User login
ITL: Physician Reviews of HM-Relevant Research
Clinical question: Does treatment with drotrecogin alfa (activated) reduce mortality in patients with septic shock?
Background: Recombinant human activated protein C, or drotrecogin alfa (activated) (DrotAA), was approved for the treatment of patients with severe sepsis in 2001 on the basis of the Prospective Recombinant Human Activated Protein C Worldwide Evaluation in Severe Sepsis (PROWESS) study. Since its approval, conflicting reports about its efficacy have surfaced.
Study design: Double-blind, randomized-controlled trial.
Setting: Multicenter, multinational trial.
Synopsis: This trial enrolled 1,697 patients with septic shock to receive either DrotAA or placebo. At 28 days, 223 of 846 patients (26.4%) in the DrotAA group and 202 of 834 (24.2%) in the placebo group had died (relative risk in the DrotAA group, 1.09; 95% confidence interval, 0.92 to 1.28; P=0.31). At 90 days, there was still no significant difference in mortality. Mortality was also unchanged in patients with severe protein C deficiency at baseline. This lack of mortality benefit with either therapy persisted across all predefined subgroups in this study.
The incidence of nonserious bleeding was more common among patients who received DrotAA than among those in the placebo group (8.6% vs. 4.8%, P=0.002), but the incidence of serious bleeding events was similar in both groups. This study was appropriately powered after adjusting the sample size when aggregate mortality was found to be lower than anticipated.
Bottom line: DrotAA does not significantly reduce mortality at 28 or 90 days in patients with septic shock.
Citation: Ranieri VM, Thompson BT, Barie PS, et al. Drotrecogin alfa (activated) in adults with septic shock. N Engl J Med. 2012;366:2055-2064.
Read more of our physician reviews of recent, HM-relevant literature.
Clinical question: Does treatment with drotrecogin alfa (activated) reduce mortality in patients with septic shock?
Background: Recombinant human activated protein C, or drotrecogin alfa (activated) (DrotAA), was approved for the treatment of patients with severe sepsis in 2001 on the basis of the Prospective Recombinant Human Activated Protein C Worldwide Evaluation in Severe Sepsis (PROWESS) study. Since its approval, conflicting reports about its efficacy have surfaced.
Study design: Double-blind, randomized-controlled trial.
Setting: Multicenter, multinational trial.
Synopsis: This trial enrolled 1,697 patients with septic shock to receive either DrotAA or placebo. At 28 days, 223 of 846 patients (26.4%) in the DrotAA group and 202 of 834 (24.2%) in the placebo group had died (relative risk in the DrotAA group, 1.09; 95% confidence interval, 0.92 to 1.28; P=0.31). At 90 days, there was still no significant difference in mortality. Mortality was also unchanged in patients with severe protein C deficiency at baseline. This lack of mortality benefit with either therapy persisted across all predefined subgroups in this study.
The incidence of nonserious bleeding was more common among patients who received DrotAA than among those in the placebo group (8.6% vs. 4.8%, P=0.002), but the incidence of serious bleeding events was similar in both groups. This study was appropriately powered after adjusting the sample size when aggregate mortality was found to be lower than anticipated.
Bottom line: DrotAA does not significantly reduce mortality at 28 or 90 days in patients with septic shock.
Citation: Ranieri VM, Thompson BT, Barie PS, et al. Drotrecogin alfa (activated) in adults with septic shock. N Engl J Med. 2012;366:2055-2064.
Read more of our physician reviews of recent, HM-relevant literature.
Clinical question: Does treatment with drotrecogin alfa (activated) reduce mortality in patients with septic shock?
Background: Recombinant human activated protein C, or drotrecogin alfa (activated) (DrotAA), was approved for the treatment of patients with severe sepsis in 2001 on the basis of the Prospective Recombinant Human Activated Protein C Worldwide Evaluation in Severe Sepsis (PROWESS) study. Since its approval, conflicting reports about its efficacy have surfaced.
Study design: Double-blind, randomized-controlled trial.
Setting: Multicenter, multinational trial.
Synopsis: This trial enrolled 1,697 patients with septic shock to receive either DrotAA or placebo. At 28 days, 223 of 846 patients (26.4%) in the DrotAA group and 202 of 834 (24.2%) in the placebo group had died (relative risk in the DrotAA group, 1.09; 95% confidence interval, 0.92 to 1.28; P=0.31). At 90 days, there was still no significant difference in mortality. Mortality was also unchanged in patients with severe protein C deficiency at baseline. This lack of mortality benefit with either therapy persisted across all predefined subgroups in this study.
The incidence of nonserious bleeding was more common among patients who received DrotAA than among those in the placebo group (8.6% vs. 4.8%, P=0.002), but the incidence of serious bleeding events was similar in both groups. This study was appropriately powered after adjusting the sample size when aggregate mortality was found to be lower than anticipated.
Bottom line: DrotAA does not significantly reduce mortality at 28 or 90 days in patients with septic shock.
Citation: Ranieri VM, Thompson BT, Barie PS, et al. Drotrecogin alfa (activated) in adults with septic shock. N Engl J Med. 2012;366:2055-2064.
Read more of our physician reviews of recent, HM-relevant literature.
ITL: Physician Reviews of HM-Relevant Research
Clinical question: Does treatment with drotrecogin alfa (activated) reduce mortality in patients with septic shock?
Background: Recombinant human activated protein C, or drotrecogin alfa (activated) (DrotAA), was approved for the treatment of patients with severe sepsis in 2001 on the basis of the Prospective Recombinant Human Activated Protein C Worldwide Evaluation in Severe Sepsis (PROWESS) study. Since approval, conflicting reports about its efficacy have surfaced.
Study design: Double-blind, randomized-controlled trial.
Setting: Multicenter, multinational trial.
Synopsis: This trial enrolled 1,697 patients with septic shock to receive either DrotAA or placebo. At 28 days, 223 of 846 patients (26.4%) in the DrotAA group and 202 of 834 (24.2%) in the placebo group had died (relative risk in the DrotAA group, 1.09; 95% confidence interval, 0.92 to 1.28; P=0.31). At 90 days, there was still no significant difference in mortality. Mortality was also unchanged in patients with severe protein C deficiency at baseline. This lack of mortality benefit with either therapy persisted across all predefined subgroups in this study.
The incidence of non-serious bleeding was more common among patients who received DrotAA than among those in the placebo group (8.6% vs. 4.8%, P=0.002), but the incidence of serious bleeding events was similar in both groups. This study was appropriately powered after adjusting the sample size when aggregate mortality was found to be lower than anticipated.
Bottom line: DrotAA does not significantly reduce mortality at 28 or 90 days in patients with septic shock.
Citation: Ranieri VM, Thompson BT, Barie PS, et al. Drotrecogin alfa (activated) in adults with septic shock. N Engl J Med. 2012;366:2055-2064.
Read more of our physician reviews of recent, HM-relevant literature.
Clinical question: Does treatment with drotrecogin alfa (activated) reduce mortality in patients with septic shock?
Background: Recombinant human activated protein C, or drotrecogin alfa (activated) (DrotAA), was approved for the treatment of patients with severe sepsis in 2001 on the basis of the Prospective Recombinant Human Activated Protein C Worldwide Evaluation in Severe Sepsis (PROWESS) study. Since approval, conflicting reports about its efficacy have surfaced.
Study design: Double-blind, randomized-controlled trial.
Setting: Multicenter, multinational trial.
Synopsis: This trial enrolled 1,697 patients with septic shock to receive either DrotAA or placebo. At 28 days, 223 of 846 patients (26.4%) in the DrotAA group and 202 of 834 (24.2%) in the placebo group had died (relative risk in the DrotAA group, 1.09; 95% confidence interval, 0.92 to 1.28; P=0.31). At 90 days, there was still no significant difference in mortality. Mortality was also unchanged in patients with severe protein C deficiency at baseline. This lack of mortality benefit with either therapy persisted across all predefined subgroups in this study.
The incidence of non-serious bleeding was more common among patients who received DrotAA than among those in the placebo group (8.6% vs. 4.8%, P=0.002), but the incidence of serious bleeding events was similar in both groups. This study was appropriately powered after adjusting the sample size when aggregate mortality was found to be lower than anticipated.
Bottom line: DrotAA does not significantly reduce mortality at 28 or 90 days in patients with septic shock.
Citation: Ranieri VM, Thompson BT, Barie PS, et al. Drotrecogin alfa (activated) in adults with septic shock. N Engl J Med. 2012;366:2055-2064.
Read more of our physician reviews of recent, HM-relevant literature.
Clinical question: Does treatment with drotrecogin alfa (activated) reduce mortality in patients with septic shock?
Background: Recombinant human activated protein C, or drotrecogin alfa (activated) (DrotAA), was approved for the treatment of patients with severe sepsis in 2001 on the basis of the Prospective Recombinant Human Activated Protein C Worldwide Evaluation in Severe Sepsis (PROWESS) study. Since approval, conflicting reports about its efficacy have surfaced.
Study design: Double-blind, randomized-controlled trial.
Setting: Multicenter, multinational trial.
Synopsis: This trial enrolled 1,697 patients with septic shock to receive either DrotAA or placebo. At 28 days, 223 of 846 patients (26.4%) in the DrotAA group and 202 of 834 (24.2%) in the placebo group had died (relative risk in the DrotAA group, 1.09; 95% confidence interval, 0.92 to 1.28; P=0.31). At 90 days, there was still no significant difference in mortality. Mortality was also unchanged in patients with severe protein C deficiency at baseline. This lack of mortality benefit with either therapy persisted across all predefined subgroups in this study.
The incidence of non-serious bleeding was more common among patients who received DrotAA than among those in the placebo group (8.6% vs. 4.8%, P=0.002), but the incidence of serious bleeding events was similar in both groups. This study was appropriately powered after adjusting the sample size when aggregate mortality was found to be lower than anticipated.
Bottom line: DrotAA does not significantly reduce mortality at 28 or 90 days in patients with septic shock.
Citation: Ranieri VM, Thompson BT, Barie PS, et al. Drotrecogin alfa (activated) in adults with septic shock. N Engl J Med. 2012;366:2055-2064.
Read more of our physician reviews of recent, HM-relevant literature.
ITL: Physician Reviews of HM-Relevant Research
In This Edition
Literature At A Glance
A guide to this month’s studies
- Warfarin vs. aspirin in heart-failure patients
- Aspirin after anticoagulation prevents VTE recurrence
- Novel oral anticoagulants vs. warfarin in afib patients
- Intravenous metronidazole for mild C. diff infection
- Frequency of Foley catheter complications vs. CAUTI
- Intensive hyperglycemia control in noncritical hospitalized patients
- Risk score predicts 30-day mortality after noncardiac surgery
- Temperature, white blood cell count are not sensitive predictors of bacteremia
Warfarin Reduces Stoke but Increases Hemorrhage Compared with Aspirin in Patients with Heart Failure and Sinus Rhythm
Clinical question: Is warfarin superior to aspirin with regard to clinical outcomes in patients with heart failure who are in sinus rhythm?
Background: Heart failure is associated with stroke and death potentially caused by atherothrombotic events. Anticoagulation is efficacious in some heart failure patients with atrial fibrillation or significant valvular disease, but the role of anticoagulation versus aspirin in patients with chronic heart failure and sinus rhythm is unclear.
Study design: Double-blind randomized controlled trial.
Setting: Multicenter, multinational trial involving outpatients.
Synopsis: This double-blind, double-dummy trial involving 2,305 patients with sinus rhythm and reduced left ventricular ejection fraction (<35%) showed no significant difference in the primary combined outcome (ischemic stroke, intracerebral hemorrhage, or death) in those treated with warfarin as compared with aspirin. Warfarin did significantly reduce the rate of ischemic stroke by 0.64 events per 100 patient-years (absolute risk reduction 2.2%, number needed to treat 45) when compared with aspirin, with no significant difference in the rate of intracerebral hemorrhage. This outcome was offset by an increased rate of major hemorrhage by 0.91 events per 100 patient-years (absolute risk increase 3.1%, number needed to harm 32).
This study included patients from all functional classes of heart failure, with a protocol to initiate treatment with other standard heart failure medications. Patients with an indication for either warfarin or aspirin were excluded. Due to recruitment difficulties, the power of this study was reduced. Other study limitations included a relatively low percentage of time that patients on warfarin were in therapeutic range and a substantial period of follow-up time in which patients did not receive the assigned study treatments.
Bottom line: The benefit of reduced stoke in patients with heart failure and sinus rhythm who take warfarin over aspirin is counteracted by an increased risk for serious bleeding outcomes.
Citation: Homma S, Thompson JLP, Pullicino PM, et al. Warfarin and aspirin in patients with heart failure and sinus rhythm. N Engl J Med. 2012;366(20):1859-1869.
Aspirin Use after Recommended Anticoagulation Treatment Prevents Recurrence in VTE Patients
Clinical question: Does aspirin prevent recurrence in patients after treatment with anticoagulation following their first episode of unprovoked VTE?
Background: VTE recurrence is common following the discontinuation of anticoagulation, particularly in patients with a history of unprovoked pulmonary embolism (PE) or DVT. Extension of treatment with vitamin K antagonists decreases recurrence but also causes more bleeding. The role of aspirin in the secondary prevention of VTE is unknown.
Study design: Double-blind randomized controlled trial.
Setting: Multicenter international trial involving outpatients.
Synopsis: This trial compared treatment with aspirin versus placebo for approximately two years in 205 patients with a history of unprovoked VTE who had completed six to 18 months of anticoagulant therapy. The relative risk reduction of recurrent VTE in the aspirin versus the placebo group was approximately 40% per year (6.6% vs. 11.2% per year; absolute risk reduction 4.6% per year; number needed to treat 22). No difference in major or clinically relevant bleeding was observed between the two groups.
This study was appropriately powered to detect the treatment effect reported by the authors. Typically, anticoagulation is discontinued in this specific patient population once the risk of bleeding and/or the patient’s perceived inconvenience of therapy outweighs the expected benefit from continuing treatment to prevent VTE recurrence. Study results suggest aspirin is effective in preventing recurrence while not conferring an increased risk for hemorrhage. It is important to note that patients with cancer and symptomatic atherosclerosis were excluded from this study.
Bottom line: Following an appropriate treatment period with standard anticoagulation, aspirin appears to be a safe and effective therapy in the secondary prevention of recurrence in patients with a history of unprovoked VTE.
Citation: Becattini C, Agnelli G, Schenone A, et al. Aspirin for preventing recurrence of venous thromboembolism. N Engl J Med. 2012;366(21):1959-1967.
Meta-Analysis Supports New Oral Anticoagulants in Patients with Atrial Fibrillation
Clinical question: Are novel oral anticoagulants both efficacious and safe in comparison to warfarin in patients with atrial fibrillation (afib)?
Background: Three large clinical trials recently evaluated novel oral anticoagulants (dabigatran, rivaroxaban, and apixaban) as alternatives to warfarin in afib patients. Although the anticoagulants all appeared efficacious for primary outcomes, results regarding secondary and safety outcomes were either inconclusive or heterogeneous.
Study design: Systematic review and meta-analysis of randomized controlled trials.
Setting: Three diverse, clinical-trial settings.
Synopsis: A systematic review and meta-analysis of randomized controlled trials comparing novel oral anticoagulants to warfarin in afib patients found three large studies examining dabigatran, rivaroxaban, and apixaban that included 44,563 patients.
Using random-effects models to pool data from these studies, the authors found a 22% relative risk (RR) reduction of stroke or systemic embolism with the use of these new anticoagulants as compared to warfarin. The risks for ischemic and unidentified stroke (RR 0.87), hemorrhagic stroke (RR 0.45), intracranial bleeding (RR 0.49), and mortality (RR 0.88) were significantly reduced in patients taking these new anticoagulants. There was no significant reduction in major bleeding.
A trend in favor of warfarin was seen for gastrointestinal bleeding, but this trend was not statistically significant (RR 1.25; 95% confidence interval, 0.91-1.72).
This meta-analysis was limited to only three randomized controlled trials, each comparing a different oral anticoagulant to warfarin and using somewhat heterogeneous study designs and patient populations.
Bottom line: Three new oral anticoagulants appear safe and more efficacious than warfarin in the prevention of stroke and systemic embolism, as well as other important clinical outcomes in patients with atrial fibrillation.
Citation: Miller CS, Grandi SM, Shimony A, Filion KB, Eisenberg MJ. Meta-analysis of efficacy and safety of new oral anticoagulants (dabigatran, rivaroxaban, apixaban) versus warfarin in patients with atrial fibrillation. Am J Cardiol. 2012;110(3):453-60.
Observational Study Suggests Intravenous Metronidazole May Be Inferior for Mild Clostridium Difficile Infection
Clinical question: How do different treatment regimens (oral metronidazole vs. intravenous metronidazole vs. oral vancomycin) for mild Clostridium difficile infection (CDI) compare with regard to clinical outcomes?
Background: CDIs are increasing. Oral metronidazole or vancomycin can be used for the initial treatment of non-severe CDI. Additionally, a paucity of clinical data exists on intravenous metronidazole, which is used in some cases, typically in combination with vancomycin and in patients with severe CDI.
Study design: Prospective cohort study.
Setting: International hospital-based study.
Synopsis: This observational study assessed three different regimens (oral metronidazole, intravenous metronidazole, and oral vancomycin) for the treatment of mild CDI in 265 inpatients. Mortality at 30 days was higher in the intravenous metronidazole group (38.1%) than in the oral metronidazole (7.4%) and vancomycin (9.5%) groups. Patients receiving intravenous metronidazole also were less likely to recover from disease (52.4% versus >80% in the oral metronidazole and vancomycin groups). No statistically significant differences for other sequelae of CDI were found, except for higher risk of dehydration in the oral vancomycin group.
After controlling for age, sex, and comorbidity severity, patients in the intravenous metronidazole group were approximately four times more likely to die than patients in either the oral vancomycin group or the oral metronidazole group. There was no significant difference in mortality between the oral metronidazole and vancomycin groups.
Although this study was limited by its observational nature, no randomized controlled trial has yet to compare these three treatment regimens for mild CDI.
Bottom line: Treatment of mild C. diff infection with intravenous metronidazole appears to be associated with higher mortality and lower disease resolution than treatment with either oral metronidazole or vancomycin.
Citation: Wenisch JM, Schmid D, Kuo HW, et al. Prospective observational study comparing three different treatment regimes in patients with Clostridium difficile infection. Antimicrob Agents Chemother. 2012;56(4):1974-1978.
Traumatic Foley Catheter Complications Occur with Similar Frequency as Catheter-Associated Urinary Tract Infections
Clinical question: How does the frequency and clinical significance of urinary tract infection (UTI) compare to genitourinary trauma when associated with Foley catheterization?
Background: Foley catheter use in hospitalized patients is common and carries many associated risks. Although the risk of UTI when using catheters often is recognized, providers should consider other important complications of catheter use, such as genitourinary trauma.
Study design: Descriptive, prospective cohort study.
Setting: Single-center study in a Veterans Affairs hospital.
Synopsis: This surveillance study of 6,513 Foley catheter days compared the incidence of catheter-associated urinary tract infections (CAUTIs) to that of genitourinary trauma. Traumatic Foley events included gross hematuria, creation of false passage, ridging causing pain and/or difficulties with catheter removal, external genital trauma, catheter misplacement (ranging from prostatic to intraperitoneal), and catheter removal with the balloon inflated.
The incidence of possible UTI episodes was 1.8% of the Foley catheter days compared with 1.5% for catheter-associated trauma. Despite the fact that 72% of the UTI cases were asymptomatic, approximately 41% of these cases were treated with antibiotics, which accounted for 70% of all UTIs treated. Of the cases of Foley catheter trauma, 32% required further interventions (i.e. prolonged catheterization or cystoscopy). Trauma prompting intervention was as common as symptomatic UTIs.
The observational study design, use of a single center with a predominantly male population, and inclusion of patients undergoing urologic procedures who might have had valid indications for treatment of asymptomatic bacteriuria limit the study findings.
Bottom line: The complication of catheter-associated genitourinary trauma is just as common as CAUTIs in hospitalized patients, with each necessitating further intervention and treatment at similar rates.
Citation: Leuck AM, Wright D, Ellingson L, et al. Complications of Foley catheters—is infection the greatest risk? J Urol. 2012;187(5):1662-1666.
Intensive Control of Hyperglycemia in Noncritical, Hospitalized Patients Decreases Infection Risk, but No Significant Effect on Other Outcomes
Clinical question: What is the effect of tight glucose control in patients hospitalized in noncritical-care settings?
Background: Hyperglycemia is associated with increased in-hospital mortality and morbidity. Several trials have demonstrated the potential benefits of intensive glycemic control for patients in intensive-care settings, but this could lead to increased hypoglycemia. The effect of intensive therapy to achieve tight glycemic control in noncritically ill patients is unclear.
Study design: Systematic review and meta-analysis.
Setting: Various study sites of hospitalized patients.
Synopsis: This meta-analysis included 19 studies (nine randomized, 10 observational) published from 1995 to 2011. Intensive glycemic control (fasting blood glucose of 100-180 mg/dL) was not associated with significant effect on risk of death, myocardial infarction (MI), or stroke. There was a nonsignificant trend for increased risk of hypoglycemia (relative risk, 1.58; 95% CI, 0.97-2.57).
Intensive glycemic control was associated with a decreased risk of infection (relative risk, 0.41; 95% CI, 0.21–0.77), but this association mainly was derived from studies in surgical settings.
Subgroup analyses demonstrated an association between achieving intensive glycemic goals and an increased risk of hypoglycemia (P=0.01). Hypoglycemia also more commonly occurred in surgical patients.
There was substantial heterogeneity across studies included for all outcomes except infection. The quality of the current evidence supporting a reduction in infection is low and appears mostly derived from patients in surgical settings. The quality of evidence relating to all the other outcomes is also low and is limited by heterogeneity and imprecision.
Bottom line: Intensive control of hyperglycemia in noncritically ill hospitalized patients might reduce the risk of infection in some patients but does not appear to be significantly associated with improvement in other important clinical outcomes.
Citation: Murad MH, Coburn JA, Coto-Yglesias F, et al. Glycemic control in non-critically ill hospitalized patients: a systematic review and meta-analysis. J Clin Endocrinol Metab. 2012;97(1):49-58.
Simple Risk Score Predicts 30-Day Mortality after Noncardiac Surgery
Clinical question: Can 30-day mortality risk after noncardiac surgery be predicted by using a simple bedside-risk index?
Background: While indices exist to quantify the risk of cardiac complications in patients undergoing noncardiac surgery, there is significant perioperative mortality due to noncardiac causes. Therefore, a need exists for a simple risk index to predict all-cause mortality after noncardiac surgery.
Study design: Retrospective cohort study.
Setting: American College of Surgeons National Surgical Quality Improvement Program database of patients in more than 200 hospitals.
Synopsis: The nine-point Surgical Mortality Probability Model (S-MPM) 30-day mortality risk index was empirically created and applied to a randomly split portion of a database, which included 298,772 patients undergoing noncardiac surgery. Three risk factors were included: American Society of Anesthesiologists (ASA) physical status, surgery risk class, and emergency status. Patients with ASA physical status I, II, III, IV, or V were assigned zero, two, four, five, or six points, respectively. Patients undergoing intermediate- or high-risk procedures were assigned one or two points, respectively. Patients undergoing emergency procedures were assigned one point. The S-MPM then was applied to the validation portion of the data set.
The 30-day predicted risk of mortality was less than 0.50% for those patients with combined risk scores of less than five (S-MPM Class I), between 1.5% and 4.0% for risk scores of five to six (Class II), and more than 10% for risk scores greater than six (Class III).
The major limitation of this derived risk score is the reliance on ASA physical status, which has imprecise definitions and might lead to inconsistent ratings.
Bottom line: The S-MPM risk index is a simple bedside scoring system, which can accurately predict 30-day mortality in patients undergoing noncardiac surgery.
Citation: Glance LG, Lustik SJ, Hannan EL, et al. The Surgical Mortality Probability Model: Derivation and validation of a simple risk prediction rule for noncardiac surgery. Ann Surg. 2012;255(4):696-702.
Temperature, White Blood Cell Count Are Not Sensitive Predictors of Bacteremia
Clinical question: In ED patients with suspected infection, are temperature, white blood cell (WBC) count, and bandemia reliable predictors of bacteremia?
Background: Sepsis is a significant cause of morbidity and mortality. Early identification and treatment of sepsis improves patient outcomes. Although systemic inflammatory response syndrome criteria aids in the prompt recognition of sepsis, these markers have variable sensitivity and specificity for true infection or bacteremia, which places patients at high risk for sepsis.
Study design: Post-hoc data analysis of a prospective cohort study.
Setting: ED patients at a single tertiary-care center.
Synopsis: A retrospective analysis was performed on 3,563 patients who presented to the ED. Blood cultures obtained on patients with suspected infection revealed bacteremia in 289 patients (8.1%). Patients with bacteremia were reviewed for the presence of normal temperature (36.1° to 38° Celsius), normal WBC count (4,000 to 12,000 cells per µL), and presence of bandemia (>5% of WBC differential).
Among patients with bacteremia, 33% had a normal body temperature (67% sensitivity) and 52% had a normal WBC count (48% sensitivity). Of the 210 bacteremic patients who had a full differential performed, bandemia was present in 82% (sensitivity 82%). Bandemia was present in 80% of culture-positive patients with a normal temperature and 79% of culture-positive patients with a normal WBC count. Approximately 17% of patients with bacteremia had neither an abnormal temperature nor an abnormal WBC. This study was limited by the retrospective nature of analysis and the subjective designation of “suspected infection” by the original providers.
Bottom line: In patients presenting to the ED with suspected infection who are found to have culture-proven bacteremia, a significant percentage have normal temperature and WBC count, but the presence of bandemia could be more useful for identifying occult bacteremia.
Citation: Seigel TA, Cocchi MN, Salciccioli J, et al. Inadequacy of temperature and white blood cell count in predicting bacteremia in patients with suspected infection. J Emerg Med. 2012;42(3):254-259.
In This Edition
Literature At A Glance
A guide to this month’s studies
- Warfarin vs. aspirin in heart-failure patients
- Aspirin after anticoagulation prevents VTE recurrence
- Novel oral anticoagulants vs. warfarin in afib patients
- Intravenous metronidazole for mild C. diff infection
- Frequency of Foley catheter complications vs. CAUTI
- Intensive hyperglycemia control in noncritical hospitalized patients
- Risk score predicts 30-day mortality after noncardiac surgery
- Temperature, white blood cell count are not sensitive predictors of bacteremia
Warfarin Reduces Stoke but Increases Hemorrhage Compared with Aspirin in Patients with Heart Failure and Sinus Rhythm
Clinical question: Is warfarin superior to aspirin with regard to clinical outcomes in patients with heart failure who are in sinus rhythm?
Background: Heart failure is associated with stroke and death potentially caused by atherothrombotic events. Anticoagulation is efficacious in some heart failure patients with atrial fibrillation or significant valvular disease, but the role of anticoagulation versus aspirin in patients with chronic heart failure and sinus rhythm is unclear.
Study design: Double-blind randomized controlled trial.
Setting: Multicenter, multinational trial involving outpatients.
Synopsis: This double-blind, double-dummy trial involving 2,305 patients with sinus rhythm and reduced left ventricular ejection fraction (<35%) showed no significant difference in the primary combined outcome (ischemic stroke, intracerebral hemorrhage, or death) in those treated with warfarin as compared with aspirin. Warfarin did significantly reduce the rate of ischemic stroke by 0.64 events per 100 patient-years (absolute risk reduction 2.2%, number needed to treat 45) when compared with aspirin, with no significant difference in the rate of intracerebral hemorrhage. This outcome was offset by an increased rate of major hemorrhage by 0.91 events per 100 patient-years (absolute risk increase 3.1%, number needed to harm 32).
This study included patients from all functional classes of heart failure, with a protocol to initiate treatment with other standard heart failure medications. Patients with an indication for either warfarin or aspirin were excluded. Due to recruitment difficulties, the power of this study was reduced. Other study limitations included a relatively low percentage of time that patients on warfarin were in therapeutic range and a substantial period of follow-up time in which patients did not receive the assigned study treatments.
Bottom line: The benefit of reduced stoke in patients with heart failure and sinus rhythm who take warfarin over aspirin is counteracted by an increased risk for serious bleeding outcomes.
Citation: Homma S, Thompson JLP, Pullicino PM, et al. Warfarin and aspirin in patients with heart failure and sinus rhythm. N Engl J Med. 2012;366(20):1859-1869.
Aspirin Use after Recommended Anticoagulation Treatment Prevents Recurrence in VTE Patients
Clinical question: Does aspirin prevent recurrence in patients after treatment with anticoagulation following their first episode of unprovoked VTE?
Background: VTE recurrence is common following the discontinuation of anticoagulation, particularly in patients with a history of unprovoked pulmonary embolism (PE) or DVT. Extension of treatment with vitamin K antagonists decreases recurrence but also causes more bleeding. The role of aspirin in the secondary prevention of VTE is unknown.
Study design: Double-blind randomized controlled trial.
Setting: Multicenter international trial involving outpatients.
Synopsis: This trial compared treatment with aspirin versus placebo for approximately two years in 205 patients with a history of unprovoked VTE who had completed six to 18 months of anticoagulant therapy. The relative risk reduction of recurrent VTE in the aspirin versus the placebo group was approximately 40% per year (6.6% vs. 11.2% per year; absolute risk reduction 4.6% per year; number needed to treat 22). No difference in major or clinically relevant bleeding was observed between the two groups.
