User login
Rivaroxaban’s single daily dose may lead to higher bleeding risk than other DOACs
The results, which were published in the Annals of Internal Medicine, could help guide DOAC selection for high-risk groups with a prior history of peptic ulcer disease or major GI bleeding, said lead study authors Arnar Bragi Ingason, MD and Einar S. Björnsson, MD, PhD, in an email.
DOACs treat conditions such as atrial fibrillation, venous thromboembolism, and ischemic stroke and are known to cause GI bleeding. Previous studies have suggested that rivaroxaban poses a higher GI-bleeding risk than other DOACs.
These studies, which used large administrative databases, “had an inherent risk of selection bias due to insurance status, age, and comorbidities due to their origin from insurance/administrative databases. In addition, they lacked phenotypic details on GI bleeding events,” said Dr. Björnsson and Dr. Ingason, who are both of Landspitali University Hospital, Reykjavik, Iceland,
Daily dosage may exacerbate risk
Rivaroxaban is administered as a single daily dose, compared with apixaban’s and dabigatran’s twice-daily regimens. “We hypothesized that this may lead to a greater variance in drug plasma concentration, making these patients more susceptible to GI bleeding,” the lead authors said.
Using data from the Icelandic Medicine Registry, a national database of outpatient prescription information, they compared rates of GI bleeding among new users of apixaban, dabigatran, and rivaroxaban from 2014 to 2019. Overall, 5,868 patients receiving one of the DOACs took part in the study. Among these participants, 3,217 received rivaroxaban, 2,157 received apixaban, and 494 received dabigatran. The researchers used inverse probability weighting, Kaplan–Meier survival estimates, and Cox regression to compare GI bleeding.
Compared with dabigatran, rivaroxaban was associated with a 63%-104% higher overall risk for GI bleeding and 39%-95% higher risk for major GI bleeding. Rivaroxaban also had a 40%-42% higher overall risk for GI bleeding and 49%-50% higher risk for major GI bleeding, compared with apixaban.
The investigators were surprised by the low rate of upper GI bleeding for dabigatran, compared with the other two drugs. “However, these results must be interpreted in the context that the dabigatran group was relatively small,” said Dr. Björnsson and Dr. Ingason via email.
Overall, the study cohort was small, compared with previous registry studies.
Investigators also did not account for account for socioeconomic status or lifestyle factors, such as alcohol consumption or smoking. “However, because the cost of all DOACs is similar in Iceland, selection bias due to socioeconomic status is unlikely,” the investigators reported in their paper. “We are currently working on comparing the rates of thromboembolisms and overall major bleeding events between the drugs,” the lead authors said.
Clinicians should consider location of bleeding
Though retrospective, the study by Ingason et. al. “is likely as close as is feasible to a randomized trial as is possible,” said Don C. Rockey, MD, a professor of medicine at the Medical University of South Carolina, Charleston, in an interview.
“From the clinician’s perspective, it is important to take away that there may be differences among the DOACs in terms of where in the GI tract the bleeding occurs,” said Dr. Rockey. In the study, the greatest differences appeared to be in the upper GI tract, with rivaroxaban outpacing apixaban and dabigatran. In patients who are at risk for upper GI bleeding, it may be reasonable to consider use of dabigatran or apixaban, he suggested.
“A limitation of the study is that it is likely underpowered overall,” said Dr. Rockey. It also wasn’t clear how many deaths occurred either directly from GI bleeding or as a complication of GI bleeding, he said.The study also didn’t differentiate major bleeding among DOACs specifically in the upper or lower GI tract, Dr. Rockey added.
Other studies yield similar results
Dr. Ingason and Dr. Björnsson said their work complements previous studies, and Neena S. Abraham, MD, MSc , who has conducted a similar investigation to the new study, agreed with that statement.
Data from the last 4 years overwhelmingly show that rivaroxaban is most likely to cause GI bleeding, said Dr. Abraham, professor of medicine and a consultant with Mayo Clinic’s division of gastroenterology and hepatology, in an interview.
A comparative safety study Dr. Abraham coauthored in 2017 of rivaroxaban, apixaban, and dabigatran in a much larger U.S. cohort of 372,380 patients revealed that rivaroxaban had the worst GI bleeding profile. Apixaban was 66% safer than rivaroxaban and 64% safer than dabigatran to prevent gastrointestinal bleeding.
“I believe our group was the first to conduct this study and show clinically significant differences in GI safety of the available direct oral anticoagulants,” she said. Other investigators have since published similar results, and the topic of the new study needs no further investigation, according to Dr. Abraham.
“It is time for physicians to choose a better choice when prescribing a direct oral anticoagulant to their atrial fibrillation patients, and that choice is not rivaroxaban,” she said.
The Icelandic Centre for Research and the Landspítali University Hospital Research Fund provided funds for this study. Dr. Ingason, Dr. Björnsson, Dr. Rockey, and Dr. Abraham reported no disclosures.
The results, which were published in the Annals of Internal Medicine, could help guide DOAC selection for high-risk groups with a prior history of peptic ulcer disease or major GI bleeding, said lead study authors Arnar Bragi Ingason, MD and Einar S. Björnsson, MD, PhD, in an email.
DOACs treat conditions such as atrial fibrillation, venous thromboembolism, and ischemic stroke and are known to cause GI bleeding. Previous studies have suggested that rivaroxaban poses a higher GI-bleeding risk than other DOACs.
These studies, which used large administrative databases, “had an inherent risk of selection bias due to insurance status, age, and comorbidities due to their origin from insurance/administrative databases. In addition, they lacked phenotypic details on GI bleeding events,” said Dr. Björnsson and Dr. Ingason, who are both of Landspitali University Hospital, Reykjavik, Iceland,
Daily dosage may exacerbate risk
Rivaroxaban is administered as a single daily dose, compared with apixaban’s and dabigatran’s twice-daily regimens. “We hypothesized that this may lead to a greater variance in drug plasma concentration, making these patients more susceptible to GI bleeding,” the lead authors said.
Using data from the Icelandic Medicine Registry, a national database of outpatient prescription information, they compared rates of GI bleeding among new users of apixaban, dabigatran, and rivaroxaban from 2014 to 2019. Overall, 5,868 patients receiving one of the DOACs took part in the study. Among these participants, 3,217 received rivaroxaban, 2,157 received apixaban, and 494 received dabigatran. The researchers used inverse probability weighting, Kaplan–Meier survival estimates, and Cox regression to compare GI bleeding.
Compared with dabigatran, rivaroxaban was associated with a 63%-104% higher overall risk for GI bleeding and 39%-95% higher risk for major GI bleeding. Rivaroxaban also had a 40%-42% higher overall risk for GI bleeding and 49%-50% higher risk for major GI bleeding, compared with apixaban.
The investigators were surprised by the low rate of upper GI bleeding for dabigatran, compared with the other two drugs. “However, these results must be interpreted in the context that the dabigatran group was relatively small,” said Dr. Björnsson and Dr. Ingason via email.
Overall, the study cohort was small, compared with previous registry studies.
Investigators also did not account for account for socioeconomic status or lifestyle factors, such as alcohol consumption or smoking. “However, because the cost of all DOACs is similar in Iceland, selection bias due to socioeconomic status is unlikely,” the investigators reported in their paper. “We are currently working on comparing the rates of thromboembolisms and overall major bleeding events between the drugs,” the lead authors said.
Clinicians should consider location of bleeding
Though retrospective, the study by Ingason et. al. “is likely as close as is feasible to a randomized trial as is possible,” said Don C. Rockey, MD, a professor of medicine at the Medical University of South Carolina, Charleston, in an interview.
“From the clinician’s perspective, it is important to take away that there may be differences among the DOACs in terms of where in the GI tract the bleeding occurs,” said Dr. Rockey. In the study, the greatest differences appeared to be in the upper GI tract, with rivaroxaban outpacing apixaban and dabigatran. In patients who are at risk for upper GI bleeding, it may be reasonable to consider use of dabigatran or apixaban, he suggested.
“A limitation of the study is that it is likely underpowered overall,” said Dr. Rockey. It also wasn’t clear how many deaths occurred either directly from GI bleeding or as a complication of GI bleeding, he said.The study also didn’t differentiate major bleeding among DOACs specifically in the upper or lower GI tract, Dr. Rockey added.
Other studies yield similar results
Dr. Ingason and Dr. Björnsson said their work complements previous studies, and Neena S. Abraham, MD, MSc , who has conducted a similar investigation to the new study, agreed with that statement.
Data from the last 4 years overwhelmingly show that rivaroxaban is most likely to cause GI bleeding, said Dr. Abraham, professor of medicine and a consultant with Mayo Clinic’s division of gastroenterology and hepatology, in an interview.
A comparative safety study Dr. Abraham coauthored in 2017 of rivaroxaban, apixaban, and dabigatran in a much larger U.S. cohort of 372,380 patients revealed that rivaroxaban had the worst GI bleeding profile. Apixaban was 66% safer than rivaroxaban and 64% safer than dabigatran to prevent gastrointestinal bleeding.
“I believe our group was the first to conduct this study and show clinically significant differences in GI safety of the available direct oral anticoagulants,” she said. Other investigators have since published similar results, and the topic of the new study needs no further investigation, according to Dr. Abraham.
“It is time for physicians to choose a better choice when prescribing a direct oral anticoagulant to their atrial fibrillation patients, and that choice is not rivaroxaban,” she said.
The Icelandic Centre for Research and the Landspítali University Hospital Research Fund provided funds for this study. Dr. Ingason, Dr. Björnsson, Dr. Rockey, and Dr. Abraham reported no disclosures.
The results, which were published in the Annals of Internal Medicine, could help guide DOAC selection for high-risk groups with a prior history of peptic ulcer disease or major GI bleeding, said lead study authors Arnar Bragi Ingason, MD and Einar S. Björnsson, MD, PhD, in an email.
DOACs treat conditions such as atrial fibrillation, venous thromboembolism, and ischemic stroke and are known to cause GI bleeding. Previous studies have suggested that rivaroxaban poses a higher GI-bleeding risk than other DOACs.
These studies, which used large administrative databases, “had an inherent risk of selection bias due to insurance status, age, and comorbidities due to their origin from insurance/administrative databases. In addition, they lacked phenotypic details on GI bleeding events,” said Dr. Björnsson and Dr. Ingason, who are both of Landspitali University Hospital, Reykjavik, Iceland,
Daily dosage may exacerbate risk
Rivaroxaban is administered as a single daily dose, compared with apixaban’s and dabigatran’s twice-daily regimens. “We hypothesized that this may lead to a greater variance in drug plasma concentration, making these patients more susceptible to GI bleeding,” the lead authors said.
Using data from the Icelandic Medicine Registry, a national database of outpatient prescription information, they compared rates of GI bleeding among new users of apixaban, dabigatran, and rivaroxaban from 2014 to 2019. Overall, 5,868 patients receiving one of the DOACs took part in the study. Among these participants, 3,217 received rivaroxaban, 2,157 received apixaban, and 494 received dabigatran. The researchers used inverse probability weighting, Kaplan–Meier survival estimates, and Cox regression to compare GI bleeding.
Compared with dabigatran, rivaroxaban was associated with a 63%-104% higher overall risk for GI bleeding and 39%-95% higher risk for major GI bleeding. Rivaroxaban also had a 40%-42% higher overall risk for GI bleeding and 49%-50% higher risk for major GI bleeding, compared with apixaban.
The investigators were surprised by the low rate of upper GI bleeding for dabigatran, compared with the other two drugs. “However, these results must be interpreted in the context that the dabigatran group was relatively small,” said Dr. Björnsson and Dr. Ingason via email.
Overall, the study cohort was small, compared with previous registry studies.
Investigators also did not account for account for socioeconomic status or lifestyle factors, such as alcohol consumption or smoking. “However, because the cost of all DOACs is similar in Iceland, selection bias due to socioeconomic status is unlikely,” the investigators reported in their paper. “We are currently working on comparing the rates of thromboembolisms and overall major bleeding events between the drugs,” the lead authors said.
Clinicians should consider location of bleeding
Though retrospective, the study by Ingason et. al. “is likely as close as is feasible to a randomized trial as is possible,” said Don C. Rockey, MD, a professor of medicine at the Medical University of South Carolina, Charleston, in an interview.
“From the clinician’s perspective, it is important to take away that there may be differences among the DOACs in terms of where in the GI tract the bleeding occurs,” said Dr. Rockey. In the study, the greatest differences appeared to be in the upper GI tract, with rivaroxaban outpacing apixaban and dabigatran. In patients who are at risk for upper GI bleeding, it may be reasonable to consider use of dabigatran or apixaban, he suggested.
“A limitation of the study is that it is likely underpowered overall,” said Dr. Rockey. It also wasn’t clear how many deaths occurred either directly from GI bleeding or as a complication of GI bleeding, he said.The study also didn’t differentiate major bleeding among DOACs specifically in the upper or lower GI tract, Dr. Rockey added.
Other studies yield similar results
Dr. Ingason and Dr. Björnsson said their work complements previous studies, and Neena S. Abraham, MD, MSc , who has conducted a similar investigation to the new study, agreed with that statement.
Data from the last 4 years overwhelmingly show that rivaroxaban is most likely to cause GI bleeding, said Dr. Abraham, professor of medicine and a consultant with Mayo Clinic’s division of gastroenterology and hepatology, in an interview.
A comparative safety study Dr. Abraham coauthored in 2017 of rivaroxaban, apixaban, and dabigatran in a much larger U.S. cohort of 372,380 patients revealed that rivaroxaban had the worst GI bleeding profile. Apixaban was 66% safer than rivaroxaban and 64% safer than dabigatran to prevent gastrointestinal bleeding.
“I believe our group was the first to conduct this study and show clinically significant differences in GI safety of the available direct oral anticoagulants,” she said. Other investigators have since published similar results, and the topic of the new study needs no further investigation, according to Dr. Abraham.
“It is time for physicians to choose a better choice when prescribing a direct oral anticoagulant to their atrial fibrillation patients, and that choice is not rivaroxaban,” she said.
The Icelandic Centre for Research and the Landspítali University Hospital Research Fund provided funds for this study. Dr. Ingason, Dr. Björnsson, Dr. Rockey, and Dr. Abraham reported no disclosures.
FROM ANNALS OF INTERNAL MEDICINE
Extraesophageal symptoms of GERD
Patients often present with symptoms that are not classic for reflux such as chronic cough, worsening asthma, sore throat, or globus.
In the upper GI section of the postgraduate course program, Rena Yadlapati, MD, and C. Prakash Gyawali, MD, MRCP, educated us about optimal strategies for diagnosis and treatment of this difficult group of patients. Dr. Gyawali reminded us of risk stratification of patients into those with high or low likelihood of reflux as contributing etiology for patients with suspected extraesophageal reflux. Dr. Yadlapti reviewed the utility of the HASBEER score in stratifying patients into these two risk categories. Patients with known reflux at baseline and/or if they have classic symptoms of reflux in addition to extraesophageal symptoms may be at higher likelihood of having abnormal esophageal acid exposure than those without classic heartburn and/or regurgitation. The low-risk group may then benefit from diagnostic testing off PPI therapy (either impedance/pH monitoring or wireless pH testing), whereas those in the high-risk group for reflux may undergo impedance pH testing on PPI therapy to ensure control of reflux while on therapy.
Dr. Yadlapati also updated the audience about lack of robust data to suggest clinical utility for oropharyngeal pH test or salivary pepsin assay testing. It was generally agreed on that the majority of patients who do not respond to aggressive acid suppressive therapy likely do not have reflux related extraesophageal symptoms and alternative etiologies may be at play.
Finally, both investigators outlined the importance of neuromodulation in those whose symptoms may be due to “irritable larynx.” They emphasized the role of tricyclics as well as gabapentin as off label uses for patients who have normal reflux testing and continue to have chronic cough or globus sensation.
Michael F. Vaezi, MD, PhD, MSc, is an associate chief and a clinical director of the division of gastroenterology, hepatology, and nutrition and director of the Clinical Research and Center for Esophageal Disorders at Vanderbilt University, Nashville, Tenn. He reports consulting for Phathom, Ironwood, Diversatek, Isothrive, and Medtronic. These remarks were made during one of the AGA Postgraduate Course sessions held at DDW 2021.
Patients often present with symptoms that are not classic for reflux such as chronic cough, worsening asthma, sore throat, or globus.
