User login
The AGA Future Leaders Program: A Mentee-Mentor Triad Perspective
Two of us (Parakkal Deepak and Edward L. Barnes) were part of the American Gastroenterological Association’s (AGA) Future Leaders Program (FLP) class of 2022-2023, and our mentor was Aasma Shaukat. We were invited to share our experiences as participants in the FLP and its impact in our careers.
Why Was the Future Leaders Program Conceived?
To understand this, one must first understand that the AGA, like all other GI professional organizations, relies on volunteer leaders to develop its long-term vision and execute this through strategic initiatives and programs. and understand the governance structure of the AGA to help lead it to face these challenges effectively.
The AGA FLP was thus conceived and launched in 2014-2015 by the founding chairs, Byron Cryer, MD, who is a professor of medicine and associate dean for faculty diversity at University of Texas Southwestern Medical School and Suzanne Rose, MD, MSEd, AGAF, who is a professor of medicine and senior vice dean for medical education at Perelman School of Medicine at the University of Pennsylvania. They envisioned a leadership pathway that would position early career GIs on a track to positively affect the AGA and the field of GI.
How Does One Apply for the Program?
Our FLP cohort applications were invited in October of 2021 and mentees accepted into the program in November 2021. The application process is competitive – applicants are encouraged to detail why they feel they would benefit from the FLP, what existing skillsets they have that can be further enhanced through the program, and what their long-term vision is for their growth as leaders, both within their institution and within the AGA. This is further accompanied by letters of support from their divisional chiefs and other key supervisors within the division who are intimately aware of their leadership potential and career trajectory. This process identified 18 future leaders for our class of 2022-2023.
What Is Involved?
Following acceptance into the AGA Future Leaders Program, we embarked on a series of virtual and in-person meetings with our mentorship triads (one mentor and two mentees) and other mentorship teams over the 18-month program (see Figure). These meetings covered highly focused topics ranging from the role of advocacy in leadership to negotiation and developing a business plan, with ample opportunities for individually tailored mentorship within the mentorship triads.

We also completed personality assessments that helped us understand our strengths and areas of improvement, and ways to use the information to hone our leadership styles.
A large portion of programming and the mentorship experience during the AGA Future Leaders Program is focused on a leadership project that is aimed at addressing a societal driver of interest for the AGA. Examples of these societal drivers of interest include maximizing the role of women in gastroenterology, the role of artificial intelligence in gastroenterology, burnout, and the impact of climate change on gastroenterology. Mentorship triads propose novel methods for addressing these critical issues, outlining the roles that the AGA and other stakeholders may embrace to address these anticipated growing challenges head on.
Our mentorship triad was asked to address the issue of ending disparities within gastroenterology. Given our research and clinical interest in inflammatory bowel disease (IBD), we immediately recognized an opportunity to evaluate and potentially offer solutions for the geographic disparities that exist in the field of IBD. These disparities affect access to care for patients with Crohn’s disease and ulcerative colitis, leading to delays in diagnosis and ultimately effective therapy decisions.
In addition to developing a proposal for the AGA to expand access to care to major IBD centers in rural areas where these disparities exist, we also initiated an examination of geographic disparities in our own multidisciplinary IBD centers (abstract accepted for presentation at Digestive Diseases Week 2024). This allowed us to expand our respective research footprints at our institutions, utilizing new methods of geocoding to directly measure factors affecting clinical outcomes in IBD. Given our in-depth evaluation of this topic as part of our Future Leaders Program training, at the suggestion of our mentor, our mentorship triad also published a commentary on geographic disparities in the Diversity, Equity, and Inclusion sections of Gastroenterology and Clinical Gastroenterology and Hepatology.1, 2
Impact on the Field and Our Careers
Our mentorship triad had the unique experience of having a mentor who had previously participated in the Future Leaders Program as a mentee. As the Future Leaders Program has now enrolled 72 participants, these occasions will likely become more frequent, given the opportunities for career development and growth within the AGA (and our field) that are available after participating in the Future Leaders Program.
To have a mentor with this insight of having been a mentee in the program was invaluable, given her direct experience and understanding of the growth opportunities available, and opportunities to maximize participation in the Future Leaders Program. Additionally, as evidenced by Dr. Shaukat’s recommendations to grow our initial assignment into published commentaries, need statements for our field, and ultimately growing research projects, her keen insights as a mentor were a critical component of our individual growth in the program and the success of our mentorship triad. We benefited from networking with peers and learning about their work, which can lead to future collaborations. We had access to the highly accomplished mentors from diverse settings and learned models of leadership, while developing skills to foster our own leadership style.
In terms of programmatic impact, more than 90% of FLP alumni are serving in AGA leadership on committees, task forces, editorial boards, and councils. What is also important is the impact of content developed by mentee-mentor triads during the FLP cohorts over time. More than 700 GIs have benefited from online leadership development content created by the FLP. Based on our experience, we highly recommend all early career GI physicians to apply!
Dr. Parakkal (@P_DeepakIBDMD) is based in the division of gastroenterology, Washington University in St. Louis (Mo.) School of Medicine. He is supported by a Junior Faculty Development Award from the American College of Gastroenterology and IBD Plexus of the Crohn’s & Colitis Foundation. He has received research support under a sponsored research agreement unrelated to the data in the paper from AbbVie, Arena Pharmaceuticals, Boehringer Ingelheim, Bristol Myers Squibb, Janssen, Prometheus Biosciences, Takeda Pharmaceuticals, Roche-Genentech, and CorEvitas LLC. He has served as a consultant for AbbVie, Boehringer Ingelheim, Bristol Myers Squibb, Scipher Medicine, Fresenius Kabi, Roche-Genentech, and CorEvitas LLC. Dr. Barnes (@EdBarnesMD) is based in the division of gastroenterology and hepatology, University of North Carolina at Chapel Hill. He is supported by National Institutes of Health K23DK127157-01, and has served as a consultant for Eli Lilly, Bristol-Meyers Squibb, and Target RWE. Dr. Shaukat (@AasmaShaukatMD) is based in the division of gastroenterology, New York University, New York. She has served as a consultant for Iterative health, Motus, Freenome, and Geneoscopy. Research support by the Steve and Alex Cohen Foundation.
References
1. Deepak P, Barnes EL, Shaukat A. Health Disparities in Inflammatory Bowel Disease Care Driven by Rural Versus Urban Residence: Challenges and Potential Solutions. Gastroenterology. 2023 July. doi: 10.1053/j.gastro.2023.05.017.
2. Deepak P, Barnes EL, Shaukat A. Health Disparities in Inflammatory Bowel Disease Care Driven by Rural Versus Urban Residence: Challenges and Potential Solutions. Clin Gastroenterol Hepatol. 2023 July. doi: 10.1016/j.cgh.2023.04.006.
Two of us (Parakkal Deepak and Edward L. Barnes) were part of the American Gastroenterological Association’s (AGA) Future Leaders Program (FLP) class of 2022-2023, and our mentor was Aasma Shaukat. We were invited to share our experiences as participants in the FLP and its impact in our careers.
Why Was the Future Leaders Program Conceived?
To understand this, one must first understand that the AGA, like all other GI professional organizations, relies on volunteer leaders to develop its long-term vision and execute this through strategic initiatives and programs. and understand the governance structure of the AGA to help lead it to face these challenges effectively.
The AGA FLP was thus conceived and launched in 2014-2015 by the founding chairs, Byron Cryer, MD, who is a professor of medicine and associate dean for faculty diversity at University of Texas Southwestern Medical School and Suzanne Rose, MD, MSEd, AGAF, who is a professor of medicine and senior vice dean for medical education at Perelman School of Medicine at the University of Pennsylvania. They envisioned a leadership pathway that would position early career GIs on a track to positively affect the AGA and the field of GI.
How Does One Apply for the Program?
Our FLP cohort applications were invited in October of 2021 and mentees accepted into the program in November 2021. The application process is competitive – applicants are encouraged to detail why they feel they would benefit from the FLP, what existing skillsets they have that can be further enhanced through the program, and what their long-term vision is for their growth as leaders, both within their institution and within the AGA. This is further accompanied by letters of support from their divisional chiefs and other key supervisors within the division who are intimately aware of their leadership potential and career trajectory. This process identified 18 future leaders for our class of 2022-2023.
What Is Involved?
Following acceptance into the AGA Future Leaders Program, we embarked on a series of virtual and in-person meetings with our mentorship triads (one mentor and two mentees) and other mentorship teams over the 18-month program (see Figure). These meetings covered highly focused topics ranging from the role of advocacy in leadership to negotiation and developing a business plan, with ample opportunities for individually tailored mentorship within the mentorship triads.

We also completed personality assessments that helped us understand our strengths and areas of improvement, and ways to use the information to hone our leadership styles.
A large portion of programming and the mentorship experience during the AGA Future Leaders Program is focused on a leadership project that is aimed at addressing a societal driver of interest for the AGA. Examples of these societal drivers of interest include maximizing the role of women in gastroenterology, the role of artificial intelligence in gastroenterology, burnout, and the impact of climate change on gastroenterology. Mentorship triads propose novel methods for addressing these critical issues, outlining the roles that the AGA and other stakeholders may embrace to address these anticipated growing challenges head on.
Our mentorship triad was asked to address the issue of ending disparities within gastroenterology. Given our research and clinical interest in inflammatory bowel disease (IBD), we immediately recognized an opportunity to evaluate and potentially offer solutions for the geographic disparities that exist in the field of IBD. These disparities affect access to care for patients with Crohn’s disease and ulcerative colitis, leading to delays in diagnosis and ultimately effective therapy decisions.
In addition to developing a proposal for the AGA to expand access to care to major IBD centers in rural areas where these disparities exist, we also initiated an examination of geographic disparities in our own multidisciplinary IBD centers (abstract accepted for presentation at Digestive Diseases Week 2024). This allowed us to expand our respective research footprints at our institutions, utilizing new methods of geocoding to directly measure factors affecting clinical outcomes in IBD. Given our in-depth evaluation of this topic as part of our Future Leaders Program training, at the suggestion of our mentor, our mentorship triad also published a commentary on geographic disparities in the Diversity, Equity, and Inclusion sections of Gastroenterology and Clinical Gastroenterology and Hepatology.1, 2
Impact on the Field and Our Careers
Our mentorship triad had the unique experience of having a mentor who had previously participated in the Future Leaders Program as a mentee. As the Future Leaders Program has now enrolled 72 participants, these occasions will likely become more frequent, given the opportunities for career development and growth within the AGA (and our field) that are available after participating in the Future Leaders Program.
To have a mentor with this insight of having been a mentee in the program was invaluable, given her direct experience and understanding of the growth opportunities available, and opportunities to maximize participation in the Future Leaders Program. Additionally, as evidenced by Dr. Shaukat’s recommendations to grow our initial assignment into published commentaries, need statements for our field, and ultimately growing research projects, her keen insights as a mentor were a critical component of our individual growth in the program and the success of our mentorship triad. We benefited from networking with peers and learning about their work, which can lead to future collaborations. We had access to the highly accomplished mentors from diverse settings and learned models of leadership, while developing skills to foster our own leadership style.
In terms of programmatic impact, more than 90% of FLP alumni are serving in AGA leadership on committees, task forces, editorial boards, and councils. What is also important is the impact of content developed by mentee-mentor triads during the FLP cohorts over time. More than 700 GIs have benefited from online leadership development content created by the FLP. Based on our experience, we highly recommend all early career GI physicians to apply!
Dr. Parakkal (@P_DeepakIBDMD) is based in the division of gastroenterology, Washington University in St. Louis (Mo.) School of Medicine. He is supported by a Junior Faculty Development Award from the American College of Gastroenterology and IBD Plexus of the Crohn’s & Colitis Foundation. He has received research support under a sponsored research agreement unrelated to the data in the paper from AbbVie, Arena Pharmaceuticals, Boehringer Ingelheim, Bristol Myers Squibb, Janssen, Prometheus Biosciences, Takeda Pharmaceuticals, Roche-Genentech, and CorEvitas LLC. He has served as a consultant for AbbVie, Boehringer Ingelheim, Bristol Myers Squibb, Scipher Medicine, Fresenius Kabi, Roche-Genentech, and CorEvitas LLC. Dr. Barnes (@EdBarnesMD) is based in the division of gastroenterology and hepatology, University of North Carolina at Chapel Hill. He is supported by National Institutes of Health K23DK127157-01, and has served as a consultant for Eli Lilly, Bristol-Meyers Squibb, and Target RWE. Dr. Shaukat (@AasmaShaukatMD) is based in the division of gastroenterology, New York University, New York. She has served as a consultant for Iterative health, Motus, Freenome, and Geneoscopy. Research support by the Steve and Alex Cohen Foundation.
References
1. Deepak P, Barnes EL, Shaukat A. Health Disparities in Inflammatory Bowel Disease Care Driven by Rural Versus Urban Residence: Challenges and Potential Solutions. Gastroenterology. 2023 July. doi: 10.1053/j.gastro.2023.05.017.
2. Deepak P, Barnes EL, Shaukat A. Health Disparities in Inflammatory Bowel Disease Care Driven by Rural Versus Urban Residence: Challenges and Potential Solutions. Clin Gastroenterol Hepatol. 2023 July. doi: 10.1016/j.cgh.2023.04.006.
Two of us (Parakkal Deepak and Edward L. Barnes) were part of the American Gastroenterological Association’s (AGA) Future Leaders Program (FLP) class of 2022-2023, and our mentor was Aasma Shaukat. We were invited to share our experiences as participants in the FLP and its impact in our careers.
Why Was the Future Leaders Program Conceived?
To understand this, one must first understand that the AGA, like all other GI professional organizations, relies on volunteer leaders to develop its long-term vision and execute this through strategic initiatives and programs. and understand the governance structure of the AGA to help lead it to face these challenges effectively.
The AGA FLP was thus conceived and launched in 2014-2015 by the founding chairs, Byron Cryer, MD, who is a professor of medicine and associate dean for faculty diversity at University of Texas Southwestern Medical School and Suzanne Rose, MD, MSEd, AGAF, who is a professor of medicine and senior vice dean for medical education at Perelman School of Medicine at the University of Pennsylvania. They envisioned a leadership pathway that would position early career GIs on a track to positively affect the AGA and the field of GI.
How Does One Apply for the Program?
Our FLP cohort applications were invited in October of 2021 and mentees accepted into the program in November 2021. The application process is competitive – applicants are encouraged to detail why they feel they would benefit from the FLP, what existing skillsets they have that can be further enhanced through the program, and what their long-term vision is for their growth as leaders, both within their institution and within the AGA. This is further accompanied by letters of support from their divisional chiefs and other key supervisors within the division who are intimately aware of their leadership potential and career trajectory. This process identified 18 future leaders for our class of 2022-2023.
What Is Involved?
Following acceptance into the AGA Future Leaders Program, we embarked on a series of virtual and in-person meetings with our mentorship triads (one mentor and two mentees) and other mentorship teams over the 18-month program (see Figure). These meetings covered highly focused topics ranging from the role of advocacy in leadership to negotiation and developing a business plan, with ample opportunities for individually tailored mentorship within the mentorship triads.

We also completed personality assessments that helped us understand our strengths and areas of improvement, and ways to use the information to hone our leadership styles.
A large portion of programming and the mentorship experience during the AGA Future Leaders Program is focused on a leadership project that is aimed at addressing a societal driver of interest for the AGA. Examples of these societal drivers of interest include maximizing the role of women in gastroenterology, the role of artificial intelligence in gastroenterology, burnout, and the impact of climate change on gastroenterology. Mentorship triads propose novel methods for addressing these critical issues, outlining the roles that the AGA and other stakeholders may embrace to address these anticipated growing challenges head on.
Our mentorship triad was asked to address the issue of ending disparities within gastroenterology. Given our research and clinical interest in inflammatory bowel disease (IBD), we immediately recognized an opportunity to evaluate and potentially offer solutions for the geographic disparities that exist in the field of IBD. These disparities affect access to care for patients with Crohn’s disease and ulcerative colitis, leading to delays in diagnosis and ultimately effective therapy decisions.
In addition to developing a proposal for the AGA to expand access to care to major IBD centers in rural areas where these disparities exist, we also initiated an examination of geographic disparities in our own multidisciplinary IBD centers (abstract accepted for presentation at Digestive Diseases Week 2024). This allowed us to expand our respective research footprints at our institutions, utilizing new methods of geocoding to directly measure factors affecting clinical outcomes in IBD. Given our in-depth evaluation of this topic as part of our Future Leaders Program training, at the suggestion of our mentor, our mentorship triad also published a commentary on geographic disparities in the Diversity, Equity, and Inclusion sections of Gastroenterology and Clinical Gastroenterology and Hepatology.1, 2
Impact on the Field and Our Careers
Our mentorship triad had the unique experience of having a mentor who had previously participated in the Future Leaders Program as a mentee. As the Future Leaders Program has now enrolled 72 participants, these occasions will likely become more frequent, given the opportunities for career development and growth within the AGA (and our field) that are available after participating in the Future Leaders Program.
To have a mentor with this insight of having been a mentee in the program was invaluable, given her direct experience and understanding of the growth opportunities available, and opportunities to maximize participation in the Future Leaders Program. Additionally, as evidenced by Dr. Shaukat’s recommendations to grow our initial assignment into published commentaries, need statements for our field, and ultimately growing research projects, her keen insights as a mentor were a critical component of our individual growth in the program and the success of our mentorship triad. We benefited from networking with peers and learning about their work, which can lead to future collaborations. We had access to the highly accomplished mentors from diverse settings and learned models of leadership, while developing skills to foster our own leadership style.
In terms of programmatic impact, more than 90% of FLP alumni are serving in AGA leadership on committees, task forces, editorial boards, and councils. What is also important is the impact of content developed by mentee-mentor triads during the FLP cohorts over time. More than 700 GIs have benefited from online leadership development content created by the FLP. Based on our experience, we highly recommend all early career GI physicians to apply!
Dr. Parakkal (@P_DeepakIBDMD) is based in the division of gastroenterology, Washington University in St. Louis (Mo.) School of Medicine. He is supported by a Junior Faculty Development Award from the American College of Gastroenterology and IBD Plexus of the Crohn’s & Colitis Foundation. He has received research support under a sponsored research agreement unrelated to the data in the paper from AbbVie, Arena Pharmaceuticals, Boehringer Ingelheim, Bristol Myers Squibb, Janssen, Prometheus Biosciences, Takeda Pharmaceuticals, Roche-Genentech, and CorEvitas LLC. He has served as a consultant for AbbVie, Boehringer Ingelheim, Bristol Myers Squibb, Scipher Medicine, Fresenius Kabi, Roche-Genentech, and CorEvitas LLC. Dr. Barnes (@EdBarnesMD) is based in the division of gastroenterology and hepatology, University of North Carolina at Chapel Hill. He is supported by National Institutes of Health K23DK127157-01, and has served as a consultant for Eli Lilly, Bristol-Meyers Squibb, and Target RWE. Dr. Shaukat (@AasmaShaukatMD) is based in the division of gastroenterology, New York University, New York. She has served as a consultant for Iterative health, Motus, Freenome, and Geneoscopy. Research support by the Steve and Alex Cohen Foundation.
References
1. Deepak P, Barnes EL, Shaukat A. Health Disparities in Inflammatory Bowel Disease Care Driven by Rural Versus Urban Residence: Challenges and Potential Solutions. Gastroenterology. 2023 July. doi: 10.1053/j.gastro.2023.05.017.
2. Deepak P, Barnes EL, Shaukat A. Health Disparities in Inflammatory Bowel Disease Care Driven by Rural Versus Urban Residence: Challenges and Potential Solutions. Clin Gastroenterol Hepatol. 2023 July. doi: 10.1016/j.cgh.2023.04.006.
Artificial Intelligence in GI and Hepatology
Dear colleagues,
Since our prior Perspectives piece on artificial intelligence (AI) in GI and Hepatology in 2022, the field has seen almost exponential growth. Expectations are high that AI will revolutionize our field and significantly improve patient care. But as the global discussion on AI has shown, there are real challenges with adoption, including issues with accuracy, reliability, and privacy.
In this issue, Dr. Nabil M. Mansour and Dr. Thomas R. McCarty explore the current and future impact of AI on gastroenterology, while Dr. Basile Njei and Yazan A. Al Ajlouni assess its role in hepatology. We hope these pieces will help your discussions in incorporating or researching AI for use in your own practices. We welcome your thoughts on this issue on X @AGA_GIHN.
Gyanprakash A. Ketwaroo, MD, MSc, is associate professor of medicine, Yale University, New Haven, Conn., and chief of endoscopy at West Haven (Conn.) VA Medical Center. He is an associate editor for GI & Hepatology News.
