User login
Stay Afloat
How does Martin Izakovic, MD, medical director of the hospitalist program at Mercy Hospital in Iowa City, Iowa, suggest keeping current with medical literature?
“Let your journals pile up in your office, including the free ones you never subscribed to, feel guilty about throwing any away, tell yourself you will get to them one day, and then watch as it almost never happens.”
Dr. Izakovic is kidding, of course, but it’s no joke trying to read the wealth of medical information published daily. In fact, some people call it impossible. So to stay afloat, many hospitalists go electronic or turn to journal clubs.
Electronic Resources to the Rescue
It’s not for lack of trying that you can’t get through all the literature out there. Most hospitalists we queried say they only skim through the major internal medicine-related journals, including the Annals of Internal Medicine, the Journal of the American Medical Association (JAMA), The New England Journal of Medicine, Lancet, the Journal of General Internal Medicine, and the Journal of Hospital Medicine.
What really keeps hospitalists apprised of the latest medical news and research, they say, comes to them by way of the World Wide Web—straight to their inboxes. To start, many register for e-mails of journal tables of contents. Others subscribe to the American College of Physicians Journal Club, which reviews and critiques journal articles, rates the relevance of each article on a five-point scale, offers a customized literature updating service, and bundles mailings with the Annals.
Some physicians, like Leora Horwitz, MD, assistant professor in the division of General Internal Medicine at Yale School of Medicine, New Haven, only wish to receive information pertinent to specific topics. To make this happen, Dr. Horwitz sets up a search through Ovid or PubMed that runs about every two weeks and flags new articles that match her criteria.
“I only do this for absolutely key areas and I make the search criteria very restrictive so I only get one to two hits a month at most,” she says. “Then I set up an alert for one or two major articles in each field I am interested in.”
Dr. Horwitz also sets up alerts for her own published articles.
Hospitalists who work at academic institutions, in particular, are inundated with information via grand rounds, lectures, and formats for topics related to hospital medicine.
“We’ll take a list of top conditions relevant to our practice, to review as a working group and then take that to the rest of the group to decide how we’ll standardize care,” says Julia S. Wright, MD, director of hospital medicine and an associate professor of medicine at the University of Wisconsin School of Medicine and Public Health, Madison.
On top of setting up specific searches, many hospitalists use their institutions’ subscriptions to services such as:
- UpToDate, the evidence-based, peer-reviewed electronic resource for doctors;
- InfoPOEMs, Patient-Oriented Evidence that Matters from Essential Evidence Plus;
- Epocrates and Micromedex, for drug-related information;
- JournalWATCH;
- The Medical Letter;
- The Hospitalist’s “In the Literature” department; and
- PubMed.
Physicians each have their favorite subscription services. Bill Stinnette, MD, a hospitalist for the Permanente Medical Group, Inc. at Kaiser Permanente San Rafael Medical Center in northern California, recommends MedPage Today daily headlines online as “an excellent source for breaking news and studies, with subspecialty areas, interactive features, FDA alerts, and CME.”
Kenneth Patrick, MD, hospitalist and ICU director of Chestnut Hill Hospital in Philadelphia, uses Medscape as his main online update method. After having completed a personalized profile of his interests, Dr. Patrick now receives e-mail links and general articles based on his criteria. “There’s no paper, it’s done at a convenient time and location, you don’t have to remember where you put that journal you were reading when you were interrupted, and there’s online CME credits,” he says.
Gatherings Become Informative Discussions
Despite enthusiasm about getting information electronically, many hospitalists continue to benefit from—and enjoy—good old-fashioned journal clubs. For example, the quarterly “Lunch and Learn” at the Hospital of St. Raphael in New Haven, Conn., developed by hospitalist Ilona Figura, MD, “has been a real hit,” says Steven Angelo, MD, director of hospitalist services there.
“On a rotating basis, each hospitalist presents an interesting case and leads our group in a discussion of the differential diagnosis, similar to what is done in the NEJM case presentations,” Dr. Angelo says. “At the end of the meeting, the presenter then provides the relevant points from the literature.”
Valerie J. Lang, MD, and her hospitalist colleagues in the division of Hospital Medicine at the University of Rochester (N.Y.) School of Medicine and Dentistry hold their own journal club twice a month. “We include the General Medicine division [their outpatient counterparts], which adds a nice perspective to our inpatient work,” she says.
Like the physicians at the Hospital of St. Raphael, these doctors also rotate topic selection and presentation. “For example, the last time [it was my turn], I presented a meta-analysis of DVT prophylaxis in medical inpatients along with a review of how to interpret meta-analyses,” Dr. Lang says.
The General Internal Medicine division at the University of Medicine and Dentistry of New Jersey in New Brunswick, where the four-person hospital medicine group (HMG) resides, takes a slightly different approach. The group has a weekly journal club, reviewing a month’s worth of four major journals, one per week, says Gabriela S. Ferreira, MD.
The Waterbury Hospital HMG, Waterbury, Conn., has its journal club once a month—at a restaurant. “One hospitalist presents an article, and then we eat and get drunk and have a generally good time,” says Rachel Lovins, MD, director of the hospitalist program.
When pressed about whether cocktail availability interferes with information retention, Dr. Lovins admits that’s the reason the presentations are made early in the evening. But she also backs down a bit: “We don’t actually get drunk but the social stuff is so important. It’s glue.”
Although the group totals 20 hospitalists, only a core group of six to 10 usually attends the dinners. Dr. Lovins makes sure everyone gets the pertinent information. “When I present an article, I always write up a summary page and hand it out at the meeting and also e-mail to the rest of the group,” she says. “But I’m a dork and no one else really does that.”
It’s All Timing
Sometimes it’s not about the method of receiving information, but about when and where you receive it. For example, when David Pressel, MD, PhD, director of Inpatient Service, General Pediatrics at Nemours Alfred I. duPont Hospital for Children in Wilmington, Del., encounters a patient with a new and different condition, he researches it immediately. “When learning is attached to a patient you see,” he says, “you’re more likely to cement that information in your mind.”
Dr. Wright uses a similar methodology. “I try to look up a couple of articles on every patient every day, with periodic reviews,” she says.
Other physicians, like Benny Gavi, MD, a hospitalist at Stanford Hospital & Clinics in California, print out articles of interest. “I take one or two articles in the pocket of my white coat to read when I have time, for example, when waiting for a meeting to start,” he says. “The pile is also near where I have lunch and I take an article when I eat.”
One hospitalist, who wishes to remain nameless, uses another time to get his literature scoop: at his daily poop, so to speak, during that block of time each day when he sits and reads. “Continuing education is a lifelong process and can happen anytime,” he says, whimsically. TH
Andrea Sattinger is a freelance writer based in North Carolina and a longtime contributor to The Hospitalist.
Reference
- Bennett, HJ. A piece of my mind. Keeping up with the literature. JAMA. 1992;267(7):920.
How does Martin Izakovic, MD, medical director of the hospitalist program at Mercy Hospital in Iowa City, Iowa, suggest keeping current with medical literature?
“Let your journals pile up in your office, including the free ones you never subscribed to, feel guilty about throwing any away, tell yourself you will get to them one day, and then watch as it almost never happens.”
Dr. Izakovic is kidding, of course, but it’s no joke trying to read the wealth of medical information published daily. In fact, some people call it impossible. So to stay afloat, many hospitalists go electronic or turn to journal clubs.
Electronic Resources to the Rescue
It’s not for lack of trying that you can’t get through all the literature out there. Most hospitalists we queried say they only skim through the major internal medicine-related journals, including the Annals of Internal Medicine, the Journal of the American Medical Association (JAMA), The New England Journal of Medicine, Lancet, the Journal of General Internal Medicine, and the Journal of Hospital Medicine.
What really keeps hospitalists apprised of the latest medical news and research, they say, comes to them by way of the World Wide Web—straight to their inboxes. To start, many register for e-mails of journal tables of contents. Others subscribe to the American College of Physicians Journal Club, which reviews and critiques journal articles, rates the relevance of each article on a five-point scale, offers a customized literature updating service, and bundles mailings with the Annals.
Some physicians, like Leora Horwitz, MD, assistant professor in the division of General Internal Medicine at Yale School of Medicine, New Haven, only wish to receive information pertinent to specific topics. To make this happen, Dr. Horwitz sets up a search through Ovid or PubMed that runs about every two weeks and flags new articles that match her criteria.
“I only do this for absolutely key areas and I make the search criteria very restrictive so I only get one to two hits a month at most,” she says. “Then I set up an alert for one or two major articles in each field I am interested in.”
Dr. Horwitz also sets up alerts for her own published articles.
Hospitalists who work at academic institutions, in particular, are inundated with information via grand rounds, lectures, and formats for topics related to hospital medicine.
“We’ll take a list of top conditions relevant to our practice, to review as a working group and then take that to the rest of the group to decide how we’ll standardize care,” says Julia S. Wright, MD, director of hospital medicine and an associate professor of medicine at the University of Wisconsin School of Medicine and Public Health, Madison.
On top of setting up specific searches, many hospitalists use their institutions’ subscriptions to services such as:
- UpToDate, the evidence-based, peer-reviewed electronic resource for doctors;
- InfoPOEMs, Patient-Oriented Evidence that Matters from Essential Evidence Plus;
- Epocrates and Micromedex, for drug-related information;
- JournalWATCH;
- The Medical Letter;
- The Hospitalist’s “In the Literature” department; and
- PubMed.
Physicians each have their favorite subscription services. Bill Stinnette, MD, a hospitalist for the Permanente Medical Group, Inc. at Kaiser Permanente San Rafael Medical Center in northern California, recommends MedPage Today daily headlines online as “an excellent source for breaking news and studies, with subspecialty areas, interactive features, FDA alerts, and CME.”
Kenneth Patrick, MD, hospitalist and ICU director of Chestnut Hill Hospital in Philadelphia, uses Medscape as his main online update method. After having completed a personalized profile of his interests, Dr. Patrick now receives e-mail links and general articles based on his criteria. “There’s no paper, it’s done at a convenient time and location, you don’t have to remember where you put that journal you were reading when you were interrupted, and there’s online CME credits,” he says.
Gatherings Become Informative Discussions
Despite enthusiasm about getting information electronically, many hospitalists continue to benefit from—and enjoy—good old-fashioned journal clubs. For example, the quarterly “Lunch and Learn” at the Hospital of St. Raphael in New Haven, Conn., developed by hospitalist Ilona Figura, MD, “has been a real hit,” says Steven Angelo, MD, director of hospitalist services there.
“On a rotating basis, each hospitalist presents an interesting case and leads our group in a discussion of the differential diagnosis, similar to what is done in the NEJM case presentations,” Dr. Angelo says. “At the end of the meeting, the presenter then provides the relevant points from the literature.”
Valerie J. Lang, MD, and her hospitalist colleagues in the division of Hospital Medicine at the University of Rochester (N.Y.) School of Medicine and Dentistry hold their own journal club twice a month. “We include the General Medicine division [their outpatient counterparts], which adds a nice perspective to our inpatient work,” she says.
Like the physicians at the Hospital of St. Raphael, these doctors also rotate topic selection and presentation. “For example, the last time [it was my turn], I presented a meta-analysis of DVT prophylaxis in medical inpatients along with a review of how to interpret meta-analyses,” Dr. Lang says.
The General Internal Medicine division at the University of Medicine and Dentistry of New Jersey in New Brunswick, where the four-person hospital medicine group (HMG) resides, takes a slightly different approach. The group has a weekly journal club, reviewing a month’s worth of four major journals, one per week, says Gabriela S. Ferreira, MD.
The Waterbury Hospital HMG, Waterbury, Conn., has its journal club once a month—at a restaurant. “One hospitalist presents an article, and then we eat and get drunk and have a generally good time,” says Rachel Lovins, MD, director of the hospitalist program.
When pressed about whether cocktail availability interferes with information retention, Dr. Lovins admits that’s the reason the presentations are made early in the evening. But she also backs down a bit: “We don’t actually get drunk but the social stuff is so important. It’s glue.”
Although the group totals 20 hospitalists, only a core group of six to 10 usually attends the dinners. Dr. Lovins makes sure everyone gets the pertinent information. “When I present an article, I always write up a summary page and hand it out at the meeting and also e-mail to the rest of the group,” she says. “But I’m a dork and no one else really does that.”
It’s All Timing
Sometimes it’s not about the method of receiving information, but about when and where you receive it. For example, when David Pressel, MD, PhD, director of Inpatient Service, General Pediatrics at Nemours Alfred I. duPont Hospital for Children in Wilmington, Del., encounters a patient with a new and different condition, he researches it immediately. “When learning is attached to a patient you see,” he says, “you’re more likely to cement that information in your mind.”
Dr. Wright uses a similar methodology. “I try to look up a couple of articles on every patient every day, with periodic reviews,” she says.
Other physicians, like Benny Gavi, MD, a hospitalist at Stanford Hospital & Clinics in California, print out articles of interest. “I take one or two articles in the pocket of my white coat to read when I have time, for example, when waiting for a meeting to start,” he says. “The pile is also near where I have lunch and I take an article when I eat.”
One hospitalist, who wishes to remain nameless, uses another time to get his literature scoop: at his daily poop, so to speak, during that block of time each day when he sits and reads. “Continuing education is a lifelong process and can happen anytime,” he says, whimsically. TH
Andrea Sattinger is a freelance writer based in North Carolina and a longtime contributor to The Hospitalist.
Reference
- Bennett, HJ. A piece of my mind. Keeping up with the literature. JAMA. 1992;267(7):920.
How does Martin Izakovic, MD, medical director of the hospitalist program at Mercy Hospital in Iowa City, Iowa, suggest keeping current with medical literature?
“Let your journals pile up in your office, including the free ones you never subscribed to, feel guilty about throwing any away, tell yourself you will get to them one day, and then watch as it almost never happens.”
Dr. Izakovic is kidding, of course, but it’s no joke trying to read the wealth of medical information published daily. In fact, some people call it impossible. So to stay afloat, many hospitalists go electronic or turn to journal clubs.
Electronic Resources to the Rescue
It’s not for lack of trying that you can’t get through all the literature out there. Most hospitalists we queried say they only skim through the major internal medicine-related journals, including the Annals of Internal Medicine, the Journal of the American Medical Association (JAMA), The New England Journal of Medicine, Lancet, the Journal of General Internal Medicine, and the Journal of Hospital Medicine.
What really keeps hospitalists apprised of the latest medical news and research, they say, comes to them by way of the World Wide Web—straight to their inboxes. To start, many register for e-mails of journal tables of contents. Others subscribe to the American College of Physicians Journal Club, which reviews and critiques journal articles, rates the relevance of each article on a five-point scale, offers a customized literature updating service, and bundles mailings with the Annals.
Some physicians, like Leora Horwitz, MD, assistant professor in the division of General Internal Medicine at Yale School of Medicine, New Haven, only wish to receive information pertinent to specific topics. To make this happen, Dr. Horwitz sets up a search through Ovid or PubMed that runs about every two weeks and flags new articles that match her criteria.
“I only do this for absolutely key areas and I make the search criteria very restrictive so I only get one to two hits a month at most,” she says. “Then I set up an alert for one or two major articles in each field I am interested in.”
Dr. Horwitz also sets up alerts for her own published articles.
Hospitalists who work at academic institutions, in particular, are inundated with information via grand rounds, lectures, and formats for topics related to hospital medicine.
“We’ll take a list of top conditions relevant to our practice, to review as a working group and then take that to the rest of the group to decide how we’ll standardize care,” says Julia S. Wright, MD, director of hospital medicine and an associate professor of medicine at the University of Wisconsin School of Medicine and Public Health, Madison.
On top of setting up specific searches, many hospitalists use their institutions’ subscriptions to services such as:
- UpToDate, the evidence-based, peer-reviewed electronic resource for doctors;
- InfoPOEMs, Patient-Oriented Evidence that Matters from Essential Evidence Plus;
- Epocrates and Micromedex, for drug-related information;
- JournalWATCH;
- The Medical Letter;
- The Hospitalist’s “In the Literature” department; and
- PubMed.
Physicians each have their favorite subscription services. Bill Stinnette, MD, a hospitalist for the Permanente Medical Group, Inc. at Kaiser Permanente San Rafael Medical Center in northern California, recommends MedPage Today daily headlines online as “an excellent source for breaking news and studies, with subspecialty areas, interactive features, FDA alerts, and CME.”
Kenneth Patrick, MD, hospitalist and ICU director of Chestnut Hill Hospital in Philadelphia, uses Medscape as his main online update method. After having completed a personalized profile of his interests, Dr. Patrick now receives e-mail links and general articles based on his criteria. “There’s no paper, it’s done at a convenient time and location, you don’t have to remember where you put that journal you were reading when you were interrupted, and there’s online CME credits,” he says.
Gatherings Become Informative Discussions
Despite enthusiasm about getting information electronically, many hospitalists continue to benefit from—and enjoy—good old-fashioned journal clubs. For example, the quarterly “Lunch and Learn” at the Hospital of St. Raphael in New Haven, Conn., developed by hospitalist Ilona Figura, MD, “has been a real hit,” says Steven Angelo, MD, director of hospitalist services there.
“On a rotating basis, each hospitalist presents an interesting case and leads our group in a discussion of the differential diagnosis, similar to what is done in the NEJM case presentations,” Dr. Angelo says. “At the end of the meeting, the presenter then provides the relevant points from the literature.”
Valerie J. Lang, MD, and her hospitalist colleagues in the division of Hospital Medicine at the University of Rochester (N.Y.) School of Medicine and Dentistry hold their own journal club twice a month. “We include the General Medicine division [their outpatient counterparts], which adds a nice perspective to our inpatient work,” she says.
Like the physicians at the Hospital of St. Raphael, these doctors also rotate topic selection and presentation. “For example, the last time [it was my turn], I presented a meta-analysis of DVT prophylaxis in medical inpatients along with a review of how to interpret meta-analyses,” Dr. Lang says.
The General Internal Medicine division at the University of Medicine and Dentistry of New Jersey in New Brunswick, where the four-person hospital medicine group (HMG) resides, takes a slightly different approach. The group has a weekly journal club, reviewing a month’s worth of four major journals, one per week, says Gabriela S. Ferreira, MD.
The Waterbury Hospital HMG, Waterbury, Conn., has its journal club once a month—at a restaurant. “One hospitalist presents an article, and then we eat and get drunk and have a generally good time,” says Rachel Lovins, MD, director of the hospitalist program.
When pressed about whether cocktail availability interferes with information retention, Dr. Lovins admits that’s the reason the presentations are made early in the evening. But she also backs down a bit: “We don’t actually get drunk but the social stuff is so important. It’s glue.”
Although the group totals 20 hospitalists, only a core group of six to 10 usually attends the dinners. Dr. Lovins makes sure everyone gets the pertinent information. “When I present an article, I always write up a summary page and hand it out at the meeting and also e-mail to the rest of the group,” she says. “But I’m a dork and no one else really does that.”
It’s All Timing
Sometimes it’s not about the method of receiving information, but about when and where you receive it. For example, when David Pressel, MD, PhD, director of Inpatient Service, General Pediatrics at Nemours Alfred I. duPont Hospital for Children in Wilmington, Del., encounters a patient with a new and different condition, he researches it immediately. “When learning is attached to a patient you see,” he says, “you’re more likely to cement that information in your mind.”
Dr. Wright uses a similar methodology. “I try to look up a couple of articles on every patient every day, with periodic reviews,” she says.
Other physicians, like Benny Gavi, MD, a hospitalist at Stanford Hospital & Clinics in California, print out articles of interest. “I take one or two articles in the pocket of my white coat to read when I have time, for example, when waiting for a meeting to start,” he says. “The pile is also near where I have lunch and I take an article when I eat.”
One hospitalist, who wishes to remain nameless, uses another time to get his literature scoop: at his daily poop, so to speak, during that block of time each day when he sits and reads. “Continuing education is a lifelong process and can happen anytime,” he says, whimsically. TH
Andrea Sattinger is a freelance writer based in North Carolina and a longtime contributor to The Hospitalist.
Reference
- Bennett, HJ. A piece of my mind. Keeping up with the literature. JAMA. 1992;267(7):920.
Hitting the Big Time
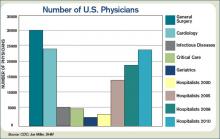
No matter how big a hospital medicine group is, the leader is likely to say “but we need a couple more.” As the fastest-growing medical specialty in the history of American medicine, there never seem to be enough hospitalists (see Figure 1, p. 28).
“The programs are getting larger and larger, ranging anywhere from 20 to 100 physicians in a hospitalist group,” says Jeffrey Hay, MD, senior vice president of medical operations for Lakeside Systems Inc. in Los Angeles.
Because of this rapid growth, two questions become apparent:
1. How is a big hospitalist group defined?
2. What does it take to manage a big group well?
How Big is Big?
Although what constitutes a big hospitalist group is relative, Leslie Flores and her partner, John Nelson, MD, of Nelson/Flores Associates, LLC, La Quinta, Calif., estimate with about 20-30 hospitalists, the role of the medical director becomes a different job than for the typical-sized practice of 10-15 hospitalists.
According to SHM Executive Advisor to the CEO Joseph Miller, this year’s “Society of Hospital Medicine 2007-08 Survey: The Authoritative Source on the State of the Hospitalist Movement” revealed only eight groups with more than 40 hospitalists (excluding the multistate hospitalist management companies). In the approximate 2,200 hospitalist groups in the U.S., Miller estimates there are perhaps 40 groups with 40 or more physicians compared with two in the previous 2005-06 survey.
Medical directors of hospital medicine groups (HMGs) ranging from 22-100 people offer varied insights about how the role of medical director changes as groups grow from big to bigger to biggest.
Big
Jeffery Kin, MD, medical director of the private-practice group Fredericks Hospitalist Group PC, manages 22 hospitalists, and about 130-140 inpatients and 45 admissions a day at Mary Washington Hospital in Fredericksburg, Va. They began as a team of three in 2000 as the outgrowth of a hospital house-doctor program.
“The medical director’s role changes and evolves with the growth of the group,” says Dr. Kin. He and other medical directors of larger groups find it more difficult to retain the informal shift arrival or departure and lunches together that were possible when the HMG was smaller. “Now that we are bigger it is more ‘protocolized,’” Dr. Kin says, “but we try to maintain a family-like atmosphere because I think it makes physicians want to stay with the group long term and not move on with every little problem or challenge that inevitably arises in the changing filed of hospital medicine.”
William Ford, MD, program medical director for Cogent Healthcare and the chief of hospital medicine at Temple University in Philadelphia, considers his group of 28 hospitalists to be a “small” big group. Dr. Ford’s group, which covers three of the four hospitals in the university health systems, grew from five hospitalists in September 2006. He devotes about half his time on personnel issues, including recruitment, retention, and staff development.
As groups grow, so does diversity, requiring more flexibility to manage leaves of absence, scheduling, and day-to-day practice. “In a large group we tend to bring on new measures,” Dr. Ford says. “We change like the wind, so if you aren’t ready for that, you will have a lot of turnover.”
Bigger
Jasen W. Gundersen, MD, MBA, division chief, hospital medicine, University of Massachusetts Memorial Medical Center, Worcester, grew his HMG from 3.6 FTEs three years ago to the 47.5 FTEs (40 physician FTEs and 7.5 FTEs nurse practitioners) they now employ. The group, which covers four hospitals ranging from a 30-bed community hospital to a 770-bed academic hospital, is the biggest HMG in New England. “Our budget numbers for charges and volume are 2.19 times what we projected in the budget,” he says.
With an average of 185 billable patient encounters per day, Dr. Gundersen attributes his successes to a management style based on a financial business model and a revision of the compensation plan. By increasing effectiveness, they reward their doctors with more free time and subsequently improved physician retention.
As the group, the budget, and the financial impact all expand, formal training becomes more important for leaders. While few HMG leaders have a background in the strategic processes of running a company, Dr. Gundersen earned his MBA and believes his training made it easier to talk to administrators, meet clients, track data, effect change, and better handle the politics inherent to the job. “The role is a lot more political than people are aware of because you are such a big presence to the hospital,” he says. “Everybody wants something from you.”
Part of that phenomenon, coined “medical creep” by one hospitalist, can best be defined as the gradual increase in workload shifted to HMGs without a proportional shift in resources to do the work. Work previously done by either surgical specialists or medical subspecialists must be shifted as they more narrowly define their workload; what is left over (more general medical care, phone calls, after-hours work, and paperwork) goes to “co-managing” hospitalists.
Asked about this phenomenon, Tom Lorence, MD, chief of hospitalist medicine for the Northwest Kaiser Permanente region, Portland, Ore., says: “The larger the hospitalist groups become, the bigger a target we are for this shifting. Most try to justify it by saying, ‘It is only a little more work.’ ”
Dr. Lorence and two colleagues began his HMG in 1990; he now manages 55 hospitalists at three facilities. “Administrators have to be convinced that it is worth the money to reshift their priorities and give more resources to the hospital medicine groups,” he says.
Mark V. Williams, MD, FACP, professor and chief, division of hospital medicine, Northwestern University Feinberg School of Medicine, Chicago, moved to his current post last September. Northwestern Memorial Hospital almost doubled its hospitalists to 42 in one year. The initial challenges at Northwestern primarily include assimilating new faculty and establishing a culture of thriving on change, says Dr. Williams, who is also editor in chief of the Journal of Hospital Medicine.
Biggest
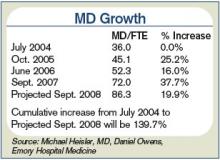
The distinction between academic and non-academic programs is an important one says Michael B. Heisler, MD, MPH, who became the interim medical director of Emory Healthcare, Atlanta, in March 2007 when Dr. Williams moved to Northwestern. Generally, the Emory group has increased in size by 20% each of the past five years. Beginning with nine hospitalists in 1999, it now exceeds 80 (see Figure 2, p. 28).
Academic hospitals have additional stakeholders and deliverables expected by those to whom the medical director reports. Whereas community hospital medicine programs are driven by patient encounters/RVUs, quality improvement, and the bottom line, academic groups also must engage in scholarly activities.
Dr. Heisler and his group have just completed a three-year strategic plan that emphasizes medical education and research and a plateau to the group’s growth.
“We can’t be the premier academic program with growth going through the roof,” Dr. Heisler says. “With some limits we are not going to increase services within our institutions and will not entertain requests to grow into any other facilities through 2010. You can’t develop faculty, define protected time, and invest in scholarly work when you are constantly in growth mode.”
Strategic planning has a different tone for Tyler Jung, MD, director of inpatient services of the multi-specialty group HealthCare Partners, who took over that position three years ago when Dr. Hay left. About 100 hospitalists are employed under the HealthCare Partners umbrella; approximately 85 are on the payroll, and 15 work in a strategic alliance. The HMG covers 14 community hospitals in Southern California, about 14 hospitals in Las Vegas, Nevada, and about five hospitals in the Tampa/Orlando area of Florida.
The full-risk California medical model drives a lot of the metrics. “We look at [relative value unit] goals for our hospitalists, but mostly to ensure proper staffing,” Dr. Jung says. “We are satisfied when our docs have 12 to 14 encounters a day. In the service market you’d go broke with that, but I’d rather have our hospitalists see our patients twice a day because it drives quality and it turns out to be more cost effective.”
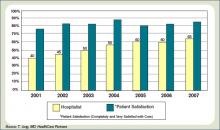
Some of the outcomes Dr. Jung regularly reviews include patient utilization per membership (admit rates, readmit data, and length of stay), and these metrics are largely unchanged as they have grown. “Additionally, maintaining high patient satisfaction can be overlooked, but is critical with the growth of any program,” he says (see Figure 3, p. 28).
Dr. Williams, who began the hospitalist group at Emory Healthcare, says the primary challenges he faced as that program grew were finding capable physicians willing to join a new or expanding program; managing the different cultures at different hospitals and working to ensure they all felt a part of the whole; having sufficient administrative support time to manage recruitment and credentialing; and keeping up constant communications with individuals and leadership at all sites. He found it helpful to occasionally rotate hospitalists, especially the more senior physicians, so they could appreciate the workload and issues at different sites.
Dr. Williams, who trained in internal medicine but later became board certified in emergency medicine, is not surprised Dr. Jung has some background in critical care, as does Dr. Heisler. He surmises they also all have well-honed administrative skills. “The experience I had in running a 65,000-visit-a-year emergency room and a 45,000-visit-a-year urgent-care center gave me the skills to run a large hospital medicine program,” Dr. Williams says. TH
Andrea M. Sattinger is a medical writer based in North Carolina.
No matter how big a hospital medicine group is, the leader is likely to say “but we need a couple more.” As the fastest-growing medical specialty in the history of American medicine, there never seem to be enough hospitalists (see Figure 1, p. 28).
“The programs are getting larger and larger, ranging anywhere from 20 to 100 physicians in a hospitalist group,” says Jeffrey Hay, MD, senior vice president of medical operations for Lakeside Systems Inc. in Los Angeles.
Because of this rapid growth, two questions become apparent:
1. How is a big hospitalist group defined?
2. What does it take to manage a big group well?
How Big is Big?
Although what constitutes a big hospitalist group is relative, Leslie Flores and her partner, John Nelson, MD, of Nelson/Flores Associates, LLC, La Quinta, Calif., estimate with about 20-30 hospitalists, the role of the medical director becomes a different job than for the typical-sized practice of 10-15 hospitalists.
According to SHM Executive Advisor to the CEO Joseph Miller, this year’s “Society of Hospital Medicine 2007-08 Survey: The Authoritative Source on the State of the Hospitalist Movement” revealed only eight groups with more than 40 hospitalists (excluding the multistate hospitalist management companies). In the approximate 2,200 hospitalist groups in the U.S., Miller estimates there are perhaps 40 groups with 40 or more physicians compared with two in the previous 2005-06 survey.
Medical directors of hospital medicine groups (HMGs) ranging from 22-100 people offer varied insights about how the role of medical director changes as groups grow from big to bigger to biggest.
Big
Jeffery Kin, MD, medical director of the private-practice group Fredericks Hospitalist Group PC, manages 22 hospitalists, and about 130-140 inpatients and 45 admissions a day at Mary Washington Hospital in Fredericksburg, Va. They began as a team of three in 2000 as the outgrowth of a hospital house-doctor program.
“The medical director’s role changes and evolves with the growth of the group,” says Dr. Kin. He and other medical directors of larger groups find it more difficult to retain the informal shift arrival or departure and lunches together that were possible when the HMG was smaller. “Now that we are bigger it is more ‘protocolized,’” Dr. Kin says, “but we try to maintain a family-like atmosphere because I think it makes physicians want to stay with the group long term and not move on with every little problem or challenge that inevitably arises in the changing filed of hospital medicine.”
William Ford, MD, program medical director for Cogent Healthcare and the chief of hospital medicine at Temple University in Philadelphia, considers his group of 28 hospitalists to be a “small” big group. Dr. Ford’s group, which covers three of the four hospitals in the university health systems, grew from five hospitalists in September 2006. He devotes about half his time on personnel issues, including recruitment, retention, and staff development.
As groups grow, so does diversity, requiring more flexibility to manage leaves of absence, scheduling, and day-to-day practice. “In a large group we tend to bring on new measures,” Dr. Ford says. “We change like the wind, so if you aren’t ready for that, you will have a lot of turnover.”
Bigger
Jasen W. Gundersen, MD, MBA, division chief, hospital medicine, University of Massachusetts Memorial Medical Center, Worcester, grew his HMG from 3.6 FTEs three years ago to the 47.5 FTEs (40 physician FTEs and 7.5 FTEs nurse practitioners) they now employ. The group, which covers four hospitals ranging from a 30-bed community hospital to a 770-bed academic hospital, is the biggest HMG in New England. “Our budget numbers for charges and volume are 2.19 times what we projected in the budget,” he says.
With an average of 185 billable patient encounters per day, Dr. Gundersen attributes his successes to a management style based on a financial business model and a revision of the compensation plan. By increasing effectiveness, they reward their doctors with more free time and subsequently improved physician retention.
As the group, the budget, and the financial impact all expand, formal training becomes more important for leaders. While few HMG leaders have a background in the strategic processes of running a company, Dr. Gundersen earned his MBA and believes his training made it easier to talk to administrators, meet clients, track data, effect change, and better handle the politics inherent to the job. “The role is a lot more political than people are aware of because you are such a big presence to the hospital,” he says. “Everybody wants something from you.”
Part of that phenomenon, coined “medical creep” by one hospitalist, can best be defined as the gradual increase in workload shifted to HMGs without a proportional shift in resources to do the work. Work previously done by either surgical specialists or medical subspecialists must be shifted as they more narrowly define their workload; what is left over (more general medical care, phone calls, after-hours work, and paperwork) goes to “co-managing” hospitalists.
Asked about this phenomenon, Tom Lorence, MD, chief of hospitalist medicine for the Northwest Kaiser Permanente region, Portland, Ore., says: “The larger the hospitalist groups become, the bigger a target we are for this shifting. Most try to justify it by saying, ‘It is only a little more work.’ ”
Dr. Lorence and two colleagues began his HMG in 1990; he now manages 55 hospitalists at three facilities. “Administrators have to be convinced that it is worth the money to reshift their priorities and give more resources to the hospital medicine groups,” he says.
Mark V. Williams, MD, FACP, professor and chief, division of hospital medicine, Northwestern University Feinberg School of Medicine, Chicago, moved to his current post last September. Northwestern Memorial Hospital almost doubled its hospitalists to 42 in one year. The initial challenges at Northwestern primarily include assimilating new faculty and establishing a culture of thriving on change, says Dr. Williams, who is also editor in chief of the Journal of Hospital Medicine.
Biggest
The distinction between academic and non-academic programs is an important one says Michael B. Heisler, MD, MPH, who became the interim medical director of Emory Healthcare, Atlanta, in March 2007 when Dr. Williams moved to Northwestern. Generally, the Emory group has increased in size by 20% each of the past five years. Beginning with nine hospitalists in 1999, it now exceeds 80 (see Figure 2, p. 28).
Academic hospitals have additional stakeholders and deliverables expected by those to whom the medical director reports. Whereas community hospital medicine programs are driven by patient encounters/RVUs, quality improvement, and the bottom line, academic groups also must engage in scholarly activities.
Dr. Heisler and his group have just completed a three-year strategic plan that emphasizes medical education and research and a plateau to the group’s growth.
