User login
MIND diet preserves cognition, new data show
Adherence to the MIND diet can improve memory and thinking skills of older adults, even in the presence of Alzheimer’s disease pathology, new data from the Rush Memory and Aging Project (MAP) show.
“The MIND diet was associated with better cognitive functions independently of brain pathologies related to Alzheimer’s disease, suggesting that diet may contribute to cognitive resilience, which ultimately indicates that it is never too late for dementia prevention,” lead author Klodian Dhana, MD, PhD, with the Rush Institute of Healthy Aging at Rush University, Chicago, said in an interview.
The study was published online Sept. 14, 2021, in the Journal of Alzheimer’s Disease.
Impact on brain pathology
“While previous investigations determined that the MIND diet is associated with a slower cognitive decline, the current study furthered the diet and brain health evidence by assessing the impact of brain pathology in the diet-cognition relationship,” Dr. Dhana said.
The MIND diet was pioneered by the late Martha Clare Morris, ScD, a Rush nutritional epidemiologist, who died in 2020 of cancer at age 64. A hybrid of the Mediterranean and DASH (Dietary Approaches to Stop Hypertension) diets, the MIND diet includes green leafy vegetables, fish, nuts, berries, beans, and whole grains and limits consumption of fried and fast foods, sweets, and pastries.
The current study focused on 569 older adults who died while participating in the MAP study, which began in 1997. Participants in the study were mostly White and were without known dementia. All of the participants agreed to undergo annual clinical evaluations. They also agreed to undergo brain autopsy after death.
Beginning in 2004, participants completed annual food frequency questionnaires, which were used to calculate a MIND diet score based on how often the participants ate specific foods.
The researchers used a series of regression analyses to examine associations of the MIND diet, dementia-related brain pathologies, and global cognition near the time of death. Analyses were adjusted for age, sex, education, apo E4, late-life cognitive activities, and total energy intake.
(beta, 0.119; P = .003).
Notably, the researchers said, neither the strength nor the significance of association changed markedly when AD pathology and other brain pathologies were included in the model (beta, 0.111; P = .003).
The relationship between better adherence to the MIND diet and better cognition remained significant when the analysis was restricted to individuals without mild cognitive impairment at baseline (beta, 0.121; P = .005) as well as to persons in whom a postmortem diagnosis of AD was made on the basis of NIA-Reagan consensus recommendations (beta, 0.114; P = .023).
The limitations of the study include the reliance on self-reported diet information and a sample made up of mostly White volunteers who agreed to annual evaluations and postmortem organ donation, thus limiting generalizability.
Strengths of the study include the prospective design with annual assessment of cognitive function using standardized tests and collection of the dietary information using validated questionnaires. Also, the neuropathologic evaluations were performed by examiners blinded to clinical data.
“Diet changes can impact cognitive functioning and risk of dementia, for better or worse. There are fairly simple diet and lifestyle changes a person could make that may help to slow cognitive decline with aging and contribute to brain health,” Dr. Dhana said in a news release.
Builds resilience
Weighing in on the study, Heather Snyder, PhD, vice president of medical and scientific relations for the Alzheimer’s Association, said this “interesting study sheds light on the impact of nutrition on cognitive function.
“The findings add to the growing literature that lifestyle factors – like access to a heart-healthy diet – may help the brain be more resilient to disease-specific changes,” Snyder said in an interview.
“The Alzheimer’s Association’s US POINTER study is investigating how lifestyle interventions, including nutrition guidance, like the MIND diet, may impact a person’s risk of cognitive decline. An ancillary study of the US POINTER will include brain imaging to investigate how these lifestyle interventions impact the biology of the brain,” Dr. Snyder noted.
The research was supported by the National Institute on Aging of the National Institutes of Health. Dr. Dhana and Dr. Snyder disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Adherence to the MIND diet can improve memory and thinking skills of older adults, even in the presence of Alzheimer’s disease pathology, new data from the Rush Memory and Aging Project (MAP) show.
“The MIND diet was associated with better cognitive functions independently of brain pathologies related to Alzheimer’s disease, suggesting that diet may contribute to cognitive resilience, which ultimately indicates that it is never too late for dementia prevention,” lead author Klodian Dhana, MD, PhD, with the Rush Institute of Healthy Aging at Rush University, Chicago, said in an interview.
The study was published online Sept. 14, 2021, in the Journal of Alzheimer’s Disease.
Impact on brain pathology
“While previous investigations determined that the MIND diet is associated with a slower cognitive decline, the current study furthered the diet and brain health evidence by assessing the impact of brain pathology in the diet-cognition relationship,” Dr. Dhana said.
The MIND diet was pioneered by the late Martha Clare Morris, ScD, a Rush nutritional epidemiologist, who died in 2020 of cancer at age 64. A hybrid of the Mediterranean and DASH (Dietary Approaches to Stop Hypertension) diets, the MIND diet includes green leafy vegetables, fish, nuts, berries, beans, and whole grains and limits consumption of fried and fast foods, sweets, and pastries.
The current study focused on 569 older adults who died while participating in the MAP study, which began in 1997. Participants in the study were mostly White and were without known dementia. All of the participants agreed to undergo annual clinical evaluations. They also agreed to undergo brain autopsy after death.
Beginning in 2004, participants completed annual food frequency questionnaires, which were used to calculate a MIND diet score based on how often the participants ate specific foods.
The researchers used a series of regression analyses to examine associations of the MIND diet, dementia-related brain pathologies, and global cognition near the time of death. Analyses were adjusted for age, sex, education, apo E4, late-life cognitive activities, and total energy intake.
(beta, 0.119; P = .003).
Notably, the researchers said, neither the strength nor the significance of association changed markedly when AD pathology and other brain pathologies were included in the model (beta, 0.111; P = .003).
The relationship between better adherence to the MIND diet and better cognition remained significant when the analysis was restricted to individuals without mild cognitive impairment at baseline (beta, 0.121; P = .005) as well as to persons in whom a postmortem diagnosis of AD was made on the basis of NIA-Reagan consensus recommendations (beta, 0.114; P = .023).
The limitations of the study include the reliance on self-reported diet information and a sample made up of mostly White volunteers who agreed to annual evaluations and postmortem organ donation, thus limiting generalizability.
Strengths of the study include the prospective design with annual assessment of cognitive function using standardized tests and collection of the dietary information using validated questionnaires. Also, the neuropathologic evaluations were performed by examiners blinded to clinical data.
“Diet changes can impact cognitive functioning and risk of dementia, for better or worse. There are fairly simple diet and lifestyle changes a person could make that may help to slow cognitive decline with aging and contribute to brain health,” Dr. Dhana said in a news release.
Builds resilience
Weighing in on the study, Heather Snyder, PhD, vice president of medical and scientific relations for the Alzheimer’s Association, said this “interesting study sheds light on the impact of nutrition on cognitive function.
“The findings add to the growing literature that lifestyle factors – like access to a heart-healthy diet – may help the brain be more resilient to disease-specific changes,” Snyder said in an interview.
“The Alzheimer’s Association’s US POINTER study is investigating how lifestyle interventions, including nutrition guidance, like the MIND diet, may impact a person’s risk of cognitive decline. An ancillary study of the US POINTER will include brain imaging to investigate how these lifestyle interventions impact the biology of the brain,” Dr. Snyder noted.
The research was supported by the National Institute on Aging of the National Institutes of Health. Dr. Dhana and Dr. Snyder disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Adherence to the MIND diet can improve memory and thinking skills of older adults, even in the presence of Alzheimer’s disease pathology, new data from the Rush Memory and Aging Project (MAP) show.
“The MIND diet was associated with better cognitive functions independently of brain pathologies related to Alzheimer’s disease, suggesting that diet may contribute to cognitive resilience, which ultimately indicates that it is never too late for dementia prevention,” lead author Klodian Dhana, MD, PhD, with the Rush Institute of Healthy Aging at Rush University, Chicago, said in an interview.
The study was published online Sept. 14, 2021, in the Journal of Alzheimer’s Disease.
Impact on brain pathology
“While previous investigations determined that the MIND diet is associated with a slower cognitive decline, the current study furthered the diet and brain health evidence by assessing the impact of brain pathology in the diet-cognition relationship,” Dr. Dhana said.
The MIND diet was pioneered by the late Martha Clare Morris, ScD, a Rush nutritional epidemiologist, who died in 2020 of cancer at age 64. A hybrid of the Mediterranean and DASH (Dietary Approaches to Stop Hypertension) diets, the MIND diet includes green leafy vegetables, fish, nuts, berries, beans, and whole grains and limits consumption of fried and fast foods, sweets, and pastries.
The current study focused on 569 older adults who died while participating in the MAP study, which began in 1997. Participants in the study were mostly White and were without known dementia. All of the participants agreed to undergo annual clinical evaluations. They also agreed to undergo brain autopsy after death.
Beginning in 2004, participants completed annual food frequency questionnaires, which were used to calculate a MIND diet score based on how often the participants ate specific foods.
The researchers used a series of regression analyses to examine associations of the MIND diet, dementia-related brain pathologies, and global cognition near the time of death. Analyses were adjusted for age, sex, education, apo E4, late-life cognitive activities, and total energy intake.
(beta, 0.119; P = .003).
Notably, the researchers said, neither the strength nor the significance of association changed markedly when AD pathology and other brain pathologies were included in the model (beta, 0.111; P = .003).
The relationship between better adherence to the MIND diet and better cognition remained significant when the analysis was restricted to individuals without mild cognitive impairment at baseline (beta, 0.121; P = .005) as well as to persons in whom a postmortem diagnosis of AD was made on the basis of NIA-Reagan consensus recommendations (beta, 0.114; P = .023).
The limitations of the study include the reliance on self-reported diet information and a sample made up of mostly White volunteers who agreed to annual evaluations and postmortem organ donation, thus limiting generalizability.
Strengths of the study include the prospective design with annual assessment of cognitive function using standardized tests and collection of the dietary information using validated questionnaires. Also, the neuropathologic evaluations were performed by examiners blinded to clinical data.
“Diet changes can impact cognitive functioning and risk of dementia, for better or worse. There are fairly simple diet and lifestyle changes a person could make that may help to slow cognitive decline with aging and contribute to brain health,” Dr. Dhana said in a news release.
Builds resilience
Weighing in on the study, Heather Snyder, PhD, vice president of medical and scientific relations for the Alzheimer’s Association, said this “interesting study sheds light on the impact of nutrition on cognitive function.
“The findings add to the growing literature that lifestyle factors – like access to a heart-healthy diet – may help the brain be more resilient to disease-specific changes,” Snyder said in an interview.
“The Alzheimer’s Association’s US POINTER study is investigating how lifestyle interventions, including nutrition guidance, like the MIND diet, may impact a person’s risk of cognitive decline. An ancillary study of the US POINTER will include brain imaging to investigate how these lifestyle interventions impact the biology of the brain,” Dr. Snyder noted.
The research was supported by the National Institute on Aging of the National Institutes of Health. Dr. Dhana and Dr. Snyder disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Military sexual trauma tied to risk for hypertension
a new study suggests.
“Understanding a patient’s trauma history is invaluable for treating the whole person,” Allison E. Gaffey, PhD, Yale University, New Haven, Conn., and the Veterans Affairs Connecticut Healthcare System, told this news organization.
“Assessing men and women’s history of trauma, including sexual trauma, is critical for recognizing nontraditional factors that contribute to their cardiovascular risk and to gain a more comprehensive understanding of their mental and physical health,” Dr. Gaffey added.
She presented her research at the joint scientific sessions of the American Heart Association Council on Hypertension, AHA Council on Kidney in Cardiovascular Disease, and American Society of Hypertension.
