User login
Point: Healthcare Providers Should Receive Treatment Priority During a Pandemic
Potential catastrophic surges in coronavirus disease 2019 (COVID-19) are leading to more patients requiring intensive care unit beds than are available, prompting hospitals to prepare to activate crisis standards of care (CSC).1,2 These guidelines manage the sobering process of determining which gravely ill patients will have access to limited ventilators, critical care specialists, and other essential hospital personnel. As a member of the CSC triage team at Brigham and Women’s Hospital, Boston, Massachusetts, during the initial surge,1 I was taught how to follow procedures that assign each patient a priority score that ranged from 1 to 8, with lower scores representing higher priority. Scoring decisions were largely based on current status of organ systems and major medical illnesses (predictive of short-term and longer-term survival, respectively), consistent with the objective of maximizing lives and life-years saved.1,3-7 Other parameters included improving the priority score of a pregnant woman with a viable fetus and breaking ties in favor of younger patients who had not lived through life’s major stages.4,7 One issue that elicited sharp disagreement among my colleagues was whether healthcare providers (HCPs; eg, physicians, nurses) should be treated any differently than other individuals.
I believe that HCPs should receive treatment priority during a pandemic because the community has a special obligation to those workers willing to risk serious illness by providing care to potentially infected patients.
THE UTILITARIAN CASE FOR TREATMENT PRIORITIZATION
The most common argument for prioritizing HCPs has been made on utilitarian grounds: save individuals who can save others.3,4,6 Such an approach is not founded on the claim that HCPs have higher intrinsic worth, but is based on the instrumental value of HCPs to keep others alive.4,6 An abiding concern for human life demands systems to ensure individuals with clinical expertise are protected so that they can use their skills to maximize the number of lives saved. A similar case has been made to justify prioritizing HCPs for early access to vaccines during a pandemic.5 To underscore these issues, imagine a scenario in which, because of serious illness among HCPs, there were not enough workers with requisite expertise to care for the rest of the community in which a virus was rapidly spreading. Prioritizing HCPs could mitigate this sequence of events by preventing them from becoming infected through early access to vaccinations or promoting their recovery from the illness, which might allow them to return to work caring for others.
THE ROLE OF SPECIAL OBLIGATIONS
Although the utilitarian argument has merit, my primary reason for advocating the prioritization of HCPs reflects a different ethical framework that emphasizes the reciprocal obligations between HCPs and the community. Obligations of physicians have been framed in terms of the commitments made to their self-chosen profession and the putative social contract that has been constructed with the community.8-10 These principles are well articulated in the American Medical Association’s (AMA’s) Code of Medical Ethics, which states, “Because of their commitment to care for the sick and injured, individual physicians have an obligation to provide urgent medical care during disasters…even in the face of greater than usual risks to their own safety, health, or life.”10,11 Although the AMA qualified its position by indicating that this obligation is not unconditional, it still formulated exceptions within the overarching structure of professional duty, allowing physicians to “balance immediate benefits to individual patients with ability to care for patients in the future.”11,12
If one accepts that HCPs have a professional obligation to take care of sick members of the community, even in perilous situations, what, if any, reciprocal obligation does the community have to its HCPs? Reciprocity is a fundamental ethical principle,13 serving as a foundation for the Golden Rule, which is a component of almost every ethical tradition.14 At its core, reciprocity asks us to treat other people as we would want to be treated. It requires endeavoring to take the perspective of others. Within this framework, a strategy for generating a just policy about treatment prioritization is to develop it under the assumption of not knowing which role one would end up playing in a situation. It is critical that if the positions of the individuals involved were reversed, the same rules and obligations would be accepted as fair.13 I suggest that if members of the community put themselves in the shoes of HCPs who are willing to risk exposure to a potentially deadly virus, they would acknowledge the legitimate expectation of HCPs to receive prioritized care if they became ill from the infection.
In most cases, reciprocity is not construed as requiring an identical exchange, but a fair one in which, for instance, sacrifice is returned in kind. Obligations can be viewed as debts that we either owe or are entitled to receive.15 In the current context, reciprocal obligations are derived from the relationship between HCPs and the community in which they serve. HCPs have a special set of obligations to carry out their work with a high degree of professionalism. If circumstances demand they take on substantial risk for their community, the community, in turn, has a special obligation to take care of them.
To highlight this perspective, imagine HCPs who become ill with COVID-19 and make claims for treatment priority despite having been unwilling to work with patients who are sick with COVID-19. We would consider such claims to be unjust because our moral intuition suggests that individuals are owed a debt for the actual risks they have taken, not for the potential ones they have avoided. A corollary of this view is that HCPs who have demonstrated a willingness to risk their lives contracting COVID-19 have a legitimate claim for prioritization.
Implementation
Acknowledgment of the community’s special obligation to HCPs does not negate competing claims for prioritization, such as trying to save the most lives or accounting for a patient’s pregnancy status and stage of life. Rather, there is a need for CSC guidelines to also include recognition of the special obligations owed HCPs by improving their priority score in the calculus used to triage care. Operationalizing the process would need to be worked out. One possibility would be for HCPs directly caring for patients ill from COVID-19 to have their priority score improve by 2 points, and HCPs directly caring for patients without known disease (but who could still be infectious) to benefit by 1 point. At a minimum, recognition of the risks taken should serve as a tiebreaker in favor of these workers.
To Whom Does the Community Have a Special Obligation?
If we acknowledge that during a pandemic, the community has a special obligation to HCPs because of the risks they are taking to serve others, by the same logic, this commitment should be extended to any personnel linked to the healthcare system (eg, employees in environmental services) or frontline workers providing essential services (eg, grocery store workers) who are taking similar risks that involve exposure to potentially infected individuals. Conversely, HCPs who are working exclusively from home via telemedicine should not receive treatment priority. An approach that extends treatment prioritization to other relevant workers mitigates concerns raised about prioritizing scarce critical care resources to an already advantaged class of individuals (ie, HCPs) as well as the negative optics of a committee of “deciders” in a hospital who are privileging care to their own members.12
CONCLUSION
Reciprocity, a critical component of our notion of justice, should be incorporated into CSC guidelines. The community’s reciprocity to HCPs and frontline workers needs to be commensurate with the sacrifice made by these groups. Although public demonstrations of gratitude may be much appreciated, such displays alone are not adequate for honoring the community’s special obligations. If, during a pandemic, HCPs or frontline workers deliver direct care or services to members of the community, despite serious risk to their own lives, the community has a reciprocal obligation to these individuals to prioritize their access to critical care. HCPs and frontline workers should be prioritized not because their lives have higher intrinsic worth or solely as a reflection of their instrumental value to the community, but out of recognition of the special debt owed them. This is not an unconditional obligation, but one that should be built into the complex, multifaceted decision-making process4,6,16 underlying the allocation of scarce medical resources in a pandemic.
Acknowledgments
The author deeply appreciates the thoughtful comments on the essay from William Snyder, PhD, Melissa Frumin, MD, Brittany McFeeley, BS, Lise Bliss, MBA, and especially Seth Gales, MD, and remains grateful for the guidance and support he received early in his academic career from his first mentors, Carol Gilligan, PhD, and Michael Walzer, PhD.
1. Milliken A, Jurchak M, Sadovnikoff N, et al. Addressing challenges associated with operationalizing a crisis standards of care protocol for the Covid-19 pandemic. NEJM Catalyst. 2020:1-14. https://doi.org/10.1056/CAT.20.0384
2. Paquette ET, Derrington S, Fry JT, et al. Shifting duties of children’s hospitals during the COVID-19 pandemic. J Hosp Med. 2020;15(10):631-633. https://doi.org/10.12788/jhm.3490
3. Emanuel EJ, Persad G, Upshur R, et al. Fair allocation of scarce medical resources in the time of Covid-19.N Engl J Med.2020;382(21):2049-2055. https://doi.org/10.1056/NEJMsb2005114
4. White DB, Lo B. A framework for rationing ventilators and critical care beds during the COVID-19 pandemic. JAMA. 2020;323(18):1773-1774. https://doi.org/10.1001/jama.2020.5046
5. Emanuel EJ, Wetheimer A. Who should get influenza vaccine when not all can? Science. 2006;312(5775):854-855. https://doi.org/10.1126/science.1125347
6. White DB, Katz MH, Luce JM, Lo B. Who should receive life support during a public health emergency? Using ethical principles to improve allocation decisions. Ann Intern Med. 2009;150(2):132-138. https://doi.org/10.7326/0003-4819-150-2-200901200-00011
7. The Commonwealth of Massachusetts Executive Office of Health and Human Services Department of Public Health. Crisis Standards of Care: Planning Guidance for the COVID-19 Pandemic. Accessed August 1, 2020. https://www.mass.gov/doc/statewide-advisory-committee-recommendations-forstandards-of-care/download?_ga=2.55928739.940920097.159299949-195847297.1590861397
8. Brody H, Avery EN. Medicine’s duty to treat pandemic illness: solidarity and vulnerability. Hastings Cent Rep. 2009;39(1):40-48. https://doi.org/10.1353/hcr.0.0104
9. Ruderman C, Tracy CS, Bensimon CM, et al. On pandemics and the duty to care: whose duty? who cares? BMC Med Ethics. 2006;7:E5. https://doi.org/10.1186/1472-6939-7-5
10. Huber SJ, Wynia MK. When pestilence prevails . . . physician responsibilities in epidemics. Am J Bioeth. 2004;4(1):W5-11. https://doi.org/10.1162/152651604773067497
11. AMA Council on Ethical and Judicial Affairs. Opinion 9.067 Physician Obligation in Disaster Preparedness and Response. Virtual Mentor. 2010;12(6):459. d10.1001/virtualmentor.2010.12.6.coet1-1006
12. Rothstein MA. Should health care providers get treatment priority in an influenza pandemic? J Law Med Ethics. 2010;38(2):412-419. https://doi.org/10.1111/j.1748-720X.2010.00499.x
13. Rawls J. A Theory of Justice. The Belknap Press: an imprint of Harvard University Press; 1971.
14. Green WS. Parsing reciprocity: questions for the Golden Rule. In: Neusner J, Chilton BD, eds. The Golden Rule: The Ethics of Reciprocity in World Religions. Continuum International Publishing Group; 2008:1-8.
15. Walzer M. Obligations: Essays on Disobedience, War and Citizenship. Harvard University Press; 1970.
16. Persad G, Wertheimer A, Emanuel EJ. Principles for allocation of scarce medical interventions. Lancet. 2009;373(9661):423-431. https://doi.org/10.1016/S0140-6736(09)60137-9
Potential catastrophic surges in coronavirus disease 2019 (COVID-19) are leading to more patients requiring intensive care unit beds than are available, prompting hospitals to prepare to activate crisis standards of care (CSC).1,2 These guidelines manage the sobering process of determining which gravely ill patients will have access to limited ventilators, critical care specialists, and other essential hospital personnel. As a member of the CSC triage team at Brigham and Women’s Hospital, Boston, Massachusetts, during the initial surge,1 I was taught how to follow procedures that assign each patient a priority score that ranged from 1 to 8, with lower scores representing higher priority. Scoring decisions were largely based on current status of organ systems and major medical illnesses (predictive of short-term and longer-term survival, respectively), consistent with the objective of maximizing lives and life-years saved.1,3-7 Other parameters included improving the priority score of a pregnant woman with a viable fetus and breaking ties in favor of younger patients who had not lived through life’s major stages.4,7 One issue that elicited sharp disagreement among my colleagues was whether healthcare providers (HCPs; eg, physicians, nurses) should be treated any differently than other individuals.
I believe that HCPs should receive treatment priority during a pandemic because the community has a special obligation to those workers willing to risk serious illness by providing care to potentially infected patients.
THE UTILITARIAN CASE FOR TREATMENT PRIORITIZATION
The most common argument for prioritizing HCPs has been made on utilitarian grounds: save individuals who can save others.3,4,6 Such an approach is not founded on the claim that HCPs have higher intrinsic worth, but is based on the instrumental value of HCPs to keep others alive.4,6 An abiding concern for human life demands systems to ensure individuals with clinical expertise are protected so that they can use their skills to maximize the number of lives saved. A similar case has been made to justify prioritizing HCPs for early access to vaccines during a pandemic.5 To underscore these issues, imagine a scenario in which, because of serious illness among HCPs, there were not enough workers with requisite expertise to care for the rest of the community in which a virus was rapidly spreading. Prioritizing HCPs could mitigate this sequence of events by preventing them from becoming infected through early access to vaccinations or promoting their recovery from the illness, which might allow them to return to work caring for others.
THE ROLE OF SPECIAL OBLIGATIONS
Although the utilitarian argument has merit, my primary reason for advocating the prioritization of HCPs reflects a different ethical framework that emphasizes the reciprocal obligations between HCPs and the community. Obligations of physicians have been framed in terms of the commitments made to their self-chosen profession and the putative social contract that has been constructed with the community.8-10 These principles are well articulated in the American Medical Association’s (AMA’s) Code of Medical Ethics, which states, “Because of their commitment to care for the sick and injured, individual physicians have an obligation to provide urgent medical care during disasters…even in the face of greater than usual risks to their own safety, health, or life.”10,11 Although the AMA qualified its position by indicating that this obligation is not unconditional, it still formulated exceptions within the overarching structure of professional duty, allowing physicians to “balance immediate benefits to individual patients with ability to care for patients in the future.”11,12
If one accepts that HCPs have a professional obligation to take care of sick members of the community, even in perilous situations, what, if any, reciprocal obligation does the community have to its HCPs? Reciprocity is a fundamental ethical principle,13 serving as a foundation for the Golden Rule, which is a component of almost every ethical tradition.14 At its core, reciprocity asks us to treat other people as we would want to be treated. It requires endeavoring to take the perspective of others. Within this framework, a strategy for generating a just policy about treatment prioritization is to develop it under the assumption of not knowing which role one would end up playing in a situation. It is critical that if the positions of the individuals involved were reversed, the same rules and obligations would be accepted as fair.13 I suggest that if members of the community put themselves in the shoes of HCPs who are willing to risk exposure to a potentially deadly virus, they would acknowledge the legitimate expectation of HCPs to receive prioritized care if they became ill from the infection.
In most cases, reciprocity is not construed as requiring an identical exchange, but a fair one in which, for instance, sacrifice is returned in kind. Obligations can be viewed as debts that we either owe or are entitled to receive.15 In the current context, reciprocal obligations are derived from the relationship between HCPs and the community in which they serve. HCPs have a special set of obligations to carry out their work with a high degree of professionalism. If circumstances demand they take on substantial risk for their community, the community, in turn, has a special obligation to take care of them.
To highlight this perspective, imagine HCPs who become ill with COVID-19 and make claims for treatment priority despite having been unwilling to work with patients who are sick with COVID-19. We would consider such claims to be unjust because our moral intuition suggests that individuals are owed a debt for the actual risks they have taken, not for the potential ones they have avoided. A corollary of this view is that HCPs who have demonstrated a willingness to risk their lives contracting COVID-19 have a legitimate claim for prioritization.
Implementation
Acknowledgment of the community’s special obligation to HCPs does not negate competing claims for prioritization, such as trying to save the most lives or accounting for a patient’s pregnancy status and stage of life. Rather, there is a need for CSC guidelines to also include recognition of the special obligations owed HCPs by improving their priority score in the calculus used to triage care. Operationalizing the process would need to be worked out. One possibility would be for HCPs directly caring for patients ill from COVID-19 to have their priority score improve by 2 points, and HCPs directly caring for patients without known disease (but who could still be infectious) to benefit by 1 point. At a minimum, recognition of the risks taken should serve as a tiebreaker in favor of these workers.
To Whom Does the Community Have a Special Obligation?
If we acknowledge that during a pandemic, the community has a special obligation to HCPs because of the risks they are taking to serve others, by the same logic, this commitment should be extended to any personnel linked to the healthcare system (eg, employees in environmental services) or frontline workers providing essential services (eg, grocery store workers) who are taking similar risks that involve exposure to potentially infected individuals. Conversely, HCPs who are working exclusively from home via telemedicine should not receive treatment priority. An approach that extends treatment prioritization to other relevant workers mitigates concerns raised about prioritizing scarce critical care resources to an already advantaged class of individuals (ie, HCPs) as well as the negative optics of a committee of “deciders” in a hospital who are privileging care to their own members.12
CONCLUSION
Reciprocity, a critical component of our notion of justice, should be incorporated into CSC guidelines. The community’s reciprocity to HCPs and frontline workers needs to be commensurate with the sacrifice made by these groups. Although public demonstrations of gratitude may be much appreciated, such displays alone are not adequate for honoring the community’s special obligations. If, during a pandemic, HCPs or frontline workers deliver direct care or services to members of the community, despite serious risk to their own lives, the community has a reciprocal obligation to these individuals to prioritize their access to critical care. HCPs and frontline workers should be prioritized not because their lives have higher intrinsic worth or solely as a reflection of their instrumental value to the community, but out of recognition of the special debt owed them. This is not an unconditional obligation, but one that should be built into the complex, multifaceted decision-making process4,6,16 underlying the allocation of scarce medical resources in a pandemic.
Acknowledgments
The author deeply appreciates the thoughtful comments on the essay from William Snyder, PhD, Melissa Frumin, MD, Brittany McFeeley, BS, Lise Bliss, MBA, and especially Seth Gales, MD, and remains grateful for the guidance and support he received early in his academic career from his first mentors, Carol Gilligan, PhD, and Michael Walzer, PhD.
Potential catastrophic surges in coronavirus disease 2019 (COVID-19) are leading to more patients requiring intensive care unit beds than are available, prompting hospitals to prepare to activate crisis standards of care (CSC).1,2 These guidelines manage the sobering process of determining which gravely ill patients will have access to limited ventilators, critical care specialists, and other essential hospital personnel. As a member of the CSC triage team at Brigham and Women’s Hospital, Boston, Massachusetts, during the initial surge,1 I was taught how to follow procedures that assign each patient a priority score that ranged from 1 to 8, with lower scores representing higher priority. Scoring decisions were largely based on current status of organ systems and major medical illnesses (predictive of short-term and longer-term survival, respectively), consistent with the objective of maximizing lives and life-years saved.1,3-7 Other parameters included improving the priority score of a pregnant woman with a viable fetus and breaking ties in favor of younger patients who had not lived through life’s major stages.4,7 One issue that elicited sharp disagreement among my colleagues was whether healthcare providers (HCPs; eg, physicians, nurses) should be treated any differently than other individuals.
I believe that HCPs should receive treatment priority during a pandemic because the community has a special obligation to those workers willing to risk serious illness by providing care to potentially infected patients.
THE UTILITARIAN CASE FOR TREATMENT PRIORITIZATION
The most common argument for prioritizing HCPs has been made on utilitarian grounds: save individuals who can save others.3,4,6 Such an approach is not founded on the claim that HCPs have higher intrinsic worth, but is based on the instrumental value of HCPs to keep others alive.4,6 An abiding concern for human life demands systems to ensure individuals with clinical expertise are protected so that they can use their skills to maximize the number of lives saved. A similar case has been made to justify prioritizing HCPs for early access to vaccines during a pandemic.5 To underscore these issues, imagine a scenario in which, because of serious illness among HCPs, there were not enough workers with requisite expertise to care for the rest of the community in which a virus was rapidly spreading. Prioritizing HCPs could mitigate this sequence of events by preventing them from becoming infected through early access to vaccinations or promoting their recovery from the illness, which might allow them to return to work caring for others.
THE ROLE OF SPECIAL OBLIGATIONS
Although the utilitarian argument has merit, my primary reason for advocating the prioritization of HCPs reflects a different ethical framework that emphasizes the reciprocal obligations between HCPs and the community. Obligations of physicians have been framed in terms of the commitments made to their self-chosen profession and the putative social contract that has been constructed with the community.8-10 These principles are well articulated in the American Medical Association’s (AMA’s) Code of Medical Ethics, which states, “Because of their commitment to care for the sick and injured, individual physicians have an obligation to provide urgent medical care during disasters…even in the face of greater than usual risks to their own safety, health, or life.”10,11 Although the AMA qualified its position by indicating that this obligation is not unconditional, it still formulated exceptions within the overarching structure of professional duty, allowing physicians to “balance immediate benefits to individual patients with ability to care for patients in the future.”11,12
If one accepts that HCPs have a professional obligation to take care of sick members of the community, even in perilous situations, what, if any, reciprocal obligation does the community have to its HCPs? Reciprocity is a fundamental ethical principle,13 serving as a foundation for the Golden Rule, which is a component of almost every ethical tradition.14 At its core, reciprocity asks us to treat other people as we would want to be treated. It requires endeavoring to take the perspective of others. Within this framework, a strategy for generating a just policy about treatment prioritization is to develop it under the assumption of not knowing which role one would end up playing in a situation. It is critical that if the positions of the individuals involved were reversed, the same rules and obligations would be accepted as fair.13 I suggest that if members of the community put themselves in the shoes of HCPs who are willing to risk exposure to a potentially deadly virus, they would acknowledge the legitimate expectation of HCPs to receive prioritized care if they became ill from the infection.
In most cases, reciprocity is not construed as requiring an identical exchange, but a fair one in which, for instance, sacrifice is returned in kind. Obligations can be viewed as debts that we either owe or are entitled to receive.15 In the current context, reciprocal obligations are derived from the relationship between HCPs and the community in which they serve. HCPs have a special set of obligations to carry out their work with a high degree of professionalism. If circumstances demand they take on substantial risk for their community, the community, in turn, has a special obligation to take care of them.
To highlight this perspective, imagine HCPs who become ill with COVID-19 and make claims for treatment priority despite having been unwilling to work with patients who are sick with COVID-19. We would consider such claims to be unjust because our moral intuition suggests that individuals are owed a debt for the actual risks they have taken, not for the potential ones they have avoided. A corollary of this view is that HCPs who have demonstrated a willingness to risk their lives contracting COVID-19 have a legitimate claim for prioritization.
Implementation
Acknowledgment of the community’s special obligation to HCPs does not negate competing claims for prioritization, such as trying to save the most lives or accounting for a patient’s pregnancy status and stage of life. Rather, there is a need for CSC guidelines to also include recognition of the special obligations owed HCPs by improving their priority score in the calculus used to triage care. Operationalizing the process would need to be worked out. One possibility would be for HCPs directly caring for patients ill from COVID-19 to have their priority score improve by 2 points, and HCPs directly caring for patients without known disease (but who could still be infectious) to benefit by 1 point. At a minimum, recognition of the risks taken should serve as a tiebreaker in favor of these workers.
To Whom Does the Community Have a Special Obligation?
If we acknowledge that during a pandemic, the community has a special obligation to HCPs because of the risks they are taking to serve others, by the same logic, this commitment should be extended to any personnel linked to the healthcare system (eg, employees in environmental services) or frontline workers providing essential services (eg, grocery store workers) who are taking similar risks that involve exposure to potentially infected individuals. Conversely, HCPs who are working exclusively from home via telemedicine should not receive treatment priority. An approach that extends treatment prioritization to other relevant workers mitigates concerns raised about prioritizing scarce critical care resources to an already advantaged class of individuals (ie, HCPs) as well as the negative optics of a committee of “deciders” in a hospital who are privileging care to their own members.12
CONCLUSION
Reciprocity, a critical component of our notion of justice, should be incorporated into CSC guidelines. The community’s reciprocity to HCPs and frontline workers needs to be commensurate with the sacrifice made by these groups. Although public demonstrations of gratitude may be much appreciated, such displays alone are not adequate for honoring the community’s special obligations. If, during a pandemic, HCPs or frontline workers deliver direct care or services to members of the community, despite serious risk to their own lives, the community has a reciprocal obligation to these individuals to prioritize their access to critical care. HCPs and frontline workers should be prioritized not because their lives have higher intrinsic worth or solely as a reflection of their instrumental value to the community, but out of recognition of the special debt owed them. This is not an unconditional obligation, but one that should be built into the complex, multifaceted decision-making process4,6,16 underlying the allocation of scarce medical resources in a pandemic.
Acknowledgments
The author deeply appreciates the thoughtful comments on the essay from William Snyder, PhD, Melissa Frumin, MD, Brittany McFeeley, BS, Lise Bliss, MBA, and especially Seth Gales, MD, and remains grateful for the guidance and support he received early in his academic career from his first mentors, Carol Gilligan, PhD, and Michael Walzer, PhD.
1. Milliken A, Jurchak M, Sadovnikoff N, et al. Addressing challenges associated with operationalizing a crisis standards of care protocol for the Covid-19 pandemic. NEJM Catalyst. 2020:1-14. https://doi.org/10.1056/CAT.20.0384
2. Paquette ET, Derrington S, Fry JT, et al. Shifting duties of children’s hospitals during the COVID-19 pandemic. J Hosp Med. 2020;15(10):631-633. https://doi.org/10.12788/jhm.3490
3. Emanuel EJ, Persad G, Upshur R, et al. Fair allocation of scarce medical resources in the time of Covid-19.N Engl J Med.2020;382(21):2049-2055. https://doi.org/10.1056/NEJMsb2005114
4. White DB, Lo B. A framework for rationing ventilators and critical care beds during the COVID-19 pandemic. JAMA. 2020;323(18):1773-1774. https://doi.org/10.1001/jama.2020.5046
5. Emanuel EJ, Wetheimer A. Who should get influenza vaccine when not all can? Science. 2006;312(5775):854-855. https://doi.org/10.1126/science.1125347
6. White DB, Katz MH, Luce JM, Lo B. Who should receive life support during a public health emergency? Using ethical principles to improve allocation decisions. Ann Intern Med. 2009;150(2):132-138. https://doi.org/10.7326/0003-4819-150-2-200901200-00011
7. The Commonwealth of Massachusetts Executive Office of Health and Human Services Department of Public Health. Crisis Standards of Care: Planning Guidance for the COVID-19 Pandemic. Accessed August 1, 2020. https://www.mass.gov/doc/statewide-advisory-committee-recommendations-forstandards-of-care/download?_ga=2.55928739.940920097.159299949-195847297.1590861397
8. Brody H, Avery EN. Medicine’s duty to treat pandemic illness: solidarity and vulnerability. Hastings Cent Rep. 2009;39(1):40-48. https://doi.org/10.1353/hcr.0.0104
9. Ruderman C, Tracy CS, Bensimon CM, et al. On pandemics and the duty to care: whose duty? who cares? BMC Med Ethics. 2006;7:E5. https://doi.org/10.1186/1472-6939-7-5
10. Huber SJ, Wynia MK. When pestilence prevails . . . physician responsibilities in epidemics. Am J Bioeth. 2004;4(1):W5-11. https://doi.org/10.1162/152651604773067497
11. AMA Council on Ethical and Judicial Affairs. Opinion 9.067 Physician Obligation in Disaster Preparedness and Response. Virtual Mentor. 2010;12(6):459. d10.1001/virtualmentor.2010.12.6.coet1-1006
12. Rothstein MA. Should health care providers get treatment priority in an influenza pandemic? J Law Med Ethics. 2010;38(2):412-419. https://doi.org/10.1111/j.1748-720X.2010.00499.x
13. Rawls J. A Theory of Justice. The Belknap Press: an imprint of Harvard University Press; 1971.
14. Green WS. Parsing reciprocity: questions for the Golden Rule. In: Neusner J, Chilton BD, eds. The Golden Rule: The Ethics of Reciprocity in World Religions. Continuum International Publishing Group; 2008:1-8.
15. Walzer M. Obligations: Essays on Disobedience, War and Citizenship. Harvard University Press; 1970.
16. Persad G, Wertheimer A, Emanuel EJ. Principles for allocation of scarce medical interventions. Lancet. 2009;373(9661):423-431. https://doi.org/10.1016/S0140-6736(09)60137-9
1. Milliken A, Jurchak M, Sadovnikoff N, et al. Addressing challenges associated with operationalizing a crisis standards of care protocol for the Covid-19 pandemic. NEJM Catalyst. 2020:1-14. https://doi.org/10.1056/CAT.20.0384
2. Paquette ET, Derrington S, Fry JT, et al. Shifting duties of children’s hospitals during the COVID-19 pandemic. J Hosp Med. 2020;15(10):631-633. https://doi.org/10.12788/jhm.3490
3. Emanuel EJ, Persad G, Upshur R, et al. Fair allocation of scarce medical resources in the time of Covid-19.N Engl J Med.2020;382(21):2049-2055. https://doi.org/10.1056/NEJMsb2005114
4. White DB, Lo B. A framework for rationing ventilators and critical care beds during the COVID-19 pandemic. JAMA. 2020;323(18):1773-1774. https://doi.org/10.1001/jama.2020.5046
5. Emanuel EJ, Wetheimer A. Who should get influenza vaccine when not all can? Science. 2006;312(5775):854-855. https://doi.org/10.1126/science.1125347
6. White DB, Katz MH, Luce JM, Lo B. Who should receive life support during a public health emergency? Using ethical principles to improve allocation decisions. Ann Intern Med. 2009;150(2):132-138. https://doi.org/10.7326/0003-4819-150-2-200901200-00011
7. The Commonwealth of Massachusetts Executive Office of Health and Human Services Department of Public Health. Crisis Standards of Care: Planning Guidance for the COVID-19 Pandemic. Accessed August 1, 2020. https://www.mass.gov/doc/statewide-advisory-committee-recommendations-forstandards-of-care/download?_ga=2.55928739.940920097.159299949-195847297.1590861397
8. Brody H, Avery EN. Medicine’s duty to treat pandemic illness: solidarity and vulnerability. Hastings Cent Rep. 2009;39(1):40-48. https://doi.org/10.1353/hcr.0.0104
9. Ruderman C, Tracy CS, Bensimon CM, et al. On pandemics and the duty to care: whose duty? who cares? BMC Med Ethics. 2006;7:E5. https://doi.org/10.1186/1472-6939-7-5
10. Huber SJ, Wynia MK. When pestilence prevails . . . physician responsibilities in epidemics. Am J Bioeth. 2004;4(1):W5-11. https://doi.org/10.1162/152651604773067497
11. AMA Council on Ethical and Judicial Affairs. Opinion 9.067 Physician Obligation in Disaster Preparedness and Response. Virtual Mentor. 2010;12(6):459. d10.1001/virtualmentor.2010.12.6.coet1-1006
12. Rothstein MA. Should health care providers get treatment priority in an influenza pandemic? J Law Med Ethics. 2010;38(2):412-419. https://doi.org/10.1111/j.1748-720X.2010.00499.x
13. Rawls J. A Theory of Justice. The Belknap Press: an imprint of Harvard University Press; 1971.
14. Green WS. Parsing reciprocity: questions for the Golden Rule. In: Neusner J, Chilton BD, eds. The Golden Rule: The Ethics of Reciprocity in World Religions. Continuum International Publishing Group; 2008:1-8.
15. Walzer M. Obligations: Essays on Disobedience, War and Citizenship. Harvard University Press; 1970.
16. Persad G, Wertheimer A, Emanuel EJ. Principles for allocation of scarce medical interventions. Lancet. 2009;373(9661):423-431. https://doi.org/10.1016/S0140-6736(09)60137-9
© 2021 Society of Hospital Medicine
Counterpoint: Prioritizing Healthcare Workers for Scarce Critical Care Resources Is Impractical and Unjust
The impact of the coronavirus disease 2019 (COVID-19) pandemic has been far reaching and devastating. As the pandemic reaches its 1-year mark, there have been more cases and deaths than most of us can comprehend: nearly 28 million cases and 497,000 deaths in the United States1 and more than 111 million cases and 2.4 million deaths globally.2 Frontline healthcare workers (HCWs) have struggled to provide compassionate care in the face of heavy workloads and risks to themselves and their loved ones. Sadly, more than 1,700 US HCWs have died from COVID-19.3 The pandemic has also taken a heavy emotional and psychological toll: HCWs have died by suicide, and others are leaving the profession in which they invested so much and formerly loved. Caring for ill colleagues and dying patients whose family members cannot visit has been particularly difficult. It is, therefore, understandable that some HCWs have called for their prioritization if it becomes necessary to implement crisis standards of care. Although Daffner’s4 reciprocity argument—HCWs should receive priority because of the risks that they have voluntarily accepted—has some appeal, it disregards several important considerations. First, it fails to consider the changing dynamics of viral transmission during the pandemic or alternative ways in which the duty of reciprocity may be fulfilled that do not involve prioritizing HCWs over others. Second, this position is both over- and underinclusive in ways that make it difficult to implement. Third, and most important, the inordinate attention to the prioritization of HCWs ignores the issues the pandemic raises regarding racism and inequity.
LIMITS OF RECIPROCITY AND ALTERNATIVES TO PRIORITIZATION
Although the reciprocity argument has some conceptual merit, there are several different ways that the duty of reciprocity can be fulfilled. One fundamental obligation of government agencies and healthcare systems is providing a safe work environment, including adequate personal protective equipment (PPE) and physical distancing. Before we understood the extent of the pandemic, modes of transmission, and effective preventative measures, hospital transmission was significant. For example, a single-center case series at Zhongan Hospital of Wuhan University, China, from January 1, 2020, to January 28, 2020, found that 29% (40 of 138) of hospitalized patients with COVID-19 were health professionals who were presumed to have been infected by patients.5 There were also significant shortages of PPE, and a number of frontline HCWs reported being dismissed for calling attention to unsafe conditions. Although professionals have an obligation to expose themselves to risk, they are not obligated to expose themselves to inordinate risk. Prioritizing HCWs in ventilator triage may have been justified during the initial surge.
