User login
Associations of Physician Empathy with Patient Anxiety and Ratings of Communication in Hospital Admission Encounters
Admission to a hospital can be a stressful event,1,2 and patients report having many concerns at the time of hospital admission.3 Over the last 20 years, the United States has widely adopted the hospitalist model of inpatient care. Although this model has clear benefits, it also has the potential to contribute to patient stress, as hospitalized patients generally lack preexisting relationships with their inpatient physicians.4,5 In this changing hospital environment, defining and promoting effective medical communication has become an essential goal of both individual practitioners and medical centers.
Successful communication and strong therapeutic relationships with physicians support patients’ coping with illness-associated stress6,7 as well as promote adherence to medical treatment plans.8 Empathy serves as an important building block of patient-centered communication and encourages a strong therapeutic alliance.9 Studies from primary care, oncology, and intensive care unit (ICU) settings indicate that physician empathy is associated with decreased emotional distress,10,11 improved ratings of communication,12 and even better medical outcomes.13
Prior work has shown that hospitalists, like other clinicians, underutilize empathy as a tool in their daily interactions with patients.14-16 Our prior qualitative analysis of audio-recorded hospitalist-patient admission encounters indicated that how hospitalists respond to patient expressions of negative emotion influences relationships with patients and alignment around care plans.17 To determine whether empathic communication is associated with patient-reported outcomes in the hospitalist model, we quantitatively analyzed coded admission encounters and survey data to examine the association between hospitalists’ responses to patient expressions of negative emotion (anxiety, sadness, and anger) and patient anxiety and ratings of communication. Given the often-limited time hospitalists have to complete admission encounters, we also examined the association between response to emotion and encounter length.
METHODS
We analyzed data collected as part of an observational study of hospitalist-patient communication during hospital admission encounters14 to assess the association between the way physicians responded to patient expressions of negative emotion and patient anxiety, ratings of communication in the encounter, and encounter length. We collected data between August 2008 and March 2009 on the general medical service at 2 urban hospitals that are part of an academic medical center. Participants were attending hospitalists (not physician trainees), and patients admitted under participating hospitalists’ care who were able to communicate verbally in English and provide informed consent for the study. The institutional review board at the University of California, San Francisco approved the study; physician and patient participants provided written informed consent.
Enrollment and data collection has been described previously.17 Our cohort for this analysis included 76 patients of 27 physicians who completed encounter audio recordings and pre- and postencounter surveys. Following enrollment, patients completed a preencounter survey to collect demographic information and to measure their baseline anxiety via the State Anxiety Scale (STAI-S), which assesses transient anxious mood using 20 items answered on a 4-point scale for a final score range of 20 to 80.10,18,19 We timed and audio-recorded admission encounters. Encounter recordings were obtained solely from patient interactions with attending hospitalists and did not take into account the time patients may have spent with other physicians, including trainees. After the encounter, patients completed postencounter surveys, which included the STAI-S and patients’ ratings of communication during the encounter. To rate communication, patients responded to 7 items on a 0- to 10-point scale that were derived from previous work (Table 1)12,20,21; the anchors were “not at all” and “completely.” To identify patients with serious illness, which we used as a covariate in regression models, we asked physicians on a postencounter survey whether or not they “would be surprised by this patient’s death or admission to the ICU in the next year.”22
We considered physician as a clustering variable in the calculation of robust standard errors for all models. In addition, we included in each model covariates that were associated with the outcome at P ≤ 0.10, including patient gender, patient age, serious illness,22 preencounter anxiety, encounter length, and hospital. We considered P values < 0.05 to be statistically significant. We used Stata SE 13 (StataCorp LLC, College Station, TX) for all statistical analyses.
RESULTS
We analyzed data from admission encounters with 76 patients (consent rate 63%) and 27 hospitalists (consent rate 91%). Their characteristics are shown in Table 3. Median encounter length was 19 minutes (mean 21 minutes, range 3-68). Patients expressed negative emotion in 190 instances across all encounters; median number of expressions per encounter was 1 (range 0-14). Hospitalists responded empathically to 32% (n = 61) of the patient expressions, neutrally to 43% (n = 81), and nonempathically to 25% (n = 48).
The STAI-S was normally distributed. The mean preencounter STAI-S score was 39 (standard deviation [SD] 8.9). Mean postencounter STAI-S score was 38 (SD 10.7). Mean change in anxiety over the course of the encounter, calculated as the postencounter minus preencounter mean was −1.2 (SD 7.6). Table 1 shows summary statistics for the patient ratings of communication items. All items were rated highly. Across the items, between 51% and 78% of patients rated the highest score of 10.
Across the range of frequencies of emotional expressions per encounter in our data set (0-14 expressions), each additional empathic hospitalist response was associated with a 1.65-point decrease in the STAI-S (95% confidence interval [CI], 0.48-2.82). We did not find significant associations between changes in the STAI-S and the number of neutral hospitalist responses (−0.65 per response; 95% CI, −1.67-0.37) or nonempathic hospitalist responses (0.61 per response; 95% CI, −0.88-2.10).
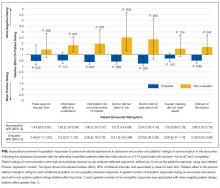
In addition, nonempathic responses were associated with more negative ratings of communication for 5 of the 7 items: ease of understanding information, covering points of interest, the doctor listening, the doctor caring, and trusting the doctor. For example, for the item “I felt this doctor cared about me,” each nonempathic hospitalist response was associated with a more than doubling of negative patient ratings (aRE: 2.3; 95% CI, 1.32-4.16). Neutral physician responses to patient expressions of negative emotion were associated with less negative patient ratings for 2 of the items: covering points of interest (aRE 0.68; 95% CI, 0.51-0.90) and trusting the doctor (aRE: 0.86; 95% CI, 0.75-0.99).
We did not find a statistical association between encounter length and the number of empathic hospitalist responses in the encounter (percent change in encounter length per response [PC]: 1%; 95% CI, −8%-10%) or the number of nonempathic responses (PC: 18%; 95% CI, −2%-42%). We did find a statistically significant association between the number of neutral responses and encounter length (PC: 13%; 95% CI, 3%-24%), corresponding to 2.5 minutes of additional encounter time per neutral response for the median encounter length of 19 minutes.
DISCUSSION
Our study set out to measure how hospitalists responded to expressions of negative emotion during admission encounters with patients and how those responses correlated with patient anxiety, ratings of communication, and encounter length. We found that empathic responses were associated with diminishing patient anxiety after the visit, as well as with better ratings of several domains of hospitalist communication. Moreover, nonempathic responses to negative emotion were associated with more strongly negative ratings of hospitalist communication. Finally, while clinicians may worry that encouraging patients to speak further about emotion will result in excessive visit lengths, we did not find a statistical association between empathic responses and encounter duration. To our knowledge, this is the first study to indicate an association between empathy and patient anxiety and communication ratings within the hospitalist model, which is rapidly becoming the predominant model for providing inpatient care in the United States.4,5
As in oncologic care, anxiety is an emotion commonly confronted by clinicians meeting admitted medical patients for the first time. Studies show that not only do patient anxiety levels remain high throughout a hospital course, patients who experience higher levels of anxiety tend to stay longer in the hospital.1,2,27-30 But unlike oncologic care or other therapy provided in an outpatient setting, the hospitalist model does not facilitate “continuity” of care, or the ability to care for the same patients over a long period of time. This reality of inpatient care makes rapid, effective rapport-building critical to establishing strong physician-patient relationships. In this setting, a simple communication tool that is potentially able to reduce inpatients’ anxiety could have a meaningful impact on hospitalist-provided care and patient outcomes.
In terms of the magnitude of the effect of empathic responses, the clinical significance of a 1.65-point decrease in the STAI-S anxiety score is not precisely clear. A prior study that examined the effect of music therapy on anxiety levels in patients with cancer found an average anxiety reduction of approximately 9.5 units on the STAIS-S scale after sensitivity analysis, suggesting a rather large meaningful effect size.31 Given we found a reduction of 1.65 points for each empathic response, however, with a range of 0-14 negative emotions expressed over a median 19-minute encounter, there is opportunity for hospitalists to achieve a clinically significant decrease in patient anxiety during an admission encounter. The potential to reduce anxiety is extended further when we consider that the impact of an empathic response may apply not just to the admission encounter alone but also to numerous other patient-clinician interactions over the course of a hospitalization.
A healthy body of communication research supports the associations we found in our study between empathy and patient ratings of communication and physicians. Families in ICU conferences rate communication more positively when physicians express empathy,12 and a number of studies indicate an association between empathy and patient satisfaction in outpatient settings.8 Given the associations we found with negative ratings on the items in our study, promoting empathic responses to expressions of emotion and, more importantly, stressing avoidance of nonempathic responses may be relevant efforts in working to improve patient satisfaction scores on surveys reporting “top box” percentages, such as Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS). More notably, evidence indicates that empathy has positive impacts beyond satisfaction surveys, such as adherence, better diagnostic and clinical outcomes, and strengthening of patient enablement.8Not all hospitalist responses to emotion were associated with patient ratings across the 7 communication items we assessed. For example, we did not find an association between how physicians responded to patient expressions of negative emotion and patient perception that enough time was spent in the visit or the degree to which talking with the doctor met a patient’s overall needs. It follows logically, and other research supports, that empathy would influence patient ratings of physician caring and trust,32 whereas other communication factors we were unable to measure (eg, physician body language, tone, and use of jargon and patient health literacy and primary language) may have a more significant association with patient ratings of the other items we assessed.
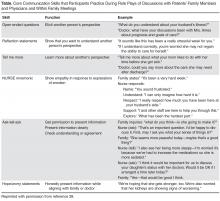
In considering the clinical application of our results, it is important to note that communication skills, including responding empathically to patient expressions of negative emotion, can be imparted through training in the same way as abdominal examination or electrocardiogram interpretation skills.33-35 However, training of hospitalists in communication skills requires time and some financial investment on the part of the physician, their hospital or group, or, ideally, both. Effective training methods, like those for other skill acquisition, involve learner-centered teaching and practicing skills with role-play and feedback.36 Given the importance of a learner-centered approach, learning would likely be better received and more effective if it was tailored to the specific needs and patient scenarios commonly encountered by hospitalist physicians. As these programs are developed, it will be important to assess the impact of any training on the patient-reported outcomes we assessed in this observational study, along with clinical outcomes.
Our study has several limitations. First, we were only able to evaluate whether hospitalists verbally responded to patient emotion and were thus not able to account for nonverbal empathy such as facial expressions, body language, or voice tone. Second, given our patient consent rate of 63%, patients who agreed to participate in the study may have had different opinions than those who declined to participate. Also, hospitalists and patients may have behaved differently as a result of being audio recorded. We only included patients who spoke English, and our patient population was predominately non-Hispanic white. Patients who spoke other languages or came from other cultural backgrounds may have had different responses. Third, we did not use a single validated scale for patient ratings of communication, and multiple analyses increase our risk of finding statistically significant associations by chance. The skewing of the communication rating items toward high scores may also have led to our results being driven by outliers, although the model we chose for analysis does penalize for this. Furthermore, our sample size was small, leading to wide CIs and potential for lack of statistical associations due to insufficient power. Our findings warrant replication in larger studies. Fourth, the setting of our study in an academic center may affect generalizability. Finally, the age of our data (collected between 2008 and 2009) is also a limitation. Given a recent focus on communication and patient experience since the initiation of HCAHPS feedback, a similar analysis of empathy and communication methods now may result in different outcomes.
In conclusion, our results suggest that enhancing hospitalists’ empathic responses to patient expressions of negative emotion could decrease patient anxiety and improve patients’ perceptions of (and thus possibly their relationships with) hospitalists, without sacrificing efficiency. Future work should focus on tailoring and implementing communication skills training programs for hospitalists and evaluating the impact of training on patient outcomes.
Acknowledgments
The authors extend their sincere thanks to the patients and physicians who participated in this study. Dr. Anderson was funded by the National Palliative Care Research Center and the University of California, San Francisco Clinical and Translational Science Institute Career Development Program, National Institutes of Health (NIH) grant number 5 KL2 RR024130-04. Project costs were funded by a grant from the University of California, San Francisco Academic Senate.
Disclosure
All coauthors have seen and agree with the contents of this manuscript. This submission is not under review by any other publication. Wendy Anderson received funding for this project from the National Palliative Care Research Center, University of California San Francisco Clinical and Translational Science Institute (NIH grant number 5KL2RR024130-04), and the University of San Francisco Academic Senate [From Section 2 of Author Disclosure Form]. Andy Auerbach has a Patient-Centered Outcomes Research Institute research grant in development [From Section 3 of the Author Disclosure Form].
1. Walker FB, Novack DH, Kaiser DL, Knight A, Oblinger P. Anxiety and depression among medical and surgical patients nearing hospital discharge. J Gen Intern Med. 1987;2(2):99-101. PubMed
2. Castillo MI, Cooke M, Macfarlane B, Aitken LM. Factors associated with anxiety in critically ill patients: A prospective observational cohort study. Int J Nurs Stud. 2016;60:225-233. PubMed
3. Anderson WG, Winters K, Auerbach AD. Patient concerns at hospital admission. Arch Intern Med. 2011;171(15):1399-1400. PubMed
4. Kuo Y-F, Sharma G, Freeman JL, Goodwin JS. Growth in the care of older patients by hospitalists in the United States. N Engl J Med. 2009;360(11):1102-1112. PubMed
5. Wachter RM, Goldman L. Zero to 50,000 - The 20th Anniversary of the Hospitalist. N Engl J Med. 2016;375(11):1009-1011. PubMed
6. Mack JW, Block SD, Nilsson M, et al. Measuring therapeutic alliance between oncologists and patients with advanced cancer: the Human Connection Scale. Cancer. 2009;115(14):3302-3311. PubMed
7. Huff NG, Nadig N, Ford DW, Cox CE. Therapeutic Alliance between the Caregivers of Critical Illness Survivors and Intensive Care Unit Clinicians. [published correction appears in Ann Am Thorac Soc. 2016;13(4):576]. Ann Am Thorac Soc. 2015;12(11):1646-1653. PubMed
8. Derksen F, Bensing J, Lagro-Janssen A. Effectiveness of empathy in general practice: a systematic review. Br J Gen Pract. 2013;63(606):e76-e84. PubMed
9. Dwamena F, Holmes-Rovner M, Gaulden CM, et al. Interventions for providers to promote a patient-centred approach in clinical consultations. Cochrane Database Syst Rev. 2012;12:CD003267. PubMed
10. Fogarty LA, Curbow BA, Wingard JR, McDonnell K, Somerfield MR. Can 40 seconds of compassion reduce patient anxiety? J Clin Oncol. 1999;17(1):371-379. PubMed
11. Roter DL, Hall JA, Kern DE, Barker LR, Cole KA, Roca RP. Improving physicians’ interviewing skills and reducing patients’ emotional distress. A randomized clinical trial. Arch Intern Med. 1995;155(17):1877-1884. PubMed
12. Stapleton RD, Engelberg RA, Wenrich MD, Goss CH, Curtis JR. Clinician statements and family satisfaction with family conferences in the intensive care unit. Crit Care Med. 2006;34(6):1679-1685. PubMed
13. Hojat M, Louis DZ, Markham FW, Wender R, Rabinowitz C, Gonnella JS. Physicians’ empathy and clinical outcomes for diabetic patients. Acad Med. 2011;86(3):359-364. PubMed
14. Anderson WG, Winters K, Arnold RM, Puntillo KA, White DB, Auerbach AD. Studying physician-patient communication in the acute care setting: the hospitalist rapport study. Patient Educ Couns. 2011;82(2):275-279. PubMed
15. Pollak KI, Arnold RM, Jeffreys AS, et al. Oncologist communication about emotion during visits with patients with advanced cancer. J Clin Oncol. 2007;25(36):5748-5752. PubMed
16. Suchman AL, Markakis K, Beckman HB, Frankel R. A model of empathic communication in the medical interview. JAMA. 1997;277(8):678-682. PubMed
17. Adams K, Cimino JEW, Arnold RM, Anderson WG. Why should I talk about emotion? Communication patterns associated with physician discussion of patient expressions of negative emotion in hospital admission encounters. Patient Educ Couns. 2012;89(1):44-50. PubMed
18. Julian LJ. Measures of anxiety: State-Trait Anxiety Inventory (STAI), Beck Anxiety Inventory (BAI), and Hospital Anxiety and Depression Scale-Anxiety (HADS-A). Arthritis Care Res (Hoboken). 2011;63 Suppl 11:S467-S472. PubMed
19. Speilberger C, Ritterband L, Sydeman S, Reheiser E, Unger K. Assessment of emotional states and personality traits: measuring psychological vital signs. In: Butcher J, editor. Clinical personality assessment: practical approaches. New York: Oxford University Press; 1995.
20. Safran DG, Kosinski M, Tarlov AR, et al. The Primary Care Assessment Survey: tests of data quality and measurement performance. Med Care. 1998;36(5):728-739. PubMed
21. Azoulay E, Pochard F, Kentish-Barnes N, et al. Risk of post-traumatic stress symptoms in family members of intensive care unit patients. Am J Respir Crit Care Med. 2005;171(9):987-994. PubMed
22. Lynn J. Perspectives on care at the close of life. Serving patients who may die soon and their families: the role of hospice and other services. JAMA. 2001;285(7):925-932. PubMed
23. Kennifer SL, Alexander SC, Pollak KI, et al. Negative emotions in cancer care: do oncologists’ responses depend on severity and type of emotion? Patient Educ Couns. 2009;76(1):51-56. PubMed
24. Butow PN, Brown RF, Cogar S, Tattersall MHN, Dunn SM. Oncologists’ reactions to cancer patients’ verbal cues. Psychooncology. 2002;11(1):47-58. PubMed
25. Levinson W, Gorawara-Bhat R, Lamb J. A study of patient clues and physician responses in primary care and surgical settings. JAMA. 2000;284(8):1021-1027. PubMed
26. Cohen J. A coefficient of agreement for nominal scales. Educ Psychol Meas. 1960;20(1):37-46.
27. Fulop G. Anxiety disorders in the general hospital setting. Psychiatr Med. 1990;8(3):187-195. PubMed
28. Gerson S, Mistry R, Bastani R, et al. Symptoms of depression and anxiety (MHI) following acute medical/surgical hospitalization and post-discharge psychiatric diagnoses (DSM) in 839 geriatric US veterans. Int J Geriatr Psychiatry. 2004;19(12):1155-1167. PubMed
29. Kathol RG, Wenzel RP. Natural history of symptoms of depression and anxiety during inpatient treatment on general medicine wards. J Gen Intern Med. 1992;7(3):287-293. PubMed
30. Unsal A, Unaldi C, Baytemir C. Anxiety and depression levels of inpatients in the city centre of Kirşehir in Turkey. Int J Nurs Pract. 2011;17(4):411-418. PubMed
31. Bradt J, Dileo C, Grocke D, Magill L. Music interventions for improving psychological and physical outcomes in cancer patients. [Update appears in Cochrane Database Syst Rev. 2016;(8):CD006911] Cochrane Database Syst Rev. 2011;(8):CD006911. PubMed
32. Kim SS, Kaplowitz S, Johnston MV. The effects of physician empathy on patient satisfaction and compliance. Eval Health Prof. 2004;27(3):237-251. PubMed
33. Tulsky JA, Arnold RM, Alexander SC, et al. Enhancing communication between oncologists and patients with a computer-based training program: a randomized trial. Ann Intern Med. 2011;155(9):593-601. PubMed
34. Bays AM, Engelberg RA, Back AL, et al. Interprofessional communication skills training for serious illness: evaluation of a small-group, simulated patient intervention. J Palliat Med. 2014;17(2):159-166. PubMed
35. Epstein RM, Duberstein PR, Fenton JJ, et al. Effect of a Patient-Centered Communication Intervention on Oncologist-Patient Communication, Quality of Life, and Health Care Utilization in Advanced Cancer: The VOICE Randomized Clinical Trial. JAMA Oncol. 2017;3(1):92-100. PubMed
36. Berkhof M, van Rijssen HJ, Schellart AJM, Anema JR, van der Beek AJ. Effective training strategies for teaching communication skills to physicians: an overview of systematic reviews. Patient Educ Couns. 2011;84(2):152-162. PubMed
Admission to a hospital can be a stressful event,1,2 and patients report having many concerns at the time of hospital admission.3 Over the last 20 years, the United States has widely adopted the hospitalist model of inpatient care. Although this model has clear benefits, it also has the potential to contribute to patient stress, as hospitalized patients generally lack preexisting relationships with their inpatient physicians.4,5 In this changing hospital environment, defining and promoting effective medical communication has become an essential goal of both individual practitioners and medical centers.
Successful communication and strong therapeutic relationships with physicians support patients’ coping with illness-associated stress6,7 as well as promote adherence to medical treatment plans.8 Empathy serves as an important building block of patient-centered communication and encourages a strong therapeutic alliance.9 Studies from primary care, oncology, and intensive care unit (ICU) settings indicate that physician empathy is associated with decreased emotional distress,10,11 improved ratings of communication,12 and even better medical outcomes.13
Prior work has shown that hospitalists, like other clinicians, underutilize empathy as a tool in their daily interactions with patients.14-16 Our prior qualitative analysis of audio-recorded hospitalist-patient admission encounters indicated that how hospitalists respond to patient expressions of negative emotion influences relationships with patients and alignment around care plans.17 To determine whether empathic communication is associated with patient-reported outcomes in the hospitalist model, we quantitatively analyzed coded admission encounters and survey data to examine the association between hospitalists’ responses to patient expressions of negative emotion (anxiety, sadness, and anger) and patient anxiety and ratings of communication. Given the often-limited time hospitalists have to complete admission encounters, we also examined the association between response to emotion and encounter length.
METHODS
We analyzed data collected as part of an observational study of hospitalist-patient communication during hospital admission encounters14 to assess the association between the way physicians responded to patient expressions of negative emotion and patient anxiety, ratings of communication in the encounter, and encounter length. We collected data between August 2008 and March 2009 on the general medical service at 2 urban hospitals that are part of an academic medical center. Participants were attending hospitalists (not physician trainees), and patients admitted under participating hospitalists’ care who were able to communicate verbally in English and provide informed consent for the study. The institutional review board at the University of California, San Francisco approved the study; physician and patient participants provided written informed consent.