Lasting impact on physical health
Dr. Gaffey and colleagues analyzed data from the VA for roughly 1.2 million veterans (mean age, 30.2 years; 12% female) who were discharged from the military after Sept. 30, 2001, and who received health care services at VA medical centers from 2001 to 2017.
All were screened for sexual harassment and assault, known as military sexual trauma (MST), when they first began receiving VA care.
During 16 years of follow-up, 33,881 veterans screened positive for MST (65% women), and 307,332 developed hypertension (15% women).
Overall, MST was associated with a 30% increase in risk for incident hypertension in unadjusted models (hazard ratio, 1.30; 95% confidence interval, 1.28-1.33; P < .001).
After adjustment for demographic characteristics, lifestyle factors, cardiovascular comorbidities, PTSD, anxiety, and depression, MST remained significantly associated with hypertension (adjusted HR, 1.10; 95% CI, 1.08-1.12; P < .001).
When women and men were examined separately, the link between MST and risk for hypertension remained for both groups, but was slightly stronger among women.
“Sexual trauma has been associated with autonomic dysfunction, inflammation, and dysregulation in the hypothalamic pituitary adrenal axis and renin-angiotensin-aldosterone system, which could lead to elevations in BP over time,” Dr. Gaffey told this news organization.
“These findings show that even many years after being discharged from military service, exposure to military sexual trauma can continue to significantly influence veterans’ physical health,” she added.
Dr. Gaffey said it will be important to determine if early treatment of MST improves hypertension risk, particularly among those showing elevated blood pressure or stage 1 hypertension.
Social determinants of health
Willie Lawrence Jr., MD, head of the AHA National Hypertension Control Initiative oversight committee, said the findings in this study are “in line with what we know about the impact of social determinants of health on high blood pressure.”
“There are studies that suggest that things that we historically don’t look at as risk factors for hypertension – lifelong racism, crime, mental health status – do in fact predict your risk of developing hypertension,” Dr. Lawrence, from Spectrum Health in Benton Harbor, Mich., told this news organization.
“It’s not just your genetics that will determine your health, and there are a lot of things that will affect your blood pressure. Your blood pressure is really just a barometer of everything that’s going on in your life and some of the things that have gone on in your life in the past,” added Dr. Lawrence, who wasn’t involved in the study.
Funding for the study was provided by the Department of Veterans Affairs. Dr. Gaffey and Dr. Lawrence have no relevant disclosures.
A version of this article first appeared on Medscape.com.
a new study suggests.
“Understanding a patient’s trauma history is invaluable for treating the whole person,” Allison E. Gaffey, PhD, Yale University, New Haven, Conn., and the Veterans Affairs Connecticut Healthcare System, told this news organization.
“Assessing men and women’s history of trauma, including sexual trauma, is critical for recognizing nontraditional factors that contribute to their cardiovascular risk and to gain a more comprehensive understanding of their mental and physical health,” Dr. Gaffey added.
She presented her research at the joint scientific sessions of the American Heart Association Council on Hypertension, AHA Council on Kidney in Cardiovascular Disease, and American Society of Hypertension.
Lasting impact on physical health
Dr. Gaffey and colleagues analyzed data from the VA for roughly 1.2 million veterans (mean age, 30.2 years; 12% female) who were discharged from the military after Sept. 30, 2001, and who received health care services at VA medical centers from 2001 to 2017.
All were screened for sexual harassment and assault, known as military sexual trauma (MST), when they first began receiving VA care.
During 16 years of follow-up, 33,881 veterans screened positive for MST (65% women), and 307,332 developed hypertension (15% women).
Overall, MST was associated with a 30% increase in risk for incident hypertension in unadjusted models (hazard ratio, 1.30; 95% confidence interval, 1.28-1.33; P < .001).
After adjustment for demographic characteristics, lifestyle factors, cardiovascular comorbidities, PTSD, anxiety, and depression, MST remained significantly associated with hypertension (adjusted HR, 1.10; 95% CI, 1.08-1.12; P < .001).
When women and men were examined separately, the link between MST and risk for hypertension remained for both groups, but was slightly stronger among women.
“Sexual trauma has been associated with autonomic dysfunction, inflammation, and dysregulation in the hypothalamic pituitary adrenal axis and renin-angiotensin-aldosterone system, which could lead to elevations in BP over time,” Dr. Gaffey told this news organization.
“These findings show that even many years after being discharged from military service, exposure to military sexual trauma can continue to significantly influence veterans’ physical health,” she added.
Dr. Gaffey said it will be important to determine if early treatment of MST improves hypertension risk, particularly among those showing elevated blood pressure or stage 1 hypertension.
Social determinants of health
Willie Lawrence Jr., MD, head of the AHA National Hypertension Control Initiative oversight committee, said the findings in this study are “in line with what we know about the impact of social determinants of health on high blood pressure.”
“There are studies that suggest that things that we historically don’t look at as risk factors for hypertension – lifelong racism, crime, mental health status – do in fact predict your risk of developing hypertension,” Dr. Lawrence, from Spectrum Health in Benton Harbor, Mich., told this news organization.
“It’s not just your genetics that will determine your health, and there are a lot of things that will affect your blood pressure. Your blood pressure is really just a barometer of everything that’s going on in your life and some of the things that have gone on in your life in the past,” added Dr. Lawrence, who wasn’t involved in the study.
Funding for the study was provided by the Department of Veterans Affairs. Dr. Gaffey and Dr. Lawrence have no relevant disclosures.
A version of this article first appeared on Medscape.com.
a new study suggests.
“Understanding a patient’s trauma history is invaluable for treating the whole person,” Allison E. Gaffey, PhD, Yale University, New Haven, Conn., and the Veterans Affairs Connecticut Healthcare System, told this news organization.
“Assessing men and women’s history of trauma, including sexual trauma, is critical for recognizing nontraditional factors that contribute to their cardiovascular risk and to gain a more comprehensive understanding of their mental and physical health,” Dr. Gaffey added.
She presented her research at the joint scientific sessions of the American Heart Association Council on Hypertension, AHA Council on Kidney in Cardiovascular Disease, and American Society of Hypertension.
Lasting impact on physical health
Dr. Gaffey and colleagues analyzed data from the VA for roughly 1.2 million veterans (mean age, 30.2 years; 12% female) who were discharged from the military after Sept. 30, 2001, and who received health care services at VA medical centers from 2001 to 2017.
All were screened for sexual harassment and assault, known as military sexual trauma (MST), when they first began receiving VA care.
During 16 years of follow-up, 33,881 veterans screened positive for MST (65% women), and 307,332 developed hypertension (15% women).
Overall, MST was associated with a 30% increase in risk for incident hypertension in unadjusted models (hazard ratio, 1.30; 95% confidence interval, 1.28-1.33; P < .001).
After adjustment for demographic characteristics, lifestyle factors, cardiovascular comorbidities, PTSD, anxiety, and depression, MST remained significantly associated with hypertension (adjusted HR, 1.10; 95% CI, 1.08-1.12; P < .001).
When women and men were examined separately, the link between MST and risk for hypertension remained for both groups, but was slightly stronger among women.
“Sexual trauma has been associated with autonomic dysfunction, inflammation, and dysregulation in the hypothalamic pituitary adrenal axis and renin-angiotensin-aldosterone system, which could lead to elevations in BP over time,” Dr. Gaffey told this news organization.
“These findings show that even many years after being discharged from military service, exposure to military sexual trauma can continue to significantly influence veterans’ physical health,” she added.
Dr. Gaffey said it will be important to determine if early treatment of MST improves hypertension risk, particularly among those showing elevated blood pressure or stage 1 hypertension.
Social determinants of health
Willie Lawrence Jr., MD, head of the AHA National Hypertension Control Initiative oversight committee, said the findings in this study are “in line with what we know about the impact of social determinants of health on high blood pressure.”
“There are studies that suggest that things that we historically don’t look at as risk factors for hypertension – lifelong racism, crime, mental health status – do in fact predict your risk of developing hypertension,” Dr. Lawrence, from Spectrum Health in Benton Harbor, Mich., told this news organization.
“It’s not just your genetics that will determine your health, and there are a lot of things that will affect your blood pressure. Your blood pressure is really just a barometer of everything that’s going on in your life and some of the things that have gone on in your life in the past,” added Dr. Lawrence, who wasn’t involved in the study.
Funding for the study was provided by the Department of Veterans Affairs. Dr. Gaffey and Dr. Lawrence have no relevant disclosures.
A version of this article first appeared on Medscape.com.
Antipsychotic effective for bipolar depression in phase 3 trial
Results of a phase 3 study show that treatment with lumateperone (Caplyta) significantly improved depressive symptoms for patients with major depressive episodes associated with both bipolar I and bipolar II disorders.
“Bipolar depression represents the most prevalent and debilitating presentation of bipolar disorder. There is a critical need for more treatments that are effective and have favorable safety profiles,” study investigator Gary S. Sachs, MD, associate clinical professor in psychiatry, Harvard Medical School, Boston, said in a company news release.
“The strong efficacy and impressive safety results reported in this trial for a broad patient population position lumateperone as a potentially important advancement in the treatment of this disorder,” said Dr. Sachs, who is also founding director of the Bipolar Clinic and Research Program at Massachusetts General Hospital, Boston.
The findings were published online September 23 in the American Journal of Psychiatry.
First-in-class antipsychotic
Lumateperone is a first-in-class antipsychotic that acts synergistically through the serotonergic, dopaminergic, and glutamatergic systems.
It was approved by the U.S. Food and Drug Administration in late 2019 for the treatment of adults with schizophrenia, as reported at the time by this news organization.
All were randomly allocated in a 1:1 ratio to receive 6 weeks of lumateperone monotherapy at 42 mg/d or matching placebo.
At day 43, lumateperone treatment was associated with significantly greater improvement from baseline in Montgomery-Åsberg Depression Rating Scale (MADRS) score in comparison with placebo (drug-placebo difference, -4.6 points; P < .0001; effect size = -0.56), which met the study’s primary endpoint.
The study drug led to significant improvement in MADRS total score as early as the first week, which was the first time point measured. Improvement continued throughout the study.
Treatment with lumateperone also led to significantly greater improvement in the key secondary endpoints of total score on the severity scale of the Clinical Global Impressions Scale–Bipolar Version (CGI-BP-S) (P < .0001; effect size = -0.46) and the CGI-BP-S depression score (P < .001; effect size = -50).
In addition, it was superior to placebo both for patients with bipolar I disorder and those with bipolar II disorder.
Somnolence and nausea were the most commonly reported adverse events associated with lumateperone. Minimal changes were observed in weight and vital signs and in results of metabolic or endocrine assessments. These findings are in line with previous studies involving patients with schizophrenia.
The incidence of extrapyramidal symptom–related events was low and was similar to those with placebo.
The company has submitted a supplemental new drug application for lumateperone for the treatment of bipolar depression, which is currently under review with the FDA. The target action date is December 17.
A version of this article first appeared on Medscape.com.
Results of a phase 3 study show that treatment with lumateperone (Caplyta) significantly improved depressive symptoms for patients with major depressive episodes associated with both bipolar I and bipolar II disorders.
“Bipolar depression represents the most prevalent and debilitating presentation of bipolar disorder. There is a critical need for more treatments that are effective and have favorable safety profiles,” study investigator Gary S. Sachs, MD, associate clinical professor in psychiatry, Harvard Medical School, Boston, said in a company news release.
“The strong efficacy and impressive safety results reported in this trial for a broad patient population position lumateperone as a potentially important advancement in the treatment of this disorder,” said Dr. Sachs, who is also founding director of the Bipolar Clinic and Research Program at Massachusetts General Hospital, Boston.