“We can’t be the premier academic program with growth going through the roof,” Dr. Heisler says. “With some limits we are not going to increase services within our institutions and will not entertain requests to grow into any other facilities through 2010. You can’t develop faculty, define protected time, and invest in scholarly work when you are constantly in growth mode.”
Strategic planning has a different tone for Tyler Jung, MD, director of inpatient services of the multi-specialty group HealthCare Partners, who took over that position three years ago when Dr. Hay left. About 100 hospitalists are employed under the HealthCare Partners umbrella; approximately 85 are on the payroll, and 15 work in a strategic alliance. The HMG covers 14 community hospitals in Southern California, about 14 hospitals in Las Vegas, Nevada, and about five hospitals in the Tampa/Orlando area of Florida.
The full-risk California medical model drives a lot of the metrics. “We look at [relative value unit] goals for our hospitalists, but mostly to ensure proper staffing,” Dr. Jung says. “We are satisfied when our docs have 12 to 14 encounters a day. In the service market you’d go broke with that, but I’d rather have our hospitalists see our patients twice a day because it drives quality and it turns out to be more cost effective.”
Some of the outcomes Dr. Jung regularly reviews include patient utilization per membership (admit rates, readmit data, and length of stay), and these metrics are largely unchanged as they have grown. “Additionally, maintaining high patient satisfaction can be overlooked, but is critical with the growth of any program,” he says (see Figure 3, p. 28).
Dr. Williams, who began the hospitalist group at Emory Healthcare, says the primary challenges he faced as that program grew were finding capable physicians willing to join a new or expanding program; managing the different cultures at different hospitals and working to ensure they all felt a part of the whole; having sufficient administrative support time to manage recruitment and credentialing; and keeping up constant communications with individuals and leadership at all sites. He found it helpful to occasionally rotate hospitalists, especially the more senior physicians, so they could appreciate the workload and issues at different sites.
Dr. Williams, who trained in internal medicine but later became board certified in emergency medicine, is not surprised Dr. Jung has some background in critical care, as does Dr. Heisler. He surmises they also all have well-honed administrative skills. “The experience I had in running a 65,000-visit-a-year emergency room and a 45,000-visit-a-year urgent-care center gave me the skills to run a large hospital medicine program,” Dr. Williams says. TH
Andrea M. Sattinger is a medical writer based in North Carolina.
No matter how big a hospital medicine group is, the leader is likely to say “but we need a couple more.” As the fastest-growing medical specialty in the history of American medicine, there never seem to be enough hospitalists (see Figure 1, p. 28).
“The programs are getting larger and larger, ranging anywhere from 20 to 100 physicians in a hospitalist group,” says Jeffrey Hay, MD, senior vice president of medical operations for Lakeside Systems Inc. in Los Angeles.
Because of this rapid growth, two questions become apparent:
1. How is a big hospitalist group defined?
2. What does it take to manage a big group well?
How Big is Big?
Although what constitutes a big hospitalist group is relative, Leslie Flores and her partner, John Nelson, MD, of Nelson/Flores Associates, LLC, La Quinta, Calif., estimate with about 20-30 hospitalists, the role of the medical director becomes a different job than for the typical-sized practice of 10-15 hospitalists.
According to SHM Executive Advisor to the CEO Joseph Miller, this year’s “Society of Hospital Medicine 2007-08 Survey: The Authoritative Source on the State of the Hospitalist Movement” revealed only eight groups with more than 40 hospitalists (excluding the multistate hospitalist management companies). In the approximate 2,200 hospitalist groups in the U.S., Miller estimates there are perhaps 40 groups with 40 or more physicians compared with two in the previous 2005-06 survey.
Medical directors of hospital medicine groups (HMGs) ranging from 22-100 people offer varied insights about how the role of medical director changes as groups grow from big to bigger to biggest.
Big
Jeffery Kin, MD, medical director of the private-practice group Fredericks Hospitalist Group PC, manages 22 hospitalists, and about 130-140 inpatients and 45 admissions a day at Mary Washington Hospital in Fredericksburg, Va. They began as a team of three in 2000 as the outgrowth of a hospital house-doctor program.
“The medical director’s role changes and evolves with the growth of the group,” says Dr. Kin. He and other medical directors of larger groups find it more difficult to retain the informal shift arrival or departure and lunches together that were possible when the HMG was smaller. “Now that we are bigger it is more ‘protocolized,’” Dr. Kin says, “but we try to maintain a family-like atmosphere because I think it makes physicians want to stay with the group long term and not move on with every little problem or challenge that inevitably arises in the changing filed of hospital medicine.”
William Ford, MD, program medical director for Cogent Healthcare and the chief of hospital medicine at Temple University in Philadelphia, considers his group of 28 hospitalists to be a “small” big group. Dr. Ford’s group, which covers three of the four hospitals in the university health systems, grew from five hospitalists in September 2006. He devotes about half his time on personnel issues, including recruitment, retention, and staff development.
As groups grow, so does diversity, requiring more flexibility to manage leaves of absence, scheduling, and day-to-day practice. “In a large group we tend to bring on new measures,” Dr. Ford says. “We change like the wind, so if you aren’t ready for that, you will have a lot of turnover.”
Bigger
Jasen W. Gundersen, MD, MBA, division chief, hospital medicine, University of Massachusetts Memorial Medical Center, Worcester, grew his HMG from 3.6 FTEs three years ago to the 47.5 FTEs (40 physician FTEs and 7.5 FTEs nurse practitioners) they now employ. The group, which covers four hospitals ranging from a 30-bed community hospital to a 770-bed academic hospital, is the biggest HMG in New England. “Our budget numbers for charges and volume are 2.19 times what we projected in the budget,” he says.
With an average of 185 billable patient encounters per day, Dr. Gundersen attributes his successes to a management style based on a financial business model and a revision of the compensation plan. By increasing effectiveness, they reward their doctors with more free time and subsequently improved physician retention.
As the group, the budget, and the financial impact all expand, formal training becomes more important for leaders. While few HMG leaders have a background in the strategic processes of running a company, Dr. Gundersen earned his MBA and believes his training made it easier to talk to administrators, meet clients, track data, effect change, and better handle the politics inherent to the job. “The role is a lot more political than people are aware of because you are such a big presence to the hospital,” he says. “Everybody wants something from you.”
Part of that phenomenon, coined “medical creep” by one hospitalist, can best be defined as the gradual increase in workload shifted to HMGs without a proportional shift in resources to do the work. Work previously done by either surgical specialists or medical subspecialists must be shifted as they more narrowly define their workload; what is left over (more general medical care, phone calls, after-hours work, and paperwork) goes to “co-managing” hospitalists.
Asked about this phenomenon, Tom Lorence, MD, chief of hospitalist medicine for the Northwest Kaiser Permanente region, Portland, Ore., says: “The larger the hospitalist groups become, the bigger a target we are for this shifting. Most try to justify it by saying, ‘It is only a little more work.’ ”
Dr. Lorence and two colleagues began his HMG in 1990; he now manages 55 hospitalists at three facilities. “Administrators have to be convinced that it is worth the money to reshift their priorities and give more resources to the hospital medicine groups,” he says.
Mark V. Williams, MD, FACP, professor and chief, division of hospital medicine, Northwestern University Feinberg School of Medicine, Chicago, moved to his current post last September. Northwestern Memorial Hospital almost doubled its hospitalists to 42 in one year. The initial challenges at Northwestern primarily include assimilating new faculty and establishing a culture of thriving on change, says Dr. Williams, who is also editor in chief of the Journal of Hospital Medicine.
Biggest
The distinction between academic and non-academic programs is an important one says Michael B. Heisler, MD, MPH, who became the interim medical director of Emory Healthcare, Atlanta, in March 2007 when Dr. Williams moved to Northwestern. Generally, the Emory group has increased in size by 20% each of the past five years. Beginning with nine hospitalists in 1999, it now exceeds 80 (see Figure 2, p. 28).
Academic hospitals have additional stakeholders and deliverables expected by those to whom the medical director reports. Whereas community hospital medicine programs are driven by patient encounters/RVUs, quality improvement, and the bottom line, academic groups also must engage in scholarly activities.
Dr. Heisler and his group have just completed a three-year strategic plan that emphasizes medical education and research and a plateau to the group’s growth.
“We can’t be the premier academic program with growth going through the roof,” Dr. Heisler says. “With some limits we are not going to increase services within our institutions and will not entertain requests to grow into any other facilities through 2010. You can’t develop faculty, define protected time, and invest in scholarly work when you are constantly in growth mode.”
Strategic planning has a different tone for Tyler Jung, MD, director of inpatient services of the multi-specialty group HealthCare Partners, who took over that position three years ago when Dr. Hay left. About 100 hospitalists are employed under the HealthCare Partners umbrella; approximately 85 are on the payroll, and 15 work in a strategic alliance. The HMG covers 14 community hospitals in Southern California, about 14 hospitals in Las Vegas, Nevada, and about five hospitals in the Tampa/Orlando area of Florida.
The full-risk California medical model drives a lot of the metrics. “We look at [relative value unit] goals for our hospitalists, but mostly to ensure proper staffing,” Dr. Jung says. “We are satisfied when our docs have 12 to 14 encounters a day. In the service market you’d go broke with that, but I’d rather have our hospitalists see our patients twice a day because it drives quality and it turns out to be more cost effective.”
Some of the outcomes Dr. Jung regularly reviews include patient utilization per membership (admit rates, readmit data, and length of stay), and these metrics are largely unchanged as they have grown. “Additionally, maintaining high patient satisfaction can be overlooked, but is critical with the growth of any program,” he says (see Figure 3, p. 28).
Dr. Williams, who began the hospitalist group at Emory Healthcare, says the primary challenges he faced as that program grew were finding capable physicians willing to join a new or expanding program; managing the different cultures at different hospitals and working to ensure they all felt a part of the whole; having sufficient administrative support time to manage recruitment and credentialing; and keeping up constant communications with individuals and leadership at all sites. He found it helpful to occasionally rotate hospitalists, especially the more senior physicians, so they could appreciate the workload and issues at different sites.
Dr. Williams, who trained in internal medicine but later became board certified in emergency medicine, is not surprised Dr. Jung has some background in critical care, as does Dr. Heisler. He surmises they also all have well-honed administrative skills. “The experience I had in running a 65,000-visit-a-year emergency room and a 45,000-visit-a-year urgent-care center gave me the skills to run a large hospital medicine program,” Dr. Williams says. TH
Andrea M. Sattinger is a medical writer based in North Carolina.
How Am I Doing?
How hospitalists assess their performance and hone their skills is critical to patient care. Continuing medical education (CME), relicensure, specialty recertification, and lifelong learning are all linked to hospitalists’ abilities to assess and meet their learning needs.
But the preponderance of evidence suggests physicians have limited ability to accurately assess their performance, according to a physician self-assessment literature review published in September 2006 in JAMA.1
“Self-assessment should be guided by tools designed by experts, based on standards, and aimed at filling gaps in knowledge, skills, and competencies—not simply the internally based self-rating of individual practitioners,” says C. Michael Fordis, MD, senior associate dean for con-
tinuing medical education at the Baylor College of Medicine in Houston, and one of the authors of the study.
“Hospitalists and other physicians are not doing themselves a service to rely on their own internal self-rated judgments of knowledge and performance,” Dr. Fordis says. “There’s too much to know, too much that’s changing, and too much that affects the implementation into practice of the knowledge that you have for any one person to be able to take care of patients and at the same time have some sense of whether there are gaps along that implementation pathway.”
“Guided” self-assessment represents the thinking of many experts who ask questions, consider guidelines, and suggest tools that can help physicians pursue the best ways of identifying those gaps that reflect differences in what they think they are doing and their actual performance.
Regular, consistent self-assessment is imperative for a self-regulating profession such as medicine. How well are hospitalists doing—and what mechanisms or tools do they use?
Group Assessment
Hospital medicine groups are increasingly able to measure their clinical competence against other hospitals’ and hospitalist groups. SHM’s Benchmarks Committee has been working on performance assessment at a program level.
“When the JCAHO [Joint Commission on Accreditation of Healthcare Organizations] Core Measures were coming out a few years back, as a whole most docs when reflecting on their practice would say they do a fine job within these measures,” says Burke T. Kealey, MD, chairman of the Benchmarks Committee from 2006-07. “For instance, [they might say] ‘I always send people out on ACE inhibitors and beta-blockers,’ or, ‘We always start people on aspirin when they come into the ER,’ but when you looked at the data, you found that their self-assessment was not as accurate as we hoped it would be.”
A lot of hard work went into discovering why their self-assessment was inaccurate. “We found there were documentation problems that they didn’t really incorporate a lot of the contraindications when giving their answer about self-assessment,” says Dr. Kealey, who leads the hospital medicine program at Regions Hospital and HealthPartners Medical Group in St. Paul, Minn.
If patients had kidney dysfunction or kidney failure, they were not discharged on ACE inhibitors.
“But we as doctors didn’t do a great job of explaining why we weren’t doing that,” Dr. Kealey says. “We were not transparent in our reasoning, but the core measures caused us to become more transparent, to explain what we were thinking and what we were doing in a way that the public could see.”
At SHM’s annual meeting in May, the Benchmarks Committee released the white paper “Measuring Hospitalist Performance: Metrics, Reports, and Dashboards” with the intent of assisting hospitals and hospital medicine programs develop or improve their performance monitoring and reporting.
“Hospitalists in general could do a better job of assessing themselves,” says Arpana Vidyarthi, MD, an assistant professor in the division of hospital medicine at the University of California, San Francisco (UCSF). “Self-assessment for those of us in cognitive specialties, like internists, is more complicated than in procedural specialties like surgery, partly because these procedural specialties have very specific outcomes that are linked to the procedure and that level of skill. With the new drivers of quality improvement and patient safety, and the dramatic increase of quality indicators for hospitals overall, this is now trickling down to thinking about how we truly assess the doctors themselves.”
The quality indicators that hospitalist groups are benchmarking may not be linked to the individual, she says. Dr. Vidyarthi, also director of quality for the Inpatient General Medicine Service at UCSF Medical Center, provides an example. “Pneumovax as a quality indicator is part of the Joint Commission core measures,” says Dr. Vidyarthi. “You can go online where it is publicly reported and choose this or other indicators to compare one hospital to another. That is the sort of benchmarking that some hospitalists groups are doing.”
But using that kind of evaluation for individual assessment misses the mark.
“Does the fact that the patient does not get Pneumovax reflect upon me and my abilities as a hospitalist? Not at all,” she says, “because my institution and those institutions who have done well with this specific indicator have taken it out of the hands of the doctors. It’s an automated sort of thing. At our hospital, the pharmacists do it.”
Although the American Board of Internal Medicine asks that the individual physician assess his or her own care as part of recredentialing, it’s more difficult for a hospitalist than for an outpatient internist. Hospitalists don’t have a panel of diabetic patients, for instance, for which the outcomes data can be easily analyzed.
Hospitalists as a group also haven’t had a tradition of self-assessment or peer assessment. Further, hospitalist groups differ as to how they handle assessments of individual physicians.
“In general if you ask our [UCSF] hospitalists, the way that we assess competency is generally through hospital privileging,” Dr. Vidyarthi says. Because the hospital as a whole reviews the competency of all the doctors that work there, the process known as “privileging” has consisted of asking a couple of colleagues to write letters of recommendation. “The division is changing this, but that is just on the cusp.
“We’ve built a new system for our quality committee in which one layer is peer assessment, looking at just the individual cases that bubble up from an incident report or a root-cause analysis or other sources. We’re looking at and identifying both systems issues and individual issues and trying to build a way to feed back those assessments.”
But that’s just half the equation, she says, the flip side being continual self-assessment for what a hospitalist is doing well.
To Dr. Kealey, self-assessment plays a significant role in helping physicians with their career goals and ensuring that their careers are on track and on target.
At HealthPartners, physicians fill out a self-evaluation form on which they list all activities they’ve been involved in over the previous year. Then they are asked what they got out of these activities, what their career goals are, and whether they are meeting them. They’re also asked how the group can help them reach those goals.
“We ask them to pause and reflect on where they’re headed with their career and their life, and put it down in writing so that in that moment they take the time to ask, ‘What is it that I’m ultimately after?’ ” says Dr. Kealey.
Day to day, they are immersed in patient care and focused on doing a good job. “But in the trajectory of where they are headed—the committees, projects, and educational activities they are involved in—are they all aligned and pointing in the same direction and the right direction?” Dr Kealey asks.
The process, which HealthPartners hospitalists have been using for about 10 years, was modified from the American College of Physician Executives course “Managing Physician Performance.”
“It is a tool to help hospitalists pause and reflect on their career and how to move it forward,” Dr. Kealey says.
Marc B. Westle, DO, FACP, president and managing partner of the Asheville Hospitalist Group, PA, in Asheville, N.C., relies on ongoing conversations. This group also uses Crimson’s Physician Management Software to track various group quality and cost indicators, looking at data from as many angles as possible.
“It’s an excellent tool to look at a group, it is a poor tool to look at an individual,” Dr. Westle says. “Although the insurance companies like to say you can apply it to the individual, in reality there is no good way to attribute that data down to the physician level.”
Within the group data, it may be possible to recognize underperformers, but still it is anecdotal, based on experience and interaction.
“Under, ‘How am I doing?’ there is an objective category in the software where there are hard end-points and measures you can look at,” says Dr. Westle
On the subjective side, Dr. Westle collects data on relative value units (RVUs), non-monetary, numeric values Medicare uses to represent the relative amount of physician time, resources, and expertise needed to provide various services to patients. They review total RVUs as well as individual-components that make up total RVUs.
“I’ll track how many simple, moderate, or complex follow-up visits were made, how many simple or moderate histories and physicals or consultations, how many procedures are they doing.” Dr. Westle says. “I’ll track every statistic that way for every individual and give them that feedback so they can see how they’re doing from a performance and a work standard, compared to their peers within the group, and nationally as published by Medicare.”
Dr. Westle uses charts and graphs to drive his points home.
“It just gives them an idea about where they are,’’ he says. “It doesn’t mean they’re doing a bad job. Our patients may be sicker than some other patients. And that is why we do it as a group, too, because their patients should be similar to the group’s patients and the group’s patients may be different than the average Medicare patient.”
They also look at hospitalists’ quality of life, their schedules, and the quantity of work the average physician is doing compared with those around the country. They discuss scheduling, income, disposable income, and the kind of work they’re doing in the hospital. “All this comes into a discussion of where they are in their lives and are they happy with what they’re doing,” Dr. Westle says. TH
Andrea Sattinger is a medical writer based in North Carolina.
Reference
- Davis DA, Mazmanian PE, Fordis M, et al. Accuracy of physician self-assessment compared with observed measures of competence: a systematic review. JAMA. 2006;296(9):1094-1102.
How hospitalists assess their performance and hone their skills is critical to patient care. Continuing medical education (CME), relicensure, specialty recertification, and lifelong learning are all linked to hospitalists’ abilities to assess and meet their learning needs.
But the preponderance of evidence suggests physicians have limited ability to accurately assess their performance, according to a physician self-assessment literature review published in September 2006 in JAMA.1
“Self-assessment should be guided by tools designed by experts, based on standards, and aimed at filling gaps in knowledge, skills, and competencies—not simply the internally based self-rating of individual practitioners,” says C. Michael Fordis, MD, senior associate dean for con-
tinuing medical education at the Baylor College of Medicine in Houston, and one of the authors of the study.
“Hospitalists and other physicians are not doing themselves a service to rely on their own internal self-rated judgments of knowledge and performance,” Dr. Fordis says. “There’s too much to know, too much that’s changing, and too much that affects the implementation into practice of the knowledge that you have for any one person to be able to take care of patients and at the same time have some sense of whether there are gaps along that implementation pathway.”
“Guided” self-assessment represents the thinking of many experts who ask questions, consider guidelines, and suggest tools that can help physicians pursue the best ways of identifying those gaps that reflect differences in what they think they are doing and their actual performance.
Regular, consistent self-assessment is imperative for a self-regulating profession such as medicine. How well are hospitalists doing—and what mechanisms or tools do they use?
Group Assessment
Hospital medicine groups are increasingly able to measure their clinical competence against other hospitals’ and hospitalist groups. SHM’s Benchmarks Committee has been working on performance assessment at a program level.
“When the JCAHO [Joint Commission on Accreditation of Healthcare Organizations] Core Measures were coming out a few years back, as a whole most docs when reflecting on their practice would say they do a fine job within these measures,” says Burke T. Kealey, MD, chairman of the Benchmarks Committee from 2006-07. “For instance, [they might say] ‘I always send people out on ACE inhibitors and beta-blockers,’ or, ‘We always start people on aspirin when they come into the ER,’ but when you looked at the data, you found that their self-assessment was not as accurate as we hoped it would be.”
A lot of hard work went into discovering why their self-assessment was inaccurate. “We found there were documentation problems that they didn’t really incorporate a lot of the contraindications when giving their answer about self-assessment,” says Dr. Kealey, who leads the hospital medicine program at Regions Hospital and HealthPartners Medical Group in St. Paul, Minn.
If patients had kidney dysfunction or kidney failure, they were not discharged on ACE inhibitors.
“But we as doctors didn’t do a great job of explaining why we weren’t doing that,” Dr. Kealey says. “We were not transparent in our reasoning, but the core measures caused us to become more transparent, to explain what we were thinking and what we were doing in a way that the public could see.”
At SHM’s annual meeting in May, the Benchmarks Committee released the white paper “Measuring Hospitalist Performance: Metrics, Reports, and Dashboards” with the intent of assisting hospitals and hospital medicine programs develop or improve their performance monitoring and reporting.
“Hospitalists in general could do a better job of assessing themselves,” says Arpana Vidyarthi, MD, an assistant professor in the division of hospital medicine at the University of California, San Francisco (UCSF). “Self-assessment for those of us in cognitive specialties, like internists, is more complicated than in procedural specialties like surgery, partly because these procedural specialties have very specific outcomes that are linked to the procedure and that level of skill. With the new drivers of quality improvement and patient safety, and the dramatic increase of quality indicators for hospitals overall, this is now trickling down to thinking about how we truly assess the doctors themselves.”
The quality indicators that hospitalist groups are benchmarking may not be linked to the individual, she says. Dr. Vidyarthi, also director of quality for the Inpatient General Medicine Service at UCSF Medical Center, provides an example. “Pneumovax as a quality indicator is part of the Joint Commission core measures,” says Dr. Vidyarthi. “You can go online where it is publicly reported and choose this or other indicators to compare one hospital to another. That is the sort of benchmarking that some hospitalists groups are doing.”
But using that kind of evaluation for individual assessment misses the mark.
“Does the fact that the patient does not get Pneumovax reflect upon me and my abilities as a hospitalist? Not at all,” she says, “because my institution and those institutions who have done well with this specific indicator have taken it out of the hands of the doctors. It’s an automated sort of thing. At our hospital, the pharmacists do it.”
Although the American Board of Internal Medicine asks that the individual physician assess his or her own care as part of recredentialing, it’s more difficult for a hospitalist than for an outpatient internist. Hospitalists don’t have a panel of diabetic patients, for instance, for which the outcomes data can be easily analyzed.
Hospitalists as a group also haven’t had a tradition of self-assessment or peer assessment. Further, hospitalist groups differ as to how they handle assessments of individual physicians.
“In general if you ask our [UCSF] hospitalists, the way that we assess competency is generally through hospital privileging,” Dr. Vidyarthi says. Because the hospital as a whole reviews the competency of all the doctors that work there, the process known as “privileging” has consisted of asking a couple of colleagues to write letters of recommendation. “The division is changing this, but that is just on the cusp.
“We’ve built a new system for our quality committee in which one layer is peer assessment, looking at just the individual cases that bubble up from an incident report or a root-cause analysis or other sources. We’re looking at and identifying both systems issues and individual issues and trying to build a way to feed back those assessments.”
But that’s just half the equation, she says, the flip side being continual self-assessment for what a hospitalist is doing well.
To Dr. Kealey, self-assessment plays a significant role in helping physicians with their career goals and ensuring that their careers are on track and on target.
At HealthPartners, physicians fill out a self-evaluation form on which they list all activities they’ve been involved in over the previous year. Then they are asked what they got out of these activities, what their career goals are, and whether they are meeting them. They’re also asked how the group can help them reach those goals.
“We ask them to pause and reflect on where they’re headed with their career and their life, and put it down in writing so that in that moment they take the time to ask, ‘What is it that I’m ultimately after?’ ” says Dr. Kealey.
Day to day, they are immersed in patient care and focused on doing a good job. “But in the trajectory of where they are headed—the committees, projects, and educational activities they are involved in—are they all aligned and pointing in the same direction and the right direction?” Dr Kealey asks.
The process, which HealthPartners hospitalists have been using for about 10 years, was modified from the American College of Physician Executives course “Managing Physician Performance.”
“It is a tool to help hospitalists pause and reflect on their career and how to move it forward,” Dr. Kealey says.
Marc B. Westle, DO, FACP, president and managing partner of the Asheville Hospitalist Group, PA, in Asheville, N.C., relies on ongoing conversations. This group also uses Crimson’s Physician Management Software to track various group quality and cost indicators, looking at data from as many angles as possible.
“It’s an excellent tool to look at a group, it is a poor tool to look at an individual,” Dr. Westle says. “Although the insurance companies like to say you can apply it to the individual, in reality there is no good way to attribute that data down to the physician level.”
Within the group data, it may be possible to recognize underperformers, but still it is anecdotal, based on experience and interaction.
“Under, ‘How am I doing?’ there is an objective category in the software where there are hard end-points and measures you can look at,” says Dr. Westle
On the subjective side, Dr. Westle collects data on relative value units (RVUs), non-monetary, numeric values Medicare uses to represent the relative amount of physician time, resources, and expertise needed to provide various services to patients. They review total RVUs as well as individual-components that make up total RVUs.
“I’ll track how many simple, moderate, or complex follow-up visits were made, how many simple or moderate histories and physicals or consultations, how many procedures are they doing.” Dr. Westle says. “I’ll track every statistic that way for every individual and give them that feedback so they can see how they’re doing from a performance and a work standard, compared to their peers within the group, and nationally as published by Medicare.”
Dr. Westle uses charts and graphs to drive his points home.
“It just gives them an idea about where they are,’’ he says. “It doesn’t mean they’re doing a bad job. Our patients may be sicker than some other patients. And that is why we do it as a group, too, because their patients should be similar to the group’s patients and the group’s patients may be different than the average Medicare patient.”
They also look at hospitalists’ quality of life, their schedules, and the quantity of work the average physician is doing compared with those around the country. They discuss scheduling, income, disposable income, and the kind of work they’re doing in the hospital. “All this comes into a discussion of where they are in their lives and are they happy with what they’re doing,” Dr. Westle says. TH
Andrea Sattinger is a medical writer based in North Carolina.
Reference
- Davis DA, Mazmanian PE, Fordis M, et al. Accuracy of physician self-assessment compared with observed measures of competence: a systematic review. JAMA. 2006;296(9):1094-1102.
How hospitalists assess their performance and hone their skills is critical to patient care. Continuing medical education (CME), relicensure, specialty recertification, and lifelong learning are all linked to hospitalists’ abilities to assess and meet their learning needs.
But the preponderance of evidence suggests physicians have limited ability to accurately assess their performance, according to a physician self-assessment literature review published in September 2006 in JAMA.1
“Self-assessment should be guided by tools designed by experts, based on standards, and aimed at filling gaps in knowledge, skills, and competencies—not simply the internally based self-rating of individual practitioners,” says C. Michael Fordis, MD, senior associate dean for con-
tinuing medical education at the Baylor College of Medicine in Houston, and one of the authors of the study.
“Hospitalists and other physicians are not doing themselves a service to rely on their own internal self-rated judgments of knowledge and performance,” Dr. Fordis says. “There’s too much to know, too much that’s changing, and too much that affects the implementation into practice of the knowledge that you have for any one person to be able to take care of patients and at the same time have some sense of whether there are gaps along that implementation pathway.”
“Guided” self-assessment represents the thinking of many experts who ask questions, consider guidelines, and suggest tools that can help physicians pursue the best ways of identifying those gaps that reflect differences in what they think they are doing and their actual performance.
Regular, consistent self-assessment is imperative for a self-regulating profession such as medicine. How well are hospitalists doing—and what mechanisms or tools do they use?
Group Assessment
Hospital medicine groups are increasingly able to measure their clinical competence against other hospitals’ and hospitalist groups. SHM’s Benchmarks Committee has been working on performance assessment at a program level.
“When the JCAHO [Joint Commission on Accreditation of Healthcare Organizations] Core Measures were coming out a few years back, as a whole most docs when reflecting on their practice would say they do a fine job within these measures,” says Burke T. Kealey, MD, chairman of the Benchmarks Committee from 2006-07. “For instance, [they might say] ‘I always send people out on ACE inhibitors and beta-blockers,’ or, ‘We always start people on aspirin when they come into the ER,’ but when you looked at the data, you found that their self-assessment was not as accurate as we hoped it would be.”
A lot of hard work went into discovering why their self-assessment was inaccurate. “We found there were documentation problems that they didn’t really incorporate a lot of the contraindications when giving their answer about self-assessment,” says Dr. Kealey, who leads the hospital medicine program at Regions Hospital and HealthPartners Medical Group in St. Paul, Minn.
If patients had kidney dysfunction or kidney failure, they were not discharged on ACE inhibitors.
“But we as doctors didn’t do a great job of explaining why we weren’t doing that,” Dr. Kealey says. “We were not transparent in our reasoning, but the core measures caused us to become more transparent, to explain what we were thinking and what we were doing in a way that the public could see.”
At SHM’s annual meeting in May, the Benchmarks Committee released the white paper “Measuring Hospitalist Performance: Metrics, Reports, and Dashboards” with the intent of assisting hospitals and hospital medicine programs develop or improve their performance monitoring and reporting.
“Hospitalists in general could do a better job of assessing themselves,” says Arpana Vidyarthi, MD, an assistant professor in the division of hospital medicine at the University of California, San Francisco (UCSF). “Self-assessment for those of us in cognitive specialties, like internists, is more complicated than in procedural specialties like surgery, partly because these procedural specialties have very specific outcomes that are linked to the procedure and that level of skill. With the new drivers of quality improvement and patient safety, and the dramatic increase of quality indicators for hospitals overall, this is now trickling down to thinking about how we truly assess the doctors themselves.”
The quality indicators that hospitalist groups are benchmarking may not be linked to the individual, she says. Dr. Vidyarthi, also director of quality for the Inpatient General Medicine Service at UCSF Medical Center, provides an example. “Pneumovax as a quality indicator is part of the Joint Commission core measures,” says Dr. Vidyarthi. “You can go online where it is publicly reported and choose this or other indicators to compare one hospital to another. That is the sort of benchmarking that some hospitalists groups are doing.”
But using that kind of evaluation for individual assessment misses the mark.
“Does the fact that the patient does not get Pneumovax reflect upon me and my abilities as a hospitalist? Not at all,” she says, “because my institution and those institutions who have done well with this specific indicator have taken it out of the hands of the doctors. It’s an automated sort of thing. At our hospital, the pharmacists do it.”
Although the American Board of Internal Medicine asks that the individual physician assess his or her own care as part of recredentialing, it’s more difficult for a hospitalist than for an outpatient internist. Hospitalists don’t have a panel of diabetic patients, for instance, for which the outcomes data can be easily analyzed.
Hospitalists as a group also haven’t had a tradition of self-assessment or peer assessment. Further, hospitalist groups differ as to how they handle assessments of individual physicians.
“In general if you ask our [UCSF] hospitalists, the way that we assess competency is generally through hospital privileging,” Dr. Vidyarthi says. Because the hospital as a whole reviews the competency of all the doctors that work there, the process known as “privileging” has consisted of asking a couple of colleagues to write letters of recommendation. “The division is changing this, but that is just on the cusp.
“We’ve built a new system for our quality committee in which one layer is peer assessment, looking at just the individual cases that bubble up from an incident report or a root-cause analysis or other sources. We’re looking at and identifying both systems issues and individual issues and trying to build a way to feed back those assessments.”
But that’s just half the equation, she says, the flip side being continual self-assessment for what a hospitalist is doing well.
To Dr. Kealey, self-assessment plays a significant role in helping physicians with their career goals and ensuring that their careers are on track and on target.
At HealthPartners, physicians fill out a self-evaluation form on which they list all activities they’ve been involved in over the previous year. Then they are asked what they got out of these activities, what their career goals are, and whether they are meeting them. They’re also asked how the group can help them reach those goals.
“We ask them to pause and reflect on where they’re headed with their career and their life, and put it down in writing so that in that moment they take the time to ask, ‘What is it that I’m ultimately after?’ ” says Dr. Kealey.
Day to day, they are immersed in patient care and focused on doing a good job. “But in the trajectory of where they are headed—the committees, projects, and educational activities they are involved in—are they all aligned and pointing in the same direction and the right direction?” Dr Kealey asks.
The process, which HealthPartners hospitalists have been using for about 10 years, was modified from the American College of Physician Executives course “Managing Physician Performance.”
“It is a tool to help hospitalists pause and reflect on their career and how to move it forward,” Dr. Kealey says.
Marc B. Westle, DO, FACP, president and managing partner of the Asheville Hospitalist Group, PA, in Asheville, N.C., relies on ongoing conversations. This group also uses Crimson’s Physician Management Software to track various group quality and cost indicators, looking at data from as many angles as possible.
“It’s an excellent tool to look at a group, it is a poor tool to look at an individual,” Dr. Westle says. “Although the insurance companies like to say you can apply it to the individual, in reality there is no good way to attribute that data down to the physician level.”
Within the group data, it may be possible to recognize underperformers, but still it is anecdotal, based on experience and interaction.
“Under, ‘How am I doing?’ there is an objective category in the software where there are hard end-points and measures you can look at,” says Dr. Westle
On the subjective side, Dr. Westle collects data on relative value units (RVUs), non-monetary, numeric values Medicare uses to represent the relative amount of physician time, resources, and expertise needed to provide various services to patients. They review total RVUs as well as individual-components that make up total RVUs.
“I’ll track how many simple, moderate, or complex follow-up visits were made, how many simple or moderate histories and physicals or consultations, how many procedures are they doing.” Dr. Westle says. “I’ll track every statistic that way for every individual and give them that feedback so they can see how they’re doing from a performance and a work standard, compared to their peers within the group, and nationally as published by Medicare.”
