User login
TBI deaths from falls on the rise
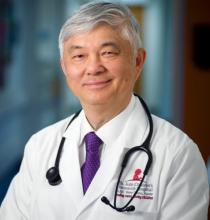
A 17% surge in mortality from fall-related traumatic brain injuries from 2008 to 2017 was driven largely by increases among those aged 75 years and older, according to investigators from the Centers for Disease Control and Prevention.
Nationally, the rate of deaths from traumatic brain injuries (TBIs) caused by unintentional falls rose from 3.86 per 100,000 population in 2008 to 4.52 per 100,000 in 2017, as the number of deaths went from 12,311 to 17,408, said Alexis B. Peterson, PhD, and Scott R. Kegler, PhD, of the CDC’s National Center for Injury Prevention and Control in Atlanta.
“This increase might be explained by longer survival following the onset of common diseases such as stroke, cancer, and heart disease or be attributable to the increasing population of older adults in the United States,” they suggested in the Mortality and Morbidity Weekly Report.
The rate of fall-related TBI among Americans aged 75 years and older increased by an average of 2.6% per year from 2008 to 2017, compared with 1.8% in those aged 55-74. Over that same time, death rates dropped for those aged 35-44 (–0.3%), 18-34 (–1.1%), and 0-17 (–4.3%), they said, based on data from the National Vital Statistics System’s multiple cause-of-death database.
The death rate increased fastest in residents of rural areas (2.9% per year), but deaths from fall-related TBI were up at all levels of urbanization. The largest central cities and fringe metro areas were up by 1.4% a year, with larger annual increases seen in medium-size cities (2.1%), small cities (2.2%), and small towns (2.1%), Dr. Peterson and Dr. Kegler said.
Rates of TBI-related mortality in general are higher in rural areas, they noted, and “heterogeneity in the availability and accessibility of resources (e.g., access to high-level trauma centers and rehabilitative services) can result in disparities in postinjury outcomes.”
State-specific rates increased in 45 states, although Alaska was excluded from the analysis because of its small number of cases (less than 20). Increases were significant in 29 states, but none of the changes were significant in the 4 states with lower rates at the end of the study period, the investigators reported.
“In older adults, evidence-based fall prevention strategies can prevent falls and avert costly medical expenditures,” Dr. Peterson and Dr. Kegler said, suggesting that health care providers “consider prescribing exercises that incorporate balance, strength and gait activities, such as tai chi, and reviewing and managing medications linked to falls.”
SOURCE: Peterson AB, Kegler SR. MMWR. 2019 Mar 6;69(9):225-30.
A 17% surge in mortality from fall-related traumatic brain injuries from 2008 to 2017 was driven largely by increases among those aged 75 years and older, according to investigators from the Centers for Disease Control and Prevention.
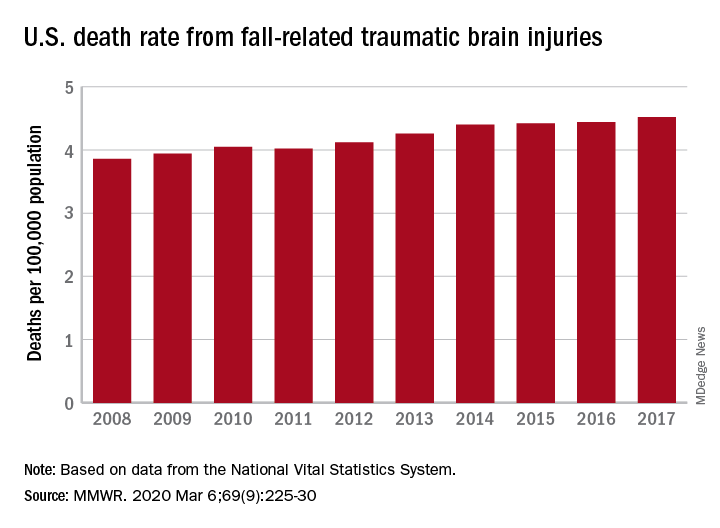
Nationally, the rate of deaths from traumatic brain injuries (TBIs) caused by unintentional falls rose from 3.86 per 100,000 population in 2008 to 4.52 per 100,000 in 2017, as the number of deaths went from 12,311 to 17,408, said Alexis B. Peterson, PhD, and Scott R. Kegler, PhD, of the CDC’s National Center for Injury Prevention and Control in Atlanta.
“This increase might be explained by longer survival following the onset of common diseases such as stroke, cancer, and heart disease or be attributable to the increasing population of older adults in the United States,” they suggested in the Mortality and Morbidity Weekly Report.
The rate of fall-related TBI among Americans aged 75 years and older increased by an average of 2.6% per year from 2008 to 2017, compared with 1.8% in those aged 55-74. Over that same time, death rates dropped for those aged 35-44 (–0.3%), 18-34 (–1.1%), and 0-17 (–4.3%), they said, based on data from the National Vital Statistics System’s multiple cause-of-death database.
The death rate increased fastest in residents of rural areas (2.9% per year), but deaths from fall-related TBI were up at all levels of urbanization. The largest central cities and fringe metro areas were up by 1.4% a year, with larger annual increases seen in medium-size cities (2.1%), small cities (2.2%), and small towns (2.1%), Dr. Peterson and Dr. Kegler said.
Rates of TBI-related mortality in general are higher in rural areas, they noted, and “heterogeneity in the availability and accessibility of resources (e.g., access to high-level trauma centers and rehabilitative services) can result in disparities in postinjury outcomes.”
State-specific rates increased in 45 states, although Alaska was excluded from the analysis because of its small number of cases (less than 20). Increases were significant in 29 states, but none of the changes were significant in the 4 states with lower rates at the end of the study period, the investigators reported.
“In older adults, evidence-based fall prevention strategies can prevent falls and avert costly medical expenditures,” Dr. Peterson and Dr. Kegler said, suggesting that health care providers “consider prescribing exercises that incorporate balance, strength and gait activities, such as tai chi, and reviewing and managing medications linked to falls.”
SOURCE: Peterson AB, Kegler SR. MMWR. 2019 Mar 6;69(9):225-30.
A 17% surge in mortality from fall-related traumatic brain injuries from 2008 to 2017 was driven largely by increases among those aged 75 years and older, according to investigators from the Centers for Disease Control and Prevention.
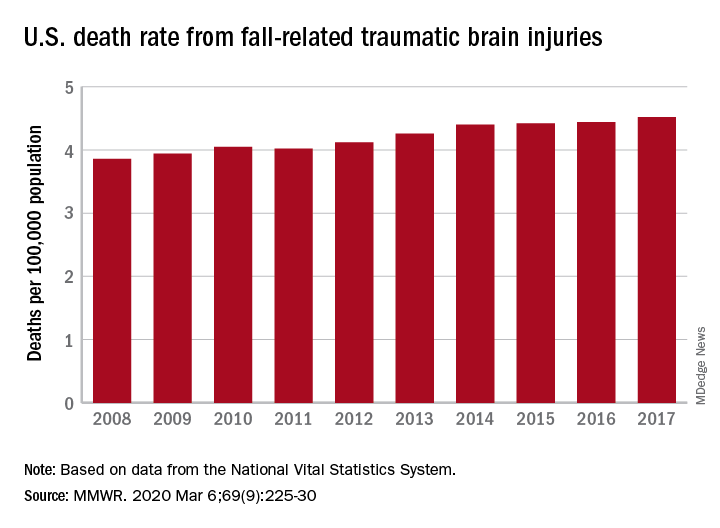
Nationally, the rate of deaths from traumatic brain injuries (TBIs) caused by unintentional falls rose from 3.86 per 100,000 population in 2008 to 4.52 per 100,000 in 2017, as the number of deaths went from 12,311 to 17,408, said Alexis B. Peterson, PhD, and Scott R. Kegler, PhD, of the CDC’s National Center for Injury Prevention and Control in Atlanta.
“This increase might be explained by longer survival following the onset of common diseases such as stroke, cancer, and heart disease or be attributable to the increasing population of older adults in the United States,” they suggested in the Mortality and Morbidity Weekly Report.
The rate of fall-related TBI among Americans aged 75 years and older increased by an average of 2.6% per year from 2008 to 2017, compared with 1.8% in those aged 55-74. Over that same time, death rates dropped for those aged 35-44 (–0.3%), 18-34 (–1.1%), and 0-17 (–4.3%), they said, based on data from the National Vital Statistics System’s multiple cause-of-death database.
The death rate increased fastest in residents of rural areas (2.9% per year), but deaths from fall-related TBI were up at all levels of urbanization. The largest central cities and fringe metro areas were up by 1.4% a year, with larger annual increases seen in medium-size cities (2.1%), small cities (2.2%), and small towns (2.1%), Dr. Peterson and Dr. Kegler said.
Rates of TBI-related mortality in general are higher in rural areas, they noted, and “heterogeneity in the availability and accessibility of resources (e.g., access to high-level trauma centers and rehabilitative services) can result in disparities in postinjury outcomes.”
State-specific rates increased in 45 states, although Alaska was excluded from the analysis because of its small number of cases (less than 20). Increases were significant in 29 states, but none of the changes were significant in the 4 states with lower rates at the end of the study period, the investigators reported.
“In older adults, evidence-based fall prevention strategies can prevent falls and avert costly medical expenditures,” Dr. Peterson and Dr. Kegler said, suggesting that health care providers “consider prescribing exercises that incorporate balance, strength and gait activities, such as tai chi, and reviewing and managing medications linked to falls.”
SOURCE: Peterson AB, Kegler SR. MMWR. 2019 Mar 6;69(9):225-30.
FROM MMWR
Adjuvant chemo emerges as new standard in upper tract urothelial cancer
(UTUC) and should therefore be a new standard of care, according to investigators from the POUT trial.
The risk of disease-free survival events was reduced by more than half for patients who started platinum-based chemotherapy within 90 days after nephroureterectomy, compared with counterparts who simply received surveillance. The treatment was generally well tolerated, with adverse events as expected for this regimen and only a transient impact on quality of life.
Alison Birtle, MD, of Lancashire Teaching Hospitals National Health Services Foundation Trust in Preston, England, and colleagues conducted this trial and reported the results in the Lancet.
“Urothelial carcinomas of the upper urinary tract … are rare, with poorer stage-for-stage prognosis than urothelial carcinomas of the urinary bladder,” the investigators wrote. “No international consensus exists on the benefit of adjuvant chemotherapy for patients with UTUCs after nephroureterectomy with curative intent.”
With this in mind, the investigators conducted the phase 3 POUT trial (NCT01993979), which is the largest trial to report outcomes exclusively in patients with UTUC. The trial included 261 patients with UTUC (transitional cell carcinoma of the ureter or renal pelvis) that was locally advanced at either pT2-T4 pN0-N3 M0 stage or pTany N1-3 M0 stage.
Patients were randomized to chemotherapy (n = 132) or surveillance (n = 129). Patients in the chemotherapy arm received four 21-day cycles of gemcitabine plus cisplatin or, when renal function was impaired, carboplatin.
With a median follow-up of 30.3 months, patients who received chemotherapy had a lower risk of disease recurrence or death, relative to counterparts who received only surveillance (hazard ratio, 0.45; P = .0001), with similar benefit across subgroups. The estimated 3-year disease-free survival rate was 71% in the chemotherapy arm and 46% in the surveillance arm. The median disease-free survival was 29.8 months and not reached, respectively.
The chemotherapy group also had a lower risk of metastasis or death when compared with the surveillance group (HR, 0.48; P = .0007). The 3-year event-free rates were 71% and 53%, respectively. Overall survival data are not yet mature.
“We acknowledge that disease-free survival is not regarded as a fully validated surrogate of overall survival after nephroureterectomy for UTUC,” the investigators wrote. “However, in a rare disease such as UTUC, a suitably powered trial with overall survival as the primary endpoint was not judged feasible. Although mature survival data (as a secondary endpoint) are not yet available, the large improvement in disease-free survival we noted for the primary endpoint, together with improved metastasis-free survival recorded as a secondary endpoint, strongly suggest that patients have better outcomes with chemotherapy than without.”
The incidence of acute grade 3 or worse treatment-emergent adverse events was 44% in the chemotherapy arm and 4% in the surveillance arm (P less than .0001). Quality of life was worse for the chemotherapy arm at 3 months (P = .0028), but that was no longer the case at 12 months (P = .20). There were no treatment-related deaths.
“[A]djuvant platinum-based chemotherapy should be adopted as a new standard of care for patients with locally advanced UTUC for whom systemic chemotherapy is not contraindicated,” the investigators recommended. “This regimen should be routinely considered for all patients in this population, and future studies should focus on combinations with novel agents in the adjuvant setting, which might further improve the prognosis for locally advanced UTUC.”
The trial was funded by Cancer Research UK. The authors disclosed relationships with numerous pharmaceutical companies.
SOURCE: Birtle A et al. Lancet. 2020 Mar 5. doi: 10.1016/S0140-6736(20)30415-3.
(UTUC) and should therefore be a new standard of care, according to investigators from the POUT trial.
The risk of disease-free survival events was reduced by more than half for patients who started platinum-based chemotherapy within 90 days after nephroureterectomy, compared with counterparts who simply received surveillance. The treatment was generally well tolerated, with adverse events as expected for this regimen and only a transient impact on quality of life.
Alison Birtle, MD, of Lancashire Teaching Hospitals National Health Services Foundation Trust in Preston, England, and colleagues conducted this trial and reported the results in the Lancet.
“Urothelial carcinomas of the upper urinary tract … are rare, with poorer stage-for-stage prognosis than urothelial carcinomas of the urinary bladder,” the investigators wrote. “No international consensus exists on the benefit of adjuvant chemotherapy for patients with UTUCs after nephroureterectomy with curative intent.”
With this in mind, the investigators conducted the phase 3 POUT trial (NCT01993979), which is the largest trial to report outcomes exclusively in patients with UTUC. The trial included 261 patients with UTUC (transitional cell carcinoma of the ureter or renal pelvis) that was locally advanced at either pT2-T4 pN0-N3 M0 stage or pTany N1-3 M0 stage.
Patients were randomized to chemotherapy (n = 132) or surveillance (n = 129). Patients in the chemotherapy arm received four 21-day cycles of gemcitabine plus cisplatin or, when renal function was impaired, carboplatin.
With a median follow-up of 30.3 months, patients who received chemotherapy had a lower risk of disease recurrence or death, relative to counterparts who received only surveillance (hazard ratio, 0.45; P = .0001), with similar benefit across subgroups. The estimated 3-year disease-free survival rate was 71% in the chemotherapy arm and 46% in the surveillance arm. The median disease-free survival was 29.8 months and not reached, respectively.