The findings were published online September 23 in the American Journal of Psychiatry.
First-in-class antipsychotic
Lumateperone is a first-in-class antipsychotic that acts synergistically through the serotonergic, dopaminergic, and glutamatergic systems.
It was approved by the U.S. Food and Drug Administration in late 2019 for the treatment of adults with schizophrenia, as reported at the time by this news organization.
All were randomly allocated in a 1:1 ratio to receive 6 weeks of lumateperone monotherapy at 42 mg/d or matching placebo.
At day 43, lumateperone treatment was associated with significantly greater improvement from baseline in Montgomery-Åsberg Depression Rating Scale (MADRS) score in comparison with placebo (drug-placebo difference, -4.6 points; P < .0001; effect size = -0.56), which met the study’s primary endpoint.
The study drug led to significant improvement in MADRS total score as early as the first week, which was the first time point measured. Improvement continued throughout the study.
Treatment with lumateperone also led to significantly greater improvement in the key secondary endpoints of total score on the severity scale of the Clinical Global Impressions Scale–Bipolar Version (CGI-BP-S) (P < .0001; effect size = -0.46) and the CGI-BP-S depression score (P < .001; effect size = -50).
In addition, it was superior to placebo both for patients with bipolar I disorder and those with bipolar II disorder.
Somnolence and nausea were the most commonly reported adverse events associated with lumateperone. Minimal changes were observed in weight and vital signs and in results of metabolic or endocrine assessments. These findings are in line with previous studies involving patients with schizophrenia.
The incidence of extrapyramidal symptom–related events was low and was similar to those with placebo.
The company has submitted a supplemental new drug application for lumateperone for the treatment of bipolar depression, which is currently under review with the FDA. The target action date is December 17.
A version of this article first appeared on Medscape.com.
Results of a phase 3 study show that treatment with lumateperone (Caplyta) significantly improved depressive symptoms for patients with major depressive episodes associated with both bipolar I and bipolar II disorders.
“Bipolar depression represents the most prevalent and debilitating presentation of bipolar disorder. There is a critical need for more treatments that are effective and have favorable safety profiles,” study investigator Gary S. Sachs, MD, associate clinical professor in psychiatry, Harvard Medical School, Boston, said in a company news release.
“The strong efficacy and impressive safety results reported in this trial for a broad patient population position lumateperone as a potentially important advancement in the treatment of this disorder,” said Dr. Sachs, who is also founding director of the Bipolar Clinic and Research Program at Massachusetts General Hospital, Boston.
The findings were published online September 23 in the American Journal of Psychiatry.
First-in-class antipsychotic
Lumateperone is a first-in-class antipsychotic that acts synergistically through the serotonergic, dopaminergic, and glutamatergic systems.
It was approved by the U.S. Food and Drug Administration in late 2019 for the treatment of adults with schizophrenia, as reported at the time by this news organization.
All were randomly allocated in a 1:1 ratio to receive 6 weeks of lumateperone monotherapy at 42 mg/d or matching placebo.
At day 43, lumateperone treatment was associated with significantly greater improvement from baseline in Montgomery-Åsberg Depression Rating Scale (MADRS) score in comparison with placebo (drug-placebo difference, -4.6 points; P < .0001; effect size = -0.56), which met the study’s primary endpoint.
The study drug led to significant improvement in MADRS total score as early as the first week, which was the first time point measured. Improvement continued throughout the study.
Treatment with lumateperone also led to significantly greater improvement in the key secondary endpoints of total score on the severity scale of the Clinical Global Impressions Scale–Bipolar Version (CGI-BP-S) (P < .0001; effect size = -0.46) and the CGI-BP-S depression score (P < .001; effect size = -50).
In addition, it was superior to placebo both for patients with bipolar I disorder and those with bipolar II disorder.
Somnolence and nausea were the most commonly reported adverse events associated with lumateperone. Minimal changes were observed in weight and vital signs and in results of metabolic or endocrine assessments. These findings are in line with previous studies involving patients with schizophrenia.
The incidence of extrapyramidal symptom–related events was low and was similar to those with placebo.
The company has submitted a supplemental new drug application for lumateperone for the treatment of bipolar depression, which is currently under review with the FDA. The target action date is December 17.
A version of this article first appeared on Medscape.com.
‘Alarming’ increase in fake pills laced with fentanyl, methamphetamine, DEA warns
The U.S. Drug Enforcement Administration has issued a public safety alert over an “alarming” increase in fake prescription pills laced with the synthetic opioid fentanyl or the stimulant methamphetamine.
“The United States is facing an unprecedented crisis of overdose deaths fueled by illegally manufactured fentanyl and methamphetamine,” DEA Administrator Anne Milgram said in the alert.
“Counterfeit pills that contain these dangerous and extremely addictive drugs are more lethal and more accessible than ever before. DEA is focusing resources on taking down the violent drug traffickers causing the greatest harm and posing the greatest threat to the safety and health of Americans,” Ms. Milgram said.
Criminal drug networks are mass-producing fake fentanyl- and methamphetamine-laced pills and deceptively marketing them as legitimate prescription pills, the DEA warns.
such as oxycodone (Oxycontin, Percocet), hydrocodone (Vicodin), and alprazolam (Xanax); or stimulants like amphetamines (Adderall).
The agency has seized fake pills in every U.S. state. More than 9.5 million fake pills have been seized so far this year – more than the last 2 years combined.
The number of seized counterfeit pills with fentanyl has jumped nearly 430% since 2019. DEA lab tests reveal that two out of every five pills with fentanyl contain a potentially lethal dose.
These deadly pills are widely accessible and often sold on social media and e-commerce platforms – making them available to anyone with a smartphone, including minors, the DEA warns.
More than 93,000 people died of a drug overdose in the United States last year, according to federal statistics, and fentanyl is the primary driver of this alarming increase in overdose deaths, the DEA says.
The agency has launched a “One Pill Can Kill” public awareness campaign to educate the public of the dangers of counterfeit pills purchased outside of a licensed pharmacy. These pills are “illegal, dangerous, and potentially lethal,” the DEA warns.
This alert does not apply to legitimate pharmaceutical medications prescribed by doctors and dispensed by licensed pharmacists, the DEA says.
“The legitimate prescription supply chain is not impacted. Anyone filling a prescription at a licensed pharmacy can be confident that the medications they receive are safe when taken as directed by a medical professional,” the agency says.
A version of this article first appeared on Medscape.com.
The U.S. Drug Enforcement Administration has issued a public safety alert over an “alarming” increase in fake prescription pills laced with the synthetic opioid fentanyl or the stimulant methamphetamine.
“The United States is facing an unprecedented crisis of overdose deaths fueled by illegally manufactured fentanyl and methamphetamine,” DEA Administrator Anne Milgram said in the alert.
“Counterfeit pills that contain these dangerous and extremely addictive drugs are more lethal and more accessible than ever before. DEA is focusing resources on taking down the violent drug traffickers causing the greatest harm and posing the greatest threat to the safety and health of Americans,” Ms. Milgram said.
Criminal drug networks are mass-producing fake fentanyl- and methamphetamine-laced pills and deceptively marketing them as legitimate prescription pills, the DEA warns.
such as oxycodone (Oxycontin, Percocet), hydrocodone (Vicodin), and alprazolam (Xanax); or stimulants like amphetamines (Adderall).
The agency has seized fake pills in every U.S. state. More than 9.5 million fake pills have been seized so far this year – more than the last 2 years combined.
The number of seized counterfeit pills with fentanyl has jumped nearly 430% since 2019. DEA lab tests reveal that two out of every five pills with fentanyl contain a potentially lethal dose.
These deadly pills are widely accessible and often sold on social media and e-commerce platforms – making them available to anyone with a smartphone, including minors, the DEA warns.
More than 93,000 people died of a drug overdose in the United States last year, according to federal statistics, and fentanyl is the primary driver of this alarming increase in overdose deaths, the DEA says.
The agency has launched a “One Pill Can Kill” public awareness campaign to educate the public of the dangers of counterfeit pills purchased outside of a licensed pharmacy. These pills are “illegal, dangerous, and potentially lethal,” the DEA warns.
This alert does not apply to legitimate pharmaceutical medications prescribed by doctors and dispensed by licensed pharmacists, the DEA says.
“The legitimate prescription supply chain is not impacted. Anyone filling a prescription at a licensed pharmacy can be confident that the medications they receive are safe when taken as directed by a medical professional,” the agency says.
A version of this article first appeared on Medscape.com.
The U.S. Drug Enforcement Administration has issued a public safety alert over an “alarming” increase in fake prescription pills laced with the synthetic opioid fentanyl or the stimulant methamphetamine.
“The United States is facing an unprecedented crisis of overdose deaths fueled by illegally manufactured fentanyl and methamphetamine,” DEA Administrator Anne Milgram said in the alert.
“Counterfeit pills that contain these dangerous and extremely addictive drugs are more lethal and more accessible than ever before. DEA is focusing resources on taking down the violent drug traffickers causing the greatest harm and posing the greatest threat to the safety and health of Americans,” Ms. Milgram said.
Criminal drug networks are mass-producing fake fentanyl- and methamphetamine-laced pills and deceptively marketing them as legitimate prescription pills, the DEA warns.
such as oxycodone (Oxycontin, Percocet), hydrocodone (Vicodin), and alprazolam (Xanax); or stimulants like amphetamines (Adderall).
The agency has seized fake pills in every U.S. state. More than 9.5 million fake pills have been seized so far this year – more than the last 2 years combined.
The number of seized counterfeit pills with fentanyl has jumped nearly 430% since 2019. DEA lab tests reveal that two out of every five pills with fentanyl contain a potentially lethal dose.
These deadly pills are widely accessible and often sold on social media and e-commerce platforms – making them available to anyone with a smartphone, including minors, the DEA warns.
More than 93,000 people died of a drug overdose in the United States last year, according to federal statistics, and fentanyl is the primary driver of this alarming increase in overdose deaths, the DEA says.
The agency has launched a “One Pill Can Kill” public awareness campaign to educate the public of the dangers of counterfeit pills purchased outside of a licensed pharmacy. These pills are “illegal, dangerous, and potentially lethal,” the DEA warns.
This alert does not apply to legitimate pharmaceutical medications prescribed by doctors and dispensed by licensed pharmacists, the DEA says.
“The legitimate prescription supply chain is not impacted. Anyone filling a prescription at a licensed pharmacy can be confident that the medications they receive are safe when taken as directed by a medical professional,” the agency says.
A version of this article first appeared on Medscape.com.
COVID-19 a rare trigger for Guillain-Barré syndrome
Although Guillain-Barré syndrome may rarely follow a recent infection with SARS-CoV-2, a strong relationship of GBS with the novel coronavirus is unlikely, say researchers with the International GBS Outcome Study (IGOS) consortium.
“Our study shows that COVID-19 may precede Guillain-Barré syndrome in rare cases, but the existence of a true association or causal relation still needs to be established,” Bart Jacobs, MD, PhD, department of neurology and immunology, Erasmus Medical Center and University Medical Center, both in Rotterdam, the Netherlands, said in a statement.
The study was published online in the journal Brain.
No uptick in pandemic cases
Since the beginning of the pandemic, there are reports of more than 90 GBS diagnoses following a possible COVID-19 infection. However, it remains unclear whether COVID-19 is another potential infectious trigger or whether the reported cases are coincidental.
To investigate further, Dr. Jacobs and the IGOS consortium reviewed 49 patients (median age, 56 years) with GBS who were added to their ongoing prospective observational cohort study between Jan. 30 and May 30, 2020.
The patients came from China, Denmark, France, Greece, Italy, Japan, the Netherlands, Spain, Switzerland, and the United Kingdom.
