User login
Benefits of High-Dose Vitamin D in Managing Cutaneous Adverse Events Induced by Chemotherapy and Radiation Therapy
Vitamin D (VD) regulates keratinocyte proliferation and differentiation, modulates inflammatory pathways, and protects against cellular damage in the skin. 1 In the setting of tissue injury and acute skin inflammation, active vitamin D—1,25(OH) 2 D—suppresses signaling from pro-inflammatory chemokines and cytokines such as IFN- γ and IL-17. 2,3 This suppression reduces proliferation of helper T cells (T H 1, T H 17) and B cells, decreasing tissue damage from reactive oxygen species release while enhancing secretion of the anti-inflammatory cytokine IL-10 by antigen-presenting cells. 2-4
Suboptimal VD levels have been associated with numerous health consequences including malignancy, prompting interest in VD supplementation for improving cancer-related outcomes.5 Beyond disease prognosis, high-dose VD supplementation has been suggested as a potential therapy for adverse events (AEs) related to cancer treatments. In one study, mice that received oral vitamin D3 supplementation of 11,500 IU/kg daily had fewer doxorubicin-induced cardiotoxic effects on ejection fraction (P<.0001) and stroke volume (P<.01) than mice that received VD supplementation of 1500 IU/kg daily.6
In this review, we examine the impact of chemoradiation on 25(OH)D levels—which more accurately reflects VD stores than 1,25(OH)2D levels—and the impact of suboptimal VD on cutaneous toxicities related to chemoradiation. To define the suboptimal VD threshold, we used the Endocrine Society’s clinical practice guidelines, which characterize suboptimal 25(OH)D levels as insufficiency (21–29 ng/mL [52.5–72.5 nmol/L]) or deficiency (<20 ng/mL [50 nmol/L])7; deficiency can be further categorized as severe deficiency (<12 ng/mL [30 nmol/L]).8 This review also evaluates the evidence for vitamin D3 supplementation to alleviate the cutaneous AEs of chemotherapy and radiation treatments.
Effects of Chemotherapy on Vitamin D Levels
A high prevalence of VD deficiency is seen in various cancers. In a retrospective review of 25(OH)D levels in 2098 adults with solid tumors of any stage (6% had metastatic disease [n=124]), suboptimal levels were found in 69% of patients with breast cancer (n=617), 75% with colorectal cancer (n=84), 72% with gynecologic cancer (n=65), 79% with kidney and bladder cancer (n=145), 83% with pancreatic and upper gastrointestinal tract cancer (n=178), 73% with lung cancer (n=73), 69% with prostate cancer (n=225), 61% with skin cancer (n=399), and 63% with thyroid cancer (n=172).5 Suboptimal VD also has been found in hematologic malignancies. In a prospective cohort study, mean serum 25(OH)D levels in 23 patients with recently diagnosed acute myeloid leukemia demonstrated VD deficiency (mean [SD], 18.6 [6.6] nmol/L).9 Given that many patients already exhibit a baseline VD deficiency at cancer diagnosis, it is important to understand the relationship between VD and cancer treatment modalities.5
In the United States, breast and colorectal cancers were estimated to be the first and fourth most common cancers, with 313,510 and 152,810 predicted new cases in 2024, respectively.10 This review will focus on breast and colorectal cancer when describing VD variation associated with chemotherapy exposure due to their high prevalence.
Effects of Chemotherapy on Vitamin D Levels in Breast Cancer—Breast cancer studies have shown suboptimal VD levels in 76% of females 75 years or younger with any T1, T2, or T3; N0 or N1; and M0 breast cancer, in which 38.5% (n=197) had insufficient and 37.5% (n=192) had deficient 25(OH)D levels.11 In a study of female patients with primary breast cancer (stage I, II, or III and T1 with high Ki67 expression [≥30%], T2, or T3), VD deficiency was seen in 60% of patients not receiving VD supplementation.12,13 A systematic review that included 7 studies of different types of breast cancer suggested that circulating 25(OH)D may be associated with improved prognosis.14 Thus, studies have investigated risk factors associated with poor or worsening VD status in individuals with breast cancer, including exposure to chemotherapy and/or radiation treatment.12,15-18
A prospective cohort study assessed 25(OH)D levels in 95 patients with any breast cancer (stages I, II, IIIA, IIIB) before and after initiating chemotherapy with docetaxel, doxorubicin, epirubicin, 5-fluorouracil, or cyclophosphamide, compared with a group of 52 females without cancer.17 In the breast cancer group, approximately 80% (76/95) had suboptimal and 50% (47/95) had deficient VD levels before chemotherapy initiation (mean [SD], 54.1 [22.8] nmol/L). In the comparison group, 60% (31/52) had suboptimal and 30% (15/52) had deficient VD at baseline (mean [SD], 66.1 [23.5] nmol/L), which was higher than the breast cancer group (P=.03). A subgroup analysis excluded participants who started, stopped, or lacked data on dietary supplements containing VD (n=39); in the remaining 56 participants, a significant decrease in 25(OH)D levels was observed shortly after finishing chemotherapy compared with the prechemotherapy baseline value (mean, −7.9 nmol/L; P=.004). Notably, 6 months after chemotherapy completion, 25(OH)D levels increased (mean, +12.8 nmol/L; P<.001). Vitamin D levels remained stable in the comparison group (P=.987).17
Consistent with these findings, a cross-sectional study assessing VD status in 394 female patients with primary breast cancer (stage I, II, or III and T1 with high Ki67 expression [≥30%], T2, or T3), found that a history of chemotherapy was associated with increased odds of 25(OH)D levels less than 20 ng/mL compared with breast cancer patients with no prior chemotherapy (odds ratio, 1.86; 95% CI, 1.03-3.38).12 Although the study data included chemotherapy history, no information was provided on specific chemotherapy agents or regimens used in this cohort, limiting the ability to detect the drugs most often implicated.
Both studies indicated a complex interplay between chemotherapy and VD levels in breast cancer patients. Although Kok et al17 suggested a transient decrease in VD levels during chemotherapy with a subsequent recovery after cessation, Fassio et al12 highlighted the increased odds of VD deficiency associated with chemotherapy. Ultimately, larger randomized controlled trials are needed to better understand the relationship between chemotherapy and VD status in breast cancer patients.
Effects of Chemotherapy on Vitamin D Levels in Colorectal Cancer—Similar to patterns seen in breast cancer, a systematic review with 6 studies of different types of colorectal cancer suggested that circulating 25(OH)D levels may be associated with prognosis.14 Studies also have investigated the relationship between colorectal chemotherapy regimens and VD status.15,16,18,19
A retrospective study assessed 25(OH)D levels in 315 patients with any colorectal cancer (stage I–IV).15 Patients were included in the analysis if they received less than 400 IU daily of VD supplementation at baseline. For the whole study sample, the mean (SD) VD level was 23.7 (13.71) ng/mL. Patients who had not received chemotherapy within 3 months of the VD level assessment were categorized as the no chemotherapy group, and the others were designated as the chemotherapy group; the latter group was exposed to various chemotherapy regimens, including combinations of irinotecan, oxaliplatin, 5-fluorouracil, leucovorin, bevacizumab, or cetuximab. Multivariate analysis showed that the chemotherapy group was 3.7 times more likely to have very low VD levels (≤15 ng/mL) compared with those in the no chemotherapy group (P<.0001).15
A separate cross-sectional study examined serum 25(OH)D concentrations in 1201 patients with any newly diagnosed colorectal carcinoma (stage I–III); 91% of cases were adenocarcinoma.18 In a multivariate analysis, chemotherapy plus surgery was associated with lower VD levels than surgery alone 6 months after diagnosis (mean, −8.74 nmol/L; 95% CI, −11.30 to −6.18 nmol/L), specifically decreasing by a mean of 6.7 nmol/L (95% CI, −9.8 to −3.8 nmol/L) after adjusting for demographic and lifestyle factors.18 However, a prospective cohort study demonstrated different findings.19 Comparing 58 patients with newly diagnosed colorectal adenocarcinoma (stages I–IV) who underwent chemotherapy and 36 patients who did not receive chemotherapy, there was no significant change in 25(OH)D levels from the time of diagnosis to 6 months later. Median VD levels decreased by 0.7 ng/mL in those who received chemotherapy, while a minimal (and not significant) increase of 1.6 ng/mL was observed in those without chemotherapy intervention (P=.26). Notably, supplementation was not restricted in this cohort, which may have resulted in higher VD levels in those taking supplements.19
Since time of year and geographic location can influence VD levels, one prospective cohort study controlled for differential sun exposure due to these factors in their analysis.16 Assessment of 25(OH)D levels was completed in 81 chemotherapy-naïve cancer patients immediately before beginning chemotherapy as well as 6 and 12 weeks into treatment. More than 8 primary cancer types were represented in this study, with breast (34% [29/81]) and colorectal (14% [12/81]) cancer being the most common, but the cancer stages of the participants were not detailed. Vitamin D levels decreased after commencing chemotherapy, with the largest drop occurring 6 weeks into treatment. From the 6- to 12-week end points, VD increased but remained below the original baseline level (baseline: mean [SD], 49.2 [22.3] nmol/L; 6 weeks: mean [SD], 40.9 [19.0] nmol/L; 12 weeks: mean [SD], 45.9 [19.7] nmol/L; P=.05).16
Although focused on breast and colorectal cancers, these studies suggest that various chemotherapy regimens may confer a higher risk for VD deficiency compared with VD status at diagnosis and/or prior to chemotherapy treatment. However, most of these studies only discussed stage-based differences, excluding analysis of the variety of cancer subtypes that comprise breast and colorectal malignancies, which may limit our ability to extrapolate from these data. Ultimately, larger randomized controlled trials are needed to better understand the relationship between chemotherapy and VD status across various primary cancer types.
Effects of Radiation Therapy on Vitamin D Levels
Unlike chemotherapy, studies on the association between radiation therapy and VD levels are minimal, with most reports in the literature discussing the use of VD to potentiate the effects of radiation therapy. In one cross-sectional analysis of 1201 patients with newly diagnosed stage I, II, or III colorectal cancer of any type (94% were adenocarcinoma), radiation plus surgery was associated with slightly lower 25(OH)D levels than surgery alone for tumor treatment 6 months after diagnosis (mean, −3.17; 95% CI, −6.07 to −0.28 nmol/L). However, after adjustment for demographic and lifestyle factors, this decrease in VD levels attributable to radiotherapy was not statistically significant compared with the surgery-only cohort (mean, −1.78; 95% CI, −5.07 to 1.52 nmol/L).18
Similarly, a cross-sectional study assessing VD status in 394 female patients with primary breast cancer (stage I, II, or III and T1 with high Ki67 expression [≥30%], T2, or T3), found that a history of radiotherapy was not associated with a difference in serum 25(OH)D levels compared with those with breast cancer without prior radiotherapy (odds ratio, 0.90; 95% CI, 0.52-1.54).12 From the limited existing literature specifically addressing variations of VD levels with radiation, radiation therapy does not appear to significantly impact VD levels.
Vitamin D Levels and the Severity of Chemotherapy- or Radiation Therapy–Induced AEs
A prospective cohort of 241 patients did not find an increase in the incidence or severity of chemotherapy-induced cutaneous toxicities in those with suboptimal 1,25(OH)2D3 levels (≤75 nmol/L).20 Eight different primary cancer types were represented, including breast and colorectal cancer; the tumor stages of the participants were not detailed. Forty-one patients had normal 1,25(OH)2D3 levels, while the remaining 200 had suboptimal levels. There was no significant association between serum VD levels and the following dermatologic toxicities: desquamation (P=.26), xerosis (P=.15), mucositis (P=.30), or painful rash (P=.87). Surprisingly, nail changes and hand-foot reactions occurred with greater frequency in patients with normal VD levels (P=.01 and P=.03, respectively).20 Hand-foot reaction is part of the toxic erythema of chemotherapy (TEC) spectrum, which is comprised of a range of cytotoxic skin injuries that typically manifest within 2 to 3 weeks of exposure to the offending chemotherapeutic agents, often characterized by erythema, pain, swelling, and blistering, particularly in intertriginous and acral areas.21-23 Recovery from TEC generally takes at least 2 to 4 weeks and may necessitate cessation of the offending chemotherapeutic agent.21,24 Notably, this study measured 1,25(OH)2D3 levels instead of 25(OH)D levels, which may not reliably indicate body stores of VD.7,20 These results underscore the complex nature between chemotherapy and VD; however, VD levels alone do not appear to be a sufficient biomarker for predicting chemotherapy-associated cutaneous AEs.
Interestingly, radiation therapy–induced AEs may be associated with VD levels. A prospective cohort study of 98 patients with prostate, bladder, or gynecologic cancers (tumor stages were not detailed) undergoing pelvic radiotherapy found that females and males with 25(OH)D levels below a threshold of 35 and 40 nmol/L, respectively, were more likely to experience higher Radiation Therapy Oncology Group (RTOG) grade acute proctitis compared with those with VD above these thresholds.25 Specifically, VD below these thresholds was associated with increased odds of RTOG grade 2 or higher radiation-induced proctitis (OR, 3.07; 95% CI, 1.27-7.50 [P=.013]). Additionally, a weak correlation was noted between VD below these thresholds and the RTOG grade, with a Spearman correlation value of −0.189 (P=.031).25
One prospective cohort study included 28 patients with any cancer of the oral cavity, oropharynx, hypopharynx, or larynx stages II, III, or IVA; 93% (26/28) were stage III or IVA.26 The 20 (71%) patients with suboptimal 25(OH)D levels (≤75 nmol/L) experienced a higher prevalence of grade II radiation dermatitis compared with the 8 (29%) patients with optimal VD levels (χ22=5.973; P=.0505). This pattern persisted with the severity of mucositis; patients from the suboptimal VD group presented with higher rates of grades II and III mucositis compared with the VD optimal group (χ22=13.627; P=.0011).26 Recognizing the small cohort evaluated in the study, we highlight the importance of further studies to clarify these associations.
Chemotherapy-Induced Cutaneous Events Treated with High-Dose Vitamin D
Chemotherapeutic agents are known to induce cellular damage, resulting in a range of cutaneous AEs that can invoke discontinuation of otherwise effective chemotherapeutic interventions.27,28 Recent research has explored the potential of high-dose vitamin D3 as a therapeutic agent to mitigate cutaneous reactions.29,30
A randomized, double-blind, placebo-controlled trial investigated the use of a single high dose of oral 25(OH)D to treat topical nitrogen mustard (NM)–induced rash.29 To characterize baseline inflammatory responses from NM injury without intervention, clinical measures, serum studies, and tissue analyses from skin biopsies were performed on 28 healthy adults after exposure to topical NM—a chemotherapeutic agent classified as a DNA alkylator. Two weeks later, participants were exposed to topical NM a second time and were split into 2 groups: 14 patients received a single 200,000-IU dose of oral 25(OH)D while the other 14 participants were given a placebo. Using the inflammatory markers induced from baseline exposure to NM alone, posttreatment analysis revealed that the punch biopsies from
Although Ernst et al29 did not observe any clinically significant improvements with VD treatment, a case series of 6 patients with either glioblastoma multiforme, acute myeloid leukemia, or aplastic anemia did demonstrate clinical improvement of TEC after receiving high-dose vitamin D3.30 The mean time to onset of TEC was noted at 8.5 days following administration of the inciting chemotherapeutic agent, which included combinations of anthracycline, antimetabolite, kinase inhibitor, B-cell lymphoma 2 inhibitor, purine analogue, and alkylating agents. A combination of clinical and histologic findings was used to diagnose TEC. Baseline 25(OH)D levels were not established prior to treatment. The treatment regimen for 1 patient included 2 doses of 50,000 IU of VD spaced 1 week apart, totaling 100,000 IU, while the remaining 5 patients received a total of 200,000 IU, also split into 2 doses given 1 week apart. All patients received their first dose of VD within a week of the cutaneous eruption. Following the initial VD dose, there was a notable improvement in pain, pruritus, or swelling by the next day. Reduction in erythema also was observed within 1 to 4 days.30
No AEs associated with VD supplementation were reported, suggesting a potential beneficial role of high-dose VD in accelerating recovery from chemotherapy-induced rashes without evident safety concerns.
Radiation Therapy–Induced Cutaneous Events Treated with High-Dose Vitamin D
Radiation dermatitis is a common and often severe complication of radiation therapy that affects more than 90% of patients undergoing treatment, with half of these individuals experiencing grade 2 toxicity, according to the National Cancer Institute’s Common Terminology Criteria for Adverse Events.31,32 Radiation damage to basal keratinocytes and hair follicle stem cells disrupts the renewal of the skin’s outer layer, while a surge of free radicals causes irreversible DNA damage.33 Symptoms of radiation dermatitis can vary from mild pink erythema to tissue ulceration and necrosis, typically within 1 to 4 weeks of radiation exposure.34 The resulting dermatitis can take 2 to 4 weeks to heal, notably impacting patient quality of life and often necessitating modifications or interruptions in cancer therapy.33
Prior studies have demonstrated the use of high-dose VD to improve the healing of UV-irradiated skin. A randomized controlled trial investigated high-dose vitamin D3 to treat experimentally induced sunburn in 20 healthy adults. Compared with those who received a placebo, participants receiving the oral dose of 200,000 IU of vitamin D3 demonstrated suppression of the pro-inflammatory mediators tumor necrosis factor α (P=.04) and inducible nitric oxide synthase (P=.02), while expression of tissue repair enhancer arginase 1 was increased (P<.005).35 The mechanism of this enhanced tissue repair was investigated using a mouse model, in which intraperitoneal 25(OH)D was administered following severe UV-induced skin injury. On immunofluorescence microscopy, mice treated with VD showed enhanced autophagy within the macrophages infiltrating UV-irradiated skin.36 The use of high-dose VD to treat UV-irradiated skin in these studies established a precedent for using VD to heal cutaneous injury caused by ionizing radiation therapy.
Some studies have focused on the role of VD for treating acute radiation dermatitis. A study of 23 patients with ductal carcinoma in situ or localized invasive ductal carcinoma breast cancer compared the effectiveness of topical calcipotriol to that of a standard hydrating ointment.37 Participants were randomized to 1 of 2 treatments before starting adjuvant radiotherapy to evaluate their potential in preventing radiation dermatitis. In 87% (20/23) of these patients, no difference in skin reaction was observed between the 2 treatments, suggesting that topical VD application may not offer any advantage over the standard hydrating ointment for the prevention of radiation dermatitis.37
Benefits of high-dose oral VD for treating radiation dermatitis also have been reported. Nguyen et al38 documented 3 cases in which patients with neuroendocrine carcinoma of the pancreas, tonsillar carcinoma, and breast cancer received 200,000 IU of oral ergocalciferol distributed over 2 doses given 7 days apart for radiation dermatitis. These patients experienced substantial improvements in pain, swelling, and redness within a week of the initial dose. Additionally, a case of radiation recall dermatitis, which occurred a week after vinorelbine chemotherapy, was treated with 2 doses totaling 100,000 IU of oral ergocalciferol. This patient also had improvement in pain and swelling but continued to have tumor-related induration and ulceration.39
Although topical VD did not show significant benefits over standard treatments for radiation dermatitis, high-dose oral VD appears promising in improving patient outcomes of pain and swelling more rapidly than current practices. Further research is needed to confirm these findings and establish standardized treatment protocols.
Final Thoughts
Suboptimal VD levels are prevalent in numerous cancer types. Chemotherapy often is associated with acute, potentially transient worsening of VD status in patients with breast and colorectal cancer. Although 25(OH)D levels have not corresponded with increased frequency of chemotherapy-related dermatologic AEs, suboptimal 25(OH)D levels appear to be associated with increased severity of radiation-induced mucositis and dermatitis.20,25,26 The use of high-dose VD as a therapeutic agent shows promise in mitigating chemotherapy-induced and radiation therapy–induced rashes in multiple cancer types with reduction of inflammatory markers and a durable anti-inflammatory impact. Although the mechanisms of cellular injury vary among chemotherapeutic agents, the anti-inflammatory and tissue repair properties of VD may make it an effective treatment for chemotherapy-induced cutaneous damage regardless of injury mechanism.2-4,35 However, reports of clinical improvement vary, and further objective studies to classify optimal dosing, administration, and outcome measures are needed. The absence of reported AEs associated with high-dose VD supplementation is encouraging, but selection of a safe and optimal dosing regimen can only occur with dedicated clinical trials.
- Bikle DD. Vitamin D and the skin: physiology and pathophysiology. Rev Endocr Metab Disord. 2012;13:3-19. doi:10.1007/s11154-011-9194-0
- Penna G, Adorini L. 1α,25-Dihydroxyvitamin D3 inhibits differentiation, maturation, activation, and survival of dendritic cells leading to impaired alloreactive T cell activation. J Immunol. 2000;164:2405-2411. doi:10.4049/jimmunol.164.5.2405
- Penna G, Amuchastegui S, Cossetti C, et al. Treatment of experimental autoimmune prostatitis in nonobese diabetic mice by the vitamin D receptor agonist elocalcitol. J Immunol. 2006;177:8504-8511. doi:10.4049/jimmunol.177.12.8504
- Heine G, Niesner U, Chang HD, et al. 1,25-dihydroxyvitamin D3 promotes IL-10 production in human B cells. Eur J Immunol. 2008;38:2210-2218. doi:10.1002/eji.200838216
- Hauser K, Walsh D, Shrotriya S, et al. Low 25-hydroxyvitamin D levels in people with a solid tumor cancer diagnosis: the tip of the iceberg? Support Care Cancer. 2014;22:1931-1939. doi:10.1007/s00520-014-2154-y
- Lee KJ, Wright G, Bryant H, et al. Cytoprotective effect of vitamin D on doxorubicin-induced cardiac toxicity in triple negative breast cancer. Int J Mol Sci. 2021;22:7439. doi:10.3390/ijms22147439
- Holick MF, Binkley NC, Bischoff-Ferrari HA, et al. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96:1911-1930. doi:10.1210/jc.2011-0385
- Amrein K, Scherkl M, Hoffmann M, et al. Vitamin D deficiency 2.0: an update on the current status worldwide. Eur J Clin Nutr. 2020;74:1498-1513. doi:10.1038/s41430-020-0558-y
- Thomas X, Chelghoum Y, Fanari N, et al. Serum 25-hydroxyvitamin D levels are associated with prognosis in hematological malignancies. Hematology. 2011;16:278-283. doi:10.1179/102453311X13085644679908
- Siegel RL, Giaquinto AN, Jemal A. Cancer statistics, 2024. CA Cancer J Clin. 2024;74:12-49. doi:10.3322/caac.21820
- Goodwin PJ, Ennis M, Pritchard KI, et al. Prognostic effects of 25-hydroxyvitamin D levels in early breast cancer. J Clin Oncol. 2009;27:3757-3763. doi:10.1200/JCO.2008.20.0725
- Fassio A, Porciello G, Carioli G, et al. Post-diagnosis serum 25-hydroxyvitamin D concentrations in women treated for breast cancer participating in a lifestyle trial in Italy. Reumatismo. 2024;76:21-34.
- Augustin LSA, Libra M, Crispo A, et al. Low glycemic index diet, exercise and vitamin D to reduce breast cancer recurrence (DEDiCa): design of a clinical trial. BMC Cancer. 2017;17:69. doi:10.1186/s12885-017-3064-4
- Toriola AT, Nguyen N, Scheitler-Ring K, et al. Circulating 25-hydroxyvitamin D levels and prognosis among cancer patients: a systematic review. Cancer Epidemiol Biomarkers Prev. 2014;23:917-933. doi:10.1158/1055-9965.EPI-14-0053
- Fakih MG, Trump DL, Johnson CS, et al. Chemotherapy is linked to severe vitamin D deficiency in patients with colorectal cancer. Int J Colorectal Dis. 2009;24:219-224. doi:10.1007/s00384-008-0593-y
- Isenring EA, Teleni L, Woodman RJ, et al. Serum vitamin D decreases during chemotherapy: an Australian prospective cohort study. Asia Pac J Clin Nutr. 2018;27:962-967. doi:10.6133/apjcn.042018.01
- Kok DE, van den Berg MMGA, Posthuma L, et al. Changes in circulating levels of 25-hydroxyvitamin D3 in breast cancer patients receiving chemotherapy. Nutr Cancer. 2019;71:756-766. doi:10.1080/01635581.2018.1559938
- Wesselink E, Bours MJL, de Wilt JHW, et al. Chemotherapy and vitamin D supplement use are determinants of serum 25-hydroxyvitamin D levels during the first six months after colorectal cancer diagnosis. J Steroid Biochem Mol Biol. 2020;199:105577. doi:10.1016/j.jsbmb.2020.105577
- Savoie MB, Paciorek A, Zhang L, et al. Vitamin D levels in patients with colorectal cancer before and after treatment initiation. J Gastrointest Cancer. 2019;50:769-779. doi:10.1007/s12029-018-0147-7
- Kitchen D, Hughes B, Gill I, et al. The relationship between vitamin D and chemotherapy-induced toxicity—a pilot study. Br J Cancer. 2012;107:158-160. doi:10.1038/bjc.2012.194
- Demircay Z, Gürbüz O, Alpdogan TB, et al. Chemotherapy-induced acral erythema in leukemic patients: a report of 15 cases. Int J Dermatol. 1997;36:593-598. doi:10.1046/j.1365-4362.1997.00040.x
- Valks R, Fraga J, Porras-Luque J, et al. Chemotherapy-induced eccrine squamous syringometaplasia. a distinctive eruption in patients receiving hematopoietic progenitor cells. Arch Dermatol. 1997;133;873-878. doi:10.1001/archderm.133.7.873
- Webber KA, Kos L, Holland KE, et al. Intertriginous eruption associated with chemotherapy in pediatric patients. Arch Dermatol. 2007;143:67-71. doi:10.1001/archderm.143.1.67
- Hunjan MK, Nowsheen S, Ramos-Rodriguez AJ, et al. Clinical and histopathological spectrum of toxic erythema of chemotherapy in patients who have undergone allogeneic hematopoietic cell transplantation. Hematol Oncol Stem Cell Ther. 2019;12:19-25. doi:10.1016/j.hemonc.2018.09.001
- Ghorbanzadeh-Moghaddam A, Gholamrezaei A, Hemati S. Vitamin D deficiency is associated with the severity of radiation-induced proctitis in cancer patients. Int J Radiat Oncol Biol Phys. 2015;92:613-618. doi:10.1016/j.ijrobp.2015.02.011
- Bhanu A, Waghmare CM, Jain VS, et al. Serum 25-hydroxy vitamin-D levels in head and neck cancer chemoradiation therapy: potential in cancer therapeutics. Indian J Cancer. Published online February 27, 2003. doi:10.4103/ijc.ijc_358_20
- Yang B, Xie X, Wu Z, et al. DNA damage-mediated cellular senescence promotes hand-foot syndrome that can be relieved by thymidine prodrug. Genes Dis. 2022;10:2557-2571. doi:10.1016/j.gendis.2022.10.004
- Lassere Y, Hoff P. Management of hand-foot syndrome in patients treated with capecitabine (Xeloda®). Eur J Oncol Nurs. 2004;8(suppl 1):S31-S40. doi:10.1016/j.ejon.2004.06.007
- Ernst MK, Evans ST, Techner JM, et al. Vitamin D3 and deconvoluting a rash. JCI Insight. 2023;8:E163789.
- Nguyen CV, Zheng L, Zhou XA, et al. High-dose vitamin d for the management of toxic erythema of chemotherapy in hospitalized patients. JAMA Dermatol. 2023;159:219-221. doi:10.1001/jamadermatol.2022.5397
- Fisher J, Scott C, Stevens R, et al. Randomized phase III study comparing best supportive care to biafine as a prophylactic agent for radiation-induced skin toxicity for women undergoing breast irradiation: Radiation Therapy Oncology Group (RTOG) 97-13. Int J Radiat Oncol Biol Phys. 2000;48:1307-1310. doi:10.1016/s0360-3016(00)00782-3
- Pignol JP, Olivotto I, Rakovitch E, et al. A multicenter randomized trial of breast intensity-modulated radiation therapy to reduce acute radiation dermatitis. J Clin Oncol. 2008;26:2085-2092. doi:10.1200/JCO.2007.15.2488
- Hymes SR, Strom EA, Fife C. Radiation dermatitis: clinical presentation, pathophysiology, and treatment 2006. J Am Acad Dermatol. 2006;54:28-46. doi:10.1016/j.jaad.2005.08.054
- Ryan JL. Ionizing radiation: the good, the bad, and the ugly. J Invest Dermatol. 2012;132(3 pt 2):985-993. doi:10.1038/jid.2011.411
- Scott JF, Das LM, Ahsanuddin S, et al. Oral vitamin D rapidly attenuates inflammation from sunburn: an interventional study. J Invest Dermatol. 2017;137:2078-2086. doi:10.1016/j.jid.2017.04.040
- Das LM, Binko AM, Traylor ZP, et al. Vitamin D improves sunburns by increasing autophagy in M2 macrophages. Autophagy. 2019;15:813-826. doi:10.1080/15548627.2019.1569298
- Nasser NJ, Fenig S, Ravid A, et al. Vitamin D ointment for prevention of radiation dermatitis in breast cancer patients. NPJ Breast Cancer. 2017;3:10. doi:10.1038/s41523-017-0006-x
- Nguyen CV, Zheng L, Lu KQ. High-dose vitamin D for the management acute radiation dermatitis. JAAD Case Rep. 2023;39:47-50. doi:10.1016/j.jdcr.2023.07.001
- Nguyen CV, Lu KQ. Vitamin D3 and its potential to ameliorate chemical and radiation-induced skin injury during cancer therapy. Disaster Med Public Health Prep. 2024;18:E4. doi:10.1017/dmp.2023.211
Vitamin D (VD) regulates keratinocyte proliferation and differentiation, modulates inflammatory pathways, and protects against cellular damage in the skin. 1 In the setting of tissue injury and acute skin inflammation, active vitamin D—1,25(OH) 2 D—suppresses signaling from pro-inflammatory chemokines and cytokines such as IFN- γ and IL-17. 2,3 This suppression reduces proliferation of helper T cells (T H 1, T H 17) and B cells, decreasing tissue damage from reactive oxygen species release while enhancing secretion of the anti-inflammatory cytokine IL-10 by antigen-presenting cells. 2-4
Suboptimal VD levels have been associated with numerous health consequences including malignancy, prompting interest in VD supplementation for improving cancer-related outcomes.5 Beyond disease prognosis, high-dose VD supplementation has been suggested as a potential therapy for adverse events (AEs) related to cancer treatments. In one study, mice that received oral vitamin D3 supplementation of 11,500 IU/kg daily had fewer doxorubicin-induced cardiotoxic effects on ejection fraction (P<.0001) and stroke volume (P<.01) than mice that received VD supplementation of 1500 IU/kg daily.6
In this review, we examine the impact of chemoradiation on 25(OH)D levels—which more accurately reflects VD stores than 1,25(OH)2D levels—and the impact of suboptimal VD on cutaneous toxicities related to chemoradiation. To define the suboptimal VD threshold, we used the Endocrine Society’s clinical practice guidelines, which characterize suboptimal 25(OH)D levels as insufficiency (21–29 ng/mL [52.5–72.5 nmol/L]) or deficiency (<20 ng/mL [50 nmol/L])7; deficiency can be further categorized as severe deficiency (<12 ng/mL [30 nmol/L]).8 This review also evaluates the evidence for vitamin D3 supplementation to alleviate the cutaneous AEs of chemotherapy and radiation treatments.
Effects of Chemotherapy on Vitamin D Levels
A high prevalence of VD deficiency is seen in various cancers. In a retrospective review of 25(OH)D levels in 2098 adults with solid tumors of any stage (6% had metastatic disease [n=124]), suboptimal levels were found in 69% of patients with breast cancer (n=617), 75% with colorectal cancer (n=84), 72% with gynecologic cancer (n=65), 79% with kidney and bladder cancer (n=145), 83% with pancreatic and upper gastrointestinal tract cancer (n=178), 73% with lung cancer (n=73), 69% with prostate cancer (n=225), 61% with skin cancer (n=399), and 63% with thyroid cancer (n=172).5 Suboptimal VD also has been found in hematologic malignancies. In a prospective cohort study, mean serum 25(OH)D levels in 23 patients with recently diagnosed acute myeloid leukemia demonstrated VD deficiency (mean [SD], 18.6 [6.6] nmol/L).9 Given that many patients already exhibit a baseline VD deficiency at cancer diagnosis, it is important to understand the relationship between VD and cancer treatment modalities.5
In the United States, breast and colorectal cancers were estimated to be the first and fourth most common cancers, with 313,510 and 152,810 predicted new cases in 2024, respectively.10 This review will focus on breast and colorectal cancer when describing VD variation associated with chemotherapy exposure due to their high prevalence.
Effects of Chemotherapy on Vitamin D Levels in Breast Cancer—Breast cancer studies have shown suboptimal VD levels in 76% of females 75 years or younger with any T1, T2, or T3; N0 or N1; and M0 breast cancer, in which 38.5% (n=197) had insufficient and 37.5% (n=192) had deficient 25(OH)D levels.11 In a study of female patients with primary breast cancer (stage I, II, or III and T1 with high Ki67 expression [≥30%], T2, or T3), VD deficiency was seen in 60% of patients not receiving VD supplementation.12,13 A systematic review that included 7 studies of different types of breast cancer suggested that circulating 25(OH)D may be associated with improved prognosis.14 Thus, studies have investigated risk factors associated with poor or worsening VD status in individuals with breast cancer, including exposure to chemotherapy and/or radiation treatment.12,15-18
A prospective cohort study assessed 25(OH)D levels in 95 patients with any breast cancer (stages I, II, IIIA, IIIB) before and after initiating chemotherapy with docetaxel, doxorubicin, epirubicin, 5-fluorouracil, or cyclophosphamide, compared with a group of 52 females without cancer.17 In the breast cancer group, approximately 80% (76/95) had suboptimal and 50% (47/95) had deficient VD levels before chemotherapy initiation (mean [SD], 54.1 [22.8] nmol/L). In the comparison group, 60% (31/52) had suboptimal and 30% (15/52) had deficient VD at baseline (mean [SD], 66.1 [23.5] nmol/L), which was higher than the breast cancer group (P=.03). A subgroup analysis excluded participants who started, stopped, or lacked data on dietary supplements containing VD (n=39); in the remaining 56 participants, a significant decrease in 25(OH)D levels was observed shortly after finishing chemotherapy compared with the prechemotherapy baseline value (mean, −7.9 nmol/L; P=.004). Notably, 6 months after chemotherapy completion, 25(OH)D levels increased (mean, +12.8 nmol/L; P<.001). Vitamin D levels remained stable in the comparison group (P=.987).17
Consistent with these findings, a cross-sectional study assessing VD status in 394 female patients with primary breast cancer (stage I, II, or III and T1 with high Ki67 expression [≥30%], T2, or T3), found that a history of chemotherapy was associated with increased odds of 25(OH)D levels less than 20 ng/mL compared with breast cancer patients with no prior chemotherapy (odds ratio, 1.86; 95% CI, 1.03-3.38).12 Although the study data included chemotherapy history, no information was provided on specific chemotherapy agents or regimens used in this cohort, limiting the ability to detect the drugs most often implicated.
Both studies indicated a complex interplay between chemotherapy and VD levels in breast cancer patients. Although Kok et al17 suggested a transient decrease in VD levels during chemotherapy with a subsequent recovery after cessation, Fassio et al12 highlighted the increased odds of VD deficiency associated with chemotherapy. Ultimately, larger randomized controlled trials are needed to better understand the relationship between chemotherapy and VD status in breast cancer patients.
Effects of Chemotherapy on Vitamin D Levels in Colorectal Cancer—Similar to patterns seen in breast cancer, a systematic review with 6 studies of different types of colorectal cancer suggested that circulating 25(OH)D levels may be associated with prognosis.14 Studies also have investigated the relationship between colorectal chemotherapy regimens and VD status.15,16,18,19
A retrospective study assessed 25(OH)D levels in 315 patients with any colorectal cancer (stage I–IV).15 Patients were included in the analysis if they received less than 400 IU daily of VD supplementation at baseline. For the whole study sample, the mean (SD) VD level was 23.7 (13.71) ng/mL. Patients who had not received chemotherapy within 3 months of the VD level assessment were categorized as the no chemotherapy group, and the others were designated as the chemotherapy group; the latter group was exposed to various chemotherapy regimens, including combinations of irinotecan, oxaliplatin, 5-fluorouracil, leucovorin, bevacizumab, or cetuximab. Multivariate analysis showed that the chemotherapy group was 3.7 times more likely to have very low VD levels (≤15 ng/mL) compared with those in the no chemotherapy group (P<.0001).15
A separate cross-sectional study examined serum 25(OH)D concentrations in 1201 patients with any newly diagnosed colorectal carcinoma (stage I–III); 91% of cases were adenocarcinoma.18 In a multivariate analysis, chemotherapy plus surgery was associated with lower VD levels than surgery alone 6 months after diagnosis (mean, −8.74 nmol/L; 95% CI, −11.30 to −6.18 nmol/L), specifically decreasing by a mean of 6.7 nmol/L (95% CI, −9.8 to −3.8 nmol/L) after adjusting for demographic and lifestyle factors.18 However, a prospective cohort study demonstrated different findings.19 Comparing 58 patients with newly diagnosed colorectal adenocarcinoma (stages I–IV) who underwent chemotherapy and 36 patients who did not receive chemotherapy, there was no significant change in 25(OH)D levels from the time of diagnosis to 6 months later. Median VD levels decreased by 0.7 ng/mL in those who received chemotherapy, while a minimal (and not significant) increase of 1.6 ng/mL was observed in those without chemotherapy intervention (P=.26). Notably, supplementation was not restricted in this cohort, which may have resulted in higher VD levels in those taking supplements.19
Since time of year and geographic location can influence VD levels, one prospective cohort study controlled for differential sun exposure due to these factors in their analysis.16 Assessment of 25(OH)D levels was completed in 81 chemotherapy-naïve cancer patients immediately before beginning chemotherapy as well as 6 and 12 weeks into treatment. More than 8 primary cancer types were represented in this study, with breast (34% [29/81]) and colorectal (14% [12/81]) cancer being the most common, but the cancer stages of the participants were not detailed. Vitamin D levels decreased after commencing chemotherapy, with the largest drop occurring 6 weeks into treatment. From the 6- to 12-week end points, VD increased but remained below the original baseline level (baseline: mean [SD], 49.2 [22.3] nmol/L; 6 weeks: mean [SD], 40.9 [19.0] nmol/L; 12 weeks: mean [SD], 45.9 [19.7] nmol/L; P=.05).16
Although focused on breast and colorectal cancers, these studies suggest that various chemotherapy regimens may confer a higher risk for VD deficiency compared with VD status at diagnosis and/or prior to chemotherapy treatment. However, most of these studies only discussed stage-based differences, excluding analysis of the variety of cancer subtypes that comprise breast and colorectal malignancies, which may limit our ability to extrapolate from these data. Ultimately, larger randomized controlled trials are needed to better understand the relationship between chemotherapy and VD status across various primary cancer types.
Effects of Radiation Therapy on Vitamin D Levels
Unlike chemotherapy, studies on the association between radiation therapy and VD levels are minimal, with most reports in the literature discussing the use of VD to potentiate the effects of radiation therapy. In one cross-sectional analysis of 1201 patients with newly diagnosed stage I, II, or III colorectal cancer of any type (94% were adenocarcinoma), radiation plus surgery was associated with slightly lower 25(OH)D levels than surgery alone for tumor treatment 6 months after diagnosis (mean, −3.17; 95% CI, −6.07 to −0.28 nmol/L). However, after adjustment for demographic and lifestyle factors, this decrease in VD levels attributable to radiotherapy was not statistically significant compared with the surgery-only cohort (mean, −1.78; 95% CI, −5.07 to 1.52 nmol/L).18
Similarly, a cross-sectional study assessing VD status in 394 female patients with primary breast cancer (stage I, II, or III and T1 with high Ki67 expression [≥30%], T2, or T3), found that a history of radiotherapy was not associated with a difference in serum 25(OH)D levels compared with those with breast cancer without prior radiotherapy (odds ratio, 0.90; 95% CI, 0.52-1.54).12 From the limited existing literature specifically addressing variations of VD levels with radiation, radiation therapy does not appear to significantly impact VD levels.
Vitamin D Levels and the Severity of Chemotherapy- or Radiation Therapy–Induced AEs
A prospective cohort of 241 patients did not find an increase in the incidence or severity of chemotherapy-induced cutaneous toxicities in those with suboptimal 1,25(OH)2D3 levels (≤75 nmol/L).20 Eight different primary cancer types were represented, including breast and colorectal cancer; the tumor stages of the participants were not detailed. Forty-one patients had normal 1,25(OH)2D3 levels, while the remaining 200 had suboptimal levels. There was no significant association between serum VD levels and the following dermatologic toxicities: desquamation (P=.26), xerosis (P=.15), mucositis (P=.30), or painful rash (P=.87). Surprisingly, nail changes and hand-foot reactions occurred with greater frequency in patients with normal VD levels (P=.01 and P=.03, respectively).20 Hand-foot reaction is part of the toxic erythema of chemotherapy (TEC) spectrum, which is comprised of a range of cytotoxic skin injuries that typically manifest within 2 to 3 weeks of exposure to the offending chemotherapeutic agents, often characterized by erythema, pain, swelling, and blistering, particularly in intertriginous and acral areas.21-23 Recovery from TEC generally takes at least 2 to 4 weeks and may necessitate cessation of the offending chemotherapeutic agent.21,24 Notably, this study measured 1,25(OH)2D3 levels instead of 25(OH)D levels, which may not reliably indicate body stores of VD.7,20 These results underscore the complex nature between chemotherapy and VD; however, VD levels alone do not appear to be a sufficient biomarker for predicting chemotherapy-associated cutaneous AEs.
Interestingly, radiation therapy–induced AEs may be associated with VD levels. A prospective cohort study of 98 patients with prostate, bladder, or gynecologic cancers (tumor stages were not detailed) undergoing pelvic radiotherapy found that females and males with 25(OH)D levels below a threshold of 35 and 40 nmol/L, respectively, were more likely to experience higher Radiation Therapy Oncology Group (RTOG) grade acute proctitis compared with those with VD above these thresholds.25 Specifically, VD below these thresholds was associated with increased odds of RTOG grade 2 or higher radiation-induced proctitis (OR, 3.07; 95% CI, 1.27-7.50 [P=.013]). Additionally, a weak correlation was noted between VD below these thresholds and the RTOG grade, with a Spearman correlation value of −0.189 (P=.031).25
One prospective cohort study included 28 patients with any cancer of the oral cavity, oropharynx, hypopharynx, or larynx stages II, III, or IVA; 93% (26/28) were stage III or IVA.26 The 20 (71%) patients with suboptimal 25(OH)D levels (≤75 nmol/L) experienced a higher prevalence of grade II radiation dermatitis compared with the 8 (29%) patients with optimal VD levels (χ22=5.973; P=.0505). This pattern persisted with the severity of mucositis; patients from the suboptimal VD group presented with higher rates of grades II and III mucositis compared with the VD optimal group (χ22=13.627; P=.0011).26 Recognizing the small cohort evaluated in the study, we highlight the importance of further studies to clarify these associations.
Chemotherapy-Induced Cutaneous Events Treated with High-Dose Vitamin D
Chemotherapeutic agents are known to induce cellular damage, resulting in a range of cutaneous AEs that can invoke discontinuation of otherwise effective chemotherapeutic interventions.27,28 Recent research has explored the potential of high-dose vitamin D3 as a therapeutic agent to mitigate cutaneous reactions.29,30
A randomized, double-blind, placebo-controlled trial investigated the use of a single high dose of oral 25(OH)D to treat topical nitrogen mustard (NM)–induced rash.29 To characterize baseline inflammatory responses from NM injury without intervention, clinical measures, serum studies, and tissue analyses from skin biopsies were performed on 28 healthy adults after exposure to topical NM—a chemotherapeutic agent classified as a DNA alkylator. Two weeks later, participants were exposed to topical NM a second time and were split into 2 groups: 14 patients received a single 200,000-IU dose of oral 25(OH)D while the other 14 participants were given a placebo. Using the inflammatory markers induced from baseline exposure to NM alone, posttreatment analysis revealed that the punch biopsies from
Although Ernst et al29 did not observe any clinically significant improvements with VD treatment, a case series of 6 patients with either glioblastoma multiforme, acute myeloid leukemia, or aplastic anemia did demonstrate clinical improvement of TEC after receiving high-dose vitamin D3.30 The mean time to onset of TEC was noted at 8.5 days following administration of the inciting chemotherapeutic agent, which included combinations of anthracycline, antimetabolite, kinase inhibitor, B-cell lymphoma 2 inhibitor, purine analogue, and alkylating agents. A combination of clinical and histologic findings was used to diagnose TEC. Baseline 25(OH)D levels were not established prior to treatment. The treatment regimen for 1 patient included 2 doses of 50,000 IU of VD spaced 1 week apart, totaling 100,000 IU, while the remaining 5 patients received a total of 200,000 IU, also split into 2 doses given 1 week apart. All patients received their first dose of VD within a week of the cutaneous eruption. Following the initial VD dose, there was a notable improvement in pain, pruritus, or swelling by the next day. Reduction in erythema also was observed within 1 to 4 days.30
No AEs associated with VD supplementation were reported, suggesting a potential beneficial role of high-dose VD in accelerating recovery from chemotherapy-induced rashes without evident safety concerns.
Radiation Therapy–Induced Cutaneous Events Treated with High-Dose Vitamin D
Radiation dermatitis is a common and often severe complication of radiation therapy that affects more than 90% of patients undergoing treatment, with half of these individuals experiencing grade 2 toxicity, according to the National Cancer Institute’s Common Terminology Criteria for Adverse Events.31,32 Radiation damage to basal keratinocytes and hair follicle stem cells disrupts the renewal of the skin’s outer layer, while a surge of free radicals causes irreversible DNA damage.33 Symptoms of radiation dermatitis can vary from mild pink erythema to tissue ulceration and necrosis, typically within 1 to 4 weeks of radiation exposure.34 The resulting dermatitis can take 2 to 4 weeks to heal, notably impacting patient quality of life and often necessitating modifications or interruptions in cancer therapy.33
Prior studies have demonstrated the use of high-dose VD to improve the healing of UV-irradiated skin. A randomized controlled trial investigated high-dose vitamin D3 to treat experimentally induced sunburn in 20 healthy adults. Compared with those who received a placebo, participants receiving the oral dose of 200,000 IU of vitamin D3 demonstrated suppression of the pro-inflammatory mediators tumor necrosis factor α (P=.04) and inducible nitric oxide synthase (P=.02), while expression of tissue repair enhancer arginase 1 was increased (P<.005).35 The mechanism of this enhanced tissue repair was investigated using a mouse model, in which intraperitoneal 25(OH)D was administered following severe UV-induced skin injury. On immunofluorescence microscopy, mice treated with VD showed enhanced autophagy within the macrophages infiltrating UV-irradiated skin.36 The use of high-dose VD to treat UV-irradiated skin in these studies established a precedent for using VD to heal cutaneous injury caused by ionizing radiation therapy.
Some studies have focused on the role of VD for treating acute radiation dermatitis. A study of 23 patients with ductal carcinoma in situ or localized invasive ductal carcinoma breast cancer compared the effectiveness of topical calcipotriol to that of a standard hydrating ointment.37 Participants were randomized to 1 of 2 treatments before starting adjuvant radiotherapy to evaluate their potential in preventing radiation dermatitis. In 87% (20/23) of these patients, no difference in skin reaction was observed between the 2 treatments, suggesting that topical VD application may not offer any advantage over the standard hydrating ointment for the prevention of radiation dermatitis.37
Benefits of high-dose oral VD for treating radiation dermatitis also have been reported. Nguyen et al38 documented 3 cases in which patients with neuroendocrine carcinoma of the pancreas, tonsillar carcinoma, and breast cancer received 200,000 IU of oral ergocalciferol distributed over 2 doses given 7 days apart for radiation dermatitis. These patients experienced substantial improvements in pain, swelling, and redness within a week of the initial dose. Additionally, a case of radiation recall dermatitis, which occurred a week after vinorelbine chemotherapy, was treated with 2 doses totaling 100,000 IU of oral ergocalciferol. This patient also had improvement in pain and swelling but continued to have tumor-related induration and ulceration.39
Although topical VD did not show significant benefits over standard treatments for radiation dermatitis, high-dose oral VD appears promising in improving patient outcomes of pain and swelling more rapidly than current practices. Further research is needed to confirm these findings and establish standardized treatment protocols.
Final Thoughts
Suboptimal VD levels are prevalent in numerous cancer types. Chemotherapy often is associated with acute, potentially transient worsening of VD status in patients with breast and colorectal cancer. Although 25(OH)D levels have not corresponded with increased frequency of chemotherapy-related dermatologic AEs, suboptimal 25(OH)D levels appear to be associated with increased severity of radiation-induced mucositis and dermatitis.20,25,26 The use of high-dose VD as a therapeutic agent shows promise in mitigating chemotherapy-induced and radiation therapy–induced rashes in multiple cancer types with reduction of inflammatory markers and a durable anti-inflammatory impact. Although the mechanisms of cellular injury vary among chemotherapeutic agents, the anti-inflammatory and tissue repair properties of VD may make it an effective treatment for chemotherapy-induced cutaneous damage regardless of injury mechanism.2-4,35 However, reports of clinical improvement vary, and further objective studies to classify optimal dosing, administration, and outcome measures are needed. The absence of reported AEs associated with high-dose VD supplementation is encouraging, but selection of a safe and optimal dosing regimen can only occur with dedicated clinical trials.
Vitamin D (VD) regulates keratinocyte proliferation and differentiation, modulates inflammatory pathways, and protects against cellular damage in the skin. 1 In the setting of tissue injury and acute skin inflammation, active vitamin D—1,25(OH) 2 D—suppresses signaling from pro-inflammatory chemokines and cytokines such as IFN- γ and IL-17. 2,3 This suppression reduces proliferation of helper T cells (T H 1, T H 17) and B cells, decreasing tissue damage from reactive oxygen species release while enhancing secretion of the anti-inflammatory cytokine IL-10 by antigen-presenting cells. 2-4
Suboptimal VD levels have been associated with numerous health consequences including malignancy, prompting interest in VD supplementation for improving cancer-related outcomes.5 Beyond disease prognosis, high-dose VD supplementation has been suggested as a potential therapy for adverse events (AEs) related to cancer treatments. In one study, mice that received oral vitamin D3 supplementation of 11,500 IU/kg daily had fewer doxorubicin-induced cardiotoxic effects on ejection fraction (P<.0001) and stroke volume (P<.01) than mice that received VD supplementation of 1500 IU/kg daily.6
In this review, we examine the impact of chemoradiation on 25(OH)D levels—which more accurately reflects VD stores than 1,25(OH)2D levels—and the impact of suboptimal VD on cutaneous toxicities related to chemoradiation. To define the suboptimal VD threshold, we used the Endocrine Society’s clinical practice guidelines, which characterize suboptimal 25(OH)D levels as insufficiency (21–29 ng/mL [52.5–72.5 nmol/L]) or deficiency (<20 ng/mL [50 nmol/L])7; deficiency can be further categorized as severe deficiency (<12 ng/mL [30 nmol/L]).8 This review also evaluates the evidence for vitamin D3 supplementation to alleviate the cutaneous AEs of chemotherapy and radiation treatments.
Effects of Chemotherapy on Vitamin D Levels
A high prevalence of VD deficiency is seen in various cancers. In a retrospective review of 25(OH)D levels in 2098 adults with solid tumors of any stage (6% had metastatic disease [n=124]), suboptimal levels were found in 69% of patients with breast cancer (n=617), 75% with colorectal cancer (n=84), 72% with gynecologic cancer (n=65), 79% with kidney and bladder cancer (n=145), 83% with pancreatic and upper gastrointestinal tract cancer (n=178), 73% with lung cancer (n=73), 69% with prostate cancer (n=225), 61% with skin cancer (n=399), and 63% with thyroid cancer (n=172).5 Suboptimal VD also has been found in hematologic malignancies. In a prospective cohort study, mean serum 25(OH)D levels in 23 patients with recently diagnosed acute myeloid leukemia demonstrated VD deficiency (mean [SD], 18.6 [6.6] nmol/L).9 Given that many patients already exhibit a baseline VD deficiency at cancer diagnosis, it is important to understand the relationship between VD and cancer treatment modalities.5
In the United States, breast and colorectal cancers were estimated to be the first and fourth most common cancers, with 313,510 and 152,810 predicted new cases in 2024, respectively.10 This review will focus on breast and colorectal cancer when describing VD variation associated with chemotherapy exposure due to their high prevalence.
Effects of Chemotherapy on Vitamin D Levels in Breast Cancer—Breast cancer studies have shown suboptimal VD levels in 76% of females 75 years or younger with any T1, T2, or T3; N0 or N1; and M0 breast cancer, in which 38.5% (n=197) had insufficient and 37.5% (n=192) had deficient 25(OH)D levels.11 In a study of female patients with primary breast cancer (stage I, II, or III and T1 with high Ki67 expression [≥30%], T2, or T3), VD deficiency was seen in 60% of patients not receiving VD supplementation.12,13 A systematic review that included 7 studies of different types of breast cancer suggested that circulating 25(OH)D may be associated with improved prognosis.14 Thus, studies have investigated risk factors associated with poor or worsening VD status in individuals with breast cancer, including exposure to chemotherapy and/or radiation treatment.12,15-18
A prospective cohort study assessed 25(OH)D levels in 95 patients with any breast cancer (stages I, II, IIIA, IIIB) before and after initiating chemotherapy with docetaxel, doxorubicin, epirubicin, 5-fluorouracil, or cyclophosphamide, compared with a group of 52 females without cancer.17 In the breast cancer group, approximately 80% (76/95) had suboptimal and 50% (47/95) had deficient VD levels before chemotherapy initiation (mean [SD], 54.1 [22.8] nmol/L). In the comparison group, 60% (31/52) had suboptimal and 30% (15/52) had deficient VD at baseline (mean [SD], 66.1 [23.5] nmol/L), which was higher than the breast cancer group (P=.03). A subgroup analysis excluded participants who started, stopped, or lacked data on dietary supplements containing VD (n=39); in the remaining 56 participants, a significant decrease in 25(OH)D levels was observed shortly after finishing chemotherapy compared with the prechemotherapy baseline value (mean, −7.9 nmol/L; P=.004). Notably, 6 months after chemotherapy completion, 25(OH)D levels increased (mean, +12.8 nmol/L; P<.001). Vitamin D levels remained stable in the comparison group (P=.987).17
Consistent with these findings, a cross-sectional study assessing VD status in 394 female patients with primary breast cancer (stage I, II, or III and T1 with high Ki67 expression [≥30%], T2, or T3), found that a history of chemotherapy was associated with increased odds of 25(OH)D levels less than 20 ng/mL compared with breast cancer patients with no prior chemotherapy (odds ratio, 1.86; 95% CI, 1.03-3.38).12 Although the study data included chemotherapy history, no information was provided on specific chemotherapy agents or regimens used in this cohort, limiting the ability to detect the drugs most often implicated.
Both studies indicated a complex interplay between chemotherapy and VD levels in breast cancer patients. Although Kok et al17 suggested a transient decrease in VD levels during chemotherapy with a subsequent recovery after cessation, Fassio et al12 highlighted the increased odds of VD deficiency associated with chemotherapy. Ultimately, larger randomized controlled trials are needed to better understand the relationship between chemotherapy and VD status in breast cancer patients.
Effects of Chemotherapy on Vitamin D Levels in Colorectal Cancer—Similar to patterns seen in breast cancer, a systematic review with 6 studies of different types of colorectal cancer suggested that circulating 25(OH)D levels may be associated with prognosis.14 Studies also have investigated the relationship between colorectal chemotherapy regimens and VD status.15,16,18,19
A retrospective study assessed 25(OH)D levels in 315 patients with any colorectal cancer (stage I–IV).15 Patients were included in the analysis if they received less than 400 IU daily of VD supplementation at baseline. For the whole study sample, the mean (SD) VD level was 23.7 (13.71) ng/mL. Patients who had not received chemotherapy within 3 months of the VD level assessment were categorized as the no chemotherapy group, and the others were designated as the chemotherapy group; the latter group was exposed to various chemotherapy regimens, including combinations of irinotecan, oxaliplatin, 5-fluorouracil, leucovorin, bevacizumab, or cetuximab. Multivariate analysis showed that the chemotherapy group was 3.7 times more likely to have very low VD levels (≤15 ng/mL) compared with those in the no chemotherapy group (P<.0001).15
A separate cross-sectional study examined serum 25(OH)D concentrations in 1201 patients with any newly diagnosed colorectal carcinoma (stage I–III); 91% of cases were adenocarcinoma.18 In a multivariate analysis, chemotherapy plus surgery was associated with lower VD levels than surgery alone 6 months after diagnosis (mean, −8.74 nmol/L; 95% CI, −11.30 to −6.18 nmol/L), specifically decreasing by a mean of 6.7 nmol/L (95% CI, −9.8 to −3.8 nmol/L) after adjusting for demographic and lifestyle factors.18 However, a prospective cohort study demonstrated different findings.19 Comparing 58 patients with newly diagnosed colorectal adenocarcinoma (stages I–IV) who underwent chemotherapy and 36 patients who did not receive chemotherapy, there was no significant change in 25(OH)D levels from the time of diagnosis to 6 months later. Median VD levels decreased by 0.7 ng/mL in those who received chemotherapy, while a minimal (and not significant) increase of 1.6 ng/mL was observed in those without chemotherapy intervention (P=.26). Notably, supplementation was not restricted in this cohort, which may have resulted in higher VD levels in those taking supplements.19
Since time of year and geographic location can influence VD levels, one prospective cohort study controlled for differential sun exposure due to these factors in their analysis.16 Assessment of 25(OH)D levels was completed in 81 chemotherapy-naïve cancer patients immediately before beginning chemotherapy as well as 6 and 12 weeks into treatment. More than 8 primary cancer types were represented in this study, with breast (34% [29/81]) and colorectal (14% [12/81]) cancer being the most common, but the cancer stages of the participants were not detailed. Vitamin D levels decreased after commencing chemotherapy, with the largest drop occurring 6 weeks into treatment. From the 6- to 12-week end points, VD increased but remained below the original baseline level (baseline: mean [SD], 49.2 [22.3] nmol/L; 6 weeks: mean [SD], 40.9 [19.0] nmol/L; 12 weeks: mean [SD], 45.9 [19.7] nmol/L; P=.05).16
Although focused on breast and colorectal cancers, these studies suggest that various chemotherapy regimens may confer a higher risk for VD deficiency compared with VD status at diagnosis and/or prior to chemotherapy treatment. However, most of these studies only discussed stage-based differences, excluding analysis of the variety of cancer subtypes that comprise breast and colorectal malignancies, which may limit our ability to extrapolate from these data. Ultimately, larger randomized controlled trials are needed to better understand the relationship between chemotherapy and VD status across various primary cancer types.
Effects of Radiation Therapy on Vitamin D Levels
Unlike chemotherapy, studies on the association between radiation therapy and VD levels are minimal, with most reports in the literature discussing the use of VD to potentiate the effects of radiation therapy. In one cross-sectional analysis of 1201 patients with newly diagnosed stage I, II, or III colorectal cancer of any type (94% were adenocarcinoma), radiation plus surgery was associated with slightly lower 25(OH)D levels than surgery alone for tumor treatment 6 months after diagnosis (mean, −3.17; 95% CI, −6.07 to −0.28 nmol/L). However, after adjustment for demographic and lifestyle factors, this decrease in VD levels attributable to radiotherapy was not statistically significant compared with the surgery-only cohort (mean, −1.78; 95% CI, −5.07 to 1.52 nmol/L).18
Similarly, a cross-sectional study assessing VD status in 394 female patients with primary breast cancer (stage I, II, or III and T1 with high Ki67 expression [≥30%], T2, or T3), found that a history of radiotherapy was not associated with a difference in serum 25(OH)D levels compared with those with breast cancer without prior radiotherapy (odds ratio, 0.90; 95% CI, 0.52-1.54).12 From the limited existing literature specifically addressing variations of VD levels with radiation, radiation therapy does not appear to significantly impact VD levels.
Vitamin D Levels and the Severity of Chemotherapy- or Radiation Therapy–Induced AEs
A prospective cohort of 241 patients did not find an increase in the incidence or severity of chemotherapy-induced cutaneous toxicities in those with suboptimal 1,25(OH)2D3 levels (≤75 nmol/L).20 Eight different primary cancer types were represented, including breast and colorectal cancer; the tumor stages of the participants were not detailed. Forty-one patients had normal 1,25(OH)2D3 levels, while the remaining 200 had suboptimal levels. There was no significant association between serum VD levels and the following dermatologic toxicities: desquamation (P=.26), xerosis (P=.15), mucositis (P=.30), or painful rash (P=.87). Surprisingly, nail changes and hand-foot reactions occurred with greater frequency in patients with normal VD levels (P=.01 and P=.03, respectively).20 Hand-foot reaction is part of the toxic erythema of chemotherapy (TEC) spectrum, which is comprised of a range of cytotoxic skin injuries that typically manifest within 2 to 3 weeks of exposure to the offending chemotherapeutic agents, often characterized by erythema, pain, swelling, and blistering, particularly in intertriginous and acral areas.21-23 Recovery from TEC generally takes at least 2 to 4 weeks and may necessitate cessation of the offending chemotherapeutic agent.21,24 Notably, this study measured 1,25(OH)2D3 levels instead of 25(OH)D levels, which may not reliably indicate body stores of VD.7,20 These results underscore the complex nature between chemotherapy and VD; however, VD levels alone do not appear to be a sufficient biomarker for predicting chemotherapy-associated cutaneous AEs.
Interestingly, radiation therapy–induced AEs may be associated with VD levels. A prospective cohort study of 98 patients with prostate, bladder, or gynecologic cancers (tumor stages were not detailed) undergoing pelvic radiotherapy found that females and males with 25(OH)D levels below a threshold of 35 and 40 nmol/L, respectively, were more likely to experience higher Radiation Therapy Oncology Group (RTOG) grade acute proctitis compared with those with VD above these thresholds.25 Specifically, VD below these thresholds was associated with increased odds of RTOG grade 2 or higher radiation-induced proctitis (OR, 3.07; 95% CI, 1.27-7.50 [P=.013]). Additionally, a weak correlation was noted between VD below these thresholds and the RTOG grade, with a Spearman correlation value of −0.189 (P=.031).25
One prospective cohort study included 28 patients with any cancer of the oral cavity, oropharynx, hypopharynx, or larynx stages II, III, or IVA; 93% (26/28) were stage III or IVA.26 The 20 (71%) patients with suboptimal 25(OH)D levels (≤75 nmol/L) experienced a higher prevalence of grade II radiation dermatitis compared with the 8 (29%) patients with optimal VD levels (χ22=5.973; P=.0505). This pattern persisted with the severity of mucositis; patients from the suboptimal VD group presented with higher rates of grades II and III mucositis compared with the VD optimal group (χ22=13.627; P=.0011).26 Recognizing the small cohort evaluated in the study, we highlight the importance of further studies to clarify these associations.
Chemotherapy-Induced Cutaneous Events Treated with High-Dose Vitamin D
Chemotherapeutic agents are known to induce cellular damage, resulting in a range of cutaneous AEs that can invoke discontinuation of otherwise effective chemotherapeutic interventions.27,28 Recent research has explored the potential of high-dose vitamin D3 as a therapeutic agent to mitigate cutaneous reactions.29,30
A randomized, double-blind, placebo-controlled trial investigated the use of a single high dose of oral 25(OH)D to treat topical nitrogen mustard (NM)–induced rash.29 To characterize baseline inflammatory responses from NM injury without intervention, clinical measures, serum studies, and tissue analyses from skin biopsies were performed on 28 healthy adults after exposure to topical NM—a chemotherapeutic agent classified as a DNA alkylator. Two weeks later, participants were exposed to topical NM a second time and were split into 2 groups: 14 patients received a single 200,000-IU dose of oral 25(OH)D while the other 14 participants were given a placebo. Using the inflammatory markers induced from baseline exposure to NM alone, posttreatment analysis revealed that the punch biopsies from
Although Ernst et al29 did not observe any clinically significant improvements with VD treatment, a case series of 6 patients with either glioblastoma multiforme, acute myeloid leukemia, or aplastic anemia did demonstrate clinical improvement of TEC after receiving high-dose vitamin D3.30 The mean time to onset of TEC was noted at 8.5 days following administration of the inciting chemotherapeutic agent, which included combinations of anthracycline, antimetabolite, kinase inhibitor, B-cell lymphoma 2 inhibitor, purine analogue, and alkylating agents. A combination of clinical and histologic findings was used to diagnose TEC. Baseline 25(OH)D levels were not established prior to treatment. The treatment regimen for 1 patient included 2 doses of 50,000 IU of VD spaced 1 week apart, totaling 100,000 IU, while the remaining 5 patients received a total of 200,000 IU, also split into 2 doses given 1 week apart. All patients received their first dose of VD within a week of the cutaneous eruption. Following the initial VD dose, there was a notable improvement in pain, pruritus, or swelling by the next day. Reduction in erythema also was observed within 1 to 4 days.30
No AEs associated with VD supplementation were reported, suggesting a potential beneficial role of high-dose VD in accelerating recovery from chemotherapy-induced rashes without evident safety concerns.
Radiation Therapy–Induced Cutaneous Events Treated with High-Dose Vitamin D
Radiation dermatitis is a common and often severe complication of radiation therapy that affects more than 90% of patients undergoing treatment, with half of these individuals experiencing grade 2 toxicity, according to the National Cancer Institute’s Common Terminology Criteria for Adverse Events.31,32 Radiation damage to basal keratinocytes and hair follicle stem cells disrupts the renewal of the skin’s outer layer, while a surge of free radicals causes irreversible DNA damage.33 Symptoms of radiation dermatitis can vary from mild pink erythema to tissue ulceration and necrosis, typically within 1 to 4 weeks of radiation exposure.34 The resulting dermatitis can take 2 to 4 weeks to heal, notably impacting patient quality of life and often necessitating modifications or interruptions in cancer therapy.33
Prior studies have demonstrated the use of high-dose VD to improve the healing of UV-irradiated skin. A randomized controlled trial investigated high-dose vitamin D3 to treat experimentally induced sunburn in 20 healthy adults. Compared with those who received a placebo, participants receiving the oral dose of 200,000 IU of vitamin D3 demonstrated suppression of the pro-inflammatory mediators tumor necrosis factor α (P=.04) and inducible nitric oxide synthase (P=.02), while expression of tissue repair enhancer arginase 1 was increased (P<.005).35 The mechanism of this enhanced tissue repair was investigated using a mouse model, in which intraperitoneal 25(OH)D was administered following severe UV-induced skin injury. On immunofluorescence microscopy, mice treated with VD showed enhanced autophagy within the macrophages infiltrating UV-irradiated skin.36 The use of high-dose VD to treat UV-irradiated skin in these studies established a precedent for using VD to heal cutaneous injury caused by ionizing radiation therapy.
Some studies have focused on the role of VD for treating acute radiation dermatitis. A study of 23 patients with ductal carcinoma in situ or localized invasive ductal carcinoma breast cancer compared the effectiveness of topical calcipotriol to that of a standard hydrating ointment.37 Participants were randomized to 1 of 2 treatments before starting adjuvant radiotherapy to evaluate their potential in preventing radiation dermatitis. In 87% (20/23) of these patients, no difference in skin reaction was observed between the 2 treatments, suggesting that topical VD application may not offer any advantage over the standard hydrating ointment for the prevention of radiation dermatitis.37
Benefits of high-dose oral VD for treating radiation dermatitis also have been reported. Nguyen et al38 documented 3 cases in which patients with neuroendocrine carcinoma of the pancreas, tonsillar carcinoma, and breast cancer received 200,000 IU of oral ergocalciferol distributed over 2 doses given 7 days apart for radiation dermatitis. These patients experienced substantial improvements in pain, swelling, and redness within a week of the initial dose. Additionally, a case of radiation recall dermatitis, which occurred a week after vinorelbine chemotherapy, was treated with 2 doses totaling 100,000 IU of oral ergocalciferol. This patient also had improvement in pain and swelling but continued to have tumor-related induration and ulceration.39
Although topical VD did not show significant benefits over standard treatments for radiation dermatitis, high-dose oral VD appears promising in improving patient outcomes of pain and swelling more rapidly than current practices. Further research is needed to confirm these findings and establish standardized treatment protocols.
Final Thoughts
Suboptimal VD levels are prevalent in numerous cancer types. Chemotherapy often is associated with acute, potentially transient worsening of VD status in patients with breast and colorectal cancer. Although 25(OH)D levels have not corresponded with increased frequency of chemotherapy-related dermatologic AEs, suboptimal 25(OH)D levels appear to be associated with increased severity of radiation-induced mucositis and dermatitis.20,25,26 The use of high-dose VD as a therapeutic agent shows promise in mitigating chemotherapy-induced and radiation therapy–induced rashes in multiple cancer types with reduction of inflammatory markers and a durable anti-inflammatory impact. Although the mechanisms of cellular injury vary among chemotherapeutic agents, the anti-inflammatory and tissue repair properties of VD may make it an effective treatment for chemotherapy-induced cutaneous damage regardless of injury mechanism.2-4,35 However, reports of clinical improvement vary, and further objective studies to classify optimal dosing, administration, and outcome measures are needed. The absence of reported AEs associated with high-dose VD supplementation is encouraging, but selection of a safe and optimal dosing regimen can only occur with dedicated clinical trials.
- Bikle DD. Vitamin D and the skin: physiology and pathophysiology. Rev Endocr Metab Disord. 2012;13:3-19. doi:10.1007/s11154-011-9194-0
- Penna G, Adorini L. 1α,25-Dihydroxyvitamin D3 inhibits differentiation, maturation, activation, and survival of dendritic cells leading to impaired alloreactive T cell activation. J Immunol. 2000;164:2405-2411. doi:10.4049/jimmunol.164.5.2405
- Penna G, Amuchastegui S, Cossetti C, et al. Treatment of experimental autoimmune prostatitis in nonobese diabetic mice by the vitamin D receptor agonist elocalcitol. J Immunol. 2006;177:8504-8511. doi:10.4049/jimmunol.177.12.8504
- Heine G, Niesner U, Chang HD, et al. 1,25-dihydroxyvitamin D3 promotes IL-10 production in human B cells. Eur J Immunol. 2008;38:2210-2218. doi:10.1002/eji.200838216
- Hauser K, Walsh D, Shrotriya S, et al. Low 25-hydroxyvitamin D levels in people with a solid tumor cancer diagnosis: the tip of the iceberg? Support Care Cancer. 2014;22:1931-1939. doi:10.1007/s00520-014-2154-y
- Lee KJ, Wright G, Bryant H, et al. Cytoprotective effect of vitamin D on doxorubicin-induced cardiac toxicity in triple negative breast cancer. Int J Mol Sci. 2021;22:7439. doi:10.3390/ijms22147439
- Holick MF, Binkley NC, Bischoff-Ferrari HA, et al. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96:1911-1930. doi:10.1210/jc.2011-0385
- Amrein K, Scherkl M, Hoffmann M, et al. Vitamin D deficiency 2.0: an update on the current status worldwide. Eur J Clin Nutr. 2020;74:1498-1513. doi:10.1038/s41430-020-0558-y
- Thomas X, Chelghoum Y, Fanari N, et al. Serum 25-hydroxyvitamin D levels are associated with prognosis in hematological malignancies. Hematology. 2011;16:278-283. doi:10.1179/102453311X13085644679908
- Siegel RL, Giaquinto AN, Jemal A. Cancer statistics, 2024. CA Cancer J Clin. 2024;74:12-49. doi:10.3322/caac.21820
- Goodwin PJ, Ennis M, Pritchard KI, et al. Prognostic effects of 25-hydroxyvitamin D levels in early breast cancer. J Clin Oncol. 2009;27:3757-3763. doi:10.1200/JCO.2008.20.0725
- Fassio A, Porciello G, Carioli G, et al. Post-diagnosis serum 25-hydroxyvitamin D concentrations in women treated for breast cancer participating in a lifestyle trial in Italy. Reumatismo. 2024;76:21-34.
- Augustin LSA, Libra M, Crispo A, et al. Low glycemic index diet, exercise and vitamin D to reduce breast cancer recurrence (DEDiCa): design of a clinical trial. BMC Cancer. 2017;17:69. doi:10.1186/s12885-017-3064-4
- Toriola AT, Nguyen N, Scheitler-Ring K, et al. Circulating 25-hydroxyvitamin D levels and prognosis among cancer patients: a systematic review. Cancer Epidemiol Biomarkers Prev. 2014;23:917-933. doi:10.1158/1055-9965.EPI-14-0053
- Fakih MG, Trump DL, Johnson CS, et al. Chemotherapy is linked to severe vitamin D deficiency in patients with colorectal cancer. Int J Colorectal Dis. 2009;24:219-224. doi:10.1007/s00384-008-0593-y
- Isenring EA, Teleni L, Woodman RJ, et al. Serum vitamin D decreases during chemotherapy: an Australian prospective cohort study. Asia Pac J Clin Nutr. 2018;27:962-967. doi:10.6133/apjcn.042018.01
- Kok DE, van den Berg MMGA, Posthuma L, et al. Changes in circulating levels of 25-hydroxyvitamin D3 in breast cancer patients receiving chemotherapy. Nutr Cancer. 2019;71:756-766. doi:10.1080/01635581.2018.1559938
- Wesselink E, Bours MJL, de Wilt JHW, et al. Chemotherapy and vitamin D supplement use are determinants of serum 25-hydroxyvitamin D levels during the first six months after colorectal cancer diagnosis. J Steroid Biochem Mol Biol. 2020;199:105577. doi:10.1016/j.jsbmb.2020.105577
- Savoie MB, Paciorek A, Zhang L, et al. Vitamin D levels in patients with colorectal cancer before and after treatment initiation. J Gastrointest Cancer. 2019;50:769-779. doi:10.1007/s12029-018-0147-7
- Kitchen D, Hughes B, Gill I, et al. The relationship between vitamin D and chemotherapy-induced toxicity—a pilot study. Br J Cancer. 2012;107:158-160. doi:10.1038/bjc.2012.194
- Demircay Z, Gürbüz O, Alpdogan TB, et al. Chemotherapy-induced acral erythema in leukemic patients: a report of 15 cases. Int J Dermatol. 1997;36:593-598. doi:10.1046/j.1365-4362.1997.00040.x
- Valks R, Fraga J, Porras-Luque J, et al. Chemotherapy-induced eccrine squamous syringometaplasia. a distinctive eruption in patients receiving hematopoietic progenitor cells. Arch Dermatol. 1997;133;873-878. doi:10.1001/archderm.133.7.873
- Webber KA, Kos L, Holland KE, et al. Intertriginous eruption associated with chemotherapy in pediatric patients. Arch Dermatol. 2007;143:67-71. doi:10.1001/archderm.143.1.67
- Hunjan MK, Nowsheen S, Ramos-Rodriguez AJ, et al. Clinical and histopathological spectrum of toxic erythema of chemotherapy in patients who have undergone allogeneic hematopoietic cell transplantation. Hematol Oncol Stem Cell Ther. 2019;12:19-25. doi:10.1016/j.hemonc.2018.09.001
- Ghorbanzadeh-Moghaddam A, Gholamrezaei A, Hemati S. Vitamin D deficiency is associated with the severity of radiation-induced proctitis in cancer patients. Int J Radiat Oncol Biol Phys. 2015;92:613-618. doi:10.1016/j.ijrobp.2015.02.011
- Bhanu A, Waghmare CM, Jain VS, et al. Serum 25-hydroxy vitamin-D levels in head and neck cancer chemoradiation therapy: potential in cancer therapeutics. Indian J Cancer. Published online February 27, 2003. doi:10.4103/ijc.ijc_358_20
- Yang B, Xie X, Wu Z, et al. DNA damage-mediated cellular senescence promotes hand-foot syndrome that can be relieved by thymidine prodrug. Genes Dis. 2022;10:2557-2571. doi:10.1016/j.gendis.2022.10.004
- Lassere Y, Hoff P. Management of hand-foot syndrome in patients treated with capecitabine (Xeloda®). Eur J Oncol Nurs. 2004;8(suppl 1):S31-S40. doi:10.1016/j.ejon.2004.06.007
- Ernst MK, Evans ST, Techner JM, et al. Vitamin D3 and deconvoluting a rash. JCI Insight. 2023;8:E163789.
- Nguyen CV, Zheng L, Zhou XA, et al. High-dose vitamin d for the management of toxic erythema of chemotherapy in hospitalized patients. JAMA Dermatol. 2023;159:219-221. doi:10.1001/jamadermatol.2022.5397
- Fisher J, Scott C, Stevens R, et al. Randomized phase III study comparing best supportive care to biafine as a prophylactic agent for radiation-induced skin toxicity for women undergoing breast irradiation: Radiation Therapy Oncology Group (RTOG) 97-13. Int J Radiat Oncol Biol Phys. 2000;48:1307-1310. doi:10.1016/s0360-3016(00)00782-3
- Pignol JP, Olivotto I, Rakovitch E, et al. A multicenter randomized trial of breast intensity-modulated radiation therapy to reduce acute radiation dermatitis. J Clin Oncol. 2008;26:2085-2092. doi:10.1200/JCO.2007.15.2488
- Hymes SR, Strom EA, Fife C. Radiation dermatitis: clinical presentation, pathophysiology, and treatment 2006. J Am Acad Dermatol. 2006;54:28-46. doi:10.1016/j.jaad.2005.08.054
- Ryan JL. Ionizing radiation: the good, the bad, and the ugly. J Invest Dermatol. 2012;132(3 pt 2):985-993. doi:10.1038/jid.2011.411
- Scott JF, Das LM, Ahsanuddin S, et al. Oral vitamin D rapidly attenuates inflammation from sunburn: an interventional study. J Invest Dermatol. 2017;137:2078-2086. doi:10.1016/j.jid.2017.04.040
- Das LM, Binko AM, Traylor ZP, et al. Vitamin D improves sunburns by increasing autophagy in M2 macrophages. Autophagy. 2019;15:813-826. doi:10.1080/15548627.2019.1569298
- Nasser NJ, Fenig S, Ravid A, et al. Vitamin D ointment for prevention of radiation dermatitis in breast cancer patients. NPJ Breast Cancer. 2017;3:10. doi:10.1038/s41523-017-0006-x
- Nguyen CV, Zheng L, Lu KQ. High-dose vitamin D for the management acute radiation dermatitis. JAAD Case Rep. 2023;39:47-50. doi:10.1016/j.jdcr.2023.07.001
- Nguyen CV, Lu KQ. Vitamin D3 and its potential to ameliorate chemical and radiation-induced skin injury during cancer therapy. Disaster Med Public Health Prep. 2024;18:E4. doi:10.1017/dmp.2023.211
- Bikle DD. Vitamin D and the skin: physiology and pathophysiology. Rev Endocr Metab Disord. 2012;13:3-19. doi:10.1007/s11154-011-9194-0
- Penna G, Adorini L. 1α,25-Dihydroxyvitamin D3 inhibits differentiation, maturation, activation, and survival of dendritic cells leading to impaired alloreactive T cell activation. J Immunol. 2000;164:2405-2411. doi:10.4049/jimmunol.164.5.2405
- Penna G, Amuchastegui S, Cossetti C, et al. Treatment of experimental autoimmune prostatitis in nonobese diabetic mice by the vitamin D receptor agonist elocalcitol. J Immunol. 2006;177:8504-8511. doi:10.4049/jimmunol.177.12.8504
- Heine G, Niesner U, Chang HD, et al. 1,25-dihydroxyvitamin D3 promotes IL-10 production in human B cells. Eur J Immunol. 2008;38:2210-2218. doi:10.1002/eji.200838216
- Hauser K, Walsh D, Shrotriya S, et al. Low 25-hydroxyvitamin D levels in people with a solid tumor cancer diagnosis: the tip of the iceberg? Support Care Cancer. 2014;22:1931-1939. doi:10.1007/s00520-014-2154-y
- Lee KJ, Wright G, Bryant H, et al. Cytoprotective effect of vitamin D on doxorubicin-induced cardiac toxicity in triple negative breast cancer. Int J Mol Sci. 2021;22:7439. doi:10.3390/ijms22147439
- Holick MF, Binkley NC, Bischoff-Ferrari HA, et al. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96:1911-1930. doi:10.1210/jc.2011-0385
- Amrein K, Scherkl M, Hoffmann M, et al. Vitamin D deficiency 2.0: an update on the current status worldwide. Eur J Clin Nutr. 2020;74:1498-1513. doi:10.1038/s41430-020-0558-y
- Thomas X, Chelghoum Y, Fanari N, et al. Serum 25-hydroxyvitamin D levels are associated with prognosis in hematological malignancies. Hematology. 2011;16:278-283. doi:10.1179/102453311X13085644679908
- Siegel RL, Giaquinto AN, Jemal A. Cancer statistics, 2024. CA Cancer J Clin. 2024;74:12-49. doi:10.3322/caac.21820
- Goodwin PJ, Ennis M, Pritchard KI, et al. Prognostic effects of 25-hydroxyvitamin D levels in early breast cancer. J Clin Oncol. 2009;27:3757-3763. doi:10.1200/JCO.2008.20.0725
- Fassio A, Porciello G, Carioli G, et al. Post-diagnosis serum 25-hydroxyvitamin D concentrations in women treated for breast cancer participating in a lifestyle trial in Italy. Reumatismo. 2024;76:21-34.
- Augustin LSA, Libra M, Crispo A, et al. Low glycemic index diet, exercise and vitamin D to reduce breast cancer recurrence (DEDiCa): design of a clinical trial. BMC Cancer. 2017;17:69. doi:10.1186/s12885-017-3064-4
- Toriola AT, Nguyen N, Scheitler-Ring K, et al. Circulating 25-hydroxyvitamin D levels and prognosis among cancer patients: a systematic review. Cancer Epidemiol Biomarkers Prev. 2014;23:917-933. doi:10.1158/1055-9965.EPI-14-0053
- Fakih MG, Trump DL, Johnson CS, et al. Chemotherapy is linked to severe vitamin D deficiency in patients with colorectal cancer. Int J Colorectal Dis. 2009;24:219-224. doi:10.1007/s00384-008-0593-y
- Isenring EA, Teleni L, Woodman RJ, et al. Serum vitamin D decreases during chemotherapy: an Australian prospective cohort study. Asia Pac J Clin Nutr. 2018;27:962-967. doi:10.6133/apjcn.042018.01
- Kok DE, van den Berg MMGA, Posthuma L, et al. Changes in circulating levels of 25-hydroxyvitamin D3 in breast cancer patients receiving chemotherapy. Nutr Cancer. 2019;71:756-766. doi:10.1080/01635581.2018.1559938
- Wesselink E, Bours MJL, de Wilt JHW, et al. Chemotherapy and vitamin D supplement use are determinants of serum 25-hydroxyvitamin D levels during the first six months after colorectal cancer diagnosis. J Steroid Biochem Mol Biol. 2020;199:105577. doi:10.1016/j.jsbmb.2020.105577
- Savoie MB, Paciorek A, Zhang L, et al. Vitamin D levels in patients with colorectal cancer before and after treatment initiation. J Gastrointest Cancer. 2019;50:769-779. doi:10.1007/s12029-018-0147-7
- Kitchen D, Hughes B, Gill I, et al. The relationship between vitamin D and chemotherapy-induced toxicity—a pilot study. Br J Cancer. 2012;107:158-160. doi:10.1038/bjc.2012.194
- Demircay Z, Gürbüz O, Alpdogan TB, et al. Chemotherapy-induced acral erythema in leukemic patients: a report of 15 cases. Int J Dermatol. 1997;36:593-598. doi:10.1046/j.1365-4362.1997.00040.x
- Valks R, Fraga J, Porras-Luque J, et al. Chemotherapy-induced eccrine squamous syringometaplasia. a distinctive eruption in patients receiving hematopoietic progenitor cells. Arch Dermatol. 1997;133;873-878. doi:10.1001/archderm.133.7.873
- Webber KA, Kos L, Holland KE, et al. Intertriginous eruption associated with chemotherapy in pediatric patients. Arch Dermatol. 2007;143:67-71. doi:10.1001/archderm.143.1.67
- Hunjan MK, Nowsheen S, Ramos-Rodriguez AJ, et al. Clinical and histopathological spectrum of toxic erythema of chemotherapy in patients who have undergone allogeneic hematopoietic cell transplantation. Hematol Oncol Stem Cell Ther. 2019;12:19-25. doi:10.1016/j.hemonc.2018.09.001
- Ghorbanzadeh-Moghaddam A, Gholamrezaei A, Hemati S. Vitamin D deficiency is associated with the severity of radiation-induced proctitis in cancer patients. Int J Radiat Oncol Biol Phys. 2015;92:613-618. doi:10.1016/j.ijrobp.2015.02.011
- Bhanu A, Waghmare CM, Jain VS, et al. Serum 25-hydroxy vitamin-D levels in head and neck cancer chemoradiation therapy: potential in cancer therapeutics. Indian J Cancer. Published online February 27, 2003. doi:10.4103/ijc.ijc_358_20
- Yang B, Xie X, Wu Z, et al. DNA damage-mediated cellular senescence promotes hand-foot syndrome that can be relieved by thymidine prodrug. Genes Dis. 2022;10:2557-2571. doi:10.1016/j.gendis.2022.10.004
- Lassere Y, Hoff P. Management of hand-foot syndrome in patients treated with capecitabine (Xeloda®). Eur J Oncol Nurs. 2004;8(suppl 1):S31-S40. doi:10.1016/j.ejon.2004.06.007
- Ernst MK, Evans ST, Techner JM, et al. Vitamin D3 and deconvoluting a rash. JCI Insight. 2023;8:E163789.
- Nguyen CV, Zheng L, Zhou XA, et al. High-dose vitamin d for the management of toxic erythema of chemotherapy in hospitalized patients. JAMA Dermatol. 2023;159:219-221. doi:10.1001/jamadermatol.2022.5397
- Fisher J, Scott C, Stevens R, et al. Randomized phase III study comparing best supportive care to biafine as a prophylactic agent for radiation-induced skin toxicity for women undergoing breast irradiation: Radiation Therapy Oncology Group (RTOG) 97-13. Int J Radiat Oncol Biol Phys. 2000;48:1307-1310. doi:10.1016/s0360-3016(00)00782-3
- Pignol JP, Olivotto I, Rakovitch E, et al. A multicenter randomized trial of breast intensity-modulated radiation therapy to reduce acute radiation dermatitis. J Clin Oncol. 2008;26:2085-2092. doi:10.1200/JCO.2007.15.2488
- Hymes SR, Strom EA, Fife C. Radiation dermatitis: clinical presentation, pathophysiology, and treatment 2006. J Am Acad Dermatol. 2006;54:28-46. doi:10.1016/j.jaad.2005.08.054
- Ryan JL. Ionizing radiation: the good, the bad, and the ugly. J Invest Dermatol. 2012;132(3 pt 2):985-993. doi:10.1038/jid.2011.411
- Scott JF, Das LM, Ahsanuddin S, et al. Oral vitamin D rapidly attenuates inflammation from sunburn: an interventional study. J Invest Dermatol. 2017;137:2078-2086. doi:10.1016/j.jid.2017.04.040
- Das LM, Binko AM, Traylor ZP, et al. Vitamin D improves sunburns by increasing autophagy in M2 macrophages. Autophagy. 2019;15:813-826. doi:10.1080/15548627.2019.1569298
- Nasser NJ, Fenig S, Ravid A, et al. Vitamin D ointment for prevention of radiation dermatitis in breast cancer patients. NPJ Breast Cancer. 2017;3:10. doi:10.1038/s41523-017-0006-x
- Nguyen CV, Zheng L, Lu KQ. High-dose vitamin D for the management acute radiation dermatitis. JAAD Case Rep. 2023;39:47-50. doi:10.1016/j.jdcr.2023.07.001
- Nguyen CV, Lu KQ. Vitamin D3 and its potential to ameliorate chemical and radiation-induced skin injury during cancer therapy. Disaster Med Public Health Prep. 2024;18:E4. doi:10.1017/dmp.2023.211
Practice Points
- High-dose vitamin D supplementation may be considered in the management of cutaneous injury from chemotherapy or ionizing radiation.
- Optimal dosing has not been established, so patients given high-dose vitamin D supplementation should have close clinical follow-up; however, adverse events from high-dose vitamin D supplementation have not been reported.
Inpatient Management of Hidradenitis Suppurativa: A Delphi Consensus Study
Hidradenitis suppurativa (HS) is a chronic inflammatory skin condition that affects approximately 0.1% of the US population.1,2 Severe disease or HS flares can lead patients to seek care through the emergency department (ED), with some requiring inpatient admission. 3 Inpatient hospitalization of patients with HS has increased over the last 2 decades, and patients with HS utilize emergency and inpatient care more frequently than those with other dermatologic conditions.4,5 Minority patients and those of lower socioeconomic status are more likely to present to the ED for HS management due to limited access to care and other existing comorbid conditions. 4 In a 2022 study of the Nationwide Readmissions Database, the authors looked at hospital readmission rates of patients with HS compared with those with heart failure—both patient populations with chronic debilitating conditions. Results indicated that the hospital readmission rates for patients with HS surpassed those of patients with heart failure for that year, highlighting the need for improved inpatient management of HS.6
Patients with HS present to the ED with severe pain, fever, wound care, or the need for surgical intervention. The ED and inpatient hospital setting are locations in which physicians may not be as familiar with the diagnosis or treatment of HS, specifically flares or severe disease. 7 The inpatient care setting provides access to certain resources that can be challenging to obtain in the outpatient clinical setting, such as social workers and pain specialists, but also can prove challenging in obtaining other resources for HS management, such as advanced medical therapies. Given the increase in hospital- based care for HS and lack of widespread inpatient access to dermatology and HS experts, consensus recommendations for management of HS in the acute hospital setting would be beneficial. In our study, we sought to generate a collection of expert consensus statements providers can refer to when managing patients with HS in the inpatient setting.
Methods
The study team at the Wake Forest University School of Medicine (Winston-Salem, North Carolina)(M.N., R.P., L.C.S.) developed an initial set of consensus statements based on current published HS treatment guidelines,8,9 publications on management of inpatient HS,3 published supportive care guidelines for Stevens-Johnson syndrome, 10 and personal clinical experience in managing inpatient HS, which resulted in 50 statements organized into the following categories: overall care, wound care, genital care, pain management, infection control, medical management, surgical management, nutrition, and transitional care guidelines. This study was approved by the Wake Forest University institutional review board (IRB00084257).
Participant Recruitment—Dermatologists were identified for participation in the study based on membership in the Society of Dermatology Hospitalists and the Hidradenitis Suppurativa Foundation or authorship of publications relevant to HS or inpatient dermatology. Dermatologists from larger academic institutions with HS specialty clinics and inpatient dermatology services also were identified. Participants were invited via email and could suggest other experts for inclusion. A total of 31 dermatologists were invited to participate in the study, with 26 agreeing to participate. All participating dermatologists were practicing in the United States.
Delphi Study—In the first round of the Delphi study, the participants were sent an online survey via REDCap in which they were asked to rank the appropriateness of each of the proposed 50 guideline statements on a scale of 1 (very inappropriate) to 9 (very appropriate). Participants also were able to provide commentary and feedback on each of the statements. Survey results were analyzed using the RAND/ UCLA Appropriateness Method.11 For each statement, the median rating for appropriateness, interpercentile range (IPR), IPR adjusted for symmetry, and disagreement index (DI) were calculated (DI=IPR/IPR adjusted for symmetry). The 30th and 70th percentiles were used in the DI calculation as the upper and lower limits, respectively. A median rating for appropriateness of 1.0 to 3.9 was considered “inappropriate,” 4.0 to 6.9 was considered “uncertain appropriateness,” and 7.0 to 9.0 was “appropriate.” A DI value greater than or equal to 1 indicated a lack of consensus regarding the appropriateness of the statement. Following each round, participants received a copy of their responses along with the group median rank of each statement. Statements that did not reach consensus in the first Delphi round were revised based on feedback received by the participants, and a second survey with 14 statements was sent via REDCap 2 weeks later. The RAND/UCLA Appropriateness Method also was applied to this second Delphi round. After the second survey, participants received a copy of anonymized comments regarding the consensus statements and were allowed to provide additional final commentary to be included in the discussion of these recommendations.
Results
Twenty-six dermatologists completed the first-round survey, and 24 participants completed the second-round survey. All participants self-identified as having expertise in either HS (n=22 [85%]) or inpatient dermatology (n=17 [65%]), and 13 (50%) participants self-identified as experts in both HS and inpatient dermatology. All participants, except 1, were affiliated with an academic health system with inpatient dermatology services. The average length of time in practice as a dermatologist was 10 years (median, 9 years [range, 3–27 years]).
Of the 50 initial proposed consensus statements, 26 (52%) achieved consensus after the first round; 21 statements revealed DI calculations that did not achieve consensus. Two statements achieved consensus but received median ratings for appropriateness, indicating uncertain appropriateness; because of this, 1 statement was removed and 1 was revised based on participant feedback, resulting in 13 revised statements (eTable 1). Controversial topics in the consensus process included obtaining wound cultures and meaningful culture data interpretation, use of specific biologic medications in the inpatient setting, and use of intravenous ertapenem. Participant responses to these topics are discussed in detail below. Of these secondround statements, all achieved consensus. The final set of consensus statements can be found in eTable 2.
Comment
Our Delphi consensus study combined the expertise of both dermatologists who care for patients with HS and those with inpatient dermatology experience to produce a set of recommendations for the management of HS in the hospital care setting. A strength of this study is inclusion of many national leaders in both HS and inpatient dermatology, with some participants having developed the previously published HS treatment guidelines and others having participated in inpatient dermatology Delphi studies.8-10 The expertise is further strengthened by the geographically diverse institutional representation within the United States.
The final consensus recommendations included 40 statements covering a range of patient care issues, including use of appropriate inpatient subspecialists (care team), supportive care measures (wound care, pain control, genital care), disease-oriented treatment (medical management, surgical management), inpatient complications (infection control, nutrition), and successful transition back to outpatient management (transitional care). These recommendations are meant to serve as a resource for providers to consider when taking care of inpatient HS flares, recognizing that the complexity and individual circumstances of each patient are unique.
Delphi Consensus Recommendations Compared to Prior Guidelines—Several recommendations in the current study align with the previously published North American clinical management guidelines for HS.8,9 Our recommendations agree with prior guidelines on the importance of disease staging and pain assessment using validated assessment tools as well as screening for HS comorbidities. There also is agreement in the potential benefit of involving pain specialists in the development of a comprehensive pain management plan. The inpatient care setting provides a unique opportunity to engage multiple specialists and collaborate on patient care in a timely manner. Our recommendations regarding surgical care also align with established guidelines in recommending incision and drainage as an acute bedside procedure best utilized for symptom relief in inflamed abscesses and relegating most other surgical management to the outpatient setting. Wound care recommendations also are similar, with our expert participants agreeing on individualizing dressing choices based on wound characteristics. A benefit of inpatient wound care is access to skilled nursing for dressing changes and potentially improved access to more sophisticated dressing materials. Our recommendations differ from the prior guidelines in our focus on severe HS, HS flares, and HS complications, which constitute the majority of inpatient disease management. We provide additional guidance on management of secondary infections, perianal fistulous disease, and importantly transitional care to optimize discharge planning.
Differing Opinions in Our Analysis—Despite the success of our Delphi consensus process, there were some differing opinions regarding certain aspects of inpatient HS management, which is to be expected given the lack of strong evidence-based research to support some of the recommended practices. There were differing opinions on the utility of wound culture data, with some participants feeling culture data could help with antibiotic susceptibility and resistance patterns, while others felt wound cultures represent bacterial colonization or biofilm formation.
Initial consensus statements in the first Delphi round were created for individual biologic medications but did not achieve consensus, and feedback on the use of biologics in the inpatient environment was mixed, largely due to logistic and insurance issues. Many participants felt biologic medication cost, difficulty obtaining inpatient reimbursement, health care resource utilization, and availability of biologics in different hospital systems prevented recommending the use of specific biologics during hospitalization. The one exception was in the case of a hospitalized patient who was already receiving infliximab for HS: there was consensus on ensuring the patient dosing was maximized, if appropriate, to 10 mg/kg.12 Ertapenem use also was controversial, with some participants using it as a bridge therapy to either outpatient biologic use or surgery, while others felt it was onerous and difficult to establish reliable access to secure intravenous administration and regular dosing once the patient left the inpatient setting.13 Others said they have experienced objections from infectious disease colleagues on the use of intravenous antibiotics, citing antibiotic stewardship concerns.
Patient Care in the Inpatient Setting—Prior literature suggests patients admitted as inpatients for HS tend to be of lower socioeconomic status and are admitted to larger urban teaching hospitals.14,15 Patients with lower socioeconomic status have increased difficulty accessing health care resources; therefore, inpatient admission serves as an opportunity to provide a holistic HS assessment and coordinate resources for chronic outpatient management.
Study Limitations—This Delphi consensus study has some limitations. The existing literature on inpatient management of HS is limited, challenging our ability to assess the extent to which these published recommendations are already being implemented. Additionally, the study included HS and inpatient dermatology experts from the United States, which means the recommendations may not be generalizable to other countries. Most participants practiced dermatology at large tertiary care academic medical centers, which may limit the ability to implement recommendations in all US inpatient care settings such as small community-based hospitals; however, many of the supportive care guidelines such as pain control, wound care, nutritional support, and social work should be achievable in most inpatient care settings.
Conclusion
Given the increase in inpatient and ED health care utilization for HS, there is an urgent need for expert consensus recommendations on inpatient management of this unique patient population, which requires complex multidisciplinary care. Our recommendations are a resource for providers to utilize and potentially improve the standard of care we provide these patients.
Acknowledgment—We thank the Wake Forest University Clinical and Translational Science Institute (Winston- Salem, North Carolina) for providing statistical help.
- Garg A, Kirby JS, Lavian J, et al. Sex- and age-adjusted population analysis of prevalence estimates for hidradenitis suppurativa in the United States. JAMA Dermatol. 2017;153:760-764.
- Ingram JR. The epidemiology of hidradenitis suppurativa. Br J Dermatol. 2020;183:990-998. doi:10.1111/bjd.19435
- Charrow A, Savage KT, Flood K, et al. Hidradenitis suppurativa for the dermatologic hospitalist. Cutis. 2019;104:276-280.
- Anzaldi L, Perkins JA, Byrd AS, et al. Characterizing inpatient hospitalizations for hidradenitis suppurativa in the United States. J Am Acad Dermatol. 2020;82:510-513. doi:10.1016/j.jaad.2019.09.019
- Khalsa A, Liu G, Kirby JS. Increased utilization of emergency department and inpatient care by patients with hidradenitis suppurativa. J Am Acad Dermatol. 2015;73:609-614. doi:10.1016/j.jaad.2015.06.053
- Edigin E, Kaul S, Eseaton PO, et al. At 180 days hidradenitis suppurativa readmission rate is comparable to heart failure: analysis of the nationwide readmissions database. J Am Acad Dermatol. 2022;87:188-192. doi:10.1016/j.jaad.2021.06.894
- Kirby JS, Miller JJ, Adams DR, et al. Health care utilization patterns and costs for patients with hidradenitis suppurativa. JAMA Dermatol. 2014;150:937-944. doi:10.1001/jamadermatol.2014.691
- Alikhan A, Sayed C, Alavi A, et al. North American clinical management guidelines for hidradenitis suppurativa: a publication from the United States and Canadian Hidradenitis Suppurativa Foundations: part I: diagnosis, evaluation, and the use of complementary and procedural management. J Am Acad Dermatol. 2019;81:76-90. doi:10.1016/j .jaad.2019.02.067
- Alikhan A, Sayed C, Alavi A, et al. North American clinical management guidelines for hidradenitis suppurativa: a publication from the United States and Canadian Hidradenitis Suppurativa Foundations: part II: topical, intralesional, and systemic medical management. J Am Acad Dermatol. 2019;81:91-101. doi:10.1016/j.jaad.2019.02.068
- Seminario-Vidal L, Kroshinsky D, Malachowski SJ, et al. Society of Dermatology Hospitalists supportive care guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults. J Am Acad Dermatol. 2020;82:1553-1567. doi:10.1016/j .jaad.2020.02.066
- Fitch K, Bernstein SJ, Burnand B, et al. The RAND/UCLA Appropriateness Method: User’s Manual. Rand; 2001.
- Oskardmay AN, Miles JA, Sayed CJ. Determining the optimal dose of infliximab for treatment of hidradenitis suppurativa. J Am Acad Dermatol. 2019;81:702-708. doi:10.1016/j.jaad.2019.05.022
- Join-Lambert O, Coignard-Biehler H, Jais JP, et al. Efficacy of ertapenem in severe hidradenitis suppurativa: a pilot study in a cohort of 30 consecutive patients. J Antimicrob Chemother. 2016;71:513-520. doi:10.1093/jac/dkv361
- Khanna R, Whang KA, Huang AH, et al. Inpatient burden of hidradenitis suppurativa in the United States: analysis of the 2016 National Inpatient Sample. J Dermatolog Treat. 2022;33:1150-1152. doi:10.1080/09 546634.2020.1773380
- Patel A, Patel A, Solanki D, et al. Hidradenitis suppurativa in the United States: insights from the national inpatient sample (2008-2017) on contemporary trends in demographics, hospitalization rates, chronic comorbid conditions, and mortality. Cureus. 2022;14:E24755. doi:10.7759/cureus.24755
Hidradenitis suppurativa (HS) is a chronic inflammatory skin condition that affects approximately 0.1% of the US population.1,2 Severe disease or HS flares can lead patients to seek care through the emergency department (ED), with some requiring inpatient admission. 3 Inpatient hospitalization of patients with HS has increased over the last 2 decades, and patients with HS utilize emergency and inpatient care more frequently than those with other dermatologic conditions.4,5 Minority patients and those of lower socioeconomic status are more likely to present to the ED for HS management due to limited access to care and other existing comorbid conditions. 4 In a 2022 study of the Nationwide Readmissions Database, the authors looked at hospital readmission rates of patients with HS compared with those with heart failure—both patient populations with chronic debilitating conditions. Results indicated that the hospital readmission rates for patients with HS surpassed those of patients with heart failure for that year, highlighting the need for improved inpatient management of HS.6
Patients with HS present to the ED with severe pain, fever, wound care, or the need for surgical intervention. The ED and inpatient hospital setting are locations in which physicians may not be as familiar with the diagnosis or treatment of HS, specifically flares or severe disease. 7 The inpatient care setting provides access to certain resources that can be challenging to obtain in the outpatient clinical setting, such as social workers and pain specialists, but also can prove challenging in obtaining other resources for HS management, such as advanced medical therapies. Given the increase in hospital- based care for HS and lack of widespread inpatient access to dermatology and HS experts, consensus recommendations for management of HS in the acute hospital setting would be beneficial. In our study, we sought to generate a collection of expert consensus statements providers can refer to when managing patients with HS in the inpatient setting.
Methods
The study team at the Wake Forest University School of Medicine (Winston-Salem, North Carolina)(M.N., R.P., L.C.S.) developed an initial set of consensus statements based on current published HS treatment guidelines,8,9 publications on management of inpatient HS,3 published supportive care guidelines for Stevens-Johnson syndrome, 10 and personal clinical experience in managing inpatient HS, which resulted in 50 statements organized into the following categories: overall care, wound care, genital care, pain management, infection control, medical management, surgical management, nutrition, and transitional care guidelines. This study was approved by the Wake Forest University institutional review board (IRB00084257).
Participant Recruitment—Dermatologists were identified for participation in the study based on membership in the Society of Dermatology Hospitalists and the Hidradenitis Suppurativa Foundation or authorship of publications relevant to HS or inpatient dermatology. Dermatologists from larger academic institutions with HS specialty clinics and inpatient dermatology services also were identified. Participants were invited via email and could suggest other experts for inclusion. A total of 31 dermatologists were invited to participate in the study, with 26 agreeing to participate. All participating dermatologists were practicing in the United States.
Delphi Study—In the first round of the Delphi study, the participants were sent an online survey via REDCap in which they were asked to rank the appropriateness of each of the proposed 50 guideline statements on a scale of 1 (very inappropriate) to 9 (very appropriate). Participants also were able to provide commentary and feedback on each of the statements. Survey results were analyzed using the RAND/ UCLA Appropriateness Method.11 For each statement, the median rating for appropriateness, interpercentile range (IPR), IPR adjusted for symmetry, and disagreement index (DI) were calculated (DI=IPR/IPR adjusted for symmetry). The 30th and 70th percentiles were used in the DI calculation as the upper and lower limits, respectively. A median rating for appropriateness of 1.0 to 3.9 was considered “inappropriate,” 4.0 to 6.9 was considered “uncertain appropriateness,” and 7.0 to 9.0 was “appropriate.” A DI value greater than or equal to 1 indicated a lack of consensus regarding the appropriateness of the statement. Following each round, participants received a copy of their responses along with the group median rank of each statement. Statements that did not reach consensus in the first Delphi round were revised based on feedback received by the participants, and a second survey with 14 statements was sent via REDCap 2 weeks later. The RAND/UCLA Appropriateness Method also was applied to this second Delphi round. After the second survey, participants received a copy of anonymized comments regarding the consensus statements and were allowed to provide additional final commentary to be included in the discussion of these recommendations.
Results
Twenty-six dermatologists completed the first-round survey, and 24 participants completed the second-round survey. All participants self-identified as having expertise in either HS (n=22 [85%]) or inpatient dermatology (n=17 [65%]), and 13 (50%) participants self-identified as experts in both HS and inpatient dermatology. All participants, except 1, were affiliated with an academic health system with inpatient dermatology services. The average length of time in practice as a dermatologist was 10 years (median, 9 years [range, 3–27 years]).
Of the 50 initial proposed consensus statements, 26 (52%) achieved consensus after the first round; 21 statements revealed DI calculations that did not achieve consensus. Two statements achieved consensus but received median ratings for appropriateness, indicating uncertain appropriateness; because of this, 1 statement was removed and 1 was revised based on participant feedback, resulting in 13 revised statements (eTable 1). Controversial topics in the consensus process included obtaining wound cultures and meaningful culture data interpretation, use of specific biologic medications in the inpatient setting, and use of intravenous ertapenem. Participant responses to these topics are discussed in detail below. Of these secondround statements, all achieved consensus. The final set of consensus statements can be found in eTable 2.
Comment
Our Delphi consensus study combined the expertise of both dermatologists who care for patients with HS and those with inpatient dermatology experience to produce a set of recommendations for the management of HS in the hospital care setting. A strength of this study is inclusion of many national leaders in both HS and inpatient dermatology, with some participants having developed the previously published HS treatment guidelines and others having participated in inpatient dermatology Delphi studies.8-10 The expertise is further strengthened by the geographically diverse institutional representation within the United States.
The final consensus recommendations included 40 statements covering a range of patient care issues, including use of appropriate inpatient subspecialists (care team), supportive care measures (wound care, pain control, genital care), disease-oriented treatment (medical management, surgical management), inpatient complications (infection control, nutrition), and successful transition back to outpatient management (transitional care). These recommendations are meant to serve as a resource for providers to consider when taking care of inpatient HS flares, recognizing that the complexity and individual circumstances of each patient are unique.
Delphi Consensus Recommendations Compared to Prior Guidelines—Several recommendations in the current study align with the previously published North American clinical management guidelines for HS.8,9 Our recommendations agree with prior guidelines on the importance of disease staging and pain assessment using validated assessment tools as well as screening for HS comorbidities. There also is agreement in the potential benefit of involving pain specialists in the development of a comprehensive pain management plan. The inpatient care setting provides a unique opportunity to engage multiple specialists and collaborate on patient care in a timely manner. Our recommendations regarding surgical care also align with established guidelines in recommending incision and drainage as an acute bedside procedure best utilized for symptom relief in inflamed abscesses and relegating most other surgical management to the outpatient setting. Wound care recommendations also are similar, with our expert participants agreeing on individualizing dressing choices based on wound characteristics. A benefit of inpatient wound care is access to skilled nursing for dressing changes and potentially improved access to more sophisticated dressing materials. Our recommendations differ from the prior guidelines in our focus on severe HS, HS flares, and HS complications, which constitute the majority of inpatient disease management. We provide additional guidance on management of secondary infections, perianal fistulous disease, and importantly transitional care to optimize discharge planning.
Differing Opinions in Our Analysis—Despite the success of our Delphi consensus process, there were some differing opinions regarding certain aspects of inpatient HS management, which is to be expected given the lack of strong evidence-based research to support some of the recommended practices. There were differing opinions on the utility of wound culture data, with some participants feeling culture data could help with antibiotic susceptibility and resistance patterns, while others felt wound cultures represent bacterial colonization or biofilm formation.
Initial consensus statements in the first Delphi round were created for individual biologic medications but did not achieve consensus, and feedback on the use of biologics in the inpatient environment was mixed, largely due to logistic and insurance issues. Many participants felt biologic medication cost, difficulty obtaining inpatient reimbursement, health care resource utilization, and availability of biologics in different hospital systems prevented recommending the use of specific biologics during hospitalization. The one exception was in the case of a hospitalized patient who was already receiving infliximab for HS: there was consensus on ensuring the patient dosing was maximized, if appropriate, to 10 mg/kg.12 Ertapenem use also was controversial, with some participants using it as a bridge therapy to either outpatient biologic use or surgery, while others felt it was onerous and difficult to establish reliable access to secure intravenous administration and regular dosing once the patient left the inpatient setting.13 Others said they have experienced objections from infectious disease colleagues on the use of intravenous antibiotics, citing antibiotic stewardship concerns.
Patient Care in the Inpatient Setting—Prior literature suggests patients admitted as inpatients for HS tend to be of lower socioeconomic status and are admitted to larger urban teaching hospitals.14,15 Patients with lower socioeconomic status have increased difficulty accessing health care resources; therefore, inpatient admission serves as an opportunity to provide a holistic HS assessment and coordinate resources for chronic outpatient management.
Study Limitations—This Delphi consensus study has some limitations. The existing literature on inpatient management of HS is limited, challenging our ability to assess the extent to which these published recommendations are already being implemented. Additionally, the study included HS and inpatient dermatology experts from the United States, which means the recommendations may not be generalizable to other countries. Most participants practiced dermatology at large tertiary care academic medical centers, which may limit the ability to implement recommendations in all US inpatient care settings such as small community-based hospitals; however, many of the supportive care guidelines such as pain control, wound care, nutritional support, and social work should be achievable in most inpatient care settings.
Conclusion
Given the increase in inpatient and ED health care utilization for HS, there is an urgent need for expert consensus recommendations on inpatient management of this unique patient population, which requires complex multidisciplinary care. Our recommendations are a resource for providers to utilize and potentially improve the standard of care we provide these patients.
