User login
Medically Unlikely Edits
Medically Unlikely Edits (MUEs) are benchmarks recognized by the Centers for Medicare & Medicaid Services (CMS) that are designed to prevent incorrect or excessive coding. Specifically, an MUE is an edit that tests medical claims for services billed in excess of the maximum number of units of service permitted for a single beneficiary on the same date of service from the same provider (eg, multiples of the same Healthcare Common Procedure Coding System [HCPCS] code listed on different claim lines).1
The MUE System
If the number of units of service billed by the same physician for the same patient on the same day exceeds the maximum number permitted by the CMS, the Medicare Administrative Contractor (MAC) will deny the code or return the claim to the provider for correction (return to provider [RTP]). Units of service billed in excess of the MUE will not be paid, but other services billed on the same claim form may still be paid. In the case of an MUE-associated RTP, the provider should resubmit a corrected claim, not an appeal; however, an appeal is possible in the case of an MUE-associated denial. An MUE-associated denial is a coding denial, not a medical necessity denial; therefore, the provider cannot use an Advance Beneficiary Notice to transfer liability for claim payment to the patient.
MUE Adjudication Indicators
In 2013, the CMS modified the MUE process to include 3 different MUE adjudication indicators (MAIs) with a value of 1, 2, or 3 so that some MUE values would be date of service edits rather than claim line edits.2 Medically Unlikely Edits for HCPCS codes with an MAI of 1 are identical to the prior claim line edits. If a provider needs to report excess units of service with an MAI of 1, appropriate modifiers should be used to report them on separate lines of a claim. Current Procedural Terminology (CPT) modifiers such as -76 (repeat procedure or service by the same physician) and -91 (repeat clinical diagnostic laboratory test) as well as anatomic modifiers (eg, RT, LT, F1, F2) may be used, with modifier -59 (distinct procedural service) used only if no other modifier suffices. An example of an MUE with an MAI of 1 is CPT code 17264 (destruction, malignant lesion [eg, laser surgery, electrosurgery, cryosurgery, chemosurgery, surgical curettement], trunk, arms or legs; lesion diameter 3.1–4.0 cm), for which the MUE threshold is 3, meaning no more than 3 destructions can be submitted per claim line without triggering an edit-based rejection or RTP.
An MAI of 2 denotes absolute date of service edits, or so-called “per day edits based on policy.” Such edits are in place because units of service billed in excess of the MUE value on the same date of service are considered to be impossible by the CMS based on regulatory guidance or anatomic considerations.2 For instance, although the same physician may destroy multiple actinic keratoses in a single patient on the same date of service, it would not be possible to code more than one unit of service as
CPT code 17000, which specifically and exclusively
refers to the first lesion destroyed. Similarly,
CPT code 13101 (repair, complex, trunk; lesion diameter 2.6–7.5 cm) could only be reported once that day, as all complex repairs at that anatomic site must be summed and smaller or larger totals would be reported with another code.
Anatomic limitations are sometimes obvious and do not require specific coding rules. For example, only 1 gallbladder can be removed per patient. Although Qualified Independent Contractors and Administrative Law Judges are not bound by MAIs, they do give particular deference to an MAI of
2 given its definitive nature.2 Because ambulatory surgical center providers (Medicare specialty code 49) cannot report modifier -50 for bilateral
procedures, the MUE value used for editing is doubled for HCPCS codes with an MAI of 2 or 3 if the bilateral surgery indicator for the HCPCS code is 1.3
An MAI of 3 describes less strict date of service edits, so-called “per day edits based on clinical benchmarks.”2 Similar to MAIs of 1, MUEs for MAIs of 3 are based on medically likely daily frequencies of services provided in most settings. To determine if an MUE with an MAI of 3 has been reached, the MAC sums the units of service billed on all claim lines of the current claim as well as all prior paid claims for the same patient billed by the same provider on the same date of service. If the total units of service obtained in this manner exceeds the MUE value, then all claim lines with the relevant code for the current claim will be denied, but prior paid claims will not be adjusted. Denials based on MUEs for codes with an MAI of 3 can be appealed to the local MAC. Successful appeals require documentation that the units of service in excess of the MUE value were actually delivered and demonstration of medical necessity.2 An example of a CPT code with an MAI of 3 is 40490 (biopsy of lip) for which the MUE value is 3.
Complications With MUE and MAI
Because MUEs are based on current coding guidelines as well as current clinical practice, they are only applicable for the time period in which they are in effect. A change made to an MUE value for a particular code is not retroactive; however, in exceptional circumstances when a retroactive effective date is applied, MACs are not directed to examine prior claims but only “claims that are brought to their attention.”2
It also is important to realize that not all MUEs are publicly available and many are confidential. When claim denials occur, particularly in the context of multiple units of a particular code, automated MUE edits should be among the issues that are suspected. Physicians may resubmit RTP claims on separate lines if a claim line edit (MAI of 1) is operative. An MAI of 2 suggests a coding error that needs to be corrected, as these coding approaches are generally impossible based on definitional issues or anatomy. If an MUE with an MAI of 3 is the reason for denial, an appeal is possible, provided there is documentation to show that the service was actually provided and that it was medically necessary.
Final Thoughts
Dermatologists should be vigilant for unexpected payment denials, which may coincide with the implementation of new MUE values. When such denials occur and MUE values are publicly available, dermatologists should consider filing an appeal if the relevant MUEs were associated with an MAI of 1 or 3. Overall, dermatologists should be aware that many MUEs that were formerly claim line edits (MAI of 1) have been recently transitioned to date of service edits (MAI of 3), which are more restrictive.
1. American Academy of Dermatology. Medicare’s expanded medically unlikely edits. https://www.aad.org/members
/practice-and-advocacy-resource-center/coding-resources
/derm-coding-consult-library/winter-2014/medicare-
s-expanded-medically-unlikely-edits. Published Winter 2014. Accessed August 6, 2015.
2. Centers for Medicare & Medicaid Services. Revised modification to the Medically Unlikely Edit (MUE) program. MLN Matters. Number MM8853. https://www.cms.gov
/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNMattersArticles/downloads/MM8853.pdf. Published January 1, 2015. Accessed August 6, 2015.
3. Centers for Medicare & Medicaid Services.
Medically Unlikely Edits (MUE) and bilateral procedures. MLN Matters. Number SE1422.
https://www.cms.gov/Regulations-and-Guidance
/Guidance/Transmittals/2014-Transmittals-Items/SE1422.html?DLPage=2&DLEntries=10&DLSort=1&DLSort
Dir=ascending. Accessed July 28, 2015.
Medically Unlikely Edits (MUEs) are benchmarks recognized by the Centers for Medicare & Medicaid Services (CMS) that are designed to prevent incorrect or excessive coding. Specifically, an MUE is an edit that tests medical claims for services billed in excess of the maximum number of units of service permitted for a single beneficiary on the same date of service from the same provider (eg, multiples of the same Healthcare Common Procedure Coding System [HCPCS] code listed on different claim lines).1
The MUE System
If the number of units of service billed by the same physician for the same patient on the same day exceeds the maximum number permitted by the CMS, the Medicare Administrative Contractor (MAC) will deny the code or return the claim to the provider for correction (return to provider [RTP]). Units of service billed in excess of the MUE will not be paid, but other services billed on the same claim form may still be paid. In the case of an MUE-associated RTP, the provider should resubmit a corrected claim, not an appeal; however, an appeal is possible in the case of an MUE-associated denial. An MUE-associated denial is a coding denial, not a medical necessity denial; therefore, the provider cannot use an Advance Beneficiary Notice to transfer liability for claim payment to the patient.
MUE Adjudication Indicators
In 2013, the CMS modified the MUE process to include 3 different MUE adjudication indicators (MAIs) with a value of 1, 2, or 3 so that some MUE values would be date of service edits rather than claim line edits.2 Medically Unlikely Edits for HCPCS codes with an MAI of 1 are identical to the prior claim line edits. If a provider needs to report excess units of service with an MAI of 1, appropriate modifiers should be used to report them on separate lines of a claim. Current Procedural Terminology (CPT) modifiers such as -76 (repeat procedure or service by the same physician) and -91 (repeat clinical diagnostic laboratory test) as well as anatomic modifiers (eg, RT, LT, F1, F2) may be used, with modifier -59 (distinct procedural service) used only if no other modifier suffices. An example of an MUE with an MAI of 1 is CPT code 17264 (destruction, malignant lesion [eg, laser surgery, electrosurgery, cryosurgery, chemosurgery, surgical curettement], trunk, arms or legs; lesion diameter 3.1–4.0 cm), for which the MUE threshold is 3, meaning no more than 3 destructions can be submitted per claim line without triggering an edit-based rejection or RTP.
An MAI of 2 denotes absolute date of service edits, or so-called “per day edits based on policy.” Such edits are in place because units of service billed in excess of the MUE value on the same date of service are considered to be impossible by the CMS based on regulatory guidance or anatomic considerations.2 For instance, although the same physician may destroy multiple actinic keratoses in a single patient on the same date of service, it would not be possible to code more than one unit of service as
CPT code 17000, which specifically and exclusively
refers to the first lesion destroyed. Similarly,
CPT code 13101 (repair, complex, trunk; lesion diameter 2.6–7.5 cm) could only be reported once that day, as all complex repairs at that anatomic site must be summed and smaller or larger totals would be reported with another code.
Anatomic limitations are sometimes obvious and do not require specific coding rules. For example, only 1 gallbladder can be removed per patient. Although Qualified Independent Contractors and Administrative Law Judges are not bound by MAIs, they do give particular deference to an MAI of
2 given its definitive nature.2 Because ambulatory surgical center providers (Medicare specialty code 49) cannot report modifier -50 for bilateral
procedures, the MUE value used for editing is doubled for HCPCS codes with an MAI of 2 or 3 if the bilateral surgery indicator for the HCPCS code is 1.3
An MAI of 3 describes less strict date of service edits, so-called “per day edits based on clinical benchmarks.”2 Similar to MAIs of 1, MUEs for MAIs of 3 are based on medically likely daily frequencies of services provided in most settings. To determine if an MUE with an MAI of 3 has been reached, the MAC sums the units of service billed on all claim lines of the current claim as well as all prior paid claims for the same patient billed by the same provider on the same date of service. If the total units of service obtained in this manner exceeds the MUE value, then all claim lines with the relevant code for the current claim will be denied, but prior paid claims will not be adjusted. Denials based on MUEs for codes with an MAI of 3 can be appealed to the local MAC. Successful appeals require documentation that the units of service in excess of the MUE value were actually delivered and demonstration of medical necessity.2 An example of a CPT code with an MAI of 3 is 40490 (biopsy of lip) for which the MUE value is 3.
Complications With MUE and MAI
Because MUEs are based on current coding guidelines as well as current clinical practice, they are only applicable for the time period in which they are in effect. A change made to an MUE value for a particular code is not retroactive; however, in exceptional circumstances when a retroactive effective date is applied, MACs are not directed to examine prior claims but only “claims that are brought to their attention.”2
It also is important to realize that not all MUEs are publicly available and many are confidential. When claim denials occur, particularly in the context of multiple units of a particular code, automated MUE edits should be among the issues that are suspected. Physicians may resubmit RTP claims on separate lines if a claim line edit (MAI of 1) is operative. An MAI of 2 suggests a coding error that needs to be corrected, as these coding approaches are generally impossible based on definitional issues or anatomy. If an MUE with an MAI of 3 is the reason for denial, an appeal is possible, provided there is documentation to show that the service was actually provided and that it was medically necessary.
Final Thoughts
Dermatologists should be vigilant for unexpected payment denials, which may coincide with the implementation of new MUE values. When such denials occur and MUE values are publicly available, dermatologists should consider filing an appeal if the relevant MUEs were associated with an MAI of 1 or 3. Overall, dermatologists should be aware that many MUEs that were formerly claim line edits (MAI of 1) have been recently transitioned to date of service edits (MAI of 3), which are more restrictive.
Medically Unlikely Edits (MUEs) are benchmarks recognized by the Centers for Medicare & Medicaid Services (CMS) that are designed to prevent incorrect or excessive coding. Specifically, an MUE is an edit that tests medical claims for services billed in excess of the maximum number of units of service permitted for a single beneficiary on the same date of service from the same provider (eg, multiples of the same Healthcare Common Procedure Coding System [HCPCS] code listed on different claim lines).1
The MUE System
If the number of units of service billed by the same physician for the same patient on the same day exceeds the maximum number permitted by the CMS, the Medicare Administrative Contractor (MAC) will deny the code or return the claim to the provider for correction (return to provider [RTP]). Units of service billed in excess of the MUE will not be paid, but other services billed on the same claim form may still be paid. In the case of an MUE-associated RTP, the provider should resubmit a corrected claim, not an appeal; however, an appeal is possible in the case of an MUE-associated denial. An MUE-associated denial is a coding denial, not a medical necessity denial; therefore, the provider cannot use an Advance Beneficiary Notice to transfer liability for claim payment to the patient.
MUE Adjudication Indicators
In 2013, the CMS modified the MUE process to include 3 different MUE adjudication indicators (MAIs) with a value of 1, 2, or 3 so that some MUE values would be date of service edits rather than claim line edits.2 Medically Unlikely Edits for HCPCS codes with an MAI of 1 are identical to the prior claim line edits. If a provider needs to report excess units of service with an MAI of 1, appropriate modifiers should be used to report them on separate lines of a claim. Current Procedural Terminology (CPT) modifiers such as -76 (repeat procedure or service by the same physician) and -91 (repeat clinical diagnostic laboratory test) as well as anatomic modifiers (eg, RT, LT, F1, F2) may be used, with modifier -59 (distinct procedural service) used only if no other modifier suffices. An example of an MUE with an MAI of 1 is CPT code 17264 (destruction, malignant lesion [eg, laser surgery, electrosurgery, cryosurgery, chemosurgery, surgical curettement], trunk, arms or legs; lesion diameter 3.1–4.0 cm), for which the MUE threshold is 3, meaning no more than 3 destructions can be submitted per claim line without triggering an edit-based rejection or RTP.
An MAI of 2 denotes absolute date of service edits, or so-called “per day edits based on policy.” Such edits are in place because units of service billed in excess of the MUE value on the same date of service are considered to be impossible by the CMS based on regulatory guidance or anatomic considerations.2 For instance, although the same physician may destroy multiple actinic keratoses in a single patient on the same date of service, it would not be possible to code more than one unit of service as
CPT code 17000, which specifically and exclusively
refers to the first lesion destroyed. Similarly,
CPT code 13101 (repair, complex, trunk; lesion diameter 2.6–7.5 cm) could only be reported once that day, as all complex repairs at that anatomic site must be summed and smaller or larger totals would be reported with another code.
Anatomic limitations are sometimes obvious and do not require specific coding rules. For example, only 1 gallbladder can be removed per patient. Although Qualified Independent Contractors and Administrative Law Judges are not bound by MAIs, they do give particular deference to an MAI of
2 given its definitive nature.2 Because ambulatory surgical center providers (Medicare specialty code 49) cannot report modifier -50 for bilateral
procedures, the MUE value used for editing is doubled for HCPCS codes with an MAI of 2 or 3 if the bilateral surgery indicator for the HCPCS code is 1.3
An MAI of 3 describes less strict date of service edits, so-called “per day edits based on clinical benchmarks.”2 Similar to MAIs of 1, MUEs for MAIs of 3 are based on medically likely daily frequencies of services provided in most settings. To determine if an MUE with an MAI of 3 has been reached, the MAC sums the units of service billed on all claim lines of the current claim as well as all prior paid claims for the same patient billed by the same provider on the same date of service. If the total units of service obtained in this manner exceeds the MUE value, then all claim lines with the relevant code for the current claim will be denied, but prior paid claims will not be adjusted. Denials based on MUEs for codes with an MAI of 3 can be appealed to the local MAC. Successful appeals require documentation that the units of service in excess of the MUE value were actually delivered and demonstration of medical necessity.2 An example of a CPT code with an MAI of 3 is 40490 (biopsy of lip) for which the MUE value is 3.
Complications With MUE and MAI
Because MUEs are based on current coding guidelines as well as current clinical practice, they are only applicable for the time period in which they are in effect. A change made to an MUE value for a particular code is not retroactive; however, in exceptional circumstances when a retroactive effective date is applied, MACs are not directed to examine prior claims but only “claims that are brought to their attention.”2
It also is important to realize that not all MUEs are publicly available and many are confidential. When claim denials occur, particularly in the context of multiple units of a particular code, automated MUE edits should be among the issues that are suspected. Physicians may resubmit RTP claims on separate lines if a claim line edit (MAI of 1) is operative. An MAI of 2 suggests a coding error that needs to be corrected, as these coding approaches are generally impossible based on definitional issues or anatomy. If an MUE with an MAI of 3 is the reason for denial, an appeal is possible, provided there is documentation to show that the service was actually provided and that it was medically necessary.
Final Thoughts
Dermatologists should be vigilant for unexpected payment denials, which may coincide with the implementation of new MUE values. When such denials occur and MUE values are publicly available, dermatologists should consider filing an appeal if the relevant MUEs were associated with an MAI of 1 or 3. Overall, dermatologists should be aware that many MUEs that were formerly claim line edits (MAI of 1) have been recently transitioned to date of service edits (MAI of 3), which are more restrictive.
1. American Academy of Dermatology. Medicare’s expanded medically unlikely edits. https://www.aad.org/members
/practice-and-advocacy-resource-center/coding-resources
/derm-coding-consult-library/winter-2014/medicare-
s-expanded-medically-unlikely-edits. Published Winter 2014. Accessed August 6, 2015.
2. Centers for Medicare & Medicaid Services. Revised modification to the Medically Unlikely Edit (MUE) program. MLN Matters. Number MM8853. https://www.cms.gov
/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNMattersArticles/downloads/MM8853.pdf. Published January 1, 2015. Accessed August 6, 2015.
3. Centers for Medicare & Medicaid Services.
Medically Unlikely Edits (MUE) and bilateral procedures. MLN Matters. Number SE1422.
https://www.cms.gov/Regulations-and-Guidance
/Guidance/Transmittals/2014-Transmittals-Items/SE1422.html?DLPage=2&DLEntries=10&DLSort=1&DLSort
Dir=ascending. Accessed July 28, 2015.
1. American Academy of Dermatology. Medicare’s expanded medically unlikely edits. https://www.aad.org/members
/practice-and-advocacy-resource-center/coding-resources
/derm-coding-consult-library/winter-2014/medicare-
s-expanded-medically-unlikely-edits. Published Winter 2014. Accessed August 6, 2015.
2. Centers for Medicare & Medicaid Services. Revised modification to the Medically Unlikely Edit (MUE) program. MLN Matters. Number MM8853. https://www.cms.gov
/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNMattersArticles/downloads/MM8853.pdf. Published January 1, 2015. Accessed August 6, 2015.
3. Centers for Medicare & Medicaid Services.
Medically Unlikely Edits (MUE) and bilateral procedures. MLN Matters. Number SE1422.
https://www.cms.gov/Regulations-and-Guidance
/Guidance/Transmittals/2014-Transmittals-Items/SE1422.html?DLPage=2&DLEntries=10&DLSort=1&DLSort
Dir=ascending. Accessed July 28, 2015.
Practice Points
- Medically Unlikely Edits (MUEs) are designed to prevent incorrect or excessive coding. Units of service billed in excess of the MUE will not be paid.
- Three different MUE adjudication indicators (MAIs) were added so that some MUE values would be date of service edits.
- Dermatologists should be vigilant for unexpected payment denials.
Is Your Electronic Health Record Putting You at Risk for a Documentation Audit?
A group of 3 busy orthopedists attended coding education each year and did their best to accurately code and document their services. As a risk-reduction strategy, the group engaged our firm to conduct an audit to determine whether they were documenting their services properly and to provide feedback about how they could improve.
What we found was shocking to the surgeons, but all too common, as we review thousands of orthopedic visit notes every year: The same examination had been documented for all visits, with physicians stating in their notes that the examination was medically necessary. In addition, their documentation supported Current Procedural Terminology (CPT) code 99214 at every visit, with visit frequencies of 2 weeks to 4 months.
