User login
Frailty tied to higher mortality after major vascular surgery
Frailty defined as functional dependence is a predictor of mortality risk in elderly patients having major vascular surgery, a meta-analysis of studies has found
“Functional dependency may be recommended for use in rapid screening for frailty in major vascular surgery because of the high quality of associated evidence. Additionally, information on central muscle mass also adds incremental predictive value to long-term survival of elderly patients after major vascular surgery,” the study investigaters stated. However, they pointed out that “other newly developed frailty tools require further validation in more studies” before they should be adopted.
The report, published in the European Journal of Vascular and Endovascular Surgery, evaluated the effect of frailty in major vascular surgery from a search of MEDLINE, Embase, Cochrane Database, and Scopus through May 2018. Data were extracted from the articles related to surgery for abdominal aortic aneurysms (AAA) and lower extremity artery disease (LEAD), and a modified Newcastle-Ottawa scale was used to assess the quality of the included studies, according to Jiarong Wang, MD, of the department of vascular surgery, Sichuan University, Sichuan Province, China, and colleagues. A total of 22 cohort studies and one randomized controlled trial was used in the final analysis. The reviewers expressed the impact of frailty on outcomes as odds ratios (OR) or hazard ratios (HR) using a random effects model.
The researchers found that frailty, in terms of functional dependence, was associated with a significantly increased 30-day mortality risk in patients with AAA without heterogeneity (OR 5.15) and also in LEAD patients (OR 3.29). Functionally dependent patients also had a significantly increased 30-day mortality risk, compared with independent patients (OR 4.49), and similar results were observed after stratifying those who underwent AAA repair (OR 5.14) or lower extremity revascularization (OR 4.18). Even for patients who underwent endovascular procedures rather than open surgery, functional dependency was also associated with a significantly increased 30-day mortality risk (OR 4.90). In addition, with regard to 30-day morbidity, frailty was associated with a significantly increased risk in both AAA (OR 2.79) and LEAD (OR 1.40) patients.
As far as long-term outcomes were concerned, frailty was associated with a significantly increased risk of long-term all-cause mortality in the overall studied population (HR 2.22), as well as in patients with AAA repair (HR 2.10) and LEAD revascularization (HR 2.46). Dr. Wang and colleagues found that central muscle mass was the only tool with moderate quality of evidence predicting long-term survival after major vascular surgery (HR .48), with other single-domain tools such as nutrition or cognition scoring being of low quality. The modified Frailty Index was the only multi-domain tool with moderate quality in predicting mortality for AAA, while others were scored as low or very low, the authors added.
“Future research is warranted to establish consensus on how to select the optimal frailty tool for certain clinical settings,” they concluded.
The authors reported that they had no conflicts of interest and no funding sources for the study.
SOURCE: Wang, J et al. Eur J Vasc Endovasc Surg. 2018;56:591-602.
Frailty defined as functional dependence is a predictor of mortality risk in elderly patients having major vascular surgery, a meta-analysis of studies has found
“Functional dependency may be recommended for use in rapid screening for frailty in major vascular surgery because of the high quality of associated evidence. Additionally, information on central muscle mass also adds incremental predictive value to long-term survival of elderly patients after major vascular surgery,” the study investigaters stated. However, they pointed out that “other newly developed frailty tools require further validation in more studies” before they should be adopted.
The report, published in the European Journal of Vascular and Endovascular Surgery, evaluated the effect of frailty in major vascular surgery from a search of MEDLINE, Embase, Cochrane Database, and Scopus through May 2018. Data were extracted from the articles related to surgery for abdominal aortic aneurysms (AAA) and lower extremity artery disease (LEAD), and a modified Newcastle-Ottawa scale was used to assess the quality of the included studies, according to Jiarong Wang, MD, of the department of vascular surgery, Sichuan University, Sichuan Province, China, and colleagues. A total of 22 cohort studies and one randomized controlled trial was used in the final analysis. The reviewers expressed the impact of frailty on outcomes as odds ratios (OR) or hazard ratios (HR) using a random effects model.
The researchers found that frailty, in terms of functional dependence, was associated with a significantly increased 30-day mortality risk in patients with AAA without heterogeneity (OR 5.15) and also in LEAD patients (OR 3.29). Functionally dependent patients also had a significantly increased 30-day mortality risk, compared with independent patients (OR 4.49), and similar results were observed after stratifying those who underwent AAA repair (OR 5.14) or lower extremity revascularization (OR 4.18). Even for patients who underwent endovascular procedures rather than open surgery, functional dependency was also associated with a significantly increased 30-day mortality risk (OR 4.90). In addition, with regard to 30-day morbidity, frailty was associated with a significantly increased risk in both AAA (OR 2.79) and LEAD (OR 1.40) patients.
As far as long-term outcomes were concerned, frailty was associated with a significantly increased risk of long-term all-cause mortality in the overall studied population (HR 2.22), as well as in patients with AAA repair (HR 2.10) and LEAD revascularization (HR 2.46). Dr. Wang and colleagues found that central muscle mass was the only tool with moderate quality of evidence predicting long-term survival after major vascular surgery (HR .48), with other single-domain tools such as nutrition or cognition scoring being of low quality. The modified Frailty Index was the only multi-domain tool with moderate quality in predicting mortality for AAA, while others were scored as low or very low, the authors added.
“Future research is warranted to establish consensus on how to select the optimal frailty tool for certain clinical settings,” they concluded.
The authors reported that they had no conflicts of interest and no funding sources for the study.
SOURCE: Wang, J et al. Eur J Vasc Endovasc Surg. 2018;56:591-602.
Frailty defined as functional dependence is a predictor of mortality risk in elderly patients having major vascular surgery, a meta-analysis of studies has found
“Functional dependency may be recommended for use in rapid screening for frailty in major vascular surgery because of the high quality of associated evidence. Additionally, information on central muscle mass also adds incremental predictive value to long-term survival of elderly patients after major vascular surgery,” the study investigaters stated. However, they pointed out that “other newly developed frailty tools require further validation in more studies” before they should be adopted.
The report, published in the European Journal of Vascular and Endovascular Surgery, evaluated the effect of frailty in major vascular surgery from a search of MEDLINE, Embase, Cochrane Database, and Scopus through May 2018. Data were extracted from the articles related to surgery for abdominal aortic aneurysms (AAA) and lower extremity artery disease (LEAD), and a modified Newcastle-Ottawa scale was used to assess the quality of the included studies, according to Jiarong Wang, MD, of the department of vascular surgery, Sichuan University, Sichuan Province, China, and colleagues. A total of 22 cohort studies and one randomized controlled trial was used in the final analysis. The reviewers expressed the impact of frailty on outcomes as odds ratios (OR) or hazard ratios (HR) using a random effects model.
The researchers found that frailty, in terms of functional dependence, was associated with a significantly increased 30-day mortality risk in patients with AAA without heterogeneity (OR 5.15) and also in LEAD patients (OR 3.29). Functionally dependent patients also had a significantly increased 30-day mortality risk, compared with independent patients (OR 4.49), and similar results were observed after stratifying those who underwent AAA repair (OR 5.14) or lower extremity revascularization (OR 4.18). Even for patients who underwent endovascular procedures rather than open surgery, functional dependency was also associated with a significantly increased 30-day mortality risk (OR 4.90). In addition, with regard to 30-day morbidity, frailty was associated with a significantly increased risk in both AAA (OR 2.79) and LEAD (OR 1.40) patients.
As far as long-term outcomes were concerned, frailty was associated with a significantly increased risk of long-term all-cause mortality in the overall studied population (HR 2.22), as well as in patients with AAA repair (HR 2.10) and LEAD revascularization (HR 2.46). Dr. Wang and colleagues found that central muscle mass was the only tool with moderate quality of evidence predicting long-term survival after major vascular surgery (HR .48), with other single-domain tools such as nutrition or cognition scoring being of low quality. The modified Frailty Index was the only multi-domain tool with moderate quality in predicting mortality for AAA, while others were scored as low or very low, the authors added.
