User login
Lost keys, missed appointments: The struggle of treating executive dysfunction
Maybe you know some of these patients: They may come late or not show up at all. They may have little to say and minimize their difficulties, often because they are ashamed of how much effort it takes to meet ordinary obligations. They may struggle to complete assignments, fail classes, or lose jobs. And being in the right place at the right time can feel monumental to them: They forget appointments, double book themselves, or sometimes sleep through important events.
It’s not just appointments. They lose their keys and valuables, forget to pay bills, and may not answer calls, texts, or emails. Their voicemail may be full and people are often frustrated with them. These are all characteristics of executive dysfunction, which together can make the routine responsibilities of life very difficult.
Treatments include stimulants, and because of their potential for abuse, these medications are more strictly regulated when it comes to prescribing. The FDA does not allow them to be phoned into a pharmacy or refills to be added to prescriptions. Patients must wait until right before they are due to run out to get the next prescription, and this can present a problem if the patient travels or takes long vacations.
And although it is not the patient’s fault that stimulants can’t be ordered with refills, this adds to the burden of treating patients who take them. It’s hard to imagine that these restrictions on stimulants and opiates (but not on benzodiazepines) do much to deter abuse or diversion.
I trained at a time when ADD and ADHD were disorders of childhood, and as an adult psychiatrist, I was not exposed to patients on these medications. Occasionally, a stimulant was prescribed in a low dose to help activate a very depressed patient, but it was thought that children outgrow issues of attention and focus, and I have never felt fully confident in the more nuanced use of these medications with adults. Most of the patients I now treat with ADD have come to me on stable doses of the medications or at least with a history that directs care.
With others, the tip-off to look for the disorder is their disorganization in the absence of a substance use or active mood disorder. Medications help, sometimes remarkably, yet patients still struggle with organization and planning, and sometimes I find myself frustrated when patients forget their appointments or the issues around prescribing stimulants become time-consuming.
David W. Goodman, MD, director of the Adult Attention Deficit Center of Maryland, Lutherville, currently treats hundreds of patients with ADD and has written and spoken extensively about treating this disorder in adults.
“There are three things that make it difficult to manage patients with ADD,” Dr. Goodman noted, referring specifically to administrative issues. “You can’t write for refills, but with e-prescribing you can write a sequence of prescriptions with ‘fill-after’ dates. Or some patients are able to get a 90-day supply from mail-order pharmacies. Still, it’s a hassle if the patient moves around, as college students often do, and there are inventory shortages when some pharmacies can’t get the medications.”
“The second issue,” he adds, “is that it’s the nature of this disorder that patients struggle with organizational issues. Yelling at someone with ADD to pay attention is like yelling at a blind person not to run into furniture when they are in a new room. They go through life with people being impatient that they can’t do the things an ordinary person can do easily.”
Finally, Dr. Goodman noted that the clinicians who treat patients with ADD may have counter-transference issues.
“You have to understand that this is a disability and be sympathetic to it. They often have comorbid disorders, including personality disorders, and this can all bleed over to cause frustrations in their care. Psychiatrists who treat patients with ADD need to know they can deal with them compassionately.”
“I am occasionally contacted by patients who already have an ADHD diagnosis and are on stimulants, and who seem like they just want to get their prescriptions filled and aren’t interested in working on their issues,” says Douglas Beech, MD, a psychiatrist in private practice in Worthington, Ohio. “The doctor in this situation can feel like they are functioning as a sort of drug dealer. There are logistical matters that are structurally inherent in trying to assist these patients, from both a regulatory perspective and from a functional perspective. Dr. Beech feels that it’s helpful to acknowledge these issues when seeing patients with ADHD, so that he is prepared when problems do arise.
“It can almost feel cruel to charge a patient for a “no-show,” when difficulty keeping appointments may be a symptom of their illness, Dr. Beech adds. But he does believe it’s important to apply any fee policy equitably to all patients. “I don’t apply the ‘missed appointment’ policy differently to a person with an ADHD diagnosis versus any other diagnosis.” Though for their first missed appointment, he does give patients a “mulligan.”
“I don’t charge, but it puts both patient and doctor on notice,” he says.
And when his patients do miss an appointment, he offers to send a reminder for the next time, which is he says is effective. “With electronic messaging, this is a quick and easy way to prevent missed appointments and the complications that arise with prescriptions and rescheduling,” says Dr. Beech.
Dr. Goodman speaks about manging a large caseload of patients, many of whom have organizational issues.
“I have a full-time office manager who handles a lot of the logistics of scheduling and prescribing. Patients are sent multiple reminders, and I charge a nominal administrative fee if prescriptions need to be sent outside of appointments. This is not to make money, but to encourage patients to consider the administrative time.”
“I charge for appointments that are not canceled 48 hours in advance, and for patients who have missed appointments, a credit card is kept on file,” he says.
In a practice similar to Dr. Beech, Dr. Goodman notes that he shows some flexibility for new patients when they miss an appointment the first time. “By the second time, they know this is the policy. Having ADHD can be financially costly.”
He notes that about 10% of his patients, roughly one a day, cancel late or don’t show up for scheduled appointments: “We keep a waitlist, and if someone cancels before the appointment, we can often fill the time with another patient in need on our waitlist.”
Dr. Goodman noted repeatedly that the clinician needs to be able to empathize with the patient’s condition and how they suffer. “This is not something people choose to have. The trap is that people think that if you’re successful you can’t have ADHD, and that’s not true. Often people with this condition work harder, are brighter, and find ways to compensate.”
If a practice is set up to accommodate the needs of patients with attention and organizational issues, treating them can be very gratifying. In settings without administrative support, the psychiatrist needs to stay cognizant of this invisible disability and the frustration that may come with this disorder, not just for the patient, but also for the family, friends, and employers, and even for the psychiatrist.
Dr. Dinah Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, Baltimore. Dr. Miller has no conflicts of interest.
A version of this article first appeared on Medscape.com.
Maybe you know some of these patients: They may come late or not show up at all. They may have little to say and minimize their difficulties, often because they are ashamed of how much effort it takes to meet ordinary obligations. They may struggle to complete assignments, fail classes, or lose jobs. And being in the right place at the right time can feel monumental to them: They forget appointments, double book themselves, or sometimes sleep through important events.
It’s not just appointments. They lose their keys and valuables, forget to pay bills, and may not answer calls, texts, or emails. Their voicemail may be full and people are often frustrated with them. These are all characteristics of executive dysfunction, which together can make the routine responsibilities of life very difficult.
Treatments include stimulants, and because of their potential for abuse, these medications are more strictly regulated when it comes to prescribing. The FDA does not allow them to be phoned into a pharmacy or refills to be added to prescriptions. Patients must wait until right before they are due to run out to get the next prescription, and this can present a problem if the patient travels or takes long vacations.
And although it is not the patient’s fault that stimulants can’t be ordered with refills, this adds to the burden of treating patients who take them. It’s hard to imagine that these restrictions on stimulants and opiates (but not on benzodiazepines) do much to deter abuse or diversion.
I trained at a time when ADD and ADHD were disorders of childhood, and as an adult psychiatrist, I was not exposed to patients on these medications. Occasionally, a stimulant was prescribed in a low dose to help activate a very depressed patient, but it was thought that children outgrow issues of attention and focus, and I have never felt fully confident in the more nuanced use of these medications with adults. Most of the patients I now treat with ADD have come to me on stable doses of the medications or at least with a history that directs care.
With others, the tip-off to look for the disorder is their disorganization in the absence of a substance use or active mood disorder. Medications help, sometimes remarkably, yet patients still struggle with organization and planning, and sometimes I find myself frustrated when patients forget their appointments or the issues around prescribing stimulants become time-consuming.
David W. Goodman, MD, director of the Adult Attention Deficit Center of Maryland, Lutherville, currently treats hundreds of patients with ADD and has written and spoken extensively about treating this disorder in adults.
“There are three things that make it difficult to manage patients with ADD,” Dr. Goodman noted, referring specifically to administrative issues. “You can’t write for refills, but with e-prescribing you can write a sequence of prescriptions with ‘fill-after’ dates. Or some patients are able to get a 90-day supply from mail-order pharmacies. Still, it’s a hassle if the patient moves around, as college students often do, and there are inventory shortages when some pharmacies can’t get the medications.”
“The second issue,” he adds, “is that it’s the nature of this disorder that patients struggle with organizational issues. Yelling at someone with ADD to pay attention is like yelling at a blind person not to run into furniture when they are in a new room. They go through life with people being impatient that they can’t do the things an ordinary person can do easily.”
Finally, Dr. Goodman noted that the clinicians who treat patients with ADD may have counter-transference issues.
“You have to understand that this is a disability and be sympathetic to it. They often have comorbid disorders, including personality disorders, and this can all bleed over to cause frustrations in their care. Psychiatrists who treat patients with ADD need to know they can deal with them compassionately.”
“I am occasionally contacted by patients who already have an ADHD diagnosis and are on stimulants, and who seem like they just want to get their prescriptions filled and aren’t interested in working on their issues,” says Douglas Beech, MD, a psychiatrist in private practice in Worthington, Ohio. “The doctor in this situation can feel like they are functioning as a sort of drug dealer. There are logistical matters that are structurally inherent in trying to assist these patients, from both a regulatory perspective and from a functional perspective. Dr. Beech feels that it’s helpful to acknowledge these issues when seeing patients with ADHD, so that he is prepared when problems do arise.
“It can almost feel cruel to charge a patient for a “no-show,” when difficulty keeping appointments may be a symptom of their illness, Dr. Beech adds. But he does believe it’s important to apply any fee policy equitably to all patients. “I don’t apply the ‘missed appointment’ policy differently to a person with an ADHD diagnosis versus any other diagnosis.” Though for their first missed appointment, he does give patients a “mulligan.”
“I don’t charge, but it puts both patient and doctor on notice,” he says.
And when his patients do miss an appointment, he offers to send a reminder for the next time, which is he says is effective. “With electronic messaging, this is a quick and easy way to prevent missed appointments and the complications that arise with prescriptions and rescheduling,” says Dr. Beech.
Dr. Goodman speaks about manging a large caseload of patients, many of whom have organizational issues.
“I have a full-time office manager who handles a lot of the logistics of scheduling and prescribing. Patients are sent multiple reminders, and I charge a nominal administrative fee if prescriptions need to be sent outside of appointments. This is not to make money, but to encourage patients to consider the administrative time.”
“I charge for appointments that are not canceled 48 hours in advance, and for patients who have missed appointments, a credit card is kept on file,” he says.
In a practice similar to Dr. Beech, Dr. Goodman notes that he shows some flexibility for new patients when they miss an appointment the first time. “By the second time, they know this is the policy. Having ADHD can be financially costly.”
He notes that about 10% of his patients, roughly one a day, cancel late or don’t show up for scheduled appointments: “We keep a waitlist, and if someone cancels before the appointment, we can often fill the time with another patient in need on our waitlist.”
Dr. Goodman noted repeatedly that the clinician needs to be able to empathize with the patient’s condition and how they suffer. “This is not something people choose to have. The trap is that people think that if you’re successful you can’t have ADHD, and that’s not true. Often people with this condition work harder, are brighter, and find ways to compensate.”
If a practice is set up to accommodate the needs of patients with attention and organizational issues, treating them can be very gratifying. In settings without administrative support, the psychiatrist needs to stay cognizant of this invisible disability and the frustration that may come with this disorder, not just for the patient, but also for the family, friends, and employers, and even for the psychiatrist.
Dr. Dinah Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, Baltimore. Dr. Miller has no conflicts of interest.
A version of this article first appeared on Medscape.com.
Maybe you know some of these patients: They may come late or not show up at all. They may have little to say and minimize their difficulties, often because they are ashamed of how much effort it takes to meet ordinary obligations. They may struggle to complete assignments, fail classes, or lose jobs. And being in the right place at the right time can feel monumental to them: They forget appointments, double book themselves, or sometimes sleep through important events.
It’s not just appointments. They lose their keys and valuables, forget to pay bills, and may not answer calls, texts, or emails. Their voicemail may be full and people are often frustrated with them. These are all characteristics of executive dysfunction, which together can make the routine responsibilities of life very difficult.
Treatments include stimulants, and because of their potential for abuse, these medications are more strictly regulated when it comes to prescribing. The FDA does not allow them to be phoned into a pharmacy or refills to be added to prescriptions. Patients must wait until right before they are due to run out to get the next prescription, and this can present a problem if the patient travels or takes long vacations.
And although it is not the patient’s fault that stimulants can’t be ordered with refills, this adds to the burden of treating patients who take them. It’s hard to imagine that these restrictions on stimulants and opiates (but not on benzodiazepines) do much to deter abuse or diversion.
I trained at a time when ADD and ADHD were disorders of childhood, and as an adult psychiatrist, I was not exposed to patients on these medications. Occasionally, a stimulant was prescribed in a low dose to help activate a very depressed patient, but it was thought that children outgrow issues of attention and focus, and I have never felt fully confident in the more nuanced use of these medications with adults. Most of the patients I now treat with ADD have come to me on stable doses of the medications or at least with a history that directs care.
With others, the tip-off to look for the disorder is their disorganization in the absence of a substance use or active mood disorder. Medications help, sometimes remarkably, yet patients still struggle with organization and planning, and sometimes I find myself frustrated when patients forget their appointments or the issues around prescribing stimulants become time-consuming.
David W. Goodman, MD, director of the Adult Attention Deficit Center of Maryland, Lutherville, currently treats hundreds of patients with ADD and has written and spoken extensively about treating this disorder in adults.
“There are three things that make it difficult to manage patients with ADD,” Dr. Goodman noted, referring specifically to administrative issues. “You can’t write for refills, but with e-prescribing you can write a sequence of prescriptions with ‘fill-after’ dates. Or some patients are able to get a 90-day supply from mail-order pharmacies. Still, it’s a hassle if the patient moves around, as college students often do, and there are inventory shortages when some pharmacies can’t get the medications.”
“The second issue,” he adds, “is that it’s the nature of this disorder that patients struggle with organizational issues. Yelling at someone with ADD to pay attention is like yelling at a blind person not to run into furniture when they are in a new room. They go through life with people being impatient that they can’t do the things an ordinary person can do easily.”
Finally, Dr. Goodman noted that the clinicians who treat patients with ADD may have counter-transference issues.
“You have to understand that this is a disability and be sympathetic to it. They often have comorbid disorders, including personality disorders, and this can all bleed over to cause frustrations in their care. Psychiatrists who treat patients with ADD need to know they can deal with them compassionately.”
“I am occasionally contacted by patients who already have an ADHD diagnosis and are on stimulants, and who seem like they just want to get their prescriptions filled and aren’t interested in working on their issues,” says Douglas Beech, MD, a psychiatrist in private practice in Worthington, Ohio. “The doctor in this situation can feel like they are functioning as a sort of drug dealer. There are logistical matters that are structurally inherent in trying to assist these patients, from both a regulatory perspective and from a functional perspective. Dr. Beech feels that it’s helpful to acknowledge these issues when seeing patients with ADHD, so that he is prepared when problems do arise.
“It can almost feel cruel to charge a patient for a “no-show,” when difficulty keeping appointments may be a symptom of their illness, Dr. Beech adds. But he does believe it’s important to apply any fee policy equitably to all patients. “I don’t apply the ‘missed appointment’ policy differently to a person with an ADHD diagnosis versus any other diagnosis.” Though for their first missed appointment, he does give patients a “mulligan.”
“I don’t charge, but it puts both patient and doctor on notice,” he says.
And when his patients do miss an appointment, he offers to send a reminder for the next time, which is he says is effective. “With electronic messaging, this is a quick and easy way to prevent missed appointments and the complications that arise with prescriptions and rescheduling,” says Dr. Beech.
Dr. Goodman speaks about manging a large caseload of patients, many of whom have organizational issues.
“I have a full-time office manager who handles a lot of the logistics of scheduling and prescribing. Patients are sent multiple reminders, and I charge a nominal administrative fee if prescriptions need to be sent outside of appointments. This is not to make money, but to encourage patients to consider the administrative time.”
“I charge for appointments that are not canceled 48 hours in advance, and for patients who have missed appointments, a credit card is kept on file,” he says.
In a practice similar to Dr. Beech, Dr. Goodman notes that he shows some flexibility for new patients when they miss an appointment the first time. “By the second time, they know this is the policy. Having ADHD can be financially costly.”
He notes that about 10% of his patients, roughly one a day, cancel late or don’t show up for scheduled appointments: “We keep a waitlist, and if someone cancels before the appointment, we can often fill the time with another patient in need on our waitlist.”
Dr. Goodman noted repeatedly that the clinician needs to be able to empathize with the patient’s condition and how they suffer. “This is not something people choose to have. The trap is that people think that if you’re successful you can’t have ADHD, and that’s not true. Often people with this condition work harder, are brighter, and find ways to compensate.”
If a practice is set up to accommodate the needs of patients with attention and organizational issues, treating them can be very gratifying. In settings without administrative support, the psychiatrist needs to stay cognizant of this invisible disability and the frustration that may come with this disorder, not just for the patient, but also for the family, friends, and employers, and even for the psychiatrist.
Dr. Dinah Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, Baltimore. Dr. Miller has no conflicts of interest.
A version of this article first appeared on Medscape.com.
Four mental health trajectories in youth: Predicting persistent psychopathology
A study that tracked psychopathology in 13,000 children and adolescents found that
Investigators also found a strong correlation between new incidence of high psychopathology and externalizing problems such as hyperactivity. “It is of paramount importance to identify factors that distinguish those with persisting problems and escalating trajectories so that resources can be appropriately directed,” wrote the authors of the study published online in JAMA Network Open.
Recent studies have shown that concurrent and sequential comorbidity of psychiatric disorders are very common in adult populations, lead author Colm Healy, PhD, a postdoctoral researcher for psychiatry with the University of Medicine and Health Sciences, Ireland, said in an interview.
The speculation is that this occurs in early life when psychiatry symptoms experience high fluidity. “This presents a complex scenario to model, where young people’s mental health appears to shift and change across development. Few investigations to date have had the data available to examine these trajectories over the full range of child development,” said Dr. Healy.
He and his colleagues attempted to map the profiles and trajectories of psychopathology in children and adolescents, using latent profile transition analysis (LPTA), a person-centered method, to assess comorbidity and movement in the various phases of childhood development.
“The idea behind person-centered methods such as LTPA is that it identifies unobserved subgroups of participants who respond similarly to specific variables – in this case responses to a broad measure of psychopathology,” explained Dr. Healy.
The study included 7,507 children from the child sample (ages 3, 5, and 9 years) and 6,039 children from the adolescent sample (ages 9, 13, and 17 or 18 years). Data analysis took place from October 2020 to September 2021.
Dr. Healy and colleagues in a supplementary investigation compared cohorts at age 9 years to look for sex and generational differences.
Four developmental profiles
Researchers identified 4 distinct developmental profies for person-centered psychopathological trajectories: no psychopathology (incidence range, 60%-70%), high psychopathology (incidence range, 3%-5%), externalizing problems (incidence range, 15%-25%), and internalizing problems (incidence range, 7%-12%).
Internalizing problems reflect issues with peers and emotional problems whereas externalizing problems more closely associate with hyperactivity and conduct.
Less than 5% of the youth studied experienced persistent symptoms. However, 48.6% in the child cohort and 44.1% in the adolescent cohort moved into one of the 3 psychopathology profiles (high psychopathology, externalizing, internalizing problems) at some point in development.
The spread of trajectories was more diverse in the child cohort, said Dr. Healy. “Children ebbed and flowed between the different profiles over time with a large proportion falling into one of the psychopathology categories and then switching between these profiles.” Switching was also evident in the adolescent cohort but to a lesser extent, he said.
Externalizing problems link to high psychopathology
Rates of remittance were higher among individuals in both cohorts for internalizing problems, compared with externalizing problems.
It’s possible that for some of these young people, internalizing problems are a reaction to environmental stressors such as bullying,” said Dr. Healy. “When that stress is relieved, the internalizing problems may dissipate.”
In a clinically relevant finding, children with externalizing problems (age 5, 129 [61.3%] and age 9, 95 [74.3%]) were more likely to present with new incidents of high psychopathology. This was also true in the adolescent group (age 13, 129 [91.1%] and age 17, 146 [89.9%]).
This suggests that a proportion of youth with externalizing problems have an escalating trajectory of psychopathology. “Thus, it may be possible to distinguish those with an escalating trajectory from a stable or remitting trajectory. The specific distinguishing factors require further investigation, but it has been observed before that some of those reporting externalizing problems in early life continue to have difficulties into later life,” noted Dr. Healy.
A combination of environmental or biological factors may explain this escalation, which could respond to early intervention, he said.
Overall, few children in the study transitioned directly from no psychopathology to high psychopathology.
Differences between boys, girls
In both cohorts, investigators noticed significant differences between the sexes.
Boys in childhood made up a larger proportion of the three psychopathology profiles. But by late adolescence, girls made up a larger proportion of the internalizing profile whereas boys made up a larger proportion of the externalizing profile. “These differences were in line with our expectations,” said Dr. Healy.
Trajectories also differed among boys and girls. In childhood, girls had a higher percentage of de-escalating trajectories relative to boys. “More girls than boys in the psychopathology profiles switched to a non or less severe profile. In adolescence, differences in trajectories were less obvious, with the exception that girls were more likely than boys to transition to internalizing problems from all of the other profiles at age 17,” said Dr. Healy.
Most young people who experience psychopathology will eventually see an improvement in symptoms, noted Dr. Healy. Next steps are to identify markers that distinguish individuals with persistent trajectories from remitting trajectories at the different phases of development, he said.
Study draws mixed reviews
Clinical psychiatrists not involved in the study had varying reactions to the results.
“This study is notable for its data-driven and powerful illustration of how childhood and adolescence are dynamic periods during which psychiatric symptoms can emerge and evolve,” said Sunny X. Tang, MD, a psychiatrist and an assistant professor at the Institute of Behavioral Science and the Feinstein Institutes for Medical Research, Manhasset, New York.
The clinical call for action is for person-centered mental health screening to be a routine part of pediatric and adolescent primary care or school-based services, noted Dr. Tang.
Paul S. Nestadt, MD, an assistant professor and public mental health researcher at Johns Hopkins University, Baltimore, did not think the study would have a significant impact on clinical practice.