Artificial Intelligence in Gastrointestinal Endoscopy
BY THOMAS R. MCCARTY, MD, MPH; NABIL M. MANSOUR, MD
The last few decades have seen an exponential increase and interest in the role of artificial intelligence (AI) and adoption of deep learning algorithms within healthcare and patient care services. The field of gastroenterology and endoscopy has similarly seen a tremendous uptake in acceptance and implementation of AI for a variety of gastrointestinal conditions. The spectrum of AI-based applications includes detection or diagnostic-based as well as therapeutic assistance tools. From the first US Food and Drug Administration (FDA)-approved device that uses machine learning to assist clinicians in detecting lesions during colonoscopy, to other more innovative machine learning techniques for small bowel, esophageal, and hepatobiliary conditions, AI has dramatically changed the landscape of gastrointestinal endoscopy.
Approved applications for colorectal cancer
In an attempt to improve colorectal cancer screening and outcomes related to screening and surveillance, efforts have been focused on procedural performance metrics, quality indicators, and tools to aid in lesion detection and improve quality of care. One such tool has been computer-aided detection (CADe), with early randomized controlled trial (RCT) data showing significantly increased adenoma detection rate (ADR) and adenomas per colonoscopy (APC).1-3
Ultimately, this data led to FDA approval of the CADe system GI Genius (Medtronic, Dublin, Ireland) in 2021.4 Additional systems have since been FDA approved or 510(k) cleared including Endoscreener (Wision AI, Shanghai, China), SKOUT (Iterative Health, Cambridge, Massachusetts), MAGENTIQ-COLO (MAGENTIQ-EYE LTD, Haifa, Israel), and CAD EYE (Fujifilm, Tokyo), all of which have shown increased ADR and/or increased APC and/or reduced adenoma miss rates in randomized trials.5
Yet despite the promise of improved quality and subsequent translation to better patient outcomes, there has been a noticeable disconnect between RCT data and more real-world literature.6 In a recent study, no improvement was seen in ADR after implementation of a CADe system for colorectal cancer screening — including both higher and lower-ADR performers. Looking at change over time after implementation, CADe had no positive effect in any group over time, divergent from early RCT data. In a more recent multicenter, community-based RCT study, again CADe did not result in a statistically significant difference in the number of adenomas detected.7 The differences between some of these more recent “real-world” studies vs the majority of data from RCTs raise important questions regarding the potential of bias (due to unblinding) in prospective trials, as well as the role of the human-AI interaction.
Importantly for RCT data, both cohorts in these studies met adequate ADR benchmarks, though it remains unclear whether a truly increased ADR necessitates better patient outcomes — is higher always better? In addition, an important consideration with evaluating any AI/CADe system is that they often undergo frequent updates, each promising improved accuracy, sensitivity, and specificity. This is an interesting dilemma and raises questions about the enduring relevance of studies conducted using an outdated version of a CADe system.
Additional unanswered questions regarding an ideal ADR for implementation, preferred patient populations for screening (especially for younger individuals), and the role and adoption of computer-aided polyp diagnosis/characterization (CADx) within the United States remain. Furthermore, questions regarding procedural withdrawal time, impact on sessile serrated lesion detection, cost-effectiveness, and preferred adoption strategies have begun to be explored, though require more data to better define a best practice approach. Ultimately, answers to some of these unknowns may explain the discordant results and help guide future implementation measures.
Innovative applications for alternative gastrointestinal conditions
Given the fervor and excitement, as well as the outcomes associated with AI-based colorectal screening, it is not surprising these techniques have been expanded to other gastrointestinal conditions. At this time, all of these are fledgling, mostly single-center tools, not yet ready for widespread adoption. Nonetheless, these represent a potentially important step forward for difficult-to-manage gastrointestinal diseases.
Machine learning CADe systems have been developed to help identify early Barrett’s neoplasia, depth and invasion of gastric cancer, as well as lesion detection in small bowel video capsule endoscopy.8-10 Endoscopic retrograde cholangiopancreatography (ERCP)-based applications for cholangiocarcinoma and indeterminate stricture diagnosis have also been studied.11 Additional AI-based algorithms have been employed for complex procedures such as endoscopic submucosal dissection (ESD) or peroral endoscopic myotomy (POEM) to delineate vessels, better define tissue planes for dissection, and visualize landmark structures.12,13 Furthermore, AI-based scope guidance/manipulation, bleeding detection, landmark identification, and lesion detection have the potential to revolutionize endoscopic training and education. The impact that generative AI can potentially have on clinical practice is also an exciting prospect that warrants further investigation.
Artificial intelligence adoption in clinical practice
Clinical practice with regard to AI and colorectal cancer screening largely mirrors the disconnect in the current literature, with “believers” and “non-believers” as well as innovators and early adopters alongside laggards. In our own academic practices, we continue to struggle with the adoption and standardized implementation of AI-based colorectal cancer CADe systems, despite the RCT data showing positive results. It is likely that AI uptake will follow the technology predictions of Amara’s Law — i.e., individuals tend to overestimate the short-term impact of new technologies while underestimating long-term effects. In the end, more widespread adoption in community practice and larger scale real-world clinical outcomes studies are likely to determine the true impact of these exciting technologies. For other, less established AI-based tools, more data are currently required.
Conclusions
Ultimately, AI-based algorithms are likely here to stay, with continued improvement and evolution to occur based on provider feedback and patient care needs. Current tools, while not all-encompassing, have the potential to dramatically change the landscape of endoscopic training, diagnostic evaluation, and therapeutic care. It is critically important that relevant stakeholders, both endoscopists and patients, be involved in future applications and design to improve efficiency and quality outcomes overall.
Dr. McCarty is based in the Lynda K. and David M. Underwood Center for Digestive Disorders, Houston Methodist Hospital. Dr. Mansour is based in the section of gastroenterology, Baylor College of Medicine, Houston. Dr. McCarty reports no conflicts of interest. Dr. Mansour reports having been a consultant for Iterative Health.
References
1. Repici A, et al. Efficacy of real-time computer-aided detection of colorectal neoplasia in a randomized trial. Gastroenterology. 2020 Aug. doi: 10.1053/j.gastro.2020.04.062.
2. Repici A, et al. Artificial intelligence and colonoscopy experience: Lessons from two randomised trials. Gut. Apr 2022. doi: 10.1136/gutjnl-2021-324471.
3. Wallace MB, et al. Impact of artificial intelligence on miss rate of colorectal neoplasia. Gastroenterology 2022 Jul. doi: 10.1053/j.gastro.2022.03.007.
4. United States Food and Drug Administration (FDA). GI Genius FDA Approval [April 9, 2021]. Accessed January 5, 2022. Available at: www.accessdata.fda.gov/cdrh_docs/pdf21/K211951.pdf.
5. Maas MHJ, et al. A computer-aided polyp detection system in screening and surveillance colonoscopy: An international, multicentre, randomised, tandem trial. Lancet Digit Health. 2024 Mar. doi: 10.1016/S2589-7500(23)00242-X.
6. Ladabaum U, et al. Computer-aided detection of polyps does not improve colonoscopist performance in a pragmatic implementation trial. Gastroenterology. 2023 Mar. doi: 10.1053/j.gastro.2022.12.004.
7. Wei MT, et al. Evaluation of computer-aided detection during colonoscopy in the community (AI-SEE): A multicenter randomized clinical trial. Am J Gastroenterol. 2023 Oct. doi: 10.14309/ajg.0000000000002239.
8. de Groof J, et al. The Argos project: The development of a computer-aided detection system to improve detection of Barrett’s neoplasia on white light endoscopy. United European Gastroenterol J. 2019 May. doi: 10.1177/2050640619837443.
9. Kanesaka T, et al. Computer-aided diagnosis for identifying and delineating early gastric cancers in magnifying narrow-band imaging. Gastrointest Endosc. 2018 May. doi: 10.1016/j.gie.2017.11.029.
10. Sahafi A, et al. Edge artificial intelligence wireless video capsule endoscopy. Sci Rep. 2022 Aug. doi: 10.1038/s41598-022-17502-7.
11. Njei B, et al. Artificial intelligence in endoscopic imaging for detection of malignant biliary strictures and cholangiocarcinoma: A systematic review. Ann Gastroenterol. 2023 Mar-Apr. doi: 10.20524/aog.2023.0779.
12. Ebigbo A, et al. Vessel and tissue recognition during third-space endoscopy using a deep learning algorithm. Gut. 2022 Dec. doi: 10.1136/gutjnl-2021-326470.
13. Cao J, et al. Intelligent surgical workflow recognition for endoscopic submucosal dissection with real-time animal study. Nat Commun. 2023 Oct. doi: 10.1038/s41467-023-42451-8.
The Promise and Challenges of AI in Hepatology
BY BASILE NJEI, MD, MPH, PHD; YAZAN A. AL-AJLOUNI, MPHIL
In the dynamic realm of medicine, artificial intelligence (AI) emerges as a transformative force, notably within hepatology. The discipline of hepatology, dedicated to liver and related organ diseases, is ripe for AI’s promise to revolutionize diagnostics and treatment, pushing toward a future of precision medicine. Yet, the path to fully realizing AI’s potential in hepatology is laced with data, ethical, and integration challenges.
The application of AI, particularly in histopathology, significantly enhances disease diagnosis and staging in hepatology. AI-driven approaches remedy traditional histopathological challenges, such as interpretative variability, providing more consistent and accurate disease analyses. This is especially evident in conditions like metabolic dysfunction-associated steatohepatitis (MASH) and hepatocellular carcinoma (HCC), where AI aids in identifying critical gene signatures, thereby refining therapy selection.
Similarly, deep learning (DL), a branch of AI, has attracted significant interest globally, particularly in image recognition. AI’s incorporation into medical imaging marks a significant advancement, enabling early detection of malignancies like HCC and improving diagnostics in steatotic liver disease through enhanced imaging analyses using convolutional neural networks (CNN). The abundance of imaging data alongside clinical outcomes has catalyzed AI’s integration into radiology, leading to the swift growth of radiomics as a novel domain in medical research.
AI has also been shown to identify nuanced alterations in electrocardiograms (EKGs) associated with liver conditions, potentially detecting the progression of liver diseases at an earlier stage than currently possible. By leveraging complex algorithms and machine learning, AI can analyze EKG patterns with a precision and depth unattainable through traditional manual interpretation. Given that liver diseases, such as cirrhosis or hepatitis, can induce subtle cardiac changes long before other clinical symptoms manifest, early detection through AI-enhanced EKG analysis could lead to timely interventions, potentially halting or reversing disease progression. This approach further enriches our understanding of the intricate interplay between liver function and cardiac health, highlighting the potential for AI to transform not just liver disease diagnostics but also to foster a more integrated approach to patient care.
Beyond diagnostics, the burgeoning field of generative AI introduces groundbreaking possibilities in treatment planning and patient education, particularly for chronic conditions like cirrhosis. Generative AI produces original content, including text, visuals, and music, by identifying and learning patterns from its training data. When it leverages large language models (LLMs), it entails training on vast collections of textual data and using AI models characterized by many parameters. A notable instance of generative AI employing LLMs is ChatGPT (General Pretrained Transformers). By simulating disease progression and treatment outcomes, generative AI can foster personalized treatment strategies and empower patients with knowledge about their health trajectories. Yet, realizing these potential demands requires overcoming data quality and interpretability challenges, and ensuring AI outputs are accessible and actionable for clinicians and patients.
Despite these advancements, leveraging AI in hepatology is not devoid of hurdles. The development and training of AI models require extensive and diverse datasets, raising concerns about data privacy and ethical use. Addressing these concerns is paramount for successfully integrating AI into clinical hepatology practice, necessitating transparent algorithmic processes and stringent ethical standards. Ethical considerations are central to AI’s integration into hepatology. Algorithmic biases, patient privacy, and the impact of AI-driven decisions underscore the need for cautious AI deployment. Developing transparent, understandable algorithms and establishing ethical guidelines for AI use are critical steps towards ethically leveraging AI in patient care.
In conclusion, AI’s integration into hepatology holds tremendous promise for advancing patient care through enhanced diagnostics, treatment planning, and patient education. Overcoming the associated challenges, including ethical concerns, data diversity, and algorithm interpretability, is crucial. As the hepatology community navigates this technological evolution, a balanced approach that marries technological advancements with ethical stewardship will be key to harnessing AI’s full potential, ensuring it serves the best interests of patients and propels the field of hepatology into the future.
We predict a trajectory of increased use and adoption of AI in hepatology. AI in hepatology is likely to meet the test of pervasiveness, improvement, and innovation. The adoption of AI in routine hepatology diagnosis and management will likely follow Amara’s law and the five stages of the hype cycle. We believe that we are still in the infant stages of adopting AI technology in hepatology, and this phase may last 5 years before there is a peak of inflated expectations. The trough of disillusionment and slopes of enlightenment may only be observed in the next decades.
Dr. Njei is based in the Section of Digestive Diseases, Yale School of Medicine, New Haven, Conn. Mr. Al-Ajlouni is a senior medical student at New York Medical College School of Medicine, Valhalla, N.Y. They have no conflicts of interest to declare.
Sources
Taylor-Weiner A, et al. A Machine Learning Approach Enables Quantitative Measurement of Liver Histology and Disease Monitoring in NASH. Hepatology. 2021 Jul. doi: 10.1002/hep.31750.
Zeng Q, et al. Artificial intelligence predicts immune and inflammatory gene signatures directly from hepatocellular carcinoma histology. J Hepatol. 2022 Jul. doi: 10.1016/j.jhep.2022.01.018.
Ahn JC, et al. Development of the AI-Cirrhosis-ECG Score: An Electrocardiogram-Based Deep Learning Model in Cirrhosis. Am J Gastroenterol. 2022 Mar. doi: 10.14309/ajg.0000000000001617.
Nduma BN, et al. The Application of Artificial Intelligence (AI)-Based Ultrasound for the Diagnosis of Fatty Liver Disease: A Systematic Review. Cureus. 2023 Dec 15. doi: 10.7759/cureus.50601.
Dear colleagues,
Since our prior Perspectives piece on artificial intelligence (AI) in GI and Hepatology in 2022, the field has seen almost exponential growth. Expectations are high that AI will revolutionize our field and significantly improve patient care. But as the global discussion on AI has shown, there are real challenges with adoption, including issues with accuracy, reliability, and privacy.
In this issue, Dr. Nabil M. Mansour and Dr. Thomas R. McCarty explore the current and future impact of AI on gastroenterology, while Dr. Basile Njei and Yazan A. Al Ajlouni assess its role in hepatology. We hope these pieces will help your discussions in incorporating or researching AI for use in your own practices. We welcome your thoughts on this issue on X @AGA_GIHN.
Gyanprakash A. Ketwaroo, MD, MSc, is associate professor of medicine, Yale University, New Haven, Conn., and chief of endoscopy at West Haven (Conn.) VA Medical Center. He is an associate editor for GI & Hepatology News.
Artificial Intelligence in Gastrointestinal Endoscopy
BY THOMAS R. MCCARTY, MD, MPH; NABIL M. MANSOUR, MD
The last few decades have seen an exponential increase and interest in the role of artificial intelligence (AI) and adoption of deep learning algorithms within healthcare and patient care services. The field of gastroenterology and endoscopy has similarly seen a tremendous uptake in acceptance and implementation of AI for a variety of gastrointestinal conditions. The spectrum of AI-based applications includes detection or diagnostic-based as well as therapeutic assistance tools. From the first US Food and Drug Administration (FDA)-approved device that uses machine learning to assist clinicians in detecting lesions during colonoscopy, to other more innovative machine learning techniques for small bowel, esophageal, and hepatobiliary conditions, AI has dramatically changed the landscape of gastrointestinal endoscopy.
Approved applications for colorectal cancer
In an attempt to improve colorectal cancer screening and outcomes related to screening and surveillance, efforts have been focused on procedural performance metrics, quality indicators, and tools to aid in lesion detection and improve quality of care. One such tool has been computer-aided detection (CADe), with early randomized controlled trial (RCT) data showing significantly increased adenoma detection rate (ADR) and adenomas per colonoscopy (APC).1-3
Ultimately, this data led to FDA approval of the CADe system GI Genius (Medtronic, Dublin, Ireland) in 2021.4 Additional systems have since been FDA approved or 510(k) cleared including Endoscreener (Wision AI, Shanghai, China), SKOUT (Iterative Health, Cambridge, Massachusetts), MAGENTIQ-COLO (MAGENTIQ-EYE LTD, Haifa, Israel), and CAD EYE (Fujifilm, Tokyo), all of which have shown increased ADR and/or increased APC and/or reduced adenoma miss rates in randomized trials.5
Yet despite the promise of improved quality and subsequent translation to better patient outcomes, there has been a noticeable disconnect between RCT data and more real-world literature.6 In a recent study, no improvement was seen in ADR after implementation of a CADe system for colorectal cancer screening — including both higher and lower-ADR performers. Looking at change over time after implementation, CADe had no positive effect in any group over time, divergent from early RCT data. In a more recent multicenter, community-based RCT study, again CADe did not result in a statistically significant difference in the number of adenomas detected.7 The differences between some of these more recent “real-world” studies vs the majority of data from RCTs raise important questions regarding the potential of bias (due to unblinding) in prospective trials, as well as the role of the human-AI interaction.
Importantly for RCT data, both cohorts in these studies met adequate ADR benchmarks, though it remains unclear whether a truly increased ADR necessitates better patient outcomes — is higher always better? In addition, an important consideration with evaluating any AI/CADe system is that they often undergo frequent updates, each promising improved accuracy, sensitivity, and specificity. This is an interesting dilemma and raises questions about the enduring relevance of studies conducted using an outdated version of a CADe system.
Additional unanswered questions regarding an ideal ADR for implementation, preferred patient populations for screening (especially for younger individuals), and the role and adoption of computer-aided polyp diagnosis/characterization (CADx) within the United States remain. Furthermore, questions regarding procedural withdrawal time, impact on sessile serrated lesion detection, cost-effectiveness, and preferred adoption strategies have begun to be explored, though require more data to better define a best practice approach. Ultimately, answers to some of these unknowns may explain the discordant results and help guide future implementation measures.
Innovative applications for alternative gastrointestinal conditions
Given the fervor and excitement, as well as the outcomes associated with AI-based colorectal screening, it is not surprising these techniques have been expanded to other gastrointestinal conditions. At this time, all of these are fledgling, mostly single-center tools, not yet ready for widespread adoption. Nonetheless, these represent a potentially important step forward for difficult-to-manage gastrointestinal diseases.
Machine learning CADe systems have been developed to help identify early Barrett’s neoplasia, depth and invasion of gastric cancer, as well as lesion detection in small bowel video capsule endoscopy.8-10 Endoscopic retrograde cholangiopancreatography (ERCP)-based applications for cholangiocarcinoma and indeterminate stricture diagnosis have also been studied.11 Additional AI-based algorithms have been employed for complex procedures such as endoscopic submucosal dissection (ESD) or peroral endoscopic myotomy (POEM) to delineate vessels, better define tissue planes for dissection, and visualize landmark structures.12,13 Furthermore, AI-based scope guidance/manipulation, bleeding detection, landmark identification, and lesion detection have the potential to revolutionize endoscopic training and education. The impact that generative AI can potentially have on clinical practice is also an exciting prospect that warrants further investigation.
Artificial intelligence adoption in clinical practice
Clinical practice with regard to AI and colorectal cancer screening largely mirrors the disconnect in the current literature, with “believers” and “non-believers” as well as innovators and early adopters alongside laggards. In our own academic practices, we continue to struggle with the adoption and standardized implementation of AI-based colorectal cancer CADe systems, despite the RCT data showing positive results. It is likely that AI uptake will follow the technology predictions of Amara’s Law — i.e., individuals tend to overestimate the short-term impact of new technologies while underestimating long-term effects. In the end, more widespread adoption in community practice and larger scale real-world clinical outcomes studies are likely to determine the true impact of these exciting technologies. For other, less established AI-based tools, more data are currently required.
Conclusions
Ultimately, AI-based algorithms are likely here to stay, with continued improvement and evolution to occur based on provider feedback and patient care needs. Current tools, while not all-encompassing, have the potential to dramatically change the landscape of endoscopic training, diagnostic evaluation, and therapeutic care. It is critically important that relevant stakeholders, both endoscopists and patients, be involved in future applications and design to improve efficiency and quality outcomes overall.
Dr. McCarty is based in the Lynda K. and David M. Underwood Center for Digestive Disorders, Houston Methodist Hospital. Dr. Mansour is based in the section of gastroenterology, Baylor College of Medicine, Houston. Dr. McCarty reports no conflicts of interest. Dr. Mansour reports having been a consultant for Iterative Health.
References
1. Repici A, et al. Efficacy of real-time computer-aided detection of colorectal neoplasia in a randomized trial. Gastroenterology. 2020 Aug. doi: 10.1053/j.gastro.2020.04.062.
2. Repici A, et al. Artificial intelligence and colonoscopy experience: Lessons from two randomised trials. Gut. Apr 2022. doi: 10.1136/gutjnl-2021-324471.
