User login
Bullied into Botched Care
Bullying, intimidation, verbal abuse—these behaviors negatively affect self-esteem, feelings of competence, and workplace morale. And they can devastate hospital professionals and their patients.
When 2,095 healthcare providers (1,565 nurses, 354 pharmacists, and 176 others) responded to an Institute for Safe Medication Practices (ISMP) survey on intimidation in their healthcare setting, remarkable data were collected.1
Perhaps the most alarming statistic in the 2003-2004 study was that 7% of respondents (n=147) reported they had been involved in a medication error allowed to occur partly because the respondents were afraid to question the prescriber’s decision. At a large urban trauma center in the northeastern United States, nurses listed intimidation as one of the barriers to implementing a sharps safety program.2
Nurses’ Perceptions
Research over the past decade has spotlighted intimidation in healthcare.3
“Bullying and harassment still happen in many areas of medicine,” says David M. Pressel, MD, PhD, hospitalist and director, Inpatient Service, Division of General Pediatrics at Alfred I. duPont Hospital for Children in Wilmington, Del. “The question is, how do you monitor yourself to make sure you aren’t falling into that hierarchical frame of mind that could intervene in great teaching and learning and great patient care?”
Dr. Pressel and his partner, David I. Rappaport, MD, also a pediatric hospitalist at duPont, have focused on the literature pertaining to nurse-physician relationships. Research shows that intimidation impedes nurse recruitment, retention, and satisfaction. In one study, 90% of nurses reported experiencing at least one episode of verbal abuse.4 A 1997 study examining the effects of intimidation on 35 pediatric nurses over a three-month period found that 25 (71.4%) of them reported being yelled at or loudly admonished. Sixteen (45.7%) had been victims of insults. Thirty (85.7%) were spoken to in a condescending manner. One-third of nurses believed that such behavior was “part of the job.”
Although studies have differed as to the most common source of this abuse—patients and families or physicians—a study of pediatric nurses reported a similar incidence from both sources.5 And, nurses are often guilty of verbally abusing each other.6
When the duPont pediatric hospitalist team began performing more family-centered rounds, they began to appreciate the nurse-physician relationship. “We have worked hard to have a charge nurse and oftentimes the bedside nurse with us when we round,” Dr. Rappaport says. Speculating that rounding with hospitalists allowed nurses to feel more part of the team, Dr. Rappaport says know the medical plan, consolidate efforts such that pages to residents were reduced, and generally improve communication. They heard from participating nurses that it made a tremendous difference. This prompted them to conduct their research.
“Our study looked at the nurse-physician relationship globally, not intimidation or abuse specifically,” says Dr. Rappaport. Along with their nurse colleague Norine Watson, RN, Drs. Pressel and Rappaport are examining the relationship between nurses and different categories of physicians: how nurses perceive interactions between nurses and surgical residents, surgical attendings, community physicians, pediatric residents, and pediatric hospitalists.
“Early data suggest that hospitalists may work more effectively with nurses because they share many of the same goals,” says Dr. Rappaport. “As hospital leaders, hospitalists can also improve working conditions for nurses by providing more accessible, efficient, and effective care. Presumably, improved collaboration will also include decreased intimidation or abuse from physicians and also probably from dissatisfied patients and families.”
Avoiding the trap of communicating in a manner that is too direct and might be construed as abusive requires self-awareness and the realization that people receive information in different ways, says Dr. Pressel. Standard professional behavior is the key. Beyond that, the challenge is giving feedback constructively and in a positive manner.
“Hospitalists [may be] more in tune with the needs of nurses than nonhospitalists,” says Dr. Rappaport. “I think that is one of our strengths. We need to continue to facilitate very strong relationships between nurses and physicians because without good nursing care, hospitalists simply cannot provide good medical care.”
There is another way hospitalists can help address verbal abuse. “Studies consistently show that nurses are hesitant to report episodes of verbal abuse,” Dr. Rappaport says, “whether it is from a family, a patient, a physician, or a fellow nurse. Fewer than one in five nurses reports these episodes. One thing that hospitalists can do is work with hospital administration to create an environment that is more proactive in addressing these concerns and allowing nurses to feel more support in this area.”
Only 60% of respondents to the ISMP survey felt their organization had clearly defined an effective process for handling disagreements with a medication order’s safety. Only about a third felt the process facilitated their bypassing an intimidating prescriber or their own supervisor if necessary. Although 70% of respondents reported that they thought their organization or manager would support them if they reported intimidating behavior, only 39% of respondents believed their organization was dealing effectively with intimidating behavior.
Untapped Source
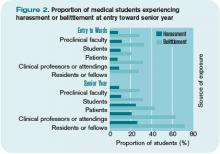
Perceptions of intimidation also occur among trainees. When 2,884 students from the class of 2003 at 16 U.S. medical schools completed questionnaires at various times during training, 27% reported having been “harassed” by house staff, 21% by faculty, and 25% by patients.7 Further, 71% reported having been “belittled” by house staff, 63% by faculty, and 43% by patients.
Mistreated students were significantly more likely to have suffered stress, be depressed or suicidal, and less likely to report being glad they trained as a physician.

—David I. Rappaport, MD, pediatric hospitalist, Alfred I. Dupont Hospital for Children, Wilmington, Del.
This may have an underlying effect on the potential to monitor for patient safety.8,9 Because errors and near misses often result from miscommunication, medical students may be adept at preventing certain types of errors. Students’ observation skills may be just as keen, if not more so, than their more clinically proficient healthcare teammates.8 In four cases from two U.S. academic health centers reported by medical students Samuel Seiden, Cynthia Galvan, and Ruth Lamm in 2006, medical students demonstrated keen attention to detail and appropriately characterized problematic situations with patients—adding another layer of defense within systems safeguarding against patient harm.8 Yet of the 76% of medical students who had observed a medical error, only about half of the students reported the errors to a resident or an attending, despite having received patient-safety training; only 7% reported having used an electronic medical error reporting system.10
By Example
Some intimidation in medical education may be the result of anger toward students and residents over a lack of medical knowledge, says Jeffery G. Wiese, MD, associate professor of Medicine at Tulane University in New Orleans and member of the SHM Board of Directors. “It is natural to feel [that anger]; people abhor in others what they most detest in themselves,’’ he says. “As physicians, a lack of medical knowledge is what we detest in ourselves. But a student’s ignorance is usually a product of where she is in her training; that’s why she is with you.”
—Jeffery G. Wiese, MD, associate professor of Medicine at Tulane University, New Orleans
Anger alienates students, absolving them of the guilt of not knowing the information, and demotivating them from learning it. “The lesson to be communicated is that it is OK not to know, but it is not OK to continue to not know,” Dr. Wiese says. “Reprimands should be reserved for the student who does not know, and then after being taught or asked to look it up, continues to not know.”
“The average physician who practices for 30 years will take care of roughly 80,000 people,” estimates Dr. Wiese. “That’s an arithmetic contribution and there is nothing wrong with that. But if you really want to change the world, teaching is the rule. The same 30 years invested in teaching will indirectly affect 400 million people,” he says. “Even better, if you can train your students and residents in the value of coaching their students and residents, well, now you’re talking about 10 billion people that you can affect over the course of a career.”
The question to ask yourself, says Dr. Wiese, is: Do you want to change the world? “If you do, this is the way to do it,” he says.
“For the 30 years in your career, focus on clinical coaching and getting others to clinically coach. That way, especially if you have the right motives in your heart, the right vision for the way you want to see the profession practiced, and the way you want patient care performed, that’s your shot at changing the world.” TH
Andrea Sattinger is a frequent contributor to The Hospitalist.
References
- Institute for Safe Medication Practice. Intimidation: practitioners speak up about this unresolved problem (Part I). Available at w.ismp.org/Newsletters/acutecare/articles/20040311_2.asp. Last accessed June 27, 2007.
- Hagstrom AM. Perceived barriers to implementation of a successful sharps safety program. AORN J. 2006;83(2):391-7.
- Porto G, Lauve R. Disruptive clinician behavior: a persistent threat to patient safety. Patient Safety Qual Healthc. 2006 Jul-Aug;3:16-24.
- Manderino MA, Berkey N. Verbal abuse of staff nurses by physicians. J Prof Nurs. 1997;13(1):48-55.
- Pejic AR. Verbal abuse: A problem for pediatric nurses. Pediatr Nurs. 2005;31(4):271-279.
- Rowe MM, Sherlock H. Stress and verbal abuse in nursing: do burned out nurses eat their young? J Nurs Manag. 2005May;13(3):242-248.
- Frank E, Carrera JS, Stratton T, et al. Experiences of belittlement and harassment and their correlates among medical students in the United States: longitudinal survey. BMJ. 2006 Sep 30;333(7570):682.
- Seiden SC, Galvan C, Lamm R. Role of medical students in preventing patient harm and enhancing patient safety. Qual Saf Health Care. 2006 Aug;15(4):272-276.
- Wood DF. Bullying and harassment in medical schools. BMJ. 2006 Sep 30;333(7570):664-665.
- Madigosky WS, Headrick LA, Nelson K, et al. Changing and sustaining medical students’ knowledge, skills, and attitudes about patient safety and medical fallibility. Acad Med. 2006 Jan;81(1):94-101.
- Institute for Safe Medication Practice. Intimidation: Mapping a plan for cultural change in healthcare (Part II). Available at www.ismp.org/Newsletters/acutecare/articles/20040325.asp Last accessed July 2, 2007.
Bullying, intimidation, verbal abuse—these behaviors negatively affect self-esteem, feelings of competence, and workplace morale. And they can devastate hospital professionals and their patients.
When 2,095 healthcare providers (1,565 nurses, 354 pharmacists, and 176 others) responded to an Institute for Safe Medication Practices (ISMP) survey on intimidation in their healthcare setting, remarkable data were collected.1
Perhaps the most alarming statistic in the 2003-2004 study was that 7% of respondents (n=147) reported they had been involved in a medication error allowed to occur partly because the respondents were afraid to question the prescriber’s decision. At a large urban trauma center in the northeastern United States, nurses listed intimidation as one of the barriers to implementing a sharps safety program.2
Nurses’ Perceptions
Research over the past decade has spotlighted intimidation in healthcare.3
“Bullying and harassment still happen in many areas of medicine,” says David M. Pressel, MD, PhD, hospitalist and director, Inpatient Service, Division of General Pediatrics at Alfred I. duPont Hospital for Children in Wilmington, Del. “The question is, how do you monitor yourself to make sure you aren’t falling into that hierarchical frame of mind that could intervene in great teaching and learning and great patient care?”
Dr. Pressel and his partner, David I. Rappaport, MD, also a pediatric hospitalist at duPont, have focused on the literature pertaining to nurse-physician relationships. Research shows that intimidation impedes nurse recruitment, retention, and satisfaction. In one study, 90% of nurses reported experiencing at least one episode of verbal abuse.4 A 1997 study examining the effects of intimidation on 35 pediatric nurses over a three-month period found that 25 (71.4%) of them reported being yelled at or loudly admonished. Sixteen (45.7%) had been victims of insults. Thirty (85.7%) were spoken to in a condescending manner. One-third of nurses believed that such behavior was “part of the job.”
Although studies have differed as to the most common source of this abuse—patients and families or physicians—a study of pediatric nurses reported a similar incidence from both sources.5 And, nurses are often guilty of verbally abusing each other.6
When the duPont pediatric hospitalist team began performing more family-centered rounds, they began to appreciate the nurse-physician relationship. “We have worked hard to have a charge nurse and oftentimes the bedside nurse with us when we round,” Dr. Rappaport says. Speculating that rounding with hospitalists allowed nurses to feel more part of the team, Dr. Rappaport says know the medical plan, consolidate efforts such that pages to residents were reduced, and generally improve communication. They heard from participating nurses that it made a tremendous difference. This prompted them to conduct their research.
“Our study looked at the nurse-physician relationship globally, not intimidation or abuse specifically,” says Dr. Rappaport. Along with their nurse colleague Norine Watson, RN, Drs. Pressel and Rappaport are examining the relationship between nurses and different categories of physicians: how nurses perceive interactions between nurses and surgical residents, surgical attendings, community physicians, pediatric residents, and pediatric hospitalists.
“Early data suggest that hospitalists may work more effectively with nurses because they share many of the same goals,” says Dr. Rappaport. “As hospital leaders, hospitalists can also improve working conditions for nurses by providing more accessible, efficient, and effective care. Presumably, improved collaboration will also include decreased intimidation or abuse from physicians and also probably from dissatisfied patients and families.”
Avoiding the trap of communicating in a manner that is too direct and might be construed as abusive requires self-awareness and the realization that people receive information in different ways, says Dr. Pressel. Standard professional behavior is the key. Beyond that, the challenge is giving feedback constructively and in a positive manner.
“Hospitalists [may be] more in tune with the needs of nurses than nonhospitalists,” says Dr. Rappaport. “I think that is one of our strengths. We need to continue to facilitate very strong relationships between nurses and physicians because without good nursing care, hospitalists simply cannot provide good medical care.”
There is another way hospitalists can help address verbal abuse. “Studies consistently show that nurses are hesitant to report episodes of verbal abuse,” Dr. Rappaport says, “whether it is from a family, a patient, a physician, or a fellow nurse. Fewer than one in five nurses reports these episodes. One thing that hospitalists can do is work with hospital administration to create an environment that is more proactive in addressing these concerns and allowing nurses to feel more support in this area.”
Only 60% of respondents to the ISMP survey felt their organization had clearly defined an effective process for handling disagreements with a medication order’s safety. Only about a third felt the process facilitated their bypassing an intimidating prescriber or their own supervisor if necessary. Although 70% of respondents reported that they thought their organization or manager would support them if they reported intimidating behavior, only 39% of respondents believed their organization was dealing effectively with intimidating behavior.
Untapped Source
Perceptions of intimidation also occur among trainees. When 2,884 students from the class of 2003 at 16 U.S. medical schools completed questionnaires at various times during training, 27% reported having been “harassed” by house staff, 21% by faculty, and 25% by patients.7 Further, 71% reported having been “belittled” by house staff, 63% by faculty, and 43% by patients.
Mistreated students were significantly more likely to have suffered stress, be depressed or suicidal, and less likely to report being glad they trained as a physician.

—David I. Rappaport, MD, pediatric hospitalist, Alfred I. Dupont Hospital for Children, Wilmington, Del.
This may have an underlying effect on the potential to monitor for patient safety.8,9 Because errors and near misses often result from miscommunication, medical students may be adept at preventing certain types of errors. Students’ observation skills may be just as keen, if not more so, than their more clinically proficient healthcare teammates.8 In four cases from two U.S. academic health centers reported by medical students Samuel Seiden, Cynthia Galvan, and Ruth Lamm in 2006, medical students demonstrated keen attention to detail and appropriately characterized problematic situations with patients—adding another layer of defense within systems safeguarding against patient harm.8 Yet of the 76% of medical students who had observed a medical error, only about half of the students reported the errors to a resident or an attending, despite having received patient-safety training; only 7% reported having used an electronic medical error reporting system.10
By Example
Some intimidation in medical education may be the result of anger toward students and residents over a lack of medical knowledge, says Jeffery G. Wiese, MD, associate professor of Medicine at Tulane University in New Orleans and member of the SHM Board of Directors. “It is natural to feel [that anger]; people abhor in others what they most detest in themselves,’’ he says. “As physicians, a lack of medical knowledge is what we detest in ourselves. But a student’s ignorance is usually a product of where she is in her training; that’s why she is with you.”
—Jeffery G. Wiese, MD, associate professor of Medicine at Tulane University, New Orleans
Anger alienates students, absolving them of the guilt of not knowing the information, and demotivating them from learning it. “The lesson to be communicated is that it is OK not to know, but it is not OK to continue to not know,” Dr. Wiese says. “Reprimands should be reserved for the student who does not know, and then after being taught or asked to look it up, continues to not know.”
“The average physician who practices for 30 years will take care of roughly 80,000 people,” estimates Dr. Wiese. “That’s an arithmetic contribution and there is nothing wrong with that. But if you really want to change the world, teaching is the rule. The same 30 years invested in teaching will indirectly affect 400 million people,” he says. “Even better, if you can train your students and residents in the value of coaching their students and residents, well, now you’re talking about 10 billion people that you can affect over the course of a career.”
The question to ask yourself, says Dr. Wiese, is: Do you want to change the world? “If you do, this is the way to do it,” he says.
“For the 30 years in your career, focus on clinical coaching and getting others to clinically coach. That way, especially if you have the right motives in your heart, the right vision for the way you want to see the profession practiced, and the way you want patient care performed, that’s your shot at changing the world.” TH
Andrea Sattinger is a frequent contributor to The Hospitalist.
References
- Institute for Safe Medication Practice. Intimidation: practitioners speak up about this unresolved problem (Part I). Available at w.ismp.org/Newsletters/acutecare/articles/20040311_2.asp. Last accessed June 27, 2007.
- Hagstrom AM. Perceived barriers to implementation of a successful sharps safety program. AORN J. 2006;83(2):391-7.
- Porto G, Lauve R. Disruptive clinician behavior: a persistent threat to patient safety. Patient Safety Qual Healthc. 2006 Jul-Aug;3:16-24.
- Manderino MA, Berkey N. Verbal abuse of staff nurses by physicians. J Prof Nurs. 1997;13(1):48-55.
- Pejic AR. Verbal abuse: A problem for pediatric nurses. Pediatr Nurs. 2005;31(4):271-279.
- Rowe MM, Sherlock H. Stress and verbal abuse in nursing: do burned out nurses eat their young? J Nurs Manag. 2005May;13(3):242-248.
- Frank E, Carrera JS, Stratton T, et al. Experiences of belittlement and harassment and their correlates among medical students in the United States: longitudinal survey. BMJ. 2006 Sep 30;333(7570):682.
- Seiden SC, Galvan C, Lamm R. Role of medical students in preventing patient harm and enhancing patient safety. Qual Saf Health Care. 2006 Aug;15(4):272-276.
- Wood DF. Bullying and harassment in medical schools. BMJ. 2006 Sep 30;333(7570):664-665.
- Madigosky WS, Headrick LA, Nelson K, et al. Changing and sustaining medical students’ knowledge, skills, and attitudes about patient safety and medical fallibility. Acad Med. 2006 Jan;81(1):94-101.
- Institute for Safe Medication Practice. Intimidation: Mapping a plan for cultural change in healthcare (Part II). Available at www.ismp.org/Newsletters/acutecare/articles/20040325.asp Last accessed July 2, 2007.
Bullying, intimidation, verbal abuse—these behaviors negatively affect self-esteem, feelings of competence, and workplace morale. And they can devastate hospital professionals and their patients.
When 2,095 healthcare providers (1,565 nurses, 354 pharmacists, and 176 others) responded to an Institute for Safe Medication Practices (ISMP) survey on intimidation in their healthcare setting, remarkable data were collected.1
Perhaps the most alarming statistic in the 2003-2004 study was that 7% of respondents (n=147) reported they had been involved in a medication error allowed to occur partly because the respondents were afraid to question the prescriber’s decision. At a large urban trauma center in the northeastern United States, nurses listed intimidation as one of the barriers to implementing a sharps safety program.2
Nurses’ Perceptions
Research over the past decade has spotlighted intimidation in healthcare.3
“Bullying and harassment still happen in many areas of medicine,” says David M. Pressel, MD, PhD, hospitalist and director, Inpatient Service, Division of General Pediatrics at Alfred I. duPont Hospital for Children in Wilmington, Del. “The question is, how do you monitor yourself to make sure you aren’t falling into that hierarchical frame of mind that could intervene in great teaching and learning and great patient care?”
Dr. Pressel and his partner, David I. Rappaport, MD, also a pediatric hospitalist at duPont, have focused on the literature pertaining to nurse-physician relationships. Research shows that intimidation impedes nurse recruitment, retention, and satisfaction. In one study, 90% of nurses reported experiencing at least one episode of verbal abuse.4 A 1997 study examining the effects of intimidation on 35 pediatric nurses over a three-month period found that 25 (71.4%) of them reported being yelled at or loudly admonished. Sixteen (45.7%) had been victims of insults. Thirty (85.7%) were spoken to in a condescending manner. One-third of nurses believed that such behavior was “part of the job.”
Although studies have differed as to the most common source of this abuse—patients and families or physicians—a study of pediatric nurses reported a similar incidence from both sources.5 And, nurses are often guilty of verbally abusing each other.6
When the duPont pediatric hospitalist team began performing more family-centered rounds, they began to appreciate the nurse-physician relationship. “We have worked hard to have a charge nurse and oftentimes the bedside nurse with us when we round,” Dr. Rappaport says. Speculating that rounding with hospitalists allowed nurses to feel more part of the team, Dr. Rappaport says know the medical plan, consolidate efforts such that pages to residents were reduced, and generally improve communication. They heard from participating nurses that it made a tremendous difference. This prompted them to conduct their research.
“Our study looked at the nurse-physician relationship globally, not intimidation or abuse specifically,” says Dr. Rappaport. Along with their nurse colleague Norine Watson, RN, Drs. Pressel and Rappaport are examining the relationship between nurses and different categories of physicians: how nurses perceive interactions between nurses and surgical residents, surgical attendings, community physicians, pediatric residents, and pediatric hospitalists.
“Early data suggest that hospitalists may work more effectively with nurses because they share many of the same goals,” says Dr. Rappaport. “As hospital leaders, hospitalists can also improve working conditions for nurses by providing more accessible, efficient, and effective care. Presumably, improved collaboration will also include decreased intimidation or abuse from physicians and also probably from dissatisfied patients and families.”
Avoiding the trap of communicating in a manner that is too direct and might be construed as abusive requires self-awareness and the realization that people receive information in different ways, says Dr. Pressel. Standard professional behavior is the key. Beyond that, the challenge is giving feedback constructively and in a positive manner.
“Hospitalists [may be] more in tune with the needs of nurses than nonhospitalists,” says Dr. Rappaport. “I think that is one of our strengths. We need to continue to facilitate very strong relationships between nurses and physicians because without good nursing care, hospitalists simply cannot provide good medical care.”
There is another way hospitalists can help address verbal abuse. “Studies consistently show that nurses are hesitant to report episodes of verbal abuse,” Dr. Rappaport says, “whether it is from a family, a patient, a physician, or a fellow nurse. Fewer than one in five nurses reports these episodes. One thing that hospitalists can do is work with hospital administration to create an environment that is more proactive in addressing these concerns and allowing nurses to feel more support in this area.”
Only 60% of respondents to the ISMP survey felt their organization had clearly defined an effective process for handling disagreements with a medication order’s safety. Only about a third felt the process facilitated their bypassing an intimidating prescriber or their own supervisor if necessary. Although 70% of respondents reported that they thought their organization or manager would support them if they reported intimidating behavior, only 39% of respondents believed their organization was dealing effectively with intimidating behavior.
Untapped Source
Perceptions of intimidation also occur among trainees. When 2,884 students from the class of 2003 at 16 U.S. medical schools completed questionnaires at various times during training, 27% reported having been “harassed” by house staff, 21% by faculty, and 25% by patients.7 Further, 71% reported having been “belittled” by house staff, 63% by faculty, and 43% by patients.
Mistreated students were significantly more likely to have suffered stress, be depressed or suicidal, and less likely to report being glad they trained as a physician.

—David I. Rappaport, MD, pediatric hospitalist, Alfred I. Dupont Hospital for Children, Wilmington, Del.
This may have an underlying effect on the potential to monitor for patient safety.8,9 Because errors and near misses often result from miscommunication, medical students may be adept at preventing certain types of errors. Students’ observation skills may be just as keen, if not more so, than their more clinically proficient healthcare teammates.8 In four cases from two U.S. academic health centers reported by medical students Samuel Seiden, Cynthia Galvan, and Ruth Lamm in 2006, medical students demonstrated keen attention to detail and appropriately characterized problematic situations with patients—adding another layer of defense within systems safeguarding against patient harm.8 Yet of the 76% of medical students who had observed a medical error, only about half of the students reported the errors to a resident or an attending, despite having received patient-safety training; only 7% reported having used an electronic medical error reporting system.10
By Example
Some intimidation in medical education may be the result of anger toward students and residents over a lack of medical knowledge, says Jeffery G. Wiese, MD, associate professor of Medicine at Tulane University in New Orleans and member of the SHM Board of Directors. “It is natural to feel [that anger]; people abhor in others what they most detest in themselves,’’ he says. “As physicians, a lack of medical knowledge is what we detest in ourselves. But a student’s ignorance is usually a product of where she is in her training; that’s why she is with you.”
—Jeffery G. Wiese, MD, associate professor of Medicine at Tulane University, New Orleans
Anger alienates students, absolving them of the guilt of not knowing the information, and demotivating them from learning it. “The lesson to be communicated is that it is OK not to know, but it is not OK to continue to not know,” Dr. Wiese says. “Reprimands should be reserved for the student who does not know, and then after being taught or asked to look it up, continues to not know.”
“The average physician who practices for 30 years will take care of roughly 80,000 people,” estimates Dr. Wiese. “That’s an arithmetic contribution and there is nothing wrong with that. But if you really want to change the world, teaching is the rule. The same 30 years invested in teaching will indirectly affect 400 million people,” he says. “Even better, if you can train your students and residents in the value of coaching their students and residents, well, now you’re talking about 10 billion people that you can affect over the course of a career.”
The question to ask yourself, says Dr. Wiese, is: Do you want to change the world? “If you do, this is the way to do it,” he says.
“For the 30 years in your career, focus on clinical coaching and getting others to clinically coach. That way, especially if you have the right motives in your heart, the right vision for the way you want to see the profession practiced, and the way you want patient care performed, that’s your shot at changing the world.” TH
Andrea Sattinger is a frequent contributor to The Hospitalist.
References
- Institute for Safe Medication Practice. Intimidation: practitioners speak up about this unresolved problem (Part I). Available at w.ismp.org/Newsletters/acutecare/articles/20040311_2.asp. Last accessed June 27, 2007.
- Hagstrom AM. Perceived barriers to implementation of a successful sharps safety program. AORN J. 2006;83(2):391-7.
- Porto G, Lauve R. Disruptive clinician behavior: a persistent threat to patient safety. Patient Safety Qual Healthc. 2006 Jul-Aug;3:16-24.
- Manderino MA, Berkey N. Verbal abuse of staff nurses by physicians. J Prof Nurs. 1997;13(1):48-55.
- Pejic AR. Verbal abuse: A problem for pediatric nurses. Pediatr Nurs. 2005;31(4):271-279.
- Rowe MM, Sherlock H. Stress and verbal abuse in nursing: do burned out nurses eat their young? J Nurs Manag. 2005May;13(3):242-248.
- Frank E, Carrera JS, Stratton T, et al. Experiences of belittlement and harassment and their correlates among medical students in the United States: longitudinal survey. BMJ. 2006 Sep 30;333(7570):682.
- Seiden SC, Galvan C, Lamm R. Role of medical students in preventing patient harm and enhancing patient safety. Qual Saf Health Care. 2006 Aug;15(4):272-276.
- Wood DF. Bullying and harassment in medical schools. BMJ. 2006 Sep 30;333(7570):664-665.
- Madigosky WS, Headrick LA, Nelson K, et al. Changing and sustaining medical students’ knowledge, skills, and attitudes about patient safety and medical fallibility. Acad Med. 2006 Jan;81(1):94-101.
- Institute for Safe Medication Practice. Intimidation: Mapping a plan for cultural change in healthcare (Part II). Available at www.ismp.org/Newsletters/acutecare/articles/20040325.asp Last accessed July 2, 2007.
The Gray Zone
In part 1 of this two-part series (July 2007, p. 16), hospitalists and emergency medicine physicians expressed their views on the relationship between their two specialties. In part 2, we look at how those relationships intersect—and what issues are at stake when they do.
One area where there is a bit of overlap between hospital medicine and emergency medicine is observational medicine,” says James W. Hoekstra, MD, professor and chairman, Department of Emergency Medicine, Wake Forest University Health Sciences Center, Winston-Salem, N.C.
Those patients who require a short stay for observation, he says, are neither in the ED or admitted to the hospital—they are in a zone of their own.
“That’s a gray zone in terms of who takes care of those patients,” he says, “and it depends on the hospital. It will be interesting to see how that works out, or whether that is ever worked out. It may just stay a shared area.”
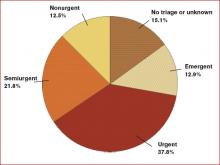
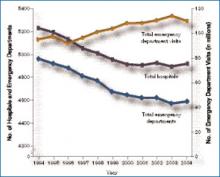
The observation conundrum is complicated by the fact that many people use emergency departments for primary care. (See Figure 1, p. 33) “ True emergencies make up only some of the patient [cases] in the ED,” says Debra L. Burgy, MD, a hospitalist at Abbott Northwestern Hospital in Minneapolis. “We do have a 23-hour observation unit of 10 beds, and, frankly, could use 10 more to [handle unpredictable volumes of patients and insufficient support staff. That unit] has certainly helped to alleviate unnecessary admissions.”
Collaboration between hospitalists and emergency medicine physicians happens a number of ways at the University of Colorado at Denver and Health Sciences Center, where Jeff Glasheen, MD, is director of both the hospital medicine program and inpatient clinical services in the department of medicine.
“One way we work closely with the ED—because we think it is the right thing to do—is by building a much more comprehensive observation unit,” Dr. Glasheen says. “In some settings the observation unit lives in the ED and is run by the ED and in others, it is run by hospitalists. The hospitalists [here] will now run the unit, but we want to help solve some of the ED’s throughput issues.”
When Dr. Glasheen arrived at his institution, the observation unit was limited to patients with chest pain. “I didn’t understand why we would get chest pain patients through efficiently and not all patients,” he says.
A team that began operating in July will be available for all patients under the admission status of observation. The team will be hospitalist-led and aim to reduce length of stay and increase quality of care for those patients.
“Right now those patients are very scattered throughout the system and they may be [covered by] six to eight different teams,” Dr. Glasheen explains. One team of caregivers will be more efficient and reduce length of stay, he says.
By nurturing their working relationship with the emergency department, hospitalists will be able to more easily say: “We understand that that workup’s not complete, but we also understand that they’re going to come into the hospital and let us know what things need to be done. We’ll be happy to take that patient a little earlier than we did in the past to get them out of the ED.”
That’s a tricky thing to do, he says, “because the benefit to us isn’t huge, we’re self-sacrificing to help the ED, and that’s what I want hospitalist groups nationally to be thinking: how we can make the whole system better and not just make our own job better.”
Dr. Glasheen believes the professional structure in his institution is representative of what other hospitals will function like in the next 10 years.
“You have a backbone structure of basically four types of physicians: emergency medicine docs, hospitalists, intensivists, and a surgical team,” Dr. Glasheen says. “Everyone else, more and more, is serving in a consultative role.” Having that backbone allows you to tackle the issues, which are primarily complex, systems-based issues, he says. “It is no longer [a matter of just] the ED trying to deal with capacity issues. Now they have an ally on the inpatient side.”
An excess of patients for the number of beds means some patients spend a disproportionate amount of their stay in the ED, and that challenges communication and efficiency. “The challenges may be simple things, such as it being harder for a hospitalist to get to the ED to see a patient than it is upstairs,” Dr. Glasheen says. “[Or] it’s harder to decide who really has ownership of that patient.” In his hospital, as soon as a patient is assigned to a hospitalist, the primary responsibility for that patient is seen as the hospitalist’s.
But there are other issues. “Even if we are able to get down [to the ED] and write orders, that is problematic for the ED and the hospitalist; as a hospitalist we don’t have the nurses with staffing ratios and skills in the ED that they have on floors and in the ICU,” says Dr. Glasheen. “It is not always possible to get things done as efficiently as they probably could if the patients were in a proper unit. Locally and globally in my experience, the biggest issue is: How do you take care of these patients who now spend their inpatient stay in the ED?”
Collaborations, Models, and Solutions
A number of hospitalists raise the issue of managing internal medicine residents doing rotations in the ED.
“We were approached recently by the ED because most of our admissions are called in directly to the medical residents,” says Jason R. Orlinick, MD, PhD, head of the section of Hospital Medicine at Norwalk Hospital, Conn. “I think the ED would like to talk directly with the medical attending assuming care for the patient. One of the things we haven’t done well is meet on a regular basis to discuss communication issues.”
The hospitalists and emergency medicine group at Dr. Orlinick’s institution have entertained the idea of setting up a direct triage system whereby medical residents are taken out of the picture. “The emergency medicine docs would page us directly—at least during the busiest hours of the day. Eventually, the hope is to make it a 24-hour, seven-days-a-week, 365 [days-a-year process],” says Dr. Orlinick. By bringing this to the emergency medicine physicians, the intent was to send the message that hospitalists recognize ED overcrowding as an institutional issue and want to improve communication with their ED colleagues to improve patient care.
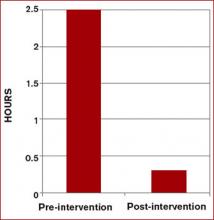
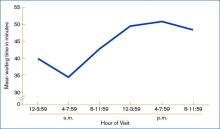
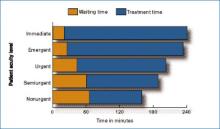
This model, devised at Johns Hopkins Bayview Medical Center in Baltimore, enabled communication between ED doctors and hospitalists, and reduced wait times by more than two hours when a bed was available.2 This triage and direct-admission protocol was not associated with increased mortality and resulted in improved patient and physician satisfaction. (See Figure 2 at right). Once the ED attending decides to admit a patient, direct communication is facilitated with a hospitalist. The approach includes monthly meetings between the department of medicine and the ED to continue to discuss improvements in admissions.
At Norwalk Hospital, the administration asked the hospitalist group to intervene in that throughput process. But Dr. Orlinick, also a clinical instructor of medicine at Yale University in New Haven, Conn., says they’ve hesitated out of sensitivity to their ED colleagues.
“We as a group have really struggled with that concept because [although] we feel like that is something we can do well, this is really within the purview of the emergency medicine docs,” says Dr. Orlinick. Adopting the Johns Hopkins model is a win-win solution where each specialty is providing its best skills to solve mutual issues. “What we can do well is look at the patients … on the floor[s], look at flow through the hospital systems in terms of getting testing; make sure that all that—and consults—happen in a timely manner, and that people leave the hospital when they’ve reached their goals of hospitalization,” he says. “It’s afterload as opposed to preload.”
Hospitalists see committee collaboration as important to solving the complex multidisciplinary systemic issues. Jasen W. Gundersen, MD, participates on a pneumonia task force with several hospitalists, a pulmonologist, and one of the heads of the ED. “We address the whole gamut from when patients come in to when they go through the hospital,” says Dr. Gundersen, head of the Hospital Medicine Division, University of Massachusetts Memorial Medical Center, Worcester. “We can learn from each other as we go through the process.”
Many of the ways hospitalists and ED physicians tackle systems-related issues are new to Dr. Glasheen’s institution because the hospital medicine program was begun in 2004. It is now common to see higher-level leadership from different specialties and areas all in the same room—talking about issues of capacity, for instance. There are also many more instances of hospitalists and ED physicians sitting on the same committees. Further, “It is relatively common for our ED to call our hospitalists to say, ‘Can you help see this patient? I’m not sure what to do,’ or, ‘I’ve got this situation with this patient, this needs to be done and I need help getting that done,’ ” Dr. Glasheen says. Even though he concedes that is more of a workaround as opposed to a solution for a faulty system, it still represents ED physicians and hospitalists co-managing that workaround.
The Future
Because he “sits on both sides of the fence” between emergency medicine and hospital medicine, Dr. Gundersen thinks it is especially important for hospitalists to train in all the different areas—including emergency medicine—when they are medical students and residents.
Emergency medicine physicians Dr. Hoekstra and Benjamin Honigman, MD, professor of surgery and head of the Division of Emergency Medicine at the University of Colorado School of Medicine, Denver, believe hospital medicine will be integral to that training. Dr. Glasheen, also the director of the longest-running internal medicine hospitalist-training program in the U.S., expects greater attention to hospitalist training. “My sense is that many hospitalists groups are in a growth phase and are trying to solve their own problems,” he says. Basically, their primary focus is staffing the hospital with good people and retaining them. He believes that once groups have been around for three to five years, they are more likely to take on bigger issues, such as hospital efficiency and capacity management.
“One of the reasons we started a hospitalist training program is that I didn’t want hospitalists to fall into the same mistakes, barriers, or issues that we’ve had in the past,” Dr. Glasheen says. He fears “this sort of continued balkanization of hospital care, where everyone silos everything out and considers such issues as throughput and ED divert as outside of their [jurisdiction]. I want to get to the place where hospitalists are looking at the whole hospital system and are justly rewarded for that either by financial incentives or time to [work on systemic issues].”
Dr. Glasheen and his team remind themselves of where their commitment resides: “This hospital is where we live—and with everything between the front door to the back door, our primary job is to make this a better place.” TH
Andrea Sattinger is a frequent contributor to The Hospitalist.
References
- Burt CW, McCaig LF. Staffing, capacity, and ambulance diversion in emergency departments: United States, 2003-04. Adv Data; US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics, Hyattsville, Md. Sept. 27, 2006. Available at: www.cdc.gov/nchs/data/ad/ad376.pdf. Last accessed June 25, 2007.
- Howell EE, Bessman ES, Rubin HR. Hospitalists and an innovative emergency department admission process. J Gen Intern Med. 2004 Mar;19(3):266-268.
In part 1 of this two-part series (July 2007, p. 16), hospitalists and emergency medicine physicians expressed their views on the relationship between their two specialties. In part 2, we look at how those relationships intersect—and what issues are at stake when they do.
One area where there is a bit of overlap between hospital medicine and emergency medicine is observational medicine,” says James W. Hoekstra, MD, professor and chairman, Department of Emergency Medicine, Wake Forest University Health Sciences Center, Winston-Salem, N.C.
Those patients who require a short stay for observation, he says, are neither in the ED or admitted to the hospital—they are in a zone of their own.
“That’s a gray zone in terms of who takes care of those patients,” he says, “and it depends on the hospital. It will be interesting to see how that works out, or whether that is ever worked out. It may just stay a shared area.”
The observation conundrum is complicated by the fact that many people use emergency departments for primary care. (See Figure 1, p. 33) “ True emergencies make up only some of the patient [cases] in the ED,” says Debra L. Burgy, MD, a hospitalist at Abbott Northwestern Hospital in Minneapolis. “We do have a 23-hour observation unit of 10 beds, and, frankly, could use 10 more to [handle unpredictable volumes of patients and insufficient support staff. That unit] has certainly helped to alleviate unnecessary admissions.”