Acknowledgment—We thank the Wake Forest University Clinical and Translational Science Institute (Winston- Salem, North Carolina) for providing statistical help.
Hidradenitis suppurativa (HS) is a chronic inflammatory skin condition that affects approximately 0.1% of the US population.1,2 Severe disease or HS flares can lead patients to seek care through the emergency department (ED), with some requiring inpatient admission. 3 Inpatient hospitalization of patients with HS has increased over the last 2 decades, and patients with HS utilize emergency and inpatient care more frequently than those with other dermatologic conditions.4,5 Minority patients and those of lower socioeconomic status are more likely to present to the ED for HS management due to limited access to care and other existing comorbid conditions. 4 In a 2022 study of the Nationwide Readmissions Database, the authors looked at hospital readmission rates of patients with HS compared with those with heart failure—both patient populations with chronic debilitating conditions. Results indicated that the hospital readmission rates for patients with HS surpassed those of patients with heart failure for that year, highlighting the need for improved inpatient management of HS.6
Patients with HS present to the ED with severe pain, fever, wound care, or the need for surgical intervention. The ED and inpatient hospital setting are locations in which physicians may not be as familiar with the diagnosis or treatment of HS, specifically flares or severe disease. 7 The inpatient care setting provides access to certain resources that can be challenging to obtain in the outpatient clinical setting, such as social workers and pain specialists, but also can prove challenging in obtaining other resources for HS management, such as advanced medical therapies. Given the increase in hospital- based care for HS and lack of widespread inpatient access to dermatology and HS experts, consensus recommendations for management of HS in the acute hospital setting would be beneficial. In our study, we sought to generate a collection of expert consensus statements providers can refer to when managing patients with HS in the inpatient setting.
Methods
The study team at the Wake Forest University School of Medicine (Winston-Salem, North Carolina)(M.N., R.P., L.C.S.) developed an initial set of consensus statements based on current published HS treatment guidelines,8,9 publications on management of inpatient HS,3 published supportive care guidelines for Stevens-Johnson syndrome, 10 and personal clinical experience in managing inpatient HS, which resulted in 50 statements organized into the following categories: overall care, wound care, genital care, pain management, infection control, medical management, surgical management, nutrition, and transitional care guidelines. This study was approved by the Wake Forest University institutional review board (IRB00084257).
Participant Recruitment—Dermatologists were identified for participation in the study based on membership in the Society of Dermatology Hospitalists and the Hidradenitis Suppurativa Foundation or authorship of publications relevant to HS or inpatient dermatology. Dermatologists from larger academic institutions with HS specialty clinics and inpatient dermatology services also were identified. Participants were invited via email and could suggest other experts for inclusion. A total of 31 dermatologists were invited to participate in the study, with 26 agreeing to participate. All participating dermatologists were practicing in the United States.
Delphi Study—In the first round of the Delphi study, the participants were sent an online survey via REDCap in which they were asked to rank the appropriateness of each of the proposed 50 guideline statements on a scale of 1 (very inappropriate) to 9 (very appropriate). Participants also were able to provide commentary and feedback on each of the statements. Survey results were analyzed using the RAND/ UCLA Appropriateness Method.11 For each statement, the median rating for appropriateness, interpercentile range (IPR), IPR adjusted for symmetry, and disagreement index (DI) were calculated (DI=IPR/IPR adjusted for symmetry). The 30th and 70th percentiles were used in the DI calculation as the upper and lower limits, respectively. A median rating for appropriateness of 1.0 to 3.9 was considered “inappropriate,” 4.0 to 6.9 was considered “uncertain appropriateness,” and 7.0 to 9.0 was “appropriate.” A DI value greater than or equal to 1 indicated a lack of consensus regarding the appropriateness of the statement. Following each round, participants received a copy of their responses along with the group median rank of each statement. Statements that did not reach consensus in the first Delphi round were revised based on feedback received by the participants, and a second survey with 14 statements was sent via REDCap 2 weeks later. The RAND/UCLA Appropriateness Method also was applied to this second Delphi round. After the second survey, participants received a copy of anonymized comments regarding the consensus statements and were allowed to provide additional final commentary to be included in the discussion of these recommendations.
Results
Twenty-six dermatologists completed the first-round survey, and 24 participants completed the second-round survey. All participants self-identified as having expertise in either HS (n=22 [85%]) or inpatient dermatology (n=17 [65%]), and 13 (50%) participants self-identified as experts in both HS and inpatient dermatology. All participants, except 1, were affiliated with an academic health system with inpatient dermatology services. The average length of time in practice as a dermatologist was 10 years (median, 9 years [range, 3–27 years]).
Of the 50 initial proposed consensus statements, 26 (52%) achieved consensus after the first round; 21 statements revealed DI calculations that did not achieve consensus. Two statements achieved consensus but received median ratings for appropriateness, indicating uncertain appropriateness; because of this, 1 statement was removed and 1 was revised based on participant feedback, resulting in 13 revised statements (eTable 1). Controversial topics in the consensus process included obtaining wound cultures and meaningful culture data interpretation, use of specific biologic medications in the inpatient setting, and use of intravenous ertapenem. Participant responses to these topics are discussed in detail below. Of these secondround statements, all achieved consensus. The final set of consensus statements can be found in eTable 2.
Comment
Our Delphi consensus study combined the expertise of both dermatologists who care for patients with HS and those with inpatient dermatology experience to produce a set of recommendations for the management of HS in the hospital care setting. A strength of this study is inclusion of many national leaders in both HS and inpatient dermatology, with some participants having developed the previously published HS treatment guidelines and others having participated in inpatient dermatology Delphi studies.8-10 The expertise is further strengthened by the geographically diverse institutional representation within the United States.
The final consensus recommendations included 40 statements covering a range of patient care issues, including use of appropriate inpatient subspecialists (care team), supportive care measures (wound care, pain control, genital care), disease-oriented treatment (medical management, surgical management), inpatient complications (infection control, nutrition), and successful transition back to outpatient management (transitional care). These recommendations are meant to serve as a resource for providers to consider when taking care of inpatient HS flares, recognizing that the complexity and individual circumstances of each patient are unique.
Delphi Consensus Recommendations Compared to Prior Guidelines—Several recommendations in the current study align with the previously published North American clinical management guidelines for HS.8,9 Our recommendations agree with prior guidelines on the importance of disease staging and pain assessment using validated assessment tools as well as screening for HS comorbidities. There also is agreement in the potential benefit of involving pain specialists in the development of a comprehensive pain management plan. The inpatient care setting provides a unique opportunity to engage multiple specialists and collaborate on patient care in a timely manner. Our recommendations regarding surgical care also align with established guidelines in recommending incision and drainage as an acute bedside procedure best utilized for symptom relief in inflamed abscesses and relegating most other surgical management to the outpatient setting. Wound care recommendations also are similar, with our expert participants agreeing on individualizing dressing choices based on wound characteristics. A benefit of inpatient wound care is access to skilled nursing for dressing changes and potentially improved access to more sophisticated dressing materials. Our recommendations differ from the prior guidelines in our focus on severe HS, HS flares, and HS complications, which constitute the majority of inpatient disease management. We provide additional guidance on management of secondary infections, perianal fistulous disease, and importantly transitional care to optimize discharge planning.
Differing Opinions in Our Analysis—Despite the success of our Delphi consensus process, there were some differing opinions regarding certain aspects of inpatient HS management, which is to be expected given the lack of strong evidence-based research to support some of the recommended practices. There were differing opinions on the utility of wound culture data, with some participants feeling culture data could help with antibiotic susceptibility and resistance patterns, while others felt wound cultures represent bacterial colonization or biofilm formation.
Initial consensus statements in the first Delphi round were created for individual biologic medications but did not achieve consensus, and feedback on the use of biologics in the inpatient environment was mixed, largely due to logistic and insurance issues. Many participants felt biologic medication cost, difficulty obtaining inpatient reimbursement, health care resource utilization, and availability of biologics in different hospital systems prevented recommending the use of specific biologics during hospitalization. The one exception was in the case of a hospitalized patient who was already receiving infliximab for HS: there was consensus on ensuring the patient dosing was maximized, if appropriate, to 10 mg/kg.12 Ertapenem use also was controversial, with some participants using it as a bridge therapy to either outpatient biologic use or surgery, while others felt it was onerous and difficult to establish reliable access to secure intravenous administration and regular dosing once the patient left the inpatient setting.13 Others said they have experienced objections from infectious disease colleagues on the use of intravenous antibiotics, citing antibiotic stewardship concerns.
Patient Care in the Inpatient Setting—Prior literature suggests patients admitted as inpatients for HS tend to be of lower socioeconomic status and are admitted to larger urban teaching hospitals.14,15 Patients with lower socioeconomic status have increased difficulty accessing health care resources; therefore, inpatient admission serves as an opportunity to provide a holistic HS assessment and coordinate resources for chronic outpatient management.
Study Limitations—This Delphi consensus study has some limitations. The existing literature on inpatient management of HS is limited, challenging our ability to assess the extent to which these published recommendations are already being implemented. Additionally, the study included HS and inpatient dermatology experts from the United States, which means the recommendations may not be generalizable to other countries. Most participants practiced dermatology at large tertiary care academic medical centers, which may limit the ability to implement recommendations in all US inpatient care settings such as small community-based hospitals; however, many of the supportive care guidelines such as pain control, wound care, nutritional support, and social work should be achievable in most inpatient care settings.
Conclusion
Given the increase in inpatient and ED health care utilization for HS, there is an urgent need for expert consensus recommendations on inpatient management of this unique patient population, which requires complex multidisciplinary care. Our recommendations are a resource for providers to utilize and potentially improve the standard of care we provide these patients.
Acknowledgment—We thank the Wake Forest University Clinical and Translational Science Institute (Winston- Salem, North Carolina) for providing statistical help.
- Garg A, Kirby JS, Lavian J, et al. Sex- and age-adjusted population analysis of prevalence estimates for hidradenitis suppurativa in the United States. JAMA Dermatol. 2017;153:760-764.
- Ingram JR. The epidemiology of hidradenitis suppurativa. Br J Dermatol. 2020;183:990-998. doi:10.1111/bjd.19435
- Charrow A, Savage KT, Flood K, et al. Hidradenitis suppurativa for the dermatologic hospitalist. Cutis. 2019;104:276-280.
- Anzaldi L, Perkins JA, Byrd AS, et al. Characterizing inpatient hospitalizations for hidradenitis suppurativa in the United States. J Am Acad Dermatol. 2020;82:510-513. doi:10.1016/j.jaad.2019.09.019
- Khalsa A, Liu G, Kirby JS. Increased utilization of emergency department and inpatient care by patients with hidradenitis suppurativa. J Am Acad Dermatol. 2015;73:609-614. doi:10.1016/j.jaad.2015.06.053
- Edigin E, Kaul S, Eseaton PO, et al. At 180 days hidradenitis suppurativa readmission rate is comparable to heart failure: analysis of the nationwide readmissions database. J Am Acad Dermatol. 2022;87:188-192. doi:10.1016/j.jaad.2021.06.894
- Kirby JS, Miller JJ, Adams DR, et al. Health care utilization patterns and costs for patients with hidradenitis suppurativa. JAMA Dermatol. 2014;150:937-944. doi:10.1001/jamadermatol.2014.691
- Alikhan A, Sayed C, Alavi A, et al. North American clinical management guidelines for hidradenitis suppurativa: a publication from the United States and Canadian Hidradenitis Suppurativa Foundations: part I: diagnosis, evaluation, and the use of complementary and procedural management. J Am Acad Dermatol. 2019;81:76-90. doi:10.1016/j .jaad.2019.02.067
- Alikhan A, Sayed C, Alavi A, et al. North American clinical management guidelines for hidradenitis suppurativa: a publication from the United States and Canadian Hidradenitis Suppurativa Foundations: part II: topical, intralesional, and systemic medical management. J Am Acad Dermatol. 2019;81:91-101. doi:10.1016/j.jaad.2019.02.068
- Seminario-Vidal L, Kroshinsky D, Malachowski SJ, et al. Society of Dermatology Hospitalists supportive care guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults. J Am Acad Dermatol. 2020;82:1553-1567. doi:10.1016/j .jaad.2020.02.066
- Fitch K, Bernstein SJ, Burnand B, et al. The RAND/UCLA Appropriateness Method: User’s Manual. Rand; 2001.
- Oskardmay AN, Miles JA, Sayed CJ. Determining the optimal dose of infliximab for treatment of hidradenitis suppurativa. J Am Acad Dermatol. 2019;81:702-708. doi:10.1016/j.jaad.2019.05.022
- Join-Lambert O, Coignard-Biehler H, Jais JP, et al. Efficacy of ertapenem in severe hidradenitis suppurativa: a pilot study in a cohort of 30 consecutive patients. J Antimicrob Chemother. 2016;71:513-520. doi:10.1093/jac/dkv361
- Khanna R, Whang KA, Huang AH, et al. Inpatient burden of hidradenitis suppurativa in the United States: analysis of the 2016 National Inpatient Sample. J Dermatolog Treat. 2022;33:1150-1152. doi:10.1080/09 546634.2020.1773380
- Patel A, Patel A, Solanki D, et al. Hidradenitis suppurativa in the United States: insights from the national inpatient sample (2008-2017) on contemporary trends in demographics, hospitalization rates, chronic comorbid conditions, and mortality. Cureus. 2022;14:E24755. doi:10.7759/cureus.24755
- Garg A, Kirby JS, Lavian J, et al. Sex- and age-adjusted population analysis of prevalence estimates for hidradenitis suppurativa in the United States. JAMA Dermatol. 2017;153:760-764.
- Ingram JR. The epidemiology of hidradenitis suppurativa. Br J Dermatol. 2020;183:990-998. doi:10.1111/bjd.19435
- Charrow A, Savage KT, Flood K, et al. Hidradenitis suppurativa for the dermatologic hospitalist. Cutis. 2019;104:276-280.
- Anzaldi L, Perkins JA, Byrd AS, et al. Characterizing inpatient hospitalizations for hidradenitis suppurativa in the United States. J Am Acad Dermatol. 2020;82:510-513. doi:10.1016/j.jaad.2019.09.019
- Khalsa A, Liu G, Kirby JS. Increased utilization of emergency department and inpatient care by patients with hidradenitis suppurativa. J Am Acad Dermatol. 2015;73:609-614. doi:10.1016/j.jaad.2015.06.053
- Edigin E, Kaul S, Eseaton PO, et al. At 180 days hidradenitis suppurativa readmission rate is comparable to heart failure: analysis of the nationwide readmissions database. J Am Acad Dermatol. 2022;87:188-192. doi:10.1016/j.jaad.2021.06.894
- Kirby JS, Miller JJ, Adams DR, et al. Health care utilization patterns and costs for patients with hidradenitis suppurativa. JAMA Dermatol. 2014;150:937-944. doi:10.1001/jamadermatol.2014.691
- Alikhan A, Sayed C, Alavi A, et al. North American clinical management guidelines for hidradenitis suppurativa: a publication from the United States and Canadian Hidradenitis Suppurativa Foundations: part I: diagnosis, evaluation, and the use of complementary and procedural management. J Am Acad Dermatol. 2019;81:76-90. doi:10.1016/j .jaad.2019.02.067
- Alikhan A, Sayed C, Alavi A, et al. North American clinical management guidelines for hidradenitis suppurativa: a publication from the United States and Canadian Hidradenitis Suppurativa Foundations: part II: topical, intralesional, and systemic medical management. J Am Acad Dermatol. 2019;81:91-101. doi:10.1016/j.jaad.2019.02.068
- Seminario-Vidal L, Kroshinsky D, Malachowski SJ, et al. Society of Dermatology Hospitalists supportive care guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults. J Am Acad Dermatol. 2020;82:1553-1567. doi:10.1016/j .jaad.2020.02.066
- Fitch K, Bernstein SJ, Burnand B, et al. The RAND/UCLA Appropriateness Method: User’s Manual. Rand; 2001.
- Oskardmay AN, Miles JA, Sayed CJ. Determining the optimal dose of infliximab for treatment of hidradenitis suppurativa. J Am Acad Dermatol. 2019;81:702-708. doi:10.1016/j.jaad.2019.05.022
- Join-Lambert O, Coignard-Biehler H, Jais JP, et al. Efficacy of ertapenem in severe hidradenitis suppurativa: a pilot study in a cohort of 30 consecutive patients. J Antimicrob Chemother. 2016;71:513-520. doi:10.1093/jac/dkv361
- Khanna R, Whang KA, Huang AH, et al. Inpatient burden of hidradenitis suppurativa in the United States: analysis of the 2016 National Inpatient Sample. J Dermatolog Treat. 2022;33:1150-1152. doi:10.1080/09 546634.2020.1773380
- Patel A, Patel A, Solanki D, et al. Hidradenitis suppurativa in the United States: insights from the national inpatient sample (2008-2017) on contemporary trends in demographics, hospitalization rates, chronic comorbid conditions, and mortality. Cureus. 2022;14:E24755. doi:10.7759/cureus.24755
Practice Points
- Given the increase in hospital-based care for hidradenitis suppurativa (HS) and the lack of widespread inpatient access to dermatology and HS experts, consensus recommendations for management of HS in the acute hospital setting would be beneficial.
- Our Delphi study yielded 40 statements that reached consensus covering a range of patient care issues (eg, appropriate inpatient subspecialists [care team]), supportive care measures (wound care, pain control, genital care), disease-oriented treatment (medical management, surgical management), inpatient complications (infection control, nutrition), and successful transition to outpatient management (transitional care).
- These recommendations serve as an important resource for providers caring for inpatients with HS and represent a successful collaboration between inpatient dermatology and HS experts.
Micronutrient Deficiencies in Patients With Inflammatory Bowel Disease
In 2023, ESPEN (the European Society for Clinical Nutrition and Metabolism) published consensus recommendations highlighting the importance of regular monitoring and treatment of nutrient deficiencies in patients with inflammatory bowel disease (IBD) for improved prognosis, mortality, and quality of life.1 Suboptimal nutrition in patients with IBD predominantly results from inflammation of the gastrointestinal (GI) tract leading to malabsorption; however, medications commonly used to manage IBD also can contribute to malnutrition.2,3 Additionally, patients may develop nausea and food avoidance due to medication or the disease itself, leading to nutritional withdrawal and eventual deficiency.4 Even with the development of diets focused on balancing nutritional needs and decreasing inflammation,5 offsetting this aversion to food can be difficult to overcome.2
Cutaneous manifestations of IBD are multifaceted and can be secondary to the disease, reactive to or associated with IBD, or effects from nutritional deficiencies. The most common vitamin and nutrient deficiencies in patients with IBD include iron; zinc; calcium; vitamin D; and vitamins B6 (pyridoxine), B9 (folic acid), and B12.6 Malnutrition may manifest with cutaneous disease, and dermatologists can be the first to identify and assess for nutritional deficiencies. In this article, we review the mechanisms of these micronutrient depletions in the context of IBD, their subsequent dermatologic manifestations (Table), and treatment and monitoring guidelines for each deficiency.
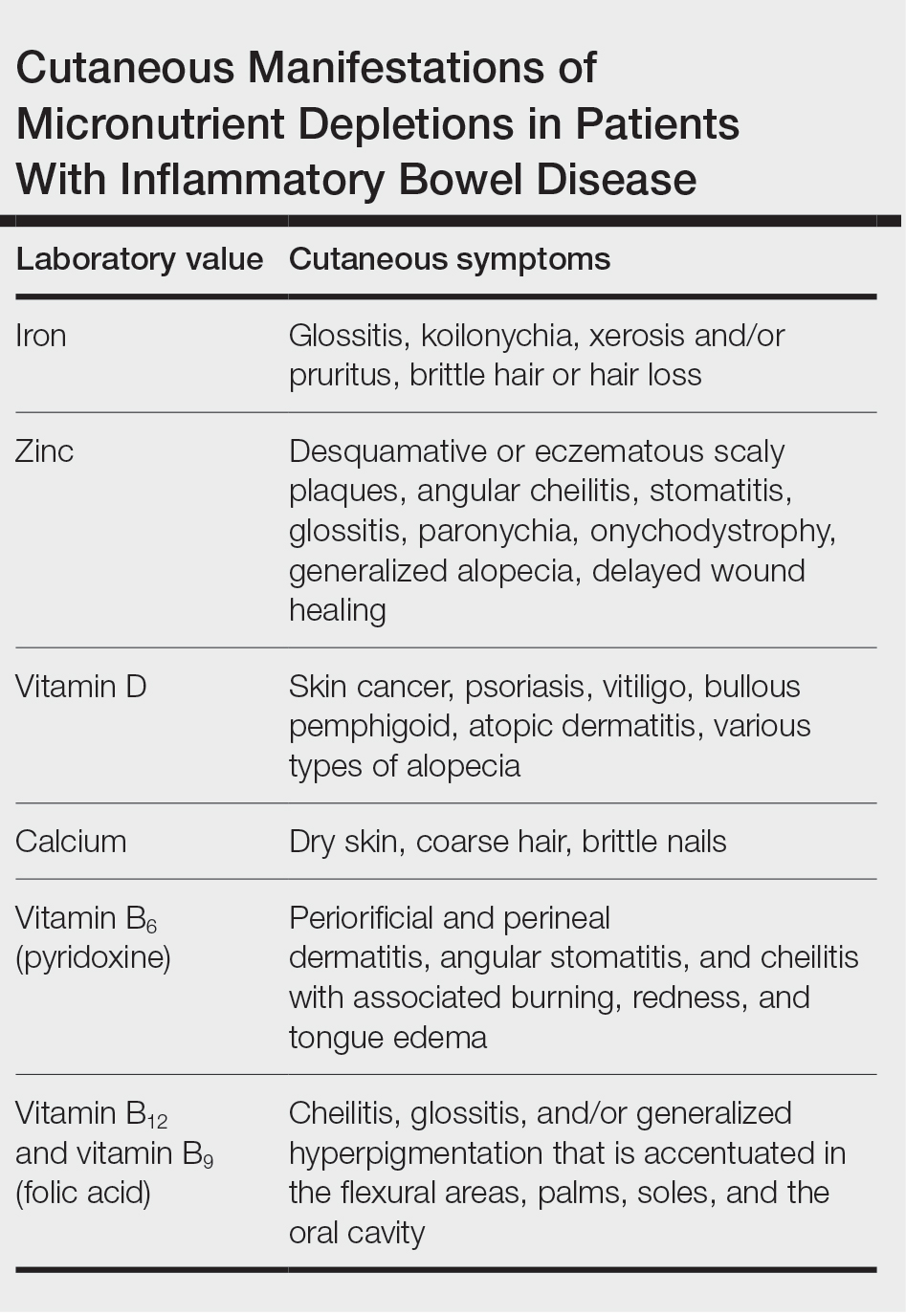
Iron
A systematic review conducted from 2007 to 2012 in European patients with IBD (N=2192) found the overall prevalence of anemia in this population to be 24% (95% CI, 18%-31%), with 57% of patients with anemia experiencing iron deficiency.7 Anemia is observed more commonly in patients hospitalized with IBD and is common in patients with both Crohn disease and ulcerative colitis.8
Pathophysiology—Iron is critically important in oxygen transportation throughout the body as a major component of hemoglobin. Physiologically, the low pH of the duodenum and proximal jejunum allows divalent metal transporter 1 to transfer dietary Fe3+ into enterocytes, where it is reduced to the transportable Fe2+.9,10 Distribution of Fe2+ ions from enterocytes relies on ferroportin, an iron-transporting protein, which is heavily regulated by the protein hepcidin.11 Hepcidin, a known acute phase reactant, will increase in the setting of active IBD, causing a depletion of ferroportin and an inability of the body to utilize the stored iron in enterocytes.12 This poor utilization of iron stores combined with blood loss caused by inflammation in the GI tract is the proposed primary mechanism of iron-deficiency anemia observed in patients with IBD.13
Cutaneous Manifestations—From a dermatologic perspective, iron-deficiency anemia can manifest with a wide range of symptoms including glossitis, koilonychia, xerosis and/or pruritus, and brittle hair or hair loss.14,15 Although the underlying pathophysiology of these cutaneous manifestations is not fully understood, there are several theories assessing the mechanisms behind the skin findings of iron deficiency.
Atrophic glossitis has been observed in many patients with iron deficiency and is thought to manifest due to low iron concentrations in the blood, thereby decreasing oxygen delivery to the papillae of the dorsal tongue with resultant atrophy.16,17 Similarly, decreased oxygen delivery to the nail bed capillaries may cause deformities in the nail called koilonychia (or “spoon nails”).18 Iron is a key co-factor in collagen lysyl hydroxylase that promotes collagen binding; iron deficiency may lead to disruptions in the epidermal barrier that can cause pruritus and xerosis.19 An observational study of 200 healthy patients with a primary concern of pruritus found a correlation between low serum ferritin and a higher degree of pruritus (r=−0.768; P<.00001).20
Evidence for iron’s role in hair growth comes from a mouse model study with a mutation in the serine protease TMPRSS6—a protein that regulates hepcidin and iron absorption—which caused an increase in hepcidin production and subsequent systemic iron deficiency. Mice at 4 weeks of age were devoid of all body hair but had substantial regrowth after initiation of a 2-week iron-rich diet, which suggests a connection between iron repletion and hair growth in mice with iron deficiency.21 Additionally, a meta-analysis analyzing the comorbidities of patients with alopecia areata found them to have higher odds (odds ratio [OR]=2.78; 95% CI, 1.23-6.29) of iron-deficiency anemia but no association with IBD (OR=1.48; 95% CI, 0.32-6.82).22
Diagnosis and Monitoring—The American Gastroenterological Association recommends a complete blood cell count (CBC), serum ferritin, transferrin saturation (TfS), and C-reactive protein (CRP) as standard evaluations for iron deficiency in patients with IBD. Patients with active IBD should be screened every 3 months,and patients with inactive disease should be screened every 6 to 12 months.23
Although ferritin and TfS often are used as markers for iron status in healthy individuals, they are positive and negative acute phase reactants, respectively. Using them to assess iron status in patients with IBD may inaccurately represent iron status in the setting of inflammation from the disease.24 The European Crohn’s and Colitis Organisation (ECCO) produced guidelines to define iron deficiency as a TfS less than 20% or a ferritin level less than 30 µg/L in patients without evidence of active IBD and a ferritin level less than 100 µg/L for patients with active inflammation.25
A 2020 multicenter observational study of 202 patients with diagnosed IBD found that the ECCO guideline of ferritin less than 30 µg/L had an area under the receiver operating characteristic (AUROC) curve of 0.69, a sensitivity of 0.43, and a specificity of 0.95 in their population.26 In a sensitivity analysis stratifying patients by CRP level (<10 or ≥10 mg/L), the authors found that for patients with ulcerative colitis and a CRP less than 10 mg/L, a cut-off value of ferritin less than 65 µg/L (AUROC=0.78) had a sensitivity of 0.78 and specificity of 0.76, and a TfS value of less than 16% (AUROC=0.88) had a sensitivity of 0.79 and a specificity of 0.9. In patients with a CRP of 10 mg/L or greater, a cut-off value of ferritin 80 µg/L (AUROC=0.76) had a sensitivity of 0.75 and a specificity of 0.82, and a TfS value of less than 11% (AUROC=0.69) had a sensitivity of 0.79 and a specificity of 0.88. There were no ferritin cut-off values associated with good diagnostic performance (defined as both sensitivity and specificity >0.70) for iron deficiency in patients with Crohn disease.26
The authors recommended using an alternative iron measurement such as soluble transferrin receptor (sTfR)/log ferritin ratio (TfR-F) that is not influenced by active inflammation and has a good correlation with ferritin values (TfR-F: r=0.66; P<.001).26 However, both sTfR and TfR-F have high costs and intermethod variability as well as differences in their reference ranges depending on which laboratory performs the analysis, limiting the accessibility and practicality of easily obtaining these tests.27 Although there may be inaccuracies for standard ferritin or TfS under ECCO guidelines, proposed alternatives have their own limitations, which may make ferritin and TfS the most reasonable evaluations of iron status as long as disease activity status at the time of testing is taken into consideration.
Treatment—Treatment of underlying iron deficiency in patients with IBD requires reversing the cause of the deficiency and supplementing iron. In patients with IBD, the options to supplement iron may be limited by active disease, making oral intake less effective. Oral iron supplementation also is associated with notable GI adverse effects that may be exacerbated in patients with IBD. A systematic review of 43 randomized controlled trials (RCTs) evaluating GI adverse effects (eg, nausea, abdominal pain, diarrhea, constipation, and black or tarry stools) of oral ferrous sulfate compared with placebo or intravenous (IV) iron supplementation in healthy nonanemic individuals found a significant increase in GI adverse effects with oral supplementation (placebo: OR=2.32; P<.0001; IV: OR=3.05; P<.0001).28
Therefore, IV iron repletion may be necessary in patients with IBD and may require numerous infusions depending on the formulation of iron. In an RCT conducted in 2011, patients with iron-deficiency anemia with quiescent or mild to moderate IBD were treated with either IV iron sulfate or ferric carboxymaltose.29 With a primary end point of hemoglobin response greater than 2 g/dL, the authors found that 150 of 240 patients responded to ferric carboxymaltose vs 118 of 235 treated with iron sulfate (P=.004). The dosing for ferric carboxymaltose was 1 to 3 infusions of 500 to 1000 mg of iron and for iron sulfate up to 11 infusions of 200 mg of iron.29
Zinc
A systematic review of zinc deficiency in patients with IBD identified 7 studies including 2413 patients and revealed those with Crohn disease had a higher prevalence of zinc deficiency compared with patients with ulcerative colitis (54% vs 41%).30
Pathophysiology—Zinc serves as a catalytic cofactor for enzymatic activity within proteins and immune cells.31 The homeostasis of zinc is tightly regulated within the brush border of the small intestine by zinc transporters ZIP4 and ZIP1 from the lumen of enterocytes into the bloodstream.32 Inflammation in the small intestine due to Crohn disease can result in zinc malabsorption.
Ranaldi et al33 exposed intestinal cells and zinc-depleted intestinal cells to tumor necrosis factor α media to simulate an inflammatory environment. They measured transepithelial electrical resistance as a surrogate for transmembrane permeability and found that zinc-depleted cells had a statistically significantly higher transepithelial electrical resistance percentage (60% reduction after 4 hours; P<1.10–6) when exposed to tumor necrosis factor α signaling compared with normal intestinal cells. They concluded that zinc deficiency can increase intestinal permeability in the presence of inflammation, creating a cycle of further nutrient malabsorption and inflammation exacerbating IBD symptoms.33
Cutaneous Manifestations—After absorption in the small intestine, approximately 5% of zinc resides in the skin, with the highest concentration in the stratum spinosum.34 A cell study found that keratinocytes in zinc-deficient environments had higher rates of apoptosis compared with cells in normal media. The authors proposed that this higher rate of apoptosis and the resulting inflammation could be a mechanism for developing the desquamative or eczematous scaly plaques that are common cutaneous manifestations of zinc deficiency.35
Other cutaneous findings may include angular cheilitis, stomatitis, glossitis, paronychia, onychodystrophy, generalized alopecia, and delayed wound healing.36 The histopathology of these skin lesions is characterized by granular layer loss, epidermal pallor, confluent parakeratosis, spongiosis, dyskeratosis, and psoriasiform hyperplasia.37
Diagnosis and Monitoring—Assessing serum zinc levels is challenging, as they may decrease during states of inflammation.38 A mouse model study showed a 3.1-fold increase (P<.001) in ZIP14 expression in wild-type mice compared with an IL-6 -/- knock-down model after IL-6 exposure. The authors concluded that the upregulation of ZIP14 in the liver due to inflammatory cytokine upregulation decreases zinc availability in serum.39 Additionally, serum zinc can overestimate the level of deficiency in IBD because approximately 75% of serum zinc is bound to albumin, which decreases in the setting of inflammation.40-42
Alternatively, alkaline phosphatase (AP), a zinc-dependent metalloenzyme, may be a better evaluator of zinc status during periods of inflammation. A study in rats evaluated zinc through serum zinc levels and AP levels after a period of induced stress to mimic a short-term inflammatory state.43 The researchers found that total body stores of zinc were unaffected throughout the experiment; only serum zinc declined throughout the experiment duration while AP did not. Because approximately 75% of serum zinc is bound to serum albumin,42 the researchers concluded the induced inflammatory state depleted serum albumin and redistributed zinc to the liver, causing the observed serum zinc changes, while total body zinc levels and AP were largely unaffected in comparison.43 Comorbid conditions such as liver or bone disease can increase AP levels, which limits the utility of AP as a surrogate for zinc in patients with comorbidities.44 However, even in the context of active IBD, serum zinc still is currently considered the best biomarker to evaluate zinc status.45
Treatment—The recommended dose for zinc supplementation is 20 to 40 mg daily with higher doses (>50 mg/d) for patients with malabsorptive syndromes such as IBD.46 It can be administered orally or parenterally. Although rare, zinc replacement therapy may be associated with diarrhea, nausea, vomiting, mild headaches, and fatigue.46 Additional considerations should be taken when repleting other micronutrients with zinc, as calcium and folate can inhibit zinc reabsorption, while zinc itself can inhibit iron and copper reabsorption.47
Vitamin D and Calcium
Low vitamin D levels (<50 nmol/L) and hypocalcemia (<8.8 mg/dL) are common in patients with IBD.48,49
Pathophysiology—Vitamin D levels are maintained via 2 mechanisms. The first mechanism is through the skin, as keratinocytes produce 7-dehydrocholesterol after exposure to UV light, which is converted into previtamin D3 and then thermally isomerizes into vitamin D3. This vitamin D3 is then transported to the liver on vitamin D–binding protein.50 The second mechanism is through oral vitamin D3 that is absorbed through vitamin D receptors in intestinal epithelium and transported to the liver, where it is hydroxylated into 25-hydroxyvitamin D (25[OH]D), then to the kidneys for hydroxylation to 1,25(OH)2D for redistribution throughout the body.50 This activated form of vitamin D regulates calcium absorption in the intestine, and optimal vitamin D levels are necessary to absorb calcium efficiently.51 Inflammation from IBD within the small intestine can downregulate vitamin D receptors, causing malabsorption and decreased serum vitamin D.52
Vitamin D signaling also is vital to maintaining the tight junctions and adherens junctions of the intestinal epithelium. Weakening the permeability of the epithelium further exacerbates malabsorption and subsequent vitamin D deficiency.52 A meta-analysis of 27 studies including 8316 patients with IBD showed low vitamin D levels were associated with increased odds of disease activity (OR=1.53; 95% CI, 1.32-1.77), mucosal inflammation (OR=1.25; 95% CI, 1.06-1.47), and future clinical relapse (OR=1.23; 95% CI, 1.03-1.47) in patients with Crohn disease. The authors concluded that low levels of vitamin D could be used as a potential biomarker of inflammatory status in Crohn disease.53
Vitamin D and calcium are further implicated in maintaining skeletal health,47 while vitamin D specifically helps maintain intestinal homeostasis54 and immune system modulation in the skin.55
Cutaneous Manifestations—Vitamin D is thought to play crucial roles in skin differentiation and proliferation, cutaneous innate immunity, hair follicle cycling, photoprotection, and wound healing.56 Vitamin D deficiency has been observed in a large range of cutaneous diseases including skin cancer, psoriasis, vitiligo, bullous pemphigoid, atopic dermatitis, and various types of alopecia.56-59 It is unclear whether vitamin D deficiency facilitates these disease processes or is merely the consequence of a disrupted cutaneous surface with the inability to complete the first step in vitamin D processing. A 2014 meta-analysis of 290 prospective cohort studies and 172 randomized trials concluded that 25(OH)D deficiency was associated with ill health and did not find causal evidence for any specific disease, dermatologic or otherwise.60 Calcium deficiency may cause epidermal changes including dry skin, coarse hair, and brittle nails.61
Diagnosis and Monitoring—The ECCO guidelines recommend obtaining serum 25(OH)D levels every 3 months in patients with IBD.62 Levels less than 75 nmol/L are considered deficient, and a value less than 30 nmol/L increases the risk for osteomalacia and nutritional rickets, constituting severe vitamin D deficiency.63-65
An observational study of 325 patients with IBD showed a statistically significant negative correlation between serum vitamin D and fecal calprotectin (r=−0.19; P<.001), a stool-based marker for gut inflammation, supporting vitamin D as a potential biomarker in IBD.66
Evaluation of calcium can be done through serum levels in patients with IBD.67 Patients with IBD are at risk for hypoalbuminemia; therefore, consideration should be taken to ensure calcium levels are corrected, as approximately 50% of calcium is bound to albumin or other ions in the body,68 which can be done by adjusting the calcium concentration by 0.02 mmol/L for every 1 g/L of albumin above or below 40 g/L. In the most critically ill patients, a direct ionized calcium blood level should be used instead because the previously mentioned correction calculations are inaccurate when albumin is critically low.69
Treatment—The ECCO guidelines recommend calcium and vitamin D repletion of 500 to 1000 mg and 800 to 1000 U, respectively, in patients with IBD on systemic corticosteroids to prevent the negative effects of bone loss.62 Calcium repletion in patients with IBD who are not on systemic steroids are the same as for the general population.65
Vitamin D repletion also may help decrease IBD activity. In a prospective study, 10,000 IU/d of vitamin D in 10 patients with IBD—adjusted over 12 weeks to a target of 100 to 125 nmol/L of serum 25(OH)D—showed a significant reduction in clinical Crohn activity (P=.019) over the study period.70 In contrast, 2000 IU/d for 3 months in an RCT of 27 patients with Crohn disease found significantly lower CRP (P=.019) and significantly higher self-reported quality of life (P=.037) but nonsignificant decreases in Crohn activity (P=.082) in patients with 25(OH)D levels of 75 nmol/L or higher compared with those with 25(OH)D levels less than 75 nmol/L.71
These discrepancies illustrate the need for expanded clinical trials to elucidate the optimal vitamin D dosing for patients with IBD. Ultimately, assessing vitamin D and calcium status and considering repletion in patients with IBD, especially those with comorbid dermatologic diseases such as poor wound healing, psoriasis, or atopic dermatitis, is important.
Vitamin B6 (Pyridoxine)
Pathophysiology—Pyridoxine is an important coenzyme for many functions including amino acid transamination, fatty acid metabolism, and conversion of tryptophan to niacin. It is absorbed in the jejunum and ileum and subsequently transported to the liver for rephosphorylation and release into its active form.36 An observational study assessing the nutritional status of patients with IBD found that only 5.7% of 105 patients with food records had inadequate dietary intake of pyridoxine, but 29% of all patients with IBD had subnormal pyridoxine levels.72 Additionally, they found no significant difference in the prevalence of subnormal pyridoxine levels in patients with active IBD vs IBD in remission. The authors suggested that the subnormal pyridoxine levels in patients with IBD likely were multifactorial and resulted from malabsorption due to active disease, inflammation, and inadequate intake.72
Cutaneous Manifestations—Cutaneous findings associated with pyridoxine deficiency include periorificial and perineal dermatitis,73 angular stomatitis, and cheilitis with associated burning, redness, and tongue edema.36 Additionally, pyridoxine is involved in the conversion of tryptophan to niacin, and its deficiency may manifest with pellagralike findings.74
Because pyridoxine is critical to protein metabolism, its deficiency may disrupt key cellular structures that rely on protein concentrations to maintain structural integrity. One such structure in the skin that heavily relies on protein concentrations is the ground substance of the extracellular matrix—the amorphous gelatinous spaces that occupy the areas between the extracellular matrix, which consists of cross-linked glycosaminoglycans and proteins.75 Without protein, ground substance increases in viscosity and can disrupt the epidermal barrier, leading to increased transepidermal water loss and ultimately inflammation.76 Although this theory has yet to be validated fully, this is a potential mechanistic explanation for the inflammation in dermal papillae that leads to dermatitis observed in pyridoxine deficiency.
Diagnosis and Monitoring—Direct biomarkers of pyridoxine status are in serum, plasma, erythrocytes, and urine, with the most common measurement in plasma as pyridoxal 5′-phosphate (PLP).77 Plasma PLP concentrations lower than 20 nmol/L are suggestive of deficiency.78 Plasma PLP has shown inverse relationships with acute phase inflammatory markers CRP79 and AP,78 thereby raising concerns for its validity to assess pyridoxine status in patients with symptomatic IBD.80
Alternative evaluations of pyridoxine include tryptophan and methionine loading tests,36 which are measured via urinary excretion and require normal kidney function to be accurate. They should be considered in IBD if necessary, but routine testing, even in patients with symptomatic IBD, is not recommended in the ECCO guidelines. Additional considerations should be taken in patients with altered nutrient requirements such as those who have undergone bowel resection due to highly active disease or those who receive parenteral nutritional supplementation.81
Treatment—Recommendations for oral pyridoxine supplementation range from 25 to 600 mg daily,82 with symptoms typically improving on 100 mg daily.36 Pyridoxine supplementation may have additional benefits for patients with IBD and potentially modulate disease severity. An IL-10 knockout mouse supplemented with pyridoxine had an approximately 60% reduction (P<.05) in inflammation compared to mice deficient in pyridoxine.83 The authors suggest that PLP-dependent enzymes can inhibit further proinflammatory signaling and T-cell migration that can exacerbate IBD. Ultimately, more data is needed before determining the efficacy of pyridoxine supplementation for active IBD.
Vitamin B12 and Vitamin B9 (Folic Acid)
Pathophysiology—Vitamin B12 is reabsorbed in the terminal ileum, the distal portion of the small intestine. The American Gastroenterological Association recommends that patients with a history of extensive ileal disease or prior ileal surgery, which is the case for many patients with Crohn disease, be monitored for vitamin B12 deficiency.23 Monitoring and rapid supplementation of vitamin B12 can prevent pernicious anemia and irreversible neurologic damage that may result from deficiency.84
Folic acid is primarily absorbed in the duodenum and jejunum of the small intestine. A meta-analysis performed in 2017 assessed studies observing folic acid and vitamin B12 levels in 1086 patients with IBD compared with 1484 healthy controls and found an average difference in serum folate concentration of 0.46 nmol/L (P<.001).84 Interestingly, this study did not find a significant difference in serum vitamin B12 levels between patients with IBD and healthy controls, highlighting the mechanism of vitamin B12 deficiency in IBD because only patients with terminal ileal involvement are at risk for malabsorption and subsequent deficiency.
Cutaneous Manifestations—Both vitamin B12 and folic acid deficiency can manifest as cheilitis, glossitis, and/or generalized hyperpigmentation that is accentuated in the flexural areas, palms, soles, and oral cavity.85,86 Systemic symptoms of patients with vitamin B12 and folic acid deficiency include megaloblastic anemia, pallor, and fatigue. A potential mechanism for the hyperpigmentation observed from vitamin B12 deficiency came from an electron microscope study that showed an increased concentration of melanosomes in a patient with deficiency.87
Diagnosis and Monitoring—In patients with suspected vitamin B12 and/or folic acid deficiency, initial evaluation should include a CBC with peripheral smear and serum vitamin B12 and folate levels. In cases for which the diagnosis still is unclear after initial testing,
Treatment—According to the Centers for Disease Control and Prevention, supplementation of vitamin B12 can be done orally with 1000 µg daily in patients with deficiency. In patients with active IBD, oral reabsorption of vitamin B12 can be less effective, making subcutaneous or intramuscular administration (1000 µg/wk for 8 weeks, then monthly for life) better options.89
Patients with IBD managed with methotrexate should be screened carefully for folate deficiency. Methotrexate is a folate analog that sometimes is used for the treatment of IBD. Reversible competitive inhibition of dihydrofolate reductase can precipitate a systemic folic acid decrease.91 Typically, oral folic acid (1 to 5 mg/d) is sufficient to treat folate deficiency, with the ESPEN recommending 5 mg once weekly 24 to 72 hours after methotrexate treatment or 1 mg daily for 5 days per week in patients with IBD.1 Alternative formulations—IV, subcutaneous, or intramuscular—are available for patients who cannot tolerate oral intake.92
Final Thoughts
Dermatologists can be the first to observe the cutaneous manifestations of micronutrient deficiencies. Although the symptoms of each micronutrient deficiency discussed may overlap, attention to small clinical clues in patients with IBD can improve patient outcomes and quality of life. For example, koilonychia with glossitis and xerosis likely is due to iron deficiency, while zinc deficiency should be suspected in patients with scaly eczematous plaques in skin folds. A high level of suspicion for micronutrient deficiencies in patients with IBD should be followed by a complete patient history, review of systems, and thorough clinical examination. A thorough laboratory evaluation can pinpoint nutritional deficiencies in patients with IBD, keeping in mind that specific biomarkers such as ferritin and serum zinc also act as acute phase reactants and should be interpreted in this context. Co-management with gastroenterologists should be a priority in patients with IBD, as gaining control of inflammatory disease is crucial for the prevention of recurrent vitamin and micronutrient deficiencies in addition to long-term health in this population.
- Bischoff SC, Bager P, Escher J, et al. ESPEN guideline on clinical nutrition in inflammatory bowel disease. Clin Nutr. 2023;42:352-379. doi:10.1016/j.clnu.2022.12.004
- Gerasimidis K, McGrogan P, Edwards CA. The aetiology and impact of malnutrition in paediatric inflammator y bowel disease. J Hum Nutr Diet. 2011;24:313-326. doi:10.1111/j.1365-277X.2011.01171.x
- Mentella MC, Scaldaferri F, Pizzoferrato M, et al. Nutrition, IBD and gut microbiota: a review. Nutrients. 2020;12:944. doi:10.3390/nu12040944
- Bonsack O, Caron B, Baumann C, et al. Food avoidance and fasting in patients with inflammatory bowel disease: experience from the Nancy IBD nutrition clinic. United European Gastroenterol J. 2023;11:361-370. doi:10.1002/ueg2.1238521
- Campmans-Kuijpers MJE, Dijkstra G. Food and food groups in inflammatory bowel disease (IBD): the design of the Groningen Anti-Inflammatory Diet (GrAID). Nutrients. 2021;13:1067. doi:10.3390/nu13041067
- Hwang C, Issokson K, Giguere-Rich C, et al. Development and pilot testing of the inflammatory bowel disease nutrition care pathway. Clin Gastroenterol Hepatol. 2020;18:2645-2649.e4. doi:10.1016/j.cgh.2020.06.039
- Filmann N, Rey J, Schneeweiss S, et al. Prevalence of anemia in inflammatory bowel diseases in European countries: a systematic review and individual patient data meta-analysis. Inflamm Bowel Dis. 2014;20:936-945. doi:10.1097/01.MIB.0000442728.74340.fd
- Stein J, Hartmann F, Dignass AU. Diagnosis and management of iron deficiency anemia in patients with IBD. Nat Rev Gastroenterol Hepatol. 2010;7:599-610. doi:10.1038/nrgastro.2010.151
- Ems T, St Lucia K, Huecker MR. Biochemistry, iron absorption. StatPearls [Internet]. Updated April 17, 2023. Accessed March 19, 2024. https://www.ncbi.nlm.nih.gov/books/NBK448204/
- Evstatiev R, Gasche C. Iron sensing and signalling. Gut. 2012;61:933-952. doi:10.1136/gut.2010.214312
- Przybyszewska J, Zekanowska E. The role of hepcidin, ferroportin, HCP1, and DMT1 protein in iron absorption in the human digestive tract. Prz Gastroenterol. 2014;9:208-213. doi:10.5114/pg.2014.45102
- Weiss G, Gasche C. Pathogenesis and treatment of anemia in inflammatory bowel disease. Haematologica. 2010;95:175-178. doi:10.3324/haematol.2009.017046
- Kaitha S, Bashir M, Ali T. Iron deficiency anemia in inflammatory bowel disease. World J Gastrointest Pathophysiol. 2015;6:62-72. doi:10.4291/wjgp.v6.i3.62
- Moiz B. Spoon nails: still seen in today’s world. Clin Case Rep. 2018;6:547-548. doi:10.1002/ccr3.1404
- St Pierre SA, Vercellotti GM, Donovan JC, et al. Iron deficiency and diffuse nonscarring scalp alopecia in women: more pieces to the puzzle. J Am Acad Dermatol. 2010;63:1070-1076. doi:10.1016/j.jaad.2009.05.054
- Chiang CP, Yu-Fong Chang J, Wang YP, et al. Anemia, hematinic deficiencies, hyperhomocysteinemia, and serum gastric parietal cell antibody positivity in atrophic glossitis patients with or without microcytosis. J Formos Med Assoc. 2019;118:1401-1407. doi:10.1016/j.jfma.2019.06.004
- Chiang CP, Chang JY, Wang YP, et al. Atrophic glossitis: Etiology, serum autoantibodies, anemia, hematinic deficiencies, hyperhomocysteinemia, and management. J Formos Med Assoc. 2020;119:774-780. doi:10.1016/j.jfma.2019.04.015
- Walker J, Baran R, Vélez N, et al. Koilonychia: an update on pathophysiology, differential diagnosis and clinical relevance. J Eur Acad Dermatol Venereol. 2016;30:1985-1991. doi:10.1111/jdv.13610
- Guo HF, Tsai CL, Terajima M, et al. Pro-metastatic collagen lysyl hydroxylase dimer assemblies stabilized by Fe2+-binding. Nat Commun. 2018;9:512. doi:10.1038/s41467-018-02859-z
- Saini S, Jain AK, Agarwal S, et al. Iron deficiency and pruritus: a cross-sectional analysis to assess its association and relationship. Indian J Dermatol. 2021;66:705. doi:10.4103/ijd.ijd_326_21
- Du X, She E, Gelbart T, et al. The serine protease TMPRSS6 is required to sense iron deficiency. Science. 2008;320:1088-1092. doi:10.1126/science.1157121
- Lee S, Lee H, Lee CH, et al. Comorbidities in alopecia areata: a systematic review and meta-analysis. J Am Acad Dermatol. 2019;80:466-477.e16. doi:10.1016/j.jaad.2018.07.013
- Hashash JG, Elkins J, Lewis JD, et al. AGA Clinical Practice Update on diet and nutritional therapies in patients with inflammatory bowel disease: expert review [published online January 23, 2024]. Gastroenterology. doi:10.1053/j.gastro.2023.11.303
- Choudhuri S, Chowdhury IH, Saha A, et al. Acute monocyte pro- inflammatory response predicts higher positive to negative acute phase reactants ratio and severe hemostatic derangement in dengue fever. Cytokine. 2021;146:155644. doi:10.1016/j.cyto.2021.155644
- Dignass AU, Gasche C, Bettenworth D, et al; European Crohn’s and Colitis Organisation. European consensus on the diagnosis and management of iron deficiency and anaemia in inflammatory bowel diseases. J Crohn’s Colitis. 2015;9:211-222. doi:10.1093/ecco-jcc/jju009
- Daude S, Remen T, Chateau T, et al. Comparative accuracy of ferritin, transferrin saturation and soluble transferrin receptor for the diagnosis of iron deficiency in inflammatory bowel disease. Aliment Pharmacol Ther. 2020;51:1087-1095. doi:10.1111/apt.15739
- Pfeiffer CM, Looker AC. Laboratory methodologies for indicators of iron status: strengths, limitations, and analytical challenges. Am J Clin Nutr. 2017;106(suppl 6):1606S-1614S. doi:10.3945/ajcn.117.155887
- Tolkien Z, Stecher L, Mander AP, et al. Ferrous sulfate supplementation causes significant gastrointestinal side-effects in adults: a systematic review and meta-analysis. PLoS One. 2015;10:e0117383. doi:10.1371/journal.pone.0117383
- Evstatiev R, Marteau P, Iqbal T, et al. FERGIcor, a randomized controlled trial on ferric carboxymaltose for iron deficiency anemia in inflammatory bowel disease. Gastroenterology. 2011;141:846-853.e8532. doi:10.1053/j.gastro.2011.06.005
- Zupo R, Sila A, Castellana F, et al. Prevalence of zinc deficiency in inflammatory bowel disease: a systematic review and meta-analysis. Nutrients. 2022;14:4052. doi:10.3390/nu14194052
- Thompson MW. Regulation of zinc-dependent enzymes by metal carrier proteins. Biometals. 2022;35:187-213. doi:10.1007/s10534-022-00373-w
- Maares M, Haase H. A guide to human zinc absorption: general overview and recent advances of in vitro intestinal models. Nutrients. 2020;12:762. doi:10.3390/nu12030762
- Ranaldi G, Ferruzza S, Canali R, et al. Intracellular zinc is required for intestinal cell survival signals triggered by the inflammatory cytokine TNFα. J Nutr Biochem. 2013;24:967-976. doi:10.1016/j.jnutbio.2012.06.020
- Ogawa Y, Kawamura T, Shimada S. Zinc and skin biology. Arch Biochem Biophys. 2016;611:113-119. doi:10.1016/j.abb.2016.06.003
- Wilson D, Varigos G, Ackland ML. Apoptosis may underlie the pathology of zinc-deficient skin. Immunol Cell Biol. 2006;84:28-37. doi:10.1111/j.1440-1711.2005.01391.x
- Jen M, Yan AC. Syndromes associated with nutritional deficiency and excess. Clin Dermatol. 2010;28:669-685. doi:10.1016/j.clindermatol.2010.03.029
- Gonzalez JR, Botet MV, Sanchez JL. The histopathology of acrodermatitis enteropathica. Am J Dermatopathol. 1982;4:303-311.
- Gammoh NZ, Rink L. Zinc in infection and inflammation. Nutrients. 2017;9:624. doi:10.3390/nu9060624
- Liuzzi JP, Lichten LA, Rivera S, et al. Interleukin-6 regulates the zinc transporter Zip14 in liver and contributes to the hypozincemia of the acute-phase response. Proc Natl Acad Sci U S A. 2005;102:6843-6848. doi:10.1073/pnas.0502257102
- Vermeire S, Van Assche G, Rutgeerts P. Laboratory markers in IBD: useful, magic, or unnecessary toys?. Gut. 2006;55:426-431. doi:10.1136/gut.2005.069476
- Morisaku M, Ito K, Ogiso A, et al. Correlation between serum albumin and serum zinc in malignant lymphoma. Fujita Med J. 2022;8:59-64. doi:10.20407/fmj.2021-006
- Falchuk KH. Effect of acute disease and ACTH on serum zinc proteins. N Engl J Med. 1977:296:1129-1134.
- Naber TH, Baadenhuysen H, Jansen JB, et al. Serum alkaline phosphatase activity during zinc deficiency and long-term inflammatory stress. Clin Chim Acta. 1996;249:109-127. doi:10.1016/0009-8981(96)06281-x
- Lowe D, Sanvictores T, Zubair M, et al. Alkaline phosphatase. StatPearls [Internet]. Updated October 29, 2023. Accessed March 19, 2024. https://www.ncbi.nlm.nih.gov/books/NBK459201/
- Krebs NF. Update on zinc deficiency and excess in clinical pediatric practice. Ann Nutr Metab. 2013;62 suppl 1:19-29. doi:10.1159/000348261
- Maxfield L, Shukla S, Crane JS. Zinc deficiency. StatPearls [Internet]. Updated June 28, 2023. Accessed March 25, 2024. https://www.ncbi.nlm.nih.gov/books/NBK493231/
- Ghishan FK, Kiela PR. Vitamins and minerals in inflammatory bowel disease. Gastroenterol Clin North Am. 2017;46:797-808. doi:10.1016/j.gtc.2017.08.011
- Caviezel D, Maissen S, Niess JH, et al. High prevalence of vitamin D deficiency among patients with inflammatory bowel disease. Inflamm Intest Dis. 2018;2:200-210. doi:10.1159/000489010
- Jasielska M, Grzybowska-Chlebowczyk U. Hypocalcemia and vitamin D deficiency in children with inflammatory bowel diseases and lactose intolerance. Nutrients. 2021;13:2583. doi:10.3390/nu13082583
- Vernia F, Valvano M, Longo S, et al. Vitamin D in inflammatory bowel diseases. Mechanisms of action and therapeutic implications. Nutrients. 2022;14:269. doi:10.3390/nu14020269
- Khazai N, Judd SE, Tangpricha V. Calcium and vitamin D: skeletal and extraskeletal health. Curr Rheumatol Rep. 2008;10:110-117. doi:10.1007/s11926-008-0020-y
- Domazetovic V, Iantomasi T, Bonanomi AG, et al. Vitamin D regulates claudin-2 and claudin-4 expression in active ulcerative colitis by p-Stat-6 and Smad-7 signaling. Int J Colorectal Dis. 2020;35:1231-1242. doi:10.1007/s00384-020-03576-0
- Gubatan J, Chou ND, Nielsen OH, et al. Systematic review with meta-analysis: association of vitamin D status with clinical outcomes in adult patients with inflammatory bowel disease. Aliment Pharmacol Ther. 2019;50:1146-1158. doi:10.1111/apt.15506
- Fakhoury HMA, Kvietys PR, AlKattan W, et al. Vitamin D and intestinal homeostasis: barrier, microbiota, and immune modulation. J Steroid Biochem Mol Biol. 2020;200:105663. doi:10.1016/j.jsbmb.2020.105663
- Liu PT, Stenger S, Li H, et al. Toll-like receptor triggering of a vitamin D-mediated human antimicrobial response. Science. 2006;311:1770-1773. doi:10.1126/science.1123933
- Mostafa WZ, Hegazy RA. Vitamin D and the skin: focus on a complex relationship: a review. J Adv Res. 2015;6:793-804. doi:10.1016/j.jare.2014.01.011
- Searing DA, Leung DY. Vitamin D in atopic dermatitis, asthma and allergic diseases. Immunol Allergy Clin North Am. 2010;30:397-409.
- Lee YH, Song GG. Association between circulating 25-hydroxyvitamin D levels and psoriasis, and correlation with disease severity: a meta-analysis. Clin Exp Dermatol. 2018;43:529-535.
- Adorini L, Penna G. Control of autoimmune diseases by the vitamin D endocrine system. Nat Clin Pract Rheumatol. 2008;4:404-412.
- Autier P, Boniol M, Pizot C, et al. Vitamin D status and ill health: a systematic review. Lancet Diabetes Endocrinol. 2014;2:76-89. doi:10.1016/S2213-8587(13)70165-7
- Schafer AL, Shoback DM. Hypocalcemia: diagnosis and treatment. In: Feingold KR, Anawalt B, Blackman MR, et al, eds. Endotext [Internet]. Updated January 3, 2016. Accessed March 19, 2024. https://www.ncbi.nlm.nih.gov/books/NBK279022/
- Magro F, Gionchetti P, Eliakim R, et al. Third European Evidence-based Consensus on Diagnosis and Management of Ulcerative Colitis. Part 1: Definitions, diagnosis, extra-intestinal manifestations, pregnancy, cancer surveillance, surgery, and ileo-anal pouch disorders. J Crohns Colitis. 2017;11:649-670. doi:10.1093/ecco-jcc/jjx008
- Amrein K, Scherkl M, Hoffmann M, et al. Vitamin D deficiency 2.0: an update on the current status worldwide. Eur J Clin Nutr. 2020;74:1498-1513. doi:10.1038/s41430-020-0558-y
- Munns CF, Shaw N, Kiely M, et al. Global consensus recommendations on prevention and management of nutritional rickets. J Clin Endocrinol Metab. 2016;101:394-415. doi:10.1210/jc.2015-2175
- Institute of Medicine (US) Committee to Review Dietary Reference Intakes for Vitamin D and Calcium; Ross AC, Taylor CL, Yaktine AL, Del Valle HB, eds. Dietary Reference Intakes for Calcium and Vitamin D. National Academies Press (US); 2011.
- Yeaman F, Nguyen A, Abasszade J, et al. Assessing vitamin D as a biomarker in inflammatory bowel disease. JGH Open. 2023;7:953-958. doi:10.1002/jgh3.13010
- Vernia P, Loizos P, Di Giuseppantonio I, et al S. Dietary calcium intake in patients with inflammatory bowel disease. J Crohns Colitis. 2014;8:312-317. doi:10.1016/j.crohns.2013.09.008
- Cooper MS, Gittoes NJ. Diagnosis and management of hypocalcaemia. BMJ. 2008;336:1298-1302. doi:10.1136/bmj.39582.589433.BE
- Kenny CM, Murphy CE, Boyce DS, et al. Things we do for no reason™: calculating a “corrected calcium” level. J Hosp Med. 2021;16:499-501. doi:10.12788/jhm.3619
- Garg M, Rosella O, Rosella G, et al. Evaluation of a 12-week targeted vitamin D supplementation regimen in patients with active inflammatory bowel disease. Clin Nutr. 2018;37:1375-1382. doi:10.1016/j.clnu.2017.06.011
- Raftery T, Martineau AR, Greiller CL, et al. Effects of vitamin D supplementation on intestinal permeability, cathelicidin and disease markers in Crohn’s disease: results from a randomised double-blind placebo-controlled study. United European Gastroenterol J. 2015;3:294-302. doi:10.1177/2050640615572176
- Vagianos K, Bector S, McConnell J, et al. Nutrition assessment of patients with inflammatory bowel disease. JPEN J Parenter Enteral Nutr. 2007;31:311-319. doi:10.1177/0148607107031004311
- Barthelemy H, Chouvet B, Cambazard F. Skin and mucosal manifestations in vitamin deficiency. J Am Acad Dermatol. 1986;15:1263-1274. doi:10.1016/s0190-9622(86)70301-0
- Galimberti F, Mesinkovska NA. Skin findings associated with nutritional deficiencies. Cleve Clin J Med. 2016;83:731-739. doi:10.3949/ccjm.83a.15061
- Elgharably N, Al Abadie M, Al Abadie M, et al. Vitamin B group levels and supplementations in dermatology. Dermatol Reports. 2022;15:9511. doi:10.4081/dr.2022.9511
- Hołubiec P, Leon´czyk M, Staszewski F, et al. Pathophysiology and clinical management of pellagra—a review. Folia Med Cracov. 2021;61:125-137. doi:10.24425/fmc.2021.138956
- Ink SL, Henderson LM. Vitamin B6 metabolism. Annu Rev Nutr. 1984;4:455-470. doi:10.1146/annurev.nu.04.070184.002323
- Brown MJ, Ameer MA, Daley SF, et al. Vitamin B6 deficiency. StatPearls [Internet]. Updated August 8, 2023. Accessed March 25, 2024. https://www.ncbi.nlm.nih.gov/books/NBK470579/.
- Vasilaki AT, McMillan DC, Kinsella J, et al. Relation between pyridoxal and pyridoxal phosphate concentrations in plasma, red cells, and white cells in patients with critical illness. Am J Clin Nutr. 2008;88:140-146. doi:10.1093/ajcn/88.1.140
- Chiang EP, Bagley PJ, Selhub J, et al. Abnormal vitamin B(6) status is associated with severity of symptoms in patients with rheumatoid arthritis. Am J Med. 2003;114:283-287. doi:10.1016/s0002-9343(02)01528-0
- Maaser C, Sturm A, Vavricka SR, et al. ECCO-ESGAR guideline for diagnostic assessment in IBD. Part 1: initial diagnosis, monitoring of known IBD, detection of complications. J Crohns Colitis. 2019;13:144-164. doi:10.1093/ecco-jcc/jjy113
- Spinneker A, Sola R, Lemmen V, et al. Vitamin B6 status, deficiency and its consequences—an overview. Nutr Hosp. 2007;22:7-24.
- Selhub J, Byun A, Liu Z, et al. Dietary vitamin B6 intake modulates colonic inflammation in the IL10-/- model of inflammatory bowel disease. J Nutr Biochem. 2013;24:2138-2143. doi:10.1016/j.jnutbio.2013.08.005
- Pan Y, Liu Y, Guo H, et al. Associations between folate and vitamin B12 levels and inflammatory bowel disease: a meta-analysis. Nutrients. 2017;9:382. doi:10.3390/nu9040382
- Brescoll J, Daveluy S. A review of vitamin B12 in dermatology. Am J Clin Dermatol. 2015;16:27-33. doi:10.1007/s40257-014-0107-3
- DiBaise M, Tarleton SM. Hair, nails, and skin: differentiating cutaneous manifestations of micronutrient deficiency. Nutr Clin Pract. 2019;34:490-503. doi:10.1002/ncp.10321
- Mori K, Ando I, Kukita A. Generalized hyperpigmentation of the skin due to vitamin B12 deficiency. J Dermatol. 2001;28:282-285. doi:10.1111/j.1346-8138.2001.tb00134.x
- Green R. Indicators for assessing folate and vitamin B-12 status and for monitoring the efficacy of intervention strategies. Am J Clin Nutr. 2011;94:666S-672S. doi:10.3945/ajcn.110.009613
- NIH Office of Dietary Supplements. Vitamin B12: fact sheet for health professionals. Updated February 27, 2024. Accessed March 19, 2024. https://ods.od.nih.gov/factsheets/VitaminB12-HealthProfessional/
- NIH Office of Dietary Supplements. Folate: fact sheet for health professionals. Updated November 20, 2023. Accessed March 19, 2024. https://ods.od.nih.gov/factsheets/Folate-HealthProfessional/.
- Saibeni S, Bollani S, Losco A, et al. The use of methotrexate for treatment of inflammatory bowel disease in clinical practice. Dig Liver Dis. 2012;44:123-127. doi:10.1016/j.dld.2011.09.015
- Khan KM, Jialal I. Folic acid deficiency. StatPearls [Internet]. Updated June 26, 2023. Accessed March 19, 2024. https://www.ncbi.nlm.nih.gov/books/NBK535377/
In 2023, ESPEN (the European Society for Clinical Nutrition and Metabolism) published consensus recommendations highlighting the importance of regular monitoring and treatment of nutrient deficiencies in patients with inflammatory bowel disease (IBD) for improved prognosis, mortality, and quality of life.1 Suboptimal nutrition in patients with IBD predominantly results from inflammation of the gastrointestinal (GI) tract leading to malabsorption; however, medications commonly used to manage IBD also can contribute to malnutrition.2,3 Additionally, patients may develop nausea and food avoidance due to medication or the disease itself, leading to nutritional withdrawal and eventual deficiency.4 Even with the development of diets focused on balancing nutritional needs and decreasing inflammation,5 offsetting this aversion to food can be difficult to overcome.2
Cutaneous manifestations of IBD are multifaceted and can be secondary to the disease, reactive to or associated with IBD, or effects from nutritional deficiencies. The most common vitamin and nutrient deficiencies in patients with IBD include iron; zinc; calcium; vitamin D; and vitamins B6 (pyridoxine), B9 (folic acid), and B12.6 Malnutrition may manifest with cutaneous disease, and dermatologists can be the first to identify and assess for nutritional deficiencies. In this article, we review the mechanisms of these micronutrient depletions in the context of IBD, their subsequent dermatologic manifestations (Table), and treatment and monitoring guidelines for each deficiency.
Iron
A systematic review conducted from 2007 to 2012 in European patients with IBD (N=2192) found the overall prevalence of anemia in this population to be 24% (95% CI, 18%-31%), with 57% of patients with anemia experiencing iron deficiency.7 Anemia is observed more commonly in patients hospitalized with IBD and is common in patients with both Crohn disease and ulcerative colitis.8
Pathophysiology—Iron is critically important in oxygen transportation throughout the body as a major component of hemoglobin. Physiologically, the low pH of the duodenum and proximal jejunum allows divalent metal transporter 1 to transfer dietary Fe3+ into enterocytes, where it is reduced to the transportable Fe2+.9,10 Distribution of Fe2+ ions from enterocytes relies on ferroportin, an iron-transporting protein, which is heavily regulated by the protein hepcidin.11 Hepcidin, a known acute phase reactant, will increase in the setting of active IBD, causing a depletion of ferroportin and an inability of the body to utilize the stored iron in enterocytes.12 This poor utilization of iron stores combined with blood loss caused by inflammation in the GI tract is the proposed primary mechanism of iron-deficiency anemia observed in patients with IBD.13
Cutaneous Manifestations—From a dermatologic perspective, iron-deficiency anemia can manifest with a wide range of symptoms including glossitis, koilonychia, xerosis and/or pruritus, and brittle hair or hair loss.14,15 Although the underlying pathophysiology of these cutaneous manifestations is not fully understood, there are several theories assessing the mechanisms behind the skin findings of iron deficiency.
Atrophic glossitis has been observed in many patients with iron deficiency and is thought to manifest due to low iron concentrations in the blood, thereby decreasing oxygen delivery to the papillae of the dorsal tongue with resultant atrophy.16,17 Similarly, decreased oxygen delivery to the nail bed capillaries may cause deformities in the nail called koilonychia (or “spoon nails”).18 Iron is a key co-factor in collagen lysyl hydroxylase that promotes collagen binding; iron deficiency may lead to disruptions in the epidermal barrier that can cause pruritus and xerosis.19 An observational study of 200 healthy patients with a primary concern of pruritus found a correlation between low serum ferritin and a higher degree of pruritus (r=−0.768; P<.00001).20
Evidence for iron’s role in hair growth comes from a mouse model study with a mutation in the serine protease TMPRSS6—a protein that regulates hepcidin and iron absorption—which caused an increase in hepcidin production and subsequent systemic iron deficiency. Mice at 4 weeks of age were devoid of all body hair but had substantial regrowth after initiation of a 2-week iron-rich diet, which suggests a connection between iron repletion and hair growth in mice with iron deficiency.21 Additionally, a meta-analysis analyzing the comorbidities of patients with alopecia areata found them to have higher odds (odds ratio [OR]=2.78; 95% CI, 1.23-6.29) of iron-deficiency anemia but no association with IBD (OR=1.48; 95% CI, 0.32-6.82).22
Diagnosis and Monitoring—The American Gastroenterological Association recommends a complete blood cell count (CBC), serum ferritin, transferrin saturation (TfS), and C-reactive protein (CRP) as standard evaluations for iron deficiency in patients with IBD. Patients with active IBD should be screened every 3 months,and patients with inactive disease should be screened every 6 to 12 months.23
Although ferritin and TfS often are used as markers for iron status in healthy individuals, they are positive and negative acute phase reactants, respectively. Using them to assess iron status in patients with IBD may inaccurately represent iron status in the setting of inflammation from the disease.24 The European Crohn’s and Colitis Organisation (ECCO) produced guidelines to define iron deficiency as a TfS less than 20% or a ferritin level less than 30 µg/L in patients without evidence of active IBD and a ferritin level less than 100 µg/L for patients with active inflammation.25
A 2020 multicenter observational study of 202 patients with diagnosed IBD found that the ECCO guideline of ferritin less than 30 µg/L had an area under the receiver operating characteristic (AUROC) curve of 0.69, a sensitivity of 0.43, and a specificity of 0.95 in their population.26 In a sensitivity analysis stratifying patients by CRP level (<10 or ≥10 mg/L), the authors found that for patients with ulcerative colitis and a CRP less than 10 mg/L, a cut-off value of ferritin less than 65 µg/L (AUROC=0.78) had a sensitivity of 0.78 and specificity of 0.76, and a TfS value of less than 16% (AUROC=0.88) had a sensitivity of 0.79 and a specificity of 0.9. In patients with a CRP of 10 mg/L or greater, a cut-off value of ferritin 80 µg/L (AUROC=0.76) had a sensitivity of 0.75 and a specificity of 0.82, and a TfS value of less than 11% (AUROC=0.69) had a sensitivity of 0.79 and a specificity of 0.88. There were no ferritin cut-off values associated with good diagnostic performance (defined as both sensitivity and specificity >0.70) for iron deficiency in patients with Crohn disease.26
The authors recommended using an alternative iron measurement such as soluble transferrin receptor (sTfR)/log ferritin ratio (TfR-F) that is not influenced by active inflammation and has a good correlation with ferritin values (TfR-F: r=0.66; P<.001).26 However, both sTfR and TfR-F have high costs and intermethod variability as well as differences in their reference ranges depending on which laboratory performs the analysis, limiting the accessibility and practicality of easily obtaining these tests.27 Although there may be inaccuracies for standard ferritin or TfS under ECCO guidelines, proposed alternatives have their own limitations, which may make ferritin and TfS the most reasonable evaluations of iron status as long as disease activity status at the time of testing is taken into consideration.
Treatment—Treatment of underlying iron deficiency in patients with IBD requires reversing the cause of the deficiency and supplementing iron. In patients with IBD, the options to supplement iron may be limited by active disease, making oral intake less effective. Oral iron supplementation also is associated with notable GI adverse effects that may be exacerbated in patients with IBD. A systematic review of 43 randomized controlled trials (RCTs) evaluating GI adverse effects (eg, nausea, abdominal pain, diarrhea, constipation, and black or tarry stools) of oral ferrous sulfate compared with placebo or intravenous (IV) iron supplementation in healthy nonanemic individuals found a significant increase in GI adverse effects with oral supplementation (placebo: OR=2.32; P<.0001; IV: OR=3.05; P<.0001).28
Therefore, IV iron repletion may be necessary in patients with IBD and may require numerous infusions depending on the formulation of iron. In an RCT conducted in 2011, patients with iron-deficiency anemia with quiescent or mild to moderate IBD were treated with either IV iron sulfate or ferric carboxymaltose.29 With a primary end point of hemoglobin response greater than 2 g/dL, the authors found that 150 of 240 patients responded to ferric carboxymaltose vs 118 of 235 treated with iron sulfate (P=.004). The dosing for ferric carboxymaltose was 1 to 3 infusions of 500 to 1000 mg of iron and for iron sulfate up to 11 infusions of 200 mg of iron.29
Zinc
A systematic review of zinc deficiency in patients with IBD identified 7 studies including 2413 patients and revealed those with Crohn disease had a higher prevalence of zinc deficiency compared with patients with ulcerative colitis (54% vs 41%).30
Pathophysiology—Zinc serves as a catalytic cofactor for enzymatic activity within proteins and immune cells.31 The homeostasis of zinc is tightly regulated within the brush border of the small intestine by zinc transporters ZIP4 and ZIP1 from the lumen of enterocytes into the bloodstream.32 Inflammation in the small intestine due to Crohn disease can result in zinc malabsorption.
Ranaldi et al33 exposed intestinal cells and zinc-depleted intestinal cells to tumor necrosis factor α media to simulate an inflammatory environment. They measured transepithelial electrical resistance as a surrogate for transmembrane permeability and found that zinc-depleted cells had a statistically significantly higher transepithelial electrical resistance percentage (60% reduction after 4 hours; P<1.10–6) when exposed to tumor necrosis factor α signaling compared with normal intestinal cells. They concluded that zinc deficiency can increase intestinal permeability in the presence of inflammation, creating a cycle of further nutrient malabsorption and inflammation exacerbating IBD symptoms.33
Cutaneous Manifestations—After absorption in the small intestine, approximately 5% of zinc resides in the skin, with the highest concentration in the stratum spinosum.34 A cell study found that keratinocytes in zinc-deficient environments had higher rates of apoptosis compared with cells in normal media. The authors proposed that this higher rate of apoptosis and the resulting inflammation could be a mechanism for developing the desquamative or eczematous scaly plaques that are common cutaneous manifestations of zinc deficiency.35
Other cutaneous findings may include angular cheilitis, stomatitis, glossitis, paronychia, onychodystrophy, generalized alopecia, and delayed wound healing.36 The histopathology of these skin lesions is characterized by granular layer loss, epidermal pallor, confluent parakeratosis, spongiosis, dyskeratosis, and psoriasiform hyperplasia.37
Diagnosis and Monitoring—Assessing serum zinc levels is challenging, as they may decrease during states of inflammation.38 A mouse model study showed a 3.1-fold increase (P<.001) in ZIP14 expression in wild-type mice compared with an IL-6 -/- knock-down model after IL-6 exposure. The authors concluded that the upregulation of ZIP14 in the liver due to inflammatory cytokine upregulation decreases zinc availability in serum.39 Additionally, serum zinc can overestimate the level of deficiency in IBD because approximately 75% of serum zinc is bound to albumin, which decreases in the setting of inflammation.40-42
Alternatively, alkaline phosphatase (AP), a zinc-dependent metalloenzyme, may be a better evaluator of zinc status during periods of inflammation. A study in rats evaluated zinc through serum zinc levels and AP levels after a period of induced stress to mimic a short-term inflammatory state.43 The researchers found that total body stores of zinc were unaffected throughout the experiment; only serum zinc declined throughout the experiment duration while AP did not. Because approximately 75% of serum zinc is bound to serum albumin,42 the researchers concluded the induced inflammatory state depleted serum albumin and redistributed zinc to the liver, causing the observed serum zinc changes, while total body zinc levels and AP were largely unaffected in comparison.43 Comorbid conditions such as liver or bone disease can increase AP levels, which limits the utility of AP as a surrogate for zinc in patients with comorbidities.44 However, even in the context of active IBD, serum zinc still is currently considered the best biomarker to evaluate zinc status.45
Treatment—The recommended dose for zinc supplementation is 20 to 40 mg daily with higher doses (>50 mg/d) for patients with malabsorptive syndromes such as IBD.46 It can be administered orally or parenterally. Although rare, zinc replacement therapy may be associated with diarrhea, nausea, vomiting, mild headaches, and fatigue.46 Additional considerations should be taken when repleting other micronutrients with zinc, as calcium and folate can inhibit zinc reabsorption, while zinc itself can inhibit iron and copper reabsorption.47
Vitamin D and Calcium
Low vitamin D levels (<50 nmol/L) and hypocalcemia (<8.8 mg/dL) are common in patients with IBD.48,49
Pathophysiology—Vitamin D levels are maintained via 2 mechanisms. The first mechanism is through the skin, as keratinocytes produce 7-dehydrocholesterol after exposure to UV light, which is converted into previtamin D3 and then thermally isomerizes into vitamin D3. This vitamin D3 is then transported to the liver on vitamin D–binding protein.50 The second mechanism is through oral vitamin D3 that is absorbed through vitamin D receptors in intestinal epithelium and transported to the liver, where it is hydroxylated into 25-hydroxyvitamin D (25[OH]D), then to the kidneys for hydroxylation to 1,25(OH)2D for redistribution throughout the body.50 This activated form of vitamin D regulates calcium absorption in the intestine, and optimal vitamin D levels are necessary to absorb calcium efficiently.51 Inflammation from IBD within the small intestine can downregulate vitamin D receptors, causing malabsorption and decreased serum vitamin D.52
Vitamin D signaling also is vital to maintaining the tight junctions and adherens junctions of the intestinal epithelium. Weakening the permeability of the epithelium further exacerbates malabsorption and subsequent vitamin D deficiency.52 A meta-analysis of 27 studies including 8316 patients with IBD showed low vitamin D levels were associated with increased odds of disease activity (OR=1.53; 95% CI, 1.32-1.77), mucosal inflammation (OR=1.25; 95% CI, 1.06-1.47), and future clinical relapse (OR=1.23; 95% CI, 1.03-1.47) in patients with Crohn disease. The authors concluded that low levels of vitamin D could be used as a potential biomarker of inflammatory status in Crohn disease.53
Vitamin D and calcium are further implicated in maintaining skeletal health,47 while vitamin D specifically helps maintain intestinal homeostasis54 and immune system modulation in the skin.55
Cutaneous Manifestations—Vitamin D is thought to play crucial roles in skin differentiation and proliferation, cutaneous innate immunity, hair follicle cycling, photoprotection, and wound healing.56 Vitamin D deficiency has been observed in a large range of cutaneous diseases including skin cancer, psoriasis, vitiligo, bullous pemphigoid, atopic dermatitis, and various types of alopecia.56-59 It is unclear whether vitamin D deficiency facilitates these disease processes or is merely the consequence of a disrupted cutaneous surface with the inability to complete the first step in vitamin D processing. A 2014 meta-analysis of 290 prospective cohort studies and 172 randomized trials concluded that 25(OH)D deficiency was associated with ill health and did not find causal evidence for any specific disease, dermatologic or otherwise.60 Calcium deficiency may cause epidermal changes including dry skin, coarse hair, and brittle nails.61
Diagnosis and Monitoring—The ECCO guidelines recommend obtaining serum 25(OH)D levels every 3 months in patients with IBD.62 Levels less than 75 nmol/L are considered deficient, and a value less than 30 nmol/L increases the risk for osteomalacia and nutritional rickets, constituting severe vitamin D deficiency.63-65
An observational study of 325 patients with IBD showed a statistically significant negative correlation between serum vitamin D and fecal calprotectin (r=−0.19; P<.001), a stool-based marker for gut inflammation, supporting vitamin D as a potential biomarker in IBD.66
Evaluation of calcium can be done through serum levels in patients with IBD.67 Patients with IBD are at risk for hypoalbuminemia; therefore, consideration should be taken to ensure calcium levels are corrected, as approximately 50% of calcium is bound to albumin or other ions in the body,68 which can be done by adjusting the calcium concentration by 0.02 mmol/L for every 1 g/L of albumin above or below 40 g/L. In the most critically ill patients, a direct ionized calcium blood level should be used instead because the previously mentioned correction calculations are inaccurate when albumin is critically low.69
Treatment—The ECCO guidelines recommend calcium and vitamin D repletion of 500 to 1000 mg and 800 to 1000 U, respectively, in patients with IBD on systemic corticosteroids to prevent the negative effects of bone loss.62 Calcium repletion in patients with IBD who are not on systemic steroids are the same as for the general population.65
Vitamin D repletion also may help decrease IBD activity. In a prospective study, 10,000 IU/d of vitamin D in 10 patients with IBD—adjusted over 12 weeks to a target of 100 to 125 nmol/L of serum 25(OH)D—showed a significant reduction in clinical Crohn activity (P=.019) over the study period.70 In contrast, 2000 IU/d for 3 months in an RCT of 27 patients with Crohn disease found significantly lower CRP (P=.019) and significantly higher self-reported quality of life (P=.037) but nonsignificant decreases in Crohn activity (P=.082) in patients with 25(OH)D levels of 75 nmol/L or higher compared with those with 25(OH)D levels less than 75 nmol/L.71
These discrepancies illustrate the need for expanded clinical trials to elucidate the optimal vitamin D dosing for patients with IBD. Ultimately, assessing vitamin D and calcium status and considering repletion in patients with IBD, especially those with comorbid dermatologic diseases such as poor wound healing, psoriasis, or atopic dermatitis, is important.
Vitamin B6 (Pyridoxine)
Pathophysiology—Pyridoxine is an important coenzyme for many functions including amino acid transamination, fatty acid metabolism, and conversion of tryptophan to niacin. It is absorbed in the jejunum and ileum and subsequently transported to the liver for rephosphorylation and release into its active form.36 An observational study assessing the nutritional status of patients with IBD found that only 5.7% of 105 patients with food records had inadequate dietary intake of pyridoxine, but 29% of all patients with IBD had subnormal pyridoxine levels.72 Additionally, they found no significant difference in the prevalence of subnormal pyridoxine levels in patients with active IBD vs IBD in remission. The authors suggested that the subnormal pyridoxine levels in patients with IBD likely were multifactorial and resulted from malabsorption due to active disease, inflammation, and inadequate intake.72
Cutaneous Manifestations—Cutaneous findings associated with pyridoxine deficiency include periorificial and perineal dermatitis,73 angular stomatitis, and cheilitis with associated burning, redness, and tongue edema.36 Additionally, pyridoxine is involved in the conversion of tryptophan to niacin, and its deficiency may manifest with pellagralike findings.74
Because pyridoxine is critical to protein metabolism, its deficiency may disrupt key cellular structures that rely on protein concentrations to maintain structural integrity. One such structure in the skin that heavily relies on protein concentrations is the ground substance of the extracellular matrix—the amorphous gelatinous spaces that occupy the areas between the extracellular matrix, which consists of cross-linked glycosaminoglycans and proteins.75 Without protein, ground substance increases in viscosity and can disrupt the epidermal barrier, leading to increased transepidermal water loss and ultimately inflammation.76 Although this theory has yet to be validated fully, this is a potential mechanistic explanation for the inflammation in dermal papillae that leads to dermatitis observed in pyridoxine deficiency.
Diagnosis and Monitoring—Direct biomarkers of pyridoxine status are in serum, plasma, erythrocytes, and urine, with the most common measurement in plasma as pyridoxal 5′-phosphate (PLP).77 Plasma PLP concentrations lower than 20 nmol/L are suggestive of deficiency.78 Plasma PLP has shown inverse relationships with acute phase inflammatory markers CRP79 and AP,78 thereby raising concerns for its validity to assess pyridoxine status in patients with symptomatic IBD.80
Alternative evaluations of pyridoxine include tryptophan and methionine loading tests,36 which are measured via urinary excretion and require normal kidney function to be accurate. They should be considered in IBD if necessary, but routine testing, even in patients with symptomatic IBD, is not recommended in the ECCO guidelines. Additional considerations should be taken in patients with altered nutrient requirements such as those who have undergone bowel resection due to highly active disease or those who receive parenteral nutritional supplementation.81
Treatment—Recommendations for oral pyridoxine supplementation range from 25 to 600 mg daily,82 with symptoms typically improving on 100 mg daily.36 Pyridoxine supplementation may have additional benefits for patients with IBD and potentially modulate disease severity. An IL-10 knockout mouse supplemented with pyridoxine had an approximately 60% reduction (P<.05) in inflammation compared to mice deficient in pyridoxine.83 The authors suggest that PLP-dependent enzymes can inhibit further proinflammatory signaling and T-cell migration that can exacerbate IBD. Ultimately, more data is needed before determining the efficacy of pyridoxine supplementation for active IBD.
Vitamin B12 and Vitamin B9 (Folic Acid)
Pathophysiology—Vitamin B12 is reabsorbed in the terminal ileum, the distal portion of the small intestine. The American Gastroenterological Association recommends that patients with a history of extensive ileal disease or prior ileal surgery, which is the case for many patients with Crohn disease, be monitored for vitamin B12 deficiency.23 Monitoring and rapid supplementation of vitamin B12 can prevent pernicious anemia and irreversible neurologic damage that may result from deficiency.84
Folic acid is primarily absorbed in the duodenum and jejunum of the small intestine. A meta-analysis performed in 2017 assessed studies observing folic acid and vitamin B12 levels in 1086 patients with IBD compared with 1484 healthy controls and found an average difference in serum folate concentration of 0.46 nmol/L (P<.001).84 Interestingly, this study did not find a significant difference in serum vitamin B12 levels between patients with IBD and healthy controls, highlighting the mechanism of vitamin B12 deficiency in IBD because only patients with terminal ileal involvement are at risk for malabsorption and subsequent deficiency.
Cutaneous Manifestations—Both vitamin B12 and folic acid deficiency can manifest as cheilitis, glossitis, and/or generalized hyperpigmentation that is accentuated in the flexural areas, palms, soles, and oral cavity.85,86 Systemic symptoms of patients with vitamin B12 and folic acid deficiency include megaloblastic anemia, pallor, and fatigue. A potential mechanism for the hyperpigmentation observed from vitamin B12 deficiency came from an electron microscope study that showed an increased concentration of melanosomes in a patient with deficiency.87
Diagnosis and Monitoring—In patients with suspected vitamin B12 and/or folic acid deficiency, initial evaluation should include a CBC with peripheral smear and serum vitamin B12 and folate levels. In cases for which the diagnosis still is unclear after initial testing,
Treatment—According to the Centers for Disease Control and Prevention, supplementation of vitamin B12 can be done orally with 1000 µg daily in patients with deficiency. In patients with active IBD, oral reabsorption of vitamin B12 can be less effective, making subcutaneous or intramuscular administration (1000 µg/wk for 8 weeks, then monthly for life) better options.89
Patients with IBD managed with methotrexate should be screened carefully for folate deficiency. Methotrexate is a folate analog that sometimes is used for the treatment of IBD. Reversible competitive inhibition of dihydrofolate reductase can precipitate a systemic folic acid decrease.91 Typically, oral folic acid (1 to 5 mg/d) is sufficient to treat folate deficiency, with the ESPEN recommending 5 mg once weekly 24 to 72 hours after methotrexate treatment or 1 mg daily for 5 days per week in patients with IBD.1 Alternative formulations—IV, subcutaneous, or intramuscular—are available for patients who cannot tolerate oral intake.92
Final Thoughts
Dermatologists can be the first to observe the cutaneous manifestations of micronutrient deficiencies. Although the symptoms of each micronutrient deficiency discussed may overlap, attention to small clinical clues in patients with IBD can improve patient outcomes and quality of life. For example, koilonychia with glossitis and xerosis likely is due to iron deficiency, while zinc deficiency should be suspected in patients with scaly eczematous plaques in skin folds. A high level of suspicion for micronutrient deficiencies in patients with IBD should be followed by a complete patient history, review of systems, and thorough clinical examination. A thorough laboratory evaluation can pinpoint nutritional deficiencies in patients with IBD, keeping in mind that specific biomarkers such as ferritin and serum zinc also act as acute phase reactants and should be interpreted in this context. Co-management with gastroenterologists should be a priority in patients with IBD, as gaining control of inflammatory disease is crucial for the prevention of recurrent vitamin and micronutrient deficiencies in addition to long-term health in this population.
In 2023, ESPEN (the European Society for Clinical Nutrition and Metabolism) published consensus recommendations highlighting the importance of regular monitoring and treatment of nutrient deficiencies in patients with inflammatory bowel disease (IBD) for improved prognosis, mortality, and quality of life.1 Suboptimal nutrition in patients with IBD predominantly results from inflammation of the gastrointestinal (GI) tract leading to malabsorption; however, medications commonly used to manage IBD also can contribute to malnutrition.2,3 Additionally, patients may develop nausea and food avoidance due to medication or the disease itself, leading to nutritional withdrawal and eventual deficiency.4 Even with the development of diets focused on balancing nutritional needs and decreasing inflammation,5 offsetting this aversion to food can be difficult to overcome.2
Cutaneous manifestations of IBD are multifaceted and can be secondary to the disease, reactive to or associated with IBD, or effects from nutritional deficiencies. The most common vitamin and nutrient deficiencies in patients with IBD include iron; zinc; calcium; vitamin D; and vitamins B6 (pyridoxine), B9 (folic acid), and B12.6 Malnutrition may manifest with cutaneous disease, and dermatologists can be the first to identify and assess for nutritional deficiencies. In this article, we review the mechanisms of these micronutrient depletions in the context of IBD, their subsequent dermatologic manifestations (Table), and treatment and monitoring guidelines for each deficiency.
Iron
A systematic review conducted from 2007 to 2012 in European patients with IBD (N=2192) found the overall prevalence of anemia in this population to be 24% (95% CI, 18%-31%), with 57% of patients with anemia experiencing iron deficiency.7 Anemia is observed more commonly in patients hospitalized with IBD and is common in patients with both Crohn disease and ulcerative colitis.8
Pathophysiology—Iron is critically important in oxygen transportation throughout the body as a major component of hemoglobin. Physiologically, the low pH of the duodenum and proximal jejunum allows divalent metal transporter 1 to transfer dietary Fe3+ into enterocytes, where it is reduced to the transportable Fe2+.9,10 Distribution of Fe2+ ions from enterocytes relies on ferroportin, an iron-transporting protein, which is heavily regulated by the protein hepcidin.11 Hepcidin, a known acute phase reactant, will increase in the setting of active IBD, causing a depletion of ferroportin and an inability of the body to utilize the stored iron in enterocytes.12 This poor utilization of iron stores combined with blood loss caused by inflammation in the GI tract is the proposed primary mechanism of iron-deficiency anemia observed in patients with IBD.13
Cutaneous Manifestations—From a dermatologic perspective, iron-deficiency anemia can manifest with a wide range of symptoms including glossitis, koilonychia, xerosis and/or pruritus, and brittle hair or hair loss.14,15 Although the underlying pathophysiology of these cutaneous manifestations is not fully understood, there are several theories assessing the mechanisms behind the skin findings of iron deficiency.
Atrophic glossitis has been observed in many patients with iron deficiency and is thought to manifest due to low iron concentrations in the blood, thereby decreasing oxygen delivery to the papillae of the dorsal tongue with resultant atrophy.16,17 Similarly, decreased oxygen delivery to the nail bed capillaries may cause deformities in the nail called koilonychia (or “spoon nails”).18 Iron is a key co-factor in collagen lysyl hydroxylase that promotes collagen binding; iron deficiency may lead to disruptions in the epidermal barrier that can cause pruritus and xerosis.19 An observational study of 200 healthy patients with a primary concern of pruritus found a correlation between low serum ferritin and a higher degree of pruritus (r=−0.768; P<.00001).20
Evidence for iron’s role in hair growth comes from a mouse model study with a mutation in the serine protease TMPRSS6—a protein that regulates hepcidin and iron absorption—which caused an increase in hepcidin production and subsequent systemic iron deficiency. Mice at 4 weeks of age were devoid of all body hair but had substantial regrowth after initiation of a 2-week iron-rich diet, which suggests a connection between iron repletion and hair growth in mice with iron deficiency.21 Additionally, a meta-analysis analyzing the comorbidities of patients with alopecia areata found them to have higher odds (odds ratio [OR]=2.78; 95% CI, 1.23-6.29) of iron-deficiency anemia but no association with IBD (OR=1.48; 95% CI, 0.32-6.82).22
Diagnosis and Monitoring—The American Gastroenterological Association recommends a complete blood cell count (CBC), serum ferritin, transferrin saturation (TfS), and C-reactive protein (CRP) as standard evaluations for iron deficiency in patients with IBD. Patients with active IBD should be screened every 3 months,and patients with inactive disease should be screened every 6 to 12 months.23
Although ferritin and TfS often are used as markers for iron status in healthy individuals, they are positive and negative acute phase reactants, respectively. Using them to assess iron status in patients with IBD may inaccurately represent iron status in the setting of inflammation from the disease.24 The European Crohn’s and Colitis Organisation (ECCO) produced guidelines to define iron deficiency as a TfS less than 20% or a ferritin level less than 30 µg/L in patients without evidence of active IBD and a ferritin level less than 100 µg/L for patients with active inflammation.25
A 2020 multicenter observational study of 202 patients with diagnosed IBD found that the ECCO guideline of ferritin less than 30 µg/L had an area under the receiver operating characteristic (AUROC) curve of 0.69, a sensitivity of 0.43, and a specificity of 0.95 in their population.26 In a sensitivity analysis stratifying patients by CRP level (<10 or ≥10 mg/L), the authors found that for patients with ulcerative colitis and a CRP less than 10 mg/L, a cut-off value of ferritin less than 65 µg/L (AUROC=0.78) had a sensitivity of 0.78 and specificity of 0.76, and a TfS value of less than 16% (AUROC=0.88) had a sensitivity of 0.79 and a specificity of 0.9. In patients with a CRP of 10 mg/L or greater, a cut-off value of ferritin 80 µg/L (AUROC=0.76) had a sensitivity of 0.75 and a specificity of 0.82, and a TfS value of less than 11% (AUROC=0.69) had a sensitivity of 0.79 and a specificity of 0.88. There were no ferritin cut-off values associated with good diagnostic performance (defined as both sensitivity and specificity >0.70) for iron deficiency in patients with Crohn disease.26
The authors recommended using an alternative iron measurement such as soluble transferrin receptor (sTfR)/log ferritin ratio (TfR-F) that is not influenced by active inflammation and has a good correlation with ferritin values (TfR-F: r=0.66; P<.001).26 However, both sTfR and TfR-F have high costs and intermethod variability as well as differences in their reference ranges depending on which laboratory performs the analysis, limiting the accessibility and practicality of easily obtaining these tests.27 Although there may be inaccuracies for standard ferritin or TfS under ECCO guidelines, proposed alternatives have their own limitations, which may make ferritin and TfS the most reasonable evaluations of iron status as long as disease activity status at the time of testing is taken into consideration.
Treatment—Treatment of underlying iron deficiency in patients with IBD requires reversing the cause of the deficiency and supplementing iron. In patients with IBD, the options to supplement iron may be limited by active disease, making oral intake less effective. Oral iron supplementation also is associated with notable GI adverse effects that may be exacerbated in patients with IBD. A systematic review of 43 randomized controlled trials (RCTs) evaluating GI adverse effects (eg, nausea, abdominal pain, diarrhea, constipation, and black or tarry stools) of oral ferrous sulfate compared with placebo or intravenous (IV) iron supplementation in healthy nonanemic individuals found a significant increase in GI adverse effects with oral supplementation (placebo: OR=2.32; P<.0001; IV: OR=3.05; P<.0001).28
Therefore, IV iron repletion may be necessary in patients with IBD and may require numerous infusions depending on the formulation of iron. In an RCT conducted in 2011, patients with iron-deficiency anemia with quiescent or mild to moderate IBD were treated with either IV iron sulfate or ferric carboxymaltose.29 With a primary end point of hemoglobin response greater than 2 g/dL, the authors found that 150 of 240 patients responded to ferric carboxymaltose vs 118 of 235 treated with iron sulfate (P=.004). The dosing for ferric carboxymaltose was 1 to 3 infusions of 500 to 1000 mg of iron and for iron sulfate up to 11 infusions of 200 mg of iron.29
Zinc
A systematic review of zinc deficiency in patients with IBD identified 7 studies including 2413 patients and revealed those with Crohn disease had a higher prevalence of zinc deficiency compared with patients with ulcerative colitis (54% vs 41%).30
Pathophysiology—Zinc serves as a catalytic cofactor for enzymatic activity within proteins and immune cells.31 The homeostasis of zinc is tightly regulated within the brush border of the small intestine by zinc transporters ZIP4 and ZIP1 from the lumen of enterocytes into the bloodstream.32 Inflammation in the small intestine due to Crohn disease can result in zinc malabsorption.
Ranaldi et al33 exposed intestinal cells and zinc-depleted intestinal cells to tumor necrosis factor α media to simulate an inflammatory environment. They measured transepithelial electrical resistance as a surrogate for transmembrane permeability and found that zinc-depleted cells had a statistically significantly higher transepithelial electrical resistance percentage (60% reduction after 4 hours; P<1.10–6) when exposed to tumor necrosis factor α signaling compared with normal intestinal cells. They concluded that zinc deficiency can increase intestinal permeability in the presence of inflammation, creating a cycle of further nutrient malabsorption and inflammation exacerbating IBD symptoms.33
Cutaneous Manifestations—After absorption in the small intestine, approximately 5% of zinc resides in the skin, with the highest concentration in the stratum spinosum.34 A cell study found that keratinocytes in zinc-deficient environments had higher rates of apoptosis compared with cells in normal media. The authors proposed that this higher rate of apoptosis and the resulting inflammation could be a mechanism for developing the desquamative or eczematous scaly plaques that are common cutaneous manifestations of zinc deficiency.35
Other cutaneous findings may include angular cheilitis, stomatitis, glossitis, paronychia, onychodystrophy, generalized alopecia, and delayed wound healing.36 The histopathology of these skin lesions is characterized by granular layer loss, epidermal pallor, confluent parakeratosis, spongiosis, dyskeratosis, and psoriasiform hyperplasia.37
Diagnosis and Monitoring—Assessing serum zinc levels is challenging, as they may decrease during states of inflammation.38 A mouse model study showed a 3.1-fold increase (P<.001) in ZIP14 expression in wild-type mice compared with an IL-6 -/- knock-down model after IL-6 exposure. The authors concluded that the upregulation of ZIP14 in the liver due to inflammatory cytokine upregulation decreases zinc availability in serum.39 Additionally, serum zinc can overestimate the level of deficiency in IBD because approximately 75% of serum zinc is bound to albumin, which decreases in the setting of inflammation.40-42
Alternatively, alkaline phosphatase (AP), a zinc-dependent metalloenzyme, may be a better evaluator of zinc status during periods of inflammation. A study in rats evaluated zinc through serum zinc levels and AP levels after a period of induced stress to mimic a short-term inflammatory state.43 The researchers found that total body stores of zinc were unaffected throughout the experiment; only serum zinc declined throughout the experiment duration while AP did not. Because approximately 75% of serum zinc is bound to serum albumin,42 the researchers concluded the induced inflammatory state depleted serum albumin and redistributed zinc to the liver, causing the observed serum zinc changes, while total body zinc levels and AP were largely unaffected in comparison.43 Comorbid conditions such as liver or bone disease can increase AP levels, which limits the utility of AP as a surrogate for zinc in patients with comorbidities.44 However, even in the context of active IBD, serum zinc still is currently considered the best biomarker to evaluate zinc status.45
Treatment—The recommended dose for zinc supplementation is 20 to 40 mg daily with higher doses (>50 mg/d) for patients with malabsorptive syndromes such as IBD.46 It can be administered orally or parenterally. Although rare, zinc replacement therapy may be associated with diarrhea, nausea, vomiting, mild headaches, and fatigue.46 Additional considerations should be taken when repleting other micronutrients with zinc, as calcium and folate can inhibit zinc reabsorption, while zinc itself can inhibit iron and copper reabsorption.47
Vitamin D and Calcium
Low vitamin D levels (<50 nmol/L) and hypocalcemia (<8.8 mg/dL) are common in patients with IBD.48,49
Pathophysiology—Vitamin D levels are maintained via 2 mechanisms. The first mechanism is through the skin, as keratinocytes produce 7-dehydrocholesterol after exposure to UV light, which is converted into previtamin D3 and then thermally isomerizes into vitamin D3. This vitamin D3 is then transported to the liver on vitamin D–binding protein.50 The second mechanism is through oral vitamin D3 that is absorbed through vitamin D receptors in intestinal epithelium and transported to the liver, where it is hydroxylated into 25-hydroxyvitamin D (25[OH]D), then to the kidneys for hydroxylation to 1,25(OH)2D for redistribution throughout the body.50 This activated form of vitamin D regulates calcium absorption in the intestine, and optimal vitamin D levels are necessary to absorb calcium efficiently.51 Inflammation from IBD within the small intestine can downregulate vitamin D receptors, causing malabsorption and decreased serum vitamin D.52
Vitamin D signaling also is vital to maintaining the tight junctions and adherens junctions of the intestinal epithelium. Weakening the permeability of the epithelium further exacerbates malabsorption and subsequent vitamin D deficiency.52 A meta-analysis of 27 studies including 8316 patients with IBD showed low vitamin D levels were associated with increased odds of disease activity (OR=1.53; 95% CI, 1.32-1.77), mucosal inflammation (OR=1.25; 95% CI, 1.06-1.47), and future clinical relapse (OR=1.23; 95% CI, 1.03-1.47) in patients with Crohn disease. The authors concluded that low levels of vitamin D could be used as a potential biomarker of inflammatory status in Crohn disease.53
Vitamin D and calcium are further implicated in maintaining skeletal health,47 while vitamin D specifically helps maintain intestinal homeostasis54 and immune system modulation in the skin.55
Cutaneous Manifestations—Vitamin D is thought to play crucial roles in skin differentiation and proliferation, cutaneous innate immunity, hair follicle cycling, photoprotection, and wound healing.56 Vitamin D deficiency has been observed in a large range of cutaneous diseases including skin cancer, psoriasis, vitiligo, bullous pemphigoid, atopic dermatitis, and various types of alopecia.56-59 It is unclear whether vitamin D deficiency facilitates these disease processes or is merely the consequence of a disrupted cutaneous surface with the inability to complete the first step in vitamin D processing. A 2014 meta-analysis of 290 prospective cohort studies and 172 randomized trials concluded that 25(OH)D deficiency was associated with ill health and did not find causal evidence for any specific disease, dermatologic or otherwise.60 Calcium deficiency may cause epidermal changes including dry skin, coarse hair, and brittle nails.61
Diagnosis and Monitoring—The ECCO guidelines recommend obtaining serum 25(OH)D levels every 3 months in patients with IBD.62 Levels less than 75 nmol/L are considered deficient, and a value less than 30 nmol/L increases the risk for osteomalacia and nutritional rickets, constituting severe vitamin D deficiency.63-65
An observational study of 325 patients with IBD showed a statistically significant negative correlation between serum vitamin D and fecal calprotectin (r=−0.19; P<.001), a stool-based marker for gut inflammation, supporting vitamin D as a potential biomarker in IBD.66
Evaluation of calcium can be done through serum levels in patients with IBD.67 Patients with IBD are at risk for hypoalbuminemia; therefore, consideration should be taken to ensure calcium levels are corrected, as approximately 50% of calcium is bound to albumin or other ions in the body,68 which can be done by adjusting the calcium concentration by 0.02 mmol/L for every 1 g/L of albumin above or below 40 g/L. In the most critically ill patients, a direct ionized calcium blood level should be used instead because the previously mentioned correction calculations are inaccurate when albumin is critically low.69
Treatment—The ECCO guidelines recommend calcium and vitamin D repletion of 500 to 1000 mg and 800 to 1000 U, respectively, in patients with IBD on systemic corticosteroids to prevent the negative effects of bone loss.62 Calcium repletion in patients with IBD who are not on systemic steroids are the same as for the general population.65
Vitamin D repletion also may help decrease IBD activity. In a prospective study, 10,000 IU/d of vitamin D in 10 patients with IBD—adjusted over 12 weeks to a target of 100 to 125 nmol/L of serum 25(OH)D—showed a significant reduction in clinical Crohn activity (P=.019) over the study period.70 In contrast, 2000 IU/d for 3 months in an RCT of 27 patients with Crohn disease found significantly lower CRP (P=.019) and significantly higher self-reported quality of life (P=.037) but nonsignificant decreases in Crohn activity (P=.082) in patients with 25(OH)D levels of 75 nmol/L or higher compared with those with 25(OH)D levels less than 75 nmol/L.71
These discrepancies illustrate the need for expanded clinical trials to elucidate the optimal vitamin D dosing for patients with IBD. Ultimately, assessing vitamin D and calcium status and considering repletion in patients with IBD, especially those with comorbid dermatologic diseases such as poor wound healing, psoriasis, or atopic dermatitis, is important.
Vitamin B6 (Pyridoxine)
Pathophysiology—Pyridoxine is an important coenzyme for many functions including amino acid transamination, fatty acid metabolism, and conversion of tryptophan to niacin. It is absorbed in the jejunum and ileum and subsequently transported to the liver for rephosphorylation and release into its active form.36 An observational study assessing the nutritional status of patients with IBD found that only 5.7% of 105 patients with food records had inadequate dietary intake of pyridoxine, but 29% of all patients with IBD had subnormal pyridoxine levels.72 Additionally, they found no significant difference in the prevalence of subnormal pyridoxine levels in patients with active IBD vs IBD in remission. The authors suggested that the subnormal pyridoxine levels in patients with IBD likely were multifactorial and resulted from malabsorption due to active disease, inflammation, and inadequate intake.72
Cutaneous Manifestations—Cutaneous findings associated with pyridoxine deficiency include periorificial and perineal dermatitis,73 angular stomatitis, and cheilitis with associated burning, redness, and tongue edema.36 Additionally, pyridoxine is involved in the conversion of tryptophan to niacin, and its deficiency may manifest with pellagralike findings.74
Because pyridoxine is critical to protein metabolism, its deficiency may disrupt key cellular structures that rely on protein concentrations to maintain structural integrity. One such structure in the skin that heavily relies on protein concentrations is the ground substance of the extracellular matrix—the amorphous gelatinous spaces that occupy the areas between the extracellular matrix, which consists of cross-linked glycosaminoglycans and proteins.75 Without protein, ground substance increases in viscosity and can disrupt the epidermal barrier, leading to increased transepidermal water loss and ultimately inflammation.76 Although this theory has yet to be validated fully, this is a potential mechanistic explanation for the inflammation in dermal papillae that leads to dermatitis observed in pyridoxine deficiency.
Diagnosis and Monitoring—Direct biomarkers of pyridoxine status are in serum, plasma, erythrocytes, and urine, with the most common measurement in plasma as pyridoxal 5′-phosphate (PLP).77 Plasma PLP concentrations lower than 20 nmol/L are suggestive of deficiency.78 Plasma PLP has shown inverse relationships with acute phase inflammatory markers CRP79 and AP,78 thereby raising concerns for its validity to assess pyridoxine status in patients with symptomatic IBD.80
Alternative evaluations of pyridoxine include tryptophan and methionine loading tests,36 which are measured via urinary excretion and require normal kidney function to be accurate. They should be considered in IBD if necessary, but routine testing, even in patients with symptomatic IBD, is not recommended in the ECCO guidelines. Additional considerations should be taken in patients with altered nutrient requirements such as those who have undergone bowel resection due to highly active disease or those who receive parenteral nutritional supplementation.81
Treatment—Recommendations for oral pyridoxine supplementation range from 25 to 600 mg daily,82 with symptoms typically improving on 100 mg daily.36 Pyridoxine supplementation may have additional benefits for patients with IBD and potentially modulate disease severity. An IL-10 knockout mouse supplemented with pyridoxine had an approximately 60% reduction (P<.05) in inflammation compared to mice deficient in pyridoxine.83 The authors suggest that PLP-dependent enzymes can inhibit further proinflammatory signaling and T-cell migration that can exacerbate IBD. Ultimately, more data is needed before determining the efficacy of pyridoxine supplementation for active IBD.
Vitamin B12 and Vitamin B9 (Folic Acid)
Pathophysiology—Vitamin B12 is reabsorbed in the terminal ileum, the distal portion of the small intestine. The American Gastroenterological Association recommends that patients with a history of extensive ileal disease or prior ileal surgery, which is the case for many patients with Crohn disease, be monitored for vitamin B12 deficiency.23 Monitoring and rapid supplementation of vitamin B12 can prevent pernicious anemia and irreversible neurologic damage that may result from deficiency.84
Folic acid is primarily absorbed in the duodenum and jejunum of the small intestine. A meta-analysis performed in 2017 assessed studies observing folic acid and vitamin B12 levels in 1086 patients with IBD compared with 1484 healthy controls and found an average difference in serum folate concentration of 0.46 nmol/L (P<.001).84 Interestingly, this study did not find a significant difference in serum vitamin B12 levels between patients with IBD and healthy controls, highlighting the mechanism of vitamin B12 deficiency in IBD because only patients with terminal ileal involvement are at risk for malabsorption and subsequent deficiency.
Cutaneous Manifestations—Both vitamin B12 and folic acid deficiency can manifest as cheilitis, glossitis, and/or generalized hyperpigmentation that is accentuated in the flexural areas, palms, soles, and oral cavity.85,86 Systemic symptoms of patients with vitamin B12 and folic acid deficiency include megaloblastic anemia, pallor, and fatigue. A potential mechanism for the hyperpigmentation observed from vitamin B12 deficiency came from an electron microscope study that showed an increased concentration of melanosomes in a patient with deficiency.87
Diagnosis and Monitoring—In patients with suspected vitamin B12 and/or folic acid deficiency, initial evaluation should include a CBC with peripheral smear and serum vitamin B12 and folate levels. In cases for which the diagnosis still is unclear after initial testing,
Treatment—According to the Centers for Disease Control and Prevention, supplementation of vitamin B12 can be done orally with 1000 µg daily in patients with deficiency. In patients with active IBD, oral reabsorption of vitamin B12 can be less effective, making subcutaneous or intramuscular administration (1000 µg/wk for 8 weeks, then monthly for life) better options.89
Patients with IBD managed with methotrexate should be screened carefully for folate deficiency. Methotrexate is a folate analog that sometimes is used for the treatment of IBD. Reversible competitive inhibition of dihydrofolate reductase can precipitate a systemic folic acid decrease.91 Typically, oral folic acid (1 to 5 mg/d) is sufficient to treat folate deficiency, with the ESPEN recommending 5 mg once weekly 24 to 72 hours after methotrexate treatment or 1 mg daily for 5 days per week in patients with IBD.1 Alternative formulations—IV, subcutaneous, or intramuscular—are available for patients who cannot tolerate oral intake.92
Final Thoughts
Dermatologists can be the first to observe the cutaneous manifestations of micronutrient deficiencies. Although the symptoms of each micronutrient deficiency discussed may overlap, attention to small clinical clues in patients with IBD can improve patient outcomes and quality of life. For example, koilonychia with glossitis and xerosis likely is due to iron deficiency, while zinc deficiency should be suspected in patients with scaly eczematous plaques in skin folds. A high level of suspicion for micronutrient deficiencies in patients with IBD should be followed by a complete patient history, review of systems, and thorough clinical examination. A thorough laboratory evaluation can pinpoint nutritional deficiencies in patients with IBD, keeping in mind that specific biomarkers such as ferritin and serum zinc also act as acute phase reactants and should be interpreted in this context. Co-management with gastroenterologists should be a priority in patients with IBD, as gaining control of inflammatory disease is crucial for the prevention of recurrent vitamin and micronutrient deficiencies in addition to long-term health in this population.
