User login
ObGyn salaries jumped in the last year
The mean income for ObGyns rose by 10% in 2015 over 2014 ($277,000 compared with $249,000), according to a recent report from Medscape.1 This jump follows a gradual increase over the last few years ($243,000 in 2013; $242,000 in 2012; $220,000 in 2011).1−3 The report included responses from 19,183 physicians across 26 specialties, 5% (nearly 1,000) of whom were ObGyns.1
The highest earners among all physician specialties were orthopedists ($443,000), cardiologists, and dermatologists. The lowest earners were pediatricians ($204,000), endocrinologists, and family physicians. The highest ObGyn earners lived in the Southwest ($307,000), the North Central region, and the West.1
Merritt Hawkins & Associates, a national physician search and consulting firm, recently evaluated the annual starting salaries and year-over-year increases of 3,342 of its physician and advanced practitioner recruiting assignments. They found that ObGyns had the second greatest increase in starting salaries among specialties, at 16%. They also found obstetrics and gynecology to be among the top 5 specialties most in demand.4
The gender picture
As in past years, male ObGyns reported higher earnings than their female counterparts: full-time male ObGyns earned $304,000 while full-time female ObGyns earned $256,000.1
According to a report published in the British Medical Journal in June 2016, there are drastic differences between the incomes of white and black male and female physicians in the United States.5 White male physicians had an adjusted median annual income of $253,042 (95% confidence interval [CI], $248,670−$257,413), compared with $188,230 ($170,844−$205,616) for black male physicians, $163,234 (95% CI, $159,912−$166,557) for white female physicians, and $152,784 (95% CI, $137,927−$167,641) for black female physicians.
How does employment status factor in? Of the self-employed, men earn $310,000 while women earn $285,000. Men who are employed report earning $293,000, with women reporting $244,000.5 (This includes full-time workers but does not control for the number of hours worked.) When Medscape evaluated full- versus part-time work (<40 hours per week), results indicated that, among primary care and most other specialties, more female physicians (25%) are part-timers than males (12%).6 However, among ObGyns, 13% of women report part-time employment versus 16% of men.1
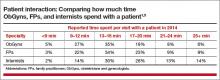
Time with patients. Medscape reports that, among all physicians, 41% of men spent 17 minutes or more with their patients, compared with 49% of women. For office-based ObGyns, 31% of men and 39% of women spent 17 minutes or more with patients.1
Can disparity in leadership positions explain gender-related salary discrepancy?
In 2015, 48% of all medical students were female.7 In residency, the ratio of men to women is similar: For 2013−2014, the Association of American Medical Colleges (AAMC) reported that 46% of all residents were female.8 For ObGyn residency, however, the AMA’s FREIDA Online specialty training search (detailing 2014 general program information) indicates that, of the 5,018 active residents and fellows in ObGyn, 81.4% are female.9
Although the ObGyn field is becoming female-dominated, leadership within the specialty remains male dominated, points out Laura E. Baecher-Lind, MD, MPH, Director of the Division of General Obstetrics & Gynecology at Tufts Medical Center, Boston, Massachusetts. Dr. Baecher-Lind authored a study in 2012 in which she explored whether the proportions of ObGyn leadership positions held by women reflect the proportion of women who entered the field at the same time as current leaders.10 She found that very few academic department chair positions in ObGyn are held by women, although that number is gradually increasing.10 In addition, her study results indicated that women should hold 71 of the total of 194 ObGyn leadership positions. In actuality, 41 of the leadership positions were held by women (21.1%, P<.001) when based on the proportion of women entering residency programs. When considering only leaders who graduated during the years in which residency matching data were available, she found that women should hold 28 of 74 leadership positions, but they actually held 20 (27.0%, P = .05).10
Could the salary discrepancy disappear if more women held leadership positions? OBG <scaps>Management</scaps> posed this question to Dr. Baecher-Lind. “I suspect that the gender pay gap would persist,” she said. “Studies indicate that women hold implicit gender bias as strongly as men. This bias leads to devaluing women’s skills and accomplishments compared with men’s and is a strong contributor to the leadership and pay gaps in this country and in our specialty. We need to be mindful of this implicit bias and work against it with policies such as salary transparency and salary audits to encourage parity.”11
Do patients have a gender preference for their ObGyn?
Although multiple surveys have been published regarding patient gender preference when choosing an ObGyn, overall results have not been analyzed. To address this literature gap, Kyle J. Tobler, MD, and colleagues at the Womack Army Medical Center in Fort Bragg, North Carolina, and Uniformed Services University of the Health Sciences in Bethesda, Maryland, searched multiple sources to provide a conglomerate analysis of patients' gender preference when choosing an ObGyn. An abstract describing their study was published in Obstetrics & Gynecology in May 2016 and presented at the American College of Obstetricians and Gynecologists 2016 Annual Clinical and Scientific Meeting, May 14−17, in Washington, DC.1
A personal impetus for studying gender preference
The impetus for this project truly was initiated for Dr. Tobler when he was a 4th-year medical student. "I was trying to decide if Obstetrics and Gynecology was the right field for me," he said. "I was discouraged by many people around me, who told me that men in ObGyn would not have a place, as female patients only wanted female ObGyns. And with the residency match at 60% to 70% women for ObGyn, it did seem that men would not have a place. Thus, I began searching the literature to verify if the question for gender preference for their ObGyn provider had been evaluated previously, and I found mixed results." After medical school Dr. Tobler pursued this current meta-analysis to address the conflict-ing results.
Details of the study
Dr. Tobler and his colleagues explored PubMed, Embase, PsycINFO (American Psychological Association's medical literature database), Cumulative Index to Nursing and Allied Health Literature (EBSCO Health's database), Scopus (Elsevier's abstract and citation database of peer-reviewed literature), and references of relevant articles. Included were 4,822 electronically identified citations of English-language studies, including surveys administered to patients that specifically asked for gender preference of their ObGyn provider.
The researchers found that 23 studies met their inclusion criteria, comprising 14,736 patients. Overall, 8.3% (95% confidence interval [CI], 0.08-0.09) of ObGyn patients reported a preference for a male provider, 50.2% (95% CI, 0.49-0.51) preferred a female provider, and 41.3% (95% CI, 0.40-0.42) reported no gender preference when choosing an ObGyn.1
What about US patients?
A subanalysis of studies (n = 9,861) conducted in the United States from 1999 to 2008 (with the last search undertaken in April 2015) showed that 8.4% (95% CI, 0.08-0.09) preferred a male ObGyn, 53.2% (95% CI, 0.52-0.54) preferred a female ObGyn, and 38.5% (95% CI, 0.38-0.39) had no gender preference.1
"We were surprised by the numbers," comments Dr. Tobler. "The general trend demonstrated a mix between no preference or a preference for female providers, but not by a large margin."
"We considered analyzing for age," he said, "but most of the studies gave a mean or median age value and were widely distributed. We were able, however, to break our analysis down into regions where one would expect a very strong preference for female providers--the Middle East and Africa. But, in fact, results were not much different than for Western countries. Our results for this subanalysis of Middle Eastern countries and Nigeria (n = 1,951) demonstrated that 8.7% of women (95% CI, 4.1-13.3) preferred a male provider, 51.2% (95% CI, 17.2-85.1) preferred a female provider, and 46.9% (95% CI, 9.3-84.5) had no gender preference."1
References
- Tobler KJ, Wu J, Khafagy AM, et al. Gender preference of the obstetrician gynecologist provider: a systematic review and meta-analysis. Obstet Gynecol. 2016;127(5)(suppl):43S. http://journals.lww.com/greenjournal/page/results.aspx?txtkeywords=Gender+preference+of+the+obstetrician+gynecologist+provider. Accessed May 18, 2016.
What are ObGyns’ greatest practice concerns?
The Medicus Firm reported in its 2016 Physician Practice Preference and Relocation Survey that the top 3 major practice concerns for practicing physicians were compensation, work-life balance, and work-related burnout and stress.12 They found that physicians in general were slightly more satisfied with their 2015 income than their 2014 income, but less optimistic about the future. Only 29% projected that their 2016 income would increase over their 2015 earnings.
With ObGyn salaries on the up in 2015, less than half (46%) of ObGyns reported to Medscape that they feel fairly compensated; these physicians made $62,000 more than those who believed their pay was unfair.1 Fifty-four percent of employed male ObGyns and 64% of employed female ObGyns reported feeling fairly compensated, compared with 43% and 32%, respectively, who were self-employed.
ObGyns indicated in the 2016 Medscape report that the prime causes of stress were bureaucratic tasks and spending too many hours at work. More than half (52%) of ObGyns spend 30 to 45 hours per week seeing patients, and 40% spend more time than that.1 According to employment status, 56% of those who are self-employed and 58% of those who are employed spend 10 hours or more per week on administrative tasks.1
Lucia DiVenere, MA, Officer, Government and Political Affairs, at the American Congress of Obstetricians and Gynecologists (ACOG) in Washington, DC, offers a brief look, with an in-depth focus to come in an upcoming issue, at the growing concern of burnout among physicians and how it can affect both ObGyns and their patients. She outlines ACOG’s efforts to help ObGyns maintain work-life balance in “ObGyn burnout: ACOG takes aim.”
ObGyn burnout: ACOG takes aim
Lucia DiVenere, MA
The good news: More women have access to coverage for health care than ever before--better insurance coverage for pregnancy, contraceptives, and well-woman care.
The bad news: America faces a shortage of ObGyns to provide that care, a shortage not likely to go away soon.
One of the imperatives of this dynamic is that we need to help every practicing ObGyn perform at his or her very best: your highest level of quality care, your best productivity, and your best ability to survive and thrive in an always changing and often challenging work environment.
This imperative is undermined when ObGyns are so stressed, overworked, overworried, and undersupported that you experience the very real effects of physician burnout.
Studies show that:
- ObGyns experience high rates of burnout
- rates of burnout are increasing over time
- women, the majority gender in obstetrics and gynecology, experience higher rates of burnout than their male counterparts.
Between 2011 and 2014, rates of physician burnout increased from 45.5% to 54.4%.1 Fifty-one percent of ObGyns reported experiencing burnout in 2015, with women reporting 55% compared to 46% for men.2
This insert is a quick look at this important issue, which can seriously erode an ObGyn's ability to provide high-quality care and continue enjoying practice. It can take a real toll on your personal health and well-being, too. In an upcoming issue of OBG Management, I will take a deeper dive, previewing the American College of Obstetricians and Gynecologists (ACOG) and American Medical Association resources to help you avoid burnout, plus highlighting ObGyns who provide insight and inspiration. I also will interview ACOG President Tom Gellhaus, MD, who is dedicating his presidency to providing you with opportunities to experience new and meaningful aspects of the ObGyn specialty. I will discuss ACOG's programs to help you combat burnout, as well as how you can:
- help underserved women around the globe through medical missions
- bring your leadership and passion for women's health to your state and national capitals
- explore your artistic side.
ObGyn burnout amounts to a public health challenge in women's health care. ACOG takes your well-being seriously, so that you can continue to ensure the well-being of women.
Lucia DiVenere, MA, is Officer, Government and Political Affairs, at the American Congress of Obstetricians and Gynecologists in Washington, DC.
Ms. DiVenere reports no financial relationships relevant to this article. .
References
- Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clinic Proceedings. 2015;90(12):1600-1613.
- Peckham C. Medscape Lifestyle Report 2016: Bias and Burnout. Medscape website. http://www.medscape.com/features/slideshow/lifestyle/2016/public/overview. Published January 13, 2016. Accessed June 14, 2016.
Effects of the ACA on ObGyns
As of February 2016, 12.7 million Americans selected plans through the Health Insurance Marketplace of the Affordable Care Act (ACA).1 Physicians often have no choice in whether or not they participate in Health Insurance Exchanges; however, in 2016, 24% of ObGyns said they plan to participate in exchanges, 25% do not, and the rest are unsure.1
It is still unclear how the ACA affects physician income.1 When ObGyns who participated in Health Insurance Exchanges in 2015 were asked whether their income was affected, approximately 60% reported no change, 30% reported a decrease, and 9% said it increased.1
Medicus reported that physicians’ approval of the ACA has declined since last year. In their 2016 report, 71% of respondents gave the ACA a passing grade (A, B, C, or D), compared with 83% in 2015 and 77% in 2014. Fewer than 3% of 2016 respondents gave the ACA an “A.”12
Medscape reported that 36% of ObGyns have seen an increase in the number of patients due to the ACA.1 A 2015 report from the Kaiser Family Foundation and The Commonwealth Fund assessing the experiences and attitudes of primary care providers after the first year of ACA coverage found no association with lower- and higher-quality care whether or not patient load had increased.13 Among those in the Medscape report who said that quality of care had worsened, 21% had a greater patient load; 18% reported no increase in patient load. Seventy-eight percent of physicians whose patient load increased said that quality had stayed the same or improved; 82% of those who experienced no increase in patient load reported that quality had stayed the same or improved.1
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
- Peckham C. Medscape Ob/Gyn Compensation Report 2016. Medscape website. http://www.medscape.com/features/slideshow/compensation/2016/womenshealth. Published April 1, 2016. Accessed June 8, 2016.
- Reale D, Yates J. ObGyn salaries continue gradual improvement. OBG Manag. 2015;27(7):34−37.
- Peckham C. Medscape Ob/Gyn Compensation Report 2014. Medscape website. http://www.medscape.com/features/slideshow/compensation/2014/womenshealth. Published April 14, 2014. Accessed June 8, 2016.
- Merritt Hawkins. Survey: Starting salaries for physicians spiking. http://www.merritthawkins.com/uploadedFiles/MerrittHawkins/Pdf/Merritt_Hawkins_Starting_Salaries_For_Physicians_Spiking.pdf. Published June 7, 2016. Accessed June 17, 2016.
- Ly DP, Seabury SA, Jena AB, Newhouse RL. Differences in incomes of physicians in the United States by race and sex: observational study [published online ahead of print June 7, 2016]. BMJ. 2016;353:i2923. http://dx.doi.org/10.1136/bmj.i2923. Accessed June 8, 2016.
- Peckham C. Medscape Physician Compensation Report 2016. Medscape website. http://www.medscape.com/features/slideshow/compensation/2016/public/overview#page=1. Published April 1, 2016. Accessed June 15, 2016.
- Kaiser Family Foundation. Distribution of medical school graduates by gender. http://kff.org/other/state-indicator/medical-school-graduates-by-gender/. Published 2016. Accessed June 22, 2016.
- Lautenberger DM, Dandar VM, Raezer CL, Sloane RA. The state of women in academic medicine, 2013-2014. Association of American Medical Colleges. 2014. https://members.aamc.org/eweb/upload/The%20State%20of%20Women%20in%20Academic%20Medicine%202013-2014%20FINAL.pdf. Accessed June 17, 2016.
- American Medical Association. FREIDA Online specialty training search: Obstetrics and Gynecology, 2014. https://freida.ama-assn.org/Freida/user/specStatisticsSearch.do?method=viewDetail&pageNumber=2&spcCd=220. Accessed June 17, 2016.
- Baecher-Lind L. Women in leadership positions within obstetrics and gynecology. Obstet Gynecol. 2012;120(6):1415−1418.
- Email correspondence with Laura E. Baecher-Lind, June 19, 2016.
- Medicus Firm. The Medicus Firm releases annual Physician Practice Preference Survey for 2016. http://www .themedicusfirm.com/the-medicus-firm-releases-annual-physician-practice-preference-survey-for-2016. Published May 4, 2016. Accessed June 10, 2016.
- Hamel L, Doty MM, Norton M, et al; Kaiser Family Foundation and The Commonwealth Fund. Experiences and attitudes of primary care providers under the first year of ACA coverage expansion. http://www.commonwealthfund.org/publications/issue-briefs/2015/jun/primary-care-providers-first-year-aca. Published June 18, 2015. Accessed June 15, 2016.
The mean income for ObGyns rose by 10% in 2015 over 2014 ($277,000 compared with $249,000), according to a recent report from Medscape.1 This jump follows a gradual increase over the last few years ($243,000 in 2013; $242,000 in 2012; $220,000 in 2011).1−3 The report included responses from 19,183 physicians across 26 specialties, 5% (nearly 1,000) of whom were ObGyns.1
The highest earners among all physician specialties were orthopedists ($443,000), cardiologists, and dermatologists. The lowest earners were pediatricians ($204,000), endocrinologists, and family physicians. The highest ObGyn earners lived in the Southwest ($307,000), the North Central region, and the West.1
Merritt Hawkins & Associates, a national physician search and consulting firm, recently evaluated the annual starting salaries and year-over-year increases of 3,342 of its physician and advanced practitioner recruiting assignments. They found that ObGyns had the second greatest increase in starting salaries among specialties, at 16%. They also found obstetrics and gynecology to be among the top 5 specialties most in demand.4
The gender picture
As in past years, male ObGyns reported higher earnings than their female counterparts: full-time male ObGyns earned $304,000 while full-time female ObGyns earned $256,000.1
According to a report published in the British Medical Journal in June 2016, there are drastic differences between the incomes of white and black male and female physicians in the United States.5 White male physicians had an adjusted median annual income of $253,042 (95% confidence interval [CI], $248,670−$257,413), compared with $188,230 ($170,844−$205,616) for black male physicians, $163,234 (95% CI, $159,912−$166,557) for white female physicians, and $152,784 (95% CI, $137,927−$167,641) for black female physicians.
How does employment status factor in? Of the self-employed, men earn $310,000 while women earn $285,000. Men who are employed report earning $293,000, with women reporting $244,000.5 (This includes full-time workers but does not control for the number of hours worked.) When Medscape evaluated full- versus part-time work (<40 hours per week), results indicated that, among primary care and most other specialties, more female physicians (25%) are part-timers than males (12%).6 However, among ObGyns, 13% of women report part-time employment versus 16% of men.1
Time with patients. Medscape reports that, among all physicians, 41% of men spent 17 minutes or more with their patients, compared with 49% of women. For office-based ObGyns, 31% of men and 39% of women spent 17 minutes or more with patients.1
Can disparity in leadership positions explain gender-related salary discrepancy?
In 2015, 48% of all medical students were female.7 In residency, the ratio of men to women is similar: For 2013−2014, the Association of American Medical Colleges (AAMC) reported that 46% of all residents were female.8 For ObGyn residency, however, the AMA’s FREIDA Online specialty training search (detailing 2014 general program information) indicates that, of the 5,018 active residents and fellows in ObGyn, 81.4% are female.9
Although the ObGyn field is becoming female-dominated, leadership within the specialty remains male dominated, points out Laura E. Baecher-Lind, MD, MPH, Director of the Division of General Obstetrics & Gynecology at Tufts Medical Center, Boston, Massachusetts. Dr. Baecher-Lind authored a study in 2012 in which she explored whether the proportions of ObGyn leadership positions held by women reflect the proportion of women who entered the field at the same time as current leaders.10 She found that very few academic department chair positions in ObGyn are held by women, although that number is gradually increasing.10 In addition, her study results indicated that women should hold 71 of the total of 194 ObGyn leadership positions. In actuality, 41 of the leadership positions were held by women (21.1%, P<.001) when based on the proportion of women entering residency programs. When considering only leaders who graduated during the years in which residency matching data were available, she found that women should hold 28 of 74 leadership positions, but they actually held 20 (27.0%, P = .05).10
Could the salary discrepancy disappear if more women held leadership positions? OBG <scaps>Management</scaps> posed this question to Dr. Baecher-Lind. “I suspect that the gender pay gap would persist,” she said. “Studies indicate that women hold implicit gender bias as strongly as men. This bias leads to devaluing women’s skills and accomplishments compared with men’s and is a strong contributor to the leadership and pay gaps in this country and in our specialty. We need to be mindful of this implicit bias and work against it with policies such as salary transparency and salary audits to encourage parity.”11
Do patients have a gender preference for their ObGyn?
Although multiple surveys have been published regarding patient gender preference when choosing an ObGyn, overall results have not been analyzed. To address this literature gap, Kyle J. Tobler, MD, and colleagues at the Womack Army Medical Center in Fort Bragg, North Carolina, and Uniformed Services University of the Health Sciences in Bethesda, Maryland, searched multiple sources to provide a conglomerate analysis of patients' gender preference when choosing an ObGyn. An abstract describing their study was published in Obstetrics & Gynecology in May 2016 and presented at the American College of Obstetricians and Gynecologists 2016 Annual Clinical and Scientific Meeting, May 14−17, in Washington, DC.1
A personal impetus for studying gender preference
The impetus for this project truly was initiated for Dr. Tobler when he was a 4th-year medical student. "I was trying to decide if Obstetrics and Gynecology was the right field for me," he said. "I was discouraged by many people around me, who told me that men in ObGyn would not have a place, as female patients only wanted female ObGyns. And with the residency match at 60% to 70% women for ObGyn, it did seem that men would not have a place. Thus, I began searching the literature to verify if the question for gender preference for their ObGyn provider had been evaluated previously, and I found mixed results." After medical school Dr. Tobler pursued this current meta-analysis to address the conflict-ing results.
Details of the study
Dr. Tobler and his colleagues explored PubMed, Embase, PsycINFO (American Psychological Association's medical literature database), Cumulative Index to Nursing and Allied Health Literature (EBSCO Health's database), Scopus (Elsevier's abstract and citation database of peer-reviewed literature), and references of relevant articles. Included were 4,822 electronically identified citations of English-language studies, including surveys administered to patients that specifically asked for gender preference of their ObGyn provider.
The researchers found that 23 studies met their inclusion criteria, comprising 14,736 patients. Overall, 8.3% (95% confidence interval [CI], 0.08-0.09) of ObGyn patients reported a preference for a male provider, 50.2% (95% CI, 0.49-0.51) preferred a female provider, and 41.3% (95% CI, 0.40-0.42) reported no gender preference when choosing an ObGyn.1
What about US patients?
A subanalysis of studies (n = 9,861) conducted in the United States from 1999 to 2008 (with the last search undertaken in April 2015) showed that 8.4% (95% CI, 0.08-0.09) preferred a male ObGyn, 53.2% (95% CI, 0.52-0.54) preferred a female ObGyn, and 38.5% (95% CI, 0.38-0.39) had no gender preference.1
"We were surprised by the numbers," comments Dr. Tobler. "The general trend demonstrated a mix between no preference or a preference for female providers, but not by a large margin."
"We considered analyzing for age," he said, "but most of the studies gave a mean or median age value and were widely distributed. We were able, however, to break our analysis down into regions where one would expect a very strong preference for female providers--the Middle East and Africa. But, in fact, results were not much different than for Western countries. Our results for this subanalysis of Middle Eastern countries and Nigeria (n = 1,951) demonstrated that 8.7% of women (95% CI, 4.1-13.3) preferred a male provider, 51.2% (95% CI, 17.2-85.1) preferred a female provider, and 46.9% (95% CI, 9.3-84.5) had no gender preference."1
References
- Tobler KJ, Wu J, Khafagy AM, et al. Gender preference of the obstetrician gynecologist provider: a systematic review and meta-analysis. Obstet Gynecol. 2016;127(5)(suppl):43S. http://journals.lww.com/greenjournal/page/results.aspx?txtkeywords=Gender+preference+of+the+obstetrician+gynecologist+provider. Accessed May 18, 2016.
What are ObGyns’ greatest practice concerns?
The Medicus Firm reported in its 2016 Physician Practice Preference and Relocation Survey that the top 3 major practice concerns for practicing physicians were compensation, work-life balance, and work-related burnout and stress.12 They found that physicians in general were slightly more satisfied with their 2015 income than their 2014 income, but less optimistic about the future. Only 29% projected that their 2016 income would increase over their 2015 earnings.
With ObGyn salaries on the up in 2015, less than half (46%) of ObGyns reported to Medscape that they feel fairly compensated; these physicians made $62,000 more than those who believed their pay was unfair.1 Fifty-four percent of employed male ObGyns and 64% of employed female ObGyns reported feeling fairly compensated, compared with 43% and 32%, respectively, who were self-employed.
ObGyns indicated in the 2016 Medscape report that the prime causes of stress were bureaucratic tasks and spending too many hours at work. More than half (52%) of ObGyns spend 30 to 45 hours per week seeing patients, and 40% spend more time than that.1 According to employment status, 56% of those who are self-employed and 58% of those who are employed spend 10 hours or more per week on administrative tasks.1
Lucia DiVenere, MA, Officer, Government and Political Affairs, at the American Congress of Obstetricians and Gynecologists (ACOG) in Washington, DC, offers a brief look, with an in-depth focus to come in an upcoming issue, at the growing concern of burnout among physicians and how it can affect both ObGyns and their patients. She outlines ACOG’s efforts to help ObGyns maintain work-life balance in “ObGyn burnout: ACOG takes aim.”
ObGyn burnout: ACOG takes aim
Lucia DiVenere, MA
The good news: More women have access to coverage for health care than ever before--better insurance coverage for pregnancy, contraceptives, and well-woman care.
The bad news: America faces a shortage of ObGyns to provide that care, a shortage not likely to go away soon.
One of the imperatives of this dynamic is that we need to help every practicing ObGyn perform at his or her very best: your highest level of quality care, your best productivity, and your best ability to survive and thrive in an always changing and often challenging work environment.
This imperative is undermined when ObGyns are so stressed, overworked, overworried, and undersupported that you experience the very real effects of physician burnout.
Studies show that:
- ObGyns experience high rates of burnout
- rates of burnout are increasing over time
- women, the majority gender in obstetrics and gynecology, experience higher rates of burnout than their male counterparts.
Between 2011 and 2014, rates of physician burnout increased from 45.5% to 54.4%.1 Fifty-one percent of ObGyns reported experiencing burnout in 2015, with women reporting 55% compared to 46% for men.2
This insert is a quick look at this important issue, which can seriously erode an ObGyn's ability to provide high-quality care and continue enjoying practice. It can take a real toll on your personal health and well-being, too. In an upcoming issue of OBG Management, I will take a deeper dive, previewing the American College of Obstetricians and Gynecologists (ACOG) and American Medical Association resources to help you avoid burnout, plus highlighting ObGyns who provide insight and inspiration. I also will interview ACOG President Tom Gellhaus, MD, who is dedicating his presidency to providing you with opportunities to experience new and meaningful aspects of the ObGyn specialty. I will discuss ACOG's programs to help you combat burnout, as well as how you can:
- help underserved women around the globe through medical missions
- bring your leadership and passion for women's health to your state and national capitals
- explore your artistic side.
ObGyn burnout amounts to a public health challenge in women's health care. ACOG takes your well-being seriously, so that you can continue to ensure the well-being of women.
Lucia DiVenere, MA, is Officer, Government and Political Affairs, at the American Congress of Obstetricians and Gynecologists in Washington, DC.
Ms. DiVenere reports no financial relationships relevant to this article. .
References
- Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clinic Proceedings. 2015;90(12):1600-1613.
- Peckham C. Medscape Lifestyle Report 2016: Bias and Burnout. Medscape website. http://www.medscape.com/features/slideshow/lifestyle/2016/public/overview. Published January 13, 2016. Accessed June 14, 2016.
Effects of the ACA on ObGyns
As of February 2016, 12.7 million Americans selected plans through the Health Insurance Marketplace of the Affordable Care Act (ACA).1 Physicians often have no choice in whether or not they participate in Health Insurance Exchanges; however, in 2016, 24% of ObGyns said they plan to participate in exchanges, 25% do not, and the rest are unsure.1
It is still unclear how the ACA affects physician income.1 When ObGyns who participated in Health Insurance Exchanges in 2015 were asked whether their income was affected, approximately 60% reported no change, 30% reported a decrease, and 9% said it increased.1
Medicus reported that physicians’ approval of the ACA has declined since last year. In their 2016 report, 71% of respondents gave the ACA a passing grade (A, B, C, or D), compared with 83% in 2015 and 77% in 2014. Fewer than 3% of 2016 respondents gave the ACA an “A.”12
Medscape reported that 36% of ObGyns have seen an increase in the number of patients due to the ACA.1 A 2015 report from the Kaiser Family Foundation and The Commonwealth Fund assessing the experiences and attitudes of primary care providers after the first year of ACA coverage found no association with lower- and higher-quality care whether or not patient load had increased.13 Among those in the Medscape report who said that quality of care had worsened, 21% had a greater patient load; 18% reported no increase in patient load. Seventy-eight percent of physicians whose patient load increased said that quality had stayed the same or improved; 82% of those who experienced no increase in patient load reported that quality had stayed the same or improved.1
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
The mean income for ObGyns rose by 10% in 2015 over 2014 ($277,000 compared with $249,000), according to a recent report from Medscape.1 This jump follows a gradual increase over the last few years ($243,000 in 2013; $242,000 in 2012; $220,000 in 2011).1−3 The report included responses from 19,183 physicians across 26 specialties, 5% (nearly 1,000) of whom were ObGyns.1
The highest earners among all physician specialties were orthopedists ($443,000), cardiologists, and dermatologists. The lowest earners were pediatricians ($204,000), endocrinologists, and family physicians. The highest ObGyn earners lived in the Southwest ($307,000), the North Central region, and the West.1
Merritt Hawkins & Associates, a national physician search and consulting firm, recently evaluated the annual starting salaries and year-over-year increases of 3,342 of its physician and advanced practitioner recruiting assignments. They found that ObGyns had the second greatest increase in starting salaries among specialties, at 16%. They also found obstetrics and gynecology to be among the top 5 specialties most in demand.4
The gender picture
As in past years, male ObGyns reported higher earnings than their female counterparts: full-time male ObGyns earned $304,000 while full-time female ObGyns earned $256,000.1
According to a report published in the British Medical Journal in June 2016, there are drastic differences between the incomes of white and black male and female physicians in the United States.5 White male physicians had an adjusted median annual income of $253,042 (95% confidence interval [CI], $248,670−$257,413), compared with $188,230 ($170,844−$205,616) for black male physicians, $163,234 (95% CI, $159,912−$166,557) for white female physicians, and $152,784 (95% CI, $137,927−$167,641) for black female physicians.
How does employment status factor in? Of the self-employed, men earn $310,000 while women earn $285,000. Men who are employed report earning $293,000, with women reporting $244,000.5 (This includes full-time workers but does not control for the number of hours worked.) When Medscape evaluated full- versus part-time work (<40 hours per week), results indicated that, among primary care and most other specialties, more female physicians (25%) are part-timers than males (12%).6 However, among ObGyns, 13% of women report part-time employment versus 16% of men.1
Time with patients. Medscape reports that, among all physicians, 41% of men spent 17 minutes or more with their patients, compared with 49% of women. For office-based ObGyns, 31% of men and 39% of women spent 17 minutes or more with patients.1
Can disparity in leadership positions explain gender-related salary discrepancy?