The use of surgical masks by all employees and patients has substantially reduced hospital transmission. A study at Duke Health, Raleigh, North Carolina, of HCWs who tested positive for SARS-CoV-2 between March 15, 2020, and June 6, 2020, found 22% of cases were healthcare acquired, 38% were community acquired, and 40% were of unknown acquisition route. Of the healthcare-acquired cases, 30% were thought to be secondary to direct patient care and 70% to exposure to another worker. The cumulative incidence rate of healthcare-acquired infections among workers decreased significantly 1 week after universal masking was implemented on March 31, 2020. The cumulative incidence rates of community-acquired cases and those with unknown acquisition routes continued to mirror incidence rates in the community.6 There is substantially less justification for prioritizing HCWs during the current phase of the pandemic; reciprocity does not justify granting HCWs infected via community spread greater priority than non-HCWs similarly infected.
There are other means of reciprocating that do not involve prioritization. COVID-19 has exacted an immense toll on the mental well-being of frontline HCWs. They should be provided robust, comprehensive, and accessible mental health services. Additionally, reciprocity can be expressed by providing alternative housing options for HCWs who are concerned about infecting their family members, especially family members at higher risk of morbidity or mortality from COVID-19. Many HCWs have also died from COVID-193; providing life insurance would recognize the sacrifice of HCWs and support their survivors. None of these interventions would require prioritizing HCWs over others.
OVER- AND UNDERINCLUSIVENESS
As Daffner4 acknowledges, the category of “healthcare provider” is both over- and underinclusive. Healthcare providers are exposed to variable risks. Some physicians, for example, are no longer involved in direct patient care. It is unclear how triage teams will identify frontline HCWs or validate claims to being a frontline HCW, especially for individuals not employed by the hospital at which they are seeking care. Hence, triage protocols prioritizing healthcare providers are likely to be substantially overinclusive, which raises significant issues of fairness.
Moreover, the category “healthcare provider” is also underinclusive. Many essential, nonclinical hospital employees expose themselves to risk, including custodial and food service staff. As Daffner4 recognizes, there are also many other occupations outside of healthcare in which individuals voluntarily expose themselves to risks for the benefit of others, including police officers, firefighters, and clerks in grocery stores. We would add that workers in the food-supply system, transportation, and education face similar risks.7 Identifying the types of jobs that should confer priority and validating an individual’s employment also makes implementation difficult and risks injustice.
EQUITY AND JUSTICE
The COVID-19 pandemic and the murder of Black people by police have brought substantial attention to racism and racial inequities in the United States. We must, however, move from merely acknowledging existing inequities to dismantling structures that perpetuate them. The prioritization of HCWs may further privilege those who already have substantial advantages. This is especially true for physicians. For example, although state and federal laws pose limitations, physicians have historically extended one another professional courtesy by providing free or discounted services. Furthermore, HCWs and their family members are more likely to receive VIP treatment. For instance, when taken to the emergency department, children of physicians are less likely to have medical students and residents involved in their care and more likely to see attending physicians and consultants.8
In contrast, other categories of essential workers do not have such advantages. These workers are more likely to be members of marginalized racial and ethnic minority groups, have substantially lower wages, have less access to PPE, and work in more crowded conditions, and are less likely to have paid sick leave compared with HCWs.7 These workers are also more likely to lack access to quality healthcare. In fact, many safety net hospitals that provide care to marginalized communities have faced significant financial hardships as a result of the pandemic, and without additional support, some may close. Prioritizing HCWs will likely widen the gaps in health, economic, and social status among these groups.
With respect to allocation criteria, Black, Latinx, and Native American communities have more severe morbidity and mortality from COVID-19 as a result of racism and its interaction with other social determinants of health. Members of marginalized communities of color have a higher likelihood of becoming infected with COVID-19, a higher prevalence of comorbidities, and less access to treatment.7 Before her untimely death, Dr Susan Moore, a Black family physician, painfully described the racism to which she was subjected while being treated for COVID-19.9 The economic devastation caused by the pandemic, including unemployment, evictions, and food insecurity, compounds the impact of social determinants of health and disproportionately affects minority communities. Purely race- and ethnicity-based approaches to allocation to redress these inequities have potential limitations and obstacles, such as omission of other social determinants of health and legal challenges.7 While currently proposed for allocation of medications or vaccines, alternatives include using the Centers for Disease Control and Prevention’s Social Vulnerability Index8 or the Area Deprivation Index10 as a priority criterion. Most importantly, healthcare systems should more broadly demonstrate themselves trustworthy and assure that marginalized communities of color have access to quality healthcare services.
CONCLUSION
The United States has failed to adequately control the COVID-19 pandemic, and increasing numbers of admissions and staffing shortages have renewed concerns that hospitals will need to implement crisis standards of care. Daffner4 argues that healthcare providers should be prioritized in the allocation of critical care based on reciprocity. In the current phase of the pandemic, HCWs are more likely to be infected by one another or in the community than by patients. There are also other ways that hospitals can discharge this duty that do not require prioritizing HCWs over patients. The category of HCW is both over- and underinclusive, and Daffner4 has not shown that prioritization can be implemented fairly. Finally, inordinate attention has been paid to this topic. Much more attention should be focused on how to redress the ways in which the pandemic has exacerbated existing racial and ethnic inequities.
1. COVID data tracker: United States COVID-19 cases and deaths by state. Centers for Disease Control and Prevention . Updated February 22, 2021. Accessed February 22, 2021. https://covid.cdc.gov/covid-data-tracker/#cases_casesper100klast7days
2. WHO coronavirus disease (COVID-19) dashboard: overview. World Health Organization. Updated February 22, 2021. Accessed February 22, 2021. https://covid19.who.int/
3. Sins of omission: how government failures to track Covid-19 data have led to more than 1,700 health care worker deaths and jeopardize public health. National Nurses United. September 2020. Accessed November 23, 2020. https://act.nationalnursesunited.org/page/-/files/graphics/0920_Covid19_SinsOfOmission_Data_Report.pdf
4. Daffner KR. Point: healthcare providers should receive treatment priority during a pandemic. J Hosp Med. Published online February 17, 2021. https://doi.org/10.12788/jhm.3596
5. Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061-1069. https://doi.org/10.1001/jama.2020.1585
6. Seidelman JL, Lewis SS, Advani SD, et al. Universal masking is an effective strategy to flatten the severe acute respiratory coronavirus virus 2 (SARS-CoV-2) healthcare worker epidemiologic curve. Infect Control Hosp Epidemiol. 2020;41(12):1466-1467. https://doi.org/10.1017/ice.2020.313
7. Gayle H, Foege W, Brown L, Kahn B, eds. Framework for Equitable Allocation of COVID-19 Vaccine. The National Academies Press; 2020. https://doi.org/10.17226/25917
8. Diekema DS, Cummings P, Quan L. Physicians’ children are treated differently in the emergency department. Am J Emerg Med. 1996;14(1):6-9. https://doi.org/10.1016/S0735-6757(96)90002-9
9. Maybank A, Jones CP, Blackstock U, Perry JC. Say her name: Dr. Susan Moore. The Washington Post. December 26, 2020. Accessed January 6, 2021. https://www.washingtonpost.com/opinions/2020/12/26/say-her-name-dr-susan-moore/
10. White DB, Schmidhofer M, McCreary E, et al. Model hospital policy for fair allocation of scarce medications to treat COVID-19. University of Pittsburgh. May 28, 2020. Accessed November 23, 2020. https://ccm.pitt.edu/sites/default/files/2020-05-28b%20Model%20hospital%20policy%20for%20allocating%20scarce%20COVID%20meds.pdf
The impact of the coronavirus disease 2019 (COVID-19) pandemic has been far reaching and devastating. As the pandemic reaches its 1-year mark, there have been more cases and deaths than most of us can comprehend: nearly 28 million cases and 497,000 deaths in the United States1 and more than 111 million cases and 2.4 million deaths globally.2 Frontline healthcare workers (HCWs) have struggled to provide compassionate care in the face of heavy workloads and risks to themselves and their loved ones. Sadly, more than 1,700 US HCWs have died from COVID-19.3 The pandemic has also taken a heavy emotional and psychological toll: HCWs have died by suicide, and others are leaving the profession in which they invested so much and formerly loved. Caring for ill colleagues and dying patients whose family members cannot visit has been particularly difficult. It is, therefore, understandable that some HCWs have called for their prioritization if it becomes necessary to implement crisis standards of care. Although Daffner’s4 reciprocity argument—HCWs should receive priority because of the risks that they have voluntarily accepted—has some appeal, it disregards several important considerations. First, it fails to consider the changing dynamics of viral transmission during the pandemic or alternative ways in which the duty of reciprocity may be fulfilled that do not involve prioritizing HCWs over others. Second, this position is both over- and underinclusive in ways that make it difficult to implement. Third, and most important, the inordinate attention to the prioritization of HCWs ignores the issues the pandemic raises regarding racism and inequity.
LIMITS OF RECIPROCITY AND ALTERNATIVES TO PRIORITIZATION
Although the reciprocity argument has some conceptual merit, there are several different ways that the duty of reciprocity can be fulfilled. One fundamental obligation of government agencies and healthcare systems is providing a safe work environment, including adequate personal protective equipment (PPE) and physical distancing. Before we understood the extent of the pandemic, modes of transmission, and effective preventative measures, hospital transmission was significant. For example, a single-center case series at Zhongan Hospital of Wuhan University, China, from January 1, 2020, to January 28, 2020, found that 29% (40 of 138) of hospitalized patients with COVID-19 were health professionals who were presumed to have been infected by patients.5 There were also significant shortages of PPE, and a number of frontline HCWs reported being dismissed for calling attention to unsafe conditions. Although professionals have an obligation to expose themselves to risk, they are not obligated to expose themselves to inordinate risk. Prioritizing HCWs in ventilator triage may have been justified during the initial surge.
The use of surgical masks by all employees and patients has substantially reduced hospital transmission. A study at Duke Health, Raleigh, North Carolina, of HCWs who tested positive for SARS-CoV-2 between March 15, 2020, and June 6, 2020, found 22% of cases were healthcare acquired, 38% were community acquired, and 40% were of unknown acquisition route. Of the healthcare-acquired cases, 30% were thought to be secondary to direct patient care and 70% to exposure to another worker. The cumulative incidence rate of healthcare-acquired infections among workers decreased significantly 1 week after universal masking was implemented on March 31, 2020. The cumulative incidence rates of community-acquired cases and those with unknown acquisition routes continued to mirror incidence rates in the community.6 There is substantially less justification for prioritizing HCWs during the current phase of the pandemic; reciprocity does not justify granting HCWs infected via community spread greater priority than non-HCWs similarly infected.
There are other means of reciprocating that do not involve prioritization. COVID-19 has exacted an immense toll on the mental well-being of frontline HCWs. They should be provided robust, comprehensive, and accessible mental health services. Additionally, reciprocity can be expressed by providing alternative housing options for HCWs who are concerned about infecting their family members, especially family members at higher risk of morbidity or mortality from COVID-19. Many HCWs have also died from COVID-193; providing life insurance would recognize the sacrifice of HCWs and support their survivors. None of these interventions would require prioritizing HCWs over others.
OVER- AND UNDERINCLUSIVENESS
As Daffner4 acknowledges, the category of “healthcare provider” is both over- and underinclusive. Healthcare providers are exposed to variable risks. Some physicians, for example, are no longer involved in direct patient care. It is unclear how triage teams will identify frontline HCWs or validate claims to being a frontline HCW, especially for individuals not employed by the hospital at which they are seeking care. Hence, triage protocols prioritizing healthcare providers are likely to be substantially overinclusive, which raises significant issues of fairness.
Moreover, the category “healthcare provider” is also underinclusive. Many essential, nonclinical hospital employees expose themselves to risk, including custodial and food service staff. As Daffner4 recognizes, there are also many other occupations outside of healthcare in which individuals voluntarily expose themselves to risks for the benefit of others, including police officers, firefighters, and clerks in grocery stores. We would add that workers in the food-supply system, transportation, and education face similar risks.7 Identifying the types of jobs that should confer priority and validating an individual’s employment also makes implementation difficult and risks injustice.
EQUITY AND JUSTICE
The COVID-19 pandemic and the murder of Black people by police have brought substantial attention to racism and racial inequities in the United States. We must, however, move from merely acknowledging existing inequities to dismantling structures that perpetuate them. The prioritization of HCWs may further privilege those who already have substantial advantages. This is especially true for physicians. For example, although state and federal laws pose limitations, physicians have historically extended one another professional courtesy by providing free or discounted services. Furthermore, HCWs and their family members are more likely to receive VIP treatment. For instance, when taken to the emergency department, children of physicians are less likely to have medical students and residents involved in their care and more likely to see attending physicians and consultants.8
In contrast, other categories of essential workers do not have such advantages. These workers are more likely to be members of marginalized racial and ethnic minority groups, have substantially lower wages, have less access to PPE, and work in more crowded conditions, and are less likely to have paid sick leave compared with HCWs.7 These workers are also more likely to lack access to quality healthcare. In fact, many safety net hospitals that provide care to marginalized communities have faced significant financial hardships as a result of the pandemic, and without additional support, some may close. Prioritizing HCWs will likely widen the gaps in health, economic, and social status among these groups.
With respect to allocation criteria, Black, Latinx, and Native American communities have more severe morbidity and mortality from COVID-19 as a result of racism and its interaction with other social determinants of health. Members of marginalized communities of color have a higher likelihood of becoming infected with COVID-19, a higher prevalence of comorbidities, and less access to treatment.7 Before her untimely death, Dr Susan Moore, a Black family physician, painfully described the racism to which she was subjected while being treated for COVID-19.9 The economic devastation caused by the pandemic, including unemployment, evictions, and food insecurity, compounds the impact of social determinants of health and disproportionately affects minority communities. Purely race- and ethnicity-based approaches to allocation to redress these inequities have potential limitations and obstacles, such as omission of other social determinants of health and legal challenges.7 While currently proposed for allocation of medications or vaccines, alternatives include using the Centers for Disease Control and Prevention’s Social Vulnerability Index8 or the Area Deprivation Index10 as a priority criterion. Most importantly, healthcare systems should more broadly demonstrate themselves trustworthy and assure that marginalized communities of color have access to quality healthcare services.
CONCLUSION
The United States has failed to adequately control the COVID-19 pandemic, and increasing numbers of admissions and staffing shortages have renewed concerns that hospitals will need to implement crisis standards of care. Daffner4 argues that healthcare providers should be prioritized in the allocation of critical care based on reciprocity. In the current phase of the pandemic, HCWs are more likely to be infected by one another or in the community than by patients. There are also other ways that hospitals can discharge this duty that do not require prioritizing HCWs over patients. The category of HCW is both over- and underinclusive, and Daffner4 has not shown that prioritization can be implemented fairly. Finally, inordinate attention has been paid to this topic. Much more attention should be focused on how to redress the ways in which the pandemic has exacerbated existing racial and ethnic inequities.
The impact of the coronavirus disease 2019 (COVID-19) pandemic has been far reaching and devastating. As the pandemic reaches its 1-year mark, there have been more cases and deaths than most of us can comprehend: nearly 28 million cases and 497,000 deaths in the United States1 and more than 111 million cases and 2.4 million deaths globally.2 Frontline healthcare workers (HCWs) have struggled to provide compassionate care in the face of heavy workloads and risks to themselves and their loved ones. Sadly, more than 1,700 US HCWs have died from COVID-19.3 The pandemic has also taken a heavy emotional and psychological toll: HCWs have died by suicide, and others are leaving the profession in which they invested so much and formerly loved. Caring for ill colleagues and dying patients whose family members cannot visit has been particularly difficult. It is, therefore, understandable that some HCWs have called for their prioritization if it becomes necessary to implement crisis standards of care. Although Daffner’s4 reciprocity argument—HCWs should receive priority because of the risks that they have voluntarily accepted—has some appeal, it disregards several important considerations. First, it fails to consider the changing dynamics of viral transmission during the pandemic or alternative ways in which the duty of reciprocity may be fulfilled that do not involve prioritizing HCWs over others. Second, this position is both over- and underinclusive in ways that make it difficult to implement. Third, and most important, the inordinate attention to the prioritization of HCWs ignores the issues the pandemic raises regarding racism and inequity.
LIMITS OF RECIPROCITY AND ALTERNATIVES TO PRIORITIZATION
Although the reciprocity argument has some conceptual merit, there are several different ways that the duty of reciprocity can be fulfilled. One fundamental obligation of government agencies and healthcare systems is providing a safe work environment, including adequate personal protective equipment (PPE) and physical distancing. Before we understood the extent of the pandemic, modes of transmission, and effective preventative measures, hospital transmission was significant. For example, a single-center case series at Zhongan Hospital of Wuhan University, China, from January 1, 2020, to January 28, 2020, found that 29% (40 of 138) of hospitalized patients with COVID-19 were health professionals who were presumed to have been infected by patients.5 There were also significant shortages of PPE, and a number of frontline HCWs reported being dismissed for calling attention to unsafe conditions. Although professionals have an obligation to expose themselves to risk, they are not obligated to expose themselves to inordinate risk. Prioritizing HCWs in ventilator triage may have been justified during the initial surge.
The use of surgical masks by all employees and patients has substantially reduced hospital transmission. A study at Duke Health, Raleigh, North Carolina, of HCWs who tested positive for SARS-CoV-2 between March 15, 2020, and June 6, 2020, found 22% of cases were healthcare acquired, 38% were community acquired, and 40% were of unknown acquisition route. Of the healthcare-acquired cases, 30% were thought to be secondary to direct patient care and 70% to exposure to another worker. The cumulative incidence rate of healthcare-acquired infections among workers decreased significantly 1 week after universal masking was implemented on March 31, 2020. The cumulative incidence rates of community-acquired cases and those with unknown acquisition routes continued to mirror incidence rates in the community.6 There is substantially less justification for prioritizing HCWs during the current phase of the pandemic; reciprocity does not justify granting HCWs infected via community spread greater priority than non-HCWs similarly infected.
There are other means of reciprocating that do not involve prioritization. COVID-19 has exacted an immense toll on the mental well-being of frontline HCWs. They should be provided robust, comprehensive, and accessible mental health services. Additionally, reciprocity can be expressed by providing alternative housing options for HCWs who are concerned about infecting their family members, especially family members at higher risk of morbidity or mortality from COVID-19. Many HCWs have also died from COVID-193; providing life insurance would recognize the sacrifice of HCWs and support their survivors. None of these interventions would require prioritizing HCWs over others.
OVER- AND UNDERINCLUSIVENESS
As Daffner4 acknowledges, the category of “healthcare provider” is both over- and underinclusive. Healthcare providers are exposed to variable risks. Some physicians, for example, are no longer involved in direct patient care. It is unclear how triage teams will identify frontline HCWs or validate claims to being a frontline HCW, especially for individuals not employed by the hospital at which they are seeking care. Hence, triage protocols prioritizing healthcare providers are likely to be substantially overinclusive, which raises significant issues of fairness.
Moreover, the category “healthcare provider” is also underinclusive. Many essential, nonclinical hospital employees expose themselves to risk, including custodial and food service staff. As Daffner4 recognizes, there are also many other occupations outside of healthcare in which individuals voluntarily expose themselves to risks for the benefit of others, including police officers, firefighters, and clerks in grocery stores. We would add that workers in the food-supply system, transportation, and education face similar risks.7 Identifying the types of jobs that should confer priority and validating an individual’s employment also makes implementation difficult and risks injustice.
EQUITY AND JUSTICE
The COVID-19 pandemic and the murder of Black people by police have brought substantial attention to racism and racial inequities in the United States. We must, however, move from merely acknowledging existing inequities to dismantling structures that perpetuate them. The prioritization of HCWs may further privilege those who already have substantial advantages. This is especially true for physicians. For example, although state and federal laws pose limitations, physicians have historically extended one another professional courtesy by providing free or discounted services. Furthermore, HCWs and their family members are more likely to receive VIP treatment. For instance, when taken to the emergency department, children of physicians are less likely to have medical students and residents involved in their care and more likely to see attending physicians and consultants.8
In contrast, other categories of essential workers do not have such advantages. These workers are more likely to be members of marginalized racial and ethnic minority groups, have substantially lower wages, have less access to PPE, and work in more crowded conditions, and are less likely to have paid sick leave compared with HCWs.7 These workers are also more likely to lack access to quality healthcare. In fact, many safety net hospitals that provide care to marginalized communities have faced significant financial hardships as a result of the pandemic, and without additional support, some may close. Prioritizing HCWs will likely widen the gaps in health, economic, and social status among these groups.
With respect to allocation criteria, Black, Latinx, and Native American communities have more severe morbidity and mortality from COVID-19 as a result of racism and its interaction with other social determinants of health. Members of marginalized communities of color have a higher likelihood of becoming infected with COVID-19, a higher prevalence of comorbidities, and less access to treatment.7 Before her untimely death, Dr Susan Moore, a Black family physician, painfully described the racism to which she was subjected while being treated for COVID-19.9 The economic devastation caused by the pandemic, including unemployment, evictions, and food insecurity, compounds the impact of social determinants of health and disproportionately affects minority communities. Purely race- and ethnicity-based approaches to allocation to redress these inequities have potential limitations and obstacles, such as omission of other social determinants of health and legal challenges.7 While currently proposed for allocation of medications or vaccines, alternatives include using the Centers for Disease Control and Prevention’s Social Vulnerability Index8 or the Area Deprivation Index10 as a priority criterion. Most importantly, healthcare systems should more broadly demonstrate themselves trustworthy and assure that marginalized communities of color have access to quality healthcare services.
CONCLUSION
The United States has failed to adequately control the COVID-19 pandemic, and increasing numbers of admissions and staffing shortages have renewed concerns that hospitals will need to implement crisis standards of care. Daffner4 argues that healthcare providers should be prioritized in the allocation of critical care based on reciprocity. In the current phase of the pandemic, HCWs are more likely to be infected by one another or in the community than by patients. There are also other ways that hospitals can discharge this duty that do not require prioritizing HCWs over patients. The category of HCW is both over- and underinclusive, and Daffner4 has not shown that prioritization can be implemented fairly. Finally, inordinate attention has been paid to this topic. Much more attention should be focused on how to redress the ways in which the pandemic has exacerbated existing racial and ethnic inequities.
1. COVID data tracker: United States COVID-19 cases and deaths by state. Centers for Disease Control and Prevention . Updated February 22, 2021. Accessed February 22, 2021. https://covid.cdc.gov/covid-data-tracker/#cases_casesper100klast7days
2. WHO coronavirus disease (COVID-19) dashboard: overview. World Health Organization. Updated February 22, 2021. Accessed February 22, 2021. https://covid19.who.int/
3. Sins of omission: how government failures to track Covid-19 data have led to more than 1,700 health care worker deaths and jeopardize public health. National Nurses United. September 2020. Accessed November 23, 2020. https://act.nationalnursesunited.org/page/-/files/graphics/0920_Covid19_SinsOfOmission_Data_Report.pdf
4. Daffner KR. Point: healthcare providers should receive treatment priority during a pandemic. J Hosp Med. Published online February 17, 2021. https://doi.org/10.12788/jhm.3596
5. Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061-1069. https://doi.org/10.1001/jama.2020.1585
6. Seidelman JL, Lewis SS, Advani SD, et al. Universal masking is an effective strategy to flatten the severe acute respiratory coronavirus virus 2 (SARS-CoV-2) healthcare worker epidemiologic curve. Infect Control Hosp Epidemiol. 2020;41(12):1466-1467. https://doi.org/10.1017/ice.2020.313
7. Gayle H, Foege W, Brown L, Kahn B, eds. Framework for Equitable Allocation of COVID-19 Vaccine. The National Academies Press; 2020. https://doi.org/10.17226/25917
8. Diekema DS, Cummings P, Quan L. Physicians’ children are treated differently in the emergency department. Am J Emerg Med. 1996;14(1):6-9. https://doi.org/10.1016/S0735-6757(96)90002-9
9. Maybank A, Jones CP, Blackstock U, Perry JC. Say her name: Dr. Susan Moore. The Washington Post. December 26, 2020. Accessed January 6, 2021. https://www.washingtonpost.com/opinions/2020/12/26/say-her-name-dr-susan-moore/
10. White DB, Schmidhofer M, McCreary E, et al. Model hospital policy for fair allocation of scarce medications to treat COVID-19. University of Pittsburgh. May 28, 2020. Accessed November 23, 2020. https://ccm.pitt.edu/sites/default/files/2020-05-28b%20Model%20hospital%20policy%20for%20allocating%20scarce%20COVID%20meds.pdf
1. COVID data tracker: United States COVID-19 cases and deaths by state. Centers for Disease Control and Prevention . Updated February 22, 2021. Accessed February 22, 2021. https://covid.cdc.gov/covid-data-tracker/#cases_casesper100klast7days
2. WHO coronavirus disease (COVID-19) dashboard: overview. World Health Organization. Updated February 22, 2021. Accessed February 22, 2021. https://covid19.who.int/
3. Sins of omission: how government failures to track Covid-19 data have led to more than 1,700 health care worker deaths and jeopardize public health. National Nurses United. September 2020. Accessed November 23, 2020. https://act.nationalnursesunited.org/page/-/files/graphics/0920_Covid19_SinsOfOmission_Data_Report.pdf
4. Daffner KR. Point: healthcare providers should receive treatment priority during a pandemic. J Hosp Med. Published online February 17, 2021. https://doi.org/10.12788/jhm.3596
5. Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061-1069. https://doi.org/10.1001/jama.2020.1585
6. Seidelman JL, Lewis SS, Advani SD, et al. Universal masking is an effective strategy to flatten the severe acute respiratory coronavirus virus 2 (SARS-CoV-2) healthcare worker epidemiologic curve. Infect Control Hosp Epidemiol. 2020;41(12):1466-1467. https://doi.org/10.1017/ice.2020.313
7. Gayle H, Foege W, Brown L, Kahn B, eds. Framework for Equitable Allocation of COVID-19 Vaccine. The National Academies Press; 2020. https://doi.org/10.17226/25917
8. Diekema DS, Cummings P, Quan L. Physicians’ children are treated differently in the emergency department. Am J Emerg Med. 1996;14(1):6-9. https://doi.org/10.1016/S0735-6757(96)90002-9
9. Maybank A, Jones CP, Blackstock U, Perry JC. Say her name: Dr. Susan Moore. The Washington Post. December 26, 2020. Accessed January 6, 2021. https://www.washingtonpost.com/opinions/2020/12/26/say-her-name-dr-susan-moore/
10. White DB, Schmidhofer M, McCreary E, et al. Model hospital policy for fair allocation of scarce medications to treat COVID-19. University of Pittsburgh. May 28, 2020. Accessed November 23, 2020. https://ccm.pitt.edu/sites/default/files/2020-05-28b%20Model%20hospital%20policy%20for%20allocating%20scarce%20COVID%20meds.pdf
© 2021 Society of Hospital Medicine
Rebuttal: Accounting for the Community’s Reciprocal Obligations to Healthcare Workers During a Pandemic
In their thoughtful response to the thesis that healthcare workers (HCWs) should be prioritized for scarce resources during a pandemic,1 Antommaria and Unaka offer compelling reasons for opposing this position.2 Common ground can be found in our shared recognition that the community has a reciprocal obligation to HCWs because of their willingness to accept the increased risk of being exposed to serious illness in caring for patients. We disagree on the most appropriate way to honor this obligation and whether HCWs currently have a greater risk of infection than others.
Antommaria and Unaka2 indicate that “prioritizing HCWs …may have been justified during the initial surge” of coronavirus disease 2019 (COVID-19), when risk was excessive. They suggest that, with universal masking and other measures, infection rates among HCWs now mirror those in the community. However, this assessment is questionable. Personal protective equipment is still inadequate in numerous healthcare settings,3,4 and many reports, including one by the National Academies, indicate that the threat to HCWs remains higher.5 In the absence of certainty, I favor erring on the side of continuing to recognize the special obligation to HCWs. Fortunately, COVID-19 vaccines should further reduce the danger of infection, and my article provides justification for prioritizing HCWs to receive them.
Antommaria and Unaka2 seem to support special obligations to HCWs based on reciprocity, but suggest alternatives to critical care prioritization, such as mental health services and life insurance. In my view, mental health care should be universal and not a means of recognizing the sacrifice of HCWs. Providing life insurance for HCWs reflects a tacit acknowledgment of the increased threat they face. However, given governmental delays approving basic COVID-19 relief, it is unlikely that resources will be appropriated for life insurance, which has not occurred since Antommaria et al made this suggestion in 2011.6
Although there may be challenges to identifying and verifying frontline HCWs at risk for exposure to COVID-19, there are always gaps between the principles underlying policies and the way they are implemented. For example, according to guidelines from the Centers for Disease Control and Prevention,7 the first wave of individuals to receive COVID-19 vaccinations should include “frontline essential workers.” Defining and identifying this group of individuals provoke similar concerns to those raised by Antommaria and Unaka2 about my proposal.
I concur that the narrow category of HCWs fails to include nonclinical and other frontline workers who are at a higher risk of being exposed to COVID-19. My article addresses this issue by suggesting the community has a similar set of obligations to these workers.1 Nonclinical hospital workers are disproportionately non-White and have substantially lower median incomes than the average US wage earner.4 Moreover, among HCWs, people of color account for a disproportionate number of COVID-19 cases and deaths.4 Inclusion of at-risk nonclinical and other frontline workers in treatment prioritization is consistent with concerns about fairness that animate Antommaria and Unaka’s article.2
The importance of directing attention to the pandemic’s exacerbation of racial and ethnic inequalities, as highlighted by Antommaria and Unaka,2 does not preclude also carefully examining whether special obligations are owed to HCWs and frontline workers. Thoughtful discussions about weighty ethical questions do not represent a zero-sum game, and, as in the current case, the issues raised during such deliberations often have much broader implications. Of note, social justice can be framed in terms of reciprocity, and efforts to confront societal inequities can reflect the special obligations owed Black Americans to address our long history of systemic racism.
In summary, fairness includes accounting for reciprocity and the duties resulting from it. Special obligations are owed HCWs and frontline workers until they are no longer at higher risk for infection. Hypothetical offers of life insurance or mental health benefits are inadequate ways to demonstrate reciprocity. The challenge of identifying HCWs and other frontline workers ought not preclude efforts to do so. HCWs and frontline workers should not automatically move to the head of the line to receive limited critical care resources. However, recognition of their willingness to risk serious infection should be included in the multidimensional calculus for triaging critical care.
1. Daffner KR. Point: healthcare providers should receive treatment priority during a pandemic. J Hosp Med. Published online February 17, 2021. https://doi.org/10.12788/jhm.3596
2. Antommaria AHM, Unaka NI. Counterpoint: prioritizing healthcare workers for scarce critical care resources is impractical and unjust. J Hosp Med. Published online February 17, 2021. https://doi.org/10.12788/jhm.3597
3. Erdman SL. As Covid-19 cases surge, health care workers say PPE is still a struggle. CNN. Updated November 24, 2020. Accessed January 6, 2021. https://www.cnn.com/2020/11/24/health/covid-surge-ppe-availability/index.html
4. Artiga S, Rae M, Pham O, Hamel L, Muñana C. COVID-19 risks and impacts among health care workers by race/ethnicity. November 11, 2020. Accessed January 6, 2021. https://www.kff.org/racial-equity-and-health-policy/issue-brief/covid-19-risks-impacts-health-care-workers-race-ethnicity/
5. Gayle H, Foege W, Brown L, Kahn B, eds. Framework for Equitable Allocation of COVID-19 Vaccine . The National Academies Press; 2020. https://doi.org/10.17226/25917
6. Antommaria AHM, Powell T, Miller JE, Christian MD, for the Task Force for Pediatric Emergency Mass Critical Care. Ethical issues in pediatric emergency mass critical care. Pediatr Crit Care Med. 2011;12(6 Suppl):S163-168. https://doi.org/10.1097/PCC.0b013e318234a88b
7. Dooling K. Phased allocation of COVID-19 vaccines. Presented at the Advisory Committee on Immunization Practices meeting. December 19-20, 2020. Atlanta, GA. Accessed February 2, 2021. https://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2020-12/slides-12-20/02-COVID-Dooling.pdf
In their thoughtful response to the thesis that healthcare workers (HCWs) should be prioritized for scarce resources during a pandemic,1 Antommaria and Unaka offer compelling reasons for opposing this position.2 Common ground can be found in our shared recognition that the community has a reciprocal obligation to HCWs because of their willingness to accept the increased risk of being exposed to serious illness in caring for patients. We disagree on the most appropriate way to honor this obligation and whether HCWs currently have a greater risk of infection than others.