He noted that Dr. Healy and coauthors found that some children stayed true to type, but many fluctuated between the four profile groups. The finding that fluctuation occurred more frequently in younger children is not surprising “and is consistent with what we know about the ‘moving targets’ that make diagnosing children so difficult,” said Dr. Nestadt.
“It would have been helpful to have identified clinical indicators of likely persistence in psychopathology, but the measure employed here did not allow that. It is also frustrating to not have any information on treatment, such that we cannot know whether the children who shifted to ‘no psychopathology’ did so because of treatment or spontaneously,” he added.
Victor M. Fornari, MD, MS, director of the Division of Child & Adolescent Psychiatry at The Zucker Hillside Hospital and Cohen’s Children’s Medical Center, New York, said the study is an important contribution to understanding the development of psychopathology during childhood.
“Generally, it is felt that nearly one in five youth will meet criteria for at least one psychiatric disorder by the age of 18. It is well known that externalizing disorders like ADHD manifest earlier in childhood and that depression often manifests later in adolescence,” he said.
No disclosures were reported.
A study that tracked psychopathology in 13,000 children and adolescents found that
Investigators also found a strong correlation between new incidence of high psychopathology and externalizing problems such as hyperactivity. “It is of paramount importance to identify factors that distinguish those with persisting problems and escalating trajectories so that resources can be appropriately directed,” wrote the authors of the study published online in JAMA Network Open.
Recent studies have shown that concurrent and sequential comorbidity of psychiatric disorders are very common in adult populations, lead author Colm Healy, PhD, a postdoctoral researcher for psychiatry with the University of Medicine and Health Sciences, Ireland, said in an interview.
The speculation is that this occurs in early life when psychiatry symptoms experience high fluidity. “This presents a complex scenario to model, where young people’s mental health appears to shift and change across development. Few investigations to date have had the data available to examine these trajectories over the full range of child development,” said Dr. Healy.
He and his colleagues attempted to map the profiles and trajectories of psychopathology in children and adolescents, using latent profile transition analysis (LPTA), a person-centered method, to assess comorbidity and movement in the various phases of childhood development.
“The idea behind person-centered methods such as LTPA is that it identifies unobserved subgroups of participants who respond similarly to specific variables – in this case responses to a broad measure of psychopathology,” explained Dr. Healy.
The study included 7,507 children from the child sample (ages 3, 5, and 9 years) and 6,039 children from the adolescent sample (ages 9, 13, and 17 or 18 years). Data analysis took place from October 2020 to September 2021.
Dr. Healy and colleagues in a supplementary investigation compared cohorts at age 9 years to look for sex and generational differences.
Four developmental profiles
Researchers identified 4 distinct developmental profies for person-centered psychopathological trajectories: no psychopathology (incidence range, 60%-70%), high psychopathology (incidence range, 3%-5%), externalizing problems (incidence range, 15%-25%), and internalizing problems (incidence range, 7%-12%).
Internalizing problems reflect issues with peers and emotional problems whereas externalizing problems more closely associate with hyperactivity and conduct.
Less than 5% of the youth studied experienced persistent symptoms. However, 48.6% in the child cohort and 44.1% in the adolescent cohort moved into one of the 3 psychopathology profiles (high psychopathology, externalizing, internalizing problems) at some point in development.
The spread of trajectories was more diverse in the child cohort, said Dr. Healy. “Children ebbed and flowed between the different profiles over time with a large proportion falling into one of the psychopathology categories and then switching between these profiles.” Switching was also evident in the adolescent cohort but to a lesser extent, he said.
Externalizing problems link to high psychopathology
Rates of remittance were higher among individuals in both cohorts for internalizing problems, compared with externalizing problems.
It’s possible that for some of these young people, internalizing problems are a reaction to environmental stressors such as bullying,” said Dr. Healy. “When that stress is relieved, the internalizing problems may dissipate.”
In a clinically relevant finding, children with externalizing problems (age 5, 129 [61.3%] and age 9, 95 [74.3%]) were more likely to present with new incidents of high psychopathology. This was also true in the adolescent group (age 13, 129 [91.1%] and age 17, 146 [89.9%]).
This suggests that a proportion of youth with externalizing problems have an escalating trajectory of psychopathology. “Thus, it may be possible to distinguish those with an escalating trajectory from a stable or remitting trajectory. The specific distinguishing factors require further investigation, but it has been observed before that some of those reporting externalizing problems in early life continue to have difficulties into later life,” noted Dr. Healy.
A combination of environmental or biological factors may explain this escalation, which could respond to early intervention, he said.
Overall, few children in the study transitioned directly from no psychopathology to high psychopathology.
Differences between boys, girls
In both cohorts, investigators noticed significant differences between the sexes.
Boys in childhood made up a larger proportion of the three psychopathology profiles. But by late adolescence, girls made up a larger proportion of the internalizing profile whereas boys made up a larger proportion of the externalizing profile. “These differences were in line with our expectations,” said Dr. Healy.
Trajectories also differed among boys and girls. In childhood, girls had a higher percentage of de-escalating trajectories relative to boys. “More girls than boys in the psychopathology profiles switched to a non or less severe profile. In adolescence, differences in trajectories were less obvious, with the exception that girls were more likely than boys to transition to internalizing problems from all of the other profiles at age 17,” said Dr. Healy.
Most young people who experience psychopathology will eventually see an improvement in symptoms, noted Dr. Healy. Next steps are to identify markers that distinguish individuals with persistent trajectories from remitting trajectories at the different phases of development, he said.
Study draws mixed reviews
Clinical psychiatrists not involved in the study had varying reactions to the results.
“This study is notable for its data-driven and powerful illustration of how childhood and adolescence are dynamic periods during which psychiatric symptoms can emerge and evolve,” said Sunny X. Tang, MD, a psychiatrist and an assistant professor at the Institute of Behavioral Science and the Feinstein Institutes for Medical Research, Manhasset, New York.
The clinical call for action is for person-centered mental health screening to be a routine part of pediatric and adolescent primary care or school-based services, noted Dr. Tang.
Paul S. Nestadt, MD, an assistant professor and public mental health researcher at Johns Hopkins University, Baltimore, did not think the study would have a significant impact on clinical practice.
He noted that Dr. Healy and coauthors found that some children stayed true to type, but many fluctuated between the four profile groups. The finding that fluctuation occurred more frequently in younger children is not surprising “and is consistent with what we know about the ‘moving targets’ that make diagnosing children so difficult,” said Dr. Nestadt.
“It would have been helpful to have identified clinical indicators of likely persistence in psychopathology, but the measure employed here did not allow that. It is also frustrating to not have any information on treatment, such that we cannot know whether the children who shifted to ‘no psychopathology’ did so because of treatment or spontaneously,” he added.
Victor M. Fornari, MD, MS, director of the Division of Child & Adolescent Psychiatry at The Zucker Hillside Hospital and Cohen’s Children’s Medical Center, New York, said the study is an important contribution to understanding the development of psychopathology during childhood.
“Generally, it is felt that nearly one in five youth will meet criteria for at least one psychiatric disorder by the age of 18. It is well known that externalizing disorders like ADHD manifest earlier in childhood and that depression often manifests later in adolescence,” he said.
No disclosures were reported.
A study that tracked psychopathology in 13,000 children and adolescents found that
Investigators also found a strong correlation between new incidence of high psychopathology and externalizing problems such as hyperactivity. “It is of paramount importance to identify factors that distinguish those with persisting problems and escalating trajectories so that resources can be appropriately directed,” wrote the authors of the study published online in JAMA Network Open.
Recent studies have shown that concurrent and sequential comorbidity of psychiatric disorders are very common in adult populations, lead author Colm Healy, PhD, a postdoctoral researcher for psychiatry with the University of Medicine and Health Sciences, Ireland, said in an interview.
The speculation is that this occurs in early life when psychiatry symptoms experience high fluidity. “This presents a complex scenario to model, where young people’s mental health appears to shift and change across development. Few investigations to date have had the data available to examine these trajectories over the full range of child development,” said Dr. Healy.
He and his colleagues attempted to map the profiles and trajectories of psychopathology in children and adolescents, using latent profile transition analysis (LPTA), a person-centered method, to assess comorbidity and movement in the various phases of childhood development.
“The idea behind person-centered methods such as LTPA is that it identifies unobserved subgroups of participants who respond similarly to specific variables – in this case responses to a broad measure of psychopathology,” explained Dr. Healy.
The study included 7,507 children from the child sample (ages 3, 5, and 9 years) and 6,039 children from the adolescent sample (ages 9, 13, and 17 or 18 years). Data analysis took place from October 2020 to September 2021.
Dr. Healy and colleagues in a supplementary investigation compared cohorts at age 9 years to look for sex and generational differences.
Four developmental profiles
Researchers identified 4 distinct developmental profies for person-centered psychopathological trajectories: no psychopathology (incidence range, 60%-70%), high psychopathology (incidence range, 3%-5%), externalizing problems (incidence range, 15%-25%), and internalizing problems (incidence range, 7%-12%).
Internalizing problems reflect issues with peers and emotional problems whereas externalizing problems more closely associate with hyperactivity and conduct.
Less than 5% of the youth studied experienced persistent symptoms. However, 48.6% in the child cohort and 44.1% in the adolescent cohort moved into one of the 3 psychopathology profiles (high psychopathology, externalizing, internalizing problems) at some point in development.
The spread of trajectories was more diverse in the child cohort, said Dr. Healy. “Children ebbed and flowed between the different profiles over time with a large proportion falling into one of the psychopathology categories and then switching between these profiles.” Switching was also evident in the adolescent cohort but to a lesser extent, he said.
Externalizing problems link to high psychopathology
Rates of remittance were higher among individuals in both cohorts for internalizing problems, compared with externalizing problems.
It’s possible that for some of these young people, internalizing problems are a reaction to environmental stressors such as bullying,” said Dr. Healy. “When that stress is relieved, the internalizing problems may dissipate.”
In a clinically relevant finding, children with externalizing problems (age 5, 129 [61.3%] and age 9, 95 [74.3%]) were more likely to present with new incidents of high psychopathology. This was also true in the adolescent group (age 13, 129 [91.1%] and age 17, 146 [89.9%]).
This suggests that a proportion of youth with externalizing problems have an escalating trajectory of psychopathology. “Thus, it may be possible to distinguish those with an escalating trajectory from a stable or remitting trajectory. The specific distinguishing factors require further investigation, but it has been observed before that some of those reporting externalizing problems in early life continue to have difficulties into later life,” noted Dr. Healy.
A combination of environmental or biological factors may explain this escalation, which could respond to early intervention, he said.
Overall, few children in the study transitioned directly from no psychopathology to high psychopathology.
Differences between boys, girls
In both cohorts, investigators noticed significant differences between the sexes.
Boys in childhood made up a larger proportion of the three psychopathology profiles. But by late adolescence, girls made up a larger proportion of the internalizing profile whereas boys made up a larger proportion of the externalizing profile. “These differences were in line with our expectations,” said Dr. Healy.
Trajectories also differed among boys and girls. In childhood, girls had a higher percentage of de-escalating trajectories relative to boys. “More girls than boys in the psychopathology profiles switched to a non or less severe profile. In adolescence, differences in trajectories were less obvious, with the exception that girls were more likely than boys to transition to internalizing problems from all of the other profiles at age 17,” said Dr. Healy.
Most young people who experience psychopathology will eventually see an improvement in symptoms, noted Dr. Healy. Next steps are to identify markers that distinguish individuals with persistent trajectories from remitting trajectories at the different phases of development, he said.
Study draws mixed reviews
Clinical psychiatrists not involved in the study had varying reactions to the results.
“This study is notable for its data-driven and powerful illustration of how childhood and adolescence are dynamic periods during which psychiatric symptoms can emerge and evolve,” said Sunny X. Tang, MD, a psychiatrist and an assistant professor at the Institute of Behavioral Science and the Feinstein Institutes for Medical Research, Manhasset, New York.
The clinical call for action is for person-centered mental health screening to be a routine part of pediatric and adolescent primary care or school-based services, noted Dr. Tang.
Paul S. Nestadt, MD, an assistant professor and public mental health researcher at Johns Hopkins University, Baltimore, did not think the study would have a significant impact on clinical practice.
He noted that Dr. Healy and coauthors found that some children stayed true to type, but many fluctuated between the four profile groups. The finding that fluctuation occurred more frequently in younger children is not surprising “and is consistent with what we know about the ‘moving targets’ that make diagnosing children so difficult,” said Dr. Nestadt.
“It would have been helpful to have identified clinical indicators of likely persistence in psychopathology, but the measure employed here did not allow that. It is also frustrating to not have any information on treatment, such that we cannot know whether the children who shifted to ‘no psychopathology’ did so because of treatment or spontaneously,” he added.
Victor M. Fornari, MD, MS, director of the Division of Child & Adolescent Psychiatry at The Zucker Hillside Hospital and Cohen’s Children’s Medical Center, New York, said the study is an important contribution to understanding the development of psychopathology during childhood.
“Generally, it is felt that nearly one in five youth will meet criteria for at least one psychiatric disorder by the age of 18. It is well known that externalizing disorders like ADHD manifest earlier in childhood and that depression often manifests later in adolescence,” he said.
No disclosures were reported.
FROM JAMA NETWORK OPEN
Adherence to ADHD meds may lower unemployment risk
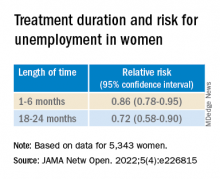
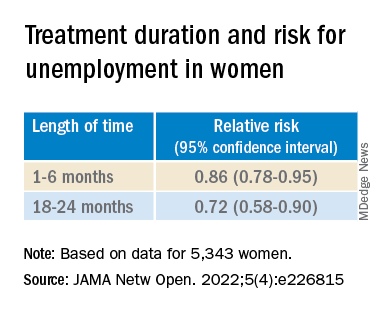
Investigators analyzed data for almost 13,000 working-age adults with ADHD and found ADHD medication use during the previous 2 years was associated with a 10% lower risk for long-term unemployment in the following year.
In addition, among the female participants, longer treatment duration was associated with a lower risk for subsequent long-term unemployment. In both genders, within-individual comparisons showed long-term unemployment was lower during periods of ADHD medication treatment, compared with nontreatment periods.
“This evidence should be considered together with the existing knowledge of risks and benefits of ADHD medications when developing treatment plans for working-aged adults,” lead author Lin Li, MSc, a doctoral candidate at the School of Medical Science, Örebro University, Sweden, told this news organization.
“However, the effect size is relatively small in magnitude, indicating that other treatment programs, such as psychotherapy, are also needed to help individuals with ADHD in work-related settings,” Ms. Li said.
The findings were published online in JAMA Network Open.
Evidence gap
Adults with ADHD “have occupational impairments, such as poor work performance, less job stability, financial problems, and increased risk for unemployment,” the investigators write.
However, “less is known about the extent to which pharmacological treatment of ADHD is associated with reductions in unemployment rates,” they add.
“People with ADHD have been reported to have problems in work-related performance,” Ms. Li noted. “ADHD medications could reduce ADHD symptoms and also help with academic achievement, but there is limited evidence on the association between ADHD medication and occupational outcomes.”
To address this gap in evidence, the researchers turned to several major Swedish registries to identify 25,358 individuals with ADHD born between 1958 and 1978 who were aged 30 to 55 years during the study period of Jan. 1, 2008, through Dec. 31, 2013).
Of these, 12,875 (41.5% women; mean age, 37.9 years) were included in the analysis. Most participants (81.19%) had more than 9 years of education.
The registers provided information not only about diagnosis, but also about prescription medications these individuals took for ADHD, including methylphenidate, amphetamine, dexamphetamine, lisdexamfetamine, and atomoxetine.
Administrative records provided data about yearly accumulated unemployment days, with long-term unemployment defined as having at least 90 days of unemployment in a calendar year.
Covariates included age at baseline, sex, country of birth, highest educational level, crime records, and psychiatric comorbidities.
Most patients (69.34%) had at least one psychiatric comorbidity, with depressive, anxiety, and substance use disorders being the most common (in 40.28%, 35.27%, and 28.77%, respectively).
Symptom reduction
The mean length of medication use was 49 days (range, 0-366 days) per year. Of participants in whom these data were available, 31.29% of women and 31.03% of men never used ADHD medications. Among participants treated with ADHD medication (68.71%), only 3.23% of the women and 3.46% of the men had persistent use during the follow-up period.
Among women and men in whom these data were available, (38.85% of the total sample), 35.70% and 41.08%, respectively, were recorded as having one or more long-term unemployment stretches across the study period. In addition, 0.15% and 0.4%, respectively, had long-term unemployment during each of those years.
Use of ADHD medications during the previous 2 years was associated with a 10% lower risk for long-term unemployment in the following year (adjusted relative risk, 0.90; 95% confidence interval, 0.87-0.95).
The researchers also found an association between use of ADHD medications and long-term unemployment among women (RR, 0.82; 95% CI, 0.76-0.89) but not among men (RR, 0.96; 95% CI, 0.91-1.01).
Among women in particular, longer treatment duration was associated with a lower risk of subsequent long-term unemployment (P < .001 for trend).
Within-individual comparisons showed the long-term unemployment rate was lower during periods when individuals were being treated with ADHD medication vs. periods of nontreatment (RR, 0.89; 95% CI, 0.85-0.94).
“Among 12,875 working-aged adults with ADHD in Sweden, we found the use of ADHD medication is associated with a lower risk of long-term unemployment, especially for women,” Ms. Li said.
“The hypothesis of this study is that ADHD medications are effective in reducing ADHD symptoms, which may in turn help to improve work performance among individuals with ADHD,” she added.
However, Ms. Li cautioned, “the information on ADHD symptoms is not available in Swedish National Registers, so more research is needed to test the hypothesis.”
The investigators also suggest that future research “should further explore the effectiveness of stimulant and nonstimulant ADHD medications” and replicate their findings in other settings.
Findings ‘make sense’
Commenting on the study, Ari Tuckman PsyD, expert spokesman for Children and Adults with Attention-Deficit/Hyperactivity Disorder, said, there is “a lot to like about this study, specifically the large sample size and within-individual comparisons that the Scandinavians’ databases allow.”
“We know that ADHD can impact both finding and keeping a job, so it absolutely makes sense that medication use would reduce duration of unemployment,” said Dr. Tuckman, who is in private practice in West Chester, Pa., and was not involved with the research.
However, “I would venture that the results would have been more robust if the authors had been able to only look at those on optimized medication regimens, which is far too few,” he added. “This lack of optimization would have been even more true 10 years ago, which is when the data was from.”
The study was supported by a grant from the Swedish Council for Health, Working Life, and Welfare, an award from the Swedish Research Council, and a grant from Shire International GmbH, a member of the Takeda group of companies. Ms. Li and Dr. Tuckman have disclosed no relevant financial relationships. The other authors’ disclosures are listed in the original paper.
A version of this article first appeared on Medscape.com.
Investigators analyzed data for almost 13,000 working-age adults with ADHD and found ADHD medication use during the previous 2 years was associated with a 10% lower risk for long-term unemployment in the following year.
In addition, among the female participants, longer treatment duration was associated with a lower risk for subsequent long-term unemployment. In both genders, within-individual comparisons showed long-term unemployment was lower during periods of ADHD medication treatment, compared with nontreatment periods.
“This evidence should be considered together with the existing knowledge of risks and benefits of ADHD medications when developing treatment plans for working-aged adults,” lead author Lin Li, MSc, a doctoral candidate at the School of Medical Science, Örebro University, Sweden, told this news organization.
“However, the effect size is relatively small in magnitude, indicating that other treatment programs, such as psychotherapy, are also needed to help individuals with ADHD in work-related settings,” Ms. Li said.
The findings were published online in JAMA Network Open.
Evidence gap
Adults with ADHD “have occupational impairments, such as poor work performance, less job stability, financial problems, and increased risk for unemployment,” the investigators write.
However, “less is known about the extent to which pharmacological treatment of ADHD is associated with reductions in unemployment rates,” they add.
“People with ADHD have been reported to have problems in work-related performance,” Ms. Li noted. “ADHD medications could reduce ADHD symptoms and also help with academic achievement, but there is limited evidence on the association between ADHD medication and occupational outcomes.”
To address this gap in evidence, the researchers turned to several major Swedish registries to identify 25,358 individuals with ADHD born between 1958 and 1978 who were aged 30 to 55 years during the study period of Jan. 1, 2008, through Dec. 31, 2013).
Of these, 12,875 (41.5% women; mean age, 37.9 years) were included in the analysis. Most participants (81.19%) had more than 9 years of education.
The registers provided information not only about diagnosis, but also about prescription medications these individuals took for ADHD, including methylphenidate, amphetamine, dexamphetamine, lisdexamfetamine, and atomoxetine.
Administrative records provided data about yearly accumulated unemployment days, with long-term unemployment defined as having at least 90 days of unemployment in a calendar year.
Covariates included age at baseline, sex, country of birth, highest educational level, crime records, and psychiatric comorbidities.
Most patients (69.34%) had at least one psychiatric comorbidity, with depressive, anxiety, and substance use disorders being the most common (in 40.28%, 35.27%, and 28.77%, respectively).
Symptom reduction
The mean length of medication use was 49 days (range, 0-366 days) per year. Of participants in whom these data were available, 31.29% of women and 31.03% of men never used ADHD medications. Among participants treated with ADHD medication (68.71%), only 3.23% of the women and 3.46% of the men had persistent use during the follow-up period.
Among women and men in whom these data were available, (38.85% of the total sample), 35.70% and 41.08%, respectively, were recorded as having one or more long-term unemployment stretches across the study period. In addition, 0.15% and 0.4%, respectively, had long-term unemployment during each of those years.
Use of ADHD medications during the previous 2 years was associated with a 10% lower risk for long-term unemployment in the following year (adjusted relative risk, 0.90; 95% confidence interval, 0.87-0.95).
The researchers also found an association between use of ADHD medications and long-term unemployment among women (RR, 0.82; 95% CI, 0.76-0.89) but not among men (RR, 0.96; 95% CI, 0.91-1.01).
Among women in particular, longer treatment duration was associated with a lower risk of subsequent long-term unemployment (P < .001 for trend).
Within-individual comparisons showed the long-term unemployment rate was lower during periods when individuals were being treated with ADHD medication vs. periods of nontreatment (RR, 0.89; 95% CI, 0.85-0.94).