The culprit of all this sameness? The practice’s electronic health record (EHR).
“Practices with EHRs often have a large volume of visit notes that look almost identical for a patient who is seen for multiple visits,” explains Mary LeGrand, RN, MA, CCS-P, CPC, KarenZupko & Associates consultant and coding educator. “And that is putting physicians at higher risk of being audited or of not passing an audit.”
According to LeGrand, this is because physicians are using the practice’s EHR to “pull forward” the patient’s previous visit note for the current visit, but failing to customize it for the current visit. The unintended consequence of this workflow efficiency is twofold:
1. It creates documentation that looks strikingly similar to, if not exactly like, the patient’s last billed visit note. This is often referred to as note “cloning.”
2. It creates documentation that includes a lot of unnecessary detail that, even if delivered and documented, doesn’t match the medical necessity of the visit, based on the history of present illness statements.
Both of these things can come back to bite you.
Zero in on the Risk
If your practice has an EHR, it is important that you evaluate whether certain workflow efficiency features are putting the practice at risk. You do not necessarily need to dump the EHR, but you may need to take action to reduce the risk of using these features.
In a pre-EHR practice, physicians began each visit with a blank piece of paper or dictated the entire visit. Then along came EHR vendors who, in an effort to make things easier and more efficient, created visit templates and the ability to “pull forward” the last visit note and use it as a basis for the current visit. The intention was always that physicians would modify it based on the current visit. But the reality is that physicians are busy, editing is time-consuming, and the unintended consequence is cloning.
“If you pull in unnecessary history or exam information from a previous visit that’s not relevant to the current visit, you can get dinged in an audit for not customizing the note to the patient’s specific presenting complaint,” LeGrand explains, “or, for attempting to bill a higher-level code by unintentionally padding the note with irrelevant information. What is documented for ‘reference’ has to be separated from what can be used to select the level of service.”
Your first documentation risk-reduction strategy is to review notes and look for signs of cloning.
LeGrand explains that a practice may be predisposed to cloning simply because of the way the EHR templates and workflow were set up when the system was implemented. “But,” she says, “‘the EHR made me do it’ defense won’t hold water, because it’s still the physician’s responsibility to customize or remove the information from templates and make the note unique to the visit.”
Yes, physician time is precious. But the reality is that the onus is on the physician to integrate EHR features with clinic workflow and to follow documentation rules.
The second documentation risk-reduction strategy is to make sure the level of evaluation and management (E/M) service billed is supported by medical necessity, not only by documentation artifacts that were relevant to the patient in the past but irrelevant to his or her current presenting complaint or condition.
“Medicare won’t pay for services that aren’t supported by medical necessity,” says LeGrand, “and you can’t achieve medical necessity by simply documenting additional E/M elements.”
This has always been the rule, LeGrand says. “But with the increased use of EHRs, and templates that automatically document visit elements and drive visits to a higher level of service, the Centers for Medicare & Medicaid Services [CMS] and private payers have added scrutiny to medical necessity reviews. They want to validate that higher-level visits billed indeed required a higher level of history and/or exam.”
To do this, the Office of the Inspector General (OIG) has supplemented its audit team with registered nurses. “The nurses assist certified coders by determining whether medical necessity has been met,” explains LeGrand.
Look at a patient who presents with toe pain. You take a detailed family history, conduct a review of systems (ROS), bill a high-level code, and document all the elements to support it. LeGrand explains, “There is no medical necessity to support doing an eye exam for a patient with toe pain in the absence of any other medical history, or performing a ROS to correlate an eye exam with toe pain. So, even if you do it and document it, the higher-level code won’t pass muster in an audit because the information documented is not medically necessary.”
According to LeGrand, the extent of the history and examination should be based on the presenting problem and the patient’s condition. “If an ankle sprain patient returns 2 weeks after the initial evaluation of the injury with a negative medical or surgical history, and the patient has been treated conservatively, it’s probably not necessary to conduct a ROS that includes 10 organ systems,” she says. “If your standard of care is to perform this level of service, no one will fault you for your care delivery; however, if you also choose a level of service based on this system review, without relevance to the presenting problem, and you bill a higher level of service than is supported by the nature of the presenting problem or the plan of care, the documentation probably won’t hold up in an audit where medical necessity is valued into the equation.”
On the other hand, LeGrand adds, if a patient presents to the emergency department after an automobile accident with an open fracture and other injuries, and the surgeon performs a complete ROS, the medical necessity would most likely be supported as the surgeon is preparing the patient for surgery.
Based on LeGrand’s work with practices, this distinction about medical necessity is news to many nonclinical billing staff. “They confuse medical necessity with medical decision-making, an E/M code documentation component, and incorrectly bill for a high-level visit because medical decision-making elements meet the documentation requirements—yet the code is not supported by medical necessity of the presenting problem.”
Talk with your billing team to make sure all staff members understand this critical difference. They must comprehend that the medically necessary level of service is determined by a number of clinical factors, not medical decision-making. Describe some of these clinical factors, which include, but are not limited to, chief complaint, clinical judgment, standards of practice, acute exacerbations/onsets of medical conditions or injuries, and comorbidities.
EHR Dos and Don’ts
LeGrand recommends the following best practices for using EHR documentation features:
1. DON’T simply cut and paste from a previous note. “This is what leads to verbose notes that have little to do with the patient you are documenting,” she says. “If you don’t cut and paste, you’ll avoid the root cause of this risk.”
2. DON’T pull forward information from previous visit notes that have nothing to do with the nature of the patient’s problem. “We understand that this takes extra time because physicians must review the previous note,” LeGrand says. “So if you don’t have time to review the past note, just don’t pull it forward. Start fresh with a new drop-down menu and select elements pertinent to the current visit. Or, dictate or type a note relevant to the current condition and presenting problems.”
How you choose to work this into your process will vary depending on which EHR system you use. “One surgeon I work with dictates everything because the drop-down menus and templates are cumbersome,” LeGrand says. “Some groups find it faster to use the EHR templates that they have customized. Others find their EHR’s point-and-click features most efficient for customizing quickly.”
3. DO customize your EHR visit templates if the use of templates is critical to your efficiency. “This is the most overlooked step in the EHR implementation process because it takes a fair amount of time to do,” LeGrand says. She suggests avoiding the use of multisystem examination templates created for medicine specialties altogether, and insists, “Don’t assume ‘that is how the vendor built it so we have to use it.’ Customize a template for each of your visit types so you can document in the EHR in the same fashion as when you used a paper system. Doing so will save you loads of documentation time.”
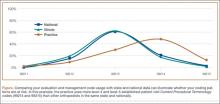
4. DO review your E/M code distribution. Generate a CPT frequency report for each physician and for the practice as a whole. Compare the data with state and national usage in orthopedics as a baseline. The American Academy of Orthopaedic Surgeon’s Code-X tool enables easy comparison of your practice’s E/M code usage with state and national data for orthopedics. Simply generate a CPT frequency report from your practice management system and enter the E/M data. Line graphs are automatically generated, making trends and patterns easy to see (Figure).
“Identify your outliers, pull charts randomly, and review the notes,” recommends LeGrand. “Make sure there is medical necessity for the level of code that’s been billed and that documentation supports it.”
You may be surprised to find you are an outlier on inpatient hospital codes, or your distribution of level-2 or -3 codes varies from your practice, state, or national data. Orthopedic surgeons don’t typically report high volumes of CPT codes 99204, 99205 or 99215, but if your practice does and you are an outlier, best to pay attention before someone else does.
5. DO select auditors with the right skill sets. Evaluating medical necessity in the note requires a clinical background. “If internal documentation reviews are conducted by the billing team, that’s fine,” LeGrand advises. “Just add a physician assistant or nurse to your internal review team. They can provide clinical oversight and review the note when necessary for medical necessity.”
If you are contracting with external auditors or consultants, verify auditor credentials and skill sets to ensure they can abstract and incorporate medical necessity into the review. “Auditors must be able to do more than count elements,” LeGrand says. “They must have clinical knowledge, and expertise in orthopedics is critical. This knowledge should be used to verify that medical necessity is present in every note.” LeGrand is quick to point out that not every note will be at risk, based on the amount of work performed and documented and the level of service billed. “But medical necessity must always be present.”
The addition of nurses to the OIG’s audit team is a big change and will refine the auditing process by adding more clinical scrutiny. The EHR documentation features are intended to improve efficiency, but only a clinician can determine and document unique visit elements and medical necessity.
Address these intersections of risk by ensuring your documentation meets medical necessity as well as E/M documentation elements. Conduct internal audits bi-annually to verify that E/M usage patterns align with peers and physician documentation is appropriate. And be sure there is clinical expertise on your audit team, whether it is internal or external. CMS now has it, and your practice should too. ◾
A group of 3 busy orthopedists attended coding education each year and did their best to accurately code and document their services. As a risk-reduction strategy, the group engaged our firm to conduct an audit to determine whether they were documenting their services properly and to provide feedback about how they could improve.
What we found was shocking to the surgeons, but all too common, as we review thousands of orthopedic visit notes every year: The same examination had been documented for all visits, with physicians stating in their notes that the examination was medically necessary. In addition, their documentation supported Current Procedural Terminology (CPT) code 99214 at every visit, with visit frequencies of 2 weeks to 4 months.
The culprit of all this sameness? The practice’s electronic health record (EHR).
“Practices with EHRs often have a large volume of visit notes that look almost identical for a patient who is seen for multiple visits,” explains Mary LeGrand, RN, MA, CCS-P, CPC, KarenZupko & Associates consultant and coding educator. “And that is putting physicians at higher risk of being audited or of not passing an audit.”
According to LeGrand, this is because physicians are using the practice’s EHR to “pull forward” the patient’s previous visit note for the current visit, but failing to customize it for the current visit. The unintended consequence of this workflow efficiency is twofold:
1. It creates documentation that looks strikingly similar to, if not exactly like, the patient’s last billed visit note. This is often referred to as note “cloning.”
2. It creates documentation that includes a lot of unnecessary detail that, even if delivered and documented, doesn’t match the medical necessity of the visit, based on the history of present illness statements.
Both of these things can come back to bite you.
Zero in on the Risk
If your practice has an EHR, it is important that you evaluate whether certain workflow efficiency features are putting the practice at risk. You do not necessarily need to dump the EHR, but you may need to take action to reduce the risk of using these features.
In a pre-EHR practice, physicians began each visit with a blank piece of paper or dictated the entire visit. Then along came EHR vendors who, in an effort to make things easier and more efficient, created visit templates and the ability to “pull forward” the last visit note and use it as a basis for the current visit. The intention was always that physicians would modify it based on the current visit. But the reality is that physicians are busy, editing is time-consuming, and the unintended consequence is cloning.
“If you pull in unnecessary history or exam information from a previous visit that’s not relevant to the current visit, you can get dinged in an audit for not customizing the note to the patient’s specific presenting complaint,” LeGrand explains, “or, for attempting to bill a higher-level code by unintentionally padding the note with irrelevant information. What is documented for ‘reference’ has to be separated from what can be used to select the level of service.”
Your first documentation risk-reduction strategy is to review notes and look for signs of cloning.
LeGrand explains that a practice may be predisposed to cloning simply because of the way the EHR templates and workflow were set up when the system was implemented. “But,” she says, “‘the EHR made me do it’ defense won’t hold water, because it’s still the physician’s responsibility to customize or remove the information from templates and make the note unique to the visit.”
Yes, physician time is precious. But the reality is that the onus is on the physician to integrate EHR features with clinic workflow and to follow documentation rules.
The second documentation risk-reduction strategy is to make sure the level of evaluation and management (E/M) service billed is supported by medical necessity, not only by documentation artifacts that were relevant to the patient in the past but irrelevant to his or her current presenting complaint or condition.
“Medicare won’t pay for services that aren’t supported by medical necessity,” says LeGrand, “and you can’t achieve medical necessity by simply documenting additional E/M elements.”
This has always been the rule, LeGrand says. “But with the increased use of EHRs, and templates that automatically document visit elements and drive visits to a higher level of service, the Centers for Medicare & Medicaid Services [CMS] and private payers have added scrutiny to medical necessity reviews. They want to validate that higher-level visits billed indeed required a higher level of history and/or exam.”
To do this, the Office of the Inspector General (OIG) has supplemented its audit team with registered nurses. “The nurses assist certified coders by determining whether medical necessity has been met,” explains LeGrand.
Look at a patient who presents with toe pain. You take a detailed family history, conduct a review of systems (ROS), bill a high-level code, and document all the elements to support it. LeGrand explains, “There is no medical necessity to support doing an eye exam for a patient with toe pain in the absence of any other medical history, or performing a ROS to correlate an eye exam with toe pain. So, even if you do it and document it, the higher-level code won’t pass muster in an audit because the information documented is not medically necessary.”
According to LeGrand, the extent of the history and examination should be based on the presenting problem and the patient’s condition. “If an ankle sprain patient returns 2 weeks after the initial evaluation of the injury with a negative medical or surgical history, and the patient has been treated conservatively, it’s probably not necessary to conduct a ROS that includes 10 organ systems,” she says. “If your standard of care is to perform this level of service, no one will fault you for your care delivery; however, if you also choose a level of service based on this system review, without relevance to the presenting problem, and you bill a higher level of service than is supported by the nature of the presenting problem or the plan of care, the documentation probably won’t hold up in an audit where medical necessity is valued into the equation.”
On the other hand, LeGrand adds, if a patient presents to the emergency department after an automobile accident with an open fracture and other injuries, and the surgeon performs a complete ROS, the medical necessity would most likely be supported as the surgeon is preparing the patient for surgery.
Based on LeGrand’s work with practices, this distinction about medical necessity is news to many nonclinical billing staff. “They confuse medical necessity with medical decision-making, an E/M code documentation component, and incorrectly bill for a high-level visit because medical decision-making elements meet the documentation requirements—yet the code is not supported by medical necessity of the presenting problem.”
Talk with your billing team to make sure all staff members understand this critical difference. They must comprehend that the medically necessary level of service is determined by a number of clinical factors, not medical decision-making. Describe some of these clinical factors, which include, but are not limited to, chief complaint, clinical judgment, standards of practice, acute exacerbations/onsets of medical conditions or injuries, and comorbidities.
EHR Dos and Don’ts
LeGrand recommends the following best practices for using EHR documentation features:
1. DON’T simply cut and paste from a previous note. “This is what leads to verbose notes that have little to do with the patient you are documenting,” she says. “If you don’t cut and paste, you’ll avoid the root cause of this risk.”
2. DON’T pull forward information from previous visit notes that have nothing to do with the nature of the patient’s problem. “We understand that this takes extra time because physicians must review the previous note,” LeGrand says. “So if you don’t have time to review the past note, just don’t pull it forward. Start fresh with a new drop-down menu and select elements pertinent to the current visit. Or, dictate or type a note relevant to the current condition and presenting problems.”
How you choose to work this into your process will vary depending on which EHR system you use. “One surgeon I work with dictates everything because the drop-down menus and templates are cumbersome,” LeGrand says. “Some groups find it faster to use the EHR templates that they have customized. Others find their EHR’s point-and-click features most efficient for customizing quickly.”
3. DO customize your EHR visit templates if the use of templates is critical to your efficiency. “This is the most overlooked step in the EHR implementation process because it takes a fair amount of time to do,” LeGrand says. She suggests avoiding the use of multisystem examination templates created for medicine specialties altogether, and insists, “Don’t assume ‘that is how the vendor built it so we have to use it.’ Customize a template for each of your visit types so you can document in the EHR in the same fashion as when you used a paper system. Doing so will save you loads of documentation time.”
4. DO review your E/M code distribution. Generate a CPT frequency report for each physician and for the practice as a whole. Compare the data with state and national usage in orthopedics as a baseline. The American Academy of Orthopaedic Surgeon’s Code-X tool enables easy comparison of your practice’s E/M code usage with state and national data for orthopedics. Simply generate a CPT frequency report from your practice management system and enter the E/M data. Line graphs are automatically generated, making trends and patterns easy to see (Figure).
“Identify your outliers, pull charts randomly, and review the notes,” recommends LeGrand. “Make sure there is medical necessity for the level of code that’s been billed and that documentation supports it.”
You may be surprised to find you are an outlier on inpatient hospital codes, or your distribution of level-2 or -3 codes varies from your practice, state, or national data. Orthopedic surgeons don’t typically report high volumes of CPT codes 99204, 99205 or 99215, but if your practice does and you are an outlier, best to pay attention before someone else does.
5. DO select auditors with the right skill sets. Evaluating medical necessity in the note requires a clinical background. “If internal documentation reviews are conducted by the billing team, that’s fine,” LeGrand advises. “Just add a physician assistant or nurse to your internal review team. They can provide clinical oversight and review the note when necessary for medical necessity.”
If you are contracting with external auditors or consultants, verify auditor credentials and skill sets to ensure they can abstract and incorporate medical necessity into the review. “Auditors must be able to do more than count elements,” LeGrand says. “They must have clinical knowledge, and expertise in orthopedics is critical. This knowledge should be used to verify that medical necessity is present in every note.” LeGrand is quick to point out that not every note will be at risk, based on the amount of work performed and documented and the level of service billed. “But medical necessity must always be present.”
The addition of nurses to the OIG’s audit team is a big change and will refine the auditing process by adding more clinical scrutiny. The EHR documentation features are intended to improve efficiency, but only a clinician can determine and document unique visit elements and medical necessity.
Address these intersections of risk by ensuring your documentation meets medical necessity as well as E/M documentation elements. Conduct internal audits bi-annually to verify that E/M usage patterns align with peers and physician documentation is appropriate. And be sure there is clinical expertise on your audit team, whether it is internal or external. CMS now has it, and your practice should too. ◾
A group of 3 busy orthopedists attended coding education each year and did their best to accurately code and document their services. As a risk-reduction strategy, the group engaged our firm to conduct an audit to determine whether they were documenting their services properly and to provide feedback about how they could improve.
What we found was shocking to the surgeons, but all too common, as we review thousands of orthopedic visit notes every year: The same examination had been documented for all visits, with physicians stating in their notes that the examination was medically necessary. In addition, their documentation supported Current Procedural Terminology (CPT) code 99214 at every visit, with visit frequencies of 2 weeks to 4 months.
The culprit of all this sameness? The practice’s electronic health record (EHR).
“Practices with EHRs often have a large volume of visit notes that look almost identical for a patient who is seen for multiple visits,” explains Mary LeGrand, RN, MA, CCS-P, CPC, KarenZupko & Associates consultant and coding educator. “And that is putting physicians at higher risk of being audited or of not passing an audit.”
According to LeGrand, this is because physicians are using the practice’s EHR to “pull forward” the patient’s previous visit note for the current visit, but failing to customize it for the current visit. The unintended consequence of this workflow efficiency is twofold:
1. It creates documentation that looks strikingly similar to, if not exactly like, the patient’s last billed visit note. This is often referred to as note “cloning.”
2. It creates documentation that includes a lot of unnecessary detail that, even if delivered and documented, doesn’t match the medical necessity of the visit, based on the history of present illness statements.
Both of these things can come back to bite you.
Zero in on the Risk
If your practice has an EHR, it is important that you evaluate whether certain workflow efficiency features are putting the practice at risk. You do not necessarily need to dump the EHR, but you may need to take action to reduce the risk of using these features.
In a pre-EHR practice, physicians began each visit with a blank piece of paper or dictated the entire visit. Then along came EHR vendors who, in an effort to make things easier and more efficient, created visit templates and the ability to “pull forward” the last visit note and use it as a basis for the current visit. The intention was always that physicians would modify it based on the current visit. But the reality is that physicians are busy, editing is time-consuming, and the unintended consequence is cloning.
“If you pull in unnecessary history or exam information from a previous visit that’s not relevant to the current visit, you can get dinged in an audit for not customizing the note to the patient’s specific presenting complaint,” LeGrand explains, “or, for attempting to bill a higher-level code by unintentionally padding the note with irrelevant information. What is documented for ‘reference’ has to be separated from what can be used to select the level of service.”