“Future research is warranted to establish consensus on how to select the optimal frailty tool for certain clinical settings,” they concluded.
The authors reported that they had no conflicts of interest and no funding sources for the study.
SOURCE: Wang, J et al. Eur J Vasc Endovasc Surg. 2018;56:591-602.
FROM EUROPEAN JOURNAL OF VASCULAR AND ENDOVASCULAR SURGERY
Key clinical point: Frailty was associated with increased short- and long-term mortality in major vascular surgery.
Major finding: Frailty was associated with a fourfold increased risk of 30-day mortality and a doubled increased risk of long-term mortality after major vascular surgery.
Study details: A meta-analysis of 22 cohort studies and one randomized controlled trial.
Disclosures: The authors reported that they had no conflicts of interest and no funding sources for the study.
Source: Wang, J et al., 2018. Eur J Vasc Endovasc Surg. 56:591-602.
Vascular emergencies on the rise, but more patients surviving
ST. LOUIS – A patient with a nontraumatic vascular emergency is significantly less likely to die today than a decade ago, with few exceptions, according to a new national analysis looking at 10 years of data. Unsurprisingly, endovascular surgery rates climbed over the study period, as did rates of acute limb ischemia, said Todd Vogel, MD, who discussed the study at the annual meeting of the Midwestern Vascular Surgical Society.
With an objective of evaluating trends for management of nontraumatic vascular emergencies in the United States, Dr. Vogel, who is chief of vascular and endovascular surgery at the University of Missouri–Columbia, and his colleagues examined frequencies of vascular emergencies, mortality rates, and how open versus endoscopic procedure technique affected the data.
To do this, the investigators used the U.S. National Inpatient Sample from 2005 to 2014 to identify nontraumatic vascular emergencies.
Using ICD-9 clinical management diagnosis and procedure codes allowed the investigators to capture a wide array of vascular emergencies, Dr. Vogel said. These included ruptured abdominal, thoracic, and thoracoabdominal aortic aneurysms (rAAAs, rTAAs, and rTAAAs, respectively), as well as acute limb ischemia, acute mesenteric ischemia, and ruptured visceral artery aneurysms.
Among the outcomes analyzed in the study were a trend analysis looking at how outcomes changed over time and an analysis of in-hospital mortality. Dr. Vogel and his colleagues also examined hospital resource utilization including length of stay and total hospital cost, inflation adjusted to 2014 costs.
The prevalence of endovascular intervention increased sharply over the study period, as one would expect, Dr. Vogel said. “At the beginning, we had about 24% of patients getting endovascular intervention for vascular emergencies, and currently, it’s 36%.” (P for trend, less than .0001).
Mortality dropped steeply overall, with overall mortality going from 13.80% to 9.14% during the study period (P less than .0001). Much of this decrease could be attributed to mortality for open procedures decreasing by over a third, from 16.5% to 10.7%, over the study period (P less than .0001). Endovascular procedure–related mortality decreased from 8.3% to 7.9% (P = .03).
Ruptured abdominal and thoracic aortic aneurysms were much less likely to be fatal in 2014 than in 2005. The overall mortality rate for rAAA went from 41.4% to 27.6% (P less than .0001) and rates for rTAAs dropped overall from 41.2% to 23.0% (P = .002).
However, endovascular rTAA repair mortality jumped from 14.9% to 27.4% (P = .0003) while mortality for open procedures plummeted from 51.3% to 16.7% (P less than .0001).
In-hospital mortality for some conditions didn’t change much over time: rTAAA mortality, for example, increased, but by a nonsignificant amount (44.7% vs. 47.6%; P = .06). “Mortality rates for rTAAA have remained static, despite the advances in treatment,” Dr. Vogel said.
Discussing these “concerning” results, Dr. Vogel noted that the increase in mortality “suggests an increased use of endovascular repair on higher-risk patients.” The mortality rate for ruptured visceral artery aneurysms did not change significantly either (16.7% vs. 6.7%, P = .09).
Overall, patients were 44% female and 66% white. “Over half of the patients were aged 70 or greater,” he said.
Acute limb ischemia was by far the most common vascular emergency, accounting for 82.4% of the total. Next most common were rAAAs, which made up just 10.79% of the vascular emergencies studied.
Looking at hospitalization trends over time, acute limb ischemia showed a slight trend up over the study period, from an occurrence rate of about 8.2 per 100,000 individuals at the beginning to about 9.0 per 100,000 by 2014.
Acute mesenteric ischemia also trended up, from an occurrence rate of about 4 per 1 million individuals in 2005 to about 6 per 1 million in 2014; rAAAs trended down, from about 13 per 1 million to a little over 9 per 1 million over the study period.
Among the other vascular emergencies incurring hospitalization, rTAAAs and ruptured visceral artery aneurysms were both rare, occurring in fewer than 7 per 10 million individuals, but both showed a slight upward trend over the study period. Slightly more common were rTAAs, which occurred at a rate of about 12 per 10 million individuals at the beginning of the study period and at slightly less than 15 per 10 million by the end.
Looking at hospital resource utilization, length of stay dropped significantly (P less than .004), but costs, unsurprisingly, increased over the study period, from about $25,000 to about $30,000 per occurrence (P less than .0001).
“The overall frequency of vascular emergencies has significantly increased over time,” Dr. Vogel said, “but in subgroup analysis ruptured abdominal [aortic] aneurysms are decreasing.” As endovascular procedures have increased, “The overall mortality has decreased, so we actually are doing better.” Some of this drop “may be due to improved perioperative care” as well as the increase in endovascular utilization, he noted.
In sum, though mortality has generally improved as endovascular procedures have become more common in vascular emergencies, “increased implementation of endovascular repair may not always improve outcomes,” Dr. Vogel said, especially in the context of an increasingly complex and aging patient population.
Dr. Vogel reported no conflicts of interest and no outside sources of funding.
ST. LOUIS – A patient with a nontraumatic vascular emergency is significantly less likely to die today than a decade ago, with few exceptions, according to a new national analysis looking at 10 years of data. Unsurprisingly, endovascular surgery rates climbed over the study period, as did rates of acute limb ischemia, said Todd Vogel, MD, who discussed the study at the annual meeting of the Midwestern Vascular Surgical Society.
With an objective of evaluating trends for management of nontraumatic vascular emergencies in the United States, Dr. Vogel, who is chief of vascular and endovascular surgery at the University of Missouri–Columbia, and his colleagues examined frequencies of vascular emergencies, mortality rates, and how open versus endoscopic procedure technique affected the data.
To do this, the investigators used the U.S. National Inpatient Sample from 2005 to 2014 to identify nontraumatic vascular emergencies.
Using ICD-9 clinical management diagnosis and procedure codes allowed the investigators to capture a wide array of vascular emergencies, Dr. Vogel said. These included ruptured abdominal, thoracic, and thoracoabdominal aortic aneurysms (rAAAs, rTAAs, and rTAAAs, respectively), as well as acute limb ischemia, acute mesenteric ischemia, and ruptured visceral artery aneurysms.
Among the outcomes analyzed in the study were a trend analysis looking at how outcomes changed over time and an analysis of in-hospital mortality. Dr. Vogel and his colleagues also examined hospital resource utilization including length of stay and total hospital cost, inflation adjusted to 2014 costs.
The prevalence of endovascular intervention increased sharply over the study period, as one would expect, Dr. Vogel said. “At the beginning, we had about 24% of patients getting endovascular intervention for vascular emergencies, and currently, it’s 36%.” (P for trend, less than .0001).