Of the 49 GBS patients, 8 (16%) had a confirmed and 3 (6%) had a probable SARS-CoV-2 infection; 15 had possible SARS-CoV-2 infection, 21 had no suspicion of SARS-CoV-2 infection, and 2 were “unclassifiable.”
Of the 11 patients with confirmed/probable SARS-CoV-2 infection, 9 had no serological evidence of any other recent preceding infection known to be associated with GBS.
The other two had serological evidence of a recent Campylobacter jejuni infection, which could have played a role in GBS onset, the researchers noted.
Most patients with a confirmed/probable SARS-CoV-2 infection had a sensorimotor GBS variant (73%), although Miller Fisher syndrome–GBS overlap (18%) and an ataxic variant (9%) were also found.
All patients with a confirmed/probable SARS-CoV-2 infection had a severe form of GBS. Common early neurologic features were facial weakness (64%), sensory deficits (82%), and autonomic dysfunction (64%), although not significantly different, compared with the other patients.
All eight patients who underwent nerve conduction study had a demyelinating subtype, which was more frequent than in the other GBS patients (47%; P = .012) as well as historical region and age-matched controls included in the IGOS cohort before the pandemic (52%, P = .016).
The median time from the onset of SARS-CoV-2 infection to neurologic symptoms was 16 days and ranged from 12 to 22 days.
More research needed
The researchers noted that the 22% frequency of a preceding SARS-CoV-2 infection in this study population was “higher than estimates of the contemporaneous background prevalence of SARS-CoV-2, which may be a result of recruitment bias during the pandemic, but could also indicate that GBS may rarely follow a recent SARS-CoV-2 infection.”
Importantly, however, they did not find more patients diagnosed with GBS during the first 4 months of the pandemic, compared with previous years, “suggesting that a strong association between SARS-CoV-2 and GBS is unlikely.”
“Should SARS-CoV-2 indeed be able to trigger GBS, our data are consistent with a postinfectious disease mechanism rather than direct viral invasion,” they noted, adding that the study was not designed to quantify a causative link between GBS and SARS-CoV-2.
“An unbiased multicenter, international, case-control study is needed to determine whether there is an association or not,” they wrote.
The IGOS is financially supported by the GBS-CIDP Foundation International, Gain, Erasmus MC University Medical Center Rotterdam, Glasgow University, CSL Behring, Grifols, Annexon and Hansa Biopharma. Dr. Jacobs received grants from Grifols, CSL-Behring, Annexon, Prinses Beatrix Spierfonds, Hansa Biopharma, and GBS-CIDP Foundation International and is on the global medical advisory board of the GBS CIDP Foundation International.
A version of this article first appeared on Medscape.com.
Although Guillain-Barré syndrome may rarely follow a recent infection with SARS-CoV-2, a strong relationship of GBS with the novel coronavirus is unlikely, say researchers with the International GBS Outcome Study (IGOS) consortium.
“Our study shows that COVID-19 may precede Guillain-Barré syndrome in rare cases, but the existence of a true association or causal relation still needs to be established,” Bart Jacobs, MD, PhD, department of neurology and immunology, Erasmus Medical Center and University Medical Center, both in Rotterdam, the Netherlands, said in a statement.
The study was published online in the journal Brain.
No uptick in pandemic cases
Since the beginning of the pandemic, there are reports of more than 90 GBS diagnoses following a possible COVID-19 infection. However, it remains unclear whether COVID-19 is another potential infectious trigger or whether the reported cases are coincidental.
To investigate further, Dr. Jacobs and the IGOS consortium reviewed 49 patients (median age, 56 years) with GBS who were added to their ongoing prospective observational cohort study between Jan. 30 and May 30, 2020.
The patients came from China, Denmark, France, Greece, Italy, Japan, the Netherlands, Spain, Switzerland, and the United Kingdom.
Of the 49 GBS patients, 8 (16%) had a confirmed and 3 (6%) had a probable SARS-CoV-2 infection; 15 had possible SARS-CoV-2 infection, 21 had no suspicion of SARS-CoV-2 infection, and 2 were “unclassifiable.”
Of the 11 patients with confirmed/probable SARS-CoV-2 infection, 9 had no serological evidence of any other recent preceding infection known to be associated with GBS.
The other two had serological evidence of a recent Campylobacter jejuni infection, which could have played a role in GBS onset, the researchers noted.
Most patients with a confirmed/probable SARS-CoV-2 infection had a sensorimotor GBS variant (73%), although Miller Fisher syndrome–GBS overlap (18%) and an ataxic variant (9%) were also found.
All patients with a confirmed/probable SARS-CoV-2 infection had a severe form of GBS. Common early neurologic features were facial weakness (64%), sensory deficits (82%), and autonomic dysfunction (64%), although not significantly different, compared with the other patients.
All eight patients who underwent nerve conduction study had a demyelinating subtype, which was more frequent than in the other GBS patients (47%; P = .012) as well as historical region and age-matched controls included in the IGOS cohort before the pandemic (52%, P = .016).
The median time from the onset of SARS-CoV-2 infection to neurologic symptoms was 16 days and ranged from 12 to 22 days.
More research needed
The researchers noted that the 22% frequency of a preceding SARS-CoV-2 infection in this study population was “higher than estimates of the contemporaneous background prevalence of SARS-CoV-2, which may be a result of recruitment bias during the pandemic, but could also indicate that GBS may rarely follow a recent SARS-CoV-2 infection.”
Importantly, however, they did not find more patients diagnosed with GBS during the first 4 months of the pandemic, compared with previous years, “suggesting that a strong association between SARS-CoV-2 and GBS is unlikely.”
“Should SARS-CoV-2 indeed be able to trigger GBS, our data are consistent with a postinfectious disease mechanism rather than direct viral invasion,” they noted, adding that the study was not designed to quantify a causative link between GBS and SARS-CoV-2.
“An unbiased multicenter, international, case-control study is needed to determine whether there is an association or not,” they wrote.
The IGOS is financially supported by the GBS-CIDP Foundation International, Gain, Erasmus MC University Medical Center Rotterdam, Glasgow University, CSL Behring, Grifols, Annexon and Hansa Biopharma. Dr. Jacobs received grants from Grifols, CSL-Behring, Annexon, Prinses Beatrix Spierfonds, Hansa Biopharma, and GBS-CIDP Foundation International and is on the global medical advisory board of the GBS CIDP Foundation International.
A version of this article first appeared on Medscape.com.
Although Guillain-Barré syndrome may rarely follow a recent infection with SARS-CoV-2, a strong relationship of GBS with the novel coronavirus is unlikely, say researchers with the International GBS Outcome Study (IGOS) consortium.
“Our study shows that COVID-19 may precede Guillain-Barré syndrome in rare cases, but the existence of a true association or causal relation still needs to be established,” Bart Jacobs, MD, PhD, department of neurology and immunology, Erasmus Medical Center and University Medical Center, both in Rotterdam, the Netherlands, said in a statement.
The study was published online in the journal Brain.
No uptick in pandemic cases
Since the beginning of the pandemic, there are reports of more than 90 GBS diagnoses following a possible COVID-19 infection. However, it remains unclear whether COVID-19 is another potential infectious trigger or whether the reported cases are coincidental.
To investigate further, Dr. Jacobs and the IGOS consortium reviewed 49 patients (median age, 56 years) with GBS who were added to their ongoing prospective observational cohort study between Jan. 30 and May 30, 2020.
The patients came from China, Denmark, France, Greece, Italy, Japan, the Netherlands, Spain, Switzerland, and the United Kingdom.
Of the 49 GBS patients, 8 (16%) had a confirmed and 3 (6%) had a probable SARS-CoV-2 infection; 15 had possible SARS-CoV-2 infection, 21 had no suspicion of SARS-CoV-2 infection, and 2 were “unclassifiable.”
Of the 11 patients with confirmed/probable SARS-CoV-2 infection, 9 had no serological evidence of any other recent preceding infection known to be associated with GBS.
The other two had serological evidence of a recent Campylobacter jejuni infection, which could have played a role in GBS onset, the researchers noted.
Most patients with a confirmed/probable SARS-CoV-2 infection had a sensorimotor GBS variant (73%), although Miller Fisher syndrome–GBS overlap (18%) and an ataxic variant (9%) were also found.
All patients with a confirmed/probable SARS-CoV-2 infection had a severe form of GBS. Common early neurologic features were facial weakness (64%), sensory deficits (82%), and autonomic dysfunction (64%), although not significantly different, compared with the other patients.
All eight patients who underwent nerve conduction study had a demyelinating subtype, which was more frequent than in the other GBS patients (47%; P = .012) as well as historical region and age-matched controls included in the IGOS cohort before the pandemic (52%, P = .016).
The median time from the onset of SARS-CoV-2 infection to neurologic symptoms was 16 days and ranged from 12 to 22 days.
More research needed
The researchers noted that the 22% frequency of a preceding SARS-CoV-2 infection in this study population was “higher than estimates of the contemporaneous background prevalence of SARS-CoV-2, which may be a result of recruitment bias during the pandemic, but could also indicate that GBS may rarely follow a recent SARS-CoV-2 infection.”
Importantly, however, they did not find more patients diagnosed with GBS during the first 4 months of the pandemic, compared with previous years, “suggesting that a strong association between SARS-CoV-2 and GBS is unlikely.”
“Should SARS-CoV-2 indeed be able to trigger GBS, our data are consistent with a postinfectious disease mechanism rather than direct viral invasion,” they noted, adding that the study was not designed to quantify a causative link between GBS and SARS-CoV-2.
“An unbiased multicenter, international, case-control study is needed to determine whether there is an association or not,” they wrote.
The IGOS is financially supported by the GBS-CIDP Foundation International, Gain, Erasmus MC University Medical Center Rotterdam, Glasgow University, CSL Behring, Grifols, Annexon and Hansa Biopharma. Dr. Jacobs received grants from Grifols, CSL-Behring, Annexon, Prinses Beatrix Spierfonds, Hansa Biopharma, and GBS-CIDP Foundation International and is on the global medical advisory board of the GBS CIDP Foundation International.
A version of this article first appeared on Medscape.com.
Sexual assault in women tied to increased stroke, dementia risk
Traumatic experiences, especially sexual assault, may put women at greater risk for poor brain health.
In the Ms Brain study, middle-aged women with trauma exposure had a greater volume of white matter hyperintensities (WMHs) than those without trauma. In addition, the differences persisted even after adjusting for depressive or post-traumatic stress symptoms.
WMHs are “an important indicator of small vessel disease in the brain and have been linked to future stroke risk, dementia risk, and mortality,” lead investigator Rebecca Thurston, PhD, from the University of Pittsburgh, told this news organization.
“What I take from this is, really, that sexual assault has implications for women’s health, far beyond exclusively mental health outcomes, but also for their cardiovascular health, as we have shown in other work and for their stroke and dementia risk as we are seeing in the present work,” Dr. Thurston added.
The study was presented at the North American Menopause Society (NAMS) Annual Meeting in Washington, D.C., and has been accepted for publication in the journal Brain Imaging and Behavior.
Beyond the usual suspects
As part of the study, 145 women (mean age, 59 years) free of clinical cardiovascular disease, stroke, or dementia provided their medical history, including history of traumatic experiences, depression, and post-traumatic stress disorder and underwent magnetic resonance brain imaging for WMHs.
More than two-thirds (68%) of the women reported at least one trauma, most commonly sexual assault (23%).
In multivariate analysis, women with trauma exposure had greater WMH volume than women without trauma (P = .01), with sexual assault most strongly associated with greater WMH volume (P = .02).
The associations persisted after adjusting for depressive or post-traumatic stress symptoms.