In 2015, 48% of all medical students were female.7 In residency, the ratio of men to women is similar: For 2013−2014, the Association of American Medical Colleges (AAMC) reported that 46% of all residents were female.8 For ObGyn residency, however, the AMA’s FREIDA Online specialty training search (detailing 2014 general program information) indicates that, of the 5,018 active residents and fellows in ObGyn, 81.4% are female.9
Although the ObGyn field is becoming female-dominated, leadership within the specialty remains male dominated, points out Laura E. Baecher-Lind, MD, MPH, Director of the Division of General Obstetrics & Gynecology at Tufts Medical Center, Boston, Massachusetts. Dr. Baecher-Lind authored a study in 2012 in which she explored whether the proportions of ObGyn leadership positions held by women reflect the proportion of women who entered the field at the same time as current leaders.10 She found that very few academic department chair positions in ObGyn are held by women, although that number is gradually increasing.10 In addition, her study results indicated that women should hold 71 of the total of 194 ObGyn leadership positions. In actuality, 41 of the leadership positions were held by women (21.1%, P<.001) when based on the proportion of women entering residency programs. When considering only leaders who graduated during the years in which residency matching data were available, she found that women should hold 28 of 74 leadership positions, but they actually held 20 (27.0%, P = .05).10
Could the salary discrepancy disappear if more women held leadership positions? OBG <scaps>Management</scaps> posed this question to Dr. Baecher-Lind. “I suspect that the gender pay gap would persist,” she said. “Studies indicate that women hold implicit gender bias as strongly as men. This bias leads to devaluing women’s skills and accomplishments compared with men’s and is a strong contributor to the leadership and pay gaps in this country and in our specialty. We need to be mindful of this implicit bias and work against it with policies such as salary transparency and salary audits to encourage parity.”11
Do patients have a gender preference for their ObGyn?
Although multiple surveys have been published regarding patient gender preference when choosing an ObGyn, overall results have not been analyzed. To address this literature gap, Kyle J. Tobler, MD, and colleagues at the Womack Army Medical Center in Fort Bragg, North Carolina, and Uniformed Services University of the Health Sciences in Bethesda, Maryland, searched multiple sources to provide a conglomerate analysis of patients' gender preference when choosing an ObGyn. An abstract describing their study was published in Obstetrics & Gynecology in May 2016 and presented at the American College of Obstetricians and Gynecologists 2016 Annual Clinical and Scientific Meeting, May 14−17, in Washington, DC.1
A personal impetus for studying gender preference
The impetus for this project truly was initiated for Dr. Tobler when he was a 4th-year medical student. "I was trying to decide if Obstetrics and Gynecology was the right field for me," he said. "I was discouraged by many people around me, who told me that men in ObGyn would not have a place, as female patients only wanted female ObGyns. And with the residency match at 60% to 70% women for ObGyn, it did seem that men would not have a place. Thus, I began searching the literature to verify if the question for gender preference for their ObGyn provider had been evaluated previously, and I found mixed results." After medical school Dr. Tobler pursued this current meta-analysis to address the conflict-ing results.
Details of the study
Dr. Tobler and his colleagues explored PubMed, Embase, PsycINFO (American Psychological Association's medical literature database), Cumulative Index to Nursing and Allied Health Literature (EBSCO Health's database), Scopus (Elsevier's abstract and citation database of peer-reviewed literature), and references of relevant articles. Included were 4,822 electronically identified citations of English-language studies, including surveys administered to patients that specifically asked for gender preference of their ObGyn provider.
The researchers found that 23 studies met their inclusion criteria, comprising 14,736 patients. Overall, 8.3% (95% confidence interval [CI], 0.08-0.09) of ObGyn patients reported a preference for a male provider, 50.2% (95% CI, 0.49-0.51) preferred a female provider, and 41.3% (95% CI, 0.40-0.42) reported no gender preference when choosing an ObGyn.1
What about US patients?
A subanalysis of studies (n = 9,861) conducted in the United States from 1999 to 2008 (with the last search undertaken in April 2015) showed that 8.4% (95% CI, 0.08-0.09) preferred a male ObGyn, 53.2% (95% CI, 0.52-0.54) preferred a female ObGyn, and 38.5% (95% CI, 0.38-0.39) had no gender preference.1
"We were surprised by the numbers," comments Dr. Tobler. "The general trend demonstrated a mix between no preference or a preference for female providers, but not by a large margin."
"We considered analyzing for age," he said, "but most of the studies gave a mean or median age value and were widely distributed. We were able, however, to break our analysis down into regions where one would expect a very strong preference for female providers--the Middle East and Africa. But, in fact, results were not much different than for Western countries. Our results for this subanalysis of Middle Eastern countries and Nigeria (n = 1,951) demonstrated that 8.7% of women (95% CI, 4.1-13.3) preferred a male provider, 51.2% (95% CI, 17.2-85.1) preferred a female provider, and 46.9% (95% CI, 9.3-84.5) had no gender preference."1
References
- Tobler KJ, Wu J, Khafagy AM, et al. Gender preference of the obstetrician gynecologist provider: a systematic review and meta-analysis. Obstet Gynecol. 2016;127(5)(suppl):43S. http://journals.lww.com/greenjournal/page/results.aspx?txtkeywords=Gender+preference+of+the+obstetrician+gynecologist+provider. Accessed May 18, 2016.
What are ObGyns’ greatest practice concerns?
The Medicus Firm reported in its 2016 Physician Practice Preference and Relocation Survey that the top 3 major practice concerns for practicing physicians were compensation, work-life balance, and work-related burnout and stress.12 They found that physicians in general were slightly more satisfied with their 2015 income than their 2014 income, but less optimistic about the future. Only 29% projected that their 2016 income would increase over their 2015 earnings.
With ObGyn salaries on the up in 2015, less than half (46%) of ObGyns reported to Medscape that they feel fairly compensated; these physicians made $62,000 more than those who believed their pay was unfair.1 Fifty-four percent of employed male ObGyns and 64% of employed female ObGyns reported feeling fairly compensated, compared with 43% and 32%, respectively, who were self-employed.
ObGyns indicated in the 2016 Medscape report that the prime causes of stress were bureaucratic tasks and spending too many hours at work. More than half (52%) of ObGyns spend 30 to 45 hours per week seeing patients, and 40% spend more time than that.1 According to employment status, 56% of those who are self-employed and 58% of those who are employed spend 10 hours or more per week on administrative tasks.1
Lucia DiVenere, MA, Officer, Government and Political Affairs, at the American Congress of Obstetricians and Gynecologists (ACOG) in Washington, DC, offers a brief look, with an in-depth focus to come in an upcoming issue, at the growing concern of burnout among physicians and how it can affect both ObGyns and their patients. She outlines ACOG’s efforts to help ObGyns maintain work-life balance in “ObGyn burnout: ACOG takes aim.”
ObGyn burnout: ACOG takes aim
Lucia DiVenere, MA
The good news: More women have access to coverage for health care than ever before--better insurance coverage for pregnancy, contraceptives, and well-woman care.
The bad news: America faces a shortage of ObGyns to provide that care, a shortage not likely to go away soon.
One of the imperatives of this dynamic is that we need to help every practicing ObGyn perform at his or her very best: your highest level of quality care, your best productivity, and your best ability to survive and thrive in an always changing and often challenging work environment.
This imperative is undermined when ObGyns are so stressed, overworked, overworried, and undersupported that you experience the very real effects of physician burnout.
Studies show that:
- ObGyns experience high rates of burnout
- rates of burnout are increasing over time
- women, the majority gender in obstetrics and gynecology, experience higher rates of burnout than their male counterparts.
Between 2011 and 2014, rates of physician burnout increased from 45.5% to 54.4%.1 Fifty-one percent of ObGyns reported experiencing burnout in 2015, with women reporting 55% compared to 46% for men.2
This insert is a quick look at this important issue, which can seriously erode an ObGyn's ability to provide high-quality care and continue enjoying practice. It can take a real toll on your personal health and well-being, too. In an upcoming issue of OBG Management, I will take a deeper dive, previewing the American College of Obstetricians and Gynecologists (ACOG) and American Medical Association resources to help you avoid burnout, plus highlighting ObGyns who provide insight and inspiration. I also will interview ACOG President Tom Gellhaus, MD, who is dedicating his presidency to providing you with opportunities to experience new and meaningful aspects of the ObGyn specialty. I will discuss ACOG's programs to help you combat burnout, as well as how you can:
- help underserved women around the globe through medical missions
- bring your leadership and passion for women's health to your state and national capitals
- explore your artistic side.
ObGyn burnout amounts to a public health challenge in women's health care. ACOG takes your well-being seriously, so that you can continue to ensure the well-being of women.
Lucia DiVenere, MA, is Officer, Government and Political Affairs, at the American Congress of Obstetricians and Gynecologists in Washington, DC.
Ms. DiVenere reports no financial relationships relevant to this article. .
References
- Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clinic Proceedings. 2015;90(12):1600-1613.
- Peckham C. Medscape Lifestyle Report 2016: Bias and Burnout. Medscape website. http://www.medscape.com/features/slideshow/lifestyle/2016/public/overview. Published January 13, 2016. Accessed June 14, 2016.
Effects of the ACA on ObGyns
As of February 2016, 12.7 million Americans selected plans through the Health Insurance Marketplace of the Affordable Care Act (ACA).1 Physicians often have no choice in whether or not they participate in Health Insurance Exchanges; however, in 2016, 24% of ObGyns said they plan to participate in exchanges, 25% do not, and the rest are unsure.1
It is still unclear how the ACA affects physician income.1 When ObGyns who participated in Health Insurance Exchanges in 2015 were asked whether their income was affected, approximately 60% reported no change, 30% reported a decrease, and 9% said it increased.1
Medicus reported that physicians’ approval of the ACA has declined since last year. In their 2016 report, 71% of respondents gave the ACA a passing grade (A, B, C, or D), compared with 83% in 2015 and 77% in 2014. Fewer than 3% of 2016 respondents gave the ACA an “A.”12
Medscape reported that 36% of ObGyns have seen an increase in the number of patients due to the ACA.1 A 2015 report from the Kaiser Family Foundation and The Commonwealth Fund assessing the experiences and attitudes of primary care providers after the first year of ACA coverage found no association with lower- and higher-quality care whether or not patient load had increased.13 Among those in the Medscape report who said that quality of care had worsened, 21% had a greater patient load; 18% reported no increase in patient load. Seventy-eight percent of physicians whose patient load increased said that quality had stayed the same or improved; 82% of those who experienced no increase in patient load reported that quality had stayed the same or improved.1
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
- Peckham C. Medscape Ob/Gyn Compensation Report 2016. Medscape website. http://www.medscape.com/features/slideshow/compensation/2016/womenshealth. Published April 1, 2016. Accessed June 8, 2016.
- Reale D, Yates J. ObGyn salaries continue gradual improvement. OBG Manag. 2015;27(7):34−37.
- Peckham C. Medscape Ob/Gyn Compensation Report 2014. Medscape website. http://www.medscape.com/features/slideshow/compensation/2014/womenshealth. Published April 14, 2014. Accessed June 8, 2016.
- Merritt Hawkins. Survey: Starting salaries for physicians spiking. http://www.merritthawkins.com/uploadedFiles/MerrittHawkins/Pdf/Merritt_Hawkins_Starting_Salaries_For_Physicians_Spiking.pdf. Published June 7, 2016. Accessed June 17, 2016.
- Ly DP, Seabury SA, Jena AB, Newhouse RL. Differences in incomes of physicians in the United States by race and sex: observational study [published online ahead of print June 7, 2016]. BMJ. 2016;353:i2923. http://dx.doi.org/10.1136/bmj.i2923. Accessed June 8, 2016.
- Peckham C. Medscape Physician Compensation Report 2016. Medscape website. http://www.medscape.com/features/slideshow/compensation/2016/public/overview#page=1. Published April 1, 2016. Accessed June 15, 2016.
- Kaiser Family Foundation. Distribution of medical school graduates by gender. http://kff.org/other/state-indicator/medical-school-graduates-by-gender/. Published 2016. Accessed June 22, 2016.
- Lautenberger DM, Dandar VM, Raezer CL, Sloane RA. The state of women in academic medicine, 2013-2014. Association of American Medical Colleges. 2014. https://members.aamc.org/eweb/upload/The%20State%20of%20Women%20in%20Academic%20Medicine%202013-2014%20FINAL.pdf. Accessed June 17, 2016.
- American Medical Association. FREIDA Online specialty training search: Obstetrics and Gynecology, 2014. https://freida.ama-assn.org/Freida/user/specStatisticsSearch.do?method=viewDetail&pageNumber=2&spcCd=220. Accessed June 17, 2016.
- Baecher-Lind L. Women in leadership positions within obstetrics and gynecology. Obstet Gynecol. 2012;120(6):1415−1418.
- Email correspondence with Laura E. Baecher-Lind, June 19, 2016.
- Medicus Firm. The Medicus Firm releases annual Physician Practice Preference Survey for 2016. http://www .themedicusfirm.com/the-medicus-firm-releases-annual-physician-practice-preference-survey-for-2016. Published May 4, 2016. Accessed June 10, 2016.
- Hamel L, Doty MM, Norton M, et al; Kaiser Family Foundation and The Commonwealth Fund. Experiences and attitudes of primary care providers under the first year of ACA coverage expansion. http://www.commonwealthfund.org/publications/issue-briefs/2015/jun/primary-care-providers-first-year-aca. Published June 18, 2015. Accessed June 15, 2016.
- Peckham C. Medscape Ob/Gyn Compensation Report 2016. Medscape website. http://www.medscape.com/features/slideshow/compensation/2016/womenshealth. Published April 1, 2016. Accessed June 8, 2016.
- Reale D, Yates J. ObGyn salaries continue gradual improvement. OBG Manag. 2015;27(7):34−37.
- Peckham C. Medscape Ob/Gyn Compensation Report 2014. Medscape website. http://www.medscape.com/features/slideshow/compensation/2014/womenshealth. Published April 14, 2014. Accessed June 8, 2016.
- Merritt Hawkins. Survey: Starting salaries for physicians spiking. http://www.merritthawkins.com/uploadedFiles/MerrittHawkins/Pdf/Merritt_Hawkins_Starting_Salaries_For_Physicians_Spiking.pdf. Published June 7, 2016. Accessed June 17, 2016.
- Ly DP, Seabury SA, Jena AB, Newhouse RL. Differences in incomes of physicians in the United States by race and sex: observational study [published online ahead of print June 7, 2016]. BMJ. 2016;353:i2923. http://dx.doi.org/10.1136/bmj.i2923. Accessed June 8, 2016.
- Peckham C. Medscape Physician Compensation Report 2016. Medscape website. http://www.medscape.com/features/slideshow/compensation/2016/public/overview#page=1. Published April 1, 2016. Accessed June 15, 2016.
- Kaiser Family Foundation. Distribution of medical school graduates by gender. http://kff.org/other/state-indicator/medical-school-graduates-by-gender/. Published 2016. Accessed June 22, 2016.
- Lautenberger DM, Dandar VM, Raezer CL, Sloane RA. The state of women in academic medicine, 2013-2014. Association of American Medical Colleges. 2014. https://members.aamc.org/eweb/upload/The%20State%20of%20Women%20in%20Academic%20Medicine%202013-2014%20FINAL.pdf. Accessed June 17, 2016.
- American Medical Association. FREIDA Online specialty training search: Obstetrics and Gynecology, 2014. https://freida.ama-assn.org/Freida/user/specStatisticsSearch.do?method=viewDetail&pageNumber=2&spcCd=220. Accessed June 17, 2016.
- Baecher-Lind L. Women in leadership positions within obstetrics and gynecology. Obstet Gynecol. 2012;120(6):1415−1418.
- Email correspondence with Laura E. Baecher-Lind, June 19, 2016.
- Medicus Firm. The Medicus Firm releases annual Physician Practice Preference Survey for 2016. http://www .themedicusfirm.com/the-medicus-firm-releases-annual-physician-practice-preference-survey-for-2016. Published May 4, 2016. Accessed June 10, 2016.
- Hamel L, Doty MM, Norton M, et al; Kaiser Family Foundation and The Commonwealth Fund. Experiences and attitudes of primary care providers under the first year of ACA coverage expansion. http://www.commonwealthfund.org/publications/issue-briefs/2015/jun/primary-care-providers-first-year-aca. Published June 18, 2015. Accessed June 15, 2016.
In this Article
- ACOG takes aim at burnout
- Considering salary and leadership disparities
- ObGyns’ greatest practice concerns
Randomized trial: When a vaginal approach is feasible, the robot offers no advantages for benign hysterectomy
When investigators compared the cost of vaginal hysterectomy with robot-assisted laparoscopic hysterectomy head to head, they found hospital costs of $4,579 and $7,059, respectively, with no other significant differences between the approaches. Accordingly, they concluded that vaginal hysterectomy should be the “first-choice” approach when it is feasible.
The randomized controlled trial by Lönnerfors and colleagues also compared “traditional” minimally invasive hysterectomy (vaginal or laparoscopic approach) with robot-assisted hysterectomy in 122 women undergoing hysterectomy for benign conditions. Women with a uterine size of 16 gestational weeks or smaller were randomly allocated to:
- traditional minimally invasive hysterectomy (n = 61) or
- robotic assisted hysterectomy (n = 61).
In the traditional group, vaginal hysterectomy was the first-choice approach when it was feasible; otherwise, laparoscopic hysterectomy was performed. Vaginal hysterectomy was possible in 41% of cases in this group.
When costs for vaginal and laparoscopic approaches were consolidated and compared with the cost of the robot-assisted approach, the differential was $993 for the robotic approach when the robot was considered a preexisting investment. The hospital cost increased by $1,607 for the robotic approach when investment costs and maintenance expenses were included.
When laparoscopic hysterectomy was compared directly with robot-assisted hysterectomy, costs were similar ($7,016 vs $7,059, respectively) when the robot was considered a preexisting investment, and the robotic approach was associated with less blood loss and fewer postoperative complications.
Investigators noted that: “per-protocol analysis indicates that laparoscopic and robotic-assisted hysterectomy can be performed at similar hospital cost because of higher robot capacity that entails excluding the cost of investment and maintenance, i.e., the basic cost of the robot. This cost differs among institutions, depending on the number of procedures performed; however, the difference becomes less pronounced when 300 to 400 procedures or more are performed annually and the cost for instruments and disposables accounts for most of the cost of the procedure.”
This randomized controlled trial was awarded the Robert B. Hunt Award at the 2015 AAGL Global Congress in Las Vegas as the best paper published over the past year in the Journal of Minimally Invasive Gynecology.
Reference
Lönnerfors C, Reynisson P, Persson J. A randomized trial comparing vaginal and laparoscopic hysterectomy vs robot-assisted hysterectomy. J Minim Invasive Gynecol. 2015;22(1):78–86.
When investigators compared the cost of vaginal hysterectomy with robot-assisted laparoscopic hysterectomy head to head, they found hospital costs of $4,579 and $7,059, respectively, with no other significant differences between the approaches. Accordingly, they concluded that vaginal hysterectomy should be the “first-choice” approach when it is feasible.
The randomized controlled trial by Lönnerfors and colleagues also compared “traditional” minimally invasive hysterectomy (vaginal or laparoscopic approach) with robot-assisted hysterectomy in 122 women undergoing hysterectomy for benign conditions. Women with a uterine size of 16 gestational weeks or smaller were randomly allocated to:
- traditional minimally invasive hysterectomy (n = 61) or
- robotic assisted hysterectomy (n = 61).
In the traditional group, vaginal hysterectomy was the first-choice approach when it was feasible; otherwise, laparoscopic hysterectomy was performed. Vaginal hysterectomy was possible in 41% of cases in this group.
When costs for vaginal and laparoscopic approaches were consolidated and compared with the cost of the robot-assisted approach, the differential was $993 for the robotic approach when the robot was considered a preexisting investment. The hospital cost increased by $1,607 for the robotic approach when investment costs and maintenance expenses were included.
When laparoscopic hysterectomy was compared directly with robot-assisted hysterectomy, costs were similar ($7,016 vs $7,059, respectively) when the robot was considered a preexisting investment, and the robotic approach was associated with less blood loss and fewer postoperative complications.
Investigators noted that: “per-protocol analysis indicates that laparoscopic and robotic-assisted hysterectomy can be performed at similar hospital cost because of higher robot capacity that entails excluding the cost of investment and maintenance, i.e., the basic cost of the robot. This cost differs among institutions, depending on the number of procedures performed; however, the difference becomes less pronounced when 300 to 400 procedures or more are performed annually and the cost for instruments and disposables accounts for most of the cost of the procedure.”
This randomized controlled trial was awarded the Robert B. Hunt Award at the 2015 AAGL Global Congress in Las Vegas as the best paper published over the past year in the Journal of Minimally Invasive Gynecology.
When investigators compared the cost of vaginal hysterectomy with robot-assisted laparoscopic hysterectomy head to head, they found hospital costs of $4,579 and $7,059, respectively, with no other significant differences between the approaches. Accordingly, they concluded that vaginal hysterectomy should be the “first-choice” approach when it is feasible.
The randomized controlled trial by Lönnerfors and colleagues also compared “traditional” minimally invasive hysterectomy (vaginal or laparoscopic approach) with robot-assisted hysterectomy in 122 women undergoing hysterectomy for benign conditions. Women with a uterine size of 16 gestational weeks or smaller were randomly allocated to:
- traditional minimally invasive hysterectomy (n = 61) or
- robotic assisted hysterectomy (n = 61).
In the traditional group, vaginal hysterectomy was the first-choice approach when it was feasible; otherwise, laparoscopic hysterectomy was performed. Vaginal hysterectomy was possible in 41% of cases in this group.
When costs for vaginal and laparoscopic approaches were consolidated and compared with the cost of the robot-assisted approach, the differential was $993 for the robotic approach when the robot was considered a preexisting investment. The hospital cost increased by $1,607 for the robotic approach when investment costs and maintenance expenses were included.
When laparoscopic hysterectomy was compared directly with robot-assisted hysterectomy, costs were similar ($7,016 vs $7,059, respectively) when the robot was considered a preexisting investment, and the robotic approach was associated with less blood loss and fewer postoperative complications.
Investigators noted that: “per-protocol analysis indicates that laparoscopic and robotic-assisted hysterectomy can be performed at similar hospital cost because of higher robot capacity that entails excluding the cost of investment and maintenance, i.e., the basic cost of the robot. This cost differs among institutions, depending on the number of procedures performed; however, the difference becomes less pronounced when 300 to 400 procedures or more are performed annually and the cost for instruments and disposables accounts for most of the cost of the procedure.”
This randomized controlled trial was awarded the Robert B. Hunt Award at the 2015 AAGL Global Congress in Las Vegas as the best paper published over the past year in the Journal of Minimally Invasive Gynecology.
Reference
Lönnerfors C, Reynisson P, Persson J. A randomized trial comparing vaginal and laparoscopic hysterectomy vs robot-assisted hysterectomy. J Minim Invasive Gynecol. 2015;22(1):78–86.
Reference
Lönnerfors C, Reynisson P, Persson J. A randomized trial comparing vaginal and laparoscopic hysterectomy vs robot-assisted hysterectomy. J Minim Invasive Gynecol. 2015;22(1):78–86.
A surge in congenital syphilis reveals gaps in obstetric practice
The rate of congenital syphilis increased to 11.6 cases per 100,000 live births in 2014 in the United States—the highest rate documented since 2001, according to a new report from the Centers for Disease Control and Prevention (CDC).1 The increase in the rate of congenital syphilis reflects a rise in the rate of primary and secondary syphilis among US women, from 0.9 to 1.1 cases per 100,000 women, during the same period.1
The rate of congenital syphilis had declined between 2008 and 2012, from 10.5 cases to 8.4 cases per 100,000 live births.
Congenital syphilis occurs when an infected mother transmits the disease to her fetus during pregnancy. Among the adverse effects of congenital syphilis are deformities, stillbirth, and early infant death. “However, among mothers identified with syphilis who deliver past 20 weeks’ gestation, treatment with penicillin at least 30 days before delivery is 98% effective at preventing [congenital syphilis],” the CDC report notes.1
For the purposes of the CDC report, congenital syphilis includes “both infants and stillbirths with clinical evidence” of the disease, “as well as those infants and stillbirths born to mothers with untreated or inadequately treated syphilis, regardless of the infant’s manifestation of clinical disease.”1
CDC recommendations
The CDC notes that most of the increases in the rates of maternal and congenital syphilis likely stem from inadequate prenatal care.
“A large percentage of [congenital syphilis] cases continue to be attributable to a lack of prenatal care; even among those receiving some prenatal care, the detection and treatment of maternal syphilis is often not early enough….At particular risk are those who are uninsured or underinsured and those with substance use issues.”1
Among the recommendations of the CDC:
- Screen all pregnant women for syphilis at their first prenatal visit.
- Screen women at elevated risk for syphilis, as well as those who live in “high-morbidity geographic areas” at the beginning of the third trimester and again at delivery.
- In cases where prenatal care has been lacking, screen the woman for syphilis using a rapid plasma reagin (RPR) card and treat the patient who tests positive at the time the pregnancy is confirmed.
- Do not discharge an infant from the hospital unless the syphilis serologic status of the mother has been tested at least once during pregnancy and, preferably, again at delivery (in high-risk cases).
- Test any woman who delivers a stillborn infant for syphilis.
Reference
1. Bowen V, Su J, Torrone E, Kidd S, Weinstock H. Increase in incidence of congenital syphilis—United States, 2008–2014. MMWR. 2015;64(44):1241–1245.
The rate of congenital syphilis increased to 11.6 cases per 100,000 live births in 2014 in the United States—the highest rate documented since 2001, according to a new report from the Centers for Disease Control and Prevention (CDC).1 The increase in the rate of congenital syphilis reflects a rise in the rate of primary and secondary syphilis among US women, from 0.9 to 1.1 cases per 100,000 women, during the same period.1
The rate of congenital syphilis had declined between 2008 and 2012, from 10.5 cases to 8.4 cases per 100,000 live births.
Congenital syphilis occurs when an infected mother transmits the disease to her fetus during pregnancy. Among the adverse effects of congenital syphilis are deformities, stillbirth, and early infant death. “However, among mothers identified with syphilis who deliver past 20 weeks’ gestation, treatment with penicillin at least 30 days before delivery is 98% effective at preventing [congenital syphilis],” the CDC report notes.1
For the purposes of the CDC report, congenital syphilis includes “both infants and stillbirths with clinical evidence” of the disease, “as well as those infants and stillbirths born to mothers with untreated or inadequately treated syphilis, regardless of the infant’s manifestation of clinical disease.”1
CDC recommendations
The CDC notes that most of the increases in the rates of maternal and congenital syphilis likely stem from inadequate prenatal care.
“A large percentage of [congenital syphilis] cases continue to be attributable to a lack of prenatal care; even among those receiving some prenatal care, the detection and treatment of maternal syphilis is often not early enough….At particular risk are those who are uninsured or underinsured and those with substance use issues.”1
Among the recommendations of the CDC:
- Screen all pregnant women for syphilis at their first prenatal visit.
- Screen women at elevated risk for syphilis, as well as those who live in “high-morbidity geographic areas” at the beginning of the third trimester and again at delivery.
- In cases where prenatal care has been lacking, screen the woman for syphilis using a rapid plasma reagin (RPR) card and treat the patient who tests positive at the time the pregnancy is confirmed.
- Do not discharge an infant from the hospital unless the syphilis serologic status of the mother has been tested at least once during pregnancy and, preferably, again at delivery (in high-risk cases).
- Test any woman who delivers a stillborn infant for syphilis.
The rate of congenital syphilis increased to 11.6 cases per 100,000 live births in 2014 in the United States—the highest rate documented since 2001, according to a new report from the Centers for Disease Control and Prevention (CDC).1 The increase in the rate of congenital syphilis reflects a rise in the rate of primary and secondary syphilis among US women, from 0.9 to 1.1 cases per 100,000 women, during the same period.1
The rate of congenital syphilis had declined between 2008 and 2012, from 10.5 cases to 8.4 cases per 100,000 live births.
Congenital syphilis occurs when an infected mother transmits the disease to her fetus during pregnancy. Among the adverse effects of congenital syphilis are deformities, stillbirth, and early infant death. “However, among mothers identified with syphilis who deliver past 20 weeks’ gestation, treatment with penicillin at least 30 days before delivery is 98% effective at preventing [congenital syphilis],” the CDC report notes.1
For the purposes of the CDC report, congenital syphilis includes “both infants and stillbirths with clinical evidence” of the disease, “as well as those infants and stillbirths born to mothers with untreated or inadequately treated syphilis, regardless of the infant’s manifestation of clinical disease.”1
CDC recommendations
The CDC notes that most of the increases in the rates of maternal and congenital syphilis likely stem from inadequate prenatal care.
“A large percentage of [congenital syphilis] cases continue to be attributable to a lack of prenatal care; even among those receiving some prenatal care, the detection and treatment of maternal syphilis is often not early enough….At particular risk are those who are uninsured or underinsured and those with substance use issues.”1
Among the recommendations of the CDC:
- Screen all pregnant women for syphilis at their first prenatal visit.
- Screen women at elevated risk for syphilis, as well as those who live in “high-morbidity geographic areas” at the beginning of the third trimester and again at delivery.
- In cases where prenatal care has been lacking, screen the woman for syphilis using a rapid plasma reagin (RPR) card and treat the patient who tests positive at the time the pregnancy is confirmed.
- Do not discharge an infant from the hospital unless the syphilis serologic status of the mother has been tested at least once during pregnancy and, preferably, again at delivery (in high-risk cases).
- Test any woman who delivers a stillborn infant for syphilis.
Reference
1. Bowen V, Su J, Torrone E, Kidd S, Weinstock H. Increase in incidence of congenital syphilis—United States, 2008–2014. MMWR. 2015;64(44):1241–1245.
Reference
1. Bowen V, Su J, Torrone E, Kidd S, Weinstock H. Increase in incidence of congenital syphilis—United States, 2008–2014. MMWR. 2015;64(44):1241–1245.
What you need to know (and do) to prescribe the new drug flibanserin
It was a long road to approval by the US Food and Drug Administration (FDA), but flibanserin (Addyi) got the nod on August 18, 2015. Its New Drug Application (NDA) originally was filed October 27, 2009. The drug launched October 17, 2015.
Although there has been a lot of fanfare about approval of this drug, most of the coverage has focused on its status as the “first female Viagra”—a less than accurate depiction. For a more realistic and practical assessment of the drug, OBG Management turned to Michael Krychman, MD, executive director of the Southern California Center for Sexual Health and Survivorship Medicine in Newport Beach, to determine the types of information clinicians need to know to begin prescribing flibanserin. This article highlights 11 questions (and answers) to help you get started.
1. How did the FDA arrive
at its approval?
In 2012, the agency determined that female sexual dysfunction was one of 20 disease areas that warranted focused attention. In October 2014, as part of its intensified look at female sexual dysfunction, the FDA convened a 2-day meeting “to advance our understanding,” reports Andrea Fischer, FDA press officer.
“During the first day of the meeting, the FDA solicited patients’ perspectives on their condition and its impact on daily life. While this meeting did not focus on flibanserin, it provided an opportunity for the FDA to hear directly from patients about the impact of their condition,” Ms. Fischer says. During the second day of the meeting, the FDA “discussed scientific issues and challenges with experts in sexual medicine.”
As a result, by the time of the FDA’s June 4, 2015 Advisory Committee meeting on the flibanserin NDA, FDA physician-scientists were well versed in many nuances of female sexual function. That meeting included an open public hearing “that provided an opportunity for members of the public, including patients, to provide input specifically on the flibanserin application,” Ms. Fischer notes.
Nuances of the deliberations
“The FDA’s regulatory decision making on any drug product is a science-based process that carefully weighs each drug in terms of its risks and benefits to the patient population for which the drug would be indicated,” says Ms. Fischer.
The challenge in the case of flibanserin was determining whether the drug provides “clinically meaningful” improvements in sexual activity and desire.
“For many conditions and diseases, what constitutes ‘clinically meaningful’ is well known and accepted,” Ms. Fischer notes, “such as when something is cured or a severe symptom that is life-altering resolves completely. For others, this is not the case. For example, a condition that has a wide range of degree of severity can offer challenges in assessing what constitutes a clinically meaningful treatment effect. Ascertaining this requires a comprehensive knowledge of the disease, affected patient population, management strategies and the drug in question, as well as an ability to look at the clinical trial data taking this all into account.”