Collaboration between hospitalists and emergency medicine physicians happens a number of ways at the University of Colorado at Denver and Health Sciences Center, where Jeff Glasheen, MD, is director of both the hospital medicine program and inpatient clinical services in the department of medicine.
“One way we work closely with the ED—because we think it is the right thing to do—is by building a much more comprehensive observation unit,” Dr. Glasheen says. “In some settings the observation unit lives in the ED and is run by the ED and in others, it is run by hospitalists. The hospitalists [here] will now run the unit, but we want to help solve some of the ED’s throughput issues.”
When Dr. Glasheen arrived at his institution, the observation unit was limited to patients with chest pain. “I didn’t understand why we would get chest pain patients through efficiently and not all patients,” he says.
A team that began operating in July will be available for all patients under the admission status of observation. The team will be hospitalist-led and aim to reduce length of stay and increase quality of care for those patients.
“Right now those patients are very scattered throughout the system and they may be [covered by] six to eight different teams,” Dr. Glasheen explains. One team of caregivers will be more efficient and reduce length of stay, he says.
By nurturing their working relationship with the emergency department, hospitalists will be able to more easily say: “We understand that that workup’s not complete, but we also understand that they’re going to come into the hospital and let us know what things need to be done. We’ll be happy to take that patient a little earlier than we did in the past to get them out of the ED.”
That’s a tricky thing to do, he says, “because the benefit to us isn’t huge, we’re self-sacrificing to help the ED, and that’s what I want hospitalist groups nationally to be thinking: how we can make the whole system better and not just make our own job better.”
Dr. Glasheen believes the professional structure in his institution is representative of what other hospitals will function like in the next 10 years.
“You have a backbone structure of basically four types of physicians: emergency medicine docs, hospitalists, intensivists, and a surgical team,” Dr. Glasheen says. “Everyone else, more and more, is serving in a consultative role.” Having that backbone allows you to tackle the issues, which are primarily complex, systems-based issues, he says. “It is no longer [a matter of just] the ED trying to deal with capacity issues. Now they have an ally on the inpatient side.”
An excess of patients for the number of beds means some patients spend a disproportionate amount of their stay in the ED, and that challenges communication and efficiency. “The challenges may be simple things, such as it being harder for a hospitalist to get to the ED to see a patient than it is upstairs,” Dr. Glasheen says. “[Or] it’s harder to decide who really has ownership of that patient.” In his hospital, as soon as a patient is assigned to a hospitalist, the primary responsibility for that patient is seen as the hospitalist’s.
But there are other issues. “Even if we are able to get down [to the ED] and write orders, that is problematic for the ED and the hospitalist; as a hospitalist we don’t have the nurses with staffing ratios and skills in the ED that they have on floors and in the ICU,” says Dr. Glasheen. “It is not always possible to get things done as efficiently as they probably could if the patients were in a proper unit. Locally and globally in my experience, the biggest issue is: How do you take care of these patients who now spend their inpatient stay in the ED?”
Collaborations, Models, and Solutions
A number of hospitalists raise the issue of managing internal medicine residents doing rotations in the ED.
“We were approached recently by the ED because most of our admissions are called in directly to the medical residents,” says Jason R. Orlinick, MD, PhD, head of the section of Hospital Medicine at Norwalk Hospital, Conn. “I think the ED would like to talk directly with the medical attending assuming care for the patient. One of the things we haven’t done well is meet on a regular basis to discuss communication issues.”
The hospitalists and emergency medicine group at Dr. Orlinick’s institution have entertained the idea of setting up a direct triage system whereby medical residents are taken out of the picture. “The emergency medicine docs would page us directly—at least during the busiest hours of the day. Eventually, the hope is to make it a 24-hour, seven-days-a-week, 365 [days-a-year process],” says Dr. Orlinick. By bringing this to the emergency medicine physicians, the intent was to send the message that hospitalists recognize ED overcrowding as an institutional issue and want to improve communication with their ED colleagues to improve patient care.
This model, devised at Johns Hopkins Bayview Medical Center in Baltimore, enabled communication between ED doctors and hospitalists, and reduced wait times by more than two hours when a bed was available.2 This triage and direct-admission protocol was not associated with increased mortality and resulted in improved patient and physician satisfaction. (See Figure 2 at right). Once the ED attending decides to admit a patient, direct communication is facilitated with a hospitalist. The approach includes monthly meetings between the department of medicine and the ED to continue to discuss improvements in admissions.
At Norwalk Hospital, the administration asked the hospitalist group to intervene in that throughput process. But Dr. Orlinick, also a clinical instructor of medicine at Yale University in New Haven, Conn., says they’ve hesitated out of sensitivity to their ED colleagues.
“We as a group have really struggled with that concept because [although] we feel like that is something we can do well, this is really within the purview of the emergency medicine docs,” says Dr. Orlinick. Adopting the Johns Hopkins model is a win-win solution where each specialty is providing its best skills to solve mutual issues. “What we can do well is look at the patients … on the floor[s], look at flow through the hospital systems in terms of getting testing; make sure that all that—and consults—happen in a timely manner, and that people leave the hospital when they’ve reached their goals of hospitalization,” he says. “It’s afterload as opposed to preload.”
Hospitalists see committee collaboration as important to solving the complex multidisciplinary systemic issues. Jasen W. Gundersen, MD, participates on a pneumonia task force with several hospitalists, a pulmonologist, and one of the heads of the ED. “We address the whole gamut from when patients come in to when they go through the hospital,” says Dr. Gundersen, head of the Hospital Medicine Division, University of Massachusetts Memorial Medical Center, Worcester. “We can learn from each other as we go through the process.”
Many of the ways hospitalists and ED physicians tackle systems-related issues are new to Dr. Glasheen’s institution because the hospital medicine program was begun in 2004. It is now common to see higher-level leadership from different specialties and areas all in the same room—talking about issues of capacity, for instance. There are also many more instances of hospitalists and ED physicians sitting on the same committees. Further, “It is relatively common for our ED to call our hospitalists to say, ‘Can you help see this patient? I’m not sure what to do,’ or, ‘I’ve got this situation with this patient, this needs to be done and I need help getting that done,’ ” Dr. Glasheen says. Even though he concedes that is more of a workaround as opposed to a solution for a faulty system, it still represents ED physicians and hospitalists co-managing that workaround.
The Future
Because he “sits on both sides of the fence” between emergency medicine and hospital medicine, Dr. Gundersen thinks it is especially important for hospitalists to train in all the different areas—including emergency medicine—when they are medical students and residents.
Emergency medicine physicians Dr. Hoekstra and Benjamin Honigman, MD, professor of surgery and head of the Division of Emergency Medicine at the University of Colorado School of Medicine, Denver, believe hospital medicine will be integral to that training. Dr. Glasheen, also the director of the longest-running internal medicine hospitalist-training program in the U.S., expects greater attention to hospitalist training. “My sense is that many hospitalists groups are in a growth phase and are trying to solve their own problems,” he says. Basically, their primary focus is staffing the hospital with good people and retaining them. He believes that once groups have been around for three to five years, they are more likely to take on bigger issues, such as hospital efficiency and capacity management.
“One of the reasons we started a hospitalist training program is that I didn’t want hospitalists to fall into the same mistakes, barriers, or issues that we’ve had in the past,” Dr. Glasheen says. He fears “this sort of continued balkanization of hospital care, where everyone silos everything out and considers such issues as throughput and ED divert as outside of their [jurisdiction]. I want to get to the place where hospitalists are looking at the whole hospital system and are justly rewarded for that either by financial incentives or time to [work on systemic issues].”
Dr. Glasheen and his team remind themselves of where their commitment resides: “This hospital is where we live—and with everything between the front door to the back door, our primary job is to make this a better place.” TH
Andrea Sattinger is a frequent contributor to The Hospitalist.
References
- Burt CW, McCaig LF. Staffing, capacity, and ambulance diversion in emergency departments: United States, 2003-04. Adv Data; US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics, Hyattsville, Md. Sept. 27, 2006. Available at: www.cdc.gov/nchs/data/ad/ad376.pdf. Last accessed June 25, 2007.
- Howell EE, Bessman ES, Rubin HR. Hospitalists and an innovative emergency department admission process. J Gen Intern Med. 2004 Mar;19(3):266-268.
In part 1 of this two-part series (July 2007, p. 16), hospitalists and emergency medicine physicians expressed their views on the relationship between their two specialties. In part 2, we look at how those relationships intersect—and what issues are at stake when they do.
One area where there is a bit of overlap between hospital medicine and emergency medicine is observational medicine,” says James W. Hoekstra, MD, professor and chairman, Department of Emergency Medicine, Wake Forest University Health Sciences Center, Winston-Salem, N.C.
Those patients who require a short stay for observation, he says, are neither in the ED or admitted to the hospital—they are in a zone of their own.
“That’s a gray zone in terms of who takes care of those patients,” he says, “and it depends on the hospital. It will be interesting to see how that works out, or whether that is ever worked out. It may just stay a shared area.”
The observation conundrum is complicated by the fact that many people use emergency departments for primary care. (See Figure 1, p. 33) “ True emergencies make up only some of the patient [cases] in the ED,” says Debra L. Burgy, MD, a hospitalist at Abbott Northwestern Hospital in Minneapolis. “We do have a 23-hour observation unit of 10 beds, and, frankly, could use 10 more to [handle unpredictable volumes of patients and insufficient support staff. That unit] has certainly helped to alleviate unnecessary admissions.”
Collaboration between hospitalists and emergency medicine physicians happens a number of ways at the University of Colorado at Denver and Health Sciences Center, where Jeff Glasheen, MD, is director of both the hospital medicine program and inpatient clinical services in the department of medicine.
“One way we work closely with the ED—because we think it is the right thing to do—is by building a much more comprehensive observation unit,” Dr. Glasheen says. “In some settings the observation unit lives in the ED and is run by the ED and in others, it is run by hospitalists. The hospitalists [here] will now run the unit, but we want to help solve some of the ED’s throughput issues.”
When Dr. Glasheen arrived at his institution, the observation unit was limited to patients with chest pain. “I didn’t understand why we would get chest pain patients through efficiently and not all patients,” he says.
A team that began operating in July will be available for all patients under the admission status of observation. The team will be hospitalist-led and aim to reduce length of stay and increase quality of care for those patients.
“Right now those patients are very scattered throughout the system and they may be [covered by] six to eight different teams,” Dr. Glasheen explains. One team of caregivers will be more efficient and reduce length of stay, he says.
By nurturing their working relationship with the emergency department, hospitalists will be able to more easily say: “We understand that that workup’s not complete, but we also understand that they’re going to come into the hospital and let us know what things need to be done. We’ll be happy to take that patient a little earlier than we did in the past to get them out of the ED.”
That’s a tricky thing to do, he says, “because the benefit to us isn’t huge, we’re self-sacrificing to help the ED, and that’s what I want hospitalist groups nationally to be thinking: how we can make the whole system better and not just make our own job better.”
Dr. Glasheen believes the professional structure in his institution is representative of what other hospitals will function like in the next 10 years.
“You have a backbone structure of basically four types of physicians: emergency medicine docs, hospitalists, intensivists, and a surgical team,” Dr. Glasheen says. “Everyone else, more and more, is serving in a consultative role.” Having that backbone allows you to tackle the issues, which are primarily complex, systems-based issues, he says. “It is no longer [a matter of just] the ED trying to deal with capacity issues. Now they have an ally on the inpatient side.”
An excess of patients for the number of beds means some patients spend a disproportionate amount of their stay in the ED, and that challenges communication and efficiency. “The challenges may be simple things, such as it being harder for a hospitalist to get to the ED to see a patient than it is upstairs,” Dr. Glasheen says. “[Or] it’s harder to decide who really has ownership of that patient.” In his hospital, as soon as a patient is assigned to a hospitalist, the primary responsibility for that patient is seen as the hospitalist’s.
But there are other issues. “Even if we are able to get down [to the ED] and write orders, that is problematic for the ED and the hospitalist; as a hospitalist we don’t have the nurses with staffing ratios and skills in the ED that they have on floors and in the ICU,” says Dr. Glasheen. “It is not always possible to get things done as efficiently as they probably could if the patients were in a proper unit. Locally and globally in my experience, the biggest issue is: How do you take care of these patients who now spend their inpatient stay in the ED?”
Collaborations, Models, and Solutions
A number of hospitalists raise the issue of managing internal medicine residents doing rotations in the ED.
“We were approached recently by the ED because most of our admissions are called in directly to the medical residents,” says Jason R. Orlinick, MD, PhD, head of the section of Hospital Medicine at Norwalk Hospital, Conn. “I think the ED would like to talk directly with the medical attending assuming care for the patient. One of the things we haven’t done well is meet on a regular basis to discuss communication issues.”
The hospitalists and emergency medicine group at Dr. Orlinick’s institution have entertained the idea of setting up a direct triage system whereby medical residents are taken out of the picture. “The emergency medicine docs would page us directly—at least during the busiest hours of the day. Eventually, the hope is to make it a 24-hour, seven-days-a-week, 365 [days-a-year process],” says Dr. Orlinick. By bringing this to the emergency medicine physicians, the intent was to send the message that hospitalists recognize ED overcrowding as an institutional issue and want to improve communication with their ED colleagues to improve patient care.
This model, devised at Johns Hopkins Bayview Medical Center in Baltimore, enabled communication between ED doctors and hospitalists, and reduced wait times by more than two hours when a bed was available.2 This triage and direct-admission protocol was not associated with increased mortality and resulted in improved patient and physician satisfaction. (See Figure 2 at right). Once the ED attending decides to admit a patient, direct communication is facilitated with a hospitalist. The approach includes monthly meetings between the department of medicine and the ED to continue to discuss improvements in admissions.
At Norwalk Hospital, the administration asked the hospitalist group to intervene in that throughput process. But Dr. Orlinick, also a clinical instructor of medicine at Yale University in New Haven, Conn., says they’ve hesitated out of sensitivity to their ED colleagues.
“We as a group have really struggled with that concept because [although] we feel like that is something we can do well, this is really within the purview of the emergency medicine docs,” says Dr. Orlinick. Adopting the Johns Hopkins model is a win-win solution where each specialty is providing its best skills to solve mutual issues. “What we can do well is look at the patients … on the floor[s], look at flow through the hospital systems in terms of getting testing; make sure that all that—and consults—happen in a timely manner, and that people leave the hospital when they’ve reached their goals of hospitalization,” he says. “It’s afterload as opposed to preload.”
Hospitalists see committee collaboration as important to solving the complex multidisciplinary systemic issues. Jasen W. Gundersen, MD, participates on a pneumonia task force with several hospitalists, a pulmonologist, and one of the heads of the ED. “We address the whole gamut from when patients come in to when they go through the hospital,” says Dr. Gundersen, head of the Hospital Medicine Division, University of Massachusetts Memorial Medical Center, Worcester. “We can learn from each other as we go through the process.”
Many of the ways hospitalists and ED physicians tackle systems-related issues are new to Dr. Glasheen’s institution because the hospital medicine program was begun in 2004. It is now common to see higher-level leadership from different specialties and areas all in the same room—talking about issues of capacity, for instance. There are also many more instances of hospitalists and ED physicians sitting on the same committees. Further, “It is relatively common for our ED to call our hospitalists to say, ‘Can you help see this patient? I’m not sure what to do,’ or, ‘I’ve got this situation with this patient, this needs to be done and I need help getting that done,’ ” Dr. Glasheen says. Even though he concedes that is more of a workaround as opposed to a solution for a faulty system, it still represents ED physicians and hospitalists co-managing that workaround.
The Future
Because he “sits on both sides of the fence” between emergency medicine and hospital medicine, Dr. Gundersen thinks it is especially important for hospitalists to train in all the different areas—including emergency medicine—when they are medical students and residents.
Emergency medicine physicians Dr. Hoekstra and Benjamin Honigman, MD, professor of surgery and head of the Division of Emergency Medicine at the University of Colorado School of Medicine, Denver, believe hospital medicine will be integral to that training. Dr. Glasheen, also the director of the longest-running internal medicine hospitalist-training program in the U.S., expects greater attention to hospitalist training. “My sense is that many hospitalists groups are in a growth phase and are trying to solve their own problems,” he says. Basically, their primary focus is staffing the hospital with good people and retaining them. He believes that once groups have been around for three to five years, they are more likely to take on bigger issues, such as hospital efficiency and capacity management.
“One of the reasons we started a hospitalist training program is that I didn’t want hospitalists to fall into the same mistakes, barriers, or issues that we’ve had in the past,” Dr. Glasheen says. He fears “this sort of continued balkanization of hospital care, where everyone silos everything out and considers such issues as throughput and ED divert as outside of their [jurisdiction]. I want to get to the place where hospitalists are looking at the whole hospital system and are justly rewarded for that either by financial incentives or time to [work on systemic issues].”
Dr. Glasheen and his team remind themselves of where their commitment resides: “This hospital is where we live—and with everything between the front door to the back door, our primary job is to make this a better place.” TH
Andrea Sattinger is a frequent contributor to The Hospitalist.
References
- Burt CW, McCaig LF. Staffing, capacity, and ambulance diversion in emergency departments: United States, 2003-04. Adv Data; US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics, Hyattsville, Md. Sept. 27, 2006. Available at: www.cdc.gov/nchs/data/ad/ad376.pdf. Last accessed June 25, 2007.
- Howell EE, Bessman ES, Rubin HR. Hospitalists and an innovative emergency department admission process. J Gen Intern Med. 2004 Mar;19(3):266-268.
Heinous Crimes
By the time a mortician in the northeast British town of Hyde, Greater Manchester, United Kingdom, noticed Dr. Harold Shipman’s patients were dying at an exorbitant rate, the doctor had probably killed close to 300 of them, according to Kenneth V. Iserson, MD, MBA, professor of emergency medicine at the University of Arizona College of Medicine and author of “Demon Doctors: Physicians as Serial Killers.”
Shipman, labeled ‘‘the most prolific serial killer in the history of the United Kingdom—and probably the world,’’ was officially convicted of killing 15 patients in 2000 and sentenced to 15 consecutive life sentences.1 In January 2004 he was found hanged in his prison cell.
Sometimes referred to as caregiver-associated serial killings, these incidents generate profound shock in the healthcare community. As repellent and relatively rare as this behavior is, and as controversial as the topic is, neither individuals nor institutions can afford to disassociate themselves from the subject. Hospitalists should not hide from this issue and should not feel they will be accused of “treason” if they educate themselves and bring suspicious behavior to the awareness of superiors, says Beatrice Crofts Yorker, JD, RN, MS, FAAN, dean of the College of Health and Human Services at California State University, Los Angeles. On the contrary, she says, “first, do no harm” also entails ensuring everyone else around you follows the same ethic.
Dr. Yorker, who has been studying this phenomenon since 1986, published the first examination of cases of serial murder by nurses in the American Journal of Nursing (AJN) in 1988. “It is a serious problem that has been under-recognized, and it is the right thing to blow the whistle when adverse patient incidents are associated with the presence of a specific healthcare provider,” says Dr. Yorker. “In fact, most of the cases came to the attention of authorities because a nurse blew the whistle. The sad thing is that some of the nurses were disciplined for their protective actions; however, they were ultimately vindicated.”
A veteran of the phenomenon urges continued vigilance. “As a general caveat, there needs to be a higher index of suspicion for these incidents,” says Kenneth W. Kizer, MD, MPH, the former head of the veterans healthcare system who had to deal with three incidents of serial murder at Veterans Affairs (VA) hospitals in the 1990s. “These incidents are grossly underreported.”
Incidence and Cause of Death
Drs. Kizer and Yorker were two of the investigators who reviewed epidemiologic studies, toxicology evidence, and court transcripts for data on healthcare professionals prosecuted between 1970 and 2006.
“Dr. Robert Forrest, who was a forensic toxicologist getting a law degree and wrote his dissertation on the topic of serial murder by healthcare providers, contacted me after the AJN article came out,” says Dr. Yorker. Dr. Forrest has been the testifying expert in most of the U.K. cases. “After the Charles Cullen case hit the news, The New York Times and Modern Healthcare contacted me regarding my study in AJN and the Journal of Nursing Law. That is how Ken Kizer and Paula Lampe found me.” (Cullen, a registered nurse, received 11 consecutive life sentences in 2006 after pleading guilty to administering lethal doses of medication to more than 40 patients in New Jersey and Pennsylvania.)
Lampe, an author, had been studying cases in Europe. “Because both Robert and Paula provided additional data on some cases, they were co-authors—as was Ken—who provided data on the VA cases and an important public policy perspective,” says Dr. Yorker.
The search showed 90 criminal prosecutions of healthcare providers who met the criteria of serial murder of patients. Of those, 54 have been convicted—45 for serial murder, four for attempted murder, and five on lesser charges. Since the publication of their study, one more of the accused has received a sentence of life in prison, another has been convicted and sentenced to 20 years, one committed suicide in prison, and two additional nurses in Germany and the Czech Republic have been arrested and confessed to serial murder of patients. In addition, Dr. Yorker is continuing to follow two large-scale murder-for-profit prosecutions. There are four defendants in each case. Further, three individuals have been found liable for wrongful death in the amounts of $27 million, $8 million, and $450,000 in damages.
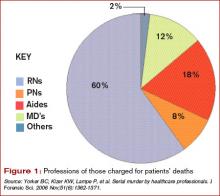
Injection was the main method used by healthcare killers, followed by suffocation, poisoning, and tampering with equipment. Prosecutions were reported in 20 countries, with 40% of the incidents taking place in the United States. Nursing personnel were 86% of the healthcare providers prosecuted; 12% were physicians, and 2% were allied health professionals. The number of patient deaths that resulted in a murder conviction is 317, and the number of suspicious patient deaths attributed to the 54 convicted caregivers is 2,113.
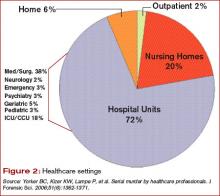
“Physicians as serial killers are remarkably uncommon,” says Dr. Iserson, who is also director of the Arizona Bioethics Program at the University of Arizona College of Medicine in Tucson. “Nurses [who are serial killers] are much more common, but of course there are more nurses in the hospital, just as there are ancillary people.” (See Figure 1, left.) Dr. Iserson, who practices emergency medicine and consults nationally on bioethics, advises maintaining caution when examining data of charges or suspicions that were never proved.
Most of these crimes (70%) occur in hospital units. (See Figure 2, left.) Victims are almost always female, as are almost half (49%) of convicted serial killers and 55% of the total number of prosecuted healthcare providers. Males are disproportionately represented among prosecuted nurses.
Motives: Who Is Always There?
Although the motives are complex, some common threads connect these crimes. “There are some classical signs, if you will,” says Dr. Kizer.
When the same person repeatedly calls a code and always seems to be in the thick of it, that is one prime indicator. These people are usually legitimately present in those settings and circumstances—for example, they are on call or working a shift—which makes it more difficult to discern when something is awry. Commonly, the perpetrators have easy access to high-alert drugs without sufficient accountability. Sometimes, once an investigation has been launched it is discovered the person has falsified his or her credentials.
In hospitals, experts say, the “rescuer” or “hero” personality is often on display in those who kill patients—the first person there to give the patient drugs or attempt to save the patient.
“What you are going to see as a pattern,” says Dr. Iserson, “is that they need to be near death.” Codes or calls for respiratory arrest are the most common; patients who have cardiac arrests are much harder to save. Being the hero is not always the motive; the converse can also apply.
Such is the case with nurse Orville Lynn Majors, LPN, convicted of six murders at the Vermillion county hospital in Clinton, Ind. The deaths were consistent with injections of potassium chloride and epinephrine according to prosecutors. Majors’ coworkers were concerned that patients were coding in alarming numbers while in his care. Although this information did not come out until after he was apprehended, his coworkers had a good idea which of his patients would not survive: Patients who were whiny, demanding, or required a lot of work. “The scuttlebutt or rumor among his coworkers,” says Dr. Kizer, “is that they could almost predict which patients would have a demise under his care.”
Although a typical profile of the serial healthcare murderer has been demonstrated in many cases, in many other cases the demographics and behaviors of these killers have deviated widely from generalized assumptions.2 Therefore, before looking at people, look at the numbers.
An unusual number of calls and codes may occur in a particular area of the hospital. “In ICUs you expect a lot of [codes and calls], but not on general post-op wards or the pediatrics MICU,” Dr. Kizer says. “When this happens in these settings it should raise a red flag.”
Unfortunately, most hospitals don’t track mortality on a monthly basis per unit or ward or ICU, so they may not recognize when something is out of line in a timely manner. Also, the hospital committee assigned to review deaths may be remiss in its duty to meet regularly or otherwise perform according to policy.
Another factor that should raise a red flag is a disproportionate number of codes or deaths on the same shift—most often the night shift. Often, someone says, “Gee, it seems like there’s an awful lot of codes lately,” explains Dr. Kizer. An unusually high rate of successful codes is another sign.
For example, in the 1995-1996 case of Kristen Gilbert, an RN convicted of four murders at the Veterans Affairs Medical Center in Northampton, Mass., she was having an extramarital affair with a hospital security guard who worked the evening shift. Protocol required that security be called to all cardiopulmonary arrests. Gilbert used stimulant epinephrine to make their hearts race out of control. The epidemiologic data later showed that suspicious codes occurred when both were on duty. “The patients always seemed to recover and she was the hero,” says Dr. Kizer. “She wanted to look good for her boyfriend.”
Similarly, Richard Angelo, a charge nurse at Good Samaritan Hospital in West Islip, Long Island, N.Y., admitted that between 1987 and 1989 he injected patients with paralyzing drugs Pavulon (pancuronium) and Anectine (succinylcholine). He wanted his colleagues to admire him for performing well in a code. During his confession, he likened himself to volunteer firefighters who set fires. In fact, Dr. Iserson makes this same parallel. “From what we can tell,” he says, “these people don’t really care whether the person dies or not. They would rather they not [die], so they can be seen as the hero. It’s all about them.” As with instances of arson, he says, the perpetrator is “the first one to show up at the fire watch, over and over again.”
Obstacles to Disclosure
Even when healthcare workers and related personnel come forward with their suspicions, law enforcement may be a barrier to prosecution.
In the United Kingdom, a Manchester mortician took her observations about the excessive deaths and cremations in Harold Shipman’s practice to her father and brother, who were also in the family business. She also obtained the support of a local female general practitioner. The two women went to the police, explaining that most patients who had died had not been critically ill and noted that the doctor had exhibited peculiar behavior when he was questioned.
But, says Dr. Iserson, the response again was typical: “‘Oh, foolish women. That can’t be happening.’ And it wasn’t until Shipman killed the wrong person [a former town mayor, mother of a prominent lawyer] that things started to unravel for him.” When police finally looked at other deaths Shipman had certified, a pattern emerged. He would overdose patients with diamorphine, sign their death certificates, then forge medical records to indicate they were in poor health.
A second common response by institutions is just as much of a barrier to bringing these crimes to light and ultimately, prosecution. “In essence,” says Dr. Iserson, “that response is, ‘Well, maybe it is happening but, boy, it sure is going to put our institution in a bad light. So let’s just not say anything.’ ”
This was the case with Michael Swango, a doctor who worked in several states and a number of countries. He was charged with five murders and may have been involved in 126 deaths. Swango confessed to the deaths that occurred in a Veterans Affairs hospital in Northport, N.Y., where he reportedly injected three veterans with a drug that stopped their hearts. He had forged “do not resuscitate” orders for the three. He was sentenced to two life sentences. It is possible that he killed as many as 35-60 people in the United States and Zimbabwe. But before it was all out in the open, “some very prominent people were involved in sweeping it under the rug,” says Dr. Iserson, “and they didn’t even get a slap on the wrist.”
Hiring Practices
One of the most shocking aspects of the Cullen case was that institutional coverup and employee privacy policies meant his prior employers never revealed the problems to prospective employers.
“Identifying potential serial killers is not at all the total problem,” says Dr. Iserson. “The problem is getting the powers that be to act. What they typically do is pass the problem on to somebody else, in effect, saying, ‘We don’t want you to work here anymore. We won’t necessarily write you a good letter of recommendation, but we will say that you worked here, and basically we just want you to go away.’ ”
An investigation revealed that Cullen had a history of reported incidents at hospitals in Pennsylvania and New Jersey, but there were no tracking or disclosure systems in place as he moved from one hospital to another. His employment history included termination from several hospitals because of misconduct, hospitalizations for mental illness, and a criminal investigation regarding improper medication administration.
In an open letter published in The New York Times on March 14, 2004, Somerset Medical Center (Somerville, N.J.) asserted: “Mr. Cullen worked at nine other healthcare facilities over a 16-year period. His former work history problems were not revealed to us. Nor were any state agencies or licensing boards able to provide us with accurate information about his employment history.”
Cullen had been investigated by three hospitals, a nursing home, and two prosecutors for suspicious patient deaths. He was fired by five hospitals and one nursing home for suspected wrongdoing. But Cullen continued to find employment and kill patients.
“Confidentiality is essential [as is] not leaking to the media, which can taint the investigation,” says Dr. Yorker. “The Charles Cullen case should motivate hospitalists to [participate in helping to stop the systemic mechanism that made possible] his killing over 40 patients in nine different hospitals and a nursing home before being stopped. This erodes the public trust in hospitals.”
The Health Care Quality Improvement Act provides some immunity for reporters of adverse information, but it applies only to physicians—not communications between employers.
The American Society for Healthcare Risk Management (ASHRM) and Dr. Kizer and his colleagues are in alignment in advocating for the provision of more comprehensive immunity to help healthcare employees and patients when they report these incidents.3
“If you have information that a worker is harming patients, the institution should be able to tell prospective employers and not worry about getting sued,” says Dr. Yorker. A number of states have passed varying forms of legislation so far, and ASHRM is recommending this be a federal matter. Dr. Kizer and his group recommend that reporting of suspected serial murderers should be considered for coverage under Good Samaritan laws.
Other Complicating Factors
Another problem in bringing legitimate cases to prosecution is when providers are accused on trumped-up charges, which in Dr. Iserson’s view amounts to prosecutorial malpractice. Examples are cases post-Hurricane Katrina, when physicians and nurses were charged with patient deaths.
Internationally, an example is the case in Libya where the main defendants—a Palestinian doctor and five Bulgarian nurses—were charged with injecting 426 children with HIV in 1998, causing an epidemic at El-Fath Children’s Hospital in Benghazi. According to World Politics Watch, dozens of foreign medical professionals were arrested, with six eventually charged and forced to confess by Libyan authorities. Subsequent research published in the journal Nature indicated that viral strains present in the infected children were present at the hospital before 1998.
“This was a case of political blackmail,” says Dr. Iserson. These cases may not be clear-cut and may be open to negative interpretations that “make people skittish. That is why institutions are prone to say, ‘Gee, maybe it’s just one of those kinds of cases. We don’t want to make that kind of mistake.’ ”
Also problematic is the variable rate at which hospitals perform autopsies.
“Autopsy rates are down in many communities to 1% or 2% or even lower,” says Dr. Kizer. “When the data point to the possibility of a crime on a particular unit, the site needs to be treated as a crime scene. In most hospitals, when someone dies, you get them off the floor and you clean up as quickly as possible. That shouldn’t be the case if it is a suspected crime scene. Ideally there should be standardized processes or protocols whenever there is suspicion. And those protocols may be different than when a patient ordinarily dies.”
Seeking Solutions
Hospitalists and other professionals—especially nurses and ancillary personnel—have an obligation to be informed and astute regarding individual characteristics and signs of suspicious patient deaths. Appropriate epidemiological, toxicological, and psychological data must be collected and analyzed routinely.
“Data about this phenomenon need to be disseminated to heighten awareness that serial murder of patients is a significant concern that extends beyond a few shocking, isolated incidents,” write Drs. Yorker and Kizer and their co-authors.
Institutional hiring practices must be changed so balance is achieved between preventing wrongful discharge or denial-of-employment lawsuits and protecting patient safety. Existing state legislation and future federal legislation for institutional immunity is an important element of patient advocacy that hospitalists can support.
Ultimately, hospitalists must be informed, aware, and alert. “Most [suspicions] will not be anything,” says Dr. Iserson. “Just pay attention to it.” TH
Andrea Sattinger is a frequent contributor to The Hospitalist.
References
- Yorker BC, Kizer KW, Lampe P, et al. Serial murder by healthcare professionals. J Forensic Sci. 2006 Nov;51(6):1362-1371.
- Wolf BC, Lavezzi WA. Paths to destruction: the lives and crimes of two serial killers. J Forensic Sci. 2007 Jan;52(1):199-203.
- ASHRM. American Society for Healthcare Risk Management. A call for federal immunity to protect health care employers … and patients. Chicago: Monograph; April 1, 2005; www.ashrm.org/ashrm/resources/files/Monograph.Immunity.pdf.
By the time a mortician in the northeast British town of Hyde, Greater Manchester, United Kingdom, noticed Dr. Harold Shipman’s patients were dying at an exorbitant rate, the doctor had probably killed close to 300 of them, according to Kenneth V. Iserson, MD, MBA, professor of emergency medicine at the University of Arizona College of Medicine and author of “Demon Doctors: Physicians as Serial Killers.”
Shipman, labeled ‘‘the most prolific serial killer in the history of the United Kingdom—and probably the world,’’ was officially convicted of killing 15 patients in 2000 and sentenced to 15 consecutive life sentences.1 In January 2004 he was found hanged in his prison cell.
Sometimes referred to as caregiver-associated serial killings, these incidents generate profound shock in the healthcare community. As repellent and relatively rare as this behavior is, and as controversial as the topic is, neither individuals nor institutions can afford to disassociate themselves from the subject. Hospitalists should not hide from this issue and should not feel they will be accused of “treason” if they educate themselves and bring suspicious behavior to the awareness of superiors, says Beatrice Crofts Yorker, JD, RN, MS, FAAN, dean of the College of Health and Human Services at California State University, Los Angeles. On the contrary, she says, “first, do no harm” also entails ensuring everyone else around you follows the same ethic.
Dr. Yorker, who has been studying this phenomenon since 1986, published the first examination of cases of serial murder by nurses in the American Journal of Nursing (AJN) in 1988. “It is a serious problem that has been under-recognized, and it is the right thing to blow the whistle when adverse patient incidents are associated with the presence of a specific healthcare provider,” says Dr. Yorker. “In fact, most of the cases came to the attention of authorities because a nurse blew the whistle. The sad thing is that some of the nurses were disciplined for their protective actions; however, they were ultimately vindicated.”
A veteran of the phenomenon urges continued vigilance. “As a general caveat, there needs to be a higher index of suspicion for these incidents,” says Kenneth W. Kizer, MD, MPH, the former head of the veterans healthcare system who had to deal with three incidents of serial murder at Veterans Affairs (VA) hospitals in the 1990s. “These incidents are grossly underreported.”
Incidence and Cause of Death
Drs. Kizer and Yorker were two of the investigators who reviewed epidemiologic studies, toxicology evidence, and court transcripts for data on healthcare professionals prosecuted between 1970 and 2006.
“Dr. Robert Forrest, who was a forensic toxicologist getting a law degree and wrote his dissertation on the topic of serial murder by healthcare providers, contacted me after the AJN article came out,” says Dr. Yorker. Dr. Forrest has been the testifying expert in most of the U.K. cases. “After the Charles Cullen case hit the news, The New York Times and Modern Healthcare contacted me regarding my study in AJN and the Journal of Nursing Law. That is how Ken Kizer and Paula Lampe found me.” (Cullen, a registered nurse, received 11 consecutive life sentences in 2006 after pleading guilty to administering lethal doses of medication to more than 40 patients in New Jersey and Pennsylvania.)
Lampe, an author, had been studying cases in Europe. “Because both Robert and Paula provided additional data on some cases, they were co-authors—as was Ken—who provided data on the VA cases and an important public policy perspective,” says Dr. Yorker.
The search showed 90 criminal prosecutions of healthcare providers who met the criteria of serial murder of patients. Of those, 54 have been convicted—45 for serial murder, four for attempted murder, and five on lesser charges. Since the publication of their study, one more of the accused has received a sentence of life in prison, another has been convicted and sentenced to 20 years, one committed suicide in prison, and two additional nurses in Germany and the Czech Republic have been arrested and confessed to serial murder of patients. In addition, Dr. Yorker is continuing to follow two large-scale murder-for-profit prosecutions. There are four defendants in each case. Further, three individuals have been found liable for wrongful death in the amounts of $27 million, $8 million, and $450,000 in damages.
Injection was the main method used by healthcare killers, followed by suffocation, poisoning, and tampering with equipment. Prosecutions were reported in 20 countries, with 40% of the incidents taking place in the United States. Nursing personnel were 86% of the healthcare providers prosecuted; 12% were physicians, and 2% were allied health professionals. The number of patient deaths that resulted in a murder conviction is 317, and the number of suspicious patient deaths attributed to the 54 convicted caregivers is 2,113.
“Physicians as serial killers are remarkably uncommon,” says Dr. Iserson, who is also director of the Arizona Bioethics Program at the University of Arizona College of Medicine in Tucson. “Nurses [who are serial killers] are much more common, but of course there are more nurses in the hospital, just as there are ancillary people.” (See Figure 1, left.) Dr. Iserson, who practices emergency medicine and consults nationally on bioethics, advises maintaining caution when examining data of charges or suspicions that were never proved.
Most of these crimes (70%) occur in hospital units. (See Figure 2, left.) Victims are almost always female, as are almost half (49%) of convicted serial killers and 55% of the total number of prosecuted healthcare providers. Males are disproportionately represented among prosecuted nurses.
Motives: Who Is Always There?
Although the motives are complex, some common threads connect these crimes. “There are some classical signs, if you will,” says Dr. Kizer.
When the same person repeatedly calls a code and always seems to be in the thick of it, that is one prime indicator. These people are usually legitimately present in those settings and circumstances—for example, they are on call or working a shift—which makes it more difficult to discern when something is awry. Commonly, the perpetrators have easy access to high-alert drugs without sufficient accountability. Sometimes, once an investigation has been launched it is discovered the person has falsified his or her credentials.
In hospitals, experts say, the “rescuer” or “hero” personality is often on display in those who kill patients—the first person there to give the patient drugs or attempt to save the patient.
“What you are going to see as a pattern,” says Dr. Iserson, “is that they need to be near death.” Codes or calls for respiratory arrest are the most common; patients who have cardiac arrests are much harder to save. Being the hero is not always the motive; the converse can also apply.