3. Wallace MB, et al. Impact of artificial intelligence on miss rate of colorectal neoplasia. Gastroenterology 2022 Jul. doi: 10.1053/j.gastro.2022.03.007.
4. United States Food and Drug Administration (FDA). GI Genius FDA Approval [April 9, 2021]. Accessed January 5, 2022. Available at: www.accessdata.fda.gov/cdrh_docs/pdf21/K211951.pdf.
5. Maas MHJ, et al. A computer-aided polyp detection system in screening and surveillance colonoscopy: An international, multicentre, randomised, tandem trial. Lancet Digit Health. 2024 Mar. doi: 10.1016/S2589-7500(23)00242-X.
6. Ladabaum U, et al. Computer-aided detection of polyps does not improve colonoscopist performance in a pragmatic implementation trial. Gastroenterology. 2023 Mar. doi: 10.1053/j.gastro.2022.12.004.
7. Wei MT, et al. Evaluation of computer-aided detection during colonoscopy in the community (AI-SEE): A multicenter randomized clinical trial. Am J Gastroenterol. 2023 Oct. doi: 10.14309/ajg.0000000000002239.
8. de Groof J, et al. The Argos project: The development of a computer-aided detection system to improve detection of Barrett’s neoplasia on white light endoscopy. United European Gastroenterol J. 2019 May. doi: 10.1177/2050640619837443.
9. Kanesaka T, et al. Computer-aided diagnosis for identifying and delineating early gastric cancers in magnifying narrow-band imaging. Gastrointest Endosc. 2018 May. doi: 10.1016/j.gie.2017.11.029.
10. Sahafi A, et al. Edge artificial intelligence wireless video capsule endoscopy. Sci Rep. 2022 Aug. doi: 10.1038/s41598-022-17502-7.
11. Njei B, et al. Artificial intelligence in endoscopic imaging for detection of malignant biliary strictures and cholangiocarcinoma: A systematic review. Ann Gastroenterol. 2023 Mar-Apr. doi: 10.20524/aog.2023.0779.
12. Ebigbo A, et al. Vessel and tissue recognition during third-space endoscopy using a deep learning algorithm. Gut. 2022 Dec. doi: 10.1136/gutjnl-2021-326470.
13. Cao J, et al. Intelligent surgical workflow recognition for endoscopic submucosal dissection with real-time animal study. Nat Commun. 2023 Oct. doi: 10.1038/s41467-023-42451-8.
The Promise and Challenges of AI in Hepatology
BY BASILE NJEI, MD, MPH, PHD; YAZAN A. AL-AJLOUNI, MPHIL
In the dynamic realm of medicine, artificial intelligence (AI) emerges as a transformative force, notably within hepatology. The discipline of hepatology, dedicated to liver and related organ diseases, is ripe for AI’s promise to revolutionize diagnostics and treatment, pushing toward a future of precision medicine. Yet, the path to fully realizing AI’s potential in hepatology is laced with data, ethical, and integration challenges.
The application of AI, particularly in histopathology, significantly enhances disease diagnosis and staging in hepatology. AI-driven approaches remedy traditional histopathological challenges, such as interpretative variability, providing more consistent and accurate disease analyses. This is especially evident in conditions like metabolic dysfunction-associated steatohepatitis (MASH) and hepatocellular carcinoma (HCC), where AI aids in identifying critical gene signatures, thereby refining therapy selection.
Similarly, deep learning (DL), a branch of AI, has attracted significant interest globally, particularly in image recognition. AI’s incorporation into medical imaging marks a significant advancement, enabling early detection of malignancies like HCC and improving diagnostics in steatotic liver disease through enhanced imaging analyses using convolutional neural networks (CNN). The abundance of imaging data alongside clinical outcomes has catalyzed AI’s integration into radiology, leading to the swift growth of radiomics as a novel domain in medical research.
AI has also been shown to identify nuanced alterations in electrocardiograms (EKGs) associated with liver conditions, potentially detecting the progression of liver diseases at an earlier stage than currently possible. By leveraging complex algorithms and machine learning, AI can analyze EKG patterns with a precision and depth unattainable through traditional manual interpretation. Given that liver diseases, such as cirrhosis or hepatitis, can induce subtle cardiac changes long before other clinical symptoms manifest, early detection through AI-enhanced EKG analysis could lead to timely interventions, potentially halting or reversing disease progression. This approach further enriches our understanding of the intricate interplay between liver function and cardiac health, highlighting the potential for AI to transform not just liver disease diagnostics but also to foster a more integrated approach to patient care.
Beyond diagnostics, the burgeoning field of generative AI introduces groundbreaking possibilities in treatment planning and patient education, particularly for chronic conditions like cirrhosis. Generative AI produces original content, including text, visuals, and music, by identifying and learning patterns from its training data. When it leverages large language models (LLMs), it entails training on vast collections of textual data and using AI models characterized by many parameters. A notable instance of generative AI employing LLMs is ChatGPT (General Pretrained Transformers). By simulating disease progression and treatment outcomes, generative AI can foster personalized treatment strategies and empower patients with knowledge about their health trajectories. Yet, realizing these potential demands requires overcoming data quality and interpretability challenges, and ensuring AI outputs are accessible and actionable for clinicians and patients.
Despite these advancements, leveraging AI in hepatology is not devoid of hurdles. The development and training of AI models require extensive and diverse datasets, raising concerns about data privacy and ethical use. Addressing these concerns is paramount for successfully integrating AI into clinical hepatology practice, necessitating transparent algorithmic processes and stringent ethical standards. Ethical considerations are central to AI’s integration into hepatology. Algorithmic biases, patient privacy, and the impact of AI-driven decisions underscore the need for cautious AI deployment. Developing transparent, understandable algorithms and establishing ethical guidelines for AI use are critical steps towards ethically leveraging AI in patient care.
In conclusion, AI’s integration into hepatology holds tremendous promise for advancing patient care through enhanced diagnostics, treatment planning, and patient education. Overcoming the associated challenges, including ethical concerns, data diversity, and algorithm interpretability, is crucial. As the hepatology community navigates this technological evolution, a balanced approach that marries technological advancements with ethical stewardship will be key to harnessing AI’s full potential, ensuring it serves the best interests of patients and propels the field of hepatology into the future.
We predict a trajectory of increased use and adoption of AI in hepatology. AI in hepatology is likely to meet the test of pervasiveness, improvement, and innovation. The adoption of AI in routine hepatology diagnosis and management will likely follow Amara’s law and the five stages of the hype cycle. We believe that we are still in the infant stages of adopting AI technology in hepatology, and this phase may last 5 years before there is a peak of inflated expectations. The trough of disillusionment and slopes of enlightenment may only be observed in the next decades.
Dr. Njei is based in the Section of Digestive Diseases, Yale School of Medicine, New Haven, Conn. Mr. Al-Ajlouni is a senior medical student at New York Medical College School of Medicine, Valhalla, N.Y. They have no conflicts of interest to declare.
Sources
Taylor-Weiner A, et al. A Machine Learning Approach Enables Quantitative Measurement of Liver Histology and Disease Monitoring in NASH. Hepatology. 2021 Jul. doi: 10.1002/hep.31750.
Zeng Q, et al. Artificial intelligence predicts immune and inflammatory gene signatures directly from hepatocellular carcinoma histology. J Hepatol. 2022 Jul. doi: 10.1016/j.jhep.2022.01.018.
Ahn JC, et al. Development of the AI-Cirrhosis-ECG Score: An Electrocardiogram-Based Deep Learning Model in Cirrhosis. Am J Gastroenterol. 2022 Mar. doi: 10.14309/ajg.0000000000001617.
Nduma BN, et al. The Application of Artificial Intelligence (AI)-Based Ultrasound for the Diagnosis of Fatty Liver Disease: A Systematic Review. Cureus. 2023 Dec 15. doi: 10.7759/cureus.50601.
Dear colleagues,
Since our prior Perspectives piece on artificial intelligence (AI) in GI and Hepatology in 2022, the field has seen almost exponential growth. Expectations are high that AI will revolutionize our field and significantly improve patient care. But as the global discussion on AI has shown, there are real challenges with adoption, including issues with accuracy, reliability, and privacy.
In this issue, Dr. Nabil M. Mansour and Dr. Thomas R. McCarty explore the current and future impact of AI on gastroenterology, while Dr. Basile Njei and Yazan A. Al Ajlouni assess its role in hepatology. We hope these pieces will help your discussions in incorporating or researching AI for use in your own practices. We welcome your thoughts on this issue on X @AGA_GIHN.
Gyanprakash A. Ketwaroo, MD, MSc, is associate professor of medicine, Yale University, New Haven, Conn., and chief of endoscopy at West Haven (Conn.) VA Medical Center. He is an associate editor for GI & Hepatology News.
Artificial Intelligence in Gastrointestinal Endoscopy
BY THOMAS R. MCCARTY, MD, MPH; NABIL M. MANSOUR, MD
The last few decades have seen an exponential increase and interest in the role of artificial intelligence (AI) and adoption of deep learning algorithms within healthcare and patient care services. The field of gastroenterology and endoscopy has similarly seen a tremendous uptake in acceptance and implementation of AI for a variety of gastrointestinal conditions. The spectrum of AI-based applications includes detection or diagnostic-based as well as therapeutic assistance tools. From the first US Food and Drug Administration (FDA)-approved device that uses machine learning to assist clinicians in detecting lesions during colonoscopy, to other more innovative machine learning techniques for small bowel, esophageal, and hepatobiliary conditions, AI has dramatically changed the landscape of gastrointestinal endoscopy.
Approved applications for colorectal cancer
In an attempt to improve colorectal cancer screening and outcomes related to screening and surveillance, efforts have been focused on procedural performance metrics, quality indicators, and tools to aid in lesion detection and improve quality of care. One such tool has been computer-aided detection (CADe), with early randomized controlled trial (RCT) data showing significantly increased adenoma detection rate (ADR) and adenomas per colonoscopy (APC).1-3
Ultimately, this data led to FDA approval of the CADe system GI Genius (Medtronic, Dublin, Ireland) in 2021.4 Additional systems have since been FDA approved or 510(k) cleared including Endoscreener (Wision AI, Shanghai, China), SKOUT (Iterative Health, Cambridge, Massachusetts), MAGENTIQ-COLO (MAGENTIQ-EYE LTD, Haifa, Israel), and CAD EYE (Fujifilm, Tokyo), all of which have shown increased ADR and/or increased APC and/or reduced adenoma miss rates in randomized trials.5
Yet despite the promise of improved quality and subsequent translation to better patient outcomes, there has been a noticeable disconnect between RCT data and more real-world literature.6 In a recent study, no improvement was seen in ADR after implementation of a CADe system for colorectal cancer screening — including both higher and lower-ADR performers. Looking at change over time after implementation, CADe had no positive effect in any group over time, divergent from early RCT data. In a more recent multicenter, community-based RCT study, again CADe did not result in a statistically significant difference in the number of adenomas detected.7 The differences between some of these more recent “real-world” studies vs the majority of data from RCTs raise important questions regarding the potential of bias (due to unblinding) in prospective trials, as well as the role of the human-AI interaction.
Importantly for RCT data, both cohorts in these studies met adequate ADR benchmarks, though it remains unclear whether a truly increased ADR necessitates better patient outcomes — is higher always better? In addition, an important consideration with evaluating any AI/CADe system is that they often undergo frequent updates, each promising improved accuracy, sensitivity, and specificity. This is an interesting dilemma and raises questions about the enduring relevance of studies conducted using an outdated version of a CADe system.
Additional unanswered questions regarding an ideal ADR for implementation, preferred patient populations for screening (especially for younger individuals), and the role and adoption of computer-aided polyp diagnosis/characterization (CADx) within the United States remain. Furthermore, questions regarding procedural withdrawal time, impact on sessile serrated lesion detection, cost-effectiveness, and preferred adoption strategies have begun to be explored, though require more data to better define a best practice approach. Ultimately, answers to some of these unknowns may explain the discordant results and help guide future implementation measures.
Innovative applications for alternative gastrointestinal conditions
Given the fervor and excitement, as well as the outcomes associated with AI-based colorectal screening, it is not surprising these techniques have been expanded to other gastrointestinal conditions. At this time, all of these are fledgling, mostly single-center tools, not yet ready for widespread adoption. Nonetheless, these represent a potentially important step forward for difficult-to-manage gastrointestinal diseases.
Machine learning CADe systems have been developed to help identify early Barrett’s neoplasia, depth and invasion of gastric cancer, as well as lesion detection in small bowel video capsule endoscopy.8-10 Endoscopic retrograde cholangiopancreatography (ERCP)-based applications for cholangiocarcinoma and indeterminate stricture diagnosis have also been studied.11 Additional AI-based algorithms have been employed for complex procedures such as endoscopic submucosal dissection (ESD) or peroral endoscopic myotomy (POEM) to delineate vessels, better define tissue planes for dissection, and visualize landmark structures.12,13 Furthermore, AI-based scope guidance/manipulation, bleeding detection, landmark identification, and lesion detection have the potential to revolutionize endoscopic training and education. The impact that generative AI can potentially have on clinical practice is also an exciting prospect that warrants further investigation.
Artificial intelligence adoption in clinical practice
Clinical practice with regard to AI and colorectal cancer screening largely mirrors the disconnect in the current literature, with “believers” and “non-believers” as well as innovators and early adopters alongside laggards. In our own academic practices, we continue to struggle with the adoption and standardized implementation of AI-based colorectal cancer CADe systems, despite the RCT data showing positive results. It is likely that AI uptake will follow the technology predictions of Amara’s Law — i.e., individuals tend to overestimate the short-term impact of new technologies while underestimating long-term effects. In the end, more widespread adoption in community practice and larger scale real-world clinical outcomes studies are likely to determine the true impact of these exciting technologies. For other, less established AI-based tools, more data are currently required.
Conclusions
Ultimately, AI-based algorithms are likely here to stay, with continued improvement and evolution to occur based on provider feedback and patient care needs. Current tools, while not all-encompassing, have the potential to dramatically change the landscape of endoscopic training, diagnostic evaluation, and therapeutic care. It is critically important that relevant stakeholders, both endoscopists and patients, be involved in future applications and design to improve efficiency and quality outcomes overall.
Dr. McCarty is based in the Lynda K. and David M. Underwood Center for Digestive Disorders, Houston Methodist Hospital. Dr. Mansour is based in the section of gastroenterology, Baylor College of Medicine, Houston. Dr. McCarty reports no conflicts of interest. Dr. Mansour reports having been a consultant for Iterative Health.
References
1. Repici A, et al. Efficacy of real-time computer-aided detection of colorectal neoplasia in a randomized trial. Gastroenterology. 2020 Aug. doi: 10.1053/j.gastro.2020.04.062.
2. Repici A, et al. Artificial intelligence and colonoscopy experience: Lessons from two randomised trials. Gut. Apr 2022. doi: 10.1136/gutjnl-2021-324471.
3. Wallace MB, et al. Impact of artificial intelligence on miss rate of colorectal neoplasia. Gastroenterology 2022 Jul. doi: 10.1053/j.gastro.2022.03.007.
4. United States Food and Drug Administration (FDA). GI Genius FDA Approval [April 9, 2021]. Accessed January 5, 2022. Available at: www.accessdata.fda.gov/cdrh_docs/pdf21/K211951.pdf.
5. Maas MHJ, et al. A computer-aided polyp detection system in screening and surveillance colonoscopy: An international, multicentre, randomised, tandem trial. Lancet Digit Health. 2024 Mar. doi: 10.1016/S2589-7500(23)00242-X.
6. Ladabaum U, et al. Computer-aided detection of polyps does not improve colonoscopist performance in a pragmatic implementation trial. Gastroenterology. 2023 Mar. doi: 10.1053/j.gastro.2022.12.004.
7. Wei MT, et al. Evaluation of computer-aided detection during colonoscopy in the community (AI-SEE): A multicenter randomized clinical trial. Am J Gastroenterol. 2023 Oct. doi: 10.14309/ajg.0000000000002239.
8. de Groof J, et al. The Argos project: The development of a computer-aided detection system to improve detection of Barrett’s neoplasia on white light endoscopy. United European Gastroenterol J. 2019 May. doi: 10.1177/2050640619837443.
9. Kanesaka T, et al. Computer-aided diagnosis for identifying and delineating early gastric cancers in magnifying narrow-band imaging. Gastrointest Endosc. 2018 May. doi: 10.1016/j.gie.2017.11.029.
10. Sahafi A, et al. Edge artificial intelligence wireless video capsule endoscopy. Sci Rep. 2022 Aug. doi: 10.1038/s41598-022-17502-7.
11. Njei B, et al. Artificial intelligence in endoscopic imaging for detection of malignant biliary strictures and cholangiocarcinoma: A systematic review. Ann Gastroenterol. 2023 Mar-Apr. doi: 10.20524/aog.2023.0779.
12. Ebigbo A, et al. Vessel and tissue recognition during third-space endoscopy using a deep learning algorithm. Gut. 2022 Dec. doi: 10.1136/gutjnl-2021-326470.
13. Cao J, et al. Intelligent surgical workflow recognition for endoscopic submucosal dissection with real-time animal study. Nat Commun. 2023 Oct. doi: 10.1038/s41467-023-42451-8.
The Promise and Challenges of AI in Hepatology
BY BASILE NJEI, MD, MPH, PHD; YAZAN A. AL-AJLOUNI, MPHIL
In the dynamic realm of medicine, artificial intelligence (AI) emerges as a transformative force, notably within hepatology. The discipline of hepatology, dedicated to liver and related organ diseases, is ripe for AI’s promise to revolutionize diagnostics and treatment, pushing toward a future of precision medicine. Yet, the path to fully realizing AI’s potential in hepatology is laced with data, ethical, and integration challenges.
The application of AI, particularly in histopathology, significantly enhances disease diagnosis and staging in hepatology. AI-driven approaches remedy traditional histopathological challenges, such as interpretative variability, providing more consistent and accurate disease analyses. This is especially evident in conditions like metabolic dysfunction-associated steatohepatitis (MASH) and hepatocellular carcinoma (HCC), where AI aids in identifying critical gene signatures, thereby refining therapy selection.
Similarly, deep learning (DL), a branch of AI, has attracted significant interest globally, particularly in image recognition. AI’s incorporation into medical imaging marks a significant advancement, enabling early detection of malignancies like HCC and improving diagnostics in steatotic liver disease through enhanced imaging analyses using convolutional neural networks (CNN). The abundance of imaging data alongside clinical outcomes has catalyzed AI’s integration into radiology, leading to the swift growth of radiomics as a novel domain in medical research.
AI has also been shown to identify nuanced alterations in electrocardiograms (EKGs) associated with liver conditions, potentially detecting the progression of liver diseases at an earlier stage than currently possible. By leveraging complex algorithms and machine learning, AI can analyze EKG patterns with a precision and depth unattainable through traditional manual interpretation. Given that liver diseases, such as cirrhosis or hepatitis, can induce subtle cardiac changes long before other clinical symptoms manifest, early detection through AI-enhanced EKG analysis could lead to timely interventions, potentially halting or reversing disease progression. This approach further enriches our understanding of the intricate interplay between liver function and cardiac health, highlighting the potential for AI to transform not just liver disease diagnostics but also to foster a more integrated approach to patient care.
Beyond diagnostics, the burgeoning field of generative AI introduces groundbreaking possibilities in treatment planning and patient education, particularly for chronic conditions like cirrhosis. Generative AI produces original content, including text, visuals, and music, by identifying and learning patterns from its training data. When it leverages large language models (LLMs), it entails training on vast collections of textual data and using AI models characterized by many parameters. A notable instance of generative AI employing LLMs is ChatGPT (General Pretrained Transformers). By simulating disease progression and treatment outcomes, generative AI can foster personalized treatment strategies and empower patients with knowledge about their health trajectories. Yet, realizing these potential demands requires overcoming data quality and interpretability challenges, and ensuring AI outputs are accessible and actionable for clinicians and patients.
Despite these advancements, leveraging AI in hepatology is not devoid of hurdles. The development and training of AI models require extensive and diverse datasets, raising concerns about data privacy and ethical use. Addressing these concerns is paramount for successfully integrating AI into clinical hepatology practice, necessitating transparent algorithmic processes and stringent ethical standards. Ethical considerations are central to AI’s integration into hepatology. Algorithmic biases, patient privacy, and the impact of AI-driven decisions underscore the need for cautious AI deployment. Developing transparent, understandable algorithms and establishing ethical guidelines for AI use are critical steps towards ethically leveraging AI in patient care.
In conclusion, AI’s integration into hepatology holds tremendous promise for advancing patient care through enhanced diagnostics, treatment planning, and patient education. Overcoming the associated challenges, including ethical concerns, data diversity, and algorithm interpretability, is crucial. As the hepatology community navigates this technological evolution, a balanced approach that marries technological advancements with ethical stewardship will be key to harnessing AI’s full potential, ensuring it serves the best interests of patients and propels the field of hepatology into the future.