This study was appropriately powered to detect the treatment effect reported by the authors. Typically, anticoagulation is discontinued in this specific patient population once the risk of bleeding and/or the patient’s perceived inconvenience of therapy outweighs the expected benefit from continuing treatment to prevent VTE recurrence. Study results suggest aspirin is effective in preventing recurrence while not conferring an increased risk for hemorrhage. It is important to note that patients with cancer and symptomatic atherosclerosis were excluded from this study.
Bottom line: Following an appropriate treatment period with standard anticoagulation, aspirin appears to be a safe and effective therapy in the secondary prevention of recurrence in patients with a history of unprovoked VTE.
Citation: Becattini C, Agnelli G, Schenone A, et al. Aspirin for preventing recurrence of venous thromboembolism. N Engl J Med. 2012;366(21):1959-1967.
Meta-Analysis Supports New Oral Anticoagulants in Patients with Atrial Fibrillation
Clinical question: Are novel oral anticoagulants both efficacious and safe in comparison to warfarin in patients with atrial fibrillation (afib)?
Background: Three large clinical trials recently evaluated novel oral anticoagulants (dabigatran, rivaroxaban, and apixaban) as alternatives to warfarin in afib patients. Although the anticoagulants all appeared efficacious for primary outcomes, results regarding secondary and safety outcomes were either inconclusive or heterogeneous.
Study design: Systematic review and meta-analysis of randomized controlled trials.
Setting: Three diverse, clinical-trial settings.
Synopsis: A systematic review and meta-analysis of randomized controlled trials comparing novel oral anticoagulants to warfarin in afib patients found three large studies examining dabigatran, rivaroxaban, and apixaban that included 44,563 patients.
Using random-effects models to pool data from these studies, the authors found a 22% relative risk (RR) reduction of stroke or systemic embolism with the use of these new anticoagulants as compared to warfarin. The risks for ischemic and unidentified stroke (RR 0.87), hemorrhagic stroke (RR 0.45), intracranial bleeding (RR 0.49), and mortality (RR 0.88) were significantly reduced in patients taking these new anticoagulants. There was no significant reduction in major bleeding.
A trend in favor of warfarin was seen for gastrointestinal bleeding, but this trend was not statistically significant (RR 1.25; 95% confidence interval, 0.91-1.72).
This meta-analysis was limited to only three randomized controlled trials, each comparing a different oral anticoagulant to warfarin and using somewhat heterogeneous study designs and patient populations.
Bottom line: Three new oral anticoagulants appear safe and more efficacious than warfarin in the prevention of stroke and systemic embolism, as well as other important clinical outcomes in patients with atrial fibrillation.
Citation: Miller CS, Grandi SM, Shimony A, Filion KB, Eisenberg MJ. Meta-analysis of efficacy and safety of new oral anticoagulants (dabigatran, rivaroxaban, apixaban) versus warfarin in patients with atrial fibrillation. Am J Cardiol. 2012;110(3):453-60.
Observational Study Suggests Intravenous Metronidazole May Be Inferior for Mild Clostridium Difficile Infection
Clinical question: How do different treatment regimens (oral metronidazole vs. intravenous metronidazole vs. oral vancomycin) for mild Clostridium difficile infection (CDI) compare with regard to clinical outcomes?
Background: CDIs are increasing. Oral metronidazole or vancomycin can be used for the initial treatment of non-severe CDI. Additionally, a paucity of clinical data exists on intravenous metronidazole, which is used in some cases, typically in combination with vancomycin and in patients with severe CDI.
Study design: Prospective cohort study.
Setting: International hospital-based study.
Synopsis: This observational study assessed three different regimens (oral metronidazole, intravenous metronidazole, and oral vancomycin) for the treatment of mild CDI in 265 inpatients. Mortality at 30 days was higher in the intravenous metronidazole group (38.1%) than in the oral metronidazole (7.4%) and vancomycin (9.5%) groups. Patients receiving intravenous metronidazole also were less likely to recover from disease (52.4% versus >80% in the oral metronidazole and vancomycin groups). No statistically significant differences for other sequelae of CDI were found, except for higher risk of dehydration in the oral vancomycin group.
After controlling for age, sex, and comorbidity severity, patients in the intravenous metronidazole group were approximately four times more likely to die than patients in either the oral vancomycin group or the oral metronidazole group. There was no significant difference in mortality between the oral metronidazole and vancomycin groups.
Although this study was limited by its observational nature, no randomized controlled trial has yet to compare these three treatment regimens for mild CDI.
Bottom line: Treatment of mild C. diff infection with intravenous metronidazole appears to be associated with higher mortality and lower disease resolution than treatment with either oral metronidazole or vancomycin.
Citation: Wenisch JM, Schmid D, Kuo HW, et al. Prospective observational study comparing three different treatment regimes in patients with Clostridium difficile infection. Antimicrob Agents Chemother. 2012;56(4):1974-1978.
Traumatic Foley Catheter Complications Occur with Similar Frequency as Catheter-Associated Urinary Tract Infections
Clinical question: How does the frequency and clinical significance of urinary tract infection (UTI) compare to genitourinary trauma when associated with Foley catheterization?
Background: Foley catheter use in hospitalized patients is common and carries many associated risks. Although the risk of UTI when using catheters often is recognized, providers should consider other important complications of catheter use, such as genitourinary trauma.
Study design: Descriptive, prospective cohort study.
Setting: Single-center study in a Veterans Affairs hospital.
Synopsis: This surveillance study of 6,513 Foley catheter days compared the incidence of catheter-associated urinary tract infections (CAUTIs) to that of genitourinary trauma. Traumatic Foley events included gross hematuria, creation of false passage, ridging causing pain and/or difficulties with catheter removal, external genital trauma, catheter misplacement (ranging from prostatic to intraperitoneal), and catheter removal with the balloon inflated.
The incidence of possible UTI episodes was 1.8% of the Foley catheter days compared with 1.5% for catheter-associated trauma. Despite the fact that 72% of the UTI cases were asymptomatic, approximately 41% of these cases were treated with antibiotics, which accounted for 70% of all UTIs treated. Of the cases of Foley catheter trauma, 32% required further interventions (i.e. prolonged catheterization or cystoscopy). Trauma prompting intervention was as common as symptomatic UTIs.
The observational study design, use of a single center with a predominantly male population, and inclusion of patients undergoing urologic procedures who might have had valid indications for treatment of asymptomatic bacteriuria limit the study findings.
Bottom line: The complication of catheter-associated genitourinary trauma is just as common as CAUTIs in hospitalized patients, with each necessitating further intervention and treatment at similar rates.
Citation: Leuck AM, Wright D, Ellingson L, et al. Complications of Foley catheters—is infection the greatest risk? J Urol. 2012;187(5):1662-1666.
Intensive Control of Hyperglycemia in Noncritical, Hospitalized Patients Decreases Infection Risk, but No Significant Effect on Other Outcomes
Clinical question: What is the effect of tight glucose control in patients hospitalized in noncritical-care settings?
Background: Hyperglycemia is associated with increased in-hospital mortality and morbidity. Several trials have demonstrated the potential benefits of intensive glycemic control for patients in intensive-care settings, but this could lead to increased hypoglycemia. The effect of intensive therapy to achieve tight glycemic control in noncritically ill patients is unclear.
Study design: Systematic review and meta-analysis.
Setting: Various study sites of hospitalized patients.
Synopsis: This meta-analysis included 19 studies (nine randomized, 10 observational) published from 1995 to 2011. Intensive glycemic control (fasting blood glucose of 100-180 mg/dL) was not associated with significant effect on risk of death, myocardial infarction (MI), or stroke. There was a nonsignificant trend for increased risk of hypoglycemia (relative risk, 1.58; 95% CI, 0.97-2.57).
Intensive glycemic control was associated with a decreased risk of infection (relative risk, 0.41; 95% CI, 0.21–0.77), but this association mainly was derived from studies in surgical settings.
Subgroup analyses demonstrated an association between achieving intensive glycemic goals and an increased risk of hypoglycemia (P=0.01). Hypoglycemia also more commonly occurred in surgical patients.
There was substantial heterogeneity across studies included for all outcomes except infection. The quality of the current evidence supporting a reduction in infection is low and appears mostly derived from patients in surgical settings. The quality of evidence relating to all the other outcomes is also low and is limited by heterogeneity and imprecision.
Bottom line: Intensive control of hyperglycemia in noncritically ill hospitalized patients might reduce the risk of infection in some patients but does not appear to be significantly associated with improvement in other important clinical outcomes.
Citation: Murad MH, Coburn JA, Coto-Yglesias F, et al. Glycemic control in non-critically ill hospitalized patients: a systematic review and meta-analysis. J Clin Endocrinol Metab. 2012;97(1):49-58.
Simple Risk Score Predicts 30-Day Mortality after Noncardiac Surgery
Clinical question: Can 30-day mortality risk after noncardiac surgery be predicted by using a simple bedside-risk index?
Background: While indices exist to quantify the risk of cardiac complications in patients undergoing noncardiac surgery, there is significant perioperative mortality due to noncardiac causes. Therefore, a need exists for a simple risk index to predict all-cause mortality after noncardiac surgery.
Study design: Retrospective cohort study.
Setting: American College of Surgeons National Surgical Quality Improvement Program database of patients in more than 200 hospitals.
Synopsis: The nine-point Surgical Mortality Probability Model (S-MPM) 30-day mortality risk index was empirically created and applied to a randomly split portion of a database, which included 298,772 patients undergoing noncardiac surgery. Three risk factors were included: American Society of Anesthesiologists (ASA) physical status, surgery risk class, and emergency status. Patients with ASA physical status I, II, III, IV, or V were assigned zero, two, four, five, or six points, respectively. Patients undergoing intermediate- or high-risk procedures were assigned one or two points, respectively. Patients undergoing emergency procedures were assigned one point. The S-MPM then was applied to the validation portion of the data set.
The 30-day predicted risk of mortality was less than 0.50% for those patients with combined risk scores of less than five (S-MPM Class I), between 1.5% and 4.0% for risk scores of five to six (Class II), and more than 10% for risk scores greater than six (Class III).
The major limitation of this derived risk score is the reliance on ASA physical status, which has imprecise definitions and might lead to inconsistent ratings.
Bottom line: The S-MPM risk index is a simple bedside scoring system, which can accurately predict 30-day mortality in patients undergoing noncardiac surgery.
Citation: Glance LG, Lustik SJ, Hannan EL, et al. The Surgical Mortality Probability Model: Derivation and validation of a simple risk prediction rule for noncardiac surgery. Ann Surg. 2012;255(4):696-702.
Temperature, White Blood Cell Count Are Not Sensitive Predictors of Bacteremia
Clinical question: In ED patients with suspected infection, are temperature, white blood cell (WBC) count, and bandemia reliable predictors of bacteremia?
Background: Sepsis is a significant cause of morbidity and mortality. Early identification and treatment of sepsis improves patient outcomes. Although systemic inflammatory response syndrome criteria aids in the prompt recognition of sepsis, these markers have variable sensitivity and specificity for true infection or bacteremia, which places patients at high risk for sepsis.
Study design: Post-hoc data analysis of a prospective cohort study.
Setting: ED patients at a single tertiary-care center.
Synopsis: A retrospective analysis was performed on 3,563 patients who presented to the ED. Blood cultures obtained on patients with suspected infection revealed bacteremia in 289 patients (8.1%). Patients with bacteremia were reviewed for the presence of normal temperature (36.1° to 38° Celsius), normal WBC count (4,000 to 12,000 cells per µL), and presence of bandemia (>5% of WBC differential).
Among patients with bacteremia, 33% had a normal body temperature (67% sensitivity) and 52% had a normal WBC count (48% sensitivity). Of the 210 bacteremic patients who had a full differential performed, bandemia was present in 82% (sensitivity 82%). Bandemia was present in 80% of culture-positive patients with a normal temperature and 79% of culture-positive patients with a normal WBC count. Approximately 17% of patients with bacteremia had neither an abnormal temperature nor an abnormal WBC. This study was limited by the retrospective nature of analysis and the subjective designation of “suspected infection” by the original providers.
Bottom line: In patients presenting to the ED with suspected infection who are found to have culture-proven bacteremia, a significant percentage have normal temperature and WBC count, but the presence of bandemia could be more useful for identifying occult bacteremia.
Citation: Seigel TA, Cocchi MN, Salciccioli J, et al. Inadequacy of temperature and white blood cell count in predicting bacteremia in patients with suspected infection. J Emerg Med. 2012;42(3):254-259.
In This Edition
Literature At A Glance
A guide to this month’s studies
- Warfarin vs. aspirin in heart-failure patients
- Aspirin after anticoagulation prevents VTE recurrence
- Novel oral anticoagulants vs. warfarin in afib patients
- Intravenous metronidazole for mild C. diff infection
- Frequency of Foley catheter complications vs. CAUTI
- Intensive hyperglycemia control in noncritical hospitalized patients
- Risk score predicts 30-day mortality after noncardiac surgery
- Temperature, white blood cell count are not sensitive predictors of bacteremia
Warfarin Reduces Stoke but Increases Hemorrhage Compared with Aspirin in Patients with Heart Failure and Sinus Rhythm
Clinical question: Is warfarin superior to aspirin with regard to clinical outcomes in patients with heart failure who are in sinus rhythm?
Background: Heart failure is associated with stroke and death potentially caused by atherothrombotic events. Anticoagulation is efficacious in some heart failure patients with atrial fibrillation or significant valvular disease, but the role of anticoagulation versus aspirin in patients with chronic heart failure and sinus rhythm is unclear.
Study design: Double-blind randomized controlled trial.
Setting: Multicenter, multinational trial involving outpatients.
Synopsis: This double-blind, double-dummy trial involving 2,305 patients with sinus rhythm and reduced left ventricular ejection fraction (<35%) showed no significant difference in the primary combined outcome (ischemic stroke, intracerebral hemorrhage, or death) in those treated with warfarin as compared with aspirin. Warfarin did significantly reduce the rate of ischemic stroke by 0.64 events per 100 patient-years (absolute risk reduction 2.2%, number needed to treat 45) when compared with aspirin, with no significant difference in the rate of intracerebral hemorrhage. This outcome was offset by an increased rate of major hemorrhage by 0.91 events per 100 patient-years (absolute risk increase 3.1%, number needed to harm 32).
This study included patients from all functional classes of heart failure, with a protocol to initiate treatment with other standard heart failure medications. Patients with an indication for either warfarin or aspirin were excluded. Due to recruitment difficulties, the power of this study was reduced. Other study limitations included a relatively low percentage of time that patients on warfarin were in therapeutic range and a substantial period of follow-up time in which patients did not receive the assigned study treatments.
Bottom line: The benefit of reduced stoke in patients with heart failure and sinus rhythm who take warfarin over aspirin is counteracted by an increased risk for serious bleeding outcomes.
Citation: Homma S, Thompson JLP, Pullicino PM, et al. Warfarin and aspirin in patients with heart failure and sinus rhythm. N Engl J Med. 2012;366(20):1859-1869.
Aspirin Use after Recommended Anticoagulation Treatment Prevents Recurrence in VTE Patients
Clinical question: Does aspirin prevent recurrence in patients after treatment with anticoagulation following their first episode of unprovoked VTE?
Background: VTE recurrence is common following the discontinuation of anticoagulation, particularly in patients with a history of unprovoked pulmonary embolism (PE) or DVT. Extension of treatment with vitamin K antagonists decreases recurrence but also causes more bleeding. The role of aspirin in the secondary prevention of VTE is unknown.
Study design: Double-blind randomized controlled trial.
Setting: Multicenter international trial involving outpatients.
Synopsis: This trial compared treatment with aspirin versus placebo for approximately two years in 205 patients with a history of unprovoked VTE who had completed six to 18 months of anticoagulant therapy. The relative risk reduction of recurrent VTE in the aspirin versus the placebo group was approximately 40% per year (6.6% vs. 11.2% per year; absolute risk reduction 4.6% per year; number needed to treat 22). No difference in major or clinically relevant bleeding was observed between the two groups.
This study was appropriately powered to detect the treatment effect reported by the authors. Typically, anticoagulation is discontinued in this specific patient population once the risk of bleeding and/or the patient’s perceived inconvenience of therapy outweighs the expected benefit from continuing treatment to prevent VTE recurrence. Study results suggest aspirin is effective in preventing recurrence while not conferring an increased risk for hemorrhage. It is important to note that patients with cancer and symptomatic atherosclerosis were excluded from this study.
Bottom line: Following an appropriate treatment period with standard anticoagulation, aspirin appears to be a safe and effective therapy in the secondary prevention of recurrence in patients with a history of unprovoked VTE.
Citation: Becattini C, Agnelli G, Schenone A, et al. Aspirin for preventing recurrence of venous thromboembolism. N Engl J Med. 2012;366(21):1959-1967.
Meta-Analysis Supports New Oral Anticoagulants in Patients with Atrial Fibrillation
Clinical question: Are novel oral anticoagulants both efficacious and safe in comparison to warfarin in patients with atrial fibrillation (afib)?
Background: Three large clinical trials recently evaluated novel oral anticoagulants (dabigatran, rivaroxaban, and apixaban) as alternatives to warfarin in afib patients. Although the anticoagulants all appeared efficacious for primary outcomes, results regarding secondary and safety outcomes were either inconclusive or heterogeneous.
Study design: Systematic review and meta-analysis of randomized controlled trials.
Setting: Three diverse, clinical-trial settings.
Synopsis: A systematic review and meta-analysis of randomized controlled trials comparing novel oral anticoagulants to warfarin in afib patients found three large studies examining dabigatran, rivaroxaban, and apixaban that included 44,563 patients.
Using random-effects models to pool data from these studies, the authors found a 22% relative risk (RR) reduction of stroke or systemic embolism with the use of these new anticoagulants as compared to warfarin. The risks for ischemic and unidentified stroke (RR 0.87), hemorrhagic stroke (RR 0.45), intracranial bleeding (RR 0.49), and mortality (RR 0.88) were significantly reduced in patients taking these new anticoagulants. There was no significant reduction in major bleeding.
A trend in favor of warfarin was seen for gastrointestinal bleeding, but this trend was not statistically significant (RR 1.25; 95% confidence interval, 0.91-1.72).
This meta-analysis was limited to only three randomized controlled trials, each comparing a different oral anticoagulant to warfarin and using somewhat heterogeneous study designs and patient populations.
Bottom line: Three new oral anticoagulants appear safe and more efficacious than warfarin in the prevention of stroke and systemic embolism, as well as other important clinical outcomes in patients with atrial fibrillation.
Citation: Miller CS, Grandi SM, Shimony A, Filion KB, Eisenberg MJ. Meta-analysis of efficacy and safety of new oral anticoagulants (dabigatran, rivaroxaban, apixaban) versus warfarin in patients with atrial fibrillation. Am J Cardiol. 2012;110(3):453-60.
Observational Study Suggests Intravenous Metronidazole May Be Inferior for Mild Clostridium Difficile Infection
Clinical question: How do different treatment regimens (oral metronidazole vs. intravenous metronidazole vs. oral vancomycin) for mild Clostridium difficile infection (CDI) compare with regard to clinical outcomes?
Background: CDIs are increasing. Oral metronidazole or vancomycin can be used for the initial treatment of non-severe CDI. Additionally, a paucity of clinical data exists on intravenous metronidazole, which is used in some cases, typically in combination with vancomycin and in patients with severe CDI.
Study design: Prospective cohort study.
Setting: International hospital-based study.
Synopsis: This observational study assessed three different regimens (oral metronidazole, intravenous metronidazole, and oral vancomycin) for the treatment of mild CDI in 265 inpatients. Mortality at 30 days was higher in the intravenous metronidazole group (38.1%) than in the oral metronidazole (7.4%) and vancomycin (9.5%) groups. Patients receiving intravenous metronidazole also were less likely to recover from disease (52.4% versus >80% in the oral metronidazole and vancomycin groups). No statistically significant differences for other sequelae of CDI were found, except for higher risk of dehydration in the oral vancomycin group.
After controlling for age, sex, and comorbidity severity, patients in the intravenous metronidazole group were approximately four times more likely to die than patients in either the oral vancomycin group or the oral metronidazole group. There was no significant difference in mortality between the oral metronidazole and vancomycin groups.
Although this study was limited by its observational nature, no randomized controlled trial has yet to compare these three treatment regimens for mild CDI.
Bottom line: Treatment of mild C. diff infection with intravenous metronidazole appears to be associated with higher mortality and lower disease resolution than treatment with either oral metronidazole or vancomycin.
Citation: Wenisch JM, Schmid D, Kuo HW, et al. Prospective observational study comparing three different treatment regimes in patients with Clostridium difficile infection. Antimicrob Agents Chemother. 2012;56(4):1974-1978.
Traumatic Foley Catheter Complications Occur with Similar Frequency as Catheter-Associated Urinary Tract Infections
Clinical question: How does the frequency and clinical significance of urinary tract infection (UTI) compare to genitourinary trauma when associated with Foley catheterization?
Background: Foley catheter use in hospitalized patients is common and carries many associated risks. Although the risk of UTI when using catheters often is recognized, providers should consider other important complications of catheter use, such as genitourinary trauma.
Study design: Descriptive, prospective cohort study.
Setting: Single-center study in a Veterans Affairs hospital.
Synopsis: This surveillance study of 6,513 Foley catheter days compared the incidence of catheter-associated urinary tract infections (CAUTIs) to that of genitourinary trauma. Traumatic Foley events included gross hematuria, creation of false passage, ridging causing pain and/or difficulties with catheter removal, external genital trauma, catheter misplacement (ranging from prostatic to intraperitoneal), and catheter removal with the balloon inflated.
The incidence of possible UTI episodes was 1.8% of the Foley catheter days compared with 1.5% for catheter-associated trauma. Despite the fact that 72% of the UTI cases were asymptomatic, approximately 41% of these cases were treated with antibiotics, which accounted for 70% of all UTIs treated. Of the cases of Foley catheter trauma, 32% required further interventions (i.e. prolonged catheterization or cystoscopy). Trauma prompting intervention was as common as symptomatic UTIs.
The observational study design, use of a single center with a predominantly male population, and inclusion of patients undergoing urologic procedures who might have had valid indications for treatment of asymptomatic bacteriuria limit the study findings.
Bottom line: The complication of catheter-associated genitourinary trauma is just as common as CAUTIs in hospitalized patients, with each necessitating further intervention and treatment at similar rates.
Citation: Leuck AM, Wright D, Ellingson L, et al. Complications of Foley catheters—is infection the greatest risk? J Urol. 2012;187(5):1662-1666.
Intensive Control of Hyperglycemia in Noncritical, Hospitalized Patients Decreases Infection Risk, but No Significant Effect on Other Outcomes
Clinical question: What is the effect of tight glucose control in patients hospitalized in noncritical-care settings?
Background: Hyperglycemia is associated with increased in-hospital mortality and morbidity. Several trials have demonstrated the potential benefits of intensive glycemic control for patients in intensive-care settings, but this could lead to increased hypoglycemia. The effect of intensive therapy to achieve tight glycemic control in noncritically ill patients is unclear.
Study design: Systematic review and meta-analysis.
Setting: Various study sites of hospitalized patients.
Synopsis: This meta-analysis included 19 studies (nine randomized, 10 observational) published from 1995 to 2011. Intensive glycemic control (fasting blood glucose of 100-180 mg/dL) was not associated with significant effect on risk of death, myocardial infarction (MI), or stroke. There was a nonsignificant trend for increased risk of hypoglycemia (relative risk, 1.58; 95% CI, 0.97-2.57).
Intensive glycemic control was associated with a decreased risk of infection (relative risk, 0.41; 95% CI, 0.21–0.77), but this association mainly was derived from studies in surgical settings.
Subgroup analyses demonstrated an association between achieving intensive glycemic goals and an increased risk of hypoglycemia (P=0.01). Hypoglycemia also more commonly occurred in surgical patients.
There was substantial heterogeneity across studies included for all outcomes except infection. The quality of the current evidence supporting a reduction in infection is low and appears mostly derived from patients in surgical settings. The quality of evidence relating to all the other outcomes is also low and is limited by heterogeneity and imprecision.
Bottom line: Intensive control of hyperglycemia in noncritically ill hospitalized patients might reduce the risk of infection in some patients but does not appear to be significantly associated with improvement in other important clinical outcomes.
Citation: Murad MH, Coburn JA, Coto-Yglesias F, et al. Glycemic control in non-critically ill hospitalized patients: a systematic review and meta-analysis. J Clin Endocrinol Metab. 2012;97(1):49-58.
Simple Risk Score Predicts 30-Day Mortality after Noncardiac Surgery
Clinical question: Can 30-day mortality risk after noncardiac surgery be predicted by using a simple bedside-risk index?
Background: While indices exist to quantify the risk of cardiac complications in patients undergoing noncardiac surgery, there is significant perioperative mortality due to noncardiac causes. Therefore, a need exists for a simple risk index to predict all-cause mortality after noncardiac surgery.
Study design: Retrospective cohort study.
Setting: American College of Surgeons National Surgical Quality Improvement Program database of patients in more than 200 hospitals.
Synopsis: The nine-point Surgical Mortality Probability Model (S-MPM) 30-day mortality risk index was empirically created and applied to a randomly split portion of a database, which included 298,772 patients undergoing noncardiac surgery. Three risk factors were included: American Society of Anesthesiologists (ASA) physical status, surgery risk class, and emergency status. Patients with ASA physical status I, II, III, IV, or V were assigned zero, two, four, five, or six points, respectively. Patients undergoing intermediate- or high-risk procedures were assigned one or two points, respectively. Patients undergoing emergency procedures were assigned one point. The S-MPM then was applied to the validation portion of the data set.
The 30-day predicted risk of mortality was less than 0.50% for those patients with combined risk scores of less than five (S-MPM Class I), between 1.5% and 4.0% for risk scores of five to six (Class II), and more than 10% for risk scores greater than six (Class III).
The major limitation of this derived risk score is the reliance on ASA physical status, which has imprecise definitions and might lead to inconsistent ratings.
Bottom line: The S-MPM risk index is a simple bedside scoring system, which can accurately predict 30-day mortality in patients undergoing noncardiac surgery.
Citation: Glance LG, Lustik SJ, Hannan EL, et al. The Surgical Mortality Probability Model: Derivation and validation of a simple risk prediction rule for noncardiac surgery. Ann Surg. 2012;255(4):696-702.
Temperature, White Blood Cell Count Are Not Sensitive Predictors of Bacteremia
Clinical question: In ED patients with suspected infection, are temperature, white blood cell (WBC) count, and bandemia reliable predictors of bacteremia?
Background: Sepsis is a significant cause of morbidity and mortality. Early identification and treatment of sepsis improves patient outcomes. Although systemic inflammatory response syndrome criteria aids in the prompt recognition of sepsis, these markers have variable sensitivity and specificity for true infection or bacteremia, which places patients at high risk for sepsis.
Study design: Post-hoc data analysis of a prospective cohort study.
Setting: ED patients at a single tertiary-care center.
Synopsis: A retrospective analysis was performed on 3,563 patients who presented to the ED. Blood cultures obtained on patients with suspected infection revealed bacteremia in 289 patients (8.1%). Patients with bacteremia were reviewed for the presence of normal temperature (36.1° to 38° Celsius), normal WBC count (4,000 to 12,000 cells per µL), and presence of bandemia (>5% of WBC differential).
Among patients with bacteremia, 33% had a normal body temperature (67% sensitivity) and 52% had a normal WBC count (48% sensitivity). Of the 210 bacteremic patients who had a full differential performed, bandemia was present in 82% (sensitivity 82%). Bandemia was present in 80% of culture-positive patients with a normal temperature and 79% of culture-positive patients with a normal WBC count. Approximately 17% of patients with bacteremia had neither an abnormal temperature nor an abnormal WBC. This study was limited by the retrospective nature of analysis and the subjective designation of “suspected infection” by the original providers.
Bottom line: In patients presenting to the ED with suspected infection who are found to have culture-proven bacteremia, a significant percentage have normal temperature and WBC count, but the presence of bandemia could be more useful for identifying occult bacteremia.
Citation: Seigel TA, Cocchi MN, Salciccioli J, et al. Inadequacy of temperature and white blood cell count in predicting bacteremia in patients with suspected infection. J Emerg Med. 2012;42(3):254-259.
ITL: Physician Reviews of HM-Relevant Research
Clinical question: Is azithromycin use associated with an increased risk of cardiovascular death?
Background: Accumulating evidence suggests that azithromycin might have pro-arrhythmic effects on the heart. Other macrolides, including erythromycin and clarithromycin, can increase the risk for serious ventricular arrhythmias and are associated with an increased risk of sudden cardiac death. The risk of cardiac death associated with azithromycin use is unclear.
Study design: Retrospective cohort study.
Setting: Statewide database of patients enrolled in the Tennessee Medicaid program.
Synopsis: This study matched patients who took a five-day course of azithromycin (347,795 prescriptions) with those who took no antibiotics (1,391,180 control periods). Patients taking azithromycin had an increased risk of cardiovascular death (hazard ratio [HR], 2.88; P<0.001) and death from any cause (HR, 1.85; P=0.002).
Additional control groups of patients taking other antibiotics were included in this study for comparison. Patients who took amoxicillin did not have an increased risk of death. Relative to amoxicillin, azithromycin was associated with a significantly increased risk of cardiovascular death, with an estimated 47 additional cardiovascular deaths per 1 million courses. The risk of cardiovascular death was greater with azithromycin than with ciprofloxacin but did not differ significantly from levofloxacin.
Importantly, patients with factors conferring a high risk of death were excluded from analysis. The increased risk of death did not appear to persist after azithromycin therapy ended. A major limitation of this study was confounding associated with antibiotic use, which the authors attempted to mitigate with the use of multiple control groups.