“A history of sexual assault was particularly related to white matter hyperintensities in the parietal lobe, and these kinds of white matter hyperintensities have been linked to Alzheimer’s disease in a fairly pronounced way,” Dr. Thurston said.
“When we think about risk factors for stroke, dementia, we need to think beyond exclusively our usual suspects and also think about women [who experienced] psychological trauma and experienced sexual assault in particular. So ask about it and consider it part of your screening regimen,” she added.
‘Burgeoning’ literature
Commenting on the findings, Charles Nemeroff, MD, PhD, professor and chair, department of psychiatry and behavioral sciences, Dell Medical School, University of Texas at Austin, and director of its Institute for Early Life Adversity Research, said the research adds to the “burgeoning literature on the long term neurobiological consequences of trauma and more specifically, sexual abuse, on brain imaging measures.”
“Our group and others reported several years ago that patients with mood disorders, more specifically bipolar disorder and major depression, had higher rates of WMH than matched controls. Those older studies did not control for a history of early life adversity such as childhood maltreatment,” Dr. Nemeroff said.
“In addition to this finding of increased WMH in subjects exposed to trauma is a very large literature documenting other central nervous system (CNS) changes in this population, including cortical thinning in certain brain areas and clearly an emerging finding that different forms of childhood maltreatment are associated with quite distinct structural brain alterations in adulthood,” he noted.
The study was supported by grants from the National Institutes of Health. Dr. Thurston and Dr. Nemeroff have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Traumatic experiences, especially sexual assault, may put women at greater risk for poor brain health.
In the Ms Brain study, middle-aged women with trauma exposure had a greater volume of white matter hyperintensities (WMHs) than those without trauma. In addition, the differences persisted even after adjusting for depressive or post-traumatic stress symptoms.
WMHs are “an important indicator of small vessel disease in the brain and have been linked to future stroke risk, dementia risk, and mortality,” lead investigator Rebecca Thurston, PhD, from the University of Pittsburgh, told this news organization.
“What I take from this is, really, that sexual assault has implications for women’s health, far beyond exclusively mental health outcomes, but also for their cardiovascular health, as we have shown in other work and for their stroke and dementia risk as we are seeing in the present work,” Dr. Thurston added.
The study was presented at the North American Menopause Society (NAMS) Annual Meeting in Washington, D.C., and has been accepted for publication in the journal Brain Imaging and Behavior.
Beyond the usual suspects
As part of the study, 145 women (mean age, 59 years) free of clinical cardiovascular disease, stroke, or dementia provided their medical history, including history of traumatic experiences, depression, and post-traumatic stress disorder and underwent magnetic resonance brain imaging for WMHs.
More than two-thirds (68%) of the women reported at least one trauma, most commonly sexual assault (23%).
In multivariate analysis, women with trauma exposure had greater WMH volume than women without trauma (P = .01), with sexual assault most strongly associated with greater WMH volume (P = .02).
The associations persisted after adjusting for depressive or post-traumatic stress symptoms.
“A history of sexual assault was particularly related to white matter hyperintensities in the parietal lobe, and these kinds of white matter hyperintensities have been linked to Alzheimer’s disease in a fairly pronounced way,” Dr. Thurston said.
“When we think about risk factors for stroke, dementia, we need to think beyond exclusively our usual suspects and also think about women [who experienced] psychological trauma and experienced sexual assault in particular. So ask about it and consider it part of your screening regimen,” she added.
‘Burgeoning’ literature
Commenting on the findings, Charles Nemeroff, MD, PhD, professor and chair, department of psychiatry and behavioral sciences, Dell Medical School, University of Texas at Austin, and director of its Institute for Early Life Adversity Research, said the research adds to the “burgeoning literature on the long term neurobiological consequences of trauma and more specifically, sexual abuse, on brain imaging measures.”
“Our group and others reported several years ago that patients with mood disorders, more specifically bipolar disorder and major depression, had higher rates of WMH than matched controls. Those older studies did not control for a history of early life adversity such as childhood maltreatment,” Dr. Nemeroff said.
“In addition to this finding of increased WMH in subjects exposed to trauma is a very large literature documenting other central nervous system (CNS) changes in this population, including cortical thinning in certain brain areas and clearly an emerging finding that different forms of childhood maltreatment are associated with quite distinct structural brain alterations in adulthood,” he noted.
The study was supported by grants from the National Institutes of Health. Dr. Thurston and Dr. Nemeroff have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Traumatic experiences, especially sexual assault, may put women at greater risk for poor brain health.
In the Ms Brain study, middle-aged women with trauma exposure had a greater volume of white matter hyperintensities (WMHs) than those without trauma. In addition, the differences persisted even after adjusting for depressive or post-traumatic stress symptoms.
WMHs are “an important indicator of small vessel disease in the brain and have been linked to future stroke risk, dementia risk, and mortality,” lead investigator Rebecca Thurston, PhD, from the University of Pittsburgh, told this news organization.
“What I take from this is, really, that sexual assault has implications for women’s health, far beyond exclusively mental health outcomes, but also for their cardiovascular health, as we have shown in other work and for their stroke and dementia risk as we are seeing in the present work,” Dr. Thurston added.
The study was presented at the North American Menopause Society (NAMS) Annual Meeting in Washington, D.C., and has been accepted for publication in the journal Brain Imaging and Behavior.
Beyond the usual suspects
As part of the study, 145 women (mean age, 59 years) free of clinical cardiovascular disease, stroke, or dementia provided their medical history, including history of traumatic experiences, depression, and post-traumatic stress disorder and underwent magnetic resonance brain imaging for WMHs.
More than two-thirds (68%) of the women reported at least one trauma, most commonly sexual assault (23%).
In multivariate analysis, women with trauma exposure had greater WMH volume than women without trauma (P = .01), with sexual assault most strongly associated with greater WMH volume (P = .02).
The associations persisted after adjusting for depressive or post-traumatic stress symptoms.
“A history of sexual assault was particularly related to white matter hyperintensities in the parietal lobe, and these kinds of white matter hyperintensities have been linked to Alzheimer’s disease in a fairly pronounced way,” Dr. Thurston said.
“When we think about risk factors for stroke, dementia, we need to think beyond exclusively our usual suspects and also think about women [who experienced] psychological trauma and experienced sexual assault in particular. So ask about it and consider it part of your screening regimen,” she added.
‘Burgeoning’ literature
Commenting on the findings, Charles Nemeroff, MD, PhD, professor and chair, department of psychiatry and behavioral sciences, Dell Medical School, University of Texas at Austin, and director of its Institute for Early Life Adversity Research, said the research adds to the “burgeoning literature on the long term neurobiological consequences of trauma and more specifically, sexual abuse, on brain imaging measures.”
“Our group and others reported several years ago that patients with mood disorders, more specifically bipolar disorder and major depression, had higher rates of WMH than matched controls. Those older studies did not control for a history of early life adversity such as childhood maltreatment,” Dr. Nemeroff said.
“In addition to this finding of increased WMH in subjects exposed to trauma is a very large literature documenting other central nervous system (CNS) changes in this population, including cortical thinning in certain brain areas and clearly an emerging finding that different forms of childhood maltreatment are associated with quite distinct structural brain alterations in adulthood,” he noted.
The study was supported by grants from the National Institutes of Health. Dr. Thurston and Dr. Nemeroff have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Nonopioid med promising for neuropathic pain
Top-line results from a phase 2 study suggest vixotrigine (BIIB074, Biogen), a nonopioid investigational oral pain medication, reduces chronic neuropathic pain caused by small fiber neuropathy (SFN) and is generally well tolerated.
“We are encouraged by the overall results of the CONVEY study, especially given the significant unmet medical need for additional agents to treat chronic painful neuropathy,” Katherine Dawson, MD, senior vice president and head of the therapeutics development unit at Biogen, said in a news release.
Vixotrigine (BIIB074) is a peripherally and centrally acting, orally administered, voltage- and use-dependent voltage-gated sodium channel blocker.
CONVEY was a phase 2, placebo-controlled, double-blind, randomized withdrawal study of 265 patients experiencing pain from confirmed idiopathic or diabetes-associated SFN.
Following a 4-week open-label run-in period, 123 responders to vixotrigine were randomly allocated to 200 mg or 350 mg vixotrigine or placebo twice daily for 12 weeks in the double-blind portion of the study.
At week 12, vixotrigine 200 mg twice daily met the primary endpoint of a statistically significant reduction from baseline in the mean average daily pain (ADP) score versus placebo (P = .0501).
A subgroup analysis showed a treatment effect in patients with diabetes-associated SFN but not in the smaller subgroup of patients with idiopathic SFN.
The 200-mg dose also led to a significant improvement over placebo in mean worst daily pain score at 12 weeks (P = .0455).
A numeric advantage of 200 mg vixotrigine over placebo was observed in additional secondary endpoints, including the proportion of patients with at least a 2-point improvement in ADP score and the proportion with at least a 30% reduction in ADP at week 12, but these failed to reach statistical significance.
Vixotrigine 350 mg twice daily did not meet the primary endpoint of mean change in ADP at 12 weeks.
However, treatment at the higher dose led to a significant increase in the proportion of patients who reported being “very much improved” or “much improved” over baseline (P = .0580), Biogen reported.
In addition, a numeric advantage of 350 mg over placebo was observed in the proportion of patients with a 2-point or greater improvement in ADP score and the proportion with at least a 30% reduction in ADP at 12 weeks, but these also did not reach statistical significance.
Both doses of vixotrigine were “generally well tolerated and the safety profile was consistent with previous studies of vixotrigine with no evidence of abuse potential,” the company said.
In the open-label period, common adverse events seen in at least 2.5% of patients were dizziness, headache, vertigo, and nausea; adverse events led 5.3% of patients to discontinue the open-label portion of the study. Across the entire study, most adverse events were mild or moderate in severity.
“The totality of data from the vixotrigine program will inform potential doses for study in future phase 3 clinical trials,” the company said.
A version of this article first appeared on Medscape.com.
Top-line results from a phase 2 study suggest vixotrigine (BIIB074, Biogen), a nonopioid investigational oral pain medication, reduces chronic neuropathic pain caused by small fiber neuropathy (SFN) and is generally well tolerated.
“We are encouraged by the overall results of the CONVEY study, especially given the significant unmet medical need for additional agents to treat chronic painful neuropathy,” Katherine Dawson, MD, senior vice president and head of the therapeutics development unit at Biogen, said in a news release.
Vixotrigine (BIIB074) is a peripherally and centrally acting, orally administered, voltage- and use-dependent voltage-gated sodium channel blocker.
CONVEY was a phase 2, placebo-controlled, double-blind, randomized withdrawal study of 265 patients experiencing pain from confirmed idiopathic or diabetes-associated SFN.
Following a 4-week open-label run-in period, 123 responders to vixotrigine were randomly allocated to 200 mg or 350 mg vixotrigine or placebo twice daily for 12 weeks in the double-blind portion of the study.
At week 12, vixotrigine 200 mg twice daily met the primary endpoint of a statistically significant reduction from baseline in the mean average daily pain (ADP) score versus placebo (P = .0501).
A subgroup analysis showed a treatment effect in patients with diabetes-associated SFN but not in the smaller subgroup of patients with idiopathic SFN.
The 200-mg dose also led to a significant improvement over placebo in mean worst daily pain score at 12 weeks (P = .0455).
A numeric advantage of 200 mg vixotrigine over placebo was observed in additional secondary endpoints, including the proportion of patients with at least a 2-point improvement in ADP score and the proportion with at least a 30% reduction in ADP at week 12, but these failed to reach statistical significance.
Vixotrigine 350 mg twice daily did not meet the primary endpoint of mean change in ADP at 12 weeks.