We predict a trajectory of increased use and adoption of AI in hepatology. AI in hepatology is likely to meet the test of pervasiveness, improvement, and innovation. The adoption of AI in routine hepatology diagnosis and management will likely follow Amara’s law and the five stages of the hype cycle. We believe that we are still in the infant stages of adopting AI technology in hepatology, and this phase may last 5 years before there is a peak of inflated expectations. The trough of disillusionment and slopes of enlightenment may only be observed in the next decades.
Dr. Njei is based in the Section of Digestive Diseases, Yale School of Medicine, New Haven, Conn. Mr. Al-Ajlouni is a senior medical student at New York Medical College School of Medicine, Valhalla, N.Y. They have no conflicts of interest to declare.
Sources
Taylor-Weiner A, et al. A Machine Learning Approach Enables Quantitative Measurement of Liver Histology and Disease Monitoring in NASH. Hepatology. 2021 Jul. doi: 10.1002/hep.31750.
Zeng Q, et al. Artificial intelligence predicts immune and inflammatory gene signatures directly from hepatocellular carcinoma histology. J Hepatol. 2022 Jul. doi: 10.1016/j.jhep.2022.01.018.
Ahn JC, et al. Development of the AI-Cirrhosis-ECG Score: An Electrocardiogram-Based Deep Learning Model in Cirrhosis. Am J Gastroenterol. 2022 Mar. doi: 10.14309/ajg.0000000000001617.
Nduma BN, et al. The Application of Artificial Intelligence (AI)-Based Ultrasound for the Diagnosis of Fatty Liver Disease: A Systematic Review. Cureus. 2023 Dec 15. doi: 10.7759/cureus.50601.
Navigating the Search for a Financial Adviser
As gastroenterologists, we spend innumerable years in medical training with an abrupt and significant increase in our earning potential upon beginning practice. The majority of us also carry a sizeable amount of student loan debt. This combination results in a unique situation that can make us hesitant about how best to set ourselves up financially while also making us vulnerable to potentially predatory financial practices.
Although your initial steps to achieve financial wellness and build wealth can be obtained on your own with some education, a financial adviser becomes indispensable when you have significant assets, a high income, complex finances, and/or are experiencing a major life change. Additionally, as there are so many avenues to invest and grow your capital, a financial adviser can assist in designing a portfolio to best accomplish specific monetary goals. Studies have demonstrated that those working with a financial adviser reduce their single-stock risk and have more significant increase in portfolio value, reducing the total cost associated with their investments’ management.1 Those working with a financial adviser will also net up to a 3% larger annual return, compared with a standard baseline investment plan.2,3
Based on this information, it may appear that working with a personal financial adviser would be a no-brainer. Unfortunately, there is a caveat: There is no legal regulation regarding who can use the title “financial adviser.” It is therefore crucial to be aware of common practices and terminology to best help you identify a reputable financial adviser and reduce your risk of excessive fees or financial loss. This is also a highly personal decision and your search should first begin with understanding why you are looking for an adviser, as this will determine the appropriate type of service to look for.
Types of Advisers
A certified financial planner (CFP) is an expert in estate planning, taxes, retirement saving, and financial planning who has a formal designation by the Certified Financial Planner Board of Standards Inc.4 They must undergo stringent licensing examinations following a 3-year course with required continuing education to maintain their credentials. CFPs are fiduciaries, meaning they must make financial decisions in your best interest, even if they may make less money with that product or investment strategy. In other words, they are beholden to give honest, impartial recommendations to their clients, and may face sanctions by the CFP Board if found to violate its Code of Ethics and Standards of Conduct, which includes failure to act in a fiduciary duty.5
CFPs evaluate your total financial picture, such as investments, insurance policies, and overall current financial position, to develop a comprehensive strategy that will successfully guide you to your financial goal. There are many individuals who may refer to themselves as financial planners without having the CFP designation; while they may offer similar services as above, they will not be required to act as a fiduciary. Hence, it is important to do your due diligence and verify they hold this certification via the CFP Board website: www.cfp.net/verify-a-cfp-professional.
An investment adviser is a legal term from the U.S. Securities and Exchange Commission (SEC) and the Financial Industry Regulatory Authority (FINRA) referring to an individual who provides recommendations and analyses for financial securities such as stock. Both of these agencies ensure investment advisers adhere to regulatory requirements designed to protect client investers. Similar to CFPs, they are held to a fiduciary standard, and their firm is required to register with the SEC or the state of practice based on the amount of assets under management.6
An individual investment adviser must also register with their state as an Investment Adviser Representative (IAR), the distinctive term referring to an individual as opposed to an investment advising firm. Investment advisers are required to pass the extensive Series 65, Uniform Investment Advisor Law Exam, or equivalent, by states requiring licensure.7 They can guide you on the selection of particular investments and portfolio management based on a discussion with you regarding your current financial standing and what fiscal ambitions you wish to achieve.
A financial adviser provides direction on a multitude of financially related topics such as investing, tax laws, and life insurance with the goal to help you reach specific financial objectives. However, this term is often used quite ubiquitously given the lack of formal regulation of the title. Essentially, those with varying types of educational background can give themselves the title of financial adviser.
If a financial adviser buys or sells financial securities such as stocks or bonds, then they must be registered as a licensed broker with the SEC and IAR and pass the Series 6 or Series 7 exam. Unlike CFPs and investment advisers, a financial adviser (if also a licensed broker) is not required to be a fiduciary, and instead works under the suitability standard.8 Suitability requires that financial recommendations made by the adviser are appropriate but not necessarily the best for the client. In fact, these recommendations do not even have to be the most suitable. This is where conflicts of interest can arise with the adviser recommending products and securities that best compensate them while not serving the best return on investment for you.
Making the search for a financial adviser more complex, an individual can be a combination of any of the above, pending the appropriate licensing. For example, a CFP can also be an asset manager and thus hold the title of a financial adviser and/or IAR. A financial adviser may also not directly manage your assets if they have a partnership with a third party or another licensed individual. Questions to ask of your potential financial adviser should therefore include the following:
- What licensure and related education do you have?
- What is your particular area of expertise?
- How long have you been in practice?
- How will you be managing my assets?
Financial Adviser Fee Schedules
Prior to working with a financial adviser, you must also inquire about their fee structure. There are two kinds of fee schedules used by financial advisers: fee-only and fee-based.
Fee-only advisers receive payment solely for the services they provide. They do not collect commissions from third parties providing the recommended products. There is variability in how this type of payment schedule is structured, encompassing flat fees, hourly rates, or the adviser charging a retainer. The Table below compares the types of fee-only structures and range of charges based on 2023 rates.9 Of note, fee-only advisers serve as fiduciaries.10
Fee-based financial advisers receive payment for services but may also receive commission on specific products they sell to you.9 Most, if not all, financial experts recommend avoiding advisers using commission-based charges given the potential conflict of interest: How can one be absolutely sure this recommended financial product is best for you, knowing your adviser has a financial stake in said item?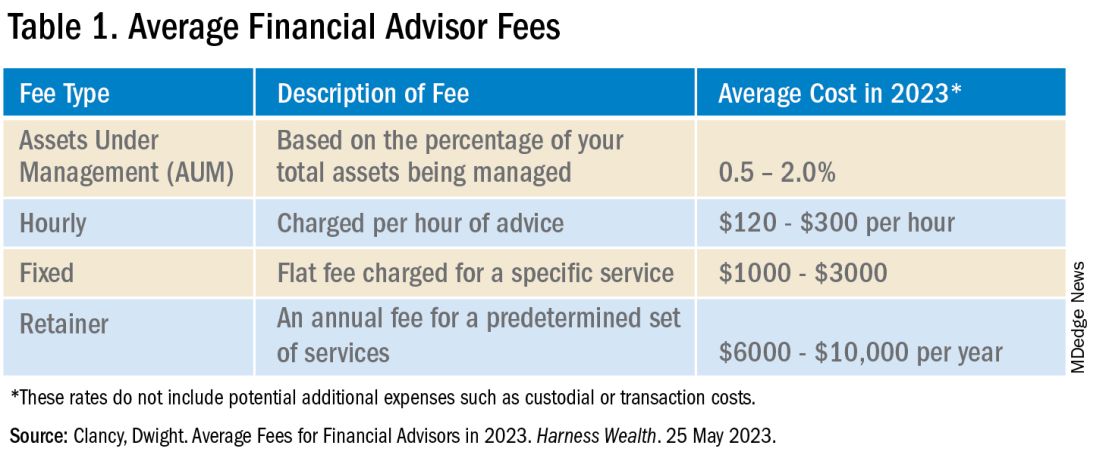
In addition to charging the fees above, your financial adviser, if they are actively managing your investment portfolio, will also charge an assets under management (AUM) fee. This is a percentage of the dollar amount within your portfolio. For example, if your adviser charges a 1% AUM rate for your account totaling $100,000, this equates to a $1,000 fee in that calendar year. AUM fees typically decrease as the size of your portfolio increases. As seen in the Table, there is a wide range of the average AUM rate (0.5%–2%); however, an AUM fee approaching 2% is unnecessarily high and consumes a significant portion of your portfolio. Thus, it is recommended to look for a money manager with an approximate 1% AUM fee.
Many of us delay or avoid working with a financial adviser due to the potential perceived risks of having poor portfolio management from an adviser not working in our best interest, along with the concern for excessive fees. In many ways, it is how we counsel our patients. While they can seek medical information on their own, their best care is under the guidance of an expert: a healthcare professional. That being said, personal finance is indeed personal, so I hope this guide helps facilitate your search and increase your financial wellness.
Dr. Luthra is a therapeutic endoscopist at Moffitt Cancer Center, Tampa, Florida, and the founder of The Scope of Finance, a financial wellness education and coaching company focused on physicians. Her interest in financial well-being is thanks to the teachings of her father, an entrepreneur and former Certified Financial Planner (CFP). She can be found on Instagram (thescopeoffinance) and X (@ScopeofFinance). She reports no financial disclosures relevant to this article.
References
1. Pagliaro CA and Utkus SP. Assessing the value of advice. Vanguard. 2019 Sept.
2. Kinniry Jr. FM et al. Putting a value on your value: Quantifying Vanguard Advisor’s Alpha. Vanguard. 2022 July.
3. Horan S. What Are the Benefits of Working with a Financial Advisor? – 2021 Study. Smart Asset. 2023 July 27.
4. Kagan J. Certified Financial PlannerTM(CFP): What It Is and How to Become One. Investopedia. 2023 Aug 3.
5. CFP Board. Our Commitment to Ethical Standards. CFP Board. 2024.
6. Staff of the Investment Adviser Regulation Office Division of Investment Management, U.S. Securities and Exchange Commission. Regulation of Investment Advisers by the U.S. Securities and Exchange Commission. 2013 Mar.
7. Hicks C. Investment Advisor vs. Financial Advisor: There is a Difference. US News & World Report. 2019 June 13.
8. Roberts K. Financial advisor vs. financial planner: What is the difference? Bankrate. 2023 Nov 21.
9. Clancy D. Average Fees for Financial Advisors in 2023. Harness Wealth. 2023 May 25.
10. Palmer B. Fee- vs. Commission-Based Advisor: What’s the Difference? Investopedia. 2023 June 20.
As gastroenterologists, we spend innumerable years in medical training with an abrupt and significant increase in our earning potential upon beginning practice. The majority of us also carry a sizeable amount of student loan debt. This combination results in a unique situation that can make us hesitant about how best to set ourselves up financially while also making us vulnerable to potentially predatory financial practices.
Although your initial steps to achieve financial wellness and build wealth can be obtained on your own with some education, a financial adviser becomes indispensable when you have significant assets, a high income, complex finances, and/or are experiencing a major life change. Additionally, as there are so many avenues to invest and grow your capital, a financial adviser can assist in designing a portfolio to best accomplish specific monetary goals. Studies have demonstrated that those working with a financial adviser reduce their single-stock risk and have more significant increase in portfolio value, reducing the total cost associated with their investments’ management.1 Those working with a financial adviser will also net up to a 3% larger annual return, compared with a standard baseline investment plan.2,3
Based on this information, it may appear that working with a personal financial adviser would be a no-brainer. Unfortunately, there is a caveat: There is no legal regulation regarding who can use the title “financial adviser.” It is therefore crucial to be aware of common practices and terminology to best help you identify a reputable financial adviser and reduce your risk of excessive fees or financial loss. This is also a highly personal decision and your search should first begin with understanding why you are looking for an adviser, as this will determine the appropriate type of service to look for.
Types of Advisers
A certified financial planner (CFP) is an expert in estate planning, taxes, retirement saving, and financial planning who has a formal designation by the Certified Financial Planner Board of Standards Inc.4 They must undergo stringent licensing examinations following a 3-year course with required continuing education to maintain their credentials. CFPs are fiduciaries, meaning they must make financial decisions in your best interest, even if they may make less money with that product or investment strategy. In other words, they are beholden to give honest, impartial recommendations to their clients, and may face sanctions by the CFP Board if found to violate its Code of Ethics and Standards of Conduct, which includes failure to act in a fiduciary duty.5
CFPs evaluate your total financial picture, such as investments, insurance policies, and overall current financial position, to develop a comprehensive strategy that will successfully guide you to your financial goal. There are many individuals who may refer to themselves as financial planners without having the CFP designation; while they may offer similar services as above, they will not be required to act as a fiduciary. Hence, it is important to do your due diligence and verify they hold this certification via the CFP Board website: www.cfp.net/verify-a-cfp-professional.
An investment adviser is a legal term from the U.S. Securities and Exchange Commission (SEC) and the Financial Industry Regulatory Authority (FINRA) referring to an individual who provides recommendations and analyses for financial securities such as stock. Both of these agencies ensure investment advisers adhere to regulatory requirements designed to protect client investers. Similar to CFPs, they are held to a fiduciary standard, and their firm is required to register with the SEC or the state of practice based on the amount of assets under management.6
An individual investment adviser must also register with their state as an Investment Adviser Representative (IAR), the distinctive term referring to an individual as opposed to an investment advising firm. Investment advisers are required to pass the extensive Series 65, Uniform Investment Advisor Law Exam, or equivalent, by states requiring licensure.7 They can guide you on the selection of particular investments and portfolio management based on a discussion with you regarding your current financial standing and what fiscal ambitions you wish to achieve.
A financial adviser provides direction on a multitude of financially related topics such as investing, tax laws, and life insurance with the goal to help you reach specific financial objectives. However, this term is often used quite ubiquitously given the lack of formal regulation of the title. Essentially, those with varying types of educational background can give themselves the title of financial adviser.
If a financial adviser buys or sells financial securities such as stocks or bonds, then they must be registered as a licensed broker with the SEC and IAR and pass the Series 6 or Series 7 exam. Unlike CFPs and investment advisers, a financial adviser (if also a licensed broker) is not required to be a fiduciary, and instead works under the suitability standard.8 Suitability requires that financial recommendations made by the adviser are appropriate but not necessarily the best for the client. In fact, these recommendations do not even have to be the most suitable. This is where conflicts of interest can arise with the adviser recommending products and securities that best compensate them while not serving the best return on investment for you.
Making the search for a financial adviser more complex, an individual can be a combination of any of the above, pending the appropriate licensing. For example, a CFP can also be an asset manager and thus hold the title of a financial adviser and/or IAR. A financial adviser may also not directly manage your assets if they have a partnership with a third party or another licensed individual. Questions to ask of your potential financial adviser should therefore include the following:
- What licensure and related education do you have?
- What is your particular area of expertise?
- How long have you been in practice?
- How will you be managing my assets?
Financial Adviser Fee Schedules
Prior to working with a financial adviser, you must also inquire about their fee structure. There are two kinds of fee schedules used by financial advisers: fee-only and fee-based.
Fee-only advisers receive payment solely for the services they provide. They do not collect commissions from third parties providing the recommended products. There is variability in how this type of payment schedule is structured, encompassing flat fees, hourly rates, or the adviser charging a retainer. The Table below compares the types of fee-only structures and range of charges based on 2023 rates.9 Of note, fee-only advisers serve as fiduciaries.10
Fee-based financial advisers receive payment for services but may also receive commission on specific products they sell to you.9 Most, if not all, financial experts recommend avoiding advisers using commission-based charges given the potential conflict of interest: How can one be absolutely sure this recommended financial product is best for you, knowing your adviser has a financial stake in said item?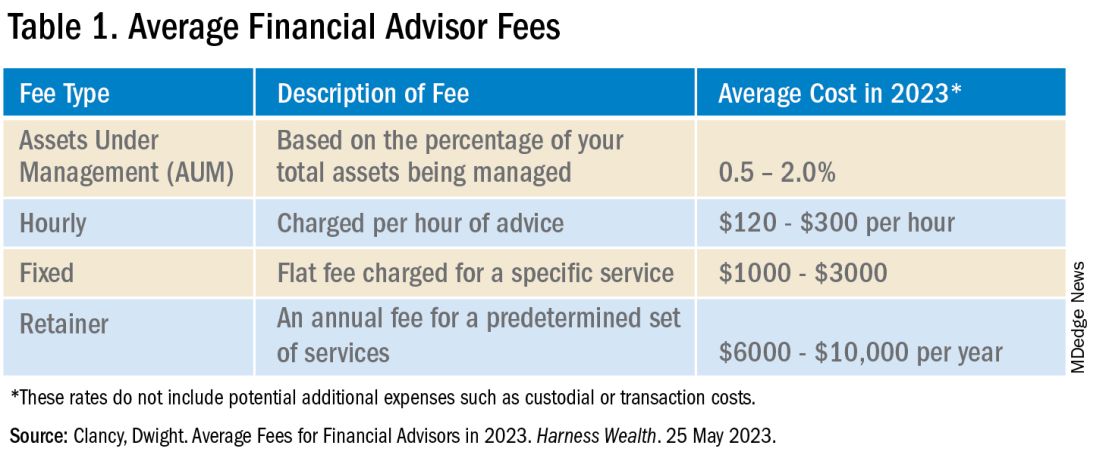
In addition to charging the fees above, your financial adviser, if they are actively managing your investment portfolio, will also charge an assets under management (AUM) fee. This is a percentage of the dollar amount within your portfolio. For example, if your adviser charges a 1% AUM rate for your account totaling $100,000, this equates to a $1,000 fee in that calendar year. AUM fees typically decrease as the size of your portfolio increases. As seen in the Table, there is a wide range of the average AUM rate (0.5%–2%); however, an AUM fee approaching 2% is unnecessarily high and consumes a significant portion of your portfolio. Thus, it is recommended to look for a money manager with an approximate 1% AUM fee.
Many of us delay or avoid working with a financial adviser due to the potential perceived risks of having poor portfolio management from an adviser not working in our best interest, along with the concern for excessive fees. In many ways, it is how we counsel our patients. While they can seek medical information on their own, their best care is under the guidance of an expert: a healthcare professional. That being said, personal finance is indeed personal, so I hope this guide helps facilitate your search and increase your financial wellness.
Dr. Luthra is a therapeutic endoscopist at Moffitt Cancer Center, Tampa, Florida, and the founder of The Scope of Finance, a financial wellness education and coaching company focused on physicians. Her interest in financial well-being is thanks to the teachings of her father, an entrepreneur and former Certified Financial Planner (CFP). She can be found on Instagram (thescopeoffinance) and X (@ScopeofFinance). She reports no financial disclosures relevant to this article.
References
1. Pagliaro CA and Utkus SP. Assessing the value of advice. Vanguard. 2019 Sept.
2. Kinniry Jr. FM et al. Putting a value on your value: Quantifying Vanguard Advisor’s Alpha. Vanguard. 2022 July.
3. Horan S. What Are the Benefits of Working with a Financial Advisor? – 2021 Study. Smart Asset. 2023 July 27.
4. Kagan J. Certified Financial PlannerTM(CFP): What It Is and How to Become One. Investopedia. 2023 Aug 3.
5. CFP Board. Our Commitment to Ethical Standards. CFP Board. 2024.
6. Staff of the Investment Adviser Regulation Office Division of Investment Management, U.S. Securities and Exchange Commission. Regulation of Investment Advisers by the U.S. Securities and Exchange Commission. 2013 Mar.
7. Hicks C. Investment Advisor vs. Financial Advisor: There is a Difference. US News & World Report. 2019 June 13.
8. Roberts K. Financial advisor vs. financial planner: What is the difference? Bankrate. 2023 Nov 21.
9. Clancy D. Average Fees for Financial Advisors in 2023. Harness Wealth. 2023 May 25.
10. Palmer B. Fee- vs. Commission-Based Advisor: What’s the Difference? Investopedia. 2023 June 20.
As gastroenterologists, we spend innumerable years in medical training with an abrupt and significant increase in our earning potential upon beginning practice. The majority of us also carry a sizeable amount of student loan debt. This combination results in a unique situation that can make us hesitant about how best to set ourselves up financially while also making us vulnerable to potentially predatory financial practices.