Your first documentation risk-reduction strategy is to review notes and look for signs of cloning.
LeGrand explains that a practice may be predisposed to cloning simply because of the way the EHR templates and workflow were set up when the system was implemented. “But,” she says, “‘the EHR made me do it’ defense won’t hold water, because it’s still the physician’s responsibility to customize or remove the information from templates and make the note unique to the visit.”
Yes, physician time is precious. But the reality is that the onus is on the physician to integrate EHR features with clinic workflow and to follow documentation rules.
The second documentation risk-reduction strategy is to make sure the level of evaluation and management (E/M) service billed is supported by medical necessity, not only by documentation artifacts that were relevant to the patient in the past but irrelevant to his or her current presenting complaint or condition.
“Medicare won’t pay for services that aren’t supported by medical necessity,” says LeGrand, “and you can’t achieve medical necessity by simply documenting additional E/M elements.”
This has always been the rule, LeGrand says. “But with the increased use of EHRs, and templates that automatically document visit elements and drive visits to a higher level of service, the Centers for Medicare & Medicaid Services [CMS] and private payers have added scrutiny to medical necessity reviews. They want to validate that higher-level visits billed indeed required a higher level of history and/or exam.”
To do this, the Office of the Inspector General (OIG) has supplemented its audit team with registered nurses. “The nurses assist certified coders by determining whether medical necessity has been met,” explains LeGrand.
Look at a patient who presents with toe pain. You take a detailed family history, conduct a review of systems (ROS), bill a high-level code, and document all the elements to support it. LeGrand explains, “There is no medical necessity to support doing an eye exam for a patient with toe pain in the absence of any other medical history, or performing a ROS to correlate an eye exam with toe pain. So, even if you do it and document it, the higher-level code won’t pass muster in an audit because the information documented is not medically necessary.”
According to LeGrand, the extent of the history and examination should be based on the presenting problem and the patient’s condition. “If an ankle sprain patient returns 2 weeks after the initial evaluation of the injury with a negative medical or surgical history, and the patient has been treated conservatively, it’s probably not necessary to conduct a ROS that includes 10 organ systems,” she says. “If your standard of care is to perform this level of service, no one will fault you for your care delivery; however, if you also choose a level of service based on this system review, without relevance to the presenting problem, and you bill a higher level of service than is supported by the nature of the presenting problem or the plan of care, the documentation probably won’t hold up in an audit where medical necessity is valued into the equation.”
On the other hand, LeGrand adds, if a patient presents to the emergency department after an automobile accident with an open fracture and other injuries, and the surgeon performs a complete ROS, the medical necessity would most likely be supported as the surgeon is preparing the patient for surgery.
Based on LeGrand’s work with practices, this distinction about medical necessity is news to many nonclinical billing staff. “They confuse medical necessity with medical decision-making, an E/M code documentation component, and incorrectly bill for a high-level visit because medical decision-making elements meet the documentation requirements—yet the code is not supported by medical necessity of the presenting problem.”
Talk with your billing team to make sure all staff members understand this critical difference. They must comprehend that the medically necessary level of service is determined by a number of clinical factors, not medical decision-making. Describe some of these clinical factors, which include, but are not limited to, chief complaint, clinical judgment, standards of practice, acute exacerbations/onsets of medical conditions or injuries, and comorbidities.
EHR Dos and Don’ts
LeGrand recommends the following best practices for using EHR documentation features:
1. DON’T simply cut and paste from a previous note. “This is what leads to verbose notes that have little to do with the patient you are documenting,” she says. “If you don’t cut and paste, you’ll avoid the root cause of this risk.”
2. DON’T pull forward information from previous visit notes that have nothing to do with the nature of the patient’s problem. “We understand that this takes extra time because physicians must review the previous note,” LeGrand says. “So if you don’t have time to review the past note, just don’t pull it forward. Start fresh with a new drop-down menu and select elements pertinent to the current visit. Or, dictate or type a note relevant to the current condition and presenting problems.”
How you choose to work this into your process will vary depending on which EHR system you use. “One surgeon I work with dictates everything because the drop-down menus and templates are cumbersome,” LeGrand says. “Some groups find it faster to use the EHR templates that they have customized. Others find their EHR’s point-and-click features most efficient for customizing quickly.”
3. DO customize your EHR visit templates if the use of templates is critical to your efficiency. “This is the most overlooked step in the EHR implementation process because it takes a fair amount of time to do,” LeGrand says. She suggests avoiding the use of multisystem examination templates created for medicine specialties altogether, and insists, “Don’t assume ‘that is how the vendor built it so we have to use it.’ Customize a template for each of your visit types so you can document in the EHR in the same fashion as when you used a paper system. Doing so will save you loads of documentation time.”
4. DO review your E/M code distribution. Generate a CPT frequency report for each physician and for the practice as a whole. Compare the data with state and national usage in orthopedics as a baseline. The American Academy of Orthopaedic Surgeon’s Code-X tool enables easy comparison of your practice’s E/M code usage with state and national data for orthopedics. Simply generate a CPT frequency report from your practice management system and enter the E/M data. Line graphs are automatically generated, making trends and patterns easy to see (Figure).
“Identify your outliers, pull charts randomly, and review the notes,” recommends LeGrand. “Make sure there is medical necessity for the level of code that’s been billed and that documentation supports it.”
You may be surprised to find you are an outlier on inpatient hospital codes, or your distribution of level-2 or -3 codes varies from your practice, state, or national data. Orthopedic surgeons don’t typically report high volumes of CPT codes 99204, 99205 or 99215, but if your practice does and you are an outlier, best to pay attention before someone else does.
5. DO select auditors with the right skill sets. Evaluating medical necessity in the note requires a clinical background. “If internal documentation reviews are conducted by the billing team, that’s fine,” LeGrand advises. “Just add a physician assistant or nurse to your internal review team. They can provide clinical oversight and review the note when necessary for medical necessity.”
If you are contracting with external auditors or consultants, verify auditor credentials and skill sets to ensure they can abstract and incorporate medical necessity into the review. “Auditors must be able to do more than count elements,” LeGrand says. “They must have clinical knowledge, and expertise in orthopedics is critical. This knowledge should be used to verify that medical necessity is present in every note.” LeGrand is quick to point out that not every note will be at risk, based on the amount of work performed and documented and the level of service billed. “But medical necessity must always be present.”
The addition of nurses to the OIG’s audit team is a big change and will refine the auditing process by adding more clinical scrutiny. The EHR documentation features are intended to improve efficiency, but only a clinician can determine and document unique visit elements and medical necessity.
Address these intersections of risk by ensuring your documentation meets medical necessity as well as E/M documentation elements. Conduct internal audits bi-annually to verify that E/M usage patterns align with peers and physician documentation is appropriate. And be sure there is clinical expertise on your audit team, whether it is internal or external. CMS now has it, and your practice should too. ◾
ICD-10 Medical Coding System Likely to Improve Documentation, Reimbursement
ICD-10 is the system that will replace ICD-9 for all parties covered by the Health Insurance Portability and Accountability Act (HIPAA). ICD-10 contains a code set used for inpatient procedural reporting and a code set used for diagnosis reporting. Physicians billing for professional services will only be affected when reporting diagnoses codes on their claims, but both physician and hospital selection of ICD-10 codes relies heavily on physician documentation. Therefore, documentation must be scrutinized. The most widely noted impact ICD-10 will have on documentation is increased specificity, with enhanced reporting of the patient’s presenting problem(s). Expanding from a pool of 14,000 3/5-digit codes to 69,000 7-digit codes, and accommodating this change, are daunting tasks. These anticipated burdens make it hard for physicians to recognize the positive effects ICD-10 may create, such as:1
- Better clinical decisions as better data is documented, collected, and evaluated;
- Improved protocol and clinical pathway design for various health conditions;
- Improved public health reporting and tracking of illnesses and severity over time;
- Better definition of patient conditions, providing improved matching of professional resources and care teams and increasing communications between providers;
- Support in practice transition to risk-sharing models with more precise data for patients and populations;
- Provision of clear objective data for credentialing and privileges, and support for professional Maintenance of Certification reporting across specialties;
- Better documentation of patient complexity and level of care, supporting reimbursement and measures for quality and efficiency reporting; and
- Reduction in audit risk exposure by encouraging the use of diagnosis codes with a greater degree of specificity as supported by the clinical documentation.
With the Oct. 1 implementation date rapidly approaching, physicians need to ask themselves, “Am I prepared?”
Getting Started
Everyone has a role and responsibility in transitioning to ICD-10. Active participation by all involved parties guarantees a more successful outcome. Practice administration must ensure that each aspect of implementation is reviewed and appropriately addressed. If not already done, immediate steps should be taken to verify the products and services that affect implementation. These include:
- Payer mix and related contracts: Entities not covered by HIPAA (e.g. workers’ compensation and auto insurance companies) may choose not to implement ICD-10. Since ICD-9 will no longer be maintained post-ICD-10 implementation, it is in the best interest of non-covered entities to use the new coding system.2 For payers who are required to transition to ICD-10, it is important to identify whether patient eligibility, claim processing, and/or payment timelines will be affected, as well as fee schedules or capitated rates.
- Vendor readiness: Physician groups may use a variety of vendors to assist with different aspects of the revenue cycle, including an electronic health record (e.g. documenting services and transmitting physician orders/prescriptions); a practice management system (e.g. scheduling and registering patients); a billing service (e.g. processing patient claims and payments); and a clearinghouse (e.g. verifying patient eligibility and obtaining authorizations). Know when software and/or hardware upgrades are available and if there are additional upgrade fees. Identify vendors that provide support services, training, and tools or templates to ease the transition. Most importantly, inquire about a testing period for products and applications to ensure functionality and adequate feedback on use of the system(s).
- Internal coding and billing resources. Identify physicians and staff who use ICD-9 codes and need to know ICD-10 codes in order to fulfill their responsibilities. Both physicians and staff can assist in identifying common clinical scenarios and the most frequently used ICD-9 codes, in order to develop a list of common ICD-10 specialty codes. Payer coverage policies currently include ICD-10 codes for provider review and comparison. Revise current forms/templates that include diagnosis codes to reflect this updated information. Schedule ICD-10 training for clinicians, office managers, billers, coders, and other key staff. Coding professionals recommend that training take place approximately six months prior to the ICD-10 compliance deadline.3 Training sessions are available from consultants, professional societies, payers, and other entities. Cost varies depending upon the type and length of training. CMS provides some free services, but in-depth training or certification for at least one practice member should be considered.
Once training is completed, dual coding is an option. Dual coding is the process by which both ICD-9 codes and ICD-10 codes are selected during the coding process. Some practices rely on independent selection of each code, while others rely on the General Equivalence Mappings (GEMs). GEMs were developed to assist industry migration to ICD-10. They are intended to be used primarily for translations of code lists or code tables used by an application or other coded data when codes in one code set are the only source of information; they are not intended as a substitution for direct use of ICD-9-CM and ICD-10-CM/PCS.4 Manual coding enhances coding efficiency and also identifies physician documentation deficiencies. Dual coding should begin as soon as possible, prior to October 1.
End-to-end testing is an opportunity to submit test claims to CMS with ICD-10 codes; providers will receive a remittance advice that explains the adjudication of the claims.5 This testing is limited to a small group of providers who were required to register in April, and its final week is July 20-24.
Provide Feedback
The importance of feedback is often understated. Many physician practices do not have the time to plan ahead and, as a result, find themselves in a reactive rather than proactive role. Over the next couple of months, find the time and resources to audit physician documentation based on ICD-10 criteria. Ask yourself whether or not the information contains enough specificity to select the best possible code, or does code selection default to an “unspecified” code?
Avoid “unspecified” codes when possible in preparation for payer policy revisions that are aimed at reducing or eliminating these types of codes. If the documentation lacks detail, educate physicians on the missing elements.
Review ICD-10 code sets with physicians to improve their understanding of the new system. For example, diabetes mellitus is identified in ICD-9 as one category (250.xx), with digits to specify Type I or Type II, controlled vs. uncontrolled, with or without complications. ICD-10 separates diabetes into categories of Type I (E10) or Type II (E11), with subcategories to identify complications and affected body systems, thereby expanding the volume of codes and corresponding documentation criteria.6
Post-implementation feedback will become even more important. Monitor claim denials for invalid codes and medical necessity issues (i.e., valid codes not included for coverage). If the medical necessity denials are a result of inaccurate code selection related to insufficient documentation details, provider education will be crucial in resolving these errors. Continuing education to strengthen and update staff skills is imperative.
CMS has developed many tools and resources to promote a successful transition and assess your ICD-10 preparedness. Physician practices can develop an “action plan,” learn basic ICD-10 concepts, and much more.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. Road to 10: the small physician practice’s route to ICD-10? Accessed June 6, 2015.
- Department of Health and Human Services. Centers for Medicare and Medicaid Services. Medicare Learning Network: ICD-10-CM/PCS Myths and Facts. Accessed June 6, 2015.
- Centers for Medicare and Medicaid Services. ICD-10: ICD-10 Basics for Medical Practices. Accessed June 6, 2015.
- American Health Information Management Association (AHIMA). Putting the ICD-10-CM/PCS GEMs into practice. Accessed June 6, 2015.
- Novitas Solutions. Medicare JL, Part B. ICD-10 Implementation. Accessed June 6, 2015.
- Centers for Medicare and Medicaid Services. ICD-10 Coding and Diabetes. Accessed June 6, 2015.
ICD-10 is the system that will replace ICD-9 for all parties covered by the Health Insurance Portability and Accountability Act (HIPAA). ICD-10 contains a code set used for inpatient procedural reporting and a code set used for diagnosis reporting. Physicians billing for professional services will only be affected when reporting diagnoses codes on their claims, but both physician and hospital selection of ICD-10 codes relies heavily on physician documentation. Therefore, documentation must be scrutinized. The most widely noted impact ICD-10 will have on documentation is increased specificity, with enhanced reporting of the patient’s presenting problem(s). Expanding from a pool of 14,000 3/5-digit codes to 69,000 7-digit codes, and accommodating this change, are daunting tasks. These anticipated burdens make it hard for physicians to recognize the positive effects ICD-10 may create, such as:1
- Better clinical decisions as better data is documented, collected, and evaluated;
- Improved protocol and clinical pathway design for various health conditions;
- Improved public health reporting and tracking of illnesses and severity over time;
- Better definition of patient conditions, providing improved matching of professional resources and care teams and increasing communications between providers;
- Support in practice transition to risk-sharing models with more precise data for patients and populations;
- Provision of clear objective data for credentialing and privileges, and support for professional Maintenance of Certification reporting across specialties;
- Better documentation of patient complexity and level of care, supporting reimbursement and measures for quality and efficiency reporting; and
- Reduction in audit risk exposure by encouraging the use of diagnosis codes with a greater degree of specificity as supported by the clinical documentation.
With the Oct. 1 implementation date rapidly approaching, physicians need to ask themselves, “Am I prepared?”
Getting Started
Everyone has a role and responsibility in transitioning to ICD-10. Active participation by all involved parties guarantees a more successful outcome. Practice administration must ensure that each aspect of implementation is reviewed and appropriately addressed. If not already done, immediate steps should be taken to verify the products and services that affect implementation. These include:
- Payer mix and related contracts: Entities not covered by HIPAA (e.g. workers’ compensation and auto insurance companies) may choose not to implement ICD-10. Since ICD-9 will no longer be maintained post-ICD-10 implementation, it is in the best interest of non-covered entities to use the new coding system.2 For payers who are required to transition to ICD-10, it is important to identify whether patient eligibility, claim processing, and/or payment timelines will be affected, as well as fee schedules or capitated rates.
- Vendor readiness: Physician groups may use a variety of vendors to assist with different aspects of the revenue cycle, including an electronic health record (e.g. documenting services and transmitting physician orders/prescriptions); a practice management system (e.g. scheduling and registering patients); a billing service (e.g. processing patient claims and payments); and a clearinghouse (e.g. verifying patient eligibility and obtaining authorizations). Know when software and/or hardware upgrades are available and if there are additional upgrade fees. Identify vendors that provide support services, training, and tools or templates to ease the transition. Most importantly, inquire about a testing period for products and applications to ensure functionality and adequate feedback on use of the system(s).
- Internal coding and billing resources. Identify physicians and staff who use ICD-9 codes and need to know ICD-10 codes in order to fulfill their responsibilities. Both physicians and staff can assist in identifying common clinical scenarios and the most frequently used ICD-9 codes, in order to develop a list of common ICD-10 specialty codes. Payer coverage policies currently include ICD-10 codes for provider review and comparison. Revise current forms/templates that include diagnosis codes to reflect this updated information. Schedule ICD-10 training for clinicians, office managers, billers, coders, and other key staff. Coding professionals recommend that training take place approximately six months prior to the ICD-10 compliance deadline.3 Training sessions are available from consultants, professional societies, payers, and other entities. Cost varies depending upon the type and length of training. CMS provides some free services, but in-depth training or certification for at least one practice member should be considered.
Once training is completed, dual coding is an option. Dual coding is the process by which both ICD-9 codes and ICD-10 codes are selected during the coding process. Some practices rely on independent selection of each code, while others rely on the General Equivalence Mappings (GEMs). GEMs were developed to assist industry migration to ICD-10. They are intended to be used primarily for translations of code lists or code tables used by an application or other coded data when codes in one code set are the only source of information; they are not intended as a substitution for direct use of ICD-9-CM and ICD-10-CM/PCS.4 Manual coding enhances coding efficiency and also identifies physician documentation deficiencies. Dual coding should begin as soon as possible, prior to October 1.
End-to-end testing is an opportunity to submit test claims to CMS with ICD-10 codes; providers will receive a remittance advice that explains the adjudication of the claims.5 This testing is limited to a small group of providers who were required to register in April, and its final week is July 20-24.
Provide Feedback
The importance of feedback is often understated. Many physician practices do not have the time to plan ahead and, as a result, find themselves in a reactive rather than proactive role. Over the next couple of months, find the time and resources to audit physician documentation based on ICD-10 criteria. Ask yourself whether or not the information contains enough specificity to select the best possible code, or does code selection default to an “unspecified” code?
Avoid “unspecified” codes when possible in preparation for payer policy revisions that are aimed at reducing or eliminating these types of codes. If the documentation lacks detail, educate physicians on the missing elements.
Review ICD-10 code sets with physicians to improve their understanding of the new system. For example, diabetes mellitus is identified in ICD-9 as one category (250.xx), with digits to specify Type I or Type II, controlled vs. uncontrolled, with or without complications. ICD-10 separates diabetes into categories of Type I (E10) or Type II (E11), with subcategories to identify complications and affected body systems, thereby expanding the volume of codes and corresponding documentation criteria.6
Post-implementation feedback will become even more important. Monitor claim denials for invalid codes and medical necessity issues (i.e., valid codes not included for coverage). If the medical necessity denials are a result of inaccurate code selection related to insufficient documentation details, provider education will be crucial in resolving these errors. Continuing education to strengthen and update staff skills is imperative.
CMS has developed many tools and resources to promote a successful transition and assess your ICD-10 preparedness. Physician practices can develop an “action plan,” learn basic ICD-10 concepts, and much more.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. Road to 10: the small physician practice’s route to ICD-10? Accessed June 6, 2015.
- Department of Health and Human Services. Centers for Medicare and Medicaid Services. Medicare Learning Network: ICD-10-CM/PCS Myths and Facts. Accessed June 6, 2015.
- Centers for Medicare and Medicaid Services. ICD-10: ICD-10 Basics for Medical Practices. Accessed June 6, 2015.
- American Health Information Management Association (AHIMA). Putting the ICD-10-CM/PCS GEMs into practice. Accessed June 6, 2015.
- Novitas Solutions. Medicare JL, Part B. ICD-10 Implementation. Accessed June 6, 2015.
- Centers for Medicare and Medicaid Services. ICD-10 Coding and Diabetes. Accessed June 6, 2015.