The chemotherapy group also had a lower risk of metastasis or death when compared with the surveillance group (HR, 0.48; P = .0007). The 3-year event-free rates were 71% and 53%, respectively. Overall survival data are not yet mature.
“We acknowledge that disease-free survival is not regarded as a fully validated surrogate of overall survival after nephroureterectomy for UTUC,” the investigators wrote. “However, in a rare disease such as UTUC, a suitably powered trial with overall survival as the primary endpoint was not judged feasible. Although mature survival data (as a secondary endpoint) are not yet available, the large improvement in disease-free survival we noted for the primary endpoint, together with improved metastasis-free survival recorded as a secondary endpoint, strongly suggest that patients have better outcomes with chemotherapy than without.”
The incidence of acute grade 3 or worse treatment-emergent adverse events was 44% in the chemotherapy arm and 4% in the surveillance arm (P less than .0001). Quality of life was worse for the chemotherapy arm at 3 months (P = .0028), but that was no longer the case at 12 months (P = .20). There were no treatment-related deaths.
“[A]djuvant platinum-based chemotherapy should be adopted as a new standard of care for patients with locally advanced UTUC for whom systemic chemotherapy is not contraindicated,” the investigators recommended. “This regimen should be routinely considered for all patients in this population, and future studies should focus on combinations with novel agents in the adjuvant setting, which might further improve the prognosis for locally advanced UTUC.”
The trial was funded by Cancer Research UK. The authors disclosed relationships with numerous pharmaceutical companies.
SOURCE: Birtle A et al. Lancet. 2020 Mar 5. doi: 10.1016/S0140-6736(20)30415-3.
(UTUC) and should therefore be a new standard of care, according to investigators from the POUT trial.
The risk of disease-free survival events was reduced by more than half for patients who started platinum-based chemotherapy within 90 days after nephroureterectomy, compared with counterparts who simply received surveillance. The treatment was generally well tolerated, with adverse events as expected for this regimen and only a transient impact on quality of life.
Alison Birtle, MD, of Lancashire Teaching Hospitals National Health Services Foundation Trust in Preston, England, and colleagues conducted this trial and reported the results in the Lancet.
“Urothelial carcinomas of the upper urinary tract … are rare, with poorer stage-for-stage prognosis than urothelial carcinomas of the urinary bladder,” the investigators wrote. “No international consensus exists on the benefit of adjuvant chemotherapy for patients with UTUCs after nephroureterectomy with curative intent.”
With this in mind, the investigators conducted the phase 3 POUT trial (NCT01993979), which is the largest trial to report outcomes exclusively in patients with UTUC. The trial included 261 patients with UTUC (transitional cell carcinoma of the ureter or renal pelvis) that was locally advanced at either pT2-T4 pN0-N3 M0 stage or pTany N1-3 M0 stage.
Patients were randomized to chemotherapy (n = 132) or surveillance (n = 129). Patients in the chemotherapy arm received four 21-day cycles of gemcitabine plus cisplatin or, when renal function was impaired, carboplatin.
With a median follow-up of 30.3 months, patients who received chemotherapy had a lower risk of disease recurrence or death, relative to counterparts who received only surveillance (hazard ratio, 0.45; P = .0001), with similar benefit across subgroups. The estimated 3-year disease-free survival rate was 71% in the chemotherapy arm and 46% in the surveillance arm. The median disease-free survival was 29.8 months and not reached, respectively.
The chemotherapy group also had a lower risk of metastasis or death when compared with the surveillance group (HR, 0.48; P = .0007). The 3-year event-free rates were 71% and 53%, respectively. Overall survival data are not yet mature.
“We acknowledge that disease-free survival is not regarded as a fully validated surrogate of overall survival after nephroureterectomy for UTUC,” the investigators wrote. “However, in a rare disease such as UTUC, a suitably powered trial with overall survival as the primary endpoint was not judged feasible. Although mature survival data (as a secondary endpoint) are not yet available, the large improvement in disease-free survival we noted for the primary endpoint, together with improved metastasis-free survival recorded as a secondary endpoint, strongly suggest that patients have better outcomes with chemotherapy than without.”
The incidence of acute grade 3 or worse treatment-emergent adverse events was 44% in the chemotherapy arm and 4% in the surveillance arm (P less than .0001). Quality of life was worse for the chemotherapy arm at 3 months (P = .0028), but that was no longer the case at 12 months (P = .20). There were no treatment-related deaths.
“[A]djuvant platinum-based chemotherapy should be adopted as a new standard of care for patients with locally advanced UTUC for whom systemic chemotherapy is not contraindicated,” the investigators recommended. “This regimen should be routinely considered for all patients in this population, and future studies should focus on combinations with novel agents in the adjuvant setting, which might further improve the prognosis for locally advanced UTUC.”
The trial was funded by Cancer Research UK. The authors disclosed relationships with numerous pharmaceutical companies.
SOURCE: Birtle A et al. Lancet. 2020 Mar 5. doi: 10.1016/S0140-6736(20)30415-3.
FROM THE LANCET
Fezolinetant safe, effective for menopausal vasomotor symptoms
The selective neurokinin 3 receptor antagonist Graeme L. Fraser, PhD, of Ogeda, a subsidiary of Astellas Pharma, and associates reported in Menopause.
The investigators conducted a randomized, double-blind, placebo-controlled, dose-ranging, parallel-group study between July 19, 2017, and Sept. 19, 2018, in 287 women who completed the full 12-week trial. The women were aged between 41 and 65 years, were menopausal, and had moderate to severe vasomotor symptoms (VMS) with an incidence of at least 50 episodes per week. The majority of the women were white, 25% were black, 1% were Asian, and 1% were “other.”
The reduction in VMS episodes in patients who received fezolinetant ranged from 1.9 to 3.5 episodes per day at week 4 and from 1.8 to 2.6 per day at week 12. The mean difference from placebo in VMS severity score was –0.4 to –1 at week 4 and was –0.2 to –0.6 at week 12. At least a 50% reduction in VMS frequency at week 12 was achieved by 81%-95% of patients who received fezolinetant, compared with 59% of those who received placebo.
Treatment-emergent adverse events were generally mild to moderate, with the most common events including nausea, diarrhea, fatigue, urinary tract infection, upper respiratory tract infections, sinusitis, headache, and cough. Of the five severe adverse events reported, only two were considered related to treatment – cholelithiasis and drug-induced liver injury. A total of 21 patients discontinued because of adverse events.
“Further evaluation of fezolinetant in larger and longer phase 3 trials of women with VMS associated with menopause is warranted to more fully characterize its efficacy and safety profile,” Dr. Fraser and colleagues concluded.
The study was funded by Astellas Pharma. The investigators reported numerous conflicts of interest with pharmaceutical companies.
SOURCE: Fraser GL et al. Menopause. 2020 Feb 24. doi: 10.1097/GME.0000000000001510.
The selective neurokinin 3 receptor antagonist Graeme L. Fraser, PhD, of Ogeda, a subsidiary of Astellas Pharma, and associates reported in Menopause.
The investigators conducted a randomized, double-blind, placebo-controlled, dose-ranging, parallel-group study between July 19, 2017, and Sept. 19, 2018, in 287 women who completed the full 12-week trial. The women were aged between 41 and 65 years, were menopausal, and had moderate to severe vasomotor symptoms (VMS) with an incidence of at least 50 episodes per week. The majority of the women were white, 25% were black, 1% were Asian, and 1% were “other.”
The reduction in VMS episodes in patients who received fezolinetant ranged from 1.9 to 3.5 episodes per day at week 4 and from 1.8 to 2.6 per day at week 12. The mean difference from placebo in VMS severity score was –0.4 to –1 at week 4 and was –0.2 to –0.6 at week 12. At least a 50% reduction in VMS frequency at week 12 was achieved by 81%-95% of patients who received fezolinetant, compared with 59% of those who received placebo.
Treatment-emergent adverse events were generally mild to moderate, with the most common events including nausea, diarrhea, fatigue, urinary tract infection, upper respiratory tract infections, sinusitis, headache, and cough. Of the five severe adverse events reported, only two were considered related to treatment – cholelithiasis and drug-induced liver injury. A total of 21 patients discontinued because of adverse events.
“Further evaluation of fezolinetant in larger and longer phase 3 trials of women with VMS associated with menopause is warranted to more fully characterize its efficacy and safety profile,” Dr. Fraser and colleagues concluded.
The study was funded by Astellas Pharma. The investigators reported numerous conflicts of interest with pharmaceutical companies.
SOURCE: Fraser GL et al. Menopause. 2020 Feb 24. doi: 10.1097/GME.0000000000001510.
The selective neurokinin 3 receptor antagonist Graeme L. Fraser, PhD, of Ogeda, a subsidiary of Astellas Pharma, and associates reported in Menopause.
The investigators conducted a randomized, double-blind, placebo-controlled, dose-ranging, parallel-group study between July 19, 2017, and Sept. 19, 2018, in 287 women who completed the full 12-week trial. The women were aged between 41 and 65 years, were menopausal, and had moderate to severe vasomotor symptoms (VMS) with an incidence of at least 50 episodes per week. The majority of the women were white, 25% were black, 1% were Asian, and 1% were “other.”
The reduction in VMS episodes in patients who received fezolinetant ranged from 1.9 to 3.5 episodes per day at week 4 and from 1.8 to 2.6 per day at week 12. The mean difference from placebo in VMS severity score was –0.4 to –1 at week 4 and was –0.2 to –0.6 at week 12. At least a 50% reduction in VMS frequency at week 12 was achieved by 81%-95% of patients who received fezolinetant, compared with 59% of those who received placebo.
Treatment-emergent adverse events were generally mild to moderate, with the most common events including nausea, diarrhea, fatigue, urinary tract infection, upper respiratory tract infections, sinusitis, headache, and cough. Of the five severe adverse events reported, only two were considered related to treatment – cholelithiasis and drug-induced liver injury. A total of 21 patients discontinued because of adverse events.
“Further evaluation of fezolinetant in larger and longer phase 3 trials of women with VMS associated with menopause is warranted to more fully characterize its efficacy and safety profile,” Dr. Fraser and colleagues concluded.
The study was funded by Astellas Pharma. The investigators reported numerous conflicts of interest with pharmaceutical companies.
SOURCE: Fraser GL et al. Menopause. 2020 Feb 24. doi: 10.1097/GME.0000000000001510.
FROM MENOPAUSE
High BMI does not complicate postpartum tubal ligation
GRAPEVINE, TEXAS – Higher body mass index is not associated with increased morbidity in women undergoing postpartum tubal ligation, according to a study of more than 1,000 patients.
John J. Byrne, MD, said at the Pregnancy Meeting. Dr. Byrne is affiliated with the department of obstetrics and gynecology at University of Texas Southwestern Medical Center in Dallas.
Physicians may recommend contraception within 6 weeks of delivery, but many patients do not attend postpartum visits. “One option for women who have completed childbearing is bilateral midsegment salpingectomy via minilaparotomy,” Dr. Byrne said at the Pregnancy Meeting, sponsored by the Society for Maternal-Fetal Medicine. “Offering this procedure immediately after delivery makes it available to women who face obstacles to follow-up care.”
The procedure entails the risk of anesthetic complications, bowel injury, and vascular injury. Subsequent pregnancy or ectopic pregnancy also may occur. Some centers will not perform the procedure if a patient’s size affects the surgeon’s ability to feel the relevant anatomy, Dr. Byrne said. “Although operative complications are presumed to be higher among obese women,” prior studies have not examined whether BMI affects rates of procedure completion, complication, or subsequent pregnancy, the researchers said.
To study this question, Dr. Byrne and colleagues examined data from women who requested postpartum sterilization following vaginal delivery at their center in 2018. The center uses the Parkland tubal ligation technique. The researchers assessed complication rates using a composite measure that included surgical complications (that is, blood transfusion, aborted procedure, or extension of incision), anesthetic complications, readmission, superficial or deep wound infection, venous thromboembolism, ileus or small bowel obstruction, incomplete transection, and subsequent pregnancy. The investigators used statistical tests to assess the relationship between BMI and morbidity.
In all, 1,014 patients underwent a postpartum tubal ligation; 17% had undergone prior abdominal surgery. The researchers classified patients’ BMI as normal (7% of the population), overweight (28%), class I obesity (38%), class II obesity (18%), or class III obesity (9%). A composite morbidity event occurred in 2%, and the proportion of patients with a complication did not significantly differ across BMI categories. No morbid events occurred in patients with normal BMI, which indicates “minimal risk” in this population, Dr. Byrne said. One incomplete transection occurred in a patient with class I obesity, and one subsequent pregnancy occurred in a patient with class II obesity. Estimated blood loss ranged from 9 mL in patients with normal BMI to 13 mL in patients with class III obesity, and length of surgery ranged from 32 minutes to 40 minutes. Neither difference is clinically significant, Dr. Byrne said.
“For the woman who desires permanent contraception, BMI should not impede her access to the procedure,” he noted.
The researchers had no relevant disclosures.
SOURCE: Byrne JJ et al. Am J Obstet Gynecol. 2020 Jan;222(1):S290, Abstract 442.
GRAPEVINE, TEXAS – Higher body mass index is not associated with increased morbidity in women undergoing postpartum tubal ligation, according to a study of more than 1,000 patients.
John J. Byrne, MD, said at the Pregnancy Meeting. Dr. Byrne is affiliated with the department of obstetrics and gynecology at University of Texas Southwestern Medical Center in Dallas.
Physicians may recommend contraception within 6 weeks of delivery, but many patients do not attend postpartum visits. “One option for women who have completed childbearing is bilateral midsegment salpingectomy via minilaparotomy,” Dr. Byrne said at the Pregnancy Meeting, sponsored by the Society for Maternal-Fetal Medicine. “Offering this procedure immediately after delivery makes it available to women who face obstacles to follow-up care.”
The procedure entails the risk of anesthetic complications, bowel injury, and vascular injury. Subsequent pregnancy or ectopic pregnancy also may occur. Some centers will not perform the procedure if a patient’s size affects the surgeon’s ability to feel the relevant anatomy, Dr. Byrne said. “Although operative complications are presumed to be higher among obese women,” prior studies have not examined whether BMI affects rates of procedure completion, complication, or subsequent pregnancy, the researchers said.
To study this question, Dr. Byrne and colleagues examined data from women who requested postpartum sterilization following vaginal delivery at their center in 2018. The center uses the Parkland tubal ligation technique. The researchers assessed complication rates using a composite measure that included surgical complications (that is, blood transfusion, aborted procedure, or extension of incision), anesthetic complications, readmission, superficial or deep wound infection, venous thromboembolism, ileus or small bowel obstruction, incomplete transection, and subsequent pregnancy. The investigators used statistical tests to assess the relationship between BMI and morbidity.
