having the following 3 skills were essential to successfully managing situations with difficult patients11,12:
- the ability to collaborate (vs opposition)
- the appropriate use of power (vs misuse of power, or violation of boundaries by either party)
- the ability to empathize, which for most physicians involves understanding and validating the patient’s subjective experiences.
Although a description of the many facets of empathy (cognitive, affective, motivational) is beyond the scope of this article, it is worth pointing out that a patient’s positive perception of their physician’s empathy improves not only patient satisfaction but health outcomes.13 The Box describes a difficult patient whose actions changed through the collaboration and empathy of his treatment team.
Box 1
Mr. L, a 60-year-old veteran, is admitted to an inpatient unit following a suicide attempt that was prompted by eviction from his apartment. Mr. L is physically disabled and has difficulty walking without assistance. His main concern is his homelessness, and he insists that the inpatient team find a suitable “Americans with Disabilities (ADA)-compliant apartment” that he can afford on his $800 monthly income. He implies that he will kill himself if the team fails in that task. He makes it clear that his problems are the team’s problems. He is prescribed an antidepressant, and both his mood and reported suicidal ideations gradually resolve.
The team’s social worker finds an opening at a well-run veterans home, but Mr. L rejects it because he doesn’t want to “give up his independence.” The social worker finds a small apartment in a nearby community that is ADA-compliant, but Mr. L complains that it is small. He asks the resident psychiatrist, “Where will I put all my things?” The next day, after insulting the attending psychiatrist for failing to find an adequate apartment, Mr. L says from under the bedsheet: “How come none of you ever help me?”
Mr. L presents a challenge to the entire team. At times, he is rude, demanding, and entitled. The team recognizes that although he had served in the military with distinction, he is now alone after having divorced many years earlier, and nearly friendless because of his increasing disability. The team surmises that Mr. L lashes out due to frustration and feelings of powerlessness.
Resolving this conflict involves treating Mr. L with respect and listening without judgment. No one ever confronts him or argues with him. The team psychologist meets with him to help him work through his many losses. Closer to discharge, he is enrolled in several post-hospitalization programs to keep him connected with other veterans. At discharge, the hospital arranges for his belongings that had been in storage to be delivered to his new home. He is pleasant and social with his peers, and although he is still concerned about the size of the apartment, he thanks the team members for their care.
Verbalize the difficulty. It is important to openly discuss the problem. For example, “We both have very different views about how your symptoms should be investigated, and that’s causing some difficulty between us. Do you agree?” This approach names the “elephant in the room” and avoids casting blame. It also creates a sense of shared ownership by externalizing the problem from both the patient and physician. Verbalizing the difficulty can help build trust and pave the way to working together toward a common solution.
Consider other explanations for the patient’s behavior. For example, anger directed at a physician could be due to anxiety about an unrelated matter, such as the patient’s recent job loss or impending divorce. Psychiatrists might understand this behavior better as displacement, which is considered a maladaptive defense mechanism. It is important to listen to the patient and offer empathy, which will help the patient feel supported and build a rapport that can help to resolve the encounter.
Continue to: When helping patients...
When helping patients with multiple issues, which is a common scenario, the physician might start by asking, “What would you like to address today?”14 Keep a list of the issues so you do not forget the patient’s concerns, and then ask: “What do you think is going on?” Give patients time to verbalize their concerns. Physicians should:
- validate concerns: “I understand where you’re coming from.”
- offer empathy: “I can see how difficult this has been for you.”
- reframe: “Let me make sure I hear you correctly.”
- refocus: “Let’s agree on what we need to do at this visit.”
Find common ground. When the patient and physician have different ideas on diagnosis or treatment, finding common ground is another way to resolve a difficult encounter. Difficulties arise when there appears to be little common ground, which often results from unrealistic expectations. Patients might be seen as “demanding” or “manipulative”’ if they push for a diagnosis or treatment the doctor is not comfortable with. As soon as there is some overlap and common ground, the difficulty rapidly subsides.
Set clear boundaries and limits. Physicians should set limits on what patient behavior might “cross the line.” A “behavioral contract” (or “treatment contract”) can help by setting explicit expectations. For example, showing up late for appointments or inappropriately seeking drugs of abuse (eg, opioids, benzodiazepines) might be identified as violations of the contract. Once the contract is set, the patient should be asked to restate key components. Clarify any confusion or barriers to compliance and define clear expectations. The patient should be informed of potential consequences of contract violations, including termination.
Staff members involved in the patient’s care should agree with the terms of any behavioral contract, and should receive a copy of it. Patients should have “buy in,” meaning that they have had an opportunity to provide input to the contract and have agreed to its elements. Both the physician and patient should sign the document.
When all else fails
When there is a breakdown in rapport that makes it difficult or impossible to continue offering treatment, consider termination. This could be due to threatening or abusive patient behavior, sexual advances, repeated no-shows, treatment noncompliance that jeopardizes patient safety, refusal to follow the treatment plan, or violating the terms of a behavioral contract. In some settings, it might be the failure to pay bills.
Continue to: If a patient is unable to...
If a patient is unable to follow the contract, the physician should explore possible extenuating circumstances. The physician should seek to remedy the problem and involve other team members if possible (eg, case manager, nurse), advising a patient about behaviors that could lead to termination.
If the problem is irremediable, notify the patient in writing, give them time to find another physician, and facilitate the transfer of care.15 Take steps to prevent the patient from running out of any medications associated with withdrawal or discontinuation syndromes (eg, selective serotonin reuptake inhibitors, benzodiazepines) during the care transition. While there is no requirement regarding the amount of time allowed, at least 30 days is typical.
Bottom Line
Difficult patient interactions are common and unavoidable. Physicians should acknowledge and recognize contributing factors in such encounters—including their own role. When handling such situations, physicians should remain calm and model appropriate behavior. Improving communication, offering empathy, and validating the patient’s concerns can help resolve factors that contribute to poor patient interactions. If efforts to remediate the physician-patient relationship fail, termination may be necessary.
Related Resources
- Koekkoek B, Berno van Meijel CNS, Hutschemaekers G. “Difficult patients” in mental health care: a review. Psychiatr Serv. 2006;57(6):795-802.
- Pereira MR, Figueiredo AF. Challenging patient-doctor interactions in psychiatry – difficult patient syndrome. European Psychiatry. 2017;41(supplement):S719. doi. org/10.1016/j.eurpsy.2017.01.1297
1. Dupont J. Ferenczi’s madness. Contemp Psychoanal. 1988;24(2):250-261.
2. Adams J, Murray R. The difficult diagnosis: the general approach to the difficult patient. Emerg Med Clin North Am. 1998;16(4):689-700.
3. Davies M. Managing challenging interactions with patients. BMJ. 2013;347:f4673. doi: https://doi.org/10.1136/bmj.f4673
4. Chou C. Dealing with the “difficult” patient. Wisc Med J. 2004;103:35-38.
5. Koekkoek B, Berno van Meijel CNS, Hutschemaekers G. “Difficult patients” in mental health care: a review. Psychiatr Serv. 2006;57(6):795-802.
6. Jackson JL, Kroenke K. Difficult patient encounter in the ambulatory clinic: clinical predictors and outcomes. Arch Intern Med 1999;159(10):1069-1075.
7. Groves JE. Taking care of the hateful patient. N Eng J Med. 1978;298:883-887.
8. Hull S, Broquet K. How to manage difficult encounters. Fam Prac Manag. 2007;14(6):30-34.
9. Hardavella G, Aamli-Gaagnat A, Frille A, et al. Top tips to deal with challenging situations: doctor patient interactions. Breathe. 2017;13(2):129-135.
10. Black DW, Balon R. Editorial: electronic medical records (EMRs) and the psychiatrist shortage. Ann Clin Psychiatry. 2018;30(4):257-259.
11. Elder N, Ricer R, Tobias B. How respected family physicians manage difficult patient encounters. J Am Board Fam Med. 2006;19(6):533-541.
12. Campbell RJ. Campbell’s Psychiatric Dictionary. 8th Edition. Oxford University Press; 2004:219-220.
13. Decety J, Fotopoulou A. Why empathy has a beneficial impact on others in medicine: unifying theories. Front Behav Neurosci. 2014;8:457. https://doi.org/10.3389/fnbeh.2014.00457
14. Klugman B. The difficult patient. Accessed May 24, 2021. https://www.umassmed.edu/globalassets/office-of-continuing-medical-education/pdfs/cme-primary-care-days/e2-the-difficult-patient.pdf
15. Mossman D, Farrell HM, Gilday E. ‘Firing’ a patient: may psychiatrists unilaterally terminate care? Current Psychiatry. 2010;9(12):18-29.
“I did not like those patients… They made me angry and I found myself irritated to experience them as they seemed so distant from myself and from all that is human. This is an astonishing intolerance which brands me a poor psychiatrist.”
Sigmund Freud, Letter to István Hollós (1928)
While Freud was referring to psychotic patients,1 his evident frustration shows that difficult and challenging patients have vexed even the best of us. All physicians and other clinicians will experience patient encounters that lead to anger or frustration, or even challenge their sense of equanimity and professional identity. In short, difficult and challenging patient interactions are unavoidable, regardless of the physician’s discipline.2-5 At times, physicians might struggle with demanding, unpleasant, ungrateful, and possibly dangerous patients, while sometimes the struggle is with the patient’s family members. No physician is immune to the problem, which makes it crucial to learn to anticipate and manage difficult patient interactions, skills which are generally not taught in medical schools or residency programs.
One prospective study of clinic patients found that up to 15% of patient encounters are deemed “difficult.”6 Common scenarios include patients (or their relatives) who seek certain tests after researching symptoms online, threats of legal or social media action in response to feeling that the physician is not listening to them, demands for a second opinion after disagreeing with the physician’s diagnosis, and mistrust of doctors after presenting with symptoms and not receiving a diagnosis. It is also common to care for patients who focus on negative outcomes or fail to adhere to treatment recommendations. These encounters can make physicians feel stressed out, disrespected, abused, or even fearful if threatened. Some physicians may come to feel they are trapped in a hostile work environment with little support from their supervisors or administrators. Patients often have a complaint office or department to turn to, but there is no equivalent for physicians, who are expected to soldier on regardless.
This article highlights a model that describes poor physician-patient encounters, factors contributing to these issues, how to manage these difficult interactions, and what to do if the relationship cannot be remediated.
Describing the ‘difficult’ patient
In a landmark 1978 paper, Groves7 provided one of the first descriptions of “difficult” patients. His colorful observations continue to provide useful insights. Groves emphasized that most medical texts ignore the issue of difficult patients and provide little or no guidance—which is still true 43 years later. He observed that physicians cannot avoid occasional negative feelings toward some patients. Further, Groves suggested that countertransference is often at the root of hateful reactions, a process he defines as “conscious or unconscious unbidden and unwanted hostile or sexual feelings toward the patient.”7Table 17 outlines how Groves divided “hateful” patients into several categories, and how physicians might respond to such patients.
A model for understanding difficult patient encounters
Adams and Murray2 created a model to help explain interactions with difficult or challenging patients that consists of 3 elements: the patient, the physician, and the system (ie, situation or environment). Hull and Broquet8 and Hardavella et al9 later adapted the model and described its components (Table 22,8,9).
Continue to: When considering...
When considering difficult interactions, it is important to be aware that all 3 components could interact, or merely 1 or 2 could come into play, but all should be explored as possible contributing factors.
Patient factors
The patient’s role in initiating or maintaining a problematic interaction should be explored. While some physicians are tempted to conclude that a personality disorder underlies difficult interactions, research shows a more complex picture. First, not all difficult patients have a psychiatric disorder, let alone a personality disorder. Jackson and Kroenke6 reported that among 74 difficult patients in an ambulatory clinic, 29% had a depressive disorder or anxiety disorder, with 11% experiencing 2 or more disorders. Major depressive disorder was present in 8.4% patients, other depressive disorders in 17.4%, panic disorder in 1.4%, and other anxiety disorders in 14.2%.6 These researchers found that difficult patient interactions were associated with the presence of a psychiatric disorder, especially depressive or anxiety disorders, and multiple physical symptoms.
Importantly, difficult patients are not unique to psychiatry, and are found in all medical disciplines and every type of practice situation. Some problematic patients have a substance use disorder, and their difficulty might stem from intoxication, withdrawal, or drug-seeking behaviors. Psychotic disorders can be the source of difficult interactions, typically resulting from the patient’s symptoms (ie, hallucinations, delusions, or bizarre behavior). Physicians tend to be forgiving toward these patients because they understand the extent of the individual’s illness. The same is true for a patient with dementia, who might be disruptive and loud, yet clearly is not in control of their behavior.
Koekkoek et al5 reviewed 94 articles that focused on difficult patients seen in mental health settings. Most patients were male (60% to 68%), and most were age 26 to 32 years. Diagnoses of psychotic disorders and personality disorders were the most frequent, while mood and other disorders were less common. In 1 of the studies reviewed, 6% of psychiatric inpatients were considered difficult. Koekkoek et al5 proposed that there are 3 groups of difficult patients:
- care avoiders: patients with psychosis who lack insight
- care seekers: patients who are chronically ill who have trouble maintaining a steady relationship with their caregivers
- care claimers: patients who do not require long-term care, but need housing, medication, or a “declaration of incompetence.”
Physician factors
Physicians are frequent contributors to bad interactions with their patients.2,7,8 They can become angry or defensive because of burnout, stress, or frustration, which might lead them to snap or otherwise respond inappropriately to their patients. Many physicians are overworked, sleep-deprived, or busier than they would prefer. Personal problems can be preoccupying and contribute to a physician being ill-tempered or distracted (eg, marital or family problems). Some physicians are simply poor communicators and might not understand the need to adapt their communication style to their patient, instead using medical jargon the patient does not understand. Ideally, physicians should modify their language to suit the patient’s level of education, degree of medical sophistication, and cultural background.
Continue to: A physician's personality traits...
A physician’s personality traits could clash with those of the patient, particularly if the physician is especially rigid or obsessional. Rather than “going with the flow,” the overly rigid physician might become impatient with patients who fail to understand diagnostic assessments or treatment recommendations. Inefficient physicians might not be able to keep up with the daily schedule, which could fuel impatience and perhaps even lead them to think that the patient is taking too much of their valuable time. Some might not know how to convey empathy, for example when giving bad news (“The tests show you have cancer…”). Others fail to make consistent eye contact with patients without understanding its importance to communication, a problem made worse by the use of electronic medical record systems (EMRs).
Systems issues
Systems issues also contribute to suboptimal physician-patient interactions, and some issues can be attributed to administrative problems. Examples of systems issues include:
- when a patient has difficulty making an appointment and is forced to listen to a confusing menu of choices
- a busy clinic that can only offer a patient an appointment 6 months away
- crowded or noisy waiting rooms
- language barriers for patients whose primary langage is not English. Not having access to an interpreter can exacerbate their frustration
- the use of EMRs is a growing threat to positive physician-patient interactions, yet their influence is often ignored. Widely disliked by physicians,10 EMRs are required in all but the smallest independent practice settings. Many busy physicians focus their attention on the computer, giving the patient the impression that the physician is not listening to them. Many patients conclude that they are less important than the process.