Mortality dropped steeply overall, with overall mortality going from 13.80% to 9.14% during the study period (P less than .0001). Much of this decrease could be attributed to mortality for open procedures decreasing by over a third, from 16.5% to 10.7%, over the study period (P less than .0001). Endovascular procedure–related mortality decreased from 8.3% to 7.9% (P = .03).
Ruptured abdominal and thoracic aortic aneurysms were much less likely to be fatal in 2014 than in 2005. The overall mortality rate for rAAA went from 41.4% to 27.6% (P less than .0001) and rates for rTAAs dropped overall from 41.2% to 23.0% (P = .002).
However, endovascular rTAA repair mortality jumped from 14.9% to 27.4% (P = .0003) while mortality for open procedures plummeted from 51.3% to 16.7% (P less than .0001).
In-hospital mortality for some conditions didn’t change much over time: rTAAA mortality, for example, increased, but by a nonsignificant amount (44.7% vs. 47.6%; P = .06). “Mortality rates for rTAAA have remained static, despite the advances in treatment,” Dr. Vogel said.
Discussing these “concerning” results, Dr. Vogel noted that the increase in mortality “suggests an increased use of endovascular repair on higher-risk patients.” The mortality rate for ruptured visceral artery aneurysms did not change significantly either (16.7% vs. 6.7%, P = .09).
Overall, patients were 44% female and 66% white. “Over half of the patients were aged 70 or greater,” he said.
Acute limb ischemia was by far the most common vascular emergency, accounting for 82.4% of the total. Next most common were rAAAs, which made up just 10.79% of the vascular emergencies studied.
Looking at hospitalization trends over time, acute limb ischemia showed a slight trend up over the study period, from an occurrence rate of about 8.2 per 100,000 individuals at the beginning to about 9.0 per 100,000 by 2014.
Acute mesenteric ischemia also trended up, from an occurrence rate of about 4 per 1 million individuals in 2005 to about 6 per 1 million in 2014; rAAAs trended down, from about 13 per 1 million to a little over 9 per 1 million over the study period.
Among the other vascular emergencies incurring hospitalization, rTAAAs and ruptured visceral artery aneurysms were both rare, occurring in fewer than 7 per 10 million individuals, but both showed a slight upward trend over the study period. Slightly more common were rTAAs, which occurred at a rate of about 12 per 10 million individuals at the beginning of the study period and at slightly less than 15 per 10 million by the end.
Looking at hospital resource utilization, length of stay dropped significantly (P less than .004), but costs, unsurprisingly, increased over the study period, from about $25,000 to about $30,000 per occurrence (P less than .0001).
“The overall frequency of vascular emergencies has significantly increased over time,” Dr. Vogel said, “but in subgroup analysis ruptured abdominal [aortic] aneurysms are decreasing.” As endovascular procedures have increased, “The overall mortality has decreased, so we actually are doing better.” Some of this drop “may be due to improved perioperative care” as well as the increase in endovascular utilization, he noted.
In sum, though mortality has generally improved as endovascular procedures have become more common in vascular emergencies, “increased implementation of endovascular repair may not always improve outcomes,” Dr. Vogel said, especially in the context of an increasingly complex and aging patient population.
Dr. Vogel reported no conflicts of interest and no outside sources of funding.
ST. LOUIS – A patient with a nontraumatic vascular emergency is significantly less likely to die today than a decade ago, with few exceptions, according to a new national analysis looking at 10 years of data. Unsurprisingly, endovascular surgery rates climbed over the study period, as did rates of acute limb ischemia, said Todd Vogel, MD, who discussed the study at the annual meeting of the Midwestern Vascular Surgical Society.
With an objective of evaluating trends for management of nontraumatic vascular emergencies in the United States, Dr. Vogel, who is chief of vascular and endovascular surgery at the University of Missouri–Columbia, and his colleagues examined frequencies of vascular emergencies, mortality rates, and how open versus endoscopic procedure technique affected the data.
To do this, the investigators used the U.S. National Inpatient Sample from 2005 to 2014 to identify nontraumatic vascular emergencies.
Using ICD-9 clinical management diagnosis and procedure codes allowed the investigators to capture a wide array of vascular emergencies, Dr. Vogel said. These included ruptured abdominal, thoracic, and thoracoabdominal aortic aneurysms (rAAAs, rTAAs, and rTAAAs, respectively), as well as acute limb ischemia, acute mesenteric ischemia, and ruptured visceral artery aneurysms.
Among the outcomes analyzed in the study were a trend analysis looking at how outcomes changed over time and an analysis of in-hospital mortality. Dr. Vogel and his colleagues also examined hospital resource utilization including length of stay and total hospital cost, inflation adjusted to 2014 costs.
The prevalence of endovascular intervention increased sharply over the study period, as one would expect, Dr. Vogel said. “At the beginning, we had about 24% of patients getting endovascular intervention for vascular emergencies, and currently, it’s 36%.” (P for trend, less than .0001).
Mortality dropped steeply overall, with overall mortality going from 13.80% to 9.14% during the study period (P less than .0001). Much of this decrease could be attributed to mortality for open procedures decreasing by over a third, from 16.5% to 10.7%, over the study period (P less than .0001). Endovascular procedure–related mortality decreased from 8.3% to 7.9% (P = .03).
Ruptured abdominal and thoracic aortic aneurysms were much less likely to be fatal in 2014 than in 2005. The overall mortality rate for rAAA went from 41.4% to 27.6% (P less than .0001) and rates for rTAAs dropped overall from 41.2% to 23.0% (P = .002).
However, endovascular rTAA repair mortality jumped from 14.9% to 27.4% (P = .0003) while mortality for open procedures plummeted from 51.3% to 16.7% (P less than .0001).
In-hospital mortality for some conditions didn’t change much over time: rTAAA mortality, for example, increased, but by a nonsignificant amount (44.7% vs. 47.6%; P = .06). “Mortality rates for rTAAA have remained static, despite the advances in treatment,” Dr. Vogel said.
Discussing these “concerning” results, Dr. Vogel noted that the increase in mortality “suggests an increased use of endovascular repair on higher-risk patients.” The mortality rate for ruptured visceral artery aneurysms did not change significantly either (16.7% vs. 6.7%, P = .09).
Overall, patients were 44% female and 66% white. “Over half of the patients were aged 70 or greater,” he said.
Acute limb ischemia was by far the most common vascular emergency, accounting for 82.4% of the total. Next most common were rAAAs, which made up just 10.79% of the vascular emergencies studied.
Looking at hospitalization trends over time, acute limb ischemia showed a slight trend up over the study period, from an occurrence rate of about 8.2 per 100,000 individuals at the beginning to about 9.0 per 100,000 by 2014.
Acute mesenteric ischemia also trended up, from an occurrence rate of about 4 per 1 million individuals in 2005 to about 6 per 1 million in 2014; rAAAs trended down, from about 13 per 1 million to a little over 9 per 1 million over the study period.
Among the other vascular emergencies incurring hospitalization, rTAAAs and ruptured visceral artery aneurysms were both rare, occurring in fewer than 7 per 10 million individuals, but both showed a slight upward trend over the study period. Slightly more common were rTAAs, which occurred at a rate of about 12 per 10 million individuals at the beginning of the study period and at slightly less than 15 per 10 million by the end.
Looking at hospital resource utilization, length of stay dropped significantly (P less than .004), but costs, unsurprisingly, increased over the study period, from about $25,000 to about $30,000 per occurrence (P less than .0001).
“The overall frequency of vascular emergencies has significantly increased over time,” Dr. Vogel said, “but in subgroup analysis ruptured abdominal [aortic] aneurysms are decreasing.” As endovascular procedures have increased, “The overall mortality has decreased, so we actually are doing better.” Some of this drop “may be due to improved perioperative care” as well as the increase in endovascular utilization, he noted.
In sum, though mortality has generally improved as endovascular procedures have become more common in vascular emergencies, “increased implementation of endovascular repair may not always improve outcomes,” Dr. Vogel said, especially in the context of an increasingly complex and aging patient population.