“Among 12,875 working-aged adults with ADHD in Sweden, we found the use of ADHD medication is associated with a lower risk of long-term unemployment, especially for women,” Ms. Li said.
“The hypothesis of this study is that ADHD medications are effective in reducing ADHD symptoms, which may in turn help to improve work performance among individuals with ADHD,” she added.
However, Ms. Li cautioned, “the information on ADHD symptoms is not available in Swedish National Registers, so more research is needed to test the hypothesis.”
The investigators also suggest that future research “should further explore the effectiveness of stimulant and nonstimulant ADHD medications” and replicate their findings in other settings.
Findings ‘make sense’
Commenting on the study, Ari Tuckman PsyD, expert spokesman for Children and Adults with Attention-Deficit/Hyperactivity Disorder, said, there is “a lot to like about this study, specifically the large sample size and within-individual comparisons that the Scandinavians’ databases allow.”
“We know that ADHD can impact both finding and keeping a job, so it absolutely makes sense that medication use would reduce duration of unemployment,” said Dr. Tuckman, who is in private practice in West Chester, Pa., and was not involved with the research.
However, “I would venture that the results would have been more robust if the authors had been able to only look at those on optimized medication regimens, which is far too few,” he added. “This lack of optimization would have been even more true 10 years ago, which is when the data was from.”
The study was supported by a grant from the Swedish Council for Health, Working Life, and Welfare, an award from the Swedish Research Council, and a grant from Shire International GmbH, a member of the Takeda group of companies. Ms. Li and Dr. Tuckman have disclosed no relevant financial relationships. The other authors’ disclosures are listed in the original paper.
A version of this article first appeared on Medscape.com.
Investigators analyzed data for almost 13,000 working-age adults with ADHD and found ADHD medication use during the previous 2 years was associated with a 10% lower risk for long-term unemployment in the following year.
In addition, among the female participants, longer treatment duration was associated with a lower risk for subsequent long-term unemployment. In both genders, within-individual comparisons showed long-term unemployment was lower during periods of ADHD medication treatment, compared with nontreatment periods.
“This evidence should be considered together with the existing knowledge of risks and benefits of ADHD medications when developing treatment plans for working-aged adults,” lead author Lin Li, MSc, a doctoral candidate at the School of Medical Science, Örebro University, Sweden, told this news organization.
“However, the effect size is relatively small in magnitude, indicating that other treatment programs, such as psychotherapy, are also needed to help individuals with ADHD in work-related settings,” Ms. Li said.
The findings were published online in JAMA Network Open.
Evidence gap
Adults with ADHD “have occupational impairments, such as poor work performance, less job stability, financial problems, and increased risk for unemployment,” the investigators write.
However, “less is known about the extent to which pharmacological treatment of ADHD is associated with reductions in unemployment rates,” they add.
“People with ADHD have been reported to have problems in work-related performance,” Ms. Li noted. “ADHD medications could reduce ADHD symptoms and also help with academic achievement, but there is limited evidence on the association between ADHD medication and occupational outcomes.”
To address this gap in evidence, the researchers turned to several major Swedish registries to identify 25,358 individuals with ADHD born between 1958 and 1978 who were aged 30 to 55 years during the study period of Jan. 1, 2008, through Dec. 31, 2013).
Of these, 12,875 (41.5% women; mean age, 37.9 years) were included in the analysis. Most participants (81.19%) had more than 9 years of education.
The registers provided information not only about diagnosis, but also about prescription medications these individuals took for ADHD, including methylphenidate, amphetamine, dexamphetamine, lisdexamfetamine, and atomoxetine.
Administrative records provided data about yearly accumulated unemployment days, with long-term unemployment defined as having at least 90 days of unemployment in a calendar year.
Covariates included age at baseline, sex, country of birth, highest educational level, crime records, and psychiatric comorbidities.
Most patients (69.34%) had at least one psychiatric comorbidity, with depressive, anxiety, and substance use disorders being the most common (in 40.28%, 35.27%, and 28.77%, respectively).
Symptom reduction
The mean length of medication use was 49 days (range, 0-366 days) per year. Of participants in whom these data were available, 31.29% of women and 31.03% of men never used ADHD medications. Among participants treated with ADHD medication (68.71%), only 3.23% of the women and 3.46% of the men had persistent use during the follow-up period.
Among women and men in whom these data were available, (38.85% of the total sample), 35.70% and 41.08%, respectively, were recorded as having one or more long-term unemployment stretches across the study period. In addition, 0.15% and 0.4%, respectively, had long-term unemployment during each of those years.
Use of ADHD medications during the previous 2 years was associated with a 10% lower risk for long-term unemployment in the following year (adjusted relative risk, 0.90; 95% confidence interval, 0.87-0.95).
The researchers also found an association between use of ADHD medications and long-term unemployment among women (RR, 0.82; 95% CI, 0.76-0.89) but not among men (RR, 0.96; 95% CI, 0.91-1.01).
Among women in particular, longer treatment duration was associated with a lower risk of subsequent long-term unemployment (P < .001 for trend).
Within-individual comparisons showed the long-term unemployment rate was lower during periods when individuals were being treated with ADHD medication vs. periods of nontreatment (RR, 0.89; 95% CI, 0.85-0.94).
“Among 12,875 working-aged adults with ADHD in Sweden, we found the use of ADHD medication is associated with a lower risk of long-term unemployment, especially for women,” Ms. Li said.
“The hypothesis of this study is that ADHD medications are effective in reducing ADHD symptoms, which may in turn help to improve work performance among individuals with ADHD,” she added.
However, Ms. Li cautioned, “the information on ADHD symptoms is not available in Swedish National Registers, so more research is needed to test the hypothesis.”
The investigators also suggest that future research “should further explore the effectiveness of stimulant and nonstimulant ADHD medications” and replicate their findings in other settings.
Findings ‘make sense’
Commenting on the study, Ari Tuckman PsyD, expert spokesman for Children and Adults with Attention-Deficit/Hyperactivity Disorder, said, there is “a lot to like about this study, specifically the large sample size and within-individual comparisons that the Scandinavians’ databases allow.”
“We know that ADHD can impact both finding and keeping a job, so it absolutely makes sense that medication use would reduce duration of unemployment,” said Dr. Tuckman, who is in private practice in West Chester, Pa., and was not involved with the research.
However, “I would venture that the results would have been more robust if the authors had been able to only look at those on optimized medication regimens, which is far too few,” he added. “This lack of optimization would have been even more true 10 years ago, which is when the data was from.”
The study was supported by a grant from the Swedish Council for Health, Working Life, and Welfare, an award from the Swedish Research Council, and a grant from Shire International GmbH, a member of the Takeda group of companies. Ms. Li and Dr. Tuckman have disclosed no relevant financial relationships. The other authors’ disclosures are listed in the original paper.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Psychodynamic factors in psychotropic prescribing
Medical noncompliance and patient resistance to treatment are frequent problems in medical practice. According to an older report by the US Office of Inspector General, approximately 125,000 people die each year in the United States because they do not take their medication properly.1 The World Health Organization reported that 10% to 25% of hospital and nursing home admissions are a result of patient noncompliance.2 In addition, approximately 50% of prescriptions filled for chronic diseases in developed nations are not taken correctly, and up to 40% of patients do not adhere to their treatment regimens.2 Among psychiatric patients, noncompliance with medications and other treatments ranges from 25% to 75%.3
In recent years, combining pharmacotherapy with psychodynamic psychotherapy has become a fairly common form of psychiatric practice. A main reason for combining these treatments is that a patient with severe psychiatric symptoms may be unable to engage in self-reflective insightful therapy until those symptoms are substantially relieved with pharmacotherapy. The efficacy of combined pharmacotherapy/psychotherapy may also be more than additive and result in a therapeutic alliance that is greater than the sum of the 2 individual treatments.4 Establishing a therapeutic alliance is critical to successful treatment, but this alliance can be distorted by the needs and expectations of both the patient and the clinician.
A psychodynamic understanding of the patient and the therapeutic alliance can facilitate combined treatment in several ways. It can lead to better communication, which in turn can lead to a realistic discussion of a patient’s fears and worries about any medications they have been prescribed. A dynamically aware clinician may better understand what the symptoms mean to the patient. Such clinicians will not only be able to explain the value of a medication, its target symptoms, and the rationale for taking it, but will also be able to discuss the psychological significance of the medication, along with its medical and biological significance.5
This article briefly reviews the therapeutic alliance and the influence of transference (the emotional reactions of the patient towards the clinician),6 countertransference (the emotional reactions of the clinician towards the patient),6 and patient resistance/nonadherence to treatment on the failure or success of pharmacotherapy. We provide case examples to illustrate how these psychodynamic factors can be at play in prescribing.
The therapeutic alliance
The therapeutic alliance is a rational agreement or contract between a patient and the clinician; it is a cornerstone of treatment in medicine.6 Its basic premise is that the patient’s rational expectation that their physician is appropriately qualified, will perform a suitable evaluation, and will prescribe relevant treatment is matched by the physician’s expectation that the patient will do their best to comply with treatment recommendations. For this to succeed, the contract needs to be straightforward, and there needs to be no covert agenda. A covert agenda may be in the form of unrealistic expectations and wishes rooted in insecure experiences in childhood by either party. A patient under stress may react to the physician with mistrust, excessive demands, and noncompliance. A physician under stress may react to a patient by becoming authoritative or indecisive, or by overmedicating or underprescribing.
Transference
Transference is a phenomenon whereby a patient’s feelings and attitudes are unconsciously transferred from a person or situation in the past to the clinician or treatment in the present.6 For example, a patient who is scared of a serious illness may adopt a helpless, childlike role and project an omnipotent, parentlike quality on the clinician (positive transference) that may be unrealistic. Positive transference may underlie a placebo response to medication in which a patient’s response is too quick or too complete, and it may be a way of unconsciously pleasing an authoritative parent figure from childhood. On the other hand, a patient may unconsciously view their physician as a controlling parent (negative transference) and react angrily or rebelliously. A patient’s flirtatious behavior toward their physician may be a form of transference from unresolved sexual trauma during childhood. However, not all patient reactions should be considered transference; a patient may be appropriately thankful and deferential, or irritated and questioning, depending on the clinician’s demeanor and treatment approach.
Countertransference
Countertransference is the response elicited in the physician by a patient’s appearance and behaviors, or by a patient’s transference projections.6 This response can be positive or negative and includes both feelings and associated thoughts related to the physician’s past experiences. For example, a physician in the emergency department may get angry with a patient with an alcohol use disorder because of the physician’s negative experiences with an alcoholic parent during childhood. On the other hand, a physician raised by a compulsive mother may order unnecessary tests on a demanding older female patient. Or, a clinician raised by a sheltering parent may react to a hapless and dependent patient by spending excessive time with them or providing additional medication samples. However, not all clinician reactions are countertransference. For example, a physician’s empathic or stoic demeanor may be an appropriate emotional response to a patient’s diagnosis such as cancer.
Continue to: Patient resistance/nonadherence
Patient resistance/nonadherence
In 1920, Freud conceptualized the psychodynamic factors in patient resistance to treatment and theorized that many patients were unconsciously reluctant to give up their symptoms or were driven, for transference reasons, to resist the physician.7 This same concept may underlie patient resistance to pharmacotherapy. When symptoms constitute an important defense mechanism, patients are likely to resist medication effects until they have developed more mature defenses or more effective ways of coping.8 Even when patients do not resist symptom relief, they may still resist the physician’s choice of treatment due to negative transference. Such patients often negotiate the type of medication, dose, timing of the dose, and start date as a way of trying to “keep control” of a “doctor they don’t quite trust.”8 They may manage their own medication regimen by taking more or less than the prescribed dose. This resistance might lead to a “nocebo” effect in which a medication trial fails not because of its ineffectiveness but instead from the unconscious mind influencing the patient’s body to resist. Nonadherence to treatment may occur in patients who have attachment difficulties that make it difficult for them to trust anyone as a result of negative childhood experiences.9 Clinicians need to recognize the dynamics of power struggles, control, and trust. A warm, collaborative and cooperative stance is likely to be more beneficial than an authoritative and detached approach.10
The following 3 case examples illustrate how psychodynamic factors such as transference and countertransference can influence the therapeutic alliance, treatment decisions, and the outcomes of pharmacotherapy.
CASE 1
Mr. A, age 63, has posttraumatic stress disorder originating from his father’s death by a self-inflicted gunshot wound when Mr. A was 19, and later from the symbolic loss of his mother when she remarried. He reported vivid memories of his father sexually assaulting his mother when he was 6. This fostered a protective nature in him for his mother, as well as for his 3 younger siblings. After his father’s suicide, Mr. A had to take on a paternal role for his 3 siblings. He often feels he grew up too quickly, and resents this. He feels his mother betrayed him when she got remarried. Mr. A attempts suicide, is admitted to a local hospital, and then follows up at a university hospital outpatient psychiatry clinic.
At the clinic, Mr. A begins psychodynamic psychotherapy with a female resident physician. They establish a good rapport. Mr. A begins working through his past traumas and looks forward to his therapy sessions. The physician views this as positive transference, perhaps because her personality style and appearance are similar to that of Mr. A’s mother. She also often notes a positive countertransference during sessions; Mr. A seemingly reminds her of her father in personality and appearance. Perhaps due to this positive transference/positive countertransference dynamic, Mr. A feels comfortable with having his medication regimen simplified after years of unsuccessful medication trials and a course of electroconvulsive therapy. His regimen soon consists of only a selective serotonin reuptake inhibitor and a glutamate modulator as an adjunct for anxiety. Psychotherapy sessions remain the mainstay of his treatment plan. Mr. A’s mood and anxiety improve significantly over a short time.
CASE 2
Ms. G, age 24, is admitted to a partial hospitalization program (PHP). Her diagnoses include seasonal affective disorder, anxiety, and attention-deficit/hyperactivity disorder (ADHD); she might have a genetic disposition to bipolar disorder. Ms. G recently had attempted suicide and was discharged from an inpatient unit. She is a middle child and was raised by emotionally and verbally abusive parents in a tumultuous household. Her father rarely kept a job for more than a few months, displayed rage, and lacked empathy. Ms. G feels unloved by her mother and says that her mother is emotionally unstable. Upon admission to the PHP, Ms. G is quick to question the credentials of every staff member she meets, and suggests the abuse and lack of trust she had experienced during her formative years have made her aggressive and paranoid.
Continue to: Since her teens...
Since her teens, Ms. G had received treatment for ADHD with various stimulant and nonstimulant medications that were prescribed by an outpatient psychiatrist. During her sophomore year of college, she was also prescribed medications for depression and anxiety. Ms. G speaks very highly of and praises the skill of her previous psychiatrist while voicing concerns about having to see new clinicians in the PHP. She had recently seen a therapist who moved out of state after a few sessions. Ms. G has abandonment fears and appears to react with anger toward new clinicians.
A negative transference towards Ms. G’s treatment team and the PHP as a whole are evident during the first week. She skips most group therapy sessions and criticizes the clinicians’ skills and training as ineffective. When her psychiatrist recommends changes in medication, she initially argues. She eventually agrees to take a new medication but soon reports intolerable adverse effects, which suggests negative transference toward the psychiatrist as an authority figure, and toward the medication as an extension of the psychiatrist. The treatment team also interprets this as nocebo effect. Ms. G engages in “splitting” by complaining about her psychiatrist to her therapist. The psychiatrist resents having been belittled. Ms. G demands to see a different psychiatrist, and when her demands are not met, she discharges herself from the PHP against medical advice. The treatment team interprets Ms. G’s resistance to treatment to have resulted from poor attachment during childhood and subsequent negative transference.
CASE 3
Ms. U, age 60, is seen at a local mental health center and diagnosed with major depressive disorder, likely resulting from grief and loss from her husband’s recent death. She was raised by her single mother and mostly absent father. Ms. U is a homemaker and had been married for more than 30 years. She participates in weekly psychotherapy with a young male psychiatrist, who prescribes an antidepressant. Ms. U is eager to please and makes every effort to be the perfect patient: she is always early for her appointments, takes her medications as prescribed, and frequently expresses her respect and appreciation for her psychiatrist. Within a few weeks, Ms. U’s depressive symptoms rapidly improve.
Ms. U is a talented and avid knit and crochet expert. At an appointment soon before Christmas, she gives her psychiatrist a pair of socks she knitted. While the gift is of little monetary value, the psychiatrist interprets this as part of transference, but the intimate nature of the gift makes him uncomfortable. He and Ms. U discuss this at length, which reveals definite transference as Ms. U says the psychiatrist perhaps reminds her of her husband, who also had brown skin. It is also apparent that Ms. U’s tendency to please perhaps comes from the lack of having a father figure, which her husband had fulfilled. The psychiatrist believes that Ms. U’s rapid response may be a placebo effect from positive transference. Upon further reflection, the psychiatrist realizes that Ms. U is a motherly figure to him, and that positive countertransference is at play in that he could not turn down the gift and had looked forward to the therapy sessions with her.
Bottom Line
Even clinicians who do not provide psychodynamic psychotherapy can use an awareness of psychodynamic factors to improve treatment. Psychodynamic factors such as transference and countertransference can influence the therapeutic alliance, treatment decisions, and patient outcomes. Patients’ experiences and difficulties with attachment during childhood should be recognized and addressed as part of pharmacotherapy.
Related Resources
- Neumann M, Silva N, Opler DJ. ARISE to supportive psychotherapy. Current Psychiatry. 2021;20(5):48-49. doi:10.12788/cp.0123
- Mintz D. Psychodynamic psychopharmacology. Psychiatric Times. 2011;28(9). https://www.psychiatrictimes.com/view/psychodynamic-psychopharmacology
1. Office of Inspector General, Office of Evaluation and Inspections. Medication Regimens: Causes of Noncompliance. 1990. Accessed April 13, 2022. https://oig.hhs.gov/oei/reports/oei-04-89-89121.pdf
2. World Health Organization. Adherence to Long Term Therapies: Evidence for Action. World Health Organization; 2003.
3. Powell AD. The medication life. J Psychother Pract Res. 2001;10(4):217-222.
4. Wright JH, Hollifield M. Combining pharmacotherapy and psychotherapy. Psychiatric Annals. 2006;36(5):302-305.
5. Summers RF, Barber JP. Psychodynamic Therapy: A Guide to Evidence-Based Practice. Guilford Press; 2013:265-290.
6. Hughes P, Kerr I. Transference and countertransference in communication between doctor and patient. Advances in Psychiatric Treatment. 2000;6(1):57-64.
7. Freud S. Resistance and suppression. In: Freud S. A General Introduction to Psychoanalysis. Boni and Liveright Publishers; 1920:248-261.
8. Vlastelica M. Psychodynamic approach as a creative factor in psychopharmacotherapy. Psychiatr Danub. 2013;25(3):316-319.
9. Alfonso CA. Understanding the psychodynamics of nonadherence. Psychiatric Times. 2011;28(5). Accessed April 13, 2022. https://www.psychiatrictimes.com/view/understanding-psychodynamics-nonadherence
10. Wallin DJ. Attachment in Psychotherapy. Guilford Press; 2007.
Medical noncompliance and patient resistance to treatment are frequent problems in medical practice. According to an older report by the US Office of Inspector General, approximately 125,000 people die each year in the United States because they do not take their medication properly.1 The World Health Organization reported that 10% to 25% of hospital and nursing home admissions are a result of patient noncompliance.2 In addition, approximately 50% of prescriptions filled for chronic diseases in developed nations are not taken correctly, and up to 40% of patients do not adhere to their treatment regimens.2 Among psychiatric patients, noncompliance with medications and other treatments ranges from 25% to 75%.3
In recent years, combining pharmacotherapy with psychodynamic psychotherapy has become a fairly common form of psychiatric practice. A main reason for combining these treatments is that a patient with severe psychiatric symptoms may be unable to engage in self-reflective insightful therapy until those symptoms are substantially relieved with pharmacotherapy. The efficacy of combined pharmacotherapy/psychotherapy may also be more than additive and result in a therapeutic alliance that is greater than the sum of the 2 individual treatments.4 Establishing a therapeutic alliance is critical to successful treatment, but this alliance can be distorted by the needs and expectations of both the patient and the clinician.
A psychodynamic understanding of the patient and the therapeutic alliance can facilitate combined treatment in several ways. It can lead to better communication, which in turn can lead to a realistic discussion of a patient’s fears and worries about any medications they have been prescribed. A dynamically aware clinician may better understand what the symptoms mean to the patient. Such clinicians will not only be able to explain the value of a medication, its target symptoms, and the rationale for taking it, but will also be able to discuss the psychological significance of the medication, along with its medical and biological significance.5
This article briefly reviews the therapeutic alliance and the influence of transference (the emotional reactions of the patient towards the clinician),6 countertransference (the emotional reactions of the clinician towards the patient),6 and patient resistance/nonadherence to treatment on the failure or success of pharmacotherapy. We provide case examples to illustrate how these psychodynamic factors can be at play in prescribing.
The therapeutic alliance
The therapeutic alliance is a rational agreement or contract between a patient and the clinician; it is a cornerstone of treatment in medicine.6 Its basic premise is that the patient’s rational expectation that their physician is appropriately qualified, will perform a suitable evaluation, and will prescribe relevant treatment is matched by the physician’s expectation that the patient will do their best to comply with treatment recommendations. For this to succeed, the contract needs to be straightforward, and there needs to be no covert agenda. A covert agenda may be in the form of unrealistic expectations and wishes rooted in insecure experiences in childhood by either party. A patient under stress may react to the physician with mistrust, excessive demands, and noncompliance. A physician under stress may react to a patient by becoming authoritative or indecisive, or by overmedicating or underprescribing.
Transference
Transference is a phenomenon whereby a patient’s feelings and attitudes are unconsciously transferred from a person or situation in the past to the clinician or treatment in the present.6 For example, a patient who is scared of a serious illness may adopt a helpless, childlike role and project an omnipotent, parentlike quality on the clinician (positive transference) that may be unrealistic. Positive transference may underlie a placebo response to medication in which a patient’s response is too quick or too complete, and it may be a way of unconsciously pleasing an authoritative parent figure from childhood. On the other hand, a patient may unconsciously view their physician as a controlling parent (negative transference) and react angrily or rebelliously. A patient’s flirtatious behavior toward their physician may be a form of transference from unresolved sexual trauma during childhood. However, not all patient reactions should be considered transference; a patient may be appropriately thankful and deferential, or irritated and questioning, depending on the clinician’s demeanor and treatment approach.