The consequences of difficult interactions
Following a bad interaction, dissatisfied patients are more likely to leave the clinic or hospital and ignore medical advice. These patients might then show up in crowded emergency departments, which may lead to poor use of health care resources. For physicians, challenging situations sap their emotional energy, cause demoralization, and interfere with their sense of job fulfillment. In extreme cases, such feelings might lead the physician to dislike and even avoid the patient.
How to manage challenging situations
Taking the following steps can help physicians work through challenging situations with their patients.
Diagnose the problem. First, recognize the difficult situation, analyze it, and identify how the patient, the physician, and the system are contributing to a bad physician-patient interaction. Diagnosing the interactional difficulty should precede the diagnosis and management of the patient’s disease. Physicians should acknowledge their own contribution through their attitude or actions. Finally, determine if there are system issues that are contributing to the problem, or if it is the clinic or inpatient setting itself (eg, noisy inpatient unit).
Continue to: Maintain your cool
Maintain your cool. With any difficult interaction, a physician’s first obligation is to remain calm and professional, while modeling appropriate behavior. If the patient is angry or emotionally intense, talking over them or interrupting them only makes the situation worse. Try to see the interaction from the patient’s perspective. Both parties should work together to find a common ground.
Collaborate, respect boundaries, and empathize. One study of a group of 100 family physicians found that having the following 3 skills were essential to successfully managing situations with difficult patients11,12:
- the ability to collaborate (vs opposition)
- the appropriate use of power (vs misuse of power, or violation of boundaries by either party)
- the ability to empathize, which for most physicians involves understanding and validating the patient’s subjective experiences.
Although a description of the many facets of empathy (cognitive, affective, motivational) is beyond the scope of this article, it is worth pointing out that a patient’s positive perception of their physician’s empathy improves not only patient satisfaction but health outcomes.13 The Box describes a difficult patient whose actions changed through the collaboration and empathy of his treatment team.
Box 1
Mr. L, a 60-year-old veteran, is admitted to an inpatient unit following a suicide attempt that was prompted by eviction from his apartment. Mr. L is physically disabled and has difficulty walking without assistance. His main concern is his homelessness, and he insists that the inpatient team find a suitable “Americans with Disabilities (ADA)-compliant apartment” that he can afford on his $800 monthly income. He implies that he will kill himself if the team fails in that task. He makes it clear that his problems are the team’s problems. He is prescribed an antidepressant, and both his mood and reported suicidal ideations gradually resolve.
The team’s social worker finds an opening at a well-run veterans home, but Mr. L rejects it because he doesn’t want to “give up his independence.” The social worker finds a small apartment in a nearby community that is ADA-compliant, but Mr. L complains that it is small. He asks the resident psychiatrist, “Where will I put all my things?” The next day, after insulting the attending psychiatrist for failing to find an adequate apartment, Mr. L says from under the bedsheet: “How come none of you ever help me?”
Mr. L presents a challenge to the entire team. At times, he is rude, demanding, and entitled. The team recognizes that although he had served in the military with distinction, he is now alone after having divorced many years earlier, and nearly friendless because of his increasing disability. The team surmises that Mr. L lashes out due to frustration and feelings of powerlessness.
Resolving this conflict involves treating Mr. L with respect and listening without judgment. No one ever confronts him or argues with him. The team psychologist meets with him to help him work through his many losses. Closer to discharge, he is enrolled in several post-hospitalization programs to keep him connected with other veterans. At discharge, the hospital arranges for his belongings that had been in storage to be delivered to his new home. He is pleasant and social with his peers, and although he is still concerned about the size of the apartment, he thanks the team members for their care.
Verbalize the difficulty. It is important to openly discuss the problem. For example, “We both have very different views about how your symptoms should be investigated, and that’s causing some difficulty between us. Do you agree?” This approach names the “elephant in the room” and avoids casting blame. It also creates a sense of shared ownership by externalizing the problem from both the patient and physician. Verbalizing the difficulty can help build trust and pave the way to working together toward a common solution.
Consider other explanations for the patient’s behavior. For example, anger directed at a physician could be due to anxiety about an unrelated matter, such as the patient’s recent job loss or impending divorce. Psychiatrists might understand this behavior better as displacement, which is considered a maladaptive defense mechanism. It is important to listen to the patient and offer empathy, which will help the patient feel supported and build a rapport that can help to resolve the encounter.
Continue to: When helping patients...
When helping patients with multiple issues, which is a common scenario, the physician might start by asking, “What would you like to address today?”14 Keep a list of the issues so you do not forget the patient’s concerns, and then ask: “What do you think is going on?” Give patients time to verbalize their concerns. Physicians should:
- validate concerns: “I understand where you’re coming from.”
- offer empathy: “I can see how difficult this has been for you.”
- reframe: “Let me make sure I hear you correctly.”
- refocus: “Let’s agree on what we need to do at this visit.”
Find common ground. When the patient and physician have different ideas on diagnosis or treatment, finding common ground is another way to resolve a difficult encounter. Difficulties arise when there appears to be little common ground, which often results from unrealistic expectations. Patients might be seen as “demanding” or “manipulative”’ if they push for a diagnosis or treatment the doctor is not comfortable with. As soon as there is some overlap and common ground, the difficulty rapidly subsides.
Set clear boundaries and limits. Physicians should set limits on what patient behavior might “cross the line.” A “behavioral contract” (or “treatment contract”) can help by setting explicit expectations. For example, showing up late for appointments or inappropriately seeking drugs of abuse (eg, opioids, benzodiazepines) might be identified as violations of the contract. Once the contract is set, the patient should be asked to restate key components. Clarify any confusion or barriers to compliance and define clear expectations. The patient should be informed of potential consequences of contract violations, including termination.
Staff members involved in the patient’s care should agree with the terms of any behavioral contract, and should receive a copy of it. Patients should have “buy in,” meaning that they have had an opportunity to provide input to the contract and have agreed to its elements. Both the physician and patient should sign the document.
When all else fails
When there is a breakdown in rapport that makes it difficult or impossible to continue offering treatment, consider termination. This could be due to threatening or abusive patient behavior, sexual advances, repeated no-shows, treatment noncompliance that jeopardizes patient safety, refusal to follow the treatment plan, or violating the terms of a behavioral contract. In some settings, it might be the failure to pay bills.
Continue to: If a patient is unable to...
If a patient is unable to follow the contract, the physician should explore possible extenuating circumstances. The physician should seek to remedy the problem and involve other team members if possible (eg, case manager, nurse), advising a patient about behaviors that could lead to termination.
If the problem is irremediable, notify the patient in writing, give them time to find another physician, and facilitate the transfer of care.15 Take steps to prevent the patient from running out of any medications associated with withdrawal or discontinuation syndromes (eg, selective serotonin reuptake inhibitors, benzodiazepines) during the care transition. While there is no requirement regarding the amount of time allowed, at least 30 days is typical.
Bottom Line
Difficult patient interactions are common and unavoidable. Physicians should acknowledge and recognize contributing factors in such encounters—including their own role. When handling such situations, physicians should remain calm and model appropriate behavior. Improving communication, offering empathy, and validating the patient’s concerns can help resolve factors that contribute to poor patient interactions. If efforts to remediate the physician-patient relationship fail, termination may be necessary.
Related Resources
- Koekkoek B, Berno van Meijel CNS, Hutschemaekers G. “Difficult patients” in mental health care: a review. Psychiatr Serv. 2006;57(6):795-802.
- Pereira MR, Figueiredo AF. Challenging patient-doctor interactions in psychiatry – difficult patient syndrome. European Psychiatry. 2017;41(supplement):S719. doi. org/10.1016/j.eurpsy.2017.01.1297
“I did not like those patients… They made me angry and I found myself irritated to experience them as they seemed so distant from myself and from all that is human. This is an astonishing intolerance which brands me a poor psychiatrist.”
Sigmund Freud, Letter to István Hollós (1928)
While Freud was referring to psychotic patients,1 his evident frustration shows that difficult and challenging patients have vexed even the best of us. All physicians and other clinicians will experience patient encounters that lead to anger or frustration, or even challenge their sense of equanimity and professional identity. In short, difficult and challenging patient interactions are unavoidable, regardless of the physician’s discipline.2-5 At times, physicians might struggle with demanding, unpleasant, ungrateful, and possibly dangerous patients, while sometimes the struggle is with the patient’s family members. No physician is immune to the problem, which makes it crucial to learn to anticipate and manage difficult patient interactions, skills which are generally not taught in medical schools or residency programs.
One prospective study of clinic patients found that up to 15% of patient encounters are deemed “difficult.”6 Common scenarios include patients (or their relatives) who seek certain tests after researching symptoms online, threats of legal or social media action in response to feeling that the physician is not listening to them, demands for a second opinion after disagreeing with the physician’s diagnosis, and mistrust of doctors after presenting with symptoms and not receiving a diagnosis. It is also common to care for patients who focus on negative outcomes or fail to adhere to treatment recommendations. These encounters can make physicians feel stressed out, disrespected, abused, or even fearful if threatened. Some physicians may come to feel they are trapped in a hostile work environment with little support from their supervisors or administrators. Patients often have a complaint office or department to turn to, but there is no equivalent for physicians, who are expected to soldier on regardless.
This article highlights a model that describes poor physician-patient encounters, factors contributing to these issues, how to manage these difficult interactions, and what to do if the relationship cannot be remediated.
Describing the ‘difficult’ patient
In a landmark 1978 paper, Groves7 provided one of the first descriptions of “difficult” patients. His colorful observations continue to provide useful insights. Groves emphasized that most medical texts ignore the issue of difficult patients and provide little or no guidance—which is still true 43 years later. He observed that physicians cannot avoid occasional negative feelings toward some patients. Further, Groves suggested that countertransference is often at the root of hateful reactions, a process he defines as “conscious or unconscious unbidden and unwanted hostile or sexual feelings toward the patient.”7Table 17 outlines how Groves divided “hateful” patients into several categories, and how physicians might respond to such patients.
A model for understanding difficult patient encounters
Adams and Murray2 created a model to help explain interactions with difficult or challenging patients that consists of 3 elements: the patient, the physician, and the system (ie, situation or environment). Hull and Broquet8 and Hardavella et al9 later adapted the model and described its components (Table 22,8,9).
Continue to: When considering...
When considering difficult interactions, it is important to be aware that all 3 components could interact, or merely 1 or 2 could come into play, but all should be explored as possible contributing factors.
Patient factors
The patient’s role in initiating or maintaining a problematic interaction should be explored. While some physicians are tempted to conclude that a personality disorder underlies difficult interactions, research shows a more complex picture. First, not all difficult patients have a psychiatric disorder, let alone a personality disorder. Jackson and Kroenke6 reported that among 74 difficult patients in an ambulatory clinic, 29% had a depressive disorder or anxiety disorder, with 11% experiencing 2 or more disorders. Major depressive disorder was present in 8.4% patients, other depressive disorders in 17.4%, panic disorder in 1.4%, and other anxiety disorders in 14.2%.6 These researchers found that difficult patient interactions were associated with the presence of a psychiatric disorder, especially depressive or anxiety disorders, and multiple physical symptoms.
Importantly, difficult patients are not unique to psychiatry, and are found in all medical disciplines and every type of practice situation. Some problematic patients have a substance use disorder, and their difficulty might stem from intoxication, withdrawal, or drug-seeking behaviors. Psychotic disorders can be the source of difficult interactions, typically resulting from the patient’s symptoms (ie, hallucinations, delusions, or bizarre behavior). Physicians tend to be forgiving toward these patients because they understand the extent of the individual’s illness. The same is true for a patient with dementia, who might be disruptive and loud, yet clearly is not in control of their behavior.
Koekkoek et al5 reviewed 94 articles that focused on difficult patients seen in mental health settings. Most patients were male (60% to 68%), and most were age 26 to 32 years. Diagnoses of psychotic disorders and personality disorders were the most frequent, while mood and other disorders were less common. In 1 of the studies reviewed, 6% of psychiatric inpatients were considered difficult. Koekkoek et al5 proposed that there are 3 groups of difficult patients:
- care avoiders: patients with psychosis who lack insight
- care seekers: patients who are chronically ill who have trouble maintaining a steady relationship with their caregivers
- care claimers: patients who do not require long-term care, but need housing, medication, or a “declaration of incompetence.”
Physician factors
Physicians are frequent contributors to bad interactions with their patients.2,7,8 They can become angry or defensive because of burnout, stress, or frustration, which might lead them to snap or otherwise respond inappropriately to their patients. Many physicians are overworked, sleep-deprived, or busier than they would prefer. Personal problems can be preoccupying and contribute to a physician being ill-tempered or distracted (eg, marital or family problems). Some physicians are simply poor communicators and might not understand the need to adapt their communication style to their patient, instead using medical jargon the patient does not understand. Ideally, physicians should modify their language to suit the patient’s level of education, degree of medical sophistication, and cultural background.
Continue to: A physician's personality traits...
A physician’s personality traits could clash with those of the patient, particularly if the physician is especially rigid or obsessional. Rather than “going with the flow,” the overly rigid physician might become impatient with patients who fail to understand diagnostic assessments or treatment recommendations. Inefficient physicians might not be able to keep up with the daily schedule, which could fuel impatience and perhaps even lead them to think that the patient is taking too much of their valuable time. Some might not know how to convey empathy, for example when giving bad news (“The tests show you have cancer…”). Others fail to make consistent eye contact with patients without understanding its importance to communication, a problem made worse by the use of electronic medical record systems (EMRs).
Systems issues
Systems issues also contribute to suboptimal physician-patient interactions, and some issues can be attributed to administrative problems. Examples of systems issues include:
- when a patient has difficulty making an appointment and is forced to listen to a confusing menu of choices
- a busy clinic that can only offer a patient an appointment 6 months away
- crowded or noisy waiting rooms
- language barriers for patients whose primary langage is not English. Not having access to an interpreter can exacerbate their frustration
- the use of EMRs is a growing threat to positive physician-patient interactions, yet their influence is often ignored. Widely disliked by physicians,10 EMRs are required in all but the smallest independent practice settings. Many busy physicians focus their attention on the computer, giving the patient the impression that the physician is not listening to them. Many patients conclude that they are less important than the process.
The consequences of difficult interactions
Following a bad interaction, dissatisfied patients are more likely to leave the clinic or hospital and ignore medical advice. These patients might then show up in crowded emergency departments, which may lead to poor use of health care resources. For physicians, challenging situations sap their emotional energy, cause demoralization, and interfere with their sense of job fulfillment. In extreme cases, such feelings might lead the physician to dislike and even avoid the patient.