Dr. Vogel reported no conflicts of interest and no outside sources of funding.
REPORTING FROM MIDWESTERN VASCULAR 2018
Key clinical point: Rates of endovascular repair for nontraumatic vascular emergencies rose sharply.
Major finding: Endovascular repair rates for nontraumatic vascular emergencies climbed from 24% to 36% of cases from 2005 to 2014 (P for trend, less than .0001).
Study details: A 10-year sample of hospitalizations for nontraumatic vascular emergencies from the U.S. National Inpatient Sample.
Disclosures: Dr. Vogel reported no outside sources of funding and no conflicts of interest.
Tracking 90-day vascular surgery outcomes: The coming new normal?
The Centers for Medicare and Medicaid Services is test driving a new quality measurement model that pushes hospital readmissions measures out from 30 to 90 days.
Previous research has identified vascular surgery as having twice as high rates of 90-day readmissions, compared with 30-day readmissions (Am J Manag Care. 2014;20[9]:e432-e438), and this could prove problematic in light of the CMS pilot project currently underway, according to Donald E. Fry, MD, of MPA Healthcare Solutions, Chicago, and his colleagues.
They performed a study that found a high level of adverse outcomes for common vascular procedures and that there was a significant variability in risk-adjusted outcomes among best- and poorest-performing hospitals in all major vascular procedures, indicating that a large opportunity exists for improvement in results.
Medicare’s value-based care Readmissions Reduction Model developed financial penalties for hospitals that fail to achieve acceptable performance scores, and in doing so shifted some of the financial risks of care to the providers based on a 30-day readmission model. In contrast, the pilot Bundled Payments for Care Improvement (BPCI) Advanced Program, which the CMS plans to launch in October 2018, will follow a 90-day period of postoperative care as its duration of financial accountability.
“While BPCI Advanced, has, until now, focused upon orthopedics, cardiovascular procedures, and high-volume medical admissions areas, it is anticipated that vascular surgery will be included in the future,” according to the investigators. Therefore, the researchers performed an in-depth analysis to examine the 90-day outcomes of common vascular surgeries across hospitals as a prelude to the vascular surgery field having to potentially confront this new CMS model (Surgery 2018 Jun 22 doi: 10.1016/j.surg.2018.03.025).
Dr. Fry and his colleagues used the Medicare Limited Data Set for 2012-2014 to follow the outcomes of major vascular surgery beginning with the inpatient stay and on through 90 days of postoperative care. A pool of more than 500 aggregated and individual candidate risk factors, including age and sex, was used in model development, based upon data from 359 hospitals with 10,815 patients in the Medicare Limited Data Set.
The researchers examined the risk-adjusted outcomes of four major groupings of vascular surgery procedures: elective open aortic; open peripheral vascular procedures; endovascular aortic; and percutaneous angioplasty procedures.
They found that the total adverse-outcome rate (AO) was 27.8% for open aortic procedures, 31.5% for open peripheral vascular procedures, 19.6% for endovascular aortic procedures, and 36.4% for percutaneous angioplasty procedures. The difference in risk-adjusted adverse-outcome rates between the best- and the poorest- performing deciles was 32.2% for open aortic procedures, 29.5% for open peripheral vascular procedures, 21.5% for endovascular aortic procedures, and 37.1% for percutaneous angioplasty procedures.
The model determined significant risk factors (P less than .001) for inpatient death (including malnutrition, intestinal ischemia, supplemental oxygen, and age greater than or equal to 85 years); prolonged length of stay (including supplemental oxygen, peritoneal adhesions, and chronic lung obstructive disease); 90-day postdischarge death (including heart failure, chronic infection, psychosis, and primary head/neck cancer); and 90-day postdischarge readmission (malnutrition, chronic obstructive lung disease, upper aerodigestive tract cancer, and skin ulceration) for these procedures.
For all cases, the total 90-day postdischarge mortality rate exceeded the inpatient death rate, and readmissions were the major driver of the total AO. They found that 22% of all patients readmitted across the entire 90-day interval had not seen a physician for follow-up after discharge. [This] “begs the question of whether more frequent physician or physician-extender follow-up can reduce this AO,” according to Dr. Fry and his colleagues. “Importantly, first readmissions during days 31-90 following discharge were almost as common as those occurring during the initial 30 days. Over 20% of total readmissions were subsequently repeat events during the 90-day interval,” they added.
They also found that the variability in risk-adjusted outcomes among the best and poorest performing hospitals was over 20% in all of the major vascular procedures and indicates a large opportunity for improvement in results.
“Understanding variables associated with higher risk can be used as a decision support tool to identify which patients will need increased vigilance to avoid AOs. Identification of very high risk may become a consideration in the assessment of the appropriateness of the surgical intervention. If providers know their outcomes and those outcomes are benchmarked against the whole population of hospitals, then clinical performance can be improved by specific care redesign initiatives,” the researchers concluded.
Dr. Fry is executive vice president of MPA Healthcare Solutions, which funded the research.
SOURCE: Fry DE et al. Surgery 2018 Jun 22. doi: 10.1016/j.surg.2018.03.025.
The Centers for Medicare and Medicaid Services is test driving a new quality measurement model that pushes hospital readmissions measures out from 30 to 90 days.
Previous research has identified vascular surgery as having twice as high rates of 90-day readmissions, compared with 30-day readmissions (Am J Manag Care. 2014;20[9]:e432-e438), and this could prove problematic in light of the CMS pilot project currently underway, according to Donald E. Fry, MD, of MPA Healthcare Solutions, Chicago, and his colleagues.
They performed a study that found a high level of adverse outcomes for common vascular procedures and that there was a significant variability in risk-adjusted outcomes among best- and poorest-performing hospitals in all major vascular procedures, indicating that a large opportunity exists for improvement in results.
Medicare’s value-based care Readmissions Reduction Model developed financial penalties for hospitals that fail to achieve acceptable performance scores, and in doing so shifted some of the financial risks of care to the providers based on a 30-day readmission model. In contrast, the pilot Bundled Payments for Care Improvement (BPCI) Advanced Program, which the CMS plans to launch in October 2018, will follow a 90-day period of postoperative care as its duration of financial accountability.
“While BPCI Advanced, has, until now, focused upon orthopedics, cardiovascular procedures, and high-volume medical admissions areas, it is anticipated that vascular surgery will be included in the future,” according to the investigators. Therefore, the researchers performed an in-depth analysis to examine the 90-day outcomes of common vascular surgeries across hospitals as a prelude to the vascular surgery field having to potentially confront this new CMS model (Surgery 2018 Jun 22 doi: 10.1016/j.surg.2018.03.025).
Dr. Fry and his colleagues used the Medicare Limited Data Set for 2012-2014 to follow the outcomes of major vascular surgery beginning with the inpatient stay and on through 90 days of postoperative care. A pool of more than 500 aggregated and individual candidate risk factors, including age and sex, was used in model development, based upon data from 359 hospitals with 10,815 patients in the Medicare Limited Data Set.
The researchers examined the risk-adjusted outcomes of four major groupings of vascular surgery procedures: elective open aortic; open peripheral vascular procedures; endovascular aortic; and percutaneous angioplasty procedures.
They found that the total adverse-outcome rate (AO) was 27.8% for open aortic procedures, 31.5% for open peripheral vascular procedures, 19.6% for endovascular aortic procedures, and 36.4% for percutaneous angioplasty procedures. The difference in risk-adjusted adverse-outcome rates between the best- and the poorest- performing deciles was 32.2% for open aortic procedures, 29.5% for open peripheral vascular procedures, 21.5% for endovascular aortic procedures, and 37.1% for percutaneous angioplasty procedures.