In the upper GI section of the postgraduate course program, Rena Yadlapati, MD, and C. Prakash Gyawali, MD, MRCP, educated us about optimal strategies for diagnosis and treatment of this difficult group of patients. Dr. Gyawali reminded us of risk stratification of patients into those with high or low likelihood of reflux as contributing etiology for patients with suspected extraesophageal reflux. Dr. Yadlapti reviewed the utility of the HASBEER score in stratifying patients into these two risk categories. Patients with known reflux at baseline and/or if they have classic symptoms of reflux in addition to extraesophageal symptoms may be at higher likelihood of having abnormal esophageal acid exposure than those without classic heartburn and/or regurgitation. The low-risk group may then benefit from diagnostic testing off PPI therapy (either impedance/pH monitoring or wireless pH testing), whereas those in the high-risk group for reflux may undergo impedance pH testing on PPI therapy to ensure control of reflux while on therapy.
Dr. Yadlapati also updated the audience about lack of robust data to suggest clinical utility for oropharyngeal pH test or salivary pepsin assay testing. It was generally agreed on that the majority of patients who do not respond to aggressive acid suppressive therapy likely do not have reflux related extraesophageal symptoms and alternative etiologies may be at play.
Finally, both investigators outlined the importance of neuromodulation in those whose symptoms may be due to “irritable larynx.” They emphasized the role of tricyclics as well as gabapentin as off label uses for patients who have normal reflux testing and continue to have chronic cough or globus sensation.
Michael F. Vaezi, MD, PhD, MSc, is an associate chief and a clinical director of the division of gastroenterology, hepatology, and nutrition and director of the Clinical Research and Center for Esophageal Disorders at Vanderbilt University, Nashville, Tenn. He reports consulting for Phathom, Ironwood, Diversatek, Isothrive, and Medtronic. These remarks were made during one of the AGA Postgraduate Course sessions held at DDW 2021.
Patients often present with symptoms that are not classic for reflux such as chronic cough, worsening asthma, sore throat, or globus.
In the upper GI section of the postgraduate course program, Rena Yadlapati, MD, and C. Prakash Gyawali, MD, MRCP, educated us about optimal strategies for diagnosis and treatment of this difficult group of patients. Dr. Gyawali reminded us of risk stratification of patients into those with high or low likelihood of reflux as contributing etiology for patients with suspected extraesophageal reflux. Dr. Yadlapti reviewed the utility of the HASBEER score in stratifying patients into these two risk categories. Patients with known reflux at baseline and/or if they have classic symptoms of reflux in addition to extraesophageal symptoms may be at higher likelihood of having abnormal esophageal acid exposure than those without classic heartburn and/or regurgitation. The low-risk group may then benefit from diagnostic testing off PPI therapy (either impedance/pH monitoring or wireless pH testing), whereas those in the high-risk group for reflux may undergo impedance pH testing on PPI therapy to ensure control of reflux while on therapy.
Dr. Yadlapati also updated the audience about lack of robust data to suggest clinical utility for oropharyngeal pH test or salivary pepsin assay testing. It was generally agreed on that the majority of patients who do not respond to aggressive acid suppressive therapy likely do not have reflux related extraesophageal symptoms and alternative etiologies may be at play.
Finally, both investigators outlined the importance of neuromodulation in those whose symptoms may be due to “irritable larynx.” They emphasized the role of tricyclics as well as gabapentin as off label uses for patients who have normal reflux testing and continue to have chronic cough or globus sensation.
Michael F. Vaezi, MD, PhD, MSc, is an associate chief and a clinical director of the division of gastroenterology, hepatology, and nutrition and director of the Clinical Research and Center for Esophageal Disorders at Vanderbilt University, Nashville, Tenn. He reports consulting for Phathom, Ironwood, Diversatek, Isothrive, and Medtronic. These remarks were made during one of the AGA Postgraduate Course sessions held at DDW 2021.
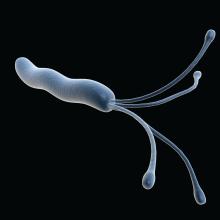
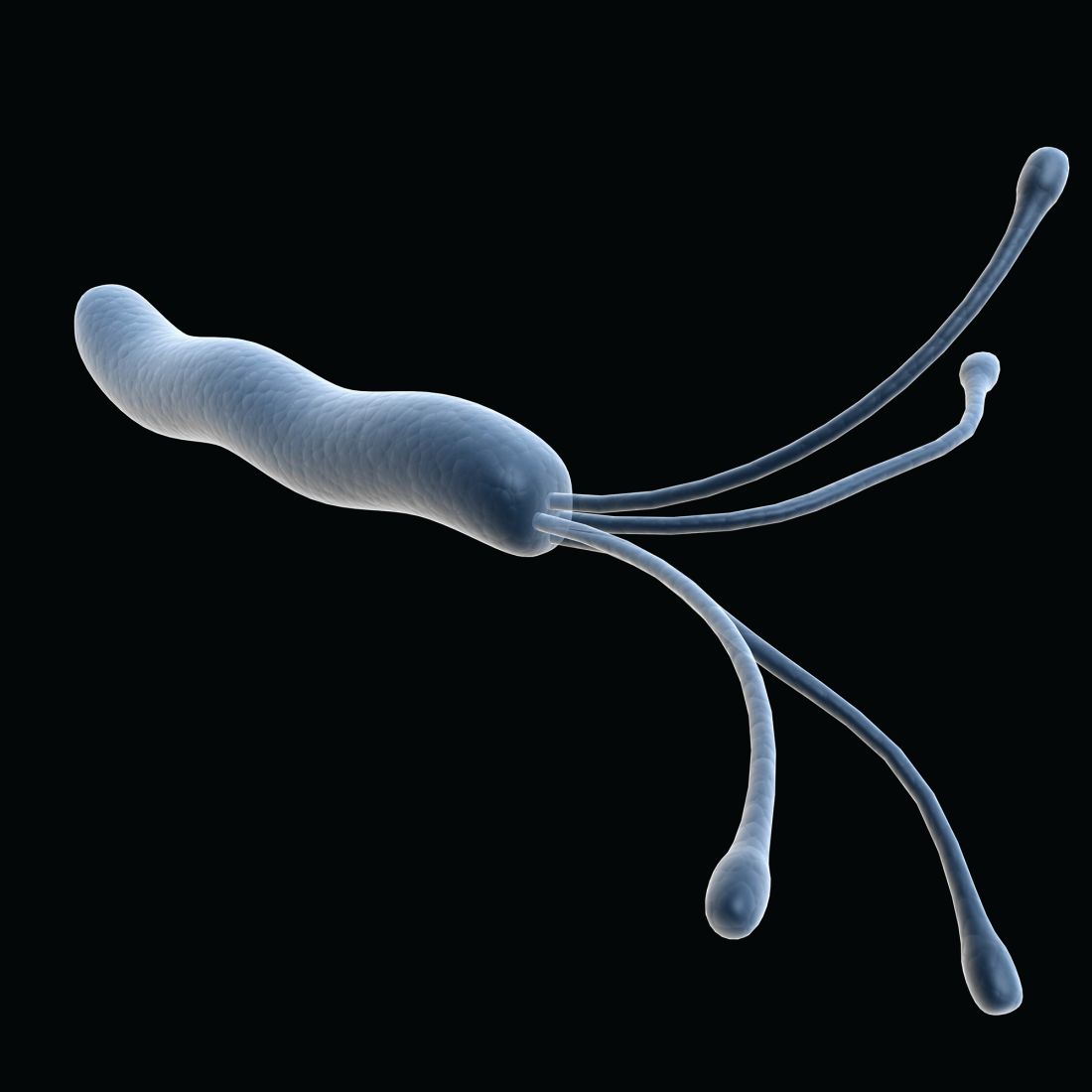
Gastric cancer: Family history–based H. pylori strategy would be cost effective
Testing for and treating Helicobacter pylori infection among individuals with a family history of gastric cancer could be a cost-effective strategy in the United States, according to a new model published in the journal Gastroenterology.
As many as 10% of gastric cancers aggregate within families, though just why this happens is unclear, according to Sheila D. Rustgi, MD, and colleagues. Shared environmental or genetic factors, or combinations of both, may be responsible. First-degree family history and H. pylori infection each raise gastric cancer risk by roughly 2.5-fold.
In the United States, universal screening for H. pylori infection is not currently recommended, but some studies have suggested a possible benefit in some high-risk populations. American Gastroenterological Association clinical practice guidelines suggest that a patient’s family history should be a factor when considering surveillance strategies for intestinal metaplasia.
Furthermore, a study by Il Ju Choi, MD, and colleagues in 2020 showed that H. pylori treatment with bismuth-based quadruple therapy reduced the risk of gastric cancer by 73% among individuals with a first-degree relative who had gastric cancer. The combination included a proton pump inhibitor, bismuth, metronidazole, and tetracycline for 10 days.
“We hypothesize that, given the dramatic reduction in GC demonstrated by Choi et al., that the screening strategy can be a cost-effective intervention,” Dr. Rustgi and colleagues wrote.
In the new study, the researchers used a Markov state-transition mode, employing a hypothetical cohort of 40-year-old U.S. men and women with a first-degree relative with gastric cancer. It simulated a follow-up period of 60 years or until death. The model assumed a 7-day treatment with triple therapy (proton pump inhibitor, clarithromycin, and amoxicillin) followed by a 14-day treatment period with quadruple therapy if needed. Although the model was analyzed from the U.S. perspective, the trial that informed the risk reduction was performed in a South Korean population.
No screening had a cost of $2,694.09 and resulted in 21.95 quality-adjusted life years (QALYs). 13C-Urea Breath Test screening had a cost of $2,105.28 and led to 22.37 QALYs. Stool antigen testing had a cost of $2,126.00 and yielded 22.30 QALYs.
In the no-screening group, an estimated 2.04% of patients would develop gastric cancer, and 1.82% would die of it. With screening, the frequency of gastric cancer dropped to 1.59%-1.65%, with a gastric cancer mortality rate of 1.41%-1.46%. Overall, screening was modeled to lead to a 19.1%-22.0% risk reduction.
The researchers validated their model by an assumption of an H. pylori infection rate of 100% and then compared the results of the model to the outcome of the study by Dr. Choi and colleagues. In the trial, there was a 55% reduction in gastric cancer among treated patients at a median of 9 years of follow-up. Those who had successful eradication of H. pylori had a 73% reduction. The new model estimated reductions from a testing and treatment strategy of 53.3%-64.5%.
The findings aren’t surprising, according to Joseph Jennings, MD, of the department of medicine at Georgetown University, Washington, and director of the Center for GI Bleeding at MedStar Georgetown University Hospital, who was not involved with the study. “Even eliminating one person getting gastric cancer, where they will then need major surgery, chemotherapy, all these very expensive interventions [is important],” said Dr. Jennings. “We have very efficient ways to test for these things that don’t involve endoscopy.”
One potential caveat to identifying and treating H. pylori infection is whether elimination of H. pylori may lead to some adverse effects. Some patients can experience increased acid reflux as a result, while others suffer no ill effects. “But when you’re dealing with the alternative, which is stomach cancer, those negatives would have to stack up really, really high to outweigh the positives of preventing a cancer that’s really hard to treat,” said Dr. Jennings.
Dr. Jennings pointed out that the model also projected testing and an intervention conducted in a South Korean population, and extrapolated it to a U.S. population, where the incidence of gastric cancer is lower. “There definitely are some questions about how well it would translate if applied to the general United States population,” said Dr. Jennings.
That question could prompt researchers to conduct a U.S.-based study modeled after the test and treat study in South Korea to see if the regimen produced similar results. The model should add weight to that argument, said Dr. Jennings: “This is raising the point that, at least from an intellectual level, it might be worth now designing the study to see if it works in our population,” said Dr. Jennings.
The authors and Dr. Jennings have no relevant financial disclosures.
Testing for and treating Helicobacter pylori infection among individuals with a family history of gastric cancer could be a cost-effective strategy in the United States, according to a new model published in the journal Gastroenterology.
As many as 10% of gastric cancers aggregate within families, though just why this happens is unclear, according to Sheila D. Rustgi, MD, and colleagues. Shared environmental or genetic factors, or combinations of both, may be responsible. First-degree family history and H. pylori infection each raise gastric cancer risk by roughly 2.5-fold.
In the United States, universal screening for H. pylori infection is not currently recommended, but some studies have suggested a possible benefit in some high-risk populations. American Gastroenterological Association clinical practice guidelines suggest that a patient’s family history should be a factor when considering surveillance strategies for intestinal metaplasia.
Furthermore, a study by Il Ju Choi, MD, and colleagues in 2020 showed that H. pylori treatment with bismuth-based quadruple therapy reduced the risk of gastric cancer by 73% among individuals with a first-degree relative who had gastric cancer. The combination included a proton pump inhibitor, bismuth, metronidazole, and tetracycline for 10 days.
“We hypothesize that, given the dramatic reduction in GC demonstrated by Choi et al., that the screening strategy can be a cost-effective intervention,” Dr. Rustgi and colleagues wrote.
In the new study, the researchers used a Markov state-transition mode, employing a hypothetical cohort of 40-year-old U.S. men and women with a first-degree relative with gastric cancer. It simulated a follow-up period of 60 years or until death. The model assumed a 7-day treatment with triple therapy (proton pump inhibitor, clarithromycin, and amoxicillin) followed by a 14-day treatment period with quadruple therapy if needed. Although the model was analyzed from the U.S. perspective, the trial that informed the risk reduction was performed in a South Korean population.
No screening had a cost of $2,694.09 and resulted in 21.95 quality-adjusted life years (QALYs). 13C-Urea Breath Test screening had a cost of $2,105.28 and led to 22.37 QALYs. Stool antigen testing had a cost of $2,126.00 and yielded 22.30 QALYs.
In the no-screening group, an estimated 2.04% of patients would develop gastric cancer, and 1.82% would die of it. With screening, the frequency of gastric cancer dropped to 1.59%-1.65%, with a gastric cancer mortality rate of 1.41%-1.46%. Overall, screening was modeled to lead to a 19.1%-22.0% risk reduction.
The researchers validated their model by an assumption of an H. pylori infection rate of 100% and then compared the results of the model to the outcome of the study by Dr. Choi and colleagues. In the trial, there was a 55% reduction in gastric cancer among treated patients at a median of 9 years of follow-up. Those who had successful eradication of H. pylori had a 73% reduction. The new model estimated reductions from a testing and treatment strategy of 53.3%-64.5%.
The findings aren’t surprising, according to Joseph Jennings, MD, of the department of medicine at Georgetown University, Washington, and director of the Center for GI Bleeding at MedStar Georgetown University Hospital, who was not involved with the study. “Even eliminating one person getting gastric cancer, where they will then need major surgery, chemotherapy, all these very expensive interventions [is important],” said Dr. Jennings. “We have very efficient ways to test for these things that don’t involve endoscopy.”
One potential caveat to identifying and treating H. pylori infection is whether elimination of H. pylori may lead to some adverse effects. Some patients can experience increased acid reflux as a result, while others suffer no ill effects. “But when you’re dealing with the alternative, which is stomach cancer, those negatives would have to stack up really, really high to outweigh the positives of preventing a cancer that’s really hard to treat,” said Dr. Jennings.
Dr. Jennings pointed out that the model also projected testing and an intervention conducted in a South Korean population, and extrapolated it to a U.S. population, where the incidence of gastric cancer is lower. “There definitely are some questions about how well it would translate if applied to the general United States population,” said Dr. Jennings.
That question could prompt researchers to conduct a U.S.-based study modeled after the test and treat study in South Korea to see if the regimen produced similar results. The model should add weight to that argument, said Dr. Jennings: “This is raising the point that, at least from an intellectual level, it might be worth now designing the study to see if it works in our population,” said Dr. Jennings.
The authors and Dr. Jennings have no relevant financial disclosures.
Testing for and treating Helicobacter pylori infection among individuals with a family history of gastric cancer could be a cost-effective strategy in the United States, according to a new model published in the journal Gastroenterology.
As many as 10% of gastric cancers aggregate within families, though just why this happens is unclear, according to Sheila D. Rustgi, MD, and colleagues. Shared environmental or genetic factors, or combinations of both, may be responsible. First-degree family history and H. pylori infection each raise gastric cancer risk by roughly 2.5-fold.
In the United States, universal screening for H. pylori infection is not currently recommended, but some studies have suggested a possible benefit in some high-risk populations. American Gastroenterological Association clinical practice guidelines suggest that a patient’s family history should be a factor when considering surveillance strategies for intestinal metaplasia.