How to manage challenging situations
Taking the following steps can help physicians work through challenging situations with their patients.
Diagnose the problem. First, recognize the difficult situation, analyze it, and identify how the patient, the physician, and the system are contributing to a bad physician-patient interaction. Diagnosing the interactional difficulty should precede the diagnosis and management of the patient’s disease. Physicians should acknowledge their own contribution through their attitude or actions. Finally, determine if there are system issues that are contributing to the problem, or if it is the clinic or inpatient setting itself (eg, noisy inpatient unit).
Continue to: Maintain your cool
Maintain your cool. With any difficult interaction, a physician’s first obligation is to remain calm and professional, while modeling appropriate behavior. If the patient is angry or emotionally intense, talking over them or interrupting them only makes the situation worse. Try to see the interaction from the patient’s perspective. Both parties should work together to find a common ground.
Collaborate, respect boundaries, and empathize. One study of a group of 100 family physicians found that having the following 3 skills were essential to successfully managing situations with difficult patients11,12:
- the ability to collaborate (vs opposition)
- the appropriate use of power (vs misuse of power, or violation of boundaries by either party)
- the ability to empathize, which for most physicians involves understanding and validating the patient’s subjective experiences.
Although a description of the many facets of empathy (cognitive, affective, motivational) is beyond the scope of this article, it is worth pointing out that a patient’s positive perception of their physician’s empathy improves not only patient satisfaction but health outcomes.13 The Box describes a difficult patient whose actions changed through the collaboration and empathy of his treatment team.
Box 1
Mr. L, a 60-year-old veteran, is admitted to an inpatient unit following a suicide attempt that was prompted by eviction from his apartment. Mr. L is physically disabled and has difficulty walking without assistance. His main concern is his homelessness, and he insists that the inpatient team find a suitable “Americans with Disabilities (ADA)-compliant apartment” that he can afford on his $800 monthly income. He implies that he will kill himself if the team fails in that task. He makes it clear that his problems are the team’s problems. He is prescribed an antidepressant, and both his mood and reported suicidal ideations gradually resolve.
The team’s social worker finds an opening at a well-run veterans home, but Mr. L rejects it because he doesn’t want to “give up his independence.” The social worker finds a small apartment in a nearby community that is ADA-compliant, but Mr. L complains that it is small. He asks the resident psychiatrist, “Where will I put all my things?” The next day, after insulting the attending psychiatrist for failing to find an adequate apartment, Mr. L says from under the bedsheet: “How come none of you ever help me?”
Mr. L presents a challenge to the entire team. At times, he is rude, demanding, and entitled. The team recognizes that although he had served in the military with distinction, he is now alone after having divorced many years earlier, and nearly friendless because of his increasing disability. The team surmises that Mr. L lashes out due to frustration and feelings of powerlessness.
Resolving this conflict involves treating Mr. L with respect and listening without judgment. No one ever confronts him or argues with him. The team psychologist meets with him to help him work through his many losses. Closer to discharge, he is enrolled in several post-hospitalization programs to keep him connected with other veterans. At discharge, the hospital arranges for his belongings that had been in storage to be delivered to his new home. He is pleasant and social with his peers, and although he is still concerned about the size of the apartment, he thanks the team members for their care.
Verbalize the difficulty. It is important to openly discuss the problem. For example, “We both have very different views about how your symptoms should be investigated, and that’s causing some difficulty between us. Do you agree?” This approach names the “elephant in the room” and avoids casting blame. It also creates a sense of shared ownership by externalizing the problem from both the patient and physician. Verbalizing the difficulty can help build trust and pave the way to working together toward a common solution.
Consider other explanations for the patient’s behavior. For example, anger directed at a physician could be due to anxiety about an unrelated matter, such as the patient’s recent job loss or impending divorce. Psychiatrists might understand this behavior better as displacement, which is considered a maladaptive defense mechanism. It is important to listen to the patient and offer empathy, which will help the patient feel supported and build a rapport that can help to resolve the encounter.
Continue to: When helping patients...
When helping patients with multiple issues, which is a common scenario, the physician might start by asking, “What would you like to address today?”14 Keep a list of the issues so you do not forget the patient’s concerns, and then ask: “What do you think is going on?” Give patients time to verbalize their concerns. Physicians should:
- validate concerns: “I understand where you’re coming from.”
- offer empathy: “I can see how difficult this has been for you.”
- reframe: “Let me make sure I hear you correctly.”
- refocus: “Let’s agree on what we need to do at this visit.”
Find common ground. When the patient and physician have different ideas on diagnosis or treatment, finding common ground is another way to resolve a difficult encounter. Difficulties arise when there appears to be little common ground, which often results from unrealistic expectations. Patients might be seen as “demanding” or “manipulative”’ if they push for a diagnosis or treatment the doctor is not comfortable with. As soon as there is some overlap and common ground, the difficulty rapidly subsides.
Set clear boundaries and limits. Physicians should set limits on what patient behavior might “cross the line.” A “behavioral contract” (or “treatment contract”) can help by setting explicit expectations. For example, showing up late for appointments or inappropriately seeking drugs of abuse (eg, opioids, benzodiazepines) might be identified as violations of the contract. Once the contract is set, the patient should be asked to restate key components. Clarify any confusion or barriers to compliance and define clear expectations. The patient should be informed of potential consequences of contract violations, including termination.
Staff members involved in the patient’s care should agree with the terms of any behavioral contract, and should receive a copy of it. Patients should have “buy in,” meaning that they have had an opportunity to provide input to the contract and have agreed to its elements. Both the physician and patient should sign the document.
When all else fails
When there is a breakdown in rapport that makes it difficult or impossible to continue offering treatment, consider termination. This could be due to threatening or abusive patient behavior, sexual advances, repeated no-shows, treatment noncompliance that jeopardizes patient safety, refusal to follow the treatment plan, or violating the terms of a behavioral contract. In some settings, it might be the failure to pay bills.
Continue to: If a patient is unable to...
If a patient is unable to follow the contract, the physician should explore possible extenuating circumstances. The physician should seek to remedy the problem and involve other team members if possible (eg, case manager, nurse), advising a patient about behaviors that could lead to termination.
If the problem is irremediable, notify the patient in writing, give them time to find another physician, and facilitate the transfer of care.15 Take steps to prevent the patient from running out of any medications associated with withdrawal or discontinuation syndromes (eg, selective serotonin reuptake inhibitors, benzodiazepines) during the care transition. While there is no requirement regarding the amount of time allowed, at least 30 days is typical.
Bottom Line
Difficult patient interactions are common and unavoidable. Physicians should acknowledge and recognize contributing factors in such encounters—including their own role. When handling such situations, physicians should remain calm and model appropriate behavior. Improving communication, offering empathy, and validating the patient’s concerns can help resolve factors that contribute to poor patient interactions. If efforts to remediate the physician-patient relationship fail, termination may be necessary.
Related Resources
- Koekkoek B, Berno van Meijel CNS, Hutschemaekers G. “Difficult patients” in mental health care: a review. Psychiatr Serv. 2006;57(6):795-802.
- Pereira MR, Figueiredo AF. Challenging patient-doctor interactions in psychiatry – difficult patient syndrome. European Psychiatry. 2017;41(supplement):S719. doi. org/10.1016/j.eurpsy.2017.01.1297
1. Dupont J. Ferenczi’s madness. Contemp Psychoanal. 1988;24(2):250-261.
2. Adams J, Murray R. The difficult diagnosis: the general approach to the difficult patient. Emerg Med Clin North Am. 1998;16(4):689-700.
3. Davies M. Managing challenging interactions with patients. BMJ. 2013;347:f4673. doi: https://doi.org/10.1136/bmj.f4673
4. Chou C. Dealing with the “difficult” patient. Wisc Med J. 2004;103:35-38.
5. Koekkoek B, Berno van Meijel CNS, Hutschemaekers G. “Difficult patients” in mental health care: a review. Psychiatr Serv. 2006;57(6):795-802.
6. Jackson JL, Kroenke K. Difficult patient encounter in the ambulatory clinic: clinical predictors and outcomes. Arch Intern Med 1999;159(10):1069-1075.
7. Groves JE. Taking care of the hateful patient. N Eng J Med. 1978;298:883-887.
8. Hull S, Broquet K. How to manage difficult encounters. Fam Prac Manag. 2007;14(6):30-34.
9. Hardavella G, Aamli-Gaagnat A, Frille A, et al. Top tips to deal with challenging situations: doctor patient interactions. Breathe. 2017;13(2):129-135.
10. Black DW, Balon R. Editorial: electronic medical records (EMRs) and the psychiatrist shortage. Ann Clin Psychiatry. 2018;30(4):257-259.
11. Elder N, Ricer R, Tobias B. How respected family physicians manage difficult patient encounters. J Am Board Fam Med. 2006;19(6):533-541.
12. Campbell RJ. Campbell’s Psychiatric Dictionary. 8th Edition. Oxford University Press; 2004:219-220.
13. Decety J, Fotopoulou A. Why empathy has a beneficial impact on others in medicine: unifying theories. Front Behav Neurosci. 2014;8:457. https://doi.org/10.3389/fnbeh.2014.00457
14. Klugman B. The difficult patient. Accessed May 24, 2021. https://www.umassmed.edu/globalassets/office-of-continuing-medical-education/pdfs/cme-primary-care-days/e2-the-difficult-patient.pdf
15. Mossman D, Farrell HM, Gilday E. ‘Firing’ a patient: may psychiatrists unilaterally terminate care? Current Psychiatry. 2010;9(12):18-29.
1. Dupont J. Ferenczi’s madness. Contemp Psychoanal. 1988;24(2):250-261.
2. Adams J, Murray R. The difficult diagnosis: the general approach to the difficult patient. Emerg Med Clin North Am. 1998;16(4):689-700.
3. Davies M. Managing challenging interactions with patients. BMJ. 2013;347:f4673. doi: https://doi.org/10.1136/bmj.f4673
4. Chou C. Dealing with the “difficult” patient. Wisc Med J. 2004;103:35-38.
5. Koekkoek B, Berno van Meijel CNS, Hutschemaekers G. “Difficult patients” in mental health care: a review. Psychiatr Serv. 2006;57(6):795-802.
6. Jackson JL, Kroenke K. Difficult patient encounter in the ambulatory clinic: clinical predictors and outcomes. Arch Intern Med 1999;159(10):1069-1075.
7. Groves JE. Taking care of the hateful patient. N Eng J Med. 1978;298:883-887.
8. Hull S, Broquet K. How to manage difficult encounters. Fam Prac Manag. 2007;14(6):30-34.
9. Hardavella G, Aamli-Gaagnat A, Frille A, et al. Top tips to deal with challenging situations: doctor patient interactions. Breathe. 2017;13(2):129-135.
10. Black DW, Balon R. Editorial: electronic medical records (EMRs) and the psychiatrist shortage. Ann Clin Psychiatry. 2018;30(4):257-259.
11. Elder N, Ricer R, Tobias B. How respected family physicians manage difficult patient encounters. J Am Board Fam Med. 2006;19(6):533-541.
12. Campbell RJ. Campbell’s Psychiatric Dictionary. 8th Edition. Oxford University Press; 2004:219-220.
13. Decety J, Fotopoulou A. Why empathy has a beneficial impact on others in medicine: unifying theories. Front Behav Neurosci. 2014;8:457. https://doi.org/10.3389/fnbeh.2014.00457
14. Klugman B. The difficult patient. Accessed May 24, 2021. https://www.umassmed.edu/globalassets/office-of-continuing-medical-education/pdfs/cme-primary-care-days/e2-the-difficult-patient.pdf
15. Mossman D, Farrell HM, Gilday E. ‘Firing’ a patient: may psychiatrists unilaterally terminate care? Current Psychiatry. 2010;9(12):18-29.
APA, AMA, others move to stop insurer from overturning mental health claims ruling
The American Psychiatric Association has joined with the American Medical Association and other medical societies to oppose United Behavioral Health’s (UBH) request that a court throw out a ruling that found the insurer unfairly denied tens of thousands of claims for mental health and substance use disorder services.
Wit v. United Behavioral Health, in litigation since 2014, is being closely watched by clinicians, patients, providers, and attorneys.
Reena Kapoor, MD, chair of the APA’s Committee on Judicial Action, said in an interview that the APA is hopeful that “whatever the court says about UBH should be applicable to all insurance companies that are providing employer-sponsored health benefits.”
In a friend of the court (amicus curiae) brief, the APA, AMA, the California Medical Association, Southern California Psychiatric Society, Northern California Psychiatric Society, Orange County Psychiatric Society, Central California Psychiatric Society, and San Diego Psychiatric Society argue that “despite the availability of professionally developed, evidence-based guidelines embodying generally accepted standards of care for mental health and substance use disorders, managed care organizations commonly base coverage decisions on internally developed ‘level of care guidelines’ that are inappropriately restrictive.”
The guidelines “may lead to denial of coverage for treatment that is recommended by a patient’s physician and even cut off coverage when treatment is already being delivered,” said the groups.
The U.S. Department of Labor also filed a brief in support of the plaintiffs who are suing UBH. Those individuals suffered injury when they were denied coverage, said the federal agency, which regulates employer-sponsored insurance plans.
California Attorney General Rob Bonta also made an amicus filing supporting the plaintiffs.
“When insurers limit access to this critical care, they leave Californians who need it feeling as if they have no other option than to try to cope alone,” said Mr. Bonta in a statement.
‘Discrimination must end’
Mr. Bonta said he agreed with a 2019 ruling by the U.S. District Court for the Northern District of California that UBH had violated its fiduciary duties by wrongfully using its internally developed coverage determination guidelines and level of care guidelines to deny care.
The court also found that UBH’s medically necessary criteria meant that only “acute” episodes would be covered. Instead, said the court last November, chronic and comorbid conditions should always be treated, according to Maureen Gammon and Kathleen Rosenow of Willis Towers Watson, a risk advisor.
In November, the same Northern California District Court ruled on the remedies it would require of United, including that the insurer reprocess more than 67,000 claims. UBH was also barred indefinitely from using any of its guidelines to make coverage determinations. Instead, it was ordered to make determinations “consistent with generally accepted standards of care,” and consistent with state laws.
The District Court denied a request by UBH to put a hold on the claims reprocessing until it appealed the overall case. But the Ninth Circuit Court of Appeals in February granted that request.
Then, in March, United appealed the District Court’s overall ruling, claiming that the plaintiffs had not proven harm.
The U.S. Chamber of Commerce has filed a brief in support of United, agreeing with its arguments.
However, the APA and other clinician groups said there is no question of harm.
“Failure to provide appropriate levels of care for treatment of mental illness and substance use disorders leads to relapse, overdose, transmission of infectious diseases, and death,” said APA CEO and Medical Director Saul Levin, MD, MPA, in a statement.