“In clinical trials, an important method for assessing the impact of a treatment on a patient’s symptoms, mental state, or functional status is through direct self-report using well developed and thoughtfully integrated patient-reported outcome (PRO) assessments,” Ms. Fischer says. “PROs can provide valuable information on the patient perspective when determining whether benefits outweigh risks, and they also are used to support medical product labeling claims, which are a key source of information for both health care providers and patients. PROs have been and continue to be a high priority as part of FDA’s commitment to advance patient-focused drug development, and we fully expect this to continue. The clinical trials in the flibanserin NDA all utilized PRO assessments.”
Those assessments found that patients taking flibanserin had a significant increase in “sexually satisfying events.” Three 24-week randomized controlled trials explored this endpoint for flibanserin (studies 1–3).
As for improvements in desire, the first 2 trials utilized an e-diary to assess this aspect of sexual function, while the 3rd trial utilized the Female Sexual Function Index (FSFI).
Although the e-diary reflected no statistically significant improvement in desire in the first 2 trials, the FSFI did find significant improvement in the 3rd trial. In addition, when the FSFI was considered across all 3 trials, results in the desire domain were consistent. (The FSFI was used as a secondary tool in the first 2 trials.)
In addition, sexual distress, as measured by the Female Sexual Distress Scale (FSDS), was decreased in the trials with use of flibanserin, notes Dr. Krychman. The Advisory Committee determined that these findings were sufficient to demonstrate clinically meaningful improvements with use of the drug.
Although the drug was approved by the FDA, the agency was sufficiently concerned about some of its potential risks (see questions 4 and 5) that it implemented rigorous mitigation strategies (see question 7). Additional investigations were requested by the agency, including drug-drug interaction, alcohol challenge, and driving studies.
2. What are the indications?
Flibanserin is intended for use in premenopausal women who have acquired, generalized hypoactive sexual desire disorder (HSDD). That diagnosis no longer is included in the 5th edition of the Diagnostic and
Statistical Manual of Mental Disorders but is described in drug package labeling as “low sexual desire that causes marked distress or interpersonal difficulty and is not due to:
- a coexisting medical or psychiatric condition,
- problems within the relationship, or
- the effects of a medication or other drug substance.”1
- the effects of a medication or other drug substance.”
Although the drug has been tested in both premenopausal and postmenopausal women, it was approved for use only in premenopausal women. Also note inclusion of the term “acquired” before the diagnosis of HSDD, indicating that the drug is inappropriate for women who have never experienced a period of normal sexual desire.
3. How is HSDD diagnosed?
One of the best screening tools is the
Decreased Sexual Desire Screener, says
Dr. Krychman. It is available at http://obgynalliance.com/files/fsd/DSDS_Pocketcard.pdf. This tool is a validated instrument to help clinicians identify what HSDD is and is not.
4. Does the drug carry
any warnings?
Yes, it carries a black box warning about the risks of hypotension and syncope:
- when alcohol is consumed by users of the drug. (Alcohol use is contraindicated.)
- when the drug is taken in conjunction with moderate or strong CYP3A4 inhibitors or by patients with hepatic impairment. (The drug is contraindicated in both circumstances.) See question 9 for a list of drugs that are CYP3A4 inhibitors.
5. Are there any other risks worth noting?
The medication can increase the risks of hypotension and syncope even without concomitant use of alcohol. For example, in clinical trials, hypotension was reported in 0.2% of flibanserin-treated women versus less than 0.1% of placebo users. And syncope was reported in 0.4% of flibanserin users versus 0.2% of placebo-treated patients. Flibanserin is prescribed as a once-daily medication that is to be taken at bedtime; the risks of hypotension and syncope are increased if flibanserin is taken during waking hours.
The risk of adverse effects when flibanserin is taken with alcohol is highlighted by one case reported in package labeling: A 54-year-old postmenopausal woman died after taking flibanserin (100 mg daily at bedtime) for 14 days. This patient had a history of hypertension and hypercholesterolemia and consumed a baseline amount of 1 to 3 alcoholic beverages daily. She died of acute alcohol intoxication, with a blood alcohol concentration of 0.289 g/dL.1 Whether this patient’s death was related to flibanserin use is unknown.1
It is interesting to note that, in the studies of flibanserin leading up to the drug’s approval, alcohol use was not an exclusion, says Dr. Krychman. “Approximately 58% of women were self-described as mild to moderate drinkers. The clinical program was extremely large—more than 11,000 women were studied.”
Flibanserin is currently not approved for use in postmenopausal women, and concomitant alcohol consumption is contraindicated.
6. What is the dose?
The recommended dose is one tablet of
100 mg daily. The drug is to be taken at
bedtime to reduce the risks of hypotension, syncope, accidental injury, and central nervous system (CNS) depression, which can occur even in the absence of alcohol.
7. Are there any requirements for clinicians who want to prescribe the drug?
Yes. Because of the risks of hypotension, syncope, and CNS depression, the drug is subject to Risk Evaluation and Mitigation Strategies (REMS), as determined by the FDA. To prescribe the drug, providers must:
- review its prescribing information
- review the Provider and Pharmacy Training Program
- complete and submit the Knowledge Assessment Form
- enroll in REMS by completing and submitting the Prescriber Enrollment Form.
Before giving a patient her initial prescription, the provider must counsel her about the risks of hypotension and syncope and the interaction with alcohol using the Patient-Provider Agreement Form. The provider must then complete that form, provide a designated portion of it to the patient, and retain the remainder for the patient’s file.
For more information and to download the relevant forms, visit https://www.addyirems.com.
8. What are the most common
adverse reactions to the drug?
According to package labeling, the most common adverse reactions, with an incidence greater than 2%, are dizziness, somnolence, nausea, fatigue, insomnia, and dry mouth.
Less common reactions include anxiety, constipation, abdominal pain, rash, sedation, and vertigo.
In studies of the drug, appendicitis was reported among 0.2% of flibanserin-treated patients, compared with no reports of appendicitis among placebo-treated patients. The FDA has requested additional investigation of the association, if any, between flibanserin and appendicitis.
9. What drug interactions are notable?
As stated earlier, the concomitant use of flibanserin with alcohol or a moderate or strong CYP3A4 inhibitor can result in severe hypotension and syncope. Flibanserin also should not be prescribed for patients who use other CNS depressants such as diphenhydramine, opioids, benzodiazepines, and hypnotic agents.
Some examples of strong CYP3A4 inhibitors are ketoconazole, itraconazole, posaconazole, clarithromycin, nefazodone, ritonavir, saquinavir, nelfinavir, indinavir, boceprevir, telaprevir, telithromycin, and conivaptan.
Moderate CYP3A4 inhibitors include amprenavir, atazanavir, ciprofloxacin, diltiazem, erythromycin, fluconazole, fosamprenavir, verapamil, and grapefruit juice.
In addition, the concomitant use of flibanserin with multiple weak CYP3A4 inhibitors—which include herbal supplements such as ginkgo and resveratrol and nonprescription drugs such as cimetidine—also may increase the risks of hypotension and syncope.
The concomitant use of flibanserin with digoxin increases the digoxin concentration and may lead to toxicity.
10. Is the drug safe in pregnancy
and lactation?
There are currently no data on the use of flibanserin in human pregnancy. In animals, fetal toxicity occurred only in the presence of significant maternal toxicity. Adverse effects included decreased fetal weight, structural anomalies, and increases in fetal loss when exposure exceeded 15 times the recommended human dosage.
As for the advisability of using flibanserin during lactation, it is unknown whether the drug is excreted in human milk, whether it might have adverse effects in the breastfed infant, or whether it affects milk production. Package labeling states: “Because of the potential for serious adverse reactions, including sedation in a breastfed infant, breastfeeding is not recommended during treatment with [flibanserin].”1
11. When should the drug
be discontinued?
If there is no improvement in sexual desire after an 8-week trial of flibanserin, the drug should be
discontinued.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
Reference
- Addyi [package insert]. Raleigh, NC: Sprout Pharmaceuticals; 2015.
It was a long road to approval by the US Food and Drug Administration (FDA), but flibanserin (Addyi) got the nod on August 18, 2015. Its New Drug Application (NDA) originally was filed October 27, 2009. The drug launched October 17, 2015.
Although there has been a lot of fanfare about approval of this drug, most of the coverage has focused on its status as the “first female Viagra”—a less than accurate depiction. For a more realistic and practical assessment of the drug, OBG Management turned to Michael Krychman, MD, executive director of the Southern California Center for Sexual Health and Survivorship Medicine in Newport Beach, to determine the types of information clinicians need to know to begin prescribing flibanserin. This article highlights 11 questions (and answers) to help you get started.
1. How did the FDA arrive
at its approval?
In 2012, the agency determined that female sexual dysfunction was one of 20 disease areas that warranted focused attention. In October 2014, as part of its intensified look at female sexual dysfunction, the FDA convened a 2-day meeting “to advance our understanding,” reports Andrea Fischer, FDA press officer.
“During the first day of the meeting, the FDA solicited patients’ perspectives on their condition and its impact on daily life. While this meeting did not focus on flibanserin, it provided an opportunity for the FDA to hear directly from patients about the impact of their condition,” Ms. Fischer says. During the second day of the meeting, the FDA “discussed scientific issues and challenges with experts in sexual medicine.”
As a result, by the time of the FDA’s June 4, 2015 Advisory Committee meeting on the flibanserin NDA, FDA physician-scientists were well versed in many nuances of female sexual function. That meeting included an open public hearing “that provided an opportunity for members of the public, including patients, to provide input specifically on the flibanserin application,” Ms. Fischer notes.
Nuances of the deliberations
“The FDA’s regulatory decision making on any drug product is a science-based process that carefully weighs each drug in terms of its risks and benefits to the patient population for which the drug would be indicated,” says Ms. Fischer.
The challenge in the case of flibanserin was determining whether the drug provides “clinically meaningful” improvements in sexual activity and desire.
“For many conditions and diseases, what constitutes ‘clinically meaningful’ is well known and accepted,” Ms. Fischer notes, “such as when something is cured or a severe symptom that is life-altering resolves completely. For others, this is not the case. For example, a condition that has a wide range of degree of severity can offer challenges in assessing what constitutes a clinically meaningful treatment effect. Ascertaining this requires a comprehensive knowledge of the disease, affected patient population, management strategies and the drug in question, as well as an ability to look at the clinical trial data taking this all into account.”
“In clinical trials, an important method for assessing the impact of a treatment on a patient’s symptoms, mental state, or functional status is through direct self-report using well developed and thoughtfully integrated patient-reported outcome (PRO) assessments,” Ms. Fischer says. “PROs can provide valuable information on the patient perspective when determining whether benefits outweigh risks, and they also are used to support medical product labeling claims, which are a key source of information for both health care providers and patients. PROs have been and continue to be a high priority as part of FDA’s commitment to advance patient-focused drug development, and we fully expect this to continue. The clinical trials in the flibanserin NDA all utilized PRO assessments.”
Those assessments found that patients taking flibanserin had a significant increase in “sexually satisfying events.” Three 24-week randomized controlled trials explored this endpoint for flibanserin (studies 1–3).
As for improvements in desire, the first 2 trials utilized an e-diary to assess this aspect of sexual function, while the 3rd trial utilized the Female Sexual Function Index (FSFI).
Although the e-diary reflected no statistically significant improvement in desire in the first 2 trials, the FSFI did find significant improvement in the 3rd trial. In addition, when the FSFI was considered across all 3 trials, results in the desire domain were consistent. (The FSFI was used as a secondary tool in the first 2 trials.)
In addition, sexual distress, as measured by the Female Sexual Distress Scale (FSDS), was decreased in the trials with use of flibanserin, notes Dr. Krychman. The Advisory Committee determined that these findings were sufficient to demonstrate clinically meaningful improvements with use of the drug.
Although the drug was approved by the FDA, the agency was sufficiently concerned about some of its potential risks (see questions 4 and 5) that it implemented rigorous mitigation strategies (see question 7). Additional investigations were requested by the agency, including drug-drug interaction, alcohol challenge, and driving studies.
2. What are the indications?
Flibanserin is intended for use in premenopausal women who have acquired, generalized hypoactive sexual desire disorder (HSDD). That diagnosis no longer is included in the 5th edition of the Diagnostic and
Statistical Manual of Mental Disorders but is described in drug package labeling as “low sexual desire that causes marked distress or interpersonal difficulty and is not due to:
- a coexisting medical or psychiatric condition,
- problems within the relationship, or
- the effects of a medication or other drug substance.”1
- the effects of a medication or other drug substance.”
Although the drug has been tested in both premenopausal and postmenopausal women, it was approved for use only in premenopausal women. Also note inclusion of the term “acquired” before the diagnosis of HSDD, indicating that the drug is inappropriate for women who have never experienced a period of normal sexual desire.
3. How is HSDD diagnosed?
One of the best screening tools is the
Decreased Sexual Desire Screener, says
Dr. Krychman. It is available at http://obgynalliance.com/files/fsd/DSDS_Pocketcard.pdf. This tool is a validated instrument to help clinicians identify what HSDD is and is not.
4. Does the drug carry
any warnings?
Yes, it carries a black box warning about the risks of hypotension and syncope:
- when alcohol is consumed by users of the drug. (Alcohol use is contraindicated.)
- when the drug is taken in conjunction with moderate or strong CYP3A4 inhibitors or by patients with hepatic impairment. (The drug is contraindicated in both circumstances.) See question 9 for a list of drugs that are CYP3A4 inhibitors.
5. Are there any other risks worth noting?
The medication can increase the risks of hypotension and syncope even without concomitant use of alcohol. For example, in clinical trials, hypotension was reported in 0.2% of flibanserin-treated women versus less than 0.1% of placebo users. And syncope was reported in 0.4% of flibanserin users versus 0.2% of placebo-treated patients. Flibanserin is prescribed as a once-daily medication that is to be taken at bedtime; the risks of hypotension and syncope are increased if flibanserin is taken during waking hours.
The risk of adverse effects when flibanserin is taken with alcohol is highlighted by one case reported in package labeling: A 54-year-old postmenopausal woman died after taking flibanserin (100 mg daily at bedtime) for 14 days. This patient had a history of hypertension and hypercholesterolemia and consumed a baseline amount of 1 to 3 alcoholic beverages daily. She died of acute alcohol intoxication, with a blood alcohol concentration of 0.289 g/dL.1 Whether this patient’s death was related to flibanserin use is unknown.1
It is interesting to note that, in the studies of flibanserin leading up to the drug’s approval, alcohol use was not an exclusion, says Dr. Krychman. “Approximately 58% of women were self-described as mild to moderate drinkers. The clinical program was extremely large—more than 11,000 women were studied.”
Flibanserin is currently not approved for use in postmenopausal women, and concomitant alcohol consumption is contraindicated.
6. What is the dose?
The recommended dose is one tablet of
100 mg daily. The drug is to be taken at
bedtime to reduce the risks of hypotension, syncope, accidental injury, and central nervous system (CNS) depression, which can occur even in the absence of alcohol.
7. Are there any requirements for clinicians who want to prescribe the drug?
Yes. Because of the risks of hypotension, syncope, and CNS depression, the drug is subject to Risk Evaluation and Mitigation Strategies (REMS), as determined by the FDA. To prescribe the drug, providers must:
- review its prescribing information
- review the Provider and Pharmacy Training Program
- complete and submit the Knowledge Assessment Form
- enroll in REMS by completing and submitting the Prescriber Enrollment Form.
Before giving a patient her initial prescription, the provider must counsel her about the risks of hypotension and syncope and the interaction with alcohol using the Patient-Provider Agreement Form. The provider must then complete that form, provide a designated portion of it to the patient, and retain the remainder for the patient’s file.
For more information and to download the relevant forms, visit https://www.addyirems.com.
8. What are the most common
adverse reactions to the drug?
According to package labeling, the most common adverse reactions, with an incidence greater than 2%, are dizziness, somnolence, nausea, fatigue, insomnia, and dry mouth.
Less common reactions include anxiety, constipation, abdominal pain, rash, sedation, and vertigo.
In studies of the drug, appendicitis was reported among 0.2% of flibanserin-treated patients, compared with no reports of appendicitis among placebo-treated patients. The FDA has requested additional investigation of the association, if any, between flibanserin and appendicitis.
9. What drug interactions are notable?
As stated earlier, the concomitant use of flibanserin with alcohol or a moderate or strong CYP3A4 inhibitor can result in severe hypotension and syncope. Flibanserin also should not be prescribed for patients who use other CNS depressants such as diphenhydramine, opioids, benzodiazepines, and hypnotic agents.
Some examples of strong CYP3A4 inhibitors are ketoconazole, itraconazole, posaconazole, clarithromycin, nefazodone, ritonavir, saquinavir, nelfinavir, indinavir, boceprevir, telaprevir, telithromycin, and conivaptan.
Moderate CYP3A4 inhibitors include amprenavir, atazanavir, ciprofloxacin, diltiazem, erythromycin, fluconazole, fosamprenavir, verapamil, and grapefruit juice.
In addition, the concomitant use of flibanserin with multiple weak CYP3A4 inhibitors—which include herbal supplements such as ginkgo and resveratrol and nonprescription drugs such as cimetidine—also may increase the risks of hypotension and syncope.
The concomitant use of flibanserin with digoxin increases the digoxin concentration and may lead to toxicity.
10. Is the drug safe in pregnancy
and lactation?
There are currently no data on the use of flibanserin in human pregnancy. In animals, fetal toxicity occurred only in the presence of significant maternal toxicity. Adverse effects included decreased fetal weight, structural anomalies, and increases in fetal loss when exposure exceeded 15 times the recommended human dosage.
As for the advisability of using flibanserin during lactation, it is unknown whether the drug is excreted in human milk, whether it might have adverse effects in the breastfed infant, or whether it affects milk production. Package labeling states: “Because of the potential for serious adverse reactions, including sedation in a breastfed infant, breastfeeding is not recommended during treatment with [flibanserin].”1
11. When should the drug
be discontinued?
If there is no improvement in sexual desire after an 8-week trial of flibanserin, the drug should be
discontinued.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
It was a long road to approval by the US Food and Drug Administration (FDA), but flibanserin (Addyi) got the nod on August 18, 2015. Its New Drug Application (NDA) originally was filed October 27, 2009. The drug launched October 17, 2015.
Although there has been a lot of fanfare about approval of this drug, most of the coverage has focused on its status as the “first female Viagra”—a less than accurate depiction. For a more realistic and practical assessment of the drug, OBG Management turned to Michael Krychman, MD, executive director of the Southern California Center for Sexual Health and Survivorship Medicine in Newport Beach, to determine the types of information clinicians need to know to begin prescribing flibanserin. This article highlights 11 questions (and answers) to help you get started.
1. How did the FDA arrive
at its approval?
In 2012, the agency determined that female sexual dysfunction was one of 20 disease areas that warranted focused attention. In October 2014, as part of its intensified look at female sexual dysfunction, the FDA convened a 2-day meeting “to advance our understanding,” reports Andrea Fischer, FDA press officer.
“During the first day of the meeting, the FDA solicited patients’ perspectives on their condition and its impact on daily life. While this meeting did not focus on flibanserin, it provided an opportunity for the FDA to hear directly from patients about the impact of their condition,” Ms. Fischer says. During the second day of the meeting, the FDA “discussed scientific issues and challenges with experts in sexual medicine.”
As a result, by the time of the FDA’s June 4, 2015 Advisory Committee meeting on the flibanserin NDA, FDA physician-scientists were well versed in many nuances of female sexual function. That meeting included an open public hearing “that provided an opportunity for members of the public, including patients, to provide input specifically on the flibanserin application,” Ms. Fischer notes.
Nuances of the deliberations
“The FDA’s regulatory decision making on any drug product is a science-based process that carefully weighs each drug in terms of its risks and benefits to the patient population for which the drug would be indicated,” says Ms. Fischer.
The challenge in the case of flibanserin was determining whether the drug provides “clinically meaningful” improvements in sexual activity and desire.
“For many conditions and diseases, what constitutes ‘clinically meaningful’ is well known and accepted,” Ms. Fischer notes, “such as when something is cured or a severe symptom that is life-altering resolves completely. For others, this is not the case. For example, a condition that has a wide range of degree of severity can offer challenges in assessing what constitutes a clinically meaningful treatment effect. Ascertaining this requires a comprehensive knowledge of the disease, affected patient population, management strategies and the drug in question, as well as an ability to look at the clinical trial data taking this all into account.”
“In clinical trials, an important method for assessing the impact of a treatment on a patient’s symptoms, mental state, or functional status is through direct self-report using well developed and thoughtfully integrated patient-reported outcome (PRO) assessments,” Ms. Fischer says. “PROs can provide valuable information on the patient perspective when determining whether benefits outweigh risks, and they also are used to support medical product labeling claims, which are a key source of information for both health care providers and patients. PROs have been and continue to be a high priority as part of FDA’s commitment to advance patient-focused drug development, and we fully expect this to continue. The clinical trials in the flibanserin NDA all utilized PRO assessments.”
Those assessments found that patients taking flibanserin had a significant increase in “sexually satisfying events.” Three 24-week randomized controlled trials explored this endpoint for flibanserin (studies 1–3).
As for improvements in desire, the first 2 trials utilized an e-diary to assess this aspect of sexual function, while the 3rd trial utilized the Female Sexual Function Index (FSFI).
Although the e-diary reflected no statistically significant improvement in desire in the first 2 trials, the FSFI did find significant improvement in the 3rd trial. In addition, when the FSFI was considered across all 3 trials, results in the desire domain were consistent. (The FSFI was used as a secondary tool in the first 2 trials.)
In addition, sexual distress, as measured by the Female Sexual Distress Scale (FSDS), was decreased in the trials with use of flibanserin, notes Dr. Krychman. The Advisory Committee determined that these findings were sufficient to demonstrate clinically meaningful improvements with use of the drug.
Although the drug was approved by the FDA, the agency was sufficiently concerned about some of its potential risks (see questions 4 and 5) that it implemented rigorous mitigation strategies (see question 7). Additional investigations were requested by the agency, including drug-drug interaction, alcohol challenge, and driving studies.
2. What are the indications?
Flibanserin is intended for use in premenopausal women who have acquired, generalized hypoactive sexual desire disorder (HSDD). That diagnosis no longer is included in the 5th edition of the Diagnostic and
Statistical Manual of Mental Disorders but is described in drug package labeling as “low sexual desire that causes marked distress or interpersonal difficulty and is not due to:
- a coexisting medical or psychiatric condition,
- problems within the relationship, or
- the effects of a medication or other drug substance.”1
- the effects of a medication or other drug substance.”
Although the drug has been tested in both premenopausal and postmenopausal women, it was approved for use only in premenopausal women. Also note inclusion of the term “acquired” before the diagnosis of HSDD, indicating that the drug is inappropriate for women who have never experienced a period of normal sexual desire.
3. How is HSDD diagnosed?
One of the best screening tools is the
Decreased Sexual Desire Screener, says
Dr. Krychman. It is available at http://obgynalliance.com/files/fsd/DSDS_Pocketcard.pdf. This tool is a validated instrument to help clinicians identify what HSDD is and is not.
4. Does the drug carry
any warnings?
Yes, it carries a black box warning about the risks of hypotension and syncope:
- when alcohol is consumed by users of the drug. (Alcohol use is contraindicated.)
- when the drug is taken in conjunction with moderate or strong CYP3A4 inhibitors or by patients with hepatic impairment. (The drug is contraindicated in both circumstances.) See question 9 for a list of drugs that are CYP3A4 inhibitors.
5. Are there any other risks worth noting?
The medication can increase the risks of hypotension and syncope even without concomitant use of alcohol. For example, in clinical trials, hypotension was reported in 0.2% of flibanserin-treated women versus less than 0.1% of placebo users. And syncope was reported in 0.4% of flibanserin users versus 0.2% of placebo-treated patients. Flibanserin is prescribed as a once-daily medication that is to be taken at bedtime; the risks of hypotension and syncope are increased if flibanserin is taken during waking hours.
The risk of adverse effects when flibanserin is taken with alcohol is highlighted by one case reported in package labeling: A 54-year-old postmenopausal woman died after taking flibanserin (100 mg daily at bedtime) for 14 days. This patient had a history of hypertension and hypercholesterolemia and consumed a baseline amount of 1 to 3 alcoholic beverages daily. She died of acute alcohol intoxication, with a blood alcohol concentration of 0.289 g/dL.1 Whether this patient’s death was related to flibanserin use is unknown.1
It is interesting to note that, in the studies of flibanserin leading up to the drug’s approval, alcohol use was not an exclusion, says Dr. Krychman. “Approximately 58% of women were self-described as mild to moderate drinkers. The clinical program was extremely large—more than 11,000 women were studied.”
Flibanserin is currently not approved for use in postmenopausal women, and concomitant alcohol consumption is contraindicated.
6. What is the dose?
The recommended dose is one tablet of
100 mg daily. The drug is to be taken at
bedtime to reduce the risks of hypotension, syncope, accidental injury, and central nervous system (CNS) depression, which can occur even in the absence of alcohol.
7. Are there any requirements for clinicians who want to prescribe the drug?
Yes. Because of the risks of hypotension, syncope, and CNS depression, the drug is subject to Risk Evaluation and Mitigation Strategies (REMS), as determined by the FDA. To prescribe the drug, providers must:
- review its prescribing information
- review the Provider and Pharmacy Training Program
- complete and submit the Knowledge Assessment Form
- enroll in REMS by completing and submitting the Prescriber Enrollment Form.
Before giving a patient her initial prescription, the provider must counsel her about the risks of hypotension and syncope and the interaction with alcohol using the Patient-Provider Agreement Form. The provider must then complete that form, provide a designated portion of it to the patient, and retain the remainder for the patient’s file.
For more information and to download the relevant forms, visit https://www.addyirems.com.
8. What are the most common
adverse reactions to the drug?
According to package labeling, the most common adverse reactions, with an incidence greater than 2%, are dizziness, somnolence, nausea, fatigue, insomnia, and dry mouth.
Less common reactions include anxiety, constipation, abdominal pain, rash, sedation, and vertigo.
In studies of the drug, appendicitis was reported among 0.2% of flibanserin-treated patients, compared with no reports of appendicitis among placebo-treated patients. The FDA has requested additional investigation of the association, if any, between flibanserin and appendicitis.
9. What drug interactions are notable?
As stated earlier, the concomitant use of flibanserin with alcohol or a moderate or strong CYP3A4 inhibitor can result in severe hypotension and syncope. Flibanserin also should not be prescribed for patients who use other CNS depressants such as diphenhydramine, opioids, benzodiazepines, and hypnotic agents.
Some examples of strong CYP3A4 inhibitors are ketoconazole, itraconazole, posaconazole, clarithromycin, nefazodone, ritonavir, saquinavir, nelfinavir, indinavir, boceprevir, telaprevir, telithromycin, and conivaptan.
Moderate CYP3A4 inhibitors include amprenavir, atazanavir, ciprofloxacin, diltiazem, erythromycin, fluconazole, fosamprenavir, verapamil, and grapefruit juice.
In addition, the concomitant use of flibanserin with multiple weak CYP3A4 inhibitors—which include herbal supplements such as ginkgo and resveratrol and nonprescription drugs such as cimetidine—also may increase the risks of hypotension and syncope.
The concomitant use of flibanserin with digoxin increases the digoxin concentration and may lead to toxicity.
10. Is the drug safe in pregnancy
and lactation?
There are currently no data on the use of flibanserin in human pregnancy. In animals, fetal toxicity occurred only in the presence of significant maternal toxicity. Adverse effects included decreased fetal weight, structural anomalies, and increases in fetal loss when exposure exceeded 15 times the recommended human dosage.
As for the advisability of using flibanserin during lactation, it is unknown whether the drug is excreted in human milk, whether it might have adverse effects in the breastfed infant, or whether it affects milk production. Package labeling states: “Because of the potential for serious adverse reactions, including sedation in a breastfed infant, breastfeeding is not recommended during treatment with [flibanserin].”1
11. When should the drug
be discontinued?
If there is no improvement in sexual desire after an 8-week trial of flibanserin, the drug should be
discontinued.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
Reference
- Addyi [package insert]. Raleigh, NC: Sprout Pharmaceuticals; 2015.
Reference
- Addyi [package insert]. Raleigh, NC: Sprout Pharmaceuticals; 2015.
In this Article
- How is HSDD diagnosed?
- What are clinicians required to do?
- Is the drug safe in pregnancy?
What you should know about the latest change in mammography screening guidelines
When the American Cancer Society (ACS) updated its guidelines for screening mammography earlier this week,1 the effect was that of a stone being tossed into a tranquil pond, generating ripples in all directions.
The new guidelines focus on women at average risk for breast cancer (TABLE 1) and were updated for the first time since 2003, based on new evidence, a new emphasis on eliminating as many screening harms as possible, and a goal of “supporting the interplay among values, preferences, informed decision making, and recommendations.”1 Earlier ACS guidelines recommended annual screening starting at age 40.
TABLE 1 What constitutes “average risk” of breast cancer?
|
The new guidelines are graded according to the strength of the rec ommendation as being either “strong” or “qualified.” The ACS defines a “strong” recommendation as one that most individuals should follow. “Adherence to this recommendation according to the guideline could be used as a quality criterion or performance indicator,” the guidelines note.1
A “qualified” recommendation indicates that “Clinicians should acknowledge that different choices will be appropriate for different patients and that clinicians must help each patient arrive at a management decision consistent with her or his values and preferences.”1
The recommendations are:
- Regular screening mammography should start at age 45 years (strong recommendation)
- Screening should be annual in women aged 45 to 54 years (qualified recommendation)
- Screening should shift to biennial intervals at age 55, unless the patient prefers to continue screening annually (qualified recommendation)
- Women who desire to initiate annual screening between the ages of 40 and 44 years should be accommodated (qualified recommendation)
- Screening mammography should continue as long as the woman is in good health and has a life expectancy of at least 10 years (qualified recommendation)
- Clinical breast examination (CBE) is not recommended at any age (qualified recommendation).1
ACOG weighs in
Shortly after publication of the new ACS guidelines, the American College of Obstetricians and Gynecologists (ACOG) issued a formal statement in response2:
Response of the USPSTF
The US Preventive Services Task Force (USPSTF) also issued a statement in response to the new ACS guidelines:
The USPSTF currently recommends biennial screening beginning at age 50.
A leader in breast health cites pros and cons of ACS recommendations
Mark Pearlman, MD, professor of obstetrics and gynecology at the University of Michigan health system, is a nationally recognized expert on breast cancer screening. He sits on the National Comprehensive Cancer Network (NCCN) breast cancer screening and diagnosis group, helped author ACOG guidelines on mammography screening, and serves as a Contributing Editor to OBG Management.
“I believe the overall ACS mammography benefit evidence synthesis is reasonable and is in keeping with both NCCN and ACOG’s current recommendations. NCCN and ACOG mammography screening recommendations have both valued lives saved more highly than the ‘harms’ such as recalls and needle biopsies,” Dr. Pearlman says.
“If one combines ACS ‘strong’ and ‘qualified’ recommendations, ACS recommendations are similar to current ACOG and NCCN recommendations for mammography,” he adds.
Dr. Pearlman finds 7 areas of agreement between NCCN/ACOG and ACS recommendations, using both strong and qualified recommendations:
- “They reaffirm that screening from age 40 to 69 years is associated with a reduction in breast cancer deaths.