Countertransference
Countertransference is the response elicited in the physician by a patient’s appearance and behaviors, or by a patient’s transference projections.6 This response can be positive or negative and includes both feelings and associated thoughts related to the physician’s past experiences. For example, a physician in the emergency department may get angry with a patient with an alcohol use disorder because of the physician’s negative experiences with an alcoholic parent during childhood. On the other hand, a physician raised by a compulsive mother may order unnecessary tests on a demanding older female patient. Or, a clinician raised by a sheltering parent may react to a hapless and dependent patient by spending excessive time with them or providing additional medication samples. However, not all clinician reactions are countertransference. For example, a physician’s empathic or stoic demeanor may be an appropriate emotional response to a patient’s diagnosis such as cancer.
Continue to: Patient resistance/nonadherence
Patient resistance/nonadherence
In 1920, Freud conceptualized the psychodynamic factors in patient resistance to treatment and theorized that many patients were unconsciously reluctant to give up their symptoms or were driven, for transference reasons, to resist the physician.7 This same concept may underlie patient resistance to pharmacotherapy. When symptoms constitute an important defense mechanism, patients are likely to resist medication effects until they have developed more mature defenses or more effective ways of coping.8 Even when patients do not resist symptom relief, they may still resist the physician’s choice of treatment due to negative transference. Such patients often negotiate the type of medication, dose, timing of the dose, and start date as a way of trying to “keep control” of a “doctor they don’t quite trust.”8 They may manage their own medication regimen by taking more or less than the prescribed dose. This resistance might lead to a “nocebo” effect in which a medication trial fails not because of its ineffectiveness but instead from the unconscious mind influencing the patient’s body to resist. Nonadherence to treatment may occur in patients who have attachment difficulties that make it difficult for them to trust anyone as a result of negative childhood experiences.9 Clinicians need to recognize the dynamics of power struggles, control, and trust. A warm, collaborative and cooperative stance is likely to be more beneficial than an authoritative and detached approach.10
The following 3 case examples illustrate how psychodynamic factors such as transference and countertransference can influence the therapeutic alliance, treatment decisions, and the outcomes of pharmacotherapy.
CASE 1
Mr. A, age 63, has posttraumatic stress disorder originating from his father’s death by a self-inflicted gunshot wound when Mr. A was 19, and later from the symbolic loss of his mother when she remarried. He reported vivid memories of his father sexually assaulting his mother when he was 6. This fostered a protective nature in him for his mother, as well as for his 3 younger siblings. After his father’s suicide, Mr. A had to take on a paternal role for his 3 siblings. He often feels he grew up too quickly, and resents this. He feels his mother betrayed him when she got remarried. Mr. A attempts suicide, is admitted to a local hospital, and then follows up at a university hospital outpatient psychiatry clinic.
At the clinic, Mr. A begins psychodynamic psychotherapy with a female resident physician. They establish a good rapport. Mr. A begins working through his past traumas and looks forward to his therapy sessions. The physician views this as positive transference, perhaps because her personality style and appearance are similar to that of Mr. A’s mother. She also often notes a positive countertransference during sessions; Mr. A seemingly reminds her of her father in personality and appearance. Perhaps due to this positive transference/positive countertransference dynamic, Mr. A feels comfortable with having his medication regimen simplified after years of unsuccessful medication trials and a course of electroconvulsive therapy. His regimen soon consists of only a selective serotonin reuptake inhibitor and a glutamate modulator as an adjunct for anxiety. Psychotherapy sessions remain the mainstay of his treatment plan. Mr. A’s mood and anxiety improve significantly over a short time.
CASE 2
Ms. G, age 24, is admitted to a partial hospitalization program (PHP). Her diagnoses include seasonal affective disorder, anxiety, and attention-deficit/hyperactivity disorder (ADHD); she might have a genetic disposition to bipolar disorder. Ms. G recently had attempted suicide and was discharged from an inpatient unit. She is a middle child and was raised by emotionally and verbally abusive parents in a tumultuous household. Her father rarely kept a job for more than a few months, displayed rage, and lacked empathy. Ms. G feels unloved by her mother and says that her mother is emotionally unstable. Upon admission to the PHP, Ms. G is quick to question the credentials of every staff member she meets, and suggests the abuse and lack of trust she had experienced during her formative years have made her aggressive and paranoid.
Continue to: Since her teens...
Since her teens, Ms. G had received treatment for ADHD with various stimulant and nonstimulant medications that were prescribed by an outpatient psychiatrist. During her sophomore year of college, she was also prescribed medications for depression and anxiety. Ms. G speaks very highly of and praises the skill of her previous psychiatrist while voicing concerns about having to see new clinicians in the PHP. She had recently seen a therapist who moved out of state after a few sessions. Ms. G has abandonment fears and appears to react with anger toward new clinicians.
A negative transference towards Ms. G’s treatment team and the PHP as a whole are evident during the first week. She skips most group therapy sessions and criticizes the clinicians’ skills and training as ineffective. When her psychiatrist recommends changes in medication, she initially argues. She eventually agrees to take a new medication but soon reports intolerable adverse effects, which suggests negative transference toward the psychiatrist as an authority figure, and toward the medication as an extension of the psychiatrist. The treatment team also interprets this as nocebo effect. Ms. G engages in “splitting” by complaining about her psychiatrist to her therapist. The psychiatrist resents having been belittled. Ms. G demands to see a different psychiatrist, and when her demands are not met, she discharges herself from the PHP against medical advice. The treatment team interprets Ms. G’s resistance to treatment to have resulted from poor attachment during childhood and subsequent negative transference.
CASE 3
Ms. U, age 60, is seen at a local mental health center and diagnosed with major depressive disorder, likely resulting from grief and loss from her husband’s recent death. She was raised by her single mother and mostly absent father. Ms. U is a homemaker and had been married for more than 30 years. She participates in weekly psychotherapy with a young male psychiatrist, who prescribes an antidepressant. Ms. U is eager to please and makes every effort to be the perfect patient: she is always early for her appointments, takes her medications as prescribed, and frequently expresses her respect and appreciation for her psychiatrist. Within a few weeks, Ms. U’s depressive symptoms rapidly improve.
Ms. U is a talented and avid knit and crochet expert. At an appointment soon before Christmas, she gives her psychiatrist a pair of socks she knitted. While the gift is of little monetary value, the psychiatrist interprets this as part of transference, but the intimate nature of the gift makes him uncomfortable. He and Ms. U discuss this at length, which reveals definite transference as Ms. U says the psychiatrist perhaps reminds her of her husband, who also had brown skin. It is also apparent that Ms. U’s tendency to please perhaps comes from the lack of having a father figure, which her husband had fulfilled. The psychiatrist believes that Ms. U’s rapid response may be a placebo effect from positive transference. Upon further reflection, the psychiatrist realizes that Ms. U is a motherly figure to him, and that positive countertransference is at play in that he could not turn down the gift and had looked forward to the therapy sessions with her.
Bottom Line
Even clinicians who do not provide psychodynamic psychotherapy can use an awareness of psychodynamic factors to improve treatment. Psychodynamic factors such as transference and countertransference can influence the therapeutic alliance, treatment decisions, and patient outcomes. Patients’ experiences and difficulties with attachment during childhood should be recognized and addressed as part of pharmacotherapy.
Related Resources
- Neumann M, Silva N, Opler DJ. ARISE to supportive psychotherapy. Current Psychiatry. 2021;20(5):48-49. doi:10.12788/cp.0123
- Mintz D. Psychodynamic psychopharmacology. Psychiatric Times. 2011;28(9). https://www.psychiatrictimes.com/view/psychodynamic-psychopharmacology
Medical noncompliance and patient resistance to treatment are frequent problems in medical practice. According to an older report by the US Office of Inspector General, approximately 125,000 people die each year in the United States because they do not take their medication properly.1 The World Health Organization reported that 10% to 25% of hospital and nursing home admissions are a result of patient noncompliance.2 In addition, approximately 50% of prescriptions filled for chronic diseases in developed nations are not taken correctly, and up to 40% of patients do not adhere to their treatment regimens.2 Among psychiatric patients, noncompliance with medications and other treatments ranges from 25% to 75%.3
In recent years, combining pharmacotherapy with psychodynamic psychotherapy has become a fairly common form of psychiatric practice. A main reason for combining these treatments is that a patient with severe psychiatric symptoms may be unable to engage in self-reflective insightful therapy until those symptoms are substantially relieved with pharmacotherapy. The efficacy of combined pharmacotherapy/psychotherapy may also be more than additive and result in a therapeutic alliance that is greater than the sum of the 2 individual treatments.4 Establishing a therapeutic alliance is critical to successful treatment, but this alliance can be distorted by the needs and expectations of both the patient and the clinician.
A psychodynamic understanding of the patient and the therapeutic alliance can facilitate combined treatment in several ways. It can lead to better communication, which in turn can lead to a realistic discussion of a patient’s fears and worries about any medications they have been prescribed. A dynamically aware clinician may better understand what the symptoms mean to the patient. Such clinicians will not only be able to explain the value of a medication, its target symptoms, and the rationale for taking it, but will also be able to discuss the psychological significance of the medication, along with its medical and biological significance.5
This article briefly reviews the therapeutic alliance and the influence of transference (the emotional reactions of the patient towards the clinician),6 countertransference (the emotional reactions of the clinician towards the patient),6 and patient resistance/nonadherence to treatment on the failure or success of pharmacotherapy. We provide case examples to illustrate how these psychodynamic factors can be at play in prescribing.
The therapeutic alliance
The therapeutic alliance is a rational agreement or contract between a patient and the clinician; it is a cornerstone of treatment in medicine.6 Its basic premise is that the patient’s rational expectation that their physician is appropriately qualified, will perform a suitable evaluation, and will prescribe relevant treatment is matched by the physician’s expectation that the patient will do their best to comply with treatment recommendations. For this to succeed, the contract needs to be straightforward, and there needs to be no covert agenda. A covert agenda may be in the form of unrealistic expectations and wishes rooted in insecure experiences in childhood by either party. A patient under stress may react to the physician with mistrust, excessive demands, and noncompliance. A physician under stress may react to a patient by becoming authoritative or indecisive, or by overmedicating or underprescribing.
Transference
Transference is a phenomenon whereby a patient’s feelings and attitudes are unconsciously transferred from a person or situation in the past to the clinician or treatment in the present.6 For example, a patient who is scared of a serious illness may adopt a helpless, childlike role and project an omnipotent, parentlike quality on the clinician (positive transference) that may be unrealistic. Positive transference may underlie a placebo response to medication in which a patient’s response is too quick or too complete, and it may be a way of unconsciously pleasing an authoritative parent figure from childhood. On the other hand, a patient may unconsciously view their physician as a controlling parent (negative transference) and react angrily or rebelliously. A patient’s flirtatious behavior toward their physician may be a form of transference from unresolved sexual trauma during childhood. However, not all patient reactions should be considered transference; a patient may be appropriately thankful and deferential, or irritated and questioning, depending on the clinician’s demeanor and treatment approach.
Countertransference
Countertransference is the response elicited in the physician by a patient’s appearance and behaviors, or by a patient’s transference projections.6 This response can be positive or negative and includes both feelings and associated thoughts related to the physician’s past experiences. For example, a physician in the emergency department may get angry with a patient with an alcohol use disorder because of the physician’s negative experiences with an alcoholic parent during childhood. On the other hand, a physician raised by a compulsive mother may order unnecessary tests on a demanding older female patient. Or, a clinician raised by a sheltering parent may react to a hapless and dependent patient by spending excessive time with them or providing additional medication samples. However, not all clinician reactions are countertransference. For example, a physician’s empathic or stoic demeanor may be an appropriate emotional response to a patient’s diagnosis such as cancer.
Continue to: Patient resistance/nonadherence
Patient resistance/nonadherence
In 1920, Freud conceptualized the psychodynamic factors in patient resistance to treatment and theorized that many patients were unconsciously reluctant to give up their symptoms or were driven, for transference reasons, to resist the physician.7 This same concept may underlie patient resistance to pharmacotherapy. When symptoms constitute an important defense mechanism, patients are likely to resist medication effects until they have developed more mature defenses or more effective ways of coping.8 Even when patients do not resist symptom relief, they may still resist the physician’s choice of treatment due to negative transference. Such patients often negotiate the type of medication, dose, timing of the dose, and start date as a way of trying to “keep control” of a “doctor they don’t quite trust.”8 They may manage their own medication regimen by taking more or less than the prescribed dose. This resistance might lead to a “nocebo” effect in which a medication trial fails not because of its ineffectiveness but instead from the unconscious mind influencing the patient’s body to resist. Nonadherence to treatment may occur in patients who have attachment difficulties that make it difficult for them to trust anyone as a result of negative childhood experiences.9 Clinicians need to recognize the dynamics of power struggles, control, and trust. A warm, collaborative and cooperative stance is likely to be more beneficial than an authoritative and detached approach.10
The following 3 case examples illustrate how psychodynamic factors such as transference and countertransference can influence the therapeutic alliance, treatment decisions, and the outcomes of pharmacotherapy.
CASE 1
Mr. A, age 63, has posttraumatic stress disorder originating from his father’s death by a self-inflicted gunshot wound when Mr. A was 19, and later from the symbolic loss of his mother when she remarried. He reported vivid memories of his father sexually assaulting his mother when he was 6. This fostered a protective nature in him for his mother, as well as for his 3 younger siblings. After his father’s suicide, Mr. A had to take on a paternal role for his 3 siblings. He often feels he grew up too quickly, and resents this. He feels his mother betrayed him when she got remarried. Mr. A attempts suicide, is admitted to a local hospital, and then follows up at a university hospital outpatient psychiatry clinic.
At the clinic, Mr. A begins psychodynamic psychotherapy with a female resident physician. They establish a good rapport. Mr. A begins working through his past traumas and looks forward to his therapy sessions. The physician views this as positive transference, perhaps because her personality style and appearance are similar to that of Mr. A’s mother. She also often notes a positive countertransference during sessions; Mr. A seemingly reminds her of her father in personality and appearance. Perhaps due to this positive transference/positive countertransference dynamic, Mr. A feels comfortable with having his medication regimen simplified after years of unsuccessful medication trials and a course of electroconvulsive therapy. His regimen soon consists of only a selective serotonin reuptake inhibitor and a glutamate modulator as an adjunct for anxiety. Psychotherapy sessions remain the mainstay of his treatment plan. Mr. A’s mood and anxiety improve significantly over a short time.
CASE 2
Ms. G, age 24, is admitted to a partial hospitalization program (PHP). Her diagnoses include seasonal affective disorder, anxiety, and attention-deficit/hyperactivity disorder (ADHD); she might have a genetic disposition to bipolar disorder. Ms. G recently had attempted suicide and was discharged from an inpatient unit. She is a middle child and was raised by emotionally and verbally abusive parents in a tumultuous household. Her father rarely kept a job for more than a few months, displayed rage, and lacked empathy. Ms. G feels unloved by her mother and says that her mother is emotionally unstable. Upon admission to the PHP, Ms. G is quick to question the credentials of every staff member she meets, and suggests the abuse and lack of trust she had experienced during her formative years have made her aggressive and paranoid.
Continue to: Since her teens...
Since her teens, Ms. G had received treatment for ADHD with various stimulant and nonstimulant medications that were prescribed by an outpatient psychiatrist. During her sophomore year of college, she was also prescribed medications for depression and anxiety. Ms. G speaks very highly of and praises the skill of her previous psychiatrist while voicing concerns about having to see new clinicians in the PHP. She had recently seen a therapist who moved out of state after a few sessions. Ms. G has abandonment fears and appears to react with anger toward new clinicians.
A negative transference towards Ms. G’s treatment team and the PHP as a whole are evident during the first week. She skips most group therapy sessions and criticizes the clinicians’ skills and training as ineffective. When her psychiatrist recommends changes in medication, she initially argues. She eventually agrees to take a new medication but soon reports intolerable adverse effects, which suggests negative transference toward the psychiatrist as an authority figure, and toward the medication as an extension of the psychiatrist. The treatment team also interprets this as nocebo effect. Ms. G engages in “splitting” by complaining about her psychiatrist to her therapist. The psychiatrist resents having been belittled. Ms. G demands to see a different psychiatrist, and when her demands are not met, she discharges herself from the PHP against medical advice. The treatment team interprets Ms. G’s resistance to treatment to have resulted from poor attachment during childhood and subsequent negative transference.
CASE 3
Ms. U, age 60, is seen at a local mental health center and diagnosed with major depressive disorder, likely resulting from grief and loss from her husband’s recent death. She was raised by her single mother and mostly absent father. Ms. U is a homemaker and had been married for more than 30 years. She participates in weekly psychotherapy with a young male psychiatrist, who prescribes an antidepressant. Ms. U is eager to please and makes every effort to be the perfect patient: she is always early for her appointments, takes her medications as prescribed, and frequently expresses her respect and appreciation for her psychiatrist. Within a few weeks, Ms. U’s depressive symptoms rapidly improve.
Ms. U is a talented and avid knit and crochet expert. At an appointment soon before Christmas, she gives her psychiatrist a pair of socks she knitted. While the gift is of little monetary value, the psychiatrist interprets this as part of transference, but the intimate nature of the gift makes him uncomfortable. He and Ms. U discuss this at length, which reveals definite transference as Ms. U says the psychiatrist perhaps reminds her of her husband, who also had brown skin. It is also apparent that Ms. U’s tendency to please perhaps comes from the lack of having a father figure, which her husband had fulfilled. The psychiatrist believes that Ms. U’s rapid response may be a placebo effect from positive transference. Upon further reflection, the psychiatrist realizes that Ms. U is a motherly figure to him, and that positive countertransference is at play in that he could not turn down the gift and had looked forward to the therapy sessions with her.
Bottom Line
Even clinicians who do not provide psychodynamic psychotherapy can use an awareness of psychodynamic factors to improve treatment. Psychodynamic factors such as transference and countertransference can influence the therapeutic alliance, treatment decisions, and patient outcomes. Patients’ experiences and difficulties with attachment during childhood should be recognized and addressed as part of pharmacotherapy.
Related Resources
- Neumann M, Silva N, Opler DJ. ARISE to supportive psychotherapy. Current Psychiatry. 2021;20(5):48-49. doi:10.12788/cp.0123
- Mintz D. Psychodynamic psychopharmacology. Psychiatric Times. 2011;28(9). https://www.psychiatrictimes.com/view/psychodynamic-psychopharmacology
1. Office of Inspector General, Office of Evaluation and Inspections. Medication Regimens: Causes of Noncompliance. 1990. Accessed April 13, 2022. https://oig.hhs.gov/oei/reports/oei-04-89-89121.pdf
2. World Health Organization. Adherence to Long Term Therapies: Evidence for Action. World Health Organization; 2003.
3. Powell AD. The medication life. J Psychother Pract Res. 2001;10(4):217-222.
4. Wright JH, Hollifield M. Combining pharmacotherapy and psychotherapy. Psychiatric Annals. 2006;36(5):302-305.
5. Summers RF, Barber JP. Psychodynamic Therapy: A Guide to Evidence-Based Practice. Guilford Press; 2013:265-290.
6. Hughes P, Kerr I. Transference and countertransference in communication between doctor and patient. Advances in Psychiatric Treatment. 2000;6(1):57-64.
7. Freud S. Resistance and suppression. In: Freud S. A General Introduction to Psychoanalysis. Boni and Liveright Publishers; 1920:248-261.
8. Vlastelica M. Psychodynamic approach as a creative factor in psychopharmacotherapy. Psychiatr Danub. 2013;25(3):316-319.
9. Alfonso CA. Understanding the psychodynamics of nonadherence. Psychiatric Times. 2011;28(5). Accessed April 13, 2022. https://www.psychiatrictimes.com/view/understanding-psychodynamics-nonadherence
10. Wallin DJ. Attachment in Psychotherapy. Guilford Press; 2007.
1. Office of Inspector General, Office of Evaluation and Inspections. Medication Regimens: Causes of Noncompliance. 1990. Accessed April 13, 2022. https://oig.hhs.gov/oei/reports/oei-04-89-89121.pdf
2. World Health Organization. Adherence to Long Term Therapies: Evidence for Action. World Health Organization; 2003.
3. Powell AD. The medication life. J Psychother Pract Res. 2001;10(4):217-222.
4. Wright JH, Hollifield M. Combining pharmacotherapy and psychotherapy. Psychiatric Annals. 2006;36(5):302-305.
5. Summers RF, Barber JP. Psychodynamic Therapy: A Guide to Evidence-Based Practice. Guilford Press; 2013:265-290.
6. Hughes P, Kerr I. Transference and countertransference in communication between doctor and patient. Advances in Psychiatric Treatment. 2000;6(1):57-64.
7. Freud S. Resistance and suppression. In: Freud S. A General Introduction to Psychoanalysis. Boni and Liveright Publishers; 1920:248-261.
8. Vlastelica M. Psychodynamic approach as a creative factor in psychopharmacotherapy. Psychiatr Danub. 2013;25(3):316-319.
9. Alfonso CA. Understanding the psychodynamics of nonadherence. Psychiatric Times. 2011;28(5). Accessed April 13, 2022. https://www.psychiatrictimes.com/view/understanding-psychodynamics-nonadherence
10. Wallin DJ. Attachment in Psychotherapy. Guilford Press; 2007.
Methylphenidate is overprescribed to children in France
The prevalence of attention-deficit/hyperactivity disorder is difficult to evaluate, and the diagnosis is based primarily on clinical criteria. In 2008, a French study estimated the prevalence to be between 3.5% and 5.6%, but the study’s design was questionable.
Treatment of this disorder consists first and foremost of educational, social, and psychotherapeutic management. Only if such treatment fails is methylphenidate (MPH), the only drug that has been approved in France for this indication, to be considered, according to the recommendations.
The drug’s short-term efficacy has been proven, but it has not shown any effect on the long-term risks for academic failure, delinquency, and drug addiction associated with ADHD. In contrast, its adverse effects are numerous. Cases of nervousness, sleep disorders, headaches, weight loss, risk for aggravation of psychiatric conditions, and progression to violent or suicidal behavior have all been documented extensively, as well as cases of cardiovascular and cerebrovascular disease. Moreover, MPH is classified as a narcotic.