Dr. Westle uses charts and graphs to drive his points home.
“It just gives them an idea about where they are,’’ he says. “It doesn’t mean they’re doing a bad job. Our patients may be sicker than some other patients. And that is why we do it as a group, too, because their patients should be similar to the group’s patients and the group’s patients may be different than the average Medicare patient.”
They also look at hospitalists’ quality of life, their schedules, and the quantity of work the average physician is doing compared with those around the country. They discuss scheduling, income, disposable income, and the kind of work they’re doing in the hospital. “All this comes into a discussion of where they are in their lives and are they happy with what they’re doing,” Dr. Westle says. TH
Andrea Sattinger is a medical writer based in North Carolina.
Reference
- Davis DA, Mazmanian PE, Fordis M, et al. Accuracy of physician self-assessment compared with observed measures of competence: a systematic review. JAMA. 2006;296(9):1094-1102.
The Surgical Surge
New limits on resident work hours and the graying of the U.S. population are putting hospitalists in the forefront of helping surgeons manage their patients.
Because the Accreditation Council for Graduate Medical Education restricted resident duty hours, surgeons can no longer rely automatically on residents to medically manage their patients on the floors, says Amir K. Jaffer, MD, a hospitalist and an associate professor of medicine at the Cleveland Clinic Lerner College of Medicine of Case Western Reserve University in Ohio.
Meanwhile, the population over age 65 will double, increasing to 70 million over the next 10 to 15 years.1
“More patients living longer means an increase in surgeries along the way,” says Dr. Jaffer, who is also the medical director of the Internal Medicine Preoperative Assessment Consultation and Treatment program in the section of hospital medicine at the Cleveland Clinic. For him, the first place hospitalists need to co-manage is in the postoperative setting.
“Studies have suggested that as patients age there is an increase in cardiological complications, noncardiological complications, pulmonary complications, and overall mortality,” he continues. “In my opinion there is going to be a crisis in regard to managing medical issues and complications surrounding surgery.” (See Table 1, p. 24)
Medications issues are another major reason hospitalists are called for surgical consults, says Benny Gavi, MD, hospitalist at Stanford Hospitals and Clinics in Calif. “I got consulted for a patient with tachycardia in the inpatient setting,” says Dr. Gavi. “By the time we saw the patient, the orthopedic surgeon had already ordered an echocardiogram and added a beta-blocker. When I looked at the patient I realized he had a gout flare; the colchicine that he took daily for his gout was never started in the inpatient setting, which ultimately delayed his physical therapy and added three additional days to his hospital stay.”
Co-management makes sense for still other reasons, he says.
“The knowledge base of both surgery and medicine is growing rapidly; no one person can remain on top of what is needed for both fields,” says Dr. Gavi. “In the last 20 years there has been a dramatic rise in the number of medications and some are very complicated. Also, physicians and surgeons both are being approached to participate more in quality initiatives and increasing throughput. As a result, physicians have to work faster and do more.”
Opportunities
In the United States, approximately 100,000 surgeries are performed each day and 36 million surgeries are performed each year at a cost of $450 billion annually. More than 1 million serious surgical adverse events each year cost $45 billion. Within two decades, the surgeries will increase by 25%, the associated cost will increase 50%, and the cost of in-hospital and long-term complications will increase 100%.
Along with postoperative care, there are increasing opportunities in the preoperative setting.
“At our institution, which is a tertiary care center with a huge surgical hospital, we determined that there was a need for hospitalists to provide medical management of surgical patients 10 years ago,” Dr. Jaffer says. “Patients were often not adequately prepared when they went to surgery, and sometimes in the morning of surgery the anesthesiologists would cancel their cases.”
The traditional model of physicians calling in consultants when problems arise might need to change.
“We are increasingly looking for ways to identify patients who have a high likelihood of developing medical problems and proactively getting involved,” says Dr. Gavi.
To co-manage, hospitalists must take ownership of some medical issues under specific conditions (diabetes, anticoagulation, blood pressure), says Dr. Jaffer.
The Benefits
To Latha Sivaprasad, MD, hospitalist at Beth Israel Medical Center in New York City, there are three main advantages of hospitalists’ involvement in perioperative co-management:
- Hospitalists typically perform comprehensive, multisystemic patient evaluations;
- Hospitalists are extremely accessible; and
- Hospitalists are up to date on inpatient medicine.
How up to date?
“Periop isn’t routinely taught in residency,” says Ali Usmani, MD, a hospitalist at the Cleveland Clinic. “In fact, I had little information about perioperative care.”
When he joined the hospitalist group after a three-year residency at Cleveland Clinic, Dr. Usmani did preparatory reading. Later, the hospitalist group gave him a helpful collection of essays.
“I was very nervous because, of course, I had never done this before,” he says. “Surprisingly, I also had not done a general medicine consult service where we see postoperative patients. It was scary to some extent, but I found out that it is easier than I thought because there are guidelines you can follow from the AHA/ACC that are fairly straightforward. It also meant a nice schedule change from being on the floors.”
Although conducting preoperative evaluations with patients was technically outpatient work, it was not like he was seeing patients with such simple illnesses as a cold or a sore throat. Also, he says, there were no new surprises postoperatively because either he or a hospitalist colleague had seen the patient preoperatively.
Dr. Usmani, also a clinical assistant professor of medicine at Cleveland Clinic Lerner College of Medicine of Case Western Reserve University, believes patients are happier when seen by hospitalists because they get a standardized, holistic preoperative assessment. And, helping to reduce the number of unnecessary tests ordered by primary care physicians or surgeons makes him feel as though he’s making a valuable contribution.
New Niche
Dr. Sivaprasad, who is also doing a one-year fellowship in quality improvement and patient safety at Beth Israel, has practiced hospital medicine in four hospitals ranging from 500 to 1,000 beds. “The primary reason we are consulted by surgeons is for perioperative cardiac risk assessment,” says Dr. Sivaprasad. “Other reasons include co-managing a patient with comorbidities such as a history of diabetes, hypertension, or renal failure.”
From 2003-2006, Dr. Sivaprasad was one of 14 hospitalists consulted often by surgeons at St. John’s Mercy Hospital in St Louis, a 1,000-bed Level I trauma center. “We were consulted for postoperative co-management, preoperative evaluation, or more urgent cases such as a patient experiencing hypotension, atrial fibrillation, shortness of breath, decreased urine output, or renal failure,” she says.
Dr. Sivaprasad recently attended the Johns Hopkins conference on Perioperative Management. The session made it easier for her to do a systems-based consult.
“All hospitalists differ to the degree of perioperative medicine they feel comfortable with,” she says. “Hospitalists understand perioperative medicine on different levels. They all can do an acceptable consult; but there is a spectrum of how detailed one can be and what service one can provide for the surgeon and the patient.”
Dr. Jaffer finds his work in perioperative care fulfilling and considers it another way hospitalists can increase their influence.
“Often when you manage medical patients in the hospital, it’s you, the medical patient, and the patient’s primary care physician,” Dr. Jaffer says. “But when you start to manage surgical patients, you are really being looked at by your surgical colleagues as an expert in managing medical problems, just as you view them as experts in managing surgical problems. What I realize from this is that I can be a perioperative medicine expert as well.”
Are there any downfalls to co-managing surgical patients?
“Sometimes the surgeons order unnecessary lab tests such as PTTs [partial thromboplastin time] because they are concerned about bleeding and complications,” Dr. Usmani says. “The next day if there is a deranged PTT, we need to figure out whether to suggest postponing the surgery or go ahead with the surgery based on the patients’ past medical/family history. We try to get our surgeons and our colleagues to work together with us in that regard because they don’t want to postpone surgery either.”
Drs. Usmani, Gavi, Jaffer, and Sivaprasad all say that when surgeons can observe firsthand their hospitalist partners exhibiting expertise in acute care it appears to improve surgeons’ attitudes about the role and value of hospitalists.
In fact, says Dr. Usmani, surgeons call him or one of his colleagues to thank them. “They say, ‘We really appreciate what you’ve done for this patient,’ ’’ he says. “Even if we suggest canceling surgery, they respect that we have seen a potential problem instead of letting it go ahead. They are happy to receive this advice.”
Another new relationship is between anesthesiologists and hospitalists. “I spend a lot of time calling anesthesiologists in regard to patient cases, and a good many of them are surprised to get a call from a hospitalist,” Dr. Gavi says. “We especially work closely together when we get complicated patients ready for surgery.”
A recent encounter proved to Dr. Gavi the complementary nature of the hospitalist-anesthesiologist relationship.2
“A patient came to the hospital two weeks ago to have an elective total knee replacement,” says Dr. Gavi. “She was an older woman with severe pulmonary disease. When the anesthesiologists saw her in the preoperative waiting area and realized how sick she is, they wanted to cancel the surgery. But the surgeon told the anesthesiologist that this patient had been seen in our own preoperative clinic and cleared by a hospitalist.”
Dr. Gavi had done what is customary for an internist. He took a more in-depth look at her pulmonology and cardiac records, called her cardiologist for further history, and reassured the anesthesiologist and surgeon. The patient had her surgery.
The Future
“Perioperative co-management is becoming more of a visible need,” says Dr. Sivaprasad. “It bridges the gap between surgeons and internists.”
To those of his hospitalist colleagues who have little information and are a bit afraid to begin perioperative care practice, Dr. Usmani recommends attending a perioperative summit conference.
The session should teach how to set up a perioperative center and what to do when managing patients with certain conditions.
“Although you meet with patients preoperatively in an office setting, you don’t feel like a primary care physician,” Dr. Usmani says. “You feel as if you are a specialist. You are respected, and you are contributing to postoperative outcomes to the benefit of the patient.”
Perioperative patient management is also financially rewarding because reimbursement is higher than customary hospital medicine duties.
Dr. Jaffer, soon to be chief of the division of hospital medicine at the University of Miami Medical Center in Florida, is proud of the work he and his colleagues have done to grow the Cleveland Clinic perioperative summit. This third summit, in September, was organized in collaboration with the Society of Perioperative Assessment and Quality Improvement.
“I think this is something that every hospitalist should try,” Dr. Usmani says. “It is definitely a niche.” TH
Andrea Sattinger is a frequent contributor to The Hospitalist.
References
- Mangano DT. Perioperative medicine: NHLBI working group deliberations and recommendations. J Cardiothorac Vasc Anesth. 2004;18(1):1-6.
- Adebola O, Adesanya AO, Joshi GP. Hospitalists and anesthesiologists as perioperative physicians: Are their roles complementary? Proc. (Bayl Univ Med Cent) 2007 April;20(2):140-142.
New limits on resident work hours and the graying of the U.S. population are putting hospitalists in the forefront of helping surgeons manage their patients.
Because the Accreditation Council for Graduate Medical Education restricted resident duty hours, surgeons can no longer rely automatically on residents to medically manage their patients on the floors, says Amir K. Jaffer, MD, a hospitalist and an associate professor of medicine at the Cleveland Clinic Lerner College of Medicine of Case Western Reserve University in Ohio.
Meanwhile, the population over age 65 will double, increasing to 70 million over the next 10 to 15 years.1
“More patients living longer means an increase in surgeries along the way,” says Dr. Jaffer, who is also the medical director of the Internal Medicine Preoperative Assessment Consultation and Treatment program in the section of hospital medicine at the Cleveland Clinic. For him, the first place hospitalists need to co-manage is in the postoperative setting.
“Studies have suggested that as patients age there is an increase in cardiological complications, noncardiological complications, pulmonary complications, and overall mortality,” he continues. “In my opinion there is going to be a crisis in regard to managing medical issues and complications surrounding surgery.” (See Table 1, p. 24)
Medications issues are another major reason hospitalists are called for surgical consults, says Benny Gavi, MD, hospitalist at Stanford Hospitals and Clinics in Calif. “I got consulted for a patient with tachycardia in the inpatient setting,” says Dr. Gavi. “By the time we saw the patient, the orthopedic surgeon had already ordered an echocardiogram and added a beta-blocker. When I looked at the patient I realized he had a gout flare; the colchicine that he took daily for his gout was never started in the inpatient setting, which ultimately delayed his physical therapy and added three additional days to his hospital stay.”
Co-management makes sense for still other reasons, he says.
“The knowledge base of both surgery and medicine is growing rapidly; no one person can remain on top of what is needed for both fields,” says Dr. Gavi. “In the last 20 years there has been a dramatic rise in the number of medications and some are very complicated. Also, physicians and surgeons both are being approached to participate more in quality initiatives and increasing throughput. As a result, physicians have to work faster and do more.”
Opportunities
In the United States, approximately 100,000 surgeries are performed each day and 36 million surgeries are performed each year at a cost of $450 billion annually. More than 1 million serious surgical adverse events each year cost $45 billion. Within two decades, the surgeries will increase by 25%, the associated cost will increase 50%, and the cost of in-hospital and long-term complications will increase 100%.
Along with postoperative care, there are increasing opportunities in the preoperative setting.
“At our institution, which is a tertiary care center with a huge surgical hospital, we determined that there was a need for hospitalists to provide medical management of surgical patients 10 years ago,” Dr. Jaffer says. “Patients were often not adequately prepared when they went to surgery, and sometimes in the morning of surgery the anesthesiologists would cancel their cases.”
The traditional model of physicians calling in consultants when problems arise might need to change.
“We are increasingly looking for ways to identify patients who have a high likelihood of developing medical problems and proactively getting involved,” says Dr. Gavi.
To co-manage, hospitalists must take ownership of some medical issues under specific conditions (diabetes, anticoagulation, blood pressure), says Dr. Jaffer.
The Benefits
To Latha Sivaprasad, MD, hospitalist at Beth Israel Medical Center in New York City, there are three main advantages of hospitalists’ involvement in perioperative co-management:
- Hospitalists typically perform comprehensive, multisystemic patient evaluations;
- Hospitalists are extremely accessible; and
- Hospitalists are up to date on inpatient medicine.
How up to date?
“Periop isn’t routinely taught in residency,” says Ali Usmani, MD, a hospitalist at the Cleveland Clinic. “In fact, I had little information about perioperative care.”
When he joined the hospitalist group after a three-year residency at Cleveland Clinic, Dr. Usmani did preparatory reading. Later, the hospitalist group gave him a helpful collection of essays.
“I was very nervous because, of course, I had never done this before,” he says. “Surprisingly, I also had not done a general medicine consult service where we see postoperative patients. It was scary to some extent, but I found out that it is easier than I thought because there are guidelines you can follow from the AHA/ACC that are fairly straightforward. It also meant a nice schedule change from being on the floors.”
Although conducting preoperative evaluations with patients was technically outpatient work, it was not like he was seeing patients with such simple illnesses as a cold or a sore throat. Also, he says, there were no new surprises postoperatively because either he or a hospitalist colleague had seen the patient preoperatively.
Dr. Usmani, also a clinical assistant professor of medicine at Cleveland Clinic Lerner College of Medicine of Case Western Reserve University, believes patients are happier when seen by hospitalists because they get a standardized, holistic preoperative assessment. And, helping to reduce the number of unnecessary tests ordered by primary care physicians or surgeons makes him feel as though he’s making a valuable contribution.
New Niche
Dr. Sivaprasad, who is also doing a one-year fellowship in quality improvement and patient safety at Beth Israel, has practiced hospital medicine in four hospitals ranging from 500 to 1,000 beds. “The primary reason we are consulted by surgeons is for perioperative cardiac risk assessment,” says Dr. Sivaprasad. “Other reasons include co-managing a patient with comorbidities such as a history of diabetes, hypertension, or renal failure.”
From 2003-2006, Dr. Sivaprasad was one of 14 hospitalists consulted often by surgeons at St. John’s Mercy Hospital in St Louis, a 1,000-bed Level I trauma center. “We were consulted for postoperative co-management, preoperative evaluation, or more urgent cases such as a patient experiencing hypotension, atrial fibrillation, shortness of breath, decreased urine output, or renal failure,” she says.
Dr. Sivaprasad recently attended the Johns Hopkins conference on Perioperative Management. The session made it easier for her to do a systems-based consult.
“All hospitalists differ to the degree of perioperative medicine they feel comfortable with,” she says. “Hospitalists understand perioperative medicine on different levels. They all can do an acceptable consult; but there is a spectrum of how detailed one can be and what service one can provide for the surgeon and the patient.”
Dr. Jaffer finds his work in perioperative care fulfilling and considers it another way hospitalists can increase their influence.
“Often when you manage medical patients in the hospital, it’s you, the medical patient, and the patient’s primary care physician,” Dr. Jaffer says. “But when you start to manage surgical patients, you are really being looked at by your surgical colleagues as an expert in managing medical problems, just as you view them as experts in managing surgical problems. What I realize from this is that I can be a perioperative medicine expert as well.”
Are there any downfalls to co-managing surgical patients?
“Sometimes the surgeons order unnecessary lab tests such as PTTs [partial thromboplastin time] because they are concerned about bleeding and complications,” Dr. Usmani says. “The next day if there is a deranged PTT, we need to figure out whether to suggest postponing the surgery or go ahead with the surgery based on the patients’ past medical/family history. We try to get our surgeons and our colleagues to work together with us in that regard because they don’t want to postpone surgery either.”
Drs. Usmani, Gavi, Jaffer, and Sivaprasad all say that when surgeons can observe firsthand their hospitalist partners exhibiting expertise in acute care it appears to improve surgeons’ attitudes about the role and value of hospitalists.
In fact, says Dr. Usmani, surgeons call him or one of his colleagues to thank them. “They say, ‘We really appreciate what you’ve done for this patient,’ ’’ he says. “Even if we suggest canceling surgery, they respect that we have seen a potential problem instead of letting it go ahead. They are happy to receive this advice.”
Another new relationship is between anesthesiologists and hospitalists. “I spend a lot of time calling anesthesiologists in regard to patient cases, and a good many of them are surprised to get a call from a hospitalist,” Dr. Gavi says. “We especially work closely together when we get complicated patients ready for surgery.”
A recent encounter proved to Dr. Gavi the complementary nature of the hospitalist-anesthesiologist relationship.2
“A patient came to the hospital two weeks ago to have an elective total knee replacement,” says Dr. Gavi. “She was an older woman with severe pulmonary disease. When the anesthesiologists saw her in the preoperative waiting area and realized how sick she is, they wanted to cancel the surgery. But the surgeon told the anesthesiologist that this patient had been seen in our own preoperative clinic and cleared by a hospitalist.”
Dr. Gavi had done what is customary for an internist. He took a more in-depth look at her pulmonology and cardiac records, called her cardiologist for further history, and reassured the anesthesiologist and surgeon. The patient had her surgery.
The Future
“Perioperative co-management is becoming more of a visible need,” says Dr. Sivaprasad. “It bridges the gap between surgeons and internists.”
To those of his hospitalist colleagues who have little information and are a bit afraid to begin perioperative care practice, Dr. Usmani recommends attending a perioperative summit conference.
The session should teach how to set up a perioperative center and what to do when managing patients with certain conditions.
“Although you meet with patients preoperatively in an office setting, you don’t feel like a primary care physician,” Dr. Usmani says. “You feel as if you are a specialist. You are respected, and you are contributing to postoperative outcomes to the benefit of the patient.”
Perioperative patient management is also financially rewarding because reimbursement is higher than customary hospital medicine duties.
Dr. Jaffer, soon to be chief of the division of hospital medicine at the University of Miami Medical Center in Florida, is proud of the work he and his colleagues have done to grow the Cleveland Clinic perioperative summit. This third summit, in September, was organized in collaboration with the Society of Perioperative Assessment and Quality Improvement.
“I think this is something that every hospitalist should try,” Dr. Usmani says. “It is definitely a niche.” TH
Andrea Sattinger is a frequent contributor to The Hospitalist.
References
- Mangano DT. Perioperative medicine: NHLBI working group deliberations and recommendations. J Cardiothorac Vasc Anesth. 2004;18(1):1-6.
- Adebola O, Adesanya AO, Joshi GP. Hospitalists and anesthesiologists as perioperative physicians: Are their roles complementary? Proc. (Bayl Univ Med Cent) 2007 April;20(2):140-142.
New limits on resident work hours and the graying of the U.S. population are putting hospitalists in the forefront of helping surgeons manage their patients.
Because the Accreditation Council for Graduate Medical Education restricted resident duty hours, surgeons can no longer rely automatically on residents to medically manage their patients on the floors, says Amir K. Jaffer, MD, a hospitalist and an associate professor of medicine at the Cleveland Clinic Lerner College of Medicine of Case Western Reserve University in Ohio.
Meanwhile, the population over age 65 will double, increasing to 70 million over the next 10 to 15 years.1
“More patients living longer means an increase in surgeries along the way,” says Dr. Jaffer, who is also the medical director of the Internal Medicine Preoperative Assessment Consultation and Treatment program in the section of hospital medicine at the Cleveland Clinic. For him, the first place hospitalists need to co-manage is in the postoperative setting.
“Studies have suggested that as patients age there is an increase in cardiological complications, noncardiological complications, pulmonary complications, and overall mortality,” he continues. “In my opinion there is going to be a crisis in regard to managing medical issues and complications surrounding surgery.” (See Table 1, p. 24)
Medications issues are another major reason hospitalists are called for surgical consults, says Benny Gavi, MD, hospitalist at Stanford Hospitals and Clinics in Calif. “I got consulted for a patient with tachycardia in the inpatient setting,” says Dr. Gavi. “By the time we saw the patient, the orthopedic surgeon had already ordered an echocardiogram and added a beta-blocker. When I looked at the patient I realized he had a gout flare; the colchicine that he took daily for his gout was never started in the inpatient setting, which ultimately delayed his physical therapy and added three additional days to his hospital stay.”
Co-management makes sense for still other reasons, he says.
“The knowledge base of both surgery and medicine is growing rapidly; no one person can remain on top of what is needed for both fields,” says Dr. Gavi. “In the last 20 years there has been a dramatic rise in the number of medications and some are very complicated. Also, physicians and surgeons both are being approached to participate more in quality initiatives and increasing throughput. As a result, physicians have to work faster and do more.”
Opportunities
In the United States, approximately 100,000 surgeries are performed each day and 36 million surgeries are performed each year at a cost of $450 billion annually. More than 1 million serious surgical adverse events each year cost $45 billion. Within two decades, the surgeries will increase by 25%, the associated cost will increase 50%, and the cost of in-hospital and long-term complications will increase 100%.
Along with postoperative care, there are increasing opportunities in the preoperative setting.
“At our institution, which is a tertiary care center with a huge surgical hospital, we determined that there was a need for hospitalists to provide medical management of surgical patients 10 years ago,” Dr. Jaffer says. “Patients were often not adequately prepared when they went to surgery, and sometimes in the morning of surgery the anesthesiologists would cancel their cases.”
The traditional model of physicians calling in consultants when problems arise might need to change.
“We are increasingly looking for ways to identify patients who have a high likelihood of developing medical problems and proactively getting involved,” says Dr. Gavi.
To co-manage, hospitalists must take ownership of some medical issues under specific conditions (diabetes, anticoagulation, blood pressure), says Dr. Jaffer.
The Benefits
To Latha Sivaprasad, MD, hospitalist at Beth Israel Medical Center in New York City, there are three main advantages of hospitalists’ involvement in perioperative co-management:
- Hospitalists typically perform comprehensive, multisystemic patient evaluations;
- Hospitalists are extremely accessible; and
- Hospitalists are up to date on inpatient medicine.
How up to date?
“Periop isn’t routinely taught in residency,” says Ali Usmani, MD, a hospitalist at the Cleveland Clinic. “In fact, I had little information about perioperative care.”
When he joined the hospitalist group after a three-year residency at Cleveland Clinic, Dr. Usmani did preparatory reading. Later, the hospitalist group gave him a helpful collection of essays.
“I was very nervous because, of course, I had never done this before,” he says. “Surprisingly, I also had not done a general medicine consult service where we see postoperative patients. It was scary to some extent, but I found out that it is easier than I thought because there are guidelines you can follow from the AHA/ACC that are fairly straightforward. It also meant a nice schedule change from being on the floors.”
Although conducting preoperative evaluations with patients was technically outpatient work, it was not like he was seeing patients with such simple illnesses as a cold or a sore throat. Also, he says, there were no new surprises postoperatively because either he or a hospitalist colleague had seen the patient preoperatively.
Dr. Usmani, also a clinical assistant professor of medicine at Cleveland Clinic Lerner College of Medicine of Case Western Reserve University, believes patients are happier when seen by hospitalists because they get a standardized, holistic preoperative assessment. And, helping to reduce the number of unnecessary tests ordered by primary care physicians or surgeons makes him feel as though he’s making a valuable contribution.
New Niche
Dr. Sivaprasad, who is also doing a one-year fellowship in quality improvement and patient safety at Beth Israel, has practiced hospital medicine in four hospitals ranging from 500 to 1,000 beds. “The primary reason we are consulted by surgeons is for perioperative cardiac risk assessment,” says Dr. Sivaprasad. “Other reasons include co-managing a patient with comorbidities such as a history of diabetes, hypertension, or renal failure.”
From 2003-2006, Dr. Sivaprasad was one of 14 hospitalists consulted often by surgeons at St. John’s Mercy Hospital in St Louis, a 1,000-bed Level I trauma center. “We were consulted for postoperative co-management, preoperative evaluation, or more urgent cases such as a patient experiencing hypotension, atrial fibrillation, shortness of breath, decreased urine output, or renal failure,” she says.
Dr. Sivaprasad recently attended the Johns Hopkins conference on Perioperative Management. The session made it easier for her to do a systems-based consult.
“All hospitalists differ to the degree of perioperative medicine they feel comfortable with,” she says. “Hospitalists understand perioperative medicine on different levels. They all can do an acceptable consult; but there is a spectrum of how detailed one can be and what service one can provide for the surgeon and the patient.”
Dr. Jaffer finds his work in perioperative care fulfilling and considers it another way hospitalists can increase their influence.
“Often when you manage medical patients in the hospital, it’s you, the medical patient, and the patient’s primary care physician,” Dr. Jaffer says. “But when you start to manage surgical patients, you are really being looked at by your surgical colleagues as an expert in managing medical problems, just as you view them as experts in managing surgical problems. What I realize from this is that I can be a perioperative medicine expert as well.”
Are there any downfalls to co-managing surgical patients?
“Sometimes the surgeons order unnecessary lab tests such as PTTs [partial thromboplastin time] because they are concerned about bleeding and complications,” Dr. Usmani says. “The next day if there is a deranged PTT, we need to figure out whether to suggest postponing the surgery or go ahead with the surgery based on the patients’ past medical/family history. We try to get our surgeons and our colleagues to work together with us in that regard because they don’t want to postpone surgery either.”
Drs. Usmani, Gavi, Jaffer, and Sivaprasad all say that when surgeons can observe firsthand their hospitalist partners exhibiting expertise in acute care it appears to improve surgeons’ attitudes about the role and value of hospitalists.
In fact, says Dr. Usmani, surgeons call him or one of his colleagues to thank them. “They say, ‘We really appreciate what you’ve done for this patient,’ ’’ he says. “Even if we suggest canceling surgery, they respect that we have seen a potential problem instead of letting it go ahead. They are happy to receive this advice.”
Another new relationship is between anesthesiologists and hospitalists. “I spend a lot of time calling anesthesiologists in regard to patient cases, and a good many of them are surprised to get a call from a hospitalist,” Dr. Gavi says. “We especially work closely together when we get complicated patients ready for surgery.”
A recent encounter proved to Dr. Gavi the complementary nature of the hospitalist-anesthesiologist relationship.2
“A patient came to the hospital two weeks ago to have an elective total knee replacement,” says Dr. Gavi. “She was an older woman with severe pulmonary disease. When the anesthesiologists saw her in the preoperative waiting area and realized how sick she is, they wanted to cancel the surgery. But the surgeon told the anesthesiologist that this patient had been seen in our own preoperative clinic and cleared by a hospitalist.”
Dr. Gavi had done what is customary for an internist. He took a more in-depth look at her pulmonology and cardiac records, called her cardiologist for further history, and reassured the anesthesiologist and surgeon. The patient had her surgery.
The Future
“Perioperative co-management is becoming more of a visible need,” says Dr. Sivaprasad. “It bridges the gap between surgeons and internists.”
To those of his hospitalist colleagues who have little information and are a bit afraid to begin perioperative care practice, Dr. Usmani recommends attending a perioperative summit conference.
The session should teach how to set up a perioperative center and what to do when managing patients with certain conditions.
“Although you meet with patients preoperatively in an office setting, you don’t feel like a primary care physician,” Dr. Usmani says. “You feel as if you are a specialist. You are respected, and you are contributing to postoperative outcomes to the benefit of the patient.”
Perioperative patient management is also financially rewarding because reimbursement is higher than customary hospital medicine duties.
Dr. Jaffer, soon to be chief of the division of hospital medicine at the University of Miami Medical Center in Florida, is proud of the work he and his colleagues have done to grow the Cleveland Clinic perioperative summit. This third summit, in September, was organized in collaboration with the Society of Perioperative Assessment and Quality Improvement.
“I think this is something that every hospitalist should try,” Dr. Usmani says. “It is definitely a niche.” TH
Andrea Sattinger is a frequent contributor to The Hospitalist.
References
- Mangano DT. Perioperative medicine: NHLBI working group deliberations and recommendations. J Cardiothorac Vasc Anesth. 2004;18(1):1-6.
- Adebola O, Adesanya AO, Joshi GP. Hospitalists and anesthesiologists as perioperative physicians: Are their roles complementary? Proc. (Bayl Univ Med Cent) 2007 April;20(2):140-142.
The Hospitalist as Teacher
In addition to being expert in acute care clinical issues, hospitalists are knowledgeable in the ways and means of the hospital.
As teachers, hospitalists are ideally situated to improve house staff’s proficiency in areas such as evidence-based medicine, effective teamwork, communication, and quality improvement.1 These areas meld with hospitalist core competencies, writes David M. Pressel, MD, PhD, director of Inpatient Service and General Pediatrics at Alfred I. duPont Hospital for Children in Wilmington, Del.
What makes a great hospitalist a great teacher? “I don’t think there is anything special about a hospitalist [that would make him or her] a great teacher as opposed to another kind of physician,” Dr. Pressel says. “The only caveat to that is that presumably the hospitalist has specialized knowledge that they can impart similarly to [how] another doc can [impart information] in their specialized knowledge.”
Good teaching in all specialties has the same core features. But the key component a hospitalist would want to impart, he says, is that the hospitalist should maintain a holistic view of the patient.
In Dr. Pressel’s view, a great teacher loves what he does, has a sense of humor and makes learning fun or enjoyable, makes his lessons interactive, continually learns alongside his students, and knows his strengths and weaknesses.
“A great teacher has a sense of self-awareness as to what they do well and what they don’t do well,” he says. “Some people can be dynamic speakers for a mass audience and hold a lecture hall of 200 in thrall, but one on one, they’re not that strong. Others are the opposite. It is easy to teach people who are smart, dynamic, and interested; it is more challenging for someone who is a bit slower and [finds it] harder to get it.”
A good teacher also models for his trainees, especially in more delicate conversations, such as when giving bad news or asking patients and families to make difficult decisions.
“Residents should be watching you have those kinds of conversations,” says Howard Epstein, MD, a hospitalist and the medical director of the palliative care program at Regions Hospital, St. Paul, Minn. “[Rather than saying], ‘I’m just going to go have a family conference so why don’t you go take care of this, that, and the other thing,’ we should be saying, ‘This is really important. You need to come in and watch me do this now. This is just as important as putting in those discharge orders or putting in that central line.’ ”
Teach versus Coach
Jeffery G. Wiese, MD, associate professor of medicine at Tulane University in New Orleans, has thought a lot about what makes a great teacher and the differences between teaching information and teaching skills. To him it is the difference between teaching and coaching.
Dr. Wiese, who is on SHM’s board of directors, believes medical education is less about the dissemination of knowledge and more about how to apply that knowledge.
“Dissemination of knowledge is requisite but not sufficient,” says Dr. Wiese. “Clinical education is about performance because ultimately it doesn’t matter if the student knows a lot if he or she can’t put it in act for the benefit of their patient. And when you change that paradigm, then you move from being a good teacher to being a great coach.”
Dr. Wiese, who is also director of the Internal Medicine Residency Program and the chief of medicine at Tulane, presented a workshop at the SHM’s annual meeting in May, titled “Great Hospitalist to Great Teacher: Clinical Coaching.”
The five main points of the presentation are represented by the mnemonic VACUM: visualization, anticipation, choosing content that has utility, and motivation.
Visualization
Great teachers empower trainees to visualize how they will use the skill or knowledge for the benefit of the patient. The average lecture on hypotension, for example, disseminates the causes of hypotension and the treatment for each. The great coaching session, however, begins with getting the student to visualize using the skill. “Picture this: You are awakened from sleep on call to see a hypotensive patient,” Dr. Wiese says. “Do you see yourself in the room? Do you see the panic, the fear of those around you? Now visualize feeling the warmth of the patient’s extremities to exclude causes of low vascular resistance. Now imagine feeling the pulse to exclude bradycardia. Are you there? Now see yourself lowering the head of the bed and starting the IV to increase his preload.” The vision makes the content stick in the student’s memory.
Anticipation
“It’s not enough to teach a trainee how to do the skill,” says Dr. Wiese. “You have to anticipate where the trainee is going to get it confused and where the pitfalls are going to be in performing that skill down the road.”
This concept is analogous to that of someone giving directions to their house. Merely giving the student the destination (i.e., what they need to know) is not sufficient. Providing a heads up on where they might take a wrong turn ensures that they arrive at the destination.
In teaching hyperosmolar nonketotic coma (HONKC), for example, a great coach will begin with the warning: “Listen, this is where you could get confused. You might be tempted to ascribe a patient’s delirium to the osmotic effects of the high glucose, and while this can happen, it does not happen with a serum osmolarity of less than 340. You could forget that the cortisol surge that comes from infection is the leading cause of HONKC. Do you see yourself in the emergency department with that patient with HONKC? OK, when it happens, make sure you check the osmolarity; if it’s less than 340, do the lumbar puncture. Meningitis may just be the cause of the delirium and the infection that has caused the HONKC.”