Furthermore, a study by Il Ju Choi, MD, and colleagues in 2020 showed that H. pylori treatment with bismuth-based quadruple therapy reduced the risk of gastric cancer by 73% among individuals with a first-degree relative who had gastric cancer. The combination included a proton pump inhibitor, bismuth, metronidazole, and tetracycline for 10 days.
“We hypothesize that, given the dramatic reduction in GC demonstrated by Choi et al., that the screening strategy can be a cost-effective intervention,” Dr. Rustgi and colleagues wrote.
In the new study, the researchers used a Markov state-transition mode, employing a hypothetical cohort of 40-year-old U.S. men and women with a first-degree relative with gastric cancer. It simulated a follow-up period of 60 years or until death. The model assumed a 7-day treatment with triple therapy (proton pump inhibitor, clarithromycin, and amoxicillin) followed by a 14-day treatment period with quadruple therapy if needed. Although the model was analyzed from the U.S. perspective, the trial that informed the risk reduction was performed in a South Korean population.
No screening had a cost of $2,694.09 and resulted in 21.95 quality-adjusted life years (QALYs). 13C-Urea Breath Test screening had a cost of $2,105.28 and led to 22.37 QALYs. Stool antigen testing had a cost of $2,126.00 and yielded 22.30 QALYs.
In the no-screening group, an estimated 2.04% of patients would develop gastric cancer, and 1.82% would die of it. With screening, the frequency of gastric cancer dropped to 1.59%-1.65%, with a gastric cancer mortality rate of 1.41%-1.46%. Overall, screening was modeled to lead to a 19.1%-22.0% risk reduction.
The researchers validated their model by an assumption of an H. pylori infection rate of 100% and then compared the results of the model to the outcome of the study by Dr. Choi and colleagues. In the trial, there was a 55% reduction in gastric cancer among treated patients at a median of 9 years of follow-up. Those who had successful eradication of H. pylori had a 73% reduction. The new model estimated reductions from a testing and treatment strategy of 53.3%-64.5%.
The findings aren’t surprising, according to Joseph Jennings, MD, of the department of medicine at Georgetown University, Washington, and director of the Center for GI Bleeding at MedStar Georgetown University Hospital, who was not involved with the study. “Even eliminating one person getting gastric cancer, where they will then need major surgery, chemotherapy, all these very expensive interventions [is important],” said Dr. Jennings. “We have very efficient ways to test for these things that don’t involve endoscopy.”
One potential caveat to identifying and treating H. pylori infection is whether elimination of H. pylori may lead to some adverse effects. Some patients can experience increased acid reflux as a result, while others suffer no ill effects. “But when you’re dealing with the alternative, which is stomach cancer, those negatives would have to stack up really, really high to outweigh the positives of preventing a cancer that’s really hard to treat,” said Dr. Jennings.
Dr. Jennings pointed out that the model also projected testing and an intervention conducted in a South Korean population, and extrapolated it to a U.S. population, where the incidence of gastric cancer is lower. “There definitely are some questions about how well it would translate if applied to the general United States population,” said Dr. Jennings.
That question could prompt researchers to conduct a U.S.-based study modeled after the test and treat study in South Korea to see if the regimen produced similar results. The model should add weight to that argument, said Dr. Jennings: “This is raising the point that, at least from an intellectual level, it might be worth now designing the study to see if it works in our population,” said Dr. Jennings.
The authors and Dr. Jennings have no relevant financial disclosures.
FROM GASTROENTEROLOGY
Is Nissen fundoplication the best we can do?
As an esophagologist that does not perform fundoplication, LINX, or TIF, I find it difficult to debate the merits of one procedure over another based on my experience. In fact, I have always stated that it is difficult to assess a procedure or test that one has not used. That being said, maybe the fact that I have not performed these procedures makes me more objective and I can only use my experience with patients and the data to make the case that we need options beyond Nissen fundoplication.
The recent VA Randomized trial in refractory GERD published by Spechler and colleagues once again highlighted the fact that there are some patients that require a mechanical solution to reflux disease.1 In this study, the authors carefully defined a patient population with refractory GERD and showed that Nissen fundoplication was superior to medical management in patients who did not respond to proton pump inhibitors. However, of the 27 patients who underwent fundoplication, one patient had major complications which required a repeat operation and prolonged hospital stay. These findings highlight the main problem with Nissen fundoplication. Dr. Watson elegantly argued in his assertion during our debate that Nissen and fundoplication are not the same. In this position, he was noting the side effects associated with Nissen fundoplication,2 and he focused his argument on the comparison between a partial wrap versus LINX and TIF to level the playing field. On that note, I agree with Dr. Watson that a well-done partial fundoplication is a great option for patients with a mechanical problem.
Nonetheless, Redo operations have an escalating risk of severe debilitating consequences and we should do everything possible to reduce that risk.3 The LINX and the TIF procedure have data to support their effectiveness, and the initial studies a more favorable side effect profile.4,5 The ability to perform these procedures in patients with hiatal hernia and the fact that these approaches do not exclude the possibility of fundoplication in the future make them an attractive alternative.
In the end, more rigorous comparative studies should be performed to truly determine which approach is better. Although we have good surgical and medical options, we all recognize that they are not perfect and we should not settle on the current state of GERD management.
John E. Pandolfino, MD, MSCI, is the Hans Popper Professor of Medicine and Division Chief, Gastroenterology and Hepatology at Northwestern University, Chicago. He disclosed relationships with Ethicon/Johnson & Johnson, Endogastric Solutions, and Medtronic. These remarks were made during one of the AGA Postgraduate Course sessions held at DDW 2021.
References
1. Spechler SJ et al. N Engl J Med. 2019 Oct 17;381[16]:1513-23.
2. Yadlapati R et al. Am J Gastroenterol. 2018 Aug;113[8]:1137-47.
3. Singhal S et al. J Gastrointest Surg. 2018 Feb;22[2]:177-86.
4. Ganz RA et al. Clin Gastroenterol Hepatol. 2016 May;14(5):671-7.
Endosc Int Open. 2019 May;7(5):E647-E654
As an esophagologist that does not perform fundoplication, LINX, or TIF, I find it difficult to debate the merits of one procedure over another based on my experience. In fact, I have always stated that it is difficult to assess a procedure or test that one has not used. That being said, maybe the fact that I have not performed these procedures makes me more objective and I can only use my experience with patients and the data to make the case that we need options beyond Nissen fundoplication.
The recent VA Randomized trial in refractory GERD published by Spechler and colleagues once again highlighted the fact that there are some patients that require a mechanical solution to reflux disease.1 In this study, the authors carefully defined a patient population with refractory GERD and showed that Nissen fundoplication was superior to medical management in patients who did not respond to proton pump inhibitors. However, of the 27 patients who underwent fundoplication, one patient had major complications which required a repeat operation and prolonged hospital stay. These findings highlight the main problem with Nissen fundoplication. Dr. Watson elegantly argued in his assertion during our debate that Nissen and fundoplication are not the same. In this position, he was noting the side effects associated with Nissen fundoplication,2 and he focused his argument on the comparison between a partial wrap versus LINX and TIF to level the playing field. On that note, I agree with Dr. Watson that a well-done partial fundoplication is a great option for patients with a mechanical problem.
Nonetheless, Redo operations have an escalating risk of severe debilitating consequences and we should do everything possible to reduce that risk.3 The LINX and the TIF procedure have data to support their effectiveness, and the initial studies a more favorable side effect profile.4,5 The ability to perform these procedures in patients with hiatal hernia and the fact that these approaches do not exclude the possibility of fundoplication in the future make them an attractive alternative.
In the end, more rigorous comparative studies should be performed to truly determine which approach is better. Although we have good surgical and medical options, we all recognize that they are not perfect and we should not settle on the current state of GERD management.
John E. Pandolfino, MD, MSCI, is the Hans Popper Professor of Medicine and Division Chief, Gastroenterology and Hepatology at Northwestern University, Chicago. He disclosed relationships with Ethicon/Johnson & Johnson, Endogastric Solutions, and Medtronic. These remarks were made during one of the AGA Postgraduate Course sessions held at DDW 2021.
References
1. Spechler SJ et al. N Engl J Med. 2019 Oct 17;381[16]:1513-23.
2. Yadlapati R et al. Am J Gastroenterol. 2018 Aug;113[8]:1137-47.
3. Singhal S et al. J Gastrointest Surg. 2018 Feb;22[2]:177-86.
4. Ganz RA et al. Clin Gastroenterol Hepatol. 2016 May;14(5):671-7.
Endosc Int Open. 2019 May;7(5):E647-E654
As an esophagologist that does not perform fundoplication, LINX, or TIF, I find it difficult to debate the merits of one procedure over another based on my experience. In fact, I have always stated that it is difficult to assess a procedure or test that one has not used. That being said, maybe the fact that I have not performed these procedures makes me more objective and I can only use my experience with patients and the data to make the case that we need options beyond Nissen fundoplication.
The recent VA Randomized trial in refractory GERD published by Spechler and colleagues once again highlighted the fact that there are some patients that require a mechanical solution to reflux disease.1 In this study, the authors carefully defined a patient population with refractory GERD and showed that Nissen fundoplication was superior to medical management in patients who did not respond to proton pump inhibitors. However, of the 27 patients who underwent fundoplication, one patient had major complications which required a repeat operation and prolonged hospital stay. These findings highlight the main problem with Nissen fundoplication. Dr. Watson elegantly argued in his assertion during our debate that Nissen and fundoplication are not the same. In this position, he was noting the side effects associated with Nissen fundoplication,2 and he focused his argument on the comparison between a partial wrap versus LINX and TIF to level the playing field. On that note, I agree with Dr. Watson that a well-done partial fundoplication is a great option for patients with a mechanical problem.
Nonetheless, Redo operations have an escalating risk of severe debilitating consequences and we should do everything possible to reduce that risk.3 The LINX and the TIF procedure have data to support their effectiveness, and the initial studies a more favorable side effect profile.4,5 The ability to perform these procedures in patients with hiatal hernia and the fact that these approaches do not exclude the possibility of fundoplication in the future make them an attractive alternative.
In the end, more rigorous comparative studies should be performed to truly determine which approach is better. Although we have good surgical and medical options, we all recognize that they are not perfect and we should not settle on the current state of GERD management.
John E. Pandolfino, MD, MSCI, is the Hans Popper Professor of Medicine and Division Chief, Gastroenterology and Hepatology at Northwestern University, Chicago. He disclosed relationships with Ethicon/Johnson & Johnson, Endogastric Solutions, and Medtronic. These remarks were made during one of the AGA Postgraduate Course sessions held at DDW 2021.
References
1. Spechler SJ et al. N Engl J Med. 2019 Oct 17;381[16]:1513-23.
2. Yadlapati R et al. Am J Gastroenterol. 2018 Aug;113[8]:1137-47.
3. Singhal S et al. J Gastrointest Surg. 2018 Feb;22[2]:177-86.
4. Ganz RA et al. Clin Gastroenterol Hepatol. 2016 May;14(5):671-7.
Endosc Int Open. 2019 May;7(5):E647-E654
Most stent misdeployments in EUS-GE are manageable
Most instances of stent misdeployment in cases of endoscopic ultrasound–guided gastroenterostomy (EUS-GE) can be managed endoscopically, based on data from 16 tertiary care centers in the United States and Europe.
EUS-GE provides a viable alternative to traditional surgical gastroenterostomy and stent placement for patients with gastric outlet obstruction (GOO), but the potential for stent misdeployment has limited adoption of the procedure because it remains the most common cause of technical failures and adverse events, Bachir Ghandour, MD, of Johns Hopkins University, Baltimore, and colleagues wrote.
However, data on outcomes and management of stent misdeployment during EUS-GE are limited, and the researchers hypothesized that most stent misdeployments could be managed endoscopically.
In a retrospective study published in Gastrointestinal Endoscopy, the researchers reviewed data from 467 EUS-GE procedures performed for gastric outlet obstruction between March 2015 and December 2020 at eight centers in the United States and eight in Europe. The primary outcome was the rate and severity of stent misdeployment.
Stent misdeployment occurred in 46 patients (9.9%). Of these, 73.2% occurred during the operators’ first 13 cases.
The researchers created a classification system of stent misdeployment according to type, depending on which flange was misdeployed.
Type I was the most common, and occurred in 29 patients; this type was defined as “the deployment of the distal flange in the peritoneum and proximal flange in the stomach without evidence of a resulting enterotomy”; type II (14 patients) was defined as “the deployment of the distal flange in the peritoneum and proximal flange in the stomach despite an enterotomy (i.e., visual confirmation of stent having penetrated targeted small bowel, under EUS or fluoroscopy, but migrated out on deployment)”; type III (1 patient) was defined as “the deployment of the distal flange in the small bowel and proximal flange in the peritoneum”; and type IV (2 patients) was defined as “the deployment of the distal flange in the colon and proximal flange in the stomach resulting in a gastrocolic anastomosis,” the researchers wrote.
The researchers also classified the stent misdeployment in terms of severity as mild (28 patients), moderate (11 patients), severe (6 cases) or fatal (1 case) based on the American Society for Gastrointestinal Endoscopy lexicon.
Overall, type I was significantly more likely to be mild in severity, compared with type II (75.9% vs. 42.9%; P = .04), although the rate of surgical repair was similar between these two types (10.3% vs. 7.1%). Rates of ICU admission were approximately 7% in patients with type I and type II stent misdeployments, and the median postprocedural stay was 4 days for these two groups.
Same-session salvage management of GOO was achieved by EUS/endoscopic-GE in 24 patients, duodenal stent placement in 6 patients, duodenal dilation in 1 patient, and gastroenterostomy with natural orifice transluminal endoscopic surgery in 3 patients. Of the remaining 12 patients, GOO was managed with subsequent EUS-GE in 6 patients and surgical GI in 6 patients.
The study findings were limited by several factors including the retrospective design and inclusion of a time period that encompassed changes and improvements in the EUS-GE, the researchers noted. The small sample size of type III and IV stent misdeployments prohibited comparison with other types.
However, the cohort size was relatively large, compared with previous studies, and included a range of centers and countries with different strategies for managing stent misdeployments. Given the steep learning curve for EUS-GE, the study findings may help endoscopists better understand the implications and potential consequences of stent misdeployment by classifying the misdeployments into types. “We believe that such a classification or categorization of the different types is important because patient outcomes vary depending on the specific [stent misdeployment] subtype and site of injury. Such a classification will also be very helpful for future research by standardizing the terminology,” the researchers said.
“Although [stent misdeployment] is not infrequent during EUS-GE, with a rate of approximately 10%, the majority of cases are mild in severity and can be managed or repaired endoscopically without ill consequences,” they concluded. “Surgical intervention is required in less than 11% of the cases.”
Data support safe stent use in GI disease
“The lines continue to be blurred between surgical and endoscopic management of gastrointestinal disease, especially with a rise in therapeutic EUS,” Gyanprakash A. Ketwaroo, MD, of Baylor College of Medicine, Houston, said in an interview.
“Stent misdeployment has been commonly reported during EUS-GE and may limit uptake of this more technically challenging procedure,” Dr. Ketwaroo said. “A comprehensive assessment of stent misdeployment, with suggestions for management and a classification system that predicts outcomes, can help practitioners to more confidently perform this procedure.”
Risks associated with misdeployed stents include “inability to perform the endoscopic management of gastric outlet obstruction, as well as adverse events such as peritonitis,” said Dr. Ketwaroo. He noted that, in most cases, the defect was closed and same-session salvage was performed, primarily by repeat EUS-GE.
Dr. Ketwaroo highlighted one challenge to endoscopic management of stent misdeployment. “If the proximal flange is deployed/slips into peritoneum (type III by currently proposed classification system), it can be more difficult to retrieve the stent,” but “this complication was treated with surgery, and it was very rare – only one case of this in the study,” he explained. “This is a large retrospective multicenter study, which adds validity to the generalizability of the study.” However, prospective studies will be needed as EUS-GE is more widely adopted, he added.
The study received no outside funding. Lead author Dr. Ghandour had no financial conflicts to disclose. Other authors disclosed industry relationships, such as consulting for Boston Scientific, Apollo, Olympus America, Medtronic, and GI Supply. Dr. Ketwaroo had no financial conflicts to disclose, but serves as a member of the GI & Hepatology News editorial advisory board.
Most instances of stent misdeployment in cases of endoscopic ultrasound–guided gastroenterostomy (EUS-GE) can be managed endoscopically, based on data from 16 tertiary care centers in the United States and Europe.