- They support annual screening for women in their 40s [although the ACS’ ‘strong’ recommendation is that regular screening begin at age 45 instead of 40].
- They support screening for women 70 and older who are in good health (10-year life expectancy).
- They support the finding that annual screening yields a larger mortality reduction than biennial screening.
- They confirm much uncertainty about the “over-diagnosis/overtreatment” issue.
- They endorse insurance coverage at all ages and intervals of screening (not just USPSTF ‘A’ or ‘B’ recommendations).
- They involve the patient in informed decision making.”
Where the ACS and ACOG/NCCN disagree is over the issue of the physical exam (abandoning CBE in average-risk women).
In regard to this last item, Dr. Pearlman says, “The ACS made a qualified recommendation against clinical breast exam. There is no high-level data to support such a marked change in practice. For example, when recommendations against breast self-examinations (BSE) were made, there were randomized controlled trials (RCTs) showing a lack of benefit and significant harms with BSE. With RCT-level data, it made sense to make a recommendation against the long-taught practice of SBE in average-risk women. That was not the case here. In fact, there are small amounts of data showing benefits of clinical breast exam.”
“One of my biggest concerns is not just the recommendation against CBE,” says Dr. Pearlman, “but that this may lead many women to interpret [this statement] as if they do not need to see their health care provider anymore. As you may recall, the American College of Physicians (ACP) recommended against annual pelvic examinations in asymptomatic patients. The ACS recommendation statement—taken together with the ACP statement—basically suggests that average-risk women don’t ever need to see a provider for a pelvic or breast examination except every 5 years for a Pap smear. That thinking does not recognize the importance of the clinical encounter (not just the CBE or pelvic exam), which is the opportunity to perform risk assessment and provide risk-reduction recommendations and healthy lifestyle recommendations.”
Radiologists resist new recommendations
Although the American College of Radiology (ACR) and the Society of Breast Imaging (SBI) agree with the ACS that mammography screening saves lives and should be available to women aged 40 and older, the 2 imaging organizations continue to recommend that annual screening begin at age 40. Their rationale: The latest ACS breast cancer screening guidelines, and earlier data used by the USPSTF to create its recommendations, both note that starting annual mammography at age 40 “saves the most lives.”
Where the organizations differ from the ACR is summed up by a formal statement on the ACR Web site: “The ACR and SBI strongly encourage women to obtain the maximum lifesaving benefits from mammography by continuing to get annual screening.”4
When OBG Management touched base with radiologist Barbara Monsees, MD, professor of radiology and Evens Professor of Women’s Health at Washington University Medical Center in St. Louis, Missouri, she expressed dismay at early news reports on the ACS guidelines.
“I’m dismayed that the headlines don’t seem to correlate with what the ACS actually recommended. The ACS did not state that women should wait until age 45 to begin screening. I believe the ACS was going for a more nuanced approach, but since that’s a bit complicated, I think that reporters have misconstrued what was intended,” Dr. Monsees says.
“The ACS guideline says that women between 40 and 44 years should have the opportunity to begin annual screening,” she says, noting that this recommendation was graded as “qualified.”
“The ACS states that a qualified recommendation indicates that ‘there is clear evidence of benefit of screening, but less certainty about the balance of benefits and harms, or about patients’ values and preferences, which could lead to different decisions about screening.’” The guideline also articulates the view “that the meaning of a qualified recommendation for patients is that the ‘majority of individuals in this situation would want the suggested course of action, but many would not.’ Therefore, I find it mind-boggling that this has been interpreted to mean that women should not begin screening until age 45.”1
“It is my opinion that it is clear that if women want to achieve the most lifesaving benefit from screening, they should adhere to a schedule of yearly mammograms beginning at age 40,” says Dr. Monsees. However, she also agrees with the ACS notation that clinicians should acknowledge that “different choices will be appropriate for different patients and that clinicians must help each patient arrive at a management decision consistent with her values and preferences.”1
The word from an expert ObGyn
“By changing its guidance to begin screening at age 45 instead of 40, and in recommending biennial rather than annual screens in women 55 years of age and older, the updated ACS guidance will reduce harms (overdiagnosis and unnecessary additional imaging and biopsies) and moves closer to USPSTF guidance,” says Andrew M. Kaunitz, MD. He is University of Florida Research Foundation Professor and Associate Chairman, Department of Obstetrics and Gynecology, at the University of Florida College of Medicine–Jacksonville. He also serves on the OBG Management Board of Editors.
“As one editorialist points out, the ACS recommendation that women begin screening at age 45 years is based on observational comparisons of screened and unscreened cohorts—a type of analysis which the USPSTF does not consider due to concerns regarding bias,” notes Dr. Kaunitz.5
“The ACS recommendation for annual screening in women aged 45 to 54 is largely based on the findings of a report showing that, for premenopausal (but not postmenopausal) women, tumor stage was higher and size larger for screen-detected lesions among women undergoing biennial screens."6
As for the recommendation against screening CBE, Dr. Kaunitz considers that “a dramatic change from prior guidance. It is based on the absence of data finding benefits with CBE (alone or with screening mammography). Furthermore, the updated ACS guidance does not change its 2003 guidance, which does not support routine performance of or instruction regarding SBE.”
“These updated ACS guidelines should result in more women starting screening mammograms later in life, and they endorse biennial screening for many women, meaning that patients following ACS guidance will have fewer lifetime screens than with earlier recommendations,” says Dr. Kaunitz.
“Another plus is that performing fewer breast examinations during well-woman visits will allow us more time to assess family history and other risk factors for breast cancer, and to discuss screening recommendations.”
The bottom line
What is one to make of the many viewpoints on screening? For now, it probably is best to adhere to either the new ACS guidelines or current ACOG guidelines (TABLE 2), says OBG Management Editor in Chief Robert L. Barbieri, MD. He is chief of the Department of Obstetrics and Gynecology at Brigham and Women’s Hospital in Boston, and Kate Macy Ladd Professor of Obstetrics, Gynecology, and Reproductive Biology at Harvard Medical School.
TABLE 2 What are ACOG’s current recommendations?
|
ACOG recommends screening mammography every year for women starting at age 40. ACOG also states that “breast self-awareness has the potential to detect palpable breast cancer and can be recommended”; it also recommends CBE every year for women aged 19 or older.
These recommendations may change early next year, after ACOG convenes a consensus conference on the subject. The aim: “To develop a consistent set of uniform guidelines for breast cancer screening that can be implemented nationwide. Major organizations and providers of women’s health care, including ACS, will gather to evaluate and interpret the data in greater detail.”2
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
- Oeffinger KC, Fontham ET, Etzioni R, et al. Breast cancer screening for women at average risk. 2015 guideline update from the American Cancer Society. JAMA. 2015;314(15):1599–1614.
- American College of Obstetricians and Gynecologists. ACOG Statement on Revised American Cancer Society Recommendations on Breast Cancer Screening. http://www.acog.org/About-ACOG/News-Room/Statements/2015/ACOG-Statement-on-Recommendations-on-Breast-Cancer-Screening. Published October 20, 2015. Accessed October 20, 2015.
- US Preventive Services Task Force. Email communication, USPSTF Newsroom, October 20, 2015.
- American College of Radiology. News Release: ACR and SBI Continue to Recommend Regular Mammography Starting at Age 40. http://www.acr.org/About-Us/Media-Center/Press-Releases/2015-Press-Releases/20151020-ACR-SBI-Recommend-Mammography-at-Age-40. Published October 20, 2015. Accessed October 21, 2015.
- Kerlikowske K. Progress toward consensus on breast cancer screening guidelines and reducing screening harms [published online ahead of print October 20, 2015]. JAMA Intern Med. doi:10.1001/jamainternmed.2015.6466.
- Miglioretti DL, Zhu W, Kerlikowske K, et al; Breast Cancer Surveillance Consortium. Breast tumor prognostic characteristics and biennial vs annual mammography, age, and menopausal status [published online ahead of print October 20, 2015]. JAMA. doi:10.1001/jamaoncol.2015.3084.
When the American Cancer Society (ACS) updated its guidelines for screening mammography earlier this week,1 the effect was that of a stone being tossed into a tranquil pond, generating ripples in all directions.
The new guidelines focus on women at average risk for breast cancer (TABLE 1) and were updated for the first time since 2003, based on new evidence, a new emphasis on eliminating as many screening harms as possible, and a goal of “supporting the interplay among values, preferences, informed decision making, and recommendations.”1 Earlier ACS guidelines recommended annual screening starting at age 40.
TABLE 1 What constitutes “average risk” of breast cancer?
|
The new guidelines are graded according to the strength of the rec ommendation as being either “strong” or “qualified.” The ACS defines a “strong” recommendation as one that most individuals should follow. “Adherence to this recommendation according to the guideline could be used as a quality criterion or performance indicator,” the guidelines note.1
A “qualified” recommendation indicates that “Clinicians should acknowledge that different choices will be appropriate for different patients and that clinicians must help each patient arrive at a management decision consistent with her or his values and preferences.”1
The recommendations are:
- Regular screening mammography should start at age 45 years (strong recommendation)
- Screening should be annual in women aged 45 to 54 years (qualified recommendation)
- Screening should shift to biennial intervals at age 55, unless the patient prefers to continue screening annually (qualified recommendation)
- Women who desire to initiate annual screening between the ages of 40 and 44 years should be accommodated (qualified recommendation)
- Screening mammography should continue as long as the woman is in good health and has a life expectancy of at least 10 years (qualified recommendation)
- Clinical breast examination (CBE) is not recommended at any age (qualified recommendation).1
ACOG weighs in
Shortly after publication of the new ACS guidelines, the American College of Obstetricians and Gynecologists (ACOG) issued a formal statement in response2:
Response of the USPSTF
The US Preventive Services Task Force (USPSTF) also issued a statement in response to the new ACS guidelines:
The USPSTF currently recommends biennial screening beginning at age 50.
A leader in breast health cites pros and cons of ACS recommendations
Mark Pearlman, MD, professor of obstetrics and gynecology at the University of Michigan health system, is a nationally recognized expert on breast cancer screening. He sits on the National Comprehensive Cancer Network (NCCN) breast cancer screening and diagnosis group, helped author ACOG guidelines on mammography screening, and serves as a Contributing Editor to OBG Management.
“I believe the overall ACS mammography benefit evidence synthesis is reasonable and is in keeping with both NCCN and ACOG’s current recommendations. NCCN and ACOG mammography screening recommendations have both valued lives saved more highly than the ‘harms’ such as recalls and needle biopsies,” Dr. Pearlman says.
“If one combines ACS ‘strong’ and ‘qualified’ recommendations, ACS recommendations are similar to current ACOG and NCCN recommendations for mammography,” he adds.
Dr. Pearlman finds 7 areas of agreement between NCCN/ACOG and ACS recommendations, using both strong and qualified recommendations:
- “They reaffirm that screening from age 40 to 69 years is associated with a reduction in breast cancer deaths.
- They support annual screening for women in their 40s [although the ACS’ ‘strong’ recommendation is that regular screening begin at age 45 instead of 40].
- They support screening for women 70 and older who are in good health (10-year life expectancy).
- They support the finding that annual screening yields a larger mortality reduction than biennial screening.
- They confirm much uncertainty about the “over-diagnosis/overtreatment” issue.
- They endorse insurance coverage at all ages and intervals of screening (not just USPSTF ‘A’ or ‘B’ recommendations).
- They involve the patient in informed decision making.”
Where the ACS and ACOG/NCCN disagree is over the issue of the physical exam (abandoning CBE in average-risk women).
In regard to this last item, Dr. Pearlman says, “The ACS made a qualified recommendation against clinical breast exam. There is no high-level data to support such a marked change in practice. For example, when recommendations against breast self-examinations (BSE) were made, there were randomized controlled trials (RCTs) showing a lack of benefit and significant harms with BSE. With RCT-level data, it made sense to make a recommendation against the long-taught practice of SBE in average-risk women. That was not the case here. In fact, there are small amounts of data showing benefits of clinical breast exam.”
“One of my biggest concerns is not just the recommendation against CBE,” says Dr. Pearlman, “but that this may lead many women to interpret [this statement] as if they do not need to see their health care provider anymore. As you may recall, the American College of Physicians (ACP) recommended against annual pelvic examinations in asymptomatic patients. The ACS recommendation statement—taken together with the ACP statement—basically suggests that average-risk women don’t ever need to see a provider for a pelvic or breast examination except every 5 years for a Pap smear. That thinking does not recognize the importance of the clinical encounter (not just the CBE or pelvic exam), which is the opportunity to perform risk assessment and provide risk-reduction recommendations and healthy lifestyle recommendations.”
Radiologists resist new recommendations
Although the American College of Radiology (ACR) and the Society of Breast Imaging (SBI) agree with the ACS that mammography screening saves lives and should be available to women aged 40 and older, the 2 imaging organizations continue to recommend that annual screening begin at age 40. Their rationale: The latest ACS breast cancer screening guidelines, and earlier data used by the USPSTF to create its recommendations, both note that starting annual mammography at age 40 “saves the most lives.”
Where the organizations differ from the ACR is summed up by a formal statement on the ACR Web site: “The ACR and SBI strongly encourage women to obtain the maximum lifesaving benefits from mammography by continuing to get annual screening.”4
When OBG Management touched base with radiologist Barbara Monsees, MD, professor of radiology and Evens Professor of Women’s Health at Washington University Medical Center in St. Louis, Missouri, she expressed dismay at early news reports on the ACS guidelines.
“I’m dismayed that the headlines don’t seem to correlate with what the ACS actually recommended. The ACS did not state that women should wait until age 45 to begin screening. I believe the ACS was going for a more nuanced approach, but since that’s a bit complicated, I think that reporters have misconstrued what was intended,” Dr. Monsees says.
“The ACS guideline says that women between 40 and 44 years should have the opportunity to begin annual screening,” she says, noting that this recommendation was graded as “qualified.”
“The ACS states that a qualified recommendation indicates that ‘there is clear evidence of benefit of screening, but less certainty about the balance of benefits and harms, or about patients’ values and preferences, which could lead to different decisions about screening.’” The guideline also articulates the view “that the meaning of a qualified recommendation for patients is that the ‘majority of individuals in this situation would want the suggested course of action, but many would not.’ Therefore, I find it mind-boggling that this has been interpreted to mean that women should not begin screening until age 45.”1
“It is my opinion that it is clear that if women want to achieve the most lifesaving benefit from screening, they should adhere to a schedule of yearly mammograms beginning at age 40,” says Dr. Monsees. However, she also agrees with the ACS notation that clinicians should acknowledge that “different choices will be appropriate for different patients and that clinicians must help each patient arrive at a management decision consistent with her values and preferences.”1
The word from an expert ObGyn
“By changing its guidance to begin screening at age 45 instead of 40, and in recommending biennial rather than annual screens in women 55 years of age and older, the updated ACS guidance will reduce harms (overdiagnosis and unnecessary additional imaging and biopsies) and moves closer to USPSTF guidance,” says Andrew M. Kaunitz, MD. He is University of Florida Research Foundation Professor and Associate Chairman, Department of Obstetrics and Gynecology, at the University of Florida College of Medicine–Jacksonville. He also serves on the OBG Management Board of Editors.
“As one editorialist points out, the ACS recommendation that women begin screening at age 45 years is based on observational comparisons of screened and unscreened cohorts—a type of analysis which the USPSTF does not consider due to concerns regarding bias,” notes Dr. Kaunitz.5
“The ACS recommendation for annual screening in women aged 45 to 54 is largely based on the findings of a report showing that, for premenopausal (but not postmenopausal) women, tumor stage was higher and size larger for screen-detected lesions among women undergoing biennial screens."6
As for the recommendation against screening CBE, Dr. Kaunitz considers that “a dramatic change from prior guidance. It is based on the absence of data finding benefits with CBE (alone or with screening mammography). Furthermore, the updated ACS guidance does not change its 2003 guidance, which does not support routine performance of or instruction regarding SBE.”
“These updated ACS guidelines should result in more women starting screening mammograms later in life, and they endorse biennial screening for many women, meaning that patients following ACS guidance will have fewer lifetime screens than with earlier recommendations,” says Dr. Kaunitz.
“Another plus is that performing fewer breast examinations during well-woman visits will allow us more time to assess family history and other risk factors for breast cancer, and to discuss screening recommendations.”
The bottom line
What is one to make of the many viewpoints on screening? For now, it probably is best to adhere to either the new ACS guidelines or current ACOG guidelines (TABLE 2), says OBG Management Editor in Chief Robert L. Barbieri, MD. He is chief of the Department of Obstetrics and Gynecology at Brigham and Women’s Hospital in Boston, and Kate Macy Ladd Professor of Obstetrics, Gynecology, and Reproductive Biology at Harvard Medical School.
TABLE 2 What are ACOG’s current recommendations?
|
ACOG recommends screening mammography every year for women starting at age 40. ACOG also states that “breast self-awareness has the potential to detect palpable breast cancer and can be recommended”; it also recommends CBE every year for women aged 19 or older.
These recommendations may change early next year, after ACOG convenes a consensus conference on the subject. The aim: “To develop a consistent set of uniform guidelines for breast cancer screening that can be implemented nationwide. Major organizations and providers of women’s health care, including ACS, will gather to evaluate and interpret the data in greater detail.”2
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
When the American Cancer Society (ACS) updated its guidelines for screening mammography earlier this week,1 the effect was that of a stone being tossed into a tranquil pond, generating ripples in all directions.
The new guidelines focus on women at average risk for breast cancer (TABLE 1) and were updated for the first time since 2003, based on new evidence, a new emphasis on eliminating as many screening harms as possible, and a goal of “supporting the interplay among values, preferences, informed decision making, and recommendations.”1 Earlier ACS guidelines recommended annual screening starting at age 40.
TABLE 1 What constitutes “average risk” of breast cancer?
|
The new guidelines are graded according to the strength of the rec ommendation as being either “strong” or “qualified.” The ACS defines a “strong” recommendation as one that most individuals should follow. “Adherence to this recommendation according to the guideline could be used as a quality criterion or performance indicator,” the guidelines note.1
A “qualified” recommendation indicates that “Clinicians should acknowledge that different choices will be appropriate for different patients and that clinicians must help each patient arrive at a management decision consistent with her or his values and preferences.”1
The recommendations are:
- Regular screening mammography should start at age 45 years (strong recommendation)
- Screening should be annual in women aged 45 to 54 years (qualified recommendation)
- Screening should shift to biennial intervals at age 55, unless the patient prefers to continue screening annually (qualified recommendation)
- Women who desire to initiate annual screening between the ages of 40 and 44 years should be accommodated (qualified recommendation)
- Screening mammography should continue as long as the woman is in good health and has a life expectancy of at least 10 years (qualified recommendation)
- Clinical breast examination (CBE) is not recommended at any age (qualified recommendation).1
ACOG weighs in
Shortly after publication of the new ACS guidelines, the American College of Obstetricians and Gynecologists (ACOG) issued a formal statement in response2:
Response of the USPSTF
The US Preventive Services Task Force (USPSTF) also issued a statement in response to the new ACS guidelines:
The USPSTF currently recommends biennial screening beginning at age 50.
A leader in breast health cites pros and cons of ACS recommendations
Mark Pearlman, MD, professor of obstetrics and gynecology at the University of Michigan health system, is a nationally recognized expert on breast cancer screening. He sits on the National Comprehensive Cancer Network (NCCN) breast cancer screening and diagnosis group, helped author ACOG guidelines on mammography screening, and serves as a Contributing Editor to OBG Management.
“I believe the overall ACS mammography benefit evidence synthesis is reasonable and is in keeping with both NCCN and ACOG’s current recommendations. NCCN and ACOG mammography screening recommendations have both valued lives saved more highly than the ‘harms’ such as recalls and needle biopsies,” Dr. Pearlman says.
“If one combines ACS ‘strong’ and ‘qualified’ recommendations, ACS recommendations are similar to current ACOG and NCCN recommendations for mammography,” he adds.
Dr. Pearlman finds 7 areas of agreement between NCCN/ACOG and ACS recommendations, using both strong and qualified recommendations:
- “They reaffirm that screening from age 40 to 69 years is associated with a reduction in breast cancer deaths.
- They support annual screening for women in their 40s [although the ACS’ ‘strong’ recommendation is that regular screening begin at age 45 instead of 40].
- They support screening for women 70 and older who are in good health (10-year life expectancy).
- They support the finding that annual screening yields a larger mortality reduction than biennial screening.
- They confirm much uncertainty about the “over-diagnosis/overtreatment” issue.
- They endorse insurance coverage at all ages and intervals of screening (not just USPSTF ‘A’ or ‘B’ recommendations).
- They involve the patient in informed decision making.”
Where the ACS and ACOG/NCCN disagree is over the issue of the physical exam (abandoning CBE in average-risk women).
In regard to this last item, Dr. Pearlman says, “The ACS made a qualified recommendation against clinical breast exam. There is no high-level data to support such a marked change in practice. For example, when recommendations against breast self-examinations (BSE) were made, there were randomized controlled trials (RCTs) showing a lack of benefit and significant harms with BSE. With RCT-level data, it made sense to make a recommendation against the long-taught practice of SBE in average-risk women. That was not the case here. In fact, there are small amounts of data showing benefits of clinical breast exam.”
“One of my biggest concerns is not just the recommendation against CBE,” says Dr. Pearlman, “but that this may lead many women to interpret [this statement] as if they do not need to see their health care provider anymore. As you may recall, the American College of Physicians (ACP) recommended against annual pelvic examinations in asymptomatic patients. The ACS recommendation statement—taken together with the ACP statement—basically suggests that average-risk women don’t ever need to see a provider for a pelvic or breast examination except every 5 years for a Pap smear. That thinking does not recognize the importance of the clinical encounter (not just the CBE or pelvic exam), which is the opportunity to perform risk assessment and provide risk-reduction recommendations and healthy lifestyle recommendations.”
Radiologists resist new recommendations
Although the American College of Radiology (ACR) and the Society of Breast Imaging (SBI) agree with the ACS that mammography screening saves lives and should be available to women aged 40 and older, the 2 imaging organizations continue to recommend that annual screening begin at age 40. Their rationale: The latest ACS breast cancer screening guidelines, and earlier data used by the USPSTF to create its recommendations, both note that starting annual mammography at age 40 “saves the most lives.”
Where the organizations differ from the ACR is summed up by a formal statement on the ACR Web site: “The ACR and SBI strongly encourage women to obtain the maximum lifesaving benefits from mammography by continuing to get annual screening.”4
When OBG Management touched base with radiologist Barbara Monsees, MD, professor of radiology and Evens Professor of Women’s Health at Washington University Medical Center in St. Louis, Missouri, she expressed dismay at early news reports on the ACS guidelines.
“I’m dismayed that the headlines don’t seem to correlate with what the ACS actually recommended. The ACS did not state that women should wait until age 45 to begin screening. I believe the ACS was going for a more nuanced approach, but since that’s a bit complicated, I think that reporters have misconstrued what was intended,” Dr. Monsees says.
“The ACS guideline says that women between 40 and 44 years should have the opportunity to begin annual screening,” she says, noting that this recommendation was graded as “qualified.”
“The ACS states that a qualified recommendation indicates that ‘there is clear evidence of benefit of screening, but less certainty about the balance of benefits and harms, or about patients’ values and preferences, which could lead to different decisions about screening.’” The guideline also articulates the view “that the meaning of a qualified recommendation for patients is that the ‘majority of individuals in this situation would want the suggested course of action, but many would not.’ Therefore, I find it mind-boggling that this has been interpreted to mean that women should not begin screening until age 45.”1
“It is my opinion that it is clear that if women want to achieve the most lifesaving benefit from screening, they should adhere to a schedule of yearly mammograms beginning at age 40,” says Dr. Monsees. However, she also agrees with the ACS notation that clinicians should acknowledge that “different choices will be appropriate for different patients and that clinicians must help each patient arrive at a management decision consistent with her values and preferences.”1
The word from an expert ObGyn
“By changing its guidance to begin screening at age 45 instead of 40, and in recommending biennial rather than annual screens in women 55 years of age and older, the updated ACS guidance will reduce harms (overdiagnosis and unnecessary additional imaging and biopsies) and moves closer to USPSTF guidance,” says Andrew M. Kaunitz, MD. He is University of Florida Research Foundation Professor and Associate Chairman, Department of Obstetrics and Gynecology, at the University of Florida College of Medicine–Jacksonville. He also serves on the OBG Management Board of Editors.
“As one editorialist points out, the ACS recommendation that women begin screening at age 45 years is based on observational comparisons of screened and unscreened cohorts—a type of analysis which the USPSTF does not consider due to concerns regarding bias,” notes Dr. Kaunitz.5
“The ACS recommendation for annual screening in women aged 45 to 54 is largely based on the findings of a report showing that, for premenopausal (but not postmenopausal) women, tumor stage was higher and size larger for screen-detected lesions among women undergoing biennial screens."6
As for the recommendation against screening CBE, Dr. Kaunitz considers that “a dramatic change from prior guidance. It is based on the absence of data finding benefits with CBE (alone or with screening mammography). Furthermore, the updated ACS guidance does not change its 2003 guidance, which does not support routine performance of or instruction regarding SBE.”
“These updated ACS guidelines should result in more women starting screening mammograms later in life, and they endorse biennial screening for many women, meaning that patients following ACS guidance will have fewer lifetime screens than with earlier recommendations,” says Dr. Kaunitz.
“Another plus is that performing fewer breast examinations during well-woman visits will allow us more time to assess family history and other risk factors for breast cancer, and to discuss screening recommendations.”
The bottom line
What is one to make of the many viewpoints on screening? For now, it probably is best to adhere to either the new ACS guidelines or current ACOG guidelines (TABLE 2), says OBG Management Editor in Chief Robert L. Barbieri, MD. He is chief of the Department of Obstetrics and Gynecology at Brigham and Women’s Hospital in Boston, and Kate Macy Ladd Professor of Obstetrics, Gynecology, and Reproductive Biology at Harvard Medical School.
TABLE 2 What are ACOG’s current recommendations?
|
ACOG recommends screening mammography every year for women starting at age 40. ACOG also states that “breast self-awareness has the potential to detect palpable breast cancer and can be recommended”; it also recommends CBE every year for women aged 19 or older.
These recommendations may change early next year, after ACOG convenes a consensus conference on the subject. The aim: “To develop a consistent set of uniform guidelines for breast cancer screening that can be implemented nationwide. Major organizations and providers of women’s health care, including ACS, will gather to evaluate and interpret the data in greater detail.”2
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
- Oeffinger KC, Fontham ET, Etzioni R, et al. Breast cancer screening for women at average risk. 2015 guideline update from the American Cancer Society. JAMA. 2015;314(15):1599–1614.
- American College of Obstetricians and Gynecologists. ACOG Statement on Revised American Cancer Society Recommendations on Breast Cancer Screening. http://www.acog.org/About-ACOG/News-Room/Statements/2015/ACOG-Statement-on-Recommendations-on-Breast-Cancer-Screening. Published October 20, 2015. Accessed October 20, 2015.
- US Preventive Services Task Force. Email communication, USPSTF Newsroom, October 20, 2015.
- American College of Radiology. News Release: ACR and SBI Continue to Recommend Regular Mammography Starting at Age 40. http://www.acr.org/About-Us/Media-Center/Press-Releases/2015-Press-Releases/20151020-ACR-SBI-Recommend-Mammography-at-Age-40. Published October 20, 2015. Accessed October 21, 2015.
- Kerlikowske K. Progress toward consensus on breast cancer screening guidelines and reducing screening harms [published online ahead of print October 20, 2015]. JAMA Intern Med. doi:10.1001/jamainternmed.2015.6466.
- Miglioretti DL, Zhu W, Kerlikowske K, et al; Breast Cancer Surveillance Consortium. Breast tumor prognostic characteristics and biennial vs annual mammography, age, and menopausal status [published online ahead of print October 20, 2015]. JAMA. doi:10.1001/jamaoncol.2015.3084.
- Oeffinger KC, Fontham ET, Etzioni R, et al. Breast cancer screening for women at average risk. 2015 guideline update from the American Cancer Society. JAMA. 2015;314(15):1599–1614.
- American College of Obstetricians and Gynecologists. ACOG Statement on Revised American Cancer Society Recommendations on Breast Cancer Screening. http://www.acog.org/About-ACOG/News-Room/Statements/2015/ACOG-Statement-on-Recommendations-on-Breast-Cancer-Screening. Published October 20, 2015. Accessed October 20, 2015.
- US Preventive Services Task Force. Email communication, USPSTF Newsroom, October 20, 2015.
- American College of Radiology. News Release: ACR and SBI Continue to Recommend Regular Mammography Starting at Age 40. http://www.acr.org/About-Us/Media-Center/Press-Releases/2015-Press-Releases/20151020-ACR-SBI-Recommend-Mammography-at-Age-40. Published October 20, 2015. Accessed October 21, 2015.
- Kerlikowske K. Progress toward consensus on breast cancer screening guidelines and reducing screening harms [published online ahead of print October 20, 2015]. JAMA Intern Med. doi:10.1001/jamainternmed.2015.6466.
- Miglioretti DL, Zhu W, Kerlikowske K, et al; Breast Cancer Surveillance Consortium. Breast tumor prognostic characteristics and biennial vs annual mammography, age, and menopausal status [published online ahead of print October 20, 2015]. JAMA. doi:10.1001/jamaoncol.2015.3084.
A survey of liability claims against obstetric providers highlights major areas of contention
An analysis of 882 obstetric claims closed between 2007 and 2014 highlighted 3 common allegationsby patients1:
- a delay in the treatment of fetal distress (22%). The term “fetal distress” remains a common allegation in malpractice claims. Cases in this category most often reflected a delay or failure to act in the face of Category II or III fetal heart-rate tracings.
- improper performance of vaginal delivery (20%). Almost half of the cases in this category involved brachial plexus injuries linked to shoulder dystocia. Patients alleged that improper maneuvers were used to resolve the dystocia. The remainder of cases in this category involved forceps and vacuum extraction deliveries.
- improper management of pregnancy (17%). Among the allegations were a failure to test for fetal abnormalities, failure to recognize complications of pregnancy, and failure to address abnormal findings.
Together, these 3 allegations accounted for 59% of claims. Other allegations included diagnosis-related claims, delay in delivery, improper performance of operative delivery, retained foreign bodies, and improper choice of delivery method.1
Where are the really big malpractice awards?
Everything may be bigger in Texas, but New York is the biggest in at least 1 area: large medical malpractice payments. New York had more than 3 times as many $1 million-plus malpractice awards as any other state in 2014, according to data from the National Practitioner Data Bank (NPDB).1
New York physicians had 210 malpractice payments of $1 million or more reported to the NPDB last year, compared with 61 for Illinois, the next-highest state. Rounding out the top 5 were Massachusetts with 49, followed by California with 43, and New Jersey with 41, the NPDB data show.
After taking population into account, New York was still the leader with 10.66 large awards per million residents. Next in this category was the New England trio of Rhode Island, which had 9.42 such payments per 1 million population; Massachusetts (7.26); and Connecticut (6.39).
In 2014, there were 4 states that had no malpractice payments of at least $1 million reported to the NPDB: Alaska, Kansas, North Dakota, and Nebraska, with Kansas having the largest population. In states with at least one $1 million-plus malpractice payment, Texas physicians had the lowest rate per million population, 0.22—just 6 awards from a population of 27 million.