In all, 1,014 patients underwent a postpartum tubal ligation; 17% had undergone prior abdominal surgery. The researchers classified patients’ BMI as normal (7% of the population), overweight (28%), class I obesity (38%), class II obesity (18%), or class III obesity (9%). A composite morbidity event occurred in 2%, and the proportion of patients with a complication did not significantly differ across BMI categories. No morbid events occurred in patients with normal BMI, which indicates “minimal risk” in this population, Dr. Byrne said. One incomplete transection occurred in a patient with class I obesity, and one subsequent pregnancy occurred in a patient with class II obesity. Estimated blood loss ranged from 9 mL in patients with normal BMI to 13 mL in patients with class III obesity, and length of surgery ranged from 32 minutes to 40 minutes. Neither difference is clinically significant, Dr. Byrne said.
“For the woman who desires permanent contraception, BMI should not impede her access to the procedure,” he noted.
The researchers had no relevant disclosures.
SOURCE: Byrne JJ et al. Am J Obstet Gynecol. 2020 Jan;222(1):S290, Abstract 442.
GRAPEVINE, TEXAS – Higher body mass index is not associated with increased morbidity in women undergoing postpartum tubal ligation, according to a study of more than 1,000 patients.
John J. Byrne, MD, said at the Pregnancy Meeting. Dr. Byrne is affiliated with the department of obstetrics and gynecology at University of Texas Southwestern Medical Center in Dallas.
Physicians may recommend contraception within 6 weeks of delivery, but many patients do not attend postpartum visits. “One option for women who have completed childbearing is bilateral midsegment salpingectomy via minilaparotomy,” Dr. Byrne said at the Pregnancy Meeting, sponsored by the Society for Maternal-Fetal Medicine. “Offering this procedure immediately after delivery makes it available to women who face obstacles to follow-up care.”
The procedure entails the risk of anesthetic complications, bowel injury, and vascular injury. Subsequent pregnancy or ectopic pregnancy also may occur. Some centers will not perform the procedure if a patient’s size affects the surgeon’s ability to feel the relevant anatomy, Dr. Byrne said. “Although operative complications are presumed to be higher among obese women,” prior studies have not examined whether BMI affects rates of procedure completion, complication, or subsequent pregnancy, the researchers said.
To study this question, Dr. Byrne and colleagues examined data from women who requested postpartum sterilization following vaginal delivery at their center in 2018. The center uses the Parkland tubal ligation technique. The researchers assessed complication rates using a composite measure that included surgical complications (that is, blood transfusion, aborted procedure, or extension of incision), anesthetic complications, readmission, superficial or deep wound infection, venous thromboembolism, ileus or small bowel obstruction, incomplete transection, and subsequent pregnancy. The investigators used statistical tests to assess the relationship between BMI and morbidity.
In all, 1,014 patients underwent a postpartum tubal ligation; 17% had undergone prior abdominal surgery. The researchers classified patients’ BMI as normal (7% of the population), overweight (28%), class I obesity (38%), class II obesity (18%), or class III obesity (9%). A composite morbidity event occurred in 2%, and the proportion of patients with a complication did not significantly differ across BMI categories. No morbid events occurred in patients with normal BMI, which indicates “minimal risk” in this population, Dr. Byrne said. One incomplete transection occurred in a patient with class I obesity, and one subsequent pregnancy occurred in a patient with class II obesity. Estimated blood loss ranged from 9 mL in patients with normal BMI to 13 mL in patients with class III obesity, and length of surgery ranged from 32 minutes to 40 minutes. Neither difference is clinically significant, Dr. Byrne said.
“For the woman who desires permanent contraception, BMI should not impede her access to the procedure,” he noted.
The researchers had no relevant disclosures.
SOURCE: Byrne JJ et al. Am J Obstet Gynecol. 2020 Jan;222(1):S290, Abstract 442.
REPORTING FROM THE PREGNANCY MEETING
Prenatal test market booms as patients grapple with results
When she was 4 months pregnant, Angela Crawley waited for 30 minutes in a private room to hear the results of her noninvasive prenatal testing. Her ultrasound had been flagged as high risk by the radiologist and she agreed to undergo further testing to gather information on the health of her unborn child.
As she waited for her genetic counseling appointment, she noticed somber expressions on the faces of her health team and picked up on hushed tones.
It had taken 2 years to become pregnant and the joy she felt attending prenatal care appointments was fading into a sense of dread as she sat in that small room and the minutes ticked by.
Crawley – a scientist in the chronic disease program at the Ottawa Hospital Research Institute, assistant professor at the University of Ottawa, and adjunct research professor at Carleton University in Ontario, Canada – is more qualified than most patients to absorb health information and make appropriate decisions.
And yet, “I was completely unprepared,” she told Medscape Medical News as she reflected on what she now refers to as some of the darkest days of her life. “It was a nightmare and it was such a confusing, scary time.”
Crawley is among the more than 6 million women from at least 90 countries who have undergone noninvasive prenatal testing. During pregnancy, a mother’s bloodstream contains a mix of cell-free DNA from her own cells and from placental cells, which is usually identical to the DNA of the fetus. Analysis of cell-free DNA can lead to the early detection of genetic disorders.
Testing is most often used to look for chromosomal disorders that are caused by the presence of an extra chromosome, like in trisomy 21 in the case of Down syndrome or extra or missing copies of the X and Y chromosomes in other disorders. The accuracy of the test tends to vary, depending on the condition being assessed.
Cell-free DNA testing has reduced the number of invasive prenatal diagnostic procedures, some of which can lead to miscarriage, and this noninvasive option made sense to Crawley and was covered by government health insurance.
With a market projected to surpass $13 billion by the year 2027, some experts speculate that prenatal genetic testing is the most rapidly adopted test in human history. Globally, noninvasive prenatal tests cost $500 to $3,000 for patients who pay out of pocket, and all those screening options are amassing valuable genetic data troves.
The pioneer of noninvasive prenatal testing, Dennis Lo, PhD, from the Chinese University of Hong Kong, told Medscape Medical News that the success of using cell-free DNA came after a long, winding road of rejected grant applications and scientific skepticism.
“Initially, people did not think this would be useful for assessing chromosomal abnormalities because the thinking at the time was that we would need to count them,” Lo said.
But he was enchanted by early glimpses of the capability of cell-free DNA, and felt driven to pursue unconventional research ideas even though there were significant hurdles to overcome in the lab.
“We were detecting fetal Y chromosomes in women. At first, it was just scientific curiosity,” said Lo. “At the time, people worried that fetal cells would persist from one pregnancy to the next, but we discovered that fetal DNA actually clears very quickly and does not progress into the next pregnancy,” he explained. “This is very important because it won’t alter the accuracy of the test.”
Gripped by the scientific mystery, the researcher put in long hours at the lab. “I’m fortunate I have a very understanding wife who is herself a scientist,” he said. After a particularly long stretch without quality time together, Lo and his spouse, Alice Wong, went to see a Harry Potter movie.
As Lo viewed the Harry Potter H through 3D glasses, he was suddenly reminded of the male human karyotype.
“I saw the vertical stripes of the H and it hit me,” he told Medscape Medical News. “There are two sets of chromosomes.” The average human karyotype contains 22 pairs of autosomal chromosomes and one pair of sex chromosomes.
“Our complex genetic conundrum was cracked in the middle of a Harry Potter movie in a moment when I felt completely relaxed,” he recalled. “My wife said: ‘You can’t even watch a movie properly.’ ”
Back at the lab, Lo shared his Harry Potter–inspired concept and the team got to work.
In December 2019, Lo received the Fudan-Zhongzhi Science Award in Shanghai from Nobel laureate physicist Samuel Chao Chung Ting, chair of the award committee. The prize honors fundamental and groundbreaking achievements in biomedicine, and the laureate receives ¥3 million (about U.S. $428,550), donated by Zhongzhi Enterprise Group.
This honor was 30 years in the making, Lo told Medscape Medical News. “I’m pleased to experience public recognition and this is a high honor in China,” he added.
“Noninvasive prenatal testing is better than anything we’ve ever had before,” said Ronald Wapner, MD, from the Columbia University Irving Medical Center in New York City, who taught a course on the transition of prenatal diagnostics from amniocentesis to whole-genome sequencing at the recent Society for Maternal–Fetal Medicine 2020 Annual Pregnancy Meeting.
“We now have the capability to improve healthcare decision-making in utero and at birth,” he told Medscape Medical News. “It’s remarkable.”
But, Wapner said, the market grew too fast. “The National Institutes of Health didn’t even play a role in these fast-paced developments. Traditional governing bodies and authorities were bypassed as cytogenetic labs marketed directly to physicians and patients,” he explained.
One of the major problems with the rapid uptake in testing is a lack of preparation for patients like Crawley.
The clinician who delivered her test results was not feeling well, so “she spoke through a surgical mask,” Crawley reported. “I was trying to understand what she was saying, but it was an uncomfortable exchange.”
Crawley had undergone prenatal genetic testing because her ultrasound had shown irregularities in fetal leg measurements. The genetic tests confirmed no anomalies in the chromosome count, but that was it.
“There was no prognosis, just vague numbers that no one seemed to know what to do with,” Crawley recalled.
With concern about growth measurements, the conversation moved quickly to options, including termination. Crawley said the dialogue felt jarring and moved too quickly for her to process all the information and possible courses of action.
She was told she could terminate and “try again to get pregnant.” But Crawley was 39 years old and had been trying to conceive for 2 years.
“It was devastating,” she said. “No one sat down with me before this appointment to learn about my values or preferences, and I left that conversation with more questions than I had before I arrived. I went home and had one the worst weekends of my life. My husband and I felt so overwhelmed, grieved, and alone.”
Pretest counseling can be as important as any subsequent genetic counseling, said Blair Stevens, a prenatal expert from the National Society of Genetic Counselors and a genetic counselor at the University of Texas Health Science Center in Houston.
“Information is valuable, but it can also be toxic, depending on what individuals intend to do with what they learn,” she explained. “We cannot unknow or unhear details, so it’s really important to work with patients in advance to make sure their preferences guide any planning.”
Uncertainty can be very unsettling, she acknowledged. “It’s important to help patients balance any ambiguity, so if there is a 20% risk, there is also an 80% chance of another, perhaps more favorable, outcome.”
Most clinicians don’t have the time to fully assess patient goals and align counseling approaches to individual needs, Stevens explained. And public interest in prenatal testing has outpaced clinical best practices as competing labs race to expand offerings and add options to screening tests to grab a piece of the global market, which is now about 130 million births per year.
“These are not scientifically sound additions and we need more evidence,” Stevens said. “There is a right way to handle this, and labs and clinicians need to collaborate on responsible methods to test and integrate expanding options.”
The blue and pink elephant in the room
“The reality is that most people don’t have a super high risk for chromosomal irregularities,” said Stevens. “Most people are more interested in learning the sex of their baby in early pregnancy than in any actual desire for genetic information.” Noninvasive prenatal testing can detect fetal sex as early as 9 weeks into a pregnancy, whereas ultrasound might not detect it until about 18 weeks.
“Honestly? I think the growing popularity of gender-reveal parties is what is actually driving the push for more prenatal testing,” she added. “The problem is that a couple eager to learn the sex of their baby may wind up with way more information than they expected and have trouble processing unanticipated risk.”
In February, five national medical organizations in the United States partnered with the Reproductive Genetics Technology Consortium to develop consensus recommendations and guidelines for prenatal genetic testing.
The National Society of Genetic Counselors and the Society for Maternal–Fetal Medicine are among the new members that will provide a forum through which commercial laboratories can communicate about new technologies and obtain input and guidance on emerging options.
Wapner, who is a member of the consortium, said he hopes thought leaders will be at the forefront to guide this next chapter of prenatal screening. “So much money is pouring into all this testing; let’s make sure we are making the right, most essential screening decisions,” he said.
“Science typically advances more rapidly than the ethical and legal framework to support decision-making, and it’s important for society to put protections in place,” Lo acknowledged.
The misuse of screening and unethical sex-selection efforts in Asia and elsewhere in the world, where males are highly valued and females are more likely to be aborted, is dismaying, he told Medscape Medical News. “These are exploitations of the science.”
In addition to scientific misuse like sex selection, data breaches are becoming a huge concern as companies amass large amounts of valuable genetic information.
Data for ransom
In Canada, where Crawley took her test, LifeLabs – the country’s largest laboratory testing company and a provider of genetic testing – paid a ransom after a major cyberattack led to the theft of lab results for 85,000 people in Ontario and the personal information of 15 million customers.
LifeLabs paid an undisclosed sum to retrieve the data, the company reported on December 17, and hired cybersecurity experts to assess the damage. The company is offering security protection services, including identity theft and fraud protection insurance, to customers.
“This has served as a reminder that we need to stay ahead of cybercrime, which has become a pervasive issue around the world in all sectors,” Charles Brown, president and chief executive officer of LifeLabs, wrote in a letter to customers. “You entrust us with important health information, and we take that responsibility very seriously.”
The United States has led the world in the commercial push for more prenatal testing. Other countries in Europe, for example, have proceeded with caution and have integrated the technologies with more controls. Hong Kong, where the inventor of the test is based, has been among the slowest to adopt the practice.
“I have been lobbying for 8 years for Hong Kong to offer testing,” said Lo. “I think Hong Kong has been too slow to integrate, but the United States probably moved too quickly. There is a balance that I think countries like the Netherlands have found; they take the aim of screening into account, along with justice and societal aspects.”
“Ideally, we will develop a great pretest model triage tool to help guide patients through this process,” Stevens said. “And we have to make sure the data they receive are clinically useful and backed up by evidence to safeguard the care of every patient.”
The practice of medicine is meticulously designed to assess and mitigate risk, “but this sensible objective can also be extremely negative in focus, with not-so-great delivery of information,” she acknowledged. Each individual’s tolerance for uncertainty and ability to cope in the face of adversity varies. “These are complex conversations that require time and empathy, and the details matter,” she added.
“In my home state of Texas, where there is a large religious base, there is not as much drive for advance prenatal genetic information,” Stevens explained. “We see a real advocacy movement emerging and a need for information from patients first because these can’t really be clinician-led decisions,” she pointed out. “Patients come to us undergoing not just the physical changes of pregnancy, but also emotional transformation as they transition to become parents. They may be nauseous or already sleep-deprived and they need our help,” she added.
Crawley could feel the fluttering of fetal movements in her womb and said she felt connected to her child, but she remembered her trip to Ireland when she and her husband drank too much and they likely conceived. Irrational thoughts crept in: “Maybe it was something we did. What about my swimming; could it have been harmful?”
Apprehensions lingered as she waited to meet her specialist. Would the child grow and be able to walk? Be held back by disabling joint pain? Crawley sat down with her doctor at the high-risk clinic to discuss the possibilities.