EUS-GE provides a viable alternative to traditional surgical gastroenterostomy and stent placement for patients with gastric outlet obstruction (GOO), but the potential for stent misdeployment has limited adoption of the procedure because it remains the most common cause of technical failures and adverse events, Bachir Ghandour, MD, of Johns Hopkins University, Baltimore, and colleagues wrote.
However, data on outcomes and management of stent misdeployment during EUS-GE are limited, and the researchers hypothesized that most stent misdeployments could be managed endoscopically.
In a retrospective study published in Gastrointestinal Endoscopy, the researchers reviewed data from 467 EUS-GE procedures performed for gastric outlet obstruction between March 2015 and December 2020 at eight centers in the United States and eight in Europe. The primary outcome was the rate and severity of stent misdeployment.
Stent misdeployment occurred in 46 patients (9.9%). Of these, 73.2% occurred during the operators’ first 13 cases.
The researchers created a classification system of stent misdeployment according to type, depending on which flange was misdeployed.
Type I was the most common, and occurred in 29 patients; this type was defined as “the deployment of the distal flange in the peritoneum and proximal flange in the stomach without evidence of a resulting enterotomy”; type II (14 patients) was defined as “the deployment of the distal flange in the peritoneum and proximal flange in the stomach despite an enterotomy (i.e., visual confirmation of stent having penetrated targeted small bowel, under EUS or fluoroscopy, but migrated out on deployment)”; type III (1 patient) was defined as “the deployment of the distal flange in the small bowel and proximal flange in the peritoneum”; and type IV (2 patients) was defined as “the deployment of the distal flange in the colon and proximal flange in the stomach resulting in a gastrocolic anastomosis,” the researchers wrote.
The researchers also classified the stent misdeployment in terms of severity as mild (28 patients), moderate (11 patients), severe (6 cases) or fatal (1 case) based on the American Society for Gastrointestinal Endoscopy lexicon.
Overall, type I was significantly more likely to be mild in severity, compared with type II (75.9% vs. 42.9%; P = .04), although the rate of surgical repair was similar between these two types (10.3% vs. 7.1%). Rates of ICU admission were approximately 7% in patients with type I and type II stent misdeployments, and the median postprocedural stay was 4 days for these two groups.
Same-session salvage management of GOO was achieved by EUS/endoscopic-GE in 24 patients, duodenal stent placement in 6 patients, duodenal dilation in 1 patient, and gastroenterostomy with natural orifice transluminal endoscopic surgery in 3 patients. Of the remaining 12 patients, GOO was managed with subsequent EUS-GE in 6 patients and surgical GI in 6 patients.
The study findings were limited by several factors including the retrospective design and inclusion of a time period that encompassed changes and improvements in the EUS-GE, the researchers noted. The small sample size of type III and IV stent misdeployments prohibited comparison with other types.
However, the cohort size was relatively large, compared with previous studies, and included a range of centers and countries with different strategies for managing stent misdeployments. Given the steep learning curve for EUS-GE, the study findings may help endoscopists better understand the implications and potential consequences of stent misdeployment by classifying the misdeployments into types. “We believe that such a classification or categorization of the different types is important because patient outcomes vary depending on the specific [stent misdeployment] subtype and site of injury. Such a classification will also be very helpful for future research by standardizing the terminology,” the researchers said.
“Although [stent misdeployment] is not infrequent during EUS-GE, with a rate of approximately 10%, the majority of cases are mild in severity and can be managed or repaired endoscopically without ill consequences,” they concluded. “Surgical intervention is required in less than 11% of the cases.”
Data support safe stent use in GI disease
“The lines continue to be blurred between surgical and endoscopic management of gastrointestinal disease, especially with a rise in therapeutic EUS,” Gyanprakash A. Ketwaroo, MD, of Baylor College of Medicine, Houston, said in an interview.
“Stent misdeployment has been commonly reported during EUS-GE and may limit uptake of this more technically challenging procedure,” Dr. Ketwaroo said. “A comprehensive assessment of stent misdeployment, with suggestions for management and a classification system that predicts outcomes, can help practitioners to more confidently perform this procedure.”
Risks associated with misdeployed stents include “inability to perform the endoscopic management of gastric outlet obstruction, as well as adverse events such as peritonitis,” said Dr. Ketwaroo. He noted that, in most cases, the defect was closed and same-session salvage was performed, primarily by repeat EUS-GE.
Dr. Ketwaroo highlighted one challenge to endoscopic management of stent misdeployment. “If the proximal flange is deployed/slips into peritoneum (type III by currently proposed classification system), it can be more difficult to retrieve the stent,” but “this complication was treated with surgery, and it was very rare – only one case of this in the study,” he explained. “This is a large retrospective multicenter study, which adds validity to the generalizability of the study.” However, prospective studies will be needed as EUS-GE is more widely adopted, he added.
The study received no outside funding. Lead author Dr. Ghandour had no financial conflicts to disclose. Other authors disclosed industry relationships, such as consulting for Boston Scientific, Apollo, Olympus America, Medtronic, and GI Supply. Dr. Ketwaroo had no financial conflicts to disclose, but serves as a member of the GI & Hepatology News editorial advisory board.
Most instances of stent misdeployment in cases of endoscopic ultrasound–guided gastroenterostomy (EUS-GE) can be managed endoscopically, based on data from 16 tertiary care centers in the United States and Europe.
EUS-GE provides a viable alternative to traditional surgical gastroenterostomy and stent placement for patients with gastric outlet obstruction (GOO), but the potential for stent misdeployment has limited adoption of the procedure because it remains the most common cause of technical failures and adverse events, Bachir Ghandour, MD, of Johns Hopkins University, Baltimore, and colleagues wrote.
However, data on outcomes and management of stent misdeployment during EUS-GE are limited, and the researchers hypothesized that most stent misdeployments could be managed endoscopically.
In a retrospective study published in Gastrointestinal Endoscopy, the researchers reviewed data from 467 EUS-GE procedures performed for gastric outlet obstruction between March 2015 and December 2020 at eight centers in the United States and eight in Europe. The primary outcome was the rate and severity of stent misdeployment.
Stent misdeployment occurred in 46 patients (9.9%). Of these, 73.2% occurred during the operators’ first 13 cases.
The researchers created a classification system of stent misdeployment according to type, depending on which flange was misdeployed.
Type I was the most common, and occurred in 29 patients; this type was defined as “the deployment of the distal flange in the peritoneum and proximal flange in the stomach without evidence of a resulting enterotomy”; type II (14 patients) was defined as “the deployment of the distal flange in the peritoneum and proximal flange in the stomach despite an enterotomy (i.e., visual confirmation of stent having penetrated targeted small bowel, under EUS or fluoroscopy, but migrated out on deployment)”; type III (1 patient) was defined as “the deployment of the distal flange in the small bowel and proximal flange in the peritoneum”; and type IV (2 patients) was defined as “the deployment of the distal flange in the colon and proximal flange in the stomach resulting in a gastrocolic anastomosis,” the researchers wrote.
The researchers also classified the stent misdeployment in terms of severity as mild (28 patients), moderate (11 patients), severe (6 cases) or fatal (1 case) based on the American Society for Gastrointestinal Endoscopy lexicon.
Overall, type I was significantly more likely to be mild in severity, compared with type II (75.9% vs. 42.9%; P = .04), although the rate of surgical repair was similar between these two types (10.3% vs. 7.1%). Rates of ICU admission were approximately 7% in patients with type I and type II stent misdeployments, and the median postprocedural stay was 4 days for these two groups.
Same-session salvage management of GOO was achieved by EUS/endoscopic-GE in 24 patients, duodenal stent placement in 6 patients, duodenal dilation in 1 patient, and gastroenterostomy with natural orifice transluminal endoscopic surgery in 3 patients. Of the remaining 12 patients, GOO was managed with subsequent EUS-GE in 6 patients and surgical GI in 6 patients.
The study findings were limited by several factors including the retrospective design and inclusion of a time period that encompassed changes and improvements in the EUS-GE, the researchers noted. The small sample size of type III and IV stent misdeployments prohibited comparison with other types.
However, the cohort size was relatively large, compared with previous studies, and included a range of centers and countries with different strategies for managing stent misdeployments. Given the steep learning curve for EUS-GE, the study findings may help endoscopists better understand the implications and potential consequences of stent misdeployment by classifying the misdeployments into types. “We believe that such a classification or categorization of the different types is important because patient outcomes vary depending on the specific [stent misdeployment] subtype and site of injury. Such a classification will also be very helpful for future research by standardizing the terminology,” the researchers said.
“Although [stent misdeployment] is not infrequent during EUS-GE, with a rate of approximately 10%, the majority of cases are mild in severity and can be managed or repaired endoscopically without ill consequences,” they concluded. “Surgical intervention is required in less than 11% of the cases.”
Data support safe stent use in GI disease
“The lines continue to be blurred between surgical and endoscopic management of gastrointestinal disease, especially with a rise in therapeutic EUS,” Gyanprakash A. Ketwaroo, MD, of Baylor College of Medicine, Houston, said in an interview.
“Stent misdeployment has been commonly reported during EUS-GE and may limit uptake of this more technically challenging procedure,” Dr. Ketwaroo said. “A comprehensive assessment of stent misdeployment, with suggestions for management and a classification system that predicts outcomes, can help practitioners to more confidently perform this procedure.”
Risks associated with misdeployed stents include “inability to perform the endoscopic management of gastric outlet obstruction, as well as adverse events such as peritonitis,” said Dr. Ketwaroo. He noted that, in most cases, the defect was closed and same-session salvage was performed, primarily by repeat EUS-GE.
Dr. Ketwaroo highlighted one challenge to endoscopic management of stent misdeployment. “If the proximal flange is deployed/slips into peritoneum (type III by currently proposed classification system), it can be more difficult to retrieve the stent,” but “this complication was treated with surgery, and it was very rare – only one case of this in the study,” he explained. “This is a large retrospective multicenter study, which adds validity to the generalizability of the study.” However, prospective studies will be needed as EUS-GE is more widely adopted, he added.
The study received no outside funding. Lead author Dr. Ghandour had no financial conflicts to disclose. Other authors disclosed industry relationships, such as consulting for Boston Scientific, Apollo, Olympus America, Medtronic, and GI Supply. Dr. Ketwaroo had no financial conflicts to disclose, but serves as a member of the GI & Hepatology News editorial advisory board.
FROM GASTROINTESTINAL ENDOSCOPY
Prebiotic in development shows promise for reducing GERD symptoms
A prebiotic therapy in development significantly reduced the number of days per month that people with gastroesophageal reflux disease (GERD) experienced heartburn.
The prebiotic treatment, maltosyl-isomalto-oligosaccharides (MIMO, ISOT-101), under development by ISOThrive, was also associated with reduced symptom severity and improved quality of life, John Selling, MD, chief medical officer at ISOThrive, said during the presentation of his study at the virtual Digestive Disease Week (DDW) 2021.
ISOT-101 is a nondigestible, nonabsorbable prebiotic carbohydrate produced by bacterial fermentation of sucrose and maltose. It was “possibly a staple of the bacterial diet that was present in the human diet during the past 10,000 years,” Dr. Selling said. He is a clinical associate professor of medicine and gastroenterology at Stanford (Calif.) University.
The prebiotic, however, “has been absent in our diet for about 50 to 100 years, driven by changes in agriculture, food production, food preservation, and dietary preferences,” he added.
Acid suppression treatments, such as proton pump inhibitors (PPIs), have long been a staple of treating GERD. However, about 40% of people taking PPIs still have symptoms, Dr. Selling said. He noted that there are concerns about the health risks associated with long-term PPI use.
A prebiotic could work because the distal esophageal microbiome in people with GERD “differs greatly” from that of healthy persons, Dr. Selling said. The prebiotic could help reduce an abnormal increase in gram-negative bacteria in these patients, for example. These bacterial strains express lipopolysaccharides on their outer cell membranes, which, in turn, alter cytokine signaling. This mechanism could lead to the hyperinflammatory state associated with GERD.
Dr. Selling and colleagues hypothesized that this treatment could help resolve GERD symptoms in two ways. The prebiotic could selectively feed the beneficial gram-positive bacteria in the distal esophagus, thereby helping to restore a healthy balance of bacteria. ISOT-101 could also produce bacteriocins that help kill the harmful gram-negative bacteria and control inflammation.
To assess the efficacy and tolerability of ISOT-101, Dr. Selling and colleagues plan to evaluate use of the agent in 110 people with GERD. The data presented at this year’s DDW are based on the first 44 participants to complete the study protocol.
Participants had to have active symptoms four or more days a week. They verbally reported symptoms to investigators and completed a daily ReQuest validated GERD symptom questionnaire.
After a week of baseline screening, participants consumed about a quarter teaspoon of ISOT-101 as the last substance swallowed before bed every night. The investigators asked participants to rate their GI symptoms, general well-being including any sleep disturbances, and quality of life on the Short Form 36 (SF-36) health survey. Participants also recorded use of any other medications during the 4-week study.
“I thought this was a very interesting study, as it proposes an alternative approach to manage patients with GERD,” Richa Shukla, MD, who was not affiliated with the research, said in an interview when asked to comment. “We see many patients with typical GERD symptoms who do not respond to PPI therapy, and perhaps considering an alternative cause and treatment may help with these patients.”
Dr. Shukla shared a couple of caveats. “This is a relatively small study, and it has not yet completed its enrollment target, so it will be helpful to see what the results are with the full study.” Also, it would be useful to know how many participants also took a PPI during the study, she said.
“Essentially, a lot remains unknown, but the study holds promise for patients,” added Dr. Shukla, assistant professor in the section of gastroenterology and hepatology at Baylor College of Medicine, Houston. “I think there is a lot of interest in the microbiome and how modulating it can impact inflammatory conditions.”
Key findings
The increase in heartburn-free days translated to more than eight additional days a month in which patients had no complaints of acid or heartburn. The difference from baseline was statistically significant (P < .001).
About two-thirds (66%) of participants were classified as “strong responders” to treatment, meaning they experienced an improvement of >50% in their ReQuest symptom scores over the 4 weeks. Again, the difference compared to baseline was statistically significant (P < .001).
The researchers also reported statistically significant improvements in quality-of-life indicators, such as well-being and sleep (P < .001).
The primary endpoint of the study was tolerability. The prebiotic was defined as tolerable if the ReQuest symptom scores and SF-36 scores remained constant or improved by the fourth week. ReQuest symptom scores improved for 89% of participants.
Two participants experienced nausea. No other adverse events related to ISOT-101 were reported. For five participants, ReQuest GI subscores worsened over time. For four participants, ReQuest total symptom scores worsened over time; that score represents a sum of GI and general well-being scores.
Unanswered questions
Inflammation in GERD is likely due to bacterial dysbiosis and acid-induced injury, Dr. Selling said.
If development of the prebiotic continues successfully, it could represent a paradigm shift in this clinical area, he said. “It suggests moving from acid reduction to also reducing dysbiosis as a treatment modality.”
But it remains unclear whether ISOT-101 would be indicated as monotherapy or for use in combination with other therapies for GERD.
Another unanswered question is whether the agent could be used to treat progressive disease. “This type of bacterial dysbiosis remains throughout the disease progression, from GERD to Barrett’s esophagus to esophageal adenocarcinoma,” Dr. Selling said.
The investigators reported that further controlled studies are forthcoming.
Dr. Selling is a co-founder and chief medical officer at ISOThrive. Dr. Shukla has disclosed no relevant financial relationships. David Johnson, MD, one of the authors of the abstract, is an advisor and contributor to Medscape.
A version of this article first appeared on Medscape.com.
A prebiotic therapy in development significantly reduced the number of days per month that people with gastroesophageal reflux disease (GERD) experienced heartburn.
The prebiotic treatment, maltosyl-isomalto-oligosaccharides (MIMO, ISOT-101), under development by ISOThrive, was also associated with reduced symptom severity and improved quality of life, John Selling, MD, chief medical officer at ISOThrive, said during the presentation of his study at the virtual Digestive Disease Week (DDW) 2021.
ISOT-101 is a nondigestible, nonabsorbable prebiotic carbohydrate produced by bacterial fermentation of sucrose and maltose. It was “possibly a staple of the bacterial diet that was present in the human diet during the past 10,000 years,” Dr. Selling said. He is a clinical associate professor of medicine and gastroenterology at Stanford (Calif.) University.
The prebiotic, however, “has been absent in our diet for about 50 to 100 years, driven by changes in agriculture, food production, food preservation, and dietary preferences,” he added.
Acid suppression treatments, such as proton pump inhibitors (PPIs), have long been a staple of treating GERD. However, about 40% of people taking PPIs still have symptoms, Dr. Selling said. He noted that there are concerns about the health risks associated with long-term PPI use.