Such is the case with nurse Orville Lynn Majors, LPN, convicted of six murders at the Vermillion county hospital in Clinton, Ind. The deaths were consistent with injections of potassium chloride and epinephrine according to prosecutors. Majors’ coworkers were concerned that patients were coding in alarming numbers while in his care. Although this information did not come out until after he was apprehended, his coworkers had a good idea which of his patients would not survive: Patients who were whiny, demanding, or required a lot of work. “The scuttlebutt or rumor among his coworkers,” says Dr. Kizer, “is that they could almost predict which patients would have a demise under his care.”
Although a typical profile of the serial healthcare murderer has been demonstrated in many cases, in many other cases the demographics and behaviors of these killers have deviated widely from generalized assumptions.2 Therefore, before looking at people, look at the numbers.
An unusual number of calls and codes may occur in a particular area of the hospital. “In ICUs you expect a lot of [codes and calls], but not on general post-op wards or the pediatrics MICU,” Dr. Kizer says. “When this happens in these settings it should raise a red flag.”
Unfortunately, most hospitals don’t track mortality on a monthly basis per unit or ward or ICU, so they may not recognize when something is out of line in a timely manner. Also, the hospital committee assigned to review deaths may be remiss in its duty to meet regularly or otherwise perform according to policy.
Another factor that should raise a red flag is a disproportionate number of codes or deaths on the same shift—most often the night shift. Often, someone says, “Gee, it seems like there’s an awful lot of codes lately,” explains Dr. Kizer. An unusually high rate of successful codes is another sign.
For example, in the 1995-1996 case of Kristen Gilbert, an RN convicted of four murders at the Veterans Affairs Medical Center in Northampton, Mass., she was having an extramarital affair with a hospital security guard who worked the evening shift. Protocol required that security be called to all cardiopulmonary arrests. Gilbert used stimulant epinephrine to make their hearts race out of control. The epidemiologic data later showed that suspicious codes occurred when both were on duty. “The patients always seemed to recover and she was the hero,” says Dr. Kizer. “She wanted to look good for her boyfriend.”
Similarly, Richard Angelo, a charge nurse at Good Samaritan Hospital in West Islip, Long Island, N.Y., admitted that between 1987 and 1989 he injected patients with paralyzing drugs Pavulon (pancuronium) and Anectine (succinylcholine). He wanted his colleagues to admire him for performing well in a code. During his confession, he likened himself to volunteer firefighters who set fires. In fact, Dr. Iserson makes this same parallel. “From what we can tell,” he says, “these people don’t really care whether the person dies or not. They would rather they not [die], so they can be seen as the hero. It’s all about them.” As with instances of arson, he says, the perpetrator is “the first one to show up at the fire watch, over and over again.”
Obstacles to Disclosure
Even when healthcare workers and related personnel come forward with their suspicions, law enforcement may be a barrier to prosecution.
In the United Kingdom, a Manchester mortician took her observations about the excessive deaths and cremations in Harold Shipman’s practice to her father and brother, who were also in the family business. She also obtained the support of a local female general practitioner. The two women went to the police, explaining that most patients who had died had not been critically ill and noted that the doctor had exhibited peculiar behavior when he was questioned.
But, says Dr. Iserson, the response again was typical: “‘Oh, foolish women. That can’t be happening.’ And it wasn’t until Shipman killed the wrong person [a former town mayor, mother of a prominent lawyer] that things started to unravel for him.” When police finally looked at other deaths Shipman had certified, a pattern emerged. He would overdose patients with diamorphine, sign their death certificates, then forge medical records to indicate they were in poor health.
A second common response by institutions is just as much of a barrier to bringing these crimes to light and ultimately, prosecution. “In essence,” says Dr. Iserson, “that response is, ‘Well, maybe it is happening but, boy, it sure is going to put our institution in a bad light. So let’s just not say anything.’ ”
This was the case with Michael Swango, a doctor who worked in several states and a number of countries. He was charged with five murders and may have been involved in 126 deaths. Swango confessed to the deaths that occurred in a Veterans Affairs hospital in Northport, N.Y., where he reportedly injected three veterans with a drug that stopped their hearts. He had forged “do not resuscitate” orders for the three. He was sentenced to two life sentences. It is possible that he killed as many as 35-60 people in the United States and Zimbabwe. But before it was all out in the open, “some very prominent people were involved in sweeping it under the rug,” says Dr. Iserson, “and they didn’t even get a slap on the wrist.”
Hiring Practices
One of the most shocking aspects of the Cullen case was that institutional coverup and employee privacy policies meant his prior employers never revealed the problems to prospective employers.
“Identifying potential serial killers is not at all the total problem,” says Dr. Iserson. “The problem is getting the powers that be to act. What they typically do is pass the problem on to somebody else, in effect, saying, ‘We don’t want you to work here anymore. We won’t necessarily write you a good letter of recommendation, but we will say that you worked here, and basically we just want you to go away.’ ”
An investigation revealed that Cullen had a history of reported incidents at hospitals in Pennsylvania and New Jersey, but there were no tracking or disclosure systems in place as he moved from one hospital to another. His employment history included termination from several hospitals because of misconduct, hospitalizations for mental illness, and a criminal investigation regarding improper medication administration.
In an open letter published in The New York Times on March 14, 2004, Somerset Medical Center (Somerville, N.J.) asserted: “Mr. Cullen worked at nine other healthcare facilities over a 16-year period. His former work history problems were not revealed to us. Nor were any state agencies or licensing boards able to provide us with accurate information about his employment history.”
Cullen had been investigated by three hospitals, a nursing home, and two prosecutors for suspicious patient deaths. He was fired by five hospitals and one nursing home for suspected wrongdoing. But Cullen continued to find employment and kill patients.
“Confidentiality is essential [as is] not leaking to the media, which can taint the investigation,” says Dr. Yorker. “The Charles Cullen case should motivate hospitalists to [participate in helping to stop the systemic mechanism that made possible] his killing over 40 patients in nine different hospitals and a nursing home before being stopped. This erodes the public trust in hospitals.”
The Health Care Quality Improvement Act provides some immunity for reporters of adverse information, but it applies only to physicians—not communications between employers.
The American Society for Healthcare Risk Management (ASHRM) and Dr. Kizer and his colleagues are in alignment in advocating for the provision of more comprehensive immunity to help healthcare employees and patients when they report these incidents.3
“If you have information that a worker is harming patients, the institution should be able to tell prospective employers and not worry about getting sued,” says Dr. Yorker. A number of states have passed varying forms of legislation so far, and ASHRM is recommending this be a federal matter. Dr. Kizer and his group recommend that reporting of suspected serial murderers should be considered for coverage under Good Samaritan laws.
Other Complicating Factors
Another problem in bringing legitimate cases to prosecution is when providers are accused on trumped-up charges, which in Dr. Iserson’s view amounts to prosecutorial malpractice. Examples are cases post-Hurricane Katrina, when physicians and nurses were charged with patient deaths.
Internationally, an example is the case in Libya where the main defendants—a Palestinian doctor and five Bulgarian nurses—were charged with injecting 426 children with HIV in 1998, causing an epidemic at El-Fath Children’s Hospital in Benghazi. According to World Politics Watch, dozens of foreign medical professionals were arrested, with six eventually charged and forced to confess by Libyan authorities. Subsequent research published in the journal Nature indicated that viral strains present in the infected children were present at the hospital before 1998.
“This was a case of political blackmail,” says Dr. Iserson. These cases may not be clear-cut and may be open to negative interpretations that “make people skittish. That is why institutions are prone to say, ‘Gee, maybe it’s just one of those kinds of cases. We don’t want to make that kind of mistake.’ ”
Also problematic is the variable rate at which hospitals perform autopsies.
“Autopsy rates are down in many communities to 1% or 2% or even lower,” says Dr. Kizer. “When the data point to the possibility of a crime on a particular unit, the site needs to be treated as a crime scene. In most hospitals, when someone dies, you get them off the floor and you clean up as quickly as possible. That shouldn’t be the case if it is a suspected crime scene. Ideally there should be standardized processes or protocols whenever there is suspicion. And those protocols may be different than when a patient ordinarily dies.”
Seeking Solutions
Hospitalists and other professionals—especially nurses and ancillary personnel—have an obligation to be informed and astute regarding individual characteristics and signs of suspicious patient deaths. Appropriate epidemiological, toxicological, and psychological data must be collected and analyzed routinely.
“Data about this phenomenon need to be disseminated to heighten awareness that serial murder of patients is a significant concern that extends beyond a few shocking, isolated incidents,” write Drs. Yorker and Kizer and their co-authors.
Institutional hiring practices must be changed so balance is achieved between preventing wrongful discharge or denial-of-employment lawsuits and protecting patient safety. Existing state legislation and future federal legislation for institutional immunity is an important element of patient advocacy that hospitalists can support.
Ultimately, hospitalists must be informed, aware, and alert. “Most [suspicions] will not be anything,” says Dr. Iserson. “Just pay attention to it.” TH
Andrea Sattinger is a frequent contributor to The Hospitalist.
References
- Yorker BC, Kizer KW, Lampe P, et al. Serial murder by healthcare professionals. J Forensic Sci. 2006 Nov;51(6):1362-1371.
- Wolf BC, Lavezzi WA. Paths to destruction: the lives and crimes of two serial killers. J Forensic Sci. 2007 Jan;52(1):199-203.
- ASHRM. American Society for Healthcare Risk Management. A call for federal immunity to protect health care employers … and patients. Chicago: Monograph; April 1, 2005; www.ashrm.org/ashrm/resources/files/Monograph.Immunity.pdf.
By the time a mortician in the northeast British town of Hyde, Greater Manchester, United Kingdom, noticed Dr. Harold Shipman’s patients were dying at an exorbitant rate, the doctor had probably killed close to 300 of them, according to Kenneth V. Iserson, MD, MBA, professor of emergency medicine at the University of Arizona College of Medicine and author of “Demon Doctors: Physicians as Serial Killers.”
Shipman, labeled ‘‘the most prolific serial killer in the history of the United Kingdom—and probably the world,’’ was officially convicted of killing 15 patients in 2000 and sentenced to 15 consecutive life sentences.1 In January 2004 he was found hanged in his prison cell.
Sometimes referred to as caregiver-associated serial killings, these incidents generate profound shock in the healthcare community. As repellent and relatively rare as this behavior is, and as controversial as the topic is, neither individuals nor institutions can afford to disassociate themselves from the subject. Hospitalists should not hide from this issue and should not feel they will be accused of “treason” if they educate themselves and bring suspicious behavior to the awareness of superiors, says Beatrice Crofts Yorker, JD, RN, MS, FAAN, dean of the College of Health and Human Services at California State University, Los Angeles. On the contrary, she says, “first, do no harm” also entails ensuring everyone else around you follows the same ethic.
Dr. Yorker, who has been studying this phenomenon since 1986, published the first examination of cases of serial murder by nurses in the American Journal of Nursing (AJN) in 1988. “It is a serious problem that has been under-recognized, and it is the right thing to blow the whistle when adverse patient incidents are associated with the presence of a specific healthcare provider,” says Dr. Yorker. “In fact, most of the cases came to the attention of authorities because a nurse blew the whistle. The sad thing is that some of the nurses were disciplined for their protective actions; however, they were ultimately vindicated.”
A veteran of the phenomenon urges continued vigilance. “As a general caveat, there needs to be a higher index of suspicion for these incidents,” says Kenneth W. Kizer, MD, MPH, the former head of the veterans healthcare system who had to deal with three incidents of serial murder at Veterans Affairs (VA) hospitals in the 1990s. “These incidents are grossly underreported.”
Incidence and Cause of Death
Drs. Kizer and Yorker were two of the investigators who reviewed epidemiologic studies, toxicology evidence, and court transcripts for data on healthcare professionals prosecuted between 1970 and 2006.
“Dr. Robert Forrest, who was a forensic toxicologist getting a law degree and wrote his dissertation on the topic of serial murder by healthcare providers, contacted me after the AJN article came out,” says Dr. Yorker. Dr. Forrest has been the testifying expert in most of the U.K. cases. “After the Charles Cullen case hit the news, The New York Times and Modern Healthcare contacted me regarding my study in AJN and the Journal of Nursing Law. That is how Ken Kizer and Paula Lampe found me.” (Cullen, a registered nurse, received 11 consecutive life sentences in 2006 after pleading guilty to administering lethal doses of medication to more than 40 patients in New Jersey and Pennsylvania.)
Lampe, an author, had been studying cases in Europe. “Because both Robert and Paula provided additional data on some cases, they were co-authors—as was Ken—who provided data on the VA cases and an important public policy perspective,” says Dr. Yorker.
The search showed 90 criminal prosecutions of healthcare providers who met the criteria of serial murder of patients. Of those, 54 have been convicted—45 for serial murder, four for attempted murder, and five on lesser charges. Since the publication of their study, one more of the accused has received a sentence of life in prison, another has been convicted and sentenced to 20 years, one committed suicide in prison, and two additional nurses in Germany and the Czech Republic have been arrested and confessed to serial murder of patients. In addition, Dr. Yorker is continuing to follow two large-scale murder-for-profit prosecutions. There are four defendants in each case. Further, three individuals have been found liable for wrongful death in the amounts of $27 million, $8 million, and $450,000 in damages.
Injection was the main method used by healthcare killers, followed by suffocation, poisoning, and tampering with equipment. Prosecutions were reported in 20 countries, with 40% of the incidents taking place in the United States. Nursing personnel were 86% of the healthcare providers prosecuted; 12% were physicians, and 2% were allied health professionals. The number of patient deaths that resulted in a murder conviction is 317, and the number of suspicious patient deaths attributed to the 54 convicted caregivers is 2,113.
“Physicians as serial killers are remarkably uncommon,” says Dr. Iserson, who is also director of the Arizona Bioethics Program at the University of Arizona College of Medicine in Tucson. “Nurses [who are serial killers] are much more common, but of course there are more nurses in the hospital, just as there are ancillary people.” (See Figure 1, left.) Dr. Iserson, who practices emergency medicine and consults nationally on bioethics, advises maintaining caution when examining data of charges or suspicions that were never proved.
Most of these crimes (70%) occur in hospital units. (See Figure 2, left.) Victims are almost always female, as are almost half (49%) of convicted serial killers and 55% of the total number of prosecuted healthcare providers. Males are disproportionately represented among prosecuted nurses.
Motives: Who Is Always There?
Although the motives are complex, some common threads connect these crimes. “There are some classical signs, if you will,” says Dr. Kizer.
When the same person repeatedly calls a code and always seems to be in the thick of it, that is one prime indicator. These people are usually legitimately present in those settings and circumstances—for example, they are on call or working a shift—which makes it more difficult to discern when something is awry. Commonly, the perpetrators have easy access to high-alert drugs without sufficient accountability. Sometimes, once an investigation has been launched it is discovered the person has falsified his or her credentials.
In hospitals, experts say, the “rescuer” or “hero” personality is often on display in those who kill patients—the first person there to give the patient drugs or attempt to save the patient.
“What you are going to see as a pattern,” says Dr. Iserson, “is that they need to be near death.” Codes or calls for respiratory arrest are the most common; patients who have cardiac arrests are much harder to save. Being the hero is not always the motive; the converse can also apply.
Such is the case with nurse Orville Lynn Majors, LPN, convicted of six murders at the Vermillion county hospital in Clinton, Ind. The deaths were consistent with injections of potassium chloride and epinephrine according to prosecutors. Majors’ coworkers were concerned that patients were coding in alarming numbers while in his care. Although this information did not come out until after he was apprehended, his coworkers had a good idea which of his patients would not survive: Patients who were whiny, demanding, or required a lot of work. “The scuttlebutt or rumor among his coworkers,” says Dr. Kizer, “is that they could almost predict which patients would have a demise under his care.”
Although a typical profile of the serial healthcare murderer has been demonstrated in many cases, in many other cases the demographics and behaviors of these killers have deviated widely from generalized assumptions.2 Therefore, before looking at people, look at the numbers.
An unusual number of calls and codes may occur in a particular area of the hospital. “In ICUs you expect a lot of [codes and calls], but not on general post-op wards or the pediatrics MICU,” Dr. Kizer says. “When this happens in these settings it should raise a red flag.”
Unfortunately, most hospitals don’t track mortality on a monthly basis per unit or ward or ICU, so they may not recognize when something is out of line in a timely manner. Also, the hospital committee assigned to review deaths may be remiss in its duty to meet regularly or otherwise perform according to policy.
Another factor that should raise a red flag is a disproportionate number of codes or deaths on the same shift—most often the night shift. Often, someone says, “Gee, it seems like there’s an awful lot of codes lately,” explains Dr. Kizer. An unusually high rate of successful codes is another sign.
For example, in the 1995-1996 case of Kristen Gilbert, an RN convicted of four murders at the Veterans Affairs Medical Center in Northampton, Mass., she was having an extramarital affair with a hospital security guard who worked the evening shift. Protocol required that security be called to all cardiopulmonary arrests. Gilbert used stimulant epinephrine to make their hearts race out of control. The epidemiologic data later showed that suspicious codes occurred when both were on duty. “The patients always seemed to recover and she was the hero,” says Dr. Kizer. “She wanted to look good for her boyfriend.”
Similarly, Richard Angelo, a charge nurse at Good Samaritan Hospital in West Islip, Long Island, N.Y., admitted that between 1987 and 1989 he injected patients with paralyzing drugs Pavulon (pancuronium) and Anectine (succinylcholine). He wanted his colleagues to admire him for performing well in a code. During his confession, he likened himself to volunteer firefighters who set fires. In fact, Dr. Iserson makes this same parallel. “From what we can tell,” he says, “these people don’t really care whether the person dies or not. They would rather they not [die], so they can be seen as the hero. It’s all about them.” As with instances of arson, he says, the perpetrator is “the first one to show up at the fire watch, over and over again.”
Obstacles to Disclosure
Even when healthcare workers and related personnel come forward with their suspicions, law enforcement may be a barrier to prosecution.
In the United Kingdom, a Manchester mortician took her observations about the excessive deaths and cremations in Harold Shipman’s practice to her father and brother, who were also in the family business. She also obtained the support of a local female general practitioner. The two women went to the police, explaining that most patients who had died had not been critically ill and noted that the doctor had exhibited peculiar behavior when he was questioned.
But, says Dr. Iserson, the response again was typical: “‘Oh, foolish women. That can’t be happening.’ And it wasn’t until Shipman killed the wrong person [a former town mayor, mother of a prominent lawyer] that things started to unravel for him.” When police finally looked at other deaths Shipman had certified, a pattern emerged. He would overdose patients with diamorphine, sign their death certificates, then forge medical records to indicate they were in poor health.
A second common response by institutions is just as much of a barrier to bringing these crimes to light and ultimately, prosecution. “In essence,” says Dr. Iserson, “that response is, ‘Well, maybe it is happening but, boy, it sure is going to put our institution in a bad light. So let’s just not say anything.’ ”
This was the case with Michael Swango, a doctor who worked in several states and a number of countries. He was charged with five murders and may have been involved in 126 deaths. Swango confessed to the deaths that occurred in a Veterans Affairs hospital in Northport, N.Y., where he reportedly injected three veterans with a drug that stopped their hearts. He had forged “do not resuscitate” orders for the three. He was sentenced to two life sentences. It is possible that he killed as many as 35-60 people in the United States and Zimbabwe. But before it was all out in the open, “some very prominent people were involved in sweeping it under the rug,” says Dr. Iserson, “and they didn’t even get a slap on the wrist.”
Hiring Practices
One of the most shocking aspects of the Cullen case was that institutional coverup and employee privacy policies meant his prior employers never revealed the problems to prospective employers.
“Identifying potential serial killers is not at all the total problem,” says Dr. Iserson. “The problem is getting the powers that be to act. What they typically do is pass the problem on to somebody else, in effect, saying, ‘We don’t want you to work here anymore. We won’t necessarily write you a good letter of recommendation, but we will say that you worked here, and basically we just want you to go away.’ ”
An investigation revealed that Cullen had a history of reported incidents at hospitals in Pennsylvania and New Jersey, but there were no tracking or disclosure systems in place as he moved from one hospital to another. His employment history included termination from several hospitals because of misconduct, hospitalizations for mental illness, and a criminal investigation regarding improper medication administration.
In an open letter published in The New York Times on March 14, 2004, Somerset Medical Center (Somerville, N.J.) asserted: “Mr. Cullen worked at nine other healthcare facilities over a 16-year period. His former work history problems were not revealed to us. Nor were any state agencies or licensing boards able to provide us with accurate information about his employment history.”
Cullen had been investigated by three hospitals, a nursing home, and two prosecutors for suspicious patient deaths. He was fired by five hospitals and one nursing home for suspected wrongdoing. But Cullen continued to find employment and kill patients.
“Confidentiality is essential [as is] not leaking to the media, which can taint the investigation,” says Dr. Yorker. “The Charles Cullen case should motivate hospitalists to [participate in helping to stop the systemic mechanism that made possible] his killing over 40 patients in nine different hospitals and a nursing home before being stopped. This erodes the public trust in hospitals.”
The Health Care Quality Improvement Act provides some immunity for reporters of adverse information, but it applies only to physicians—not communications between employers.
The American Society for Healthcare Risk Management (ASHRM) and Dr. Kizer and his colleagues are in alignment in advocating for the provision of more comprehensive immunity to help healthcare employees and patients when they report these incidents.3
“If you have information that a worker is harming patients, the institution should be able to tell prospective employers and not worry about getting sued,” says Dr. Yorker. A number of states have passed varying forms of legislation so far, and ASHRM is recommending this be a federal matter. Dr. Kizer and his group recommend that reporting of suspected serial murderers should be considered for coverage under Good Samaritan laws.
Other Complicating Factors
Another problem in bringing legitimate cases to prosecution is when providers are accused on trumped-up charges, which in Dr. Iserson’s view amounts to prosecutorial malpractice. Examples are cases post-Hurricane Katrina, when physicians and nurses were charged with patient deaths.
Internationally, an example is the case in Libya where the main defendants—a Palestinian doctor and five Bulgarian nurses—were charged with injecting 426 children with HIV in 1998, causing an epidemic at El-Fath Children’s Hospital in Benghazi. According to World Politics Watch, dozens of foreign medical professionals were arrested, with six eventually charged and forced to confess by Libyan authorities. Subsequent research published in the journal Nature indicated that viral strains present in the infected children were present at the hospital before 1998.
“This was a case of political blackmail,” says Dr. Iserson. These cases may not be clear-cut and may be open to negative interpretations that “make people skittish. That is why institutions are prone to say, ‘Gee, maybe it’s just one of those kinds of cases. We don’t want to make that kind of mistake.’ ”
Also problematic is the variable rate at which hospitals perform autopsies.
“Autopsy rates are down in many communities to 1% or 2% or even lower,” says Dr. Kizer. “When the data point to the possibility of a crime on a particular unit, the site needs to be treated as a crime scene. In most hospitals, when someone dies, you get them off the floor and you clean up as quickly as possible. That shouldn’t be the case if it is a suspected crime scene. Ideally there should be standardized processes or protocols whenever there is suspicion. And those protocols may be different than when a patient ordinarily dies.”
Seeking Solutions
Hospitalists and other professionals—especially nurses and ancillary personnel—have an obligation to be informed and astute regarding individual characteristics and signs of suspicious patient deaths. Appropriate epidemiological, toxicological, and psychological data must be collected and analyzed routinely.
“Data about this phenomenon need to be disseminated to heighten awareness that serial murder of patients is a significant concern that extends beyond a few shocking, isolated incidents,” write Drs. Yorker and Kizer and their co-authors.
Institutional hiring practices must be changed so balance is achieved between preventing wrongful discharge or denial-of-employment lawsuits and protecting patient safety. Existing state legislation and future federal legislation for institutional immunity is an important element of patient advocacy that hospitalists can support.
Ultimately, hospitalists must be informed, aware, and alert. “Most [suspicions] will not be anything,” says Dr. Iserson. “Just pay attention to it.” TH
Andrea Sattinger is a frequent contributor to The Hospitalist.
References
- Yorker BC, Kizer KW, Lampe P, et al. Serial murder by healthcare professionals. J Forensic Sci. 2006 Nov;51(6):1362-1371.
- Wolf BC, Lavezzi WA. Paths to destruction: the lives and crimes of two serial killers. J Forensic Sci. 2007 Jan;52(1):199-203.
- ASHRM. American Society for Healthcare Risk Management. A call for federal immunity to protect health care employers … and patients. Chicago: Monograph; April 1, 2005; www.ashrm.org/ashrm/resources/files/Monograph.Immunity.pdf.
Smoke Screens
Nobody thought it was possible. Could all indoor workplaces in Ireland—including pubs—be made smoke-free? Now, a law enacted in 2004 is seen as a triumph for public health policy worldwide.1
Smoking kills 438,000 people a year in the United States, and 8.6 million have a serious smoking-related illness.2 Research shows many outpatient physicians do not judge it worthwhile to talk with their patients about quitting smoking because they assume they will have no effect. The assumption is that even if patients quit, they will relapse.
Yet ample evidence suggests hospitalists can have a positive effect by intervening during a patient’s hospital visit.
Data also show that an individual will relapse an average of seven times before being able to take the step for the long term. Relapse is a part of the process, each time teaching an individual something about his or her motivation and behavior.
“Doctors who address smoking with patients can double or even triple the chances of their quitting,” says Shawn Ralston, MD, pediatric hospitalist at Presbyterian Hospital in Albuquerque, N.M. A few pointed questions and a show of compassion to the patient in the hospital could make a world of difference.
Golden Opportunity
Stephen Liu, MD, MPH, a hospitalist and an assistant program director at Dartmouth-Hitchcock Medical Center (DHMC) in Lebanon, N.H., has been interested in smoking-cessation interventions since his residency in DHMC’s Leadership Preventive Medicine Residency Program in 2003, where he worked on improving care for pneumonia patients. His efforts took off as a result of the Centers for Medicare and Medicaid Services (CMS) pay-for-performance measures, which made smoking-cessation counseling a key component of admission and discharge documentation for a number of disease states.
The approach used with adult patients at DHMC is the brainchild of Colleen Warren, a registered nurse on the medicine unit on which Dr. Liu worked.
“The more times that smokers hear the message [about quitting], the more likely they are to try to quit,” says Dr. Liu. “We capitalized on that [point when] we developed a tobacco treatment team in our hospital. The team, which includes two to five motivated nurses, social workers, or care managers in most units of the hospital, pursued training including an online tobacco treatment course through U Mass Medical Center.”
In January 2006, DHMC was awarded a grant from the New Hampshire Department of Health and Human Services to standardize the treatment of hospitalized smokers. This includes conducting tobacco screening, assessing a patient’s readiness to quit, providing brief counseling, documenting the status and stage of change into the electronic medical record, and referring the patient to community resources upon discharge. The funding allowed the institution to support Warren and Dr. Liu as they coordinated the team and its work. These efforts, including counseling, nicotine replacement therapy, and cessation medications, are also available free to DHMC employees.
DHMC is participating in the CMS demonstration project, in which the hospital publicly reports performance measures for several conditions on the CMS Web site. In addition, many more performance measures are publicly reported on the DHMC quality-measures Web site. Although the team initially targeted the intervention to performance measures related to pneumonia and heart failure hospitalizations, they decided to offer interventions to all patients admitted to the hospital. Of these patients, about 20% are smokers, Dr. Liu says.
Because financial support wasn’t available at first and staff time was voluntary, the work was more difficult. Data from a six-month pilot intervention on two inpatient floors at DHMC showed patient assessments increased from 2% to 85%. In addition, the percentage of eligible heart failure and pneumonia patients receiving smoking cessation advice or counseling prior to discharge has risen from 30% before 2005 to 80% to 90%.
“We have found that hospitalization is a golden opportunity to address smoking cessation in patients in that they become acutely aware of how the smoking has affected their health,” says Dr. Liu. Because patients frequently go without smoking for several days while hospitalized, they learn they can live without smoking and feel much better.
“The key for our kind of intervention is not only assessing it and addressing it while they are hospitalized, but making sure that we link them to resources after they leave,” Dr. Liu says. Those resources include telephone quit lines or local support groups and/or local cessation clinics.
Counseling patients can be personally and professionally fulfilling, says Dr. Liu. He recalls a 50-year-old man—a lifelong smoker—admitted for pancreatitis. The day he was discharged, he showed Dr. Liu a hospital-produced packet of information. The patient said he had been reading it during his stay, decided he was motivated to quit, and had called the quit line.
Dr. Liu and his team use what they call the five A’s:
- Ask (does the patient smoke and has he/she tried to quit?);
- Advise the patient to quit;
- Assess (if the patient is ready to try to quit);
- Assist (the patient in planning treatment and referrals); and
- Arrange for a follow-up visit.
As part of their counseling, DHMC team members ask patients whether they have used assistive medication, such as nicotine-replacement therapy, bupropion (Wellbutrin) or varenicline (Chantix), in their attempts. They find out what patients have and have not tried. Then they ask, “How can we as a hospital help so that you will not restart smoking when you get home?”
A slightly longer counseling session with a motivated patient means a provider can explore whether they know their triggers for smoking, such as stress, alcohol use, or being around other smokers, and help the patient develop a proactive plan for when they are re-exposed to triggers upon discharge.
Counseling Parents of Hospitalized Children
In Dr. Ralston’s case, her research and the research of others inspired her to begin counseling the parents of hospitalized children.3-4 She was conducting research on respiratory illness, specifically bronchiolitis—the most common reason children are hospitalized.
She noticed the vast majority of children had had secondary smoke exposure. The work of C. Andrew Aligne, MD, formerly in the department of general pediatrics at the University of Rochester (N.Y.) Medical Center, inspired her.5-6 His analyses of attributable risk data revealed that the major and preventable cause of death in children is secondary smoke from parents.
But the issue really crystallized for Dr. Ralston when she encountered the work of Jonathan Winickoff, MD, MPH, an assistant professor of pediatrics at Harvard Medical School and a researcher with the Massachusetts General Hospital Center for Child and Adolescent Health Policy in Boston.
“The AHRQ guidelines show a huge amount of literature that say hospitalization is a great time to address smoking in adults,” says Dr. Ralston. “The [quit rate in office patients] will move from 5% to 12% or 15%, depending on the message. But in hospitalized adults, the quit rate can rise to 25% or 27%. Dr. Winickoff said, ‘Why can’t hospitalization for children be a teachable moment for parents?’ ”7
Another researcher who inspired Dr. Ralston was William R. Miller, PhD, who created the motivational interviewing model. Motivational interviewing is used with individuals to elicit and examine the ambivalence surrounding their unhealthy behaviors. Dr. Miller, retiring this year from the University of New Mexico (Albuquerque), began his work in the area of alcohol abuse. He and his colleagues have increasingly used motivational interviewing in other areas of addiction.
Dr. Ralston says what she has learned from motivational interviewing—and how she counsels parents of hospitalized children differently because of it—primarily pertains to her willingness to talk to people about a difficult subject. Instead of bombarding parents with facts about how smoking is bad for their children—which they already believe but don’t want to talk about—she learned to focus on the parents’ needs instead of the effects on the child.
“And there is the issue of bringing it up when this is not technically your patient,” she says. But after fine-tuning and developing her technique, she now assumes a value-neutral, nonjudgmental, open-ended approach using motivational interviewing. “Eventually it becomes easy to do.”
When approaching a parent to offer help, says Dr. Ralston, “I will lead by acknowledging that the experience the parent is having is extremely stressful. Then, after addressing the primary illness of the child and what the plan is for that, I say, ‘I see [from our records] that you are smoking. Have you tried to quit? Are you interested in quitting now? What might I be able to do to help you?’ If there is an opening, then I’ll go into more extensive counseling.
“You don’t need all the data behind you. I use my expertise more to motivate pediatricians, not the parents.” Another tack she takes to motivate pediatricians to empathically address smoking is to ask them to think of something they do that they know is bad for them but that they continue to do.
Conclusion
“There have been some studies that have shown [disappointing] outcomes when we intervene with hospitalized patients, but I’m more optimistic,” says Dr. Liu. “I feel that as long as we can make a difference in some people’s lives and get them to quit after they leave the hospital, then it’s worth the effort.”
Look at what you are willing to do, advises Dr. Ralston. “If that is a brief message and then a referral to a quit line, that’s fabulous,” she says. “You still might double the quit rate.” Given the temporal nature of the hospitalist-patient relationship, there may be a good number of ways hospitalists could effect change by offering a few encouraging words. TH
Andrea Sattinger is a frequent contributor to The Hospitalist.
References
- Koh HK, Joossens LX, Connolly GN. Making smoking history worldwide. N Engl J Med. 2007 Apr 12;356(15):1496-1498.
- Centers for Disease Control and Prevention. Targeting Tobacco Use: The Nation’s Leading Cause of Preventable Death, 2007. Available at www.cdc.gov/Tobacco/basic_information/00_pdfs/AAGTobacco2007.pdf. Last accessed June 18, 2007.
- Ralston S, Kellett N, Williams RL, et al. Practice-based assessment of tobacco usage in southwestern primary care patients: a Research Involving Outpatient Settings Network (RIOS Net) study. J Am Board Fam Med. 2007;20(2):174-180.
- Ralston S, Mahshid R. The pediatric hospitalist and the smoking parent. Pediatric Research Day 2006. Available at http://hsc.unm.edu/pedsresearch/ORAL%20PRESENTATIONS.htm Albuquerque: Office of Research and Creative Endeavors, Department of Pediatrics, University of New Mexico Health Sciences Center; 2006. Last accessed June 18, 2007.
- Aligne CA, Stoddard JJ. Tobacco and children. An economic evaluation of the medical effects of parental smoking. Arch Pediatr Adolesc Med. 1997 Jul;151(7):648-653. Erratum in: Arch Pediatr Adolesc Med 1997 Oct;151(10):988. Comment in: Arch Pediatr Adolesc Med. 1997 Dec;151(12):1269. Arch Pediatr Adolesc Med. 2000 Aug;154(8):850.
- Leonard K, Mosquera M, Aligne CA. Pediatrics in the community: Taking a collective breath to help children who have asthma. Pediatr Rev. 2007;28:152-153.
- Winickoff JP, Hillis VJ, Palfrey JS, et al. A smoking cessation intervention for parents of children who are hospitalized for respiratory illness: the stop tobacco outreach program. Pediatrics. 2003 Jan;111(1):140-145.
Nobody thought it was possible. Could all indoor workplaces in Ireland—including pubs—be made smoke-free? Now, a law enacted in 2004 is seen as a triumph for public health policy worldwide.1
Smoking kills 438,000 people a year in the United States, and 8.6 million have a serious smoking-related illness.2 Research shows many outpatient physicians do not judge it worthwhile to talk with their patients about quitting smoking because they assume they will have no effect. The assumption is that even if patients quit, they will relapse.
Yet ample evidence suggests hospitalists can have a positive effect by intervening during a patient’s hospital visit.
Data also show that an individual will relapse an average of seven times before being able to take the step for the long term. Relapse is a part of the process, each time teaching an individual something about his or her motivation and behavior.
“Doctors who address smoking with patients can double or even triple the chances of their quitting,” says Shawn Ralston, MD, pediatric hospitalist at Presbyterian Hospital in Albuquerque, N.M. A few pointed questions and a show of compassion to the patient in the hospital could make a world of difference.
Golden Opportunity
Stephen Liu, MD, MPH, a hospitalist and an assistant program director at Dartmouth-Hitchcock Medical Center (DHMC) in Lebanon, N.H., has been interested in smoking-cessation interventions since his residency in DHMC’s Leadership Preventive Medicine Residency Program in 2003, where he worked on improving care for pneumonia patients. His efforts took off as a result of the Centers for Medicare and Medicaid Services (CMS) pay-for-performance measures, which made smoking-cessation counseling a key component of admission and discharge documentation for a number of disease states.
The approach used with adult patients at DHMC is the brainchild of Colleen Warren, a registered nurse on the medicine unit on which Dr. Liu worked.
“The more times that smokers hear the message [about quitting], the more likely they are to try to quit,” says Dr. Liu. “We capitalized on that [point when] we developed a tobacco treatment team in our hospital. The team, which includes two to five motivated nurses, social workers, or care managers in most units of the hospital, pursued training including an online tobacco treatment course through U Mass Medical Center.”
In January 2006, DHMC was awarded a grant from the New Hampshire Department of Health and Human Services to standardize the treatment of hospitalized smokers. This includes conducting tobacco screening, assessing a patient’s readiness to quit, providing brief counseling, documenting the status and stage of change into the electronic medical record, and referring the patient to community resources upon discharge. The funding allowed the institution to support Warren and Dr. Liu as they coordinated the team and its work. These efforts, including counseling, nicotine replacement therapy, and cessation medications, are also available free to DHMC employees.
DHMC is participating in the CMS demonstration project, in which the hospital publicly reports performance measures for several conditions on the CMS Web site. In addition, many more performance measures are publicly reported on the DHMC quality-measures Web site. Although the team initially targeted the intervention to performance measures related to pneumonia and heart failure hospitalizations, they decided to offer interventions to all patients admitted to the hospital. Of these patients, about 20% are smokers, Dr. Liu says.
Because financial support wasn’t available at first and staff time was voluntary, the work was more difficult. Data from a six-month pilot intervention on two inpatient floors at DHMC showed patient assessments increased from 2% to 85%. In addition, the percentage of eligible heart failure and pneumonia patients receiving smoking cessation advice or counseling prior to discharge has risen from 30% before 2005 to 80% to 90%.
“We have found that hospitalization is a golden opportunity to address smoking cessation in patients in that they become acutely aware of how the smoking has affected their health,” says Dr. Liu. Because patients frequently go without smoking for several days while hospitalized, they learn they can live without smoking and feel much better.
“The key for our kind of intervention is not only assessing it and addressing it while they are hospitalized, but making sure that we link them to resources after they leave,” Dr. Liu says. Those resources include telephone quit lines or local support groups and/or local cessation clinics.
Counseling patients can be personally and professionally fulfilling, says Dr. Liu. He recalls a 50-year-old man—a lifelong smoker—admitted for pancreatitis. The day he was discharged, he showed Dr. Liu a hospital-produced packet of information. The patient said he had been reading it during his stay, decided he was motivated to quit, and had called the quit line.
Dr. Liu and his team use what they call the five A’s:
- Ask (does the patient smoke and has he/she tried to quit?);
- Advise the patient to quit;
- Assess (if the patient is ready to try to quit);
- Assist (the patient in planning treatment and referrals); and
- Arrange for a follow-up visit.