Although your initial steps to achieve financial wellness and build wealth can be obtained on your own with some education, a financial adviser becomes indispensable when you have significant assets, a high income, complex finances, and/or are experiencing a major life change. Additionally, as there are so many avenues to invest and grow your capital, a financial adviser can assist in designing a portfolio to best accomplish specific monetary goals. Studies have demonstrated that those working with a financial adviser reduce their single-stock risk and have more significant increase in portfolio value, reducing the total cost associated with their investments’ management.1 Those working with a financial adviser will also net up to a 3% larger annual return, compared with a standard baseline investment plan.2,3
Based on this information, it may appear that working with a personal financial adviser would be a no-brainer. Unfortunately, there is a caveat: There is no legal regulation regarding who can use the title “financial adviser.” It is therefore crucial to be aware of common practices and terminology to best help you identify a reputable financial adviser and reduce your risk of excessive fees or financial loss. This is also a highly personal decision and your search should first begin with understanding why you are looking for an adviser, as this will determine the appropriate type of service to look for.
Types of Advisers
A certified financial planner (CFP) is an expert in estate planning, taxes, retirement saving, and financial planning who has a formal designation by the Certified Financial Planner Board of Standards Inc.4 They must undergo stringent licensing examinations following a 3-year course with required continuing education to maintain their credentials. CFPs are fiduciaries, meaning they must make financial decisions in your best interest, even if they may make less money with that product or investment strategy. In other words, they are beholden to give honest, impartial recommendations to their clients, and may face sanctions by the CFP Board if found to violate its Code of Ethics and Standards of Conduct, which includes failure to act in a fiduciary duty.5
CFPs evaluate your total financial picture, such as investments, insurance policies, and overall current financial position, to develop a comprehensive strategy that will successfully guide you to your financial goal. There are many individuals who may refer to themselves as financial planners without having the CFP designation; while they may offer similar services as above, they will not be required to act as a fiduciary. Hence, it is important to do your due diligence and verify they hold this certification via the CFP Board website: www.cfp.net/verify-a-cfp-professional.
An investment adviser is a legal term from the U.S. Securities and Exchange Commission (SEC) and the Financial Industry Regulatory Authority (FINRA) referring to an individual who provides recommendations and analyses for financial securities such as stock. Both of these agencies ensure investment advisers adhere to regulatory requirements designed to protect client investers. Similar to CFPs, they are held to a fiduciary standard, and their firm is required to register with the SEC or the state of practice based on the amount of assets under management.6
An individual investment adviser must also register with their state as an Investment Adviser Representative (IAR), the distinctive term referring to an individual as opposed to an investment advising firm. Investment advisers are required to pass the extensive Series 65, Uniform Investment Advisor Law Exam, or equivalent, by states requiring licensure.7 They can guide you on the selection of particular investments and portfolio management based on a discussion with you regarding your current financial standing and what fiscal ambitions you wish to achieve.
A financial adviser provides direction on a multitude of financially related topics such as investing, tax laws, and life insurance with the goal to help you reach specific financial objectives. However, this term is often used quite ubiquitously given the lack of formal regulation of the title. Essentially, those with varying types of educational background can give themselves the title of financial adviser.
If a financial adviser buys or sells financial securities such as stocks or bonds, then they must be registered as a licensed broker with the SEC and IAR and pass the Series 6 or Series 7 exam. Unlike CFPs and investment advisers, a financial adviser (if also a licensed broker) is not required to be a fiduciary, and instead works under the suitability standard.8 Suitability requires that financial recommendations made by the adviser are appropriate but not necessarily the best for the client. In fact, these recommendations do not even have to be the most suitable. This is where conflicts of interest can arise with the adviser recommending products and securities that best compensate them while not serving the best return on investment for you.
Making the search for a financial adviser more complex, an individual can be a combination of any of the above, pending the appropriate licensing. For example, a CFP can also be an asset manager and thus hold the title of a financial adviser and/or IAR. A financial adviser may also not directly manage your assets if they have a partnership with a third party or another licensed individual. Questions to ask of your potential financial adviser should therefore include the following:
- What licensure and related education do you have?
- What is your particular area of expertise?
- How long have you been in practice?
- How will you be managing my assets?
Financial Adviser Fee Schedules
Prior to working with a financial adviser, you must also inquire about their fee structure. There are two kinds of fee schedules used by financial advisers: fee-only and fee-based.
Fee-only advisers receive payment solely for the services they provide. They do not collect commissions from third parties providing the recommended products. There is variability in how this type of payment schedule is structured, encompassing flat fees, hourly rates, or the adviser charging a retainer. The Table below compares the types of fee-only structures and range of charges based on 2023 rates.9 Of note, fee-only advisers serve as fiduciaries.10
Fee-based financial advisers receive payment for services but may also receive commission on specific products they sell to you.9 Most, if not all, financial experts recommend avoiding advisers using commission-based charges given the potential conflict of interest: How can one be absolutely sure this recommended financial product is best for you, knowing your adviser has a financial stake in said item?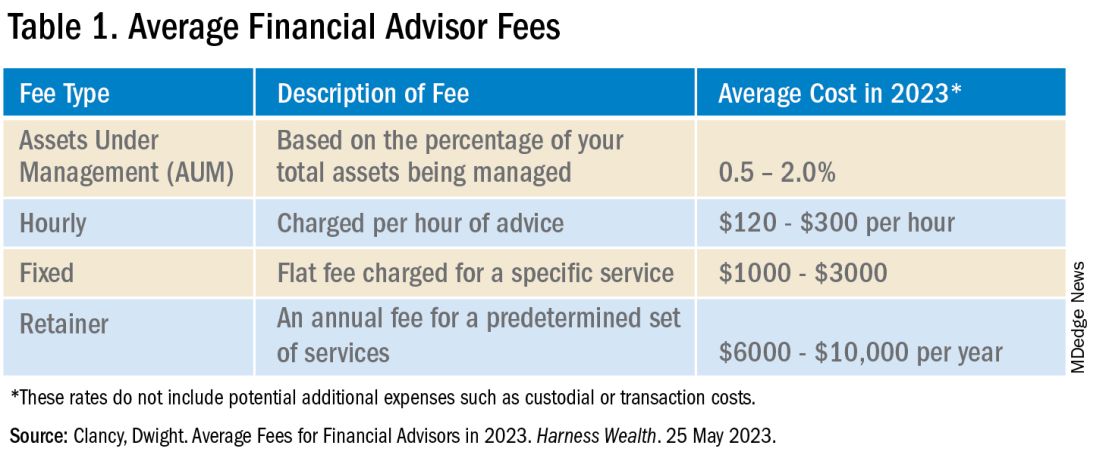
In addition to charging the fees above, your financial adviser, if they are actively managing your investment portfolio, will also charge an assets under management (AUM) fee. This is a percentage of the dollar amount within your portfolio. For example, if your adviser charges a 1% AUM rate for your account totaling $100,000, this equates to a $1,000 fee in that calendar year. AUM fees typically decrease as the size of your portfolio increases. As seen in the Table, there is a wide range of the average AUM rate (0.5%–2%); however, an AUM fee approaching 2% is unnecessarily high and consumes a significant portion of your portfolio. Thus, it is recommended to look for a money manager with an approximate 1% AUM fee.
Many of us delay or avoid working with a financial adviser due to the potential perceived risks of having poor portfolio management from an adviser not working in our best interest, along with the concern for excessive fees. In many ways, it is how we counsel our patients. While they can seek medical information on their own, their best care is under the guidance of an expert: a healthcare professional. That being said, personal finance is indeed personal, so I hope this guide helps facilitate your search and increase your financial wellness.
Dr. Luthra is a therapeutic endoscopist at Moffitt Cancer Center, Tampa, Florida, and the founder of The Scope of Finance, a financial wellness education and coaching company focused on physicians. Her interest in financial well-being is thanks to the teachings of her father, an entrepreneur and former Certified Financial Planner (CFP). She can be found on Instagram (thescopeoffinance) and X (@ScopeofFinance). She reports no financial disclosures relevant to this article.
References
1. Pagliaro CA and Utkus SP. Assessing the value of advice. Vanguard. 2019 Sept.
2. Kinniry Jr. FM et al. Putting a value on your value: Quantifying Vanguard Advisor’s Alpha. Vanguard. 2022 July.
3. Horan S. What Are the Benefits of Working with a Financial Advisor? – 2021 Study. Smart Asset. 2023 July 27.
4. Kagan J. Certified Financial PlannerTM(CFP): What It Is and How to Become One. Investopedia. 2023 Aug 3.
5. CFP Board. Our Commitment to Ethical Standards. CFP Board. 2024.
6. Staff of the Investment Adviser Regulation Office Division of Investment Management, U.S. Securities and Exchange Commission. Regulation of Investment Advisers by the U.S. Securities and Exchange Commission. 2013 Mar.
7. Hicks C. Investment Advisor vs. Financial Advisor: There is a Difference. US News & World Report. 2019 June 13.
8. Roberts K. Financial advisor vs. financial planner: What is the difference? Bankrate. 2023 Nov 21.
9. Clancy D. Average Fees for Financial Advisors in 2023. Harness Wealth. 2023 May 25.
10. Palmer B. Fee- vs. Commission-Based Advisor: What’s the Difference? Investopedia. 2023 June 20.
Achieving Promotion for Junior Faculty in Academic Medicine: An Interview With Experts
Academic medicine plays a crucial role at the crossroads of medical practice, education, and research, influencing the future landscape of healthcare. Many physicians aspire to pursue and sustain a career in academic medicine to contribute to the advancement of medical knowledge, enhance patient care, and influence the trajectory of the medical field. Opting for a career in academic medicine can offer benefits such as increased autonomy and scheduling flexibility, which can significantly improve the quality of life. In addition, engagement in scholarly activities and working in a dynamic environment with continuous learning opportunities can help mitigate burnout.
However, embarking on an academic career can be daunting for junior faculty members who face the challenge of providing clinical care while excelling in research and dedicating time to mentorship and teaching trainees. According to a report by the Association of American Medical Colleges, 38% of physicians leave academic medicine within a decade of obtaining a faculty position. Barriers to promotion and retention within academic medicine include ineffective mentorship, unclear or inconsistent promotion criteria, and disparities in gender/ethnic representation.
In this article, we interview two accomplished physicians in academic medicine who have attained the rank of professors.
Interview with Sophie Balzora, MD
Dr. Balzora is a professor of medicine at NYU Grossman School of Medicine and a practicing gastroenterologist specializing in the care of patients with inflammatory bowel disease at NYU Langone Health. She serves as the American College of Gastroenterology’s Diversity, Equity, and Inclusion Committee Chair, on the Advisory Board of ACG’s Leadership, Ethics, and Equity (LE&E) Center, and is president and cofounder of the Association of Black Gastroenterologists and Hepatologists (ABGH). Dr. Balzora was promoted to full professor 11 years after graduating from fellowship.
What would you identify as some of the most important factors that led to your success in achieving a promotion to professor of medicine?
Surround yourself with individuals whose professional and personal priorities align with yours. To achieve this, it is essential to gain an understanding of what is important to you, what you envision your success to look like, and establish a timeline to achieve it. The concept of personal success and how to best achieve it will absolutely change as you grow, and that is okay and expected. Connecting with those outside of your clinical interests, at other institutions, and even outside of the medical field, can help you achieve these goals and better shape how you see your career unfolding and how you want it to look.
Historically, the proportion of physicians who achieve professorship is lower among women compared with men. What do you believe are some of the barriers involved in this, and how would you counsel women who are interested in pursuing the rank of professor?
Systemic gender bias and discrimination, over-mentorship and under-sponsorship, inconsistent parental leave, and delayed parenthood are a few of the factors that contribute to the observed disparities in academic rank. Predictably, for women from underrepresented backgrounds in medicine, the chasm grows.
What has helped me most is to keep my eyes on the prize, and to recognize that the prize is different for everyone. It’s important not to make direct comparisons to any other individual, because they are not you. Harness what makes you different and drown out the naysayers — the “we’ve never seen this done before” camp, the “it’s too soon [for someone like you] to go up for promotion” folks. While these voices are sometimes well intentioned, they can distract you from your goals and ambitions because they are rooted in bias and adherence to traditional expectations. To do something new, and to change the game, requires going against the grain and utilizing your skills and talents to achieve what you want to achieve in a way that works for you.
What are some practical tips you have for junior gastroenterologists to track their promotion in academia?
- Keep your curriculum vitae (CV) up to date and formatted to your institutional guidelines. Ensure that you document your academic activities, even if it doesn’t seem important in the moment. When it’s time to submit that promotion portfolio, you want to be ready and organized.
- Remember: “No” is a full sentence, and saying it takes practice and time and confidence. It is a skill I still struggle to adopt at times, but it’s important to recognize the power of no, for it opens opportunities to say yes to other things.
- Lift as you climb — a critical part of changing the status quo is fostering the future of those underrepresented in medicine. A professional goal of mine that keeps me steady and passionate is to create supporting and enriching systemic and institutional changes that work to dismantle the obstacles perpetuating disparities in academic rank for women and those underrepresented in medicine. Discovering your “why” is a complex, difficult, and rewarding journey.
Interview with Mark Schattner, MD, AGAF
Dr. Schattner is a professor of clinical medicine at Weill Cornell College of Medicine and chief of the gastroenterology, hepatology, and nutrition service at Memorial Sloan Kettering Cancer Center, both in New York. He is a former president of the New York Society for Gastrointestinal Endoscopy and a fellow of the AGA and ASGE.
In your role as chief, you serve as a mentor for early career gastroenterologists for pursuing career promotion. What advice do you have for achieving this?
Promoting junior faculty is one of the prime responsibilities of a service chief. Generally, the early steps of promotion are straightforward, with criteria becoming more stringent as you progress. I think it is critical to understand the criteria used by promotion committees and to be aware of the various available tracks. I believe every meeting a junior faculty member has with their service chief should include, at the least, a brief check-in on where they are in the promotion process and plans (both short term and long term) to move forward. Successful promotion is facilitated when done upon a solid foundation of production and accomplishment. It is very challenging or even impossible when trying to piece together a package from discordant activities.
Most institutions require or encourage academic involvement at both national and international levels for career promotion. Do you have advice for junior faculty about how to achieve this type of recognition or experience?
The easiest place to start is with regional professional societies. Active involvement in these local societies fosters valuable networking and lays the groundwork for involvement at the national or international level. I would strongly encourage junior faculty to seek opportunities for a leadership position at any level in these societies and move up the ladder as their career matures. This is also a very good avenue to network and get invited to join collaborative research projects, which can be a fruitful means to enhance your academic productivity.
In your opinion, what factors are likely to hinder or delay an individual’s promotion?
I think it is crucial to consider the career track you are on. If you are very clinically productive and love to teach, that is completely appropriate, and most institutions will recognize the value of that and promote you along a clinical-educator tract. On the other hand, if you have a passion for research and can successfully lead research and compete for grants, then you would move along a traditional tenure track. It is also critical to think ahead, know the criteria on which you will be judged, and incorporate that into your practice early. Trying to scramble to enhance your CV in a short time just for promotion will likely prove ineffective.
Do you have advice for junior faculty who have families about how to manage career goals but also prioritize time with family?
There is no one-size-fits-all approach to this. I think this requires a lot of shared decision-making with your family. Compromise will undoubtedly be required. For example, I always chose to live in close proximity to my workplace, eliminating any commuting time. This choice really allowed me spend time with my family.
In conclusion, a career in academic medicine presents both opportunities and challenges. A successful academic career, and achieving promotion to the rank of professor of medicine, requires a combination of factors including understanding institution-specific criteria for promotion, proactive engagement at the regional and national level, and envisioning your career goals and creating a timeline to achieve them. There are challenges to promotion, including navigating systemic biases and balancing career goals with family commitments, which also requires consideration and open communication. Ultimately, we hope these insights provide valuable guidance and advice for junior faculty who are navigating this complex environment of academic medicine and are motivated toward achieving professional fulfillment and satisfaction in their careers.
Dr. Rolston is based in the Department of Gastroenterology, Hepatology, and Nutrition, Memorial Sloan Kettering Cancer Center, New York. She reports no conflicts in relation this article. Dr. Balzora and Dr. Schattner are based in the Division of Gastroenterology and Hepatology, New York University Langone Health, New York. Dr. Schattner is a consultant for Boston Scientific and Novo Nordisk. Dr. Balzora reports no conflicts in relation to this article.
References
Campbell KM. Mitigating the isolation of minoritized faculty in academic medicine. J Gen Intern Med. 2023 May. doi: 10.1007/s11606-022-07982-8.
Howard-Anderson JR et al. Strategies for developing a successful career in academic medicine. Am J Med Sci. 2024 Apr. doi: 10.1016/j.amjms.2023.12.010.
Murphy M et al. Women’s experiences of promotion and tenure in academic medicine and potential implications for gender disparities in career advancement: A qualitative analysis. JAMA Netw Open. 2021 Sep 1. doi: 10.1001/jamanetworkopen.2021.25843.
Sambunjak D et al. Mentoring in academic medicine: A systematic review. JAMA. 2006 Sep 6. doi: 10.1001/jama.296.9.1103.
Shen MR et al. Impact of mentoring on academic career success for women in medicine: A systematic review. Acad Med. 2022 Mar 1. doi: 10.1097/ACM.0000000000004563.
Academic medicine plays a crucial role at the crossroads of medical practice, education, and research, influencing the future landscape of healthcare. Many physicians aspire to pursue and sustain a career in academic medicine to contribute to the advancement of medical knowledge, enhance patient care, and influence the trajectory of the medical field. Opting for a career in academic medicine can offer benefits such as increased autonomy and scheduling flexibility, which can significantly improve the quality of life. In addition, engagement in scholarly activities and working in a dynamic environment with continuous learning opportunities can help mitigate burnout.
However, embarking on an academic career can be daunting for junior faculty members who face the challenge of providing clinical care while excelling in research and dedicating time to mentorship and teaching trainees. According to a report by the Association of American Medical Colleges, 38% of physicians leave academic medicine within a decade of obtaining a faculty position. Barriers to promotion and retention within academic medicine include ineffective mentorship, unclear or inconsistent promotion criteria, and disparities in gender/ethnic representation.
In this article, we interview two accomplished physicians in academic medicine who have attained the rank of professors.
Interview with Sophie Balzora, MD
Dr. Balzora is a professor of medicine at NYU Grossman School of Medicine and a practicing gastroenterologist specializing in the care of patients with inflammatory bowel disease at NYU Langone Health. She serves as the American College of Gastroenterology’s Diversity, Equity, and Inclusion Committee Chair, on the Advisory Board of ACG’s Leadership, Ethics, and Equity (LE&E) Center, and is president and cofounder of the Association of Black Gastroenterologists and Hepatologists (ABGH). Dr. Balzora was promoted to full professor 11 years after graduating from fellowship.
What would you identify as some of the most important factors that led to your success in achieving a promotion to professor of medicine?
Surround yourself with individuals whose professional and personal priorities align with yours. To achieve this, it is essential to gain an understanding of what is important to you, what you envision your success to look like, and establish a timeline to achieve it. The concept of personal success and how to best achieve it will absolutely change as you grow, and that is okay and expected. Connecting with those outside of your clinical interests, at other institutions, and even outside of the medical field, can help you achieve these goals and better shape how you see your career unfolding and how you want it to look.
Historically, the proportion of physicians who achieve professorship is lower among women compared with men. What do you believe are some of the barriers involved in this, and how would you counsel women who are interested in pursuing the rank of professor?
Systemic gender bias and discrimination, over-mentorship and under-sponsorship, inconsistent parental leave, and delayed parenthood are a few of the factors that contribute to the observed disparities in academic rank. Predictably, for women from underrepresented backgrounds in medicine, the chasm grows.
What has helped me most is to keep my eyes on the prize, and to recognize that the prize is different for everyone. It’s important not to make direct comparisons to any other individual, because they are not you. Harness what makes you different and drown out the naysayers — the “we’ve never seen this done before” camp, the “it’s too soon [for someone like you] to go up for promotion” folks. While these voices are sometimes well intentioned, they can distract you from your goals and ambitions because they are rooted in bias and adherence to traditional expectations. To do something new, and to change the game, requires going against the grain and utilizing your skills and talents to achieve what you want to achieve in a way that works for you.
What are some practical tips you have for junior gastroenterologists to track their promotion in academia?
- Keep your curriculum vitae (CV) up to date and formatted to your institutional guidelines. Ensure that you document your academic activities, even if it doesn’t seem important in the moment. When it’s time to submit that promotion portfolio, you want to be ready and organized.