“I don’t see anything to be alarmed about. She’s probably going to be small,” said the obstetrician.
“She?!” Crawley had opted not to learn the sex of her baby, unlike so many other parents she knew, but her hope for her baby’s good health soared above the accidental disclosure.
“Everything changed in that moment,” Crawley said. “I knew that we were going to be okay no matter what happened next.”
Crawley’s pregnancy progressed to term and she gave birth to a healthy baby girl who is now 3 years old and dances ballet. Her beloved daughter is shorter than some of the other dancers in her class, but her mom says she hasn’t missed a beat. “The world is a better place because my daughter is in it,” Crawley said. “This, I know for sure.”
This article first appeared on Medscape.com.
When she was 4 months pregnant, Angela Crawley waited for 30 minutes in a private room to hear the results of her noninvasive prenatal testing. Her ultrasound had been flagged as high risk by the radiologist and she agreed to undergo further testing to gather information on the health of her unborn child.
As she waited for her genetic counseling appointment, she noticed somber expressions on the faces of her health team and picked up on hushed tones.
It had taken 2 years to become pregnant and the joy she felt attending prenatal care appointments was fading into a sense of dread as she sat in that small room and the minutes ticked by.
Crawley – a scientist in the chronic disease program at the Ottawa Hospital Research Institute, assistant professor at the University of Ottawa, and adjunct research professor at Carleton University in Ontario, Canada – is more qualified than most patients to absorb health information and make appropriate decisions.
And yet, “I was completely unprepared,” she told Medscape Medical News as she reflected on what she now refers to as some of the darkest days of her life. “It was a nightmare and it was such a confusing, scary time.”
Crawley is among the more than 6 million women from at least 90 countries who have undergone noninvasive prenatal testing. During pregnancy, a mother’s bloodstream contains a mix of cell-free DNA from her own cells and from placental cells, which is usually identical to the DNA of the fetus. Analysis of cell-free DNA can lead to the early detection of genetic disorders.
Testing is most often used to look for chromosomal disorders that are caused by the presence of an extra chromosome, like in trisomy 21 in the case of Down syndrome or extra or missing copies of the X and Y chromosomes in other disorders. The accuracy of the test tends to vary, depending on the condition being assessed.
Cell-free DNA testing has reduced the number of invasive prenatal diagnostic procedures, some of which can lead to miscarriage, and this noninvasive option made sense to Crawley and was covered by government health insurance.
With a market projected to surpass $13 billion by the year 2027, some experts speculate that prenatal genetic testing is the most rapidly adopted test in human history. Globally, noninvasive prenatal tests cost $500 to $3,000 for patients who pay out of pocket, and all those screening options are amassing valuable genetic data troves.
The pioneer of noninvasive prenatal testing, Dennis Lo, PhD, from the Chinese University of Hong Kong, told Medscape Medical News that the success of using cell-free DNA came after a long, winding road of rejected grant applications and scientific skepticism.
“Initially, people did not think this would be useful for assessing chromosomal abnormalities because the thinking at the time was that we would need to count them,” Lo said.
But he was enchanted by early glimpses of the capability of cell-free DNA, and felt driven to pursue unconventional research ideas even though there were significant hurdles to overcome in the lab.
“We were detecting fetal Y chromosomes in women. At first, it was just scientific curiosity,” said Lo. “At the time, people worried that fetal cells would persist from one pregnancy to the next, but we discovered that fetal DNA actually clears very quickly and does not progress into the next pregnancy,” he explained. “This is very important because it won’t alter the accuracy of the test.”
Gripped by the scientific mystery, the researcher put in long hours at the lab. “I’m fortunate I have a very understanding wife who is herself a scientist,” he said. After a particularly long stretch without quality time together, Lo and his spouse, Alice Wong, went to see a Harry Potter movie.
As Lo viewed the Harry Potter H through 3D glasses, he was suddenly reminded of the male human karyotype.
“I saw the vertical stripes of the H and it hit me,” he told Medscape Medical News. “There are two sets of chromosomes.” The average human karyotype contains 22 pairs of autosomal chromosomes and one pair of sex chromosomes.
“Our complex genetic conundrum was cracked in the middle of a Harry Potter movie in a moment when I felt completely relaxed,” he recalled. “My wife said: ‘You can’t even watch a movie properly.’ ”
Back at the lab, Lo shared his Harry Potter–inspired concept and the team got to work.
In December 2019, Lo received the Fudan-Zhongzhi Science Award in Shanghai from Nobel laureate physicist Samuel Chao Chung Ting, chair of the award committee. The prize honors fundamental and groundbreaking achievements in biomedicine, and the laureate receives ¥3 million (about U.S. $428,550), donated by Zhongzhi Enterprise Group.
This honor was 30 years in the making, Lo told Medscape Medical News. “I’m pleased to experience public recognition and this is a high honor in China,” he added.
“Noninvasive prenatal testing is better than anything we’ve ever had before,” said Ronald Wapner, MD, from the Columbia University Irving Medical Center in New York City, who taught a course on the transition of prenatal diagnostics from amniocentesis to whole-genome sequencing at the recent Society for Maternal–Fetal Medicine 2020 Annual Pregnancy Meeting.
“We now have the capability to improve healthcare decision-making in utero and at birth,” he told Medscape Medical News. “It’s remarkable.”
But, Wapner said, the market grew too fast. “The National Institutes of Health didn’t even play a role in these fast-paced developments. Traditional governing bodies and authorities were bypassed as cytogenetic labs marketed directly to physicians and patients,” he explained.
One of the major problems with the rapid uptake in testing is a lack of preparation for patients like Crawley.
The clinician who delivered her test results was not feeling well, so “she spoke through a surgical mask,” Crawley reported. “I was trying to understand what she was saying, but it was an uncomfortable exchange.”
Crawley had undergone prenatal genetic testing because her ultrasound had shown irregularities in fetal leg measurements. The genetic tests confirmed no anomalies in the chromosome count, but that was it.
“There was no prognosis, just vague numbers that no one seemed to know what to do with,” Crawley recalled.
With concern about growth measurements, the conversation moved quickly to options, including termination. Crawley said the dialogue felt jarring and moved too quickly for her to process all the information and possible courses of action.
She was told she could terminate and “try again to get pregnant.” But Crawley was 39 years old and had been trying to conceive for 2 years.
“It was devastating,” she said. “No one sat down with me before this appointment to learn about my values or preferences, and I left that conversation with more questions than I had before I arrived. I went home and had one the worst weekends of my life. My husband and I felt so overwhelmed, grieved, and alone.”
Pretest counseling can be as important as any subsequent genetic counseling, said Blair Stevens, a prenatal expert from the National Society of Genetic Counselors and a genetic counselor at the University of Texas Health Science Center in Houston.
“Information is valuable, but it can also be toxic, depending on what individuals intend to do with what they learn,” she explained. “We cannot unknow or unhear details, so it’s really important to work with patients in advance to make sure their preferences guide any planning.”
Uncertainty can be very unsettling, she acknowledged. “It’s important to help patients balance any ambiguity, so if there is a 20% risk, there is also an 80% chance of another, perhaps more favorable, outcome.”
Most clinicians don’t have the time to fully assess patient goals and align counseling approaches to individual needs, Stevens explained. And public interest in prenatal testing has outpaced clinical best practices as competing labs race to expand offerings and add options to screening tests to grab a piece of the global market, which is now about 130 million births per year.
“These are not scientifically sound additions and we need more evidence,” Stevens said. “There is a right way to handle this, and labs and clinicians need to collaborate on responsible methods to test and integrate expanding options.”
The blue and pink elephant in the room
“The reality is that most people don’t have a super high risk for chromosomal irregularities,” said Stevens. “Most people are more interested in learning the sex of their baby in early pregnancy than in any actual desire for genetic information.” Noninvasive prenatal testing can detect fetal sex as early as 9 weeks into a pregnancy, whereas ultrasound might not detect it until about 18 weeks.
“Honestly? I think the growing popularity of gender-reveal parties is what is actually driving the push for more prenatal testing,” she added. “The problem is that a couple eager to learn the sex of their baby may wind up with way more information than they expected and have trouble processing unanticipated risk.”
In February, five national medical organizations in the United States partnered with the Reproductive Genetics Technology Consortium to develop consensus recommendations and guidelines for prenatal genetic testing.
The National Society of Genetic Counselors and the Society for Maternal–Fetal Medicine are among the new members that will provide a forum through which commercial laboratories can communicate about new technologies and obtain input and guidance on emerging options.
Wapner, who is a member of the consortium, said he hopes thought leaders will be at the forefront to guide this next chapter of prenatal screening. “So much money is pouring into all this testing; let’s make sure we are making the right, most essential screening decisions,” he said.
“Science typically advances more rapidly than the ethical and legal framework to support decision-making, and it’s important for society to put protections in place,” Lo acknowledged.
The misuse of screening and unethical sex-selection efforts in Asia and elsewhere in the world, where males are highly valued and females are more likely to be aborted, is dismaying, he told Medscape Medical News. “These are exploitations of the science.”
In addition to scientific misuse like sex selection, data breaches are becoming a huge concern as companies amass large amounts of valuable genetic information.
Data for ransom
In Canada, where Crawley took her test, LifeLabs – the country’s largest laboratory testing company and a provider of genetic testing – paid a ransom after a major cyberattack led to the theft of lab results for 85,000 people in Ontario and the personal information of 15 million customers.
LifeLabs paid an undisclosed sum to retrieve the data, the company reported on December 17, and hired cybersecurity experts to assess the damage. The company is offering security protection services, including identity theft and fraud protection insurance, to customers.
“This has served as a reminder that we need to stay ahead of cybercrime, which has become a pervasive issue around the world in all sectors,” Charles Brown, president and chief executive officer of LifeLabs, wrote in a letter to customers. “You entrust us with important health information, and we take that responsibility very seriously.”
The United States has led the world in the commercial push for more prenatal testing. Other countries in Europe, for example, have proceeded with caution and have integrated the technologies with more controls. Hong Kong, where the inventor of the test is based, has been among the slowest to adopt the practice.
“I have been lobbying for 8 years for Hong Kong to offer testing,” said Lo. “I think Hong Kong has been too slow to integrate, but the United States probably moved too quickly. There is a balance that I think countries like the Netherlands have found; they take the aim of screening into account, along with justice and societal aspects.”
“Ideally, we will develop a great pretest model triage tool to help guide patients through this process,” Stevens said. “And we have to make sure the data they receive are clinically useful and backed up by evidence to safeguard the care of every patient.”
The practice of medicine is meticulously designed to assess and mitigate risk, “but this sensible objective can also be extremely negative in focus, with not-so-great delivery of information,” she acknowledged. Each individual’s tolerance for uncertainty and ability to cope in the face of adversity varies. “These are complex conversations that require time and empathy, and the details matter,” she added.
“In my home state of Texas, where there is a large religious base, there is not as much drive for advance prenatal genetic information,” Stevens explained. “We see a real advocacy movement emerging and a need for information from patients first because these can’t really be clinician-led decisions,” she pointed out. “Patients come to us undergoing not just the physical changes of pregnancy, but also emotional transformation as they transition to become parents. They may be nauseous or already sleep-deprived and they need our help,” she added.
Crawley could feel the fluttering of fetal movements in her womb and said she felt connected to her child, but she remembered her trip to Ireland when she and her husband drank too much and they likely conceived. Irrational thoughts crept in: “Maybe it was something we did. What about my swimming; could it have been harmful?”
Apprehensions lingered as she waited to meet her specialist. Would the child grow and be able to walk? Be held back by disabling joint pain? Crawley sat down with her doctor at the high-risk clinic to discuss the possibilities.
“I don’t see anything to be alarmed about. She’s probably going to be small,” said the obstetrician.
“She?!” Crawley had opted not to learn the sex of her baby, unlike so many other parents she knew, but her hope for her baby’s good health soared above the accidental disclosure.
“Everything changed in that moment,” Crawley said. “I knew that we were going to be okay no matter what happened next.”
Crawley’s pregnancy progressed to term and she gave birth to a healthy baby girl who is now 3 years old and dances ballet. Her beloved daughter is shorter than some of the other dancers in her class, but her mom says she hasn’t missed a beat. “The world is a better place because my daughter is in it,” Crawley said. “This, I know for sure.”
This article first appeared on Medscape.com.
When she was 4 months pregnant, Angela Crawley waited for 30 minutes in a private room to hear the results of her noninvasive prenatal testing. Her ultrasound had been flagged as high risk by the radiologist and she agreed to undergo further testing to gather information on the health of her unborn child.
As she waited for her genetic counseling appointment, she noticed somber expressions on the faces of her health team and picked up on hushed tones.
It had taken 2 years to become pregnant and the joy she felt attending prenatal care appointments was fading into a sense of dread as she sat in that small room and the minutes ticked by.
Crawley – a scientist in the chronic disease program at the Ottawa Hospital Research Institute, assistant professor at the University of Ottawa, and adjunct research professor at Carleton University in Ontario, Canada – is more qualified than most patients to absorb health information and make appropriate decisions.
And yet, “I was completely unprepared,” she told Medscape Medical News as she reflected on what she now refers to as some of the darkest days of her life. “It was a nightmare and it was such a confusing, scary time.”
Crawley is among the more than 6 million women from at least 90 countries who have undergone noninvasive prenatal testing. During pregnancy, a mother’s bloodstream contains a mix of cell-free DNA from her own cells and from placental cells, which is usually identical to the DNA of the fetus. Analysis of cell-free DNA can lead to the early detection of genetic disorders.
Testing is most often used to look for chromosomal disorders that are caused by the presence of an extra chromosome, like in trisomy 21 in the case of Down syndrome or extra or missing copies of the X and Y chromosomes in other disorders. The accuracy of the test tends to vary, depending on the condition being assessed.
Cell-free DNA testing has reduced the number of invasive prenatal diagnostic procedures, some of which can lead to miscarriage, and this noninvasive option made sense to Crawley and was covered by government health insurance.
With a market projected to surpass $13 billion by the year 2027, some experts speculate that prenatal genetic testing is the most rapidly adopted test in human history. Globally, noninvasive prenatal tests cost $500 to $3,000 for patients who pay out of pocket, and all those screening options are amassing valuable genetic data troves.
The pioneer of noninvasive prenatal testing, Dennis Lo, PhD, from the Chinese University of Hong Kong, told Medscape Medical News that the success of using cell-free DNA came after a long, winding road of rejected grant applications and scientific skepticism.
“Initially, people did not think this would be useful for assessing chromosomal abnormalities because the thinking at the time was that we would need to count them,” Lo said.
But he was enchanted by early glimpses of the capability of cell-free DNA, and felt driven to pursue unconventional research ideas even though there were significant hurdles to overcome in the lab.