- Bischoff SC, Bager P, Escher J, et al. ESPEN guideline on clinical nutrition in inflammatory bowel disease. Clin Nutr. 2023;42:352-379. doi:10.1016/j.clnu.2022.12.004
- Gerasimidis K, McGrogan P, Edwards CA. The aetiology and impact of malnutrition in paediatric inflammator y bowel disease. J Hum Nutr Diet. 2011;24:313-326. doi:10.1111/j.1365-277X.2011.01171.x
- Mentella MC, Scaldaferri F, Pizzoferrato M, et al. Nutrition, IBD and gut microbiota: a review. Nutrients. 2020;12:944. doi:10.3390/nu12040944
- Bonsack O, Caron B, Baumann C, et al. Food avoidance and fasting in patients with inflammatory bowel disease: experience from the Nancy IBD nutrition clinic. United European Gastroenterol J. 2023;11:361-370. doi:10.1002/ueg2.1238521
- Campmans-Kuijpers MJE, Dijkstra G. Food and food groups in inflammatory bowel disease (IBD): the design of the Groningen Anti-Inflammatory Diet (GrAID). Nutrients. 2021;13:1067. doi:10.3390/nu13041067
- Hwang C, Issokson K, Giguere-Rich C, et al. Development and pilot testing of the inflammatory bowel disease nutrition care pathway. Clin Gastroenterol Hepatol. 2020;18:2645-2649.e4. doi:10.1016/j.cgh.2020.06.039
- Filmann N, Rey J, Schneeweiss S, et al. Prevalence of anemia in inflammatory bowel diseases in European countries: a systematic review and individual patient data meta-analysis. Inflamm Bowel Dis. 2014;20:936-945. doi:10.1097/01.MIB.0000442728.74340.fd
- Stein J, Hartmann F, Dignass AU. Diagnosis and management of iron deficiency anemia in patients with IBD. Nat Rev Gastroenterol Hepatol. 2010;7:599-610. doi:10.1038/nrgastro.2010.151
- Ems T, St Lucia K, Huecker MR. Biochemistry, iron absorption. StatPearls [Internet]. Updated April 17, 2023. Accessed March 19, 2024. https://www.ncbi.nlm.nih.gov/books/NBK448204/
- Evstatiev R, Gasche C. Iron sensing and signalling. Gut. 2012;61:933-952. doi:10.1136/gut.2010.214312
- Przybyszewska J, Zekanowska E. The role of hepcidin, ferroportin, HCP1, and DMT1 protein in iron absorption in the human digestive tract. Prz Gastroenterol. 2014;9:208-213. doi:10.5114/pg.2014.45102
- Weiss G, Gasche C. Pathogenesis and treatment of anemia in inflammatory bowel disease. Haematologica. 2010;95:175-178. doi:10.3324/haematol.2009.017046
- Kaitha S, Bashir M, Ali T. Iron deficiency anemia in inflammatory bowel disease. World J Gastrointest Pathophysiol. 2015;6:62-72. doi:10.4291/wjgp.v6.i3.62
- Moiz B. Spoon nails: still seen in today’s world. Clin Case Rep. 2018;6:547-548. doi:10.1002/ccr3.1404
- St Pierre SA, Vercellotti GM, Donovan JC, et al. Iron deficiency and diffuse nonscarring scalp alopecia in women: more pieces to the puzzle. J Am Acad Dermatol. 2010;63:1070-1076. doi:10.1016/j.jaad.2009.05.054
- Chiang CP, Yu-Fong Chang J, Wang YP, et al. Anemia, hematinic deficiencies, hyperhomocysteinemia, and serum gastric parietal cell antibody positivity in atrophic glossitis patients with or without microcytosis. J Formos Med Assoc. 2019;118:1401-1407. doi:10.1016/j.jfma.2019.06.004
- Chiang CP, Chang JY, Wang YP, et al. Atrophic glossitis: Etiology, serum autoantibodies, anemia, hematinic deficiencies, hyperhomocysteinemia, and management. J Formos Med Assoc. 2020;119:774-780. doi:10.1016/j.jfma.2019.04.015
- Walker J, Baran R, Vélez N, et al. Koilonychia: an update on pathophysiology, differential diagnosis and clinical relevance. J Eur Acad Dermatol Venereol. 2016;30:1985-1991. doi:10.1111/jdv.13610
- Guo HF, Tsai CL, Terajima M, et al. Pro-metastatic collagen lysyl hydroxylase dimer assemblies stabilized by Fe2+-binding. Nat Commun. 2018;9:512. doi:10.1038/s41467-018-02859-z
- Saini S, Jain AK, Agarwal S, et al. Iron deficiency and pruritus: a cross-sectional analysis to assess its association and relationship. Indian J Dermatol. 2021;66:705. doi:10.4103/ijd.ijd_326_21
- Du X, She E, Gelbart T, et al. The serine protease TMPRSS6 is required to sense iron deficiency. Science. 2008;320:1088-1092. doi:10.1126/science.1157121
- Lee S, Lee H, Lee CH, et al. Comorbidities in alopecia areata: a systematic review and meta-analysis. J Am Acad Dermatol. 2019;80:466-477.e16. doi:10.1016/j.jaad.2018.07.013
- Hashash JG, Elkins J, Lewis JD, et al. AGA Clinical Practice Update on diet and nutritional therapies in patients with inflammatory bowel disease: expert review [published online January 23, 2024]. Gastroenterology. doi:10.1053/j.gastro.2023.11.303
- Choudhuri S, Chowdhury IH, Saha A, et al. Acute monocyte pro- inflammatory response predicts higher positive to negative acute phase reactants ratio and severe hemostatic derangement in dengue fever. Cytokine. 2021;146:155644. doi:10.1016/j.cyto.2021.155644
- Dignass AU, Gasche C, Bettenworth D, et al; European Crohn’s and Colitis Organisation. European consensus on the diagnosis and management of iron deficiency and anaemia in inflammatory bowel diseases. J Crohn’s Colitis. 2015;9:211-222. doi:10.1093/ecco-jcc/jju009
- Daude S, Remen T, Chateau T, et al. Comparative accuracy of ferritin, transferrin saturation and soluble transferrin receptor for the diagnosis of iron deficiency in inflammatory bowel disease. Aliment Pharmacol Ther. 2020;51:1087-1095. doi:10.1111/apt.15739
- Pfeiffer CM, Looker AC. Laboratory methodologies for indicators of iron status: strengths, limitations, and analytical challenges. Am J Clin Nutr. 2017;106(suppl 6):1606S-1614S. doi:10.3945/ajcn.117.155887
- Tolkien Z, Stecher L, Mander AP, et al. Ferrous sulfate supplementation causes significant gastrointestinal side-effects in adults: a systematic review and meta-analysis. PLoS One. 2015;10:e0117383. doi:10.1371/journal.pone.0117383
- Evstatiev R, Marteau P, Iqbal T, et al. FERGIcor, a randomized controlled trial on ferric carboxymaltose for iron deficiency anemia in inflammatory bowel disease. Gastroenterology. 2011;141:846-853.e8532. doi:10.1053/j.gastro.2011.06.005
- Zupo R, Sila A, Castellana F, et al. Prevalence of zinc deficiency in inflammatory bowel disease: a systematic review and meta-analysis. Nutrients. 2022;14:4052. doi:10.3390/nu14194052
- Thompson MW. Regulation of zinc-dependent enzymes by metal carrier proteins. Biometals. 2022;35:187-213. doi:10.1007/s10534-022-00373-w
- Maares M, Haase H. A guide to human zinc absorption: general overview and recent advances of in vitro intestinal models. Nutrients. 2020;12:762. doi:10.3390/nu12030762
- Ranaldi G, Ferruzza S, Canali R, et al. Intracellular zinc is required for intestinal cell survival signals triggered by the inflammatory cytokine TNFα. J Nutr Biochem. 2013;24:967-976. doi:10.1016/j.jnutbio.2012.06.020
- Ogawa Y, Kawamura T, Shimada S. Zinc and skin biology. Arch Biochem Biophys. 2016;611:113-119. doi:10.1016/j.abb.2016.06.003
- Wilson D, Varigos G, Ackland ML. Apoptosis may underlie the pathology of zinc-deficient skin. Immunol Cell Biol. 2006;84:28-37. doi:10.1111/j.1440-1711.2005.01391.x
- Jen M, Yan AC. Syndromes associated with nutritional deficiency and excess. Clin Dermatol. 2010;28:669-685. doi:10.1016/j.clindermatol.2010.03.029
- Gonzalez JR, Botet MV, Sanchez JL. The histopathology of acrodermatitis enteropathica. Am J Dermatopathol. 1982;4:303-311.
- Gammoh NZ, Rink L. Zinc in infection and inflammation. Nutrients. 2017;9:624. doi:10.3390/nu9060624
- Liuzzi JP, Lichten LA, Rivera S, et al. Interleukin-6 regulates the zinc transporter Zip14 in liver and contributes to the hypozincemia of the acute-phase response. Proc Natl Acad Sci U S A. 2005;102:6843-6848. doi:10.1073/pnas.0502257102
- Vermeire S, Van Assche G, Rutgeerts P. Laboratory markers in IBD: useful, magic, or unnecessary toys?. Gut. 2006;55:426-431. doi:10.1136/gut.2005.069476
- Morisaku M, Ito K, Ogiso A, et al. Correlation between serum albumin and serum zinc in malignant lymphoma. Fujita Med J. 2022;8:59-64. doi:10.20407/fmj.2021-006
- Falchuk KH. Effect of acute disease and ACTH on serum zinc proteins. N Engl J Med. 1977:296:1129-1134.
- Naber TH, Baadenhuysen H, Jansen JB, et al. Serum alkaline phosphatase activity during zinc deficiency and long-term inflammatory stress. Clin Chim Acta. 1996;249:109-127. doi:10.1016/0009-8981(96)06281-x
- Lowe D, Sanvictores T, Zubair M, et al. Alkaline phosphatase. StatPearls [Internet]. Updated October 29, 2023. Accessed March 19, 2024. https://www.ncbi.nlm.nih.gov/books/NBK459201/
- Krebs NF. Update on zinc deficiency and excess in clinical pediatric practice. Ann Nutr Metab. 2013;62 suppl 1:19-29. doi:10.1159/000348261
- Maxfield L, Shukla S, Crane JS. Zinc deficiency. StatPearls [Internet]. Updated June 28, 2023. Accessed March 25, 2024. https://www.ncbi.nlm.nih.gov/books/NBK493231/
- Ghishan FK, Kiela PR. Vitamins and minerals in inflammatory bowel disease. Gastroenterol Clin North Am. 2017;46:797-808. doi:10.1016/j.gtc.2017.08.011
- Caviezel D, Maissen S, Niess JH, et al. High prevalence of vitamin D deficiency among patients with inflammatory bowel disease. Inflamm Intest Dis. 2018;2:200-210. doi:10.1159/000489010
- Jasielska M, Grzybowska-Chlebowczyk U. Hypocalcemia and vitamin D deficiency in children with inflammatory bowel diseases and lactose intolerance. Nutrients. 2021;13:2583. doi:10.3390/nu13082583
- Vernia F, Valvano M, Longo S, et al. Vitamin D in inflammatory bowel diseases. Mechanisms of action and therapeutic implications. Nutrients. 2022;14:269. doi:10.3390/nu14020269
- Khazai N, Judd SE, Tangpricha V. Calcium and vitamin D: skeletal and extraskeletal health. Curr Rheumatol Rep. 2008;10:110-117. doi:10.1007/s11926-008-0020-y
- Domazetovic V, Iantomasi T, Bonanomi AG, et al. Vitamin D regulates claudin-2 and claudin-4 expression in active ulcerative colitis by p-Stat-6 and Smad-7 signaling. Int J Colorectal Dis. 2020;35:1231-1242. doi:10.1007/s00384-020-03576-0
- Gubatan J, Chou ND, Nielsen OH, et al. Systematic review with meta-analysis: association of vitamin D status with clinical outcomes in adult patients with inflammatory bowel disease. Aliment Pharmacol Ther. 2019;50:1146-1158. doi:10.1111/apt.15506
- Fakhoury HMA, Kvietys PR, AlKattan W, et al. Vitamin D and intestinal homeostasis: barrier, microbiota, and immune modulation. J Steroid Biochem Mol Biol. 2020;200:105663. doi:10.1016/j.jsbmb.2020.105663
- Liu PT, Stenger S, Li H, et al. Toll-like receptor triggering of a vitamin D-mediated human antimicrobial response. Science. 2006;311:1770-1773. doi:10.1126/science.1123933
- Mostafa WZ, Hegazy RA. Vitamin D and the skin: focus on a complex relationship: a review. J Adv Res. 2015;6:793-804. doi:10.1016/j.jare.2014.01.011
- Searing DA, Leung DY. Vitamin D in atopic dermatitis, asthma and allergic diseases. Immunol Allergy Clin North Am. 2010;30:397-409.
- Lee YH, Song GG. Association between circulating 25-hydroxyvitamin D levels and psoriasis, and correlation with disease severity: a meta-analysis. Clin Exp Dermatol. 2018;43:529-535.
- Adorini L, Penna G. Control of autoimmune diseases by the vitamin D endocrine system. Nat Clin Pract Rheumatol. 2008;4:404-412.
- Autier P, Boniol M, Pizot C, et al. Vitamin D status and ill health: a systematic review. Lancet Diabetes Endocrinol. 2014;2:76-89. doi:10.1016/S2213-8587(13)70165-7
- Schafer AL, Shoback DM. Hypocalcemia: diagnosis and treatment. In: Feingold KR, Anawalt B, Blackman MR, et al, eds. Endotext [Internet]. Updated January 3, 2016. Accessed March 19, 2024. https://www.ncbi.nlm.nih.gov/books/NBK279022/
- Magro F, Gionchetti P, Eliakim R, et al. Third European Evidence-based Consensus on Diagnosis and Management of Ulcerative Colitis. Part 1: Definitions, diagnosis, extra-intestinal manifestations, pregnancy, cancer surveillance, surgery, and ileo-anal pouch disorders. J Crohns Colitis. 2017;11:649-670. doi:10.1093/ecco-jcc/jjx008
- Amrein K, Scherkl M, Hoffmann M, et al. Vitamin D deficiency 2.0: an update on the current status worldwide. Eur J Clin Nutr. 2020;74:1498-1513. doi:10.1038/s41430-020-0558-y
- Munns CF, Shaw N, Kiely M, et al. Global consensus recommendations on prevention and management of nutritional rickets. J Clin Endocrinol Metab. 2016;101:394-415. doi:10.1210/jc.2015-2175
- Institute of Medicine (US) Committee to Review Dietary Reference Intakes for Vitamin D and Calcium; Ross AC, Taylor CL, Yaktine AL, Del Valle HB, eds. Dietary Reference Intakes for Calcium and Vitamin D. National Academies Press (US); 2011.
- Yeaman F, Nguyen A, Abasszade J, et al. Assessing vitamin D as a biomarker in inflammatory bowel disease. JGH Open. 2023;7:953-958. doi:10.1002/jgh3.13010
- Vernia P, Loizos P, Di Giuseppantonio I, et al S. Dietary calcium intake in patients with inflammatory bowel disease. J Crohns Colitis. 2014;8:312-317. doi:10.1016/j.crohns.2013.09.008
- Cooper MS, Gittoes NJ. Diagnosis and management of hypocalcaemia. BMJ. 2008;336:1298-1302. doi:10.1136/bmj.39582.589433.BE
- Kenny CM, Murphy CE, Boyce DS, et al. Things we do for no reason™: calculating a “corrected calcium” level. J Hosp Med. 2021;16:499-501. doi:10.12788/jhm.3619
- Garg M, Rosella O, Rosella G, et al. Evaluation of a 12-week targeted vitamin D supplementation regimen in patients with active inflammatory bowel disease. Clin Nutr. 2018;37:1375-1382. doi:10.1016/j.clnu.2017.06.011
- Raftery T, Martineau AR, Greiller CL, et al. Effects of vitamin D supplementation on intestinal permeability, cathelicidin and disease markers in Crohn’s disease: results from a randomised double-blind placebo-controlled study. United European Gastroenterol J. 2015;3:294-302. doi:10.1177/2050640615572176
- Vagianos K, Bector S, McConnell J, et al. Nutrition assessment of patients with inflammatory bowel disease. JPEN J Parenter Enteral Nutr. 2007;31:311-319. doi:10.1177/0148607107031004311
- Barthelemy H, Chouvet B, Cambazard F. Skin and mucosal manifestations in vitamin deficiency. J Am Acad Dermatol. 1986;15:1263-1274. doi:10.1016/s0190-9622(86)70301-0
- Galimberti F, Mesinkovska NA. Skin findings associated with nutritional deficiencies. Cleve Clin J Med. 2016;83:731-739. doi:10.3949/ccjm.83a.15061
- Elgharably N, Al Abadie M, Al Abadie M, et al. Vitamin B group levels and supplementations in dermatology. Dermatol Reports. 2022;15:9511. doi:10.4081/dr.2022.9511
- Hołubiec P, Leon´czyk M, Staszewski F, et al. Pathophysiology and clinical management of pellagra—a review. Folia Med Cracov. 2021;61:125-137. doi:10.24425/fmc.2021.138956
- Ink SL, Henderson LM. Vitamin B6 metabolism. Annu Rev Nutr. 1984;4:455-470. doi:10.1146/annurev.nu.04.070184.002323
- Brown MJ, Ameer MA, Daley SF, et al. Vitamin B6 deficiency. StatPearls [Internet]. Updated August 8, 2023. Accessed March 25, 2024. https://www.ncbi.nlm.nih.gov/books/NBK470579/.
- Vasilaki AT, McMillan DC, Kinsella J, et al. Relation between pyridoxal and pyridoxal phosphate concentrations in plasma, red cells, and white cells in patients with critical illness. Am J Clin Nutr. 2008;88:140-146. doi:10.1093/ajcn/88.1.140
- Chiang EP, Bagley PJ, Selhub J, et al. Abnormal vitamin B(6) status is associated with severity of symptoms in patients with rheumatoid arthritis. Am J Med. 2003;114:283-287. doi:10.1016/s0002-9343(02)01528-0
- Maaser C, Sturm A, Vavricka SR, et al. ECCO-ESGAR guideline for diagnostic assessment in IBD. Part 1: initial diagnosis, monitoring of known IBD, detection of complications. J Crohns Colitis. 2019;13:144-164. doi:10.1093/ecco-jcc/jjy113
- Spinneker A, Sola R, Lemmen V, et al. Vitamin B6 status, deficiency and its consequences—an overview. Nutr Hosp. 2007;22:7-24.
- Selhub J, Byun A, Liu Z, et al. Dietary vitamin B6 intake modulates colonic inflammation in the IL10-/- model of inflammatory bowel disease. J Nutr Biochem. 2013;24:2138-2143. doi:10.1016/j.jnutbio.2013.08.005
- Pan Y, Liu Y, Guo H, et al. Associations between folate and vitamin B12 levels and inflammatory bowel disease: a meta-analysis. Nutrients. 2017;9:382. doi:10.3390/nu9040382
- Brescoll J, Daveluy S. A review of vitamin B12 in dermatology. Am J Clin Dermatol. 2015;16:27-33. doi:10.1007/s40257-014-0107-3
- DiBaise M, Tarleton SM. Hair, nails, and skin: differentiating cutaneous manifestations of micronutrient deficiency. Nutr Clin Pract. 2019;34:490-503. doi:10.1002/ncp.10321
- Mori K, Ando I, Kukita A. Generalized hyperpigmentation of the skin due to vitamin B12 deficiency. J Dermatol. 2001;28:282-285. doi:10.1111/j.1346-8138.2001.tb00134.x
- Green R. Indicators for assessing folate and vitamin B-12 status and for monitoring the efficacy of intervention strategies. Am J Clin Nutr. 2011;94:666S-672S. doi:10.3945/ajcn.110.009613
- NIH Office of Dietary Supplements. Vitamin B12: fact sheet for health professionals. Updated February 27, 2024. Accessed March 19, 2024. https://ods.od.nih.gov/factsheets/VitaminB12-HealthProfessional/
- NIH Office of Dietary Supplements. Folate: fact sheet for health professionals. Updated November 20, 2023. Accessed March 19, 2024. https://ods.od.nih.gov/factsheets/Folate-HealthProfessional/.
- Saibeni S, Bollani S, Losco A, et al. The use of methotrexate for treatment of inflammatory bowel disease in clinical practice. Dig Liver Dis. 2012;44:123-127. doi:10.1016/j.dld.2011.09.015
- Khan KM, Jialal I. Folic acid deficiency. StatPearls [Internet]. Updated June 26, 2023. Accessed March 19, 2024. https://www.ncbi.nlm.nih.gov/books/NBK535377/
- Bischoff SC, Bager P, Escher J, et al. ESPEN guideline on clinical nutrition in inflammatory bowel disease. Clin Nutr. 2023;42:352-379. doi:10.1016/j.clnu.2022.12.004
- Gerasimidis K, McGrogan P, Edwards CA. The aetiology and impact of malnutrition in paediatric inflammator y bowel disease. J Hum Nutr Diet. 2011;24:313-326. doi:10.1111/j.1365-277X.2011.01171.x
- Mentella MC, Scaldaferri F, Pizzoferrato M, et al. Nutrition, IBD and gut microbiota: a review. Nutrients. 2020;12:944. doi:10.3390/nu12040944
- Bonsack O, Caron B, Baumann C, et al. Food avoidance and fasting in patients with inflammatory bowel disease: experience from the Nancy IBD nutrition clinic. United European Gastroenterol J. 2023;11:361-370. doi:10.1002/ueg2.1238521
- Campmans-Kuijpers MJE, Dijkstra G. Food and food groups in inflammatory bowel disease (IBD): the design of the Groningen Anti-Inflammatory Diet (GrAID). Nutrients. 2021;13:1067. doi:10.3390/nu13041067
- Hwang C, Issokson K, Giguere-Rich C, et al. Development and pilot testing of the inflammatory bowel disease nutrition care pathway. Clin Gastroenterol Hepatol. 2020;18:2645-2649.e4. doi:10.1016/j.cgh.2020.06.039
- Filmann N, Rey J, Schneeweiss S, et al. Prevalence of anemia in inflammatory bowel diseases in European countries: a systematic review and individual patient data meta-analysis. Inflamm Bowel Dis. 2014;20:936-945. doi:10.1097/01.MIB.0000442728.74340.fd
- Stein J, Hartmann F, Dignass AU. Diagnosis and management of iron deficiency anemia in patients with IBD. Nat Rev Gastroenterol Hepatol. 2010;7:599-610. doi:10.1038/nrgastro.2010.151
- Ems T, St Lucia K, Huecker MR. Biochemistry, iron absorption. StatPearls [Internet]. Updated April 17, 2023. Accessed March 19, 2024. https://www.ncbi.nlm.nih.gov/books/NBK448204/
- Evstatiev R, Gasche C. Iron sensing and signalling. Gut. 2012;61:933-952. doi:10.1136/gut.2010.214312
- Przybyszewska J, Zekanowska E. The role of hepcidin, ferroportin, HCP1, and DMT1 protein in iron absorption in the human digestive tract. Prz Gastroenterol. 2014;9:208-213. doi:10.5114/pg.2014.45102
- Weiss G, Gasche C. Pathogenesis and treatment of anemia in inflammatory bowel disease. Haematologica. 2010;95:175-178. doi:10.3324/haematol.2009.017046
- Kaitha S, Bashir M, Ali T. Iron deficiency anemia in inflammatory bowel disease. World J Gastrointest Pathophysiol. 2015;6:62-72. doi:10.4291/wjgp.v6.i3.62
- Moiz B. Spoon nails: still seen in today’s world. Clin Case Rep. 2018;6:547-548. doi:10.1002/ccr3.1404
- St Pierre SA, Vercellotti GM, Donovan JC, et al. Iron deficiency and diffuse nonscarring scalp alopecia in women: more pieces to the puzzle. J Am Acad Dermatol. 2010;63:1070-1076. doi:10.1016/j.jaad.2009.05.054
- Chiang CP, Yu-Fong Chang J, Wang YP, et al. Anemia, hematinic deficiencies, hyperhomocysteinemia, and serum gastric parietal cell antibody positivity in atrophic glossitis patients with or without microcytosis. J Formos Med Assoc. 2019;118:1401-1407. doi:10.1016/j.jfma.2019.06.004
- Chiang CP, Chang JY, Wang YP, et al. Atrophic glossitis: Etiology, serum autoantibodies, anemia, hematinic deficiencies, hyperhomocysteinemia, and management. J Formos Med Assoc. 2020;119:774-780. doi:10.1016/j.jfma.2019.04.015
- Walker J, Baran R, Vélez N, et al. Koilonychia: an update on pathophysiology, differential diagnosis and clinical relevance. J Eur Acad Dermatol Venereol. 2016;30:1985-1991. doi:10.1111/jdv.13610
- Guo HF, Tsai CL, Terajima M, et al. Pro-metastatic collagen lysyl hydroxylase dimer assemblies stabilized by Fe2+-binding. Nat Commun. 2018;9:512. doi:10.1038/s41467-018-02859-z
- Saini S, Jain AK, Agarwal S, et al. Iron deficiency and pruritus: a cross-sectional analysis to assess its association and relationship. Indian J Dermatol. 2021;66:705. doi:10.4103/ijd.ijd_326_21
- Du X, She E, Gelbart T, et al. The serine protease TMPRSS6 is required to sense iron deficiency. Science. 2008;320:1088-1092. doi:10.1126/science.1157121
- Lee S, Lee H, Lee CH, et al. Comorbidities in alopecia areata: a systematic review and meta-analysis. J Am Acad Dermatol. 2019;80:466-477.e16. doi:10.1016/j.jaad.2018.07.013
- Hashash JG, Elkins J, Lewis JD, et al. AGA Clinical Practice Update on diet and nutritional therapies in patients with inflammatory bowel disease: expert review [published online January 23, 2024]. Gastroenterology. doi:10.1053/j.gastro.2023.11.303
- Choudhuri S, Chowdhury IH, Saha A, et al. Acute monocyte pro- inflammatory response predicts higher positive to negative acute phase reactants ratio and severe hemostatic derangement in dengue fever. Cytokine. 2021;146:155644. doi:10.1016/j.cyto.2021.155644
- Dignass AU, Gasche C, Bettenworth D, et al; European Crohn’s and Colitis Organisation. European consensus on the diagnosis and management of iron deficiency and anaemia in inflammatory bowel diseases. J Crohn’s Colitis. 2015;9:211-222. doi:10.1093/ecco-jcc/jju009
- Daude S, Remen T, Chateau T, et al. Comparative accuracy of ferritin, transferrin saturation and soluble transferrin receptor for the diagnosis of iron deficiency in inflammatory bowel disease. Aliment Pharmacol Ther. 2020;51:1087-1095. doi:10.1111/apt.15739
- Pfeiffer CM, Looker AC. Laboratory methodologies for indicators of iron status: strengths, limitations, and analytical challenges. Am J Clin Nutr. 2017;106(suppl 6):1606S-1614S. doi:10.3945/ajcn.117.155887
- Tolkien Z, Stecher L, Mander AP, et al. Ferrous sulfate supplementation causes significant gastrointestinal side-effects in adults: a systematic review and meta-analysis. PLoS One. 2015;10:e0117383. doi:10.1371/journal.pone.0117383
- Evstatiev R, Marteau P, Iqbal T, et al. FERGIcor, a randomized controlled trial on ferric carboxymaltose for iron deficiency anemia in inflammatory bowel disease. Gastroenterology. 2011;141:846-853.e8532. doi:10.1053/j.gastro.2011.06.005
- Zupo R, Sila A, Castellana F, et al. Prevalence of zinc deficiency in inflammatory bowel disease: a systematic review and meta-analysis. Nutrients. 2022;14:4052. doi:10.3390/nu14194052
- Thompson MW. Regulation of zinc-dependent enzymes by metal carrier proteins. Biometals. 2022;35:187-213. doi:10.1007/s10534-022-00373-w
- Maares M, Haase H. A guide to human zinc absorption: general overview and recent advances of in vitro intestinal models. Nutrients. 2020;12:762. doi:10.3390/nu12030762
- Ranaldi G, Ferruzza S, Canali R, et al. Intracellular zinc is required for intestinal cell survival signals triggered by the inflammatory cytokine TNFα. J Nutr Biochem. 2013;24:967-976. doi:10.1016/j.jnutbio.2012.06.020
- Ogawa Y, Kawamura T, Shimada S. Zinc and skin biology. Arch Biochem Biophys. 2016;611:113-119. doi:10.1016/j.abb.2016.06.003
- Wilson D, Varigos G, Ackland ML. Apoptosis may underlie the pathology of zinc-deficient skin. Immunol Cell Biol. 2006;84:28-37. doi:10.1111/j.1440-1711.2005.01391.x
- Jen M, Yan AC. Syndromes associated with nutritional deficiency and excess. Clin Dermatol. 2010;28:669-685. doi:10.1016/j.clindermatol.2010.03.029
- Gonzalez JR, Botet MV, Sanchez JL. The histopathology of acrodermatitis enteropathica. Am J Dermatopathol. 1982;4:303-311.
- Gammoh NZ, Rink L. Zinc in infection and inflammation. Nutrients. 2017;9:624. doi:10.3390/nu9060624
- Liuzzi JP, Lichten LA, Rivera S, et al. Interleukin-6 regulates the zinc transporter Zip14 in liver and contributes to the hypozincemia of the acute-phase response. Proc Natl Acad Sci U S A. 2005;102:6843-6848. doi:10.1073/pnas.0502257102
- Vermeire S, Van Assche G, Rutgeerts P. Laboratory markers in IBD: useful, magic, or unnecessary toys?. Gut. 2006;55:426-431. doi:10.1136/gut.2005.069476
- Morisaku M, Ito K, Ogiso A, et al. Correlation between serum albumin and serum zinc in malignant lymphoma. Fujita Med J. 2022;8:59-64. doi:10.20407/fmj.2021-006
- Falchuk KH. Effect of acute disease and ACTH on serum zinc proteins. N Engl J Med. 1977:296:1129-1134.
- Naber TH, Baadenhuysen H, Jansen JB, et al. Serum alkaline phosphatase activity during zinc deficiency and long-term inflammatory stress. Clin Chim Acta. 1996;249:109-127. doi:10.1016/0009-8981(96)06281-x
- Lowe D, Sanvictores T, Zubair M, et al. Alkaline phosphatase. StatPearls [Internet]. Updated October 29, 2023. Accessed March 19, 2024. https://www.ncbi.nlm.nih.gov/books/NBK459201/
- Krebs NF. Update on zinc deficiency and excess in clinical pediatric practice. Ann Nutr Metab. 2013;62 suppl 1:19-29. doi:10.1159/000348261
- Maxfield L, Shukla S, Crane JS. Zinc deficiency. StatPearls [Internet]. Updated June 28, 2023. Accessed March 25, 2024. https://www.ncbi.nlm.nih.gov/books/NBK493231/
- Ghishan FK, Kiela PR. Vitamins and minerals in inflammatory bowel disease. Gastroenterol Clin North Am. 2017;46:797-808. doi:10.1016/j.gtc.2017.08.011
- Caviezel D, Maissen S, Niess JH, et al. High prevalence of vitamin D deficiency among patients with inflammatory bowel disease. Inflamm Intest Dis. 2018;2:200-210. doi:10.1159/000489010
- Jasielska M, Grzybowska-Chlebowczyk U. Hypocalcemia and vitamin D deficiency in children with inflammatory bowel diseases and lactose intolerance. Nutrients. 2021;13:2583. doi:10.3390/nu13082583
- Vernia F, Valvano M, Longo S, et al. Vitamin D in inflammatory bowel diseases. Mechanisms of action and therapeutic implications. Nutrients. 2022;14:269. doi:10.3390/nu14020269
- Khazai N, Judd SE, Tangpricha V. Calcium and vitamin D: skeletal and extraskeletal health. Curr Rheumatol Rep. 2008;10:110-117. doi:10.1007/s11926-008-0020-y
- Domazetovic V, Iantomasi T, Bonanomi AG, et al. Vitamin D regulates claudin-2 and claudin-4 expression in active ulcerative colitis by p-Stat-6 and Smad-7 signaling. Int J Colorectal Dis. 2020;35:1231-1242. doi:10.1007/s00384-020-03576-0
- Gubatan J, Chou ND, Nielsen OH, et al. Systematic review with meta-analysis: association of vitamin D status with clinical outcomes in adult patients with inflammatory bowel disease. Aliment Pharmacol Ther. 2019;50:1146-1158. doi:10.1111/apt.15506
- Fakhoury HMA, Kvietys PR, AlKattan W, et al. Vitamin D and intestinal homeostasis: barrier, microbiota, and immune modulation. J Steroid Biochem Mol Biol. 2020;200:105663. doi:10.1016/j.jsbmb.2020.105663
- Liu PT, Stenger S, Li H, et al. Toll-like receptor triggering of a vitamin D-mediated human antimicrobial response. Science. 2006;311:1770-1773. doi:10.1126/science.1123933
- Mostafa WZ, Hegazy RA. Vitamin D and the skin: focus on a complex relationship: a review. J Adv Res. 2015;6:793-804. doi:10.1016/j.jare.2014.01.011
- Searing DA, Leung DY. Vitamin D in atopic dermatitis, asthma and allergic diseases. Immunol Allergy Clin North Am. 2010;30:397-409.
- Lee YH, Song GG. Association between circulating 25-hydroxyvitamin D levels and psoriasis, and correlation with disease severity: a meta-analysis. Clin Exp Dermatol. 2018;43:529-535.
- Adorini L, Penna G. Control of autoimmune diseases by the vitamin D endocrine system. Nat Clin Pract Rheumatol. 2008;4:404-412.
- Autier P, Boniol M, Pizot C, et al. Vitamin D status and ill health: a systematic review. Lancet Diabetes Endocrinol. 2014;2:76-89. doi:10.1016/S2213-8587(13)70165-7
- Schafer AL, Shoback DM. Hypocalcemia: diagnosis and treatment. In: Feingold KR, Anawalt B, Blackman MR, et al, eds. Endotext [Internet]. Updated January 3, 2016. Accessed March 19, 2024. https://www.ncbi.nlm.nih.gov/books/NBK279022/
- Magro F, Gionchetti P, Eliakim R, et al. Third European Evidence-based Consensus on Diagnosis and Management of Ulcerative Colitis. Part 1: Definitions, diagnosis, extra-intestinal manifestations, pregnancy, cancer surveillance, surgery, and ileo-anal pouch disorders. J Crohns Colitis. 2017;11:649-670. doi:10.1093/ecco-jcc/jjx008
- Amrein K, Scherkl M, Hoffmann M, et al. Vitamin D deficiency 2.0: an update on the current status worldwide. Eur J Clin Nutr. 2020;74:1498-1513. doi:10.1038/s41430-020-0558-y
- Munns CF, Shaw N, Kiely M, et al. Global consensus recommendations on prevention and management of nutritional rickets. J Clin Endocrinol Metab. 2016;101:394-415. doi:10.1210/jc.2015-2175
- Institute of Medicine (US) Committee to Review Dietary Reference Intakes for Vitamin D and Calcium; Ross AC, Taylor CL, Yaktine AL, Del Valle HB, eds. Dietary Reference Intakes for Calcium and Vitamin D. National Academies Press (US); 2011.
- Yeaman F, Nguyen A, Abasszade J, et al. Assessing vitamin D as a biomarker in inflammatory bowel disease. JGH Open. 2023;7:953-958. doi:10.1002/jgh3.13010
- Vernia P, Loizos P, Di Giuseppantonio I, et al S. Dietary calcium intake in patients with inflammatory bowel disease. J Crohns Colitis. 2014;8:312-317. doi:10.1016/j.crohns.2013.09.008
- Cooper MS, Gittoes NJ. Diagnosis and management of hypocalcaemia. BMJ. 2008;336:1298-1302. doi:10.1136/bmj.39582.589433.BE
- Kenny CM, Murphy CE, Boyce DS, et al. Things we do for no reason™: calculating a “corrected calcium” level. J Hosp Med. 2021;16:499-501. doi:10.12788/jhm.3619
- Garg M, Rosella O, Rosella G, et al. Evaluation of a 12-week targeted vitamin D supplementation regimen in patients with active inflammatory bowel disease. Clin Nutr. 2018;37:1375-1382. doi:10.1016/j.clnu.2017.06.011
- Raftery T, Martineau AR, Greiller CL, et al. Effects of vitamin D supplementation on intestinal permeability, cathelicidin and disease markers in Crohn’s disease: results from a randomised double-blind placebo-controlled study. United European Gastroenterol J. 2015;3:294-302. doi:10.1177/2050640615572176
- Vagianos K, Bector S, McConnell J, et al. Nutrition assessment of patients with inflammatory bowel disease. JPEN J Parenter Enteral Nutr. 2007;31:311-319. doi:10.1177/0148607107031004311
- Barthelemy H, Chouvet B, Cambazard F. Skin and mucosal manifestations in vitamin deficiency. J Am Acad Dermatol. 1986;15:1263-1274. doi:10.1016/s0190-9622(86)70301-0
- Galimberti F, Mesinkovska NA. Skin findings associated with nutritional deficiencies. Cleve Clin J Med. 2016;83:731-739. doi:10.3949/ccjm.83a.15061
- Elgharably N, Al Abadie M, Al Abadie M, et al. Vitamin B group levels and supplementations in dermatology. Dermatol Reports. 2022;15:9511. doi:10.4081/dr.2022.9511
- Hołubiec P, Leon´czyk M, Staszewski F, et al. Pathophysiology and clinical management of pellagra—a review. Folia Med Cracov. 2021;61:125-137. doi:10.24425/fmc.2021.138956
- Ink SL, Henderson LM. Vitamin B6 metabolism. Annu Rev Nutr. 1984;4:455-470. doi:10.1146/annurev.nu.04.070184.002323
- Brown MJ, Ameer MA, Daley SF, et al. Vitamin B6 deficiency. StatPearls [Internet]. Updated August 8, 2023. Accessed March 25, 2024. https://www.ncbi.nlm.nih.gov/books/NBK470579/.
- Vasilaki AT, McMillan DC, Kinsella J, et al. Relation between pyridoxal and pyridoxal phosphate concentrations in plasma, red cells, and white cells in patients with critical illness. Am J Clin Nutr. 2008;88:140-146. doi:10.1093/ajcn/88.1.140
- Chiang EP, Bagley PJ, Selhub J, et al. Abnormal vitamin B(6) status is associated with severity of symptoms in patients with rheumatoid arthritis. Am J Med. 2003;114:283-287. doi:10.1016/s0002-9343(02)01528-0
- Maaser C, Sturm A, Vavricka SR, et al. ECCO-ESGAR guideline for diagnostic assessment in IBD. Part 1: initial diagnosis, monitoring of known IBD, detection of complications. J Crohns Colitis. 2019;13:144-164. doi:10.1093/ecco-jcc/jjy113
- Spinneker A, Sola R, Lemmen V, et al. Vitamin B6 status, deficiency and its consequences—an overview. Nutr Hosp. 2007;22:7-24.
- Selhub J, Byun A, Liu Z, et al. Dietary vitamin B6 intake modulates colonic inflammation in the IL10-/- model of inflammatory bowel disease. J Nutr Biochem. 2013;24:2138-2143. doi:10.1016/j.jnutbio.2013.08.005
- Pan Y, Liu Y, Guo H, et al. Associations between folate and vitamin B12 levels and inflammatory bowel disease: a meta-analysis. Nutrients. 2017;9:382. doi:10.3390/nu9040382
- Brescoll J, Daveluy S. A review of vitamin B12 in dermatology. Am J Clin Dermatol. 2015;16:27-33. doi:10.1007/s40257-014-0107-3
- DiBaise M, Tarleton SM. Hair, nails, and skin: differentiating cutaneous manifestations of micronutrient deficiency. Nutr Clin Pract. 2019;34:490-503. doi:10.1002/ncp.10321
- Mori K, Ando I, Kukita A. Generalized hyperpigmentation of the skin due to vitamin B12 deficiency. J Dermatol. 2001;28:282-285. doi:10.1111/j.1346-8138.2001.tb00134.x
- Green R. Indicators for assessing folate and vitamin B-12 status and for monitoring the efficacy of intervention strategies. Am J Clin Nutr. 2011;94:666S-672S. doi:10.3945/ajcn.110.009613
- NIH Office of Dietary Supplements. Vitamin B12: fact sheet for health professionals. Updated February 27, 2024. Accessed March 19, 2024. https://ods.od.nih.gov/factsheets/VitaminB12-HealthProfessional/
- NIH Office of Dietary Supplements. Folate: fact sheet for health professionals. Updated November 20, 2023. Accessed March 19, 2024. https://ods.od.nih.gov/factsheets/Folate-HealthProfessional/.
- Saibeni S, Bollani S, Losco A, et al. The use of methotrexate for treatment of inflammatory bowel disease in clinical practice. Dig Liver Dis. 2012;44:123-127. doi:10.1016/j.dld.2011.09.015
- Khan KM, Jialal I. Folic acid deficiency. StatPearls [Internet]. Updated June 26, 2023. Accessed March 19, 2024. https://www.ncbi.nlm.nih.gov/books/NBK535377/
Practice Points
- Patients with inflammatory bowel disease (IBD) are at increased risk for vitamin and nutrient deficiencies that may be identified first through cutaneous manifestations.
- Because active inflammation in IBD may skew routine laboratory values used for screening of micronutrient deficiencies, be cautious when interpreting these values.
- Patients taking systemic therapies for IBD such as corticosteroids and methotrexate are at higher risk for nutritional deficiencies.
Culprits of Medication-Induced Telogen Effluvium, Part 2
Medication-induced telogen effluvium (TE) is a nonscarring alopecia that typically is reversible. Appropriate management requires identification of the underlying trigger and cessation of potential culprit medications. In part 2 of this series, we review anticoagulant and antihypertensive medications as potential contributors to TE.
Anticoagulants
Anticoagulants target various parts of the coagulation cascade to prevent clot formation in patients with conditions that increase their risk for thromboembolic events. Common indications for initiating anticoagulant therapy include atrial fibrillation,1 venous thromboembolism,2 acute myocardial infarction,3 malignancy,4 and hypercoagulable states.5 Traditional anticoagulants include heparin and warfarin. Heparin is a glycosaminoglycan that exerts its anticoagulant effects through binding with antithrombin, greatly increasing its inactivation of thrombin and factor Xa of the coagulation cascade.6 Warfarin is a coumarin derivative that inhibits activation of vitamin K, subsequently limiting the function of vitamin K–dependent factors II, VII, IX, and X.7,8 Watras et al9 noted that heparin and warfarin were implicated in alopecia as their clinical use became widespread throughout the mid-20th century. Onset of alopecia following the use of heparin or warfarin was reported at 3 weeks to 3 months following medication initiation, with most cases clinically consistent with TE.9 Heparin and warfarin both have alopecia reported as a potential adverse effect in their structured product labeling documents.10,11
Heparin is further classified into unfractionated heparin (UFH) and low-molecular-weight heparin (LMWH); the latter is a heterogeneous group of medications derived from chemical or enzymatic depolymerization of UFH.12 In contrast to UFH, LMWH exerts its anticoagulant effects through inactivation of factor Xa without the ability to bind thrombin.12 An animal study using anagen-induced mice demonstrated that intraperitoneal administration of heparin inhibited the development of anagen follicles, while in vitro studies showed that the addition of heparin inhibited mouse dermal papilla cell proliferation.13 Other animal and in vitro studies have examined the inhibitory effects of heparin on signaling pathways in tumor lymphangiogenesis, including the vascular endothelial growth factor C/vascular endothelial growth factor receptor 3 axis.14,15 Clinically, it has been demonstrated that heparin, especially LMWHs, may be associated with a survival benefit among certain cancer patients,16,17 with the impact of LMWHs attributed to antimitotic and antimetastatic effects of heparin on tumor growth.14 It is hypothesized that such antiangiogenic and antimitotic effects also are involved in the pathomechanisms of heparin-induced alopecia.18
More recently, the use of direct oral anticoagulants (DOACs) such as dabigatran, rivaroxaban, and apixaban has increased due to their more favorable adverse-effect profile and minimal monitoring requirements. Bonaldo et al19 conducted an analysis of reports submitted to the World Health Organization’s VigiBase database of alopecia associated with DOACs until May 2, 2018. They found 1316 nonduplicate DOAC-induced cases of alopecia, with rivaroxaban as the most reported drug associated with alopecia development (58.8% [774/1316]). Only 4 cases demonstrated alopecia with DOAC rechallenge, suggesting onset of alopecia may have been unrelated to DOAC use or caused by a different trigger. Among 243 cases with a documented time to onset of alopecia, the median was 28 days, with an interquartile range of 63 days. Because TE most commonly occurs 3 to 4 months after the inciting event or medication trigger, there is little evidence to suggest DOACs as the cause of TE, and the observed cases of alopecia may be attributable to another preceding medical event and/or medication exposure.19 More studies are needed to examine the impact of anticoagulant medications on the hair cycle.
Antihypertensives
Hypertension is a modifiable risk factor for several cardiovascular diseases.20 According to the 2019 American College of Cardiology/American Heart Association Guideline on the Primary Prevention of Cardiovascular Disease,21 first-line medications include thiazide diuretics, calcium channel blockers, angiotensin-converting enzyme (ACE) inhibitors, and angiotensin receptor blockers (ARBs).
Angiotensin-converting enzyme inhibitors exert their antihypertensive effects by reducing conversion of angiotensin I to angiotensin II, thereby limiting the downstream effects of vasoconstriction as well as sodium and water retention. Given the proven mortality benefit of ACE inhibition in patients with congestive heart failure, ACE inhibitors are used as first-line therapy in these patients.22,23 Alopecia associated with ACE inhibitors is rare and limited to case reports following their introduction and approval in 1981.24-28 In one case, a woman in her 60s with congestive heart failure initiated captopril with development of an erythematous pruritic rash on the extremities and diffuse scalp hair loss 2 months later; spontaneous hair growth resumed 1 month following captopril discontinuation.25 In this case, the hair loss may be secondary to the drug eruption rather than true medication-induced TE. Initiation of enalapril in a woman in her 30s with hypertension was associated with diffuse scalp alopecia 4 weeks later that resolved with cessation of the suspected culprit, enalapril; rechallenge with enalapril several months later reproduced the hair loss.27 Given limited reports of ACE inhibitor–associated hair loss relative to their pervasive use, a direct causal role between ACE inhibition and TE is unlikely, or it has not been rigorously identified. The structured product labeling for captopril includes alopecia in its list of adverse effects reported in approximately 0.5% to 2% of patients but did not appear at increased frequency compared to placebo or other treatments used in controlled trials.29 Alternative inciting causes of alopecia in patients prescribed ACE inhibitors may include use of other medications, hospitalization, or metabolic derangements related to their underlying cardiac disease.
Although not indicated as a primary treatment for hypertension, β-blockers have US Food and Drug Administration approval for the treatment of certain arrhythmias, hypertension, heart failure, myocardial infarction, hyperthyroidism, and other conditions.30β-Blockers are competitive antagonists of β-adrenergic receptors that limit the production of intracellular cyclic adenosine monophosphate, but the mechanism of β-blockers as antihypertensives is unclear.31 Evidence supporting the role of β-adrenergic antagonists in TE is limited to case reports. Widespread alopecia across the scalp and arms was noted in a man in his 30s several months after starting propranolol.32 Biopsy of an affected area of the scalp demonstrated an increased number of telogen follicles with no other abnormalities. Near-complete resolution of alopecia was seen 4 months following cessation of propranolol, which recurred within 4 weeks of rechallenge.
Minoxidil—Oral minoxidil originally was approved for use in patients with resistant hypertension, defined as blood pressure elevated above goal despite concurrent use of the maximum dose of 3 classes of antihypertensives.36 Unlike other antihypertensive medications, minoxidil appears to cause reversible hypertrichosis that affects nearly all patients using oral minoxidil for longer than 1 month.37 This common adverse effect was a desired outcome in patients affected by hair loss, and a topical formulation of minoxidil was approved for androgenetic alopecia in men and women in 1988 and 1991, respectively.38 Since its approval, topical minoxidil has been commonly prescribed in the treatment of several types of alopecia, though evidence of its efficacy in the treatment of TE is limited.39,40 Low-dose oral minoxidil also has been reported to aid hair growth in androgenetic alopecia and TE.41 Taken orally, minoxidil is converted by sulfotransferases in the liver to minoxidil sulfate, which causes opening of plasma membrane adenosine triphosphate–sensitive potassium channels.42-44 The subsequent membrane hyperpolarization reduces calcium ion influx, which also reduces cell excitability, and inhibits contraction in vascular smooth muscle cells, which results in the arteriolar vasodilatory and antihypertensive effects of minoxidil.43,45 The potassium channel–opening effects of minoxidil may underly its hair growth stimulatory action. Unrelated potassium channel openers such as diazoxide and pinacidil also cause hypertrichosis.46-48 An animal study showed that topical minoxidil, cromakalim (potassium channel opener), and P1075 (pinacidil analog) applied daily to the scalps of balding stump-tailed macaques led to significant increases in hair weight over a 20-week treatment period compared with the vehicle control group (P<.05 for minoxidil 100 mM and 250 mM, cromakalim 100 mM, and P1075 100 mM and 250 mM).50 For minoxidil, this effect on hair growth appears to be dose dependent, as cumulative hair weights for the study period were significantly greater in the 250-mM concentration compared with 100-mM minoxidil (P<.05).49 The potassium channel–opening activity of minoxidil may induce stimulation of microcirculation around hair follicles conducive to hair growth.50 Other proposed mechanisms for hair growth with minoxidil include effects on keratinocyte and fibroblast cell proliferation,51-53 collagen synthesis,52,54 and prostaglandin activity.44,55
Final Thoughts
Medication-induced TE is an undesired adverse effect of many commonly used medications, including retinoids, azole antifungals, mood stabilizers, anticoagulants, and antihypertensives. In part 156 of this 2-part series, we reviewed the existing literature on hair loss from retinoids, antifungals, and psychotropic medications. Herein, we focused on anticoagulant and antihypertensive medications as potential culprits of TE. Heparin and its derivatives have been associated with development of diffuse alopecia weeks to months after the start of treatment. Alopecia associated with ACE inhibitors and β-blockers has been described only in case reports, suggesting that they may be unlikely causes of TE. In contrast, minoxidil is an antihypertensive that can result in hypertrichosis and is used in the treatment of androgenetic alopecia. It should not be assumed that medications that share an indication or are part of the same medication class would similarly induce TE. The development of diffuse nonscarring alopecia should prompt suspicion for TE and thorough investigation of medications initiated 1 to 6 months prior to onset of clinically apparent alopecia. Suspected culprit medications should be carefully assessed for their likelihood of inducing TE.
- Angiolillo DJ, Bhatt DL, Cannon CP, et al. Antithrombotic therapy in patients with atrial fibrillation treated with oral anticoagulation undergoing percutaneous coronary intervention: a North American perspective: 2021 update. Circulation. 2021;143:583-596. doi:10.1161 /circulationaha.120.050438
- Kearon C, Kahn SR. Long-term treatment of venous thromboembolism. Blood. 2020;135:317-325. doi:10.1182/blood.2019002364
- Frishman WH, Ribner HS. Anticoagulation in myocardial infarction: modern approach to an old problem. Am J Cardiol. 1979;43:1207-1213. doi:10.1016/0002-9149(79)90155-3
- Khorana AA, Mackman N, Falanga A, et al. Cancer-associated venous thromboembolism. Nat Rev Dis Primers. 2022;8:11. doi:10.1038 /s41572-022-00336-y
- Umerah CO, Momodu, II. Anticoagulation. StatPearls [Internet]. StatPearls Publishing; 2023. Accessed December 11, 2023. https://www.ncbi.nlm.nih.gov/books/NBK560651/
- Beurskens DMH, Huckriede JP, Schrijver R, et al. The anticoagulant and nonanticoagulant properties of heparin. Thromb Haemost. 2020;120:1371-1383. doi:10.1055/s-0040-1715460
- Hirsh J, Dalen J, Anderson DR, et al. Oral anticoagulants: mechanism of action, clinical effectiveness, and optimal therapeutic range. Chest. 2001;119(1 suppl):8S-21S. doi:10.1378/chest.119.1_suppl.8s
- Holbrook AM, Pereira JA, Labiris R, et al. Systematic overview of warfarin and its drug and food interactions. Arch Intern Med. 2005;165:1095-1106. doi:10.1001/archinte.165.10.1095
- Watras MM, Patel JP, Arya R. Traditional anticoagulants and hair loss: a role for direct oral anticoagulants? a review of the literature. Drugs Real World Outcomes. 2016;3:1-6. doi:10.1007/s40801-015-0056-z
- Heparin sodium. Product information. Hepalink USA Inc; January 2022. Accessed December 11, 2023. https://nctr-crs.fda.gov/fdalabel/services/spl/set-ids/c4c6bc1f-e0c7-fd0d-e053-2995a90abdef/spl-doc?hl=heparin
- Warfarin sodium. Product information. Bryant Ranch Prepack; April 2023. Accessed December 11, 2023. https://nctr-crs.fda.gov/fdalabel/services/spl/set-ids/c41b7c23-8053-428a-ac1d-8395e714c2f1/spl-doc?hl=alopecia%7Cwarfarin#section-6
- Hirsh J. Low-molecular-weight heparin. Circulation. 1998;98:1575-1582. doi:10.1161/01.CIR.98.15.1575
- Paus R. Hair growth inhibition by heparin in mice: a model system for studying the modulation of epithelial cell growth by glycosaminoglycans? Br J Dermatol. 1991;124:415-422. doi:10.1111/j.1365-2133.1991.tb00618.x
- Ma SN, Mao ZX, Wu Y, et al. The anti-cancer properties of heparin and its derivatives: a review and prospect. Cell Adh Migr. 2020;14:118-128. doi:10.1080/19336918.2020.1767489
- Choi JU, Chung SW, Al-Hilal TA, et al. A heparin conjugate, LHbisD4, inhibits lymphangiogenesis and attenuates lymph node metastasis by blocking VEGF-C signaling pathway. Biomaterials. 2017;139:56-66. doi:0.1016/j.biomaterials.2017.05.026
- Klerk CP, Smorenburg SM, Otten HM, et al. The effect of low molecular weight heparin on survival in patients with advanced malignancy. J Clin Oncol. 2005;23:2130-2135. doi:10.1200/jco.2005.03.134
- Altinbas M, Coskun HS, Er O, et al. A randomized clinical trial of combination chemotherapy with and without low-molecular-weight heparin in small cell lung cancer. J Thromb Haemost. 2004;2:1266-1271. doi:10.1111/j.1538-7836.2004.00871.x
- Weyand AC, Shavit JA. Agent specific effects of anticoagulant induced alopecia. Res Pract Thromb Haemost. 2017;1:90-92. doi:10.1002 /rth2.12001
- Bonaldo G, Vaccheri A, Motola D. Direct-acting oral anticoagulants and alopecia: the valuable support of postmarketing data. Br J Clin Pharmacol. 2020;86:1654-1660. doi:10.1111/bcp.14221
- Fuchs FD, Whelton PK. High blood pressure and cardiovascular disease. Hypertension. 2020;75:285-292. doi:10.1161 /HYPERTENSIONAHA.119.14240
- Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;140:E596-E646. doi:10.1161/CIR.0000000000000678
- Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013;128:E240-E327. doi:10.1161 /CIR.0b013e31829e8776
- Effects of enalapril on mortality in severe congestive heart failure. results of the Cooperative North Scandinavian Enalapril Survival Study (CONSENSUS). N Engl J Med. 1987;316:1429-1435. doi:10.1056 /nejm198706043162301
- Kataria V, Wang H, Wald JW, et al. Lisinopril-induced alopecia: a case report. J Pharm Pract. 2017;30:562-566. doi:10.1177/0897190016652554
- Motel PJ. Captopril and alopecia: a case report and review of known cutaneous reactions in captopril use. J Am Acad Dermatol. 1990;23:124-125. doi:10.1016/s0190-9622(08)81205-4
- Leaker B, Whitworth JA. Alopecia associated with captopril treatment. Aust N Z J Med. 1984;14:866. doi:10.1111/j.1445-5994.1984.tb03797.x
- Ahmad S. Enalapril and reversible alopecia. Arch Intern Med. 1991;151:404.
- Bicket DP. Using ACE inhibitors appropriately. Am Fam Physician. 2002;66:461-468.
- Captopril. Product information. Bryant Ranch Prepack; May 2023. Accessed December 11, 2023. https://nctr-crs.fda.gov/fdalabel/services/spl/set-ids/563737c5-4d63-4957-8022-e3bc3112dfac/spl-doc?hl=captopril
- Farzam K, Jan A. Beta blockers. StatPearls Publishing; 2023. https://www.ncbi.nlm.nih.gov/books/NBK532906/
- Mason RP, Giles TD, Sowers JR. Evolving mechanisms of action of beta blockers: focus on nebivolol. J Cardiovasc Pharmacol. 2009; 54:123-128.
- Martin CM, Southwick EG, Maibach HI. Propranolol induced alopecia. Am Heart J. 1973;86:236-237. doi:10.1016/0002-8703(73)90250-0
- Graeber CW, Lapkin RA. Metoprolol and alopecia. Cutis. 1981; 28:633-634.
- Hilder RJ. Propranolol and alopecia. Cutis. 1979;24:63-64.
- Coreg. Prescribing information. Woodward Pharma Services LLC; 2023. Accessed December 11, 2023. https://www.accessdata.fda.gov/spl/data/34aa881a-3df4-460b-acad-fb9975ca3a06/34aa881a-3df4-460b-acad-fb9975ca3a06.xml
- Carey RM, Calhoun DA, Bakris GL, et al. Resistant hypertension: detection, evaluation, and management: a scientific statement from the American Heart Association. Hypertension. 2018;72:E53-E90. doi:10.1161/hyp.0000000000000084
- Campese VM. Minoxidil: a review of its pharmacological properties and therapeutic use. Drugs. 1981;22:257-278. doi:10.2165/00003495-198122040-00001
- Heymann WR. Coming full circle (almost): low dose oral minoxidil for alopecia. J Am Acad Dermatol. 2021;84:613-614. doi:10.1016/j .jaad.2020.12.053
- Yin S, Zhang B, Lin J, et al. Development of purification process for dual-function recombinant human heavy-chain ferritin by the investigation of genetic modification impact on conformation. Eng Life Sci. 2021;21:630-642. doi:10.1002/elsc.202000105
- Mysore V, Parthasaradhi A, Kharkar RD, et al. Expert consensus on the management of telogen effluvium in India. Int J Trichology. 2019;11:107-112.
- Gupta AK, Talukder M, Shemar A, et al. Low-dose oral minoxidil for alopecia: a comprehensive review [published online September 27, 2023]. Skin Appendage Disord. doi:10.1159/000531890
- Meisheri KD, Cipkus LA, Taylor CJ. Mechanism of action of minoxidil sulfate-induced vasodilation: a role for increased K+ permeability. J Pharmacol Exp Ther. 1988;245:751-760.
- Winquist RJ, Heaney LA, Wallace AA, et al. Glyburide blocks the relaxation response to BRL 34915 (cromakalim), minoxidil sulfate and diazoxide in vascular smooth muscle. J Pharmacol Exp Ther. 1989;248:149-56.
- Messenger AG, Rundegren J. Minoxidil: mechanisms of action on hair growth. Br J Dermatol. 2004;150:186-194. doi:10.1111/j .1365-2133.2004.05785.x
- Alijotas-Reig J, García GV, Velthuis PJ, et al. Inflammatory immunemediated adverse reactions induced by COVID-19 vaccines in previously injected patients with soft tissue fillers: a case series of 20 patients. J Cosmet Dermatol. 2022;21:3181-3187. doi: 10.1111/jocd.15117
- Boskabadi SJ, Ramezaninejad S, Sohrab M, et al. Diazoxideinduced hypertrichosis in a neonate with transient hyperinsulinism. Clin Med Insights Case Rep. 2023;16:11795476231151330. doi:10.1177/11795476231151330
- Burton JL, Schutt WH, Caldwell IW. Hypertrichosis due to diazoxide. Br J Dermatol. 1975;93:707-711. doi:10.1111/j.1365-2133.1975.tb05123.x
- Goldberg MR. Clinical pharmacology of pinacidil, a prototype for drugs that affect potassium channels. J Cardiovasc Pharmacol. 1988;12 suppl 2:S41-S47. doi: 10.1097/00005344-198812002-00008
- Buhl AE, Waldon DJ, Conrad SJ, et al. Potassium channel conductance: a mechanism affecting hair growth both in vitro and in vivo. J Invest Dermatol. 1992;98:315-319. doi:10.1111/1523-1747.ep12499788
- Patel P, Nessel TA, Kumar DD. Minoxidil. StatPearls [Internet]. StatPearls Publishing; 2023. Accessed December 11, 2023. https://www.ncbi.nlm.nih.gov/books/NBK482378/
- O’Keefe E, Payne RE Jr. Minoxidil: inhibition of proliferation of keratinocytes in vitro. J Invest Dermatol. 1991;97:534-536. doi:10.1111/1523-1747.ep12481560
- Murad S, Pinnell SR. Suppression of fibroblast proliferation and lysyl hydroxylase activity by minoxidil. J Biol Chem. 1987;262:11973-11978.
- Baden HP, Kubilus J. Effect of minoxidil on cultured keratinocytes. J Invest Dermatol. 1983;81:558-560. doi:10.1111/1523-1747.ep12523220
- Murad S, Walker LC, Tajima S, et al. Minimum structural requirements for minoxidil inhibition of lysyl hydroxylase in cultured fibroblasts. Arch Biochem Biophys. 1994;308:42-47. doi:10.1006/abbi.1994.1006
- Kvedar JC, Baden HP, Levine L. Selective inhibition by minoxidil of prostacyclin production by cells in culture. Biochem Pharmacol. 1988;37:867-874. doi:0.1016/0006-2952(88)90174-8
- Zhang D, LaSenna C, Shields BE. Culprits of medication-induced telogen effluvium, part 1. Cutis. 2023;112:267-271.
Medication-induced telogen effluvium (TE) is a nonscarring alopecia that typically is reversible. Appropriate management requires identification of the underlying trigger and cessation of potential culprit medications. In part 2 of this series, we review anticoagulant and antihypertensive medications as potential contributors to TE.
Anticoagulants
Anticoagulants target various parts of the coagulation cascade to prevent clot formation in patients with conditions that increase their risk for thromboembolic events. Common indications for initiating anticoagulant therapy include atrial fibrillation,1 venous thromboembolism,2 acute myocardial infarction,3 malignancy,4 and hypercoagulable states.5 Traditional anticoagulants include heparin and warfarin. Heparin is a glycosaminoglycan that exerts its anticoagulant effects through binding with antithrombin, greatly increasing its inactivation of thrombin and factor Xa of the coagulation cascade.6 Warfarin is a coumarin derivative that inhibits activation of vitamin K, subsequently limiting the function of vitamin K–dependent factors II, VII, IX, and X.7,8 Watras et al9 noted that heparin and warfarin were implicated in alopecia as their clinical use became widespread throughout the mid-20th century. Onset of alopecia following the use of heparin or warfarin was reported at 3 weeks to 3 months following medication initiation, with most cases clinically consistent with TE.9 Heparin and warfarin both have alopecia reported as a potential adverse effect in their structured product labeling documents.10,11
Heparin is further classified into unfractionated heparin (UFH) and low-molecular-weight heparin (LMWH); the latter is a heterogeneous group of medications derived from chemical or enzymatic depolymerization of UFH.12 In contrast to UFH, LMWH exerts its anticoagulant effects through inactivation of factor Xa without the ability to bind thrombin.12 An animal study using anagen-induced mice demonstrated that intraperitoneal administration of heparin inhibited the development of anagen follicles, while in vitro studies showed that the addition of heparin inhibited mouse dermal papilla cell proliferation.13 Other animal and in vitro studies have examined the inhibitory effects of heparin on signaling pathways in tumor lymphangiogenesis, including the vascular endothelial growth factor C/vascular endothelial growth factor receptor 3 axis.14,15 Clinically, it has been demonstrated that heparin, especially LMWHs, may be associated with a survival benefit among certain cancer patients,16,17 with the impact of LMWHs attributed to antimitotic and antimetastatic effects of heparin on tumor growth.14 It is hypothesized that such antiangiogenic and antimitotic effects also are involved in the pathomechanisms of heparin-induced alopecia.18
More recently, the use of direct oral anticoagulants (DOACs) such as dabigatran, rivaroxaban, and apixaban has increased due to their more favorable adverse-effect profile and minimal monitoring requirements. Bonaldo et al19 conducted an analysis of reports submitted to the World Health Organization’s VigiBase database of alopecia associated with DOACs until May 2, 2018. They found 1316 nonduplicate DOAC-induced cases of alopecia, with rivaroxaban as the most reported drug associated with alopecia development (58.8% [774/1316]). Only 4 cases demonstrated alopecia with DOAC rechallenge, suggesting onset of alopecia may have been unrelated to DOAC use or caused by a different trigger. Among 243 cases with a documented time to onset of alopecia, the median was 28 days, with an interquartile range of 63 days. Because TE most commonly occurs 3 to 4 months after the inciting event or medication trigger, there is little evidence to suggest DOACs as the cause of TE, and the observed cases of alopecia may be attributable to another preceding medical event and/or medication exposure.19 More studies are needed to examine the impact of anticoagulant medications on the hair cycle.
Antihypertensives
Hypertension is a modifiable risk factor for several cardiovascular diseases.20 According to the 2019 American College of Cardiology/American Heart Association Guideline on the Primary Prevention of Cardiovascular Disease,21 first-line medications include thiazide diuretics, calcium channel blockers, angiotensin-converting enzyme (ACE) inhibitors, and angiotensin receptor blockers (ARBs).
Angiotensin-converting enzyme inhibitors exert their antihypertensive effects by reducing conversion of angiotensin I to angiotensin II, thereby limiting the downstream effects of vasoconstriction as well as sodium and water retention. Given the proven mortality benefit of ACE inhibition in patients with congestive heart failure, ACE inhibitors are used as first-line therapy in these patients.22,23 Alopecia associated with ACE inhibitors is rare and limited to case reports following their introduction and approval in 1981.24-28 In one case, a woman in her 60s with congestive heart failure initiated captopril with development of an erythematous pruritic rash on the extremities and diffuse scalp hair loss 2 months later; spontaneous hair growth resumed 1 month following captopril discontinuation.25 In this case, the hair loss may be secondary to the drug eruption rather than true medication-induced TE. Initiation of enalapril in a woman in her 30s with hypertension was associated with diffuse scalp alopecia 4 weeks later that resolved with cessation of the suspected culprit, enalapril; rechallenge with enalapril several months later reproduced the hair loss.27 Given limited reports of ACE inhibitor–associated hair loss relative to their pervasive use, a direct causal role between ACE inhibition and TE is unlikely, or it has not been rigorously identified. The structured product labeling for captopril includes alopecia in its list of adverse effects reported in approximately 0.5% to 2% of patients but did not appear at increased frequency compared to placebo or other treatments used in controlled trials.29 Alternative inciting causes of alopecia in patients prescribed ACE inhibitors may include use of other medications, hospitalization, or metabolic derangements related to their underlying cardiac disease.
Although not indicated as a primary treatment for hypertension, β-blockers have US Food and Drug Administration approval for the treatment of certain arrhythmias, hypertension, heart failure, myocardial infarction, hyperthyroidism, and other conditions.30β-Blockers are competitive antagonists of β-adrenergic receptors that limit the production of intracellular cyclic adenosine monophosphate, but the mechanism of β-blockers as antihypertensives is unclear.31 Evidence supporting the role of β-adrenergic antagonists in TE is limited to case reports. Widespread alopecia across the scalp and arms was noted in a man in his 30s several months after starting propranolol.32 Biopsy of an affected area of the scalp demonstrated an increased number of telogen follicles with no other abnormalities. Near-complete resolution of alopecia was seen 4 months following cessation of propranolol, which recurred within 4 weeks of rechallenge.
Minoxidil—Oral minoxidil originally was approved for use in patients with resistant hypertension, defined as blood pressure elevated above goal despite concurrent use of the maximum dose of 3 classes of antihypertensives.36 Unlike other antihypertensive medications, minoxidil appears to cause reversible hypertrichosis that affects nearly all patients using oral minoxidil for longer than 1 month.37 This common adverse effect was a desired outcome in patients affected by hair loss, and a topical formulation of minoxidil was approved for androgenetic alopecia in men and women in 1988 and 1991, respectively.38 Since its approval, topical minoxidil has been commonly prescribed in the treatment of several types of alopecia, though evidence of its efficacy in the treatment of TE is limited.39,40 Low-dose oral minoxidil also has been reported to aid hair growth in androgenetic alopecia and TE.41 Taken orally, minoxidil is converted by sulfotransferases in the liver to minoxidil sulfate, which causes opening of plasma membrane adenosine triphosphate–sensitive potassium channels.42-44 The subsequent membrane hyperpolarization reduces calcium ion influx, which also reduces cell excitability, and inhibits contraction in vascular smooth muscle cells, which results in the arteriolar vasodilatory and antihypertensive effects of minoxidil.43,45 The potassium channel–opening effects of minoxidil may underly its hair growth stimulatory action. Unrelated potassium channel openers such as diazoxide and pinacidil also cause hypertrichosis.46-48 An animal study showed that topical minoxidil, cromakalim (potassium channel opener), and P1075 (pinacidil analog) applied daily to the scalps of balding stump-tailed macaques led to significant increases in hair weight over a 20-week treatment period compared with the vehicle control group (P<.05 for minoxidil 100 mM and 250 mM, cromakalim 100 mM, and P1075 100 mM and 250 mM).50 For minoxidil, this effect on hair growth appears to be dose dependent, as cumulative hair weights for the study period were significantly greater in the 250-mM concentration compared with 100-mM minoxidil (P<.05).49 The potassium channel–opening activity of minoxidil may induce stimulation of microcirculation around hair follicles conducive to hair growth.50 Other proposed mechanisms for hair growth with minoxidil include effects on keratinocyte and fibroblast cell proliferation,51-53 collagen synthesis,52,54 and prostaglandin activity.44,55
Final Thoughts
Medication-induced TE is an undesired adverse effect of many commonly used medications, including retinoids, azole antifungals, mood stabilizers, anticoagulants, and antihypertensives. In part 156 of this 2-part series, we reviewed the existing literature on hair loss from retinoids, antifungals, and psychotropic medications. Herein, we focused on anticoagulant and antihypertensive medications as potential culprits of TE. Heparin and its derivatives have been associated with development of diffuse alopecia weeks to months after the start of treatment. Alopecia associated with ACE inhibitors and β-blockers has been described only in case reports, suggesting that they may be unlikely causes of TE. In contrast, minoxidil is an antihypertensive that can result in hypertrichosis and is used in the treatment of androgenetic alopecia. It should not be assumed that medications that share an indication or are part of the same medication class would similarly induce TE. The development of diffuse nonscarring alopecia should prompt suspicion for TE and thorough investigation of medications initiated 1 to 6 months prior to onset of clinically apparent alopecia. Suspected culprit medications should be carefully assessed for their likelihood of inducing TE.
Medication-induced telogen effluvium (TE) is a nonscarring alopecia that typically is reversible. Appropriate management requires identification of the underlying trigger and cessation of potential culprit medications. In part 2 of this series, we review anticoagulant and antihypertensive medications as potential contributors to TE.
Anticoagulants
Anticoagulants target various parts of the coagulation cascade to prevent clot formation in patients with conditions that increase their risk for thromboembolic events. Common indications for initiating anticoagulant therapy include atrial fibrillation,1 venous thromboembolism,2 acute myocardial infarction,3 malignancy,4 and hypercoagulable states.5 Traditional anticoagulants include heparin and warfarin. Heparin is a glycosaminoglycan that exerts its anticoagulant effects through binding with antithrombin, greatly increasing its inactivation of thrombin and factor Xa of the coagulation cascade.6 Warfarin is a coumarin derivative that inhibits activation of vitamin K, subsequently limiting the function of vitamin K–dependent factors II, VII, IX, and X.7,8 Watras et al9 noted that heparin and warfarin were implicated in alopecia as their clinical use became widespread throughout the mid-20th century. Onset of alopecia following the use of heparin or warfarin was reported at 3 weeks to 3 months following medication initiation, with most cases clinically consistent with TE.9 Heparin and warfarin both have alopecia reported as a potential adverse effect in their structured product labeling documents.10,11
Heparin is further classified into unfractionated heparin (UFH) and low-molecular-weight heparin (LMWH); the latter is a heterogeneous group of medications derived from chemical or enzymatic depolymerization of UFH.12 In contrast to UFH, LMWH exerts its anticoagulant effects through inactivation of factor Xa without the ability to bind thrombin.12 An animal study using anagen-induced mice demonstrated that intraperitoneal administration of heparin inhibited the development of anagen follicles, while in vitro studies showed that the addition of heparin inhibited mouse dermal papilla cell proliferation.13 Other animal and in vitro studies have examined the inhibitory effects of heparin on signaling pathways in tumor lymphangiogenesis, including the vascular endothelial growth factor C/vascular endothelial growth factor receptor 3 axis.14,15 Clinically, it has been demonstrated that heparin, especially LMWHs, may be associated with a survival benefit among certain cancer patients,16,17 with the impact of LMWHs attributed to antimitotic and antimetastatic effects of heparin on tumor growth.14 It is hypothesized that such antiangiogenic and antimitotic effects also are involved in the pathomechanisms of heparin-induced alopecia.18
More recently, the use of direct oral anticoagulants (DOACs) such as dabigatran, rivaroxaban, and apixaban has increased due to their more favorable adverse-effect profile and minimal monitoring requirements. Bonaldo et al19 conducted an analysis of reports submitted to the World Health Organization’s VigiBase database of alopecia associated with DOACs until May 2, 2018. They found 1316 nonduplicate DOAC-induced cases of alopecia, with rivaroxaban as the most reported drug associated with alopecia development (58.8% [774/1316]). Only 4 cases demonstrated alopecia with DOAC rechallenge, suggesting onset of alopecia may have been unrelated to DOAC use or caused by a different trigger. Among 243 cases with a documented time to onset of alopecia, the median was 28 days, with an interquartile range of 63 days. Because TE most commonly occurs 3 to 4 months after the inciting event or medication trigger, there is little evidence to suggest DOACs as the cause of TE, and the observed cases of alopecia may be attributable to another preceding medical event and/or medication exposure.19 More studies are needed to examine the impact of anticoagulant medications on the hair cycle.
Antihypertensives
Hypertension is a modifiable risk factor for several cardiovascular diseases.20 According to the 2019 American College of Cardiology/American Heart Association Guideline on the Primary Prevention of Cardiovascular Disease,21 first-line medications include thiazide diuretics, calcium channel blockers, angiotensin-converting enzyme (ACE) inhibitors, and angiotensin receptor blockers (ARBs).
Angiotensin-converting enzyme inhibitors exert their antihypertensive effects by reducing conversion of angiotensin I to angiotensin II, thereby limiting the downstream effects of vasoconstriction as well as sodium and water retention. Given the proven mortality benefit of ACE inhibition in patients with congestive heart failure, ACE inhibitors are used as first-line therapy in these patients.22,23 Alopecia associated with ACE inhibitors is rare and limited to case reports following their introduction and approval in 1981.24-28 In one case, a woman in her 60s with congestive heart failure initiated captopril with development of an erythematous pruritic rash on the extremities and diffuse scalp hair loss 2 months later; spontaneous hair growth resumed 1 month following captopril discontinuation.25 In this case, the hair loss may be secondary to the drug eruption rather than true medication-induced TE. Initiation of enalapril in a woman in her 30s with hypertension was associated with diffuse scalp alopecia 4 weeks later that resolved with cessation of the suspected culprit, enalapril; rechallenge with enalapril several months later reproduced the hair loss.27 Given limited reports of ACE inhibitor–associated hair loss relative to their pervasive use, a direct causal role between ACE inhibition and TE is unlikely, or it has not been rigorously identified. The structured product labeling for captopril includes alopecia in its list of adverse effects reported in approximately 0.5% to 2% of patients but did not appear at increased frequency compared to placebo or other treatments used in controlled trials.29 Alternative inciting causes of alopecia in patients prescribed ACE inhibitors may include use of other medications, hospitalization, or metabolic derangements related to their underlying cardiac disease.
Although not indicated as a primary treatment for hypertension, β-blockers have US Food and Drug Administration approval for the treatment of certain arrhythmias, hypertension, heart failure, myocardial infarction, hyperthyroidism, and other conditions.30β-Blockers are competitive antagonists of β-adrenergic receptors that limit the production of intracellular cyclic adenosine monophosphate, but the mechanism of β-blockers as antihypertensives is unclear.31 Evidence supporting the role of β-adrenergic antagonists in TE is limited to case reports. Widespread alopecia across the scalp and arms was noted in a man in his 30s several months after starting propranolol.32 Biopsy of an affected area of the scalp demonstrated an increased number of telogen follicles with no other abnormalities. Near-complete resolution of alopecia was seen 4 months following cessation of propranolol, which recurred within 4 weeks of rechallenge.
Minoxidil—Oral minoxidil originally was approved for use in patients with resistant hypertension, defined as blood pressure elevated above goal despite concurrent use of the maximum dose of 3 classes of antihypertensives.36 Unlike other antihypertensive medications, minoxidil appears to cause reversible hypertrichosis that affects nearly all patients using oral minoxidil for longer than 1 month.37 This common adverse effect was a desired outcome in patients affected by hair loss, and a topical formulation of minoxidil was approved for androgenetic alopecia in men and women in 1988 and 1991, respectively.38 Since its approval, topical minoxidil has been commonly prescribed in the treatment of several types of alopecia, though evidence of its efficacy in the treatment of TE is limited.39,40 Low-dose oral minoxidil also has been reported to aid hair growth in androgenetic alopecia and TE.41 Taken orally, minoxidil is converted by sulfotransferases in the liver to minoxidil sulfate, which causes opening of plasma membrane adenosine triphosphate–sensitive potassium channels.42-44 The subsequent membrane hyperpolarization reduces calcium ion influx, which also reduces cell excitability, and inhibits contraction in vascular smooth muscle cells, which results in the arteriolar vasodilatory and antihypertensive effects of minoxidil.43,45 The potassium channel–opening effects of minoxidil may underly its hair growth stimulatory action. Unrelated potassium channel openers such as diazoxide and pinacidil also cause hypertrichosis.46-48 An animal study showed that topical minoxidil, cromakalim (potassium channel opener), and P1075 (pinacidil analog) applied daily to the scalps of balding stump-tailed macaques led to significant increases in hair weight over a 20-week treatment period compared with the vehicle control group (P<.05 for minoxidil 100 mM and 250 mM, cromakalim 100 mM, and P1075 100 mM and 250 mM).50 For minoxidil, this effect on hair growth appears to be dose dependent, as cumulative hair weights for the study period were significantly greater in the 250-mM concentration compared with 100-mM minoxidil (P<.05).49 The potassium channel–opening activity of minoxidil may induce stimulation of microcirculation around hair follicles conducive to hair growth.50 Other proposed mechanisms for hair growth with minoxidil include effects on keratinocyte and fibroblast cell proliferation,51-53 collagen synthesis,52,54 and prostaglandin activity.44,55
Final Thoughts
Medication-induced TE is an undesired adverse effect of many commonly used medications, including retinoids, azole antifungals, mood stabilizers, anticoagulants, and antihypertensives. In part 156 of this 2-part series, we reviewed the existing literature on hair loss from retinoids, antifungals, and psychotropic medications. Herein, we focused on anticoagulant and antihypertensive medications as potential culprits of TE. Heparin and its derivatives have been associated with development of diffuse alopecia weeks to months after the start of treatment. Alopecia associated with ACE inhibitors and β-blockers has been described only in case reports, suggesting that they may be unlikely causes of TE. In contrast, minoxidil is an antihypertensive that can result in hypertrichosis and is used in the treatment of androgenetic alopecia. It should not be assumed that medications that share an indication or are part of the same medication class would similarly induce TE. The development of diffuse nonscarring alopecia should prompt suspicion for TE and thorough investigation of medications initiated 1 to 6 months prior to onset of clinically apparent alopecia. Suspected culprit medications should be carefully assessed for their likelihood of inducing TE.
- Angiolillo DJ, Bhatt DL, Cannon CP, et al. Antithrombotic therapy in patients with atrial fibrillation treated with oral anticoagulation undergoing percutaneous coronary intervention: a North American perspective: 2021 update. Circulation. 2021;143:583-596. doi:10.1161 /circulationaha.120.050438
- Kearon C, Kahn SR. Long-term treatment of venous thromboembolism. Blood. 2020;135:317-325. doi:10.1182/blood.2019002364
- Frishman WH, Ribner HS. Anticoagulation in myocardial infarction: modern approach to an old problem. Am J Cardiol. 1979;43:1207-1213. doi:10.1016/0002-9149(79)90155-3
- Khorana AA, Mackman N, Falanga A, et al. Cancer-associated venous thromboembolism. Nat Rev Dis Primers. 2022;8:11. doi:10.1038 /s41572-022-00336-y
- Umerah CO, Momodu, II. Anticoagulation. StatPearls [Internet]. StatPearls Publishing; 2023. Accessed December 11, 2023. https://www.ncbi.nlm.nih.gov/books/NBK560651/
- Beurskens DMH, Huckriede JP, Schrijver R, et al. The anticoagulant and nonanticoagulant properties of heparin. Thromb Haemost. 2020;120:1371-1383. doi:10.1055/s-0040-1715460
- Hirsh J, Dalen J, Anderson DR, et al. Oral anticoagulants: mechanism of action, clinical effectiveness, and optimal therapeutic range. Chest. 2001;119(1 suppl):8S-21S. doi:10.1378/chest.119.1_suppl.8s
- Holbrook AM, Pereira JA, Labiris R, et al. Systematic overview of warfarin and its drug and food interactions. Arch Intern Med. 2005;165:1095-1106. doi:10.1001/archinte.165.10.1095
- Watras MM, Patel JP, Arya R. Traditional anticoagulants and hair loss: a role for direct oral anticoagulants? a review of the literature. Drugs Real World Outcomes. 2016;3:1-6. doi:10.1007/s40801-015-0056-z
- Heparin sodium. Product information. Hepalink USA Inc; January 2022. Accessed December 11, 2023. https://nctr-crs.fda.gov/fdalabel/services/spl/set-ids/c4c6bc1f-e0c7-fd0d-e053-2995a90abdef/spl-doc?hl=heparin
- Warfarin sodium. Product information. Bryant Ranch Prepack; April 2023. Accessed December 11, 2023. https://nctr-crs.fda.gov/fdalabel/services/spl/set-ids/c41b7c23-8053-428a-ac1d-8395e714c2f1/spl-doc?hl=alopecia%7Cwarfarin#section-6
- Hirsh J. Low-molecular-weight heparin. Circulation. 1998;98:1575-1582. doi:10.1161/01.CIR.98.15.1575
- Paus R. Hair growth inhibition by heparin in mice: a model system for studying the modulation of epithelial cell growth by glycosaminoglycans? Br J Dermatol. 1991;124:415-422. doi:10.1111/j.1365-2133.1991.tb00618.x
- Ma SN, Mao ZX, Wu Y, et al. The anti-cancer properties of heparin and its derivatives: a review and prospect. Cell Adh Migr. 2020;14:118-128. doi:10.1080/19336918.2020.1767489
- Choi JU, Chung SW, Al-Hilal TA, et al. A heparin conjugate, LHbisD4, inhibits lymphangiogenesis and attenuates lymph node metastasis by blocking VEGF-C signaling pathway. Biomaterials. 2017;139:56-66. doi:0.1016/j.biomaterials.2017.05.026
- Klerk CP, Smorenburg SM, Otten HM, et al. The effect of low molecular weight heparin on survival in patients with advanced malignancy. J Clin Oncol. 2005;23:2130-2135. doi:10.1200/jco.2005.03.134
- Altinbas M, Coskun HS, Er O, et al. A randomized clinical trial of combination chemotherapy with and without low-molecular-weight heparin in small cell lung cancer. J Thromb Haemost. 2004;2:1266-1271. doi:10.1111/j.1538-7836.2004.00871.x
- Weyand AC, Shavit JA. Agent specific effects of anticoagulant induced alopecia. Res Pract Thromb Haemost. 2017;1:90-92. doi:10.1002 /rth2.12001
- Bonaldo G, Vaccheri A, Motola D. Direct-acting oral anticoagulants and alopecia: the valuable support of postmarketing data. Br J Clin Pharmacol. 2020;86:1654-1660. doi:10.1111/bcp.14221
- Fuchs FD, Whelton PK. High blood pressure and cardiovascular disease. Hypertension. 2020;75:285-292. doi:10.1161 /HYPERTENSIONAHA.119.14240
- Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;140:E596-E646. doi:10.1161/CIR.0000000000000678
- Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013;128:E240-E327. doi:10.1161 /CIR.0b013e31829e8776
- Effects of enalapril on mortality in severe congestive heart failure. results of the Cooperative North Scandinavian Enalapril Survival Study (CONSENSUS). N Engl J Med. 1987;316:1429-1435. doi:10.1056 /nejm198706043162301
- Kataria V, Wang H, Wald JW, et al. Lisinopril-induced alopecia: a case report. J Pharm Pract. 2017;30:562-566. doi:10.1177/0897190016652554
- Motel PJ. Captopril and alopecia: a case report and review of known cutaneous reactions in captopril use. J Am Acad Dermatol. 1990;23:124-125. doi:10.1016/s0190-9622(08)81205-4
- Leaker B, Whitworth JA. Alopecia associated with captopril treatment. Aust N Z J Med. 1984;14:866. doi:10.1111/j.1445-5994.1984.tb03797.x
- Ahmad S. Enalapril and reversible alopecia. Arch Intern Med. 1991;151:404.
- Bicket DP. Using ACE inhibitors appropriately. Am Fam Physician. 2002;66:461-468.
- Captopril. Product information. Bryant Ranch Prepack; May 2023. Accessed December 11, 2023. https://nctr-crs.fda.gov/fdalabel/services/spl/set-ids/563737c5-4d63-4957-8022-e3bc3112dfac/spl-doc?hl=captopril
- Farzam K, Jan A. Beta blockers. StatPearls Publishing; 2023. https://www.ncbi.nlm.nih.gov/books/NBK532906/
- Mason RP, Giles TD, Sowers JR. Evolving mechanisms of action of beta blockers: focus on nebivolol. J Cardiovasc Pharmacol. 2009; 54:123-128.
- Martin CM, Southwick EG, Maibach HI. Propranolol induced alopecia. Am Heart J. 1973;86:236-237. doi:10.1016/0002-8703(73)90250-0
- Graeber CW, Lapkin RA. Metoprolol and alopecia. Cutis. 1981; 28:633-634.
- Hilder RJ. Propranolol and alopecia. Cutis. 1979;24:63-64.
- Coreg. Prescribing information. Woodward Pharma Services LLC; 2023. Accessed December 11, 2023. https://www.accessdata.fda.gov/spl/data/34aa881a-3df4-460b-acad-fb9975ca3a06/34aa881a-3df4-460b-acad-fb9975ca3a06.xml
- Carey RM, Calhoun DA, Bakris GL, et al. Resistant hypertension: detection, evaluation, and management: a scientific statement from the American Heart Association. Hypertension. 2018;72:E53-E90. doi:10.1161/hyp.0000000000000084
- Campese VM. Minoxidil: a review of its pharmacological properties and therapeutic use. Drugs. 1981;22:257-278. doi:10.2165/00003495-198122040-00001
- Heymann WR. Coming full circle (almost): low dose oral minoxidil for alopecia. J Am Acad Dermatol. 2021;84:613-614. doi:10.1016/j .jaad.2020.12.053
- Yin S, Zhang B, Lin J, et al. Development of purification process for dual-function recombinant human heavy-chain ferritin by the investigation of genetic modification impact on conformation. Eng Life Sci. 2021;21:630-642. doi:10.1002/elsc.202000105
- Mysore V, Parthasaradhi A, Kharkar RD, et al. Expert consensus on the management of telogen effluvium in India. Int J Trichology. 2019;11:107-112.
- Gupta AK, Talukder M, Shemar A, et al. Low-dose oral minoxidil for alopecia: a comprehensive review [published online September 27, 2023]. Skin Appendage Disord. doi:10.1159/000531890
- Meisheri KD, Cipkus LA, Taylor CJ. Mechanism of action of minoxidil sulfate-induced vasodilation: a role for increased K+ permeability. J Pharmacol Exp Ther. 1988;245:751-760.
- Winquist RJ, Heaney LA, Wallace AA, et al. Glyburide blocks the relaxation response to BRL 34915 (cromakalim), minoxidil sulfate and diazoxide in vascular smooth muscle. J Pharmacol Exp Ther. 1989;248:149-56.
- Messenger AG, Rundegren J. Minoxidil: mechanisms of action on hair growth. Br J Dermatol. 2004;150:186-194. doi:10.1111/j .1365-2133.2004.05785.x
- Alijotas-Reig J, García GV, Velthuis PJ, et al. Inflammatory immunemediated adverse reactions induced by COVID-19 vaccines in previously injected patients with soft tissue fillers: a case series of 20 patients. J Cosmet Dermatol. 2022;21:3181-3187. doi: 10.1111/jocd.15117
- Boskabadi SJ, Ramezaninejad S, Sohrab M, et al. Diazoxideinduced hypertrichosis in a neonate with transient hyperinsulinism. Clin Med Insights Case Rep. 2023;16:11795476231151330. doi:10.1177/11795476231151330
- Burton JL, Schutt WH, Caldwell IW. Hypertrichosis due to diazoxide. Br J Dermatol. 1975;93:707-711. doi:10.1111/j.1365-2133.1975.tb05123.x
- Goldberg MR. Clinical pharmacology of pinacidil, a prototype for drugs that affect potassium channels. J Cardiovasc Pharmacol. 1988;12 suppl 2:S41-S47. doi: 10.1097/00005344-198812002-00008
- Buhl AE, Waldon DJ, Conrad SJ, et al. Potassium channel conductance: a mechanism affecting hair growth both in vitro and in vivo. J Invest Dermatol. 1992;98:315-319. doi:10.1111/1523-1747.ep12499788
- Patel P, Nessel TA, Kumar DD. Minoxidil. StatPearls [Internet]. StatPearls Publishing; 2023. Accessed December 11, 2023. https://www.ncbi.nlm.nih.gov/books/NBK482378/
- O’Keefe E, Payne RE Jr. Minoxidil: inhibition of proliferation of keratinocytes in vitro. J Invest Dermatol. 1991;97:534-536. doi:10.1111/1523-1747.ep12481560
- Murad S, Pinnell SR. Suppression of fibroblast proliferation and lysyl hydroxylase activity by minoxidil. J Biol Chem. 1987;262:11973-11978.
- Baden HP, Kubilus J. Effect of minoxidil on cultured keratinocytes. J Invest Dermatol. 1983;81:558-560. doi:10.1111/1523-1747.ep12523220
- Murad S, Walker LC, Tajima S, et al. Minimum structural requirements for minoxidil inhibition of lysyl hydroxylase in cultured fibroblasts. Arch Biochem Biophys. 1994;308:42-47. doi:10.1006/abbi.1994.1006
- Kvedar JC, Baden HP, Levine L. Selective inhibition by minoxidil of prostacyclin production by cells in culture. Biochem Pharmacol. 1988;37:867-874. doi:0.1016/0006-2952(88)90174-8
- Zhang D, LaSenna C, Shields BE. Culprits of medication-induced telogen effluvium, part 1. Cutis. 2023;112:267-271.
- Angiolillo DJ, Bhatt DL, Cannon CP, et al. Antithrombotic therapy in patients with atrial fibrillation treated with oral anticoagulation undergoing percutaneous coronary intervention: a North American perspective: 2021 update. Circulation. 2021;143:583-596. doi:10.1161 /circulationaha.120.050438
- Kearon C, Kahn SR. Long-term treatment of venous thromboembolism. Blood. 2020;135:317-325. doi:10.1182/blood.2019002364
- Frishman WH, Ribner HS. Anticoagulation in myocardial infarction: modern approach to an old problem. Am J Cardiol. 1979;43:1207-1213. doi:10.1016/0002-9149(79)90155-3
- Khorana AA, Mackman N, Falanga A, et al. Cancer-associated venous thromboembolism. Nat Rev Dis Primers. 2022;8:11. doi:10.1038 /s41572-022-00336-y
- Umerah CO, Momodu, II. Anticoagulation. StatPearls [Internet]. StatPearls Publishing; 2023. Accessed December 11, 2023. https://www.ncbi.nlm.nih.gov/books/NBK560651/
- Beurskens DMH, Huckriede JP, Schrijver R, et al. The anticoagulant and nonanticoagulant properties of heparin. Thromb Haemost. 2020;120:1371-1383. doi:10.1055/s-0040-1715460
- Hirsh J, Dalen J, Anderson DR, et al. Oral anticoagulants: mechanism of action, clinical effectiveness, and optimal therapeutic range. Chest. 2001;119(1 suppl):8S-21S. doi:10.1378/chest.119.1_suppl.8s
- Holbrook AM, Pereira JA, Labiris R, et al. Systematic overview of warfarin and its drug and food interactions. Arch Intern Med. 2005;165:1095-1106. doi:10.1001/archinte.165.10.1095
- Watras MM, Patel JP, Arya R. Traditional anticoagulants and hair loss: a role for direct oral anticoagulants? a review of the literature. Drugs Real World Outcomes. 2016;3:1-6. doi:10.1007/s40801-015-0056-z
- Heparin sodium. Product information. Hepalink USA Inc; January 2022. Accessed December 11, 2023. https://nctr-crs.fda.gov/fdalabel/services/spl/set-ids/c4c6bc1f-e0c7-fd0d-e053-2995a90abdef/spl-doc?hl=heparin
- Warfarin sodium. Product information. Bryant Ranch Prepack; April 2023. Accessed December 11, 2023. https://nctr-crs.fda.gov/fdalabel/services/spl/set-ids/c41b7c23-8053-428a-ac1d-8395e714c2f1/spl-doc?hl=alopecia%7Cwarfarin#section-6
- Hirsh J. Low-molecular-weight heparin. Circulation. 1998;98:1575-1582. doi:10.1161/01.CIR.98.15.1575
- Paus R. Hair growth inhibition by heparin in mice: a model system for studying the modulation of epithelial cell growth by glycosaminoglycans? Br J Dermatol. 1991;124:415-422. doi:10.1111/j.1365-2133.1991.tb00618.x
- Ma SN, Mao ZX, Wu Y, et al. The anti-cancer properties of heparin and its derivatives: a review and prospect. Cell Adh Migr. 2020;14:118-128. doi:10.1080/19336918.2020.1767489
- Choi JU, Chung SW, Al-Hilal TA, et al. A heparin conjugate, LHbisD4, inhibits lymphangiogenesis and attenuates lymph node metastasis by blocking VEGF-C signaling pathway. Biomaterials. 2017;139:56-66. doi:0.1016/j.biomaterials.2017.05.026
- Klerk CP, Smorenburg SM, Otten HM, et al. The effect of low molecular weight heparin on survival in patients with advanced malignancy. J Clin Oncol. 2005;23:2130-2135. doi:10.1200/jco.2005.03.134
- Altinbas M, Coskun HS, Er O, et al. A randomized clinical trial of combination chemotherapy with and without low-molecular-weight heparin in small cell lung cancer. J Thromb Haemost. 2004;2:1266-1271. doi:10.1111/j.1538-7836.2004.00871.x
- Weyand AC, Shavit JA. Agent specific effects of anticoagulant induced alopecia. Res Pract Thromb Haemost. 2017;1:90-92. doi:10.1002 /rth2.12001
- Bonaldo G, Vaccheri A, Motola D. Direct-acting oral anticoagulants and alopecia: the valuable support of postmarketing data. Br J Clin Pharmacol. 2020;86:1654-1660. doi:10.1111/bcp.14221
- Fuchs FD, Whelton PK. High blood pressure and cardiovascular disease. Hypertension. 2020;75:285-292. doi:10.1161 /HYPERTENSIONAHA.119.14240
- Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;140:E596-E646. doi:10.1161/CIR.0000000000000678
- Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013;128:E240-E327. doi:10.1161 /CIR.0b013e31829e8776
- Effects of enalapril on mortality in severe congestive heart failure. results of the Cooperative North Scandinavian Enalapril Survival Study (CONSENSUS). N Engl J Med. 1987;316:1429-1435. doi:10.1056 /nejm198706043162301
- Kataria V, Wang H, Wald JW, et al. Lisinopril-induced alopecia: a case report. J Pharm Pract. 2017;30:562-566. doi:10.1177/0897190016652554
- Motel PJ. Captopril and alopecia: a case report and review of known cutaneous reactions in captopril use. J Am Acad Dermatol. 1990;23:124-125. doi:10.1016/s0190-9622(08)81205-4
- Leaker B, Whitworth JA. Alopecia associated with captopril treatment. Aust N Z J Med. 1984;14:866. doi:10.1111/j.1445-5994.1984.tb03797.x
- Ahmad S. Enalapril and reversible alopecia. Arch Intern Med. 1991;151:404.
- Bicket DP. Using ACE inhibitors appropriately. Am Fam Physician. 2002;66:461-468.
- Captopril. Product information. Bryant Ranch Prepack; May 2023. Accessed December 11, 2023. https://nctr-crs.fda.gov/fdalabel/services/spl/set-ids/563737c5-4d63-4957-8022-e3bc3112dfac/spl-doc?hl=captopril
- Farzam K, Jan A. Beta blockers. StatPearls Publishing; 2023. https://www.ncbi.nlm.nih.gov/books/NBK532906/
- Mason RP, Giles TD, Sowers JR. Evolving mechanisms of action of beta blockers: focus on nebivolol. J Cardiovasc Pharmacol. 2009; 54:123-128.
- Martin CM, Southwick EG, Maibach HI. Propranolol induced alopecia. Am Heart J. 1973;86:236-237. doi:10.1016/0002-8703(73)90250-0
- Graeber CW, Lapkin RA. Metoprolol and alopecia. Cutis. 1981; 28:633-634.
- Hilder RJ. Propranolol and alopecia. Cutis. 1979;24:63-64.
- Coreg. Prescribing information. Woodward Pharma Services LLC; 2023. Accessed December 11, 2023. https://www.accessdata.fda.gov/spl/data/34aa881a-3df4-460b-acad-fb9975ca3a06/34aa881a-3df4-460b-acad-fb9975ca3a06.xml
- Carey RM, Calhoun DA, Bakris GL, et al. Resistant hypertension: detection, evaluation, and management: a scientific statement from the American Heart Association. Hypertension. 2018;72:E53-E90. doi:10.1161/hyp.0000000000000084
- Campese VM. Minoxidil: a review of its pharmacological properties and therapeutic use. Drugs. 1981;22:257-278. doi:10.2165/00003495-198122040-00001
- Heymann WR. Coming full circle (almost): low dose oral minoxidil for alopecia. J Am Acad Dermatol. 2021;84:613-614. doi:10.1016/j .jaad.2020.12.053
- Yin S, Zhang B, Lin J, et al. Development of purification process for dual-function recombinant human heavy-chain ferritin by the investigation of genetic modification impact on conformation. Eng Life Sci. 2021;21:630-642. doi:10.1002/elsc.202000105
- Mysore V, Parthasaradhi A, Kharkar RD, et al. Expert consensus on the management of telogen effluvium in India. Int J Trichology. 2019;11:107-112.
- Gupta AK, Talukder M, Shemar A, et al. Low-dose oral minoxidil for alopecia: a comprehensive review [published online September 27, 2023]. Skin Appendage Disord. doi:10.1159/000531890
- Meisheri KD, Cipkus LA, Taylor CJ. Mechanism of action of minoxidil sulfate-induced vasodilation: a role for increased K+ permeability. J Pharmacol Exp Ther. 1988;245:751-760.
- Winquist RJ, Heaney LA, Wallace AA, et al. Glyburide blocks the relaxation response to BRL 34915 (cromakalim), minoxidil sulfate and diazoxide in vascular smooth muscle. J Pharmacol Exp Ther. 1989;248:149-56.
- Messenger AG, Rundegren J. Minoxidil: mechanisms of action on hair growth. Br J Dermatol. 2004;150:186-194. doi:10.1111/j .1365-2133.2004.05785.x
- Alijotas-Reig J, García GV, Velthuis PJ, et al. Inflammatory immunemediated adverse reactions induced by COVID-19 vaccines in previously injected patients with soft tissue fillers: a case series of 20 patients. J Cosmet Dermatol. 2022;21:3181-3187. doi: 10.1111/jocd.15117
- Boskabadi SJ, Ramezaninejad S, Sohrab M, et al. Diazoxideinduced hypertrichosis in a neonate with transient hyperinsulinism. Clin Med Insights Case Rep. 2023;16:11795476231151330. doi:10.1177/11795476231151330
- Burton JL, Schutt WH, Caldwell IW. Hypertrichosis due to diazoxide. Br J Dermatol. 1975;93:707-711. doi:10.1111/j.1365-2133.1975.tb05123.x
- Goldberg MR. Clinical pharmacology of pinacidil, a prototype for drugs that affect potassium channels. J Cardiovasc Pharmacol. 1988;12 suppl 2:S41-S47. doi: 10.1097/00005344-198812002-00008
- Buhl AE, Waldon DJ, Conrad SJ, et al. Potassium channel conductance: a mechanism affecting hair growth both in vitro and in vivo. J Invest Dermatol. 1992;98:315-319. doi:10.1111/1523-1747.ep12499788
- Patel P, Nessel TA, Kumar DD. Minoxidil. StatPearls [Internet]. StatPearls Publishing; 2023. Accessed December 11, 2023. https://www.ncbi.nlm.nih.gov/books/NBK482378/
- O’Keefe E, Payne RE Jr. Minoxidil: inhibition of proliferation of keratinocytes in vitro. J Invest Dermatol. 1991;97:534-536. doi:10.1111/1523-1747.ep12481560
- Murad S, Pinnell SR. Suppression of fibroblast proliferation and lysyl hydroxylase activity by minoxidil. J Biol Chem. 1987;262:11973-11978.
- Baden HP, Kubilus J. Effect of minoxidil on cultured keratinocytes. J Invest Dermatol. 1983;81:558-560. doi:10.1111/1523-1747.ep12523220
- Murad S, Walker LC, Tajima S, et al. Minimum structural requirements for minoxidil inhibition of lysyl hydroxylase in cultured fibroblasts. Arch Biochem Biophys. 1994;308:42-47. doi:10.1006/abbi.1994.1006
- Kvedar JC, Baden HP, Levine L. Selective inhibition by minoxidil of prostacyclin production by cells in culture. Biochem Pharmacol. 1988;37:867-874. doi:0.1016/0006-2952(88)90174-8
- Zhang D, LaSenna C, Shields BE. Culprits of medication-induced telogen effluvium, part 1. Cutis. 2023;112:267-271.
Practice Points
- Medications are a common culprit of telogen effluvium (TE), and medication-induced TE should be suspected in patients presenting with diffuse nonscarring alopecia who are taking systemic medication(s) such as heparin and its derivatives.
- Infection, illness, or hospitalization around the time of initiation of the suspected culprit medication may complicate identification of the inciting cause and may contribute to TE.
- Angiotensin-converting enzyme inhibitors and β-blockers are unlikely culprits of medication-induced TE, and the benefits of discontinuing a suspected culprit medication should be weighed carefully against the risks of medication cessation.
Culprits of Medication-Induced Telogen Effluvium, Part 1
Alopecia is a commonly reported side effect of various medications. Anagen effluvium and telogen effluvium (TE) are considered the most common mechanisms underlying medication-related hair loss. Anagen effluvium is associated with chemotherapeutic agents and radiation therapy, with anagen shedding typically occurring within 2 weeks of medication administration.1,2 Medication-induced TE is a diffuse nonscarring alopecia that is a reversible reactive process.3-5 Telogen effluvium is clinically apparent as a generalized shedding of scalp hair 1 to 6 months after an inciting cause.6 The underlying cause of TE may be multifactorial and difficult to identify given the delay between the trigger and the onset of clinically apparent hair loss. Other known triggers of TE include acute illness,7,8 nutritional deficiencies,4,9 and/or major surgery.10
Each hair follicle independently and sequentially progresses through anagen growth, catagen transition, and telogen resting phases. In the human scalp, the telogen phase typically lasts 3 months, at the end of which the telogen hair is extruded from the scalp. Anagen and telogen follicles typically account for an average of 90% and 10% of follicles on the human scalp, respectively.11 Immediate anagen release is hypothesized to be the mechanism underlying medication-induced TE.12 This theory suggests that an increased percentage of anagen follicles prematurely enter the telogen phase, with a notable increase in hair shedding at the conclusion of the telogen phase approximately 1 to 6 months later.12 First-line management of medication-induced TE is identification and cessation of the causative agent, if possible. Notable regrowth of hair is expected several months after removal of the inciting medication. In part 1 of this 2-part series, we review the existing literature to identify common culprits of medication-induced TE, including retinoids, antifungals, and psychotropic medications.
Retinoids
Retinoids are vitamin A derivatives used in the treatment of a myriad of dermatologic and nondermatologic conditions.13,14 Retinoids modulate sebum production,15 keratinocyte proliferation,16 and epithelial differentiation through signal transduction downstream of the ligand-activated nuclear retinoic acid receptors and retinoid X receptors.13,14,17 The recommended daily dosage of retinol is 900 µg retinol activity equivalent (3000 IU) for men and 700 µg retinol activity equivalent (2333 IU) for women. Retinoids are used in the treatment of acne vulgaris,18 psoriasis,19 and ichthyosis.20 The most commonly reported adverse effects of systemic retinoid therapy include cheilitis, alopecia, and xerosis.21 Retinoid-associated alopecia is dose and duration dependent.19,21-24 A prospective study of acitretin therapy in plaque psoriasis reported that more than 63% (42/66) of patients on 50 mg or more of acitretin daily for 6 months or longer experienced alopecia that reversed with discontinuation.23 A systematic review of isotretinoin use in acne showed alopecia was seen in 3.2% (18/565) of patients on less than 0.5 mg/kg/d of isotretinoin and in 5.7% (192/3375) of patients on 0.5 mg/kg/d or less of isotretinoin.24 In a phase 2 clinical trial of orally administered 9-cis-retinoic acid (alitretinoin) in the treatment of Kaposi sarcoma related to AIDS, 42% (24/57) of adult male patients receiving 60, 100, or 140 mg/m2 alitretinoin daily (median treatment duration, 15.1 weeks) reported alopecia as an adverse effect of treatment.25 In one case report, a patient who ingested 500,000 IU of vitamin A daily for 4 months and then 100,000 IU monthly for 6 months experienced diffusely increased shedding of scalp hair along with muscle soreness, nail dystrophy, diffuse skin rash, and refractory ascites; he was found to have severe liver damage secondary to hypervitaminosis A that required liver transplantation.26 Regarding the pathomechanism of retinoid-induced alopecia, animal and in vitro studies similarly have demonstrated that all-trans-retinoic acid appears to exert its inhibitory effects on hair follicle growth via the influence of the transforming growth factor β2 and SMAD2/3 pathway influence on dermal papillae cells.14,27 Development of hair loss secondary to systemic retinoid therapy may be managed with dose reduction or cessation.
Antifungals
Azole medications have broad-spectrum fungistatic activity against a wide range of yeast and filamentous fungi. Azoles inhibit sterol 14α-demethylase activity, impairing ergosterol synthesis and thereby disrupting plasma membrane synthesis and activity of membrane-bound enzymes.28 Fluconazole is a systemic oral agent in this class that was first approved by the US Food and Drug Administration (FDA) for use in the 1990s.29 A retrospective study by the National Institute of Allergy and Infectious Disease Mycoses Study Group followed the clinical course of 33 patients who developed alopecia while receiving fluconazole therapy for various mycoses.30 The majority (88% [29/33]) of patients received 400 mg or more of fluconazole daily. The median time to hair loss after starting fluconazole was 3 months, and the scalp was involved in all cases. In 97% (32/33) of patients, resolution of alopecia was noted following discontinuation of fluconazole or a dose reduction of 50% or more. In 85% (28/33) of patients, complete resolution of alopecia occurred within 6 months of fluconazole cessation or dose reduction.30 Fluconazole-induced TE was reproducible in an animal model using Wistar rats31; however, further studies are required to clarify the molecular pathways of its effect on hair growth.