Antommaria and Unaka2 indicate that “prioritizing HCWs …may have been justified during the initial surge” of coronavirus disease 2019 (COVID-19), when risk was excessive. They suggest that, with universal masking and other measures, infection rates among HCWs now mirror those in the community. However, this assessment is questionable. Personal protective equipment is still inadequate in numerous healthcare settings,3,4 and many reports, including one by the National Academies, indicate that the threat to HCWs remains higher.5 In the absence of certainty, I favor erring on the side of continuing to recognize the special obligation to HCWs. Fortunately, COVID-19 vaccines should further reduce the danger of infection, and my article provides justification for prioritizing HCWs to receive them.
Antommaria and Unaka2 seem to support special obligations to HCWs based on reciprocity, but suggest alternatives to critical care prioritization, such as mental health services and life insurance. In my view, mental health care should be universal and not a means of recognizing the sacrifice of HCWs. Providing life insurance for HCWs reflects a tacit acknowledgment of the increased threat they face. However, given governmental delays approving basic COVID-19 relief, it is unlikely that resources will be appropriated for life insurance, which has not occurred since Antommaria et al made this suggestion in 2011.6
Although there may be challenges to identifying and verifying frontline HCWs at risk for exposure to COVID-19, there are always gaps between the principles underlying policies and the way they are implemented. For example, according to guidelines from the Centers for Disease Control and Prevention,7 the first wave of individuals to receive COVID-19 vaccinations should include “frontline essential workers.” Defining and identifying this group of individuals provoke similar concerns to those raised by Antommaria and Unaka2 about my proposal.
I concur that the narrow category of HCWs fails to include nonclinical and other frontline workers who are at a higher risk of being exposed to COVID-19. My article addresses this issue by suggesting the community has a similar set of obligations to these workers.1 Nonclinical hospital workers are disproportionately non-White and have substantially lower median incomes than the average US wage earner.4 Moreover, among HCWs, people of color account for a disproportionate number of COVID-19 cases and deaths.4 Inclusion of at-risk nonclinical and other frontline workers in treatment prioritization is consistent with concerns about fairness that animate Antommaria and Unaka’s article.2
The importance of directing attention to the pandemic’s exacerbation of racial and ethnic inequalities, as highlighted by Antommaria and Unaka,2 does not preclude also carefully examining whether special obligations are owed to HCWs and frontline workers. Thoughtful discussions about weighty ethical questions do not represent a zero-sum game, and, as in the current case, the issues raised during such deliberations often have much broader implications. Of note, social justice can be framed in terms of reciprocity, and efforts to confront societal inequities can reflect the special obligations owed Black Americans to address our long history of systemic racism.
In summary, fairness includes accounting for reciprocity and the duties resulting from it. Special obligations are owed HCWs and frontline workers until they are no longer at higher risk for infection. Hypothetical offers of life insurance or mental health benefits are inadequate ways to demonstrate reciprocity. The challenge of identifying HCWs and other frontline workers ought not preclude efforts to do so. HCWs and frontline workers should not automatically move to the head of the line to receive limited critical care resources. However, recognition of their willingness to risk serious infection should be included in the multidimensional calculus for triaging critical care.
In their thoughtful response to the thesis that healthcare workers (HCWs) should be prioritized for scarce resources during a pandemic,1 Antommaria and Unaka offer compelling reasons for opposing this position.2 Common ground can be found in our shared recognition that the community has a reciprocal obligation to HCWs because of their willingness to accept the increased risk of being exposed to serious illness in caring for patients. We disagree on the most appropriate way to honor this obligation and whether HCWs currently have a greater risk of infection than others.
Antommaria and Unaka2 indicate that “prioritizing HCWs …may have been justified during the initial surge” of coronavirus disease 2019 (COVID-19), when risk was excessive. They suggest that, with universal masking and other measures, infection rates among HCWs now mirror those in the community. However, this assessment is questionable. Personal protective equipment is still inadequate in numerous healthcare settings,3,4 and many reports, including one by the National Academies, indicate that the threat to HCWs remains higher.5 In the absence of certainty, I favor erring on the side of continuing to recognize the special obligation to HCWs. Fortunately, COVID-19 vaccines should further reduce the danger of infection, and my article provides justification for prioritizing HCWs to receive them.
Antommaria and Unaka2 seem to support special obligations to HCWs based on reciprocity, but suggest alternatives to critical care prioritization, such as mental health services and life insurance. In my view, mental health care should be universal and not a means of recognizing the sacrifice of HCWs. Providing life insurance for HCWs reflects a tacit acknowledgment of the increased threat they face. However, given governmental delays approving basic COVID-19 relief, it is unlikely that resources will be appropriated for life insurance, which has not occurred since Antommaria et al made this suggestion in 2011.6
Although there may be challenges to identifying and verifying frontline HCWs at risk for exposure to COVID-19, there are always gaps between the principles underlying policies and the way they are implemented. For example, according to guidelines from the Centers for Disease Control and Prevention,7 the first wave of individuals to receive COVID-19 vaccinations should include “frontline essential workers.” Defining and identifying this group of individuals provoke similar concerns to those raised by Antommaria and Unaka2 about my proposal.
I concur that the narrow category of HCWs fails to include nonclinical and other frontline workers who are at a higher risk of being exposed to COVID-19. My article addresses this issue by suggesting the community has a similar set of obligations to these workers.1 Nonclinical hospital workers are disproportionately non-White and have substantially lower median incomes than the average US wage earner.4 Moreover, among HCWs, people of color account for a disproportionate number of COVID-19 cases and deaths.4 Inclusion of at-risk nonclinical and other frontline workers in treatment prioritization is consistent with concerns about fairness that animate Antommaria and Unaka’s article.2
The importance of directing attention to the pandemic’s exacerbation of racial and ethnic inequalities, as highlighted by Antommaria and Unaka,2 does not preclude also carefully examining whether special obligations are owed to HCWs and frontline workers. Thoughtful discussions about weighty ethical questions do not represent a zero-sum game, and, as in the current case, the issues raised during such deliberations often have much broader implications. Of note, social justice can be framed in terms of reciprocity, and efforts to confront societal inequities can reflect the special obligations owed Black Americans to address our long history of systemic racism.
In summary, fairness includes accounting for reciprocity and the duties resulting from it. Special obligations are owed HCWs and frontline workers until they are no longer at higher risk for infection. Hypothetical offers of life insurance or mental health benefits are inadequate ways to demonstrate reciprocity. The challenge of identifying HCWs and other frontline workers ought not preclude efforts to do so. HCWs and frontline workers should not automatically move to the head of the line to receive limited critical care resources. However, recognition of their willingness to risk serious infection should be included in the multidimensional calculus for triaging critical care.
1. Daffner KR. Point: healthcare providers should receive treatment priority during a pandemic. J Hosp Med. Published online February 17, 2021. https://doi.org/10.12788/jhm.3596
2. Antommaria AHM, Unaka NI. Counterpoint: prioritizing healthcare workers for scarce critical care resources is impractical and unjust. J Hosp Med. Published online February 17, 2021. https://doi.org/10.12788/jhm.3597
3. Erdman SL. As Covid-19 cases surge, health care workers say PPE is still a struggle. CNN. Updated November 24, 2020. Accessed January 6, 2021. https://www.cnn.com/2020/11/24/health/covid-surge-ppe-availability/index.html
4. Artiga S, Rae M, Pham O, Hamel L, Muñana C. COVID-19 risks and impacts among health care workers by race/ethnicity. November 11, 2020. Accessed January 6, 2021. https://www.kff.org/racial-equity-and-health-policy/issue-brief/covid-19-risks-impacts-health-care-workers-race-ethnicity/
5. Gayle H, Foege W, Brown L, Kahn B, eds. Framework for Equitable Allocation of COVID-19 Vaccine . The National Academies Press; 2020. https://doi.org/10.17226/25917
6. Antommaria AHM, Powell T, Miller JE, Christian MD, for the Task Force for Pediatric Emergency Mass Critical Care. Ethical issues in pediatric emergency mass critical care. Pediatr Crit Care Med. 2011;12(6 Suppl):S163-168. https://doi.org/10.1097/PCC.0b013e318234a88b
7. Dooling K. Phased allocation of COVID-19 vaccines. Presented at the Advisory Committee on Immunization Practices meeting. December 19-20, 2020. Atlanta, GA. Accessed February 2, 2021. https://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2020-12/slides-12-20/02-COVID-Dooling.pdf
1. Daffner KR. Point: healthcare providers should receive treatment priority during a pandemic. J Hosp Med. Published online February 17, 2021. https://doi.org/10.12788/jhm.3596
2. Antommaria AHM, Unaka NI. Counterpoint: prioritizing healthcare workers for scarce critical care resources is impractical and unjust. J Hosp Med. Published online February 17, 2021. https://doi.org/10.12788/jhm.3597
3. Erdman SL. As Covid-19 cases surge, health care workers say PPE is still a struggle. CNN. Updated November 24, 2020. Accessed January 6, 2021. https://www.cnn.com/2020/11/24/health/covid-surge-ppe-availability/index.html
4. Artiga S, Rae M, Pham O, Hamel L, Muñana C. COVID-19 risks and impacts among health care workers by race/ethnicity. November 11, 2020. Accessed January 6, 2021. https://www.kff.org/racial-equity-and-health-policy/issue-brief/covid-19-risks-impacts-health-care-workers-race-ethnicity/
5. Gayle H, Foege W, Brown L, Kahn B, eds. Framework for Equitable Allocation of COVID-19 Vaccine . The National Academies Press; 2020. https://doi.org/10.17226/25917
6. Antommaria AHM, Powell T, Miller JE, Christian MD, for the Task Force for Pediatric Emergency Mass Critical Care. Ethical issues in pediatric emergency mass critical care. Pediatr Crit Care Med. 2011;12(6 Suppl):S163-168. https://doi.org/10.1097/PCC.0b013e318234a88b
7. Dooling K. Phased allocation of COVID-19 vaccines. Presented at the Advisory Committee on Immunization Practices meeting. December 19-20, 2020. Atlanta, GA. Accessed February 2, 2021. https://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2020-12/slides-12-20/02-COVID-Dooling.pdf
© 2021 Society of Hospital Medicine
Dearth of Hospitalist Investigators in Academic Medicine: A Call to Action
In their report celebrating the increase in the number of hospitalists from a few hundred in the 1990s to more than 50,000 in 2016, Drs Robert Wachter and Lee Goldman also noted the stunted growth of productive hospital medicine research programs, which presents a challenge to academic credibility in hospital medicine.1 Given the substantial increase in the number of hospitalists over the past two decades, we surveyed adult academic hospital medicine groups to quantify the number of hospitalist clinician investigators and identify gaps in resources for researchers. The number of clinician investigators supported at academic medical centers (AMCs) remains disturbingly low despite the rapid growth of our specialty. Some programs also reported a lack of access to fundamental research services. We report selected results from our survey and provide recommendations to support and facilitate the development of clinician investigators in hospital medicine.
DEARTH OF CLINICIAN INVESTIGATORS IN HOSPITAL MEDICINE
We performed a survey of hospital medicine programs at AMCs in the United States through the Hospital Medicine Reengineering Network (HOMERuN), a hospital medicine research collaborative that facilitates and conducts multisite research studies.2 The purpose of this survey was to obtain a profile of adult academic hospital medicine groups. Surveys were distributed via email to directors and/or senior leaders of each hospital medicine group between January and August 2019. In the survey, a clinician investigator was defined as “faculty whose primary nonclinical focus is scientific papers and grant writing.”
We received responses from 43 of the 86 invitees (50%), each of whom represented a unique hospital medicine group; 41 of the representatives responded to the questions concerning available research services. Collectively, these 43 programs represented 2,503 hospitalists. There were 79 clinician investigators reported among all surveyed hospital medicine groups (3.1% of all hospitalists). The median number of clinician investigators per hospital medicine group was 0 (range 0-12) (Appendix Figure 1), and 22 of 43 (51.2%) hospital medicine groups reported having no clinician investigators. Two of the hospital medicine groups, however, reported having 12 clinician investigators at their respective institutions, comprising nearly one third of the total number of clinician investigators reported in the survey.
Many of the programs reported lack of access to resources such as research assistants (56.1%) and dedicated research fellowships (53.7%) (Appendix Figure 2). A number of groups reported a need for more support for various junior faculty development activities, including research mentoring (53.5%), networking with other researchers (60.5%), and access to clinical data from multiple sites (62.8%).
One of the limitations of this survey was the manner in which the participating hospital medicine groups were chosen. Selection was based on groups affiliated with HOMERuN; among those chosen were highly visible US AMCs, including 70% of the top 20 AMCs based on National Institutes of Health (NIH) funding.3 Therefore, our results likely overestimate the research presence of hospital medicine across all AMCs in the United States.
LACK OF GROWTH OVER TIME: CONTEXTUALIZATION AND IMPLICATIONS
Despite the substantial growth of hospital medicine over the past 2 decades, there has been no proportional increase in the number of hospitalist clinician investigators, with earlier surveys also demonstrating low numbers.4,5 Along with the survey by Chopra and colleagues published in 2019,6 our survey provides an additional contemporary appraisal of research activities for adult academic hospital medicine groups. In the survey by Chopra et al, only 54% (15 of 28) of responding programs reported having any faculty with research as their major activity (ie, >50% effort), and 3% of total faculty reported having funding for >50% effort toward research.6 Our study expands upon these findings by providing more detailed data on the number of clinician investigators per hospital medicine group. Results of our survey showed a concentration of hospitalists within a small number of programs, which may have contributed to the observed lack of growth. We also expand on prior work by identifying a lack of resources and services to support hospitalist researchers.
The findings of our survey have important implications for the field of hospital medicine. Without a critical mass of hospitalist clinician investigators, the quality of research that addresses important questions in our field will suffer. It will also limit academic credibility of the field, as well as individual academic achievement; previous studies have consistently demonstrated that few hospitalists at AMCs achieve the rank of associate or full professor.5-9
POTENTIAL EXPLANATIONS FOR LACK OF RESEARCH GROWTH
The results of our study additionally offer possible explanations for the dearth of clinician investigators in hospital medicine. The limited access to research resources and fellowship training identified in our survey are critical domains that must be addressed in order to develop successful academic hospital medicine programs.4,6,8,10
Regarding dedicated hospital medicine research fellowships, there are only a handful across the country. The small number of existing research fellowships only have one or two fellows per year, and these positions often go unfilled because of a lack of applicants and lower salaries compared to full-time clinical positions.11 The lack of applicants for adult hospital medicine fellowship positions is also integrally linked to board certification requirements. Unlike pediatric hospital medicine where additional fellowship training is required to become board-certified, no such fellowship is required in adult hospital medicine. In pediatrics, this requirement has led to a rapid increase in the number of fellowships with scholarly work requirements (more than 60 fellowships, plus additional programs in development) and greater standardization among training experiences.12,13
The lack of fellowship applicants may also stem from the fact that many trainees are not aware of a potential career as a hospitalist clinician investigator due to limited exposure to this career at most AMCs. Our results revealed that nearly half of sites in our survey had zero clinician investigators, depriving trainees at these programs of role models and thus perpetuating a negative feedback loop. Lastly, although unfilled fellowship positions may indicate that demand is a larger problem than supply, it is also true that fellowship programs generate their own demand through recruitment efforts and the gradual establishment of a positive reputation.
Another potential explanation could relate to the development of hospital medicine in response to rising clinical demands at hospitals: compared with other medical specialties, AMCs may regard hospitalists as being clinicians first and academicians second.1,7,10 Also, hospitalists may be perceived as being beholden to hospitals and less engaged with their surrounding communities than other general medicine fields. With a small footprint in health equity research, academic hospital medicine may be less of a draw to generalists interested in pursuing this area of research. Further, there are very few underrepresented in medicine (URiM) hospital medicine research faculty.5
Another challenge to the career development of hospitalist researchers is the lack of available funding for the type of research typically conducted by hospitalists (eg, rigorous quality improvement implementation and evaluation, optimizing best evidence-based care delivery models, evaluation of patient safety in the hospital setting). As hospitalists tend to be system-level thinkers, this lack of funding may steer potential researchers away from externally funded research careers and into hospital operations and quality improvement positions. Also, unlike other medical specialties, there is no dedicated NIH funding source for hospital medicine research (eg, cardiology and the National Heart, Lung, and Blood Institute), placing hospitalists at a disadvantage in seeking funding compared to subspecialists.
STRATEGIES TO ENHANCE RESEARCH PRESENCE
We recommend several approaches—ones that should be pursued simultaneously—to increase the number of clinician investigators in hospital medicine. First, hospital medicine groups and their respective divisions, departments, and hospitals should allocate funding to support research resources; this includes investing in research assistants, data analysts, statisticians, and administrative support. Through the funding of such research infrastructure programs, AMCs could incentivize hospitalists to research best approaches to improve the value of healthcare delivery, ultimately leading to cost savings.
With 60% of respondents identifying the need for improved access to data across multiple sites, our survey also emphasizes the requirement for further collaboration among hospital medicine groups. Such collaboration could lead to high-powered observational studies and the evaluation of interventions across multiple sites, thus improving the generalizability of study findings.
The Society of Hospital Medicine (SHM) and its research committee can continue to expand the research footprint of hospital medicine. To date, the committee has achieved this by highlighting hospitalist research activity at the SHM Annual Conference Scientific Abstract and Poster Competition and developing a visiting professorship exchange program. In addition to these efforts, SHM could foster collaboration and networking between institutions, as well as take advantage of the current political push for expanded Medicare access by lobbying for robust funding for the Agency for Healthcare Research and Quality, which could provide more opportunities for hospitalists to study the effects of healthcare policy reform on the delivery of inpatient care.
Another strategy to increase the number of hospitalist clinician investigators is to expand hospital medicine research fellowships and recruit trainees for these programs. Fellowships could be internally funded wherein a fellow’s clinical productivity is used to offset the costs associated with obtaining advanced degrees. As an incentive to encourage applicants to temporarily forego a full-time clinical salary during fellowship, hospital medicine groups could offer expanded moonlighting opportunities and contribute to repayment of medical school loans. Hospital medicine groups should also advocate for NIH-funded T32 or K12 training grants for hospital medicine. (There are, however, challenges with this approach because the number of T32 spots per NIH institute is usually fixed). The success of academic emergency medicine offers a precedent for such efforts: After the development of a K12 research training program in emergency medicine, the number of NIH-sponsored principal investigators in this specialty increased by 40% in 6 years.14 Additionally, now that fellowships are required for the pediatric hospital medicine clinician investigators, it would be revealing to track the growth of this workforce.12,13
Structured and formalized mentorship is an essential part of the development of clinician investigators in hospital medicine.4,7,8,10 One successful strategy for mentorship has been the partnering of hospital medicine groups with faculty of general internal medicine and other subspecialty divisions with robust research programs.7,8,15 In addition to developing sustainable mentorship programs, hospital medicine researchers must increase their visibility to trainees. Therefore, it is essential that the majority of academic hospital medicine groups not only hire clinician investigators but also invest in their development, rather than rely on the few programs that have several such faculty members. With this strategy, we could dramatically increase the number of hospitalist clinician investigators from a diverse background of training institutions.
SHM could also play a greater role in organizing events for networking and mentoring for trainees and medical students interested in pursuing a career in hospital medicine research. It is also critically important that hospital medicine groups actively recruit, retain, and develop URiM hospital medicine research faculty in order to attract talented researchers and actively participate in the necessary effort to mitigate the inequities prevalent throughout our healthcare system.
CONCLUSION
Despite the growth of hospital medicine over the past decade, there remains a dearth of hospitalist clinician investigators at major AMCs in the United States. This may be due in part to lack of research resources and mentorship within hospital medicine groups. We believe that investment in these resources, expanded funding opportunities, mentorship development, research fellowship programs, and greater exposure of trainees to hospitalist researchers are solutions that should be strongly considered to develop hospitalist clinician investigators.
Acknowledgments
The authors thank HOMERuN executive committee members, including Grant Fletcher, MD, James Harrison, PhD, BSC, MPH, Peter K. Lindenauer, MD, Melissa Mattison, MD, David Meltzer, MD, PhD, Joshua Metlay, MD, PhD, Jennifer Myers, MD, Sumant Ranji, MD, Gregory Ruhnke, MD, MPH, Edmondo Robinson, MD, MBA, and Neil Sehgal, MPH PhD, for their assistance in developing the survey. They also thank Tiffany Lee, MA, for her project management assistance for HOMERuN.
1. Wachter RM, Goldman L. Zero to 50,000 – The 20th anniversary of the hospitalist. N Engl J Med. 2016;375(11):1009-1011. https://doi.org/10.1056/NEJMp1607958
2. Auerbach AD, Patel MS, Metlay JP, et al. The Hospital Medicine Reengineering Network (HOMERuN): a learning organization focused on improving hospital care. Acad Med. 2014;89(3):415-420. https://doi.org/10.1097/acm.0000000000000139
3. Roskoski R Jr, Parslow TG. Ranking Tables of NIH funding to US medical schools in 2019. Blue Ridge Institute for Medical Research. Published 2020. Updated July 14, 2020. Accessed July 30, 2020. http://www.brimr.org/NIH_Awards/2019/NIH_Awards_2019.htm
4. Reid MB, Misky GJ, Harrison RA, Sharpe B, Auerbach A, Glasheen JJ. Mentorship, productivity, and promotion among academic hospitalists. J Gen Intern Med. 2012;27(1):23-27. https://doi.org/10.1007/s11606-011-1892-5
5. Miller CS, Fogerty RL, Gann J, Bruti CP, Klein R; The Society of General Internal Medicine Membership Committee. The growth of hospitalists and the future of the society of general internal medicine: results from the 2014 membership survey. J Gen Intern Med. 2017;32(11):1179-1185. https://doi.org/10.1007/s11606-017-4126-7
6. Chopra V, Burden M, Jones CD, et al; Society of Hospital Medicine Research Committee. State of research in adult hospital medicine: results of a national survey. J Hosp Med. 2019;14(4):207-211. https://doi.org/10.12788/jhm.3136
7. Seymann GB, Southern W, Burger A, et al. Features of successful academic hospitalist programs: insights from the SCHOLAR (SuCcessful HOspitaLists in academics and research) project. J Hosp Med. 2016;11(10):708-713. https://doi.org/10.1002/jhm.2603
8. Harrison R, Hunter AJ, Sharpe B, Auerbach AD. Survey of US academic hospitalist leaders about mentorship and academic activities in hospitalist groups. J Hosp Med. 2011;6(1):5-9. https://doi.org/10.1002/jhm.836
9. Dang Do AN, Munchhof AM, Terry C, Emmett T, Kara A. Research and publication trends in hospital medicine. J Hosp Med. 2014;9(3):148-154. https://doi.org/10.1002/jhm.2148
10. Sehgal NL, Sharpe BA, Auerbach AA, Wachter RM. Investing in the future: building an academic hospitalist faculty development program. J Hosp Med. 2011;6(3):161-166. https://doi.org/10.1002/jhm.845
11. Ranji SR, Rosenman DJ, Amin AN, Kripalani S. Hospital medicine fellowships: works in progress. Am J Med. 2006;119(1):72.e1-72.e7. https://doi.org/10.1016/j.amjmed.2005.07.061
12. Shah NH, Rhim HJ, Maniscalco J, Wilson K, Rassbach C. The current state of pediatric hospital medicine fellowships: a survey of program directors. J Hosp Med. 2016;11(5):324-328. https://doi.org/10.1002/jhm.2571
13. Jerardi KE, Fisher E, Rassbach C, et al; Council of Pediatric Hospital Medicine Fellowship Directors. Development of a curricular framework for pediatric hospital medicine fellowships. Pediatrics. 2017;140(1):e20170698. https://doi.org/10.1542/peds.2017-0698
14. Lewis RJ, Neumar RW. Research in emergency medicine: building the investigator pipeline. Ann Emerg Med. 2018;72(6):691-695. https://doi.org/10.1016/j.annemergmed.2018.10.019
15. Flanders SA, Kaufman SR, Nallamothu BK, Saint S. The University of Michigan Specialist-Hospitalist Allied Research Program: jumpstarting hospital medicine research. J Hosp Med. 2008;3(4):308-313. https://doi.org/10.1002/jhm.342
In their report celebrating the increase in the number of hospitalists from a few hundred in the 1990s to more than 50,000 in 2016, Drs Robert Wachter and Lee Goldman also noted the stunted growth of productive hospital medicine research programs, which presents a challenge to academic credibility in hospital medicine.1 Given the substantial increase in the number of hospitalists over the past two decades, we surveyed adult academic hospital medicine groups to quantify the number of hospitalist clinician investigators and identify gaps in resources for researchers. The number of clinician investigators supported at academic medical centers (AMCs) remains disturbingly low despite the rapid growth of our specialty. Some programs also reported a lack of access to fundamental research services. We report selected results from our survey and provide recommendations to support and facilitate the development of clinician investigators in hospital medicine.
DEARTH OF CLINICIAN INVESTIGATORS IN HOSPITAL MEDICINE
We performed a survey of hospital medicine programs at AMCs in the United States through the Hospital Medicine Reengineering Network (HOMERuN), a hospital medicine research collaborative that facilitates and conducts multisite research studies.2 The purpose of this survey was to obtain a profile of adult academic hospital medicine groups. Surveys were distributed via email to directors and/or senior leaders of each hospital medicine group between January and August 2019. In the survey, a clinician investigator was defined as “faculty whose primary nonclinical focus is scientific papers and grant writing.”
We received responses from 43 of the 86 invitees (50%), each of whom represented a unique hospital medicine group; 41 of the representatives responded to the questions concerning available research services. Collectively, these 43 programs represented 2,503 hospitalists. There were 79 clinician investigators reported among all surveyed hospital medicine groups (3.1% of all hospitalists). The median number of clinician investigators per hospital medicine group was 0 (range 0-12) (Appendix Figure 1), and 22 of 43 (51.2%) hospital medicine groups reported having no clinician investigators. Two of the hospital medicine groups, however, reported having 12 clinician investigators at their respective institutions, comprising nearly one third of the total number of clinician investigators reported in the survey.
Many of the programs reported lack of access to resources such as research assistants (56.1%) and dedicated research fellowships (53.7%) (Appendix Figure 2). A number of groups reported a need for more support for various junior faculty development activities, including research mentoring (53.5%), networking with other researchers (60.5%), and access to clinical data from multiple sites (62.8%).
One of the limitations of this survey was the manner in which the participating hospital medicine groups were chosen. Selection was based on groups affiliated with HOMERuN; among those chosen were highly visible US AMCs, including 70% of the top 20 AMCs based on National Institutes of Health (NIH) funding.3 Therefore, our results likely overestimate the research presence of hospital medicine across all AMCs in the United States.
LACK OF GROWTH OVER TIME: CONTEXTUALIZATION AND IMPLICATIONS
Despite the substantial growth of hospital medicine over the past 2 decades, there has been no proportional increase in the number of hospitalist clinician investigators, with earlier surveys also demonstrating low numbers.4,5 Along with the survey by Chopra and colleagues published in 2019,6 our survey provides an additional contemporary appraisal of research activities for adult academic hospital medicine groups. In the survey by Chopra et al, only 54% (15 of 28) of responding programs reported having any faculty with research as their major activity (ie, >50% effort), and 3% of total faculty reported having funding for >50% effort toward research.6 Our study expands upon these findings by providing more detailed data on the number of clinician investigators per hospital medicine group. Results of our survey showed a concentration of hospitalists within a small number of programs, which may have contributed to the observed lack of growth. We also expand on prior work by identifying a lack of resources and services to support hospitalist researchers.
The findings of our survey have important implications for the field of hospital medicine. Without a critical mass of hospitalist clinician investigators, the quality of research that addresses important questions in our field will suffer. It will also limit academic credibility of the field, as well as individual academic achievement; previous studies have consistently demonstrated that few hospitalists at AMCs achieve the rank of associate or full professor.5-9
POTENTIAL EXPLANATIONS FOR LACK OF RESEARCH GROWTH
The results of our study additionally offer possible explanations for the dearth of clinician investigators in hospital medicine. The limited access to research resources and fellowship training identified in our survey are critical domains that must be addressed in order to develop successful academic hospital medicine programs.4,6,8,10
Regarding dedicated hospital medicine research fellowships, there are only a handful across the country. The small number of existing research fellowships only have one or two fellows per year, and these positions often go unfilled because of a lack of applicants and lower salaries compared to full-time clinical positions.11 The lack of applicants for adult hospital medicine fellowship positions is also integrally linked to board certification requirements. Unlike pediatric hospital medicine where additional fellowship training is required to become board-certified, no such fellowship is required in adult hospital medicine. In pediatrics, this requirement has led to a rapid increase in the number of fellowships with scholarly work requirements (more than 60 fellowships, plus additional programs in development) and greater standardization among training experiences.12,13
The lack of fellowship applicants may also stem from the fact that many trainees are not aware of a potential career as a hospitalist clinician investigator due to limited exposure to this career at most AMCs. Our results revealed that nearly half of sites in our survey had zero clinician investigators, depriving trainees at these programs of role models and thus perpetuating a negative feedback loop. Lastly, although unfilled fellowship positions may indicate that demand is a larger problem than supply, it is also true that fellowship programs generate their own demand through recruitment efforts and the gradual establishment of a positive reputation.
Another potential explanation could relate to the development of hospital medicine in response to rising clinical demands at hospitals: compared with other medical specialties, AMCs may regard hospitalists as being clinicians first and academicians second.1,7,10 Also, hospitalists may be perceived as being beholden to hospitals and less engaged with their surrounding communities than other general medicine fields. With a small footprint in health equity research, academic hospital medicine may be less of a draw to generalists interested in pursuing this area of research. Further, there are very few underrepresented in medicine (URiM) hospital medicine research faculty.5
Another challenge to the career development of hospitalist researchers is the lack of available funding for the type of research typically conducted by hospitalists (eg, rigorous quality improvement implementation and evaluation, optimizing best evidence-based care delivery models, evaluation of patient safety in the hospital setting). As hospitalists tend to be system-level thinkers, this lack of funding may steer potential researchers away from externally funded research careers and into hospital operations and quality improvement positions. Also, unlike other medical specialties, there is no dedicated NIH funding source for hospital medicine research (eg, cardiology and the National Heart, Lung, and Blood Institute), placing hospitalists at a disadvantage in seeking funding compared to subspecialists.
STRATEGIES TO ENHANCE RESEARCH PRESENCE
We recommend several approaches—ones that should be pursued simultaneously—to increase the number of clinician investigators in hospital medicine. First, hospital medicine groups and their respective divisions, departments, and hospitals should allocate funding to support research resources; this includes investing in research assistants, data analysts, statisticians, and administrative support. Through the funding of such research infrastructure programs, AMCs could incentivize hospitalists to research best approaches to improve the value of healthcare delivery, ultimately leading to cost savings.
With 60% of respondents identifying the need for improved access to data across multiple sites, our survey also emphasizes the requirement for further collaboration among hospital medicine groups. Such collaboration could lead to high-powered observational studies and the evaluation of interventions across multiple sites, thus improving the generalizability of study findings.
The Society of Hospital Medicine (SHM) and its research committee can continue to expand the research footprint of hospital medicine. To date, the committee has achieved this by highlighting hospitalist research activity at the SHM Annual Conference Scientific Abstract and Poster Competition and developing a visiting professorship exchange program. In addition to these efforts, SHM could foster collaboration and networking between institutions, as well as take advantage of the current political push for expanded Medicare access by lobbying for robust funding for the Agency for Healthcare Research and Quality, which could provide more opportunities for hospitalists to study the effects of healthcare policy reform on the delivery of inpatient care.
Another strategy to increase the number of hospitalist clinician investigators is to expand hospital medicine research fellowships and recruit trainees for these programs. Fellowships could be internally funded wherein a fellow’s clinical productivity is used to offset the costs associated with obtaining advanced degrees. As an incentive to encourage applicants to temporarily forego a full-time clinical salary during fellowship, hospital medicine groups could offer expanded moonlighting opportunities and contribute to repayment of medical school loans. Hospital medicine groups should also advocate for NIH-funded T32 or K12 training grants for hospital medicine. (There are, however, challenges with this approach because the number of T32 spots per NIH institute is usually fixed). The success of academic emergency medicine offers a precedent for such efforts: After the development of a K12 research training program in emergency medicine, the number of NIH-sponsored principal investigators in this specialty increased by 40% in 6 years.14 Additionally, now that fellowships are required for the pediatric hospital medicine clinician investigators, it would be revealing to track the growth of this workforce.12,13
Structured and formalized mentorship is an essential part of the development of clinician investigators in hospital medicine.4,7,8,10 One successful strategy for mentorship has been the partnering of hospital medicine groups with faculty of general internal medicine and other subspecialty divisions with robust research programs.7,8,15 In addition to developing sustainable mentorship programs, hospital medicine researchers must increase their visibility to trainees. Therefore, it is essential that the majority of academic hospital medicine groups not only hire clinician investigators but also invest in their development, rather than rely on the few programs that have several such faculty members. With this strategy, we could dramatically increase the number of hospitalist clinician investigators from a diverse background of training institutions.
SHM could also play a greater role in organizing events for networking and mentoring for trainees and medical students interested in pursuing a career in hospital medicine research. It is also critically important that hospital medicine groups actively recruit, retain, and develop URiM hospital medicine research faculty in order to attract talented researchers and actively participate in the necessary effort to mitigate the inequities prevalent throughout our healthcare system.