However, treatment at the higher dose led to a significant increase in the proportion of patients who reported being “very much improved” or “much improved” over baseline (P = .0580), Biogen reported.
In addition, a numeric advantage of 350 mg over placebo was observed in the proportion of patients with a 2-point or greater improvement in ADP score and the proportion with at least a 30% reduction in ADP at 12 weeks, but these also did not reach statistical significance.
Both doses of vixotrigine were “generally well tolerated and the safety profile was consistent with previous studies of vixotrigine with no evidence of abuse potential,” the company said.
In the open-label period, common adverse events seen in at least 2.5% of patients were dizziness, headache, vertigo, and nausea; adverse events led 5.3% of patients to discontinue the open-label portion of the study. Across the entire study, most adverse events were mild or moderate in severity.
“The totality of data from the vixotrigine program will inform potential doses for study in future phase 3 clinical trials,” the company said.
A version of this article first appeared on Medscape.com.
Top-line results from a phase 2 study suggest vixotrigine (BIIB074, Biogen), a nonopioid investigational oral pain medication, reduces chronic neuropathic pain caused by small fiber neuropathy (SFN) and is generally well tolerated.
“We are encouraged by the overall results of the CONVEY study, especially given the significant unmet medical need for additional agents to treat chronic painful neuropathy,” Katherine Dawson, MD, senior vice president and head of the therapeutics development unit at Biogen, said in a news release.
Vixotrigine (BIIB074) is a peripherally and centrally acting, orally administered, voltage- and use-dependent voltage-gated sodium channel blocker.
CONVEY was a phase 2, placebo-controlled, double-blind, randomized withdrawal study of 265 patients experiencing pain from confirmed idiopathic or diabetes-associated SFN.
Following a 4-week open-label run-in period, 123 responders to vixotrigine were randomly allocated to 200 mg or 350 mg vixotrigine or placebo twice daily for 12 weeks in the double-blind portion of the study.
At week 12, vixotrigine 200 mg twice daily met the primary endpoint of a statistically significant reduction from baseline in the mean average daily pain (ADP) score versus placebo (P = .0501).
A subgroup analysis showed a treatment effect in patients with diabetes-associated SFN but not in the smaller subgroup of patients with idiopathic SFN.
The 200-mg dose also led to a significant improvement over placebo in mean worst daily pain score at 12 weeks (P = .0455).
A numeric advantage of 200 mg vixotrigine over placebo was observed in additional secondary endpoints, including the proportion of patients with at least a 2-point improvement in ADP score and the proportion with at least a 30% reduction in ADP at week 12, but these failed to reach statistical significance.
Vixotrigine 350 mg twice daily did not meet the primary endpoint of mean change in ADP at 12 weeks.
However, treatment at the higher dose led to a significant increase in the proportion of patients who reported being “very much improved” or “much improved” over baseline (P = .0580), Biogen reported.
In addition, a numeric advantage of 350 mg over placebo was observed in the proportion of patients with a 2-point or greater improvement in ADP score and the proportion with at least a 30% reduction in ADP at 12 weeks, but these also did not reach statistical significance.
Both doses of vixotrigine were “generally well tolerated and the safety profile was consistent with previous studies of vixotrigine with no evidence of abuse potential,” the company said.
In the open-label period, common adverse events seen in at least 2.5% of patients were dizziness, headache, vertigo, and nausea; adverse events led 5.3% of patients to discontinue the open-label portion of the study. Across the entire study, most adverse events were mild or moderate in severity.
“The totality of data from the vixotrigine program will inform potential doses for study in future phase 3 clinical trials,” the company said.
A version of this article first appeared on Medscape.com.
ADHD a new risk factor for Alzheimer’s?
results from a large, multigenerational study show.
“The findings suggest there are common genetic and/or environmental contributions to the association between ADHD and dementia,” study investigator Zheng Chang, PhD, from the department of medical epidemiology and biostatistics at Karolinska Institute, Stockholm, said in a statement.
“There have been few studies previously on the link between ADHD and dementia, all with limited sample size,” Dr. Chang said in an interview.
“This is the first study to look at ADHD and dementia within extended families. It’s a large population-based study including over 2 million individuals and their over 5 million biological relatives,” he noted.
The study was published online Sept. 9, 2021, in the journal Alzheimer’s & Dementia.
Shared familial risk
The researchers identified roughly 2.1 million people born in Sweden between 1980 and 2001. Overall, 3.2% of the cohort had a diagnosis of ADHD.
Using national registries, they linked these individuals to more than 5 million of their biological relatives including parents, grandparents, uncles, and aunts and determined which of these relatives developed dementia over time.
In adjusted analyses, parents of individuals with ADHD had 34% higher risk for any dementia than parents of those without ADHD (hazard ratio, 1.34; 95% CI, 1.11-1.63).
The risk for AD, the most common type of dementia, was 55% higher in parents of individuals with ADHD (HR, 1.55; 95% CI, 1.26-1.89).
Individuals with ADHD were more likely to have parents with early-onset dementia rather than late-onset dementia. However, the absolute risk for dementia was low for the parent cohort: Only 0.17% of the parents were diagnosed with dementia during follow-up.
The association between ADHD and dementia was not as strong for second-degree relatives of individuals with ADHD. For example, grandparents of individuals with ADHD had a 10% increased risk for dementia, compared with grandparents of individuals without ADHD.
The finding of attenuated associations with decreasing genetic relatedness (parents > grandparents and uncles/aunts), points to shared familial risk between ADHD and AD, the researchers said.
There could be “undiscovered genetic variants that contribute to either traits or family-wide environmental risk factors, such as socioeconomic status, that may have an impact on the association,” Dr. Chang said in the news release.
“There are no direct clinical implications from this study, but research like this could lead to further research with goals for improved detection, prevention, and treatment,” he said in an interview.
More questions than answers
Heather Snyder, PhD, vice president of medical and scientific relations for the Alzheimer’s Association that the way different brain diseases are linked “is a question the Alzheimer’s Association is often asked, and it is a part of our funding portfolio to get that question answered.”
This study looking at ADHD and dementia is “intriguing,” Dr. Snyder said, “because, right now, there is limited information available. That said, this is an association study; it shows that two things are somehow connected. Because of how the study was conducted, it does not – and cannot – prove causation,” Dr. Snyder said. “But it is interesting all the same. More research is needed to uncover specifically why and how these two diseases are related. That might eventually give us insight into how to manage risk or even improve treatment.”
The study was supported by grants from the Swedish Council for Health, Working Life and Welfare, the Swedish Research Council, the Swedish Brain Foundation, the European Union’s Horizon 2020 research and innovation program under the Marie Skłodowska-Curie, the Fredrik & Ingrid Thurings Stiftelse, and the Karolinska Institutet Research Foundation. Dr. Chang and Dr. Snyder disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
results from a large, multigenerational study show.
“The findings suggest there are common genetic and/or environmental contributions to the association between ADHD and dementia,” study investigator Zheng Chang, PhD, from the department of medical epidemiology and biostatistics at Karolinska Institute, Stockholm, said in a statement.
“There have been few studies previously on the link between ADHD and dementia, all with limited sample size,” Dr. Chang said in an interview.
“This is the first study to look at ADHD and dementia within extended families. It’s a large population-based study including over 2 million individuals and their over 5 million biological relatives,” he noted.
The study was published online Sept. 9, 2021, in the journal Alzheimer’s & Dementia.
Shared familial risk
The researchers identified roughly 2.1 million people born in Sweden between 1980 and 2001. Overall, 3.2% of the cohort had a diagnosis of ADHD.
Using national registries, they linked these individuals to more than 5 million of their biological relatives including parents, grandparents, uncles, and aunts and determined which of these relatives developed dementia over time.
In adjusted analyses, parents of individuals with ADHD had 34% higher risk for any dementia than parents of those without ADHD (hazard ratio, 1.34; 95% CI, 1.11-1.63).
The risk for AD, the most common type of dementia, was 55% higher in parents of individuals with ADHD (HR, 1.55; 95% CI, 1.26-1.89).
Individuals with ADHD were more likely to have parents with early-onset dementia rather than late-onset dementia. However, the absolute risk for dementia was low for the parent cohort: Only 0.17% of the parents were diagnosed with dementia during follow-up.
The association between ADHD and dementia was not as strong for second-degree relatives of individuals with ADHD. For example, grandparents of individuals with ADHD had a 10% increased risk for dementia, compared with grandparents of individuals without ADHD.
The finding of attenuated associations with decreasing genetic relatedness (parents > grandparents and uncles/aunts), points to shared familial risk between ADHD and AD, the researchers said.
There could be “undiscovered genetic variants that contribute to either traits or family-wide environmental risk factors, such as socioeconomic status, that may have an impact on the association,” Dr. Chang said in the news release.
“There are no direct clinical implications from this study, but research like this could lead to further research with goals for improved detection, prevention, and treatment,” he said in an interview.
More questions than answers
Heather Snyder, PhD, vice president of medical and scientific relations for the Alzheimer’s Association that the way different brain diseases are linked “is a question the Alzheimer’s Association is often asked, and it is a part of our funding portfolio to get that question answered.”
This study looking at ADHD and dementia is “intriguing,” Dr. Snyder said, “because, right now, there is limited information available. That said, this is an association study; it shows that two things are somehow connected. Because of how the study was conducted, it does not – and cannot – prove causation,” Dr. Snyder said. “But it is interesting all the same. More research is needed to uncover specifically why and how these two diseases are related. That might eventually give us insight into how to manage risk or even improve treatment.”
The study was supported by grants from the Swedish Council for Health, Working Life and Welfare, the Swedish Research Council, the Swedish Brain Foundation, the European Union’s Horizon 2020 research and innovation program under the Marie Skłodowska-Curie, the Fredrik & Ingrid Thurings Stiftelse, and the Karolinska Institutet Research Foundation. Dr. Chang and Dr. Snyder disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
results from a large, multigenerational study show.
“The findings suggest there are common genetic and/or environmental contributions to the association between ADHD and dementia,” study investigator Zheng Chang, PhD, from the department of medical epidemiology and biostatistics at Karolinska Institute, Stockholm, said in a statement.
“There have been few studies previously on the link between ADHD and dementia, all with limited sample size,” Dr. Chang said in an interview.
“This is the first study to look at ADHD and dementia within extended families. It’s a large population-based study including over 2 million individuals and their over 5 million biological relatives,” he noted.
The study was published online Sept. 9, 2021, in the journal Alzheimer’s & Dementia.
Shared familial risk
The researchers identified roughly 2.1 million people born in Sweden between 1980 and 2001. Overall, 3.2% of the cohort had a diagnosis of ADHD.
Using national registries, they linked these individuals to more than 5 million of their biological relatives including parents, grandparents, uncles, and aunts and determined which of these relatives developed dementia over time.
In adjusted analyses, parents of individuals with ADHD had 34% higher risk for any dementia than parents of those without ADHD (hazard ratio, 1.34; 95% CI, 1.11-1.63).
The risk for AD, the most common type of dementia, was 55% higher in parents of individuals with ADHD (HR, 1.55; 95% CI, 1.26-1.89).
Individuals with ADHD were more likely to have parents with early-onset dementia rather than late-onset dementia. However, the absolute risk for dementia was low for the parent cohort: Only 0.17% of the parents were diagnosed with dementia during follow-up.
The association between ADHD and dementia was not as strong for second-degree relatives of individuals with ADHD. For example, grandparents of individuals with ADHD had a 10% increased risk for dementia, compared with grandparents of individuals without ADHD.
The finding of attenuated associations with decreasing genetic relatedness (parents > grandparents and uncles/aunts), points to shared familial risk between ADHD and AD, the researchers said.