Inappropriate prescribing conditions
A study that appeared in the French journal of neuropsychiatry in minors, Neuropsychiatrie de l’Enfance et de l’Adolescence, investigated the prescribing procedures for this drug in France. Researchers examined Social Security data for 144,509 patients between the ages of 0 and 17 years who had received at least one prescription between 2010 and 2019. The researchers made the following observations about prescribing patterns and usage during this period:
- New MPH prescriptions increased by 56% per year, and the total number of annual prescriptions increased by 116%. In 3- to 17-year-olds, the prevalence was estimated at 0.61% to 0.75% of the pediatric population in 2019. Boys accounted for most of this consumption (82.5% to 80.8% over this period).
- In 2011, the median duration of consumption by children 6 years of age and older was 5.5 years. For 25% of those children, it was more than 8 years.
- Contrary to the labeling, some prescriptions were written for children younger than 6 years.
- Twenty-five percent of initial prescriptions and 50% of annual renewals were not written by a hospital specialist, in violation of the regulatory requirements in effect until Sept. 13, 2021. On that date, the French National Authority for Health (HAS) decided that initial hospital prescription of MPH should end.
- Eighty-four percent of children did not have any medical consultations at the prescribing hospital department in the 13 months after starting MPH. While the prevalence of ADHD has more than doubled, the number of consultations at specialist French medical, psychological, and educational centers for minors (CMPPs) is now less than a fourth of what it was – a drop from 4.1% to 0.8%.
- The prescribing of MPH is not always associated with an ADHD diagnosis, even though ADHD is its only indication.
- Of children and adolescents who use MPH, 22.8% received one or more other psychotropic drugs in the year following the initial prescription, including the following: neuroleptics (64.5%), anxiolytics (35.5%), antidepressants (16.2%), antiepileptics (11%), hypnotics (4.8%), and antiparkinsonian drugs (3%). “These co-prescriptions are often way off-label and are not within HAS recommendations,” according to the authors.
- For the youngest children in school classes (those born in December rather than in January), between 2010 and 2019, there was on average a 54% increased risk of being medicated.
- In 2019, 21.7% of children who received MPH lived in families with Universal Health Coverage or a similar plan. Yet, according to the French National Institute of Statistics and Economic Studies, only 7.8% of the French population had this type of assistance.
A minority of practitioners
The authors of this article state that “the distribution of consumption suggests a predominant role of a minority of practitioners and hospital departments in the prescription of methylphenidate.” They note that “in European countries and in North America, the prescription rate of psychotropic drugs for ADHD has stabilized or shown a clear trend toward stabilization since 2008. The same cannot be said for France, where this rate is continuously increasing; so much so that in 2019, it reached a higher level than in other European countries like Great Britain.” The reasons for this are disputed.
A version of this article first appeared on Medscape.com.
The prevalence of attention-deficit/hyperactivity disorder is difficult to evaluate, and the diagnosis is based primarily on clinical criteria. In 2008, a French study estimated the prevalence to be between 3.5% and 5.6%, but the study’s design was questionable.
Treatment of this disorder consists first and foremost of educational, social, and psychotherapeutic management. Only if such treatment fails is methylphenidate (MPH), the only drug that has been approved in France for this indication, to be considered, according to the recommendations.
The drug’s short-term efficacy has been proven, but it has not shown any effect on the long-term risks for academic failure, delinquency, and drug addiction associated with ADHD. In contrast, its adverse effects are numerous. Cases of nervousness, sleep disorders, headaches, weight loss, risk for aggravation of psychiatric conditions, and progression to violent or suicidal behavior have all been documented extensively, as well as cases of cardiovascular and cerebrovascular disease. Moreover, MPH is classified as a narcotic.
Inappropriate prescribing conditions
A study that appeared in the French journal of neuropsychiatry in minors, Neuropsychiatrie de l’Enfance et de l’Adolescence, investigated the prescribing procedures for this drug in France. Researchers examined Social Security data for 144,509 patients between the ages of 0 and 17 years who had received at least one prescription between 2010 and 2019. The researchers made the following observations about prescribing patterns and usage during this period:
- New MPH prescriptions increased by 56% per year, and the total number of annual prescriptions increased by 116%. In 3- to 17-year-olds, the prevalence was estimated at 0.61% to 0.75% of the pediatric population in 2019. Boys accounted for most of this consumption (82.5% to 80.8% over this period).
- In 2011, the median duration of consumption by children 6 years of age and older was 5.5 years. For 25% of those children, it was more than 8 years.
- Contrary to the labeling, some prescriptions were written for children younger than 6 years.
- Twenty-five percent of initial prescriptions and 50% of annual renewals were not written by a hospital specialist, in violation of the regulatory requirements in effect until Sept. 13, 2021. On that date, the French National Authority for Health (HAS) decided that initial hospital prescription of MPH should end.
- Eighty-four percent of children did not have any medical consultations at the prescribing hospital department in the 13 months after starting MPH. While the prevalence of ADHD has more than doubled, the number of consultations at specialist French medical, psychological, and educational centers for minors (CMPPs) is now less than a fourth of what it was – a drop from 4.1% to 0.8%.
- The prescribing of MPH is not always associated with an ADHD diagnosis, even though ADHD is its only indication.
- Of children and adolescents who use MPH, 22.8% received one or more other psychotropic drugs in the year following the initial prescription, including the following: neuroleptics (64.5%), anxiolytics (35.5%), antidepressants (16.2%), antiepileptics (11%), hypnotics (4.8%), and antiparkinsonian drugs (3%). “These co-prescriptions are often way off-label and are not within HAS recommendations,” according to the authors.
- For the youngest children in school classes (those born in December rather than in January), between 2010 and 2019, there was on average a 54% increased risk of being medicated.
- In 2019, 21.7% of children who received MPH lived in families with Universal Health Coverage or a similar plan. Yet, according to the French National Institute of Statistics and Economic Studies, only 7.8% of the French population had this type of assistance.
A minority of practitioners
The authors of this article state that “the distribution of consumption suggests a predominant role of a minority of practitioners and hospital departments in the prescription of methylphenidate.” They note that “in European countries and in North America, the prescription rate of psychotropic drugs for ADHD has stabilized or shown a clear trend toward stabilization since 2008. The same cannot be said for France, where this rate is continuously increasing; so much so that in 2019, it reached a higher level than in other European countries like Great Britain.” The reasons for this are disputed.
A version of this article first appeared on Medscape.com.
The prevalence of attention-deficit/hyperactivity disorder is difficult to evaluate, and the diagnosis is based primarily on clinical criteria. In 2008, a French study estimated the prevalence to be between 3.5% and 5.6%, but the study’s design was questionable.
Treatment of this disorder consists first and foremost of educational, social, and psychotherapeutic management. Only if such treatment fails is methylphenidate (MPH), the only drug that has been approved in France for this indication, to be considered, according to the recommendations.
The drug’s short-term efficacy has been proven, but it has not shown any effect on the long-term risks for academic failure, delinquency, and drug addiction associated with ADHD. In contrast, its adverse effects are numerous. Cases of nervousness, sleep disorders, headaches, weight loss, risk for aggravation of psychiatric conditions, and progression to violent or suicidal behavior have all been documented extensively, as well as cases of cardiovascular and cerebrovascular disease. Moreover, MPH is classified as a narcotic.
Inappropriate prescribing conditions
A study that appeared in the French journal of neuropsychiatry in minors, Neuropsychiatrie de l’Enfance et de l’Adolescence, investigated the prescribing procedures for this drug in France. Researchers examined Social Security data for 144,509 patients between the ages of 0 and 17 years who had received at least one prescription between 2010 and 2019. The researchers made the following observations about prescribing patterns and usage during this period:
- New MPH prescriptions increased by 56% per year, and the total number of annual prescriptions increased by 116%. In 3- to 17-year-olds, the prevalence was estimated at 0.61% to 0.75% of the pediatric population in 2019. Boys accounted for most of this consumption (82.5% to 80.8% over this period).
- In 2011, the median duration of consumption by children 6 years of age and older was 5.5 years. For 25% of those children, it was more than 8 years.
- Contrary to the labeling, some prescriptions were written for children younger than 6 years.
- Twenty-five percent of initial prescriptions and 50% of annual renewals were not written by a hospital specialist, in violation of the regulatory requirements in effect until Sept. 13, 2021. On that date, the French National Authority for Health (HAS) decided that initial hospital prescription of MPH should end.
- Eighty-four percent of children did not have any medical consultations at the prescribing hospital department in the 13 months after starting MPH. While the prevalence of ADHD has more than doubled, the number of consultations at specialist French medical, psychological, and educational centers for minors (CMPPs) is now less than a fourth of what it was – a drop from 4.1% to 0.8%.
- The prescribing of MPH is not always associated with an ADHD diagnosis, even though ADHD is its only indication.
- Of children and adolescents who use MPH, 22.8% received one or more other psychotropic drugs in the year following the initial prescription, including the following: neuroleptics (64.5%), anxiolytics (35.5%), antidepressants (16.2%), antiepileptics (11%), hypnotics (4.8%), and antiparkinsonian drugs (3%). “These co-prescriptions are often way off-label and are not within HAS recommendations,” according to the authors.
- For the youngest children in school classes (those born in December rather than in January), between 2010 and 2019, there was on average a 54% increased risk of being medicated.
- In 2019, 21.7% of children who received MPH lived in families with Universal Health Coverage or a similar plan. Yet, according to the French National Institute of Statistics and Economic Studies, only 7.8% of the French population had this type of assistance.
A minority of practitioners
The authors of this article state that “the distribution of consumption suggests a predominant role of a minority of practitioners and hospital departments in the prescription of methylphenidate.” They note that “in European countries and in North America, the prescription rate of psychotropic drugs for ADHD has stabilized or shown a clear trend toward stabilization since 2008. The same cannot be said for France, where this rate is continuously increasing; so much so that in 2019, it reached a higher level than in other European countries like Great Britain.” The reasons for this are disputed.
A version of this article first appeared on Medscape.com.
ADHD link to prenatal opioid exposure shifts with other substances
Children prenatally exposed to opioids alone have an increased risk of attention-deficit/hyperactivity disorder (ADHD), but interactions between opioids and both cannabis use and alcohol use were linked to varying levels of ADHD risk as well, according to findings published March 11 in JAMA Network Open.
While many prenatal exposure studies examine associations with one substance, the results of this case-control study “suggest that it is important to consider prenatal exposure to multiple substances and the interactions between these substances when counseling women regarding substance use during pregnancy,” wrote Henri M. Garrison-Desany of the Johns Hopkins University, Baltimore, and colleagues.
Using data from children in the prospective Boston Birth Cohort between 1998 and 2019, the researchers did a secondary analysis on the 3,138 children (50.4% of whom were male) with at least 2 years of follow-up, excluding children from multiple-gestation pregnancies, in vitro fertilization pregnancies, and deliveries involving major maternal trauma or major chromosomal anomalies. Mothers answered a questionnaire within 24-72 hours of delivery regarding their demographics, substance use, pregnancy history, and health status. Among the mothers, 58.6% were Black, 22.3% were Hispanic, 7.2% were White, 1.5% were Asian, and 10.4% were other races/ethnicities.
The children’s electronic medical records were used to identify those with ADHD diagnoses. The researchers did not assess prescription opioid exposure during pregnancy, but they based opioid exposure on mothers’ reports of recreationally using heroin or oxycodone, mothers’ reports of receiving methadone treatment, or a newborn diagnosis of neonatal abstinence syndrome or neonatal opioid withdrawal syndrome.
Just under a quarter of the women (24.2%) reported using at least one substance during pregnancy. After tobacco smoking (18.5%), the next most reported substances were alcohol (8.1%), cannabis (3.9%), and opioids (1.9%). With a median 12 years of follow-up, 15.5% of the children had been diagnosed with ADHD, most of whom (71.6%) were male.
Before considering interaction of different substances, children exposed to opioids had a little over twice the risk of ADHD (hazard ratio [HR], 2.19) compared to those with no prenatal substance exposure. Although neither cannabis nor alcohol was independently associated with ADHD, smoking had a 40% increased risk, and researchers found a 21% increase in risk of ADHD with each additional substance mothers used during pregnancy. The researchers had adjusted these findings for maternal age, race/ethnicity, marital status, educational level, annual household income, parity, number of perinatal visits, and general stress during pregnancy, based on a structured interview.
When the researchers considered all the substances together, opioid exposure increased risk of ADHD by 60% (HR, 1.6), opioids with cannabis increased risk by 42%, opioids with alcohol increased risk by 15%, and opioids with smoking increased risk by 17%.
”Our findings suggest opioids may interact with other substances (including cannabis), which may be particularly deleterious,” the researchers reported. “It is not clear whether this interaction is owing to biological or environmental factors, such as whether individuals with illicit polysubstance use are more likely to use more substances or whether they have other characteristics that may impact child development.”
The authors noted that cannabis exposure has been linked to other neurodevelopmental outcomes, including reduced executive and motor function in infants. ”Notably, although we did not find a significant independent association between cannabis exposure and ADHD, children exposed to both cannabis and opioids had a 23% greater risk than expected from either exposure individually,” they reported.
The researchers suggest that their findings provide data for considering harm reduction approaches that reduce use of any single substance during pregnancy. “Focusing on the most obviously harmful exposures may be a useful way to reduce the risk of ADHD,” they wrote. “Further work is needed to directly investigate this hypothesis and examine whether reduction in the use of any substance among those with polysubstance use could be acceptable compared with abstinence.”
In an invited commentary, Angela Lupattelli, PhD, and Nhung T. H. Trinh, PhD, both of the department of pharmacy at the University of Oslo, noted the methodological challenges of assessing exposures and associations from multiple different substances during pregnancy.
“First, how can we disentangle the consequences of individual and/or combined substance exposures during pregnancy from the underlying risks?” they asked. In addition to differences in baseline characteristic between those who use opioids or cannabis, Dr. Lupattelli and Dr. Trinh noted that other important unmeasured factors, such as genetics and family environment, may confound the effect size estimates for ADHD.
They also noted the need to consider intensity, dose, duration, and timing of substance use during pregnancy.
“Understanding the longer-term safety of substance use during pregnancy is paramount to inform prevention policy and shape counseling strategies. Observational studies, despite their limitations, are a necessary piece of the puzzle,” they wrote. “However, the study findings should be interpreted with caution, as the use of advanced analytical methods cannot overcome the unavailability of some important confounding factors and exposure information.”
The research was funded by the U.S. Department of Health and Human Services and the National Institutes of Health. The authors had no industry-related disclosures.
Children prenatally exposed to opioids alone have an increased risk of attention-deficit/hyperactivity disorder (ADHD), but interactions between opioids and both cannabis use and alcohol use were linked to varying levels of ADHD risk as well, according to findings published March 11 in JAMA Network Open.
While many prenatal exposure studies examine associations with one substance, the results of this case-control study “suggest that it is important to consider prenatal exposure to multiple substances and the interactions between these substances when counseling women regarding substance use during pregnancy,” wrote Henri M. Garrison-Desany of the Johns Hopkins University, Baltimore, and colleagues.
Using data from children in the prospective Boston Birth Cohort between 1998 and 2019, the researchers did a secondary analysis on the 3,138 children (50.4% of whom were male) with at least 2 years of follow-up, excluding children from multiple-gestation pregnancies, in vitro fertilization pregnancies, and deliveries involving major maternal trauma or major chromosomal anomalies. Mothers answered a questionnaire within 24-72 hours of delivery regarding their demographics, substance use, pregnancy history, and health status. Among the mothers, 58.6% were Black, 22.3% were Hispanic, 7.2% were White, 1.5% were Asian, and 10.4% were other races/ethnicities.
The children’s electronic medical records were used to identify those with ADHD diagnoses. The researchers did not assess prescription opioid exposure during pregnancy, but they based opioid exposure on mothers’ reports of recreationally using heroin or oxycodone, mothers’ reports of receiving methadone treatment, or a newborn diagnosis of neonatal abstinence syndrome or neonatal opioid withdrawal syndrome.
Just under a quarter of the women (24.2%) reported using at least one substance during pregnancy. After tobacco smoking (18.5%), the next most reported substances were alcohol (8.1%), cannabis (3.9%), and opioids (1.9%). With a median 12 years of follow-up, 15.5% of the children had been diagnosed with ADHD, most of whom (71.6%) were male.
Before considering interaction of different substances, children exposed to opioids had a little over twice the risk of ADHD (hazard ratio [HR], 2.19) compared to those with no prenatal substance exposure. Although neither cannabis nor alcohol was independently associated with ADHD, smoking had a 40% increased risk, and researchers found a 21% increase in risk of ADHD with each additional substance mothers used during pregnancy. The researchers had adjusted these findings for maternal age, race/ethnicity, marital status, educational level, annual household income, parity, number of perinatal visits, and general stress during pregnancy, based on a structured interview.
When the researchers considered all the substances together, opioid exposure increased risk of ADHD by 60% (HR, 1.6), opioids with cannabis increased risk by 42%, opioids with alcohol increased risk by 15%, and opioids with smoking increased risk by 17%.
”Our findings suggest opioids may interact with other substances (including cannabis), which may be particularly deleterious,” the researchers reported. “It is not clear whether this interaction is owing to biological or environmental factors, such as whether individuals with illicit polysubstance use are more likely to use more substances or whether they have other characteristics that may impact child development.”
The authors noted that cannabis exposure has been linked to other neurodevelopmental outcomes, including reduced executive and motor function in infants. ”Notably, although we did not find a significant independent association between cannabis exposure and ADHD, children exposed to both cannabis and opioids had a 23% greater risk than expected from either exposure individually,” they reported.
The researchers suggest that their findings provide data for considering harm reduction approaches that reduce use of any single substance during pregnancy. “Focusing on the most obviously harmful exposures may be a useful way to reduce the risk of ADHD,” they wrote. “Further work is needed to directly investigate this hypothesis and examine whether reduction in the use of any substance among those with polysubstance use could be acceptable compared with abstinence.”
In an invited commentary, Angela Lupattelli, PhD, and Nhung T. H. Trinh, PhD, both of the department of pharmacy at the University of Oslo, noted the methodological challenges of assessing exposures and associations from multiple different substances during pregnancy.
“First, how can we disentangle the consequences of individual and/or combined substance exposures during pregnancy from the underlying risks?” they asked. In addition to differences in baseline characteristic between those who use opioids or cannabis, Dr. Lupattelli and Dr. Trinh noted that other important unmeasured factors, such as genetics and family environment, may confound the effect size estimates for ADHD.
They also noted the need to consider intensity, dose, duration, and timing of substance use during pregnancy.
“Understanding the longer-term safety of substance use during pregnancy is paramount to inform prevention policy and shape counseling strategies. Observational studies, despite their limitations, are a necessary piece of the puzzle,” they wrote. “However, the study findings should be interpreted with caution, as the use of advanced analytical methods cannot overcome the unavailability of some important confounding factors and exposure information.”
The research was funded by the U.S. Department of Health and Human Services and the National Institutes of Health. The authors had no industry-related disclosures.
Children prenatally exposed to opioids alone have an increased risk of attention-deficit/hyperactivity disorder (ADHD), but interactions between opioids and both cannabis use and alcohol use were linked to varying levels of ADHD risk as well, according to findings published March 11 in JAMA Network Open.
While many prenatal exposure studies examine associations with one substance, the results of this case-control study “suggest that it is important to consider prenatal exposure to multiple substances and the interactions between these substances when counseling women regarding substance use during pregnancy,” wrote Henri M. Garrison-Desany of the Johns Hopkins University, Baltimore, and colleagues.
Using data from children in the prospective Boston Birth Cohort between 1998 and 2019, the researchers did a secondary analysis on the 3,138 children (50.4% of whom were male) with at least 2 years of follow-up, excluding children from multiple-gestation pregnancies, in vitro fertilization pregnancies, and deliveries involving major maternal trauma or major chromosomal anomalies. Mothers answered a questionnaire within 24-72 hours of delivery regarding their demographics, substance use, pregnancy history, and health status. Among the mothers, 58.6% were Black, 22.3% were Hispanic, 7.2% were White, 1.5% were Asian, and 10.4% were other races/ethnicities.
The children’s electronic medical records were used to identify those with ADHD diagnoses. The researchers did not assess prescription opioid exposure during pregnancy, but they based opioid exposure on mothers’ reports of recreationally using heroin or oxycodone, mothers’ reports of receiving methadone treatment, or a newborn diagnosis of neonatal abstinence syndrome or neonatal opioid withdrawal syndrome.
Just under a quarter of the women (24.2%) reported using at least one substance during pregnancy. After tobacco smoking (18.5%), the next most reported substances were alcohol (8.1%), cannabis (3.9%), and opioids (1.9%). With a median 12 years of follow-up, 15.5% of the children had been diagnosed with ADHD, most of whom (71.6%) were male.
Before considering interaction of different substances, children exposed to opioids had a little over twice the risk of ADHD (hazard ratio [HR], 2.19) compared to those with no prenatal substance exposure. Although neither cannabis nor alcohol was independently associated with ADHD, smoking had a 40% increased risk, and researchers found a 21% increase in risk of ADHD with each additional substance mothers used during pregnancy. The researchers had adjusted these findings for maternal age, race/ethnicity, marital status, educational level, annual household income, parity, number of perinatal visits, and general stress during pregnancy, based on a structured interview.
When the researchers considered all the substances together, opioid exposure increased risk of ADHD by 60% (HR, 1.6), opioids with cannabis increased risk by 42%, opioids with alcohol increased risk by 15%, and opioids with smoking increased risk by 17%.
”Our findings suggest opioids may interact with other substances (including cannabis), which may be particularly deleterious,” the researchers reported. “It is not clear whether this interaction is owing to biological or environmental factors, such as whether individuals with illicit polysubstance use are more likely to use more substances or whether they have other characteristics that may impact child development.”
The authors noted that cannabis exposure has been linked to other neurodevelopmental outcomes, including reduced executive and motor function in infants. ”Notably, although we did not find a significant independent association between cannabis exposure and ADHD, children exposed to both cannabis and opioids had a 23% greater risk than expected from either exposure individually,” they reported.