—Jeffery G. Wiese, MD, associate professor of medicine, Tulane University Health Sciences Center, New Orleans
Content With Utility
Teaching the oppressive details about a disease beyond what the student learns from textbooks probably does not have the same utility for them as learning the fundamental principles of how to diagnose, treat, and prognosticate a disease, says Dr. Wiese.
Although most hospitalists train in internal medicine, with a lesser number training in pediatrics or family practice, all hospitalist instructors are still responsible for all students—including those who may be headed for radiology or orthopedics, for instance.
“I can teach the medical content that is of utility to that student’s performance,” Dr. Wiese says, “and I still share responsibility for their performance as an orthopedic surgeon, particularly with respect to how they manage medical disease.” The important lesson is that utility is defined by the learner. “If my student has chosen a future career in orthopedics, the content of the lectures will shift away from high-end internal medicine topics and toward what I think the future orthopedist before me needs to know.”
Motivation
“Should we have to motivate students to be great physicians both professionally and in terms of patient care and knowledge competence?” asks Dr. Wiese. “At the end of the day, the answer should be no; everyone has responsibility for motivating themselves. But, like a great coach, it is still the coach’s responsibly to ensure that when the players are tired, when they’re hungry, when they’ve got other things on their mind, they will stay motivated to want to learn the skill—even before we begin to teach the skill.
“A big portion of that motivation comes from figuring out what their career goals are and helping to link the medical knowledge or the skill that you’re teaching to those hooks, those things that are going to be of interest to them.”
There are four key components to motivation, says Dr. Wiese.
“First, remember the student’s name and use it often,” he says. “Remember that they will not care what you know, until they know that you care. Second, be physical. Reach out with the handshake or pat on the shoulder when things get done correctly. Third, stay focused on their hooks: Couch all content in terms of how they will use it in their future careers, and focus your analogies on their personal interests. For example, if a student likes music, my teaching of heart murmurs is going to use analogies of the song writer and performer.”
Game Time
“The medical knowledge is analogous to the play that the team will run or the skill of throwing the ball, but [there are a lot of other factors that influence what’s needed for] the game-time scenario,” Dr. Wiese says. “It’s how you interact with the clock for the game, how you interact with the referees, how you interact with your team mates, how you interact against the defense.”
To teach in order to prepare your “players” for the realities of the challenge—or the challenges of reality, as the case may be—teachers need to do more than unwittingly repeat the methods used when they were students.
“A student who is learning about a disease from Harrison’s or Cecil’s [textbooks] can focus on all the details and knowledge they need to know,” says Dr. Wiese. “But the thing that they can’t get out of the book and that they really need from the hospitalist coach is all that game-time instruction.”
In other words, hospitalists must consider with their students how to integrate their knowledge into their interactions with the hospital system.
In this era of PDAs, wireless networking, and access to the Internet, hospitalists are way past the point of having to keep all their acquired information in their heads, Dr. Wiese says. “The issue now is how do you ask the right questions and then access that knowledge—and then more importantly, how do you take that knowledge and put it into the ‘play’ that is the patient?” And that is what a student can’t get out of a book, he says—and what they need to get from their coach.
Be an Agent for Change
Don’t automatically transfer the way you learned or the ways you were taught into how you teach your own students. “Learning and teaching are very different,” says Dr. Wiese. “Learning knowledge is focused on the details. Teaching is much more [about] how you put that knowledge into play.”
That kind of transference is easily recognizable in a situation where a student asks “Can you teach me something this afternoon?” and the hospitalist replies, “Well, let me go home tonight and prepare, and then I’ll teach you.”
“What they’re saying is, ‘Let me read up, make a list of facts—maybe worse, maybe put it in PowerPoint,’ ” says Dr. Wiese. “The student could have done that on his or her own.”
Because hospitalists are intimately familiar with the hospital system, they serve as agents of change, Dr. Wiese says.
“Hospitalists are the key group at the first level of being able to take a student or resident or fellow and say, ‘These are the patients, we’re on hospital wards, and let me show you how to put in action the knowledge and skills you have to make a success for your patients,’ ” he says.
Hospitalists know where the system doesn’t work. “The great hospitalist doesn’t [face a problem and think], ‘Oh, woe is me; I’m hopelessly at the whim of the system that is broken,” says Dr. Wiese. “A great hospitalist consistently looks at [the situation] and asks, ‘How can I improve this system?’ The only way that medical students and residents can move out of the helpless role where [they see themselves as] servants of the system is to have hospitalist teachers who have a perspective of themselves as owners and who take responsibility for improving the system. Nothing has to be the way that it is,” says Dr. Wiese. TH
Andrea Sattinger is a frequent contributor to The Hospitalist.
References
- Pressel DM. Hospitalists in medical education: coming to an academic medical center near you. J Natl Med Assoc. 2006 Sep;98(9):1501-1504.
In addition to being expert in acute care clinical issues, hospitalists are knowledgeable in the ways and means of the hospital.
As teachers, hospitalists are ideally situated to improve house staff’s proficiency in areas such as evidence-based medicine, effective teamwork, communication, and quality improvement.1 These areas meld with hospitalist core competencies, writes David M. Pressel, MD, PhD, director of Inpatient Service and General Pediatrics at Alfred I. duPont Hospital for Children in Wilmington, Del.
What makes a great hospitalist a great teacher? “I don’t think there is anything special about a hospitalist [that would make him or her] a great teacher as opposed to another kind of physician,” Dr. Pressel says. “The only caveat to that is that presumably the hospitalist has specialized knowledge that they can impart similarly to [how] another doc can [impart information] in their specialized knowledge.”
Good teaching in all specialties has the same core features. But the key component a hospitalist would want to impart, he says, is that the hospitalist should maintain a holistic view of the patient.
In Dr. Pressel’s view, a great teacher loves what he does, has a sense of humor and makes learning fun or enjoyable, makes his lessons interactive, continually learns alongside his students, and knows his strengths and weaknesses.
“A great teacher has a sense of self-awareness as to what they do well and what they don’t do well,” he says. “Some people can be dynamic speakers for a mass audience and hold a lecture hall of 200 in thrall, but one on one, they’re not that strong. Others are the opposite. It is easy to teach people who are smart, dynamic, and interested; it is more challenging for someone who is a bit slower and [finds it] harder to get it.”
A good teacher also models for his trainees, especially in more delicate conversations, such as when giving bad news or asking patients and families to make difficult decisions.
“Residents should be watching you have those kinds of conversations,” says Howard Epstein, MD, a hospitalist and the medical director of the palliative care program at Regions Hospital, St. Paul, Minn. “[Rather than saying], ‘I’m just going to go have a family conference so why don’t you go take care of this, that, and the other thing,’ we should be saying, ‘This is really important. You need to come in and watch me do this now. This is just as important as putting in those discharge orders or putting in that central line.’ ”
Teach versus Coach
Jeffery G. Wiese, MD, associate professor of medicine at Tulane University in New Orleans, has thought a lot about what makes a great teacher and the differences between teaching information and teaching skills. To him it is the difference between teaching and coaching.
Dr. Wiese, who is on SHM’s board of directors, believes medical education is less about the dissemination of knowledge and more about how to apply that knowledge.
“Dissemination of knowledge is requisite but not sufficient,” says Dr. Wiese. “Clinical education is about performance because ultimately it doesn’t matter if the student knows a lot if he or she can’t put it in act for the benefit of their patient. And when you change that paradigm, then you move from being a good teacher to being a great coach.”
Dr. Wiese, who is also director of the Internal Medicine Residency Program and the chief of medicine at Tulane, presented a workshop at the SHM’s annual meeting in May, titled “Great Hospitalist to Great Teacher: Clinical Coaching.”
The five main points of the presentation are represented by the mnemonic VACUM: visualization, anticipation, choosing content that has utility, and motivation.
Visualization
Great teachers empower trainees to visualize how they will use the skill or knowledge for the benefit of the patient. The average lecture on hypotension, for example, disseminates the causes of hypotension and the treatment for each. The great coaching session, however, begins with getting the student to visualize using the skill. “Picture this: You are awakened from sleep on call to see a hypotensive patient,” Dr. Wiese says. “Do you see yourself in the room? Do you see the panic, the fear of those around you? Now visualize feeling the warmth of the patient’s extremities to exclude causes of low vascular resistance. Now imagine feeling the pulse to exclude bradycardia. Are you there? Now see yourself lowering the head of the bed and starting the IV to increase his preload.” The vision makes the content stick in the student’s memory.
Anticipation
“It’s not enough to teach a trainee how to do the skill,” says Dr. Wiese. “You have to anticipate where the trainee is going to get it confused and where the pitfalls are going to be in performing that skill down the road.”
This concept is analogous to that of someone giving directions to their house. Merely giving the student the destination (i.e., what they need to know) is not sufficient. Providing a heads up on where they might take a wrong turn ensures that they arrive at the destination.
In teaching hyperosmolar nonketotic coma (HONKC), for example, a great coach will begin with the warning: “Listen, this is where you could get confused. You might be tempted to ascribe a patient’s delirium to the osmotic effects of the high glucose, and while this can happen, it does not happen with a serum osmolarity of less than 340. You could forget that the cortisol surge that comes from infection is the leading cause of HONKC. Do you see yourself in the emergency department with that patient with HONKC? OK, when it happens, make sure you check the osmolarity; if it’s less than 340, do the lumbar puncture. Meningitis may just be the cause of the delirium and the infection that has caused the HONKC.”
—Jeffery G. Wiese, MD, associate professor of medicine, Tulane University Health Sciences Center, New Orleans
Content With Utility
Teaching the oppressive details about a disease beyond what the student learns from textbooks probably does not have the same utility for them as learning the fundamental principles of how to diagnose, treat, and prognosticate a disease, says Dr. Wiese.
Although most hospitalists train in internal medicine, with a lesser number training in pediatrics or family practice, all hospitalist instructors are still responsible for all students—including those who may be headed for radiology or orthopedics, for instance.
“I can teach the medical content that is of utility to that student’s performance,” Dr. Wiese says, “and I still share responsibility for their performance as an orthopedic surgeon, particularly with respect to how they manage medical disease.” The important lesson is that utility is defined by the learner. “If my student has chosen a future career in orthopedics, the content of the lectures will shift away from high-end internal medicine topics and toward what I think the future orthopedist before me needs to know.”
Motivation
“Should we have to motivate students to be great physicians both professionally and in terms of patient care and knowledge competence?” asks Dr. Wiese. “At the end of the day, the answer should be no; everyone has responsibility for motivating themselves. But, like a great coach, it is still the coach’s responsibly to ensure that when the players are tired, when they’re hungry, when they’ve got other things on their mind, they will stay motivated to want to learn the skill—even before we begin to teach the skill.
“A big portion of that motivation comes from figuring out what their career goals are and helping to link the medical knowledge or the skill that you’re teaching to those hooks, those things that are going to be of interest to them.”
There are four key components to motivation, says Dr. Wiese.
“First, remember the student’s name and use it often,” he says. “Remember that they will not care what you know, until they know that you care. Second, be physical. Reach out with the handshake or pat on the shoulder when things get done correctly. Third, stay focused on their hooks: Couch all content in terms of how they will use it in their future careers, and focus your analogies on their personal interests. For example, if a student likes music, my teaching of heart murmurs is going to use analogies of the song writer and performer.”
Game Time
“The medical knowledge is analogous to the play that the team will run or the skill of throwing the ball, but [there are a lot of other factors that influence what’s needed for] the game-time scenario,” Dr. Wiese says. “It’s how you interact with the clock for the game, how you interact with the referees, how you interact with your team mates, how you interact against the defense.”
To teach in order to prepare your “players” for the realities of the challenge—or the challenges of reality, as the case may be—teachers need to do more than unwittingly repeat the methods used when they were students.
“A student who is learning about a disease from Harrison’s or Cecil’s [textbooks] can focus on all the details and knowledge they need to know,” says Dr. Wiese. “But the thing that they can’t get out of the book and that they really need from the hospitalist coach is all that game-time instruction.”
In other words, hospitalists must consider with their students how to integrate their knowledge into their interactions with the hospital system.
In this era of PDAs, wireless networking, and access to the Internet, hospitalists are way past the point of having to keep all their acquired information in their heads, Dr. Wiese says. “The issue now is how do you ask the right questions and then access that knowledge—and then more importantly, how do you take that knowledge and put it into the ‘play’ that is the patient?” And that is what a student can’t get out of a book, he says—and what they need to get from their coach.
Be an Agent for Change
Don’t automatically transfer the way you learned or the ways you were taught into how you teach your own students. “Learning and teaching are very different,” says Dr. Wiese. “Learning knowledge is focused on the details. Teaching is much more [about] how you put that knowledge into play.”
That kind of transference is easily recognizable in a situation where a student asks “Can you teach me something this afternoon?” and the hospitalist replies, “Well, let me go home tonight and prepare, and then I’ll teach you.”
“What they’re saying is, ‘Let me read up, make a list of facts—maybe worse, maybe put it in PowerPoint,’ ” says Dr. Wiese. “The student could have done that on his or her own.”
Because hospitalists are intimately familiar with the hospital system, they serve as agents of change, Dr. Wiese says.
“Hospitalists are the key group at the first level of being able to take a student or resident or fellow and say, ‘These are the patients, we’re on hospital wards, and let me show you how to put in action the knowledge and skills you have to make a success for your patients,’ ” he says.
Hospitalists know where the system doesn’t work. “The great hospitalist doesn’t [face a problem and think], ‘Oh, woe is me; I’m hopelessly at the whim of the system that is broken,” says Dr. Wiese. “A great hospitalist consistently looks at [the situation] and asks, ‘How can I improve this system?’ The only way that medical students and residents can move out of the helpless role where [they see themselves as] servants of the system is to have hospitalist teachers who have a perspective of themselves as owners and who take responsibility for improving the system. Nothing has to be the way that it is,” says Dr. Wiese. TH
Andrea Sattinger is a frequent contributor to The Hospitalist.
References
- Pressel DM. Hospitalists in medical education: coming to an academic medical center near you. J Natl Med Assoc. 2006 Sep;98(9):1501-1504.
In addition to being expert in acute care clinical issues, hospitalists are knowledgeable in the ways and means of the hospital.
As teachers, hospitalists are ideally situated to improve house staff’s proficiency in areas such as evidence-based medicine, effective teamwork, communication, and quality improvement.1 These areas meld with hospitalist core competencies, writes David M. Pressel, MD, PhD, director of Inpatient Service and General Pediatrics at Alfred I. duPont Hospital for Children in Wilmington, Del.
What makes a great hospitalist a great teacher? “I don’t think there is anything special about a hospitalist [that would make him or her] a great teacher as opposed to another kind of physician,” Dr. Pressel says. “The only caveat to that is that presumably the hospitalist has specialized knowledge that they can impart similarly to [how] another doc can [impart information] in their specialized knowledge.”
Good teaching in all specialties has the same core features. But the key component a hospitalist would want to impart, he says, is that the hospitalist should maintain a holistic view of the patient.
In Dr. Pressel’s view, a great teacher loves what he does, has a sense of humor and makes learning fun or enjoyable, makes his lessons interactive, continually learns alongside his students, and knows his strengths and weaknesses.
“A great teacher has a sense of self-awareness as to what they do well and what they don’t do well,” he says. “Some people can be dynamic speakers for a mass audience and hold a lecture hall of 200 in thrall, but one on one, they’re not that strong. Others are the opposite. It is easy to teach people who are smart, dynamic, and interested; it is more challenging for someone who is a bit slower and [finds it] harder to get it.”
A good teacher also models for his trainees, especially in more delicate conversations, such as when giving bad news or asking patients and families to make difficult decisions.
“Residents should be watching you have those kinds of conversations,” says Howard Epstein, MD, a hospitalist and the medical director of the palliative care program at Regions Hospital, St. Paul, Minn. “[Rather than saying], ‘I’m just going to go have a family conference so why don’t you go take care of this, that, and the other thing,’ we should be saying, ‘This is really important. You need to come in and watch me do this now. This is just as important as putting in those discharge orders or putting in that central line.’ ”
Teach versus Coach
Jeffery G. Wiese, MD, associate professor of medicine at Tulane University in New Orleans, has thought a lot about what makes a great teacher and the differences between teaching information and teaching skills. To him it is the difference between teaching and coaching.
Dr. Wiese, who is on SHM’s board of directors, believes medical education is less about the dissemination of knowledge and more about how to apply that knowledge.
“Dissemination of knowledge is requisite but not sufficient,” says Dr. Wiese. “Clinical education is about performance because ultimately it doesn’t matter if the student knows a lot if he or she can’t put it in act for the benefit of their patient. And when you change that paradigm, then you move from being a good teacher to being a great coach.”
Dr. Wiese, who is also director of the Internal Medicine Residency Program and the chief of medicine at Tulane, presented a workshop at the SHM’s annual meeting in May, titled “Great Hospitalist to Great Teacher: Clinical Coaching.”
The five main points of the presentation are represented by the mnemonic VACUM: visualization, anticipation, choosing content that has utility, and motivation.
Visualization
Great teachers empower trainees to visualize how they will use the skill or knowledge for the benefit of the patient. The average lecture on hypotension, for example, disseminates the causes of hypotension and the treatment for each. The great coaching session, however, begins with getting the student to visualize using the skill. “Picture this: You are awakened from sleep on call to see a hypotensive patient,” Dr. Wiese says. “Do you see yourself in the room? Do you see the panic, the fear of those around you? Now visualize feeling the warmth of the patient’s extremities to exclude causes of low vascular resistance. Now imagine feeling the pulse to exclude bradycardia. Are you there? Now see yourself lowering the head of the bed and starting the IV to increase his preload.” The vision makes the content stick in the student’s memory.
Anticipation
“It’s not enough to teach a trainee how to do the skill,” says Dr. Wiese. “You have to anticipate where the trainee is going to get it confused and where the pitfalls are going to be in performing that skill down the road.”
This concept is analogous to that of someone giving directions to their house. Merely giving the student the destination (i.e., what they need to know) is not sufficient. Providing a heads up on where they might take a wrong turn ensures that they arrive at the destination.
In teaching hyperosmolar nonketotic coma (HONKC), for example, a great coach will begin with the warning: “Listen, this is where you could get confused. You might be tempted to ascribe a patient’s delirium to the osmotic effects of the high glucose, and while this can happen, it does not happen with a serum osmolarity of less than 340. You could forget that the cortisol surge that comes from infection is the leading cause of HONKC. Do you see yourself in the emergency department with that patient with HONKC? OK, when it happens, make sure you check the osmolarity; if it’s less than 340, do the lumbar puncture. Meningitis may just be the cause of the delirium and the infection that has caused the HONKC.”
—Jeffery G. Wiese, MD, associate professor of medicine, Tulane University Health Sciences Center, New Orleans
Content With Utility
Teaching the oppressive details about a disease beyond what the student learns from textbooks probably does not have the same utility for them as learning the fundamental principles of how to diagnose, treat, and prognosticate a disease, says Dr. Wiese.
Although most hospitalists train in internal medicine, with a lesser number training in pediatrics or family practice, all hospitalist instructors are still responsible for all students—including those who may be headed for radiology or orthopedics, for instance.
“I can teach the medical content that is of utility to that student’s performance,” Dr. Wiese says, “and I still share responsibility for their performance as an orthopedic surgeon, particularly with respect to how they manage medical disease.” The important lesson is that utility is defined by the learner. “If my student has chosen a future career in orthopedics, the content of the lectures will shift away from high-end internal medicine topics and toward what I think the future orthopedist before me needs to know.”
Motivation
“Should we have to motivate students to be great physicians both professionally and in terms of patient care and knowledge competence?” asks Dr. Wiese. “At the end of the day, the answer should be no; everyone has responsibility for motivating themselves. But, like a great coach, it is still the coach’s responsibly to ensure that when the players are tired, when they’re hungry, when they’ve got other things on their mind, they will stay motivated to want to learn the skill—even before we begin to teach the skill.
“A big portion of that motivation comes from figuring out what their career goals are and helping to link the medical knowledge or the skill that you’re teaching to those hooks, those things that are going to be of interest to them.”
There are four key components to motivation, says Dr. Wiese.
“First, remember the student’s name and use it often,” he says. “Remember that they will not care what you know, until they know that you care. Second, be physical. Reach out with the handshake or pat on the shoulder when things get done correctly. Third, stay focused on their hooks: Couch all content in terms of how they will use it in their future careers, and focus your analogies on their personal interests. For example, if a student likes music, my teaching of heart murmurs is going to use analogies of the song writer and performer.”
Game Time
“The medical knowledge is analogous to the play that the team will run or the skill of throwing the ball, but [there are a lot of other factors that influence what’s needed for] the game-time scenario,” Dr. Wiese says. “It’s how you interact with the clock for the game, how you interact with the referees, how you interact with your team mates, how you interact against the defense.”
To teach in order to prepare your “players” for the realities of the challenge—or the challenges of reality, as the case may be—teachers need to do more than unwittingly repeat the methods used when they were students.
“A student who is learning about a disease from Harrison’s or Cecil’s [textbooks] can focus on all the details and knowledge they need to know,” says Dr. Wiese. “But the thing that they can’t get out of the book and that they really need from the hospitalist coach is all that game-time instruction.”
In other words, hospitalists must consider with their students how to integrate their knowledge into their interactions with the hospital system.
In this era of PDAs, wireless networking, and access to the Internet, hospitalists are way past the point of having to keep all their acquired information in their heads, Dr. Wiese says. “The issue now is how do you ask the right questions and then access that knowledge—and then more importantly, how do you take that knowledge and put it into the ‘play’ that is the patient?” And that is what a student can’t get out of a book, he says—and what they need to get from their coach.
Be an Agent for Change
Don’t automatically transfer the way you learned or the ways you were taught into how you teach your own students. “Learning and teaching are very different,” says Dr. Wiese. “Learning knowledge is focused on the details. Teaching is much more [about] how you put that knowledge into play.”
That kind of transference is easily recognizable in a situation where a student asks “Can you teach me something this afternoon?” and the hospitalist replies, “Well, let me go home tonight and prepare, and then I’ll teach you.”
“What they’re saying is, ‘Let me read up, make a list of facts—maybe worse, maybe put it in PowerPoint,’ ” says Dr. Wiese. “The student could have done that on his or her own.”
Because hospitalists are intimately familiar with the hospital system, they serve as agents of change, Dr. Wiese says.
“Hospitalists are the key group at the first level of being able to take a student or resident or fellow and say, ‘These are the patients, we’re on hospital wards, and let me show you how to put in action the knowledge and skills you have to make a success for your patients,’ ” he says.
Hospitalists know where the system doesn’t work. “The great hospitalist doesn’t [face a problem and think], ‘Oh, woe is me; I’m hopelessly at the whim of the system that is broken,” says Dr. Wiese. “A great hospitalist consistently looks at [the situation] and asks, ‘How can I improve this system?’ The only way that medical students and residents can move out of the helpless role where [they see themselves as] servants of the system is to have hospitalist teachers who have a perspective of themselves as owners and who take responsibility for improving the system. Nothing has to be the way that it is,” says Dr. Wiese. TH
Andrea Sattinger is a frequent contributor to The Hospitalist.
References
- Pressel DM. Hospitalists in medical education: coming to an academic medical center near you. J Natl Med Assoc. 2006 Sep;98(9):1501-1504.
Close the Loop
This is the second of a two-part series examining medical errors. Part 1 addressed thought processes hospitalists use that may lead to mistaken diagnoses (October 2007, p. 36). Part 2 examines what healthcare corporations are doing to improve diagnoses and reduce errors.
Pilots taking off, Swiss cheese, low-hanging fruit. Talk to hospitalists about the issue of medical errors and the analogies come quickly.
Ever since 2000’s landmark Institute of Medicine report “To Err is Human: Building a Safer Health System” found that anywhere from 40,000 to 100,000 patients incur injury or die every year because of medical errors, debate has been constant.
Medical literature is abundant on this topic. The Joint Commission, National Center for Patient Safety, Agency for Health Care Research and Quality, and myriad other organizations and institutions, including SHM, are all helping providers and hospitals solve the problems by establishing goals, standards, guidelines, and policies.
—Evan Falchuk, president, Best Doctors Inc., Boston
Definitions and Paradigms
Best-practice recommendations for reducing errors are generally based on two essential principles: using a systems-based approach to patient safety and creating an environment that supports open dialogue about errors, their causes, and strategies for prevention.
Terminology is a key factor. The terms “error” and “mistake” carry an emotional component associated with embarrassment and shame. Healthcare providers don’t like to be associated with errors. There is an accompanying fear of litigation, and people, perhaps especially physicians, don’t want to be known as someone who was sued.
“The language we use to talk about these issues is important,” says Janet Nagamine, MD, part-time hospitalist at Kaiser Permanente Santa Clara Medical Center in Calif. and current chair of SHM’s quality and patient safety committee. In fact, because of the negativity around the terms “misdiagnosis” and “delay in diagnosis” she advocates using the term “unintended adverse event” in order to appear more neutral.
“The term error is extremely threatening and scary to any health professional because it implies a personal failure,” says Dr. Nagamine. The goal when it comes to errors is essentially to look for the how—not the who.
Reporting medical errors is one thing, but reporting misdiagnoses is another, says Lakshmi Halasyamani, MD, vice chair for the department of internal medicine at St. Joseph’s Mercy Hospital in Ann Arbor, Mich., and SHM board member. “We don’t really talk about misdiagnosis,” she says. “That’s partly because we have tended to assign more individual blame for misdiagnoses.”
Drs. Nagamine and Halasyamani agree that altering the way of viewing errors means nurturing culture change.
“We have made very little headway helping physicians understand that in the course of their careers there will be misdiagnoses and the best of physicians have misdiagnoses,” says Dr. Halasyamani. “We are not developmentally at the same stage that we are with talking about medical errors.”
She believes this is largely a professionalism issue that first means normalizing the issue of misdiagnosis. “It is kind of ludicrous to think that you will practice medicine over 40 years and not have a misdiagnosis,” she says. “But we don’t look at it from that perspective when we begin to orient trainees.”
National Efforts
To the people at the U.S. Pharmacopeia Center for the Advancement of Patient Safety (USP), the arrival of universal electronic medical records (EMR) in the coming decade will be a boon to the error-reduction effort.
“Eventually we will all have our health information stored electronically for easy retrieval,” says Rodney W. Hicks, PhD, ARNP, manager, patient safety research and practice for the USP and first author on its most recent report. The beginning of regional networks for EMR is taking hold.
“Even before the IOM report, the USP was familiar with intensivists,” says Dr. Hicks. “We recognize hospitalists as experts who bring efficiency and effectiveness to the healthcare system.”
The USP maintains perhaps the largest database of medication errors in the world.1 Each year the USP issues a report that focuses on one topic and builds its knowledge base.
This year’s report focuses exclusively on the perioperative continuum of care. Last year’s covered ICU- and radiology-related errors. Two years ago the report was a five-year data summary of errors occurring primarily in hospitals.
“The area of errors due to breakdowns in handoffs remains a huge problem for diagnosis and the continuity of care,” says Shawn C. Becker, MS, BSN, RN, director of patient safety initiatives for the USP.
Classification
In general, errors are divided into those that stem from individual factors and those that are system-related, which include environmental and organizational factors.
Environmental risks are often related to human factors. Dr. Nagamine offers an aviation analogy to demonstrate the many pulls on caregivers’ attention.
“What happens in a cockpit at take off is that you are not allowed to talk about anything other than the take-off checklist,” she says. “In medicine, we have nurses’ stations or medication carts in the middle of the hallway, so nurses are preparing meds and people are tugging on their shoulder and interrupting them during a critical task.”
Organizational factors involve culture and priorities. If your organization says it values quality and safety but doesn’t put in place policies and processes to support it, that affects diagnostics and error-free performance.
Market Drivers
“The discussion about quality is driven by medical error,” says Evan Falchuk, president of Best Doctors Inc., based in Boston. “But the issue is more interesting than simply looking for mistakes.”
Best Doctors partners with employers and health plans to help members with serious illnesses make sure they have the right diagnosis and treatment. Members can consult with specialists who assess diagnoses and can recommend treatment. The firm believes this is the best way to measure quality, and consumers around the world increasingly agree: The company serves more than 10 million people in 30 countries.
Best Doctors was founded in 1989 by two internists: Falchuk’s father, Kenneth H. Falchuk, MD, a professor of medicine at Harvard University Medical School, and Jose Halperin, MD, an associate professor of medicine at Harvard. The service they created is one in which doctors review a patient’s medical information, identify the important issues, and consult with leading experts from their peer-reviewed database. The company then has clinicians work with the patient and his or her doctor to ensure that the patient is getting appropriate care. The process has identified incorrect diagnosis or treatment in more than half of reviewed cases.
“Hospitalists should think about quality in terms of things happening outside the hospital,” says Falchuk. “The informed, demanding consumer is coming to healthcare, and their expectations are clear: to be paid attention to, to have all of their questions answered, and to be certain that their diagnosis and treatment are correct.” These sentiments affect how hospitals do business.
The increasing amount of medical information patients can find on the Internet can raise questions in their minds. “Patients want to trust their doctors,” Falchuk says. “But when the patient has lots of information and questions and finds it difficult to spend as much time as they would like with their doctor, trust is eroded—and patients start to wonder if their doctor is doing the right thing.”
The complexity of modern medicine, with new diagnoses, treatments, and testing, and ultra-specialized experts, can sometimes—ironically—lead to lesser quality.
“It is more important than ever before that doctors with differing perspectives discuss each case,” says Falchuk. “But doctors complain that the system, often because of constraints imposed by managed care, only allows for episodic interactions like that. If that kind of interaction can be made the norm, it will give patients an extraordinary amount of comfort as to the quality of their care.”
Falchuk believes the tipping point for combating errors is being reached—at least from the business point of view.
“With major employers, as many as one in 200 employees call us for help,” he says. “That is close to the incidence rate of the illnesses we commonly see: cancer, heart problems, and undiagnosed situations. When you see this flood of demand, you say, ‘Something is going on that is driving this.’ ”
These market-based factors are driving hospitals to publish and compare rates for process of care and mortality, and many medical centers are publishing report cards. With the advent of advanced technology, hospital and provider performance will be increasingly apparent and transparent. Corporations and institutions will have to be less guarded about what they share publicly as their public accountability is increased.
Interventions, Feedback
The healthcare industry has embraced British psychologist James Reason’s 1990 Swiss cheese model of error as a means of tackling the cumulative effects that cause adverse events. The model conceptualizes the factors that contributed to an error as holes in slices of Swiss cheese. Only when the holes line up does the adverse event occur; placing barriers at one or more of the holes “traps the error” from being realized.
For instance, Best Doctors notes “potholes” in the reading stage of pathology.
“We see many cases of underdiagnosis or even misdiagnosis based on one of the most difficult steps: a pathology review,” says Falchuk. “With new, specifically targeted treatments, getting that right is extremely significant.” Best Doctors experts often recommend having pathology re-reviewed. “I wouldn’t call this error, but patients view it as a question of quality,” he says.
Integrating technology with observation skills is an important way hospitals are working to improve diagnostics and reduce error.
Because the same factors contribute to a near miss as to an actual event, studying the patterns of near misses can provide a wealth of information.
“I heard some statistics that for every 19 near misses, you’re going to have one event,” says Dr. Nagamine. If on a particular day, a provider was fatigued or overtaxed and didn’t catch a contributing factor that is a risk—termed a “latent condition”—that’s when the holes line up. “An event is never just the result of one thing or one person; it is a combination of factors,” says Dr. Nagamine.
One example of this concerns an element in the policy for discharge bundles that institutions establish to better manage transfer of care. When lab results become available only after a patient’s discharge, it increases the risk for delays in diagnosis. Electronically placing the test results into the primary care physician’s e-mail inbox helps to “close the loop,” says Dr. Nagamine. “That information gets to somebody, and we’re clear on who that somebody is. We are putting in place those types of interventions—which are really the low-hanging fruit.”
Culture Change
Opening up about adverse events and providing feedback creates a different awareness about the risks surrounding the event.
“The look-alike, sound-alike medications are an example,” Dr. Nagamine says. “I went up to the unit and said, ‘A nurse recorded that she almost gave hydralazine instead of hydroxyzine—has that ever happened to you?’ The first three nurses I asked said, ‘Yes,’ ‘Yes,’ ‘Yes.’ Until I ask these types of questions, I don’t know. And until you can make it safe for your staff to talk, you will not have good information.”
Although this is the approach most of the safety world and quality world is embracing, it is not how most clinicians on the frontline view it.
“We are trying to educate people about a framework in which to think about this,” says Dr. Nagamine. “It is not constructive to point fingers, but it is important to give people feedback about how the event happened. It is far more constructive to look at the entire system and ask, ‘How did we fail here? What was your piece of it? What was the system’s piece of it?’ ”
Because of the connection between litigation and adverse events, changing the culture is a complex imperative. But providers must recognize that systems failures are involved in about 75% to 80% of medical malpractice cases—whether that involves communication breakdowns, inadequate availability of information, or a host of other factors. The individual, environment, and organization are linked.
Reducing negativity and sensitivity around the terms associated with error and reframing thinking toward prevention are important.
“There is a richness of information that comes once you change the culture from blaming to fixing,” says Dr. Nagamine. Providing feedback to frontline practitioners is key, as is thanking those who report. “It increases providers’ awareness about where the hot spots and vulnerabilities are and how to stay out of trouble. Simply by giving them information about an event raises their awareness of the magnitude of certain types of issues,” she explains.
When Dr. Nagamine led a safety initiative on the ICU floor consisting of human factors training and a new system for reporting events, the number of reports “went through roof,” she says. “My new problem was not that people were not reporting; it was being overwhelmed with the information that was coming in. We were able to create a culture of safety that made it safe to report and consequently had much better information from which we could devise prevention strategies.”
SHM, in planning to co-create standards for focused practice with the American Board of Internal Medicine, intends to promote the standards of professionalism along with other standards. The issue of personal accountability, although a part of that, has been less of a focus to date. In the future, all institutions may have technology hospitalists can use to learn whether the discharge diagnosis was correct in the months and years that followed. Will the culture be emotionally ready to handle what technology can offer?
“We will need to own it when things go well and when things don’t go well or when we are wrong,” says Dr. Halasyamani. “We need to be able to investigate the distribution of the reasons for misdiagnosis, determine how many of those problems are systems issues, and devise strategies to address them.” In a sense, she says, everything can be viewed as a system issue unless actions are egregious and malicious.