ICD-10 is the system that will replace ICD-9 for all parties covered by the Health Insurance Portability and Accountability Act (HIPAA). ICD-10 contains a code set used for inpatient procedural reporting and a code set used for diagnosis reporting. Physicians billing for professional services will only be affected when reporting diagnoses codes on their claims, but both physician and hospital selection of ICD-10 codes relies heavily on physician documentation. Therefore, documentation must be scrutinized. The most widely noted impact ICD-10 will have on documentation is increased specificity, with enhanced reporting of the patient’s presenting problem(s). Expanding from a pool of 14,000 3/5-digit codes to 69,000 7-digit codes, and accommodating this change, are daunting tasks. These anticipated burdens make it hard for physicians to recognize the positive effects ICD-10 may create, such as:1
- Better clinical decisions as better data is documented, collected, and evaluated;
- Improved protocol and clinical pathway design for various health conditions;
- Improved public health reporting and tracking of illnesses and severity over time;
- Better definition of patient conditions, providing improved matching of professional resources and care teams and increasing communications between providers;
- Support in practice transition to risk-sharing models with more precise data for patients and populations;
- Provision of clear objective data for credentialing and privileges, and support for professional Maintenance of Certification reporting across specialties;
- Better documentation of patient complexity and level of care, supporting reimbursement and measures for quality and efficiency reporting; and
- Reduction in audit risk exposure by encouraging the use of diagnosis codes with a greater degree of specificity as supported by the clinical documentation.
With the Oct. 1 implementation date rapidly approaching, physicians need to ask themselves, “Am I prepared?”
Getting Started
Everyone has a role and responsibility in transitioning to ICD-10. Active participation by all involved parties guarantees a more successful outcome. Practice administration must ensure that each aspect of implementation is reviewed and appropriately addressed. If not already done, immediate steps should be taken to verify the products and services that affect implementation. These include:
- Payer mix and related contracts: Entities not covered by HIPAA (e.g. workers’ compensation and auto insurance companies) may choose not to implement ICD-10. Since ICD-9 will no longer be maintained post-ICD-10 implementation, it is in the best interest of non-covered entities to use the new coding system.2 For payers who are required to transition to ICD-10, it is important to identify whether patient eligibility, claim processing, and/or payment timelines will be affected, as well as fee schedules or capitated rates.
- Vendor readiness: Physician groups may use a variety of vendors to assist with different aspects of the revenue cycle, including an electronic health record (e.g. documenting services and transmitting physician orders/prescriptions); a practice management system (e.g. scheduling and registering patients); a billing service (e.g. processing patient claims and payments); and a clearinghouse (e.g. verifying patient eligibility and obtaining authorizations). Know when software and/or hardware upgrades are available and if there are additional upgrade fees. Identify vendors that provide support services, training, and tools or templates to ease the transition. Most importantly, inquire about a testing period for products and applications to ensure functionality and adequate feedback on use of the system(s).
- Internal coding and billing resources. Identify physicians and staff who use ICD-9 codes and need to know ICD-10 codes in order to fulfill their responsibilities. Both physicians and staff can assist in identifying common clinical scenarios and the most frequently used ICD-9 codes, in order to develop a list of common ICD-10 specialty codes. Payer coverage policies currently include ICD-10 codes for provider review and comparison. Revise current forms/templates that include diagnosis codes to reflect this updated information. Schedule ICD-10 training for clinicians, office managers, billers, coders, and other key staff. Coding professionals recommend that training take place approximately six months prior to the ICD-10 compliance deadline.3 Training sessions are available from consultants, professional societies, payers, and other entities. Cost varies depending upon the type and length of training. CMS provides some free services, but in-depth training or certification for at least one practice member should be considered.
Once training is completed, dual coding is an option. Dual coding is the process by which both ICD-9 codes and ICD-10 codes are selected during the coding process. Some practices rely on independent selection of each code, while others rely on the General Equivalence Mappings (GEMs). GEMs were developed to assist industry migration to ICD-10. They are intended to be used primarily for translations of code lists or code tables used by an application or other coded data when codes in one code set are the only source of information; they are not intended as a substitution for direct use of ICD-9-CM and ICD-10-CM/PCS.4 Manual coding enhances coding efficiency and also identifies physician documentation deficiencies. Dual coding should begin as soon as possible, prior to October 1.
End-to-end testing is an opportunity to submit test claims to CMS with ICD-10 codes; providers will receive a remittance advice that explains the adjudication of the claims.5 This testing is limited to a small group of providers who were required to register in April, and its final week is July 20-24.
Provide Feedback
The importance of feedback is often understated. Many physician practices do not have the time to plan ahead and, as a result, find themselves in a reactive rather than proactive role. Over the next couple of months, find the time and resources to audit physician documentation based on ICD-10 criteria. Ask yourself whether or not the information contains enough specificity to select the best possible code, or does code selection default to an “unspecified” code?
Avoid “unspecified” codes when possible in preparation for payer policy revisions that are aimed at reducing or eliminating these types of codes. If the documentation lacks detail, educate physicians on the missing elements.
Review ICD-10 code sets with physicians to improve their understanding of the new system. For example, diabetes mellitus is identified in ICD-9 as one category (250.xx), with digits to specify Type I or Type II, controlled vs. uncontrolled, with or without complications. ICD-10 separates diabetes into categories of Type I (E10) or Type II (E11), with subcategories to identify complications and affected body systems, thereby expanding the volume of codes and corresponding documentation criteria.6
Post-implementation feedback will become even more important. Monitor claim denials for invalid codes and medical necessity issues (i.e., valid codes not included for coverage). If the medical necessity denials are a result of inaccurate code selection related to insufficient documentation details, provider education will be crucial in resolving these errors. Continuing education to strengthen and update staff skills is imperative.
CMS has developed many tools and resources to promote a successful transition and assess your ICD-10 preparedness. Physician practices can develop an “action plan,” learn basic ICD-10 concepts, and much more.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. Road to 10: the small physician practice’s route to ICD-10? Accessed June 6, 2015.
- Department of Health and Human Services. Centers for Medicare and Medicaid Services. Medicare Learning Network: ICD-10-CM/PCS Myths and Facts. Accessed June 6, 2015.
- Centers for Medicare and Medicaid Services. ICD-10: ICD-10 Basics for Medical Practices. Accessed June 6, 2015.
- American Health Information Management Association (AHIMA). Putting the ICD-10-CM/PCS GEMs into practice. Accessed June 6, 2015.
- Novitas Solutions. Medicare JL, Part B. ICD-10 Implementation. Accessed June 6, 2015.
- Centers for Medicare and Medicaid Services. ICD-10 Coding and Diabetes. Accessed June 6, 2015.
ICD-10 Race to the Finish: 8 High Priorities in the 11th Hour
As late as mid-April 2015, a survey of 121 orthopedic practices indicated that 30% had done nothing to start preparing for ICD-10 (International Classification of Diseases, Tenth Revision).1 That’s scary. And even the practices that had begun to prepare had not completed a number of key tasks (Figure 1).
Certainly, the will-they-or-won’t-they possibility of another congressional delay had many practices sitting on their hands this year. But now that the October 1, 2015, implementation is set in stone, this lack of inertia has many practices woefully behind. If your practice is one of many that hasn’t mapped your common ICD-9 (International Classification of Diseases, Ninth Revision) codes to ICD-10 codes, completed payer testing, or attended training, it’s time for a “full-court press.”
Being unprepared for ICD-10 will cause more than just an increase in claim denials. If your surgery schedule is booked a few months out, your staff will need to pre-authorize cases using ICD-10 as early as August 1—and they won’t be able to do that if you haven’t dictated the clinical terms required to choose an ICD-10 code. Without an understanding of ICD-10, severity of illness coding will suffer, and that will affect your bundled and value-based payments. And, if you don’t provide an adequate diagnosis when sending patients off-site for physical therapy, you’ll soon be getting phone calls from their billing staff demanding more specifics.
The clock is ticking and time is short. Here’s a prioritized list of what needs to get done.
1. Generate an ICD-9 frequency report
Identifying which diagnosis codes are the most frequently used, and therefore drive a significant portion of practice revenue, is an absolute must. The data will help prioritize training and code-mapping activities.
Most practices generate Current Procedural Terminology (CPT) code-frequency reports regularly, but few have ever run an ICD-9 code-frequency report. Call your vendor and ask for assistance, as there are multiple ways to run this report and they vary by practice management system. Sort the data elements and generate the ICD-9 frequency report by:
- Primary diagnosis.
- Unique patient.
- Revenue. (If your practice management system can’t give you diagnosis data by revenue, which enables you to focus on the codes that generate the most revenue, generate it by charges.)
The result should be a report that identifies the 20 to 25 diagnosis codes (or charges, depending on the reports generated) that drive the most revenue for the practice. Use the data to focus and prioritize your training and code-mapping activities.
2. Schedule training
Forget about “general” ICD-10 training courses. You need orthopedic-specific guidance. That’s because ICD-10 for orthopedics is more complex than for other specialties. Dictating fractures under ICD-10 is not so simple. Selecting an injury code requires confidence in correctly using the seventh character.
“Everyone who uses diagnosis codes must have baseline knowledge: surgeons, billing staff, surgical coordinators, and clinical team,” according to Sarah Wiskerchen, MBA, CPC, consultant and ICD-10 educator with KarenZupko & Associates (KZA). Training must include the practical details of ICD-10, such as assigning laterality, understanding the system architecture, and limiting the use of unspecified codes.
The American Academy of Orthopaedic Surgeons (AAOS) offers a self-paced, online training series that provides details for the top 3 diagnosis codes for each subspecialty. The 10-program course, ICD-10-CM: By the Numbers, is available at www.aaos.org ($299 for members, $399 for nonmembers). If you prefer live instruction, there is one more AAOS-sponsored, regional ICD-10 workshop left before the October 1 deadline, and more may be added. (Details at www.karenzupko.com)
These courses provide highly specific and granular ICD-10 knowledge and incorporate the use of Code-X, an AAOS-developed software tool. They also feature tools for handling the complexities of fractures and injury codes, such as Leo C. Far, an acronym developed by KZA consultant and coding educator Margie Maley, BSN, MS, to make ICD-10 diagnosis coding for fractures easier (Figure 2).
Some subspecialty societies also offer ICD-10 training. The American Society for Surgery of the Hand (www.assh.org), for example, offers a series of webinars and member-developed ICD-9-to-ICD-10 code maps.
3. Crosswalk your common codes from ICD-9 to ICD-10
Crosswalking is the process of mapping your most commonly used ICD-9 codes to their equivalent ICD-10 codes. This exercise familiarizes your team with ICD-10 language and terms, and gives a sense of which ICD-9 codes expand to just 1 or 2 ICD-10 codes and which codes expand into 10 or more codes—as some injury codes do (Table).
“Attempting to map the codes before completing ICD-10 training is like trying to write a letter in Greek when you only speak English,” Wiskerchen warns. “So start this process after at least some of your team have grasped the fundamentals of ICD-10.” This is where the data from your ICD-9 frequency report comes in. Use it to prioritize which codes to map first with a goal of mapping your top 25 ICD-9 codes to their ICD-10 equivalents by August 31.
Invest in good tools to support your mapping efforts. Avoid general mapping equivalent (GEM) coding tools, which are free for a good reason—they are incomplete and don’t always lead you to the correct ICD-10 code. Instead, purchase resources from credible sources, such as the American Medical Association (AMA; www.ama-assn.org). The AMA publishes ICD-10-CM 2016: The Complete Official Codebook as well as ICD-10-CM Mappings 2016, which links ICD-9 codes to all valid ICD-10 alternatives. The AMA also offers electronic ICD-10-CM Express Reference Mapping Cards for multiple specialties.
Practice makes perfect and crosswalking from ICD-9 to ICD-10 is one of the best ways for your team to become aware of the nuances in the new coding system. Like learning a new language, “speaking” ICD-10 does not become automatic just because you’ve attended training or completed the coding maps. Training teaches the architecture of the new coding system. Mapping provides a structured way to become familiar with the codes the practice will use most often. Once these 2 primary pieces are understood and assimilated, most physicians find that dictating the necessary new terms becomes quite easy.
4. Conduct a gap analysis to identify the ICD-10 terms missing from each provider’s current documentation
Conduct the gap analysis after your team has completed training, and once you’ve at least begun the process of mapping codes from ICD-9 to ICD-10. Here’s how:
- Generate a CPT frequency report.
- Select the top 5 procedures for each physician.
- Pull 2 patients’ notes for each of the top procedures.
- Review the notes and try to select ICD-10 code(s).
If key ICD-10 terms are not included in current documentation, physicians should modify the templates or macros they rely on for dictation.
“This simple exercise makes it obvious which clinical information physicians must add for ICD-10,” Wiskerchen says. For example, if the patient had an arthroscopy, but the note doesn’t specify on which leg, that’s a clear indication that the physician must dictate laterality. “The gap analysis is a great way to coach physicians about the clinical details to document, so staff can bill under ICD-10,” Wiskerchen says.
5. Contact technology vendors
Given the number of new ICD-10 codes in orthopedics, paper cheat sheets will be obsolete. Instead, you’ll need to rely on pull-down menus and/or search fields in the electronic health record (EHR) and practice management systems.
“Get clarity about how the new features and workflow processes will work in your systems,” suggests Wiskerchen. “Ask questions such as: Which features will be added or changed to accommodate the new codes? Will there be new screens or pick lists for ICD-10, or search fields? How will new screens and features change our current workflow? And schedule any necessary training as soon as possible.”
In addition to software upgrades and training, vendors and clearinghouses offer an array of services to help practices make the transition. Some vendors even provide help coordinating your internal plan with their new product features and training. Contact vendors to find out what they offer.
6. Use completed code maps to build diagnosis code databases, EHR templates, charge tickets, pick lists, prompters, and other coding tools
“Provide the code crosswalks and results of your documentation gap analysis to the IT [information technology] team so they can get started,” Wiskerchen advises. “And assign a physician or midlevel provider to work with IT so that the tools are clinically accurate.”
7. Schedule testing with clearinghouses and payers
“Successful testing indicates that your hard work has paid off, and that claims will be processed with few, if any, ICD-10–related hiccups,” Wiskerchen says. Essentially, the testing confirms that your ICD-10 code database, pick lists, vendor features, and other coding fields are working properly. “Testing with a clearinghouse is good. Testing directly with the payer is even better, if you are a direct submitter and it is allowed,” Wiskerchen suggests. Contact your clearinghouse and/or payers for testing opportunities prior to October 1.
8. Develop a plan for a potential cash flow crunch
So what happens if your best efforts in the 11th hour still aren’t enough to get your practice to the ICD-10 finish line? Prepare for the possibility of increased claim denials and temporary cash flow stalls, and put a plan in place to deal with them.
Start now by cleaning up as much of the accounts receivable as possible, and moving patient collections up front. Ask the billing team for a weekly status update of the largest unpaid balances in the 60-day aging column, and what has been done to appeal or otherwise address them. Analyze denial patterns and trends and fix their causes at the source—some may be ICD-10–related, others may simply be a gap in the reimbursement process that needs improvement.
Use payer cost estimators to calculate patient out-of-pocket cost and to collect unmet deductibles, coinsurance, and noncovered services prior to surgery. The surgeon-developed iPhone app Health Insurance Arithmetic2 ($1.99 in the iTunes Store) can help staff do this math on one, simple screen.
Finally, secure a line of credit to guard against a claim denial pile up this fall. A line of credit mitigates financial risk by making cash available quickly, should you need it to cover temporary revenue shortfalls, meet payroll, or pay operational expenses. It’s not too late to meet with your banker and apply for this protection, and the peace of mind may even help you sleep better.
1. KarenZupko & Associates, Inc. Pre-course survey of Q1 2015 coding and reimbursement workshop attendees. [Workshops are cosponsored by the American Academy of Orthopaedic Surgeons.] Unpublished data, April 2015.
2. Health Insurance Arithmetic. iTunes Store website. https://itunes.apple.com/us/app/healthinsurancearithmetic/id953262818. Accessed May 12, 2015.
As late as mid-April 2015, a survey of 121 orthopedic practices indicated that 30% had done nothing to start preparing for ICD-10 (International Classification of Diseases, Tenth Revision).1 That’s scary. And even the practices that had begun to prepare had not completed a number of key tasks (Figure 1).
Certainly, the will-they-or-won’t-they possibility of another congressional delay had many practices sitting on their hands this year. But now that the October 1, 2015, implementation is set in stone, this lack of inertia has many practices woefully behind. If your practice is one of many that hasn’t mapped your common ICD-9 (International Classification of Diseases, Ninth Revision) codes to ICD-10 codes, completed payer testing, or attended training, it’s time for a “full-court press.”
Being unprepared for ICD-10 will cause more than just an increase in claim denials. If your surgery schedule is booked a few months out, your staff will need to pre-authorize cases using ICD-10 as early as August 1—and they won’t be able to do that if you haven’t dictated the clinical terms required to choose an ICD-10 code. Without an understanding of ICD-10, severity of illness coding will suffer, and that will affect your bundled and value-based payments. And, if you don’t provide an adequate diagnosis when sending patients off-site for physical therapy, you’ll soon be getting phone calls from their billing staff demanding more specifics.
The clock is ticking and time is short. Here’s a prioritized list of what needs to get done.
1. Generate an ICD-9 frequency report
Identifying which diagnosis codes are the most frequently used, and therefore drive a significant portion of practice revenue, is an absolute must. The data will help prioritize training and code-mapping activities.
Most practices generate Current Procedural Terminology (CPT) code-frequency reports regularly, but few have ever run an ICD-9 code-frequency report. Call your vendor and ask for assistance, as there are multiple ways to run this report and they vary by practice management system. Sort the data elements and generate the ICD-9 frequency report by:
- Primary diagnosis.
- Unique patient.
- Revenue. (If your practice management system can’t give you diagnosis data by revenue, which enables you to focus on the codes that generate the most revenue, generate it by charges.)
The result should be a report that identifies the 20 to 25 diagnosis codes (or charges, depending on the reports generated) that drive the most revenue for the practice. Use the data to focus and prioritize your training and code-mapping activities.
2. Schedule training
Forget about “general” ICD-10 training courses. You need orthopedic-specific guidance. That’s because ICD-10 for orthopedics is more complex than for other specialties. Dictating fractures under ICD-10 is not so simple. Selecting an injury code requires confidence in correctly using the seventh character.
“Everyone who uses diagnosis codes must have baseline knowledge: surgeons, billing staff, surgical coordinators, and clinical team,” according to Sarah Wiskerchen, MBA, CPC, consultant and ICD-10 educator with KarenZupko & Associates (KZA). Training must include the practical details of ICD-10, such as assigning laterality, understanding the system architecture, and limiting the use of unspecified codes.
The American Academy of Orthopaedic Surgeons (AAOS) offers a self-paced, online training series that provides details for the top 3 diagnosis codes for each subspecialty. The 10-program course, ICD-10-CM: By the Numbers, is available at www.aaos.org ($299 for members, $399 for nonmembers). If you prefer live instruction, there is one more AAOS-sponsored, regional ICD-10 workshop left before the October 1 deadline, and more may be added. (Details at www.karenzupko.com)
These courses provide highly specific and granular ICD-10 knowledge and incorporate the use of Code-X, an AAOS-developed software tool. They also feature tools for handling the complexities of fractures and injury codes, such as Leo C. Far, an acronym developed by KZA consultant and coding educator Margie Maley, BSN, MS, to make ICD-10 diagnosis coding for fractures easier (Figure 2).
Some subspecialty societies also offer ICD-10 training. The American Society for Surgery of the Hand (www.assh.org), for example, offers a series of webinars and member-developed ICD-9-to-ICD-10 code maps.
3. Crosswalk your common codes from ICD-9 to ICD-10
Crosswalking is the process of mapping your most commonly used ICD-9 codes to their equivalent ICD-10 codes. This exercise familiarizes your team with ICD-10 language and terms, and gives a sense of which ICD-9 codes expand to just 1 or 2 ICD-10 codes and which codes expand into 10 or more codes—as some injury codes do (Table).