The model determined significant risk factors (P less than .001) for inpatient death (including malnutrition, intestinal ischemia, supplemental oxygen, and age greater than or equal to 85 years); prolonged length of stay (including supplemental oxygen, peritoneal adhesions, and chronic lung obstructive disease); 90-day postdischarge death (including heart failure, chronic infection, psychosis, and primary head/neck cancer); and 90-day postdischarge readmission (malnutrition, chronic obstructive lung disease, upper aerodigestive tract cancer, and skin ulceration) for these procedures.
For all cases, the total 90-day postdischarge mortality rate exceeded the inpatient death rate, and readmissions were the major driver of the total AO. They found that 22% of all patients readmitted across the entire 90-day interval had not seen a physician for follow-up after discharge. [This] “begs the question of whether more frequent physician or physician-extender follow-up can reduce this AO,” according to Dr. Fry and his colleagues. “Importantly, first readmissions during days 31-90 following discharge were almost as common as those occurring during the initial 30 days. Over 20% of total readmissions were subsequently repeat events during the 90-day interval,” they added.
They also found that the variability in risk-adjusted outcomes among the best and poorest performing hospitals was over 20% in all of the major vascular procedures and indicates a large opportunity for improvement in results.
“Understanding variables associated with higher risk can be used as a decision support tool to identify which patients will need increased vigilance to avoid AOs. Identification of very high risk may become a consideration in the assessment of the appropriateness of the surgical intervention. If providers know their outcomes and those outcomes are benchmarked against the whole population of hospitals, then clinical performance can be improved by specific care redesign initiatives,” the researchers concluded.
Dr. Fry is executive vice president of MPA Healthcare Solutions, which funded the research.
SOURCE: Fry DE et al. Surgery 2018 Jun 22. doi: 10.1016/j.surg.2018.03.025.
The Centers for Medicare and Medicaid Services is test driving a new quality measurement model that pushes hospital readmissions measures out from 30 to 90 days.
Previous research has identified vascular surgery as having twice as high rates of 90-day readmissions, compared with 30-day readmissions (Am J Manag Care. 2014;20[9]:e432-e438), and this could prove problematic in light of the CMS pilot project currently underway, according to Donald E. Fry, MD, of MPA Healthcare Solutions, Chicago, and his colleagues.
They performed a study that found a high level of adverse outcomes for common vascular procedures and that there was a significant variability in risk-adjusted outcomes among best- and poorest-performing hospitals in all major vascular procedures, indicating that a large opportunity exists for improvement in results.
Medicare’s value-based care Readmissions Reduction Model developed financial penalties for hospitals that fail to achieve acceptable performance scores, and in doing so shifted some of the financial risks of care to the providers based on a 30-day readmission model. In contrast, the pilot Bundled Payments for Care Improvement (BPCI) Advanced Program, which the CMS plans to launch in October 2018, will follow a 90-day period of postoperative care as its duration of financial accountability.
“While BPCI Advanced, has, until now, focused upon orthopedics, cardiovascular procedures, and high-volume medical admissions areas, it is anticipated that vascular surgery will be included in the future,” according to the investigators. Therefore, the researchers performed an in-depth analysis to examine the 90-day outcomes of common vascular surgeries across hospitals as a prelude to the vascular surgery field having to potentially confront this new CMS model (Surgery 2018 Jun 22 doi: 10.1016/j.surg.2018.03.025).
Dr. Fry and his colleagues used the Medicare Limited Data Set for 2012-2014 to follow the outcomes of major vascular surgery beginning with the inpatient stay and on through 90 days of postoperative care. A pool of more than 500 aggregated and individual candidate risk factors, including age and sex, was used in model development, based upon data from 359 hospitals with 10,815 patients in the Medicare Limited Data Set.
The researchers examined the risk-adjusted outcomes of four major groupings of vascular surgery procedures: elective open aortic; open peripheral vascular procedures; endovascular aortic; and percutaneous angioplasty procedures.
They found that the total adverse-outcome rate (AO) was 27.8% for open aortic procedures, 31.5% for open peripheral vascular procedures, 19.6% for endovascular aortic procedures, and 36.4% for percutaneous angioplasty procedures. The difference in risk-adjusted adverse-outcome rates between the best- and the poorest- performing deciles was 32.2% for open aortic procedures, 29.5% for open peripheral vascular procedures, 21.5% for endovascular aortic procedures, and 37.1% for percutaneous angioplasty procedures.
The model determined significant risk factors (P less than .001) for inpatient death (including malnutrition, intestinal ischemia, supplemental oxygen, and age greater than or equal to 85 years); prolonged length of stay (including supplemental oxygen, peritoneal adhesions, and chronic lung obstructive disease); 90-day postdischarge death (including heart failure, chronic infection, psychosis, and primary head/neck cancer); and 90-day postdischarge readmission (malnutrition, chronic obstructive lung disease, upper aerodigestive tract cancer, and skin ulceration) for these procedures.
For all cases, the total 90-day postdischarge mortality rate exceeded the inpatient death rate, and readmissions were the major driver of the total AO. They found that 22% of all patients readmitted across the entire 90-day interval had not seen a physician for follow-up after discharge. [This] “begs the question of whether more frequent physician or physician-extender follow-up can reduce this AO,” according to Dr. Fry and his colleagues. “Importantly, first readmissions during days 31-90 following discharge were almost as common as those occurring during the initial 30 days. Over 20% of total readmissions were subsequently repeat events during the 90-day interval,” they added.
They also found that the variability in risk-adjusted outcomes among the best and poorest performing hospitals was over 20% in all of the major vascular procedures and indicates a large opportunity for improvement in results.
“Understanding variables associated with higher risk can be used as a decision support tool to identify which patients will need increased vigilance to avoid AOs. Identification of very high risk may become a consideration in the assessment of the appropriateness of the surgical intervention. If providers know their outcomes and those outcomes are benchmarked against the whole population of hospitals, then clinical performance can be improved by specific care redesign initiatives,” the researchers concluded.
Dr. Fry is executive vice president of MPA Healthcare Solutions, which funded the research.
SOURCE: Fry DE et al. Surgery 2018 Jun 22. doi: 10.1016/j.surg.2018.03.025.
FROM SURGERY
Key clinical point: The variability in risk-adjusted outcomes among the best and poorest performing hospitals was over 20% in all of the major vascular procedures.
Major finding: The total adverse-outcome rate was 27.8% for open aortic procedures, 31.5% for open peripheral artery, 19.6% for endovascular aortic, and 36.4% for percutaneous angioplasty.
Study details: The Medicare Limited Data Set for 2012-2014 was used to follow the outcomes of major vascular surgery beginning with the inpatient stay and on through 90 days of postop care.
Disclosures: Dr. Fry is executive vice president of MPA Healthcare Solutions, which funded the research.
Source: Fry DE et al. Surgery 2018 Jun 22. doi: 10.1016/j.surg.2018.03.025.
Open AAA and peripheral bypass surgery patients among the highest users of post-acute care
in Medicare spending, according to the findings of a study that used data from the National Inpatient Sample (NIS) and the Veterans Affairs health system (VA) regarding surgical patients.
PAC, including skilled nursing facilities and inpatient rehabilitation, accounts for 73% of regional variation in Medicare spending, and studies on hospital variation in this area have typically focused on nonsurgical patients or been limited to Medicare data. However, a high degree of variation also appears to hold for surgical patients, according to the authors of this large database study of more than 4 million patients who had aortic aneurysm repair, peripheral vascular bypass, colorectal surgery, hepatectomy, pancreatectomy, or coronary bypass.
“We found that there is significant variation in use of PAC and rates of home discharge following complex cardiac, abdominal, and vascular surgery,” Courtney J. Balentine, MD, of the University of Alabama at Birmingham and his colleagues wrote in their report in the Journal of Surgical Research.