Yet when physicians are associated with an adverse event, research shows they feel they have little support to talk about it.
“The system we have in place has begun to try to address some of the issues related to system errors,” says Dr. Halasyamani. “But what if an individual does have an error? What systems do we have in place to support that person in the recovery? And along the way if we find people who are having these issues over and over again, we need to design processes to deal with that.”
One particular focus of SHM’s transfer-of-care initiative concerns communication surrounding handoffs. “We are setting those standards and thinking about what kinds of technology tools can help make those standards easier to adhere to and easier to implement,” says Dr. Halasyamani. TH
Andrea Sattinger is a frequent contributor to The Hospitalist.
This is the second of a two-part series examining medical errors. Part 1 addressed thought processes hospitalists use that may lead to mistaken diagnoses (October 2007, p. 36). Part 2 examines what healthcare corporations are doing to improve diagnoses and reduce errors.
Pilots taking off, Swiss cheese, low-hanging fruit. Talk to hospitalists about the issue of medical errors and the analogies come quickly.
Ever since 2000’s landmark Institute of Medicine report “To Err is Human: Building a Safer Health System” found that anywhere from 40,000 to 100,000 patients incur injury or die every year because of medical errors, debate has been constant.
Medical literature is abundant on this topic. The Joint Commission, National Center for Patient Safety, Agency for Health Care Research and Quality, and myriad other organizations and institutions, including SHM, are all helping providers and hospitals solve the problems by establishing goals, standards, guidelines, and policies.
—Evan Falchuk, president, Best Doctors Inc., Boston
Definitions and Paradigms
Best-practice recommendations for reducing errors are generally based on two essential principles: using a systems-based approach to patient safety and creating an environment that supports open dialogue about errors, their causes, and strategies for prevention.
Terminology is a key factor. The terms “error” and “mistake” carry an emotional component associated with embarrassment and shame. Healthcare providers don’t like to be associated with errors. There is an accompanying fear of litigation, and people, perhaps especially physicians, don’t want to be known as someone who was sued.
“The language we use to talk about these issues is important,” says Janet Nagamine, MD, part-time hospitalist at Kaiser Permanente Santa Clara Medical Center in Calif. and current chair of SHM’s quality and patient safety committee. In fact, because of the negativity around the terms “misdiagnosis” and “delay in diagnosis” she advocates using the term “unintended adverse event” in order to appear more neutral.
“The term error is extremely threatening and scary to any health professional because it implies a personal failure,” says Dr. Nagamine. The goal when it comes to errors is essentially to look for the how—not the who.
Reporting medical errors is one thing, but reporting misdiagnoses is another, says Lakshmi Halasyamani, MD, vice chair for the department of internal medicine at St. Joseph’s Mercy Hospital in Ann Arbor, Mich., and SHM board member. “We don’t really talk about misdiagnosis,” she says. “That’s partly because we have tended to assign more individual blame for misdiagnoses.”
Drs. Nagamine and Halasyamani agree that altering the way of viewing errors means nurturing culture change.
“We have made very little headway helping physicians understand that in the course of their careers there will be misdiagnoses and the best of physicians have misdiagnoses,” says Dr. Halasyamani. “We are not developmentally at the same stage that we are with talking about medical errors.”
She believes this is largely a professionalism issue that first means normalizing the issue of misdiagnosis. “It is kind of ludicrous to think that you will practice medicine over 40 years and not have a misdiagnosis,” she says. “But we don’t look at it from that perspective when we begin to orient trainees.”
National Efforts
To the people at the U.S. Pharmacopeia Center for the Advancement of Patient Safety (USP), the arrival of universal electronic medical records (EMR) in the coming decade will be a boon to the error-reduction effort.
“Eventually we will all have our health information stored electronically for easy retrieval,” says Rodney W. Hicks, PhD, ARNP, manager, patient safety research and practice for the USP and first author on its most recent report. The beginning of regional networks for EMR is taking hold.
“Even before the IOM report, the USP was familiar with intensivists,” says Dr. Hicks. “We recognize hospitalists as experts who bring efficiency and effectiveness to the healthcare system.”
The USP maintains perhaps the largest database of medication errors in the world.1 Each year the USP issues a report that focuses on one topic and builds its knowledge base.
This year’s report focuses exclusively on the perioperative continuum of care. Last year’s covered ICU- and radiology-related errors. Two years ago the report was a five-year data summary of errors occurring primarily in hospitals.
“The area of errors due to breakdowns in handoffs remains a huge problem for diagnosis and the continuity of care,” says Shawn C. Becker, MS, BSN, RN, director of patient safety initiatives for the USP.
Classification
In general, errors are divided into those that stem from individual factors and those that are system-related, which include environmental and organizational factors.
Environmental risks are often related to human factors. Dr. Nagamine offers an aviation analogy to demonstrate the many pulls on caregivers’ attention.
“What happens in a cockpit at take off is that you are not allowed to talk about anything other than the take-off checklist,” she says. “In medicine, we have nurses’ stations or medication carts in the middle of the hallway, so nurses are preparing meds and people are tugging on their shoulder and interrupting them during a critical task.”
Organizational factors involve culture and priorities. If your organization says it values quality and safety but doesn’t put in place policies and processes to support it, that affects diagnostics and error-free performance.
Market Drivers
“The discussion about quality is driven by medical error,” says Evan Falchuk, president of Best Doctors Inc., based in Boston. “But the issue is more interesting than simply looking for mistakes.”
Best Doctors partners with employers and health plans to help members with serious illnesses make sure they have the right diagnosis and treatment. Members can consult with specialists who assess diagnoses and can recommend treatment. The firm believes this is the best way to measure quality, and consumers around the world increasingly agree: The company serves more than 10 million people in 30 countries.
Best Doctors was founded in 1989 by two internists: Falchuk’s father, Kenneth H. Falchuk, MD, a professor of medicine at Harvard University Medical School, and Jose Halperin, MD, an associate professor of medicine at Harvard. The service they created is one in which doctors review a patient’s medical information, identify the important issues, and consult with leading experts from their peer-reviewed database. The company then has clinicians work with the patient and his or her doctor to ensure that the patient is getting appropriate care. The process has identified incorrect diagnosis or treatment in more than half of reviewed cases.
“Hospitalists should think about quality in terms of things happening outside the hospital,” says Falchuk. “The informed, demanding consumer is coming to healthcare, and their expectations are clear: to be paid attention to, to have all of their questions answered, and to be certain that their diagnosis and treatment are correct.” These sentiments affect how hospitals do business.
The increasing amount of medical information patients can find on the Internet can raise questions in their minds. “Patients want to trust their doctors,” Falchuk says. “But when the patient has lots of information and questions and finds it difficult to spend as much time as they would like with their doctor, trust is eroded—and patients start to wonder if their doctor is doing the right thing.”
The complexity of modern medicine, with new diagnoses, treatments, and testing, and ultra-specialized experts, can sometimes—ironically—lead to lesser quality.
“It is more important than ever before that doctors with differing perspectives discuss each case,” says Falchuk. “But doctors complain that the system, often because of constraints imposed by managed care, only allows for episodic interactions like that. If that kind of interaction can be made the norm, it will give patients an extraordinary amount of comfort as to the quality of their care.”
Falchuk believes the tipping point for combating errors is being reached—at least from the business point of view.
“With major employers, as many as one in 200 employees call us for help,” he says. “That is close to the incidence rate of the illnesses we commonly see: cancer, heart problems, and undiagnosed situations. When you see this flood of demand, you say, ‘Something is going on that is driving this.’ ”
These market-based factors are driving hospitals to publish and compare rates for process of care and mortality, and many medical centers are publishing report cards. With the advent of advanced technology, hospital and provider performance will be increasingly apparent and transparent. Corporations and institutions will have to be less guarded about what they share publicly as their public accountability is increased.
Interventions, Feedback
The healthcare industry has embraced British psychologist James Reason’s 1990 Swiss cheese model of error as a means of tackling the cumulative effects that cause adverse events. The model conceptualizes the factors that contributed to an error as holes in slices of Swiss cheese. Only when the holes line up does the adverse event occur; placing barriers at one or more of the holes “traps the error” from being realized.
For instance, Best Doctors notes “potholes” in the reading stage of pathology.
“We see many cases of underdiagnosis or even misdiagnosis based on one of the most difficult steps: a pathology review,” says Falchuk. “With new, specifically targeted treatments, getting that right is extremely significant.” Best Doctors experts often recommend having pathology re-reviewed. “I wouldn’t call this error, but patients view it as a question of quality,” he says.
Integrating technology with observation skills is an important way hospitals are working to improve diagnostics and reduce error.
Because the same factors contribute to a near miss as to an actual event, studying the patterns of near misses can provide a wealth of information.
“I heard some statistics that for every 19 near misses, you’re going to have one event,” says Dr. Nagamine. If on a particular day, a provider was fatigued or overtaxed and didn’t catch a contributing factor that is a risk—termed a “latent condition”—that’s when the holes line up. “An event is never just the result of one thing or one person; it is a combination of factors,” says Dr. Nagamine.
One example of this concerns an element in the policy for discharge bundles that institutions establish to better manage transfer of care. When lab results become available only after a patient’s discharge, it increases the risk for delays in diagnosis. Electronically placing the test results into the primary care physician’s e-mail inbox helps to “close the loop,” says Dr. Nagamine. “That information gets to somebody, and we’re clear on who that somebody is. We are putting in place those types of interventions—which are really the low-hanging fruit.”
Culture Change
Opening up about adverse events and providing feedback creates a different awareness about the risks surrounding the event.
“The look-alike, sound-alike medications are an example,” Dr. Nagamine says. “I went up to the unit and said, ‘A nurse recorded that she almost gave hydralazine instead of hydroxyzine—has that ever happened to you?’ The first three nurses I asked said, ‘Yes,’ ‘Yes,’ ‘Yes.’ Until I ask these types of questions, I don’t know. And until you can make it safe for your staff to talk, you will not have good information.”
Although this is the approach most of the safety world and quality world is embracing, it is not how most clinicians on the frontline view it.
“We are trying to educate people about a framework in which to think about this,” says Dr. Nagamine. “It is not constructive to point fingers, but it is important to give people feedback about how the event happened. It is far more constructive to look at the entire system and ask, ‘How did we fail here? What was your piece of it? What was the system’s piece of it?’ ”
Because of the connection between litigation and adverse events, changing the culture is a complex imperative. But providers must recognize that systems failures are involved in about 75% to 80% of medical malpractice cases—whether that involves communication breakdowns, inadequate availability of information, or a host of other factors. The individual, environment, and organization are linked.
Reducing negativity and sensitivity around the terms associated with error and reframing thinking toward prevention are important.
“There is a richness of information that comes once you change the culture from blaming to fixing,” says Dr. Nagamine. Providing feedback to frontline practitioners is key, as is thanking those who report. “It increases providers’ awareness about where the hot spots and vulnerabilities are and how to stay out of trouble. Simply by giving them information about an event raises their awareness of the magnitude of certain types of issues,” she explains.
When Dr. Nagamine led a safety initiative on the ICU floor consisting of human factors training and a new system for reporting events, the number of reports “went through roof,” she says. “My new problem was not that people were not reporting; it was being overwhelmed with the information that was coming in. We were able to create a culture of safety that made it safe to report and consequently had much better information from which we could devise prevention strategies.”
SHM, in planning to co-create standards for focused practice with the American Board of Internal Medicine, intends to promote the standards of professionalism along with other standards. The issue of personal accountability, although a part of that, has been less of a focus to date. In the future, all institutions may have technology hospitalists can use to learn whether the discharge diagnosis was correct in the months and years that followed. Will the culture be emotionally ready to handle what technology can offer?
“We will need to own it when things go well and when things don’t go well or when we are wrong,” says Dr. Halasyamani. “We need to be able to investigate the distribution of the reasons for misdiagnosis, determine how many of those problems are systems issues, and devise strategies to address them.” In a sense, she says, everything can be viewed as a system issue unless actions are egregious and malicious.
Yet when physicians are associated with an adverse event, research shows they feel they have little support to talk about it.
“The system we have in place has begun to try to address some of the issues related to system errors,” says Dr. Halasyamani. “But what if an individual does have an error? What systems do we have in place to support that person in the recovery? And along the way if we find people who are having these issues over and over again, we need to design processes to deal with that.”
One particular focus of SHM’s transfer-of-care initiative concerns communication surrounding handoffs. “We are setting those standards and thinking about what kinds of technology tools can help make those standards easier to adhere to and easier to implement,” says Dr. Halasyamani. TH
Andrea Sattinger is a frequent contributor to The Hospitalist.
This is the second of a two-part series examining medical errors. Part 1 addressed thought processes hospitalists use that may lead to mistaken diagnoses (October 2007, p. 36). Part 2 examines what healthcare corporations are doing to improve diagnoses and reduce errors.
Pilots taking off, Swiss cheese, low-hanging fruit. Talk to hospitalists about the issue of medical errors and the analogies come quickly.
Ever since 2000’s landmark Institute of Medicine report “To Err is Human: Building a Safer Health System” found that anywhere from 40,000 to 100,000 patients incur injury or die every year because of medical errors, debate has been constant.
Medical literature is abundant on this topic. The Joint Commission, National Center for Patient Safety, Agency for Health Care Research and Quality, and myriad other organizations and institutions, including SHM, are all helping providers and hospitals solve the problems by establishing goals, standards, guidelines, and policies.
—Evan Falchuk, president, Best Doctors Inc., Boston
Definitions and Paradigms
Best-practice recommendations for reducing errors are generally based on two essential principles: using a systems-based approach to patient safety and creating an environment that supports open dialogue about errors, their causes, and strategies for prevention.
Terminology is a key factor. The terms “error” and “mistake” carry an emotional component associated with embarrassment and shame. Healthcare providers don’t like to be associated with errors. There is an accompanying fear of litigation, and people, perhaps especially physicians, don’t want to be known as someone who was sued.
“The language we use to talk about these issues is important,” says Janet Nagamine, MD, part-time hospitalist at Kaiser Permanente Santa Clara Medical Center in Calif. and current chair of SHM’s quality and patient safety committee. In fact, because of the negativity around the terms “misdiagnosis” and “delay in diagnosis” she advocates using the term “unintended adverse event” in order to appear more neutral.
“The term error is extremely threatening and scary to any health professional because it implies a personal failure,” says Dr. Nagamine. The goal when it comes to errors is essentially to look for the how—not the who.
Reporting medical errors is one thing, but reporting misdiagnoses is another, says Lakshmi Halasyamani, MD, vice chair for the department of internal medicine at St. Joseph’s Mercy Hospital in Ann Arbor, Mich., and SHM board member. “We don’t really talk about misdiagnosis,” she says. “That’s partly because we have tended to assign more individual blame for misdiagnoses.”
Drs. Nagamine and Halasyamani agree that altering the way of viewing errors means nurturing culture change.
“We have made very little headway helping physicians understand that in the course of their careers there will be misdiagnoses and the best of physicians have misdiagnoses,” says Dr. Halasyamani. “We are not developmentally at the same stage that we are with talking about medical errors.”
She believes this is largely a professionalism issue that first means normalizing the issue of misdiagnosis. “It is kind of ludicrous to think that you will practice medicine over 40 years and not have a misdiagnosis,” she says. “But we don’t look at it from that perspective when we begin to orient trainees.”
National Efforts
To the people at the U.S. Pharmacopeia Center for the Advancement of Patient Safety (USP), the arrival of universal electronic medical records (EMR) in the coming decade will be a boon to the error-reduction effort.
“Eventually we will all have our health information stored electronically for easy retrieval,” says Rodney W. Hicks, PhD, ARNP, manager, patient safety research and practice for the USP and first author on its most recent report. The beginning of regional networks for EMR is taking hold.
“Even before the IOM report, the USP was familiar with intensivists,” says Dr. Hicks. “We recognize hospitalists as experts who bring efficiency and effectiveness to the healthcare system.”
The USP maintains perhaps the largest database of medication errors in the world.1 Each year the USP issues a report that focuses on one topic and builds its knowledge base.
This year’s report focuses exclusively on the perioperative continuum of care. Last year’s covered ICU- and radiology-related errors. Two years ago the report was a five-year data summary of errors occurring primarily in hospitals.
“The area of errors due to breakdowns in handoffs remains a huge problem for diagnosis and the continuity of care,” says Shawn C. Becker, MS, BSN, RN, director of patient safety initiatives for the USP.
Classification
In general, errors are divided into those that stem from individual factors and those that are system-related, which include environmental and organizational factors.
Environmental risks are often related to human factors. Dr. Nagamine offers an aviation analogy to demonstrate the many pulls on caregivers’ attention.
“What happens in a cockpit at take off is that you are not allowed to talk about anything other than the take-off checklist,” she says. “In medicine, we have nurses’ stations or medication carts in the middle of the hallway, so nurses are preparing meds and people are tugging on their shoulder and interrupting them during a critical task.”
Organizational factors involve culture and priorities. If your organization says it values quality and safety but doesn’t put in place policies and processes to support it, that affects diagnostics and error-free performance.
Market Drivers
“The discussion about quality is driven by medical error,” says Evan Falchuk, president of Best Doctors Inc., based in Boston. “But the issue is more interesting than simply looking for mistakes.”
Best Doctors partners with employers and health plans to help members with serious illnesses make sure they have the right diagnosis and treatment. Members can consult with specialists who assess diagnoses and can recommend treatment. The firm believes this is the best way to measure quality, and consumers around the world increasingly agree: The company serves more than 10 million people in 30 countries.
Best Doctors was founded in 1989 by two internists: Falchuk’s father, Kenneth H. Falchuk, MD, a professor of medicine at Harvard University Medical School, and Jose Halperin, MD, an associate professor of medicine at Harvard. The service they created is one in which doctors review a patient’s medical information, identify the important issues, and consult with leading experts from their peer-reviewed database. The company then has clinicians work with the patient and his or her doctor to ensure that the patient is getting appropriate care. The process has identified incorrect diagnosis or treatment in more than half of reviewed cases.
“Hospitalists should think about quality in terms of things happening outside the hospital,” says Falchuk. “The informed, demanding consumer is coming to healthcare, and their expectations are clear: to be paid attention to, to have all of their questions answered, and to be certain that their diagnosis and treatment are correct.” These sentiments affect how hospitals do business.
The increasing amount of medical information patients can find on the Internet can raise questions in their minds. “Patients want to trust their doctors,” Falchuk says. “But when the patient has lots of information and questions and finds it difficult to spend as much time as they would like with their doctor, trust is eroded—and patients start to wonder if their doctor is doing the right thing.”
The complexity of modern medicine, with new diagnoses, treatments, and testing, and ultra-specialized experts, can sometimes—ironically—lead to lesser quality.
“It is more important than ever before that doctors with differing perspectives discuss each case,” says Falchuk. “But doctors complain that the system, often because of constraints imposed by managed care, only allows for episodic interactions like that. If that kind of interaction can be made the norm, it will give patients an extraordinary amount of comfort as to the quality of their care.”
Falchuk believes the tipping point for combating errors is being reached—at least from the business point of view.
“With major employers, as many as one in 200 employees call us for help,” he says. “That is close to the incidence rate of the illnesses we commonly see: cancer, heart problems, and undiagnosed situations. When you see this flood of demand, you say, ‘Something is going on that is driving this.’ ”
These market-based factors are driving hospitals to publish and compare rates for process of care and mortality, and many medical centers are publishing report cards. With the advent of advanced technology, hospital and provider performance will be increasingly apparent and transparent. Corporations and institutions will have to be less guarded about what they share publicly as their public accountability is increased.
Interventions, Feedback
The healthcare industry has embraced British psychologist James Reason’s 1990 Swiss cheese model of error as a means of tackling the cumulative effects that cause adverse events. The model conceptualizes the factors that contributed to an error as holes in slices of Swiss cheese. Only when the holes line up does the adverse event occur; placing barriers at one or more of the holes “traps the error” from being realized.
For instance, Best Doctors notes “potholes” in the reading stage of pathology.
“We see many cases of underdiagnosis or even misdiagnosis based on one of the most difficult steps: a pathology review,” says Falchuk. “With new, specifically targeted treatments, getting that right is extremely significant.” Best Doctors experts often recommend having pathology re-reviewed. “I wouldn’t call this error, but patients view it as a question of quality,” he says.
Integrating technology with observation skills is an important way hospitals are working to improve diagnostics and reduce error.
Because the same factors contribute to a near miss as to an actual event, studying the patterns of near misses can provide a wealth of information.
“I heard some statistics that for every 19 near misses, you’re going to have one event,” says Dr. Nagamine. If on a particular day, a provider was fatigued or overtaxed and didn’t catch a contributing factor that is a risk—termed a “latent condition”—that’s when the holes line up. “An event is never just the result of one thing or one person; it is a combination of factors,” says Dr. Nagamine.
One example of this concerns an element in the policy for discharge bundles that institutions establish to better manage transfer of care. When lab results become available only after a patient’s discharge, it increases the risk for delays in diagnosis. Electronically placing the test results into the primary care physician’s e-mail inbox helps to “close the loop,” says Dr. Nagamine. “That information gets to somebody, and we’re clear on who that somebody is. We are putting in place those types of interventions—which are really the low-hanging fruit.”
Culture Change
Opening up about adverse events and providing feedback creates a different awareness about the risks surrounding the event.
“The look-alike, sound-alike medications are an example,” Dr. Nagamine says. “I went up to the unit and said, ‘A nurse recorded that she almost gave hydralazine instead of hydroxyzine—has that ever happened to you?’ The first three nurses I asked said, ‘Yes,’ ‘Yes,’ ‘Yes.’ Until I ask these types of questions, I don’t know. And until you can make it safe for your staff to talk, you will not have good information.”
Although this is the approach most of the safety world and quality world is embracing, it is not how most clinicians on the frontline view it.
“We are trying to educate people about a framework in which to think about this,” says Dr. Nagamine. “It is not constructive to point fingers, but it is important to give people feedback about how the event happened. It is far more constructive to look at the entire system and ask, ‘How did we fail here? What was your piece of it? What was the system’s piece of it?’ ”
Because of the connection between litigation and adverse events, changing the culture is a complex imperative. But providers must recognize that systems failures are involved in about 75% to 80% of medical malpractice cases—whether that involves communication breakdowns, inadequate availability of information, or a host of other factors. The individual, environment, and organization are linked.
Reducing negativity and sensitivity around the terms associated with error and reframing thinking toward prevention are important.
“There is a richness of information that comes once you change the culture from blaming to fixing,” says Dr. Nagamine. Providing feedback to frontline practitioners is key, as is thanking those who report. “It increases providers’ awareness about where the hot spots and vulnerabilities are and how to stay out of trouble. Simply by giving them information about an event raises their awareness of the magnitude of certain types of issues,” she explains.
When Dr. Nagamine led a safety initiative on the ICU floor consisting of human factors training and a new system for reporting events, the number of reports “went through roof,” she says. “My new problem was not that people were not reporting; it was being overwhelmed with the information that was coming in. We were able to create a culture of safety that made it safe to report and consequently had much better information from which we could devise prevention strategies.”
SHM, in planning to co-create standards for focused practice with the American Board of Internal Medicine, intends to promote the standards of professionalism along with other standards. The issue of personal accountability, although a part of that, has been less of a focus to date. In the future, all institutions may have technology hospitalists can use to learn whether the discharge diagnosis was correct in the months and years that followed. Will the culture be emotionally ready to handle what technology can offer?
“We will need to own it when things go well and when things don’t go well or when we are wrong,” says Dr. Halasyamani. “We need to be able to investigate the distribution of the reasons for misdiagnosis, determine how many of those problems are systems issues, and devise strategies to address them.” In a sense, she says, everything can be viewed as a system issue unless actions are egregious and malicious.
Yet when physicians are associated with an adverse event, research shows they feel they have little support to talk about it.
“The system we have in place has begun to try to address some of the issues related to system errors,” says Dr. Halasyamani. “But what if an individual does have an error? What systems do we have in place to support that person in the recovery? And along the way if we find people who are having these issues over and over again, we need to design processes to deal with that.”
One particular focus of SHM’s transfer-of-care initiative concerns communication surrounding handoffs. “We are setting those standards and thinking about what kinds of technology tools can help make those standards easier to adhere to and easier to implement,” says Dr. Halasyamani. TH
Andrea Sattinger is a frequent contributor to The Hospitalist.
Video Interpreters Help Hospitals, Patients Connect
Twenty years ago, when Andrew Panos’ brother was involved in a car crash during a vacation in Puerto Vallarta, Mexico, there were no interpretation services available at the hospital where he was taken.
When the family was finally able to get him to Los Angeles, doctors concluded that if he had stayed in Mexico another eight hours he would have died from blood poisoning.
This experience—and the realization that even in his hometown of Columbus, Ohio, there was a serious need for fast, accurate healthcare interpretation services—prompted Andrew Panos to create the Language Access Network (LAN), a face-to-face live audio-video interpretation service, in 2003.
The system, My Accessible Real-Time Trusted Interpreter (MARTTI) is available in 23 hospitals. The system centralizes video interpretation into a center staffed by medically trained interpreter. In a hospital subscribing to the service, a provider can call LAN’s center in Columbus, Ohio, 24 hours a day, seven days a week. Users can choose among 150 languages, including a range of Chinese dialects and American Sign Language, and access an on-screen interpreter.
To use the system, a hospital purchases a block of minutes each month; charges are incurred when interpretations are sought.
“Some people have referred to it as the OnStar of interpreting,” says Panos, referring to the vehicle security system. “They are finding it more affordable than the cost of having on-site interpreters or calling an agency and having to pay a two-hour minimum and then having a wait time of upward of an hour.”
LAN’s system is a boon for hospitals that deal daily with Americans with Disabilities Act compliance.
“For instance, in New York they’re demanding that interpreters be provided within 10 minutes,” Panos says. “Having an American Sign Language interpreter in that short a time has really put quite a burden on their hospitals. With our system, since it is available with the push of a button, the result has been amazing.”
At Boston Medical Center (BMC), implementing MARTTI has meant synchronizing the institution’s wireless system with LAN’s system.
“It’s been a marriage of the two,” says Oscar Arocha, director of interpreter services and guest support services at BMC. Its 44 full-time interpreters were already providing in-person interpreting wherever possible. Then the hospital began telephone interpretation, and has since installed MARTTI units.
It was crucial to Arocha and BMC’s administrators that the service be available wirelessly so video units could be wheeled from place to place. Desktop units are also available from LAN.
“The user turns the video unit on and waits two or three seconds for the operator to come up on screen,” says Arocha. “You ask for the language you want, and they connect you within seconds to minutes, depending on the requested language.”
If the requested language or dialect is not one available on video, LAN automatically seeks an interpreter who connects via audio.
At Texas Children’s Hospital in Houston, a pilot program with the LAN system was set to go live in the emergency centers Nov. 1. Hospitalists and other providers can use this system in addition to personal and commercial telephone interpreters.
Yong S. Han, MD, a hospitalist at that institution, hopes the service enhances communication with patients and families. “Given that we have adopted family-centered rounding, this will also allow everyone to hear the conversation,” he says. “Additionally, it is pretty cumbersome and problematic switching the phone between the patient and the provider, so MARTTI should allow improvements in this arena.”
Information about the LAN system is available at www.languageaccessnetwork.com. TH
Andrea Sattinger is a medical journalist based in North Carolina
Twenty years ago, when Andrew Panos’ brother was involved in a car crash during a vacation in Puerto Vallarta, Mexico, there were no interpretation services available at the hospital where he was taken.
When the family was finally able to get him to Los Angeles, doctors concluded that if he had stayed in Mexico another eight hours he would have died from blood poisoning.
This experience—and the realization that even in his hometown of Columbus, Ohio, there was a serious need for fast, accurate healthcare interpretation services—prompted Andrew Panos to create the Language Access Network (LAN), a face-to-face live audio-video interpretation service, in 2003.
The system, My Accessible Real-Time Trusted Interpreter (MARTTI) is available in 23 hospitals. The system centralizes video interpretation into a center staffed by medically trained interpreter. In a hospital subscribing to the service, a provider can call LAN’s center in Columbus, Ohio, 24 hours a day, seven days a week. Users can choose among 150 languages, including a range of Chinese dialects and American Sign Language, and access an on-screen interpreter.
To use the system, a hospital purchases a block of minutes each month; charges are incurred when interpretations are sought.
“Some people have referred to it as the OnStar of interpreting,” says Panos, referring to the vehicle security system. “They are finding it more affordable than the cost of having on-site interpreters or calling an agency and having to pay a two-hour minimum and then having a wait time of upward of an hour.”
LAN’s system is a boon for hospitals that deal daily with Americans with Disabilities Act compliance.
“For instance, in New York they’re demanding that interpreters be provided within 10 minutes,” Panos says. “Having an American Sign Language interpreter in that short a time has really put quite a burden on their hospitals. With our system, since it is available with the push of a button, the result has been amazing.”
At Boston Medical Center (BMC), implementing MARTTI has meant synchronizing the institution’s wireless system with LAN’s system.
“It’s been a marriage of the two,” says Oscar Arocha, director of interpreter services and guest support services at BMC. Its 44 full-time interpreters were already providing in-person interpreting wherever possible. Then the hospital began telephone interpretation, and has since installed MARTTI units.
It was crucial to Arocha and BMC’s administrators that the service be available wirelessly so video units could be wheeled from place to place. Desktop units are also available from LAN.
“The user turns the video unit on and waits two or three seconds for the operator to come up on screen,” says Arocha. “You ask for the language you want, and they connect you within seconds to minutes, depending on the requested language.”
If the requested language or dialect is not one available on video, LAN automatically seeks an interpreter who connects via audio.
At Texas Children’s Hospital in Houston, a pilot program with the LAN system was set to go live in the emergency centers Nov. 1. Hospitalists and other providers can use this system in addition to personal and commercial telephone interpreters.
Yong S. Han, MD, a hospitalist at that institution, hopes the service enhances communication with patients and families. “Given that we have adopted family-centered rounding, this will also allow everyone to hear the conversation,” he says. “Additionally, it is pretty cumbersome and problematic switching the phone between the patient and the provider, so MARTTI should allow improvements in this arena.”
Information about the LAN system is available at www.languageaccessnetwork.com. TH
Andrea Sattinger is a medical journalist based in North Carolina
Twenty years ago, when Andrew Panos’ brother was involved in a car crash during a vacation in Puerto Vallarta, Mexico, there were no interpretation services available at the hospital where he was taken.
When the family was finally able to get him to Los Angeles, doctors concluded that if he had stayed in Mexico another eight hours he would have died from blood poisoning.
This experience—and the realization that even in his hometown of Columbus, Ohio, there was a serious need for fast, accurate healthcare interpretation services—prompted Andrew Panos to create the Language Access Network (LAN), a face-to-face live audio-video interpretation service, in 2003.
The system, My Accessible Real-Time Trusted Interpreter (MARTTI) is available in 23 hospitals. The system centralizes video interpretation into a center staffed by medically trained interpreter. In a hospital subscribing to the service, a provider can call LAN’s center in Columbus, Ohio, 24 hours a day, seven days a week. Users can choose among 150 languages, including a range of Chinese dialects and American Sign Language, and access an on-screen interpreter.
To use the system, a hospital purchases a block of minutes each month; charges are incurred when interpretations are sought.
“Some people have referred to it as the OnStar of interpreting,” says Panos, referring to the vehicle security system. “They are finding it more affordable than the cost of having on-site interpreters or calling an agency and having to pay a two-hour minimum and then having a wait time of upward of an hour.”
LAN’s system is a boon for hospitals that deal daily with Americans with Disabilities Act compliance.
“For instance, in New York they’re demanding that interpreters be provided within 10 minutes,” Panos says. “Having an American Sign Language interpreter in that short a time has really put quite a burden on their hospitals. With our system, since it is available with the push of a button, the result has been amazing.”
At Boston Medical Center (BMC), implementing MARTTI has meant synchronizing the institution’s wireless system with LAN’s system.
“It’s been a marriage of the two,” says Oscar Arocha, director of interpreter services and guest support services at BMC. Its 44 full-time interpreters were already providing in-person interpreting wherever possible. Then the hospital began telephone interpretation, and has since installed MARTTI units.
It was crucial to Arocha and BMC’s administrators that the service be available wirelessly so video units could be wheeled from place to place. Desktop units are also available from LAN.
“The user turns the video unit on and waits two or three seconds for the operator to come up on screen,” says Arocha. “You ask for the language you want, and they connect you within seconds to minutes, depending on the requested language.”
If the requested language or dialect is not one available on video, LAN automatically seeks an interpreter who connects via audio.
At Texas Children’s Hospital in Houston, a pilot program with the LAN system was set to go live in the emergency centers Nov. 1. Hospitalists and other providers can use this system in addition to personal and commercial telephone interpreters.
Yong S. Han, MD, a hospitalist at that institution, hopes the service enhances communication with patients and families. “Given that we have adopted family-centered rounding, this will also allow everyone to hear the conversation,” he says. “Additionally, it is pretty cumbersome and problematic switching the phone between the patient and the provider, so MARTTI should allow improvements in this arena.”
Information about the LAN system is available at www.languageaccessnetwork.com. TH
Andrea Sattinger is a medical journalist based in North Carolina
Diagnose Misdiagnosis
This is the first of a two-part series examining medical errors. This article addresses thought processes hospitalists use that may lead to mistaken diagnoses. Part 2 will look at what healthcare corporations are doing to improve diagnoses and reduce errors.
When talking about tough diagnoses, academic hospitalist David Feinbloom, MD, recalls the story of a female patient seen by his hospitalist group whose diagnosis took some time to nail down.
This woman had been in and out of the hospital for several years with nonspecific abdominal pain and intermittent diarrhea. She had been seen by numerous doctors and tested extensively. Increasingly her doctors concluded that there was some psychiatric overlay—she was depressed or somatic.
“Patients like these are very common and often end up on the hospitalist service,” says Dr. Feinbloom, who works at Beth Israel Deaconess Medical Center in Boston.
But to Joseph Li, MD, director of the hospital medicine program at Beth Israel, this patient seemed normal. There was something about the symptoms she described that reminded him of a patient he had seen who had been diagnosed with a metastatic neuroendocrine tumor.