“Attempting to map the codes before completing ICD-10 training is like trying to write a letter in Greek when you only speak English,” Wiskerchen warns. “So start this process after at least some of your team have grasped the fundamentals of ICD-10.” This is where the data from your ICD-9 frequency report comes in. Use it to prioritize which codes to map first with a goal of mapping your top 25 ICD-9 codes to their ICD-10 equivalents by August 31.
Invest in good tools to support your mapping efforts. Avoid general mapping equivalent (GEM) coding tools, which are free for a good reason—they are incomplete and don’t always lead you to the correct ICD-10 code. Instead, purchase resources from credible sources, such as the American Medical Association (AMA; www.ama-assn.org). The AMA publishes ICD-10-CM 2016: The Complete Official Codebook as well as ICD-10-CM Mappings 2016, which links ICD-9 codes to all valid ICD-10 alternatives. The AMA also offers electronic ICD-10-CM Express Reference Mapping Cards for multiple specialties.
Practice makes perfect and crosswalking from ICD-9 to ICD-10 is one of the best ways for your team to become aware of the nuances in the new coding system. Like learning a new language, “speaking” ICD-10 does not become automatic just because you’ve attended training or completed the coding maps. Training teaches the architecture of the new coding system. Mapping provides a structured way to become familiar with the codes the practice will use most often. Once these 2 primary pieces are understood and assimilated, most physicians find that dictating the necessary new terms becomes quite easy.
4. Conduct a gap analysis to identify the ICD-10 terms missing from each provider’s current documentation
Conduct the gap analysis after your team has completed training, and once you’ve at least begun the process of mapping codes from ICD-9 to ICD-10. Here’s how:
- Generate a CPT frequency report.
- Select the top 5 procedures for each physician.
- Pull 2 patients’ notes for each of the top procedures.
- Review the notes and try to select ICD-10 code(s).
If key ICD-10 terms are not included in current documentation, physicians should modify the templates or macros they rely on for dictation.
“This simple exercise makes it obvious which clinical information physicians must add for ICD-10,” Wiskerchen says. For example, if the patient had an arthroscopy, but the note doesn’t specify on which leg, that’s a clear indication that the physician must dictate laterality. “The gap analysis is a great way to coach physicians about the clinical details to document, so staff can bill under ICD-10,” Wiskerchen says.
5. Contact technology vendors
Given the number of new ICD-10 codes in orthopedics, paper cheat sheets will be obsolete. Instead, you’ll need to rely on pull-down menus and/or search fields in the electronic health record (EHR) and practice management systems.
“Get clarity about how the new features and workflow processes will work in your systems,” suggests Wiskerchen. “Ask questions such as: Which features will be added or changed to accommodate the new codes? Will there be new screens or pick lists for ICD-10, or search fields? How will new screens and features change our current workflow? And schedule any necessary training as soon as possible.”
In addition to software upgrades and training, vendors and clearinghouses offer an array of services to help practices make the transition. Some vendors even provide help coordinating your internal plan with their new product features and training. Contact vendors to find out what they offer.
6. Use completed code maps to build diagnosis code databases, EHR templates, charge tickets, pick lists, prompters, and other coding tools
“Provide the code crosswalks and results of your documentation gap analysis to the IT [information technology] team so they can get started,” Wiskerchen advises. “And assign a physician or midlevel provider to work with IT so that the tools are clinically accurate.”
7. Schedule testing with clearinghouses and payers
“Successful testing indicates that your hard work has paid off, and that claims will be processed with few, if any, ICD-10–related hiccups,” Wiskerchen says. Essentially, the testing confirms that your ICD-10 code database, pick lists, vendor features, and other coding fields are working properly. “Testing with a clearinghouse is good. Testing directly with the payer is even better, if you are a direct submitter and it is allowed,” Wiskerchen suggests. Contact your clearinghouse and/or payers for testing opportunities prior to October 1.
8. Develop a plan for a potential cash flow crunch
So what happens if your best efforts in the 11th hour still aren’t enough to get your practice to the ICD-10 finish line? Prepare for the possibility of increased claim denials and temporary cash flow stalls, and put a plan in place to deal with them.
Start now by cleaning up as much of the accounts receivable as possible, and moving patient collections up front. Ask the billing team for a weekly status update of the largest unpaid balances in the 60-day aging column, and what has been done to appeal or otherwise address them. Analyze denial patterns and trends and fix their causes at the source—some may be ICD-10–related, others may simply be a gap in the reimbursement process that needs improvement.
Use payer cost estimators to calculate patient out-of-pocket cost and to collect unmet deductibles, coinsurance, and noncovered services prior to surgery. The surgeon-developed iPhone app Health Insurance Arithmetic2 ($1.99 in the iTunes Store) can help staff do this math on one, simple screen.
Finally, secure a line of credit to guard against a claim denial pile up this fall. A line of credit mitigates financial risk by making cash available quickly, should you need it to cover temporary revenue shortfalls, meet payroll, or pay operational expenses. It’s not too late to meet with your banker and apply for this protection, and the peace of mind may even help you sleep better.
As late as mid-April 2015, a survey of 121 orthopedic practices indicated that 30% had done nothing to start preparing for ICD-10 (International Classification of Diseases, Tenth Revision).1 That’s scary. And even the practices that had begun to prepare had not completed a number of key tasks (Figure 1).
Certainly, the will-they-or-won’t-they possibility of another congressional delay had many practices sitting on their hands this year. But now that the October 1, 2015, implementation is set in stone, this lack of inertia has many practices woefully behind. If your practice is one of many that hasn’t mapped your common ICD-9 (International Classification of Diseases, Ninth Revision) codes to ICD-10 codes, completed payer testing, or attended training, it’s time for a “full-court press.”
Being unprepared for ICD-10 will cause more than just an increase in claim denials. If your surgery schedule is booked a few months out, your staff will need to pre-authorize cases using ICD-10 as early as August 1—and they won’t be able to do that if you haven’t dictated the clinical terms required to choose an ICD-10 code. Without an understanding of ICD-10, severity of illness coding will suffer, and that will affect your bundled and value-based payments. And, if you don’t provide an adequate diagnosis when sending patients off-site for physical therapy, you’ll soon be getting phone calls from their billing staff demanding more specifics.
The clock is ticking and time is short. Here’s a prioritized list of what needs to get done.
1. Generate an ICD-9 frequency report
Identifying which diagnosis codes are the most frequently used, and therefore drive a significant portion of practice revenue, is an absolute must. The data will help prioritize training and code-mapping activities.
Most practices generate Current Procedural Terminology (CPT) code-frequency reports regularly, but few have ever run an ICD-9 code-frequency report. Call your vendor and ask for assistance, as there are multiple ways to run this report and they vary by practice management system. Sort the data elements and generate the ICD-9 frequency report by:
- Primary diagnosis.
- Unique patient.
- Revenue. (If your practice management system can’t give you diagnosis data by revenue, which enables you to focus on the codes that generate the most revenue, generate it by charges.)
The result should be a report that identifies the 20 to 25 diagnosis codes (or charges, depending on the reports generated) that drive the most revenue for the practice. Use the data to focus and prioritize your training and code-mapping activities.
2. Schedule training
Forget about “general” ICD-10 training courses. You need orthopedic-specific guidance. That’s because ICD-10 for orthopedics is more complex than for other specialties. Dictating fractures under ICD-10 is not so simple. Selecting an injury code requires confidence in correctly using the seventh character.
“Everyone who uses diagnosis codes must have baseline knowledge: surgeons, billing staff, surgical coordinators, and clinical team,” according to Sarah Wiskerchen, MBA, CPC, consultant and ICD-10 educator with KarenZupko & Associates (KZA). Training must include the practical details of ICD-10, such as assigning laterality, understanding the system architecture, and limiting the use of unspecified codes.
The American Academy of Orthopaedic Surgeons (AAOS) offers a self-paced, online training series that provides details for the top 3 diagnosis codes for each subspecialty. The 10-program course, ICD-10-CM: By the Numbers, is available at www.aaos.org ($299 for members, $399 for nonmembers). If you prefer live instruction, there is one more AAOS-sponsored, regional ICD-10 workshop left before the October 1 deadline, and more may be added. (Details at www.karenzupko.com)
These courses provide highly specific and granular ICD-10 knowledge and incorporate the use of Code-X, an AAOS-developed software tool. They also feature tools for handling the complexities of fractures and injury codes, such as Leo C. Far, an acronym developed by KZA consultant and coding educator Margie Maley, BSN, MS, to make ICD-10 diagnosis coding for fractures easier (Figure 2).
Some subspecialty societies also offer ICD-10 training. The American Society for Surgery of the Hand (www.assh.org), for example, offers a series of webinars and member-developed ICD-9-to-ICD-10 code maps.
3. Crosswalk your common codes from ICD-9 to ICD-10
Crosswalking is the process of mapping your most commonly used ICD-9 codes to their equivalent ICD-10 codes. This exercise familiarizes your team with ICD-10 language and terms, and gives a sense of which ICD-9 codes expand to just 1 or 2 ICD-10 codes and which codes expand into 10 or more codes—as some injury codes do (Table).
“Attempting to map the codes before completing ICD-10 training is like trying to write a letter in Greek when you only speak English,” Wiskerchen warns. “So start this process after at least some of your team have grasped the fundamentals of ICD-10.” This is where the data from your ICD-9 frequency report comes in. Use it to prioritize which codes to map first with a goal of mapping your top 25 ICD-9 codes to their ICD-10 equivalents by August 31.
Invest in good tools to support your mapping efforts. Avoid general mapping equivalent (GEM) coding tools, which are free for a good reason—they are incomplete and don’t always lead you to the correct ICD-10 code. Instead, purchase resources from credible sources, such as the American Medical Association (AMA; www.ama-assn.org). The AMA publishes ICD-10-CM 2016: The Complete Official Codebook as well as ICD-10-CM Mappings 2016, which links ICD-9 codes to all valid ICD-10 alternatives. The AMA also offers electronic ICD-10-CM Express Reference Mapping Cards for multiple specialties.
Practice makes perfect and crosswalking from ICD-9 to ICD-10 is one of the best ways for your team to become aware of the nuances in the new coding system. Like learning a new language, “speaking” ICD-10 does not become automatic just because you’ve attended training or completed the coding maps. Training teaches the architecture of the new coding system. Mapping provides a structured way to become familiar with the codes the practice will use most often. Once these 2 primary pieces are understood and assimilated, most physicians find that dictating the necessary new terms becomes quite easy.
4. Conduct a gap analysis to identify the ICD-10 terms missing from each provider’s current documentation
Conduct the gap analysis after your team has completed training, and once you’ve at least begun the process of mapping codes from ICD-9 to ICD-10. Here’s how:
- Generate a CPT frequency report.
- Select the top 5 procedures for each physician.
- Pull 2 patients’ notes for each of the top procedures.
- Review the notes and try to select ICD-10 code(s).
If key ICD-10 terms are not included in current documentation, physicians should modify the templates or macros they rely on for dictation.
“This simple exercise makes it obvious which clinical information physicians must add for ICD-10,” Wiskerchen says. For example, if the patient had an arthroscopy, but the note doesn’t specify on which leg, that’s a clear indication that the physician must dictate laterality. “The gap analysis is a great way to coach physicians about the clinical details to document, so staff can bill under ICD-10,” Wiskerchen says.
5. Contact technology vendors
Given the number of new ICD-10 codes in orthopedics, paper cheat sheets will be obsolete. Instead, you’ll need to rely on pull-down menus and/or search fields in the electronic health record (EHR) and practice management systems.
“Get clarity about how the new features and workflow processes will work in your systems,” suggests Wiskerchen. “Ask questions such as: Which features will be added or changed to accommodate the new codes? Will there be new screens or pick lists for ICD-10, or search fields? How will new screens and features change our current workflow? And schedule any necessary training as soon as possible.”
In addition to software upgrades and training, vendors and clearinghouses offer an array of services to help practices make the transition. Some vendors even provide help coordinating your internal plan with their new product features and training. Contact vendors to find out what they offer.
6. Use completed code maps to build diagnosis code databases, EHR templates, charge tickets, pick lists, prompters, and other coding tools
“Provide the code crosswalks and results of your documentation gap analysis to the IT [information technology] team so they can get started,” Wiskerchen advises. “And assign a physician or midlevel provider to work with IT so that the tools are clinically accurate.”
7. Schedule testing with clearinghouses and payers
“Successful testing indicates that your hard work has paid off, and that claims will be processed with few, if any, ICD-10–related hiccups,” Wiskerchen says. Essentially, the testing confirms that your ICD-10 code database, pick lists, vendor features, and other coding fields are working properly. “Testing with a clearinghouse is good. Testing directly with the payer is even better, if you are a direct submitter and it is allowed,” Wiskerchen suggests. Contact your clearinghouse and/or payers for testing opportunities prior to October 1.
8. Develop a plan for a potential cash flow crunch
So what happens if your best efforts in the 11th hour still aren’t enough to get your practice to the ICD-10 finish line? Prepare for the possibility of increased claim denials and temporary cash flow stalls, and put a plan in place to deal with them.
Start now by cleaning up as much of the accounts receivable as possible, and moving patient collections up front. Ask the billing team for a weekly status update of the largest unpaid balances in the 60-day aging column, and what has been done to appeal or otherwise address them. Analyze denial patterns and trends and fix their causes at the source—some may be ICD-10–related, others may simply be a gap in the reimbursement process that needs improvement.
Use payer cost estimators to calculate patient out-of-pocket cost and to collect unmet deductibles, coinsurance, and noncovered services prior to surgery. The surgeon-developed iPhone app Health Insurance Arithmetic2 ($1.99 in the iTunes Store) can help staff do this math on one, simple screen.
Finally, secure a line of credit to guard against a claim denial pile up this fall. A line of credit mitigates financial risk by making cash available quickly, should you need it to cover temporary revenue shortfalls, meet payroll, or pay operational expenses. It’s not too late to meet with your banker and apply for this protection, and the peace of mind may even help you sleep better.
1. KarenZupko & Associates, Inc. Pre-course survey of Q1 2015 coding and reimbursement workshop attendees. [Workshops are cosponsored by the American Academy of Orthopaedic Surgeons.] Unpublished data, April 2015.
2. Health Insurance Arithmetic. iTunes Store website. https://itunes.apple.com/us/app/healthinsurancearithmetic/id953262818. Accessed May 12, 2015.
1. KarenZupko & Associates, Inc. Pre-course survey of Q1 2015 coding and reimbursement workshop attendees. [Workshops are cosponsored by the American Academy of Orthopaedic Surgeons.] Unpublished data, April 2015.
2. Health Insurance Arithmetic. iTunes Store website. https://itunes.apple.com/us/app/healthinsurancearithmetic/id953262818. Accessed May 12, 2015.
Coding for “Incident-to” Services
Services that physicians bill to Medicare but do not perform themselves are called “incident-to” services. These services usually are performed by nonphysician medical providers under close physician supervision. The authorization to bill for these incident-to services derives from the Social Security Act,1 which provides for Medicare coverage of services and supplies offered incident to the professional services of a physician. The underlying logic is that incident-to services are delivered as a necessary but incidental part of the physician’s professional services during diagnosis or treatment.
Eligibility Criteria
One key qualification for incident-to services is direct supervision of a nonphysician provider by a physician. When services are delivered in an office setting (place of service 11), the physician must be present in the office and immediately available to offer direction to nonphysician providers. Some states do include telecommunication in their definition of direct supervision, wherein the physician is accessible by telephone or some similar medium.
Another element necessary in the criteria for incident-to services is that initial care must be personally provided by the physician who also writes orders for ongoing care. In general, incident-to services include ongoing physician involvement in the provision of care. Importantly, the physician who first saw a patient, initiated service, or ordered a test is not the only one who can supervise subsequent incident-to visits with a nonphysician provider. In office settings where several physicians are responsible for overseeing a nonphysician provider, any of these physicians who are in clinic at the time can act as the supervising physician. In such cases, each of the other physicians should be listed in appropriate documentation as substitute physicians for the nonphysician provider.
The Centers for Medicare & Medicaid Services recognize a variety of nonphysician providers, but in dermatology these providers typically include physician assistants, certified registered nurse practitioners, or clinical nurse specialists. When services offered by these nonphysician providers are reported as incident-to services, Medicare reimburses them at 100% of the physician fee schedule; conversely, a non–incident-to service reported under a nonphysician provider’s National Provider Identifier (NPI) number is reimbursed at 85%. Only approved mid-level nonphysician providers may bill evaluation and management services with codes above 99211 under incident-to guidelines. Even then, the services delivered must be appropriate for the given nonphysician provider based on training and licensure.
Not every type of visit is eligible for coding as an incident-to service. For instance, it is not appropriate to code new patient visits or new services provided to existing patients as incident-to services. Similarly, visits with established patients that address new diagnoses or problems cannot be considered incident-to services. The only visits or services that may potentially be classified as incident to are those that address existing problems in established patients with an established care plan.
When an established patient presents with a new problem, there are at least 2 coding approaches that may be appropriate. First, the physician could choose to see the patient and code the visit as a standard physician visit under the physician’s own NPI number. Alternatively, if the supervising physician in the practice is not available to see the patient, the nonphysician provider could code the entire service, including new and old problems, under his/her own NPI number as a non–incident-to service.
Regulations by State and Payer
State regulations and rules promulgated by specific payers also must be considered to ensure incident-to coding is proper. Each state may have guidelines that define the scope of practice of particular nonphysician providers, including what services can or cannot be coded as incident-to services. Additionally, states typically regulate the number of nonphysician providers that a physician can supervise; by extension, no more than this number of nonphysician providers could bill incident-to services under a given physician’s NPI number. Private payers may have comparable rules, and specific Medicare guidelines apply to Medicare patients. When there is ambiguity regarding incident-to coding, it may be prudent to check with major payers regarding relevant guidelines. It also may be helpful to confirm when supervision via telecommunication is acceptable.
Billing Tips
Common sense also can guide appropriate use of incident-to coding. Although occasional coding errors are likely unavoidable, periodic review of billing patterns will keep these errors to a minimum. For instance, if a nonphysician provider is the only provider of any type seeing patients in the office during particular days of the week, then incident-to coding would be unlikely. In another example, the number of nonphysician providers working with a given dermatologist and billing incident-to services should not exceed the number of nonphysician providers allowed per physician in that state. An interesting twist is the case in which a dermatologist is working in an ambulatory surgery center while a nonphysician provider is seeing patients in an adjacent office suite. Even when the 2 sites of service are physically contiguous, the physician in the surgery center generally is not deemed to be in office and is not able to supervise the nonphysician provider, unless telecommunication is allowed.
Final Thoughts
Attention to correct coding for incident-to services is particularly salient, as the Office of Inspector General (OIG) for the US Department of Health & Human Services has expressed concern that these services may be routinely coded incorrectly. Specifically, the OIG work plan for the 2013 fiscal year stated, “We will review physician billing for ‘incident-to’ services to determine whether payment for such services had a higher error rate than that for non–incident-to services.” The same report also cited a 2009 OIG review that found that “unqualified nonphysicians performed 21 percent of the services that physicians did not personally perform.”2 In short, coding for incident-to services is under scrutiny, and it may be useful for dermatologists to review their internal policies regarding incident-to services.
1. Social Security Act, 42 USC §1861 (1935).
2. Work plan for fiscal year 2013. Office of Inspector General, US Department of Health & Human Services Web site. http://oig.hhs.gov/reports-and-publications/archives/workplan/2013/Work-Plan-2013.pdf. Accessed May 5, 2015.
Services that physicians bill to Medicare but do not perform themselves are called “incident-to” services. These services usually are performed by nonphysician medical providers under close physician supervision. The authorization to bill for these incident-to services derives from the Social Security Act,1 which provides for Medicare coverage of services and supplies offered incident to the professional services of a physician. The underlying logic is that incident-to services are delivered as a necessary but incidental part of the physician’s professional services during diagnosis or treatment.