CONCLUSION
Despite the growth of hospital medicine over the past decade, there remains a dearth of hospitalist clinician investigators at major AMCs in the United States. This may be due in part to lack of research resources and mentorship within hospital medicine groups. We believe that investment in these resources, expanded funding opportunities, mentorship development, research fellowship programs, and greater exposure of trainees to hospitalist researchers are solutions that should be strongly considered to develop hospitalist clinician investigators.
Acknowledgments
The authors thank HOMERuN executive committee members, including Grant Fletcher, MD, James Harrison, PhD, BSC, MPH, Peter K. Lindenauer, MD, Melissa Mattison, MD, David Meltzer, MD, PhD, Joshua Metlay, MD, PhD, Jennifer Myers, MD, Sumant Ranji, MD, Gregory Ruhnke, MD, MPH, Edmondo Robinson, MD, MBA, and Neil Sehgal, MPH PhD, for their assistance in developing the survey. They also thank Tiffany Lee, MA, for her project management assistance for HOMERuN.
In their report celebrating the increase in the number of hospitalists from a few hundred in the 1990s to more than 50,000 in 2016, Drs Robert Wachter and Lee Goldman also noted the stunted growth of productive hospital medicine research programs, which presents a challenge to academic credibility in hospital medicine.1 Given the substantial increase in the number of hospitalists over the past two decades, we surveyed adult academic hospital medicine groups to quantify the number of hospitalist clinician investigators and identify gaps in resources for researchers. The number of clinician investigators supported at academic medical centers (AMCs) remains disturbingly low despite the rapid growth of our specialty. Some programs also reported a lack of access to fundamental research services. We report selected results from our survey and provide recommendations to support and facilitate the development of clinician investigators in hospital medicine.
DEARTH OF CLINICIAN INVESTIGATORS IN HOSPITAL MEDICINE
We performed a survey of hospital medicine programs at AMCs in the United States through the Hospital Medicine Reengineering Network (HOMERuN), a hospital medicine research collaborative that facilitates and conducts multisite research studies.2 The purpose of this survey was to obtain a profile of adult academic hospital medicine groups. Surveys were distributed via email to directors and/or senior leaders of each hospital medicine group between January and August 2019. In the survey, a clinician investigator was defined as “faculty whose primary nonclinical focus is scientific papers and grant writing.”
We received responses from 43 of the 86 invitees (50%), each of whom represented a unique hospital medicine group; 41 of the representatives responded to the questions concerning available research services. Collectively, these 43 programs represented 2,503 hospitalists. There were 79 clinician investigators reported among all surveyed hospital medicine groups (3.1% of all hospitalists). The median number of clinician investigators per hospital medicine group was 0 (range 0-12) (Appendix Figure 1), and 22 of 43 (51.2%) hospital medicine groups reported having no clinician investigators. Two of the hospital medicine groups, however, reported having 12 clinician investigators at their respective institutions, comprising nearly one third of the total number of clinician investigators reported in the survey.
Many of the programs reported lack of access to resources such as research assistants (56.1%) and dedicated research fellowships (53.7%) (Appendix Figure 2). A number of groups reported a need for more support for various junior faculty development activities, including research mentoring (53.5%), networking with other researchers (60.5%), and access to clinical data from multiple sites (62.8%).
One of the limitations of this survey was the manner in which the participating hospital medicine groups were chosen. Selection was based on groups affiliated with HOMERuN; among those chosen were highly visible US AMCs, including 70% of the top 20 AMCs based on National Institutes of Health (NIH) funding.3 Therefore, our results likely overestimate the research presence of hospital medicine across all AMCs in the United States.
LACK OF GROWTH OVER TIME: CONTEXTUALIZATION AND IMPLICATIONS
Despite the substantial growth of hospital medicine over the past 2 decades, there has been no proportional increase in the number of hospitalist clinician investigators, with earlier surveys also demonstrating low numbers.4,5 Along with the survey by Chopra and colleagues published in 2019,6 our survey provides an additional contemporary appraisal of research activities for adult academic hospital medicine groups. In the survey by Chopra et al, only 54% (15 of 28) of responding programs reported having any faculty with research as their major activity (ie, >50% effort), and 3% of total faculty reported having funding for >50% effort toward research.6 Our study expands upon these findings by providing more detailed data on the number of clinician investigators per hospital medicine group. Results of our survey showed a concentration of hospitalists within a small number of programs, which may have contributed to the observed lack of growth. We also expand on prior work by identifying a lack of resources and services to support hospitalist researchers.
The findings of our survey have important implications for the field of hospital medicine. Without a critical mass of hospitalist clinician investigators, the quality of research that addresses important questions in our field will suffer. It will also limit academic credibility of the field, as well as individual academic achievement; previous studies have consistently demonstrated that few hospitalists at AMCs achieve the rank of associate or full professor.5-9
POTENTIAL EXPLANATIONS FOR LACK OF RESEARCH GROWTH
The results of our study additionally offer possible explanations for the dearth of clinician investigators in hospital medicine. The limited access to research resources and fellowship training identified in our survey are critical domains that must be addressed in order to develop successful academic hospital medicine programs.4,6,8,10
Regarding dedicated hospital medicine research fellowships, there are only a handful across the country. The small number of existing research fellowships only have one or two fellows per year, and these positions often go unfilled because of a lack of applicants and lower salaries compared to full-time clinical positions.11 The lack of applicants for adult hospital medicine fellowship positions is also integrally linked to board certification requirements. Unlike pediatric hospital medicine where additional fellowship training is required to become board-certified, no such fellowship is required in adult hospital medicine. In pediatrics, this requirement has led to a rapid increase in the number of fellowships with scholarly work requirements (more than 60 fellowships, plus additional programs in development) and greater standardization among training experiences.12,13
The lack of fellowship applicants may also stem from the fact that many trainees are not aware of a potential career as a hospitalist clinician investigator due to limited exposure to this career at most AMCs. Our results revealed that nearly half of sites in our survey had zero clinician investigators, depriving trainees at these programs of role models and thus perpetuating a negative feedback loop. Lastly, although unfilled fellowship positions may indicate that demand is a larger problem than supply, it is also true that fellowship programs generate their own demand through recruitment efforts and the gradual establishment of a positive reputation.
Another potential explanation could relate to the development of hospital medicine in response to rising clinical demands at hospitals: compared with other medical specialties, AMCs may regard hospitalists as being clinicians first and academicians second.1,7,10 Also, hospitalists may be perceived as being beholden to hospitals and less engaged with their surrounding communities than other general medicine fields. With a small footprint in health equity research, academic hospital medicine may be less of a draw to generalists interested in pursuing this area of research. Further, there are very few underrepresented in medicine (URiM) hospital medicine research faculty.5
Another challenge to the career development of hospitalist researchers is the lack of available funding for the type of research typically conducted by hospitalists (eg, rigorous quality improvement implementation and evaluation, optimizing best evidence-based care delivery models, evaluation of patient safety in the hospital setting). As hospitalists tend to be system-level thinkers, this lack of funding may steer potential researchers away from externally funded research careers and into hospital operations and quality improvement positions. Also, unlike other medical specialties, there is no dedicated NIH funding source for hospital medicine research (eg, cardiology and the National Heart, Lung, and Blood Institute), placing hospitalists at a disadvantage in seeking funding compared to subspecialists.
STRATEGIES TO ENHANCE RESEARCH PRESENCE
We recommend several approaches—ones that should be pursued simultaneously—to increase the number of clinician investigators in hospital medicine. First, hospital medicine groups and their respective divisions, departments, and hospitals should allocate funding to support research resources; this includes investing in research assistants, data analysts, statisticians, and administrative support. Through the funding of such research infrastructure programs, AMCs could incentivize hospitalists to research best approaches to improve the value of healthcare delivery, ultimately leading to cost savings.
With 60% of respondents identifying the need for improved access to data across multiple sites, our survey also emphasizes the requirement for further collaboration among hospital medicine groups. Such collaboration could lead to high-powered observational studies and the evaluation of interventions across multiple sites, thus improving the generalizability of study findings.
The Society of Hospital Medicine (SHM) and its research committee can continue to expand the research footprint of hospital medicine. To date, the committee has achieved this by highlighting hospitalist research activity at the SHM Annual Conference Scientific Abstract and Poster Competition and developing a visiting professorship exchange program. In addition to these efforts, SHM could foster collaboration and networking between institutions, as well as take advantage of the current political push for expanded Medicare access by lobbying for robust funding for the Agency for Healthcare Research and Quality, which could provide more opportunities for hospitalists to study the effects of healthcare policy reform on the delivery of inpatient care.
Another strategy to increase the number of hospitalist clinician investigators is to expand hospital medicine research fellowships and recruit trainees for these programs. Fellowships could be internally funded wherein a fellow’s clinical productivity is used to offset the costs associated with obtaining advanced degrees. As an incentive to encourage applicants to temporarily forego a full-time clinical salary during fellowship, hospital medicine groups could offer expanded moonlighting opportunities and contribute to repayment of medical school loans. Hospital medicine groups should also advocate for NIH-funded T32 or K12 training grants for hospital medicine. (There are, however, challenges with this approach because the number of T32 spots per NIH institute is usually fixed). The success of academic emergency medicine offers a precedent for such efforts: After the development of a K12 research training program in emergency medicine, the number of NIH-sponsored principal investigators in this specialty increased by 40% in 6 years.14 Additionally, now that fellowships are required for the pediatric hospital medicine clinician investigators, it would be revealing to track the growth of this workforce.12,13
Structured and formalized mentorship is an essential part of the development of clinician investigators in hospital medicine.4,7,8,10 One successful strategy for mentorship has been the partnering of hospital medicine groups with faculty of general internal medicine and other subspecialty divisions with robust research programs.7,8,15 In addition to developing sustainable mentorship programs, hospital medicine researchers must increase their visibility to trainees. Therefore, it is essential that the majority of academic hospital medicine groups not only hire clinician investigators but also invest in their development, rather than rely on the few programs that have several such faculty members. With this strategy, we could dramatically increase the number of hospitalist clinician investigators from a diverse background of training institutions.
SHM could also play a greater role in organizing events for networking and mentoring for trainees and medical students interested in pursuing a career in hospital medicine research. It is also critically important that hospital medicine groups actively recruit, retain, and develop URiM hospital medicine research faculty in order to attract talented researchers and actively participate in the necessary effort to mitigate the inequities prevalent throughout our healthcare system.
CONCLUSION
Despite the growth of hospital medicine over the past decade, there remains a dearth of hospitalist clinician investigators at major AMCs in the United States. This may be due in part to lack of research resources and mentorship within hospital medicine groups. We believe that investment in these resources, expanded funding opportunities, mentorship development, research fellowship programs, and greater exposure of trainees to hospitalist researchers are solutions that should be strongly considered to develop hospitalist clinician investigators.
Acknowledgments
The authors thank HOMERuN executive committee members, including Grant Fletcher, MD, James Harrison, PhD, BSC, MPH, Peter K. Lindenauer, MD, Melissa Mattison, MD, David Meltzer, MD, PhD, Joshua Metlay, MD, PhD, Jennifer Myers, MD, Sumant Ranji, MD, Gregory Ruhnke, MD, MPH, Edmondo Robinson, MD, MBA, and Neil Sehgal, MPH PhD, for their assistance in developing the survey. They also thank Tiffany Lee, MA, for her project management assistance for HOMERuN.
1. Wachter RM, Goldman L. Zero to 50,000 – The 20th anniversary of the hospitalist. N Engl J Med. 2016;375(11):1009-1011. https://doi.org/10.1056/NEJMp1607958
2. Auerbach AD, Patel MS, Metlay JP, et al. The Hospital Medicine Reengineering Network (HOMERuN): a learning organization focused on improving hospital care. Acad Med. 2014;89(3):415-420. https://doi.org/10.1097/acm.0000000000000139
3. Roskoski R Jr, Parslow TG. Ranking Tables of NIH funding to US medical schools in 2019. Blue Ridge Institute for Medical Research. Published 2020. Updated July 14, 2020. Accessed July 30, 2020. http://www.brimr.org/NIH_Awards/2019/NIH_Awards_2019.htm
4. Reid MB, Misky GJ, Harrison RA, Sharpe B, Auerbach A, Glasheen JJ. Mentorship, productivity, and promotion among academic hospitalists. J Gen Intern Med. 2012;27(1):23-27. https://doi.org/10.1007/s11606-011-1892-5
5. Miller CS, Fogerty RL, Gann J, Bruti CP, Klein R; The Society of General Internal Medicine Membership Committee. The growth of hospitalists and the future of the society of general internal medicine: results from the 2014 membership survey. J Gen Intern Med. 2017;32(11):1179-1185. https://doi.org/10.1007/s11606-017-4126-7
6. Chopra V, Burden M, Jones CD, et al; Society of Hospital Medicine Research Committee. State of research in adult hospital medicine: results of a national survey. J Hosp Med. 2019;14(4):207-211. https://doi.org/10.12788/jhm.3136
7. Seymann GB, Southern W, Burger A, et al. Features of successful academic hospitalist programs: insights from the SCHOLAR (SuCcessful HOspitaLists in academics and research) project. J Hosp Med. 2016;11(10):708-713. https://doi.org/10.1002/jhm.2603
8. Harrison R, Hunter AJ, Sharpe B, Auerbach AD. Survey of US academic hospitalist leaders about mentorship and academic activities in hospitalist groups. J Hosp Med. 2011;6(1):5-9. https://doi.org/10.1002/jhm.836
9. Dang Do AN, Munchhof AM, Terry C, Emmett T, Kara A. Research and publication trends in hospital medicine. J Hosp Med. 2014;9(3):148-154. https://doi.org/10.1002/jhm.2148
10. Sehgal NL, Sharpe BA, Auerbach AA, Wachter RM. Investing in the future: building an academic hospitalist faculty development program. J Hosp Med. 2011;6(3):161-166. https://doi.org/10.1002/jhm.845
11. Ranji SR, Rosenman DJ, Amin AN, Kripalani S. Hospital medicine fellowships: works in progress. Am J Med. 2006;119(1):72.e1-72.e7. https://doi.org/10.1016/j.amjmed.2005.07.061
12. Shah NH, Rhim HJ, Maniscalco J, Wilson K, Rassbach C. The current state of pediatric hospital medicine fellowships: a survey of program directors. J Hosp Med. 2016;11(5):324-328. https://doi.org/10.1002/jhm.2571
13. Jerardi KE, Fisher E, Rassbach C, et al; Council of Pediatric Hospital Medicine Fellowship Directors. Development of a curricular framework for pediatric hospital medicine fellowships. Pediatrics. 2017;140(1):e20170698. https://doi.org/10.1542/peds.2017-0698
14. Lewis RJ, Neumar RW. Research in emergency medicine: building the investigator pipeline. Ann Emerg Med. 2018;72(6):691-695. https://doi.org/10.1016/j.annemergmed.2018.10.019
15. Flanders SA, Kaufman SR, Nallamothu BK, Saint S. The University of Michigan Specialist-Hospitalist Allied Research Program: jumpstarting hospital medicine research. J Hosp Med. 2008;3(4):308-313. https://doi.org/10.1002/jhm.342
1. Wachter RM, Goldman L. Zero to 50,000 – The 20th anniversary of the hospitalist. N Engl J Med. 2016;375(11):1009-1011. https://doi.org/10.1056/NEJMp1607958
2. Auerbach AD, Patel MS, Metlay JP, et al. The Hospital Medicine Reengineering Network (HOMERuN): a learning organization focused on improving hospital care. Acad Med. 2014;89(3):415-420. https://doi.org/10.1097/acm.0000000000000139
3. Roskoski R Jr, Parslow TG. Ranking Tables of NIH funding to US medical schools in 2019. Blue Ridge Institute for Medical Research. Published 2020. Updated July 14, 2020. Accessed July 30, 2020. http://www.brimr.org/NIH_Awards/2019/NIH_Awards_2019.htm
4. Reid MB, Misky GJ, Harrison RA, Sharpe B, Auerbach A, Glasheen JJ. Mentorship, productivity, and promotion among academic hospitalists. J Gen Intern Med. 2012;27(1):23-27. https://doi.org/10.1007/s11606-011-1892-5
5. Miller CS, Fogerty RL, Gann J, Bruti CP, Klein R; The Society of General Internal Medicine Membership Committee. The growth of hospitalists and the future of the society of general internal medicine: results from the 2014 membership survey. J Gen Intern Med. 2017;32(11):1179-1185. https://doi.org/10.1007/s11606-017-4126-7
6. Chopra V, Burden M, Jones CD, et al; Society of Hospital Medicine Research Committee. State of research in adult hospital medicine: results of a national survey. J Hosp Med. 2019;14(4):207-211. https://doi.org/10.12788/jhm.3136
7. Seymann GB, Southern W, Burger A, et al. Features of successful academic hospitalist programs: insights from the SCHOLAR (SuCcessful HOspitaLists in academics and research) project. J Hosp Med. 2016;11(10):708-713. https://doi.org/10.1002/jhm.2603
8. Harrison R, Hunter AJ, Sharpe B, Auerbach AD. Survey of US academic hospitalist leaders about mentorship and academic activities in hospitalist groups. J Hosp Med. 2011;6(1):5-9. https://doi.org/10.1002/jhm.836
9. Dang Do AN, Munchhof AM, Terry C, Emmett T, Kara A. Research and publication trends in hospital medicine. J Hosp Med. 2014;9(3):148-154. https://doi.org/10.1002/jhm.2148
10. Sehgal NL, Sharpe BA, Auerbach AA, Wachter RM. Investing in the future: building an academic hospitalist faculty development program. J Hosp Med. 2011;6(3):161-166. https://doi.org/10.1002/jhm.845
11. Ranji SR, Rosenman DJ, Amin AN, Kripalani S. Hospital medicine fellowships: works in progress. Am J Med. 2006;119(1):72.e1-72.e7. https://doi.org/10.1016/j.amjmed.2005.07.061
12. Shah NH, Rhim HJ, Maniscalco J, Wilson K, Rassbach C. The current state of pediatric hospital medicine fellowships: a survey of program directors. J Hosp Med. 2016;11(5):324-328. https://doi.org/10.1002/jhm.2571
13. Jerardi KE, Fisher E, Rassbach C, et al; Council of Pediatric Hospital Medicine Fellowship Directors. Development of a curricular framework for pediatric hospital medicine fellowships. Pediatrics. 2017;140(1):e20170698. https://doi.org/10.1542/peds.2017-0698
14. Lewis RJ, Neumar RW. Research in emergency medicine: building the investigator pipeline. Ann Emerg Med. 2018;72(6):691-695. https://doi.org/10.1016/j.annemergmed.2018.10.019
15. Flanders SA, Kaufman SR, Nallamothu BK, Saint S. The University of Michigan Specialist-Hospitalist Allied Research Program: jumpstarting hospital medicine research. J Hosp Med. 2008;3(4):308-313. https://doi.org/10.1002/jhm.342
© 2021 Society of Hospital Medicine
Unmasked: How the COVID-19 Pandemic Exacerbates Disparities for People With Communication-Based Disabilities
Adults with communication-based disabilities struggle with healthcare inequities,1-4 largely secondary to poor healthcare provider-patient communication. The prevalence of communication-based disabilities, which include speech, language, voice, and/or hearing disabilities, is relatively high yet difficult to ascertain. Ten percent of adults in the United States report having had a speech, language, or voice disability within the past year,5 and hearing loss also affects 17% of the US population.6 These individuals’ collective communication difficulties have been exacerbated by the coronavirus disease 2019 (COVID-19) pandemic, with healthcare systems mandating personal protective equipment (PPE), including face masks, to ensure the safety of workers and patients. This change has placed patients with communication-based disabilities at even greater risk for communication breakdowns.7,8
Hospitals pose challenging communicative environments due to multiple factors (eg, noisy equipment alarms, harried healthcare teams spending less time with patients, PPE use obstructing faces and muffling sounds). Adverse communication among those with communication-based disabilities results in poorer healthcare outcomes, including higher rates of readmission and preventable adverse medical events, as well as lower healthcare satisfaction.7,9,10 Ineffective communication leads to reduced adherence, longer hospitalizations, and worse health outcomes in general.11-13 This is problematic because those with communication-based disabilities are more likely to require hospitalization due to higher rates of associated comorbidities, including frailty, cardiovascular disease, cognitive decline, and falls.4,14-16 Yet hospitals rarely screen and implement best practices to ensure effective and accessible communication for those with communication-based disabilities. The COVID-19 pandemic has exacerbated existing barriers, despite feasible solutions. Importantly, the Americans with Disabilities Act (ADA) remains in effect despite the pandemic. Therefore, hospitals should review existing policies and approaches to ensure adherence to ADA mandates. We address commonly encountered COVID-19-related communication barriers and recommend potential solutions.17
KEY COMMUNICATION BARRIERS
Limited Time or Support
Patients with communication-based disabilities may need more time than others to communicate their needs, values, and preferences effectively, whether due to slower articulation (eg, movement disorders) or communicating via an intermediary (eg, family member who understands them well) or an interpreter. Due to capacity or patient acuity issues, or even concerns about minimizing time in the room of a patient infected with COVID-19, hospital staff may inadvertently spend less time than needed to develop the necessary therapeutic relationships. This concern is magnified when restrictive visitor policies limit the availability of caregivers, such as loved ones, who assist at the bedside with communication.18
Universal Masking and Face Shields
Standard face masks, now required for all in-person encounters regardless of the patient’s COVID-19 status, obstruct the view of the lips and many facial expressions. Facial cues are an important form of nonverbal communication and are critical to conveying meaning in sign language. Face masks, particularly N95 respirators, substantially degrade speech perception.19 Masking increases the difficulty of acoustically and visually understanding patients who have disorders that decrease speech intelligibility, such as dysphonia, dysarthria, or
Interpreters
For deaf and hard-of-hearing people who use American Sign Language (ASL) as their preferred healthcare communication method, interpreters play a critical role in ensuring accessible healthcare communication. Signed language interpretation can occur in person or remotely by video. For in-person interpretation, interpreters must likewise wear PPE. The use of PPE, including face masks, can obscure many of the facial cues important to ASL grammar. Similarly, patients’ face masks can make it more challenging for interpreters to interpret effectively. With remote video interpretation, technological difficulties (eg, dropped WiFi connections) and the loss of environmental cues (eg, interpreter at a remote location unable to see or hear patient surroundings) often mar opportunities for accessible and effective communication. For the DeafBlind community, the use of remote video interpretation is not feasible. DeafBlind people rely on tactile forms of ASL, requiring interpreters’ physical touch throughout the communication encounter. This potentially increases COVID-19 transmission risk.
POTENTIAL OR IMPLEMENTED SOLUTIONS
While some of the solutions listed below also apply to communication in nonpandemic times, identifying high-risk patients and anticipatory planning for communication has become even more important during the COVID-19 outbreak.
Identification and Assessment of
Hospital staff should systematically review admission and transfer protocols to ensure every patient is asked about their communication preferences, necessary accommodations, and specific needs. Any communication needs or accommodation requests (eg, interpreters, communication boards) should be documented and flagged in highly visible areas of the electronic health record. These patients should be assessed regularly to ensure their communication needs are being met and documented throughout their hospital stay.
Assistive Communication Steps
Some steps can be performed in advance. Careful consideration should be given to healthcare providers’ ability to spend additional time with patients with communication-based disabilities. Even if providers are limited physically in the room, they can still work to optimize mindful, high-quality communication by calling into the patient’s room by phone or video. The additional time is important especially when establishing rapport with patients and identifying their preferred communication approaches, as well as engaging their support networks. Patients with communication-based disabilities and their support team often have expertise on their ideal communication strategies. Healthcare providers and staff should inquire about communication preferences. Patients should also be oriented to hospital team structure and members, which could include simple solutions such as legible name tags. Hearing aids, batteries, and other assistive technology should have designated places to prevent loss and ensure ongoing working status. In addition, nurse stations should have a communication toolbox that includes replacement batteries for hearing aids along with other assistive technology devices, such as a personal sound amplification product.
Communication Strategies
Healthcare teams should be trained and reminded to use patient-centered communication strategies, including assessing their comprehension of shared health information through teach-back principles. Strategies vary by patient and may require teams’ flexibility in meeting the patient’s needs and preferences. Examples include ensuring one has the patient’s attention and uses good eye contact. Using a projected “radio voice,” which emphasizes clarity and articulation rather than volume, is helpful for those with hearing loss. For some, meaningful gestures (eg, pointing to one’s own head when asking about headaches) can aid communication. Another strategy when having difficulty understanding patients with decreased speech intelligibility is to repeat the audible speech so that the patient only needs to repeat the inaudible portions that were missed. Patients should have secure access to personal assistive devices, such as hearing aids and even smartphones with communication apps (eg, speech-to-text apps) to facilitate interpersonal communication.
Clear Face Masks
Face masks with transparent windows have been developed. Deaf and hard of hearing people’s speech perception increases when speakers use transparent versus conventional masks. The Food and Drug Administration has approved two clear face masks as American Society for Testing Materials Level 1 (Table). These two masks have limited utility for high-risk situations, such as aerosolizing procedures; in such cases, a powered air purifying respirator with a clear viewing window will be needed instead. Notably, clear mask supply has lagged behind demand, creating limited mask availability during the pandemic; their use may need to be restricted to those working with patients with communication-based disabilities.
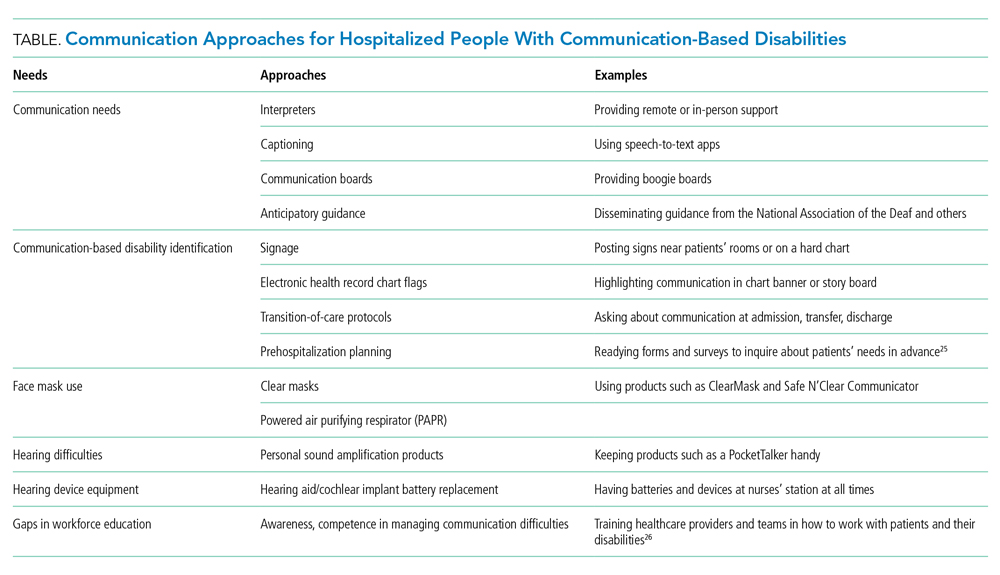
Tools for Communicating Within the Patient’s Room
Erasable whiteboards and communication boards are useful tools for simple exchanges as long as patients’ literacy and fluency are adequate. “PocketTalkers” or personalized sound amplification products may allow providers to speak into a microphone, providing amplified speech via a patient’s headphones. These amplification products are typically useful for those with mild to moderate hearing loss who are not using a hearing aid. Automatic speech recognition apps are device-based apps for converting speech to text. Speakers hold the device near the mouth to maximize accuracy while the patient reads the captions on their screen. With social distancing, lavalier microphones can increase text accuracy, but higher rates of error may still occur due to background noises or accents. For increased reliability and accuracy, Computer Access Realtime Translation stenographers can provide live speech to text on a computer screen from off-site via a computer or smartphone.
Tools for Isolation-Limited Communication
Team members can call an intermediary service to communicate with the patient via the patient’s smartphone or hospital-provided remote video interpreting service, depending on the patient’s preferred communication modality. For oral and spoken language, some services (Table) use remote stenographers to convert speech to text or sign language interpreters for those who use sign language. For both communication modes, smartphone-based videoconferencing may be beneficial while maintaining isolation precautions.
Interpreter Accessibility
Conceptualize interpreters as consulting healthcare team members. They should receive the same PPE training and monitoring as other healthcare workers. For patients using remote video interpretation, this technology needs to be optimized for best results. The room should be in a location with a strong Wi-Fi signal. Equipment should be consistently charged when not in use and rapidly accessible, even remaining in the patients’ room if possible. Healthcare teams need training to appropriately locate and set up the equipment with appropriate support from information technology staff.
Signage
Signage is useful to remind healthcare teams of the patients’ and/or caregivers’ communication-based disability. The most commonly used disability signage shows a line across an ear to indicate hearing loss (Appendix Figure).22 Appropriate signage use, even simple printed sheets documenting a communication issue, can remind healthcare team members of patients’ needs to ensure that communication is accessible and avoid misconceptions toward the patient (eg, noncompliance or cognitive issues). Chart banners, patient room doorways, and over the patients’ beds are good signage locations.
Systematic Noise Reduction
Consistent with previous calls to reduce inpatient noise,23 hospitals should systematically review and monitor protocols to reduce noise pollution. If intra-unit noise varies, patients relying on acoustic-based communication due to hearing loss or speech, language, or voice disability should be placed in quieter rooms.
Communication Concordance
Healthcare professionals and staff with disabilities are an increasingly recognized workforce segment,24 and often are experienced innovators in communicating effectively with patients with communication-based disabilities. Healthcare systems can explore whether they have healthcare team members, employees, disability resource professionals, and/or trainees with these backgrounds and, if they are available, recruit them into developing effective inpatient communication policies and processes.
CONCLUSION
People with communication disabilities experience significant healthcare disparities, now further exacerbated by COVID-19. As clinicians, staff and hospitals work to fuse safety with high-quality communication and care, we should capitalize on multipronged opportunities at the system and individual levels to identify barriers and ensure accessible and effective communication with patients who have communication-based disabilities.
1. McKee MM, Moreland C, Atcherson SR, Zazove P. Hearing loss: communicating with the patient who is deaf or hard of hearing. FP Essent. 2015;434:24-28.
2. Morris MA, Dudgeon BJ, Yorkston K. A qualitative study of adult AAC users’ experiences communicating with medical providers. Disabil Rehabil Assist Technol. 2013;8(6):472-481. https://doi.org/10.3109/17483107.2012.746398
3. Steinberg AG, Barnett S, Meador HE, Wiggins EA, Zazove P. Health care system accessibility. experiences and perceptions of deaf people. J Gen Intern Med. 2006;21(3):260-266. https://doi.org/10.1111/j.1525-1497.2006.00340.x
4. Stransky ML, Jensen KM, Morris MA. Adults with communication disabilities experience poorer health and healthcare outcomes compared to persons without communication disabilities. J Gen Intern Med. 2018;33(12):2147-2155. https://doi.org/10.1007/s11606-018-4625-1
5. Morris MA, Meier SK, Griffin JM, Branda ME, Phelan SM. Prevalence and etiologies of adult communication disabilities in the United States: results from the 2012 National Health Interview Survey. Disabil Health J. 2016;9(1):140-144. https://doi.org/10.1016/j.dhjo.2015.07.004
6. Blackwell DL, Lucas JW, Clarke TC. Summary health statistics for U.S. adults: National Health Interview Survey, 2012. Vital Health Stat. 2014(260):1-161.