Although this patient’s past MRI had been negative, Dr. Li remembered that if you don’t perform the right MRI protocol, you’ll miss something. He asked the team to obtain a panel looking for specific markers and to repeat the MRI with the correct protocol. It was accepted as fact that there was no pathology to explain her symptoms but that she had had every test. He requested another gastrointestinal (GI) consult.
“It seemed so far out there, and then everything he said was completely correct,” says Dr. Feinbloom. “She had Zollinger-Ellison syndrome.”
Clues from Sherlock
In his book How Doctors Think, Jerome Groopman, MD, discusses Sir Arthur Conan Doyle, physician and creator of the brilliant detective Sherlock Holmes. When it comes to solving crimes, Holmes’ superior observation and logic, intellectual prowess, and pristine reasoning help him observe and interpret the most obscure and arcane clues. He is, in the end, a consummate diagnostician.
One of the first rules a great diagnostician must follow is to not get boxed into one way of thinking, says Dr. Groopman, the Dina and Raphael Recanati chair of medicine at the Harvard Medical School and chief of experimental medicine at the Beth Israel Deaconess Medical Center, Boston. That is one of the downsides of a too-easy attachment to using clinical practice guidelines, he says.
“Guidelines are valuable reference points, but in order to use a guideline effectively, you have to have the correct diagnosis,” he says. “Studies over decades with hospitalized patients show that the misdiagnosis rate is at least 15% and hasn’t changed.1 A great deal of effort needs to be put into improving our accuracy in making diagnoses.”
Compared with other kinds of medical errors, diagnostic errors have not gotten a great deal of attention. The hospital patient safety movement has been more focused on preventing medication errors, surgical errors, handoff communications, nosocomial infections, falls, and blood clots.2 There have been few studies pertaining exclusively to diagnostic errors—but the topic is gaining headway.3
Think about Thinking
Diagnostic errors are usually multifactorial in origin and typically involve system-related and individual factors. The systems-based piece includes environmental and organizational factors. Medical researchers conclude the majority of diagnostic errors arise from flaws in physician thinking, not technical mistakes.
Cognitive errors involve instances where knowledge, data gathering, data processing, or verification (such as by lab testing) are faulty. Improving diagnostics will require better accountability by institutions and individuals. To do the latter, experts say, physicians would do well to familiarize themselves with their diagnostic weaknesses.
Thinking about thinking is the science of cognitive psychology and addresses the cognitive aspects of clinical reasoning underlying diagnostic decision-making. It is an area of study in which few medical professionals are versed. “Except for a few of these guys who trained in psych or were voices in the wilderness that have been largely ignored,” most physicians are unaware of the cognitive psychology literature, Dr. Groopman says.
Common biases and errors in clinical reasoning are presented in Table 1 (right).4,5 These are largely individual mistakes for which physicians traditionally have been accountable.
Patterns and Heuristics
The following factors contribute to how shortcuts are used: the pressures of working in medicine, the degrees of uncertainty a physician may feel, and the fact that hospitalists rarely have all the information they need about a patient.
“That’s just the nature of medicine,” says Dr. Groopman. “These shortcuts are natural ways of thinking under those conditions. They succeed about 85% of the time; they fail up to 10-20% of the time. The first thing we need to educate ourselves about is that this is how our minds work as doctors.”
Dr. Groopman and those he interviewed for his book have a razor-sharp overview of clinical practice within hospitals throughout the U.S. and Canada, including academic centers, community centers, affluent areas, suburbs, inner cities, and Native American reservations. But except for Pat Croskerry, MD, PhD, in the department of emergency medicine at Dalhousie University’s Queen Elizabeth II Health Sciences Center in Halifax, Nova Scotia, none of the experts he interviewed had rigorous training in cognitive science.
Although how to think is a priority in physicians’ training, how to think about one’s thinking is not.
“We are not given a vocabulary during medical training, or later through CME courses, in this emerging science—and yet this science involves how our mind works successfully and when we make mistakes,” Dr. Groopman says.
The data back this assertion. In a study of 100 cases of diagnostic error, 90 involved injury, including 33 deaths; 74% were attributed to errors in cognitive reasoning (see Figure 1, right).1 Failure to consider reasonable alternatives after an initial diagnosis was the most common cause. Other common causes included faulty context generation, misjudging the salience of findings, faulty perception, and errors connected with the use of heuristics. In this study, faulty or inadequate knowledge was uncommon.
Underlying contributions to error fell into three categories: “no fault,” system-related, and cognitive. Only seven cases reflected no-fault errors alone. In the remaining 93 cases, 548 errors were identified as system-related or cognitive factors (5.9 per case). System-related factors contributed to the diagnostic error in 65% of the cases and cognitive factors in 74%. The most common system-related factors involved problems with policies and procedures, inefficient processes, teamwork, and communication. The most common cognitive problems involved faulty synthesis.
Dr. Groopman believes it is important for physicians to be more introspective about the thinking patterns they employ and learn the traps to which they are susceptible. He also feels it is imperative to develop curricula at different stages of medical training so this new knowledge can be used to reduce error rates. Because the names for these traps can vary, the development of a universal and comprehensive taxonomy for classifying diagnostic errors is also needed.
“It’s impossible to be perfect; we’re never going to be 100%,” Dr. Groopman says. “But I deeply believe that it is quite feasible to think about your thinking and to assess how your mind came to a conclusion about a diagnosis and treatment plan.”
When phy-sicians think about errors in cognitive reasoning, they often focus on the “don’t-miss diagnoses” or the uncommon variant missed by recall or anchoring errors.
“When I reflect on the errors I have made, they mostly fall into the categories that Dr. Groopman describes in his book,” Dr. Feinbloom says. “Interestingly, the errors that I see most often stem from the fear of making an error of omission.”
It is paradoxical, but in order to ensure that no possible diagnosis is missed, doctors often feel the need to rule out all possible diagnoses.
“While it makes us feel that we are doing the best for our patients, this approach leads to an inordinate amount of unnecessary testing and potentially harmful interventions,” says Dr. Feinbloom. “Understanding how cognitive errors occur should allow us to be judicious in our approach, with the confidence to hold back when the diagnosis is clear, and push harder when we know that something does not fit.”
Emotional Dimension
Although many diagnostic errors are attributable to mistakes in thinking, emotions, and feelings—which may not be easy to detect or admit—also contribute to decision-making.
As hypothesized by noted neurologist and author Antonio Damasio in Descartes’ Error: Emotion, Reason, and the Human Brain, some feelings—visceral signals he calls somatic markers—deter us from or attract us to certain images and decisions.6 Remaining cognizant of those feelings helps clarify how they may inform a medical decision—for good and bad.
The emotional dimension of decision-making cannot be disregarded, says Dr. Groopman. “We need to take our emotional temperature; there are patients we like more and patients we like less,” he says. “There are times when we are tremendously motivated to succeed with a very complicated and daunting patient in the hospital, and there are times when we retreat from that for whatever psychological reason. Sometimes it’s fear of failure, sometimes it’s stereotyping. Regardless, we need to have a level of self-awareness.”
The stressful atmosphere of hospital-based medicine contributes to a high level of anxiety. “Physicians use a telegraphic language full of sound bytes with each other that may contribute to the way heuristics are passed from one generation of doctors to the next,” Dr. Groopman says. “That language is enormously powerful in guiding our thinking and the kinds of shortcuts that we use.”
Pitfalls in Reasoning
Of all the bias errors in clinical reasoning, two of the most influential on physicians are anchoring and attribution. Bound-ed rationality—the failure to continue considering reasonable alternatives after an initial diagnosis is reached—is also a pitfall. The difference between the latter and anchoring is whether the clinician adjusts the diagnosis when new data emerge.
Anchoring errors may arise from seizing the first bits of data and allowing them to guide all future questioning. “It happens every day,” says Dr. Feinbloom. “The diagnosis kind of feels right. There is something about the speed with which it comes to mind, the familiarity with the diagnosis in question, [that] reinforces your confidence.”
Dr. Feinbloom teaches his young trainees to trust no one. “I mean that in a good-hearted way,” he says. “Never assume what you’re told is accurate. You have to review everything yourself, interview the patient again; skepticism is a powerful tool.”
With the woman who was ultimately diagnosed with Zollinger-Ellison syndrome, Dr. Li’s skepticism paid off—and the hospitalist team benefited from deconstructing its clinical thinking to see where it went awry.
“If someone had gotten the gastrin level earlier,” says Dr. Feinbloom, “they would have caught it, but it was not on anyone’s radar. When imaging was negative, the team assumed it wasn’t a tumor.”
Lessons Learned
There are lots of lessons here, says Dr. Feinbloom. “You could spin it any one of five different ways with heuristic lessons, but what jumped out at me was that if you don’t know it, you don’t know it, and you can’t diagnose it,’’ he says. “And that gives you a sense of confidence that you’ve covered everything.”
No one had a familiarity with the subtle manifestations of that diagnosis until Dr. Li stepped in. “One lesson is that if you think the patient is on the up and up, and you haven’t yet made a diagnosis,” says Dr. Feinbloom, “it doesn’t mean there’s no diagnosis to be made.”
Dr. Li gives this lesson to his students this way: You may not have seen diagnosis X, but has diagnosis X seen you?
Andrea Sattinger is a frequent contributor to The Hospitalist.
References
- Graber ML, Franklin N, Gordon R. Diagnostic error in internal medicine. Arch Intern Med. 2005;165(13):1493-1499.
- Wachter RM. Is ambulatory patient safety just like hospital safety, only without the ‘‘stat’’? Ann Intern Med. 2006;145(7):547-549.
- Schiff GD, Kim S, Abrams R, et al. Diagnosing diagnosis errors: lessons from a multi-institutional collaborative project. Rockville, MD: Agency for Healthcare Research and Quality (AHRQ Publication No.050021-2.); 2005.
- Kempainen RR, Migeon MB, Wolf FM. Understanding our mistakes: a primer on errors in clinical reasoning. Med Teach. 2003;25(2):177-181.
- Redelmeier DA. Improving patient care. The cognitive psychology of missed diagnoses. Ann Intern Med. 2005;142(2):115-120.
- Damasio AR. Descartes’ Error: Emotion, Reason, and the Human Brain. New York: GP Putnam’s Sons; 1995.
This is the first of a two-part series examining medical errors. This article addresses thought processes hospitalists use that may lead to mistaken diagnoses. Part 2 will look at what healthcare corporations are doing to improve diagnoses and reduce errors.
When talking about tough diagnoses, academic hospitalist David Feinbloom, MD, recalls the story of a female patient seen by his hospitalist group whose diagnosis took some time to nail down.
This woman had been in and out of the hospital for several years with nonspecific abdominal pain and intermittent diarrhea. She had been seen by numerous doctors and tested extensively. Increasingly her doctors concluded that there was some psychiatric overlay—she was depressed or somatic.
“Patients like these are very common and often end up on the hospitalist service,” says Dr. Feinbloom, who works at Beth Israel Deaconess Medical Center in Boston.
But to Joseph Li, MD, director of the hospital medicine program at Beth Israel, this patient seemed normal. There was something about the symptoms she described that reminded him of a patient he had seen who had been diagnosed with a metastatic neuroendocrine tumor.
Although this patient’s past MRI had been negative, Dr. Li remembered that if you don’t perform the right MRI protocol, you’ll miss something. He asked the team to obtain a panel looking for specific markers and to repeat the MRI with the correct protocol. It was accepted as fact that there was no pathology to explain her symptoms but that she had had every test. He requested another gastrointestinal (GI) consult.
“It seemed so far out there, and then everything he said was completely correct,” says Dr. Feinbloom. “She had Zollinger-Ellison syndrome.”
Clues from Sherlock
In his book How Doctors Think, Jerome Groopman, MD, discusses Sir Arthur Conan Doyle, physician and creator of the brilliant detective Sherlock Holmes. When it comes to solving crimes, Holmes’ superior observation and logic, intellectual prowess, and pristine reasoning help him observe and interpret the most obscure and arcane clues. He is, in the end, a consummate diagnostician.
One of the first rules a great diagnostician must follow is to not get boxed into one way of thinking, says Dr. Groopman, the Dina and Raphael Recanati chair of medicine at the Harvard Medical School and chief of experimental medicine at the Beth Israel Deaconess Medical Center, Boston. That is one of the downsides of a too-easy attachment to using clinical practice guidelines, he says.
“Guidelines are valuable reference points, but in order to use a guideline effectively, you have to have the correct diagnosis,” he says. “Studies over decades with hospitalized patients show that the misdiagnosis rate is at least 15% and hasn’t changed.1 A great deal of effort needs to be put into improving our accuracy in making diagnoses.”
Compared with other kinds of medical errors, diagnostic errors have not gotten a great deal of attention. The hospital patient safety movement has been more focused on preventing medication errors, surgical errors, handoff communications, nosocomial infections, falls, and blood clots.2 There have been few studies pertaining exclusively to diagnostic errors—but the topic is gaining headway.3
Think about Thinking
Diagnostic errors are usually multifactorial in origin and typically involve system-related and individual factors. The systems-based piece includes environmental and organizational factors. Medical researchers conclude the majority of diagnostic errors arise from flaws in physician thinking, not technical mistakes.
Cognitive errors involve instances where knowledge, data gathering, data processing, or verification (such as by lab testing) are faulty. Improving diagnostics will require better accountability by institutions and individuals. To do the latter, experts say, physicians would do well to familiarize themselves with their diagnostic weaknesses.
Thinking about thinking is the science of cognitive psychology and addresses the cognitive aspects of clinical reasoning underlying diagnostic decision-making. It is an area of study in which few medical professionals are versed. “Except for a few of these guys who trained in psych or were voices in the wilderness that have been largely ignored,” most physicians are unaware of the cognitive psychology literature, Dr. Groopman says.
Common biases and errors in clinical reasoning are presented in Table 1 (right).4,5 These are largely individual mistakes for which physicians traditionally have been accountable.
Patterns and Heuristics
The following factors contribute to how shortcuts are used: the pressures of working in medicine, the degrees of uncertainty a physician may feel, and the fact that hospitalists rarely have all the information they need about a patient.
“That’s just the nature of medicine,” says Dr. Groopman. “These shortcuts are natural ways of thinking under those conditions. They succeed about 85% of the time; they fail up to 10-20% of the time. The first thing we need to educate ourselves about is that this is how our minds work as doctors.”
Dr. Groopman and those he interviewed for his book have a razor-sharp overview of clinical practice within hospitals throughout the U.S. and Canada, including academic centers, community centers, affluent areas, suburbs, inner cities, and Native American reservations. But except for Pat Croskerry, MD, PhD, in the department of emergency medicine at Dalhousie University’s Queen Elizabeth II Health Sciences Center in Halifax, Nova Scotia, none of the experts he interviewed had rigorous training in cognitive science.
Although how to think is a priority in physicians’ training, how to think about one’s thinking is not.
“We are not given a vocabulary during medical training, or later through CME courses, in this emerging science—and yet this science involves how our mind works successfully and when we make mistakes,” Dr. Groopman says.
The data back this assertion. In a study of 100 cases of diagnostic error, 90 involved injury, including 33 deaths; 74% were attributed to errors in cognitive reasoning (see Figure 1, right).1 Failure to consider reasonable alternatives after an initial diagnosis was the most common cause. Other common causes included faulty context generation, misjudging the salience of findings, faulty perception, and errors connected with the use of heuristics. In this study, faulty or inadequate knowledge was uncommon.
Underlying contributions to error fell into three categories: “no fault,” system-related, and cognitive. Only seven cases reflected no-fault errors alone. In the remaining 93 cases, 548 errors were identified as system-related or cognitive factors (5.9 per case). System-related factors contributed to the diagnostic error in 65% of the cases and cognitive factors in 74%. The most common system-related factors involved problems with policies and procedures, inefficient processes, teamwork, and communication. The most common cognitive problems involved faulty synthesis.
Dr. Groopman believes it is important for physicians to be more introspective about the thinking patterns they employ and learn the traps to which they are susceptible. He also feels it is imperative to develop curricula at different stages of medical training so this new knowledge can be used to reduce error rates. Because the names for these traps can vary, the development of a universal and comprehensive taxonomy for classifying diagnostic errors is also needed.
“It’s impossible to be perfect; we’re never going to be 100%,” Dr. Groopman says. “But I deeply believe that it is quite feasible to think about your thinking and to assess how your mind came to a conclusion about a diagnosis and treatment plan.”
When phy-sicians think about errors in cognitive reasoning, they often focus on the “don’t-miss diagnoses” or the uncommon variant missed by recall or anchoring errors.
“When I reflect on the errors I have made, they mostly fall into the categories that Dr. Groopman describes in his book,” Dr. Feinbloom says. “Interestingly, the errors that I see most often stem from the fear of making an error of omission.”
It is paradoxical, but in order to ensure that no possible diagnosis is missed, doctors often feel the need to rule out all possible diagnoses.
“While it makes us feel that we are doing the best for our patients, this approach leads to an inordinate amount of unnecessary testing and potentially harmful interventions,” says Dr. Feinbloom. “Understanding how cognitive errors occur should allow us to be judicious in our approach, with the confidence to hold back when the diagnosis is clear, and push harder when we know that something does not fit.”
Emotional Dimension
Although many diagnostic errors are attributable to mistakes in thinking, emotions, and feelings—which may not be easy to detect or admit—also contribute to decision-making.
As hypothesized by noted neurologist and author Antonio Damasio in Descartes’ Error: Emotion, Reason, and the Human Brain, some feelings—visceral signals he calls somatic markers—deter us from or attract us to certain images and decisions.6 Remaining cognizant of those feelings helps clarify how they may inform a medical decision—for good and bad.
The emotional dimension of decision-making cannot be disregarded, says Dr. Groopman. “We need to take our emotional temperature; there are patients we like more and patients we like less,” he says. “There are times when we are tremendously motivated to succeed with a very complicated and daunting patient in the hospital, and there are times when we retreat from that for whatever psychological reason. Sometimes it’s fear of failure, sometimes it’s stereotyping. Regardless, we need to have a level of self-awareness.”
The stressful atmosphere of hospital-based medicine contributes to a high level of anxiety. “Physicians use a telegraphic language full of sound bytes with each other that may contribute to the way heuristics are passed from one generation of doctors to the next,” Dr. Groopman says. “That language is enormously powerful in guiding our thinking and the kinds of shortcuts that we use.”
Pitfalls in Reasoning
Of all the bias errors in clinical reasoning, two of the most influential on physicians are anchoring and attribution. Bound-ed rationality—the failure to continue considering reasonable alternatives after an initial diagnosis is reached—is also a pitfall. The difference between the latter and anchoring is whether the clinician adjusts the diagnosis when new data emerge.
Anchoring errors may arise from seizing the first bits of data and allowing them to guide all future questioning. “It happens every day,” says Dr. Feinbloom. “The diagnosis kind of feels right. There is something about the speed with which it comes to mind, the familiarity with the diagnosis in question, [that] reinforces your confidence.”
Dr. Feinbloom teaches his young trainees to trust no one. “I mean that in a good-hearted way,” he says. “Never assume what you’re told is accurate. You have to review everything yourself, interview the patient again; skepticism is a powerful tool.”
With the woman who was ultimately diagnosed with Zollinger-Ellison syndrome, Dr. Li’s skepticism paid off—and the hospitalist team benefited from deconstructing its clinical thinking to see where it went awry.
“If someone had gotten the gastrin level earlier,” says Dr. Feinbloom, “they would have caught it, but it was not on anyone’s radar. When imaging was negative, the team assumed it wasn’t a tumor.”
Lessons Learned
There are lots of lessons here, says Dr. Feinbloom. “You could spin it any one of five different ways with heuristic lessons, but what jumped out at me was that if you don’t know it, you don’t know it, and you can’t diagnose it,’’ he says. “And that gives you a sense of confidence that you’ve covered everything.”
No one had a familiarity with the subtle manifestations of that diagnosis until Dr. Li stepped in. “One lesson is that if you think the patient is on the up and up, and you haven’t yet made a diagnosis,” says Dr. Feinbloom, “it doesn’t mean there’s no diagnosis to be made.”
Dr. Li gives this lesson to his students this way: You may not have seen diagnosis X, but has diagnosis X seen you?
Andrea Sattinger is a frequent contributor to The Hospitalist.
References
- Graber ML, Franklin N, Gordon R. Diagnostic error in internal medicine. Arch Intern Med. 2005;165(13):1493-1499.
- Wachter RM. Is ambulatory patient safety just like hospital safety, only without the ‘‘stat’’? Ann Intern Med. 2006;145(7):547-549.
- Schiff GD, Kim S, Abrams R, et al. Diagnosing diagnosis errors: lessons from a multi-institutional collaborative project. Rockville, MD: Agency for Healthcare Research and Quality (AHRQ Publication No.050021-2.); 2005.
- Kempainen RR, Migeon MB, Wolf FM. Understanding our mistakes: a primer on errors in clinical reasoning. Med Teach. 2003;25(2):177-181.
- Redelmeier DA. Improving patient care. The cognitive psychology of missed diagnoses. Ann Intern Med. 2005;142(2):115-120.
- Damasio AR. Descartes’ Error: Emotion, Reason, and the Human Brain. New York: GP Putnam’s Sons; 1995.
This is the first of a two-part series examining medical errors. This article addresses thought processes hospitalists use that may lead to mistaken diagnoses. Part 2 will look at what healthcare corporations are doing to improve diagnoses and reduce errors.
When talking about tough diagnoses, academic hospitalist David Feinbloom, MD, recalls the story of a female patient seen by his hospitalist group whose diagnosis took some time to nail down.
This woman had been in and out of the hospital for several years with nonspecific abdominal pain and intermittent diarrhea. She had been seen by numerous doctors and tested extensively. Increasingly her doctors concluded that there was some psychiatric overlay—she was depressed or somatic.
“Patients like these are very common and often end up on the hospitalist service,” says Dr. Feinbloom, who works at Beth Israel Deaconess Medical Center in Boston.
But to Joseph Li, MD, director of the hospital medicine program at Beth Israel, this patient seemed normal. There was something about the symptoms she described that reminded him of a patient he had seen who had been diagnosed with a metastatic neuroendocrine tumor.
Although this patient’s past MRI had been negative, Dr. Li remembered that if you don’t perform the right MRI protocol, you’ll miss something. He asked the team to obtain a panel looking for specific markers and to repeat the MRI with the correct protocol. It was accepted as fact that there was no pathology to explain her symptoms but that she had had every test. He requested another gastrointestinal (GI) consult.
“It seemed so far out there, and then everything he said was completely correct,” says Dr. Feinbloom. “She had Zollinger-Ellison syndrome.”
Clues from Sherlock
In his book How Doctors Think, Jerome Groopman, MD, discusses Sir Arthur Conan Doyle, physician and creator of the brilliant detective Sherlock Holmes. When it comes to solving crimes, Holmes’ superior observation and logic, intellectual prowess, and pristine reasoning help him observe and interpret the most obscure and arcane clues. He is, in the end, a consummate diagnostician.
One of the first rules a great diagnostician must follow is to not get boxed into one way of thinking, says Dr. Groopman, the Dina and Raphael Recanati chair of medicine at the Harvard Medical School and chief of experimental medicine at the Beth Israel Deaconess Medical Center, Boston. That is one of the downsides of a too-easy attachment to using clinical practice guidelines, he says.
“Guidelines are valuable reference points, but in order to use a guideline effectively, you have to have the correct diagnosis,” he says. “Studies over decades with hospitalized patients show that the misdiagnosis rate is at least 15% and hasn’t changed.1 A great deal of effort needs to be put into improving our accuracy in making diagnoses.”
Compared with other kinds of medical errors, diagnostic errors have not gotten a great deal of attention. The hospital patient safety movement has been more focused on preventing medication errors, surgical errors, handoff communications, nosocomial infections, falls, and blood clots.2 There have been few studies pertaining exclusively to diagnostic errors—but the topic is gaining headway.3
Think about Thinking
Diagnostic errors are usually multifactorial in origin and typically involve system-related and individual factors. The systems-based piece includes environmental and organizational factors. Medical researchers conclude the majority of diagnostic errors arise from flaws in physician thinking, not technical mistakes.
Cognitive errors involve instances where knowledge, data gathering, data processing, or verification (such as by lab testing) are faulty. Improving diagnostics will require better accountability by institutions and individuals. To do the latter, experts say, physicians would do well to familiarize themselves with their diagnostic weaknesses.
Thinking about thinking is the science of cognitive psychology and addresses the cognitive aspects of clinical reasoning underlying diagnostic decision-making. It is an area of study in which few medical professionals are versed. “Except for a few of these guys who trained in psych or were voices in the wilderness that have been largely ignored,” most physicians are unaware of the cognitive psychology literature, Dr. Groopman says.
Common biases and errors in clinical reasoning are presented in Table 1 (right).4,5 These are largely individual mistakes for which physicians traditionally have been accountable.
Patterns and Heuristics
The following factors contribute to how shortcuts are used: the pressures of working in medicine, the degrees of uncertainty a physician may feel, and the fact that hospitalists rarely have all the information they need about a patient.
“That’s just the nature of medicine,” says Dr. Groopman. “These shortcuts are natural ways of thinking under those conditions. They succeed about 85% of the time; they fail up to 10-20% of the time. The first thing we need to educate ourselves about is that this is how our minds work as doctors.”
Dr. Groopman and those he interviewed for his book have a razor-sharp overview of clinical practice within hospitals throughout the U.S. and Canada, including academic centers, community centers, affluent areas, suburbs, inner cities, and Native American reservations. But except for Pat Croskerry, MD, PhD, in the department of emergency medicine at Dalhousie University’s Queen Elizabeth II Health Sciences Center in Halifax, Nova Scotia, none of the experts he interviewed had rigorous training in cognitive science.
Although how to think is a priority in physicians’ training, how to think about one’s thinking is not.
“We are not given a vocabulary during medical training, or later through CME courses, in this emerging science—and yet this science involves how our mind works successfully and when we make mistakes,” Dr. Groopman says.
The data back this assertion. In a study of 100 cases of diagnostic error, 90 involved injury, including 33 deaths; 74% were attributed to errors in cognitive reasoning (see Figure 1, right).1 Failure to consider reasonable alternatives after an initial diagnosis was the most common cause. Other common causes included faulty context generation, misjudging the salience of findings, faulty perception, and errors connected with the use of heuristics. In this study, faulty or inadequate knowledge was uncommon.
Underlying contributions to error fell into three categories: “no fault,” system-related, and cognitive. Only seven cases reflected no-fault errors alone. In the remaining 93 cases, 548 errors were identified as system-related or cognitive factors (5.9 per case). System-related factors contributed to the diagnostic error in 65% of the cases and cognitive factors in 74%. The most common system-related factors involved problems with policies and procedures, inefficient processes, teamwork, and communication. The most common cognitive problems involved faulty synthesis.
Dr. Groopman believes it is important for physicians to be more introspective about the thinking patterns they employ and learn the traps to which they are susceptible. He also feels it is imperative to develop curricula at different stages of medical training so this new knowledge can be used to reduce error rates. Because the names for these traps can vary, the development of a universal and comprehensive taxonomy for classifying diagnostic errors is also needed.
“It’s impossible to be perfect; we’re never going to be 100%,” Dr. Groopman says. “But I deeply believe that it is quite feasible to think about your thinking and to assess how your mind came to a conclusion about a diagnosis and treatment plan.”
When phy-sicians think about errors in cognitive reasoning, they often focus on the “don’t-miss diagnoses” or the uncommon variant missed by recall or anchoring errors.
“When I reflect on the errors I have made, they mostly fall into the categories that Dr. Groopman describes in his book,” Dr. Feinbloom says. “Interestingly, the errors that I see most often stem from the fear of making an error of omission.”
It is paradoxical, but in order to ensure that no possible diagnosis is missed, doctors often feel the need to rule out all possible diagnoses.
“While it makes us feel that we are doing the best for our patients, this approach leads to an inordinate amount of unnecessary testing and potentially harmful interventions,” says Dr. Feinbloom. “Understanding how cognitive errors occur should allow us to be judicious in our approach, with the confidence to hold back when the diagnosis is clear, and push harder when we know that something does not fit.”
Emotional Dimension
Although many diagnostic errors are attributable to mistakes in thinking, emotions, and feelings—which may not be easy to detect or admit—also contribute to decision-making.
As hypothesized by noted neurologist and author Antonio Damasio in Descartes’ Error: Emotion, Reason, and the Human Brain, some feelings—visceral signals he calls somatic markers—deter us from or attract us to certain images and decisions.6 Remaining cognizant of those feelings helps clarify how they may inform a medical decision—for good and bad.
The emotional dimension of decision-making cannot be disregarded, says Dr. Groopman. “We need to take our emotional temperature; there are patients we like more and patients we like less,” he says. “There are times when we are tremendously motivated to succeed with a very complicated and daunting patient in the hospital, and there are times when we retreat from that for whatever psychological reason. Sometimes it’s fear of failure, sometimes it’s stereotyping. Regardless, we need to have a level of self-awareness.”
The stressful atmosphere of hospital-based medicine contributes to a high level of anxiety. “Physicians use a telegraphic language full of sound bytes with each other that may contribute to the way heuristics are passed from one generation of doctors to the next,” Dr. Groopman says. “That language is enormously powerful in guiding our thinking and the kinds of shortcuts that we use.”
Pitfalls in Reasoning
Of all the bias errors in clinical reasoning, two of the most influential on physicians are anchoring and attribution. Bound-ed rationality—the failure to continue considering reasonable alternatives after an initial diagnosis is reached—is also a pitfall. The difference between the latter and anchoring is whether the clinician adjusts the diagnosis when new data emerge.
Anchoring errors may arise from seizing the first bits of data and allowing them to guide all future questioning. “It happens every day,” says Dr. Feinbloom. “The diagnosis kind of feels right. There is something about the speed with which it comes to mind, the familiarity with the diagnosis in question, [that] reinforces your confidence.”
Dr. Feinbloom teaches his young trainees to trust no one. “I mean that in a good-hearted way,” he says. “Never assume what you’re told is accurate. You have to review everything yourself, interview the patient again; skepticism is a powerful tool.”
With the woman who was ultimately diagnosed with Zollinger-Ellison syndrome, Dr. Li’s skepticism paid off—and the hospitalist team benefited from deconstructing its clinical thinking to see where it went awry.
“If someone had gotten the gastrin level earlier,” says Dr. Feinbloom, “they would have caught it, but it was not on anyone’s radar. When imaging was negative, the team assumed it wasn’t a tumor.”
Lessons Learned
There are lots of lessons here, says Dr. Feinbloom. “You could spin it any one of five different ways with heuristic lessons, but what jumped out at me was that if you don’t know it, you don’t know it, and you can’t diagnose it,’’ he says. “And that gives you a sense of confidence that you’ve covered everything.”
No one had a familiarity with the subtle manifestations of that diagnosis until Dr. Li stepped in. “One lesson is that if you think the patient is on the up and up, and you haven’t yet made a diagnosis,” says Dr. Feinbloom, “it doesn’t mean there’s no diagnosis to be made.”
Dr. Li gives this lesson to his students this way: You may not have seen diagnosis X, but has diagnosis X seen you?
Andrea Sattinger is a frequent contributor to The Hospitalist.
References
- Graber ML, Franklin N, Gordon R. Diagnostic error in internal medicine. Arch Intern Med. 2005;165(13):1493-1499.
- Wachter RM. Is ambulatory patient safety just like hospital safety, only without the ‘‘stat’’? Ann Intern Med. 2006;145(7):547-549.
- Schiff GD, Kim S, Abrams R, et al. Diagnosing diagnosis errors: lessons from a multi-institutional collaborative project. Rockville, MD: Agency for Healthcare Research and Quality (AHRQ Publication No.050021-2.); 2005.
- Kempainen RR, Migeon MB, Wolf FM. Understanding our mistakes: a primer on errors in clinical reasoning. Med Teach. 2003;25(2):177-181.
- Redelmeier DA. Improving patient care. The cognitive psychology of missed diagnoses. Ann Intern Med. 2005;142(2):115-120.
- Damasio AR. Descartes’ Error: Emotion, Reason, and the Human Brain. New York: GP Putnam’s Sons; 1995.
Transfer Training
When attendings at Denver Health Medical Center (DHMC) were asked to be available to help supervise the teams of residents and interns with the hand-off process, Eugene Chu, MD, director of the hospital medicine program, quickly knew there was a problem.
“They didn’t really know what they were teaching,” says Dr. Chu. “They had an idea of how to do a hand-off, but they had never explicitly learned what a good hand-off was because it had never been described before. Some of our attendings fell back on what they did best—teach medicine. But that was not necessarily what the house staff wanted at that time of day.”
The house staff did want to learn to give safe, effective, and efficient hand-offs. “Giving a lecture on renal failure was not really the point of the hand-off,” says Dr. Chu.
Time for Training
“Sign outs serve a lot of purposes, not just information [transfer],” says Leora Horwitz, MD, an assistant professor in the division of general internal medicine at Yale School of Medicine, New Haven, Conn. “Signout is also a time for training. It is a time for socialization in terms of how we talk about patients and what is expected. And it is a time for catching errors and for rethinking plans and diagnoses because as you are describing something to someone, they might pick up on gaps or inconsistencies or things that should be done differently.”
Dr. Horwitz, who is also associate medical director of the Center for Outcomes Research and Evaluation at Yale-New Haven Hospital, has researched training for transfer of care over the past three years.1
“The most important thing is that hospitalists should not assume that residents have any skills [pertaining to transfer of care],” says Dr. Horwitz. “In medical schools, students are taught over and over how to present a patient for the first time. There’s a rigid order in which the information is supposed to flow, and there is a rigid list of categories of information that should be conveyed. People are taught that same order and that same flow and that same list of categories at all med schools. Consequently, as residents, everybody has the same sense of how to represent an initial history and physical. There is no such thing for hand-offs.”
Resident duty-hour limitations have increased the number of hand-offs, which creates greater risks for discontinuity of care and patient safety.2, 3 “Hand-offs occur two or three times a day and a patient presentation only occurs once—when the patient shows up,” says Dr. Horwitz. On top of that, when residents appear in their clinical duties, the attendings tend to forget residents don’t have the skills to execute a comprehensive and well-communicated hand-off. “The first thing to remember is that people need to be trained,” she says.