“We were detecting fetal Y chromosomes in women. At first, it was just scientific curiosity,” said Lo. “At the time, people worried that fetal cells would persist from one pregnancy to the next, but we discovered that fetal DNA actually clears very quickly and does not progress into the next pregnancy,” he explained. “This is very important because it won’t alter the accuracy of the test.”
Gripped by the scientific mystery, the researcher put in long hours at the lab. “I’m fortunate I have a very understanding wife who is herself a scientist,” he said. After a particularly long stretch without quality time together, Lo and his spouse, Alice Wong, went to see a Harry Potter movie.
As Lo viewed the Harry Potter H through 3D glasses, he was suddenly reminded of the male human karyotype.
“I saw the vertical stripes of the H and it hit me,” he told Medscape Medical News. “There are two sets of chromosomes.” The average human karyotype contains 22 pairs of autosomal chromosomes and one pair of sex chromosomes.
“Our complex genetic conundrum was cracked in the middle of a Harry Potter movie in a moment when I felt completely relaxed,” he recalled. “My wife said: ‘You can’t even watch a movie properly.’ ”
Back at the lab, Lo shared his Harry Potter–inspired concept and the team got to work.
In December 2019, Lo received the Fudan-Zhongzhi Science Award in Shanghai from Nobel laureate physicist Samuel Chao Chung Ting, chair of the award committee. The prize honors fundamental and groundbreaking achievements in biomedicine, and the laureate receives ¥3 million (about U.S. $428,550), donated by Zhongzhi Enterprise Group.
This honor was 30 years in the making, Lo told Medscape Medical News. “I’m pleased to experience public recognition and this is a high honor in China,” he added.
“Noninvasive prenatal testing is better than anything we’ve ever had before,” said Ronald Wapner, MD, from the Columbia University Irving Medical Center in New York City, who taught a course on the transition of prenatal diagnostics from amniocentesis to whole-genome sequencing at the recent Society for Maternal–Fetal Medicine 2020 Annual Pregnancy Meeting.
“We now have the capability to improve healthcare decision-making in utero and at birth,” he told Medscape Medical News. “It’s remarkable.”
But, Wapner said, the market grew too fast. “The National Institutes of Health didn’t even play a role in these fast-paced developments. Traditional governing bodies and authorities were bypassed as cytogenetic labs marketed directly to physicians and patients,” he explained.
One of the major problems with the rapid uptake in testing is a lack of preparation for patients like Crawley.
The clinician who delivered her test results was not feeling well, so “she spoke through a surgical mask,” Crawley reported. “I was trying to understand what she was saying, but it was an uncomfortable exchange.”
Crawley had undergone prenatal genetic testing because her ultrasound had shown irregularities in fetal leg measurements. The genetic tests confirmed no anomalies in the chromosome count, but that was it.
“There was no prognosis, just vague numbers that no one seemed to know what to do with,” Crawley recalled.
With concern about growth measurements, the conversation moved quickly to options, including termination. Crawley said the dialogue felt jarring and moved too quickly for her to process all the information and possible courses of action.
She was told she could terminate and “try again to get pregnant.” But Crawley was 39 years old and had been trying to conceive for 2 years.
“It was devastating,” she said. “No one sat down with me before this appointment to learn about my values or preferences, and I left that conversation with more questions than I had before I arrived. I went home and had one the worst weekends of my life. My husband and I felt so overwhelmed, grieved, and alone.”
Pretest counseling can be as important as any subsequent genetic counseling, said Blair Stevens, a prenatal expert from the National Society of Genetic Counselors and a genetic counselor at the University of Texas Health Science Center in Houston.
“Information is valuable, but it can also be toxic, depending on what individuals intend to do with what they learn,” she explained. “We cannot unknow or unhear details, so it’s really important to work with patients in advance to make sure their preferences guide any planning.”
Uncertainty can be very unsettling, she acknowledged. “It’s important to help patients balance any ambiguity, so if there is a 20% risk, there is also an 80% chance of another, perhaps more favorable, outcome.”
Most clinicians don’t have the time to fully assess patient goals and align counseling approaches to individual needs, Stevens explained. And public interest in prenatal testing has outpaced clinical best practices as competing labs race to expand offerings and add options to screening tests to grab a piece of the global market, which is now about 130 million births per year.
“These are not scientifically sound additions and we need more evidence,” Stevens said. “There is a right way to handle this, and labs and clinicians need to collaborate on responsible methods to test and integrate expanding options.”
The blue and pink elephant in the room
“The reality is that most people don’t have a super high risk for chromosomal irregularities,” said Stevens. “Most people are more interested in learning the sex of their baby in early pregnancy than in any actual desire for genetic information.” Noninvasive prenatal testing can detect fetal sex as early as 9 weeks into a pregnancy, whereas ultrasound might not detect it until about 18 weeks.
“Honestly? I think the growing popularity of gender-reveal parties is what is actually driving the push for more prenatal testing,” she added. “The problem is that a couple eager to learn the sex of their baby may wind up with way more information than they expected and have trouble processing unanticipated risk.”
In February, five national medical organizations in the United States partnered with the Reproductive Genetics Technology Consortium to develop consensus recommendations and guidelines for prenatal genetic testing.
The National Society of Genetic Counselors and the Society for Maternal–Fetal Medicine are among the new members that will provide a forum through which commercial laboratories can communicate about new technologies and obtain input and guidance on emerging options.
Wapner, who is a member of the consortium, said he hopes thought leaders will be at the forefront to guide this next chapter of prenatal screening. “So much money is pouring into all this testing; let’s make sure we are making the right, most essential screening decisions,” he said.
“Science typically advances more rapidly than the ethical and legal framework to support decision-making, and it’s important for society to put protections in place,” Lo acknowledged.
The misuse of screening and unethical sex-selection efforts in Asia and elsewhere in the world, where males are highly valued and females are more likely to be aborted, is dismaying, he told Medscape Medical News. “These are exploitations of the science.”
In addition to scientific misuse like sex selection, data breaches are becoming a huge concern as companies amass large amounts of valuable genetic information.
Data for ransom
In Canada, where Crawley took her test, LifeLabs – the country’s largest laboratory testing company and a provider of genetic testing – paid a ransom after a major cyberattack led to the theft of lab results for 85,000 people in Ontario and the personal information of 15 million customers.
LifeLabs paid an undisclosed sum to retrieve the data, the company reported on December 17, and hired cybersecurity experts to assess the damage. The company is offering security protection services, including identity theft and fraud protection insurance, to customers.
“This has served as a reminder that we need to stay ahead of cybercrime, which has become a pervasive issue around the world in all sectors,” Charles Brown, president and chief executive officer of LifeLabs, wrote in a letter to customers. “You entrust us with important health information, and we take that responsibility very seriously.”
The United States has led the world in the commercial push for more prenatal testing. Other countries in Europe, for example, have proceeded with caution and have integrated the technologies with more controls. Hong Kong, where the inventor of the test is based, has been among the slowest to adopt the practice.
“I have been lobbying for 8 years for Hong Kong to offer testing,” said Lo. “I think Hong Kong has been too slow to integrate, but the United States probably moved too quickly. There is a balance that I think countries like the Netherlands have found; they take the aim of screening into account, along with justice and societal aspects.”
“Ideally, we will develop a great pretest model triage tool to help guide patients through this process,” Stevens said. “And we have to make sure the data they receive are clinically useful and backed up by evidence to safeguard the care of every patient.”
The practice of medicine is meticulously designed to assess and mitigate risk, “but this sensible objective can also be extremely negative in focus, with not-so-great delivery of information,” she acknowledged. Each individual’s tolerance for uncertainty and ability to cope in the face of adversity varies. “These are complex conversations that require time and empathy, and the details matter,” she added.
“In my home state of Texas, where there is a large religious base, there is not as much drive for advance prenatal genetic information,” Stevens explained. “We see a real advocacy movement emerging and a need for information from patients first because these can’t really be clinician-led decisions,” she pointed out. “Patients come to us undergoing not just the physical changes of pregnancy, but also emotional transformation as they transition to become parents. They may be nauseous or already sleep-deprived and they need our help,” she added.
Crawley could feel the fluttering of fetal movements in her womb and said she felt connected to her child, but she remembered her trip to Ireland when she and her husband drank too much and they likely conceived. Irrational thoughts crept in: “Maybe it was something we did. What about my swimming; could it have been harmful?”
Apprehensions lingered as she waited to meet her specialist. Would the child grow and be able to walk? Be held back by disabling joint pain? Crawley sat down with her doctor at the high-risk clinic to discuss the possibilities.
“I don’t see anything to be alarmed about. She’s probably going to be small,” said the obstetrician.
“She?!” Crawley had opted not to learn the sex of her baby, unlike so many other parents she knew, but her hope for her baby’s good health soared above the accidental disclosure.
“Everything changed in that moment,” Crawley said. “I knew that we were going to be okay no matter what happened next.”
Crawley’s pregnancy progressed to term and she gave birth to a healthy baby girl who is now 3 years old and dances ballet. Her beloved daughter is shorter than some of the other dancers in her class, but her mom says she hasn’t missed a beat. “The world is a better place because my daughter is in it,” Crawley said. “This, I know for sure.”
This article first appeared on Medscape.com.
Colorectal cancer burden rises in younger age groups
Current trends in the incidence and mortality of colorectal cancer (CRC) in the United States suggest CRC will become a disease that largely affects young and middle-aged adults, according to a report published in CA: A Cancer Journal for Clinicians.
As the second leading cause of cancer-related death in the United States, and with modifiable risk factors accounting for over 50% of cases and deaths, CRC is largely a preventable disease, explained study author Rebecca L. Siegel, of the American Cancer Society, and colleagues.
According to the investigators, CRC incidence dropped by 3.3% per year from 2011 through 2016 among individuals aged 65 years or older, but the opposite was observed for those aged 50-64 years, with rates increasing by 1% per year. The increase was even greater for those younger than 50 years, with an increase of 2.2% per year.
The CRC incidence from 2012 through 2016 was highest among Alaska Natives (89 cases per 100,000 persons) and lowest among Asian/Pacific Islanders (30 cases per 100,000 persons).
“CRC has been the most commonly diagnosed cancer in Alaska Natives since the early 1970s for reasons that are unknown but may include a higher prevalence of risk factors,” the investigators wrote.
The risk of developing CRC is related to several factors, including obesity, vitamin D deficiency, diabetes, smoking, and other dietary factors, the team further explained.
Among those aged 65 years or older, CRC death rates decreased by 3% per year from 2008 through 2017. For those aged 50-64 years, death rates dropped by 0.6% per year. In contrast, death rates rose by 1.3% per year for those younger than 50 years.
“The uptick in young adults, which is most rapid among non-Hispanic whites (2% per year), began around 2004 and was preceded by declines of 1% to 2% per year since at least 1975,” the investigators wrote.
The reduction in incidence and mortality among older adults is partially attributable to higher uptake of CRC screening. According to recent data, CRC screening rates were lower for those aged 50-64 years compared with individuals aged 65 years and older.
Based on current recommendations from the American Cancer Society, CRC screening should begin at age 45, with some higher-risk patients starting at age 40.
“Progress against CRC can be accelerated by increasing access to guideline-recommended screening and high quality treatment, particularly among Alaska Natives, and elucidating causes for rising incidence in young and middle-aged adults,” the investigators concluded.
The authors disclosed financial affiliations with the American Cancer Society, which funded the study, as well as Array Biopharma, Bayer, RGenix, Tesaro, and Seattle Genetics.
SOURCE: Siegel RL et al. CA Cancer J Clin. 2020 Mar 5. doi: 10.3322/caac.21601.
Current trends in the incidence and mortality of colorectal cancer (CRC) in the United States suggest CRC will become a disease that largely affects young and middle-aged adults, according to a report published in CA: A Cancer Journal for Clinicians.
As the second leading cause of cancer-related death in the United States, and with modifiable risk factors accounting for over 50% of cases and deaths, CRC is largely a preventable disease, explained study author Rebecca L. Siegel, of the American Cancer Society, and colleagues.
According to the investigators, CRC incidence dropped by 3.3% per year from 2011 through 2016 among individuals aged 65 years or older, but the opposite was observed for those aged 50-64 years, with rates increasing by 1% per year. The increase was even greater for those younger than 50 years, with an increase of 2.2% per year.
The CRC incidence from 2012 through 2016 was highest among Alaska Natives (89 cases per 100,000 persons) and lowest among Asian/Pacific Islanders (30 cases per 100,000 persons).
“CRC has been the most commonly diagnosed cancer in Alaska Natives since the early 1970s for reasons that are unknown but may include a higher prevalence of risk factors,” the investigators wrote.
The risk of developing CRC is related to several factors, including obesity, vitamin D deficiency, diabetes, smoking, and other dietary factors, the team further explained.
Among those aged 65 years or older, CRC death rates decreased by 3% per year from 2008 through 2017. For those aged 50-64 years, death rates dropped by 0.6% per year. In contrast, death rates rose by 1.3% per year for those younger than 50 years.
“The uptick in young adults, which is most rapid among non-Hispanic whites (2% per year), began around 2004 and was preceded by declines of 1% to 2% per year since at least 1975,” the investigators wrote.
The reduction in incidence and mortality among older adults is partially attributable to higher uptake of CRC screening. According to recent data, CRC screening rates were lower for those aged 50-64 years compared with individuals aged 65 years and older.
Based on current recommendations from the American Cancer Society, CRC screening should begin at age 45, with some higher-risk patients starting at age 40.
“Progress against CRC can be accelerated by increasing access to guideline-recommended screening and high quality treatment, particularly among Alaska Natives, and elucidating causes for rising incidence in young and middle-aged adults,” the investigators concluded.
The authors disclosed financial affiliations with the American Cancer Society, which funded the study, as well as Array Biopharma, Bayer, RGenix, Tesaro, and Seattle Genetics.
SOURCE: Siegel RL et al. CA Cancer J Clin. 2020 Mar 5. doi: 10.3322/caac.21601.
Current trends in the incidence and mortality of colorectal cancer (CRC) in the United States suggest CRC will become a disease that largely affects young and middle-aged adults, according to a report published in CA: A Cancer Journal for Clinicians.
As the second leading cause of cancer-related death in the United States, and with modifiable risk factors accounting for over 50% of cases and deaths, CRC is largely a preventable disease, explained study author Rebecca L. Siegel, of the American Cancer Society, and colleagues.
According to the investigators, CRC incidence dropped by 3.3% per year from 2011 through 2016 among individuals aged 65 years or older, but the opposite was observed for those aged 50-64 years, with rates increasing by 1% per year. The increase was even greater for those younger than 50 years, with an increase of 2.2% per year.