7. Chang JE, Weinstein B, Chodosh J, Blustein J. Hospital readmission risk for patients with self-reported hearing loss and communication trouble. J Am Geriatr Soc. 2018;66(11):2227-2228. https://doi.org/10.1111/jgs.15545
8. McKee M, Moran C, Zazove P. Overcoming additional barriers to care for deaf and hard of hearing patients during COVID-19. JAMA Otolaryngol Head Neck Surg. 2020;146(9):781-782. https://doi.org/10.1001/jamaoto.2020.1705
9. Bartlett G, Blais R, Tamblyn R, Clermont RJ, MacGibbon B. Impact of patient communication problems on the risk of preventable adverse events in acute care settings. CMAJ. 2008;178(12):1555-1562. https://doi.org/10.1503/cmaj.070690
10. Hoffman JM, Yorkston KM, Shumway-Cook A, Ciol MA, Dudgeon BJ, Chan L. Effect of communication disability on satisfaction with health care: a survey of medicare beneficiaries. Am J Speech Lang Pathol. 2005;14(3):221-228. https://doi.org/10.1044/1058-0360(2005/022)
11. Kelley JM, Kraft-Todd G, Schapira L, Kossowsky J, Riess H. The influence of the patient-clinician relationship on healthcare outcomes: a systematic review and meta-analysis of randomized controlled trials. PLoS One. 2014;9(4):e94207. https://doi.org/10.1371/journal.pone.0094207
12. Mast MS. On the importance of nonverbal communication in the physician-patient interaction. Patient Educ Couns. 2007;67(3):315-318. https://doi.org/10.1016/j.pec.2007.03.005
13. Street RL Jr, Makoul G, Arora NK, Epstein RM. How does communication heal? pathways linking clinician-patient communication to health outcomes. Patient Educ Couns. 2009;74(3):295-301. https://doi.org/10.1016/j.pec.2008.11.015
14. Genther DJ, Frick KD, Chen D, Betz J, Lin FR. Association of hearing loss with hospitalization and burden of disease in older adults. JAMA. 2013;309(22):2322-2324. https://doi.org/10.1001/jama.2013.5912
15. Lin FR, Yaffe K, Xia J, et al. Hearing loss and cognitive decline in older adults. JAMA Intern Med. 2013;173(4):293-299. https://doi.org/10.1001/jamainternmed.2013.1868
16. McKee MM, Stransky ML, Reichard A. Hearing loss and associated medical conditions among individuals 65 years and older. Disabil Health J. 2018;11(1):122-125. https://doi.org/10.1016/j.dhjo.2017.05.007
17. ADA requirements: effective communication. U.S. Department of Justice. January 31, 2014. Accessed February 12, 2021. https://www.ada.gov/effective-comm.htm
18. OCR resolves complaints after State of Connecticut and private hospital safeguard the rights of persons with disabilities to have reasonable access to support persons in hospital settings during COVID-19. Press Release. US Department of Health and Human Services; June 9, 2020. Accessed September 19, 2020. https://www.hhs.gov/about/news/2020/06/09/ocr-resolves-complaints-after-state-connecticut-private-hospital-safeguard-rights-persons.html
19. Goldin A, Weinstein B, Shiman N. How do medical masks degrade speech perception? The Hearing Review. April 1, 2020. Accessed September 30, 2020. https://www.hearingreview.com/hearing-loss/health-wellness/how-do-medical-masks-degrade-speech-reception
20. Mendel LL, Gardino JA, Atcherson SR. Speech understanding using surgical masks: a problem in health care? J Am Acad Audiol. 2008;19(9):686-695. https://doi.org/10.3766/jaaa.19.9.4
21. Atcherson SR, Finley ET, McDowell BR, Watson C. More speech degradations and considerations in the search for transparent face coverings during the COVID-19 pandemic. American Academy of Audiology. November/December 2020. Accessed September 19, 2020. https://www.audiology.org/audiology-today-julyaugust-2020/online-feature-more-speech-degradations-and-considerations-search
22. Hearing Loss. Wikipedia. Accessed October 28, 2020. https://en.wikipedia.org/wiki/Hearing_loss
23. Kamdar BB, Martin JL, Needham DM. Noise and light pollution in the hospital: a call for action. J Hosp Med. 2017;12(10):861-862. https://doi.org/10.12788/jhm.2838
24. Meeks LM, Herzer K, Jain NR. Removing barriers and facilitating access: increasing the number of physicians with disabilities. Acad Med. 2018;93(4):540-543. https://doi.org/10.1097/acm.0000000000002112
25. Communication Access Plan (CAP): Instructions for Patients and Providers. Hearing Loss Association of America (HLAA). Accessed September 30, 2020. https://www.hearingloss.org/wp-content/uploads/HLAA_HC_CAP_Form_and_Instructions.pdf
26. How Do I Communicate with Doctors, Nurses, and Staff at the Hospital During COVID-19? Hearing Loss Association of America (HLAA). May 8, 2020. Accessed September 30, 2020. https://www.hearingloss.org/communication-access-recommendations-hospitals-covid-19/
Adults with communication-based disabilities struggle with healthcare inequities,1-4 largely secondary to poor healthcare provider-patient communication. The prevalence of communication-based disabilities, which include speech, language, voice, and/or hearing disabilities, is relatively high yet difficult to ascertain. Ten percent of adults in the United States report having had a speech, language, or voice disability within the past year,5 and hearing loss also affects 17% of the US population.6 These individuals’ collective communication difficulties have been exacerbated by the coronavirus disease 2019 (COVID-19) pandemic, with healthcare systems mandating personal protective equipment (PPE), including face masks, to ensure the safety of workers and patients. This change has placed patients with communication-based disabilities at even greater risk for communication breakdowns.7,8
Hospitals pose challenging communicative environments due to multiple factors (eg, noisy equipment alarms, harried healthcare teams spending less time with patients, PPE use obstructing faces and muffling sounds). Adverse communication among those with communication-based disabilities results in poorer healthcare outcomes, including higher rates of readmission and preventable adverse medical events, as well as lower healthcare satisfaction.7,9,10 Ineffective communication leads to reduced adherence, longer hospitalizations, and worse health outcomes in general.11-13 This is problematic because those with communication-based disabilities are more likely to require hospitalization due to higher rates of associated comorbidities, including frailty, cardiovascular disease, cognitive decline, and falls.4,14-16 Yet hospitals rarely screen and implement best practices to ensure effective and accessible communication for those with communication-based disabilities. The COVID-19 pandemic has exacerbated existing barriers, despite feasible solutions. Importantly, the Americans with Disabilities Act (ADA) remains in effect despite the pandemic. Therefore, hospitals should review existing policies and approaches to ensure adherence to ADA mandates. We address commonly encountered COVID-19-related communication barriers and recommend potential solutions.17
KEY COMMUNICATION BARRIERS
Limited Time or Support
Patients with communication-based disabilities may need more time than others to communicate their needs, values, and preferences effectively, whether due to slower articulation (eg, movement disorders) or communicating via an intermediary (eg, family member who understands them well) or an interpreter. Due to capacity or patient acuity issues, or even concerns about minimizing time in the room of a patient infected with COVID-19, hospital staff may inadvertently spend less time than needed to develop the necessary therapeutic relationships. This concern is magnified when restrictive visitor policies limit the availability of caregivers, such as loved ones, who assist at the bedside with communication.18
Universal Masking and Face Shields
Standard face masks, now required for all in-person encounters regardless of the patient’s COVID-19 status, obstruct the view of the lips and many facial expressions. Facial cues are an important form of nonverbal communication and are critical to conveying meaning in sign language. Face masks, particularly N95 respirators, substantially degrade speech perception.19 Masking increases the difficulty of acoustically and visually understanding patients who have disorders that decrease speech intelligibility, such as dysphonia, dysarthria, or
Interpreters
For deaf and hard-of-hearing people who use American Sign Language (ASL) as their preferred healthcare communication method, interpreters play a critical role in ensuring accessible healthcare communication. Signed language interpretation can occur in person or remotely by video. For in-person interpretation, interpreters must likewise wear PPE. The use of PPE, including face masks, can obscure many of the facial cues important to ASL grammar. Similarly, patients’ face masks can make it more challenging for interpreters to interpret effectively. With remote video interpretation, technological difficulties (eg, dropped WiFi connections) and the loss of environmental cues (eg, interpreter at a remote location unable to see or hear patient surroundings) often mar opportunities for accessible and effective communication. For the DeafBlind community, the use of remote video interpretation is not feasible. DeafBlind people rely on tactile forms of ASL, requiring interpreters’ physical touch throughout the communication encounter. This potentially increases COVID-19 transmission risk.
POTENTIAL OR IMPLEMENTED SOLUTIONS
While some of the solutions listed below also apply to communication in nonpandemic times, identifying high-risk patients and anticipatory planning for communication has become even more important during the COVID-19 outbreak.
Identification and Assessment of
Hospital staff should systematically review admission and transfer protocols to ensure every patient is asked about their communication preferences, necessary accommodations, and specific needs. Any communication needs or accommodation requests (eg, interpreters, communication boards) should be documented and flagged in highly visible areas of the electronic health record. These patients should be assessed regularly to ensure their communication needs are being met and documented throughout their hospital stay.
Assistive Communication Steps
Some steps can be performed in advance. Careful consideration should be given to healthcare providers’ ability to spend additional time with patients with communication-based disabilities. Even if providers are limited physically in the room, they can still work to optimize mindful, high-quality communication by calling into the patient’s room by phone or video. The additional time is important especially when establishing rapport with patients and identifying their preferred communication approaches, as well as engaging their support networks. Patients with communication-based disabilities and their support team often have expertise on their ideal communication strategies. Healthcare providers and staff should inquire about communication preferences. Patients should also be oriented to hospital team structure and members, which could include simple solutions such as legible name tags. Hearing aids, batteries, and other assistive technology should have designated places to prevent loss and ensure ongoing working status. In addition, nurse stations should have a communication toolbox that includes replacement batteries for hearing aids along with other assistive technology devices, such as a personal sound amplification product.
Communication Strategies
Healthcare teams should be trained and reminded to use patient-centered communication strategies, including assessing their comprehension of shared health information through teach-back principles. Strategies vary by patient and may require teams’ flexibility in meeting the patient’s needs and preferences. Examples include ensuring one has the patient’s attention and uses good eye contact. Using a projected “radio voice,” which emphasizes clarity and articulation rather than volume, is helpful for those with hearing loss. For some, meaningful gestures (eg, pointing to one’s own head when asking about headaches) can aid communication. Another strategy when having difficulty understanding patients with decreased speech intelligibility is to repeat the audible speech so that the patient only needs to repeat the inaudible portions that were missed. Patients should have secure access to personal assistive devices, such as hearing aids and even smartphones with communication apps (eg, speech-to-text apps) to facilitate interpersonal communication.
Clear Face Masks
Face masks with transparent windows have been developed. Deaf and hard of hearing people’s speech perception increases when speakers use transparent versus conventional masks. The Food and Drug Administration has approved two clear face masks as American Society for Testing Materials Level 1 (Table). These two masks have limited utility for high-risk situations, such as aerosolizing procedures; in such cases, a powered air purifying respirator with a clear viewing window will be needed instead. Notably, clear mask supply has lagged behind demand, creating limited mask availability during the pandemic; their use may need to be restricted to those working with patients with communication-based disabilities.
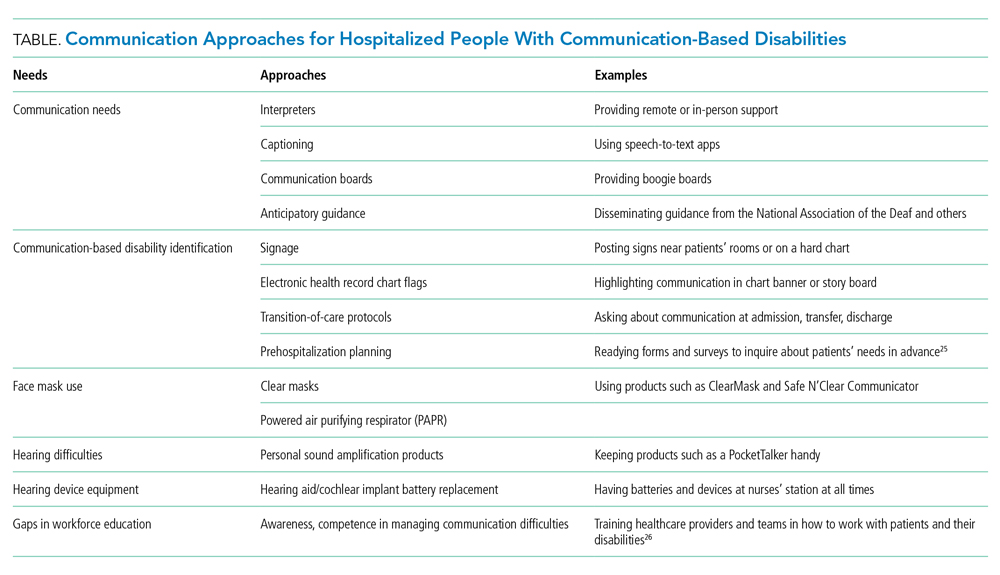
Tools for Communicating Within the Patient’s Room
Erasable whiteboards and communication boards are useful tools for simple exchanges as long as patients’ literacy and fluency are adequate. “PocketTalkers” or personalized sound amplification products may allow providers to speak into a microphone, providing amplified speech via a patient’s headphones. These amplification products are typically useful for those with mild to moderate hearing loss who are not using a hearing aid. Automatic speech recognition apps are device-based apps for converting speech to text. Speakers hold the device near the mouth to maximize accuracy while the patient reads the captions on their screen. With social distancing, lavalier microphones can increase text accuracy, but higher rates of error may still occur due to background noises or accents. For increased reliability and accuracy, Computer Access Realtime Translation stenographers can provide live speech to text on a computer screen from off-site via a computer or smartphone.
Tools for Isolation-Limited Communication
Team members can call an intermediary service to communicate with the patient via the patient’s smartphone or hospital-provided remote video interpreting service, depending on the patient’s preferred communication modality. For oral and spoken language, some services (Table) use remote stenographers to convert speech to text or sign language interpreters for those who use sign language. For both communication modes, smartphone-based videoconferencing may be beneficial while maintaining isolation precautions.
Interpreter Accessibility
Conceptualize interpreters as consulting healthcare team members. They should receive the same PPE training and monitoring as other healthcare workers. For patients using remote video interpretation, this technology needs to be optimized for best results. The room should be in a location with a strong Wi-Fi signal. Equipment should be consistently charged when not in use and rapidly accessible, even remaining in the patients’ room if possible. Healthcare teams need training to appropriately locate and set up the equipment with appropriate support from information technology staff.
Signage
Signage is useful to remind healthcare teams of the patients’ and/or caregivers’ communication-based disability. The most commonly used disability signage shows a line across an ear to indicate hearing loss (Appendix Figure).22 Appropriate signage use, even simple printed sheets documenting a communication issue, can remind healthcare team members of patients’ needs to ensure that communication is accessible and avoid misconceptions toward the patient (eg, noncompliance or cognitive issues). Chart banners, patient room doorways, and over the patients’ beds are good signage locations.
Systematic Noise Reduction
Consistent with previous calls to reduce inpatient noise,23 hospitals should systematically review and monitor protocols to reduce noise pollution. If intra-unit noise varies, patients relying on acoustic-based communication due to hearing loss or speech, language, or voice disability should be placed in quieter rooms.
Communication Concordance
Healthcare professionals and staff with disabilities are an increasingly recognized workforce segment,24 and often are experienced innovators in communicating effectively with patients with communication-based disabilities. Healthcare systems can explore whether they have healthcare team members, employees, disability resource professionals, and/or trainees with these backgrounds and, if they are available, recruit them into developing effective inpatient communication policies and processes.
CONCLUSION
People with communication disabilities experience significant healthcare disparities, now further exacerbated by COVID-19. As clinicians, staff and hospitals work to fuse safety with high-quality communication and care, we should capitalize on multipronged opportunities at the system and individual levels to identify barriers and ensure accessible and effective communication with patients who have communication-based disabilities.
Adults with communication-based disabilities struggle with healthcare inequities,1-4 largely secondary to poor healthcare provider-patient communication. The prevalence of communication-based disabilities, which include speech, language, voice, and/or hearing disabilities, is relatively high yet difficult to ascertain. Ten percent of adults in the United States report having had a speech, language, or voice disability within the past year,5 and hearing loss also affects 17% of the US population.6 These individuals’ collective communication difficulties have been exacerbated by the coronavirus disease 2019 (COVID-19) pandemic, with healthcare systems mandating personal protective equipment (PPE), including face masks, to ensure the safety of workers and patients. This change has placed patients with communication-based disabilities at even greater risk for communication breakdowns.7,8
Hospitals pose challenging communicative environments due to multiple factors (eg, noisy equipment alarms, harried healthcare teams spending less time with patients, PPE use obstructing faces and muffling sounds). Adverse communication among those with communication-based disabilities results in poorer healthcare outcomes, including higher rates of readmission and preventable adverse medical events, as well as lower healthcare satisfaction.7,9,10 Ineffective communication leads to reduced adherence, longer hospitalizations, and worse health outcomes in general.11-13 This is problematic because those with communication-based disabilities are more likely to require hospitalization due to higher rates of associated comorbidities, including frailty, cardiovascular disease, cognitive decline, and falls.4,14-16 Yet hospitals rarely screen and implement best practices to ensure effective and accessible communication for those with communication-based disabilities. The COVID-19 pandemic has exacerbated existing barriers, despite feasible solutions. Importantly, the Americans with Disabilities Act (ADA) remains in effect despite the pandemic. Therefore, hospitals should review existing policies and approaches to ensure adherence to ADA mandates. We address commonly encountered COVID-19-related communication barriers and recommend potential solutions.17
KEY COMMUNICATION BARRIERS
Limited Time or Support
Patients with communication-based disabilities may need more time than others to communicate their needs, values, and preferences effectively, whether due to slower articulation (eg, movement disorders) or communicating via an intermediary (eg, family member who understands them well) or an interpreter. Due to capacity or patient acuity issues, or even concerns about minimizing time in the room of a patient infected with COVID-19, hospital staff may inadvertently spend less time than needed to develop the necessary therapeutic relationships. This concern is magnified when restrictive visitor policies limit the availability of caregivers, such as loved ones, who assist at the bedside with communication.18
Universal Masking and Face Shields
Standard face masks, now required for all in-person encounters regardless of the patient’s COVID-19 status, obstruct the view of the lips and many facial expressions. Facial cues are an important form of nonverbal communication and are critical to conveying meaning in sign language. Face masks, particularly N95 respirators, substantially degrade speech perception.19 Masking increases the difficulty of acoustically and visually understanding patients who have disorders that decrease speech intelligibility, such as dysphonia, dysarthria, or
Interpreters
For deaf and hard-of-hearing people who use American Sign Language (ASL) as their preferred healthcare communication method, interpreters play a critical role in ensuring accessible healthcare communication. Signed language interpretation can occur in person or remotely by video. For in-person interpretation, interpreters must likewise wear PPE. The use of PPE, including face masks, can obscure many of the facial cues important to ASL grammar. Similarly, patients’ face masks can make it more challenging for interpreters to interpret effectively. With remote video interpretation, technological difficulties (eg, dropped WiFi connections) and the loss of environmental cues (eg, interpreter at a remote location unable to see or hear patient surroundings) often mar opportunities for accessible and effective communication. For the DeafBlind community, the use of remote video interpretation is not feasible. DeafBlind people rely on tactile forms of ASL, requiring interpreters’ physical touch throughout the communication encounter. This potentially increases COVID-19 transmission risk.
POTENTIAL OR IMPLEMENTED SOLUTIONS
While some of the solutions listed below also apply to communication in nonpandemic times, identifying high-risk patients and anticipatory planning for communication has become even more important during the COVID-19 outbreak.
Identification and Assessment of
Hospital staff should systematically review admission and transfer protocols to ensure every patient is asked about their communication preferences, necessary accommodations, and specific needs. Any communication needs or accommodation requests (eg, interpreters, communication boards) should be documented and flagged in highly visible areas of the electronic health record. These patients should be assessed regularly to ensure their communication needs are being met and documented throughout their hospital stay.
Assistive Communication Steps
Some steps can be performed in advance. Careful consideration should be given to healthcare providers’ ability to spend additional time with patients with communication-based disabilities. Even if providers are limited physically in the room, they can still work to optimize mindful, high-quality communication by calling into the patient’s room by phone or video. The additional time is important especially when establishing rapport with patients and identifying their preferred communication approaches, as well as engaging their support networks. Patients with communication-based disabilities and their support team often have expertise on their ideal communication strategies. Healthcare providers and staff should inquire about communication preferences. Patients should also be oriented to hospital team structure and members, which could include simple solutions such as legible name tags. Hearing aids, batteries, and other assistive technology should have designated places to prevent loss and ensure ongoing working status. In addition, nurse stations should have a communication toolbox that includes replacement batteries for hearing aids along with other assistive technology devices, such as a personal sound amplification product.
Communication Strategies
Healthcare teams should be trained and reminded to use patient-centered communication strategies, including assessing their comprehension of shared health information through teach-back principles. Strategies vary by patient and may require teams’ flexibility in meeting the patient’s needs and preferences. Examples include ensuring one has the patient’s attention and uses good eye contact. Using a projected “radio voice,” which emphasizes clarity and articulation rather than volume, is helpful for those with hearing loss. For some, meaningful gestures (eg, pointing to one’s own head when asking about headaches) can aid communication. Another strategy when having difficulty understanding patients with decreased speech intelligibility is to repeat the audible speech so that the patient only needs to repeat the inaudible portions that were missed. Patients should have secure access to personal assistive devices, such as hearing aids and even smartphones with communication apps (eg, speech-to-text apps) to facilitate interpersonal communication.
Clear Face Masks
Face masks with transparent windows have been developed. Deaf and hard of hearing people’s speech perception increases when speakers use transparent versus conventional masks. The Food and Drug Administration has approved two clear face masks as American Society for Testing Materials Level 1 (Table). These two masks have limited utility for high-risk situations, such as aerosolizing procedures; in such cases, a powered air purifying respirator with a clear viewing window will be needed instead. Notably, clear mask supply has lagged behind demand, creating limited mask availability during the pandemic; their use may need to be restricted to those working with patients with communication-based disabilities.
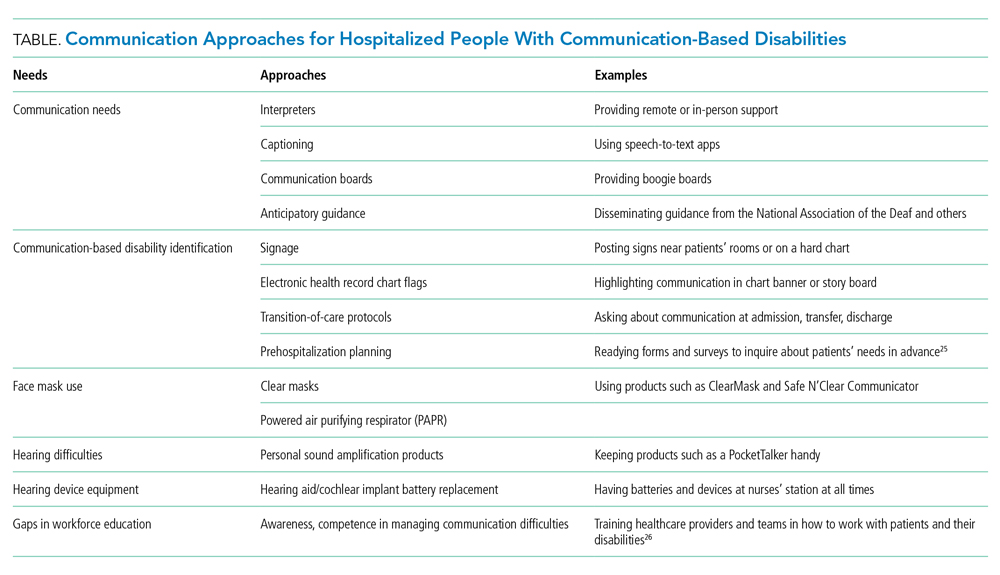
Tools for Communicating Within the Patient’s Room
Erasable whiteboards and communication boards are useful tools for simple exchanges as long as patients’ literacy and fluency are adequate. “PocketTalkers” or personalized sound amplification products may allow providers to speak into a microphone, providing amplified speech via a patient’s headphones. These amplification products are typically useful for those with mild to moderate hearing loss who are not using a hearing aid. Automatic speech recognition apps are device-based apps for converting speech to text. Speakers hold the device near the mouth to maximize accuracy while the patient reads the captions on their screen. With social distancing, lavalier microphones can increase text accuracy, but higher rates of error may still occur due to background noises or accents. For increased reliability and accuracy, Computer Access Realtime Translation stenographers can provide live speech to text on a computer screen from off-site via a computer or smartphone.
Tools for Isolation-Limited Communication
Team members can call an intermediary service to communicate with the patient via the patient’s smartphone or hospital-provided remote video interpreting service, depending on the patient’s preferred communication modality. For oral and spoken language, some services (Table) use remote stenographers to convert speech to text or sign language interpreters for those who use sign language. For both communication modes, smartphone-based videoconferencing may be beneficial while maintaining isolation precautions.
Interpreter Accessibility
Conceptualize interpreters as consulting healthcare team members. They should receive the same PPE training and monitoring as other healthcare workers. For patients using remote video interpretation, this technology needs to be optimized for best results. The room should be in a location with a strong Wi-Fi signal. Equipment should be consistently charged when not in use and rapidly accessible, even remaining in the patients’ room if possible. Healthcare teams need training to appropriately locate and set up the equipment with appropriate support from information technology staff.
Signage
Signage is useful to remind healthcare teams of the patients’ and/or caregivers’ communication-based disability. The most commonly used disability signage shows a line across an ear to indicate hearing loss (Appendix Figure).22 Appropriate signage use, even simple printed sheets documenting a communication issue, can remind healthcare team members of patients’ needs to ensure that communication is accessible and avoid misconceptions toward the patient (eg, noncompliance or cognitive issues). Chart banners, patient room doorways, and over the patients’ beds are good signage locations.
Systematic Noise Reduction
Consistent with previous calls to reduce inpatient noise,23 hospitals should systematically review and monitor protocols to reduce noise pollution. If intra-unit noise varies, patients relying on acoustic-based communication due to hearing loss or speech, language, or voice disability should be placed in quieter rooms.
Communication Concordance
Healthcare professionals and staff with disabilities are an increasingly recognized workforce segment,24 and often are experienced innovators in communicating effectively with patients with communication-based disabilities. Healthcare systems can explore whether they have healthcare team members, employees, disability resource professionals, and/or trainees with these backgrounds and, if they are available, recruit them into developing effective inpatient communication policies and processes.
CONCLUSION
People with communication disabilities experience significant healthcare disparities, now further exacerbated by COVID-19. As clinicians, staff and hospitals work to fuse safety with high-quality communication and care, we should capitalize on multipronged opportunities at the system and individual levels to identify barriers and ensure accessible and effective communication with patients who have communication-based disabilities.
1. McKee MM, Moreland C, Atcherson SR, Zazove P. Hearing loss: communicating with the patient who is deaf or hard of hearing. FP Essent. 2015;434:24-28.
2. Morris MA, Dudgeon BJ, Yorkston K. A qualitative study of adult AAC users’ experiences communicating with medical providers. Disabil Rehabil Assist Technol. 2013;8(6):472-481. https://doi.org/10.3109/17483107.2012.746398
3. Steinberg AG, Barnett S, Meador HE, Wiggins EA, Zazove P. Health care system accessibility. experiences and perceptions of deaf people. J Gen Intern Med. 2006;21(3):260-266. https://doi.org/10.1111/j.1525-1497.2006.00340.x
4. Stransky ML, Jensen KM, Morris MA. Adults with communication disabilities experience poorer health and healthcare outcomes compared to persons without communication disabilities. J Gen Intern Med. 2018;33(12):2147-2155. https://doi.org/10.1007/s11606-018-4625-1
5. Morris MA, Meier SK, Griffin JM, Branda ME, Phelan SM. Prevalence and etiologies of adult communication disabilities in the United States: results from the 2012 National Health Interview Survey. Disabil Health J. 2016;9(1):140-144. https://doi.org/10.1016/j.dhjo.2015.07.004
6. Blackwell DL, Lucas JW, Clarke TC. Summary health statistics for U.S. adults: National Health Interview Survey, 2012. Vital Health Stat. 2014(260):1-161.
7. Chang JE, Weinstein B, Chodosh J, Blustein J. Hospital readmission risk for patients with self-reported hearing loss and communication trouble. J Am Geriatr Soc. 2018;66(11):2227-2228. https://doi.org/10.1111/jgs.15545
8. McKee M, Moran C, Zazove P. Overcoming additional barriers to care for deaf and hard of hearing patients during COVID-19. JAMA Otolaryngol Head Neck Surg. 2020;146(9):781-782. https://doi.org/10.1001/jamaoto.2020.1705
9. Bartlett G, Blais R, Tamblyn R, Clermont RJ, MacGibbon B. Impact of patient communication problems on the risk of preventable adverse events in acute care settings. CMAJ. 2008;178(12):1555-1562. https://doi.org/10.1503/cmaj.070690
10. Hoffman JM, Yorkston KM, Shumway-Cook A, Ciol MA, Dudgeon BJ, Chan L. Effect of communication disability on satisfaction with health care: a survey of medicare beneficiaries. Am J Speech Lang Pathol. 2005;14(3):221-228. https://doi.org/10.1044/1058-0360(2005/022)
11. Kelley JM, Kraft-Todd G, Schapira L, Kossowsky J, Riess H. The influence of the patient-clinician relationship on healthcare outcomes: a systematic review and meta-analysis of randomized controlled trials. PLoS One. 2014;9(4):e94207. https://doi.org/10.1371/journal.pone.0094207
12. Mast MS. On the importance of nonverbal communication in the physician-patient interaction. Patient Educ Couns. 2007;67(3):315-318. https://doi.org/10.1016/j.pec.2007.03.005
13. Street RL Jr, Makoul G, Arora NK, Epstein RM. How does communication heal? pathways linking clinician-patient communication to health outcomes. Patient Educ Couns. 2009;74(3):295-301. https://doi.org/10.1016/j.pec.2008.11.015
14. Genther DJ, Frick KD, Chen D, Betz J, Lin FR. Association of hearing loss with hospitalization and burden of disease in older adults. JAMA. 2013;309(22):2322-2324. https://doi.org/10.1001/jama.2013.5912
15. Lin FR, Yaffe K, Xia J, et al. Hearing loss and cognitive decline in older adults. JAMA Intern Med. 2013;173(4):293-299. https://doi.org/10.1001/jamainternmed.2013.1868
16. McKee MM, Stransky ML, Reichard A. Hearing loss and associated medical conditions among individuals 65 years and older. Disabil Health J. 2018;11(1):122-125. https://doi.org/10.1016/j.dhjo.2017.05.007
17. ADA requirements: effective communication. U.S. Department of Justice. January 31, 2014. Accessed February 12, 2021. https://www.ada.gov/effective-comm.htm
18. OCR resolves complaints after State of Connecticut and private hospital safeguard the rights of persons with disabilities to have reasonable access to support persons in hospital settings during COVID-19. Press Release. US Department of Health and Human Services; June 9, 2020. Accessed September 19, 2020. https://www.hhs.gov/about/news/2020/06/09/ocr-resolves-complaints-after-state-connecticut-private-hospital-safeguard-rights-persons.html
19. Goldin A, Weinstein B, Shiman N. How do medical masks degrade speech perception? The Hearing Review. April 1, 2020. Accessed September 30, 2020. https://www.hearingreview.com/hearing-loss/health-wellness/how-do-medical-masks-degrade-speech-reception
20. Mendel LL, Gardino JA, Atcherson SR. Speech understanding using surgical masks: a problem in health care? J Am Acad Audiol. 2008;19(9):686-695. https://doi.org/10.3766/jaaa.19.9.4
21. Atcherson SR, Finley ET, McDowell BR, Watson C. More speech degradations and considerations in the search for transparent face coverings during the COVID-19 pandemic. American Academy of Audiology. November/December 2020. Accessed September 19, 2020. https://www.audiology.org/audiology-today-julyaugust-2020/online-feature-more-speech-degradations-and-considerations-search
22. Hearing Loss. Wikipedia. Accessed October 28, 2020. https://en.wikipedia.org/wiki/Hearing_loss
23. Kamdar BB, Martin JL, Needham DM. Noise and light pollution in the hospital: a call for action. J Hosp Med. 2017;12(10):861-862. https://doi.org/10.12788/jhm.2838
24. Meeks LM, Herzer K, Jain NR. Removing barriers and facilitating access: increasing the number of physicians with disabilities. Acad Med. 2018;93(4):540-543. https://doi.org/10.1097/acm.0000000000002112
25. Communication Access Plan (CAP): Instructions for Patients and Providers. Hearing Loss Association of America (HLAA). Accessed September 30, 2020. https://www.hearingloss.org/wp-content/uploads/HLAA_HC_CAP_Form_and_Instructions.pdf
26. How Do I Communicate with Doctors, Nurses, and Staff at the Hospital During COVID-19? Hearing Loss Association of America (HLAA). May 8, 2020. Accessed September 30, 2020. https://www.hearingloss.org/communication-access-recommendations-hospitals-covid-19/
1. McKee MM, Moreland C, Atcherson SR, Zazove P. Hearing loss: communicating with the patient who is deaf or hard of hearing. FP Essent. 2015;434:24-28.
2. Morris MA, Dudgeon BJ, Yorkston K. A qualitative study of adult AAC users’ experiences communicating with medical providers. Disabil Rehabil Assist Technol. 2013;8(6):472-481. https://doi.org/10.3109/17483107.2012.746398
3. Steinberg AG, Barnett S, Meador HE, Wiggins EA, Zazove P. Health care system accessibility. experiences and perceptions of deaf people. J Gen Intern Med. 2006;21(3):260-266. https://doi.org/10.1111/j.1525-1497.2006.00340.x
4. Stransky ML, Jensen KM, Morris MA. Adults with communication disabilities experience poorer health and healthcare outcomes compared to persons without communication disabilities. J Gen Intern Med. 2018;33(12):2147-2155. https://doi.org/10.1007/s11606-018-4625-1
5. Morris MA, Meier SK, Griffin JM, Branda ME, Phelan SM. Prevalence and etiologies of adult communication disabilities in the United States: results from the 2012 National Health Interview Survey. Disabil Health J. 2016;9(1):140-144. https://doi.org/10.1016/j.dhjo.2015.07.004
6. Blackwell DL, Lucas JW, Clarke TC. Summary health statistics for U.S. adults: National Health Interview Survey, 2012. Vital Health Stat. 2014(260):1-161.