To explore hospital variation in post-surgery PAC, they evaluated 3,487,365 patients from the NIS (39% were aged 70 years or older, and 60% were men) and 60,666 from the VA (32% were aged 70 years or older, and 98% were men) who had surgery during 2008-2011.
Within the NIS, 631,199 patients (18%) were discharged to PAC facilities, and among the 60,666 veterans, 4744 (7.8%) were discharged to PAC facilities. In addition, hospital rates of discharge to PAC facilities varied from 1% to 36% for VA hospitals and from 1% to 59% for non-VA hospitals, according to the researchers. They found that some VA hospitals were four times more likely to discharge patients to PAC facilities than would be expected from their patients’ characteristics, while others were 90% more likely to send patients home than would be expected, according to Dr. Balentine and his colleagues.
Procedure-specific rates of discharge to PAC facilities from VA hospitals ranged from 2% following endovascular aneurysm repair to 10% after pancreatectomy and peripheral vascular bypass. Among the NIS hospitals, in contrast, rates of discharge to PAC facilities ranged from 6% following hepatectomy to as high as 44% following open aneurysm repair.
“These data could be used to characterize practices that promote more effective recovery from surgery and minimize the need for PAC,” the authors wrote. “Given that skilled nursing facilities and inpatient rehabilitation cost [$5,000]-$24,000 more than treatment at home, even minor reductions in the need for PAC facilities could result in substantial cost savings,” they stated.
“Our findings suggest that there is considerable room for improvement in the use of PAC after surgery and that we still have a long way to go in terms of using PAC to help patients recover and regain their independence,” the researchers concluded.
The authors reported that they had no conflicts of interest.
SOURCE: Balentine CJ et al. J Surg Res. 2018 Oct;230:61-70.
in Medicare spending, according to the findings of a study that used data from the National Inpatient Sample (NIS) and the Veterans Affairs health system (VA) regarding surgical patients.
PAC, including skilled nursing facilities and inpatient rehabilitation, accounts for 73% of regional variation in Medicare spending, and studies on hospital variation in this area have typically focused on nonsurgical patients or been limited to Medicare data. However, a high degree of variation also appears to hold for surgical patients, according to the authors of this large database study of more than 4 million patients who had aortic aneurysm repair, peripheral vascular bypass, colorectal surgery, hepatectomy, pancreatectomy, or coronary bypass.
“We found that there is significant variation in use of PAC and rates of home discharge following complex cardiac, abdominal, and vascular surgery,” Courtney J. Balentine, MD, of the University of Alabama at Birmingham and his colleagues wrote in their report in the Journal of Surgical Research.
To explore hospital variation in post-surgery PAC, they evaluated 3,487,365 patients from the NIS (39% were aged 70 years or older, and 60% were men) and 60,666 from the VA (32% were aged 70 years or older, and 98% were men) who had surgery during 2008-2011.
Within the NIS, 631,199 patients (18%) were discharged to PAC facilities, and among the 60,666 veterans, 4744 (7.8%) were discharged to PAC facilities. In addition, hospital rates of discharge to PAC facilities varied from 1% to 36% for VA hospitals and from 1% to 59% for non-VA hospitals, according to the researchers. They found that some VA hospitals were four times more likely to discharge patients to PAC facilities than would be expected from their patients’ characteristics, while others were 90% more likely to send patients home than would be expected, according to Dr. Balentine and his colleagues.
Procedure-specific rates of discharge to PAC facilities from VA hospitals ranged from 2% following endovascular aneurysm repair to 10% after pancreatectomy and peripheral vascular bypass. Among the NIS hospitals, in contrast, rates of discharge to PAC facilities ranged from 6% following hepatectomy to as high as 44% following open aneurysm repair.
“These data could be used to characterize practices that promote more effective recovery from surgery and minimize the need for PAC,” the authors wrote. “Given that skilled nursing facilities and inpatient rehabilitation cost [$5,000]-$24,000 more than treatment at home, even minor reductions in the need for PAC facilities could result in substantial cost savings,” they stated.
“Our findings suggest that there is considerable room for improvement in the use of PAC after surgery and that we still have a long way to go in terms of using PAC to help patients recover and regain their independence,” the researchers concluded.
The authors reported that they had no conflicts of interest.
SOURCE: Balentine CJ et al. J Surg Res. 2018 Oct;230:61-70.
in Medicare spending, according to the findings of a study that used data from the National Inpatient Sample (NIS) and the Veterans Affairs health system (VA) regarding surgical patients.
PAC, including skilled nursing facilities and inpatient rehabilitation, accounts for 73% of regional variation in Medicare spending, and studies on hospital variation in this area have typically focused on nonsurgical patients or been limited to Medicare data. However, a high degree of variation also appears to hold for surgical patients, according to the authors of this large database study of more than 4 million patients who had aortic aneurysm repair, peripheral vascular bypass, colorectal surgery, hepatectomy, pancreatectomy, or coronary bypass.
“We found that there is significant variation in use of PAC and rates of home discharge following complex cardiac, abdominal, and vascular surgery,” Courtney J. Balentine, MD, of the University of Alabama at Birmingham and his colleagues wrote in their report in the Journal of Surgical Research.
To explore hospital variation in post-surgery PAC, they evaluated 3,487,365 patients from the NIS (39% were aged 70 years or older, and 60% were men) and 60,666 from the VA (32% were aged 70 years or older, and 98% were men) who had surgery during 2008-2011.
Within the NIS, 631,199 patients (18%) were discharged to PAC facilities, and among the 60,666 veterans, 4744 (7.8%) were discharged to PAC facilities. In addition, hospital rates of discharge to PAC facilities varied from 1% to 36% for VA hospitals and from 1% to 59% for non-VA hospitals, according to the researchers. They found that some VA hospitals were four times more likely to discharge patients to PAC facilities than would be expected from their patients’ characteristics, while others were 90% more likely to send patients home than would be expected, according to Dr. Balentine and his colleagues.
Procedure-specific rates of discharge to PAC facilities from VA hospitals ranged from 2% following endovascular aneurysm repair to 10% after pancreatectomy and peripheral vascular bypass. Among the NIS hospitals, in contrast, rates of discharge to PAC facilities ranged from 6% following hepatectomy to as high as 44% following open aneurysm repair.
“These data could be used to characterize practices that promote more effective recovery from surgery and minimize the need for PAC,” the authors wrote. “Given that skilled nursing facilities and inpatient rehabilitation cost [$5,000]-$24,000 more than treatment at home, even minor reductions in the need for PAC facilities could result in substantial cost savings,” they stated.
“Our findings suggest that there is considerable room for improvement in the use of PAC after surgery and that we still have a long way to go in terms of using PAC to help patients recover and regain their independence,” the researchers concluded.
The authors reported that they had no conflicts of interest.
SOURCE: Balentine CJ et al. J Surg Res. 2018 Oct;230:61-70.
FROM THE JOURNAL OF SURGICAL RESEARCH
Key clinical point: The wide disparity among hospitals in their rates of postsurgery discharge to post-acute care (PAC) could be an area of focus for cost containment in Medicare spending.
Major finding: Rates of discharge to PAC facilities varied from 1% to 36% for VA hospitals and from 1% to 59% for non-VA hospitals.
Study details: A database analysis of 3,487,365 National Inpatient Sample patients and 60,666 VA patients who had surgery during 2008-2011.
Disclosures: The authors reported that they had no conflicts of interest.
Source: Balentine CJ et al. J Surg Res. 2018 Oct;230:61-70.
ACR and EULAR to review new criteria for classifying vasculitis
AMSTERDAM – New classification criteria for antineutrophil cytoplasmic antibody (ANCA)–associated vasculitides have been drafted and now need formal review by the American College of Rheumatology and the European League Against Rheumatism before they can be put into practice.
According to Joanna Robson, MBBS, PhD, the chair of the DCVAS steering committee, these new criteria better “reflect current practice by incorporating, but not relying on, ANCA testing and advanced imaging.”