Enrollment and data collection has been described previously.17 Our cohort for this analysis included 76 patients of 27 physicians who completed encounter audio recordings and pre- and postencounter surveys. Following enrollment, patients completed a preencounter survey to collect demographic information and to measure their baseline anxiety via the State Anxiety Scale (STAI-S), which assesses transient anxious mood using 20 items answered on a 4-point scale for a final score range of 20 to 80.10,18,19 We timed and audio-recorded admission encounters. Encounter recordings were obtained solely from patient interactions with attending hospitalists and did not take into account the time patients may have spent with other physicians, including trainees. After the encounter, patients completed postencounter surveys, which included the STAI-S and patients’ ratings of communication during the encounter. To rate communication, patients responded to 7 items on a 0- to 10-point scale that were derived from previous work (Table 1)12,20,21; the anchors were “not at all” and “completely.” To identify patients with serious illness, which we used as a covariate in regression models, we asked physicians on a postencounter survey whether or not they “would be surprised by this patient’s death or admission to the ICU in the next year.”22
We considered physician as a clustering variable in the calculation of robust standard errors for all models. In addition, we included in each model covariates that were associated with the outcome at P ≤ 0.10, including patient gender, patient age, serious illness,22 preencounter anxiety, encounter length, and hospital. We considered P values < 0.05 to be statistically significant. We used Stata SE 13 (StataCorp LLC, College Station, TX) for all statistical analyses.
RESULTS
We analyzed data from admission encounters with 76 patients (consent rate 63%) and 27 hospitalists (consent rate 91%). Their characteristics are shown in Table 3. Median encounter length was 19 minutes (mean 21 minutes, range 3-68). Patients expressed negative emotion in 190 instances across all encounters; median number of expressions per encounter was 1 (range 0-14). Hospitalists responded empathically to 32% (n = 61) of the patient expressions, neutrally to 43% (n = 81), and nonempathically to 25% (n = 48).
The STAI-S was normally distributed. The mean preencounter STAI-S score was 39 (standard deviation [SD] 8.9). Mean postencounter STAI-S score was 38 (SD 10.7). Mean change in anxiety over the course of the encounter, calculated as the postencounter minus preencounter mean was −1.2 (SD 7.6). Table 1 shows summary statistics for the patient ratings of communication items. All items were rated highly. Across the items, between 51% and 78% of patients rated the highest score of 10.
Across the range of frequencies of emotional expressions per encounter in our data set (0-14 expressions), each additional empathic hospitalist response was associated with a 1.65-point decrease in the STAI-S (95% confidence interval [CI], 0.48-2.82). We did not find significant associations between changes in the STAI-S and the number of neutral hospitalist responses (−0.65 per response; 95% CI, −1.67-0.37) or nonempathic hospitalist responses (0.61 per response; 95% CI, −0.88-2.10).
In addition, nonempathic responses were associated with more negative ratings of communication for 5 of the 7 items: ease of understanding information, covering points of interest, the doctor listening, the doctor caring, and trusting the doctor. For example, for the item “I felt this doctor cared about me,” each nonempathic hospitalist response was associated with a more than doubling of negative patient ratings (aRE: 2.3; 95% CI, 1.32-4.16). Neutral physician responses to patient expressions of negative emotion were associated with less negative patient ratings for 2 of the items: covering points of interest (aRE 0.68; 95% CI, 0.51-0.90) and trusting the doctor (aRE: 0.86; 95% CI, 0.75-0.99).
We did not find a statistical association between encounter length and the number of empathic hospitalist responses in the encounter (percent change in encounter length per response [PC]: 1%; 95% CI, −8%-10%) or the number of nonempathic responses (PC: 18%; 95% CI, −2%-42%). We did find a statistically significant association between the number of neutral responses and encounter length (PC: 13%; 95% CI, 3%-24%), corresponding to 2.5 minutes of additional encounter time per neutral response for the median encounter length of 19 minutes.
DISCUSSION
Our study set out to measure how hospitalists responded to expressions of negative emotion during admission encounters with patients and how those responses correlated with patient anxiety, ratings of communication, and encounter length. We found that empathic responses were associated with diminishing patient anxiety after the visit, as well as with better ratings of several domains of hospitalist communication. Moreover, nonempathic responses to negative emotion were associated with more strongly negative ratings of hospitalist communication. Finally, while clinicians may worry that encouraging patients to speak further about emotion will result in excessive visit lengths, we did not find a statistical association between empathic responses and encounter duration. To our knowledge, this is the first study to indicate an association between empathy and patient anxiety and communication ratings within the hospitalist model, which is rapidly becoming the predominant model for providing inpatient care in the United States.4,5
As in oncologic care, anxiety is an emotion commonly confronted by clinicians meeting admitted medical patients for the first time. Studies show that not only do patient anxiety levels remain high throughout a hospital course, patients who experience higher levels of anxiety tend to stay longer in the hospital.1,2,27-30 But unlike oncologic care or other therapy provided in an outpatient setting, the hospitalist model does not facilitate “continuity” of care, or the ability to care for the same patients over a long period of time. This reality of inpatient care makes rapid, effective rapport-building critical to establishing strong physician-patient relationships. In this setting, a simple communication tool that is potentially able to reduce inpatients’ anxiety could have a meaningful impact on hospitalist-provided care and patient outcomes.
In terms of the magnitude of the effect of empathic responses, the clinical significance of a 1.65-point decrease in the STAI-S anxiety score is not precisely clear. A prior study that examined the effect of music therapy on anxiety levels in patients with cancer found an average anxiety reduction of approximately 9.5 units on the STAIS-S scale after sensitivity analysis, suggesting a rather large meaningful effect size.31 Given we found a reduction of 1.65 points for each empathic response, however, with a range of 0-14 negative emotions expressed over a median 19-minute encounter, there is opportunity for hospitalists to achieve a clinically significant decrease in patient anxiety during an admission encounter. The potential to reduce anxiety is extended further when we consider that the impact of an empathic response may apply not just to the admission encounter alone but also to numerous other patient-clinician interactions over the course of a hospitalization.
A healthy body of communication research supports the associations we found in our study between empathy and patient ratings of communication and physicians. Families in ICU conferences rate communication more positively when physicians express empathy,12 and a number of studies indicate an association between empathy and patient satisfaction in outpatient settings.8 Given the associations we found with negative ratings on the items in our study, promoting empathic responses to expressions of emotion and, more importantly, stressing avoidance of nonempathic responses may be relevant efforts in working to improve patient satisfaction scores on surveys reporting “top box” percentages, such as Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS). More notably, evidence indicates that empathy has positive impacts beyond satisfaction surveys, such as adherence, better diagnostic and clinical outcomes, and strengthening of patient enablement.8Not all hospitalist responses to emotion were associated with patient ratings across the 7 communication items we assessed. For example, we did not find an association between how physicians responded to patient expressions of negative emotion and patient perception that enough time was spent in the visit or the degree to which talking with the doctor met a patient’s overall needs. It follows logically, and other research supports, that empathy would influence patient ratings of physician caring and trust,32 whereas other communication factors we were unable to measure (eg, physician body language, tone, and use of jargon and patient health literacy and primary language) may have a more significant association with patient ratings of the other items we assessed.
In considering the clinical application of our results, it is important to note that communication skills, including responding empathically to patient expressions of negative emotion, can be imparted through training in the same way as abdominal examination or electrocardiogram interpretation skills.33-35 However, training of hospitalists in communication skills requires time and some financial investment on the part of the physician, their hospital or group, or, ideally, both. Effective training methods, like those for other skill acquisition, involve learner-centered teaching and practicing skills with role-play and feedback.36 Given the importance of a learner-centered approach, learning would likely be better received and more effective if it was tailored to the specific needs and patient scenarios commonly encountered by hospitalist physicians. As these programs are developed, it will be important to assess the impact of any training on the patient-reported outcomes we assessed in this observational study, along with clinical outcomes.
Our study has several limitations. First, we were only able to evaluate whether hospitalists verbally responded to patient emotion and were thus not able to account for nonverbal empathy such as facial expressions, body language, or voice tone. Second, given our patient consent rate of 63%, patients who agreed to participate in the study may have had different opinions than those who declined to participate. Also, hospitalists and patients may have behaved differently as a result of being audio recorded. We only included patients who spoke English, and our patient population was predominately non-Hispanic white. Patients who spoke other languages or came from other cultural backgrounds may have had different responses. Third, we did not use a single validated scale for patient ratings of communication, and multiple analyses increase our risk of finding statistically significant associations by chance. The skewing of the communication rating items toward high scores may also have led to our results being driven by outliers, although the model we chose for analysis does penalize for this. Furthermore, our sample size was small, leading to wide CIs and potential for lack of statistical associations due to insufficient power. Our findings warrant replication in larger studies. Fourth, the setting of our study in an academic center may affect generalizability. Finally, the age of our data (collected between 2008 and 2009) is also a limitation. Given a recent focus on communication and patient experience since the initiation of HCAHPS feedback, a similar analysis of empathy and communication methods now may result in different outcomes.
In conclusion, our results suggest that enhancing hospitalists’ empathic responses to patient expressions of negative emotion could decrease patient anxiety and improve patients’ perceptions of (and thus possibly their relationships with) hospitalists, without sacrificing efficiency. Future work should focus on tailoring and implementing communication skills training programs for hospitalists and evaluating the impact of training on patient outcomes.
Acknowledgments
The authors extend their sincere thanks to the patients and physicians who participated in this study. Dr. Anderson was funded by the National Palliative Care Research Center and the University of California, San Francisco Clinical and Translational Science Institute Career Development Program, National Institutes of Health (NIH) grant number 5 KL2 RR024130-04. Project costs were funded by a grant from the University of California, San Francisco Academic Senate.
Disclosure
All coauthors have seen and agree with the contents of this manuscript. This submission is not under review by any other publication. Wendy Anderson received funding for this project from the National Palliative Care Research Center, University of California San Francisco Clinical and Translational Science Institute (NIH grant number 5KL2RR024130-04), and the University of San Francisco Academic Senate [From Section 2 of Author Disclosure Form]. Andy Auerbach has a Patient-Centered Outcomes Research Institute research grant in development [From Section 3 of the Author Disclosure Form].
Admission to a hospital can be a stressful event,1,2 and patients report having many concerns at the time of hospital admission.3 Over the last 20 years, the United States has widely adopted the hospitalist model of inpatient care. Although this model has clear benefits, it also has the potential to contribute to patient stress, as hospitalized patients generally lack preexisting relationships with their inpatient physicians.4,5 In this changing hospital environment, defining and promoting effective medical communication has become an essential goal of both individual practitioners and medical centers.
Successful communication and strong therapeutic relationships with physicians support patients’ coping with illness-associated stress6,7 as well as promote adherence to medical treatment plans.8 Empathy serves as an important building block of patient-centered communication and encourages a strong therapeutic alliance.9 Studies from primary care, oncology, and intensive care unit (ICU) settings indicate that physician empathy is associated with decreased emotional distress,10,11 improved ratings of communication,12 and even better medical outcomes.13
Prior work has shown that hospitalists, like other clinicians, underutilize empathy as a tool in their daily interactions with patients.14-16 Our prior qualitative analysis of audio-recorded hospitalist-patient admission encounters indicated that how hospitalists respond to patient expressions of negative emotion influences relationships with patients and alignment around care plans.17 To determine whether empathic communication is associated with patient-reported outcomes in the hospitalist model, we quantitatively analyzed coded admission encounters and survey data to examine the association between hospitalists’ responses to patient expressions of negative emotion (anxiety, sadness, and anger) and patient anxiety and ratings of communication. Given the often-limited time hospitalists have to complete admission encounters, we also examined the association between response to emotion and encounter length.
METHODS
We analyzed data collected as part of an observational study of hospitalist-patient communication during hospital admission encounters14 to assess the association between the way physicians responded to patient expressions of negative emotion and patient anxiety, ratings of communication in the encounter, and encounter length. We collected data between August 2008 and March 2009 on the general medical service at 2 urban hospitals that are part of an academic medical center. Participants were attending hospitalists (not physician trainees), and patients admitted under participating hospitalists’ care who were able to communicate verbally in English and provide informed consent for the study. The institutional review board at the University of California, San Francisco approved the study; physician and patient participants provided written informed consent.
Enrollment and data collection has been described previously.17 Our cohort for this analysis included 76 patients of 27 physicians who completed encounter audio recordings and pre- and postencounter surveys. Following enrollment, patients completed a preencounter survey to collect demographic information and to measure their baseline anxiety via the State Anxiety Scale (STAI-S), which assesses transient anxious mood using 20 items answered on a 4-point scale for a final score range of 20 to 80.10,18,19 We timed and audio-recorded admission encounters. Encounter recordings were obtained solely from patient interactions with attending hospitalists and did not take into account the time patients may have spent with other physicians, including trainees. After the encounter, patients completed postencounter surveys, which included the STAI-S and patients’ ratings of communication during the encounter. To rate communication, patients responded to 7 items on a 0- to 10-point scale that were derived from previous work (Table 1)12,20,21; the anchors were “not at all” and “completely.” To identify patients with serious illness, which we used as a covariate in regression models, we asked physicians on a postencounter survey whether or not they “would be surprised by this patient’s death or admission to the ICU in the next year.”22
We considered physician as a clustering variable in the calculation of robust standard errors for all models. In addition, we included in each model covariates that were associated with the outcome at P ≤ 0.10, including patient gender, patient age, serious illness,22 preencounter anxiety, encounter length, and hospital. We considered P values < 0.05 to be statistically significant. We used Stata SE 13 (StataCorp LLC, College Station, TX) for all statistical analyses.
RESULTS
We analyzed data from admission encounters with 76 patients (consent rate 63%) and 27 hospitalists (consent rate 91%). Their characteristics are shown in Table 3. Median encounter length was 19 minutes (mean 21 minutes, range 3-68). Patients expressed negative emotion in 190 instances across all encounters; median number of expressions per encounter was 1 (range 0-14). Hospitalists responded empathically to 32% (n = 61) of the patient expressions, neutrally to 43% (n = 81), and nonempathically to 25% (n = 48).
The STAI-S was normally distributed. The mean preencounter STAI-S score was 39 (standard deviation [SD] 8.9). Mean postencounter STAI-S score was 38 (SD 10.7). Mean change in anxiety over the course of the encounter, calculated as the postencounter minus preencounter mean was −1.2 (SD 7.6). Table 1 shows summary statistics for the patient ratings of communication items. All items were rated highly. Across the items, between 51% and 78% of patients rated the highest score of 10.
Across the range of frequencies of emotional expressions per encounter in our data set (0-14 expressions), each additional empathic hospitalist response was associated with a 1.65-point decrease in the STAI-S (95% confidence interval [CI], 0.48-2.82). We did not find significant associations between changes in the STAI-S and the number of neutral hospitalist responses (−0.65 per response; 95% CI, −1.67-0.37) or nonempathic hospitalist responses (0.61 per response; 95% CI, −0.88-2.10).
In addition, nonempathic responses were associated with more negative ratings of communication for 5 of the 7 items: ease of understanding information, covering points of interest, the doctor listening, the doctor caring, and trusting the doctor. For example, for the item “I felt this doctor cared about me,” each nonempathic hospitalist response was associated with a more than doubling of negative patient ratings (aRE: 2.3; 95% CI, 1.32-4.16). Neutral physician responses to patient expressions of negative emotion were associated with less negative patient ratings for 2 of the items: covering points of interest (aRE 0.68; 95% CI, 0.51-0.90) and trusting the doctor (aRE: 0.86; 95% CI, 0.75-0.99).
We did not find a statistical association between encounter length and the number of empathic hospitalist responses in the encounter (percent change in encounter length per response [PC]: 1%; 95% CI, −8%-10%) or the number of nonempathic responses (PC: 18%; 95% CI, −2%-42%). We did find a statistically significant association between the number of neutral responses and encounter length (PC: 13%; 95% CI, 3%-24%), corresponding to 2.5 minutes of additional encounter time per neutral response for the median encounter length of 19 minutes.
DISCUSSION
Our study set out to measure how hospitalists responded to expressions of negative emotion during admission encounters with patients and how those responses correlated with patient anxiety, ratings of communication, and encounter length. We found that empathic responses were associated with diminishing patient anxiety after the visit, as well as with better ratings of several domains of hospitalist communication. Moreover, nonempathic responses to negative emotion were associated with more strongly negative ratings of hospitalist communication. Finally, while clinicians may worry that encouraging patients to speak further about emotion will result in excessive visit lengths, we did not find a statistical association between empathic responses and encounter duration. To our knowledge, this is the first study to indicate an association between empathy and patient anxiety and communication ratings within the hospitalist model, which is rapidly becoming the predominant model for providing inpatient care in the United States.4,5
As in oncologic care, anxiety is an emotion commonly confronted by clinicians meeting admitted medical patients for the first time. Studies show that not only do patient anxiety levels remain high throughout a hospital course, patients who experience higher levels of anxiety tend to stay longer in the hospital.1,2,27-30 But unlike oncologic care or other therapy provided in an outpatient setting, the hospitalist model does not facilitate “continuity” of care, or the ability to care for the same patients over a long period of time. This reality of inpatient care makes rapid, effective rapport-building critical to establishing strong physician-patient relationships. In this setting, a simple communication tool that is potentially able to reduce inpatients’ anxiety could have a meaningful impact on hospitalist-provided care and patient outcomes.
In terms of the magnitude of the effect of empathic responses, the clinical significance of a 1.65-point decrease in the STAI-S anxiety score is not precisely clear. A prior study that examined the effect of music therapy on anxiety levels in patients with cancer found an average anxiety reduction of approximately 9.5 units on the STAIS-S scale after sensitivity analysis, suggesting a rather large meaningful effect size.31 Given we found a reduction of 1.65 points for each empathic response, however, with a range of 0-14 negative emotions expressed over a median 19-minute encounter, there is opportunity for hospitalists to achieve a clinically significant decrease in patient anxiety during an admission encounter. The potential to reduce anxiety is extended further when we consider that the impact of an empathic response may apply not just to the admission encounter alone but also to numerous other patient-clinician interactions over the course of a hospitalization.
A healthy body of communication research supports the associations we found in our study between empathy and patient ratings of communication and physicians. Families in ICU conferences rate communication more positively when physicians express empathy,12 and a number of studies indicate an association between empathy and patient satisfaction in outpatient settings.8 Given the associations we found with negative ratings on the items in our study, promoting empathic responses to expressions of emotion and, more importantly, stressing avoidance of nonempathic responses may be relevant efforts in working to improve patient satisfaction scores on surveys reporting “top box” percentages, such as Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS). More notably, evidence indicates that empathy has positive impacts beyond satisfaction surveys, such as adherence, better diagnostic and clinical outcomes, and strengthening of patient enablement.8Not all hospitalist responses to emotion were associated with patient ratings across the 7 communication items we assessed. For example, we did not find an association between how physicians responded to patient expressions of negative emotion and patient perception that enough time was spent in the visit or the degree to which talking with the doctor met a patient’s overall needs. It follows logically, and other research supports, that empathy would influence patient ratings of physician caring and trust,32 whereas other communication factors we were unable to measure (eg, physician body language, tone, and use of jargon and patient health literacy and primary language) may have a more significant association with patient ratings of the other items we assessed.
In considering the clinical application of our results, it is important to note that communication skills, including responding empathically to patient expressions of negative emotion, can be imparted through training in the same way as abdominal examination or electrocardiogram interpretation skills.33-35 However, training of hospitalists in communication skills requires time and some financial investment on the part of the physician, their hospital or group, or, ideally, both. Effective training methods, like those for other skill acquisition, involve learner-centered teaching and practicing skills with role-play and feedback.36 Given the importance of a learner-centered approach, learning would likely be better received and more effective if it was tailored to the specific needs and patient scenarios commonly encountered by hospitalist physicians. As these programs are developed, it will be important to assess the impact of any training on the patient-reported outcomes we assessed in this observational study, along with clinical outcomes.
Our study has several limitations. First, we were only able to evaluate whether hospitalists verbally responded to patient emotion and were thus not able to account for nonverbal empathy such as facial expressions, body language, or voice tone. Second, given our patient consent rate of 63%, patients who agreed to participate in the study may have had different opinions than those who declined to participate. Also, hospitalists and patients may have behaved differently as a result of being audio recorded. We only included patients who spoke English, and our patient population was predominately non-Hispanic white. Patients who spoke other languages or came from other cultural backgrounds may have had different responses. Third, we did not use a single validated scale for patient ratings of communication, and multiple analyses increase our risk of finding statistically significant associations by chance. The skewing of the communication rating items toward high scores may also have led to our results being driven by outliers, although the model we chose for analysis does penalize for this. Furthermore, our sample size was small, leading to wide CIs and potential for lack of statistical associations due to insufficient power. Our findings warrant replication in larger studies. Fourth, the setting of our study in an academic center may affect generalizability. Finally, the age of our data (collected between 2008 and 2009) is also a limitation. Given a recent focus on communication and patient experience since the initiation of HCAHPS feedback, a similar analysis of empathy and communication methods now may result in different outcomes.
In conclusion, our results suggest that enhancing hospitalists’ empathic responses to patient expressions of negative emotion could decrease patient anxiety and improve patients’ perceptions of (and thus possibly their relationships with) hospitalists, without sacrificing efficiency. Future work should focus on tailoring and implementing communication skills training programs for hospitalists and evaluating the impact of training on patient outcomes.
Acknowledgments
The authors extend their sincere thanks to the patients and physicians who participated in this study. Dr. Anderson was funded by the National Palliative Care Research Center and the University of California, San Francisco Clinical and Translational Science Institute Career Development Program, National Institutes of Health (NIH) grant number 5 KL2 RR024130-04. Project costs were funded by a grant from the University of California, San Francisco Academic Senate.
Disclosure
All coauthors have seen and agree with the contents of this manuscript. This submission is not under review by any other publication. Wendy Anderson received funding for this project from the National Palliative Care Research Center, University of California San Francisco Clinical and Translational Science Institute (NIH grant number 5KL2RR024130-04), and the University of San Francisco Academic Senate [From Section 2 of Author Disclosure Form]. Andy Auerbach has a Patient-Centered Outcomes Research Institute research grant in development [From Section 3 of the Author Disclosure Form].