There could be “undiscovered genetic variants that contribute to either traits or family-wide environmental risk factors, such as socioeconomic status, that may have an impact on the association,” Dr. Chang said in the news release.
“There are no direct clinical implications from this study, but research like this could lead to further research with goals for improved detection, prevention, and treatment,” he said in an interview.
More questions than answers
Heather Snyder, PhD, vice president of medical and scientific relations for the Alzheimer’s Association that the way different brain diseases are linked “is a question the Alzheimer’s Association is often asked, and it is a part of our funding portfolio to get that question answered.”
This study looking at ADHD and dementia is “intriguing,” Dr. Snyder said, “because, right now, there is limited information available. That said, this is an association study; it shows that two things are somehow connected. Because of how the study was conducted, it does not – and cannot – prove causation,” Dr. Snyder said. “But it is interesting all the same. More research is needed to uncover specifically why and how these two diseases are related. That might eventually give us insight into how to manage risk or even improve treatment.”
The study was supported by grants from the Swedish Council for Health, Working Life and Welfare, the Swedish Research Council, the Swedish Brain Foundation, the European Union’s Horizon 2020 research and innovation program under the Marie Skłodowska-Curie, the Fredrik & Ingrid Thurings Stiftelse, and the Karolinska Institutet Research Foundation. Dr. Chang and Dr. Snyder disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
New guidance on preventing cutaneous SCC in solid organ transplant patients
An expert panel of 48 dermatologists from 13 countries has developed recommendations to guide efforts aimed at preventing cutaneous squamous cell carcinoma (CSCC) in solid organ transplant recipients.
The recommendations were published online on Sept. 1 in JAMA Dermatology.
Because of lifelong immunosuppression, solid organ transplant recipients (SOTRs) have a risk of CSCC that is 20-200 times higher than in the general population and despite a growing literature on prevention of CSCC in these patients, uncertainty remains regarding best practices for various patient scenarios.
Paul Massey, MD, MPH, of the department of dermatology, Brigham and Women’s Hospital, Boston, and colleagues used a Delphi process to identify consensus-based medical management recommendations for prevention of CSCC in SOTRs.
The survey design was guided by a novel actinic damage and skin cancer index (AD-SCI) made up of six ordinal stages corresponding to an increasing burden of actinic damage and CSCC.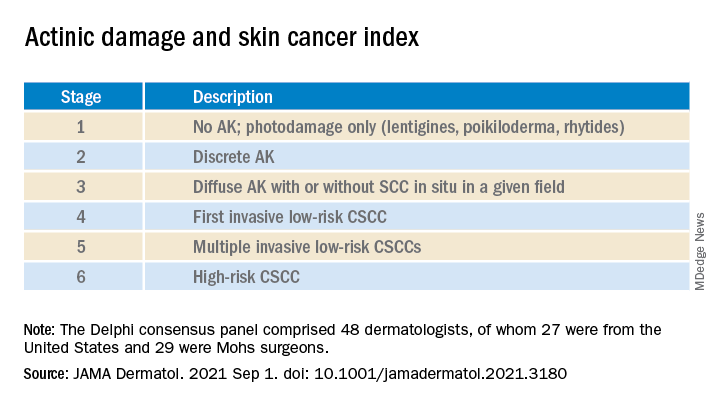
The AD-SCI stage-based recommendations were established when consensus was reached (80% or higher concordance) or near consensus was reached (70%-80% concordance) among panel members.
For five of the six AD-SCI stages, the panel was able to make recommendations. Key recommendations include:
- Cryotherapy for scattered AK.
- Field therapy for AK when grouped in one site, unless AKs are thick, in which case field therapy and cryotherapy are recommended.
- Combination lesion-directed and field therapy with fluorouracil for field cancerized skin.
- Initiation of acitretin therapy and discussion of immunosuppression reduction or modification for patients who develop multiple CSCCs at a high rate (10 per year) or develop high-risk CSCC (defined by a tumor with roughly ≥20% risk of nodal metastasis). The panel did not make a recommendation as to the best immunosuppression modification strategy to pursue.
Lingering questions
The panel was unable to reach consensus on a recommendation for SOTRs with a first low-risk CSCC, reflecting “clinical equipoise” in this situation and the need for further study in this clinical scenario, they say.
The panel did not make a recommendation for use of nicotinamide or capecitabine in any of the six stages, which is “notable,” they acknowledge, given results of a double-blind randomized controlled trial in immunocompetent patients demonstrating benefit in preventing AKs and CSCCs, as reported previously.
Nearly three-quarters of the panel felt that a lack of efficacy data specifically for the SOTR population limited their use of nicotinamide. “Given the low cost, high safety, and demonstration of CSCC reduction in non-SOTRs, nicotinamide administration may be an area for further consideration and expanded study,” the panel wrote.
As for capecitabine, the panel notes that case series in SOTRs have found efficacy for chemoprevention, but randomized controlled studies are lacking. More than half of the panel noted that they did not have routine access to capecitabine in their practice.
The panel recommended routine skin surveillance and sunscreen use for all patients.
“These recommendations reflect consensus among expert transplant dermatologists and the incorporation of limited and sometimes contradictory evidence into real-world clinical experience across a range of CSCC disease severity,” the panel said.
“Areas of consensus may aid physicians in establishing best practices regarding prevention of CSCC in SOTRs in the setting of limited high level of evidence data in this population,” they added.
This research had no specific funding. Author disclosures included serving as a consultant to Regeneron, Sanofi, and receiving research funding from Castle Biosciences, Regeneron, Novartis, and Genentech. A complete list of disclosures for panel members is available with the original article.
An expert panel of 48 dermatologists from 13 countries has developed recommendations to guide efforts aimed at preventing cutaneous squamous cell carcinoma (CSCC) in solid organ transplant recipients.
The recommendations were published online on Sept. 1 in JAMA Dermatology.
Because of lifelong immunosuppression, solid organ transplant recipients (SOTRs) have a risk of CSCC that is 20-200 times higher than in the general population and despite a growing literature on prevention of CSCC in these patients, uncertainty remains regarding best practices for various patient scenarios.
Paul Massey, MD, MPH, of the department of dermatology, Brigham and Women’s Hospital, Boston, and colleagues used a Delphi process to identify consensus-based medical management recommendations for prevention of CSCC in SOTRs.
The survey design was guided by a novel actinic damage and skin cancer index (AD-SCI) made up of six ordinal stages corresponding to an increasing burden of actinic damage and CSCC.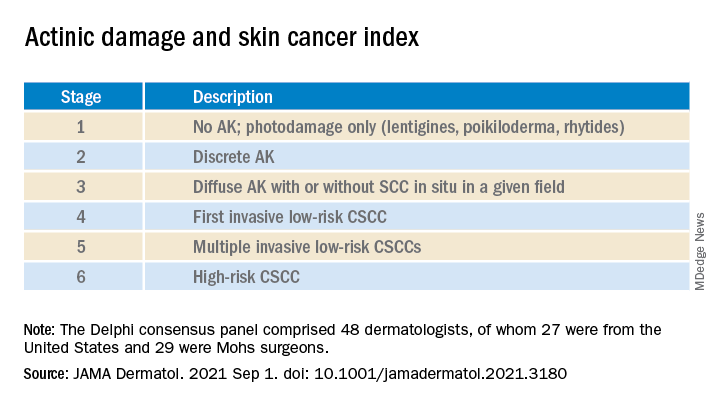
The AD-SCI stage-based recommendations were established when consensus was reached (80% or higher concordance) or near consensus was reached (70%-80% concordance) among panel members.
For five of the six AD-SCI stages, the panel was able to make recommendations. Key recommendations include:
- Cryotherapy for scattered AK.
- Field therapy for AK when grouped in one site, unless AKs are thick, in which case field therapy and cryotherapy are recommended.
- Combination lesion-directed and field therapy with fluorouracil for field cancerized skin.
- Initiation of acitretin therapy and discussion of immunosuppression reduction or modification for patients who develop multiple CSCCs at a high rate (10 per year) or develop high-risk CSCC (defined by a tumor with roughly ≥20% risk of nodal metastasis). The panel did not make a recommendation as to the best immunosuppression modification strategy to pursue.
Lingering questions
The panel was unable to reach consensus on a recommendation for SOTRs with a first low-risk CSCC, reflecting “clinical equipoise” in this situation and the need for further study in this clinical scenario, they say.
The panel did not make a recommendation for use of nicotinamide or capecitabine in any of the six stages, which is “notable,” they acknowledge, given results of a double-blind randomized controlled trial in immunocompetent patients demonstrating benefit in preventing AKs and CSCCs, as reported previously.
Nearly three-quarters of the panel felt that a lack of efficacy data specifically for the SOTR population limited their use of nicotinamide. “Given the low cost, high safety, and demonstration of CSCC reduction in non-SOTRs, nicotinamide administration may be an area for further consideration and expanded study,” the panel wrote.
As for capecitabine, the panel notes that case series in SOTRs have found efficacy for chemoprevention, but randomized controlled studies are lacking. More than half of the panel noted that they did not have routine access to capecitabine in their practice.
The panel recommended routine skin surveillance and sunscreen use for all patients.
“These recommendations reflect consensus among expert transplant dermatologists and the incorporation of limited and sometimes contradictory evidence into real-world clinical experience across a range of CSCC disease severity,” the panel said.
“Areas of consensus may aid physicians in establishing best practices regarding prevention of CSCC in SOTRs in the setting of limited high level of evidence data in this population,” they added.
This research had no specific funding. Author disclosures included serving as a consultant to Regeneron, Sanofi, and receiving research funding from Castle Biosciences, Regeneron, Novartis, and Genentech. A complete list of disclosures for panel members is available with the original article.
An expert panel of 48 dermatologists from 13 countries has developed recommendations to guide efforts aimed at preventing cutaneous squamous cell carcinoma (CSCC) in solid organ transplant recipients.
The recommendations were published online on Sept. 1 in JAMA Dermatology.
Because of lifelong immunosuppression, solid organ transplant recipients (SOTRs) have a risk of CSCC that is 20-200 times higher than in the general population and despite a growing literature on prevention of CSCC in these patients, uncertainty remains regarding best practices for various patient scenarios.
Paul Massey, MD, MPH, of the department of dermatology, Brigham and Women’s Hospital, Boston, and colleagues used a Delphi process to identify consensus-based medical management recommendations for prevention of CSCC in SOTRs.
The survey design was guided by a novel actinic damage and skin cancer index (AD-SCI) made up of six ordinal stages corresponding to an increasing burden of actinic damage and CSCC.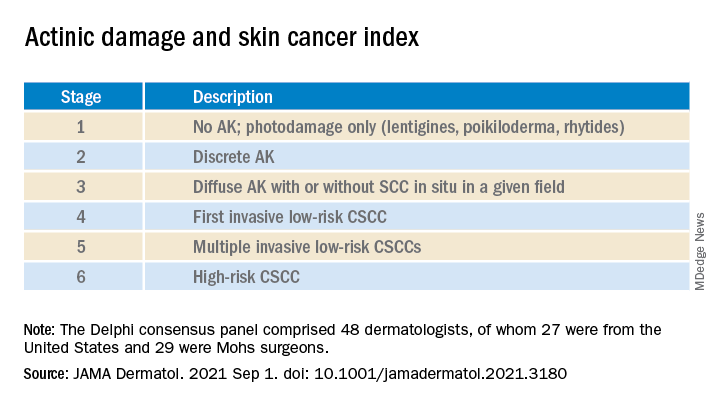
The AD-SCI stage-based recommendations were established when consensus was reached (80% or higher concordance) or near consensus was reached (70%-80% concordance) among panel members.