“The old criteria were actually produced in the early 1990s and since then we’ve had further thinking about the different subtypes of systemic vasculitis,” explained Dr. Robson of the University of the West of England in Bristol. There has also been a consensus conference held at Chapel Hill (Arthritis Rheum 2013;65[1]:1-11) which identified MPA as a separate entity, and ANCA testing has become routine practice. Computed tomography and magnetic resonance imaging are also now used to help differentiate between the different vasculitides.
“This really has been a collaborative, multinational effort,” Dr. Robson said at the European Congress of Rheumatology. To develop the draft criteria, data collated from 135 sites in 32 countries on more than 2,000 patients were used. These had been collected as part of the ACR/EULAR–run DCVAS study, which has been coordinated at the University of Oxford since 2011.
Three phases were used to develop these criteria: first an expert panel reviewed all cases in the DCVAS to identify those that they felt were attributable to small vessel vasculitis. Second, variables that might be appropriate to use in the models were examined, with more than 8,000 individual DVCAS items considered and then whittled down to 91 items and then sifted again to form a clear set of 10 or fewer items. Third, statistical analyses combined with expert review were used to develop the criteria and then validate these.
Dr. Robson reported that of 2,871 cases identified as ANCA-associated vasculitis, 2,072 (72%) were agreed upon by the expert review panel. Of these, there were 724 cases of GPA, 291 of MPA, 226 of EGPA, and around 300 cases of other small vessel vasculitis or polyarteritis nodosa. To develop the criteria the GPA cases were used as the “cases” and the other types of vasculitis as the comparators, Dr. Robson explained.
For GPA, MPA, and EGPA a set of items (10, 6, and 7, respectively) were derived and scored, positively or negatively, and a cutoff determined at which a classification of the particular vasculitis could be made. During discussion, Dr. Robson noted that the threshold score for a classification of EGPA (greater than or equal to 6) had been set slightly higher than for GPA or MPA (both greater than or equal to 5) “because of the clinical problem of there being very close comparators which can actually mimic EGPA.” This is where the negative scoring of some items used in these criteria are very important, she said.
The 10-item GPA criteria included three clinical (such as the presence of bloody nasal discharge upon examination) and seven investigational (such as cANCA positivity) items. These criteria were found to have a high sensitivity (92%) and specificity (94%) for identifying GPA.
The six-item MPA criteria included one clinical item (bloody nasal discharge, which was this time attributed a negative score) and five investigational items (with ANCA testing given a higher positive score than for GPA). The sensitivity and specificity of these criteria were a respective 91% and 94%.
Finally, the seven-item EGPA criteria included three clinical items (including obstructive airways disease and nasal polyps) and four investigational items (with ANCA positivity given a negative score). These criteria had an 85% sensitivity and 99% specificity for EGPA.
Dr. Robson emphasized that all of these classification criteria were to be used only after exclusion of other possible causes of vasculitis, such as infection, malignancy, or other autoimmune diseases such as inflammatory bowel disease, and a “diagnosis of small- or medium-vessel vasculitis has been made.”
These criteria are to help classify into the subtypes of vasculitis “primarily for the purpose of clinical trials,” she said. “The next steps are review by the EULAR and ACR committee, and only on final approval will these criteria be ready to use.”
DCVAS is sponsored by the University of Oxford (England) with funding from the European League Against Rheumatism, the American College of Rheumatology, and the Vasculitis Foundation. Dr. Robson had no relevant financial disclosures.
SOURCE: Robson JC et al. EULAR 2018. Abstract OP0021.
AMSTERDAM – New classification criteria for antineutrophil cytoplasmic antibody (ANCA)–associated vasculitides have been drafted and now need formal review by the American College of Rheumatology and the European League Against Rheumatism before they can be put into practice.
According to Joanna Robson, MBBS, PhD, the chair of the DCVAS steering committee, these new criteria better “reflect current practice by incorporating, but not relying on, ANCA testing and advanced imaging.”
“The old criteria were actually produced in the early 1990s and since then we’ve had further thinking about the different subtypes of systemic vasculitis,” explained Dr. Robson of the University of the West of England in Bristol. There has also been a consensus conference held at Chapel Hill (Arthritis Rheum 2013;65[1]:1-11) which identified MPA as a separate entity, and ANCA testing has become routine practice. Computed tomography and magnetic resonance imaging are also now used to help differentiate between the different vasculitides.
“This really has been a collaborative, multinational effort,” Dr. Robson said at the European Congress of Rheumatology. To develop the draft criteria, data collated from 135 sites in 32 countries on more than 2,000 patients were used. These had been collected as part of the ACR/EULAR–run DCVAS study, which has been coordinated at the University of Oxford since 2011.
Three phases were used to develop these criteria: first an expert panel reviewed all cases in the DCVAS to identify those that they felt were attributable to small vessel vasculitis. Second, variables that might be appropriate to use in the models were examined, with more than 8,000 individual DVCAS items considered and then whittled down to 91 items and then sifted again to form a clear set of 10 or fewer items. Third, statistical analyses combined with expert review were used to develop the criteria and then validate these.
Dr. Robson reported that of 2,871 cases identified as ANCA-associated vasculitis, 2,072 (72%) were agreed upon by the expert review panel. Of these, there were 724 cases of GPA, 291 of MPA, 226 of EGPA, and around 300 cases of other small vessel vasculitis or polyarteritis nodosa. To develop the criteria the GPA cases were used as the “cases” and the other types of vasculitis as the comparators, Dr. Robson explained.
For GPA, MPA, and EGPA a set of items (10, 6, and 7, respectively) were derived and scored, positively or negatively, and a cutoff determined at which a classification of the particular vasculitis could be made. During discussion, Dr. Robson noted that the threshold score for a classification of EGPA (greater than or equal to 6) had been set slightly higher than for GPA or MPA (both greater than or equal to 5) “because of the clinical problem of there being very close comparators which can actually mimic EGPA.” This is where the negative scoring of some items used in these criteria are very important, she said.
The 10-item GPA criteria included three clinical (such as the presence of bloody nasal discharge upon examination) and seven investigational (such as cANCA positivity) items. These criteria were found to have a high sensitivity (92%) and specificity (94%) for identifying GPA.
The six-item MPA criteria included one clinical item (bloody nasal discharge, which was this time attributed a negative score) and five investigational items (with ANCA testing given a higher positive score than for GPA). The sensitivity and specificity of these criteria were a respective 91% and 94%.
Finally, the seven-item EGPA criteria included three clinical items (including obstructive airways disease and nasal polyps) and four investigational items (with ANCA positivity given a negative score). These criteria had an 85% sensitivity and 99% specificity for EGPA.
Dr. Robson emphasized that all of these classification criteria were to be used only after exclusion of other possible causes of vasculitis, such as infection, malignancy, or other autoimmune diseases such as inflammatory bowel disease, and a “diagnosis of small- or medium-vessel vasculitis has been made.”
These criteria are to help classify into the subtypes of vasculitis “primarily for the purpose of clinical trials,” she said. “The next steps are review by the EULAR and ACR committee, and only on final approval will these criteria be ready to use.”
DCVAS is sponsored by the University of Oxford (England) with funding from the European League Against Rheumatism, the American College of Rheumatology, and the Vasculitis Foundation. Dr. Robson had no relevant financial disclosures.
SOURCE: Robson JC et al. EULAR 2018. Abstract OP0021.
AMSTERDAM – New classification criteria for antineutrophil cytoplasmic antibody (ANCA)–associated vasculitides have been drafted and now need formal review by the American College of Rheumatology and the European League Against Rheumatism before they can be put into practice.
According to Joanna Robson, MBBS, PhD, the chair of the DCVAS steering committee, these new criteria better “reflect current practice by incorporating, but not relying on, ANCA testing and advanced imaging.”