Reference
1. NPDB Research Statistics. National Practitioner Data Bank. http://www.npdb.hrsa.gov/resources/npdbstats/npdbStatistics.jsp. Accessed
July 17, 2015.
Copyright © 2015 Ob.Gyn. News Digital Network, Frontline Medical Communications. Available at: http://www.obgynews.com/?id=11146&tx_ttnews[tt_news]=417377&cHash=5cc8cd69fa7c8a1186aaeec0e814e4e4
The Obstetrics Closed Claims Study findings were released earlier this spring by the Napa, California−based Doctors Company, the nation’s largest physician-owned medical malpractice insurer.1 Susan Mann, MD,a spokesperson for the company, provided expert commentary on the study at the 2015 Annual Clinical Meeting of the American College of Obstetricians and Gynecologists in San Francisco (see “Frequent sources of malpractice claims” below).
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel |
Frequent sources of malpractice claims
Communication breakdowns and treatment delays are frequent sources of malpractice claims. Susan Mann, MD, spokesperson for The Doctors Company, the nation’s largest physician-owned medical malpractice insurer, discusses the underlying practice vulnerabilities revealed by the Obstetrics Closed Claims Study.
Dr. Mann practices obstetrics and gynecology in Brookline, Massachusetts, and at Beth Israel Deaconess Medical Center in Boston. She is president of the QualBridge Institute, a consulting firm focused on issues of quality and safety.
Top 7 factors contributing to patient injury
The Doctors Company identified specific factors that contributed to patient injury in the closed claims1:
- Selection and management of therapy(34%). Among the issues here were decisions involving augmentation of labor, route of delivery, and the timing of interventions. This factor also related to medications—for example, a failure to order antibiotics for Group A and Group B strep, a failure to order Rho(D) immune globulin for Rh-negative mothers, and a failure to provide magnesium sulfate for women with eclampsia.
- Patient-assessment issues (32%). The Doctors Company reviewers found that physicians frequently failed to consider information that was available, or overlooked abnormal findings.
- Technical performance (18%). This factor involved problems associated with known risks of various procedures, such as postpartum hemorrhage and brachial plexus injuries. It also included poor technique.
- Communication problems among providers (17%).
- Patient factors (16%). These factors included a failure to comply with therapy or to show up for appointments.
- Insufficient notes or a lack of documentation (14%).
- Communication problems between patient/family and provider (14%).
“Studying obstetrical medical malpractice claims sheds light on the wide array of problems that may arise during pregnancy and in labor and delivery,” the study authors conclude. “Many of these cases reflect unusual maternal or neonatal conditions that can be diagnosed only with vigilance. Examples include protein deficiencies, clotting abnormalities, placental abruptions, infections, and genetic abnormalities. More common conditions should be identified with close attention to vital signs, laboratory studies, changes to maternal and neonatal conditions, and patient complaints.”1 See “Tips for reducing malpractice claims in obstetrics” below.
Tips for reducing malpractice claims in obstetrics1
The Obstetrics Closed Claim Study identified a number of “underlying vulnerabilities” that place patients at risk and increase liability for clinicians. The Doctors Company offers the following tips to help reduce these claims:
Require periodic training and certification for physicians and nurses to maintain competency and facilitate conversations about fetal heart-rate (FHR) tracing interpretation. Both parties should use the same terminology when discussing the strips.
Use technology that allows physicians to review FHR patterns from remote locations so that physicians and nurses are able to see the same information when discussing next steps.
When operative vaginal delivery is attempted in the face of a Category III FHR tracing, a contingency team should be available for possible emergent cesarean delivery.
Foster a culture in which caregivers feel comfortable speaking up if they have a concern. Ensure that the organization has a well-defined escalation guideline.
“Obstetric departments must plan for clinical emergencies by developing and maintaining physician and staff competencies through mock drills and simulations that reduce the likelihood of injuries to mothers and their infants,” the study authors conclude.1
Share your thoughts on this article! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
Reference
1. The Doctors Company. Obstetrics Closed Claim Study. http://www.thedoctors.com/KnowledgeCenter/Pa tient Safety/articles/CON_ID_011803. Published April 2015. Accessed May 6, 2015.
An analysis of 882 obstetric claims closed between 2007 and 2014 highlighted 3 common allegationsby patients1:
- a delay in the treatment of fetal distress (22%). The term “fetal distress” remains a common allegation in malpractice claims. Cases in this category most often reflected a delay or failure to act in the face of Category II or III fetal heart-rate tracings.
- improper performance of vaginal delivery (20%). Almost half of the cases in this category involved brachial plexus injuries linked to shoulder dystocia. Patients alleged that improper maneuvers were used to resolve the dystocia. The remainder of cases in this category involved forceps and vacuum extraction deliveries.
- improper management of pregnancy (17%). Among the allegations were a failure to test for fetal abnormalities, failure to recognize complications of pregnancy, and failure to address abnormal findings.
Together, these 3 allegations accounted for 59% of claims. Other allegations included diagnosis-related claims, delay in delivery, improper performance of operative delivery, retained foreign bodies, and improper choice of delivery method.1
Where are the really big malpractice awards?
Everything may be bigger in Texas, but New York is the biggest in at least 1 area: large medical malpractice payments. New York had more than 3 times as many $1 million-plus malpractice awards as any other state in 2014, according to data from the National Practitioner Data Bank (NPDB).1
New York physicians had 210 malpractice payments of $1 million or more reported to the NPDB last year, compared with 61 for Illinois, the next-highest state. Rounding out the top 5 were Massachusetts with 49, followed by California with 43, and New Jersey with 41, the NPDB data show.
After taking population into account, New York was still the leader with 10.66 large awards per million residents. Next in this category was the New England trio of Rhode Island, which had 9.42 such payments per 1 million population; Massachusetts (7.26); and Connecticut (6.39).
In 2014, there were 4 states that had no malpractice payments of at least $1 million reported to the NPDB: Alaska, Kansas, North Dakota, and Nebraska, with Kansas having the largest population. In states with at least one $1 million-plus malpractice payment, Texas physicians had the lowest rate per million population, 0.22—just 6 awards from a population of 27 million.
Reference
1. NPDB Research Statistics. National Practitioner Data Bank. http://www.npdb.hrsa.gov/resources/npdbstats/npdbStatistics.jsp. Accessed
July 17, 2015.
Copyright © 2015 Ob.Gyn. News Digital Network, Frontline Medical Communications. Available at: http://www.obgynews.com/?id=11146&tx_ttnews[tt_news]=417377&cHash=5cc8cd69fa7c8a1186aaeec0e814e4e4
The Obstetrics Closed Claims Study findings were released earlier this spring by the Napa, California−based Doctors Company, the nation’s largest physician-owned medical malpractice insurer.1 Susan Mann, MD,a spokesperson for the company, provided expert commentary on the study at the 2015 Annual Clinical Meeting of the American College of Obstetricians and Gynecologists in San Francisco (see “Frequent sources of malpractice claims” below).
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel |
Frequent sources of malpractice claims
Communication breakdowns and treatment delays are frequent sources of malpractice claims. Susan Mann, MD, spokesperson for The Doctors Company, the nation’s largest physician-owned medical malpractice insurer, discusses the underlying practice vulnerabilities revealed by the Obstetrics Closed Claims Study.
Dr. Mann practices obstetrics and gynecology in Brookline, Massachusetts, and at Beth Israel Deaconess Medical Center in Boston. She is president of the QualBridge Institute, a consulting firm focused on issues of quality and safety.
Top 7 factors contributing to patient injury
The Doctors Company identified specific factors that contributed to patient injury in the closed claims1:
- Selection and management of therapy(34%). Among the issues here were decisions involving augmentation of labor, route of delivery, and the timing of interventions. This factor also related to medications—for example, a failure to order antibiotics for Group A and Group B strep, a failure to order Rho(D) immune globulin for Rh-negative mothers, and a failure to provide magnesium sulfate for women with eclampsia.
- Patient-assessment issues (32%). The Doctors Company reviewers found that physicians frequently failed to consider information that was available, or overlooked abnormal findings.
- Technical performance (18%). This factor involved problems associated with known risks of various procedures, such as postpartum hemorrhage and brachial plexus injuries. It also included poor technique.
- Communication problems among providers (17%).
- Patient factors (16%). These factors included a failure to comply with therapy or to show up for appointments.
- Insufficient notes or a lack of documentation (14%).
- Communication problems between patient/family and provider (14%).
“Studying obstetrical medical malpractice claims sheds light on the wide array of problems that may arise during pregnancy and in labor and delivery,” the study authors conclude. “Many of these cases reflect unusual maternal or neonatal conditions that can be diagnosed only with vigilance. Examples include protein deficiencies, clotting abnormalities, placental abruptions, infections, and genetic abnormalities. More common conditions should be identified with close attention to vital signs, laboratory studies, changes to maternal and neonatal conditions, and patient complaints.”1 See “Tips for reducing malpractice claims in obstetrics” below.
Tips for reducing malpractice claims in obstetrics1
The Obstetrics Closed Claim Study identified a number of “underlying vulnerabilities” that place patients at risk and increase liability for clinicians. The Doctors Company offers the following tips to help reduce these claims:
Require periodic training and certification for physicians and nurses to maintain competency and facilitate conversations about fetal heart-rate (FHR) tracing interpretation. Both parties should use the same terminology when discussing the strips.
Use technology that allows physicians to review FHR patterns from remote locations so that physicians and nurses are able to see the same information when discussing next steps.
When operative vaginal delivery is attempted in the face of a Category III FHR tracing, a contingency team should be available for possible emergent cesarean delivery.
Foster a culture in which caregivers feel comfortable speaking up if they have a concern. Ensure that the organization has a well-defined escalation guideline.
“Obstetric departments must plan for clinical emergencies by developing and maintaining physician and staff competencies through mock drills and simulations that reduce the likelihood of injuries to mothers and their infants,” the study authors conclude.1
Share your thoughts on this article! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
An analysis of 882 obstetric claims closed between 2007 and 2014 highlighted 3 common allegationsby patients1:
- a delay in the treatment of fetal distress (22%). The term “fetal distress” remains a common allegation in malpractice claims. Cases in this category most often reflected a delay or failure to act in the face of Category II or III fetal heart-rate tracings.
- improper performance of vaginal delivery (20%). Almost half of the cases in this category involved brachial plexus injuries linked to shoulder dystocia. Patients alleged that improper maneuvers were used to resolve the dystocia. The remainder of cases in this category involved forceps and vacuum extraction deliveries.
- improper management of pregnancy (17%). Among the allegations were a failure to test for fetal abnormalities, failure to recognize complications of pregnancy, and failure to address abnormal findings.
Together, these 3 allegations accounted for 59% of claims. Other allegations included diagnosis-related claims, delay in delivery, improper performance of operative delivery, retained foreign bodies, and improper choice of delivery method.1
Where are the really big malpractice awards?
Everything may be bigger in Texas, but New York is the biggest in at least 1 area: large medical malpractice payments. New York had more than 3 times as many $1 million-plus malpractice awards as any other state in 2014, according to data from the National Practitioner Data Bank (NPDB).1
New York physicians had 210 malpractice payments of $1 million or more reported to the NPDB last year, compared with 61 for Illinois, the next-highest state. Rounding out the top 5 were Massachusetts with 49, followed by California with 43, and New Jersey with 41, the NPDB data show.
After taking population into account, New York was still the leader with 10.66 large awards per million residents. Next in this category was the New England trio of Rhode Island, which had 9.42 such payments per 1 million population; Massachusetts (7.26); and Connecticut (6.39).
In 2014, there were 4 states that had no malpractice payments of at least $1 million reported to the NPDB: Alaska, Kansas, North Dakota, and Nebraska, with Kansas having the largest population. In states with at least one $1 million-plus malpractice payment, Texas physicians had the lowest rate per million population, 0.22—just 6 awards from a population of 27 million.
Reference
1. NPDB Research Statistics. National Practitioner Data Bank. http://www.npdb.hrsa.gov/resources/npdbstats/npdbStatistics.jsp. Accessed
July 17, 2015.
Copyright © 2015 Ob.Gyn. News Digital Network, Frontline Medical Communications. Available at: http://www.obgynews.com/?id=11146&tx_ttnews[tt_news]=417377&cHash=5cc8cd69fa7c8a1186aaeec0e814e4e4
The Obstetrics Closed Claims Study findings were released earlier this spring by the Napa, California−based Doctors Company, the nation’s largest physician-owned medical malpractice insurer.1 Susan Mann, MD,a spokesperson for the company, provided expert commentary on the study at the 2015 Annual Clinical Meeting of the American College of Obstetricians and Gynecologists in San Francisco (see “Frequent sources of malpractice claims” below).
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel |
Frequent sources of malpractice claims
Communication breakdowns and treatment delays are frequent sources of malpractice claims. Susan Mann, MD, spokesperson for The Doctors Company, the nation’s largest physician-owned medical malpractice insurer, discusses the underlying practice vulnerabilities revealed by the Obstetrics Closed Claims Study.
Dr. Mann practices obstetrics and gynecology in Brookline, Massachusetts, and at Beth Israel Deaconess Medical Center in Boston. She is president of the QualBridge Institute, a consulting firm focused on issues of quality and safety.
Top 7 factors contributing to patient injury
The Doctors Company identified specific factors that contributed to patient injury in the closed claims1:
- Selection and management of therapy(34%). Among the issues here were decisions involving augmentation of labor, route of delivery, and the timing of interventions. This factor also related to medications—for example, a failure to order antibiotics for Group A and Group B strep, a failure to order Rho(D) immune globulin for Rh-negative mothers, and a failure to provide magnesium sulfate for women with eclampsia.
- Patient-assessment issues (32%). The Doctors Company reviewers found that physicians frequently failed to consider information that was available, or overlooked abnormal findings.
- Technical performance (18%). This factor involved problems associated with known risks of various procedures, such as postpartum hemorrhage and brachial plexus injuries. It also included poor technique.
- Communication problems among providers (17%).
- Patient factors (16%). These factors included a failure to comply with therapy or to show up for appointments.
- Insufficient notes or a lack of documentation (14%).
- Communication problems between patient/family and provider (14%).
“Studying obstetrical medical malpractice claims sheds light on the wide array of problems that may arise during pregnancy and in labor and delivery,” the study authors conclude. “Many of these cases reflect unusual maternal or neonatal conditions that can be diagnosed only with vigilance. Examples include protein deficiencies, clotting abnormalities, placental abruptions, infections, and genetic abnormalities. More common conditions should be identified with close attention to vital signs, laboratory studies, changes to maternal and neonatal conditions, and patient complaints.”1 See “Tips for reducing malpractice claims in obstetrics” below.
Tips for reducing malpractice claims in obstetrics1
The Obstetrics Closed Claim Study identified a number of “underlying vulnerabilities” that place patients at risk and increase liability for clinicians. The Doctors Company offers the following tips to help reduce these claims:
Require periodic training and certification for physicians and nurses to maintain competency and facilitate conversations about fetal heart-rate (FHR) tracing interpretation. Both parties should use the same terminology when discussing the strips.
Use technology that allows physicians to review FHR patterns from remote locations so that physicians and nurses are able to see the same information when discussing next steps.
When operative vaginal delivery is attempted in the face of a Category III FHR tracing, a contingency team should be available for possible emergent cesarean delivery.
Foster a culture in which caregivers feel comfortable speaking up if they have a concern. Ensure that the organization has a well-defined escalation guideline.
“Obstetric departments must plan for clinical emergencies by developing and maintaining physician and staff competencies through mock drills and simulations that reduce the likelihood of injuries to mothers and their infants,” the study authors conclude.1
Share your thoughts on this article! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
Reference
1. The Doctors Company. Obstetrics Closed Claim Study. http://www.thedoctors.com/KnowledgeCenter/Pa tient Safety/articles/CON_ID_011803. Published April 2015. Accessed May 6, 2015.
Reference
1. The Doctors Company. Obstetrics Closed Claim Study. http://www.thedoctors.com/KnowledgeCenter/Pa tient Safety/articles/CON_ID_011803. Published April 2015. Accessed May 6, 2015.
In this Article
- Tips for reducing malpractice claims in obstetrics
- Where are the really big malpractice awards?
- Top 7 factors contributing topatient injury
ObGyn salaries continue gradual improvement
The mean income for ObGyns rose by 2% in 2014 over 2013 to $249,000, according to the 2015 Medscape Compensation Report.1 This slight rise continues a gradual increase over the past few years ($242,000 in 2012; $220,000 in 2011).1–4 The 2015 report took into account survey responses from 19,657 physicians across 26 specialties, 5% (982) of whom were ObGyns.
The highest earners among all physician specialties were orthopedists ($421,000), cardiologists, and gastroenterologists. The lowest earners were pediatricians, family physicians, endocrinologists, and internists ($196,000). The highest ObGyn earners lived in the Northwest ($289,000) and Great Lakes ($268,000) regions; the lowest earners lived in the Mid-Atlantic ($230,000) and Northeast ($235,000) areas.1
Survey findings
Career satisfaction for ObGyns is dipping
In 2011, 69%, 53%, and 48% of ObGyns indicated they would choose a career in medicine again, select the same specialty, and pick the same practice setting, respectively.4 In the 2015 survey, 67% of ObGyns reported that they would still choose medicine; however, only 40% would pick obstetrics and gynecology as their specialty, and only 22% would select the same practice setting.1
Employment over private practice: Who feels best compensated?
Overall, 63% of all physicians are now employed, with only 23% reporting to be in private practice. Employment appears to be more popular for women: 59% of men and 72% of women responded that they work for a salary. Slightly more than a third (36%) of men and about a quarter (23%) of women are self-employed.5
The gender picture. Half of all ObGyns are women, and almost half of medical school graduates are women, yet male ObGyns continue to make more money than their female counterparts.1,5,6 The 9% difference between compensation rates for self-employed male and female ObGyns ($265,000 vs $242,000, respectively) is less than the 14% difference between their employed colleagues ($266,000 vs $229,000, respectively).1 Women tend to work shorter hours, fewer weeks, and see fewer patients than men, which could account for the lower compensation rate for female ObGyns. Studies suggest that greater schedule flexibility and fewer hours are key factors that improve satisfaction rates for female physicians.5
Male and female ObGyns tend to agree on their income satisfaction: less than half are satisfied (male, 44%; female, 46%). Many more employed ObGyns (55%) than self-employed ObGyns (31%) believe that they are fairly compensated.1
Which practice settings pay better?
Compensation rates for ObGyns in 2015 are greatest for those in office-based multispecialty group practice ($280,000), followed by those who work in1:
- health care organizations ($269,000)
- office-based single-specialty group practices ($266,000)
- outpatient clinics ($223,000)
- academic settings (nonhospital), research, military, and government ($219,000).
The lowest paid practice settings are office-based solo practices ($218,000) and hospital-employed ObGyns ($209,000).
In 2013, ObGyns who earned the most worked for health care organizations ($273,000); those who earned the least worked for outpatient clinics ($207,000).1
Do you take insurance, Medicare, Medicaid?
More employed (82%) than self-employed (53%) ObGyns will continue to take new and current Medicare or Medicaid patients, which is a rise from data published in the 2014 report (employed, 72%; self-employed, 46%).1
More than half (58%) of all physicians received less than $100 from private insurers for a new-patient office visit in 2014. Among ObGyns, 26% said they would drop insurers that pay poorly; 29% replied that they would not drop an insurer because they need all payers.1
The rate of participation in Accountable Care Organizations (ACOs) has increased from 25% in 2013 to 35% in 2014, with 8% more expecting to join an ACO in 2015. Concierge practice (2%) and cash-only practice (5%) were reportedly not significant payment models for ObGyns in 2014.1
Only 26% of ObGyns are planning to participate in health insurance exchanges; 23% said they are not participating, and 51% are not sure whether they will participate. Close to half (41%) of ObGyns believe their income will decrease because of health insurance exchanges, whereas 54% do not anticipate a change in income.1
Do you offer ancillary services?
When asked, 11% of employed ObGyns and 28% of self-employed ObGyns revealed that they have offered new ancillary services within the past 3 years. These ancillary services can include mammography, bone density testing, ultrasound, in-house laboratory services, bioidentical hormone replacement therapy, and weight management.1
How much time do you spend with patients?
In 2014, 62% of ObGyns reported spending 9 to 16 minutes with a patient during a visit. This is compared to 56% of family physicians and 44% of internists (TABLE).1,5
More than one-half (52%) of ObGynsspend 30 to 45 hours per week seeing patients. Fewer (38%) spend more than 45 hours per week, and 9% spend less than 30 hours per week with patients. This decline may be due to the increasing proportion of women and older physicians who tend to work shorter hours and fewer weeks.1
In the general physician population, 24% of women and 13% of men work part time, whereas 16% of both male and female ObGyns work part time. ObGyns aged 65 years or older constitute 35% of part-timers; 9% of those aged 35 to 49 years, and 11% of those aged 50 to 64 years, work part time. Only 2% of those younger than age 35 work part time.1
Would you select a career in obstetrics and gynecology all over again?
If given a second chance, would you rather choose orthopedic surgery as your specialty, or even choose medicine as a career again? OBG Management recently asked readers to weigh in, through its Quick Poll posted at obgmanagement.com, on whether or not they would choose ObGyn all over again. Ninety-one readers answered “yes” and 70 answered “no,” for a total of 161 respondents.
When this same question was posed to OBG Management’s Virtual Board of Editors (VBE), the perspectives were as split as the Quick Poll results:
- “No, no, no, I would not choose ObGyn all over again.”
- “Yes, I still love what I do.”
- “Yes, it is still the most unique specialty in medicine because it involves both surgery and primary care.”
- “Yes, for all the reasons I first loved the specialty: every week’s schedule, and every day is different. There is a mix of office care, surgery, and call.”
- “No! There is constant concern of litigation for complications, poor reimbursement, and compromised lifestyle.”
“There are much easier ways to make a living,” said one respondent, and another replied, “Work is very tough right now and the payment is too low.”
“The specialty has changed,” said Mary Vanko, MD, who practices in the suburbs of “blue collar Indiana.” “The public has very little idea of the breadth of our knowledge. The ObGyn generalist has the ability to serve as a woman’s doctor throughout her lifetime, not just perform the deliveries and surgeries. All of a sudden we are excluded from primary care status and people have to fight to see us. The newbies will never experience what it used to be as an ObGyn, the woman’s primary. Now we are the doctors to see when someone wants an IUD or is bleeding or pregnant. Big difference.”
Wesley Hambright, MD, practices in a small community hospital, but feels that “a larger hospital with more specialties may offer more flexibility and support in dealing with external pressures.” Tameka O’Neal, MD, is currently hospital employed but feels “as though I have little say in my practice.” Shaukat Ashai, MD, who is retired after 35 years in practice, says he would have preferred an academic setting on a full-time basis, citing long hours and poor compensation.
Robert del Rosario, MD, is in a large single-specialty suburban practice and would choose this practice setting again, although he would not choose a career as an ObGyn again. “The work demands have taken away too much from family,” he says. In addition, “as a male ObGyn, I am regularly faced with patients who choose their doctors based on gender rather than on skill. Our colleagues are no better. Early in my career and until the present, I hear people say, ‘Oh, I can’t hire Dr. X because we’re looking to hire a female.’”
Joe Walsh, MD, of Philadelphia, Pennsylvania, expresses similar discontent as a male ObGyn practicing in today’s female-populated specialty. In a letter to the editor in response to Editor in Chief Robert L. Barbieri, MD’s Editorial in the May 2015 issue, “Why is obstetrics and gynecology a popular choice for medical students?” Dr. Walsh states: “The unaddressed question is why is it unpopular for half of medical students? Ninety-three percent of resident graduates in the field are women, while women account for half of medical student graduates. Men rarely go into the field today. Perhaps job advertisements touting physician opportunities in ‘all female groups’ discourage men. Perhaps hospitals’ ‘Women’s Health Centers’ with such slogans as ‘Women taking care of women’ discourage men. Perhaps receptionists’ asking patients whether they prefer a male or female physician discourages male ObGyns.”
Many VBE members express some frustrations—with their practice setting, compensation, and longer work hours—but say that the patient relationships are the most rewarding aspect of their jobs. After 29 years in practice, Patrick Pevoto, MD, says the most rewarding aspect of his job is “being part of the legacy in people’s lives.”
Others say what keeps them engaged is:
- Enjoying “good outcomes.”
- “The patient contact. It’s fun having someone come up to me in the grocery store and introduce me to a teenager that I delivered 15 years ago.”
- “Surgery.”
- “Helping patients and teaching fellows.”
- “Knowing that I am making a difference in people’s lives.”
What is most rewarding?
When given several choices to select as the most rewarding aspect of their jobs, more female ObGyns (47%) than males (41%) reported that their physician-patient relationships are the major source of satisfaction. More men (10%) than women (7%) cite that making good money at a job they like is most gratifying. Only 3% of men and 2% of women reported no reward to being an ObGyn.1
Survey methodology
Medscape reports that the recruitment period for the 2015 Physician Compensation Report was from December 30, 2014, through March 11, 2015. Data were collected via a third-party online survey collection site. The margin of error for the survey was ±0.69%.1
Share your thoughts on this article! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
1. Peckham C. Medscape OB/GYN Compensation Report 2015. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2015/womenshealth. Published April 21, 2015. Accessed May 13, 2015.
2. Peckham C. Medscape OB/GYN Compensation Report 2014. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2014/womenshealth. Published April 15, 2014. Accessed June 2, 2014.
3. Medscape News. Ob/Gyn Compensation Report 2013. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2013/womenshealth. Accessed June 30, 2013.
4. Reale D. Mean income for ObGyns increased in 2012. OBG Manag. 2013;25(8):34–36.
5. Peckham C. Medscape Physician Compensation Report 2015. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2015/public/overview. Published April 21, 2015. Accessed May 13, 2015.
6. Distribution of medical school graduates by gender. Henry Kaiser Family Foundation Web site. http://kff.org/other/state-indicator/medical-school-graduates-by-gender/. Accessed May 13, 2015.
The mean income for ObGyns rose by 2% in 2014 over 2013 to $249,000, according to the 2015 Medscape Compensation Report.1 This slight rise continues a gradual increase over the past few years ($242,000 in 2012; $220,000 in 2011).1–4 The 2015 report took into account survey responses from 19,657 physicians across 26 specialties, 5% (982) of whom were ObGyns.
The highest earners among all physician specialties were orthopedists ($421,000), cardiologists, and gastroenterologists. The lowest earners were pediatricians, family physicians, endocrinologists, and internists ($196,000). The highest ObGyn earners lived in the Northwest ($289,000) and Great Lakes ($268,000) regions; the lowest earners lived in the Mid-Atlantic ($230,000) and Northeast ($235,000) areas.1
Survey findings
Career satisfaction for ObGyns is dipping
In 2011, 69%, 53%, and 48% of ObGyns indicated they would choose a career in medicine again, select the same specialty, and pick the same practice setting, respectively.4 In the 2015 survey, 67% of ObGyns reported that they would still choose medicine; however, only 40% would pick obstetrics and gynecology as their specialty, and only 22% would select the same practice setting.1
Employment over private practice: Who feels best compensated?
Overall, 63% of all physicians are now employed, with only 23% reporting to be in private practice. Employment appears to be more popular for women: 59% of men and 72% of women responded that they work for a salary. Slightly more than a third (36%) of men and about a quarter (23%) of women are self-employed.5
The gender picture. Half of all ObGyns are women, and almost half of medical school graduates are women, yet male ObGyns continue to make more money than their female counterparts.1,5,6 The 9% difference between compensation rates for self-employed male and female ObGyns ($265,000 vs $242,000, respectively) is less than the 14% difference between their employed colleagues ($266,000 vs $229,000, respectively).1 Women tend to work shorter hours, fewer weeks, and see fewer patients than men, which could account for the lower compensation rate for female ObGyns. Studies suggest that greater schedule flexibility and fewer hours are key factors that improve satisfaction rates for female physicians.5
Male and female ObGyns tend to agree on their income satisfaction: less than half are satisfied (male, 44%; female, 46%). Many more employed ObGyns (55%) than self-employed ObGyns (31%) believe that they are fairly compensated.1
Which practice settings pay better?
Compensation rates for ObGyns in 2015 are greatest for those in office-based multispecialty group practice ($280,000), followed by those who work in1:
- health care organizations ($269,000)
- office-based single-specialty group practices ($266,000)
- outpatient clinics ($223,000)
- academic settings (nonhospital), research, military, and government ($219,000).
The lowest paid practice settings are office-based solo practices ($218,000) and hospital-employed ObGyns ($209,000).
In 2013, ObGyns who earned the most worked for health care organizations ($273,000); those who earned the least worked for outpatient clinics ($207,000).1
Do you take insurance, Medicare, Medicaid?
More employed (82%) than self-employed (53%) ObGyns will continue to take new and current Medicare or Medicaid patients, which is a rise from data published in the 2014 report (employed, 72%; self-employed, 46%).1
More than half (58%) of all physicians received less than $100 from private insurers for a new-patient office visit in 2014. Among ObGyns, 26% said they would drop insurers that pay poorly; 29% replied that they would not drop an insurer because they need all payers.1
The rate of participation in Accountable Care Organizations (ACOs) has increased from 25% in 2013 to 35% in 2014, with 8% more expecting to join an ACO in 2015. Concierge practice (2%) and cash-only practice (5%) were reportedly not significant payment models for ObGyns in 2014.1
Only 26% of ObGyns are planning to participate in health insurance exchanges; 23% said they are not participating, and 51% are not sure whether they will participate. Close to half (41%) of ObGyns believe their income will decrease because of health insurance exchanges, whereas 54% do not anticipate a change in income.1
Do you offer ancillary services?
When asked, 11% of employed ObGyns and 28% of self-employed ObGyns revealed that they have offered new ancillary services within the past 3 years. These ancillary services can include mammography, bone density testing, ultrasound, in-house laboratory services, bioidentical hormone replacement therapy, and weight management.1
How much time do you spend with patients?
In 2014, 62% of ObGyns reported spending 9 to 16 minutes with a patient during a visit. This is compared to 56% of family physicians and 44% of internists (TABLE).1,5
More than one-half (52%) of ObGynsspend 30 to 45 hours per week seeing patients. Fewer (38%) spend more than 45 hours per week, and 9% spend less than 30 hours per week with patients. This decline may be due to the increasing proportion of women and older physicians who tend to work shorter hours and fewer weeks.1
In the general physician population, 24% of women and 13% of men work part time, whereas 16% of both male and female ObGyns work part time. ObGyns aged 65 years or older constitute 35% of part-timers; 9% of those aged 35 to 49 years, and 11% of those aged 50 to 64 years, work part time. Only 2% of those younger than age 35 work part time.1
Would you select a career in obstetrics and gynecology all over again?
If given a second chance, would you rather choose orthopedic surgery as your specialty, or even choose medicine as a career again? OBG Management recently asked readers to weigh in, through its Quick Poll posted at obgmanagement.com, on whether or not they would choose ObGyn all over again. Ninety-one readers answered “yes” and 70 answered “no,” for a total of 161 respondents.
When this same question was posed to OBG Management’s Virtual Board of Editors (VBE), the perspectives were as split as the Quick Poll results:
- “No, no, no, I would not choose ObGyn all over again.”
- “Yes, I still love what I do.”
- “Yes, it is still the most unique specialty in medicine because it involves both surgery and primary care.”
- “Yes, for all the reasons I first loved the specialty: every week’s schedule, and every day is different. There is a mix of office care, surgery, and call.”