Eligibility Criteria
One key qualification for incident-to services is direct supervision of a nonphysician provider by a physician. When services are delivered in an office setting (place of service 11), the physician must be present in the office and immediately available to offer direction to nonphysician providers. Some states do include telecommunication in their definition of direct supervision, wherein the physician is accessible by telephone or some similar medium.
Another element necessary in the criteria for incident-to services is that initial care must be personally provided by the physician who also writes orders for ongoing care. In general, incident-to services include ongoing physician involvement in the provision of care. Importantly, the physician who first saw a patient, initiated service, or ordered a test is not the only one who can supervise subsequent incident-to visits with a nonphysician provider. In office settings where several physicians are responsible for overseeing a nonphysician provider, any of these physicians who are in clinic at the time can act as the supervising physician. In such cases, each of the other physicians should be listed in appropriate documentation as substitute physicians for the nonphysician provider.
The Centers for Medicare & Medicaid Services recognize a variety of nonphysician providers, but in dermatology these providers typically include physician assistants, certified registered nurse practitioners, or clinical nurse specialists. When services offered by these nonphysician providers are reported as incident-to services, Medicare reimburses them at 100% of the physician fee schedule; conversely, a non–incident-to service reported under a nonphysician provider’s National Provider Identifier (NPI) number is reimbursed at 85%. Only approved mid-level nonphysician providers may bill evaluation and management services with codes above 99211 under incident-to guidelines. Even then, the services delivered must be appropriate for the given nonphysician provider based on training and licensure.
Not every type of visit is eligible for coding as an incident-to service. For instance, it is not appropriate to code new patient visits or new services provided to existing patients as incident-to services. Similarly, visits with established patients that address new diagnoses or problems cannot be considered incident-to services. The only visits or services that may potentially be classified as incident to are those that address existing problems in established patients with an established care plan.
When an established patient presents with a new problem, there are at least 2 coding approaches that may be appropriate. First, the physician could choose to see the patient and code the visit as a standard physician visit under the physician’s own NPI number. Alternatively, if the supervising physician in the practice is not available to see the patient, the nonphysician provider could code the entire service, including new and old problems, under his/her own NPI number as a non–incident-to service.
Regulations by State and Payer
State regulations and rules promulgated by specific payers also must be considered to ensure incident-to coding is proper. Each state may have guidelines that define the scope of practice of particular nonphysician providers, including what services can or cannot be coded as incident-to services. Additionally, states typically regulate the number of nonphysician providers that a physician can supervise; by extension, no more than this number of nonphysician providers could bill incident-to services under a given physician’s NPI number. Private payers may have comparable rules, and specific Medicare guidelines apply to Medicare patients. When there is ambiguity regarding incident-to coding, it may be prudent to check with major payers regarding relevant guidelines. It also may be helpful to confirm when supervision via telecommunication is acceptable.
Billing Tips
Common sense also can guide appropriate use of incident-to coding. Although occasional coding errors are likely unavoidable, periodic review of billing patterns will keep these errors to a minimum. For instance, if a nonphysician provider is the only provider of any type seeing patients in the office during particular days of the week, then incident-to coding would be unlikely. In another example, the number of nonphysician providers working with a given dermatologist and billing incident-to services should not exceed the number of nonphysician providers allowed per physician in that state. An interesting twist is the case in which a dermatologist is working in an ambulatory surgery center while a nonphysician provider is seeing patients in an adjacent office suite. Even when the 2 sites of service are physically contiguous, the physician in the surgery center generally is not deemed to be in office and is not able to supervise the nonphysician provider, unless telecommunication is allowed.
Final Thoughts
Attention to correct coding for incident-to services is particularly salient, as the Office of Inspector General (OIG) for the US Department of Health & Human Services has expressed concern that these services may be routinely coded incorrectly. Specifically, the OIG work plan for the 2013 fiscal year stated, “We will review physician billing for ‘incident-to’ services to determine whether payment for such services had a higher error rate than that for non–incident-to services.” The same report also cited a 2009 OIG review that found that “unqualified nonphysicians performed 21 percent of the services that physicians did not personally perform.”2 In short, coding for incident-to services is under scrutiny, and it may be useful for dermatologists to review their internal policies regarding incident-to services.
Services that physicians bill to Medicare but do not perform themselves are called “incident-to” services. These services usually are performed by nonphysician medical providers under close physician supervision. The authorization to bill for these incident-to services derives from the Social Security Act,1 which provides for Medicare coverage of services and supplies offered incident to the professional services of a physician. The underlying logic is that incident-to services are delivered as a necessary but incidental part of the physician’s professional services during diagnosis or treatment.
Eligibility Criteria
One key qualification for incident-to services is direct supervision of a nonphysician provider by a physician. When services are delivered in an office setting (place of service 11), the physician must be present in the office and immediately available to offer direction to nonphysician providers. Some states do include telecommunication in their definition of direct supervision, wherein the physician is accessible by telephone or some similar medium.
Another element necessary in the criteria for incident-to services is that initial care must be personally provided by the physician who also writes orders for ongoing care. In general, incident-to services include ongoing physician involvement in the provision of care. Importantly, the physician who first saw a patient, initiated service, or ordered a test is not the only one who can supervise subsequent incident-to visits with a nonphysician provider. In office settings where several physicians are responsible for overseeing a nonphysician provider, any of these physicians who are in clinic at the time can act as the supervising physician. In such cases, each of the other physicians should be listed in appropriate documentation as substitute physicians for the nonphysician provider.
The Centers for Medicare & Medicaid Services recognize a variety of nonphysician providers, but in dermatology these providers typically include physician assistants, certified registered nurse practitioners, or clinical nurse specialists. When services offered by these nonphysician providers are reported as incident-to services, Medicare reimburses them at 100% of the physician fee schedule; conversely, a non–incident-to service reported under a nonphysician provider’s National Provider Identifier (NPI) number is reimbursed at 85%. Only approved mid-level nonphysician providers may bill evaluation and management services with codes above 99211 under incident-to guidelines. Even then, the services delivered must be appropriate for the given nonphysician provider based on training and licensure.
Not every type of visit is eligible for coding as an incident-to service. For instance, it is not appropriate to code new patient visits or new services provided to existing patients as incident-to services. Similarly, visits with established patients that address new diagnoses or problems cannot be considered incident-to services. The only visits or services that may potentially be classified as incident to are those that address existing problems in established patients with an established care plan.
When an established patient presents with a new problem, there are at least 2 coding approaches that may be appropriate. First, the physician could choose to see the patient and code the visit as a standard physician visit under the physician’s own NPI number. Alternatively, if the supervising physician in the practice is not available to see the patient, the nonphysician provider could code the entire service, including new and old problems, under his/her own NPI number as a non–incident-to service.
Regulations by State and Payer
State regulations and rules promulgated by specific payers also must be considered to ensure incident-to coding is proper. Each state may have guidelines that define the scope of practice of particular nonphysician providers, including what services can or cannot be coded as incident-to services. Additionally, states typically regulate the number of nonphysician providers that a physician can supervise; by extension, no more than this number of nonphysician providers could bill incident-to services under a given physician’s NPI number. Private payers may have comparable rules, and specific Medicare guidelines apply to Medicare patients. When there is ambiguity regarding incident-to coding, it may be prudent to check with major payers regarding relevant guidelines. It also may be helpful to confirm when supervision via telecommunication is acceptable.
Billing Tips
Common sense also can guide appropriate use of incident-to coding. Although occasional coding errors are likely unavoidable, periodic review of billing patterns will keep these errors to a minimum. For instance, if a nonphysician provider is the only provider of any type seeing patients in the office during particular days of the week, then incident-to coding would be unlikely. In another example, the number of nonphysician providers working with a given dermatologist and billing incident-to services should not exceed the number of nonphysician providers allowed per physician in that state. An interesting twist is the case in which a dermatologist is working in an ambulatory surgery center while a nonphysician provider is seeing patients in an adjacent office suite. Even when the 2 sites of service are physically contiguous, the physician in the surgery center generally is not deemed to be in office and is not able to supervise the nonphysician provider, unless telecommunication is allowed.
Final Thoughts
Attention to correct coding for incident-to services is particularly salient, as the Office of Inspector General (OIG) for the US Department of Health & Human Services has expressed concern that these services may be routinely coded incorrectly. Specifically, the OIG work plan for the 2013 fiscal year stated, “We will review physician billing for ‘incident-to’ services to determine whether payment for such services had a higher error rate than that for non–incident-to services.” The same report also cited a 2009 OIG review that found that “unqualified nonphysicians performed 21 percent of the services that physicians did not personally perform.”2 In short, coding for incident-to services is under scrutiny, and it may be useful for dermatologists to review their internal policies regarding incident-to services.
1. Social Security Act, 42 USC §1861 (1935).
2. Work plan for fiscal year 2013. Office of Inspector General, US Department of Health & Human Services Web site. http://oig.hhs.gov/reports-and-publications/archives/workplan/2013/Work-Plan-2013.pdf. Accessed May 5, 2015.
1. Social Security Act, 42 USC §1861 (1935).
2. Work plan for fiscal year 2013. Office of Inspector General, US Department of Health & Human Services Web site. http://oig.hhs.gov/reports-and-publications/archives/workplan/2013/Work-Plan-2013.pdf. Accessed May 5, 2015.
Practice Points
- Direct supervision of a nonphysician provider by a physician must be demonstrated for incident-to services. Not every type of visit is eligible for incident-to billing.
- Only management of established problems on established patients by nonphysician providers may qualify as incident-to services.
- Refer to state and payer regulations and rules for proper incident-to coding.
Implementing Physician Value-Based Purchasing in Your Practice: HM15 Session Analysis
HM15 Session: Putting Your Nickel Down: The What, Why, and How of Implementing Physician Value-Based Purchasing in Your Practice
Presenters: Stephen Besch, Simone Karp RPh, Patrick Torcson MD MMM SFHM, Gregory Seymann MD SFHM
Medicare is transforming itself from a “passive payer” to an “active purchaser” of high quality, efficient healthcare. As such- active participation by physicians, physician groups, and hospitals is required for payment eligibility.
At the physician/group level, hospitalists should be reporting PQRS measures. Incentive payments for PQRS ended in 2014, Medicare is now making “negative payment adjustments.” Penalties are equal to a percentage of all Medicare Part B FFS (Fee-for-Service) charges and there is a 2-year delay between reporting or performance failure and penalization.
Physician Value-Based Purchasing (P-VBP) affects all Eligible Providers (EPs) in 2015. P4P (Pay for Performance) assesses both quality and cost. Aim is for budget neutrality via “quality tiering” which rewards “high quality/low cost” practices with penalties from “low quality/high cost” practices. As of now (2015) ACPs and therapists can be penalized under P-VBP.
Key Points/HM Takeaways:
- Hospitalists should be reporting PQRS measures- penalty phase has begun
- Key PQRS Changes for 2015:
- 6 measures applicable to inpatient billing removed
- no useful inpatient measures added
- penalty avoidance requires 9 measures at 50% or higher rates, covering at least 3 of the 6 NQS (National Quality Strategy) domains- including 1 cross-cutting measure
- all 2015 PQRS data will be posted to Physician Compare website in 2016
- 3 Examples of hospitalist applicable “cross-cutting measures” are
- 47-advance care plan
- 130-documentation of current medications
- 317-preventative care: bp screening
- PQRS data must be reported with respect to MAV clusters (Measure Applicability Validation)- reporting only measure that have no MAV cluster is a safe strategy so long as one of the measures is “cross-cutting”
- Maximum P-VBP penalties automatically apply if group does not report enough PQRS data
- visit CMS website for more information
HM15 Session: Putting Your Nickel Down: The What, Why, and How of Implementing Physician Value-Based Purchasing in Your Practice
Presenters: Stephen Besch, Simone Karp RPh, Patrick Torcson MD MMM SFHM, Gregory Seymann MD SFHM
Medicare is transforming itself from a “passive payer” to an “active purchaser” of high quality, efficient healthcare. As such- active participation by physicians, physician groups, and hospitals is required for payment eligibility.
At the physician/group level, hospitalists should be reporting PQRS measures. Incentive payments for PQRS ended in 2014, Medicare is now making “negative payment adjustments.” Penalties are equal to a percentage of all Medicare Part B FFS (Fee-for-Service) charges and there is a 2-year delay between reporting or performance failure and penalization.
Physician Value-Based Purchasing (P-VBP) affects all Eligible Providers (EPs) in 2015. P4P (Pay for Performance) assesses both quality and cost. Aim is for budget neutrality via “quality tiering” which rewards “high quality/low cost” practices with penalties from “low quality/high cost” practices. As of now (2015) ACPs and therapists can be penalized under P-VBP.
Key Points/HM Takeaways:
- Hospitalists should be reporting PQRS measures- penalty phase has begun
- Key PQRS Changes for 2015:
- 6 measures applicable to inpatient billing removed
- no useful inpatient measures added
- penalty avoidance requires 9 measures at 50% or higher rates, covering at least 3 of the 6 NQS (National Quality Strategy) domains- including 1 cross-cutting measure
- all 2015 PQRS data will be posted to Physician Compare website in 2016
- 3 Examples of hospitalist applicable “cross-cutting measures” are
- 47-advance care plan
- 130-documentation of current medications
- 317-preventative care: bp screening
- PQRS data must be reported with respect to MAV clusters (Measure Applicability Validation)- reporting only measure that have no MAV cluster is a safe strategy so long as one of the measures is “cross-cutting”
- Maximum P-VBP penalties automatically apply if group does not report enough PQRS data
- visit CMS website for more information
HM15 Session: Putting Your Nickel Down: The What, Why, and How of Implementing Physician Value-Based Purchasing in Your Practice
Presenters: Stephen Besch, Simone Karp RPh, Patrick Torcson MD MMM SFHM, Gregory Seymann MD SFHM
Medicare is transforming itself from a “passive payer” to an “active purchaser” of high quality, efficient healthcare. As such- active participation by physicians, physician groups, and hospitals is required for payment eligibility.
At the physician/group level, hospitalists should be reporting PQRS measures. Incentive payments for PQRS ended in 2014, Medicare is now making “negative payment adjustments.” Penalties are equal to a percentage of all Medicare Part B FFS (Fee-for-Service) charges and there is a 2-year delay between reporting or performance failure and penalization.
Physician Value-Based Purchasing (P-VBP) affects all Eligible Providers (EPs) in 2015. P4P (Pay for Performance) assesses both quality and cost. Aim is for budget neutrality via “quality tiering” which rewards “high quality/low cost” practices with penalties from “low quality/high cost” practices. As of now (2015) ACPs and therapists can be penalized under P-VBP.
Key Points/HM Takeaways:
- Hospitalists should be reporting PQRS measures- penalty phase has begun
- Key PQRS Changes for 2015:
- 6 measures applicable to inpatient billing removed
- no useful inpatient measures added
- penalty avoidance requires 9 measures at 50% or higher rates, covering at least 3 of the 6 NQS (National Quality Strategy) domains- including 1 cross-cutting measure
- all 2015 PQRS data will be posted to Physician Compare website in 2016
- 3 Examples of hospitalist applicable “cross-cutting measures” are
- 47-advance care plan
- 130-documentation of current medications
- 317-preventative care: bp screening
- PQRS data must be reported with respect to MAV clusters (Measure Applicability Validation)- reporting only measure that have no MAV cluster is a safe strategy so long as one of the measures is “cross-cutting”
- Maximum P-VBP penalties automatically apply if group does not report enough PQRS data
- visit CMS website for more information
Hot Topics in Practice Management; HM15 Session Analysis
HM15 Presenters: Roy Sittig MD SFHM, Jeffrey Frank MD MBA, Jodi Braun
Summation: Speakers covered timely topics regarding the Accountable Care Act, namely Medicaid Expansion and Bundled Payment arrangements; and reviewed the seminal paper on “Key Principals and Characteristics of an Effective Hospitalist Medicine Group” and lessons learned in implementing those 10 Key Principles.
Medicaid Expansion: EDs serving the 29 Medicaid expansion states are reporting higher volumes, likely due to 11.4million new lives now insured under the ACA. While the ACA does provide for higher Medicaid payment rates thus far, only 34% of providers accept Medicaid, a 21% drop since the ACA went into effect.
Bundled Payment Arrangements:
- Bundled Payment Care Initiative (BPCI) lexicon:
- Model 2-Episode Anchor (anchor admission) AND 90days post d/c; Medicare pays 98% of usual cost
- Model 3-90days post d/c AFTER anchor admission; Medicare pays 97% of usual cost
- Convener-entity that brings providers together and enters into CMS agreement to bear risk for bundles
- Awardee (entity having agreement with Medicare to assume risk and receive payment via BPCI) and Convener own the Bundle
- Episode initiator (EI) triggers “bundle period”
- Bundles based on DRG
10-Key Principles of an Effective Hospitalist Medicine Group:
- Effective Leadership
- Engaged Hospitalists
- Adequate Resources
- Planning and Management Infrastructure
- Alignment with Hospital/Health System
- Care Coordination Across Settings
- Leadership in Key Clinical Issues in the Hospital/Health System
- Thoughtful Approach to Scope of Activity
- Patient/Family-Centered, Team-Based Care; Effective Communication
- Recruiting/Retaining Qualified Clinicians
Key Points/HM Takeaways:
Medicaid Expansion- many of the 11.4M newly insured lives under the ACA have moved into Medicaid. Only about 1/3 of providers now accept Medicaid- 1 in 5 covered persons now have Medicaid, nearly 20% increase since 2013.
Bundled Payments- Majority of savings opportunity lies in Post-Acute Care. Awardee and Convener make profit is total cost is less than 98% of Target Price. In gainsharing agreements individuals can be reimbursed up to 150% usual Medicare rate. Pay occurs in usual Medicare fashion but is reconciled 60-90 days after end of bundle. For more information: http://innovation.cms.gov/initiatives/bundled-payments/
Effective HM Groups- Three important areas for focus when beginning to address group performance are: engaged hospitalists, planning and management infrastructure, care coordination across settings. These three topics have broad reaching implications into the hospitalist practice and patient care. [Cawley P, et al. Journal of Hospital Medicine 2014; 9(2):123-128]
HM15 Presenters: Roy Sittig MD SFHM, Jeffrey Frank MD MBA, Jodi Braun
Summation: Speakers covered timely topics regarding the Accountable Care Act, namely Medicaid Expansion and Bundled Payment arrangements; and reviewed the seminal paper on “Key Principals and Characteristics of an Effective Hospitalist Medicine Group” and lessons learned in implementing those 10 Key Principles.
Medicaid Expansion: EDs serving the 29 Medicaid expansion states are reporting higher volumes, likely due to 11.4million new lives now insured under the ACA. While the ACA does provide for higher Medicaid payment rates thus far, only 34% of providers accept Medicaid, a 21% drop since the ACA went into effect.
Bundled Payment Arrangements:
- Bundled Payment Care Initiative (BPCI) lexicon:
- Model 2-Episode Anchor (anchor admission) AND 90days post d/c; Medicare pays 98% of usual cost
- Model 3-90days post d/c AFTER anchor admission; Medicare pays 97% of usual cost
- Convener-entity that brings providers together and enters into CMS agreement to bear risk for bundles
- Awardee (entity having agreement with Medicare to assume risk and receive payment via BPCI) and Convener own the Bundle
- Episode initiator (EI) triggers “bundle period”
- Bundles based on DRG
10-Key Principles of an Effective Hospitalist Medicine Group:
- Effective Leadership
- Engaged Hospitalists
- Adequate Resources
- Planning and Management Infrastructure
- Alignment with Hospital/Health System
- Care Coordination Across Settings
- Leadership in Key Clinical Issues in the Hospital/Health System
- Thoughtful Approach to Scope of Activity
- Patient/Family-Centered, Team-Based Care; Effective Communication
- Recruiting/Retaining Qualified Clinicians
Key Points/HM Takeaways:
Medicaid Expansion- many of the 11.4M newly insured lives under the ACA have moved into Medicaid. Only about 1/3 of providers now accept Medicaid- 1 in 5 covered persons now have Medicaid, nearly 20% increase since 2013.