1. Walker FB, Novack DH, Kaiser DL, Knight A, Oblinger P. Anxiety and depression among medical and surgical patients nearing hospital discharge. J Gen Intern Med. 1987;2(2):99-101. PubMed
2. Castillo MI, Cooke M, Macfarlane B, Aitken LM. Factors associated with anxiety in critically ill patients: A prospective observational cohort study. Int J Nurs Stud. 2016;60:225-233. PubMed
3. Anderson WG, Winters K, Auerbach AD. Patient concerns at hospital admission. Arch Intern Med. 2011;171(15):1399-1400. PubMed
4. Kuo Y-F, Sharma G, Freeman JL, Goodwin JS. Growth in the care of older patients by hospitalists in the United States. N Engl J Med. 2009;360(11):1102-1112. PubMed
5. Wachter RM, Goldman L. Zero to 50,000 - The 20th Anniversary of the Hospitalist. N Engl J Med. 2016;375(11):1009-1011. PubMed
6. Mack JW, Block SD, Nilsson M, et al. Measuring therapeutic alliance between oncologists and patients with advanced cancer: the Human Connection Scale. Cancer. 2009;115(14):3302-3311. PubMed
7. Huff NG, Nadig N, Ford DW, Cox CE. Therapeutic Alliance between the Caregivers of Critical Illness Survivors and Intensive Care Unit Clinicians. [published correction appears in Ann Am Thorac Soc. 2016;13(4):576]. Ann Am Thorac Soc. 2015;12(11):1646-1653. PubMed
8. Derksen F, Bensing J, Lagro-Janssen A. Effectiveness of empathy in general practice: a systematic review. Br J Gen Pract. 2013;63(606):e76-e84. PubMed
9. Dwamena F, Holmes-Rovner M, Gaulden CM, et al. Interventions for providers to promote a patient-centred approach in clinical consultations. Cochrane Database Syst Rev. 2012;12:CD003267. PubMed
10. Fogarty LA, Curbow BA, Wingard JR, McDonnell K, Somerfield MR. Can 40 seconds of compassion reduce patient anxiety? J Clin Oncol. 1999;17(1):371-379. PubMed
11. Roter DL, Hall JA, Kern DE, Barker LR, Cole KA, Roca RP. Improving physicians’ interviewing skills and reducing patients’ emotional distress. A randomized clinical trial. Arch Intern Med. 1995;155(17):1877-1884. PubMed
12. Stapleton RD, Engelberg RA, Wenrich MD, Goss CH, Curtis JR. Clinician statements and family satisfaction with family conferences in the intensive care unit. Crit Care Med. 2006;34(6):1679-1685. PubMed
13. Hojat M, Louis DZ, Markham FW, Wender R, Rabinowitz C, Gonnella JS. Physicians’ empathy and clinical outcomes for diabetic patients. Acad Med. 2011;86(3):359-364. PubMed
14. Anderson WG, Winters K, Arnold RM, Puntillo KA, White DB, Auerbach AD. Studying physician-patient communication in the acute care setting: the hospitalist rapport study. Patient Educ Couns. 2011;82(2):275-279. PubMed
15. Pollak KI, Arnold RM, Jeffreys AS, et al. Oncologist communication about emotion during visits with patients with advanced cancer. J Clin Oncol. 2007;25(36):5748-5752. PubMed
16. Suchman AL, Markakis K, Beckman HB, Frankel R. A model of empathic communication in the medical interview. JAMA. 1997;277(8):678-682. PubMed
17. Adams K, Cimino JEW, Arnold RM, Anderson WG. Why should I talk about emotion? Communication patterns associated with physician discussion of patient expressions of negative emotion in hospital admission encounters. Patient Educ Couns. 2012;89(1):44-50. PubMed
18. Julian LJ. Measures of anxiety: State-Trait Anxiety Inventory (STAI), Beck Anxiety Inventory (BAI), and Hospital Anxiety and Depression Scale-Anxiety (HADS-A). Arthritis Care Res (Hoboken). 2011;63 Suppl 11:S467-S472. PubMed
19. Speilberger C, Ritterband L, Sydeman S, Reheiser E, Unger K. Assessment of emotional states and personality traits: measuring psychological vital signs. In: Butcher J, editor. Clinical personality assessment: practical approaches. New York: Oxford University Press; 1995.
20. Safran DG, Kosinski M, Tarlov AR, et al. The Primary Care Assessment Survey: tests of data quality and measurement performance. Med Care. 1998;36(5):728-739. PubMed
21. Azoulay E, Pochard F, Kentish-Barnes N, et al. Risk of post-traumatic stress symptoms in family members of intensive care unit patients. Am J Respir Crit Care Med. 2005;171(9):987-994. PubMed
22. Lynn J. Perspectives on care at the close of life. Serving patients who may die soon and their families: the role of hospice and other services. JAMA. 2001;285(7):925-932. PubMed
23. Kennifer SL, Alexander SC, Pollak KI, et al. Negative emotions in cancer care: do oncologists’ responses depend on severity and type of emotion? Patient Educ Couns. 2009;76(1):51-56. PubMed
24. Butow PN, Brown RF, Cogar S, Tattersall MHN, Dunn SM. Oncologists’ reactions to cancer patients’ verbal cues. Psychooncology. 2002;11(1):47-58. PubMed
25. Levinson W, Gorawara-Bhat R, Lamb J. A study of patient clues and physician responses in primary care and surgical settings. JAMA. 2000;284(8):1021-1027. PubMed
26. Cohen J. A coefficient of agreement for nominal scales. Educ Psychol Meas. 1960;20(1):37-46.
27. Fulop G. Anxiety disorders in the general hospital setting. Psychiatr Med. 1990;8(3):187-195. PubMed
28. Gerson S, Mistry R, Bastani R, et al. Symptoms of depression and anxiety (MHI) following acute medical/surgical hospitalization and post-discharge psychiatric diagnoses (DSM) in 839 geriatric US veterans. Int J Geriatr Psychiatry. 2004;19(12):1155-1167. PubMed
29. Kathol RG, Wenzel RP. Natural history of symptoms of depression and anxiety during inpatient treatment on general medicine wards. J Gen Intern Med. 1992;7(3):287-293. PubMed
30. Unsal A, Unaldi C, Baytemir C. Anxiety and depression levels of inpatients in the city centre of Kirşehir in Turkey. Int J Nurs Pract. 2011;17(4):411-418. PubMed
31. Bradt J, Dileo C, Grocke D, Magill L. Music interventions for improving psychological and physical outcomes in cancer patients. [Update appears in Cochrane Database Syst Rev. 2016;(8):CD006911] Cochrane Database Syst Rev. 2011;(8):CD006911. PubMed
32. Kim SS, Kaplowitz S, Johnston MV. The effects of physician empathy on patient satisfaction and compliance. Eval Health Prof. 2004;27(3):237-251. PubMed
33. Tulsky JA, Arnold RM, Alexander SC, et al. Enhancing communication between oncologists and patients with a computer-based training program: a randomized trial. Ann Intern Med. 2011;155(9):593-601. PubMed
34. Bays AM, Engelberg RA, Back AL, et al. Interprofessional communication skills training for serious illness: evaluation of a small-group, simulated patient intervention. J Palliat Med. 2014;17(2):159-166. PubMed
35. Epstein RM, Duberstein PR, Fenton JJ, et al. Effect of a Patient-Centered Communication Intervention on Oncologist-Patient Communication, Quality of Life, and Health Care Utilization in Advanced Cancer: The VOICE Randomized Clinical Trial. JAMA Oncol. 2017;3(1):92-100. PubMed
36. Berkhof M, van Rijssen HJ, Schellart AJM, Anema JR, van der Beek AJ. Effective training strategies for teaching communication skills to physicians: an overview of systematic reviews. Patient Educ Couns. 2011;84(2):152-162. PubMed
1. Walker FB, Novack DH, Kaiser DL, Knight A, Oblinger P. Anxiety and depression among medical and surgical patients nearing hospital discharge. J Gen Intern Med. 1987;2(2):99-101. PubMed
2. Castillo MI, Cooke M, Macfarlane B, Aitken LM. Factors associated with anxiety in critically ill patients: A prospective observational cohort study. Int J Nurs Stud. 2016;60:225-233. PubMed
3. Anderson WG, Winters K, Auerbach AD. Patient concerns at hospital admission. Arch Intern Med. 2011;171(15):1399-1400. PubMed
4. Kuo Y-F, Sharma G, Freeman JL, Goodwin JS. Growth in the care of older patients by hospitalists in the United States. N Engl J Med. 2009;360(11):1102-1112. PubMed
5. Wachter RM, Goldman L. Zero to 50,000 - The 20th Anniversary of the Hospitalist. N Engl J Med. 2016;375(11):1009-1011. PubMed
6. Mack JW, Block SD, Nilsson M, et al. Measuring therapeutic alliance between oncologists and patients with advanced cancer: the Human Connection Scale. Cancer. 2009;115(14):3302-3311. PubMed
7. Huff NG, Nadig N, Ford DW, Cox CE. Therapeutic Alliance between the Caregivers of Critical Illness Survivors and Intensive Care Unit Clinicians. [published correction appears in Ann Am Thorac Soc. 2016;13(4):576]. Ann Am Thorac Soc. 2015;12(11):1646-1653. PubMed
8. Derksen F, Bensing J, Lagro-Janssen A. Effectiveness of empathy in general practice: a systematic review. Br J Gen Pract. 2013;63(606):e76-e84. PubMed
9. Dwamena F, Holmes-Rovner M, Gaulden CM, et al. Interventions for providers to promote a patient-centred approach in clinical consultations. Cochrane Database Syst Rev. 2012;12:CD003267. PubMed
10. Fogarty LA, Curbow BA, Wingard JR, McDonnell K, Somerfield MR. Can 40 seconds of compassion reduce patient anxiety? J Clin Oncol. 1999;17(1):371-379. PubMed
11. Roter DL, Hall JA, Kern DE, Barker LR, Cole KA, Roca RP. Improving physicians’ interviewing skills and reducing patients’ emotional distress. A randomized clinical trial. Arch Intern Med. 1995;155(17):1877-1884. PubMed
12. Stapleton RD, Engelberg RA, Wenrich MD, Goss CH, Curtis JR. Clinician statements and family satisfaction with family conferences in the intensive care unit. Crit Care Med. 2006;34(6):1679-1685. PubMed
13. Hojat M, Louis DZ, Markham FW, Wender R, Rabinowitz C, Gonnella JS. Physicians’ empathy and clinical outcomes for diabetic patients. Acad Med. 2011;86(3):359-364. PubMed
14. Anderson WG, Winters K, Arnold RM, Puntillo KA, White DB, Auerbach AD. Studying physician-patient communication in the acute care setting: the hospitalist rapport study. Patient Educ Couns. 2011;82(2):275-279. PubMed
15. Pollak KI, Arnold RM, Jeffreys AS, et al. Oncologist communication about emotion during visits with patients with advanced cancer. J Clin Oncol. 2007;25(36):5748-5752. PubMed
16. Suchman AL, Markakis K, Beckman HB, Frankel R. A model of empathic communication in the medical interview. JAMA. 1997;277(8):678-682. PubMed
17. Adams K, Cimino JEW, Arnold RM, Anderson WG. Why should I talk about emotion? Communication patterns associated with physician discussion of patient expressions of negative emotion in hospital admission encounters. Patient Educ Couns. 2012;89(1):44-50. PubMed
18. Julian LJ. Measures of anxiety: State-Trait Anxiety Inventory (STAI), Beck Anxiety Inventory (BAI), and Hospital Anxiety and Depression Scale-Anxiety (HADS-A). Arthritis Care Res (Hoboken). 2011;63 Suppl 11:S467-S472. PubMed
19. Speilberger C, Ritterband L, Sydeman S, Reheiser E, Unger K. Assessment of emotional states and personality traits: measuring psychological vital signs. In: Butcher J, editor. Clinical personality assessment: practical approaches. New York: Oxford University Press; 1995.
20. Safran DG, Kosinski M, Tarlov AR, et al. The Primary Care Assessment Survey: tests of data quality and measurement performance. Med Care. 1998;36(5):728-739. PubMed
21. Azoulay E, Pochard F, Kentish-Barnes N, et al. Risk of post-traumatic stress symptoms in family members of intensive care unit patients. Am J Respir Crit Care Med. 2005;171(9):987-994. PubMed
22. Lynn J. Perspectives on care at the close of life. Serving patients who may die soon and their families: the role of hospice and other services. JAMA. 2001;285(7):925-932. PubMed
23. Kennifer SL, Alexander SC, Pollak KI, et al. Negative emotions in cancer care: do oncologists’ responses depend on severity and type of emotion? Patient Educ Couns. 2009;76(1):51-56. PubMed
24. Butow PN, Brown RF, Cogar S, Tattersall MHN, Dunn SM. Oncologists’ reactions to cancer patients’ verbal cues. Psychooncology. 2002;11(1):47-58. PubMed
25. Levinson W, Gorawara-Bhat R, Lamb J. A study of patient clues and physician responses in primary care and surgical settings. JAMA. 2000;284(8):1021-1027. PubMed
26. Cohen J. A coefficient of agreement for nominal scales. Educ Psychol Meas. 1960;20(1):37-46.
27. Fulop G. Anxiety disorders in the general hospital setting. Psychiatr Med. 1990;8(3):187-195. PubMed
28. Gerson S, Mistry R, Bastani R, et al. Symptoms of depression and anxiety (MHI) following acute medical/surgical hospitalization and post-discharge psychiatric diagnoses (DSM) in 839 geriatric US veterans. Int J Geriatr Psychiatry. 2004;19(12):1155-1167. PubMed
29. Kathol RG, Wenzel RP. Natural history of symptoms of depression and anxiety during inpatient treatment on general medicine wards. J Gen Intern Med. 1992;7(3):287-293. PubMed
30. Unsal A, Unaldi C, Baytemir C. Anxiety and depression levels of inpatients in the city centre of Kirşehir in Turkey. Int J Nurs Pract. 2011;17(4):411-418. PubMed
31. Bradt J, Dileo C, Grocke D, Magill L. Music interventions for improving psychological and physical outcomes in cancer patients. [Update appears in Cochrane Database Syst Rev. 2016;(8):CD006911] Cochrane Database Syst Rev. 2011;(8):CD006911. PubMed
32. Kim SS, Kaplowitz S, Johnston MV. The effects of physician empathy on patient satisfaction and compliance. Eval Health Prof. 2004;27(3):237-251. PubMed
33. Tulsky JA, Arnold RM, Alexander SC, et al. Enhancing communication between oncologists and patients with a computer-based training program: a randomized trial. Ann Intern Med. 2011;155(9):593-601. PubMed
34. Bays AM, Engelberg RA, Back AL, et al. Interprofessional communication skills training for serious illness: evaluation of a small-group, simulated patient intervention. J Palliat Med. 2014;17(2):159-166. PubMed
35. Epstein RM, Duberstein PR, Fenton JJ, et al. Effect of a Patient-Centered Communication Intervention on Oncologist-Patient Communication, Quality of Life, and Health Care Utilization in Advanced Cancer: The VOICE Randomized Clinical Trial. JAMA Oncol. 2017;3(1):92-100. PubMed
36. Berkhof M, van Rijssen HJ, Schellart AJM, Anema JR, van der Beek AJ. Effective training strategies for teaching communication skills to physicians: an overview of systematic reviews. Patient Educ Couns. 2011;84(2):152-162. PubMed
© 2017 Society of Hospital Medicine
Filling the gap: Hospitalists & palliative care
Most Americans diagnosed with serious illness will be hospitalized in their last months. During these hospitalizations, hospitalists direct their care.
For seriously ill patients, consultation with palliative care specialists has been shown to promote patient- and family-centered care, ensuring that care is consistent with patients’ goals, values, and preferences. Yet, many hospitalized patients lack access to palliative care consultation, and specialists have identified key domains of primary palliative care that can be delivered by nonspecialists.
To fill this gap, SHM’s Center for Quality Improvement partnered with The Hastings Center, a world-renowned bioethics research institution, to develop a resource room focused on hospitalists’ role in providing high-quality communication about prognosis and goals of care. The resource room presents a Prognosis and Goals of Care Communication Pathway, which highlights key processes and maps them onto the daily workflows of hospitalist physicians.
The care pathway is grounded in palliative care communication research and the consensus guidance of The Hastings Center Guidelines for Decisions on Life-Sustaining Treatment and Care Near the End of Life. It was informed by a national stakeholder meeting of hospitalists, other hospital clinicians, patient and family advocates, bioethicists, social scientists, and other experts, who identified professional values of hospital medicine aligned with communication as part of good care for seriously ill patients.
A collaborative interdisciplinary work group convened by SHM and including hospitalists, palliative medicine physicians, a bioethicist, and a palliative nursing specialist constructed the care pathway in terms of key processes occurring at admission, during hospitalization, and in discharge planning to support primary palliative care integration into normal workflow. The resource room also includes skills-building tools and resources for individual hospitals, teams, and institutions.
The work group will present a workshop on the care pathway at Hospital Medicine 2017: “Demystifying Difficult Decisions: Strategies and Skills to Equip Hospitalists for High-Quality Goals of Care Conversations with Seriously Ill Patients and Their Families.” For more information on the resource room, visit www.hospitalmedicine.org/EOL.
Dr. Anderson is associate professor in residence in the division of hospital medicine at the University of California, San Francisco. She also serves as attending physician in the Palliative Care Program and codirector of the School of Nursing Interprofessional Palliative Care Training Program at UCSF.
Most Americans diagnosed with serious illness will be hospitalized in their last months. During these hospitalizations, hospitalists direct their care.
For seriously ill patients, consultation with palliative care specialists has been shown to promote patient- and family-centered care, ensuring that care is consistent with patients’ goals, values, and preferences. Yet, many hospitalized patients lack access to palliative care consultation, and specialists have identified key domains of primary palliative care that can be delivered by nonspecialists.
To fill this gap, SHM’s Center for Quality Improvement partnered with The Hastings Center, a world-renowned bioethics research institution, to develop a resource room focused on hospitalists’ role in providing high-quality communication about prognosis and goals of care. The resource room presents a Prognosis and Goals of Care Communication Pathway, which highlights key processes and maps them onto the daily workflows of hospitalist physicians.
The care pathway is grounded in palliative care communication research and the consensus guidance of The Hastings Center Guidelines for Decisions on Life-Sustaining Treatment and Care Near the End of Life. It was informed by a national stakeholder meeting of hospitalists, other hospital clinicians, patient and family advocates, bioethicists, social scientists, and other experts, who identified professional values of hospital medicine aligned with communication as part of good care for seriously ill patients.
A collaborative interdisciplinary work group convened by SHM and including hospitalists, palliative medicine physicians, a bioethicist, and a palliative nursing specialist constructed the care pathway in terms of key processes occurring at admission, during hospitalization, and in discharge planning to support primary palliative care integration into normal workflow. The resource room also includes skills-building tools and resources for individual hospitals, teams, and institutions.
The work group will present a workshop on the care pathway at Hospital Medicine 2017: “Demystifying Difficult Decisions: Strategies and Skills to Equip Hospitalists for High-Quality Goals of Care Conversations with Seriously Ill Patients and Their Families.” For more information on the resource room, visit www.hospitalmedicine.org/EOL.
Dr. Anderson is associate professor in residence in the division of hospital medicine at the University of California, San Francisco. She also serves as attending physician in the Palliative Care Program and codirector of the School of Nursing Interprofessional Palliative Care Training Program at UCSF.
Most Americans diagnosed with serious illness will be hospitalized in their last months. During these hospitalizations, hospitalists direct their care.
For seriously ill patients, consultation with palliative care specialists has been shown to promote patient- and family-centered care, ensuring that care is consistent with patients’ goals, values, and preferences. Yet, many hospitalized patients lack access to palliative care consultation, and specialists have identified key domains of primary palliative care that can be delivered by nonspecialists.
To fill this gap, SHM’s Center for Quality Improvement partnered with The Hastings Center, a world-renowned bioethics research institution, to develop a resource room focused on hospitalists’ role in providing high-quality communication about prognosis and goals of care. The resource room presents a Prognosis and Goals of Care Communication Pathway, which highlights key processes and maps them onto the daily workflows of hospitalist physicians.
The care pathway is grounded in palliative care communication research and the consensus guidance of The Hastings Center Guidelines for Decisions on Life-Sustaining Treatment and Care Near the End of Life. It was informed by a national stakeholder meeting of hospitalists, other hospital clinicians, patient and family advocates, bioethicists, social scientists, and other experts, who identified professional values of hospital medicine aligned with communication as part of good care for seriously ill patients.
A collaborative interdisciplinary work group convened by SHM and including hospitalists, palliative medicine physicians, a bioethicist, and a palliative nursing specialist constructed the care pathway in terms of key processes occurring at admission, during hospitalization, and in discharge planning to support primary palliative care integration into normal workflow. The resource room also includes skills-building tools and resources for individual hospitals, teams, and institutions.
The work group will present a workshop on the care pathway at Hospital Medicine 2017: “Demystifying Difficult Decisions: Strategies and Skills to Equip Hospitalists for High-Quality Goals of Care Conversations with Seriously Ill Patients and Their Families.” For more information on the resource room, visit www.hospitalmedicine.org/EOL.
Dr. Anderson is associate professor in residence in the division of hospital medicine at the University of California, San Francisco. She also serves as attending physician in the Palliative Care Program and codirector of the School of Nursing Interprofessional Palliative Care Training Program at UCSF.
Enhancing the Communication Skills of Critical Care Nurses: Focus on Prognosis and Goals of Care Discussions
From the University of California Irvine Health/Chao Family Comprehensive Cancer Center Orange, CA (Ms. Boyle) and the University of California San Francisco Medical Center, San Francisco, CA (Dr. Anderson).
Abstract
- Objective: To describe components of a unique interactive workshop focusing on the enhancement of critical care nurses’ communication skills within the realm of prognosis and goals of care discussions with family members and physicians.
- Methods: A series of one-day workshops were offered to critical care nurses practicing in the 5 University of California hospital settings. After workshop attendance, nurse participants were followed by workshop facilitators in their units to ensure new communication skills were being integrated into practice and to problem solve if barriers were met.
- Results: Improvement in nurses’ self-confidence in engaging in these discussions was seen. This confidence was sustained months following workshop participation.
- Conclusion: The combination of critical care nurse workshop participation that involved skill enhancement through role-playing, in combination with clinical follow-up with attendees, resulted in positive affirmation of nurse communication skills specific to prognosis and goals of care discussions with family members and physicians.
There is increasing evidence that in the absence of quality communication between professional caregivers and those they care for, negative outcomes may prevail, such as reduced patient/family satisfaction, lower health status awareness, and a decreased sense of being cared about and cared for [1–5]. Communication skill competency is a critical corollary of nursing practice. In the intensive care unit (ICU) setting, patients and families have cited skilled communication as a core element of high-quality care [3,6]. Proficiency in this realm enhances nurses’ understanding of the patient and family’s encounter with health care and provides a vehicle to gather information, inform, teach, and offer emotional support. Additionally, it identifies values, goals, health care preferences, worries and concerns, and facilitates the nurses’ coordination of care [7]. Despite this skill’s importance, however, it is generally not taught in basic education and until recently has been overlooked as a key competency [8,9].