A prebiotic could work because the distal esophageal microbiome in people with GERD “differs greatly” from that of healthy persons, Dr. Selling said. The prebiotic could help reduce an abnormal increase in gram-negative bacteria in these patients, for example. These bacterial strains express lipopolysaccharides on their outer cell membranes, which, in turn, alter cytokine signaling. This mechanism could lead to the hyperinflammatory state associated with GERD.
Dr. Selling and colleagues hypothesized that this treatment could help resolve GERD symptoms in two ways. The prebiotic could selectively feed the beneficial gram-positive bacteria in the distal esophagus, thereby helping to restore a healthy balance of bacteria. ISOT-101 could also produce bacteriocins that help kill the harmful gram-negative bacteria and control inflammation.
To assess the efficacy and tolerability of ISOT-101, Dr. Selling and colleagues plan to evaluate use of the agent in 110 people with GERD. The data presented at this year’s DDW are based on the first 44 participants to complete the study protocol.
Participants had to have active symptoms four or more days a week. They verbally reported symptoms to investigators and completed a daily ReQuest validated GERD symptom questionnaire.
After a week of baseline screening, participants consumed about a quarter teaspoon of ISOT-101 as the last substance swallowed before bed every night. The investigators asked participants to rate their GI symptoms, general well-being including any sleep disturbances, and quality of life on the Short Form 36 (SF-36) health survey. Participants also recorded use of any other medications during the 4-week study.
“I thought this was a very interesting study, as it proposes an alternative approach to manage patients with GERD,” Richa Shukla, MD, who was not affiliated with the research, said in an interview when asked to comment. “We see many patients with typical GERD symptoms who do not respond to PPI therapy, and perhaps considering an alternative cause and treatment may help with these patients.”
Dr. Shukla shared a couple of caveats. “This is a relatively small study, and it has not yet completed its enrollment target, so it will be helpful to see what the results are with the full study.” Also, it would be useful to know how many participants also took a PPI during the study, she said.
“Essentially, a lot remains unknown, but the study holds promise for patients,” added Dr. Shukla, assistant professor in the section of gastroenterology and hepatology at Baylor College of Medicine, Houston. “I think there is a lot of interest in the microbiome and how modulating it can impact inflammatory conditions.”
Key findings
The increase in heartburn-free days translated to more than eight additional days a month in which patients had no complaints of acid or heartburn. The difference from baseline was statistically significant (P < .001).
About two-thirds (66%) of participants were classified as “strong responders” to treatment, meaning they experienced an improvement of >50% in their ReQuest symptom scores over the 4 weeks. Again, the difference compared to baseline was statistically significant (P < .001).
The researchers also reported statistically significant improvements in quality-of-life indicators, such as well-being and sleep (P < .001).
The primary endpoint of the study was tolerability. The prebiotic was defined as tolerable if the ReQuest symptom scores and SF-36 scores remained constant or improved by the fourth week. ReQuest symptom scores improved for 89% of participants.
Two participants experienced nausea. No other adverse events related to ISOT-101 were reported. For five participants, ReQuest GI subscores worsened over time. For four participants, ReQuest total symptom scores worsened over time; that score represents a sum of GI and general well-being scores.
Unanswered questions
Inflammation in GERD is likely due to bacterial dysbiosis and acid-induced injury, Dr. Selling said.
If development of the prebiotic continues successfully, it could represent a paradigm shift in this clinical area, he said. “It suggests moving from acid reduction to also reducing dysbiosis as a treatment modality.”
But it remains unclear whether ISOT-101 would be indicated as monotherapy or for use in combination with other therapies for GERD.
Another unanswered question is whether the agent could be used to treat progressive disease. “This type of bacterial dysbiosis remains throughout the disease progression, from GERD to Barrett’s esophagus to esophageal adenocarcinoma,” Dr. Selling said.
The investigators reported that further controlled studies are forthcoming.
Dr. Selling is a co-founder and chief medical officer at ISOThrive. Dr. Shukla has disclosed no relevant financial relationships. David Johnson, MD, one of the authors of the abstract, is an advisor and contributor to Medscape.
A version of this article first appeared on Medscape.com.
A prebiotic therapy in development significantly reduced the number of days per month that people with gastroesophageal reflux disease (GERD) experienced heartburn.
The prebiotic treatment, maltosyl-isomalto-oligosaccharides (MIMO, ISOT-101), under development by ISOThrive, was also associated with reduced symptom severity and improved quality of life, John Selling, MD, chief medical officer at ISOThrive, said during the presentation of his study at the virtual Digestive Disease Week (DDW) 2021.
ISOT-101 is a nondigestible, nonabsorbable prebiotic carbohydrate produced by bacterial fermentation of sucrose and maltose. It was “possibly a staple of the bacterial diet that was present in the human diet during the past 10,000 years,” Dr. Selling said. He is a clinical associate professor of medicine and gastroenterology at Stanford (Calif.) University.
The prebiotic, however, “has been absent in our diet for about 50 to 100 years, driven by changes in agriculture, food production, food preservation, and dietary preferences,” he added.
Acid suppression treatments, such as proton pump inhibitors (PPIs), have long been a staple of treating GERD. However, about 40% of people taking PPIs still have symptoms, Dr. Selling said. He noted that there are concerns about the health risks associated with long-term PPI use.
A prebiotic could work because the distal esophageal microbiome in people with GERD “differs greatly” from that of healthy persons, Dr. Selling said. The prebiotic could help reduce an abnormal increase in gram-negative bacteria in these patients, for example. These bacterial strains express lipopolysaccharides on their outer cell membranes, which, in turn, alter cytokine signaling. This mechanism could lead to the hyperinflammatory state associated with GERD.
Dr. Selling and colleagues hypothesized that this treatment could help resolve GERD symptoms in two ways. The prebiotic could selectively feed the beneficial gram-positive bacteria in the distal esophagus, thereby helping to restore a healthy balance of bacteria. ISOT-101 could also produce bacteriocins that help kill the harmful gram-negative bacteria and control inflammation.
To assess the efficacy and tolerability of ISOT-101, Dr. Selling and colleagues plan to evaluate use of the agent in 110 people with GERD. The data presented at this year’s DDW are based on the first 44 participants to complete the study protocol.
Participants had to have active symptoms four or more days a week. They verbally reported symptoms to investigators and completed a daily ReQuest validated GERD symptom questionnaire.
After a week of baseline screening, participants consumed about a quarter teaspoon of ISOT-101 as the last substance swallowed before bed every night. The investigators asked participants to rate their GI symptoms, general well-being including any sleep disturbances, and quality of life on the Short Form 36 (SF-36) health survey. Participants also recorded use of any other medications during the 4-week study.
“I thought this was a very interesting study, as it proposes an alternative approach to manage patients with GERD,” Richa Shukla, MD, who was not affiliated with the research, said in an interview when asked to comment. “We see many patients with typical GERD symptoms who do not respond to PPI therapy, and perhaps considering an alternative cause and treatment may help with these patients.”
Dr. Shukla shared a couple of caveats. “This is a relatively small study, and it has not yet completed its enrollment target, so it will be helpful to see what the results are with the full study.” Also, it would be useful to know how many participants also took a PPI during the study, she said.
“Essentially, a lot remains unknown, but the study holds promise for patients,” added Dr. Shukla, assistant professor in the section of gastroenterology and hepatology at Baylor College of Medicine, Houston. “I think there is a lot of interest in the microbiome and how modulating it can impact inflammatory conditions.”
Key findings
The increase in heartburn-free days translated to more than eight additional days a month in which patients had no complaints of acid or heartburn. The difference from baseline was statistically significant (P < .001).
About two-thirds (66%) of participants were classified as “strong responders” to treatment, meaning they experienced an improvement of >50% in their ReQuest symptom scores over the 4 weeks. Again, the difference compared to baseline was statistically significant (P < .001).
The researchers also reported statistically significant improvements in quality-of-life indicators, such as well-being and sleep (P < .001).
The primary endpoint of the study was tolerability. The prebiotic was defined as tolerable if the ReQuest symptom scores and SF-36 scores remained constant or improved by the fourth week. ReQuest symptom scores improved for 89% of participants.
Two participants experienced nausea. No other adverse events related to ISOT-101 were reported. For five participants, ReQuest GI subscores worsened over time. For four participants, ReQuest total symptom scores worsened over time; that score represents a sum of GI and general well-being scores.
Unanswered questions
Inflammation in GERD is likely due to bacterial dysbiosis and acid-induced injury, Dr. Selling said.
If development of the prebiotic continues successfully, it could represent a paradigm shift in this clinical area, he said. “It suggests moving from acid reduction to also reducing dysbiosis as a treatment modality.”
But it remains unclear whether ISOT-101 would be indicated as monotherapy or for use in combination with other therapies for GERD.
Another unanswered question is whether the agent could be used to treat progressive disease. “This type of bacterial dysbiosis remains throughout the disease progression, from GERD to Barrett’s esophagus to esophageal adenocarcinoma,” Dr. Selling said.
The investigators reported that further controlled studies are forthcoming.
Dr. Selling is a co-founder and chief medical officer at ISOThrive. Dr. Shukla has disclosed no relevant financial relationships. David Johnson, MD, one of the authors of the abstract, is an advisor and contributor to Medscape.
A version of this article first appeared on Medscape.com.
Upper GI bleed guidelines say endoscopy within 24 hours of bleed
Updated guidelines from the American College of Gastroenterology address upper gastrointestinal and ulcer bleeding. Many recommendations are similar to the 2012 version, but some important changes place an emphasis on risk-stratification tools to reduce hospitalization in low-risk patients, and the timing of endoscopy for patients who are admitted to the hospital.
The guidelines were published in the American Journal of Gastroenterology.
One key change was the expansion of the Glasgow-Blatchford score (GBS) that could be used to identify patients at very low risk for a hospital intervention, from 0 in the 2012 guidelines to 0-1 in the current version. That expands the group of patients that could be discharged with outpatient follow-up.
A cutoff score of 0 identifies very few people, said Neil Sengupta, MD, who is an assistant professor of medicine at University of Chicago Medicine. Although expanding the qualification to 0-1 can increase the number of patients sent home, “which is certainly a good thing,” Dr. Sengupta said, it may be difficult to put into practice – especially in EDs. In most situations, GBS requires manual inputs. A few hospital systems have implemented automatic calculation of GBS from medical records, but the practice is not widespread.
“No. 1, the compliance of measuring the score is pretty low. No. 2, it’s difficult for an emergency room physician to discharge a patient with upper GI bleeding if patients don’t have good social support, or if they don’t have a good follow-up plan. So it’s hard to know whether this will really make a difference in terms of the number of people being discharged,” said Dr. Sengupta, who served as a monitor for the ACG committee that produced this guideline, and will become chair of the ACG guideline committee in October.
Another key message in the updated guidelines centers around timing of endoscopy. The 2012 guidelines recommended considering endoscopy within 12 hours for patients with high-risk clinical features. The new guidelines recommend that all patients should undergo endoscopy within 24 hours, and they do not specifically recommend endoscopy within 12 hours. Earlier endoscopy can lead to a more accurate prognosis, but can also cause mortality or complications if resuscitation and management of active comorbidities is insufficient, and outcomes can be worse during after-hours endoscopies. The change is based on a recent randomized, controlled trial that showed no 30-day mortality benefit to endoscopy performed within 6 hours of a consult, versus endoscopy performed between 6 and 24 hours.
That change still leaves uncertainty, because there may be some patients who would potentially benefit from earlier endoscopy. “I think that’s kind of the unknown: Whether there’s a subset of people who may benefit from going in very early and limiting the amount of resuscitation they get,” Dr. Sengupta said.
Another important message in the new guideline addresses proton pump inhibitor (PPI) therapy before endoscopy. Although the 2012 guidelines recommended considering pre-endoscopy PPI infusions, the new version states that there is no clear benefit for clinical outcomes. The authors of the guidelines did not recommend against it, either, because it is associated with a modest reduction in the need to perform endoscopic therapy. “And there’s a theoretical possibility that PPIs may benefit a minority of patients in whom endoscopy may not be possible in a timely fashion,” he said.
This advice may generate some controversy, since PPI use is very common prior to endoscopy, and in some places in the world, it might not be possible to complete an endoscopy within 24 hours. “As such, a lot of providers use PPIs routinely prior to endoscopy. It’s a little challenging just because this is such a common clinical scenario, and PPI use is so widespread that I don’t think it’s likely that practice is going to change based on this guideline,” Dr. Sengupta said. He did suggest that the benefit of PPIs after endoscopic therapy is well established, “so it’s going to be important to identify people who are at high risk (after an endoscopic treatment).
“The other the other thing is that you don’t really have too much guidance on whether there’s a benefit of using a continuous intravenous PPI versus intermittent PPI [either oral or intravenous] after endoscopy in high-risk patients, primarily [because of] the lack of high-quality data,” Dr. Sengupta said.
There is also good evidence that patients with ulcers and high-risk stigmata should receive endoscopic therapy, and these patients can benefit from posttherapy high-dose PPIs for 3 days.
Some guideline authors reported relationships with Phathom Pharmaceuticals, Olympus, and Cook. Dr. Sengupta is the upcoming chair of the ACG Practice Parameters Committees, which oversees the commissioning, updating, and review of all ACG clinical practice guidelines.
Updated guidelines from the American College of Gastroenterology address upper gastrointestinal and ulcer bleeding. Many recommendations are similar to the 2012 version, but some important changes place an emphasis on risk-stratification tools to reduce hospitalization in low-risk patients, and the timing of endoscopy for patients who are admitted to the hospital.
The guidelines were published in the American Journal of Gastroenterology.
One key change was the expansion of the Glasgow-Blatchford score (GBS) that could be used to identify patients at very low risk for a hospital intervention, from 0 in the 2012 guidelines to 0-1 in the current version. That expands the group of patients that could be discharged with outpatient follow-up.
A cutoff score of 0 identifies very few people, said Neil Sengupta, MD, who is an assistant professor of medicine at University of Chicago Medicine. Although expanding the qualification to 0-1 can increase the number of patients sent home, “which is certainly a good thing,” Dr. Sengupta said, it may be difficult to put into practice – especially in EDs. In most situations, GBS requires manual inputs. A few hospital systems have implemented automatic calculation of GBS from medical records, but the practice is not widespread.
“No. 1, the compliance of measuring the score is pretty low. No. 2, it’s difficult for an emergency room physician to discharge a patient with upper GI bleeding if patients don’t have good social support, or if they don’t have a good follow-up plan. So it’s hard to know whether this will really make a difference in terms of the number of people being discharged,” said Dr. Sengupta, who served as a monitor for the ACG committee that produced this guideline, and will become chair of the ACG guideline committee in October.
Another key message in the updated guidelines centers around timing of endoscopy. The 2012 guidelines recommended considering endoscopy within 12 hours for patients with high-risk clinical features. The new guidelines recommend that all patients should undergo endoscopy within 24 hours, and they do not specifically recommend endoscopy within 12 hours. Earlier endoscopy can lead to a more accurate prognosis, but can also cause mortality or complications if resuscitation and management of active comorbidities is insufficient, and outcomes can be worse during after-hours endoscopies. The change is based on a recent randomized, controlled trial that showed no 30-day mortality benefit to endoscopy performed within 6 hours of a consult, versus endoscopy performed between 6 and 24 hours.
That change still leaves uncertainty, because there may be some patients who would potentially benefit from earlier endoscopy. “I think that’s kind of the unknown: Whether there’s a subset of people who may benefit from going in very early and limiting the amount of resuscitation they get,” Dr. Sengupta said.
Another important message in the new guideline addresses proton pump inhibitor (PPI) therapy before endoscopy. Although the 2012 guidelines recommended considering pre-endoscopy PPI infusions, the new version states that there is no clear benefit for clinical outcomes. The authors of the guidelines did not recommend against it, either, because it is associated with a modest reduction in the need to perform endoscopic therapy. “And there’s a theoretical possibility that PPIs may benefit a minority of patients in whom endoscopy may not be possible in a timely fashion,” he said.
This advice may generate some controversy, since PPI use is very common prior to endoscopy, and in some places in the world, it might not be possible to complete an endoscopy within 24 hours. “As such, a lot of providers use PPIs routinely prior to endoscopy. It’s a little challenging just because this is such a common clinical scenario, and PPI use is so widespread that I don’t think it’s likely that practice is going to change based on this guideline,” Dr. Sengupta said. He did suggest that the benefit of PPIs after endoscopic therapy is well established, “so it’s going to be important to identify people who are at high risk (after an endoscopic treatment).