Voriconazole is an azole approved for the treatment of invasive aspergillosis, candidemia, and fungal infections caused by Scedosporium apiospermum and Fusarium species. A retrospective survey study of patients who received voriconazole for 1 month or longer found a considerable proportion of patients developed diffuse reversible hair loss.32 Scalp alopecia was noted in 79% (120/152) of patients who completed the survey, with a mean (SD) time to alopecia of 75 (54) days after initiation of voriconazole. Notable regrowth was reported in 69% (79/114) of patients who discontinued voriconazole for at least 3 months. A subgroup of 32 patients were changed to itraconazole or posaconazole, and hair loss stopped in 84% (27/32) with regrowth noted in 69% (22/32) of patients.32 Voriconazole and fluconazole share structural similarity not present with other triazoles.33,34 Because voriconazole-associated alopecia was reversed in the majority of patients who switched to itraconazole or posaconazole, the authors hypothesized that structural similarity of fluconazole and voriconazole may underly the greater risk for TE that is not a class effect of azole medications.31
Psychotropic Medications
Various psychotropic medications have been associated with hair loss. Valproic acid (or sodium valproate) is an anticonvulsant and mood-stabilizing agent used for the treatment of seizures, bipolar disorder (BD), migraines, and neuropathic pain.35,36 Divalproex sodium (or divalproex) is an enteric-coated formulation of sodium valproate and valproic acid with similar indications. Valproate is a notorious culprit of medication-induced hair loss, with alopecia listed among the most common adverse reactions (reported >5%) on its structure product labeling document.37 A systemic review and meta-analysis by Wang et al38 estimated the overall incidence of valproate-related alopecia to be 11% (95% CI, 0.08-0.13). Although this meta-analysis did not find an association between incidence of alopecia and dose or duration of valproate therapy,38 a separate review suggested that valproate-induced alopecia is dose dependent and can be managed with dose reduction.39 A 12-month, randomized, double-blind study of treatment of BD with divalproex (valproate derivative), lithium, or placebo (2:1:1 ratio) showed a significantly higher frequency of alopecia in the divalproex group compared with placebo (16% [30/187] vs 6% [6/94]; P=.03).40 Valproate-related hair loss is characteristically diffuse and nonscarring, often noted 3 to 6 months following initiation of valproate.41,42 The proposed mechanism of valproate-induced alopecia includes chelation of zinc and selenium,43 and a reduction in serum biotinidase activity, thereby decreasing the availability of these essential micronutrients required for hair growth.41 Studies examining the effects of valproate administration and serum biotinidase activity in patients have yielded conflicting results.44-46 In a study of children with seizures including 57 patients treated with valproic acid, 17 treated with carbamazepine, and 75 age- and sex-matched healthy controls, the authors found no significant differences in serum biotinidase enzyme activity across the 3 groups.44 In contrast, a study of 75 children with seizures on valproic acid therapy stratified by dose (mean [SD])—group A: 28.7 [8.5] mg/kg/d; group B: 41.6 [4.9] mg/kg/d; group C: 64.5 [5.8] mg/kg/d—found that patients receiving higher doses (groups B and C) had significantly reduced serum biotinidase activity (1.22
Lithium carbonate (lithium) is used in the treatment of BD. Despite its efficacy and low cost, its potential for adverse effects, narrow therapeutic index, and subsequent need for routine monitoring are factors that limit its use.48 Some reported dermatologic adverse reactions on its structure product labeling include xerosis, thinning of hair, alopecia, xerosis cutis, psoriasis onset/exacerbation, and generalized pruritus.49 A systematic review and meta-analysis of 385 studies identified 24 publications reporting adverse effects of lithium on hair with no significantly increased risk of alopecia overall.50 The analysis included 2 randomized controlled trials comparing the effects of lithium and placebo on hair loss in patients with BD. Hair loss was reported in 7% (7/94) of patients taking lithium and 6% (6/94) of the placebo group in the 12-month study40 and in 3% (1/32) of the lithium group and 0% (0/28) of the divalproex group in the 20-month study.51 Despite anecdotal reports of alopecia associated with lithium, there is a lack of high-quality evidence to support this claim. Of note, hypothyroidism is a known complication of lithium use, and serum testing of thyroid function at 6-month intervals is recommended for patients on lithium treatment.52 Because thyroid abnormalities can cause alopecia distinct from TE, new-onset alopecia during lithium use should prompt serum testing of thyroid function. The development of hypothyroidism secondary to lithium is not a direct contraindication to its use53; rather, treatment should be focused on correction with thyroid replacement therapy (eg, supplementation with thyroxine).54
Commonly prescribed antidepressant medications include selective serotonin reuptake inhibitors (SSRIs) and bupropion. Selective serotonin reuptake inhibitors affect the neuronal serotonin transporter, increasing the concentration of serotonin in the synaptic cleft available for stimulation of postsynaptic serotonin receptors55,56; bupropion is an antidepressant medication that inhibits norepinephrine and dopamine reuptake at the synaptic cleft.57 Alopecia is an infrequent (1 in 100 to 1 in 1000 patients) adverse effect for several SSRIs.58-62 A recent systematic review identified a total of 71 cases of alopecia associated with SSRI use including citalopram (n=11), escitalopram (n=7), fluoxetine (n=27), fluoxvamine (n=5), paroxetine (n=4), and sertraline (n=20), with a median time to onset of hair shedding of 8.6 weeks (range, 3 days to 5 years). Discontinuation of the suspected culprit SSRI led to improvement and/or resolution in 63% (51/81) episodes of alopecia, with a median time to improvement and/or resolution of 4 weeks.63 A comparative retrospective cohort study using a large US health claims database from 2006 to 2014 included more than 1 million new and mutually exclusive patients taking fluoxetine, fluvoxamine, sertraline, citalopram, escitalopram, paroxetine, duloxetine, venlafaxine, desvenlafaxine, and bupropion.64 Overall, 1% (1569/150,404) of patients treated with bupropion received 1 or more physician visits for alopecia. Patients on SSRIs generally had a lower risk for hair loss compared with patients using bupropion (citalopram: hazard ratio [HR], 0.80 [95% CI, 0.74-0.86]; escitalopram: HR, 0.79 [95% CI, 0.74-0.86]; fluoxetine: HR, 0.68 [95% CI, 0.63-0.74]; paroxetine: HR, 0.68 [95% CI, 0.62-0.74]; sertraline: HR, 0.74 [95% CI, 0.69-0.79]), with the exception of fluvoxamine (HR, 0.93 [95% CI, 0.64-1.37]). However, the type of alopecia, time to onset, and time to resolution were not reported, making it difficult to assess whether the reported hair loss was consistent with medication-induced TE. Additionally, the authors acknowledged that bupropion may have been prescribed for smoking cessation, which may carry a different risk profile for the development of alopecia.64 Several other case reports have described alopecia following treatment with SSRIs, including sertraline,65 fluvoxamine,66 paroxetine,67 fluoxetine,68 and escitalopram.69
Overall, it appears that the use of SSRIs portends relatively low risk for alopecia and medication-induced TE. Little is known regarding the molecular effects of SSRIs on hair growth and the pathomechanism of SSRI-induced TE. The potential benefits of discontinuing a suspected culprit medication should be carefully weighed against the risks of medication cessation, and consideration should be given to alternative medications in the same class that also may be associated with TE. In patients requiring antidepressant therapy with suspected medication-induced TE, consider transitioning to a different class of medication with lower risk of medication-induced alopecia; for example, discontinuing bupropion in favor of an SSRI.
Final Thoughts
Medication-induced alopecia is an undesired side effect of many commonly used drugs and drug classes, including retinoids, azole antifungals, and mood stabilizers. Although the precise pathomechanisms of medication-induced TE remain unclear, the recommended management often requires identification of the likely causative agent and its discontinuation, if possible. Suspicion for medication-induced TE should prompt a thorough history of recent changes to medications, risk factors for nutritional deficiencies, underlying illnesses, and recent surgical procedures. Underlying nutritional, electrolyte, and/or metabolic disturbances should be corrected. In part 2 of this series, we will discuss medication-induced alopecia associated with anticoagulant and antihypertensive medications.
- Saleh D, Nassereddin A, Cook C. Anagen effluvium. StatPearls. StatPearls Publishing; 2023. https://www.ncbi.nlm.nih.gov/books/NBK482293/
- Guerrero-Putz MD, Flores-Dominguez AC, Castillo-de la Garza RJ, et al. Anagen effluvium after neurointerventional radiation: trichoscopy as a diagnostic ally. Skin Appendage Disord. 2021;8:102-107. doi:10.1159/000518743
- Patel M, Harrison S, Sinclair R. Drugs and hair loss. Dermatol Clin. 2013;31:67-73. doi:https://doi.org/10.1016/j.det.2012.08.002
- Chen V, Strazzulla L, Asbeck SM, et al. Etiology, management, and outcomes of pediatric telogen effluvium: a single-center study in the United States. Pediatr Dermatol. 2023;40:120-124. doi:10.1111/pde.15154
- Watras MM, Patel JP, Arya R. Traditional anticoagulants and hair loss: a role for direct oral anticoagulants? a review of the literature. Drugs Real World Outcomes. 2016;3:1-6. doi:10.1007/s40801-015-0056-z
- Hughes EC, Saleh D. Telogen effluvium. StatPearls. StatPearls Publishing; 2023. https://www.ncbi.nlm.nih.gov/books/NBK430848/
- Nguyen B, Tosti A. Alopecia in patients with COVID-19: a systematic review and meta-analysis. JAAD Int. 2022;7:67-77. doi:10.1016/j.jdin.2022.02.006
- Starace M, Piraccini BM, Evangelista V, et al. Acute telogen effluvium due to dengue fever mimicking androgenetic alopecia. Ital J Dermatol Venerol. 2023;158:66-67. doi:10.23736/s2784-8671.22.07369-8
- Patel KV, Farrant P, Sanderson JD, et al. Hair loss in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2013;19:1753-1763. doi:10.1097/MIB.0b013e31828132de
- Cohen-Kurzrock RA, Cohen PR. Bariatric surgery–induced telogen effluvium (bar site): case report and a review of hair loss following weight loss surgery. Cureus. 2021;13:E14617. doi:10.7759/cureus.14617
- Price VH. Treatment of hair loss. N Engl J Med. 1999;341:964-973. doi:10.1056/nejm199909233411307
- Headington JT. Telogen effluvium: new concepts and review. Arch Dermatol. 1993;129:356-363. doi:10.1001/arcderm.1993.01680240096017
- Lee DD, Stojadinovic O, Krzyzanowska A, et al. Retinoid-responsive transcriptional changes in epidermal keratinocytes. J Cell Physiol. 2009;220:427-439. doi:10.1002/jcp.21784
- Foitzik K, Spexard T, Nakamura M, et al. Towards dissecting the pathogenesis of retinoid-induced hair loss: all-trans retinoic acid induces premature hair follicle regression (catagen) by upregulation of transforming growth factor-beta2 in the dermal papilla. J Invest Dermatol. 2005;124:1119-1126. doi:10.1111/j.0022-202X.2005.23686.x
- Karlsson T, Vahlquist A, Kedishvili N, et al. 13-cis-retinoic acid competitively inhibits 3 alpha-hydroxysteroid oxidation by retinol dehydrogenase RoDH-4: a mechanism for its anti-androgenic effects in sebaceous glands? Biochem Biophys Res Commun. 2003;303:273-278. doi:10.1016/s0006-291x(03)00332-2
- Chapellier B, Mark M, Messaddeq N, et al. Physiological and retinoid-induced proliferations of epidermis basal keratinocytes are differently controlled. EMBO J. 2002;21:3402-3413. doi:10.1093/emboj/cdf331
- Geiger JM. Retinoids and sebaceous gland activity. Dermatology. 1995;191:305-310. doi:10.1159/000246581
- Oge LK, Broussard A, Marshall MD. Acne vulgaris: diagnosis and treatment. Am Fam Physician. 2019;100:475-484.
- Pilkington T, Brogden RN. Acitretin. Drugs. 1992;43:597-627. doi:10.2165/00003495-199243040-00010
- Zaenglein AL, Levy ML, Stefanko NS, et al. Consensus recommendations for the use of retinoids in ichthyosis and other disorders of cornification in children and adolescents. Pediatr Dermatol. 2021;38:164-180. doi:10.1111/pde.14408
- Katz HI, Waalen J, Leach EE. Acitretin in psoriasis: an overview of adverse effects. J Am Acad Dermatol. 1999;41(3 suppl):S7-S12. doi:10.1016/s0190-9622(99)70359-2
- Tran PT, Evron E, Goh C. Characteristics of patients with hair loss after isotretinoin treatment: a retrospective review study. Int J Trichology. 2022;14:125-127. doi:10.4103/ijt.ijt_80_20
- Gupta AK, Goldfarb MT, Ellis CN, et al. Side-effect profile of acitretin therapy in psoriasis. J Am Acad Dermatol. 1989;20:1088-1093. doi:10.1016/s0190-9622(89)70138-9
- Lytvyn Y, McDonald K, Mufti A, et al. Comparing the frequency of isotretinoin-induced hair loss at <0.5-mg/kg/d versus ≥0.5-mg/kg/d dosing in acne patients: a systematic review. JAAD Int. 2022;6:125-142. doi:10.1016/j.jdin.2022.01.002
- Aboulafia DM, Norris D, Henry D, et al. 9-cis-Retinoic acid capsules in the treatment of AIDS-related Kaposi sarcoma: results of a phase 2 multicenter clinical trial. Arch Dermatol. 2003;139:178-186. doi:10.1001/archderm.139.2.178
- Cheruvattath R, Orrego M, Gautam M, et al. Vitamin A toxicity: when one a day doesn’t keep the doctor away. Liver Transpl. 2006;12:1888-1891. doi:10.1002/lt.21007
- Nan W, Li G, Si H, et al. All-trans-retinoic acid inhibits mink hair follicle growth via inhibiting proliferation and inducing apoptosis of dermal papilla cells through TGF-β2/Smad2/3 pathway. Acta Histochem. 2020;122:151603. doi:10.1016/j.acthis.2020.151603
- Georgopapadakou NH, Walsh TJ. Antifungal agents: chemotherapeutic targets and immunologic strategies. Antimicrob Agents Chemother. 1996;40:279-291. doi:10.1128/aac.40.2.279
- Sheehan DJ, Hitchcock CA, Sibley CM. Current and emerging azole antifungal agents. Clin Microbiol Rev. 1999;12:40-79. doi:10.1128/cmr.12.1.40
- Pappas PG, Kauffman CA, Perfect J, et al. Alopecia associated with fluconazole therapy. Ann Intern Med. 1995;123:354-357. doi:10.7326/0003-4819-123-5-199509010-00006
- Thompson GR 3rd, Krois CR, Affolter VK, et al. Examination of fluconazole-induced alopecia in an animal model and human cohort. Antimicrob Agents Chemother. 2019;63:e01384-18. doi:10.1128/aac.01384-18
- Malani AN, Kerr L, Obear J, et al. Alopecia and nail changes associated with voriconazole therapy. Clin Infect Dis. 2014;59:E61-E65. doi:10.1093/cid/ciu275
- Greer ND. Voriconazole: the newest triazole antifungal agent. Proc (Bayl Univ Med Cent). 2003;16:241-248. doi:10.1080/08998280.2003.11927910
- Drabin´ska B, Dettlaff K, Kossakowski K, et al. Structural and spectroscopic properties of voriconazole and fluconazole—experimental and theoretical studies. Open Chemistry. 2022;20:1575-1590. doi:10.1515/chem-2022-0253
- Löscher W. Valproate: a reappraisal of its pharmacodynamic properties and mechanisms of action. Prog Neurobiol. 1999;58:31-59. doi:10.1016/s0301-0082(98)00075-6
- Gill D, Derry S, Wiffen PJ, et al. Valproic acid and sodium valproate for neuropathic pain and fibromyalgia in adults. Cochrane Database Syst Rev. 2011;2011:CD009183. doi:10.1002/14651858.CD009183.pub2
- Depakote, Prescribing information. Abbott Laboratories; 2011. Accessed November 20, 2023. https://www.accessdata.fda.gov/drugsatfda_docs/label/2011/018723s037lbl.pdf
- Wang X, Wang H, Xu D, et al. Risk of valproic acid-related alopecia: a systematic review and meta-analysis. Seizure. 2019;69:61-69. doi:10.1016/j.seizure.2019.04.003
- Mercke Y, Sheng H, Khan T, et al. Hair loss in psychopharmacology. Ann Clin Psychiatry. 2000;12:35-42. doi:10.1023/a:1009074926921
- Bowden CL, Calabrese JR, McElroy SL, et al. A randomized, placebo-controlled 12-month trial of divalproex and lithium in treatment of outpatients with bipolar I disorder. Divalproex Maintenance Study Group. Arch Gen Psychiatry. 2000;57:481-489. doi:10.1001/archpsyc.57.5.481
- Praharaj SK, Munoli RN, Udupa ST, et al. Valproate-associated hair abnormalities: pathophysiology and management strategies. Hum Psychopharmacol. 2022;37:E2814. doi:10.1002/hup.2814
- Wilting I, van Laarhoven JH, de Koning-Verest IF, et al. Valproic acid-induced hair-texture changes in a white woman. Epilepsia. 2007;48:400-401. doi:10.1111/j.1528-1167.2006.00933.x
- Potter WZ, Ketter TA. Pharmacological issues in the treatment of bipolar disorder: focus on mood-stabilizing compounds. Can J Psychiatry. 1993;38(3 suppl 2):S51-S56.
- Castro-Gago M, Gómez-Lado C, Eirís-Pun´al J, et al. Serum biotinidase activity in children treated with valproic acid and carbamazepine. J Child Neurol. 2009;25:32-35. doi:10.1177/0883073809336118
- Schulpis KH, Karikas GA, Tjamouranis J, et al. Low serum biotinidase activity in children with valproic acid monotherapy. Epilepsia. 2001;42:1359-1362. doi:10.1046/j.1528-1157.2001.47000.x
- Yilmaz Y, Tasdemir HA, Paksu MS. The influence of valproic acid treatment on hair and serum zinc levels and serum biotinidase activity. Eur J Paediatr Neurol. 2009;13:439-443. doi:10.1016/j.ejpn.2008.08.007
- Henriksen O, Johannessen SI. Clinical and pharmacokinetic observations on sodium valproate—a 5-year follow-up study in 100 children with epilepsy. Acta Neurol Scand. 1982;65:504-523. doi:10.1111/j.1600-0404.1982.tb03106.x
- Fountoulakis KN, Tohen M, Zarate CA Jr. Lithium treatment of bipolar disorder in adults: a systematic review of randomized trials and meta-analyses. Eur Neuropsychopharmacol. 2022;54:100-115. doi:10.1016/j.euroneuro.2021.10.003
- Lithium carbonate. Prescribing information. West-Ward Pharmaceuticals; 2018. Accessed November 20, 2023. https://ww.accessdata.fda.gov/drugsatfda_docs/label/2018/017812s033,018421s032,018558s027lbl.pdf
- McKnight RF, Adida M, Budge K, et al. Lithium toxicity profile: a systematic review and meta-analysis. Lancet. 2012;379:721-728. doi:10.1016/s0140-6736(11)61516-x
- Calabrese JR, Shelton MD, Rapport DJ, et al. A 20-month, double-blind, maintenance trial of lithium versus divalproex in rapid-cycling bipolar disorder. Am J Psychiatry. 2005;162:2152-2161. doi:10.1176/appi.ajp.162.11.2152.
- Duce HL, Duff CJ, Zaidi S, et al. Evaluation of thyroid function monitoring in people treated with lithium: advice based on real-world data. Bipolar Disord. 2023;25:402-409. doi:10.1111/bdi.13298
- Bocchetta A, Loviselli A. Lithium treatment and thyroid abnormalities. Clin Pract Epidemiol Ment Health. 2006;2:23. doi:10.1186/1745-0179-2-23.
- Joffe RT. How should lithium-induced thyroid dysfunction be managed in patients with bipolar disorder? J Psychiatry Neurosci. 2002;27:392.
- Preskorn SH. Clinically relevant pharmacology of selective serotonin reuptake inhibitors. an overview with emphasis on pharmacokinetics and effects on oxidative drug metabolism. Clin Pharmacokinet. 1997;32(suppl 1):1-21. doi:10.2165/00003088-199700321-00003
- Chu A, Wadhwa R. Selective serotonin reuptake inhibitors. StatPearls. StatPearls Publishing; 2023.
- Stahl SM, Pradko JF, Haight BR, et al. A review of the neuropharmacology of bupropion, a dual norepinephrine and dopamine reuptake inhibitor. Prim Care Companion J Clin Psychiatry. 2004;6:159-166. doi:10.4088/pcc.v06n0403
- Escitalopram. Prescribing information. Solco Healthcare US, LLC; 2022. Accessed November 20, 2023. https://nctr-crs.fda.gov/fdalabel/services/spl/set-ids/2ffc6ec3-830f-46bc-9b3f-7c42cefa39b2/spl-doc
- Fluoxetine. Eli Lilly & Company; 2017. Prescribing information. Accessed November 20, 2023. https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/018936s108lbl.pdf
- Paxil. Prescribing information. GlaxoSmithKline; 2012. Accessed November 20, 2023. https://www.accessdata.fda.gov/drugsatfda_docs/label/2012/020031s067,020710s031.pdf
- Zoloft. Prescribing information. Pfizer; 2016. Accessed November 20, 2023. https://www.accessdata.fda.gov/drugsatfda_docs/label/2016/019839s74s86s87_20990s35s44s45lbl.pdf
- Celexa. Prescribing information. Allergan; 2022. Accessed November 20, 2023. https://www.accessdata.fda.gov/drugsatfda_docs/label/2022/020822s041lbl.pdf
- Pejcic AV, Paudel V. Alopecia associated with the use of selective serotonin reuptake inhibitors: systematic review. Psychiatry Res. 2022;313:114620. 10.1016/j.psychres.2022.114620
- Etminan M, Sodhi M, Procyshyn RM, et al. Risk of hair loss with different antidepressants: a comparative retrospective cohort study. Int Clin Psychopharmacol. 2018;33:44-48.
- Ghanizadeh A. Sertraline-associated hair loss. J Drugs Dermatol. 2008;7:693-694.
- Parameshwar E. Hair loss associated with fluvoxamine use. Am J Psychiatry. 1996;153:581-582. doi:10.1176/ajp.153.4.581
- Zalsman G, Sever J, Munitz H. Hair loss associated with paroxetine treatment: a case report. Clin Neuropharmacol. 1999;22:246-247.
- Ananth J, Elmishaugh A. Hair loss associated with fluoxetinetreatment. Can J Psychiatry. 1991;36:621. doi:10.1177/070674379103600824
- Tirmazi SI, Imran H, Rasheed A, et al. Escitalopram-induced hair loss. Prim Care Companion CNS Disord. 2020;22:19l02496. doi:10.4088/PCC.19l02496
Alopecia is a commonly reported side effect of various medications. Anagen effluvium and telogen effluvium (TE) are considered the most common mechanisms underlying medication-related hair loss. Anagen effluvium is associated with chemotherapeutic agents and radiation therapy, with anagen shedding typically occurring within 2 weeks of medication administration.1,2 Medication-induced TE is a diffuse nonscarring alopecia that is a reversible reactive process.3-5 Telogen effluvium is clinically apparent as a generalized shedding of scalp hair 1 to 6 months after an inciting cause.6 The underlying cause of TE may be multifactorial and difficult to identify given the delay between the trigger and the onset of clinically apparent hair loss. Other known triggers of TE include acute illness,7,8 nutritional deficiencies,4,9 and/or major surgery.10
Each hair follicle independently and sequentially progresses through anagen growth, catagen transition, and telogen resting phases. In the human scalp, the telogen phase typically lasts 3 months, at the end of which the telogen hair is extruded from the scalp. Anagen and telogen follicles typically account for an average of 90% and 10% of follicles on the human scalp, respectively.11 Immediate anagen release is hypothesized to be the mechanism underlying medication-induced TE.12 This theory suggests that an increased percentage of anagen follicles prematurely enter the telogen phase, with a notable increase in hair shedding at the conclusion of the telogen phase approximately 1 to 6 months later.12 First-line management of medication-induced TE is identification and cessation of the causative agent, if possible. Notable regrowth of hair is expected several months after removal of the inciting medication. In part 1 of this 2-part series, we review the existing literature to identify common culprits of medication-induced TE, including retinoids, antifungals, and psychotropic medications.
Retinoids
Retinoids are vitamin A derivatives used in the treatment of a myriad of dermatologic and nondermatologic conditions.13,14 Retinoids modulate sebum production,15 keratinocyte proliferation,16 and epithelial differentiation through signal transduction downstream of the ligand-activated nuclear retinoic acid receptors and retinoid X receptors.13,14,17 The recommended daily dosage of retinol is 900 µg retinol activity equivalent (3000 IU) for men and 700 µg retinol activity equivalent (2333 IU) for women. Retinoids are used in the treatment of acne vulgaris,18 psoriasis,19 and ichthyosis.20 The most commonly reported adverse effects of systemic retinoid therapy include cheilitis, alopecia, and xerosis.21 Retinoid-associated alopecia is dose and duration dependent.19,21-24 A prospective study of acitretin therapy in plaque psoriasis reported that more than 63% (42/66) of patients on 50 mg or more of acitretin daily for 6 months or longer experienced alopecia that reversed with discontinuation.23 A systematic review of isotretinoin use in acne showed alopecia was seen in 3.2% (18/565) of patients on less than 0.5 mg/kg/d of isotretinoin and in 5.7% (192/3375) of patients on 0.5 mg/kg/d or less of isotretinoin.24 In a phase 2 clinical trial of orally administered 9-cis-retinoic acid (alitretinoin) in the treatment of Kaposi sarcoma related to AIDS, 42% (24/57) of adult male patients receiving 60, 100, or 140 mg/m2 alitretinoin daily (median treatment duration, 15.1 weeks) reported alopecia as an adverse effect of treatment.25 In one case report, a patient who ingested 500,000 IU of vitamin A daily for 4 months and then 100,000 IU monthly for 6 months experienced diffusely increased shedding of scalp hair along with muscle soreness, nail dystrophy, diffuse skin rash, and refractory ascites; he was found to have severe liver damage secondary to hypervitaminosis A that required liver transplantation.26 Regarding the pathomechanism of retinoid-induced alopecia, animal and in vitro studies similarly have demonstrated that all-trans-retinoic acid appears to exert its inhibitory effects on hair follicle growth via the influence of the transforming growth factor β2 and SMAD2/3 pathway influence on dermal papillae cells.14,27 Development of hair loss secondary to systemic retinoid therapy may be managed with dose reduction or cessation.
Antifungals
Azole medications have broad-spectrum fungistatic activity against a wide range of yeast and filamentous fungi. Azoles inhibit sterol 14α-demethylase activity, impairing ergosterol synthesis and thereby disrupting plasma membrane synthesis and activity of membrane-bound enzymes.28 Fluconazole is a systemic oral agent in this class that was first approved by the US Food and Drug Administration (FDA) for use in the 1990s.29 A retrospective study by the National Institute of Allergy and Infectious Disease Mycoses Study Group followed the clinical course of 33 patients who developed alopecia while receiving fluconazole therapy for various mycoses.30 The majority (88% [29/33]) of patients received 400 mg or more of fluconazole daily. The median time to hair loss after starting fluconazole was 3 months, and the scalp was involved in all cases. In 97% (32/33) of patients, resolution of alopecia was noted following discontinuation of fluconazole or a dose reduction of 50% or more. In 85% (28/33) of patients, complete resolution of alopecia occurred within 6 months of fluconazole cessation or dose reduction.30 Fluconazole-induced TE was reproducible in an animal model using Wistar rats31; however, further studies are required to clarify the molecular pathways of its effect on hair growth.
Voriconazole is an azole approved for the treatment of invasive aspergillosis, candidemia, and fungal infections caused by Scedosporium apiospermum and Fusarium species. A retrospective survey study of patients who received voriconazole for 1 month or longer found a considerable proportion of patients developed diffuse reversible hair loss.32 Scalp alopecia was noted in 79% (120/152) of patients who completed the survey, with a mean (SD) time to alopecia of 75 (54) days after initiation of voriconazole. Notable regrowth was reported in 69% (79/114) of patients who discontinued voriconazole for at least 3 months. A subgroup of 32 patients were changed to itraconazole or posaconazole, and hair loss stopped in 84% (27/32) with regrowth noted in 69% (22/32) of patients.32 Voriconazole and fluconazole share structural similarity not present with other triazoles.33,34 Because voriconazole-associated alopecia was reversed in the majority of patients who switched to itraconazole or posaconazole, the authors hypothesized that structural similarity of fluconazole and voriconazole may underly the greater risk for TE that is not a class effect of azole medications.31
Psychotropic Medications
Various psychotropic medications have been associated with hair loss. Valproic acid (or sodium valproate) is an anticonvulsant and mood-stabilizing agent used for the treatment of seizures, bipolar disorder (BD), migraines, and neuropathic pain.35,36 Divalproex sodium (or divalproex) is an enteric-coated formulation of sodium valproate and valproic acid with similar indications. Valproate is a notorious culprit of medication-induced hair loss, with alopecia listed among the most common adverse reactions (reported >5%) on its structure product labeling document.37 A systemic review and meta-analysis by Wang et al38 estimated the overall incidence of valproate-related alopecia to be 11% (95% CI, 0.08-0.13). Although this meta-analysis did not find an association between incidence of alopecia and dose or duration of valproate therapy,38 a separate review suggested that valproate-induced alopecia is dose dependent and can be managed with dose reduction.39 A 12-month, randomized, double-blind study of treatment of BD with divalproex (valproate derivative), lithium, or placebo (2:1:1 ratio) showed a significantly higher frequency of alopecia in the divalproex group compared with placebo (16% [30/187] vs 6% [6/94]; P=.03).40 Valproate-related hair loss is characteristically diffuse and nonscarring, often noted 3 to 6 months following initiation of valproate.41,42 The proposed mechanism of valproate-induced alopecia includes chelation of zinc and selenium,43 and a reduction in serum biotinidase activity, thereby decreasing the availability of these essential micronutrients required for hair growth.41 Studies examining the effects of valproate administration and serum biotinidase activity in patients have yielded conflicting results.44-46 In a study of children with seizures including 57 patients treated with valproic acid, 17 treated with carbamazepine, and 75 age- and sex-matched healthy controls, the authors found no significant differences in serum biotinidase enzyme activity across the 3 groups.44 In contrast, a study of 75 children with seizures on valproic acid therapy stratified by dose (mean [SD])—group A: 28.7 [8.5] mg/kg/d; group B: 41.6 [4.9] mg/kg/d; group C: 64.5 [5.8] mg/kg/d—found that patients receiving higher doses (groups B and C) had significantly reduced serum biotinidase activity (1.22
Lithium carbonate (lithium) is used in the treatment of BD. Despite its efficacy and low cost, its potential for adverse effects, narrow therapeutic index, and subsequent need for routine monitoring are factors that limit its use.48 Some reported dermatologic adverse reactions on its structure product labeling include xerosis, thinning of hair, alopecia, xerosis cutis, psoriasis onset/exacerbation, and generalized pruritus.49 A systematic review and meta-analysis of 385 studies identified 24 publications reporting adverse effects of lithium on hair with no significantly increased risk of alopecia overall.50 The analysis included 2 randomized controlled trials comparing the effects of lithium and placebo on hair loss in patients with BD. Hair loss was reported in 7% (7/94) of patients taking lithium and 6% (6/94) of the placebo group in the 12-month study40 and in 3% (1/32) of the lithium group and 0% (0/28) of the divalproex group in the 20-month study.51 Despite anecdotal reports of alopecia associated with lithium, there is a lack of high-quality evidence to support this claim. Of note, hypothyroidism is a known complication of lithium use, and serum testing of thyroid function at 6-month intervals is recommended for patients on lithium treatment.52 Because thyroid abnormalities can cause alopecia distinct from TE, new-onset alopecia during lithium use should prompt serum testing of thyroid function. The development of hypothyroidism secondary to lithium is not a direct contraindication to its use53; rather, treatment should be focused on correction with thyroid replacement therapy (eg, supplementation with thyroxine).54
Commonly prescribed antidepressant medications include selective serotonin reuptake inhibitors (SSRIs) and bupropion. Selective serotonin reuptake inhibitors affect the neuronal serotonin transporter, increasing the concentration of serotonin in the synaptic cleft available for stimulation of postsynaptic serotonin receptors55,56; bupropion is an antidepressant medication that inhibits norepinephrine and dopamine reuptake at the synaptic cleft.57 Alopecia is an infrequent (1 in 100 to 1 in 1000 patients) adverse effect for several SSRIs.58-62 A recent systematic review identified a total of 71 cases of alopecia associated with SSRI use including citalopram (n=11), escitalopram (n=7), fluoxetine (n=27), fluoxvamine (n=5), paroxetine (n=4), and sertraline (n=20), with a median time to onset of hair shedding of 8.6 weeks (range, 3 days to 5 years). Discontinuation of the suspected culprit SSRI led to improvement and/or resolution in 63% (51/81) episodes of alopecia, with a median time to improvement and/or resolution of 4 weeks.63 A comparative retrospective cohort study using a large US health claims database from 2006 to 2014 included more than 1 million new and mutually exclusive patients taking fluoxetine, fluvoxamine, sertraline, citalopram, escitalopram, paroxetine, duloxetine, venlafaxine, desvenlafaxine, and bupropion.64 Overall, 1% (1569/150,404) of patients treated with bupropion received 1 or more physician visits for alopecia. Patients on SSRIs generally had a lower risk for hair loss compared with patients using bupropion (citalopram: hazard ratio [HR], 0.80 [95% CI, 0.74-0.86]; escitalopram: HR, 0.79 [95% CI, 0.74-0.86]; fluoxetine: HR, 0.68 [95% CI, 0.63-0.74]; paroxetine: HR, 0.68 [95% CI, 0.62-0.74]; sertraline: HR, 0.74 [95% CI, 0.69-0.79]), with the exception of fluvoxamine (HR, 0.93 [95% CI, 0.64-1.37]). However, the type of alopecia, time to onset, and time to resolution were not reported, making it difficult to assess whether the reported hair loss was consistent with medication-induced TE. Additionally, the authors acknowledged that bupropion may have been prescribed for smoking cessation, which may carry a different risk profile for the development of alopecia.64 Several other case reports have described alopecia following treatment with SSRIs, including sertraline,65 fluvoxamine,66 paroxetine,67 fluoxetine,68 and escitalopram.69
Overall, it appears that the use of SSRIs portends relatively low risk for alopecia and medication-induced TE. Little is known regarding the molecular effects of SSRIs on hair growth and the pathomechanism of SSRI-induced TE. The potential benefits of discontinuing a suspected culprit medication should be carefully weighed against the risks of medication cessation, and consideration should be given to alternative medications in the same class that also may be associated with TE. In patients requiring antidepressant therapy with suspected medication-induced TE, consider transitioning to a different class of medication with lower risk of medication-induced alopecia; for example, discontinuing bupropion in favor of an SSRI.
Final Thoughts
Medication-induced alopecia is an undesired side effect of many commonly used drugs and drug classes, including retinoids, azole antifungals, and mood stabilizers. Although the precise pathomechanisms of medication-induced TE remain unclear, the recommended management often requires identification of the likely causative agent and its discontinuation, if possible. Suspicion for medication-induced TE should prompt a thorough history of recent changes to medications, risk factors for nutritional deficiencies, underlying illnesses, and recent surgical procedures. Underlying nutritional, electrolyte, and/or metabolic disturbances should be corrected. In part 2 of this series, we will discuss medication-induced alopecia associated with anticoagulant and antihypertensive medications.
Alopecia is a commonly reported side effect of various medications. Anagen effluvium and telogen effluvium (TE) are considered the most common mechanisms underlying medication-related hair loss. Anagen effluvium is associated with chemotherapeutic agents and radiation therapy, with anagen shedding typically occurring within 2 weeks of medication administration.1,2 Medication-induced TE is a diffuse nonscarring alopecia that is a reversible reactive process.3-5 Telogen effluvium is clinically apparent as a generalized shedding of scalp hair 1 to 6 months after an inciting cause.6 The underlying cause of TE may be multifactorial and difficult to identify given the delay between the trigger and the onset of clinically apparent hair loss. Other known triggers of TE include acute illness,7,8 nutritional deficiencies,4,9 and/or major surgery.10
Each hair follicle independently and sequentially progresses through anagen growth, catagen transition, and telogen resting phases. In the human scalp, the telogen phase typically lasts 3 months, at the end of which the telogen hair is extruded from the scalp. Anagen and telogen follicles typically account for an average of 90% and 10% of follicles on the human scalp, respectively.11 Immediate anagen release is hypothesized to be the mechanism underlying medication-induced TE.12 This theory suggests that an increased percentage of anagen follicles prematurely enter the telogen phase, with a notable increase in hair shedding at the conclusion of the telogen phase approximately 1 to 6 months later.12 First-line management of medication-induced TE is identification and cessation of the causative agent, if possible. Notable regrowth of hair is expected several months after removal of the inciting medication. In part 1 of this 2-part series, we review the existing literature to identify common culprits of medication-induced TE, including retinoids, antifungals, and psychotropic medications.
Retinoids
Retinoids are vitamin A derivatives used in the treatment of a myriad of dermatologic and nondermatologic conditions.13,14 Retinoids modulate sebum production,15 keratinocyte proliferation,16 and epithelial differentiation through signal transduction downstream of the ligand-activated nuclear retinoic acid receptors and retinoid X receptors.13,14,17 The recommended daily dosage of retinol is 900 µg retinol activity equivalent (3000 IU) for men and 700 µg retinol activity equivalent (2333 IU) for women. Retinoids are used in the treatment of acne vulgaris,18 psoriasis,19 and ichthyosis.20 The most commonly reported adverse effects of systemic retinoid therapy include cheilitis, alopecia, and xerosis.21 Retinoid-associated alopecia is dose and duration dependent.19,21-24 A prospective study of acitretin therapy in plaque psoriasis reported that more than 63% (42/66) of patients on 50 mg or more of acitretin daily for 6 months or longer experienced alopecia that reversed with discontinuation.23 A systematic review of isotretinoin use in acne showed alopecia was seen in 3.2% (18/565) of patients on less than 0.5 mg/kg/d of isotretinoin and in 5.7% (192/3375) of patients on 0.5 mg/kg/d or less of isotretinoin.24 In a phase 2 clinical trial of orally administered 9-cis-retinoic acid (alitretinoin) in the treatment of Kaposi sarcoma related to AIDS, 42% (24/57) of adult male patients receiving 60, 100, or 140 mg/m2 alitretinoin daily (median treatment duration, 15.1 weeks) reported alopecia as an adverse effect of treatment.25 In one case report, a patient who ingested 500,000 IU of vitamin A daily for 4 months and then 100,000 IU monthly for 6 months experienced diffusely increased shedding of scalp hair along with muscle soreness, nail dystrophy, diffuse skin rash, and refractory ascites; he was found to have severe liver damage secondary to hypervitaminosis A that required liver transplantation.26 Regarding the pathomechanism of retinoid-induced alopecia, animal and in vitro studies similarly have demonstrated that all-trans-retinoic acid appears to exert its inhibitory effects on hair follicle growth via the influence of the transforming growth factor β2 and SMAD2/3 pathway influence on dermal papillae cells.14,27 Development of hair loss secondary to systemic retinoid therapy may be managed with dose reduction or cessation.
Antifungals
Azole medications have broad-spectrum fungistatic activity against a wide range of yeast and filamentous fungi. Azoles inhibit sterol 14α-demethylase activity, impairing ergosterol synthesis and thereby disrupting plasma membrane synthesis and activity of membrane-bound enzymes.28 Fluconazole is a systemic oral agent in this class that was first approved by the US Food and Drug Administration (FDA) for use in the 1990s.29 A retrospective study by the National Institute of Allergy and Infectious Disease Mycoses Study Group followed the clinical course of 33 patients who developed alopecia while receiving fluconazole therapy for various mycoses.30 The majority (88% [29/33]) of patients received 400 mg or more of fluconazole daily. The median time to hair loss after starting fluconazole was 3 months, and the scalp was involved in all cases. In 97% (32/33) of patients, resolution of alopecia was noted following discontinuation of fluconazole or a dose reduction of 50% or more. In 85% (28/33) of patients, complete resolution of alopecia occurred within 6 months of fluconazole cessation or dose reduction.30 Fluconazole-induced TE was reproducible in an animal model using Wistar rats31; however, further studies are required to clarify the molecular pathways of its effect on hair growth.
Voriconazole is an azole approved for the treatment of invasive aspergillosis, candidemia, and fungal infections caused by Scedosporium apiospermum and Fusarium species. A retrospective survey study of patients who received voriconazole for 1 month or longer found a considerable proportion of patients developed diffuse reversible hair loss.32 Scalp alopecia was noted in 79% (120/152) of patients who completed the survey, with a mean (SD) time to alopecia of 75 (54) days after initiation of voriconazole. Notable regrowth was reported in 69% (79/114) of patients who discontinued voriconazole for at least 3 months. A subgroup of 32 patients were changed to itraconazole or posaconazole, and hair loss stopped in 84% (27/32) with regrowth noted in 69% (22/32) of patients.32 Voriconazole and fluconazole share structural similarity not present with other triazoles.33,34 Because voriconazole-associated alopecia was reversed in the majority of patients who switched to itraconazole or posaconazole, the authors hypothesized that structural similarity of fluconazole and voriconazole may underly the greater risk for TE that is not a class effect of azole medications.31
Psychotropic Medications
Various psychotropic medications have been associated with hair loss. Valproic acid (or sodium valproate) is an anticonvulsant and mood-stabilizing agent used for the treatment of seizures, bipolar disorder (BD), migraines, and neuropathic pain.35,36 Divalproex sodium (or divalproex) is an enteric-coated formulation of sodium valproate and valproic acid with similar indications. Valproate is a notorious culprit of medication-induced hair loss, with alopecia listed among the most common adverse reactions (reported >5%) on its structure product labeling document.37 A systemic review and meta-analysis by Wang et al38 estimated the overall incidence of valproate-related alopecia to be 11% (95% CI, 0.08-0.13). Although this meta-analysis did not find an association between incidence of alopecia and dose or duration of valproate therapy,38 a separate review suggested that valproate-induced alopecia is dose dependent and can be managed with dose reduction.39 A 12-month, randomized, double-blind study of treatment of BD with divalproex (valproate derivative), lithium, or placebo (2:1:1 ratio) showed a significantly higher frequency of alopecia in the divalproex group compared with placebo (16% [30/187] vs 6% [6/94]; P=.03).40 Valproate-related hair loss is characteristically diffuse and nonscarring, often noted 3 to 6 months following initiation of valproate.41,42 The proposed mechanism of valproate-induced alopecia includes chelation of zinc and selenium,43 and a reduction in serum biotinidase activity, thereby decreasing the availability of these essential micronutrients required for hair growth.41 Studies examining the effects of valproate administration and serum biotinidase activity in patients have yielded conflicting results.44-46 In a study of children with seizures including 57 patients treated with valproic acid, 17 treated with carbamazepine, and 75 age- and sex-matched healthy controls, the authors found no significant differences in serum biotinidase enzyme activity across the 3 groups.44 In contrast, a study of 75 children with seizures on valproic acid therapy stratified by dose (mean [SD])—group A: 28.7 [8.5] mg/kg/d; group B: 41.6 [4.9] mg/kg/d; group C: 64.5 [5.8] mg/kg/d—found that patients receiving higher doses (groups B and C) had significantly reduced serum biotinidase activity (1.22
Lithium carbonate (lithium) is used in the treatment of BD. Despite its efficacy and low cost, its potential for adverse effects, narrow therapeutic index, and subsequent need for routine monitoring are factors that limit its use.48 Some reported dermatologic adverse reactions on its structure product labeling include xerosis, thinning of hair, alopecia, xerosis cutis, psoriasis onset/exacerbation, and generalized pruritus.49 A systematic review and meta-analysis of 385 studies identified 24 publications reporting adverse effects of lithium on hair with no significantly increased risk of alopecia overall.50 The analysis included 2 randomized controlled trials comparing the effects of lithium and placebo on hair loss in patients with BD. Hair loss was reported in 7% (7/94) of patients taking lithium and 6% (6/94) of the placebo group in the 12-month study40 and in 3% (1/32) of the lithium group and 0% (0/28) of the divalproex group in the 20-month study.51 Despite anecdotal reports of alopecia associated with lithium, there is a lack of high-quality evidence to support this claim. Of note, hypothyroidism is a known complication of lithium use, and serum testing of thyroid function at 6-month intervals is recommended for patients on lithium treatment.52 Because thyroid abnormalities can cause alopecia distinct from TE, new-onset alopecia during lithium use should prompt serum testing of thyroid function. The development of hypothyroidism secondary to lithium is not a direct contraindication to its use53; rather, treatment should be focused on correction with thyroid replacement therapy (eg, supplementation with thyroxine).54
Commonly prescribed antidepressant medications include selective serotonin reuptake inhibitors (SSRIs) and bupropion. Selective serotonin reuptake inhibitors affect the neuronal serotonin transporter, increasing the concentration of serotonin in the synaptic cleft available for stimulation of postsynaptic serotonin receptors55,56; bupropion is an antidepressant medication that inhibits norepinephrine and dopamine reuptake at the synaptic cleft.57 Alopecia is an infrequent (1 in 100 to 1 in 1000 patients) adverse effect for several SSRIs.58-62 A recent systematic review identified a total of 71 cases of alopecia associated with SSRI use including citalopram (n=11), escitalopram (n=7), fluoxetine (n=27), fluoxvamine (n=5), paroxetine (n=4), and sertraline (n=20), with a median time to onset of hair shedding of 8.6 weeks (range, 3 days to 5 years). Discontinuation of the suspected culprit SSRI led to improvement and/or resolution in 63% (51/81) episodes of alopecia, with a median time to improvement and/or resolution of 4 weeks.63 A comparative retrospective cohort study using a large US health claims database from 2006 to 2014 included more than 1 million new and mutually exclusive patients taking fluoxetine, fluvoxamine, sertraline, citalopram, escitalopram, paroxetine, duloxetine, venlafaxine, desvenlafaxine, and bupropion.64 Overall, 1% (1569/150,404) of patients treated with bupropion received 1 or more physician visits for alopecia. Patients on SSRIs generally had a lower risk for hair loss compared with patients using bupropion (citalopram: hazard ratio [HR], 0.80 [95% CI, 0.74-0.86]; escitalopram: HR, 0.79 [95% CI, 0.74-0.86]; fluoxetine: HR, 0.68 [95% CI, 0.63-0.74]; paroxetine: HR, 0.68 [95% CI, 0.62-0.74]; sertraline: HR, 0.74 [95% CI, 0.69-0.79]), with the exception of fluvoxamine (HR, 0.93 [95% CI, 0.64-1.37]). However, the type of alopecia, time to onset, and time to resolution were not reported, making it difficult to assess whether the reported hair loss was consistent with medication-induced TE. Additionally, the authors acknowledged that bupropion may have been prescribed for smoking cessation, which may carry a different risk profile for the development of alopecia.64 Several other case reports have described alopecia following treatment with SSRIs, including sertraline,65 fluvoxamine,66 paroxetine,67 fluoxetine,68 and escitalopram.69
Overall, it appears that the use of SSRIs portends relatively low risk for alopecia and medication-induced TE. Little is known regarding the molecular effects of SSRIs on hair growth and the pathomechanism of SSRI-induced TE. The potential benefits of discontinuing a suspected culprit medication should be carefully weighed against the risks of medication cessation, and consideration should be given to alternative medications in the same class that also may be associated with TE. In patients requiring antidepressant therapy with suspected medication-induced TE, consider transitioning to a different class of medication with lower risk of medication-induced alopecia; for example, discontinuing bupropion in favor of an SSRI.
Final Thoughts
Medication-induced alopecia is an undesired side effect of many commonly used drugs and drug classes, including retinoids, azole antifungals, and mood stabilizers. Although the precise pathomechanisms of medication-induced TE remain unclear, the recommended management often requires identification of the likely causative agent and its discontinuation, if possible. Suspicion for medication-induced TE should prompt a thorough history of recent changes to medications, risk factors for nutritional deficiencies, underlying illnesses, and recent surgical procedures. Underlying nutritional, electrolyte, and/or metabolic disturbances should be corrected. In part 2 of this series, we will discuss medication-induced alopecia associated with anticoagulant and antihypertensive medications.
- Saleh D, Nassereddin A, Cook C. Anagen effluvium. StatPearls. StatPearls Publishing; 2023. https://www.ncbi.nlm.nih.gov/books/NBK482293/
- Guerrero-Putz MD, Flores-Dominguez AC, Castillo-de la Garza RJ, et al. Anagen effluvium after neurointerventional radiation: trichoscopy as a diagnostic ally. Skin Appendage Disord. 2021;8:102-107. doi:10.1159/000518743
- Patel M, Harrison S, Sinclair R. Drugs and hair loss. Dermatol Clin. 2013;31:67-73. doi:https://doi.org/10.1016/j.det.2012.08.002
- Chen V, Strazzulla L, Asbeck SM, et al. Etiology, management, and outcomes of pediatric telogen effluvium: a single-center study in the United States. Pediatr Dermatol. 2023;40:120-124. doi:10.1111/pde.15154
- Watras MM, Patel JP, Arya R. Traditional anticoagulants and hair loss: a role for direct oral anticoagulants? a review of the literature. Drugs Real World Outcomes. 2016;3:1-6. doi:10.1007/s40801-015-0056-z
- Hughes EC, Saleh D. Telogen effluvium. StatPearls. StatPearls Publishing; 2023. https://www.ncbi.nlm.nih.gov/books/NBK430848/
- Nguyen B, Tosti A. Alopecia in patients with COVID-19: a systematic review and meta-analysis. JAAD Int. 2022;7:67-77. doi:10.1016/j.jdin.2022.02.006
- Starace M, Piraccini BM, Evangelista V, et al. Acute telogen effluvium due to dengue fever mimicking androgenetic alopecia. Ital J Dermatol Venerol. 2023;158:66-67. doi:10.23736/s2784-8671.22.07369-8
- Patel KV, Farrant P, Sanderson JD, et al. Hair loss in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2013;19:1753-1763. doi:10.1097/MIB.0b013e31828132de
- Cohen-Kurzrock RA, Cohen PR. Bariatric surgery–induced telogen effluvium (bar site): case report and a review of hair loss following weight loss surgery. Cureus. 2021;13:E14617. doi:10.7759/cureus.14617
- Price VH. Treatment of hair loss. N Engl J Med. 1999;341:964-973. doi:10.1056/nejm199909233411307
- Headington JT. Telogen effluvium: new concepts and review. Arch Dermatol. 1993;129:356-363. doi:10.1001/arcderm.1993.01680240096017
- Lee DD, Stojadinovic O, Krzyzanowska A, et al. Retinoid-responsive transcriptional changes in epidermal keratinocytes. J Cell Physiol. 2009;220:427-439. doi:10.1002/jcp.21784
- Foitzik K, Spexard T, Nakamura M, et al. Towards dissecting the pathogenesis of retinoid-induced hair loss: all-trans retinoic acid induces premature hair follicle regression (catagen) by upregulation of transforming growth factor-beta2 in the dermal papilla. J Invest Dermatol. 2005;124:1119-1126. doi:10.1111/j.0022-202X.2005.23686.x
- Karlsson T, Vahlquist A, Kedishvili N, et al. 13-cis-retinoic acid competitively inhibits 3 alpha-hydroxysteroid oxidation by retinol dehydrogenase RoDH-4: a mechanism for its anti-androgenic effects in sebaceous glands? Biochem Biophys Res Commun. 2003;303:273-278. doi:10.1016/s0006-291x(03)00332-2
- Chapellier B, Mark M, Messaddeq N, et al. Physiological and retinoid-induced proliferations of epidermis basal keratinocytes are differently controlled. EMBO J. 2002;21:3402-3413. doi:10.1093/emboj/cdf331
- Geiger JM. Retinoids and sebaceous gland activity. Dermatology. 1995;191:305-310. doi:10.1159/000246581
- Oge LK, Broussard A, Marshall MD. Acne vulgaris: diagnosis and treatment. Am Fam Physician. 2019;100:475-484.
- Pilkington T, Brogden RN. Acitretin. Drugs. 1992;43:597-627. doi:10.2165/00003495-199243040-00010
- Zaenglein AL, Levy ML, Stefanko NS, et al. Consensus recommendations for the use of retinoids in ichthyosis and other disorders of cornification in children and adolescents. Pediatr Dermatol. 2021;38:164-180. doi:10.1111/pde.14408
- Katz HI, Waalen J, Leach EE. Acitretin in psoriasis: an overview of adverse effects. J Am Acad Dermatol. 1999;41(3 suppl):S7-S12. doi:10.1016/s0190-9622(99)70359-2
- Tran PT, Evron E, Goh C. Characteristics of patients with hair loss after isotretinoin treatment: a retrospective review study. Int J Trichology. 2022;14:125-127. doi:10.4103/ijt.ijt_80_20
- Gupta AK, Goldfarb MT, Ellis CN, et al. Side-effect profile of acitretin therapy in psoriasis. J Am Acad Dermatol. 1989;20:1088-1093. doi:10.1016/s0190-9622(89)70138-9
- Lytvyn Y, McDonald K, Mufti A, et al. Comparing the frequency of isotretinoin-induced hair loss at <0.5-mg/kg/d versus ≥0.5-mg/kg/d dosing in acne patients: a systematic review. JAAD Int. 2022;6:125-142. doi:10.1016/j.jdin.2022.01.002
- Aboulafia DM, Norris D, Henry D, et al. 9-cis-Retinoic acid capsules in the treatment of AIDS-related Kaposi sarcoma: results of a phase 2 multicenter clinical trial. Arch Dermatol. 2003;139:178-186. doi:10.1001/archderm.139.2.178
- Cheruvattath R, Orrego M, Gautam M, et al. Vitamin A toxicity: when one a day doesn’t keep the doctor away. Liver Transpl. 2006;12:1888-1891. doi:10.1002/lt.21007
- Nan W, Li G, Si H, et al. All-trans-retinoic acid inhibits mink hair follicle growth via inhibiting proliferation and inducing apoptosis of dermal papilla cells through TGF-β2/Smad2/3 pathway. Acta Histochem. 2020;122:151603. doi:10.1016/j.acthis.2020.151603
- Georgopapadakou NH, Walsh TJ. Antifungal agents: chemotherapeutic targets and immunologic strategies. Antimicrob Agents Chemother. 1996;40:279-291. doi:10.1128/aac.40.2.279
- Sheehan DJ, Hitchcock CA, Sibley CM. Current and emerging azole antifungal agents. Clin Microbiol Rev. 1999;12:40-79. doi:10.1128/cmr.12.1.40
- Pappas PG, Kauffman CA, Perfect J, et al. Alopecia associated with fluconazole therapy. Ann Intern Med. 1995;123:354-357. doi:10.7326/0003-4819-123-5-199509010-00006
- Thompson GR 3rd, Krois CR, Affolter VK, et al. Examination of fluconazole-induced alopecia in an animal model and human cohort. Antimicrob Agents Chemother. 2019;63:e01384-18. doi:10.1128/aac.01384-18
- Malani AN, Kerr L, Obear J, et al. Alopecia and nail changes associated with voriconazole therapy. Clin Infect Dis. 2014;59:E61-E65. doi:10.1093/cid/ciu275
- Greer ND. Voriconazole: the newest triazole antifungal agent. Proc (Bayl Univ Med Cent). 2003;16:241-248. doi:10.1080/08998280.2003.11927910
- Drabin´ska B, Dettlaff K, Kossakowski K, et al. Structural and spectroscopic properties of voriconazole and fluconazole—experimental and theoretical studies. Open Chemistry. 2022;20:1575-1590. doi:10.1515/chem-2022-0253
- Löscher W. Valproate: a reappraisal of its pharmacodynamic properties and mechanisms of action. Prog Neurobiol. 1999;58:31-59. doi:10.1016/s0301-0082(98)00075-6
- Gill D, Derry S, Wiffen PJ, et al. Valproic acid and sodium valproate for neuropathic pain and fibromyalgia in adults. Cochrane Database Syst Rev. 2011;2011:CD009183. doi:10.1002/14651858.CD009183.pub2
- Depakote, Prescribing information. Abbott Laboratories; 2011. Accessed November 20, 2023. https://www.accessdata.fda.gov/drugsatfda_docs/label/2011/018723s037lbl.pdf
- Wang X, Wang H, Xu D, et al. Risk of valproic acid-related alopecia: a systematic review and meta-analysis. Seizure. 2019;69:61-69. doi:10.1016/j.seizure.2019.04.003
- Mercke Y, Sheng H, Khan T, et al. Hair loss in psychopharmacology. Ann Clin Psychiatry. 2000;12:35-42. doi:10.1023/a:1009074926921
- Bowden CL, Calabrese JR, McElroy SL, et al. A randomized, placebo-controlled 12-month trial of divalproex and lithium in treatment of outpatients with bipolar I disorder. Divalproex Maintenance Study Group. Arch Gen Psychiatry. 2000;57:481-489. doi:10.1001/archpsyc.57.5.481
- Praharaj SK, Munoli RN, Udupa ST, et al. Valproate-associated hair abnormalities: pathophysiology and management strategies. Hum Psychopharmacol. 2022;37:E2814. doi:10.1002/hup.2814
- Wilting I, van Laarhoven JH, de Koning-Verest IF, et al. Valproic acid-induced hair-texture changes in a white woman. Epilepsia. 2007;48:400-401. doi:10.1111/j.1528-1167.2006.00933.x
- Potter WZ, Ketter TA. Pharmacological issues in the treatment of bipolar disorder: focus on mood-stabilizing compounds. Can J Psychiatry. 1993;38(3 suppl 2):S51-S56.
- Castro-Gago M, Gómez-Lado C, Eirís-Pun´al J, et al. Serum biotinidase activity in children treated with valproic acid and carbamazepine. J Child Neurol. 2009;25:32-35. doi:10.1177/0883073809336118
- Schulpis KH, Karikas GA, Tjamouranis J, et al. Low serum biotinidase activity in children with valproic acid monotherapy. Epilepsia. 2001;42:1359-1362. doi:10.1046/j.1528-1157.2001.47000.x
- Yilmaz Y, Tasdemir HA, Paksu MS. The influence of valproic acid treatment on hair and serum zinc levels and serum biotinidase activity. Eur J Paediatr Neurol. 2009;13:439-443. doi:10.1016/j.ejpn.2008.08.007
- Henriksen O, Johannessen SI. Clinical and pharmacokinetic observations on sodium valproate—a 5-year follow-up study in 100 children with epilepsy. Acta Neurol Scand. 1982;65:504-523. doi:10.1111/j.1600-0404.1982.tb03106.x
- Fountoulakis KN, Tohen M, Zarate CA Jr. Lithium treatment of bipolar disorder in adults: a systematic review of randomized trials and meta-analyses. Eur Neuropsychopharmacol. 2022;54:100-115. doi:10.1016/j.euroneuro.2021.10.003
- Lithium carbonate. Prescribing information. West-Ward Pharmaceuticals; 2018. Accessed November 20, 2023. https://ww.accessdata.fda.gov/drugsatfda_docs/label/2018/017812s033,018421s032,018558s027lbl.pdf
- McKnight RF, Adida M, Budge K, et al. Lithium toxicity profile: a systematic review and meta-analysis. Lancet. 2012;379:721-728. doi:10.1016/s0140-6736(11)61516-x
- Calabrese JR, Shelton MD, Rapport DJ, et al. A 20-month, double-blind, maintenance trial of lithium versus divalproex in rapid-cycling bipolar disorder. Am J Psychiatry. 2005;162:2152-2161. doi:10.1176/appi.ajp.162.11.2152.
- Duce HL, Duff CJ, Zaidi S, et al. Evaluation of thyroid function monitoring in people treated with lithium: advice based on real-world data. Bipolar Disord. 2023;25:402-409. doi:10.1111/bdi.13298
- Bocchetta A, Loviselli A. Lithium treatment and thyroid abnormalities. Clin Pract Epidemiol Ment Health. 2006;2:23. doi:10.1186/1745-0179-2-23.
- Joffe RT. How should lithium-induced thyroid dysfunction be managed in patients with bipolar disorder? J Psychiatry Neurosci. 2002;27:392.
- Preskorn SH. Clinically relevant pharmacology of selective serotonin reuptake inhibitors. an overview with emphasis on pharmacokinetics and effects on oxidative drug metabolism. Clin Pharmacokinet. 1997;32(suppl 1):1-21. doi:10.2165/00003088-199700321-00003
- Chu A, Wadhwa R. Selective serotonin reuptake inhibitors. StatPearls. StatPearls Publishing; 2023.
- Stahl SM, Pradko JF, Haight BR, et al. A review of the neuropharmacology of bupropion, a dual norepinephrine and dopamine reuptake inhibitor. Prim Care Companion J Clin Psychiatry. 2004;6:159-166. doi:10.4088/pcc.v06n0403
- Escitalopram. Prescribing information. Solco Healthcare US, LLC; 2022. Accessed November 20, 2023. https://nctr-crs.fda.gov/fdalabel/services/spl/set-ids/2ffc6ec3-830f-46bc-9b3f-7c42cefa39b2/spl-doc
- Fluoxetine. Eli Lilly & Company; 2017. Prescribing information. Accessed November 20, 2023. https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/018936s108lbl.pdf
- Paxil. Prescribing information. GlaxoSmithKline; 2012. Accessed November 20, 2023. https://www.accessdata.fda.gov/drugsatfda_docs/label/2012/020031s067,020710s031.pdf
- Zoloft. Prescribing information. Pfizer; 2016. Accessed November 20, 2023. https://www.accessdata.fda.gov/drugsatfda_docs/label/2016/019839s74s86s87_20990s35s44s45lbl.pdf
- Celexa. Prescribing information. Allergan; 2022. Accessed November 20, 2023. https://www.accessdata.fda.gov/drugsatfda_docs/label/2022/020822s041lbl.pdf
- Pejcic AV, Paudel V. Alopecia associated with the use of selective serotonin reuptake inhibitors: systematic review. Psychiatry Res. 2022;313:114620. 10.1016/j.psychres.2022.114620
- Etminan M, Sodhi M, Procyshyn RM, et al. Risk of hair loss with different antidepressants: a comparative retrospective cohort study. Int Clin Psychopharmacol. 2018;33:44-48.
- Ghanizadeh A. Sertraline-associated hair loss. J Drugs Dermatol. 2008;7:693-694.
- Parameshwar E. Hair loss associated with fluvoxamine use. Am J Psychiatry. 1996;153:581-582. doi:10.1176/ajp.153.4.581
- Zalsman G, Sever J, Munitz H. Hair loss associated with paroxetine treatment: a case report. Clin Neuropharmacol. 1999;22:246-247.
- Ananth J, Elmishaugh A. Hair loss associated with fluoxetinetreatment. Can J Psychiatry. 1991;36:621. doi:10.1177/070674379103600824
- Tirmazi SI, Imran H, Rasheed A, et al. Escitalopram-induced hair loss. Prim Care Companion CNS Disord. 2020;22:19l02496. doi:10.4088/PCC.19l02496
- Saleh D, Nassereddin A, Cook C. Anagen effluvium. StatPearls. StatPearls Publishing; 2023. https://www.ncbi.nlm.nih.gov/books/NBK482293/
- Guerrero-Putz MD, Flores-Dominguez AC, Castillo-de la Garza RJ, et al. Anagen effluvium after neurointerventional radiation: trichoscopy as a diagnostic ally. Skin Appendage Disord. 2021;8:102-107. doi:10.1159/000518743
- Patel M, Harrison S, Sinclair R. Drugs and hair loss. Dermatol Clin. 2013;31:67-73. doi:https://doi.org/10.1016/j.det.2012.08.002
- Chen V, Strazzulla L, Asbeck SM, et al. Etiology, management, and outcomes of pediatric telogen effluvium: a single-center study in the United States. Pediatr Dermatol. 2023;40:120-124. doi:10.1111/pde.15154
- Watras MM, Patel JP, Arya R. Traditional anticoagulants and hair loss: a role for direct oral anticoagulants? a review of the literature. Drugs Real World Outcomes. 2016;3:1-6. doi:10.1007/s40801-015-0056-z
- Hughes EC, Saleh D. Telogen effluvium. StatPearls. StatPearls Publishing; 2023. https://www.ncbi.nlm.nih.gov/books/NBK430848/
- Nguyen B, Tosti A. Alopecia in patients with COVID-19: a systematic review and meta-analysis. JAAD Int. 2022;7:67-77. doi:10.1016/j.jdin.2022.02.006
- Starace M, Piraccini BM, Evangelista V, et al. Acute telogen effluvium due to dengue fever mimicking androgenetic alopecia. Ital J Dermatol Venerol. 2023;158:66-67. doi:10.23736/s2784-8671.22.07369-8
- Patel KV, Farrant P, Sanderson JD, et al. Hair loss in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2013;19:1753-1763. doi:10.1097/MIB.0b013e31828132de
- Cohen-Kurzrock RA, Cohen PR. Bariatric surgery–induced telogen effluvium (bar site): case report and a review of hair loss following weight loss surgery. Cureus. 2021;13:E14617. doi:10.7759/cureus.14617
- Price VH. Treatment of hair loss. N Engl J Med. 1999;341:964-973. doi:10.1056/nejm199909233411307
- Headington JT. Telogen effluvium: new concepts and review. Arch Dermatol. 1993;129:356-363. doi:10.1001/arcderm.1993.01680240096017
- Lee DD, Stojadinovic O, Krzyzanowska A, et al. Retinoid-responsive transcriptional changes in epidermal keratinocytes. J Cell Physiol. 2009;220:427-439. doi:10.1002/jcp.21784
- Foitzik K, Spexard T, Nakamura M, et al. Towards dissecting the pathogenesis of retinoid-induced hair loss: all-trans retinoic acid induces premature hair follicle regression (catagen) by upregulation of transforming growth factor-beta2 in the dermal papilla. J Invest Dermatol. 2005;124:1119-1126. doi:10.1111/j.0022-202X.2005.23686.x
- Karlsson T, Vahlquist A, Kedishvili N, et al. 13-cis-retinoic acid competitively inhibits 3 alpha-hydroxysteroid oxidation by retinol dehydrogenase RoDH-4: a mechanism for its anti-androgenic effects in sebaceous glands? Biochem Biophys Res Commun. 2003;303:273-278. doi:10.1016/s0006-291x(03)00332-2
- Chapellier B, Mark M, Messaddeq N, et al. Physiological and retinoid-induced proliferations of epidermis basal keratinocytes are differently controlled. EMBO J. 2002;21:3402-3413. doi:10.1093/emboj/cdf331
- Geiger JM. Retinoids and sebaceous gland activity. Dermatology. 1995;191:305-310. doi:10.1159/000246581
- Oge LK, Broussard A, Marshall MD. Acne vulgaris: diagnosis and treatment. Am Fam Physician. 2019;100:475-484.
- Pilkington T, Brogden RN. Acitretin. Drugs. 1992;43:597-627. doi:10.2165/00003495-199243040-00010
- Zaenglein AL, Levy ML, Stefanko NS, et al. Consensus recommendations for the use of retinoids in ichthyosis and other disorders of cornification in children and adolescents. Pediatr Dermatol. 2021;38:164-180. doi:10.1111/pde.14408
- Katz HI, Waalen J, Leach EE. Acitretin in psoriasis: an overview of adverse effects. J Am Acad Dermatol. 1999;41(3 suppl):S7-S12. doi:10.1016/s0190-9622(99)70359-2
- Tran PT, Evron E, Goh C. Characteristics of patients with hair loss after isotretinoin treatment: a retrospective review study. Int J Trichology. 2022;14:125-127. doi:10.4103/ijt.ijt_80_20
- Gupta AK, Goldfarb MT, Ellis CN, et al. Side-effect profile of acitretin therapy in psoriasis. J Am Acad Dermatol. 1989;20:1088-1093. doi:10.1016/s0190-9622(89)70138-9
- Lytvyn Y, McDonald K, Mufti A, et al. Comparing the frequency of isotretinoin-induced hair loss at <0.5-mg/kg/d versus ≥0.5-mg/kg/d dosing in acne patients: a systematic review. JAAD Int. 2022;6:125-142. doi:10.1016/j.jdin.2022.01.002
- Aboulafia DM, Norris D, Henry D, et al. 9-cis-Retinoic acid capsules in the treatment of AIDS-related Kaposi sarcoma: results of a phase 2 multicenter clinical trial. Arch Dermatol. 2003;139:178-186. doi:10.1001/archderm.139.2.178
- Cheruvattath R, Orrego M, Gautam M, et al. Vitamin A toxicity: when one a day doesn’t keep the doctor away. Liver Transpl. 2006;12:1888-1891. doi:10.1002/lt.21007
- Nan W, Li G, Si H, et al. All-trans-retinoic acid inhibits mink hair follicle growth via inhibiting proliferation and inducing apoptosis of dermal papilla cells through TGF-β2/Smad2/3 pathway. Acta Histochem. 2020;122:151603. doi:10.1016/j.acthis.2020.151603
- Georgopapadakou NH, Walsh TJ. Antifungal agents: chemotherapeutic targets and immunologic strategies. Antimicrob Agents Chemother. 1996;40:279-291. doi:10.1128/aac.40.2.279
- Sheehan DJ, Hitchcock CA, Sibley CM. Current and emerging azole antifungal agents. Clin Microbiol Rev. 1999;12:40-79. doi:10.1128/cmr.12.1.40
- Pappas PG, Kauffman CA, Perfect J, et al. Alopecia associated with fluconazole therapy. Ann Intern Med. 1995;123:354-357. doi:10.7326/0003-4819-123-5-199509010-00006
- Thompson GR 3rd, Krois CR, Affolter VK, et al. Examination of fluconazole-induced alopecia in an animal model and human cohort. Antimicrob Agents Chemother. 2019;63:e01384-18. doi:10.1128/aac.01384-18
- Malani AN, Kerr L, Obear J, et al. Alopecia and nail changes associated with voriconazole therapy. Clin Infect Dis. 2014;59:E61-E65. doi:10.1093/cid/ciu275
- Greer ND. Voriconazole: the newest triazole antifungal agent. Proc (Bayl Univ Med Cent). 2003;16:241-248. doi:10.1080/08998280.2003.11927910
- Drabin´ska B, Dettlaff K, Kossakowski K, et al. Structural and spectroscopic properties of voriconazole and fluconazole—experimental and theoretical studies. Open Chemistry. 2022;20:1575-1590. doi:10.1515/chem-2022-0253
- Löscher W. Valproate: a reappraisal of its pharmacodynamic properties and mechanisms of action. Prog Neurobiol. 1999;58:31-59. doi:10.1016/s0301-0082(98)00075-6
- Gill D, Derry S, Wiffen PJ, et al. Valproic acid and sodium valproate for neuropathic pain and fibromyalgia in adults. Cochrane Database Syst Rev. 2011;2011:CD009183. doi:10.1002/14651858.CD009183.pub2
- Depakote, Prescribing information. Abbott Laboratories; 2011. Accessed November 20, 2023. https://www.accessdata.fda.gov/drugsatfda_docs/label/2011/018723s037lbl.pdf
- Wang X, Wang H, Xu D, et al. Risk of valproic acid-related alopecia: a systematic review and meta-analysis. Seizure. 2019;69:61-69. doi:10.1016/j.seizure.2019.04.003
- Mercke Y, Sheng H, Khan T, et al. Hair loss in psychopharmacology. Ann Clin Psychiatry. 2000;12:35-42. doi:10.1023/a:1009074926921
- Bowden CL, Calabrese JR, McElroy SL, et al. A randomized, placebo-controlled 12-month trial of divalproex and lithium in treatment of outpatients with bipolar I disorder. Divalproex Maintenance Study Group. Arch Gen Psychiatry. 2000;57:481-489. doi:10.1001/archpsyc.57.5.481
- Praharaj SK, Munoli RN, Udupa ST, et al. Valproate-associated hair abnormalities: pathophysiology and management strategies. Hum Psychopharmacol. 2022;37:E2814. doi:10.1002/hup.2814
- Wilting I, van Laarhoven JH, de Koning-Verest IF, et al. Valproic acid-induced hair-texture changes in a white woman. Epilepsia. 2007;48:400-401. doi:10.1111/j.1528-1167.2006.00933.x
- Potter WZ, Ketter TA. Pharmacological issues in the treatment of bipolar disorder: focus on mood-stabilizing compounds. Can J Psychiatry. 1993;38(3 suppl 2):S51-S56.
- Castro-Gago M, Gómez-Lado C, Eirís-Pun´al J, et al. Serum biotinidase activity in children treated with valproic acid and carbamazepine. J Child Neurol. 2009;25:32-35. doi:10.1177/0883073809336118
- Schulpis KH, Karikas GA, Tjamouranis J, et al. Low serum biotinidase activity in children with valproic acid monotherapy. Epilepsia. 2001;42:1359-1362. doi:10.1046/j.1528-1157.2001.47000.x
- Yilmaz Y, Tasdemir HA, Paksu MS. The influence of valproic acid treatment on hair and serum zinc levels and serum biotinidase activity. Eur J Paediatr Neurol. 2009;13:439-443. doi:10.1016/j.ejpn.2008.08.007
- Henriksen O, Johannessen SI. Clinical and pharmacokinetic observations on sodium valproate—a 5-year follow-up study in 100 children with epilepsy. Acta Neurol Scand. 1982;65:504-523. doi:10.1111/j.1600-0404.1982.tb03106.x
- Fountoulakis KN, Tohen M, Zarate CA Jr. Lithium treatment of bipolar disorder in adults: a systematic review of randomized trials and meta-analyses. Eur Neuropsychopharmacol. 2022;54:100-115. doi:10.1016/j.euroneuro.2021.10.003
- Lithium carbonate. Prescribing information. West-Ward Pharmaceuticals; 2018. Accessed November 20, 2023. https://ww.accessdata.fda.gov/drugsatfda_docs/label/2018/017812s033,018421s032,018558s027lbl.pdf
- McKnight RF, Adida M, Budge K, et al. Lithium toxicity profile: a systematic review and meta-analysis. Lancet. 2012;379:721-728. doi:10.1016/s0140-6736(11)61516-x
- Calabrese JR, Shelton MD, Rapport DJ, et al. A 20-month, double-blind, maintenance trial of lithium versus divalproex in rapid-cycling bipolar disorder. Am J Psychiatry. 2005;162:2152-2161. doi:10.1176/appi.ajp.162.11.2152.
- Duce HL, Duff CJ, Zaidi S, et al. Evaluation of thyroid function monitoring in people treated with lithium: advice based on real-world data. Bipolar Disord. 2023;25:402-409. doi:10.1111/bdi.13298
- Bocchetta A, Loviselli A. Lithium treatment and thyroid abnormalities. Clin Pract Epidemiol Ment Health. 2006;2:23. doi:10.1186/1745-0179-2-23.
- Joffe RT. How should lithium-induced thyroid dysfunction be managed in patients with bipolar disorder? J Psychiatry Neurosci. 2002;27:392.
- Preskorn SH. Clinically relevant pharmacology of selective serotonin reuptake inhibitors. an overview with emphasis on pharmacokinetics and effects on oxidative drug metabolism. Clin Pharmacokinet. 1997;32(suppl 1):1-21. doi:10.2165/00003088-199700321-00003
- Chu A, Wadhwa R. Selective serotonin reuptake inhibitors. StatPearls. StatPearls Publishing; 2023.
- Stahl SM, Pradko JF, Haight BR, et al. A review of the neuropharmacology of bupropion, a dual norepinephrine and dopamine reuptake inhibitor. Prim Care Companion J Clin Psychiatry. 2004;6:159-166. doi:10.4088/pcc.v06n0403
- Escitalopram. Prescribing information. Solco Healthcare US, LLC; 2022. Accessed November 20, 2023. https://nctr-crs.fda.gov/fdalabel/services/spl/set-ids/2ffc6ec3-830f-46bc-9b3f-7c42cefa39b2/spl-doc
- Fluoxetine. Eli Lilly & Company; 2017. Prescribing information. Accessed November 20, 2023. https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/018936s108lbl.pdf
- Paxil. Prescribing information. GlaxoSmithKline; 2012. Accessed November 20, 2023. https://www.accessdata.fda.gov/drugsatfda_docs/label/2012/020031s067,020710s031.pdf
- Zoloft. Prescribing information. Pfizer; 2016. Accessed November 20, 2023. https://www.accessdata.fda.gov/drugsatfda_docs/label/2016/019839s74s86s87_20990s35s44s45lbl.pdf
- Celexa. Prescribing information. Allergan; 2022. Accessed November 20, 2023. https://www.accessdata.fda.gov/drugsatfda_docs/label/2022/020822s041lbl.pdf
- Pejcic AV, Paudel V. Alopecia associated with the use of selective serotonin reuptake inhibitors: systematic review. Psychiatry Res. 2022;313:114620. 10.1016/j.psychres.2022.114620
- Etminan M, Sodhi M, Procyshyn RM, et al. Risk of hair loss with different antidepressants: a comparative retrospective cohort study. Int Clin Psychopharmacol. 2018;33:44-48.
- Ghanizadeh A. Sertraline-associated hair loss. J Drugs Dermatol. 2008;7:693-694.
- Parameshwar E. Hair loss associated with fluvoxamine use. Am J Psychiatry. 1996;153:581-582. doi:10.1176/ajp.153.4.581
- Zalsman G, Sever J, Munitz H. Hair loss associated with paroxetine treatment: a case report. Clin Neuropharmacol. 1999;22:246-247.
- Ananth J, Elmishaugh A. Hair loss associated with fluoxetinetreatment. Can J Psychiatry. 1991;36:621. doi:10.1177/070674379103600824
- Tirmazi SI, Imran H, Rasheed A, et al. Escitalopram-induced hair loss. Prim Care Companion CNS Disord. 2020;22:19l02496. doi:10.4088/PCC.19l02496
Practice Points
- Medications are a common culprit of telogen effluvium (TE), and medication-induced TE should be suspected in patients presenting with diffuse nonscarring alopecia who are taking systemic medication(s).
- A careful history of new medications and dose adjustments 1 to 6 months prior to notable hair loss may identify the most likely inciting cause.
- Medication-induced TE often improves with cessation or dose reduction of the culprit medication.
Serum Ferritin Levels: A Clinical Guide in Patients With Hair Loss
Ferritin is an iron storage protein crucial to human iron homeostasis. Because serum ferritin levels are in dynamic equilibrium with the body’s iron stores, ferritin often is measured as a reflection of iron status; however, ferritin also is an acute-phase reactant whose levels may be nonspecifically elevated in a wide range of inflammatory conditions. The various processes that alter serum ferritin levels complicate the clinical interpretation of this laboratory value. In this article, we review the structure and function of ferritin and provide a guide for clinical use.
Overview of Iron
Iron is an essential element of key biologic functions including DNA synthesis and repair, oxygen transport, and oxidative phosphorylation. The body’s iron stores are mainly derived from internal iron recycling following red blood cell breakdown, while 5% to 10% is supplied by dietary intake.1-3 Iron metabolism is of particular importance in cells of the reticuloendothelial system (eg, spleen, liver, bone marrow), where excess iron must be appropriately sequestered and from which iron can be mobilized.4 Sufficient iron stores are necessary for proper cellular function and survival, as iron is a necessary component of hemoglobin for oxygen delivery, iron-sulfur clusters in electron transport, and enzyme cofactors in other cellular processes.
Although labile pools of biologically active free iron exist in limited amounts within cells, excess free iron can generate free radicals that damage cellular proteins, lipids, and nucleic acids.5-7 As such, most intracellular iron is captured within ferritin molecules. The excretion of iron is unregulated and occurs through loss in sweat, menstruation, hair shedding, skin desquamation, and enterocyte turnover.8 The lack of regulated excretion highlights the need for a tightly regulated system of uptake, transportation, storage, and sequestration to maintain iron homeostasis.
Overview of Ferritin Structure and Function
Ferritin is a key regulator of iron homeostasis that also serves as an important clinical indicator of body iron status. Ferritin mainly is found as an intracellular cytosolic iron storage and detoxification protein structured as a hollow 24-subunit polymer shell that can sequester up to 4500 atoms of iron within its core.9,10 The 24-mer is composed of both ferritin L (FTL) and ferritin H (FTH) subunits, with dynamic regulation of the H:L ratio dependent on the context and tissue in which ferritin is found.6
Ferritin H possesses ferroxidase, which facilitates oxidation of ferrous (Fe2+) iron into ferric (Fe3+) iron, which can then be incorporated into the mineral core of the ferritin heteropolymer.11 Ferritin L is more abundant in the spleen and liver, while FTH is found predominantly in the heart and kidneys where the increased ferroxidase activity may confer an increased ability to oxidize Fe2+ and limit oxidative stress.6
Regulation of Ferritin Synthesis and Secretion
Ferritin synthesis is regulated by intracellular nonheme iron levels, governed mainly by an iron response element (IRE) and iron response protein (IRP) translational repression system. Both FTH and FTL messenger RNA (mRNA) contain an IRE that is a regulatory stem-loop structure in the 5´ untranslated region. When the IRE is bound by IRP1 or IRP2, mRNA translation of ferritin subunits is suppressed.6 In low iron conditions, IRPs have greater affinity for IRE, and binding suppresses ferritin translation.12 In high iron conditions, IRPs have a decreased affinity for IRE, and ferritin mRNA synthesis is increased.13 Additionally, inflammatory cytokines such as tumor necrosis factor α and IL-1α transcriptionally induce FTH synthesis, resulting in an increased population of H-rich ferritins.11,14-16 A study using cultured human primary skin fibroblasts demonstrated UV radiation–induced increases in free intracellular iron content.17,18 Pourzand et al18 suggested that UV-mediated damage of lysosomal membranes results in leakage of lysosomal proteases into the cytosol, contributing to degradation of intracellular ferritin and subsequent release of iron within skin fibroblasts. The increased intracellular iron downregulates IRPs and increases ferritin mRNA synthesis,18 consistent with prior findings of increased ferritin synthesis in skin that is induced by UV radiation.19
Molecular analysis of serum ferritin in iron-overloaded mice revealed that extracellular ferritin found in the serum is composed of a greater fraction of FTL and has lower iron content than intracellular ferritin. The low iron content of serum ferritin compared with intracellular ferritin and transferrin suggests that serum ferritin is not a major pathway of systemic iron transport.10 However, locally secreted ferritins may play a greater role in iron transport and release in selected tissues. Additionally, in vitro studies of cell cultures from humans and mice have demonstrated the ability of macrophages to secrete ferritin, suggesting that macrophages are an important cellular source of serum ferritin.10,20 As such, serum ferritin generally may reflect body iron status but more specifically reflects macrophage iron status.10 Although the exact pathways of ferritin release are unknown, it is hypothesized that ferritin secretion occurs through cytosolic autophagy followed by secretion of proteins from the lysosomal compartment.10,18,21
Clinical Utility of Serum Ferritin
Low Ferritin and Iron Deficiency—Although bone marrow biopsy with iron staining remains the gold standard for diagnosis of iron deficiency, serum ferritin is a much more accessible and less invasive tool for evaluation of iron status. A serum ferritin level below 12 μg/L is highly specific for iron depletion,22 with a higher cutoff recommended in clinical practice to improve diagnostic sensitivity.23,24 Conditions independent of iron deficiency that may reduce serum ferritin include hypothyroidism and ascorbate deficiency, though neither condition has been reported to interfere with appropriate diagnosis of iron deficiency.25 Guyatt et al26 conducted a systematic review of laboratory tests used in the diagnosis of iron deficiency anemia and identified 55 studies suitable for inclusion. Based on an area under the receiver operating characteristic curve (AUROC) of 0.95, serum ferritin values were superior to transferrin saturation (AUROC, 0.74), red cell protoporphyrin (AUROC, 0.77), red cell volume distribution width (AUROC, 0.62), and mean cell volume (AUROC, 0.76) for diagnosis of IDA, verified by histologic examination of aspirated bone marrow.26 The likelihood ratio of iron deficiency begins to decrease for serum ferritin values of 40 μg/L or greater. For patients with inflammatory conditions—patients with concomitant chronic renal failure, inflammatory disease, infection, rheumatoid arthritis, liver disease, inflammatory bowel disease, and malignancy—the likelihood of iron deficiency begins to decrease at serum ferritin levels of 70 μg/L or greater.26 Similarly, the World Health Organization recommends that in adults with infection or inflammation, serum ferritin levels lower than 70 μg/L may be used to indicate iron deficiency.24 A serum ferritin level of 41 μg/L or lower was found to have a sensitivity and specificity of 98% for discriminating between iron-deficiency anemia and anemia of chronic disease (diagnosed based on bone marrow biopsy with iron staining), with an AUROC of 0.98.27 As such, we recommend using a serum ferritin level of 40 μg/L or lower in patients who are otherwise healthy as an indicator of iron deficiency.
The threshold for iron supplementation may vary based on age, sex, and race. In women, ferritin levels increase during menopause and peak after menopause; ferritin levels are higher in men than in women.28-30 A multisite longitudinal cohort study of 70 women in the United States found that the mean (SD) ferritin valuewas 69.5 (81.7) μg/L premenopause and 128.8 (125.7) μg/L postmenopause (P<.01).31 A separate longitudinal survey study of 8564 patients in China found that the mean (SE) ferritin value was 201.55 (3.60) μg/L for men and 80.46 (1.64) μg/L for women (P<.0001).32 Analysis of serum ferritin levels of 3554 male patients from the third National Health and Nutrition Examination Survey demonstrated that patients who self-reported as non-Hispanic Black (n=1616) had significantly higher serum ferritin levels than non-Hispanic White patients (n=1938)(serum ferritin difference of 37.1 μg/L)(P<.0001).33 The British Society for Haematology guidelines recommend that the threshold of serum ferritin for diagnosing iron deficiency should take into account age-, sex-, and race-based differences.34 Ferritin and Hair—Cutaneous manifestations of iron deficiency include koilonychia, glossitis, pruritus, angular cheilitis, and telogen effluvium (TE).1 A case-control study of 30 females aged 15 to 45 years demonstrated that the mean (SD) ferritin level was significantly lower in patients with TE than those with no hair loss (16.3 [12.6] ng/mL vs 60.3 [50.1] ng/mL; P<.0001). Using a threshold of 30 μg/L or lower, the investigators found that the odds ratio for TE was 21.0 (95% CI, 4.2-105.0) in patients with low serum ferritin.35
Another retrospective review of 54 patients with diffuse hair loss and 55 controls compared serum vitamin B12, folate, thyroid-stimulating hormone, zinc, ferritin, and 25-hydroxy vitamin D levels between the 2 groups.36 Exclusion criteria were clinical diagnoses of female pattern hair loss (androgenetic alopecia), pregnancy, menopause, metabolic and endocrine disorders, hormone replacement therapy, chemotherapy, immunosuppressive therapy, vitamin and mineral supplementation, scarring alopecia, eating disorders, and restrictive diets. Compared with controls, patients with diffuse nonscarring hair loss were found to have significantly lower ferritin (mean [SD], 14.72 [10.70] ng/mL vs 25.30 [14.41] ng/mL; P<.001) and 25-hydroxy vitamin D levels (mean [SD], 14.03 [8.09] ng/mL vs 17.01 [8.59] ng/mL; P=.01).36
In contrast, a separate case-control study of 381 cases and 76 controls found no increase in the rate of iron deficiency—defined as ferritin ≤15 μg/L or ≤40 μg/L—among women with female pattern hair loss or chronic TE vs controls.37 Taken together, these studies suggest that iron status may play a role in TE, a process that may result from nutritional deficiency, trauma, or physical or psychological stress38; however, there is insufficient evidence to suggest that low iron status impacts androgenetic alopecia, in which its multifactorial pathogenesis implicates genetic and hormonal factors.39 More research is needed to clarify the potential associations between iron deficiency and types of hair loss. Additionally, it is unclear whether iron supplementation improves hair growth parameters such as density and caliber.40
Low serum ferritin (<40 μg/L) with concurrent symptoms of iron deficiency, including fatigue, pallor, dyspnea on exertion, or hair loss, should prompt treatment with supplemental iron.41-43 Generally, ferrous (Fe2+) salts are preferred to ferric (Fe3+) salts, as the former is more readily absorbed through the duodenal mucosa44 and is the more common formulation in commercially available supplements in the United States.45 Oral supplementation with ferrous sulfate 325 mg (65 mg elemental iron) tablets is the first-line therapy for iron deficiency anemia.1 Alternatively, ferrous gluconate 324 mg (38 mg elemental iron) over-the-counter and its liquid form has demonstrated superior absorption compared to ferrous sulfate tablets in a clinical study with peritoneal dialysis patients.1,46 One study suggested that oral iron 40 to 80 mg should be taken every other day to increase absorption.47 Due to improved bioavailability, intravenous iron may be utilized in patients with malabsorption, renal failure, or intolerance to oral iron (including those with gastric ulcers or active inflammatory bowel disease), with the formulation chosen based on underlying comorbidities and potential risks.1,48 The theoretical risk for potentiating bacterial growth by increasing the amount of unbound iron in the blood raises concerns of iron supplementation in patients with infection or sepsis. Although far from definitive, existing data suggest that risk for infection is greater with intravenous iron supplementation and should be carefully considered prior to use.49,50Elevated Ferritin—Elevated ferritin may be difficult to interpret given the multitude of conditions that can cause it.23,51,52 Elevated serum ferritin can be broadly characterized by increased synthesis due to iron overload, increased synthesis due to inflammation, or increased ferritin release from cellular damage.34 Further complicating interpretation is the potential diurnal fluctuations in serum iron levels dependent on dietary intake and timing of laboratory evaluation, choice of assay, differences in reference standards, and variations in calibration procedures that can lead to analytic variability in the measurement of ferritin.23,53,54
Among healthy patients, serum ferritin is directly proportional to iron status.9,51 A study utilizing weekly phlebotomy of 22 healthy participants to measure serum ferritin and calculate mobilizable storage iron found a strong positive correlation between the 2 variables (r=0.83, P<.001), with each 1-μg/L increase of serum ferritin corresponding to approximately an 8-mg increase of storage iron; the initial serum ferritin values ranged from 2 to 83 μg/L in females and 36 to 224 μg/L in males.55 The correlation of ferritin with iron status also was supported by the significant correlation between the number of transfusions received in patients with transfusion-related iron overload and serum ferritin levels (r=0.89, P<.001), with an average increase of 60 μg/L per transfusion.51
Clinical guidelines on the interpretation of serum ferritin levels by Cullis et al34 recommend a normal upper limit of 200 μg/L for healthy females and 300 μg/L for healthy males. Outside of clinical syndromes associated with iron overload, Lee and Means56 found that serum ferritin of 1000 μg/L or higher was a nonspecific marker of disease, including infection and/or neoplastic disorders. We have adapted these guidelines to propose a workflow for evaluation of serum ferritin levels (Figure). In patients with inflammatory conditions or those affected by metabolic syndrome, elevated serum ferritin does not correlate with body iron status.57,58 It is believed that inflammatory cytokines, including tumor necrosis factor α and IL-1α, can upregulate ferritin synthesis independent of cellular iron stores.15,16 Several studies have examined the relationship between insulin resistance and/or metabolic syndrome with serum ferritin levels.31,32 Han et al32 found that elevated serum ferritin was significantly associated with higher risk for metabolic syndrome in men (P<.0001) but not in women.
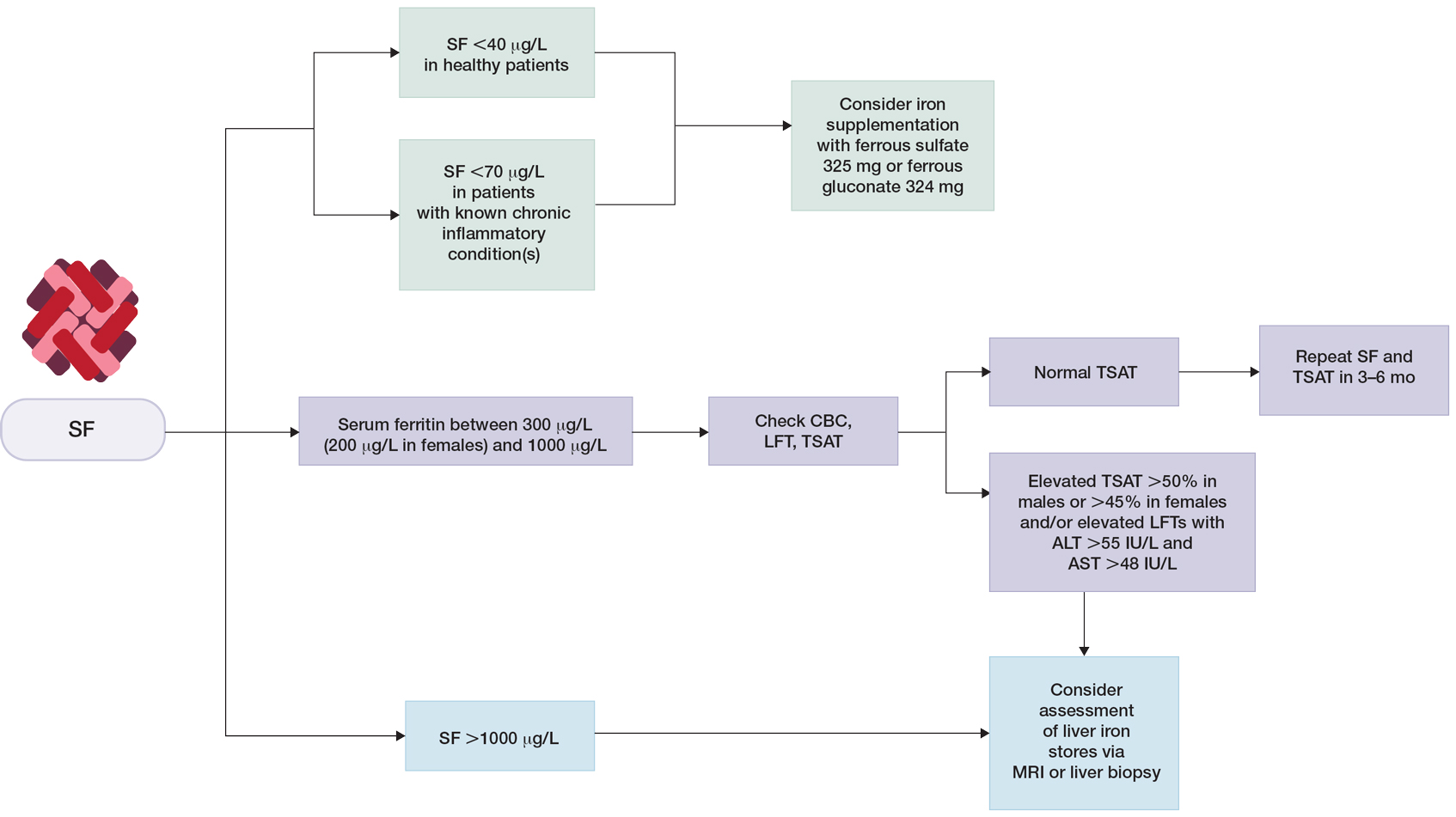
Although cutaneous manifestations of iron overload can be seen as skin hyperpigmentation due to increased iron deposits and increased melanin production,22 the effects of elevated ferritin on the skin and hair are not well known. Iron overload is a known trigger of porphyria cutanea tarda (PCT),59 a condition in which reduced or absent enzymatic activity of uroporphyrinogen decarboxylase (UROD) leads to build up of toxic porphyrins in various organs.60 In the skin, PCT manifests as a blistering photosensitive eruption that may resolve as dyspigmentation, scarring, and milia.61 Phlebotomy is first-line therapy in PCT to reduce serum iron and subsequent formation of UROD inhibitors, with guidelines suggesting discontinuation of phlebotomy when serum ferritin levels reach 20 ng/mL or lower.60 Hyperferritinemia (serum ferritin >500 μg/L) is a common finding in several inflammatory disorders often accompanied by clinically apparent cutaneous symptoms such as adult-onset Still disease,62 hemophagocytic lymphohistiocytosis,63,64 and anti-melanoma differentiation-associated gene 5 dermatomyositis.65 Among these conditions, serum ferritin levels have been reported to correlate with disease activity, raising the question of whether ferritin is a bystander or a driver of the underlying pathology.62,66,67 However, rapid decline of serum ferritin levels with treatment and control of inflammatory cytokines suggest that ferritin is unlikely to contribute to pathology.62,67
Final Thoughts
Many clinical studies have examined the association between hair health and body iron status, the collective findings of which suggest that iron deficiency may be associated with TE. Among commonly measured serum iron parameters, low ferritin is a highly specific and sensitive marker for diagnosing iron deficiency. Serum ferritin may be a clinically useful tool for ruling out underlying iron deficiency in patients presenting with hair loss. Despite advances in our understanding of the molecular mechanisms of ferritin synthesis and regulation, whether ferritin itself contributes to cutaneous pathology is poorly understood.35,36,68-74 For patients who are otherwise healthy with low suspicion for inflammatory disorders, chronic systemic illnesses, or malignancy, serum ferritin can be used as an indicator of body iron status. The workup for slightly elevated serum ferritin should be interpreted in the context of other laboratory findings and should be reassessed over time. Serum ferritin levels above 1000 μg/L warrant further investigation into causes such as iron overload conditions and underlying inflammatory conditions or malignancy.
- Hoffman M, Micheletti RG, Shields BE. Nutritional dermatoses in the hospitalized patient. Cutis. 2020;105:296, 302-308, E1-E5.
- Ganz T. Macrophages and systemic iron homeostasis. J Innate Immun. 2012;4:446-453. doi:10.1159/000336423
- Slusarczyk P, Mandal PK, Zurawska G, et al. Impaired iron recycling from erythrocytes is an early hallmark of aging. eLife. 2023;12:E79196. doi:10.7554/eLife.79196
- Crichton RR. Ferritin: structure, synthesis and function. N Engl J Med. 1971;284:1413-1422. doi:10.1056/nejm197106242842506
- Sandnes M, Ulvik RJ, Vorland M, et al. Hyperferritinemia—a clinical overview. J Clin Med. 2021;10:2008. doi:10.3390/jcm10092008
- Kernan KF, Carcillo JA. Hyperferritinemia and inflammation. Int Immunol. 2017;29:401-409. doi:10.1093/intimm/dxx031
- Wright JA, Richards T, Srai SKS. The role of iron in the skin and cutaneous wound healing. review. Front Pharmacol. 2014;5:156. doi:10.3389/fphar.2014.00156
- Ems T, St Lucia K, Huecker MR. Biochemistry, iron absorption. StatPearls Publishing; 2022.
- Crichton RR. Ferritin: structure, synthesis and function. N Engl J Med. 1971;284:1413-1422. doi:10.1056/nejm197106242842506
- Cohen LA, Gutierrez L, Weiss A, et al. Serum ferritin is derived primarily from macrophages through a nonclassical secretory pathway. Blood. 2010;116:1574-1584. doi:10.1182/blood-2009-11-253815
- Briat JF, Ravet K, Arnaud N, et al. New insights into ferritin synthesis and function highlight a link between iron homeostasis and oxidative stress in plants. Ann Bot. 2010;105:811-822. doi:10.1093/aob/mcp128
- Kato J, Kobune M, Ohkubo S, et al. Iron/IRP-1-dependent regulation of mRNA expression for transferrin receptor, DMT1 and ferritin during human erythroid differentiation. Exp Hematol. 2007;35:879-887. doi:10.1016/j.exphem.2007.03.005
- Gozzelino R, Soares MP. Coupling heme and iron metabolism via ferritin H chain. Antioxid Redox Signal. 2014;20:1754-1769. doi:10.1089/ars.2013.5666
- Torti FM, Torti SV. Regulation of ferritin genes and protein. Blood. 2002;99:3505-3516. doi:10.1182/blood.V99.10.3505
- Torti SV, Kwak EL, Miller SC, et al. The molecular cloning and characterization of murine ferritin heavy chain, a tumor necrosis factor-inducible gene. J Biol Chem. 1988;263:12638-12644.
- Wei Y, Miller SC, Tsuji Y, et al. Interleukin 1 induces ferritin heavy chain in human muscle cells. Biochem Biophys Res Commun. 1990;169:289-296. doi:10.1016/0006-291x(90)91466-6
- Bissett DL, Chatterjee R, Hannon DP. Chronic ultraviolet radiation–induced increase in skin iron and the photoprotective effect of topically applied iron chelators. Photochem Photobiol. 1991;54:215-223. https://doi.org/10.1111/j.1751-1097.1991.tb02009.x
- Pourzand C, Watkin RD, Brown JE, et al. Ultraviolet A radiation induces immediate release of iron in human primary skin fibroblasts: the role of ferritin. Proc Natl Acad Sci U S A. 1999;96:6751-6756. doi:10.1073/pnas.96.12.6751
- Applegate LA, Scaletta C, Panizzon R, et al. Evidence that ferritin is UV inducible in human skin: part of a putative defense mechanism. J Invest Dermatol. 1998;111:159-163. https://doi.org/10.1046/j.1523-1747.1998.00254.x
- Wesselius LJ, Nelson ME, Skikne BS. Increased release of ferritin and iron by iron-loaded alveolar macrophages in cigarette smokers. Am J Respir Crit Care Med. 1994;150:690-695. doi:10.1164/ajrccm.150.3.8087339
- De Domenico I, Ward DM, Kaplan J. Specific iron chelators determine the route of ferritin degradation. Blood. 2009;114:4546-4551. doi:10.1182/blood-2009-05-224188
- Knovich MA, Storey JA, Coffman LG, et al. Ferritin for the clinician. Blood Rev. 2009;23:95-104. doi:10.1016/j.blre.2008.08.001
- Dignass A, Farrag K, Stein J. Limitations of serum ferritin in diagnosing iron deficiency in inflammatory conditions. Int J Chronic Dis. 2018;2018:9394060. doi:10.1155/2018/9394060
- World Health Organization. WHO guideline on use of ferritin concentrations to assess iron status in individuals and populations. Published April 21, 2020. Accessed July 23, 2023. https://www.who.int/publications/i/item/9789240000124
- Finch CA, Bellotti V, Stray S, et al. Plasma ferritin determination as a diagnostic tool. West J Med. 1986;145:657-663.
- Guyatt GH, Oxman AD, Ali M, et al. Laboratory diagnosis of iron-deficiency anemia. J Gen Intern Med. 1992;7:145-153. doi:10.1007/BF02598003
- Punnonen K, Irjala K, Rajamäki A. Serum transferrin receptor and its ratio to serum ferritin in the diagnosis of iron deficiency. Blood. 1997;89:1052-1057. https://doi.org/10.1182/blood.V89.3.1052
- Zacharski LR, Ornstein DL, Woloshin S, et al. Association of age, sex, and race with body iron stores in adults: analysis of NHANES III data. American Heart Journal. 2000;140:98-104. https://doi.org/10.1067/mhj.2000.106646
- Milman N, Kirchhoff M. Iron stores in 1359, 30- to 60-year-old Danish women: evaluation by serum ferritin and hemoglobin. Ann Hematol. 1992;64:22-27. doi:10.1007/bf01811467
- Liu J-M, Hankinson SE, Stampfer MJ, et al. Body iron stores and their determinants in healthy postmenopausal US women. Am J Clin Nutr. 2003;78:1160-1167. doi:10.1093/ajcn/78.6.1160
- Kim C, Nan B, Kong S, et al. Changes in iron measures over menopause and associations with insulin resistance. J Womens Health (Larchmt). 2012;21:872-877. doi:10.1089/jwh.2012.3549
- Han LL, Wang YX, Li J, et al. Gender differences in associations of serum ferritin and diabetes, metabolic syndrome, and obesity in the China Health and Nutrition Survey. Mol Nutr Food Res. 2014;58:2189-2195. doi:10.1002/mnfr.201400088
- Pan Y, Jackson RT. Insights into the ethnic differences in serum ferritin between black and white US adult men. Am J Hum Biol. 2008;20:406-416. https://doi.org/10.1002/ajhb.20745
- Cullis JO, Fitzsimons EJ, Griffiths WJ, et al. Investigation and management of a raised serum ferritin. Br J Haematol. 2018;181:331-340. doi:10.1111/bjh.15166
- Moeinvaziri M, Mansoori P, Holakooee K, et al. Iron status in diffuse telogen hair loss among women. Acta Dermatovenerol Croat. 2009;17:279-284.
- Tamer F, Yuksel ME, Karabag Y. Serum ferritin and vitamin D levels should be evaluated in patients with diffuse hair loss prior to treatment. Postepy Dermatol Alergol. 2020;37:407-411. doi:10.5114/ada.2020.96251
- Olsen EA, Reed KB, Cacchio PB, et al. Iron deficiency in female pattern hair loss, chronic telogen effluvium, and control groups. J Am Acad Dermatol. 2010;63:991-999. doi:10.1016/j.jaad.2009.12.006
- Asghar F, Shamim N, Farooque U, et al. Telogen effluvium: a review of the literature. Cureus. 2020;12:E8320. doi:10.7759/cureus.8320
- Brough KR, Torgerson RR. Hormonal therapy in female pattern hair loss. Int J Womens Dermatol. 2017;3:53-57. doi:10.1016/j.ijwd.2017.01.001
- Klein EJ, Karim M, Li X, et al. Supplementation and hair growth: a retrospective chart review of patients with alopecia and laboratory abnormalities. JAAD Int. 2022;9:69-71. doi:10.1016/j.jdin.2022.08.013
- Goksin S. Retrospective evaluation of clinical profile and comorbidities in patients with alopecia areata. North Clin Istanb. 2022;9:451-458. doi:10.14744/nci.2022.78790
- Beatrix J, Piales C, Berland P, et al. Non-anemic iron deficiency: correlations between symptoms and iron status parameters. Eur J Clin Nutr. 2022;76:835-840. doi:10.1038/s41430-021-01047-5
- Treister-Goltzman Y, Yarza S, Peleg R. Iron deficiency and nonscarring alopecia in women: systematic review and meta-analysis. Skin Appendage Disord. 2022;8:83-92. doi:10.1159/000519952
- Santiago P. Ferrous versus ferric oral iron formulations for the treatment of iron deficiency: a clinical overview. ScientificWorldJournal. 2012;2012:846824. doi:10.1100/2012/846824
- Lo JO, Benson AE, Martens KL, et al. The role of oral iron in the treatment of adults with iron deficiency. Eur J Haematol. 2023;110:123-130. doi:10.1111/ejh.13892
- Lausevic´ M, Jovanovic´ N, Ignjatovic´ S, et al. Resorption and tolerance of the high doses of ferrous sulfate and ferrous gluconate in the patients on peritoneal dialysis. Vojnosanit Pregl. 2006;63:143-147. doi:10.2298/vsp0602143l
- Stoffel NU, Zeder C, Brittenham GM, et al. Iron absorption from supplements is greater with alternate day than with consecutive day dosing in iron-deficient anemic women. Haematologica. 2020;105:1232-1239. doi:10.3324/haematol.2019.220830
- Jimenez KM, Gasche C. Management of iron deficiency anaemia in inflammatory bowel disease. Acta Haematologica. 2019;142:30-36. doi:10.1159/000496728
- Shah AA, Donovan K, Seeley C, et al. Risk of infection associated with administration of intravenous iron: a systematic review and meta-analysis. JAMA Netw Open. 2021;4:E2133935-E2133935. doi:10.1001/jamanetworkopen.2021.33935
- Ganz T, Aronoff GR, Gaillard CAJM, et al. Iron administration, infection, and anemia management in ckd: untangling the effects of intravenous iron therapy on immunity and infection risk. Kidney Med. 2020/05/01/ 2020;2:341-353. doi: 10.1016/j.xkme.2020.01.006
- Lipschitz DA, Cook JD, Finch CA. A clinical evaluation of serum ferritin as an index of iron stores. N Engl J Med. 1974;290:1213-1216. doi:10.1056/nejm197405302902201
- Loveikyte R, Bourgonje AR, van der Reijden JJ, et al. Hepcidin and iron status in patients with inflammatory bowel disease undergoing induction therapy with vedolizumab or infliximab [published online February 7, 2023]. Inflamm Bowel Dis. doi:10.1093/ibd/izad010
- Borel MJ, Smith SM, Derr J, et al. Day-to-day variation in iron-status indices in healthy men and women. Am J Clin Nutr. 1991;54:729-735. doi:10.1093/ajcn/54.4.729
- Ford BA, Coyne DW, Eby CS, et al. Variability of ferritin measurements in chronic kidney disease; implications for iron management. Kidney International. 2009;75:104-110. doi:10.1038/ki.2008.526
- Walters GO, Miller FM, Worwood M. Serum ferritin concentration and iron stores in normal subjects. J Clin Pathol. 1973;26:770-772. doi:10.1136/jcp.26.10.770
- Lee MH, Means RT Jr. Extremely elevated serum ferritin levels in a university hospital: associated diseases and clinical significance. Am J Med. Jun 1995;98:566-571. doi:10.1016/s0002-9343(99)80015-1
- Theil EC. Ferritin: structure, gene regulation, and cellular function in animals, plants, and microorganisms. Annu Rev Biochem. 1987;56:289-315. doi:10.1146/annurev.bi.56.070187.001445
- Chen LY, Chang SD, Sreenivasan GM, et al. Dysmetabolic hyperferritinemia is associated with normal transferrin saturation, mild hepatic iron overload, and elevated hepcidin. Ann Hematol. 2011;90:139-143. doi:10.1007/s00277-010-1050-x
- Sampietro M, Fiorelli G, Fargion S. Iron overload in porphyria cutanea tarda. Haematologica. 1999;84:248-253.
- Singal AK. Porphyria cutanea tarda: recent update. Mol Genet Metab. 2019;128:271-281. doi:10.1016/j.ymgme.2019.01.004
- Frank J, Poblete-Gutiérrez P. Porphyria cutanea tarda—when skin meets liver. Best Pract Res Clin Gastroenterol. 2010;24:735-745. doi:10.1016/j.bpg.2010.07.002
- Mehta B, Efthimiou P. Ferritin in adult-onset Still’s disease: just a useful innocent bystander? Int J Inflam. 2012;2012:298405. doi:10.1155/2012/298405
- Ma AD, Fedoriw YD, Roehrs P. Hyperferritinemia and hemophagocytic lymphohistiocytosis. single institution experience in adult and pediatric patients. Blood. 2012;120:2135-2135. doi:10.1182/blood.V120.21.2135.2135
- Basu S, Maji B, Barman S, et al. Hyperferritinemia in hemophagocytic lymphohistiocytosis: a single institution experience in pediatric patients. Indian J Clin Biochem. 2018;33:108-112. doi:10.1007/s12291-017-0655-4
- Yamada K, Asai K, Okamoto A, et al. Correlation between disease activity and serum ferritin in clinically amyopathic dermatomyositis with rapidly-progressive interstitial lung disease: a case report. BMC Res Notes. 2018;11:34. doi:10.1186/s13104-018-3146-7
- Zohar DN, Seluk L, Yonath H, et al. Anti-MDA5 positive dermatomyositis associated with rapidly progressive interstitial lung disease and correlation between serum ferritin level and treatment response. Mediterr J Rheumatol. 2020;31:75-77. doi:10.31138/mjr.31.1.75
- Lin TF, Ferlic-Stark LL, Allen CE, et al. Rate of decline of ferritin in patients with hemophagocytic lymphohistiocytosis as a prognostic variable for mortality. Pediatr Blood Cancer. 2011;56:154-155. doi:10.1002/pbc.22774
- Bregy A, Trueb RM. No association between serum ferritin levels >10 microg/l and hair loss activity in women. Dermatology. 2008;217:1-6. doi:10.1159/000118505
- de Queiroz M, Vaske TM, Boza JC. Serum ferritin and vitamin D levels in women with non-scarring alopecia. J Cosmet Dermatol. 2022;21:2688-2690. doi:10.1111/jocd.14472
- El-Husseiny R, Alrgig NT, Abdel Fattah NSA. Epidemiological and biochemical factors (serum ferritin and vitamin D) associated with premature hair graying in Egyptian population. J Cosmet Dermatol. 2021;20:1860-1866. doi:10.1111/jocd.13747
- Enitan AO, Olasode OA, Onayemi EO, et al. Serum ferritin levels amongst individuals with androgenetic alopecia in Ile-Ife, Nigeria. West Afr J Med. 2022;39:1026-1031.