Skilled communication in palliative and end-of-life care is pivotal for discussing prognosis and care planning. In the acute care setting this is particularly relevant as the majority of Americans die in hospitals versus their preferred site of home [10]. Additionally, 1 in 5 Americans die during or shortly after receiving care in an ICU [11]. Hence, while the ICU is a setting in which intensive effort to save lives is employed, it is also a setting where death frequently occurs. The complexity and highly emotive nature of critical care often results in family needs for information and support not being met [12]. A number of reasons for this occurrence have been proposed. In this paper, we will delineate barriers to critical care nurses’ involvement in prognosis and goals of care discussions, identify why nurse involvement in this communication is needed, describe a unique workshop exemplar with a sample role play that characterizes the workshop, and offer recommendations for colleagues interested in replicating similar education offerings.
Barriers to Communication
In the ICU, the sheer number of professionals families interact with may cause confusion. In particular, numerous medical consultants commonly offer opposing opinions. Additionally, each specialist may provide information that focuses on their area of expertise such that the “big picture” is not relayed to the patient and family. Emotional discomfort on the part of the health professional around discussions of poor prognosis, goals of care, and code status may prompt limiting discussion time with patients and families and even the avoidance of interpersonal exchanges [13–15]. Health professionals have also reported concern that end-of-life discussions will increase patient distress [16]. Among health care professionals, the subject of mortality may prompt personal anxiety, trigger unresolved grief, or fear that they will “become emotional” in front of the patient/family [7]. Lack of knowledge about cultural and religious norms has been cited as a barrier, as has time constraints [17,18]. Most frequently, inadequate or absent communication skill training is noted as a significant barrier [19,20]. Many ICU nurses also report feeling marginalized due their exclusion from goals of care and decision-making discussions with patients and families they know well [21,22].
Nurses As Key Palliative Care Communicators
Education efforts that foster communication proficiency during serious illness have traditionally focused on training physicians. Recently, nursing has become a focus of communication skill enhancement in recognition of nurses’ intense and protracted interactions with patients and families in the acute care setting. Nurses are the ‘constant’ in the patient and family’s journey through the fragmented health care system [21,23]. They often have the best knowledge of, and strongest relationship with, the family and often have had extensive discussions with them about their loved one’s status [24]. Nurses are aware of the patients’ symptom experiences and are privy to valuable information about the concerns and priorities of patients and families [12]. Additionally, having the most continuous presence, nurses have seen and heard interactions with clinicians from numerous disciplines. Nurses are the most visible, constant resource for patient and family education, information and support, and thus they perceive one of their most important roles to be that of advocate for the patient and family [20,21].
Communication Training Programs for Critical Care Nurses
Education is critical to enhance communication skills within palliative care [7,15,17,20,21,24]. The preferred teaching style within this realm is role play, where skills can be practiced and the affective component of engaging in sensitive discussions can be addressed [25–27]. Role play also demonstrates firsthand the importance of nonverbal communication (eg, body language, proximity, use of gestures, tone of voice) [7,20] and facilitates nurses’ gaining a sense of comfort with wordless communication [18].
Communication skills training programs have been designed to provide bedside critical care nurses with the tools they need to be active participants in discussions of prognosis, goals of care, and palliative care with families and physicians [27,28]. These programs have demonstrated improvement in nurses’ confidence to engage in key palliative care-related discussions. Essential elements of these programs include (1) delineation of the role of the bedside nurse in palliative care communication; (2) presentation and learner-centered practice of communication skills using role play; and (3) a reflection session focused on self-care and sustainability.
Across the 5 academic University of California medical centers (San Francisco, Davis, Los Angeles, Irvine, and San Diego), a communication training program based on this work has been implemented [29]. The one-day workshop, entitled IMPACT-ICU (Integrating Multidisciplinary Palliative Care into the ICU), has taught a total of 527 critical care nurses across the 5 centers. In addition to classroom training, the IMPACT-ICU program also includes proactive specialty palliative nursing support for bedside nurses by facilitating the availability of palliative care advanced practice nurses and nurse educators resources. This support helps nurses to apply the skills learned in the workshop in their practice. During rounds at the bedside, the nurse resources coach the bedside staff on the “how” and “when” of addressing palliative care needs. Education and support on a range of topics are offered, including clarifying goals and interventions provided by palliative care teams, the specifics of how to provide family emotional support and delivery of understandable information, the assessment and management of symptoms distress, and the nurses’ role in organizing and participating in family meetings. Case-specific consultations are also offered that address how to interface with resistant medical staff. The importance of nurse documentation of these varied exchanges is also emphasized.
IMPACT-ICU Workshop
A maximum of 15 nurses participate in each 8-hour workshop. The session begins with introductions and small group discussions about what the participants perceive to be the greatest barriers to goals of care discussions and fostering patient/family decision-making in the ICU. Participants are also asked to reflect on what they want to learn as a result of their workshop attendance.
A short didactic session then reviews the definition of palliative care and its core components, addresses the nurses’ role in communication within palliative care, a social worker’s perspective of what it is like to be a family member in the ICU, and the outline of the day. This includes delineation of expectations for involvement within the role plays and the various roles to be enacted. An emphasis is placed on the workshop being a safe place to explore and trial skills with the support of colleagues, and that practice is the optimum way to integrate communication expertise into the nurses’ skill set.
The “4 Cs” serves as the instructional basis for nurse communication skill enhancement [27]. This model outlines 4 key nursing roles in optimizing communication within palliative care:
Convening: Making sure multidisciplinary patient/family/clinician communication occurs.
Checking: Identifying the patient and family needs for information; ensuring that patients and families clearly receive desired information; ensuring that clinicians understand patient and family perspectives.
Caring: Naming emotions and responding to feeling.
Continuing: Following up after discussions to clarify and reinforce information and provide support.
Sample Role Play
Facilitator: So our first role play is focused on eliciting patient and family perspectives and needs. I need a learner and someone to play the role of the family member.
Learner: I’ll give it a try.
Facilitator: Lisa, you’re going to do great. Who wants to play the family member?
Workshop Participant: I’ll do it.
Facilitator: So Mary (who has agreed to play the role of the wife), why don’t you read us the scenario. (She reads it out loud to the group).
Facilitator: Lisa, as the nurse, I want you to look at your guide and tell me what your goal is for this conversation with Mrs. Ames and then which skill you want to practice.
Learner: I think I want to try eliciting the patient and family’s needs for information and I’ll try “Tell Me More” statements.
Facilitator: Alright. So remember Lisa, if you feel the conversation isn’t going well, you can call a “time out.” I can do this as well if I feel you need to start over. I’ll also call a time out when I feel you have met your goal. Sound OK? Mary, do you have any questions playing the part of Mrs. Ames?
Wife Role: Well, how hard should I make this for her? Should I be one of those “difficult” family members?
Facilitator: Our goal here is not to “stump” you or make it particularly difficult. We want you to try out these skills and get a sense of your “comfort zone.” So let’s start with some basic communication skills, OK?
Wife Role: Alright.
Facilitator: Why don’t we set the stage, such that Lisa, you are Mr. Ames’ nurse assessing him at the start of your shift, when Mrs. Ames enters. This is the first time you have taken care of him. The night nurse has told you that he has been requiring increasing ventilator support and his renal function is declining. Per Mrs. Ames’ request, the night nurse called her to let her know how he was doing and Mrs. Ames told her she would be in shortly.
Wife Role: (nervously enters the room and grasps her husband’s hand and looks at the nurse). How’s he doing? Is he better? The night nurse called me and I was so worried I rushed over here.
Learner: (Turns to Mrs. Ames and extends her hand). Are you Mrs. Ames? I’m Lisa and I am going to be taking care of Mr. Ames today. Let me just finish my assessment and how about we talk then? Will that be OK? It will be just a few minutes.
Wife Role: Alright, I’ll be in the waiting area but please come get me as soon as you can.
Learner: I will. (Nurse then shortly comes into the waiting area and asks Mrs. Ames to come back into the ICU where she invites her to sit just outside Mr. Ames’ room). Mrs. Ames, how are you doing? This must be so stressful for you, having your husband in the ICU.
Wife Role: It’s awful. He’s never been in the hospital before this and look at him, all hooked up to machines. I’m so worried. He seems to be getting worse instead of better.
Learner: What’s your understanding of what is going on?
Wife Role: I really don’t know. One doctor comes in and says one thing and then another comes in and tells me the opposite. I’m so confused I don’t know what to think.
Learner: Would having a better idea of his condition from the doctors who are treating him help you have a better understanding?
Wife Role: Oh, yes, but they always seem in such a hurry.
Learner: What exactly would you like to know?
Wife: Well, I want to know when he can get off that breathing machine because we have been planning to go to our son’s house for Thanksgiving.
Facilitator: Time out. Lisa, did you meet your conversation goal?
Learner: Um, I’m not sure, I guess so.
Facilitator: (Turns to Observers). What do you think, did she meet her goal?
Observer: Yes, she determined Mrs. Ames’ need for more information and she asked her what she wanted to know exactly.
Facilitator: What else did we see Lisa do to enhance communication with Mrs. Ames?
Observer: Well, when Mrs. Ames rushed into the room and asked her for information, Lisa didn’t just jump in and spout out values for the ventilator and his output. She took the time to introduce herself and de-escalate Mrs. Ames’ anxiety and she followed up on her promise to come get her in the waiting room as soon as she could.
Facilitator: Why do you think was important?
Observer: It helps establish trust.
Facilitator: Did Lisa use the skill she wanted to try out?
Observer: Yes.
Facilitator: How do you know? What did you hear her say?
Observer: She said, “What’s your understanding of what is going on with Mr. Ames?”
Facilitator: Absolutely. Great job, Lisa. And who wants to take a guess at how long Lisa’s exchange with Mrs. Ames took?
Observer: Less than two minutes?
Facilitator: That’s right. So just as you consider how long it takes, and how proficient you are, in starting an IV or inserting a Foley catheter, when you have a goal in mind and have practiced the skills to do it well, any skill can be mastered.
Feedback
Participants in the workshops uniformly report an enhanced sense of self-confidence in their palliative care communication skills as a result of their participation [29]. Key to the success of the workshop is the ongoing contact by the workshop facilitators with participants. Rounding is routinely planned such that each participant is visited weekly by a workshop facilitator in their clinical area to determine if the bedside nurse has practiced the new skills and if so, how the interaction transpired. Positive feedback is given for attempts to engage in new behaviors and participants are reminded that with any new skill, repetitive trials are necessary to foster success.
Lessons Learned and Next Steps
One of our major lessons learned was recognizing that it was difficult for many critical care nurses to practice the new communication skills. Nurses are trained to fix problems and perform medico-technical tasks; “listening” has not always been recognized as real work [18]. We needed to reinforce that skills like eliciting another’s perspective or making reflection statements are equally important to those associated with behavioral/technical proficiency.
While our program has been successful, we recognize that the next step in fostering ideal palliative care communication is to provide education within an interdisciplinary context. We recommend that colleagues interested in replicating this or a similar education intervention, survey nurse participants prior to and following workshop participation to measure attitudes, self confidence and perceived barriers over time [30]. We hope to translate our positive experience into a program that engages multiple professionals in the enhancement of optimum palliative care communication proficiency.
Corresponding author: Deborah A. Boyle MSN, RN, AOCNS, Department of Nursing Quality, Research and Education, University of California, Irvine Health, 101 The City Drive, Bldg 22A, Room 3104, Orange, CA 92868.
1. Leung JM, Udris EM, Uman J, et al. The effect of end-of-life discussions on perceived quality of care and health status among patients with COPD. Chest 2012;142:128–33.
2. Osborn TR, Curtis JR, Nielsen EL, et al. Identifying elements of ICU care that families report as important but unsatisfactory: decision-making, control and ICU atmosphere. Chest 2012;142:1185–92.
3. Nelson JE, Puntillo K, Pronovost PJ, et al. In their own words: patients and families define high-quality palliative care in the ICU. Crit Care Med 2010;38:808–18.
4. Nels W, Gabrijel S, Kiss S, et al. Communication skill training significantly improves lung cancer patients understanding. J Palliat Care Med 2014;4:182.
5. Van Vliet LM, Epstein AS. Current state of the art and science of patient-clinician communication in progressive disease: patients’ need to know and feel known. J Clin Oncol 2014;32:3474-8.
6. Troug RD, Campbell ML, Curtis JR, et al. Recommendations for end of life care in the intensive care unit: a consensus statement by the American College of Critical Care Medicine. Crit Care Med 2008;36:953–63.
7. Dahlin CM, Wittenberg E. Communication in palliative care. In: Ferrell BR, Coyle N, Paice J, editors. Oxford textbook of palliative nursing. 4th ed. Oxford: Oxford University Press; 2014:81–109.
8. Baer L, Weinstein E. Improving oncology nurses’ communication skills for difficult conversations. Clin J Oncol Nurs 2013;17:E45–E51.
9. Treece PD. Communication in the intensive care unit about end of life care. AACN Adv Crit Care 2007;18:406–14.
10. Teno JM, Clarridge BR, Casey V, et al. Family perspectives on end of life care at the last place of care. JAMA 2004;291:88–92.
11. Angus DC, Barnato AE, Linde-Zwirble WT, et al. Robert Wood Johnson Foundation ICU End-of-Life Peer Group. Use of intensive care at the end of life in the United States: an epidemiologic study. Crit Care Med 2004;32:638–43.
12. Hamric AB, Blackhall LJ. Nurse-physician perspectives on the care of dying patients in intensive care units: collaboration, moral distress, and ethical climate. Crit Care Med 2007;35:422–9.
13. Back AL, Trinidad SB, Hopley EK, Edwards KA. Reframing the goals of care conversation: “We’re in a different place.” J Palliat Med 2014;17:1010–24.
14. Aslakson RA, Wyskiel R, Thornton I, et al. Nurse perceived barriers to effective communication regarding prognosis and optimal end of life care for surgical ICU patients: a qualitative exploration. J Palliat Med 2012;15:910–5.
15. Erickson J. Bedside nurse involvement in end of life decision-making. Dimens Crit Care Nurs 2013;32:65–8.
16. Bernacki RE, Block SD for the American College of Physicians High Value Care Task Force. Communication about serious illness care goals: a review and synthesis of best practices. JAMA Intern Med 2014;174:1994–2003.
17. You JJ, Downar J, Fowler RA, et al. Barriers to goals of care discussion with ‘seriously’ ill hospitalized patients and their families: a multicenter survey of clinicians. JAMA Intern Med 2015;175:549–56.
18. Strang S, Henoch I, Danielson E, et al. Communication about existential issues with patients close to death: nurses’ reflections on content, process, and meaning. Psychooncology 2014;23:562–8.
19. Slatore CG, Hensen L, Gauzine L, et al. Communication by nurses in the intensive care unit: qualitative analysis of domains in patient-centered care. Am J Crit Care 2012;21:410–8.
20. Wittenberg-Lyles E, Goldsmith J, Platt CS. Palliative care communication. Sem Oncol Nurs 2014;30:280–6.
21. Fox MY. Improving communication with patients and families in the ICU: palliative care strategies for intensive care unit nurses. J Hospice Palliat Nurs 2014;16:93–8.
22. Beckstrand RL, Callister LC, Kirchhoff KT. Providing a ‘good death’: critical care nurses’ suggestions for improving end of life care. Am J Crit Care 2006;15:38–45.
23. Peereboom K, Coyle N. Facilitating goals of care discus.sions for patients with life-limiting disease: communication strategies for nurses. J Hospice Palliat Nurs 2012; 14:251–8.
24. Nelson JE, Cortez TB, Curtis JR, et al. Integrating palliative care in the ICU: the nurse in the leading role. J Hospice Palliat Nurs 2011;13:89–94.
25. Jors K, Seibel K, Bardenheuer H, et al. Education in end of life care: what do experienced professionals find important? J Cancer Educ 2015 March 15.
26. Roze des Ordons AL, Sharma N, Heyland DK, et al. Strategies for effective goals of care discussions and decision-making: perspective from a multi-centre survey of Canadian hospital-based health care providers. BMC Palliat Care 2015;14:38.
27. Krimshtein NS, Luhrs CA, Puntillo KA, et al. Training nurses for interdisciplinary communication with families in the ICU. J Palliat Med 2011;14:1325–32.
28. Milic MM, Puntillo K, Turner K, et al. Communicating with patients’ families and physicians about prognosis and goals of care. Am J Crit Care 2015;24:e56–e64.
29. Anderson W, Puntillo K, Barbour S, et al. The IMPACT-ICU Project: expanding palliative care nursing across University of California Centers ICUs to advance palliative care. Center to Advance Palliative Care (CAPC) national seminar. Nov 7–9, 2013. Dallas, TX.
30. Anderson WG, Puntillo K, Boyle D, et al. ICU bedside nurses’ involvement in palliative care communication: a multicenter survey. J Pain Symptom Manage. In press.
From the University of California Irvine Health/Chao Family Comprehensive Cancer Center Orange, CA (Ms. Boyle) and the University of California San Francisco Medical Center, San Francisco, CA (Dr. Anderson).
Abstract
- Objective: To describe components of a unique interactive workshop focusing on the enhancement of critical care nurses’ communication skills within the realm of prognosis and goals of care discussions with family members and physicians.
- Methods: A series of one-day workshops were offered to critical care nurses practicing in the 5 University of California hospital settings. After workshop attendance, nurse participants were followed by workshop facilitators in their units to ensure new communication skills were being integrated into practice and to problem solve if barriers were met.
- Results: Improvement in nurses’ self-confidence in engaging in these discussions was seen. This confidence was sustained months following workshop participation.
- Conclusion: The combination of critical care nurse workshop participation that involved skill enhancement through role-playing, in combination with clinical follow-up with attendees, resulted in positive affirmation of nurse communication skills specific to prognosis and goals of care discussions with family members and physicians.
There is increasing evidence that in the absence of quality communication between professional caregivers and those they care for, negative outcomes may prevail, such as reduced patient/family satisfaction, lower health status awareness, and a decreased sense of being cared about and cared for [1–5]. Communication skill competency is a critical corollary of nursing practice. In the intensive care unit (ICU) setting, patients and families have cited skilled communication as a core element of high-quality care [3,6]. Proficiency in this realm enhances nurses’ understanding of the patient and family’s encounter with health care and provides a vehicle to gather information, inform, teach, and offer emotional support. Additionally, it identifies values, goals, health care preferences, worries and concerns, and facilitates the nurses’ coordination of care [7]. Despite this skill’s importance, however, it is generally not taught in basic education and until recently has been overlooked as a key competency [8,9].
Skilled communication in palliative and end-of-life care is pivotal for discussing prognosis and care planning. In the acute care setting this is particularly relevant as the majority of Americans die in hospitals versus their preferred site of home [10]. Additionally, 1 in 5 Americans die during or shortly after receiving care in an ICU [11]. Hence, while the ICU is a setting in which intensive effort to save lives is employed, it is also a setting where death frequently occurs. The complexity and highly emotive nature of critical care often results in family needs for information and support not being met [12]. A number of reasons for this occurrence have been proposed. In this paper, we will delineate barriers to critical care nurses’ involvement in prognosis and goals of care discussions, identify why nurse involvement in this communication is needed, describe a unique workshop exemplar with a sample role play that characterizes the workshop, and offer recommendations for colleagues interested in replicating similar education offerings.
Barriers to Communication
In the ICU, the sheer number of professionals families interact with may cause confusion. In particular, numerous medical consultants commonly offer opposing opinions. Additionally, each specialist may provide information that focuses on their area of expertise such that the “big picture” is not relayed to the patient and family. Emotional discomfort on the part of the health professional around discussions of poor prognosis, goals of care, and code status may prompt limiting discussion time with patients and families and even the avoidance of interpersonal exchanges [13–15]. Health professionals have also reported concern that end-of-life discussions will increase patient distress [16]. Among health care professionals, the subject of mortality may prompt personal anxiety, trigger unresolved grief, or fear that they will “become emotional” in front of the patient/family [7]. Lack of knowledge about cultural and religious norms has been cited as a barrier, as has time constraints [17,18]. Most frequently, inadequate or absent communication skill training is noted as a significant barrier [19,20]. Many ICU nurses also report feeling marginalized due their exclusion from goals of care and decision-making discussions with patients and families they know well [21,22].
Nurses As Key Palliative Care Communicators
Education efforts that foster communication proficiency during serious illness have traditionally focused on training physicians. Recently, nursing has become a focus of communication skill enhancement in recognition of nurses’ intense and protracted interactions with patients and families in the acute care setting. Nurses are the ‘constant’ in the patient and family’s journey through the fragmented health care system [21,23]. They often have the best knowledge of, and strongest relationship with, the family and often have had extensive discussions with them about their loved one’s status [24]. Nurses are aware of the patients’ symptom experiences and are privy to valuable information about the concerns and priorities of patients and families [12]. Additionally, having the most continuous presence, nurses have seen and heard interactions with clinicians from numerous disciplines. Nurses are the most visible, constant resource for patient and family education, information and support, and thus they perceive one of their most important roles to be that of advocate for the patient and family [20,21].
Communication Training Programs for Critical Care Nurses
Education is critical to enhance communication skills within palliative care [7,15,17,20,21,24]. The preferred teaching style within this realm is role play, where skills can be practiced and the affective component of engaging in sensitive discussions can be addressed [25–27]. Role play also demonstrates firsthand the importance of nonverbal communication (eg, body language, proximity, use of gestures, tone of voice) [7,20] and facilitates nurses’ gaining a sense of comfort with wordless communication [18].
Communication skills training programs have been designed to provide bedside critical care nurses with the tools they need to be active participants in discussions of prognosis, goals of care, and palliative care with families and physicians [27,28]. These programs have demonstrated improvement in nurses’ confidence to engage in key palliative care-related discussions. Essential elements of these programs include (1) delineation of the role of the bedside nurse in palliative care communication; (2) presentation and learner-centered practice of communication skills using role play; and (3) a reflection session focused on self-care and sustainability.
Across the 5 academic University of California medical centers (San Francisco, Davis, Los Angeles, Irvine, and San Diego), a communication training program based on this work has been implemented [29]. The one-day workshop, entitled IMPACT-ICU (Integrating Multidisciplinary Palliative Care into the ICU), has taught a total of 527 critical care nurses across the 5 centers. In addition to classroom training, the IMPACT-ICU program also includes proactive specialty palliative nursing support for bedside nurses by facilitating the availability of palliative care advanced practice nurses and nurse educators resources. This support helps nurses to apply the skills learned in the workshop in their practice. During rounds at the bedside, the nurse resources coach the bedside staff on the “how” and “when” of addressing palliative care needs. Education and support on a range of topics are offered, including clarifying goals and interventions provided by palliative care teams, the specifics of how to provide family emotional support and delivery of understandable information, the assessment and management of symptoms distress, and the nurses’ role in organizing and participating in family meetings. Case-specific consultations are also offered that address how to interface with resistant medical staff. The importance of nurse documentation of these varied exchanges is also emphasized.