APA President Vivian Pender, MD, said guidelines that “are overly focused on stabilizing acute symptoms of mental health and substance use disorders” are not treating the underlying disease. “When the injury is physical, insurers treat the underlying disease and not just the symptoms. Discrimination against patients with mental illness must end,” she said.
No court has ever recognized the type of claims reprocessing ordered by the District Court judge, said attorneys Nathaniel Cohen and Joseph Laska of Manatt, Phelps & Phillips, in an analysis of the case.
Mr. Cohen and Mr. Laska write. “Practitioners, health plans, and health insurers would be wise to track UBH’s long-awaited appeal to the Ninth Circuit.”
This article first appeared on Medscape.com.
The American Psychiatric Association has joined with the American Medical Association and other medical societies to oppose United Behavioral Health’s (UBH) request that a court throw out a ruling that found the insurer unfairly denied tens of thousands of claims for mental health and substance use disorder services.
Wit v. United Behavioral Health, in litigation since 2014, is being closely watched by clinicians, patients, providers, and attorneys.
Reena Kapoor, MD, chair of the APA’s Committee on Judicial Action, said in an interview that the APA is hopeful that “whatever the court says about UBH should be applicable to all insurance companies that are providing employer-sponsored health benefits.”
In a friend of the court (amicus curiae) brief, the APA, AMA, the California Medical Association, Southern California Psychiatric Society, Northern California Psychiatric Society, Orange County Psychiatric Society, Central California Psychiatric Society, and San Diego Psychiatric Society argue that “despite the availability of professionally developed, evidence-based guidelines embodying generally accepted standards of care for mental health and substance use disorders, managed care organizations commonly base coverage decisions on internally developed ‘level of care guidelines’ that are inappropriately restrictive.”
The guidelines “may lead to denial of coverage for treatment that is recommended by a patient’s physician and even cut off coverage when treatment is already being delivered,” said the groups.
The U.S. Department of Labor also filed a brief in support of the plaintiffs who are suing UBH. Those individuals suffered injury when they were denied coverage, said the federal agency, which regulates employer-sponsored insurance plans.
California Attorney General Rob Bonta also made an amicus filing supporting the plaintiffs.
“When insurers limit access to this critical care, they leave Californians who need it feeling as if they have no other option than to try to cope alone,” said Mr. Bonta in a statement.
‘Discrimination must end’
Mr. Bonta said he agreed with a 2019 ruling by the U.S. District Court for the Northern District of California that UBH had violated its fiduciary duties by wrongfully using its internally developed coverage determination guidelines and level of care guidelines to deny care.
The court also found that UBH’s medically necessary criteria meant that only “acute” episodes would be covered. Instead, said the court last November, chronic and comorbid conditions should always be treated, according to Maureen Gammon and Kathleen Rosenow of Willis Towers Watson, a risk advisor.
In November, the same Northern California District Court ruled on the remedies it would require of United, including that the insurer reprocess more than 67,000 claims. UBH was also barred indefinitely from using any of its guidelines to make coverage determinations. Instead, it was ordered to make determinations “consistent with generally accepted standards of care,” and consistent with state laws.
The District Court denied a request by UBH to put a hold on the claims reprocessing until it appealed the overall case. But the Ninth Circuit Court of Appeals in February granted that request.
Then, in March, United appealed the District Court’s overall ruling, claiming that the plaintiffs had not proven harm.
The U.S. Chamber of Commerce has filed a brief in support of United, agreeing with its arguments.
However, the APA and other clinician groups said there is no question of harm.
“Failure to provide appropriate levels of care for treatment of mental illness and substance use disorders leads to relapse, overdose, transmission of infectious diseases, and death,” said APA CEO and Medical Director Saul Levin, MD, MPA, in a statement.
APA President Vivian Pender, MD, said guidelines that “are overly focused on stabilizing acute symptoms of mental health and substance use disorders” are not treating the underlying disease. “When the injury is physical, insurers treat the underlying disease and not just the symptoms. Discrimination against patients with mental illness must end,” she said.
No court has ever recognized the type of claims reprocessing ordered by the District Court judge, said attorneys Nathaniel Cohen and Joseph Laska of Manatt, Phelps & Phillips, in an analysis of the case.
Mr. Cohen and Mr. Laska write. “Practitioners, health plans, and health insurers would be wise to track UBH’s long-awaited appeal to the Ninth Circuit.”
This article first appeared on Medscape.com.
The American Psychiatric Association has joined with the American Medical Association and other medical societies to oppose United Behavioral Health’s (UBH) request that a court throw out a ruling that found the insurer unfairly denied tens of thousands of claims for mental health and substance use disorder services.
Wit v. United Behavioral Health, in litigation since 2014, is being closely watched by clinicians, patients, providers, and attorneys.
Reena Kapoor, MD, chair of the APA’s Committee on Judicial Action, said in an interview that the APA is hopeful that “whatever the court says about UBH should be applicable to all insurance companies that are providing employer-sponsored health benefits.”
In a friend of the court (amicus curiae) brief, the APA, AMA, the California Medical Association, Southern California Psychiatric Society, Northern California Psychiatric Society, Orange County Psychiatric Society, Central California Psychiatric Society, and San Diego Psychiatric Society argue that “despite the availability of professionally developed, evidence-based guidelines embodying generally accepted standards of care for mental health and substance use disorders, managed care organizations commonly base coverage decisions on internally developed ‘level of care guidelines’ that are inappropriately restrictive.”
The guidelines “may lead to denial of coverage for treatment that is recommended by a patient’s physician and even cut off coverage when treatment is already being delivered,” said the groups.
The U.S. Department of Labor also filed a brief in support of the plaintiffs who are suing UBH. Those individuals suffered injury when they were denied coverage, said the federal agency, which regulates employer-sponsored insurance plans.
California Attorney General Rob Bonta also made an amicus filing supporting the plaintiffs.
“When insurers limit access to this critical care, they leave Californians who need it feeling as if they have no other option than to try to cope alone,” said Mr. Bonta in a statement.
‘Discrimination must end’
Mr. Bonta said he agreed with a 2019 ruling by the U.S. District Court for the Northern District of California that UBH had violated its fiduciary duties by wrongfully using its internally developed coverage determination guidelines and level of care guidelines to deny care.
The court also found that UBH’s medically necessary criteria meant that only “acute” episodes would be covered. Instead, said the court last November, chronic and comorbid conditions should always be treated, according to Maureen Gammon and Kathleen Rosenow of Willis Towers Watson, a risk advisor.
In November, the same Northern California District Court ruled on the remedies it would require of United, including that the insurer reprocess more than 67,000 claims. UBH was also barred indefinitely from using any of its guidelines to make coverage determinations. Instead, it was ordered to make determinations “consistent with generally accepted standards of care,” and consistent with state laws.
The District Court denied a request by UBH to put a hold on the claims reprocessing until it appealed the overall case. But the Ninth Circuit Court of Appeals in February granted that request.
Then, in March, United appealed the District Court’s overall ruling, claiming that the plaintiffs had not proven harm.
The U.S. Chamber of Commerce has filed a brief in support of United, agreeing with its arguments.
However, the APA and other clinician groups said there is no question of harm.
“Failure to provide appropriate levels of care for treatment of mental illness and substance use disorders leads to relapse, overdose, transmission of infectious diseases, and death,” said APA CEO and Medical Director Saul Levin, MD, MPA, in a statement.
APA President Vivian Pender, MD, said guidelines that “are overly focused on stabilizing acute symptoms of mental health and substance use disorders” are not treating the underlying disease. “When the injury is physical, insurers treat the underlying disease and not just the symptoms. Discrimination against patients with mental illness must end,” she said.
No court has ever recognized the type of claims reprocessing ordered by the District Court judge, said attorneys Nathaniel Cohen and Joseph Laska of Manatt, Phelps & Phillips, in an analysis of the case.
Mr. Cohen and Mr. Laska write. “Practitioners, health plans, and health insurers would be wise to track UBH’s long-awaited appeal to the Ninth Circuit.”
This article first appeared on Medscape.com.
Prevalence of psychiatric disorders higher in adult cerebral palsy patients
Adults with cerebral palsy, especially those with intellectual disabilities, are significantly more likely to be diagnosed with a psychiatric disorder, compared with the general population, a review of seven datasets shows.
The body of literature on psychiatric issues in children with cerebral palsy (CP) is increasing, but population-based studies of psychiatric issues in adults with CP have been limited in number and in scope. Most of those studies focus mainly on anxiety and depression, rather than on other issues such as psychosis or schizophrenia, Carly A. McMorris, PhD, of the University of Calgary (Alta.) and colleagues wrote.
In a retrospective, cross-sectional study published in Research in Developmental Disabilities, the researchers reviewed information from five health data sets, one registry, and census data for adults aged 18-64 years with a CP diagnosis living in Ontario, including those with and without diagnosed intellectual disabilities (ID) and a comparison group of individuals in the general population. The researchers examined the proportion of individuals with a psychiatric disorder in each of four groups: total CP, CP without ID, CP with ID, and the general population.
The study participants included 9,388 individuals with CP, 4,767 individuals with CP and ID, and a general population of 2,757,744 individuals. About half of the participants were male, and at least 85% lived in urban areas.
Overall, compared with the general population group, over a 2-year period (33.7 % vs. 24.7%). Also, the CP group was more than twice as likely to be diagnosed with a psychotic disorder, schizophrenia, personality disorder, or bipolar disorder, compared with the general population. Individuals with CP were significantly more likely to suffer from mood or affective disorders, and depression and anxiety disorders, compared with the general population, but less likely to suffer from substance use disorders.
When the data were assessed by ID status, disorders such as psychotic disorders, bipolar disorders, and schizophrenia were six times more common among individuals with CP and ID, compared with the general population (adjusted prevalence ratios, 6.26 and 6.46, respectively).
Individuals with CP and ID also had a notably higher prevalence of bipolar disorder (confidence interval, 2.06-2.89) and personality disorder, compared with the general population (aPR, 2.44 and 4.22, respectively), but this subgroup also was less likely than the general population to engage in substance use (aPR, 0.44).
The study findings were limited by several factors, including the absence of universal definitions for some of the conditions studied, potential misclassification of ID, the inclusion of data on specific psychiatric diagnoses but not elevated symptoms, and by the challenges of diagnosing psychiatric disorders in individuals with ID, the researchers noted.
However, “the present study contributes important information to the existing literature, highlighting that psychiatric issues are common in adults with CP, similar to what has been reported in children and youth,” they said. “Further research is needed to determine the validity and reliability of mental health assessment measures for this population, the efficacy of evidence-based psychotherapeutic approaches ... and the underlying causes or mechanisms of psychiatric issues in individuals with CP.”
The findings also highlight the need for health care clinicians to screen for psychiatric issues in CP patients, they said.
The study was supported in part by the Province of Ontario research grants and the Institute for Clinical Evaluative Sciences, funded by an annual grant from the Ontario Ministry of Health and Long-Term Care. The researchers had no disclosures.
Adults with cerebral palsy, especially those with intellectual disabilities, are significantly more likely to be diagnosed with a psychiatric disorder, compared with the general population, a review of seven datasets shows.
The body of literature on psychiatric issues in children with cerebral palsy (CP) is increasing, but population-based studies of psychiatric issues in adults with CP have been limited in number and in scope. Most of those studies focus mainly on anxiety and depression, rather than on other issues such as psychosis or schizophrenia, Carly A. McMorris, PhD, of the University of Calgary (Alta.) and colleagues wrote.
In a retrospective, cross-sectional study published in Research in Developmental Disabilities, the researchers reviewed information from five health data sets, one registry, and census data for adults aged 18-64 years with a CP diagnosis living in Ontario, including those with and without diagnosed intellectual disabilities (ID) and a comparison group of individuals in the general population. The researchers examined the proportion of individuals with a psychiatric disorder in each of four groups: total CP, CP without ID, CP with ID, and the general population.
The study participants included 9,388 individuals with CP, 4,767 individuals with CP and ID, and a general population of 2,757,744 individuals. About half of the participants were male, and at least 85% lived in urban areas.
Overall, compared with the general population group, over a 2-year period (33.7 % vs. 24.7%). Also, the CP group was more than twice as likely to be diagnosed with a psychotic disorder, schizophrenia, personality disorder, or bipolar disorder, compared with the general population. Individuals with CP were significantly more likely to suffer from mood or affective disorders, and depression and anxiety disorders, compared with the general population, but less likely to suffer from substance use disorders.
When the data were assessed by ID status, disorders such as psychotic disorders, bipolar disorders, and schizophrenia were six times more common among individuals with CP and ID, compared with the general population (adjusted prevalence ratios, 6.26 and 6.46, respectively).
Individuals with CP and ID also had a notably higher prevalence of bipolar disorder (confidence interval, 2.06-2.89) and personality disorder, compared with the general population (aPR, 2.44 and 4.22, respectively), but this subgroup also was less likely than the general population to engage in substance use (aPR, 0.44).
The study findings were limited by several factors, including the absence of universal definitions for some of the conditions studied, potential misclassification of ID, the inclusion of data on specific psychiatric diagnoses but not elevated symptoms, and by the challenges of diagnosing psychiatric disorders in individuals with ID, the researchers noted.
However, “the present study contributes important information to the existing literature, highlighting that psychiatric issues are common in adults with CP, similar to what has been reported in children and youth,” they said. “Further research is needed to determine the validity and reliability of mental health assessment measures for this population, the efficacy of evidence-based psychotherapeutic approaches ... and the underlying causes or mechanisms of psychiatric issues in individuals with CP.”
The findings also highlight the need for health care clinicians to screen for psychiatric issues in CP patients, they said.
The study was supported in part by the Province of Ontario research grants and the Institute for Clinical Evaluative Sciences, funded by an annual grant from the Ontario Ministry of Health and Long-Term Care. The researchers had no disclosures.
Adults with cerebral palsy, especially those with intellectual disabilities, are significantly more likely to be diagnosed with a psychiatric disorder, compared with the general population, a review of seven datasets shows.
The body of literature on psychiatric issues in children with cerebral palsy (CP) is increasing, but population-based studies of psychiatric issues in adults with CP have been limited in number and in scope. Most of those studies focus mainly on anxiety and depression, rather than on other issues such as psychosis or schizophrenia, Carly A. McMorris, PhD, of the University of Calgary (Alta.) and colleagues wrote.
In a retrospective, cross-sectional study published in Research in Developmental Disabilities, the researchers reviewed information from five health data sets, one registry, and census data for adults aged 18-64 years with a CP diagnosis living in Ontario, including those with and without diagnosed intellectual disabilities (ID) and a comparison group of individuals in the general population. The researchers examined the proportion of individuals with a psychiatric disorder in each of four groups: total CP, CP without ID, CP with ID, and the general population.
The study participants included 9,388 individuals with CP, 4,767 individuals with CP and ID, and a general population of 2,757,744 individuals. About half of the participants were male, and at least 85% lived in urban areas.