- Remember: “No” is a full sentence, and saying it takes practice and time and confidence. It is a skill I still struggle to adopt at times, but it’s important to recognize the power of no, for it opens opportunities to say yes to other things.
- Lift as you climb — a critical part of changing the status quo is fostering the future of those underrepresented in medicine. A professional goal of mine that keeps me steady and passionate is to create supporting and enriching systemic and institutional changes that work to dismantle the obstacles perpetuating disparities in academic rank for women and those underrepresented in medicine. Discovering your “why” is a complex, difficult, and rewarding journey.
Interview with Mark Schattner, MD, AGAF
Dr. Schattner is a professor of clinical medicine at Weill Cornell College of Medicine and chief of the gastroenterology, hepatology, and nutrition service at Memorial Sloan Kettering Cancer Center, both in New York. He is a former president of the New York Society for Gastrointestinal Endoscopy and a fellow of the AGA and ASGE.
In your role as chief, you serve as a mentor for early career gastroenterologists for pursuing career promotion. What advice do you have for achieving this?
Promoting junior faculty is one of the prime responsibilities of a service chief. Generally, the early steps of promotion are straightforward, with criteria becoming more stringent as you progress. I think it is critical to understand the criteria used by promotion committees and to be aware of the various available tracks. I believe every meeting a junior faculty member has with their service chief should include, at the least, a brief check-in on where they are in the promotion process and plans (both short term and long term) to move forward. Successful promotion is facilitated when done upon a solid foundation of production and accomplishment. It is very challenging or even impossible when trying to piece together a package from discordant activities.
Most institutions require or encourage academic involvement at both national and international levels for career promotion. Do you have advice for junior faculty about how to achieve this type of recognition or experience?
The easiest place to start is with regional professional societies. Active involvement in these local societies fosters valuable networking and lays the groundwork for involvement at the national or international level. I would strongly encourage junior faculty to seek opportunities for a leadership position at any level in these societies and move up the ladder as their career matures. This is also a very good avenue to network and get invited to join collaborative research projects, which can be a fruitful means to enhance your academic productivity.
In your opinion, what factors are likely to hinder or delay an individual’s promotion?
I think it is crucial to consider the career track you are on. If you are very clinically productive and love to teach, that is completely appropriate, and most institutions will recognize the value of that and promote you along a clinical-educator tract. On the other hand, if you have a passion for research and can successfully lead research and compete for grants, then you would move along a traditional tenure track. It is also critical to think ahead, know the criteria on which you will be judged, and incorporate that into your practice early. Trying to scramble to enhance your CV in a short time just for promotion will likely prove ineffective.
Do you have advice for junior faculty who have families about how to manage career goals but also prioritize time with family?
There is no one-size-fits-all approach to this. I think this requires a lot of shared decision-making with your family. Compromise will undoubtedly be required. For example, I always chose to live in close proximity to my workplace, eliminating any commuting time. This choice really allowed me spend time with my family.
In conclusion, a career in academic medicine presents both opportunities and challenges. A successful academic career, and achieving promotion to the rank of professor of medicine, requires a combination of factors including understanding institution-specific criteria for promotion, proactive engagement at the regional and national level, and envisioning your career goals and creating a timeline to achieve them. There are challenges to promotion, including navigating systemic biases and balancing career goals with family commitments, which also requires consideration and open communication. Ultimately, we hope these insights provide valuable guidance and advice for junior faculty who are navigating this complex environment of academic medicine and are motivated toward achieving professional fulfillment and satisfaction in their careers.
Dr. Rolston is based in the Department of Gastroenterology, Hepatology, and Nutrition, Memorial Sloan Kettering Cancer Center, New York. She reports no conflicts in relation this article. Dr. Balzora and Dr. Schattner are based in the Division of Gastroenterology and Hepatology, New York University Langone Health, New York. Dr. Schattner is a consultant for Boston Scientific and Novo Nordisk. Dr. Balzora reports no conflicts in relation to this article.
References
Campbell KM. Mitigating the isolation of minoritized faculty in academic medicine. J Gen Intern Med. 2023 May. doi: 10.1007/s11606-022-07982-8.
Howard-Anderson JR et al. Strategies for developing a successful career in academic medicine. Am J Med Sci. 2024 Apr. doi: 10.1016/j.amjms.2023.12.010.
Murphy M et al. Women’s experiences of promotion and tenure in academic medicine and potential implications for gender disparities in career advancement: A qualitative analysis. JAMA Netw Open. 2021 Sep 1. doi: 10.1001/jamanetworkopen.2021.25843.
Sambunjak D et al. Mentoring in academic medicine: A systematic review. JAMA. 2006 Sep 6. doi: 10.1001/jama.296.9.1103.
Shen MR et al. Impact of mentoring on academic career success for women in medicine: A systematic review. Acad Med. 2022 Mar 1. doi: 10.1097/ACM.0000000000004563.
Academic medicine plays a crucial role at the crossroads of medical practice, education, and research, influencing the future landscape of healthcare. Many physicians aspire to pursue and sustain a career in academic medicine to contribute to the advancement of medical knowledge, enhance patient care, and influence the trajectory of the medical field. Opting for a career in academic medicine can offer benefits such as increased autonomy and scheduling flexibility, which can significantly improve the quality of life. In addition, engagement in scholarly activities and working in a dynamic environment with continuous learning opportunities can help mitigate burnout.
However, embarking on an academic career can be daunting for junior faculty members who face the challenge of providing clinical care while excelling in research and dedicating time to mentorship and teaching trainees. According to a report by the Association of American Medical Colleges, 38% of physicians leave academic medicine within a decade of obtaining a faculty position. Barriers to promotion and retention within academic medicine include ineffective mentorship, unclear or inconsistent promotion criteria, and disparities in gender/ethnic representation.
In this article, we interview two accomplished physicians in academic medicine who have attained the rank of professors.
Interview with Sophie Balzora, MD
Dr. Balzora is a professor of medicine at NYU Grossman School of Medicine and a practicing gastroenterologist specializing in the care of patients with inflammatory bowel disease at NYU Langone Health. She serves as the American College of Gastroenterology’s Diversity, Equity, and Inclusion Committee Chair, on the Advisory Board of ACG’s Leadership, Ethics, and Equity (LE&E) Center, and is president and cofounder of the Association of Black Gastroenterologists and Hepatologists (ABGH). Dr. Balzora was promoted to full professor 11 years after graduating from fellowship.
What would you identify as some of the most important factors that led to your success in achieving a promotion to professor of medicine?
Surround yourself with individuals whose professional and personal priorities align with yours. To achieve this, it is essential to gain an understanding of what is important to you, what you envision your success to look like, and establish a timeline to achieve it. The concept of personal success and how to best achieve it will absolutely change as you grow, and that is okay and expected. Connecting with those outside of your clinical interests, at other institutions, and even outside of the medical field, can help you achieve these goals and better shape how you see your career unfolding and how you want it to look.
Historically, the proportion of physicians who achieve professorship is lower among women compared with men. What do you believe are some of the barriers involved in this, and how would you counsel women who are interested in pursuing the rank of professor?
Systemic gender bias and discrimination, over-mentorship and under-sponsorship, inconsistent parental leave, and delayed parenthood are a few of the factors that contribute to the observed disparities in academic rank. Predictably, for women from underrepresented backgrounds in medicine, the chasm grows.
What has helped me most is to keep my eyes on the prize, and to recognize that the prize is different for everyone. It’s important not to make direct comparisons to any other individual, because they are not you. Harness what makes you different and drown out the naysayers — the “we’ve never seen this done before” camp, the “it’s too soon [for someone like you] to go up for promotion” folks. While these voices are sometimes well intentioned, they can distract you from your goals and ambitions because they are rooted in bias and adherence to traditional expectations. To do something new, and to change the game, requires going against the grain and utilizing your skills and talents to achieve what you want to achieve in a way that works for you.
What are some practical tips you have for junior gastroenterologists to track their promotion in academia?
- Keep your curriculum vitae (CV) up to date and formatted to your institutional guidelines. Ensure that you document your academic activities, even if it doesn’t seem important in the moment. When it’s time to submit that promotion portfolio, you want to be ready and organized.
- Remember: “No” is a full sentence, and saying it takes practice and time and confidence. It is a skill I still struggle to adopt at times, but it’s important to recognize the power of no, for it opens opportunities to say yes to other things.
- Lift as you climb — a critical part of changing the status quo is fostering the future of those underrepresented in medicine. A professional goal of mine that keeps me steady and passionate is to create supporting and enriching systemic and institutional changes that work to dismantle the obstacles perpetuating disparities in academic rank for women and those underrepresented in medicine. Discovering your “why” is a complex, difficult, and rewarding journey.
Interview with Mark Schattner, MD, AGAF
Dr. Schattner is a professor of clinical medicine at Weill Cornell College of Medicine and chief of the gastroenterology, hepatology, and nutrition service at Memorial Sloan Kettering Cancer Center, both in New York. He is a former president of the New York Society for Gastrointestinal Endoscopy and a fellow of the AGA and ASGE.
In your role as chief, you serve as a mentor for early career gastroenterologists for pursuing career promotion. What advice do you have for achieving this?
Promoting junior faculty is one of the prime responsibilities of a service chief. Generally, the early steps of promotion are straightforward, with criteria becoming more stringent as you progress. I think it is critical to understand the criteria used by promotion committees and to be aware of the various available tracks. I believe every meeting a junior faculty member has with their service chief should include, at the least, a brief check-in on where they are in the promotion process and plans (both short term and long term) to move forward. Successful promotion is facilitated when done upon a solid foundation of production and accomplishment. It is very challenging or even impossible when trying to piece together a package from discordant activities.
Most institutions require or encourage academic involvement at both national and international levels for career promotion. Do you have advice for junior faculty about how to achieve this type of recognition or experience?
The easiest place to start is with regional professional societies. Active involvement in these local societies fosters valuable networking and lays the groundwork for involvement at the national or international level. I would strongly encourage junior faculty to seek opportunities for a leadership position at any level in these societies and move up the ladder as their career matures. This is also a very good avenue to network and get invited to join collaborative research projects, which can be a fruitful means to enhance your academic productivity.
In your opinion, what factors are likely to hinder or delay an individual’s promotion?
I think it is crucial to consider the career track you are on. If you are very clinically productive and love to teach, that is completely appropriate, and most institutions will recognize the value of that and promote you along a clinical-educator tract. On the other hand, if you have a passion for research and can successfully lead research and compete for grants, then you would move along a traditional tenure track. It is also critical to think ahead, know the criteria on which you will be judged, and incorporate that into your practice early. Trying to scramble to enhance your CV in a short time just for promotion will likely prove ineffective.
Do you have advice for junior faculty who have families about how to manage career goals but also prioritize time with family?
There is no one-size-fits-all approach to this. I think this requires a lot of shared decision-making with your family. Compromise will undoubtedly be required. For example, I always chose to live in close proximity to my workplace, eliminating any commuting time. This choice really allowed me spend time with my family.
In conclusion, a career in academic medicine presents both opportunities and challenges. A successful academic career, and achieving promotion to the rank of professor of medicine, requires a combination of factors including understanding institution-specific criteria for promotion, proactive engagement at the regional and national level, and envisioning your career goals and creating a timeline to achieve them. There are challenges to promotion, including navigating systemic biases and balancing career goals with family commitments, which also requires consideration and open communication. Ultimately, we hope these insights provide valuable guidance and advice for junior faculty who are navigating this complex environment of academic medicine and are motivated toward achieving professional fulfillment and satisfaction in their careers.
Dr. Rolston is based in the Department of Gastroenterology, Hepatology, and Nutrition, Memorial Sloan Kettering Cancer Center, New York. She reports no conflicts in relation this article. Dr. Balzora and Dr. Schattner are based in the Division of Gastroenterology and Hepatology, New York University Langone Health, New York. Dr. Schattner is a consultant for Boston Scientific and Novo Nordisk. Dr. Balzora reports no conflicts in relation to this article.
References
Campbell KM. Mitigating the isolation of minoritized faculty in academic medicine. J Gen Intern Med. 2023 May. doi: 10.1007/s11606-022-07982-8.
Howard-Anderson JR et al. Strategies for developing a successful career in academic medicine. Am J Med Sci. 2024 Apr. doi: 10.1016/j.amjms.2023.12.010.
Murphy M et al. Women’s experiences of promotion and tenure in academic medicine and potential implications for gender disparities in career advancement: A qualitative analysis. JAMA Netw Open. 2021 Sep 1. doi: 10.1001/jamanetworkopen.2021.25843.
Sambunjak D et al. Mentoring in academic medicine: A systematic review. JAMA. 2006 Sep 6. doi: 10.1001/jama.296.9.1103.
Shen MR et al. Impact of mentoring on academic career success for women in medicine: A systematic review. Acad Med. 2022 Mar 1. doi: 10.1097/ACM.0000000000004563.
Defining Your ‘Success’
Dear Friends,
The prevailing theme of this issue is “Success.” I have learned that “success” is personal and personalized. What “success” looked like 10, or even 5, years ago to me is very different from how I perceive it now; and I know it may be different 5 years from now. My definition of success should not look like another’s — that was the best advice I have gotten over the years and it has kept me constantly redefining what is important to me and placing value on where I want to allocate my time and efforts, at work and at home.
This issue of The New Gastroenterologist highlights topics from successful GIs within their own realms of expertise, offering insights on advancing in academic medicine, navigating financial wellness with a financial adviser, and becoming a future leader in GI.
In this issue’s clinically-focused articles, we spotlight two very nuanced and challenging topics. Dr. Sachin Srinivasan and Dr. Prateek Sharma review Barrett’s esophagus management for our “In Focus” section, with a particular emphasis on Barrett’s endoscopic therapy modalities for dysplasia and early neoplasia. Dr. Brooke Corning and team simplify their approach to pelvic floor dysfunction (PFD) in our “Short Clinical Reviews.” They suggest validated ways to assess patient history, pros and cons of various diagnostic tests, and stepwise management of PFD.
Navigating academic promotion can be overwhelming and may not be at the forefront with our early career GIs’ priorities. In our “Early Career” section, Dr. Vineet Rolston interviews two highly accomplished professors in academic medicine, Dr. Sophie Balzora and Dr. Mark Schattner, for their insights into the promotion process and recommendations for junior faculty.
Dr. Anjuli K. Luthra, a therapeutic endoscopist and founder of The Scope of Finance, emphasizes financial wellness for physicians. She breaks down the search for a financial adviser, including the different types, what to ask when searching for the right fit, and what to expect.
Lastly, this issue highlights an AGA program that invests in the development of leaders for the field — the Future Leaders Program (FLP). Dr. Parakkal Deepak and Dr. Edward L. Barnes, along with their mentor, Dr. Aasma Shaukat, describe their experience as a mentee-mentor triad of FLP and how this program has impacted their careers.
If you are interested in contributing or have ideas for future TNG topics, please contact me (tjudy@wustl.edu), or Danielle Kiefer (dkiefer@gastro.org), managing editor of TNG.
Until next time, I leave you with a historical fun fact because we would not be where we are now without appreciating where we were: Dr. C.G. Stockton was the first AGA president in 1897, a Professor of the Principles and Practice of Medicine and Clinical Medicine at the University of Buffalo in New York, and published on the relationship between GI/Hepatology and gout in the Journal of the American Medical Association the same year of his presidency.
Yours truly,
Judy A. Trieu, MD, MPH
Editor-in-Chief
Interventional Endoscopy, Division of Gastroenterology
Washington University in St. Louis
Dear Friends,
The prevailing theme of this issue is “Success.” I have learned that “success” is personal and personalized. What “success” looked like 10, or even 5, years ago to me is very different from how I perceive it now; and I know it may be different 5 years from now. My definition of success should not look like another’s — that was the best advice I have gotten over the years and it has kept me constantly redefining what is important to me and placing value on where I want to allocate my time and efforts, at work and at home.
This issue of The New Gastroenterologist highlights topics from successful GIs within their own realms of expertise, offering insights on advancing in academic medicine, navigating financial wellness with a financial adviser, and becoming a future leader in GI.
In this issue’s clinically-focused articles, we spotlight two very nuanced and challenging topics. Dr. Sachin Srinivasan and Dr. Prateek Sharma review Barrett’s esophagus management for our “In Focus” section, with a particular emphasis on Barrett’s endoscopic therapy modalities for dysplasia and early neoplasia. Dr. Brooke Corning and team simplify their approach to pelvic floor dysfunction (PFD) in our “Short Clinical Reviews.” They suggest validated ways to assess patient history, pros and cons of various diagnostic tests, and stepwise management of PFD.
Navigating academic promotion can be overwhelming and may not be at the forefront with our early career GIs’ priorities. In our “Early Career” section, Dr. Vineet Rolston interviews two highly accomplished professors in academic medicine, Dr. Sophie Balzora and Dr. Mark Schattner, for their insights into the promotion process and recommendations for junior faculty.
Dr. Anjuli K. Luthra, a therapeutic endoscopist and founder of The Scope of Finance, emphasizes financial wellness for physicians. She breaks down the search for a financial adviser, including the different types, what to ask when searching for the right fit, and what to expect.
Lastly, this issue highlights an AGA program that invests in the development of leaders for the field — the Future Leaders Program (FLP). Dr. Parakkal Deepak and Dr. Edward L. Barnes, along with their mentor, Dr. Aasma Shaukat, describe their experience as a mentee-mentor triad of FLP and how this program has impacted their careers.
If you are interested in contributing or have ideas for future TNG topics, please contact me (tjudy@wustl.edu), or Danielle Kiefer (dkiefer@gastro.org), managing editor of TNG.
Until next time, I leave you with a historical fun fact because we would not be where we are now without appreciating where we were: Dr. C.G. Stockton was the first AGA president in 1897, a Professor of the Principles and Practice of Medicine and Clinical Medicine at the University of Buffalo in New York, and published on the relationship between GI/Hepatology and gout in the Journal of the American Medical Association the same year of his presidency.
Yours truly,
Judy A. Trieu, MD, MPH
Editor-in-Chief
Interventional Endoscopy, Division of Gastroenterology
Washington University in St. Louis
Dear Friends,
The prevailing theme of this issue is “Success.” I have learned that “success” is personal and personalized. What “success” looked like 10, or even 5, years ago to me is very different from how I perceive it now; and I know it may be different 5 years from now. My definition of success should not look like another’s — that was the best advice I have gotten over the years and it has kept me constantly redefining what is important to me and placing value on where I want to allocate my time and efforts, at work and at home.
This issue of The New Gastroenterologist highlights topics from successful GIs within their own realms of expertise, offering insights on advancing in academic medicine, navigating financial wellness with a financial adviser, and becoming a future leader in GI.
In this issue’s clinically-focused articles, we spotlight two very nuanced and challenging topics. Dr. Sachin Srinivasan and Dr. Prateek Sharma review Barrett’s esophagus management for our “In Focus” section, with a particular emphasis on Barrett’s endoscopic therapy modalities for dysplasia and early neoplasia. Dr. Brooke Corning and team simplify their approach to pelvic floor dysfunction (PFD) in our “Short Clinical Reviews.” They suggest validated ways to assess patient history, pros and cons of various diagnostic tests, and stepwise management of PFD.
Navigating academic promotion can be overwhelming and may not be at the forefront with our early career GIs’ priorities. In our “Early Career” section, Dr. Vineet Rolston interviews two highly accomplished professors in academic medicine, Dr. Sophie Balzora and Dr. Mark Schattner, for their insights into the promotion process and recommendations for junior faculty.
Dr. Anjuli K. Luthra, a therapeutic endoscopist and founder of The Scope of Finance, emphasizes financial wellness for physicians. She breaks down the search for a financial adviser, including the different types, what to ask when searching for the right fit, and what to expect.
Lastly, this issue highlights an AGA program that invests in the development of leaders for the field — the Future Leaders Program (FLP). Dr. Parakkal Deepak and Dr. Edward L. Barnes, along with their mentor, Dr. Aasma Shaukat, describe their experience as a mentee-mentor triad of FLP and how this program has impacted their careers.
If you are interested in contributing or have ideas for future TNG topics, please contact me (tjudy@wustl.edu), or Danielle Kiefer (dkiefer@gastro.org), managing editor of TNG.
Until next time, I leave you with a historical fun fact because we would not be where we are now without appreciating where we were: Dr. C.G. Stockton was the first AGA president in 1897, a Professor of the Principles and Practice of Medicine and Clinical Medicine at the University of Buffalo in New York, and published on the relationship between GI/Hepatology and gout in the Journal of the American Medical Association the same year of his presidency.
Yours truly,
Judy A. Trieu, MD, MPH
Editor-in-Chief
Interventional Endoscopy, Division of Gastroenterology
Washington University in St. Louis
Converging on Our Nation’s Capital
Release of our May issue coincides with our annual pilgrimage to Digestive Disease Week® (DDW), this year held in our nation’s capital of Washington, D.C.