As part of their counseling, DHMC team members ask patients whether they have used assistive medication, such as nicotine-replacement therapy, bupropion (Wellbutrin) or varenicline (Chantix), in their attempts. They find out what patients have and have not tried. Then they ask, “How can we as a hospital help so that you will not restart smoking when you get home?”
A slightly longer counseling session with a motivated patient means a provider can explore whether they know their triggers for smoking, such as stress, alcohol use, or being around other smokers, and help the patient develop a proactive plan for when they are re-exposed to triggers upon discharge.
Counseling Parents of Hospitalized Children
In Dr. Ralston’s case, her research and the research of others inspired her to begin counseling the parents of hospitalized children.3-4 She was conducting research on respiratory illness, specifically bronchiolitis—the most common reason children are hospitalized.
She noticed the vast majority of children had had secondary smoke exposure. The work of C. Andrew Aligne, MD, formerly in the department of general pediatrics at the University of Rochester (N.Y.) Medical Center, inspired her.5-6 His analyses of attributable risk data revealed that the major and preventable cause of death in children is secondary smoke from parents.
But the issue really crystallized for Dr. Ralston when she encountered the work of Jonathan Winickoff, MD, MPH, an assistant professor of pediatrics at Harvard Medical School and a researcher with the Massachusetts General Hospital Center for Child and Adolescent Health Policy in Boston.
“The AHRQ guidelines show a huge amount of literature that say hospitalization is a great time to address smoking in adults,” says Dr. Ralston. “The [quit rate in office patients] will move from 5% to 12% or 15%, depending on the message. But in hospitalized adults, the quit rate can rise to 25% or 27%. Dr. Winickoff said, ‘Why can’t hospitalization for children be a teachable moment for parents?’ ”7
Another researcher who inspired Dr. Ralston was William R. Miller, PhD, who created the motivational interviewing model. Motivational interviewing is used with individuals to elicit and examine the ambivalence surrounding their unhealthy behaviors. Dr. Miller, retiring this year from the University of New Mexico (Albuquerque), began his work in the area of alcohol abuse. He and his colleagues have increasingly used motivational interviewing in other areas of addiction.
Dr. Ralston says what she has learned from motivational interviewing—and how she counsels parents of hospitalized children differently because of it—primarily pertains to her willingness to talk to people about a difficult subject. Instead of bombarding parents with facts about how smoking is bad for their children—which they already believe but don’t want to talk about—she learned to focus on the parents’ needs instead of the effects on the child.
“And there is the issue of bringing it up when this is not technically your patient,” she says. But after fine-tuning and developing her technique, she now assumes a value-neutral, nonjudgmental, open-ended approach using motivational interviewing. “Eventually it becomes easy to do.”
When approaching a parent to offer help, says Dr. Ralston, “I will lead by acknowledging that the experience the parent is having is extremely stressful. Then, after addressing the primary illness of the child and what the plan is for that, I say, ‘I see [from our records] that you are smoking. Have you tried to quit? Are you interested in quitting now? What might I be able to do to help you?’ If there is an opening, then I’ll go into more extensive counseling.
“You don’t need all the data behind you. I use my expertise more to motivate pediatricians, not the parents.” Another tack she takes to motivate pediatricians to empathically address smoking is to ask them to think of something they do that they know is bad for them but that they continue to do.
Conclusion
“There have been some studies that have shown [disappointing] outcomes when we intervene with hospitalized patients, but I’m more optimistic,” says Dr. Liu. “I feel that as long as we can make a difference in some people’s lives and get them to quit after they leave the hospital, then it’s worth the effort.”
Look at what you are willing to do, advises Dr. Ralston. “If that is a brief message and then a referral to a quit line, that’s fabulous,” she says. “You still might double the quit rate.” Given the temporal nature of the hospitalist-patient relationship, there may be a good number of ways hospitalists could effect change by offering a few encouraging words. TH
Andrea Sattinger is a frequent contributor to The Hospitalist.
References
- Koh HK, Joossens LX, Connolly GN. Making smoking history worldwide. N Engl J Med. 2007 Apr 12;356(15):1496-1498.
- Centers for Disease Control and Prevention. Targeting Tobacco Use: The Nation’s Leading Cause of Preventable Death, 2007. Available at www.cdc.gov/Tobacco/basic_information/00_pdfs/AAGTobacco2007.pdf. Last accessed June 18, 2007.
- Ralston S, Kellett N, Williams RL, et al. Practice-based assessment of tobacco usage in southwestern primary care patients: a Research Involving Outpatient Settings Network (RIOS Net) study. J Am Board Fam Med. 2007;20(2):174-180.
- Ralston S, Mahshid R. The pediatric hospitalist and the smoking parent. Pediatric Research Day 2006. Available at http://hsc.unm.edu/pedsresearch/ORAL%20PRESENTATIONS.htm Albuquerque: Office of Research and Creative Endeavors, Department of Pediatrics, University of New Mexico Health Sciences Center; 2006. Last accessed June 18, 2007.
- Aligne CA, Stoddard JJ. Tobacco and children. An economic evaluation of the medical effects of parental smoking. Arch Pediatr Adolesc Med. 1997 Jul;151(7):648-653. Erratum in: Arch Pediatr Adolesc Med 1997 Oct;151(10):988. Comment in: Arch Pediatr Adolesc Med. 1997 Dec;151(12):1269. Arch Pediatr Adolesc Med. 2000 Aug;154(8):850.
- Leonard K, Mosquera M, Aligne CA. Pediatrics in the community: Taking a collective breath to help children who have asthma. Pediatr Rev. 2007;28:152-153.
- Winickoff JP, Hillis VJ, Palfrey JS, et al. A smoking cessation intervention for parents of children who are hospitalized for respiratory illness: the stop tobacco outreach program. Pediatrics. 2003 Jan;111(1):140-145.
Nobody thought it was possible. Could all indoor workplaces in Ireland—including pubs—be made smoke-free? Now, a law enacted in 2004 is seen as a triumph for public health policy worldwide.1
Smoking kills 438,000 people a year in the United States, and 8.6 million have a serious smoking-related illness.2 Research shows many outpatient physicians do not judge it worthwhile to talk with their patients about quitting smoking because they assume they will have no effect. The assumption is that even if patients quit, they will relapse.
Yet ample evidence suggests hospitalists can have a positive effect by intervening during a patient’s hospital visit.
Data also show that an individual will relapse an average of seven times before being able to take the step for the long term. Relapse is a part of the process, each time teaching an individual something about his or her motivation and behavior.
“Doctors who address smoking with patients can double or even triple the chances of their quitting,” says Shawn Ralston, MD, pediatric hospitalist at Presbyterian Hospital in Albuquerque, N.M. A few pointed questions and a show of compassion to the patient in the hospital could make a world of difference.
Golden Opportunity
Stephen Liu, MD, MPH, a hospitalist and an assistant program director at Dartmouth-Hitchcock Medical Center (DHMC) in Lebanon, N.H., has been interested in smoking-cessation interventions since his residency in DHMC’s Leadership Preventive Medicine Residency Program in 2003, where he worked on improving care for pneumonia patients. His efforts took off as a result of the Centers for Medicare and Medicaid Services (CMS) pay-for-performance measures, which made smoking-cessation counseling a key component of admission and discharge documentation for a number of disease states.
The approach used with adult patients at DHMC is the brainchild of Colleen Warren, a registered nurse on the medicine unit on which Dr. Liu worked.
“The more times that smokers hear the message [about quitting], the more likely they are to try to quit,” says Dr. Liu. “We capitalized on that [point when] we developed a tobacco treatment team in our hospital. The team, which includes two to five motivated nurses, social workers, or care managers in most units of the hospital, pursued training including an online tobacco treatment course through U Mass Medical Center.”
In January 2006, DHMC was awarded a grant from the New Hampshire Department of Health and Human Services to standardize the treatment of hospitalized smokers. This includes conducting tobacco screening, assessing a patient’s readiness to quit, providing brief counseling, documenting the status and stage of change into the electronic medical record, and referring the patient to community resources upon discharge. The funding allowed the institution to support Warren and Dr. Liu as they coordinated the team and its work. These efforts, including counseling, nicotine replacement therapy, and cessation medications, are also available free to DHMC employees.
DHMC is participating in the CMS demonstration project, in which the hospital publicly reports performance measures for several conditions on the CMS Web site. In addition, many more performance measures are publicly reported on the DHMC quality-measures Web site. Although the team initially targeted the intervention to performance measures related to pneumonia and heart failure hospitalizations, they decided to offer interventions to all patients admitted to the hospital. Of these patients, about 20% are smokers, Dr. Liu says.
Because financial support wasn’t available at first and staff time was voluntary, the work was more difficult. Data from a six-month pilot intervention on two inpatient floors at DHMC showed patient assessments increased from 2% to 85%. In addition, the percentage of eligible heart failure and pneumonia patients receiving smoking cessation advice or counseling prior to discharge has risen from 30% before 2005 to 80% to 90%.
“We have found that hospitalization is a golden opportunity to address smoking cessation in patients in that they become acutely aware of how the smoking has affected their health,” says Dr. Liu. Because patients frequently go without smoking for several days while hospitalized, they learn they can live without smoking and feel much better.
“The key for our kind of intervention is not only assessing it and addressing it while they are hospitalized, but making sure that we link them to resources after they leave,” Dr. Liu says. Those resources include telephone quit lines or local support groups and/or local cessation clinics.
Counseling patients can be personally and professionally fulfilling, says Dr. Liu. He recalls a 50-year-old man—a lifelong smoker—admitted for pancreatitis. The day he was discharged, he showed Dr. Liu a hospital-produced packet of information. The patient said he had been reading it during his stay, decided he was motivated to quit, and had called the quit line.
Dr. Liu and his team use what they call the five A’s:
- Ask (does the patient smoke and has he/she tried to quit?);
- Advise the patient to quit;
- Assess (if the patient is ready to try to quit);
- Assist (the patient in planning treatment and referrals); and
- Arrange for a follow-up visit.
As part of their counseling, DHMC team members ask patients whether they have used assistive medication, such as nicotine-replacement therapy, bupropion (Wellbutrin) or varenicline (Chantix), in their attempts. They find out what patients have and have not tried. Then they ask, “How can we as a hospital help so that you will not restart smoking when you get home?”
A slightly longer counseling session with a motivated patient means a provider can explore whether they know their triggers for smoking, such as stress, alcohol use, or being around other smokers, and help the patient develop a proactive plan for when they are re-exposed to triggers upon discharge.
Counseling Parents of Hospitalized Children
In Dr. Ralston’s case, her research and the research of others inspired her to begin counseling the parents of hospitalized children.3-4 She was conducting research on respiratory illness, specifically bronchiolitis—the most common reason children are hospitalized.
She noticed the vast majority of children had had secondary smoke exposure. The work of C. Andrew Aligne, MD, formerly in the department of general pediatrics at the University of Rochester (N.Y.) Medical Center, inspired her.5-6 His analyses of attributable risk data revealed that the major and preventable cause of death in children is secondary smoke from parents.
But the issue really crystallized for Dr. Ralston when she encountered the work of Jonathan Winickoff, MD, MPH, an assistant professor of pediatrics at Harvard Medical School and a researcher with the Massachusetts General Hospital Center for Child and Adolescent Health Policy in Boston.
“The AHRQ guidelines show a huge amount of literature that say hospitalization is a great time to address smoking in adults,” says Dr. Ralston. “The [quit rate in office patients] will move from 5% to 12% or 15%, depending on the message. But in hospitalized adults, the quit rate can rise to 25% or 27%. Dr. Winickoff said, ‘Why can’t hospitalization for children be a teachable moment for parents?’ ”7
Another researcher who inspired Dr. Ralston was William R. Miller, PhD, who created the motivational interviewing model. Motivational interviewing is used with individuals to elicit and examine the ambivalence surrounding their unhealthy behaviors. Dr. Miller, retiring this year from the University of New Mexico (Albuquerque), began his work in the area of alcohol abuse. He and his colleagues have increasingly used motivational interviewing in other areas of addiction.
Dr. Ralston says what she has learned from motivational interviewing—and how she counsels parents of hospitalized children differently because of it—primarily pertains to her willingness to talk to people about a difficult subject. Instead of bombarding parents with facts about how smoking is bad for their children—which they already believe but don’t want to talk about—she learned to focus on the parents’ needs instead of the effects on the child.
“And there is the issue of bringing it up when this is not technically your patient,” she says. But after fine-tuning and developing her technique, she now assumes a value-neutral, nonjudgmental, open-ended approach using motivational interviewing. “Eventually it becomes easy to do.”
When approaching a parent to offer help, says Dr. Ralston, “I will lead by acknowledging that the experience the parent is having is extremely stressful. Then, after addressing the primary illness of the child and what the plan is for that, I say, ‘I see [from our records] that you are smoking. Have you tried to quit? Are you interested in quitting now? What might I be able to do to help you?’ If there is an opening, then I’ll go into more extensive counseling.
“You don’t need all the data behind you. I use my expertise more to motivate pediatricians, not the parents.” Another tack she takes to motivate pediatricians to empathically address smoking is to ask them to think of something they do that they know is bad for them but that they continue to do.
Conclusion
“There have been some studies that have shown [disappointing] outcomes when we intervene with hospitalized patients, but I’m more optimistic,” says Dr. Liu. “I feel that as long as we can make a difference in some people’s lives and get them to quit after they leave the hospital, then it’s worth the effort.”
Look at what you are willing to do, advises Dr. Ralston. “If that is a brief message and then a referral to a quit line, that’s fabulous,” she says. “You still might double the quit rate.” Given the temporal nature of the hospitalist-patient relationship, there may be a good number of ways hospitalists could effect change by offering a few encouraging words. TH
Andrea Sattinger is a frequent contributor to The Hospitalist.
References
- Koh HK, Joossens LX, Connolly GN. Making smoking history worldwide. N Engl J Med. 2007 Apr 12;356(15):1496-1498.
- Centers for Disease Control and Prevention. Targeting Tobacco Use: The Nation’s Leading Cause of Preventable Death, 2007. Available at www.cdc.gov/Tobacco/basic_information/00_pdfs/AAGTobacco2007.pdf. Last accessed June 18, 2007.
- Ralston S, Kellett N, Williams RL, et al. Practice-based assessment of tobacco usage in southwestern primary care patients: a Research Involving Outpatient Settings Network (RIOS Net) study. J Am Board Fam Med. 2007;20(2):174-180.
- Ralston S, Mahshid R. The pediatric hospitalist and the smoking parent. Pediatric Research Day 2006. Available at http://hsc.unm.edu/pedsresearch/ORAL%20PRESENTATIONS.htm Albuquerque: Office of Research and Creative Endeavors, Department of Pediatrics, University of New Mexico Health Sciences Center; 2006. Last accessed June 18, 2007.
- Aligne CA, Stoddard JJ. Tobacco and children. An economic evaluation of the medical effects of parental smoking. Arch Pediatr Adolesc Med. 1997 Jul;151(7):648-653. Erratum in: Arch Pediatr Adolesc Med 1997 Oct;151(10):988. Comment in: Arch Pediatr Adolesc Med. 1997 Dec;151(12):1269. Arch Pediatr Adolesc Med. 2000 Aug;154(8):850.
- Leonard K, Mosquera M, Aligne CA. Pediatrics in the community: Taking a collective breath to help children who have asthma. Pediatr Rev. 2007;28:152-153.
- Winickoff JP, Hillis VJ, Palfrey JS, et al. A smoking cessation intervention for parents of children who are hospitalized for respiratory illness: the stop tobacco outreach program. Pediatrics. 2003 Jan;111(1):140-145.
Kindred Spirits
Emergency care in the U.S. has been called a system in crisis, and the data are startling. From 1994 to 2004, the number of hospitals and emergency departments (EDs) decreased, the latter by 9%, but the number of ED visits increased by more than 1 million annually.1 (See Figure 1, p. 17)
According to the Centers for Disease Control and Prevention’s (CDC) National Center for Health Statistics, between 40% and 50% of U.S. hospitals experience crowded conditions in the ED, with almost two-thirds of metropolitan EDs experiencing crowding at times.2
Hospitalists and emergency medicine physicians asked about their complex relationship—the good, the bad, and the not yet solved—praised their ability to work together.
“In general, our relationship with hospitalists has been fantastic,” says James Hoekstra, MD, president of the Society of Academic Emergency Medicine. “To have physicians who are willing to take patients with a lot of different disease states that are not necessarily procedure oriented, don’t necessarily fit into a specific specialty, or are somewhat undifferentiated in their presentation—for us that is an absolute joy.”
The number of hospitalists and emergency medicine physicians might be said to be running in parallel, says Alpesh Amin, MD, MBA, FACP, executive director of the hospitalist program and vice chair for clinical affairs and quality in the department of medicine at the University of California, Irvine. He tends to refer to this ratio as 30-30, meaning that, within a few years, there will be roughly 30,000 hospitalists, while there are currently that many emergency medicine physicians.3 In addition, emergency medicine and hospital medicine are site-based specialties, says Dr. Amin, so bridging their separateness is crucial to patient care.
“Aside from a small proportion of direct [patient] admissions,” says Jasen W. Gundersen, MD, chief of hospital medicine at the U. Mass. Medical Center in Worcester, “we are an extension of the ER, and the ER is an extension of us. We need to all be on the same page so that what’s said in the ER matches what happens on the floor, which matches what we send out to the primary [care physician].”
Optimizing patient flow is primarily a function of communication, says Marc Newquist, MD, FACEP, a hospitalist, an emergency medicine physician, and program director of the hospitalist division of The Schumacher Group in Lafayette, La. “The better that these communication systems can be standardized, the better hospitalists and their emergency medicine colleagues can promote a seamless integration between the two specialties as patients journey through their hospital stays,” he says.
“As medicine becomes more fragmented and hospital medicine does, let’s face it, fragment care,” adds Dr. Gundersen. “We also have to make sure that information flows from the primary-care physician who may send the patient to the ER. Everybody is a partner, and everybody needs to communicate back and forth and understand that if the ER wants to get someone admitted, timely communication with the hospitalist and understanding how the flow of the hospital works is really important.”
Interactions and Roles
“Far and away the most common type of interaction between hospitalists and ED docs is admissions,” says David M. Pressel, MD, PhD, director, Inpatient Service, General Pediatrics at Alfred I. duPont Hospital for Children in Wilmington, Del. The next most common interaction will depend upon the institution and its style, but, primarily, interactions include consults, and—in some institutions—patient discharge.
Dr. Pressel works at a tertiary-care referral center where residents staff the ED and his unit. “But at a community hospital where you generally have ED medicine-trained docs—not pediatricians who have ED
medicine fellowships—they have less experience with pediatrics, so they may be more likely to consult us on a patient,” he says. The development of care pathways to facilitate care is another important interaction between emergency medicine physicians and hospitalists.
An example of a protocol development the hospitalist and the ED should do together, says Dr. Pressel, is when patients come in with certain symptoms that would indicate a possible communicable disease for which the patient might need special isolation on an inpatient unit. That issue may more likely be foremost in hospitalist’s mind, and he or she can perform an evaluation early to determine what isolation may be needed. If the hospitalist suspects a patient has varicella or active pulmonary tuberculosis, for instance, “those kinds of [isolation] rooms are limited,” says Dr. Pressel. “Hospitals don’t have a lot of them, so you have to make sure you’re getting beds assigned well.”
Our interviews say the major roles of the hospitalist in managing relationships with emergency medicine physicians involve professionalism. “The hospitalist needs to understand the needs of the ER physician in terms of the needs of the [overall] ER: timing, flow, and getting patients seen in a prompt manner,” says Dr. Gundersen. “There’s a give and take, and both sides need to understand the other side of the job to maximize that collegiality and to maximize that sense of teamwork.”
Dr. Gundersen, who works full time as a hospitalist and moonlights as an ED physician, says that “what at times the ED doesn’t realize is that the time it takes for them to do something in the ED is not the same as it takes for us to do something on the floor. If they order a CT scan in the ED, it happens right away. If they say, ‘You can just get the CT scan on the floor,’ well, we don’t have as much priority in terms of getting lab draws and diagnostic tests done as fast as they do.”
—Debra L. Burgy, MD, hospitalist, Abbott Northwestern Hospital, Minneapolis, Minn.
Stepping on toes is always a danger.
“One of the key things for the relationship is to realize that you’re not walking in the other person’s shoes,” says Dr. Pressel. “I’ve witnessed [situations] where a hospitalist on the receiving end scoffs at the management in the ED—either because, number one, the patient was perceived to be not sick enough to merit hospitalization according to the hospitalist, or, number two, because of over-workup and overdiagnosis or under-workup and under- or misdiagnosis.”
Both groups need to realize that the patient’s condition evolves over time. “What the ED saw three hours ago may not be what’s being seen now, and that’s true in the reverse,” he says. “If the patient looked great three hours ago, now [their condition may be life-threatening].”
Therefore, feedback between ED doctors and hospitalists should be provided in a “respectful, collegial, follow-up type of manner,” says Dr. Pressel. A beneficial means of communication involves feedback that is “telling it as an evolving story,” he says, as opposed to assuming the ED doctor is wrong. That is, “collaborating and adding to the story and the end diagnosis and recognizing that the ED doc’s job is not necessarily to make the final diagnosis.”
Dr. Pressel thinks it comes down to politeness, plain and simple. “I hope that when I miss something, someone will be kind enough to [be polite] to me, [to phrase it as] ‘I’m sure you were thinking of this but the clues looked this way and we went on to do further evaluation.’ ”
That kind of interaction happens all the time, he says. “And ultimately it’s best for the patient, number one, because everybody learns that way, and, number two, if you make yourself obnoxious with your colleagues, they’re not necessarily going to want to call you.”
The Nature of the Beast
Most interactions with their ED colleagues go smoothly, our hospitalists say, but sometimes there are bumps in the road—most often involving flow and the transfer of care.
Jason R. Orlinick, MD, PhD, chief, Section of Hospital Medicine at Norwalk Hospital, Conn., and clinical instructor of medicine at Yale University (New Haven, Conn.), probably represents the bulk of his hospitalist colleagues when he says he and the emergency medicine physicians with whom he works have a cordial relationship overall. But “there is always some level of tension between the hospitalists and the emergency department—at least at the institutions I’ve been at. To some extent, it depends on the mentality of the ED docs where you’re working.”
Debra L. Burgy, MD, a hospitalist at Abbott Northwestern Hospital in Minneapolis, puts it this way: “The interface between hospitalists and the ED is sometimes tense because the ED physicians are regularly bombarded with patients, which is completely unpredictable, and they do not have adequate support staff, such as social workers and psychiatric assessment workers, to create a safe disposition for patients who could otherwise go home.
“The path of least resistance, and the least time-consuming route, is to admit patients. The chain reaction continues with the hospitalist service being overwhelmed.”
It is common for the ED to get a large volume of patients in the afternoon, our hospitalists remark. (See Figure 2, left) “We sometimes get hit with this huge bolus of patients,” Dr. Gundersen says. The biggest challenges involve “promptly identifying those patients who are identified for admission and maintaining a more open communication because when we get three, four, five admissions at once, we have difficulty working down that backlog.”
In the medical residency program at Dr. Orlinick’s institution, the bolus phenomenon can overwhelm residents’ and attendings’ capacities to see patients in a timely manner. “Unfortunately, we’ve not had a lot of success with that,” he says, and recently, his institution approached the hospitalists to work on a solution.
The timing of handoffs represents a large part of the breakdown in patient flow. “This is because of the ED physician who works until 4 p.m. or 6 p.m. and then tries to get all their patients whom they’re not sending home admitted right away before [the hospitalists] go off service,” Dr. Gundersen says. “It’s not uncommon that I get called or paged every three minutes—if I don’t answer right away—because they are trying to get someone admitted seconds after they call. The ER needs the beds, we haven’t been able to discharge the patients, everything gets bottlenecked.”
Although Dr. Gundersen recognizes that this problem is unavoidable at times, he suggests it would help “if the ED physicians were cognizant that there may be just one or two hospitalists who are admitting for the day, and giving them five admissions all at once, for instance, is going to take time to get through.”
On the other side, “Hospitalists rely on ED physicians to have the patient worked up and know which service they belong to,” explains Dr. Gundersen. “Succinct transfer of care is [paramount] so that critical information is brought to the attention of the accepting physician.” For the most part, he says, his ED colleagues do a good job.
Because the ED is always in a rush to get patients admitted and a disposition made, “there is the tendency to hamstring what’s happening on the floor. I think that big downstream effect from everything that begins in the ER transitions through the patient’s whole length of stay in the hospital,” says Dr. Gundersen.
All the interviewed hospitalists realize that the hospitalists and ED physicians need to have an understanding of what the other group faces. “We have to be understanding of the ER position that there are a lot of patients to be seen, and they’re trying to do the best they can in that period of time,” says Dr. Gundersen. A 2006 study revealed that interruptions within the ED were prevalent and diverse in nature and—on average—there was an interruption every nine and 14 minutes, respectively, for the attending emergency medicine physicians and residents.5
“And ED physicians have to realize that whatever patient they give to us, we then deal with,” says Dr. Gundersen, “and we [continue] to deal with all the issues, moving them through tests and studies [and] getting them discharged, so sometimes there are delays on both ends. It’s just the nature of the beast.”
A Sense of Control
The benefits of maintaining collegiality with ED physicians go beyond the norm, says Jeff Glasheen, MD, director of both the hospital medicine program and inpatient clinical services in the department of medicine at the University of Colorado at Denver Health Sciences Center. Dr. Glasheen has conducted some research on burnout—mostly in residents.6-7
“One of the main things that leads to burnout is lack of control and feeling like you don’t have control over your daily job,” he says. “One of the things that comes out of this relationship with the ER is that it’s no longer like someone’s just dumping on us. They’re very reasonable when we say, ‘That sounds like somebody who could go home; let me come down and see the patient, and let’s see if we can get this patient discharged.’ You begin to feel like you have control over your day, control over the patients who are admitted to you, and—quite honestly—it’s more fun. That kind of professional interaction is hard to put a price on, but I think it’s priceless.”TH
Andrea Sattinger is a frequent contributor to The Hospitalist.
References
- Kellermann AL. Crisis in the emergency department. N Engl J Med. 2006 Sep 28;355(13):1300-1303.
- Burt CW, McCaig LF. Staffing, capacity, and ambulance diversion in emergency departments: United States, 2003-04. Adv Data. 2006 Sep 27;(376):1-23. Available at www.cdc.gov/nchs/data/ad/ad376.pdf. Last accessed April 10, 2007.
- Freed DH. Hospitalists: evolution, evidence, and eventualities. Health Care Manag. 2004 Jul-Sep;23(3):238-256;1-38.
- McCaig LF, Burt CW. National Hospital Ambulatory Medical Care Survey: 2003 emergency department summary. Adv Data. 2005;(358):1-38. Available at www.cdc.gov/nchs/data/ad/ad358.pdf. Last accessed April 10, 2007.
- Laxmisan A, Hakimzada F, Sayan OR, et al. The multitasking clinician: decision-making and cognitive demand during and after team handoffs in emergency care. Int J Med Inform. 2006 Oct 21. [Epub ahead of print.]
- Gopal RK, Carreira F, Baker WA, et al. Internal medicine residents reject “longer and gentler” training. J Gen Intern Med. 2007 Jan;22(1):102-106.
- Gopal R, Glasheen JJ, Miyoshi TJ, et al. Burnout and internal medicine resident work-hour restrictions. Arch Intern Med. 2005 Dec 12-26;165(22):2595-2600. Comment in Arch Intern Med. 2005 Dec 12-26; 165(22):2561-2562. Arch Intern Med. 2006 Jul 10;166(13):1423; author reply 1423-1425.
Emergency care in the U.S. has been called a system in crisis, and the data are startling. From 1994 to 2004, the number of hospitals and emergency departments (EDs) decreased, the latter by 9%, but the number of ED visits increased by more than 1 million annually.1 (See Figure 1, p. 17)
According to the Centers for Disease Control and Prevention’s (CDC) National Center for Health Statistics, between 40% and 50% of U.S. hospitals experience crowded conditions in the ED, with almost two-thirds of metropolitan EDs experiencing crowding at times.2
Hospitalists and emergency medicine physicians asked about their complex relationship—the good, the bad, and the not yet solved—praised their ability to work together.
“In general, our relationship with hospitalists has been fantastic,” says James Hoekstra, MD, president of the Society of Academic Emergency Medicine. “To have physicians who are willing to take patients with a lot of different disease states that are not necessarily procedure oriented, don’t necessarily fit into a specific specialty, or are somewhat undifferentiated in their presentation—for us that is an absolute joy.”
The number of hospitalists and emergency medicine physicians might be said to be running in parallel, says Alpesh Amin, MD, MBA, FACP, executive director of the hospitalist program and vice chair for clinical affairs and quality in the department of medicine at the University of California, Irvine. He tends to refer to this ratio as 30-30, meaning that, within a few years, there will be roughly 30,000 hospitalists, while there are currently that many emergency medicine physicians.3 In addition, emergency medicine and hospital medicine are site-based specialties, says Dr. Amin, so bridging their separateness is crucial to patient care.
“Aside from a small proportion of direct [patient] admissions,” says Jasen W. Gundersen, MD, chief of hospital medicine at the U. Mass. Medical Center in Worcester, “we are an extension of the ER, and the ER is an extension of us. We need to all be on the same page so that what’s said in the ER matches what happens on the floor, which matches what we send out to the primary [care physician].”
Optimizing patient flow is primarily a function of communication, says Marc Newquist, MD, FACEP, a hospitalist, an emergency medicine physician, and program director of the hospitalist division of The Schumacher Group in Lafayette, La. “The better that these communication systems can be standardized, the better hospitalists and their emergency medicine colleagues can promote a seamless integration between the two specialties as patients journey through their hospital stays,” he says.
“As medicine becomes more fragmented and hospital medicine does, let’s face it, fragment care,” adds Dr. Gundersen. “We also have to make sure that information flows from the primary-care physician who may send the patient to the ER. Everybody is a partner, and everybody needs to communicate back and forth and understand that if the ER wants to get someone admitted, timely communication with the hospitalist and understanding how the flow of the hospital works is really important.”
Interactions and Roles
“Far and away the most common type of interaction between hospitalists and ED docs is admissions,” says David M. Pressel, MD, PhD, director, Inpatient Service, General Pediatrics at Alfred I. duPont Hospital for Children in Wilmington, Del. The next most common interaction will depend upon the institution and its style, but, primarily, interactions include consults, and—in some institutions—patient discharge.
Dr. Pressel works at a tertiary-care referral center where residents staff the ED and his unit. “But at a community hospital where you generally have ED medicine-trained docs—not pediatricians who have ED
medicine fellowships—they have less experience with pediatrics, so they may be more likely to consult us on a patient,” he says. The development of care pathways to facilitate care is another important interaction between emergency medicine physicians and hospitalists.
An example of a protocol development the hospitalist and the ED should do together, says Dr. Pressel, is when patients come in with certain symptoms that would indicate a possible communicable disease for which the patient might need special isolation on an inpatient unit. That issue may more likely be foremost in hospitalist’s mind, and he or she can perform an evaluation early to determine what isolation may be needed. If the hospitalist suspects a patient has varicella or active pulmonary tuberculosis, for instance, “those kinds of [isolation] rooms are limited,” says Dr. Pressel. “Hospitals don’t have a lot of them, so you have to make sure you’re getting beds assigned well.”
Our interviews say the major roles of the hospitalist in managing relationships with emergency medicine physicians involve professionalism. “The hospitalist needs to understand the needs of the ER physician in terms of the needs of the [overall] ER: timing, flow, and getting patients seen in a prompt manner,” says Dr. Gundersen. “There’s a give and take, and both sides need to understand the other side of the job to maximize that collegiality and to maximize that sense of teamwork.”
Dr. Gundersen, who works full time as a hospitalist and moonlights as an ED physician, says that “what at times the ED doesn’t realize is that the time it takes for them to do something in the ED is not the same as it takes for us to do something on the floor. If they order a CT scan in the ED, it happens right away. If they say, ‘You can just get the CT scan on the floor,’ well, we don’t have as much priority in terms of getting lab draws and diagnostic tests done as fast as they do.”
—Debra L. Burgy, MD, hospitalist, Abbott Northwestern Hospital, Minneapolis, Minn.
Stepping on toes is always a danger.
“One of the key things for the relationship is to realize that you’re not walking in the other person’s shoes,” says Dr. Pressel. “I’ve witnessed [situations] where a hospitalist on the receiving end scoffs at the management in the ED—either because, number one, the patient was perceived to be not sick enough to merit hospitalization according to the hospitalist, or, number two, because of over-workup and overdiagnosis or under-workup and under- or misdiagnosis.”
Both groups need to realize that the patient’s condition evolves over time. “What the ED saw three hours ago may not be what’s being seen now, and that’s true in the reverse,” he says. “If the patient looked great three hours ago, now [their condition may be life-threatening].”
Therefore, feedback between ED doctors and hospitalists should be provided in a “respectful, collegial, follow-up type of manner,” says Dr. Pressel. A beneficial means of communication involves feedback that is “telling it as an evolving story,” he says, as opposed to assuming the ED doctor is wrong. That is, “collaborating and adding to the story and the end diagnosis and recognizing that the ED doc’s job is not necessarily to make the final diagnosis.”
Dr. Pressel thinks it comes down to politeness, plain and simple. “I hope that when I miss something, someone will be kind enough to [be polite] to me, [to phrase it as] ‘I’m sure you were thinking of this but the clues looked this way and we went on to do further evaluation.’ ”
That kind of interaction happens all the time, he says. “And ultimately it’s best for the patient, number one, because everybody learns that way, and, number two, if you make yourself obnoxious with your colleagues, they’re not necessarily going to want to call you.”
The Nature of the Beast
Most interactions with their ED colleagues go smoothly, our hospitalists say, but sometimes there are bumps in the road—most often involving flow and the transfer of care.
Jason R. Orlinick, MD, PhD, chief, Section of Hospital Medicine at Norwalk Hospital, Conn., and clinical instructor of medicine at Yale University (New Haven, Conn.), probably represents the bulk of his hospitalist colleagues when he says he and the emergency medicine physicians with whom he works have a cordial relationship overall. But “there is always some level of tension between the hospitalists and the emergency department—at least at the institutions I’ve been at. To some extent, it depends on the mentality of the ED docs where you’re working.”
Debra L. Burgy, MD, a hospitalist at Abbott Northwestern Hospital in Minneapolis, puts it this way: “The interface between hospitalists and the ED is sometimes tense because the ED physicians are regularly bombarded with patients, which is completely unpredictable, and they do not have adequate support staff, such as social workers and psychiatric assessment workers, to create a safe disposition for patients who could otherwise go home.
“The path of least resistance, and the least time-consuming route, is to admit patients. The chain reaction continues with the hospitalist service being overwhelmed.”
It is common for the ED to get a large volume of patients in the afternoon, our hospitalists remark. (See Figure 2, left) “We sometimes get hit with this huge bolus of patients,” Dr. Gundersen says. The biggest challenges involve “promptly identifying those patients who are identified for admission and maintaining a more open communication because when we get three, four, five admissions at once, we have difficulty working down that backlog.”
In the medical residency program at Dr. Orlinick’s institution, the bolus phenomenon can overwhelm residents’ and attendings’ capacities to see patients in a timely manner. “Unfortunately, we’ve not had a lot of success with that,” he says, and recently, his institution approached the hospitalists to work on a solution.
The timing of handoffs represents a large part of the breakdown in patient flow. “This is because of the ED physician who works until 4 p.m. or 6 p.m. and then tries to get all their patients whom they’re not sending home admitted right away before [the hospitalists] go off service,” Dr. Gundersen says. “It’s not uncommon that I get called or paged every three minutes—if I don’t answer right away—because they are trying to get someone admitted seconds after they call. The ER needs the beds, we haven’t been able to discharge the patients, everything gets bottlenecked.”
Although Dr. Gundersen recognizes that this problem is unavoidable at times, he suggests it would help “if the ED physicians were cognizant that there may be just one or two hospitalists who are admitting for the day, and giving them five admissions all at once, for instance, is going to take time to get through.”
On the other side, “Hospitalists rely on ED physicians to have the patient worked up and know which service they belong to,” explains Dr. Gundersen. “Succinct transfer of care is [paramount] so that critical information is brought to the attention of the accepting physician.” For the most part, he says, his ED colleagues do a good job.
Because the ED is always in a rush to get patients admitted and a disposition made, “there is the tendency to hamstring what’s happening on the floor. I think that big downstream effect from everything that begins in the ER transitions through the patient’s whole length of stay in the hospital,” says Dr. Gundersen.
All the interviewed hospitalists realize that the hospitalists and ED physicians need to have an understanding of what the other group faces. “We have to be understanding of the ER position that there are a lot of patients to be seen, and they’re trying to do the best they can in that period of time,” says Dr. Gundersen. A 2006 study revealed that interruptions within the ED were prevalent and diverse in nature and—on average—there was an interruption every nine and 14 minutes, respectively, for the attending emergency medicine physicians and residents.5
“And ED physicians have to realize that whatever patient they give to us, we then deal with,” says Dr. Gundersen, “and we [continue] to deal with all the issues, moving them through tests and studies [and] getting them discharged, so sometimes there are delays on both ends. It’s just the nature of the beast.”
A Sense of Control
The benefits of maintaining collegiality with ED physicians go beyond the norm, says Jeff Glasheen, MD, director of both the hospital medicine program and inpatient clinical services in the department of medicine at the University of Colorado at Denver Health Sciences Center. Dr. Glasheen has conducted some research on burnout—mostly in residents.6-7
“One of the main things that leads to burnout is lack of control and feeling like you don’t have control over your daily job,” he says. “One of the things that comes out of this relationship with the ER is that it’s no longer like someone’s just dumping on us. They’re very reasonable when we say, ‘That sounds like somebody who could go home; let me come down and see the patient, and let’s see if we can get this patient discharged.’ You begin to feel like you have control over your day, control over the patients who are admitted to you, and—quite honestly—it’s more fun. That kind of professional interaction is hard to put a price on, but I think it’s priceless.”TH
Andrea Sattinger is a frequent contributor to The Hospitalist.
References
- Kellermann AL. Crisis in the emergency department. N Engl J Med. 2006 Sep 28;355(13):1300-1303.
- Burt CW, McCaig LF. Staffing, capacity, and ambulance diversion in emergency departments: United States, 2003-04. Adv Data. 2006 Sep 27;(376):1-23. Available at www.cdc.gov/nchs/data/ad/ad376.pdf. Last accessed April 10, 2007.