Bottom line: A five-day treatment course of azithromycin is associated with a small absolute increase in cardiovascular deaths and deaths from any cause.
Citation: Ray WA, Murray KT, Hall K, Arbogast PG, Stein CM. Azithromycin and the risk of cardiovascular death. N Engl J Med. 2012;366:1881-1890.
Clinical question: Is azithromycin use associated with an increased risk of cardiovascular death?
Background: Accumulating evidence suggests that azithromycin might have pro-arrhythmic effects on the heart. Other macrolides, including erythromycin and clarithromycin, can increase the risk for serious ventricular arrhythmias and are associated with an increased risk of sudden cardiac death. The risk of cardiac death associated with azithromycin use is unclear.
Study design: Retrospective cohort study.
Setting: Statewide database of patients enrolled in the Tennessee Medicaid program.
Synopsis: This study matched patients who took a five-day course of azithromycin (347,795 prescriptions) with those who took no antibiotics (1,391,180 control periods). Patients taking azithromycin had an increased risk of cardiovascular death (hazard ratio [HR], 2.88; P<0.001) and death from any cause (HR, 1.85; P=0.002).
Additional control groups of patients taking other antibiotics were included in this study for comparison. Patients who took amoxicillin did not have an increased risk of death. Relative to amoxicillin, azithromycin was associated with a significantly increased risk of cardiovascular death, with an estimated 47 additional cardiovascular deaths per 1 million courses. The risk of cardiovascular death was greater with azithromycin than with ciprofloxacin but did not differ significantly from levofloxacin.
Importantly, patients with factors conferring a high risk of death were excluded from analysis. The increased risk of death did not appear to persist after azithromycin therapy ended. A major limitation of this study was confounding associated with antibiotic use, which the authors attempted to mitigate with the use of multiple control groups.
Bottom line: A five-day treatment course of azithromycin is associated with a small absolute increase in cardiovascular deaths and deaths from any cause.
Citation: Ray WA, Murray KT, Hall K, Arbogast PG, Stein CM. Azithromycin and the risk of cardiovascular death. N Engl J Med. 2012;366:1881-1890.
Clinical question: Is azithromycin use associated with an increased risk of cardiovascular death?
Background: Accumulating evidence suggests that azithromycin might have pro-arrhythmic effects on the heart. Other macrolides, including erythromycin and clarithromycin, can increase the risk for serious ventricular arrhythmias and are associated with an increased risk of sudden cardiac death. The risk of cardiac death associated with azithromycin use is unclear.
Study design: Retrospective cohort study.
Setting: Statewide database of patients enrolled in the Tennessee Medicaid program.
Synopsis: This study matched patients who took a five-day course of azithromycin (347,795 prescriptions) with those who took no antibiotics (1,391,180 control periods). Patients taking azithromycin had an increased risk of cardiovascular death (hazard ratio [HR], 2.88; P<0.001) and death from any cause (HR, 1.85; P=0.002).
Additional control groups of patients taking other antibiotics were included in this study for comparison. Patients who took amoxicillin did not have an increased risk of death. Relative to amoxicillin, azithromycin was associated with a significantly increased risk of cardiovascular death, with an estimated 47 additional cardiovascular deaths per 1 million courses. The risk of cardiovascular death was greater with azithromycin than with ciprofloxacin but did not differ significantly from levofloxacin.
Importantly, patients with factors conferring a high risk of death were excluded from analysis. The increased risk of death did not appear to persist after azithromycin therapy ended. A major limitation of this study was confounding associated with antibiotic use, which the authors attempted to mitigate with the use of multiple control groups.
Bottom line: A five-day treatment course of azithromycin is associated with a small absolute increase in cardiovascular deaths and deaths from any cause.
Citation: Ray WA, Murray KT, Hall K, Arbogast PG, Stein CM. Azithromycin and the risk of cardiovascular death. N Engl J Med. 2012;366:1881-1890.
In the Literature: Research You Need to Know
In This Edition
Literature At A Glance
A guide to this month’s studies
- Screening for AAA
- Adverse events in atrial fibrillation
- Biological treatment of inflammatory bowel diseases
- Steroid treatment of inflammatory bowel diseases
- Levofloxacin for H. pylori
- Natural history of tako-tsubo cardiomyopathy
- Predicting postoperative pulmonary complications
- Code status and goals of care in the ICU
New Screening Strategy To Identify Large Abdominal Aortic Aneurysms
Clinical question: Can an effective scoring system be developed to better identify patients at risk for large abdominal aortic aneurysms (AAA)?
Background: Screening reduces AAA-related mortality by about half in men aged >65. The United States Preventive Services Task Force (USPSTF) has recommended screening for AAA in men aged 65 to 75 with a history of smoking. However, more than 50% of AAA ruptures occur in individuals outside this patient cohort, and only some AAAs detected are large enough to warrant surgery.
Study design: Retrospective, observational cohort study.
Setting: More than 20,000 screening sites across the U.S.
Synopsis: Researchers collected demographics and risk factors from 3.1 million people undergoing ultrasound screening for AAA by Life Line Screening Inc. At the screening visit, subjects completed a questionnaire about their health status and medical history. Screening data also included diameter of the infrarenal abdominal aorta. To construct and test a risk model, the screened individuals were randomly allocated into two equal groups: a data set used for model development and one for validation.
Most of the AAAs greater than 5 cm in diameter discovered were in males (84.4%) and among subjects with a smoking history (83%). Other risk factors for large AAAs included advanced age, peripheral arterial disease, and obesity. The authors estimate that there are about 121,000 people with >5.0 cm aneurysms in the general population. Current guidelines would detect only 33.7% of the existing large AAAs. Study limitations include possible selection bias, as a majority of patients were self-referred. Also, the database did not include all comorbidities that could affect the risk of AAA. The self-reported nature of health data might cause misclassification of a patient’s true health status.
Bottom line: A screening strategy based on a newly developed scoring system is an effective way to identify patients at risk of large abdominal aortic aneurysms.
Citation: Greco G, Egorova NN, Gelijns AC, et al. Development of a novel scoring tool for the identification of large >5 cm abdominal aortic aneurysms. Ann Surg. 2010;252(4):675-682.
Risk Factors for Adverse Events in Patients with Symptomatic Atrial Fibrillation
Clinical question: What are the predictors of 30-day adverse events in ED patients evaluated for symptomatic atrial fibrillation?
Background: Atrial fibrillation (AF) affects more than 2 million people in the U.S. and accounts for nearly 1% of ED visits. Physicians have little information to guide risk stratification, and they admit more than 65% of patients. A strategy to better define the ED management of patients presenting with atrial fibrillation is required.
Study design: Retrospective, observational cohort study.
Setting: Urban academic tertiary-care referral center with an adult ED.
Synopsis: A systematic review of the electronic medical records of all ED patients presenting with symptomatic atrial fibrillation over a three-year period was performed. Predefined adverse outcomes included 30-day ED return visits, unscheduled hospitalizations, cardiovascular complications, or death.
Of 832 eligible patients, 216 (25.9%) experienced at least one of the 30-day adverse events. Adverse events occurred in 181 of the 638 (28.4%) admitted patients and 35 of the 192 (18.2%) patients discharged from the ED. Increasing age, complaint of dyspnea, smoking history, inadequate ventricular rate control, and patients receiving beta-blockers were factors independently associated with higher risk for adverse events.
Study results were limited by a number of factors. This was a single-center, retrospective, observational study, with all of its inherent limitations. The predictor model did not include laboratory data, such as BNP or troponin. Patients might have experienced additional events within the 30 days that were treated at other hospitals and not recorded in the database. Patient disposition might have affected the results, as patients initially admitted from the ED had a higher rate of 30-day adverse events than patients who were discharged from the ED.
Bottom line: Patients with increased age, smoking history, complaints of dyspnea, inadequate ventricular rate control in the ED, and home beta-blocker therapy are more likely to experience an atrial-fibrillation-related adverse event within 30 days.
Citation: Barrett TW, Martin AR, Storrow AB, et al. A clinical prediction model to estimate risk for 30-day adverse events in emergency department patients with symptomatic atrial fibrillation. Ann Emerg Med. 2011;57 (1):1-12.
Biological Therapies Are Effective in Inducing Remission in Inflammatory Bowel Disease
Clinical question: Are biological therapies useful in the treatment of ulcerative colitis (UC) and Crohn’s disease (CD)?
Background: Patients with CD and UC often experience flares of disease activity, despite maintenance therapy with 5-aminosalicylic acid compounds. These flares are usually treated with corticosteroids, which carry numerous adverse side effects. The role of biological therapies in inducing remission is uncertain.
Study design: Systematic review and meta-analysis.
Setting: Twenty-seven randomized controlled trials involving 7,416 patients.
Synopsis: Anti-TNF α antibodies and natalizumab were both superior to placebo in inducing remission of luminal CD (RR of no remission 0.87 and 0.88, respectively). Anti-TNF antibodies also were superior to placebo in preventing relapse of luminal CD (RR of relapse=0.71). Infliximab was superior to placebo in inducing remission of moderate to severely active UC (RR=0.72; 95% CI, 0.57-0.91). There were no significantly increased adverse drug effects with anti-TNF α antibodies or with infliximab compared with placebo. Natalizumab caused significantly higher rates of headache.
Limitations include risk of publication bias inherent in meta-analyses. There also was evidence of moderate heterogeneity in the studies analyzed. Finally, not every study was consistent in reporting adverse drug effects.
Bottom line: Biological therapies are superior to placebo in inducing remission of active UC and CD, as well as preventing relapse of quiescent CD.
Citation: Ford AC, Sandborn WJ, Khan KJ, Hanauer SB, Talley NJ, Moayyedi P. Efficacy of biological therapies in inflammatory bowel disease: systematic review and meta-analysis. Am J Gastroenterol. 2011; 106(4):644-659.
Glucocorticosteroids Probably Effective in Treatment of Inflammatory Bowel Disease, Primarily in Active Ulcerative Colitis
Clinical question: Is glucocorticosteroid therapy effective in the treatment of active IBD and in preventing relapses?
Background: Crohn’s disease (CD) and ulcerative colitis (UC) are chronic inflammatory bowel diseases of unclear etiology. Use of standard glucocorticosteroids and budesonide is widespread in inflammatory bowel disease (IBD) treatment. To date, there has been no large-scale meta-analysis to examine the effectiveness of both treatments in CD and UC.
Study design: Systematic review and meta-analysis.
Setting: Twenty randomized controlled trials totaling 2,398 patients.
Synopsis: Standard glucocorticosteroids were superior to placebo for UC remission (RR of no remission=0.65; 95% CI, 0.45-0.93). Both trials of standard glucocorticosteroids in CD remission reported a statistically significant effect, but the overall effect was not significant due to heterogeneity of the studies. Budesonide was superior to placebo for CD remission (RR=0.73; 95% CI, 0.63-0.84) but not in preventing CD relapse (RR=0.93; 95% CI, 0.83-1.04). Standard glucocorticosteroids were superior to budesonide for CD remission (RR=0.82; 95% CI, 0.68-0.98) but with more adverse effects (RR=1.64; 95% CI, 1.34-2.00).
The limitations of the study include the poor overall quality of the studies included in the meta-analysis, with only one study judged as low risk of bias. There was intermediate to high heterogeneity between study results.
Bottom line: Standard glucocorticosteroids are likely effective in inducing remission in UC and, possibly, in CD. Budesonide probably is effective at inducing remission in active CD. Neither therapy was recommended in preventing relapse of UC and CD.
Citation: Ford AC, Bernstein CN, Khan KJ, et al. Glucocorticosteroid therapy in inflammatory bowel disease: systematic review and meta-analysis. Am J Gastroenterol. 2011;106(4):590-599.
Levofloxacin Effective in Treatment of H. Pylori in Settings of High Clarithromycin Resistance
Clinical question: In areas with high H. pylori clarithromycin resistance rates, is levofloxacin more effective in eradicating H. pylori than standard clarithromycin, based treatment regimens?
Background: The rise in antimicrobial drug resistance is a major cause for the decreasing rate of H. pylori eradication. In areas with higher than 15% H. pyloriclarithromycin-resistant strains, quadruple therapy has been suggested as first-line therapy. The efficacy of a levofloxacin-based sequential therapy in eradicating H. pylori is undetermined.
Study design: Prospective, randomized, controlled multicenter study with a parallel-group design.
Setting: Five gastroenterology clinics in Italy.
Synopsis: Researchers randomly assigned 375 patients who were infected with H. pylori and naive to treatment to one of three groups. All three treatment groups received an initial five days of omeprazole 20 mg BID and amoxicillin 1 gm BID, then five days of omeprazole 20 mg BID and tinidazole 500 mg BID. The groups also received either clarithromycin 500 mg BID, levofloxacin 250 mg BID, or levofloxacin 500 mg BID, respectively, during the second five days of treatment.
Eradication rates were 80.8% (95% CI, 72.8% to 87.3%) with clarithromycin sequential therapy, 96.0% (95% CI, 90.9% to 98.7%) with levofloxacin-250 sequential therapy, and 96.8% (95% CI, 92.0% to 99.1%) with levofloxacin-500 sequential therapy.
The clarithromycin-group eradication rate was significantly lower than both levofloxacin groups. No significant difference was observed between the levofloxacin-250 and levofloxacin-500 groups. No differences in prevalence of antimicrobial resistance or incidence of adverse events were observed between the groups. Levofloxacin-250 therapy does offer cost savings when compared with clarithromycin sequential therapy.
A potential limitation to the study is referral bias, as each of the patients first were sent by their primary physicians to a specialized GI clinic.
Bottom line: In areas with a high prevalence of clarithromycin-resistant strains of H. pylori levofloxacin-containing sequential therapy should be considered for a first-line eradication regimen.
Citation: Romano M, Cuomo A, Gravina AG, et al. Empirical levofloxacin-containing versus clarithromycin-containing sequential therapy for Helicobacter pylori eradication: a randomised trial. Gut. 2010;59(11):1465-1470.
Tako-Tsubo Cardiomyopathy Is Associated with Higher Hospital Readmission Rates and Long-Term Mortality
Clinical question: What is the natural history of patients who develop tako-tsubo cardiomyopathy?
Background: Stress-induced or tako-tsubo cardiomyopathy (TTC) is a rare acute cardiac syndrome, characterized by chest pain or dyspnea, ischemic electrocardiographic changes, transient left ventricular (LV) dysfunction, and limited release of cardiac injury markers, in the absence of epicardial coronary artery disease (CAD). The long-term outcome of this condition is unknown.
Study design: Prospective, case-control study.
Setting: Five urban-based hospitals in Italy.
Synopsis: One hundred-sixteen patients with TTC were included in the five-year study period. Patients were followed up at one and six months, then annually thereafter. Primary endpoints were death, TTC recurrence, and rehospitalization for any cause.
Mean initial LV ejection fraction (LVEF) was 36%. Two patients died of refractory heart failure during hospitalization. Of the patients who were discharged alive, all except one showed complete LV functional recovery.
At follow-up (mean two years), only 64 (55%) patients were asymptomatic. Rehospitalization rate was high (25%), with chest pain and dyspnea the most common causes. Only two patients had a recurrence of TTC. Eleven patients died (seven from cardiovascular causes). There was no significant difference in mortality or in other clinical events between patients with and without severe LV dysfunction at presentation. The standardized mortality ratio was 3.40 (95% CI, 1.83-6.34) in the TTC population, compared with the age- and sex-specific mortality of the general population.
The study is limited by a lack of patients with subclinical TTC disease and those who might have suffered from sudden cardiac death prior to enrollment, leading to a possible sampling bias, as well as the nonrandomized use of beta-blockers.
Bottom line: Tako-tsubo disease is associated with rare recurrence of the disease, common recurrence of chest pain and dyspnea, and three times the mortality rate of the general population.
Citation: Parodi G, Bellandi B, Del Pace S, et al. Natural history of tako-tsubo cardiomyopathy. Chest. 2011;139(4):887-892.
Seven Independent Risk Factors Predict Postoperative Pulmonary Complications
Clinical question: What are the clinical risk factors that predict higher rates of postoperative pulmonary complications?
Background: Postoperative pulmonary complications (PPCs) are a major cause of postoperative morbidity, mortality, and prolonged hospital stays. Previous studies looking at risk factors for PPCs were limited by sampling bias and small sample sizes.
Study design: Prospective, randomized-sample cohort study.
Setting: Fifty-nine participating Spanish hospitals (community, intermediate referral, or major tertiary-care facilities).
Synopsis: Patients undergoing surgical procedures with general, neuraxial, or regional anesthesia were selected randomly. The main outcome was the development of at least one of the following: respiratory infection, respiratory failure, bronchospasm, atelectasis, pleural effusion, pneumothorax, or aspiration pneumonitis. Of 2,464 patients enrolled, 252 events were observed in 123 patients (5%). The 30-day mortality rate was significantly higher in patients suffering a PPC than those who did not (19.5% vs. 0.5%). Additionally, regression modeling identified seven independent risk factors: low preoperative arterial oxygen saturation, acute respiratory infection within one month of surgery, advanced age, preoperative anemia, upper abdominal or intrathoracic surgery, surgical duration more than two hours, and emergency surgery.
The study was underpowered to assess the significance of all potential risk factors for PPCs. Also, given the number of centers involved in the study, variation in assessing development of PPCs is likely.
Bottom line: Postoperative pulmonary complications are a major cause of morbidity and mortality. Seven independent risk factors were identified for the development of PPCs, which could be useful in preoperative risk stratification.
Citation: Canet J, Gallart L, Gomar C, et al. Prediction of postoperative pulmonary complications in a population-based surgical cohort. Anesthesiology. 2010;113(6):1338-1350.
Code Status Orders and Goals of Medical ICU Care
Clinical question: How familiar are patients in the medical ICU (MICU) or their surrogates regarding code-status orders and goals of care, what are their preferences, and to what extent do they and their physicians differ?
Background: Discussions about code-status orders and goals of care carry great import in the MICU. However, little data exist on patients’ code-status preferences and goals of care. More knowledge of these issues can help physicians deliver more patient-centered care.
Study design: Prospective interviews.
Setting: Twenty-six-bed MICU at a large Midwestern academic medical center.
Synopsis: Data were collected from December 2008 to December 2009 on a random sample of patients—or their surrogates—admitted to the MICU. Of 135 eligible patients/surrogates, 100 completed interviews. Patients primarily were white (95%) and from the ages of 41 to 80 (79%).
Only 28% of participants recalled having a discussion about CPR and one goal of care, while 27% recalled no discussion at all; 83% preferred full code status but had limited knowledge of CPR and its outcomes in the hospital setting. Only 4% were able to identify all components of CPR, and they estimated the mean probability of survival following in-hospital arrest with CPR to be 71.8%, although data suggest survival is closer to 18%. There was a correlation between a higher estimation of survival following CPR and preference for it. After learning about the evidence-based likelihood of a good neurologic outcome following CPR, 8% of the participants became less interested.
Discrepancies between patients’ stated code status and that in the medical record was identified 16% of the time. Additionally, 67.7% of participants differed with their physicians regarding the most important goal of care.
Bottom line: Discussions about code status and goals of care in the MICU occur less frequently than recommended, leading to widespread discrepancies between patients/surrogates and their physicians regarding the most important goal of care. This is compounded by the fact that patients and their surrogates have limited knowledge about in-hospital CPR and its likelihood of success.
Citation: Gehlbach TG, Shinkunas LA, Forman-Hoffman VL, Thomas KW, Schmidt GA, Kaldjian LC. Code status orders and goals of care in the medical ICU. Chest. 2011;139:802-809. TH
In This Edition
Literature At A Glance
A guide to this month’s studies
- Screening for AAA
- Adverse events in atrial fibrillation
- Biological treatment of inflammatory bowel diseases
- Steroid treatment of inflammatory bowel diseases
- Levofloxacin for H. pylori
- Natural history of tako-tsubo cardiomyopathy
- Predicting postoperative pulmonary complications
- Code status and goals of care in the ICU
New Screening Strategy To Identify Large Abdominal Aortic Aneurysms
Clinical question: Can an effective scoring system be developed to better identify patients at risk for large abdominal aortic aneurysms (AAA)?
Background: Screening reduces AAA-related mortality by about half in men aged >65. The United States Preventive Services Task Force (USPSTF) has recommended screening for AAA in men aged 65 to 75 with a history of smoking. However, more than 50% of AAA ruptures occur in individuals outside this patient cohort, and only some AAAs detected are large enough to warrant surgery.
Study design: Retrospective, observational cohort study.
Setting: More than 20,000 screening sites across the U.S.
Synopsis: Researchers collected demographics and risk factors from 3.1 million people undergoing ultrasound screening for AAA by Life Line Screening Inc. At the screening visit, subjects completed a questionnaire about their health status and medical history. Screening data also included diameter of the infrarenal abdominal aorta. To construct and test a risk model, the screened individuals were randomly allocated into two equal groups: a data set used for model development and one for validation.
Most of the AAAs greater than 5 cm in diameter discovered were in males (84.4%) and among subjects with a smoking history (83%). Other risk factors for large AAAs included advanced age, peripheral arterial disease, and obesity. The authors estimate that there are about 121,000 people with >5.0 cm aneurysms in the general population. Current guidelines would detect only 33.7% of the existing large AAAs. Study limitations include possible selection bias, as a majority of patients were self-referred. Also, the database did not include all comorbidities that could affect the risk of AAA. The self-reported nature of health data might cause misclassification of a patient’s true health status.
Bottom line: A screening strategy based on a newly developed scoring system is an effective way to identify patients at risk of large abdominal aortic aneurysms.
Citation: Greco G, Egorova NN, Gelijns AC, et al. Development of a novel scoring tool for the identification of large >5 cm abdominal aortic aneurysms. Ann Surg. 2010;252(4):675-682.
Risk Factors for Adverse Events in Patients with Symptomatic Atrial Fibrillation
Clinical question: What are the predictors of 30-day adverse events in ED patients evaluated for symptomatic atrial fibrillation?
Background: Atrial fibrillation (AF) affects more than 2 million people in the U.S. and accounts for nearly 1% of ED visits. Physicians have little information to guide risk stratification, and they admit more than 65% of patients. A strategy to better define the ED management of patients presenting with atrial fibrillation is required.
Study design: Retrospective, observational cohort study.
Setting: Urban academic tertiary-care referral center with an adult ED.
Synopsis: A systematic review of the electronic medical records of all ED patients presenting with symptomatic atrial fibrillation over a three-year period was performed. Predefined adverse outcomes included 30-day ED return visits, unscheduled hospitalizations, cardiovascular complications, or death.
Of 832 eligible patients, 216 (25.9%) experienced at least one of the 30-day adverse events. Adverse events occurred in 181 of the 638 (28.4%) admitted patients and 35 of the 192 (18.2%) patients discharged from the ED. Increasing age, complaint of dyspnea, smoking history, inadequate ventricular rate control, and patients receiving beta-blockers were factors independently associated with higher risk for adverse events.
Study results were limited by a number of factors. This was a single-center, retrospective, observational study, with all of its inherent limitations. The predictor model did not include laboratory data, such as BNP or troponin. Patients might have experienced additional events within the 30 days that were treated at other hospitals and not recorded in the database. Patient disposition might have affected the results, as patients initially admitted from the ED had a higher rate of 30-day adverse events than patients who were discharged from the ED.
Bottom line: Patients with increased age, smoking history, complaints of dyspnea, inadequate ventricular rate control in the ED, and home beta-blocker therapy are more likely to experience an atrial-fibrillation-related adverse event within 30 days.
Citation: Barrett TW, Martin AR, Storrow AB, et al. A clinical prediction model to estimate risk for 30-day adverse events in emergency department patients with symptomatic atrial fibrillation. Ann Emerg Med. 2011;57 (1):1-12.
Biological Therapies Are Effective in Inducing Remission in Inflammatory Bowel Disease
Clinical question: Are biological therapies useful in the treatment of ulcerative colitis (UC) and Crohn’s disease (CD)?
Background: Patients with CD and UC often experience flares of disease activity, despite maintenance therapy with 5-aminosalicylic acid compounds. These flares are usually treated with corticosteroids, which carry numerous adverse side effects. The role of biological therapies in inducing remission is uncertain.
Study design: Systematic review and meta-analysis.
Setting: Twenty-seven randomized controlled trials involving 7,416 patients.
Synopsis: Anti-TNF α antibodies and natalizumab were both superior to placebo in inducing remission of luminal CD (RR of no remission 0.87 and 0.88, respectively). Anti-TNF antibodies also were superior to placebo in preventing relapse of luminal CD (RR of relapse=0.71). Infliximab was superior to placebo in inducing remission of moderate to severely active UC (RR=0.72; 95% CI, 0.57-0.91). There were no significantly increased adverse drug effects with anti-TNF α antibodies or with infliximab compared with placebo. Natalizumab caused significantly higher rates of headache.
Limitations include risk of publication bias inherent in meta-analyses. There also was evidence of moderate heterogeneity in the studies analyzed. Finally, not every study was consistent in reporting adverse drug effects.
Bottom line: Biological therapies are superior to placebo in inducing remission of active UC and CD, as well as preventing relapse of quiescent CD.
Citation: Ford AC, Sandborn WJ, Khan KJ, Hanauer SB, Talley NJ, Moayyedi P. Efficacy of biological therapies in inflammatory bowel disease: systematic review and meta-analysis. Am J Gastroenterol. 2011; 106(4):644-659.
Glucocorticosteroids Probably Effective in Treatment of Inflammatory Bowel Disease, Primarily in Active Ulcerative Colitis
Clinical question: Is glucocorticosteroid therapy effective in the treatment of active IBD and in preventing relapses?
Background: Crohn’s disease (CD) and ulcerative colitis (UC) are chronic inflammatory bowel diseases of unclear etiology. Use of standard glucocorticosteroids and budesonide is widespread in inflammatory bowel disease (IBD) treatment. To date, there has been no large-scale meta-analysis to examine the effectiveness of both treatments in CD and UC.
Study design: Systematic review and meta-analysis.
Setting: Twenty randomized controlled trials totaling 2,398 patients.
Synopsis: Standard glucocorticosteroids were superior to placebo for UC remission (RR of no remission=0.65; 95% CI, 0.45-0.93). Both trials of standard glucocorticosteroids in CD remission reported a statistically significant effect, but the overall effect was not significant due to heterogeneity of the studies. Budesonide was superior to placebo for CD remission (RR=0.73; 95% CI, 0.63-0.84) but not in preventing CD relapse (RR=0.93; 95% CI, 0.83-1.04). Standard glucocorticosteroids were superior to budesonide for CD remission (RR=0.82; 95% CI, 0.68-0.98) but with more adverse effects (RR=1.64; 95% CI, 1.34-2.00).
The limitations of the study include the poor overall quality of the studies included in the meta-analysis, with only one study judged as low risk of bias. There was intermediate to high heterogeneity between study results.
Bottom line: Standard glucocorticosteroids are likely effective in inducing remission in UC and, possibly, in CD. Budesonide probably is effective at inducing remission in active CD. Neither therapy was recommended in preventing relapse of UC and CD.
Citation: Ford AC, Bernstein CN, Khan KJ, et al. Glucocorticosteroid therapy in inflammatory bowel disease: systematic review and meta-analysis. Am J Gastroenterol. 2011;106(4):590-599.
Levofloxacin Effective in Treatment of H. Pylori in Settings of High Clarithromycin Resistance
Clinical question: In areas with high H. pylori clarithromycin resistance rates, is levofloxacin more effective in eradicating H. pylori than standard clarithromycin, based treatment regimens?
Background: The rise in antimicrobial drug resistance is a major cause for the decreasing rate of H. pylori eradication. In areas with higher than 15% H. pyloriclarithromycin-resistant strains, quadruple therapy has been suggested as first-line therapy. The efficacy of a levofloxacin-based sequential therapy in eradicating H. pylori is undetermined.
Study design: Prospective, randomized, controlled multicenter study with a parallel-group design.
Setting: Five gastroenterology clinics in Italy.
Synopsis: Researchers randomly assigned 375 patients who were infected with H. pylori and naive to treatment to one of three groups. All three treatment groups received an initial five days of omeprazole 20 mg BID and amoxicillin 1 gm BID, then five days of omeprazole 20 mg BID and tinidazole 500 mg BID. The groups also received either clarithromycin 500 mg BID, levofloxacin 250 mg BID, or levofloxacin 500 mg BID, respectively, during the second five days of treatment.
Eradication rates were 80.8% (95% CI, 72.8% to 87.3%) with clarithromycin sequential therapy, 96.0% (95% CI, 90.9% to 98.7%) with levofloxacin-250 sequential therapy, and 96.8% (95% CI, 92.0% to 99.1%) with levofloxacin-500 sequential therapy.
The clarithromycin-group eradication rate was significantly lower than both levofloxacin groups. No significant difference was observed between the levofloxacin-250 and levofloxacin-500 groups. No differences in prevalence of antimicrobial resistance or incidence of adverse events were observed between the groups. Levofloxacin-250 therapy does offer cost savings when compared with clarithromycin sequential therapy.
A potential limitation to the study is referral bias, as each of the patients first were sent by their primary physicians to a specialized GI clinic.
Bottom line: In areas with a high prevalence of clarithromycin-resistant strains of H. pylori levofloxacin-containing sequential therapy should be considered for a first-line eradication regimen.
Citation: Romano M, Cuomo A, Gravina AG, et al. Empirical levofloxacin-containing versus clarithromycin-containing sequential therapy for Helicobacter pylori eradication: a randomised trial. Gut. 2010;59(11):1465-1470.
Tako-Tsubo Cardiomyopathy Is Associated with Higher Hospital Readmission Rates and Long-Term Mortality
Clinical question: What is the natural history of patients who develop tako-tsubo cardiomyopathy?