Bundled Payments- Majority of savings opportunity lies in Post-Acute Care. Awardee and Convener make profit is total cost is less than 98% of Target Price. In gainsharing agreements individuals can be reimbursed up to 150% usual Medicare rate. Pay occurs in usual Medicare fashion but is reconciled 60-90 days after end of bundle. For more information: http://innovation.cms.gov/initiatives/bundled-payments/
Effective HM Groups- Three important areas for focus when beginning to address group performance are: engaged hospitalists, planning and management infrastructure, care coordination across settings. These three topics have broad reaching implications into the hospitalist practice and patient care. [Cawley P, et al. Journal of Hospital Medicine 2014; 9(2):123-128]
HM15 Presenters: Roy Sittig MD SFHM, Jeffrey Frank MD MBA, Jodi Braun
Summation: Speakers covered timely topics regarding the Accountable Care Act, namely Medicaid Expansion and Bundled Payment arrangements; and reviewed the seminal paper on “Key Principals and Characteristics of an Effective Hospitalist Medicine Group” and lessons learned in implementing those 10 Key Principles.
Medicaid Expansion: EDs serving the 29 Medicaid expansion states are reporting higher volumes, likely due to 11.4million new lives now insured under the ACA. While the ACA does provide for higher Medicaid payment rates thus far, only 34% of providers accept Medicaid, a 21% drop since the ACA went into effect.
Bundled Payment Arrangements:
- Bundled Payment Care Initiative (BPCI) lexicon:
- Model 2-Episode Anchor (anchor admission) AND 90days post d/c; Medicare pays 98% of usual cost
- Model 3-90days post d/c AFTER anchor admission; Medicare pays 97% of usual cost
- Convener-entity that brings providers together and enters into CMS agreement to bear risk for bundles
- Awardee (entity having agreement with Medicare to assume risk and receive payment via BPCI) and Convener own the Bundle
- Episode initiator (EI) triggers “bundle period”
- Bundles based on DRG
10-Key Principles of an Effective Hospitalist Medicine Group:
- Effective Leadership
- Engaged Hospitalists
- Adequate Resources
- Planning and Management Infrastructure
- Alignment with Hospital/Health System
- Care Coordination Across Settings
- Leadership in Key Clinical Issues in the Hospital/Health System
- Thoughtful Approach to Scope of Activity
- Patient/Family-Centered, Team-Based Care; Effective Communication
- Recruiting/Retaining Qualified Clinicians
Key Points/HM Takeaways:
Medicaid Expansion- many of the 11.4M newly insured lives under the ACA have moved into Medicaid. Only about 1/3 of providers now accept Medicaid- 1 in 5 covered persons now have Medicaid, nearly 20% increase since 2013.
Bundled Payments- Majority of savings opportunity lies in Post-Acute Care. Awardee and Convener make profit is total cost is less than 98% of Target Price. In gainsharing agreements individuals can be reimbursed up to 150% usual Medicare rate. Pay occurs in usual Medicare fashion but is reconciled 60-90 days after end of bundle. For more information: http://innovation.cms.gov/initiatives/bundled-payments/
Effective HM Groups- Three important areas for focus when beginning to address group performance are: engaged hospitalists, planning and management infrastructure, care coordination across settings. These three topics have broad reaching implications into the hospitalist practice and patient care. [Cawley P, et al. Journal of Hospital Medicine 2014; 9(2):123-128]
Cloning and Chart Similarity
Health care providers select Current Procedural Terminology codes based on the service provided and then document to support the level of service reported.1 According to the Office of Inspector General (OIG) for the US Department of Health and Human Services, “Medicare contractors have noted an increased frequency of medical records with identical documentation across services,” which may under certain circumstances be considered inappropriate.2 Regarding this practice, the OIG work plan for the 2014 fiscal year stated: "We will determine the extent to which selected payments for evaluation and management (E/M) services were inappropriate. We will also review multiple E/M services associated with the same providers and beneficiaries to determine the extent to which electronic or paper medical records had documentation vulnerabilities."2The OIG’s annual work plan reflects areas of concern that will be investigated in the coming years. These investigations may result in audits of specific Medicare and Medicaid providers, including physicians.
Concerns about physicians providing identical documentation across services has evinced an ongoing focus on the so-called cloning of medical records. Cloning is not well defined but generally refers to inappropriate use of the same exact documentation, perhaps via cutting and pasting, in different patient encounters. This type of cloning could occur in office visits with the same patient or different patients. The advent of electronic health records has made such duplication easier, and the concern is that duplicated notes in a medical record for a particular encounter may not accurately reflect the services that were provided in another encounter; in some cases, services may be overdocumented, with this creating a risk that that they may also be overcoded.
How can dermatologists minimize the risk for being flagged for cloning records? If you use templates for procedures, you may consider reviewing the completed template before filing the record to ensure that the details are consistent with the procedure that was performed. If you use abbreviations or other unique documentation that may not be easily understandable to an outside authority, you may want to keep a manual somewhere in your office that defines or describes such abbreviations and notations. Also, be aware that scribing is different than cloning, and scribing is not under scrutiny by OIG. A scribe writes word for word as a physician dictates and cannot act independently to alter or embellish the notes; once scribing is complete, both the scribe and the physician should sign the notes.
The American Academy of Dermatology has been concerned that an imprecise definition of so-called cloning can unfairly marginalize appropriate coding practices. In particular, when similar procedures or E/M services are performed by the same physician, the documentation may be very similar, even identical, while still being accurate and appropriately descriptive of the services provided. To help explain when similar notes are an acceptable practice in dermatology and when notes should be different, the American Academy of Dermatology has developed a guidance document that has been approved by its board of directors.3
Current Procedural Terminology coding guidelines clearly indicate that documentation cannot drive the level of coding and that excessive documentation cannot be used to justify a higher-level code, such as a higher-level E/M code. Instead, the level of service delivered should be appropriate for the patient’s condition and should be documented accordingly.4
It is important for dermatologists to document patient encounters as accurately and completely as is necessary for good patient care. Documentation will often vary substantially from patient to patient and encounter to encounter, but sometimes routine procedures or E/M visits may be coded similarly. For instance, a shave biopsy on the cheek to rule out nonmelanoma skin cancer may be performed by a particular practitioner with a standard instrument and after standard preparation and infiltration of local anesthetic; postoperative care may also be the same. To minimize regulatory scrutiny when similar descriptions are used, review the documentation for accuracy and to confirm that important specific information has not been inadvertently omitted or that wrong information has not been appended.
Unfortunately, there are dermatologists who have been audited for cloning during the last year. As with any audit, it is important to be vigilant regarding deadlines and to file appeals in a timely manner. Keep all the notifications you receive safely and explain to your staff that any communications should be promptly forwarded to you. If you are audited for suspected cloning, you may wish to contact the coding staff of professional dermatology societies for general guidance.
1. Centers for Medicare & Medicaid Services. Medicare claim processing manual: chapter 12 – physicians/nonphysician practitioners. http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c12.pdf. Revised October 17, 2014. Accessed March 4, 2015.
2. Work plan for fiscal year 2014. Office of Inspector General, US Department of Health and Human Services Web site. https://oig.hhs.gov/reports-and-publications/archives/workplan/2014/Work-Plan-2014.pdf. Accessed March 4, 2015.
3. American Academy of Dermatology and AAD Association. Guidance statement: documentation of patient encounters and procedures. https://www.aad.org/forms/policies/Uploads/PS/Guidance%20Statement%20on%20Charting%20Practices.pdf. Approved October 23, 2014. Accessed March 6, 2015.
4. Evaluation and management services guide. Centers for Medicare & Medicaid Services Web site. http://www.cms.gov/outreach-and-education/medicare-learning-network-mln/mlnproducts/downloads/eval_mgmt_serv_guide-icn006764.pdf. Published November 2014. Accessed March 5, 2015.
Health care providers select Current Procedural Terminology codes based on the service provided and then document to support the level of service reported.1 According to the Office of Inspector General (OIG) for the US Department of Health and Human Services, “Medicare contractors have noted an increased frequency of medical records with identical documentation across services,” which may under certain circumstances be considered inappropriate.2 Regarding this practice, the OIG work plan for the 2014 fiscal year stated: "We will determine the extent to which selected payments for evaluation and management (E/M) services were inappropriate. We will also review multiple E/M services associated with the same providers and beneficiaries to determine the extent to which electronic or paper medical records had documentation vulnerabilities."2The OIG’s annual work plan reflects areas of concern that will be investigated in the coming years. These investigations may result in audits of specific Medicare and Medicaid providers, including physicians.
Concerns about physicians providing identical documentation across services has evinced an ongoing focus on the so-called cloning of medical records. Cloning is not well defined but generally refers to inappropriate use of the same exact documentation, perhaps via cutting and pasting, in different patient encounters. This type of cloning could occur in office visits with the same patient or different patients. The advent of electronic health records has made such duplication easier, and the concern is that duplicated notes in a medical record for a particular encounter may not accurately reflect the services that were provided in another encounter; in some cases, services may be overdocumented, with this creating a risk that that they may also be overcoded.
How can dermatologists minimize the risk for being flagged for cloning records? If you use templates for procedures, you may consider reviewing the completed template before filing the record to ensure that the details are consistent with the procedure that was performed. If you use abbreviations or other unique documentation that may not be easily understandable to an outside authority, you may want to keep a manual somewhere in your office that defines or describes such abbreviations and notations. Also, be aware that scribing is different than cloning, and scribing is not under scrutiny by OIG. A scribe writes word for word as a physician dictates and cannot act independently to alter or embellish the notes; once scribing is complete, both the scribe and the physician should sign the notes.
The American Academy of Dermatology has been concerned that an imprecise definition of so-called cloning can unfairly marginalize appropriate coding practices. In particular, when similar procedures or E/M services are performed by the same physician, the documentation may be very similar, even identical, while still being accurate and appropriately descriptive of the services provided. To help explain when similar notes are an acceptable practice in dermatology and when notes should be different, the American Academy of Dermatology has developed a guidance document that has been approved by its board of directors.3
Current Procedural Terminology coding guidelines clearly indicate that documentation cannot drive the level of coding and that excessive documentation cannot be used to justify a higher-level code, such as a higher-level E/M code. Instead, the level of service delivered should be appropriate for the patient’s condition and should be documented accordingly.4
It is important for dermatologists to document patient encounters as accurately and completely as is necessary for good patient care. Documentation will often vary substantially from patient to patient and encounter to encounter, but sometimes routine procedures or E/M visits may be coded similarly. For instance, a shave biopsy on the cheek to rule out nonmelanoma skin cancer may be performed by a particular practitioner with a standard instrument and after standard preparation and infiltration of local anesthetic; postoperative care may also be the same. To minimize regulatory scrutiny when similar descriptions are used, review the documentation for accuracy and to confirm that important specific information has not been inadvertently omitted or that wrong information has not been appended.
Unfortunately, there are dermatologists who have been audited for cloning during the last year. As with any audit, it is important to be vigilant regarding deadlines and to file appeals in a timely manner. Keep all the notifications you receive safely and explain to your staff that any communications should be promptly forwarded to you. If you are audited for suspected cloning, you may wish to contact the coding staff of professional dermatology societies for general guidance.
Health care providers select Current Procedural Terminology codes based on the service provided and then document to support the level of service reported.1 According to the Office of Inspector General (OIG) for the US Department of Health and Human Services, “Medicare contractors have noted an increased frequency of medical records with identical documentation across services,” which may under certain circumstances be considered inappropriate.2 Regarding this practice, the OIG work plan for the 2014 fiscal year stated: "We will determine the extent to which selected payments for evaluation and management (E/M) services were inappropriate. We will also review multiple E/M services associated with the same providers and beneficiaries to determine the extent to which electronic or paper medical records had documentation vulnerabilities."2The OIG’s annual work plan reflects areas of concern that will be investigated in the coming years. These investigations may result in audits of specific Medicare and Medicaid providers, including physicians.
Concerns about physicians providing identical documentation across services has evinced an ongoing focus on the so-called cloning of medical records. Cloning is not well defined but generally refers to inappropriate use of the same exact documentation, perhaps via cutting and pasting, in different patient encounters. This type of cloning could occur in office visits with the same patient or different patients. The advent of electronic health records has made such duplication easier, and the concern is that duplicated notes in a medical record for a particular encounter may not accurately reflect the services that were provided in another encounter; in some cases, services may be overdocumented, with this creating a risk that that they may also be overcoded.
How can dermatologists minimize the risk for being flagged for cloning records? If you use templates for procedures, you may consider reviewing the completed template before filing the record to ensure that the details are consistent with the procedure that was performed. If you use abbreviations or other unique documentation that may not be easily understandable to an outside authority, you may want to keep a manual somewhere in your office that defines or describes such abbreviations and notations. Also, be aware that scribing is different than cloning, and scribing is not under scrutiny by OIG. A scribe writes word for word as a physician dictates and cannot act independently to alter or embellish the notes; once scribing is complete, both the scribe and the physician should sign the notes.
The American Academy of Dermatology has been concerned that an imprecise definition of so-called cloning can unfairly marginalize appropriate coding practices. In particular, when similar procedures or E/M services are performed by the same physician, the documentation may be very similar, even identical, while still being accurate and appropriately descriptive of the services provided. To help explain when similar notes are an acceptable practice in dermatology and when notes should be different, the American Academy of Dermatology has developed a guidance document that has been approved by its board of directors.3
Current Procedural Terminology coding guidelines clearly indicate that documentation cannot drive the level of coding and that excessive documentation cannot be used to justify a higher-level code, such as a higher-level E/M code. Instead, the level of service delivered should be appropriate for the patient’s condition and should be documented accordingly.4
It is important for dermatologists to document patient encounters as accurately and completely as is necessary for good patient care. Documentation will often vary substantially from patient to patient and encounter to encounter, but sometimes routine procedures or E/M visits may be coded similarly. For instance, a shave biopsy on the cheek to rule out nonmelanoma skin cancer may be performed by a particular practitioner with a standard instrument and after standard preparation and infiltration of local anesthetic; postoperative care may also be the same. To minimize regulatory scrutiny when similar descriptions are used, review the documentation for accuracy and to confirm that important specific information has not been inadvertently omitted or that wrong information has not been appended.
Unfortunately, there are dermatologists who have been audited for cloning during the last year. As with any audit, it is important to be vigilant regarding deadlines and to file appeals in a timely manner. Keep all the notifications you receive safely and explain to your staff that any communications should be promptly forwarded to you. If you are audited for suspected cloning, you may wish to contact the coding staff of professional dermatology societies for general guidance.
1. Centers for Medicare & Medicaid Services. Medicare claim processing manual: chapter 12 – physicians/nonphysician practitioners. http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c12.pdf. Revised October 17, 2014. Accessed March 4, 2015.
2. Work plan for fiscal year 2014. Office of Inspector General, US Department of Health and Human Services Web site. https://oig.hhs.gov/reports-and-publications/archives/workplan/2014/Work-Plan-2014.pdf. Accessed March 4, 2015.
3. American Academy of Dermatology and AAD Association. Guidance statement: documentation of patient encounters and procedures. https://www.aad.org/forms/policies/Uploads/PS/Guidance%20Statement%20on%20Charting%20Practices.pdf. Approved October 23, 2014. Accessed March 6, 2015.
4. Evaluation and management services guide. Centers for Medicare & Medicaid Services Web site. http://www.cms.gov/outreach-and-education/medicare-learning-network-mln/mlnproducts/downloads/eval_mgmt_serv_guide-icn006764.pdf. Published November 2014. Accessed March 5, 2015.
1. Centers for Medicare & Medicaid Services. Medicare claim processing manual: chapter 12 – physicians/nonphysician practitioners. http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c12.pdf. Revised October 17, 2014. Accessed March 4, 2015.
2. Work plan for fiscal year 2014. Office of Inspector General, US Department of Health and Human Services Web site. https://oig.hhs.gov/reports-and-publications/archives/workplan/2014/Work-Plan-2014.pdf. Accessed March 4, 2015.
3. American Academy of Dermatology and AAD Association. Guidance statement: documentation of patient encounters and procedures. https://www.aad.org/forms/policies/Uploads/PS/Guidance%20Statement%20on%20Charting%20Practices.pdf. Approved October 23, 2014. Accessed March 6, 2015.
4. Evaluation and management services guide. Centers for Medicare & Medicaid Services Web site. http://www.cms.gov/outreach-and-education/medicare-learning-network-mln/mlnproducts/downloads/eval_mgmt_serv_guide-icn006764.pdf. Published November 2014. Accessed March 5, 2015.
Practice Points
- Medical record documentation for evaluation and management services includes information relevant to the patient encounter. Providing identical documentation for different patients may under certain circumstances be considered cloning and hence inappropriate.
- Following best practices can minimize the risk for being flagged for cloning.
Medicare Standard Practical Solution to Medical Coding Complexity
In the article “Common Coding Mistakes Hospitalists Should Avoid” in the August 2014 issue of The Hospitalist, the author states:
“For inpatient care, an established problem is defined as one in which a care plan has been generated by the physician (or same specialty group practice member) during the current hospitalization.”
This definition contradicts what I have been told in other coding courses regarding new vs. established problems relative to the examiner. It has been my understanding that when [I am] rotating on service and I have not seen that particular patient during the current admission, all of the current problems are new to me, even if previously identified by another member of my group. This [situation] results in a higher complexity of medical decision-making, which is reflective of the increased time spent learning a new patient when coming on service. I would appreciate clarification from the author.
–Matt George, MD,
medical director, MBHS Hospitalists
Billing and coding expert Carol Pohlig, BSN, RN, CPC, ACS, explains:
Be mindful when attending coding courses that are not contractor sponsored, as they may not validate the geographical interpretations of the rules for providers. There are several factors to consider when crediting the physician with “new” or “established” problems.
CMS documentation guidelines state: “Decision making with respect to a diagnosed problem is easier than that for an identified but undiagnosed problem.1
- For a presenting problem with an established diagnosis, the record should reflect whether the problem is:
- Improved, well-controlled, resolving, or resolved or
- Inadequately controlled, worsening, or failing to change as expected.
- For a presenting problem without an established diagnosis, the assessment or clinical impression may be stated in the form of differential diagnoses or as a “possible,” “probable,” or “rule out” diagnosis.
Although Medicare contractors utilize the Marshfield Clinic Scoring Tool when reviewing evaluation and management (E/M) services, a tool that historically refers to the “examiner” when considering the patient’s diagnoses, not all accept this tool-inspired standard, particularly in the advent of electronic health record accessibility and the idea that same-specialty physicians in a group practice are viewed as an individual physician.2,3
Reviewing information and familiarization of patients is often considered pre-service work and factored into the payment for E/M services. More importantly, the feasibility of an auditor being able to distinguish new vs. established problems at the level of the “examiner” is decreased when auditing a single date of service. Non-Medicare payers who audit E/M services do not necessarily follow contractor-specific guidelines but, rather, general CMS guidelines.
Therefore, without knowing the insurer or their interpretation at the time of service or visit level selection, the CMS-developed standard is the most practical application when considering the complexity of the encounter.
References
- Centers for Medicare and Medicaid Services. Department of Health and Human Services. Evaluation and management services guide. Available at: http://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/downloads//eval_mgmt_serv_guide-ICN006764.pdf. Accessed November 13, 2014.
- National Government Services. Evaluation and management documentation training too. Available at: http://www.ngsmedicare.com/ngs/wcm/connect/3632a905-b697-4266-8fc0-2aa2a84fedb2/1074_0514_EM_Documentation_Training_Tool_508.pdf?MOD=AJPERES. Accessed November 13, 2014.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual. Chapter 12 – Physicians/nonphysician practitioners. Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c12.pdf. Accessed November 13, 2014.
In the article “Common Coding Mistakes Hospitalists Should Avoid” in the August 2014 issue of The Hospitalist, the author states:
“For inpatient care, an established problem is defined as one in which a care plan has been generated by the physician (or same specialty group practice member) during the current hospitalization.”