The researchers suggest that their findings provide data for considering harm reduction approaches that reduce use of any single substance during pregnancy. “Focusing on the most obviously harmful exposures may be a useful way to reduce the risk of ADHD,” they wrote. “Further work is needed to directly investigate this hypothesis and examine whether reduction in the use of any substance among those with polysubstance use could be acceptable compared with abstinence.”
In an invited commentary, Angela Lupattelli, PhD, and Nhung T. H. Trinh, PhD, both of the department of pharmacy at the University of Oslo, noted the methodological challenges of assessing exposures and associations from multiple different substances during pregnancy.
“First, how can we disentangle the consequences of individual and/or combined substance exposures during pregnancy from the underlying risks?” they asked. In addition to differences in baseline characteristic between those who use opioids or cannabis, Dr. Lupattelli and Dr. Trinh noted that other important unmeasured factors, such as genetics and family environment, may confound the effect size estimates for ADHD.
They also noted the need to consider intensity, dose, duration, and timing of substance use during pregnancy.
“Understanding the longer-term safety of substance use during pregnancy is paramount to inform prevention policy and shape counseling strategies. Observational studies, despite their limitations, are a necessary piece of the puzzle,” they wrote. “However, the study findings should be interpreted with caution, as the use of advanced analytical methods cannot overcome the unavailability of some important confounding factors and exposure information.”
The research was funded by the U.S. Department of Health and Human Services and the National Institutes of Health. The authors had no industry-related disclosures.
FROM JAMA NETWORK OPEN
Prescription video game focuses attention in ADHD
Investigators found children who used the video game-based therapy (EndeavorRx) experienced increased brain activity related to attention function, as measured by EEG, which correlated with improvements in objective behavioral measures of attention.
“While the previous multicenter trials show attention improvement for children using EndeavorRx, this is the first study to look at the brain activity in children with a primary concern of ADHD,” principal investigator Elysa Marco, MD, clinical executive for neurodevelopmental medicine at Cortica Healthcare, San Rafael, Calif., said in news release.
“It is exciting to see measurable improvement on the EEGs that correlates with the behavioral benefits,” said Dr. Marco.
The study was recently published online in PLOS ONE.
Measurable changes
As previously reported by this news organization, the Food and Drug Administration approved EndeavorRx in June 2020 as a prescription video game–based therapeutic device for children aged 8-12 years with primarily inattentive or combined-type ADHD, who have a demonstrated attention issue.
“The device is intended for use as part of a therapeutic program that may include clinician-directed therapy, medication, and/or educational programs, which further address symptoms of the disorder,” the FDA said upon approval.
In the current unblinded, single-arm study, the researchers assessed 25 children (aged 8-12 years) with a confirmed diagnosis of ADHD on neural, behavioral, and clinical metrics of attention before and after a 4-week at-home intervention.
Participants were instructed to use EndeavorRx for about 25 minutes a day at least 5 days a week for 4 weeks, as recommended by the FDA.
“EndeavorRx enhanced midline frontal theta (MFT) activity, suggesting that patients who used EndeavorRx for 4 weeks showed changes in measurable brain function,” Anil S. Jina, MD, chief medical officer of Akili Interactive, told this news organization. Dr. Jina was not involved with the study.
There was also a correlation between MFT activity and attention functioning, “suggesting that children who experienced the largest gains in MFT activity as measured by EEG also showed the greatest improvements in computerized performance tests designed to measure attention,” Dr. Jina said.
In addition, parents reported significantly fewer inattention symptoms in children after EndeavorRx treatment, as measured by the Vanderbilt ADHD Diagnostic Rating Scale.
‘Not just another video game’
EndeavorRx has been evaluated in five clinical studies involving more than 600 children with ADHD, including the STARS-ADHD trial, a prospective, randomized, controlled study published in The Lancet Digital Health.
The STARS-ADHD trial randomly allocated 348 children to either EndeavorRx treatment or a controlled intervention, which was a word game.
The researchers reported statistically significant improvements in attentional functioning in the EndeavorRx group as rated by test of variables of attention.
“This is not just another video game,” STARS-ADHD trialist Scott H. Kollins, PhD, MS, a clinical psychologist at Duke Health’s ADHD Clinic in Durham, N.C., who helped developed it, previously told this news organization.
The tool’s adaptive algorithms adjust and monitor task difficulty based on performance, using a video game format and rewards to engage users, he explained. EndeavorRx is a challenge to play by design.
“The treatment was programmed into the gameplay experience and designed to challenge a child’s attentional control during gameplay, requiring focus and flexibility to manage tasks at the same time,” Dr. Jina said in an interview.
“Unlike a video game that is designed only for entertainment purposes, to drive efficacy, EndeavorRx is designed to be challenging and can therefore sometimes feel repetitive, and frustrating to some children,” Dr. Jina said.
Commenting on the study, Stephen Faraone, PhD, distinguished professor of psychiatry and vice chair of research, department of psychiatry, State University of New York, Syracuse, said this study “supports the idea that EndeavorRx improves a neural measure of attention.
“The limitation is that we don’t know if this translates into clinically relevant outcomes,” cautioned Dr. Faraone, who was not associated with the current study.
“The main caveat about EndeavorRx is that it was cleared by the FDA for improving a computer-based measure of inattention, not inattentive symptoms as reported by the parents of children with ADHD,” he noted.
Several authors have disclosed financial relationships with Akili Interactive Labs, which funded the study. Dr. Faraone was an investigator on the STARS-ADHD trial.
A version of this article first appeared on Medscape.com.
Investigators found children who used the video game-based therapy (EndeavorRx) experienced increased brain activity related to attention function, as measured by EEG, which correlated with improvements in objective behavioral measures of attention.
“While the previous multicenter trials show attention improvement for children using EndeavorRx, this is the first study to look at the brain activity in children with a primary concern of ADHD,” principal investigator Elysa Marco, MD, clinical executive for neurodevelopmental medicine at Cortica Healthcare, San Rafael, Calif., said in news release.
“It is exciting to see measurable improvement on the EEGs that correlates with the behavioral benefits,” said Dr. Marco.
The study was recently published online in PLOS ONE.
Measurable changes
As previously reported by this news organization, the Food and Drug Administration approved EndeavorRx in June 2020 as a prescription video game–based therapeutic device for children aged 8-12 years with primarily inattentive or combined-type ADHD, who have a demonstrated attention issue.
“The device is intended for use as part of a therapeutic program that may include clinician-directed therapy, medication, and/or educational programs, which further address symptoms of the disorder,” the FDA said upon approval.
In the current unblinded, single-arm study, the researchers assessed 25 children (aged 8-12 years) with a confirmed diagnosis of ADHD on neural, behavioral, and clinical metrics of attention before and after a 4-week at-home intervention.
Participants were instructed to use EndeavorRx for about 25 minutes a day at least 5 days a week for 4 weeks, as recommended by the FDA.
“EndeavorRx enhanced midline frontal theta (MFT) activity, suggesting that patients who used EndeavorRx for 4 weeks showed changes in measurable brain function,” Anil S. Jina, MD, chief medical officer of Akili Interactive, told this news organization. Dr. Jina was not involved with the study.
There was also a correlation between MFT activity and attention functioning, “suggesting that children who experienced the largest gains in MFT activity as measured by EEG also showed the greatest improvements in computerized performance tests designed to measure attention,” Dr. Jina said.
In addition, parents reported significantly fewer inattention symptoms in children after EndeavorRx treatment, as measured by the Vanderbilt ADHD Diagnostic Rating Scale.
‘Not just another video game’
EndeavorRx has been evaluated in five clinical studies involving more than 600 children with ADHD, including the STARS-ADHD trial, a prospective, randomized, controlled study published in The Lancet Digital Health.
The STARS-ADHD trial randomly allocated 348 children to either EndeavorRx treatment or a controlled intervention, which was a word game.
The researchers reported statistically significant improvements in attentional functioning in the EndeavorRx group as rated by test of variables of attention.
“This is not just another video game,” STARS-ADHD trialist Scott H. Kollins, PhD, MS, a clinical psychologist at Duke Health’s ADHD Clinic in Durham, N.C., who helped developed it, previously told this news organization.
The tool’s adaptive algorithms adjust and monitor task difficulty based on performance, using a video game format and rewards to engage users, he explained. EndeavorRx is a challenge to play by design.
“The treatment was programmed into the gameplay experience and designed to challenge a child’s attentional control during gameplay, requiring focus and flexibility to manage tasks at the same time,” Dr. Jina said in an interview.
“Unlike a video game that is designed only for entertainment purposes, to drive efficacy, EndeavorRx is designed to be challenging and can therefore sometimes feel repetitive, and frustrating to some children,” Dr. Jina said.
Commenting on the study, Stephen Faraone, PhD, distinguished professor of psychiatry and vice chair of research, department of psychiatry, State University of New York, Syracuse, said this study “supports the idea that EndeavorRx improves a neural measure of attention.
“The limitation is that we don’t know if this translates into clinically relevant outcomes,” cautioned Dr. Faraone, who was not associated with the current study.
“The main caveat about EndeavorRx is that it was cleared by the FDA for improving a computer-based measure of inattention, not inattentive symptoms as reported by the parents of children with ADHD,” he noted.
Several authors have disclosed financial relationships with Akili Interactive Labs, which funded the study. Dr. Faraone was an investigator on the STARS-ADHD trial.
A version of this article first appeared on Medscape.com.
Investigators found children who used the video game-based therapy (EndeavorRx) experienced increased brain activity related to attention function, as measured by EEG, which correlated with improvements in objective behavioral measures of attention.
“While the previous multicenter trials show attention improvement for children using EndeavorRx, this is the first study to look at the brain activity in children with a primary concern of ADHD,” principal investigator Elysa Marco, MD, clinical executive for neurodevelopmental medicine at Cortica Healthcare, San Rafael, Calif., said in news release.
“It is exciting to see measurable improvement on the EEGs that correlates with the behavioral benefits,” said Dr. Marco.
The study was recently published online in PLOS ONE.
Measurable changes
As previously reported by this news organization, the Food and Drug Administration approved EndeavorRx in June 2020 as a prescription video game–based therapeutic device for children aged 8-12 years with primarily inattentive or combined-type ADHD, who have a demonstrated attention issue.
“The device is intended for use as part of a therapeutic program that may include clinician-directed therapy, medication, and/or educational programs, which further address symptoms of the disorder,” the FDA said upon approval.
In the current unblinded, single-arm study, the researchers assessed 25 children (aged 8-12 years) with a confirmed diagnosis of ADHD on neural, behavioral, and clinical metrics of attention before and after a 4-week at-home intervention.
Participants were instructed to use EndeavorRx for about 25 minutes a day at least 5 days a week for 4 weeks, as recommended by the FDA.
“EndeavorRx enhanced midline frontal theta (MFT) activity, suggesting that patients who used EndeavorRx for 4 weeks showed changes in measurable brain function,” Anil S. Jina, MD, chief medical officer of Akili Interactive, told this news organization. Dr. Jina was not involved with the study.
There was also a correlation between MFT activity and attention functioning, “suggesting that children who experienced the largest gains in MFT activity as measured by EEG also showed the greatest improvements in computerized performance tests designed to measure attention,” Dr. Jina said.
In addition, parents reported significantly fewer inattention symptoms in children after EndeavorRx treatment, as measured by the Vanderbilt ADHD Diagnostic Rating Scale.
‘Not just another video game’
EndeavorRx has been evaluated in five clinical studies involving more than 600 children with ADHD, including the STARS-ADHD trial, a prospective, randomized, controlled study published in The Lancet Digital Health.
The STARS-ADHD trial randomly allocated 348 children to either EndeavorRx treatment or a controlled intervention, which was a word game.
The researchers reported statistically significant improvements in attentional functioning in the EndeavorRx group as rated by test of variables of attention.
“This is not just another video game,” STARS-ADHD trialist Scott H. Kollins, PhD, MS, a clinical psychologist at Duke Health’s ADHD Clinic in Durham, N.C., who helped developed it, previously told this news organization.
The tool’s adaptive algorithms adjust and monitor task difficulty based on performance, using a video game format and rewards to engage users, he explained. EndeavorRx is a challenge to play by design.
“The treatment was programmed into the gameplay experience and designed to challenge a child’s attentional control during gameplay, requiring focus and flexibility to manage tasks at the same time,” Dr. Jina said in an interview.
“Unlike a video game that is designed only for entertainment purposes, to drive efficacy, EndeavorRx is designed to be challenging and can therefore sometimes feel repetitive, and frustrating to some children,” Dr. Jina said.
Commenting on the study, Stephen Faraone, PhD, distinguished professor of psychiatry and vice chair of research, department of psychiatry, State University of New York, Syracuse, said this study “supports the idea that EndeavorRx improves a neural measure of attention.
“The limitation is that we don’t know if this translates into clinically relevant outcomes,” cautioned Dr. Faraone, who was not associated with the current study.
“The main caveat about EndeavorRx is that it was cleared by the FDA for improving a computer-based measure of inattention, not inattentive symptoms as reported by the parents of children with ADHD,” he noted.
Several authors have disclosed financial relationships with Akili Interactive Labs, which funded the study. Dr. Faraone was an investigator on the STARS-ADHD trial.
A version of this article first appeared on Medscape.com.
Routine pharmacogenetic testing in psychiatry not indicated
LAS VEGAS –
“It’s misleading to rely on results of genetic tests to drive clinical treatment,” Dr. Nurmi, a child and adolescent psychiatrist in the department of psychiatry and biobehavioral sciences at the University of California, Los Angeles, said during an annual psychopharmacology update held by the Nevada Psychiatric Association. “There’s a lot of hope and promise there. But currently, we only know the tip of the iceberg about how drugs work and the genetics influencing these effects. Current testing is probably a very poor reflection of the complexity of drug effects.”
According to Dr. Nurmi, there are at least 165 Food and Drug Administration–approved drugs with pharmacogenetic information on 64 different biomarkers – 37% with CYP p450 notations. Of these, 32 psychiatric drugs have pharmacogenetic information, and most of them are dosing recommendations based on whether a patient has the variant. However, there is wide public acceptance of genetic testing in preventing the wrong drug from being used, in selecting the best drug dose, and avoiding side effects (Pharmacogenomics 2012;12[3]:197-204). “Most people have a lot of hope [for genetic testing in psychiatry],” Dr. Nurmi said. “But is the science really there? It doesn’t matter, because these companies are doing it, and you are being shown these reports from patients. Whether or not the science supports it, we’re going to have to interpret these reports and explain them to our patients – even if we don’t order them.”
Currently, she continued, clinicians practice trial and error prescribing where they might try one treatment in a class that they think that will work based on previous literature. If nothing works, they try another one. If that’s intolerable, they try a third treatment, and so on. “When we finally find the right treatment, it can take some time to get the dosing right,” Dr. Nurmi said. “So, it can take many months to get a child on the right medication. Precision treatment, on the other hand, would start off by taking a saliva or blood sample to get a printout that lets physicians know which drugs might be used with caution because they might lack efficacy at standard doses, which ones would likely have adverse effects at standard doses, and which are the best choices and what are the dosing recommendations for those choices. If we could get all the information to guide us, that would be a useful product, but right now, we don’t know enough to be able to make these determinations.”
Current evidence-based genetic testing supports a limited role for CYP2D6 and CYP2C19 genotyping because most psychiatric drugs are metabolized by those two enzymes. Poor metabolizers have two dysfunctional copies of the enzyme-encoding gene. This results in increased drug plasma levels with a potentially increased rate of adverse effects.
“Intermediate and extensive metabolizers usually have a normal phenotype, but you can also have ultrarapid metabolizers who have duplications or other enhancing mutations of the CYP gene,” Dr. Nurmi said. “This can result in lower bioavailability and possibly efficacy. Psychiatrists treat poor metabolizers and ultrarapid metabolizers all the time, because the variants are very common.” An estimated 10% of White people are poor metabolizers at the CYP2D6 gene while about 7% are ultrarapid metabolizers. At the same time, an estimated 20% of Asians, Africans, and Whites are poor metabolizers at the CYP2C19 gene. “So, you’re seeing a lot of this in your practice, and you’re probably changing dosing based on genetic differences in metabolism,” she said.
The only FDA pharmacodynamic treatment guideline is for the risk of Stevens-Johnson syndrome (SJS) with the use of carbamazepine. In a study of 44 patients with SJS, all were positive for the HLA-B*1502 variant, compared with 3% of carbamazepine-tolerant patients (Nature 2004;428[6982]:486). The frequency of carrying this variant is an estimated 1:10,000 among Whites and 1:1,000 among Asians. In 2007, the FDA recommended that patients of Asian ancestry should be screened for HLA-B*1502 prior to starting carbamazepine.
Genetic variation also predicts clinical outcome with atomoxetine use. “Most child psychiatrists I know think atomoxetine doesn’t work as a second-line nonstimulant medication for ADHD,” Dr. Nurmi said. “I’d like to convince you that why you think it doesn’t work is because of the genetics.” In a study published in 2019, Dr. Nurmi and colleagues reviewed medical literature and provided therapeutic recommendations for atomoxetine therapy based on CYP2D6 genotype (Clin Pharmacol Ther 2019 Jul;106[1]:94-102). They observed 10- to 30-fold plasma differences in drug exposure between normal metabolizers and poor metabolizers.
“Poor metabolizers therefore get more benefit, but they are also going to get more side effects,” she said. “FDA recommended doses are inadequate for normal metabolizers, so they had to make guidelines based on poor metabolizers because there would be too much risk for them at higher doses. One-third of individuals require doses above the FDA limit to achieve a therapeutic drug level.”
Dr. Nurmi warned that the existing evidence base for using these genetic tests in children “is really poor. There is no data in adults with any diagnosis other than depression, and even those studies are plagued by concerns. When you’re implementing decision support tools in your practice, the key factors are patient presentation, history and symptoms, your clinical skills, the evidence base, FDA recommendations, and patient autonomy. Appropriate incorporation of genetic data should include avoiding a medication with high toxicity (like SJS), titration planning (dose and titration speed adjustments), and choosing between medications in the same class with an indication or evidence base for the target disorder.” She added that while the benefit of current genetic testing is limited, it may help some patients feel more comfortable tolerating a medication. “For example, being able to tell someone with anxiety that their genetics suggests that they will not have side effects could be very powerful,” she said.
In a 2018 safety communication, the FDA warned the public about its concerns with companies making claims about how to use genetic test results to manage medication treatments that are not supported by recommendations in the FDA-approved drug labeling or other scientific evidence. The American Academy of Child and Adolescent Psychiatry also published a guide for patients and families.
Dr. Nurmi disclosed that she is an unpaid advisory board member for Myriad Genetics and the Tourette Association of America, a paid adviser for Teva Pharmaceuticals, and a recipient of research support from Emalex Pharmaceuticals. She has received research funding from the National Institutes Health, the International OCD Foundation, the Tourette Association of America, and the Brain & Behavior Research Foundation.
LAS VEGAS –
“It’s misleading to rely on results of genetic tests to drive clinical treatment,” Dr. Nurmi, a child and adolescent psychiatrist in the department of psychiatry and biobehavioral sciences at the University of California, Los Angeles, said during an annual psychopharmacology update held by the Nevada Psychiatric Association. “There’s a lot of hope and promise there. But currently, we only know the tip of the iceberg about how drugs work and the genetics influencing these effects. Current testing is probably a very poor reflection of the complexity of drug effects.”
According to Dr. Nurmi, there are at least 165 Food and Drug Administration–approved drugs with pharmacogenetic information on 64 different biomarkers – 37% with CYP p450 notations. Of these, 32 psychiatric drugs have pharmacogenetic information, and most of them are dosing recommendations based on whether a patient has the variant. However, there is wide public acceptance of genetic testing in preventing the wrong drug from being used, in selecting the best drug dose, and avoiding side effects (Pharmacogenomics 2012;12[3]:197-204). “Most people have a lot of hope [for genetic testing in psychiatry],” Dr. Nurmi said. “But is the science really there? It doesn’t matter, because these companies are doing it, and you are being shown these reports from patients. Whether or not the science supports it, we’re going to have to interpret these reports and explain them to our patients – even if we don’t order them.”
Currently, she continued, clinicians practice trial and error prescribing where they might try one treatment in a class that they think that will work based on previous literature. If nothing works, they try another one. If that’s intolerable, they try a third treatment, and so on. “When we finally find the right treatment, it can take some time to get the dosing right,” Dr. Nurmi said. “So, it can take many months to get a child on the right medication. Precision treatment, on the other hand, would start off by taking a saliva or blood sample to get a printout that lets physicians know which drugs might be used with caution because they might lack efficacy at standard doses, which ones would likely have adverse effects at standard doses, and which are the best choices and what are the dosing recommendations for those choices. If we could get all the information to guide us, that would be a useful product, but right now, we don’t know enough to be able to make these determinations.”
Current evidence-based genetic testing supports a limited role for CYP2D6 and CYP2C19 genotyping because most psychiatric drugs are metabolized by those two enzymes. Poor metabolizers have two dysfunctional copies of the enzyme-encoding gene. This results in increased drug plasma levels with a potentially increased rate of adverse effects.
“Intermediate and extensive metabolizers usually have a normal phenotype, but you can also have ultrarapid metabolizers who have duplications or other enhancing mutations of the CYP gene,” Dr. Nurmi said. “This can result in lower bioavailability and possibly efficacy. Psychiatrists treat poor metabolizers and ultrarapid metabolizers all the time, because the variants are very common.” An estimated 10% of White people are poor metabolizers at the CYP2D6 gene while about 7% are ultrarapid metabolizers. At the same time, an estimated 20% of Asians, Africans, and Whites are poor metabolizers at the CYP2C19 gene. “So, you’re seeing a lot of this in your practice, and you’re probably changing dosing based on genetic differences in metabolism,” she said.
The only FDA pharmacodynamic treatment guideline is for the risk of Stevens-Johnson syndrome (SJS) with the use of carbamazepine. In a study of 44 patients with SJS, all were positive for the HLA-B*1502 variant, compared with 3% of carbamazepine-tolerant patients (Nature 2004;428[6982]:486). The frequency of carrying this variant is an estimated 1:10,000 among Whites and 1:1,000 among Asians. In 2007, the FDA recommended that patients of Asian ancestry should be screened for HLA-B*1502 prior to starting carbamazepine.