- Freed DH. Hospitalists: evolution, evidence, and eventualities. Health Care Manag. 2004 Jul-Sep;23(3):238-256;1-38.
- McCaig LF, Burt CW. National Hospital Ambulatory Medical Care Survey: 2003 emergency department summary. Adv Data. 2005;(358):1-38. Available at www.cdc.gov/nchs/data/ad/ad358.pdf. Last accessed April 10, 2007.
- Laxmisan A, Hakimzada F, Sayan OR, et al. The multitasking clinician: decision-making and cognitive demand during and after team handoffs in emergency care. Int J Med Inform. 2006 Oct 21. [Epub ahead of print.]
- Gopal RK, Carreira F, Baker WA, et al. Internal medicine residents reject “longer and gentler” training. J Gen Intern Med. 2007 Jan;22(1):102-106.
- Gopal R, Glasheen JJ, Miyoshi TJ, et al. Burnout and internal medicine resident work-hour restrictions. Arch Intern Med. 2005 Dec 12-26;165(22):2595-2600. Comment in Arch Intern Med. 2005 Dec 12-26; 165(22):2561-2562. Arch Intern Med. 2006 Jul 10;166(13):1423; author reply 1423-1425.
Emergency care in the U.S. has been called a system in crisis, and the data are startling. From 1994 to 2004, the number of hospitals and emergency departments (EDs) decreased, the latter by 9%, but the number of ED visits increased by more than 1 million annually.1 (See Figure 1, p. 17)
According to the Centers for Disease Control and Prevention’s (CDC) National Center for Health Statistics, between 40% and 50% of U.S. hospitals experience crowded conditions in the ED, with almost two-thirds of metropolitan EDs experiencing crowding at times.2
Hospitalists and emergency medicine physicians asked about their complex relationship—the good, the bad, and the not yet solved—praised their ability to work together.
“In general, our relationship with hospitalists has been fantastic,” says James Hoekstra, MD, president of the Society of Academic Emergency Medicine. “To have physicians who are willing to take patients with a lot of different disease states that are not necessarily procedure oriented, don’t necessarily fit into a specific specialty, or are somewhat undifferentiated in their presentation—for us that is an absolute joy.”
The number of hospitalists and emergency medicine physicians might be said to be running in parallel, says Alpesh Amin, MD, MBA, FACP, executive director of the hospitalist program and vice chair for clinical affairs and quality in the department of medicine at the University of California, Irvine. He tends to refer to this ratio as 30-30, meaning that, within a few years, there will be roughly 30,000 hospitalists, while there are currently that many emergency medicine physicians.3 In addition, emergency medicine and hospital medicine are site-based specialties, says Dr. Amin, so bridging their separateness is crucial to patient care.
“Aside from a small proportion of direct [patient] admissions,” says Jasen W. Gundersen, MD, chief of hospital medicine at the U. Mass. Medical Center in Worcester, “we are an extension of the ER, and the ER is an extension of us. We need to all be on the same page so that what’s said in the ER matches what happens on the floor, which matches what we send out to the primary [care physician].”
Optimizing patient flow is primarily a function of communication, says Marc Newquist, MD, FACEP, a hospitalist, an emergency medicine physician, and program director of the hospitalist division of The Schumacher Group in Lafayette, La. “The better that these communication systems can be standardized, the better hospitalists and their emergency medicine colleagues can promote a seamless integration between the two specialties as patients journey through their hospital stays,” he says.
“As medicine becomes more fragmented and hospital medicine does, let’s face it, fragment care,” adds Dr. Gundersen. “We also have to make sure that information flows from the primary-care physician who may send the patient to the ER. Everybody is a partner, and everybody needs to communicate back and forth and understand that if the ER wants to get someone admitted, timely communication with the hospitalist and understanding how the flow of the hospital works is really important.”
Interactions and Roles
“Far and away the most common type of interaction between hospitalists and ED docs is admissions,” says David M. Pressel, MD, PhD, director, Inpatient Service, General Pediatrics at Alfred I. duPont Hospital for Children in Wilmington, Del. The next most common interaction will depend upon the institution and its style, but, primarily, interactions include consults, and—in some institutions—patient discharge.
Dr. Pressel works at a tertiary-care referral center where residents staff the ED and his unit. “But at a community hospital where you generally have ED medicine-trained docs—not pediatricians who have ED
medicine fellowships—they have less experience with pediatrics, so they may be more likely to consult us on a patient,” he says. The development of care pathways to facilitate care is another important interaction between emergency medicine physicians and hospitalists.
An example of a protocol development the hospitalist and the ED should do together, says Dr. Pressel, is when patients come in with certain symptoms that would indicate a possible communicable disease for which the patient might need special isolation on an inpatient unit. That issue may more likely be foremost in hospitalist’s mind, and he or she can perform an evaluation early to determine what isolation may be needed. If the hospitalist suspects a patient has varicella or active pulmonary tuberculosis, for instance, “those kinds of [isolation] rooms are limited,” says Dr. Pressel. “Hospitals don’t have a lot of them, so you have to make sure you’re getting beds assigned well.”
Our interviews say the major roles of the hospitalist in managing relationships with emergency medicine physicians involve professionalism. “The hospitalist needs to understand the needs of the ER physician in terms of the needs of the [overall] ER: timing, flow, and getting patients seen in a prompt manner,” says Dr. Gundersen. “There’s a give and take, and both sides need to understand the other side of the job to maximize that collegiality and to maximize that sense of teamwork.”
Dr. Gundersen, who works full time as a hospitalist and moonlights as an ED physician, says that “what at times the ED doesn’t realize is that the time it takes for them to do something in the ED is not the same as it takes for us to do something on the floor. If they order a CT scan in the ED, it happens right away. If they say, ‘You can just get the CT scan on the floor,’ well, we don’t have as much priority in terms of getting lab draws and diagnostic tests done as fast as they do.”
—Debra L. Burgy, MD, hospitalist, Abbott Northwestern Hospital, Minneapolis, Minn.
Stepping on toes is always a danger.
“One of the key things for the relationship is to realize that you’re not walking in the other person’s shoes,” says Dr. Pressel. “I’ve witnessed [situations] where a hospitalist on the receiving end scoffs at the management in the ED—either because, number one, the patient was perceived to be not sick enough to merit hospitalization according to the hospitalist, or, number two, because of over-workup and overdiagnosis or under-workup and under- or misdiagnosis.”
Both groups need to realize that the patient’s condition evolves over time. “What the ED saw three hours ago may not be what’s being seen now, and that’s true in the reverse,” he says. “If the patient looked great three hours ago, now [their condition may be life-threatening].”
Therefore, feedback between ED doctors and hospitalists should be provided in a “respectful, collegial, follow-up type of manner,” says Dr. Pressel. A beneficial means of communication involves feedback that is “telling it as an evolving story,” he says, as opposed to assuming the ED doctor is wrong. That is, “collaborating and adding to the story and the end diagnosis and recognizing that the ED doc’s job is not necessarily to make the final diagnosis.”
Dr. Pressel thinks it comes down to politeness, plain and simple. “I hope that when I miss something, someone will be kind enough to [be polite] to me, [to phrase it as] ‘I’m sure you were thinking of this but the clues looked this way and we went on to do further evaluation.’ ”
That kind of interaction happens all the time, he says. “And ultimately it’s best for the patient, number one, because everybody learns that way, and, number two, if you make yourself obnoxious with your colleagues, they’re not necessarily going to want to call you.”
The Nature of the Beast
Most interactions with their ED colleagues go smoothly, our hospitalists say, but sometimes there are bumps in the road—most often involving flow and the transfer of care.
Jason R. Orlinick, MD, PhD, chief, Section of Hospital Medicine at Norwalk Hospital, Conn., and clinical instructor of medicine at Yale University (New Haven, Conn.), probably represents the bulk of his hospitalist colleagues when he says he and the emergency medicine physicians with whom he works have a cordial relationship overall. But “there is always some level of tension between the hospitalists and the emergency department—at least at the institutions I’ve been at. To some extent, it depends on the mentality of the ED docs where you’re working.”
Debra L. Burgy, MD, a hospitalist at Abbott Northwestern Hospital in Minneapolis, puts it this way: “The interface between hospitalists and the ED is sometimes tense because the ED physicians are regularly bombarded with patients, which is completely unpredictable, and they do not have adequate support staff, such as social workers and psychiatric assessment workers, to create a safe disposition for patients who could otherwise go home.
“The path of least resistance, and the least time-consuming route, is to admit patients. The chain reaction continues with the hospitalist service being overwhelmed.”
It is common for the ED to get a large volume of patients in the afternoon, our hospitalists remark. (See Figure 2, left) “We sometimes get hit with this huge bolus of patients,” Dr. Gundersen says. The biggest challenges involve “promptly identifying those patients who are identified for admission and maintaining a more open communication because when we get three, four, five admissions at once, we have difficulty working down that backlog.”
In the medical residency program at Dr. Orlinick’s institution, the bolus phenomenon can overwhelm residents’ and attendings’ capacities to see patients in a timely manner. “Unfortunately, we’ve not had a lot of success with that,” he says, and recently, his institution approached the hospitalists to work on a solution.
The timing of handoffs represents a large part of the breakdown in patient flow. “This is because of the ED physician who works until 4 p.m. or 6 p.m. and then tries to get all their patients whom they’re not sending home admitted right away before [the hospitalists] go off service,” Dr. Gundersen says. “It’s not uncommon that I get called or paged every three minutes—if I don’t answer right away—because they are trying to get someone admitted seconds after they call. The ER needs the beds, we haven’t been able to discharge the patients, everything gets bottlenecked.”
Although Dr. Gundersen recognizes that this problem is unavoidable at times, he suggests it would help “if the ED physicians were cognizant that there may be just one or two hospitalists who are admitting for the day, and giving them five admissions all at once, for instance, is going to take time to get through.”
On the other side, “Hospitalists rely on ED physicians to have the patient worked up and know which service they belong to,” explains Dr. Gundersen. “Succinct transfer of care is [paramount] so that critical information is brought to the attention of the accepting physician.” For the most part, he says, his ED colleagues do a good job.
Because the ED is always in a rush to get patients admitted and a disposition made, “there is the tendency to hamstring what’s happening on the floor. I think that big downstream effect from everything that begins in the ER transitions through the patient’s whole length of stay in the hospital,” says Dr. Gundersen.
All the interviewed hospitalists realize that the hospitalists and ED physicians need to have an understanding of what the other group faces. “We have to be understanding of the ER position that there are a lot of patients to be seen, and they’re trying to do the best they can in that period of time,” says Dr. Gundersen. A 2006 study revealed that interruptions within the ED were prevalent and diverse in nature and—on average—there was an interruption every nine and 14 minutes, respectively, for the attending emergency medicine physicians and residents.5
“And ED physicians have to realize that whatever patient they give to us, we then deal with,” says Dr. Gundersen, “and we [continue] to deal with all the issues, moving them through tests and studies [and] getting them discharged, so sometimes there are delays on both ends. It’s just the nature of the beast.”
A Sense of Control
The benefits of maintaining collegiality with ED physicians go beyond the norm, says Jeff Glasheen, MD, director of both the hospital medicine program and inpatient clinical services in the department of medicine at the University of Colorado at Denver Health Sciences Center. Dr. Glasheen has conducted some research on burnout—mostly in residents.6-7
“One of the main things that leads to burnout is lack of control and feeling like you don’t have control over your daily job,” he says. “One of the things that comes out of this relationship with the ER is that it’s no longer like someone’s just dumping on us. They’re very reasonable when we say, ‘That sounds like somebody who could go home; let me come down and see the patient, and let’s see if we can get this patient discharged.’ You begin to feel like you have control over your day, control over the patients who are admitted to you, and—quite honestly—it’s more fun. That kind of professional interaction is hard to put a price on, but I think it’s priceless.”TH
Andrea Sattinger is a frequent contributor to The Hospitalist.
References
- Kellermann AL. Crisis in the emergency department. N Engl J Med. 2006 Sep 28;355(13):1300-1303.
- Burt CW, McCaig LF. Staffing, capacity, and ambulance diversion in emergency departments: United States, 2003-04. Adv Data. 2006 Sep 27;(376):1-23. Available at www.cdc.gov/nchs/data/ad/ad376.pdf. Last accessed April 10, 2007.
- Freed DH. Hospitalists: evolution, evidence, and eventualities. Health Care Manag. 2004 Jul-Sep;23(3):238-256;1-38.
- McCaig LF, Burt CW. National Hospital Ambulatory Medical Care Survey: 2003 emergency department summary. Adv Data. 2005;(358):1-38. Available at www.cdc.gov/nchs/data/ad/ad358.pdf. Last accessed April 10, 2007.
- Laxmisan A, Hakimzada F, Sayan OR, et al. The multitasking clinician: decision-making and cognitive demand during and after team handoffs in emergency care. Int J Med Inform. 2006 Oct 21. [Epub ahead of print.]
- Gopal RK, Carreira F, Baker WA, et al. Internal medicine residents reject “longer and gentler” training. J Gen Intern Med. 2007 Jan;22(1):102-106.
- Gopal R, Glasheen JJ, Miyoshi TJ, et al. Burnout and internal medicine resident work-hour restrictions. Arch Intern Med. 2005 Dec 12-26;165(22):2595-2600. Comment in Arch Intern Med. 2005 Dec 12-26; 165(22):2561-2562. Arch Intern Med. 2006 Jul 10;166(13):1423; author reply 1423-1425.
Googling for Diagnoses
Googling—the use of search-engines such as Google—is a new diagnostic tool in the modern clinician’s armamentarium.
A 2006 study published in The British Medical Journal examined how often searching with Google leads physicians to a correct diagnosis.1 The investigators were blinded to the correct diagnoses and compared the results of diagnostic cases published in the 2005 case records of The New England Journal of Medicine (NEJM) with diagnoses made using Google searches. Their results indicated that Google searches revealed the correct diagnosis in 15 of 26 cases, or 58% of the time. (See Table 1, p. 34.)
The limitations of the study are important to recognize when considering how well a Web-searched diagnosis can compare with one made without Web searching.
In some cases, although Google supplied information that approximated the diagnoses made in NEJM, the researchers thought the diagnoses were not specific enough.
For instance, one case for which Google suggested a diagnosis of extrinsic allergic alveolitis was described in the NEJM case record as extrinsic allergic alveolitis caused by Mycobacterium avium, also known as “hot tub lung.” This exemplifies the point that search engines don’t make diagnoses—people do. Expert knowledge is required to choose the best search words and select among the results.
Experts agree that using search engines for a diagnosis is likely to be more effective for conditions with unique symptoms and most useful in a certain class of diagnostic challenges in which clinical experts are at the helm of diagnostic deliberations.1,2
The choice of search engines is important and will increasingly affect accurate diagnoses as the technology develops.
“Hospitalists may utilize [Google] less; they are often working in environments [hospitals] that have ready access to more thoroughly vetted sources such as UpToDate, Medline, or MDConsult,” says Joshua Lee, MD, a hospitalist and medical director of Information Services at the University of California at San Diego. “Within Google there are variations on a theme, such as GoogleScholar, which accesses many of the same academic journals as Medline. Given that they are accessing the same journals, many would feel that searching with GoogleScholar is just as accurate as [searching with] Medline—at least as far as the source material is concerned.”
Search engines offer an impressive volume of new scientific material that is indexed daily. But, current search engines cannot identify differences of meaning in symptoms, drug names, anatomic features, or diagnoses.
“The key drawback to using open Google is that you cannot guarantee that the information comes from peer-reviewed journals,” Dr. Lee says. “When a search with ‘regular’ Google brings back untested medical information that is not peer reviewed, it gets dicey, and thus less reliable.”
Current Web technologies may merely be a first step in creating a much more powerful infrastructure for Web-based diagnostics. The so-called semantic Web will allow computers to process meaning in documentation.3 Two key elements of this revolution are the resource description framework (RDF) and Web ontology language (OWL) technologies. These next-generation search tools are being beta tested and will be freely available within the next decade.
There are a number of caveats to using and trusting information from search-engine investigations. Google stands up much better than other search engines in simple diagnostic searches. Also, diagnostic problems are not solved on a linear scale of difficulty.2 Research and development of the benefits of the semantic Web in clinical practice will help maximize this tool for diagnostics. TH
Andrea Sattinger is a frequent contributor to The Hospitalist.
References
- Tang H, Ng JHK. Googling for a diagnosis—use of Google as a diagnostic aid: internet based study. BMJ. 2006 Dec 2;333(7579):1143-1145.
- Gardner M. Diagnosis using search engines. BMJ. 2006 Dec 2;333(7579):1131.
- Berners-Lee T, Hendler J, Lassila O. The semantic web. Sci Am. 2001 May 1;34-43.
Googling—the use of search-engines such as Google—is a new diagnostic tool in the modern clinician’s armamentarium.
A 2006 study published in The British Medical Journal examined how often searching with Google leads physicians to a correct diagnosis.1 The investigators were blinded to the correct diagnoses and compared the results of diagnostic cases published in the 2005 case records of The New England Journal of Medicine (NEJM) with diagnoses made using Google searches. Their results indicated that Google searches revealed the correct diagnosis in 15 of 26 cases, or 58% of the time. (See Table 1, p. 34.)
The limitations of the study are important to recognize when considering how well a Web-searched diagnosis can compare with one made without Web searching.
In some cases, although Google supplied information that approximated the diagnoses made in NEJM, the researchers thought the diagnoses were not specific enough.
For instance, one case for which Google suggested a diagnosis of extrinsic allergic alveolitis was described in the NEJM case record as extrinsic allergic alveolitis caused by Mycobacterium avium, also known as “hot tub lung.” This exemplifies the point that search engines don’t make diagnoses—people do. Expert knowledge is required to choose the best search words and select among the results.
Experts agree that using search engines for a diagnosis is likely to be more effective for conditions with unique symptoms and most useful in a certain class of diagnostic challenges in which clinical experts are at the helm of diagnostic deliberations.1,2
The choice of search engines is important and will increasingly affect accurate diagnoses as the technology develops.
“Hospitalists may utilize [Google] less; they are often working in environments [hospitals] that have ready access to more thoroughly vetted sources such as UpToDate, Medline, or MDConsult,” says Joshua Lee, MD, a hospitalist and medical director of Information Services at the University of California at San Diego. “Within Google there are variations on a theme, such as GoogleScholar, which accesses many of the same academic journals as Medline. Given that they are accessing the same journals, many would feel that searching with GoogleScholar is just as accurate as [searching with] Medline—at least as far as the source material is concerned.”
Search engines offer an impressive volume of new scientific material that is indexed daily. But, current search engines cannot identify differences of meaning in symptoms, drug names, anatomic features, or diagnoses.
“The key drawback to using open Google is that you cannot guarantee that the information comes from peer-reviewed journals,” Dr. Lee says. “When a search with ‘regular’ Google brings back untested medical information that is not peer reviewed, it gets dicey, and thus less reliable.”
Current Web technologies may merely be a first step in creating a much more powerful infrastructure for Web-based diagnostics. The so-called semantic Web will allow computers to process meaning in documentation.3 Two key elements of this revolution are the resource description framework (RDF) and Web ontology language (OWL) technologies. These next-generation search tools are being beta tested and will be freely available within the next decade.
There are a number of caveats to using and trusting information from search-engine investigations. Google stands up much better than other search engines in simple diagnostic searches. Also, diagnostic problems are not solved on a linear scale of difficulty.2 Research and development of the benefits of the semantic Web in clinical practice will help maximize this tool for diagnostics. TH
Andrea Sattinger is a frequent contributor to The Hospitalist.
References
- Tang H, Ng JHK. Googling for a diagnosis—use of Google as a diagnostic aid: internet based study. BMJ. 2006 Dec 2;333(7579):1143-1145.
- Gardner M. Diagnosis using search engines. BMJ. 2006 Dec 2;333(7579):1131.
- Berners-Lee T, Hendler J, Lassila O. The semantic web. Sci Am. 2001 May 1;34-43.
Googling—the use of search-engines such as Google—is a new diagnostic tool in the modern clinician’s armamentarium.
A 2006 study published in The British Medical Journal examined how often searching with Google leads physicians to a correct diagnosis.1 The investigators were blinded to the correct diagnoses and compared the results of diagnostic cases published in the 2005 case records of The New England Journal of Medicine (NEJM) with diagnoses made using Google searches. Their results indicated that Google searches revealed the correct diagnosis in 15 of 26 cases, or 58% of the time. (See Table 1, p. 34.)
The limitations of the study are important to recognize when considering how well a Web-searched diagnosis can compare with one made without Web searching.
In some cases, although Google supplied information that approximated the diagnoses made in NEJM, the researchers thought the diagnoses were not specific enough.
For instance, one case for which Google suggested a diagnosis of extrinsic allergic alveolitis was described in the NEJM case record as extrinsic allergic alveolitis caused by Mycobacterium avium, also known as “hot tub lung.” This exemplifies the point that search engines don’t make diagnoses—people do. Expert knowledge is required to choose the best search words and select among the results.
Experts agree that using search engines for a diagnosis is likely to be more effective for conditions with unique symptoms and most useful in a certain class of diagnostic challenges in which clinical experts are at the helm of diagnostic deliberations.1,2
The choice of search engines is important and will increasingly affect accurate diagnoses as the technology develops.
“Hospitalists may utilize [Google] less; they are often working in environments [hospitals] that have ready access to more thoroughly vetted sources such as UpToDate, Medline, or MDConsult,” says Joshua Lee, MD, a hospitalist and medical director of Information Services at the University of California at San Diego. “Within Google there are variations on a theme, such as GoogleScholar, which accesses many of the same academic journals as Medline. Given that they are accessing the same journals, many would feel that searching with GoogleScholar is just as accurate as [searching with] Medline—at least as far as the source material is concerned.”
Search engines offer an impressive volume of new scientific material that is indexed daily. But, current search engines cannot identify differences of meaning in symptoms, drug names, anatomic features, or diagnoses.
“The key drawback to using open Google is that you cannot guarantee that the information comes from peer-reviewed journals,” Dr. Lee says. “When a search with ‘regular’ Google brings back untested medical information that is not peer reviewed, it gets dicey, and thus less reliable.”
Current Web technologies may merely be a first step in creating a much more powerful infrastructure for Web-based diagnostics. The so-called semantic Web will allow computers to process meaning in documentation.3 Two key elements of this revolution are the resource description framework (RDF) and Web ontology language (OWL) technologies. These next-generation search tools are being beta tested and will be freely available within the next decade.
There are a number of caveats to using and trusting information from search-engine investigations. Google stands up much better than other search engines in simple diagnostic searches. Also, diagnostic problems are not solved on a linear scale of difficulty.2 Research and development of the benefits of the semantic Web in clinical practice will help maximize this tool for diagnostics. TH
Andrea Sattinger is a frequent contributor to The Hospitalist.
References
- Tang H, Ng JHK. Googling for a diagnosis—use of Google as a diagnostic aid: internet based study. BMJ. 2006 Dec 2;333(7579):1143-1145.
- Gardner M. Diagnosis using search engines. BMJ. 2006 Dec 2;333(7579):1131.
- Berners-Lee T, Hendler J, Lassila O. The semantic web. Sci Am. 2001 May 1;34-43.
Vigilant Awareness
In hospitals, clinicians constantly encounter conflicting and ambiguous information,” says Ronald M. Epstein, MD, professor of family medicine, psychiatry, and oncology at the University of Rochester Medical Center (URMC) N.Y. “This information often gets processed tacitly, outside of awareness, and often results in various undesired consequences. For example, premature closure of diagnostic thinking or ordering a test rather than inquiring further of the patient.” In the average hospital, distractions and sensory inputs, including smells, sights, sounds, and tactile sensations, as well as multiple tasks to complete, can all seem pretty overwhelming. Faced with so much data, says Dr. Epstein, the tendency of the mind is to simplify and reduce it in some way. And that’s when error can rear its ugly head.
“Simplification is often arbitrary and unconscious,” he says, and thus “the trick of working in hospital is to develop a vigilant awareness of the ambient stimuli that are all around you, making choices as to what you attend to, relegating other stimuli to the background, and in that way avoiding becoming overwhelmed or controlled by them. In that way, you have the capacity for making better judgments.”
Some clinical decisions can be made fairly easily and routinely (low-level decisions), he says, whereas other patient situations require a fair bit of deliberation (high-level decisions). (See Tables 1 and 2, right.) The human mind tends to avoid the unpleasant and to give more attention to what is compelling. Also, the ambiguity of role and responsibility—especially in large hospitals—may further confound a hospitalist’s mental capacity. Keen attention to each moment also boosts physician well being.
“Hospitalists are often working in crowded, stressful, high-paced, windowless environments in which there is no natural form of respite,” says Dr. Epstein. Therefore, all physicians need ways of keeping themselves from being overwhelmed by the challenges of sensory input and intense emotions caused by exposure to suffering, conflicts, imperatives for critical thinking, and so on.
“If practitioners were able to be more mindful,” he says, “they might experience greater well-being, because they would be able to make more choices about what they attend to and how they react to them.”
Dr. Epstein and his colleagues at the University of Rochester Medical Center—Timothy Quill, MD, Michael Krasner, MD, and Howard Beckman, MD—have studied the qualities of mind required to exercise that awareness extensively, especially as they relate to clinical practice and education.2 They were recently awarded three complementary grants to teach mindfulness to physicians: one from the Arthur Vining Davis Foundations, another from the Physicians’ Foundation for Health Systems Excellence, and the Mannix Award for Excellence in Medical Education.
But just what does mindfulness in medicine entail?
Defining Mindful Practice
“Mindful practice is recognizing where you are at every moment. If you’re distressed, if you’re content or unhappy, if you’re comfortable or in pain, if you’re experiencing some kind of positive or negative effect, if you’re feeling in tune or disconnected from yourself. It’s that monitoring function to be able to say, I’m angry or I’m uncomfortable, or, possibly, I’m in the flow,” says Dr. Epstein.
For physicians to be able to exercise those qualities of mind, to watch and deconstruct their own behavior (what Dr. Epstein describes as “the ability to observe the observer observing the observed”) is something that goes back a long way for him.3 “There’s nothing really mystical about it,” he says. “People do this all the time. It’s part of being an excellent professional in lots of fields. It’s just that no one has organized the science of doing so in the context of medical training.”
In the late 1990s, Dr. Epstein and his coworkers implemented a curriculum reform process at URMC, and his particular charge was to assess the competence of medical students. To accomplish this, he did two things. First, he reviewed the literature on the assessment and definitions of special competence. Second, he turned the magnifying glass on himself. “I thought that it might be a useful exercise to try to understand what made me practice at my best and what barriers there were to doing so.”
The resulting article from this self-monitoring and evaluation was published in JAMA in 1999, before the review article on defining and assessing professional competence appeared in that same journal.3,4 Exploring the nature of his own mindful practice reacquainted him with two areas in which he had participated as a teenager: music and the study of mind—particularly the use of meditation to enhance mental capacities. Those inquiries led him to explore the psychology of a number of qualities of mind: attentiveness, curiosity, decision-making, and the use of cognitive knowledge. The literature was convergent in a number of ways, he says, and “seemed to point to the fact that a lot of competence is not a matter of book knowledge or the kind of knowledge we can explain but tacit knowledge, things we do semi-automatically that really take some effort to deconstruct.”
He realized that “what distinguished an excellent clinician from someone who wasn’t quite so excellent had to do with some of those same qualities that one sees in accomplished musicians, athletes, and meditators, which is the ability to make fine distinctions, lower one’s own level of reactivity, respond in a more conscious way, and pay attention to the unexpected—the surprises that are part of everyday work but that we often ignore.”
All of this rather radicalized his view of what medical education should be doing. He came to believe that—on top of a foundation of knowledge and skills—physicians need to be attentive to their own mental processes and alert to the effects of bias or prior experience.
Writing about excellent clinical practice in this way drew a crescendo of response from readers of the JAMA. The JAMA editors had thoroughly engaged in helping him refine and present the ideas in a way that would really speak to clinical practitioners and educators.3 After publication, he was amazed to receive hundreds of letters from all over the world from physicians in different specialties expressing their appreciation “for having articulated something that was really at the heart of medicine,” he says. “For me, that was incredibly gratifying.”
Hospitalist Qualities of Mind
What qualities of mind are important for a hospitalist to have?
“You have to be enthusiastic, fast-paced individuals,” says Yousaf Ali, MD, hospitalist at URMC and assistant professor of medicine in the Hospital Medicine Division. You also have to be able to immediately connect with patients and families and to have the knowledge and passion that makes that possible. Further, he says, you need to quickly access knowledge pertaining to caring for patients with multiple problems.
Traci Ferguson, MD, is a hospitalist at Boca Raton Community Hospital in Florida, which, by affiliating with Florida Atlantic University (the regional campus for the University of Miami School of Medicine), is moving from community hospital to teaching hospital. Dr. Ferguson believes the qualities of mind necessary to be a good hospitalist are the capacity to be aware of reactions and biases toward patients in order to avoid being judgmental.
“I think the major thing is being present and being attentive when you are caring for patients,” she says, “and that occurs when you’re writing a chart, when you’re talking to family members, [and] when you’re talking to nurses, just as it does when you’re at the bedside.”
Other qualities of mind, in Dr. Ferguson’s view, include the whole spectrum of empathy and compassion, being personable in the sense of being open to what patients and families have to say, and being patient. She also believes the quality of mind necessary to express a human touch is sometimes missing.
Valerie Lang, MD, is also a hospitalist at URMC and has studied mindfulness with Dr. Epstein. She is enrolled in Dr. Krasner’s class for healthcare providers on being mindful. What qualities of mind does she think are important for a hospitalist to have?
“I want to say an open mind, but that’s such a broad term,” she says. “Dr. Epstein uses the term ‘beginner’s mind’ [to refer to] when you’re willing to consider many alternatives, where you don’t necessarily jump to a conclusion and then just stick with it. As a hospitalist, you start making those conclusions as soon as you hear what the patient’s chief complaint is. I think that having [a] beginner’s mind … is so important because we don’t know these patients, and it’s easy to jump to conclusions because we have to make decisions very quickly and … repeatedly.” She also believes that “being able to reflect on how you are communicating with another person is incredibly important to their care.”
—Valerie Lang, MD, hospitalist, University of Rochester Medical Center
Operationalizing Mindfulness
In 2004, after the publication of two of Dr. Epstein’s articles on mindful practice in action, the Arthur Vining Davis Foundation approached him and requested a proposal.5,6 At that time, he was in the process of writing an article on reflection and mindfulness in the context of preventing errors.1 (See Table 3, left.)
“This [proposal] was an intriguing possibility,” says Dr. Epstein, “and galvanized my putting together a curriculum that would not just be elective experiences for preclinical students, which is what the offerings related to mindfulness currently are, but something that was really going to influence clinical training.”
In Dr. Epstein’s view, placing educational reform in the first two years of medical school is teaching it when it matters the least. “Where it matters the most is when students are interacting with patients and using the knowledge and skills and doing work that they’ll ultimately end up doing for the next 30 or 40 years,” says Dr. Epstein.
One project plan is to train practicing primary care physicians to communicate more mindfully with their patients. Outcomes of the intervention will be measured by how it has affected the physicians as well as the patients’ ratings of their physicians and their practice styles.
The second project is a series of annual workshops for 100 third-year medical students and about 250 residents in the nine largest programs at the medical center. All participants will take five seminars that include mindfulness techniques to improve the capacity for paying attention and observing, and narrative exercises, whose themes will include, for instance, suffering, meaningful experience, professionalism, physician self-care, and avoiding burnout. The coursework, which will include both cognitive and experiential content, will also involve training a cadre of about 20 faculty members to teach these sessions, and educational outcomes will ultimately be measured for all participants.
Focus on Metacognition
Dr. Epstein, director of The Rochester Center to Improve Communication in Health Care, says metacognition builds on other approaches, such as the Healer’s Art, a course designed by Rachel Remen, MD, and colleagues, which a number of medical centers are incorporating into their curricula.7
“We are building on Dr. Remen’s wonderful work,” he says. Both curricula include self-awareness, humanism, caring, compassion, meaningful experiences, and physician well being. Both address the “informal curriculum”—a term used to refer to the social environment in which medical trainees adopt values, expectations, and clinical habits. In addition, Dr. Epstein and his colleagues focus on quality of clinical care, including medical decision-making and preventing errors.
“Importantly, our initiative is part of the required curriculum,” says Dr. Epstein. “It targets students and residents working in clinical settings at an advanced level, and it also has a faculty component. … We are trying to transform and heal the informal curriculum, not just immunize students against its toxicity.”
In the Thick of It
All this sounds as if it might benefit hospital practice, according to the hospitalists interviewed for this story. All three believe that mindfulness can be cultivated. Dr. Ali believes the aforementioned forces acting on hospitalists require that hospitalists work at their top capacities, but prioritizing remains essential. He believes one way a hospitalist can cultivate mindfulness in the patient-physician relationship is to avoid burnout in any way that works. Having been a hospitalist for almost 10 years, he discusses this with his medical students and residents. In addition to his hospitalist practice and teaching, Dr. Ali does patient-related quality work, which refreshes his energy.
Dr. Ferguson also thinks mindful practice can be cultivated. “I took cues from the nursing profession in realizing that you do have to care for all aspects of the patient,” she says. “But you can learn this from mentors and people who are successful: people you can emulate, shadow, and follow.”
For her, such a person is Lisa Cooper, MD, MPH, an associate professor in the department of medicine at Johns Hopkins University School of Medicine. Dr. Cooper, both a practicing internist and a researcher, studies and teaches about communication between physicians and minorities—that is, how physicians interact with people of the same or different races and ethnicities. Dr. Ferguson says she feels fortunate to have adopted a mindful awareness in that regard.
As director of the medicine clerkship, Dr. Lang came into contact with Dr. Epstein’s project through her Dean’s Teaching Fellowship, a competitive program at the URSM for faculty members who have a special interest in education.
“The discussions with other educators and clinicians really got me thinking about how my own feelings, whether they had to do with a patient or anything else in life, affect my decision-making,” says Dr. Lang. “You see the phenomenon in residency where you’re in morning report when the residents present a patient and everyone is sitting around a table—not involved with the patient—making judgments about what they should have done. It’s so much easier when you’re not involved [in the situation].”
Though Dr. Lang thinks there are a lot of reasons for that, “part of it is that you are not in the excitement of the moment. And the other factor is that when you’re presenting a patient to a group, you wouldn’t convey your own emotions, what else was going on, what were the competing pressures. Even if you have a wonderful intellect and clinical reasoning skills, you might make the wrong decision when you’re in the thick of the situation.”
Mindful Hospital Practice
Dr. Lang has seen a number of outcomes from her study of mindful practice. It has made her aware of her biases and has taught her to say, in certain cases, “OK, I need to think through the problem again to make sure I’m not changing my judgment about what we should be doing clinically based on how I’m feeling about a patient.”
Dr. Lang sometimes asks herself, “How am I feeling about this? Did that wear me down?” Or, sometimes the opposite can occur. A patient can make you feel “puffed up, where they are so complimentary and make you feel so good that you think that every decision you make is perfect,” she explains.
What Dr. Lang has learned about herself has helped her recognize when she might have prematurely closed a differential diagnosis or come to a conclusion too quickly simply because the patient appeared to agree with her clinical assessment.
Dr. Lang also thinks being a mindful physician has made her a better physician and that she is providing better care that results in better outcomes. “I definitely communicate better with my patients. … I think my relationships with my patients have significantly improved.”
What is her recommendation for how her hospitalist colleagues can learn to practice mindfully? “It’s a practice, and it’s a matter of practice,” says Dr. Lang. “It’s not something you get overnight. It’s a matter of every day, every encounter, taking the time before entering the patient’s room to pause, put things aside, and be present with the patient. And then, at the end of the day, take some time to reflect.”
How does education for mindfulness differ from her original medical training? “I don’t think you’re really ever taught how to manage your emotions when you’ve just made a medical error and you are distraught,” says Dr. Lang, “or how to manage doing that when your pager is going off like crazy and yet you need to sit down and be present with your patient. And that’s the kind of thing that ends up being in your way of being the best physician you can be.” TH
References
- Borrell-Carrió F, Epstein RM. Preventing errors in clinical practice: a call for self-awareness. Ann Fam Med. 2004;2:310-316.
- Epstein RM. Assessment in medical education. N Engl J Med. 2007;356(4):387-396.
- Epstein RM. Mindful practice. JAMA. 1999 Sep;282(9):833-839.
- Epstein RM, Hundert EM. Defining and assessing professional competence. JAMA. 2002 Jan 9;287(2):226-235.
- Epstein RM. Mindful practice in action (I): technical competence, evidence-based medicine and relationship-centered care. Fam Syst Health. 2003;21:1-9.
- Epstein RM. Mindful practice in action (II): cultivating habits of mind. Fam Syst Health. 2003;21:11-17.
- O’Donnell JF, Rabow MW, Remen RN. The healer’s art: awakening the heart of medicine. Medical Encounter: Newsletter of the American Academy on Communication in Healthcare. 2007;21, No 1.
In hospitals, clinicians constantly encounter conflicting and ambiguous information,” says Ronald M. Epstein, MD, professor of family medicine, psychiatry, and oncology at the University of Rochester Medical Center (URMC) N.Y. “This information often gets processed tacitly, outside of awareness, and often results in various undesired consequences. For example, premature closure of diagnostic thinking or ordering a test rather than inquiring further of the patient.” In the average hospital, distractions and sensory inputs, including smells, sights, sounds, and tactile sensations, as well as multiple tasks to complete, can all seem pretty overwhelming. Faced with so much data, says Dr. Epstein, the tendency of the mind is to simplify and reduce it in some way. And that’s when error can rear its ugly head.
“Simplification is often arbitrary and unconscious,” he says, and thus “the trick of working in hospital is to develop a vigilant awareness of the ambient stimuli that are all around you, making choices as to what you attend to, relegating other stimuli to the background, and in that way avoiding becoming overwhelmed or controlled by them. In that way, you have the capacity for making better judgments.”
Some clinical decisions can be made fairly easily and routinely (low-level decisions), he says, whereas other patient situations require a fair bit of deliberation (high-level decisions). (See Tables 1 and 2, right.) The human mind tends to avoid the unpleasant and to give more attention to what is compelling. Also, the ambiguity of role and responsibility—especially in large hospitals—may further confound a hospitalist’s mental capacity. Keen attention to each moment also boosts physician well being.