Overall, compared with the general population group, over a 2-year period (33.7 % vs. 24.7%). Also, the CP group was more than twice as likely to be diagnosed with a psychotic disorder, schizophrenia, personality disorder, or bipolar disorder, compared with the general population. Individuals with CP were significantly more likely to suffer from mood or affective disorders, and depression and anxiety disorders, compared with the general population, but less likely to suffer from substance use disorders.
When the data were assessed by ID status, disorders such as psychotic disorders, bipolar disorders, and schizophrenia were six times more common among individuals with CP and ID, compared with the general population (adjusted prevalence ratios, 6.26 and 6.46, respectively).
Individuals with CP and ID also had a notably higher prevalence of bipolar disorder (confidence interval, 2.06-2.89) and personality disorder, compared with the general population (aPR, 2.44 and 4.22, respectively), but this subgroup also was less likely than the general population to engage in substance use (aPR, 0.44).
The study findings were limited by several factors, including the absence of universal definitions for some of the conditions studied, potential misclassification of ID, the inclusion of data on specific psychiatric diagnoses but not elevated symptoms, and by the challenges of diagnosing psychiatric disorders in individuals with ID, the researchers noted.
However, “the present study contributes important information to the existing literature, highlighting that psychiatric issues are common in adults with CP, similar to what has been reported in children and youth,” they said. “Further research is needed to determine the validity and reliability of mental health assessment measures for this population, the efficacy of evidence-based psychotherapeutic approaches ... and the underlying causes or mechanisms of psychiatric issues in individuals with CP.”
The findings also highlight the need for health care clinicians to screen for psychiatric issues in CP patients, they said.
The study was supported in part by the Province of Ontario research grants and the Institute for Clinical Evaluative Sciences, funded by an annual grant from the Ontario Ministry of Health and Long-Term Care. The researchers had no disclosures.
FROM RESEARCH IN DEVELOPMENTAL DISABILITIES
Two key suicide risk factors identified in borderline personality disorder
Feelings of chronic emptiness and self-injury have been identified as two key risk factors for suicide attempts (SAs) in patients with borderline personality disorder (BPD), a new cross-sectional, nationally representative study suggests.
The findings also show lifetime and past-year SAs are common among patients with BPD, even when excluding self-injurious behaviors.
The results suggest that in addition to asking patients about self-harm during suicide risk screenings and assessments, clinicians should query them about “longstanding” feelings of emptiness, study investigator Carlos M. Grilo, PhD, professor of psychiatry and psychology, Yale University, New Haven, Conn., said in an interview.
Although related, chronic emptiness “is distinct and goes beyond feelings of sadness, loneliness, and hopelessness,” explained Dr. Grilo. he said.
The study was published online May 11 in JAMA Network Open.
Filling a research gap
While BPD and other psychiatric disorders are associated with suicide, the authors noted there is a “dearth of epidemiological research” examining the link between BPD and suicide.
Criteria for BPD diagnosis requires any five of the following criteria: relationships, affective instability, abandonment fear, anger, identity disturbance, emptiness, disassociation/paranoia, self-injurious behavior, and impulsivity, along with social-occupation dysfunction.
To determine SA risk with specific BPD diagnostic criteria, the investigators examined data on 36,309 individuals who participated in the third wave of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC-III), conducted from 2012 to 2013.
During computer-assisted, face-to-face interviews, study participants answered questions based on the Alcohol Use Disorder and Associated Disabilities Interview Schedule-5 (AUDADIS-5) of the National Institute on Alcohol Abuse and Alcoholism.
This structured interview assesses a range of DSM-5–defined psychiatric disorders and their criteria. In addition to BPD, the AUDADIS-5 generates diagnoses for mood disorders, anxiety disorders, posttraumatic stress disorder, substance use disorders, antisocial personality disorder, schizotypal disorder, and conduct disorder.
During the interviews, respondents were asked if they had ever attempted suicide. For those who had, interviewers recorded the total number of lifetime attempts.
Participants also answered questions about childhood maltreatment including physical neglect, emotional neglect, physical abuse, emotional abuse, and sexual abuse by parents or caregivers and other adverse events occurring before the age of 18.
Childhood trauma common
Patients with BPD frequently report a history of childhood trauma, noted Dr. Grilo, adding that such trauma is associated with self-harm and suicide attempts. Sociodemographic information, including age, sex, and ethnicity/race, education level, and income, was also gathered.
Investigators examined data on suicide attempts using relatively stringent coding that required serious dysfunction in at least five BPD criteria.
Using this definition, investigators found the lifetime SA prevalence in patients with BPD was 30.4%, and 3.2% for past-year SAs. This compared with a rate of 3.7% for lifetime SAs and 0.2% for past-year SAs in those without a BPD diagnosis.
The authors examined SA rates using diagnostic codes in the NESARC-III that required seriously impaired function in only 1 or 2 BPD criteria. Rates were higher using the 5-criteria definition.
When the researchers excluded the BPD criterion of self-injurious behavior, the prevalence was 28.1% for lifetime and 3.0% for past-year SAs among the BPD group, with corresponding rates of 3.8% and 0.2% in those without a BPD diagnosis.
It’s important to look at this, said Dr. Grilo, as some patients with BPD who engage in self-harm have suicidal intent while others don’t.
“We tested whether BPD had heightened risk for suicide attempts if we eliminated the self-injurious criterion and we found that heightened risk was still there,” he explained.
Looking at individual criteria for BPD, a model that adjusted for sociodemographic characteristics, other psychiatric disorders, age at BPD onset, and history of childhood adverse events uncovered two criteria that were significantly associated with increased odds of SAs.
One was emptiness. For lifetime suicide attempts, the adjusted odds ratio (aOR) was 1.58 (95% confidence interval, 1.16-2.14) and for past-year attempts, the aOR was 1.99 (95% CI, 1.08-3.66).
The second was self-injurious behavior. For lifetime attempts, the aOR was 24.28 (95% CI, 16.83-32.03) and for past-year attempts, the aOR was 19.32 (95% CI, 5.22-71.58).
In a model in which all BPD-specific criteria were entered while excluding self-injurious behavior, the aORs for emptiness were 1.66 (95% CI, 1.23-2.24) for lifetime suicide attempts and 2.45 (95% CI, 1.18-5.08) for past year attempts.
Unlike another recent study that included more than 700 treatment-seeking patients with BPD who were followed for 10 years, the current study did not show significant associations with SAs for two other BPD criteria – identity disturbance and frantic attempts to avoid abandonment.
Dr. Grilo explained this might be because the earlier study included treatment-seeking patients instead of community cases, or because of differences in assessment interviews or other factors.
‘Compelling evidence’
“Our epidemiological sample has much broader generalizability and fewer potential confounds than the clinical treatment-seeking sample,” said Dr. Grilo.
However, he noted that the two studies “converge strongly and provide compelling evidence that BPD is associated with substantially heightened risk for suicide attempts over the lifetime.”
The two studies “also converge in finding that the presence of symptoms such as repeated self-harm and feelings of chronic emptiness are also associated with risk for suicide attempts.”
The new findings highlight the need to ask potentially at-risk patients about feelings of emptiness as well as self-injurious behaviors. Clinicians could, for example, ask: “Have you often felt like your life had no purpose or meaning?” or “Have you often felt empty inside?”
Limitations of the study include reliance on retrospective self-reports and use of lay interviewers, although these interviewers were trained and had an average of 5 years of experience conducting health-related surveys.
Although the study included a representative sample of U.S. adults, the sample did not include groups known to have high rates of suicide and self-harm behaviors, such as institutionalized, incarcerated, or homeless individuals.
In addition, the study did not evaluate severity and duration of BPD, although the authors noted they did adjust for age at BPD onset, this did not alter the findings.
Often misdiagnosed
Commenting on the study, John M. Oldham, MD, Distinguished Emeritus Professor, Menninger Department of Psychiatry and Behavioral Sciences, Baylor College of Medicine, Houston, and past-president, American Psychiatric Association, and an expert on BPD, had high praise for the research.
BPD is often misdiagnosed, Dr. Oldham said in an interview. Many patients seek help from primary care doctors who may label the symptoms as an anxiety disorder or a mood disorder, he said.
Although medications can help treat some BPD symptoms, “the primary, core evidence-based treatment for BPD is psychotherapy,” said Dr. Oldham, who some years ago helped develop evidence-based practice guidelines for BPD.
“It’s a clear and very well-designed study, and I don’t see any major limitations or problems with it,” he said. “The authors kept their focus rigorously on their goals and they used really careful methodology.”
He noted the “huge” numbers of patients included in the data and the relatively large percentage of men (43.7%).
“There’s a general belief that it’s mostly females who have BPD, but that’s not true; it’s females who come to treatment,” said Dr. Oldham.
Requiring that all five criteria lead to seriously impaired functioning “is a much more rigorous diagnostic methodology” than requiring only one or two criteria to lead to such impairment, said Dr. Oldham. “This is really important” and makes it “a much stronger study.”
The finding that self-harm behavior was linked to suicide attempts isn’t that surprising as this association has been well documented, but the finding that chronic emptiness is also predictive of future suicide attempts “is news,” said Dr. Oldham.
“We have not paid enough attention to this criterion in the clinical world or in the research world.”
Dr. Oldham said one patient with BPD gave him an ideal metaphor for emptiness. “She said it’s like there’s just nobody home. Think of it as an empty house that may look fine on the outside but you go inside and nobody lives there; there’s no furniture; no favorite things; no photos; no possessions.”
The authors have “important messages we need to pay attention to, and the main one is to explore this sense of chronic ‘nobody home’ emptiness,” said Dr. Oldham.
Dr. Grilo has reported receiving research grants from the National Institutes of Health; serving as a consultant for Sunovion and Weight Watchers; receiving honoraria for lectures, continuing medical education activities, and presentations at scientific conferences; and receiving royalties from Guilford Press and Taylor & Francis, all outside the submitted work.
A version of this article first appeared on Medscape.com.
Feelings of chronic emptiness and self-injury have been identified as two key risk factors for suicide attempts (SAs) in patients with borderline personality disorder (BPD), a new cross-sectional, nationally representative study suggests.
The findings also show lifetime and past-year SAs are common among patients with BPD, even when excluding self-injurious behaviors.
The results suggest that in addition to asking patients about self-harm during suicide risk screenings and assessments, clinicians should query them about “longstanding” feelings of emptiness, study investigator Carlos M. Grilo, PhD, professor of psychiatry and psychology, Yale University, New Haven, Conn., said in an interview.
Although related, chronic emptiness “is distinct and goes beyond feelings of sadness, loneliness, and hopelessness,” explained Dr. Grilo. he said.
The study was published online May 11 in JAMA Network Open.
Filling a research gap
While BPD and other psychiatric disorders are associated with suicide, the authors noted there is a “dearth of epidemiological research” examining the link between BPD and suicide.
Criteria for BPD diagnosis requires any five of the following criteria: relationships, affective instability, abandonment fear, anger, identity disturbance, emptiness, disassociation/paranoia, self-injurious behavior, and impulsivity, along with social-occupation dysfunction.
To determine SA risk with specific BPD diagnostic criteria, the investigators examined data on 36,309 individuals who participated in the third wave of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC-III), conducted from 2012 to 2013.
During computer-assisted, face-to-face interviews, study participants answered questions based on the Alcohol Use Disorder and Associated Disabilities Interview Schedule-5 (AUDADIS-5) of the National Institute on Alcohol Abuse and Alcoholism.
This structured interview assesses a range of DSM-5–defined psychiatric disorders and their criteria. In addition to BPD, the AUDADIS-5 generates diagnoses for mood disorders, anxiety disorders, posttraumatic stress disorder, substance use disorders, antisocial personality disorder, schizotypal disorder, and conduct disorder.
During the interviews, respondents were asked if they had ever attempted suicide. For those who had, interviewers recorded the total number of lifetime attempts.
Participants also answered questions about childhood maltreatment including physical neglect, emotional neglect, physical abuse, emotional abuse, and sexual abuse by parents or caregivers and other adverse events occurring before the age of 18.
Childhood trauma common
Patients with BPD frequently report a history of childhood trauma, noted Dr. Grilo, adding that such trauma is associated with self-harm and suicide attempts. Sociodemographic information, including age, sex, and ethnicity/race, education level, and income, was also gathered.
Investigators examined data on suicide attempts using relatively stringent coding that required serious dysfunction in at least five BPD criteria.
Using this definition, investigators found the lifetime SA prevalence in patients with BPD was 30.4%, and 3.2% for past-year SAs. This compared with a rate of 3.7% for lifetime SAs and 0.2% for past-year SAs in those without a BPD diagnosis.
The authors examined SA rates using diagnostic codes in the NESARC-III that required seriously impaired function in only 1 or 2 BPD criteria. Rates were higher using the 5-criteria definition.
When the researchers excluded the BPD criterion of self-injurious behavior, the prevalence was 28.1% for lifetime and 3.0% for past-year SAs among the BPD group, with corresponding rates of 3.8% and 0.2% in those without a BPD diagnosis.
It’s important to look at this, said Dr. Grilo, as some patients with BPD who engage in self-harm have suicidal intent while others don’t.
“We tested whether BPD had heightened risk for suicide attempts if we eliminated the self-injurious criterion and we found that heightened risk was still there,” he explained.
Looking at individual criteria for BPD, a model that adjusted for sociodemographic characteristics, other psychiatric disorders, age at BPD onset, and history of childhood adverse events uncovered two criteria that were significantly associated with increased odds of SAs.
One was emptiness. For lifetime suicide attempts, the adjusted odds ratio (aOR) was 1.58 (95% confidence interval, 1.16-2.14) and for past-year attempts, the aOR was 1.99 (95% CI, 1.08-3.66).
The second was self-injurious behavior. For lifetime attempts, the aOR was 24.28 (95% CI, 16.83-32.03) and for past-year attempts, the aOR was 19.32 (95% CI, 5.22-71.58).
In a model in which all BPD-specific criteria were entered while excluding self-injurious behavior, the aORs for emptiness were 1.66 (95% CI, 1.23-2.24) for lifetime suicide attempts and 2.45 (95% CI, 1.18-5.08) for past year attempts.
Unlike another recent study that included more than 700 treatment-seeking patients with BPD who were followed for 10 years, the current study did not show significant associations with SAs for two other BPD criteria – identity disturbance and frantic attempts to avoid abandonment.
Dr. Grilo explained this might be because the earlier study included treatment-seeking patients instead of community cases, or because of differences in assessment interviews or other factors.
‘Compelling evidence’
“Our epidemiological sample has much broader generalizability and fewer potential confounds than the clinical treatment-seeking sample,” said Dr. Grilo.
However, he noted that the two studies “converge strongly and provide compelling evidence that BPD is associated with substantially heightened risk for suicide attempts over the lifetime.”
The two studies “also converge in finding that the presence of symptoms such as repeated self-harm and feelings of chronic emptiness are also associated with risk for suicide attempts.”