7. Chang JE, Weinstein B, Chodosh J, Blustein J. Hospital readmission risk for patients with self-reported hearing loss and communication trouble. J Am Geriatr Soc. 2018;66(11):2227-2228. https://doi.org/10.1111/jgs.15545
8. McKee M, Moran C, Zazove P. Overcoming additional barriers to care for deaf and hard of hearing patients during COVID-19. JAMA Otolaryngol Head Neck Surg. 2020;146(9):781-782. https://doi.org/10.1001/jamaoto.2020.1705
9. Bartlett G, Blais R, Tamblyn R, Clermont RJ, MacGibbon B. Impact of patient communication problems on the risk of preventable adverse events in acute care settings. CMAJ. 2008;178(12):1555-1562. https://doi.org/10.1503/cmaj.070690
10. Hoffman JM, Yorkston KM, Shumway-Cook A, Ciol MA, Dudgeon BJ, Chan L. Effect of communication disability on satisfaction with health care: a survey of medicare beneficiaries. Am J Speech Lang Pathol. 2005;14(3):221-228. https://doi.org/10.1044/1058-0360(2005/022)
11. Kelley JM, Kraft-Todd G, Schapira L, Kossowsky J, Riess H. The influence of the patient-clinician relationship on healthcare outcomes: a systematic review and meta-analysis of randomized controlled trials. PLoS One. 2014;9(4):e94207. https://doi.org/10.1371/journal.pone.0094207
12. Mast MS. On the importance of nonverbal communication in the physician-patient interaction. Patient Educ Couns. 2007;67(3):315-318. https://doi.org/10.1016/j.pec.2007.03.005
13. Street RL Jr, Makoul G, Arora NK, Epstein RM. How does communication heal? pathways linking clinician-patient communication to health outcomes. Patient Educ Couns. 2009;74(3):295-301. https://doi.org/10.1016/j.pec.2008.11.015
14. Genther DJ, Frick KD, Chen D, Betz J, Lin FR. Association of hearing loss with hospitalization and burden of disease in older adults. JAMA. 2013;309(22):2322-2324. https://doi.org/10.1001/jama.2013.5912
15. Lin FR, Yaffe K, Xia J, et al. Hearing loss and cognitive decline in older adults. JAMA Intern Med. 2013;173(4):293-299. https://doi.org/10.1001/jamainternmed.2013.1868
16. McKee MM, Stransky ML, Reichard A. Hearing loss and associated medical conditions among individuals 65 years and older. Disabil Health J. 2018;11(1):122-125. https://doi.org/10.1016/j.dhjo.2017.05.007
17. ADA requirements: effective communication. U.S. Department of Justice. January 31, 2014. Accessed February 12, 2021. https://www.ada.gov/effective-comm.htm
18. OCR resolves complaints after State of Connecticut and private hospital safeguard the rights of persons with disabilities to have reasonable access to support persons in hospital settings during COVID-19. Press Release. US Department of Health and Human Services; June 9, 2020. Accessed September 19, 2020. https://www.hhs.gov/about/news/2020/06/09/ocr-resolves-complaints-after-state-connecticut-private-hospital-safeguard-rights-persons.html
19. Goldin A, Weinstein B, Shiman N. How do medical masks degrade speech perception? The Hearing Review. April 1, 2020. Accessed September 30, 2020. https://www.hearingreview.com/hearing-loss/health-wellness/how-do-medical-masks-degrade-speech-reception
20. Mendel LL, Gardino JA, Atcherson SR. Speech understanding using surgical masks: a problem in health care? J Am Acad Audiol. 2008;19(9):686-695. https://doi.org/10.3766/jaaa.19.9.4
21. Atcherson SR, Finley ET, McDowell BR, Watson C. More speech degradations and considerations in the search for transparent face coverings during the COVID-19 pandemic. American Academy of Audiology. November/December 2020. Accessed September 19, 2020. https://www.audiology.org/audiology-today-julyaugust-2020/online-feature-more-speech-degradations-and-considerations-search
22. Hearing Loss. Wikipedia. Accessed October 28, 2020. https://en.wikipedia.org/wiki/Hearing_loss
23. Kamdar BB, Martin JL, Needham DM. Noise and light pollution in the hospital: a call for action. J Hosp Med. 2017;12(10):861-862. https://doi.org/10.12788/jhm.2838
24. Meeks LM, Herzer K, Jain NR. Removing barriers and facilitating access: increasing the number of physicians with disabilities. Acad Med. 2018;93(4):540-543. https://doi.org/10.1097/acm.0000000000002112
25. Communication Access Plan (CAP): Instructions for Patients and Providers. Hearing Loss Association of America (HLAA). Accessed September 30, 2020. https://www.hearingloss.org/wp-content/uploads/HLAA_HC_CAP_Form_and_Instructions.pdf
26. How Do I Communicate with Doctors, Nurses, and Staff at the Hospital During COVID-19? Hearing Loss Association of America (HLAA). May 8, 2020. Accessed September 30, 2020. https://www.hearingloss.org/communication-access-recommendations-hospitals-covid-19/
© 2021 Society of Hospital Medicine
Protecting Children by Healing Their Caregivers
It was a busy night in the emergency department. EMS called to give a heads up—they were on their way with a girl who was “pretty banged up.” They warned us that the story seemed a little fishy. We thought we were ready. The trauma bay was organized; supplies were at the ready and everyone had a role. Within seconds of her arrival, it was clear that no one could ever have been truly prepared. She was unresponsive and unstable. Her injuries were widespread, brutal, and long term. My seasoned attendings would describe it as no less than horrific. There was no question—someone had done this to her.
After she was stabilized, her wounds were gently tended, her body was bathed, her hair was combed. She died several days later. While distressed, many members of her team took consolation in the idea that, after years of torture, she finally got to be loved.
It’s no wonder that every person involved with her care during her hospitalization was so deeply affected by her. How could anyone do this to another person? Or even worse, to an innocent child? “What a monster,” we said. “Only a monster could have done this.”
While anyone would agree that what this abuser—the girl’s mother—did was brutal and wrong, I would also argue that the underlying danger is much more systemic. We call her the “monster,” but I sense that the real monster is still lurking in the shadows, unnamed. I can’t help but try to understand this woman; it is unfair to condemn her without first learning her story. How were her actions guided by her own history of trauma, abuse, and violent discipline as a child? We preach to each other and to our learners that trauma-informed care is essential; you must not ask what’s wrong with you, but what happened to you. Founder and Director of the Equal Justice Initiative Bryan Stevenson has said that “each of us is more than the worst thing we’ve ever done.”1 It’s inhumane of us to dehumanize her for this atrocity, especially without pausing to ask how her environment, personal trauma, and understanding of child development set the risk.
It is important to understand the cycle of trauma and abuse. Traumatic experiences have been shown to alter neurodevelopment and the body’s stress response, particularly when experiences take place early in life, when they are repeated and long term, and when they are severe. We know that adverse childhood experiences are cumulative and result in adverse outcomes as adults, including increased likelihood of violent or criminal activity. We know that prior history of trauma, specifically child abuse, sexual abuse, or domestic violence, is associated with higher potential for child abuse later on.
The effect of experiencing trauma is such that only 22% of adults who experienced abuse or neglect as children will achieve resiliency.2 In a world in which social distancing and isolation have become the new normal, we must be even more aware of the effects of trauma on families. The COVID-19 pandemic has increased known risk factors for child abuse, including financial hardship, unemployment, increased anxiety, increased caregiver responsibilities, and decreased access to mental health services and community resources.3 Furthermore, virtual learning environments may have significant implications on the reporting of child abuse. Among cases of maltreatment of children that received an investigation or alternative response in 2018, 20.5% were reported by education personnel.4 While remote learning options may be necessary to minimize risk of viral spread, fewer interactions between children and mandatory reporters may result in child maltreatment going undetected. In the face of these challenges, I urge our healthcare system to use current constraints as fuel for creative interventions including the following:
- Applying advances in telemedicine to create a new opportunity to interface with families, provide mental health support, connect them with resources, and offer gentle guidance about safe parenting.
- Improving both screening methods for parental trauma and distress and referrals for support services.
- Advocating for adequate access to life-sustaining resources including shelter, food, and healthcare for all families. This is a necessary foundation for building resilience.
- Providing bias training for mandatory reporters to ensure that all children and their families are approached with respect and compassion.
- Prioritizing innovation that provides long-lasting, sustainable, and equitable access to support and healing.
To best protect our children, we must heal their adult caregivers; we must help them to conquer their monsters.
Our patient and her family have since visited me in my thoughts and dreams, less often now than before. While I never truly knew her, she has left an open void where there should have been the promise of a healthy, growing, and developing child. Within that void resides fear. I fear for other “hidden children” and the abuse they are at risk for experiencing. I fear that her siblings, now living without their mother, will become victims of the instability of being “in the system.” I fear that by turning to punishment as our only solution, we miss opportunities to prevent such tragedy. Despite the darkness, she also brings me hope. I hope that her siblings can rely on each other as a foundation for resilience. I hope that we as a healthcare system can continue to love our patients without question or condition. I hope that we as a society can invest in breaking the cycle of trauma and in supporting parents. I hope that we can create a system in which children can grow up free from abuse.
1. Stevenson B. Just Mercy: A Story of Justice and Redemption. Spiegel & Grau; 2015.
2. De Bellis MD, Zisk A. The biological effects of childhood trauma. Child Adolesc Psychiatr Clin N Am. 2014;23(2):185-222. https://doi.org/10.1016/j.chc.2014.01.002
3. Schneider W, Waldfogel J, Brooks-Gunn J. The Great Recession and risk for child abuse and neglect. Child Youth Serv Rev. 2017;72:71-81. https://doi.org/10.1016/j.childyouth.2016.10.016
4. Child Maltreatment 2018. Children’s Bureau, Youth and Families, Administration on Children, Administration for Children and Families, U.S. Department of Health & Human Services; January 15, 2020. Accessed May 10, 2020. https://www.acf.hhs.gov/cb/resource/child-maltreatment-2018
It was a busy night in the emergency department. EMS called to give a heads up—they were on their way with a girl who was “pretty banged up.” They warned us that the story seemed a little fishy. We thought we were ready. The trauma bay was organized; supplies were at the ready and everyone had a role. Within seconds of her arrival, it was clear that no one could ever have been truly prepared. She was unresponsive and unstable. Her injuries were widespread, brutal, and long term. My seasoned attendings would describe it as no less than horrific. There was no question—someone had done this to her.
After she was stabilized, her wounds were gently tended, her body was bathed, her hair was combed. She died several days later. While distressed, many members of her team took consolation in the idea that, after years of torture, she finally got to be loved.
It’s no wonder that every person involved with her care during her hospitalization was so deeply affected by her. How could anyone do this to another person? Or even worse, to an innocent child? “What a monster,” we said. “Only a monster could have done this.”
While anyone would agree that what this abuser—the girl’s mother—did was brutal and wrong, I would also argue that the underlying danger is much more systemic. We call her the “monster,” but I sense that the real monster is still lurking in the shadows, unnamed. I can’t help but try to understand this woman; it is unfair to condemn her without first learning her story. How were her actions guided by her own history of trauma, abuse, and violent discipline as a child? We preach to each other and to our learners that trauma-informed care is essential; you must not ask what’s wrong with you, but what happened to you. Founder and Director of the Equal Justice Initiative Bryan Stevenson has said that “each of us is more than the worst thing we’ve ever done.”1 It’s inhumane of us to dehumanize her for this atrocity, especially without pausing to ask how her environment, personal trauma, and understanding of child development set the risk.
It is important to understand the cycle of trauma and abuse. Traumatic experiences have been shown to alter neurodevelopment and the body’s stress response, particularly when experiences take place early in life, when they are repeated and long term, and when they are severe. We know that adverse childhood experiences are cumulative and result in adverse outcomes as adults, including increased likelihood of violent or criminal activity. We know that prior history of trauma, specifically child abuse, sexual abuse, or domestic violence, is associated with higher potential for child abuse later on.
The effect of experiencing trauma is such that only 22% of adults who experienced abuse or neglect as children will achieve resiliency.2 In a world in which social distancing and isolation have become the new normal, we must be even more aware of the effects of trauma on families. The COVID-19 pandemic has increased known risk factors for child abuse, including financial hardship, unemployment, increased anxiety, increased caregiver responsibilities, and decreased access to mental health services and community resources.3 Furthermore, virtual learning environments may have significant implications on the reporting of child abuse. Among cases of maltreatment of children that received an investigation or alternative response in 2018, 20.5% were reported by education personnel.4 While remote learning options may be necessary to minimize risk of viral spread, fewer interactions between children and mandatory reporters may result in child maltreatment going undetected. In the face of these challenges, I urge our healthcare system to use current constraints as fuel for creative interventions including the following:
- Applying advances in telemedicine to create a new opportunity to interface with families, provide mental health support, connect them with resources, and offer gentle guidance about safe parenting.
- Improving both screening methods for parental trauma and distress and referrals for support services.
- Advocating for adequate access to life-sustaining resources including shelter, food, and healthcare for all families. This is a necessary foundation for building resilience.
- Providing bias training for mandatory reporters to ensure that all children and their families are approached with respect and compassion.
- Prioritizing innovation that provides long-lasting, sustainable, and equitable access to support and healing.
To best protect our children, we must heal their adult caregivers; we must help them to conquer their monsters.
Our patient and her family have since visited me in my thoughts and dreams, less often now than before. While I never truly knew her, she has left an open void where there should have been the promise of a healthy, growing, and developing child. Within that void resides fear. I fear for other “hidden children” and the abuse they are at risk for experiencing. I fear that her siblings, now living without their mother, will become victims of the instability of being “in the system.” I fear that by turning to punishment as our only solution, we miss opportunities to prevent such tragedy. Despite the darkness, she also brings me hope. I hope that her siblings can rely on each other as a foundation for resilience. I hope that we as a healthcare system can continue to love our patients without question or condition. I hope that we as a society can invest in breaking the cycle of trauma and in supporting parents. I hope that we can create a system in which children can grow up free from abuse.
It was a busy night in the emergency department. EMS called to give a heads up—they were on their way with a girl who was “pretty banged up.” They warned us that the story seemed a little fishy. We thought we were ready. The trauma bay was organized; supplies were at the ready and everyone had a role. Within seconds of her arrival, it was clear that no one could ever have been truly prepared. She was unresponsive and unstable. Her injuries were widespread, brutal, and long term. My seasoned attendings would describe it as no less than horrific. There was no question—someone had done this to her.
After she was stabilized, her wounds were gently tended, her body was bathed, her hair was combed. She died several days later. While distressed, many members of her team took consolation in the idea that, after years of torture, she finally got to be loved.
It’s no wonder that every person involved with her care during her hospitalization was so deeply affected by her. How could anyone do this to another person? Or even worse, to an innocent child? “What a monster,” we said. “Only a monster could have done this.”
While anyone would agree that what this abuser—the girl’s mother—did was brutal and wrong, I would also argue that the underlying danger is much more systemic. We call her the “monster,” but I sense that the real monster is still lurking in the shadows, unnamed. I can’t help but try to understand this woman; it is unfair to condemn her without first learning her story. How were her actions guided by her own history of trauma, abuse, and violent discipline as a child? We preach to each other and to our learners that trauma-informed care is essential; you must not ask what’s wrong with you, but what happened to you. Founder and Director of the Equal Justice Initiative Bryan Stevenson has said that “each of us is more than the worst thing we’ve ever done.”1 It’s inhumane of us to dehumanize her for this atrocity, especially without pausing to ask how her environment, personal trauma, and understanding of child development set the risk.
It is important to understand the cycle of trauma and abuse. Traumatic experiences have been shown to alter neurodevelopment and the body’s stress response, particularly when experiences take place early in life, when they are repeated and long term, and when they are severe. We know that adverse childhood experiences are cumulative and result in adverse outcomes as adults, including increased likelihood of violent or criminal activity. We know that prior history of trauma, specifically child abuse, sexual abuse, or domestic violence, is associated with higher potential for child abuse later on.
The effect of experiencing trauma is such that only 22% of adults who experienced abuse or neglect as children will achieve resiliency.2 In a world in which social distancing and isolation have become the new normal, we must be even more aware of the effects of trauma on families. The COVID-19 pandemic has increased known risk factors for child abuse, including financial hardship, unemployment, increased anxiety, increased caregiver responsibilities, and decreased access to mental health services and community resources.3 Furthermore, virtual learning environments may have significant implications on the reporting of child abuse. Among cases of maltreatment of children that received an investigation or alternative response in 2018, 20.5% were reported by education personnel.4 While remote learning options may be necessary to minimize risk of viral spread, fewer interactions between children and mandatory reporters may result in child maltreatment going undetected. In the face of these challenges, I urge our healthcare system to use current constraints as fuel for creative interventions including the following:
- Applying advances in telemedicine to create a new opportunity to interface with families, provide mental health support, connect them with resources, and offer gentle guidance about safe parenting.
- Improving both screening methods for parental trauma and distress and referrals for support services.
- Advocating for adequate access to life-sustaining resources including shelter, food, and healthcare for all families. This is a necessary foundation for building resilience.
- Providing bias training for mandatory reporters to ensure that all children and their families are approached with respect and compassion.
- Prioritizing innovation that provides long-lasting, sustainable, and equitable access to support and healing.
To best protect our children, we must heal their adult caregivers; we must help them to conquer their monsters.
Our patient and her family have since visited me in my thoughts and dreams, less often now than before. While I never truly knew her, she has left an open void where there should have been the promise of a healthy, growing, and developing child. Within that void resides fear. I fear for other “hidden children” and the abuse they are at risk for experiencing. I fear that her siblings, now living without their mother, will become victims of the instability of being “in the system.” I fear that by turning to punishment as our only solution, we miss opportunities to prevent such tragedy. Despite the darkness, she also brings me hope. I hope that her siblings can rely on each other as a foundation for resilience. I hope that we as a healthcare system can continue to love our patients without question or condition. I hope that we as a society can invest in breaking the cycle of trauma and in supporting parents. I hope that we can create a system in which children can grow up free from abuse.
1. Stevenson B. Just Mercy: A Story of Justice and Redemption. Spiegel & Grau; 2015.
2. De Bellis MD, Zisk A. The biological effects of childhood trauma. Child Adolesc Psychiatr Clin N Am. 2014;23(2):185-222. https://doi.org/10.1016/j.chc.2014.01.002
3. Schneider W, Waldfogel J, Brooks-Gunn J. The Great Recession and risk for child abuse and neglect. Child Youth Serv Rev. 2017;72:71-81. https://doi.org/10.1016/j.childyouth.2016.10.016
4. Child Maltreatment 2018. Children’s Bureau, Youth and Families, Administration on Children, Administration for Children and Families, U.S. Department of Health & Human Services; January 15, 2020. Accessed May 10, 2020. https://www.acf.hhs.gov/cb/resource/child-maltreatment-2018
1. Stevenson B. Just Mercy: A Story of Justice and Redemption. Spiegel & Grau; 2015.
2. De Bellis MD, Zisk A. The biological effects of childhood trauma. Child Adolesc Psychiatr Clin N Am. 2014;23(2):185-222. https://doi.org/10.1016/j.chc.2014.01.002
3. Schneider W, Waldfogel J, Brooks-Gunn J. The Great Recession and risk for child abuse and neglect. Child Youth Serv Rev. 2017;72:71-81. https://doi.org/10.1016/j.childyouth.2016.10.016
4. Child Maltreatment 2018. Children’s Bureau, Youth and Families, Administration on Children, Administration for Children and Families, U.S. Department of Health & Human Services; January 15, 2020. Accessed May 10, 2020. https://www.acf.hhs.gov/cb/resource/child-maltreatment-2018
© 2021 Society of Hospital Medicine
Prioritizing High-Value, Equitable Care After the COVID-19 Shutdown: An Opportunity for a Healthcare Renaissance
The day after Memorial Day 2020 marked an important transition in the United States’ experience with coronavirus disease 2019 (COVID-19), with many states making initial plans to reopen.
This year’s widespread healthcare closures were necessary to reduce COVID-19 transmission and prepare for a future patient surge, but these closures had unintended consequences. Nearly half of adults polled said they or someone in their household had foregone or delayed care since the outbreak began.1 This was especially true for visits to emergency departments and doctors’ offices for strokes, heart attacks, and routine medical care.2 In a survey across 49 states, only 7% of primary care practices considered scheduling preventive visits as a high priority.3 Eleven percent of polled adults reported delaying care worsened their condition,1 and in hard-hit areas such as New York City, non-COVID mortality was 22% higher than expected.4
Avoidance of the medical system decreased not only use of necessary, high-value care but also use of low-value care. Low-value services are those in which the “potential for harms exceed the potential benefits,”5 such as unnecessary hospitalizations, avoidable emergency department or clinic visits, unwarranted or excessive diagnostic testing (eg, annual physicals), and certain procedures (eg, spinal fusion surgery for low-back pain).
KEEP PATIENTS CENTRAL IN REOPENING SERVICES TO DELIVER HIGH-VALUE CARE
Medical centers can better focus on high-value care by defining their high-risk patient populations; high-value treatments, procedures, and preventive care; and phases of reopening. During the first pandemic wave, medical centers tried to reassure patients about emergency care, such as coming in for chest pain or neurologic symptoms, through personal outreach and media campaigns. Outpatient virtual visits also continued, including primary care, specialty services, mental health treatment, and physical therapy. While reopening, some medical centers have assessed disparities by relying on their data analytics and, if available, embedded health services researchers to understand what care was stopped and what populations were most affected.
The University of California health systems, for example, had a learning collaborative focused on sharing methods to restore care delivery that prioritizes patient needs. Some campuses conducted analyses using both electronic health record data and input from patients and their care teams to identify clinical needs and determine patient outreach plans. Some approaches used machine learning models to identify patients at highest risk of hospitalization or emergency department visits over the next 12 months and to conduct additional outreach to schedule these patients in primary and specialty care if clinically appropriate. Similarly, surgical specialties identified the highest-priority nonemergent surgeries for scheduling, including cancer resection, radiation therapy, and pain-management procedures. Similar guidance toward the most meaningful care has been prioritized within the United States Department of Veterans Affairs.
The rapid deployment of telehealth and payment models that reimburse video and in-clinic visits equally created new opportunities for medical centers to expand high-value care in lower-cost home settings. Similarly, new infrastructure is being developed to help define smarter use of virtual visits and home-based lab collection and monitoring.
Medical centers also must pay careful attention to redeploying service capacity for underused, high-value services. The pandemic uncovered existing staff that could be redeployed to support these changes. For example, with an “all hands on deck” mentality during the pandemic, in some medical centers, analysts or care managers from less-prioritized or duplicative areas were reassigned to vital COVID-19 efforts. Medical centers may realize that this staff can provide more value in the future by supporting increased high-value, affordable healthcare.
DELIBERATELY AVOID LOW-VALUE CARE
During the intial wave of the pandemic, medical centers greatly reduced the care they provided, often focusing on delivering essential care. This preparation for a surge of COVID patients had the effect of halting many unnecessary services by moving care from the clinic to home under new reimbursement changes, such as those affecting telehealth payments. The experience of reducing low-value medical services and visits can be extended to limiting unnecessary diagnostic testing. Medical centers could, for example, focus only on tests that advance care plans; reduce unnecessary blood draws, procedures, and vital sign checks on stable patients; shift to medications with less-frequent dosing intervals; and consolidate visits by treatment teams.10,11
Medical centers, however, now face continued pressures to increase revenue because 75% report their organization’s top priority is focused on increasing patient volume.12
PROACTIVELY AVOID WORSENING HEALTHCARE DISPARITIES
As medical centers reboot, operational and clinical leaders must proactively view changes through an equity lens to avoid exacerbating health disparities among vulnerable populations. The pandemic has focused national attention on the severity and pervasiveness of disparities and created an imperative for substantive action to evaluate how every decision will affect health equity. For example, medical centers are expanding use of telehealth to improve patient outreach. However, in a survey of primary care physicians, 72% said they have patients who are unable to access telehealth because they do not have access to technology.3 Exclusion of these patients from programs risks worsening health disparities. In a recent survey, nearly 65% of medical centers report reexamining existing policies, protocols, and practices for patients at risk of disparities.12
REFORM TO SUPPORT HIGH-VALUE CARE DELIVERY
Medical centers nationwide will need payment reform that provides greater financial stability beyond the pandemic to support high-value care delivery. They also will need flexibility to invest in prevention and to deliver the appropriate intensity of care to meet patients’ and communities’ needs.15-17 Options to provide this support include prospective population-based payments that may create more resilience in protecting access to care when it is most needed. Models can include fully capitated payment for physician practices.19,20 For example, after Vermont entered a single accountable care organization (ACO) model with the Centers for Medicare & Medicaid Services (CMS) in 2018, they not only generated a $97 million Medicaid savings, but also had a financial cushion that was later used in their COVID-19 response.21,22 The advanced payments allowed primary care practices and community agencies to invest in a digital tool to support outreach to patient at high risk for virus complications.
Hospitals similarly can adapt global budgets that incentivize financial stewardship by encouraging clinicians to resume necessary services and not unnecessary ones.16 For example, CMS partnered with Pennsylvania’s Department of Health to provide prospective all-payer global budgets for rural hospitals and Maryland’s Health Services Cost Review Commission that negotiates a budget with each hospital. During the COVID-19 pandemic, hospitals in these programs have had more financial protection from fluctuating finances by allowing for easier shifts in service delivery location and adjustments in rates to compensate for declines in visits and procedures.23
Policy makers and payers also can hold medical centers accountable to evidence-based guidelines and appropriate use of care, especially when necessary but expensive (eg, percutaneous coronary interventions, spinal surgeries, or cancer care). Funding agencies, additionally, can support these efforts by focusing on research, dissemination, and reliable implementation of these practices.
CONCLUSION
The COVID-19 crisis presents a tremendous opportunity for each medical center to revitalize healthcare. This opportunity can be seized only with reform by policy makers, payers, and regulatory agencies who encourage restarting high-value care without low-value services. We must take deliberate action so the nation’s medical centers can better meet patients’ needs to make healthcare more resilient, efficient, and fair.
1. Hamel L, Kearney A, Kirzinger A, Lopes L, Muñana C, Brodie M. KFF Health Tracking Poll - May 2020: Impact of Coronavirus on Personal Health, Economic and Food Security, and Medicaid. Kaiser Family Foundation; May 27, 2020. Accessed August 9, 2020. https://www.kff.org/report-section/kff-health-tracking-poll-may-2020-health-and-economic-impacts/
2. McFarling UL. ‘Where are all our patients?’: Covid phobia is keeping people with serious heart symptoms away from ERs. STAT. April 23, 2020. Accessed August 9, 2020. https://www.statnews.com/2020/04/23/coronavirus-phobia-keeping-heart-patients-away-from-er/
3. Primary Care & COVID-19: Week 4 Survey. Primary Care Collaborative; April 9, 2020. Accessed August 9, 2020. https://www.pcpcc.org/2020/04/08/primary-care-covid-19-week-4-survey
4. Olson DR, Huynh M, Fine A, et al. New York City Department of Health and Mental Hygiene (DOHMH) COVID-19 Response Team. Preliminary estimate of excess mortality during the COVID-19 outbreak — New York City, March 11–May 2, 2020. Morbidity and Mortality Weekly Report. May 11, 2020. Accessed August 9, 2020. https://stacks.cdc.gov/view/cdc/87858
5. Chassin MR, Galvin RW. The urgent need to improve health care quality. Institute of Medicine National Roundtable on Health Care Quality. JAMA. 1998;280(11):1000-1005. https://doi.org/10.1001/jama.280.11.1000
6. Shrank WH, Rogstad TL, Parekh N. Waste in the US health care system: estimated costs and potential for savings. JAMA. 2019;322(15):1501-1509. https://doi.org/10.1001/jama.2019.13978
7. Collins SR, Gunja MZ, Doty MM, Bhupal HK. Americans’ confidence in their ability to pay for health care is falling. To The Point blog. May 10, 2018. The Commonwealth Fund. Accessed August 9, 2020. https://www.commonwealthfund.org/blog/2018/americans-confidence-their-ability-pay-health-care-falling
8. Saad L. More Americans delaying medical treatment due to cost. Gallup News. December 9, 2019. Accessed August 9, 2020. https://news.gallup.com/poll/269138/americans-delaying-medical-treatment-due-cost.aspx
9. Lee VS. Fee for service is a terrible way to pay for health care. Try a subscription model instead. STAT. June 12, 2020. Accessed August 9, 2020. https://www.statnews.com/2020/06/12/fee-for-service-is-a-terrible-way-to-pay-for-health-care-try-a-subscription-model-instead/
10. Moriates C, Shah NT, Arora VM. A framework for the frontline: how hospitalists can improve healthcare value. J Hosp Med. 2016;11(4):297-302. https://doi.org/10.1002/jhm.2494
11. Seymann G, Komsoukaniants A, Bouland D, Jenkins I. The Silver Linings Playbook for Covid-19. KevinMD. June 12, 2020. Accessed August 9, 2020. https://www.kevinmd.com/blog/2020/06/the-silver-linings-playbook-for-covid-19.html
12. Advis In The News. Industry Professionals Weigh In: Future of Healthcare Survey. Advis. Accessed August 9, 2020. https://advis.com/advis-in-the-news/post-pandemic-survey-june2020/
13. APM Measurement Effort. Healthcare Learning Payment and Action Network; 2019. Accessed August 9, 2020. https://hcp-lan.org/workproducts/apm-infographic-2019.pdf
14. Mosley D, DeBehnke D. Rural hospital sustainability: new analysis shows worsening situation for rural hospitals, residents. Navigant; February 2019. Accessed August 9, 2020. https://guidehouse.com/-/media/www/site/insights/healthcare/2019/navigant-rural-hospital-analysis-22019.pdf
15. Gondi S, Chokshi DA. Financial stability as a goal of payment reform—a lesson from COVID-19. JAMA Health Forum. August 6, 2020. Accessed August 9, 2020. https://jamanetwork.com/channels/health-forum/fullarticle/2769307
16. Murphy K, Koski-Vacirca R, Sharfstein J. Resilience in health care financing. JAMA. 2020;324(2):126-127. https://doi.org/10.1001/jama.2020.10417
17. Khullar D, Bond AM, Schpero WL. COVID-19 and the financial health of US hospitals. JAMA. 2020;323(21):2127-2128. https://doi.org/10.1001/jama.2020.6269
18. Weiss AJ, Elixhauser A, Andrews RM. Statistical Brief #170: Characteristics of Operating Room Procedures in U.S. Hospitals, 2011. Healthcare Costs and Utilization Project, Agency for Healthcare Research and Quality; February 2014. Accessed August 9, 2020: https://www.hcup-us.ahrq.gov/reports/statbriefs/sb170-Operating-Room-Procedures-United-States-2011.pdf
19. Crook HL, Saunders RS, Bleser WK, Broome T, Muhlestein D, McLellan MB. Leveraging Payment Reforms For COVID-19 And Beyond: Recommendations For Medicare ACOs And CMS’s Interim Final Rule. Health Affairs Blog. May 29, 2020. Accessed August 9, 2020. https://www.healthaffairs.org/do/10.1377/hblog20200528.402208/full/
20. Blue Cross NC Launches Comprehensive Program to Help Independent Primary Care Practices Stay in Business. Press release. BlueCross BlueShield of North Carolina; June 24, 2020. Accessed August 9, 2020. https://mediacenter.bcbsnc.com/news/blue-cross-nc-launches-comprehensive-program-to-help-independent-primary-care-practices-stay-in-business
21. RTI International. State Innovation Models (SIM) Initiative Evaluation: Model Test Year Five Annual Report. Centers for Medicaid & Medicare Services; December 2019. Accessed August 9, 2020. https://downloads.cms.gov/files/cmmi/sim-rd1-mt-fifthannrpt.pdf
22. Wack A. A Message from OneCare CEO Vicki Loner: OneCare’s Response to the Pandemic. OneCare Vermont. May 1, 2020. Accessed August 9, 2020. https://www.onecarevt.org/20200501-covid19/
23. Haber S, Bell H, Morrison M, et al. Evaluation of the Maryland All-Payer Model: Vol 1: Final Report. Centers for Medicare & Medicaid Services; November 2019. Accessed August 9, 2020. https://downloads.cms.gov/files/md-allpayer-finalevalrpt.pdf
The day after Memorial Day 2020 marked an important transition in the United States’ experience with coronavirus disease 2019 (COVID-19), with many states making initial plans to reopen.