Background: Stress-induced or tako-tsubo cardiomyopathy (TTC) is a rare acute cardiac syndrome, characterized by chest pain or dyspnea, ischemic electrocardiographic changes, transient left ventricular (LV) dysfunction, and limited release of cardiac injury markers, in the absence of epicardial coronary artery disease (CAD). The long-term outcome of this condition is unknown.
Study design: Prospective, case-control study.
Setting: Five urban-based hospitals in Italy.
Synopsis: One hundred-sixteen patients with TTC were included in the five-year study period. Patients were followed up at one and six months, then annually thereafter. Primary endpoints were death, TTC recurrence, and rehospitalization for any cause.
Mean initial LV ejection fraction (LVEF) was 36%. Two patients died of refractory heart failure during hospitalization. Of the patients who were discharged alive, all except one showed complete LV functional recovery.
At follow-up (mean two years), only 64 (55%) patients were asymptomatic. Rehospitalization rate was high (25%), with chest pain and dyspnea the most common causes. Only two patients had a recurrence of TTC. Eleven patients died (seven from cardiovascular causes). There was no significant difference in mortality or in other clinical events between patients with and without severe LV dysfunction at presentation. The standardized mortality ratio was 3.40 (95% CI, 1.83-6.34) in the TTC population, compared with the age- and sex-specific mortality of the general population.
The study is limited by a lack of patients with subclinical TTC disease and those who might have suffered from sudden cardiac death prior to enrollment, leading to a possible sampling bias, as well as the nonrandomized use of beta-blockers.
Bottom line: Tako-tsubo disease is associated with rare recurrence of the disease, common recurrence of chest pain and dyspnea, and three times the mortality rate of the general population.
Citation: Parodi G, Bellandi B, Del Pace S, et al. Natural history of tako-tsubo cardiomyopathy. Chest. 2011;139(4):887-892.
Seven Independent Risk Factors Predict Postoperative Pulmonary Complications
Clinical question: What are the clinical risk factors that predict higher rates of postoperative pulmonary complications?
Background: Postoperative pulmonary complications (PPCs) are a major cause of postoperative morbidity, mortality, and prolonged hospital stays. Previous studies looking at risk factors for PPCs were limited by sampling bias and small sample sizes.
Study design: Prospective, randomized-sample cohort study.
Setting: Fifty-nine participating Spanish hospitals (community, intermediate referral, or major tertiary-care facilities).
Synopsis: Patients undergoing surgical procedures with general, neuraxial, or regional anesthesia were selected randomly. The main outcome was the development of at least one of the following: respiratory infection, respiratory failure, bronchospasm, atelectasis, pleural effusion, pneumothorax, or aspiration pneumonitis. Of 2,464 patients enrolled, 252 events were observed in 123 patients (5%). The 30-day mortality rate was significantly higher in patients suffering a PPC than those who did not (19.5% vs. 0.5%). Additionally, regression modeling identified seven independent risk factors: low preoperative arterial oxygen saturation, acute respiratory infection within one month of surgery, advanced age, preoperative anemia, upper abdominal or intrathoracic surgery, surgical duration more than two hours, and emergency surgery.
The study was underpowered to assess the significance of all potential risk factors for PPCs. Also, given the number of centers involved in the study, variation in assessing development of PPCs is likely.
Bottom line: Postoperative pulmonary complications are a major cause of morbidity and mortality. Seven independent risk factors were identified for the development of PPCs, which could be useful in preoperative risk stratification.
Citation: Canet J, Gallart L, Gomar C, et al. Prediction of postoperative pulmonary complications in a population-based surgical cohort. Anesthesiology. 2010;113(6):1338-1350.
Code Status Orders and Goals of Medical ICU Care
Clinical question: How familiar are patients in the medical ICU (MICU) or their surrogates regarding code-status orders and goals of care, what are their preferences, and to what extent do they and their physicians differ?
Background: Discussions about code-status orders and goals of care carry great import in the MICU. However, little data exist on patients’ code-status preferences and goals of care. More knowledge of these issues can help physicians deliver more patient-centered care.
Study design: Prospective interviews.
Setting: Twenty-six-bed MICU at a large Midwestern academic medical center.
Synopsis: Data were collected from December 2008 to December 2009 on a random sample of patients—or their surrogates—admitted to the MICU. Of 135 eligible patients/surrogates, 100 completed interviews. Patients primarily were white (95%) and from the ages of 41 to 80 (79%).
Only 28% of participants recalled having a discussion about CPR and one goal of care, while 27% recalled no discussion at all; 83% preferred full code status but had limited knowledge of CPR and its outcomes in the hospital setting. Only 4% were able to identify all components of CPR, and they estimated the mean probability of survival following in-hospital arrest with CPR to be 71.8%, although data suggest survival is closer to 18%. There was a correlation between a higher estimation of survival following CPR and preference for it. After learning about the evidence-based likelihood of a good neurologic outcome following CPR, 8% of the participants became less interested.
Discrepancies between patients’ stated code status and that in the medical record was identified 16% of the time. Additionally, 67.7% of participants differed with their physicians regarding the most important goal of care.
Bottom line: Discussions about code status and goals of care in the MICU occur less frequently than recommended, leading to widespread discrepancies between patients/surrogates and their physicians regarding the most important goal of care. This is compounded by the fact that patients and their surrogates have limited knowledge about in-hospital CPR and its likelihood of success.
Citation: Gehlbach TG, Shinkunas LA, Forman-Hoffman VL, Thomas KW, Schmidt GA, Kaldjian LC. Code status orders and goals of care in the medical ICU. Chest. 2011;139:802-809. TH
In This Edition
Literature At A Glance
A guide to this month’s studies
- Screening for AAA
- Adverse events in atrial fibrillation
- Biological treatment of inflammatory bowel diseases
- Steroid treatment of inflammatory bowel diseases
- Levofloxacin for H. pylori
- Natural history of tako-tsubo cardiomyopathy
- Predicting postoperative pulmonary complications
- Code status and goals of care in the ICU
New Screening Strategy To Identify Large Abdominal Aortic Aneurysms
Clinical question: Can an effective scoring system be developed to better identify patients at risk for large abdominal aortic aneurysms (AAA)?
Background: Screening reduces AAA-related mortality by about half in men aged >65. The United States Preventive Services Task Force (USPSTF) has recommended screening for AAA in men aged 65 to 75 with a history of smoking. However, more than 50% of AAA ruptures occur in individuals outside this patient cohort, and only some AAAs detected are large enough to warrant surgery.
Study design: Retrospective, observational cohort study.
Setting: More than 20,000 screening sites across the U.S.
Synopsis: Researchers collected demographics and risk factors from 3.1 million people undergoing ultrasound screening for AAA by Life Line Screening Inc. At the screening visit, subjects completed a questionnaire about their health status and medical history. Screening data also included diameter of the infrarenal abdominal aorta. To construct and test a risk model, the screened individuals were randomly allocated into two equal groups: a data set used for model development and one for validation.
Most of the AAAs greater than 5 cm in diameter discovered were in males (84.4%) and among subjects with a smoking history (83%). Other risk factors for large AAAs included advanced age, peripheral arterial disease, and obesity. The authors estimate that there are about 121,000 people with >5.0 cm aneurysms in the general population. Current guidelines would detect only 33.7% of the existing large AAAs. Study limitations include possible selection bias, as a majority of patients were self-referred. Also, the database did not include all comorbidities that could affect the risk of AAA. The self-reported nature of health data might cause misclassification of a patient’s true health status.
Bottom line: A screening strategy based on a newly developed scoring system is an effective way to identify patients at risk of large abdominal aortic aneurysms.
Citation: Greco G, Egorova NN, Gelijns AC, et al. Development of a novel scoring tool for the identification of large >5 cm abdominal aortic aneurysms. Ann Surg. 2010;252(4):675-682.
Risk Factors for Adverse Events in Patients with Symptomatic Atrial Fibrillation
Clinical question: What are the predictors of 30-day adverse events in ED patients evaluated for symptomatic atrial fibrillation?
Background: Atrial fibrillation (AF) affects more than 2 million people in the U.S. and accounts for nearly 1% of ED visits. Physicians have little information to guide risk stratification, and they admit more than 65% of patients. A strategy to better define the ED management of patients presenting with atrial fibrillation is required.
Study design: Retrospective, observational cohort study.
Setting: Urban academic tertiary-care referral center with an adult ED.
Synopsis: A systematic review of the electronic medical records of all ED patients presenting with symptomatic atrial fibrillation over a three-year period was performed. Predefined adverse outcomes included 30-day ED return visits, unscheduled hospitalizations, cardiovascular complications, or death.
Of 832 eligible patients, 216 (25.9%) experienced at least one of the 30-day adverse events. Adverse events occurred in 181 of the 638 (28.4%) admitted patients and 35 of the 192 (18.2%) patients discharged from the ED. Increasing age, complaint of dyspnea, smoking history, inadequate ventricular rate control, and patients receiving beta-blockers were factors independently associated with higher risk for adverse events.
Study results were limited by a number of factors. This was a single-center, retrospective, observational study, with all of its inherent limitations. The predictor model did not include laboratory data, such as BNP or troponin. Patients might have experienced additional events within the 30 days that were treated at other hospitals and not recorded in the database. Patient disposition might have affected the results, as patients initially admitted from the ED had a higher rate of 30-day adverse events than patients who were discharged from the ED.
Bottom line: Patients with increased age, smoking history, complaints of dyspnea, inadequate ventricular rate control in the ED, and home beta-blocker therapy are more likely to experience an atrial-fibrillation-related adverse event within 30 days.
Citation: Barrett TW, Martin AR, Storrow AB, et al. A clinical prediction model to estimate risk for 30-day adverse events in emergency department patients with symptomatic atrial fibrillation. Ann Emerg Med. 2011;57 (1):1-12.
Biological Therapies Are Effective in Inducing Remission in Inflammatory Bowel Disease
Clinical question: Are biological therapies useful in the treatment of ulcerative colitis (UC) and Crohn’s disease (CD)?
Background: Patients with CD and UC often experience flares of disease activity, despite maintenance therapy with 5-aminosalicylic acid compounds. These flares are usually treated with corticosteroids, which carry numerous adverse side effects. The role of biological therapies in inducing remission is uncertain.
Study design: Systematic review and meta-analysis.
Setting: Twenty-seven randomized controlled trials involving 7,416 patients.
Synopsis: Anti-TNF α antibodies and natalizumab were both superior to placebo in inducing remission of luminal CD (RR of no remission 0.87 and 0.88, respectively). Anti-TNF antibodies also were superior to placebo in preventing relapse of luminal CD (RR of relapse=0.71). Infliximab was superior to placebo in inducing remission of moderate to severely active UC (RR=0.72; 95% CI, 0.57-0.91). There were no significantly increased adverse drug effects with anti-TNF α antibodies or with infliximab compared with placebo. Natalizumab caused significantly higher rates of headache.
Limitations include risk of publication bias inherent in meta-analyses. There also was evidence of moderate heterogeneity in the studies analyzed. Finally, not every study was consistent in reporting adverse drug effects.
Bottom line: Biological therapies are superior to placebo in inducing remission of active UC and CD, as well as preventing relapse of quiescent CD.
Citation: Ford AC, Sandborn WJ, Khan KJ, Hanauer SB, Talley NJ, Moayyedi P. Efficacy of biological therapies in inflammatory bowel disease: systematic review and meta-analysis. Am J Gastroenterol. 2011; 106(4):644-659.
Glucocorticosteroids Probably Effective in Treatment of Inflammatory Bowel Disease, Primarily in Active Ulcerative Colitis
Clinical question: Is glucocorticosteroid therapy effective in the treatment of active IBD and in preventing relapses?
Background: Crohn’s disease (CD) and ulcerative colitis (UC) are chronic inflammatory bowel diseases of unclear etiology. Use of standard glucocorticosteroids and budesonide is widespread in inflammatory bowel disease (IBD) treatment. To date, there has been no large-scale meta-analysis to examine the effectiveness of both treatments in CD and UC.
Study design: Systematic review and meta-analysis.
Setting: Twenty randomized controlled trials totaling 2,398 patients.
Synopsis: Standard glucocorticosteroids were superior to placebo for UC remission (RR of no remission=0.65; 95% CI, 0.45-0.93). Both trials of standard glucocorticosteroids in CD remission reported a statistically significant effect, but the overall effect was not significant due to heterogeneity of the studies. Budesonide was superior to placebo for CD remission (RR=0.73; 95% CI, 0.63-0.84) but not in preventing CD relapse (RR=0.93; 95% CI, 0.83-1.04). Standard glucocorticosteroids were superior to budesonide for CD remission (RR=0.82; 95% CI, 0.68-0.98) but with more adverse effects (RR=1.64; 95% CI, 1.34-2.00).
The limitations of the study include the poor overall quality of the studies included in the meta-analysis, with only one study judged as low risk of bias. There was intermediate to high heterogeneity between study results.
Bottom line: Standard glucocorticosteroids are likely effective in inducing remission in UC and, possibly, in CD. Budesonide probably is effective at inducing remission in active CD. Neither therapy was recommended in preventing relapse of UC and CD.
Citation: Ford AC, Bernstein CN, Khan KJ, et al. Glucocorticosteroid therapy in inflammatory bowel disease: systematic review and meta-analysis. Am J Gastroenterol. 2011;106(4):590-599.
Levofloxacin Effective in Treatment of H. Pylori in Settings of High Clarithromycin Resistance
Clinical question: In areas with high H. pylori clarithromycin resistance rates, is levofloxacin more effective in eradicating H. pylori than standard clarithromycin, based treatment regimens?
Background: The rise in antimicrobial drug resistance is a major cause for the decreasing rate of H. pylori eradication. In areas with higher than 15% H. pyloriclarithromycin-resistant strains, quadruple therapy has been suggested as first-line therapy. The efficacy of a levofloxacin-based sequential therapy in eradicating H. pylori is undetermined.
Study design: Prospective, randomized, controlled multicenter study with a parallel-group design.
Setting: Five gastroenterology clinics in Italy.
Synopsis: Researchers randomly assigned 375 patients who were infected with H. pylori and naive to treatment to one of three groups. All three treatment groups received an initial five days of omeprazole 20 mg BID and amoxicillin 1 gm BID, then five days of omeprazole 20 mg BID and tinidazole 500 mg BID. The groups also received either clarithromycin 500 mg BID, levofloxacin 250 mg BID, or levofloxacin 500 mg BID, respectively, during the second five days of treatment.
Eradication rates were 80.8% (95% CI, 72.8% to 87.3%) with clarithromycin sequential therapy, 96.0% (95% CI, 90.9% to 98.7%) with levofloxacin-250 sequential therapy, and 96.8% (95% CI, 92.0% to 99.1%) with levofloxacin-500 sequential therapy.
The clarithromycin-group eradication rate was significantly lower than both levofloxacin groups. No significant difference was observed between the levofloxacin-250 and levofloxacin-500 groups. No differences in prevalence of antimicrobial resistance or incidence of adverse events were observed between the groups. Levofloxacin-250 therapy does offer cost savings when compared with clarithromycin sequential therapy.
A potential limitation to the study is referral bias, as each of the patients first were sent by their primary physicians to a specialized GI clinic.
Bottom line: In areas with a high prevalence of clarithromycin-resistant strains of H. pylori levofloxacin-containing sequential therapy should be considered for a first-line eradication regimen.
Citation: Romano M, Cuomo A, Gravina AG, et al. Empirical levofloxacin-containing versus clarithromycin-containing sequential therapy for Helicobacter pylori eradication: a randomised trial. Gut. 2010;59(11):1465-1470.
Tako-Tsubo Cardiomyopathy Is Associated with Higher Hospital Readmission Rates and Long-Term Mortality
Clinical question: What is the natural history of patients who develop tako-tsubo cardiomyopathy?
Background: Stress-induced or tako-tsubo cardiomyopathy (TTC) is a rare acute cardiac syndrome, characterized by chest pain or dyspnea, ischemic electrocardiographic changes, transient left ventricular (LV) dysfunction, and limited release of cardiac injury markers, in the absence of epicardial coronary artery disease (CAD). The long-term outcome of this condition is unknown.
Study design: Prospective, case-control study.
Setting: Five urban-based hospitals in Italy.
Synopsis: One hundred-sixteen patients with TTC were included in the five-year study period. Patients were followed up at one and six months, then annually thereafter. Primary endpoints were death, TTC recurrence, and rehospitalization for any cause.
Mean initial LV ejection fraction (LVEF) was 36%. Two patients died of refractory heart failure during hospitalization. Of the patients who were discharged alive, all except one showed complete LV functional recovery.
At follow-up (mean two years), only 64 (55%) patients were asymptomatic. Rehospitalization rate was high (25%), with chest pain and dyspnea the most common causes. Only two patients had a recurrence of TTC. Eleven patients died (seven from cardiovascular causes). There was no significant difference in mortality or in other clinical events between patients with and without severe LV dysfunction at presentation. The standardized mortality ratio was 3.40 (95% CI, 1.83-6.34) in the TTC population, compared with the age- and sex-specific mortality of the general population.
The study is limited by a lack of patients with subclinical TTC disease and those who might have suffered from sudden cardiac death prior to enrollment, leading to a possible sampling bias, as well as the nonrandomized use of beta-blockers.
Bottom line: Tako-tsubo disease is associated with rare recurrence of the disease, common recurrence of chest pain and dyspnea, and three times the mortality rate of the general population.
Citation: Parodi G, Bellandi B, Del Pace S, et al. Natural history of tako-tsubo cardiomyopathy. Chest. 2011;139(4):887-892.
Seven Independent Risk Factors Predict Postoperative Pulmonary Complications
Clinical question: What are the clinical risk factors that predict higher rates of postoperative pulmonary complications?
Background: Postoperative pulmonary complications (PPCs) are a major cause of postoperative morbidity, mortality, and prolonged hospital stays. Previous studies looking at risk factors for PPCs were limited by sampling bias and small sample sizes.
Study design: Prospective, randomized-sample cohort study.
Setting: Fifty-nine participating Spanish hospitals (community, intermediate referral, or major tertiary-care facilities).
Synopsis: Patients undergoing surgical procedures with general, neuraxial, or regional anesthesia were selected randomly. The main outcome was the development of at least one of the following: respiratory infection, respiratory failure, bronchospasm, atelectasis, pleural effusion, pneumothorax, or aspiration pneumonitis. Of 2,464 patients enrolled, 252 events were observed in 123 patients (5%). The 30-day mortality rate was significantly higher in patients suffering a PPC than those who did not (19.5% vs. 0.5%). Additionally, regression modeling identified seven independent risk factors: low preoperative arterial oxygen saturation, acute respiratory infection within one month of surgery, advanced age, preoperative anemia, upper abdominal or intrathoracic surgery, surgical duration more than two hours, and emergency surgery.
The study was underpowered to assess the significance of all potential risk factors for PPCs. Also, given the number of centers involved in the study, variation in assessing development of PPCs is likely.
Bottom line: Postoperative pulmonary complications are a major cause of morbidity and mortality. Seven independent risk factors were identified for the development of PPCs, which could be useful in preoperative risk stratification.
Citation: Canet J, Gallart L, Gomar C, et al. Prediction of postoperative pulmonary complications in a population-based surgical cohort. Anesthesiology. 2010;113(6):1338-1350.
Code Status Orders and Goals of Medical ICU Care
Clinical question: How familiar are patients in the medical ICU (MICU) or their surrogates regarding code-status orders and goals of care, what are their preferences, and to what extent do they and their physicians differ?
Background: Discussions about code-status orders and goals of care carry great import in the MICU. However, little data exist on patients’ code-status preferences and goals of care. More knowledge of these issues can help physicians deliver more patient-centered care.
Study design: Prospective interviews.
Setting: Twenty-six-bed MICU at a large Midwestern academic medical center.
Synopsis: Data were collected from December 2008 to December 2009 on a random sample of patients—or their surrogates—admitted to the MICU. Of 135 eligible patients/surrogates, 100 completed interviews. Patients primarily were white (95%) and from the ages of 41 to 80 (79%).
Only 28% of participants recalled having a discussion about CPR and one goal of care, while 27% recalled no discussion at all; 83% preferred full code status but had limited knowledge of CPR and its outcomes in the hospital setting. Only 4% were able to identify all components of CPR, and they estimated the mean probability of survival following in-hospital arrest with CPR to be 71.8%, although data suggest survival is closer to 18%. There was a correlation between a higher estimation of survival following CPR and preference for it. After learning about the evidence-based likelihood of a good neurologic outcome following CPR, 8% of the participants became less interested.
Discrepancies between patients’ stated code status and that in the medical record was identified 16% of the time. Additionally, 67.7% of participants differed with their physicians regarding the most important goal of care.
Bottom line: Discussions about code status and goals of care in the MICU occur less frequently than recommended, leading to widespread discrepancies between patients/surrogates and their physicians regarding the most important goal of care. This is compounded by the fact that patients and their surrogates have limited knowledge about in-hospital CPR and its likelihood of success.
Citation: Gehlbach TG, Shinkunas LA, Forman-Hoffman VL, Thomas KW, Schmidt GA, Kaldjian LC. Code status orders and goals of care in the medical ICU. Chest. 2011;139:802-809. TH
In the Literature: Research You Need to Know
Clinical question: What is the effect of corticosteroid therapy on survival in severe alcoholic hepatitis?
Background: Previous meta-analyses have suggested a survival benefit of corticosteroid treatment restricted only to those patients with severe alcoholic hepatitis (AH), with little or no benefit in less severe disease. Other meta-analyses, however, have questioned the efficacy in AH regardless of disease severity.
Study design: Meta-analysis of individual patient data.
Setting: Five randomized controlled trials (RCT) enrolling 418 patients.
Synopsis: Individual patient data were obtained from five RCTs comparing corticosteroid treatment with placebo (n3), enteral nutrition (n1), or an antioxidant cocktail (n1). Researchers analyzed 221 patients allocated to corticosteroid treatment and 197 allocated to noncorticosteroid treatment. Twenty-eight-day survival was higher in corticosteroid treated patients than in noncorticosteroid-treated patients (79.97% vs. 65.76%, P=0.0005). A subgroup analysis was performed according to the Lille score. Patients were classified as complete responders, partial responders, and null responders. Corticosteroids had a significant effect on 28-day survival in complete responders and in partial responders, but not in null responders (91.16% vs. 79.46% vs. 53.36%, P<0.0001)
Bottom line: Corticosteroids significantly improve 28-day survival in patients with severe alcoholic hepatitis. The survival benefit is mainly observed in patients classified as responders by the Lille model.
Citation: Mathurin P, O'Grady J, Carithers RL et al. Corticosteroids improve short-term survival in patients with severe alcoholic hepatitis: meta-analysis of individual patient data. Gut. 2011;60(2):255-260.
For more physician reviews of HM-related research, visit our website.
Clinical question: What is the effect of corticosteroid therapy on survival in severe alcoholic hepatitis?
Background: Previous meta-analyses have suggested a survival benefit of corticosteroid treatment restricted only to those patients with severe alcoholic hepatitis (AH), with little or no benefit in less severe disease. Other meta-analyses, however, have questioned the efficacy in AH regardless of disease severity.
Study design: Meta-analysis of individual patient data.
Setting: Five randomized controlled trials (RCT) enrolling 418 patients.
Synopsis: Individual patient data were obtained from five RCTs comparing corticosteroid treatment with placebo (n3), enteral nutrition (n1), or an antioxidant cocktail (n1). Researchers analyzed 221 patients allocated to corticosteroid treatment and 197 allocated to noncorticosteroid treatment. Twenty-eight-day survival was higher in corticosteroid treated patients than in noncorticosteroid-treated patients (79.97% vs. 65.76%, P=0.0005). A subgroup analysis was performed according to the Lille score. Patients were classified as complete responders, partial responders, and null responders. Corticosteroids had a significant effect on 28-day survival in complete responders and in partial responders, but not in null responders (91.16% vs. 79.46% vs. 53.36%, P<0.0001)
Bottom line: Corticosteroids significantly improve 28-day survival in patients with severe alcoholic hepatitis. The survival benefit is mainly observed in patients classified as responders by the Lille model.
Citation: Mathurin P, O'Grady J, Carithers RL et al. Corticosteroids improve short-term survival in patients with severe alcoholic hepatitis: meta-analysis of individual patient data. Gut. 2011;60(2):255-260.
For more physician reviews of HM-related research, visit our website.
Clinical question: What is the effect of corticosteroid therapy on survival in severe alcoholic hepatitis?
Background: Previous meta-analyses have suggested a survival benefit of corticosteroid treatment restricted only to those patients with severe alcoholic hepatitis (AH), with little or no benefit in less severe disease. Other meta-analyses, however, have questioned the efficacy in AH regardless of disease severity.
Study design: Meta-analysis of individual patient data.
Setting: Five randomized controlled trials (RCT) enrolling 418 patients.
Synopsis: Individual patient data were obtained from five RCTs comparing corticosteroid treatment with placebo (n3), enteral nutrition (n1), or an antioxidant cocktail (n1). Researchers analyzed 221 patients allocated to corticosteroid treatment and 197 allocated to noncorticosteroid treatment. Twenty-eight-day survival was higher in corticosteroid treated patients than in noncorticosteroid-treated patients (79.97% vs. 65.76%, P=0.0005). A subgroup analysis was performed according to the Lille score. Patients were classified as complete responders, partial responders, and null responders. Corticosteroids had a significant effect on 28-day survival in complete responders and in partial responders, but not in null responders (91.16% vs. 79.46% vs. 53.36%, P<0.0001)
Bottom line: Corticosteroids significantly improve 28-day survival in patients with severe alcoholic hepatitis. The survival benefit is mainly observed in patients classified as responders by the Lille model.
Citation: Mathurin P, O'Grady J, Carithers RL et al. Corticosteroids improve short-term survival in patients with severe alcoholic hepatitis: meta-analysis of individual patient data. Gut. 2011;60(2):255-260.
For more physician reviews of HM-related research, visit our website.
Short of breath, not short of diagnoses
The approach to clinical conundrums by an expert clinician is revealed through presentation of an actual patient's case in an approach typical of morning report. Similar to patient care, sequential pieces of information are provided to the clinician who is unfamiliar with the case. The focus is on the thought processes of both the clinical team caring for the patient and the discussant.
A 71‐year‐old African‐American woman presented to the emergency department with chest pain, shortness of breath, and cough. She had initially presented to her primary care physician 2 weeks previously complaining of worsening cough and shortness of breath and was told to continue her inhaled albuterol and glucocorticoids and was prescribed a prednisone taper and an unknown course of antibiotics. She noted no improvement in her symptoms despite compliance with this treatment. Three days prior to admission she described the gradual onset of left‐sided pleuritic chest pain with continued cough, associated with yellow sputum and worsening dyspnea. Review of systems was remarkable for generalized weakness and malaise. She denied fever, chills, orthopnea, paroxysmal nocturnal dyspnea, lower extremity edema, diarrhea, nausea, vomiting, or abdominal pain.
Her past medical history included a diagnosis of chronic obstructive pulmonary disease (COPD) but pulmonary function tests 7 years prior to admission showed an forced expiratory volume in the first second (FEV1)/forced vital capacity (FVC) ratio of 81%. She had a 30 pack‐year history of smoking, but quit 35 years ago. The patient also carried a diagnosis of heart failure, but an echocardiogram done 1 year ago demonstrated a left ventricular ejection fraction of 65% to 70% without diastolic dysfunction but mild right ventricular dilation and hypertrophy. Additionally, she had known nonobstructive coronary atherosclerotic heart disease, dyslipidemia, hypertension, morbid obesity, depression, and a documented chronic right hemidiaphragm elevation.
At this point the history suggests that the patient does not have a clear diagnosis of COPD. The lack of definitive spirometry evidence of chronic airway obstruction concerns me; I think that she may have been mistakenly treated with chronic inhaled steroids and doses of antibiotics for an acute exacerbation of chronic lung disease. Additional review of her history gives some indication of advanced lung disease, with her recent echocardiogram showing strain on the right ventricle with right ventricular hypertrophy and dilation, but there is no mention of the presence or severity of pulmonary hypertension. Nonetheless, I would be concerned that she probably has underlying significant cor pulmonale.
The patient now re‐presents with a worsening of her pulmonary symptoms. Her left‐sided pleuritic pain would make me concerned that she had a pulmonary embolus (PE). This morbidly obese patient with new pulmonary symptoms, right ventricular strain on her previous echocardiogram, and a persistent elevated right hemidiaphragm suggests a presentation of another PE.
At this time I cannot rule out other common possibilities such as infectious pneumonia. If she does have pneumonia, I would be concerned she could be harboring a multidrug‐resistant bacterial infection given her recent course of antibiotics in addition to her use of both chronic inhaled and intermittent oral glucocorticoids.
After gathering the rest of her full medical history, I would focus my physical exam on looking for evidence of parenchymal lung disease, signs of pulmonary hypertension, and pneumonia.
Her surgical history includes a previous hysterectomy, cholecystectomy, hernia repair, and left hepatic lobectomy for a benign mass. Her outpatient medications were ibuprofen, bupropion, fluvastatin, atenolol, potassium, aspirin, clopidogrel, albuterol inhaler, fluticasone/salmeterol inhaler, and omeprazole. She reports an allergy to penicillin and to sulfa drugs. Her mother died of an unknown cancer at age 77 years. She denied any international travel and she has always lived in Georgia.
The patient has been retired since 1992, having previously worked for the U.S. Postal Service. She admits to occasional alcohol intake (2 to 3 drinks a month). No recent travel, surgery, or prolonged immobilization was noted.