As we peruse the preliminary program in planning our meeting coverage, I am always amazed at the breadth and depth of programming offered as part of a relatively brief, 4-day meeting — this is a testament to the hard work of the AGA Council and DDW organizing committees, who have the gargantuan task of ensuring an engaging, seamless meeting each year.
This year’s conference features over 400 original scientific sessions and 4,300 oral abstract and poster presentations, in addition to the always well-attended AGA Postgraduate Course. This year’s AGA Presidential Plenary, which will feature a series of thought-provoking panel discussions on the future of GI healthcare and innovations in how we treat, disseminate, and teach, also is not to be missed. Beyond DDW, I hope you will join me in taking advantage of some of D.C.’s amazing cultural offerings, including the Smithsonian museums, National Gallery, Kennedy Center for the Performing Arts, and many others.
In this month’s issue of GIHN, we highlight an important AGA expert consensus commentary published in Clinical Gastroenterology and Hepatology examining the role of blood-based tests (“liquid biopsy”) in colorectal cancer screening. This guidance, which recognizes the promise of such tests but also urges caution in their adoption, is particularly important considering recently published data from the ECLIPSE study (also covered in this issue) evaluating the performance of Guardant’s ctDNA liquid biopsy compared to a screening colonoscopy. Also relevant to CRC screening, we highlight data on the performance of the “next gen” Cologuard test compared with FIT, which was recently published in NEJM. In our May Member Spotlight, we feature gastroenterologist Adjoa Anyane-Yeboa, MD, MPH, who shares her passion for addressing barriers to CRC screening for Black patients. Finally, GIHN Associate Editor Dr. Avi Ketwaroo introduces our quarterly Perspectives column highlighting emerging applications of AI in GI endoscopy and hepatology. We hope you enjoy all the exciting content featured in this issue and look forward to seeing you in Washington, D.C. (or virtually) for DDW.
Megan A. Adams, MD, JD, MSc
Editor-in-Chief
Release of our May issue coincides with our annual pilgrimage to Digestive Disease Week® (DDW), this year held in our nation’s capital of Washington, D.C.
As we peruse the preliminary program in planning our meeting coverage, I am always amazed at the breadth and depth of programming offered as part of a relatively brief, 4-day meeting — this is a testament to the hard work of the AGA Council and DDW organizing committees, who have the gargantuan task of ensuring an engaging, seamless meeting each year.
This year’s conference features over 400 original scientific sessions and 4,300 oral abstract and poster presentations, in addition to the always well-attended AGA Postgraduate Course. This year’s AGA Presidential Plenary, which will feature a series of thought-provoking panel discussions on the future of GI healthcare and innovations in how we treat, disseminate, and teach, also is not to be missed. Beyond DDW, I hope you will join me in taking advantage of some of D.C.’s amazing cultural offerings, including the Smithsonian museums, National Gallery, Kennedy Center for the Performing Arts, and many others.
In this month’s issue of GIHN, we highlight an important AGA expert consensus commentary published in Clinical Gastroenterology and Hepatology examining the role of blood-based tests (“liquid biopsy”) in colorectal cancer screening. This guidance, which recognizes the promise of such tests but also urges caution in their adoption, is particularly important considering recently published data from the ECLIPSE study (also covered in this issue) evaluating the performance of Guardant’s ctDNA liquid biopsy compared to a screening colonoscopy. Also relevant to CRC screening, we highlight data on the performance of the “next gen” Cologuard test compared with FIT, which was recently published in NEJM. In our May Member Spotlight, we feature gastroenterologist Adjoa Anyane-Yeboa, MD, MPH, who shares her passion for addressing barriers to CRC screening for Black patients. Finally, GIHN Associate Editor Dr. Avi Ketwaroo introduces our quarterly Perspectives column highlighting emerging applications of AI in GI endoscopy and hepatology. We hope you enjoy all the exciting content featured in this issue and look forward to seeing you in Washington, D.C. (or virtually) for DDW.
Megan A. Adams, MD, JD, MSc
Editor-in-Chief
Release of our May issue coincides with our annual pilgrimage to Digestive Disease Week® (DDW), this year held in our nation’s capital of Washington, D.C.
As we peruse the preliminary program in planning our meeting coverage, I am always amazed at the breadth and depth of programming offered as part of a relatively brief, 4-day meeting — this is a testament to the hard work of the AGA Council and DDW organizing committees, who have the gargantuan task of ensuring an engaging, seamless meeting each year.
This year’s conference features over 400 original scientific sessions and 4,300 oral abstract and poster presentations, in addition to the always well-attended AGA Postgraduate Course. This year’s AGA Presidential Plenary, which will feature a series of thought-provoking panel discussions on the future of GI healthcare and innovations in how we treat, disseminate, and teach, also is not to be missed. Beyond DDW, I hope you will join me in taking advantage of some of D.C.’s amazing cultural offerings, including the Smithsonian museums, National Gallery, Kennedy Center for the Performing Arts, and many others.
In this month’s issue of GIHN, we highlight an important AGA expert consensus commentary published in Clinical Gastroenterology and Hepatology examining the role of blood-based tests (“liquid biopsy”) in colorectal cancer screening. This guidance, which recognizes the promise of such tests but also urges caution in their adoption, is particularly important considering recently published data from the ECLIPSE study (also covered in this issue) evaluating the performance of Guardant’s ctDNA liquid biopsy compared to a screening colonoscopy. Also relevant to CRC screening, we highlight data on the performance of the “next gen” Cologuard test compared with FIT, which was recently published in NEJM. In our May Member Spotlight, we feature gastroenterologist Adjoa Anyane-Yeboa, MD, MPH, who shares her passion for addressing barriers to CRC screening for Black patients. Finally, GIHN Associate Editor Dr. Avi Ketwaroo introduces our quarterly Perspectives column highlighting emerging applications of AI in GI endoscopy and hepatology. We hope you enjoy all the exciting content featured in this issue and look forward to seeing you in Washington, D.C. (or virtually) for DDW.
Megan A. Adams, MD, JD, MSc
Editor-in-Chief
Do No Harm: What Smoldering Myeloma Teaches Us
My approach to treating SMM takes into account what its history can teach us about 1) how advancements in imaging and diagnostic reclassifications can revise the entire natural history of a disease, and 2) how evidence generated by even the best of studies may have an expiration date.
Much of what we know about SMM today dates to a pivotal study by Robert A. Kyle, MD, and colleagues, published in 2007. That inspirational team of investigators followed people diagnosed with SMM from 1970 to 1995 and established the first natural history of the condition. Their monumental effort and the data and conclusions it generated (eg,10% risk annually of SMM becoming MM for the first 5 years) are still cited today in references, papers, and slide sets.
Despite the seminal importance of this work, from today’s perspective the 2007 study might just as well have been describing a different disease. Back then people were diagnosed with SMM if their blood work detected a monoclonal protein and a follow-up bone marrow biopsy found at least 10% plasma cells (or a monoclonal protein exceeding 3g/dL). If there were no signs of end-organ damage (ie, no anemia or kidney problems) and an x-ray showed no fractures or lesions in the bones, the diagnosis was determined to be SMM.
What’s different in 2024? First and foremost: advanced, highly sensitive imaging techniques. MRIs can pick up small lytic lesions (and even the precursor to lytic lesions) that would not appear on an x-ray. In fact, relying solely on x-rays risks missing half of the lytic lesions.
Therefore, using the same criteria, many people who in the past were diagnosed with SMM would today be diagnosed with MM. Furthermore, in 2014 a diagnostic change reclassified people’s diagnosis from the highest risk category of SMM to the category of active MM.
Due to these scientific advances and classification changes, I believe that the natural history of SMM is unknown. Risk stratification models for SMM derived from data sets of people who had not undergone rigorous advanced imaging likely are skewed by data from people who had MM. In addition, current risk stratification models have very poor concordance with each other. I routinely see people whose 2-year risk according to different models varies by more than 30%-40%.
All this information tells us that SMM today is more indolent than the SMM of the past. Paradoxically, however, our therapies keep getting more and more aggressive, exposing this vulnerable group of people to intense treatment regimens that they may not require. Therapies tested on people diagnosed with SMM include an aggressive three-drug regimen, autologous stem cell transplant, and 2 years of additional therapy, as well as, more recently CAR T-cell therapy which so far has at least a 4%-5% treatment-related mortality risk in people with myeloma and a strong signal for secondary cancer risk. Other trials are testing bispecific therapies such as talquetamab, a drug which in my experience causes horrendous skin toxicity, profound weight loss, and one’s nails to fall off.
Doctors routinely keep showing slides from Kyle’s pivotal work to describe the natural history of SMM and to justify the need for treatment, and trials continue to use outdated progression prediction models. In my opinion, as people with MM keep living longer and treatments for MM keep getting better, the threshold for intervening with asymptomatic, healthy people with SMM should be getting higher, not lower.
I strongly believe that the current landscape of SMM treatment exemplifies good intentions leading to bad outcomes. A routine blood test in a completely healthy person that finds elevated total protein in the blood could culminate in well-intentioned but aggressive therapies that can lead to many serious side effects. (I repeat: Secondary cancers and deaths from infections have all occurred in SMM trials.)
With no control arm, we simply don’t know how well these people might have fared without any therapy. For all we know, treatment may have shortened their lives due to complications up to and including death — all because of a blood test often conducted for reasons that have no evidentiary basis.
For example, plasma cell diseases are not linked to low bone density or auto-immune diseases, yet these labs are sent routinely as part of a workup for those conditions, leading to increasing anxiety and costs.
So, what is my approach? When treating people with SMM, I hold nuanced discussions of this data to help prioritize and reach informed decisions. After our honest conversation about the limitations of SMM models, older data, and the limitations of prospective data studying pharmacological treatment, almost no one signs up for treatment.
I want these people to stay safe, and I’m proud to be a part of a trial (SPOTLIGHT, NCT06212323) that aims to show prospectively that these people can be watched off treatment with monitoring via advanced imaging modalities.
In conclusion: SMM teaches us how, even in the absence of pharmacological interventions, the natural history of a disease can change over time, simply via better imaging techniques and changes in diagnostic classifications. Unfortunately, SMM also illustrates how good intentions can lead to harm.
Dr. Mohyuddin is assistant professor in the multiple myeloma program at the Huntsman Cancer Institute at the University of Utah in Salt Lake City.
My approach to treating SMM takes into account what its history can teach us about 1) how advancements in imaging and diagnostic reclassifications can revise the entire natural history of a disease, and 2) how evidence generated by even the best of studies may have an expiration date.
Much of what we know about SMM today dates to a pivotal study by Robert A. Kyle, MD, and colleagues, published in 2007. That inspirational team of investigators followed people diagnosed with SMM from 1970 to 1995 and established the first natural history of the condition. Their monumental effort and the data and conclusions it generated (eg,10% risk annually of SMM becoming MM for the first 5 years) are still cited today in references, papers, and slide sets.
Despite the seminal importance of this work, from today’s perspective the 2007 study might just as well have been describing a different disease. Back then people were diagnosed with SMM if their blood work detected a monoclonal protein and a follow-up bone marrow biopsy found at least 10% plasma cells (or a monoclonal protein exceeding 3g/dL). If there were no signs of end-organ damage (ie, no anemia or kidney problems) and an x-ray showed no fractures or lesions in the bones, the diagnosis was determined to be SMM.
What’s different in 2024? First and foremost: advanced, highly sensitive imaging techniques. MRIs can pick up small lytic lesions (and even the precursor to lytic lesions) that would not appear on an x-ray. In fact, relying solely on x-rays risks missing half of the lytic lesions.
Therefore, using the same criteria, many people who in the past were diagnosed with SMM would today be diagnosed with MM. Furthermore, in 2014 a diagnostic change reclassified people’s diagnosis from the highest risk category of SMM to the category of active MM.
Due to these scientific advances and classification changes, I believe that the natural history of SMM is unknown. Risk stratification models for SMM derived from data sets of people who had not undergone rigorous advanced imaging likely are skewed by data from people who had MM. In addition, current risk stratification models have very poor concordance with each other. I routinely see people whose 2-year risk according to different models varies by more than 30%-40%.
All this information tells us that SMM today is more indolent than the SMM of the past. Paradoxically, however, our therapies keep getting more and more aggressive, exposing this vulnerable group of people to intense treatment regimens that they may not require. Therapies tested on people diagnosed with SMM include an aggressive three-drug regimen, autologous stem cell transplant, and 2 years of additional therapy, as well as, more recently CAR T-cell therapy which so far has at least a 4%-5% treatment-related mortality risk in people with myeloma and a strong signal for secondary cancer risk. Other trials are testing bispecific therapies such as talquetamab, a drug which in my experience causes horrendous skin toxicity, profound weight loss, and one’s nails to fall off.
Doctors routinely keep showing slides from Kyle’s pivotal work to describe the natural history of SMM and to justify the need for treatment, and trials continue to use outdated progression prediction models. In my opinion, as people with MM keep living longer and treatments for MM keep getting better, the threshold for intervening with asymptomatic, healthy people with SMM should be getting higher, not lower.
I strongly believe that the current landscape of SMM treatment exemplifies good intentions leading to bad outcomes. A routine blood test in a completely healthy person that finds elevated total protein in the blood could culminate in well-intentioned but aggressive therapies that can lead to many serious side effects. (I repeat: Secondary cancers and deaths from infections have all occurred in SMM trials.)
With no control arm, we simply don’t know how well these people might have fared without any therapy. For all we know, treatment may have shortened their lives due to complications up to and including death — all because of a blood test often conducted for reasons that have no evidentiary basis.
For example, plasma cell diseases are not linked to low bone density or auto-immune diseases, yet these labs are sent routinely as part of a workup for those conditions, leading to increasing anxiety and costs.
So, what is my approach? When treating people with SMM, I hold nuanced discussions of this data to help prioritize and reach informed decisions. After our honest conversation about the limitations of SMM models, older data, and the limitations of prospective data studying pharmacological treatment, almost no one signs up for treatment.
I want these people to stay safe, and I’m proud to be a part of a trial (SPOTLIGHT, NCT06212323) that aims to show prospectively that these people can be watched off treatment with monitoring via advanced imaging modalities.
In conclusion: SMM teaches us how, even in the absence of pharmacological interventions, the natural history of a disease can change over time, simply via better imaging techniques and changes in diagnostic classifications. Unfortunately, SMM also illustrates how good intentions can lead to harm.
Dr. Mohyuddin is assistant professor in the multiple myeloma program at the Huntsman Cancer Institute at the University of Utah in Salt Lake City.
My approach to treating SMM takes into account what its history can teach us about 1) how advancements in imaging and diagnostic reclassifications can revise the entire natural history of a disease, and 2) how evidence generated by even the best of studies may have an expiration date.
Much of what we know about SMM today dates to a pivotal study by Robert A. Kyle, MD, and colleagues, published in 2007. That inspirational team of investigators followed people diagnosed with SMM from 1970 to 1995 and established the first natural history of the condition. Their monumental effort and the data and conclusions it generated (eg,10% risk annually of SMM becoming MM for the first 5 years) are still cited today in references, papers, and slide sets.
Despite the seminal importance of this work, from today’s perspective the 2007 study might just as well have been describing a different disease. Back then people were diagnosed with SMM if their blood work detected a monoclonal protein and a follow-up bone marrow biopsy found at least 10% plasma cells (or a monoclonal protein exceeding 3g/dL). If there were no signs of end-organ damage (ie, no anemia or kidney problems) and an x-ray showed no fractures or lesions in the bones, the diagnosis was determined to be SMM.
What’s different in 2024? First and foremost: advanced, highly sensitive imaging techniques. MRIs can pick up small lytic lesions (and even the precursor to lytic lesions) that would not appear on an x-ray. In fact, relying solely on x-rays risks missing half of the lytic lesions.
Therefore, using the same criteria, many people who in the past were diagnosed with SMM would today be diagnosed with MM. Furthermore, in 2014 a diagnostic change reclassified people’s diagnosis from the highest risk category of SMM to the category of active MM.
Due to these scientific advances and classification changes, I believe that the natural history of SMM is unknown. Risk stratification models for SMM derived from data sets of people who had not undergone rigorous advanced imaging likely are skewed by data from people who had MM. In addition, current risk stratification models have very poor concordance with each other. I routinely see people whose 2-year risk according to different models varies by more than 30%-40%.
All this information tells us that SMM today is more indolent than the SMM of the past. Paradoxically, however, our therapies keep getting more and more aggressive, exposing this vulnerable group of people to intense treatment regimens that they may not require. Therapies tested on people diagnosed with SMM include an aggressive three-drug regimen, autologous stem cell transplant, and 2 years of additional therapy, as well as, more recently CAR T-cell therapy which so far has at least a 4%-5% treatment-related mortality risk in people with myeloma and a strong signal for secondary cancer risk. Other trials are testing bispecific therapies such as talquetamab, a drug which in my experience causes horrendous skin toxicity, profound weight loss, and one’s nails to fall off.
Doctors routinely keep showing slides from Kyle’s pivotal work to describe the natural history of SMM and to justify the need for treatment, and trials continue to use outdated progression prediction models. In my opinion, as people with MM keep living longer and treatments for MM keep getting better, the threshold for intervening with asymptomatic, healthy people with SMM should be getting higher, not lower.
I strongly believe that the current landscape of SMM treatment exemplifies good intentions leading to bad outcomes. A routine blood test in a completely healthy person that finds elevated total protein in the blood could culminate in well-intentioned but aggressive therapies that can lead to many serious side effects. (I repeat: Secondary cancers and deaths from infections have all occurred in SMM trials.)
With no control arm, we simply don’t know how well these people might have fared without any therapy. For all we know, treatment may have shortened their lives due to complications up to and including death — all because of a blood test often conducted for reasons that have no evidentiary basis.
For example, plasma cell diseases are not linked to low bone density or auto-immune diseases, yet these labs are sent routinely as part of a workup for those conditions, leading to increasing anxiety and costs.
So, what is my approach? When treating people with SMM, I hold nuanced discussions of this data to help prioritize and reach informed decisions. After our honest conversation about the limitations of SMM models, older data, and the limitations of prospective data studying pharmacological treatment, almost no one signs up for treatment.
I want these people to stay safe, and I’m proud to be a part of a trial (SPOTLIGHT, NCT06212323) that aims to show prospectively that these people can be watched off treatment with monitoring via advanced imaging modalities.
In conclusion: SMM teaches us how, even in the absence of pharmacological interventions, the natural history of a disease can change over time, simply via better imaging techniques and changes in diagnostic classifications. Unfortunately, SMM also illustrates how good intentions can lead to harm.
Dr. Mohyuddin is assistant professor in the multiple myeloma program at the Huntsman Cancer Institute at the University of Utah in Salt Lake City.
PCP Compensation, Part 1
I recently read an op-ed piece in which the author wondered if any young people entering the practice of medicine felt that they were answering a “calling.” I suspect that there will continue to be, and will always be, idealists whose primary motivation for choosing medicine is that they will be healing the sick or at least providing comfort to the suffering. I occasionally hear that about a former patient who has been inspired by a personal or familial experience with a serious illness.
Unfortunately, I suspect those who feel called are the providers most likely to feel discouraged and frustrated by the current state of primary care. Luckily, I never felt a calling. For me, primary care pediatrics was a job. One that l felt obligated to perform to the best of my ability. Mine was not a calling but an inherited philosophy that work in itself was virtuous. A work ethic, if you will. Pediatrics offered the additional reward that, if well done, it might help some parents and their children feel a little better.
Fifty years ago I was not alone in treating medicine as a job. Most physicians were self-employed. Although there were exceptions like Albert Schweitzer, even those of us with a calling had to obey the basic rules of business as it applied to medicine. We were employer and employee and had to understand the critical factors of overhead, profit, and loss.
I have burdened you with this little history recitation not to suggest that things were better in the good old days, but to provide a stepping stone into the murky and uncomfortable topic of primary care physician (PCP) compensation. Because almost three quarters of you work for a hospital, health system, or corporate entity, I am going to illuminate our journey by leaning on the advice of an international company with 7000 employees and revenue of 2.5 billion dollars that considers itself a “global leader” in management consulting. Your employer is listening to some management consultant and it may help us to view your compensation from someone on their side of the table.
First, you should be aware that “most health systems lose money on their primary care operations — up to $200,000 or more per primary care physician.” This may help explain why despite being in short supply, you and most PCPs feel undervalued. However, if we are such losers, we must provide something(s) that the systems are seeking. It is likely that the system is looking to tout its ability to provide comprehensive care and demonstrate that it has a patient base broad enough to warrant attention and provide bargaining leverage on volume discounts.
The system also may want to minimize competition by absorbing the remaining PCPs in the community into their system. With you outside of the system, it had less control over your compensation than it does when you are under its umbrella.