This definition contradicts what I have been told in other coding courses regarding new vs. established problems relative to the examiner. It has been my understanding that when [I am] rotating on service and I have not seen that particular patient during the current admission, all of the current problems are new to me, even if previously identified by another member of my group. This [situation] results in a higher complexity of medical decision-making, which is reflective of the increased time spent learning a new patient when coming on service. I would appreciate clarification from the author.
–Matt George, MD,
medical director, MBHS Hospitalists
Billing and coding expert Carol Pohlig, BSN, RN, CPC, ACS, explains:
Be mindful when attending coding courses that are not contractor sponsored, as they may not validate the geographical interpretations of the rules for providers. There are several factors to consider when crediting the physician with “new” or “established” problems.
CMS documentation guidelines state: “Decision making with respect to a diagnosed problem is easier than that for an identified but undiagnosed problem.1
- For a presenting problem with an established diagnosis, the record should reflect whether the problem is:
- Improved, well-controlled, resolving, or resolved or
- Inadequately controlled, worsening, or failing to change as expected.
- For a presenting problem without an established diagnosis, the assessment or clinical impression may be stated in the form of differential diagnoses or as a “possible,” “probable,” or “rule out” diagnosis.
Although Medicare contractors utilize the Marshfield Clinic Scoring Tool when reviewing evaluation and management (E/M) services, a tool that historically refers to the “examiner” when considering the patient’s diagnoses, not all accept this tool-inspired standard, particularly in the advent of electronic health record accessibility and the idea that same-specialty physicians in a group practice are viewed as an individual physician.2,3
Reviewing information and familiarization of patients is often considered pre-service work and factored into the payment for E/M services. More importantly, the feasibility of an auditor being able to distinguish new vs. established problems at the level of the “examiner” is decreased when auditing a single date of service. Non-Medicare payers who audit E/M services do not necessarily follow contractor-specific guidelines but, rather, general CMS guidelines.
Therefore, without knowing the insurer or their interpretation at the time of service or visit level selection, the CMS-developed standard is the most practical application when considering the complexity of the encounter.
References
- Centers for Medicare and Medicaid Services. Department of Health and Human Services. Evaluation and management services guide. Available at: http://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/downloads//eval_mgmt_serv_guide-ICN006764.pdf. Accessed November 13, 2014.
- National Government Services. Evaluation and management documentation training too. Available at: http://www.ngsmedicare.com/ngs/wcm/connect/3632a905-b697-4266-8fc0-2aa2a84fedb2/1074_0514_EM_Documentation_Training_Tool_508.pdf?MOD=AJPERES. Accessed November 13, 2014.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual. Chapter 12 – Physicians/nonphysician practitioners. Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c12.pdf. Accessed November 13, 2014.
In the article “Common Coding Mistakes Hospitalists Should Avoid” in the August 2014 issue of The Hospitalist, the author states:
“For inpatient care, an established problem is defined as one in which a care plan has been generated by the physician (or same specialty group practice member) during the current hospitalization.”
This definition contradicts what I have been told in other coding courses regarding new vs. established problems relative to the examiner. It has been my understanding that when [I am] rotating on service and I have not seen that particular patient during the current admission, all of the current problems are new to me, even if previously identified by another member of my group. This [situation] results in a higher complexity of medical decision-making, which is reflective of the increased time spent learning a new patient when coming on service. I would appreciate clarification from the author.
–Matt George, MD,
medical director, MBHS Hospitalists
Billing and coding expert Carol Pohlig, BSN, RN, CPC, ACS, explains:
Be mindful when attending coding courses that are not contractor sponsored, as they may not validate the geographical interpretations of the rules for providers. There are several factors to consider when crediting the physician with “new” or “established” problems.
CMS documentation guidelines state: “Decision making with respect to a diagnosed problem is easier than that for an identified but undiagnosed problem.1
- For a presenting problem with an established diagnosis, the record should reflect whether the problem is:
- Improved, well-controlled, resolving, or resolved or
- Inadequately controlled, worsening, or failing to change as expected.
- For a presenting problem without an established diagnosis, the assessment or clinical impression may be stated in the form of differential diagnoses or as a “possible,” “probable,” or “rule out” diagnosis.
Although Medicare contractors utilize the Marshfield Clinic Scoring Tool when reviewing evaluation and management (E/M) services, a tool that historically refers to the “examiner” when considering the patient’s diagnoses, not all accept this tool-inspired standard, particularly in the advent of electronic health record accessibility and the idea that same-specialty physicians in a group practice are viewed as an individual physician.2,3
Reviewing information and familiarization of patients is often considered pre-service work and factored into the payment for E/M services. More importantly, the feasibility of an auditor being able to distinguish new vs. established problems at the level of the “examiner” is decreased when auditing a single date of service. Non-Medicare payers who audit E/M services do not necessarily follow contractor-specific guidelines but, rather, general CMS guidelines.
Therefore, without knowing the insurer or their interpretation at the time of service or visit level selection, the CMS-developed standard is the most practical application when considering the complexity of the encounter.
References
- Centers for Medicare and Medicaid Services. Department of Health and Human Services. Evaluation and management services guide. Available at: http://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/downloads//eval_mgmt_serv_guide-ICN006764.pdf. Accessed November 13, 2014.
- National Government Services. Evaluation and management documentation training too. Available at: http://www.ngsmedicare.com/ngs/wcm/connect/3632a905-b697-4266-8fc0-2aa2a84fedb2/1074_0514_EM_Documentation_Training_Tool_508.pdf?MOD=AJPERES. Accessed November 13, 2014.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual. Chapter 12 – Physicians/nonphysician practitioners. Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c12.pdf. Accessed November 13, 2014.
Service Distinction Crucial for Medical Claim Submissions
Hospitalists often are tasked with coordinating and overseeing patient care throughout a hospitalization. Depending on the care model and the availability of varying specialists, a patient could see several specialists throughout the stay, and even during a single day. A recurring issue for many hospitalists is justifying the medical necessity of their services, because payers do not want to reimburse overlapping care (i.e., multiple providers caring for the same patient problem) when more than one physician provides care on the same service date.
Payers often consider two key principles before reimbursing multiple visits on the same date:1
- Does the patient’s condition warrant the services of more than one physician?
- Are the individual services provided by each physician reasonable and necessary?
Consider the following example: A 65-year-old female patient is admitted with a hip fracture (820.8) after slipping on the ice outside her home. The patient also has hypertension (401.1) and type II diabetes (250.00). The surgeon manages the patient’s peri-operative course for the fracture, while the hospitalist manages the patient’s medical issues.
Payers must be sure that the services of one physician do not duplicate those provided by another.1 For the above scenario, it is imperative that the hospitalist understand which services are considered the surgeon’s responsibility. The global surgical package includes payment for the surgical procedure and the completion of its corresponding facility-required paperwork (e.g. pre-operative history and physical exam, operative consent forms, pre-operative orders), in addition to the following services:2
- Pre-operative visits after making the decision for surgery beginning one day prior to surgery;
- All additional post-operative medical or surgical services provided by the surgeon related to complications but not requiring additional trips to the operating room;
- Post-operative visits by the surgeon related to recovery from surgery, including but not limited to dressing changes, local incisional care, removal of cutaneous sutures and staples, line removals, changes and removal of tracheostomy tubes, and discharge services; and
- Post-operative pain management provided by the surgeon.
Another physician who performs any component of the global package will not receive separate payment unless the surgeon is willing to forego a portion of the payment. For example, a hospitalist admits a patient who has no other identifiable medical conditions aside from the problem prompting surgery. The hospitalist’s role may be dictated by facility policy—quality of care or risk reduction, for example—and administrative requirements (history and physical exam, discharge services, coordination of care) rather than what a payer would perceive as necessary “medical” management. Similarly, if the hospitalist’s post-op care is limited to ordering routine post-op labs or maintaining appropriate pain management, the hospitalist’s service will likely be denied as incidental to the surgical package.
Remember, if the hospitalist’s claim is submitted and paid, it doesn’t mean that the payer won’t retract the payment upon review if an erroneous payment is suspected. A payer review may be triggered when the diagnosis listed on the hospitalist’s claim matches the diagnosis listed on the surgeon’s claim (e.g. 820.8). If too many claims are considered “not medically necessary” due to overlapping care, hospitalists may need to negotiate other terms of payment with the facility to recoup unpaid time and effort when involved in this type of care.
When more than one medical condition exists and several physicians participate in the patient’s care, medical necessity is easily established for each physician. Each physician manages the condition related to his/her expertise. In the above example, the surgeon cares for the patient’s fracture, while the hospitalist oversees diabetes and hypertension management. Service distinction is crucial during the claim submission process. The hospitalist should report a subsequent hospital care code (99231-99233) with a primary diagnosis corresponding to his/her specialty-related care (i.e., 9923x with 250.00, 401.1).3
When more specialists are involved, claim submission becomes more complex. A cardiologist who was also involved in patient management would report his or her service using 401.1. When a different primary diagnosis is assigned to the visit code to indicate the reason for each physician’s involvement, all claims are more likely to be paid.4 As long as the hospitalist maintains care over one of the patients’ conditions, concurrent care is justified.
Because these physicians are in different specialties and different provider groups, most payers do not require the modifier 25 (separately identifiable evaluation/management [E/M] service on the same day as a procedure or other service) with the visit code; however, some managed care payers may have a general claim edit that pays the first claim and denies the second unless modifier 25 is appended to the concurrent E/M visit code (i.e., 99232-25) as an attestation that the service is distinct from any other provider’s service that day, despite claim submission under different tax identification numbers. This may not be identified until the claim is rejected or denied. If appropriate modifier use does not yield payment, appeal the denied concurrent care claims with supporting documentation from each physician visit, if possible. This demonstrates each physician’s contribution to care.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. Medicare Benefit Policy Manual: Chapter 15—Covered Medical and Other Health Services. Section 30.E. Available at: www.cms.gov/manuals/Downloads/bp102c15.pdf. Accessed March 5, 2015.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12—Physicians/Nonphysician Practitioners. Section 40.A. Available at: www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c12.pdf. Accessed March 5, 2015.
- American Medical Association. Current Procedural Terminology 2015 Professional Edition. Chicago: American Medical Association Press; 2014.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12—Physicians/Nonphysician Practitioners. Section 30.6.9.C. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed March 5, 2015.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12—Physicians/Nonphysician Practitioners. Section 30.6.5. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed March 5, 2015.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 26—Completing and Processing Form CMS-1500 Data Set. Section 10.8.2. Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/clm104c26.pdf. Accessed March 5, 2015.
Hospitalists often are tasked with coordinating and overseeing patient care throughout a hospitalization. Depending on the care model and the availability of varying specialists, a patient could see several specialists throughout the stay, and even during a single day. A recurring issue for many hospitalists is justifying the medical necessity of their services, because payers do not want to reimburse overlapping care (i.e., multiple providers caring for the same patient problem) when more than one physician provides care on the same service date.
Payers often consider two key principles before reimbursing multiple visits on the same date:1
- Does the patient’s condition warrant the services of more than one physician?
- Are the individual services provided by each physician reasonable and necessary?
Consider the following example: A 65-year-old female patient is admitted with a hip fracture (820.8) after slipping on the ice outside her home. The patient also has hypertension (401.1) and type II diabetes (250.00). The surgeon manages the patient’s peri-operative course for the fracture, while the hospitalist manages the patient’s medical issues.
Payers must be sure that the services of one physician do not duplicate those provided by another.1 For the above scenario, it is imperative that the hospitalist understand which services are considered the surgeon’s responsibility. The global surgical package includes payment for the surgical procedure and the completion of its corresponding facility-required paperwork (e.g. pre-operative history and physical exam, operative consent forms, pre-operative orders), in addition to the following services:2
- Pre-operative visits after making the decision for surgery beginning one day prior to surgery;
- All additional post-operative medical or surgical services provided by the surgeon related to complications but not requiring additional trips to the operating room;
- Post-operative visits by the surgeon related to recovery from surgery, including but not limited to dressing changes, local incisional care, removal of cutaneous sutures and staples, line removals, changes and removal of tracheostomy tubes, and discharge services; and
- Post-operative pain management provided by the surgeon.
Another physician who performs any component of the global package will not receive separate payment unless the surgeon is willing to forego a portion of the payment. For example, a hospitalist admits a patient who has no other identifiable medical conditions aside from the problem prompting surgery. The hospitalist’s role may be dictated by facility policy—quality of care or risk reduction, for example—and administrative requirements (history and physical exam, discharge services, coordination of care) rather than what a payer would perceive as necessary “medical” management. Similarly, if the hospitalist’s post-op care is limited to ordering routine post-op labs or maintaining appropriate pain management, the hospitalist’s service will likely be denied as incidental to the surgical package.
Remember, if the hospitalist’s claim is submitted and paid, it doesn’t mean that the payer won’t retract the payment upon review if an erroneous payment is suspected. A payer review may be triggered when the diagnosis listed on the hospitalist’s claim matches the diagnosis listed on the surgeon’s claim (e.g. 820.8). If too many claims are considered “not medically necessary” due to overlapping care, hospitalists may need to negotiate other terms of payment with the facility to recoup unpaid time and effort when involved in this type of care.
When more than one medical condition exists and several physicians participate in the patient’s care, medical necessity is easily established for each physician. Each physician manages the condition related to his/her expertise. In the above example, the surgeon cares for the patient’s fracture, while the hospitalist oversees diabetes and hypertension management. Service distinction is crucial during the claim submission process. The hospitalist should report a subsequent hospital care code (99231-99233) with a primary diagnosis corresponding to his/her specialty-related care (i.e., 9923x with 250.00, 401.1).3
When more specialists are involved, claim submission becomes more complex. A cardiologist who was also involved in patient management would report his or her service using 401.1. When a different primary diagnosis is assigned to the visit code to indicate the reason for each physician’s involvement, all claims are more likely to be paid.4 As long as the hospitalist maintains care over one of the patients’ conditions, concurrent care is justified.
Because these physicians are in different specialties and different provider groups, most payers do not require the modifier 25 (separately identifiable evaluation/management [E/M] service on the same day as a procedure or other service) with the visit code; however, some managed care payers may have a general claim edit that pays the first claim and denies the second unless modifier 25 is appended to the concurrent E/M visit code (i.e., 99232-25) as an attestation that the service is distinct from any other provider’s service that day, despite claim submission under different tax identification numbers. This may not be identified until the claim is rejected or denied. If appropriate modifier use does not yield payment, appeal the denied concurrent care claims with supporting documentation from each physician visit, if possible. This demonstrates each physician’s contribution to care.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. Medicare Benefit Policy Manual: Chapter 15—Covered Medical and Other Health Services. Section 30.E. Available at: www.cms.gov/manuals/Downloads/bp102c15.pdf. Accessed March 5, 2015.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12—Physicians/Nonphysician Practitioners. Section 40.A. Available at: www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c12.pdf. Accessed March 5, 2015.
- American Medical Association. Current Procedural Terminology 2015 Professional Edition. Chicago: American Medical Association Press; 2014.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12—Physicians/Nonphysician Practitioners. Section 30.6.9.C. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed March 5, 2015.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12—Physicians/Nonphysician Practitioners. Section 30.6.5. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed March 5, 2015.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 26—Completing and Processing Form CMS-1500 Data Set. Section 10.8.2. Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/clm104c26.pdf. Accessed March 5, 2015.
Hospitalists often are tasked with coordinating and overseeing patient care throughout a hospitalization. Depending on the care model and the availability of varying specialists, a patient could see several specialists throughout the stay, and even during a single day. A recurring issue for many hospitalists is justifying the medical necessity of their services, because payers do not want to reimburse overlapping care (i.e., multiple providers caring for the same patient problem) when more than one physician provides care on the same service date.
Payers often consider two key principles before reimbursing multiple visits on the same date:1
- Does the patient’s condition warrant the services of more than one physician?
- Are the individual services provided by each physician reasonable and necessary?
Consider the following example: A 65-year-old female patient is admitted with a hip fracture (820.8) after slipping on the ice outside her home. The patient also has hypertension (401.1) and type II diabetes (250.00). The surgeon manages the patient’s peri-operative course for the fracture, while the hospitalist manages the patient’s medical issues.
Payers must be sure that the services of one physician do not duplicate those provided by another.1 For the above scenario, it is imperative that the hospitalist understand which services are considered the surgeon’s responsibility. The global surgical package includes payment for the surgical procedure and the completion of its corresponding facility-required paperwork (e.g. pre-operative history and physical exam, operative consent forms, pre-operative orders), in addition to the following services:2
- Pre-operative visits after making the decision for surgery beginning one day prior to surgery;
- All additional post-operative medical or surgical services provided by the surgeon related to complications but not requiring additional trips to the operating room;
- Post-operative visits by the surgeon related to recovery from surgery, including but not limited to dressing changes, local incisional care, removal of cutaneous sutures and staples, line removals, changes and removal of tracheostomy tubes, and discharge services; and
- Post-operative pain management provided by the surgeon.
Another physician who performs any component of the global package will not receive separate payment unless the surgeon is willing to forego a portion of the payment. For example, a hospitalist admits a patient who has no other identifiable medical conditions aside from the problem prompting surgery. The hospitalist’s role may be dictated by facility policy—quality of care or risk reduction, for example—and administrative requirements (history and physical exam, discharge services, coordination of care) rather than what a payer would perceive as necessary “medical” management. Similarly, if the hospitalist’s post-op care is limited to ordering routine post-op labs or maintaining appropriate pain management, the hospitalist’s service will likely be denied as incidental to the surgical package.
Remember, if the hospitalist’s claim is submitted and paid, it doesn’t mean that the payer won’t retract the payment upon review if an erroneous payment is suspected. A payer review may be triggered when the diagnosis listed on the hospitalist’s claim matches the diagnosis listed on the surgeon’s claim (e.g. 820.8). If too many claims are considered “not medically necessary” due to overlapping care, hospitalists may need to negotiate other terms of payment with the facility to recoup unpaid time and effort when involved in this type of care.
When more than one medical condition exists and several physicians participate in the patient’s care, medical necessity is easily established for each physician. Each physician manages the condition related to his/her expertise. In the above example, the surgeon cares for the patient’s fracture, while the hospitalist oversees diabetes and hypertension management. Service distinction is crucial during the claim submission process. The hospitalist should report a subsequent hospital care code (99231-99233) with a primary diagnosis corresponding to his/her specialty-related care (i.e., 9923x with 250.00, 401.1).3
When more specialists are involved, claim submission becomes more complex. A cardiologist who was also involved in patient management would report his or her service using 401.1. When a different primary diagnosis is assigned to the visit code to indicate the reason for each physician’s involvement, all claims are more likely to be paid.4 As long as the hospitalist maintains care over one of the patients’ conditions, concurrent care is justified.
Because these physicians are in different specialties and different provider groups, most payers do not require the modifier 25 (separately identifiable evaluation/management [E/M] service on the same day as a procedure or other service) with the visit code; however, some managed care payers may have a general claim edit that pays the first claim and denies the second unless modifier 25 is appended to the concurrent E/M visit code (i.e., 99232-25) as an attestation that the service is distinct from any other provider’s service that day, despite claim submission under different tax identification numbers. This may not be identified until the claim is rejected or denied. If appropriate modifier use does not yield payment, appeal the denied concurrent care claims with supporting documentation from each physician visit, if possible. This demonstrates each physician’s contribution to care.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. Medicare Benefit Policy Manual: Chapter 15—Covered Medical and Other Health Services. Section 30.E. Available at: www.cms.gov/manuals/Downloads/bp102c15.pdf. Accessed March 5, 2015.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12—Physicians/Nonphysician Practitioners. Section 40.A. Available at: www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c12.pdf. Accessed March 5, 2015.
- American Medical Association. Current Procedural Terminology 2015 Professional Edition. Chicago: American Medical Association Press; 2014.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12—Physicians/Nonphysician Practitioners. Section 30.6.9.C. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed March 5, 2015.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12—Physicians/Nonphysician Practitioners. Section 30.6.5. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed March 5, 2015.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 26—Completing and Processing Form CMS-1500 Data Set. Section 10.8.2. Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/clm104c26.pdf. Accessed March 5, 2015.