Genetic variation also predicts clinical outcome with atomoxetine use. “Most child psychiatrists I know think atomoxetine doesn’t work as a second-line nonstimulant medication for ADHD,” Dr. Nurmi said. “I’d like to convince you that why you think it doesn’t work is because of the genetics.” In a study published in 2019, Dr. Nurmi and colleagues reviewed medical literature and provided therapeutic recommendations for atomoxetine therapy based on CYP2D6 genotype (Clin Pharmacol Ther 2019 Jul;106[1]:94-102). They observed 10- to 30-fold plasma differences in drug exposure between normal metabolizers and poor metabolizers.
“Poor metabolizers therefore get more benefit, but they are also going to get more side effects,” she said. “FDA recommended doses are inadequate for normal metabolizers, so they had to make guidelines based on poor metabolizers because there would be too much risk for them at higher doses. One-third of individuals require doses above the FDA limit to achieve a therapeutic drug level.”
Dr. Nurmi warned that the existing evidence base for using these genetic tests in children “is really poor. There is no data in adults with any diagnosis other than depression, and even those studies are plagued by concerns. When you’re implementing decision support tools in your practice, the key factors are patient presentation, history and symptoms, your clinical skills, the evidence base, FDA recommendations, and patient autonomy. Appropriate incorporation of genetic data should include avoiding a medication with high toxicity (like SJS), titration planning (dose and titration speed adjustments), and choosing between medications in the same class with an indication or evidence base for the target disorder.” She added that while the benefit of current genetic testing is limited, it may help some patients feel more comfortable tolerating a medication. “For example, being able to tell someone with anxiety that their genetics suggests that they will not have side effects could be very powerful,” she said.
In a 2018 safety communication, the FDA warned the public about its concerns with companies making claims about how to use genetic test results to manage medication treatments that are not supported by recommendations in the FDA-approved drug labeling or other scientific evidence. The American Academy of Child and Adolescent Psychiatry also published a guide for patients and families.
Dr. Nurmi disclosed that she is an unpaid advisory board member for Myriad Genetics and the Tourette Association of America, a paid adviser for Teva Pharmaceuticals, and a recipient of research support from Emalex Pharmaceuticals. She has received research funding from the National Institutes Health, the International OCD Foundation, the Tourette Association of America, and the Brain & Behavior Research Foundation.
LAS VEGAS –
“It’s misleading to rely on results of genetic tests to drive clinical treatment,” Dr. Nurmi, a child and adolescent psychiatrist in the department of psychiatry and biobehavioral sciences at the University of California, Los Angeles, said during an annual psychopharmacology update held by the Nevada Psychiatric Association. “There’s a lot of hope and promise there. But currently, we only know the tip of the iceberg about how drugs work and the genetics influencing these effects. Current testing is probably a very poor reflection of the complexity of drug effects.”
According to Dr. Nurmi, there are at least 165 Food and Drug Administration–approved drugs with pharmacogenetic information on 64 different biomarkers – 37% with CYP p450 notations. Of these, 32 psychiatric drugs have pharmacogenetic information, and most of them are dosing recommendations based on whether a patient has the variant. However, there is wide public acceptance of genetic testing in preventing the wrong drug from being used, in selecting the best drug dose, and avoiding side effects (Pharmacogenomics 2012;12[3]:197-204). “Most people have a lot of hope [for genetic testing in psychiatry],” Dr. Nurmi said. “But is the science really there? It doesn’t matter, because these companies are doing it, and you are being shown these reports from patients. Whether or not the science supports it, we’re going to have to interpret these reports and explain them to our patients – even if we don’t order them.”
Currently, she continued, clinicians practice trial and error prescribing where they might try one treatment in a class that they think that will work based on previous literature. If nothing works, they try another one. If that’s intolerable, they try a third treatment, and so on. “When we finally find the right treatment, it can take some time to get the dosing right,” Dr. Nurmi said. “So, it can take many months to get a child on the right medication. Precision treatment, on the other hand, would start off by taking a saliva or blood sample to get a printout that lets physicians know which drugs might be used with caution because they might lack efficacy at standard doses, which ones would likely have adverse effects at standard doses, and which are the best choices and what are the dosing recommendations for those choices. If we could get all the information to guide us, that would be a useful product, but right now, we don’t know enough to be able to make these determinations.”
Current evidence-based genetic testing supports a limited role for CYP2D6 and CYP2C19 genotyping because most psychiatric drugs are metabolized by those two enzymes. Poor metabolizers have two dysfunctional copies of the enzyme-encoding gene. This results in increased drug plasma levels with a potentially increased rate of adverse effects.
“Intermediate and extensive metabolizers usually have a normal phenotype, but you can also have ultrarapid metabolizers who have duplications or other enhancing mutations of the CYP gene,” Dr. Nurmi said. “This can result in lower bioavailability and possibly efficacy. Psychiatrists treat poor metabolizers and ultrarapid metabolizers all the time, because the variants are very common.” An estimated 10% of White people are poor metabolizers at the CYP2D6 gene while about 7% are ultrarapid metabolizers. At the same time, an estimated 20% of Asians, Africans, and Whites are poor metabolizers at the CYP2C19 gene. “So, you’re seeing a lot of this in your practice, and you’re probably changing dosing based on genetic differences in metabolism,” she said.
The only FDA pharmacodynamic treatment guideline is for the risk of Stevens-Johnson syndrome (SJS) with the use of carbamazepine. In a study of 44 patients with SJS, all were positive for the HLA-B*1502 variant, compared with 3% of carbamazepine-tolerant patients (Nature 2004;428[6982]:486). The frequency of carrying this variant is an estimated 1:10,000 among Whites and 1:1,000 among Asians. In 2007, the FDA recommended that patients of Asian ancestry should be screened for HLA-B*1502 prior to starting carbamazepine.
Genetic variation also predicts clinical outcome with atomoxetine use. “Most child psychiatrists I know think atomoxetine doesn’t work as a second-line nonstimulant medication for ADHD,” Dr. Nurmi said. “I’d like to convince you that why you think it doesn’t work is because of the genetics.” In a study published in 2019, Dr. Nurmi and colleagues reviewed medical literature and provided therapeutic recommendations for atomoxetine therapy based on CYP2D6 genotype (Clin Pharmacol Ther 2019 Jul;106[1]:94-102). They observed 10- to 30-fold plasma differences in drug exposure between normal metabolizers and poor metabolizers.
“Poor metabolizers therefore get more benefit, but they are also going to get more side effects,” she said. “FDA recommended doses are inadequate for normal metabolizers, so they had to make guidelines based on poor metabolizers because there would be too much risk for them at higher doses. One-third of individuals require doses above the FDA limit to achieve a therapeutic drug level.”
Dr. Nurmi warned that the existing evidence base for using these genetic tests in children “is really poor. There is no data in adults with any diagnosis other than depression, and even those studies are plagued by concerns. When you’re implementing decision support tools in your practice, the key factors are patient presentation, history and symptoms, your clinical skills, the evidence base, FDA recommendations, and patient autonomy. Appropriate incorporation of genetic data should include avoiding a medication with high toxicity (like SJS), titration planning (dose and titration speed adjustments), and choosing between medications in the same class with an indication or evidence base for the target disorder.” She added that while the benefit of current genetic testing is limited, it may help some patients feel more comfortable tolerating a medication. “For example, being able to tell someone with anxiety that their genetics suggests that they will not have side effects could be very powerful,” she said.
In a 2018 safety communication, the FDA warned the public about its concerns with companies making claims about how to use genetic test results to manage medication treatments that are not supported by recommendations in the FDA-approved drug labeling or other scientific evidence. The American Academy of Child and Adolescent Psychiatry also published a guide for patients and families.
Dr. Nurmi disclosed that she is an unpaid advisory board member for Myriad Genetics and the Tourette Association of America, a paid adviser for Teva Pharmaceuticals, and a recipient of research support from Emalex Pharmaceuticals. She has received research funding from the National Institutes Health, the International OCD Foundation, the Tourette Association of America, and the Brain & Behavior Research Foundation.
REPORTING FROM NPA 2022
New AAD guidelines eye comorbidities in adults with atopic dermatitis
While it’s well established that atopic dermatitis (AD) in adults is associated with asthma, allergic rhinitis, and other atopic conditions, the links between AD and other comorbidities are coming into clearer focus.
, published evidence supports an association between AD and comorbidities that may not be on the radar of clinicians and patients, including substance use, attention-deficit/hyperactivity disorder (ADHD), elements of metabolic syndrome, and various cardiovascular conditions.
“There are more comorbidities with AD than we anticipated, that are supported by data in the literature,” Dawn M.R. Davis, MD, cochair and an author of the guidelines, told this news organization. “We are learning more about the interconnectivity of various medical conditions,” she continued. “Many skin diseases over time have been noted to be impactful to the whole person and not only the skin. A classic example of that is psoriasis. We now understand that psoriasis is a multisystem inflammatory disorder.”
As for AD, “we’ve always appreciated that AD patients tend to be at higher risk for other atopic diseases such as asthma, allergic rhinoconjunctivitis, and food allergies,” said Dr. Davis, of the departments of dermatology and pediatrics at the Mayo Clinic, Rochester, Minn. “With further research, we are now able to delineate those associations more intimately and have data to support our suspicions. Additionally, we’re now understanding that these inflammatory conditions can impact more than the end organ involved, such as the skin and AD. We wanted to look at how AD can affect the whole patient.”
For the guidelines, which are the first of their kind and were published online in the Journal of the American Academy of Dermatology, Dr. Davis and project cochair Robert Sidbury, MD, MPH, chief of dermatology at Seattle Children’s Hospital, led a multidisciplinary group of 12 experts to review the association between AD and selected comorbidities. They applied the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) for prognosis approach for assessing the certainty of the evidence and provided statements of association based on the available evidence.
With respect to highlights for atopic and allergic conditions, the guideline authors found high-quality evidence that AD in adults is associated with food allergies, moderate-quality evidence that AD is associated with asthma, and low-quality evidence that AD in adults may be associated with eosinophilic esophagitis.
In the realm of mental health and substance use, ample evidence exists to support an association between AD and mental health conditions such as depression and anxiety, the guidelines state. “For many patients, low mood may be driven by the symptoms of AD, including chronic itch and poor sleep,” Dr. Davis and her coauthors wrote. “Successfully treating AD may alleviate depressive symptoms for some patients; for others, assessment and treatment specific to their mental health may be needed.”
The guidelines also state that low-quality evidence exists to suggest that AD in adults may be associated with alcohol abuse disorders and cigarette smoking.
The authors noted “limited but consistent evidence” supporting a link between AD and adverse bone health, including osteoporosis and fractures, while associations between AD and cardiovascular risk factors and comorbidities, including hypertension, myocardial infarction, and stroke, are more controversial.
“I have published on bone health and AD so that was not as surprising to me,” Dr. Davis said in the interview. “I found a lot of the evidence in the guidelines to be validating of patterns that we see in our patients. The most significant learning point for me was [the link to] cardiovascular disease and the link to specific mental health and substance use disorders. It validates how impactful AD is to the individual.”
According to the guidelines, moderate-quality evidence exists linking AD in adults to both alopecia areata and urticaria. “Because we are dermatologists and take care of both of those diseases, be mindful of that in your daily practice,” Dr. Davis advised. “I would also encourage our colleagues to remember to educate patients on the comorbidities of AD so that they are empowered, and to screen for those comorbidities in your office based on the patient and their history and physical exam, to the level that you think is appropriate for that person’s individual’s care.”
Christine Ko, MD, who was asked to comment on the guidelines, characterized some of the reported comorbidity associations as predictable, such as asthma, food allergy, allergic rhinitis, and skin infections. “As the authors comment, ‘associations between AD and other atopic and allergic conditions have been recognized for decades and even contribute to diagnostic criteria for AD,’ ” said Dr. Ko, professor of dermatology and pathology at Yale University, New Haven, Conn, who was not involved with the guidelines. “I was a bit surprised to see that atopic dermatitis in adults is associated with osteoporosis and fractures. As the authors suggest, this could be secondary to treatment with oral prednisone, and it is possible that use of dupilumab and JAK inhibitors may lessen this association.”
Shawn G. Kwatra, MD, of the department of dermatology at Johns Hopkins University, Baltimore, who was not involved with the guidelines, and was also asked to comment, said that the guidelines underscore the importance of informing adults with AD “of the risks of unchecked inflammation and the potential for multiple disease comorbidities.” Dr. Kwatra, who has AD, added that “these results make me want to be more proactive in treating my eczema to reduce the potential for development of these comorbidities.”
He pointed out that the guidelines did not address racial and ethnic differences in the observed comorbidities. “Unfortunately, minority populations have a greater comorbidity burden in many inflammatory skin diseases so this will be another area needing further investigation,” he said. “As an example, our group found from multicenter data that black patients with atopic dermatitis have higher levels of C-reactive protein, blood eosinophils, and other inflammatory biomarkers.”
The AAD guidelines are the first in a four-part series on AD expected to be published over the next 1-2 years, Dr. Davis said. The subsequent guidelines will address topicals, phototherapy/systemics, and pediatrics.
The study was funded by internal funds from the AAD. Dr. Davis reported having no financial disclosures. Dr. Sidbury disclosed that he serves as an advisory board member for Pfizer, a principal investigator for Regeneron, and an investigator for Brickell Biotech and Galderma. He is also a consultant for Galderma Global and Microes. Dr. Ko reported having no financial disclosures. Dr. Kwatra is a member of the board of directors of the Skin of Color Society. He is also an advisory board member/consultant for AbbVie, Galderma, Incyte, Pfizer, Regeneron Pharmaceuticals, and Sanofi, and has served as an investigator for Galderma, Pfizer, and Sanofi.
While it’s well established that atopic dermatitis (AD) in adults is associated with asthma, allergic rhinitis, and other atopic conditions, the links between AD and other comorbidities are coming into clearer focus.
, published evidence supports an association between AD and comorbidities that may not be on the radar of clinicians and patients, including substance use, attention-deficit/hyperactivity disorder (ADHD), elements of metabolic syndrome, and various cardiovascular conditions.
“There are more comorbidities with AD than we anticipated, that are supported by data in the literature,” Dawn M.R. Davis, MD, cochair and an author of the guidelines, told this news organization. “We are learning more about the interconnectivity of various medical conditions,” she continued. “Many skin diseases over time have been noted to be impactful to the whole person and not only the skin. A classic example of that is psoriasis. We now understand that psoriasis is a multisystem inflammatory disorder.”
As for AD, “we’ve always appreciated that AD patients tend to be at higher risk for other atopic diseases such as asthma, allergic rhinoconjunctivitis, and food allergies,” said Dr. Davis, of the departments of dermatology and pediatrics at the Mayo Clinic, Rochester, Minn. “With further research, we are now able to delineate those associations more intimately and have data to support our suspicions. Additionally, we’re now understanding that these inflammatory conditions can impact more than the end organ involved, such as the skin and AD. We wanted to look at how AD can affect the whole patient.”
For the guidelines, which are the first of their kind and were published online in the Journal of the American Academy of Dermatology, Dr. Davis and project cochair Robert Sidbury, MD, MPH, chief of dermatology at Seattle Children’s Hospital, led a multidisciplinary group of 12 experts to review the association between AD and selected comorbidities. They applied the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) for prognosis approach for assessing the certainty of the evidence and provided statements of association based on the available evidence.
With respect to highlights for atopic and allergic conditions, the guideline authors found high-quality evidence that AD in adults is associated with food allergies, moderate-quality evidence that AD is associated with asthma, and low-quality evidence that AD in adults may be associated with eosinophilic esophagitis.
In the realm of mental health and substance use, ample evidence exists to support an association between AD and mental health conditions such as depression and anxiety, the guidelines state. “For many patients, low mood may be driven by the symptoms of AD, including chronic itch and poor sleep,” Dr. Davis and her coauthors wrote. “Successfully treating AD may alleviate depressive symptoms for some patients; for others, assessment and treatment specific to their mental health may be needed.”
The guidelines also state that low-quality evidence exists to suggest that AD in adults may be associated with alcohol abuse disorders and cigarette smoking.
The authors noted “limited but consistent evidence” supporting a link between AD and adverse bone health, including osteoporosis and fractures, while associations between AD and cardiovascular risk factors and comorbidities, including hypertension, myocardial infarction, and stroke, are more controversial.
“I have published on bone health and AD so that was not as surprising to me,” Dr. Davis said in the interview. “I found a lot of the evidence in the guidelines to be validating of patterns that we see in our patients. The most significant learning point for me was [the link to] cardiovascular disease and the link to specific mental health and substance use disorders. It validates how impactful AD is to the individual.”
According to the guidelines, moderate-quality evidence exists linking AD in adults to both alopecia areata and urticaria. “Because we are dermatologists and take care of both of those diseases, be mindful of that in your daily practice,” Dr. Davis advised. “I would also encourage our colleagues to remember to educate patients on the comorbidities of AD so that they are empowered, and to screen for those comorbidities in your office based on the patient and their history and physical exam, to the level that you think is appropriate for that person’s individual’s care.”
Christine Ko, MD, who was asked to comment on the guidelines, characterized some of the reported comorbidity associations as predictable, such as asthma, food allergy, allergic rhinitis, and skin infections. “As the authors comment, ‘associations between AD and other atopic and allergic conditions have been recognized for decades and even contribute to diagnostic criteria for AD,’ ” said Dr. Ko, professor of dermatology and pathology at Yale University, New Haven, Conn, who was not involved with the guidelines. “I was a bit surprised to see that atopic dermatitis in adults is associated with osteoporosis and fractures. As the authors suggest, this could be secondary to treatment with oral prednisone, and it is possible that use of dupilumab and JAK inhibitors may lessen this association.”
Shawn G. Kwatra, MD, of the department of dermatology at Johns Hopkins University, Baltimore, who was not involved with the guidelines, and was also asked to comment, said that the guidelines underscore the importance of informing adults with AD “of the risks of unchecked inflammation and the potential for multiple disease comorbidities.” Dr. Kwatra, who has AD, added that “these results make me want to be more proactive in treating my eczema to reduce the potential for development of these comorbidities.”
He pointed out that the guidelines did not address racial and ethnic differences in the observed comorbidities. “Unfortunately, minority populations have a greater comorbidity burden in many inflammatory skin diseases so this will be another area needing further investigation,” he said. “As an example, our group found from multicenter data that black patients with atopic dermatitis have higher levels of C-reactive protein, blood eosinophils, and other inflammatory biomarkers.”
The AAD guidelines are the first in a four-part series on AD expected to be published over the next 1-2 years, Dr. Davis said. The subsequent guidelines will address topicals, phototherapy/systemics, and pediatrics.
The study was funded by internal funds from the AAD. Dr. Davis reported having no financial disclosures. Dr. Sidbury disclosed that he serves as an advisory board member for Pfizer, a principal investigator for Regeneron, and an investigator for Brickell Biotech and Galderma. He is also a consultant for Galderma Global and Microes. Dr. Ko reported having no financial disclosures. Dr. Kwatra is a member of the board of directors of the Skin of Color Society. He is also an advisory board member/consultant for AbbVie, Galderma, Incyte, Pfizer, Regeneron Pharmaceuticals, and Sanofi, and has served as an investigator for Galderma, Pfizer, and Sanofi.
While it’s well established that atopic dermatitis (AD) in adults is associated with asthma, allergic rhinitis, and other atopic conditions, the links between AD and other comorbidities are coming into clearer focus.
, published evidence supports an association between AD and comorbidities that may not be on the radar of clinicians and patients, including substance use, attention-deficit/hyperactivity disorder (ADHD), elements of metabolic syndrome, and various cardiovascular conditions.
“There are more comorbidities with AD than we anticipated, that are supported by data in the literature,” Dawn M.R. Davis, MD, cochair and an author of the guidelines, told this news organization. “We are learning more about the interconnectivity of various medical conditions,” she continued. “Many skin diseases over time have been noted to be impactful to the whole person and not only the skin. A classic example of that is psoriasis. We now understand that psoriasis is a multisystem inflammatory disorder.”
As for AD, “we’ve always appreciated that AD patients tend to be at higher risk for other atopic diseases such as asthma, allergic rhinoconjunctivitis, and food allergies,” said Dr. Davis, of the departments of dermatology and pediatrics at the Mayo Clinic, Rochester, Minn. “With further research, we are now able to delineate those associations more intimately and have data to support our suspicions. Additionally, we’re now understanding that these inflammatory conditions can impact more than the end organ involved, such as the skin and AD. We wanted to look at how AD can affect the whole patient.”
For the guidelines, which are the first of their kind and were published online in the Journal of the American Academy of Dermatology, Dr. Davis and project cochair Robert Sidbury, MD, MPH, chief of dermatology at Seattle Children’s Hospital, led a multidisciplinary group of 12 experts to review the association between AD and selected comorbidities. They applied the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) for prognosis approach for assessing the certainty of the evidence and provided statements of association based on the available evidence.
With respect to highlights for atopic and allergic conditions, the guideline authors found high-quality evidence that AD in adults is associated with food allergies, moderate-quality evidence that AD is associated with asthma, and low-quality evidence that AD in adults may be associated with eosinophilic esophagitis.
In the realm of mental health and substance use, ample evidence exists to support an association between AD and mental health conditions such as depression and anxiety, the guidelines state. “For many patients, low mood may be driven by the symptoms of AD, including chronic itch and poor sleep,” Dr. Davis and her coauthors wrote. “Successfully treating AD may alleviate depressive symptoms for some patients; for others, assessment and treatment specific to their mental health may be needed.”
The guidelines also state that low-quality evidence exists to suggest that AD in adults may be associated with alcohol abuse disorders and cigarette smoking.
The authors noted “limited but consistent evidence” supporting a link between AD and adverse bone health, including osteoporosis and fractures, while associations between AD and cardiovascular risk factors and comorbidities, including hypertension, myocardial infarction, and stroke, are more controversial.
“I have published on bone health and AD so that was not as surprising to me,” Dr. Davis said in the interview. “I found a lot of the evidence in the guidelines to be validating of patterns that we see in our patients. The most significant learning point for me was [the link to] cardiovascular disease and the link to specific mental health and substance use disorders. It validates how impactful AD is to the individual.”
According to the guidelines, moderate-quality evidence exists linking AD in adults to both alopecia areata and urticaria. “Because we are dermatologists and take care of both of those diseases, be mindful of that in your daily practice,” Dr. Davis advised. “I would also encourage our colleagues to remember to educate patients on the comorbidities of AD so that they are empowered, and to screen for those comorbidities in your office based on the patient and their history and physical exam, to the level that you think is appropriate for that person’s individual’s care.”