This year’s widespread healthcare closures were necessary to reduce COVID-19 transmission and prepare for a future patient surge, but these closures had unintended consequences. Nearly half of adults polled said they or someone in their household had foregone or delayed care since the outbreak began.1 This was especially true for visits to emergency departments and doctors’ offices for strokes, heart attacks, and routine medical care.2 In a survey across 49 states, only 7% of primary care practices considered scheduling preventive visits as a high priority.3 Eleven percent of polled adults reported delaying care worsened their condition,1 and in hard-hit areas such as New York City, non-COVID mortality was 22% higher than expected.4
Avoidance of the medical system decreased not only use of necessary, high-value care but also use of low-value care. Low-value services are those in which the “potential for harms exceed the potential benefits,”5 such as unnecessary hospitalizations, avoidable emergency department or clinic visits, unwarranted or excessive diagnostic testing (eg, annual physicals), and certain procedures (eg, spinal fusion surgery for low-back pain).
KEEP PATIENTS CENTRAL IN REOPENING SERVICES TO DELIVER HIGH-VALUE CARE
Medical centers can better focus on high-value care by defining their high-risk patient populations; high-value treatments, procedures, and preventive care; and phases of reopening. During the first pandemic wave, medical centers tried to reassure patients about emergency care, such as coming in for chest pain or neurologic symptoms, through personal outreach and media campaigns. Outpatient virtual visits also continued, including primary care, specialty services, mental health treatment, and physical therapy. While reopening, some medical centers have assessed disparities by relying on their data analytics and, if available, embedded health services researchers to understand what care was stopped and what populations were most affected.
The University of California health systems, for example, had a learning collaborative focused on sharing methods to restore care delivery that prioritizes patient needs. Some campuses conducted analyses using both electronic health record data and input from patients and their care teams to identify clinical needs and determine patient outreach plans. Some approaches used machine learning models to identify patients at highest risk of hospitalization or emergency department visits over the next 12 months and to conduct additional outreach to schedule these patients in primary and specialty care if clinically appropriate. Similarly, surgical specialties identified the highest-priority nonemergent surgeries for scheduling, including cancer resection, radiation therapy, and pain-management procedures. Similar guidance toward the most meaningful care has been prioritized within the United States Department of Veterans Affairs.
The rapid deployment of telehealth and payment models that reimburse video and in-clinic visits equally created new opportunities for medical centers to expand high-value care in lower-cost home settings. Similarly, new infrastructure is being developed to help define smarter use of virtual visits and home-based lab collection and monitoring.
Medical centers also must pay careful attention to redeploying service capacity for underused, high-value services. The pandemic uncovered existing staff that could be redeployed to support these changes. For example, with an “all hands on deck” mentality during the pandemic, in some medical centers, analysts or care managers from less-prioritized or duplicative areas were reassigned to vital COVID-19 efforts. Medical centers may realize that this staff can provide more value in the future by supporting increased high-value, affordable healthcare.
DELIBERATELY AVOID LOW-VALUE CARE
During the intial wave of the pandemic, medical centers greatly reduced the care they provided, often focusing on delivering essential care. This preparation for a surge of COVID patients had the effect of halting many unnecessary services by moving care from the clinic to home under new reimbursement changes, such as those affecting telehealth payments. The experience of reducing low-value medical services and visits can be extended to limiting unnecessary diagnostic testing. Medical centers could, for example, focus only on tests that advance care plans; reduce unnecessary blood draws, procedures, and vital sign checks on stable patients; shift to medications with less-frequent dosing intervals; and consolidate visits by treatment teams.10,11
Medical centers, however, now face continued pressures to increase revenue because 75% report their organization’s top priority is focused on increasing patient volume.12
PROACTIVELY AVOID WORSENING HEALTHCARE DISPARITIES
As medical centers reboot, operational and clinical leaders must proactively view changes through an equity lens to avoid exacerbating health disparities among vulnerable populations. The pandemic has focused national attention on the severity and pervasiveness of disparities and created an imperative for substantive action to evaluate how every decision will affect health equity. For example, medical centers are expanding use of telehealth to improve patient outreach. However, in a survey of primary care physicians, 72% said they have patients who are unable to access telehealth because they do not have access to technology.3 Exclusion of these patients from programs risks worsening health disparities. In a recent survey, nearly 65% of medical centers report reexamining existing policies, protocols, and practices for patients at risk of disparities.12
REFORM TO SUPPORT HIGH-VALUE CARE DELIVERY
Medical centers nationwide will need payment reform that provides greater financial stability beyond the pandemic to support high-value care delivery. They also will need flexibility to invest in prevention and to deliver the appropriate intensity of care to meet patients’ and communities’ needs.15-17 Options to provide this support include prospective population-based payments that may create more resilience in protecting access to care when it is most needed. Models can include fully capitated payment for physician practices.19,20 For example, after Vermont entered a single accountable care organization (ACO) model with the Centers for Medicare & Medicaid Services (CMS) in 2018, they not only generated a $97 million Medicaid savings, but also had a financial cushion that was later used in their COVID-19 response.21,22 The advanced payments allowed primary care practices and community agencies to invest in a digital tool to support outreach to patient at high risk for virus complications.
Hospitals similarly can adapt global budgets that incentivize financial stewardship by encouraging clinicians to resume necessary services and not unnecessary ones.16 For example, CMS partnered with Pennsylvania’s Department of Health to provide prospective all-payer global budgets for rural hospitals and Maryland’s Health Services Cost Review Commission that negotiates a budget with each hospital. During the COVID-19 pandemic, hospitals in these programs have had more financial protection from fluctuating finances by allowing for easier shifts in service delivery location and adjustments in rates to compensate for declines in visits and procedures.23
Policy makers and payers also can hold medical centers accountable to evidence-based guidelines and appropriate use of care, especially when necessary but expensive (eg, percutaneous coronary interventions, spinal surgeries, or cancer care). Funding agencies, additionally, can support these efforts by focusing on research, dissemination, and reliable implementation of these practices.
CONCLUSION
The COVID-19 crisis presents a tremendous opportunity for each medical center to revitalize healthcare. This opportunity can be seized only with reform by policy makers, payers, and regulatory agencies who encourage restarting high-value care without low-value services. We must take deliberate action so the nation’s medical centers can better meet patients’ needs to make healthcare more resilient, efficient, and fair.
The day after Memorial Day 2020 marked an important transition in the United States’ experience with coronavirus disease 2019 (COVID-19), with many states making initial plans to reopen.
This year’s widespread healthcare closures were necessary to reduce COVID-19 transmission and prepare for a future patient surge, but these closures had unintended consequences. Nearly half of adults polled said they or someone in their household had foregone or delayed care since the outbreak began.1 This was especially true for visits to emergency departments and doctors’ offices for strokes, heart attacks, and routine medical care.2 In a survey across 49 states, only 7% of primary care practices considered scheduling preventive visits as a high priority.3 Eleven percent of polled adults reported delaying care worsened their condition,1 and in hard-hit areas such as New York City, non-COVID mortality was 22% higher than expected.4
Avoidance of the medical system decreased not only use of necessary, high-value care but also use of low-value care. Low-value services are those in which the “potential for harms exceed the potential benefits,”5 such as unnecessary hospitalizations, avoidable emergency department or clinic visits, unwarranted or excessive diagnostic testing (eg, annual physicals), and certain procedures (eg, spinal fusion surgery for low-back pain).
KEEP PATIENTS CENTRAL IN REOPENING SERVICES TO DELIVER HIGH-VALUE CARE
Medical centers can better focus on high-value care by defining their high-risk patient populations; high-value treatments, procedures, and preventive care; and phases of reopening. During the first pandemic wave, medical centers tried to reassure patients about emergency care, such as coming in for chest pain or neurologic symptoms, through personal outreach and media campaigns. Outpatient virtual visits also continued, including primary care, specialty services, mental health treatment, and physical therapy. While reopening, some medical centers have assessed disparities by relying on their data analytics and, if available, embedded health services researchers to understand what care was stopped and what populations were most affected.
The University of California health systems, for example, had a learning collaborative focused on sharing methods to restore care delivery that prioritizes patient needs. Some campuses conducted analyses using both electronic health record data and input from patients and their care teams to identify clinical needs and determine patient outreach plans. Some approaches used machine learning models to identify patients at highest risk of hospitalization or emergency department visits over the next 12 months and to conduct additional outreach to schedule these patients in primary and specialty care if clinically appropriate. Similarly, surgical specialties identified the highest-priority nonemergent surgeries for scheduling, including cancer resection, radiation therapy, and pain-management procedures. Similar guidance toward the most meaningful care has been prioritized within the United States Department of Veterans Affairs.
The rapid deployment of telehealth and payment models that reimburse video and in-clinic visits equally created new opportunities for medical centers to expand high-value care in lower-cost home settings. Similarly, new infrastructure is being developed to help define smarter use of virtual visits and home-based lab collection and monitoring.
Medical centers also must pay careful attention to redeploying service capacity for underused, high-value services. The pandemic uncovered existing staff that could be redeployed to support these changes. For example, with an “all hands on deck” mentality during the pandemic, in some medical centers, analysts or care managers from less-prioritized or duplicative areas were reassigned to vital COVID-19 efforts. Medical centers may realize that this staff can provide more value in the future by supporting increased high-value, affordable healthcare.
DELIBERATELY AVOID LOW-VALUE CARE
During the intial wave of the pandemic, medical centers greatly reduced the care they provided, often focusing on delivering essential care. This preparation for a surge of COVID patients had the effect of halting many unnecessary services by moving care from the clinic to home under new reimbursement changes, such as those affecting telehealth payments. The experience of reducing low-value medical services and visits can be extended to limiting unnecessary diagnostic testing. Medical centers could, for example, focus only on tests that advance care plans; reduce unnecessary blood draws, procedures, and vital sign checks on stable patients; shift to medications with less-frequent dosing intervals; and consolidate visits by treatment teams.10,11
Medical centers, however, now face continued pressures to increase revenue because 75% report their organization’s top priority is focused on increasing patient volume.12
PROACTIVELY AVOID WORSENING HEALTHCARE DISPARITIES
As medical centers reboot, operational and clinical leaders must proactively view changes through an equity lens to avoid exacerbating health disparities among vulnerable populations. The pandemic has focused national attention on the severity and pervasiveness of disparities and created an imperative for substantive action to evaluate how every decision will affect health equity. For example, medical centers are expanding use of telehealth to improve patient outreach. However, in a survey of primary care physicians, 72% said they have patients who are unable to access telehealth because they do not have access to technology.3 Exclusion of these patients from programs risks worsening health disparities. In a recent survey, nearly 65% of medical centers report reexamining existing policies, protocols, and practices for patients at risk of disparities.12
REFORM TO SUPPORT HIGH-VALUE CARE DELIVERY
Medical centers nationwide will need payment reform that provides greater financial stability beyond the pandemic to support high-value care delivery. They also will need flexibility to invest in prevention and to deliver the appropriate intensity of care to meet patients’ and communities’ needs.15-17 Options to provide this support include prospective population-based payments that may create more resilience in protecting access to care when it is most needed. Models can include fully capitated payment for physician practices.19,20 For example, after Vermont entered a single accountable care organization (ACO) model with the Centers for Medicare & Medicaid Services (CMS) in 2018, they not only generated a $97 million Medicaid savings, but also had a financial cushion that was later used in their COVID-19 response.21,22 The advanced payments allowed primary care practices and community agencies to invest in a digital tool to support outreach to patient at high risk for virus complications.
Hospitals similarly can adapt global budgets that incentivize financial stewardship by encouraging clinicians to resume necessary services and not unnecessary ones.16 For example, CMS partnered with Pennsylvania’s Department of Health to provide prospective all-payer global budgets for rural hospitals and Maryland’s Health Services Cost Review Commission that negotiates a budget with each hospital. During the COVID-19 pandemic, hospitals in these programs have had more financial protection from fluctuating finances by allowing for easier shifts in service delivery location and adjustments in rates to compensate for declines in visits and procedures.23
Policy makers and payers also can hold medical centers accountable to evidence-based guidelines and appropriate use of care, especially when necessary but expensive (eg, percutaneous coronary interventions, spinal surgeries, or cancer care). Funding agencies, additionally, can support these efforts by focusing on research, dissemination, and reliable implementation of these practices.
CONCLUSION
The COVID-19 crisis presents a tremendous opportunity for each medical center to revitalize healthcare. This opportunity can be seized only with reform by policy makers, payers, and regulatory agencies who encourage restarting high-value care without low-value services. We must take deliberate action so the nation’s medical centers can better meet patients’ needs to make healthcare more resilient, efficient, and fair.
1. Hamel L, Kearney A, Kirzinger A, Lopes L, Muñana C, Brodie M. KFF Health Tracking Poll - May 2020: Impact of Coronavirus on Personal Health, Economic and Food Security, and Medicaid. Kaiser Family Foundation; May 27, 2020. Accessed August 9, 2020. https://www.kff.org/report-section/kff-health-tracking-poll-may-2020-health-and-economic-impacts/
2. McFarling UL. ‘Where are all our patients?’: Covid phobia is keeping people with serious heart symptoms away from ERs. STAT. April 23, 2020. Accessed August 9, 2020. https://www.statnews.com/2020/04/23/coronavirus-phobia-keeping-heart-patients-away-from-er/
3. Primary Care & COVID-19: Week 4 Survey. Primary Care Collaborative; April 9, 2020. Accessed August 9, 2020. https://www.pcpcc.org/2020/04/08/primary-care-covid-19-week-4-survey
4. Olson DR, Huynh M, Fine A, et al. New York City Department of Health and Mental Hygiene (DOHMH) COVID-19 Response Team. Preliminary estimate of excess mortality during the COVID-19 outbreak — New York City, March 11–May 2, 2020. Morbidity and Mortality Weekly Report. May 11, 2020. Accessed August 9, 2020. https://stacks.cdc.gov/view/cdc/87858
5. Chassin MR, Galvin RW. The urgent need to improve health care quality. Institute of Medicine National Roundtable on Health Care Quality. JAMA. 1998;280(11):1000-1005. https://doi.org/10.1001/jama.280.11.1000
6. Shrank WH, Rogstad TL, Parekh N. Waste in the US health care system: estimated costs and potential for savings. JAMA. 2019;322(15):1501-1509. https://doi.org/10.1001/jama.2019.13978
7. Collins SR, Gunja MZ, Doty MM, Bhupal HK. Americans’ confidence in their ability to pay for health care is falling. To The Point blog. May 10, 2018. The Commonwealth Fund. Accessed August 9, 2020. https://www.commonwealthfund.org/blog/2018/americans-confidence-their-ability-pay-health-care-falling
8. Saad L. More Americans delaying medical treatment due to cost. Gallup News. December 9, 2019. Accessed August 9, 2020. https://news.gallup.com/poll/269138/americans-delaying-medical-treatment-due-cost.aspx
9. Lee VS. Fee for service is a terrible way to pay for health care. Try a subscription model instead. STAT. June 12, 2020. Accessed August 9, 2020. https://www.statnews.com/2020/06/12/fee-for-service-is-a-terrible-way-to-pay-for-health-care-try-a-subscription-model-instead/
10. Moriates C, Shah NT, Arora VM. A framework for the frontline: how hospitalists can improve healthcare value. J Hosp Med. 2016;11(4):297-302. https://doi.org/10.1002/jhm.2494
11. Seymann G, Komsoukaniants A, Bouland D, Jenkins I. The Silver Linings Playbook for Covid-19. KevinMD. June 12, 2020. Accessed August 9, 2020. https://www.kevinmd.com/blog/2020/06/the-silver-linings-playbook-for-covid-19.html
12. Advis In The News. Industry Professionals Weigh In: Future of Healthcare Survey. Advis. Accessed August 9, 2020. https://advis.com/advis-in-the-news/post-pandemic-survey-june2020/
13. APM Measurement Effort. Healthcare Learning Payment and Action Network; 2019. Accessed August 9, 2020. https://hcp-lan.org/workproducts/apm-infographic-2019.pdf
14. Mosley D, DeBehnke D. Rural hospital sustainability: new analysis shows worsening situation for rural hospitals, residents. Navigant; February 2019. Accessed August 9, 2020. https://guidehouse.com/-/media/www/site/insights/healthcare/2019/navigant-rural-hospital-analysis-22019.pdf
15. Gondi S, Chokshi DA. Financial stability as a goal of payment reform—a lesson from COVID-19. JAMA Health Forum. August 6, 2020. Accessed August 9, 2020. https://jamanetwork.com/channels/health-forum/fullarticle/2769307
16. Murphy K, Koski-Vacirca R, Sharfstein J. Resilience in health care financing. JAMA. 2020;324(2):126-127. https://doi.org/10.1001/jama.2020.10417
17. Khullar D, Bond AM, Schpero WL. COVID-19 and the financial health of US hospitals. JAMA. 2020;323(21):2127-2128. https://doi.org/10.1001/jama.2020.6269
18. Weiss AJ, Elixhauser A, Andrews RM. Statistical Brief #170: Characteristics of Operating Room Procedures in U.S. Hospitals, 2011. Healthcare Costs and Utilization Project, Agency for Healthcare Research and Quality; February 2014. Accessed August 9, 2020: https://www.hcup-us.ahrq.gov/reports/statbriefs/sb170-Operating-Room-Procedures-United-States-2011.pdf
19. Crook HL, Saunders RS, Bleser WK, Broome T, Muhlestein D, McLellan MB. Leveraging Payment Reforms For COVID-19 And Beyond: Recommendations For Medicare ACOs And CMS’s Interim Final Rule. Health Affairs Blog. May 29, 2020. Accessed August 9, 2020. https://www.healthaffairs.org/do/10.1377/hblog20200528.402208/full/
20. Blue Cross NC Launches Comprehensive Program to Help Independent Primary Care Practices Stay in Business. Press release. BlueCross BlueShield of North Carolina; June 24, 2020. Accessed August 9, 2020. https://mediacenter.bcbsnc.com/news/blue-cross-nc-launches-comprehensive-program-to-help-independent-primary-care-practices-stay-in-business
21. RTI International. State Innovation Models (SIM) Initiative Evaluation: Model Test Year Five Annual Report. Centers for Medicaid & Medicare Services; December 2019. Accessed August 9, 2020. https://downloads.cms.gov/files/cmmi/sim-rd1-mt-fifthannrpt.pdf
22. Wack A. A Message from OneCare CEO Vicki Loner: OneCare’s Response to the Pandemic. OneCare Vermont. May 1, 2020. Accessed August 9, 2020. https://www.onecarevt.org/20200501-covid19/
23. Haber S, Bell H, Morrison M, et al. Evaluation of the Maryland All-Payer Model: Vol 1: Final Report. Centers for Medicare & Medicaid Services; November 2019. Accessed August 9, 2020. https://downloads.cms.gov/files/md-allpayer-finalevalrpt.pdf
1. Hamel L, Kearney A, Kirzinger A, Lopes L, Muñana C, Brodie M. KFF Health Tracking Poll - May 2020: Impact of Coronavirus on Personal Health, Economic and Food Security, and Medicaid. Kaiser Family Foundation; May 27, 2020. Accessed August 9, 2020. https://www.kff.org/report-section/kff-health-tracking-poll-may-2020-health-and-economic-impacts/
2. McFarling UL. ‘Where are all our patients?’: Covid phobia is keeping people with serious heart symptoms away from ERs. STAT. April 23, 2020. Accessed August 9, 2020. https://www.statnews.com/2020/04/23/coronavirus-phobia-keeping-heart-patients-away-from-er/
3. Primary Care & COVID-19: Week 4 Survey. Primary Care Collaborative; April 9, 2020. Accessed August 9, 2020. https://www.pcpcc.org/2020/04/08/primary-care-covid-19-week-4-survey
4. Olson DR, Huynh M, Fine A, et al. New York City Department of Health and Mental Hygiene (DOHMH) COVID-19 Response Team. Preliminary estimate of excess mortality during the COVID-19 outbreak — New York City, March 11–May 2, 2020. Morbidity and Mortality Weekly Report. May 11, 2020. Accessed August 9, 2020. https://stacks.cdc.gov/view/cdc/87858
5. Chassin MR, Galvin RW. The urgent need to improve health care quality. Institute of Medicine National Roundtable on Health Care Quality. JAMA. 1998;280(11):1000-1005. https://doi.org/10.1001/jama.280.11.1000
6. Shrank WH, Rogstad TL, Parekh N. Waste in the US health care system: estimated costs and potential for savings. JAMA. 2019;322(15):1501-1509. https://doi.org/10.1001/jama.2019.13978
7. Collins SR, Gunja MZ, Doty MM, Bhupal HK. Americans’ confidence in their ability to pay for health care is falling. To The Point blog. May 10, 2018. The Commonwealth Fund. Accessed August 9, 2020. https://www.commonwealthfund.org/blog/2018/americans-confidence-their-ability-pay-health-care-falling
8. Saad L. More Americans delaying medical treatment due to cost. Gallup News. December 9, 2019. Accessed August 9, 2020. https://news.gallup.com/poll/269138/americans-delaying-medical-treatment-due-cost.aspx
9. Lee VS. Fee for service is a terrible way to pay for health care. Try a subscription model instead. STAT. June 12, 2020. Accessed August 9, 2020. https://www.statnews.com/2020/06/12/fee-for-service-is-a-terrible-way-to-pay-for-health-care-try-a-subscription-model-instead/
10. Moriates C, Shah NT, Arora VM. A framework for the frontline: how hospitalists can improve healthcare value. J Hosp Med. 2016;11(4):297-302. https://doi.org/10.1002/jhm.2494
11. Seymann G, Komsoukaniants A, Bouland D, Jenkins I. The Silver Linings Playbook for Covid-19. KevinMD. June 12, 2020. Accessed August 9, 2020. https://www.kevinmd.com/blog/2020/06/the-silver-linings-playbook-for-covid-19.html
12. Advis In The News. Industry Professionals Weigh In: Future of Healthcare Survey. Advis. Accessed August 9, 2020. https://advis.com/advis-in-the-news/post-pandemic-survey-june2020/
13. APM Measurement Effort. Healthcare Learning Payment and Action Network; 2019. Accessed August 9, 2020. https://hcp-lan.org/workproducts/apm-infographic-2019.pdf
14. Mosley D, DeBehnke D. Rural hospital sustainability: new analysis shows worsening situation for rural hospitals, residents. Navigant; February 2019. Accessed August 9, 2020. https://guidehouse.com/-/media/www/site/insights/healthcare/2019/navigant-rural-hospital-analysis-22019.pdf
15. Gondi S, Chokshi DA. Financial stability as a goal of payment reform—a lesson from COVID-19. JAMA Health Forum. August 6, 2020. Accessed August 9, 2020. https://jamanetwork.com/channels/health-forum/fullarticle/2769307
16. Murphy K, Koski-Vacirca R, Sharfstein J. Resilience in health care financing. JAMA. 2020;324(2):126-127. https://doi.org/10.1001/jama.2020.10417
17. Khullar D, Bond AM, Schpero WL. COVID-19 and the financial health of US hospitals. JAMA. 2020;323(21):2127-2128. https://doi.org/10.1001/jama.2020.6269
18. Weiss AJ, Elixhauser A, Andrews RM. Statistical Brief #170: Characteristics of Operating Room Procedures in U.S. Hospitals, 2011. Healthcare Costs and Utilization Project, Agency for Healthcare Research and Quality; February 2014. Accessed August 9, 2020: https://www.hcup-us.ahrq.gov/reports/statbriefs/sb170-Operating-Room-Procedures-United-States-2011.pdf
19. Crook HL, Saunders RS, Bleser WK, Broome T, Muhlestein D, McLellan MB. Leveraging Payment Reforms For COVID-19 And Beyond: Recommendations For Medicare ACOs And CMS’s Interim Final Rule. Health Affairs Blog. May 29, 2020. Accessed August 9, 2020. https://www.healthaffairs.org/do/10.1377/hblog20200528.402208/full/
20. Blue Cross NC Launches Comprehensive Program to Help Independent Primary Care Practices Stay in Business. Press release. BlueCross BlueShield of North Carolina; June 24, 2020. Accessed August 9, 2020. https://mediacenter.bcbsnc.com/news/blue-cross-nc-launches-comprehensive-program-to-help-independent-primary-care-practices-stay-in-business
21. RTI International. State Innovation Models (SIM) Initiative Evaluation: Model Test Year Five Annual Report. Centers for Medicaid & Medicare Services; December 2019. Accessed August 9, 2020. https://downloads.cms.gov/files/cmmi/sim-rd1-mt-fifthannrpt.pdf
22. Wack A. A Message from OneCare CEO Vicki Loner: OneCare’s Response to the Pandemic. OneCare Vermont. May 1, 2020. Accessed August 9, 2020. https://www.onecarevt.org/20200501-covid19/
23. Haber S, Bell H, Morrison M, et al. Evaluation of the Maryland All-Payer Model: Vol 1: Final Report. Centers for Medicare & Medicaid Services; November 2019. Accessed August 9, 2020. https://downloads.cms.gov/files/md-allpayer-finalevalrpt.pdf
© 2021 Society of Hospital Medicine
Leveling the Playing Field: Accounting for Academic Productivity During the COVID-19 Pandemic
Professional upheavals caused by the coronavirus disease 2019 (COVID-19) pandemic have affected the academic productivity of many physicians. This is due in part to rapid changes in clinical care and medical education: physician-researchers have been redeployed to frontline clinical care; clinician-educators have been forced to rapidly transition in-person curricula to virtual platforms; and primary care physicians and subspecialists have been forced to transition to telehealth-based practices. In addition to these changes in clinical and educational responsibilities, the COVID-19 pandemic has substantially altered the personal lives of physicians. During the height of the pandemic, clinicians simultaneously wrestled with a lack of available childcare, unexpected home-schooling responsibilities, decreased income, and many other COVID-19-related stresses.1 Additionally, the ever-present “second pandemic” of structural racism, persistent health disparities, and racial inequity has further increased the personal and professional demands facing academic faculty.2
In particular, the pandemic has placed personal and professional pressure on female and minority faculty members. In spite of these pressures, however, the academic promotions process still requires rigid accounting of scholarly productivity. As the focus of academic practices has shifted to support clinical care during the pandemic, scholarly productivity has suffered for clinicians on the frontline. As a result, academic clinical faculty have expressed significant stress and concerns about failing to meet benchmarks for promotion (eg, publications, curricula development, national presentations). To counter these shifts (and the inherent inequity that they create for female clinicians and for men and women who are Black, Indigenous, and/or of color), academic institutions should not only recognize the effects the COVID-19 pandemic has had on faculty, but also adopt immediate solutions to more equitably account for such disruptions to academic portfolios. In this paper, we explore populations whose career trajectories are most at-risk and propose a framework to capture novel and nontraditional contributions while also acknowledging the rapid changes the COVID-19 pandemic has brought to academic medicine.
POPULATIONS AT RISK FOR CAREER DISRUPTION
Even before the COVID-19 pandemic, physician mothers, underrepresented racial/ethnic minority groups, and junior faculty were most at-risk for career disruptions. The closure of daycare facilities and schools and shift to online learning resulting from the pandemic, along with the common challenges of parenting, have taken a significant toll on the lives of working parents. Because women tend to carry a disproportionate share of childcare and household responsibilities, these changes have inequitably leveraged themselves as a “mommy tax” on working women.3,4
As underrepresented medicine faculty (particularly Black, Hispanic, Latino, and Native American clinicians) comprise only 8% of the academic medical workforce,they currently face a variety of personal and professional challenges.5 This is especially true for Black and Latinx physicians who have been experiencing an increased COVID-19 burden in their communities, while concurrently fighting entrenched structural racism and police violence. In academia, these challenges have worsened because of the “minority tax”—the toll of often uncompensated extra responsibilities (time or money) placed on minority faculty in the name of achieving diversity. The unintended consequences of these responsibilities result in having fewer mentors,6 caring for underserved populations,7 and performing more clinical care8 than non-underrepresented minority faculty. Because minority faculty are unlikely to be in leadership positions, it is reasonable to conclude they have been shouldering heavier clinical obligations and facing greater career disruption of scholarly work due to the COVID-19 pandemic.
Junior faculty (eg, instructors and assistant professors) also remain professionally vulnerable during the COVID-19 pandemic. Because junior faculty are often more clinically focused and less likely to hold leadership positions than senior faculty, they are more likely to have assumed frontline clinical positions, which come at the expense of academic work. Junior faculty are also at a critical building phase in their academic career—a time when they benefit from the opportunity to share their scholarly work and network at conferences. Unfortunately, many conferences have been canceled or moved to a virtual platform. Given that some institutions may be freezing academic funding for conferences due to budgetary shortfalls from the pandemic, junior faculty may be particularly at risk if they are not able to present their work. In addition, junior faculty often face disproportionate struggles at home, trying to balance demands of work and caring for young children. Considering the unique needs of each of these groups, it is especially important to consider intersectionality, or the compounded issues for individuals who exist in multiple disproportionately affected groups (eg, a Black female junior faculty member who is also a mother).
THE COVID-19-CURRICULUM VITAE MATRIX
The typical format of a professional curriculum vitae (CV) at most academic institutions does not allow one to document potential disruptions or novel contributions, including those that occurred during the COVID-19 pandemic. As a group of academic clinicians, educators, and researchers whose careers have been affected by the pandemic, we created a COVID-19 CV matrix, a potential framework to serve as a supplement for faculty. In this matrix, faculty members may document their contributions, disruptions that affected their work, and caregiving responsibilities during this time period, while also providing a rubric for promotions and tenure committees to equitably evaluate the pandemic period on an academic CV. Our COVID-19 CV matrix consists of six domains: (1) clinical care, (2) research, (3) education, (4) service, (5) advocacy/media, and (6) social media. These domains encompass traditional and nontraditional contributions made by healthcare professionals during the pandemic (Table). This matrix broadens the ability of both faculty and institutions to determine the actual impact of individuals during the pandemic.
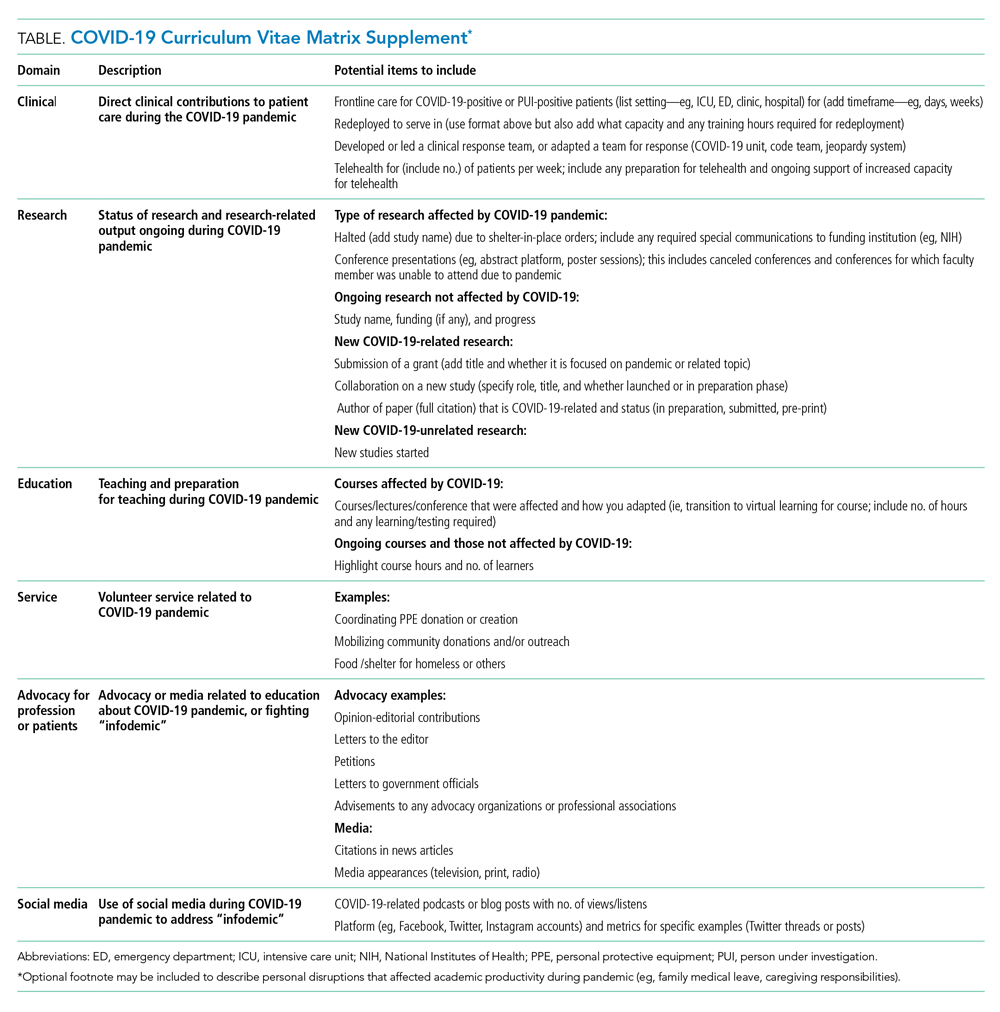
ACCOUNT FOR YOUR (NEW) IMPACT
Throughout the COVID-19 pandemic, academic faculty have been innovative, contributing in novel ways not routinely captured by promotions committees—eg, the digital health researcher who now directs the telemedicine response for their institution and the health disparities researcher who now leads daily webinar sessions on structural racism to medical students. Other novel contributions include advancing COVID-19 innovations and engaging in media and community advocacy (eg, organizing large-scale donations of equipment and funds to support organizations in need). While such nontraditional contributions may not have been readily captured or thought “CV worthy” in the past, faculty should now account for them. More importantly, promotions committees need to recognize that these pivots or alterations in career paths are not signals of professional failure, but rather evidence of a shifting landscape and the respective response of the individual. Furthermore, because these pivots often help fulfill an institutional mission, they are impactful.