IMPACT-ICU Workshop
A maximum of 15 nurses participate in each 8-hour workshop. The session begins with introductions and small group discussions about what the participants perceive to be the greatest barriers to goals of care discussions and fostering patient/family decision-making in the ICU. Participants are also asked to reflect on what they want to learn as a result of their workshop attendance.
A short didactic session then reviews the definition of palliative care and its core components, addresses the nurses’ role in communication within palliative care, a social worker’s perspective of what it is like to be a family member in the ICU, and the outline of the day. This includes delineation of expectations for involvement within the role plays and the various roles to be enacted. An emphasis is placed on the workshop being a safe place to explore and trial skills with the support of colleagues, and that practice is the optimum way to integrate communication expertise into the nurses’ skill set.
The “4 Cs” serves as the instructional basis for nurse communication skill enhancement [27]. This model outlines 4 key nursing roles in optimizing communication within palliative care:
Convening: Making sure multidisciplinary patient/family/clinician communication occurs.
Checking: Identifying the patient and family needs for information; ensuring that patients and families clearly receive desired information; ensuring that clinicians understand patient and family perspectives.
Caring: Naming emotions and responding to feeling.
Continuing: Following up after discussions to clarify and reinforce information and provide support.
Sample Role Play
Facilitator: So our first role play is focused on eliciting patient and family perspectives and needs. I need a learner and someone to play the role of the family member.
Learner: I’ll give it a try.
Facilitator: Lisa, you’re going to do great. Who wants to play the family member?
Workshop Participant: I’ll do it.
Facilitator: So Mary (who has agreed to play the role of the wife), why don’t you read us the scenario. (She reads it out loud to the group).
Facilitator: Lisa, as the nurse, I want you to look at your guide and tell me what your goal is for this conversation with Mrs. Ames and then which skill you want to practice.
Learner: I think I want to try eliciting the patient and family’s needs for information and I’ll try “Tell Me More” statements.
Facilitator: Alright. So remember Lisa, if you feel the conversation isn’t going well, you can call a “time out.” I can do this as well if I feel you need to start over. I’ll also call a time out when I feel you have met your goal. Sound OK? Mary, do you have any questions playing the part of Mrs. Ames?
Wife Role: Well, how hard should I make this for her? Should I be one of those “difficult” family members?
Facilitator: Our goal here is not to “stump” you or make it particularly difficult. We want you to try out these skills and get a sense of your “comfort zone.” So let’s start with some basic communication skills, OK?
Wife Role: Alright.
Facilitator: Why don’t we set the stage, such that Lisa, you are Mr. Ames’ nurse assessing him at the start of your shift, when Mrs. Ames enters. This is the first time you have taken care of him. The night nurse has told you that he has been requiring increasing ventilator support and his renal function is declining. Per Mrs. Ames’ request, the night nurse called her to let her know how he was doing and Mrs. Ames told her she would be in shortly.
Wife Role: (nervously enters the room and grasps her husband’s hand and looks at the nurse). How’s he doing? Is he better? The night nurse called me and I was so worried I rushed over here.
Learner: (Turns to Mrs. Ames and extends her hand). Are you Mrs. Ames? I’m Lisa and I am going to be taking care of Mr. Ames today. Let me just finish my assessment and how about we talk then? Will that be OK? It will be just a few minutes.
Wife Role: Alright, I’ll be in the waiting area but please come get me as soon as you can.
Learner: I will. (Nurse then shortly comes into the waiting area and asks Mrs. Ames to come back into the ICU where she invites her to sit just outside Mr. Ames’ room). Mrs. Ames, how are you doing? This must be so stressful for you, having your husband in the ICU.
Wife Role: It’s awful. He’s never been in the hospital before this and look at him, all hooked up to machines. I’m so worried. He seems to be getting worse instead of better.
Learner: What’s your understanding of what is going on?
Wife Role: I really don’t know. One doctor comes in and says one thing and then another comes in and tells me the opposite. I’m so confused I don’t know what to think.
Learner: Would having a better idea of his condition from the doctors who are treating him help you have a better understanding?
Wife Role: Oh, yes, but they always seem in such a hurry.
Learner: What exactly would you like to know?
Wife: Well, I want to know when he can get off that breathing machine because we have been planning to go to our son’s house for Thanksgiving.
Facilitator: Time out. Lisa, did you meet your conversation goal?
Learner: Um, I’m not sure, I guess so.
Facilitator: (Turns to Observers). What do you think, did she meet her goal?
Observer: Yes, she determined Mrs. Ames’ need for more information and she asked her what she wanted to know exactly.
Facilitator: What else did we see Lisa do to enhance communication with Mrs. Ames?
Observer: Well, when Mrs. Ames rushed into the room and asked her for information, Lisa didn’t just jump in and spout out values for the ventilator and his output. She took the time to introduce herself and de-escalate Mrs. Ames’ anxiety and she followed up on her promise to come get her in the waiting room as soon as she could.
Facilitator: Why do you think was important?
Observer: It helps establish trust.
Facilitator: Did Lisa use the skill she wanted to try out?
Observer: Yes.
Facilitator: How do you know? What did you hear her say?
Observer: She said, “What’s your understanding of what is going on with Mr. Ames?”
Facilitator: Absolutely. Great job, Lisa. And who wants to take a guess at how long Lisa’s exchange with Mrs. Ames took?
Observer: Less than two minutes?
Facilitator: That’s right. So just as you consider how long it takes, and how proficient you are, in starting an IV or inserting a Foley catheter, when you have a goal in mind and have practiced the skills to do it well, any skill can be mastered.
Feedback
Participants in the workshops uniformly report an enhanced sense of self-confidence in their palliative care communication skills as a result of their participation [29]. Key to the success of the workshop is the ongoing contact by the workshop facilitators with participants. Rounding is routinely planned such that each participant is visited weekly by a workshop facilitator in their clinical area to determine if the bedside nurse has practiced the new skills and if so, how the interaction transpired. Positive feedback is given for attempts to engage in new behaviors and participants are reminded that with any new skill, repetitive trials are necessary to foster success.
Lessons Learned and Next Steps
One of our major lessons learned was recognizing that it was difficult for many critical care nurses to practice the new communication skills. Nurses are trained to fix problems and perform medico-technical tasks; “listening” has not always been recognized as real work [18]. We needed to reinforce that skills like eliciting another’s perspective or making reflection statements are equally important to those associated with behavioral/technical proficiency.
While our program has been successful, we recognize that the next step in fostering ideal palliative care communication is to provide education within an interdisciplinary context. We recommend that colleagues interested in replicating this or a similar education intervention, survey nurse participants prior to and following workshop participation to measure attitudes, self confidence and perceived barriers over time [30]. We hope to translate our positive experience into a program that engages multiple professionals in the enhancement of optimum palliative care communication proficiency.
Corresponding author: Deborah A. Boyle MSN, RN, AOCNS, Department of Nursing Quality, Research and Education, University of California, Irvine Health, 101 The City Drive, Bldg 22A, Room 3104, Orange, CA 92868.
From the University of California Irvine Health/Chao Family Comprehensive Cancer Center Orange, CA (Ms. Boyle) and the University of California San Francisco Medical Center, San Francisco, CA (Dr. Anderson).
Abstract
- Objective: To describe components of a unique interactive workshop focusing on the enhancement of critical care nurses’ communication skills within the realm of prognosis and goals of care discussions with family members and physicians.
- Methods: A series of one-day workshops were offered to critical care nurses practicing in the 5 University of California hospital settings. After workshop attendance, nurse participants were followed by workshop facilitators in their units to ensure new communication skills were being integrated into practice and to problem solve if barriers were met.
- Results: Improvement in nurses’ self-confidence in engaging in these discussions was seen. This confidence was sustained months following workshop participation.
- Conclusion: The combination of critical care nurse workshop participation that involved skill enhancement through role-playing, in combination with clinical follow-up with attendees, resulted in positive affirmation of nurse communication skills specific to prognosis and goals of care discussions with family members and physicians.
There is increasing evidence that in the absence of quality communication between professional caregivers and those they care for, negative outcomes may prevail, such as reduced patient/family satisfaction, lower health status awareness, and a decreased sense of being cared about and cared for [1–5]. Communication skill competency is a critical corollary of nursing practice. In the intensive care unit (ICU) setting, patients and families have cited skilled communication as a core element of high-quality care [3,6]. Proficiency in this realm enhances nurses’ understanding of the patient and family’s encounter with health care and provides a vehicle to gather information, inform, teach, and offer emotional support. Additionally, it identifies values, goals, health care preferences, worries and concerns, and facilitates the nurses’ coordination of care [7]. Despite this skill’s importance, however, it is generally not taught in basic education and until recently has been overlooked as a key competency [8,9].
Skilled communication in palliative and end-of-life care is pivotal for discussing prognosis and care planning. In the acute care setting this is particularly relevant as the majority of Americans die in hospitals versus their preferred site of home [10]. Additionally, 1 in 5 Americans die during or shortly after receiving care in an ICU [11]. Hence, while the ICU is a setting in which intensive effort to save lives is employed, it is also a setting where death frequently occurs. The complexity and highly emotive nature of critical care often results in family needs for information and support not being met [12]. A number of reasons for this occurrence have been proposed. In this paper, we will delineate barriers to critical care nurses’ involvement in prognosis and goals of care discussions, identify why nurse involvement in this communication is needed, describe a unique workshop exemplar with a sample role play that characterizes the workshop, and offer recommendations for colleagues interested in replicating similar education offerings.
Barriers to Communication
In the ICU, the sheer number of professionals families interact with may cause confusion. In particular, numerous medical consultants commonly offer opposing opinions. Additionally, each specialist may provide information that focuses on their area of expertise such that the “big picture” is not relayed to the patient and family. Emotional discomfort on the part of the health professional around discussions of poor prognosis, goals of care, and code status may prompt limiting discussion time with patients and families and even the avoidance of interpersonal exchanges [13–15]. Health professionals have also reported concern that end-of-life discussions will increase patient distress [16]. Among health care professionals, the subject of mortality may prompt personal anxiety, trigger unresolved grief, or fear that they will “become emotional” in front of the patient/family [7]. Lack of knowledge about cultural and religious norms has been cited as a barrier, as has time constraints [17,18]. Most frequently, inadequate or absent communication skill training is noted as a significant barrier [19,20]. Many ICU nurses also report feeling marginalized due their exclusion from goals of care and decision-making discussions with patients and families they know well [21,22].
Nurses As Key Palliative Care Communicators
Education efforts that foster communication proficiency during serious illness have traditionally focused on training physicians. Recently, nursing has become a focus of communication skill enhancement in recognition of nurses’ intense and protracted interactions with patients and families in the acute care setting. Nurses are the ‘constant’ in the patient and family’s journey through the fragmented health care system [21,23]. They often have the best knowledge of, and strongest relationship with, the family and often have had extensive discussions with them about their loved one’s status [24]. Nurses are aware of the patients’ symptom experiences and are privy to valuable information about the concerns and priorities of patients and families [12]. Additionally, having the most continuous presence, nurses have seen and heard interactions with clinicians from numerous disciplines. Nurses are the most visible, constant resource for patient and family education, information and support, and thus they perceive one of their most important roles to be that of advocate for the patient and family [20,21].
Communication Training Programs for Critical Care Nurses
Education is critical to enhance communication skills within palliative care [7,15,17,20,21,24]. The preferred teaching style within this realm is role play, where skills can be practiced and the affective component of engaging in sensitive discussions can be addressed [25–27]. Role play also demonstrates firsthand the importance of nonverbal communication (eg, body language, proximity, use of gestures, tone of voice) [7,20] and facilitates nurses’ gaining a sense of comfort with wordless communication [18].
Communication skills training programs have been designed to provide bedside critical care nurses with the tools they need to be active participants in discussions of prognosis, goals of care, and palliative care with families and physicians [27,28]. These programs have demonstrated improvement in nurses’ confidence to engage in key palliative care-related discussions. Essential elements of these programs include (1) delineation of the role of the bedside nurse in palliative care communication; (2) presentation and learner-centered practice of communication skills using role play; and (3) a reflection session focused on self-care and sustainability.
Across the 5 academic University of California medical centers (San Francisco, Davis, Los Angeles, Irvine, and San Diego), a communication training program based on this work has been implemented [29]. The one-day workshop, entitled IMPACT-ICU (Integrating Multidisciplinary Palliative Care into the ICU), has taught a total of 527 critical care nurses across the 5 centers. In addition to classroom training, the IMPACT-ICU program also includes proactive specialty palliative nursing support for bedside nurses by facilitating the availability of palliative care advanced practice nurses and nurse educators resources. This support helps nurses to apply the skills learned in the workshop in their practice. During rounds at the bedside, the nurse resources coach the bedside staff on the “how” and “when” of addressing palliative care needs. Education and support on a range of topics are offered, including clarifying goals and interventions provided by palliative care teams, the specifics of how to provide family emotional support and delivery of understandable information, the assessment and management of symptoms distress, and the nurses’ role in organizing and participating in family meetings. Case-specific consultations are also offered that address how to interface with resistant medical staff. The importance of nurse documentation of these varied exchanges is also emphasized.
IMPACT-ICU Workshop
A maximum of 15 nurses participate in each 8-hour workshop. The session begins with introductions and small group discussions about what the participants perceive to be the greatest barriers to goals of care discussions and fostering patient/family decision-making in the ICU. Participants are also asked to reflect on what they want to learn as a result of their workshop attendance.
A short didactic session then reviews the definition of palliative care and its core components, addresses the nurses’ role in communication within palliative care, a social worker’s perspective of what it is like to be a family member in the ICU, and the outline of the day. This includes delineation of expectations for involvement within the role plays and the various roles to be enacted. An emphasis is placed on the workshop being a safe place to explore and trial skills with the support of colleagues, and that practice is the optimum way to integrate communication expertise into the nurses’ skill set.
The “4 Cs” serves as the instructional basis for nurse communication skill enhancement [27]. This model outlines 4 key nursing roles in optimizing communication within palliative care:
Convening: Making sure multidisciplinary patient/family/clinician communication occurs.
Checking: Identifying the patient and family needs for information; ensuring that patients and families clearly receive desired information; ensuring that clinicians understand patient and family perspectives.
Caring: Naming emotions and responding to feeling.
Continuing: Following up after discussions to clarify and reinforce information and provide support.
Sample Role Play
Facilitator: So our first role play is focused on eliciting patient and family perspectives and needs. I need a learner and someone to play the role of the family member.
Learner: I’ll give it a try.
Facilitator: Lisa, you’re going to do great. Who wants to play the family member?
Workshop Participant: I’ll do it.
Facilitator: So Mary (who has agreed to play the role of the wife), why don’t you read us the scenario. (She reads it out loud to the group).
Facilitator: Lisa, as the nurse, I want you to look at your guide and tell me what your goal is for this conversation with Mrs. Ames and then which skill you want to practice.
Learner: I think I want to try eliciting the patient and family’s needs for information and I’ll try “Tell Me More” statements.
Facilitator: Alright. So remember Lisa, if you feel the conversation isn’t going well, you can call a “time out.” I can do this as well if I feel you need to start over. I’ll also call a time out when I feel you have met your goal. Sound OK? Mary, do you have any questions playing the part of Mrs. Ames?
Wife Role: Well, how hard should I make this for her? Should I be one of those “difficult” family members?
Facilitator: Our goal here is not to “stump” you or make it particularly difficult. We want you to try out these skills and get a sense of your “comfort zone.” So let’s start with some basic communication skills, OK?
Wife Role: Alright.
Facilitator: Why don’t we set the stage, such that Lisa, you are Mr. Ames’ nurse assessing him at the start of your shift, when Mrs. Ames enters. This is the first time you have taken care of him. The night nurse has told you that he has been requiring increasing ventilator support and his renal function is declining. Per Mrs. Ames’ request, the night nurse called her to let her know how he was doing and Mrs. Ames told her she would be in shortly.
Wife Role: (nervously enters the room and grasps her husband’s hand and looks at the nurse). How’s he doing? Is he better? The night nurse called me and I was so worried I rushed over here.
Learner: (Turns to Mrs. Ames and extends her hand). Are you Mrs. Ames? I’m Lisa and I am going to be taking care of Mr. Ames today. Let me just finish my assessment and how about we talk then? Will that be OK? It will be just a few minutes.
Wife Role: Alright, I’ll be in the waiting area but please come get me as soon as you can.
Learner: I will. (Nurse then shortly comes into the waiting area and asks Mrs. Ames to come back into the ICU where she invites her to sit just outside Mr. Ames’ room). Mrs. Ames, how are you doing? This must be so stressful for you, having your husband in the ICU.
Wife Role: It’s awful. He’s never been in the hospital before this and look at him, all hooked up to machines. I’m so worried. He seems to be getting worse instead of better.
Learner: What’s your understanding of what is going on?
Wife Role: I really don’t know. One doctor comes in and says one thing and then another comes in and tells me the opposite. I’m so confused I don’t know what to think.
Learner: Would having a better idea of his condition from the doctors who are treating him help you have a better understanding?
Wife Role: Oh, yes, but they always seem in such a hurry.
Learner: What exactly would you like to know?
Wife: Well, I want to know when he can get off that breathing machine because we have been planning to go to our son’s house for Thanksgiving.
Facilitator: Time out. Lisa, did you meet your conversation goal?
Learner: Um, I’m not sure, I guess so.
Facilitator: (Turns to Observers). What do you think, did she meet her goal?
Observer: Yes, she determined Mrs. Ames’ need for more information and she asked her what she wanted to know exactly.
Facilitator: What else did we see Lisa do to enhance communication with Mrs. Ames?
Observer: Well, when Mrs. Ames rushed into the room and asked her for information, Lisa didn’t just jump in and spout out values for the ventilator and his output. She took the time to introduce herself and de-escalate Mrs. Ames’ anxiety and she followed up on her promise to come get her in the waiting room as soon as she could.
Facilitator: Why do you think was important?
Observer: It helps establish trust.
Facilitator: Did Lisa use the skill she wanted to try out?
Observer: Yes.
Facilitator: How do you know? What did you hear her say?
Observer: She said, “What’s your understanding of what is going on with Mr. Ames?”
Facilitator: Absolutely. Great job, Lisa. And who wants to take a guess at how long Lisa’s exchange with Mrs. Ames took?
Observer: Less than two minutes?
Facilitator: That’s right. So just as you consider how long it takes, and how proficient you are, in starting an IV or inserting a Foley catheter, when you have a goal in mind and have practiced the skills to do it well, any skill can be mastered.
Feedback
Participants in the workshops uniformly report an enhanced sense of self-confidence in their palliative care communication skills as a result of their participation [29]. Key to the success of the workshop is the ongoing contact by the workshop facilitators with participants. Rounding is routinely planned such that each participant is visited weekly by a workshop facilitator in their clinical area to determine if the bedside nurse has practiced the new skills and if so, how the interaction transpired. Positive feedback is given for attempts to engage in new behaviors and participants are reminded that with any new skill, repetitive trials are necessary to foster success.
Lessons Learned and Next Steps
One of our major lessons learned was recognizing that it was difficult for many critical care nurses to practice the new communication skills. Nurses are trained to fix problems and perform medico-technical tasks; “listening” has not always been recognized as real work [18]. We needed to reinforce that skills like eliciting another’s perspective or making reflection statements are equally important to those associated with behavioral/technical proficiency.
While our program has been successful, we recognize that the next step in fostering ideal palliative care communication is to provide education within an interdisciplinary context. We recommend that colleagues interested in replicating this or a similar education intervention, survey nurse participants prior to and following workshop participation to measure attitudes, self confidence and perceived barriers over time [30]. We hope to translate our positive experience into a program that engages multiple professionals in the enhancement of optimum palliative care communication proficiency.
Corresponding author: Deborah A. Boyle MSN, RN, AOCNS, Department of Nursing Quality, Research and Education, University of California, Irvine Health, 101 The City Drive, Bldg 22A, Room 3104, Orange, CA 92868.
1. Leung JM, Udris EM, Uman J, et al. The effect of end-of-life discussions on perceived quality of care and health status among patients with COPD. Chest 2012;142:128–33.
2. Osborn TR, Curtis JR, Nielsen EL, et al. Identifying elements of ICU care that families report as important but unsatisfactory: decision-making, control and ICU atmosphere. Chest 2012;142:1185–92.
3. Nelson JE, Puntillo K, Pronovost PJ, et al. In their own words: patients and families define high-quality palliative care in the ICU. Crit Care Med 2010;38:808–18.
4. Nels W, Gabrijel S, Kiss S, et al. Communication skill training significantly improves lung cancer patients understanding. J Palliat Care Med 2014;4:182.
5. Van Vliet LM, Epstein AS. Current state of the art and science of patient-clinician communication in progressive disease: patients’ need to know and feel known. J Clin Oncol 2014;32:3474-8.
6. Troug RD, Campbell ML, Curtis JR, et al. Recommendations for end of life care in the intensive care unit: a consensus statement by the American College of Critical Care Medicine. Crit Care Med 2008;36:953–63.
7. Dahlin CM, Wittenberg E. Communication in palliative care. In: Ferrell BR, Coyle N, Paice J, editors. Oxford textbook of palliative nursing. 4th ed. Oxford: Oxford University Press; 2014:81–109.
8. Baer L, Weinstein E. Improving oncology nurses’ communication skills for difficult conversations. Clin J Oncol Nurs 2013;17:E45–E51.
9. Treece PD. Communication in the intensive care unit about end of life care. AACN Adv Crit Care 2007;18:406–14.
10. Teno JM, Clarridge BR, Casey V, et al. Family perspectives on end of life care at the last place of care. JAMA 2004;291:88–92.
11. Angus DC, Barnato AE, Linde-Zwirble WT, et al. Robert Wood Johnson Foundation ICU End-of-Life Peer Group. Use of intensive care at the end of life in the United States: an epidemiologic study. Crit Care Med 2004;32:638–43.
12. Hamric AB, Blackhall LJ. Nurse-physician perspectives on the care of dying patients in intensive care units: collaboration, moral distress, and ethical climate. Crit Care Med 2007;35:422–9.
13. Back AL, Trinidad SB, Hopley EK, Edwards KA. Reframing the goals of care conversation: “We’re in a different place.” J Palliat Med 2014;17:1010–24.