- I˙bis¸ S, Aksoy Sarac¸ G, Akdag˘ T. Evaluation of MCV/RDW ratio and correlations with ferritin in telogen effluvium patients. Dermatol Pract Concept. 2022;12:E2022151. doi:10.5826/dpc.1203a151
- Kakpovbia E, Ogbechie-Godec OA, Shapiro J, et al. Laboratory testing in telogen effluvium. J Drugs Dermatol. 2021;20:110-111. doi:10.36849/jdd.5771
- Rasheed H, Mahgoub D, Hegazy R, et al. Serum ferritin and vitamin D in female hair loss: do they play a role? Skin Pharmacol Physiol. 2013;26:101-107. doi:10.1159/000346698
Ferritin is an iron storage protein crucial to human iron homeostasis. Because serum ferritin levels are in dynamic equilibrium with the body’s iron stores, ferritin often is measured as a reflection of iron status; however, ferritin also is an acute-phase reactant whose levels may be nonspecifically elevated in a wide range of inflammatory conditions. The various processes that alter serum ferritin levels complicate the clinical interpretation of this laboratory value. In this article, we review the structure and function of ferritin and provide a guide for clinical use.
Overview of Iron
Iron is an essential element of key biologic functions including DNA synthesis and repair, oxygen transport, and oxidative phosphorylation. The body’s iron stores are mainly derived from internal iron recycling following red blood cell breakdown, while 5% to 10% is supplied by dietary intake.1-3 Iron metabolism is of particular importance in cells of the reticuloendothelial system (eg, spleen, liver, bone marrow), where excess iron must be appropriately sequestered and from which iron can be mobilized.4 Sufficient iron stores are necessary for proper cellular function and survival, as iron is a necessary component of hemoglobin for oxygen delivery, iron-sulfur clusters in electron transport, and enzyme cofactors in other cellular processes.
Although labile pools of biologically active free iron exist in limited amounts within cells, excess free iron can generate free radicals that damage cellular proteins, lipids, and nucleic acids.5-7 As such, most intracellular iron is captured within ferritin molecules. The excretion of iron is unregulated and occurs through loss in sweat, menstruation, hair shedding, skin desquamation, and enterocyte turnover.8 The lack of regulated excretion highlights the need for a tightly regulated system of uptake, transportation, storage, and sequestration to maintain iron homeostasis.
Overview of Ferritin Structure and Function
Ferritin is a key regulator of iron homeostasis that also serves as an important clinical indicator of body iron status. Ferritin mainly is found as an intracellular cytosolic iron storage and detoxification protein structured as a hollow 24-subunit polymer shell that can sequester up to 4500 atoms of iron within its core.9,10 The 24-mer is composed of both ferritin L (FTL) and ferritin H (FTH) subunits, with dynamic regulation of the H:L ratio dependent on the context and tissue in which ferritin is found.6
Ferritin H possesses ferroxidase, which facilitates oxidation of ferrous (Fe2+) iron into ferric (Fe3+) iron, which can then be incorporated into the mineral core of the ferritin heteropolymer.11 Ferritin L is more abundant in the spleen and liver, while FTH is found predominantly in the heart and kidneys where the increased ferroxidase activity may confer an increased ability to oxidize Fe2+ and limit oxidative stress.6
Regulation of Ferritin Synthesis and Secretion
Ferritin synthesis is regulated by intracellular nonheme iron levels, governed mainly by an iron response element (IRE) and iron response protein (IRP) translational repression system. Both FTH and FTL messenger RNA (mRNA) contain an IRE that is a regulatory stem-loop structure in the 5´ untranslated region. When the IRE is bound by IRP1 or IRP2, mRNA translation of ferritin subunits is suppressed.6 In low iron conditions, IRPs have greater affinity for IRE, and binding suppresses ferritin translation.12 In high iron conditions, IRPs have a decreased affinity for IRE, and ferritin mRNA synthesis is increased.13 Additionally, inflammatory cytokines such as tumor necrosis factor α and IL-1α transcriptionally induce FTH synthesis, resulting in an increased population of H-rich ferritins.11,14-16 A study using cultured human primary skin fibroblasts demonstrated UV radiation–induced increases in free intracellular iron content.17,18 Pourzand et al18 suggested that UV-mediated damage of lysosomal membranes results in leakage of lysosomal proteases into the cytosol, contributing to degradation of intracellular ferritin and subsequent release of iron within skin fibroblasts. The increased intracellular iron downregulates IRPs and increases ferritin mRNA synthesis,18 consistent with prior findings of increased ferritin synthesis in skin that is induced by UV radiation.19
Molecular analysis of serum ferritin in iron-overloaded mice revealed that extracellular ferritin found in the serum is composed of a greater fraction of FTL and has lower iron content than intracellular ferritin. The low iron content of serum ferritin compared with intracellular ferritin and transferrin suggests that serum ferritin is not a major pathway of systemic iron transport.10 However, locally secreted ferritins may play a greater role in iron transport and release in selected tissues. Additionally, in vitro studies of cell cultures from humans and mice have demonstrated the ability of macrophages to secrete ferritin, suggesting that macrophages are an important cellular source of serum ferritin.10,20 As such, serum ferritin generally may reflect body iron status but more specifically reflects macrophage iron status.10 Although the exact pathways of ferritin release are unknown, it is hypothesized that ferritin secretion occurs through cytosolic autophagy followed by secretion of proteins from the lysosomal compartment.10,18,21
Clinical Utility of Serum Ferritin
Low Ferritin and Iron Deficiency—Although bone marrow biopsy with iron staining remains the gold standard for diagnosis of iron deficiency, serum ferritin is a much more accessible and less invasive tool for evaluation of iron status. A serum ferritin level below 12 μg/L is highly specific for iron depletion,22 with a higher cutoff recommended in clinical practice to improve diagnostic sensitivity.23,24 Conditions independent of iron deficiency that may reduce serum ferritin include hypothyroidism and ascorbate deficiency, though neither condition has been reported to interfere with appropriate diagnosis of iron deficiency.25 Guyatt et al26 conducted a systematic review of laboratory tests used in the diagnosis of iron deficiency anemia and identified 55 studies suitable for inclusion. Based on an area under the receiver operating characteristic curve (AUROC) of 0.95, serum ferritin values were superior to transferrin saturation (AUROC, 0.74), red cell protoporphyrin (AUROC, 0.77), red cell volume distribution width (AUROC, 0.62), and mean cell volume (AUROC, 0.76) for diagnosis of IDA, verified by histologic examination of aspirated bone marrow.26 The likelihood ratio of iron deficiency begins to decrease for serum ferritin values of 40 μg/L or greater. For patients with inflammatory conditions—patients with concomitant chronic renal failure, inflammatory disease, infection, rheumatoid arthritis, liver disease, inflammatory bowel disease, and malignancy—the likelihood of iron deficiency begins to decrease at serum ferritin levels of 70 μg/L or greater.26 Similarly, the World Health Organization recommends that in adults with infection or inflammation, serum ferritin levels lower than 70 μg/L may be used to indicate iron deficiency.24 A serum ferritin level of 41 μg/L or lower was found to have a sensitivity and specificity of 98% for discriminating between iron-deficiency anemia and anemia of chronic disease (diagnosed based on bone marrow biopsy with iron staining), with an AUROC of 0.98.27 As such, we recommend using a serum ferritin level of 40 μg/L or lower in patients who are otherwise healthy as an indicator of iron deficiency.
The threshold for iron supplementation may vary based on age, sex, and race. In women, ferritin levels increase during menopause and peak after menopause; ferritin levels are higher in men than in women.28-30 A multisite longitudinal cohort study of 70 women in the United States found that the mean (SD) ferritin valuewas 69.5 (81.7) μg/L premenopause and 128.8 (125.7) μg/L postmenopause (P<.01).31 A separate longitudinal survey study of 8564 patients in China found that the mean (SE) ferritin value was 201.55 (3.60) μg/L for men and 80.46 (1.64) μg/L for women (P<.0001).32 Analysis of serum ferritin levels of 3554 male patients from the third National Health and Nutrition Examination Survey demonstrated that patients who self-reported as non-Hispanic Black (n=1616) had significantly higher serum ferritin levels than non-Hispanic White patients (n=1938)(serum ferritin difference of 37.1 μg/L)(P<.0001).33 The British Society for Haematology guidelines recommend that the threshold of serum ferritin for diagnosing iron deficiency should take into account age-, sex-, and race-based differences.34 Ferritin and Hair—Cutaneous manifestations of iron deficiency include koilonychia, glossitis, pruritus, angular cheilitis, and telogen effluvium (TE).1 A case-control study of 30 females aged 15 to 45 years demonstrated that the mean (SD) ferritin level was significantly lower in patients with TE than those with no hair loss (16.3 [12.6] ng/mL vs 60.3 [50.1] ng/mL; P<.0001). Using a threshold of 30 μg/L or lower, the investigators found that the odds ratio for TE was 21.0 (95% CI, 4.2-105.0) in patients with low serum ferritin.35
Another retrospective review of 54 patients with diffuse hair loss and 55 controls compared serum vitamin B12, folate, thyroid-stimulating hormone, zinc, ferritin, and 25-hydroxy vitamin D levels between the 2 groups.36 Exclusion criteria were clinical diagnoses of female pattern hair loss (androgenetic alopecia), pregnancy, menopause, metabolic and endocrine disorders, hormone replacement therapy, chemotherapy, immunosuppressive therapy, vitamin and mineral supplementation, scarring alopecia, eating disorders, and restrictive diets. Compared with controls, patients with diffuse nonscarring hair loss were found to have significantly lower ferritin (mean [SD], 14.72 [10.70] ng/mL vs 25.30 [14.41] ng/mL; P<.001) and 25-hydroxy vitamin D levels (mean [SD], 14.03 [8.09] ng/mL vs 17.01 [8.59] ng/mL; P=.01).36
In contrast, a separate case-control study of 381 cases and 76 controls found no increase in the rate of iron deficiency—defined as ferritin ≤15 μg/L or ≤40 μg/L—among women with female pattern hair loss or chronic TE vs controls.37 Taken together, these studies suggest that iron status may play a role in TE, a process that may result from nutritional deficiency, trauma, or physical or psychological stress38; however, there is insufficient evidence to suggest that low iron status impacts androgenetic alopecia, in which its multifactorial pathogenesis implicates genetic and hormonal factors.39 More research is needed to clarify the potential associations between iron deficiency and types of hair loss. Additionally, it is unclear whether iron supplementation improves hair growth parameters such as density and caliber.40
Low serum ferritin (<40 μg/L) with concurrent symptoms of iron deficiency, including fatigue, pallor, dyspnea on exertion, or hair loss, should prompt treatment with supplemental iron.41-43 Generally, ferrous (Fe2+) salts are preferred to ferric (Fe3+) salts, as the former is more readily absorbed through the duodenal mucosa44 and is the more common formulation in commercially available supplements in the United States.45 Oral supplementation with ferrous sulfate 325 mg (65 mg elemental iron) tablets is the first-line therapy for iron deficiency anemia.1 Alternatively, ferrous gluconate 324 mg (38 mg elemental iron) over-the-counter and its liquid form has demonstrated superior absorption compared to ferrous sulfate tablets in a clinical study with peritoneal dialysis patients.1,46 One study suggested that oral iron 40 to 80 mg should be taken every other day to increase absorption.47 Due to improved bioavailability, intravenous iron may be utilized in patients with malabsorption, renal failure, or intolerance to oral iron (including those with gastric ulcers or active inflammatory bowel disease), with the formulation chosen based on underlying comorbidities and potential risks.1,48 The theoretical risk for potentiating bacterial growth by increasing the amount of unbound iron in the blood raises concerns of iron supplementation in patients with infection or sepsis. Although far from definitive, existing data suggest that risk for infection is greater with intravenous iron supplementation and should be carefully considered prior to use.49,50Elevated Ferritin—Elevated ferritin may be difficult to interpret given the multitude of conditions that can cause it.23,51,52 Elevated serum ferritin can be broadly characterized by increased synthesis due to iron overload, increased synthesis due to inflammation, or increased ferritin release from cellular damage.34 Further complicating interpretation is the potential diurnal fluctuations in serum iron levels dependent on dietary intake and timing of laboratory evaluation, choice of assay, differences in reference standards, and variations in calibration procedures that can lead to analytic variability in the measurement of ferritin.23,53,54
Among healthy patients, serum ferritin is directly proportional to iron status.9,51 A study utilizing weekly phlebotomy of 22 healthy participants to measure serum ferritin and calculate mobilizable storage iron found a strong positive correlation between the 2 variables (r=0.83, P<.001), with each 1-μg/L increase of serum ferritin corresponding to approximately an 8-mg increase of storage iron; the initial serum ferritin values ranged from 2 to 83 μg/L in females and 36 to 224 μg/L in males.55 The correlation of ferritin with iron status also was supported by the significant correlation between the number of transfusions received in patients with transfusion-related iron overload and serum ferritin levels (r=0.89, P<.001), with an average increase of 60 μg/L per transfusion.51
Clinical guidelines on the interpretation of serum ferritin levels by Cullis et al34 recommend a normal upper limit of 200 μg/L for healthy females and 300 μg/L for healthy males. Outside of clinical syndromes associated with iron overload, Lee and Means56 found that serum ferritin of 1000 μg/L or higher was a nonspecific marker of disease, including infection and/or neoplastic disorders. We have adapted these guidelines to propose a workflow for evaluation of serum ferritin levels (Figure). In patients with inflammatory conditions or those affected by metabolic syndrome, elevated serum ferritin does not correlate with body iron status.57,58 It is believed that inflammatory cytokines, including tumor necrosis factor α and IL-1α, can upregulate ferritin synthesis independent of cellular iron stores.15,16 Several studies have examined the relationship between insulin resistance and/or metabolic syndrome with serum ferritin levels.31,32 Han et al32 found that elevated serum ferritin was significantly associated with higher risk for metabolic syndrome in men (P<.0001) but not in women.
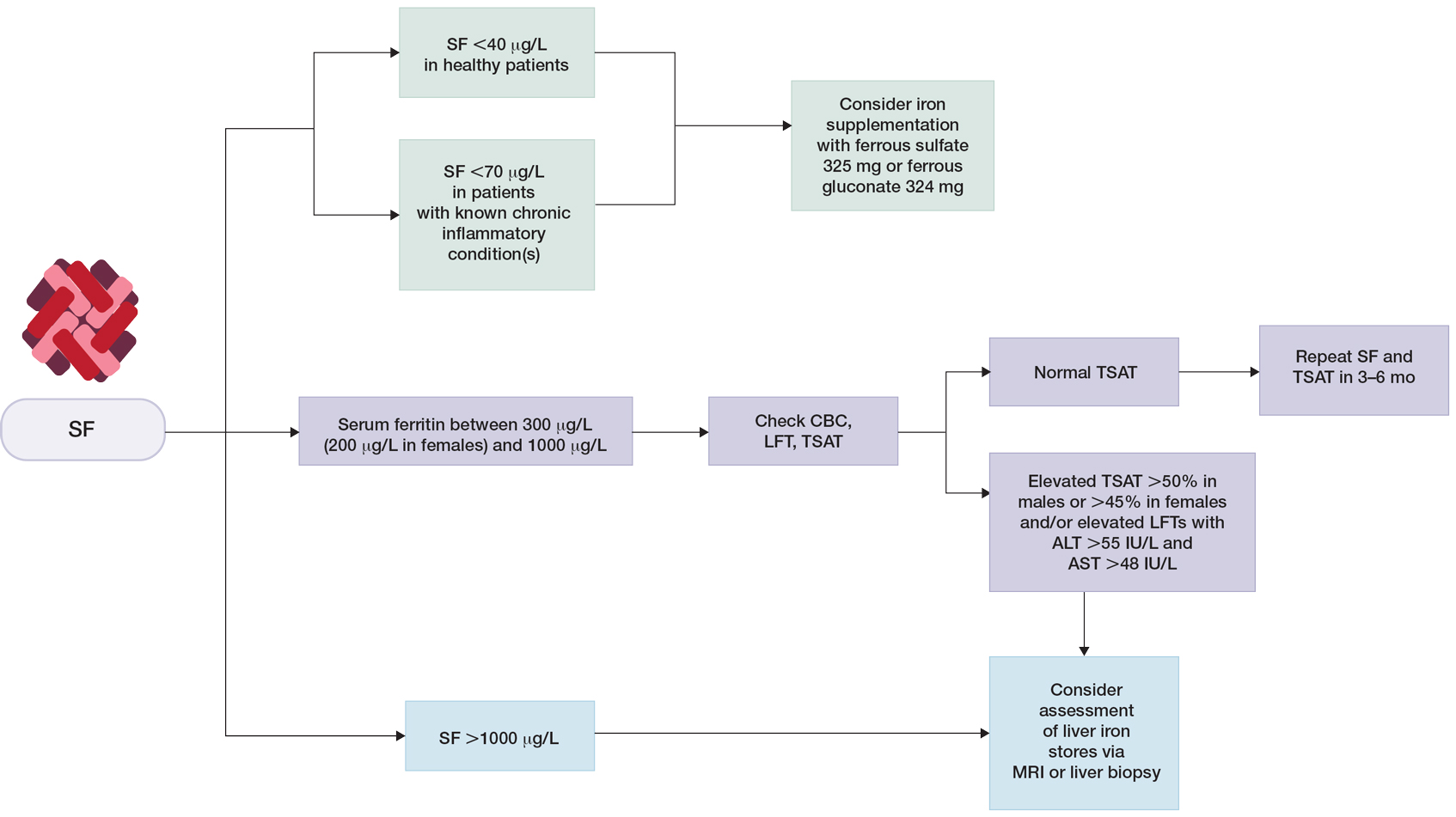
Although cutaneous manifestations of iron overload can be seen as skin hyperpigmentation due to increased iron deposits and increased melanin production,22 the effects of elevated ferritin on the skin and hair are not well known. Iron overload is a known trigger of porphyria cutanea tarda (PCT),59 a condition in which reduced or absent enzymatic activity of uroporphyrinogen decarboxylase (UROD) leads to build up of toxic porphyrins in various organs.60 In the skin, PCT manifests as a blistering photosensitive eruption that may resolve as dyspigmentation, scarring, and milia.61 Phlebotomy is first-line therapy in PCT to reduce serum iron and subsequent formation of UROD inhibitors, with guidelines suggesting discontinuation of phlebotomy when serum ferritin levels reach 20 ng/mL or lower.60 Hyperferritinemia (serum ferritin >500 μg/L) is a common finding in several inflammatory disorders often accompanied by clinically apparent cutaneous symptoms such as adult-onset Still disease,62 hemophagocytic lymphohistiocytosis,63,64 and anti-melanoma differentiation-associated gene 5 dermatomyositis.65 Among these conditions, serum ferritin levels have been reported to correlate with disease activity, raising the question of whether ferritin is a bystander or a driver of the underlying pathology.62,66,67 However, rapid decline of serum ferritin levels with treatment and control of inflammatory cytokines suggest that ferritin is unlikely to contribute to pathology.62,67
Final Thoughts
Many clinical studies have examined the association between hair health and body iron status, the collective findings of which suggest that iron deficiency may be associated with TE. Among commonly measured serum iron parameters, low ferritin is a highly specific and sensitive marker for diagnosing iron deficiency. Serum ferritin may be a clinically useful tool for ruling out underlying iron deficiency in patients presenting with hair loss. Despite advances in our understanding of the molecular mechanisms of ferritin synthesis and regulation, whether ferritin itself contributes to cutaneous pathology is poorly understood.35,36,68-74 For patients who are otherwise healthy with low suspicion for inflammatory disorders, chronic systemic illnesses, or malignancy, serum ferritin can be used as an indicator of body iron status. The workup for slightly elevated serum ferritin should be interpreted in the context of other laboratory findings and should be reassessed over time. Serum ferritin levels above 1000 μg/L warrant further investigation into causes such as iron overload conditions and underlying inflammatory conditions or malignancy.
Ferritin is an iron storage protein crucial to human iron homeostasis. Because serum ferritin levels are in dynamic equilibrium with the body’s iron stores, ferritin often is measured as a reflection of iron status; however, ferritin also is an acute-phase reactant whose levels may be nonspecifically elevated in a wide range of inflammatory conditions. The various processes that alter serum ferritin levels complicate the clinical interpretation of this laboratory value. In this article, we review the structure and function of ferritin and provide a guide for clinical use.
Overview of Iron
Iron is an essential element of key biologic functions including DNA synthesis and repair, oxygen transport, and oxidative phosphorylation. The body’s iron stores are mainly derived from internal iron recycling following red blood cell breakdown, while 5% to 10% is supplied by dietary intake.1-3 Iron metabolism is of particular importance in cells of the reticuloendothelial system (eg, spleen, liver, bone marrow), where excess iron must be appropriately sequestered and from which iron can be mobilized.4 Sufficient iron stores are necessary for proper cellular function and survival, as iron is a necessary component of hemoglobin for oxygen delivery, iron-sulfur clusters in electron transport, and enzyme cofactors in other cellular processes.
Although labile pools of biologically active free iron exist in limited amounts within cells, excess free iron can generate free radicals that damage cellular proteins, lipids, and nucleic acids.5-7 As such, most intracellular iron is captured within ferritin molecules. The excretion of iron is unregulated and occurs through loss in sweat, menstruation, hair shedding, skin desquamation, and enterocyte turnover.8 The lack of regulated excretion highlights the need for a tightly regulated system of uptake, transportation, storage, and sequestration to maintain iron homeostasis.
Overview of Ferritin Structure and Function
Ferritin is a key regulator of iron homeostasis that also serves as an important clinical indicator of body iron status. Ferritin mainly is found as an intracellular cytosolic iron storage and detoxification protein structured as a hollow 24-subunit polymer shell that can sequester up to 4500 atoms of iron within its core.9,10 The 24-mer is composed of both ferritin L (FTL) and ferritin H (FTH) subunits, with dynamic regulation of the H:L ratio dependent on the context and tissue in which ferritin is found.6
Ferritin H possesses ferroxidase, which facilitates oxidation of ferrous (Fe2+) iron into ferric (Fe3+) iron, which can then be incorporated into the mineral core of the ferritin heteropolymer.11 Ferritin L is more abundant in the spleen and liver, while FTH is found predominantly in the heart and kidneys where the increased ferroxidase activity may confer an increased ability to oxidize Fe2+ and limit oxidative stress.6
Regulation of Ferritin Synthesis and Secretion
Ferritin synthesis is regulated by intracellular nonheme iron levels, governed mainly by an iron response element (IRE) and iron response protein (IRP) translational repression system. Both FTH and FTL messenger RNA (mRNA) contain an IRE that is a regulatory stem-loop structure in the 5´ untranslated region. When the IRE is bound by IRP1 or IRP2, mRNA translation of ferritin subunits is suppressed.6 In low iron conditions, IRPs have greater affinity for IRE, and binding suppresses ferritin translation.12 In high iron conditions, IRPs have a decreased affinity for IRE, and ferritin mRNA synthesis is increased.13 Additionally, inflammatory cytokines such as tumor necrosis factor α and IL-1α transcriptionally induce FTH synthesis, resulting in an increased population of H-rich ferritins.11,14-16 A study using cultured human primary skin fibroblasts demonstrated UV radiation–induced increases in free intracellular iron content.17,18 Pourzand et al18 suggested that UV-mediated damage of lysosomal membranes results in leakage of lysosomal proteases into the cytosol, contributing to degradation of intracellular ferritin and subsequent release of iron within skin fibroblasts. The increased intracellular iron downregulates IRPs and increases ferritin mRNA synthesis,18 consistent with prior findings of increased ferritin synthesis in skin that is induced by UV radiation.19
Molecular analysis of serum ferritin in iron-overloaded mice revealed that extracellular ferritin found in the serum is composed of a greater fraction of FTL and has lower iron content than intracellular ferritin. The low iron content of serum ferritin compared with intracellular ferritin and transferrin suggests that serum ferritin is not a major pathway of systemic iron transport.10 However, locally secreted ferritins may play a greater role in iron transport and release in selected tissues. Additionally, in vitro studies of cell cultures from humans and mice have demonstrated the ability of macrophages to secrete ferritin, suggesting that macrophages are an important cellular source of serum ferritin.10,20 As such, serum ferritin generally may reflect body iron status but more specifically reflects macrophage iron status.10 Although the exact pathways of ferritin release are unknown, it is hypothesized that ferritin secretion occurs through cytosolic autophagy followed by secretion of proteins from the lysosomal compartment.10,18,21
Clinical Utility of Serum Ferritin
Low Ferritin and Iron Deficiency—Although bone marrow biopsy with iron staining remains the gold standard for diagnosis of iron deficiency, serum ferritin is a much more accessible and less invasive tool for evaluation of iron status. A serum ferritin level below 12 μg/L is highly specific for iron depletion,22 with a higher cutoff recommended in clinical practice to improve diagnostic sensitivity.23,24 Conditions independent of iron deficiency that may reduce serum ferritin include hypothyroidism and ascorbate deficiency, though neither condition has been reported to interfere with appropriate diagnosis of iron deficiency.25 Guyatt et al26 conducted a systematic review of laboratory tests used in the diagnosis of iron deficiency anemia and identified 55 studies suitable for inclusion. Based on an area under the receiver operating characteristic curve (AUROC) of 0.95, serum ferritin values were superior to transferrin saturation (AUROC, 0.74), red cell protoporphyrin (AUROC, 0.77), red cell volume distribution width (AUROC, 0.62), and mean cell volume (AUROC, 0.76) for diagnosis of IDA, verified by histologic examination of aspirated bone marrow.26 The likelihood ratio of iron deficiency begins to decrease for serum ferritin values of 40 μg/L or greater. For patients with inflammatory conditions—patients with concomitant chronic renal failure, inflammatory disease, infection, rheumatoid arthritis, liver disease, inflammatory bowel disease, and malignancy—the likelihood of iron deficiency begins to decrease at serum ferritin levels of 70 μg/L or greater.26 Similarly, the World Health Organization recommends that in adults with infection or inflammation, serum ferritin levels lower than 70 μg/L may be used to indicate iron deficiency.24 A serum ferritin level of 41 μg/L or lower was found to have a sensitivity and specificity of 98% for discriminating between iron-deficiency anemia and anemia of chronic disease (diagnosed based on bone marrow biopsy with iron staining), with an AUROC of 0.98.27 As such, we recommend using a serum ferritin level of 40 μg/L or lower in patients who are otherwise healthy as an indicator of iron deficiency.
The threshold for iron supplementation may vary based on age, sex, and race. In women, ferritin levels increase during menopause and peak after menopause; ferritin levels are higher in men than in women.28-30 A multisite longitudinal cohort study of 70 women in the United States found that the mean (SD) ferritin valuewas 69.5 (81.7) μg/L premenopause and 128.8 (125.7) μg/L postmenopause (P<.01).31 A separate longitudinal survey study of 8564 patients in China found that the mean (SE) ferritin value was 201.55 (3.60) μg/L for men and 80.46 (1.64) μg/L for women (P<.0001).32 Analysis of serum ferritin levels of 3554 male patients from the third National Health and Nutrition Examination Survey demonstrated that patients who self-reported as non-Hispanic Black (n=1616) had significantly higher serum ferritin levels than non-Hispanic White patients (n=1938)(serum ferritin difference of 37.1 μg/L)(P<.0001).33 The British Society for Haematology guidelines recommend that the threshold of serum ferritin for diagnosing iron deficiency should take into account age-, sex-, and race-based differences.34 Ferritin and Hair—Cutaneous manifestations of iron deficiency include koilonychia, glossitis, pruritus, angular cheilitis, and telogen effluvium (TE).1 A case-control study of 30 females aged 15 to 45 years demonstrated that the mean (SD) ferritin level was significantly lower in patients with TE than those with no hair loss (16.3 [12.6] ng/mL vs 60.3 [50.1] ng/mL; P<.0001). Using a threshold of 30 μg/L or lower, the investigators found that the odds ratio for TE was 21.0 (95% CI, 4.2-105.0) in patients with low serum ferritin.35
Another retrospective review of 54 patients with diffuse hair loss and 55 controls compared serum vitamin B12, folate, thyroid-stimulating hormone, zinc, ferritin, and 25-hydroxy vitamin D levels between the 2 groups.36 Exclusion criteria were clinical diagnoses of female pattern hair loss (androgenetic alopecia), pregnancy, menopause, metabolic and endocrine disorders, hormone replacement therapy, chemotherapy, immunosuppressive therapy, vitamin and mineral supplementation, scarring alopecia, eating disorders, and restrictive diets. Compared with controls, patients with diffuse nonscarring hair loss were found to have significantly lower ferritin (mean [SD], 14.72 [10.70] ng/mL vs 25.30 [14.41] ng/mL; P<.001) and 25-hydroxy vitamin D levels (mean [SD], 14.03 [8.09] ng/mL vs 17.01 [8.59] ng/mL; P=.01).36
In contrast, a separate case-control study of 381 cases and 76 controls found no increase in the rate of iron deficiency—defined as ferritin ≤15 μg/L or ≤40 μg/L—among women with female pattern hair loss or chronic TE vs controls.37 Taken together, these studies suggest that iron status may play a role in TE, a process that may result from nutritional deficiency, trauma, or physical or psychological stress38; however, there is insufficient evidence to suggest that low iron status impacts androgenetic alopecia, in which its multifactorial pathogenesis implicates genetic and hormonal factors.39 More research is needed to clarify the potential associations between iron deficiency and types of hair loss. Additionally, it is unclear whether iron supplementation improves hair growth parameters such as density and caliber.40
Low serum ferritin (<40 μg/L) with concurrent symptoms of iron deficiency, including fatigue, pallor, dyspnea on exertion, or hair loss, should prompt treatment with supplemental iron.41-43 Generally, ferrous (Fe2+) salts are preferred to ferric (Fe3+) salts, as the former is more readily absorbed through the duodenal mucosa44 and is the more common formulation in commercially available supplements in the United States.45 Oral supplementation with ferrous sulfate 325 mg (65 mg elemental iron) tablets is the first-line therapy for iron deficiency anemia.1 Alternatively, ferrous gluconate 324 mg (38 mg elemental iron) over-the-counter and its liquid form has demonstrated superior absorption compared to ferrous sulfate tablets in a clinical study with peritoneal dialysis patients.1,46 One study suggested that oral iron 40 to 80 mg should be taken every other day to increase absorption.47 Due to improved bioavailability, intravenous iron may be utilized in patients with malabsorption, renal failure, or intolerance to oral iron (including those with gastric ulcers or active inflammatory bowel disease), with the formulation chosen based on underlying comorbidities and potential risks.1,48 The theoretical risk for potentiating bacterial growth by increasing the amount of unbound iron in the blood raises concerns of iron supplementation in patients with infection or sepsis. Although far from definitive, existing data suggest that risk for infection is greater with intravenous iron supplementation and should be carefully considered prior to use.49,50Elevated Ferritin—Elevated ferritin may be difficult to interpret given the multitude of conditions that can cause it.23,51,52 Elevated serum ferritin can be broadly characterized by increased synthesis due to iron overload, increased synthesis due to inflammation, or increased ferritin release from cellular damage.34 Further complicating interpretation is the potential diurnal fluctuations in serum iron levels dependent on dietary intake and timing of laboratory evaluation, choice of assay, differences in reference standards, and variations in calibration procedures that can lead to analytic variability in the measurement of ferritin.23,53,54
Among healthy patients, serum ferritin is directly proportional to iron status.9,51 A study utilizing weekly phlebotomy of 22 healthy participants to measure serum ferritin and calculate mobilizable storage iron found a strong positive correlation between the 2 variables (r=0.83, P<.001), with each 1-μg/L increase of serum ferritin corresponding to approximately an 8-mg increase of storage iron; the initial serum ferritin values ranged from 2 to 83 μg/L in females and 36 to 224 μg/L in males.55 The correlation of ferritin with iron status also was supported by the significant correlation between the number of transfusions received in patients with transfusion-related iron overload and serum ferritin levels (r=0.89, P<.001), with an average increase of 60 μg/L per transfusion.51
Clinical guidelines on the interpretation of serum ferritin levels by Cullis et al34 recommend a normal upper limit of 200 μg/L for healthy females and 300 μg/L for healthy males. Outside of clinical syndromes associated with iron overload, Lee and Means56 found that serum ferritin of 1000 μg/L or higher was a nonspecific marker of disease, including infection and/or neoplastic disorders. We have adapted these guidelines to propose a workflow for evaluation of serum ferritin levels (Figure). In patients with inflammatory conditions or those affected by metabolic syndrome, elevated serum ferritin does not correlate with body iron status.57,58 It is believed that inflammatory cytokines, including tumor necrosis factor α and IL-1α, can upregulate ferritin synthesis independent of cellular iron stores.15,16 Several studies have examined the relationship between insulin resistance and/or metabolic syndrome with serum ferritin levels.31,32 Han et al32 found that elevated serum ferritin was significantly associated with higher risk for metabolic syndrome in men (P<.0001) but not in women.
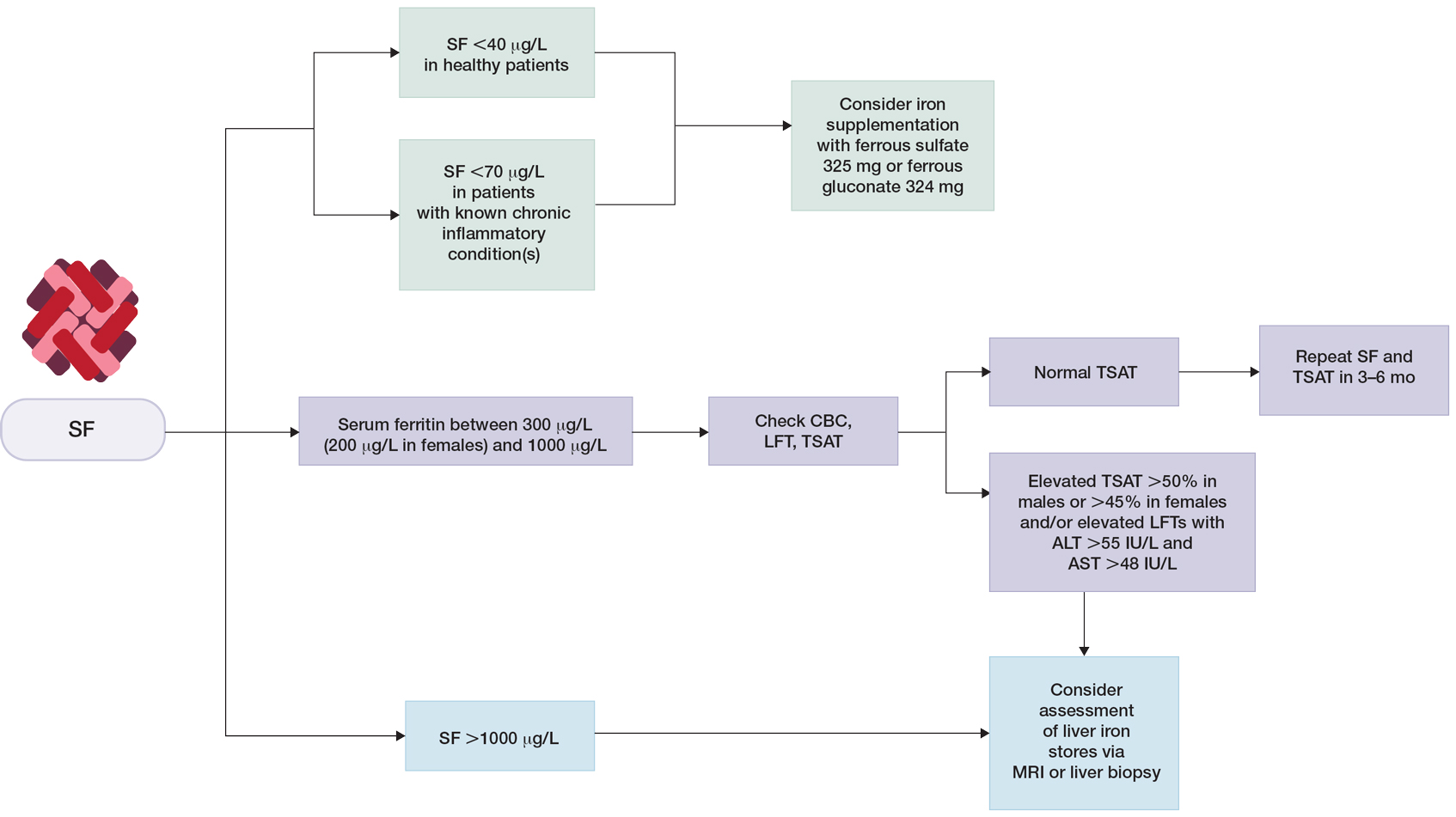
Although cutaneous manifestations of iron overload can be seen as skin hyperpigmentation due to increased iron deposits and increased melanin production,22 the effects of elevated ferritin on the skin and hair are not well known. Iron overload is a known trigger of porphyria cutanea tarda (PCT),59 a condition in which reduced or absent enzymatic activity of uroporphyrinogen decarboxylase (UROD) leads to build up of toxic porphyrins in various organs.60 In the skin, PCT manifests as a blistering photosensitive eruption that may resolve as dyspigmentation, scarring, and milia.61 Phlebotomy is first-line therapy in PCT to reduce serum iron and subsequent formation of UROD inhibitors, with guidelines suggesting discontinuation of phlebotomy when serum ferritin levels reach 20 ng/mL or lower.60 Hyperferritinemia (serum ferritin >500 μg/L) is a common finding in several inflammatory disorders often accompanied by clinically apparent cutaneous symptoms such as adult-onset Still disease,62 hemophagocytic lymphohistiocytosis,63,64 and anti-melanoma differentiation-associated gene 5 dermatomyositis.65 Among these conditions, serum ferritin levels have been reported to correlate with disease activity, raising the question of whether ferritin is a bystander or a driver of the underlying pathology.62,66,67 However, rapid decline of serum ferritin levels with treatment and control of inflammatory cytokines suggest that ferritin is unlikely to contribute to pathology.62,67
Final Thoughts
Many clinical studies have examined the association between hair health and body iron status, the collective findings of which suggest that iron deficiency may be associated with TE. Among commonly measured serum iron parameters, low ferritin is a highly specific and sensitive marker for diagnosing iron deficiency. Serum ferritin may be a clinically useful tool for ruling out underlying iron deficiency in patients presenting with hair loss. Despite advances in our understanding of the molecular mechanisms of ferritin synthesis and regulation, whether ferritin itself contributes to cutaneous pathology is poorly understood.35,36,68-74 For patients who are otherwise healthy with low suspicion for inflammatory disorders, chronic systemic illnesses, or malignancy, serum ferritin can be used as an indicator of body iron status. The workup for slightly elevated serum ferritin should be interpreted in the context of other laboratory findings and should be reassessed over time. Serum ferritin levels above 1000 μg/L warrant further investigation into causes such as iron overload conditions and underlying inflammatory conditions or malignancy.
- Hoffman M, Micheletti RG, Shields BE. Nutritional dermatoses in the hospitalized patient. Cutis. 2020;105:296, 302-308, E1-E5.
- Ganz T. Macrophages and systemic iron homeostasis. J Innate Immun. 2012;4:446-453. doi:10.1159/000336423
- Slusarczyk P, Mandal PK, Zurawska G, et al. Impaired iron recycling from erythrocytes is an early hallmark of aging. eLife. 2023;12:E79196. doi:10.7554/eLife.79196
- Crichton RR. Ferritin: structure, synthesis and function. N Engl J Med. 1971;284:1413-1422. doi:10.1056/nejm197106242842506
- Sandnes M, Ulvik RJ, Vorland M, et al. Hyperferritinemia—a clinical overview. J Clin Med. 2021;10:2008. doi:10.3390/jcm10092008
- Kernan KF, Carcillo JA. Hyperferritinemia and inflammation. Int Immunol. 2017;29:401-409. doi:10.1093/intimm/dxx031
- Wright JA, Richards T, Srai SKS. The role of iron in the skin and cutaneous wound healing. review. Front Pharmacol. 2014;5:156. doi:10.3389/fphar.2014.00156
- Ems T, St Lucia K, Huecker MR. Biochemistry, iron absorption. StatPearls Publishing; 2022.
- Crichton RR. Ferritin: structure, synthesis and function. N Engl J Med. 1971;284:1413-1422. doi:10.1056/nejm197106242842506
- Cohen LA, Gutierrez L, Weiss A, et al. Serum ferritin is derived primarily from macrophages through a nonclassical secretory pathway. Blood. 2010;116:1574-1584. doi:10.1182/blood-2009-11-253815
- Briat JF, Ravet K, Arnaud N, et al. New insights into ferritin synthesis and function highlight a link between iron homeostasis and oxidative stress in plants. Ann Bot. 2010;105:811-822. doi:10.1093/aob/mcp128
- Kato J, Kobune M, Ohkubo S, et al. Iron/IRP-1-dependent regulation of mRNA expression for transferrin receptor, DMT1 and ferritin during human erythroid differentiation. Exp Hematol. 2007;35:879-887. doi:10.1016/j.exphem.2007.03.005
- Gozzelino R, Soares MP. Coupling heme and iron metabolism via ferritin H chain. Antioxid Redox Signal. 2014;20:1754-1769. doi:10.1089/ars.2013.5666
- Torti FM, Torti SV. Regulation of ferritin genes and protein. Blood. 2002;99:3505-3516. doi:10.1182/blood.V99.10.3505
- Torti SV, Kwak EL, Miller SC, et al. The molecular cloning and characterization of murine ferritin heavy chain, a tumor necrosis factor-inducible gene. J Biol Chem. 1988;263:12638-12644.
- Wei Y, Miller SC, Tsuji Y, et al. Interleukin 1 induces ferritin heavy chain in human muscle cells. Biochem Biophys Res Commun. 1990;169:289-296. doi:10.1016/0006-291x(90)91466-6
- Bissett DL, Chatterjee R, Hannon DP. Chronic ultraviolet radiation–induced increase in skin iron and the photoprotective effect of topically applied iron chelators. Photochem Photobiol. 1991;54:215-223. https://doi.org/10.1111/j.1751-1097.1991.tb02009.x
- Pourzand C, Watkin RD, Brown JE, et al. Ultraviolet A radiation induces immediate release of iron in human primary skin fibroblasts: the role of ferritin. Proc Natl Acad Sci U S A. 1999;96:6751-6756. doi:10.1073/pnas.96.12.6751
- Applegate LA, Scaletta C, Panizzon R, et al. Evidence that ferritin is UV inducible in human skin: part of a putative defense mechanism. J Invest Dermatol. 1998;111:159-163. https://doi.org/10.1046/j.1523-1747.1998.00254.x
- Wesselius LJ, Nelson ME, Skikne BS. Increased release of ferritin and iron by iron-loaded alveolar macrophages in cigarette smokers. Am J Respir Crit Care Med. 1994;150:690-695. doi:10.1164/ajrccm.150.3.8087339
- De Domenico I, Ward DM, Kaplan J. Specific iron chelators determine the route of ferritin degradation. Blood. 2009;114:4546-4551. doi:10.1182/blood-2009-05-224188
- Knovich MA, Storey JA, Coffman LG, et al. Ferritin for the clinician. Blood Rev. 2009;23:95-104. doi:10.1016/j.blre.2008.08.001
- Dignass A, Farrag K, Stein J. Limitations of serum ferritin in diagnosing iron deficiency in inflammatory conditions. Int J Chronic Dis. 2018;2018:9394060. doi:10.1155/2018/9394060
- World Health Organization. WHO guideline on use of ferritin concentrations to assess iron status in individuals and populations. Published April 21, 2020. Accessed July 23, 2023. https://www.who.int/publications/i/item/9789240000124
- Finch CA, Bellotti V, Stray S, et al. Plasma ferritin determination as a diagnostic tool. West J Med. 1986;145:657-663.
- Guyatt GH, Oxman AD, Ali M, et al. Laboratory diagnosis of iron-deficiency anemia. J Gen Intern Med. 1992;7:145-153. doi:10.1007/BF02598003
- Punnonen K, Irjala K, Rajamäki A. Serum transferrin receptor and its ratio to serum ferritin in the diagnosis of iron deficiency. Blood. 1997;89:1052-1057. https://doi.org/10.1182/blood.V89.3.1052
- Zacharski LR, Ornstein DL, Woloshin S, et al. Association of age, sex, and race with body iron stores in adults: analysis of NHANES III data. American Heart Journal. 2000;140:98-104. https://doi.org/10.1067/mhj.2000.106646
- Milman N, Kirchhoff M. Iron stores in 1359, 30- to 60-year-old Danish women: evaluation by serum ferritin and hemoglobin. Ann Hematol. 1992;64:22-27. doi:10.1007/bf01811467
- Liu J-M, Hankinson SE, Stampfer MJ, et al. Body iron stores and their determinants in healthy postmenopausal US women. Am J Clin Nutr. 2003;78:1160-1167. doi:10.1093/ajcn/78.6.1160
- Kim C, Nan B, Kong S, et al. Changes in iron measures over menopause and associations with insulin resistance. J Womens Health (Larchmt). 2012;21:872-877. doi:10.1089/jwh.2012.3549
- Han LL, Wang YX, Li J, et al. Gender differences in associations of serum ferritin and diabetes, metabolic syndrome, and obesity in the China Health and Nutrition Survey. Mol Nutr Food Res. 2014;58:2189-2195. doi:10.1002/mnfr.201400088
- Pan Y, Jackson RT. Insights into the ethnic differences in serum ferritin between black and white US adult men. Am J Hum Biol. 2008;20:406-416. https://doi.org/10.1002/ajhb.20745
- Cullis JO, Fitzsimons EJ, Griffiths WJ, et al. Investigation and management of a raised serum ferritin. Br J Haematol. 2018;181:331-340. doi:10.1111/bjh.15166
- Moeinvaziri M, Mansoori P, Holakooee K, et al. Iron status in diffuse telogen hair loss among women. Acta Dermatovenerol Croat. 2009;17:279-284.
- Tamer F, Yuksel ME, Karabag Y. Serum ferritin and vitamin D levels should be evaluated in patients with diffuse hair loss prior to treatment. Postepy Dermatol Alergol. 2020;37:407-411. doi:10.5114/ada.2020.96251
- Olsen EA, Reed KB, Cacchio PB, et al. Iron deficiency in female pattern hair loss, chronic telogen effluvium, and control groups. J Am Acad Dermatol. 2010;63:991-999. doi:10.1016/j.jaad.2009.12.006
- Asghar F, Shamim N, Farooque U, et al. Telogen effluvium: a review of the literature. Cureus. 2020;12:E8320. doi:10.7759/cureus.8320
- Brough KR, Torgerson RR. Hormonal therapy in female pattern hair loss. Int J Womens Dermatol. 2017;3:53-57. doi:10.1016/j.ijwd.2017.01.001
- Klein EJ, Karim M, Li X, et al. Supplementation and hair growth: a retrospective chart review of patients with alopecia and laboratory abnormalities. JAAD Int. 2022;9:69-71. doi:10.1016/j.jdin.2022.08.013
- Goksin S. Retrospective evaluation of clinical profile and comorbidities in patients with alopecia areata. North Clin Istanb. 2022;9:451-458. doi:10.14744/nci.2022.78790
- Beatrix J, Piales C, Berland P, et al. Non-anemic iron deficiency: correlations between symptoms and iron status parameters. Eur J Clin Nutr. 2022;76:835-840. doi:10.1038/s41430-021-01047-5
- Treister-Goltzman Y, Yarza S, Peleg R. Iron deficiency and nonscarring alopecia in women: systematic review and meta-analysis. Skin Appendage Disord. 2022;8:83-92. doi:10.1159/000519952
- Santiago P. Ferrous versus ferric oral iron formulations for the treatment of iron deficiency: a clinical overview. ScientificWorldJournal. 2012;2012:846824. doi:10.1100/2012/846824
- Lo JO, Benson AE, Martens KL, et al. The role of oral iron in the treatment of adults with iron deficiency. Eur J Haematol. 2023;110:123-130. doi:10.1111/ejh.13892
- Lausevic´ M, Jovanovic´ N, Ignjatovic´ S, et al. Resorption and tolerance of the high doses of ferrous sulfate and ferrous gluconate in the patients on peritoneal dialysis. Vojnosanit Pregl. 2006;63:143-147. doi:10.2298/vsp0602143l
- Stoffel NU, Zeder C, Brittenham GM, et al. Iron absorption from supplements is greater with alternate day than with consecutive day dosing in iron-deficient anemic women. Haematologica. 2020;105:1232-1239. doi:10.3324/haematol.2019.220830
- Jimenez KM, Gasche C. Management of iron deficiency anaemia in inflammatory bowel disease. Acta Haematologica. 2019;142:30-36. doi:10.1159/000496728
- Shah AA, Donovan K, Seeley C, et al. Risk of infection associated with administration of intravenous iron: a systematic review and meta-analysis. JAMA Netw Open. 2021;4:E2133935-E2133935. doi:10.1001/jamanetworkopen.2021.33935
- Ganz T, Aronoff GR, Gaillard CAJM, et al. Iron administration, infection, and anemia management in ckd: untangling the effects of intravenous iron therapy on immunity and infection risk. Kidney Med. 2020/05/01/ 2020;2:341-353. doi: 10.1016/j.xkme.2020.01.006
- Lipschitz DA, Cook JD, Finch CA. A clinical evaluation of serum ferritin as an index of iron stores. N Engl J Med. 1974;290:1213-1216. doi:10.1056/nejm197405302902201
- Loveikyte R, Bourgonje AR, van der Reijden JJ, et al. Hepcidin and iron status in patients with inflammatory bowel disease undergoing induction therapy with vedolizumab or infliximab [published online February 7, 2023]. Inflamm Bowel Dis. doi:10.1093/ibd/izad010
- Borel MJ, Smith SM, Derr J, et al. Day-to-day variation in iron-status indices in healthy men and women. Am J Clin Nutr. 1991;54:729-735. doi:10.1093/ajcn/54.4.729
- Ford BA, Coyne DW, Eby CS, et al. Variability of ferritin measurements in chronic kidney disease; implications for iron management. Kidney International. 2009;75:104-110. doi:10.1038/ki.2008.526
- Walters GO, Miller FM, Worwood M. Serum ferritin concentration and iron stores in normal subjects. J Clin Pathol. 1973;26:770-772. doi:10.1136/jcp.26.10.770
- Lee MH, Means RT Jr. Extremely elevated serum ferritin levels in a university hospital: associated diseases and clinical significance. Am J Med. Jun 1995;98:566-571. doi:10.1016/s0002-9343(99)80015-1
- Theil EC. Ferritin: structure, gene regulation, and cellular function in animals, plants, and microorganisms. Annu Rev Biochem. 1987;56:289-315. doi:10.1146/annurev.bi.56.070187.001445
- Chen LY, Chang SD, Sreenivasan GM, et al. Dysmetabolic hyperferritinemia is associated with normal transferrin saturation, mild hepatic iron overload, and elevated hepcidin. Ann Hematol. 2011;90:139-143. doi:10.1007/s00277-010-1050-x
- Sampietro M, Fiorelli G, Fargion S. Iron overload in porphyria cutanea tarda. Haematologica. 1999;84:248-253.
- Singal AK. Porphyria cutanea tarda: recent update. Mol Genet Metab. 2019;128:271-281. doi:10.1016/j.ymgme.2019.01.004
- Frank J, Poblete-Gutiérrez P. Porphyria cutanea tarda—when skin meets liver. Best Pract Res Clin Gastroenterol. 2010;24:735-745. doi:10.1016/j.bpg.2010.07.002
- Mehta B, Efthimiou P. Ferritin in adult-onset Still’s disease: just a useful innocent bystander? Int J Inflam. 2012;2012:298405. doi:10.1155/2012/298405
- Ma AD, Fedoriw YD, Roehrs P. Hyperferritinemia and hemophagocytic lymphohistiocytosis. single institution experience in adult and pediatric patients. Blood. 2012;120:2135-2135. doi:10.1182/blood.V120.21.2135.2135
- Basu S, Maji B, Barman S, et al. Hyperferritinemia in hemophagocytic lymphohistiocytosis: a single institution experience in pediatric patients. Indian J Clin Biochem. 2018;33:108-112. doi:10.1007/s12291-017-0655-4
- Yamada K, Asai K, Okamoto A, et al. Correlation between disease activity and serum ferritin in clinically amyopathic dermatomyositis with rapidly-progressive interstitial lung disease: a case report. BMC Res Notes. 2018;11:34. doi:10.1186/s13104-018-3146-7
- Zohar DN, Seluk L, Yonath H, et al. Anti-MDA5 positive dermatomyositis associated with rapidly progressive interstitial lung disease and correlation between serum ferritin level and treatment response. Mediterr J Rheumatol. 2020;31:75-77. doi:10.31138/mjr.31.1.75
- Lin TF, Ferlic-Stark LL, Allen CE, et al. Rate of decline of ferritin in patients with hemophagocytic lymphohistiocytosis as a prognostic variable for mortality. Pediatr Blood Cancer. 2011;56:154-155. doi:10.1002/pbc.22774
- Bregy A, Trueb RM. No association between serum ferritin levels >10 microg/l and hair loss activity in women. Dermatology. 2008;217:1-6. doi:10.1159/000118505
- de Queiroz M, Vaske TM, Boza JC. Serum ferritin and vitamin D levels in women with non-scarring alopecia. J Cosmet Dermatol. 2022;21:2688-2690. doi:10.1111/jocd.14472
- El-Husseiny R, Alrgig NT, Abdel Fattah NSA. Epidemiological and biochemical factors (serum ferritin and vitamin D) associated with premature hair graying in Egyptian population. J Cosmet Dermatol. 2021;20:1860-1866. doi:10.1111/jocd.13747
- Enitan AO, Olasode OA, Onayemi EO, et al. Serum ferritin levels amongst individuals with androgenetic alopecia in Ile-Ife, Nigeria. West Afr J Med. 2022;39:1026-1031.
- I˙bis¸ S, Aksoy Sarac¸ G, Akdag˘ T. Evaluation of MCV/RDW ratio and correlations with ferritin in telogen effluvium patients. Dermatol Pract Concept. 2022;12:E2022151. doi:10.5826/dpc.1203a151
- Kakpovbia E, Ogbechie-Godec OA, Shapiro J, et al. Laboratory testing in telogen effluvium. J Drugs Dermatol. 2021;20:110-111. doi:10.36849/jdd.5771
- Rasheed H, Mahgoub D, Hegazy R, et al. Serum ferritin and vitamin D in female hair loss: do they play a role? Skin Pharmacol Physiol. 2013;26:101-107. doi:10.1159/000346698
- Hoffman M, Micheletti RG, Shields BE. Nutritional dermatoses in the hospitalized patient. Cutis. 2020;105:296, 302-308, E1-E5.
- Ganz T. Macrophages and systemic iron homeostasis. J Innate Immun. 2012;4:446-453. doi:10.1159/000336423
- Slusarczyk P, Mandal PK, Zurawska G, et al. Impaired iron recycling from erythrocytes is an early hallmark of aging. eLife. 2023;12:E79196. doi:10.7554/eLife.79196
- Crichton RR. Ferritin: structure, synthesis and function. N Engl J Med. 1971;284:1413-1422. doi:10.1056/nejm197106242842506
- Sandnes M, Ulvik RJ, Vorland M, et al. Hyperferritinemia—a clinical overview. J Clin Med. 2021;10:2008. doi:10.3390/jcm10092008
- Kernan KF, Carcillo JA. Hyperferritinemia and inflammation. Int Immunol. 2017;29:401-409. doi:10.1093/intimm/dxx031
- Wright JA, Richards T, Srai SKS. The role of iron in the skin and cutaneous wound healing. review. Front Pharmacol. 2014;5:156. doi:10.3389/fphar.2014.00156
- Ems T, St Lucia K, Huecker MR. Biochemistry, iron absorption. StatPearls Publishing; 2022.
- Crichton RR. Ferritin: structure, synthesis and function. N Engl J Med. 1971;284:1413-1422. doi:10.1056/nejm197106242842506
- Cohen LA, Gutierrez L, Weiss A, et al. Serum ferritin is derived primarily from macrophages through a nonclassical secretory pathway. Blood. 2010;116:1574-1584. doi:10.1182/blood-2009-11-253815
- Briat JF, Ravet K, Arnaud N, et al. New insights into ferritin synthesis and function highlight a link between iron homeostasis and oxidative stress in plants. Ann Bot. 2010;105:811-822. doi:10.1093/aob/mcp128
- Kato J, Kobune M, Ohkubo S, et al. Iron/IRP-1-dependent regulation of mRNA expression for transferrin receptor, DMT1 and ferritin during human erythroid differentiation. Exp Hematol. 2007;35:879-887. doi:10.1016/j.exphem.2007.03.005
- Gozzelino R, Soares MP. Coupling heme and iron metabolism via ferritin H chain. Antioxid Redox Signal. 2014;20:1754-1769. doi:10.1089/ars.2013.5666
- Torti FM, Torti SV. Regulation of ferritin genes and protein. Blood. 2002;99:3505-3516. doi:10.1182/blood.V99.10.3505
- Torti SV, Kwak EL, Miller SC, et al. The molecular cloning and characterization of murine ferritin heavy chain, a tumor necrosis factor-inducible gene. J Biol Chem. 1988;263:12638-12644.
- Wei Y, Miller SC, Tsuji Y, et al. Interleukin 1 induces ferritin heavy chain in human muscle cells. Biochem Biophys Res Commun. 1990;169:289-296. doi:10.1016/0006-291x(90)91466-6
- Bissett DL, Chatterjee R, Hannon DP. Chronic ultraviolet radiation–induced increase in skin iron and the photoprotective effect of topically applied iron chelators. Photochem Photobiol. 1991;54:215-223. https://doi.org/10.1111/j.1751-1097.1991.tb02009.x
- Pourzand C, Watkin RD, Brown JE, et al. Ultraviolet A radiation induces immediate release of iron in human primary skin fibroblasts: the role of ferritin. Proc Natl Acad Sci U S A. 1999;96:6751-6756. doi:10.1073/pnas.96.12.6751
- Applegate LA, Scaletta C, Panizzon R, et al. Evidence that ferritin is UV inducible in human skin: part of a putative defense mechanism. J Invest Dermatol. 1998;111:159-163. https://doi.org/10.1046/j.1523-1747.1998.00254.x
- Wesselius LJ, Nelson ME, Skikne BS. Increased release of ferritin and iron by iron-loaded alveolar macrophages in cigarette smokers. Am J Respir Crit Care Med. 1994;150:690-695. doi:10.1164/ajrccm.150.3.8087339
- De Domenico I, Ward DM, Kaplan J. Specific iron chelators determine the route of ferritin degradation. Blood. 2009;114:4546-4551. doi:10.1182/blood-2009-05-224188
- Knovich MA, Storey JA, Coffman LG, et al. Ferritin for the clinician. Blood Rev. 2009;23:95-104. doi:10.1016/j.blre.2008.08.001
- Dignass A, Farrag K, Stein J. Limitations of serum ferritin in diagnosing iron deficiency in inflammatory conditions. Int J Chronic Dis. 2018;2018:9394060. doi:10.1155/2018/9394060
- World Health Organization. WHO guideline on use of ferritin concentrations to assess iron status in individuals and populations. Published April 21, 2020. Accessed July 23, 2023. https://www.who.int/publications/i/item/9789240000124
- Finch CA, Bellotti V, Stray S, et al. Plasma ferritin determination as a diagnostic tool. West J Med. 1986;145:657-663.
- Guyatt GH, Oxman AD, Ali M, et al. Laboratory diagnosis of iron-deficiency anemia. J Gen Intern Med. 1992;7:145-153. doi:10.1007/BF02598003
- Punnonen K, Irjala K, Rajamäki A. Serum transferrin receptor and its ratio to serum ferritin in the diagnosis of iron deficiency. Blood. 1997;89:1052-1057. https://doi.org/10.1182/blood.V89.3.1052
- Zacharski LR, Ornstein DL, Woloshin S, et al. Association of age, sex, and race with body iron stores in adults: analysis of NHANES III data. American Heart Journal. 2000;140:98-104. https://doi.org/10.1067/mhj.2000.106646
- Milman N, Kirchhoff M. Iron stores in 1359, 30- to 60-year-old Danish women: evaluation by serum ferritin and hemoglobin. Ann Hematol. 1992;64:22-27. doi:10.1007/bf01811467
- Liu J-M, Hankinson SE, Stampfer MJ, et al. Body iron stores and their determinants in healthy postmenopausal US women. Am J Clin Nutr. 2003;78:1160-1167. doi:10.1093/ajcn/78.6.1160
- Kim C, Nan B, Kong S, et al. Changes in iron measures over menopause and associations with insulin resistance. J Womens Health (Larchmt). 2012;21:872-877. doi:10.1089/jwh.2012.3549
- Han LL, Wang YX, Li J, et al. Gender differences in associations of serum ferritin and diabetes, metabolic syndrome, and obesity in the China Health and Nutrition Survey. Mol Nutr Food Res. 2014;58:2189-2195. doi:10.1002/mnfr.201400088
- Pan Y, Jackson RT. Insights into the ethnic differences in serum ferritin between black and white US adult men. Am J Hum Biol. 2008;20:406-416. https://doi.org/10.1002/ajhb.20745
- Cullis JO, Fitzsimons EJ, Griffiths WJ, et al. Investigation and management of a raised serum ferritin. Br J Haematol. 2018;181:331-340. doi:10.1111/bjh.15166
- Moeinvaziri M, Mansoori P, Holakooee K, et al. Iron status in diffuse telogen hair loss among women. Acta Dermatovenerol Croat. 2009;17:279-284.
- Tamer F, Yuksel ME, Karabag Y. Serum ferritin and vitamin D levels should be evaluated in patients with diffuse hair loss prior to treatment. Postepy Dermatol Alergol. 2020;37:407-411. doi:10.5114/ada.2020.96251
- Olsen EA, Reed KB, Cacchio PB, et al. Iron deficiency in female pattern hair loss, chronic telogen effluvium, and control groups. J Am Acad Dermatol. 2010;63:991-999. doi:10.1016/j.jaad.2009.12.006
- Asghar F, Shamim N, Farooque U, et al. Telogen effluvium: a review of the literature. Cureus. 2020;12:E8320. doi:10.7759/cureus.8320
- Brough KR, Torgerson RR. Hormonal therapy in female pattern hair loss. Int J Womens Dermatol. 2017;3:53-57. doi:10.1016/j.ijwd.2017.01.001
- Klein EJ, Karim M, Li X, et al. Supplementation and hair growth: a retrospective chart review of patients with alopecia and laboratory abnormalities. JAAD Int. 2022;9:69-71. doi:10.1016/j.jdin.2022.08.013
- Goksin S. Retrospective evaluation of clinical profile and comorbidities in patients with alopecia areata. North Clin Istanb. 2022;9:451-458. doi:10.14744/nci.2022.78790
- Beatrix J, Piales C, Berland P, et al. Non-anemic iron deficiency: correlations between symptoms and iron status parameters. Eur J Clin Nutr. 2022;76:835-840. doi:10.1038/s41430-021-01047-5
- Treister-Goltzman Y, Yarza S, Peleg R. Iron deficiency and nonscarring alopecia in women: systematic review and meta-analysis. Skin Appendage Disord. 2022;8:83-92. doi:10.1159/000519952
- Santiago P. Ferrous versus ferric oral iron formulations for the treatment of iron deficiency: a clinical overview. ScientificWorldJournal. 2012;2012:846824. doi:10.1100/2012/846824
- Lo JO, Benson AE, Martens KL, et al. The role of oral iron in the treatment of adults with iron deficiency. Eur J Haematol. 2023;110:123-130. doi:10.1111/ejh.13892
- Lausevic´ M, Jovanovic´ N, Ignjatovic´ S, et al. Resorption and tolerance of the high doses of ferrous sulfate and ferrous gluconate in the patients on peritoneal dialysis. Vojnosanit Pregl. 2006;63:143-147. doi:10.2298/vsp0602143l
- Stoffel NU, Zeder C, Brittenham GM, et al. Iron absorption from supplements is greater with alternate day than with consecutive day dosing in iron-deficient anemic women. Haematologica. 2020;105:1232-1239. doi:10.3324/haematol.2019.220830
- Jimenez KM, Gasche C. Management of iron deficiency anaemia in inflammatory bowel disease. Acta Haematologica. 2019;142:30-36. doi:10.1159/000496728
- Shah AA, Donovan K, Seeley C, et al. Risk of infection associated with administration of intravenous iron: a systematic review and meta-analysis. JAMA Netw Open. 2021;4:E2133935-E2133935. doi:10.1001/jamanetworkopen.2021.33935
- Ganz T, Aronoff GR, Gaillard CAJM, et al. Iron administration, infection, and anemia management in ckd: untangling the effects of intravenous iron therapy on immunity and infection risk. Kidney Med. 2020/05/01/ 2020;2:341-353. doi: 10.1016/j.xkme.2020.01.006
- Lipschitz DA, Cook JD, Finch CA. A clinical evaluation of serum ferritin as an index of iron stores. N Engl J Med. 1974;290:1213-1216. doi:10.1056/nejm197405302902201
- Loveikyte R, Bourgonje AR, van der Reijden JJ, et al. Hepcidin and iron status in patients with inflammatory bowel disease undergoing induction therapy with vedolizumab or infliximab [published online February 7, 2023]. Inflamm Bowel Dis. doi:10.1093/ibd/izad010
- Borel MJ, Smith SM, Derr J, et al. Day-to-day variation in iron-status indices in healthy men and women. Am J Clin Nutr. 1991;54:729-735. doi:10.1093/ajcn/54.4.729
- Ford BA, Coyne DW, Eby CS, et al. Variability of ferritin measurements in chronic kidney disease; implications for iron management. Kidney International. 2009;75:104-110. doi:10.1038/ki.2008.526
- Walters GO, Miller FM, Worwood M. Serum ferritin concentration and iron stores in normal subjects. J Clin Pathol. 1973;26:770-772. doi:10.1136/jcp.26.10.770
- Lee MH, Means RT Jr. Extremely elevated serum ferritin levels in a university hospital: associated diseases and clinical significance. Am J Med. Jun 1995;98:566-571. doi:10.1016/s0002-9343(99)80015-1
- Theil EC. Ferritin: structure, gene regulation, and cellular function in animals, plants, and microorganisms. Annu Rev Biochem. 1987;56:289-315. doi:10.1146/annurev.bi.56.070187.001445
- Chen LY, Chang SD, Sreenivasan GM, et al. Dysmetabolic hyperferritinemia is associated with normal transferrin saturation, mild hepatic iron overload, and elevated hepcidin. Ann Hematol. 2011;90:139-143. doi:10.1007/s00277-010-1050-x
- Sampietro M, Fiorelli G, Fargion S. Iron overload in porphyria cutanea tarda. Haematologica. 1999;84:248-253.
- Singal AK. Porphyria cutanea tarda: recent update. Mol Genet Metab. 2019;128:271-281. doi:10.1016/j.ymgme.2019.01.004
- Frank J, Poblete-Gutiérrez P. Porphyria cutanea tarda—when skin meets liver. Best Pract Res Clin Gastroenterol. 2010;24:735-745. doi:10.1016/j.bpg.2010.07.002
- Mehta B, Efthimiou P. Ferritin in adult-onset Still’s disease: just a useful innocent bystander? Int J Inflam. 2012;2012:298405. doi:10.1155/2012/298405
- Ma AD, Fedoriw YD, Roehrs P. Hyperferritinemia and hemophagocytic lymphohistiocytosis. single institution experience in adult and pediatric patients. Blood. 2012;120:2135-2135. doi:10.1182/blood.V120.21.2135.2135
- Basu S, Maji B, Barman S, et al. Hyperferritinemia in hemophagocytic lymphohistiocytosis: a single institution experience in pediatric patients. Indian J Clin Biochem. 2018;33:108-112. doi:10.1007/s12291-017-0655-4
- Yamada K, Asai K, Okamoto A, et al. Correlation between disease activity and serum ferritin in clinically amyopathic dermatomyositis with rapidly-progressive interstitial lung disease: a case report. BMC Res Notes. 2018;11:34. doi:10.1186/s13104-018-3146-7
- Zohar DN, Seluk L, Yonath H, et al. Anti-MDA5 positive dermatomyositis associated with rapidly progressive interstitial lung disease and correlation between serum ferritin level and treatment response. Mediterr J Rheumatol. 2020;31:75-77. doi:10.31138/mjr.31.1.75
- Lin TF, Ferlic-Stark LL, Allen CE, et al. Rate of decline of ferritin in patients with hemophagocytic lymphohistiocytosis as a prognostic variable for mortality. Pediatr Blood Cancer. 2011;56:154-155. doi:10.1002/pbc.22774
- Bregy A, Trueb RM. No association between serum ferritin levels >10 microg/l and hair loss activity in women. Dermatology. 2008;217:1-6. doi:10.1159/000118505
- de Queiroz M, Vaske TM, Boza JC. Serum ferritin and vitamin D levels in women with non-scarring alopecia. J Cosmet Dermatol. 2022;21:2688-2690. doi:10.1111/jocd.14472
- El-Husseiny R, Alrgig NT, Abdel Fattah NSA. Epidemiological and biochemical factors (serum ferritin and vitamin D) associated with premature hair graying in Egyptian population. J Cosmet Dermatol. 2021;20:1860-1866. doi:10.1111/jocd.13747
- Enitan AO, Olasode OA, Onayemi EO, et al. Serum ferritin levels amongst individuals with androgenetic alopecia in Ile-Ife, Nigeria. West Afr J Med. 2022;39:1026-1031.
- I˙bis¸ S, Aksoy Sarac¸ G, Akdag˘ T. Evaluation of MCV/RDW ratio and correlations with ferritin in telogen effluvium patients. Dermatol Pract Concept. 2022;12:E2022151. doi:10.5826/dpc.1203a151
- Kakpovbia E, Ogbechie-Godec OA, Shapiro J, et al. Laboratory testing in telogen effluvium. J Drugs Dermatol. 2021;20:110-111. doi:10.36849/jdd.5771
- Rasheed H, Mahgoub D, Hegazy R, et al. Serum ferritin and vitamin D in female hair loss: do they play a role? Skin Pharmacol Physiol. 2013;26:101-107. doi:10.1159/000346698
Practice Points
- In patients who are otherwise healthy without chronic systemic disease, hepatic disease, or inflammatory disorders, serum ferritin levels directly correlate with body iron status.
- Elevated serum ferritin should be interpreted in the context of other indicators of iron status, including transferrin saturation, complete blood cell count, and/or liver function panel.
- Low serum ferritin is a specific marker for iron deficiency, and iron supplementation should be initiated based on age-, sex-, and condition-specific thresholds.
Cutaneous Signs of Malnutrition Secondary to Eating Disorders
Eating disorders (EDs) and feeding disorders refer to a wide spectrum of complex biopsychosocial illnesses. The spectrum of EDs encompasses anorexia nervosa (AN), bulimia nervosa (BN), binge eating disorder, and other specified feeding or eating disorders. Feeding disorders, distinguished from EDs based on the absence of body image disturbance, include pica, rumination syndrome, and avoidant/restrictive food intake disorder (ARFID).1
This spectrum of illnesses predominantly affect young females aged 15 to 45 years, with recent increases in the rates of EDs among males, patients with skin of color, and adolescent females.2-5 Patients with EDs are at an elevated lifetime risk of suicidal ideation, suicide attempts, and other psychiatric comorbidities compared to the general population.6 Specifically, AN and BN are associated with high psychiatric morbidity and mortality. A meta-analysis by Arcelus et al7 demonstrated the weighted annual mortality for AN was 5.10 deaths per 1000 person-years (95% CI, 3.57-7.59) among patients with EDs and 4.55 deaths for studies that selected inpatients (95% CI, 3.09-6.28); for BN, the weighted mortality was 1.74 deaths per 1000 person-years (95% CI, 1.09-2.44). Unfortunately, ED diagnoses often are delayed or missed in clinical settings. Patients may lack insight into the severity of their illness, experience embarrassment about their eating behaviors, or actively avoid treatment for their ED.8
Pica—compulsive eating of nonnutritive substances outside the cultural norm—and rumination syndrome—regurgitation of undigested food—are feeding disorders more commonly recognized in childhood.9-11 Pregnancy, intellectual disability, iron deficiency, and lead poisoning are other conditions associated with pica.6,9,10 Avoidant/restrictive food intake disorder, a new diagnosis added to the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5)1 in 2013, is an eating or feeding disturbance resulting in persistent failure to meet nutritional or energy needs. Etiologies of ARFID may include sensory sensitivities and/or a traumatic event related to eating, leading to avoidance of associated foods.12
Patients with an ED or a feeding disorder frequently experience malnutrition, including deficiencies, excesses, or imbalances in nutritional intake, which may lead to nutritional dermatoses.13 As a result, the skin may present the first visible clues to an ED diagnosis.8,14-19 Gupta et al18 organized the skin signs of EDs into 4 categories: (1) those secondary to starvation or malnutrition; (2) cutaneous injury related to self-induced vomiting; (3) dermatoses due to laxative, diuretic, or emetic use; and (4) other concomitant psychiatric illnesses (eg, hand dermatitis from compulsive handwashing, dermatodaxia, onychophagia, trichotillomania). This review will focus on the effects of malnutrition and starvation on the skin.
Skin findings in patients with EDs offer the treating dermatologist a special opportunity for early diagnosis and appropriate consultation with specialists trained in ED treatment. It is important for dermatologists to be vigilant in looking for skin findings of nutritional dermatoses, especially in populations at an increased risk for developing an ED, such as young female patients. The approach to therapy and treatment must occur through a collaborative multidisciplinary effort in a thoughtful and nonjudgmental environment.
Xerosis
Xerosis, or dry skin, is the most common dermatologic finding in both adult and pediatric patients with AN and BN.14,19 It presents as skin roughness, tightness, flaking, and scaling, which may be complicated by fissuring, itching, and bleeding.20 In healthy skin, moisture is maintained by the stratum corneum and its lipids such as ceramides, cholesterol, and free fatty acids.21 Natural moisturizing factor (NMF) within the skin is composed of amino acids, ammonia, urea, uric acid, inorganic salts, lactic acid derivatives, and pyrrolidine-3-carboxylic acid.20-22 Disruptions to this system result in increased transepidermal water loss and impaired barrier function.23
In patients with ED, xerosis arises through several mechanisms. Chronic illness or starvation can lead to euthyroid sick syndrome with decreased peripheral conversion of thyroxine (T4) to triiodothyronine (T3).24,25 In the context of functional hypothyroidism, xerosis can arise from decreased eccrine gland secretion.26 Secretions of water, lactate, urea, sodium, and potassium from eccrine glands help to maintain NMF for skin hydration.27 Persistent laxative or diuretic abuse and fluid intake restriction, which are common behaviors across the spectrum of EDs, lead to dehydration and electrolyte imbalances that can manifest as skin dryness.20 Disrupted keratinocyte differentiation due to insufficient stores of vitamins and minerals involved in keratinocyte differentiation, such as vitamins A and C, selenium, and zinc, also may contribute to xerosis.25,28,29
Severely restrictive eating patterns may lead to development of protein energy malnutrition (PEM). Cutaneous findings in PEM occur due to dysmaturation of epidermal keratinocytes and epidermal atrophy.30 Patients with severe persistent depletion of macronutrients—carbohydrates, fat, and protein—may experience marasmus, resulting in loss of subcutaneous fat that causes the appearance of dry loose skin.29,31
Xerosis is exceedingly common in the general population and has no predictive value in ED diagnosis; however, this finding should be noted in the context of other signs suggestive of an ED. Treatment of xerosis in the setting of an ED should focus on correction of the underlying malnutrition. Symptomatic alleviation requires improving skin hydration and repairing barrier function. Mild xerosis may not need treatment or can be ameliorated with over-the-counter moisturizers and emollients. Scaling secondary to dry skin can be improved by ingredients such as glycerol, urea, lactic acid, and dexpanthenol.20,32 Glycerol and urea are small hydrophilic molecules that penetrate the stratum corneum and help to bind moisture within the skin to reduce transepidermal water loss. Urea and lactic acid are keratolytics of NMF commonly found in moisturizers and emollients.33,34 Dexpanthenol may be used for soothing fissures and pruritus; in vitro and in vivo studies have demonstrated its ability to upregulate dermal fibroblast proliferation and epidermal re-epithelization to promote faster wound healing.35
Lanugo
Lanugo is clinically apparent as a layer of fine, minimally pigmented hair. It is physiologically present on the skin surface of fetuses and newborns. In utero, lanugo plays an essential role in fetal skin protection from amniotic fluid, as well as promotion of proper hydration, thermoregulation, and innate immune development.36-38 Although it may be found on approximately 30% of newborns as normal variation, its presence beyond the neonatal period signals underlying systemic disease and severe undernutrition.16,36,39 Rarely, hypertrichosis lanuginosa acquisita has been reported in association with malignancy.40,41 The finding of lanugo beyond the neonatal period should prompt exclusion of other medical disorders, including neoplasms, chronic infections, hyperthyroidism, malabsorption syndromes, and inflammatory bowel disease.41-47
There is a limited understanding of the pathomechanism behind lanugo development in the context of malnutrition. Intentional starvation leads to loss of subcutaneous fat and a state of functional hypothyroidism.48 Studies hypothesize that lanugo develops as a response to hypothermia, regulated by dermal papillae cell–derived exosomes that may stimulate hair growth via paracrine signaling to outer root sheath cells.36,49 Molecular studies have found that T3 impacts skin and hair differentiation and proliferation by modulating thyroid hormone receptor regulation of keratin expression in epithelial cells.50,51 Lanugo may be a clinical indicator of severe malnutrition among ED patients, especially children and adolescents. A study of 30 patients aged 8 to 17 years with AN and BN who underwent a standard dermatologic examination found significant positive correlation between the presence of lanugo hair growth and concomitant amenorrhea (P<.01) as well as between lanugo hair and body mass index lower than 16 kg/m2 (P<.05).19 Discovery of lanugo in the dermatology clinical setting should prompt a thorough history, including screening questions about eating patterns; attitudes on eating, exercise, and appearance; personal and family history of EDs or other psychiatric disorders; and screening for depression and anxiety. Given its association with other signs of severe malnutrition, a clinical finding of lanugo should prompt close physical examination for other potential signs of an ED and laboratory evaluation for electrolyte levels and blood counts.52 Resolution of lanugo secondary to an ED is achieved with restoration of normal total body fat.18 Treatment should be focused on appropriate weight gain with the guidance of an ED specialist.
Pruritus
The prevalence and pathomechanism of pruritus secondary to EDs remains unclear.16,53,54 There have been limited reports of pruritus secondary to ED, with Gupta et al53 providing a case series of 6 patients with generalized pruritus in association with starvation and/or rapid weight loss. The study reported remission of pruritus with nutritional rehabilitation and/or weight gain of 5 to 10 pounds. Laboratory evaluation ruled out other causes of pruritus such as cholestasis and uremia.53 Other case reports have associated pruritus with iron deficiency, with anecdotal evidence of pruritus resolution following iron supplementation.55-59 Although we found no studies specifically relating iron deficiency, EDs, and pruritus, iron deficiency routinely is seen in ED patients and has a known association with pica.9,10,60 As such, iron deficiency may be a contributing factor in pruritus in ED patients. A UK study of 19 women with AN and a body mass index lower than 16 kg/m2 found that more than half of the patients (11/19 [57.9%]) described pruritus on the St. Thomas’ Itch Questionnaire, postulating that pruritus may be a clinical feature of AN.61 Limited studies with small samples make it difficult to conclude whether pruritus arises as a direct consequence of malnutrition.
Treatment of pruritus should address the underlying ED, as the pathophysiology of itch as it relates to malnutrition is poorly understood. Correction of existing nutritional imbalances by iron supplementation and appropriate weight gain may lead to symptom resolution. Because xerosis may be a contributing factor to pruritus, correction of the xerosis also may be therapeutic. More studies are needed on the connection between pruritus and the nutritional imbalances encountered in patients with EDs.
Acrocyanosis
Acrocyanosis is clinically seen as bluish-dusky discoloration most commonly affecting the hands and feet but also may affect the nose, ears, and nipples. Acrocyanosis typically is a sign of cold intolerance, hypothesized to occur in the context of AN due to shunting of blood centrally in response to hypothermia.39,62 The diminished oxyhemoglobin delivery to extremity sites leads to the characteristic blue color.63 In a study of 211 adolescent females (age range, 13–17 years) with AN, physical examination revealed peripheral hypothermia and peripheral cyanosis in 80% and 43% of patients, respectively.48 Cold intolerance seen in EDs may be secondary to a functional hypothyroid state similar to euthyroid sick syndrome seen in conditions of severe caloric deficit.25
It is possible that anemia and dehydration can worsen acrocyanosis due to impaired delivery of oxyhemoglobin to the body’s periphery.63 In a study of 14 ED patients requiring inpatient care, 6 were found to have underlying anemia following intravenous fluid supplementation.64 On admission, the mean (SD) hemoglobin and hematocrit across 14 patients was 12.74 (2.19) and 37.42 (5.99), respectively. Following intravenous fluid supplementation, the mean (SD) hemoglobin and hematocrit decreased to 9.88 (1.79)(P<.001) and 29.56 (4.91)(P=.008), respectively. Most cases reported intentional restriction of dietary sodium and fluid intake, with 2 patients reporting a history of diuretic misuse.64 These findings demonstrate that hemoglobin and hematocrit may be falsely normal in patients with AN due to hemoconcentration, suggesting that anemia may be underdiagnosed in inpatients with AN.
Beyond treatment of the underlying ED, acrocyanosis therapy is focused on improvement of circulation and avoidance of exacerbating factors. Pharmacologic intervention rarely is needed. Patients should be reassured that acrocyanosis is a benign condition and often can be improved by dressing warmly and avoiding exposure to cold. Severe cases may warrant trial treatment with nicotinic acid derivatives, α-adrenergic blockade, and topical minoxidil, which have demonstrated limited benefit in treating primary idiopathic acrocyanosis.63
Carotenoderma
Carotenoderma—the presence of a yellow discoloration to skin secondary to hypercarotenemia—has been described in patients with EDs since the 1960s.65,66 Beyond its clinical appearance, carotenoderma is asymptomatic. Carotenoids are lipid-soluble compounds present in the diet that are metabolized by the intestinal mucosa and liver to the primary conversion product, retinaldehyde, which is further converted to retinol, retinyl esters, and other retinoid metabolites.67,68 Retinol is bound by lipoproteins and transported in the plasma, then deposited in peripheral tissues,69 including in intercellular lipids in the stratum corneum, resulting in an orange hue that is most apparent in sites of increased skin thickness and sweating (eg, palms, soles, nasolabial folds).70 In an observational study of ED patients, Glorio et al14 found that carotenoderma was present in 23.77% (29/122) and 25% (4/16) of patients with BN and other specified feeding or eating disorder, respectively; it was not noted among patients with AN. Prior case reports have provided anecdotal evidence of carotenoderma in AN patients.66,71 In the setting of an ED, increased serum carotenoids likely are due to increased ingestion of carotene-rich foods, leading to increased levels of carotenoid-bound lipoproteins in the serum.70 Resolution of xanthoderma requires restriction of carotenoid intake and may take 2 to 3 months to be clinically apparent. The lipophilic nature of carotenoids allows storage in body fat, prolonging resolution.71
Hair Changes
Telogen effluvium (TE) and hair pigmentary changes are clinical findings that have been reported in association with EDs.14,16,19,72 Telogen effluvium occurs when physiologic stress causes a large portion of hairs in the anagen phase of growth to prematurely shift into the catagen then telogen phase. Approximately 2 to 3 months following the initial insult, there is clinically apparent excessive hair shedding compared to baseline.73 Studies have demonstrated that patients with EDs commonly have psychiatric comorbidities such as mood and anxiety disorders, obsessive compulsive disorder, posttraumatic stress disorder, and panic disorder compared to the general population.6,74-76 As such, stress experienced by ED patients may contribute to TE. Despite TE being commonly reported in ED patients,16-18 there is a lack of controlled studies of TE in human subjects with ED. An animal model for TE demonstrated that stressed mice exhibited further progression in the hair cycle compared with nonstressed mice (P<.01); the majority of hair follicles in stressed mice were in the catagen phase, while the majority of hair follicles in nonstressed mice were in the anagen phase.77 Stressed mice demonstrated an increased number of major histocompatibility complex class II+ cell clusters, composed mostly of activated macrophages, per 12.5-mm epidermal length compared to nonstressed mice (mean [SEM], 7.0 [1.1] vs 2.0 [0.3][P<.05]). This study illustrated that stress can lead to inflammatory cell recruitment and activation in the hair follicle microenvironment with growth-inhibitory effects.77
The flag sign, or alternating bands of lesser and greater pigmentation in the hair, has been reported in cases of severe PEM.31 In addition, PEM may lead to scalp alopecia, dry and brittle hair, and/or hypopigmentation with periods of inadequate nutrition.29,78 Scalp hair hypopigmentation, brittleness, and alopecia have been reported in pediatric patients with highly selective eating and/or ARFID.79,80 Maruo et al80 described a 3-year-old boy with ASD who consumed only potato chips for more than a year. Physical examination revealed reduced skin turgor overall and sparse red-brown hair on the scalp; laboratory testing showed deficiencies of protein, vitamin A, vitamin D, copper, and zinc. The patient was admitted for nutritional rehabilitation via nasogastric tube feeding, leading to resolution of laboratory abnormalities and growth of thicker black scalp hair over the course of several months.80
Neuroendocrine control of keratin expression by thyroid-stimulating hormone (TSH) and thyroid hormones likely plays a role in the regulation of hair follicle activities, including hair growth, structure, and stem cell differentiation.81,82 Altered thyroid hormone activity, which commonly is seen in patients with EDs,24,25 may contribute to impaired hair growth and pigmentation.26,51,83-85 Using tissue cultures of human anagen hair follicles, van Beek et al85 provided in vitro evidence that T3 and T4 modulate scalp hair follicle growth and pigmentation. Both T3- and T4-treated tissue exhibited increased numbers of anagen and decreased numbers of catagen hair follicles in organ cultures compared with control (P<.01); on quantitative Fontana-Masson histochemistry, T3 and T4 significantly stimulated hair follicle melanin synthesis compared with control (P<.001 and P<.01, respectively).85 Molecular studies by Bodó et al83 have shown that the human scalp epidermis expresses TSH at the messenger RNA and protein levels. Both studies showed that intraepidermal TSH expression is downregulated by thyroid hormones.83,85 Further studies are needed to examine the impact of malnutrition on local thyroid hormone signaling and action at the level of the dermis, epidermis, and hair follicle.
Discovery of TE, hair loss, and/or hair hypopigmentation should prompt close investigation for other signs of thyroid dysfunction, specifically secondary to malnutrition. Imbalances in TSH, T3, and T4 should be corrected. Nutritional deficiencies and dietary habits should be addressed through careful nutritional rehabilitation and targeted ED treatment.
Oral and Mucosal Symptoms
Symptoms of the oral cavity that may arise secondary to EDs and feeding disorders include glossitis, stomatitis, cheilitis, and dental erosions. Mucosal symptoms have been observed in patients with vitamin B deficiencies, inflammatory bowel disease, and other malabsorptive disorders, including patients with EDs.86-88 Patients following restrictive diets, specifically strict vegan diets, without additional supplementation are at risk for developing vitamin B12 deficiency. Because vitamin B12 is stored in the liver, symptoms of deficiency appear when hepatic stores are depleted over the course of several years.89 Insufficient vitamin B12 prevents the proper functioning of methionine synthase, which is required for the conversion of homocysteine to methionine and for the conversion of methyl-tetrahydrofolate to tetrahydrofolate.89 Impairment of this process impedes the synthesis of pyrimidine bases of DNA, disrupting the production of rapidly proliferating cells such as myeloid cells or mucosal lining cells. In cases of glossitis and/or stomatitis due to vitamin B12 deficiency, resolution of lesions was achieved within 4 weeks of daily oral supplementation with vitamin B12 at 2 μg daily.90,91 Iron deficiency, a common finding in EDs, also may contribute to glossitis and angular cheilitis.29 If uncovered, iron deficiency should be corrected by supplementation based on total deficit, age, and sex. Oral supplementation may be done with oral ferrous sulfate (325 mg provides 65 mg elemental iron) or with other iron salts such as ferrous gluconate (325 mg provides 38 mg elemental iron).29 Mucosal symptoms of cheilitis and labial erythema may arise from irritation due to self-induced vomiting.88
Dental erosion refers to loss of tooth structure via a chemical process that does not involve bacteria; in contrast, dental caries refer to tooth damage secondary to bacterial acid production. Patients with EDs who repeatedly self-induce vomiting have persistent introduction of gastric acids into the oral cavity, resulting in dissolution of the tooth enamel, which occurs when teeth are persistently exposed to a pH less than 5.5.92 Feeding disorders also may predispose patients to dental pathology. In a study of 60 pediatric patients, those with rumination syndrome were significantly more likely to have dental erosions than age- and sex-matched healthy controls (23/30 [77%] vs 4/30 [13%][P<.001]). The same study found no difference in the frequency of dental caries between children with and without rumination syndrome.92 These findings suggest that rumination syndrome increases the risk for dental erosions but not dental caries. The distribution of teeth affected by dental erosions may differ between EDs and feeding disorders. Patients with BN are more likely to experience involvement of the palatal surfaces of maxillary teeth, while patients with rumination syndrome had equal involvement of maxillary and mandibular teeth.92
There is limited literature on the role of dentists in the care of patients with EDs and feeding disorders, though existing studies suggest inclusion of a dental care professional in multidisciplinary treatment along with emphasis on education around a home dental care regimen and frequent dental follow-up.76,93,94 Prevention of further damage requires correction of the underlying behaviors and ED.
Other Dermatologic Findings
Russell sign refers to the development of calluses on the dorsal metacarpophalangeal joints of the dominant hand due to self-induced vomiting. Due to its specificity in purging-type EDs, the discovery of Russell sign should greatly increase suspicion for an ED.17 Patients with EDs also are at an increased risk for self-harming and body-focused repetitive behaviors, including skin cutting, superficial burning, onychophagia, and trichotillomania.19 It is important to recognize these signs in patients for whom an ED is suspected. The role of the dermatologist should include careful examination of the skin and documentation of findings that may aid in the diagnosis of an underlying ED.
Final Thoughts
A major limitation of this review is the reliance on small case reports and case series reporting cutaneous manifestations of ED. Controlled studies with larger cohorts are challenging in this population but are needed to substantiate the dermatologic signs commonly associated with EDs. Translational studies may help elucidate the pathomechanisms underlying dermatologic diseases such as lanugo, pruritus, and alopecia in the context of EDs and malnutrition. The known association between thyroid dysfunction and skin disease has been substantiated by clinical and basic science investigation, suggesting a notable role of thyroid hormone and TSH signaling in the skin local environment. Further investigation into nutritional and neuroendocrine regulation of skin health will aid in the diagnosis and treatment of patients impacted by EDs.
The treatment of the underlying ED is key in correcting associated skin disease, which requires interdisciplinary collaboration that addresses the psychological, behavioral, and social components of the condition. Following a diagnosis of ED, assessment should be made of the nutritional rehabilitation required to restore weight and nutritional status. Inpatient treatment may be indicated for patients requiring close monitoring to avoid refeeding syndrome, or those who meet the criteria for extreme AN in the DSM-5 (ie, body mass index <15 kg/m2),1 or demonstrate signs of medical instability or organ failure secondary to malnutrition.62 Long-term recovery for ED patients should focus on behavioral therapy with a multidisciplinary team consisting of a psychiatrist, therapist, dietitian, and primary care provider. Comparative studies in large-scale trials of cognitive behavioral therapy, focal psychodynamic psychotherapy, and specialist supportive clinical management have shown little to no difference in efficacy in treating EDs.75,95,96
Dermatologists may be the first providers to observe sequelae of nutritional and behavioral derangement in patients with EDs. Existing literature on the dermatologic findings of EDs report great heterogeneity of skin signs, with a very limited number of controlled studies available. Each cutaneous symptom described in this review should not be interpreted as an isolated pathology but should be placed in the context of patient predisposing risk factors and the constellation of other skin findings that may be suggestive of disordered eating behavior or other psychiatric illness. The observation of multiple signs and symptoms at the same time, especially of symptoms uncommonly encountered or suggestive of a severe and prolonged imbalance (eg, xanthoderma with vitamin A excess, aphthous stomatitis with vitamin B deficiency), should heighten clinical suspicion for an underlying ED. A clinician’s highest priority should be to resolve life-threatening medical emergencies and address nutritional derangements with the assistance of experts who are well versed in EDs. The patient should undergo workup to rule out organic causes of their nutritional dermatoses. Given the high psychiatric morbidity and mortality of patients with an ED and the demonstrated benefit of early intervention, recognition of cutaneous manifestations of malnutrition and EDs may be paramount to improving outcomes.
- Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Association; 2013.
- Siddiqui A, Ramsay B, Leonard J. The cutaneous signs of eating disorders. Acta Derm Venereol. 1994;74:68-69. doi:10.2340/00015555746869
- Cheng ZH, Perko VL, Fuller-Marashi L, et al. Ethnic differences in eating disorder prevalence, risk factors, and predictive effects of risk factors among young women. Eat Behav. 2019;32:23-30. doi:10.1016/j. eatbeh.2018.11.004
- Smink FR, van Hoeken D, Hoek HW. Epidemiology of eating disorders: incidence, prevalence and mortality rates. Curr Psychiatry Rep. 2012;14:406-414. doi:10.1007/s11920-012-0282-y
- Campbell K, Peebles R. Eating disorders in children and adolescents: state of the art review. Pediatrics. 2014;134:582-592. doi:10.1542/peds.2014-0194
- Herpertz-Dahlmann B. Adolescent eating disorders: definitions, symptomatology, epidemiology and comorbidity. Child Adolesc Psychiatr Clin N Am. 2009;18:31-47. doi:10.1016/j.chc.2008.07.005
- Arcelus J, Mitchell AJ, Wales J, et al. Mortality rates in patients with anorexia nervosa and other eating disorders: a meta-analysis of 3 6 studies. Arch General Psychiatry. 2011;68:724-731. doi:10.1001 /archgenpsychiatry.2011.74
- Tyler I, Wiseman MC, Crawford RI, et al. Cutaneous manifestations of eating disorders. J Cutan Med Surg. 2002;6:345-353. doi:10.1177/120347540200600407
- Al Nasser Y, Muco E, Alsaad AJ. Pica. StatPearls. StatPearls Publishing; 2023.
- Borgna-Pignatti C, Zanella S. Pica as a manifestation of iron deficiency. Expert Rev Hematol. 2016;9:1075-1080. doi:10.1080/1747408 6.2016.1245136
- Talley NJ. Rumination syndrome. Gastroenterol Hepatol (N Y). 2011;7:117- 118.
- Sanchez-Cerezo J, Nagularaj L, Gledhill J, et al. What do we know about the epidemiology of avoidant/restrictive food intake disorder in children and adolescents? a systematic review of the literature. Eur Eat Disord Rev. 2023;31:226-246. doi:10.1002/erv.2964
- World Health Organization. Malnutrition. Published June 9, 2021. Accessed April 20, 2023. https://www.who.int/news-room/fact-sheets/detail/malnutrition
- Glorio R, Allevato M, De Pablo A, et al. Prevalence of cutaneous manifestations in 200 patients with eating disorders. Int J Dermatol. 2000;39:348-353. doi:10.1046/j.1365-4362.2000.00924.x
- Strumia R, Manzato E, Gualandi M. Is there a role for dermatologists in eating disorders? Expert Rev Dermatol. 2007;2:109-112. doi:10.1586/17469872.2.2.109
- Strumia R. Skin signs in anorexia nervosa. Dermatoendocrinol. 2009;1:268-270. doi:10.4161/derm.1.5.10193
- Strumia R. Eating disorders and the skin. Clin Dermatol. 2013;31:80-85. doi:http://doi.org/10.1016/j.clindermatol.2011.11.011
- Gupta MA, Gupta AK, Haberman HF. Dermatologic signs in anorexia nervosa and bulimia nervosa. Arch Dermatol. 1987;123:1386-1390. doi:10.1001/archderm.1987.01660340159040
- Schulze UM, Pettke-Rank CV, Kreienkamp M, et al. Dermatologic findings in anorexia and bulimia nervosa of childhood and adolescence. Pediatr Dermatol. 1999;16:90-94. doi:10.1046/j.1525-1470.1999.00022.x
- Augustin M, Wilsmann-Theis D, Körber A, et al. Diagnosis and treatment of xerosis cutis—a position paper. J Dtsch Dermatol Ges. 2019;17(suppl 7):3-33. doi:10.1111/ddg.13906
- Grubauer G, Feingold KR, Harris RM, et al. Lipid content and lipid type as determinants of the epidermal permeability barrier. J Lipid Res. 1989;30:89-96.
- Feingold KR, Man MQ, Menon GK, et al. Cholesterol synthesis is required for cutaneous barrier function in mice. J Clin Invest. 1990;86:1738-1745. doi:10.1172/jci114899
- Madison KC. Barrier function of the skin: “la raison d’être” of the epidermis. J Invest Dermatol. 2003;121:231-241. doi:10.106 /j.1523-1747.2003.12359.x
- Usdan LS, Khaodhiar L, Apovian CM. The endocrinopathies of anorexia nervosa. Endocr Pract. 2008;14:1055-1063. doi:10.4158/ep.14.8.1055
- Warren MP. Endocrine manifestations of eating disorders. J Clin Endocrinol Metabol. 2011;96:333-343. doi:10.1210/jc.2009-2304
- Safer JD. Thyroid hormone action on skin. Dermatoendocrinol. 2011;3:211-215. doi:10.4161/derm.3.3.17027
- Cui CY, Schlessinger D. Eccrine sweat gland development and sweat secretion. Exp Dermatol. 2015;24:644-650. doi:10.1111/exd.12773
- Nosewicz J, Spaccarelli N, Roberts KM, et al. The epidemiology, impact, and diagnosis of micronutrient nutritional dermatoses part 1: zinc, selenium, copper, vitamin A, and vitamin C. J Am Acad Dermatol. 2022;86:267-278. doi:10.1016/j.jaad.2021.07.079
- Hoffman M, Micheletti RG, Shields BE. Nutritional dermatoses in the hospitalized patient. Cutis. 2020;105:296;302-308, E1-E5.
- Cox JA, Beachkofsky T, Dominguez A. Flaky paint dermatosis. kwashiorkor. JAMA Dermatol. 2014;150:85-86. doi:10.1001 /jamadermatol.2013.5520
- Bradfield RB. Hair tissue as a medium for the differential diagnosis of protein-calorie malnutrition: a commentary. J Pediatr. 1974;84:294-296.
- Proksch E, Lachapelle J-M. The management of dry skin with topical emollients—recent perspectives. J Dtsch Dermatol Ges. 2005;3:768-774. doi:10.1111/j.1610-0387.2005.05068.x
- Watabe A, Sugawara T, Kikuchi K, et al. Sweat constitutes several natural moisturizing factors, lactate, urea, sodium, and potassium. J Dermatol Sci. 2013;72:177-182. doi:10.1016/j.jdermsci.2013.06.005
- Sugawara T, Kikuchi K, Tagami H, et al. Decreased lactate and potassium levels in natural moisturizing factor from the stratum corneum of mild atopic dermatitis patients are involved with the reduced hydration state. J Dermatol Sci. 2012;66:154-159. doi:10.1016/j .jdermsci.2012.02.011
- Gorski J, Proksch E, Baron JM, et al. Dexpanthenol in wound healing after medical and cosmetic interventions (postprocedure wound healing). Pharmaceuticals (Basel). 2020;13:138. doi:10.3390 /ph13070138
- Verhave BL, Nassereddin A, Lappin SL. Embryology, lanugo. StatPearls. StatPearls Publishing; 2022.
- Faist T. Vernix caseoza—composition and function. Ceska Gynekol. 2020;85:263-267.
- Bystrova K. Novel mechanism of human fetal growth regulation: a potential role of lanugo, vernix caseosa and a second tactile system of unmyelinated low-threshold C-afferents. Med Hypotheses. 2009;72:143-146. doi:10.1016/j.mehy.2008.09.033
- Mitchell JE, Crow S. Medical complications of anorexia nervosa and bulimia nervosa. Curr Opin Psychiatry. 2006;19:438-443. doi:10.1097/01.yco.0000228768.79097.3e
- Dalcin D, Manser C, Mahler R. Malignant down: hypertrichosis lanuginosa acquisita associated with endometrial adenocarcinoma. J Cutan Med Surg. 2015;19:507-510. doi:10.1177/1203475415582319
- Slee PH, van der Waal RI, Schagen van Leeuwen JH, et al. Paraneoplastic hypertrichosis lanuginosa acquisita: uncommon or overlooked? Br J Dermatol. 2007;157:1087-1092. doi:10.1111/j.1365-2133.2007.08253.x
- Lause M, Kamboj A, Fernandez Faith E. Dermatologic manifestations of endocrine disorders. Transl Pediatr. 2017;6:300-312. doi:10.21037 /tp.2017.09.08
- Vulink AJ, ten Bokkel Huinink D. Acquired hypertrichosis lanuginosa: a rare cutaneous paraneoplastic syndrome. J Clin Oncol. 2007;25:1625-1626. doi:10.1200/jco.2007.10.6963
- Wyatt JP, Anderson HF, Greer KE, et al. Acquired hypertrichosis lanuginosa as a presenting sign of metastatic prostate cancer with rapid resolution after treatment. J Am Acad Dermatol. 2007;56 (2 suppl):S45-S47. doi:10.1016/j.jaad.2006.07.011
- Saad N, Hot A, Ninet J, et al. Acquired hypertrichosis lanuginosa and gastric adenocarcinoma [in French]. Ann Dermatol Venereol. 2007;134:55-58. doi:10.1016/s0151-9638(07)88991-5
- Pruijm MC, van Houtum WH. An unusual cause of hypertrichosis. Neth J Med. 2007;65:42, 45.
- Lorette G, Maruani A. Images in clinical medicine. acquired hypertrichosis lanuginosa. N Engl J Med. 2006;354:2696. doi:10.1056 /NEJMicm050344
- Swenne I, Engström I. Medical assessment of adolescent girls with eating disorders: an evaluation of symptoms and signs of starvation. Acta Paediatr. 2005;94:1363-1371. doi:10.1111/j.1651-2227.2005.tb01805.x
- Zhou L, Wang H, Jing J, et al. Regulation of hair follicle development by exosomes derived from dermal papilla cells. Biochem Biophys Res Comm. 2018;500:325-332. doi:10.1016/j.bbrc.2018.04.067
- Tomic-Canic M, Day D, Samuels HH, et al. Novel regulation of keratin gene expression by thyroid hormone and retinoid receptors. J Biol Chem. 1996;271:1416-1423. doi:10.1074/jbc.271.3.1416
- Contreras-Jurado C, Lorz C, García-Serrano L, et al. Thyroid hormone signaling controls hair follicle stem cell function. Mol Biol Cell. 2015;26:1263-1272. doi:10.1091/mbc.E14-07-1251
- Hornberger LL, Lane MA. Identification and management of eating disorders in children and adolescents [published online December 20, 2021]. Pediatrics. doi:10.1542/peds.2020-040279
- Gupta MA, Gupta AK, Voorhees JJ. Starvation-associated pruritus: a clinical feature of eating disorders. J Am Acad Dermatol. 1992; 27:118-120. doi:10.1016/s0190-9622(08)80824-9
- Cevikbas F, Lerner EA. Physiology and pathophysiology of itch. Physiol Rev. 2020;100:945-982. doi:10.1152/physrev.00017.2019
- Stäubli M. Pruritus—a little known iron-deficiency symptom [in German]. Schweiz Med Wochenschr. 1981;111:1394-1398.
- Saini S, Jain AK, Agarwal S, et al. Iron deficiency and pruritus: a cross-sectional analysis to assess its association and relationship. Indian J Dermatol. 2021;66:705. doi:10.4103/ijd.ijd_326_21
- Tammaro A, Chello C, Di Fraia M, et al. Iron-deficiency and pruritus: a possible explanation of their relationship. Int J Research Dermatol. 2018;4:605. doi:10.18203/issn.2455-4529.IntJResDermatol20184470
- Takkunen H. Iron-deficiency pruritus. JAMA. 1978;239:1394.
- Lewiecki EM, Rahman F. Pruritus. a manifestation of iron deficiency. JAMA. 1976;236:2319-2320. doi:10.1001/jama.236.20.2319
- Kennedy A, Kohn M, Lammi A, et al. Iron status and haematological changes in adolescent female inpatients with anorexia nervosa. J Paediatr Child Health. 2004;40:430-432. doi:10.1111/j.1440-1754.2004.00432.x
- Morgan JF, Lacey JH. Scratching and fasting: a study of pruritus and anorexia nervosa. Br J Dermatol. 1999;140:453-456. doi:10.1046/j.1365- 2133.1999.02708.x
- Mehler PS. Anorexia nervosa in adults: evaluation for medical complications and criteria for hospitalization to manage these complications. UpToDate. Updated August 3, 2022. Accessed April 20, 2023. https://www.uptodate.com/contents/anorexia-nervosa-in-adults-evaluation-for-medical-complications-and-criteria-for -hospitalization-to-manage-these-complications
- Das S, Maiti A. Acrocyanosis: an overview. Indian J Dermatol. 2013;58:417-420. doi:10.4103/0019-5154.119946
- Caregaro L, Di Pascoli L, Favaro A, et al. Sodium depletion and hemoconcentration: overlooked complications in patients with anorexia nervosa? Nutrition. 2005;21:438-445. doi:10.1016/j.nut.2004.08.022
- Crisp AH, Stonehill E. Hypercarotenaemia as a symptom of weight phobia. Postgrad Med J. 1967;43:721. doi:10.1136/pgmj.43.505.721
- Pops MA, Schwabe AD. Hypercarotenemia in anorexia nervosa. JAMA. 1968;205:533-534. doi:10.1001/jama.1968.03140330075020.
- Bohn T, Desmarchelier C, El SN, et al. β-Carotene in the human body: metabolic bioactivation pathways—from digestion to tissue distribution and excretion. Proc Nutr Soc. 2019;78:68-87. doi:10.1017/S0029665118002641
- von Lintig J, Moon J, Lee J, et al. Carotenoid metabolism at the intestinal barrier. Biochim Biophys Acta Mol Cell Biol Lipids. 2020;1865:158580. doi:10.1016/j.bbalip.2019.158580
- Kanai M, Raz A, Goodman DS. Retinol-binding protein: the transport protein for vitamin A in human plasma. J Clin Invest. 1968;47:2025-2044. doi:10.1172/jci105889
- Haught JM, Patel S, English JC. Xanthoderma: a clinical review. J Am Acad Dermatol. 2007;57:1051-1058. doi:10.1016/j.jaad.2007.06.011
- Tung EE, Drage LA, Ghosh AK. Carotenoderma and hypercarotenemia: markers for disordered eating habits. J Eur Acad Dermatol Venereol. 2006;20:1147-1148. doi:10.1111/j.1468-3083.2006.01643.x
- Heilskov S, Vestergaard C, Babirekere E, et al. Characterization and scoring of skin changes in severe acute malnutrition in children between 6 months and 5 years of age. J Eur Acad Dermatol Venereol. 2015;29:2463-2469. doi:10.1111/jdv.13328
- Malkud S. Telogen effluvium: a review. J Clin Diagn Res. 2015;9:We01-3. doi:10.7860/jcdr/2015/15219.6492
- Filipponi C, Visentini C, Filippini T, et al. The follow-up of eating disorders from adolescence to early adulthood: a systematic review. Int J Environ Res Public Health. 2022;19:16237. doi:10.3390/ijerph192316237
- Byrne S, Wade T, Hay P, et al. A randomised controlled trial of three psychological treatments for anorexia nervosa. Psychol Med. 2017;47:2823-2833. doi:10.1017/s0033291717001349
- Ranalli DN, Studen-Pavlovich D. Eating disorders in the adolescent patient. Dent Clin North Am. 2021;65:689-703. doi:10.1016/j. cden.2021.06.009
- Arck PC, Handjiski B, Peters EM, et al. Stress inhibits hair growth in mice by induction of premature catagen development and deleterious perifollicular inflammatory events via neuropeptide substance P-dependent pathways. Am J Pathol. 2003;162:803-814. doi:10.1016/s0002-9440(10)63877-1
- Roy SK. Achromotrichia in tropical malnutrition. Br Med J. 1947;1:392. doi:10.1136/bmj.1.4498.392-c
- Swed-Tobia R, Haj A, Militianu D, et al. Highly selective eating in autism spectrum disorder leading to scurvy: a series of three patients. Pediatr Neurol. 2019;94:61-63. doi:10.1016/j.pediatrneurol.2018.12.011
- Maruo Y, Uetake K, Egawa K, et al. Selective eating in autism spectrum disorder leading to hair color change. Pediatr Neurol. 2021;120:1-2. doi:10.1016/j.pediatrneurol.2021.03.001
- Paus R, Langan EA, Vidali S, et al. Neuroendocrinology of the hair follicle: principles and clinical perspectives. Trends Mol Med. 2014;20:559-570. doi:10.1016/j.molmed.2014.06.002
- Antonini D, Sibilio A, Dentice M, et al. An intimate relationship between thyroid hormone and skin: regulation of gene expression. Front Endocrinol (Lausanne). 2013;4:104. doi: 10.3389/fendo.2013.00104
- Bodó E, Kany B, Gáspár E, et al. Thyroid-stimulating hormone, a novel, locally produced modulator of human epidermal functions, is regulated by thyrotropin-releasing hormone and thyroid hormones. Endocrinology. 2010;151:1633-1642. doi:10.1210/en.2009-0306
- Taguchi T. Brittle nails and hair loss in hypothyroidism. N Engl J Med. 2018;379:1363-1363. doi:10.1056/NEJMicm1801633
- van Beek N, Bodó E, Kromminga A, et al. Thyroid hormones directly alter human hair follicle functions: anagen prolongation and stimulation of both hair matrix keratinocyte proliferation and hair pigmentation. J Clin Endocrinol Metab. 2008;93:4381-4388. doi:10.1210/jc.2008-0283
- Zippi M, Corrado C, Pica R, et al. Extraintestinal manifestations in a large series of Italian inflammatory bowel disease patients. World J Gastroenterol. 2014;20:17463-7467. doi:10.3748/wjg.v20.i46.17463.
- Gutierrez Gossweiler A, Martinez-Mier EA. Chapter 6: vitamins and oral health. Monogr Oral Sci. 2020;28:59-67. doi:10.1159/000455372
- Monda M, Costacurta M, Maffei L, et al. Oral manifestations of eating disorders in adolescent patients. a review. Eur J Paediatr Dent. 2021;22:155-158. doi:10.23804/ejpd.2021.22.02.13
- Ankar A, Kumar A. Vitamin B12 deficiency. StatPearls. StatPearls Publishing; 2022.