“Hospitalists are often working in crowded, stressful, high-paced, windowless environments in which there is no natural form of respite,” says Dr. Epstein. Therefore, all physicians need ways of keeping themselves from being overwhelmed by the challenges of sensory input and intense emotions caused by exposure to suffering, conflicts, imperatives for critical thinking, and so on.
“If practitioners were able to be more mindful,” he says, “they might experience greater well-being, because they would be able to make more choices about what they attend to and how they react to them.”
Dr. Epstein and his colleagues at the University of Rochester Medical Center—Timothy Quill, MD, Michael Krasner, MD, and Howard Beckman, MD—have studied the qualities of mind required to exercise that awareness extensively, especially as they relate to clinical practice and education.2 They were recently awarded three complementary grants to teach mindfulness to physicians: one from the Arthur Vining Davis Foundations, another from the Physicians’ Foundation for Health Systems Excellence, and the Mannix Award for Excellence in Medical Education.
But just what does mindfulness in medicine entail?
Defining Mindful Practice
“Mindful practice is recognizing where you are at every moment. If you’re distressed, if you’re content or unhappy, if you’re comfortable or in pain, if you’re experiencing some kind of positive or negative effect, if you’re feeling in tune or disconnected from yourself. It’s that monitoring function to be able to say, I’m angry or I’m uncomfortable, or, possibly, I’m in the flow,” says Dr. Epstein.
For physicians to be able to exercise those qualities of mind, to watch and deconstruct their own behavior (what Dr. Epstein describes as “the ability to observe the observer observing the observed”) is something that goes back a long way for him.3 “There’s nothing really mystical about it,” he says. “People do this all the time. It’s part of being an excellent professional in lots of fields. It’s just that no one has organized the science of doing so in the context of medical training.”
In the late 1990s, Dr. Epstein and his coworkers implemented a curriculum reform process at URMC, and his particular charge was to assess the competence of medical students. To accomplish this, he did two things. First, he reviewed the literature on the assessment and definitions of special competence. Second, he turned the magnifying glass on himself. “I thought that it might be a useful exercise to try to understand what made me practice at my best and what barriers there were to doing so.”
The resulting article from this self-monitoring and evaluation was published in JAMA in 1999, before the review article on defining and assessing professional competence appeared in that same journal.3,4 Exploring the nature of his own mindful practice reacquainted him with two areas in which he had participated as a teenager: music and the study of mind—particularly the use of meditation to enhance mental capacities. Those inquiries led him to explore the psychology of a number of qualities of mind: attentiveness, curiosity, decision-making, and the use of cognitive knowledge. The literature was convergent in a number of ways, he says, and “seemed to point to the fact that a lot of competence is not a matter of book knowledge or the kind of knowledge we can explain but tacit knowledge, things we do semi-automatically that really take some effort to deconstruct.”
He realized that “what distinguished an excellent clinician from someone who wasn’t quite so excellent had to do with some of those same qualities that one sees in accomplished musicians, athletes, and meditators, which is the ability to make fine distinctions, lower one’s own level of reactivity, respond in a more conscious way, and pay attention to the unexpected—the surprises that are part of everyday work but that we often ignore.”
All of this rather radicalized his view of what medical education should be doing. He came to believe that—on top of a foundation of knowledge and skills—physicians need to be attentive to their own mental processes and alert to the effects of bias or prior experience.
Writing about excellent clinical practice in this way drew a crescendo of response from readers of the JAMA. The JAMA editors had thoroughly engaged in helping him refine and present the ideas in a way that would really speak to clinical practitioners and educators.3 After publication, he was amazed to receive hundreds of letters from all over the world from physicians in different specialties expressing their appreciation “for having articulated something that was really at the heart of medicine,” he says. “For me, that was incredibly gratifying.”
Hospitalist Qualities of Mind
What qualities of mind are important for a hospitalist to have?
“You have to be enthusiastic, fast-paced individuals,” says Yousaf Ali, MD, hospitalist at URMC and assistant professor of medicine in the Hospital Medicine Division. You also have to be able to immediately connect with patients and families and to have the knowledge and passion that makes that possible. Further, he says, you need to quickly access knowledge pertaining to caring for patients with multiple problems.
Traci Ferguson, MD, is a hospitalist at Boca Raton Community Hospital in Florida, which, by affiliating with Florida Atlantic University (the regional campus for the University of Miami School of Medicine), is moving from community hospital to teaching hospital. Dr. Ferguson believes the qualities of mind necessary to be a good hospitalist are the capacity to be aware of reactions and biases toward patients in order to avoid being judgmental.
“I think the major thing is being present and being attentive when you are caring for patients,” she says, “and that occurs when you’re writing a chart, when you’re talking to family members, [and] when you’re talking to nurses, just as it does when you’re at the bedside.”
Other qualities of mind, in Dr. Ferguson’s view, include the whole spectrum of empathy and compassion, being personable in the sense of being open to what patients and families have to say, and being patient. She also believes the quality of mind necessary to express a human touch is sometimes missing.
Valerie Lang, MD, is also a hospitalist at URMC and has studied mindfulness with Dr. Epstein. She is enrolled in Dr. Krasner’s class for healthcare providers on being mindful. What qualities of mind does she think are important for a hospitalist to have?
“I want to say an open mind, but that’s such a broad term,” she says. “Dr. Epstein uses the term ‘beginner’s mind’ [to refer to] when you’re willing to consider many alternatives, where you don’t necessarily jump to a conclusion and then just stick with it. As a hospitalist, you start making those conclusions as soon as you hear what the patient’s chief complaint is. I think that having [a] beginner’s mind … is so important because we don’t know these patients, and it’s easy to jump to conclusions because we have to make decisions very quickly and … repeatedly.” She also believes that “being able to reflect on how you are communicating with another person is incredibly important to their care.”
—Valerie Lang, MD, hospitalist, University of Rochester Medical Center
Operationalizing Mindfulness
In 2004, after the publication of two of Dr. Epstein’s articles on mindful practice in action, the Arthur Vining Davis Foundation approached him and requested a proposal.5,6 At that time, he was in the process of writing an article on reflection and mindfulness in the context of preventing errors.1 (See Table 3, left.)
“This [proposal] was an intriguing possibility,” says Dr. Epstein, “and galvanized my putting together a curriculum that would not just be elective experiences for preclinical students, which is what the offerings related to mindfulness currently are, but something that was really going to influence clinical training.”
In Dr. Epstein’s view, placing educational reform in the first two years of medical school is teaching it when it matters the least. “Where it matters the most is when students are interacting with patients and using the knowledge and skills and doing work that they’ll ultimately end up doing for the next 30 or 40 years,” says Dr. Epstein.
One project plan is to train practicing primary care physicians to communicate more mindfully with their patients. Outcomes of the intervention will be measured by how it has affected the physicians as well as the patients’ ratings of their physicians and their practice styles.
The second project is a series of annual workshops for 100 third-year medical students and about 250 residents in the nine largest programs at the medical center. All participants will take five seminars that include mindfulness techniques to improve the capacity for paying attention and observing, and narrative exercises, whose themes will include, for instance, suffering, meaningful experience, professionalism, physician self-care, and avoiding burnout. The coursework, which will include both cognitive and experiential content, will also involve training a cadre of about 20 faculty members to teach these sessions, and educational outcomes will ultimately be measured for all participants.
Focus on Metacognition
Dr. Epstein, director of The Rochester Center to Improve Communication in Health Care, says metacognition builds on other approaches, such as the Healer’s Art, a course designed by Rachel Remen, MD, and colleagues, which a number of medical centers are incorporating into their curricula.7
“We are building on Dr. Remen’s wonderful work,” he says. Both curricula include self-awareness, humanism, caring, compassion, meaningful experiences, and physician well being. Both address the “informal curriculum”—a term used to refer to the social environment in which medical trainees adopt values, expectations, and clinical habits. In addition, Dr. Epstein and his colleagues focus on quality of clinical care, including medical decision-making and preventing errors.
“Importantly, our initiative is part of the required curriculum,” says Dr. Epstein. “It targets students and residents working in clinical settings at an advanced level, and it also has a faculty component. … We are trying to transform and heal the informal curriculum, not just immunize students against its toxicity.”
In the Thick of It
All this sounds as if it might benefit hospital practice, according to the hospitalists interviewed for this story. All three believe that mindfulness can be cultivated. Dr. Ali believes the aforementioned forces acting on hospitalists require that hospitalists work at their top capacities, but prioritizing remains essential. He believes one way a hospitalist can cultivate mindfulness in the patient-physician relationship is to avoid burnout in any way that works. Having been a hospitalist for almost 10 years, he discusses this with his medical students and residents. In addition to his hospitalist practice and teaching, Dr. Ali does patient-related quality work, which refreshes his energy.
Dr. Ferguson also thinks mindful practice can be cultivated. “I took cues from the nursing profession in realizing that you do have to care for all aspects of the patient,” she says. “But you can learn this from mentors and people who are successful: people you can emulate, shadow, and follow.”
For her, such a person is Lisa Cooper, MD, MPH, an associate professor in the department of medicine at Johns Hopkins University School of Medicine. Dr. Cooper, both a practicing internist and a researcher, studies and teaches about communication between physicians and minorities—that is, how physicians interact with people of the same or different races and ethnicities. Dr. Ferguson says she feels fortunate to have adopted a mindful awareness in that regard.
As director of the medicine clerkship, Dr. Lang came into contact with Dr. Epstein’s project through her Dean’s Teaching Fellowship, a competitive program at the URSM for faculty members who have a special interest in education.
“The discussions with other educators and clinicians really got me thinking about how my own feelings, whether they had to do with a patient or anything else in life, affect my decision-making,” says Dr. Lang. “You see the phenomenon in residency where you’re in morning report when the residents present a patient and everyone is sitting around a table—not involved with the patient—making judgments about what they should have done. It’s so much easier when you’re not involved [in the situation].”
Though Dr. Lang thinks there are a lot of reasons for that, “part of it is that you are not in the excitement of the moment. And the other factor is that when you’re presenting a patient to a group, you wouldn’t convey your own emotions, what else was going on, what were the competing pressures. Even if you have a wonderful intellect and clinical reasoning skills, you might make the wrong decision when you’re in the thick of the situation.”
Mindful Hospital Practice
Dr. Lang has seen a number of outcomes from her study of mindful practice. It has made her aware of her biases and has taught her to say, in certain cases, “OK, I need to think through the problem again to make sure I’m not changing my judgment about what we should be doing clinically based on how I’m feeling about a patient.”
Dr. Lang sometimes asks herself, “How am I feeling about this? Did that wear me down?” Or, sometimes the opposite can occur. A patient can make you feel “puffed up, where they are so complimentary and make you feel so good that you think that every decision you make is perfect,” she explains.
What Dr. Lang has learned about herself has helped her recognize when she might have prematurely closed a differential diagnosis or come to a conclusion too quickly simply because the patient appeared to agree with her clinical assessment.
Dr. Lang also thinks being a mindful physician has made her a better physician and that she is providing better care that results in better outcomes. “I definitely communicate better with my patients. … I think my relationships with my patients have significantly improved.”
What is her recommendation for how her hospitalist colleagues can learn to practice mindfully? “It’s a practice, and it’s a matter of practice,” says Dr. Lang. “It’s not something you get overnight. It’s a matter of every day, every encounter, taking the time before entering the patient’s room to pause, put things aside, and be present with the patient. And then, at the end of the day, take some time to reflect.”
How does education for mindfulness differ from her original medical training? “I don’t think you’re really ever taught how to manage your emotions when you’ve just made a medical error and you are distraught,” says Dr. Lang, “or how to manage doing that when your pager is going off like crazy and yet you need to sit down and be present with your patient. And that’s the kind of thing that ends up being in your way of being the best physician you can be.” TH
References
- Borrell-Carrió F, Epstein RM. Preventing errors in clinical practice: a call for self-awareness. Ann Fam Med. 2004;2:310-316.
- Epstein RM. Assessment in medical education. N Engl J Med. 2007;356(4):387-396.
- Epstein RM. Mindful practice. JAMA. 1999 Sep;282(9):833-839.
- Epstein RM, Hundert EM. Defining and assessing professional competence. JAMA. 2002 Jan 9;287(2):226-235.
- Epstein RM. Mindful practice in action (I): technical competence, evidence-based medicine and relationship-centered care. Fam Syst Health. 2003;21:1-9.
- Epstein RM. Mindful practice in action (II): cultivating habits of mind. Fam Syst Health. 2003;21:11-17.
- O’Donnell JF, Rabow MW, Remen RN. The healer’s art: awakening the heart of medicine. Medical Encounter: Newsletter of the American Academy on Communication in Healthcare. 2007;21, No 1.
In hospitals, clinicians constantly encounter conflicting and ambiguous information,” says Ronald M. Epstein, MD, professor of family medicine, psychiatry, and oncology at the University of Rochester Medical Center (URMC) N.Y. “This information often gets processed tacitly, outside of awareness, and often results in various undesired consequences. For example, premature closure of diagnostic thinking or ordering a test rather than inquiring further of the patient.” In the average hospital, distractions and sensory inputs, including smells, sights, sounds, and tactile sensations, as well as multiple tasks to complete, can all seem pretty overwhelming. Faced with so much data, says Dr. Epstein, the tendency of the mind is to simplify and reduce it in some way. And that’s when error can rear its ugly head.
“Simplification is often arbitrary and unconscious,” he says, and thus “the trick of working in hospital is to develop a vigilant awareness of the ambient stimuli that are all around you, making choices as to what you attend to, relegating other stimuli to the background, and in that way avoiding becoming overwhelmed or controlled by them. In that way, you have the capacity for making better judgments.”
Some clinical decisions can be made fairly easily and routinely (low-level decisions), he says, whereas other patient situations require a fair bit of deliberation (high-level decisions). (See Tables 1 and 2, right.) The human mind tends to avoid the unpleasant and to give more attention to what is compelling. Also, the ambiguity of role and responsibility—especially in large hospitals—may further confound a hospitalist’s mental capacity. Keen attention to each moment also boosts physician well being.
“Hospitalists are often working in crowded, stressful, high-paced, windowless environments in which there is no natural form of respite,” says Dr. Epstein. Therefore, all physicians need ways of keeping themselves from being overwhelmed by the challenges of sensory input and intense emotions caused by exposure to suffering, conflicts, imperatives for critical thinking, and so on.
“If practitioners were able to be more mindful,” he says, “they might experience greater well-being, because they would be able to make more choices about what they attend to and how they react to them.”
Dr. Epstein and his colleagues at the University of Rochester Medical Center—Timothy Quill, MD, Michael Krasner, MD, and Howard Beckman, MD—have studied the qualities of mind required to exercise that awareness extensively, especially as they relate to clinical practice and education.2 They were recently awarded three complementary grants to teach mindfulness to physicians: one from the Arthur Vining Davis Foundations, another from the Physicians’ Foundation for Health Systems Excellence, and the Mannix Award for Excellence in Medical Education.
But just what does mindfulness in medicine entail?
Defining Mindful Practice
“Mindful practice is recognizing where you are at every moment. If you’re distressed, if you’re content or unhappy, if you’re comfortable or in pain, if you’re experiencing some kind of positive or negative effect, if you’re feeling in tune or disconnected from yourself. It’s that monitoring function to be able to say, I’m angry or I’m uncomfortable, or, possibly, I’m in the flow,” says Dr. Epstein.
For physicians to be able to exercise those qualities of mind, to watch and deconstruct their own behavior (what Dr. Epstein describes as “the ability to observe the observer observing the observed”) is something that goes back a long way for him.3 “There’s nothing really mystical about it,” he says. “People do this all the time. It’s part of being an excellent professional in lots of fields. It’s just that no one has organized the science of doing so in the context of medical training.”
In the late 1990s, Dr. Epstein and his coworkers implemented a curriculum reform process at URMC, and his particular charge was to assess the competence of medical students. To accomplish this, he did two things. First, he reviewed the literature on the assessment and definitions of special competence. Second, he turned the magnifying glass on himself. “I thought that it might be a useful exercise to try to understand what made me practice at my best and what barriers there were to doing so.”
The resulting article from this self-monitoring and evaluation was published in JAMA in 1999, before the review article on defining and assessing professional competence appeared in that same journal.3,4 Exploring the nature of his own mindful practice reacquainted him with two areas in which he had participated as a teenager: music and the study of mind—particularly the use of meditation to enhance mental capacities. Those inquiries led him to explore the psychology of a number of qualities of mind: attentiveness, curiosity, decision-making, and the use of cognitive knowledge. The literature was convergent in a number of ways, he says, and “seemed to point to the fact that a lot of competence is not a matter of book knowledge or the kind of knowledge we can explain but tacit knowledge, things we do semi-automatically that really take some effort to deconstruct.”
He realized that “what distinguished an excellent clinician from someone who wasn’t quite so excellent had to do with some of those same qualities that one sees in accomplished musicians, athletes, and meditators, which is the ability to make fine distinctions, lower one’s own level of reactivity, respond in a more conscious way, and pay attention to the unexpected—the surprises that are part of everyday work but that we often ignore.”
All of this rather radicalized his view of what medical education should be doing. He came to believe that—on top of a foundation of knowledge and skills—physicians need to be attentive to their own mental processes and alert to the effects of bias or prior experience.
Writing about excellent clinical practice in this way drew a crescendo of response from readers of the JAMA. The JAMA editors had thoroughly engaged in helping him refine and present the ideas in a way that would really speak to clinical practitioners and educators.3 After publication, he was amazed to receive hundreds of letters from all over the world from physicians in different specialties expressing their appreciation “for having articulated something that was really at the heart of medicine,” he says. “For me, that was incredibly gratifying.”
Hospitalist Qualities of Mind
What qualities of mind are important for a hospitalist to have?
“You have to be enthusiastic, fast-paced individuals,” says Yousaf Ali, MD, hospitalist at URMC and assistant professor of medicine in the Hospital Medicine Division. You also have to be able to immediately connect with patients and families and to have the knowledge and passion that makes that possible. Further, he says, you need to quickly access knowledge pertaining to caring for patients with multiple problems.
Traci Ferguson, MD, is a hospitalist at Boca Raton Community Hospital in Florida, which, by affiliating with Florida Atlantic University (the regional campus for the University of Miami School of Medicine), is moving from community hospital to teaching hospital. Dr. Ferguson believes the qualities of mind necessary to be a good hospitalist are the capacity to be aware of reactions and biases toward patients in order to avoid being judgmental.
“I think the major thing is being present and being attentive when you are caring for patients,” she says, “and that occurs when you’re writing a chart, when you’re talking to family members, [and] when you’re talking to nurses, just as it does when you’re at the bedside.”
Other qualities of mind, in Dr. Ferguson’s view, include the whole spectrum of empathy and compassion, being personable in the sense of being open to what patients and families have to say, and being patient. She also believes the quality of mind necessary to express a human touch is sometimes missing.
Valerie Lang, MD, is also a hospitalist at URMC and has studied mindfulness with Dr. Epstein. She is enrolled in Dr. Krasner’s class for healthcare providers on being mindful. What qualities of mind does she think are important for a hospitalist to have?
“I want to say an open mind, but that’s such a broad term,” she says. “Dr. Epstein uses the term ‘beginner’s mind’ [to refer to] when you’re willing to consider many alternatives, where you don’t necessarily jump to a conclusion and then just stick with it. As a hospitalist, you start making those conclusions as soon as you hear what the patient’s chief complaint is. I think that having [a] beginner’s mind … is so important because we don’t know these patients, and it’s easy to jump to conclusions because we have to make decisions very quickly and … repeatedly.” She also believes that “being able to reflect on how you are communicating with another person is incredibly important to their care.”
—Valerie Lang, MD, hospitalist, University of Rochester Medical Center
Operationalizing Mindfulness
In 2004, after the publication of two of Dr. Epstein’s articles on mindful practice in action, the Arthur Vining Davis Foundation approached him and requested a proposal.5,6 At that time, he was in the process of writing an article on reflection and mindfulness in the context of preventing errors.1 (See Table 3, left.)
“This [proposal] was an intriguing possibility,” says Dr. Epstein, “and galvanized my putting together a curriculum that would not just be elective experiences for preclinical students, which is what the offerings related to mindfulness currently are, but something that was really going to influence clinical training.”
In Dr. Epstein’s view, placing educational reform in the first two years of medical school is teaching it when it matters the least. “Where it matters the most is when students are interacting with patients and using the knowledge and skills and doing work that they’ll ultimately end up doing for the next 30 or 40 years,” says Dr. Epstein.
One project plan is to train practicing primary care physicians to communicate more mindfully with their patients. Outcomes of the intervention will be measured by how it has affected the physicians as well as the patients’ ratings of their physicians and their practice styles.
The second project is a series of annual workshops for 100 third-year medical students and about 250 residents in the nine largest programs at the medical center. All participants will take five seminars that include mindfulness techniques to improve the capacity for paying attention and observing, and narrative exercises, whose themes will include, for instance, suffering, meaningful experience, professionalism, physician self-care, and avoiding burnout. The coursework, which will include both cognitive and experiential content, will also involve training a cadre of about 20 faculty members to teach these sessions, and educational outcomes will ultimately be measured for all participants.
Focus on Metacognition
Dr. Epstein, director of The Rochester Center to Improve Communication in Health Care, says metacognition builds on other approaches, such as the Healer’s Art, a course designed by Rachel Remen, MD, and colleagues, which a number of medical centers are incorporating into their curricula.7
“We are building on Dr. Remen’s wonderful work,” he says. Both curricula include self-awareness, humanism, caring, compassion, meaningful experiences, and physician well being. Both address the “informal curriculum”—a term used to refer to the social environment in which medical trainees adopt values, expectations, and clinical habits. In addition, Dr. Epstein and his colleagues focus on quality of clinical care, including medical decision-making and preventing errors.
“Importantly, our initiative is part of the required curriculum,” says Dr. Epstein. “It targets students and residents working in clinical settings at an advanced level, and it also has a faculty component. … We are trying to transform and heal the informal curriculum, not just immunize students against its toxicity.”
In the Thick of It
All this sounds as if it might benefit hospital practice, according to the hospitalists interviewed for this story. All three believe that mindfulness can be cultivated. Dr. Ali believes the aforementioned forces acting on hospitalists require that hospitalists work at their top capacities, but prioritizing remains essential. He believes one way a hospitalist can cultivate mindfulness in the patient-physician relationship is to avoid burnout in any way that works. Having been a hospitalist for almost 10 years, he discusses this with his medical students and residents. In addition to his hospitalist practice and teaching, Dr. Ali does patient-related quality work, which refreshes his energy.
Dr. Ferguson also thinks mindful practice can be cultivated. “I took cues from the nursing profession in realizing that you do have to care for all aspects of the patient,” she says. “But you can learn this from mentors and people who are successful: people you can emulate, shadow, and follow.”
For her, such a person is Lisa Cooper, MD, MPH, an associate professor in the department of medicine at Johns Hopkins University School of Medicine. Dr. Cooper, both a practicing internist and a researcher, studies and teaches about communication between physicians and minorities—that is, how physicians interact with people of the same or different races and ethnicities. Dr. Ferguson says she feels fortunate to have adopted a mindful awareness in that regard.
As director of the medicine clerkship, Dr. Lang came into contact with Dr. Epstein’s project through her Dean’s Teaching Fellowship, a competitive program at the URSM for faculty members who have a special interest in education.
“The discussions with other educators and clinicians really got me thinking about how my own feelings, whether they had to do with a patient or anything else in life, affect my decision-making,” says Dr. Lang. “You see the phenomenon in residency where you’re in morning report when the residents present a patient and everyone is sitting around a table—not involved with the patient—making judgments about what they should have done. It’s so much easier when you’re not involved [in the situation].”
Though Dr. Lang thinks there are a lot of reasons for that, “part of it is that you are not in the excitement of the moment. And the other factor is that when you’re presenting a patient to a group, you wouldn’t convey your own emotions, what else was going on, what were the competing pressures. Even if you have a wonderful intellect and clinical reasoning skills, you might make the wrong decision when you’re in the thick of the situation.”
Mindful Hospital Practice
Dr. Lang has seen a number of outcomes from her study of mindful practice. It has made her aware of her biases and has taught her to say, in certain cases, “OK, I need to think through the problem again to make sure I’m not changing my judgment about what we should be doing clinically based on how I’m feeling about a patient.”
Dr. Lang sometimes asks herself, “How am I feeling about this? Did that wear me down?” Or, sometimes the opposite can occur. A patient can make you feel “puffed up, where they are so complimentary and make you feel so good that you think that every decision you make is perfect,” she explains.
What Dr. Lang has learned about herself has helped her recognize when she might have prematurely closed a differential diagnosis or come to a conclusion too quickly simply because the patient appeared to agree with her clinical assessment.
Dr. Lang also thinks being a mindful physician has made her a better physician and that she is providing better care that results in better outcomes. “I definitely communicate better with my patients. … I think my relationships with my patients have significantly improved.”
What is her recommendation for how her hospitalist colleagues can learn to practice mindfully? “It’s a practice, and it’s a matter of practice,” says Dr. Lang. “It’s not something you get overnight. It’s a matter of every day, every encounter, taking the time before entering the patient’s room to pause, put things aside, and be present with the patient. And then, at the end of the day, take some time to reflect.”
How does education for mindfulness differ from her original medical training? “I don’t think you’re really ever taught how to manage your emotions when you’ve just made a medical error and you are distraught,” says Dr. Lang, “or how to manage doing that when your pager is going off like crazy and yet you need to sit down and be present with your patient. And that’s the kind of thing that ends up being in your way of being the best physician you can be.” TH
References
- Borrell-Carrió F, Epstein RM. Preventing errors in clinical practice: a call for self-awareness. Ann Fam Med. 2004;2:310-316.
- Epstein RM. Assessment in medical education. N Engl J Med. 2007;356(4):387-396.
- Epstein RM. Mindful practice. JAMA. 1999 Sep;282(9):833-839.
- Epstein RM, Hundert EM. Defining and assessing professional competence. JAMA. 2002 Jan 9;287(2):226-235.
- Epstein RM. Mindful practice in action (I): technical competence, evidence-based medicine and relationship-centered care. Fam Syst Health. 2003;21:1-9.
- Epstein RM. Mindful practice in action (II): cultivating habits of mind. Fam Syst Health. 2003;21:11-17.
- O’Donnell JF, Rabow MW, Remen RN. The healer’s art: awakening the heart of medicine. Medical Encounter: Newsletter of the American Academy on Communication in Healthcare. 2007;21, No 1.
Final Exam?
You enter a patient’s room with all your senses on alert. You absorb the environment quickly—even before addressing the patient. It is perhaps these “small moments in medicine,” the under-the-radar information, that a physician may best remember about individual people or cases, says Andrew Bomback, MD, a first-year fellow in nephrology at the University of North Carolina at Chapel Hill. “Not the details of a specific disease state,” he elaborates, “but the visceral memory, such as how someone smells.”
In his article, “The Physical Exam and the Sense of Smell,” published in the New England Journal of Medicine in January 2006, Dr. Bomback writes that his training by doctors who “preached the gospel of the physical exam” was intended so that he and his fellow students “would not forget that the best doctors help their patients with their eyes, ears, and hands, not just with numbers posted on a computer screen.”1
Those small moments are often usurped from doctors as they deal with the demands and obligations of their jobs in an often-hurried environment. Let’s face it, he says, “The physical exam has just been truncated to very brief encounters.”
In fact, facing this dilemma is one of the first remedies he would prescribe. In response to the article, “I got a lot of nice letters from [physicians] who related similar incidents that happened in their training, where they used smell to learn more about a patient,” he says.
In contrast, he also received “somewhat negative letters where the message from those mostly retired physicians was, ‘You’re just not spending enough time with patients.’ I think that is a very unrealistic piece of advice,” says Dr. Bomback. “It would be very interesting to see whether they could carry the pager of a hospitalist or resident for 12 hours and actually be able to do what that hospitalist or resident does.”
Physicians today must first acknowledge the reality “that we don’t have as much time as we need,” says Dr. Bomback. “And once you admit that you’re not going to be able to spend as much time as you ideally would like … that we only have a 12-hour work shift if you are a hospitalist or a 30-hour call shift if you are a resident,” you have to maximize the time with the patient by giving “a focused physical that it is well done, accurate, and respectful to the patient.”
—Tim Creamer, MD, director, hospital medicine program, Community General Hospital, Syracuse, NY
Crisis or Evolution?
Sandeep Jauhar, MD, director of the Heart Failure Program at Long Island Jewish Medical Center, New Hyde Park, N.Y., also had an article in last year’s NEJM “Perspective” series.1-4 In that piece, “The Demise of the Physical Exam,”2 Dr. Jauhar posed a question: Is the demise of physical diagnosis a crisis or a natural evolution? Now, a year later, The Hospitalist asked him that same question.
“I don’t view it as a crisis,” he says, “but maybe that’s because of my vantage point as a cardiologist. Cardiology is very technology-driven; very few diagnoses are made on the basis of the physical exam.”
Dr. Jauhar believes that the greatest benefit of performing a thorough physical exam is not necessarily to pin down a diagnosis, though it can expedite that process, but to limit the tests that are ordered.
William Dickey, MD, hospitalist and director of quality at Abbott Northwestern Medical Center, Minneapolis, Minn., agrees that the decision of what testing to do, if any, is still guided by the physical exam.
“The high-tech diagnostic testing doesn’t demean the importance of the exam of all,” he says, but its role may have changed.
Are the intricate skills of performing a physical exam imperative, or have they mostly been replaced by technology? “I would say they’re not fully imperative under the assumption that you have the technology and you want to get the job done,” says Dr. Bomback. “Are they desired? Absolutely. A good physical exam and a remarkable finding are about showing what goes on inside the body and manifests itself outside the body.”
The ability to adequately hear a heart murmur or detect tetany is based on the physiologic understanding of why that murmur occurs or how calcium metabolism works. With that in mind, Dr. Bomback believes all patients would want their doctors to have those skills. “But,” he quickly qualifies, “could you have a functioning doctor get through his or her workday without knowing that? Absolutely. Could a cardiologist treat CHF without being able to hear a murmur? Of course. … So it’s desirable, but it’s not totally necessary.”
One reason for the desirability of maintaining those skills, which require physicians to “get up close,” as Dr. Dickey puts it, pertains to the importance of touching, seeing, and listening and to the quality of the patient-physician interaction itself.4 All the physicians interviewed for this article concur that getting that physical sense of the patient will tell you things that other information will not, and involving this true sensitivity in the interaction will most likely put the patient at greater ease.
“Because, in addition to all the information that a physician can discover from doing a physical exam, there is also a sense of rapport that the physical exam builds,” says C. Martin Buchanan, MD, FACP, a hospitalist at Penrose Hospital in Colorado Springs, Colo. “The therapy of being there, being present at the patient’s side, touching the patient, doing something for them, having a kind of healing energy, if you will, that we … transmit to the patient and [which essentially communicates], ‘I’m here to help you, I accept you as a human being even though you’re ill; I’m willing to touch you, and I’m here to help you feel better.’”
Not a Demise, but Compromised
“The physical exam is compromised during patient assessment because of where it ranks in importance,” says Tim Creamer, MD, director of the hospital medicine program at Community General Hospital in Syracuse, N.Y. “There are people who say that history is 80% of the diagnosis, which makes the physical exam 20% of the diagnosis. Although you try to emphasize that diagnostics, such as X-rays and labs, should only confirm your history and physical, we still depend too much on the technology to diagnose for us.”
The physical exam is not emphasized after medical school, says Dr. Creamer, who teaches second-year family practice residents. The emphasis now has become the patient-doctor interface: educating and talking with the patient and family. “And even in the lay literature, they encourage consumers to ‘Get your doctor to spend time with you,’” he says. “They mean talking to you, not checking your neck veins for A, C, and V waves.” Hospitalists may also minimize the physical exam, he adds, “because we feel pressured to maximize the talking and listening.”
The Focused Physical
The newest title in the 2006 edition of the Medical Knowledge Self-Assessment Program (MKSAP), published by the American College of Physicians, “Foundations of Internal Medicine,” includes an extensive discussion about the evidence-based physical exam. A good deal of recent research has addressed the topic of which physical findings are truly important to assess various conditions.
“If internists will pay attention to what’s in the medical literature about reliable physical findings,” says Dr. Buchanan, “we can tailor our physical exam a bit better, make more efficient use of the [interview] time, and provide very useful information for our diagnostic assessment and treatment planning.”
The MKSAP-14 offers 11 print books, a CD-ROM, and a new online version. Information is available at www.acponline.org/catalog/mksap/14/.
Powers of Observation
Performing a good physical exam is “something that we all aspire to and something we always try to improve,” says Dr. Bomback. “Anytime I hear of someone with a good physical exam finding I will try to see that patient.” It’s one of the reasons he likes working in an academic center. “There are always interesting cases, and there is always someone who wants to teach someone else what they’re seeing. It’s a constant learning process.”
Dr. Creamer agrees. He used to veer from his day-to-day routine and “follow around Max Kutzer, an internist at Crouse Hospital here at Syracuse, who practiced for years and who taught the physical exam to medical students at Harvard in 1954,” a time—he points out—when little-to-no diagnostic technology existed. Accompanying this master of medical observation, he says, was a Zen-like experience. The elder doctor “would walk to a patient’s doorway and stand there and watch the person breathe and watch how disheveled the bed was, whether the chair had been sat in, and [after] a couple of minutes he would walk out and say, ‘Now tell me what you noticed.’ ”
Dr. Creamer remembers naming “two or three things. But [Dr. Kutzer] would say, ‘OK, but let me tell you 10 more.’ ” Dr. Kutzer, now 96 and still productive, Dr. Creamer says, has written a book, Observation and the Physical Exam, which is in the editing stage.
Because physicians are pressed for time, those powers of observation may be, if not lost, at least largely neglected or ignored. “But I still do those things,” says Dr. Creamer. “I’ll walk to the door and watch a person breathe while they’re sleeping … . You lose the anxiety overtones when you’re watching someone sleeping. ... In order to learn, you need to listen. Listening takes time. You’ve got to step back and take the time to learn, and that’s where it gets tricky.”
Dr. Bomback believes technology will never replace the power of observation. “Those are the unique skills that come with being a hospitalist or any physician … and a lot of the reason why most people become physicians,” he says. “It is a skill that [they have had] from early on. It’s empathy, that you can observe a patient and understand what’s going on—maybe not completely, and not totally consciously, but there is an empathic sensation.”
Conclusion
The traditional use of the physical exam may have changed, but its value is still important to patient care.
“The physical exam is part of the culture of medicine,” says Dr. Jauhar. “It may have started to lose some of its utility as we get more technology, but it can limit the use of technology and help us make diagnoses more quickly.”
Providers might also sometimes be in a place “where you don’t have a CT scan or an MRI machine,” he adds. The provider discovers things that machines can’t supply, and the contributions of even a brief physical exam can communicate humanity to the patient.
“I have always wondered how physicians can do telemedicine,” says Dr. Dickey, “because there is something about being there and being with the patient in terms of judging the severity of illness that is very important.”
“For all these reasons, it’s important for hospitalists to maintain their skills,” says Dr. Jauhar, “because otherwise we’re losing a big part of what it is to be a doctor. We’re just becoming technicians.” TH
Andrea Sattinger is a frequent contributor to The Hospitalist.
References
- Bomback A. The physical exam and the sense of smell. N Engl J Med. 2006 Jan 26;354(4):327-329.
- Jauhar S. The demise of the physical exam. N Engl J Med. 2006;354(6):548-551.
- Markel H. The stethoscope and the art of listening. N Engl J Med. 2006;354(6):551-553.
- Treadway K. Becoming a physician: heart sounds. N Engl J Med. 2006 Mar 16;354(11):1112-1113.
You enter a patient’s room with all your senses on alert. You absorb the environment quickly—even before addressing the patient. It is perhaps these “small moments in medicine,” the under-the-radar information, that a physician may best remember about individual people or cases, says Andrew Bomback, MD, a first-year fellow in nephrology at the University of North Carolina at Chapel Hill. “Not the details of a specific disease state,” he elaborates, “but the visceral memory, such as how someone smells.”
In his article, “The Physical Exam and the Sense of Smell,” published in the New England Journal of Medicine in January 2006, Dr. Bomback writes that his training by doctors who “preached the gospel of the physical exam” was intended so that he and his fellow students “would not forget that the best doctors help their patients with their eyes, ears, and hands, not just with numbers posted on a computer screen.”1
Those small moments are often usurped from doctors as they deal with the demands and obligations of their jobs in an often-hurried environment. Let’s face it, he says, “The physical exam has just been truncated to very brief encounters.”
In fact, facing this dilemma is one of the first remedies he would prescribe. In response to the article, “I got a lot of nice letters from [physicians] who related similar incidents that happened in their training, where they used smell to learn more about a patient,” he says.
In contrast, he also received “somewhat negative letters where the message from those mostly retired physicians was, ‘You’re just not spending enough time with patients.’ I think that is a very unrealistic piece of advice,” says Dr. Bomback. “It would be very interesting to see whether they could carry the pager of a hospitalist or resident for 12 hours and actually be able to do what that hospitalist or resident does.”
Physicians today must first acknowledge the reality “that we don’t have as much time as we need,” says Dr. Bomback. “And once you admit that you’re not going to be able to spend as much time as you ideally would like … that we only have a 12-hour work shift if you are a hospitalist or a 30-hour call shift if you are a resident,” you have to maximize the time with the patient by giving “a focused physical that it is well done, accurate, and respectful to the patient.”
—Tim Creamer, MD, director, hospital medicine program, Community General Hospital, Syracuse, NY
Crisis or Evolution?
Sandeep Jauhar, MD, director of the Heart Failure Program at Long Island Jewish Medical Center, New Hyde Park, N.Y., also had an article in last year’s NEJM “Perspective” series.1-4 In that piece, “The Demise of the Physical Exam,”2 Dr. Jauhar posed a question: Is the demise of physical diagnosis a crisis or a natural evolution? Now, a year later, The Hospitalist asked him that same question.
“I don’t view it as a crisis,” he says, “but maybe that’s because of my vantage point as a cardiologist. Cardiology is very technology-driven; very few diagnoses are made on the basis of the physical exam.”
Dr. Jauhar believes that the greatest benefit of performing a thorough physical exam is not necessarily to pin down a diagnosis, though it can expedite that process, but to limit the tests that are ordered.
William Dickey, MD, hospitalist and director of quality at Abbott Northwestern Medical Center, Minneapolis, Minn., agrees that the decision of what testing to do, if any, is still guided by the physical exam.