The new findings highlight the need to ask potentially at-risk patients about feelings of emptiness as well as self-injurious behaviors. Clinicians could, for example, ask: “Have you often felt like your life had no purpose or meaning?” or “Have you often felt empty inside?”
Limitations of the study include reliance on retrospective self-reports and use of lay interviewers, although these interviewers were trained and had an average of 5 years of experience conducting health-related surveys.
Although the study included a representative sample of U.S. adults, the sample did not include groups known to have high rates of suicide and self-harm behaviors, such as institutionalized, incarcerated, or homeless individuals.
In addition, the study did not evaluate severity and duration of BPD, although the authors noted they did adjust for age at BPD onset, this did not alter the findings.
Often misdiagnosed
Commenting on the study, John M. Oldham, MD, Distinguished Emeritus Professor, Menninger Department of Psychiatry and Behavioral Sciences, Baylor College of Medicine, Houston, and past-president, American Psychiatric Association, and an expert on BPD, had high praise for the research.
BPD is often misdiagnosed, Dr. Oldham said in an interview. Many patients seek help from primary care doctors who may label the symptoms as an anxiety disorder or a mood disorder, he said.
Although medications can help treat some BPD symptoms, “the primary, core evidence-based treatment for BPD is psychotherapy,” said Dr. Oldham, who some years ago helped develop evidence-based practice guidelines for BPD.
“It’s a clear and very well-designed study, and I don’t see any major limitations or problems with it,” he said. “The authors kept their focus rigorously on their goals and they used really careful methodology.”
He noted the “huge” numbers of patients included in the data and the relatively large percentage of men (43.7%).
“There’s a general belief that it’s mostly females who have BPD, but that’s not true; it’s females who come to treatment,” said Dr. Oldham.
Requiring that all five criteria lead to seriously impaired functioning “is a much more rigorous diagnostic methodology” than requiring only one or two criteria to lead to such impairment, said Dr. Oldham. “This is really important” and makes it “a much stronger study.”
The finding that self-harm behavior was linked to suicide attempts isn’t that surprising as this association has been well documented, but the finding that chronic emptiness is also predictive of future suicide attempts “is news,” said Dr. Oldham.
“We have not paid enough attention to this criterion in the clinical world or in the research world.”
Dr. Oldham said one patient with BPD gave him an ideal metaphor for emptiness. “She said it’s like there’s just nobody home. Think of it as an empty house that may look fine on the outside but you go inside and nobody lives there; there’s no furniture; no favorite things; no photos; no possessions.”
The authors have “important messages we need to pay attention to, and the main one is to explore this sense of chronic ‘nobody home’ emptiness,” said Dr. Oldham.
Dr. Grilo has reported receiving research grants from the National Institutes of Health; serving as a consultant for Sunovion and Weight Watchers; receiving honoraria for lectures, continuing medical education activities, and presentations at scientific conferences; and receiving royalties from Guilford Press and Taylor & Francis, all outside the submitted work.
A version of this article first appeared on Medscape.com.
Feelings of chronic emptiness and self-injury have been identified as two key risk factors for suicide attempts (SAs) in patients with borderline personality disorder (BPD), a new cross-sectional, nationally representative study suggests.
The findings also show lifetime and past-year SAs are common among patients with BPD, even when excluding self-injurious behaviors.
The results suggest that in addition to asking patients about self-harm during suicide risk screenings and assessments, clinicians should query them about “longstanding” feelings of emptiness, study investigator Carlos M. Grilo, PhD, professor of psychiatry and psychology, Yale University, New Haven, Conn., said in an interview.
Although related, chronic emptiness “is distinct and goes beyond feelings of sadness, loneliness, and hopelessness,” explained Dr. Grilo. he said.
The study was published online May 11 in JAMA Network Open.
Filling a research gap
While BPD and other psychiatric disorders are associated with suicide, the authors noted there is a “dearth of epidemiological research” examining the link between BPD and suicide.
Criteria for BPD diagnosis requires any five of the following criteria: relationships, affective instability, abandonment fear, anger, identity disturbance, emptiness, disassociation/paranoia, self-injurious behavior, and impulsivity, along with social-occupation dysfunction.
To determine SA risk with specific BPD diagnostic criteria, the investigators examined data on 36,309 individuals who participated in the third wave of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC-III), conducted from 2012 to 2013.
During computer-assisted, face-to-face interviews, study participants answered questions based on the Alcohol Use Disorder and Associated Disabilities Interview Schedule-5 (AUDADIS-5) of the National Institute on Alcohol Abuse and Alcoholism.
This structured interview assesses a range of DSM-5–defined psychiatric disorders and their criteria. In addition to BPD, the AUDADIS-5 generates diagnoses for mood disorders, anxiety disorders, posttraumatic stress disorder, substance use disorders, antisocial personality disorder, schizotypal disorder, and conduct disorder.
During the interviews, respondents were asked if they had ever attempted suicide. For those who had, interviewers recorded the total number of lifetime attempts.
Participants also answered questions about childhood maltreatment including physical neglect, emotional neglect, physical abuse, emotional abuse, and sexual abuse by parents or caregivers and other adverse events occurring before the age of 18.
Childhood trauma common
Patients with BPD frequently report a history of childhood trauma, noted Dr. Grilo, adding that such trauma is associated with self-harm and suicide attempts. Sociodemographic information, including age, sex, and ethnicity/race, education level, and income, was also gathered.
Investigators examined data on suicide attempts using relatively stringent coding that required serious dysfunction in at least five BPD criteria.
Using this definition, investigators found the lifetime SA prevalence in patients with BPD was 30.4%, and 3.2% for past-year SAs. This compared with a rate of 3.7% for lifetime SAs and 0.2% for past-year SAs in those without a BPD diagnosis.
The authors examined SA rates using diagnostic codes in the NESARC-III that required seriously impaired function in only 1 or 2 BPD criteria. Rates were higher using the 5-criteria definition.
When the researchers excluded the BPD criterion of self-injurious behavior, the prevalence was 28.1% for lifetime and 3.0% for past-year SAs among the BPD group, with corresponding rates of 3.8% and 0.2% in those without a BPD diagnosis.
It’s important to look at this, said Dr. Grilo, as some patients with BPD who engage in self-harm have suicidal intent while others don’t.
“We tested whether BPD had heightened risk for suicide attempts if we eliminated the self-injurious criterion and we found that heightened risk was still there,” he explained.
Looking at individual criteria for BPD, a model that adjusted for sociodemographic characteristics, other psychiatric disorders, age at BPD onset, and history of childhood adverse events uncovered two criteria that were significantly associated with increased odds of SAs.
One was emptiness. For lifetime suicide attempts, the adjusted odds ratio (aOR) was 1.58 (95% confidence interval, 1.16-2.14) and for past-year attempts, the aOR was 1.99 (95% CI, 1.08-3.66).
The second was self-injurious behavior. For lifetime attempts, the aOR was 24.28 (95% CI, 16.83-32.03) and for past-year attempts, the aOR was 19.32 (95% CI, 5.22-71.58).
In a model in which all BPD-specific criteria were entered while excluding self-injurious behavior, the aORs for emptiness were 1.66 (95% CI, 1.23-2.24) for lifetime suicide attempts and 2.45 (95% CI, 1.18-5.08) for past year attempts.
Unlike another recent study that included more than 700 treatment-seeking patients with BPD who were followed for 10 years, the current study did not show significant associations with SAs for two other BPD criteria – identity disturbance and frantic attempts to avoid abandonment.
Dr. Grilo explained this might be because the earlier study included treatment-seeking patients instead of community cases, or because of differences in assessment interviews or other factors.
‘Compelling evidence’
“Our epidemiological sample has much broader generalizability and fewer potential confounds than the clinical treatment-seeking sample,” said Dr. Grilo.
However, he noted that the two studies “converge strongly and provide compelling evidence that BPD is associated with substantially heightened risk for suicide attempts over the lifetime.”
The two studies “also converge in finding that the presence of symptoms such as repeated self-harm and feelings of chronic emptiness are also associated with risk for suicide attempts.”
The new findings highlight the need to ask potentially at-risk patients about feelings of emptiness as well as self-injurious behaviors. Clinicians could, for example, ask: “Have you often felt like your life had no purpose or meaning?” or “Have you often felt empty inside?”
Limitations of the study include reliance on retrospective self-reports and use of lay interviewers, although these interviewers were trained and had an average of 5 years of experience conducting health-related surveys.
Although the study included a representative sample of U.S. adults, the sample did not include groups known to have high rates of suicide and self-harm behaviors, such as institutionalized, incarcerated, or homeless individuals.
In addition, the study did not evaluate severity and duration of BPD, although the authors noted they did adjust for age at BPD onset, this did not alter the findings.
Often misdiagnosed
Commenting on the study, John M. Oldham, MD, Distinguished Emeritus Professor, Menninger Department of Psychiatry and Behavioral Sciences, Baylor College of Medicine, Houston, and past-president, American Psychiatric Association, and an expert on BPD, had high praise for the research.
BPD is often misdiagnosed, Dr. Oldham said in an interview. Many patients seek help from primary care doctors who may label the symptoms as an anxiety disorder or a mood disorder, he said.
Although medications can help treat some BPD symptoms, “the primary, core evidence-based treatment for BPD is psychotherapy,” said Dr. Oldham, who some years ago helped develop evidence-based practice guidelines for BPD.
“It’s a clear and very well-designed study, and I don’t see any major limitations or problems with it,” he said. “The authors kept their focus rigorously on their goals and they used really careful methodology.”
He noted the “huge” numbers of patients included in the data and the relatively large percentage of men (43.7%).
“There’s a general belief that it’s mostly females who have BPD, but that’s not true; it’s females who come to treatment,” said Dr. Oldham.
Requiring that all five criteria lead to seriously impaired functioning “is a much more rigorous diagnostic methodology” than requiring only one or two criteria to lead to such impairment, said Dr. Oldham. “This is really important” and makes it “a much stronger study.”
The finding that self-harm behavior was linked to suicide attempts isn’t that surprising as this association has been well documented, but the finding that chronic emptiness is also predictive of future suicide attempts “is news,” said Dr. Oldham.
“We have not paid enough attention to this criterion in the clinical world or in the research world.”
Dr. Oldham said one patient with BPD gave him an ideal metaphor for emptiness. “She said it’s like there’s just nobody home. Think of it as an empty house that may look fine on the outside but you go inside and nobody lives there; there’s no furniture; no favorite things; no photos; no possessions.”
The authors have “important messages we need to pay attention to, and the main one is to explore this sense of chronic ‘nobody home’ emptiness,” said Dr. Oldham.
Dr. Grilo has reported receiving research grants from the National Institutes of Health; serving as a consultant for Sunovion and Weight Watchers; receiving honoraria for lectures, continuing medical education activities, and presentations at scientific conferences; and receiving royalties from Guilford Press and Taylor & Francis, all outside the submitted work.
A version of this article first appeared on Medscape.com.
Contradictions abound in ‘The End of Mental Illness’
Daniel G. Amen, MD, is an American psychiatrist well-known for his eponymous clinics, television appearances, and series of books on mental health. One of his latest books, “The End of Mental Illness,” summarizes many of his views on the causes of and treatments for mental illnesses.
Dr. Amen’s approaches – such as his advocacy for the widespread use of single photon emission computed tomography (SPECT) imaging – are somewhat controversial and at times fall outside the mainstream of current psychiatric thought. So does “The End of Mental Illness” contain anything of value to the average practicing psychiatrist? (It should be noted that I listened to this as an audiobook and took notes as I listened. This does limit my ability to directly quote portions of the text, but I believe my notes are reliable.)
He begins the book by pointing out that the term “mental illness” might be better replaced with the term “brain illness.” With this shift in terminology, Dr. Amen introduces a theme that recurs throughout the book: That mental illnesses ultimately stem from various ways in which the brain can be harmed. While the suggested change in terminology might help reduce the stigma associated with psychiatric illnesses, Dr. Amen is surprisingly timid about implementing this term in his own book. He repeatedly refers to “brain health/mental health” issues instead of discarding the “mental” term altogether. Even his BRIGHT MINDS acronym for risk factors for mental illnesses includes the term “mind” instead of “brain.”
Continuing the theme of challenging terminology, Dr. Amen goes on to decry the weaknesses of the DSM system of nosology. This is a valid point, because under the current system, the same patient may receive differing diagnoses depending on which provider is seen and how certain symptoms are interpreted. Yet, here again, Dr. Amen does not seem to adhere to his own advice: He uses DSM terminology throughout the book, speaking of depression, anxiety, bipolar disorder, and ADHD. An oddity (which, admittedly, could have been the audiobook reader’s mistake rather than an error in the original text) is that the DSM is referred to as the “Diagnostic and Structural Manual” rather than the Diagnostic and Statistical Manual. He criticizes the DSM for its imprecision, pointing out the variety of symptom combinations that can produce the same diagnoses and how similar symptoms may overlap between differing diagnoses. Yet, his descriptions of common SPECT patterns (his preferred tool to assist in diagnosis) make it clear that here, too, there is a lot of overlap. As an example, ADHD was associated with at least three of the imaging patterns he described. It is also somewhat ironic how Dr. Amen obliquely criticizes the American Psychiatric Association for profiting from the use of the DSM, when SPECT imaging is expensive and profits his own organization.
Dr. Amen repeatedly asserts that psychiatry is unique among medical specialties for making diagnoses based on symptom clusters rather than direct visualization of the affected organ. Yet, psychiatry is not, in fact, unique in making diagnoses in this way. Some examples of diagnoses based on symptom clusters from other medical specialties are systemic lupus erythematosus, fibromyalgia, and chronic fatigue syndrome. Although he asserts that SPECT imaging better demonstrates the root cause of mental illnesses, it is unclear from his book whether this is actually the case.
The descriptions for the ways in which Dr. Amen uses SPECT (which, admittedly, are vague and presumably simplified for a general audience) suggest that he has made observations correlating specific imaging patterns with certain emotional/behavioral outcomes. However, the imaging patterns he describes in the book can be interpreted to represent multiple different mental conditions, making it clear that SPECT is not a laserlike diagnostic tool that produces a single, indisputable diagnosis. Accuracy with SPECT seems especially questionable in light of two case examples he shares where brain imaging was interpreted as representing illness, but the patients were not demonstrating any signs of mental dysfunction. In one case, Dr. Amen opined that the patient’s vibrant spiritual life “overrode” the sick brain, but if this is true,
Patient testimonials are provided, asserting that SPECT imaging helped them know “exactly” what treatment would help them. One cannot help but wonder whether part of the benefit of SPECT imaging is a placebo effect, boosting the confidence of patients that the treatment they are receiving is personalized and scientifically sound. A similar trend is currently seen more broadly in psychiatry with the widespread promotion of pharmacogenetic testing. Such testing may bolster patient confidence in their medication, but its value in improving patient outcomes has not been established.1
Dr. Amen outlines a brief history of mental health care, including differing approaches and therapies from the time of Sigmund Freud up to the present. His outline is somewhat critical of the perceived shortcomings of his psychiatric forebears, yet this seems entirely unnecessary. All scientific disciplines must start somewhere and build from limited knowledge to greater. Is it necessary to belittle Freud for not being able to do SPECT imaging in the 1800s?