14. Aslakson RA, Wyskiel R, Thornton I, et al. Nurse perceived barriers to effective communication regarding prognosis and optimal end of life care for surgical ICU patients: a qualitative exploration. J Palliat Med 2012;15:910–5.
15. Erickson J. Bedside nurse involvement in end of life decision-making. Dimens Crit Care Nurs 2013;32:65–8.
16. Bernacki RE, Block SD for the American College of Physicians High Value Care Task Force. Communication about serious illness care goals: a review and synthesis of best practices. JAMA Intern Med 2014;174:1994–2003.
17. You JJ, Downar J, Fowler RA, et al. Barriers to goals of care discussion with ‘seriously’ ill hospitalized patients and their families: a multicenter survey of clinicians. JAMA Intern Med 2015;175:549–56.
18. Strang S, Henoch I, Danielson E, et al. Communication about existential issues with patients close to death: nurses’ reflections on content, process, and meaning. Psychooncology 2014;23:562–8.
19. Slatore CG, Hensen L, Gauzine L, et al. Communication by nurses in the intensive care unit: qualitative analysis of domains in patient-centered care. Am J Crit Care 2012;21:410–8.
20. Wittenberg-Lyles E, Goldsmith J, Platt CS. Palliative care communication. Sem Oncol Nurs 2014;30:280–6.
21. Fox MY. Improving communication with patients and families in the ICU: palliative care strategies for intensive care unit nurses. J Hospice Palliat Nurs 2014;16:93–8.
22. Beckstrand RL, Callister LC, Kirchhoff KT. Providing a ‘good death’: critical care nurses’ suggestions for improving end of life care. Am J Crit Care 2006;15:38–45.
23. Peereboom K, Coyle N. Facilitating goals of care discus.sions for patients with life-limiting disease: communication strategies for nurses. J Hospice Palliat Nurs 2012; 14:251–8.
24. Nelson JE, Cortez TB, Curtis JR, et al. Integrating palliative care in the ICU: the nurse in the leading role. J Hospice Palliat Nurs 2011;13:89–94.
25. Jors K, Seibel K, Bardenheuer H, et al. Education in end of life care: what do experienced professionals find important? J Cancer Educ 2015 March 15.
26. Roze des Ordons AL, Sharma N, Heyland DK, et al. Strategies for effective goals of care discussions and decision-making: perspective from a multi-centre survey of Canadian hospital-based health care providers. BMC Palliat Care 2015;14:38.
27. Krimshtein NS, Luhrs CA, Puntillo KA, et al. Training nurses for interdisciplinary communication with families in the ICU. J Palliat Med 2011;14:1325–32.
28. Milic MM, Puntillo K, Turner K, et al. Communicating with patients’ families and physicians about prognosis and goals of care. Am J Crit Care 2015;24:e56–e64.
29. Anderson W, Puntillo K, Barbour S, et al. The IMPACT-ICU Project: expanding palliative care nursing across University of California Centers ICUs to advance palliative care. Center to Advance Palliative Care (CAPC) national seminar. Nov 7–9, 2013. Dallas, TX.
30. Anderson WG, Puntillo K, Boyle D, et al. ICU bedside nurses’ involvement in palliative care communication: a multicenter survey. J Pain Symptom Manage. In press.
1. Leung JM, Udris EM, Uman J, et al. The effect of end-of-life discussions on perceived quality of care and health status among patients with COPD. Chest 2012;142:128–33.
2. Osborn TR, Curtis JR, Nielsen EL, et al. Identifying elements of ICU care that families report as important but unsatisfactory: decision-making, control and ICU atmosphere. Chest 2012;142:1185–92.
3. Nelson JE, Puntillo K, Pronovost PJ, et al. In their own words: patients and families define high-quality palliative care in the ICU. Crit Care Med 2010;38:808–18.
4. Nels W, Gabrijel S, Kiss S, et al. Communication skill training significantly improves lung cancer patients understanding. J Palliat Care Med 2014;4:182.
5. Van Vliet LM, Epstein AS. Current state of the art and science of patient-clinician communication in progressive disease: patients’ need to know and feel known. J Clin Oncol 2014;32:3474-8.
6. Troug RD, Campbell ML, Curtis JR, et al. Recommendations for end of life care in the intensive care unit: a consensus statement by the American College of Critical Care Medicine. Crit Care Med 2008;36:953–63.
7. Dahlin CM, Wittenberg E. Communication in palliative care. In: Ferrell BR, Coyle N, Paice J, editors. Oxford textbook of palliative nursing. 4th ed. Oxford: Oxford University Press; 2014:81–109.
8. Baer L, Weinstein E. Improving oncology nurses’ communication skills for difficult conversations. Clin J Oncol Nurs 2013;17:E45–E51.
9. Treece PD. Communication in the intensive care unit about end of life care. AACN Adv Crit Care 2007;18:406–14.
10. Teno JM, Clarridge BR, Casey V, et al. Family perspectives on end of life care at the last place of care. JAMA 2004;291:88–92.
11. Angus DC, Barnato AE, Linde-Zwirble WT, et al. Robert Wood Johnson Foundation ICU End-of-Life Peer Group. Use of intensive care at the end of life in the United States: an epidemiologic study. Crit Care Med 2004;32:638–43.
12. Hamric AB, Blackhall LJ. Nurse-physician perspectives on the care of dying patients in intensive care units: collaboration, moral distress, and ethical climate. Crit Care Med 2007;35:422–9.
13. Back AL, Trinidad SB, Hopley EK, Edwards KA. Reframing the goals of care conversation: “We’re in a different place.” J Palliat Med 2014;17:1010–24.
14. Aslakson RA, Wyskiel R, Thornton I, et al. Nurse perceived barriers to effective communication regarding prognosis and optimal end of life care for surgical ICU patients: a qualitative exploration. J Palliat Med 2012;15:910–5.
15. Erickson J. Bedside nurse involvement in end of life decision-making. Dimens Crit Care Nurs 2013;32:65–8.
16. Bernacki RE, Block SD for the American College of Physicians High Value Care Task Force. Communication about serious illness care goals: a review and synthesis of best practices. JAMA Intern Med 2014;174:1994–2003.
17. You JJ, Downar J, Fowler RA, et al. Barriers to goals of care discussion with ‘seriously’ ill hospitalized patients and their families: a multicenter survey of clinicians. JAMA Intern Med 2015;175:549–56.
18. Strang S, Henoch I, Danielson E, et al. Communication about existential issues with patients close to death: nurses’ reflections on content, process, and meaning. Psychooncology 2014;23:562–8.
19. Slatore CG, Hensen L, Gauzine L, et al. Communication by nurses in the intensive care unit: qualitative analysis of domains in patient-centered care. Am J Crit Care 2012;21:410–8.
20. Wittenberg-Lyles E, Goldsmith J, Platt CS. Palliative care communication. Sem Oncol Nurs 2014;30:280–6.
21. Fox MY. Improving communication with patients and families in the ICU: palliative care strategies for intensive care unit nurses. J Hospice Palliat Nurs 2014;16:93–8.
22. Beckstrand RL, Callister LC, Kirchhoff KT. Providing a ‘good death’: critical care nurses’ suggestions for improving end of life care. Am J Crit Care 2006;15:38–45.
23. Peereboom K, Coyle N. Facilitating goals of care discus.sions for patients with life-limiting disease: communication strategies for nurses. J Hospice Palliat Nurs 2012; 14:251–8.
24. Nelson JE, Cortez TB, Curtis JR, et al. Integrating palliative care in the ICU: the nurse in the leading role. J Hospice Palliat Nurs 2011;13:89–94.
25. Jors K, Seibel K, Bardenheuer H, et al. Education in end of life care: what do experienced professionals find important? J Cancer Educ 2015 March 15.
26. Roze des Ordons AL, Sharma N, Heyland DK, et al. Strategies for effective goals of care discussions and decision-making: perspective from a multi-centre survey of Canadian hospital-based health care providers. BMC Palliat Care 2015;14:38.
27. Krimshtein NS, Luhrs CA, Puntillo KA, et al. Training nurses for interdisciplinary communication with families in the ICU. J Palliat Med 2011;14:1325–32.
28. Milic MM, Puntillo K, Turner K, et al. Communicating with patients’ families and physicians about prognosis and goals of care. Am J Crit Care 2015;24:e56–e64.
29. Anderson W, Puntillo K, Barbour S, et al. The IMPACT-ICU Project: expanding palliative care nursing across University of California Centers ICUs to advance palliative care. Center to Advance Palliative Care (CAPC) national seminar. Nov 7–9, 2013. Dallas, TX.
30. Anderson WG, Puntillo K, Boyle D, et al. ICU bedside nurses’ involvement in palliative care communication: a multicenter survey. J Pain Symptom Manage. In press.
Update in Hospital Palliative Care
Seriously ill patients frequently receive care in hospitals,[1, 2, 3] and palliative care is a core competency for hospitalists.[4, 5] The goal of this update was to summarize and critique recently published research that has the highest potential to impact the clinical practice of palliative care in the hospital. We reviewed articles published between January 2012 and May 2013. To identify articles, we hand‐searched 22 leading journals (see Appendix) and the Cochrane Database of Systematic Reviews, and performed a PubMed keyword search using the terms hospice and palliative care. We evaluated identified articles based on scientific rigor and relevance to hospital practice. In this review, we summarize 9 articles that were collectively selected as having the highest impact on the clinical practice of hospital palliative care. We summarize each article and its findings and note cautions and implications for practice.
SYMPTOM MANAGEMENT
Indwelling Pleural Catheters and Talc Pleurodesis Provide Similar Dyspnea Relief in Patients With Malignant Pleural Effusions
Davies HE, Mishra EK, Kahan BC, et al. Effect of an indwelling pleural catheter vs chest tube and talc pleurodesis for relieving dyspnea in patients with malignant pleural effusion. JAMA. 2012;307:23832389.
Background
Expert guidelines recommend chest‐tube insertion and talc pleurodesis as a first‐line therapy for symptomatic malignant pleural effusions, but indwelling pleural catheters are gaining in popularity.[6] The optimal management is unknown.
Findings
A total of 106 patients with newly diagnosed symptomatic malignant pleural effusion were randomized to undergo talc pleurodesis or placement of an indwelling pleural catheter. Most patients had metastatic breast or lung cancer. Overall, there were no differences in relief of dyspnea at 42 days between patients who received indwelling catheters and pleurodesis; importantly, more than 75% of patients in both groups reported improved shortness of breath. The initial hospitalization was much shorter in the indwelling catheter group (0 days vs 4 days). There was no difference in quality of life, but in surviving patients, dyspnea at 6 months was better with the indwelling catheter. In the talc group, 22% of patients required further pleural procedures compared with 6% in the indwelling catheter group. Patients in the talc group had a higher frequency of adverse events than in the catheter group (40% vs 13%). In the catheter group, the most common adverse events were pleural infection, cellulitis, and catheter obstruction.
Cautions
The study was small and unblinded, and the primary outcome was subjective dyspnea. The study occurred at 7 hospitals, and the impact of institutional or provider experience was not taken into account. Last, overall costs of care, which could impact the choice of intervention, were not calculated.
Implications
This was a small but well‐done study showing that indwelling catheters and talc pleurodesis provide similar relief of dyspnea 42 days postintervention. Given these results, both interventions seem to be acceptable options. Clinicians and patients could select the best option based on local procedural expertise and patient factors such as preference, ability to manage a catheter, and life expectancy.
Most Dying Patients Do Not Experience Increased Respiratory Distress When Oxygen is Withdrawn
Campbell ML, Yarandi H, Dove‐Medows E. Oxygen is nonbeneficial for most patients who are near death. J Pain Symptom Manage. 2013;45(3):517523.
Background
Oxygen is frequently administered to patients at the end of life, yet there is limited evidence evaluating whether oxygen reduces respiratory distress in dying patients.
Findings
In this double‐blind, repeated‐measure study, patients served as their own controls as the investigators evaluated respiratory distress with and without oxygen therapy. The study included 32 patients who were enrolled in hospice or seen in palliative care consultation and had a diagnosis such as lung cancer or heart failure that might cause dyspnea. Medical air (nasal cannula with air flow), supplemental oxygen, and no flow were randomly alternated every 10 minutes for 1 hour. Blinded research assistants used a validated observation scale to compare respiratory distress under each condition. At baseline, 27 of 32 (84%) patients were on oxygen. Three patients, all of whom were conscious and on oxygen at baseline, experienced increased respiratory distress without oxygen; reapplication of supplemental oxygen relieved their distress. The other 29 patients had no change in respiratory distress under the oxygen, medical air, and no flow conditions.
Cautions
All patients in this study were near death as measured by the Palliative Performance Scale, which assesses prognosis based on functional status and level of consciousness. Patients were excluded if they were receiving high‐flow oxygen by face mask or were experiencing respiratory distress at the time of initial evaluation. Some patients experienced increased discomfort after withdrawal of oxygen. Close observation is needed to determine which patients will experience distress.
Implications
The majority of patients who were receiving oxygen at baseline experienced no change in respiratory comfort when oxygen was withdrawn, supporting previous evidence that oxygen provides little benefit in nonhypoxemic patients. Oxygen may be an unnecessary intervention near death and has the potential to add to discomfort through nasal dryness and decreased mobility.
Sennosides Performed Similarly to Docusate Plus Sennosides in Managing Opioid‐Induced Constipation in Seriously Ill Patients
Tarumi Y, Wilson MP, Szafran O, Spooner GR. Randomized, double‐blind, placebo‐controlled trial of oral docusate in the management of constipation in hospice patients. J Pain Symptom Manage. 2013;45:213.
Background
Seriously ill patients frequently suffer from constipation, often as a result of opioid analgesics. Hospital clinicians should seek to optimize bowel regimens to prevent opioid‐induced constipation. A combination of the stimulant laxative sennoside and the stool softener docusate is often recommended to treat and prevent constipation. Docusate may not have additional benefit to sennoside, and may have significant burdens, including disturbing the absorption of other medications, adding to patients' pill burden and increasing nurse workload.[7]
Findings
In this double‐blinded trial, 74 patients in 3 inpatient hospices in Canada were randomized to receive sennoside plus either docusate 100 mg, or placebo tablets twice daily, or sennoside plus placebo for 10 days. Most patients had cancer as a life‐limiting diagnosis and received opioids during the study period. All were able to tolerate pills and food or sips of fluid. There was no significant difference between the 2 groups in stool frequency, volume, consistency, or patients' perceptions of difficulty with defecation. The percentage of patients who had a bowel movement at least every 3 days was 71% in the docusate plus sennoside group and 81% in the sennoside only group (P=0.45). There was also no significant difference between the groups in sennoside dose (which ranged between 13, 8.6 mg tablets daily), mean morphine equivalent daily dosage, or other bowel interventions.
Cautions
The trial was small, though it was adequately powered to detect a clinically meaningful difference between the 2 groups of 0.5 in the average number of bowel movements per day. The consent rate was low (26%); the authors do not detail reasons patients were not randomized. Patients who did not participate might have had different responses.
Implications
Consistent with previous work,[7] these results indicate that docusate is probably not needed for routine management of opioid‐induced constipation in seriously ill patients.
Sublingual Atropine Performed Similarly to Placebo in Reducing Noise Associated With Respiratory Rattle Near Death
Heisler M, Hamilton G, Abbott A, et al. Randomized double‐blind trial of sublingual atropine vs. placebo for the management of death rattle. J Pain Symptom Manage. 2012;45(1):1422.
Background
Increased respiratory tract secretions in patients near death can cause noisy breathing, often referred to as a death rattle. Antimuscarinic medications, such as atropine, are frequently used to decrease audible respirations and family distress, though little evidence exists to support this practice.
Findings
In this double‐blind, placebo‐controlled, parallel group trial at 3 inpatient hospices, 177 terminally ill patients with audible respiratory secretions were randomized to 2 drops of sublingual atropine 1% solution or placebo drops. Bedside nurses rated patients' respiratory secretions at enrollment, and 2 and 4 hours after receiving atropine or placebo. There were no differences in noise score between subjects treated with atropine and placebo at 2 hours (37.8% vs. 41.3%, P=0.24) or at 4 hours (39.7% and 51.7%, P=0.21). There were no differences in the safety end point of change in heart rate (P=0.47).
Cautions
Previous studies comparing different anticholinergic medications and routes of administration to manage audible respiratory secretions had variable response rates but suggested a benefit to antimuscarinic medications. However, these trials had significant methodological limitations including lack of randomization and blinding. The improvement in death rattle over time in other studies may suggest a favorable natural course for respiratory secretions rather than a treatment effect.
Implications
Although generalizability to other antimuscarinic medications and routes of administration is limited, in a randomized, double‐blind, placebo‐controlled trial, sublingual atropine did not reduce the noise from respiratory secretions when compared to placebo.
PATIENT AND FAMILY OUTCOMES AFTER CARDIOPULMONARY RESUSCITATION
Over Half of Older Adult Survivors of In‐Hospital Cardiopulmonary Resuscitation Were Alive At 1 Year
Chan PS, Krumholz HM, Spertus JA, et al. Long‐term outcomes in elderly survivors of in‐hospital cardiac arrest. N Engl J Med. 2013;368:10191026.
Background
Studies of cardiopulmonary resuscitation (CPR) outcomes have focused on survival to hospital discharge. Little is known about long‐term outcomes following in‐hospital cardiac arrest in older adults.
Findings
The authors analyzed data from the Get With the GuidelinesResuscitation registry from 2000 to 2008 and Medicare inpatient files from 2000 to 2010. The cohort included 6972 patients at 401 hospitals who were discharged after surviving in‐hospital arrest. Outcomes were survival and freedom from hospital readmission at 1 year after discharge. At discharge, 48% of patients had either no or mild neurologic disability at discharge; the remainder had moderate to severe neurologic disability. Overall, 58% of patients who were discharged were still alive at 1 year. Survival rates were lowest for patients who were discharged in coma or vegetative state (8% at 1 year), and highest for those discharged with mild or no disability (73% at 1 year). Older patients had lower survival rates than younger patients, as did men compared with women and blacks compared with whites. At 1 year, 34.4% of the patients had not been readmitted. Predictors of readmission were similar to those for lower survival rates.
Cautions
This study only analyzed survival data from patients who survived to hospital discharge after receiving in‐hospital CPR, not all patients who had a cardiac arrest. Thus, the survival rates reported here do not include patients who died during the original arrest, or who survived the arrest but died during their hospitalization. The 1‐year survival rate for people aged 65 years and above following a cardiac arrest is not reported but is likely to be about 10%, based on data from this registry.[8] Data were not available for health status, neurologic status, or quality of life of the survivors at 1 year.
Implications
Older patients who receive in‐hospital CPR and have a good neurologic status at hospital discharge have good long‐term outcomes. In counseling patients about CPR, it is important to note that most patients who receive CPR do not survive to hospital discharge.
Families Who Were Present During CPR Had Decreased Post‐traumatic Stress Symptoms
Jabre P, Belpomme V, Azoulay E, et al. Family presence during cardiopulmonary resuscitation. N Engl J Med. 2013;368:10081018.
Background
Family members who watch their loved ones undergo (CPR) might have increased emotional distress. Alternatively, observing CPR may allow for appreciation of the efforts taken for their loved one and provide comfort at a challenging time. The right balance of benefit and harm is unclear.
Findings
Between 2009 and 2011, 15 prehospital emergency medical service units in France were randomized to offer adult family members the opportunity to observe CPR or follow their usual practice. A total of 570 relatives were enrolled. In the intervention group, 79% of relatives observed CPR, compared to 43% in the control group. There was no difference in the effectiveness of CPR between the 2 groups. At 90 days, post‐traumatic stress symptoms were more common in the control group (adjusted odds ratio [OR]: 1.7; 95% confidence interval [CI]: 1.2‐2.5). At 90 days, those who were present for the resuscitation also had fewer symptoms of anxiety and fewer symptoms of depression (P<0.009 for both). Stress of the medical teams involved in the CPR was not different between the 2 groups. No malpractice claims were filed in either group.
Cautions
The study was conducted only in France, so the results may not be generalizable outside of France. In addition, the observed resuscitation was for patients who suffered a cardiac arrest in the home; it is unclear if the same results would be found in the emergency department or hospital.
Implications
This is the highest quality study to date in this area that argues for actively inviting family members to be present for resuscitation efforts in the home. Further studies are needed to determine if hospitals should implement standard protocols. In the meantime, providers who perform CPR should consider inviting families to observe, as it may result in less emotional distress for family members.
COMMUNICATION AND DECISION MAKING
Surrogate Decision Makers Interpreted Prognostic Information Optimistically
Zier LS, Sottile PD, Hong SY, et al. Surrogate decision makers' interpretation of prognostic information: a mixed‐methods study. Ann Intern Med. 2012;156:360366.
Background
Surrogates of critically ill patients often have beliefs about prognosis that are discordant from what is told to them by providers. Little is known about why this is the case.
Findings
Eighty surrogates of patients in intensive care units (ICUs) were given questionnaires with hypothetical prognostic statements and asked to identify a survival probability associated with each statement on a 0% to 100% scale. Interviewers examined the questionnaires to identify responses that were not concordant with the given prognostic statements. They then interviewed participants to determine why the answers were discordant. The researchers found that surrogates were more likely to offer an overoptimistic interpretation of statements communicating a high risk of death, compared to statements communicating a low risk of death. The qualitative interviews revealed that surrogates felt they needed to express ongoing optimism and that patient factors not known to the medical team would lead to better outcomes.
Cautions
The participants were surrogates who were present in the ICU at the time when study investigators were there, and thus the results may not be generalizable to all surrogates. Only a subset of participants completed qualitative interviews. Prognostic statements were hypothetical. Written prognostic statements may be interpreted differently than spoken statements.
Implications
Surrogate decision makers may interpret prognostic statements optimistically, especially when a high risk of death is estimated. Inaccurate interpretation may be related to personal beliefs about the patients' strengths and a need to hold onto hope for a positive outcome. When communicating with surrogates of critically ill patients, providers should be aware that, beyond the actual information shared, many other factors influence surrogates' beliefs about prognosis.
A Majority of Patients With Metastatic Cancer Felt That Chemotherapy Might Cure Their Disease
Weeks JC, Catalano PJ, Chronin A, et al. Patients' expectations about effects of chemotherapy for advanced cancer. N Engl J Med. 2012;367:16161625.
Background
Chemotherapy for advanced cancer is not curative, and many cancer patients overestimate their prognosis. Little is known about patients' understanding of the goals of chemotherapy when cancer is advanced.