In a study in the Archives of Internal Medicine in 2006 (for which Dr. Horwitz is first author), the investigators asked internal medicine chief residents whether their program provides direct training in how to perform sign outs. Sign-out training varied considerably, and fewer than half the 202 programs that responded (62% of all U.S. residency programs) provided formal sign-out skill training: 40% of the programs taught sign-out skills through a lecture or workshop, 45% supervised oral sign outs, and 38% reviewed written sign outs.4 Residents in 27% of the programs received no training or supervision. Further, in more than one-third of training programs they found hand-offs were left to interns. “Residency programs need to recognize the problem and address it in some way,” Dr. Horwitz says.
Be Explicit, Create a Model
“Many residency programs have a standardized form that residents use to sign out to the cross-covering physician,” says Sunil Kripalani, MD, MSc, director of the Section of Hospital Medicine at Vanderbilt University in Nashville, Tenn. “However, there is often not much attention given to the actual process of transferring patient information to another physician.”
For example, residents may tack the form up to a wall or leave it on a computer, he says, because this may be more convenient than meeting for a verbal, face-to-face sign out. “It is important that residents receive training about how to best sign out patients, so it is viewed as a priority area,” he says.
The initial training should cover best practices for hand-offs, says Dr. Kripalani. “It may not be intuitive, especially to new residents, that poorly executed hand-offs can be perilous,” he says.
It is also important to teach trainees how to best convey that information. “Sometimes you’ll think more is better,” says Dr. Horwitz, “but that’s not the case; people turn off or get distracted. There is a tension between providing enough information to take care of the person overnight versus providing too much information.”
Modeling best behaviors is also an important part of training, says Jay Routson, MD, a teaching hospitalist and clinical assistant professor of medicine in the Idaho State University Department of Family Medicine in Pocatello, Idaho. Dr. Routson, trained in internal medicine, thinks opportunities to train residents and students in transfer of care are also a chance to model what you expect of them.
This is particularly important in Dr. Routson’s circumstances because of the nature of his university’s family medicine residency: It is conducted at a number of locations. At morning report on the first day of a block, residents who have been on the previous rotation are to transfer patient care to the incoming residents. But they may have already left for their new pediatrics or NICU assignments, for instance, not only elsewhere in Pocatello but perhaps in Boise or Logan.
Another problem in his program’s training for transfer of care, says Dr. Routson, is that less-experienced residents are not always aware of the important things to check. What one resident thinks is important to follow up on the next resident may put at the bottom of his or her list.
“I think that you have to model the importance you place on [hand-offs],” says Dr. Routson. “You have to set aside time during the day and make it a priority. Model the behavior when you’re checking out to a new attending, make sure the residents and interns know it’s a priority, especially early in the academic year.”
Supervision and Feedback
Supervised evaluation of performance and feedback are key aspects of training for transfer of care.
“Training residents means supervising them,” says Dr. Horwitz. “Are they getting the concepts? Are they incorporating the key points into everyday communication and actions?” Having more senior and experienced doctors present during sign out or at the very least prepare people for sign out is crucial, she says, because an issue such as anticipatory guidance/contingency planning is difficult for less-experienced residents.
“As a chief resident I made a point of periodically going around and observing sign outs,” she says. “Nobody ever watches sign out because it happens at the odd hours of the day; nobody gets feedback or evaluation. Ideally an attending should, at least now and again, be involved.”
Questions to ask include:
- Do the residents meet face to face in a dedicated time and place?
- Do they fill out a standardized template and updating it appropriately, especially with regard to medications?
- Do residents measure aspects of hand-offs to ensure they are being done?
Two-Way Street
Just as the DHMC team recognized that communication for hand-offs is a two-way street, the same is true for performing a discharge communication exchange. Are primary care providers considering best practices to train themselves in this integral aspect of patient care and safety?5, 6
“I don’t think the primary care community has gotten together and come up with a consensus of what they want to know and how much interaction they want,” Dr. Horwitz says. “There should be a standard for that.”
That is a first step to encourage greater training all around. She urges collaboration between SHM and a national organization, such as the American Academy on Family Practice, and hopes SHM will open that dialogue.
In that regard, some steps have been taken.7 Dr. Kripalani is a member of the SHM Hand-off and Communication Standards Task Force, which is developing national standards (The Hospitalist, August 2007, p. 17). There is a working list of nine best practices for hand-offs at shift changes or rotation ends, and the group plans to publish a final list in the upcoming year. The list is designed primarily for practicing hospitalists but will also be suitable for residents. The task force hopes other groups, such as internal medicine program directors and chief residents, will disseminate the best practices to trainees. National best practices are also likely to affect providers in the community.
“My suspicion is that a lot of community-based programs are interested in improving hand-offs, but each program may develop a different set of procedures,” says Dr. Kripalani. “One of the main reasons for developing national standards is so that both academic and community groups can refer to a list of evidence-based best practices.”
Evolution of Training
“Training for transfer of care and transfer of care are very different things, says Dr. Chu, “but they’re interrelated.” He and his colleague Gregory Misky, MD, a hospitalist and instructor with the University of Colorado Health Sciences Center (UCHSC), have been disseminating that training program throughout the UCHSC internal medicine residency program for the past three years.
In order to develop a structured, standard method for patient hand-offs, they took on teaching and supervising interns during their internal medicine ward rotations. Although much of the literature advocates the SBAR (situation, background, assessment, and recommendation) communication technique, the UCHSC team has developed a verbal structure specifically for hand-offs that differs from the SBAR model.8
Having learned many lessons their first year of training the trainers and the trainees, the Colorado hospitalists regrouped the next year. Because there were two interns coming on duty each evening, both taking cross cover, one attending could supervise only one of the interns. And, those hospitalists were getting called away to handle their clinical responsibilities.
“We felt it was important that attendings were available to guide the process safely,” says Dr. Chu. Therefore, because the evening hand-offs were conducted at 6 p.m. and a hospitalist was in house daily at that time, they began having the evening person, who was on each night until about 11, supervise the interns.
To improve the quality and consistency of the teaching, only four of the Division of Hospital Medicine’s eight attendings focused on supervising intern hand-offs. Also, in a series of focus-group meetings with attendings and house staff, they discussed supervision and identified several structures and standards for teaching hand-offs.
In addition to determining a consistent time and place for hand-off exchanges, they developed a consistent written template and a standard for verbal communication that provides an order of thinking and presenting, just as they use for presenting patient history and physical or daily patient progress updates. “The written template and the verbal are not necessarily the same thing,” says Dr. Chu. “We distinguished them as being two separate standards, just as they are with the written and verbal of morning rounds.”
With these protocols in place, attendings now had distinctions to watch for and a clear-cut means by which to supervise. In the third year of training at UCHSC, the hospitalist attendings provided training and feedback on the first night of call for the first four months beginning in July and in small-group sessions during the first week of the ward month.
The Reviews Are In
In response to a survey, the vast majority of UCHSC internal medicine residents said the new protocols were useful or extremely useful. Responses also revealed that training increased interns’ self-perceived hand-off skills and knowledge. The common denominator of a same time and place for hand-offs was judged the most useful element of the program; lectures were considered the least useful element.
Word got around of the program’s success. Eva Aagaard, MD, associate chair for education in the department of medicine, approached the originators to incorporate the program into the medical school’s interclinical curriculum, given to students between the third and fourth years as additional skills they would need in their sub-internships. Originally offered as an elective, demand for the course exceeded the class limit. Plans are under way to make this course mandatory.
“This past year, for the first time, we specifically taught our medical students hand-offs,” says Dr. Chu. He and his colleagues presented an abstract at SHM’s annual meeting in Dallas and are preparing a manuscript for publication.
Until now, all physicians have managed to do hand-offs without formal training. “Most residents figure out their own way of doing things after a while, but what we’re trying to do is not let it be a random evolution of learning,” says Dr. Chu. “It’s like learning to drive or ski with no lesson s: If you point your skis downhill, eventually you’ll learn how to ski, but you’ll have a lot of crashes. In hand-offs, that means communication failures, and a patient may suffer morbidity. We want to train and supervise [residents] so they learn in a progressive fashion and have fewer crashes.” TH
Andrea Sattinger is a frequent contributor to The Hospitalist.
References
- Horwitz LI, Moin T, Green ML. Development and implementation of an oral sign-out skills curriculum. J Gen Intern Med. 2007 Aug 3.
- Kripalani S, LeFevre F, Phillips CO, et al. Deficits in communication and information transfer between hospital-based and primary care physicians: implications for patient safety and continuity of care. JAMA. 2007;297(8):831-841.
- Vidyarthi AR, Arora V, Schnipper JL, et al. Managing discontinuity in academic medical centers: strategies for a safe and effective resident sign-out. J Hosp Med. 2006;1(4):257-266.
- Horwitz LI, Krumholz HM, Green ML,. Transfers of patient care between house staff on internal medicine wards: a national survey. Arch Intern Med. 2006 Jun;166(11):1173-1177.
- Coleman EA, Berenson RA. Lost in transition: challenges and opportunities for improving the quality of transitional care. Ann Intern Med. 2004 Oct;141(7):533-536.
- Halasyamani L, Kripalani S, Coleman E, et al. Transition of care for hospitalized elderly patients—development of a discharge checklist for hospitalists. J Hosp Med. 2006 Nov;1(6):354-360.
- Pantilat SZ, Lindenauer PK, Katz PP, et al. Primary care physician attitudes regarding communication with hospitalists. Am J Med. 2001;111(9, Supplement 2):15-20.
- SBAR initiative to improve staff communication. Healthcare Benchmarks Qual Improv. 2005;12(4):40-41.
When attendings at Denver Health Medical Center (DHMC) were asked to be available to help supervise the teams of residents and interns with the hand-off process, Eugene Chu, MD, director of the hospital medicine program, quickly knew there was a problem.
“They didn’t really know what they were teaching,” says Dr. Chu. “They had an idea of how to do a hand-off, but they had never explicitly learned what a good hand-off was because it had never been described before. Some of our attendings fell back on what they did best—teach medicine. But that was not necessarily what the house staff wanted at that time of day.”
The house staff did want to learn to give safe, effective, and efficient hand-offs. “Giving a lecture on renal failure was not really the point of the hand-off,” says Dr. Chu.
Time for Training
“Sign outs serve a lot of purposes, not just information [transfer],” says Leora Horwitz, MD, an assistant professor in the division of general internal medicine at Yale School of Medicine, New Haven, Conn. “Signout is also a time for training. It is a time for socialization in terms of how we talk about patients and what is expected. And it is a time for catching errors and for rethinking plans and diagnoses because as you are describing something to someone, they might pick up on gaps or inconsistencies or things that should be done differently.”
Dr. Horwitz, who is also associate medical director of the Center for Outcomes Research and Evaluation at Yale-New Haven Hospital, has researched training for transfer of care over the past three years.1
“The most important thing is that hospitalists should not assume that residents have any skills [pertaining to transfer of care],” says Dr. Horwitz. “In medical schools, students are taught over and over how to present a patient for the first time. There’s a rigid order in which the information is supposed to flow, and there is a rigid list of categories of information that should be conveyed. People are taught that same order and that same flow and that same list of categories at all med schools. Consequently, as residents, everybody has the same sense of how to represent an initial history and physical. There is no such thing for hand-offs.”
Resident duty-hour limitations have increased the number of hand-offs, which creates greater risks for discontinuity of care and patient safety.2, 3 “Hand-offs occur two or three times a day and a patient presentation only occurs once—when the patient shows up,” says Dr. Horwitz. On top of that, when residents appear in their clinical duties, the attendings tend to forget residents don’t have the skills to execute a comprehensive and well-communicated hand-off. “The first thing to remember is that people need to be trained,” she says.
In a study in the Archives of Internal Medicine in 2006 (for which Dr. Horwitz is first author), the investigators asked internal medicine chief residents whether their program provides direct training in how to perform sign outs. Sign-out training varied considerably, and fewer than half the 202 programs that responded (62% of all U.S. residency programs) provided formal sign-out skill training: 40% of the programs taught sign-out skills through a lecture or workshop, 45% supervised oral sign outs, and 38% reviewed written sign outs.4 Residents in 27% of the programs received no training or supervision. Further, in more than one-third of training programs they found hand-offs were left to interns. “Residency programs need to recognize the problem and address it in some way,” Dr. Horwitz says.
Be Explicit, Create a Model
“Many residency programs have a standardized form that residents use to sign out to the cross-covering physician,” says Sunil Kripalani, MD, MSc, director of the Section of Hospital Medicine at Vanderbilt University in Nashville, Tenn. “However, there is often not much attention given to the actual process of transferring patient information to another physician.”
For example, residents may tack the form up to a wall or leave it on a computer, he says, because this may be more convenient than meeting for a verbal, face-to-face sign out. “It is important that residents receive training about how to best sign out patients, so it is viewed as a priority area,” he says.
The initial training should cover best practices for hand-offs, says Dr. Kripalani. “It may not be intuitive, especially to new residents, that poorly executed hand-offs can be perilous,” he says.
It is also important to teach trainees how to best convey that information. “Sometimes you’ll think more is better,” says Dr. Horwitz, “but that’s not the case; people turn off or get distracted. There is a tension between providing enough information to take care of the person overnight versus providing too much information.”
Modeling best behaviors is also an important part of training, says Jay Routson, MD, a teaching hospitalist and clinical assistant professor of medicine in the Idaho State University Department of Family Medicine in Pocatello, Idaho. Dr. Routson, trained in internal medicine, thinks opportunities to train residents and students in transfer of care are also a chance to model what you expect of them.
This is particularly important in Dr. Routson’s circumstances because of the nature of his university’s family medicine residency: It is conducted at a number of locations. At morning report on the first day of a block, residents who have been on the previous rotation are to transfer patient care to the incoming residents. But they may have already left for their new pediatrics or NICU assignments, for instance, not only elsewhere in Pocatello but perhaps in Boise or Logan.
Another problem in his program’s training for transfer of care, says Dr. Routson, is that less-experienced residents are not always aware of the important things to check. What one resident thinks is important to follow up on the next resident may put at the bottom of his or her list.
“I think that you have to model the importance you place on [hand-offs],” says Dr. Routson. “You have to set aside time during the day and make it a priority. Model the behavior when you’re checking out to a new attending, make sure the residents and interns know it’s a priority, especially early in the academic year.”
Supervision and Feedback
Supervised evaluation of performance and feedback are key aspects of training for transfer of care.
“Training residents means supervising them,” says Dr. Horwitz. “Are they getting the concepts? Are they incorporating the key points into everyday communication and actions?” Having more senior and experienced doctors present during sign out or at the very least prepare people for sign out is crucial, she says, because an issue such as anticipatory guidance/contingency planning is difficult for less-experienced residents.
“As a chief resident I made a point of periodically going around and observing sign outs,” she says. “Nobody ever watches sign out because it happens at the odd hours of the day; nobody gets feedback or evaluation. Ideally an attending should, at least now and again, be involved.”
Questions to ask include:
- Do the residents meet face to face in a dedicated time and place?
- Do they fill out a standardized template and updating it appropriately, especially with regard to medications?
- Do residents measure aspects of hand-offs to ensure they are being done?
Two-Way Street
Just as the DHMC team recognized that communication for hand-offs is a two-way street, the same is true for performing a discharge communication exchange. Are primary care providers considering best practices to train themselves in this integral aspect of patient care and safety?5, 6
“I don’t think the primary care community has gotten together and come up with a consensus of what they want to know and how much interaction they want,” Dr. Horwitz says. “There should be a standard for that.”
That is a first step to encourage greater training all around. She urges collaboration between SHM and a national organization, such as the American Academy on Family Practice, and hopes SHM will open that dialogue.
In that regard, some steps have been taken.7 Dr. Kripalani is a member of the SHM Hand-off and Communication Standards Task Force, which is developing national standards (The Hospitalist, August 2007, p. 17). There is a working list of nine best practices for hand-offs at shift changes or rotation ends, and the group plans to publish a final list in the upcoming year. The list is designed primarily for practicing hospitalists but will also be suitable for residents. The task force hopes other groups, such as internal medicine program directors and chief residents, will disseminate the best practices to trainees. National best practices are also likely to affect providers in the community.
“My suspicion is that a lot of community-based programs are interested in improving hand-offs, but each program may develop a different set of procedures,” says Dr. Kripalani. “One of the main reasons for developing national standards is so that both academic and community groups can refer to a list of evidence-based best practices.”
Evolution of Training
“Training for transfer of care and transfer of care are very different things, says Dr. Chu, “but they’re interrelated.” He and his colleague Gregory Misky, MD, a hospitalist and instructor with the University of Colorado Health Sciences Center (UCHSC), have been disseminating that training program throughout the UCHSC internal medicine residency program for the past three years.
In order to develop a structured, standard method for patient hand-offs, they took on teaching and supervising interns during their internal medicine ward rotations. Although much of the literature advocates the SBAR (situation, background, assessment, and recommendation) communication technique, the UCHSC team has developed a verbal structure specifically for hand-offs that differs from the SBAR model.8
Having learned many lessons their first year of training the trainers and the trainees, the Colorado hospitalists regrouped the next year. Because there were two interns coming on duty each evening, both taking cross cover, one attending could supervise only one of the interns. And, those hospitalists were getting called away to handle their clinical responsibilities.
“We felt it was important that attendings were available to guide the process safely,” says Dr. Chu. Therefore, because the evening hand-offs were conducted at 6 p.m. and a hospitalist was in house daily at that time, they began having the evening person, who was on each night until about 11, supervise the interns.
To improve the quality and consistency of the teaching, only four of the Division of Hospital Medicine’s eight attendings focused on supervising intern hand-offs. Also, in a series of focus-group meetings with attendings and house staff, they discussed supervision and identified several structures and standards for teaching hand-offs.
In addition to determining a consistent time and place for hand-off exchanges, they developed a consistent written template and a standard for verbal communication that provides an order of thinking and presenting, just as they use for presenting patient history and physical or daily patient progress updates. “The written template and the verbal are not necessarily the same thing,” says Dr. Chu. “We distinguished them as being two separate standards, just as they are with the written and verbal of morning rounds.”
With these protocols in place, attendings now had distinctions to watch for and a clear-cut means by which to supervise. In the third year of training at UCHSC, the hospitalist attendings provided training and feedback on the first night of call for the first four months beginning in July and in small-group sessions during the first week of the ward month.
The Reviews Are In
In response to a survey, the vast majority of UCHSC internal medicine residents said the new protocols were useful or extremely useful. Responses also revealed that training increased interns’ self-perceived hand-off skills and knowledge. The common denominator of a same time and place for hand-offs was judged the most useful element of the program; lectures were considered the least useful element.
Word got around of the program’s success. Eva Aagaard, MD, associate chair for education in the department of medicine, approached the originators to incorporate the program into the medical school’s interclinical curriculum, given to students between the third and fourth years as additional skills they would need in their sub-internships. Originally offered as an elective, demand for the course exceeded the class limit. Plans are under way to make this course mandatory.
“This past year, for the first time, we specifically taught our medical students hand-offs,” says Dr. Chu. He and his colleagues presented an abstract at SHM’s annual meeting in Dallas and are preparing a manuscript for publication.
Until now, all physicians have managed to do hand-offs without formal training. “Most residents figure out their own way of doing things after a while, but what we’re trying to do is not let it be a random evolution of learning,” says Dr. Chu. “It’s like learning to drive or ski with no lesson s: If you point your skis downhill, eventually you’ll learn how to ski, but you’ll have a lot of crashes. In hand-offs, that means communication failures, and a patient may suffer morbidity. We want to train and supervise [residents] so they learn in a progressive fashion and have fewer crashes.” TH
Andrea Sattinger is a frequent contributor to The Hospitalist.
References
- Horwitz LI, Moin T, Green ML. Development and implementation of an oral sign-out skills curriculum. J Gen Intern Med. 2007 Aug 3.
- Kripalani S, LeFevre F, Phillips CO, et al. Deficits in communication and information transfer between hospital-based and primary care physicians: implications for patient safety and continuity of care. JAMA. 2007;297(8):831-841.
- Vidyarthi AR, Arora V, Schnipper JL, et al. Managing discontinuity in academic medical centers: strategies for a safe and effective resident sign-out. J Hosp Med. 2006;1(4):257-266.
- Horwitz LI, Krumholz HM, Green ML,. Transfers of patient care between house staff on internal medicine wards: a national survey. Arch Intern Med. 2006 Jun;166(11):1173-1177.
- Coleman EA, Berenson RA. Lost in transition: challenges and opportunities for improving the quality of transitional care. Ann Intern Med. 2004 Oct;141(7):533-536.
- Halasyamani L, Kripalani S, Coleman E, et al. Transition of care for hospitalized elderly patients—development of a discharge checklist for hospitalists. J Hosp Med. 2006 Nov;1(6):354-360.
- Pantilat SZ, Lindenauer PK, Katz PP, et al. Primary care physician attitudes regarding communication with hospitalists. Am J Med. 2001;111(9, Supplement 2):15-20.
- SBAR initiative to improve staff communication. Healthcare Benchmarks Qual Improv. 2005;12(4):40-41.
When attendings at Denver Health Medical Center (DHMC) were asked to be available to help supervise the teams of residents and interns with the hand-off process, Eugene Chu, MD, director of the hospital medicine program, quickly knew there was a problem.
“They didn’t really know what they were teaching,” says Dr. Chu. “They had an idea of how to do a hand-off, but they had never explicitly learned what a good hand-off was because it had never been described before. Some of our attendings fell back on what they did best—teach medicine. But that was not necessarily what the house staff wanted at that time of day.”
The house staff did want to learn to give safe, effective, and efficient hand-offs. “Giving a lecture on renal failure was not really the point of the hand-off,” says Dr. Chu.
Time for Training
“Sign outs serve a lot of purposes, not just information [transfer],” says Leora Horwitz, MD, an assistant professor in the division of general internal medicine at Yale School of Medicine, New Haven, Conn. “Signout is also a time for training. It is a time for socialization in terms of how we talk about patients and what is expected. And it is a time for catching errors and for rethinking plans and diagnoses because as you are describing something to someone, they might pick up on gaps or inconsistencies or things that should be done differently.”
Dr. Horwitz, who is also associate medical director of the Center for Outcomes Research and Evaluation at Yale-New Haven Hospital, has researched training for transfer of care over the past three years.1
“The most important thing is that hospitalists should not assume that residents have any skills [pertaining to transfer of care],” says Dr. Horwitz. “In medical schools, students are taught over and over how to present a patient for the first time. There’s a rigid order in which the information is supposed to flow, and there is a rigid list of categories of information that should be conveyed. People are taught that same order and that same flow and that same list of categories at all med schools. Consequently, as residents, everybody has the same sense of how to represent an initial history and physical. There is no such thing for hand-offs.”
Resident duty-hour limitations have increased the number of hand-offs, which creates greater risks for discontinuity of care and patient safety.2, 3 “Hand-offs occur two or three times a day and a patient presentation only occurs once—when the patient shows up,” says Dr. Horwitz. On top of that, when residents appear in their clinical duties, the attendings tend to forget residents don’t have the skills to execute a comprehensive and well-communicated hand-off. “The first thing to remember is that people need to be trained,” she says.
In a study in the Archives of Internal Medicine in 2006 (for which Dr. Horwitz is first author), the investigators asked internal medicine chief residents whether their program provides direct training in how to perform sign outs. Sign-out training varied considerably, and fewer than half the 202 programs that responded (62% of all U.S. residency programs) provided formal sign-out skill training: 40% of the programs taught sign-out skills through a lecture or workshop, 45% supervised oral sign outs, and 38% reviewed written sign outs.4 Residents in 27% of the programs received no training or supervision. Further, in more than one-third of training programs they found hand-offs were left to interns. “Residency programs need to recognize the problem and address it in some way,” Dr. Horwitz says.
Be Explicit, Create a Model
“Many residency programs have a standardized form that residents use to sign out to the cross-covering physician,” says Sunil Kripalani, MD, MSc, director of the Section of Hospital Medicine at Vanderbilt University in Nashville, Tenn. “However, there is often not much attention given to the actual process of transferring patient information to another physician.”
For example, residents may tack the form up to a wall or leave it on a computer, he says, because this may be more convenient than meeting for a verbal, face-to-face sign out. “It is important that residents receive training about how to best sign out patients, so it is viewed as a priority area,” he says.
The initial training should cover best practices for hand-offs, says Dr. Kripalani. “It may not be intuitive, especially to new residents, that poorly executed hand-offs can be perilous,” he says.
It is also important to teach trainees how to best convey that information. “Sometimes you’ll think more is better,” says Dr. Horwitz, “but that’s not the case; people turn off or get distracted. There is a tension between providing enough information to take care of the person overnight versus providing too much information.”
Modeling best behaviors is also an important part of training, says Jay Routson, MD, a teaching hospitalist and clinical assistant professor of medicine in the Idaho State University Department of Family Medicine in Pocatello, Idaho. Dr. Routson, trained in internal medicine, thinks opportunities to train residents and students in transfer of care are also a chance to model what you expect of them.
This is particularly important in Dr. Routson’s circumstances because of the nature of his university’s family medicine residency: It is conducted at a number of locations. At morning report on the first day of a block, residents who have been on the previous rotation are to transfer patient care to the incoming residents. But they may have already left for their new pediatrics or NICU assignments, for instance, not only elsewhere in Pocatello but perhaps in Boise or Logan.
Another problem in his program’s training for transfer of care, says Dr. Routson, is that less-experienced residents are not always aware of the important things to check. What one resident thinks is important to follow up on the next resident may put at the bottom of his or her list.
“I think that you have to model the importance you place on [hand-offs],” says Dr. Routson. “You have to set aside time during the day and make it a priority. Model the behavior when you’re checking out to a new attending, make sure the residents and interns know it’s a priority, especially early in the academic year.”
Supervision and Feedback
Supervised evaluation of performance and feedback are key aspects of training for transfer of care.
“Training residents means supervising them,” says Dr. Horwitz. “Are they getting the concepts? Are they incorporating the key points into everyday communication and actions?” Having more senior and experienced doctors present during sign out or at the very least prepare people for sign out is crucial, she says, because an issue such as anticipatory guidance/contingency planning is difficult for less-experienced residents.
“As a chief resident I made a point of periodically going around and observing sign outs,” she says. “Nobody ever watches sign out because it happens at the odd hours of the day; nobody gets feedback or evaluation. Ideally an attending should, at least now and again, be involved.”
Questions to ask include:
- Do the residents meet face to face in a dedicated time and place?
- Do they fill out a standardized template and updating it appropriately, especially with regard to medications?
- Do residents measure aspects of hand-offs to ensure they are being done?
Two-Way Street
Just as the DHMC team recognized that communication for hand-offs is a two-way street, the same is true for performing a discharge communication exchange. Are primary care providers considering best practices to train themselves in this integral aspect of patient care and safety?5, 6
“I don’t think the primary care community has gotten together and come up with a consensus of what they want to know and how much interaction they want,” Dr. Horwitz says. “There should be a standard for that.”
That is a first step to encourage greater training all around. She urges collaboration between SHM and a national organization, such as the American Academy on Family Practice, and hopes SHM will open that dialogue.
In that regard, some steps have been taken.7 Dr. Kripalani is a member of the SHM Hand-off and Communication Standards Task Force, which is developing national standards (The Hospitalist, August 2007, p. 17). There is a working list of nine best practices for hand-offs at shift changes or rotation ends, and the group plans to publish a final list in the upcoming year. The list is designed primarily for practicing hospitalists but will also be suitable for residents. The task force hopes other groups, such as internal medicine program directors and chief residents, will disseminate the best practices to trainees. National best practices are also likely to affect providers in the community.
“My suspicion is that a lot of community-based programs are interested in improving hand-offs, but each program may develop a different set of procedures,” says Dr. Kripalani. “One of the main reasons for developing national standards is so that both academic and community groups can refer to a list of evidence-based best practices.”
Evolution of Training
“Training for transfer of care and transfer of care are very different things, says Dr. Chu, “but they’re interrelated.” He and his colleague Gregory Misky, MD, a hospitalist and instructor with the University of Colorado Health Sciences Center (UCHSC), have been disseminating that training program throughout the UCHSC internal medicine residency program for the past three years.
In order to develop a structured, standard method for patient hand-offs, they took on teaching and supervising interns during their internal medicine ward rotations. Although much of the literature advocates the SBAR (situation, background, assessment, and recommendation) communication technique, the UCHSC team has developed a verbal structure specifically for hand-offs that differs from the SBAR model.8
Having learned many lessons their first year of training the trainers and the trainees, the Colorado hospitalists regrouped the next year. Because there were two interns coming on duty each evening, both taking cross cover, one attending could supervise only one of the interns. And, those hospitalists were getting called away to handle their clinical responsibilities.
“We felt it was important that attendings were available to guide the process safely,” says Dr. Chu. Therefore, because the evening hand-offs were conducted at 6 p.m. and a hospitalist was in house daily at that time, they began having the evening person, who was on each night until about 11, supervise the interns.
To improve the quality and consistency of the teaching, only four of the Division of Hospital Medicine’s eight attendings focused on supervising intern hand-offs. Also, in a series of focus-group meetings with attendings and house staff, they discussed supervision and identified several structures and standards for teaching hand-offs.
In addition to determining a consistent time and place for hand-off exchanges, they developed a consistent written template and a standard for verbal communication that provides an order of thinking and presenting, just as they use for presenting patient history and physical or daily patient progress updates. “The written template and the verbal are not necessarily the same thing,” says Dr. Chu. “We distinguished them as being two separate standards, just as they are with the written and verbal of morning rounds.”
With these protocols in place, attendings now had distinctions to watch for and a clear-cut means by which to supervise. In the third year of training at UCHSC, the hospitalist attendings provided training and feedback on the first night of call for the first four months beginning in July and in small-group sessions during the first week of the ward month.
The Reviews Are In
In response to a survey, the vast majority of UCHSC internal medicine residents said the new protocols were useful or extremely useful. Responses also revealed that training increased interns’ self-perceived hand-off skills and knowledge. The common denominator of a same time and place for hand-offs was judged the most useful element of the program; lectures were considered the least useful element.
Word got around of the program’s success. Eva Aagaard, MD, associate chair for education in the department of medicine, approached the originators to incorporate the program into the medical school’s interclinical curriculum, given to students between the third and fourth years as additional skills they would need in their sub-internships. Originally offered as an elective, demand for the course exceeded the class limit. Plans are under way to make this course mandatory.
“This past year, for the first time, we specifically taught our medical students hand-offs,” says Dr. Chu. He and his colleagues presented an abstract at SHM’s annual meeting in Dallas and are preparing a manuscript for publication.
Until now, all physicians have managed to do hand-offs without formal training. “Most residents figure out their own way of doing things after a while, but what we’re trying to do is not let it be a random evolution of learning,” says Dr. Chu. “It’s like learning to drive or ski with no lesson s: If you point your skis downhill, eventually you’ll learn how to ski, but you’ll have a lot of crashes. In hand-offs, that means communication failures, and a patient may suffer morbidity. We want to train and supervise [residents] so they learn in a progressive fashion and have fewer crashes.” TH
Andrea Sattinger is a frequent contributor to The Hospitalist.
References
- Horwitz LI, Moin T, Green ML. Development and implementation of an oral sign-out skills curriculum. J Gen Intern Med. 2007 Aug 3.
- Kripalani S, LeFevre F, Phillips CO, et al. Deficits in communication and information transfer between hospital-based and primary care physicians: implications for patient safety and continuity of care. JAMA. 2007;297(8):831-841.
- Vidyarthi AR, Arora V, Schnipper JL, et al. Managing discontinuity in academic medical centers: strategies for a safe and effective resident sign-out. J Hosp Med. 2006;1(4):257-266.
- Horwitz LI, Krumholz HM, Green ML,. Transfers of patient care between house staff on internal medicine wards: a national survey. Arch Intern Med. 2006 Jun;166(11):1173-1177.
- Coleman EA, Berenson RA. Lost in transition: challenges and opportunities for improving the quality of transitional care. Ann Intern Med. 2004 Oct;141(7):533-536.
- Halasyamani L, Kripalani S, Coleman E, et al. Transition of care for hospitalized elderly patients—development of a discharge checklist for hospitalists. J Hosp Med. 2006 Nov;1(6):354-360.
- Pantilat SZ, Lindenauer PK, Katz PP, et al. Primary care physician attitudes regarding communication with hospitalists. Am J Med. 2001;111(9, Supplement 2):15-20.
- SBAR initiative to improve staff communication. Healthcare Benchmarks Qual Improv. 2005;12(4):40-41.
Fly Solo
Lone hospitalist. It sounds adventurous. It might mean having the chance to set the stage for a hospital medicine program—working exactly the way one wants to and enjoying the feeling of indispensability.
But it’s not for the faint of heart, as those who’d done it attest. There’s the potential for having no starting patient base, or being overwhelmed because there are few to no physicians to share coverage. Having the chance to educate the hospital and its staff about hospital medicine can be a blessing—and a curse.
An example of a lone hospitalist who has experienced the joys and pains of her position is Patricia M. Hopkins-Braddock, MD, an assistant professor of pediatrics at Albany Medical College in N.Y. She was hired as the only pediatric hospitalist in the pediatrics intensive care unit (PICU) at Albany Medical Center. This is her fourth year in that position. Having become the residency program director at her institution in January, she works every day plus one weekend a month, alternating weekly between a pediatrics floor and a long-term care facility and sedation service for children.
“I like the fact that I have turned into the go-to person for problems within the hospital continuum,” Dr. Hopkins-Braddock says. “I also have to say that that is probably one of the things I like least. I have that presence in the hospital and the understanding of the way the floor works. I also do pediatrics sedation. Somehow I become the solution for every problem. It’s good in its own sense, but it can also become very overwhelming.”
A Perfect World?
“If we could figure out a way for one person to function productively and efficiently by themselves, it would be wonderful,” says Cary Ward, MD, who works with hospitalist programs that are part of Catholic Health Initiatives, based in Denver, and is the chief medical officer at St. Elizabeth Regional Medicine Center in Lincoln, Neb. “There is a large group of hospitals that wants to have a hospitalist program, and those are the critical access hospitals.” At these hospitals, which never have more than 25 patients, several community physicians round at the hospital in the morning, finishing by 7 or 7:30 a.m., and return to their primary office bases. “These hospitals are often clamoring for someone to be in the hospital the majority of the day,” he says.