On initial examination she was alert and mentally appropriate, but appeared to be in mild respiratory distress with a respiratory rate of 28 breaths/minute. Her blood pressure (BP) was 99/70, heart rate 102, temperature of 38.2C, and oxygen saturation of 93% on room air and 97% on 2 L of oxygen via nasal cannula. Auscultation of her lungs revealed crackles over her left anterior lung field, bronchial breath sounds in the left posterior midlung, and bibasilar crackles. No wheezing was noted. Her cardiovascular exam and the remainder of her physical exam were unremarkable except for morbid obesity.
While my initial thoughts were leaning toward an exacerbation of chronic lung disease or possibly a new PE, at this moment, infection seems more likely. Indeed, her pulmonary findings suggest a left‐sided inflammatory process, and her vital signs meet criteria for systemic inflammatory response syndrome (SIRS). My primary concern is sepsis due to a drug‐resistant bacterial infection, including Staphylococcus aureus or gram‐negative bacteria or possibly more unusual organisms such as Nocardia or fungi, due to her recent use of antibiotics and chronic inhaled steroid use and recent course of oral glucocorticoids.
Conversely, the SIRS could be a manifestation of a noninfectious lung process such as acute interstitial pneumonia or an eosinophilic pneumonia. Given the diagnostic complexity, I would strongly consider consulting a pulmonologist if the patient did not improve quickly. At this point, I would like to review a posterior‐anterior (PA) and lateral chest radiograph, and room air arterial blood gas (ABG) in addition to basic laboratory test values.
Laboratory data obtained on admission was remarkable for a white blood cell (WBC) count of 26,500/L with 75% neutrophils and 6% eosinophils. Hemoglobin was 14.4 gm/dL. Platelet count was 454,000/L. Serum chemistries showed a sodium of 137 mEq/dL, potassium 4.3 mEq/dL, Cl 108 mEq/dL, bicarbonate 19 mEq/dL, blood urea nitrogen (BUN) 8 mg/dL, creatinine 1.0 mg/dL, and glucose 137 mg/dL. Cardiac enzymes were normal. Calcium was 9.8 mg/dL, albumin 2.7 gm/dL, total protein 6.9 gm/dL, AST 36 U/L, ALT 54 U/L and the bilirubin was normal. Chest radiograph (Figure 1) demonstrated a left perihilar infiltrate with air bronchograms and marked right hemidiaphragm elevation as seen on previous films. Unchanged increased interstitial markings were also present. Her electrocardiogram (ECG) showed normal sinus rhythm, normal axis, and QRS duration with nonspecific diffuse T‐wave abnormalities.
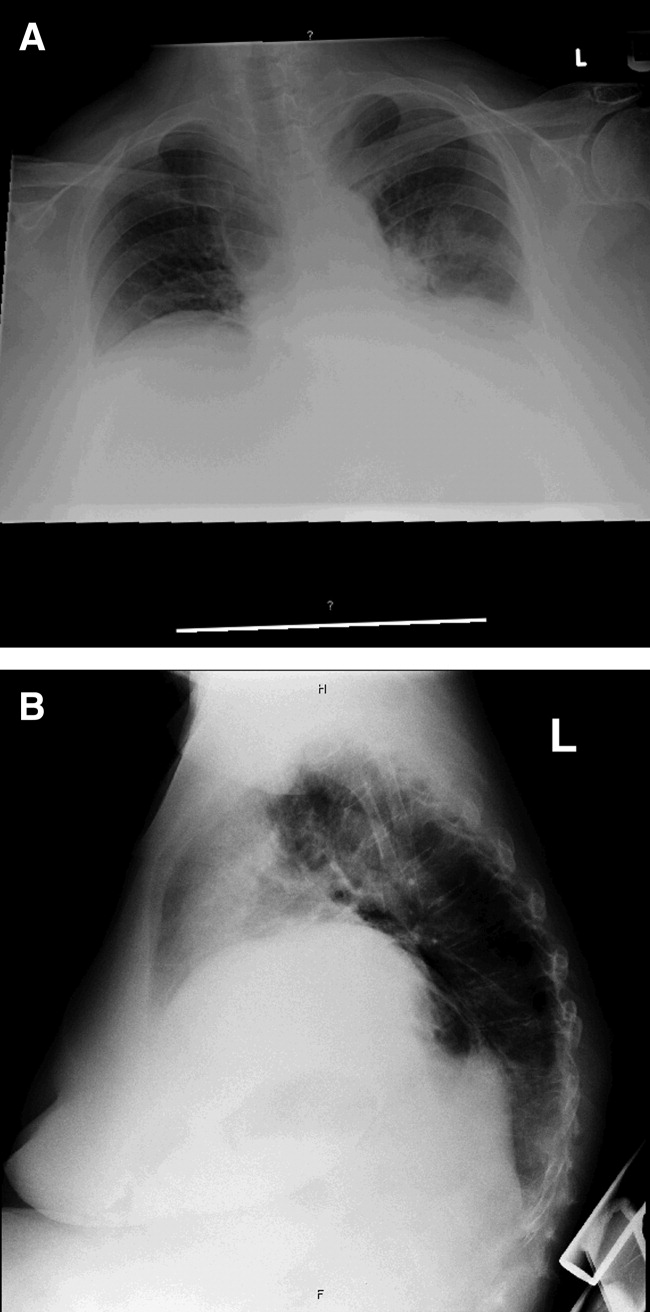
Given her presentation, I am worried about how well she is oxygenating and ventilating. An ABG should be done to assess her status more accurately. An albumin of 2.7 gm/dL indicates that she is fairly sick. I would not hesitate to consider testing the patient for human immunodeficiency virus (HIV) given how this information would dramatically change the differential diagnoses of her pulmonary process.
I am still most concerned about sepsis secondary to pneumonia in this patient with multiple chronic comorbidities, underlying chronic lung disease, receiving chronic inhaled glucocorticoids and a recent course of oral glucocorticoids and antibiotics. While I would initiate hydration I do not see a clear indication for early goal‐directed therapy for severe sepsis. In addition to obtaining an ABG and starting intravenous fluids, I would also draw blood cultures, send sputum for gram stain, culture, and sensitivity, and perform a urinalysis. I would also administer empiric antibiotics as quickly as possible based on a number of pneumonia clinical studies suggesting improved outcomes with early antibiotic administration. Because of her use of antibiotics and both inhaled and oral glucocorticoids, she is at higher risk for potentially multidrug‐resistant bacterial pathogens, including Staphyloccocus aureus and gram‐negative bacteria such as Pseudomonas and Klebsiella (Table 1). Therefore, I would initially cover her broadly for these organisms.
| Meets Any of the Following |
|---|
| Antimicrobial therapy in the preceding 90 days |
| Current hospitalization of 5 days or more |
| High frequency of antibiotic resistance in the community or in the specific hospital unit |
| Presence of risk factors for healthcare‐associated pneumonia (HCAP) |
| Hospitalization for >2 days in the preceding 90 days |
| Residence in nursing home or long‐term care facility (LTAC) for at least 5 days in last 90 days |
| Home infusion therapy including intravenous antibiotics within 30 days |
| Home wound care within 30 days |
| Chronic hemodialysis in hospital or clinic within 30 days |
| Family member with multidrug‐resistant pathogen |
| Immunosuppressive disease and/or therapy |
In addition to initial treatment choice, the inpatient triage decision is another important issue, especially at a community hospital where intensive care unit (ICU) resources are rare and often the admission decision is between sending a moderately sick patient to a regular floor bed or the medical ICU. Both the American Thoracic Society and Infectious Diseases Society of America support an ICU triage protocol in their guidelines for the management of community‐acquired pneumonia in adults that utilizes the following 9 minor criteria, of which the presence of at least 3 should support ICU admission: respiratory rate 30 breaths/minute; oxygenation index (pressure of oxygen [PaO2]/fraction of inspired oxygen [FiO2] ratio) 250; multilobar infiltrates; confusion/disorientation; uremia (BUN level 20 mg/dL); leukopenia (WBC count <4,000 cells/mm3); thrombocytopenia (platelet count <100,000 cells/mm3); hypothermia (core temperature <36C); and hypotension requiring aggressive fluid. Despite the absence of these criteria in this patient, it is important to note that no triage protocol has been adequately prospectively validated. Retrospective study of the minor criteria has found that the presence of at least 2 of the following 3 clinical criteria to have the highest specificity for predicting cardiopulmonary decompensation and subsequent need for ICU care: (1) initial hypotension (BP <90/60) on presentation with response to initial intravenous fluids to a BP >90/60; (2) oxygenation failure as indicated by PaO2/FiO2 ratio less than 250; or (3) the presence of multilobar or bilateral infiltrates on chest radiography.
I also want to comment on the relative elevation of her calcium, especially given the low albumin. This may simply be due to volume depletion, as many older patients have asymptomatic mild primary hyperparathyroidism. However, this elevated calcium may be a clue to the underlying lung process. Granulomatous lung disease due to tuberculosis or fungal infection could yield elevated calcium levels via increases in macrophage production of the active vitamin D metabolite calcitriol. This will need to be followed and a parathormone (PTH) level would be the best first test to request if the calcium level remains elevated. If the PTH level is suppressed, granulomatous disease or malignancy would be the more likely cause.
The patient was admitted with a presumptive diagnosis of community‐acquired pneumonia, was started on ceftriaxone and azithromycin, and given intravenous fluids, oxygen, and continued on inhaled salmeterol/fluticasone. Sputum was ordered for gram stain, culture, and sensitivity, and blood cultures were obtained. Urinalysis showed 1‐5 WBCs/high‐power field. Venous thromboembolism prophylaxis was initiated with subcutaneous heparin 5,000 units 8 hours. Her blood pressure normalized rapidly and during the next few days she stated she was feeling better. Despite continued significant wheezing her oxygen saturation remained at 98% on 2 L of oxygen via nasal cannula and she was less tachypneic. Attempts at obtaining an ABG were unsuccessful, and the patient subsequently refused additional attempts. Over the first few days her WBC count remained elevated above 20,000/L, with worsening bandemia (11%), and fever ranging from 38C to 39C. Sputum analysis was initially unsuccessful and blood cultures remained negative.
I am concerned about the persistent fever and elevated WBC count, and want to emphasize that I might have treated her with broader spectrum antibiotics to cover additional multidrug‐resistant bacterial organisms. I would have initially ordered vancomycin to cover methicillin resistant Staphylococcus aureus (MRSA) plus 2 additional antibiotics that cover multidrug‐resistant gram negative pathogens including Pseudomonas aeruginosa.
On the fifth hospital day, her WBC count dropped to 13,400/L and she defervesced. However, her respiratory status worsened during that same day with increased tachypnea. Of note, no results were reported from the initial sputum cultures and they were reordered and a noncontrast chest computed tomography (CT) was also ordered.
I think at this point, even though she has remained stable hemodynamically and oxygenating easily with supplemental oxygen, the question of whether or not her primary process is infectious or noninfectious lingers. I agree with obtaining a chest CT scan.
I am not surprised that sputum was not evaluated despite the orders. Among hospitalized patients with pneumonia, we frequently find that about a third of the time sputum cannot be obtained, about a third of the time it is obtained but the quality is unsatisfactory, and only a third of the time does the sputum sample meet criteria (less than 5 squamous epithelial cells per high‐power field) for adequate interpretation of the gram‐stain and culture result. Unfortunately, no one has developed a better way to improve this process. Nonetheless, I believe we do not try hard enough to obtain sputum in the first hours of evaluating our patients. I joke with our internal medicine residents that they should carry a sputum cup with them when they evaluate a patient with possible pneumonia. One recent prospective study of the value of sputum gram‐staining in community‐acquired pneumonia has found it to be highly specific for identifying Streptococcus pneumoniae or Haemophilus influenzae pneumonia.
The CT scan (Figure 2) performed on hospital day 6 demonstrated consolidation in the left upper lobe with areas of cavitation. There was also interstitial infiltrate extending into the lingula. Elevation of the right hemidiaphragm with atelectasis in both lung bases was also noted. A small effusion was present on the left and possibly a minimal effusion on the right as well. There was no pericardial effusion and only a few small pretracheal and periaortic lymph nodes were noted.

Given her failure to improve significantly after 6 days of antibiotic treatment, and her recent use of glucocorticoids, I would expand my diagnostic considerations to include other necrotizing bacterial infections, tuberculosis, fungus, and Nocardia.
Given the results of the CT scan she was placed in respiratory isolation to rule out active pulmonary tuberculosis. Though tachypneic, her blood pressure and pulse remained stable. However, her oxygen saturation deteriorated, declining to 92% on 2 L of oxygen via nasal cannula during hospital days 6 and 7. Subsequent successful attempts at collecting sputum yielded rapid growth of yeast (not Cryptococcus spp.). Pulmonary and infectious disease consultations were obtained and vancomycin was added to her regimen. The patient subsequently agreed to undergo diagnostic bronchoscopy.
I agree with obtaining input from expert consultants. I think we too often underutilize consultation in patients that are better but not completely better when we are not entirely sure what is going on. Evidence of noncryptococcus yeast in sputum may sometimes indicate colonization with Candida spp. without any significant clinical consequence. This finding may alternatively suggest the possibility of a true fungal pneumonia caused by 1 of the dimorphic fungi, including Histoplasma capsulatum, Paracoccidioides brasiliensis, Blastomyces dermatitides, or Coccidioides immitis. However, in this case there is not a strong epidemiologic patient history of exposure to any of these types of fungi.
Three sputum smears were negative for acid fast bacilli (AFB). Bronchoscopy revealed grossly abnormal mucosa in the left upper lobe and bronchomalacia, but no obstructive lesions. A transthoracic echocardiogram was ordered to evaluate her degree of pulmonary hypertension.
The 3 sputum specimens that were negative for AFB despite cavitary lung disease have high sensitivity for ruling out pulmonary tuberculosis. In addition, given the absence of any bacterial pathogen isolated from these specimens, I would pursue the possibility of other potential fungal pathogens given the patient's subacute course, history of using inhaled and oral corticosteroids, sputum results, and the presence of a cavitary lesion on her CT scan images.
Cytologic examination of the bronchoalveolar lavage (BAL) sample showed a cell differential of 1% bands, 58% neutrophils, 9% lymphs, and 27% eosinophils. The routine postbronchoscopy chest radiograph showed complete opacification of the left lung. The patient's WBC count rose to 26,000/L but she remained afebrile. Echocardiogram was reported to be of very poor quality due to her obesity. The cardiologist reviewing the echocardiogram called the attending physicians and stated there was possibly something in the left pulmonary artery and aortic dissection could not be ruled out.
The presence of eosinophilia on BAL may be a very important clue as to what lung pathology she has. In fact, eosinophilia in this setting may indicate the possibility of parasitic or fungal infection of the lung, or inflammation of the airway associated to drug toxicity, asthma, or environmental toxin exposure. With this additional information, I am concerned that she may be harboring an atypical infection such as an invasive fungus. The echocardiogram results are unclear to me but will need to be clarified with additional testing.
The interpretation of the transbronchial biopsy specimen was limited but suggested invasive pseudomembranous tracheal bronchitis due to aspergillosis. The routine hematoxylin and eosin stain showed portions of alveolar lung tissue and some collapsed submucosal bronchial glands with relatively normal‐looking lung tissue but along the edge of the spaces were obvious fungal organisms. The Gomori's methenamine silver (GMS) stain suggested the presence of Aspergillus organisms (Figure 3). Fungal cultures were also negative for any of the other dimorphic fungi or for molds.
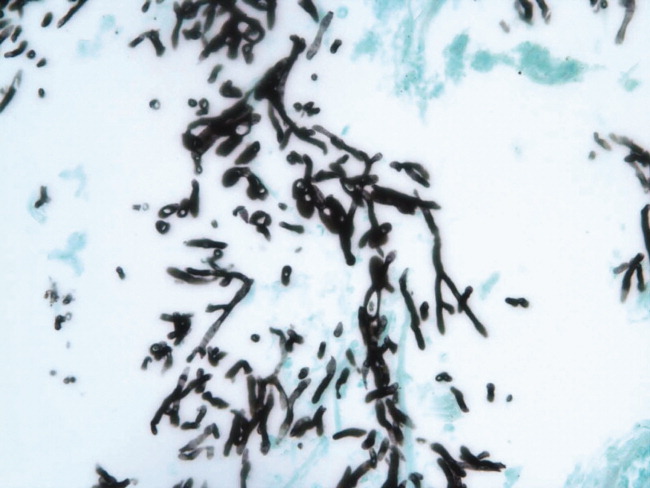
Despite the negative culture results, the overall clinical picture suggests a necrotizing pneumonia caused by an invasive Aspergillus affecting both the bronchial tree and the lower respiratory tract. Generally, necrotizing pneumonias usually have a slow response to antimicrobial therapy. Given the inherent difficulty in differentiating clearly between invasive and noninvasive disease based on a transbronchial biopsy specimen, initiating antifungal therapy for invasive aspergillosis is appropriate in this patient. This patient's recent use of oral glucocorticoids and chronic use of inhaled glucocorticoids are both potential risk factors that predisposed this patient to develop invasive aspergillosis.
Many times we simply follow treatment guidelines for different categories of pneumonia, and have limited or inadequate clinical information to make more definitive diagnoses. While we need these treatment protocols, physicians must avoid falling into the trap that antibiotics treat all infectious etiologies in the lung and we should make reasonable efforts to pin down the etiology. All of us have been fooled by atypical presentations of tuberculosis, fungus, and noninfectious diseases of the lung. I think it behooves us to be vigilant about alternative diagnoses and consider pursuing additional studies whenever the clinical response to initial treatment does not meet our expectations.
Subsequently, the patient's additional cultures remained negative. The official echocardiogram report was read as questionable PE in the pulmonary artery. A spiral CT angiogram revealed a pulmonary artery embolus in the left upper lobe and she was treated with anticoagulation. Her shortness of breath improved steadily and she was successfully discharged after receiving 9 days of oral voriconazole. Outpatient pulmonary function testing documented the presence of chronic obstructive lung disease. She completed a 5‐month course of voriconazole therapy with significant clinical and radiologic improvement of her pulmonary infiltrate. She also completed a 12‐month treatment with warfarin for the concomitant pulmonary embolism. On follow‐up at 12 months she was doing well.
COMMENTARY
Aspergillosis caused particularly by Aspergillus fumigatus is considered an emerging infectious disease that frequently produces significant morbidity and mortality among immunocompromised patients.1, 2 The most frequently‐affected organs by this fungal pathogen include the lung and the central nervous system. There are 3 pathogenic mechanisms of Aspergillus infection of the lung: colonization, hypersensitivity reaction, and invasive aspergillosis.1
Invasive pulmonary aspergillosis is predominantly seen among individuals with severe degrees of immunosuppression as a result of solid‐organ transplantation, immunosuppressive therapies for autoimmune diseases, systemic glucocorticoids, and chemotherapy for hematologic malignancies. Mortality due to invasive aspergillosis continues to be very high (>58%) despite our improved ability to diagnose this condition and newer therapies to treat immunocompromised individuals.1 Invasive aspergillosis can manifest clinically in multiple ways. These include: (1) an invasive vascular process in which fungal organisms invade blood vessels, causing a rapidly progressive and often fatal illness; (2) necrotizing pseudomembranous tracheal bronchitis; (3) chronic necrotizing aspergillosis; (4) bronchopleural fistula; or (5) empyema.35 In our case, while the pathologic findings were most suggestive of an invasive pseudomembranous tracheal bronchitis, the overall clinical picture was most compatible with a necrotizing pneumonia due to invasive aspergillosis.
In addition to the traditional identified risk factors for invasive pulmonary aspergillosis, a number of reports during the last decade have demonstrated the occurrence of invasive aspergillosis in patients with COPD.14 A systematic review of the literature demonstrated that among 1,941 patients with invasive aspergillosis, 26 (1.3%) had evidence of COPD as the main risk factor for developing invasive aspergillosis.1 A single report has associated the potential use of inhaled steroids with the occurrence of invasive aspergillosis in this patient population.2 However, other factors that may promote increased susceptibility to invasive fungal infection among patients with COPD include the use of long‐term or repeated short‐term glucocorticoid treatments, and the presence of multiple additional comorbidities, which may be found in this same population such as diabetes, malnutrition, or end‐stage renal disease.3, 4 Most reported series have demonstrated a high mortality rate of invasive pulmonary aspergillosis in patients with COPD.14
The diagnosis of invasive pulmonary aspergillosis represents a significant clinical challenge. Diagnostic algorithms incorporating CT, antigen detection testing (for serum galactomannan and ‐glucan) as well as polymerase chain reaction diagnostic testing appear to be beneficial in the early diagnosis of invasive aspergillosis in particular settings such as in allogeneic hematopoietic stem cell transplantation.5 The role of antigen testing to identify early invasive aspergillosis in patients with COPD remains uncertain since it has been evaluated in a limited number of patients and therefore clinical suspicion is critical to push clinicians to pursue invasive tissue biopsy and cultures to confirm the diagnosis.3, 4
Based on the available clinical case series and in our case, invasive pulmonary aspergillosis should be suspected in COPD patients with rapidly progressive pneumonia not responding to antibacterial therapy and who have received oral or inhaled glucocorticoids in the recent past. In addition, this case also illustrates that occasionally, patients present with more than 1 life‐threatening diagnosis. This patient was also diagnosed with PE despite adequate prophylaxis. In addition to the well‐known clinical risk factors of obesity and lung disease, the underlying infection may have contributed to a systemic or local hypercoagulable condition that further increased her risk for venous thromboembolism.
KEY TEACHING POINTS
-
Clinicians should remember to consider a broad differential in patients presenting with pneumonia, including the possibility of fungal pathogens in patients with known risk factors and in patients with multiple, potentially immunosuppressive comorbidities, or in patients who do not improve on standard antibiotic therapy.
-
There is some evidence of an association between COPD and invasive aspergillosis, likely due to the frequent use of oral corticosteroids and/or chronic inhaled steroids in this population.
- ,,.Aspergillosis case‐fatality rate: systematic review of the literature.Clin Infect Dis.2001;32:358–366.
- ,,,,.Invasive pulmonary filamentous fungal infection in a patient receiving inhaled corticosteroid therapy.Clin Infect Dis.2002;35:e54–e56.
- ,,, et al.Invasive pulmonary aspergillosis in chronic obstructive pulmonary disease: an emerging fungal pathogen.Clin Microbiol Infect.2005;11:427–429.
- ,,,,,.Invasive pulmonary aspergillosis in patients with chronic obstructive pulmonary disease: report of eight cases and review.Clin Infect Dis.1998;26:1473–1475.
- ,.Current approaches to diagnosis and treatment to invasive aspergillosis.Am J Respir Crit Care Med.2006;173:707–717.
The approach to clinical conundrums by an expert clinician is revealed through presentation of an actual patient's case in an approach typical of morning report. Similar to patient care, sequential pieces of information are provided to the clinician who is unfamiliar with the case. The focus is on the thought processes of both the clinical team caring for the patient and the discussant.
A 71‐year‐old African‐American woman presented to the emergency department with chest pain, shortness of breath, and cough. She had initially presented to her primary care physician 2 weeks previously complaining of worsening cough and shortness of breath and was told to continue her inhaled albuterol and glucocorticoids and was prescribed a prednisone taper and an unknown course of antibiotics. She noted no improvement in her symptoms despite compliance with this treatment. Three days prior to admission she described the gradual onset of left‐sided pleuritic chest pain with continued cough, associated with yellow sputum and worsening dyspnea. Review of systems was remarkable for generalized weakness and malaise. She denied fever, chills, orthopnea, paroxysmal nocturnal dyspnea, lower extremity edema, diarrhea, nausea, vomiting, or abdominal pain.
Her past medical history included a diagnosis of chronic obstructive pulmonary disease (COPD) but pulmonary function tests 7 years prior to admission showed an forced expiratory volume in the first second (FEV1)/forced vital capacity (FVC) ratio of 81%. She had a 30 pack‐year history of smoking, but quit 35 years ago. The patient also carried a diagnosis of heart failure, but an echocardiogram done 1 year ago demonstrated a left ventricular ejection fraction of 65% to 70% without diastolic dysfunction but mild right ventricular dilation and hypertrophy. Additionally, she had known nonobstructive coronary atherosclerotic heart disease, dyslipidemia, hypertension, morbid obesity, depression, and a documented chronic right hemidiaphragm elevation.
At this point the history suggests that the patient does not have a clear diagnosis of COPD. The lack of definitive spirometry evidence of chronic airway obstruction concerns me; I think that she may have been mistakenly treated with chronic inhaled steroids and doses of antibiotics for an acute exacerbation of chronic lung disease. Additional review of her history gives some indication of advanced lung disease, with her recent echocardiogram showing strain on the right ventricle with right ventricular hypertrophy and dilation, but there is no mention of the presence or severity of pulmonary hypertension. Nonetheless, I would be concerned that she probably has underlying significant cor pulmonale.
The patient now re‐presents with a worsening of her pulmonary symptoms. Her left‐sided pleuritic pain would make me concerned that she had a pulmonary embolus (PE). This morbidly obese patient with new pulmonary symptoms, right ventricular strain on her previous echocardiogram, and a persistent elevated right hemidiaphragm suggests a presentation of another PE.
At this time I cannot rule out other common possibilities such as infectious pneumonia. If she does have pneumonia, I would be concerned she could be harboring a multidrug‐resistant bacterial infection given her recent course of antibiotics in addition to her use of both chronic inhaled and intermittent oral glucocorticoids.
After gathering the rest of her full medical history, I would focus my physical exam on looking for evidence of parenchymal lung disease, signs of pulmonary hypertension, and pneumonia.
Her surgical history includes a previous hysterectomy, cholecystectomy, hernia repair, and left hepatic lobectomy for a benign mass. Her outpatient medications were ibuprofen, bupropion, fluvastatin, atenolol, potassium, aspirin, clopidogrel, albuterol inhaler, fluticasone/salmeterol inhaler, and omeprazole. She reports an allergy to penicillin and to sulfa drugs. Her mother died of an unknown cancer at age 77 years. She denied any international travel and she has always lived in Georgia.
The patient has been retired since 1992, having previously worked for the U.S. Postal Service. She admits to occasional alcohol intake (2 to 3 drinks a month). No recent travel, surgery, or prolonged immobilization was noted.
On initial examination she was alert and mentally appropriate, but appeared to be in mild respiratory distress with a respiratory rate of 28 breaths/minute. Her blood pressure (BP) was 99/70, heart rate 102, temperature of 38.2C, and oxygen saturation of 93% on room air and 97% on 2 L of oxygen via nasal cannula. Auscultation of her lungs revealed crackles over her left anterior lung field, bronchial breath sounds in the left posterior midlung, and bibasilar crackles. No wheezing was noted. Her cardiovascular exam and the remainder of her physical exam were unremarkable except for morbid obesity.
While my initial thoughts were leaning toward an exacerbation of chronic lung disease or possibly a new PE, at this moment, infection seems more likely. Indeed, her pulmonary findings suggest a left‐sided inflammatory process, and her vital signs meet criteria for systemic inflammatory response syndrome (SIRS). My primary concern is sepsis due to a drug‐resistant bacterial infection, including Staphylococcus aureus or gram‐negative bacteria or possibly more unusual organisms such as Nocardia or fungi, due to her recent use of antibiotics and chronic inhaled steroid use and recent course of oral glucocorticoids.
Conversely, the SIRS could be a manifestation of a noninfectious lung process such as acute interstitial pneumonia or an eosinophilic pneumonia. Given the diagnostic complexity, I would strongly consider consulting a pulmonologist if the patient did not improve quickly. At this point, I would like to review a posterior‐anterior (PA) and lateral chest radiograph, and room air arterial blood gas (ABG) in addition to basic laboratory test values.
Laboratory data obtained on admission was remarkable for a white blood cell (WBC) count of 26,500/L with 75% neutrophils and 6% eosinophils. Hemoglobin was 14.4 gm/dL. Platelet count was 454,000/L. Serum chemistries showed a sodium of 137 mEq/dL, potassium 4.3 mEq/dL, Cl 108 mEq/dL, bicarbonate 19 mEq/dL, blood urea nitrogen (BUN) 8 mg/dL, creatinine 1.0 mg/dL, and glucose 137 mg/dL. Cardiac enzymes were normal. Calcium was 9.8 mg/dL, albumin 2.7 gm/dL, total protein 6.9 gm/dL, AST 36 U/L, ALT 54 U/L and the bilirubin was normal. Chest radiograph (Figure 1) demonstrated a left perihilar infiltrate with air bronchograms and marked right hemidiaphragm elevation as seen on previous films. Unchanged increased interstitial markings were also present. Her electrocardiogram (ECG) showed normal sinus rhythm, normal axis, and QRS duration with nonspecific diffuse T‐wave abnormalities.