- Graells J, Ojeda RM, Muniesa C, et al. Glossitis with linear lesions: an early sign of vitamin B12 deficiency. J Am Acad Dermatol. 2009;60:498- 500. doi:10.1016/j.jaad.2008.09.011
- Pétavy-Catala C, Fontès V, Gironet N, et al. Clinical manifestations of the mouth revealing vitamin B12 deficiency before the onset of anemia [in French]. Ann Dermatol Venereol. 2003;130(2 pt 1):191-194.
- Monagas J, Ritwik P, Kolomensky A, et al. Rumination syndrome and dental erosions in children. J Pediatr Gastroenterol Nutr. 2017; 64:930-932. doi:10.1097/mpg.0000000000001395
- Silverstein LS, Haggerty C, Sams L, et al. Impact of an oral health education intervention among a group of patients with eating disorders (anorexia nervosa and bulimia nervosa). J Eat Disord. 2019;7:29. doi:10.1186/s40337-019-0259-x
- Rangé H, Colon P, Godart N, et al. Eating disorders through the periodontal lens. Periodontol 2000. 2021;87:17-31. doi:10.1111 /prd.12391
- Zipfel S, Wild B, Groß G, et al. Focal psychodynamic therapy, cognitive behaviour therapy, and optimised treatment as usual in outpatients with anorexia nervosa (ANTOP study): randomised controlled trial. Lancet Psychiatry. 2014;383:127-137. doi:10.1016 /S2215-0366(22)00028-1
- Schmidt U, Ryan EG, Bartholdy S, et al. Two-year follow-up of the MOSAIC trial: a multicenter randomized controlled trial comparing two psychological treatments in adult outpatients with broadly defined anorexia nervosa. Int J Eat Disord. 2016;49:793-800. doi:10.1002/eat.22523
Eating disorders (EDs) and feeding disorders refer to a wide spectrum of complex biopsychosocial illnesses. The spectrum of EDs encompasses anorexia nervosa (AN), bulimia nervosa (BN), binge eating disorder, and other specified feeding or eating disorders. Feeding disorders, distinguished from EDs based on the absence of body image disturbance, include pica, rumination syndrome, and avoidant/restrictive food intake disorder (ARFID).1
This spectrum of illnesses predominantly affect young females aged 15 to 45 years, with recent increases in the rates of EDs among males, patients with skin of color, and adolescent females.2-5 Patients with EDs are at an elevated lifetime risk of suicidal ideation, suicide attempts, and other psychiatric comorbidities compared to the general population.6 Specifically, AN and BN are associated with high psychiatric morbidity and mortality. A meta-analysis by Arcelus et al7 demonstrated the weighted annual mortality for AN was 5.10 deaths per 1000 person-years (95% CI, 3.57-7.59) among patients with EDs and 4.55 deaths for studies that selected inpatients (95% CI, 3.09-6.28); for BN, the weighted mortality was 1.74 deaths per 1000 person-years (95% CI, 1.09-2.44). Unfortunately, ED diagnoses often are delayed or missed in clinical settings. Patients may lack insight into the severity of their illness, experience embarrassment about their eating behaviors, or actively avoid treatment for their ED.8
Pica—compulsive eating of nonnutritive substances outside the cultural norm—and rumination syndrome—regurgitation of undigested food—are feeding disorders more commonly recognized in childhood.9-11 Pregnancy, intellectual disability, iron deficiency, and lead poisoning are other conditions associated with pica.6,9,10 Avoidant/restrictive food intake disorder, a new diagnosis added to the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5)1 in 2013, is an eating or feeding disturbance resulting in persistent failure to meet nutritional or energy needs. Etiologies of ARFID may include sensory sensitivities and/or a traumatic event related to eating, leading to avoidance of associated foods.12
Patients with an ED or a feeding disorder frequently experience malnutrition, including deficiencies, excesses, or imbalances in nutritional intake, which may lead to nutritional dermatoses.13 As a result, the skin may present the first visible clues to an ED diagnosis.8,14-19 Gupta et al18 organized the skin signs of EDs into 4 categories: (1) those secondary to starvation or malnutrition; (2) cutaneous injury related to self-induced vomiting; (3) dermatoses due to laxative, diuretic, or emetic use; and (4) other concomitant psychiatric illnesses (eg, hand dermatitis from compulsive handwashing, dermatodaxia, onychophagia, trichotillomania). This review will focus on the effects of malnutrition and starvation on the skin.
Skin findings in patients with EDs offer the treating dermatologist a special opportunity for early diagnosis and appropriate consultation with specialists trained in ED treatment. It is important for dermatologists to be vigilant in looking for skin findings of nutritional dermatoses, especially in populations at an increased risk for developing an ED, such as young female patients. The approach to therapy and treatment must occur through a collaborative multidisciplinary effort in a thoughtful and nonjudgmental environment.
Xerosis
Xerosis, or dry skin, is the most common dermatologic finding in both adult and pediatric patients with AN and BN.14,19 It presents as skin roughness, tightness, flaking, and scaling, which may be complicated by fissuring, itching, and bleeding.20 In healthy skin, moisture is maintained by the stratum corneum and its lipids such as ceramides, cholesterol, and free fatty acids.21 Natural moisturizing factor (NMF) within the skin is composed of amino acids, ammonia, urea, uric acid, inorganic salts, lactic acid derivatives, and pyrrolidine-3-carboxylic acid.20-22 Disruptions to this system result in increased transepidermal water loss and impaired barrier function.23
In patients with ED, xerosis arises through several mechanisms. Chronic illness or starvation can lead to euthyroid sick syndrome with decreased peripheral conversion of thyroxine (T4) to triiodothyronine (T3).24,25 In the context of functional hypothyroidism, xerosis can arise from decreased eccrine gland secretion.26 Secretions of water, lactate, urea, sodium, and potassium from eccrine glands help to maintain NMF for skin hydration.27 Persistent laxative or diuretic abuse and fluid intake restriction, which are common behaviors across the spectrum of EDs, lead to dehydration and electrolyte imbalances that can manifest as skin dryness.20 Disrupted keratinocyte differentiation due to insufficient stores of vitamins and minerals involved in keratinocyte differentiation, such as vitamins A and C, selenium, and zinc, also may contribute to xerosis.25,28,29
Severely restrictive eating patterns may lead to development of protein energy malnutrition (PEM). Cutaneous findings in PEM occur due to dysmaturation of epidermal keratinocytes and epidermal atrophy.30 Patients with severe persistent depletion of macronutrients—carbohydrates, fat, and protein—may experience marasmus, resulting in loss of subcutaneous fat that causes the appearance of dry loose skin.29,31
Xerosis is exceedingly common in the general population and has no predictive value in ED diagnosis; however, this finding should be noted in the context of other signs suggestive of an ED. Treatment of xerosis in the setting of an ED should focus on correction of the underlying malnutrition. Symptomatic alleviation requires improving skin hydration and repairing barrier function. Mild xerosis may not need treatment or can be ameliorated with over-the-counter moisturizers and emollients. Scaling secondary to dry skin can be improved by ingredients such as glycerol, urea, lactic acid, and dexpanthenol.20,32 Glycerol and urea are small hydrophilic molecules that penetrate the stratum corneum and help to bind moisture within the skin to reduce transepidermal water loss. Urea and lactic acid are keratolytics of NMF commonly found in moisturizers and emollients.33,34 Dexpanthenol may be used for soothing fissures and pruritus; in vitro and in vivo studies have demonstrated its ability to upregulate dermal fibroblast proliferation and epidermal re-epithelization to promote faster wound healing.35
Lanugo
Lanugo is clinically apparent as a layer of fine, minimally pigmented hair. It is physiologically present on the skin surface of fetuses and newborns. In utero, lanugo plays an essential role in fetal skin protection from amniotic fluid, as well as promotion of proper hydration, thermoregulation, and innate immune development.36-38 Although it may be found on approximately 30% of newborns as normal variation, its presence beyond the neonatal period signals underlying systemic disease and severe undernutrition.16,36,39 Rarely, hypertrichosis lanuginosa acquisita has been reported in association with malignancy.40,41 The finding of lanugo beyond the neonatal period should prompt exclusion of other medical disorders, including neoplasms, chronic infections, hyperthyroidism, malabsorption syndromes, and inflammatory bowel disease.41-47
There is a limited understanding of the pathomechanism behind lanugo development in the context of malnutrition. Intentional starvation leads to loss of subcutaneous fat and a state of functional hypothyroidism.48 Studies hypothesize that lanugo develops as a response to hypothermia, regulated by dermal papillae cell–derived exosomes that may stimulate hair growth via paracrine signaling to outer root sheath cells.36,49 Molecular studies have found that T3 impacts skin and hair differentiation and proliferation by modulating thyroid hormone receptor regulation of keratin expression in epithelial cells.50,51 Lanugo may be a clinical indicator of severe malnutrition among ED patients, especially children and adolescents. A study of 30 patients aged 8 to 17 years with AN and BN who underwent a standard dermatologic examination found significant positive correlation between the presence of lanugo hair growth and concomitant amenorrhea (P<.01) as well as between lanugo hair and body mass index lower than 16 kg/m2 (P<.05).19 Discovery of lanugo in the dermatology clinical setting should prompt a thorough history, including screening questions about eating patterns; attitudes on eating, exercise, and appearance; personal and family history of EDs or other psychiatric disorders; and screening for depression and anxiety. Given its association with other signs of severe malnutrition, a clinical finding of lanugo should prompt close physical examination for other potential signs of an ED and laboratory evaluation for electrolyte levels and blood counts.52 Resolution of lanugo secondary to an ED is achieved with restoration of normal total body fat.18 Treatment should be focused on appropriate weight gain with the guidance of an ED specialist.
Pruritus
The prevalence and pathomechanism of pruritus secondary to EDs remains unclear.16,53,54 There have been limited reports of pruritus secondary to ED, with Gupta et al53 providing a case series of 6 patients with generalized pruritus in association with starvation and/or rapid weight loss. The study reported remission of pruritus with nutritional rehabilitation and/or weight gain of 5 to 10 pounds. Laboratory evaluation ruled out other causes of pruritus such as cholestasis and uremia.53 Other case reports have associated pruritus with iron deficiency, with anecdotal evidence of pruritus resolution following iron supplementation.55-59 Although we found no studies specifically relating iron deficiency, EDs, and pruritus, iron deficiency routinely is seen in ED patients and has a known association with pica.9,10,60 As such, iron deficiency may be a contributing factor in pruritus in ED patients. A UK study of 19 women with AN and a body mass index lower than 16 kg/m2 found that more than half of the patients (11/19 [57.9%]) described pruritus on the St. Thomas’ Itch Questionnaire, postulating that pruritus may be a clinical feature of AN.61 Limited studies with small samples make it difficult to conclude whether pruritus arises as a direct consequence of malnutrition.
Treatment of pruritus should address the underlying ED, as the pathophysiology of itch as it relates to malnutrition is poorly understood. Correction of existing nutritional imbalances by iron supplementation and appropriate weight gain may lead to symptom resolution. Because xerosis may be a contributing factor to pruritus, correction of the xerosis also may be therapeutic. More studies are needed on the connection between pruritus and the nutritional imbalances encountered in patients with EDs.
Acrocyanosis
Acrocyanosis is clinically seen as bluish-dusky discoloration most commonly affecting the hands and feet but also may affect the nose, ears, and nipples. Acrocyanosis typically is a sign of cold intolerance, hypothesized to occur in the context of AN due to shunting of blood centrally in response to hypothermia.39,62 The diminished oxyhemoglobin delivery to extremity sites leads to the characteristic blue color.63 In a study of 211 adolescent females (age range, 13–17 years) with AN, physical examination revealed peripheral hypothermia and peripheral cyanosis in 80% and 43% of patients, respectively.48 Cold intolerance seen in EDs may be secondary to a functional hypothyroid state similar to euthyroid sick syndrome seen in conditions of severe caloric deficit.25
It is possible that anemia and dehydration can worsen acrocyanosis due to impaired delivery of oxyhemoglobin to the body’s periphery.63 In a study of 14 ED patients requiring inpatient care, 6 were found to have underlying anemia following intravenous fluid supplementation.64 On admission, the mean (SD) hemoglobin and hematocrit across 14 patients was 12.74 (2.19) and 37.42 (5.99), respectively. Following intravenous fluid supplementation, the mean (SD) hemoglobin and hematocrit decreased to 9.88 (1.79)(P<.001) and 29.56 (4.91)(P=.008), respectively. Most cases reported intentional restriction of dietary sodium and fluid intake, with 2 patients reporting a history of diuretic misuse.64 These findings demonstrate that hemoglobin and hematocrit may be falsely normal in patients with AN due to hemoconcentration, suggesting that anemia may be underdiagnosed in inpatients with AN.
Beyond treatment of the underlying ED, acrocyanosis therapy is focused on improvement of circulation and avoidance of exacerbating factors. Pharmacologic intervention rarely is needed. Patients should be reassured that acrocyanosis is a benign condition and often can be improved by dressing warmly and avoiding exposure to cold. Severe cases may warrant trial treatment with nicotinic acid derivatives, α-adrenergic blockade, and topical minoxidil, which have demonstrated limited benefit in treating primary idiopathic acrocyanosis.63
Carotenoderma
Carotenoderma—the presence of a yellow discoloration to skin secondary to hypercarotenemia—has been described in patients with EDs since the 1960s.65,66 Beyond its clinical appearance, carotenoderma is asymptomatic. Carotenoids are lipid-soluble compounds present in the diet that are metabolized by the intestinal mucosa and liver to the primary conversion product, retinaldehyde, which is further converted to retinol, retinyl esters, and other retinoid metabolites.67,68 Retinol is bound by lipoproteins and transported in the plasma, then deposited in peripheral tissues,69 including in intercellular lipids in the stratum corneum, resulting in an orange hue that is most apparent in sites of increased skin thickness and sweating (eg, palms, soles, nasolabial folds).70 In an observational study of ED patients, Glorio et al14 found that carotenoderma was present in 23.77% (29/122) and 25% (4/16) of patients with BN and other specified feeding or eating disorder, respectively; it was not noted among patients with AN. Prior case reports have provided anecdotal evidence of carotenoderma in AN patients.66,71 In the setting of an ED, increased serum carotenoids likely are due to increased ingestion of carotene-rich foods, leading to increased levels of carotenoid-bound lipoproteins in the serum.70 Resolution of xanthoderma requires restriction of carotenoid intake and may take 2 to 3 months to be clinically apparent. The lipophilic nature of carotenoids allows storage in body fat, prolonging resolution.71
Hair Changes
Telogen effluvium (TE) and hair pigmentary changes are clinical findings that have been reported in association with EDs.14,16,19,72 Telogen effluvium occurs when physiologic stress causes a large portion of hairs in the anagen phase of growth to prematurely shift into the catagen then telogen phase. Approximately 2 to 3 months following the initial insult, there is clinically apparent excessive hair shedding compared to baseline.73 Studies have demonstrated that patients with EDs commonly have psychiatric comorbidities such as mood and anxiety disorders, obsessive compulsive disorder, posttraumatic stress disorder, and panic disorder compared to the general population.6,74-76 As such, stress experienced by ED patients may contribute to TE. Despite TE being commonly reported in ED patients,16-18 there is a lack of controlled studies of TE in human subjects with ED. An animal model for TE demonstrated that stressed mice exhibited further progression in the hair cycle compared with nonstressed mice (P<.01); the majority of hair follicles in stressed mice were in the catagen phase, while the majority of hair follicles in nonstressed mice were in the anagen phase.77 Stressed mice demonstrated an increased number of major histocompatibility complex class II+ cell clusters, composed mostly of activated macrophages, per 12.5-mm epidermal length compared to nonstressed mice (mean [SEM], 7.0 [1.1] vs 2.0 [0.3][P<.05]). This study illustrated that stress can lead to inflammatory cell recruitment and activation in the hair follicle microenvironment with growth-inhibitory effects.77
The flag sign, or alternating bands of lesser and greater pigmentation in the hair, has been reported in cases of severe PEM.31 In addition, PEM may lead to scalp alopecia, dry and brittle hair, and/or hypopigmentation with periods of inadequate nutrition.29,78 Scalp hair hypopigmentation, brittleness, and alopecia have been reported in pediatric patients with highly selective eating and/or ARFID.79,80 Maruo et al80 described a 3-year-old boy with ASD who consumed only potato chips for more than a year. Physical examination revealed reduced skin turgor overall and sparse red-brown hair on the scalp; laboratory testing showed deficiencies of protein, vitamin A, vitamin D, copper, and zinc. The patient was admitted for nutritional rehabilitation via nasogastric tube feeding, leading to resolution of laboratory abnormalities and growth of thicker black scalp hair over the course of several months.80
Neuroendocrine control of keratin expression by thyroid-stimulating hormone (TSH) and thyroid hormones likely plays a role in the regulation of hair follicle activities, including hair growth, structure, and stem cell differentiation.81,82 Altered thyroid hormone activity, which commonly is seen in patients with EDs,24,25 may contribute to impaired hair growth and pigmentation.26,51,83-85 Using tissue cultures of human anagen hair follicles, van Beek et al85 provided in vitro evidence that T3 and T4 modulate scalp hair follicle growth and pigmentation. Both T3- and T4-treated tissue exhibited increased numbers of anagen and decreased numbers of catagen hair follicles in organ cultures compared with control (P<.01); on quantitative Fontana-Masson histochemistry, T3 and T4 significantly stimulated hair follicle melanin synthesis compared with control (P<.001 and P<.01, respectively).85 Molecular studies by Bodó et al83 have shown that the human scalp epidermis expresses TSH at the messenger RNA and protein levels. Both studies showed that intraepidermal TSH expression is downregulated by thyroid hormones.83,85 Further studies are needed to examine the impact of malnutrition on local thyroid hormone signaling and action at the level of the dermis, epidermis, and hair follicle.
Discovery of TE, hair loss, and/or hair hypopigmentation should prompt close investigation for other signs of thyroid dysfunction, specifically secondary to malnutrition. Imbalances in TSH, T3, and T4 should be corrected. Nutritional deficiencies and dietary habits should be addressed through careful nutritional rehabilitation and targeted ED treatment.
Oral and Mucosal Symptoms
Symptoms of the oral cavity that may arise secondary to EDs and feeding disorders include glossitis, stomatitis, cheilitis, and dental erosions. Mucosal symptoms have been observed in patients with vitamin B deficiencies, inflammatory bowel disease, and other malabsorptive disorders, including patients with EDs.86-88 Patients following restrictive diets, specifically strict vegan diets, without additional supplementation are at risk for developing vitamin B12 deficiency. Because vitamin B12 is stored in the liver, symptoms of deficiency appear when hepatic stores are depleted over the course of several years.89 Insufficient vitamin B12 prevents the proper functioning of methionine synthase, which is required for the conversion of homocysteine to methionine and for the conversion of methyl-tetrahydrofolate to tetrahydrofolate.89 Impairment of this process impedes the synthesis of pyrimidine bases of DNA, disrupting the production of rapidly proliferating cells such as myeloid cells or mucosal lining cells. In cases of glossitis and/or stomatitis due to vitamin B12 deficiency, resolution of lesions was achieved within 4 weeks of daily oral supplementation with vitamin B12 at 2 μg daily.90,91 Iron deficiency, a common finding in EDs, also may contribute to glossitis and angular cheilitis.29 If uncovered, iron deficiency should be corrected by supplementation based on total deficit, age, and sex. Oral supplementation may be done with oral ferrous sulfate (325 mg provides 65 mg elemental iron) or with other iron salts such as ferrous gluconate (325 mg provides 38 mg elemental iron).29 Mucosal symptoms of cheilitis and labial erythema may arise from irritation due to self-induced vomiting.88
Dental erosion refers to loss of tooth structure via a chemical process that does not involve bacteria; in contrast, dental caries refer to tooth damage secondary to bacterial acid production. Patients with EDs who repeatedly self-induce vomiting have persistent introduction of gastric acids into the oral cavity, resulting in dissolution of the tooth enamel, which occurs when teeth are persistently exposed to a pH less than 5.5.92 Feeding disorders also may predispose patients to dental pathology. In a study of 60 pediatric patients, those with rumination syndrome were significantly more likely to have dental erosions than age- and sex-matched healthy controls (23/30 [77%] vs 4/30 [13%][P<.001]). The same study found no difference in the frequency of dental caries between children with and without rumination syndrome.92 These findings suggest that rumination syndrome increases the risk for dental erosions but not dental caries. The distribution of teeth affected by dental erosions may differ between EDs and feeding disorders. Patients with BN are more likely to experience involvement of the palatal surfaces of maxillary teeth, while patients with rumination syndrome had equal involvement of maxillary and mandibular teeth.92
There is limited literature on the role of dentists in the care of patients with EDs and feeding disorders, though existing studies suggest inclusion of a dental care professional in multidisciplinary treatment along with emphasis on education around a home dental care regimen and frequent dental follow-up.76,93,94 Prevention of further damage requires correction of the underlying behaviors and ED.
Other Dermatologic Findings
Russell sign refers to the development of calluses on the dorsal metacarpophalangeal joints of the dominant hand due to self-induced vomiting. Due to its specificity in purging-type EDs, the discovery of Russell sign should greatly increase suspicion for an ED.17 Patients with EDs also are at an increased risk for self-harming and body-focused repetitive behaviors, including skin cutting, superficial burning, onychophagia, and trichotillomania.19 It is important to recognize these signs in patients for whom an ED is suspected. The role of the dermatologist should include careful examination of the skin and documentation of findings that may aid in the diagnosis of an underlying ED.
Final Thoughts
A major limitation of this review is the reliance on small case reports and case series reporting cutaneous manifestations of ED. Controlled studies with larger cohorts are challenging in this population but are needed to substantiate the dermatologic signs commonly associated with EDs. Translational studies may help elucidate the pathomechanisms underlying dermatologic diseases such as lanugo, pruritus, and alopecia in the context of EDs and malnutrition. The known association between thyroid dysfunction and skin disease has been substantiated by clinical and basic science investigation, suggesting a notable role of thyroid hormone and TSH signaling in the skin local environment. Further investigation into nutritional and neuroendocrine regulation of skin health will aid in the diagnosis and treatment of patients impacted by EDs.
The treatment of the underlying ED is key in correcting associated skin disease, which requires interdisciplinary collaboration that addresses the psychological, behavioral, and social components of the condition. Following a diagnosis of ED, assessment should be made of the nutritional rehabilitation required to restore weight and nutritional status. Inpatient treatment may be indicated for patients requiring close monitoring to avoid refeeding syndrome, or those who meet the criteria for extreme AN in the DSM-5 (ie, body mass index <15 kg/m2),1 or demonstrate signs of medical instability or organ failure secondary to malnutrition.62 Long-term recovery for ED patients should focus on behavioral therapy with a multidisciplinary team consisting of a psychiatrist, therapist, dietitian, and primary care provider. Comparative studies in large-scale trials of cognitive behavioral therapy, focal psychodynamic psychotherapy, and specialist supportive clinical management have shown little to no difference in efficacy in treating EDs.75,95,96
Dermatologists may be the first providers to observe sequelae of nutritional and behavioral derangement in patients with EDs. Existing literature on the dermatologic findings of EDs report great heterogeneity of skin signs, with a very limited number of controlled studies available. Each cutaneous symptom described in this review should not be interpreted as an isolated pathology but should be placed in the context of patient predisposing risk factors and the constellation of other skin findings that may be suggestive of disordered eating behavior or other psychiatric illness. The observation of multiple signs and symptoms at the same time, especially of symptoms uncommonly encountered or suggestive of a severe and prolonged imbalance (eg, xanthoderma with vitamin A excess, aphthous stomatitis with vitamin B deficiency), should heighten clinical suspicion for an underlying ED. A clinician’s highest priority should be to resolve life-threatening medical emergencies and address nutritional derangements with the assistance of experts who are well versed in EDs. The patient should undergo workup to rule out organic causes of their nutritional dermatoses. Given the high psychiatric morbidity and mortality of patients with an ED and the demonstrated benefit of early intervention, recognition of cutaneous manifestations of malnutrition and EDs may be paramount to improving outcomes.
Eating disorders (EDs) and feeding disorders refer to a wide spectrum of complex biopsychosocial illnesses. The spectrum of EDs encompasses anorexia nervosa (AN), bulimia nervosa (BN), binge eating disorder, and other specified feeding or eating disorders. Feeding disorders, distinguished from EDs based on the absence of body image disturbance, include pica, rumination syndrome, and avoidant/restrictive food intake disorder (ARFID).1
This spectrum of illnesses predominantly affect young females aged 15 to 45 years, with recent increases in the rates of EDs among males, patients with skin of color, and adolescent females.2-5 Patients with EDs are at an elevated lifetime risk of suicidal ideation, suicide attempts, and other psychiatric comorbidities compared to the general population.6 Specifically, AN and BN are associated with high psychiatric morbidity and mortality. A meta-analysis by Arcelus et al7 demonstrated the weighted annual mortality for AN was 5.10 deaths per 1000 person-years (95% CI, 3.57-7.59) among patients with EDs and 4.55 deaths for studies that selected inpatients (95% CI, 3.09-6.28); for BN, the weighted mortality was 1.74 deaths per 1000 person-years (95% CI, 1.09-2.44). Unfortunately, ED diagnoses often are delayed or missed in clinical settings. Patients may lack insight into the severity of their illness, experience embarrassment about their eating behaviors, or actively avoid treatment for their ED.8
Pica—compulsive eating of nonnutritive substances outside the cultural norm—and rumination syndrome—regurgitation of undigested food—are feeding disorders more commonly recognized in childhood.9-11 Pregnancy, intellectual disability, iron deficiency, and lead poisoning are other conditions associated with pica.6,9,10 Avoidant/restrictive food intake disorder, a new diagnosis added to the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5)1 in 2013, is an eating or feeding disturbance resulting in persistent failure to meet nutritional or energy needs. Etiologies of ARFID may include sensory sensitivities and/or a traumatic event related to eating, leading to avoidance of associated foods.12
Patients with an ED or a feeding disorder frequently experience malnutrition, including deficiencies, excesses, or imbalances in nutritional intake, which may lead to nutritional dermatoses.13 As a result, the skin may present the first visible clues to an ED diagnosis.8,14-19 Gupta et al18 organized the skin signs of EDs into 4 categories: (1) those secondary to starvation or malnutrition; (2) cutaneous injury related to self-induced vomiting; (3) dermatoses due to laxative, diuretic, or emetic use; and (4) other concomitant psychiatric illnesses (eg, hand dermatitis from compulsive handwashing, dermatodaxia, onychophagia, trichotillomania). This review will focus on the effects of malnutrition and starvation on the skin.
Skin findings in patients with EDs offer the treating dermatologist a special opportunity for early diagnosis and appropriate consultation with specialists trained in ED treatment. It is important for dermatologists to be vigilant in looking for skin findings of nutritional dermatoses, especially in populations at an increased risk for developing an ED, such as young female patients. The approach to therapy and treatment must occur through a collaborative multidisciplinary effort in a thoughtful and nonjudgmental environment.
Xerosis
Xerosis, or dry skin, is the most common dermatologic finding in both adult and pediatric patients with AN and BN.14,19 It presents as skin roughness, tightness, flaking, and scaling, which may be complicated by fissuring, itching, and bleeding.20 In healthy skin, moisture is maintained by the stratum corneum and its lipids such as ceramides, cholesterol, and free fatty acids.21 Natural moisturizing factor (NMF) within the skin is composed of amino acids, ammonia, urea, uric acid, inorganic salts, lactic acid derivatives, and pyrrolidine-3-carboxylic acid.20-22 Disruptions to this system result in increased transepidermal water loss and impaired barrier function.23
In patients with ED, xerosis arises through several mechanisms. Chronic illness or starvation can lead to euthyroid sick syndrome with decreased peripheral conversion of thyroxine (T4) to triiodothyronine (T3).24,25 In the context of functional hypothyroidism, xerosis can arise from decreased eccrine gland secretion.26 Secretions of water, lactate, urea, sodium, and potassium from eccrine glands help to maintain NMF for skin hydration.27 Persistent laxative or diuretic abuse and fluid intake restriction, which are common behaviors across the spectrum of EDs, lead to dehydration and electrolyte imbalances that can manifest as skin dryness.20 Disrupted keratinocyte differentiation due to insufficient stores of vitamins and minerals involved in keratinocyte differentiation, such as vitamins A and C, selenium, and zinc, also may contribute to xerosis.25,28,29
Severely restrictive eating patterns may lead to development of protein energy malnutrition (PEM). Cutaneous findings in PEM occur due to dysmaturation of epidermal keratinocytes and epidermal atrophy.30 Patients with severe persistent depletion of macronutrients—carbohydrates, fat, and protein—may experience marasmus, resulting in loss of subcutaneous fat that causes the appearance of dry loose skin.29,31
Xerosis is exceedingly common in the general population and has no predictive value in ED diagnosis; however, this finding should be noted in the context of other signs suggestive of an ED. Treatment of xerosis in the setting of an ED should focus on correction of the underlying malnutrition. Symptomatic alleviation requires improving skin hydration and repairing barrier function. Mild xerosis may not need treatment or can be ameliorated with over-the-counter moisturizers and emollients. Scaling secondary to dry skin can be improved by ingredients such as glycerol, urea, lactic acid, and dexpanthenol.20,32 Glycerol and urea are small hydrophilic molecules that penetrate the stratum corneum and help to bind moisture within the skin to reduce transepidermal water loss. Urea and lactic acid are keratolytics of NMF commonly found in moisturizers and emollients.33,34 Dexpanthenol may be used for soothing fissures and pruritus; in vitro and in vivo studies have demonstrated its ability to upregulate dermal fibroblast proliferation and epidermal re-epithelization to promote faster wound healing.35
Lanugo
Lanugo is clinically apparent as a layer of fine, minimally pigmented hair. It is physiologically present on the skin surface of fetuses and newborns. In utero, lanugo plays an essential role in fetal skin protection from amniotic fluid, as well as promotion of proper hydration, thermoregulation, and innate immune development.36-38 Although it may be found on approximately 30% of newborns as normal variation, its presence beyond the neonatal period signals underlying systemic disease and severe undernutrition.16,36,39 Rarely, hypertrichosis lanuginosa acquisita has been reported in association with malignancy.40,41 The finding of lanugo beyond the neonatal period should prompt exclusion of other medical disorders, including neoplasms, chronic infections, hyperthyroidism, malabsorption syndromes, and inflammatory bowel disease.41-47
There is a limited understanding of the pathomechanism behind lanugo development in the context of malnutrition. Intentional starvation leads to loss of subcutaneous fat and a state of functional hypothyroidism.48 Studies hypothesize that lanugo develops as a response to hypothermia, regulated by dermal papillae cell–derived exosomes that may stimulate hair growth via paracrine signaling to outer root sheath cells.36,49 Molecular studies have found that T3 impacts skin and hair differentiation and proliferation by modulating thyroid hormone receptor regulation of keratin expression in epithelial cells.50,51 Lanugo may be a clinical indicator of severe malnutrition among ED patients, especially children and adolescents. A study of 30 patients aged 8 to 17 years with AN and BN who underwent a standard dermatologic examination found significant positive correlation between the presence of lanugo hair growth and concomitant amenorrhea (P<.01) as well as between lanugo hair and body mass index lower than 16 kg/m2 (P<.05).19 Discovery of lanugo in the dermatology clinical setting should prompt a thorough history, including screening questions about eating patterns; attitudes on eating, exercise, and appearance; personal and family history of EDs or other psychiatric disorders; and screening for depression and anxiety. Given its association with other signs of severe malnutrition, a clinical finding of lanugo should prompt close physical examination for other potential signs of an ED and laboratory evaluation for electrolyte levels and blood counts.52 Resolution of lanugo secondary to an ED is achieved with restoration of normal total body fat.18 Treatment should be focused on appropriate weight gain with the guidance of an ED specialist.
Pruritus
The prevalence and pathomechanism of pruritus secondary to EDs remains unclear.16,53,54 There have been limited reports of pruritus secondary to ED, with Gupta et al53 providing a case series of 6 patients with generalized pruritus in association with starvation and/or rapid weight loss. The study reported remission of pruritus with nutritional rehabilitation and/or weight gain of 5 to 10 pounds. Laboratory evaluation ruled out other causes of pruritus such as cholestasis and uremia.53 Other case reports have associated pruritus with iron deficiency, with anecdotal evidence of pruritus resolution following iron supplementation.55-59 Although we found no studies specifically relating iron deficiency, EDs, and pruritus, iron deficiency routinely is seen in ED patients and has a known association with pica.9,10,60 As such, iron deficiency may be a contributing factor in pruritus in ED patients. A UK study of 19 women with AN and a body mass index lower than 16 kg/m2 found that more than half of the patients (11/19 [57.9%]) described pruritus on the St. Thomas’ Itch Questionnaire, postulating that pruritus may be a clinical feature of AN.61 Limited studies with small samples make it difficult to conclude whether pruritus arises as a direct consequence of malnutrition.
Treatment of pruritus should address the underlying ED, as the pathophysiology of itch as it relates to malnutrition is poorly understood. Correction of existing nutritional imbalances by iron supplementation and appropriate weight gain may lead to symptom resolution. Because xerosis may be a contributing factor to pruritus, correction of the xerosis also may be therapeutic. More studies are needed on the connection between pruritus and the nutritional imbalances encountered in patients with EDs.
Acrocyanosis
Acrocyanosis is clinically seen as bluish-dusky discoloration most commonly affecting the hands and feet but also may affect the nose, ears, and nipples. Acrocyanosis typically is a sign of cold intolerance, hypothesized to occur in the context of AN due to shunting of blood centrally in response to hypothermia.39,62 The diminished oxyhemoglobin delivery to extremity sites leads to the characteristic blue color.63 In a study of 211 adolescent females (age range, 13–17 years) with AN, physical examination revealed peripheral hypothermia and peripheral cyanosis in 80% and 43% of patients, respectively.48 Cold intolerance seen in EDs may be secondary to a functional hypothyroid state similar to euthyroid sick syndrome seen in conditions of severe caloric deficit.25
It is possible that anemia and dehydration can worsen acrocyanosis due to impaired delivery of oxyhemoglobin to the body’s periphery.63 In a study of 14 ED patients requiring inpatient care, 6 were found to have underlying anemia following intravenous fluid supplementation.64 On admission, the mean (SD) hemoglobin and hematocrit across 14 patients was 12.74 (2.19) and 37.42 (5.99), respectively. Following intravenous fluid supplementation, the mean (SD) hemoglobin and hematocrit decreased to 9.88 (1.79)(P<.001) and 29.56 (4.91)(P=.008), respectively. Most cases reported intentional restriction of dietary sodium and fluid intake, with 2 patients reporting a history of diuretic misuse.64 These findings demonstrate that hemoglobin and hematocrit may be falsely normal in patients with AN due to hemoconcentration, suggesting that anemia may be underdiagnosed in inpatients with AN.
Beyond treatment of the underlying ED, acrocyanosis therapy is focused on improvement of circulation and avoidance of exacerbating factors. Pharmacologic intervention rarely is needed. Patients should be reassured that acrocyanosis is a benign condition and often can be improved by dressing warmly and avoiding exposure to cold. Severe cases may warrant trial treatment with nicotinic acid derivatives, α-adrenergic blockade, and topical minoxidil, which have demonstrated limited benefit in treating primary idiopathic acrocyanosis.63
Carotenoderma
Carotenoderma—the presence of a yellow discoloration to skin secondary to hypercarotenemia—has been described in patients with EDs since the 1960s.65,66 Beyond its clinical appearance, carotenoderma is asymptomatic. Carotenoids are lipid-soluble compounds present in the diet that are metabolized by the intestinal mucosa and liver to the primary conversion product, retinaldehyde, which is further converted to retinol, retinyl esters, and other retinoid metabolites.67,68 Retinol is bound by lipoproteins and transported in the plasma, then deposited in peripheral tissues,69 including in intercellular lipids in the stratum corneum, resulting in an orange hue that is most apparent in sites of increased skin thickness and sweating (eg, palms, soles, nasolabial folds).70 In an observational study of ED patients, Glorio et al14 found that carotenoderma was present in 23.77% (29/122) and 25% (4/16) of patients with BN and other specified feeding or eating disorder, respectively; it was not noted among patients with AN. Prior case reports have provided anecdotal evidence of carotenoderma in AN patients.66,71 In the setting of an ED, increased serum carotenoids likely are due to increased ingestion of carotene-rich foods, leading to increased levels of carotenoid-bound lipoproteins in the serum.70 Resolution of xanthoderma requires restriction of carotenoid intake and may take 2 to 3 months to be clinically apparent. The lipophilic nature of carotenoids allows storage in body fat, prolonging resolution.71
Hair Changes
Telogen effluvium (TE) and hair pigmentary changes are clinical findings that have been reported in association with EDs.14,16,19,72 Telogen effluvium occurs when physiologic stress causes a large portion of hairs in the anagen phase of growth to prematurely shift into the catagen then telogen phase. Approximately 2 to 3 months following the initial insult, there is clinically apparent excessive hair shedding compared to baseline.73 Studies have demonstrated that patients with EDs commonly have psychiatric comorbidities such as mood and anxiety disorders, obsessive compulsive disorder, posttraumatic stress disorder, and panic disorder compared to the general population.6,74-76 As such, stress experienced by ED patients may contribute to TE. Despite TE being commonly reported in ED patients,16-18 there is a lack of controlled studies of TE in human subjects with ED. An animal model for TE demonstrated that stressed mice exhibited further progression in the hair cycle compared with nonstressed mice (P<.01); the majority of hair follicles in stressed mice were in the catagen phase, while the majority of hair follicles in nonstressed mice were in the anagen phase.77 Stressed mice demonstrated an increased number of major histocompatibility complex class II+ cell clusters, composed mostly of activated macrophages, per 12.5-mm epidermal length compared to nonstressed mice (mean [SEM], 7.0 [1.1] vs 2.0 [0.3][P<.05]). This study illustrated that stress can lead to inflammatory cell recruitment and activation in the hair follicle microenvironment with growth-inhibitory effects.77
The flag sign, or alternating bands of lesser and greater pigmentation in the hair, has been reported in cases of severe PEM.31 In addition, PEM may lead to scalp alopecia, dry and brittle hair, and/or hypopigmentation with periods of inadequate nutrition.29,78 Scalp hair hypopigmentation, brittleness, and alopecia have been reported in pediatric patients with highly selective eating and/or ARFID.79,80 Maruo et al80 described a 3-year-old boy with ASD who consumed only potato chips for more than a year. Physical examination revealed reduced skin turgor overall and sparse red-brown hair on the scalp; laboratory testing showed deficiencies of protein, vitamin A, vitamin D, copper, and zinc. The patient was admitted for nutritional rehabilitation via nasogastric tube feeding, leading to resolution of laboratory abnormalities and growth of thicker black scalp hair over the course of several months.80
Neuroendocrine control of keratin expression by thyroid-stimulating hormone (TSH) and thyroid hormones likely plays a role in the regulation of hair follicle activities, including hair growth, structure, and stem cell differentiation.81,82 Altered thyroid hormone activity, which commonly is seen in patients with EDs,24,25 may contribute to impaired hair growth and pigmentation.26,51,83-85 Using tissue cultures of human anagen hair follicles, van Beek et al85 provided in vitro evidence that T3 and T4 modulate scalp hair follicle growth and pigmentation. Both T3- and T4-treated tissue exhibited increased numbers of anagen and decreased numbers of catagen hair follicles in organ cultures compared with control (P<.01); on quantitative Fontana-Masson histochemistry, T3 and T4 significantly stimulated hair follicle melanin synthesis compared with control (P<.001 and P<.01, respectively).85 Molecular studies by Bodó et al83 have shown that the human scalp epidermis expresses TSH at the messenger RNA and protein levels. Both studies showed that intraepidermal TSH expression is downregulated by thyroid hormones.83,85 Further studies are needed to examine the impact of malnutrition on local thyroid hormone signaling and action at the level of the dermis, epidermis, and hair follicle.
Discovery of TE, hair loss, and/or hair hypopigmentation should prompt close investigation for other signs of thyroid dysfunction, specifically secondary to malnutrition. Imbalances in TSH, T3, and T4 should be corrected. Nutritional deficiencies and dietary habits should be addressed through careful nutritional rehabilitation and targeted ED treatment.
Oral and Mucosal Symptoms
Symptoms of the oral cavity that may arise secondary to EDs and feeding disorders include glossitis, stomatitis, cheilitis, and dental erosions. Mucosal symptoms have been observed in patients with vitamin B deficiencies, inflammatory bowel disease, and other malabsorptive disorders, including patients with EDs.86-88 Patients following restrictive diets, specifically strict vegan diets, without additional supplementation are at risk for developing vitamin B12 deficiency. Because vitamin B12 is stored in the liver, symptoms of deficiency appear when hepatic stores are depleted over the course of several years.89 Insufficient vitamin B12 prevents the proper functioning of methionine synthase, which is required for the conversion of homocysteine to methionine and for the conversion of methyl-tetrahydrofolate to tetrahydrofolate.89 Impairment of this process impedes the synthesis of pyrimidine bases of DNA, disrupting the production of rapidly proliferating cells such as myeloid cells or mucosal lining cells. In cases of glossitis and/or stomatitis due to vitamin B12 deficiency, resolution of lesions was achieved within 4 weeks of daily oral supplementation with vitamin B12 at 2 μg daily.90,91 Iron deficiency, a common finding in EDs, also may contribute to glossitis and angular cheilitis.29 If uncovered, iron deficiency should be corrected by supplementation based on total deficit, age, and sex. Oral supplementation may be done with oral ferrous sulfate (325 mg provides 65 mg elemental iron) or with other iron salts such as ferrous gluconate (325 mg provides 38 mg elemental iron).29 Mucosal symptoms of cheilitis and labial erythema may arise from irritation due to self-induced vomiting.88
Dental erosion refers to loss of tooth structure via a chemical process that does not involve bacteria; in contrast, dental caries refer to tooth damage secondary to bacterial acid production. Patients with EDs who repeatedly self-induce vomiting have persistent introduction of gastric acids into the oral cavity, resulting in dissolution of the tooth enamel, which occurs when teeth are persistently exposed to a pH less than 5.5.92 Feeding disorders also may predispose patients to dental pathology. In a study of 60 pediatric patients, those with rumination syndrome were significantly more likely to have dental erosions than age- and sex-matched healthy controls (23/30 [77%] vs 4/30 [13%][P<.001]). The same study found no difference in the frequency of dental caries between children with and without rumination syndrome.92 These findings suggest that rumination syndrome increases the risk for dental erosions but not dental caries. The distribution of teeth affected by dental erosions may differ between EDs and feeding disorders. Patients with BN are more likely to experience involvement of the palatal surfaces of maxillary teeth, while patients with rumination syndrome had equal involvement of maxillary and mandibular teeth.92
There is limited literature on the role of dentists in the care of patients with EDs and feeding disorders, though existing studies suggest inclusion of a dental care professional in multidisciplinary treatment along with emphasis on education around a home dental care regimen and frequent dental follow-up.76,93,94 Prevention of further damage requires correction of the underlying behaviors and ED.
Other Dermatologic Findings
Russell sign refers to the development of calluses on the dorsal metacarpophalangeal joints of the dominant hand due to self-induced vomiting. Due to its specificity in purging-type EDs, the discovery of Russell sign should greatly increase suspicion for an ED.17 Patients with EDs also are at an increased risk for self-harming and body-focused repetitive behaviors, including skin cutting, superficial burning, onychophagia, and trichotillomania.19 It is important to recognize these signs in patients for whom an ED is suspected. The role of the dermatologist should include careful examination of the skin and documentation of findings that may aid in the diagnosis of an underlying ED.
Final Thoughts
A major limitation of this review is the reliance on small case reports and case series reporting cutaneous manifestations of ED. Controlled studies with larger cohorts are challenging in this population but are needed to substantiate the dermatologic signs commonly associated with EDs. Translational studies may help elucidate the pathomechanisms underlying dermatologic diseases such as lanugo, pruritus, and alopecia in the context of EDs and malnutrition. The known association between thyroid dysfunction and skin disease has been substantiated by clinical and basic science investigation, suggesting a notable role of thyroid hormone and TSH signaling in the skin local environment. Further investigation into nutritional and neuroendocrine regulation of skin health will aid in the diagnosis and treatment of patients impacted by EDs.
The treatment of the underlying ED is key in correcting associated skin disease, which requires interdisciplinary collaboration that addresses the psychological, behavioral, and social components of the condition. Following a diagnosis of ED, assessment should be made of the nutritional rehabilitation required to restore weight and nutritional status. Inpatient treatment may be indicated for patients requiring close monitoring to avoid refeeding syndrome, or those who meet the criteria for extreme AN in the DSM-5 (ie, body mass index <15 kg/m2),1 or demonstrate signs of medical instability or organ failure secondary to malnutrition.62 Long-term recovery for ED patients should focus on behavioral therapy with a multidisciplinary team consisting of a psychiatrist, therapist, dietitian, and primary care provider. Comparative studies in large-scale trials of cognitive behavioral therapy, focal psychodynamic psychotherapy, and specialist supportive clinical management have shown little to no difference in efficacy in treating EDs.75,95,96
Dermatologists may be the first providers to observe sequelae of nutritional and behavioral derangement in patients with EDs. Existing literature on the dermatologic findings of EDs report great heterogeneity of skin signs, with a very limited number of controlled studies available. Each cutaneous symptom described in this review should not be interpreted as an isolated pathology but should be placed in the context of patient predisposing risk factors and the constellation of other skin findings that may be suggestive of disordered eating behavior or other psychiatric illness. The observation of multiple signs and symptoms at the same time, especially of symptoms uncommonly encountered or suggestive of a severe and prolonged imbalance (eg, xanthoderma with vitamin A excess, aphthous stomatitis with vitamin B deficiency), should heighten clinical suspicion for an underlying ED. A clinician’s highest priority should be to resolve life-threatening medical emergencies and address nutritional derangements with the assistance of experts who are well versed in EDs. The patient should undergo workup to rule out organic causes of their nutritional dermatoses. Given the high psychiatric morbidity and mortality of patients with an ED and the demonstrated benefit of early intervention, recognition of cutaneous manifestations of malnutrition and EDs may be paramount to improving outcomes.
- Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Association; 2013.
- Siddiqui A, Ramsay B, Leonard J. The cutaneous signs of eating disorders. Acta Derm Venereol. 1994;74:68-69. doi:10.2340/00015555746869
- Cheng ZH, Perko VL, Fuller-Marashi L, et al. Ethnic differences in eating disorder prevalence, risk factors, and predictive effects of risk factors among young women. Eat Behav. 2019;32:23-30. doi:10.1016/j. eatbeh.2018.11.004
- Smink FR, van Hoeken D, Hoek HW. Epidemiology of eating disorders: incidence, prevalence and mortality rates. Curr Psychiatry Rep. 2012;14:406-414. doi:10.1007/s11920-012-0282-y
- Campbell K, Peebles R. Eating disorders in children and adolescents: state of the art review. Pediatrics. 2014;134:582-592. doi:10.1542/peds.2014-0194
- Herpertz-Dahlmann B. Adolescent eating disorders: definitions, symptomatology, epidemiology and comorbidity. Child Adolesc Psychiatr Clin N Am. 2009;18:31-47. doi:10.1016/j.chc.2008.07.005
- Arcelus J, Mitchell AJ, Wales J, et al. Mortality rates in patients with anorexia nervosa and other eating disorders: a meta-analysis of 3 6 studies. Arch General Psychiatry. 2011;68:724-731. doi:10.1001 /archgenpsychiatry.2011.74
- Tyler I, Wiseman MC, Crawford RI, et al. Cutaneous manifestations of eating disorders. J Cutan Med Surg. 2002;6:345-353. doi:10.1177/120347540200600407
- Al Nasser Y, Muco E, Alsaad AJ. Pica. StatPearls. StatPearls Publishing; 2023.
- Borgna-Pignatti C, Zanella S. Pica as a manifestation of iron deficiency. Expert Rev Hematol. 2016;9:1075-1080. doi:10.1080/1747408 6.2016.1245136
- Talley NJ. Rumination syndrome. Gastroenterol Hepatol (N Y). 2011;7:117- 118.
- Sanchez-Cerezo J, Nagularaj L, Gledhill J, et al. What do we know about the epidemiology of avoidant/restrictive food intake disorder in children and adolescents? a systematic review of the literature. Eur Eat Disord Rev. 2023;31:226-246. doi:10.1002/erv.2964
- World Health Organization. Malnutrition. Published June 9, 2021. Accessed April 20, 2023. https://www.who.int/news-room/fact-sheets/detail/malnutrition
- Glorio R, Allevato M, De Pablo A, et al. Prevalence of cutaneous manifestations in 200 patients with eating disorders. Int J Dermatol. 2000;39:348-353. doi:10.1046/j.1365-4362.2000.00924.x
- Strumia R, Manzato E, Gualandi M. Is there a role for dermatologists in eating disorders? Expert Rev Dermatol. 2007;2:109-112. doi:10.1586/17469872.2.2.109
- Strumia R. Skin signs in anorexia nervosa. Dermatoendocrinol. 2009;1:268-270. doi:10.4161/derm.1.5.10193
- Strumia R. Eating disorders and the skin. Clin Dermatol. 2013;31:80-85. doi:http://doi.org/10.1016/j.clindermatol.2011.11.011
- Gupta MA, Gupta AK, Haberman HF. Dermatologic signs in anorexia nervosa and bulimia nervosa. Arch Dermatol. 1987;123:1386-1390. doi:10.1001/archderm.1987.01660340159040
- Schulze UM, Pettke-Rank CV, Kreienkamp M, et al. Dermatologic findings in anorexia and bulimia nervosa of childhood and adolescence. Pediatr Dermatol. 1999;16:90-94. doi:10.1046/j.1525-1470.1999.00022.x
- Augustin M, Wilsmann-Theis D, Körber A, et al. Diagnosis and treatment of xerosis cutis—a position paper. J Dtsch Dermatol Ges. 2019;17(suppl 7):3-33. doi:10.1111/ddg.13906
- Grubauer G, Feingold KR, Harris RM, et al. Lipid content and lipid type as determinants of the epidermal permeability barrier. J Lipid Res. 1989;30:89-96.
- Feingold KR, Man MQ, Menon GK, et al. Cholesterol synthesis is required for cutaneous barrier function in mice. J Clin Invest. 1990;86:1738-1745. doi:10.1172/jci114899
- Madison KC. Barrier function of the skin: “la raison d’être” of the epidermis. J Invest Dermatol. 2003;121:231-241. doi:10.106 /j.1523-1747.2003.12359.x
- Usdan LS, Khaodhiar L, Apovian CM. The endocrinopathies of anorexia nervosa. Endocr Pract. 2008;14:1055-1063. doi:10.4158/ep.14.8.1055
- Warren MP. Endocrine manifestations of eating disorders. J Clin Endocrinol Metabol. 2011;96:333-343. doi:10.1210/jc.2009-2304
- Safer JD. Thyroid hormone action on skin. Dermatoendocrinol. 2011;3:211-215. doi:10.4161/derm.3.3.17027
- Cui CY, Schlessinger D. Eccrine sweat gland development and sweat secretion. Exp Dermatol. 2015;24:644-650. doi:10.1111/exd.12773
- Nosewicz J, Spaccarelli N, Roberts KM, et al. The epidemiology, impact, and diagnosis of micronutrient nutritional dermatoses part 1: zinc, selenium, copper, vitamin A, and vitamin C. J Am Acad Dermatol. 2022;86:267-278. doi:10.1016/j.jaad.2021.07.079
- Hoffman M, Micheletti RG, Shields BE. Nutritional dermatoses in the hospitalized patient. Cutis. 2020;105:296;302-308, E1-E5.
- Cox JA, Beachkofsky T, Dominguez A. Flaky paint dermatosis. kwashiorkor. JAMA Dermatol. 2014;150:85-86. doi:10.1001 /jamadermatol.2013.5520
- Bradfield RB. Hair tissue as a medium for the differential diagnosis of protein-calorie malnutrition: a commentary. J Pediatr. 1974;84:294-296.
- Proksch E, Lachapelle J-M. The management of dry skin with topical emollients—recent perspectives. J Dtsch Dermatol Ges. 2005;3:768-774. doi:10.1111/j.1610-0387.2005.05068.x
- Watabe A, Sugawara T, Kikuchi K, et al. Sweat constitutes several natural moisturizing factors, lactate, urea, sodium, and potassium. J Dermatol Sci. 2013;72:177-182. doi:10.1016/j.jdermsci.2013.06.005
- Sugawara T, Kikuchi K, Tagami H, et al. Decreased lactate and potassium levels in natural moisturizing factor from the stratum corneum of mild atopic dermatitis patients are involved with the reduced hydration state. J Dermatol Sci. 2012;66:154-159. doi:10.1016/j .jdermsci.2012.02.011
- Gorski J, Proksch E, Baron JM, et al. Dexpanthenol in wound healing after medical and cosmetic interventions (postprocedure wound healing). Pharmaceuticals (Basel). 2020;13:138. doi:10.3390 /ph13070138
- Verhave BL, Nassereddin A, Lappin SL. Embryology, lanugo. StatPearls. StatPearls Publishing; 2022.
- Faist T. Vernix caseoza—composition and function. Ceska Gynekol. 2020;85:263-267.
- Bystrova K. Novel mechanism of human fetal growth regulation: a potential role of lanugo, vernix caseosa and a second tactile system of unmyelinated low-threshold C-afferents. Med Hypotheses. 2009;72:143-146. doi:10.1016/j.mehy.2008.09.033
- Mitchell JE, Crow S. Medical complications of anorexia nervosa and bulimia nervosa. Curr Opin Psychiatry. 2006;19:438-443. doi:10.1097/01.yco.0000228768.79097.3e
- Dalcin D, Manser C, Mahler R. Malignant down: hypertrichosis lanuginosa acquisita associated with endometrial adenocarcinoma. J Cutan Med Surg. 2015;19:507-510. doi:10.1177/1203475415582319
- Slee PH, van der Waal RI, Schagen van Leeuwen JH, et al. Paraneoplastic hypertrichosis lanuginosa acquisita: uncommon or overlooked? Br J Dermatol. 2007;157:1087-1092. doi:10.1111/j.1365-2133.2007.08253.x
- Lause M, Kamboj A, Fernandez Faith E. Dermatologic manifestations of endocrine disorders. Transl Pediatr. 2017;6:300-312. doi:10.21037 /tp.2017.09.08
- Vulink AJ, ten Bokkel Huinink D. Acquired hypertrichosis lanuginosa: a rare cutaneous paraneoplastic syndrome. J Clin Oncol. 2007;25:1625-1626. doi:10.1200/jco.2007.10.6963
- Wyatt JP, Anderson HF, Greer KE, et al. Acquired hypertrichosis lanuginosa as a presenting sign of metastatic prostate cancer with rapid resolution after treatment. J Am Acad Dermatol. 2007;56 (2 suppl):S45-S47. doi:10.1016/j.jaad.2006.07.011
- Saad N, Hot A, Ninet J, et al. Acquired hypertrichosis lanuginosa and gastric adenocarcinoma [in French]. Ann Dermatol Venereol. 2007;134:55-58. doi:10.1016/s0151-9638(07)88991-5
- Pruijm MC, van Houtum WH. An unusual cause of hypertrichosis. Neth J Med. 2007;65:42, 45.
- Lorette G, Maruani A. Images in clinical medicine. acquired hypertrichosis lanuginosa. N Engl J Med. 2006;354:2696. doi:10.1056 /NEJMicm050344
- Swenne I, Engström I. Medical assessment of adolescent girls with eating disorders: an evaluation of symptoms and signs of starvation. Acta Paediatr. 2005;94:1363-1371. doi:10.1111/j.1651-2227.2005.tb01805.x
- Zhou L, Wang H, Jing J, et al. Regulation of hair follicle development by exosomes derived from dermal papilla cells. Biochem Biophys Res Comm. 2018;500:325-332. doi:10.1016/j.bbrc.2018.04.067
- Tomic-Canic M, Day D, Samuels HH, et al. Novel regulation of keratin gene expression by thyroid hormone and retinoid receptors. J Biol Chem. 1996;271:1416-1423. doi:10.1074/jbc.271.3.1416
- Contreras-Jurado C, Lorz C, García-Serrano L, et al. Thyroid hormone signaling controls hair follicle stem cell function. Mol Biol Cell. 2015;26:1263-1272. doi:10.1091/mbc.E14-07-1251
- Hornberger LL, Lane MA. Identification and management of eating disorders in children and adolescents [published online December 20, 2021]. Pediatrics. doi:10.1542/peds.2020-040279
- Gupta MA, Gupta AK, Voorhees JJ. Starvation-associated pruritus: a clinical feature of eating disorders. J Am Acad Dermatol. 1992; 27:118-120. doi:10.1016/s0190-9622(08)80824-9
- Cevikbas F, Lerner EA. Physiology and pathophysiology of itch. Physiol Rev. 2020;100:945-982. doi:10.1152/physrev.00017.2019
- Stäubli M. Pruritus—a little known iron-deficiency symptom [in German]. Schweiz Med Wochenschr. 1981;111:1394-1398.
- Saini S, Jain AK, Agarwal S, et al. Iron deficiency and pruritus: a cross-sectional analysis to assess its association and relationship. Indian J Dermatol. 2021;66:705. doi:10.4103/ijd.ijd_326_21
- Tammaro A, Chello C, Di Fraia M, et al. Iron-deficiency and pruritus: a possible explanation of their relationship. Int J Research Dermatol. 2018;4:605. doi:10.18203/issn.2455-4529.IntJResDermatol20184470
- Takkunen H. Iron-deficiency pruritus. JAMA. 1978;239:1394.
- Lewiecki EM, Rahman F. Pruritus. a manifestation of iron deficiency. JAMA. 1976;236:2319-2320. doi:10.1001/jama.236.20.2319
- Kennedy A, Kohn M, Lammi A, et al. Iron status and haematological changes in adolescent female inpatients with anorexia nervosa. J Paediatr Child Health. 2004;40:430-432. doi:10.1111/j.1440-1754.2004.00432.x
- Morgan JF, Lacey JH. Scratching and fasting: a study of pruritus and anorexia nervosa. Br J Dermatol. 1999;140:453-456. doi:10.1046/j.1365- 2133.1999.02708.x
- Mehler PS. Anorexia nervosa in adults: evaluation for medical complications and criteria for hospitalization to manage these complications. UpToDate. Updated August 3, 2022. Accessed April 20, 2023. https://www.uptodate.com/contents/anorexia-nervosa-in-adults-evaluation-for-medical-complications-and-criteria-for -hospitalization-to-manage-these-complications
- Das S, Maiti A. Acrocyanosis: an overview. Indian J Dermatol. 2013;58:417-420. doi:10.4103/0019-5154.119946
- Caregaro L, Di Pascoli L, Favaro A, et al. Sodium depletion and hemoconcentration: overlooked complications in patients with anorexia nervosa? Nutrition. 2005;21:438-445. doi:10.1016/j.nut.2004.08.022
- Crisp AH, Stonehill E. Hypercarotenaemia as a symptom of weight phobia. Postgrad Med J. 1967;43:721. doi:10.1136/pgmj.43.505.721
- Pops MA, Schwabe AD. Hypercarotenemia in anorexia nervosa. JAMA. 1968;205:533-534. doi:10.1001/jama.1968.03140330075020.
- Bohn T, Desmarchelier C, El SN, et al. β-Carotene in the human body: metabolic bioactivation pathways—from digestion to tissue distribution and excretion. Proc Nutr Soc. 2019;78:68-87. doi:10.1017/S0029665118002641
- von Lintig J, Moon J, Lee J, et al. Carotenoid metabolism at the intestinal barrier. Biochim Biophys Acta Mol Cell Biol Lipids. 2020;1865:158580. doi:10.1016/j.bbalip.2019.158580
- Kanai M, Raz A, Goodman DS. Retinol-binding protein: the transport protein for vitamin A in human plasma. J Clin Invest. 1968;47:2025-2044. doi:10.1172/jci105889
- Haught JM, Patel S, English JC. Xanthoderma: a clinical review. J Am Acad Dermatol. 2007;57:1051-1058. doi:10.1016/j.jaad.2007.06.011
- Tung EE, Drage LA, Ghosh AK. Carotenoderma and hypercarotenemia: markers for disordered eating habits. J Eur Acad Dermatol Venereol. 2006;20:1147-1148. doi:10.1111/j.1468-3083.2006.01643.x
- Heilskov S, Vestergaard C, Babirekere E, et al. Characterization and scoring of skin changes in severe acute malnutrition in children between 6 months and 5 years of age. J Eur Acad Dermatol Venereol. 2015;29:2463-2469. doi:10.1111/jdv.13328
- Malkud S. Telogen effluvium: a review. J Clin Diagn Res. 2015;9:We01-3. doi:10.7860/jcdr/2015/15219.6492
- Filipponi C, Visentini C, Filippini T, et al. The follow-up of eating disorders from adolescence to early adulthood: a systematic review. Int J Environ Res Public Health. 2022;19:16237. doi:10.3390/ijerph192316237
- Byrne S, Wade T, Hay P, et al. A randomised controlled trial of three psychological treatments for anorexia nervosa. Psychol Med. 2017;47:2823-2833. doi:10.1017/s0033291717001349
- Ranalli DN, Studen-Pavlovich D. Eating disorders in the adolescent patient. Dent Clin North Am. 2021;65:689-703. doi:10.1016/j. cden.2021.06.009
- Arck PC, Handjiski B, Peters EM, et al. Stress inhibits hair growth in mice by induction of premature catagen development and deleterious perifollicular inflammatory events via neuropeptide substance P-dependent pathways. Am J Pathol. 2003;162:803-814. doi:10.1016/s0002-9440(10)63877-1
- Roy SK. Achromotrichia in tropical malnutrition. Br Med J. 1947;1:392. doi:10.1136/bmj.1.4498.392-c
- Swed-Tobia R, Haj A, Militianu D, et al. Highly selective eating in autism spectrum disorder leading to scurvy: a series of three patients. Pediatr Neurol. 2019;94:61-63. doi:10.1016/j.pediatrneurol.2018.12.011
- Maruo Y, Uetake K, Egawa K, et al. Selective eating in autism spectrum disorder leading to hair color change. Pediatr Neurol. 2021;120:1-2. doi:10.1016/j.pediatrneurol.2021.03.001
- Paus R, Langan EA, Vidali S, et al. Neuroendocrinology of the hair follicle: principles and clinical perspectives. Trends Mol Med. 2014;20:559-570. doi:10.1016/j.molmed.2014.06.002
- Antonini D, Sibilio A, Dentice M, et al. An intimate relationship between thyroid hormone and skin: regulation of gene expression. Front Endocrinol (Lausanne). 2013;4:104. doi: 10.3389/fendo.2013.00104
- Bodó E, Kany B, Gáspár E, et al. Thyroid-stimulating hormone, a novel, locally produced modulator of human epidermal functions, is regulated by thyrotropin-releasing hormone and thyroid hormones. Endocrinology. 2010;151:1633-1642. doi:10.1210/en.2009-0306
- Taguchi T. Brittle nails and hair loss in hypothyroidism. N Engl J Med. 2018;379:1363-1363. doi:10.1056/NEJMicm1801633
- van Beek N, Bodó E, Kromminga A, et al. Thyroid hormones directly alter human hair follicle functions: anagen prolongation and stimulation of both hair matrix keratinocyte proliferation and hair pigmentation. J Clin Endocrinol Metab. 2008;93:4381-4388. doi:10.1210/jc.2008-0283
- Zippi M, Corrado C, Pica R, et al. Extraintestinal manifestations in a large series of Italian inflammatory bowel disease patients. World J Gastroenterol. 2014;20:17463-7467. doi:10.3748/wjg.v20.i46.17463.
- Gutierrez Gossweiler A, Martinez-Mier EA. Chapter 6: vitamins and oral health. Monogr Oral Sci. 2020;28:59-67. doi:10.1159/000455372
- Monda M, Costacurta M, Maffei L, et al. Oral manifestations of eating disorders in adolescent patients. a review. Eur J Paediatr Dent. 2021;22:155-158. doi:10.23804/ejpd.2021.22.02.13
- Ankar A, Kumar A. Vitamin B12 deficiency. StatPearls. StatPearls Publishing; 2022.
- Graells J, Ojeda RM, Muniesa C, et al. Glossitis with linear lesions: an early sign of vitamin B12 deficiency. J Am Acad Dermatol. 2009;60:498- 500. doi:10.1016/j.jaad.2008.09.011
- Pétavy-Catala C, Fontès V, Gironet N, et al. Clinical manifestations of the mouth revealing vitamin B12 deficiency before the onset of anemia [in French]. Ann Dermatol Venereol. 2003;130(2 pt 1):191-194.
- Monagas J, Ritwik P, Kolomensky A, et al. Rumination syndrome and dental erosions in children. J Pediatr Gastroenterol Nutr. 2017; 64:930-932. doi:10.1097/mpg.0000000000001395
- Silverstein LS, Haggerty C, Sams L, et al. Impact of an oral health education intervention among a group of patients with eating disorders (anorexia nervosa and bulimia nervosa). J Eat Disord. 2019;7:29. doi:10.1186/s40337-019-0259-x
- Rangé H, Colon P, Godart N, et al. Eating disorders through the periodontal lens. Periodontol 2000. 2021;87:17-31. doi:10.1111 /prd.12391
- Zipfel S, Wild B, Groß G, et al. Focal psychodynamic therapy, cognitive behaviour therapy, and optimised treatment as usual in outpatients with anorexia nervosa (ANTOP study): randomised controlled trial. Lancet Psychiatry. 2014;383:127-137. doi:10.1016 /S2215-0366(22)00028-1
- Schmidt U, Ryan EG, Bartholdy S, et al. Two-year follow-up of the MOSAIC trial: a multicenter randomized controlled trial comparing two psychological treatments in adult outpatients with broadly defined anorexia nervosa. Int J Eat Disord. 2016;49:793-800. doi:10.1002/eat.22523
- Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Association; 2013.
- Siddiqui A, Ramsay B, Leonard J. The cutaneous signs of eating disorders. Acta Derm Venereol. 1994;74:68-69. doi:10.2340/00015555746869
- Cheng ZH, Perko VL, Fuller-Marashi L, et al. Ethnic differences in eating disorder prevalence, risk factors, and predictive effects of risk factors among young women. Eat Behav. 2019;32:23-30. doi:10.1016/j. eatbeh.2018.11.004
- Smink FR, van Hoeken D, Hoek HW. Epidemiology of eating disorders: incidence, prevalence and mortality rates. Curr Psychiatry Rep. 2012;14:406-414. doi:10.1007/s11920-012-0282-y
- Campbell K, Peebles R. Eating disorders in children and adolescents: state of the art review. Pediatrics. 2014;134:582-592. doi:10.1542/peds.2014-0194
- Herpertz-Dahlmann B. Adolescent eating disorders: definitions, symptomatology, epidemiology and comorbidity. Child Adolesc Psychiatr Clin N Am. 2009;18:31-47. doi:10.1016/j.chc.2008.07.005
- Arcelus J, Mitchell AJ, Wales J, et al. Mortality rates in patients with anorexia nervosa and other eating disorders: a meta-analysis of 3 6 studies. Arch General Psychiatry. 2011;68:724-731. doi:10.1001 /archgenpsychiatry.2011.74
- Tyler I, Wiseman MC, Crawford RI, et al. Cutaneous manifestations of eating disorders. J Cutan Med Surg. 2002;6:345-353. doi:10.1177/120347540200600407
- Al Nasser Y, Muco E, Alsaad AJ. Pica. StatPearls. StatPearls Publishing; 2023.
- Borgna-Pignatti C, Zanella S. Pica as a manifestation of iron deficiency. Expert Rev Hematol. 2016;9:1075-1080. doi:10.1080/1747408 6.2016.1245136
- Talley NJ. Rumination syndrome. Gastroenterol Hepatol (N Y). 2011;7:117- 118.
- Sanchez-Cerezo J, Nagularaj L, Gledhill J, et al. What do we know about the epidemiology of avoidant/restrictive food intake disorder in children and adolescents? a systematic review of the literature. Eur Eat Disord Rev. 2023;31:226-246. doi:10.1002/erv.2964
- World Health Organization. Malnutrition. Published June 9, 2021. Accessed April 20, 2023. https://www.who.int/news-room/fact-sheets/detail/malnutrition
- Glorio R, Allevato M, De Pablo A, et al. Prevalence of cutaneous manifestations in 200 patients with eating disorders. Int J Dermatol. 2000;39:348-353. doi:10.1046/j.1365-4362.2000.00924.x
- Strumia R, Manzato E, Gualandi M. Is there a role for dermatologists in eating disorders? Expert Rev Dermatol. 2007;2:109-112. doi:10.1586/17469872.2.2.109
- Strumia R. Skin signs in anorexia nervosa. Dermatoendocrinol. 2009;1:268-270. doi:10.4161/derm.1.5.10193
- Strumia R. Eating disorders and the skin. Clin Dermatol. 2013;31:80-85. doi:http://doi.org/10.1016/j.clindermatol.2011.11.011
- Gupta MA, Gupta AK, Haberman HF. Dermatologic signs in anorexia nervosa and bulimia nervosa. Arch Dermatol. 1987;123:1386-1390. doi:10.1001/archderm.1987.01660340159040
- Schulze UM, Pettke-Rank CV, Kreienkamp M, et al. Dermatologic findings in anorexia and bulimia nervosa of childhood and adolescence. Pediatr Dermatol. 1999;16:90-94. doi:10.1046/j.1525-1470.1999.00022.x
- Augustin M, Wilsmann-Theis D, Körber A, et al. Diagnosis and treatment of xerosis cutis—a position paper. J Dtsch Dermatol Ges. 2019;17(suppl 7):3-33. doi:10.1111/ddg.13906
- Grubauer G, Feingold KR, Harris RM, et al. Lipid content and lipid type as determinants of the epidermal permeability barrier. J Lipid Res. 1989;30:89-96.
- Feingold KR, Man MQ, Menon GK, et al. Cholesterol synthesis is required for cutaneous barrier function in mice. J Clin Invest. 1990;86:1738-1745. doi:10.1172/jci114899
- Madison KC. Barrier function of the skin: “la raison d’être” of the epidermis. J Invest Dermatol. 2003;121:231-241. doi:10.106 /j.1523-1747.2003.12359.x
- Usdan LS, Khaodhiar L, Apovian CM. The endocrinopathies of anorexia nervosa. Endocr Pract. 2008;14:1055-1063. doi:10.4158/ep.14.8.1055
- Warren MP. Endocrine manifestations of eating disorders. J Clin Endocrinol Metabol. 2011;96:333-343. doi:10.1210/jc.2009-2304
- Safer JD. Thyroid hormone action on skin. Dermatoendocrinol. 2011;3:211-215. doi:10.4161/derm.3.3.17027
- Cui CY, Schlessinger D. Eccrine sweat gland development and sweat secretion. Exp Dermatol. 2015;24:644-650. doi:10.1111/exd.12773
- Nosewicz J, Spaccarelli N, Roberts KM, et al. The epidemiology, impact, and diagnosis of micronutrient nutritional dermatoses part 1: zinc, selenium, copper, vitamin A, and vitamin C. J Am Acad Dermatol. 2022;86:267-278. doi:10.1016/j.jaad.2021.07.079
- Hoffman M, Micheletti RG, Shields BE. Nutritional dermatoses in the hospitalized patient. Cutis. 2020;105:296;302-308, E1-E5.
- Cox JA, Beachkofsky T, Dominguez A. Flaky paint dermatosis. kwashiorkor. JAMA Dermatol. 2014;150:85-86. doi:10.1001 /jamadermatol.2013.5520
- Bradfield RB. Hair tissue as a medium for the differential diagnosis of protein-calorie malnutrition: a commentary. J Pediatr. 1974;84:294-296.
- Proksch E, Lachapelle J-M. The management of dry skin with topical emollients—recent perspectives. J Dtsch Dermatol Ges. 2005;3:768-774. doi:10.1111/j.1610-0387.2005.05068.x
- Watabe A, Sugawara T, Kikuchi K, et al. Sweat constitutes several natural moisturizing factors, lactate, urea, sodium, and potassium. J Dermatol Sci. 2013;72:177-182. doi:10.1016/j.jdermsci.2013.06.005
- Sugawara T, Kikuchi K, Tagami H, et al. Decreased lactate and potassium levels in natural moisturizing factor from the stratum corneum of mild atopic dermatitis patients are involved with the reduced hydration state. J Dermatol Sci. 2012;66:154-159. doi:10.1016/j .jdermsci.2012.02.011
- Gorski J, Proksch E, Baron JM, et al. Dexpanthenol in wound healing after medical and cosmetic interventions (postprocedure wound healing). Pharmaceuticals (Basel). 2020;13:138. doi:10.3390 /ph13070138
- Verhave BL, Nassereddin A, Lappin SL. Embryology, lanugo. StatPearls. StatPearls Publishing; 2022.
- Faist T. Vernix caseoza—composition and function. Ceska Gynekol. 2020;85:263-267.
- Bystrova K. Novel mechanism of human fetal growth regulation: a potential role of lanugo, vernix caseosa and a second tactile system of unmyelinated low-threshold C-afferents. Med Hypotheses. 2009;72:143-146. doi:10.1016/j.mehy.2008.09.033
- Mitchell JE, Crow S. Medical complications of anorexia nervosa and bulimia nervosa. Curr Opin Psychiatry. 2006;19:438-443. doi:10.1097/01.yco.0000228768.79097.3e
- Dalcin D, Manser C, Mahler R. Malignant down: hypertrichosis lanuginosa acquisita associated with endometrial adenocarcinoma. J Cutan Med Surg. 2015;19:507-510. doi:10.1177/1203475415582319
- Slee PH, van der Waal RI, Schagen van Leeuwen JH, et al. Paraneoplastic hypertrichosis lanuginosa acquisita: uncommon or overlooked? Br J Dermatol. 2007;157:1087-1092. doi:10.1111/j.1365-2133.2007.08253.x
- Lause M, Kamboj A, Fernandez Faith E. Dermatologic manifestations of endocrine disorders. Transl Pediatr. 2017;6:300-312. doi:10.21037 /tp.2017.09.08
- Vulink AJ, ten Bokkel Huinink D. Acquired hypertrichosis lanuginosa: a rare cutaneous paraneoplastic syndrome. J Clin Oncol. 2007;25:1625-1626. doi:10.1200/jco.2007.10.6963
- Wyatt JP, Anderson HF, Greer KE, et al. Acquired hypertrichosis lanuginosa as a presenting sign of metastatic prostate cancer with rapid resolution after treatment. J Am Acad Dermatol. 2007;56 (2 suppl):S45-S47. doi:10.1016/j.jaad.2006.07.011
- Saad N, Hot A, Ninet J, et al. Acquired hypertrichosis lanuginosa and gastric adenocarcinoma [in French]. Ann Dermatol Venereol. 2007;134:55-58. doi:10.1016/s0151-9638(07)88991-5
- Pruijm MC, van Houtum WH. An unusual cause of hypertrichosis. Neth J Med. 2007;65:42, 45.
- Lorette G, Maruani A. Images in clinical medicine. acquired hypertrichosis lanuginosa. N Engl J Med. 2006;354:2696. doi:10.1056 /NEJMicm050344
- Swenne I, Engström I. Medical assessment of adolescent girls with eating disorders: an evaluation of symptoms and signs of starvation. Acta Paediatr. 2005;94:1363-1371. doi:10.1111/j.1651-2227.2005.tb01805.x
- Zhou L, Wang H, Jing J, et al. Regulation of hair follicle development by exosomes derived from dermal papilla cells. Biochem Biophys Res Comm. 2018;500:325-332. doi:10.1016/j.bbrc.2018.04.067
- Tomic-Canic M, Day D, Samuels HH, et al. Novel regulation of keratin gene expression by thyroid hormone and retinoid receptors. J Biol Chem. 1996;271:1416-1423. doi:10.1074/jbc.271.3.1416
- Contreras-Jurado C, Lorz C, García-Serrano L, et al. Thyroid hormone signaling controls hair follicle stem cell function. Mol Biol Cell. 2015;26:1263-1272. doi:10.1091/mbc.E14-07-1251
- Hornberger LL, Lane MA. Identification and management of eating disorders in children and adolescents [published online December 20, 2021]. Pediatrics. doi:10.1542/peds.2020-040279
- Gupta MA, Gupta AK, Voorhees JJ. Starvation-associated pruritus: a clinical feature of eating disorders. J Am Acad Dermatol. 1992; 27:118-120. doi:10.1016/s0190-9622(08)80824-9
- Cevikbas F, Lerner EA. Physiology and pathophysiology of itch. Physiol Rev. 2020;100:945-982. doi:10.1152/physrev.00017.2019
- Stäubli M. Pruritus—a little known iron-deficiency symptom [in German]. Schweiz Med Wochenschr. 1981;111:1394-1398.
- Saini S, Jain AK, Agarwal S, et al. Iron deficiency and pruritus: a cross-sectional analysis to assess its association and relationship. Indian J Dermatol. 2021;66:705. doi:10.4103/ijd.ijd_326_21
- Tammaro A, Chello C, Di Fraia M, et al. Iron-deficiency and pruritus: a possible explanation of their relationship. Int J Research Dermatol. 2018;4:605. doi:10.18203/issn.2455-4529.IntJResDermatol20184470
- Takkunen H. Iron-deficiency pruritus. JAMA. 1978;239:1394.
- Lewiecki EM, Rahman F. Pruritus. a manifestation of iron deficiency. JAMA. 1976;236:2319-2320. doi:10.1001/jama.236.20.2319
- Kennedy A, Kohn M, Lammi A, et al. Iron status and haematological changes in adolescent female inpatients with anorexia nervosa. J Paediatr Child Health. 2004;40:430-432. doi:10.1111/j.1440-1754.2004.00432.x
- Morgan JF, Lacey JH. Scratching and fasting: a study of pruritus and anorexia nervosa. Br J Dermatol. 1999;140:453-456. doi:10.1046/j.1365- 2133.1999.02708.x
- Mehler PS. Anorexia nervosa in adults: evaluation for medical complications and criteria for hospitalization to manage these complications. UpToDate. Updated August 3, 2022. Accessed April 20, 2023. https://www.uptodate.com/contents/anorexia-nervosa-in-adults-evaluation-for-medical-complications-and-criteria-for -hospitalization-to-manage-these-complications
- Das S, Maiti A. Acrocyanosis: an overview. Indian J Dermatol. 2013;58:417-420. doi:10.4103/0019-5154.119946
- Caregaro L, Di Pascoli L, Favaro A, et al. Sodium depletion and hemoconcentration: overlooked complications in patients with anorexia nervosa? Nutrition. 2005;21:438-445. doi:10.1016/j.nut.2004.08.022
- Crisp AH, Stonehill E. Hypercarotenaemia as a symptom of weight phobia. Postgrad Med J. 1967;43:721. doi:10.1136/pgmj.43.505.721
- Pops MA, Schwabe AD. Hypercarotenemia in anorexia nervosa. JAMA. 1968;205:533-534. doi:10.1001/jama.1968.03140330075020.
- Bohn T, Desmarchelier C, El SN, et al. β-Carotene in the human body: metabolic bioactivation pathways—from digestion to tissue distribution and excretion. Proc Nutr Soc. 2019;78:68-87. doi:10.1017/S0029665118002641
- von Lintig J, Moon J, Lee J, et al. Carotenoid metabolism at the intestinal barrier. Biochim Biophys Acta Mol Cell Biol Lipids. 2020;1865:158580. doi:10.1016/j.bbalip.2019.158580
- Kanai M, Raz A, Goodman DS. Retinol-binding protein: the transport protein for vitamin A in human plasma. J Clin Invest. 1968;47:2025-2044. doi:10.1172/jci105889
- Haught JM, Patel S, English JC. Xanthoderma: a clinical review. J Am Acad Dermatol. 2007;57:1051-1058. doi:10.1016/j.jaad.2007.06.011
- Tung EE, Drage LA, Ghosh AK. Carotenoderma and hypercarotenemia: markers for disordered eating habits. J Eur Acad Dermatol Venereol. 2006;20:1147-1148. doi:10.1111/j.1468-3083.2006.01643.x
- Heilskov S, Vestergaard C, Babirekere E, et al. Characterization and scoring of skin changes in severe acute malnutrition in children between 6 months and 5 years of age. J Eur Acad Dermatol Venereol. 2015;29:2463-2469. doi:10.1111/jdv.13328
- Malkud S. Telogen effluvium: a review. J Clin Diagn Res. 2015;9:We01-3. doi:10.7860/jcdr/2015/15219.6492
- Filipponi C, Visentini C, Filippini T, et al. The follow-up of eating disorders from adolescence to early adulthood: a systematic review. Int J Environ Res Public Health. 2022;19:16237. doi:10.3390/ijerph192316237
- Byrne S, Wade T, Hay P, et al. A randomised controlled trial of three psychological treatments for anorexia nervosa. Psychol Med. 2017;47:2823-2833. doi:10.1017/s0033291717001349
- Ranalli DN, Studen-Pavlovich D. Eating disorders in the adolescent patient. Dent Clin North Am. 2021;65:689-703. doi:10.1016/j. cden.2021.06.009
- Arck PC, Handjiski B, Peters EM, et al. Stress inhibits hair growth in mice by induction of premature catagen development and deleterious perifollicular inflammatory events via neuropeptide substance P-dependent pathways. Am J Pathol. 2003;162:803-814. doi:10.1016/s0002-9440(10)63877-1
- Roy SK. Achromotrichia in tropical malnutrition. Br Med J. 1947;1:392. doi:10.1136/bmj.1.4498.392-c
- Swed-Tobia R, Haj A, Militianu D, et al. Highly selective eating in autism spectrum disorder leading to scurvy: a series of three patients. Pediatr Neurol. 2019;94:61-63. doi:10.1016/j.pediatrneurol.2018.12.011
- Maruo Y, Uetake K, Egawa K, et al. Selective eating in autism spectrum disorder leading to hair color change. Pediatr Neurol. 2021;120:1-2. doi:10.1016/j.pediatrneurol.2021.03.001
- Paus R, Langan EA, Vidali S, et al. Neuroendocrinology of the hair follicle: principles and clinical perspectives. Trends Mol Med. 2014;20:559-570. doi:10.1016/j.molmed.2014.06.002
- Antonini D, Sibilio A, Dentice M, et al. An intimate relationship between thyroid hormone and skin: regulation of gene expression. Front Endocrinol (Lausanne). 2013;4:104. doi: 10.3389/fendo.2013.00104
- Bodó E, Kany B, Gáspár E, et al. Thyroid-stimulating hormone, a novel, locally produced modulator of human epidermal functions, is regulated by thyrotropin-releasing hormone and thyroid hormones. Endocrinology. 2010;151:1633-1642. doi:10.1210/en.2009-0306
- Taguchi T. Brittle nails and hair loss in hypothyroidism. N Engl J Med. 2018;379:1363-1363. doi:10.1056/NEJMicm1801633
- van Beek N, Bodó E, Kromminga A, et al. Thyroid hormones directly alter human hair follicle functions: anagen prolongation and stimulation of both hair matrix keratinocyte proliferation and hair pigmentation. J Clin Endocrinol Metab. 2008;93:4381-4388. doi:10.1210/jc.2008-0283
- Zippi M, Corrado C, Pica R, et al. Extraintestinal manifestations in a large series of Italian inflammatory bowel disease patients. World J Gastroenterol. 2014;20:17463-7467. doi:10.3748/wjg.v20.i46.17463.
- Gutierrez Gossweiler A, Martinez-Mier EA. Chapter 6: vitamins and oral health. Monogr Oral Sci. 2020;28:59-67. doi:10.1159/000455372
- Monda M, Costacurta M, Maffei L, et al. Oral manifestations of eating disorders in adolescent patients. a review. Eur J Paediatr Dent. 2021;22:155-158. doi:10.23804/ejpd.2021.22.02.13
- Ankar A, Kumar A. Vitamin B12 deficiency. StatPearls. StatPearls Publishing; 2022.
- Graells J, Ojeda RM, Muniesa C, et al. Glossitis with linear lesions: an early sign of vitamin B12 deficiency. J Am Acad Dermatol. 2009;60:498- 500. doi:10.1016/j.jaad.2008.09.011
- Pétavy-Catala C, Fontès V, Gironet N, et al. Clinical manifestations of the mouth revealing vitamin B12 deficiency before the onset of anemia [in French]. Ann Dermatol Venereol. 2003;130(2 pt 1):191-194.
- Monagas J, Ritwik P, Kolomensky A, et al. Rumination syndrome and dental erosions in children. J Pediatr Gastroenterol Nutr. 2017; 64:930-932. doi:10.1097/mpg.0000000000001395
- Silverstein LS, Haggerty C, Sams L, et al. Impact of an oral health education intervention among a group of patients with eating disorders (anorexia nervosa and bulimia nervosa). J Eat Disord. 2019;7:29. doi:10.1186/s40337-019-0259-x
- Rangé H, Colon P, Godart N, et al. Eating disorders through the periodontal lens. Periodontol 2000. 2021;87:17-31. doi:10.1111 /prd.12391
- Zipfel S, Wild B, Groß G, et al. Focal psychodynamic therapy, cognitive behaviour therapy, and optimised treatment as usual in outpatients with anorexia nervosa (ANTOP study): randomised controlled trial. Lancet Psychiatry. 2014;383:127-137. doi:10.1016 /S2215-0366(22)00028-1
- Schmidt U, Ryan EG, Bartholdy S, et al. Two-year follow-up of the MOSAIC trial: a multicenter randomized controlled trial comparing two psychological treatments in adult outpatients with broadly defined anorexia nervosa. Int J Eat Disord. 2016;49:793-800. doi:10.1002/eat.22523
Practice Points
- Cutaneous manifestations of malnutrition may be the presenting sign of disordered eating.
- Dermatologists have a unique opportunity for early recognition and intervention in patients with eating disorders (EDs).
- Rapid identification and multidisciplinary management of EDs may improve patient outcomes and potentially attenuate the risk of irreversible damage from malnutrition.
The Role of Dietary Antioxidants in Melanoma and Nonmelanoma Skin Cancer
Nonmelanoma skin cancer (NMSC) is the most common cancer in the United States, and cutaneous melanoma is projected to be the fifth most common form of cancer in 2022, with increasing incidence and high potential for mortality.1-3 Estimates indicate that 35% to 45% of all cancers in White patients are cutaneous, with 4% to 5% occurring in Hispanic patients, 2% to 4% in Asian patients, and 1% to 2% in Black patients.4 Of the keratinocyte carcinomas, basal cell carcinoma (BCC) is the most prevalent, projected to affect approximately 33% to 39% of White males and 23% to 28% of White females in the United States during their lifetimes. Squamous cell carcinoma (SCC) is the second most common skin malignancy, with a lifetime risk of 9% to 14% for White males and 4% to 9% for White females in the United States.5 The incidence of melanoma continues to increase, with approximately 99,780 new cases expected in the United States in 2022.1
UV-induced DNA damage plays a key role in the pathogenesis and development of various skin malignancies.6 UV radiation from sunlight or tanning devices causes photocarcinogenesis due to molecular and cellular effects, including the generation of reactive oxygen species, DNA damage due to the formation of cyclobutane pyrimidine dimers and pyrimidine-pyrimidone, melanogenesis, apoptosis, and the increased expression of harmful genes and proteins.6 The summation of this damage can result in skin malignancies, including NMSC and melanoma.6,7 Dietary antioxidants theoretically help prevent oxidative reactions from occurring within the body, and it has been suggested that intake of dietary antioxidants may decrease DNA damage and prevent tumorigenesis secondary to UV radiation.8 Antioxidants exist naturally in the body but can be acquired exogenously. Investigators have studied dietary antioxidants in preventing skin cancer formation with promising results in the laboratory setting.8-11 Recently, more robust human studies have been initiated to further delineate this relationship. We present clinical evidence of several frequently utilized antioxidant vitamins and their effects on melanoma and NMSC.
Antioxidants
Vitamin A—Vitamin A is a fat-soluble vitamin found in animal sources, including fish, liver, and eggs. Carotenoids, such as beta carotene, are provitamin A plant derivatives found in fruits and vegetables that are converted into biologically active retinol and retinoic acid.12 Retinols play a key role in cellular growth and differentiation and are thought to be protective against skin cancer via the inactivation of free radicals and immunologic enhancement due to their antiproliferative, antioxidative, and antiapoptotic effects.13-16 Animal studies have demonstrated this protective effect and the ability of retinoids to suppress carcinogenesis; however, human studies reveal conflicting results.17,18
Greenberg et al19 investigated the use of beta carotene in preventing the formation of NMSC. Patients (N=1805) were randomized to receive 50 mg of beta carotene daily or placebo. Over a 5-year period, there was no significant reduction in the occurrence of NMSC (relative risk [RR], 1.05; 95% CI, 0.91-1.22).19 Frieling et al20 conducted a similar randomized, double-blind, placebo-controlled trial investigating beta carotene for primary prevention of NMSC in 22,071 healthy male physicians. The study group received 50 mg of beta carotene every other day for 12 years’ duration, and there was no significant effect on the incidence of first NMSC development (RR, 0.98; 95% CI, 0.92-1.05).20
A case-control study by Naldi et al21 found an inverse association between vitamin A intake and development of melanoma. Study participants were stratified into quartiles based on level of dietary intake and found an odds ratio (OR) of 0.71 for beta carotene (95% CI, 0.50-1.02), 0.57 for retinol (95% CI, 0.39-0.83), and 0.51 for total vitamin A (95% CI, 0.35-0.75) when comparing the upper quartile of vitamin A intake to the lower quartile. Upper-quartile cutoff values of vitamin A intake were 214 µg/d for beta carotene, 149 µg/d for retinol, and 359 µg/d for total vitamin A.21 More recently, a meta-analysis by Zhang et al22 pooled data from 8 case-control studies and 2 prospective studies. Intake of retinol but not total vitamin A or beta carotene was associated with a reduced risk for development of melanoma (retinol: OR, 0.80; 95% CI, 0.69-0.92; total vitamin A: OR, 0.86; 95% CI, 0.59-1.25; beta carotene: OR, 0.87; 95% CI, 0.62-1.20).22 Feskanich et al23 demonstrated similar findings with use of food-frequency questionnaires in White women, suggesting that retinol intake from food combined with supplements may be protective for women who were otherwise at a low risk for melanoma based on nondietary factors. These factors included painful or blistering sunburns during childhood, history of more than 6 sunburns, more than 3 moles on the left arm, having red or blonde hair, and having a parent or sibling with melanoma (P=.01). However, this relationship did not hold true when looking at women at an intermediate or high risk for melanoma (P=.16 and P=.46).23
When looking at high-risk patients, such as transplant patients, oral retinoids have been beneficial in preventing NMSC.24-27 Bavinck et al24 investigated 44 renal transplant patients with a history of more than 10 NMSCs treated with 30 mg of acitretin daily vs placebo. Patients receiving oral retinoid supplementation developed fewer NMSCs over a 6-month treatment period (P=.01).24 Similarly, George et al25 investigated acitretin in renal transplant patients and found a statistically significant decrease in number of SCCs in patients on supplementation (P=.002). Solomon-Cohen et al26 performed a retrospective case-crossover study in solid organ transplant recipients and found that those treated with 10 mg of acitretin daily for 2 years had a significant reduction in the number of new keratinocyte carcinomas (P=.002). Other investigators have demonstrated similar results, and in 2006, Otley et al27 proposed standardized dosing of acitretin for chemoprevention in high-risk patients, including patients developing 5 to 10 NMSCs per year, solid organ transplant recipients, and those with syndromes associated with the development of NMSC.28,29 Overall, in the general population, vitamin A and related compounds have not demonstrated a significant association with decreased development of NMSC; however, oral retinoids have proven useful for high-risk patients. Furthermore, several studies have suggested a negative association between vitamin A levels and the incidence of melanoma, specifically in the retinol formulation.
Vitamin B3—Nicotinamide (also known as niacinamide) is a water-soluble form of vitamin B3 and is obtained from animal-based and plant-based foods, such as meat, fish, and legumes.30 Nicotinamide plays a key role in cellular metabolism, cellular signaling, and DNA repair, including protection from UV damage within keratinocytes.31,32 Early mouse models demonstrated decreased formation of skin tumors in mice treated with topical or oral nicotinamide.32,33 A number of human studies have revealed similar results.34-36
Chen et al34 conducted the ONTRAC study, a phase 3, double-blind, randomized controlled trial (RCT) looking at 386 participants with a history of at least 2 NMSCs in the preceding 5 years. At 12 months, those treated with 500 mg of nicotinamide twice daily demonstrated a statistically significant decreased rate of SCC formation (P=.05). A decreased incidence of BCC development was noted; however, this trend did not reach statistical significance (P=.12). Precancerous skin lesions also were found to be decreased in the treatment group, with 20% lower incidence of actinic keratoses (AKs) after 9 months of treatment (P<.001).34 Drago et al35 specifically studied the incidence of AKs in 38 transplant recipients—8 liver and 30 kidney—and found that previously noted AKs had decreased in size for 18 of 19 patients taking 500 mg of nicotinamide daily when originally photographed AKs were remeasured at 6-month follow-up, with 7 of these 18 patients demonstrating complete clinical regression. Of those on nicotinamide supplementation, no new AKs developed compared to the control group, which demonstrated increased size of AKs or development of new AKs in 91% of patients, with 7 AKs progressing into SCC.35
Nicotinamide has been demonstrated to be useful in preventing skin cancer in high-risk populations, such as transplant patients or those with a high incidence of NMSC.34,36 Despite promising results within the laboratory setting, nicotinamide’s effects on melanoma in humans remains less clear.31,37 Studies suggest that nicotinamide enhances tumor-infiltrating lymphocytes and DNA repair mechanisms in melanocytes, which may translate into nicotinamide, providing chemoprevention for melanoma, but research in human patients is limited.31,37
Vitamin B9—Folate, the natural form of vitamin B9, is a water-soluble compound that is found in many foods, especially green leafy vegetables, and often is supplemented because of its health benefits.38,39 In the skin, folic acid plays a key role in cellular replication and proliferation.38 Controversy exists regarding folate’s effects on cellular growth and turnover with respect to cancer incidence.38,40 Donnenfeld et al41 conducted a prospective study assessing dietary folic acid intake and development of NMSC. A total of 5880 participants completed dietary records throughout the first 2 years of the study. After an average follow-up period of 12.6 years, there was an overall increased incidence of skin cancer in those with increased dietary folate (P=.03). Furthermore, when striating by skin cancer type, there was an increased incidence of NMSC overall as well as BCC when analyzing by type of NMSC (P=.03 for NMSC; P=.05 for BCC). However, when stratifying by gender, these findings only held true for women.41 Similar effects were observed by Fung et al,42 who prospectively studied the intake of various vitamins in relationship to the development of BCC in women. During 12 years of follow-up, a positive association was observed between folate intake and BCC development (OR, 1.2; 95% CI, 1.10-1.31).42 Fung et al43 also investigated the role of several vitamins in the development of SCC and found that folate showed a negative association, which did not reach statistical significance (RR, 0.79; 95% CI, 0.56-1.11). Furthermore, Vollset et al40 conducted a meta-analysis comparing folic acid to placebo in the incidence of various types of cancer. The study excluded NMSC but reported no significant association between the development of melanoma and folic acid supplementation.40 In summary, the effects of folate have diverse consequences, potentially promoting the formation of NMSC, but studies suggest that an individual’s gender and other genetic and environmental factors also may play a role.
Vitamin C—Vitamin C (also known as ascorbic acid) is a water-soluble vitamin with antioxidant immune-mediating effects. It is found in various fruits and vegetables and serves as a cofactor for enzymes within the body playing a key role in immune function and collagen formation.44,45 It has been postulated that ascorbic acid can provide protection from UV radiation damage via its intracellular activity but conversely can contribute to oxidative damage.44 Multiple in vitro laboratory studies and animal models have demonstrated photoprotective effects of ascorbic acid.46-48 Despite these findings, minimal photoprotective effects have been found in the human population.
Kune et al49 performed a case-control study of 88 males with previously diagnosed NMSC undergoing surgical removal and investigated patients’ prior dietary habits. Patients with NMSC had a statistically significantly lower level of vitamin C–containing food in their diet than those without NMSC (P=.004).49 In addition, Vural et al50 analyzed plasma samples and blood cells of patients with AK and BCC and found a significant decrease in ascorbic acid levels in both the AK (P<.001) and BCC (P<.001) groups compared with controls. However, studies have found that consumption of certain dietary compounds can rapidly increase plasma concentration levels, which may serve as a major confounding variable in this study. Plasma concentrations of ascorbic acid and beta carotene were found to be significantly increased following consumption of a high-antioxidant diet for as short a duration as 2 weeks (P<.05).51 More recently, Heinen et al52 performed a prospective study on 1001 adults. In patients without a history of skin cancer, they found that vitamin C from food sources plus dietary supplements was positively associated with the development of BCC (P=.03).52 Similarly, Fung et al42 performed a study in women and found a positive association between vitamin C intake and the development of BCC (OR, 1.13; 95% CI, 1.03-1.23).
The relationship between vitamin C intake—either in dietary or supplemental form—and melanoma remains controversial. Mice-based studies found that high concentrations of orally administered vitamin C induce cytotoxicity in melanoma cell lines, but at low concentrations they promote tumor growth of malignant melanoma.53 Feskanich et al23 examined the relationship between vitamin C intake and melanoma development via food frequency questionnaires in White women and found that vitamin C was associated with a higher risk for melanoma (P=.05), and furthermore, a positive dose response with frequency of orange juice intake was observed (P=.008). Overall, despite promising laboratory studies, there is a lack of RCTs investigating the use of vitamin C supplementation for prevention of NMSC and melanoma in humans, and the oral benefits of vitamin C for chemoprevention remain unclear.
Vitamin D—Vitamin D is a fat-soluble vitamin that is found in fish, liver, egg, and cheese, and is endogenously produced when UV radiation from sun exposure interacts with the skin, triggering the synthesis of vitamin D.54 Vitamin D is biologically inactive and must be converted to its active form 1,25-dihydroxyvitamin D after entering the body. Vitamin D modulates many genes involved in cellular proliferation and differentiation.54 Vitamin D receptors are expressed on keratinocytes and melanocytes.55 Animal studies have demonstrated a potentially protective effect of vitamin D in the development of NMSC.56 In a mouse model, Ellison et al56 found that mice without vitamin D receptors developed skin tumors more rapidly than those with vitamin D receptors.
Unfortunately, these findings have not been demonstrated in humans, and studies have even reported an increased risk for development of NMSC in patients with normal or increased vitamin D levels compared with those with low levels of vitamin D.57-60 Eide et al57 studied 3223 patients seeking advice for low bone density by recording their vitamin D levels at the time of presentation and monitoring development of NMSC. Vitamin D levels greater than 15 ng/mL were positively associated with the development of NMSC (OR, 1.7; 95% CI, 1.04-2.7). This association held true for both SCC and BCC, with a higher risk estimated for SCC (OR, 3.2; 95% CI, 0.4-24.0 for SCC; OR, 1.7; 95% CI, 0.5-5.8 for BCC).57 An increased vitamin D serum level also was found to be significantly associated with a higher risk for BCC and melanoma by van der Pols et al.58 This prospective study looked at the incidence of skin cancer over 11 years. Study participants with vitamin D levels over 75 nmol/L more frequently developed BCC (P=.01) and melanoma (P=.05). In contrast, SCC was less frequently observed in participants with these high levels of vitamin D (P=.07).58 Furthermore, Park et al60 looked at vitamin D and skin cancer risk for men and women in the United States and found no association with risk for SCC or melanoma but a positive association with BCC (P=.05 for total vitamin D; P<.01 for dietary vitamin D). Additional studies have been performed with inconsistent results, and multiple authors suggest the possible confounding relationship between vitamin D levels and UV radiation exposure.59-62 Furthermore, some studies have even demonstrated a negative association between vitamin D and NMSC. Tang et al63 performed a retrospective case-control study in elderly males, investigating serum levels of vitamin D and patients’ self-reported history of NMSC, which demonstrated that higher levels of vitamin D were associated with a decreased risk for NMSC. Overall, the relationship between vitamin D and skin cancer development remains unclear for both melanoma and NMSC.
Vitamin E—Vitamin E is a fat-soluble vitamin that is found in plant-based oils, nuts, seeds, fruits, and vegetables.64 It works as an antioxidant to protect against free radicals and heighten immune function, and it also serves as a pro-oxidant.65,66 Vitamin E naturally exists in 8 chemical forms, of which gamma-tocopherol is the most frequently obtained form in the diet, and alpha-tocopherol is the most abundant form found in the body.64,65
Early animal studies demonstrated the inhibition of UV-induced damage in mice receiving vitamin E supplementation.67,68 Human studies have not consistently shown these effects. Vural et al50 investigated plasma samples and blood cells of patients with AKs and BCCs and reported a significant decrease in alpha-tocopherol levels in both the AK (P<.05) and BCC (P<.001) groups compared with controls. However, studies also have demonstrated a positive association between vitamin E intake and the development of BCC, including one by Fung et al,42 which found a significant association in women (OR, 1.15; 95% CI, 1.06-1.26).
Vitamin E has been found to inhibit melanin synthesis in the laboratory, suggesting a potentially protective effect in melanoma.69,70 However, in the study performed by Feskanich et al23 examining vitamin intake and melanoma incidence via food-frequency questionnaires, vitamin E was not associated with a lower risk for melanoma. Despite promising laboratory studies, the data surrounding the use of a vitamin E supplement for prevention of melanoma and NMSC in humans remains unclear.
Selenium—Selenium is a trace mineral found in plants, meat, and fish. It plays a key role in reproduction, hormone metabolism, DNA synthesis, and protection from oxidative damage.71 In mice studies, lack of selenium-containing proteins resulted in skin abnormalities, including the development of a hyperplastic epidermis and aberrant hair follicle morphogenesis with alopecia after birth, and numerous experimental studies have demonstrated a negative association between selenium intake and cancer.72,73 However, human studies have yielded alternative results.
The Nutritional Prevention of Cancer Study Group analyzed 1312 dermatology patients with a history of NMSC.74 The study population was obtained from 7 dermatology clinics with randomization to control for confounding variables. Study participants received either 200 μg of selenium daily or placebo.74 Baseline characteristics of each study group were overall balanced. Selenium intake was found to have no effect on the development of BCC (hazard ratio [HR], 1.09; 95% CI, 0.94-1.26) but an increased risk for developing SCC (HR, 1.25; 95% CI, 1.03-1.51) and total NMSC (HR, 1.17; 95% CI, 1.02-1.34).74,75 Similarly, Reid et al76 performed an RCT comparing patients treated with 400 μg/d of selenium to those treated with 200 μg/d of selenium. When compared with placebo, those treated with 200 μg/d of selenium had a statistically significantly increased incidence of NMSC (P=.006); however, those treated with 400 μg/d of selenium had no significant change in total incidence of NMSC (P=.51).76 Furthermore, Vinceti et al77 performed a review of 83 studies from the literature investigating the effect of dietary selenium, and from the RCTs, there was no beneficial effect of selenium in reducing cancer risk in general; however, some studies demonstrated an increased incidence of other types of cancer, including melanoma. Of the RCTs included in the study investigating NMSC incidence specifically, it was found that the incidence was not affected by selenium administration (RR, 1.16; 95% CI, 0.30-4.42; 2 studies, 2027 participants).77 Despite data from several studies demonstrating an increased risk for NMSC, the effects of selenium on the risk for NMSC and melanoma remain unclear.
Combination Antioxidant Studies
In addition to investigating the use of single antioxidants in skin cancer prevention, studies utilizing the combination of various antioxidants or other dietary minerals have been conducted. Hercberg et al78 performed a randomized, double-blinded, placebo-controlled trial of 13,017 adults (7876 women and 5141 men) receiving a combination of 120 mg vitamin C, 30 mg vitamin E, 100 μg selenium, 6 mg beta carotene, and 20 mg zinc. Study participants were followed for an average of 7.5 years, and the development of skin cancers were recorded. Overall, the incidence rate of skin cancer did not differ between the 2 treatment groups; however, when segregated by gender, the study found that there was an increased risk for developing skin cancer in women taking the antioxidant supplement combination compared with placebo (P=.03). This difference was not observed in the 2 treatment groups of male patients (P=.11). When looking specifically at NMSC, there was no difference between treatment groups for male or female patients (P=.39 for males; P=.15 for females). In contrast, there was a higher incidence of melanoma identified in female patients taking the combination antioxidant supplement (P=.01), but this was not seen within the male study population (P=.51).78 In addition, Chang et al79 performed a meta-analysis of 10 previously published RCTs. Analysis revealed that treatment with a variety of supplements, including vitamins A, C, E, and beta carotene, were found to have no preventative effects on the incidence of skin cancer development (RR, 0.98; CI, 0.98-1.03). Notable limitations to this study included the variability in protocols of the studies included in this meta-analysis, the limited number of RCTs investigating vitamin supplementation and the risk for skin cancer development, and the influence of dietary intake on study outcomes.79
Other Dietary Agents
Furocoumarins—Furocoumarins are botanical substances found in various fruits and plants, including many citrus products. Furocoumarins are activated by UV light radiation and can lead to development of a phototoxic eruption. Several studies have suggested a pharmacogenetic effect of furocoumarins.80 Sun et al80 collected dietary data from 47,453 men and 75,291 women on furocoumarin intake and correlation with the development of NMSC. Overall, the study suggested that the intake of furocoumarins may lead to an increase in the development of BCC (HR, 1.16; 95% CI, 1.11-1.21; P=.002); however, there was no significant association identified between total intake of furocoumarins in the risk for SCC or melanoma.80 Furthermore, Sakaki et al81 conducted a survey study looking at the consumption of citrus products and the development of NMSC. The group found that there was an increased risk for NMSC in those consuming an increased amount of citrus products (P=.007).81
Conclusion
Dietary antioxidants have been investigated for their potential role in the prevention of tumorigenesis. Specific antioxidant vitamins, such as vitamin A derivatives and niacinamide, have demonstrated clinical utility in the prevention of NMSC in high-risk populations. Retinol also has been associated with a reduced incidence of melanoma. Numerous antioxidants have demonstrated promising data within the laboratory setting; however, inconsistent results have been appreciated in humans. Furthermore, several research studies suggest that folate, vitamin D, and furocoumarins may be associated with an increased risk for skin cancer development; however, these studies are inconclusive, and dietary studies are challenging to conduct. Overall, RCTs investigating the role of antioxidants for chemoprevention are limited. Moreover, the study of dietary antioxidants and vitamins may be affected by various confounding variables that can be difficult to account for because of patients’ potentially poor recall of dietary intake and the effect of dietary intake in supplemental studies. Given the increasing prevalence of skin cancer worldwide, further research into the clinical utility of antioxidants in skin cancer prevention is warranted.
- Siegel RL, Miller KD, Fuchs HE, et al. Cancer statistics, 2022. CA Cancer J Clin. 2022;72:7-33.
- Global Burden of Disease Cancer Collaboration; Fitzmaurice C, Abate D, Abbasi N, et al. Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 29 cancer groups, 1990 to 2017: a systematic analysis for the Global Burden of Disease Study. JAMA Oncol. 2019;5:1749-1768.
- Leiter U, Keim U, Garbe C. Epidemiology of skin cancer: update 2019. In: Reichrath J, ed. Sunlight, Vitamin D and Skin Cancer. Springer International Publishing; 2020:123-139.
- Bradford PT. Skin cancer in skin of color. Dermatol Nurs. 2009;21:170-177, 206; quiz 178.
- Miller DL, Weinstock MA. Nonmelanoma skin cancer in the United States: incidence. J Am Acad Dermatol. 1994;30:774-778.
- Young AR, Claveau J, Rossi AB. Ultraviolet radiation and the skin: photobiology and sunscreen photoprotection. J Am Acad Dermatol. 2017;76(3S1):S100-S109.
- Pleasance ED, Cheetham RK, Stephens PJ, et al. A comprehensive catalogue of somatic mutations from a human cancer genome. Nature. 2010;463:191-196.
- Baek J, Lee MG. Oxidative stress and antioxidant strategies in dermatology. Redox Rep. 2016;21:164-169.
- Katta R, Brown DN. Diet and skin cancer: the potential role of dietary antioxidants in nonmelanoma skin cancer prevention. J Skin Cancer. 2015;2015:893149.
- Stoj V, Shahriari N, Shao K, et al. Nutrition and nonmelanoma skin cancers. Clin Dermatol. 2022;40:173-185.
- O’Connor EA, Evans CV, Ivlev I, et al. Vitamin and mineral supplements for the primary prevention of cardiovascular disease and cancer: updated evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2022;327:2334-2347.
- National Institutes of Health Office of Dietary Supplements. Vitamin A and carotenoids. fact sheet for health professionals. Updated June 15, 2022. Accessed November 14, 2022. https://ods.od.nih.gov/factsheets/VitaminA-HealthProfessional/
- Keller KL, Fenske NA. Uses of vitamins A, C, and E and related compounds in dermatology: a review. J Am Acad Dermatol. 1998;39:611-625.
- Wright TI, Spencer JM, Flowers FP. Chemoprevention of nonmelanoma skin cancer. J Am Acad Dermatol. 2006;54:933-946; quiz 947-950.
- Bushue N, Wan YJY. Retinoid pathway and cancer therapeutics. Adv Drug Deliv Rev. 2010;62:1285-1298.
- Stahl W, Sies H. β-Carotene and other carotenoids in protection from sunlight. Am J Clin Nutr. 2012;96:1179S-1184S.
- Bukhari MH, Qureshi SS, Niazi S, et al. Chemotherapeutic/chemopreventive role of retinoids in chemically induced skin carcinogenesis in albino mice. Int J Dermatol. 2007;46:1160-1165.
- Lambert LA, Wamer WG, Wei RR, et al. The protective but nonsynergistic effect of dietary beta-carotene and vitamin E on skin tumorigenesis in Skh mice. Nutr Cancer. 1994;21:1-12.
- Greenberg ER, Baron JA, Stukel TA, et al. A clinical trial of beta carotene to prevent basal-cell and squamous-cell cancers of the skin. The Skin Cancer Prevention Study Group. N Engl J Med. 1990;323:789-795.
- Frieling UM, Schaumberg DA, Kupper TS, et al. A randomized, 12-year primary-prevention trial of beta carotene supplementation for nonmelanoma skin cancer in the physician’s health study. Arch Dermatol. 2000;136:179-184.
- Naldi L, Gallus S, Tavani A, et al; Oncology Study Group of the Italian Group for Epidemiologic Research in Dermatology. Risk of melanoma and vitamin A, coffee and alcohol: a case-control study from Italy. Eur J Cancer Prev. 2004;13:503-508.
- Zhang YP, Chu RX, Liu H. Vitamin A intake and risk of melanoma: a meta-analysis. PloS One. 2014;9:e102527.