For five of the six AD-SCI stages, the panel was able to make recommendations. Key recommendations include:
- Cryotherapy for scattered AK.
- Field therapy for AK when grouped in one site, unless AKs are thick, in which case field therapy and cryotherapy are recommended.
- Combination lesion-directed and field therapy with fluorouracil for field cancerized skin.
- Initiation of acitretin therapy and discussion of immunosuppression reduction or modification for patients who develop multiple CSCCs at a high rate (10 per year) or develop high-risk CSCC (defined by a tumor with roughly ≥20% risk of nodal metastasis). The panel did not make a recommendation as to the best immunosuppression modification strategy to pursue.
Lingering questions
The panel was unable to reach consensus on a recommendation for SOTRs with a first low-risk CSCC, reflecting “clinical equipoise” in this situation and the need for further study in this clinical scenario, they say.
The panel did not make a recommendation for use of nicotinamide or capecitabine in any of the six stages, which is “notable,” they acknowledge, given results of a double-blind randomized controlled trial in immunocompetent patients demonstrating benefit in preventing AKs and CSCCs, as reported previously.
Nearly three-quarters of the panel felt that a lack of efficacy data specifically for the SOTR population limited their use of nicotinamide. “Given the low cost, high safety, and demonstration of CSCC reduction in non-SOTRs, nicotinamide administration may be an area for further consideration and expanded study,” the panel wrote.
As for capecitabine, the panel notes that case series in SOTRs have found efficacy for chemoprevention, but randomized controlled studies are lacking. More than half of the panel noted that they did not have routine access to capecitabine in their practice.
The panel recommended routine skin surveillance and sunscreen use for all patients.
“These recommendations reflect consensus among expert transplant dermatologists and the incorporation of limited and sometimes contradictory evidence into real-world clinical experience across a range of CSCC disease severity,” the panel said.
“Areas of consensus may aid physicians in establishing best practices regarding prevention of CSCC in SOTRs in the setting of limited high level of evidence data in this population,” they added.
This research had no specific funding. Author disclosures included serving as a consultant to Regeneron, Sanofi, and receiving research funding from Castle Biosciences, Regeneron, Novartis, and Genentech. A complete list of disclosures for panel members is available with the original article.
Seizure a first sign of COVID in kids?
Unlike in adults, seizures, including status epilepticus (SE), may be the first and main manifestation of COVID-19 in children, new research suggests.
Seizures may occur even in children with no history of epilepsy and in the absence of fever or severe COVID-19 illness, necessitating a “high index” of suspicion for the virus to make an early diagnosis and allow for appropriate infection control measures, say the researchers.
“We hope to increase physicians’ awareness of noninfluenza-like presentations of COVID in children. In areas with a high prevalence of COVID, we suggest that children with seizures be tested for COVID,” Tal Gilboa, MD, director of the child neurology unit and codirector of epilepsy, Hadassah Medical Center, Jerusalem, told this news organization.
The study was published online August 27 in the journal Seizure.
Presenting symptom
Among 175 children diagnosed with acute SARS-CoV-2 infection in the emergency department over 10 months in 2020, 11 (6%) presented with seizures. Studies in adults with COVID-19 have reported seizures in 0% to 2% of cases, the investigators note.
The 11 children with seizures (seven boys) ranged in age from 6 months to 17 years (median age, 11.5 years). All of them had seizures as the presenting sign of infection and none had severe COVID-19 requiring ventilatory or hemodynamic support. Six of the 11 children presented with fever.
Seven of the children had a prior history of neurological disorder: Five had epilepsy, one had a single unprovoked seizure 3 years before admission, and one had an intellectual disability. Three of the children had uncontrolled seizures despite appropriate treatment with antiseizure medication.
Nine of the 11 children presented with generalized tonic-clonic seizures. One child with a prior history of uncontrolled epilepsy with multiple seizure types had a focal tonic seizure. The youngest patient, a 5-month-old infant, presented with bilateral asymmetrical tonic-clonic seizure.
Of note, say the investigators, five of the 11 children presented with convulsive SE; none had a history of prior SE, and one had no history of seizures.
Although young age, especially under 12 months, is a known risk factor for SE, four of the five patients with SE were between 5 and 17 years old. All five children with SE responded to treatment with antiseizure medications.
All 11 children made a full recovery while in hospital, although further follow-up is essential to determine long-term outcomes, the researchers report.
“Children with no prior history of epilepsy and those with well-controlled epilepsy who present with breakthrough seizures, regardless of their body temperature, should be considered as potentially infected by SARS-CoV-2,” said Dr. Gilboa.
“It is possible, however unlikely, that a child, especially with prior epilepsy, may have an unprovoked seizure while being asymptomatically infected by SARS-CoV-2; in any case, infection control measures should be taken,” Dr. Gilboa added.
Need for replication
Weighing in on the study, Carl E. Stafstrom, MD, PhD, professor of neurology and pediatrics, Johns Hopkins University, Baltimore, said it’s important to note that “about half of the children had had epilepsy already, and for whatever reason, had a seizure, which required an ED visit, and then they found COVID.”
“Nevertheless, this article is interesting and surprising in what they found because nobody else has found nearly as frequent a seizure presentation,” said Dr. Stafstrom, director of the John M. Freeman Pediatric Epilepsy Center, Johns Hopkins Medicine.
“We would want to see some replication from other institutions and other populations,” he added.
The study had no specific funding. Dr. Gilboa and Dr. Stafstrom have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Unlike in adults, seizures, including status epilepticus (SE), may be the first and main manifestation of COVID-19 in children, new research suggests.
Seizures may occur even in children with no history of epilepsy and in the absence of fever or severe COVID-19 illness, necessitating a “high index” of suspicion for the virus to make an early diagnosis and allow for appropriate infection control measures, say the researchers.
“We hope to increase physicians’ awareness of noninfluenza-like presentations of COVID in children. In areas with a high prevalence of COVID, we suggest that children with seizures be tested for COVID,” Tal Gilboa, MD, director of the child neurology unit and codirector of epilepsy, Hadassah Medical Center, Jerusalem, told this news organization.
The study was published online August 27 in the journal Seizure.
Presenting symptom
Among 175 children diagnosed with acute SARS-CoV-2 infection in the emergency department over 10 months in 2020, 11 (6%) presented with seizures. Studies in adults with COVID-19 have reported seizures in 0% to 2% of cases, the investigators note.
The 11 children with seizures (seven boys) ranged in age from 6 months to 17 years (median age, 11.5 years). All of them had seizures as the presenting sign of infection and none had severe COVID-19 requiring ventilatory or hemodynamic support. Six of the 11 children presented with fever.
Seven of the children had a prior history of neurological disorder: Five had epilepsy, one had a single unprovoked seizure 3 years before admission, and one had an intellectual disability. Three of the children had uncontrolled seizures despite appropriate treatment with antiseizure medication.
Nine of the 11 children presented with generalized tonic-clonic seizures. One child with a prior history of uncontrolled epilepsy with multiple seizure types had a focal tonic seizure. The youngest patient, a 5-month-old infant, presented with bilateral asymmetrical tonic-clonic seizure.
Of note, say the investigators, five of the 11 children presented with convulsive SE; none had a history of prior SE, and one had no history of seizures.
Although young age, especially under 12 months, is a known risk factor for SE, four of the five patients with SE were between 5 and 17 years old. All five children with SE responded to treatment with antiseizure medications.
All 11 children made a full recovery while in hospital, although further follow-up is essential to determine long-term outcomes, the researchers report.
“Children with no prior history of epilepsy and those with well-controlled epilepsy who present with breakthrough seizures, regardless of their body temperature, should be considered as potentially infected by SARS-CoV-2,” said Dr. Gilboa.
“It is possible, however unlikely, that a child, especially with prior epilepsy, may have an unprovoked seizure while being asymptomatically infected by SARS-CoV-2; in any case, infection control measures should be taken,” Dr. Gilboa added.
Need for replication
Weighing in on the study, Carl E. Stafstrom, MD, PhD, professor of neurology and pediatrics, Johns Hopkins University, Baltimore, said it’s important to note that “about half of the children had had epilepsy already, and for whatever reason, had a seizure, which required an ED visit, and then they found COVID.”
“Nevertheless, this article is interesting and surprising in what they found because nobody else has found nearly as frequent a seizure presentation,” said Dr. Stafstrom, director of the John M. Freeman Pediatric Epilepsy Center, Johns Hopkins Medicine.
“We would want to see some replication from other institutions and other populations,” he added.
The study had no specific funding. Dr. Gilboa and Dr. Stafstrom have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Unlike in adults, seizures, including status epilepticus (SE), may be the first and main manifestation of COVID-19 in children, new research suggests.
Seizures may occur even in children with no history of epilepsy and in the absence of fever or severe COVID-19 illness, necessitating a “high index” of suspicion for the virus to make an early diagnosis and allow for appropriate infection control measures, say the researchers.
“We hope to increase physicians’ awareness of noninfluenza-like presentations of COVID in children. In areas with a high prevalence of COVID, we suggest that children with seizures be tested for COVID,” Tal Gilboa, MD, director of the child neurology unit and codirector of epilepsy, Hadassah Medical Center, Jerusalem, told this news organization.
The study was published online August 27 in the journal Seizure.
Presenting symptom
Among 175 children diagnosed with acute SARS-CoV-2 infection in the emergency department over 10 months in 2020, 11 (6%) presented with seizures. Studies in adults with COVID-19 have reported seizures in 0% to 2% of cases, the investigators note.
The 11 children with seizures (seven boys) ranged in age from 6 months to 17 years (median age, 11.5 years). All of them had seizures as the presenting sign of infection and none had severe COVID-19 requiring ventilatory or hemodynamic support. Six of the 11 children presented with fever.
Seven of the children had a prior history of neurological disorder: Five had epilepsy, one had a single unprovoked seizure 3 years before admission, and one had an intellectual disability. Three of the children had uncontrolled seizures despite appropriate treatment with antiseizure medication.
Nine of the 11 children presented with generalized tonic-clonic seizures. One child with a prior history of uncontrolled epilepsy with multiple seizure types had a focal tonic seizure. The youngest patient, a 5-month-old infant, presented with bilateral asymmetrical tonic-clonic seizure.
Of note, say the investigators, five of the 11 children presented with convulsive SE; none had a history of prior SE, and one had no history of seizures.
Although young age, especially under 12 months, is a known risk factor for SE, four of the five patients with SE were between 5 and 17 years old. All five children with SE responded to treatment with antiseizure medications.
All 11 children made a full recovery while in hospital, although further follow-up is essential to determine long-term outcomes, the researchers report.
“Children with no prior history of epilepsy and those with well-controlled epilepsy who present with breakthrough seizures, regardless of their body temperature, should be considered as potentially infected by SARS-CoV-2,” said Dr. Gilboa.
“It is possible, however unlikely, that a child, especially with prior epilepsy, may have an unprovoked seizure while being asymptomatically infected by SARS-CoV-2; in any case, infection control measures should be taken,” Dr. Gilboa added.
Need for replication
Weighing in on the study, Carl E. Stafstrom, MD, PhD, professor of neurology and pediatrics, Johns Hopkins University, Baltimore, said it’s important to note that “about half of the children had had epilepsy already, and for whatever reason, had a seizure, which required an ED visit, and then they found COVID.”
“Nevertheless, this article is interesting and surprising in what they found because nobody else has found nearly as frequent a seizure presentation,” said Dr. Stafstrom, director of the John M. Freeman Pediatric Epilepsy Center, Johns Hopkins Medicine.
“We would want to see some replication from other institutions and other populations,” he added.
The study had no specific funding. Dr. Gilboa and Dr. Stafstrom have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.