The CRC incidence from 2012 through 2016 was highest among Alaska Natives (89 cases per 100,000 persons) and lowest among Asian/Pacific Islanders (30 cases per 100,000 persons).
“CRC has been the most commonly diagnosed cancer in Alaska Natives since the early 1970s for reasons that are unknown but may include a higher prevalence of risk factors,” the investigators wrote.
The risk of developing CRC is related to several factors, including obesity, vitamin D deficiency, diabetes, smoking, and other dietary factors, the team further explained.
Among those aged 65 years or older, CRC death rates decreased by 3% per year from 2008 through 2017. For those aged 50-64 years, death rates dropped by 0.6% per year. In contrast, death rates rose by 1.3% per year for those younger than 50 years.
“The uptick in young adults, which is most rapid among non-Hispanic whites (2% per year), began around 2004 and was preceded by declines of 1% to 2% per year since at least 1975,” the investigators wrote.
The reduction in incidence and mortality among older adults is partially attributable to higher uptake of CRC screening. According to recent data, CRC screening rates were lower for those aged 50-64 years compared with individuals aged 65 years and older.
Based on current recommendations from the American Cancer Society, CRC screening should begin at age 45, with some higher-risk patients starting at age 40.
“Progress against CRC can be accelerated by increasing access to guideline-recommended screening and high quality treatment, particularly among Alaska Natives, and elucidating causes for rising incidence in young and middle-aged adults,” the investigators concluded.
The authors disclosed financial affiliations with the American Cancer Society, which funded the study, as well as Array Biopharma, Bayer, RGenix, Tesaro, and Seattle Genetics.
SOURCE: Siegel RL et al. CA Cancer J Clin. 2020 Mar 5. doi: 10.3322/caac.21601.
FROM CA: A CANCER JOURNAL FOR CLINICIANS
Researchers honored by ACS, IASLC
The International Association for the Study of Lung Cancer (IASLC) is naming the Translational Research Lectureship Award after Fred R. Hirsch, MD, PhD, of the Tisch Cancer Institute and Icahn School of Medicine at Mount Sinai, New York.
Dr. Hirsch was a longtime member of the IASLC and served as chief executive officer of the association from 2013 through October 2018. During this time, Dr. Hirsch grew the IASLC staff from 5 to 23 people and doubled the organization’s membership. The IASLC World Conference on Lung Cancer became an annual meeting under Dr. Hirsch’s direction and reported record attendance, according to their website.
The recipient of the Fred R. Hirsch Lectureship Award for Translational Research will be recognized at the IASLC 2020 World Conference on Lung Cancer, which is set to take place in Singapore on August 9-12, 2020.
In other news, the American Cancer Society (ACS) announced that it has awarded the 2020 Medal of Honor to three researchers. The recipients will be recognized at a black-tie ceremony in New York on Nov. 11, 2020.
Lewis C. Cantley, PhD, of Weill Cornell Medicine, New York, won the Medal of Honor for Basic Research. This award honors researchers whose work will have a “lasting impact on the cancer field” or who have made important discoveries or inventions within the field, according to the ACS.
Dr. Cantley won the award for research that has improved our understanding of cancer metabolism. He is known for his contributions to the discovery and study of phosphoinositide 3-kinase, which plays a role in many cancers and has become a target for therapies.
Leslie Bernstein, PhD, of City of Hope National Medical Center in Duarte, Calif., has won the Medal of Honor in Cancer Control. This award honors individuals who have made strides in public health, public communication, or public policy that have had an impact on cancer control.
Dr. Bernstein won the award for her work linking physical activity to a reduced risk of breast cancer. She is currently investigating links between hormone exposures, physical activity, obesity, and cancer, as well as examining how breast cancer impacts patients’ lives after treatment.
Ching-Hon Pui, MD, of St. Jude Children’s Research Hospital in Memphis, Tenn., has won the Medal of Honor in Clinical Research. This award honors researchers whose work has significantly improved cancer patients’ outcomes.
Dr. Pui won the award for his work in childhood acute lymphoblastic leukemia. Dr. Pui’s work has led to increased global treatment access, improved survival rates, and better quality of life for patients with childhood acute lymphoblastic leukemia.
The International Association for the Study of Lung Cancer (IASLC) is naming the Translational Research Lectureship Award after Fred R. Hirsch, MD, PhD, of the Tisch Cancer Institute and Icahn School of Medicine at Mount Sinai, New York.
Dr. Hirsch was a longtime member of the IASLC and served as chief executive officer of the association from 2013 through October 2018. During this time, Dr. Hirsch grew the IASLC staff from 5 to 23 people and doubled the organization’s membership. The IASLC World Conference on Lung Cancer became an annual meeting under Dr. Hirsch’s direction and reported record attendance, according to their website.
The recipient of the Fred R. Hirsch Lectureship Award for Translational Research will be recognized at the IASLC 2020 World Conference on Lung Cancer, which is set to take place in Singapore on August 9-12, 2020.
In other news, the American Cancer Society (ACS) announced that it has awarded the 2020 Medal of Honor to three researchers. The recipients will be recognized at a black-tie ceremony in New York on Nov. 11, 2020.
Lewis C. Cantley, PhD, of Weill Cornell Medicine, New York, won the Medal of Honor for Basic Research. This award honors researchers whose work will have a “lasting impact on the cancer field” or who have made important discoveries or inventions within the field, according to the ACS.
Dr. Cantley won the award for research that has improved our understanding of cancer metabolism. He is known for his contributions to the discovery and study of phosphoinositide 3-kinase, which plays a role in many cancers and has become a target for therapies.
Leslie Bernstein, PhD, of City of Hope National Medical Center in Duarte, Calif., has won the Medal of Honor in Cancer Control. This award honors individuals who have made strides in public health, public communication, or public policy that have had an impact on cancer control.
Dr. Bernstein won the award for her work linking physical activity to a reduced risk of breast cancer. She is currently investigating links between hormone exposures, physical activity, obesity, and cancer, as well as examining how breast cancer impacts patients’ lives after treatment.
Ching-Hon Pui, MD, of St. Jude Children’s Research Hospital in Memphis, Tenn., has won the Medal of Honor in Clinical Research. This award honors researchers whose work has significantly improved cancer patients’ outcomes.
Dr. Pui won the award for his work in childhood acute lymphoblastic leukemia. Dr. Pui’s work has led to increased global treatment access, improved survival rates, and better quality of life for patients with childhood acute lymphoblastic leukemia.
The International Association for the Study of Lung Cancer (IASLC) is naming the Translational Research Lectureship Award after Fred R. Hirsch, MD, PhD, of the Tisch Cancer Institute and Icahn School of Medicine at Mount Sinai, New York.
Dr. Hirsch was a longtime member of the IASLC and served as chief executive officer of the association from 2013 through October 2018. During this time, Dr. Hirsch grew the IASLC staff from 5 to 23 people and doubled the organization’s membership. The IASLC World Conference on Lung Cancer became an annual meeting under Dr. Hirsch’s direction and reported record attendance, according to their website.
The recipient of the Fred R. Hirsch Lectureship Award for Translational Research will be recognized at the IASLC 2020 World Conference on Lung Cancer, which is set to take place in Singapore on August 9-12, 2020.
In other news, the American Cancer Society (ACS) announced that it has awarded the 2020 Medal of Honor to three researchers. The recipients will be recognized at a black-tie ceremony in New York on Nov. 11, 2020.
Lewis C. Cantley, PhD, of Weill Cornell Medicine, New York, won the Medal of Honor for Basic Research. This award honors researchers whose work will have a “lasting impact on the cancer field” or who have made important discoveries or inventions within the field, according to the ACS.
Dr. Cantley won the award for research that has improved our understanding of cancer metabolism. He is known for his contributions to the discovery and study of phosphoinositide 3-kinase, which plays a role in many cancers and has become a target for therapies.
Leslie Bernstein, PhD, of City of Hope National Medical Center in Duarte, Calif., has won the Medal of Honor in Cancer Control. This award honors individuals who have made strides in public health, public communication, or public policy that have had an impact on cancer control.
Dr. Bernstein won the award for her work linking physical activity to a reduced risk of breast cancer. She is currently investigating links between hormone exposures, physical activity, obesity, and cancer, as well as examining how breast cancer impacts patients’ lives after treatment.
Ching-Hon Pui, MD, of St. Jude Children’s Research Hospital in Memphis, Tenn., has won the Medal of Honor in Clinical Research. This award honors researchers whose work has significantly improved cancer patients’ outcomes.
Dr. Pui won the award for his work in childhood acute lymphoblastic leukemia. Dr. Pui’s work has led to increased global treatment access, improved survival rates, and better quality of life for patients with childhood acute lymphoblastic leukemia.
Stress-related disorders linked to later neurodegenerative diseases
Individuals with posttraumatic stress disorder (PTSD), acute stress reaction, adjustment disorder, or other stress reactions had an 80% increased risk of vascular neurodegenerative diseases, according to results of the study, which was based on Swedish population registry data.
Risk of primary neurodegenerative diseases was increased as well in people with those conditions, but only by 31%, according to lead author Huan Song, MD, PhD, of Sichuan University in Chengdu, China.
“The stronger association observed for neurodegenerative diseases with a vascular component, compared with primary neurodegenerative diseases, suggested a considerable role of a possible cerebrovascular pathway,” Dr. Song and coauthors said in a report on the study appearing in JAMA Neurology.
While some previous studies have linked stress-related disorders to neurodegenerative diseases – particularly PTSD and dementia – this is believed to be the first, according to the investigators, to comprehensively evaluate all stress-related disorders in relation to the most common neurodegenerative conditions.
When considering neurodegenerative conditions separately, they found a statistically significant association between stress-related disorders and Alzheimer’s disease, while linkages with Parkinson’s disease and amyotrophic lateral sclerosis (ALS) were “comparable” but associations did not reach statistical significance, according to investigators.
Based on these findings, stress reduction should be recommended in addition to daily physical activity, mental activity, and a heart-healthy diet to potentially reduce risk of onset or worsening of cognitive decline, according to Chun Lim, MD, PhD, medical director of the cognitive neurology unit at Beth Israel Deaconess Medical Center in Boston.
“We don’t really have great evidence that anything slows down the progression of Alzheimer’s disease, but there are some suggestions that for people who lead heart-healthy lifestyles or adhere to a Mediterranean diet, fewer develop cognitive issues over 5-10 years,” Dr. Lim said in an interview. “Because of this paper, stress reduction may be one additional way to hopefully help these patients these patients that have or are concerned about cognitive issues.”
The population-matched cohort of the study included 61,748 individuals with stress-related disorders and 595,335 matched individuals without those disorders, while the sibling-matched cohort included 44,839 individuals with those disorders and 78,482 without. The median age at the start of follow-up was 47 years and 39.4% of those with stress-related disorders were male.
During follow-up, the incidence of neurodegenerative diseases per 1,000 person-years was 1.50 for individuals with stress-related disorders, versus 0.82 for those without stress-related disorders, according to the report. Risk of primary neurodegenerative diseases was increased among those with stress-related disorders, compared with those without, with a hazard ratio of 1.31 (95% confidence interval, 1.15-1.48). However, the risk of vascular neurodegenerative diseases was significantly higher, with an HR of 1.80 (95% CI, 1.40-2.31; P = .03 for the difference between hazard ratios).
Results of the matched sibling cohort supported results of the population-matched cohort, though the elevated risk of vascular neurodegenerative diseases among those with stress-related disorders was “slightly lower” than in the population-based cohort, Dr. Song and coauthors wrote in their report.
Beyond causing a host of hormonal and medical issues, stress can lead to sleep issues that may have long-term consequences, Dr. Lim noted in the interview.
“There’s some thought that quality sleep is important for memory formation, and if people are under a fair amount of stress and they have really poor sleep, that can also lead to cognitive issues including memory impairment,” he said.
“There are these multiple avenues that may be contributing to the accelerated development of these kinds of issues,” he added, “so I think this paper suggests more ways to counsel the patients about using lifestyle modifications to slow down the development of these cognitive impairments.”
Funding for the study came from the Swedish Research Council, Icelandic Research Fund; ,European Research Council the Karolinska Institutet, Swedish Research Council, and West China Hospital. Authors of the study provided disclosures related to those organizations as well as Shire/Takeda and Evolan.
SOURCE: Song H et al. JAMA Neurol. 2020 Mar 9. doi: 10.1001/jamaneurol.2020.0117.
Individuals with posttraumatic stress disorder (PTSD), acute stress reaction, adjustment disorder, or other stress reactions had an 80% increased risk of vascular neurodegenerative diseases, according to results of the study, which was based on Swedish population registry data.
Risk of primary neurodegenerative diseases was increased as well in people with those conditions, but only by 31%, according to lead author Huan Song, MD, PhD, of Sichuan University in Chengdu, China.
“The stronger association observed for neurodegenerative diseases with a vascular component, compared with primary neurodegenerative diseases, suggested a considerable role of a possible cerebrovascular pathway,” Dr. Song and coauthors said in a report on the study appearing in JAMA Neurology.
While some previous studies have linked stress-related disorders to neurodegenerative diseases – particularly PTSD and dementia – this is believed to be the first, according to the investigators, to comprehensively evaluate all stress-related disorders in relation to the most common neurodegenerative conditions.
When considering neurodegenerative conditions separately, they found a statistically significant association between stress-related disorders and Alzheimer’s disease, while linkages with Parkinson’s disease and amyotrophic lateral sclerosis (ALS) were “comparable” but associations did not reach statistical significance, according to investigators.
Based on these findings, stress reduction should be recommended in addition to daily physical activity, mental activity, and a heart-healthy diet to potentially reduce risk of onset or worsening of cognitive decline, according to Chun Lim, MD, PhD, medical director of the cognitive neurology unit at Beth Israel Deaconess Medical Center in Boston.
“We don’t really have great evidence that anything slows down the progression of Alzheimer’s disease, but there are some suggestions that for people who lead heart-healthy lifestyles or adhere to a Mediterranean diet, fewer develop cognitive issues over 5-10 years,” Dr. Lim said in an interview. “Because of this paper, stress reduction may be one additional way to hopefully help these patients these patients that have or are concerned about cognitive issues.”
The population-matched cohort of the study included 61,748 individuals with stress-related disorders and 595,335 matched individuals without those disorders, while the sibling-matched cohort included 44,839 individuals with those disorders and 78,482 without. The median age at the start of follow-up was 47 years and 39.4% of those with stress-related disorders were male.