Christine Ko, MD, who was asked to comment on the guidelines, characterized some of the reported comorbidity associations as predictable, such as asthma, food allergy, allergic rhinitis, and skin infections. “As the authors comment, ‘associations between AD and other atopic and allergic conditions have been recognized for decades and even contribute to diagnostic criteria for AD,’ ” said Dr. Ko, professor of dermatology and pathology at Yale University, New Haven, Conn, who was not involved with the guidelines. “I was a bit surprised to see that atopic dermatitis in adults is associated with osteoporosis and fractures. As the authors suggest, this could be secondary to treatment with oral prednisone, and it is possible that use of dupilumab and JAK inhibitors may lessen this association.”
Shawn G. Kwatra, MD, of the department of dermatology at Johns Hopkins University, Baltimore, who was not involved with the guidelines, and was also asked to comment, said that the guidelines underscore the importance of informing adults with AD “of the risks of unchecked inflammation and the potential for multiple disease comorbidities.” Dr. Kwatra, who has AD, added that “these results make me want to be more proactive in treating my eczema to reduce the potential for development of these comorbidities.”
He pointed out that the guidelines did not address racial and ethnic differences in the observed comorbidities. “Unfortunately, minority populations have a greater comorbidity burden in many inflammatory skin diseases so this will be another area needing further investigation,” he said. “As an example, our group found from multicenter data that black patients with atopic dermatitis have higher levels of C-reactive protein, blood eosinophils, and other inflammatory biomarkers.”
The AAD guidelines are the first in a four-part series on AD expected to be published over the next 1-2 years, Dr. Davis said. The subsequent guidelines will address topicals, phototherapy/systemics, and pediatrics.
The study was funded by internal funds from the AAD. Dr. Davis reported having no financial disclosures. Dr. Sidbury disclosed that he serves as an advisory board member for Pfizer, a principal investigator for Regeneron, and an investigator for Brickell Biotech and Galderma. He is also a consultant for Galderma Global and Microes. Dr. Ko reported having no financial disclosures. Dr. Kwatra is a member of the board of directors of the Skin of Color Society. He is also an advisory board member/consultant for AbbVie, Galderma, Incyte, Pfizer, Regeneron Pharmaceuticals, and Sanofi, and has served as an investigator for Galderma, Pfizer, and Sanofi.
FROM JOURNAL OF THE AMERICAN ACADEMY OF DERMATOLOGY
Experts plead for more pediatric telehealth
A specialty group is asking federal and state governments to preserve and expand access to telehealth services for children with developmental and behavioral problems.
Citing the success during the COVID-19 pandemic of telehealth for these patients, the Society for Developmental and Behavioral Pediatrics (SDBP) has issued a position statement in its official journal calling for continued use of video and telephone for home-based diagnostic assessments, medication management follow-ups, and therapeutic interventions for children with autism spectrum disorder, attention-deficit/hyperactivity disorder, and other neurodevelopmental conditions.
“Telehealth offers plenty of opportunities for quick check-ins. It can offer some crisis management opportunities ... to address a parent’s concern about challenging behaviors or navigating school system issues or developmental needs,” lead author Robert D. Keder, MD, assistant professor of pediatrics at University of Connecticut, Farmington, and cochair of SDBP’s Advocacy Committee, told this news organization.
“The video visit does really offer us so much more. It’s so enriching and lets us as providers meet the child in their natural home environment. The real magic of a video visit is we haven’t done house calls as a medical society for decades. But now, literally, the power of telehealth lets us do a house call.”
In the face of the pandemic, emergency government policies allowed care to continue remotely via telehealth, including video and phone calls. The policies have allowed patients to have video visits in their own home, lifted provider licensure requirements for visits across state lines, and allowed reimbursement not only for video visits but also for telephone encounters.
As a result, the field of developmental and behavioral pediatrics (DBP) has recognized telehealth as a viable and useful model of care for children with neurodevelopmental disorders, said Neelkamal Soares, MD, a member of the society’s board and a coauthor of the position paper.
“Telehealth has been helpful in mitigating barriers families often face when attending in-person visits,” such as the lack of transportation and child care, missed work hours, and other issues, said Dr. Soares, professor of pediatric and adolescent medicine at Western Michigan University Stryker in Kalamazoo. At the same time, the growth in the use of the technology has highlighted additional obstacles to equitable access to care, including broadband connectivity, digital literacy, and the availability of interpretation and sign language services, he said.
Dr. Keder said telehealth has enabled him to better help with behavior management by observing children where they are most comfortable. Remote visits also allow him to consider information such as furniture arrangements and how that can affect the patient’s living conditions, and also sibling interactions, learning and homework, eating, and sleep.
Telemedicine conferences enable DBP specialists to facilitate care collaboration with different members of the patient’s care team. Consent from a family and a click of a button allows for therapists, early intervention specialists, teachers, school nurses, or even primary care providers the capacity to participate in a telehealth visit, he said.
Dr. Keder said the future of telehealth is uncertain. The policies from the pandemic may expire in the near term and vary from state to state. The goal of the policy statement is to advocate for legislation and policies that support ongoing, equitable, home-based telehealth care for patients seen by DBP providers while ensuring equitable access to DBP in general.
Kate Benton, PhD, a clinical psychologist with Lurie Children’s Hospital at Northwestern Medicine Central DuPage Hospital in Winfield, Ill., said the society has done an excellent job of explaining the need to maintain telehealth in light of the shortage of pediatricians, clinical psychologists, and other professionals in the field.
“Telehealth has opened new avenues for these patients who otherwise have difficulty seeing specialists. This is a population of children who without telehealth have significant challenges in getting access to care,” she said.
Wendy Fournier, mother of an autistic child and president of the National Autism Association, said telehealth can be beneficial for some individuals with the disorder.
“There are many aspects of in-person doctor visits that can be overwhelming, including bright lights, many people talking, waiting for the doctor, being comfortable with the doctor’s touch, etc.,” Ms. Fournier said in an interview. “All of these things can cause sensory and emotional dysregulation leading to overwhelming anxiety and fear.”
Visits to the doctor can be especially difficult for people who are nonverbal and unable to express their discomfort, said.
“At my daughter’s last medical appointment, she could not stay in the exam room and pulled me out the door. Thankfully, we have an understanding and compassionate physician who finished our appointment in our car. I believe that telehealth visits should remain available as a necessary and vital accommodation for people with disabilities,” Ms. Fournier said.
False equivalence?
Dr. Soares said researchers have attempted to assess the evidence of telehealth benefits in such situations as ADHD, cognitive behavioral therapy, and parent training.
“There is a paucity of published studies that specifically look at different conditions and compare in-person to telehealth visits, but these are ongoing in autism diagnostics and other areas by several SDBP members,” he said. “Stay tuned.”
Dr. Keder added that telehealth will never replace in-person visits, but the availability of this new option gives developmental pediatricians flexibility in strategies in treating and evaluating patients.
“Both are helpful and viable models. In the pandemic, we were forced out of necessity to embrace telehealth,” he said. “Because of this, we are seeing the power and benefits telehealth offers. Now many families like a mixture of alternating in person with telehealth visits.”
The policy statement cites research that finds patients are highly satisfied with telehealth and that telehealth may cost less than in-office visits.
The report stresses that equitable access to devices needed for telehealth visits is a concern because there is disproportionate access to required technology, especially in rural and underserved communities. The Federal Communications Commission has provided grants to eligible families to offset the cost, in part, for a laptop, desktop computer, or tablet. However, more is still needed, the group said.
The position paper calls for:
- Equitable access to the infrastructure and technology for telehealth, including greater access to broadband services in rural and underserved areas.
- Increased access to devices needed to connect children with neurodevelopmental disorders with critical health care services.
- Reimbursement of interpretation services for the people who are deaf and/or have limited English proficiency.
- Mitigation of geographic barriers to accessing DBP care.
- Permitting patients to access telehealth from their home or whichever physical location provides opportunities for safe and timely care, especially for established patients.
- Ensuring more engagement by state medical licensing boards to join the Interstate Medical Licensing Compact to provide care by telehealth when there is already an insufficient geographic distribution of that type of provider in a state, as is being conducted in the field of psychology.
- Ensuring ongoing reimbursement.
- Parity in reimbursement for telehealth in-person visits.
- Increased funding for research looking into outcomes, quality, and effectiveness of telehealth services at the federal and state levels.
“Our organization can work with families to educate lawmakers, insurance administrators, and organizational leaders about the value that telehealth holds in the care of their child and family,” Dr. Soares said. “We can also conduct research to add to the evidence based around the topic to further the science around telehealth outcomes and equivalency to in-person settings.”
“With the current workforce shortage in DBP and behavioral health it is more critical than ever to maintain access to care,” Dr. Keder added. “The pandemic has provided an opportunity to better harness the amazing power of telehealth to allow for access to equitable care for families. We hope that this statement moves legislators, leaders, and voters to continue to advocate for ongoing telehealth at both the state, federal, and organizational levels.”
Dr. Benton, Dr. Keder, and Dr. Soares have disclosed no financial conflicts of interest.
A version of this article first appeared on Medscape.com.
A specialty group is asking federal and state governments to preserve and expand access to telehealth services for children with developmental and behavioral problems.
Citing the success during the COVID-19 pandemic of telehealth for these patients, the Society for Developmental and Behavioral Pediatrics (SDBP) has issued a position statement in its official journal calling for continued use of video and telephone for home-based diagnostic assessments, medication management follow-ups, and therapeutic interventions for children with autism spectrum disorder, attention-deficit/hyperactivity disorder, and other neurodevelopmental conditions.
“Telehealth offers plenty of opportunities for quick check-ins. It can offer some crisis management opportunities ... to address a parent’s concern about challenging behaviors or navigating school system issues or developmental needs,” lead author Robert D. Keder, MD, assistant professor of pediatrics at University of Connecticut, Farmington, and cochair of SDBP’s Advocacy Committee, told this news organization.
“The video visit does really offer us so much more. It’s so enriching and lets us as providers meet the child in their natural home environment. The real magic of a video visit is we haven’t done house calls as a medical society for decades. But now, literally, the power of telehealth lets us do a house call.”
In the face of the pandemic, emergency government policies allowed care to continue remotely via telehealth, including video and phone calls. The policies have allowed patients to have video visits in their own home, lifted provider licensure requirements for visits across state lines, and allowed reimbursement not only for video visits but also for telephone encounters.
As a result, the field of developmental and behavioral pediatrics (DBP) has recognized telehealth as a viable and useful model of care for children with neurodevelopmental disorders, said Neelkamal Soares, MD, a member of the society’s board and a coauthor of the position paper.
“Telehealth has been helpful in mitigating barriers families often face when attending in-person visits,” such as the lack of transportation and child care, missed work hours, and other issues, said Dr. Soares, professor of pediatric and adolescent medicine at Western Michigan University Stryker in Kalamazoo. At the same time, the growth in the use of the technology has highlighted additional obstacles to equitable access to care, including broadband connectivity, digital literacy, and the availability of interpretation and sign language services, he said.
Dr. Keder said telehealth has enabled him to better help with behavior management by observing children where they are most comfortable. Remote visits also allow him to consider information such as furniture arrangements and how that can affect the patient’s living conditions, and also sibling interactions, learning and homework, eating, and sleep.
Telemedicine conferences enable DBP specialists to facilitate care collaboration with different members of the patient’s care team. Consent from a family and a click of a button allows for therapists, early intervention specialists, teachers, school nurses, or even primary care providers the capacity to participate in a telehealth visit, he said.
Dr. Keder said the future of telehealth is uncertain. The policies from the pandemic may expire in the near term and vary from state to state. The goal of the policy statement is to advocate for legislation and policies that support ongoing, equitable, home-based telehealth care for patients seen by DBP providers while ensuring equitable access to DBP in general.
Kate Benton, PhD, a clinical psychologist with Lurie Children’s Hospital at Northwestern Medicine Central DuPage Hospital in Winfield, Ill., said the society has done an excellent job of explaining the need to maintain telehealth in light of the shortage of pediatricians, clinical psychologists, and other professionals in the field.
“Telehealth has opened new avenues for these patients who otherwise have difficulty seeing specialists. This is a population of children who without telehealth have significant challenges in getting access to care,” she said.
Wendy Fournier, mother of an autistic child and president of the National Autism Association, said telehealth can be beneficial for some individuals with the disorder.
“There are many aspects of in-person doctor visits that can be overwhelming, including bright lights, many people talking, waiting for the doctor, being comfortable with the doctor’s touch, etc.,” Ms. Fournier said in an interview. “All of these things can cause sensory and emotional dysregulation leading to overwhelming anxiety and fear.”
Visits to the doctor can be especially difficult for people who are nonverbal and unable to express their discomfort, said.
“At my daughter’s last medical appointment, she could not stay in the exam room and pulled me out the door. Thankfully, we have an understanding and compassionate physician who finished our appointment in our car. I believe that telehealth visits should remain available as a necessary and vital accommodation for people with disabilities,” Ms. Fournier said.
False equivalence?
Dr. Soares said researchers have attempted to assess the evidence of telehealth benefits in such situations as ADHD, cognitive behavioral therapy, and parent training.
“There is a paucity of published studies that specifically look at different conditions and compare in-person to telehealth visits, but these are ongoing in autism diagnostics and other areas by several SDBP members,” he said. “Stay tuned.”
Dr. Keder added that telehealth will never replace in-person visits, but the availability of this new option gives developmental pediatricians flexibility in strategies in treating and evaluating patients.
“Both are helpful and viable models. In the pandemic, we were forced out of necessity to embrace telehealth,” he said. “Because of this, we are seeing the power and benefits telehealth offers. Now many families like a mixture of alternating in person with telehealth visits.”
The policy statement cites research that finds patients are highly satisfied with telehealth and that telehealth may cost less than in-office visits.
The report stresses that equitable access to devices needed for telehealth visits is a concern because there is disproportionate access to required technology, especially in rural and underserved communities. The Federal Communications Commission has provided grants to eligible families to offset the cost, in part, for a laptop, desktop computer, or tablet. However, more is still needed, the group said.
The position paper calls for:
- Equitable access to the infrastructure and technology for telehealth, including greater access to broadband services in rural and underserved areas.
- Increased access to devices needed to connect children with neurodevelopmental disorders with critical health care services.
- Reimbursement of interpretation services for the people who are deaf and/or have limited English proficiency.
- Mitigation of geographic barriers to accessing DBP care.
- Permitting patients to access telehealth from their home or whichever physical location provides opportunities for safe and timely care, especially for established patients.
- Ensuring more engagement by state medical licensing boards to join the Interstate Medical Licensing Compact to provide care by telehealth when there is already an insufficient geographic distribution of that type of provider in a state, as is being conducted in the field of psychology.
- Ensuring ongoing reimbursement.
- Parity in reimbursement for telehealth in-person visits.
- Increased funding for research looking into outcomes, quality, and effectiveness of telehealth services at the federal and state levels.
“Our organization can work with families to educate lawmakers, insurance administrators, and organizational leaders about the value that telehealth holds in the care of their child and family,” Dr. Soares said. “We can also conduct research to add to the evidence based around the topic to further the science around telehealth outcomes and equivalency to in-person settings.”
“With the current workforce shortage in DBP and behavioral health it is more critical than ever to maintain access to care,” Dr. Keder added. “The pandemic has provided an opportunity to better harness the amazing power of telehealth to allow for access to equitable care for families. We hope that this statement moves legislators, leaders, and voters to continue to advocate for ongoing telehealth at both the state, federal, and organizational levels.”
Dr. Benton, Dr. Keder, and Dr. Soares have disclosed no financial conflicts of interest.
A version of this article first appeared on Medscape.com.
A specialty group is asking federal and state governments to preserve and expand access to telehealth services for children with developmental and behavioral problems.
Citing the success during the COVID-19 pandemic of telehealth for these patients, the Society for Developmental and Behavioral Pediatrics (SDBP) has issued a position statement in its official journal calling for continued use of video and telephone for home-based diagnostic assessments, medication management follow-ups, and therapeutic interventions for children with autism spectrum disorder, attention-deficit/hyperactivity disorder, and other neurodevelopmental conditions.
“Telehealth offers plenty of opportunities for quick check-ins. It can offer some crisis management opportunities ... to address a parent’s concern about challenging behaviors or navigating school system issues or developmental needs,” lead author Robert D. Keder, MD, assistant professor of pediatrics at University of Connecticut, Farmington, and cochair of SDBP’s Advocacy Committee, told this news organization.
“The video visit does really offer us so much more. It’s so enriching and lets us as providers meet the child in their natural home environment. The real magic of a video visit is we haven’t done house calls as a medical society for decades. But now, literally, the power of telehealth lets us do a house call.”
In the face of the pandemic, emergency government policies allowed care to continue remotely via telehealth, including video and phone calls. The policies have allowed patients to have video visits in their own home, lifted provider licensure requirements for visits across state lines, and allowed reimbursement not only for video visits but also for telephone encounters.
As a result, the field of developmental and behavioral pediatrics (DBP) has recognized telehealth as a viable and useful model of care for children with neurodevelopmental disorders, said Neelkamal Soares, MD, a member of the society’s board and a coauthor of the position paper.
“Telehealth has been helpful in mitigating barriers families often face when attending in-person visits,” such as the lack of transportation and child care, missed work hours, and other issues, said Dr. Soares, professor of pediatric and adolescent medicine at Western Michigan University Stryker in Kalamazoo. At the same time, the growth in the use of the technology has highlighted additional obstacles to equitable access to care, including broadband connectivity, digital literacy, and the availability of interpretation and sign language services, he said.
Dr. Keder said telehealth has enabled him to better help with behavior management by observing children where they are most comfortable. Remote visits also allow him to consider information such as furniture arrangements and how that can affect the patient’s living conditions, and also sibling interactions, learning and homework, eating, and sleep.
Telemedicine conferences enable DBP specialists to facilitate care collaboration with different members of the patient’s care team. Consent from a family and a click of a button allows for therapists, early intervention specialists, teachers, school nurses, or even primary care providers the capacity to participate in a telehealth visit, he said.
Dr. Keder said the future of telehealth is uncertain. The policies from the pandemic may expire in the near term and vary from state to state. The goal of the policy statement is to advocate for legislation and policies that support ongoing, equitable, home-based telehealth care for patients seen by DBP providers while ensuring equitable access to DBP in general.
Kate Benton, PhD, a clinical psychologist with Lurie Children’s Hospital at Northwestern Medicine Central DuPage Hospital in Winfield, Ill., said the society has done an excellent job of explaining the need to maintain telehealth in light of the shortage of pediatricians, clinical psychologists, and other professionals in the field.
“Telehealth has opened new avenues for these patients who otherwise have difficulty seeing specialists. This is a population of children who without telehealth have significant challenges in getting access to care,” she said.
Wendy Fournier, mother of an autistic child and president of the National Autism Association, said telehealth can be beneficial for some individuals with the disorder.
“There are many aspects of in-person doctor visits that can be overwhelming, including bright lights, many people talking, waiting for the doctor, being comfortable with the doctor’s touch, etc.,” Ms. Fournier said in an interview. “All of these things can cause sensory and emotional dysregulation leading to overwhelming anxiety and fear.”
Visits to the doctor can be especially difficult for people who are nonverbal and unable to express their discomfort, said.
“At my daughter’s last medical appointment, she could not stay in the exam room and pulled me out the door. Thankfully, we have an understanding and compassionate physician who finished our appointment in our car. I believe that telehealth visits should remain available as a necessary and vital accommodation for people with disabilities,” Ms. Fournier said.
False equivalence?
Dr. Soares said researchers have attempted to assess the evidence of telehealth benefits in such situations as ADHD, cognitive behavioral therapy, and parent training.
“There is a paucity of published studies that specifically look at different conditions and compare in-person to telehealth visits, but these are ongoing in autism diagnostics and other areas by several SDBP members,” he said. “Stay tuned.”
Dr. Keder added that telehealth will never replace in-person visits, but the availability of this new option gives developmental pediatricians flexibility in strategies in treating and evaluating patients.
“Both are helpful and viable models. In the pandemic, we were forced out of necessity to embrace telehealth,” he said. “Because of this, we are seeing the power and benefits telehealth offers. Now many families like a mixture of alternating in person with telehealth visits.”
The policy statement cites research that finds patients are highly satisfied with telehealth and that telehealth may cost less than in-office visits.
The report stresses that equitable access to devices needed for telehealth visits is a concern because there is disproportionate access to required technology, especially in rural and underserved communities. The Federal Communications Commission has provided grants to eligible families to offset the cost, in part, for a laptop, desktop computer, or tablet. However, more is still needed, the group said.
The position paper calls for:
- Equitable access to the infrastructure and technology for telehealth, including greater access to broadband services in rural and underserved areas.
- Increased access to devices needed to connect children with neurodevelopmental disorders with critical health care services.
- Reimbursement of interpretation services for the people who are deaf and/or have limited English proficiency.
- Mitigation of geographic barriers to accessing DBP care.
- Permitting patients to access telehealth from their home or whichever physical location provides opportunities for safe and timely care, especially for established patients.
- Ensuring more engagement by state medical licensing boards to join the Interstate Medical Licensing Compact to provide care by telehealth when there is already an insufficient geographic distribution of that type of provider in a state, as is being conducted in the field of psychology.
- Ensuring ongoing reimbursement.
- Parity in reimbursement for telehealth in-person visits.
- Increased funding for research looking into outcomes, quality, and effectiveness of telehealth services at the federal and state levels.
“Our organization can work with families to educate lawmakers, insurance administrators, and organizational leaders about the value that telehealth holds in the care of their child and family,” Dr. Soares said. “We can also conduct research to add to the evidence based around the topic to further the science around telehealth outcomes and equivalency to in-person settings.”
“With the current workforce shortage in DBP and behavioral health it is more critical than ever to maintain access to care,” Dr. Keder added. “The pandemic has provided an opportunity to better harness the amazing power of telehealth to allow for access to equitable care for families. We hope that this statement moves legislators, leaders, and voters to continue to advocate for ongoing telehealth at both the state, federal, and organizational levels.”
Dr. Benton, Dr. Keder, and Dr. Soares have disclosed no financial conflicts of interest.
A version of this article first appeared on Medscape.com.