Findings
Participants were part of the Cancer Care Outcomes Research and Surveillance study. Patients with stage IV lung or colon cancer who opted to receive chemotherapy (n=1193) were asked how likely they thought it was that the chemotherapy would cure their cancer. A majority (69% of lung cancer patients and 81% of colon cancer patients) felt that chemotherapy might cure their disease. Those who rated their physicians very favorably in satisfaction surveys were more likely to feel that that chemotherapy might be curative, compared to those who rated their physician less favorably (OR: 1.90; 95% CI: 1.33‐2.72).
Cautions
The study did not include patients who died soon after diagnosis and thus does not provide information about those who opted for chemotherapy but did not survive to the interview. It is possible that responses were influenced by participants' need to express optimism (social desirability bias). It is not clear how or whether prognostic disclosure by physicians caused the lower satisfaction ratings.
Implications
Despite the fact that stage IV lung and colon cancer are not curable with chemotherapy, a majority of patients reported believing that chemotherapy might cure their disease. Hospital clinicians should be aware that many patients who they view as terminally ill believe their illness may be cured.
Older Patients Who Viewed a Goals‐of‐Care Video at Admission to a Skilled Nursing Facility Were More Likely to Prefer Comfort Care
Volandes AE, Brandeis GH, Davis AD, et al. A randomized controlled trial of a goals‐of‐care video for elderly patients admitted to skilled nursing facilities. J Palliat Med. 2012;15:805811.
Background
Seriously ill older patients are frequently discharged from hospitals to skilled nursing facilities (SNFs). It is important to clarify and document patients' goals for care at the time of admission to SNFs, to ensure that care provided there is consistent with patients' preferences. Previous work has shown promise using videos to assist patients in advance‐care planning, providing realistic and standardized portrayals of different treatment options.[9, 10]
Findings
English‐speaking patients at least 65 years of age who did not have altered mental status were randomized to hear a verbal description (n=51) or view a 6‐minute video (n=50) that presented the same information accompanied by pictures of patients of 3 possible goals of medical care: life‐prolonging care, limited medical care, and comfort care. After the video or narrative, patients were asked what their care preference would be if they became more ill while at the SNF. Patients who viewed the video were more likely to report a preference for comfort care, compared to patients who received the narrative, 80% vs 57%, P=0.02. In a review of medical records, only 31% of patients who reported a preference for comfort care had a do not resuscitate order at the SNF.
Cautions
The study was conducted at 2 nursing homes located in the Boston, Massachusetts area, which may limit generalizability. Assessors were not blinded to whether the patient saw the video or received the narrative, which may have introduced bias. The authors note that the video aimed to present the different care options without valuing one over the other, though it may have inadvertently presented one option in a more favorable light.
Implications
Videos may be powerful tools for helping nursing home patients to clarify goals of care, and might be applied in the hospital setting prior to transferring patients to nursing homes. There is a significant opportunity to improve concordance of care with preferences through better documentation and implementation of code status orders when transferring patients to SNFs.
Acknowledgments
Disclosures: Drs. Anderson and Johnson and Mr. Horton received an honorarium and support for travel to present findings resulting from the literature review at the Annual Assembly of the American Academy of Hospice and Palliative Medicine and Hospice and Palliative Nurses Association on March 16, 2013 in New Orleans, Louisiana. Dr. Anderson was funded by the National Center for Advancing Translational Sciences, National Institutes of Health, through UCSF‐CTSI grant number KL2TR000143. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH. The authors report no conflicts of interest.
APPENDIX
Journals That Were Hand Searched to Identify Articles, By Topic Area
General:
- British Medical Journal
- Journal of the American Medical Association
- Lancet
- New England Journal of Medicine
Internal medicine:
- Annals Internal Medicine
- Archives Internal Medicine
- Journal of General Internal Medicine
- Journal of Hospital Medicine
Palliative care and symptom management:
- Journal Pain and Symptom Management
- Journal of Palliative Care
- Journal of Palliative Medicine
- Palliative Medicine
- Pain
Oncology:
- Journal of Clinical Oncology
- Supportive Care in Cancer
Critical care:
- American Journal of Respiratory and Critical Care Medicine
- Critical Care Medicine
Pediatrics:
- Pediatrics
Geriatrics:
- Journal of the American Geriatrics Society
Education:
- Academic Medicine
Nursing:
- Journal of Hospice and Palliative Nursing
- Oncology Nursing Forum
- The Dartmouth Atlas of Health Care. Percent of Medicare decedents hospitalized at least once during the last six months of life 2007. Available at: http://www.dartmouthatlas.org/data/table.aspx?ind=133. Accessed October 30, 2013.
- , , , et al. Change in end‐of‐life care for Medicare beneficiaries: site of death, place of care, and health care transitions in 2000, 2005, and 2009. JAMA. 2013;309(5):470–477.
- , , , et al. End‐of‐life care for lung cancer patients in the United States and Ontario. J Natl Cancer Inst. 2011;103(11):853–862.
- , , , , . Core competencies in hospital medicine: development and methodology. J Hosp Med. 2006;1(suppl 1):48–56.
- Society of Hospital Medicine; 2008.The core competencies in hospital medicine. http://www.hospitalmedicine.org/Content/NavigationMenu/Education/CoreCurriculum/Core_Competencies.htm. Accessed October 30, 2013.
- , , , , . Management of a malignant pleural effusion: British Thoracic Society Pleural Disease Guideline. Thorax. 2010;65:ii32–ii40.
- , . A comparison of sennosides‐based bowel protocols with and without docusate in hospitalized patients with cancer. J Palliat Med. 2008;11(4):575–581.
- , , , , , . Trends in survival after In‐hospital cardiac arrest. N Engl J Med. 2012;367:1912–1920.
- , , , et al. Use of video to facilitate end‐of‐life discussions with patients with cancer: a randomized controlled trial. J Clin Oncol. 2010;28(2):305–310.
- , , , et al. Augmenting advance care planning in poor prognosis cancer with a video decision aid: a preintervention‐postintervention study. Cancer. 2012;118(17):4331–4338.
Seriously ill patients frequently receive care in hospitals,[1, 2, 3] and palliative care is a core competency for hospitalists.[4, 5] The goal of this update was to summarize and critique recently published research that has the highest potential to impact the clinical practice of palliative care in the hospital. We reviewed articles published between January 2012 and May 2013. To identify articles, we hand‐searched 22 leading journals (see Appendix) and the Cochrane Database of Systematic Reviews, and performed a PubMed keyword search using the terms hospice and palliative care. We evaluated identified articles based on scientific rigor and relevance to hospital practice. In this review, we summarize 9 articles that were collectively selected as having the highest impact on the clinical practice of hospital palliative care. We summarize each article and its findings and note cautions and implications for practice.
SYMPTOM MANAGEMENT
Indwelling Pleural Catheters and Talc Pleurodesis Provide Similar Dyspnea Relief in Patients With Malignant Pleural Effusions
Davies HE, Mishra EK, Kahan BC, et al. Effect of an indwelling pleural catheter vs chest tube and talc pleurodesis for relieving dyspnea in patients with malignant pleural effusion. JAMA. 2012;307:23832389.
Background
Expert guidelines recommend chest‐tube insertion and talc pleurodesis as a first‐line therapy for symptomatic malignant pleural effusions, but indwelling pleural catheters are gaining in popularity.[6] The optimal management is unknown.
Findings
A total of 106 patients with newly diagnosed symptomatic malignant pleural effusion were randomized to undergo talc pleurodesis or placement of an indwelling pleural catheter. Most patients had metastatic breast or lung cancer. Overall, there were no differences in relief of dyspnea at 42 days between patients who received indwelling catheters and pleurodesis; importantly, more than 75% of patients in both groups reported improved shortness of breath. The initial hospitalization was much shorter in the indwelling catheter group (0 days vs 4 days). There was no difference in quality of life, but in surviving patients, dyspnea at 6 months was better with the indwelling catheter. In the talc group, 22% of patients required further pleural procedures compared with 6% in the indwelling catheter group. Patients in the talc group had a higher frequency of adverse events than in the catheter group (40% vs 13%). In the catheter group, the most common adverse events were pleural infection, cellulitis, and catheter obstruction.
Cautions
The study was small and unblinded, and the primary outcome was subjective dyspnea. The study occurred at 7 hospitals, and the impact of institutional or provider experience was not taken into account. Last, overall costs of care, which could impact the choice of intervention, were not calculated.
Implications
This was a small but well‐done study showing that indwelling catheters and talc pleurodesis provide similar relief of dyspnea 42 days postintervention. Given these results, both interventions seem to be acceptable options. Clinicians and patients could select the best option based on local procedural expertise and patient factors such as preference, ability to manage a catheter, and life expectancy.
Most Dying Patients Do Not Experience Increased Respiratory Distress When Oxygen is Withdrawn
Campbell ML, Yarandi H, Dove‐Medows E. Oxygen is nonbeneficial for most patients who are near death. J Pain Symptom Manage. 2013;45(3):517523.
Background
Oxygen is frequently administered to patients at the end of life, yet there is limited evidence evaluating whether oxygen reduces respiratory distress in dying patients.
Findings
In this double‐blind, repeated‐measure study, patients served as their own controls as the investigators evaluated respiratory distress with and without oxygen therapy. The study included 32 patients who were enrolled in hospice or seen in palliative care consultation and had a diagnosis such as lung cancer or heart failure that might cause dyspnea. Medical air (nasal cannula with air flow), supplemental oxygen, and no flow were randomly alternated every 10 minutes for 1 hour. Blinded research assistants used a validated observation scale to compare respiratory distress under each condition. At baseline, 27 of 32 (84%) patients were on oxygen. Three patients, all of whom were conscious and on oxygen at baseline, experienced increased respiratory distress without oxygen; reapplication of supplemental oxygen relieved their distress. The other 29 patients had no change in respiratory distress under the oxygen, medical air, and no flow conditions.
Cautions
All patients in this study were near death as measured by the Palliative Performance Scale, which assesses prognosis based on functional status and level of consciousness. Patients were excluded if they were receiving high‐flow oxygen by face mask or were experiencing respiratory distress at the time of initial evaluation. Some patients experienced increased discomfort after withdrawal of oxygen. Close observation is needed to determine which patients will experience distress.
Implications
The majority of patients who were receiving oxygen at baseline experienced no change in respiratory comfort when oxygen was withdrawn, supporting previous evidence that oxygen provides little benefit in nonhypoxemic patients. Oxygen may be an unnecessary intervention near death and has the potential to add to discomfort through nasal dryness and decreased mobility.
Sennosides Performed Similarly to Docusate Plus Sennosides in Managing Opioid‐Induced Constipation in Seriously Ill Patients
Tarumi Y, Wilson MP, Szafran O, Spooner GR. Randomized, double‐blind, placebo‐controlled trial of oral docusate in the management of constipation in hospice patients. J Pain Symptom Manage. 2013;45:213.
Background
Seriously ill patients frequently suffer from constipation, often as a result of opioid analgesics. Hospital clinicians should seek to optimize bowel regimens to prevent opioid‐induced constipation. A combination of the stimulant laxative sennoside and the stool softener docusate is often recommended to treat and prevent constipation. Docusate may not have additional benefit to sennoside, and may have significant burdens, including disturbing the absorption of other medications, adding to patients' pill burden and increasing nurse workload.[7]
Findings
In this double‐blinded trial, 74 patients in 3 inpatient hospices in Canada were randomized to receive sennoside plus either docusate 100 mg, or placebo tablets twice daily, or sennoside plus placebo for 10 days. Most patients had cancer as a life‐limiting diagnosis and received opioids during the study period. All were able to tolerate pills and food or sips of fluid. There was no significant difference between the 2 groups in stool frequency, volume, consistency, or patients' perceptions of difficulty with defecation. The percentage of patients who had a bowel movement at least every 3 days was 71% in the docusate plus sennoside group and 81% in the sennoside only group (P=0.45). There was also no significant difference between the groups in sennoside dose (which ranged between 13, 8.6 mg tablets daily), mean morphine equivalent daily dosage, or other bowel interventions.
Cautions
The trial was small, though it was adequately powered to detect a clinically meaningful difference between the 2 groups of 0.5 in the average number of bowel movements per day. The consent rate was low (26%); the authors do not detail reasons patients were not randomized. Patients who did not participate might have had different responses.
Implications
Consistent with previous work,[7] these results indicate that docusate is probably not needed for routine management of opioid‐induced constipation in seriously ill patients.
Sublingual Atropine Performed Similarly to Placebo in Reducing Noise Associated With Respiratory Rattle Near Death
Heisler M, Hamilton G, Abbott A, et al. Randomized double‐blind trial of sublingual atropine vs. placebo for the management of death rattle. J Pain Symptom Manage. 2012;45(1):1422.
Background
Increased respiratory tract secretions in patients near death can cause noisy breathing, often referred to as a death rattle. Antimuscarinic medications, such as atropine, are frequently used to decrease audible respirations and family distress, though little evidence exists to support this practice.
Findings
In this double‐blind, placebo‐controlled, parallel group trial at 3 inpatient hospices, 177 terminally ill patients with audible respiratory secretions were randomized to 2 drops of sublingual atropine 1% solution or placebo drops. Bedside nurses rated patients' respiratory secretions at enrollment, and 2 and 4 hours after receiving atropine or placebo. There were no differences in noise score between subjects treated with atropine and placebo at 2 hours (37.8% vs. 41.3%, P=0.24) or at 4 hours (39.7% and 51.7%, P=0.21). There were no differences in the safety end point of change in heart rate (P=0.47).
Cautions
Previous studies comparing different anticholinergic medications and routes of administration to manage audible respiratory secretions had variable response rates but suggested a benefit to antimuscarinic medications. However, these trials had significant methodological limitations including lack of randomization and blinding. The improvement in death rattle over time in other studies may suggest a favorable natural course for respiratory secretions rather than a treatment effect.
Implications
Although generalizability to other antimuscarinic medications and routes of administration is limited, in a randomized, double‐blind, placebo‐controlled trial, sublingual atropine did not reduce the noise from respiratory secretions when compared to placebo.
PATIENT AND FAMILY OUTCOMES AFTER CARDIOPULMONARY RESUSCITATION
Over Half of Older Adult Survivors of In‐Hospital Cardiopulmonary Resuscitation Were Alive At 1 Year
Chan PS, Krumholz HM, Spertus JA, et al. Long‐term outcomes in elderly survivors of in‐hospital cardiac arrest. N Engl J Med. 2013;368:10191026.
Background
Studies of cardiopulmonary resuscitation (CPR) outcomes have focused on survival to hospital discharge. Little is known about long‐term outcomes following in‐hospital cardiac arrest in older adults.
Findings
The authors analyzed data from the Get With the GuidelinesResuscitation registry from 2000 to 2008 and Medicare inpatient files from 2000 to 2010. The cohort included 6972 patients at 401 hospitals who were discharged after surviving in‐hospital arrest. Outcomes were survival and freedom from hospital readmission at 1 year after discharge. At discharge, 48% of patients had either no or mild neurologic disability at discharge; the remainder had moderate to severe neurologic disability. Overall, 58% of patients who were discharged were still alive at 1 year. Survival rates were lowest for patients who were discharged in coma or vegetative state (8% at 1 year), and highest for those discharged with mild or no disability (73% at 1 year). Older patients had lower survival rates than younger patients, as did men compared with women and blacks compared with whites. At 1 year, 34.4% of the patients had not been readmitted. Predictors of readmission were similar to those for lower survival rates.
Cautions
This study only analyzed survival data from patients who survived to hospital discharge after receiving in‐hospital CPR, not all patients who had a cardiac arrest. Thus, the survival rates reported here do not include patients who died during the original arrest, or who survived the arrest but died during their hospitalization. The 1‐year survival rate for people aged 65 years and above following a cardiac arrest is not reported but is likely to be about 10%, based on data from this registry.[8] Data were not available for health status, neurologic status, or quality of life of the survivors at 1 year.
Implications
Older patients who receive in‐hospital CPR and have a good neurologic status at hospital discharge have good long‐term outcomes. In counseling patients about CPR, it is important to note that most patients who receive CPR do not survive to hospital discharge.
Families Who Were Present During CPR Had Decreased Post‐traumatic Stress Symptoms
Jabre P, Belpomme V, Azoulay E, et al. Family presence during cardiopulmonary resuscitation. N Engl J Med. 2013;368:10081018.
Background
Family members who watch their loved ones undergo (CPR) might have increased emotional distress. Alternatively, observing CPR may allow for appreciation of the efforts taken for their loved one and provide comfort at a challenging time. The right balance of benefit and harm is unclear.
Findings
Between 2009 and 2011, 15 prehospital emergency medical service units in France were randomized to offer adult family members the opportunity to observe CPR or follow their usual practice. A total of 570 relatives were enrolled. In the intervention group, 79% of relatives observed CPR, compared to 43% in the control group. There was no difference in the effectiveness of CPR between the 2 groups. At 90 days, post‐traumatic stress symptoms were more common in the control group (adjusted odds ratio [OR]: 1.7; 95% confidence interval [CI]: 1.2‐2.5). At 90 days, those who were present for the resuscitation also had fewer symptoms of anxiety and fewer symptoms of depression (P<0.009 for both). Stress of the medical teams involved in the CPR was not different between the 2 groups. No malpractice claims were filed in either group.
Cautions
The study was conducted only in France, so the results may not be generalizable outside of France. In addition, the observed resuscitation was for patients who suffered a cardiac arrest in the home; it is unclear if the same results would be found in the emergency department or hospital.
Implications
This is the highest quality study to date in this area that argues for actively inviting family members to be present for resuscitation efforts in the home. Further studies are needed to determine if hospitals should implement standard protocols. In the meantime, providers who perform CPR should consider inviting families to observe, as it may result in less emotional distress for family members.
COMMUNICATION AND DECISION MAKING
Surrogate Decision Makers Interpreted Prognostic Information Optimistically
Zier LS, Sottile PD, Hong SY, et al. Surrogate decision makers' interpretation of prognostic information: a mixed‐methods study. Ann Intern Med. 2012;156:360366.
Background
Surrogates of critically ill patients often have beliefs about prognosis that are discordant from what is told to them by providers. Little is known about why this is the case.
Findings
Eighty surrogates of patients in intensive care units (ICUs) were given questionnaires with hypothetical prognostic statements and asked to identify a survival probability associated with each statement on a 0% to 100% scale. Interviewers examined the questionnaires to identify responses that were not concordant with the given prognostic statements. They then interviewed participants to determine why the answers were discordant. The researchers found that surrogates were more likely to offer an overoptimistic interpretation of statements communicating a high risk of death, compared to statements communicating a low risk of death. The qualitative interviews revealed that surrogates felt they needed to express ongoing optimism and that patient factors not known to the medical team would lead to better outcomes.
Cautions
The participants were surrogates who were present in the ICU at the time when study investigators were there, and thus the results may not be generalizable to all surrogates. Only a subset of participants completed qualitative interviews. Prognostic statements were hypothetical. Written prognostic statements may be interpreted differently than spoken statements.
Implications
Surrogate decision makers may interpret prognostic statements optimistically, especially when a high risk of death is estimated. Inaccurate interpretation may be related to personal beliefs about the patients' strengths and a need to hold onto hope for a positive outcome. When communicating with surrogates of critically ill patients, providers should be aware that, beyond the actual information shared, many other factors influence surrogates' beliefs about prognosis.
A Majority of Patients With Metastatic Cancer Felt That Chemotherapy Might Cure Their Disease
Weeks JC, Catalano PJ, Chronin A, et al. Patients' expectations about effects of chemotherapy for advanced cancer. N Engl J Med. 2012;367:16161625.
Background
Chemotherapy for advanced cancer is not curative, and many cancer patients overestimate their prognosis. Little is known about patients' understanding of the goals of chemotherapy when cancer is advanced.
Findings
Participants were part of the Cancer Care Outcomes Research and Surveillance study. Patients with stage IV lung or colon cancer who opted to receive chemotherapy (n=1193) were asked how likely they thought it was that the chemotherapy would cure their cancer. A majority (69% of lung cancer patients and 81% of colon cancer patients) felt that chemotherapy might cure their disease. Those who rated their physicians very favorably in satisfaction surveys were more likely to feel that that chemotherapy might be curative, compared to those who rated their physician less favorably (OR: 1.90; 95% CI: 1.33‐2.72).
Cautions
The study did not include patients who died soon after diagnosis and thus does not provide information about those who opted for chemotherapy but did not survive to the interview. It is possible that responses were influenced by participants' need to express optimism (social desirability bias). It is not clear how or whether prognostic disclosure by physicians caused the lower satisfaction ratings.
Implications
Despite the fact that stage IV lung and colon cancer are not curable with chemotherapy, a majority of patients reported believing that chemotherapy might cure their disease. Hospital clinicians should be aware that many patients who they view as terminally ill believe their illness may be cured.
Older Patients Who Viewed a Goals‐of‐Care Video at Admission to a Skilled Nursing Facility Were More Likely to Prefer Comfort Care
Volandes AE, Brandeis GH, Davis AD, et al. A randomized controlled trial of a goals‐of‐care video for elderly patients admitted to skilled nursing facilities. J Palliat Med. 2012;15:805811.
Background
Seriously ill older patients are frequently discharged from hospitals to skilled nursing facilities (SNFs). It is important to clarify and document patients' goals for care at the time of admission to SNFs, to ensure that care provided there is consistent with patients' preferences. Previous work has shown promise using videos to assist patients in advance‐care planning, providing realistic and standardized portrayals of different treatment options.[9, 10]
Findings
English‐speaking patients at least 65 years of age who did not have altered mental status were randomized to hear a verbal description (n=51) or view a 6‐minute video (n=50) that presented the same information accompanied by pictures of patients of 3 possible goals of medical care: life‐prolonging care, limited medical care, and comfort care. After the video or narrative, patients were asked what their care preference would be if they became more ill while at the SNF. Patients who viewed the video were more likely to report a preference for comfort care, compared to patients who received the narrative, 80% vs 57%, P=0.02. In a review of medical records, only 31% of patients who reported a preference for comfort care had a do not resuscitate order at the SNF.
Cautions
The study was conducted at 2 nursing homes located in the Boston, Massachusetts area, which may limit generalizability. Assessors were not blinded to whether the patient saw the video or received the narrative, which may have introduced bias. The authors note that the video aimed to present the different care options without valuing one over the other, though it may have inadvertently presented one option in a more favorable light.
Implications
Videos may be powerful tools for helping nursing home patients to clarify goals of care, and might be applied in the hospital setting prior to transferring patients to nursing homes. There is a significant opportunity to improve concordance of care with preferences through better documentation and implementation of code status orders when transferring patients to SNFs.