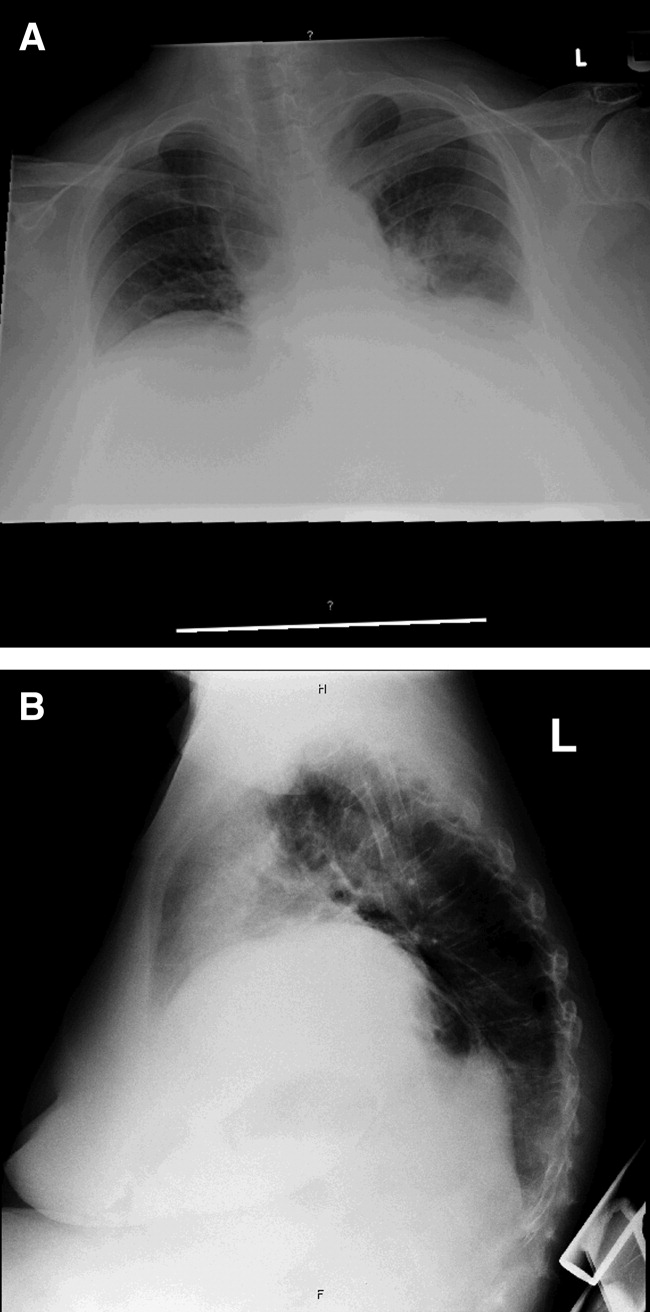
Given her presentation, I am worried about how well she is oxygenating and ventilating. An ABG should be done to assess her status more accurately. An albumin of 2.7 gm/dL indicates that she is fairly sick. I would not hesitate to consider testing the patient for human immunodeficiency virus (HIV) given how this information would dramatically change the differential diagnoses of her pulmonary process.
I am still most concerned about sepsis secondary to pneumonia in this patient with multiple chronic comorbidities, underlying chronic lung disease, receiving chronic inhaled glucocorticoids and a recent course of oral glucocorticoids and antibiotics. While I would initiate hydration I do not see a clear indication for early goal‐directed therapy for severe sepsis. In addition to obtaining an ABG and starting intravenous fluids, I would also draw blood cultures, send sputum for gram stain, culture, and sensitivity, and perform a urinalysis. I would also administer empiric antibiotics as quickly as possible based on a number of pneumonia clinical studies suggesting improved outcomes with early antibiotic administration. Because of her use of antibiotics and both inhaled and oral glucocorticoids, she is at higher risk for potentially multidrug‐resistant bacterial pathogens, including Staphyloccocus aureus and gram‐negative bacteria such as Pseudomonas and Klebsiella (Table 1). Therefore, I would initially cover her broadly for these organisms.
| Meets Any of the Following |
|---|
| Antimicrobial therapy in the preceding 90 days |
| Current hospitalization of 5 days or more |
| High frequency of antibiotic resistance in the community or in the specific hospital unit |
| Presence of risk factors for healthcare‐associated pneumonia (HCAP) |
| Hospitalization for >2 days in the preceding 90 days |
| Residence in nursing home or long‐term care facility (LTAC) for at least 5 days in last 90 days |
| Home infusion therapy including intravenous antibiotics within 30 days |
| Home wound care within 30 days |
| Chronic hemodialysis in hospital or clinic within 30 days |
| Family member with multidrug‐resistant pathogen |
| Immunosuppressive disease and/or therapy |
In addition to initial treatment choice, the inpatient triage decision is another important issue, especially at a community hospital where intensive care unit (ICU) resources are rare and often the admission decision is between sending a moderately sick patient to a regular floor bed or the medical ICU. Both the American Thoracic Society and Infectious Diseases Society of America support an ICU triage protocol in their guidelines for the management of community‐acquired pneumonia in adults that utilizes the following 9 minor criteria, of which the presence of at least 3 should support ICU admission: respiratory rate 30 breaths/minute; oxygenation index (pressure of oxygen [PaO2]/fraction of inspired oxygen [FiO2] ratio) 250; multilobar infiltrates; confusion/disorientation; uremia (BUN level 20 mg/dL); leukopenia (WBC count <4,000 cells/mm3); thrombocytopenia (platelet count <100,000 cells/mm3); hypothermia (core temperature <36C); and hypotension requiring aggressive fluid. Despite the absence of these criteria in this patient, it is important to note that no triage protocol has been adequately prospectively validated. Retrospective study of the minor criteria has found that the presence of at least 2 of the following 3 clinical criteria to have the highest specificity for predicting cardiopulmonary decompensation and subsequent need for ICU care: (1) initial hypotension (BP <90/60) on presentation with response to initial intravenous fluids to a BP >90/60; (2) oxygenation failure as indicated by PaO2/FiO2 ratio less than 250; or (3) the presence of multilobar or bilateral infiltrates on chest radiography.
I also want to comment on the relative elevation of her calcium, especially given the low albumin. This may simply be due to volume depletion, as many older patients have asymptomatic mild primary hyperparathyroidism. However, this elevated calcium may be a clue to the underlying lung process. Granulomatous lung disease due to tuberculosis or fungal infection could yield elevated calcium levels via increases in macrophage production of the active vitamin D metabolite calcitriol. This will need to be followed and a parathormone (PTH) level would be the best first test to request if the calcium level remains elevated. If the PTH level is suppressed, granulomatous disease or malignancy would be the more likely cause.
The patient was admitted with a presumptive diagnosis of community‐acquired pneumonia, was started on ceftriaxone and azithromycin, and given intravenous fluids, oxygen, and continued on inhaled salmeterol/fluticasone. Sputum was ordered for gram stain, culture, and sensitivity, and blood cultures were obtained. Urinalysis showed 1‐5 WBCs/high‐power field. Venous thromboembolism prophylaxis was initiated with subcutaneous heparin 5,000 units 8 hours. Her blood pressure normalized rapidly and during the next few days she stated she was feeling better. Despite continued significant wheezing her oxygen saturation remained at 98% on 2 L of oxygen via nasal cannula and she was less tachypneic. Attempts at obtaining an ABG were unsuccessful, and the patient subsequently refused additional attempts. Over the first few days her WBC count remained elevated above 20,000/L, with worsening bandemia (11%), and fever ranging from 38C to 39C. Sputum analysis was initially unsuccessful and blood cultures remained negative.
I am concerned about the persistent fever and elevated WBC count, and want to emphasize that I might have treated her with broader spectrum antibiotics to cover additional multidrug‐resistant bacterial organisms. I would have initially ordered vancomycin to cover methicillin resistant Staphylococcus aureus (MRSA) plus 2 additional antibiotics that cover multidrug‐resistant gram negative pathogens including Pseudomonas aeruginosa.
On the fifth hospital day, her WBC count dropped to 13,400/L and she defervesced. However, her respiratory status worsened during that same day with increased tachypnea. Of note, no results were reported from the initial sputum cultures and they were reordered and a noncontrast chest computed tomography (CT) was also ordered.
I think at this point, even though she has remained stable hemodynamically and oxygenating easily with supplemental oxygen, the question of whether or not her primary process is infectious or noninfectious lingers. I agree with obtaining a chest CT scan.
I am not surprised that sputum was not evaluated despite the orders. Among hospitalized patients with pneumonia, we frequently find that about a third of the time sputum cannot be obtained, about a third of the time it is obtained but the quality is unsatisfactory, and only a third of the time does the sputum sample meet criteria (less than 5 squamous epithelial cells per high‐power field) for adequate interpretation of the gram‐stain and culture result. Unfortunately, no one has developed a better way to improve this process. Nonetheless, I believe we do not try hard enough to obtain sputum in the first hours of evaluating our patients. I joke with our internal medicine residents that they should carry a sputum cup with them when they evaluate a patient with possible pneumonia. One recent prospective study of the value of sputum gram‐staining in community‐acquired pneumonia has found it to be highly specific for identifying Streptococcus pneumoniae or Haemophilus influenzae pneumonia.
The CT scan (Figure 2) performed on hospital day 6 demonstrated consolidation in the left upper lobe with areas of cavitation. There was also interstitial infiltrate extending into the lingula. Elevation of the right hemidiaphragm with atelectasis in both lung bases was also noted. A small effusion was present on the left and possibly a minimal effusion on the right as well. There was no pericardial effusion and only a few small pretracheal and periaortic lymph nodes were noted.

Given her failure to improve significantly after 6 days of antibiotic treatment, and her recent use of glucocorticoids, I would expand my diagnostic considerations to include other necrotizing bacterial infections, tuberculosis, fungus, and Nocardia.
Given the results of the CT scan she was placed in respiratory isolation to rule out active pulmonary tuberculosis. Though tachypneic, her blood pressure and pulse remained stable. However, her oxygen saturation deteriorated, declining to 92% on 2 L of oxygen via nasal cannula during hospital days 6 and 7. Subsequent successful attempts at collecting sputum yielded rapid growth of yeast (not Cryptococcus spp.). Pulmonary and infectious disease consultations were obtained and vancomycin was added to her regimen. The patient subsequently agreed to undergo diagnostic bronchoscopy.
I agree with obtaining input from expert consultants. I think we too often underutilize consultation in patients that are better but not completely better when we are not entirely sure what is going on. Evidence of noncryptococcus yeast in sputum may sometimes indicate colonization with Candida spp. without any significant clinical consequence. This finding may alternatively suggest the possibility of a true fungal pneumonia caused by 1 of the dimorphic fungi, including Histoplasma capsulatum, Paracoccidioides brasiliensis, Blastomyces dermatitides, or Coccidioides immitis. However, in this case there is not a strong epidemiologic patient history of exposure to any of these types of fungi.
Three sputum smears were negative for acid fast bacilli (AFB). Bronchoscopy revealed grossly abnormal mucosa in the left upper lobe and bronchomalacia, but no obstructive lesions. A transthoracic echocardiogram was ordered to evaluate her degree of pulmonary hypertension.
The 3 sputum specimens that were negative for AFB despite cavitary lung disease have high sensitivity for ruling out pulmonary tuberculosis. In addition, given the absence of any bacterial pathogen isolated from these specimens, I would pursue the possibility of other potential fungal pathogens given the patient's subacute course, history of using inhaled and oral corticosteroids, sputum results, and the presence of a cavitary lesion on her CT scan images.
Cytologic examination of the bronchoalveolar lavage (BAL) sample showed a cell differential of 1% bands, 58% neutrophils, 9% lymphs, and 27% eosinophils. The routine postbronchoscopy chest radiograph showed complete opacification of the left lung. The patient's WBC count rose to 26,000/L but she remained afebrile. Echocardiogram was reported to be of very poor quality due to her obesity. The cardiologist reviewing the echocardiogram called the attending physicians and stated there was possibly something in the left pulmonary artery and aortic dissection could not be ruled out.
The presence of eosinophilia on BAL may be a very important clue as to what lung pathology she has. In fact, eosinophilia in this setting may indicate the possibility of parasitic or fungal infection of the lung, or inflammation of the airway associated to drug toxicity, asthma, or environmental toxin exposure. With this additional information, I am concerned that she may be harboring an atypical infection such as an invasive fungus. The echocardiogram results are unclear to me but will need to be clarified with additional testing.
The interpretation of the transbronchial biopsy specimen was limited but suggested invasive pseudomembranous tracheal bronchitis due to aspergillosis. The routine hematoxylin and eosin stain showed portions of alveolar lung tissue and some collapsed submucosal bronchial glands with relatively normal‐looking lung tissue but along the edge of the spaces were obvious fungal organisms. The Gomori's methenamine silver (GMS) stain suggested the presence of Aspergillus organisms (Figure 3). Fungal cultures were also negative for any of the other dimorphic fungi or for molds.
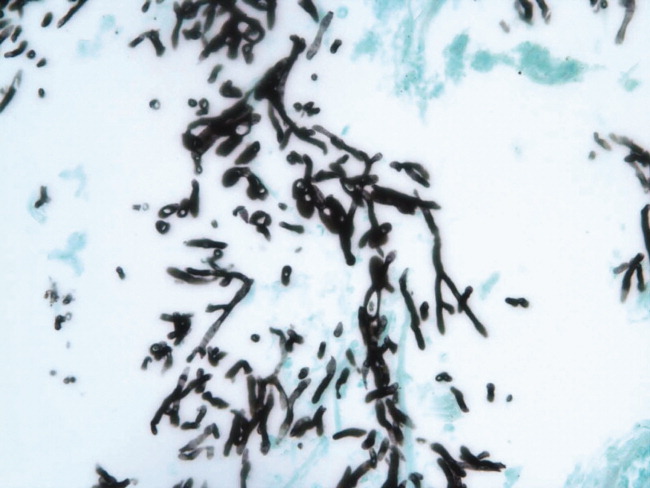
Despite the negative culture results, the overall clinical picture suggests a necrotizing pneumonia caused by an invasive Aspergillus affecting both the bronchial tree and the lower respiratory tract. Generally, necrotizing pneumonias usually have a slow response to antimicrobial therapy. Given the inherent difficulty in differentiating clearly between invasive and noninvasive disease based on a transbronchial biopsy specimen, initiating antifungal therapy for invasive aspergillosis is appropriate in this patient. This patient's recent use of oral glucocorticoids and chronic use of inhaled glucocorticoids are both potential risk factors that predisposed this patient to develop invasive aspergillosis.
Many times we simply follow treatment guidelines for different categories of pneumonia, and have limited or inadequate clinical information to make more definitive diagnoses. While we need these treatment protocols, physicians must avoid falling into the trap that antibiotics treat all infectious etiologies in the lung and we should make reasonable efforts to pin down the etiology. All of us have been fooled by atypical presentations of tuberculosis, fungus, and noninfectious diseases of the lung. I think it behooves us to be vigilant about alternative diagnoses and consider pursuing additional studies whenever the clinical response to initial treatment does not meet our expectations.
Subsequently, the patient's additional cultures remained negative. The official echocardiogram report was read as questionable PE in the pulmonary artery. A spiral CT angiogram revealed a pulmonary artery embolus in the left upper lobe and she was treated with anticoagulation. Her shortness of breath improved steadily and she was successfully discharged after receiving 9 days of oral voriconazole. Outpatient pulmonary function testing documented the presence of chronic obstructive lung disease. She completed a 5‐month course of voriconazole therapy with significant clinical and radiologic improvement of her pulmonary infiltrate. She also completed a 12‐month treatment with warfarin for the concomitant pulmonary embolism. On follow‐up at 12 months she was doing well.
COMMENTARY
Aspergillosis caused particularly by Aspergillus fumigatus is considered an emerging infectious disease that frequently produces significant morbidity and mortality among immunocompromised patients.1, 2 The most frequently‐affected organs by this fungal pathogen include the lung and the central nervous system. There are 3 pathogenic mechanisms of Aspergillus infection of the lung: colonization, hypersensitivity reaction, and invasive aspergillosis.1
Invasive pulmonary aspergillosis is predominantly seen among individuals with severe degrees of immunosuppression as a result of solid‐organ transplantation, immunosuppressive therapies for autoimmune diseases, systemic glucocorticoids, and chemotherapy for hematologic malignancies. Mortality due to invasive aspergillosis continues to be very high (>58%) despite our improved ability to diagnose this condition and newer therapies to treat immunocompromised individuals.1 Invasive aspergillosis can manifest clinically in multiple ways. These include: (1) an invasive vascular process in which fungal organisms invade blood vessels, causing a rapidly progressive and often fatal illness; (2) necrotizing pseudomembranous tracheal bronchitis; (3) chronic necrotizing aspergillosis; (4) bronchopleural fistula; or (5) empyema.35 In our case, while the pathologic findings were most suggestive of an invasive pseudomembranous tracheal bronchitis, the overall clinical picture was most compatible with a necrotizing pneumonia due to invasive aspergillosis.
In addition to the traditional identified risk factors for invasive pulmonary aspergillosis, a number of reports during the last decade have demonstrated the occurrence of invasive aspergillosis in patients with COPD.14 A systematic review of the literature demonstrated that among 1,941 patients with invasive aspergillosis, 26 (1.3%) had evidence of COPD as the main risk factor for developing invasive aspergillosis.1 A single report has associated the potential use of inhaled steroids with the occurrence of invasive aspergillosis in this patient population.2 However, other factors that may promote increased susceptibility to invasive fungal infection among patients with COPD include the use of long‐term or repeated short‐term glucocorticoid treatments, and the presence of multiple additional comorbidities, which may be found in this same population such as diabetes, malnutrition, or end‐stage renal disease.3, 4 Most reported series have demonstrated a high mortality rate of invasive pulmonary aspergillosis in patients with COPD.14
The diagnosis of invasive pulmonary aspergillosis represents a significant clinical challenge. Diagnostic algorithms incorporating CT, antigen detection testing (for serum galactomannan and ‐glucan) as well as polymerase chain reaction diagnostic testing appear to be beneficial in the early diagnosis of invasive aspergillosis in particular settings such as in allogeneic hematopoietic stem cell transplantation.5 The role of antigen testing to identify early invasive aspergillosis in patients with COPD remains uncertain since it has been evaluated in a limited number of patients and therefore clinical suspicion is critical to push clinicians to pursue invasive tissue biopsy and cultures to confirm the diagnosis.3, 4
Based on the available clinical case series and in our case, invasive pulmonary aspergillosis should be suspected in COPD patients with rapidly progressive pneumonia not responding to antibacterial therapy and who have received oral or inhaled glucocorticoids in the recent past. In addition, this case also illustrates that occasionally, patients present with more than 1 life‐threatening diagnosis. This patient was also diagnosed with PE despite adequate prophylaxis. In addition to the well‐known clinical risk factors of obesity and lung disease, the underlying infection may have contributed to a systemic or local hypercoagulable condition that further increased her risk for venous thromboembolism.
KEY TEACHING POINTS
-
Clinicians should remember to consider a broad differential in patients presenting with pneumonia, including the possibility of fungal pathogens in patients with known risk factors and in patients with multiple, potentially immunosuppressive comorbidities, or in patients who do not improve on standard antibiotic therapy.
-
There is some evidence of an association between COPD and invasive aspergillosis, likely due to the frequent use of oral corticosteroids and/or chronic inhaled steroids in this population.
The approach to clinical conundrums by an expert clinician is revealed through presentation of an actual patient's case in an approach typical of morning report. Similar to patient care, sequential pieces of information are provided to the clinician who is unfamiliar with the case. The focus is on the thought processes of both the clinical team caring for the patient and the discussant.
A 71‐year‐old African‐American woman presented to the emergency department with chest pain, shortness of breath, and cough. She had initially presented to her primary care physician 2 weeks previously complaining of worsening cough and shortness of breath and was told to continue her inhaled albuterol and glucocorticoids and was prescribed a prednisone taper and an unknown course of antibiotics. She noted no improvement in her symptoms despite compliance with this treatment. Three days prior to admission she described the gradual onset of left‐sided pleuritic chest pain with continued cough, associated with yellow sputum and worsening dyspnea. Review of systems was remarkable for generalized weakness and malaise. She denied fever, chills, orthopnea, paroxysmal nocturnal dyspnea, lower extremity edema, diarrhea, nausea, vomiting, or abdominal pain.
Her past medical history included a diagnosis of chronic obstructive pulmonary disease (COPD) but pulmonary function tests 7 years prior to admission showed an forced expiratory volume in the first second (FEV1)/forced vital capacity (FVC) ratio of 81%. She had a 30 pack‐year history of smoking, but quit 35 years ago. The patient also carried a diagnosis of heart failure, but an echocardiogram done 1 year ago demonstrated a left ventricular ejection fraction of 65% to 70% without diastolic dysfunction but mild right ventricular dilation and hypertrophy. Additionally, she had known nonobstructive coronary atherosclerotic heart disease, dyslipidemia, hypertension, morbid obesity, depression, and a documented chronic right hemidiaphragm elevation.
At this point the history suggests that the patient does not have a clear diagnosis of COPD. The lack of definitive spirometry evidence of chronic airway obstruction concerns me; I think that she may have been mistakenly treated with chronic inhaled steroids and doses of antibiotics for an acute exacerbation of chronic lung disease. Additional review of her history gives some indication of advanced lung disease, with her recent echocardiogram showing strain on the right ventricle with right ventricular hypertrophy and dilation, but there is no mention of the presence or severity of pulmonary hypertension. Nonetheless, I would be concerned that she probably has underlying significant cor pulmonale.
The patient now re‐presents with a worsening of her pulmonary symptoms. Her left‐sided pleuritic pain would make me concerned that she had a pulmonary embolus (PE). This morbidly obese patient with new pulmonary symptoms, right ventricular strain on her previous echocardiogram, and a persistent elevated right hemidiaphragm suggests a presentation of another PE.
At this time I cannot rule out other common possibilities such as infectious pneumonia. If she does have pneumonia, I would be concerned she could be harboring a multidrug‐resistant bacterial infection given her recent course of antibiotics in addition to her use of both chronic inhaled and intermittent oral glucocorticoids.
After gathering the rest of her full medical history, I would focus my physical exam on looking for evidence of parenchymal lung disease, signs of pulmonary hypertension, and pneumonia.
Her surgical history includes a previous hysterectomy, cholecystectomy, hernia repair, and left hepatic lobectomy for a benign mass. Her outpatient medications were ibuprofen, bupropion, fluvastatin, atenolol, potassium, aspirin, clopidogrel, albuterol inhaler, fluticasone/salmeterol inhaler, and omeprazole. She reports an allergy to penicillin and to sulfa drugs. Her mother died of an unknown cancer at age 77 years. She denied any international travel and she has always lived in Georgia.
The patient has been retired since 1992, having previously worked for the U.S. Postal Service. She admits to occasional alcohol intake (2 to 3 drinks a month). No recent travel, surgery, or prolonged immobilization was noted.
On initial examination she was alert and mentally appropriate, but appeared to be in mild respiratory distress with a respiratory rate of 28 breaths/minute. Her blood pressure (BP) was 99/70, heart rate 102, temperature of 38.2C, and oxygen saturation of 93% on room air and 97% on 2 L of oxygen via nasal cannula. Auscultation of her lungs revealed crackles over her left anterior lung field, bronchial breath sounds in the left posterior midlung, and bibasilar crackles. No wheezing was noted. Her cardiovascular exam and the remainder of her physical exam were unremarkable except for morbid obesity.
While my initial thoughts were leaning toward an exacerbation of chronic lung disease or possibly a new PE, at this moment, infection seems more likely. Indeed, her pulmonary findings suggest a left‐sided inflammatory process, and her vital signs meet criteria for systemic inflammatory response syndrome (SIRS). My primary concern is sepsis due to a drug‐resistant bacterial infection, including Staphylococcus aureus or gram‐negative bacteria or possibly more unusual organisms such as Nocardia or fungi, due to her recent use of antibiotics and chronic inhaled steroid use and recent course of oral glucocorticoids.
Conversely, the SIRS could be a manifestation of a noninfectious lung process such as acute interstitial pneumonia or an eosinophilic pneumonia. Given the diagnostic complexity, I would strongly consider consulting a pulmonologist if the patient did not improve quickly. At this point, I would like to review a posterior‐anterior (PA) and lateral chest radiograph, and room air arterial blood gas (ABG) in addition to basic laboratory test values.
Laboratory data obtained on admission was remarkable for a white blood cell (WBC) count of 26,500/L with 75% neutrophils and 6% eosinophils. Hemoglobin was 14.4 gm/dL. Platelet count was 454,000/L. Serum chemistries showed a sodium of 137 mEq/dL, potassium 4.3 mEq/dL, Cl 108 mEq/dL, bicarbonate 19 mEq/dL, blood urea nitrogen (BUN) 8 mg/dL, creatinine 1.0 mg/dL, and glucose 137 mg/dL. Cardiac enzymes were normal. Calcium was 9.8 mg/dL, albumin 2.7 gm/dL, total protein 6.9 gm/dL, AST 36 U/L, ALT 54 U/L and the bilirubin was normal. Chest radiograph (Figure 1) demonstrated a left perihilar infiltrate with air bronchograms and marked right hemidiaphragm elevation as seen on previous films. Unchanged increased interstitial markings were also present. Her electrocardiogram (ECG) showed normal sinus rhythm, normal axis, and QRS duration with nonspecific diffuse T‐wave abnormalities.
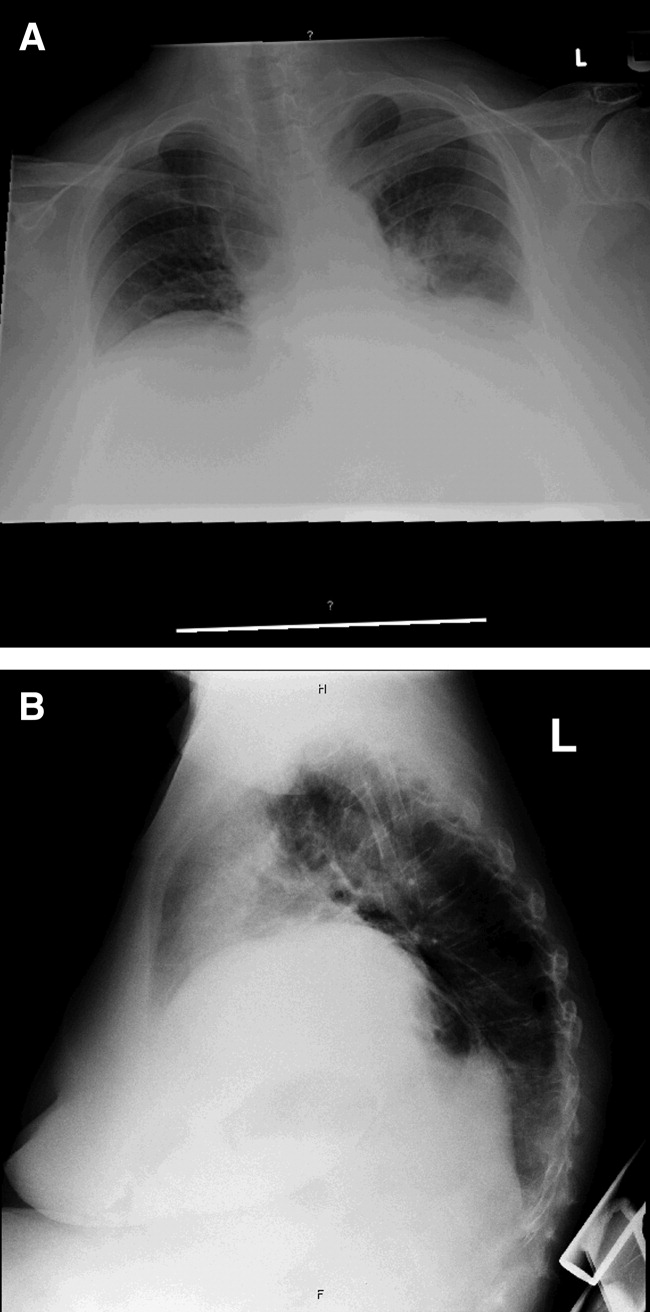
Given her presentation, I am worried about how well she is oxygenating and ventilating. An ABG should be done to assess her status more accurately. An albumin of 2.7 gm/dL indicates that she is fairly sick. I would not hesitate to consider testing the patient for human immunodeficiency virus (HIV) given how this information would dramatically change the differential diagnoses of her pulmonary process.
I am still most concerned about sepsis secondary to pneumonia in this patient with multiple chronic comorbidities, underlying chronic lung disease, receiving chronic inhaled glucocorticoids and a recent course of oral glucocorticoids and antibiotics. While I would initiate hydration I do not see a clear indication for early goal‐directed therapy for severe sepsis. In addition to obtaining an ABG and starting intravenous fluids, I would also draw blood cultures, send sputum for gram stain, culture, and sensitivity, and perform a urinalysis. I would also administer empiric antibiotics as quickly as possible based on a number of pneumonia clinical studies suggesting improved outcomes with early antibiotic administration. Because of her use of antibiotics and both inhaled and oral glucocorticoids, she is at higher risk for potentially multidrug‐resistant bacterial pathogens, including Staphyloccocus aureus and gram‐negative bacteria such as Pseudomonas and Klebsiella (Table 1). Therefore, I would initially cover her broadly for these organisms.
| Meets Any of the Following |
|---|
| Antimicrobial therapy in the preceding 90 days |
| Current hospitalization of 5 days or more |
| High frequency of antibiotic resistance in the community or in the specific hospital unit |
| Presence of risk factors for healthcare‐associated pneumonia (HCAP) |
| Hospitalization for >2 days in the preceding 90 days |
| Residence in nursing home or long‐term care facility (LTAC) for at least 5 days in last 90 days |
| Home infusion therapy including intravenous antibiotics within 30 days |
| Home wound care within 30 days |
| Chronic hemodialysis in hospital or clinic within 30 days |
| Family member with multidrug‐resistant pathogen |
| Immunosuppressive disease and/or therapy |
In addition to initial treatment choice, the inpatient triage decision is another important issue, especially at a community hospital where intensive care unit (ICU) resources are rare and often the admission decision is between sending a moderately sick patient to a regular floor bed or the medical ICU. Both the American Thoracic Society and Infectious Diseases Society of America support an ICU triage protocol in their guidelines for the management of community‐acquired pneumonia in adults that utilizes the following 9 minor criteria, of which the presence of at least 3 should support ICU admission: respiratory rate 30 breaths/minute; oxygenation index (pressure of oxygen [PaO2]/fraction of inspired oxygen [FiO2] ratio) 250; multilobar infiltrates; confusion/disorientation; uremia (BUN level 20 mg/dL); leukopenia (WBC count <4,000 cells/mm3); thrombocytopenia (platelet count <100,000 cells/mm3); hypothermia (core temperature <36C); and hypotension requiring aggressive fluid. Despite the absence of these criteria in this patient, it is important to note that no triage protocol has been adequately prospectively validated. Retrospective study of the minor criteria has found that the presence of at least 2 of the following 3 clinical criteria to have the highest specificity for predicting cardiopulmonary decompensation and subsequent need for ICU care: (1) initial hypotension (BP <90/60) on presentation with response to initial intravenous fluids to a BP >90/60; (2) oxygenation failure as indicated by PaO2/FiO2 ratio less than 250; or (3) the presence of multilobar or bilateral infiltrates on chest radiography.