“The high-tech diagnostic testing doesn’t demean the importance of the exam of all,” he says, but its role may have changed.
Are the intricate skills of performing a physical exam imperative, or have they mostly been replaced by technology? “I would say they’re not fully imperative under the assumption that you have the technology and you want to get the job done,” says Dr. Bomback. “Are they desired? Absolutely. A good physical exam and a remarkable finding are about showing what goes on inside the body and manifests itself outside the body.”
The ability to adequately hear a heart murmur or detect tetany is based on the physiologic understanding of why that murmur occurs or how calcium metabolism works. With that in mind, Dr. Bomback believes all patients would want their doctors to have those skills. “But,” he quickly qualifies, “could you have a functioning doctor get through his or her workday without knowing that? Absolutely. Could a cardiologist treat CHF without being able to hear a murmur? Of course. … So it’s desirable, but it’s not totally necessary.”
One reason for the desirability of maintaining those skills, which require physicians to “get up close,” as Dr. Dickey puts it, pertains to the importance of touching, seeing, and listening and to the quality of the patient-physician interaction itself.4 All the physicians interviewed for this article concur that getting that physical sense of the patient will tell you things that other information will not, and involving this true sensitivity in the interaction will most likely put the patient at greater ease.
“Because, in addition to all the information that a physician can discover from doing a physical exam, there is also a sense of rapport that the physical exam builds,” says C. Martin Buchanan, MD, FACP, a hospitalist at Penrose Hospital in Colorado Springs, Colo. “The therapy of being there, being present at the patient’s side, touching the patient, doing something for them, having a kind of healing energy, if you will, that we … transmit to the patient and [which essentially communicates], ‘I’m here to help you, I accept you as a human being even though you’re ill; I’m willing to touch you, and I’m here to help you feel better.’”
Not a Demise, but Compromised
“The physical exam is compromised during patient assessment because of where it ranks in importance,” says Tim Creamer, MD, director of the hospital medicine program at Community General Hospital in Syracuse, N.Y. “There are people who say that history is 80% of the diagnosis, which makes the physical exam 20% of the diagnosis. Although you try to emphasize that diagnostics, such as X-rays and labs, should only confirm your history and physical, we still depend too much on the technology to diagnose for us.”
The physical exam is not emphasized after medical school, says Dr. Creamer, who teaches second-year family practice residents. The emphasis now has become the patient-doctor interface: educating and talking with the patient and family. “And even in the lay literature, they encourage consumers to ‘Get your doctor to spend time with you,’” he says. “They mean talking to you, not checking your neck veins for A, C, and V waves.” Hospitalists may also minimize the physical exam, he adds, “because we feel pressured to maximize the talking and listening.”
The Focused Physical
The newest title in the 2006 edition of the Medical Knowledge Self-Assessment Program (MKSAP), published by the American College of Physicians, “Foundations of Internal Medicine,” includes an extensive discussion about the evidence-based physical exam. A good deal of recent research has addressed the topic of which physical findings are truly important to assess various conditions.
“If internists will pay attention to what’s in the medical literature about reliable physical findings,” says Dr. Buchanan, “we can tailor our physical exam a bit better, make more efficient use of the [interview] time, and provide very useful information for our diagnostic assessment and treatment planning.”
The MKSAP-14 offers 11 print books, a CD-ROM, and a new online version. Information is available at www.acponline.org/catalog/mksap/14/.
Powers of Observation
Performing a good physical exam is “something that we all aspire to and something we always try to improve,” says Dr. Bomback. “Anytime I hear of someone with a good physical exam finding I will try to see that patient.” It’s one of the reasons he likes working in an academic center. “There are always interesting cases, and there is always someone who wants to teach someone else what they’re seeing. It’s a constant learning process.”
Dr. Creamer agrees. He used to veer from his day-to-day routine and “follow around Max Kutzer, an internist at Crouse Hospital here at Syracuse, who practiced for years and who taught the physical exam to medical students at Harvard in 1954,” a time—he points out—when little-to-no diagnostic technology existed. Accompanying this master of medical observation, he says, was a Zen-like experience. The elder doctor “would walk to a patient’s doorway and stand there and watch the person breathe and watch how disheveled the bed was, whether the chair had been sat in, and [after] a couple of minutes he would walk out and say, ‘Now tell me what you noticed.’ ”
Dr. Creamer remembers naming “two or three things. But [Dr. Kutzer] would say, ‘OK, but let me tell you 10 more.’ ” Dr. Kutzer, now 96 and still productive, Dr. Creamer says, has written a book, Observation and the Physical Exam, which is in the editing stage.
Because physicians are pressed for time, those powers of observation may be, if not lost, at least largely neglected or ignored. “But I still do those things,” says Dr. Creamer. “I’ll walk to the door and watch a person breathe while they’re sleeping … . You lose the anxiety overtones when you’re watching someone sleeping. ... In order to learn, you need to listen. Listening takes time. You’ve got to step back and take the time to learn, and that’s where it gets tricky.”
Dr. Bomback believes technology will never replace the power of observation. “Those are the unique skills that come with being a hospitalist or any physician … and a lot of the reason why most people become physicians,” he says. “It is a skill that [they have had] from early on. It’s empathy, that you can observe a patient and understand what’s going on—maybe not completely, and not totally consciously, but there is an empathic sensation.”
Conclusion
The traditional use of the physical exam may have changed, but its value is still important to patient care.
“The physical exam is part of the culture of medicine,” says Dr. Jauhar. “It may have started to lose some of its utility as we get more technology, but it can limit the use of technology and help us make diagnoses more quickly.”
Providers might also sometimes be in a place “where you don’t have a CT scan or an MRI machine,” he adds. The provider discovers things that machines can’t supply, and the contributions of even a brief physical exam can communicate humanity to the patient.
“I have always wondered how physicians can do telemedicine,” says Dr. Dickey, “because there is something about being there and being with the patient in terms of judging the severity of illness that is very important.”
“For all these reasons, it’s important for hospitalists to maintain their skills,” says Dr. Jauhar, “because otherwise we’re losing a big part of what it is to be a doctor. We’re just becoming technicians.” TH
Andrea Sattinger is a frequent contributor to The Hospitalist.
References
- Bomback A. The physical exam and the sense of smell. N Engl J Med. 2006 Jan 26;354(4):327-329.
- Jauhar S. The demise of the physical exam. N Engl J Med. 2006;354(6):548-551.
- Markel H. The stethoscope and the art of listening. N Engl J Med. 2006;354(6):551-553.
- Treadway K. Becoming a physician: heart sounds. N Engl J Med. 2006 Mar 16;354(11):1112-1113.
You enter a patient’s room with all your senses on alert. You absorb the environment quickly—even before addressing the patient. It is perhaps these “small moments in medicine,” the under-the-radar information, that a physician may best remember about individual people or cases, says Andrew Bomback, MD, a first-year fellow in nephrology at the University of North Carolina at Chapel Hill. “Not the details of a specific disease state,” he elaborates, “but the visceral memory, such as how someone smells.”
In his article, “The Physical Exam and the Sense of Smell,” published in the New England Journal of Medicine in January 2006, Dr. Bomback writes that his training by doctors who “preached the gospel of the physical exam” was intended so that he and his fellow students “would not forget that the best doctors help their patients with their eyes, ears, and hands, not just with numbers posted on a computer screen.”1
Those small moments are often usurped from doctors as they deal with the demands and obligations of their jobs in an often-hurried environment. Let’s face it, he says, “The physical exam has just been truncated to very brief encounters.”
In fact, facing this dilemma is one of the first remedies he would prescribe. In response to the article, “I got a lot of nice letters from [physicians] who related similar incidents that happened in their training, where they used smell to learn more about a patient,” he says.
In contrast, he also received “somewhat negative letters where the message from those mostly retired physicians was, ‘You’re just not spending enough time with patients.’ I think that is a very unrealistic piece of advice,” says Dr. Bomback. “It would be very interesting to see whether they could carry the pager of a hospitalist or resident for 12 hours and actually be able to do what that hospitalist or resident does.”
Physicians today must first acknowledge the reality “that we don’t have as much time as we need,” says Dr. Bomback. “And once you admit that you’re not going to be able to spend as much time as you ideally would like … that we only have a 12-hour work shift if you are a hospitalist or a 30-hour call shift if you are a resident,” you have to maximize the time with the patient by giving “a focused physical that it is well done, accurate, and respectful to the patient.”
—Tim Creamer, MD, director, hospital medicine program, Community General Hospital, Syracuse, NY
Crisis or Evolution?
Sandeep Jauhar, MD, director of the Heart Failure Program at Long Island Jewish Medical Center, New Hyde Park, N.Y., also had an article in last year’s NEJM “Perspective” series.1-4 In that piece, “The Demise of the Physical Exam,”2 Dr. Jauhar posed a question: Is the demise of physical diagnosis a crisis or a natural evolution? Now, a year later, The Hospitalist asked him that same question.
“I don’t view it as a crisis,” he says, “but maybe that’s because of my vantage point as a cardiologist. Cardiology is very technology-driven; very few diagnoses are made on the basis of the physical exam.”
Dr. Jauhar believes that the greatest benefit of performing a thorough physical exam is not necessarily to pin down a diagnosis, though it can expedite that process, but to limit the tests that are ordered.
William Dickey, MD, hospitalist and director of quality at Abbott Northwestern Medical Center, Minneapolis, Minn., agrees that the decision of what testing to do, if any, is still guided by the physical exam.
“The high-tech diagnostic testing doesn’t demean the importance of the exam of all,” he says, but its role may have changed.
Are the intricate skills of performing a physical exam imperative, or have they mostly been replaced by technology? “I would say they’re not fully imperative under the assumption that you have the technology and you want to get the job done,” says Dr. Bomback. “Are they desired? Absolutely. A good physical exam and a remarkable finding are about showing what goes on inside the body and manifests itself outside the body.”
The ability to adequately hear a heart murmur or detect tetany is based on the physiologic understanding of why that murmur occurs or how calcium metabolism works. With that in mind, Dr. Bomback believes all patients would want their doctors to have those skills. “But,” he quickly qualifies, “could you have a functioning doctor get through his or her workday without knowing that? Absolutely. Could a cardiologist treat CHF without being able to hear a murmur? Of course. … So it’s desirable, but it’s not totally necessary.”
One reason for the desirability of maintaining those skills, which require physicians to “get up close,” as Dr. Dickey puts it, pertains to the importance of touching, seeing, and listening and to the quality of the patient-physician interaction itself.4 All the physicians interviewed for this article concur that getting that physical sense of the patient will tell you things that other information will not, and involving this true sensitivity in the interaction will most likely put the patient at greater ease.
“Because, in addition to all the information that a physician can discover from doing a physical exam, there is also a sense of rapport that the physical exam builds,” says C. Martin Buchanan, MD, FACP, a hospitalist at Penrose Hospital in Colorado Springs, Colo. “The therapy of being there, being present at the patient’s side, touching the patient, doing something for them, having a kind of healing energy, if you will, that we … transmit to the patient and [which essentially communicates], ‘I’m here to help you, I accept you as a human being even though you’re ill; I’m willing to touch you, and I’m here to help you feel better.’”
Not a Demise, but Compromised
“The physical exam is compromised during patient assessment because of where it ranks in importance,” says Tim Creamer, MD, director of the hospital medicine program at Community General Hospital in Syracuse, N.Y. “There are people who say that history is 80% of the diagnosis, which makes the physical exam 20% of the diagnosis. Although you try to emphasize that diagnostics, such as X-rays and labs, should only confirm your history and physical, we still depend too much on the technology to diagnose for us.”
The physical exam is not emphasized after medical school, says Dr. Creamer, who teaches second-year family practice residents. The emphasis now has become the patient-doctor interface: educating and talking with the patient and family. “And even in the lay literature, they encourage consumers to ‘Get your doctor to spend time with you,’” he says. “They mean talking to you, not checking your neck veins for A, C, and V waves.” Hospitalists may also minimize the physical exam, he adds, “because we feel pressured to maximize the talking and listening.”
The Focused Physical
The newest title in the 2006 edition of the Medical Knowledge Self-Assessment Program (MKSAP), published by the American College of Physicians, “Foundations of Internal Medicine,” includes an extensive discussion about the evidence-based physical exam. A good deal of recent research has addressed the topic of which physical findings are truly important to assess various conditions.
“If internists will pay attention to what’s in the medical literature about reliable physical findings,” says Dr. Buchanan, “we can tailor our physical exam a bit better, make more efficient use of the [interview] time, and provide very useful information for our diagnostic assessment and treatment planning.”
The MKSAP-14 offers 11 print books, a CD-ROM, and a new online version. Information is available at www.acponline.org/catalog/mksap/14/.
Powers of Observation
Performing a good physical exam is “something that we all aspire to and something we always try to improve,” says Dr. Bomback. “Anytime I hear of someone with a good physical exam finding I will try to see that patient.” It’s one of the reasons he likes working in an academic center. “There are always interesting cases, and there is always someone who wants to teach someone else what they’re seeing. It’s a constant learning process.”
Dr. Creamer agrees. He used to veer from his day-to-day routine and “follow around Max Kutzer, an internist at Crouse Hospital here at Syracuse, who practiced for years and who taught the physical exam to medical students at Harvard in 1954,” a time—he points out—when little-to-no diagnostic technology existed. Accompanying this master of medical observation, he says, was a Zen-like experience. The elder doctor “would walk to a patient’s doorway and stand there and watch the person breathe and watch how disheveled the bed was, whether the chair had been sat in, and [after] a couple of minutes he would walk out and say, ‘Now tell me what you noticed.’ ”
Dr. Creamer remembers naming “two or three things. But [Dr. Kutzer] would say, ‘OK, but let me tell you 10 more.’ ” Dr. Kutzer, now 96 and still productive, Dr. Creamer says, has written a book, Observation and the Physical Exam, which is in the editing stage.
Because physicians are pressed for time, those powers of observation may be, if not lost, at least largely neglected or ignored. “But I still do those things,” says Dr. Creamer. “I’ll walk to the door and watch a person breathe while they’re sleeping … . You lose the anxiety overtones when you’re watching someone sleeping. ... In order to learn, you need to listen. Listening takes time. You’ve got to step back and take the time to learn, and that’s where it gets tricky.”
Dr. Bomback believes technology will never replace the power of observation. “Those are the unique skills that come with being a hospitalist or any physician … and a lot of the reason why most people become physicians,” he says. “It is a skill that [they have had] from early on. It’s empathy, that you can observe a patient and understand what’s going on—maybe not completely, and not totally consciously, but there is an empathic sensation.”
Conclusion
The traditional use of the physical exam may have changed, but its value is still important to patient care.
“The physical exam is part of the culture of medicine,” says Dr. Jauhar. “It may have started to lose some of its utility as we get more technology, but it can limit the use of technology and help us make diagnoses more quickly.”
Providers might also sometimes be in a place “where you don’t have a CT scan or an MRI machine,” he adds. The provider discovers things that machines can’t supply, and the contributions of even a brief physical exam can communicate humanity to the patient.
“I have always wondered how physicians can do telemedicine,” says Dr. Dickey, “because there is something about being there and being with the patient in terms of judging the severity of illness that is very important.”
“For all these reasons, it’s important for hospitalists to maintain their skills,” says Dr. Jauhar, “because otherwise we’re losing a big part of what it is to be a doctor. We’re just becoming technicians.” TH
Andrea Sattinger is a frequent contributor to The Hospitalist.
References
- Bomback A. The physical exam and the sense of smell. N Engl J Med. 2006 Jan 26;354(4):327-329.
- Jauhar S. The demise of the physical exam. N Engl J Med. 2006;354(6):548-551.
- Markel H. The stethoscope and the art of listening. N Engl J Med. 2006;354(6):551-553.
- Treadway K. Becoming a physician: heart sounds. N Engl J Med. 2006 Mar 16;354(11):1112-1113.
Get Smart
In YOU: The Smart Patient: An Insider's Handbook for Getting the Best Treatment, authors Michael F. Roizen, MD, and Mehmet C. Oz, MD, well-credentialed celebrity physicians, tell the reader that being a smart patient may make the difference between good and poor care and may even save your life. Everyone can be a “medical detective,” they suggest, seeking and supplying the facts that providers and administrators need in order to avoid errors or mix-ups.
The Joint Commission Resources, a collaborator on this publication, announces on its Web site that this book “empowers patients” (www.jcrinc.com/generic.asp?durki=11727&site=11&return=405.). Dr. Oz, in a Web post to customers who might purchase the book, puts it this way: “[T]he Joint Commission, our nation’s healthcare safety advocate, approached us to help with a big problem. Medical errors cost us 98,000 lives per year, and the Joint Commission could not squash this crazily large number without pulling in the biggest ally of all, the Smart Patient.” It’s a “scary statistic,” but true, he writes, “You have a two in five chance of being affected by a major medical complication in your life.” (For more information on the book, visit www.amazon.com/YOU-Insiders-Handbook-Getting-Treatment/dp/0743293010.)
The Hospitalist asked some hospitalists what they would recommend to a friend or relative headed for a hospital stay. Do they have any tips that only an insider would know? As might be expected, some of their advice echoes that already available in print, in broadcasts, and on the Web. And some things that were mentioned in these publications were also on our hospitalists’ list, including bringing along statistics, dates, and other healthcare specifics that might be crucial to providers. In fact, Drs. Roizen and Oz recommend assembling a thorough health history and bringing two copies of it to hospital admission—one especially for “the admitting nurse who welcomes you to your bed.”
Assume Nothing
In their book chapter on hospital stays, Drs. Oz and Roizen emphasize that patients and their visitors should keep an eye out to make certain hospital staff wash their hands and give the patient the right treatments, tests, and medications. “It’s astounding the amount of diligence you and your family will have to exercise during a hospital stay,” a reader-reviewer writes on the book’s Web page on the Amazon.com site. Some of the warnings posted in a book excerpt at the Joint Commission on Accreditation of Healthcare Organizations (JCAHO)’s site include “Don’t touch that remote!” and “wear rubber gloves” if you do want to watch TV. Readers are told that “a study found that the TV remote control is one of the most germ-infested things in a hospital room.”
Patients are also cautioned to “insist on being scanned,” to “insist on a clean stethoscope,” and to keep “an industrial-sized jug of alcohol hand-sanitizing gel” by the bed. In fact, the authors write: “Stethoscopes are filthy from being used on several patients an hour. Most doc[tor]s now wash their stethoscopes with alcohol between patients, but we’d always ask.” Our hospitalists agreed.
Ian Jenkins, MD, a hospitalist with the University of California at San Diego, would tell his friends and family to remind providers to wash their hands. “Don’t let anyone touch you unless you’ve seen them wash or gel their hands correctly—and their stethoscopes, too.”
Drs. Oz and Roizen say, “You might even post a sign that reads ‘Thank You for Washing Your Hands’ as a gentle reminder.”
Trust your intuition, one hospitalist tells people facing hospitalization. “If you sense that something is awry, it probably is,” says Jeanne Farnan, MD, a hospitalist scholar at The University of Chicago Hospitals. “Discuss concerns with physicians/nurses. Write down your questions in case they come to you spontaneously.”
On the other hand, she tells friends and relatives, “Patients, when asked questions, will often respond, ‘it’s in my chart.’ We often don't have access to a primary MD’s notes/chart, and not all documentation is pristine. When we are asking questions regarding your medical history, it is only to provide you with the best care—not to be a nuisance.”
Be Selective about Your Providers and Hospital
One recommendation from JCAHO’s patient education Web pages is a section entitled “Finding Dr. Right.” “Choose wisely and you could rest easy for many years to come,” it says.
Sandeep Sachdeva, MD, lead hospitalist at Swedish Medical Center’s Stroke Program and clinical instructor at the University of Washington at Seattle, says this may apply even to a patient’s relationship with a hospitalist.
“Sometimes patients come in and tell us their stories [about how providers treat them]. It’s just amazing; I think patients who have family members providing close supervision seem to get better care than somebody [who] is not asking questions,” he says. “And some care providers find questions intimidating, but the patient should not get discouraged by that. … If they feel that the care provider is not listening to them or not being attentive to them, they can always have a recourse: They can talk to the supervisor of that provider or somebody else [to get] a different provider. Patients sometimes have the fear that if they speak up against somebody that their care might be jeopardized.”
Dr. Sachdeva advises friends and relatives that they talk to the nursing supervisor or ask for the physician supervisor or an administrative person or social worker so that they get the attention they need.
Dr. Jenkins agrees. “Informed consent” is one of his tips for friends and family: “If your doctor won't talk to you about the risks and benefits of your treatments, and alternatives to them, you need a new doctor.”
Our hospitalists suggest being discriminating, savvy, and proactive:
- “Find one hospital you are comfortable with, [where] your family physician is on staff, and use it exclusively if possible,” says David M. Grace, MD, a hospitalist with The Schumacher Group in Lafayette, La. “By utilizing one hospital, all of your previous records and test results are immediately available when needed. Often this translates into a much shorter hospitalization as there are no delays in obtaining old records, and it minimizes the chance of duplicate tests/procedures being performed.”
- “Know who your doctors are [and] what their role is, and understand their input into your healthcare,” says Dr. Farnan, who is extensively involved in medical residents’ training. And “be cognizant of the physician work hours,” she advises. “We often have families who demand to speak with ‘their’ doctor at all hours of the early morning and night.” She tells friends and relatives, “I think more patients need to understand the nature [and] structure of the system [and] what kind of information a covering physician can provide. If the family of the patient has questions [and] wants to speak with the primary MD, it may be best to attempt in the daytime when the primary service is more likely to be present.”
- “Know the full names, and preferably [the] phone numbers, of all your outpatient physicians,” says Dr. Grace. “One area will often have multiple doctors with the same last name, and, frequently, records need to be requested from them. Up-to-date contact information on your physicians helps us request the right records from the right physicians with minimal delay.”
What to Bring to the Hospital
Some hospital Web sites advise patients on what to bring with them for their hospital stay, suggesting everything from your own robe, slippers, pajamas, or nightgown to an advance directive. Definitely, the latter is an important point.
“Whether it’s an elective or emergent admission,” says Dr. Grace, “there are a few things [you] can do to ensure [your] hospitalization is as safe, efficient, and productive as possible,” he tells friends and relatives. Among them, he says, is to “have a Living Will or advance directives completed, ensure the hospital has a copy, and discuss your wishes with your family prior to admission. Clear and concise plans, coupled with good family awareness, will help ensure your wishes and values are honored appropriately.”
And, as several of his hospitalist colleagues suggest, “Bring all of the medications you are currently using, including any over-the-counter medicines and herbs or homeopathic treatments. It’s imperative that physicians know what medications you are taking [because] many cannot be stopped abruptly, and [they may] have interactions with medications you may receive in the hospital.”
In addition, “know what medications you’re truly allergic to [e.g., hives, swelling, breathing problems],” Dr. Grace advises, “and which medications you have had side effects from [e.g., stomach upset, sleepiness, and so on]. Many patients confuse the two. Occasionally the best or only option involves using medications with potential unwanted side effects. Rarely do we use medications to which the patient has a true allergy.”
Communication: The Key to the Hospital Kingdom
Dr. Sachdeva recommends being ready to communicate even before going to the hospital. “In the case of an emergency admission,” he says, “they should have all their information readily available because at the time for a needed hospitalization, they may be sick and confused.” Have it “on their person” or in “an easily identifiable place,” he says, and, like his colleagues, he reiterates that this information should include a list of medications, problems, doctors, and phone numbers, along with a list of patient advocates and their phone numbers.
“Most of the time, patients are able to notify a family member, but if that doesn’t happen, then the ER can notify the appropriate person to be present to supervise and oversee the care from a patient perspective,” he says.
Communication was mentioned by all the hospitalists we interviewed. “Be prepared to ask questions and take an active role in your healthcare,” says Dr. Grace. “Ask your nurse what each medication you receive is and what it’s for. Ensure you know what medications to continue taking when you return home and which ones to stop. If you don’t understand your diagnosis, prognosis, or treatment plan, make sure you ask.”
One hospitalist’s advice pertained to the patient’s and family’s behavior and is based on an experience in her own family: “Be really nice to everybody,” Alison Holmes, MD, a hospitalist with Concord Hospital, Concord, N.H., advises friends and family. “This is hard to do when you’re sick and scared, but it’s incredibly important.”
Dr. Holmes speaks of her own parents’ experience: “My mother was admitted to the hospital for pneumonia about a year ago. She had very long wait in the emergency room. My father got very upset and called me and said, ‘Oh, they were so angry at me, I was yelling at everybody.’
“That won’t get you anywhere!” I told him. “That will get you worse care.” I asked, “Where is she now?” and he said, ‘Oh, she’s still in the emergency room,’ and I said, “You’re at home? You left her there?” Dr. Holmes then advised her father to return to the hospital right away.
Finally, all the hospitalists we interviewed emphasized that they would tell their family members to designate a point person for communication. And you can’t assume that that would be their doctor son or daughter, even if they happened to be in the same locale.
“When possible, don’t stay in the hospital alone,” says Dr. Holmes. “Try to always have a family member present so that there is someone available for questions. It’s not always clear where [the physician] can reach someone or how far away [that person is]. It can take a little coordination and multiple people to do it,” she says.
Also, Dr. Farnan points out, “It is often difficult [because of time limitations] for [physicians] to repeat the same information to multiple family members.”
All patients, but especially the elderly, says Dr. Sachdeva, should have a patient advocate with them at the hospital. If they don’t have family close by, they should have “a close friend or neighbor who is willing to take on that job, someone who can be there in the room and ask these questions: What medicine are you giving me? What’s the next step? What are the options?”
Dr. Sachdeva advises relatives that they might be distressed or unable to focus, so having a healthy advocate with them may be extremely important, “the difference between life and death,” although, no doubt, he’d leave that last comment out of his advice to family. “Because a lot of the time, it is not that we don’t try to do a good job, but it’s just [that] the advocate might bring something to our attention that we might not have otherwise noticed.” TH
Andrea Sattinger has been writing for The Hospitalist since 2005.
In YOU: The Smart Patient: An Insider's Handbook for Getting the Best Treatment, authors Michael F. Roizen, MD, and Mehmet C. Oz, MD, well-credentialed celebrity physicians, tell the reader that being a smart patient may make the difference between good and poor care and may even save your life. Everyone can be a “medical detective,” they suggest, seeking and supplying the facts that providers and administrators need in order to avoid errors or mix-ups.
The Joint Commission Resources, a collaborator on this publication, announces on its Web site that this book “empowers patients” (www.jcrinc.com/generic.asp?durki=11727&site=11&return=405.). Dr. Oz, in a Web post to customers who might purchase the book, puts it this way: “[T]he Joint Commission, our nation’s healthcare safety advocate, approached us to help with a big problem. Medical errors cost us 98,000 lives per year, and the Joint Commission could not squash this crazily large number without pulling in the biggest ally of all, the Smart Patient.” It’s a “scary statistic,” but true, he writes, “You have a two in five chance of being affected by a major medical complication in your life.” (For more information on the book, visit www.amazon.com/YOU-Insiders-Handbook-Getting-Treatment/dp/0743293010.)
The Hospitalist asked some hospitalists what they would recommend to a friend or relative headed for a hospital stay. Do they have any tips that only an insider would know? As might be expected, some of their advice echoes that already available in print, in broadcasts, and on the Web. And some things that were mentioned in these publications were also on our hospitalists’ list, including bringing along statistics, dates, and other healthcare specifics that might be crucial to providers. In fact, Drs. Roizen and Oz recommend assembling a thorough health history and bringing two copies of it to hospital admission—one especially for “the admitting nurse who welcomes you to your bed.”
Assume Nothing
In their book chapter on hospital stays, Drs. Oz and Roizen emphasize that patients and their visitors should keep an eye out to make certain hospital staff wash their hands and give the patient the right treatments, tests, and medications. “It’s astounding the amount of diligence you and your family will have to exercise during a hospital stay,” a reader-reviewer writes on the book’s Web page on the Amazon.com site. Some of the warnings posted in a book excerpt at the Joint Commission on Accreditation of Healthcare Organizations (JCAHO)’s site include “Don’t touch that remote!” and “wear rubber gloves” if you do want to watch TV. Readers are told that “a study found that the TV remote control is one of the most germ-infested things in a hospital room.”
Patients are also cautioned to “insist on being scanned,” to “insist on a clean stethoscope,” and to keep “an industrial-sized jug of alcohol hand-sanitizing gel” by the bed. In fact, the authors write: “Stethoscopes are filthy from being used on several patients an hour. Most doc[tor]s now wash their stethoscopes with alcohol between patients, but we’d always ask.” Our hospitalists agreed.
Ian Jenkins, MD, a hospitalist with the University of California at San Diego, would tell his friends and family to remind providers to wash their hands. “Don’t let anyone touch you unless you’ve seen them wash or gel their hands correctly—and their stethoscopes, too.”
Drs. Oz and Roizen say, “You might even post a sign that reads ‘Thank You for Washing Your Hands’ as a gentle reminder.”
Trust your intuition, one hospitalist tells people facing hospitalization. “If you sense that something is awry, it probably is,” says Jeanne Farnan, MD, a hospitalist scholar at The University of Chicago Hospitals. “Discuss concerns with physicians/nurses. Write down your questions in case they come to you spontaneously.”
On the other hand, she tells friends and relatives, “Patients, when asked questions, will often respond, ‘it’s in my chart.’ We often don't have access to a primary MD’s notes/chart, and not all documentation is pristine. When we are asking questions regarding your medical history, it is only to provide you with the best care—not to be a nuisance.”
Be Selective about Your Providers and Hospital
One recommendation from JCAHO’s patient education Web pages is a section entitled “Finding Dr. Right.” “Choose wisely and you could rest easy for many years to come,” it says.
Sandeep Sachdeva, MD, lead hospitalist at Swedish Medical Center’s Stroke Program and clinical instructor at the University of Washington at Seattle, says this may apply even to a patient’s relationship with a hospitalist.
“Sometimes patients come in and tell us their stories [about how providers treat them]. It’s just amazing; I think patients who have family members providing close supervision seem to get better care than somebody [who] is not asking questions,” he says. “And some care providers find questions intimidating, but the patient should not get discouraged by that. … If they feel that the care provider is not listening to them or not being attentive to them, they can always have a recourse: They can talk to the supervisor of that provider or somebody else [to get] a different provider. Patients sometimes have the fear that if they speak up against somebody that their care might be jeopardized.”
Dr. Sachdeva advises friends and relatives that they talk to the nursing supervisor or ask for the physician supervisor or an administrative person or social worker so that they get the attention they need.
Dr. Jenkins agrees. “Informed consent” is one of his tips for friends and family: “If your doctor won't talk to you about the risks and benefits of your treatments, and alternatives to them, you need a new doctor.”
Our hospitalists suggest being discriminating, savvy, and proactive:
- “Find one hospital you are comfortable with, [where] your family physician is on staff, and use it exclusively if possible,” says David M. Grace, MD, a hospitalist with The Schumacher Group in Lafayette, La. “By utilizing one hospital, all of your previous records and test results are immediately available when needed. Often this translates into a much shorter hospitalization as there are no delays in obtaining old records, and it minimizes the chance of duplicate tests/procedures being performed.”
- “Know who your doctors are [and] what their role is, and understand their input into your healthcare,” says Dr. Farnan, who is extensively involved in medical residents’ training. And “be cognizant of the physician work hours,” she advises. “We often have families who demand to speak with ‘their’ doctor at all hours of the early morning and night.” She tells friends and relatives, “I think more patients need to understand the nature [and] structure of the system [and] what kind of information a covering physician can provide. If the family of the patient has questions [and] wants to speak with the primary MD, it may be best to attempt in the daytime when the primary service is more likely to be present.”
- “Know the full names, and preferably [the] phone numbers, of all your outpatient physicians,” says Dr. Grace. “One area will often have multiple doctors with the same last name, and, frequently, records need to be requested from them. Up-to-date contact information on your physicians helps us request the right records from the right physicians with minimal delay.”
What to Bring to the Hospital
Some hospital Web sites advise patients on what to bring with them for their hospital stay, suggesting everything from your own robe, slippers, pajamas, or nightgown to an advance directive. Definitely, the latter is an important point.
“Whether it’s an elective or emergent admission,” says Dr. Grace, “there are a few things [you] can do to ensure [your] hospitalization is as safe, efficient, and productive as possible,” he tells friends and relatives. Among them, he says, is to “have a Living Will or advance directives completed, ensure the hospital has a copy, and discuss your wishes with your family prior to admission. Clear and concise plans, coupled with good family awareness, will help ensure your wishes and values are honored appropriately.”
And, as several of his hospitalist colleagues suggest, “Bring all of the medications you are currently using, including any over-the-counter medicines and herbs or homeopathic treatments. It’s imperative that physicians know what medications you are taking [because] many cannot be stopped abruptly, and [they may] have interactions with medications you may receive in the hospital.”
In addition, “know what medications you’re truly allergic to [e.g., hives, swelling, breathing problems],” Dr. Grace advises, “and which medications you have had side effects from [e.g., stomach upset, sleepiness, and so on]. Many patients confuse the two. Occasionally the best or only option involves using medications with potential unwanted side effects. Rarely do we use medications to which the patient has a true allergy.”
Communication: The Key to the Hospital Kingdom
Dr. Sachdeva recommends being ready to communicate even before going to the hospital. “In the case of an emergency admission,” he says, “they should have all their information readily available because at the time for a needed hospitalization, they may be sick and confused.” Have it “on their person” or in “an easily identifiable place,” he says, and, like his colleagues, he reiterates that this information should include a list of medications, problems, doctors, and phone numbers, along with a list of patient advocates and their phone numbers.
“Most of the time, patients are able to notify a family member, but if that doesn’t happen, then the ER can notify the appropriate person to be present to supervise and oversee the care from a patient perspective,” he says.
Communication was mentioned by all the hospitalists we interviewed. “Be prepared to ask questions and take an active role in your healthcare,” says Dr. Grace. “Ask your nurse what each medication you receive is and what it’s for. Ensure you know what medications to continue taking when you return home and which ones to stop. If you don’t understand your diagnosis, prognosis, or treatment plan, make sure you ask.”
One hospitalist’s advice pertained to the patient’s and family’s behavior and is based on an experience in her own family: “Be really nice to everybody,” Alison Holmes, MD, a hospitalist with Concord Hospital, Concord, N.H., advises friends and family. “This is hard to do when you’re sick and scared, but it’s incredibly important.”
Dr. Holmes speaks of her own parents’ experience: “My mother was admitted to the hospital for pneumonia about a year ago. She had very long wait in the emergency room. My father got very upset and called me and said, ‘Oh, they were so angry at me, I was yelling at everybody.’
“That won’t get you anywhere!” I told him. “That will get you worse care.” I asked, “Where is she now?” and he said, ‘Oh, she’s still in the emergency room,’ and I said, “You’re at home? You left her there?” Dr. Holmes then advised her father to return to the hospital right away.
Finally, all the hospitalists we interviewed emphasized that they would tell their family members to designate a point person for communication. And you can’t assume that that would be their doctor son or daughter, even if they happened to be in the same locale.
“When possible, don’t stay in the hospital alone,” says Dr. Holmes. “Try to always have a family member present so that there is someone available for questions. It’s not always clear where [the physician] can reach someone or how far away [that person is]. It can take a little coordination and multiple people to do it,” she says.
Also, Dr. Farnan points out, “It is often difficult [because of time limitations] for [physicians] to repeat the same information to multiple family members.”
All patients, but especially the elderly, says Dr. Sachdeva, should have a patient advocate with them at the hospital. If they don’t have family close by, they should have “a close friend or neighbor who is willing to take on that job, someone who can be there in the room and ask these questions: What medicine are you giving me? What’s the next step? What are the options?”
Dr. Sachdeva advises relatives that they might be distressed or unable to focus, so having a healthy advocate with them may be extremely important, “the difference between life and death,” although, no doubt, he’d leave that last comment out of his advice to family. “Because a lot of the time, it is not that we don’t try to do a good job, but it’s just [that] the advocate might bring something to our attention that we might not have otherwise noticed.” TH
Andrea Sattinger has been writing for The Hospitalist since 2005.
In YOU: The Smart Patient: An Insider's Handbook for Getting the Best Treatment, authors Michael F. Roizen, MD, and Mehmet C. Oz, MD, well-credentialed celebrity physicians, tell the reader that being a smart patient may make the difference between good and poor care and may even save your life. Everyone can be a “medical detective,” they suggest, seeking and supplying the facts that providers and administrators need in order to avoid errors or mix-ups.
The Joint Commission Resources, a collaborator on this publication, announces on its Web site that this book “empowers patients” (www.jcrinc.com/generic.asp?durki=11727&site=11&return=405.). Dr. Oz, in a Web post to customers who might purchase the book, puts it this way: “[T]he Joint Commission, our nation’s healthcare safety advocate, approached us to help with a big problem. Medical errors cost us 98,000 lives per year, and the Joint Commission could not squash this crazily large number without pulling in the biggest ally of all, the Smart Patient.” It’s a “scary statistic,” but true, he writes, “You have a two in five chance of being affected by a major medical complication in your life.” (For more information on the book, visit www.amazon.com/YOU-Insiders-Handbook-Getting-Treatment/dp/0743293010.)
The Hospitalist asked some hospitalists what they would recommend to a friend or relative headed for a hospital stay. Do they have any tips that only an insider would know? As might be expected, some of their advice echoes that already available in print, in broadcasts, and on the Web. And some things that were mentioned in these publications were also on our hospitalists’ list, including bringing along statistics, dates, and other healthcare specifics that might be crucial to providers. In fact, Drs. Roizen and Oz recommend assembling a thorough health history and bringing two copies of it to hospital admission—one especially for “the admitting nurse who welcomes you to your bed.”
Assume Nothing
In their book chapter on hospital stays, Drs. Oz and Roizen emphasize that patients and their visitors should keep an eye out to make certain hospital staff wash their hands and give the patient the right treatments, tests, and medications. “It’s astounding the amount of diligence you and your family will have to exercise during a hospital stay,” a reader-reviewer writes on the book’s Web page on the Amazon.com site. Some of the warnings posted in a book excerpt at the Joint Commission on Accreditation of Healthcare Organizations (JCAHO)’s site include “Don’t touch that remote!” and “wear rubber gloves” if you do want to watch TV. Readers are told that “a study found that the TV remote control is one of the most germ-infested things in a hospital room.”