- “No! There is constant concern of litigation for complications, poor reimbursement, and compromised lifestyle.”
“There are much easier ways to make a living,” said one respondent, and another replied, “Work is very tough right now and the payment is too low.”
“The specialty has changed,” said Mary Vanko, MD, who practices in the suburbs of “blue collar Indiana.” “The public has very little idea of the breadth of our knowledge. The ObGyn generalist has the ability to serve as a woman’s doctor throughout her lifetime, not just perform the deliveries and surgeries. All of a sudden we are excluded from primary care status and people have to fight to see us. The newbies will never experience what it used to be as an ObGyn, the woman’s primary. Now we are the doctors to see when someone wants an IUD or is bleeding or pregnant. Big difference.”
Wesley Hambright, MD, practices in a small community hospital, but feels that “a larger hospital with more specialties may offer more flexibility and support in dealing with external pressures.” Tameka O’Neal, MD, is currently hospital employed but feels “as though I have little say in my practice.” Shaukat Ashai, MD, who is retired after 35 years in practice, says he would have preferred an academic setting on a full-time basis, citing long hours and poor compensation.
Robert del Rosario, MD, is in a large single-specialty suburban practice and would choose this practice setting again, although he would not choose a career as an ObGyn again. “The work demands have taken away too much from family,” he says. In addition, “as a male ObGyn, I am regularly faced with patients who choose their doctors based on gender rather than on skill. Our colleagues are no better. Early in my career and until the present, I hear people say, ‘Oh, I can’t hire Dr. X because we’re looking to hire a female.’”
Joe Walsh, MD, of Philadelphia, Pennsylvania, expresses similar discontent as a male ObGyn practicing in today’s female-populated specialty. In a letter to the editor in response to Editor in Chief Robert L. Barbieri, MD’s Editorial in the May 2015 issue, “Why is obstetrics and gynecology a popular choice for medical students?” Dr. Walsh states: “The unaddressed question is why is it unpopular for half of medical students? Ninety-three percent of resident graduates in the field are women, while women account for half of medical student graduates. Men rarely go into the field today. Perhaps job advertisements touting physician opportunities in ‘all female groups’ discourage men. Perhaps hospitals’ ‘Women’s Health Centers’ with such slogans as ‘Women taking care of women’ discourage men. Perhaps receptionists’ asking patients whether they prefer a male or female physician discourages male ObGyns.”
Many VBE members express some frustrations—with their practice setting, compensation, and longer work hours—but say that the patient relationships are the most rewarding aspect of their jobs. After 29 years in practice, Patrick Pevoto, MD, says the most rewarding aspect of his job is “being part of the legacy in people’s lives.”
Others say what keeps them engaged is:
- Enjoying “good outcomes.”
- “The patient contact. It’s fun having someone come up to me in the grocery store and introduce me to a teenager that I delivered 15 years ago.”
- “Surgery.”
- “Helping patients and teaching fellows.”
- “Knowing that I am making a difference in people’s lives.”
What is most rewarding?
When given several choices to select as the most rewarding aspect of their jobs, more female ObGyns (47%) than males (41%) reported that their physician-patient relationships are the major source of satisfaction. More men (10%) than women (7%) cite that making good money at a job they like is most gratifying. Only 3% of men and 2% of women reported no reward to being an ObGyn.1
Survey methodology
Medscape reports that the recruitment period for the 2015 Physician Compensation Report was from December 30, 2014, through March 11, 2015. Data were collected via a third-party online survey collection site. The margin of error for the survey was ±0.69%.1
Share your thoughts on this article! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
The mean income for ObGyns rose by 2% in 2014 over 2013 to $249,000, according to the 2015 Medscape Compensation Report.1 This slight rise continues a gradual increase over the past few years ($242,000 in 2012; $220,000 in 2011).1–4 The 2015 report took into account survey responses from 19,657 physicians across 26 specialties, 5% (982) of whom were ObGyns.
The highest earners among all physician specialties were orthopedists ($421,000), cardiologists, and gastroenterologists. The lowest earners were pediatricians, family physicians, endocrinologists, and internists ($196,000). The highest ObGyn earners lived in the Northwest ($289,000) and Great Lakes ($268,000) regions; the lowest earners lived in the Mid-Atlantic ($230,000) and Northeast ($235,000) areas.1
Survey findings
Career satisfaction for ObGyns is dipping
In 2011, 69%, 53%, and 48% of ObGyns indicated they would choose a career in medicine again, select the same specialty, and pick the same practice setting, respectively.4 In the 2015 survey, 67% of ObGyns reported that they would still choose medicine; however, only 40% would pick obstetrics and gynecology as their specialty, and only 22% would select the same practice setting.1
Employment over private practice: Who feels best compensated?
Overall, 63% of all physicians are now employed, with only 23% reporting to be in private practice. Employment appears to be more popular for women: 59% of men and 72% of women responded that they work for a salary. Slightly more than a third (36%) of men and about a quarter (23%) of women are self-employed.5
The gender picture. Half of all ObGyns are women, and almost half of medical school graduates are women, yet male ObGyns continue to make more money than their female counterparts.1,5,6 The 9% difference between compensation rates for self-employed male and female ObGyns ($265,000 vs $242,000, respectively) is less than the 14% difference between their employed colleagues ($266,000 vs $229,000, respectively).1 Women tend to work shorter hours, fewer weeks, and see fewer patients than men, which could account for the lower compensation rate for female ObGyns. Studies suggest that greater schedule flexibility and fewer hours are key factors that improve satisfaction rates for female physicians.5
Male and female ObGyns tend to agree on their income satisfaction: less than half are satisfied (male, 44%; female, 46%). Many more employed ObGyns (55%) than self-employed ObGyns (31%) believe that they are fairly compensated.1
Which practice settings pay better?
Compensation rates for ObGyns in 2015 are greatest for those in office-based multispecialty group practice ($280,000), followed by those who work in1:
- health care organizations ($269,000)
- office-based single-specialty group practices ($266,000)
- outpatient clinics ($223,000)
- academic settings (nonhospital), research, military, and government ($219,000).
The lowest paid practice settings are office-based solo practices ($218,000) and hospital-employed ObGyns ($209,000).
In 2013, ObGyns who earned the most worked for health care organizations ($273,000); those who earned the least worked for outpatient clinics ($207,000).1
Do you take insurance, Medicare, Medicaid?
More employed (82%) than self-employed (53%) ObGyns will continue to take new and current Medicare or Medicaid patients, which is a rise from data published in the 2014 report (employed, 72%; self-employed, 46%).1
More than half (58%) of all physicians received less than $100 from private insurers for a new-patient office visit in 2014. Among ObGyns, 26% said they would drop insurers that pay poorly; 29% replied that they would not drop an insurer because they need all payers.1
The rate of participation in Accountable Care Organizations (ACOs) has increased from 25% in 2013 to 35% in 2014, with 8% more expecting to join an ACO in 2015. Concierge practice (2%) and cash-only practice (5%) were reportedly not significant payment models for ObGyns in 2014.1
Only 26% of ObGyns are planning to participate in health insurance exchanges; 23% said they are not participating, and 51% are not sure whether they will participate. Close to half (41%) of ObGyns believe their income will decrease because of health insurance exchanges, whereas 54% do not anticipate a change in income.1
Do you offer ancillary services?
When asked, 11% of employed ObGyns and 28% of self-employed ObGyns revealed that they have offered new ancillary services within the past 3 years. These ancillary services can include mammography, bone density testing, ultrasound, in-house laboratory services, bioidentical hormone replacement therapy, and weight management.1
How much time do you spend with patients?
In 2014, 62% of ObGyns reported spending 9 to 16 minutes with a patient during a visit. This is compared to 56% of family physicians and 44% of internists (TABLE).1,5
More than one-half (52%) of ObGynsspend 30 to 45 hours per week seeing patients. Fewer (38%) spend more than 45 hours per week, and 9% spend less than 30 hours per week with patients. This decline may be due to the increasing proportion of women and older physicians who tend to work shorter hours and fewer weeks.1
In the general physician population, 24% of women and 13% of men work part time, whereas 16% of both male and female ObGyns work part time. ObGyns aged 65 years or older constitute 35% of part-timers; 9% of those aged 35 to 49 years, and 11% of those aged 50 to 64 years, work part time. Only 2% of those younger than age 35 work part time.1
Would you select a career in obstetrics and gynecology all over again?
If given a second chance, would you rather choose orthopedic surgery as your specialty, or even choose medicine as a career again? OBG Management recently asked readers to weigh in, through its Quick Poll posted at obgmanagement.com, on whether or not they would choose ObGyn all over again. Ninety-one readers answered “yes” and 70 answered “no,” for a total of 161 respondents.
When this same question was posed to OBG Management’s Virtual Board of Editors (VBE), the perspectives were as split as the Quick Poll results:
- “No, no, no, I would not choose ObGyn all over again.”
- “Yes, I still love what I do.”
- “Yes, it is still the most unique specialty in medicine because it involves both surgery and primary care.”
- “Yes, for all the reasons I first loved the specialty: every week’s schedule, and every day is different. There is a mix of office care, surgery, and call.”
- “No! There is constant concern of litigation for complications, poor reimbursement, and compromised lifestyle.”
“There are much easier ways to make a living,” said one respondent, and another replied, “Work is very tough right now and the payment is too low.”
“The specialty has changed,” said Mary Vanko, MD, who practices in the suburbs of “blue collar Indiana.” “The public has very little idea of the breadth of our knowledge. The ObGyn generalist has the ability to serve as a woman’s doctor throughout her lifetime, not just perform the deliveries and surgeries. All of a sudden we are excluded from primary care status and people have to fight to see us. The newbies will never experience what it used to be as an ObGyn, the woman’s primary. Now we are the doctors to see when someone wants an IUD or is bleeding or pregnant. Big difference.”
Wesley Hambright, MD, practices in a small community hospital, but feels that “a larger hospital with more specialties may offer more flexibility and support in dealing with external pressures.” Tameka O’Neal, MD, is currently hospital employed but feels “as though I have little say in my practice.” Shaukat Ashai, MD, who is retired after 35 years in practice, says he would have preferred an academic setting on a full-time basis, citing long hours and poor compensation.
Robert del Rosario, MD, is in a large single-specialty suburban practice and would choose this practice setting again, although he would not choose a career as an ObGyn again. “The work demands have taken away too much from family,” he says. In addition, “as a male ObGyn, I am regularly faced with patients who choose their doctors based on gender rather than on skill. Our colleagues are no better. Early in my career and until the present, I hear people say, ‘Oh, I can’t hire Dr. X because we’re looking to hire a female.’”
Joe Walsh, MD, of Philadelphia, Pennsylvania, expresses similar discontent as a male ObGyn practicing in today’s female-populated specialty. In a letter to the editor in response to Editor in Chief Robert L. Barbieri, MD’s Editorial in the May 2015 issue, “Why is obstetrics and gynecology a popular choice for medical students?” Dr. Walsh states: “The unaddressed question is why is it unpopular for half of medical students? Ninety-three percent of resident graduates in the field are women, while women account for half of medical student graduates. Men rarely go into the field today. Perhaps job advertisements touting physician opportunities in ‘all female groups’ discourage men. Perhaps hospitals’ ‘Women’s Health Centers’ with such slogans as ‘Women taking care of women’ discourage men. Perhaps receptionists’ asking patients whether they prefer a male or female physician discourages male ObGyns.”
Many VBE members express some frustrations—with their practice setting, compensation, and longer work hours—but say that the patient relationships are the most rewarding aspect of their jobs. After 29 years in practice, Patrick Pevoto, MD, says the most rewarding aspect of his job is “being part of the legacy in people’s lives.”
Others say what keeps them engaged is:
- Enjoying “good outcomes.”
- “The patient contact. It’s fun having someone come up to me in the grocery store and introduce me to a teenager that I delivered 15 years ago.”
- “Surgery.”
- “Helping patients and teaching fellows.”
- “Knowing that I am making a difference in people’s lives.”
What is most rewarding?
When given several choices to select as the most rewarding aspect of their jobs, more female ObGyns (47%) than males (41%) reported that their physician-patient relationships are the major source of satisfaction. More men (10%) than women (7%) cite that making good money at a job they like is most gratifying. Only 3% of men and 2% of women reported no reward to being an ObGyn.1
Survey methodology
Medscape reports that the recruitment period for the 2015 Physician Compensation Report was from December 30, 2014, through March 11, 2015. Data were collected via a third-party online survey collection site. The margin of error for the survey was ±0.69%.1
Share your thoughts on this article! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
1. Peckham C. Medscape OB/GYN Compensation Report 2015. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2015/womenshealth. Published April 21, 2015. Accessed May 13, 2015.
2. Peckham C. Medscape OB/GYN Compensation Report 2014. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2014/womenshealth. Published April 15, 2014. Accessed June 2, 2014.
3. Medscape News. Ob/Gyn Compensation Report 2013. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2013/womenshealth. Accessed June 30, 2013.
4. Reale D. Mean income for ObGyns increased in 2012. OBG Manag. 2013;25(8):34–36.
5. Peckham C. Medscape Physician Compensation Report 2015. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2015/public/overview. Published April 21, 2015. Accessed May 13, 2015.
6. Distribution of medical school graduates by gender. Henry Kaiser Family Foundation Web site. http://kff.org/other/state-indicator/medical-school-graduates-by-gender/. Accessed May 13, 2015.
1. Peckham C. Medscape OB/GYN Compensation Report 2015. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2015/womenshealth. Published April 21, 2015. Accessed May 13, 2015.
2. Peckham C. Medscape OB/GYN Compensation Report 2014. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2014/womenshealth. Published April 15, 2014. Accessed June 2, 2014.
3. Medscape News. Ob/Gyn Compensation Report 2013. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2013/womenshealth. Accessed June 30, 2013.
4. Reale D. Mean income for ObGyns increased in 2012. OBG Manag. 2013;25(8):34–36.
5. Peckham C. Medscape Physician Compensation Report 2015. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2015/public/overview. Published April 21, 2015. Accessed May 13, 2015.
6. Distribution of medical school graduates by gender. Henry Kaiser Family Foundation Web site. http://kff.org/other/state-indicator/medical-school-graduates-by-gender/. Accessed May 13, 2015.
In this article
- Which practice settings pay better?
- Would you select a career in ObGyn again?
- Comparing time spent with patients
ACOG, SMFM, and others address safety concerns in labor and delivery
At least half of all cases of maternal morbidity and mortality could be prevented, or so studies suggest.1,2
The main stumbling block?
Faulty communication.
That’s the word from the American College of Obstetricians and Gynecologists, the Society for Maternal-Fetal Medicine, the American College of Nurse-Midwives, and the Association of Women’s Health, Obstetric and Neonatal Nurses.3
In a joint “blueprint” to transform communication and enhance the safety culture in intrapartum care, these organizations, led by Audrey Lyndon, PhD, RN, from the University of California, San Francisco, School of Nursing, describe the extent of the problem, steps that various team members can take to improve safety, notable success stories, and communication strategies.3 In this article, the joint blueprint is summarized, with a focus on steps obstetricians can take to improve the intrapartum safety culture.
Scope of the problem
A study of more than 3,282 physicians, midwives, and registered nurses produced a troubling statistic: More than 90% of respondents said that they had “witnessed shortcuts, missing competencies, disrespect, or performance problems” during the preceding year of practice.4 Few of these clinicians reported that they had discussed their concerns with the parties involved.
A second study of 1,932 clinicians found that 34% of physicians, 40% of midwives, and 56% of registered nurses had witnessed patients being put at risk within the preceding 2 years by other team members’ inattentiveness or lack of responsiveness.5
These findings suggest that health care providers often witness weak links in intrapartum safety but do not always address or report them. Among the reasons team members may be hesitant to speak up when they perceive a potential problem:
- feelings of resignation or inability to change the situation
- fear of retribution or ridicule
- fear of interpersonal or intrateam conflict.
Although Lyndon and colleagues acknowledge that it is impossible to eliminate adverse outcomes entirely or completely eradicate human error, they argue that significant improvements can be made by adopting a number of manageable strategies.3
Recommended strategies
Lyndon and colleagues describe some of the challenges of effective communication in a health care setting:
Lyndon and colleagues go on to mention a number of strategies to improve communication, boost safety, and reduce medical errors.3
1. Remember that the patient is part of the team
The patient and her family play a key role in identifying the potential for harm during labor and delivery, Lyndon and colleagues assert. Patients should be considered members of the intrapartum team, care should be patient-focused, and any communications from the patient should not only be heard but fully considered. In fact, explicit elicitation of her experience and concerns is recommended.3
2. Consider that you might be part of the problem
It is human nature to attribute a communication problem to the other people involved, rather than take responsibility for it oneself. One potential solution to this mindset is team training, where all members are encouraged to communicate clearly and listen attentively. Organizations that have been successful at improving their culture of safety have implemented such training, as well as the use of checklists, training in fetal heart-rate monitoring, formation of a patient safety committee, external review of safety practices, and designation of a key clinicianto lead the safety program and oversee team training.
3. Structure handoffs
The team should standardize handoffs so that they occur smoothly and all channels of communication remain open and clear.
“Having structured formats for debriefing and handoffs are steps in the right direction, but solving the problem of communication breakdowns is more complicated than standardizing the flow and format of information transfer,” Lyndon and colleagues assert. “Indeed, solving communication breakdowns is a matter of individual, group, organizational, and professional responsibility for creating and sustaining an environment of mutual respect, curiosity, and accountability for behavior and performance.”3
4. Learn to communicate responsibly
“Differences of opinion about clinical assessments, goals of care, and the pathway to optimal outcomes are bound to occur with some regularity in the dynamic environment of labor and delivery,” note Lyndon and colleagues. “Every person has the responsibility to contribute to improving how we relate to and communicate with each other. Collectively, we must create environments in which every team member (woman, family member, physician, midwife, nurse, unit clerk, patient care assistant, or scrub tech) is comfortable expressing and discussing concerns about safety or performance, is encouraged to do so, and has the support of the team to articulate the rationale for and urgency of the concern without fear of put-downs, retribution, or receiving poor-quality care.”3
5. Be persistent and proactive
When team members have differing expectations and communication styles, useful approaches include structured communication tools such as situation, background, assessment, recommendation (SBAR); structured handoffs; board rounds; huddles; attentive listening; and explicit elicitation of the patient’s concerns and desires.3
If someone fails to pay attention to a concern you raise, be persistent about restating that concern until you elicit a response.
If someone exhibits disruptive behavior, point to or establish a code of conduct that clearly describes professional behavior.
If there is a difference of opinion on patient management, such as fetal monitoring and interpretation, conduct regular case reviews and standardize a plan for notification of complications.
6. If you’re a team leader, set clear goals
Then ask team members what will be needed to achieve the outcomes desired.
“Team leaders need to develop outstanding skills for listening and eliciting feedback and cross-monitoring (being aware of each other’s actions and performance) from other team members,” note Lyndon and colleagues.3
7. Increase public awareness of safety concepts
When these concepts and best practices are made known to the public, women and families become “empowered” to speak up when they have concerns about care.
And when they do speak up, it pays to listen.
Share your thoughts on this article! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
1. Geller SE, Rosenberg D, Cox SM, et al. The continuum of maternal morbidity and mortality: factors associated with severity. Am J Obstet Gynecol. 2004;191(3):939–944.
2. Mitchell C, Lawton E, Morton C, McCain C, Holtby S, Main E. California Pregnancy-Associated Mortality Review: mixed methods approach for improved case identification, cause of death analyses and translation of findings. Matern Child Health J. 2014;18(3):518–526.
3. Lyndon A, Johnson MC, Bingham D, et al. Transforming communication and safety culture in intrapartum care: a multi-organization blueprint. Obstet Gynecol. 2015;125(5):1049–1055.
4. Maxfield DG, Lyndon A, Kennedy HP, O’Keeffe DF, Ziatnik MG. Confronting safety gaps across labor and delivery teams. Am J Obstet Gynecol. 2013;209(5):402–408.e3.
5. Lyndon A, Zlatnik MG, Maxfield DG, Lewis A, McMillan C, Kennedy HP. Contributions of clinical disconnections and unresolved conflict to failures in intrapartum safety. J Obstet Gynecol Neonatal Nurs. 2014;43(1):2–12.
At least half of all cases of maternal morbidity and mortality could be prevented, or so studies suggest.1,2
The main stumbling block?
Faulty communication.
That’s the word from the American College of Obstetricians and Gynecologists, the Society for Maternal-Fetal Medicine, the American College of Nurse-Midwives, and the Association of Women’s Health, Obstetric and Neonatal Nurses.3
In a joint “blueprint” to transform communication and enhance the safety culture in intrapartum care, these organizations, led by Audrey Lyndon, PhD, RN, from the University of California, San Francisco, School of Nursing, describe the extent of the problem, steps that various team members can take to improve safety, notable success stories, and communication strategies.3 In this article, the joint blueprint is summarized, with a focus on steps obstetricians can take to improve the intrapartum safety culture.
Scope of the problem
A study of more than 3,282 physicians, midwives, and registered nurses produced a troubling statistic: More than 90% of respondents said that they had “witnessed shortcuts, missing competencies, disrespect, or performance problems” during the preceding year of practice.4 Few of these clinicians reported that they had discussed their concerns with the parties involved.
A second study of 1,932 clinicians found that 34% of physicians, 40% of midwives, and 56% of registered nurses had witnessed patients being put at risk within the preceding 2 years by other team members’ inattentiveness or lack of responsiveness.5
These findings suggest that health care providers often witness weak links in intrapartum safety but do not always address or report them. Among the reasons team members may be hesitant to speak up when they perceive a potential problem:
- feelings of resignation or inability to change the situation
- fear of retribution or ridicule
- fear of interpersonal or intrateam conflict.
Although Lyndon and colleagues acknowledge that it is impossible to eliminate adverse outcomes entirely or completely eradicate human error, they argue that significant improvements can be made by adopting a number of manageable strategies.3
Recommended strategies
Lyndon and colleagues describe some of the challenges of effective communication in a health care setting:
Lyndon and colleagues go on to mention a number of strategies to improve communication, boost safety, and reduce medical errors.3
1. Remember that the patient is part of the team
The patient and her family play a key role in identifying the potential for harm during labor and delivery, Lyndon and colleagues assert. Patients should be considered members of the intrapartum team, care should be patient-focused, and any communications from the patient should not only be heard but fully considered. In fact, explicit elicitation of her experience and concerns is recommended.3
2. Consider that you might be part of the problem
It is human nature to attribute a communication problem to the other people involved, rather than take responsibility for it oneself. One potential solution to this mindset is team training, where all members are encouraged to communicate clearly and listen attentively. Organizations that have been successful at improving their culture of safety have implemented such training, as well as the use of checklists, training in fetal heart-rate monitoring, formation of a patient safety committee, external review of safety practices, and designation of a key clinicianto lead the safety program and oversee team training.
3. Structure handoffs
The team should standardize handoffs so that they occur smoothly and all channels of communication remain open and clear.
“Having structured formats for debriefing and handoffs are steps in the right direction, but solving the problem of communication breakdowns is more complicated than standardizing the flow and format of information transfer,” Lyndon and colleagues assert. “Indeed, solving communication breakdowns is a matter of individual, group, organizational, and professional responsibility for creating and sustaining an environment of mutual respect, curiosity, and accountability for behavior and performance.”3
4. Learn to communicate responsibly
“Differences of opinion about clinical assessments, goals of care, and the pathway to optimal outcomes are bound to occur with some regularity in the dynamic environment of labor and delivery,” note Lyndon and colleagues. “Every person has the responsibility to contribute to improving how we relate to and communicate with each other. Collectively, we must create environments in which every team member (woman, family member, physician, midwife, nurse, unit clerk, patient care assistant, or scrub tech) is comfortable expressing and discussing concerns about safety or performance, is encouraged to do so, and has the support of the team to articulate the rationale for and urgency of the concern without fear of put-downs, retribution, or receiving poor-quality care.”3
5. Be persistent and proactive
When team members have differing expectations and communication styles, useful approaches include structured communication tools such as situation, background, assessment, recommendation (SBAR); structured handoffs; board rounds; huddles; attentive listening; and explicit elicitation of the patient’s concerns and desires.3
If someone fails to pay attention to a concern you raise, be persistent about restating that concern until you elicit a response.
If someone exhibits disruptive behavior, point to or establish a code of conduct that clearly describes professional behavior.
If there is a difference of opinion on patient management, such as fetal monitoring and interpretation, conduct regular case reviews and standardize a plan for notification of complications.
6. If you’re a team leader, set clear goals
Then ask team members what will be needed to achieve the outcomes desired.
“Team leaders need to develop outstanding skills for listening and eliciting feedback and cross-monitoring (being aware of each other’s actions and performance) from other team members,” note Lyndon and colleagues.3
7. Increase public awareness of safety concepts
When these concepts and best practices are made known to the public, women and families become “empowered” to speak up when they have concerns about care.
And when they do speak up, it pays to listen.
Share your thoughts on this article! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
At least half of all cases of maternal morbidity and mortality could be prevented, or so studies suggest.1,2
The main stumbling block?
Faulty communication.
That’s the word from the American College of Obstetricians and Gynecologists, the Society for Maternal-Fetal Medicine, the American College of Nurse-Midwives, and the Association of Women’s Health, Obstetric and Neonatal Nurses.3
In a joint “blueprint” to transform communication and enhance the safety culture in intrapartum care, these organizations, led by Audrey Lyndon, PhD, RN, from the University of California, San Francisco, School of Nursing, describe the extent of the problem, steps that various team members can take to improve safety, notable success stories, and communication strategies.3 In this article, the joint blueprint is summarized, with a focus on steps obstetricians can take to improve the intrapartum safety culture.
Scope of the problem
A study of more than 3,282 physicians, midwives, and registered nurses produced a troubling statistic: More than 90% of respondents said that they had “witnessed shortcuts, missing competencies, disrespect, or performance problems” during the preceding year of practice.4 Few of these clinicians reported that they had discussed their concerns with the parties involved.
A second study of 1,932 clinicians found that 34% of physicians, 40% of midwives, and 56% of registered nurses had witnessed patients being put at risk within the preceding 2 years by other team members’ inattentiveness or lack of responsiveness.5
These findings suggest that health care providers often witness weak links in intrapartum safety but do not always address or report them. Among the reasons team members may be hesitant to speak up when they perceive a potential problem:
- feelings of resignation or inability to change the situation
- fear of retribution or ridicule
- fear of interpersonal or intrateam conflict.
Although Lyndon and colleagues acknowledge that it is impossible to eliminate adverse outcomes entirely or completely eradicate human error, they argue that significant improvements can be made by adopting a number of manageable strategies.3
Recommended strategies
Lyndon and colleagues describe some of the challenges of effective communication in a health care setting:
Lyndon and colleagues go on to mention a number of strategies to improve communication, boost safety, and reduce medical errors.3
1. Remember that the patient is part of the team
The patient and her family play a key role in identifying the potential for harm during labor and delivery, Lyndon and colleagues assert. Patients should be considered members of the intrapartum team, care should be patient-focused, and any communications from the patient should not only be heard but fully considered. In fact, explicit elicitation of her experience and concerns is recommended.3
2. Consider that you might be part of the problem
It is human nature to attribute a communication problem to the other people involved, rather than take responsibility for it oneself. One potential solution to this mindset is team training, where all members are encouraged to communicate clearly and listen attentively. Organizations that have been successful at improving their culture of safety have implemented such training, as well as the use of checklists, training in fetal heart-rate monitoring, formation of a patient safety committee, external review of safety practices, and designation of a key clinicianto lead the safety program and oversee team training.
3. Structure handoffs
The team should standardize handoffs so that they occur smoothly and all channels of communication remain open and clear.
“Having structured formats for debriefing and handoffs are steps in the right direction, but solving the problem of communication breakdowns is more complicated than standardizing the flow and format of information transfer,” Lyndon and colleagues assert. “Indeed, solving communication breakdowns is a matter of individual, group, organizational, and professional responsibility for creating and sustaining an environment of mutual respect, curiosity, and accountability for behavior and performance.”3
4. Learn to communicate responsibly
“Differences of opinion about clinical assessments, goals of care, and the pathway to optimal outcomes are bound to occur with some regularity in the dynamic environment of labor and delivery,” note Lyndon and colleagues. “Every person has the responsibility to contribute to improving how we relate to and communicate with each other. Collectively, we must create environments in which every team member (woman, family member, physician, midwife, nurse, unit clerk, patient care assistant, or scrub tech) is comfortable expressing and discussing concerns about safety or performance, is encouraged to do so, and has the support of the team to articulate the rationale for and urgency of the concern without fear of put-downs, retribution, or receiving poor-quality care.”3
5. Be persistent and proactive
When team members have differing expectations and communication styles, useful approaches include structured communication tools such as situation, background, assessment, recommendation (SBAR); structured handoffs; board rounds; huddles; attentive listening; and explicit elicitation of the patient’s concerns and desires.3
If someone fails to pay attention to a concern you raise, be persistent about restating that concern until you elicit a response.
If someone exhibits disruptive behavior, point to or establish a code of conduct that clearly describes professional behavior.
If there is a difference of opinion on patient management, such as fetal monitoring and interpretation, conduct regular case reviews and standardize a plan for notification of complications.
6. If you’re a team leader, set clear goals
Then ask team members what will be needed to achieve the outcomes desired.
“Team leaders need to develop outstanding skills for listening and eliciting feedback and cross-monitoring (being aware of each other’s actions and performance) from other team members,” note Lyndon and colleagues.3
7. Increase public awareness of safety concepts
When these concepts and best practices are made known to the public, women and families become “empowered” to speak up when they have concerns about care.
And when they do speak up, it pays to listen.
Share your thoughts on this article! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
1. Geller SE, Rosenberg D, Cox SM, et al. The continuum of maternal morbidity and mortality: factors associated with severity. Am J Obstet Gynecol. 2004;191(3):939–944.
2. Mitchell C, Lawton E, Morton C, McCain C, Holtby S, Main E. California Pregnancy-Associated Mortality Review: mixed methods approach for improved case identification, cause of death analyses and translation of findings. Matern Child Health J. 2014;18(3):518–526.
3. Lyndon A, Johnson MC, Bingham D, et al. Transforming communication and safety culture in intrapartum care: a multi-organization blueprint. Obstet Gynecol. 2015;125(5):1049–1055.
4. Maxfield DG, Lyndon A, Kennedy HP, O’Keeffe DF, Ziatnik MG. Confronting safety gaps across labor and delivery teams. Am J Obstet Gynecol. 2013;209(5):402–408.e3.
5. Lyndon A, Zlatnik MG, Maxfield DG, Lewis A, McMillan C, Kennedy HP. Contributions of clinical disconnections and unresolved conflict to failures in intrapartum safety. J Obstet Gynecol Neonatal Nurs. 2014;43(1):2–12.
1. Geller SE, Rosenberg D, Cox SM, et al. The continuum of maternal morbidity and mortality: factors associated with severity. Am J Obstet Gynecol. 2004;191(3):939–944.
2. Mitchell C, Lawton E, Morton C, McCain C, Holtby S, Main E. California Pregnancy-Associated Mortality Review: mixed methods approach for improved case identification, cause of death analyses and translation of findings. Matern Child Health J. 2014;18(3):518–526.
3. Lyndon A, Johnson MC, Bingham D, et al. Transforming communication and safety culture in intrapartum care: a multi-organization blueprint. Obstet Gynecol. 2015;125(5):1049–1055.