“The other the other thing is that you don’t really have too much guidance on whether there’s a benefit of using a continuous intravenous PPI versus intermittent PPI [either oral or intravenous] after endoscopy in high-risk patients, primarily [because of] the lack of high-quality data,” Dr. Sengupta said.
There is also good evidence that patients with ulcers and high-risk stigmata should receive endoscopic therapy, and these patients can benefit from posttherapy high-dose PPIs for 3 days.
Some guideline authors reported relationships with Phathom Pharmaceuticals, Olympus, and Cook. Dr. Sengupta is the upcoming chair of the ACG Practice Parameters Committees, which oversees the commissioning, updating, and review of all ACG clinical practice guidelines.
Updated guidelines from the American College of Gastroenterology address upper gastrointestinal and ulcer bleeding. Many recommendations are similar to the 2012 version, but some important changes place an emphasis on risk-stratification tools to reduce hospitalization in low-risk patients, and the timing of endoscopy for patients who are admitted to the hospital.
The guidelines were published in the American Journal of Gastroenterology.
One key change was the expansion of the Glasgow-Blatchford score (GBS) that could be used to identify patients at very low risk for a hospital intervention, from 0 in the 2012 guidelines to 0-1 in the current version. That expands the group of patients that could be discharged with outpatient follow-up.
A cutoff score of 0 identifies very few people, said Neil Sengupta, MD, who is an assistant professor of medicine at University of Chicago Medicine. Although expanding the qualification to 0-1 can increase the number of patients sent home, “which is certainly a good thing,” Dr. Sengupta said, it may be difficult to put into practice – especially in EDs. In most situations, GBS requires manual inputs. A few hospital systems have implemented automatic calculation of GBS from medical records, but the practice is not widespread.
“No. 1, the compliance of measuring the score is pretty low. No. 2, it’s difficult for an emergency room physician to discharge a patient with upper GI bleeding if patients don’t have good social support, or if they don’t have a good follow-up plan. So it’s hard to know whether this will really make a difference in terms of the number of people being discharged,” said Dr. Sengupta, who served as a monitor for the ACG committee that produced this guideline, and will become chair of the ACG guideline committee in October.
Another key message in the updated guidelines centers around timing of endoscopy. The 2012 guidelines recommended considering endoscopy within 12 hours for patients with high-risk clinical features. The new guidelines recommend that all patients should undergo endoscopy within 24 hours, and they do not specifically recommend endoscopy within 12 hours. Earlier endoscopy can lead to a more accurate prognosis, but can also cause mortality or complications if resuscitation and management of active comorbidities is insufficient, and outcomes can be worse during after-hours endoscopies. The change is based on a recent randomized, controlled trial that showed no 30-day mortality benefit to endoscopy performed within 6 hours of a consult, versus endoscopy performed between 6 and 24 hours.
That change still leaves uncertainty, because there may be some patients who would potentially benefit from earlier endoscopy. “I think that’s kind of the unknown: Whether there’s a subset of people who may benefit from going in very early and limiting the amount of resuscitation they get,” Dr. Sengupta said.
Another important message in the new guideline addresses proton pump inhibitor (PPI) therapy before endoscopy. Although the 2012 guidelines recommended considering pre-endoscopy PPI infusions, the new version states that there is no clear benefit for clinical outcomes. The authors of the guidelines did not recommend against it, either, because it is associated with a modest reduction in the need to perform endoscopic therapy. “And there’s a theoretical possibility that PPIs may benefit a minority of patients in whom endoscopy may not be possible in a timely fashion,” he said.
This advice may generate some controversy, since PPI use is very common prior to endoscopy, and in some places in the world, it might not be possible to complete an endoscopy within 24 hours. “As such, a lot of providers use PPIs routinely prior to endoscopy. It’s a little challenging just because this is such a common clinical scenario, and PPI use is so widespread that I don’t think it’s likely that practice is going to change based on this guideline,” Dr. Sengupta said. He did suggest that the benefit of PPIs after endoscopic therapy is well established, “so it’s going to be important to identify people who are at high risk (after an endoscopic treatment).
“The other the other thing is that you don’t really have too much guidance on whether there’s a benefit of using a continuous intravenous PPI versus intermittent PPI [either oral or intravenous] after endoscopy in high-risk patients, primarily [because of] the lack of high-quality data,” Dr. Sengupta said.
There is also good evidence that patients with ulcers and high-risk stigmata should receive endoscopic therapy, and these patients can benefit from posttherapy high-dose PPIs for 3 days.
Some guideline authors reported relationships with Phathom Pharmaceuticals, Olympus, and Cook. Dr. Sengupta is the upcoming chair of the ACG Practice Parameters Committees, which oversees the commissioning, updating, and review of all ACG clinical practice guidelines.
FROM THE AMERICAN JOURNAL OF GASTROENTEROLOGY
Sporebiotics improve functional dyspepsia symptoms
Compared with placebo, sporebiotics significantly reduced postprandial distress, epigastric pain, and several other symptoms of functional dyspepsia, reported lead author Lucas Wauters, MD, PhD, of University Hospitals Leuven (Belgium), and colleagues.
“Acid suppressive or first-line therapy with PPIs [proton pump inhibitors] for functional dyspepsia has limited efficacy and potential long-term side effects,” the investigators reported at the annual Digestive Disease Week® (DDW). “Spore-forming bacteria or sporebiotics may be effective for postprandial distress and epigastric pain or burning symptoms, offering benefits which may differ in relation to PPI intake.”
Sporebiotics improve variety of symptoms
To test this hypothesis, the investigators recruited 68 patients with functional dyspepsia who had similar characteristics at baseline. Half of the participants (n = 34) were taking PPIs.
Patients were randomized in a 1:1 ratio to receive 2.5 x 109 CFU of Bacillus coagulans MY01 and B. subtilis MY02 twice daily for 8 weeks, or matching placebo. Following this period, an additional 8-week open-label regimen was instituted, during which time all patients received sporebiotics. Throughout the study, a daily diary was used to self-report symptoms.
The primary outcome, measured at 8 weeks, was clinical response, defined by a decrease in weekly postprandial distress symptoms greater than 0.7 among patients who had a baseline score greater than 1.0. Secondary outcomes included change in postprandial distress symptoms greater than 0.5 (minimal clinical response), as well as changes in cardinal epigastric pain, cardinal postprandial distress, and other symptoms. At baseline and 8 weeks, patients taking PPIs underwent a 14C-glycocolic acid breath test to detect changes in small intestinal bacterial overgrowth.
At 8 weeks, a clinical response was observed in 48% of patients taking sporebiotics, compared with 20% of those in the placebo group (P = .03). At the same time point, 56% of patients in the treatment group had a minimal clinical response versus 27% in the control group (P = .03).
Spore-forming probiotics were also associated with significantly greater improvements in cardinal postprandial distress, cardinal epigastric pain, postprandial fullness, and upper abdominal pain. A trend toward improvement in upper abdominal bloating was also seen (P = .07).
Among patients taking PPIs, baseline rates of positivity for bile acid breath testing were similar between those in the sporebiotic and placebo group, at 18% and 25%, respectively (P = .29). After 8 weeks, however, patients taking spore-forming probiotics had a significantly lower rate of bile acid breath test positivity (7% vs. 36%; P = .04), suggesting improvements in small intestinal bacterial overgrowth.
In the open-label portion of the trial, patients in the treatment group maintained improvements in postprandial distress. Patients who switched from placebo to sporebiotics had a significant reduction in postprandial distress symptoms.
At 8 weeks, sporebiotics were associated with a trend toward fewer side effects of any kind (16% vs. 33%; P = .09), while rates of GI-specific side effects were comparable between groups, at 3% and 15% for sporebiotics and placebo, respectively (P = .2).“Spore-forming probiotics are effective and safe in patients with functional dyspepsia, decreasing both postprandial distress and epigastric pain symptoms,” the investigators concluded. “In patients [taking PPIs], sporebiotics decrease the percentage of positive bile acid breath tests, suggesting a reduction of small intestinal bacterial overgrowth.”
Results are promising, but big questions remain
Pankaj Jay Pasricha, MBBS, MD, vice chair of medicine innovation and commercialization at Johns Hopkins and director of the Johns Hopkins Center for Neurogastroenterology, Baltimore, called the results “very encouraging.”
“This [study] is the first of its kind for this condition,” Dr. Pasricha said in an interview. “It will be very interesting to see whether others can reproduce these findings, and whether [these improvements] are sustained beyond the first few weeks or months.”
He noted that determining associated mechanisms of action could potentially open up new lines of therapy, and provide greater understanding of pathophysiology, which is currently lacking.
“We don’t fully understand the pathophysiology [of functional dyspepsia],” Dr. Pasricha said. “If you don’t understand the pathophysiology, then it’s difficult to identify the right molecular target to address the root cause. Instead, we use a variety of symptomatic treatments that aren’t actually addressing the root cause, but studies like this may help us gain some insight into the cause of the problem, and if it is in fact a fundamental imbalance in the intestinal microbiota, then this would be a rational approach.”
It’s unclear how sporebiotics may improve functional dyspepsia, Dr. Pasricha noted. He proposed three possible mechanisms: the bacteria could be colonizing the intestine, they could be releasing products as they pass through the intestine that have a therapeutic effect, or they may be altering bile acid metabolism in the colon or having some other effect there.
“It’s speculative on my part to say how it works,” Dr. Pasricha said. “All the dots remain to be connected. But it’s a good start, and an outstanding group of investigators.”Dr. Wauters and colleagues reported no conflicts of interest. Dr. Pasricha disclosed a relationship with Pendulum Therapeutics.
Compared with placebo, sporebiotics significantly reduced postprandial distress, epigastric pain, and several other symptoms of functional dyspepsia, reported lead author Lucas Wauters, MD, PhD, of University Hospitals Leuven (Belgium), and colleagues.
“Acid suppressive or first-line therapy with PPIs [proton pump inhibitors] for functional dyspepsia has limited efficacy and potential long-term side effects,” the investigators reported at the annual Digestive Disease Week® (DDW). “Spore-forming bacteria or sporebiotics may be effective for postprandial distress and epigastric pain or burning symptoms, offering benefits which may differ in relation to PPI intake.”
Sporebiotics improve variety of symptoms
To test this hypothesis, the investigators recruited 68 patients with functional dyspepsia who had similar characteristics at baseline. Half of the participants (n = 34) were taking PPIs.
Patients were randomized in a 1:1 ratio to receive 2.5 x 109 CFU of Bacillus coagulans MY01 and B. subtilis MY02 twice daily for 8 weeks, or matching placebo. Following this period, an additional 8-week open-label regimen was instituted, during which time all patients received sporebiotics. Throughout the study, a daily diary was used to self-report symptoms.
The primary outcome, measured at 8 weeks, was clinical response, defined by a decrease in weekly postprandial distress symptoms greater than 0.7 among patients who had a baseline score greater than 1.0. Secondary outcomes included change in postprandial distress symptoms greater than 0.5 (minimal clinical response), as well as changes in cardinal epigastric pain, cardinal postprandial distress, and other symptoms. At baseline and 8 weeks, patients taking PPIs underwent a 14C-glycocolic acid breath test to detect changes in small intestinal bacterial overgrowth.
At 8 weeks, a clinical response was observed in 48% of patients taking sporebiotics, compared with 20% of those in the placebo group (P = .03). At the same time point, 56% of patients in the treatment group had a minimal clinical response versus 27% in the control group (P = .03).
Spore-forming probiotics were also associated with significantly greater improvements in cardinal postprandial distress, cardinal epigastric pain, postprandial fullness, and upper abdominal pain. A trend toward improvement in upper abdominal bloating was also seen (P = .07).
Among patients taking PPIs, baseline rates of positivity for bile acid breath testing were similar between those in the sporebiotic and placebo group, at 18% and 25%, respectively (P = .29). After 8 weeks, however, patients taking spore-forming probiotics had a significantly lower rate of bile acid breath test positivity (7% vs. 36%; P = .04), suggesting improvements in small intestinal bacterial overgrowth.
In the open-label portion of the trial, patients in the treatment group maintained improvements in postprandial distress. Patients who switched from placebo to sporebiotics had a significant reduction in postprandial distress symptoms.
At 8 weeks, sporebiotics were associated with a trend toward fewer side effects of any kind (16% vs. 33%; P = .09), while rates of GI-specific side effects were comparable between groups, at 3% and 15% for sporebiotics and placebo, respectively (P = .2).“Spore-forming probiotics are effective and safe in patients with functional dyspepsia, decreasing both postprandial distress and epigastric pain symptoms,” the investigators concluded. “In patients [taking PPIs], sporebiotics decrease the percentage of positive bile acid breath tests, suggesting a reduction of small intestinal bacterial overgrowth.”
Results are promising, but big questions remain
Pankaj Jay Pasricha, MBBS, MD, vice chair of medicine innovation and commercialization at Johns Hopkins and director of the Johns Hopkins Center for Neurogastroenterology, Baltimore, called the results “very encouraging.”
“This [study] is the first of its kind for this condition,” Dr. Pasricha said in an interview. “It will be very interesting to see whether others can reproduce these findings, and whether [these improvements] are sustained beyond the first few weeks or months.”
He noted that determining associated mechanisms of action could potentially open up new lines of therapy, and provide greater understanding of pathophysiology, which is currently lacking.
“We don’t fully understand the pathophysiology [of functional dyspepsia],” Dr. Pasricha said. “If you don’t understand the pathophysiology, then it’s difficult to identify the right molecular target to address the root cause. Instead, we use a variety of symptomatic treatments that aren’t actually addressing the root cause, but studies like this may help us gain some insight into the cause of the problem, and if it is in fact a fundamental imbalance in the intestinal microbiota, then this would be a rational approach.”
It’s unclear how sporebiotics may improve functional dyspepsia, Dr. Pasricha noted. He proposed three possible mechanisms: the bacteria could be colonizing the intestine, they could be releasing products as they pass through the intestine that have a therapeutic effect, or they may be altering bile acid metabolism in the colon or having some other effect there.
“It’s speculative on my part to say how it works,” Dr. Pasricha said. “All the dots remain to be connected. But it’s a good start, and an outstanding group of investigators.”Dr. Wauters and colleagues reported no conflicts of interest. Dr. Pasricha disclosed a relationship with Pendulum Therapeutics.
Compared with placebo, sporebiotics significantly reduced postprandial distress, epigastric pain, and several other symptoms of functional dyspepsia, reported lead author Lucas Wauters, MD, PhD, of University Hospitals Leuven (Belgium), and colleagues.
“Acid suppressive or first-line therapy with PPIs [proton pump inhibitors] for functional dyspepsia has limited efficacy and potential long-term side effects,” the investigators reported at the annual Digestive Disease Week® (DDW). “Spore-forming bacteria or sporebiotics may be effective for postprandial distress and epigastric pain or burning symptoms, offering benefits which may differ in relation to PPI intake.”
Sporebiotics improve variety of symptoms
To test this hypothesis, the investigators recruited 68 patients with functional dyspepsia who had similar characteristics at baseline. Half of the participants (n = 34) were taking PPIs.
Patients were randomized in a 1:1 ratio to receive 2.5 x 109 CFU of Bacillus coagulans MY01 and B. subtilis MY02 twice daily for 8 weeks, or matching placebo. Following this period, an additional 8-week open-label regimen was instituted, during which time all patients received sporebiotics. Throughout the study, a daily diary was used to self-report symptoms.
The primary outcome, measured at 8 weeks, was clinical response, defined by a decrease in weekly postprandial distress symptoms greater than 0.7 among patients who had a baseline score greater than 1.0. Secondary outcomes included change in postprandial distress symptoms greater than 0.5 (minimal clinical response), as well as changes in cardinal epigastric pain, cardinal postprandial distress, and other symptoms. At baseline and 8 weeks, patients taking PPIs underwent a 14C-glycocolic acid breath test to detect changes in small intestinal bacterial overgrowth.
At 8 weeks, a clinical response was observed in 48% of patients taking sporebiotics, compared with 20% of those in the placebo group (P = .03). At the same time point, 56% of patients in the treatment group had a minimal clinical response versus 27% in the control group (P = .03).
Spore-forming probiotics were also associated with significantly greater improvements in cardinal postprandial distress, cardinal epigastric pain, postprandial fullness, and upper abdominal pain. A trend toward improvement in upper abdominal bloating was also seen (P = .07).