During follow-up, the incidence of neurodegenerative diseases per 1,000 person-years was 1.50 for individuals with stress-related disorders, versus 0.82 for those without stress-related disorders, according to the report. Risk of primary neurodegenerative diseases was increased among those with stress-related disorders, compared with those without, with a hazard ratio of 1.31 (95% confidence interval, 1.15-1.48). However, the risk of vascular neurodegenerative diseases was significantly higher, with an HR of 1.80 (95% CI, 1.40-2.31; P = .03 for the difference between hazard ratios).
Results of the matched sibling cohort supported results of the population-matched cohort, though the elevated risk of vascular neurodegenerative diseases among those with stress-related disorders was “slightly lower” than in the population-based cohort, Dr. Song and coauthors wrote in their report.
Beyond causing a host of hormonal and medical issues, stress can lead to sleep issues that may have long-term consequences, Dr. Lim noted in the interview.
“There’s some thought that quality sleep is important for memory formation, and if people are under a fair amount of stress and they have really poor sleep, that can also lead to cognitive issues including memory impairment,” he said.
“There are these multiple avenues that may be contributing to the accelerated development of these kinds of issues,” he added, “so I think this paper suggests more ways to counsel the patients about using lifestyle modifications to slow down the development of these cognitive impairments.”
Funding for the study came from the Swedish Research Council, Icelandic Research Fund; ,European Research Council the Karolinska Institutet, Swedish Research Council, and West China Hospital. Authors of the study provided disclosures related to those organizations as well as Shire/Takeda and Evolan.
SOURCE: Song H et al. JAMA Neurol. 2020 Mar 9. doi: 10.1001/jamaneurol.2020.0117.
Individuals with posttraumatic stress disorder (PTSD), acute stress reaction, adjustment disorder, or other stress reactions had an 80% increased risk of vascular neurodegenerative diseases, according to results of the study, which was based on Swedish population registry data.
Risk of primary neurodegenerative diseases was increased as well in people with those conditions, but only by 31%, according to lead author Huan Song, MD, PhD, of Sichuan University in Chengdu, China.
“The stronger association observed for neurodegenerative diseases with a vascular component, compared with primary neurodegenerative diseases, suggested a considerable role of a possible cerebrovascular pathway,” Dr. Song and coauthors said in a report on the study appearing in JAMA Neurology.
While some previous studies have linked stress-related disorders to neurodegenerative diseases – particularly PTSD and dementia – this is believed to be the first, according to the investigators, to comprehensively evaluate all stress-related disorders in relation to the most common neurodegenerative conditions.
When considering neurodegenerative conditions separately, they found a statistically significant association between stress-related disorders and Alzheimer’s disease, while linkages with Parkinson’s disease and amyotrophic lateral sclerosis (ALS) were “comparable” but associations did not reach statistical significance, according to investigators.
Based on these findings, stress reduction should be recommended in addition to daily physical activity, mental activity, and a heart-healthy diet to potentially reduce risk of onset or worsening of cognitive decline, according to Chun Lim, MD, PhD, medical director of the cognitive neurology unit at Beth Israel Deaconess Medical Center in Boston.
“We don’t really have great evidence that anything slows down the progression of Alzheimer’s disease, but there are some suggestions that for people who lead heart-healthy lifestyles or adhere to a Mediterranean diet, fewer develop cognitive issues over 5-10 years,” Dr. Lim said in an interview. “Because of this paper, stress reduction may be one additional way to hopefully help these patients these patients that have or are concerned about cognitive issues.”
The population-matched cohort of the study included 61,748 individuals with stress-related disorders and 595,335 matched individuals without those disorders, while the sibling-matched cohort included 44,839 individuals with those disorders and 78,482 without. The median age at the start of follow-up was 47 years and 39.4% of those with stress-related disorders were male.
During follow-up, the incidence of neurodegenerative diseases per 1,000 person-years was 1.50 for individuals with stress-related disorders, versus 0.82 for those without stress-related disorders, according to the report. Risk of primary neurodegenerative diseases was increased among those with stress-related disorders, compared with those without, with a hazard ratio of 1.31 (95% confidence interval, 1.15-1.48). However, the risk of vascular neurodegenerative diseases was significantly higher, with an HR of 1.80 (95% CI, 1.40-2.31; P = .03 for the difference between hazard ratios).
Results of the matched sibling cohort supported results of the population-matched cohort, though the elevated risk of vascular neurodegenerative diseases among those with stress-related disorders was “slightly lower” than in the population-based cohort, Dr. Song and coauthors wrote in their report.
Beyond causing a host of hormonal and medical issues, stress can lead to sleep issues that may have long-term consequences, Dr. Lim noted in the interview.
“There’s some thought that quality sleep is important for memory formation, and if people are under a fair amount of stress and they have really poor sleep, that can also lead to cognitive issues including memory impairment,” he said.
“There are these multiple avenues that may be contributing to the accelerated development of these kinds of issues,” he added, “so I think this paper suggests more ways to counsel the patients about using lifestyle modifications to slow down the development of these cognitive impairments.”
Funding for the study came from the Swedish Research Council, Icelandic Research Fund; ,European Research Council the Karolinska Institutet, Swedish Research Council, and West China Hospital. Authors of the study provided disclosures related to those organizations as well as Shire/Takeda and Evolan.
SOURCE: Song H et al. JAMA Neurol. 2020 Mar 9. doi: 10.1001/jamaneurol.2020.0117.
FROM JAMA NEUROLOGY
Sexual-minority youth at greater risk for physical, sexual violence
U.S. high school students who identify as gay, lesbian, bisexual, or questioning – “sexual minorities” – faced twice the risk of physical or sexual assault in the past year compared with their heterosexual peers, according to findings reported in a research letter.
Sexual-minority females were particularly more likely to experience physical violence while sexual-minority boys had a fourfold increased risk of sexual violence.
“The results of our study suggest the existence of a crisis of violence against sexual minority adolescents,” Theodore L. Caputi, MPH, of Harvard Medical School, Boston, and colleagues reported in JAMA Pediatrics. “Given the substantial physical and emotional consequences of violence for those subjected to it and the large existing health disparities among sexual minority adolescents, addressing both physical and sexual violence against sexual minority adolescents should become a public health priority.”
Joshua D. Safer, MD, executive director of the Center for Transgender Medicine and Surgery in the Mount Sinai Health System, New York, said he was not surprised by the findings because adolescents who may feel more vulnerable relative to their peers are likely to be more of a target. They may not have the supports they need, he said, which will affect their resiliency and their ability to push back.
“These patients are at ages where their parents might be among their supporters,” Dr. Safer said in an interview. “People in their circle may not be aware of their circumstances.”
He emphasized the need for physicians to ensure their offices are safe places for sexual-minority youth to talk to adolescent patients about their gender and sexual identity as well as any history of victimization, and to involve parents in being an ally of their child.
The researchers analyzed data from the nationally representative 2015 and 2017 National Youth Risk Behavior Surveys administered to public and private high school students in grades 9-12 by the Centers for Disease Control and Prevention. The 28,811 total respondents represented a 60% response rate both years.
After indicating their sex as male or female and their sexual orientation, respondents reported whether, in the past year, they had experienced a physical fight at school, a physical fight anywhere, or physical violence from a romantic partner. They also reported whether they had been sexually assaulted in the past year by a romantic partner or ever been forced to have intercourse. The 2017 survey included an additional question about sexual assault by anyone in the past year.
Most youth (87%) identified themselves as heterosexual while 2% were gay/lesbian, 7% were bisexual, and 4% were unsure. Sexual minorities reported a higher prevalence of all forms of violence and assault, compared with their heterosexual counterparts. Although risk of a physical fight in the past year differed by a small amount (28% of sexual-minority youth vs. 22% of heterosexual youth), the gap was considerably greater for risk of physical violence by a romantic partner (12% of sexual-minority youth vs. 5% of heterosexual youth).
More than three times as many sexual-minority adolescents (18%) as heterosexual adolescents (5%) said they had ever been forced to have intercourse, and a similarly high proportion of sexual-minority students (21%) had been sexually assaulted in the past year, compared with heterosexual students (8%). After accounting for survey year, sex, age, race/ethnicity, English language proficiency, and grade level, youth who identified as anything other than heterosexual were about twice as likely as their heterosexual counterparts to have experienced physical or sexual violence, including physical violence by a romantic partner (adjusted risk ratio, 1.97) or sexual assault by anyone (aRR, 2.10), in the past year. The risk of physical violence by a romantic partner or sexual assault by anyone was even greater for bisexual youth (aRR, 2.22 and aRR, 2.36, respectively).
The increased likelihood of physical violence and sexual violence differed by sex. Girls who identified as lesbian, bisexual, or questioning were more likely than heterosexual girls to have been in a fight at school or anywhere else (aRR, 1.91 and aRR, 1.74, respectively). Boys who were gay, bisexual, or questioning, meanwhile, were over four times more likely than heterosexual boys to have had forced intercourse or any kind of sexual assault (aRR, 4.70 and aRR, 4.64, respectively).
These findings point to the need for physicians to be “specifically talking to youth about gender identity and sexual orientation. Validating what kids are feeling is important,” Dr. Safer said in an interview.
Key to that process is making sure the physician’s office feels like a safe place for LGBTQ youth to have these kinds of conversations. “Most primary care and pediatric and adolescent care practices are not feeling well equipped to take care of these kids and are not necessarily serving as a good resource for these kids,” Dr. Safer said.
It’s also important for physicians to ask youth about potential violence or abuse they have experienced, including depression and sequelae from lack of support, for which gender- and sexual-minority youth are at greater risk, he said. Finally, doctors need to engage parents in the conversation.
“As a medical professional, you need to be asking the questions and really be out there as an ally, especially for pediatric and adolescent patients, and you need to be helping the parents of your patients be allies too,” Dr. Safer said.
The study was limited by having a binary question only about respondent’s sex and no data collection about transgender youth. The study’s cross-sectional design also precludes the ability to claim causation about any of the associations.
The research was funded by the Marshall Aid Commemoration Commission, Stanford (Calif.) University, and the National Institutes of Health. The authors had no disclosures.
SOURCE: Caputi TL et al. JAMA Pediatr. 2019 Mar 9. doi: 10.1001/jamapediatrics.2019.6291.
U.S. high school students who identify as gay, lesbian, bisexual, or questioning – “sexual minorities” – faced twice the risk of physical or sexual assault in the past year compared with their heterosexual peers, according to findings reported in a research letter.
Sexual-minority females were particularly more likely to experience physical violence while sexual-minority boys had a fourfold increased risk of sexual violence.
“The results of our study suggest the existence of a crisis of violence against sexual minority adolescents,” Theodore L. Caputi, MPH, of Harvard Medical School, Boston, and colleagues reported in JAMA Pediatrics. “Given the substantial physical and emotional consequences of violence for those subjected to it and the large existing health disparities among sexual minority adolescents, addressing both physical and sexual violence against sexual minority adolescents should become a public health priority.”
Joshua D. Safer, MD, executive director of the Center for Transgender Medicine and Surgery in the Mount Sinai Health System, New York, said he was not surprised by the findings because adolescents who may feel more vulnerable relative to their peers are likely to be more of a target. They may not have the supports they need, he said, which will affect their resiliency and their ability to push back.
“These patients are at ages where their parents might be among their supporters,” Dr. Safer said in an interview. “People in their circle may not be aware of their circumstances.”
He emphasized the need for physicians to ensure their offices are safe places for sexual-minority youth to talk to adolescent patients about their gender and sexual identity as well as any history of victimization, and to involve parents in being an ally of their child.
The researchers analyzed data from the nationally representative 2015 and 2017 National Youth Risk Behavior Surveys administered to public and private high school students in grades 9-12 by the Centers for Disease Control and Prevention. The 28,811 total respondents represented a 60% response rate both years.
After indicating their sex as male or female and their sexual orientation, respondents reported whether, in the past year, they had experienced a physical fight at school, a physical fight anywhere, or physical violence from a romantic partner. They also reported whether they had been sexually assaulted in the past year by a romantic partner or ever been forced to have intercourse. The 2017 survey included an additional question about sexual assault by anyone in the past year.
Most youth (87%) identified themselves as heterosexual while 2% were gay/lesbian, 7% were bisexual, and 4% were unsure. Sexual minorities reported a higher prevalence of all forms of violence and assault, compared with their heterosexual counterparts. Although risk of a physical fight in the past year differed by a small amount (28% of sexual-minority youth vs. 22% of heterosexual youth), the gap was considerably greater for risk of physical violence by a romantic partner (12% of sexual-minority youth vs. 5% of heterosexual youth).
More than three times as many sexual-minority adolescents (18%) as heterosexual adolescents (5%) said they had ever been forced to have intercourse, and a similarly high proportion of sexual-minority students (21%) had been sexually assaulted in the past year, compared with heterosexual students (8%). After accounting for survey year, sex, age, race/ethnicity, English language proficiency, and grade level, youth who identified as anything other than heterosexual were about twice as likely as their heterosexual counterparts to have experienced physical or sexual violence, including physical violence by a romantic partner (adjusted risk ratio, 1.97) or sexual assault by anyone (aRR, 2.10), in the past year. The risk of physical violence by a romantic partner or sexual assault by anyone was even greater for bisexual youth (aRR, 2.22 and aRR, 2.36, respectively).
The increased likelihood of physical violence and sexual violence differed by sex. Girls who identified as lesbian, bisexual, or questioning were more likely than heterosexual girls to have been in a fight at school or anywhere else (aRR, 1.91 and aRR, 1.74, respectively). Boys who were gay, bisexual, or questioning, meanwhile, were over four times more likely than heterosexual boys to have had forced intercourse or any kind of sexual assault (aRR, 4.70 and aRR, 4.64, respectively).
These findings point to the need for physicians to be “specifically talking to youth about gender identity and sexual orientation. Validating what kids are feeling is important,” Dr. Safer said in an interview.
Key to that process is making sure the physician’s office feels like a safe place for LGBTQ youth to have these kinds of conversations. “Most primary care and pediatric and adolescent care practices are not feeling well equipped to take care of these kids and are not necessarily serving as a good resource for these kids,” Dr. Safer said.
It’s also important for physicians to ask youth about potential violence or abuse they have experienced, including depression and sequelae from lack of support, for which gender- and sexual-minority youth are at greater risk, he said. Finally, doctors need to engage parents in the conversation.
“As a medical professional, you need to be asking the questions and really be out there as an ally, especially for pediatric and adolescent patients, and you need to be helping the parents of your patients be allies too,” Dr. Safer said.
The study was limited by having a binary question only about respondent’s sex and no data collection about transgender youth. The study’s cross-sectional design also precludes the ability to claim causation about any of the associations.
The research was funded by the Marshall Aid Commemoration Commission, Stanford (Calif.) University, and the National Institutes of Health. The authors had no disclosures.
SOURCE: Caputi TL et al. JAMA Pediatr. 2019 Mar 9. doi: 10.1001/jamapediatrics.2019.6291.