4. Maxfield DG, Lyndon A, Kennedy HP, O’Keeffe DF, Ziatnik MG. Confronting safety gaps across labor and delivery teams. Am J Obstet Gynecol. 2013;209(5):402–408.e3.
5. Lyndon A, Zlatnik MG, Maxfield DG, Lewis A, McMillan C, Kennedy HP. Contributions of clinical disconnections and unresolved conflict to failures in intrapartum safety. J Obstet Gynecol Neonatal Nurs. 2014;43(1):2–12.
In this article
- Why handoffs should be structured
- Goals for teamleaders
Endometriosis and infertility: Expert answers to 6 questions to help pinpoint the best route to pregnancy
Although endometriosis and infertility are clearly linked—in life as well as the medical literature—no causal relationship has been established. Nevertheless, data suggest that 25% to 50% of infertile women have endometriosis, and that as many as 30% to 50% of women who have endometriosis are infertile.1
Among the mechanisms that have been proposed to explain this link are:
- distorted pelvic anatomy
- endocrine and ovulatory abnormalities
- impaired implantation
- impaired quality of the oocyte and embryo
- altered peritoneal function
- altered hormonal and cell-mediated function
- abnormal uterotubal transport.2
Recent studies by Kao and colleagues and Giudice and colleagues have led to new findings in regard to endometriosis and infertility, says Ceana Nezhat, MD.3,4 Dr. Nezhat is Director of the Nezhat Medical Center in Atlanta, Georgia, and Medical Director of Training and Education at Northside Hospital in Atlanta. “These researchers have discovered that endometriosis causes changes to the endometrium that contribute to infertility.”
“There are no studies that have specifically assessed whether one anatomic site is associated with increased infertility over another,” says Tommaso Falcone, MD. “However, it is assumed that disease that involves the tubes and ovaries would impede fertility the most. Adhesive disease and endometriomas around the tubes and ovaries are associated with a worsening prognosis. Although peritoneal disease probably influences fertility solely on the basis of inflammation, disease around the tubes and ovaries is thought to have a mechanical effect as well.” Dr. Falcone is Professor and Chair of Obstetrics and Gynecology at the Cleveland Clinic in Cleveland, Ohio.
“Endometriosis is a chronic and heterogeneous disease process,” says Stephanie J. Estes, MD, Director of Robotic Surgical Services and Associate Professor, Division of Reproductive Endocrinology and Infertility, Department of Obstetrics and Gynecology, at Penn State Hershey Medical Center in Hershey, Pennsylvania.
“It is likely that no single site is the causative factor,” Dr. Estes says. “Endometriosis alters prostaglandins, cytokines, and proteases that may adversely affect eggs, sperm, or embryo development. In addition, altered endometrial receptivity may play a role. It has been shown that, when donor oocytes from women with endometriosis are transferred to women without endometriosis, there are lower implantation rates and poorer embryo quality.”5
Does it follow, then, that eradication of endometriosis improves fertility?
The answer is not clear. Rather, it depends on a number of variables, including the stage of the disease, its location, the presence of symptoms, and more.
“The approach for endometiosis-associated infertility is completely different from the approach for pain,” says Dr. Nezhat. “In a patient with pain, complete eradication of endometriosis is necessary. However, when addressing infertility, a surgeon must be cautious in the vicinity of the reproductive organs, even if a multistage approach is required. Fertility preservation is the goal.6,7 However, thorough treatment of endometriosis improves fertility rates even in cases of failed in vitro fertilization” (IVF).8
In this article, the focus is on 6 critical questions concerning endometriosis and infertility, including the role of medical therapy, when surgery is indicated, and whether an endometrioma warrants removal or referral for IVF.
In Part 1 of this 3-part series, which appeared in the April 2015 issue of OBG Management, the subject was diagnosis of endometriosis. In Part 2, which appeared in May 2015, the focus was endometriosis and pain.
1. Is there a role for medical therapy?
In women who have endometriosis-related infertility, medical therapy does not appear to produce any benefit. In its committee opinion on the subject, the American Society for Reproductive Medicine (ASRM) states as much: “There is no evidence that medical treatment of endometriosis improves fertility.”2
In fact, observes Dr. Estes, trials of medical treatment, involving such medications as combined estrogen-progestin therapy, danazol, progestins, or gonadotropin-releasing hormone (GnRH) agonists, may cause an unnecessary “delay in the use of more effective treatments that could result in pregnancy.”
Dr. Nezhat believes that medical therapy is effective in patients who have adenomyosis in addition to endometriosis. “Three months of treatment with a GnRH agonist will improve fertility rates in these patients,” he says.
“Medical treatments inhibit ovulation,” notes Dr. Estes. “These therapies have no role in pretreatment of patients with endometriosis prior to infertility treatment. On the other hand, medical therapy with GnRH agonists for 3 to 6 months prior to an IVF cycle does result in increased pregnancy rates.”9
2. What is the role of clomiphene and intrauterine insemination?
Should women who have endometriosis, open fallopian tubes, and infertility be treated with clomiphene and intrauterine insemination (IUI) prior to a cycle of IVF?
“This is a complex question,” says Dr. Estes, “as clinical parameters such as age, symptoms, duration of infertility, and the ability to proceed with IVF are important, as well as stage of disease.”
“Overall, in patients younger than 35 years, clomiphene-IUI is an option and has an increased pregnancy rate over timed intercourse” (9% vs 3%), she says.10 “However, clearly IVF is much more successful and is the most effective treatment, with pregnancy rates of approximately 46% for women younger than 35 years (3% of whom have a ‘diagnosis’ of endometriosis, and 13% of whom have an ‘unknown’ infertility factor).11 Women who are older than 35 or who have additional infertility factors, such as male factor, should consider IVF first.”
3. When is surgery indicated?
“Patients who have significant pain associated with their infertility will benefit from surgery, which offers both pain relief and an improvement in the spontaneous pregnancy rate,” says Dr. Falcone. “Patients who are infertile and desire spontaneous pregnancy without pharmacologic intervention or assisted reproductive technology (ART) also benefit from surgery.”
The benefit of surgery in asymptomatic women with minimal to mild endometriosis is unclear. In a randomized controlled trial of 341 women (aged 20–39 years) with infertility and minimal to mild endometriosis, laparoscopic resection or ablation of visible lesions resulted in pregnancy in 30.7% of women, compared with 17.7% of women who underwent diagnostic laparoscopy only.12
Another randomized study of 96 women with minimal to mild endometriosis who underwent resection/ablation or diagnostic laparoscopy found no difference in the birth rate at 1 year.13
When the results of these 2 studies are combined, the number needed to treat is 12 laparoscopies in women with endometriosis, says Dr. Falcone. “So 1 additional pregnancy would be gained from performing endometriosis surgery in 12 patients. If we assume a prevalence of 30% in asymptomatic women with infertility, then you need to perform 40 diagnostic laparoscopies to achieve an extra pregnancy.”
For women with infertility and severe endometriosis, a nonrandomized study found cumulative pregnancy rates of 45% and 63% after laparoscopy and laparotomy, respectively, in 216 women followed for up to 2 years.14 The difference in rates was not statistically significant.
“Although surgery is indicated to diagnose endometriosis, multiple repeat procedures are not an effective treatment for infertility,” says Dr. Estes. “Plus, especially for stage I and II endometriosis [according to the ASRM classification system], approximately 12 patients will need surgery for 1 additional pregnancy—and many more will have needed the procedure to even get to those who have endometriosis. While patients often want us to ‘do something’—often a covered service such as surgery—we need to consider that surgery for early disease does not provide a significant or long-lasting enhancement to women’s ability to conceive.”
In the absence of male-factor infertility, surgical diagnosis with conservative and precise treatment of endometriosis at the same time is better than going directly to IVF, says Dr. Nezhat. Younger patients who undergo surgical treatment have a better chance of achieving more than 1 spontaneous pregnancy than they do with IVF. And older patients also will have an improved conception rate with ART when they are treated surgically, he says.8
Coding and reimbursement
For endometriosis, the correct diagnostic code helps establish the medical necessity of later treatments
Several diagnostic codes are available to describe the location of endometriotic implants, but the fact remains that these codes can be reported only after a definitive diagnosis is made, which generally comes after confirmatory surgery has been performed. When the patient is in the diagnostic phase, she may present with complaints of pelvic pain, dyspareunia, dysmenorrhea, or infertility. Knowing which codes to use at the time of evaluation goes a long way toward establishing medical necessity for any later surgery or medical treatment.
In the TABLE, you will find common diagnostic codes that can be reported during evaluation of endometriosis, including both International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) and ICD-10-CM equivalents. Note that, with ICD-10-CM, payers are looking for a more specific type of dysmenorrhea in the documentation. In the case of painful menstruation suspected to arise from endometriosis, the code for secondary dysmenorrhea should be reported.
Diagnostic coding in cases in which the patient first presents with a complaint of infertility in the absence of other symptoms can be problematic, as many insurers still do not cover the treatment of infertility. However, in the diagnostic stage, codes for fertility testing can be reported instead of codes that confirm infertility when no other symptoms are present. Once the clinician has verified that endometriosis is the source of the infertility and begins treatment, the primary code for the type of endometriosis would be reported, not a diagnosis of infertility.
The procedure performed to diagnose endometriosis would be diagnostic laparoscopy (Current Procedure Terminology [CPT] code 49320, Laparoscopy, abdomen, peritoneum, and omentum, diagnostic, with or without collection of specimen[s] by brushing or washing [separate procedure]) if medical treatment is being pursued. If the plan is to confirm and then immediately remove the implants, the CPT codes would be either 58662, Laparoscopy, surgical; with fulguration or excision of lesions of the ovary, pelvic viscera, or peritoneal surface by any method, or 49203–49205, Excision or destruction, open, intra-abdominal tumors, cysts or endometriomas, 1 or more peritoneal, mesenteric, or retroperitoneal primary or secondary tumors, based on the largest tumor diameter, if they are removed via an abdominal incision.
—Melanie Witt, RN, CPC, COBGC, MA
Ms. Witt is an independent coding and documentation consultant and former program manager, department of coding and nomenclature, American Congress of Obstetricians and Gynecologists.
4. Surgery or IVF for endometriomas?
When an endometrioma is present, should it be surgically treated or should the patient go straight to IVF? And does the optimal approach depend on the size of the endometrioma?
“The answer to this question ultimately depends on the skill and experience of the surgeon and the type of endometrioma,” says Dr. Nezhat, “because improper removal of an endometrioma may compromise the function of the ovary.”
“I recommend removal of the endometrioma by a skilled surgeon experienced in the management of ovarian cysts and preservation of ovarian function, especially in patients who have failed IVF,” he says.6,15
According to the ASRM committee opinion on endometriosis and infertility, laparoscopic cystectomy for endometriomas larger than 4 cm improves fertility, compared with cyst drainage and coagulation, which is associated with a high risk of cyst recurrence.2 However, no randomized trials have compared laparoscopic excision of an endometrioma to expectant management prior to IVF/intracytoplasmic sperm injection (ICSI). One case-control study found that laparoscopic cystectomy prior to IVF had no effect on fertility outcomes.16 At the same time, however, “conservative surgical treatment in symptomatic patients did not impair the success rates of IVF or ICSI,” notes the ASRM.2 Therefore, “evidence suggests that surgery does not benefit asymptomatic women with an endometrioma prior to scheduled IVF/ICSI,” the ASRM concludes.2
Dr. Nezhat cautions against the practice of indiscriminate IVF in the setting of ovarian endometriomas because he has seen patients who developed tubo-ovarian abscess and infected endometriomas after transvaginal egg retrieval. He notes that there are additional case reports of similar findings from other surgeons.
As far as excision versus ablation is concerned, all studies have shown some effect on ovarian function after excision, says Dr. Falcone. “The studies assessed this parameter using several endpoints, such as the number of oocytes retrieved at IVF. Recently, anti-Müllerian hormone has been used and has confirmed this observation. The decreased ovarian reserve is especially problematic with bilateral ovarian disease. The extent of the decreased ovarian function is dependent on several parameters, especially how much energy is used to achieve hemostasis. Several techniques have been proposed to reduce damage, including less traumatic ways of achieving hemostasis in the ovarian hilus.”
“The dilemma is that, if we excise the disease, the pregnancy rates are better than with ablation, but if we excise, there is more damage to the ovary. In my practice, I excise if there is minimal associated disease, such as adhesions, because the pregnancy rate after surgery is good. If, however, there are extensive adhesions with a low chance of spontaneous pregnancy, I minimize excision,” Dr. Falcone says.
As for going straight to IVF, “many patients cannot afford IVF; therefore, surgery is their only option. Furthermore, many patients have severe associated pain; therefore, surgery is required to improve quality of life. However, if the decision is made to proceed to IVF, there is no evidence that cystectomy prior to treatment with ART improves the pregnancy rate,” Dr. Falcone says.
“Basically, if a woman has no pain and no endometrioma, and infertility alone is the issue, I treat her in the same manner as I would a patient with idiopathic infertility—no surgery,” Dr. Falcone says. “If a patient has severe pain and infertility, I treat her surgically but conservatively, especially when an endometrioma is present. The patient will get pain relief but also derive fertility benefit. If a patient has had previous surgery for endometriosis-associated infertility, additional surgery is not the next step—as our study has shown that pregnancy rates are better with IVF than repeat surgery.”17
5. Is surgery ever effective after failed IVF?
To answer this question, Dr. Nezhat points to a retrospective case series by Littman and colleagues in which 29 women with a history of failed IVF underwent laparoscopic evaluation and treatment of endometriosis (by the same surgeon).8 Of 29 patients, 22 conceived after laparoscopic treatment of endometriosis, including 15 “non-IVF” pregnancies and 7 IVF pregnancies, the study results show.8
“It is not unusual for patients and health care providers to perceive IVF as the final treatment for infertility,” Littman and colleagues write. “When this definitive therapy fails repeatedly, clinicians and patients may be inclined to pursue oocyte donation or elect to forego further treatment altogether. This is especially true in women of advanced age and in patients with borderline embryo quality. Presently, as a result of our clinical observation in patients with failed IVF, before egg donation or adoption, we offer the option to have meticulous laparoscopic evaluation and treatment by a skilled surgeon. Furthermore, we would not classify an infertility condition as unexplained without confirming the absence of endometriosis by a thorough laparoscopy. In our experience, patients under 35 years old with unexplained infertility who are found to have endometriosis at the time of laparoscopy have an excellent chance of pregnancy following surgical treatment without ART.”8
6. Is repeat surgery ever helpful?
In the treatment of endometriosis-associated infertility, repeat surgery should be avoided if no symptoms are present, says Dr. Estes. “In women with continued symptoms, the benefits of repeat surgery are small, with known risks, including the potential for adhesive disease and the iatrogenic detrimental effect on ovarian function—often in a setting of already-present decreased ovarian reserve.”
Dr. Nezhat agrees that multiple surgeries carry the potential for harm. “However, there is one caveat,” he says. “What was done at the previous surgery and how? The skill and experience of the surgeon and proper technique are of paramount importance to the surgical outcome.”
Share your thoughts on this article! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
1. Missmer SA, Hankinson SE, Spiegelman D, Barbieri RL, Marshall LM, Hunter DJ. Incidence of laparoscopically confirmed endometriosis by demographic, anthropometric, and lifestyle factors. Am J Epidemiol. 2004;160(8):784–796.
2. Practice Committee of the American Society for Reproductive Medicine. Endometriosis and infertility: a committee opinion. Fertil Steril. 2012;98(3):591–598.
3. Kao LC, Germeyer A, Tulac S, et al. Expression profiling of endometrium from women with endometriosis reveals candidate genes for disease-based implantation failure and infertility. Endocrinology. 2003;144(7):2870–2881.
4. Giudice LC, Telles TL, Lobo S, Kao L. The molecular basis for implantation failure in endometriosis: on the road to discovery. Ann N Y Acad Sci. 2002;955:252–264; discussion 293–295, 396–406.
5. Garrido N, Navarro J, Garcia-Velasco J, et al. The endometrium versus embryonic quality in endometriosis-related infertility. Hum Reprod Update. 2012;8(1):95-103.
6. Lewis M, Baker V, Nezhat C. The impact on ovarian reserve after laparoscopic ovarian cystectomy versus three-stage management in patients with endometriomas: a prospective randomized study. Fertil Steril. 2010;94(6):e81–83.
7. Tsolakidis D, Pados G, Vavilis D, et al. The impact on ovarian reserve after laparoscopic ovarian cystectomy versus three-stage management in patients with endometriomas: a prospective randomized study. Fertil Steril. 2010;94(1):71–77.
8. Littman E, Giudice L, Lathi R, Berker B, Milki A, Nezhat C. Role of laparoscopic treatment of endometriosis in patients with failed in vitro fertilization cycles. Fertil Steril. 2005;84(6):1574–1578.
9. Sallam HN, Garcia-Velasco JA, Dias S, Arici A. Long-term pituitary down-regulation before in vitro fertilization (IVF) for women with endometriosis. Cochrane Database Syst Rev. 2006;(1):CD004635.
10. Deaton JL, Gibson M, Blackmer KM, et al. A randomized, controlled trial of clomiphene citrate and intrauterine insemination in couples with unexplained infertility or surgically corrected endometriosis. Fertil Steril. 1990; 54:1083–1088.
11. Society for Assisted Reproductive Technology. Clinic Summary Report [all member clinics]: 2013. https://www.sartcorsonline.com/rptCSR_PublicMultYear.aspx?ClinicPKID=0. Accessed May 13, 2015.
12. Marcoux S, Maheux R, Bérubé S. Laparoscopic surgery in infertile women with minimal or mild endometriosis. Canadian Collaborative Group on Endometriosis. N Engl J Med. 1997;337(4):217–222.
13. Parazzini F. Ablation of lesions or no treatment in minimal-mild endometriosis in infertile women: a randomized trial. Gruppo Italiano per lo Studio dell’Endometriosi. Hum Reprod. 1999;14(5):1332–1334.
14. Crosignani PG, Vercellini P, Biffignandi F, Costantini W, Cortesi I, Imparato E. Laparoscopy versus laparotomy in conservative surgical treatment for severe endometriosis. Fertil Steril. 1996;66(5):706–711.
15. Nezhat F, Nezhat C, Allan CJ, Metzger DA, Sears DL. Clinical and histologic classification of endometriomas. Implications for a mechanism of pathogenesis. J Reprod Med. 1992;37(9):771–776.
16. Garcia-Velasco JA, Mahutte NG, Corona J, et al. Removal of endometriomas before in vitro fertilization does not improve fertility outcomes: a matched, case-control study. Fertil Steril. 2004;81(5):1194–1197.
17. Pagidas K, Falcone T, Hemmings R, Miron R. Comparison of surgical treatment of moderate (stage III) and severe (stage IV) endometriosis-related infertility with IVF–embryo transfer. Fertil Steril. 1996;65(4):791–795.
Although endometriosis and infertility are clearly linked—in life as well as the medical literature—no causal relationship has been established. Nevertheless, data suggest that 25% to 50% of infertile women have endometriosis, and that as many as 30% to 50% of women who have endometriosis are infertile.1
Among the mechanisms that have been proposed to explain this link are:
- distorted pelvic anatomy
- endocrine and ovulatory abnormalities
- impaired implantation
- impaired quality of the oocyte and embryo
- altered peritoneal function
- altered hormonal and cell-mediated function
- abnormal uterotubal transport.2
Recent studies by Kao and colleagues and Giudice and colleagues have led to new findings in regard to endometriosis and infertility, says Ceana Nezhat, MD.3,4 Dr. Nezhat is Director of the Nezhat Medical Center in Atlanta, Georgia, and Medical Director of Training and Education at Northside Hospital in Atlanta. “These researchers have discovered that endometriosis causes changes to the endometrium that contribute to infertility.”
“There are no studies that have specifically assessed whether one anatomic site is associated with increased infertility over another,” says Tommaso Falcone, MD. “However, it is assumed that disease that involves the tubes and ovaries would impede fertility the most. Adhesive disease and endometriomas around the tubes and ovaries are associated with a worsening prognosis. Although peritoneal disease probably influences fertility solely on the basis of inflammation, disease around the tubes and ovaries is thought to have a mechanical effect as well.” Dr. Falcone is Professor and Chair of Obstetrics and Gynecology at the Cleveland Clinic in Cleveland, Ohio.
“Endometriosis is a chronic and heterogeneous disease process,” says Stephanie J. Estes, MD, Director of Robotic Surgical Services and Associate Professor, Division of Reproductive Endocrinology and Infertility, Department of Obstetrics and Gynecology, at Penn State Hershey Medical Center in Hershey, Pennsylvania.
“It is likely that no single site is the causative factor,” Dr. Estes says. “Endometriosis alters prostaglandins, cytokines, and proteases that may adversely affect eggs, sperm, or embryo development. In addition, altered endometrial receptivity may play a role. It has been shown that, when donor oocytes from women with endometriosis are transferred to women without endometriosis, there are lower implantation rates and poorer embryo quality.”5
Does it follow, then, that eradication of endometriosis improves fertility?
The answer is not clear. Rather, it depends on a number of variables, including the stage of the disease, its location, the presence of symptoms, and more.
“The approach for endometiosis-associated infertility is completely different from the approach for pain,” says Dr. Nezhat. “In a patient with pain, complete eradication of endometriosis is necessary. However, when addressing infertility, a surgeon must be cautious in the vicinity of the reproductive organs, even if a multistage approach is required. Fertility preservation is the goal.6,7 However, thorough treatment of endometriosis improves fertility rates even in cases of failed in vitro fertilization” (IVF).8
In this article, the focus is on 6 critical questions concerning endometriosis and infertility, including the role of medical therapy, when surgery is indicated, and whether an endometrioma warrants removal or referral for IVF.
In Part 1 of this 3-part series, which appeared in the April 2015 issue of OBG Management, the subject was diagnosis of endometriosis. In Part 2, which appeared in May 2015, the focus was endometriosis and pain.
1. Is there a role for medical therapy?
In women who have endometriosis-related infertility, medical therapy does not appear to produce any benefit. In its committee opinion on the subject, the American Society for Reproductive Medicine (ASRM) states as much: “There is no evidence that medical treatment of endometriosis improves fertility.”2
In fact, observes Dr. Estes, trials of medical treatment, involving such medications as combined estrogen-progestin therapy, danazol, progestins, or gonadotropin-releasing hormone (GnRH) agonists, may cause an unnecessary “delay in the use of more effective treatments that could result in pregnancy.”
Dr. Nezhat believes that medical therapy is effective in patients who have adenomyosis in addition to endometriosis. “Three months of treatment with a GnRH agonist will improve fertility rates in these patients,” he says.
“Medical treatments inhibit ovulation,” notes Dr. Estes. “These therapies have no role in pretreatment of patients with endometriosis prior to infertility treatment. On the other hand, medical therapy with GnRH agonists for 3 to 6 months prior to an IVF cycle does result in increased pregnancy rates.”9
2. What is the role of clomiphene and intrauterine insemination?
Should women who have endometriosis, open fallopian tubes, and infertility be treated with clomiphene and intrauterine insemination (IUI) prior to a cycle of IVF?
“This is a complex question,” says Dr. Estes, “as clinical parameters such as age, symptoms, duration of infertility, and the ability to proceed with IVF are important, as well as stage of disease.”
“Overall, in patients younger than 35 years, clomiphene-IUI is an option and has an increased pregnancy rate over timed intercourse” (9% vs 3%), she says.10 “However, clearly IVF is much more successful and is the most effective treatment, with pregnancy rates of approximately 46% for women younger than 35 years (3% of whom have a ‘diagnosis’ of endometriosis, and 13% of whom have an ‘unknown’ infertility factor).11 Women who are older than 35 or who have additional infertility factors, such as male factor, should consider IVF first.”
3. When is surgery indicated?
“Patients who have significant pain associated with their infertility will benefit from surgery, which offers both pain relief and an improvement in the spontaneous pregnancy rate,” says Dr. Falcone. “Patients who are infertile and desire spontaneous pregnancy without pharmacologic intervention or assisted reproductive technology (ART) also benefit from surgery.”
The benefit of surgery in asymptomatic women with minimal to mild endometriosis is unclear. In a randomized controlled trial of 341 women (aged 20–39 years) with infertility and minimal to mild endometriosis, laparoscopic resection or ablation of visible lesions resulted in pregnancy in 30.7% of women, compared with 17.7% of women who underwent diagnostic laparoscopy only.12
Another randomized study of 96 women with minimal to mild endometriosis who underwent resection/ablation or diagnostic laparoscopy found no difference in the birth rate at 1 year.13
When the results of these 2 studies are combined, the number needed to treat is 12 laparoscopies in women with endometriosis, says Dr. Falcone. “So 1 additional pregnancy would be gained from performing endometriosis surgery in 12 patients. If we assume a prevalence of 30% in asymptomatic women with infertility, then you need to perform 40 diagnostic laparoscopies to achieve an extra pregnancy.”
For women with infertility and severe endometriosis, a nonrandomized study found cumulative pregnancy rates of 45% and 63% after laparoscopy and laparotomy, respectively, in 216 women followed for up to 2 years.14 The difference in rates was not statistically significant.
“Although surgery is indicated to diagnose endometriosis, multiple repeat procedures are not an effective treatment for infertility,” says Dr. Estes. “Plus, especially for stage I and II endometriosis [according to the ASRM classification system], approximately 12 patients will need surgery for 1 additional pregnancy—and many more will have needed the procedure to even get to those who have endometriosis. While patients often want us to ‘do something’—often a covered service such as surgery—we need to consider that surgery for early disease does not provide a significant or long-lasting enhancement to women’s ability to conceive.”
In the absence of male-factor infertility, surgical diagnosis with conservative and precise treatment of endometriosis at the same time is better than going directly to IVF, says Dr. Nezhat. Younger patients who undergo surgical treatment have a better chance of achieving more than 1 spontaneous pregnancy than they do with IVF. And older patients also will have an improved conception rate with ART when they are treated surgically, he says.8
Coding and reimbursement
For endometriosis, the correct diagnostic code helps establish the medical necessity of later treatments
Several diagnostic codes are available to describe the location of endometriotic implants, but the fact remains that these codes can be reported only after a definitive diagnosis is made, which generally comes after confirmatory surgery has been performed. When the patient is in the diagnostic phase, she may present with complaints of pelvic pain, dyspareunia, dysmenorrhea, or infertility. Knowing which codes to use at the time of evaluation goes a long way toward establishing medical necessity for any later surgery or medical treatment.
In the TABLE, you will find common diagnostic codes that can be reported during evaluation of endometriosis, including both International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) and ICD-10-CM equivalents. Note that, with ICD-10-CM, payers are looking for a more specific type of dysmenorrhea in the documentation. In the case of painful menstruation suspected to arise from endometriosis, the code for secondary dysmenorrhea should be reported.
Diagnostic coding in cases in which the patient first presents with a complaint of infertility in the absence of other symptoms can be problematic, as many insurers still do not cover the treatment of infertility. However, in the diagnostic stage, codes for fertility testing can be reported instead of codes that confirm infertility when no other symptoms are present. Once the clinician has verified that endometriosis is the source of the infertility and begins treatment, the primary code for the type of endometriosis would be reported, not a diagnosis of infertility.
The procedure performed to diagnose endometriosis would be diagnostic laparoscopy (Current Procedure Terminology [CPT] code 49320, Laparoscopy, abdomen, peritoneum, and omentum, diagnostic, with or without collection of specimen[s] by brushing or washing [separate procedure]) if medical treatment is being pursued. If the plan is to confirm and then immediately remove the implants, the CPT codes would be either 58662, Laparoscopy, surgical; with fulguration or excision of lesions of the ovary, pelvic viscera, or peritoneal surface by any method, or 49203–49205, Excision or destruction, open, intra-abdominal tumors, cysts or endometriomas, 1 or more peritoneal, mesenteric, or retroperitoneal primary or secondary tumors, based on the largest tumor diameter, if they are removed via an abdominal incision.
—Melanie Witt, RN, CPC, COBGC, MA
Ms. Witt is an independent coding and documentation consultant and former program manager, department of coding and nomenclature, American Congress of Obstetricians and Gynecologists.
4. Surgery or IVF for endometriomas?
When an endometrioma is present, should it be surgically treated or should the patient go straight to IVF? And does the optimal approach depend on the size of the endometrioma?
“The answer to this question ultimately depends on the skill and experience of the surgeon and the type of endometrioma,” says Dr. Nezhat, “because improper removal of an endometrioma may compromise the function of the ovary.”
“I recommend removal of the endometrioma by a skilled surgeon experienced in the management of ovarian cysts and preservation of ovarian function, especially in patients who have failed IVF,” he says.6,15
According to the ASRM committee opinion on endometriosis and infertility, laparoscopic cystectomy for endometriomas larger than 4 cm improves fertility, compared with cyst drainage and coagulation, which is associated with a high risk of cyst recurrence.2 However, no randomized trials have compared laparoscopic excision of an endometrioma to expectant management prior to IVF/intracytoplasmic sperm injection (ICSI). One case-control study found that laparoscopic cystectomy prior to IVF had no effect on fertility outcomes.16 At the same time, however, “conservative surgical treatment in symptomatic patients did not impair the success rates of IVF or ICSI,” notes the ASRM.2 Therefore, “evidence suggests that surgery does not benefit asymptomatic women with an endometrioma prior to scheduled IVF/ICSI,” the ASRM concludes.2
Dr. Nezhat cautions against the practice of indiscriminate IVF in the setting of ovarian endometriomas because he has seen patients who developed tubo-ovarian abscess and infected endometriomas after transvaginal egg retrieval. He notes that there are additional case reports of similar findings from other surgeons.
As far as excision versus ablation is concerned, all studies have shown some effect on ovarian function after excision, says Dr. Falcone. “The studies assessed this parameter using several endpoints, such as the number of oocytes retrieved at IVF. Recently, anti-Müllerian hormone has been used and has confirmed this observation. The decreased ovarian reserve is especially problematic with bilateral ovarian disease. The extent of the decreased ovarian function is dependent on several parameters, especially how much energy is used to achieve hemostasis. Several techniques have been proposed to reduce damage, including less traumatic ways of achieving hemostasis in the ovarian hilus.”
“The dilemma is that, if we excise the disease, the pregnancy rates are better than with ablation, but if we excise, there is more damage to the ovary. In my practice, I excise if there is minimal associated disease, such as adhesions, because the pregnancy rate after surgery is good. If, however, there are extensive adhesions with a low chance of spontaneous pregnancy, I minimize excision,” Dr. Falcone says.
As for going straight to IVF, “many patients cannot afford IVF; therefore, surgery is their only option. Furthermore, many patients have severe associated pain; therefore, surgery is required to improve quality of life. However, if the decision is made to proceed to IVF, there is no evidence that cystectomy prior to treatment with ART improves the pregnancy rate,” Dr. Falcone says.