I also want to comment on the relative elevation of her calcium, especially given the low albumin. This may simply be due to volume depletion, as many older patients have asymptomatic mild primary hyperparathyroidism. However, this elevated calcium may be a clue to the underlying lung process. Granulomatous lung disease due to tuberculosis or fungal infection could yield elevated calcium levels via increases in macrophage production of the active vitamin D metabolite calcitriol. This will need to be followed and a parathormone (PTH) level would be the best first test to request if the calcium level remains elevated. If the PTH level is suppressed, granulomatous disease or malignancy would be the more likely cause.
The patient was admitted with a presumptive diagnosis of community‐acquired pneumonia, was started on ceftriaxone and azithromycin, and given intravenous fluids, oxygen, and continued on inhaled salmeterol/fluticasone. Sputum was ordered for gram stain, culture, and sensitivity, and blood cultures were obtained. Urinalysis showed 1‐5 WBCs/high‐power field. Venous thromboembolism prophylaxis was initiated with subcutaneous heparin 5,000 units 8 hours. Her blood pressure normalized rapidly and during the next few days she stated she was feeling better. Despite continued significant wheezing her oxygen saturation remained at 98% on 2 L of oxygen via nasal cannula and she was less tachypneic. Attempts at obtaining an ABG were unsuccessful, and the patient subsequently refused additional attempts. Over the first few days her WBC count remained elevated above 20,000/L, with worsening bandemia (11%), and fever ranging from 38C to 39C. Sputum analysis was initially unsuccessful and blood cultures remained negative.
I am concerned about the persistent fever and elevated WBC count, and want to emphasize that I might have treated her with broader spectrum antibiotics to cover additional multidrug‐resistant bacterial organisms. I would have initially ordered vancomycin to cover methicillin resistant Staphylococcus aureus (MRSA) plus 2 additional antibiotics that cover multidrug‐resistant gram negative pathogens including Pseudomonas aeruginosa.
On the fifth hospital day, her WBC count dropped to 13,400/L and she defervesced. However, her respiratory status worsened during that same day with increased tachypnea. Of note, no results were reported from the initial sputum cultures and they were reordered and a noncontrast chest computed tomography (CT) was also ordered.
I think at this point, even though she has remained stable hemodynamically and oxygenating easily with supplemental oxygen, the question of whether or not her primary process is infectious or noninfectious lingers. I agree with obtaining a chest CT scan.
I am not surprised that sputum was not evaluated despite the orders. Among hospitalized patients with pneumonia, we frequently find that about a third of the time sputum cannot be obtained, about a third of the time it is obtained but the quality is unsatisfactory, and only a third of the time does the sputum sample meet criteria (less than 5 squamous epithelial cells per high‐power field) for adequate interpretation of the gram‐stain and culture result. Unfortunately, no one has developed a better way to improve this process. Nonetheless, I believe we do not try hard enough to obtain sputum in the first hours of evaluating our patients. I joke with our internal medicine residents that they should carry a sputum cup with them when they evaluate a patient with possible pneumonia. One recent prospective study of the value of sputum gram‐staining in community‐acquired pneumonia has found it to be highly specific for identifying Streptococcus pneumoniae or Haemophilus influenzae pneumonia.
The CT scan (Figure 2) performed on hospital day 6 demonstrated consolidation in the left upper lobe with areas of cavitation. There was also interstitial infiltrate extending into the lingula. Elevation of the right hemidiaphragm with atelectasis in both lung bases was also noted. A small effusion was present on the left and possibly a minimal effusion on the right as well. There was no pericardial effusion and only a few small pretracheal and periaortic lymph nodes were noted.

Given her failure to improve significantly after 6 days of antibiotic treatment, and her recent use of glucocorticoids, I would expand my diagnostic considerations to include other necrotizing bacterial infections, tuberculosis, fungus, and Nocardia.
Given the results of the CT scan she was placed in respiratory isolation to rule out active pulmonary tuberculosis. Though tachypneic, her blood pressure and pulse remained stable. However, her oxygen saturation deteriorated, declining to 92% on 2 L of oxygen via nasal cannula during hospital days 6 and 7. Subsequent successful attempts at collecting sputum yielded rapid growth of yeast (not Cryptococcus spp.). Pulmonary and infectious disease consultations were obtained and vancomycin was added to her regimen. The patient subsequently agreed to undergo diagnostic bronchoscopy.
I agree with obtaining input from expert consultants. I think we too often underutilize consultation in patients that are better but not completely better when we are not entirely sure what is going on. Evidence of noncryptococcus yeast in sputum may sometimes indicate colonization with Candida spp. without any significant clinical consequence. This finding may alternatively suggest the possibility of a true fungal pneumonia caused by 1 of the dimorphic fungi, including Histoplasma capsulatum, Paracoccidioides brasiliensis, Blastomyces dermatitides, or Coccidioides immitis. However, in this case there is not a strong epidemiologic patient history of exposure to any of these types of fungi.
Three sputum smears were negative for acid fast bacilli (AFB). Bronchoscopy revealed grossly abnormal mucosa in the left upper lobe and bronchomalacia, but no obstructive lesions. A transthoracic echocardiogram was ordered to evaluate her degree of pulmonary hypertension.
The 3 sputum specimens that were negative for AFB despite cavitary lung disease have high sensitivity for ruling out pulmonary tuberculosis. In addition, given the absence of any bacterial pathogen isolated from these specimens, I would pursue the possibility of other potential fungal pathogens given the patient's subacute course, history of using inhaled and oral corticosteroids, sputum results, and the presence of a cavitary lesion on her CT scan images.
Cytologic examination of the bronchoalveolar lavage (BAL) sample showed a cell differential of 1% bands, 58% neutrophils, 9% lymphs, and 27% eosinophils. The routine postbronchoscopy chest radiograph showed complete opacification of the left lung. The patient's WBC count rose to 26,000/L but she remained afebrile. Echocardiogram was reported to be of very poor quality due to her obesity. The cardiologist reviewing the echocardiogram called the attending physicians and stated there was possibly something in the left pulmonary artery and aortic dissection could not be ruled out.
The presence of eosinophilia on BAL may be a very important clue as to what lung pathology she has. In fact, eosinophilia in this setting may indicate the possibility of parasitic or fungal infection of the lung, or inflammation of the airway associated to drug toxicity, asthma, or environmental toxin exposure. With this additional information, I am concerned that she may be harboring an atypical infection such as an invasive fungus. The echocardiogram results are unclear to me but will need to be clarified with additional testing.
The interpretation of the transbronchial biopsy specimen was limited but suggested invasive pseudomembranous tracheal bronchitis due to aspergillosis. The routine hematoxylin and eosin stain showed portions of alveolar lung tissue and some collapsed submucosal bronchial glands with relatively normal‐looking lung tissue but along the edge of the spaces were obvious fungal organisms. The Gomori's methenamine silver (GMS) stain suggested the presence of Aspergillus organisms (Figure 3). Fungal cultures were also negative for any of the other dimorphic fungi or for molds.
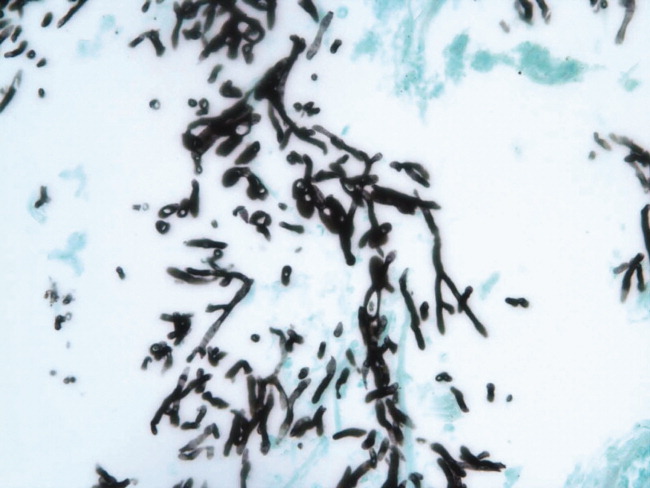
Despite the negative culture results, the overall clinical picture suggests a necrotizing pneumonia caused by an invasive Aspergillus affecting both the bronchial tree and the lower respiratory tract. Generally, necrotizing pneumonias usually have a slow response to antimicrobial therapy. Given the inherent difficulty in differentiating clearly between invasive and noninvasive disease based on a transbronchial biopsy specimen, initiating antifungal therapy for invasive aspergillosis is appropriate in this patient. This patient's recent use of oral glucocorticoids and chronic use of inhaled glucocorticoids are both potential risk factors that predisposed this patient to develop invasive aspergillosis.
Many times we simply follow treatment guidelines for different categories of pneumonia, and have limited or inadequate clinical information to make more definitive diagnoses. While we need these treatment protocols, physicians must avoid falling into the trap that antibiotics treat all infectious etiologies in the lung and we should make reasonable efforts to pin down the etiology. All of us have been fooled by atypical presentations of tuberculosis, fungus, and noninfectious diseases of the lung. I think it behooves us to be vigilant about alternative diagnoses and consider pursuing additional studies whenever the clinical response to initial treatment does not meet our expectations.
Subsequently, the patient's additional cultures remained negative. The official echocardiogram report was read as questionable PE in the pulmonary artery. A spiral CT angiogram revealed a pulmonary artery embolus in the left upper lobe and she was treated with anticoagulation. Her shortness of breath improved steadily and she was successfully discharged after receiving 9 days of oral voriconazole. Outpatient pulmonary function testing documented the presence of chronic obstructive lung disease. She completed a 5‐month course of voriconazole therapy with significant clinical and radiologic improvement of her pulmonary infiltrate. She also completed a 12‐month treatment with warfarin for the concomitant pulmonary embolism. On follow‐up at 12 months she was doing well.
COMMENTARY
Aspergillosis caused particularly by Aspergillus fumigatus is considered an emerging infectious disease that frequently produces significant morbidity and mortality among immunocompromised patients.1, 2 The most frequently‐affected organs by this fungal pathogen include the lung and the central nervous system. There are 3 pathogenic mechanisms of Aspergillus infection of the lung: colonization, hypersensitivity reaction, and invasive aspergillosis.1
Invasive pulmonary aspergillosis is predominantly seen among individuals with severe degrees of immunosuppression as a result of solid‐organ transplantation, immunosuppressive therapies for autoimmune diseases, systemic glucocorticoids, and chemotherapy for hematologic malignancies. Mortality due to invasive aspergillosis continues to be very high (>58%) despite our improved ability to diagnose this condition and newer therapies to treat immunocompromised individuals.1 Invasive aspergillosis can manifest clinically in multiple ways. These include: (1) an invasive vascular process in which fungal organisms invade blood vessels, causing a rapidly progressive and often fatal illness; (2) necrotizing pseudomembranous tracheal bronchitis; (3) chronic necrotizing aspergillosis; (4) bronchopleural fistula; or (5) empyema.35 In our case, while the pathologic findings were most suggestive of an invasive pseudomembranous tracheal bronchitis, the overall clinical picture was most compatible with a necrotizing pneumonia due to invasive aspergillosis.
In addition to the traditional identified risk factors for invasive pulmonary aspergillosis, a number of reports during the last decade have demonstrated the occurrence of invasive aspergillosis in patients with COPD.14 A systematic review of the literature demonstrated that among 1,941 patients with invasive aspergillosis, 26 (1.3%) had evidence of COPD as the main risk factor for developing invasive aspergillosis.1 A single report has associated the potential use of inhaled steroids with the occurrence of invasive aspergillosis in this patient population.2 However, other factors that may promote increased susceptibility to invasive fungal infection among patients with COPD include the use of long‐term or repeated short‐term glucocorticoid treatments, and the presence of multiple additional comorbidities, which may be found in this same population such as diabetes, malnutrition, or end‐stage renal disease.3, 4 Most reported series have demonstrated a high mortality rate of invasive pulmonary aspergillosis in patients with COPD.14
The diagnosis of invasive pulmonary aspergillosis represents a significant clinical challenge. Diagnostic algorithms incorporating CT, antigen detection testing (for serum galactomannan and ‐glucan) as well as polymerase chain reaction diagnostic testing appear to be beneficial in the early diagnosis of invasive aspergillosis in particular settings such as in allogeneic hematopoietic stem cell transplantation.5 The role of antigen testing to identify early invasive aspergillosis in patients with COPD remains uncertain since it has been evaluated in a limited number of patients and therefore clinical suspicion is critical to push clinicians to pursue invasive tissue biopsy and cultures to confirm the diagnosis.3, 4
Based on the available clinical case series and in our case, invasive pulmonary aspergillosis should be suspected in COPD patients with rapidly progressive pneumonia not responding to antibacterial therapy and who have received oral or inhaled glucocorticoids in the recent past. In addition, this case also illustrates that occasionally, patients present with more than 1 life‐threatening diagnosis. This patient was also diagnosed with PE despite adequate prophylaxis. In addition to the well‐known clinical risk factors of obesity and lung disease, the underlying infection may have contributed to a systemic or local hypercoagulable condition that further increased her risk for venous thromboembolism.
KEY TEACHING POINTS
-
Clinicians should remember to consider a broad differential in patients presenting with pneumonia, including the possibility of fungal pathogens in patients with known risk factors and in patients with multiple, potentially immunosuppressive comorbidities, or in patients who do not improve on standard antibiotic therapy.
-
There is some evidence of an association between COPD and invasive aspergillosis, likely due to the frequent use of oral corticosteroids and/or chronic inhaled steroids in this population.
- ,,.Aspergillosis case‐fatality rate: systematic review of the literature.Clin Infect Dis.2001;32:358–366.
- ,,,,.Invasive pulmonary filamentous fungal infection in a patient receiving inhaled corticosteroid therapy.Clin Infect Dis.2002;35:e54–e56.
- ,,, et al.Invasive pulmonary aspergillosis in chronic obstructive pulmonary disease: an emerging fungal pathogen.Clin Microbiol Infect.2005;11:427–429.
- ,,,,,.Invasive pulmonary aspergillosis in patients with chronic obstructive pulmonary disease: report of eight cases and review.Clin Infect Dis.1998;26:1473–1475.
- ,.Current approaches to diagnosis and treatment to invasive aspergillosis.Am J Respir Crit Care Med.2006;173:707–717.
- ,,.Aspergillosis case‐fatality rate: systematic review of the literature.Clin Infect Dis.2001;32:358–366.
- ,,,,.Invasive pulmonary filamentous fungal infection in a patient receiving inhaled corticosteroid therapy.Clin Infect Dis.2002;35:e54–e56.
- ,,, et al.Invasive pulmonary aspergillosis in chronic obstructive pulmonary disease: an emerging fungal pathogen.Clin Microbiol Infect.2005;11:427–429.
- ,,,,,.Invasive pulmonary aspergillosis in patients with chronic obstructive pulmonary disease: report of eight cases and review.Clin Infect Dis.1998;26:1473–1475.
- ,.Current approaches to diagnosis and treatment to invasive aspergillosis.Am J Respir Crit Care Med.2006;173:707–717.
The latest research you need to know
In This Edition
- Aspirin plus extended-release dipyridamole and clopidogrel provide similar outcomes in stroke.
- Traditional readings of bedside chest radiographs are insensitive in detecting intraatrial central venous catheter placement.
- Improved outcomes with bortezomib in myeloma treatment.
- ICD firings in cardiomyopathy patients are associated with worse outcomes.
- The clinical dehydration scale rapidly assesses the severity of dehydration in children.
- Liberal red blood cell transfusions may be harming patients.
- Five-year risk of colorectal neoplasia is low in patients with negative screening colonoscopy.
- Vital sign instability and oxygenation predict prognosis following hospitalization for community acquired pneumonia.
Is aspirin plus extended release dipyridamole more efficacious and safer than clopidogrel in preventing recurrent stroke?
Background: Recurrent stroke is a frequent (7% to 8% thrombotic stroke recurrence in first year) and disabling event after ischemic stroke. Multiple randomized trials demonstrate efficacy of anti-platelet agents for the prevention of recurrent stroke after non-cardioembolic stroke. However, direct comparisons and relative benefits of various antiplatelet agents are not well defined.
Study design: Randomized, double-blinded, two-by-two factorial design with intention-to-treat analysis.
Setting: A total of 20,333 patients from 695 centers in 35 countries, including the U.S.
Synopsis: This study directly compared aspirin plus extended-release dipyridamole to clopidogrel within the PRoFESS trial. A total of 20,333 patients were enrolled and followed up for a mean duration of 2.5 years. Eligible patients randomly were assigned to receive either 25 mg aspirin plus 200 mg extended-release twice a day, or clopidogrel 75 mg a day; and either telmisartan 80 mg once a day or placebo. Groups were similar at baseline.
The primary outcome of recurrent stroke was similar in both the aspirin plus extended-release dipyrimadole group and the clopidogrel group (9.0% vs. 8.8%). The composite secondary outcome of stroke, myocardial infarction or vascular death, and tertiary outcomes were similar in both groups. The trial showed statistical equivalence in the rates of recurrent stroke in the two groups.
Despite more frequent hemorrhagic strokes in the group receiving aspirin plus extended-release dipyridamole (4.1% vs. 3.6%), there was no significant difference in the risk of fatal or disabling stroke between both the groups.
Bottom line: Aspirin plus extended-release dipyridamole is equivalent to clopidogrel in the prevention of recurrent stroke, in terms of relevant efficacy and safety parameters.
Citation: Sacco RL, Diener H, Yusuf S, et.al. Aspirin and extended-release dipyridamole versus clopidogrel for recurrent stroke. N Engl J Med. 2008:359:1238-1251.
Is there a better method to judge the placement of central venous catheters?
Background: Placement of central venous catheters is common, particularly in critical care settings. Correct placement is usually confirmed by bedside chest radiography. The recommended location of the distal catheter tip is superior to the superior vena cava and right atria junction. However, determining this landmark on traditional bedside chest radiographs is frequently inaccurate.
Study design: Prospective, blinded study.
Setting: University hospital in Germany.
Synopsis: The researchers enrolled 212 patients scheduled for elective cardiac surgery. Either left or right internal jugular vein central lines were placed via EKG guidance, and more precisely evaluated by transesophageal echocardiography. Bedside chest radiographs were performed within three hours of admission to the ICU.
The radiologists were able to detect between 40% and 60% of incorrect central venous catheter placements when compared to transesophageal echocardiography. The researchers concluded TC-distance (tip of catheter to carina) of greater than 55 mm on chest X-ray performed better (98% accurate) in the detection of intra-atrial catheter placement, compared to conventional judgment by attending (93% accurate) or resident (53% accurate) radiologists. Limitations of the study include the use of only one attending radiologist. Secondly, the chest radiographs and echocardiograms were not done simultaneously, allowing for possible movement of the catheters between studies.
Bottom line: A TC distance of greater than 55 mm on chest X-ray should be further investigated as an accurate method to detect intra-atrial central venous catheters.
Citation: Wirsing M, Schummer C, Neumann R, et al. Is traditional reading of the bedside chest radiograph appropriate to detect intra-atrial central venous catheter position? Chest. 2008;134:527-533.
Does adding bortezomib to melphalan and prednisone improve outcomes in newly diagnosed myeloma?
Background: More than 50% of newly diagnosed myeloma patients are older than 65 and cannot receive optimal treatment with high-dose chemotherapy and stem-cell transplant. Previous trials have demonstrated patients with relapsed or refractory myeloma benefit from the administration of bortezomib, which sensitizes the myeloma cell lines to melphalan.
Study design: Randomized, open-label (unblinded) phase 3 study.
Setting: 151 centers, 22 countries in Asia, Europe, South and North America.
Synopsis: 682 patients with untreated multiple myeloma, who were ineligible for high-dose chemotherapy and stem cell transplant, were treated with bortezomib in combination with standard melphalan and prednisone, or melphalan and prednisone alone. The bortezomib group had improved partial or complete response (71% vs. 35%; NNT=3; p<0.001), increased median time to progression of disease (19.9 months vs. 13.1 months), and improved overall survival (87% vs. 78% over a 16-month median follow up; NNT=11; p=0.008). There were increased grade 3 adverse effects with the intervention, but no increase in grade 4 events or treatment related deaths compared to control. Limitations of the study include lack of blinding and involvement of the pharmaceutical company in data collection analysis, writing and editing of the manuscript.
Bottom line: Bortezomib is a valuable adjunct to standard treatment of multiple myeloma in patients over the age of 65 who may be ineligible for high-dose chemotherapy and stem cell transplant.
Citation: San Miguel JF, Schlag R, Khuageva NK, et al. Bortezomib plus melphalan and prednisone for the initial treatment of multiple myeloma. NEJM. 2008;359:906-917.
Does the occurrence of a shock increase the risk of death in cardiomyopathy patients with defibrillators?
Background: The SCD-HeFT trial, originally published in 2005, was instrumental in demonstrating the utility of defibrillators in the primary prevention of sudden cardiac deaths in patients with either ischemic or non-ischemic cardiomyopathy, NYHA class II or III, ejection fraction <35%, and no history of sustained ventricular tachycardia or fibrillation. This study re-examined the data derived from the SCD-HeFT trial to better understand the long-term prognosis of these patients with defibrillators who receive either appropriate shocks (ventricular fibrillation, sustained ventricular tachycardia), inappropriate shocks, or no shocks. Inappropriate shocks were defined as defibrillations due to supraventricular tachycardia, oversensing P or T waves as R waves, double counting of R waves, and artifact.
Study design: Retrospective cohort (analysis of patients randomized to implantable cardioverter-defibrillator (ICD) group in SCD-HeFT).
Setting: Multicenter trial.
Synopsis: The analysis demonstrated patients who received shocks were 11 times more likely to die compared with those who had no defibrillations (Hazard Ratio [HR]=11.3, p<0.001). These shocked patients were at more risk (HR=5.7, p<0.001) than those with inappropriate shocks (HR=2.0, p=0.002). Therefore, even inappropriate shocks themselves doubled the risk of death. Patients who received more than one shock, either appropriate or not, were at even higher odds of death (HR=8.3, p<0.001). The results highlight the higher mortality risk when patients with ICDs have received a shock (appropriate or inappropriate) and the need for further therapies to modify outcome in these patients.
Bottom Line: Appropriate or inappropriate defibrillations are associated with a poorer prognosis in patients with cardiomyopathy.
Citation: Poole JE, Johnson GW, Hellkamp AS, et al. Prognostic importance of defibrillator shocks in patients with heart failure. N Engl J Med. 2008(359):1009-1017.
Can a simple physical exam tool assess the degree of dehydration in children?
Background: Despite the frequency and the associated cost of acute gastroenteritis (AGE) in the pediatric population, there is no unified scale to assess the severity of dehydration. The authors of this paper previously reported a clinical dehydration scale (CDS) and applied it prospectively in a new cohort of patients ages 1 month to 5 years.
Study design: Prospective, observational study.
Setting: Single, tertiary care emergency department (ED) in Canada.
Synopsis: The CDS score is based purely on the physical findings of the child, including a) general appearance, b) eyes, c) mucous membranes, and d) amount of tears. On a point system, the patient is placed in one of three categories: no dehydration, some dehydration, moderate/severe dehydration. The trial enrolled 205 children and the CDS was applied by the triaging nurse. The attending ED pediatricians were blinded from this assessment. The CDS was able to predict the length of stay (mean + SD: no dehyrdation 245 + 181 mins; some dehydration, 397 + 302 mins; mod/severe dehydration, 501 + 389 mins), need for intravenous rehydration (none, 15%; some, 49%; mod/severe, 80%), and frequency of emesis/diarrhea as reported by the parents (none, 8.4 + 7.7; some, 13 + 10.7; mod/severe, 30.2 + 14.8). Only five children were categorized in the moderate/severe dehydration category, which may limit the ability to generalize the scoring system to that group of patients.
Bottom line: The CDS is an easy to use and promising tool to assess the severity of illness, expected ED length of stay, and need for intravenous rehydration in children with acute gastroenteritis.
Citation: Goldman RD, Friedman JN, Parkin PC. Validation of the clinical dehydration scale for children with acute gastroenteritis. Pediatrics. 2008;122(3):545-549.
Does maintaining a higher hemoglobin level benefit critical care patients?
Background: Historically, medical and surgical critical care patients liberally were transfused with little prospective evidence to support this approach. However, recent evidence has led to the use of a more-restricted transfusion threshold.
Study design: Systematic review and meta-analysis of cohort studies evaluating the effect of red blood cell (RBC) transfusion on patient outcomes.
Setting: Data sources include MEDLINE, Embase, and Cochrane databases.
Synopsis: The 45 cohort studies, including more than 272,000 patients, were selected due to focus on outcome measures, such as mortality, multiorgan dysfunction, acute respiratory distress syndrome, and infections. Primary studies were then placed into one of three categories: benefits outweigh the risk, neutral, or risks outweigh the benefit. Forty-two of these studies found the risks outweigh the benefits; two were neutral; and only one sub-study (in elderly patients with acute myocardial infarctions) suggested benefit outweighs the risk.
Although a systematic review of cohort studies has inherent limitations, the overwhelming direction of the results suggests statistically significant harm due to liberal transfusion practices (Summary Odd Ratios [OR] for a) death, OR = 1.69; b) infection, OR = 1.88; and c) Acute Respiratory Distress Syndrome, OR = 2.5). Due to the observational nature of the cohort studies, one might suspect RBC transfusions could simply reflect patient severity of illness. Thus, the harm suggested by the more liberal transfusion standards could just reflect the fact these patients carried a worse prognosis due to their respective illnesses.
Bottom Line: The preponderance of evidence suggests liberal transfusion practice is associated with increased morbidity and mortality of ICU patients. When considering RBC transfusions, the risks and benefits to each individual patient should be considered carefully.
Citation: Marik PE, Corwin HL. Efficacy of red blood cell transfusion in the critically ill: a systematic review of the literature. Crit Care Med. 2008; 36(9);2667-2674.
What is the appropriate frequency of rescreening for patients with initial screening colonoscopies negative for adenomas?
Background: Colonoscopy is the preferred primary screening method for the detection of colorectal cancer and precancerous polyps. Data suggest colonoscopy may be performed too frequently and for inappropriate indications.
Study design: Retrospective cohort study.
Setting: Seven sites in central Indiana.
Synopsis: In this study of 2,436 persons with no adenomas on baseline screening colonoscopies, 1,256 of them (51.6%) were rescreened a mean of 5.34 + 1.34 years later. No cancers were found on rescreening. One or more adenomas were found in 201 persons (16.0%). Nineteen advanced adenomas were found in 16 persons (1.3%). Patients in this study were relatively young (mean age at baseline was 56.7 years). Men were more likely than women to have adenomas (RR 1.88; 95% CI 1.42-2.51) and to have advanced adenomas (RR 3.31; 95% CI 1.02-10.8).
Limitations included a small cohort sample size, as well as incomplete information on persons who did not follow up with the five-year examination. Also, there is uncertainty about the clinical significance of advanced adenomas.
Bottom Line: Among persons previously screened with colonoscopy who have no colorectal adenomas, the five-year risk of detecting an advanced adenoma is extremely low (1.3%), supporting a rescreening interval of more than five years after a normal colonoscopy. Men have greater risk, and may deserve a shorter interval screening.
Citation: Imperiale TF, Glowinski EA, Lin-Cooper C, et al. Five-year risk of colorectal neoplasia after negative screening colonoscopy. N Engl J Med. 2008;359:1218-1224.
Can validated discharge instability criteria predict mortality or readmission within 30 days of hospital discharge for community acquired pneumonia (CAP)?
Background: Prior prospective cohort data have delineated instability criteria utilizing vital sign criteria at hospital discharge for CAP. However, guidelines for determining patient readiness for discharge remain largely unstudied.
Study design: Prospective, observational cohort study.
Setting: A single, non-urban teaching hospital in Spain.
Synopsis: In this study, 870 adults with CAP were evaluated following discharge. Abnormal oxygenation and vital signs were utilized to calculate an instability score. Criteria for instability were defined as temperature >37.5° C, heart rate <100, respiratory rate >24, systolic blood pressure (SBP) <90 (or diastolic blood pressure, DBP <60), and oxygen saturation <90% (or PaO2 <60).
Of all the instability criteria, only low oxygenation predicted readmission at 30 days (Hazard Ratio [HR] 1.4, p=0.03). However, mortality was significantly increased when instability criteria of temperature (HR 4.5, p=0.04), blood pressure (HR 2.6, p=0.02), respiratory rate (HR 2.4, p=0.03), or oxygenation (HR 2.4, p=0.03) were met. Elevated heart rate was not found to predict death.