“You’ve heard the saying, ‘You’ve seen one hospitalist program, you’ve seen one hospitalist program,’ ” continues Dr. Ward. “I’ve been amazed at all the hybrid programs out there. At most small hospitalist groups, even those programs under the smallest census of 12 or 13 patients, hospitals still often bring in two doctors with alternate week rotations. “Many consider this the most feasible way to try to cover one hospital census at all times; however, some worry that this ‘feast or famine’ schedule may lead to burnout and this can be expensive for the hospital. To get only one physician to cover that kind of responsibility is a real challenge.”
And yet, some hospitals and hospitalists manage to do it. Of the 362 hospitalist groups that responded to SHM’s 2005-2006 survey “Bi-Annual Survey on the State of the Hospital Medicine Movement,” only nine groups (2.5%) consisted of one physician. Joseph A. Miller, MD, who staffs SHM’s Benchmarks Task Force and has been helping SHM build a national hospitalist database, estimates that of the 2,500 hospitalist groups in the U.S., 62 groups might have just one hospitalist.
Pluses and Minuses
Martin C. Johns, MD, a rural internal medicine and pediatrics hospitalist at Gifford Medical Center in Randolph, Vt., sees some definite advantages to being a lone hospitalist, a post he has held for the 1 1/2 years. “It allowed me the time to interact with all the other modalities and to establish with physician therapy, occupational therapy, care management, pharmacy, what was lacking in the previous model with a variety of docs covering,” Dr. Johns says. “I was trying to create standards that made sense for everyone. The establishment of my being the only hospitalist was determinant primarily on my ability to create those relationships and ensure that they were solid, and also to have the support of all the primary care doctors.”
Gifford’s administration was also supportive. “Because we are a critical access hospital, there are certain restrictions and requirements that we have to take into consideration with Medicare and Medicaid,” Dr. Johns says. “Being the sole hospitalist as we’re expanding allowed me to set the stage: what was lacking, what was missing, what we could improve on, what was already working quite well. [I incorporated] the help of the administration to fill in the gaps of what we needed.”
The primary nonclinical challenge for the lone hospitalist is finding patients to care for and doctors to share coverage. Christopher Farrar, MD, lead hospitalist at Anderson Hospital in Maryville, Ill., began the program there. His employer, the hospitalist company Inpatient Management Inc., based in St. Louis, Mo., manages 18 hospitalist programs in 12 states. “As I was ending my primary care role,” says Dr. Farrar, “this opportunity came available. I think that they weren’t expecting someone to jump in so quickly. They didn’t have the luxury of time to find another physician right away.”
There are now two physicians in the program there, and they are on the verge of getting a third. Dr. Farrar said he doesn’t think there are a lot of pluses to being the lone hospitalist. The most difficult part is avoiding burnout, he warns. Although there were plenty of patients and work for him when he first started at his institution, he wasn’t overwhelmed. But he was relieved when the company brought in a second physician with whom to share call. “I could have easily become overwhelmed quickly had it gone down that road,” he says.
Finding a patient base and physician call backup were not issues for J. Stewart Fulton, DO, medical director of the hospitalist program at Southern New Hampshire Medical Center in Nashua, when he began five years ago as the lone hospitalist. Foundation Medical Partners, a multispecialty group of 27 doctors directly affiliated with the hospital, recruited Dr. Fulton to start a hospitalist program. “I walked into an ideal situation,” he says. “I stepped into a group that had a patient base, that knew they needed hospital coverage, and were willing to support me as I grew to provide 24/7 coverage for myself.”
Culture Shock
In July 1998, Joseph Li, MD, director of the hospital medicine program at Beth Israel Deaconess Medical Center, Boston, was the chief medical resident at that institution when his chief of medicine approached him about starting a hospitalist program.
In the late 1990s there was no model of that kind in Boston. “He hired me as our first full-time hospitalist, and I was referred to as a hospitalist—but nobody really understood what that meant,” says Dr. Li. “Looking back now, I didn’t even really understand what that meant.”
Tin M. Oo, MD, medical director for the hospitalist program at St. Mary’s Health Center in Jefferson City, Mo., practiced for seven months as a lone hospitalist but was hardly a new physician. He has been practicing medicine for 34 years in the U.S. and four other countries: Burma (now Myanmar, his native country), Sri Lanka, Malaysia, and Brunei Darussalam. Since he emigrated to the U.S. 15 years ago, he has served as an epidemiologist with the state Department of Health in Minnesota, matriculated into a three-year internal medicine residency program in New York and practiced there, and was in private practice in Chattanooga, Tenn.
When Dr. Oo first came to St. Mary’s, he taught his co-workers, the patients, and their families. “The hospital [and nurses] didn’t have any experience with hospitalists so they didn’t know when to call me and when not to call me,” he says. Dr. Oo got his first hospitalist experience in Chattanooga, Tenn., when he worked with outpatients and some inpatients. His prior experience moonlighting as a hospitalist as well as an emergency physician has helped him greatly as a lone hospitalist. “It was a good thing that I wasn’t just a hospitalist; that I had been in private practice and worked in the ER and as a hospitalist. I knew what the private doctors were facing, and what was coming across from the ER.”
For those who have not yet practiced medicine, Dr. Oo would dissuade them from taking a position as a lone hospitalist. “You have to have a feel for what the ER physicians or what the family practice/ internists, and what the specialists do,” he says. “You also have to be in the hospitalist’s shoes, at least from time to time.”
Be Flexible
While all hospitalists need to be flexible, this may be particularly true for the lone hospitalist. Dr. Johns finds his dual internal medicine/pediatrics training serves him well. “I assist with patients, especially pediatrics, in the emergency department [ED], go up to [resuscitate the infant in] C sections, deal with all the pediatric issues and ER consultations during the day plus do all the general internal medicine care and adult care, which does make up the majority of what I do during the day,” he says. Two physician assistants have been brought on board to improve continuity on nights and weekends and decrease the workload of all physician providers.
Dr. Johns, whose title is associate medical director in charge of hospitalist services, finds the biggest challenge has been attaining and maintaining a commitment to quality on opposite shifts. Sharing coverage with several primary care physicians, he says, means there are differences in concepts of protocols for admissions, commitment to caring for the extra patients, and the physician’s comfort in his or her inpatient knowledge base.
Taking over after a previous night’s coverage, Dr. Johns is unsure which orders were carried out and which patients received what therapy, for instance. “The covering providers take care and make sure patients make it through to next day but often hesitate to alter the plan too much because they are not covering the following day as the inpatient provider.” A newly instated Thursday-through-Monday hospitalist service schedule has helped improve continuity of care and transfer of information through the weekend. But it is still not a perfect situation.
After 15 months as the lone hospitalist, Dr. Johns’ position has changed. He cares for patients during the day and during the opposite shift takes on administrative responsibilities, such as deciding on protocols and expanding services. That kind of juggling—without hospitalist colleagues—has required flexibility as well.
Plan and Set Boundaries
Educating the hospital taught Dr. Fulton a good deal as well, especially about his and their expectations. “The group that grasps the whole concept the quickest is the ancillary services (case management) and the nursing staff,” he says. He likens their receptivity to having a hospitalist to the workings of a pendulum: “There is nothing before this better way, and then they want more of it and they want it all the time. It really means needing to create boundaries”
Dr. Oo agrees that as a lone hospitalist it is important to set boundaries for your accountabilities. The administration of his hospital asked him whether he would take charge of rapid response calls. He declined, leaving that traditional role to the ED.
The year Dr. Fulton practiced as a lone hospitalist gave him a window of time to plan. “It really allowed me to hit the bumps in the road and figure things out so when I added partners, I was able to get them up to speed more quickly,” he says. “Hospitals continue to get busier and busier and that requires planning. I was tracking and trending the volume [of patients that] these 27 doctors were generating in the hospital so that I could anticipate how many doctors I needed. Hospitals continue to increase in volume. The intensity of medicine continues to increase. You always need to plan for one or two more docs than you think you need.”
Coverage
For many lone hospitalists, sharing schedule coverage is a dilemma. Dr. Li, an assistant professor of medicine at Harvard Medical School in Boston and a board member of SHM, spent one year as a lone hospitalist before another full-timer joined him. “Everybody understands that as sole physician you really can’t be expected to see patients 24/7/365,” says Dr. Li.
Dr. Li’s recommendation for any hospitalist group of any size—but particularly early on when the hospitalist is alone or in a small group—is to match volume with staffing. “With every program that I have seen or been involved with, early on there is always a massive shift of primary care providers who want to refer patients to you after the program is up and running, Dr. Li says.
Another recommendation Dr. Li has for the lone hospitalist is to identify how you will quickly get help in urgent circumstances. “There is a real benefit to the whole service for having more than one physician on any given day,” he says. It takes only one critically ill patient to cause an upheaval in the schedule.
Committee Work
As recent SHM data show, a large proportion of hospitalists serve on hospital committees. But during his year as a lone hospitalist, Dr. Li focused on taking care of patients, relying upon consultants, and getting through the day.
“I certainly had very little insight at that point of the hospitalist model in terms of communications and leading a team and being the leader of quality in the institution,” he says. “Those were the furthest things from my mind.”
Dr. Fulton participated on committees even though he was a lone hospitalist. “I was involved because I was willing to do the extra work and to use that opportunity to educate and establish who we were in the hospital,” he says. When he was joined by his first two partners, he protected them from committee work because that wasn’t their initial responsibility,” he says.
For lone hospitalists, “you either need to anticipate being on committees and protecting time for it, or you need to anticipate protecting yourself from the committees in order to provide your service,” says Dr. Fulton. “That’s sort of a slippery slope because if you lose the opportunity to become involved in committees, someone else will do it and then they’re making decisions for you that affect your practice of medicine in the hospital.”
Because Dr. Fulton would not sit in hourlong meetings, he took an indirect route—discussing issues with case managers on the floors in between patients or when they shared a patient.
Dr. Fulton advises the lone hospitalist to consider “who is boss” when he or she considers allocating time for committee involvement. Employment by a hospital versus a multispecialty group versus going out as a solo practitioner or working in a private group will determine whose agenda you have to fulfill. “If you are owned by the hospital, the hospital calls the shots; and you have to negotiate … where you put your efforts and your service. If they want you to be on committees, you need to negotiate less patient interaction. You can’t do both; you’ll begin to lose your mind.” TH
Andrea Sattinger is a frequent contributor to The Hospitalist.
Lone hospitalist. It sounds adventurous. It might mean having the chance to set the stage for a hospital medicine program—working exactly the way one wants to and enjoying the feeling of indispensability.
But it’s not for the faint of heart, as those who’d done it attest. There’s the potential for having no starting patient base, or being overwhelmed because there are few to no physicians to share coverage. Having the chance to educate the hospital and its staff about hospital medicine can be a blessing—and a curse.
An example of a lone hospitalist who has experienced the joys and pains of her position is Patricia M. Hopkins-Braddock, MD, an assistant professor of pediatrics at Albany Medical College in N.Y. She was hired as the only pediatric hospitalist in the pediatrics intensive care unit (PICU) at Albany Medical Center. This is her fourth year in that position. Having become the residency program director at her institution in January, she works every day plus one weekend a month, alternating weekly between a pediatrics floor and a long-term care facility and sedation service for children.
“I like the fact that I have turned into the go-to person for problems within the hospital continuum,” Dr. Hopkins-Braddock says. “I also have to say that that is probably one of the things I like least. I have that presence in the hospital and the understanding of the way the floor works. I also do pediatrics sedation. Somehow I become the solution for every problem. It’s good in its own sense, but it can also become very overwhelming.”
A Perfect World?
“If we could figure out a way for one person to function productively and efficiently by themselves, it would be wonderful,” says Cary Ward, MD, who works with hospitalist programs that are part of Catholic Health Initiatives, based in Denver, and is the chief medical officer at St. Elizabeth Regional Medicine Center in Lincoln, Neb. “There is a large group of hospitals that wants to have a hospitalist program, and those are the critical access hospitals.” At these hospitals, which never have more than 25 patients, several community physicians round at the hospital in the morning, finishing by 7 or 7:30 a.m., and return to their primary office bases. “These hospitals are often clamoring for someone to be in the hospital the majority of the day,” he says.
“You’ve heard the saying, ‘You’ve seen one hospitalist program, you’ve seen one hospitalist program,’ ” continues Dr. Ward. “I’ve been amazed at all the hybrid programs out there. At most small hospitalist groups, even those programs under the smallest census of 12 or 13 patients, hospitals still often bring in two doctors with alternate week rotations. “Many consider this the most feasible way to try to cover one hospital census at all times; however, some worry that this ‘feast or famine’ schedule may lead to burnout and this can be expensive for the hospital. To get only one physician to cover that kind of responsibility is a real challenge.”
And yet, some hospitals and hospitalists manage to do it. Of the 362 hospitalist groups that responded to SHM’s 2005-2006 survey “Bi-Annual Survey on the State of the Hospital Medicine Movement,” only nine groups (2.5%) consisted of one physician. Joseph A. Miller, MD, who staffs SHM’s Benchmarks Task Force and has been helping SHM build a national hospitalist database, estimates that of the 2,500 hospitalist groups in the U.S., 62 groups might have just one hospitalist.
Pluses and Minuses
Martin C. Johns, MD, a rural internal medicine and pediatrics hospitalist at Gifford Medical Center in Randolph, Vt., sees some definite advantages to being a lone hospitalist, a post he has held for the 1 1/2 years. “It allowed me the time to interact with all the other modalities and to establish with physician therapy, occupational therapy, care management, pharmacy, what was lacking in the previous model with a variety of docs covering,” Dr. Johns says. “I was trying to create standards that made sense for everyone. The establishment of my being the only hospitalist was determinant primarily on my ability to create those relationships and ensure that they were solid, and also to have the support of all the primary care doctors.”
Gifford’s administration was also supportive. “Because we are a critical access hospital, there are certain restrictions and requirements that we have to take into consideration with Medicare and Medicaid,” Dr. Johns says. “Being the sole hospitalist as we’re expanding allowed me to set the stage: what was lacking, what was missing, what we could improve on, what was already working quite well. [I incorporated] the help of the administration to fill in the gaps of what we needed.”
The primary nonclinical challenge for the lone hospitalist is finding patients to care for and doctors to share coverage. Christopher Farrar, MD, lead hospitalist at Anderson Hospital in Maryville, Ill., began the program there. His employer, the hospitalist company Inpatient Management Inc., based in St. Louis, Mo., manages 18 hospitalist programs in 12 states. “As I was ending my primary care role,” says Dr. Farrar, “this opportunity came available. I think that they weren’t expecting someone to jump in so quickly. They didn’t have the luxury of time to find another physician right away.”
There are now two physicians in the program there, and they are on the verge of getting a third. Dr. Farrar said he doesn’t think there are a lot of pluses to being the lone hospitalist. The most difficult part is avoiding burnout, he warns. Although there were plenty of patients and work for him when he first started at his institution, he wasn’t overwhelmed. But he was relieved when the company brought in a second physician with whom to share call. “I could have easily become overwhelmed quickly had it gone down that road,” he says.
Finding a patient base and physician call backup were not issues for J. Stewart Fulton, DO, medical director of the hospitalist program at Southern New Hampshire Medical Center in Nashua, when he began five years ago as the lone hospitalist. Foundation Medical Partners, a multispecialty group of 27 doctors directly affiliated with the hospital, recruited Dr. Fulton to start a hospitalist program. “I walked into an ideal situation,” he says. “I stepped into a group that had a patient base, that knew they needed hospital coverage, and were willing to support me as I grew to provide 24/7 coverage for myself.”
Culture Shock
In July 1998, Joseph Li, MD, director of the hospital medicine program at Beth Israel Deaconess Medical Center, Boston, was the chief medical resident at that institution when his chief of medicine approached him about starting a hospitalist program.
In the late 1990s there was no model of that kind in Boston. “He hired me as our first full-time hospitalist, and I was referred to as a hospitalist—but nobody really understood what that meant,” says Dr. Li. “Looking back now, I didn’t even really understand what that meant.”
Tin M. Oo, MD, medical director for the hospitalist program at St. Mary’s Health Center in Jefferson City, Mo., practiced for seven months as a lone hospitalist but was hardly a new physician. He has been practicing medicine for 34 years in the U.S. and four other countries: Burma (now Myanmar, his native country), Sri Lanka, Malaysia, and Brunei Darussalam. Since he emigrated to the U.S. 15 years ago, he has served as an epidemiologist with the state Department of Health in Minnesota, matriculated into a three-year internal medicine residency program in New York and practiced there, and was in private practice in Chattanooga, Tenn.
When Dr. Oo first came to St. Mary’s, he taught his co-workers, the patients, and their families. “The hospital [and nurses] didn’t have any experience with hospitalists so they didn’t know when to call me and when not to call me,” he says. Dr. Oo got his first hospitalist experience in Chattanooga, Tenn., when he worked with outpatients and some inpatients. His prior experience moonlighting as a hospitalist as well as an emergency physician has helped him greatly as a lone hospitalist. “It was a good thing that I wasn’t just a hospitalist; that I had been in private practice and worked in the ER and as a hospitalist. I knew what the private doctors were facing, and what was coming across from the ER.”
For those who have not yet practiced medicine, Dr. Oo would dissuade them from taking a position as a lone hospitalist. “You have to have a feel for what the ER physicians or what the family practice/ internists, and what the specialists do,” he says. “You also have to be in the hospitalist’s shoes, at least from time to time.”
Be Flexible
While all hospitalists need to be flexible, this may be particularly true for the lone hospitalist. Dr. Johns finds his dual internal medicine/pediatrics training serves him well. “I assist with patients, especially pediatrics, in the emergency department [ED], go up to [resuscitate the infant in] C sections, deal with all the pediatric issues and ER consultations during the day plus do all the general internal medicine care and adult care, which does make up the majority of what I do during the day,” he says. Two physician assistants have been brought on board to improve continuity on nights and weekends and decrease the workload of all physician providers.
Dr. Johns, whose title is associate medical director in charge of hospitalist services, finds the biggest challenge has been attaining and maintaining a commitment to quality on opposite shifts. Sharing coverage with several primary care physicians, he says, means there are differences in concepts of protocols for admissions, commitment to caring for the extra patients, and the physician’s comfort in his or her inpatient knowledge base.
Taking over after a previous night’s coverage, Dr. Johns is unsure which orders were carried out and which patients received what therapy, for instance. “The covering providers take care and make sure patients make it through to next day but often hesitate to alter the plan too much because they are not covering the following day as the inpatient provider.” A newly instated Thursday-through-Monday hospitalist service schedule has helped improve continuity of care and transfer of information through the weekend. But it is still not a perfect situation.
After 15 months as the lone hospitalist, Dr. Johns’ position has changed. He cares for patients during the day and during the opposite shift takes on administrative responsibilities, such as deciding on protocols and expanding services. That kind of juggling—without hospitalist colleagues—has required flexibility as well.
Plan and Set Boundaries
Educating the hospital taught Dr. Fulton a good deal as well, especially about his and their expectations. “The group that grasps the whole concept the quickest is the ancillary services (case management) and the nursing staff,” he says. He likens their receptivity to having a hospitalist to the workings of a pendulum: “There is nothing before this better way, and then they want more of it and they want it all the time. It really means needing to create boundaries”
Dr. Oo agrees that as a lone hospitalist it is important to set boundaries for your accountabilities. The administration of his hospital asked him whether he would take charge of rapid response calls. He declined, leaving that traditional role to the ED.
The year Dr. Fulton practiced as a lone hospitalist gave him a window of time to plan. “It really allowed me to hit the bumps in the road and figure things out so when I added partners, I was able to get them up to speed more quickly,” he says. “Hospitals continue to get busier and busier and that requires planning. I was tracking and trending the volume [of patients that] these 27 doctors were generating in the hospital so that I could anticipate how many doctors I needed. Hospitals continue to increase in volume. The intensity of medicine continues to increase. You always need to plan for one or two more docs than you think you need.”
Coverage
For many lone hospitalists, sharing schedule coverage is a dilemma. Dr. Li, an assistant professor of medicine at Harvard Medical School in Boston and a board member of SHM, spent one year as a lone hospitalist before another full-timer joined him. “Everybody understands that as sole physician you really can’t be expected to see patients 24/7/365,” says Dr. Li.
Dr. Li’s recommendation for any hospitalist group of any size—but particularly early on when the hospitalist is alone or in a small group—is to match volume with staffing. “With every program that I have seen or been involved with, early on there is always a massive shift of primary care providers who want to refer patients to you after the program is up and running, Dr. Li says.
Another recommendation Dr. Li has for the lone hospitalist is to identify how you will quickly get help in urgent circumstances. “There is a real benefit to the whole service for having more than one physician on any given day,” he says. It takes only one critically ill patient to cause an upheaval in the schedule.
Committee Work
As recent SHM data show, a large proportion of hospitalists serve on hospital committees. But during his year as a lone hospitalist, Dr. Li focused on taking care of patients, relying upon consultants, and getting through the day.
“I certainly had very little insight at that point of the hospitalist model in terms of communications and leading a team and being the leader of quality in the institution,” he says. “Those were the furthest things from my mind.”
Dr. Fulton participated on committees even though he was a lone hospitalist. “I was involved because I was willing to do the extra work and to use that opportunity to educate and establish who we were in the hospital,” he says. When he was joined by his first two partners, he protected them from committee work because that wasn’t their initial responsibility,” he says.
For lone hospitalists, “you either need to anticipate being on committees and protecting time for it, or you need to anticipate protecting yourself from the committees in order to provide your service,” says Dr. Fulton. “That’s sort of a slippery slope because if you lose the opportunity to become involved in committees, someone else will do it and then they’re making decisions for you that affect your practice of medicine in the hospital.”
Because Dr. Fulton would not sit in hourlong meetings, he took an indirect route—discussing issues with case managers on the floors in between patients or when they shared a patient.
Dr. Fulton advises the lone hospitalist to consider “who is boss” when he or she considers allocating time for committee involvement. Employment by a hospital versus a multispecialty group versus going out as a solo practitioner or working in a private group will determine whose agenda you have to fulfill. “If you are owned by the hospital, the hospital calls the shots; and you have to negotiate … where you put your efforts and your service. If they want you to be on committees, you need to negotiate less patient interaction. You can’t do both; you’ll begin to lose your mind.” TH
Andrea Sattinger is a frequent contributor to The Hospitalist.
Lone hospitalist. It sounds adventurous. It might mean having the chance to set the stage for a hospital medicine program—working exactly the way one wants to and enjoying the feeling of indispensability.
But it’s not for the faint of heart, as those who’d done it attest. There’s the potential for having no starting patient base, or being overwhelmed because there are few to no physicians to share coverage. Having the chance to educate the hospital and its staff about hospital medicine can be a blessing—and a curse.
An example of a lone hospitalist who has experienced the joys and pains of her position is Patricia M. Hopkins-Braddock, MD, an assistant professor of pediatrics at Albany Medical College in N.Y. She was hired as the only pediatric hospitalist in the pediatrics intensive care unit (PICU) at Albany Medical Center. This is her fourth year in that position. Having become the residency program director at her institution in January, she works every day plus one weekend a month, alternating weekly between a pediatrics floor and a long-term care facility and sedation service for children.
“I like the fact that I have turned into the go-to person for problems within the hospital continuum,” Dr. Hopkins-Braddock says. “I also have to say that that is probably one of the things I like least. I have that presence in the hospital and the understanding of the way the floor works. I also do pediatrics sedation. Somehow I become the solution for every problem. It’s good in its own sense, but it can also become very overwhelming.”
A Perfect World?
“If we could figure out a way for one person to function productively and efficiently by themselves, it would be wonderful,” says Cary Ward, MD, who works with hospitalist programs that are part of Catholic Health Initiatives, based in Denver, and is the chief medical officer at St. Elizabeth Regional Medicine Center in Lincoln, Neb. “There is a large group of hospitals that wants to have a hospitalist program, and those are the critical access hospitals.” At these hospitals, which never have more than 25 patients, several community physicians round at the hospital in the morning, finishing by 7 or 7:30 a.m., and return to their primary office bases. “These hospitals are often clamoring for someone to be in the hospital the majority of the day,” he says.
“You’ve heard the saying, ‘You’ve seen one hospitalist program, you’ve seen one hospitalist program,’ ” continues Dr. Ward. “I’ve been amazed at all the hybrid programs out there. At most small hospitalist groups, even those programs under the smallest census of 12 or 13 patients, hospitals still often bring in two doctors with alternate week rotations. “Many consider this the most feasible way to try to cover one hospital census at all times; however, some worry that this ‘feast or famine’ schedule may lead to burnout and this can be expensive for the hospital. To get only one physician to cover that kind of responsibility is a real challenge.”
And yet, some hospitals and hospitalists manage to do it. Of the 362 hospitalist groups that responded to SHM’s 2005-2006 survey “Bi-Annual Survey on the State of the Hospital Medicine Movement,” only nine groups (2.5%) consisted of one physician. Joseph A. Miller, MD, who staffs SHM’s Benchmarks Task Force and has been helping SHM build a national hospitalist database, estimates that of the 2,500 hospitalist groups in the U.S., 62 groups might have just one hospitalist.
Pluses and Minuses
Martin C. Johns, MD, a rural internal medicine and pediatrics hospitalist at Gifford Medical Center in Randolph, Vt., sees some definite advantages to being a lone hospitalist, a post he has held for the 1 1/2 years. “It allowed me the time to interact with all the other modalities and to establish with physician therapy, occupational therapy, care management, pharmacy, what was lacking in the previous model with a variety of docs covering,” Dr. Johns says. “I was trying to create standards that made sense for everyone. The establishment of my being the only hospitalist was determinant primarily on my ability to create those relationships and ensure that they were solid, and also to have the support of all the primary care doctors.”
Gifford’s administration was also supportive. “Because we are a critical access hospital, there are certain restrictions and requirements that we have to take into consideration with Medicare and Medicaid,” Dr. Johns says. “Being the sole hospitalist as we’re expanding allowed me to set the stage: what was lacking, what was missing, what we could improve on, what was already working quite well. [I incorporated] the help of the administration to fill in the gaps of what we needed.”
The primary nonclinical challenge for the lone hospitalist is finding patients to care for and doctors to share coverage. Christopher Farrar, MD, lead hospitalist at Anderson Hospital in Maryville, Ill., began the program there. His employer, the hospitalist company Inpatient Management Inc., based in St. Louis, Mo., manages 18 hospitalist programs in 12 states. “As I was ending my primary care role,” says Dr. Farrar, “this opportunity came available. I think that they weren’t expecting someone to jump in so quickly. They didn’t have the luxury of time to find another physician right away.”
There are now two physicians in the program there, and they are on the verge of getting a third. Dr. Farrar said he doesn’t think there are a lot of pluses to being the lone hospitalist. The most difficult part is avoiding burnout, he warns. Although there were plenty of patients and work for him when he first started at his institution, he wasn’t overwhelmed. But he was relieved when the company brought in a second physician with whom to share call. “I could have easily become overwhelmed quickly had it gone down that road,” he says.
Finding a patient base and physician call backup were not issues for J. Stewart Fulton, DO, medical director of the hospitalist program at Southern New Hampshire Medical Center in Nashua, when he began five years ago as the lone hospitalist. Foundation Medical Partners, a multispecialty group of 27 doctors directly affiliated with the hospital, recruited Dr. Fulton to start a hospitalist program. “I walked into an ideal situation,” he says. “I stepped into a group that had a patient base, that knew they needed hospital coverage, and were willing to support me as I grew to provide 24/7 coverage for myself.”
Culture Shock
In July 1998, Joseph Li, MD, director of the hospital medicine program at Beth Israel Deaconess Medical Center, Boston, was the chief medical resident at that institution when his chief of medicine approached him about starting a hospitalist program.
In the late 1990s there was no model of that kind in Boston. “He hired me as our first full-time hospitalist, and I was referred to as a hospitalist—but nobody really understood what that meant,” says Dr. Li. “Looking back now, I didn’t even really understand what that meant.”
Tin M. Oo, MD, medical director for the hospitalist program at St. Mary’s Health Center in Jefferson City, Mo., practiced for seven months as a lone hospitalist but was hardly a new physician. He has been practicing medicine for 34 years in the U.S. and four other countries: Burma (now Myanmar, his native country), Sri Lanka, Malaysia, and Brunei Darussalam. Since he emigrated to the U.S. 15 years ago, he has served as an epidemiologist with the state Department of Health in Minnesota, matriculated into a three-year internal medicine residency program in New York and practiced there, and was in private practice in Chattanooga, Tenn.
When Dr. Oo first came to St. Mary’s, he taught his co-workers, the patients, and their families. “The hospital [and nurses] didn’t have any experience with hospitalists so they didn’t know when to call me and when not to call me,” he says. Dr. Oo got his first hospitalist experience in Chattanooga, Tenn., when he worked with outpatients and some inpatients. His prior experience moonlighting as a hospitalist as well as an emergency physician has helped him greatly as a lone hospitalist. “It was a good thing that I wasn’t just a hospitalist; that I had been in private practice and worked in the ER and as a hospitalist. I knew what the private doctors were facing, and what was coming across from the ER.”
For those who have not yet practiced medicine, Dr. Oo would dissuade them from taking a position as a lone hospitalist. “You have to have a feel for what the ER physicians or what the family practice/ internists, and what the specialists do,” he says. “You also have to be in the hospitalist’s shoes, at least from time to time.”
Be Flexible
While all hospitalists need to be flexible, this may be particularly true for the lone hospitalist. Dr. Johns finds his dual internal medicine/pediatrics training serves him well. “I assist with patients, especially pediatrics, in the emergency department [ED], go up to [resuscitate the infant in] C sections, deal with all the pediatric issues and ER consultations during the day plus do all the general internal medicine care and adult care, which does make up the majority of what I do during the day,” he says. Two physician assistants have been brought on board to improve continuity on nights and weekends and decrease the workload of all physician providers.
Dr. Johns, whose title is associate medical director in charge of hospitalist services, finds the biggest challenge has been attaining and maintaining a commitment to quality on opposite shifts. Sharing coverage with several primary care physicians, he says, means there are differences in concepts of protocols for admissions, commitment to caring for the extra patients, and the physician’s comfort in his or her inpatient knowledge base.
Taking over after a previous night’s coverage, Dr. Johns is unsure which orders were carried out and which patients received what therapy, for instance. “The covering providers take care and make sure patients make it through to next day but often hesitate to alter the plan too much because they are not covering the following day as the inpatient provider.” A newly instated Thursday-through-Monday hospitalist service schedule has helped improve continuity of care and transfer of information through the weekend. But it is still not a perfect situation.
After 15 months as the lone hospitalist, Dr. Johns’ position has changed. He cares for patients during the day and during the opposite shift takes on administrative responsibilities, such as deciding on protocols and expanding services. That kind of juggling—without hospitalist colleagues—has required flexibility as well.
Plan and Set Boundaries
Educating the hospital taught Dr. Fulton a good deal as well, especially about his and their expectations. “The group that grasps the whole concept the quickest is the ancillary services (case management) and the nursing staff,” he says. He likens their receptivity to having a hospitalist to the workings of a pendulum: “There is nothing before this better way, and then they want more of it and they want it all the time. It really means needing to create boundaries”
Dr. Oo agrees that as a lone hospitalist it is important to set boundaries for your accountabilities. The administration of his hospital asked him whether he would take charge of rapid response calls. He declined, leaving that traditional role to the ED.
The year Dr. Fulton practiced as a lone hospitalist gave him a window of time to plan. “It really allowed me to hit the bumps in the road and figure things out so when I added partners, I was able to get them up to speed more quickly,” he says. “Hospitals continue to get busier and busier and that requires planning. I was tracking and trending the volume [of patients that] these 27 doctors were generating in the hospital so that I could anticipate how many doctors I needed. Hospitals continue to increase in volume. The intensity of medicine continues to increase. You always need to plan for one or two more docs than you think you need.”
Coverage
For many lone hospitalists, sharing schedule coverage is a dilemma. Dr. Li, an assistant professor of medicine at Harvard Medical School in Boston and a board member of SHM, spent one year as a lone hospitalist before another full-timer joined him. “Everybody understands that as sole physician you really can’t be expected to see patients 24/7/365,” says Dr. Li.
Dr. Li’s recommendation for any hospitalist group of any size—but particularly early on when the hospitalist is alone or in a small group—is to match volume with staffing. “With every program that I have seen or been involved with, early on there is always a massive shift of primary care providers who want to refer patients to you after the program is up and running, Dr. Li says.
Another recommendation Dr. Li has for the lone hospitalist is to identify how you will quickly get help in urgent circumstances. “There is a real benefit to the whole service for having more than one physician on any given day,” he says. It takes only one critically ill patient to cause an upheaval in the schedule.
Committee Work
As recent SHM data show, a large proportion of hospitalists serve on hospital committees. But during his year as a lone hospitalist, Dr. Li focused on taking care of patients, relying upon consultants, and getting through the day.
“I certainly had very little insight at that point of the hospitalist model in terms of communications and leading a team and being the leader of quality in the institution,” he says. “Those were the furthest things from my mind.”
Dr. Fulton participated on committees even though he was a lone hospitalist. “I was involved because I was willing to do the extra work and to use that opportunity to educate and establish who we were in the hospital,” he says. When he was joined by his first two partners, he protected them from committee work because that wasn’t their initial responsibility,” he says.
For lone hospitalists, “you either need to anticipate being on committees and protecting time for it, or you need to anticipate protecting yourself from the committees in order to provide your service,” says Dr. Fulton. “That’s sort of a slippery slope because if you lose the opportunity to become involved in committees, someone else will do it and then they’re making decisions for you that affect your practice of medicine in the hospital.”
Because Dr. Fulton would not sit in hourlong meetings, he took an indirect route—discussing issues with case managers on the floors in between patients or when they shared a patient.
Dr. Fulton advises the lone hospitalist to consider “who is boss” when he or she considers allocating time for committee involvement. Employment by a hospital versus a multispecialty group versus going out as a solo practitioner or working in a private group will determine whose agenda you have to fulfill. “If you are owned by the hospital, the hospital calls the shots; and you have to negotiate … where you put your efforts and your service. If they want you to be on committees, you need to negotiate less patient interaction. You can’t do both; you’ll begin to lose your mind.” TH
Andrea Sattinger is a frequent contributor to The Hospitalist.