“Basically, if a woman has no pain and no endometrioma, and infertility alone is the issue, I treat her in the same manner as I would a patient with idiopathic infertility—no surgery,” Dr. Falcone says. “If a patient has severe pain and infertility, I treat her surgically but conservatively, especially when an endometrioma is present. The patient will get pain relief but also derive fertility benefit. If a patient has had previous surgery for endometriosis-associated infertility, additional surgery is not the next step—as our study has shown that pregnancy rates are better with IVF than repeat surgery.”17
5. Is surgery ever effective after failed IVF?
To answer this question, Dr. Nezhat points to a retrospective case series by Littman and colleagues in which 29 women with a history of failed IVF underwent laparoscopic evaluation and treatment of endometriosis (by the same surgeon).8 Of 29 patients, 22 conceived after laparoscopic treatment of endometriosis, including 15 “non-IVF” pregnancies and 7 IVF pregnancies, the study results show.8
“It is not unusual for patients and health care providers to perceive IVF as the final treatment for infertility,” Littman and colleagues write. “When this definitive therapy fails repeatedly, clinicians and patients may be inclined to pursue oocyte donation or elect to forego further treatment altogether. This is especially true in women of advanced age and in patients with borderline embryo quality. Presently, as a result of our clinical observation in patients with failed IVF, before egg donation or adoption, we offer the option to have meticulous laparoscopic evaluation and treatment by a skilled surgeon. Furthermore, we would not classify an infertility condition as unexplained without confirming the absence of endometriosis by a thorough laparoscopy. In our experience, patients under 35 years old with unexplained infertility who are found to have endometriosis at the time of laparoscopy have an excellent chance of pregnancy following surgical treatment without ART.”8
6. Is repeat surgery ever helpful?
In the treatment of endometriosis-associated infertility, repeat surgery should be avoided if no symptoms are present, says Dr. Estes. “In women with continued symptoms, the benefits of repeat surgery are small, with known risks, including the potential for adhesive disease and the iatrogenic detrimental effect on ovarian function—often in a setting of already-present decreased ovarian reserve.”
Dr. Nezhat agrees that multiple surgeries carry the potential for harm. “However, there is one caveat,” he says. “What was done at the previous surgery and how? The skill and experience of the surgeon and proper technique are of paramount importance to the surgical outcome.”
Share your thoughts on this article! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
Although endometriosis and infertility are clearly linked—in life as well as the medical literature—no causal relationship has been established. Nevertheless, data suggest that 25% to 50% of infertile women have endometriosis, and that as many as 30% to 50% of women who have endometriosis are infertile.1
Among the mechanisms that have been proposed to explain this link are:
- distorted pelvic anatomy
- endocrine and ovulatory abnormalities
- impaired implantation
- impaired quality of the oocyte and embryo
- altered peritoneal function
- altered hormonal and cell-mediated function
- abnormal uterotubal transport.2
Recent studies by Kao and colleagues and Giudice and colleagues have led to new findings in regard to endometriosis and infertility, says Ceana Nezhat, MD.3,4 Dr. Nezhat is Director of the Nezhat Medical Center in Atlanta, Georgia, and Medical Director of Training and Education at Northside Hospital in Atlanta. “These researchers have discovered that endometriosis causes changes to the endometrium that contribute to infertility.”
“There are no studies that have specifically assessed whether one anatomic site is associated with increased infertility over another,” says Tommaso Falcone, MD. “However, it is assumed that disease that involves the tubes and ovaries would impede fertility the most. Adhesive disease and endometriomas around the tubes and ovaries are associated with a worsening prognosis. Although peritoneal disease probably influences fertility solely on the basis of inflammation, disease around the tubes and ovaries is thought to have a mechanical effect as well.” Dr. Falcone is Professor and Chair of Obstetrics and Gynecology at the Cleveland Clinic in Cleveland, Ohio.
“Endometriosis is a chronic and heterogeneous disease process,” says Stephanie J. Estes, MD, Director of Robotic Surgical Services and Associate Professor, Division of Reproductive Endocrinology and Infertility, Department of Obstetrics and Gynecology, at Penn State Hershey Medical Center in Hershey, Pennsylvania.
“It is likely that no single site is the causative factor,” Dr. Estes says. “Endometriosis alters prostaglandins, cytokines, and proteases that may adversely affect eggs, sperm, or embryo development. In addition, altered endometrial receptivity may play a role. It has been shown that, when donor oocytes from women with endometriosis are transferred to women without endometriosis, there are lower implantation rates and poorer embryo quality.”5
Does it follow, then, that eradication of endometriosis improves fertility?
The answer is not clear. Rather, it depends on a number of variables, including the stage of the disease, its location, the presence of symptoms, and more.
“The approach for endometiosis-associated infertility is completely different from the approach for pain,” says Dr. Nezhat. “In a patient with pain, complete eradication of endometriosis is necessary. However, when addressing infertility, a surgeon must be cautious in the vicinity of the reproductive organs, even if a multistage approach is required. Fertility preservation is the goal.6,7 However, thorough treatment of endometriosis improves fertility rates even in cases of failed in vitro fertilization” (IVF).8
In this article, the focus is on 6 critical questions concerning endometriosis and infertility, including the role of medical therapy, when surgery is indicated, and whether an endometrioma warrants removal or referral for IVF.
In Part 1 of this 3-part series, which appeared in the April 2015 issue of OBG Management, the subject was diagnosis of endometriosis. In Part 2, which appeared in May 2015, the focus was endometriosis and pain.
1. Is there a role for medical therapy?
In women who have endometriosis-related infertility, medical therapy does not appear to produce any benefit. In its committee opinion on the subject, the American Society for Reproductive Medicine (ASRM) states as much: “There is no evidence that medical treatment of endometriosis improves fertility.”2
In fact, observes Dr. Estes, trials of medical treatment, involving such medications as combined estrogen-progestin therapy, danazol, progestins, or gonadotropin-releasing hormone (GnRH) agonists, may cause an unnecessary “delay in the use of more effective treatments that could result in pregnancy.”
Dr. Nezhat believes that medical therapy is effective in patients who have adenomyosis in addition to endometriosis. “Three months of treatment with a GnRH agonist will improve fertility rates in these patients,” he says.
“Medical treatments inhibit ovulation,” notes Dr. Estes. “These therapies have no role in pretreatment of patients with endometriosis prior to infertility treatment. On the other hand, medical therapy with GnRH agonists for 3 to 6 months prior to an IVF cycle does result in increased pregnancy rates.”9
2. What is the role of clomiphene and intrauterine insemination?
Should women who have endometriosis, open fallopian tubes, and infertility be treated with clomiphene and intrauterine insemination (IUI) prior to a cycle of IVF?
“This is a complex question,” says Dr. Estes, “as clinical parameters such as age, symptoms, duration of infertility, and the ability to proceed with IVF are important, as well as stage of disease.”
“Overall, in patients younger than 35 years, clomiphene-IUI is an option and has an increased pregnancy rate over timed intercourse” (9% vs 3%), she says.10 “However, clearly IVF is much more successful and is the most effective treatment, with pregnancy rates of approximately 46% for women younger than 35 years (3% of whom have a ‘diagnosis’ of endometriosis, and 13% of whom have an ‘unknown’ infertility factor).11 Women who are older than 35 or who have additional infertility factors, such as male factor, should consider IVF first.”
3. When is surgery indicated?
“Patients who have significant pain associated with their infertility will benefit from surgery, which offers both pain relief and an improvement in the spontaneous pregnancy rate,” says Dr. Falcone. “Patients who are infertile and desire spontaneous pregnancy without pharmacologic intervention or assisted reproductive technology (ART) also benefit from surgery.”
The benefit of surgery in asymptomatic women with minimal to mild endometriosis is unclear. In a randomized controlled trial of 341 women (aged 20–39 years) with infertility and minimal to mild endometriosis, laparoscopic resection or ablation of visible lesions resulted in pregnancy in 30.7% of women, compared with 17.7% of women who underwent diagnostic laparoscopy only.12
Another randomized study of 96 women with minimal to mild endometriosis who underwent resection/ablation or diagnostic laparoscopy found no difference in the birth rate at 1 year.13
When the results of these 2 studies are combined, the number needed to treat is 12 laparoscopies in women with endometriosis, says Dr. Falcone. “So 1 additional pregnancy would be gained from performing endometriosis surgery in 12 patients. If we assume a prevalence of 30% in asymptomatic women with infertility, then you need to perform 40 diagnostic laparoscopies to achieve an extra pregnancy.”
For women with infertility and severe endometriosis, a nonrandomized study found cumulative pregnancy rates of 45% and 63% after laparoscopy and laparotomy, respectively, in 216 women followed for up to 2 years.14 The difference in rates was not statistically significant.
“Although surgery is indicated to diagnose endometriosis, multiple repeat procedures are not an effective treatment for infertility,” says Dr. Estes. “Plus, especially for stage I and II endometriosis [according to the ASRM classification system], approximately 12 patients will need surgery for 1 additional pregnancy—and many more will have needed the procedure to even get to those who have endometriosis. While patients often want us to ‘do something’—often a covered service such as surgery—we need to consider that surgery for early disease does not provide a significant or long-lasting enhancement to women’s ability to conceive.”
In the absence of male-factor infertility, surgical diagnosis with conservative and precise treatment of endometriosis at the same time is better than going directly to IVF, says Dr. Nezhat. Younger patients who undergo surgical treatment have a better chance of achieving more than 1 spontaneous pregnancy than they do with IVF. And older patients also will have an improved conception rate with ART when they are treated surgically, he says.8
Coding and reimbursement
For endometriosis, the correct diagnostic code helps establish the medical necessity of later treatments
Several diagnostic codes are available to describe the location of endometriotic implants, but the fact remains that these codes can be reported only after a definitive diagnosis is made, which generally comes after confirmatory surgery has been performed. When the patient is in the diagnostic phase, she may present with complaints of pelvic pain, dyspareunia, dysmenorrhea, or infertility. Knowing which codes to use at the time of evaluation goes a long way toward establishing medical necessity for any later surgery or medical treatment.
In the TABLE, you will find common diagnostic codes that can be reported during evaluation of endometriosis, including both International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) and ICD-10-CM equivalents. Note that, with ICD-10-CM, payers are looking for a more specific type of dysmenorrhea in the documentation. In the case of painful menstruation suspected to arise from endometriosis, the code for secondary dysmenorrhea should be reported.
Diagnostic coding in cases in which the patient first presents with a complaint of infertility in the absence of other symptoms can be problematic, as many insurers still do not cover the treatment of infertility. However, in the diagnostic stage, codes for fertility testing can be reported instead of codes that confirm infertility when no other symptoms are present. Once the clinician has verified that endometriosis is the source of the infertility and begins treatment, the primary code for the type of endometriosis would be reported, not a diagnosis of infertility.
The procedure performed to diagnose endometriosis would be diagnostic laparoscopy (Current Procedure Terminology [CPT] code 49320, Laparoscopy, abdomen, peritoneum, and omentum, diagnostic, with or without collection of specimen[s] by brushing or washing [separate procedure]) if medical treatment is being pursued. If the plan is to confirm and then immediately remove the implants, the CPT codes would be either 58662, Laparoscopy, surgical; with fulguration or excision of lesions of the ovary, pelvic viscera, or peritoneal surface by any method, or 49203–49205, Excision or destruction, open, intra-abdominal tumors, cysts or endometriomas, 1 or more peritoneal, mesenteric, or retroperitoneal primary or secondary tumors, based on the largest tumor diameter, if they are removed via an abdominal incision.
—Melanie Witt, RN, CPC, COBGC, MA
Ms. Witt is an independent coding and documentation consultant and former program manager, department of coding and nomenclature, American Congress of Obstetricians and Gynecologists.
4. Surgery or IVF for endometriomas?
When an endometrioma is present, should it be surgically treated or should the patient go straight to IVF? And does the optimal approach depend on the size of the endometrioma?
“The answer to this question ultimately depends on the skill and experience of the surgeon and the type of endometrioma,” says Dr. Nezhat, “because improper removal of an endometrioma may compromise the function of the ovary.”
“I recommend removal of the endometrioma by a skilled surgeon experienced in the management of ovarian cysts and preservation of ovarian function, especially in patients who have failed IVF,” he says.6,15
According to the ASRM committee opinion on endometriosis and infertility, laparoscopic cystectomy for endometriomas larger than 4 cm improves fertility, compared with cyst drainage and coagulation, which is associated with a high risk of cyst recurrence.2 However, no randomized trials have compared laparoscopic excision of an endometrioma to expectant management prior to IVF/intracytoplasmic sperm injection (ICSI). One case-control study found that laparoscopic cystectomy prior to IVF had no effect on fertility outcomes.16 At the same time, however, “conservative surgical treatment in symptomatic patients did not impair the success rates of IVF or ICSI,” notes the ASRM.2 Therefore, “evidence suggests that surgery does not benefit asymptomatic women with an endometrioma prior to scheduled IVF/ICSI,” the ASRM concludes.2
Dr. Nezhat cautions against the practice of indiscriminate IVF in the setting of ovarian endometriomas because he has seen patients who developed tubo-ovarian abscess and infected endometriomas after transvaginal egg retrieval. He notes that there are additional case reports of similar findings from other surgeons.
As far as excision versus ablation is concerned, all studies have shown some effect on ovarian function after excision, says Dr. Falcone. “The studies assessed this parameter using several endpoints, such as the number of oocytes retrieved at IVF. Recently, anti-Müllerian hormone has been used and has confirmed this observation. The decreased ovarian reserve is especially problematic with bilateral ovarian disease. The extent of the decreased ovarian function is dependent on several parameters, especially how much energy is used to achieve hemostasis. Several techniques have been proposed to reduce damage, including less traumatic ways of achieving hemostasis in the ovarian hilus.”
“The dilemma is that, if we excise the disease, the pregnancy rates are better than with ablation, but if we excise, there is more damage to the ovary. In my practice, I excise if there is minimal associated disease, such as adhesions, because the pregnancy rate after surgery is good. If, however, there are extensive adhesions with a low chance of spontaneous pregnancy, I minimize excision,” Dr. Falcone says.
As for going straight to IVF, “many patients cannot afford IVF; therefore, surgery is their only option. Furthermore, many patients have severe associated pain; therefore, surgery is required to improve quality of life. However, if the decision is made to proceed to IVF, there is no evidence that cystectomy prior to treatment with ART improves the pregnancy rate,” Dr. Falcone says.
“Basically, if a woman has no pain and no endometrioma, and infertility alone is the issue, I treat her in the same manner as I would a patient with idiopathic infertility—no surgery,” Dr. Falcone says. “If a patient has severe pain and infertility, I treat her surgically but conservatively, especially when an endometrioma is present. The patient will get pain relief but also derive fertility benefit. If a patient has had previous surgery for endometriosis-associated infertility, additional surgery is not the next step—as our study has shown that pregnancy rates are better with IVF than repeat surgery.”17
5. Is surgery ever effective after failed IVF?
To answer this question, Dr. Nezhat points to a retrospective case series by Littman and colleagues in which 29 women with a history of failed IVF underwent laparoscopic evaluation and treatment of endometriosis (by the same surgeon).8 Of 29 patients, 22 conceived after laparoscopic treatment of endometriosis, including 15 “non-IVF” pregnancies and 7 IVF pregnancies, the study results show.8
“It is not unusual for patients and health care providers to perceive IVF as the final treatment for infertility,” Littman and colleagues write. “When this definitive therapy fails repeatedly, clinicians and patients may be inclined to pursue oocyte donation or elect to forego further treatment altogether. This is especially true in women of advanced age and in patients with borderline embryo quality. Presently, as a result of our clinical observation in patients with failed IVF, before egg donation or adoption, we offer the option to have meticulous laparoscopic evaluation and treatment by a skilled surgeon. Furthermore, we would not classify an infertility condition as unexplained without confirming the absence of endometriosis by a thorough laparoscopy. In our experience, patients under 35 years old with unexplained infertility who are found to have endometriosis at the time of laparoscopy have an excellent chance of pregnancy following surgical treatment without ART.”8
6. Is repeat surgery ever helpful?
In the treatment of endometriosis-associated infertility, repeat surgery should be avoided if no symptoms are present, says Dr. Estes. “In women with continued symptoms, the benefits of repeat surgery are small, with known risks, including the potential for adhesive disease and the iatrogenic detrimental effect on ovarian function—often in a setting of already-present decreased ovarian reserve.”
Dr. Nezhat agrees that multiple surgeries carry the potential for harm. “However, there is one caveat,” he says. “What was done at the previous surgery and how? The skill and experience of the surgeon and proper technique are of paramount importance to the surgical outcome.”
Share your thoughts on this article! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
1. Missmer SA, Hankinson SE, Spiegelman D, Barbieri RL, Marshall LM, Hunter DJ. Incidence of laparoscopically confirmed endometriosis by demographic, anthropometric, and lifestyle factors. Am J Epidemiol. 2004;160(8):784–796.
2. Practice Committee of the American Society for Reproductive Medicine. Endometriosis and infertility: a committee opinion. Fertil Steril. 2012;98(3):591–598.
3. Kao LC, Germeyer A, Tulac S, et al. Expression profiling of endometrium from women with endometriosis reveals candidate genes for disease-based implantation failure and infertility. Endocrinology. 2003;144(7):2870–2881.
4. Giudice LC, Telles TL, Lobo S, Kao L. The molecular basis for implantation failure in endometriosis: on the road to discovery. Ann N Y Acad Sci. 2002;955:252–264; discussion 293–295, 396–406.
5. Garrido N, Navarro J, Garcia-Velasco J, et al. The endometrium versus embryonic quality in endometriosis-related infertility. Hum Reprod Update. 2012;8(1):95-103.
6. Lewis M, Baker V, Nezhat C. The impact on ovarian reserve after laparoscopic ovarian cystectomy versus three-stage management in patients with endometriomas: a prospective randomized study. Fertil Steril. 2010;94(6):e81–83.
7. Tsolakidis D, Pados G, Vavilis D, et al. The impact on ovarian reserve after laparoscopic ovarian cystectomy versus three-stage management in patients with endometriomas: a prospective randomized study. Fertil Steril. 2010;94(1):71–77.
8. Littman E, Giudice L, Lathi R, Berker B, Milki A, Nezhat C. Role of laparoscopic treatment of endometriosis in patients with failed in vitro fertilization cycles. Fertil Steril. 2005;84(6):1574–1578.
9. Sallam HN, Garcia-Velasco JA, Dias S, Arici A. Long-term pituitary down-regulation before in vitro fertilization (IVF) for women with endometriosis. Cochrane Database Syst Rev. 2006;(1):CD004635.
10. Deaton JL, Gibson M, Blackmer KM, et al. A randomized, controlled trial of clomiphene citrate and intrauterine insemination in couples with unexplained infertility or surgically corrected endometriosis. Fertil Steril. 1990; 54:1083–1088.
11. Society for Assisted Reproductive Technology. Clinic Summary Report [all member clinics]: 2013. https://www.sartcorsonline.com/rptCSR_PublicMultYear.aspx?ClinicPKID=0. Accessed May 13, 2015.
12. Marcoux S, Maheux R, Bérubé S. Laparoscopic surgery in infertile women with minimal or mild endometriosis. Canadian Collaborative Group on Endometriosis. N Engl J Med. 1997;337(4):217–222.
13. Parazzini F. Ablation of lesions or no treatment in minimal-mild endometriosis in infertile women: a randomized trial. Gruppo Italiano per lo Studio dell’Endometriosi. Hum Reprod. 1999;14(5):1332–1334.
14. Crosignani PG, Vercellini P, Biffignandi F, Costantini W, Cortesi I, Imparato E. Laparoscopy versus laparotomy in conservative surgical treatment for severe endometriosis. Fertil Steril. 1996;66(5):706–711.
15. Nezhat F, Nezhat C, Allan CJ, Metzger DA, Sears DL. Clinical and histologic classification of endometriomas. Implications for a mechanism of pathogenesis. J Reprod Med. 1992;37(9):771–776.
16. Garcia-Velasco JA, Mahutte NG, Corona J, et al. Removal of endometriomas before in vitro fertilization does not improve fertility outcomes: a matched, case-control study. Fertil Steril. 2004;81(5):1194–1197.
17. Pagidas K, Falcone T, Hemmings R, Miron R. Comparison of surgical treatment of moderate (stage III) and severe (stage IV) endometriosis-related infertility with IVF–embryo transfer. Fertil Steril. 1996;65(4):791–795.
1. Missmer SA, Hankinson SE, Spiegelman D, Barbieri RL, Marshall LM, Hunter DJ. Incidence of laparoscopically confirmed endometriosis by demographic, anthropometric, and lifestyle factors. Am J Epidemiol. 2004;160(8):784–796.
2. Practice Committee of the American Society for Reproductive Medicine. Endometriosis and infertility: a committee opinion. Fertil Steril. 2012;98(3):591–598.
3. Kao LC, Germeyer A, Tulac S, et al. Expression profiling of endometrium from women with endometriosis reveals candidate genes for disease-based implantation failure and infertility. Endocrinology. 2003;144(7):2870–2881.
4. Giudice LC, Telles TL, Lobo S, Kao L. The molecular basis for implantation failure in endometriosis: on the road to discovery. Ann N Y Acad Sci. 2002;955:252–264; discussion 293–295, 396–406.
5. Garrido N, Navarro J, Garcia-Velasco J, et al. The endometrium versus embryonic quality in endometriosis-related infertility. Hum Reprod Update. 2012;8(1):95-103.
6. Lewis M, Baker V, Nezhat C. The impact on ovarian reserve after laparoscopic ovarian cystectomy versus three-stage management in patients with endometriomas: a prospective randomized study. Fertil Steril. 2010;94(6):e81–83.
7. Tsolakidis D, Pados G, Vavilis D, et al. The impact on ovarian reserve after laparoscopic ovarian cystectomy versus three-stage management in patients with endometriomas: a prospective randomized study. Fertil Steril. 2010;94(1):71–77.
8. Littman E, Giudice L, Lathi R, Berker B, Milki A, Nezhat C. Role of laparoscopic treatment of endometriosis in patients with failed in vitro fertilization cycles. Fertil Steril. 2005;84(6):1574–1578.
9. Sallam HN, Garcia-Velasco JA, Dias S, Arici A. Long-term pituitary down-regulation before in vitro fertilization (IVF) for women with endometriosis. Cochrane Database Syst Rev. 2006;(1):CD004635.
10. Deaton JL, Gibson M, Blackmer KM, et al. A randomized, controlled trial of clomiphene citrate and intrauterine insemination in couples with unexplained infertility or surgically corrected endometriosis. Fertil Steril. 1990; 54:1083–1088.
11. Society for Assisted Reproductive Technology. Clinic Summary Report [all member clinics]: 2013. https://www.sartcorsonline.com/rptCSR_PublicMultYear.aspx?ClinicPKID=0. Accessed May 13, 2015.
12. Marcoux S, Maheux R, Bérubé S. Laparoscopic surgery in infertile women with minimal or mild endometriosis. Canadian Collaborative Group on Endometriosis. N Engl J Med. 1997;337(4):217–222.
13. Parazzini F. Ablation of lesions or no treatment in minimal-mild endometriosis in infertile women: a randomized trial. Gruppo Italiano per lo Studio dell’Endometriosi. Hum Reprod. 1999;14(5):1332–1334.
14. Crosignani PG, Vercellini P, Biffignandi F, Costantini W, Cortesi I, Imparato E. Laparoscopy versus laparotomy in conservative surgical treatment for severe endometriosis. Fertil Steril. 1996;66(5):706–711.
15. Nezhat F, Nezhat C, Allan CJ, Metzger DA, Sears DL. Clinical and histologic classification of endometriomas. Implications for a mechanism of pathogenesis. J Reprod Med. 1992;37(9):771–776.
16. Garcia-Velasco JA, Mahutte NG, Corona J, et al. Removal of endometriomas before in vitro fertilization does not improve fertility outcomes: a matched, case-control study. Fertil Steril. 2004;81(5):1194–1197.
17. Pagidas K, Falcone T, Hemmings R, Miron R. Comparison of surgical treatment of moderate (stage III) and severe (stage IV) endometriosis-related infertility with IVF–embryo transfer. Fertil Steril. 1996;65(4):791–795.
In This Article
- The role of medical therapy
- When is surgery indicated?
- Coding and reimbursement
- Is surgery ever effective after failed IVF?
ACOG presidents highlight their visions for the College at the 2015 clinical meeting
The 65th and 66th presidents of the American College of Obstetricians and Gynecologists (ACOG) met May 4 at the College’s 2015 Annual Clinical Meeting in San Francisco to discuss highlights of the past and upcoming years. John C. Jennings, MD, outgoing president, described the “dynamic time we live in” and said his focus has been on shifting to efficient value-based health-care delivery based on ObGyns’ ability to work in multidisciplinary teams.
“What we’ve done this year is to bring together a collaborative practice task force to look at how we develop efficiently operating health care teams. And in doing that, I think, we’re going to be able to produce a model that is transportable to other specialties—not just obstetrics and gynecology but the overall delivery of women’s health care,” he said.
“We’ve had at the table with us the American College of Physicians, the American Academy of Pediatrics, colleagues in pharmacy, advanced nurse practitioners, and certified nurse midwives. We’ve also had representatives from the lay public. We have developed a document that will be polished off and published later this year,” he said. “Obviously I want that to be a living document that helps guide us—in particular, our Fellows—in developing effective team-based practice for the future.”
Mark S. DeFrancesco, MD, MBA, incoming president, noted that, with a team-based focus on practice, he will be able to “take it to the next level” and approach population health. “We need to recognize that many women patients—certainly, between the ages of 18 and 50—see their ObGyn primarily for health care. Short of an acute illness, they tend to not see other doctors.” Among the health issues that merit special attention among these women are obesity and smoking, Dr. DeFrancesco said.
“These two areas kill 780,000 people per year in this country. That’s compared to 70,000 who die from breast, uterine, ovarian, and cervical cancers. That’s a tenfold increase in deaths just from smoking and obesity. I’m saying let’s focus some of our zeal for healing on these issues, particularly if we build the teams that John’s talking about and, with our advanced practice RNs and nurse midwives, see patients more efficiently. Let’s do some real screening and attack these problems,” Dr. DeFrancesco said.
Obesity is an especially critical issue to address in obstetric care, Dr. DeFrancesco noted.
“Now there’s a whole body of knowledge developing about genetic changes that are driven by maternal and even paternal obesity,” he said. “I think that may be a lever to help us help our patients lose weight when we remind them that it’s not just about avoiding cesarean section but it’s about preventing a newborn from having a medically complicated life.”
Other issues Dr. DeFrancesco plans to address include physician burnout and dissatisfaction. “Unhappy doctors cannot provide high-quality care,” he noted.
“We’re also going to be doing a total review of our strategic plan,” he said. “It’s an awful lot to do and I’m going to see a few patients in between all these things. Fortunately, ACOG has fantastic senior management and staff, so it’s easier for me to kind of set the course and let the troops bring it the rest of the way.”
The 65th and 66th presidents of the American College of Obstetricians and Gynecologists (ACOG) met May 4 at the College’s 2015 Annual Clinical Meeting in San Francisco to discuss highlights of the past and upcoming years. John C. Jennings, MD, outgoing president, described the “dynamic time we live in” and said his focus has been on shifting to efficient value-based health-care delivery based on ObGyns’ ability to work in multidisciplinary teams.
“What we’ve done this year is to bring together a collaborative practice task force to look at how we develop efficiently operating health care teams. And in doing that, I think, we’re going to be able to produce a model that is transportable to other specialties—not just obstetrics and gynecology but the overall delivery of women’s health care,” he said.
“We’ve had at the table with us the American College of Physicians, the American Academy of Pediatrics, colleagues in pharmacy, advanced nurse practitioners, and certified nurse midwives. We’ve also had representatives from the lay public. We have developed a document that will be polished off and published later this year,” he said. “Obviously I want that to be a living document that helps guide us—in particular, our Fellows—in developing effective team-based practice for the future.”
Mark S. DeFrancesco, MD, MBA, incoming president, noted that, with a team-based focus on practice, he will be able to “take it to the next level” and approach population health. “We need to recognize that many women patients—certainly, between the ages of 18 and 50—see their ObGyn primarily for health care. Short of an acute illness, they tend to not see other doctors.” Among the health issues that merit special attention among these women are obesity and smoking, Dr. DeFrancesco said.
“These two areas kill 780,000 people per year in this country. That’s compared to 70,000 who die from breast, uterine, ovarian, and cervical cancers. That’s a tenfold increase in deaths just from smoking and obesity. I’m saying let’s focus some of our zeal for healing on these issues, particularly if we build the teams that John’s talking about and, with our advanced practice RNs and nurse midwives, see patients more efficiently. Let’s do some real screening and attack these problems,” Dr. DeFrancesco said.
Obesity is an especially critical issue to address in obstetric care, Dr. DeFrancesco noted.
“Now there’s a whole body of knowledge developing about genetic changes that are driven by maternal and even paternal obesity,” he said. “I think that may be a lever to help us help our patients lose weight when we remind them that it’s not just about avoiding cesarean section but it’s about preventing a newborn from having a medically complicated life.”
Other issues Dr. DeFrancesco plans to address include physician burnout and dissatisfaction. “Unhappy doctors cannot provide high-quality care,” he noted.
“We’re also going to be doing a total review of our strategic plan,” he said. “It’s an awful lot to do and I’m going to see a few patients in between all these things. Fortunately, ACOG has fantastic senior management and staff, so it’s easier for me to kind of set the course and let the troops bring it the rest of the way.”
The 65th and 66th presidents of the American College of Obstetricians and Gynecologists (ACOG) met May 4 at the College’s 2015 Annual Clinical Meeting in San Francisco to discuss highlights of the past and upcoming years. John C. Jennings, MD, outgoing president, described the “dynamic time we live in” and said his focus has been on shifting to efficient value-based health-care delivery based on ObGyns’ ability to work in multidisciplinary teams.
“What we’ve done this year is to bring together a collaborative practice task force to look at how we develop efficiently operating health care teams. And in doing that, I think, we’re going to be able to produce a model that is transportable to other specialties—not just obstetrics and gynecology but the overall delivery of women’s health care,” he said.
“We’ve had at the table with us the American College of Physicians, the American Academy of Pediatrics, colleagues in pharmacy, advanced nurse practitioners, and certified nurse midwives. We’ve also had representatives from the lay public. We have developed a document that will be polished off and published later this year,” he said. “Obviously I want that to be a living document that helps guide us—in particular, our Fellows—in developing effective team-based practice for the future.”
Mark S. DeFrancesco, MD, MBA, incoming president, noted that, with a team-based focus on practice, he will be able to “take it to the next level” and approach population health. “We need to recognize that many women patients—certainly, between the ages of 18 and 50—see their ObGyn primarily for health care. Short of an acute illness, they tend to not see other doctors.” Among the health issues that merit special attention among these women are obesity and smoking, Dr. DeFrancesco said.
“These two areas kill 780,000 people per year in this country. That’s compared to 70,000 who die from breast, uterine, ovarian, and cervical cancers. That’s a tenfold increase in deaths just from smoking and obesity. I’m saying let’s focus some of our zeal for healing on these issues, particularly if we build the teams that John’s talking about and, with our advanced practice RNs and nurse midwives, see patients more efficiently. Let’s do some real screening and attack these problems,” Dr. DeFrancesco said.
Obesity is an especially critical issue to address in obstetric care, Dr. DeFrancesco noted.
“Now there’s a whole body of knowledge developing about genetic changes that are driven by maternal and even paternal obesity,” he said. “I think that may be a lever to help us help our patients lose weight when we remind them that it’s not just about avoiding cesarean section but it’s about preventing a newborn from having a medically complicated life.”
Other issues Dr. DeFrancesco plans to address include physician burnout and dissatisfaction. “Unhappy doctors cannot provide high-quality care,” he noted.
“We’re also going to be doing a total review of our strategic plan,” he said. “It’s an awful lot to do and I’m going to see a few patients in between all these things. Fortunately, ACOG has fantastic senior management and staff, so it’s easier for me to kind of set the course and let the troops bring it the rest of the way.”