Among patients taking PPIs, baseline rates of positivity for bile acid breath testing were similar between those in the sporebiotic and placebo group, at 18% and 25%, respectively (P = .29). After 8 weeks, however, patients taking spore-forming probiotics had a significantly lower rate of bile acid breath test positivity (7% vs. 36%; P = .04), suggesting improvements in small intestinal bacterial overgrowth.
In the open-label portion of the trial, patients in the treatment group maintained improvements in postprandial distress. Patients who switched from placebo to sporebiotics had a significant reduction in postprandial distress symptoms.
At 8 weeks, sporebiotics were associated with a trend toward fewer side effects of any kind (16% vs. 33%; P = .09), while rates of GI-specific side effects were comparable between groups, at 3% and 15% for sporebiotics and placebo, respectively (P = .2).“Spore-forming probiotics are effective and safe in patients with functional dyspepsia, decreasing both postprandial distress and epigastric pain symptoms,” the investigators concluded. “In patients [taking PPIs], sporebiotics decrease the percentage of positive bile acid breath tests, suggesting a reduction of small intestinal bacterial overgrowth.”
Results are promising, but big questions remain
Pankaj Jay Pasricha, MBBS, MD, vice chair of medicine innovation and commercialization at Johns Hopkins and director of the Johns Hopkins Center for Neurogastroenterology, Baltimore, called the results “very encouraging.”
“This [study] is the first of its kind for this condition,” Dr. Pasricha said in an interview. “It will be very interesting to see whether others can reproduce these findings, and whether [these improvements] are sustained beyond the first few weeks or months.”
He noted that determining associated mechanisms of action could potentially open up new lines of therapy, and provide greater understanding of pathophysiology, which is currently lacking.
“We don’t fully understand the pathophysiology [of functional dyspepsia],” Dr. Pasricha said. “If you don’t understand the pathophysiology, then it’s difficult to identify the right molecular target to address the root cause. Instead, we use a variety of symptomatic treatments that aren’t actually addressing the root cause, but studies like this may help us gain some insight into the cause of the problem, and if it is in fact a fundamental imbalance in the intestinal microbiota, then this would be a rational approach.”
It’s unclear how sporebiotics may improve functional dyspepsia, Dr. Pasricha noted. He proposed three possible mechanisms: the bacteria could be colonizing the intestine, they could be releasing products as they pass through the intestine that have a therapeutic effect, or they may be altering bile acid metabolism in the colon or having some other effect there.
“It’s speculative on my part to say how it works,” Dr. Pasricha said. “All the dots remain to be connected. But it’s a good start, and an outstanding group of investigators.”Dr. Wauters and colleagues reported no conflicts of interest. Dr. Pasricha disclosed a relationship with Pendulum Therapeutics.
FROM DDW 2021
Some nasogastric intubation procedures lead to less aerosolization than feared
Nasogastric intubation for esophageal manometry or impedance monitoring does not generate significant aerosol particles and is associated with minimal droplet spread, according to a Belgian study presented at the annual Digestive Disease Week® (DDW). These findings suggest that standard personal protective equipment and appropriate patient positioning are likely sufficient to protect health care workers from increased risk of coronavirus transmission during tube placement and removal, reported lead author Wout Verbeure, PhD, of Leuven University Hospital, Belgium, and colleagues.
“Subsequent to the COVID-19 peak, [nasogastric tube insertion and extraction] were scaled back based on the assumption that they generate respiratory aerosol particles and droplet spread,” the investigators reported. “However, there is no scientific evidence for this theory.”
To address this knowledge gap, the investigators conducted an observational trial involving SARS-CoV-2-negative patients and including 21 insertions and removals for high-resolution manometry (HRM), plus 12 insertions and 10 removals for 24-hour multichannel intraluminal impedance-pH monitoring (MII-pH). During the study, a Camfil City M Air Purifier was added to the examination room. This was present during 13 of the 21 HRM insertions and removals, allowing for comparison of aerosol particle measurements before and after introduction of the device.
The mechanics of the study
Aerosol particles (0.3-10 mcm) were measured with a Particle Measuring Systems LASAIR II Particle Counter positioned 1 cm away from the patient’s face. For both procedures, measurements were taken before, during, and up to 5 minutes after each nasogastric tube placement and removal. Additional measurements were taken while the HRM examination was being conducted.
To measure droplet spread, 1% medical fluorescein in saline was applied to each patient’s nasal cavity; droplets were visualized on a white sheet covering the patient and a white apron worn by the health care worker. The patients’ masks were kept below their noses but were covering their mouths.
“During the placement and removal of the catheter, the health care worker was always standing sideways or even behind the patient, and they always stood higher relative to the patient to ensure that when there was aerosol or droplet spread, it was not in their direction,” Dr. Verbeure said during his virtual presentation.
During placement for HRM and removal for MII-pH, aerosol particles (excluding those that were 0.3 mcm), decreased significantly. Otherwise, particle counts remained stable. “This shows that these investigations do not generate additional aerosol [particles], which is good news,” Dr. Verbeure said.
When the air purifier was present, placement and examination for HRM were associated with significant reductions in aerosol particles (excluding those that were 0.3 mcm or 0.5 mcm), whereas removal caused a slight uptick in aerosol particles (excluding those that were 0.3 mcm or 0.5 mcm) that did not decline after 5 minutes. “This was actually a surprise to us,” Dr. Verbeure said. “Because we now had an air purifier present, and we expected an even lower number of particles.”
He suggested that the purifier may have been reducing particle counts during HRM examination, thereby lowering baseline values before removal, making small changes more noticeable; or the purifier may have been causing turbulence that spread particles during removal. Whether either of these hypotheses is true, Dr. Verbeure noted that particle counts were never higher than at the start of the examination. Fluorescein visualization showed “surprisingly little droplet spread,” Dr. Verbeure said, apart from some contamination around the patient’s neck.
“Esophageal investigations do not seem to generate additional [aerosol] particles,” Dr. Verbeure concluded. “So wearing the recommended protective gear and also considering the right positioning of the health care worker relative to the patient is important to keep performing this daily clinical routine.” To avoid droplet spread, health care workers should “be aware of the [patient’s] neck region and the direction of the catheter,” Dr. Verbeure added.
SORTing the results
According to Mahdi Najafi, MD, associate professor in the department of anesthesiology at Tehran University of Medical Sciences, Iran, and adjunct professor at Schulich School of Medicine & Dentistry, Western University, London, Ontario, the findings offer valuable insights. “[This study] is very important for at least two reasons: The extent of using this procedure in patient care, especially in the critical care setting, and the paucity of information for COVID-19 transmission and route of transmission as well,” Dr. Najafi said in an interview.
Yet he cautioned against generalizing the results. “We cannot extend the results to all nasogastric tube intubations,” Dr. Najafi said. “There are reasons for that. The tube for manometry is delicate and flexible, while the nasogastric tube used for drainage and GI pressure release – which is used commonly in intensive care and the operating room – is larger and rather rigid. Moreover, the patient is awake and conscious for manometry while the other procedures are done in sedated or unconscious patients.”
He noted that nasogastric intubation is more challenging in unconscious patients, and often requires a laryngoscope and/or Magill forceps. “The result [of using these instruments] is coughing, which is undoubtedly the most important cause of aerosol generation,” Dr. Najafi said. “It can be regarded as a drawback to this study as well. The authors would be better to report the number and/or severity of the airway reactions during the procedures, which are the main source of droplets and aerosols.”
To reduce risk of coronavirus transmission during nasogastric intubation of unconscious patients, Dr. Najafi recommended the SORT (Sniffing position, nasogastric tube Orientation, contralateral Rotation, and Twisting movement) maneuver, which he introduced in 2016 for use in critical care and operating room settings.
“The employment of anatomical approach and avoiding equipment for intubation were devised to increase the level of safety and decrease hazards and adverse effects,” Dr. Najafi said of the SORT maneuver. “The procedure needs to be done step-by-step and as smooth as possible.”
In a recent study, the SORT maneuver was compared with nasogastric intubation using neck flexion lateral pressure in critically ill patients. The investigators concluded that the SORT maneuver is “a promising method” notable for its simple technique, and suggested that more trials are needed.
The investigators and Dr. Najafi reported no conflicts of interest.
Nasogastric intubation for esophageal manometry or impedance monitoring does not generate significant aerosol particles and is associated with minimal droplet spread, according to a Belgian study presented at the annual Digestive Disease Week® (DDW). These findings suggest that standard personal protective equipment and appropriate patient positioning are likely sufficient to protect health care workers from increased risk of coronavirus transmission during tube placement and removal, reported lead author Wout Verbeure, PhD, of Leuven University Hospital, Belgium, and colleagues.
“Subsequent to the COVID-19 peak, [nasogastric tube insertion and extraction] were scaled back based on the assumption that they generate respiratory aerosol particles and droplet spread,” the investigators reported. “However, there is no scientific evidence for this theory.”
To address this knowledge gap, the investigators conducted an observational trial involving SARS-CoV-2-negative patients and including 21 insertions and removals for high-resolution manometry (HRM), plus 12 insertions and 10 removals for 24-hour multichannel intraluminal impedance-pH monitoring (MII-pH). During the study, a Camfil City M Air Purifier was added to the examination room. This was present during 13 of the 21 HRM insertions and removals, allowing for comparison of aerosol particle measurements before and after introduction of the device.
The mechanics of the study
Aerosol particles (0.3-10 mcm) were measured with a Particle Measuring Systems LASAIR II Particle Counter positioned 1 cm away from the patient’s face. For both procedures, measurements were taken before, during, and up to 5 minutes after each nasogastric tube placement and removal. Additional measurements were taken while the HRM examination was being conducted.
To measure droplet spread, 1% medical fluorescein in saline was applied to each patient’s nasal cavity; droplets were visualized on a white sheet covering the patient and a white apron worn by the health care worker. The patients’ masks were kept below their noses but were covering their mouths.
“During the placement and removal of the catheter, the health care worker was always standing sideways or even behind the patient, and they always stood higher relative to the patient to ensure that when there was aerosol or droplet spread, it was not in their direction,” Dr. Verbeure said during his virtual presentation.
During placement for HRM and removal for MII-pH, aerosol particles (excluding those that were 0.3 mcm), decreased significantly. Otherwise, particle counts remained stable. “This shows that these investigations do not generate additional aerosol [particles], which is good news,” Dr. Verbeure said.
When the air purifier was present, placement and examination for HRM were associated with significant reductions in aerosol particles (excluding those that were 0.3 mcm or 0.5 mcm), whereas removal caused a slight uptick in aerosol particles (excluding those that were 0.3 mcm or 0.5 mcm) that did not decline after 5 minutes. “This was actually a surprise to us,” Dr. Verbeure said. “Because we now had an air purifier present, and we expected an even lower number of particles.”
He suggested that the purifier may have been reducing particle counts during HRM examination, thereby lowering baseline values before removal, making small changes more noticeable; or the purifier may have been causing turbulence that spread particles during removal. Whether either of these hypotheses is true, Dr. Verbeure noted that particle counts were never higher than at the start of the examination. Fluorescein visualization showed “surprisingly little droplet spread,” Dr. Verbeure said, apart from some contamination around the patient’s neck.
“Esophageal investigations do not seem to generate additional [aerosol] particles,” Dr. Verbeure concluded. “So wearing the recommended protective gear and also considering the right positioning of the health care worker relative to the patient is important to keep performing this daily clinical routine.” To avoid droplet spread, health care workers should “be aware of the [patient’s] neck region and the direction of the catheter,” Dr. Verbeure added.
SORTing the results
According to Mahdi Najafi, MD, associate professor in the department of anesthesiology at Tehran University of Medical Sciences, Iran, and adjunct professor at Schulich School of Medicine & Dentistry, Western University, London, Ontario, the findings offer valuable insights. “[This study] is very important for at least two reasons: The extent of using this procedure in patient care, especially in the critical care setting, and the paucity of information for COVID-19 transmission and route of transmission as well,” Dr. Najafi said in an interview.
Yet he cautioned against generalizing the results. “We cannot extend the results to all nasogastric tube intubations,” Dr. Najafi said. “There are reasons for that. The tube for manometry is delicate and flexible, while the nasogastric tube used for drainage and GI pressure release – which is used commonly in intensive care and the operating room – is larger and rather rigid. Moreover, the patient is awake and conscious for manometry while the other procedures are done in sedated or unconscious patients.”
He noted that nasogastric intubation is more challenging in unconscious patients, and often requires a laryngoscope and/or Magill forceps. “The result [of using these instruments] is coughing, which is undoubtedly the most important cause of aerosol generation,” Dr. Najafi said. “It can be regarded as a drawback to this study as well. The authors would be better to report the number and/or severity of the airway reactions during the procedures, which are the main source of droplets and aerosols.”
To reduce risk of coronavirus transmission during nasogastric intubation of unconscious patients, Dr. Najafi recommended the SORT (Sniffing position, nasogastric tube Orientation, contralateral Rotation, and Twisting movement) maneuver, which he introduced in 2016 for use in critical care and operating room settings.
“The employment of anatomical approach and avoiding equipment for intubation were devised to increase the level of safety and decrease hazards and adverse effects,” Dr. Najafi said of the SORT maneuver. “The procedure needs to be done step-by-step and as smooth as possible.”
In a recent study, the SORT maneuver was compared with nasogastric intubation using neck flexion lateral pressure in critically ill patients. The investigators concluded that the SORT maneuver is “a promising method” notable for its simple technique, and suggested that more trials are needed.
The investigators and Dr. Najafi reported no conflicts of interest.
Nasogastric intubation for esophageal manometry or impedance monitoring does not generate significant aerosol particles and is associated with minimal droplet spread, according to a Belgian study presented at the annual Digestive Disease Week® (DDW). These findings suggest that standard personal protective equipment and appropriate patient positioning are likely sufficient to protect health care workers from increased risk of coronavirus transmission during tube placement and removal, reported lead author Wout Verbeure, PhD, of Leuven University Hospital, Belgium, and colleagues.
“Subsequent to the COVID-19 peak, [nasogastric tube insertion and extraction] were scaled back based on the assumption that they generate respiratory aerosol particles and droplet spread,” the investigators reported. “However, there is no scientific evidence for this theory.”
To address this knowledge gap, the investigators conducted an observational trial involving SARS-CoV-2-negative patients and including 21 insertions and removals for high-resolution manometry (HRM), plus 12 insertions and 10 removals for 24-hour multichannel intraluminal impedance-pH monitoring (MII-pH). During the study, a Camfil City M Air Purifier was added to the examination room. This was present during 13 of the 21 HRM insertions and removals, allowing for comparison of aerosol particle measurements before and after introduction of the device.
The mechanics of the study
Aerosol particles (0.3-10 mcm) were measured with a Particle Measuring Systems LASAIR II Particle Counter positioned 1 cm away from the patient’s face. For both procedures, measurements were taken before, during, and up to 5 minutes after each nasogastric tube placement and removal. Additional measurements were taken while the HRM examination was being conducted.
To measure droplet spread, 1% medical fluorescein in saline was applied to each patient’s nasal cavity; droplets were visualized on a white sheet covering the patient and a white apron worn by the health care worker. The patients’ masks were kept below their noses but were covering their mouths.
“During the placement and removal of the catheter, the health care worker was always standing sideways or even behind the patient, and they always stood higher relative to the patient to ensure that when there was aerosol or droplet spread, it was not in their direction,” Dr. Verbeure said during his virtual presentation.
During placement for HRM and removal for MII-pH, aerosol particles (excluding those that were 0.3 mcm), decreased significantly. Otherwise, particle counts remained stable. “This shows that these investigations do not generate additional aerosol [particles], which is good news,” Dr. Verbeure said.
When the air purifier was present, placement and examination for HRM were associated with significant reductions in aerosol particles (excluding those that were 0.3 mcm or 0.5 mcm), whereas removal caused a slight uptick in aerosol particles (excluding those that were 0.3 mcm or 0.5 mcm) that did not decline after 5 minutes. “This was actually a surprise to us,” Dr. Verbeure said. “Because we now had an air purifier present, and we expected an even lower number of particles.”
He suggested that the purifier may have been reducing particle counts during HRM examination, thereby lowering baseline values before removal, making small changes more noticeable; or the purifier may have been causing turbulence that spread particles during removal. Whether either of these hypotheses is true, Dr. Verbeure noted that particle counts were never higher than at the start of the examination. Fluorescein visualization showed “surprisingly little droplet spread,” Dr. Verbeure said, apart from some contamination around the patient’s neck.