Interestingly, Dr. Amen leaves cognitive-behavioral therapy (CBT), a landmark, evidence-based form of psychotherapy, out of his overview of the history of psychiatry. He does go on to mention CBT as part of the treatment offerings of the Amen Clinics, which could leave the lay reader with the incorrect impression that CBT is a treatment unique to Amen Clinics. Similarly, at one point Dr. Amen writes about “what I call automatic negative thoughts.” This phrasing could confuse readers who might not know that automatic thoughts are a concept endemic to CBT.
Dr. Amen writes repeatedly about the Amen Clinics 4 Circles, four key areas of life that can contribute to mental health. These areas are biological, psychological, social, and spiritual. While Amen Clinics may have come up with the term “4 Circles,” the biopsychosocial model of understanding illness was developed by George Engel, MD, in 1977, and current discussions of this model frequently incorporate a spiritual dimension as well.2
Dr. Amen’s writing at times mischaracterizes psychotropic medications in unhelpful ways. He speaks of psychotropic medications generally as being addictive. While this is certainly true for stimulants and benzodiazepines, most would agree that this does not apply to many other commonly used medications in psychiatry, including selective serotonin reuptake inhibitors (SSRIs), tricyclic antidepressants, antipsychotics, and mood stabilizers. He also paints with a broad brush when he states that anxiety medications can cause dementia. A concerning link has been demonstrated between benzodiazepine use and dementia,3 but SSRIs (which are considered first-line medications for anxiety) are not known to cause dementia and may actually delay progression from mild cognitive impairment to Alzheimer’s dementia.4 His mention of medication use affecting a patient’s insurability could have the unfortunate effect of scaring away suffering individuals from seeking help. The one category of psychiatric medication he does not seem concerned about is psychostimulants, which is odd – given the addictive, cardiovascular, and other risks associated with that medication class.
In contrast to his skepticism regarding many psychotropic medications, Dr. Amen expresses significant enthusiasm regarding nutraceutical use. While there has been research in this area supporting a role for some nutraceutical interventions, there is still a need for more rigorous studies.5 To support his endorsement of natural remedies, Dr. Amen mentions that Hippocrates recommended herbs and spices for many health conditions. But Hippocrates lived more than 2,000 years ago, and the state of medicine has advanced significantly since then.
Dr. Amen also mentions that 80% of the developing world relies upon natural or herbal remedies as the primary source of medicine. While he frames this statement as supporting his endorsement of such remedies, it could conversely be said that this is evidence of the need to make pharmacological interventions more widely available in the developing world.
Much of “The End of Mental Illness” is dedicated to reviewing specific risk factors that could cause harm to a person’s mental well-being. One example is head trauma. Dr. Amen documents at least one instance in which he was convinced that his patient had experienced head trauma, and questioned the patient again and again about possible brain injuries. One must wonder whether the positive results of such focused, repetitive questioning might be evidence of confirmation bias, as a search to confirm the preexisting belief of head trauma could lead to overlooking alternative explanations for a patient’s symptoms.
Another risk factor dwelt upon is exposure to toxins. One toxin Dr. Amen rightly recommends avoiding is tobacco smoke. Yet, his approach to advocate for a tobacco-free lifestyle is somewhat problematic. He lists chemicals contained in tobacco smoke, and then names unpleasant items that share those ingredients, such as paint. This smacks of the same sloppy logic manifested in social media memes decrying the use of vaccines by listing their ingredients alongside scary-sounding products that contain identical ingredients (for example, vaccines contain formaldehyde, which is used to embalm dead bodies!). This is analogous to saying that water is bad for you because it contains hydrogen, which is also an ingredient in atomic bombs.
Dr. Amen makes the blanket recommendation to avoid products containing “chemicals.” This is a difficult recommendation to interpret, since literally all matter is made of chemicals. It seems that Dr. Amen is leaning into the vague idea of a “chemical” as something artificially created in a lab, which must, therefore, be dangerous.
Along these lines, Dr. Amen suggests that if a person doesn’t know what is in a specific food item, it should not be eaten. Although this sounds reasonable on the surface, if people were told the names of the proteins and chemical compounds that make up many naturally occurring plants or meats, they would likely not recognize many of them. Dr. Amen dedicates space to list seemingly benign exposures – such as eating nonorganic produce, using two or more beauty products each day, or touching grocery store receipts – as possible “toxins.” By contrast, there is a certain irony in the absence of any mention of the risks associated with radiation from the SPECT imaging he staunchly advocates for. One potential risk of the book listing so many “toxins” to avoid is that patients could waste valuable time and energy eliminating exposures that pose little or no risk, rather than focusing efforts on well-established treatments.
In light of the observations and critiques offered above, one might come away with the impression that I would not recommend “The End of Mental Illness.” However, although one can nitpick details in the book, some of its bigger ideas make it worth commending to readers. Dr. Amen rightfully emphasizes the need for psychiatrists and patients to think more broadly about mental health issues beyond the use of pills. He justifiably criticizes the “15-minute med check” model of practice and the idea that medications are the end-all, be-all of treatment. He demonstrates an appropriate appreciation for the serious risks of reliance on benzodiazepines.6 Dr. Amen points out important contributions from Viktor Frankl, MD, to the field of psychiatry, which may go overlooked today. He also helpfully points out that bipolar disorder may often be misdiagnosed (although he attributes the misdiagnosis to traumatic brain injury, whereas other psychiatrists might say the misdiagnosis is due to borderline personality disorder).
Much of what Dr. Amen writes is sensible, and psychiatrists would do well to adopt the following steps he advocates for: Taking a comprehensive biopsychosocial-spiritual approach to the assessment and treatment of patients; thinking broadly in their differential diagnoses and not forgetting their medical training; understanding that medication alone is often not sufficient to make lasting, positive change in a person’s life; paying attention to healthy habits such as diet, exercise, sleep, and social activity; and knowing that CBT is a valuable tool that can change lives.
There is much to appreciate in “The End of Mental Illness,” especially the overarching idea that psychiatry isn’t just a symptom checklist and a prescription pad. Rather, achieving mental well-being often requires broader thinking and sustained lifestyle changes.
Although I did not agree with everything in the book, it did cause me to think and reflect on my own practice. I read “The End of Mental Illness” with colleagues in my department, and it stimulated a lively discussion. Isn’t that ultimately what a psychiatrist would want from a book like this – the opportunity to reflect, discuss, and potentially improve one’s own practice?
Dr. Weber is physician lead in the department of psychiatry at Intermountain Healthcare Budge Clinic, Logan (Utah) Psychiatry. He disclosed no relevant financial relationships.
References
1. JAMA Netw Open. 2020;3(12). doi: 10.1001/jamanetworkopen.2020.27909.
2. Curr Opin Psychiatry. 2014;27:358-63.
3. BMJ 2014. doi: 10.1136/bmj.g5205.
4. Am J Psychiatry. 2018 Mar 1;175:232-41.
5. Am J Psychiatry. 2016 Jun 1;173:575-87.
6. Current Psychiatry. 2018 Feb;17(2):22-7.
Daniel G. Amen, MD, is an American psychiatrist well-known for his eponymous clinics, television appearances, and series of books on mental health. One of his latest books, “The End of Mental Illness,” summarizes many of his views on the causes of and treatments for mental illnesses.
Dr. Amen’s approaches – such as his advocacy for the widespread use of single photon emission computed tomography (SPECT) imaging – are somewhat controversial and at times fall outside the mainstream of current psychiatric thought. So does “The End of Mental Illness” contain anything of value to the average practicing psychiatrist? (It should be noted that I listened to this as an audiobook and took notes as I listened. This does limit my ability to directly quote portions of the text, but I believe my notes are reliable.)
He begins the book by pointing out that the term “mental illness” might be better replaced with the term “brain illness.” With this shift in terminology, Dr. Amen introduces a theme that recurs throughout the book: That mental illnesses ultimately stem from various ways in which the brain can be harmed. While the suggested change in terminology might help reduce the stigma associated with psychiatric illnesses, Dr. Amen is surprisingly timid about implementing this term in his own book. He repeatedly refers to “brain health/mental health” issues instead of discarding the “mental” term altogether. Even his BRIGHT MINDS acronym for risk factors for mental illnesses includes the term “mind” instead of “brain.”
Continuing the theme of challenging terminology, Dr. Amen goes on to decry the weaknesses of the DSM system of nosology. This is a valid point, because under the current system, the same patient may receive differing diagnoses depending on which provider is seen and how certain symptoms are interpreted. Yet, here again, Dr. Amen does not seem to adhere to his own advice: He uses DSM terminology throughout the book, speaking of depression, anxiety, bipolar disorder, and ADHD. An oddity (which, admittedly, could have been the audiobook reader’s mistake rather than an error in the original text) is that the DSM is referred to as the “Diagnostic and Structural Manual” rather than the Diagnostic and Statistical Manual. He criticizes the DSM for its imprecision, pointing out the variety of symptom combinations that can produce the same diagnoses and how similar symptoms may overlap between differing diagnoses. Yet, his descriptions of common SPECT patterns (his preferred tool to assist in diagnosis) make it clear that here, too, there is a lot of overlap. As an example, ADHD was associated with at least three of the imaging patterns he described. It is also somewhat ironic how Dr. Amen obliquely criticizes the American Psychiatric Association for profiting from the use of the DSM, when SPECT imaging is expensive and profits his own organization.
Dr. Amen repeatedly asserts that psychiatry is unique among medical specialties for making diagnoses based on symptom clusters rather than direct visualization of the affected organ. Yet, psychiatry is not, in fact, unique in making diagnoses in this way. Some examples of diagnoses based on symptom clusters from other medical specialties are systemic lupus erythematosus, fibromyalgia, and chronic fatigue syndrome. Although he asserts that SPECT imaging better demonstrates the root cause of mental illnesses, it is unclear from his book whether this is actually the case.
The descriptions for the ways in which Dr. Amen uses SPECT (which, admittedly, are vague and presumably simplified for a general audience) suggest that he has made observations correlating specific imaging patterns with certain emotional/behavioral outcomes. However, the imaging patterns he describes in the book can be interpreted to represent multiple different mental conditions, making it clear that SPECT is not a laserlike diagnostic tool that produces a single, indisputable diagnosis. Accuracy with SPECT seems especially questionable in light of two case examples he shares where brain imaging was interpreted as representing illness, but the patients were not demonstrating any signs of mental dysfunction. In one case, Dr. Amen opined that the patient’s vibrant spiritual life “overrode” the sick brain, but if this is true,
Patient testimonials are provided, asserting that SPECT imaging helped them know “exactly” what treatment would help them. One cannot help but wonder whether part of the benefit of SPECT imaging is a placebo effect, boosting the confidence of patients that the treatment they are receiving is personalized and scientifically sound. A similar trend is currently seen more broadly in psychiatry with the widespread promotion of pharmacogenetic testing. Such testing may bolster patient confidence in their medication, but its value in improving patient outcomes has not been established.1
Dr. Amen outlines a brief history of mental health care, including differing approaches and therapies from the time of Sigmund Freud up to the present. His outline is somewhat critical of the perceived shortcomings of his psychiatric forebears, yet this seems entirely unnecessary. All scientific disciplines must start somewhere and build from limited knowledge to greater. Is it necessary to belittle Freud for not being able to do SPECT imaging in the 1800s?
Interestingly, Dr. Amen leaves cognitive-behavioral therapy (CBT), a landmark, evidence-based form of psychotherapy, out of his overview of the history of psychiatry. He does go on to mention CBT as part of the treatment offerings of the Amen Clinics, which could leave the lay reader with the incorrect impression that CBT is a treatment unique to Amen Clinics. Similarly, at one point Dr. Amen writes about “what I call automatic negative thoughts.” This phrasing could confuse readers who might not know that automatic thoughts are a concept endemic to CBT.
Dr. Amen writes repeatedly about the Amen Clinics 4 Circles, four key areas of life that can contribute to mental health. These areas are biological, psychological, social, and spiritual. While Amen Clinics may have come up with the term “4 Circles,” the biopsychosocial model of understanding illness was developed by George Engel, MD, in 1977, and current discussions of this model frequently incorporate a spiritual dimension as well.2
Dr. Amen’s writing at times mischaracterizes psychotropic medications in unhelpful ways. He speaks of psychotropic medications generally as being addictive. While this is certainly true for stimulants and benzodiazepines, most would agree that this does not apply to many other commonly used medications in psychiatry, including selective serotonin reuptake inhibitors (SSRIs), tricyclic antidepressants, antipsychotics, and mood stabilizers. He also paints with a broad brush when he states that anxiety medications can cause dementia. A concerning link has been demonstrated between benzodiazepine use and dementia,3 but SSRIs (which are considered first-line medications for anxiety) are not known to cause dementia and may actually delay progression from mild cognitive impairment to Alzheimer’s dementia.4 His mention of medication use affecting a patient’s insurability could have the unfortunate effect of scaring away suffering individuals from seeking help. The one category of psychiatric medication he does not seem concerned about is psychostimulants, which is odd – given the addictive, cardiovascular, and other risks associated with that medication class.
In contrast to his skepticism regarding many psychotropic medications, Dr. Amen expresses significant enthusiasm regarding nutraceutical use. While there has been research in this area supporting a role for some nutraceutical interventions, there is still a need for more rigorous studies.5 To support his endorsement of natural remedies, Dr. Amen mentions that Hippocrates recommended herbs and spices for many health conditions. But Hippocrates lived more than 2,000 years ago, and the state of medicine has advanced significantly since then.
Dr. Amen also mentions that 80% of the developing world relies upon natural or herbal remedies as the primary source of medicine. While he frames this statement as supporting his endorsement of such remedies, it could conversely be said that this is evidence of the need to make pharmacological interventions more widely available in the developing world.
Much of “The End of Mental Illness” is dedicated to reviewing specific risk factors that could cause harm to a person’s mental well-being. One example is head trauma. Dr. Amen documents at least one instance in which he was convinced that his patient had experienced head trauma, and questioned the patient again and again about possible brain injuries. One must wonder whether the positive results of such focused, repetitive questioning might be evidence of confirmation bias, as a search to confirm the preexisting belief of head trauma could lead to overlooking alternative explanations for a patient’s symptoms.
Another risk factor dwelt upon is exposure to toxins. One toxin Dr. Amen rightly recommends avoiding is tobacco smoke. Yet, his approach to advocate for a tobacco-free lifestyle is somewhat problematic. He lists chemicals contained in tobacco smoke, and then names unpleasant items that share those ingredients, such as paint. This smacks of the same sloppy logic manifested in social media memes decrying the use of vaccines by listing their ingredients alongside scary-sounding products that contain identical ingredients (for example, vaccines contain formaldehyde, which is used to embalm dead bodies!). This is analogous to saying that water is bad for you because it contains hydrogen, which is also an ingredient in atomic bombs.