Acknowledgments
Disclosures: Drs. Anderson and Johnson and Mr. Horton received an honorarium and support for travel to present findings resulting from the literature review at the Annual Assembly of the American Academy of Hospice and Palliative Medicine and Hospice and Palliative Nurses Association on March 16, 2013 in New Orleans, Louisiana. Dr. Anderson was funded by the National Center for Advancing Translational Sciences, National Institutes of Health, through UCSF‐CTSI grant number KL2TR000143. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH. The authors report no conflicts of interest.
APPENDIX
Journals That Were Hand Searched to Identify Articles, By Topic Area
General:
- British Medical Journal
- Journal of the American Medical Association
- Lancet
- New England Journal of Medicine
Internal medicine:
- Annals Internal Medicine
- Archives Internal Medicine
- Journal of General Internal Medicine
- Journal of Hospital Medicine
Palliative care and symptom management:
- Journal Pain and Symptom Management
- Journal of Palliative Care
- Journal of Palliative Medicine
- Palliative Medicine
- Pain
Oncology:
- Journal of Clinical Oncology
- Supportive Care in Cancer
Critical care:
- American Journal of Respiratory and Critical Care Medicine
- Critical Care Medicine
Pediatrics:
- Pediatrics
Geriatrics:
- Journal of the American Geriatrics Society
Education:
- Academic Medicine
Nursing:
- Journal of Hospice and Palliative Nursing
- Oncology Nursing Forum
Seriously ill patients frequently receive care in hospitals,[1, 2, 3] and palliative care is a core competency for hospitalists.[4, 5] The goal of this update was to summarize and critique recently published research that has the highest potential to impact the clinical practice of palliative care in the hospital. We reviewed articles published between January 2012 and May 2013. To identify articles, we hand‐searched 22 leading journals (see Appendix) and the Cochrane Database of Systematic Reviews, and performed a PubMed keyword search using the terms hospice and palliative care. We evaluated identified articles based on scientific rigor and relevance to hospital practice. In this review, we summarize 9 articles that were collectively selected as having the highest impact on the clinical practice of hospital palliative care. We summarize each article and its findings and note cautions and implications for practice.
SYMPTOM MANAGEMENT
Indwelling Pleural Catheters and Talc Pleurodesis Provide Similar Dyspnea Relief in Patients With Malignant Pleural Effusions
Davies HE, Mishra EK, Kahan BC, et al. Effect of an indwelling pleural catheter vs chest tube and talc pleurodesis for relieving dyspnea in patients with malignant pleural effusion. JAMA. 2012;307:23832389.
Background
Expert guidelines recommend chest‐tube insertion and talc pleurodesis as a first‐line therapy for symptomatic malignant pleural effusions, but indwelling pleural catheters are gaining in popularity.[6] The optimal management is unknown.
Findings
A total of 106 patients with newly diagnosed symptomatic malignant pleural effusion were randomized to undergo talc pleurodesis or placement of an indwelling pleural catheter. Most patients had metastatic breast or lung cancer. Overall, there were no differences in relief of dyspnea at 42 days between patients who received indwelling catheters and pleurodesis; importantly, more than 75% of patients in both groups reported improved shortness of breath. The initial hospitalization was much shorter in the indwelling catheter group (0 days vs 4 days). There was no difference in quality of life, but in surviving patients, dyspnea at 6 months was better with the indwelling catheter. In the talc group, 22% of patients required further pleural procedures compared with 6% in the indwelling catheter group. Patients in the talc group had a higher frequency of adverse events than in the catheter group (40% vs 13%). In the catheter group, the most common adverse events were pleural infection, cellulitis, and catheter obstruction.
Cautions
The study was small and unblinded, and the primary outcome was subjective dyspnea. The study occurred at 7 hospitals, and the impact of institutional or provider experience was not taken into account. Last, overall costs of care, which could impact the choice of intervention, were not calculated.
Implications
This was a small but well‐done study showing that indwelling catheters and talc pleurodesis provide similar relief of dyspnea 42 days postintervention. Given these results, both interventions seem to be acceptable options. Clinicians and patients could select the best option based on local procedural expertise and patient factors such as preference, ability to manage a catheter, and life expectancy.
Most Dying Patients Do Not Experience Increased Respiratory Distress When Oxygen is Withdrawn
Campbell ML, Yarandi H, Dove‐Medows E. Oxygen is nonbeneficial for most patients who are near death. J Pain Symptom Manage. 2013;45(3):517523.
Background
Oxygen is frequently administered to patients at the end of life, yet there is limited evidence evaluating whether oxygen reduces respiratory distress in dying patients.
Findings
In this double‐blind, repeated‐measure study, patients served as their own controls as the investigators evaluated respiratory distress with and without oxygen therapy. The study included 32 patients who were enrolled in hospice or seen in palliative care consultation and had a diagnosis such as lung cancer or heart failure that might cause dyspnea. Medical air (nasal cannula with air flow), supplemental oxygen, and no flow were randomly alternated every 10 minutes for 1 hour. Blinded research assistants used a validated observation scale to compare respiratory distress under each condition. At baseline, 27 of 32 (84%) patients were on oxygen. Three patients, all of whom were conscious and on oxygen at baseline, experienced increased respiratory distress without oxygen; reapplication of supplemental oxygen relieved their distress. The other 29 patients had no change in respiratory distress under the oxygen, medical air, and no flow conditions.
Cautions
All patients in this study were near death as measured by the Palliative Performance Scale, which assesses prognosis based on functional status and level of consciousness. Patients were excluded if they were receiving high‐flow oxygen by face mask or were experiencing respiratory distress at the time of initial evaluation. Some patients experienced increased discomfort after withdrawal of oxygen. Close observation is needed to determine which patients will experience distress.
Implications
The majority of patients who were receiving oxygen at baseline experienced no change in respiratory comfort when oxygen was withdrawn, supporting previous evidence that oxygen provides little benefit in nonhypoxemic patients. Oxygen may be an unnecessary intervention near death and has the potential to add to discomfort through nasal dryness and decreased mobility.
Sennosides Performed Similarly to Docusate Plus Sennosides in Managing Opioid‐Induced Constipation in Seriously Ill Patients
Tarumi Y, Wilson MP, Szafran O, Spooner GR. Randomized, double‐blind, placebo‐controlled trial of oral docusate in the management of constipation in hospice patients. J Pain Symptom Manage. 2013;45:213.
Background
Seriously ill patients frequently suffer from constipation, often as a result of opioid analgesics. Hospital clinicians should seek to optimize bowel regimens to prevent opioid‐induced constipation. A combination of the stimulant laxative sennoside and the stool softener docusate is often recommended to treat and prevent constipation. Docusate may not have additional benefit to sennoside, and may have significant burdens, including disturbing the absorption of other medications, adding to patients' pill burden and increasing nurse workload.[7]
Findings
In this double‐blinded trial, 74 patients in 3 inpatient hospices in Canada were randomized to receive sennoside plus either docusate 100 mg, or placebo tablets twice daily, or sennoside plus placebo for 10 days. Most patients had cancer as a life‐limiting diagnosis and received opioids during the study period. All were able to tolerate pills and food or sips of fluid. There was no significant difference between the 2 groups in stool frequency, volume, consistency, or patients' perceptions of difficulty with defecation. The percentage of patients who had a bowel movement at least every 3 days was 71% in the docusate plus sennoside group and 81% in the sennoside only group (P=0.45). There was also no significant difference between the groups in sennoside dose (which ranged between 13, 8.6 mg tablets daily), mean morphine equivalent daily dosage, or other bowel interventions.
Cautions
The trial was small, though it was adequately powered to detect a clinically meaningful difference between the 2 groups of 0.5 in the average number of bowel movements per day. The consent rate was low (26%); the authors do not detail reasons patients were not randomized. Patients who did not participate might have had different responses.
Implications
Consistent with previous work,[7] these results indicate that docusate is probably not needed for routine management of opioid‐induced constipation in seriously ill patients.
Sublingual Atropine Performed Similarly to Placebo in Reducing Noise Associated With Respiratory Rattle Near Death
Heisler M, Hamilton G, Abbott A, et al. Randomized double‐blind trial of sublingual atropine vs. placebo for the management of death rattle. J Pain Symptom Manage. 2012;45(1):1422.
Background
Increased respiratory tract secretions in patients near death can cause noisy breathing, often referred to as a death rattle. Antimuscarinic medications, such as atropine, are frequently used to decrease audible respirations and family distress, though little evidence exists to support this practice.
Findings
In this double‐blind, placebo‐controlled, parallel group trial at 3 inpatient hospices, 177 terminally ill patients with audible respiratory secretions were randomized to 2 drops of sublingual atropine 1% solution or placebo drops. Bedside nurses rated patients' respiratory secretions at enrollment, and 2 and 4 hours after receiving atropine or placebo. There were no differences in noise score between subjects treated with atropine and placebo at 2 hours (37.8% vs. 41.3%, P=0.24) or at 4 hours (39.7% and 51.7%, P=0.21). There were no differences in the safety end point of change in heart rate (P=0.47).
Cautions
Previous studies comparing different anticholinergic medications and routes of administration to manage audible respiratory secretions had variable response rates but suggested a benefit to antimuscarinic medications. However, these trials had significant methodological limitations including lack of randomization and blinding. The improvement in death rattle over time in other studies may suggest a favorable natural course for respiratory secretions rather than a treatment effect.
Implications
Although generalizability to other antimuscarinic medications and routes of administration is limited, in a randomized, double‐blind, placebo‐controlled trial, sublingual atropine did not reduce the noise from respiratory secretions when compared to placebo.
PATIENT AND FAMILY OUTCOMES AFTER CARDIOPULMONARY RESUSCITATION
Over Half of Older Adult Survivors of In‐Hospital Cardiopulmonary Resuscitation Were Alive At 1 Year
Chan PS, Krumholz HM, Spertus JA, et al. Long‐term outcomes in elderly survivors of in‐hospital cardiac arrest. N Engl J Med. 2013;368:10191026.
Background
Studies of cardiopulmonary resuscitation (CPR) outcomes have focused on survival to hospital discharge. Little is known about long‐term outcomes following in‐hospital cardiac arrest in older adults.
Findings
The authors analyzed data from the Get With the GuidelinesResuscitation registry from 2000 to 2008 and Medicare inpatient files from 2000 to 2010. The cohort included 6972 patients at 401 hospitals who were discharged after surviving in‐hospital arrest. Outcomes were survival and freedom from hospital readmission at 1 year after discharge. At discharge, 48% of patients had either no or mild neurologic disability at discharge; the remainder had moderate to severe neurologic disability. Overall, 58% of patients who were discharged were still alive at 1 year. Survival rates were lowest for patients who were discharged in coma or vegetative state (8% at 1 year), and highest for those discharged with mild or no disability (73% at 1 year). Older patients had lower survival rates than younger patients, as did men compared with women and blacks compared with whites. At 1 year, 34.4% of the patients had not been readmitted. Predictors of readmission were similar to those for lower survival rates.
Cautions
This study only analyzed survival data from patients who survived to hospital discharge after receiving in‐hospital CPR, not all patients who had a cardiac arrest. Thus, the survival rates reported here do not include patients who died during the original arrest, or who survived the arrest but died during their hospitalization. The 1‐year survival rate for people aged 65 years and above following a cardiac arrest is not reported but is likely to be about 10%, based on data from this registry.[8] Data were not available for health status, neurologic status, or quality of life of the survivors at 1 year.
Implications
Older patients who receive in‐hospital CPR and have a good neurologic status at hospital discharge have good long‐term outcomes. In counseling patients about CPR, it is important to note that most patients who receive CPR do not survive to hospital discharge.
Families Who Were Present During CPR Had Decreased Post‐traumatic Stress Symptoms
Jabre P, Belpomme V, Azoulay E, et al. Family presence during cardiopulmonary resuscitation. N Engl J Med. 2013;368:10081018.
Background
Family members who watch their loved ones undergo (CPR) might have increased emotional distress. Alternatively, observing CPR may allow for appreciation of the efforts taken for their loved one and provide comfort at a challenging time. The right balance of benefit and harm is unclear.
Findings
Between 2009 and 2011, 15 prehospital emergency medical service units in France were randomized to offer adult family members the opportunity to observe CPR or follow their usual practice. A total of 570 relatives were enrolled. In the intervention group, 79% of relatives observed CPR, compared to 43% in the control group. There was no difference in the effectiveness of CPR between the 2 groups. At 90 days, post‐traumatic stress symptoms were more common in the control group (adjusted odds ratio [OR]: 1.7; 95% confidence interval [CI]: 1.2‐2.5). At 90 days, those who were present for the resuscitation also had fewer symptoms of anxiety and fewer symptoms of depression (P<0.009 for both). Stress of the medical teams involved in the CPR was not different between the 2 groups. No malpractice claims were filed in either group.
Cautions
The study was conducted only in France, so the results may not be generalizable outside of France. In addition, the observed resuscitation was for patients who suffered a cardiac arrest in the home; it is unclear if the same results would be found in the emergency department or hospital.
Implications
This is the highest quality study to date in this area that argues for actively inviting family members to be present for resuscitation efforts in the home. Further studies are needed to determine if hospitals should implement standard protocols. In the meantime, providers who perform CPR should consider inviting families to observe, as it may result in less emotional distress for family members.
COMMUNICATION AND DECISION MAKING
Surrogate Decision Makers Interpreted Prognostic Information Optimistically
Zier LS, Sottile PD, Hong SY, et al. Surrogate decision makers' interpretation of prognostic information: a mixed‐methods study. Ann Intern Med. 2012;156:360366.
Background
Surrogates of critically ill patients often have beliefs about prognosis that are discordant from what is told to them by providers. Little is known about why this is the case.
Findings
Eighty surrogates of patients in intensive care units (ICUs) were given questionnaires with hypothetical prognostic statements and asked to identify a survival probability associated with each statement on a 0% to 100% scale. Interviewers examined the questionnaires to identify responses that were not concordant with the given prognostic statements. They then interviewed participants to determine why the answers were discordant. The researchers found that surrogates were more likely to offer an overoptimistic interpretation of statements communicating a high risk of death, compared to statements communicating a low risk of death. The qualitative interviews revealed that surrogates felt they needed to express ongoing optimism and that patient factors not known to the medical team would lead to better outcomes.
Cautions
The participants were surrogates who were present in the ICU at the time when study investigators were there, and thus the results may not be generalizable to all surrogates. Only a subset of participants completed qualitative interviews. Prognostic statements were hypothetical. Written prognostic statements may be interpreted differently than spoken statements.
Implications
Surrogate decision makers may interpret prognostic statements optimistically, especially when a high risk of death is estimated. Inaccurate interpretation may be related to personal beliefs about the patients' strengths and a need to hold onto hope for a positive outcome. When communicating with surrogates of critically ill patients, providers should be aware that, beyond the actual information shared, many other factors influence surrogates' beliefs about prognosis.
A Majority of Patients With Metastatic Cancer Felt That Chemotherapy Might Cure Their Disease
Weeks JC, Catalano PJ, Chronin A, et al. Patients' expectations about effects of chemotherapy for advanced cancer. N Engl J Med. 2012;367:16161625.
Background
Chemotherapy for advanced cancer is not curative, and many cancer patients overestimate their prognosis. Little is known about patients' understanding of the goals of chemotherapy when cancer is advanced.
Findings
Participants were part of the Cancer Care Outcomes Research and Surveillance study. Patients with stage IV lung or colon cancer who opted to receive chemotherapy (n=1193) were asked how likely they thought it was that the chemotherapy would cure their cancer. A majority (69% of lung cancer patients and 81% of colon cancer patients) felt that chemotherapy might cure their disease. Those who rated their physicians very favorably in satisfaction surveys were more likely to feel that that chemotherapy might be curative, compared to those who rated their physician less favorably (OR: 1.90; 95% CI: 1.33‐2.72).
Cautions
The study did not include patients who died soon after diagnosis and thus does not provide information about those who opted for chemotherapy but did not survive to the interview. It is possible that responses were influenced by participants' need to express optimism (social desirability bias). It is not clear how or whether prognostic disclosure by physicians caused the lower satisfaction ratings.
Implications
Despite the fact that stage IV lung and colon cancer are not curable with chemotherapy, a majority of patients reported believing that chemotherapy might cure their disease. Hospital clinicians should be aware that many patients who they view as terminally ill believe their illness may be cured.
Older Patients Who Viewed a Goals‐of‐Care Video at Admission to a Skilled Nursing Facility Were More Likely to Prefer Comfort Care
Volandes AE, Brandeis GH, Davis AD, et al. A randomized controlled trial of a goals‐of‐care video for elderly patients admitted to skilled nursing facilities. J Palliat Med. 2012;15:805811.
Background
Seriously ill older patients are frequently discharged from hospitals to skilled nursing facilities (SNFs). It is important to clarify and document patients' goals for care at the time of admission to SNFs, to ensure that care provided there is consistent with patients' preferences. Previous work has shown promise using videos to assist patients in advance‐care planning, providing realistic and standardized portrayals of different treatment options.[9, 10]
Findings
English‐speaking patients at least 65 years of age who did not have altered mental status were randomized to hear a verbal description (n=51) or view a 6‐minute video (n=50) that presented the same information accompanied by pictures of patients of 3 possible goals of medical care: life‐prolonging care, limited medical care, and comfort care. After the video or narrative, patients were asked what their care preference would be if they became more ill while at the SNF. Patients who viewed the video were more likely to report a preference for comfort care, compared to patients who received the narrative, 80% vs 57%, P=0.02. In a review of medical records, only 31% of patients who reported a preference for comfort care had a do not resuscitate order at the SNF.
Cautions
The study was conducted at 2 nursing homes located in the Boston, Massachusetts area, which may limit generalizability. Assessors were not blinded to whether the patient saw the video or received the narrative, which may have introduced bias. The authors note that the video aimed to present the different care options without valuing one over the other, though it may have inadvertently presented one option in a more favorable light.
Implications
Videos may be powerful tools for helping nursing home patients to clarify goals of care, and might be applied in the hospital setting prior to transferring patients to nursing homes. There is a significant opportunity to improve concordance of care with preferences through better documentation and implementation of code status orders when transferring patients to SNFs.
Acknowledgments
Disclosures: Drs. Anderson and Johnson and Mr. Horton received an honorarium and support for travel to present findings resulting from the literature review at the Annual Assembly of the American Academy of Hospice and Palliative Medicine and Hospice and Palliative Nurses Association on March 16, 2013 in New Orleans, Louisiana. Dr. Anderson was funded by the National Center for Advancing Translational Sciences, National Institutes of Health, through UCSF‐CTSI grant number KL2TR000143. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH. The authors report no conflicts of interest.
APPENDIX
Journals That Were Hand Searched to Identify Articles, By Topic Area
General:
- British Medical Journal
- Journal of the American Medical Association
- Lancet
- New England Journal of Medicine
Internal medicine:
- Annals Internal Medicine
- Archives Internal Medicine
- Journal of General Internal Medicine
- Journal of Hospital Medicine
Palliative care and symptom management:
- Journal Pain and Symptom Management
- Journal of Palliative Care
- Journal of Palliative Medicine
- Palliative Medicine
- Pain
Oncology:
- Journal of Clinical Oncology
- Supportive Care in Cancer
Critical care:
- American Journal of Respiratory and Critical Care Medicine
- Critical Care Medicine
Pediatrics:
- Pediatrics
Geriatrics:
- Journal of the American Geriatrics Society
Education:
- Academic Medicine
Nursing:
- Journal of Hospice and Palliative Nursing
- Oncology Nursing Forum
- The Dartmouth Atlas of Health Care. Percent of Medicare decedents hospitalized at least once during the last six months of life 2007. Available at: http://www.dartmouthatlas.org/data/table.aspx?ind=133. Accessed October 30, 2013.
- , , , et al. Change in end‐of‐life care for Medicare beneficiaries: site of death, place of care, and health care transitions in 2000, 2005, and 2009. JAMA. 2013;309(5):470–477.
- , , , et al. End‐of‐life care for lung cancer patients in the United States and Ontario. J Natl Cancer Inst. 2011;103(11):853–862.
- , , , , . Core competencies in hospital medicine: development and methodology. J Hosp Med. 2006;1(suppl 1):48–56.
- Society of Hospital Medicine; 2008.The core competencies in hospital medicine. http://www.hospitalmedicine.org/Content/NavigationMenu/Education/CoreCurriculum/Core_Competencies.htm. Accessed October 30, 2013.
- , , , , . Management of a malignant pleural effusion: British Thoracic Society Pleural Disease Guideline. Thorax. 2010;65:ii32–ii40.
- , . A comparison of sennosides‐based bowel protocols with and without docusate in hospitalized patients with cancer. J Palliat Med. 2008;11(4):575–581.
- , , , , , . Trends in survival after In‐hospital cardiac arrest. N Engl J Med. 2012;367:1912–1920.
- , , , et al. Use of video to facilitate end‐of‐life discussions with patients with cancer: a randomized controlled trial. J Clin Oncol. 2010;28(2):305–310.
- , , , et al. Augmenting advance care planning in poor prognosis cancer with a video decision aid: a preintervention‐postintervention study. Cancer. 2012;118(17):4331–4338.
- The Dartmouth Atlas of Health Care. Percent of Medicare decedents hospitalized at least once during the last six months of life 2007. Available at: http://www.dartmouthatlas.org/data/table.aspx?ind=133. Accessed October 30, 2013.
- , , , et al. Change in end‐of‐life care for Medicare beneficiaries: site of death, place of care, and health care transitions in 2000, 2005, and 2009. JAMA. 2013;309(5):470–477.
- , , , et al. End‐of‐life care for lung cancer patients in the United States and Ontario. J Natl Cancer Inst. 2011;103(11):853–862.
- , , , , . Core competencies in hospital medicine: development and methodology. J Hosp Med. 2006;1(suppl 1):48–56.
- Society of Hospital Medicine; 2008.The core competencies in hospital medicine. http://www.hospitalmedicine.org/Content/NavigationMenu/Education/CoreCurriculum/Core_Competencies.htm. Accessed October 30, 2013.
- , , , , . Management of a malignant pleural effusion: British Thoracic Society Pleural Disease Guideline. Thorax. 2010;65:ii32–ii40.
- , . A comparison of sennosides‐based bowel protocols with and without docusate in hospitalized patients with cancer. J Palliat Med. 2008;11(4):575–581.
- , , , , , . Trends in survival after In‐hospital cardiac arrest. N Engl J Med. 2012;367:1912–1920.
- , , , et al. Use of video to facilitate end‐of‐life discussions with patients with cancer: a randomized controlled trial. J Clin Oncol. 2010;28(2):305–310.
- , , , et al. Augmenting advance care planning in poor prognosis cancer with a video decision aid: a preintervention‐postintervention study. Cancer. 2012;118(17):4331–4338.