- Feskanich D, Willett WC, Hunter DJ, et al. Dietary intakes of vitamins A, C, and E and risk of melanoma in two cohorts of women. Br J Cancer. 2003;88:1381-1387.
- Bavinck JN, Tieben LM, Van der Woude FJ, et al. Prevention of skin cancer and reduction of keratotic skin lesions during acitretin therapy in renal transplant recipients: a double-blind, placebo-controlled study. J Clin Oncol. 1995;13:1933-1938.
- George R, Weightman W, Russ GR, et al. Acitretin for chemoprevention of non-melanoma skin cancers in renal transplant recipients. Australas J Dermatol. 2002;43:269-273.
- Solomon-Cohen E, Reiss-Huss S, Hodak E, et al. Low-dose acitretin for secondary prevention of keratinocyte carcinomas in solid-organ transplant recipients. Dermatology. 2022;238:161-166.
- Otley CC, Stasko T, Tope WD, et al. Chemoprevention of nonmelanoma skin cancer with systemic retinoids: practical dosing and management of adverse effects. Dermatol Surg. 2006;32:562-568.
- Kadakia KC, Barton DL, Loprinzi CL, et al. Randomized controlled trial of acitretin versus placebo in patients at high-risk for basal cell or squamous cell carcinoma of the skin (North Central Cancer Treatment Group Study 969251). Cancer. 2012;118:2128-2137.
- McKenna DB, Murphy GM. Skin cancer chemoprophylaxis in renal transplant recipients: 5 years of experience using low-dose acitretin. Br J Dermatol. 1999;140:656-660.
- National Institutes of Health Office of Dietary Supplements. Niacin: fact sheet for health professionals. Updated August 23, 2022. Accessed November 14, 2022. https://ods.od.nih.gov/factsheets/Niacin-HealthProfessional/
- Malesu R, Martin AJ, Lyons JG, et al. Nicotinamide for skin cancer chemoprevention: effects of nicotinamide on melanoma in vitro and in vivo. Photochem Photobiol Sci. 2020;19:171-179.
- Gensler HL. Prevention of photoimmunosuppression and photocarcinogenesis by topical nicotinamide. Nutr Cancer. 1997;29:157-162.
- Gensler HL, Williams T, Huang AC, et al. Oral niacin prevents photocarcinogenesis and photoimmunosuppression in mice. Nutr Cancer. 1999;34:36-41.
- Chen AC, Martin AJ, Choy B, et al. A phase 3 randomized trial of nicotinamide for skin-cancer chemoprevention. N Engl J Med. 2015;373:1618-1626.
- Drago F, Ciccarese G, Cogorno L, et al. Prevention of non-melanoma skin cancers with nicotinamide in transplant recipients: a case-control study. Eur J Dermatol. 2017;27:382-385.
- Yélamos O, Halpern AC, Weinstock MA. Reply to “A phase II randomized controlled trial of nicotinamide for skin cancer chemoprevention in renal transplant recipients.” Br J Dermatol. 2017;176:551-552.
- Scatozza F, Moschella F, D’Arcangelo D, et al. Nicotinamide inhibits melanoma in vitro and in vivo. J Exp Clin Cancer Res. 2020;39:211.
- National Institutes of Health Office of Dietary Supplements. Folate: fact sheet for health professionals. Updated November 1, 2022. Accessed November 14, 2022. https://ods.od.nih.gov/factsheets/Folate-HealthProfessional/
- Butzbach K, Epe B. Photogenotoxicity of folic acid. Free Radic Biol Med. 2013;65:821-827.
- Vollset SE, Clarke R, Lewington S, et al. Effects of folic acid supplementation on overall and site-specific cancer incidence during the randomised trials: meta-analyses of data on 50,000 individuals. Lancet. 2013;381:1029-1036.
- Donnenfeld M, Deschasaux M, Latino-Martel P, et al. Prospective association between dietary folate intake and skin cancer risk: results from the Supplémentation en Vitamines et Minéraux Antioxydants cohort. Am J Clin Nutr. 2015;102:471-478.
- Fung TT, Hunter DJ, Spiegelman D, et al. Vitamins and carotenoids intake and the risk of basal cell carcinoma of the skin in women (United States). Cancer Causes Control. 2002;13:221-230.
- Fung TT, Spiegelman D, Egan KM, et al. Vitamin and carotenoid intake and risk of squamous cell carcinoma of the skin. Int J Cancer. 2003;103:110-115.
- National Institutes of Health Office of Dietary Supplements. Vitamin C: fact sheet for health professionals. Updated March 26, 2021. Accessed November 14, 2022. https://ods.od.nih.gov/factsheets/VitaminC-HealthProfessional/
- Spoelstra-de Man AME, Elbers PWG, Oudemans-Van Straaten HM. Vitamin C: should we supplement? Curr Opin Crit Care. 2018;24:248-255.
- Moison RMW, Beijersbergen van Henegouwen GMJ. Topical antioxidant vitamins C and E prevent UVB-radiation-induced peroxidation of eicosapentaenoic acid in pig skin. Radiat Res. 2002;157:402-409.
- Lin JY, Selim MA, Shea CR, et al. UV photoprotection by combination topical antioxidants vitamin C and vitamin E. J Am Acad Dermatol. 2003;48:866-874.
- Pauling L, Willoughby R, Reynolds R, et al. Incidence of squamous cell carcinoma in hairless mice irradiated with ultraviolet light in relation to intake of ascorbic acid (vitamin C) and of D, L-alpha-tocopheryl acetate (vitamin E). Int J Vitam Nutr Res Suppl. 1982;23:53-82.
- Kune GA, Bannerman S, Field B, et al. Diet, alcohol, smoking, serum beta-carotene, and vitamin A in male nonmelanocytic skin cancer patients and controls. Nutr Cancer. 1992;18:237-244.
- Vural P, Canbaz M, Selçuki D. Plasma antioxidant defense in actinic keratosis and basal cell carcinoma. J Eur Acad Dermatol Venereol. 1999;13:96-101.
- Record IR, Dreosti IE, McInerney JK. Changes in plasma antioxidant status following consumption of diets high or low in fruit and vegetables or following dietary supplementation with an antioxidant mixture. Br J Nutr. 2001;85:459-464.
- Heinen MM, Hughes MC, Ibiebele TI, et al. Intake of antioxidant nutrients and the risk of skin cancer. Eur J Cancer. 2007;43:2707-2716.
- Yang G, Yan Y, Ma Y, et al. Vitamin C at high concentrations induces cytotoxicity in malignant melanoma but promotes tumor growth at low concentrations. Mol Carcinog. 2017;56:1965-1976.
- National Institutes of Health Office of Dietary Supplements. Vitamin D: fact sheet for health professionals. Updated August 12, 2022. Accessed November 14, 2022. https://ods.od.nih.gov/factsheets/VitaminD-HealthProfessional/
- Reichrath J, Saternus R, Vogt T. Endocrine actions of vitamin D in skin: relevance for photocarcinogenesis of non-melanoma skin cancer, and beyond. Mol Cell Endocrinol. 2017;453:96-102.
- Ellison TI, Smith MK, Gilliam AC, et al. Inactivation of the vitamin D receptor enhances susceptibility of murine skin to UV-induced tumorigenesis. J Invest Dermatol. 2008;128:2508-2517.
- Eide MJ, Johnson DA, Jacobsen GR, et al. Vitamin D and nonmelanoma skin cancer in a health maintenance organization cohort. Arch Dermatol. 2011;147:1379-1384.
- van der Pols JC, Russell A, Bauer U, et al. Vitamin D status and skin cancer risk independent of time outdoors: 11-year prospective study in an Australian community. J Invest Dermatol. 2013;133:637-641.
- Caini S, Gnagnarella P, Stanganelli I, et al. Vitamin D and the risk of non-melanoma skin cancer: a systematic literature review and meta-analysis on behalf of the Italian Melanoma Intergroup. Cancers (Basel). 2021;13:4815.
- Park SM, Li T, Wu S, et al. Vitamin D intake and risk of skin cancer in US women and men. PLoS One. 2016;11:e0160308.
- Afzal S, Nordestgaard BG, Bojesen SE. Plasma 25-hydroxyvitamin D and risk of non-melanoma and melanoma skin cancer: a prospective cohort study. J Invest Dermatol. 2013;133:629-636.
- Asgari MM, Tang J, Warton ME, et al. Association of prediagnostic serum vitamin D levels with the development of basal cell carcinoma. J Invest Dermatol. 2010;130:1438-1443.
- Tang JY, Parimi N, Wu A, et al. Inverse association between serum 25(OH) vitamin D levels and non-melanoma skin cancer in elderly men. Cancer Causes Control. 2010;21:387-391.
- Keen MA, Hassan I. Vitamin E in dermatology. Indian Dermatol Online J. 2016;7:311-315.
- National Institutes of Health Office of Dietary Supplements. Vitamin E: fact sheet for health professionals. Updated March 26, 2021. Accessed November 14, 2022. https://ods.od.nih.gov/factsheets/VitaminE-HealthProfessional/
- Pearson P, Lewis SA, Britton J, et al. The pro-oxidant activity of high-dose vitamin E supplements in vivo. BioDrugs. 2006;20:271-273.
- Gerrish KE, Gensler HL. Prevention of photocarcinogenesis by dietary vitamin E. Nutr Cancer. 1993;19:125-133.
- McVean M, Liebler DC. Prevention of DNA photodamage by vitamin E compounds and sunscreens: roles of ultraviolet absorbance and cellular uptake. Mol Carcinog. 1999;24:169-176.
- Prasad KN, Cohrs RJ, Sharma OK. Decreased expressions of c-myc and H-ras oncogenes in vitamin E succinate induced morphologically differentiated murine B-16 melanoma cells in culture. Biochem Cell Biol. 1990;68:1250-1255.
- Funasaka Y, Komoto M, Ichihashi M. Depigmenting effect of alpha-tocopheryl ferulate on normal human melanocytes. Pigment Cell Res. 2000;13(suppl 8):170-174.
- National Institutes of Health Office of Dietary Supplements. Selenium: fact sheet for health professionals. Updated March 26, 2021. Accessed November 14, 2022. https://ods.od.nih.gov/factsheets/Selenium-HealthProfessional/
- Sengupta A, Lichti UF, Carlson BA, et al. Selenoproteins are essential for proper keratinocyte function and skin development. PLoS One. 2010;5:e12249.
- Das RK, Hossain SKU, Bhattacharya S. Diphenylmethyl selenocyanate inhibits DMBA-croton oil induced two-stage mouse skin carcinogenesis by inducing apoptosis and inhibiting cutaneous cell proliferation. Cancer Lett. 2005;230:90-101.
- Clark LC, Combs GF Jr, Turnbull BW, et al. Effects of selenium supplementation for cancer prevention in patients with carcinoma of the skin. A randomized controlled trial. Nutritional Prevention of Cancer Study Group. JAMA. 1996;276:1957-1963.
- Duffield-Lillico AJ, Slate EH, Reid ME, et al. Selenium supplementation and secondary prevention of nonmelanoma skin cancer in a randomized trial. J Natl Cancer Inst. 2003;95:1477-1481.
- Reid ME, Duffield-Lillico AJ, Slate E, et al. The nutritional prevention of cancer: 400 mcg per day selenium treatment. Nutr Cancer. 2008;60:155-163.
- Vinceti M, Filippini T, Del Giovane C, et al. Selenium for preventing cancer. Cochrane Database Syst Rev. 2018;1:CD005195.
- Hercberg S, Ezzedine K, Guinot C, et al. Antioxidant supplementation increases the risk of skin cancers in women but not in men. J Nutr. 2007;137:2098-2105.
- Chang YJ, Myung SK, Chung ST, et al. Effects of vitamin treatment or supplements with purported antioxidant properties on skin cancer prevention: a meta-analysis of randomized controlled trials. Dermatology. 2011;223:36-44.
- Sun W, Rice MS, Park MK, et al. Intake of furocoumarins and risk of skin cancer in 2 prospective US cohort studies. J Nutr. 2020;150:1535-1544.
- Sakaki JR, Melough MM, Roberts MB, et al. Citrus consumption and the risk of non-melanoma skin cancer in the Women’s Health Initiative. Cancers (Basel). 2021;13:2173.
Nonmelanoma skin cancer (NMSC) is the most common cancer in the United States, and cutaneous melanoma is projected to be the fifth most common form of cancer in 2022, with increasing incidence and high potential for mortality.1-3 Estimates indicate that 35% to 45% of all cancers in White patients are cutaneous, with 4% to 5% occurring in Hispanic patients, 2% to 4% in Asian patients, and 1% to 2% in Black patients.4 Of the keratinocyte carcinomas, basal cell carcinoma (BCC) is the most prevalent, projected to affect approximately 33% to 39% of White males and 23% to 28% of White females in the United States during their lifetimes. Squamous cell carcinoma (SCC) is the second most common skin malignancy, with a lifetime risk of 9% to 14% for White males and 4% to 9% for White females in the United States.5 The incidence of melanoma continues to increase, with approximately 99,780 new cases expected in the United States in 2022.1
UV-induced DNA damage plays a key role in the pathogenesis and development of various skin malignancies.6 UV radiation from sunlight or tanning devices causes photocarcinogenesis due to molecular and cellular effects, including the generation of reactive oxygen species, DNA damage due to the formation of cyclobutane pyrimidine dimers and pyrimidine-pyrimidone, melanogenesis, apoptosis, and the increased expression of harmful genes and proteins.6 The summation of this damage can result in skin malignancies, including NMSC and melanoma.6,7 Dietary antioxidants theoretically help prevent oxidative reactions from occurring within the body, and it has been suggested that intake of dietary antioxidants may decrease DNA damage and prevent tumorigenesis secondary to UV radiation.8 Antioxidants exist naturally in the body but can be acquired exogenously. Investigators have studied dietary antioxidants in preventing skin cancer formation with promising results in the laboratory setting.8-11 Recently, more robust human studies have been initiated to further delineate this relationship. We present clinical evidence of several frequently utilized antioxidant vitamins and their effects on melanoma and NMSC.
Antioxidants
Vitamin A—Vitamin A is a fat-soluble vitamin found in animal sources, including fish, liver, and eggs. Carotenoids, such as beta carotene, are provitamin A plant derivatives found in fruits and vegetables that are converted into biologically active retinol and retinoic acid.12 Retinols play a key role in cellular growth and differentiation and are thought to be protective against skin cancer via the inactivation of free radicals and immunologic enhancement due to their antiproliferative, antioxidative, and antiapoptotic effects.13-16 Animal studies have demonstrated this protective effect and the ability of retinoids to suppress carcinogenesis; however, human studies reveal conflicting results.17,18
Greenberg et al19 investigated the use of beta carotene in preventing the formation of NMSC. Patients (N=1805) were randomized to receive 50 mg of beta carotene daily or placebo. Over a 5-year period, there was no significant reduction in the occurrence of NMSC (relative risk [RR], 1.05; 95% CI, 0.91-1.22).19 Frieling et al20 conducted a similar randomized, double-blind, placebo-controlled trial investigating beta carotene for primary prevention of NMSC in 22,071 healthy male physicians. The study group received 50 mg of beta carotene every other day for 12 years’ duration, and there was no significant effect on the incidence of first NMSC development (RR, 0.98; 95% CI, 0.92-1.05).20
A case-control study by Naldi et al21 found an inverse association between vitamin A intake and development of melanoma. Study participants were stratified into quartiles based on level of dietary intake and found an odds ratio (OR) of 0.71 for beta carotene (95% CI, 0.50-1.02), 0.57 for retinol (95% CI, 0.39-0.83), and 0.51 for total vitamin A (95% CI, 0.35-0.75) when comparing the upper quartile of vitamin A intake to the lower quartile. Upper-quartile cutoff values of vitamin A intake were 214 µg/d for beta carotene, 149 µg/d for retinol, and 359 µg/d for total vitamin A.21 More recently, a meta-analysis by Zhang et al22 pooled data from 8 case-control studies and 2 prospective studies. Intake of retinol but not total vitamin A or beta carotene was associated with a reduced risk for development of melanoma (retinol: OR, 0.80; 95% CI, 0.69-0.92; total vitamin A: OR, 0.86; 95% CI, 0.59-1.25; beta carotene: OR, 0.87; 95% CI, 0.62-1.20).22 Feskanich et al23 demonstrated similar findings with use of food-frequency questionnaires in White women, suggesting that retinol intake from food combined with supplements may be protective for women who were otherwise at a low risk for melanoma based on nondietary factors. These factors included painful or blistering sunburns during childhood, history of more than 6 sunburns, more than 3 moles on the left arm, having red or blonde hair, and having a parent or sibling with melanoma (P=.01). However, this relationship did not hold true when looking at women at an intermediate or high risk for melanoma (P=.16 and P=.46).23
When looking at high-risk patients, such as transplant patients, oral retinoids have been beneficial in preventing NMSC.24-27 Bavinck et al24 investigated 44 renal transplant patients with a history of more than 10 NMSCs treated with 30 mg of acitretin daily vs placebo. Patients receiving oral retinoid supplementation developed fewer NMSCs over a 6-month treatment period (P=.01).24 Similarly, George et al25 investigated acitretin in renal transplant patients and found a statistically significant decrease in number of SCCs in patients on supplementation (P=.002). Solomon-Cohen et al26 performed a retrospective case-crossover study in solid organ transplant recipients and found that those treated with 10 mg of acitretin daily for 2 years had a significant reduction in the number of new keratinocyte carcinomas (P=.002). Other investigators have demonstrated similar results, and in 2006, Otley et al27 proposed standardized dosing of acitretin for chemoprevention in high-risk patients, including patients developing 5 to 10 NMSCs per year, solid organ transplant recipients, and those with syndromes associated with the development of NMSC.28,29 Overall, in the general population, vitamin A and related compounds have not demonstrated a significant association with decreased development of NMSC; however, oral retinoids have proven useful for high-risk patients. Furthermore, several studies have suggested a negative association between vitamin A levels and the incidence of melanoma, specifically in the retinol formulation.
Vitamin B3—Nicotinamide (also known as niacinamide) is a water-soluble form of vitamin B3 and is obtained from animal-based and plant-based foods, such as meat, fish, and legumes.30 Nicotinamide plays a key role in cellular metabolism, cellular signaling, and DNA repair, including protection from UV damage within keratinocytes.31,32 Early mouse models demonstrated decreased formation of skin tumors in mice treated with topical or oral nicotinamide.32,33 A number of human studies have revealed similar results.34-36
Chen et al34 conducted the ONTRAC study, a phase 3, double-blind, randomized controlled trial (RCT) looking at 386 participants with a history of at least 2 NMSCs in the preceding 5 years. At 12 months, those treated with 500 mg of nicotinamide twice daily demonstrated a statistically significant decreased rate of SCC formation (P=.05). A decreased incidence of BCC development was noted; however, this trend did not reach statistical significance (P=.12). Precancerous skin lesions also were found to be decreased in the treatment group, with 20% lower incidence of actinic keratoses (AKs) after 9 months of treatment (P<.001).34 Drago et al35 specifically studied the incidence of AKs in 38 transplant recipients—8 liver and 30 kidney—and found that previously noted AKs had decreased in size for 18 of 19 patients taking 500 mg of nicotinamide daily when originally photographed AKs were remeasured at 6-month follow-up, with 7 of these 18 patients demonstrating complete clinical regression. Of those on nicotinamide supplementation, no new AKs developed compared to the control group, which demonstrated increased size of AKs or development of new AKs in 91% of patients, with 7 AKs progressing into SCC.35
Nicotinamide has been demonstrated to be useful in preventing skin cancer in high-risk populations, such as transplant patients or those with a high incidence of NMSC.34,36 Despite promising results within the laboratory setting, nicotinamide’s effects on melanoma in humans remains less clear.31,37 Studies suggest that nicotinamide enhances tumor-infiltrating lymphocytes and DNA repair mechanisms in melanocytes, which may translate into nicotinamide, providing chemoprevention for melanoma, but research in human patients is limited.31,37
Vitamin B9—Folate, the natural form of vitamin B9, is a water-soluble compound that is found in many foods, especially green leafy vegetables, and often is supplemented because of its health benefits.38,39 In the skin, folic acid plays a key role in cellular replication and proliferation.38 Controversy exists regarding folate’s effects on cellular growth and turnover with respect to cancer incidence.38,40 Donnenfeld et al41 conducted a prospective study assessing dietary folic acid intake and development of NMSC. A total of 5880 participants completed dietary records throughout the first 2 years of the study. After an average follow-up period of 12.6 years, there was an overall increased incidence of skin cancer in those with increased dietary folate (P=.03). Furthermore, when striating by skin cancer type, there was an increased incidence of NMSC overall as well as BCC when analyzing by type of NMSC (P=.03 for NMSC; P=.05 for BCC). However, when stratifying by gender, these findings only held true for women.41 Similar effects were observed by Fung et al,42 who prospectively studied the intake of various vitamins in relationship to the development of BCC in women. During 12 years of follow-up, a positive association was observed between folate intake and BCC development (OR, 1.2; 95% CI, 1.10-1.31).42 Fung et al43 also investigated the role of several vitamins in the development of SCC and found that folate showed a negative association, which did not reach statistical significance (RR, 0.79; 95% CI, 0.56-1.11). Furthermore, Vollset et al40 conducted a meta-analysis comparing folic acid to placebo in the incidence of various types of cancer. The study excluded NMSC but reported no significant association between the development of melanoma and folic acid supplementation.40 In summary, the effects of folate have diverse consequences, potentially promoting the formation of NMSC, but studies suggest that an individual’s gender and other genetic and environmental factors also may play a role.
Vitamin C—Vitamin C (also known as ascorbic acid) is a water-soluble vitamin with antioxidant immune-mediating effects. It is found in various fruits and vegetables and serves as a cofactor for enzymes within the body playing a key role in immune function and collagen formation.44,45 It has been postulated that ascorbic acid can provide protection from UV radiation damage via its intracellular activity but conversely can contribute to oxidative damage.44 Multiple in vitro laboratory studies and animal models have demonstrated photoprotective effects of ascorbic acid.46-48 Despite these findings, minimal photoprotective effects have been found in the human population.
Kune et al49 performed a case-control study of 88 males with previously diagnosed NMSC undergoing surgical removal and investigated patients’ prior dietary habits. Patients with NMSC had a statistically significantly lower level of vitamin C–containing food in their diet than those without NMSC (P=.004).49 In addition, Vural et al50 analyzed plasma samples and blood cells of patients with AK and BCC and found a significant decrease in ascorbic acid levels in both the AK (P<.001) and BCC (P<.001) groups compared with controls. However, studies have found that consumption of certain dietary compounds can rapidly increase plasma concentration levels, which may serve as a major confounding variable in this study. Plasma concentrations of ascorbic acid and beta carotene were found to be significantly increased following consumption of a high-antioxidant diet for as short a duration as 2 weeks (P<.05).51 More recently, Heinen et al52 performed a prospective study on 1001 adults. In patients without a history of skin cancer, they found that vitamin C from food sources plus dietary supplements was positively associated with the development of BCC (P=.03).52 Similarly, Fung et al42 performed a study in women and found a positive association between vitamin C intake and the development of BCC (OR, 1.13; 95% CI, 1.03-1.23).
The relationship between vitamin C intake—either in dietary or supplemental form—and melanoma remains controversial. Mice-based studies found that high concentrations of orally administered vitamin C induce cytotoxicity in melanoma cell lines, but at low concentrations they promote tumor growth of malignant melanoma.53 Feskanich et al23 examined the relationship between vitamin C intake and melanoma development via food frequency questionnaires in White women and found that vitamin C was associated with a higher risk for melanoma (P=.05), and furthermore, a positive dose response with frequency of orange juice intake was observed (P=.008). Overall, despite promising laboratory studies, there is a lack of RCTs investigating the use of vitamin C supplementation for prevention of NMSC and melanoma in humans, and the oral benefits of vitamin C for chemoprevention remain unclear.
Vitamin D—Vitamin D is a fat-soluble vitamin that is found in fish, liver, egg, and cheese, and is endogenously produced when UV radiation from sun exposure interacts with the skin, triggering the synthesis of vitamin D.54 Vitamin D is biologically inactive and must be converted to its active form 1,25-dihydroxyvitamin D after entering the body. Vitamin D modulates many genes involved in cellular proliferation and differentiation.54 Vitamin D receptors are expressed on keratinocytes and melanocytes.55 Animal studies have demonstrated a potentially protective effect of vitamin D in the development of NMSC.56 In a mouse model, Ellison et al56 found that mice without vitamin D receptors developed skin tumors more rapidly than those with vitamin D receptors.
Unfortunately, these findings have not been demonstrated in humans, and studies have even reported an increased risk for development of NMSC in patients with normal or increased vitamin D levels compared with those with low levels of vitamin D.57-60 Eide et al57 studied 3223 patients seeking advice for low bone density by recording their vitamin D levels at the time of presentation and monitoring development of NMSC. Vitamin D levels greater than 15 ng/mL were positively associated with the development of NMSC (OR, 1.7; 95% CI, 1.04-2.7). This association held true for both SCC and BCC, with a higher risk estimated for SCC (OR, 3.2; 95% CI, 0.4-24.0 for SCC; OR, 1.7; 95% CI, 0.5-5.8 for BCC).57 An increased vitamin D serum level also was found to be significantly associated with a higher risk for BCC and melanoma by van der Pols et al.58 This prospective study looked at the incidence of skin cancer over 11 years. Study participants with vitamin D levels over 75 nmol/L more frequently developed BCC (P=.01) and melanoma (P=.05). In contrast, SCC was less frequently observed in participants with these high levels of vitamin D (P=.07).58 Furthermore, Park et al60 looked at vitamin D and skin cancer risk for men and women in the United States and found no association with risk for SCC or melanoma but a positive association with BCC (P=.05 for total vitamin D; P<.01 for dietary vitamin D). Additional studies have been performed with inconsistent results, and multiple authors suggest the possible confounding relationship between vitamin D levels and UV radiation exposure.59-62 Furthermore, some studies have even demonstrated a negative association between vitamin D and NMSC. Tang et al63 performed a retrospective case-control study in elderly males, investigating serum levels of vitamin D and patients’ self-reported history of NMSC, which demonstrated that higher levels of vitamin D were associated with a decreased risk for NMSC. Overall, the relationship between vitamin D and skin cancer development remains unclear for both melanoma and NMSC.
Vitamin E—Vitamin E is a fat-soluble vitamin that is found in plant-based oils, nuts, seeds, fruits, and vegetables.64 It works as an antioxidant to protect against free radicals and heighten immune function, and it also serves as a pro-oxidant.65,66 Vitamin E naturally exists in 8 chemical forms, of which gamma-tocopherol is the most frequently obtained form in the diet, and alpha-tocopherol is the most abundant form found in the body.64,65
Early animal studies demonstrated the inhibition of UV-induced damage in mice receiving vitamin E supplementation.67,68 Human studies have not consistently shown these effects. Vural et al50 investigated plasma samples and blood cells of patients with AKs and BCCs and reported a significant decrease in alpha-tocopherol levels in both the AK (P<.05) and BCC (P<.001) groups compared with controls. However, studies also have demonstrated a positive association between vitamin E intake and the development of BCC, including one by Fung et al,42 which found a significant association in women (OR, 1.15; 95% CI, 1.06-1.26).
Vitamin E has been found to inhibit melanin synthesis in the laboratory, suggesting a potentially protective effect in melanoma.69,70 However, in the study performed by Feskanich et al23 examining vitamin intake and melanoma incidence via food-frequency questionnaires, vitamin E was not associated with a lower risk for melanoma. Despite promising laboratory studies, the data surrounding the use of a vitamin E supplement for prevention of melanoma and NMSC in humans remains unclear.
Selenium—Selenium is a trace mineral found in plants, meat, and fish. It plays a key role in reproduction, hormone metabolism, DNA synthesis, and protection from oxidative damage.71 In mice studies, lack of selenium-containing proteins resulted in skin abnormalities, including the development of a hyperplastic epidermis and aberrant hair follicle morphogenesis with alopecia after birth, and numerous experimental studies have demonstrated a negative association between selenium intake and cancer.72,73 However, human studies have yielded alternative results.
The Nutritional Prevention of Cancer Study Group analyzed 1312 dermatology patients with a history of NMSC.74 The study population was obtained from 7 dermatology clinics with randomization to control for confounding variables. Study participants received either 200 μg of selenium daily or placebo.74 Baseline characteristics of each study group were overall balanced. Selenium intake was found to have no effect on the development of BCC (hazard ratio [HR], 1.09; 95% CI, 0.94-1.26) but an increased risk for developing SCC (HR, 1.25; 95% CI, 1.03-1.51) and total NMSC (HR, 1.17; 95% CI, 1.02-1.34).74,75 Similarly, Reid et al76 performed an RCT comparing patients treated with 400 μg/d of selenium to those treated with 200 μg/d of selenium. When compared with placebo, those treated with 200 μg/d of selenium had a statistically significantly increased incidence of NMSC (P=.006); however, those treated with 400 μg/d of selenium had no significant change in total incidence of NMSC (P=.51).76 Furthermore, Vinceti et al77 performed a review of 83 studies from the literature investigating the effect of dietary selenium, and from the RCTs, there was no beneficial effect of selenium in reducing cancer risk in general; however, some studies demonstrated an increased incidence of other types of cancer, including melanoma. Of the RCTs included in the study investigating NMSC incidence specifically, it was found that the incidence was not affected by selenium administration (RR, 1.16; 95% CI, 0.30-4.42; 2 studies, 2027 participants).77 Despite data from several studies demonstrating an increased risk for NMSC, the effects of selenium on the risk for NMSC and melanoma remain unclear.
Combination Antioxidant Studies
In addition to investigating the use of single antioxidants in skin cancer prevention, studies utilizing the combination of various antioxidants or other dietary minerals have been conducted. Hercberg et al78 performed a randomized, double-blinded, placebo-controlled trial of 13,017 adults (7876 women and 5141 men) receiving a combination of 120 mg vitamin C, 30 mg vitamin E, 100 μg selenium, 6 mg beta carotene, and 20 mg zinc. Study participants were followed for an average of 7.5 years, and the development of skin cancers were recorded. Overall, the incidence rate of skin cancer did not differ between the 2 treatment groups; however, when segregated by gender, the study found that there was an increased risk for developing skin cancer in women taking the antioxidant supplement combination compared with placebo (P=.03). This difference was not observed in the 2 treatment groups of male patients (P=.11). When looking specifically at NMSC, there was no difference between treatment groups for male or female patients (P=.39 for males; P=.15 for females). In contrast, there was a higher incidence of melanoma identified in female patients taking the combination antioxidant supplement (P=.01), but this was not seen within the male study population (P=.51).78 In addition, Chang et al79 performed a meta-analysis of 10 previously published RCTs. Analysis revealed that treatment with a variety of supplements, including vitamins A, C, E, and beta carotene, were found to have no preventative effects on the incidence of skin cancer development (RR, 0.98; CI, 0.98-1.03). Notable limitations to this study included the variability in protocols of the studies included in this meta-analysis, the limited number of RCTs investigating vitamin supplementation and the risk for skin cancer development, and the influence of dietary intake on study outcomes.79
Other Dietary Agents
Furocoumarins—Furocoumarins are botanical substances found in various fruits and plants, including many citrus products. Furocoumarins are activated by UV light radiation and can lead to development of a phototoxic eruption. Several studies have suggested a pharmacogenetic effect of furocoumarins.80 Sun et al80 collected dietary data from 47,453 men and 75,291 women on furocoumarin intake and correlation with the development of NMSC. Overall, the study suggested that the intake of furocoumarins may lead to an increase in the development of BCC (HR, 1.16; 95% CI, 1.11-1.21; P=.002); however, there was no significant association identified between total intake of furocoumarins in the risk for SCC or melanoma.80 Furthermore, Sakaki et al81 conducted a survey study looking at the consumption of citrus products and the development of NMSC. The group found that there was an increased risk for NMSC in those consuming an increased amount of citrus products (P=.007).81
Conclusion
Dietary antioxidants have been investigated for their potential role in the prevention of tumorigenesis. Specific antioxidant vitamins, such as vitamin A derivatives and niacinamide, have demonstrated clinical utility in the prevention of NMSC in high-risk populations. Retinol also has been associated with a reduced incidence of melanoma. Numerous antioxidants have demonstrated promising data within the laboratory setting; however, inconsistent results have been appreciated in humans. Furthermore, several research studies suggest that folate, vitamin D, and furocoumarins may be associated with an increased risk for skin cancer development; however, these studies are inconclusive, and dietary studies are challenging to conduct. Overall, RCTs investigating the role of antioxidants for chemoprevention are limited. Moreover, the study of dietary antioxidants and vitamins may be affected by various confounding variables that can be difficult to account for because of patients’ potentially poor recall of dietary intake and the effect of dietary intake in supplemental studies. Given the increasing prevalence of skin cancer worldwide, further research into the clinical utility of antioxidants in skin cancer prevention is warranted.
Nonmelanoma skin cancer (NMSC) is the most common cancer in the United States, and cutaneous melanoma is projected to be the fifth most common form of cancer in 2022, with increasing incidence and high potential for mortality.1-3 Estimates indicate that 35% to 45% of all cancers in White patients are cutaneous, with 4% to 5% occurring in Hispanic patients, 2% to 4% in Asian patients, and 1% to 2% in Black patients.4 Of the keratinocyte carcinomas, basal cell carcinoma (BCC) is the most prevalent, projected to affect approximately 33% to 39% of White males and 23% to 28% of White females in the United States during their lifetimes. Squamous cell carcinoma (SCC) is the second most common skin malignancy, with a lifetime risk of 9% to 14% for White males and 4% to 9% for White females in the United States.5 The incidence of melanoma continues to increase, with approximately 99,780 new cases expected in the United States in 2022.1
UV-induced DNA damage plays a key role in the pathogenesis and development of various skin malignancies.6 UV radiation from sunlight or tanning devices causes photocarcinogenesis due to molecular and cellular effects, including the generation of reactive oxygen species, DNA damage due to the formation of cyclobutane pyrimidine dimers and pyrimidine-pyrimidone, melanogenesis, apoptosis, and the increased expression of harmful genes and proteins.6 The summation of this damage can result in skin malignancies, including NMSC and melanoma.6,7 Dietary antioxidants theoretically help prevent oxidative reactions from occurring within the body, and it has been suggested that intake of dietary antioxidants may decrease DNA damage and prevent tumorigenesis secondary to UV radiation.8 Antioxidants exist naturally in the body but can be acquired exogenously. Investigators have studied dietary antioxidants in preventing skin cancer formation with promising results in the laboratory setting.8-11 Recently, more robust human studies have been initiated to further delineate this relationship. We present clinical evidence of several frequently utilized antioxidant vitamins and their effects on melanoma and NMSC.
Antioxidants
Vitamin A—Vitamin A is a fat-soluble vitamin found in animal sources, including fish, liver, and eggs. Carotenoids, such as beta carotene, are provitamin A plant derivatives found in fruits and vegetables that are converted into biologically active retinol and retinoic acid.12 Retinols play a key role in cellular growth and differentiation and are thought to be protective against skin cancer via the inactivation of free radicals and immunologic enhancement due to their antiproliferative, antioxidative, and antiapoptotic effects.13-16 Animal studies have demonstrated this protective effect and the ability of retinoids to suppress carcinogenesis; however, human studies reveal conflicting results.17,18
Greenberg et al19 investigated the use of beta carotene in preventing the formation of NMSC. Patients (N=1805) were randomized to receive 50 mg of beta carotene daily or placebo. Over a 5-year period, there was no significant reduction in the occurrence of NMSC (relative risk [RR], 1.05; 95% CI, 0.91-1.22).19 Frieling et al20 conducted a similar randomized, double-blind, placebo-controlled trial investigating beta carotene for primary prevention of NMSC in 22,071 healthy male physicians. The study group received 50 mg of beta carotene every other day for 12 years’ duration, and there was no significant effect on the incidence of first NMSC development (RR, 0.98; 95% CI, 0.92-1.05).20
A case-control study by Naldi et al21 found an inverse association between vitamin A intake and development of melanoma. Study participants were stratified into quartiles based on level of dietary intake and found an odds ratio (OR) of 0.71 for beta carotene (95% CI, 0.50-1.02), 0.57 for retinol (95% CI, 0.39-0.83), and 0.51 for total vitamin A (95% CI, 0.35-0.75) when comparing the upper quartile of vitamin A intake to the lower quartile. Upper-quartile cutoff values of vitamin A intake were 214 µg/d for beta carotene, 149 µg/d for retinol, and 359 µg/d for total vitamin A.21 More recently, a meta-analysis by Zhang et al22 pooled data from 8 case-control studies and 2 prospective studies. Intake of retinol but not total vitamin A or beta carotene was associated with a reduced risk for development of melanoma (retinol: OR, 0.80; 95% CI, 0.69-0.92; total vitamin A: OR, 0.86; 95% CI, 0.59-1.25; beta carotene: OR, 0.87; 95% CI, 0.62-1.20).22 Feskanich et al23 demonstrated similar findings with use of food-frequency questionnaires in White women, suggesting that retinol intake from food combined with supplements may be protective for women who were otherwise at a low risk for melanoma based on nondietary factors. These factors included painful or blistering sunburns during childhood, history of more than 6 sunburns, more than 3 moles on the left arm, having red or blonde hair, and having a parent or sibling with melanoma (P=.01). However, this relationship did not hold true when looking at women at an intermediate or high risk for melanoma (P=.16 and P=.46).23
When looking at high-risk patients, such as transplant patients, oral retinoids have been beneficial in preventing NMSC.24-27 Bavinck et al24 investigated 44 renal transplant patients with a history of more than 10 NMSCs treated with 30 mg of acitretin daily vs placebo. Patients receiving oral retinoid supplementation developed fewer NMSCs over a 6-month treatment period (P=.01).24 Similarly, George et al25 investigated acitretin in renal transplant patients and found a statistically significant decrease in number of SCCs in patients on supplementation (P=.002). Solomon-Cohen et al26 performed a retrospective case-crossover study in solid organ transplant recipients and found that those treated with 10 mg of acitretin daily for 2 years had a significant reduction in the number of new keratinocyte carcinomas (P=.002). Other investigators have demonstrated similar results, and in 2006, Otley et al27 proposed standardized dosing of acitretin for chemoprevention in high-risk patients, including patients developing 5 to 10 NMSCs per year, solid organ transplant recipients, and those with syndromes associated with the development of NMSC.28,29 Overall, in the general population, vitamin A and related compounds have not demonstrated a significant association with decreased development of NMSC; however, oral retinoids have proven useful for high-risk patients. Furthermore, several studies have suggested a negative association between vitamin A levels and the incidence of melanoma, specifically in the retinol formulation.
Vitamin B3—Nicotinamide (also known as niacinamide) is a water-soluble form of vitamin B3 and is obtained from animal-based and plant-based foods, such as meat, fish, and legumes.30 Nicotinamide plays a key role in cellular metabolism, cellular signaling, and DNA repair, including protection from UV damage within keratinocytes.31,32 Early mouse models demonstrated decreased formation of skin tumors in mice treated with topical or oral nicotinamide.32,33 A number of human studies have revealed similar results.34-36
Chen et al34 conducted the ONTRAC study, a phase 3, double-blind, randomized controlled trial (RCT) looking at 386 participants with a history of at least 2 NMSCs in the preceding 5 years. At 12 months, those treated with 500 mg of nicotinamide twice daily demonstrated a statistically significant decreased rate of SCC formation (P=.05). A decreased incidence of BCC development was noted; however, this trend did not reach statistical significance (P=.12). Precancerous skin lesions also were found to be decreased in the treatment group, with 20% lower incidence of actinic keratoses (AKs) after 9 months of treatment (P<.001).34 Drago et al35 specifically studied the incidence of AKs in 38 transplant recipients—8 liver and 30 kidney—and found that previously noted AKs had decreased in size for 18 of 19 patients taking 500 mg of nicotinamide daily when originally photographed AKs were remeasured at 6-month follow-up, with 7 of these 18 patients demonstrating complete clinical regression. Of those on nicotinamide supplementation, no new AKs developed compared to the control group, which demonstrated increased size of AKs or development of new AKs in 91% of patients, with 7 AKs progressing into SCC.35
Nicotinamide has been demonstrated to be useful in preventing skin cancer in high-risk populations, such as transplant patients or those with a high incidence of NMSC.34,36 Despite promising results within the laboratory setting, nicotinamide’s effects on melanoma in humans remains less clear.31,37 Studies suggest that nicotinamide enhances tumor-infiltrating lymphocytes and DNA repair mechanisms in melanocytes, which may translate into nicotinamide, providing chemoprevention for melanoma, but research in human patients is limited.31,37
Vitamin B9—Folate, the natural form of vitamin B9, is a water-soluble compound that is found in many foods, especially green leafy vegetables, and often is supplemented because of its health benefits.38,39 In the skin, folic acid plays a key role in cellular replication and proliferation.38 Controversy exists regarding folate’s effects on cellular growth and turnover with respect to cancer incidence.38,40 Donnenfeld et al41 conducted a prospective study assessing dietary folic acid intake and development of NMSC. A total of 5880 participants completed dietary records throughout the first 2 years of the study. After an average follow-up period of 12.6 years, there was an overall increased incidence of skin cancer in those with increased dietary folate (P=.03). Furthermore, when striating by skin cancer type, there was an increased incidence of NMSC overall as well as BCC when analyzing by type of NMSC (P=.03 for NMSC; P=.05 for BCC). However, when stratifying by gender, these findings only held true for women.41 Similar effects were observed by Fung et al,42 who prospectively studied the intake of various vitamins in relationship to the development of BCC in women. During 12 years of follow-up, a positive association was observed between folate intake and BCC development (OR, 1.2; 95% CI, 1.10-1.31).42 Fung et al43 also investigated the role of several vitamins in the development of SCC and found that folate showed a negative association, which did not reach statistical significance (RR, 0.79; 95% CI, 0.56-1.11). Furthermore, Vollset et al40 conducted a meta-analysis comparing folic acid to placebo in the incidence of various types of cancer. The study excluded NMSC but reported no significant association between the development of melanoma and folic acid supplementation.40 In summary, the effects of folate have diverse consequences, potentially promoting the formation of NMSC, but studies suggest that an individual’s gender and other genetic and environmental factors also may play a role.
Vitamin C—Vitamin C (also known as ascorbic acid) is a water-soluble vitamin with antioxidant immune-mediating effects. It is found in various fruits and vegetables and serves as a cofactor for enzymes within the body playing a key role in immune function and collagen formation.44,45 It has been postulated that ascorbic acid can provide protection from UV radiation damage via its intracellular activity but conversely can contribute to oxidative damage.44 Multiple in vitro laboratory studies and animal models have demonstrated photoprotective effects of ascorbic acid.46-48 Despite these findings, minimal photoprotective effects have been found in the human population.
Kune et al49 performed a case-control study of 88 males with previously diagnosed NMSC undergoing surgical removal and investigated patients’ prior dietary habits. Patients with NMSC had a statistically significantly lower level of vitamin C–containing food in their diet than those without NMSC (P=.004).49 In addition, Vural et al50 analyzed plasma samples and blood cells of patients with AK and BCC and found a significant decrease in ascorbic acid levels in both the AK (P<.001) and BCC (P<.001) groups compared with controls. However, studies have found that consumption of certain dietary compounds can rapidly increase plasma concentration levels, which may serve as a major confounding variable in this study. Plasma concentrations of ascorbic acid and beta carotene were found to be significantly increased following consumption of a high-antioxidant diet for as short a duration as 2 weeks (P<.05).51 More recently, Heinen et al52 performed a prospective study on 1001 adults. In patients without a history of skin cancer, they found that vitamin C from food sources plus dietary supplements was positively associated with the development of BCC (P=.03).52 Similarly, Fung et al42 performed a study in women and found a positive association between vitamin C intake and the development of BCC (OR, 1.13; 95% CI, 1.03-1.23).
The relationship between vitamin C intake—either in dietary or supplemental form—and melanoma remains controversial. Mice-based studies found that high concentrations of orally administered vitamin C induce cytotoxicity in melanoma cell lines, but at low concentrations they promote tumor growth of malignant melanoma.53 Feskanich et al23 examined the relationship between vitamin C intake and melanoma development via food frequency questionnaires in White women and found that vitamin C was associated with a higher risk for melanoma (P=.05), and furthermore, a positive dose response with frequency of orange juice intake was observed (P=.008). Overall, despite promising laboratory studies, there is a lack of RCTs investigating the use of vitamin C supplementation for prevention of NMSC and melanoma in humans, and the oral benefits of vitamin C for chemoprevention remain unclear.
Vitamin D—Vitamin D is a fat-soluble vitamin that is found in fish, liver, egg, and cheese, and is endogenously produced when UV radiation from sun exposure interacts with the skin, triggering the synthesis of vitamin D.54 Vitamin D is biologically inactive and must be converted to its active form 1,25-dihydroxyvitamin D after entering the body. Vitamin D modulates many genes involved in cellular proliferation and differentiation.54 Vitamin D receptors are expressed on keratinocytes and melanocytes.55 Animal studies have demonstrated a potentially protective effect of vitamin D in the development of NMSC.56 In a mouse model, Ellison et al56 found that mice without vitamin D receptors developed skin tumors more rapidly than those with vitamin D receptors.
Unfortunately, these findings have not been demonstrated in humans, and studies have even reported an increased risk for development of NMSC in patients with normal or increased vitamin D levels compared with those with low levels of vitamin D.57-60 Eide et al57 studied 3223 patients seeking advice for low bone density by recording their vitamin D levels at the time of presentation and monitoring development of NMSC. Vitamin D levels greater than 15 ng/mL were positively associated with the development of NMSC (OR, 1.7; 95% CI, 1.04-2.7). This association held true for both SCC and BCC, with a higher risk estimated for SCC (OR, 3.2; 95% CI, 0.4-24.0 for SCC; OR, 1.7; 95% CI, 0.5-5.8 for BCC).57 An increased vitamin D serum level also was found to be significantly associated with a higher risk for BCC and melanoma by van der Pols et al.58 This prospective study looked at the incidence of skin cancer over 11 years. Study participants with vitamin D levels over 75 nmol/L more frequently developed BCC (P=.01) and melanoma (P=.05). In contrast, SCC was less frequently observed in participants with these high levels of vitamin D (P=.07).58 Furthermore, Park et al60 looked at vitamin D and skin cancer risk for men and women in the United States and found no association with risk for SCC or melanoma but a positive association with BCC (P=.05 for total vitamin D; P<.01 for dietary vitamin D). Additional studies have been performed with inconsistent results, and multiple authors suggest the possible confounding relationship between vitamin D levels and UV radiation exposure.59-62 Furthermore, some studies have even demonstrated a negative association between vitamin D and NMSC. Tang et al63 performed a retrospective case-control study in elderly males, investigating serum levels of vitamin D and patients’ self-reported history of NMSC, which demonstrated that higher levels of vitamin D were associated with a decreased risk for NMSC. Overall, the relationship between vitamin D and skin cancer development remains unclear for both melanoma and NMSC.
Vitamin E—Vitamin E is a fat-soluble vitamin that is found in plant-based oils, nuts, seeds, fruits, and vegetables.64 It works as an antioxidant to protect against free radicals and heighten immune function, and it also serves as a pro-oxidant.65,66 Vitamin E naturally exists in 8 chemical forms, of which gamma-tocopherol is the most frequently obtained form in the diet, and alpha-tocopherol is the most abundant form found in the body.64,65
Early animal studies demonstrated the inhibition of UV-induced damage in mice receiving vitamin E supplementation.67,68 Human studies have not consistently shown these effects. Vural et al50 investigated plasma samples and blood cells of patients with AKs and BCCs and reported a significant decrease in alpha-tocopherol levels in both the AK (P<.05) and BCC (P<.001) groups compared with controls. However, studies also have demonstrated a positive association between vitamin E intake and the development of BCC, including one by Fung et al,42 which found a significant association in women (OR, 1.15; 95% CI, 1.06-1.26).
Vitamin E has been found to inhibit melanin synthesis in the laboratory, suggesting a potentially protective effect in melanoma.69,70 However, in the study performed by Feskanich et al23 examining vitamin intake and melanoma incidence via food-frequency questionnaires, vitamin E was not associated with a lower risk for melanoma. Despite promising laboratory studies, the data surrounding the use of a vitamin E supplement for prevention of melanoma and NMSC in humans remains unclear.
Selenium—Selenium is a trace mineral found in plants, meat, and fish. It plays a key role in reproduction, hormone metabolism, DNA synthesis, and protection from oxidative damage.71 In mice studies, lack of selenium-containing proteins resulted in skin abnormalities, including the development of a hyperplastic epidermis and aberrant hair follicle morphogenesis with alopecia after birth, and numerous experimental studies have demonstrated a negative association between selenium intake and cancer.72,73 However, human studies have yielded alternative results.
The Nutritional Prevention of Cancer Study Group analyzed 1312 dermatology patients with a history of NMSC.74 The study population was obtained from 7 dermatology clinics with randomization to control for confounding variables. Study participants received either 200 μg of selenium daily or placebo.74 Baseline characteristics of each study group were overall balanced. Selenium intake was found to have no effect on the development of BCC (hazard ratio [HR], 1.09; 95% CI, 0.94-1.26) but an increased risk for developing SCC (HR, 1.25; 95% CI, 1.03-1.51) and total NMSC (HR, 1.17; 95% CI, 1.02-1.34).74,75 Similarly, Reid et al76 performed an RCT comparing patients treated with 400 μg/d of selenium to those treated with 200 μg/d of selenium. When compared with placebo, those treated with 200 μg/d of selenium had a statistically significantly increased incidence of NMSC (P=.006); however, those treated with 400 μg/d of selenium had no significant change in total incidence of NMSC (P=.51).76 Furthermore, Vinceti et al77 performed a review of 83 studies from the literature investigating the effect of dietary selenium, and from the RCTs, there was no beneficial effect of selenium in reducing cancer risk in general; however, some studies demonstrated an increased incidence of other types of cancer, including melanoma. Of the RCTs included in the study investigating NMSC incidence specifically, it was found that the incidence was not affected by selenium administration (RR, 1.16; 95% CI, 0.30-4.42; 2 studies, 2027 participants).77 Despite data from several studies demonstrating an increased risk for NMSC, the effects of selenium on the risk for NMSC and melanoma remain unclear.
Combination Antioxidant Studies
In addition to investigating the use of single antioxidants in skin cancer prevention, studies utilizing the combination of various antioxidants or other dietary minerals have been conducted. Hercberg et al78 performed a randomized, double-blinded, placebo-controlled trial of 13,017 adults (7876 women and 5141 men) receiving a combination of 120 mg vitamin C, 30 mg vitamin E, 100 μg selenium, 6 mg beta carotene, and 20 mg zinc. Study participants were followed for an average of 7.5 years, and the development of skin cancers were recorded. Overall, the incidence rate of skin cancer did not differ between the 2 treatment groups; however, when segregated by gender, the study found that there was an increased risk for developing skin cancer in women taking the antioxidant supplement combination compared with placebo (P=.03). This difference was not observed in the 2 treatment groups of male patients (P=.11). When looking specifically at NMSC, there was no difference between treatment groups for male or female patients (P=.39 for males; P=.15 for females). In contrast, there was a higher incidence of melanoma identified in female patients taking the combination antioxidant supplement (P=.01), but this was not seen within the male study population (P=.51).78 In addition, Chang et al79 performed a meta-analysis of 10 previously published RCTs. Analysis revealed that treatment with a variety of supplements, including vitamins A, C, E, and beta carotene, were found to have no preventative effects on the incidence of skin cancer development (RR, 0.98; CI, 0.98-1.03). Notable limitations to this study included the variability in protocols of the studies included in this meta-analysis, the limited number of RCTs investigating vitamin supplementation and the risk for skin cancer development, and the influence of dietary intake on study outcomes.79
Other Dietary Agents
Furocoumarins—Furocoumarins are botanical substances found in various fruits and plants, including many citrus products. Furocoumarins are activated by UV light radiation and can lead to development of a phototoxic eruption. Several studies have suggested a pharmacogenetic effect of furocoumarins.80 Sun et al80 collected dietary data from 47,453 men and 75,291 women on furocoumarin intake and correlation with the development of NMSC. Overall, the study suggested that the intake of furocoumarins may lead to an increase in the development of BCC (HR, 1.16; 95% CI, 1.11-1.21; P=.002); however, there was no significant association identified between total intake of furocoumarins in the risk for SCC or melanoma.80 Furthermore, Sakaki et al81 conducted a survey study looking at the consumption of citrus products and the development of NMSC. The group found that there was an increased risk for NMSC in those consuming an increased amount of citrus products (P=.007).81
Conclusion
Dietary antioxidants have been investigated for their potential role in the prevention of tumorigenesis. Specific antioxidant vitamins, such as vitamin A derivatives and niacinamide, have demonstrated clinical utility in the prevention of NMSC in high-risk populations. Retinol also has been associated with a reduced incidence of melanoma. Numerous antioxidants have demonstrated promising data within the laboratory setting; however, inconsistent results have been appreciated in humans. Furthermore, several research studies suggest that folate, vitamin D, and furocoumarins may be associated with an increased risk for skin cancer development; however, these studies are inconclusive, and dietary studies are challenging to conduct. Overall, RCTs investigating the role of antioxidants for chemoprevention are limited. Moreover, the study of dietary antioxidants and vitamins may be affected by various confounding variables that can be difficult to account for because of patients’ potentially poor recall of dietary intake and the effect of dietary intake in supplemental studies. Given the increasing prevalence of skin cancer worldwide, further research into the clinical utility of antioxidants in skin cancer prevention is warranted.
- Siegel RL, Miller KD, Fuchs HE, et al. Cancer statistics, 2022. CA Cancer J Clin. 2022;72:7-33.
- Global Burden of Disease Cancer Collaboration; Fitzmaurice C, Abate D, Abbasi N, et al. Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 29 cancer groups, 1990 to 2017: a systematic analysis for the Global Burden of Disease Study. JAMA Oncol. 2019;5:1749-1768.
- Leiter U, Keim U, Garbe C. Epidemiology of skin cancer: update 2019. In: Reichrath J, ed. Sunlight, Vitamin D and Skin Cancer. Springer International Publishing; 2020:123-139.
- Bradford PT. Skin cancer in skin of color. Dermatol Nurs. 2009;21:170-177, 206; quiz 178.
- Miller DL, Weinstock MA. Nonmelanoma skin cancer in the United States: incidence. J Am Acad Dermatol. 1994;30:774-778.
- Young AR, Claveau J, Rossi AB. Ultraviolet radiation and the skin: photobiology and sunscreen photoprotection. J Am Acad Dermatol. 2017;76(3S1):S100-S109.
- Pleasance ED, Cheetham RK, Stephens PJ, et al. A comprehensive catalogue of somatic mutations from a human cancer genome. Nature. 2010;463:191-196.
- Baek J, Lee MG. Oxidative stress and antioxidant strategies in dermatology. Redox Rep. 2016;21:164-169.
- Katta R, Brown DN. Diet and skin cancer: the potential role of dietary antioxidants in nonmelanoma skin cancer prevention. J Skin Cancer. 2015;2015:893149.
- Stoj V, Shahriari N, Shao K, et al. Nutrition and nonmelanoma skin cancers. Clin Dermatol. 2022;40:173-185.
- O’Connor EA, Evans CV, Ivlev I, et al. Vitamin and mineral supplements for the primary prevention of cardiovascular disease and cancer: updated evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2022;327:2334-2347.
- National Institutes of Health Office of Dietary Supplements. Vitamin A and carotenoids. fact sheet for health professionals. Updated June 15, 2022. Accessed November 14, 2022. https://ods.od.nih.gov/factsheets/VitaminA-HealthProfessional/
- Keller KL, Fenske NA. Uses of vitamins A, C, and E and related compounds in dermatology: a review. J Am Acad Dermatol. 1998;39:611-625.
- Wright TI, Spencer JM, Flowers FP. Chemoprevention of nonmelanoma skin cancer. J Am Acad Dermatol. 2006;54:933-946; quiz 947-950.
- Bushue N, Wan YJY. Retinoid pathway and cancer therapeutics. Adv Drug Deliv Rev. 2010;62:1285-1298.
- Stahl W, Sies H. β-Carotene and other carotenoids in protection from sunlight. Am J Clin Nutr. 2012;96:1179S-1184S.
- Bukhari MH, Qureshi SS, Niazi S, et al. Chemotherapeutic/chemopreventive role of retinoids in chemically induced skin carcinogenesis in albino mice. Int J Dermatol. 2007;46:1160-1165.
- Lambert LA, Wamer WG, Wei RR, et al. The protective but nonsynergistic effect of dietary beta-carotene and vitamin E on skin tumorigenesis in Skh mice. Nutr Cancer. 1994;21:1-12.
- Greenberg ER, Baron JA, Stukel TA, et al. A clinical trial of beta carotene to prevent basal-cell and squamous-cell cancers of the skin. The Skin Cancer Prevention Study Group. N Engl J Med. 1990;323:789-795.
- Frieling UM, Schaumberg DA, Kupper TS, et al. A randomized, 12-year primary-prevention trial of beta carotene supplementation for nonmelanoma skin cancer in the physician’s health study. Arch Dermatol. 2000;136:179-184.
- Naldi L, Gallus S, Tavani A, et al; Oncology Study Group of the Italian Group for Epidemiologic Research in Dermatology. Risk of melanoma and vitamin A, coffee and alcohol: a case-control study from Italy. Eur J Cancer Prev. 2004;13:503-508.
- Zhang YP, Chu RX, Liu H. Vitamin A intake and risk of melanoma: a meta-analysis. PloS One. 2014;9:e102527.
- Feskanich D, Willett WC, Hunter DJ, et al. Dietary intakes of vitamins A, C, and E and risk of melanoma in two cohorts of women. Br J Cancer. 2003;88:1381-1387.
- Bavinck JN, Tieben LM, Van der Woude FJ, et al. Prevention of skin cancer and reduction of keratotic skin lesions during acitretin therapy in renal transplant recipients: a double-blind, placebo-controlled study. J Clin Oncol. 1995;13:1933-1938.
- George R, Weightman W, Russ GR, et al. Acitretin for chemoprevention of non-melanoma skin cancers in renal transplant recipients. Australas J Dermatol. 2002;43:269-273.
- Solomon-Cohen E, Reiss-Huss S, Hodak E, et al. Low-dose acitretin for secondary prevention of keratinocyte carcinomas in solid-organ transplant recipients. Dermatology. 2022;238:161-166.
- Otley CC, Stasko T, Tope WD, et al. Chemoprevention of nonmelanoma skin cancer with systemic retinoids: practical dosing and management of adverse effects. Dermatol Surg. 2006;32:562-568.
- Kadakia KC, Barton DL, Loprinzi CL, et al. Randomized controlled trial of acitretin versus placebo in patients at high-risk for basal cell or squamous cell carcinoma of the skin (North Central Cancer Treatment Group Study 969251). Cancer. 2012;118:2128-2137.
- McKenna DB, Murphy GM. Skin cancer chemoprophylaxis in renal transplant recipients: 5 years of experience using low-dose acitretin. Br J Dermatol. 1999;140:656-660.
- National Institutes of Health Office of Dietary Supplements. Niacin: fact sheet for health professionals. Updated August 23, 2022. Accessed November 14, 2022. https://ods.od.nih.gov/factsheets/Niacin-HealthProfessional/
- Malesu R, Martin AJ, Lyons JG, et al. Nicotinamide for skin cancer chemoprevention: effects of nicotinamide on melanoma in vitro and in vivo. Photochem Photobiol Sci. 2020;19:171-179.
- Gensler HL. Prevention of photoimmunosuppression and photocarcinogenesis by topical nicotinamide. Nutr Cancer. 1997;29:157-162.
- Gensler HL, Williams T, Huang AC, et al. Oral niacin prevents photocarcinogenesis and photoimmunosuppression in mice. Nutr Cancer. 1999;34:36-41.
- Chen AC, Martin AJ, Choy B, et al. A phase 3 randomized trial of nicotinamide for skin-cancer chemoprevention. N Engl J Med. 2015;373:1618-1626.
- Drago F, Ciccarese G, Cogorno L, et al. Prevention of non-melanoma skin cancers with nicotinamide in transplant recipients: a case-control study. Eur J Dermatol. 2017;27:382-385.
- Yélamos O, Halpern AC, Weinstock MA. Reply to “A phase II randomized controlled trial of nicotinamide for skin cancer chemoprevention in renal transplant recipients.” Br J Dermatol. 2017;176:551-552.
- Scatozza F, Moschella F, D’Arcangelo D, et al. Nicotinamide inhibits melanoma in vitro and in vivo. J Exp Clin Cancer Res. 2020;39:211.
- National Institutes of Health Office of Dietary Supplements. Folate: fact sheet for health professionals. Updated November 1, 2022. Accessed November 14, 2022. https://ods.od.nih.gov/factsheets/Folate-HealthProfessional/
- Butzbach K, Epe B. Photogenotoxicity of folic acid. Free Radic Biol Med. 2013;65:821-827.
- Vollset SE, Clarke R, Lewington S, et al. Effects of folic acid supplementation on overall and site-specific cancer incidence during the randomised trials: meta-analyses of data on 50,000 individuals. Lancet. 2013;381:1029-1036.
- Donnenfeld M, Deschasaux M, Latino-Martel P, et al. Prospective association between dietary folate intake and skin cancer risk: results from the Supplémentation en Vitamines et Minéraux Antioxydants cohort. Am J Clin Nutr. 2015;102:471-478.
- Fung TT, Hunter DJ, Spiegelman D, et al. Vitamins and carotenoids intake and the risk of basal cell carcinoma of the skin in women (United States). Cancer Causes Control. 2002;13:221-230.
- Fung TT, Spiegelman D, Egan KM, et al. Vitamin and carotenoid intake and risk of squamous cell carcinoma of the skin. Int J Cancer. 2003;103:110-115.
- National Institutes of Health Office of Dietary Supplements. Vitamin C: fact sheet for health professionals. Updated March 26, 2021. Accessed November 14, 2022. https://ods.od.nih.gov/factsheets/VitaminC-HealthProfessional/
- Spoelstra-de Man AME, Elbers PWG, Oudemans-Van Straaten HM. Vitamin C: should we supplement? Curr Opin Crit Care. 2018;24:248-255.
- Moison RMW, Beijersbergen van Henegouwen GMJ. Topical antioxidant vitamins C and E prevent UVB-radiation-induced peroxidation of eicosapentaenoic acid in pig skin. Radiat Res. 2002;157:402-409.
- Lin JY, Selim MA, Shea CR, et al. UV photoprotection by combination topical antioxidants vitamin C and vitamin E. J Am Acad Dermatol. 2003;48:866-874.
- Pauling L, Willoughby R, Reynolds R, et al. Incidence of squamous cell carcinoma in hairless mice irradiated with ultraviolet light in relation to intake of ascorbic acid (vitamin C) and of D, L-alpha-tocopheryl acetate (vitamin E). Int J Vitam Nutr Res Suppl. 1982;23:53-82.
- Kune GA, Bannerman S, Field B, et al. Diet, alcohol, smoking, serum beta-carotene, and vitamin A in male nonmelanocytic skin cancer patients and controls. Nutr Cancer. 1992;18:237-244.
- Vural P, Canbaz M, Selçuki D. Plasma antioxidant defense in actinic keratosis and basal cell carcinoma. J Eur Acad Dermatol Venereol. 1999;13:96-101.
- Record IR, Dreosti IE, McInerney JK. Changes in plasma antioxidant status following consumption of diets high or low in fruit and vegetables or following dietary supplementation with an antioxidant mixture. Br J Nutr. 2001;85:459-464.
- Heinen MM, Hughes MC, Ibiebele TI, et al. Intake of antioxidant nutrients and the risk of skin cancer. Eur J Cancer. 2007;43:2707-2716.
- Yang G, Yan Y, Ma Y, et al. Vitamin C at high concentrations induces cytotoxicity in malignant melanoma but promotes tumor growth at low concentrations. Mol Carcinog. 2017;56:1965-1976.
- National Institutes of Health Office of Dietary Supplements. Vitamin D: fact sheet for health professionals. Updated August 12, 2022. Accessed November 14, 2022. https://ods.od.nih.gov/factsheets/VitaminD-HealthProfessional/
- Reichrath J, Saternus R, Vogt T. Endocrine actions of vitamin D in skin: relevance for photocarcinogenesis of non-melanoma skin cancer, and beyond. Mol Cell Endocrinol. 2017;453:96-102.
- Ellison TI, Smith MK, Gilliam AC, et al. Inactivation of the vitamin D receptor enhances susceptibility of murine skin to UV-induced tumorigenesis. J Invest Dermatol. 2008;128:2508-2517.
- Eide MJ, Johnson DA, Jacobsen GR, et al. Vitamin D and nonmelanoma skin cancer in a health maintenance organization cohort. Arch Dermatol. 2011;147:1379-1384.
- van der Pols JC, Russell A, Bauer U, et al. Vitamin D status and skin cancer risk independent of time outdoors: 11-year prospective study in an Australian community. J Invest Dermatol. 2013;133:637-641.
- Caini S, Gnagnarella P, Stanganelli I, et al. Vitamin D and the risk of non-melanoma skin cancer: a systematic literature review and meta-analysis on behalf of the Italian Melanoma Intergroup. Cancers (Basel). 2021;13:4815.
- Park SM, Li T, Wu S, et al. Vitamin D intake and risk of skin cancer in US women and men. PLoS One. 2016;11:e0160308.
- Afzal S, Nordestgaard BG, Bojesen SE. Plasma 25-hydroxyvitamin D and risk of non-melanoma and melanoma skin cancer: a prospective cohort study. J Invest Dermatol. 2013;133:629-636.
- Asgari MM, Tang J, Warton ME, et al. Association of prediagnostic serum vitamin D levels with the development of basal cell carcinoma. J Invest Dermatol. 2010;130:1438-1443.
- Tang JY, Parimi N, Wu A, et al. Inverse association between serum 25(OH) vitamin D levels and non-melanoma skin cancer in elderly men. Cancer Causes Control. 2010;21:387-391.
- Keen MA, Hassan I. Vitamin E in dermatology. Indian Dermatol Online J. 2016;7:311-315.
- National Institutes of Health Office of Dietary Supplements. Vitamin E: fact sheet for health professionals. Updated March 26, 2021. Accessed November 14, 2022. https://ods.od.nih.gov/factsheets/VitaminE-HealthProfessional/
- Pearson P, Lewis SA, Britton J, et al. The pro-oxidant activity of high-dose vitamin E supplements in vivo. BioDrugs. 2006;20:271-273.
- Gerrish KE, Gensler HL. Prevention of photocarcinogenesis by dietary vitamin E. Nutr Cancer. 1993;19:125-133.
- McVean M, Liebler DC. Prevention of DNA photodamage by vitamin E compounds and sunscreens: roles of ultraviolet absorbance and cellular uptake. Mol Carcinog. 1999;24:169-176.
- Prasad KN, Cohrs RJ, Sharma OK. Decreased expressions of c-myc and H-ras oncogenes in vitamin E succinate induced morphologically differentiated murine B-16 melanoma cells in culture. Biochem Cell Biol. 1990;68:1250-1255.
- Funasaka Y, Komoto M, Ichihashi M. Depigmenting effect of alpha-tocopheryl ferulate on normal human melanocytes. Pigment Cell Res. 2000;13(suppl 8):170-174.
- National Institutes of Health Office of Dietary Supplements. Selenium: fact sheet for health professionals. Updated March 26, 2021. Accessed November 14, 2022. https://ods.od.nih.gov/factsheets/Selenium-HealthProfessional/
- Sengupta A, Lichti UF, Carlson BA, et al. Selenoproteins are essential for proper keratinocyte function and skin development. PLoS One. 2010;5:e12249.
- Das RK, Hossain SKU, Bhattacharya S. Diphenylmethyl selenocyanate inhibits DMBA-croton oil induced two-stage mouse skin carcinogenesis by inducing apoptosis and inhibiting cutaneous cell proliferation. Cancer Lett. 2005;230:90-101.
- Clark LC, Combs GF Jr, Turnbull BW, et al. Effects of selenium supplementation for cancer prevention in patients with carcinoma of the skin. A randomized controlled trial. Nutritional Prevention of Cancer Study Group. JAMA. 1996;276:1957-1963.
- Duffield-Lillico AJ, Slate EH, Reid ME, et al. Selenium supplementation and secondary prevention of nonmelanoma skin cancer in a randomized trial. J Natl Cancer Inst. 2003;95:1477-1481.
- Reid ME, Duffield-Lillico AJ, Slate E, et al. The nutritional prevention of cancer: 400 mcg per day selenium treatment. Nutr Cancer. 2008;60:155-163.
- Vinceti M, Filippini T, Del Giovane C, et al. Selenium for preventing cancer. Cochrane Database Syst Rev. 2018;1:CD005195.
- Hercberg S, Ezzedine K, Guinot C, et al. Antioxidant supplementation increases the risk of skin cancers in women but not in men. J Nutr. 2007;137:2098-2105.
- Chang YJ, Myung SK, Chung ST, et al. Effects of vitamin treatment or supplements with purported antioxidant properties on skin cancer prevention: a meta-analysis of randomized controlled trials. Dermatology. 2011;223:36-44.
- Sun W, Rice MS, Park MK, et al. Intake of furocoumarins and risk of skin cancer in 2 prospective US cohort studies. J Nutr. 2020;150:1535-1544.
- Sakaki JR, Melough MM, Roberts MB, et al. Citrus consumption and the risk of non-melanoma skin cancer in the Women’s Health Initiative. Cancers (Basel). 2021;13:2173.
- Siegel RL, Miller KD, Fuchs HE, et al. Cancer statistics, 2022. CA Cancer J Clin. 2022;72:7-33.
- Global Burden of Disease Cancer Collaboration; Fitzmaurice C, Abate D, Abbasi N, et al. Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 29 cancer groups, 1990 to 2017: a systematic analysis for the Global Burden of Disease Study. JAMA Oncol. 2019;5:1749-1768.
- Leiter U, Keim U, Garbe C. Epidemiology of skin cancer: update 2019. In: Reichrath J, ed. Sunlight, Vitamin D and Skin Cancer. Springer International Publishing; 2020:123-139.
- Bradford PT. Skin cancer in skin of color. Dermatol Nurs. 2009;21:170-177, 206; quiz 178.
- Miller DL, Weinstock MA. Nonmelanoma skin cancer in the United States: incidence. J Am Acad Dermatol. 1994;30:774-778.
- Young AR, Claveau J, Rossi AB. Ultraviolet radiation and the skin: photobiology and sunscreen photoprotection. J Am Acad Dermatol. 2017;76(3S1):S100-S109.
- Pleasance ED, Cheetham RK, Stephens PJ, et al. A comprehensive catalogue of somatic mutations from a human cancer genome. Nature. 2010;463:191-196.
- Baek J, Lee MG. Oxidative stress and antioxidant strategies in dermatology. Redox Rep. 2016;21:164-169.
- Katta R, Brown DN. Diet and skin cancer: the potential role of dietary antioxidants in nonmelanoma skin cancer prevention. J Skin Cancer. 2015;2015:893149.
- Stoj V, Shahriari N, Shao K, et al. Nutrition and nonmelanoma skin cancers. Clin Dermatol. 2022;40:173-185.
- O’Connor EA, Evans CV, Ivlev I, et al. Vitamin and mineral supplements for the primary prevention of cardiovascular disease and cancer: updated evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2022;327:2334-2347.
- National Institutes of Health Office of Dietary Supplements. Vitamin A and carotenoids. fact sheet for health professionals. Updated June 15, 2022. Accessed November 14, 2022. https://ods.od.nih.gov/factsheets/VitaminA-HealthProfessional/
- Keller KL, Fenske NA. Uses of vitamins A, C, and E and related compounds in dermatology: a review. J Am Acad Dermatol. 1998;39:611-625.
- Wright TI, Spencer JM, Flowers FP. Chemoprevention of nonmelanoma skin cancer. J Am Acad Dermatol. 2006;54:933-946; quiz 947-950.
- Bushue N, Wan YJY. Retinoid pathway and cancer therapeutics. Adv Drug Deliv Rev. 2010;62:1285-1298.
- Stahl W, Sies H. β-Carotene and other carotenoids in protection from sunlight. Am J Clin Nutr. 2012;96:1179S-1184S.
- Bukhari MH, Qureshi SS, Niazi S, et al. Chemotherapeutic/chemopreventive role of retinoids in chemically induced skin carcinogenesis in albino mice. Int J Dermatol. 2007;46:1160-1165.
- Lambert LA, Wamer WG, Wei RR, et al. The protective but nonsynergistic effect of dietary beta-carotene and vitamin E on skin tumorigenesis in Skh mice. Nutr Cancer. 1994;21:1-12.
- Greenberg ER, Baron JA, Stukel TA, et al. A clinical trial of beta carotene to prevent basal-cell and squamous-cell cancers of the skin. The Skin Cancer Prevention Study Group. N Engl J Med. 1990;323:789-795.
- Frieling UM, Schaumberg DA, Kupper TS, et al. A randomized, 12-year primary-prevention trial of beta carotene supplementation for nonmelanoma skin cancer in the physician’s health study. Arch Dermatol. 2000;136:179-184.
- Naldi L, Gallus S, Tavani A, et al; Oncology Study Group of the Italian Group for Epidemiologic Research in Dermatology. Risk of melanoma and vitamin A, coffee and alcohol: a case-control study from Italy. Eur J Cancer Prev. 2004;13:503-508.
- Zhang YP, Chu RX, Liu H. Vitamin A intake and risk of melanoma: a meta-analysis. PloS One. 2014;9:e102527.
- Feskanich D, Willett WC, Hunter DJ, et al. Dietary intakes of vitamins A, C, and E and risk of melanoma in two cohorts of women. Br J Cancer. 2003;88:1381-1387.
- Bavinck JN, Tieben LM, Van der Woude FJ, et al. Prevention of skin cancer and reduction of keratotic skin lesions during acitretin therapy in renal transplant recipients: a double-blind, placebo-controlled study. J Clin Oncol. 1995;13:1933-1938.
- George R, Weightman W, Russ GR, et al. Acitretin for chemoprevention of non-melanoma skin cancers in renal transplant recipients. Australas J Dermatol. 2002;43:269-273.
- Solomon-Cohen E, Reiss-Huss S, Hodak E, et al. Low-dose acitretin for secondary prevention of keratinocyte carcinomas in solid-organ transplant recipients. Dermatology. 2022;238:161-166.
- Otley CC, Stasko T, Tope WD, et al. Chemoprevention of nonmelanoma skin cancer with systemic retinoids: practical dosing and management of adverse effects. Dermatol Surg. 2006;32:562-568.
- Kadakia KC, Barton DL, Loprinzi CL, et al. Randomized controlled trial of acitretin versus placebo in patients at high-risk for basal cell or squamous cell carcinoma of the skin (North Central Cancer Treatment Group Study 969251). Cancer. 2012;118:2128-2137.
- McKenna DB, Murphy GM. Skin cancer chemoprophylaxis in renal transplant recipients: 5 years of experience using low-dose acitretin. Br J Dermatol. 1999;140:656-660.
- National Institutes of Health Office of Dietary Supplements. Niacin: fact sheet for health professionals. Updated August 23, 2022. Accessed November 14, 2022. https://ods.od.nih.gov/factsheets/Niacin-HealthProfessional/
- Malesu R, Martin AJ, Lyons JG, et al. Nicotinamide for skin cancer chemoprevention: effects of nicotinamide on melanoma in vitro and in vivo. Photochem Photobiol Sci. 2020;19:171-179.
- Gensler HL. Prevention of photoimmunosuppression and photocarcinogenesis by topical nicotinamide. Nutr Cancer. 1997;29:157-162.
- Gensler HL, Williams T, Huang AC, et al. Oral niacin prevents photocarcinogenesis and photoimmunosuppression in mice. Nutr Cancer. 1999;34:36-41.
- Chen AC, Martin AJ, Choy B, et al. A phase 3 randomized trial of nicotinamide for skin-cancer chemoprevention. N Engl J Med. 2015;373:1618-1626.
- Drago F, Ciccarese G, Cogorno L, et al. Prevention of non-melanoma skin cancers with nicotinamide in transplant recipients: a case-control study. Eur J Dermatol. 2017;27:382-385.
- Yélamos O, Halpern AC, Weinstock MA. Reply to “A phase II randomized controlled trial of nicotinamide for skin cancer chemoprevention in renal transplant recipients.” Br J Dermatol. 2017;176:551-552.
- Scatozza F, Moschella F, D’Arcangelo D, et al. Nicotinamide inhibits melanoma in vitro and in vivo. J Exp Clin Cancer Res. 2020;39:211.
- National Institutes of Health Office of Dietary Supplements. Folate: fact sheet for health professionals. Updated November 1, 2022. Accessed November 14, 2022. https://ods.od.nih.gov/factsheets/Folate-HealthProfessional/
- Butzbach K, Epe B. Photogenotoxicity of folic acid. Free Radic Biol Med. 2013;65:821-827.
- Vollset SE, Clarke R, Lewington S, et al. Effects of folic acid supplementation on overall and site-specific cancer incidence during the randomised trials: meta-analyses of data on 50,000 individuals. Lancet. 2013;381:1029-1036.
- Donnenfeld M, Deschasaux M, Latino-Martel P, et al. Prospective association between dietary folate intake and skin cancer risk: results from the Supplémentation en Vitamines et Minéraux Antioxydants cohort. Am J Clin Nutr. 2015;102:471-478.
- Fung TT, Hunter DJ, Spiegelman D, et al. Vitamins and carotenoids intake and the risk of basal cell carcinoma of the skin in women (United States). Cancer Causes Control. 2002;13:221-230.
- Fung TT, Spiegelman D, Egan KM, et al. Vitamin and carotenoid intake and risk of squamous cell carcinoma of the skin. Int J Cancer. 2003;103:110-115.
- National Institutes of Health Office of Dietary Supplements. Vitamin C: fact sheet for health professionals. Updated March 26, 2021. Accessed November 14, 2022. https://ods.od.nih.gov/factsheets/VitaminC-HealthProfessional/
- Spoelstra-de Man AME, Elbers PWG, Oudemans-Van Straaten HM. Vitamin C: should we supplement? Curr Opin Crit Care. 2018;24:248-255.
- Moison RMW, Beijersbergen van Henegouwen GMJ. Topical antioxidant vitamins C and E prevent UVB-radiation-induced peroxidation of eicosapentaenoic acid in pig skin. Radiat Res. 2002;157:402-409.
- Lin JY, Selim MA, Shea CR, et al. UV photoprotection by combination topical antioxidants vitamin C and vitamin E. J Am Acad Dermatol. 2003;48:866-874.
- Pauling L, Willoughby R, Reynolds R, et al. Incidence of squamous cell carcinoma in hairless mice irradiated with ultraviolet light in relation to intake of ascorbic acid (vitamin C) and of D, L-alpha-tocopheryl acetate (vitamin E). Int J Vitam Nutr Res Suppl. 1982;23:53-82.
- Kune GA, Bannerman S, Field B, et al. Diet, alcohol, smoking, serum beta-carotene, and vitamin A in male nonmelanocytic skin cancer patients and controls. Nutr Cancer. 1992;18:237-244.
- Vural P, Canbaz M, Selçuki D. Plasma antioxidant defense in actinic keratosis and basal cell carcinoma. J Eur Acad Dermatol Venereol. 1999;13:96-101.
- Record IR, Dreosti IE, McInerney JK. Changes in plasma antioxidant status following consumption of diets high or low in fruit and vegetables or following dietary supplementation with an antioxidant mixture. Br J Nutr. 2001;85:459-464.
- Heinen MM, Hughes MC, Ibiebele TI, et al. Intake of antioxidant nutrients and the risk of skin cancer. Eur J Cancer. 2007;43:2707-2716.
- Yang G, Yan Y, Ma Y, et al. Vitamin C at high concentrations induces cytotoxicity in malignant melanoma but promotes tumor growth at low concentrations. Mol Carcinog. 2017;56:1965-1976.
- National Institutes of Health Office of Dietary Supplements. Vitamin D: fact sheet for health professionals. Updated August 12, 2022. Accessed November 14, 2022. https://ods.od.nih.gov/factsheets/VitaminD-HealthProfessional/
- Reichrath J, Saternus R, Vogt T. Endocrine actions of vitamin D in skin: relevance for photocarcinogenesis of non-melanoma skin cancer, and beyond. Mol Cell Endocrinol. 2017;453:96-102.
- Ellison TI, Smith MK, Gilliam AC, et al. Inactivation of the vitamin D receptor enhances susceptibility of murine skin to UV-induced tumorigenesis. J Invest Dermatol. 2008;128:2508-2517.
- Eide MJ, Johnson DA, Jacobsen GR, et al. Vitamin D and nonmelanoma skin cancer in a health maintenance organization cohort. Arch Dermatol. 2011;147:1379-1384.
- van der Pols JC, Russell A, Bauer U, et al. Vitamin D status and skin cancer risk independent of time outdoors: 11-year prospective study in an Australian community. J Invest Dermatol. 2013;133:637-641.
- Caini S, Gnagnarella P, Stanganelli I, et al. Vitamin D and the risk of non-melanoma skin cancer: a systematic literature review and meta-analysis on behalf of the Italian Melanoma Intergroup. Cancers (Basel). 2021;13:4815.
- Park SM, Li T, Wu S, et al. Vitamin D intake and risk of skin cancer in US women and men. PLoS One. 2016;11:e0160308.
- Afzal S, Nordestgaard BG, Bojesen SE. Plasma 25-hydroxyvitamin D and risk of non-melanoma and melanoma skin cancer: a prospective cohort study. J Invest Dermatol. 2013;133:629-636.
- Asgari MM, Tang J, Warton ME, et al. Association of prediagnostic serum vitamin D levels with the development of basal cell carcinoma. J Invest Dermatol. 2010;130:1438-1443.
- Tang JY, Parimi N, Wu A, et al. Inverse association between serum 25(OH) vitamin D levels and non-melanoma skin cancer in elderly men. Cancer Causes Control. 2010;21:387-391.
- Keen MA, Hassan I. Vitamin E in dermatology. Indian Dermatol Online J. 2016;7:311-315.
- National Institutes of Health Office of Dietary Supplements. Vitamin E: fact sheet for health professionals. Updated March 26, 2021. Accessed November 14, 2022. https://ods.od.nih.gov/factsheets/VitaminE-HealthProfessional/
- Pearson P, Lewis SA, Britton J, et al. The pro-oxidant activity of high-dose vitamin E supplements in vivo. BioDrugs. 2006;20:271-273.
- Gerrish KE, Gensler HL. Prevention of photocarcinogenesis by dietary vitamin E. Nutr Cancer. 1993;19:125-133.
- McVean M, Liebler DC. Prevention of DNA photodamage by vitamin E compounds and sunscreens: roles of ultraviolet absorbance and cellular uptake. Mol Carcinog. 1999;24:169-176.
- Prasad KN, Cohrs RJ, Sharma OK. Decreased expressions of c-myc and H-ras oncogenes in vitamin E succinate induced morphologically differentiated murine B-16 melanoma cells in culture. Biochem Cell Biol. 1990;68:1250-1255.
- Funasaka Y, Komoto M, Ichihashi M. Depigmenting effect of alpha-tocopheryl ferulate on normal human melanocytes. Pigment Cell Res. 2000;13(suppl 8):170-174.
- National Institutes of Health Office of Dietary Supplements. Selenium: fact sheet for health professionals. Updated March 26, 2021. Accessed November 14, 2022. https://ods.od.nih.gov/factsheets/Selenium-HealthProfessional/
- Sengupta A, Lichti UF, Carlson BA, et al. Selenoproteins are essential for proper keratinocyte function and skin development. PLoS One. 2010;5:e12249.
- Das RK, Hossain SKU, Bhattacharya S. Diphenylmethyl selenocyanate inhibits DMBA-croton oil induced two-stage mouse skin carcinogenesis by inducing apoptosis and inhibiting cutaneous cell proliferation. Cancer Lett. 2005;230:90-101.
- Clark LC, Combs GF Jr, Turnbull BW, et al. Effects of selenium supplementation for cancer prevention in patients with carcinoma of the skin. A randomized controlled trial. Nutritional Prevention of Cancer Study Group. JAMA. 1996;276:1957-1963.
- Duffield-Lillico AJ, Slate EH, Reid ME, et al. Selenium supplementation and secondary prevention of nonmelanoma skin cancer in a randomized trial. J Natl Cancer Inst. 2003;95:1477-1481.
- Reid ME, Duffield-Lillico AJ, Slate E, et al. The nutritional prevention of cancer: 400 mcg per day selenium treatment. Nutr Cancer. 2008;60:155-163.
- Vinceti M, Filippini T, Del Giovane C, et al. Selenium for preventing cancer. Cochrane Database Syst Rev. 2018;1:CD005195.
- Hercberg S, Ezzedine K, Guinot C, et al. Antioxidant supplementation increases the risk of skin cancers in women but not in men. J Nutr. 2007;137:2098-2105.
- Chang YJ, Myung SK, Chung ST, et al. Effects of vitamin treatment or supplements with purported antioxidant properties on skin cancer prevention: a meta-analysis of randomized controlled trials. Dermatology. 2011;223:36-44.
- Sun W, Rice MS, Park MK, et al. Intake of furocoumarins and risk of skin cancer in 2 prospective US cohort studies. J Nutr. 2020;150:1535-1544.
- Sakaki JR, Melough MM, Roberts MB, et al. Citrus consumption and the risk of non-melanoma skin cancer in the Women’s Health Initiative. Cancers (Basel). 2021;13:2173.
Practice Points
- Melanoma and nonmelanoma skin cancer (NMSC) are 2 of the most frequently diagnosed cancers in the United States. UV radiation plays a key role in the pathogenesis of both.
- Dietary antioxidants may mechanistically decrease DNA damage caused by UV radiation and could play a potential role in the prevention or development of melanoma and NMSC.
What’s Diet Got to Do With It? Basic and Clinical Science Behind Diet and Acne
The current understanding of the pathogenesis of acne includes altered keratinization, follicular obstruction, overproduction of sebum, and microbial colonization ( Cutibacterium acnes ) of the pilosebaceous unit resulting in perifollicular inflammation. 1 A deeper dive into the hormonal and molecular drivers of acne have implicated insulin, insulinlike growth factor 1 (IGF-1), corticotropin-releasing hormone, the phosphoinositide 3 -kinase/Akt pathway, mitogen-activated protein kinase pathway, and the nuclear factor κ B pathway. 2-4 A Western diet comprised of high glycemic index foods, carbohydrates, and dairy enhances the production of insulin and IGF-1. A downstream effect of excess insulin and IGF-1 is overactivity of the mammalian target of rapamycin complex 1 (mTORC1), a major promoter of cellular growth and proliferation that primarily is regulated through nutrient availability. 5 This article will review our understanding of the impact of the Western diet on acne pathogenesis and highlight the existing evidence behind the contributions of the mTORC1 pathway in this process. Although quality randomized controlled trials analyzing these effects are limited, dermatologists should understand the existing evidence supporting the potential impacts of diet on acne.
The Western Diet
Glycemic Index—To assess the impact of a high glycemic index diet on acne, Kwon et al6 evaluated 32 patients with mild to moderate acne and placed them on a low or high glycemic index diet for 10 weeks. The low glycemic index diet group was found to have a 70% reduction in the mean number of inflammatory acne lesions from baseline (P<.05), while the high glycemic index diet group had no significant reduction. Noninflammatory lesion counts remained statistically unchanged.6 Smith et al7 studied 43 male patients with acne on either a low glycemic index diet or a self-directed high glycemic diet that was carbohydrate dense. The low glycemic index group showed greater improvement in lesion count as well as improved insulin sensitivity at 12 weeks. Specifically, the mean lesion count (SEM) decreased by 23.5 (3.9) in the low glycemic index group and by only 12.0 (3.5) in the control group (P=.03).7 Observational studies also have supported this hypothesis. After adjustment, an analysis of 24,452 participants in the NutriNet-Santé cohort found significant associations between current acne and the consumption of sugary beverages (adjusted OR, 1.18; 95% CI, 1.01-1.38) and the consumption of fatty and sugary products (adjusted OR, 1.54; 95% CI, 1.09-2.16).8 A Cochrane review that included only 2 studies (Kwon et al6 and Smith et al7) did not find evidence to suggest a low glycemic index diet for noninflammatory lesion count reduction but did note possible benefit for a reduction in inflammatory and total lesion counts; however, Kwon et al6 had incomplete data.9
Dairy—A large retrospective study including 47,355 nurses noted the frequency of milk intake was significantly associated with increased prevalence of acne in adolescence (prevalence ratio, 1.22; 95% CI, 1.03-1.44; P=.002).10 A 2019 meta-analysis further suggested a significant relationship between acne and milk in highest vs lowest intake groups (OR, 1.48; 95% CI, 1.31-1.66) with no significant heterogeneity between the studies (I2=23.6%, P=.24 for heterogeneity), as well as a positive relationship between the highest vs lowest intake of low-fat milk (OR, 1.25; 95% CI, 1.10-1.43) and skim milk (OR, 1.82; 95% CI, 1.34-2.47). In this meta-analysis, yogurt and cheese consumption were not significantly associated with acne (OR, 0.90; 95% CI, 0.73-1.11).11 One non–evidence-based explanation for this may be that fermented dairy products have different biological actions. Pasteurized milk allows microRNAs that directly activate mTORC1 to persist, whereas the bacteria present in the fermentation process may augment this.12 A separate meta-analysis from 2018 did find that yogurt consumption was positively associated with acne (OR, 1.36; 95% CI, 1.05-1.77; P=.022), highlighting the need for larger, more rigorous studies on this topic.13
Insulin and IGF-1—As reviewed above, acne has been considered a disease of Western society, with the Western diet at the center of this association.14 A typical Western diet consists of high glycemic index foods, carbohydrates, and dairy, all of which enhance the production of insulin and IGF-1. Insulin levels increase secondary to high blood glucose and to a lesser degree by protein intake.15 Insulinlike growth factor 1 production is most influenced by age and peaks during puberty; however, high protein diets also increase liver IGF-1 production and release.16 When present in excess, insulin can function as a growth factor. Insulin exerts its anabolic effects through the IGF-1 pathway; however, insulin and IGF-1 are produced in response to different signals.17 Endocrine production of IGF-1 represents 70% of blood levels, peaks at puberty, and rapidly declines in the third decade of life.18 Insulin is produced by the pancreas, and levels correspond to lifestyle and genetically induced insulin resistance.19
Adolescents have elevated levels of IGF-1 as a major driver of puberty-associated growth.20 Despite the natural decrease in IGF-1 following puberty, acne persists in many patients and can even develop for the first time in adulthood in a subset of patients. A study of 40 acne patients and 20 controls found that patients with acne who consumed a high glycemic–load diet was significantly higher than the number of controls consuming a similar diet (P=.008). Additionally, significantly higher levels of mean (SD) serum IGF-1 on quantitative sandwich enzyme-linked immunosorbent assay in acne patients vs controls (543.2 [174.7] ng/mL vs 316.9 [95.7] ng/mL; P<.001) was identified, and these levels correlated significantly with high glycemic–load diet consumption.21 In another study, Kartal et al22 found that basal and fasting insulin levels and homeostasis model assessment scores evaluating for insulin resistance were significantly higher in 36 women compared with 24 age/sex-matched controls (P<.05). This finding remained significant even after excluding women with hyperandrogenemia (P<.05).22
Highlighting the importance of IGF-1 in the pathogenesis of acne, patients with genetic disorders characterized by IGF-1 deficiency, such as Laron syndrome, do not develop acne despite having a functional androgen receptor. Treatment with IGF-1 in these patients induces acne, further supporting the role of IGF-1 in the pathogenesis of this condition.23
The mTORC1 Pathway
Comprised of mTOR in addition to other proteins, mTORC1 is a nutrient-sensitive regulator of cellular growth, proliferation, lipid synthesis, and protein translation.5 Increased activity of mTORC1 has been described in diabetes, neurodegenerative disease, and cancer,14,24 while decreased activity may promote longevity.25 Regulation of mTORC1 occurs through several mechanisms. Growth factors such as insulin and IGF-1 promote mTORC1 activation through the PI3K/Akt pathway. Several amino acids—specifically branched chain amino acids such as alanine, arginine, asparagine, glutamine, histidine, leucine, methionine, serine, threonine, and valine—also can activate mTORC1 independently.26 Excess glucose leads to decreased adenosine monophosphate–activated protein kinase and increased activity of mTORC1, which occurs separately from insulin or IGF-1.27 Starvation blocks mTORC1 via increased adenosine monophosphate–activated protein kinase and starvation-induced hypoxia.26,28 To activate mTORC1, both the IGF-1 or insulin signal and amino acid excess must be present.29 Although not studied in acne, altering the dietary protein content in obese mice has been shown to perturb the mTORC1 pathway, leading to pathologic changes in the mTORC1-autophagy signaling axis, increased amino acid release into the blood, and an acute elevation in mTORC1 signaling.30
Another major regulator of mTORC1 is Forkhead box protein O1 (FOXO1), which is a transcription factor that regulates mTORC1 through sestrin 3.31,32 Sestrin 3 is a stress-induced protein that helps regulate blood glucose and promote insulin sensitivity.33 When FOXO1 is translocated to the cell nucleus, it upregulates the expression of sestrin 3, resulting in mTORC1 inhibition.31,32 Insulin, IGF-1, and nutrient excess lead to FOXO1 translocation to the cell cytoplasm where it can no longer mitigate mTORC1 activity, while the fasted state leads to translocation to the nucleus.34 A single study evaluated the association between FOXO1, mTORC1, a high glycemic–load diet, and acne development. Immunohistochemical detection of mTORC1 assessed by digital image analysis revealed significantly greater expression in inflamed pilosebaceous units found in acne patients (P<.001). Immunohistochemical cytoplasmic expression of FOXO1 and mTOR (used as a proxy for mTORC1) was significantly higher in patients on a high glycemic–load diet (P=.021 and P=.009, respectively) as well as in patients with more severe forms of acne (P=.005 and P=.015, respectively) and elevated IGF-1 levels (P=.004 and P=.003, respectively).21
mTORC1 contributes to the proliferation of keratinocytes and excess sebum production, both independently and through androgen-mediated processes.35-40 Insulinlike growth factor 1 binding the IGF-1 receptor leads to proliferation of keratinocytes lining the sebaceous gland and hair follicle in vivo.35 In mice with epidermis-specific deletion of mTOR, keratinocyte proliferation was decreased and hair follicles were diminished both in number and development. Genetic loss of mTOR in the epidermis led to attenuated signaling pathways of mTORC1 and mTORC2.36
Androgen function is augmented by mTORC1, FOXO1, and IGF-1 through several mechanisms, which may partially explain the hormonal relationship to acne. Androgens increase IGF-1 within the hair follicle.37 In prostate cancer cells, IGF-1 then facilitates movement of FOXO1 to the cytoplasm, preventing it from blocking mTORC1. This effective inactivation of FOXO1 thus further augments the impact of androgens by both allowing unchecked mTORC1 pathway activity and increasing translocation of the androgen receptor (AR) to the nucleus where it exerts its effects.38 Interestingly, genetic polymorphisms of the AR have been shown to cause variable affinity of FOXO1 for the AR; specifically, shorter CAG (cytosine, adenine, guanine) repeat length may lead to decreased FOXO1 binding and is associated with an increased risk for acne.41-43 In addition to its effects on the hair follicle, IGF-1 stimulates production of testosterone and dehydroepiandrosterone as well as activates 5α-reductase, leading to higher dihydrotestosterone levels, which activate the AR with higher affinity than testosterone.44 In some tissues, androgens help regulate the mTORC1 pathway through positive feedback loops.45,46 At this time, we do not know if this occurs in the pathogenesis of acne.
Isotretinoin is the treatment of choice for refractory acne. It has been hypothesized that isotretinoin induces sebocyte apoptosis via the upregulation of FOXO transcription factors and p53.47 Elevated levels of nuclear FOXO1 have been found in the sebaceous glands of patients following initiation of treatment with isotretinoin and are hypothesized to play a major role in the drug’s effectiveness. Specifically, biopsies from 14 acne patients before and after 6 weeks of isotretinoin therapy were analyzed with immunohistochemical staining and found to have a significantly improved nuclear to cytoplasmic ratio of nonphosphorylated FOXO1 (P<.001).47
Practical Recommendations
Given the available evidence, it is important for dermatologists to address dietary recommendations in acne patients. Although large randomized controlled trials on diet and acne severity are challenging to conduct in this population, the existing literature suggests that patients should avoid high glycemic index simple sugars and processed grains, and patients should focus on eating more complex carbohydrates in the form of legumes, vegetables, fruits, and tubers.6-8 With regard to dairy, milk (especially skim) has been associated with increased risks for acne.11,13 Fermented dairy products may have less impact on acne severity and include cheese, yogurt (unsweetened to keep glycemic index low), and sour cream.12
- Zaenglein AL. Acne vulgaris. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. Elsevier; 2017:588-603.
- Ganceviciene R, Graziene V, Fimmel S, et al. Involvement of the corticotropin-releasing hormone system in the pathogenesis of acne vulgaris. Br J Dermatol. 2009;160:345-352.
- Kang S, Cho S, Chung JH, et al. Inflammation and extracellular matrix degradation mediated by activated transcription factors nuclear factor-kappaB and activator protein-1 in inflammatory acne lesions in vivo. Am J Pathol. 2005;166:1691-1699.
- Cong TX, Hao D, Wen X, et al. From pathogenesis of acne vulgaris to anti-acne agents. Arch Dermatol Res. 2019;311:337-349.
- Pópulo H, Lopes JM, Soares P. The mTOR signalling pathway in human cancer. Int J Mol Sci. 2012;13:1886-1918.
- Kwon HH, Yoon JY, Hong JS, et al. Clinical and histological effect of a low glycaemic load diet in treatment of acne vulgaris in Korean patients: a randomized, controlled trial. Acta Derm Venereol. 2012;92:241-246.
- Smith RN, Mann NJ, Braue A, et al. A low-glycemic-load diet improves symptoms in acne vulgaris patients: a randomized controlled trial. Am J Clin Nutr. 2007;86:107-115.
- Penso L, Touvier M, Deschasaux M, et al. Association between adult acne and dietary behaviors: findings from the NutriNet-Santé prospective cohort study. JAMA Dermatol. 2020;156:854-862.
- Cao H, Yang G, Wang Y, et al. Complementary therapies for acne vulgaris. Cochrane Database Syst Rev. 2015;1:CD009436.
- Adebamowo CA, Spiegelman D, Danby FW, et al. High school dietary dairy intake and teenage acne. J Am Acad Dermatol. 2005;52:207-214.
- Aghasi M, Golzarand M, Shab-Bidar S, et al. Dairy intake and acne development: a meta-analysis of observational studies. Clin Nutr. 2019;38:1067-1075.
- Melnik BC, Schmitz G. Pasteurized non-fermented cow’s milk but not fermented milk is a promoter of mTORC1-driven aging and increased mortality. Ageing Res Rev. 2021;67:101270.
- Juhl CR, Bergholdt HKM, Miller IM, et al. Dairy intake and acne vulgaris: a systematic review and meta-analysis of 78,529 children, adolescents, and young adults. Nutrients. 2018;10:1049. doi:10.3390/nu10081049
- Melnik BC. Linking diet to acne metabolomics, inflammation, and comedogenesis: an update. Clin Cosmet Investig Dermatol. 2015;8:371-388.
- Smart CEM, King BR, Lopez PE. Insulin dosing for fat and protein: is it time? Diabetes Care. 2020;43:13-15.
- Wan X, Wang S, Xu J, et al. Dietary protein-induced hepatic IGF-1 secretion mediated by PPARγ activation. PLoS One. 2017;12:E0173174.
- Bedinger DH, Adams SH. Metabolic, anabolic, and mitogenic insulin responses: a tissue-specific perspective for insulin receptor activators. Mol Cell Endocrinol. 2015;415:143-156.
- Gubbi S, Quipildor GF, Barzilai N, et al. 40 YEARS of IGF1: IGF1: the Jekyll and Hyde of the aging brain. J Mol Endocrinol. 2018;61:T171-T185.
- Kolb H, Kempf K, Röhling M, et al. Insulin: too much of a good thing is bad. BMC Med. 2020;18:224.
- Wood CL, Lane LC, Cheetham T. Puberty: normal physiology (brief overview). Best Pract Res Clin Endocrinol Metab. 2019;33:101265.
- Agamia NF, Abdallah DM, Sorour O, et al. Skin expression of mammalian target of rapamycin and forkhead box transcription factor O1, and serum insulin-like growth factor-1 in patients with acne vulgaris and their relationship with diet. Br J Dermatol. 2016;174:1299-1307.
- Kartal D, Yildiz H, Ertas R, et al. Association between isolated female acne and insulin resistance: a prospective study. G Ital Dermatol Venereol. 2016;151:353-357.
- Ben-Amitai D, Laron Z. Effect of insulin-like growth factor-1 deficiency or administration on the occurrence of acne. J Eur Acad Dermatol Venereol. 2011;25:950-954.
- Kim LC, Cook RS, Chen J. mTORC1 and mTORC2 in cancer and the tumor microenvironment. Oncogene. 2017;36:2191-2201.
- Weichhart T. mTOR as regulator of lifespan, aging, and cellular senescence: a mini-review. Gerontology. 2018;64:127-134.
- Melick CH, Jewell JL. Regulation of mTORC1 by upstream stimuli. Genes. 2020;11:989. doi:10.3390/genes11090989
- Li M, Zhang CS, Feng JW, et al. Aldolase is a sensor for both low and high glucose, linking to AMPK and mTORC1. Cell Res. 2021;31:478-481.
- Yan T, Zhang J, Tang D, et al. Hypoxia regulates mTORC1-mediated keratinocyte motility and migration via the AMPK pathway. PLoS One. 2017;12:E0169155.
- Dennis MD, Baum JI, Kimball SR, et al. Mechanisms involved in the coordinate regulation of mTORC1 by insulin and amino acids. J Biol Chem. 2011;286:8287-8296.
- Choi BSY, Daniel N, Houde VP, et al. Feeding diversified protein sources exacerbates hepatic insulin resistance via increased gut microbial branched-chain fatty acids and mTORC1 signaling in obese mice. Nat Commun. 2021;12:3377.
- Chen CC, Jeon SM, Bhaskar PT, et al. FoxOs inhibit mTORC1 and activate Akt by inducing the expression of Sestrin3 and Rictor. Dev Cell. 2010;18:592-604.
- Chen Y, Huang T, Yu Z, et al. The functions and roles of sestrins in regulating human diseases. Cell Mol Biol Lett. 2022;27:2.
- Tao R, Xiong X, Liangpunsakul S, et al. Sestrin 3 protein enhances hepatic insulin sensitivity by direct activation of the mTORC2-Akt signaling. Diabetes. 2015;64:1211-1223.
- Gross DN, Wan M, Birnbaum MJ. The role of FOXO in the regulation of metabolism. Curr Diab Rep. 2009;9:208-214.
- Gilhar A, Ish-Shalom S, Pillar T, et al. Effect of anti–insulin-like growth factor 1 on epidermal proliferation of human skin transplanted onto nude mice treated with growth hormone. Endocrinology. 1994;134:229-232.
- Ding X, Bloch W, Iden S, et al. mTORC1 and mTORC2 regulate skin morphogenesis and epidermal barrier formation. Nat Commun. 2016;7:13226.
- Inui S, Itami S. Androgen actions on the human hair follicle: perspectives. Exp Dermatol. 2013;22:168-171.
- Fan W, Yanase T, Morinaga H, et al. Insulin-like growth factor 1/insulin signaling activates androgen signaling through direct interactions of Foxo1 with androgen receptor. J Biol Chem. 2007;282:7329-7338.
- Alestas T, Ganceviciene R, Fimmel S, et al. Enzymes involved in the biosynthesis of leukotriene B4 and prostaglandin E2 are active in sebaceous glands. J Mol Med. 2006;84:75-87.
- Smith TM, Gilliland K, Clawson GA, et al. IGF-1 induces SREBP-1 expression and lipogenesis in SEB-1 sebocytes via activation of the phosphoinositide 3-kinase/Akt pathway. J Invest Dermatol. 2008;128:1286-1293.
- Furtado GV, Yang J, Wu D, et al. FOXO1 controls protein synthesis and transcript abundance of mutant polyglutamine proteins, preventing protein aggregation. Hum Mol Genet. 2021;30:996-1005.
- Melnik BC. Isotretinoin and FoxO1: a scientific hypothesis. Dermatoendocrinol. 2011;3:141-165.
- Heng AHS, Say YH, Sio YY, et al. Gene variants associated with acne vulgaris presentation and severity: a systematic review and meta-analysis. BMC Med Genomics. 2021;14:103.
- Li J, Al-Azzawi F. Mechanism of androgen receptor action. Maturitas. 2009;63:142-148.
- Zhao Y, Tindall DJ, Huang H. Modulation of androgen receptor by FOXA1 and FOXO1 factors in prostate cancer. Int J Biol Sci. 2014;10:614-619.
- Hamdi MM, Mutungi G. Dihydrotestosterone stimulates amino acid uptake and the expression of LAT2 in mouse skeletal muscle fibres through an ERK1/2-dependent mechanism. J Physiol. 2011;589(pt 14):3623-3640.
- Agamia NF, Hussein OM, Abdelmaksoud RE, et al. Effect of oral isotretinoin on the nucleocytoplasmic distribution of FoxO1 and FoxO3 proteins in sebaceous glands of patients with acne vulgaris. Exp Dermatol. 2018;27:1344-1351.
- Kolovou GD, Watts GF, Mikhailidis DP, et al. Postprandial hypertriglyceridaemia revisited in the era of non-fasting lipid profile testing: a 2019 expert panel statement, main text. Curr Vasc Pharmacol. 2019;17:498-514.
- Svoboda SA, Shields BE. Cutaneous manifestations of nutritional excess: pathophysiologic effects of hyperglycemia and hyperinsulinemia on the skin. Cutis. 2021;107:74-78.
- González-González JG, Mancillas-Adame LG, Fernández-Reyes M, et al. Androgenetic alopecia and insulin resistance in young men. Clin Endocrinol . 2009;71:494-499.
- Livadas S, Anagnostis P, Bosdou JK, et al. Polycystic ovary syndrome and type 2 diabetes mellitus: a state-of-the-art review. World J Diabetes. 2022;13:5-26.
The current understanding of the pathogenesis of acne includes altered keratinization, follicular obstruction, overproduction of sebum, and microbial colonization ( Cutibacterium acnes ) of the pilosebaceous unit resulting in perifollicular inflammation. 1 A deeper dive into the hormonal and molecular drivers of acne have implicated insulin, insulinlike growth factor 1 (IGF-1), corticotropin-releasing hormone, the phosphoinositide 3 -kinase/Akt pathway, mitogen-activated protein kinase pathway, and the nuclear factor κ B pathway. 2-4 A Western diet comprised of high glycemic index foods, carbohydrates, and dairy enhances the production of insulin and IGF-1. A downstream effect of excess insulin and IGF-1 is overactivity of the mammalian target of rapamycin complex 1 (mTORC1), a major promoter of cellular growth and proliferation that primarily is regulated through nutrient availability. 5 This article will review our understanding of the impact of the Western diet on acne pathogenesis and highlight the existing evidence behind the contributions of the mTORC1 pathway in this process. Although quality randomized controlled trials analyzing these effects are limited, dermatologists should understand the existing evidence supporting the potential impacts of diet on acne.