U.S. high school students who identify as gay, lesbian, bisexual, or questioning – “sexual minorities” – faced twice the risk of physical or sexual assault in the past year compared with their heterosexual peers, according to findings reported in a research letter.
Sexual-minority females were particularly more likely to experience physical violence while sexual-minority boys had a fourfold increased risk of sexual violence.
“The results of our study suggest the existence of a crisis of violence against sexual minority adolescents,” Theodore L. Caputi, MPH, of Harvard Medical School, Boston, and colleagues reported in JAMA Pediatrics. “Given the substantial physical and emotional consequences of violence for those subjected to it and the large existing health disparities among sexual minority adolescents, addressing both physical and sexual violence against sexual minority adolescents should become a public health priority.”
Joshua D. Safer, MD, executive director of the Center for Transgender Medicine and Surgery in the Mount Sinai Health System, New York, said he was not surprised by the findings because adolescents who may feel more vulnerable relative to their peers are likely to be more of a target. They may not have the supports they need, he said, which will affect their resiliency and their ability to push back.
“These patients are at ages where their parents might be among their supporters,” Dr. Safer said in an interview. “People in their circle may not be aware of their circumstances.”
He emphasized the need for physicians to ensure their offices are safe places for sexual-minority youth to talk to adolescent patients about their gender and sexual identity as well as any history of victimization, and to involve parents in being an ally of their child.
The researchers analyzed data from the nationally representative 2015 and 2017 National Youth Risk Behavior Surveys administered to public and private high school students in grades 9-12 by the Centers for Disease Control and Prevention. The 28,811 total respondents represented a 60% response rate both years.
After indicating their sex as male or female and their sexual orientation, respondents reported whether, in the past year, they had experienced a physical fight at school, a physical fight anywhere, or physical violence from a romantic partner. They also reported whether they had been sexually assaulted in the past year by a romantic partner or ever been forced to have intercourse. The 2017 survey included an additional question about sexual assault by anyone in the past year.
Most youth (87%) identified themselves as heterosexual while 2% were gay/lesbian, 7% were bisexual, and 4% were unsure. Sexual minorities reported a higher prevalence of all forms of violence and assault, compared with their heterosexual counterparts. Although risk of a physical fight in the past year differed by a small amount (28% of sexual-minority youth vs. 22% of heterosexual youth), the gap was considerably greater for risk of physical violence by a romantic partner (12% of sexual-minority youth vs. 5% of heterosexual youth).
More than three times as many sexual-minority adolescents (18%) as heterosexual adolescents (5%) said they had ever been forced to have intercourse, and a similarly high proportion of sexual-minority students (21%) had been sexually assaulted in the past year, compared with heterosexual students (8%). After accounting for survey year, sex, age, race/ethnicity, English language proficiency, and grade level, youth who identified as anything other than heterosexual were about twice as likely as their heterosexual counterparts to have experienced physical or sexual violence, including physical violence by a romantic partner (adjusted risk ratio, 1.97) or sexual assault by anyone (aRR, 2.10), in the past year. The risk of physical violence by a romantic partner or sexual assault by anyone was even greater for bisexual youth (aRR, 2.22 and aRR, 2.36, respectively).
The increased likelihood of physical violence and sexual violence differed by sex. Girls who identified as lesbian, bisexual, or questioning were more likely than heterosexual girls to have been in a fight at school or anywhere else (aRR, 1.91 and aRR, 1.74, respectively). Boys who were gay, bisexual, or questioning, meanwhile, were over four times more likely than heterosexual boys to have had forced intercourse or any kind of sexual assault (aRR, 4.70 and aRR, 4.64, respectively).
These findings point to the need for physicians to be “specifically talking to youth about gender identity and sexual orientation. Validating what kids are feeling is important,” Dr. Safer said in an interview.
Key to that process is making sure the physician’s office feels like a safe place for LGBTQ youth to have these kinds of conversations. “Most primary care and pediatric and adolescent care practices are not feeling well equipped to take care of these kids and are not necessarily serving as a good resource for these kids,” Dr. Safer said.
It’s also important for physicians to ask youth about potential violence or abuse they have experienced, including depression and sequelae from lack of support, for which gender- and sexual-minority youth are at greater risk, he said. Finally, doctors need to engage parents in the conversation.
“As a medical professional, you need to be asking the questions and really be out there as an ally, especially for pediatric and adolescent patients, and you need to be helping the parents of your patients be allies too,” Dr. Safer said.
The study was limited by having a binary question only about respondent’s sex and no data collection about transgender youth. The study’s cross-sectional design also precludes the ability to claim causation about any of the associations.
The research was funded by the Marshall Aid Commemoration Commission, Stanford (Calif.) University, and the National Institutes of Health. The authors had no disclosures.
SOURCE: Caputi TL et al. JAMA Pediatr. 2019 Mar 9. doi: 10.1001/jamapediatrics.2019.6291.
FROM JAMA PEDIATRICS
Rotavirus vaccination is not a risk factor for type 1 diabetes
published in JAMA Pediatrics.
Previous findings from a number of studies have indicated a possible association between rotavirus and type 1 diabetes, according to Jason M. Glanz, PhD, and colleagues. “Epidemiologic data suggest an association between gastrointestinal infection and incidence of type 1 diabetes in children followed from birth to age 10 years. Given these findings, it is biologically plausible that live, attenuated rotavirus vaccine could either increase or decrease the risk for type 1 diabetes in early childhood,” they wrote.
To examine the association between rotavirus vaccination and the incidence of type 1 diabetes in a cohort of U.S. children, Dr. Glanz, a senior investigator at the Kaiser Permanente Colorado Institute for Health Research in Aurora, and colleagues retrospectively analyzed data from seven health care organizations that participate in the Vaccine Safety Datalink.
The researchers identified children born between 2006 and 2014 who had continuous enrollment from age 6 weeks to 2 years. They excluded children with a medical contraindication to vaccination or fewer than two well-child visits by age 12 months. They followed children until a type 1 diabetes diagnosis, disenrollment, or Dec. 31, 2017. The researchers adjusted for sex, birth year, mother’s age, birth weight, gestational age, and race or ethnicity.
The cohort included 386,937 children who were followed up a median of 5.4 years for a total person-time follow-up of 2,253,879 years. In all, 386,937 children (93.1%) were fully exposed to rotavirus vaccination; 15,765 (4.1%) were partially exposed to rotavirus vaccination, meaning that they received some, but not all, vaccine doses; and 11,003 (2.8%) were unexposed to rotavirus vaccination but had received all other recommended vaccines.
There were 464 cases of type 1 diabetes in the cohort, with an incidence rate of 20 cases per 100,000 person-years in the fully exposed group, 31.2 cases per 100,000 person-years in the partially exposed group, and 22.4 cases per 100,000 person-years in the unexposed group.
The incidence of type 1 diabetes was not significantly different across the rotavirus vaccine–exposure groups. The researchers reported that, compared with children unexposed to rotavirus vaccination, the adjusted hazard ratio for children fully exposed to rotavirus vaccination was 1.03 (95% confidence interval, 0.62-1.72), and for those partially exposed to the vaccination, it was 1.50 (95% CI, 0.81-2.77).
“Since licensure, rotavirus vaccination has been associated with a reduction in morbidity and mortality due to rotavirus infection in the United States and worldwide. ... Although rotavirus vaccination may not prevent type 1 diabetes, these results should provide additional reassurance to the public that rotavirus vaccination can be safely administered to infants,” they wrote.
The limited follow-up duration and relatively small proportion of patients unexposed to rotavirus vaccination are limitations of the study, the authors noted.
The Centers for Disease Control and Prevention funded the study. Several authors reported having received grants from the CDC. One author received grants from the National Institute of Diabetes and Digestive and Kidney Diseases, and another from pharmaceutical companies not involved in the study.
SOURCE: Glanz JM et al. JAMA Pediatr. 2020 Mar 9. doi: 10.1001/jamapediatrics.2019.6324.
published in JAMA Pediatrics.
Previous findings from a number of studies have indicated a possible association between rotavirus and type 1 diabetes, according to Jason M. Glanz, PhD, and colleagues. “Epidemiologic data suggest an association between gastrointestinal infection and incidence of type 1 diabetes in children followed from birth to age 10 years. Given these findings, it is biologically plausible that live, attenuated rotavirus vaccine could either increase or decrease the risk for type 1 diabetes in early childhood,” they wrote.
To examine the association between rotavirus vaccination and the incidence of type 1 diabetes in a cohort of U.S. children, Dr. Glanz, a senior investigator at the Kaiser Permanente Colorado Institute for Health Research in Aurora, and colleagues retrospectively analyzed data from seven health care organizations that participate in the Vaccine Safety Datalink.
The researchers identified children born between 2006 and 2014 who had continuous enrollment from age 6 weeks to 2 years. They excluded children with a medical contraindication to vaccination or fewer than two well-child visits by age 12 months. They followed children until a type 1 diabetes diagnosis, disenrollment, or Dec. 31, 2017. The researchers adjusted for sex, birth year, mother’s age, birth weight, gestational age, and race or ethnicity.
The cohort included 386,937 children who were followed up a median of 5.4 years for a total person-time follow-up of 2,253,879 years. In all, 386,937 children (93.1%) were fully exposed to rotavirus vaccination; 15,765 (4.1%) were partially exposed to rotavirus vaccination, meaning that they received some, but not all, vaccine doses; and 11,003 (2.8%) were unexposed to rotavirus vaccination but had received all other recommended vaccines.
There were 464 cases of type 1 diabetes in the cohort, with an incidence rate of 20 cases per 100,000 person-years in the fully exposed group, 31.2 cases per 100,000 person-years in the partially exposed group, and 22.4 cases per 100,000 person-years in the unexposed group.
The incidence of type 1 diabetes was not significantly different across the rotavirus vaccine–exposure groups. The researchers reported that, compared with children unexposed to rotavirus vaccination, the adjusted hazard ratio for children fully exposed to rotavirus vaccination was 1.03 (95% confidence interval, 0.62-1.72), and for those partially exposed to the vaccination, it was 1.50 (95% CI, 0.81-2.77).
“Since licensure, rotavirus vaccination has been associated with a reduction in morbidity and mortality due to rotavirus infection in the United States and worldwide. ... Although rotavirus vaccination may not prevent type 1 diabetes, these results should provide additional reassurance to the public that rotavirus vaccination can be safely administered to infants,” they wrote.
The limited follow-up duration and relatively small proportion of patients unexposed to rotavirus vaccination are limitations of the study, the authors noted.
The Centers for Disease Control and Prevention funded the study. Several authors reported having received grants from the CDC. One author received grants from the National Institute of Diabetes and Digestive and Kidney Diseases, and another from pharmaceutical companies not involved in the study.
SOURCE: Glanz JM et al. JAMA Pediatr. 2020 Mar 9. doi: 10.1001/jamapediatrics.2019.6324.
published in JAMA Pediatrics.
Previous findings from a number of studies have indicated a possible association between rotavirus and type 1 diabetes, according to Jason M. Glanz, PhD, and colleagues. “Epidemiologic data suggest an association between gastrointestinal infection and incidence of type 1 diabetes in children followed from birth to age 10 years. Given these findings, it is biologically plausible that live, attenuated rotavirus vaccine could either increase or decrease the risk for type 1 diabetes in early childhood,” they wrote.
To examine the association between rotavirus vaccination and the incidence of type 1 diabetes in a cohort of U.S. children, Dr. Glanz, a senior investigator at the Kaiser Permanente Colorado Institute for Health Research in Aurora, and colleagues retrospectively analyzed data from seven health care organizations that participate in the Vaccine Safety Datalink.
The researchers identified children born between 2006 and 2014 who had continuous enrollment from age 6 weeks to 2 years. They excluded children with a medical contraindication to vaccination or fewer than two well-child visits by age 12 months. They followed children until a type 1 diabetes diagnosis, disenrollment, or Dec. 31, 2017. The researchers adjusted for sex, birth year, mother’s age, birth weight, gestational age, and race or ethnicity.
The cohort included 386,937 children who were followed up a median of 5.4 years for a total person-time follow-up of 2,253,879 years. In all, 386,937 children (93.1%) were fully exposed to rotavirus vaccination; 15,765 (4.1%) were partially exposed to rotavirus vaccination, meaning that they received some, but not all, vaccine doses; and 11,003 (2.8%) were unexposed to rotavirus vaccination but had received all other recommended vaccines.
There were 464 cases of type 1 diabetes in the cohort, with an incidence rate of 20 cases per 100,000 person-years in the fully exposed group, 31.2 cases per 100,000 person-years in the partially exposed group, and 22.4 cases per 100,000 person-years in the unexposed group.
The incidence of type 1 diabetes was not significantly different across the rotavirus vaccine–exposure groups. The researchers reported that, compared with children unexposed to rotavirus vaccination, the adjusted hazard ratio for children fully exposed to rotavirus vaccination was 1.03 (95% confidence interval, 0.62-1.72), and for those partially exposed to the vaccination, it was 1.50 (95% CI, 0.81-2.77).
“Since licensure, rotavirus vaccination has been associated with a reduction in morbidity and mortality due to rotavirus infection in the United States and worldwide. ... Although rotavirus vaccination may not prevent type 1 diabetes, these results should provide additional reassurance to the public that rotavirus vaccination can be safely administered to infants,” they wrote.
The limited follow-up duration and relatively small proportion of patients unexposed to rotavirus vaccination are limitations of the study, the authors noted.
The Centers for Disease Control and Prevention funded the study. Several authors reported having received grants from the CDC. One author received grants from the National Institute of Diabetes and Digestive and Kidney Diseases, and another from pharmaceutical companies not involved in the study.
SOURCE: Glanz JM et al. JAMA Pediatr. 2020 Mar 9. doi: 10.1001/jamapediatrics.2019.6324.
FROM JAMA PEDIATRICS
Key clinical point: Rotavirus vaccination is not associated with the incidence of type 1 diabetes and can be safely administered to infants.
Major finding: Compared with children unexposed to rotavirus vaccination, the adjusted hazard ratio for developing type 1 diabetes for children fully exposed to the vaccination was 1.03 (95% confidence interval, 0.62-1.72), and for those partially exposed to it, the aHR was 1.50 (95% CI, 0.81-2.77).
Study details: A retrospective cohort study of 386,937 children using data from the Vaccine Safety Datalink.
Disclosures: The Centers for Disease Control and Prevention funded the study. Several authors reported having received grants from the CDC. One author received grants from the National Institute of Diabetes and Digestive and Kidney Diseases, and another from pharmaceutical companies not involved in the study.
Source: Glanz JM et al. JAMA Pediatr. 2020 Mar 9. doi: 10.1001/jamapediatrics.2019.6324.