The authors assigned each of the significant instability criteria a score of one or two (based on the weight of its hazard ratio), with respiratory rate, low blood pressure, and low oxygenation each assigned one point, and temperature assigned two points. Patients with an instability score of two or more had a six-fold increased risk of death (HR 5.8; 95%, p=0.0001). The negative predictive value (NPV) of an instability score less than two was very helpful (NPV=98%) in identifying patients with low mortality risk; however, the positive predictive value (PPV) of an instability score >2 is not necessarily helpful (PPV=13%) clinically.
Bottom line: Patients with a temperature >37.5° C or any combination of RR >24, SBP <90 (or DBP <60), and SpO2 <90% (or Pa02 <60) are at increased risk of death. Identifying a low instability score is most helpful in clinical practice.
Citation: Capelastegui A, Espana P, Bilbao A, et al. Pneumonia: criteria for patient instability on hospital discharge. Chest. 2008;34:595-600.
In This Edition
- Aspirin plus extended-release dipyridamole and clopidogrel provide similar outcomes in stroke.
- Traditional readings of bedside chest radiographs are insensitive in detecting intraatrial central venous catheter placement.
- Improved outcomes with bortezomib in myeloma treatment.
- ICD firings in cardiomyopathy patients are associated with worse outcomes.
- The clinical dehydration scale rapidly assesses the severity of dehydration in children.
- Liberal red blood cell transfusions may be harming patients.
- Five-year risk of colorectal neoplasia is low in patients with negative screening colonoscopy.
- Vital sign instability and oxygenation predict prognosis following hospitalization for community acquired pneumonia.
Is aspirin plus extended release dipyridamole more efficacious and safer than clopidogrel in preventing recurrent stroke?
Background: Recurrent stroke is a frequent (7% to 8% thrombotic stroke recurrence in first year) and disabling event after ischemic stroke. Multiple randomized trials demonstrate efficacy of anti-platelet agents for the prevention of recurrent stroke after non-cardioembolic stroke. However, direct comparisons and relative benefits of various antiplatelet agents are not well defined.
Study design: Randomized, double-blinded, two-by-two factorial design with intention-to-treat analysis.
Setting: A total of 20,333 patients from 695 centers in 35 countries, including the U.S.
Synopsis: This study directly compared aspirin plus extended-release dipyridamole to clopidogrel within the PRoFESS trial. A total of 20,333 patients were enrolled and followed up for a mean duration of 2.5 years. Eligible patients randomly were assigned to receive either 25 mg aspirin plus 200 mg extended-release twice a day, or clopidogrel 75 mg a day; and either telmisartan 80 mg once a day or placebo. Groups were similar at baseline.
The primary outcome of recurrent stroke was similar in both the aspirin plus extended-release dipyrimadole group and the clopidogrel group (9.0% vs. 8.8%). The composite secondary outcome of stroke, myocardial infarction or vascular death, and tertiary outcomes were similar in both groups. The trial showed statistical equivalence in the rates of recurrent stroke in the two groups.
Despite more frequent hemorrhagic strokes in the group receiving aspirin plus extended-release dipyridamole (4.1% vs. 3.6%), there was no significant difference in the risk of fatal or disabling stroke between both the groups.
Bottom line: Aspirin plus extended-release dipyridamole is equivalent to clopidogrel in the prevention of recurrent stroke, in terms of relevant efficacy and safety parameters.
Citation: Sacco RL, Diener H, Yusuf S, et.al. Aspirin and extended-release dipyridamole versus clopidogrel for recurrent stroke. N Engl J Med. 2008:359:1238-1251.
Is there a better method to judge the placement of central venous catheters?
Background: Placement of central venous catheters is common, particularly in critical care settings. Correct placement is usually confirmed by bedside chest radiography. The recommended location of the distal catheter tip is superior to the superior vena cava and right atria junction. However, determining this landmark on traditional bedside chest radiographs is frequently inaccurate.
Study design: Prospective, blinded study.
Setting: University hospital in Germany.
Synopsis: The researchers enrolled 212 patients scheduled for elective cardiac surgery. Either left or right internal jugular vein central lines were placed via EKG guidance, and more precisely evaluated by transesophageal echocardiography. Bedside chest radiographs were performed within three hours of admission to the ICU.
The radiologists were able to detect between 40% and 60% of incorrect central venous catheter placements when compared to transesophageal echocardiography. The researchers concluded TC-distance (tip of catheter to carina) of greater than 55 mm on chest X-ray performed better (98% accurate) in the detection of intra-atrial catheter placement, compared to conventional judgment by attending (93% accurate) or resident (53% accurate) radiologists. Limitations of the study include the use of only one attending radiologist. Secondly, the chest radiographs and echocardiograms were not done simultaneously, allowing for possible movement of the catheters between studies.
Bottom line: A TC distance of greater than 55 mm on chest X-ray should be further investigated as an accurate method to detect intra-atrial central venous catheters.
Citation: Wirsing M, Schummer C, Neumann R, et al. Is traditional reading of the bedside chest radiograph appropriate to detect intra-atrial central venous catheter position? Chest. 2008;134:527-533.
Does adding bortezomib to melphalan and prednisone improve outcomes in newly diagnosed myeloma?
Background: More than 50% of newly diagnosed myeloma patients are older than 65 and cannot receive optimal treatment with high-dose chemotherapy and stem-cell transplant. Previous trials have demonstrated patients with relapsed or refractory myeloma benefit from the administration of bortezomib, which sensitizes the myeloma cell lines to melphalan.
Study design: Randomized, open-label (unblinded) phase 3 study.
Setting: 151 centers, 22 countries in Asia, Europe, South and North America.
Synopsis: 682 patients with untreated multiple myeloma, who were ineligible for high-dose chemotherapy and stem cell transplant, were treated with bortezomib in combination with standard melphalan and prednisone, or melphalan and prednisone alone. The bortezomib group had improved partial or complete response (71% vs. 35%; NNT=3; p<0.001), increased median time to progression of disease (19.9 months vs. 13.1 months), and improved overall survival (87% vs. 78% over a 16-month median follow up; NNT=11; p=0.008). There were increased grade 3 adverse effects with the intervention, but no increase in grade 4 events or treatment related deaths compared to control. Limitations of the study include lack of blinding and involvement of the pharmaceutical company in data collection analysis, writing and editing of the manuscript.
Bottom line: Bortezomib is a valuable adjunct to standard treatment of multiple myeloma in patients over the age of 65 who may be ineligible for high-dose chemotherapy and stem cell transplant.
Citation: San Miguel JF, Schlag R, Khuageva NK, et al. Bortezomib plus melphalan and prednisone for the initial treatment of multiple myeloma. NEJM. 2008;359:906-917.
Does the occurrence of a shock increase the risk of death in cardiomyopathy patients with defibrillators?
Background: The SCD-HeFT trial, originally published in 2005, was instrumental in demonstrating the utility of defibrillators in the primary prevention of sudden cardiac deaths in patients with either ischemic or non-ischemic cardiomyopathy, NYHA class II or III, ejection fraction <35%, and no history of sustained ventricular tachycardia or fibrillation. This study re-examined the data derived from the SCD-HeFT trial to better understand the long-term prognosis of these patients with defibrillators who receive either appropriate shocks (ventricular fibrillation, sustained ventricular tachycardia), inappropriate shocks, or no shocks. Inappropriate shocks were defined as defibrillations due to supraventricular tachycardia, oversensing P or T waves as R waves, double counting of R waves, and artifact.
Study design: Retrospective cohort (analysis of patients randomized to implantable cardioverter-defibrillator (ICD) group in SCD-HeFT).
Setting: Multicenter trial.
Synopsis: The analysis demonstrated patients who received shocks were 11 times more likely to die compared with those who had no defibrillations (Hazard Ratio [HR]=11.3, p<0.001). These shocked patients were at more risk (HR=5.7, p<0.001) than those with inappropriate shocks (HR=2.0, p=0.002). Therefore, even inappropriate shocks themselves doubled the risk of death. Patients who received more than one shock, either appropriate or not, were at even higher odds of death (HR=8.3, p<0.001). The results highlight the higher mortality risk when patients with ICDs have received a shock (appropriate or inappropriate) and the need for further therapies to modify outcome in these patients.
Bottom Line: Appropriate or inappropriate defibrillations are associated with a poorer prognosis in patients with cardiomyopathy.
Citation: Poole JE, Johnson GW, Hellkamp AS, et al. Prognostic importance of defibrillator shocks in patients with heart failure. N Engl J Med. 2008(359):1009-1017.
Can a simple physical exam tool assess the degree of dehydration in children?
Background: Despite the frequency and the associated cost of acute gastroenteritis (AGE) in the pediatric population, there is no unified scale to assess the severity of dehydration. The authors of this paper previously reported a clinical dehydration scale (CDS) and applied it prospectively in a new cohort of patients ages 1 month to 5 years.
Study design: Prospective, observational study.
Setting: Single, tertiary care emergency department (ED) in Canada.
Synopsis: The CDS score is based purely on the physical findings of the child, including a) general appearance, b) eyes, c) mucous membranes, and d) amount of tears. On a point system, the patient is placed in one of three categories: no dehydration, some dehydration, moderate/severe dehydration. The trial enrolled 205 children and the CDS was applied by the triaging nurse. The attending ED pediatricians were blinded from this assessment. The CDS was able to predict the length of stay (mean + SD: no dehyrdation 245 + 181 mins; some dehydration, 397 + 302 mins; mod/severe dehydration, 501 + 389 mins), need for intravenous rehydration (none, 15%; some, 49%; mod/severe, 80%), and frequency of emesis/diarrhea as reported by the parents (none, 8.4 + 7.7; some, 13 + 10.7; mod/severe, 30.2 + 14.8). Only five children were categorized in the moderate/severe dehydration category, which may limit the ability to generalize the scoring system to that group of patients.
Bottom line: The CDS is an easy to use and promising tool to assess the severity of illness, expected ED length of stay, and need for intravenous rehydration in children with acute gastroenteritis.
Citation: Goldman RD, Friedman JN, Parkin PC. Validation of the clinical dehydration scale for children with acute gastroenteritis. Pediatrics. 2008;122(3):545-549.
Does maintaining a higher hemoglobin level benefit critical care patients?
Background: Historically, medical and surgical critical care patients liberally were transfused with little prospective evidence to support this approach. However, recent evidence has led to the use of a more-restricted transfusion threshold.
Study design: Systematic review and meta-analysis of cohort studies evaluating the effect of red blood cell (RBC) transfusion on patient outcomes.
Setting: Data sources include MEDLINE, Embase, and Cochrane databases.
Synopsis: The 45 cohort studies, including more than 272,000 patients, were selected due to focus on outcome measures, such as mortality, multiorgan dysfunction, acute respiratory distress syndrome, and infections. Primary studies were then placed into one of three categories: benefits outweigh the risk, neutral, or risks outweigh the benefit. Forty-two of these studies found the risks outweigh the benefits; two were neutral; and only one sub-study (in elderly patients with acute myocardial infarctions) suggested benefit outweighs the risk.
Although a systematic review of cohort studies has inherent limitations, the overwhelming direction of the results suggests statistically significant harm due to liberal transfusion practices (Summary Odd Ratios [OR] for a) death, OR = 1.69; b) infection, OR = 1.88; and c) Acute Respiratory Distress Syndrome, OR = 2.5). Due to the observational nature of the cohort studies, one might suspect RBC transfusions could simply reflect patient severity of illness. Thus, the harm suggested by the more liberal transfusion standards could just reflect the fact these patients carried a worse prognosis due to their respective illnesses.
Bottom Line: The preponderance of evidence suggests liberal transfusion practice is associated with increased morbidity and mortality of ICU patients. When considering RBC transfusions, the risks and benefits to each individual patient should be considered carefully.
Citation: Marik PE, Corwin HL. Efficacy of red blood cell transfusion in the critically ill: a systematic review of the literature. Crit Care Med. 2008; 36(9);2667-2674.
What is the appropriate frequency of rescreening for patients with initial screening colonoscopies negative for adenomas?
Background: Colonoscopy is the preferred primary screening method for the detection of colorectal cancer and precancerous polyps. Data suggest colonoscopy may be performed too frequently and for inappropriate indications.
Study design: Retrospective cohort study.
Setting: Seven sites in central Indiana.
Synopsis: In this study of 2,436 persons with no adenomas on baseline screening colonoscopies, 1,256 of them (51.6%) were rescreened a mean of 5.34 + 1.34 years later. No cancers were found on rescreening. One or more adenomas were found in 201 persons (16.0%). Nineteen advanced adenomas were found in 16 persons (1.3%). Patients in this study were relatively young (mean age at baseline was 56.7 years). Men were more likely than women to have adenomas (RR 1.88; 95% CI 1.42-2.51) and to have advanced adenomas (RR 3.31; 95% CI 1.02-10.8).
Limitations included a small cohort sample size, as well as incomplete information on persons who did not follow up with the five-year examination. Also, there is uncertainty about the clinical significance of advanced adenomas.
Bottom Line: Among persons previously screened with colonoscopy who have no colorectal adenomas, the five-year risk of detecting an advanced adenoma is extremely low (1.3%), supporting a rescreening interval of more than five years after a normal colonoscopy. Men have greater risk, and may deserve a shorter interval screening.
Citation: Imperiale TF, Glowinski EA, Lin-Cooper C, et al. Five-year risk of colorectal neoplasia after negative screening colonoscopy. N Engl J Med. 2008;359:1218-1224.
Can validated discharge instability criteria predict mortality or readmission within 30 days of hospital discharge for community acquired pneumonia (CAP)?
Background: Prior prospective cohort data have delineated instability criteria utilizing vital sign criteria at hospital discharge for CAP. However, guidelines for determining patient readiness for discharge remain largely unstudied.
Study design: Prospective, observational cohort study.
Setting: A single, non-urban teaching hospital in Spain.
Synopsis: In this study, 870 adults with CAP were evaluated following discharge. Abnormal oxygenation and vital signs were utilized to calculate an instability score. Criteria for instability were defined as temperature >37.5° C, heart rate <100, respiratory rate >24, systolic blood pressure (SBP) <90 (or diastolic blood pressure, DBP <60), and oxygen saturation <90% (or PaO2 <60).
Of all the instability criteria, only low oxygenation predicted readmission at 30 days (Hazard Ratio [HR] 1.4, p=0.03). However, mortality was significantly increased when instability criteria of temperature (HR 4.5, p=0.04), blood pressure (HR 2.6, p=0.02), respiratory rate (HR 2.4, p=0.03), or oxygenation (HR 2.4, p=0.03) were met. Elevated heart rate was not found to predict death.
The authors assigned each of the significant instability criteria a score of one or two (based on the weight of its hazard ratio), with respiratory rate, low blood pressure, and low oxygenation each assigned one point, and temperature assigned two points. Patients with an instability score of two or more had a six-fold increased risk of death (HR 5.8; 95%, p=0.0001). The negative predictive value (NPV) of an instability score less than two was very helpful (NPV=98%) in identifying patients with low mortality risk; however, the positive predictive value (PPV) of an instability score >2 is not necessarily helpful (PPV=13%) clinically.
Bottom line: Patients with a temperature >37.5° C or any combination of RR >24, SBP <90 (or DBP <60), and SpO2 <90% (or Pa02 <60) are at increased risk of death. Identifying a low instability score is most helpful in clinical practice.
Citation: Capelastegui A, Espana P, Bilbao A, et al. Pneumonia: criteria for patient instability on hospital discharge. Chest. 2008;34:595-600.
In This Edition
- Aspirin plus extended-release dipyridamole and clopidogrel provide similar outcomes in stroke.
- Traditional readings of bedside chest radiographs are insensitive in detecting intraatrial central venous catheter placement.
- Improved outcomes with bortezomib in myeloma treatment.
- ICD firings in cardiomyopathy patients are associated with worse outcomes.
- The clinical dehydration scale rapidly assesses the severity of dehydration in children.
- Liberal red blood cell transfusions may be harming patients.
- Five-year risk of colorectal neoplasia is low in patients with negative screening colonoscopy.
- Vital sign instability and oxygenation predict prognosis following hospitalization for community acquired pneumonia.
Is aspirin plus extended release dipyridamole more efficacious and safer than clopidogrel in preventing recurrent stroke?
Background: Recurrent stroke is a frequent (7% to 8% thrombotic stroke recurrence in first year) and disabling event after ischemic stroke. Multiple randomized trials demonstrate efficacy of anti-platelet agents for the prevention of recurrent stroke after non-cardioembolic stroke. However, direct comparisons and relative benefits of various antiplatelet agents are not well defined.
Study design: Randomized, double-blinded, two-by-two factorial design with intention-to-treat analysis.
Setting: A total of 20,333 patients from 695 centers in 35 countries, including the U.S.
Synopsis: This study directly compared aspirin plus extended-release dipyridamole to clopidogrel within the PRoFESS trial. A total of 20,333 patients were enrolled and followed up for a mean duration of 2.5 years. Eligible patients randomly were assigned to receive either 25 mg aspirin plus 200 mg extended-release twice a day, or clopidogrel 75 mg a day; and either telmisartan 80 mg once a day or placebo. Groups were similar at baseline.
The primary outcome of recurrent stroke was similar in both the aspirin plus extended-release dipyrimadole group and the clopidogrel group (9.0% vs. 8.8%). The composite secondary outcome of stroke, myocardial infarction or vascular death, and tertiary outcomes were similar in both groups. The trial showed statistical equivalence in the rates of recurrent stroke in the two groups.
Despite more frequent hemorrhagic strokes in the group receiving aspirin plus extended-release dipyridamole (4.1% vs. 3.6%), there was no significant difference in the risk of fatal or disabling stroke between both the groups.
Bottom line: Aspirin plus extended-release dipyridamole is equivalent to clopidogrel in the prevention of recurrent stroke, in terms of relevant efficacy and safety parameters.
Citation: Sacco RL, Diener H, Yusuf S, et.al. Aspirin and extended-release dipyridamole versus clopidogrel for recurrent stroke. N Engl J Med. 2008:359:1238-1251.
Is there a better method to judge the placement of central venous catheters?
Background: Placement of central venous catheters is common, particularly in critical care settings. Correct placement is usually confirmed by bedside chest radiography. The recommended location of the distal catheter tip is superior to the superior vena cava and right atria junction. However, determining this landmark on traditional bedside chest radiographs is frequently inaccurate.
Study design: Prospective, blinded study.
Setting: University hospital in Germany.
Synopsis: The researchers enrolled 212 patients scheduled for elective cardiac surgery. Either left or right internal jugular vein central lines were placed via EKG guidance, and more precisely evaluated by transesophageal echocardiography. Bedside chest radiographs were performed within three hours of admission to the ICU.
The radiologists were able to detect between 40% and 60% of incorrect central venous catheter placements when compared to transesophageal echocardiography. The researchers concluded TC-distance (tip of catheter to carina) of greater than 55 mm on chest X-ray performed better (98% accurate) in the detection of intra-atrial catheter placement, compared to conventional judgment by attending (93% accurate) or resident (53% accurate) radiologists. Limitations of the study include the use of only one attending radiologist. Secondly, the chest radiographs and echocardiograms were not done simultaneously, allowing for possible movement of the catheters between studies.
Bottom line: A TC distance of greater than 55 mm on chest X-ray should be further investigated as an accurate method to detect intra-atrial central venous catheters.
Citation: Wirsing M, Schummer C, Neumann R, et al. Is traditional reading of the bedside chest radiograph appropriate to detect intra-atrial central venous catheter position? Chest. 2008;134:527-533.
Does adding bortezomib to melphalan and prednisone improve outcomes in newly diagnosed myeloma?
Background: More than 50% of newly diagnosed myeloma patients are older than 65 and cannot receive optimal treatment with high-dose chemotherapy and stem-cell transplant. Previous trials have demonstrated patients with relapsed or refractory myeloma benefit from the administration of bortezomib, which sensitizes the myeloma cell lines to melphalan.
Study design: Randomized, open-label (unblinded) phase 3 study.
Setting: 151 centers, 22 countries in Asia, Europe, South and North America.
Synopsis: 682 patients with untreated multiple myeloma, who were ineligible for high-dose chemotherapy and stem cell transplant, were treated with bortezomib in combination with standard melphalan and prednisone, or melphalan and prednisone alone. The bortezomib group had improved partial or complete response (71% vs. 35%; NNT=3; p<0.001), increased median time to progression of disease (19.9 months vs. 13.1 months), and improved overall survival (87% vs. 78% over a 16-month median follow up; NNT=11; p=0.008). There were increased grade 3 adverse effects with the intervention, but no increase in grade 4 events or treatment related deaths compared to control. Limitations of the study include lack of blinding and involvement of the pharmaceutical company in data collection analysis, writing and editing of the manuscript.
Bottom line: Bortezomib is a valuable adjunct to standard treatment of multiple myeloma in patients over the age of 65 who may be ineligible for high-dose chemotherapy and stem cell transplant.
Citation: San Miguel JF, Schlag R, Khuageva NK, et al. Bortezomib plus melphalan and prednisone for the initial treatment of multiple myeloma. NEJM. 2008;359:906-917.
Does the occurrence of a shock increase the risk of death in cardiomyopathy patients with defibrillators?
Background: The SCD-HeFT trial, originally published in 2005, was instrumental in demonstrating the utility of defibrillators in the primary prevention of sudden cardiac deaths in patients with either ischemic or non-ischemic cardiomyopathy, NYHA class II or III, ejection fraction <35%, and no history of sustained ventricular tachycardia or fibrillation. This study re-examined the data derived from the SCD-HeFT trial to better understand the long-term prognosis of these patients with defibrillators who receive either appropriate shocks (ventricular fibrillation, sustained ventricular tachycardia), inappropriate shocks, or no shocks. Inappropriate shocks were defined as defibrillations due to supraventricular tachycardia, oversensing P or T waves as R waves, double counting of R waves, and artifact.
Study design: Retrospective cohort (analysis of patients randomized to implantable cardioverter-defibrillator (ICD) group in SCD-HeFT).
Setting: Multicenter trial.
Synopsis: The analysis demonstrated patients who received shocks were 11 times more likely to die compared with those who had no defibrillations (Hazard Ratio [HR]=11.3, p<0.001). These shocked patients were at more risk (HR=5.7, p<0.001) than those with inappropriate shocks (HR=2.0, p=0.002). Therefore, even inappropriate shocks themselves doubled the risk of death. Patients who received more than one shock, either appropriate or not, were at even higher odds of death (HR=8.3, p<0.001). The results highlight the higher mortality risk when patients with ICDs have received a shock (appropriate or inappropriate) and the need for further therapies to modify outcome in these patients.
Bottom Line: Appropriate or inappropriate defibrillations are associated with a poorer prognosis in patients with cardiomyopathy.
Citation: Poole JE, Johnson GW, Hellkamp AS, et al. Prognostic importance of defibrillator shocks in patients with heart failure. N Engl J Med. 2008(359):1009-1017.
Can a simple physical exam tool assess the degree of dehydration in children?
Background: Despite the frequency and the associated cost of acute gastroenteritis (AGE) in the pediatric population, there is no unified scale to assess the severity of dehydration. The authors of this paper previously reported a clinical dehydration scale (CDS) and applied it prospectively in a new cohort of patients ages 1 month to 5 years.
Study design: Prospective, observational study.
Setting: Single, tertiary care emergency department (ED) in Canada.
Synopsis: The CDS score is based purely on the physical findings of the child, including a) general appearance, b) eyes, c) mucous membranes, and d) amount of tears. On a point system, the patient is placed in one of three categories: no dehydration, some dehydration, moderate/severe dehydration. The trial enrolled 205 children and the CDS was applied by the triaging nurse. The attending ED pediatricians were blinded from this assessment. The CDS was able to predict the length of stay (mean + SD: no dehyrdation 245 + 181 mins; some dehydration, 397 + 302 mins; mod/severe dehydration, 501 + 389 mins), need for intravenous rehydration (none, 15%; some, 49%; mod/severe, 80%), and frequency of emesis/diarrhea as reported by the parents (none, 8.4 + 7.7; some, 13 + 10.7; mod/severe, 30.2 + 14.8). Only five children were categorized in the moderate/severe dehydration category, which may limit the ability to generalize the scoring system to that group of patients.
Bottom line: The CDS is an easy to use and promising tool to assess the severity of illness, expected ED length of stay, and need for intravenous rehydration in children with acute gastroenteritis.
Citation: Goldman RD, Friedman JN, Parkin PC. Validation of the clinical dehydration scale for children with acute gastroenteritis. Pediatrics. 2008;122(3):545-549.
Does maintaining a higher hemoglobin level benefit critical care patients?
Background: Historically, medical and surgical critical care patients liberally were transfused with little prospective evidence to support this approach. However, recent evidence has led to the use of a more-restricted transfusion threshold.
Study design: Systematic review and meta-analysis of cohort studies evaluating the effect of red blood cell (RBC) transfusion on patient outcomes.
Setting: Data sources include MEDLINE, Embase, and Cochrane databases.
Synopsis: The 45 cohort studies, including more than 272,000 patients, were selected due to focus on outcome measures, such as mortality, multiorgan dysfunction, acute respiratory distress syndrome, and infections. Primary studies were then placed into one of three categories: benefits outweigh the risk, neutral, or risks outweigh the benefit. Forty-two of these studies found the risks outweigh the benefits; two were neutral; and only one sub-study (in elderly patients with acute myocardial infarctions) suggested benefit outweighs the risk.
Although a systematic review of cohort studies has inherent limitations, the overwhelming direction of the results suggests statistically significant harm due to liberal transfusion practices (Summary Odd Ratios [OR] for a) death, OR = 1.69; b) infection, OR = 1.88; and c) Acute Respiratory Distress Syndrome, OR = 2.5). Due to the observational nature of the cohort studies, one might suspect RBC transfusions could simply reflect patient severity of illness. Thus, the harm suggested by the more liberal transfusion standards could just reflect the fact these patients carried a worse prognosis due to their respective illnesses.
Bottom Line: The preponderance of evidence suggests liberal transfusion practice is associated with increased morbidity and mortality of ICU patients. When considering RBC transfusions, the risks and benefits to each individual patient should be considered carefully.
Citation: Marik PE, Corwin HL. Efficacy of red blood cell transfusion in the critically ill: a systematic review of the literature. Crit Care Med. 2008; 36(9);2667-2674.
What is the appropriate frequency of rescreening for patients with initial screening colonoscopies negative for adenomas?
Background: Colonoscopy is the preferred primary screening method for the detection of colorectal cancer and precancerous polyps. Data suggest colonoscopy may be performed too frequently and for inappropriate indications.
Study design: Retrospective cohort study.
Setting: Seven sites in central Indiana.
Synopsis: In this study of 2,436 persons with no adenomas on baseline screening colonoscopies, 1,256 of them (51.6%) were rescreened a mean of 5.34 + 1.34 years later. No cancers were found on rescreening. One or more adenomas were found in 201 persons (16.0%). Nineteen advanced adenomas were found in 16 persons (1.3%). Patients in this study were relatively young (mean age at baseline was 56.7 years). Men were more likely than women to have adenomas (RR 1.88; 95% CI 1.42-2.51) and to have advanced adenomas (RR 3.31; 95% CI 1.02-10.8).
Limitations included a small cohort sample size, as well as incomplete information on persons who did not follow up with the five-year examination. Also, there is uncertainty about the clinical significance of advanced adenomas.
Bottom Line: Among persons previously screened with colonoscopy who have no colorectal adenomas, the five-year risk of detecting an advanced adenoma is extremely low (1.3%), supporting a rescreening interval of more than five years after a normal colonoscopy. Men have greater risk, and may deserve a shorter interval screening.
Citation: Imperiale TF, Glowinski EA, Lin-Cooper C, et al. Five-year risk of colorectal neoplasia after negative screening colonoscopy. N Engl J Med. 2008;359:1218-1224.
Can validated discharge instability criteria predict mortality or readmission within 30 days of hospital discharge for community acquired pneumonia (CAP)?
Background: Prior prospective cohort data have delineated instability criteria utilizing vital sign criteria at hospital discharge for CAP. However, guidelines for determining patient readiness for discharge remain largely unstudied.
Study design: Prospective, observational cohort study.
Setting: A single, non-urban teaching hospital in Spain.
Synopsis: In this study, 870 adults with CAP were evaluated following discharge. Abnormal oxygenation and vital signs were utilized to calculate an instability score. Criteria for instability were defined as temperature >37.5° C, heart rate <100, respiratory rate >24, systolic blood pressure (SBP) <90 (or diastolic blood pressure, DBP <60), and oxygen saturation <90% (or PaO2 <60).
Of all the instability criteria, only low oxygenation predicted readmission at 30 days (Hazard Ratio [HR] 1.4, p=0.03). However, mortality was significantly increased when instability criteria of temperature (HR 4.5, p=0.04), blood pressure (HR 2.6, p=0.02), respiratory rate (HR 2.4, p=0.03), or oxygenation (HR 2.4, p=0.03) were met. Elevated heart rate was not found to predict death.
The authors assigned each of the significant instability criteria a score of one or two (based on the weight of its hazard ratio), with respiratory rate, low blood pressure, and low oxygenation each assigned one point, and temperature assigned two points. Patients with an instability score of two or more had a six-fold increased risk of death (HR 5.8; 95%, p=0.0001). The negative predictive value (NPV) of an instability score less than two was very helpful (NPV=98%) in identifying patients with low mortality risk; however, the positive predictive value (PPV) of an instability score >2 is not necessarily helpful (PPV=13%) clinically.
Bottom line: Patients with a temperature >37.5° C or any combination of RR >24, SBP <90 (or DBP <60), and SpO2 <90% (or Pa02 <60) are at increased risk of death. Identifying a low instability score is most helpful in clinical practice.
Citation: Capelastegui A, Espana P, Bilbao A, et al. Pneumonia: criteria for patient instability on hospital discharge. Chest. 2008;34:595-600.