The Western Diet
Glycemic Index—To assess the impact of a high glycemic index diet on acne, Kwon et al6 evaluated 32 patients with mild to moderate acne and placed them on a low or high glycemic index diet for 10 weeks. The low glycemic index diet group was found to have a 70% reduction in the mean number of inflammatory acne lesions from baseline (P<.05), while the high glycemic index diet group had no significant reduction. Noninflammatory lesion counts remained statistically unchanged.6 Smith et al7 studied 43 male patients with acne on either a low glycemic index diet or a self-directed high glycemic diet that was carbohydrate dense. The low glycemic index group showed greater improvement in lesion count as well as improved insulin sensitivity at 12 weeks. Specifically, the mean lesion count (SEM) decreased by 23.5 (3.9) in the low glycemic index group and by only 12.0 (3.5) in the control group (P=.03).7 Observational studies also have supported this hypothesis. After adjustment, an analysis of 24,452 participants in the NutriNet-Santé cohort found significant associations between current acne and the consumption of sugary beverages (adjusted OR, 1.18; 95% CI, 1.01-1.38) and the consumption of fatty and sugary products (adjusted OR, 1.54; 95% CI, 1.09-2.16).8 A Cochrane review that included only 2 studies (Kwon et al6 and Smith et al7) did not find evidence to suggest a low glycemic index diet for noninflammatory lesion count reduction but did note possible benefit for a reduction in inflammatory and total lesion counts; however, Kwon et al6 had incomplete data.9
Dairy—A large retrospective study including 47,355 nurses noted the frequency of milk intake was significantly associated with increased prevalence of acne in adolescence (prevalence ratio, 1.22; 95% CI, 1.03-1.44; P=.002).10 A 2019 meta-analysis further suggested a significant relationship between acne and milk in highest vs lowest intake groups (OR, 1.48; 95% CI, 1.31-1.66) with no significant heterogeneity between the studies (I2=23.6%, P=.24 for heterogeneity), as well as a positive relationship between the highest vs lowest intake of low-fat milk (OR, 1.25; 95% CI, 1.10-1.43) and skim milk (OR, 1.82; 95% CI, 1.34-2.47). In this meta-analysis, yogurt and cheese consumption were not significantly associated with acne (OR, 0.90; 95% CI, 0.73-1.11).11 One non–evidence-based explanation for this may be that fermented dairy products have different biological actions. Pasteurized milk allows microRNAs that directly activate mTORC1 to persist, whereas the bacteria present in the fermentation process may augment this.12 A separate meta-analysis from 2018 did find that yogurt consumption was positively associated with acne (OR, 1.36; 95% CI, 1.05-1.77; P=.022), highlighting the need for larger, more rigorous studies on this topic.13
Insulin and IGF-1—As reviewed above, acne has been considered a disease of Western society, with the Western diet at the center of this association.14 A typical Western diet consists of high glycemic index foods, carbohydrates, and dairy, all of which enhance the production of insulin and IGF-1. Insulin levels increase secondary to high blood glucose and to a lesser degree by protein intake.15 Insulinlike growth factor 1 production is most influenced by age and peaks during puberty; however, high protein diets also increase liver IGF-1 production and release.16 When present in excess, insulin can function as a growth factor. Insulin exerts its anabolic effects through the IGF-1 pathway; however, insulin and IGF-1 are produced in response to different signals.17 Endocrine production of IGF-1 represents 70% of blood levels, peaks at puberty, and rapidly declines in the third decade of life.18 Insulin is produced by the pancreas, and levels correspond to lifestyle and genetically induced insulin resistance.19
Adolescents have elevated levels of IGF-1 as a major driver of puberty-associated growth.20 Despite the natural decrease in IGF-1 following puberty, acne persists in many patients and can even develop for the first time in adulthood in a subset of patients. A study of 40 acne patients and 20 controls found that patients with acne who consumed a high glycemic–load diet was significantly higher than the number of controls consuming a similar diet (P=.008). Additionally, significantly higher levels of mean (SD) serum IGF-1 on quantitative sandwich enzyme-linked immunosorbent assay in acne patients vs controls (543.2 [174.7] ng/mL vs 316.9 [95.7] ng/mL; P<.001) was identified, and these levels correlated significantly with high glycemic–load diet consumption.21 In another study, Kartal et al22 found that basal and fasting insulin levels and homeostasis model assessment scores evaluating for insulin resistance were significantly higher in 36 women compared with 24 age/sex-matched controls (P<.05). This finding remained significant even after excluding women with hyperandrogenemia (P<.05).22
Highlighting the importance of IGF-1 in the pathogenesis of acne, patients with genetic disorders characterized by IGF-1 deficiency, such as Laron syndrome, do not develop acne despite having a functional androgen receptor. Treatment with IGF-1 in these patients induces acne, further supporting the role of IGF-1 in the pathogenesis of this condition.23
The mTORC1 Pathway
Comprised of mTOR in addition to other proteins, mTORC1 is a nutrient-sensitive regulator of cellular growth, proliferation, lipid synthesis, and protein translation.5 Increased activity of mTORC1 has been described in diabetes, neurodegenerative disease, and cancer,14,24 while decreased activity may promote longevity.25 Regulation of mTORC1 occurs through several mechanisms. Growth factors such as insulin and IGF-1 promote mTORC1 activation through the PI3K/Akt pathway. Several amino acids—specifically branched chain amino acids such as alanine, arginine, asparagine, glutamine, histidine, leucine, methionine, serine, threonine, and valine—also can activate mTORC1 independently.26 Excess glucose leads to decreased adenosine monophosphate–activated protein kinase and increased activity of mTORC1, which occurs separately from insulin or IGF-1.27 Starvation blocks mTORC1 via increased adenosine monophosphate–activated protein kinase and starvation-induced hypoxia.26,28 To activate mTORC1, both the IGF-1 or insulin signal and amino acid excess must be present.29 Although not studied in acne, altering the dietary protein content in obese mice has been shown to perturb the mTORC1 pathway, leading to pathologic changes in the mTORC1-autophagy signaling axis, increased amino acid release into the blood, and an acute elevation in mTORC1 signaling.30
Another major regulator of mTORC1 is Forkhead box protein O1 (FOXO1), which is a transcription factor that regulates mTORC1 through sestrin 3.31,32 Sestrin 3 is a stress-induced protein that helps regulate blood glucose and promote insulin sensitivity.33 When FOXO1 is translocated to the cell nucleus, it upregulates the expression of sestrin 3, resulting in mTORC1 inhibition.31,32 Insulin, IGF-1, and nutrient excess lead to FOXO1 translocation to the cell cytoplasm where it can no longer mitigate mTORC1 activity, while the fasted state leads to translocation to the nucleus.34 A single study evaluated the association between FOXO1, mTORC1, a high glycemic–load diet, and acne development. Immunohistochemical detection of mTORC1 assessed by digital image analysis revealed significantly greater expression in inflamed pilosebaceous units found in acne patients (P<.001). Immunohistochemical cytoplasmic expression of FOXO1 and mTOR (used as a proxy for mTORC1) was significantly higher in patients on a high glycemic–load diet (P=.021 and P=.009, respectively) as well as in patients with more severe forms of acne (P=.005 and P=.015, respectively) and elevated IGF-1 levels (P=.004 and P=.003, respectively).21
mTORC1 contributes to the proliferation of keratinocytes and excess sebum production, both independently and through androgen-mediated processes.35-40 Insulinlike growth factor 1 binding the IGF-1 receptor leads to proliferation of keratinocytes lining the sebaceous gland and hair follicle in vivo.35 In mice with epidermis-specific deletion of mTOR, keratinocyte proliferation was decreased and hair follicles were diminished both in number and development. Genetic loss of mTOR in the epidermis led to attenuated signaling pathways of mTORC1 and mTORC2.36
Androgen function is augmented by mTORC1, FOXO1, and IGF-1 through several mechanisms, which may partially explain the hormonal relationship to acne. Androgens increase IGF-1 within the hair follicle.37 In prostate cancer cells, IGF-1 then facilitates movement of FOXO1 to the cytoplasm, preventing it from blocking mTORC1. This effective inactivation of FOXO1 thus further augments the impact of androgens by both allowing unchecked mTORC1 pathway activity and increasing translocation of the androgen receptor (AR) to the nucleus where it exerts its effects.38 Interestingly, genetic polymorphisms of the AR have been shown to cause variable affinity of FOXO1 for the AR; specifically, shorter CAG (cytosine, adenine, guanine) repeat length may lead to decreased FOXO1 binding and is associated with an increased risk for acne.41-43 In addition to its effects on the hair follicle, IGF-1 stimulates production of testosterone and dehydroepiandrosterone as well as activates 5α-reductase, leading to higher dihydrotestosterone levels, which activate the AR with higher affinity than testosterone.44 In some tissues, androgens help regulate the mTORC1 pathway through positive feedback loops.45,46 At this time, we do not know if this occurs in the pathogenesis of acne.
Isotretinoin is the treatment of choice for refractory acne. It has been hypothesized that isotretinoin induces sebocyte apoptosis via the upregulation of FOXO transcription factors and p53.47 Elevated levels of nuclear FOXO1 have been found in the sebaceous glands of patients following initiation of treatment with isotretinoin and are hypothesized to play a major role in the drug’s effectiveness. Specifically, biopsies from 14 acne patients before and after 6 weeks of isotretinoin therapy were analyzed with immunohistochemical staining and found to have a significantly improved nuclear to cytoplasmic ratio of nonphosphorylated FOXO1 (P<.001).47
Practical Recommendations
Given the available evidence, it is important for dermatologists to address dietary recommendations in acne patients. Although large randomized controlled trials on diet and acne severity are challenging to conduct in this population, the existing literature suggests that patients should avoid high glycemic index simple sugars and processed grains, and patients should focus on eating more complex carbohydrates in the form of legumes, vegetables, fruits, and tubers.6-8 With regard to dairy, milk (especially skim) has been associated with increased risks for acne.11,13 Fermented dairy products may have less impact on acne severity and include cheese, yogurt (unsweetened to keep glycemic index low), and sour cream.12
The current understanding of the pathogenesis of acne includes altered keratinization, follicular obstruction, overproduction of sebum, and microbial colonization ( Cutibacterium acnes ) of the pilosebaceous unit resulting in perifollicular inflammation. 1 A deeper dive into the hormonal and molecular drivers of acne have implicated insulin, insulinlike growth factor 1 (IGF-1), corticotropin-releasing hormone, the phosphoinositide 3 -kinase/Akt pathway, mitogen-activated protein kinase pathway, and the nuclear factor κ B pathway. 2-4 A Western diet comprised of high glycemic index foods, carbohydrates, and dairy enhances the production of insulin and IGF-1. A downstream effect of excess insulin and IGF-1 is overactivity of the mammalian target of rapamycin complex 1 (mTORC1), a major promoter of cellular growth and proliferation that primarily is regulated through nutrient availability. 5 This article will review our understanding of the impact of the Western diet on acne pathogenesis and highlight the existing evidence behind the contributions of the mTORC1 pathway in this process. Although quality randomized controlled trials analyzing these effects are limited, dermatologists should understand the existing evidence supporting the potential impacts of diet on acne.
The Western Diet
Glycemic Index—To assess the impact of a high glycemic index diet on acne, Kwon et al6 evaluated 32 patients with mild to moderate acne and placed them on a low or high glycemic index diet for 10 weeks. The low glycemic index diet group was found to have a 70% reduction in the mean number of inflammatory acne lesions from baseline (P<.05), while the high glycemic index diet group had no significant reduction. Noninflammatory lesion counts remained statistically unchanged.6 Smith et al7 studied 43 male patients with acne on either a low glycemic index diet or a self-directed high glycemic diet that was carbohydrate dense. The low glycemic index group showed greater improvement in lesion count as well as improved insulin sensitivity at 12 weeks. Specifically, the mean lesion count (SEM) decreased by 23.5 (3.9) in the low glycemic index group and by only 12.0 (3.5) in the control group (P=.03).7 Observational studies also have supported this hypothesis. After adjustment, an analysis of 24,452 participants in the NutriNet-Santé cohort found significant associations between current acne and the consumption of sugary beverages (adjusted OR, 1.18; 95% CI, 1.01-1.38) and the consumption of fatty and sugary products (adjusted OR, 1.54; 95% CI, 1.09-2.16).8 A Cochrane review that included only 2 studies (Kwon et al6 and Smith et al7) did not find evidence to suggest a low glycemic index diet for noninflammatory lesion count reduction but did note possible benefit for a reduction in inflammatory and total lesion counts; however, Kwon et al6 had incomplete data.9
Dairy—A large retrospective study including 47,355 nurses noted the frequency of milk intake was significantly associated with increased prevalence of acne in adolescence (prevalence ratio, 1.22; 95% CI, 1.03-1.44; P=.002).10 A 2019 meta-analysis further suggested a significant relationship between acne and milk in highest vs lowest intake groups (OR, 1.48; 95% CI, 1.31-1.66) with no significant heterogeneity between the studies (I2=23.6%, P=.24 for heterogeneity), as well as a positive relationship between the highest vs lowest intake of low-fat milk (OR, 1.25; 95% CI, 1.10-1.43) and skim milk (OR, 1.82; 95% CI, 1.34-2.47). In this meta-analysis, yogurt and cheese consumption were not significantly associated with acne (OR, 0.90; 95% CI, 0.73-1.11).11 One non–evidence-based explanation for this may be that fermented dairy products have different biological actions. Pasteurized milk allows microRNAs that directly activate mTORC1 to persist, whereas the bacteria present in the fermentation process may augment this.12 A separate meta-analysis from 2018 did find that yogurt consumption was positively associated with acne (OR, 1.36; 95% CI, 1.05-1.77; P=.022), highlighting the need for larger, more rigorous studies on this topic.13
Insulin and IGF-1—As reviewed above, acne has been considered a disease of Western society, with the Western diet at the center of this association.14 A typical Western diet consists of high glycemic index foods, carbohydrates, and dairy, all of which enhance the production of insulin and IGF-1. Insulin levels increase secondary to high blood glucose and to a lesser degree by protein intake.15 Insulinlike growth factor 1 production is most influenced by age and peaks during puberty; however, high protein diets also increase liver IGF-1 production and release.16 When present in excess, insulin can function as a growth factor. Insulin exerts its anabolic effects through the IGF-1 pathway; however, insulin and IGF-1 are produced in response to different signals.17 Endocrine production of IGF-1 represents 70% of blood levels, peaks at puberty, and rapidly declines in the third decade of life.18 Insulin is produced by the pancreas, and levels correspond to lifestyle and genetically induced insulin resistance.19
Adolescents have elevated levels of IGF-1 as a major driver of puberty-associated growth.20 Despite the natural decrease in IGF-1 following puberty, acne persists in many patients and can even develop for the first time in adulthood in a subset of patients. A study of 40 acne patients and 20 controls found that patients with acne who consumed a high glycemic–load diet was significantly higher than the number of controls consuming a similar diet (P=.008). Additionally, significantly higher levels of mean (SD) serum IGF-1 on quantitative sandwich enzyme-linked immunosorbent assay in acne patients vs controls (543.2 [174.7] ng/mL vs 316.9 [95.7] ng/mL; P<.001) was identified, and these levels correlated significantly with high glycemic–load diet consumption.21 In another study, Kartal et al22 found that basal and fasting insulin levels and homeostasis model assessment scores evaluating for insulin resistance were significantly higher in 36 women compared with 24 age/sex-matched controls (P<.05). This finding remained significant even after excluding women with hyperandrogenemia (P<.05).22
Highlighting the importance of IGF-1 in the pathogenesis of acne, patients with genetic disorders characterized by IGF-1 deficiency, such as Laron syndrome, do not develop acne despite having a functional androgen receptor. Treatment with IGF-1 in these patients induces acne, further supporting the role of IGF-1 in the pathogenesis of this condition.23
The mTORC1 Pathway
Comprised of mTOR in addition to other proteins, mTORC1 is a nutrient-sensitive regulator of cellular growth, proliferation, lipid synthesis, and protein translation.5 Increased activity of mTORC1 has been described in diabetes, neurodegenerative disease, and cancer,14,24 while decreased activity may promote longevity.25 Regulation of mTORC1 occurs through several mechanisms. Growth factors such as insulin and IGF-1 promote mTORC1 activation through the PI3K/Akt pathway. Several amino acids—specifically branched chain amino acids such as alanine, arginine, asparagine, glutamine, histidine, leucine, methionine, serine, threonine, and valine—also can activate mTORC1 independently.26 Excess glucose leads to decreased adenosine monophosphate–activated protein kinase and increased activity of mTORC1, which occurs separately from insulin or IGF-1.27 Starvation blocks mTORC1 via increased adenosine monophosphate–activated protein kinase and starvation-induced hypoxia.26,28 To activate mTORC1, both the IGF-1 or insulin signal and amino acid excess must be present.29 Although not studied in acne, altering the dietary protein content in obese mice has been shown to perturb the mTORC1 pathway, leading to pathologic changes in the mTORC1-autophagy signaling axis, increased amino acid release into the blood, and an acute elevation in mTORC1 signaling.30
Another major regulator of mTORC1 is Forkhead box protein O1 (FOXO1), which is a transcription factor that regulates mTORC1 through sestrin 3.31,32 Sestrin 3 is a stress-induced protein that helps regulate blood glucose and promote insulin sensitivity.33 When FOXO1 is translocated to the cell nucleus, it upregulates the expression of sestrin 3, resulting in mTORC1 inhibition.31,32 Insulin, IGF-1, and nutrient excess lead to FOXO1 translocation to the cell cytoplasm where it can no longer mitigate mTORC1 activity, while the fasted state leads to translocation to the nucleus.34 A single study evaluated the association between FOXO1, mTORC1, a high glycemic–load diet, and acne development. Immunohistochemical detection of mTORC1 assessed by digital image analysis revealed significantly greater expression in inflamed pilosebaceous units found in acne patients (P<.001). Immunohistochemical cytoplasmic expression of FOXO1 and mTOR (used as a proxy for mTORC1) was significantly higher in patients on a high glycemic–load diet (P=.021 and P=.009, respectively) as well as in patients with more severe forms of acne (P=.005 and P=.015, respectively) and elevated IGF-1 levels (P=.004 and P=.003, respectively).21
mTORC1 contributes to the proliferation of keratinocytes and excess sebum production, both independently and through androgen-mediated processes.35-40 Insulinlike growth factor 1 binding the IGF-1 receptor leads to proliferation of keratinocytes lining the sebaceous gland and hair follicle in vivo.35 In mice with epidermis-specific deletion of mTOR, keratinocyte proliferation was decreased and hair follicles were diminished both in number and development. Genetic loss of mTOR in the epidermis led to attenuated signaling pathways of mTORC1 and mTORC2.36
Androgen function is augmented by mTORC1, FOXO1, and IGF-1 through several mechanisms, which may partially explain the hormonal relationship to acne. Androgens increase IGF-1 within the hair follicle.37 In prostate cancer cells, IGF-1 then facilitates movement of FOXO1 to the cytoplasm, preventing it from blocking mTORC1. This effective inactivation of FOXO1 thus further augments the impact of androgens by both allowing unchecked mTORC1 pathway activity and increasing translocation of the androgen receptor (AR) to the nucleus where it exerts its effects.38 Interestingly, genetic polymorphisms of the AR have been shown to cause variable affinity of FOXO1 for the AR; specifically, shorter CAG (cytosine, adenine, guanine) repeat length may lead to decreased FOXO1 binding and is associated with an increased risk for acne.41-43 In addition to its effects on the hair follicle, IGF-1 stimulates production of testosterone and dehydroepiandrosterone as well as activates 5α-reductase, leading to higher dihydrotestosterone levels, which activate the AR with higher affinity than testosterone.44 In some tissues, androgens help regulate the mTORC1 pathway through positive feedback loops.45,46 At this time, we do not know if this occurs in the pathogenesis of acne.
Isotretinoin is the treatment of choice for refractory acne. It has been hypothesized that isotretinoin induces sebocyte apoptosis via the upregulation of FOXO transcription factors and p53.47 Elevated levels of nuclear FOXO1 have been found in the sebaceous glands of patients following initiation of treatment with isotretinoin and are hypothesized to play a major role in the drug’s effectiveness. Specifically, biopsies from 14 acne patients before and after 6 weeks of isotretinoin therapy were analyzed with immunohistochemical staining and found to have a significantly improved nuclear to cytoplasmic ratio of nonphosphorylated FOXO1 (P<.001).47
Practical Recommendations
Given the available evidence, it is important for dermatologists to address dietary recommendations in acne patients. Although large randomized controlled trials on diet and acne severity are challenging to conduct in this population, the existing literature suggests that patients should avoid high glycemic index simple sugars and processed grains, and patients should focus on eating more complex carbohydrates in the form of legumes, vegetables, fruits, and tubers.6-8 With regard to dairy, milk (especially skim) has been associated with increased risks for acne.11,13 Fermented dairy products may have less impact on acne severity and include cheese, yogurt (unsweetened to keep glycemic index low), and sour cream.12
- Zaenglein AL. Acne vulgaris. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. Elsevier; 2017:588-603.
- Ganceviciene R, Graziene V, Fimmel S, et al. Involvement of the corticotropin-releasing hormone system in the pathogenesis of acne vulgaris. Br J Dermatol. 2009;160:345-352.
- Kang S, Cho S, Chung JH, et al. Inflammation and extracellular matrix degradation mediated by activated transcription factors nuclear factor-kappaB and activator protein-1 in inflammatory acne lesions in vivo. Am J Pathol. 2005;166:1691-1699.
- Cong TX, Hao D, Wen X, et al. From pathogenesis of acne vulgaris to anti-acne agents. Arch Dermatol Res. 2019;311:337-349.
- Pópulo H, Lopes JM, Soares P. The mTOR signalling pathway in human cancer. Int J Mol Sci. 2012;13:1886-1918.
- Kwon HH, Yoon JY, Hong JS, et al. Clinical and histological effect of a low glycaemic load diet in treatment of acne vulgaris in Korean patients: a randomized, controlled trial. Acta Derm Venereol. 2012;92:241-246.
- Smith RN, Mann NJ, Braue A, et al. A low-glycemic-load diet improves symptoms in acne vulgaris patients: a randomized controlled trial. Am J Clin Nutr. 2007;86:107-115.
- Penso L, Touvier M, Deschasaux M, et al. Association between adult acne and dietary behaviors: findings from the NutriNet-Santé prospective cohort study. JAMA Dermatol. 2020;156:854-862.
- Cao H, Yang G, Wang Y, et al. Complementary therapies for acne vulgaris. Cochrane Database Syst Rev. 2015;1:CD009436.
- Adebamowo CA, Spiegelman D, Danby FW, et al. High school dietary dairy intake and teenage acne. J Am Acad Dermatol. 2005;52:207-214.
- Aghasi M, Golzarand M, Shab-Bidar S, et al. Dairy intake and acne development: a meta-analysis of observational studies. Clin Nutr. 2019;38:1067-1075.
- Melnik BC, Schmitz G. Pasteurized non-fermented cow’s milk but not fermented milk is a promoter of mTORC1-driven aging and increased mortality. Ageing Res Rev. 2021;67:101270.
- Juhl CR, Bergholdt HKM, Miller IM, et al. Dairy intake and acne vulgaris: a systematic review and meta-analysis of 78,529 children, adolescents, and young adults. Nutrients. 2018;10:1049. doi:10.3390/nu10081049
- Melnik BC. Linking diet to acne metabolomics, inflammation, and comedogenesis: an update. Clin Cosmet Investig Dermatol. 2015;8:371-388.
- Smart CEM, King BR, Lopez PE. Insulin dosing for fat and protein: is it time? Diabetes Care. 2020;43:13-15.
- Wan X, Wang S, Xu J, et al. Dietary protein-induced hepatic IGF-1 secretion mediated by PPARγ activation. PLoS One. 2017;12:E0173174.
- Bedinger DH, Adams SH. Metabolic, anabolic, and mitogenic insulin responses: a tissue-specific perspective for insulin receptor activators. Mol Cell Endocrinol. 2015;415:143-156.
- Gubbi S, Quipildor GF, Barzilai N, et al. 40 YEARS of IGF1: IGF1: the Jekyll and Hyde of the aging brain. J Mol Endocrinol. 2018;61:T171-T185.
- Kolb H, Kempf K, Röhling M, et al. Insulin: too much of a good thing is bad. BMC Med. 2020;18:224.
- Wood CL, Lane LC, Cheetham T. Puberty: normal physiology (brief overview). Best Pract Res Clin Endocrinol Metab. 2019;33:101265.
- Agamia NF, Abdallah DM, Sorour O, et al. Skin expression of mammalian target of rapamycin and forkhead box transcription factor O1, and serum insulin-like growth factor-1 in patients with acne vulgaris and their relationship with diet. Br J Dermatol. 2016;174:1299-1307.
- Kartal D, Yildiz H, Ertas R, et al. Association between isolated female acne and insulin resistance: a prospective study. G Ital Dermatol Venereol. 2016;151:353-357.
- Ben-Amitai D, Laron Z. Effect of insulin-like growth factor-1 deficiency or administration on the occurrence of acne. J Eur Acad Dermatol Venereol. 2011;25:950-954.
- Kim LC, Cook RS, Chen J. mTORC1 and mTORC2 in cancer and the tumor microenvironment. Oncogene. 2017;36:2191-2201.
- Weichhart T. mTOR as regulator of lifespan, aging, and cellular senescence: a mini-review. Gerontology. 2018;64:127-134.
- Melick CH, Jewell JL. Regulation of mTORC1 by upstream stimuli. Genes. 2020;11:989. doi:10.3390/genes11090989
- Li M, Zhang CS, Feng JW, et al. Aldolase is a sensor for both low and high glucose, linking to AMPK and mTORC1. Cell Res. 2021;31:478-481.
- Yan T, Zhang J, Tang D, et al. Hypoxia regulates mTORC1-mediated keratinocyte motility and migration via the AMPK pathway. PLoS One. 2017;12:E0169155.
- Dennis MD, Baum JI, Kimball SR, et al. Mechanisms involved in the coordinate regulation of mTORC1 by insulin and amino acids. J Biol Chem. 2011;286:8287-8296.
- Choi BSY, Daniel N, Houde VP, et al. Feeding diversified protein sources exacerbates hepatic insulin resistance via increased gut microbial branched-chain fatty acids and mTORC1 signaling in obese mice. Nat Commun. 2021;12:3377.
- Chen CC, Jeon SM, Bhaskar PT, et al. FoxOs inhibit mTORC1 and activate Akt by inducing the expression of Sestrin3 and Rictor. Dev Cell. 2010;18:592-604.
- Chen Y, Huang T, Yu Z, et al. The functions and roles of sestrins in regulating human diseases. Cell Mol Biol Lett. 2022;27:2.
- Tao R, Xiong X, Liangpunsakul S, et al. Sestrin 3 protein enhances hepatic insulin sensitivity by direct activation of the mTORC2-Akt signaling. Diabetes. 2015;64:1211-1223.
- Gross DN, Wan M, Birnbaum MJ. The role of FOXO in the regulation of metabolism. Curr Diab Rep. 2009;9:208-214.
- Gilhar A, Ish-Shalom S, Pillar T, et al. Effect of anti–insulin-like growth factor 1 on epidermal proliferation of human skin transplanted onto nude mice treated with growth hormone. Endocrinology. 1994;134:229-232.
- Ding X, Bloch W, Iden S, et al. mTORC1 and mTORC2 regulate skin morphogenesis and epidermal barrier formation. Nat Commun. 2016;7:13226.
- Inui S, Itami S. Androgen actions on the human hair follicle: perspectives. Exp Dermatol. 2013;22:168-171.
- Fan W, Yanase T, Morinaga H, et al. Insulin-like growth factor 1/insulin signaling activates androgen signaling through direct interactions of Foxo1 with androgen receptor. J Biol Chem. 2007;282:7329-7338.
- Alestas T, Ganceviciene R, Fimmel S, et al. Enzymes involved in the biosynthesis of leukotriene B4 and prostaglandin E2 are active in sebaceous glands. J Mol Med. 2006;84:75-87.
- Smith TM, Gilliland K, Clawson GA, et al. IGF-1 induces SREBP-1 expression and lipogenesis in SEB-1 sebocytes via activation of the phosphoinositide 3-kinase/Akt pathway. J Invest Dermatol. 2008;128:1286-1293.
- Furtado GV, Yang J, Wu D, et al. FOXO1 controls protein synthesis and transcript abundance of mutant polyglutamine proteins, preventing protein aggregation. Hum Mol Genet. 2021;30:996-1005.
- Melnik BC. Isotretinoin and FoxO1: a scientific hypothesis. Dermatoendocrinol. 2011;3:141-165.
- Heng AHS, Say YH, Sio YY, et al. Gene variants associated with acne vulgaris presentation and severity: a systematic review and meta-analysis. BMC Med Genomics. 2021;14:103.
- Li J, Al-Azzawi F. Mechanism of androgen receptor action. Maturitas. 2009;63:142-148.
- Zhao Y, Tindall DJ, Huang H. Modulation of androgen receptor by FOXA1 and FOXO1 factors in prostate cancer. Int J Biol Sci. 2014;10:614-619.
- Hamdi MM, Mutungi G. Dihydrotestosterone stimulates amino acid uptake and the expression of LAT2 in mouse skeletal muscle fibres through an ERK1/2-dependent mechanism. J Physiol. 2011;589(pt 14):3623-3640.
- Agamia NF, Hussein OM, Abdelmaksoud RE, et al. Effect of oral isotretinoin on the nucleocytoplasmic distribution of FoxO1 and FoxO3 proteins in sebaceous glands of patients with acne vulgaris. Exp Dermatol. 2018;27:1344-1351.
- Kolovou GD, Watts GF, Mikhailidis DP, et al. Postprandial hypertriglyceridaemia revisited in the era of non-fasting lipid profile testing: a 2019 expert panel statement, main text. Curr Vasc Pharmacol. 2019;17:498-514.
- Svoboda SA, Shields BE. Cutaneous manifestations of nutritional excess: pathophysiologic effects of hyperglycemia and hyperinsulinemia on the skin. Cutis. 2021;107:74-78.
- González-González JG, Mancillas-Adame LG, Fernández-Reyes M, et al. Androgenetic alopecia and insulin resistance in young men. Clin Endocrinol . 2009;71:494-499.
- Livadas S, Anagnostis P, Bosdou JK, et al. Polycystic ovary syndrome and type 2 diabetes mellitus: a state-of-the-art review. World J Diabetes. 2022;13:5-26.
- Zaenglein AL. Acne vulgaris. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. Elsevier; 2017:588-603.
- Ganceviciene R, Graziene V, Fimmel S, et al. Involvement of the corticotropin-releasing hormone system in the pathogenesis of acne vulgaris. Br J Dermatol. 2009;160:345-352.
- Kang S, Cho S, Chung JH, et al. Inflammation and extracellular matrix degradation mediated by activated transcription factors nuclear factor-kappaB and activator protein-1 in inflammatory acne lesions in vivo. Am J Pathol. 2005;166:1691-1699.
- Cong TX, Hao D, Wen X, et al. From pathogenesis of acne vulgaris to anti-acne agents. Arch Dermatol Res. 2019;311:337-349.
- Pópulo H, Lopes JM, Soares P. The mTOR signalling pathway in human cancer. Int J Mol Sci. 2012;13:1886-1918.
- Kwon HH, Yoon JY, Hong JS, et al. Clinical and histological effect of a low glycaemic load diet in treatment of acne vulgaris in Korean patients: a randomized, controlled trial. Acta Derm Venereol. 2012;92:241-246.
- Smith RN, Mann NJ, Braue A, et al. A low-glycemic-load diet improves symptoms in acne vulgaris patients: a randomized controlled trial. Am J Clin Nutr. 2007;86:107-115.
- Penso L, Touvier M, Deschasaux M, et al. Association between adult acne and dietary behaviors: findings from the NutriNet-Santé prospective cohort study. JAMA Dermatol. 2020;156:854-862.
- Cao H, Yang G, Wang Y, et al. Complementary therapies for acne vulgaris. Cochrane Database Syst Rev. 2015;1:CD009436.
- Adebamowo CA, Spiegelman D, Danby FW, et al. High school dietary dairy intake and teenage acne. J Am Acad Dermatol. 2005;52:207-214.
- Aghasi M, Golzarand M, Shab-Bidar S, et al. Dairy intake and acne development: a meta-analysis of observational studies. Clin Nutr. 2019;38:1067-1075.
- Melnik BC, Schmitz G. Pasteurized non-fermented cow’s milk but not fermented milk is a promoter of mTORC1-driven aging and increased mortality. Ageing Res Rev. 2021;67:101270.
- Juhl CR, Bergholdt HKM, Miller IM, et al. Dairy intake and acne vulgaris: a systematic review and meta-analysis of 78,529 children, adolescents, and young adults. Nutrients. 2018;10:1049. doi:10.3390/nu10081049
- Melnik BC. Linking diet to acne metabolomics, inflammation, and comedogenesis: an update. Clin Cosmet Investig Dermatol. 2015;8:371-388.
- Smart CEM, King BR, Lopez PE. Insulin dosing for fat and protein: is it time? Diabetes Care. 2020;43:13-15.
- Wan X, Wang S, Xu J, et al. Dietary protein-induced hepatic IGF-1 secretion mediated by PPARγ activation. PLoS One. 2017;12:E0173174.
- Bedinger DH, Adams SH. Metabolic, anabolic, and mitogenic insulin responses: a tissue-specific perspective for insulin receptor activators. Mol Cell Endocrinol. 2015;415:143-156.
- Gubbi S, Quipildor GF, Barzilai N, et al. 40 YEARS of IGF1: IGF1: the Jekyll and Hyde of the aging brain. J Mol Endocrinol. 2018;61:T171-T185.
- Kolb H, Kempf K, Röhling M, et al. Insulin: too much of a good thing is bad. BMC Med. 2020;18:224.
- Wood CL, Lane LC, Cheetham T. Puberty: normal physiology (brief overview). Best Pract Res Clin Endocrinol Metab. 2019;33:101265.
- Agamia NF, Abdallah DM, Sorour O, et al. Skin expression of mammalian target of rapamycin and forkhead box transcription factor O1, and serum insulin-like growth factor-1 in patients with acne vulgaris and their relationship with diet. Br J Dermatol. 2016;174:1299-1307.
- Kartal D, Yildiz H, Ertas R, et al. Association between isolated female acne and insulin resistance: a prospective study. G Ital Dermatol Venereol. 2016;151:353-357.
- Ben-Amitai D, Laron Z. Effect of insulin-like growth factor-1 deficiency or administration on the occurrence of acne. J Eur Acad Dermatol Venereol. 2011;25:950-954.
- Kim LC, Cook RS, Chen J. mTORC1 and mTORC2 in cancer and the tumor microenvironment. Oncogene. 2017;36:2191-2201.
- Weichhart T. mTOR as regulator of lifespan, aging, and cellular senescence: a mini-review. Gerontology. 2018;64:127-134.
- Melick CH, Jewell JL. Regulation of mTORC1 by upstream stimuli. Genes. 2020;11:989. doi:10.3390/genes11090989
- Li M, Zhang CS, Feng JW, et al. Aldolase is a sensor for both low and high glucose, linking to AMPK and mTORC1. Cell Res. 2021;31:478-481.
- Yan T, Zhang J, Tang D, et al. Hypoxia regulates mTORC1-mediated keratinocyte motility and migration via the AMPK pathway. PLoS One. 2017;12:E0169155.
- Dennis MD, Baum JI, Kimball SR, et al. Mechanisms involved in the coordinate regulation of mTORC1 by insulin and amino acids. J Biol Chem. 2011;286:8287-8296.
- Choi BSY, Daniel N, Houde VP, et al. Feeding diversified protein sources exacerbates hepatic insulin resistance via increased gut microbial branched-chain fatty acids and mTORC1 signaling in obese mice. Nat Commun. 2021;12:3377.
- Chen CC, Jeon SM, Bhaskar PT, et al. FoxOs inhibit mTORC1 and activate Akt by inducing the expression of Sestrin3 and Rictor. Dev Cell. 2010;18:592-604.
- Chen Y, Huang T, Yu Z, et al. The functions and roles of sestrins in regulating human diseases. Cell Mol Biol Lett. 2022;27:2.
- Tao R, Xiong X, Liangpunsakul S, et al. Sestrin 3 protein enhances hepatic insulin sensitivity by direct activation of the mTORC2-Akt signaling. Diabetes. 2015;64:1211-1223.
- Gross DN, Wan M, Birnbaum MJ. The role of FOXO in the regulation of metabolism. Curr Diab Rep. 2009;9:208-214.
- Gilhar A, Ish-Shalom S, Pillar T, et al. Effect of anti–insulin-like growth factor 1 on epidermal proliferation of human skin transplanted onto nude mice treated with growth hormone. Endocrinology. 1994;134:229-232.
- Ding X, Bloch W, Iden S, et al. mTORC1 and mTORC2 regulate skin morphogenesis and epidermal barrier formation. Nat Commun. 2016;7:13226.
- Inui S, Itami S. Androgen actions on the human hair follicle: perspectives. Exp Dermatol. 2013;22:168-171.
- Fan W, Yanase T, Morinaga H, et al. Insulin-like growth factor 1/insulin signaling activates androgen signaling through direct interactions of Foxo1 with androgen receptor. J Biol Chem. 2007;282:7329-7338.
- Alestas T, Ganceviciene R, Fimmel S, et al. Enzymes involved in the biosynthesis of leukotriene B4 and prostaglandin E2 are active in sebaceous glands. J Mol Med. 2006;84:75-87.
- Smith TM, Gilliland K, Clawson GA, et al. IGF-1 induces SREBP-1 expression and lipogenesis in SEB-1 sebocytes via activation of the phosphoinositide 3-kinase/Akt pathway. J Invest Dermatol. 2008;128:1286-1293.
- Furtado GV, Yang J, Wu D, et al. FOXO1 controls protein synthesis and transcript abundance of mutant polyglutamine proteins, preventing protein aggregation. Hum Mol Genet. 2021;30:996-1005.
- Melnik BC. Isotretinoin and FoxO1: a scientific hypothesis. Dermatoendocrinol. 2011;3:141-165.
- Heng AHS, Say YH, Sio YY, et al. Gene variants associated with acne vulgaris presentation and severity: a systematic review and meta-analysis. BMC Med Genomics. 2021;14:103.
- Li J, Al-Azzawi F. Mechanism of androgen receptor action. Maturitas. 2009;63:142-148.
- Zhao Y, Tindall DJ, Huang H. Modulation of androgen receptor by FOXA1 and FOXO1 factors in prostate cancer. Int J Biol Sci. 2014;10:614-619.
- Hamdi MM, Mutungi G. Dihydrotestosterone stimulates amino acid uptake and the expression of LAT2 in mouse skeletal muscle fibres through an ERK1/2-dependent mechanism. J Physiol. 2011;589(pt 14):3623-3640.
- Agamia NF, Hussein OM, Abdelmaksoud RE, et al. Effect of oral isotretinoin on the nucleocytoplasmic distribution of FoxO1 and FoxO3 proteins in sebaceous glands of patients with acne vulgaris. Exp Dermatol. 2018;27:1344-1351.
- Kolovou GD, Watts GF, Mikhailidis DP, et al. Postprandial hypertriglyceridaemia revisited in the era of non-fasting lipid profile testing: a 2019 expert panel statement, main text. Curr Vasc Pharmacol. 2019;17:498-514.
- Svoboda SA, Shields BE. Cutaneous manifestations of nutritional excess: pathophysiologic effects of hyperglycemia and hyperinsulinemia on the skin. Cutis. 2021;107:74-78.
- González-González JG, Mancillas-Adame LG, Fernández-Reyes M, et al. Androgenetic alopecia and insulin resistance in young men. Clin Endocrinol . 2009;71:494-499.
- Livadas S, Anagnostis P, Bosdou JK, et al. Polycystic ovary syndrome and type 2 diabetes mellitus: a state-of-the-art review. World J Diabetes. 2022;13:5-26.
Practice Points
- Patients are frequently interested in the role that diet plays in acne, and dermatologists should be aware of the current evidence to answer these questions effectively.
- One of the primary pathways in acne pathogenesis, mTORC1 (mammalian target of rapamycin complex 1), is partially regulated by nutrient availability, insulin, and insulinlike growth factor 1.
- Dietary recommendations for acne based on available evidence may include a low glycemic index diet and avoidance of certain dairy products.
- Insulin resistance may underlie the pathogenesis of acne in a subset of patients, and assessing insulin resistance in acne patients should be considered.
The Impact of Prenatal Nutrition on the Development of Atopic Dermatitis in Infancy and Childhood
Atopic dermatitis (AD) is an inflammatory skin disease characterized by skin barrier disruption, skin inflammation, and pruritus.1 It is a common and often chronic skin condition associated with the development of food allergies, asthma, and allergic rhinitis, known as the atopic march.2 Atopic dermatitis is estimated to affect 10% to 25% of children, most with onset before 5 years of age, and up to 7% of adults worldwide.3 Most patients improve with time, but multiple disease trajectories are possible. Several studies have demonstrated that fewer than 4% of children develop the classic atopic march—AD followed by food allergies, asthma, and finally allergic rhinitis—with recent evidence pointing to a more complex heterogeneous progression of disease and allergic comorbidities often occurring together.4,5 The prevalence of AD has been increasing globally over the last 30 years,6 with a marked increase in developed countries.6,7 It is well accepted that AD is based on an interplay between genetic predisposition and environmental factors,8 but many suspect that the rapid rise in prevalence cannot be attributed to genetic factors alone.9 The precipitant triggers for AD remain an area of intense investigation, with ongoing debate between the “inside out” and “outside in” hypotheses; these revolve around whether abnormalities in the immune system trigger barrier dysfunction or barrier dysfunction triggers immune programming to atopy.8 Ongoing research related to genetic predisposition of AD has identified candidate genes implicated in both impaired skin barrier function and altered immune system pathways, further supporting that both theories may contribute to disease pathogenesis.
The increasing prevalence of AD, with increasing disease burden within socioeconomically advantaged countries, raises the possibility of early modifiable environmental factors that may contribute to the disease process.10 Many studies point to the influence of the 21st century lifestyle and Western diet as primary contributing factors.9,11 However, it is not clear how these factors may influence the development of allergic atopic disease. Several studies have suggested that nonheritable influences in utero can alter fetus immune function and influence the subsequent development of allergic disease.12,13 Although many studies have examined environmental factors contributing to the development of AD in infancy and childhood, less is understood about the influence of prenatal factors. Currently, in utero exposure to tobacco smoke, phthalates, and maternal distress have been potentially implicated in the development of AD.14,15 Several studies have examined the role of maternal diet and nutrition on the development of AD in offspring; however, formal recommendations and robust trial data are lacking. In this article, we examine the existing literature surrounding maternal diet on the development of AD in infancy and childhood.
Allergen Avoidance
Extrapolating from the food allergy literature, it was once suggested that allergen avoidance in early childhood had a protective effect on the subsequent development of allergies; however, more recent research has found that early exposure to common food allergens, such as peanuts or eggs, may actually reduce a child’s risk for developing these allergies later in life.16 Among infants at high risk for food allergy, sustained consumption of peanut products beginning in the first 11 months of life resulted in an 81% lower rate of peanut allergy at 60 months of age than the rate among children who avoided peanuts.17 Given the results that antigen avoidance during infancy/childhood does not protect against the development of allergies and may actually be counterproductive, it is not surprising that research studying antigen avoidance during pregnancy on the development of AD also has demonstrated limited efficacy. A systematic review of 5 trials on maternal dietary antigen avoidance (N=952) suggested no protective effects of avoiding antigenic foods during pregnancy on the development of AD in the first 18 months of life.18 Another meta-analysis evaluating 12 intervention trials looked at the effects of maternal allergenic food avoidance during pregnancy or lactation and found no reduced risk for subsequent development of allergic disease, including AD.19 The American Academy of Pediatrics 2019 consensus statement does not support maternal dietary restrictions in pregnancy for the prevention of atopic disease and makes note that the data remain limited, which complicates drawing any firm conclusions.20
Probiotic Supplementation
One of the most investigated dietary supplements for the prevention of atopic disease is probiotics, with possible benefits noted in both the prenatal and postnatal periods. Baquerizo Nole et al21 examined several studies looking at the various benefits of probiotics in AD, which included inhibition of the helper T cell (TH2) response, stimulation of the TH1 response, upregulation of regulatory T cells, acceleration of skin and mucosal barrier function, increase in intestinal microflora diversity, suppression of toxic fermentation products in the intestinal lumen from increased production of short-chain fatty acids, and inhibition of Staphylococcus aureus attachment on epidermal keratinocytes. It is unclear how this may affect infants prenatally; however, transfer of maternal intestinal microflora during delivery and shortly thereafter has demonstrated that probiotic strains remain detectable in the infant’s stool up to 6 months after delivery, even if the mother has discontinued use.22 A 2008 meta-analysis of 10 double-bind, randomized, controlled trials (N=1880) looking at the use of maternal prenatal and postnatal probiotic supplementation in the prevention of pediatric AD found a relative risk (RR) ratio of 0.69 (95% CI, 0.57-0.83) using a fixed effects model and RR ratio of 0.66 (95% CI, 0.49-0.89) using a random effects model. After exclusion of one study that evaluated the effect of postnatal probiotic supplementation only, the RR ratio decreased to 0.61 for both the fixed effects and random effects models.23 A systematic review by Panduru et al24 noted similar findings with a subgroup meta-analysis of 11 studies of prenatal supplementation followed by postnatal supplementation of probiotics, which demonstrated a protective effect on the development of AD (odds ratio [OR]=0.61, P<.001). Postnatal supplementation alone (4 studies) did not have the same association (OR=0.95, P<.82).24 A 2012 meta-analysis by Doege et al25 evaluated 7 randomized, double-blinded, placebo-controlled trials that assessed probiotic supplementation during pregnancy (without incorporation of postnatal supplementation) and found a significant risk reduction of 5.7% (P=.022) for AD in children aged 2 to 7 years. Interestingly, this was only significant for Lactobacillus and not for other bacterial strains, even if a mixture of strains included Lactobacillus. However, Panduru et al24 found both maternal Lactobacillus supplementation alone (8 studies) and in combination with Bifidobacterium (9 studies) was protective against AD development in children (OR=0.70, P=.004; OR=0.62, P<.001). A more recent 2015 meta-analysis of 17 studies (N=4755) evaluating the use of maternal probiotic supplementation in pregnancy and/or through the infant’s first 3 months of life found a significantly lower RR (0.78 [95% CI, 0.69-0.89], P=.0003) for the development of AD in infants treated with probiotics and found this risk to be even further decreased when a mixture of probiotics including both Lactobacillus and Bifidobacterium was used (RR=0.54 [95% CI, 0.43-0.68], P<.00001).26
Antioxidants
The Westernization of many developing countries’ diets—diets high in saturated fats, protein, sucrose, salt, and processed foods and low in fresh fruits and green vegetables—has led to a reduced intake of antioxidants and an increase in susceptibility to oxidative damage.27,28 One hypothesis suggests that a reduction in nutritional antioxidants and subsequent oxidative damage leads to airway inflammation that may contribute to an increased prevalence of asthma.27 In vitro data suggest that antioxidant deficiency may influence the differentiation of helper T cells to a TH2 phenotype, which can increase susceptibility to the development of asthma and allergies.29 Vitamin E specifically has been shown to inhibit IL-4 gene expression, which drives type 2 immunity and decreases expression of multiple genes that regulate epidermal barrier function, subsequently increasing susceptibility to allergic inflammation and AD.29,30 Regardless of the proposed mechanisms for antioxidant deficiency increasing susceptibility to allergic disease, studies evaluating the benefits of antioxidant intake during pregnancy in relation to AD have not been promising. Several studies have found no association between prenatal vitamin E intake and the risk for AD development in infants and children.31,32 Another study found a statistically significant inverse relationship between vitamin E intake in mothers with a history of atopy and the development of AD in their children at 2 years of age but not at 1 year of age (P-trend=.024).33 It has been suggested that varying vitamin E isoforms may contribute to the discrepant results previously discussed, with the γ-tocopherol isoform (found frequently in Westernized diets)34 as a driver of inflammation in murine models.35 West et al31 noted an association between vitamin C intake and development of “any allergic disease”—AD, IgE-mediated food allergy, or asthma—with a crude OR of 0.48 (95% CI, 0.25-0.93). However, the P-trend and adjusted OR were not statistically significant. The investigators found no association between maternal intake of beta-carotene, vitamin E, or zinc, but they did find copper supplementation to be protective on the development of AD at 1 year of age (P-trend=0.03). Interestingly, when the data for total antioxidant intake—vitamin C, vitamin E, zinc, beta-carotene, and copper from both diet and supplementation—were combined and analyzed, no statistically significant associations for any of the antioxidants were found.31 Another study of 763 Japanese mother-child pairs found a reduced risk for AD at 16 to 24 months of age with high maternal intake of beta-carotene but found no statistically significant exposure-response associations with other antioxidants, including alpha-carotene, vitamin C, or zinc from dietary intake alone.32 These results were substantiated by 2 meta-analyses evaluating a total of 93 combined intervention trials and cohorts where no association was found between vitamin or mineral intake during pregnancy and/or during infancy and the development of AD.19,36
Fatty Acids
Other dietary changes that are associated with an increased prevalence of atopic diseases in children include excess consumption of omega-6 (n-6) long-chain polyunsaturated fatty acids (LC-PUFA) and insufficient omega-3 (n-3) LC-PUFA consumption.37 Given prior evidence that allergic immune responses in infants may be primed before birth,38 researchers have questioned whether the anti-inflammatory properties of n-3 LC-PUFA when supplemented during pregnancy may have immunomodulatory effects on infants that could alter their predisposition to develop allergic disease, including AD.39 A systematic review and meta-analysis of randomized controlled trials found a statistically significant RR of 0.53 (95% CI, 0.35-0.81; P=.004) for the incidence of AD at 12 months of age with maternal supplementation of n-3 LC-PUFA.9 Another trial of 145 pregnant women randomized to supplementation with fish oil vs placebo starting at gestational week 25 and continuing through 3.5 months of breastfeeding found a reduced cumulative incidence of AD in the intervention group compared to controls at 2 years of age, with a statistically significant crude OR of 0.33 (95% CI, 0.11-0.97; P=.04).40 However, the adjusted OR was not statistically significant. In addition, they found that mothers and infants with higher proportions of docosahexaenoic acid and eicosapentaenoic acid in plasma phospholipids have been noted to have a lower prevalence of IgE-associated disease in a dose-dependent manner (P<.05 and P<.05, respectively).40 In another trial of 98 pregnant women randomized to fish oil supplementation or placebo from 20 weeks’ gestation to delivery found no difference in the frequency of AD but did note that infants in the exposure group had significantly less severe AD compared to controls (OR=0.09 [95% CI, 0.1-0.94]; P=.045).39 A prospective birth cohort study of 2641 children evaluated dietary composition during the last 4 weeks of pregnancy and found that consumption of foods rich in n-6 LC-PUFAs (eg, margarine, vegetable oil) increased the risk for developing AD, while foods rich in n-3 LC-PUFAs (eg, fish) decreased the risk for developing AD in offspring at 2 years of age. All P values for margarine, vegetable oil, and fish were statistically significant on logistic regression at P<.05.41 A longitudinal analysis of follow-up data from a randomized controlled trial looking at maternal prenatal n-3 LC-PUFA intake and the development of allergic disease (including AD) found no differences in the development of disease at 1-, 3-, or 6-year follow-up.42 Despite several studies demonstrating a possible benefit of omega-3 fatty acid intake on the development of AD in offspring, the longitudinal analysis by Best et al42 reminds us that long-term follow-up is critical in establishing benefit of any intervention given the heterogeneous and progressive nature of the atopic march and AD.
Specific Diets
Several studies have evaluated the role of dietary patterns and their influence on atopic disease. Studies evaluating dietary patterns or supplement intake can be challenging, as data often are derived from questionnaires with bias in response to families with higher socioeconomic status.9 Further, analysis of any one food group does not account for the potential interplay between nutrients.43 Studies should focus more on dietary patterns vs individual foods to assess true risk.43,44 Given these limitations, study results on diet should be carefully scrutinized; however, there are still some positive findings that deserve further investigation. Chatzi et al44 followed 460 children for 6.5 years and found a protective effect for the development of atopy in the offspring of women who had high adherence to the Mediterranean diet (OR 0.55 [95% CI, 0.31-0.97]). Another cohort study evaluating the effects of the Mediterranean diet and risk for AD in the first year of life in 2516 mother-child pairs from Spain and Greece found no statistically significant association with consumption of the Mediterranean diet and AD. The investigators also evaluated intake of fruits, nuts, vegetables, meats, processed meats, dairy products, and cereal and found no statistically significant protective benefit.45 Another systematic review of more than 90 observational studies identified no significant relationship between prenatal dietary exposures of fruits, vegetables, nuts, fat, fatty acids, eggs, cereal, milk, alcohol, tea, or coffee and risk for allergic disease in offspring, including AD.19
A Chinese prospective cohort study evaluated the dietary protein patterns of 713 mother-child pairs and the incidence of infant AD at 6 months of age.46 Dietary protein patterns were characterized as predominantly poultry, plant based, dairy and eggs, and red meat and fish. The investigators found a statistically significant reduced risk for AD in mothers who consumed plant-based or dairy and eggs protein patterns when compared to a poultry protein pattern with an adjusted OR of 0.572 (95% CI, 0.330-0.992) and 0.478 (95% CI, 0.274-0.837), respectively. This protective effect was not seen with the red meat and fish protein patterns.46 Similar results were seen in a 2020 Canadian study that evaluated the effects of a Western (fats, meats, processed foods, and starchy vegetables), balanced (diverse sources of animal proteins [especially fish], fruits, vegetables, nuts, and seeds), or plant-based (dairy, legumes, vegetables, whole grains, and an aversion to meats) diet in more than 2000 mother-infant pairs from 24 to 28 weeks’ gestation to 1 year of age. The investigators found a lower OR of AD in mothers who followed a mostly plant-based diet compared to other dietary patterns (OR 0.65 [95% CI, 0.55-0.76]; P<.001).10 Another prospective Japanese study looking at healthy (high intake of green and yellow vegetables, seaweed, mushrooms, white vegetables, pulses, potatoes, fish, sea products, fruit, and shellfish, and low intake of confectioneries and soft drinks), Western (high intake of vegetable oil, salt-containing seasonings, beef, pork, processed meat, eggs, chicken, and white vegetables, and low intake of fruit, soft drinks, and confectioneries), or Japanese (high intake of rice, miso soup, sea products, and fish, and low intake of bread, confectioneries, and dairy products) dietary patterns in 763 mother-child pairs found no association between diet during pregnancy and development of AD in offspring at 16 to 24 months.47 Unfortunately, a longitudinal data analysis has not been performed for this study.
Final Thoughts
Atopic dermatitis is a complex, progressive, and heterogeneous disease with both genetic and environmental influences. Studying the effects of diet on the development, progression, or severity of disease can be very difficult due to the heterogeneity of study designs, lack of long-term follow-up, and high potential for residual confounding. Studies evaluating dietary patterns or supplement intake can be equally challenging, as data often are derived from questionnaires with bias in response to families with higher socioeconomic status.9 Very few studies have looked specifically at maternal dietary composition and the development of AD alone (without inclusion of asthma or food allergy). Ultimately, the inconsistency of the data makes it difficult to draw conclusions and make formal recommendations for this vulnerable population. Additional evidence from well-powered trials with comparable methodology and objective outcome measures will be imperative to make formal recommendations. In addition, longitudinal follow-up will be essential to determine long-term benefit and influence on the atopic march.
- Nutten S. Atopic dermatitis: global epidemiology and risk factors. Ann Nutr Metab. 2015;66(suppl 1):8-16.
- Kapoor R, Menon C, Hoffstad O, et al. The prevalence of atopic triad in children with physician-confirmed atopic dermatitis. J Am Acad Dermatol. 2008;58:68-73.
- Abuabara K, Magyari A, McCulloch CE, et al. Prevalence of atopic eczema among patients seen in primary care: data from the Health Improvement Network. Ann Intern Med. 2019;170:354-356.
- Belgrave DC, Granell R, Simpson A, et al. Developmental profiles of eczema, wheeze, and rhinitis: two population-based birth cohort studies. PLoS Medicine. 2014;11:E1001748.
- Aguilar D, Pinart M, Koppelman GH, et al. Computational analysis of multimorbidity between asthma, eczema and rhinitis. PloS One. 2017;12:E0179125.
- Deckers IA, McLean S, Linssen S, et al. Investigating international time trends in the incidence and prevalence of atopic eczema 1990-2010: a systematic review of epidemiological studies. PloS One. 2012;7:E39803.
- Williams H, Stewart A, von Mutius E, et al. Is eczema really on the increase worldwide? J Allergy Clin Immunol. 2008;121:947-954.
- Sullivan M, Silverberg NB. Current and emerging concepts in atopic dermatitis pathogenesis. Clin Dermatol. 2017;35:349-353.
- Best KP, Gold M, Kennedy D, et al. Omega-3 long-chain PUFA intake during pregnancy and allergic disease outcomes in the offspring: a systematic review and meta-analysis of observational studies and randomized controlled trials. Am J Clin Nutr. 2016;103:128-143.
- Zulyniak MA, de Souza RJ, Shaikh M, et al. Ethnic differences in maternal diet in pregnancy and infant eczema. PloS One. 2020;15:E0232170.
- Jena PK, Sheng L, Mcneil K, et al. Long-term Western diet intake leads to dysregulated bile acid signaling and dermatitis with Th2 and Th17 pathway features in mice. J Dermatol Sci. 2019;95:13-20.
- Grieger JA, Clifton VL, Tuck AR, et al. In utero programming of allergic susceptibility. Int Arch Allergy Immunol. 2016;169:80-92. doi:10.1159/000443961
- Khan TK, Palmer DJ, Prescott SL. In-utero exposures and the evolving epidemiology of paediatric allergy. Curr Opin Allergy Clin Immunol. 2015;15:402-408. doi:10.1097/ACI.0000000000000209
- Bauer SM. Atopic eczema: genetic associations and potential links to developmental exposures. Int J Toxicol. 2017;36:187-198.
- Shinohara M, Saito H, Matsumoto K. Different timings of prenatal or postnatal tobacco smoke exposure have different effects on the development of atopic eczema/dermatitis syndrome (AEDS) during infancy. J Allergy Clin Immunol. 2012;129:AB40.
- Lerodiakonou D, Garcia-Larsen V, Logan A, et al. Timing of allergenic food introduction to the infant diet and risk of allergic or autoimmune disease: a systematic review and meta-analysis. JAMA. 2016;316:1181-1192.
- Du Toit G, Roberts G, Sayre PH, et al. Randomized trial of peanut consumption in infants at risk for peanut allergy. N Engl J Med. 2015;372:803-813.
- Kramer MS, Kakuma R. Maternal dietary antigen avoidance during pregnancy or lactation, or both, for preventing or treating atopic disease in the child. Evid Based Child Health. 2014;9:447-483.
- Garcia-Larsen V, Ierodiakonou D, Jarrold K, et al. Diet during pregnancy and infancy and risk of allergic or autoimmune disease: a systematic review and meta-analysis. PLoS Med. 2018;15:E1002507.
- Greer FR, Sicherer SH, Burks AW; Committee on Nutrition, Section on Allergy and Immunology. The effects of early nutritional interventions on the development of atopic disease in infants and children: the role of maternal dietary restriction, breastfeeding, timing of introduction of complementary foods, and hydrolyzed formulas. Pediatrics. 2019;143:e20190281.
- Baquerizo Nole KL, Yim E, Keri JE. Probiotics and prebiotics in dermatology. J Am Acad Dermatol. 2014;71:814-821.
- Schultz M, Göttl C, Young RJ, et al. Administration of oral probiotic bacteria to pregnant women causes temporary infantile colonization. J Pediatr Gastroenterol Nutr. 2004;38:293-297.
- Lee J, Seto D, Bielory L. Meta-analysis of clinical trials of probiotics for prevention and treatment of pediatric atopic dermatitis. J Allergy Clin Immunol. 2008;121:116-121.
- Panduru M, Panduru NM, Sa˘la˘va˘stru CM, et al. Probiotics and primary prevention of atopic dermatitis: a meta‐analysis of randomized controlled studies. J Eur Acad Dermatol Venereol. 2015;29:232-242.
- Doege K, Grajecki D, Zyriax BC, et al. Impact of maternal supplementation with probiotics during pregnancy on atopic eczema in childhood—a meta-analysis. Br J Nutr. 2012;107:1-6.
- Zuccotti G, Meneghin F, Aceti A, et al. Probiotics for prevention of atopic diseases in infants: systematic review and meta‐analysis. Allergy. 2015;70:1356-1371.
- Seaton A, Godden DJ, Brown K. Increase in asthma: a more toxic environment or a more susceptible population? Thorax. 1994;49:171-174.
- Manzel A, Muller DN, Hafler DA, et al. Role of “Western diet” in inflammatory autoimmune diseases. Curr Allergy Asthma Rep. 2014;14:1-8.
- Li-Weber M, Giasisi M, Trieber MK, et al. Vitamin E inhibits IL-4 gene expression in peripheral blood T cells. Eur J Immunol. 2002;32:2401-2408.
- Sehra S, Yao Y, Howell MD, et al. IL-4 regulates skin homeostasis and the predisposition toward allergic skin inflammation. J Immunol. 2010;184:3186-3190.
- West CE, Dunstan J, McCarthy S, et al. Associations between maternal antioxidant intakes in pregnancy and infant allergic outcomes. Nutrients. 2012;4:1747-1758.
- Miyake Y, Sasaki S, Tanaka K, et al. Consumption of vegetables, fruit, and antioxidants during pregnancy and wheeze and eczema in infants. Allergy. 2010;65:758-765.
- Martindale S, McNeill G, Devereux G, et al. Antioxidant intake in pregnancy in relation to wheeze and eczema in the first two years of life. Am J Respir Crit Care Med. 2005;171:121-128.
- Robison R, Kumar R. The effect of prenatal and postnatal dietary exposures on childhood development of atopic disease. Curr Opin Allergy Clin Immunol. 2010;10:139-144.
- Berdnikovs S, Abdala-Valencia H, McCary C, et al. Isoforms of vitamin E have opposing immunoregulatory functions during inflammation by regulating leukocyte recruitment. J Immunol. 2009;182:4395-4405.
- Beckhaus AA, Garcia‐Marcos L, Forno E, et al. Maternal nutrition during pregnancy and risk of asthma, wheeze, and atopic diseases during childhood: a systematic review and meta‐analysis. Allergy. 2015;70:1588-1604.
- Calder PC, Miles EA. Fatty acids and atopic disease. Pediatr Allergy Immunol. 2000;11(suppl 13):29-36.
- Prescott S, Macaubas C, Holt B, et al. Transplacental priming of the human immune system to environmental allergens: universal skewing of initial T-cell responses towards Th-2 cytokine profile. J Immunol. 1998;160:4730-4737.
- Dunstan JA, Mori TA, Barden A, et al. Fish oil supplementation in pregnancy modifies neonatal allergen-specific immune responses and clinical outcomes in infants at high risk of atopy: a randomized, controlled trial. J Allergy Clin Immunol. 2003;112:1178-1184.
- Furuhjelm C, Warstedt K, Fagerås M, et al. Allergic disease in infants up to 2 years of age in relation to plasma omega‐3 fatty acids and maternal fish oil supplementation in pregnancy and lactation. Pediatr Allergy Immunol. 2011;22:505-514.
- Sausenthaler S, Koletzko S, Schaaf B, et al; LISA Study Group. Maternal diet during pregnancy in relation to eczema and allergic sensitization in the offspring at 2 y of age. Am J Clin Nutr. 2007;85:530-537.
- Best KP, Sullivan TR, Palmer DJ, et al. Prenatal omega-3 LCPUFA and symptoms of allergic disease and sensitization throughout early childhood—a longitudinal analysis of long-term follow-up of a randomized controlled trial. World Allergy Organ J. 2018;11:10.
- Jacobs DR Jr, Steffen LM. Nutrients, foods, and dietary patterns as exposures in research: a framework for food synergy. Am J Clin Nutr. 2003;78:508-513.
- Chatzi L, Torrent M, Romieu I, et al. Mediterranean diet in pregnancy is protective for wheeze and atopy in childhood. Thorax. 2008;63:507-513.
- Chatzi L, Garcia R, Roumeliotaki T, et al. Mediterranean diet adherence during pregnancy and risk of wheeze and eczema in the first year of life: INMA (Spain) and RHEA (Greece) mother-child cohort studies. Br J Nutr. 2013;110:2058-2068.
- Zeng J, Wu W, Chen Y, et al. Maternal dietary protein patterns during pregnancy and the risk of infant eczema: a cohort study. Front Nutr. 2021;8:294.
- Miyake Y, Okubo H, Sasaki S, et al. Maternal dietary patterns during pregnancy and risk of wheeze and eczema in Japanese infants aged 16–24 months: the Osaka Maternal and Child Health Study. Pediatr Allergy Immunol. 2011;22:734-741.
Atopic dermatitis (AD) is an inflammatory skin disease characterized by skin barrier disruption, skin inflammation, and pruritus.1 It is a common and often chronic skin condition associated with the development of food allergies, asthma, and allergic rhinitis, known as the atopic march.2 Atopic dermatitis is estimated to affect 10% to 25% of children, most with onset before 5 years of age, and up to 7% of adults worldwide.3 Most patients improve with time, but multiple disease trajectories are possible. Several studies have demonstrated that fewer than 4% of children develop the classic atopic march—AD followed by food allergies, asthma, and finally allergic rhinitis—with recent evidence pointing to a more complex heterogeneous progression of disease and allergic comorbidities often occurring together.4,5 The prevalence of AD has been increasing globally over the last 30 years,6 with a marked increase in developed countries.6,7 It is well accepted that AD is based on an interplay between genetic predisposition and environmental factors,8 but many suspect that the rapid rise in prevalence cannot be attributed to genetic factors alone.9 The precipitant triggers for AD remain an area of intense investigation, with ongoing debate between the “inside out” and “outside in” hypotheses; these revolve around whether abnormalities in the immune system trigger barrier dysfunction or barrier dysfunction triggers immune programming to atopy.8 Ongoing research related to genetic predisposition of AD has identified candidate genes implicated in both impaired skin barrier function and altered immune system pathways, further supporting that both theories may contribute to disease pathogenesis.
The increasing prevalence of AD, with increasing disease burden within socioeconomically advantaged countries, raises the possibility of early modifiable environmental factors that may contribute to the disease process.10 Many studies point to the influence of the 21st century lifestyle and Western diet as primary contributing factors.9,11 However, it is not clear how these factors may influence the development of allergic atopic disease. Several studies have suggested that nonheritable influences in utero can alter fetus immune function and influence the subsequent development of allergic disease.12,13 Although many studies have examined environmental factors contributing to the development of AD in infancy and childhood, less is understood about the influence of prenatal factors. Currently, in utero exposure to tobacco smoke, phthalates, and maternal distress have been potentially implicated in the development of AD.14,15 Several studies have examined the role of maternal diet and nutrition on the development of AD in offspring; however, formal recommendations and robust trial data are lacking. In this article, we examine the existing literature surrounding maternal diet on the development of AD in infancy and childhood.
Allergen Avoidance
Extrapolating from the food allergy literature, it was once suggested that allergen avoidance in early childhood had a protective effect on the subsequent development of allergies; however, more recent research has found that early exposure to common food allergens, such as peanuts or eggs, may actually reduce a child’s risk for developing these allergies later in life.16 Among infants at high risk for food allergy, sustained consumption of peanut products beginning in the first 11 months of life resulted in an 81% lower rate of peanut allergy at 60 months of age than the rate among children who avoided peanuts.17 Given the results that antigen avoidance during infancy/childhood does not protect against the development of allergies and may actually be counterproductive, it is not surprising that research studying antigen avoidance during pregnancy on the development of AD also has demonstrated limited efficacy. A systematic review of 5 trials on maternal dietary antigen avoidance (N=952) suggested no protective effects of avoiding antigenic foods during pregnancy on the development of AD in the first 18 months of life.18 Another meta-analysis evaluating 12 intervention trials looked at the effects of maternal allergenic food avoidance during pregnancy or lactation and found no reduced risk for subsequent development of allergic disease, including AD.19 The American Academy of Pediatrics 2019 consensus statement does not support maternal dietary restrictions in pregnancy for the prevention of atopic disease and makes note that the data remain limited, which complicates drawing any firm conclusions.20
Probiotic Supplementation
One of the most investigated dietary supplements for the prevention of atopic disease is probiotics, with possible benefits noted in both the prenatal and postnatal periods. Baquerizo Nole et al21 examined several studies looking at the various benefits of probiotics in AD, which included inhibition of the helper T cell (TH2) response, stimulation of the TH1 response, upregulation of regulatory T cells, acceleration of skin and mucosal barrier function, increase in intestinal microflora diversity, suppression of toxic fermentation products in the intestinal lumen from increased production of short-chain fatty acids, and inhibition of Staphylococcus aureus attachment on epidermal keratinocytes. It is unclear how this may affect infants prenatally; however, transfer of maternal intestinal microflora during delivery and shortly thereafter has demonstrated that probiotic strains remain detectable in the infant’s stool up to 6 months after delivery, even if the mother has discontinued use.22 A 2008 meta-analysis of 10 double-bind, randomized, controlled trials (N=1880) looking at the use of maternal prenatal and postnatal probiotic supplementation in the prevention of pediatric AD found a relative risk (RR) ratio of 0.69 (95% CI, 0.57-0.83) using a fixed effects model and RR ratio of 0.66 (95% CI, 0.49-0.89) using a random effects model. After exclusion of one study that evaluated the effect of postnatal probiotic supplementation only, the RR ratio decreased to 0.61 for both the fixed effects and random effects models.23 A systematic review by Panduru et al24 noted similar findings with a subgroup meta-analysis of 11 studies of prenatal supplementation followed by postnatal supplementation of probiotics, which demonstrated a protective effect on the development of AD (odds ratio [OR]=0.61, P<.001). Postnatal supplementation alone (4 studies) did not have the same association (OR=0.95, P<.82).24 A 2012 meta-analysis by Doege et al25 evaluated 7 randomized, double-blinded, placebo-controlled trials that assessed probiotic supplementation during pregnancy (without incorporation of postnatal supplementation) and found a significant risk reduction of 5.7% (P=.022) for AD in children aged 2 to 7 years. Interestingly, this was only significant for Lactobacillus and not for other bacterial strains, even if a mixture of strains included Lactobacillus. However, Panduru et al24 found both maternal Lactobacillus supplementation alone (8 studies) and in combination with Bifidobacterium (9 studies) was protective against AD development in children (OR=0.70, P=.004; OR=0.62, P<.001). A more recent 2015 meta-analysis of 17 studies (N=4755) evaluating the use of maternal probiotic supplementation in pregnancy and/or through the infant’s first 3 months of life found a significantly lower RR (0.78 [95% CI, 0.69-0.89], P=.0003) for the development of AD in infants treated with probiotics and found this risk to be even further decreased when a mixture of probiotics including both Lactobacillus and Bifidobacterium was used (RR=0.54 [95% CI, 0.43-0.68], P<.00001).26
Antioxidants
The Westernization of many developing countries’ diets—diets high in saturated fats, protein, sucrose, salt, and processed foods and low in fresh fruits and green vegetables—has led to a reduced intake of antioxidants and an increase in susceptibility to oxidative damage.27,28 One hypothesis suggests that a reduction in nutritional antioxidants and subsequent oxidative damage leads to airway inflammation that may contribute to an increased prevalence of asthma.27 In vitro data suggest that antioxidant deficiency may influence the differentiation of helper T cells to a TH2 phenotype, which can increase susceptibility to the development of asthma and allergies.29 Vitamin E specifically has been shown to inhibit IL-4 gene expression, which drives type 2 immunity and decreases expression of multiple genes that regulate epidermal barrier function, subsequently increasing susceptibility to allergic inflammation and AD.29,30 Regardless of the proposed mechanisms for antioxidant deficiency increasing susceptibility to allergic disease, studies evaluating the benefits of antioxidant intake during pregnancy in relation to AD have not been promising. Several studies have found no association between prenatal vitamin E intake and the risk for AD development in infants and children.31,32 Another study found a statistically significant inverse relationship between vitamin E intake in mothers with a history of atopy and the development of AD in their children at 2 years of age but not at 1 year of age (P-trend=.024).33 It has been suggested that varying vitamin E isoforms may contribute to the discrepant results previously discussed, with the γ-tocopherol isoform (found frequently in Westernized diets)34 as a driver of inflammation in murine models.35 West et al31 noted an association between vitamin C intake and development of “any allergic disease”—AD, IgE-mediated food allergy, or asthma—with a crude OR of 0.48 (95% CI, 0.25-0.93). However, the P-trend and adjusted OR were not statistically significant. The investigators found no association between maternal intake of beta-carotene, vitamin E, or zinc, but they did find copper supplementation to be protective on the development of AD at 1 year of age (P-trend=0.03). Interestingly, when the data for total antioxidant intake—vitamin C, vitamin E, zinc, beta-carotene, and copper from both diet and supplementation—were combined and analyzed, no statistically significant associations for any of the antioxidants were found.31 Another study of 763 Japanese mother-child pairs found a reduced risk for AD at 16 to 24 months of age with high maternal intake of beta-carotene but found no statistically significant exposure-response associations with other antioxidants, including alpha-carotene, vitamin C, or zinc from dietary intake alone.32 These results were substantiated by 2 meta-analyses evaluating a total of 93 combined intervention trials and cohorts where no association was found between vitamin or mineral intake during pregnancy and/or during infancy and the development of AD.19,36
Fatty Acids
Other dietary changes that are associated with an increased prevalence of atopic diseases in children include excess consumption of omega-6 (n-6) long-chain polyunsaturated fatty acids (LC-PUFA) and insufficient omega-3 (n-3) LC-PUFA consumption.37 Given prior evidence that allergic immune responses in infants may be primed before birth,38 researchers have questioned whether the anti-inflammatory properties of n-3 LC-PUFA when supplemented during pregnancy may have immunomodulatory effects on infants that could alter their predisposition to develop allergic disease, including AD.39 A systematic review and meta-analysis of randomized controlled trials found a statistically significant RR of 0.53 (95% CI, 0.35-0.81; P=.004) for the incidence of AD at 12 months of age with maternal supplementation of n-3 LC-PUFA.9 Another trial of 145 pregnant women randomized to supplementation with fish oil vs placebo starting at gestational week 25 and continuing through 3.5 months of breastfeeding found a reduced cumulative incidence of AD in the intervention group compared to controls at 2 years of age, with a statistically significant crude OR of 0.33 (95% CI, 0.11-0.97; P=.04).40 However, the adjusted OR was not statistically significant. In addition, they found that mothers and infants with higher proportions of docosahexaenoic acid and eicosapentaenoic acid in plasma phospholipids have been noted to have a lower prevalence of IgE-associated disease in a dose-dependent manner (P<.05 and P<.05, respectively).40 In another trial of 98 pregnant women randomized to fish oil supplementation or placebo from 20 weeks’ gestation to delivery found no difference in the frequency of AD but did note that infants in the exposure group had significantly less severe AD compared to controls (OR=0.09 [95% CI, 0.1-0.94]; P=.045).39 A prospective birth cohort study of 2641 children evaluated dietary composition during the last 4 weeks of pregnancy and found that consumption of foods rich in n-6 LC-PUFAs (eg, margarine, vegetable oil) increased the risk for developing AD, while foods rich in n-3 LC-PUFAs (eg, fish) decreased the risk for developing AD in offspring at 2 years of age. All P values for margarine, vegetable oil, and fish were statistically significant on logistic regression at P<.05.41 A longitudinal analysis of follow-up data from a randomized controlled trial looking at maternal prenatal n-3 LC-PUFA intake and the development of allergic disease (including AD) found no differences in the development of disease at 1-, 3-, or 6-year follow-up.42 Despite several studies demonstrating a possible benefit of omega-3 fatty acid intake on the development of AD in offspring, the longitudinal analysis by Best et al42 reminds us that long-term follow-up is critical in establishing benefit of any intervention given the heterogeneous and progressive nature of the atopic march and AD.
Specific Diets
Several studies have evaluated the role of dietary patterns and their influence on atopic disease. Studies evaluating dietary patterns or supplement intake can be challenging, as data often are derived from questionnaires with bias in response to families with higher socioeconomic status.9 Further, analysis of any one food group does not account for the potential interplay between nutrients.43 Studies should focus more on dietary patterns vs individual foods to assess true risk.43,44 Given these limitations, study results on diet should be carefully scrutinized; however, there are still some positive findings that deserve further investigation. Chatzi et al44 followed 460 children for 6.5 years and found a protective effect for the development of atopy in the offspring of women who had high adherence to the Mediterranean diet (OR 0.55 [95% CI, 0.31-0.97]). Another cohort study evaluating the effects of the Mediterranean diet and risk for AD in the first year of life in 2516 mother-child pairs from Spain and Greece found no statistically significant association with consumption of the Mediterranean diet and AD. The investigators also evaluated intake of fruits, nuts, vegetables, meats, processed meats, dairy products, and cereal and found no statistically significant protective benefit.45 Another systematic review of more than 90 observational studies identified no significant relationship between prenatal dietary exposures of fruits, vegetables, nuts, fat, fatty acids, eggs, cereal, milk, alcohol, tea, or coffee and risk for allergic disease in offspring, including AD.19
A Chinese prospective cohort study evaluated the dietary protein patterns of 713 mother-child pairs and the incidence of infant AD at 6 months of age.46 Dietary protein patterns were characterized as predominantly poultry, plant based, dairy and eggs, and red meat and fish. The investigators found a statistically significant reduced risk for AD in mothers who consumed plant-based or dairy and eggs protein patterns when compared to a poultry protein pattern with an adjusted OR of 0.572 (95% CI, 0.330-0.992) and 0.478 (95% CI, 0.274-0.837), respectively. This protective effect was not seen with the red meat and fish protein patterns.46 Similar results were seen in a 2020 Canadian study that evaluated the effects of a Western (fats, meats, processed foods, and starchy vegetables), balanced (diverse sources of animal proteins [especially fish], fruits, vegetables, nuts, and seeds), or plant-based (dairy, legumes, vegetables, whole grains, and an aversion to meats) diet in more than 2000 mother-infant pairs from 24 to 28 weeks’ gestation to 1 year of age. The investigators found a lower OR of AD in mothers who followed a mostly plant-based diet compared to other dietary patterns (OR 0.65 [95% CI, 0.55-0.76]; P<.001).10 Another prospective Japanese study looking at healthy (high intake of green and yellow vegetables, seaweed, mushrooms, white vegetables, pulses, potatoes, fish, sea products, fruit, and shellfish, and low intake of confectioneries and soft drinks), Western (high intake of vegetable oil, salt-containing seasonings, beef, pork, processed meat, eggs, chicken, and white vegetables, and low intake of fruit, soft drinks, and confectioneries), or Japanese (high intake of rice, miso soup, sea products, and fish, and low intake of bread, confectioneries, and dairy products) dietary patterns in 763 mother-child pairs found no association between diet during pregnancy and development of AD in offspring at 16 to 24 months.47 Unfortunately, a longitudinal data analysis has not been performed for this study.
Final Thoughts
Atopic dermatitis is a complex, progressive, and heterogeneous disease with both genetic and environmental influences. Studying the effects of diet on the development, progression, or severity of disease can be very difficult due to the heterogeneity of study designs, lack of long-term follow-up, and high potential for residual confounding. Studies evaluating dietary patterns or supplement intake can be equally challenging, as data often are derived from questionnaires with bias in response to families with higher socioeconomic status.9 Very few studies have looked specifically at maternal dietary composition and the development of AD alone (without inclusion of asthma or food allergy). Ultimately, the inconsistency of the data makes it difficult to draw conclusions and make formal recommendations for this vulnerable population. Additional evidence from well-powered trials with comparable methodology and objective outcome measures will be imperative to make formal recommendations. In addition, longitudinal follow-up will be essential to determine long-term benefit and influence on the atopic march.
Atopic dermatitis (AD) is an inflammatory skin disease characterized by skin barrier disruption, skin inflammation, and pruritus.1 It is a common and often chronic skin condition associated with the development of food allergies, asthma, and allergic rhinitis, known as the atopic march.2 Atopic dermatitis is estimated to affect 10% to 25% of children, most with onset before 5 years of age, and up to 7% of adults worldwide.3 Most patients improve with time, but multiple disease trajectories are possible. Several studies have demonstrated that fewer than 4% of children develop the classic atopic march—AD followed by food allergies, asthma, and finally allergic rhinitis—with recent evidence pointing to a more complex heterogeneous progression of disease and allergic comorbidities often occurring together.4,5 The prevalence of AD has been increasing globally over the last 30 years,6 with a marked increase in developed countries.6,7 It is well accepted that AD is based on an interplay between genetic predisposition and environmental factors,8 but many suspect that the rapid rise in prevalence cannot be attributed to genetic factors alone.9 The precipitant triggers for AD remain an area of intense investigation, with ongoing debate between the “inside out” and “outside in” hypotheses; these revolve around whether abnormalities in the immune system trigger barrier dysfunction or barrier dysfunction triggers immune programming to atopy.8 Ongoing research related to genetic predisposition of AD has identified candidate genes implicated in both impaired skin barrier function and altered immune system pathways, further supporting that both theories may contribute to disease pathogenesis.
The increasing prevalence of AD, with increasing disease burden within socioeconomically advantaged countries, raises the possibility of early modifiable environmental factors that may contribute to the disease process.10 Many studies point to the influence of the 21st century lifestyle and Western diet as primary contributing factors.9,11 However, it is not clear how these factors may influence the development of allergic atopic disease. Several studies have suggested that nonheritable influences in utero can alter fetus immune function and influence the subsequent development of allergic disease.12,13 Although many studies have examined environmental factors contributing to the development of AD in infancy and childhood, less is understood about the influence of prenatal factors. Currently, in utero exposure to tobacco smoke, phthalates, and maternal distress have been potentially implicated in the development of AD.14,15 Several studies have examined the role of maternal diet and nutrition on the development of AD in offspring; however, formal recommendations and robust trial data are lacking. In this article, we examine the existing literature surrounding maternal diet on the development of AD in infancy and childhood.
Allergen Avoidance
Extrapolating from the food allergy literature, it was once suggested that allergen avoidance in early childhood had a protective effect on the subsequent development of allergies; however, more recent research has found that early exposure to common food allergens, such as peanuts or eggs, may actually reduce a child’s risk for developing these allergies later in life.16 Among infants at high risk for food allergy, sustained consumption of peanut products beginning in the first 11 months of life resulted in an 81% lower rate of peanut allergy at 60 months of age than the rate among children who avoided peanuts.17 Given the results that antigen avoidance during infancy/childhood does not protect against the development of allergies and may actually be counterproductive, it is not surprising that research studying antigen avoidance during pregnancy on the development of AD also has demonstrated limited efficacy. A systematic review of 5 trials on maternal dietary antigen avoidance (N=952) suggested no protective effects of avoiding antigenic foods during pregnancy on the development of AD in the first 18 months of life.18 Another meta-analysis evaluating 12 intervention trials looked at the effects of maternal allergenic food avoidance during pregnancy or lactation and found no reduced risk for subsequent development of allergic disease, including AD.19 The American Academy of Pediatrics 2019 consensus statement does not support maternal dietary restrictions in pregnancy for the prevention of atopic disease and makes note that the data remain limited, which complicates drawing any firm conclusions.20
Probiotic Supplementation
One of the most investigated dietary supplements for the prevention of atopic disease is probiotics, with possible benefits noted in both the prenatal and postnatal periods. Baquerizo Nole et al21 examined several studies looking at the various benefits of probiotics in AD, which included inhibition of the helper T cell (TH2) response, stimulation of the TH1 response, upregulation of regulatory T cells, acceleration of skin and mucosal barrier function, increase in intestinal microflora diversity, suppression of toxic fermentation products in the intestinal lumen from increased production of short-chain fatty acids, and inhibition of Staphylococcus aureus attachment on epidermal keratinocytes. It is unclear how this may affect infants prenatally; however, transfer of maternal intestinal microflora during delivery and shortly thereafter has demonstrated that probiotic strains remain detectable in the infant’s stool up to 6 months after delivery, even if the mother has discontinued use.22 A 2008 meta-analysis of 10 double-bind, randomized, controlled trials (N=1880) looking at the use of maternal prenatal and postnatal probiotic supplementation in the prevention of pediatric AD found a relative risk (RR) ratio of 0.69 (95% CI, 0.57-0.83) using a fixed effects model and RR ratio of 0.66 (95% CI, 0.49-0.89) using a random effects model. After exclusion of one study that evaluated the effect of postnatal probiotic supplementation only, the RR ratio decreased to 0.61 for both the fixed effects and random effects models.23 A systematic review by Panduru et al24 noted similar findings with a subgroup meta-analysis of 11 studies of prenatal supplementation followed by postnatal supplementation of probiotics, which demonstrated a protective effect on the development of AD (odds ratio [OR]=0.61, P<.001). Postnatal supplementation alone (4 studies) did not have the same association (OR=0.95, P<.82).24 A 2012 meta-analysis by Doege et al25 evaluated 7 randomized, double-blinded, placebo-controlled trials that assessed probiotic supplementation during pregnancy (without incorporation of postnatal supplementation) and found a significant risk reduction of 5.7% (P=.022) for AD in children aged 2 to 7 years. Interestingly, this was only significant for Lactobacillus and not for other bacterial strains, even if a mixture of strains included Lactobacillus. However, Panduru et al24 found both maternal Lactobacillus supplementation alone (8 studies) and in combination with Bifidobacterium (9 studies) was protective against AD development in children (OR=0.70, P=.004; OR=0.62, P<.001). A more recent 2015 meta-analysis of 17 studies (N=4755) evaluating the use of maternal probiotic supplementation in pregnancy and/or through the infant’s first 3 months of life found a significantly lower RR (0.78 [95% CI, 0.69-0.89], P=.0003) for the development of AD in infants treated with probiotics and found this risk to be even further decreased when a mixture of probiotics including both Lactobacillus and Bifidobacterium was used (RR=0.54 [95% CI, 0.43-0.68], P<.00001).26
Antioxidants
The Westernization of many developing countries’ diets—diets high in saturated fats, protein, sucrose, salt, and processed foods and low in fresh fruits and green vegetables—has led to a reduced intake of antioxidants and an increase in susceptibility to oxidative damage.27,28 One hypothesis suggests that a reduction in nutritional antioxidants and subsequent oxidative damage leads to airway inflammation that may contribute to an increased prevalence of asthma.27 In vitro data suggest that antioxidant deficiency may influence the differentiation of helper T cells to a TH2 phenotype, which can increase susceptibility to the development of asthma and allergies.29 Vitamin E specifically has been shown to inhibit IL-4 gene expression, which drives type 2 immunity and decreases expression of multiple genes that regulate epidermal barrier function, subsequently increasing susceptibility to allergic inflammation and AD.29,30 Regardless of the proposed mechanisms for antioxidant deficiency increasing susceptibility to allergic disease, studies evaluating the benefits of antioxidant intake during pregnancy in relation to AD have not been promising. Several studies have found no association between prenatal vitamin E intake and the risk for AD development in infants and children.31,32 Another study found a statistically significant inverse relationship between vitamin E intake in mothers with a history of atopy and the development of AD in their children at 2 years of age but not at 1 year of age (P-trend=.024).33 It has been suggested that varying vitamin E isoforms may contribute to the discrepant results previously discussed, with the γ-tocopherol isoform (found frequently in Westernized diets)34 as a driver of inflammation in murine models.35 West et al31 noted an association between vitamin C intake and development of “any allergic disease”—AD, IgE-mediated food allergy, or asthma—with a crude OR of 0.48 (95% CI, 0.25-0.93). However, the P-trend and adjusted OR were not statistically significant. The investigators found no association between maternal intake of beta-carotene, vitamin E, or zinc, but they did find copper supplementation to be protective on the development of AD at 1 year of age (P-trend=0.03). Interestingly, when the data for total antioxidant intake—vitamin C, vitamin E, zinc, beta-carotene, and copper from both diet and supplementation—were combined and analyzed, no statistically significant associations for any of the antioxidants were found.31 Another study of 763 Japanese mother-child pairs found a reduced risk for AD at 16 to 24 months of age with high maternal intake of beta-carotene but found no statistically significant exposure-response associations with other antioxidants, including alpha-carotene, vitamin C, or zinc from dietary intake alone.32 These results were substantiated by 2 meta-analyses evaluating a total of 93 combined intervention trials and cohorts where no association was found between vitamin or mineral intake during pregnancy and/or during infancy and the development of AD.19,36
Fatty Acids
Other dietary changes that are associated with an increased prevalence of atopic diseases in children include excess consumption of omega-6 (n-6) long-chain polyunsaturated fatty acids (LC-PUFA) and insufficient omega-3 (n-3) LC-PUFA consumption.37 Given prior evidence that allergic immune responses in infants may be primed before birth,38 researchers have questioned whether the anti-inflammatory properties of n-3 LC-PUFA when supplemented during pregnancy may have immunomodulatory effects on infants that could alter their predisposition to develop allergic disease, including AD.39 A systematic review and meta-analysis of randomized controlled trials found a statistically significant RR of 0.53 (95% CI, 0.35-0.81; P=.004) for the incidence of AD at 12 months of age with maternal supplementation of n-3 LC-PUFA.9 Another trial of 145 pregnant women randomized to supplementation with fish oil vs placebo starting at gestational week 25 and continuing through 3.5 months of breastfeeding found a reduced cumulative incidence of AD in the intervention group compared to controls at 2 years of age, with a statistically significant crude OR of 0.33 (95% CI, 0.11-0.97; P=.04).40 However, the adjusted OR was not statistically significant. In addition, they found that mothers and infants with higher proportions of docosahexaenoic acid and eicosapentaenoic acid in plasma phospholipids have been noted to have a lower prevalence of IgE-associated disease in a dose-dependent manner (P<.05 and P<.05, respectively).40 In another trial of 98 pregnant women randomized to fish oil supplementation or placebo from 20 weeks’ gestation to delivery found no difference in the frequency of AD but did note that infants in the exposure group had significantly less severe AD compared to controls (OR=0.09 [95% CI, 0.1-0.94]; P=.045).39 A prospective birth cohort study of 2641 children evaluated dietary composition during the last 4 weeks of pregnancy and found that consumption of foods rich in n-6 LC-PUFAs (eg, margarine, vegetable oil) increased the risk for developing AD, while foods rich in n-3 LC-PUFAs (eg, fish) decreased the risk for developing AD in offspring at 2 years of age. All P values for margarine, vegetable oil, and fish were statistically significant on logistic regression at P<.05.41 A longitudinal analysis of follow-up data from a randomized controlled trial looking at maternal prenatal n-3 LC-PUFA intake and the development of allergic disease (including AD) found no differences in the development of disease at 1-, 3-, or 6-year follow-up.42 Despite several studies demonstrating a possible benefit of omega-3 fatty acid intake on the development of AD in offspring, the longitudinal analysis by Best et al42 reminds us that long-term follow-up is critical in establishing benefit of any intervention given the heterogeneous and progressive nature of the atopic march and AD.
Specific Diets
Several studies have evaluated the role of dietary patterns and their influence on atopic disease. Studies evaluating dietary patterns or supplement intake can be challenging, as data often are derived from questionnaires with bias in response to families with higher socioeconomic status.9 Further, analysis of any one food group does not account for the potential interplay between nutrients.43 Studies should focus more on dietary patterns vs individual foods to assess true risk.43,44 Given these limitations, study results on diet should be carefully scrutinized; however, there are still some positive findings that deserve further investigation. Chatzi et al44 followed 460 children for 6.5 years and found a protective effect for the development of atopy in the offspring of women who had high adherence to the Mediterranean diet (OR 0.55 [95% CI, 0.31-0.97]). Another cohort study evaluating the effects of the Mediterranean diet and risk for AD in the first year of life in 2516 mother-child pairs from Spain and Greece found no statistically significant association with consumption of the Mediterranean diet and AD. The investigators also evaluated intake of fruits, nuts, vegetables, meats, processed meats, dairy products, and cereal and found no statistically significant protective benefit.45 Another systematic review of more than 90 observational studies identified no significant relationship between prenatal dietary exposures of fruits, vegetables, nuts, fat, fatty acids, eggs, cereal, milk, alcohol, tea, or coffee and risk for allergic disease in offspring, including AD.19
A Chinese prospective cohort study evaluated the dietary protein patterns of 713 mother-child pairs and the incidence of infant AD at 6 months of age.46 Dietary protein patterns were characterized as predominantly poultry, plant based, dairy and eggs, and red meat and fish. The investigators found a statistically significant reduced risk for AD in mothers who consumed plant-based or dairy and eggs protein patterns when compared to a poultry protein pattern with an adjusted OR of 0.572 (95% CI, 0.330-0.992) and 0.478 (95% CI, 0.274-0.837), respectively. This protective effect was not seen with the red meat and fish protein patterns.46 Similar results were seen in a 2020 Canadian study that evaluated the effects of a Western (fats, meats, processed foods, and starchy vegetables), balanced (diverse sources of animal proteins [especially fish], fruits, vegetables, nuts, and seeds), or plant-based (dairy, legumes, vegetables, whole grains, and an aversion to meats) diet in more than 2000 mother-infant pairs from 24 to 28 weeks’ gestation to 1 year of age. The investigators found a lower OR of AD in mothers who followed a mostly plant-based diet compared to other dietary patterns (OR 0.65 [95% CI, 0.55-0.76]; P<.001).10 Another prospective Japanese study looking at healthy (high intake of green and yellow vegetables, seaweed, mushrooms, white vegetables, pulses, potatoes, fish, sea products, fruit, and shellfish, and low intake of confectioneries and soft drinks), Western (high intake of vegetable oil, salt-containing seasonings, beef, pork, processed meat, eggs, chicken, and white vegetables, and low intake of fruit, soft drinks, and confectioneries), or Japanese (high intake of rice, miso soup, sea products, and fish, and low intake of bread, confectioneries, and dairy products) dietary patterns in 763 mother-child pairs found no association between diet during pregnancy and development of AD in offspring at 16 to 24 months.47 Unfortunately, a longitudinal data analysis has not been performed for this study.
Final Thoughts
Atopic dermatitis is a complex, progressive, and heterogeneous disease with both genetic and environmental influences. Studying the effects of diet on the development, progression, or severity of disease can be very difficult due to the heterogeneity of study designs, lack of long-term follow-up, and high potential for residual confounding. Studies evaluating dietary patterns or supplement intake can be equally challenging, as data often are derived from questionnaires with bias in response to families with higher socioeconomic status.9 Very few studies have looked specifically at maternal dietary composition and the development of AD alone (without inclusion of asthma or food allergy). Ultimately, the inconsistency of the data makes it difficult to draw conclusions and make formal recommendations for this vulnerable population. Additional evidence from well-powered trials with comparable methodology and objective outcome measures will be imperative to make formal recommendations. In addition, longitudinal follow-up will be essential to determine long-term benefit and influence on the atopic march.
- Nutten S. Atopic dermatitis: global epidemiology and risk factors. Ann Nutr Metab. 2015;66(suppl 1):8-16.
- Kapoor R, Menon C, Hoffstad O, et al. The prevalence of atopic triad in children with physician-confirmed atopic dermatitis. J Am Acad Dermatol. 2008;58:68-73.
- Abuabara K, Magyari A, McCulloch CE, et al. Prevalence of atopic eczema among patients seen in primary care: data from the Health Improvement Network. Ann Intern Med. 2019;170:354-356.
- Belgrave DC, Granell R, Simpson A, et al. Developmental profiles of eczema, wheeze, and rhinitis: two population-based birth cohort studies. PLoS Medicine. 2014;11:E1001748.
- Aguilar D, Pinart M, Koppelman GH, et al. Computational analysis of multimorbidity between asthma, eczema and rhinitis. PloS One. 2017;12:E0179125.
- Deckers IA, McLean S, Linssen S, et al. Investigating international time trends in the incidence and prevalence of atopic eczema 1990-2010: a systematic review of epidemiological studies. PloS One. 2012;7:E39803.
- Williams H, Stewart A, von Mutius E, et al. Is eczema really on the increase worldwide? J Allergy Clin Immunol. 2008;121:947-954.
- Sullivan M, Silverberg NB. Current and emerging concepts in atopic dermatitis pathogenesis. Clin Dermatol. 2017;35:349-353.
- Best KP, Gold M, Kennedy D, et al. Omega-3 long-chain PUFA intake during pregnancy and allergic disease outcomes in the offspring: a systematic review and meta-analysis of observational studies and randomized controlled trials. Am J Clin Nutr. 2016;103:128-143.
- Zulyniak MA, de Souza RJ, Shaikh M, et al. Ethnic differences in maternal diet in pregnancy and infant eczema. PloS One. 2020;15:E0232170.
- Jena PK, Sheng L, Mcneil K, et al. Long-term Western diet intake leads to dysregulated bile acid signaling and dermatitis with Th2 and Th17 pathway features in mice. J Dermatol Sci. 2019;95:13-20.
- Grieger JA, Clifton VL, Tuck AR, et al. In utero programming of allergic susceptibility. Int Arch Allergy Immunol. 2016;169:80-92. doi:10.1159/000443961
- Khan TK, Palmer DJ, Prescott SL. In-utero exposures and the evolving epidemiology of paediatric allergy. Curr Opin Allergy Clin Immunol. 2015;15:402-408. doi:10.1097/ACI.0000000000000209
- Bauer SM. Atopic eczema: genetic associations and potential links to developmental exposures. Int J Toxicol. 2017;36:187-198.
- Shinohara M, Saito H, Matsumoto K. Different timings of prenatal or postnatal tobacco smoke exposure have different effects on the development of atopic eczema/dermatitis syndrome (AEDS) during infancy. J Allergy Clin Immunol. 2012;129:AB40.
- Lerodiakonou D, Garcia-Larsen V, Logan A, et al. Timing of allergenic food introduction to the infant diet and risk of allergic or autoimmune disease: a systematic review and meta-analysis. JAMA. 2016;316:1181-1192.
- Du Toit G, Roberts G, Sayre PH, et al. Randomized trial of peanut consumption in infants at risk for peanut allergy. N Engl J Med. 2015;372:803-813.
- Kramer MS, Kakuma R. Maternal dietary antigen avoidance during pregnancy or lactation, or both, for preventing or treating atopic disease in the child. Evid Based Child Health. 2014;9:447-483.
- Garcia-Larsen V, Ierodiakonou D, Jarrold K, et al. Diet during pregnancy and infancy and risk of allergic or autoimmune disease: a systematic review and meta-analysis. PLoS Med. 2018;15:E1002507.
- Greer FR, Sicherer SH, Burks AW; Committee on Nutrition, Section on Allergy and Immunology. The effects of early nutritional interventions on the development of atopic disease in infants and children: the role of maternal dietary restriction, breastfeeding, timing of introduction of complementary foods, and hydrolyzed formulas. Pediatrics. 2019;143:e20190281.
- Baquerizo Nole KL, Yim E, Keri JE. Probiotics and prebiotics in dermatology. J Am Acad Dermatol. 2014;71:814-821.
- Schultz M, Göttl C, Young RJ, et al. Administration of oral probiotic bacteria to pregnant women causes temporary infantile colonization. J Pediatr Gastroenterol Nutr. 2004;38:293-297.
- Lee J, Seto D, Bielory L. Meta-analysis of clinical trials of probiotics for prevention and treatment of pediatric atopic dermatitis. J Allergy Clin Immunol. 2008;121:116-121.
- Panduru M, Panduru NM, Sa˘la˘va˘stru CM, et al. Probiotics and primary prevention of atopic dermatitis: a meta‐analysis of randomized controlled studies. J Eur Acad Dermatol Venereol. 2015;29:232-242.
- Doege K, Grajecki D, Zyriax BC, et al. Impact of maternal supplementation with probiotics during pregnancy on atopic eczema in childhood—a meta-analysis. Br J Nutr. 2012;107:1-6.
- Zuccotti G, Meneghin F, Aceti A, et al. Probiotics for prevention of atopic diseases in infants: systematic review and meta‐analysis. Allergy. 2015;70:1356-1371.
- Seaton A, Godden DJ, Brown K. Increase in asthma: a more toxic environment or a more susceptible population? Thorax. 1994;49:171-174.
- Manzel A, Muller DN, Hafler DA, et al. Role of “Western diet” in inflammatory autoimmune diseases. Curr Allergy Asthma Rep. 2014;14:1-8.
- Li-Weber M, Giasisi M, Trieber MK, et al. Vitamin E inhibits IL-4 gene expression in peripheral blood T cells. Eur J Immunol. 2002;32:2401-2408.
- Sehra S, Yao Y, Howell MD, et al. IL-4 regulates skin homeostasis and the predisposition toward allergic skin inflammation. J Immunol. 2010;184:3186-3190.
- West CE, Dunstan J, McCarthy S, et al. Associations between maternal antioxidant intakes in pregnancy and infant allergic outcomes. Nutrients. 2012;4:1747-1758.
- Miyake Y, Sasaki S, Tanaka K, et al. Consumption of vegetables, fruit, and antioxidants during pregnancy and wheeze and eczema in infants. Allergy. 2010;65:758-765.
- Martindale S, McNeill G, Devereux G, et al. Antioxidant intake in pregnancy in relation to wheeze and eczema in the first two years of life. Am J Respir Crit Care Med. 2005;171:121-128.
- Robison R, Kumar R. The effect of prenatal and postnatal dietary exposures on childhood development of atopic disease. Curr Opin Allergy Clin Immunol. 2010;10:139-144.
- Berdnikovs S, Abdala-Valencia H, McCary C, et al. Isoforms of vitamin E have opposing immunoregulatory functions during inflammation by regulating leukocyte recruitment. J Immunol. 2009;182:4395-4405.
- Beckhaus AA, Garcia‐Marcos L, Forno E, et al. Maternal nutrition during pregnancy and risk of asthma, wheeze, and atopic diseases during childhood: a systematic review and meta‐analysis. Allergy. 2015;70:1588-1604.
- Calder PC, Miles EA. Fatty acids and atopic disease. Pediatr Allergy Immunol. 2000;11(suppl 13):29-36.
- Prescott S, Macaubas C, Holt B, et al. Transplacental priming of the human immune system to environmental allergens: universal skewing of initial T-cell responses towards Th-2 cytokine profile. J Immunol. 1998;160:4730-4737.
- Dunstan JA, Mori TA, Barden A, et al. Fish oil supplementation in pregnancy modifies neonatal allergen-specific immune responses and clinical outcomes in infants at high risk of atopy: a randomized, controlled trial. J Allergy Clin Immunol. 2003;112:1178-1184.
- Furuhjelm C, Warstedt K, Fagerås M, et al. Allergic disease in infants up to 2 years of age in relation to plasma omega‐3 fatty acids and maternal fish oil supplementation in pregnancy and lactation. Pediatr Allergy Immunol. 2011;22:505-514.
- Sausenthaler S, Koletzko S, Schaaf B, et al; LISA Study Group. Maternal diet during pregnancy in relation to eczema and allergic sensitization in the offspring at 2 y of age. Am J Clin Nutr. 2007;85:530-537.
- Best KP, Sullivan TR, Palmer DJ, et al. Prenatal omega-3 LCPUFA and symptoms of allergic disease and sensitization throughout early childhood—a longitudinal analysis of long-term follow-up of a randomized controlled trial. World Allergy Organ J. 2018;11:10.
- Jacobs DR Jr, Steffen LM. Nutrients, foods, and dietary patterns as exposures in research: a framework for food synergy. Am J Clin Nutr. 2003;78:508-513.
- Chatzi L, Torrent M, Romieu I, et al. Mediterranean diet in pregnancy is protective for wheeze and atopy in childhood. Thorax. 2008;63:507-513.
- Chatzi L, Garcia R, Roumeliotaki T, et al. Mediterranean diet adherence during pregnancy and risk of wheeze and eczema in the first year of life: INMA (Spain) and RHEA (Greece) mother-child cohort studies. Br J Nutr. 2013;110:2058-2068.
- Zeng J, Wu W, Chen Y, et al. Maternal dietary protein patterns during pregnancy and the risk of infant eczema: a cohort study. Front Nutr. 2021;8:294.
- Miyake Y, Okubo H, Sasaki S, et al. Maternal dietary patterns during pregnancy and risk of wheeze and eczema in Japanese infants aged 16–24 months: the Osaka Maternal and Child Health Study. Pediatr Allergy Immunol. 2011;22:734-741.
- Nutten S. Atopic dermatitis: global epidemiology and risk factors. Ann Nutr Metab. 2015;66(suppl 1):8-16.
- Kapoor R, Menon C, Hoffstad O, et al. The prevalence of atopic triad in children with physician-confirmed atopic dermatitis. J Am Acad Dermatol. 2008;58:68-73.
- Abuabara K, Magyari A, McCulloch CE, et al. Prevalence of atopic eczema among patients seen in primary care: data from the Health Improvement Network. Ann Intern Med. 2019;170:354-356.
- Belgrave DC, Granell R, Simpson A, et al. Developmental profiles of eczema, wheeze, and rhinitis: two population-based birth cohort studies. PLoS Medicine. 2014;11:E1001748.
- Aguilar D, Pinart M, Koppelman GH, et al. Computational analysis of multimorbidity between asthma, eczema and rhinitis. PloS One. 2017;12:E0179125.
- Deckers IA, McLean S, Linssen S, et al. Investigating international time trends in the incidence and prevalence of atopic eczema 1990-2010: a systematic review of epidemiological studies. PloS One. 2012;7:E39803.
- Williams H, Stewart A, von Mutius E, et al. Is eczema really on the increase worldwide? J Allergy Clin Immunol. 2008;121:947-954.
- Sullivan M, Silverberg NB. Current and emerging concepts in atopic dermatitis pathogenesis. Clin Dermatol. 2017;35:349-353.
- Best KP, Gold M, Kennedy D, et al. Omega-3 long-chain PUFA intake during pregnancy and allergic disease outcomes in the offspring: a systematic review and meta-analysis of observational studies and randomized controlled trials. Am J Clin Nutr. 2016;103:128-143.
- Zulyniak MA, de Souza RJ, Shaikh M, et al. Ethnic differences in maternal diet in pregnancy and infant eczema. PloS One. 2020;15:E0232170.
- Jena PK, Sheng L, Mcneil K, et al. Long-term Western diet intake leads to dysregulated bile acid signaling and dermatitis with Th2 and Th17 pathway features in mice. J Dermatol Sci. 2019;95:13-20.
- Grieger JA, Clifton VL, Tuck AR, et al. In utero programming of allergic susceptibility. Int Arch Allergy Immunol. 2016;169:80-92. doi:10.1159/000443961
- Khan TK, Palmer DJ, Prescott SL. In-utero exposures and the evolving epidemiology of paediatric allergy. Curr Opin Allergy Clin Immunol. 2015;15:402-408. doi:10.1097/ACI.0000000000000209
- Bauer SM. Atopic eczema: genetic associations and potential links to developmental exposures. Int J Toxicol. 2017;36:187-198.
- Shinohara M, Saito H, Matsumoto K. Different timings of prenatal or postnatal tobacco smoke exposure have different effects on the development of atopic eczema/dermatitis syndrome (AEDS) during infancy. J Allergy Clin Immunol. 2012;129:AB40.
- Lerodiakonou D, Garcia-Larsen V, Logan A, et al. Timing of allergenic food introduction to the infant diet and risk of allergic or autoimmune disease: a systematic review and meta-analysis. JAMA. 2016;316:1181-1192.
- Du Toit G, Roberts G, Sayre PH, et al. Randomized trial of peanut consumption in infants at risk for peanut allergy. N Engl J Med. 2015;372:803-813.
- Kramer MS, Kakuma R. Maternal dietary antigen avoidance during pregnancy or lactation, or both, for preventing or treating atopic disease in the child. Evid Based Child Health. 2014;9:447-483.
- Garcia-Larsen V, Ierodiakonou D, Jarrold K, et al. Diet during pregnancy and infancy and risk of allergic or autoimmune disease: a systematic review and meta-analysis. PLoS Med. 2018;15:E1002507.
- Greer FR, Sicherer SH, Burks AW; Committee on Nutrition, Section on Allergy and Immunology. The effects of early nutritional interventions on the development of atopic disease in infants and children: the role of maternal dietary restriction, breastfeeding, timing of introduction of complementary foods, and hydrolyzed formulas. Pediatrics. 2019;143:e20190281.
- Baquerizo Nole KL, Yim E, Keri JE. Probiotics and prebiotics in dermatology. J Am Acad Dermatol. 2014;71:814-821.
- Schultz M, Göttl C, Young RJ, et al. Administration of oral probiotic bacteria to pregnant women causes temporary infantile colonization. J Pediatr Gastroenterol Nutr. 2004;38:293-297.
- Lee J, Seto D, Bielory L. Meta-analysis of clinical trials of probiotics for prevention and treatment of pediatric atopic dermatitis. J Allergy Clin Immunol. 2008;121:116-121.
- Panduru M, Panduru NM, Sa˘la˘va˘stru CM, et al. Probiotics and primary prevention of atopic dermatitis: a meta‐analysis of randomized controlled studies. J Eur Acad Dermatol Venereol. 2015;29:232-242.
- Doege K, Grajecki D, Zyriax BC, et al. Impact of maternal supplementation with probiotics during pregnancy on atopic eczema in childhood—a meta-analysis. Br J Nutr. 2012;107:1-6.
- Zuccotti G, Meneghin F, Aceti A, et al. Probiotics for prevention of atopic diseases in infants: systematic review and meta‐analysis. Allergy. 2015;70:1356-1371.
- Seaton A, Godden DJ, Brown K. Increase in asthma: a more toxic environment or a more susceptible population? Thorax. 1994;49:171-174.
- Manzel A, Muller DN, Hafler DA, et al. Role of “Western diet” in inflammatory autoimmune diseases. Curr Allergy Asthma Rep. 2014;14:1-8.
- Li-Weber M, Giasisi M, Trieber MK, et al. Vitamin E inhibits IL-4 gene expression in peripheral blood T cells. Eur J Immunol. 2002;32:2401-2408.
- Sehra S, Yao Y, Howell MD, et al. IL-4 regulates skin homeostasis and the predisposition toward allergic skin inflammation. J Immunol. 2010;184:3186-3190.
- West CE, Dunstan J, McCarthy S, et al. Associations between maternal antioxidant intakes in pregnancy and infant allergic outcomes. Nutrients. 2012;4:1747-1758.
- Miyake Y, Sasaki S, Tanaka K, et al. Consumption of vegetables, fruit, and antioxidants during pregnancy and wheeze and eczema in infants. Allergy. 2010;65:758-765.
- Martindale S, McNeill G, Devereux G, et al. Antioxidant intake in pregnancy in relation to wheeze and eczema in the first two years of life. Am J Respir Crit Care Med. 2005;171:121-128.
- Robison R, Kumar R. The effect of prenatal and postnatal dietary exposures on childhood development of atopic disease. Curr Opin Allergy Clin Immunol. 2010;10:139-144.
- Berdnikovs S, Abdala-Valencia H, McCary C, et al. Isoforms of vitamin E have opposing immunoregulatory functions during inflammation by regulating leukocyte recruitment. J Immunol. 2009;182:4395-4405.
- Beckhaus AA, Garcia‐Marcos L, Forno E, et al. Maternal nutrition during pregnancy and risk of asthma, wheeze, and atopic diseases during childhood: a systematic review and meta‐analysis. Allergy. 2015;70:1588-1604.
- Calder PC, Miles EA. Fatty acids and atopic disease. Pediatr Allergy Immunol. 2000;11(suppl 13):29-36.
- Prescott S, Macaubas C, Holt B, et al. Transplacental priming of the human immune system to environmental allergens: universal skewing of initial T-cell responses towards Th-2 cytokine profile. J Immunol. 1998;160:4730-4737.
- Dunstan JA, Mori TA, Barden A, et al. Fish oil supplementation in pregnancy modifies neonatal allergen-specific immune responses and clinical outcomes in infants at high risk of atopy: a randomized, controlled trial. J Allergy Clin Immunol. 2003;112:1178-1184.
- Furuhjelm C, Warstedt K, Fagerås M, et al. Allergic disease in infants up to 2 years of age in relation to plasma omega‐3 fatty acids and maternal fish oil supplementation in pregnancy and lactation. Pediatr Allergy Immunol. 2011;22:505-514.
- Sausenthaler S, Koletzko S, Schaaf B, et al; LISA Study Group. Maternal diet during pregnancy in relation to eczema and allergic sensitization in the offspring at 2 y of age. Am J Clin Nutr. 2007;85:530-537.
- Best KP, Sullivan TR, Palmer DJ, et al. Prenatal omega-3 LCPUFA and symptoms of allergic disease and sensitization throughout early childhood—a longitudinal analysis of long-term follow-up of a randomized controlled trial. World Allergy Organ J. 2018;11:10.
- Jacobs DR Jr, Steffen LM. Nutrients, foods, and dietary patterns as exposures in research: a framework for food synergy. Am J Clin Nutr. 2003;78:508-513.
- Chatzi L, Torrent M, Romieu I, et al. Mediterranean diet in pregnancy is protective for wheeze and atopy in childhood. Thorax. 2008;63:507-513.
- Chatzi L, Garcia R, Roumeliotaki T, et al. Mediterranean diet adherence during pregnancy and risk of wheeze and eczema in the first year of life: INMA (Spain) and RHEA (Greece) mother-child cohort studies. Br J Nutr. 2013;110:2058-2068.
- Zeng J, Wu W, Chen Y, et al. Maternal dietary protein patterns during pregnancy and the risk of infant eczema: a cohort study. Front Nutr. 2021;8:294.
- Miyake Y, Okubo H, Sasaki S, et al. Maternal dietary patterns during pregnancy and risk of wheeze and eczema in Japanese infants aged 16–24 months: the Osaka Maternal and Child Health Study. Pediatr Allergy Immunol. 2011;22:734-741.
Practice Points
- The prevalence of atopic dermatitis (AD) has been increasing globally, with a marked increase in developed countries.
- Maternal dietary restriction is not recommended in pregnancy for the prevention of atopic disease in infancy and childhood based on the existing literature.
- There is mixed evidence to support probiotic supplementation in the prenatal period.
- The recommendations supporting antioxidant and fatty acid supplementation as well as specific prenatal diets for the prevention of AD in infants and children are limited due to the heterogeneity of study designs.