Dr. Amen makes the blanket recommendation to avoid products containing “chemicals.” This is a difficult recommendation to interpret, since literally all matter is made of chemicals. It seems that Dr. Amen is leaning into the vague idea of a “chemical” as something artificially created in a lab, which must, therefore, be dangerous.
Along these lines, Dr. Amen suggests that if a person doesn’t know what is in a specific food item, it should not be eaten. Although this sounds reasonable on the surface, if people were told the names of the proteins and chemical compounds that make up many naturally occurring plants or meats, they would likely not recognize many of them. Dr. Amen dedicates space to list seemingly benign exposures – such as eating nonorganic produce, using two or more beauty products each day, or touching grocery store receipts – as possible “toxins.” By contrast, there is a certain irony in the absence of any mention of the risks associated with radiation from the SPECT imaging he staunchly advocates for. One potential risk of the book listing so many “toxins” to avoid is that patients could waste valuable time and energy eliminating exposures that pose little or no risk, rather than focusing efforts on well-established treatments.
In light of the observations and critiques offered above, one might come away with the impression that I would not recommend “The End of Mental Illness.” However, although one can nitpick details in the book, some of its bigger ideas make it worth commending to readers. Dr. Amen rightfully emphasizes the need for psychiatrists and patients to think more broadly about mental health issues beyond the use of pills. He justifiably criticizes the “15-minute med check” model of practice and the idea that medications are the end-all, be-all of treatment. He demonstrates an appropriate appreciation for the serious risks of reliance on benzodiazepines.6 Dr. Amen points out important contributions from Viktor Frankl, MD, to the field of psychiatry, which may go overlooked today. He also helpfully points out that bipolar disorder may often be misdiagnosed (although he attributes the misdiagnosis to traumatic brain injury, whereas other psychiatrists might say the misdiagnosis is due to borderline personality disorder).
Much of what Dr. Amen writes is sensible, and psychiatrists would do well to adopt the following steps he advocates for: Taking a comprehensive biopsychosocial-spiritual approach to the assessment and treatment of patients; thinking broadly in their differential diagnoses and not forgetting their medical training; understanding that medication alone is often not sufficient to make lasting, positive change in a person’s life; paying attention to healthy habits such as diet, exercise, sleep, and social activity; and knowing that CBT is a valuable tool that can change lives.
There is much to appreciate in “The End of Mental Illness,” especially the overarching idea that psychiatry isn’t just a symptom checklist and a prescription pad. Rather, achieving mental well-being often requires broader thinking and sustained lifestyle changes.
Although I did not agree with everything in the book, it did cause me to think and reflect on my own practice. I read “The End of Mental Illness” with colleagues in my department, and it stimulated a lively discussion. Isn’t that ultimately what a psychiatrist would want from a book like this – the opportunity to reflect, discuss, and potentially improve one’s own practice?
Dr. Weber is physician lead in the department of psychiatry at Intermountain Healthcare Budge Clinic, Logan (Utah) Psychiatry. He disclosed no relevant financial relationships.
References
1. JAMA Netw Open. 2020;3(12). doi: 10.1001/jamanetworkopen.2020.27909.
2. Curr Opin Psychiatry. 2014;27:358-63.
3. BMJ 2014. doi: 10.1136/bmj.g5205.
4. Am J Psychiatry. 2018 Mar 1;175:232-41.
5. Am J Psychiatry. 2016 Jun 1;173:575-87.
6. Current Psychiatry. 2018 Feb;17(2):22-7.
Daniel G. Amen, MD, is an American psychiatrist well-known for his eponymous clinics, television appearances, and series of books on mental health. One of his latest books, “The End of Mental Illness,” summarizes many of his views on the causes of and treatments for mental illnesses.
Dr. Amen’s approaches – such as his advocacy for the widespread use of single photon emission computed tomography (SPECT) imaging – are somewhat controversial and at times fall outside the mainstream of current psychiatric thought. So does “The End of Mental Illness” contain anything of value to the average practicing psychiatrist? (It should be noted that I listened to this as an audiobook and took notes as I listened. This does limit my ability to directly quote portions of the text, but I believe my notes are reliable.)
He begins the book by pointing out that the term “mental illness” might be better replaced with the term “brain illness.” With this shift in terminology, Dr. Amen introduces a theme that recurs throughout the book: That mental illnesses ultimately stem from various ways in which the brain can be harmed. While the suggested change in terminology might help reduce the stigma associated with psychiatric illnesses, Dr. Amen is surprisingly timid about implementing this term in his own book. He repeatedly refers to “brain health/mental health” issues instead of discarding the “mental” term altogether. Even his BRIGHT MINDS acronym for risk factors for mental illnesses includes the term “mind” instead of “brain.”
Continuing the theme of challenging terminology, Dr. Amen goes on to decry the weaknesses of the DSM system of nosology. This is a valid point, because under the current system, the same patient may receive differing diagnoses depending on which provider is seen and how certain symptoms are interpreted. Yet, here again, Dr. Amen does not seem to adhere to his own advice: He uses DSM terminology throughout the book, speaking of depression, anxiety, bipolar disorder, and ADHD. An oddity (which, admittedly, could have been the audiobook reader’s mistake rather than an error in the original text) is that the DSM is referred to as the “Diagnostic and Structural Manual” rather than the Diagnostic and Statistical Manual. He criticizes the DSM for its imprecision, pointing out the variety of symptom combinations that can produce the same diagnoses and how similar symptoms may overlap between differing diagnoses. Yet, his descriptions of common SPECT patterns (his preferred tool to assist in diagnosis) make it clear that here, too, there is a lot of overlap. As an example, ADHD was associated with at least three of the imaging patterns he described. It is also somewhat ironic how Dr. Amen obliquely criticizes the American Psychiatric Association for profiting from the use of the DSM, when SPECT imaging is expensive and profits his own organization.
Dr. Amen repeatedly asserts that psychiatry is unique among medical specialties for making diagnoses based on symptom clusters rather than direct visualization of the affected organ. Yet, psychiatry is not, in fact, unique in making diagnoses in this way. Some examples of diagnoses based on symptom clusters from other medical specialties are systemic lupus erythematosus, fibromyalgia, and chronic fatigue syndrome. Although he asserts that SPECT imaging better demonstrates the root cause of mental illnesses, it is unclear from his book whether this is actually the case.
The descriptions for the ways in which Dr. Amen uses SPECT (which, admittedly, are vague and presumably simplified for a general audience) suggest that he has made observations correlating specific imaging patterns with certain emotional/behavioral outcomes. However, the imaging patterns he describes in the book can be interpreted to represent multiple different mental conditions, making it clear that SPECT is not a laserlike diagnostic tool that produces a single, indisputable diagnosis. Accuracy with SPECT seems especially questionable in light of two case examples he shares where brain imaging was interpreted as representing illness, but the patients were not demonstrating any signs of mental dysfunction. In one case, Dr. Amen opined that the patient’s vibrant spiritual life “overrode” the sick brain, but if this is true,
Patient testimonials are provided, asserting that SPECT imaging helped them know “exactly” what treatment would help them. One cannot help but wonder whether part of the benefit of SPECT imaging is a placebo effect, boosting the confidence of patients that the treatment they are receiving is personalized and scientifically sound. A similar trend is currently seen more broadly in psychiatry with the widespread promotion of pharmacogenetic testing. Such testing may bolster patient confidence in their medication, but its value in improving patient outcomes has not been established.1
Dr. Amen outlines a brief history of mental health care, including differing approaches and therapies from the time of Sigmund Freud up to the present. His outline is somewhat critical of the perceived shortcomings of his psychiatric forebears, yet this seems entirely unnecessary. All scientific disciplines must start somewhere and build from limited knowledge to greater. Is it necessary to belittle Freud for not being able to do SPECT imaging in the 1800s?
Interestingly, Dr. Amen leaves cognitive-behavioral therapy (CBT), a landmark, evidence-based form of psychotherapy, out of his overview of the history of psychiatry. He does go on to mention CBT as part of the treatment offerings of the Amen Clinics, which could leave the lay reader with the incorrect impression that CBT is a treatment unique to Amen Clinics. Similarly, at one point Dr. Amen writes about “what I call automatic negative thoughts.” This phrasing could confuse readers who might not know that automatic thoughts are a concept endemic to CBT.
Dr. Amen writes repeatedly about the Amen Clinics 4 Circles, four key areas of life that can contribute to mental health. These areas are biological, psychological, social, and spiritual. While Amen Clinics may have come up with the term “4 Circles,” the biopsychosocial model of understanding illness was developed by George Engel, MD, in 1977, and current discussions of this model frequently incorporate a spiritual dimension as well.2
Dr. Amen’s writing at times mischaracterizes psychotropic medications in unhelpful ways. He speaks of psychotropic medications generally as being addictive. While this is certainly true for stimulants and benzodiazepines, most would agree that this does not apply to many other commonly used medications in psychiatry, including selective serotonin reuptake inhibitors (SSRIs), tricyclic antidepressants, antipsychotics, and mood stabilizers. He also paints with a broad brush when he states that anxiety medications can cause dementia. A concerning link has been demonstrated between benzodiazepine use and dementia,3 but SSRIs (which are considered first-line medications for anxiety) are not known to cause dementia and may actually delay progression from mild cognitive impairment to Alzheimer’s dementia.4 His mention of medication use affecting a patient’s insurability could have the unfortunate effect of scaring away suffering individuals from seeking help. The one category of psychiatric medication he does not seem concerned about is psychostimulants, which is odd – given the addictive, cardiovascular, and other risks associated with that medication class.
In contrast to his skepticism regarding many psychotropic medications, Dr. Amen expresses significant enthusiasm regarding nutraceutical use. While there has been research in this area supporting a role for some nutraceutical interventions, there is still a need for more rigorous studies.5 To support his endorsement of natural remedies, Dr. Amen mentions that Hippocrates recommended herbs and spices for many health conditions. But Hippocrates lived more than 2,000 years ago, and the state of medicine has advanced significantly since then.
Dr. Amen also mentions that 80% of the developing world relies upon natural or herbal remedies as the primary source of medicine. While he frames this statement as supporting his endorsement of such remedies, it could conversely be said that this is evidence of the need to make pharmacological interventions more widely available in the developing world.
Much of “The End of Mental Illness” is dedicated to reviewing specific risk factors that could cause harm to a person’s mental well-being. One example is head trauma. Dr. Amen documents at least one instance in which he was convinced that his patient had experienced head trauma, and questioned the patient again and again about possible brain injuries. One must wonder whether the positive results of such focused, repetitive questioning might be evidence of confirmation bias, as a search to confirm the preexisting belief of head trauma could lead to overlooking alternative explanations for a patient’s symptoms.
Another risk factor dwelt upon is exposure to toxins. One toxin Dr. Amen rightly recommends avoiding is tobacco smoke. Yet, his approach to advocate for a tobacco-free lifestyle is somewhat problematic. He lists chemicals contained in tobacco smoke, and then names unpleasant items that share those ingredients, such as paint. This smacks of the same sloppy logic manifested in social media memes decrying the use of vaccines by listing their ingredients alongside scary-sounding products that contain identical ingredients (for example, vaccines contain formaldehyde, which is used to embalm dead bodies!). This is analogous to saying that water is bad for you because it contains hydrogen, which is also an ingredient in atomic bombs.
Dr. Amen makes the blanket recommendation to avoid products containing “chemicals.” This is a difficult recommendation to interpret, since literally all matter is made of chemicals. It seems that Dr. Amen is leaning into the vague idea of a “chemical” as something artificially created in a lab, which must, therefore, be dangerous.
Along these lines, Dr. Amen suggests that if a person doesn’t know what is in a specific food item, it should not be eaten. Although this sounds reasonable on the surface, if people were told the names of the proteins and chemical compounds that make up many naturally occurring plants or meats, they would likely not recognize many of them. Dr. Amen dedicates space to list seemingly benign exposures – such as eating nonorganic produce, using two or more beauty products each day, or touching grocery store receipts – as possible “toxins.” By contrast, there is a certain irony in the absence of any mention of the risks associated with radiation from the SPECT imaging he staunchly advocates for. One potential risk of the book listing so many “toxins” to avoid is that patients could waste valuable time and energy eliminating exposures that pose little or no risk, rather than focusing efforts on well-established treatments.
In light of the observations and critiques offered above, one might come away with the impression that I would not recommend “The End of Mental Illness.” However, although one can nitpick details in the book, some of its bigger ideas make it worth commending to readers. Dr. Amen rightfully emphasizes the need for psychiatrists and patients to think more broadly about mental health issues beyond the use of pills. He justifiably criticizes the “15-minute med check” model of practice and the idea that medications are the end-all, be-all of treatment. He demonstrates an appropriate appreciation for the serious risks of reliance on benzodiazepines.6 Dr. Amen points out important contributions from Viktor Frankl, MD, to the field of psychiatry, which may go overlooked today. He also helpfully points out that bipolar disorder may often be misdiagnosed (although he attributes the misdiagnosis to traumatic brain injury, whereas other psychiatrists might say the misdiagnosis is due to borderline personality disorder).
Much of what Dr. Amen writes is sensible, and psychiatrists would do well to adopt the following steps he advocates for: Taking a comprehensive biopsychosocial-spiritual approach to the assessment and treatment of patients; thinking broadly in their differential diagnoses and not forgetting their medical training; understanding that medication alone is often not sufficient to make lasting, positive change in a person’s life; paying attention to healthy habits such as diet, exercise, sleep, and social activity; and knowing that CBT is a valuable tool that can change lives.
There is much to appreciate in “The End of Mental Illness,” especially the overarching idea that psychiatry isn’t just a symptom checklist and a prescription pad. Rather, achieving mental well-being often requires broader thinking and sustained lifestyle changes.
Although I did not agree with everything in the book, it did cause me to think and reflect on my own practice. I read “The End of Mental Illness” with colleagues in my department, and it stimulated a lively discussion. Isn’t that ultimately what a psychiatrist would want from a book like this – the opportunity to reflect, discuss, and potentially improve one’s own practice?
Dr. Weber is physician lead in the department of psychiatry at Intermountain Healthcare Budge Clinic, Logan (Utah) Psychiatry. He disclosed no relevant financial relationships.
References
1. JAMA Netw Open. 2020;3(12). doi: 10.1001/jamanetworkopen.2020.27909.
2. Curr Opin Psychiatry. 2014;27:358-63.
3. BMJ 2014. doi: 10.1136/bmj.g5205.
4. Am J Psychiatry. 2018 Mar 1;175:232-41.
5. Am J Psychiatry. 2016 Jun 1;173:575-87.
6. Current Psychiatry. 2018 Feb;17(2):22-7.