“Esophageal investigations do not seem to generate additional [aerosol] particles,” Dr. Verbeure concluded. “So wearing the recommended protective gear and also considering the right positioning of the health care worker relative to the patient is important to keep performing this daily clinical routine.” To avoid droplet spread, health care workers should “be aware of the [patient’s] neck region and the direction of the catheter,” Dr. Verbeure added.
SORTing the results
According to Mahdi Najafi, MD, associate professor in the department of anesthesiology at Tehran University of Medical Sciences, Iran, and adjunct professor at Schulich School of Medicine & Dentistry, Western University, London, Ontario, the findings offer valuable insights. “[This study] is very important for at least two reasons: The extent of using this procedure in patient care, especially in the critical care setting, and the paucity of information for COVID-19 transmission and route of transmission as well,” Dr. Najafi said in an interview.
Yet he cautioned against generalizing the results. “We cannot extend the results to all nasogastric tube intubations,” Dr. Najafi said. “There are reasons for that. The tube for manometry is delicate and flexible, while the nasogastric tube used for drainage and GI pressure release – which is used commonly in intensive care and the operating room – is larger and rather rigid. Moreover, the patient is awake and conscious for manometry while the other procedures are done in sedated or unconscious patients.”
He noted that nasogastric intubation is more challenging in unconscious patients, and often requires a laryngoscope and/or Magill forceps. “The result [of using these instruments] is coughing, which is undoubtedly the most important cause of aerosol generation,” Dr. Najafi said. “It can be regarded as a drawback to this study as well. The authors would be better to report the number and/or severity of the airway reactions during the procedures, which are the main source of droplets and aerosols.”
To reduce risk of coronavirus transmission during nasogastric intubation of unconscious patients, Dr. Najafi recommended the SORT (Sniffing position, nasogastric tube Orientation, contralateral Rotation, and Twisting movement) maneuver, which he introduced in 2016 for use in critical care and operating room settings.
“The employment of anatomical approach and avoiding equipment for intubation were devised to increase the level of safety and decrease hazards and adverse effects,” Dr. Najafi said of the SORT maneuver. “The procedure needs to be done step-by-step and as smooth as possible.”
In a recent study, the SORT maneuver was compared with nasogastric intubation using neck flexion lateral pressure in critically ill patients. The investigators concluded that the SORT maneuver is “a promising method” notable for its simple technique, and suggested that more trials are needed.
The investigators and Dr. Najafi reported no conflicts of interest.
FROM DDW 2021
High eradication, fewer adverse events with hybrid therapy for H. pylori
A 14-day course of hybrid therapy was as effective as 10-day bismuth quadruple therapy, but with fewer side effects, according to results of a randomized trial conducted in Taiwan.
“However, the former had fewer adverse events than the latter,” investigator Ping-I Hsu, MD, of An Nan Hospital, China Medical University, Taiwan said in a virtual presentation at the annual Digestive Disease Week® (DDW). Some patients in the trial received 14-day high-dose dual therapy, which also had a lower rate of adverse events but a lower eradication rate, compared with quadruple therapy, Dr. Hsu added.
This study confirms previous data showing that hybrid therapy has high eradication rates and a lower frequency of adverse events compared with bismuth quadruple therapy, noted Joseph Adrian L. Buensalido, MD, clinical associate professor of medicine in the division of infectious diseases at the University of the Philippines–Philippine General Hospital in Manila. “Clinicians and specialty/guideline groups may need to start looking at moving to first-line hybrid therapy as opposed to the traditional approach,” Dr. Buensalido said in an interview.
Current guidelines and data to date
An American College of Gastroenterology clinical guideline published in 2017 strongly recommends bismuth quadruple therapy, with a duration of 10-14 days, as a first-line treatment option. Hybrid therapy is conditionally recommended as a first-line option in the ACG guideline, while high-dose dual therapy is conditionally recommended as a salvage regimen.
In a prospective, randomized comparative study published in 2017, the eradication rates (93.9%) in patients receiving 14-day bismuth quadruple therapy (pantoprazole, bismuth subcitrate, tetracycline, and metronidazole) were comparable with eradication rates (92.8%) with 14-day hybrid therapy (dual therapy with pantoprazole plus amoxicillin for 7 days, followed by quadruple therapy with pantoprazole, amoxicillin, clarithromycin, and metronidazole for 7 days).
Quadruple therapy had a higher frequency of adverse events, at 55%, compared with 15.7% for hybrid therapy (P < .001). “Whether shortening the treatment duration of bismuth quadruple therapy from 14 days to 10 days can reduce the frequency of adverse effects remains unclear,” Dr. Hsu said in introductory comments to his study.
Comparing three approaches
In the multicenter, randomized, open-label superiority trial presented at DDW, Dr. Hsu and colleagues randomly assigned 600 Helicobacter pylori–infected participants in equal numbers to receive 14-day hybrid therapy, 14-day high-dose dual therapy, or 10-day bismuth quadruple therapy.
The hybrid therapy regimen consisted of rabeprazole 20 mg twice a day plus amoxicillin 1 g twice a day for 14 days, with clarithromycin 500 mg and metronidazole 500 mg twice a day in the final 7 days. The high-dose dual therapy regimen consisted of rabeprazole 20 mg and amoxicillin 750 mg four times a day for 14 days. The bismuth quadruple therapy regimen consisted of rabeprazole 20 mg twice a day, tripotassium dicitrato bismuthate 300 mg four times a day, tetracycline 500 mg twice a day, and metronidazole 250 mg four times a day for 10 days.
Investigators assessed H. pylori status 6 weeks following the end of therapy. In an intention-to-treat analysis, the hybrid therapy regimen yielded an eradication rate of 96.5%, which was comparable with the 93.5% eradication rate seen with bismuth quadruple therapy and was significantly higher than the 86.0% eradication rate seen with high-dose dual therapy (P < .001), according to Dr. Hsu. Similar efficacy outcomes were seen in per-protocol analysis.
The frequency of adverse events was lowest with high-dose dual therapy, at 13.0%, according to Dr. Hsu. That was significantly lower than the 25.5% frequency of adverse events with hybrid therapy. Bismuth quadruple therapy had a rate of 34.0%.
Antibiotic resistance results
Antibiotic resistance was most common for metronidazole, seen in approximately 28% of the quadruple-therapy group, 34% of the hybrid group, and 37% of the high-dose therapy groups. Clarithromycin resistance occurred in about 23% of quadruple therapy recipients, 16% of hybrid recipients, and 16% of high-dose therapy recipients. Amoxicillin and tetracycline resistance was rare, occurring in approximately 0%-3% of groups.
In the quadruple therapy arm, metronidazole resistance was associated with H. pylori eradication failure, according to Dr. Hsu. The eradication rate was about 96% for those subjects with no metronidazole resistance, and 88% for those with resistance (P = .05). Amoxicillin resistance, although rare in the study, independently predicted eradication failure of high-dose dual therapy, Dr. Hsu said. The eradication rate with high-dose dual therapy was 87.6% for individuals without amoxicillin resistance, and 40.0% in individuals with resistance, according to presented data.
The authors reported no financial disclosures related to their research. Dr. Buensalido has been a speaker for Unilab, BSV Bioscience, and Philcare Pharma, and has received sponsorship from Pfizer.
A 14-day course of hybrid therapy was as effective as 10-day bismuth quadruple therapy, but with fewer side effects, according to results of a randomized trial conducted in Taiwan.
“However, the former had fewer adverse events than the latter,” investigator Ping-I Hsu, MD, of An Nan Hospital, China Medical University, Taiwan said in a virtual presentation at the annual Digestive Disease Week® (DDW). Some patients in the trial received 14-day high-dose dual therapy, which also had a lower rate of adverse events but a lower eradication rate, compared with quadruple therapy, Dr. Hsu added.
This study confirms previous data showing that hybrid therapy has high eradication rates and a lower frequency of adverse events compared with bismuth quadruple therapy, noted Joseph Adrian L. Buensalido, MD, clinical associate professor of medicine in the division of infectious diseases at the University of the Philippines–Philippine General Hospital in Manila. “Clinicians and specialty/guideline groups may need to start looking at moving to first-line hybrid therapy as opposed to the traditional approach,” Dr. Buensalido said in an interview.
Current guidelines and data to date
An American College of Gastroenterology clinical guideline published in 2017 strongly recommends bismuth quadruple therapy, with a duration of 10-14 days, as a first-line treatment option. Hybrid therapy is conditionally recommended as a first-line option in the ACG guideline, while high-dose dual therapy is conditionally recommended as a salvage regimen.
In a prospective, randomized comparative study published in 2017, the eradication rates (93.9%) in patients receiving 14-day bismuth quadruple therapy (pantoprazole, bismuth subcitrate, tetracycline, and metronidazole) were comparable with eradication rates (92.8%) with 14-day hybrid therapy (dual therapy with pantoprazole plus amoxicillin for 7 days, followed by quadruple therapy with pantoprazole, amoxicillin, clarithromycin, and metronidazole for 7 days).
Quadruple therapy had a higher frequency of adverse events, at 55%, compared with 15.7% for hybrid therapy (P < .001). “Whether shortening the treatment duration of bismuth quadruple therapy from 14 days to 10 days can reduce the frequency of adverse effects remains unclear,” Dr. Hsu said in introductory comments to his study.
Comparing three approaches
In the multicenter, randomized, open-label superiority trial presented at DDW, Dr. Hsu and colleagues randomly assigned 600 Helicobacter pylori–infected participants in equal numbers to receive 14-day hybrid therapy, 14-day high-dose dual therapy, or 10-day bismuth quadruple therapy.
The hybrid therapy regimen consisted of rabeprazole 20 mg twice a day plus amoxicillin 1 g twice a day for 14 days, with clarithromycin 500 mg and metronidazole 500 mg twice a day in the final 7 days. The high-dose dual therapy regimen consisted of rabeprazole 20 mg and amoxicillin 750 mg four times a day for 14 days. The bismuth quadruple therapy regimen consisted of rabeprazole 20 mg twice a day, tripotassium dicitrato bismuthate 300 mg four times a day, tetracycline 500 mg twice a day, and metronidazole 250 mg four times a day for 10 days.
Investigators assessed H. pylori status 6 weeks following the end of therapy. In an intention-to-treat analysis, the hybrid therapy regimen yielded an eradication rate of 96.5%, which was comparable with the 93.5% eradication rate seen with bismuth quadruple therapy and was significantly higher than the 86.0% eradication rate seen with high-dose dual therapy (P < .001), according to Dr. Hsu. Similar efficacy outcomes were seen in per-protocol analysis.
The frequency of adverse events was lowest with high-dose dual therapy, at 13.0%, according to Dr. Hsu. That was significantly lower than the 25.5% frequency of adverse events with hybrid therapy. Bismuth quadruple therapy had a rate of 34.0%.
Antibiotic resistance results
Antibiotic resistance was most common for metronidazole, seen in approximately 28% of the quadruple-therapy group, 34% of the hybrid group, and 37% of the high-dose therapy groups. Clarithromycin resistance occurred in about 23% of quadruple therapy recipients, 16% of hybrid recipients, and 16% of high-dose therapy recipients. Amoxicillin and tetracycline resistance was rare, occurring in approximately 0%-3% of groups.
In the quadruple therapy arm, metronidazole resistance was associated with H. pylori eradication failure, according to Dr. Hsu. The eradication rate was about 96% for those subjects with no metronidazole resistance, and 88% for those with resistance (P = .05). Amoxicillin resistance, although rare in the study, independently predicted eradication failure of high-dose dual therapy, Dr. Hsu said. The eradication rate with high-dose dual therapy was 87.6% for individuals without amoxicillin resistance, and 40.0% in individuals with resistance, according to presented data.
The authors reported no financial disclosures related to their research. Dr. Buensalido has been a speaker for Unilab, BSV Bioscience, and Philcare Pharma, and has received sponsorship from Pfizer.
A 14-day course of hybrid therapy was as effective as 10-day bismuth quadruple therapy, but with fewer side effects, according to results of a randomized trial conducted in Taiwan.
“However, the former had fewer adverse events than the latter,” investigator Ping-I Hsu, MD, of An Nan Hospital, China Medical University, Taiwan said in a virtual presentation at the annual Digestive Disease Week® (DDW). Some patients in the trial received 14-day high-dose dual therapy, which also had a lower rate of adverse events but a lower eradication rate, compared with quadruple therapy, Dr. Hsu added.
This study confirms previous data showing that hybrid therapy has high eradication rates and a lower frequency of adverse events compared with bismuth quadruple therapy, noted Joseph Adrian L. Buensalido, MD, clinical associate professor of medicine in the division of infectious diseases at the University of the Philippines–Philippine General Hospital in Manila. “Clinicians and specialty/guideline groups may need to start looking at moving to first-line hybrid therapy as opposed to the traditional approach,” Dr. Buensalido said in an interview.
Current guidelines and data to date
An American College of Gastroenterology clinical guideline published in 2017 strongly recommends bismuth quadruple therapy, with a duration of 10-14 days, as a first-line treatment option. Hybrid therapy is conditionally recommended as a first-line option in the ACG guideline, while high-dose dual therapy is conditionally recommended as a salvage regimen.
In a prospective, randomized comparative study published in 2017, the eradication rates (93.9%) in patients receiving 14-day bismuth quadruple therapy (pantoprazole, bismuth subcitrate, tetracycline, and metronidazole) were comparable with eradication rates (92.8%) with 14-day hybrid therapy (dual therapy with pantoprazole plus amoxicillin for 7 days, followed by quadruple therapy with pantoprazole, amoxicillin, clarithromycin, and metronidazole for 7 days).
Quadruple therapy had a higher frequency of adverse events, at 55%, compared with 15.7% for hybrid therapy (P < .001). “Whether shortening the treatment duration of bismuth quadruple therapy from 14 days to 10 days can reduce the frequency of adverse effects remains unclear,” Dr. Hsu said in introductory comments to his study.
Comparing three approaches
In the multicenter, randomized, open-label superiority trial presented at DDW, Dr. Hsu and colleagues randomly assigned 600 Helicobacter pylori–infected participants in equal numbers to receive 14-day hybrid therapy, 14-day high-dose dual therapy, or 10-day bismuth quadruple therapy.
The hybrid therapy regimen consisted of rabeprazole 20 mg twice a day plus amoxicillin 1 g twice a day for 14 days, with clarithromycin 500 mg and metronidazole 500 mg twice a day in the final 7 days. The high-dose dual therapy regimen consisted of rabeprazole 20 mg and amoxicillin 750 mg four times a day for 14 days. The bismuth quadruple therapy regimen consisted of rabeprazole 20 mg twice a day, tripotassium dicitrato bismuthate 300 mg four times a day, tetracycline 500 mg twice a day, and metronidazole 250 mg four times a day for 10 days.
Investigators assessed H. pylori status 6 weeks following the end of therapy. In an intention-to-treat analysis, the hybrid therapy regimen yielded an eradication rate of 96.5%, which was comparable with the 93.5% eradication rate seen with bismuth quadruple therapy and was significantly higher than the 86.0% eradication rate seen with high-dose dual therapy (P < .001), according to Dr. Hsu. Similar efficacy outcomes were seen in per-protocol analysis.
The frequency of adverse events was lowest with high-dose dual therapy, at 13.0%, according to Dr. Hsu. That was significantly lower than the 25.5% frequency of adverse events with hybrid therapy. Bismuth quadruple therapy had a rate of 34.0%.
Antibiotic resistance results
Antibiotic resistance was most common for metronidazole, seen in approximately 28% of the quadruple-therapy group, 34% of the hybrid group, and 37% of the high-dose therapy groups. Clarithromycin resistance occurred in about 23% of quadruple therapy recipients, 16% of hybrid recipients, and 16% of high-dose therapy recipients. Amoxicillin and tetracycline resistance was rare, occurring in approximately 0%-3% of groups.
In the quadruple therapy arm, metronidazole resistance was associated with H. pylori eradication failure, according to Dr. Hsu. The eradication rate was about 96% for those subjects with no metronidazole resistance, and 88% for those with resistance (P = .05). Amoxicillin resistance, although rare in the study, independently predicted eradication failure of high-dose dual therapy, Dr. Hsu said. The eradication rate with high-dose dual therapy was 87.6% for individuals without amoxicillin resistance, and 40.0% in individuals with resistance, according to presented data.
The authors reported no financial disclosures related to their research. Dr. Buensalido has been a speaker for Unilab, BSV Bioscience, and Philcare Pharma, and has received sponsorship from Pfizer.
FROM DDW 2021