Your employer may want to grow and feed its specialty care network, and it sees PCPs as having the fuel stored in their patient volume to do just that. In simplest and most cynical terms, the systems are willing to take a loss on us less profitable high-volume grunts in order to reap the profits of the lower-volume high-profitability specialties and subspecialties.
So that’s why you as a PCP have any value at all to a large healthcare system. But, it means that to maintain your value to the system you must continue to provide the volume it anticipates and needs. While the system may have been willing to accept some degrees of unprofitability when it hired you, there are limits. And, we shouldn’t be surprised if they continue to urge or demand that we narrow the gap between the revenue we generate and the costs that we incur, ie, our overhead.
In Part 2 of this series, I’m going to discuss the collateral damage that occurs when volume and overhead collide in an environment that claims to be committed to patient care.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
I recently read an op-ed piece in which the author wondered if any young people entering the practice of medicine felt that they were answering a “calling.” I suspect that there will continue to be, and will always be, idealists whose primary motivation for choosing medicine is that they will be healing the sick or at least providing comfort to the suffering. I occasionally hear that about a former patient who has been inspired by a personal or familial experience with a serious illness.
Unfortunately, I suspect those who feel called are the providers most likely to feel discouraged and frustrated by the current state of primary care. Luckily, I never felt a calling. For me, primary care pediatrics was a job. One that l felt obligated to perform to the best of my ability. Mine was not a calling but an inherited philosophy that work in itself was virtuous. A work ethic, if you will. Pediatrics offered the additional reward that, if well done, it might help some parents and their children feel a little better.
Fifty years ago I was not alone in treating medicine as a job. Most physicians were self-employed. Although there were exceptions like Albert Schweitzer, even those of us with a calling had to obey the basic rules of business as it applied to medicine. We were employer and employee and had to understand the critical factors of overhead, profit, and loss.
I have burdened you with this little history recitation not to suggest that things were better in the good old days, but to provide a stepping stone into the murky and uncomfortable topic of primary care physician (PCP) compensation. Because almost three quarters of you work for a hospital, health system, or corporate entity, I am going to illuminate our journey by leaning on the advice of an international company with 7000 employees and revenue of 2.5 billion dollars that considers itself a “global leader” in management consulting. Your employer is listening to some management consultant and it may help us to view your compensation from someone on their side of the table.
First, you should be aware that “most health systems lose money on their primary care operations — up to $200,000 or more per primary care physician.” This may help explain why despite being in short supply, you and most PCPs feel undervalued. However, if we are such losers, we must provide something(s) that the systems are seeking. It is likely that the system is looking to tout its ability to provide comprehensive care and demonstrate that it has a patient base broad enough to warrant attention and provide bargaining leverage on volume discounts.
The system also may want to minimize competition by absorbing the remaining PCPs in the community into their system. With you outside of the system, it had less control over your compensation than it does when you are under its umbrella.
Your employer may want to grow and feed its specialty care network, and it sees PCPs as having the fuel stored in their patient volume to do just that. In simplest and most cynical terms, the systems are willing to take a loss on us less profitable high-volume grunts in order to reap the profits of the lower-volume high-profitability specialties and subspecialties.
So that’s why you as a PCP have any value at all to a large healthcare system. But, it means that to maintain your value to the system you must continue to provide the volume it anticipates and needs. While the system may have been willing to accept some degrees of unprofitability when it hired you, there are limits. And, we shouldn’t be surprised if they continue to urge or demand that we narrow the gap between the revenue we generate and the costs that we incur, ie, our overhead.
In Part 2 of this series, I’m going to discuss the collateral damage that occurs when volume and overhead collide in an environment that claims to be committed to patient care.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
I recently read an op-ed piece in which the author wondered if any young people entering the practice of medicine felt that they were answering a “calling.” I suspect that there will continue to be, and will always be, idealists whose primary motivation for choosing medicine is that they will be healing the sick or at least providing comfort to the suffering. I occasionally hear that about a former patient who has been inspired by a personal or familial experience with a serious illness.
Unfortunately, I suspect those who feel called are the providers most likely to feel discouraged and frustrated by the current state of primary care. Luckily, I never felt a calling. For me, primary care pediatrics was a job. One that l felt obligated to perform to the best of my ability. Mine was not a calling but an inherited philosophy that work in itself was virtuous. A work ethic, if you will. Pediatrics offered the additional reward that, if well done, it might help some parents and their children feel a little better.
Fifty years ago I was not alone in treating medicine as a job. Most physicians were self-employed. Although there were exceptions like Albert Schweitzer, even those of us with a calling had to obey the basic rules of business as it applied to medicine. We were employer and employee and had to understand the critical factors of overhead, profit, and loss.
I have burdened you with this little history recitation not to suggest that things were better in the good old days, but to provide a stepping stone into the murky and uncomfortable topic of primary care physician (PCP) compensation. Because almost three quarters of you work for a hospital, health system, or corporate entity, I am going to illuminate our journey by leaning on the advice of an international company with 7000 employees and revenue of 2.5 billion dollars that considers itself a “global leader” in management consulting. Your employer is listening to some management consultant and it may help us to view your compensation from someone on their side of the table.
First, you should be aware that “most health systems lose money on their primary care operations — up to $200,000 or more per primary care physician.” This may help explain why despite being in short supply, you and most PCPs feel undervalued. However, if we are such losers, we must provide something(s) that the systems are seeking. It is likely that the system is looking to tout its ability to provide comprehensive care and demonstrate that it has a patient base broad enough to warrant attention and provide bargaining leverage on volume discounts.
The system also may want to minimize competition by absorbing the remaining PCPs in the community into their system. With you outside of the system, it had less control over your compensation than it does when you are under its umbrella.
Your employer may want to grow and feed its specialty care network, and it sees PCPs as having the fuel stored in their patient volume to do just that. In simplest and most cynical terms, the systems are willing to take a loss on us less profitable high-volume grunts in order to reap the profits of the lower-volume high-profitability specialties and subspecialties.
So that’s why you as a PCP have any value at all to a large healthcare system. But, it means that to maintain your value to the system you must continue to provide the volume it anticipates and needs. While the system may have been willing to accept some degrees of unprofitability when it hired you, there are limits. And, we shouldn’t be surprised if they continue to urge or demand that we narrow the gap between the revenue we generate and the costs that we incur, ie, our overhead.
In Part 2 of this series, I’m going to discuss the collateral damage that occurs when volume and overhead collide in an environment that claims to be committed to patient care.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
‘We Need to Rethink Our Options’: Lung Cancer Recurrence
This transcript has been edited for clarity.
Hello. It’s Mark Kris reporting back after attending the New York Lung Cancer Foundation Summit here in New York. A large amount of discussion went on, but as usual, I was most interested in the perioperative space.
In previous videos, I’ve talked about this ongoing discussion of whether you should operate and give adjuvant therapy or give neoadjuvant therapy, and I’ve addressed that already. One thing I want to bring up – and as we move off of that argument, which frankly doesn’t have an answer today, with neoadjuvant therapy, having all the data to support it – is
I was taught early on by my surgical mentors that the issue here was systemic control. While they could do very successful surgery to get high levels of local control, they could not control systemic disease. Sadly, the tools we had early on with chemotherapy were just not good enough. Suddenly, we have better tools to control systemic spread. In the past, the vast majority of occurrences were systemic; they’re now local.
What I think we need to do as a group of practitioners trying to deal with the problems getting in the way of curing our patients is look at what the issue is now. Frankly, the big issue now, as systemic therapy has controlled metastatic disease, is recurrence in the chest.
We give adjuvant osimertinib. Please remember what the numbers are. In the osimertinib arm, of the 11 recurrences reported in the European Society for Medical Oncology presentation a few years back, nine of them were in the chest or mediastinal nodes. In the arm that got no osimertinib afterward, there were 46 recurrences, and 32 of those 46 recurrences were in the chest, either the lung or mediastinal nodes. Therefore, 74% of the recurrences are suddenly in the chest. What’s the issue here?
The issue is we need to find strategies to give better disease control in the chest, as we have made inroads in controlling systemic disease with the targeted therapies in the endothelial growth factor receptor space, and very likely the checkpoint inhibitors, too, as that data kind of filters out. We need to think about how better to get local control.
I think rather than continue to get into this argument of neoadjuvant vs adjuvant, we should move to what’s really hurting our patients. Again, the data I quoted you was from the ADAURA trial, which was adjuvant therapy, and I’m sure the neoadjuvant is going to show the same thing. It’s better systemic therapy but now, more trouble in the chest.
How are we going to deal with that? I’d like to throw out one strategy, and that is to rethink the role of radiation in these patients. Again, if the problem is local in the chest, lung, and lymph nodes, we have to think about local therapy. Yes, we’re not recommending it routinely for everybody, but now that we have better systemic control, we need to rethink our options. The obvious one to rethink is about giving radiotherapy.
We should also use what we learned in the earlier trials, which is that there is harm in giving excessive radiation to the heart. If you avoid the heart, you avoid the harm. We have better planning strategies for stereotactic body radiotherapy and more traditional radiation, and of course, we have proton therapy as well.
As we continue to struggle with the idea of that patient with stage II or III disease, whether to give adjuvant vs neoadjuvant therapy, please remember to consider their risk in 2024. Their risk for first recurrence is in the chest.
What are we going to do to better control disease in the chest? We have a challenge. I’m sure we can meet it if we put our heads together.
Dr. Kris is professor of medicine at Weill Cornell Medical College, and attending physician, Thoracic Oncology Service, Memorial Sloan Kettering Cancer Center, New York. He disclosed ties with AstraZeneca, Roche/Genentech, Ariad Pharmaceuticals, Pfizer, and PUMA.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
Hello. It’s Mark Kris reporting back after attending the New York Lung Cancer Foundation Summit here in New York. A large amount of discussion went on, but as usual, I was most interested in the perioperative space.
In previous videos, I’ve talked about this ongoing discussion of whether you should operate and give adjuvant therapy or give neoadjuvant therapy, and I’ve addressed that already. One thing I want to bring up – and as we move off of that argument, which frankly doesn’t have an answer today, with neoadjuvant therapy, having all the data to support it – is
I was taught early on by my surgical mentors that the issue here was systemic control. While they could do very successful surgery to get high levels of local control, they could not control systemic disease. Sadly, the tools we had early on with chemotherapy were just not good enough. Suddenly, we have better tools to control systemic spread. In the past, the vast majority of occurrences were systemic; they’re now local.
What I think we need to do as a group of practitioners trying to deal with the problems getting in the way of curing our patients is look at what the issue is now. Frankly, the big issue now, as systemic therapy has controlled metastatic disease, is recurrence in the chest.
We give adjuvant osimertinib. Please remember what the numbers are. In the osimertinib arm, of the 11 recurrences reported in the European Society for Medical Oncology presentation a few years back, nine of them were in the chest or mediastinal nodes. In the arm that got no osimertinib afterward, there were 46 recurrences, and 32 of those 46 recurrences were in the chest, either the lung or mediastinal nodes. Therefore, 74% of the recurrences are suddenly in the chest. What’s the issue here?
The issue is we need to find strategies to give better disease control in the chest, as we have made inroads in controlling systemic disease with the targeted therapies in the endothelial growth factor receptor space, and very likely the checkpoint inhibitors, too, as that data kind of filters out. We need to think about how better to get local control.
I think rather than continue to get into this argument of neoadjuvant vs adjuvant, we should move to what’s really hurting our patients. Again, the data I quoted you was from the ADAURA trial, which was adjuvant therapy, and I’m sure the neoadjuvant is going to show the same thing. It’s better systemic therapy but now, more trouble in the chest.
How are we going to deal with that? I’d like to throw out one strategy, and that is to rethink the role of radiation in these patients. Again, if the problem is local in the chest, lung, and lymph nodes, we have to think about local therapy. Yes, we’re not recommending it routinely for everybody, but now that we have better systemic control, we need to rethink our options. The obvious one to rethink is about giving radiotherapy.
We should also use what we learned in the earlier trials, which is that there is harm in giving excessive radiation to the heart. If you avoid the heart, you avoid the harm. We have better planning strategies for stereotactic body radiotherapy and more traditional radiation, and of course, we have proton therapy as well.
As we continue to struggle with the idea of that patient with stage II or III disease, whether to give adjuvant vs neoadjuvant therapy, please remember to consider their risk in 2024. Their risk for first recurrence is in the chest.
What are we going to do to better control disease in the chest? We have a challenge. I’m sure we can meet it if we put our heads together.
Dr. Kris is professor of medicine at Weill Cornell Medical College, and attending physician, Thoracic Oncology Service, Memorial Sloan Kettering Cancer Center, New York. He disclosed ties with AstraZeneca, Roche/Genentech, Ariad Pharmaceuticals, Pfizer, and PUMA.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
Hello. It’s Mark Kris reporting back after attending the New York Lung Cancer Foundation Summit here in New York. A large amount of discussion went on, but as usual, I was most interested in the perioperative space.
In previous videos, I’ve talked about this ongoing discussion of whether you should operate and give adjuvant therapy or give neoadjuvant therapy, and I’ve addressed that already. One thing I want to bring up – and as we move off of that argument, which frankly doesn’t have an answer today, with neoadjuvant therapy, having all the data to support it – is
I was taught early on by my surgical mentors that the issue here was systemic control. While they could do very successful surgery to get high levels of local control, they could not control systemic disease. Sadly, the tools we had early on with chemotherapy were just not good enough. Suddenly, we have better tools to control systemic spread. In the past, the vast majority of occurrences were systemic; they’re now local.
What I think we need to do as a group of practitioners trying to deal with the problems getting in the way of curing our patients is look at what the issue is now. Frankly, the big issue now, as systemic therapy has controlled metastatic disease, is recurrence in the chest.
We give adjuvant osimertinib. Please remember what the numbers are. In the osimertinib arm, of the 11 recurrences reported in the European Society for Medical Oncology presentation a few years back, nine of them were in the chest or mediastinal nodes. In the arm that got no osimertinib afterward, there were 46 recurrences, and 32 of those 46 recurrences were in the chest, either the lung or mediastinal nodes. Therefore, 74% of the recurrences are suddenly in the chest. What’s the issue here?
The issue is we need to find strategies to give better disease control in the chest, as we have made inroads in controlling systemic disease with the targeted therapies in the endothelial growth factor receptor space, and very likely the checkpoint inhibitors, too, as that data kind of filters out. We need to think about how better to get local control.
I think rather than continue to get into this argument of neoadjuvant vs adjuvant, we should move to what’s really hurting our patients. Again, the data I quoted you was from the ADAURA trial, which was adjuvant therapy, and I’m sure the neoadjuvant is going to show the same thing. It’s better systemic therapy but now, more trouble in the chest.
How are we going to deal with that? I’d like to throw out one strategy, and that is to rethink the role of radiation in these patients. Again, if the problem is local in the chest, lung, and lymph nodes, we have to think about local therapy. Yes, we’re not recommending it routinely for everybody, but now that we have better systemic control, we need to rethink our options. The obvious one to rethink is about giving radiotherapy.
We should also use what we learned in the earlier trials, which is that there is harm in giving excessive radiation to the heart. If you avoid the heart, you avoid the harm. We have better planning strategies for stereotactic body radiotherapy and more traditional radiation, and of course, we have proton therapy as well.
As we continue to struggle with the idea of that patient with stage II or III disease, whether to give adjuvant vs neoadjuvant therapy, please remember to consider their risk in 2024. Their risk for first recurrence is in the chest.
What are we going to do to better control disease in the chest? We have a challenge. I’m sure we can meet it if we put our heads together.
Dr. Kris is professor of medicine at Weill Cornell Medical College, and attending physician, Thoracic Oncology Service, Memorial Sloan Kettering Cancer Center, New York. He disclosed ties with AstraZeneca, Roche/Genentech, Ariad Pharmaceuticals, Pfizer, and PUMA.
A version of this article appeared on Medscape.com.
A Welcome Trade-off
At the end of March, in an anniversary no one but I noticed, I passed 4 years since I’d last rounded at the hospital.
It’s hard to comprehend that. I was at the hospital regularly for the first 22 years of my career, though admittedly it had dwindled from daily (1998-2011) to 1-2 weekends a month at the end.
Looking back, I still don’t miss it, and have no desire to go back. That’s not to say I don’t keep up on inpatient neurology, in case circumstances change, but at this point, honestly, I don’t want to. I’ve become accustomed to my non-hospital world, no late-night consults, no weekends spent rounding, no taking separate cars to restaurants or family events in case I get called in.
There are certainly things I miss about it. As odd as it may seem (and as much as I’d complain about it) I liked the wee hours of the really late night and early morning. It was quieter. Less chasing patients to tests or therapy. Pleasant idle chatter with staff and the few others docs around. Sitting at the computer and trying to think out a case on the fly. There was always junk food lying around.
But at this point in my life I’ll take the quiet of being home and my routine office hours. I know when my office day starts and ends. Aside from the occasional stop at Costco, I won’t be going anywhere else on my way home. I still get the occasional after-hours call, but none that require me to run to the ER.
On Fridays I’m glad the week is over, and don’t dread the 5:00 answering service switchover, or my call partner giving me the patient list.
There’s some revenue lost in the deal, but I’ll still take the trade-off.
It’s not like I ever had some grand plan to leave the hospital — I actually had thought I’d be there, at least occasionally, until retirement. But here I am.
Not to say there aren’t docs my age (and older) who still do it. Certainly our experience makes us good at it. But younger docs are closer to residency, which is primarily inpatient, so it’s an easier transition for many.
They probably have more energy, too.
Dr. Block has a solo neurology practice in Scottsdale, Arizona.
At the end of March, in an anniversary no one but I noticed, I passed 4 years since I’d last rounded at the hospital.
It’s hard to comprehend that. I was at the hospital regularly for the first 22 years of my career, though admittedly it had dwindled from daily (1998-2011) to 1-2 weekends a month at the end.
Looking back, I still don’t miss it, and have no desire to go back. That’s not to say I don’t keep up on inpatient neurology, in case circumstances change, but at this point, honestly, I don’t want to. I’ve become accustomed to my non-hospital world, no late-night consults, no weekends spent rounding, no taking separate cars to restaurants or family events in case I get called in.
There are certainly things I miss about it. As odd as it may seem (and as much as I’d complain about it) I liked the wee hours of the really late night and early morning. It was quieter. Less chasing patients to tests or therapy. Pleasant idle chatter with staff and the few others docs around. Sitting at the computer and trying to think out a case on the fly. There was always junk food lying around.
But at this point in my life I’ll take the quiet of being home and my routine office hours. I know when my office day starts and ends. Aside from the occasional stop at Costco, I won’t be going anywhere else on my way home. I still get the occasional after-hours call, but none that require me to run to the ER.
On Fridays I’m glad the week is over, and don’t dread the 5:00 answering service switchover, or my call partner giving me the patient list.
There’s some revenue lost in the deal, but I’ll still take the trade-off.
It’s not like I ever had some grand plan to leave the hospital — I actually had thought I’d be there, at least occasionally, until retirement. But here I am.
Not to say there aren’t docs my age (and older) who still do it. Certainly our experience makes us good at it. But younger docs are closer to residency, which is primarily inpatient, so it’s an easier transition for many.
They probably have more energy, too.
Dr. Block has a solo neurology practice in Scottsdale, Arizona.
At the end of March, in an anniversary no one but I noticed, I passed 4 years since I’d last rounded at the hospital.
It’s hard to comprehend that. I was at the hospital regularly for the first 22 years of my career, though admittedly it had dwindled from daily (1998-2011) to 1-2 weekends a month at the end.
Looking back, I still don’t miss it, and have no desire to go back. That’s not to say I don’t keep up on inpatient neurology, in case circumstances change, but at this point, honestly, I don’t want to. I’ve become accustomed to my non-hospital world, no late-night consults, no weekends spent rounding, no taking separate cars to restaurants or family events in case I get called in.
There are certainly things I miss about it. As odd as it may seem (and as much as I’d complain about it) I liked the wee hours of the really late night and early morning. It was quieter. Less chasing patients to tests or therapy. Pleasant idle chatter with staff and the few others docs around. Sitting at the computer and trying to think out a case on the fly. There was always junk food lying around.
But at this point in my life I’ll take the quiet of being home and my routine office hours. I know when my office day starts and ends. Aside from the occasional stop at Costco, I won’t be going anywhere else on my way home. I still get the occasional after-hours call, but none that require me to run to the ER.
On Fridays I’m glad the week is over, and don’t dread the 5:00 answering service switchover, or my call partner giving me the patient list.
There’s some revenue lost in the deal, but I’ll still take the trade-off.
It’s not like I ever had some grand plan to leave the hospital — I actually had thought I’d be there, at least occasionally, until retirement. But here I am.
Not to say there aren’t docs my age (and older) who still do it. Certainly our experience makes us good at it. But younger docs are closer to residency, which is primarily inpatient, so it’s an easier transition for many.
They probably have more energy, too.
Dr. Block has a solo neurology practice in Scottsdale, Arizona.