Patients are also cautioned to “insist on being scanned,” to “insist on a clean stethoscope,” and to keep “an industrial-sized jug of alcohol hand-sanitizing gel” by the bed. In fact, the authors write: “Stethoscopes are filthy from being used on several patients an hour. Most doc[tor]s now wash their stethoscopes with alcohol between patients, but we’d always ask.” Our hospitalists agreed.
Ian Jenkins, MD, a hospitalist with the University of California at San Diego, would tell his friends and family to remind providers to wash their hands. “Don’t let anyone touch you unless you’ve seen them wash or gel their hands correctly—and their stethoscopes, too.”
Drs. Oz and Roizen say, “You might even post a sign that reads ‘Thank You for Washing Your Hands’ as a gentle reminder.”
Trust your intuition, one hospitalist tells people facing hospitalization. “If you sense that something is awry, it probably is,” says Jeanne Farnan, MD, a hospitalist scholar at The University of Chicago Hospitals. “Discuss concerns with physicians/nurses. Write down your questions in case they come to you spontaneously.”
On the other hand, she tells friends and relatives, “Patients, when asked questions, will often respond, ‘it’s in my chart.’ We often don't have access to a primary MD’s notes/chart, and not all documentation is pristine. When we are asking questions regarding your medical history, it is only to provide you with the best care—not to be a nuisance.”
Be Selective about Your Providers and Hospital
One recommendation from JCAHO’s patient education Web pages is a section entitled “Finding Dr. Right.” “Choose wisely and you could rest easy for many years to come,” it says.
Sandeep Sachdeva, MD, lead hospitalist at Swedish Medical Center’s Stroke Program and clinical instructor at the University of Washington at Seattle, says this may apply even to a patient’s relationship with a hospitalist.
“Sometimes patients come in and tell us their stories [about how providers treat them]. It’s just amazing; I think patients who have family members providing close supervision seem to get better care than somebody [who] is not asking questions,” he says. “And some care providers find questions intimidating, but the patient should not get discouraged by that. … If they feel that the care provider is not listening to them or not being attentive to them, they can always have a recourse: They can talk to the supervisor of that provider or somebody else [to get] a different provider. Patients sometimes have the fear that if they speak up against somebody that their care might be jeopardized.”
Dr. Sachdeva advises friends and relatives that they talk to the nursing supervisor or ask for the physician supervisor or an administrative person or social worker so that they get the attention they need.
Dr. Jenkins agrees. “Informed consent” is one of his tips for friends and family: “If your doctor won't talk to you about the risks and benefits of your treatments, and alternatives to them, you need a new doctor.”
Our hospitalists suggest being discriminating, savvy, and proactive:
- “Find one hospital you are comfortable with, [where] your family physician is on staff, and use it exclusively if possible,” says David M. Grace, MD, a hospitalist with The Schumacher Group in Lafayette, La. “By utilizing one hospital, all of your previous records and test results are immediately available when needed. Often this translates into a much shorter hospitalization as there are no delays in obtaining old records, and it minimizes the chance of duplicate tests/procedures being performed.”
- “Know who your doctors are [and] what their role is, and understand their input into your healthcare,” says Dr. Farnan, who is extensively involved in medical residents’ training. And “be cognizant of the physician work hours,” she advises. “We often have families who demand to speak with ‘their’ doctor at all hours of the early morning and night.” She tells friends and relatives, “I think more patients need to understand the nature [and] structure of the system [and] what kind of information a covering physician can provide. If the family of the patient has questions [and] wants to speak with the primary MD, it may be best to attempt in the daytime when the primary service is more likely to be present.”
- “Know the full names, and preferably [the] phone numbers, of all your outpatient physicians,” says Dr. Grace. “One area will often have multiple doctors with the same last name, and, frequently, records need to be requested from them. Up-to-date contact information on your physicians helps us request the right records from the right physicians with minimal delay.”
What to Bring to the Hospital
Some hospital Web sites advise patients on what to bring with them for their hospital stay, suggesting everything from your own robe, slippers, pajamas, or nightgown to an advance directive. Definitely, the latter is an important point.
“Whether it’s an elective or emergent admission,” says Dr. Grace, “there are a few things [you] can do to ensure [your] hospitalization is as safe, efficient, and productive as possible,” he tells friends and relatives. Among them, he says, is to “have a Living Will or advance directives completed, ensure the hospital has a copy, and discuss your wishes with your family prior to admission. Clear and concise plans, coupled with good family awareness, will help ensure your wishes and values are honored appropriately.”
And, as several of his hospitalist colleagues suggest, “Bring all of the medications you are currently using, including any over-the-counter medicines and herbs or homeopathic treatments. It’s imperative that physicians know what medications you are taking [because] many cannot be stopped abruptly, and [they may] have interactions with medications you may receive in the hospital.”
In addition, “know what medications you’re truly allergic to [e.g., hives, swelling, breathing problems],” Dr. Grace advises, “and which medications you have had side effects from [e.g., stomach upset, sleepiness, and so on]. Many patients confuse the two. Occasionally the best or only option involves using medications with potential unwanted side effects. Rarely do we use medications to which the patient has a true allergy.”
Communication: The Key to the Hospital Kingdom
Dr. Sachdeva recommends being ready to communicate even before going to the hospital. “In the case of an emergency admission,” he says, “they should have all their information readily available because at the time for a needed hospitalization, they may be sick and confused.” Have it “on their person” or in “an easily identifiable place,” he says, and, like his colleagues, he reiterates that this information should include a list of medications, problems, doctors, and phone numbers, along with a list of patient advocates and their phone numbers.
“Most of the time, patients are able to notify a family member, but if that doesn’t happen, then the ER can notify the appropriate person to be present to supervise and oversee the care from a patient perspective,” he says.
Communication was mentioned by all the hospitalists we interviewed. “Be prepared to ask questions and take an active role in your healthcare,” says Dr. Grace. “Ask your nurse what each medication you receive is and what it’s for. Ensure you know what medications to continue taking when you return home and which ones to stop. If you don’t understand your diagnosis, prognosis, or treatment plan, make sure you ask.”
One hospitalist’s advice pertained to the patient’s and family’s behavior and is based on an experience in her own family: “Be really nice to everybody,” Alison Holmes, MD, a hospitalist with Concord Hospital, Concord, N.H., advises friends and family. “This is hard to do when you’re sick and scared, but it’s incredibly important.”
Dr. Holmes speaks of her own parents’ experience: “My mother was admitted to the hospital for pneumonia about a year ago. She had very long wait in the emergency room. My father got very upset and called me and said, ‘Oh, they were so angry at me, I was yelling at everybody.’
“That won’t get you anywhere!” I told him. “That will get you worse care.” I asked, “Where is she now?” and he said, ‘Oh, she’s still in the emergency room,’ and I said, “You’re at home? You left her there?” Dr. Holmes then advised her father to return to the hospital right away.
Finally, all the hospitalists we interviewed emphasized that they would tell their family members to designate a point person for communication. And you can’t assume that that would be their doctor son or daughter, even if they happened to be in the same locale.
“When possible, don’t stay in the hospital alone,” says Dr. Holmes. “Try to always have a family member present so that there is someone available for questions. It’s not always clear where [the physician] can reach someone or how far away [that person is]. It can take a little coordination and multiple people to do it,” she says.
Also, Dr. Farnan points out, “It is often difficult [because of time limitations] for [physicians] to repeat the same information to multiple family members.”
All patients, but especially the elderly, says Dr. Sachdeva, should have a patient advocate with them at the hospital. If they don’t have family close by, they should have “a close friend or neighbor who is willing to take on that job, someone who can be there in the room and ask these questions: What medicine are you giving me? What’s the next step? What are the options?”
Dr. Sachdeva advises relatives that they might be distressed or unable to focus, so having a healthy advocate with them may be extremely important, “the difference between life and death,” although, no doubt, he’d leave that last comment out of his advice to family. “Because a lot of the time, it is not that we don’t try to do a good job, but it’s just [that] the advocate might bring something to our attention that we might not have otherwise noticed.” TH
Andrea Sattinger has been writing for The Hospitalist since 2005.
Unforgettable
Recently The Hospitalist asked readers to share their reminiscences of patients who had left their mark in some special way on the docs’ lives. Here are those stories.
Patient al Dente
Sandi Verbin, MD, pediatric hospitalist at Temple University Children's Hospital, Philadelphia, and part-time pediatric hospitalist at Holy Redeemer Hospital, Meadowbrook, Pa.
It was midnight in the ER. My shift was ending, and I had to be up early in the morning to drive to my niece’s third birthday party about two hours away. The ER showed no signs of slowing, however, and one of the nurses approached me, asking if I could see the “quick” patient in Room 4: a child with a piece of macaroni stuck up his nose.
In over 10 years of pediatric practice, the allure of placing foreign objects in body orifices has eluded me. Why is this fun? Nevertheless, a parade of toddlers have presented themselves to me with such varied objects as crayons, tissue paper, beads, coffee beans, Play-Doh, M&Ms, rocks, and magnets in their ears and nostrils. (This doesn’t count the unfortunate innocent bystanders who presented with insects having claimed “squatter’s rights” to the patients’ auditory canals.)
Invariably, when asked, the children deny knowing how the object came to be there—at best, a lame “it just fell in” is offered. When questioned as to how the offending object came so close to the involved area, I am met with silence or a shrug. One memorable child told me he did not believe I was the doctor because I was a girl. I let it pass, considering he had put a rabbit food pellet in his ear after being dared to do so by his older brother. I felt his overall judgment was somewhat questionable.
I entered Room 4, prepared to see the usual anxious—or, as in some cases, oblivious—toddler. Instead, to my surprise, a sheepish-looking eight-year-old boy sat on the table, accompanied by his exasperated mother. The pair had been waiting for several hours for the anticipated pasta-ectomy.
Unable to stop myself, I blurted out, “What is a big boy like you doing putting macaroni up his nose? I expect to see this in little kids, but not eight-year-old boys!” The child answered that he had put the macaroni up his nose “when I was in preschool.”
“You mean five or six years ago?” I asked incredulously. When he reluctantly said yes, I explained that I would look up his nose, but that that piece of macaroni was long gone—dissolved or swallowed lo these many years ago. Sure enough, an exam revealed turbinates and mucus but no complex carbohydrates.
I explained to the mother again that there was no way the food item could have survived in the child’s nose for five years, that he would have presented with sinusitis years ago had the macaroni not been swallowed, dissolved, or sneezed out, and that there was no place else to which it could have migrated.
My best diagnosis was that the child had an unusually dry, sharp-feeling piece of mucus in his nose. The discomfort of this had caused him to admit his transgression, committed in the reckless days of toddlerhood, one which had clearly been a source of guilt for him ever since. After some saline nose drops, and no doubt due in no small part to the soul-cleansing effects of confession, the boy felt better. He and mom went home.
I left the ER to contemplate what antics the next day’s group of three-year-olds would cook up. I vowed to keep a close eye on the Jelly Beans.
Great Foster Mom
Alison Holmes, MD, MPH, pediatric hospitalist, Concord Hospital, Concord, N.H., and assistant professor of Community and Family Medicine, Dartmouth Medical School, contributed two stories.
When I was a resident, there was one chronically ill baby who was born at 34 weeks and had significant cyanotic heart disease. He would need a number of high-risk cardiac surgeries, and he also had a portion of his small intestine removed for necrotizing enterocolitis [caused by] his prematurity. After that it can be hard to absorb [nutrients] and grow. The baby had a lot of trouble with diarrhea and dehydration. We put him on the GI service, and the fluid overload from rehydration caused him to go into heart failure, and nobody could ever get the balance right.
He’d go back and forth between the GI service and the cardiology service. All the residents knew him, and he was in a horrible social situation. His mother was a drug user, and after his birth she never visited; we didn’t know anything about the father. The baby was this high-risk infant who basically had laid in the hospital with the TV on for the first five months of his life. Nobody paid attention to him, and I remember thinking, “This is horrible. He’s not going to get any love or nurturing. He’s not going to be normal, because nobody picks him up and holds him and talks to him.”
He was discharged into foster care, and I became his primary doctor. He just had the greatest foster mother in the world. She didn’t care that he had these medical problems; she was so glad to have a baby. She had been a foster parent for a while and had cared for troubled older children and had had enough of that, and she had her own 11-year-old. She was so thrilled to have this baby, and she just loved him and loved him and loved him.
I watched over the next year as he regained normal development despite all his early setbacks—both medical and social. Eventually his father did get involved; he went back into the father’s care, and the father rallied his whole family. The foster mother stays in touch with the family and is the child’s godmother.
By the time I finished residency, he was about three and a half years old, had been through three major cardiac surgeries, and was completely developmentally normal. I’ll never forget that no matter what we do medically, it’s people like that foster mother who make a difference for children.
Doing Wonders
I cared for a growth-retarded baby whose mother was in her late 30s. She was a drug user, and she had lost custody of her three prior children. Here she was with a fourth child, without any supports. She had used cocaine until about the fifth month of her pregnancy, when she decided to get some help.
I thought, “What are this baby’s chances?” But [the mom] did it. She did not go back to using drugs. She stayed clean and reconciled with the father. Life wasn’t always so kind to her. She couldn’t always hold down the same job, but at least she always had a job. She did wonders for this little girl, and she was able to turn her own life around.
Yet One More Challenge
Sandeep Sachdeva, MD, hospitalist at Swedish Medical Center; lead hospitalist, Swedish Medical Center’s Stroke Program; and clinical instructor, University of Washington, Seattle.
The patient I was most impressed by was a lady who came into the hospital about a year ago. I think she was in her mid 60s and had been blind and deaf from birth. She had obviously faced huge challenges and was living alone.
She had a very good support system: a non-governmental organization (NGO) here that provides close support for people in this type of situation. Even though she didn’t have any family support, these volunteers from the NGO would come out to make sure she was doing OK.
As I recall, she had tripped over something and had fallen and broken her hip, and she was admitted to the hospital for hip surgery. Just looking after her was a tremendous learning experience for me: She couldn't see me; she couldn’t hear me; and the only way we could communicate was through a sign language interpreter, where she had to feel the hands of the person doing sign language. She was very involved in her own care; she would ask questions, and there was no dearth of communication.
It was fascinating to deal with this lady who is—in essence—in a different universe with no sound and no sight, and who was facing the challenge of being in the hospital and recovering from her surgery. It felt very satisfying to look after her and to be inspired by her—a patient who was able to overcome yet another challenge when she is already disadvantaged. She did very well, and I believe she went home. I could still feel that she was trying to be independent and be the take-charge person that she had always been.
Patient in a Pickle
Eric Kupersmith, MD, assistant professor of medicine and director of the Hospitalist Program at Cooper Hospital, Camden, N.J. Dr. Kupersmith has plenty of patients he’ll never forget. Here are the stories of few.
There was a patient who would get admitted every month with congestive heart failure. He would develop pulmonary edema as an acute event like clockwork, and no one could figure out what was causing this. The seventh consecutive time, he was placed on my service. We eventually discovered that each month he would buy a jar of pickles and eat the whole jar. Then—at the end of the month when he finished the pickles—he would drink the entire jar full of juice.
The salt in the pickle juice caused the acute pulmonary edema, but until this piece of history was taken no one could pin down the problem. It really was a medical mystery. Figuring it out prevented his readmissions and is just the kind of thing that represents how hospitalists sometimes have to serve as diagnostic detectives.
You and Who Else?
An old woman was brought in by someone and was admitted to my service. When I entered the room, the daughter who lives [with] and cares for her said, “I know she has cancer, I know she’s demented, I think it is time to let her go. I live with her. I’m her power of attorney. There’s no document, but I’m her only daughter.”
What do I do? I figure hospice care; she’s dying in the hospital. I don’t cure her pneumonia. I let her go, and—three days later [after she had died]—I get a phone call from her two sons.
They say, “Hi Doctor, we brought our mother in. What’s the plan of care?” It turns out there was no power of attorney. The daughter did live with the patient, but apparently the daughter was mad at her two brothers, so she didn’t tell me the whole story. The sons threatened me—not with malpractice—but with going to tell the district attorney that I committed murder. And one of the sons mentioned murdering me.
Both threats resolved with tears and empathy as I met with them and acknowledged the error; after full explanations, they agreed with the final decision.
Put Bar Codes on Families, Too!
A mildly demented older man was admitted for something small. In comes another man and says, “This is my brother, and he’s ready to go.”
“Really?” I asked. “That’s your brother?”
“Yes,” he answered. “That’s my brother Jim.”
“OK, great,” I replied. And Jim takes him home.
Two hours later, the family shows up and tells me he doesn’t have a brother. It turns out that at the church the patient attends, they call each other “brother.’”
When They Know, They Know
I got called to see a patient. “What is the matter?” I asked him.
“I’m dying,” he said.
“What do you mean?” I asked. “Do you have chest pain?”
“No,” he replied.
“Are you short of breath?” I asked.
“No,” he said.
“Are you feeling a fever?” I asked.
“No! I’m dying!” he exclaimed.
I found nothing from the interview. I did a physical exam and found nothing. I called other physicians in who were seeing the patient. Everyone said, “I don’t know what he means.” The patient died within the hour.
I’ve had this happen to me four times. In three of those cases, they said, “I’m going to die today.”
In the other case, the patient said, “I don’t feel right.” When I asked him what he meant, he said, “I don’t know. I just feel weird.” And then he died that day.
Ask the Patient Why
I have a number of patients with sickle cell disease who have chronic pain syndrome. I had a female patient—about 26 years old—who basically stayed immobile for two weeks. The staff was upset with her about that.
To each other, they referred to her as noncompliant, and we wondered, “Why won’t she get up? She won’t even try to get out of bed.”
When I was assigned her case, I said to her, “Everyone says you won’t get out of bed. Will you tell me why?”
“You’re the first person to ask me that,” she said.
“Well, then,” I asked, “why?”
“I have an artificial hip,” she said, “and it is dislocated.”
When the physicians and other staff had urged her to get up, she had simply said, “My hip hurts.” It turns out that she was clinically depressed and was angry because she felt frustrated that she was always being judged.
Ultimately, she died two years later from the same problem in another hospital where she had developed DVT. In that other hospital, she’d done the same thing: She had refused to move, and the staff had told her she had to move—but no one had asked her why she hadn’t. TH
Andrea Sattinger writes frequently for The Hospitalist.
Recently The Hospitalist asked readers to share their reminiscences of patients who had left their mark in some special way on the docs’ lives. Here are those stories.
Patient al Dente
Sandi Verbin, MD, pediatric hospitalist at Temple University Children's Hospital, Philadelphia, and part-time pediatric hospitalist at Holy Redeemer Hospital, Meadowbrook, Pa.
It was midnight in the ER. My shift was ending, and I had to be up early in the morning to drive to my niece’s third birthday party about two hours away. The ER showed no signs of slowing, however, and one of the nurses approached me, asking if I could see the “quick” patient in Room 4: a child with a piece of macaroni stuck up his nose.
In over 10 years of pediatric practice, the allure of placing foreign objects in body orifices has eluded me. Why is this fun? Nevertheless, a parade of toddlers have presented themselves to me with such varied objects as crayons, tissue paper, beads, coffee beans, Play-Doh, M&Ms, rocks, and magnets in their ears and nostrils. (This doesn’t count the unfortunate innocent bystanders who presented with insects having claimed “squatter’s rights” to the patients’ auditory canals.)
Invariably, when asked, the children deny knowing how the object came to be there—at best, a lame “it just fell in” is offered. When questioned as to how the offending object came so close to the involved area, I am met with silence or a shrug. One memorable child told me he did not believe I was the doctor because I was a girl. I let it pass, considering he had put a rabbit food pellet in his ear after being dared to do so by his older brother. I felt his overall judgment was somewhat questionable.
I entered Room 4, prepared to see the usual anxious—or, as in some cases, oblivious—toddler. Instead, to my surprise, a sheepish-looking eight-year-old boy sat on the table, accompanied by his exasperated mother. The pair had been waiting for several hours for the anticipated pasta-ectomy.
Unable to stop myself, I blurted out, “What is a big boy like you doing putting macaroni up his nose? I expect to see this in little kids, but not eight-year-old boys!” The child answered that he had put the macaroni up his nose “when I was in preschool.”
“You mean five or six years ago?” I asked incredulously. When he reluctantly said yes, I explained that I would look up his nose, but that that piece of macaroni was long gone—dissolved or swallowed lo these many years ago. Sure enough, an exam revealed turbinates and mucus but no complex carbohydrates.
I explained to the mother again that there was no way the food item could have survived in the child’s nose for five years, that he would have presented with sinusitis years ago had the macaroni not been swallowed, dissolved, or sneezed out, and that there was no place else to which it could have migrated.
My best diagnosis was that the child had an unusually dry, sharp-feeling piece of mucus in his nose. The discomfort of this had caused him to admit his transgression, committed in the reckless days of toddlerhood, one which had clearly been a source of guilt for him ever since. After some saline nose drops, and no doubt due in no small part to the soul-cleansing effects of confession, the boy felt better. He and mom went home.
I left the ER to contemplate what antics the next day’s group of three-year-olds would cook up. I vowed to keep a close eye on the Jelly Beans.
Great Foster Mom
Alison Holmes, MD, MPH, pediatric hospitalist, Concord Hospital, Concord, N.H., and assistant professor of Community and Family Medicine, Dartmouth Medical School, contributed two stories.
When I was a resident, there was one chronically ill baby who was born at 34 weeks and had significant cyanotic heart disease. He would need a number of high-risk cardiac surgeries, and he also had a portion of his small intestine removed for necrotizing enterocolitis [caused by] his prematurity. After that it can be hard to absorb [nutrients] and grow. The baby had a lot of trouble with diarrhea and dehydration. We put him on the GI service, and the fluid overload from rehydration caused him to go into heart failure, and nobody could ever get the balance right.
He’d go back and forth between the GI service and the cardiology service. All the residents knew him, and he was in a horrible social situation. His mother was a drug user, and after his birth she never visited; we didn’t know anything about the father. The baby was this high-risk infant who basically had laid in the hospital with the TV on for the first five months of his life. Nobody paid attention to him, and I remember thinking, “This is horrible. He’s not going to get any love or nurturing. He’s not going to be normal, because nobody picks him up and holds him and talks to him.”
He was discharged into foster care, and I became his primary doctor. He just had the greatest foster mother in the world. She didn’t care that he had these medical problems; she was so glad to have a baby. She had been a foster parent for a while and had cared for troubled older children and had had enough of that, and she had her own 11-year-old. She was so thrilled to have this baby, and she just loved him and loved him and loved him.
I watched over the next year as he regained normal development despite all his early setbacks—both medical and social. Eventually his father did get involved; he went back into the father’s care, and the father rallied his whole family. The foster mother stays in touch with the family and is the child’s godmother.
By the time I finished residency, he was about three and a half years old, had been through three major cardiac surgeries, and was completely developmentally normal. I’ll never forget that no matter what we do medically, it’s people like that foster mother who make a difference for children.
Doing Wonders
I cared for a growth-retarded baby whose mother was in her late 30s. She was a drug user, and she had lost custody of her three prior children. Here she was with a fourth child, without any supports. She had used cocaine until about the fifth month of her pregnancy, when she decided to get some help.
I thought, “What are this baby’s chances?” But [the mom] did it. She did not go back to using drugs. She stayed clean and reconciled with the father. Life wasn’t always so kind to her. She couldn’t always hold down the same job, but at least she always had a job. She did wonders for this little girl, and she was able to turn her own life around.
Yet One More Challenge
Sandeep Sachdeva, MD, hospitalist at Swedish Medical Center; lead hospitalist, Swedish Medical Center’s Stroke Program; and clinical instructor, University of Washington, Seattle.
The patient I was most impressed by was a lady who came into the hospital about a year ago. I think she was in her mid 60s and had been blind and deaf from birth. She had obviously faced huge challenges and was living alone.
She had a very good support system: a non-governmental organization (NGO) here that provides close support for people in this type of situation. Even though she didn’t have any family support, these volunteers from the NGO would come out to make sure she was doing OK.
As I recall, she had tripped over something and had fallen and broken her hip, and she was admitted to the hospital for hip surgery. Just looking after her was a tremendous learning experience for me: She couldn't see me; she couldn’t hear me; and the only way we could communicate was through a sign language interpreter, where she had to feel the hands of the person doing sign language. She was very involved in her own care; she would ask questions, and there was no dearth of communication.
It was fascinating to deal with this lady who is—in essence—in a different universe with no sound and no sight, and who was facing the challenge of being in the hospital and recovering from her surgery. It felt very satisfying to look after her and to be inspired by her—a patient who was able to overcome yet another challenge when she is already disadvantaged. She did very well, and I believe she went home. I could still feel that she was trying to be independent and be the take-charge person that she had always been.
Patient in a Pickle
Eric Kupersmith, MD, assistant professor of medicine and director of the Hospitalist Program at Cooper Hospital, Camden, N.J. Dr. Kupersmith has plenty of patients he’ll never forget. Here are the stories of few.
There was a patient who would get admitted every month with congestive heart failure. He would develop pulmonary edema as an acute event like clockwork, and no one could figure out what was causing this. The seventh consecutive time, he was placed on my service. We eventually discovered that each month he would buy a jar of pickles and eat the whole jar. Then—at the end of the month when he finished the pickles—he would drink the entire jar full of juice.
The salt in the pickle juice caused the acute pulmonary edema, but until this piece of history was taken no one could pin down the problem. It really was a medical mystery. Figuring it out prevented his readmissions and is just the kind of thing that represents how hospitalists sometimes have to serve as diagnostic detectives.
You and Who Else?
An old woman was brought in by someone and was admitted to my service. When I entered the room, the daughter who lives [with] and cares for her said, “I know she has cancer, I know she’s demented, I think it is time to let her go. I live with her. I’m her power of attorney. There’s no document, but I’m her only daughter.”
What do I do? I figure hospice care; she’s dying in the hospital. I don’t cure her pneumonia. I let her go, and—three days later [after she had died]—I get a phone call from her two sons.
They say, “Hi Doctor, we brought our mother in. What’s the plan of care?” It turns out there was no power of attorney. The daughter did live with the patient, but apparently the daughter was mad at her two brothers, so she didn’t tell me the whole story. The sons threatened me—not with malpractice—but with going to tell the district attorney that I committed murder. And one of the sons mentioned murdering me.
Both threats resolved with tears and empathy as I met with them and acknowledged the error; after full explanations, they agreed with the final decision.
Put Bar Codes on Families, Too!
A mildly demented older man was admitted for something small. In comes another man and says, “This is my brother, and he’s ready to go.”
“Really?” I asked. “That’s your brother?”
“Yes,” he answered. “That’s my brother Jim.”
“OK, great,” I replied. And Jim takes him home.
Two hours later, the family shows up and tells me he doesn’t have a brother. It turns out that at the church the patient attends, they call each other “brother.’”
When They Know, They Know
I got called to see a patient. “What is the matter?” I asked him.
“I’m dying,” he said.
“What do you mean?” I asked. “Do you have chest pain?”
“No,” he replied.
“Are you short of breath?” I asked.
“No,” he said.
“Are you feeling a fever?” I asked.
“No! I’m dying!” he exclaimed.
I found nothing from the interview. I did a physical exam and found nothing. I called other physicians in who were seeing the patient. Everyone said, “I don’t know what he means.” The patient died within the hour.
I’ve had this happen to me four times. In three of those cases, they said, “I’m going to die today.”
In the other case, the patient said, “I don’t feel right.” When I asked him what he meant, he said, “I don’t know. I just feel weird.” And then he died that day.
Ask the Patient Why
I have a number of patients with sickle cell disease who have chronic pain syndrome. I had a female patient—about 26 years old—who basically stayed immobile for two weeks. The staff was upset with her about that.
To each other, they referred to her as noncompliant, and we wondered, “Why won’t she get up? She won’t even try to get out of bed.”
When I was assigned her case, I said to her, “Everyone says you won’t get out of bed. Will you tell me why?”
“You’re the first person to ask me that,” she said.
“Well, then,” I asked, “why?”
“I have an artificial hip,” she said, “and it is dislocated.”
When the physicians and other staff had urged her to get up, she had simply said, “My hip hurts.” It turns out that she was clinically depressed and was angry because she felt frustrated that she was always being judged.
Ultimately, she died two years later from the same problem in another hospital where she had developed DVT. In that other hospital, she’d done the same thing: She had refused to move, and the staff had told her she had to move—but no one had asked her why she hadn’t. TH
Andrea Sattinger writes frequently for The Hospitalist.
Recently The Hospitalist asked readers to share their reminiscences of patients who had left their mark in some special way on the docs’ lives. Here are those stories.
Patient al Dente
Sandi Verbin, MD, pediatric hospitalist at Temple University Children's Hospital, Philadelphia, and part-time pediatric hospitalist at Holy Redeemer Hospital, Meadowbrook, Pa.
It was midnight in the ER. My shift was ending, and I had to be up early in the morning to drive to my niece’s third birthday party about two hours away. The ER showed no signs of slowing, however, and one of the nurses approached me, asking if I could see the “quick” patient in Room 4: a child with a piece of macaroni stuck up his nose.
In over 10 years of pediatric practice, the allure of placing foreign objects in body orifices has eluded me. Why is this fun? Nevertheless, a parade of toddlers have presented themselves to me with such varied objects as crayons, tissue paper, beads, coffee beans, Play-Doh, M&Ms, rocks, and magnets in their ears and nostrils. (This doesn’t count the unfortunate innocent bystanders who presented with insects having claimed “squatter’s rights” to the patients’ auditory canals.)
Invariably, when asked, the children deny knowing how the object came to be there—at best, a lame “it just fell in” is offered. When questioned as to how the offending object came so close to the involved area, I am met with silence or a shrug. One memorable child told me he did not believe I was the doctor because I was a girl. I let it pass, considering he had put a rabbit food pellet in his ear after being dared to do so by his older brother. I felt his overall judgment was somewhat questionable.
I entered Room 4, prepared to see the usual anxious—or, as in some cases, oblivious—toddler. Instead, to my surprise, a sheepish-looking eight-year-old boy sat on the table, accompanied by his exasperated mother. The pair had been waiting for several hours for the anticipated pasta-ectomy.
Unable to stop myself, I blurted out, “What is a big boy like you doing putting macaroni up his nose? I expect to see this in little kids, but not eight-year-old boys!” The child answered that he had put the macaroni up his nose “when I was in preschool.”
“You mean five or six years ago?” I asked incredulously. When he reluctantly said yes, I explained that I would look up his nose, but that that piece of macaroni was long gone—dissolved or swallowed lo these many years ago. Sure enough, an exam revealed turbinates and mucus but no complex carbohydrates.
I explained to the mother again that there was no way the food item could have survived in the child’s nose for five years, that he would have presented with sinusitis years ago had the macaroni not been swallowed, dissolved, or sneezed out, and that there was no place else to which it could have migrated.
My best diagnosis was that the child had an unusually dry, sharp-feeling piece of mucus in his nose. The discomfort of this had caused him to admit his transgression, committed in the reckless days of toddlerhood, one which had clearly been a source of guilt for him ever since. After some saline nose drops, and no doubt due in no small part to the soul-cleansing effects of confession, the boy felt better. He and mom went home.
I left the ER to contemplate what antics the next day’s group of three-year-olds would cook up. I vowed to keep a close eye on the Jelly Beans.
Great Foster Mom
Alison Holmes, MD, MPH, pediatric hospitalist, Concord Hospital, Concord, N.H., and assistant professor of Community and Family Medicine, Dartmouth Medical School, contributed two stories.
When I was a resident, there was one chronically ill baby who was born at 34 weeks and had significant cyanotic heart disease. He would need a number of high-risk cardiac surgeries, and he also had a portion of his small intestine removed for necrotizing enterocolitis [caused by] his prematurity. After that it can be hard to absorb [nutrients] and grow. The baby had a lot of trouble with diarrhea and dehydration. We put him on the GI service, and the fluid overload from rehydration caused him to go into heart failure, and nobody could ever get the balance right.
He’d go back and forth between the GI service and the cardiology service. All the residents knew him, and he was in a horrible social situation. His mother was a drug user, and after his birth she never visited; we didn’t know anything about the father. The baby was this high-risk infant who basically had laid in the hospital with the TV on for the first five months of his life. Nobody paid attention to him, and I remember thinking, “This is horrible. He’s not going to get any love or nurturing. He’s not going to be normal, because nobody picks him up and holds him and talks to him.”
He was discharged into foster care, and I became his primary doctor. He just had the greatest foster mother in the world. She didn’t care that he had these medical problems; she was so glad to have a baby. She had been a foster parent for a while and had cared for troubled older children and had had enough of that, and she had her own 11-year-old. She was so thrilled to have this baby, and she just loved him and loved him and loved him.
I watched over the next year as he regained normal development despite all his early setbacks—both medical and social. Eventually his father did get involved; he went back into the father’s care, and the father rallied his whole family. The foster mother stays in touch with the family and is the child’s godmother.
By the time I finished residency, he was about three and a half years old, had been through three major cardiac surgeries, and was completely developmentally normal. I’ll never forget that no matter what we do medically, it’s people like that foster mother who make a difference for children.
Doing Wonders
I cared for a growth-retarded baby whose mother was in her late 30s. She was a drug user, and she had lost custody of her three prior children. Here she was with a fourth child, without any supports. She had used cocaine until about the fifth month of her pregnancy, when she decided to get some help.
I thought, “What are this baby’s chances?” But [the mom] did it. She did not go back to using drugs. She stayed clean and reconciled with the father. Life wasn’t always so kind to her. She couldn’t always hold down the same job, but at least she always had a job. She did wonders for this little girl, and she was able to turn her own life around.
Yet One More Challenge
Sandeep Sachdeva, MD, hospitalist at Swedish Medical Center; lead hospitalist, Swedish Medical Center’s Stroke Program; and clinical instructor, University of Washington, Seattle.
The patient I was most impressed by was a lady who came into the hospital about a year ago. I think she was in her mid 60s and had been blind and deaf from birth. She had obviously faced huge challenges and was living alone.
She had a very good support system: a non-governmental organization (NGO) here that provides close support for people in this type of situation. Even though she didn’t have any family support, these volunteers from the NGO would come out to make sure she was doing OK.
As I recall, she had tripped over something and had fallen and broken her hip, and she was admitted to the hospital for hip surgery. Just looking after her was a tremendous learning experience for me: She couldn't see me; she couldn’t hear me; and the only way we could communicate was through a sign language interpreter, where she had to feel the hands of the person doing sign language. She was very involved in her own care; she would ask questions, and there was no dearth of communication.
It was fascinating to deal with this lady who is—in essence—in a different universe with no sound and no sight, and who was facing the challenge of being in the hospital and recovering from her surgery. It felt very satisfying to look after her and to be inspired by her—a patient who was able to overcome yet another challenge when she is already disadvantaged. She did very well, and I believe she went home. I could still feel that she was trying to be independent and be the take-charge person that she had always been.
Patient in a Pickle
Eric Kupersmith, MD, assistant professor of medicine and director of the Hospitalist Program at Cooper Hospital, Camden, N.J. Dr. Kupersmith has plenty of patients he’ll never forget. Here are the stories of few.
There was a patient who would get admitted every month with congestive heart failure. He would develop pulmonary edema as an acute event like clockwork, and no one could figure out what was causing this. The seventh consecutive time, he was placed on my service. We eventually discovered that each month he would buy a jar of pickles and eat the whole jar. Then—at the end of the month when he finished the pickles—he would drink the entire jar full of juice.
The salt in the pickle juice caused the acute pulmonary edema, but until this piece of history was taken no one could pin down the problem. It really was a medical mystery. Figuring it out prevented his readmissions and is just the kind of thing that represents how hospitalists sometimes have to serve as diagnostic detectives.
You and Who Else?
An old woman was brought in by someone and was admitted to my service. When I entered the room, the daughter who lives [with] and cares for her said, “I know she has cancer, I know she’s demented, I think it is time to let her go. I live with her. I’m her power of attorney. There’s no document, but I’m her only daughter.”
What do I do? I figure hospice care; she’s dying in the hospital. I don’t cure her pneumonia. I let her go, and—three days later [after she had died]—I get a phone call from her two sons.
They say, “Hi Doctor, we brought our mother in. What’s the plan of care?” It turns out there was no power of attorney. The daughter did live with the patient, but apparently the daughter was mad at her two brothers, so she didn’t tell me the whole story. The sons threatened me—not with malpractice—but with going to tell the district attorney that I committed murder. And one of the sons mentioned murdering me.
Both threats resolved with tears and empathy as I met with them and acknowledged the error; after full explanations, they agreed with the final decision.
Put Bar Codes on Families, Too!
A mildly demented older man was admitted for something small. In comes another man and says, “This is my brother, and he’s ready to go.”
“Really?” I asked. “That’s your brother?”
“Yes,” he answered. “That’s my brother Jim.”
“OK, great,” I replied. And Jim takes him home.
Two hours later, the family shows up and tells me he doesn’t have a brother. It turns out that at the church the patient attends, they call each other “brother.’”
When They Know, They Know
I got called to see a patient. “What is the matter?” I asked him.
“I’m dying,” he said.
“What do you mean?” I asked. “Do you have chest pain?”
“No,” he replied.
“Are you short of breath?” I asked.
“No,” he said.
“Are you feeling a fever?” I asked.
“No! I’m dying!” he exclaimed.
I found nothing from the interview. I did a physical exam and found nothing. I called other physicians in who were seeing the patient. Everyone said, “I don’t know what he means.” The patient died within the hour.
I’ve had this happen to me four times. In three of those cases, they said, “I’m going to die today.”
In the other case, the patient said, “I don’t feel right.” When I asked him what he meant, he said, “I don’t know. I just feel weird.” And then he died that day.
Ask the Patient Why
I have a number of patients with sickle cell disease who have chronic pain syndrome. I had a female patient—about 26 years old—who basically stayed immobile for two weeks. The staff was upset with her about that.
To each other, they referred to her as noncompliant, and we wondered, “Why won’t she get up? She won’t even try to get out of bed.”
When I was assigned her case, I said to her, “Everyone says you won’t get out of bed. Will you tell me why?”
“You’re the first person to ask me that,” she said.
“Well, then,” I asked, “why?”
“I have an artificial hip,” she said, “and it is dislocated.”
When the physicians and other staff had urged her to get up, she had simply said, “My hip hurts.” It turns out that she was clinically depressed and was angry because she felt frustrated that she was always being judged.
Ultimately, she died two years later from the same problem in another hospital where she had developed DVT. In that other hospital, she’d done the same thing: She had refused to move, and the staff had told her she had to move—but no one had asked her why she hadn’t. TH
Andrea Sattinger writes frequently for The Hospitalist.