ACKNOWLEDGE THE DISRUPTION
It is important for promotions and tenure committees to recognize the impact and disruption COVID-19 has had on traditional academic work, acknowledging the time and energy required for a faculty member to make needed work adjustments. This enables a leader to better assess how a faculty member’s academic portfolio has been affected. For example, researchers have had to halt studies, medical educators have had to redevelop and transition curricula to virtual platforms, and physicians have had to discontinue clinician quality improvement initiatives due to competing hospital priorities. Faculty members who document such unintentional alterations in their academic career path can explain to their institution how they have continued to positively influence their field and the community during the pandemic. This approach is analogous to the current model of accounting for clinical time when judging faculty members’ contributions in scholarly achievement.
The COVID-19 CV matrix has the potential to be annotated to explain the burden of one’s personal situation, which is often “invisible” in the professional environment. For example, many physicians have had to assume additional childcare responsibilities, tend to sick family members, friends, and even themselves. It is also possible that a faculty member has a partner who is also an essential worker, one who had to self-isolate due to COVID-19 exposure or illness, or who has been working overtime due to high patient volumes.
INSTITUTIONAL RESPONSE
How can institutions respond to the altered academic landscape caused by the COVID-19 pandemic? Promotions committees typically have two main tools at their disposal: adjusting the tenure clock or the benchmarks. Extending the period of time available to qualify for tenure is commonplace in the “publish-or-perish” academic tracks of university research professors. Clock adjustments are typically granted to faculty following the birth of a child or for other specific family- or health-related hardships, in accordance with the Family and Medical Leave Act. Unfortunately, tenure-clock extensions for female faculty members can exacerbate gender inequity: Data on tenure-clock extensions show a higher rate of tenure granted to male faculty compared to female faculty.9 For this reason, it is also important to explore adjustments or modifications to benchmark criteria. This could be accomplished by broadening the criteria for promotion, recognizing that impact occurs in many forms, thereby enabling meeting a benchmark. It can also occur by examining the trajectory of an individual within a promotion pathway before it was disrupted to determine impact. To avoid exacerbating social and gender inequities within academia, institutions should use these professional levers and create new ones to provide parity and equality across the promotional playing field. While the CV matrix openly acknowledges the disruptions and tangents the COVID-19 pandemic has had on academic careers, it remains important for academic institutions to recognize these disruptions and innovate the manner in which they acknowledge scholarly contributions.
Conclusion
While academic rigidity and known social taxes (minority and mommy taxes) are particularly problematic in the current climate, these issues have always been at play in evaluating academic success. Improved documentation of novel contributions, disruptions, caregiving, and other challenges can enable more holistic and timely professional advancement for all faculty, regardless of their sex, race, ethnicity, or social background. Ultimately, we hope this framework initiates further conversations among academic institutions on how to define productivity in an age where journal impact factor or number of publications is not the fullest measure of one’s impact in their field.
1. Jones Y, Durand V, Morton K, et al; ADVANCE PHM Steering Committee. Collateral damage: how covid-19 is adversely impacting women physicians. J Hosp Med. 2020;15(8):507-509. https://doi.org/10.12788/jhm.3470
2. Manning KD. When grief and crises intersect: perspectives of a black physician in the time of two pandemics. J Hosp Med. 2020;15(9):566-567. https://doi.org/10.12788/jhm.3481
3. Cohen P, Hsu T. Pandemic could scar a generation of working mothers. New York Times. Published June 3, 2020. Updated June 30, 2020. Accessed November 11, 2020. https://www.nytimes.com/2020/06/03/business/economy/coronavirus-working-women.html
4. Cain Miller C. Nearly half of men say they do most of the home schooling. 3 percent of women agree. Published May 6, 2020. Updated May 8, 2020. Accessed November 11, 2020. New York Times. https://www.nytimes.com/2020/05/06/upshot/pandemic-chores-homeschooling-gender.html
5. Rodríguez JE, Campbell KM, Pololi LH. Addressing disparities in academic medicine: what of the minority tax? BMC Med Educ. 2015;15:6. https://doi.org/10.1186/s12909-015-0290-9
6. Lewellen-Williams C, Johnson VA, Deloney LA, Thomas BR, Goyol A, Henry-Tillman R. The POD: a new model for mentoring underrepresented minority faculty. Acad Med. 2006;81(3):275-279. https://doi.org/10.1097/00001888-200603000-00020
7. Pololi LH, Evans AT, Gibbs BK, Krupat E, Brennan RT, Civian JT. The experience of minority faculty who are underrepresented in medicine, at 26 representative U.S. medical schools. Acad Med. 2013;88(9):1308-1314. https://doi.org/10.1097/acm.0b013e31829eefff
8. Richert A, Campbell K, Rodríguez J, Borowsky IW, Parikh R, Colwell A. ACU workforce column: expanding and supporting the health care workforce. J Health Care Poor Underserved. 2013;24(4):1423-1431. https://doi.org/10.1353/hpu.2013.0162
9. Woitowich NC, Jain S, Arora VM, Joffe H. COVID-19 threatens progress toward gender equity within academic medicine. Acad Med. 2020;29:10.1097/ACM.0000000000003782. https://doi.org/10.1097/acm.0000000000003782
Professional upheavals caused by the coronavirus disease 2019 (COVID-19) pandemic have affected the academic productivity of many physicians. This is due in part to rapid changes in clinical care and medical education: physician-researchers have been redeployed to frontline clinical care; clinician-educators have been forced to rapidly transition in-person curricula to virtual platforms; and primary care physicians and subspecialists have been forced to transition to telehealth-based practices. In addition to these changes in clinical and educational responsibilities, the COVID-19 pandemic has substantially altered the personal lives of physicians. During the height of the pandemic, clinicians simultaneously wrestled with a lack of available childcare, unexpected home-schooling responsibilities, decreased income, and many other COVID-19-related stresses.1 Additionally, the ever-present “second pandemic” of structural racism, persistent health disparities, and racial inequity has further increased the personal and professional demands facing academic faculty.2
In particular, the pandemic has placed personal and professional pressure on female and minority faculty members. In spite of these pressures, however, the academic promotions process still requires rigid accounting of scholarly productivity. As the focus of academic practices has shifted to support clinical care during the pandemic, scholarly productivity has suffered for clinicians on the frontline. As a result, academic clinical faculty have expressed significant stress and concerns about failing to meet benchmarks for promotion (eg, publications, curricula development, national presentations). To counter these shifts (and the inherent inequity that they create for female clinicians and for men and women who are Black, Indigenous, and/or of color), academic institutions should not only recognize the effects the COVID-19 pandemic has had on faculty, but also adopt immediate solutions to more equitably account for such disruptions to academic portfolios. In this paper, we explore populations whose career trajectories are most at-risk and propose a framework to capture novel and nontraditional contributions while also acknowledging the rapid changes the COVID-19 pandemic has brought to academic medicine.
POPULATIONS AT RISK FOR CAREER DISRUPTION
Even before the COVID-19 pandemic, physician mothers, underrepresented racial/ethnic minority groups, and junior faculty were most at-risk for career disruptions. The closure of daycare facilities and schools and shift to online learning resulting from the pandemic, along with the common challenges of parenting, have taken a significant toll on the lives of working parents. Because women tend to carry a disproportionate share of childcare and household responsibilities, these changes have inequitably leveraged themselves as a “mommy tax” on working women.3,4
As underrepresented medicine faculty (particularly Black, Hispanic, Latino, and Native American clinicians) comprise only 8% of the academic medical workforce,they currently face a variety of personal and professional challenges.5 This is especially true for Black and Latinx physicians who have been experiencing an increased COVID-19 burden in their communities, while concurrently fighting entrenched structural racism and police violence. In academia, these challenges have worsened because of the “minority tax”—the toll of often uncompensated extra responsibilities (time or money) placed on minority faculty in the name of achieving diversity. The unintended consequences of these responsibilities result in having fewer mentors,6 caring for underserved populations,7 and performing more clinical care8 than non-underrepresented minority faculty. Because minority faculty are unlikely to be in leadership positions, it is reasonable to conclude they have been shouldering heavier clinical obligations and facing greater career disruption of scholarly work due to the COVID-19 pandemic.
Junior faculty (eg, instructors and assistant professors) also remain professionally vulnerable during the COVID-19 pandemic. Because junior faculty are often more clinically focused and less likely to hold leadership positions than senior faculty, they are more likely to have assumed frontline clinical positions, which come at the expense of academic work. Junior faculty are also at a critical building phase in their academic career—a time when they benefit from the opportunity to share their scholarly work and network at conferences. Unfortunately, many conferences have been canceled or moved to a virtual platform. Given that some institutions may be freezing academic funding for conferences due to budgetary shortfalls from the pandemic, junior faculty may be particularly at risk if they are not able to present their work. In addition, junior faculty often face disproportionate struggles at home, trying to balance demands of work and caring for young children. Considering the unique needs of each of these groups, it is especially important to consider intersectionality, or the compounded issues for individuals who exist in multiple disproportionately affected groups (eg, a Black female junior faculty member who is also a mother).
THE COVID-19-CURRICULUM VITAE MATRIX
The typical format of a professional curriculum vitae (CV) at most academic institutions does not allow one to document potential disruptions or novel contributions, including those that occurred during the COVID-19 pandemic. As a group of academic clinicians, educators, and researchers whose careers have been affected by the pandemic, we created a COVID-19 CV matrix, a potential framework to serve as a supplement for faculty. In this matrix, faculty members may document their contributions, disruptions that affected their work, and caregiving responsibilities during this time period, while also providing a rubric for promotions and tenure committees to equitably evaluate the pandemic period on an academic CV. Our COVID-19 CV matrix consists of six domains: (1) clinical care, (2) research, (3) education, (4) service, (5) advocacy/media, and (6) social media. These domains encompass traditional and nontraditional contributions made by healthcare professionals during the pandemic (Table). This matrix broadens the ability of both faculty and institutions to determine the actual impact of individuals during the pandemic.
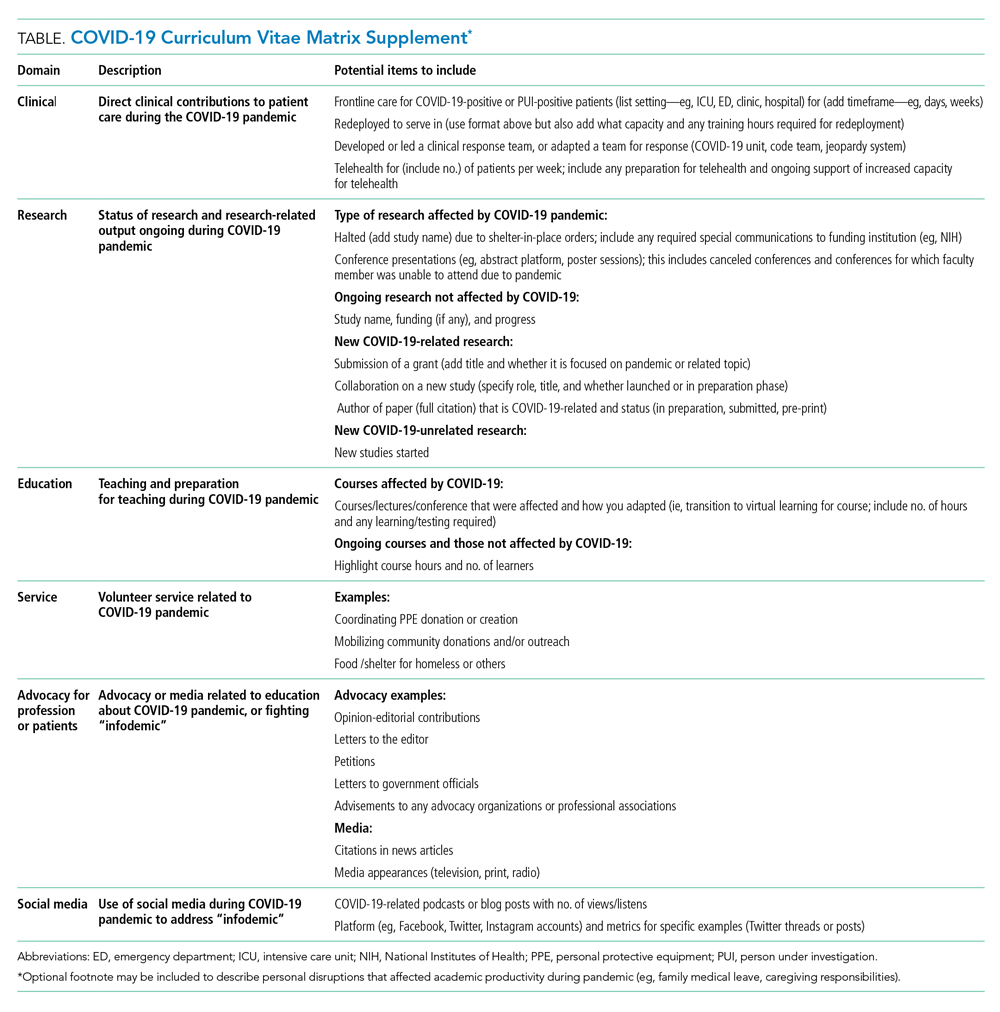
ACCOUNT FOR YOUR (NEW) IMPACT
Throughout the COVID-19 pandemic, academic faculty have been innovative, contributing in novel ways not routinely captured by promotions committees—eg, the digital health researcher who now directs the telemedicine response for their institution and the health disparities researcher who now leads daily webinar sessions on structural racism to medical students. Other novel contributions include advancing COVID-19 innovations and engaging in media and community advocacy (eg, organizing large-scale donations of equipment and funds to support organizations in need). While such nontraditional contributions may not have been readily captured or thought “CV worthy” in the past, faculty should now account for them. More importantly, promotions committees need to recognize that these pivots or alterations in career paths are not signals of professional failure, but rather evidence of a shifting landscape and the respective response of the individual. Furthermore, because these pivots often help fulfill an institutional mission, they are impactful.
ACKNOWLEDGE THE DISRUPTION
It is important for promotions and tenure committees to recognize the impact and disruption COVID-19 has had on traditional academic work, acknowledging the time and energy required for a faculty member to make needed work adjustments. This enables a leader to better assess how a faculty member’s academic portfolio has been affected. For example, researchers have had to halt studies, medical educators have had to redevelop and transition curricula to virtual platforms, and physicians have had to discontinue clinician quality improvement initiatives due to competing hospital priorities. Faculty members who document such unintentional alterations in their academic career path can explain to their institution how they have continued to positively influence their field and the community during the pandemic. This approach is analogous to the current model of accounting for clinical time when judging faculty members’ contributions in scholarly achievement.
The COVID-19 CV matrix has the potential to be annotated to explain the burden of one’s personal situation, which is often “invisible” in the professional environment. For example, many physicians have had to assume additional childcare responsibilities, tend to sick family members, friends, and even themselves. It is also possible that a faculty member has a partner who is also an essential worker, one who had to self-isolate due to COVID-19 exposure or illness, or who has been working overtime due to high patient volumes.
INSTITUTIONAL RESPONSE
How can institutions respond to the altered academic landscape caused by the COVID-19 pandemic? Promotions committees typically have two main tools at their disposal: adjusting the tenure clock or the benchmarks. Extending the period of time available to qualify for tenure is commonplace in the “publish-or-perish” academic tracks of university research professors. Clock adjustments are typically granted to faculty following the birth of a child or for other specific family- or health-related hardships, in accordance with the Family and Medical Leave Act. Unfortunately, tenure-clock extensions for female faculty members can exacerbate gender inequity: Data on tenure-clock extensions show a higher rate of tenure granted to male faculty compared to female faculty.9 For this reason, it is also important to explore adjustments or modifications to benchmark criteria. This could be accomplished by broadening the criteria for promotion, recognizing that impact occurs in many forms, thereby enabling meeting a benchmark. It can also occur by examining the trajectory of an individual within a promotion pathway before it was disrupted to determine impact. To avoid exacerbating social and gender inequities within academia, institutions should use these professional levers and create new ones to provide parity and equality across the promotional playing field. While the CV matrix openly acknowledges the disruptions and tangents the COVID-19 pandemic has had on academic careers, it remains important for academic institutions to recognize these disruptions and innovate the manner in which they acknowledge scholarly contributions.
Conclusion
While academic rigidity and known social taxes (minority and mommy taxes) are particularly problematic in the current climate, these issues have always been at play in evaluating academic success. Improved documentation of novel contributions, disruptions, caregiving, and other challenges can enable more holistic and timely professional advancement for all faculty, regardless of their sex, race, ethnicity, or social background. Ultimately, we hope this framework initiates further conversations among academic institutions on how to define productivity in an age where journal impact factor or number of publications is not the fullest measure of one’s impact in their field.
Professional upheavals caused by the coronavirus disease 2019 (COVID-19) pandemic have affected the academic productivity of many physicians. This is due in part to rapid changes in clinical care and medical education: physician-researchers have been redeployed to frontline clinical care; clinician-educators have been forced to rapidly transition in-person curricula to virtual platforms; and primary care physicians and subspecialists have been forced to transition to telehealth-based practices. In addition to these changes in clinical and educational responsibilities, the COVID-19 pandemic has substantially altered the personal lives of physicians. During the height of the pandemic, clinicians simultaneously wrestled with a lack of available childcare, unexpected home-schooling responsibilities, decreased income, and many other COVID-19-related stresses.1 Additionally, the ever-present “second pandemic” of structural racism, persistent health disparities, and racial inequity has further increased the personal and professional demands facing academic faculty.2
In particular, the pandemic has placed personal and professional pressure on female and minority faculty members. In spite of these pressures, however, the academic promotions process still requires rigid accounting of scholarly productivity. As the focus of academic practices has shifted to support clinical care during the pandemic, scholarly productivity has suffered for clinicians on the frontline. As a result, academic clinical faculty have expressed significant stress and concerns about failing to meet benchmarks for promotion (eg, publications, curricula development, national presentations). To counter these shifts (and the inherent inequity that they create for female clinicians and for men and women who are Black, Indigenous, and/or of color), academic institutions should not only recognize the effects the COVID-19 pandemic has had on faculty, but also adopt immediate solutions to more equitably account for such disruptions to academic portfolios. In this paper, we explore populations whose career trajectories are most at-risk and propose a framework to capture novel and nontraditional contributions while also acknowledging the rapid changes the COVID-19 pandemic has brought to academic medicine.
POPULATIONS AT RISK FOR CAREER DISRUPTION
Even before the COVID-19 pandemic, physician mothers, underrepresented racial/ethnic minority groups, and junior faculty were most at-risk for career disruptions. The closure of daycare facilities and schools and shift to online learning resulting from the pandemic, along with the common challenges of parenting, have taken a significant toll on the lives of working parents. Because women tend to carry a disproportionate share of childcare and household responsibilities, these changes have inequitably leveraged themselves as a “mommy tax” on working women.3,4
As underrepresented medicine faculty (particularly Black, Hispanic, Latino, and Native American clinicians) comprise only 8% of the academic medical workforce,they currently face a variety of personal and professional challenges.5 This is especially true for Black and Latinx physicians who have been experiencing an increased COVID-19 burden in their communities, while concurrently fighting entrenched structural racism and police violence. In academia, these challenges have worsened because of the “minority tax”—the toll of often uncompensated extra responsibilities (time or money) placed on minority faculty in the name of achieving diversity. The unintended consequences of these responsibilities result in having fewer mentors,6 caring for underserved populations,7 and performing more clinical care8 than non-underrepresented minority faculty. Because minority faculty are unlikely to be in leadership positions, it is reasonable to conclude they have been shouldering heavier clinical obligations and facing greater career disruption of scholarly work due to the COVID-19 pandemic.
Junior faculty (eg, instructors and assistant professors) also remain professionally vulnerable during the COVID-19 pandemic. Because junior faculty are often more clinically focused and less likely to hold leadership positions than senior faculty, they are more likely to have assumed frontline clinical positions, which come at the expense of academic work. Junior faculty are also at a critical building phase in their academic career—a time when they benefit from the opportunity to share their scholarly work and network at conferences. Unfortunately, many conferences have been canceled or moved to a virtual platform. Given that some institutions may be freezing academic funding for conferences due to budgetary shortfalls from the pandemic, junior faculty may be particularly at risk if they are not able to present their work. In addition, junior faculty often face disproportionate struggles at home, trying to balance demands of work and caring for young children. Considering the unique needs of each of these groups, it is especially important to consider intersectionality, or the compounded issues for individuals who exist in multiple disproportionately affected groups (eg, a Black female junior faculty member who is also a mother).
THE COVID-19-CURRICULUM VITAE MATRIX
The typical format of a professional curriculum vitae (CV) at most academic institutions does not allow one to document potential disruptions or novel contributions, including those that occurred during the COVID-19 pandemic. As a group of academic clinicians, educators, and researchers whose careers have been affected by the pandemic, we created a COVID-19 CV matrix, a potential framework to serve as a supplement for faculty. In this matrix, faculty members may document their contributions, disruptions that affected their work, and caregiving responsibilities during this time period, while also providing a rubric for promotions and tenure committees to equitably evaluate the pandemic period on an academic CV. Our COVID-19 CV matrix consists of six domains: (1) clinical care, (2) research, (3) education, (4) service, (5) advocacy/media, and (6) social media. These domains encompass traditional and nontraditional contributions made by healthcare professionals during the pandemic (Table). This matrix broadens the ability of both faculty and institutions to determine the actual impact of individuals during the pandemic.
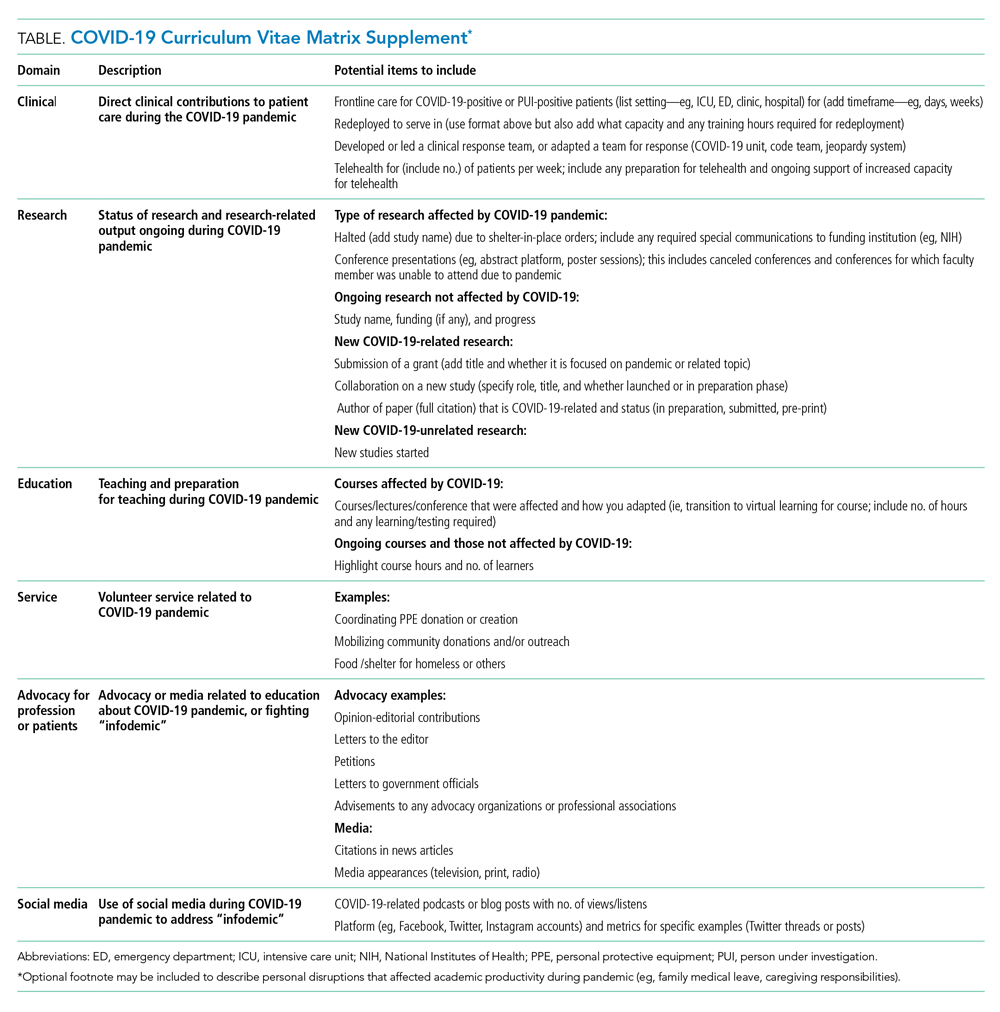
ACCOUNT FOR YOUR (NEW) IMPACT
Throughout the COVID-19 pandemic, academic faculty have been innovative, contributing in novel ways not routinely captured by promotions committees—eg, the digital health researcher who now directs the telemedicine response for their institution and the health disparities researcher who now leads daily webinar sessions on structural racism to medical students. Other novel contributions include advancing COVID-19 innovations and engaging in media and community advocacy (eg, organizing large-scale donations of equipment and funds to support organizations in need). While such nontraditional contributions may not have been readily captured or thought “CV worthy” in the past, faculty should now account for them. More importantly, promotions committees need to recognize that these pivots or alterations in career paths are not signals of professional failure, but rather evidence of a shifting landscape and the respective response of the individual. Furthermore, because these pivots often help fulfill an institutional mission, they are impactful.
ACKNOWLEDGE THE DISRUPTION
It is important for promotions and tenure committees to recognize the impact and disruption COVID-19 has had on traditional academic work, acknowledging the time and energy required for a faculty member to make needed work adjustments. This enables a leader to better assess how a faculty member’s academic portfolio has been affected. For example, researchers have had to halt studies, medical educators have had to redevelop and transition curricula to virtual platforms, and physicians have had to discontinue clinician quality improvement initiatives due to competing hospital priorities. Faculty members who document such unintentional alterations in their academic career path can explain to their institution how they have continued to positively influence their field and the community during the pandemic. This approach is analogous to the current model of accounting for clinical time when judging faculty members’ contributions in scholarly achievement.
The COVID-19 CV matrix has the potential to be annotated to explain the burden of one’s personal situation, which is often “invisible” in the professional environment. For example, many physicians have had to assume additional childcare responsibilities, tend to sick family members, friends, and even themselves. It is also possible that a faculty member has a partner who is also an essential worker, one who had to self-isolate due to COVID-19 exposure or illness, or who has been working overtime due to high patient volumes.
INSTITUTIONAL RESPONSE
How can institutions respond to the altered academic landscape caused by the COVID-19 pandemic? Promotions committees typically have two main tools at their disposal: adjusting the tenure clock or the benchmarks. Extending the period of time available to qualify for tenure is commonplace in the “publish-or-perish” academic tracks of university research professors. Clock adjustments are typically granted to faculty following the birth of a child or for other specific family- or health-related hardships, in accordance with the Family and Medical Leave Act. Unfortunately, tenure-clock extensions for female faculty members can exacerbate gender inequity: Data on tenure-clock extensions show a higher rate of tenure granted to male faculty compared to female faculty.9 For this reason, it is also important to explore adjustments or modifications to benchmark criteria. This could be accomplished by broadening the criteria for promotion, recognizing that impact occurs in many forms, thereby enabling meeting a benchmark. It can also occur by examining the trajectory of an individual within a promotion pathway before it was disrupted to determine impact. To avoid exacerbating social and gender inequities within academia, institutions should use these professional levers and create new ones to provide parity and equality across the promotional playing field. While the CV matrix openly acknowledges the disruptions and tangents the COVID-19 pandemic has had on academic careers, it remains important for academic institutions to recognize these disruptions and innovate the manner in which they acknowledge scholarly contributions.
Conclusion
While academic rigidity and known social taxes (minority and mommy taxes) are particularly problematic in the current climate, these issues have always been at play in evaluating academic success. Improved documentation of novel contributions, disruptions, caregiving, and other challenges can enable more holistic and timely professional advancement for all faculty, regardless of their sex, race, ethnicity, or social background. Ultimately, we hope this framework initiates further conversations among academic institutions on how to define productivity in an age where journal impact factor or number of publications is not the fullest measure of one’s impact in their field.
1. Jones Y, Durand V, Morton K, et al; ADVANCE PHM Steering Committee. Collateral damage: how covid-19 is adversely impacting women physicians. J Hosp Med. 2020;15(8):507-509. https://doi.org/10.12788/jhm.3470
2. Manning KD. When grief and crises intersect: perspectives of a black physician in the time of two pandemics. J Hosp Med. 2020;15(9):566-567. https://doi.org/10.12788/jhm.3481
3. Cohen P, Hsu T. Pandemic could scar a generation of working mothers. New York Times. Published June 3, 2020. Updated June 30, 2020. Accessed November 11, 2020. https://www.nytimes.com/2020/06/03/business/economy/coronavirus-working-women.html
4. Cain Miller C. Nearly half of men say they do most of the home schooling. 3 percent of women agree. Published May 6, 2020. Updated May 8, 2020. Accessed November 11, 2020. New York Times. https://www.nytimes.com/2020/05/06/upshot/pandemic-chores-homeschooling-gender.html
5. Rodríguez JE, Campbell KM, Pololi LH. Addressing disparities in academic medicine: what of the minority tax? BMC Med Educ. 2015;15:6. https://doi.org/10.1186/s12909-015-0290-9
6. Lewellen-Williams C, Johnson VA, Deloney LA, Thomas BR, Goyol A, Henry-Tillman R. The POD: a new model for mentoring underrepresented minority faculty. Acad Med. 2006;81(3):275-279. https://doi.org/10.1097/00001888-200603000-00020
7. Pololi LH, Evans AT, Gibbs BK, Krupat E, Brennan RT, Civian JT. The experience of minority faculty who are underrepresented in medicine, at 26 representative U.S. medical schools. Acad Med. 2013;88(9):1308-1314. https://doi.org/10.1097/acm.0b013e31829eefff
8. Richert A, Campbell K, Rodríguez J, Borowsky IW, Parikh R, Colwell A. ACU workforce column: expanding and supporting the health care workforce. J Health Care Poor Underserved. 2013;24(4):1423-1431. https://doi.org/10.1353/hpu.2013.0162
9. Woitowich NC, Jain S, Arora VM, Joffe H. COVID-19 threatens progress toward gender equity within academic medicine. Acad Med. 2020;29:10.1097/ACM.0000000000003782. https://doi.org/10.1097/acm.0000000000003782
1. Jones Y, Durand V, Morton K, et al; ADVANCE PHM Steering Committee. Collateral damage: how covid-19 is adversely impacting women physicians. J Hosp Med. 2020;15(8):507-509. https://doi.org/10.12788/jhm.3470
2. Manning KD. When grief and crises intersect: perspectives of a black physician in the time of two pandemics. J Hosp Med. 2020;15(9):566-567. https://doi.org/10.12788/jhm.3481
3. Cohen P, Hsu T. Pandemic could scar a generation of working mothers. New York Times. Published June 3, 2020. Updated June 30, 2020. Accessed November 11, 2020. https://www.nytimes.com/2020/06/03/business/economy/coronavirus-working-women.html
4. Cain Miller C. Nearly half of men say they do most of the home schooling. 3 percent of women agree. Published May 6, 2020. Updated May 8, 2020. Accessed November 11, 2020. New York Times. https://www.nytimes.com/2020/05/06/upshot/pandemic-chores-homeschooling-gender.html
5. Rodríguez JE, Campbell KM, Pololi LH. Addressing disparities in academic medicine: what of the minority tax? BMC Med Educ. 2015;15:6. https://doi.org/10.1186/s12909-015-0290-9
6. Lewellen-Williams C, Johnson VA, Deloney LA, Thomas BR, Goyol A, Henry-Tillman R. The POD: a new model for mentoring underrepresented minority faculty. Acad Med. 2006;81(3):275-279. https://doi.org/10.1097/00001888-200603000-00020
7. Pololi LH, Evans AT, Gibbs BK, Krupat E, Brennan RT, Civian JT. The experience of minority faculty who are underrepresented in medicine, at 26 representative U.S. medical schools. Acad Med. 2013;88(9):1308-1314. https://doi.org/10.1097/acm.0b013e31829eefff
8. Richert A, Campbell K, Rodríguez J, Borowsky IW, Parikh R, Colwell A. ACU workforce column: expanding and supporting the health care workforce. J Health Care Poor Underserved. 2013;24(4):1423-1431. https://doi.org/10.1353/hpu.2013.0162
9. Woitowich NC, Jain S, Arora VM, Joffe H. COVID-19 threatens progress toward gender equity within academic medicine. Acad Med. 2020;29:10.1097/ACM.0000000000003782. https://doi.org/10.1097/acm.0000000000003782
© 2021 Society of Hospital Medicine