“The old criteria were actually produced in the early 1990s and since then we’ve had further thinking about the different subtypes of systemic vasculitis,” explained Dr. Robson of the University of the West of England in Bristol. There has also been a consensus conference held at Chapel Hill (Arthritis Rheum 2013;65[1]:1-11) which identified MPA as a separate entity, and ANCA testing has become routine practice. Computed tomography and magnetic resonance imaging are also now used to help differentiate between the different vasculitides.
“This really has been a collaborative, multinational effort,” Dr. Robson said at the European Congress of Rheumatology. To develop the draft criteria, data collated from 135 sites in 32 countries on more than 2,000 patients were used. These had been collected as part of the ACR/EULAR–run DCVAS study, which has been coordinated at the University of Oxford since 2011.
Three phases were used to develop these criteria: first an expert panel reviewed all cases in the DCVAS to identify those that they felt were attributable to small vessel vasculitis. Second, variables that might be appropriate to use in the models were examined, with more than 8,000 individual DVCAS items considered and then whittled down to 91 items and then sifted again to form a clear set of 10 or fewer items. Third, statistical analyses combined with expert review were used to develop the criteria and then validate these.
Dr. Robson reported that of 2,871 cases identified as ANCA-associated vasculitis, 2,072 (72%) were agreed upon by the expert review panel. Of these, there were 724 cases of GPA, 291 of MPA, 226 of EGPA, and around 300 cases of other small vessel vasculitis or polyarteritis nodosa. To develop the criteria the GPA cases were used as the “cases” and the other types of vasculitis as the comparators, Dr. Robson explained.
For GPA, MPA, and EGPA a set of items (10, 6, and 7, respectively) were derived and scored, positively or negatively, and a cutoff determined at which a classification of the particular vasculitis could be made. During discussion, Dr. Robson noted that the threshold score for a classification of EGPA (greater than or equal to 6) had been set slightly higher than for GPA or MPA (both greater than or equal to 5) “because of the clinical problem of there being very close comparators which can actually mimic EGPA.” This is where the negative scoring of some items used in these criteria are very important, she said.
The 10-item GPA criteria included three clinical (such as the presence of bloody nasal discharge upon examination) and seven investigational (such as cANCA positivity) items. These criteria were found to have a high sensitivity (92%) and specificity (94%) for identifying GPA.
The six-item MPA criteria included one clinical item (bloody nasal discharge, which was this time attributed a negative score) and five investigational items (with ANCA testing given a higher positive score than for GPA). The sensitivity and specificity of these criteria were a respective 91% and 94%.
Finally, the seven-item EGPA criteria included three clinical items (including obstructive airways disease and nasal polyps) and four investigational items (with ANCA positivity given a negative score). These criteria had an 85% sensitivity and 99% specificity for EGPA.
Dr. Robson emphasized that all of these classification criteria were to be used only after exclusion of other possible causes of vasculitis, such as infection, malignancy, or other autoimmune diseases such as inflammatory bowel disease, and a “diagnosis of small- or medium-vessel vasculitis has been made.”
These criteria are to help classify into the subtypes of vasculitis “primarily for the purpose of clinical trials,” she said. “The next steps are review by the EULAR and ACR committee, and only on final approval will these criteria be ready to use.”
DCVAS is sponsored by the University of Oxford (England) with funding from the European League Against Rheumatism, the American College of Rheumatology, and the Vasculitis Foundation. Dr. Robson had no relevant financial disclosures.
SOURCE: Robson JC et al. EULAR 2018. Abstract OP0021.
REPORTING FROM THE EULAR 2018 CONGRESS
Key clinical point: New classification criteria for ANCA-associated vasculitides have been drafted and now need formal review before they are ready to use.
Major finding: Analysis of the 10-, 6-, and 7-item GPA, MPA, and EGPA criteria showed a respective 92%, 94%, and 91% sensitivity and 94%, 85%, and 99% specificity.
Study details: The Diagnostic and Classification Criteria in Vasculitis (DCVAS) observational study of more than 6,000 cases of vasculitides and comparators.
Disclosures: DCVAS is sponsored by the University of Oxford (England) with funding from the American College of Rheumatology, the European League Against Rheumatism, and the Vasculitis Foundation. Dr. Robson had no relevant financial disclosures.
Source: Robson JC et al. EULAR 2018. Abstract OP0021.
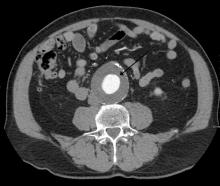
Routine screening for AAA in older men may harm more than help
Deaths from abdominal aortic aneurysm among Swedish men are going down – but not because they’re being screened for the potentially fatal condition.
Although the death rate has decreased by 70% since the early 2000s, screening only saved 2 lives per 10,000 men screened. It did, however, increase by 59% the risk of unnecessary surgery, Minna Johansson, MD, and colleagues wrote in the June 16 issue of the Lancet.
“Screening had only a minor effect on AAA mortality,” wrote Dr. Johansson of the University of Gothenburg (Sweden). “In absolute numbers, only 7% of the benefit estimated in the largest trial of AAA screening was observed. The observed large reductions in AAA mortality were present in both the screened and nonscreened cohorts and were thus mainly caused by other factors – probably reduced smoking. … Our results call the continued justification of AAA screening into question.”
In Sweden, all men aged 65 years are invited to a one-time ultrasound abdominal aorta screening. Most participate. Anyone with an aneurysm is followed up at a vascular surgery clinic, with surgery considered if the aortic diameter is 55 mm or larger.
Dr. Johansson and her colleagues plumbed national health records to estimate the risks and benefits of this routine screening. The study comprised 25,265 men invited to join the AAA screening program in Sweden from 2006 to 2009. Mortality data were compared with those from a contemporaneous cohort of 106,087 men of similar age who were not invited to screen. Finally, the mortality data were compared with national trends in AAA mortality in all Swedish men aged 40-99 years from 1987 to 2015.
A multivariate analysis adjusted for cohort year, marital status, educational level, income, and whether the patient already had an AAA diagnosis at baseline.
From the early 2000s to 2015, AAA mortality among men aged 65-74 years declined from 36 to10 deaths per 100,000. This 70% reduction was similar in both screened and unscreened populations; in fact, the decline began about a decade before population-based screening was introduced and continued to decrease at a steady rate afterward.
After 6 years of screening, there was a 30% reduction of AAA mortality in the screened population, compared with the unscreened, translating to an absolute mortality reduction of two deaths per 10,000 men offered screening.
Screening increased by 52% the number of AAAs detected. The absolute difference in incidence after 6 years of screening translated to an additional 49 overdiagnoses per 10,000 screened men.
Looking back into the mid-1990s, the investigators saw the numbers of elective AAA surgeries rise steadily. In the adjusted model, screened men were 59% more likely to have this procedure than unscreened. The increased risk didn’t come with an equally increased benefit, though. There was a 10% decrease in AAA ruptures, “rendering a risk of overtreatment of 19%, or 19 potentially avoidable elective surgeries per 10,000 men,” the team noted. “Sixty-three percent of all additional elective surgeries for AAA might therefore have constituted overtreat.”
The findings are at odds with large published studies that found a consistent benefit to screening.
“Compared with results at 7-year follow-up of the largest trial of screening for abdominal aortic aneurysm [Multicentre Aneurysm Screening Study (MASS)], we found about half of the benefit in terms of a relative effect and 7% of the estimated benefit in terms of absolute numbers [2 vs. 27 avoided deaths from AAA per 10,000 invited men]. Compared with previous estimates of overdiagnosis and overtreatment, we found a lower absolute number of over-diagnosed cases [49 vs.176 per 10,000 invited men] and fewer overtreated cases [19 vs. 37 per 10,000 invited men]. However, since the harms of screening decreased less than the benefit, the balance between benefits and harms seems much less appealing in today’s setting.”
None of the authors had any financial disclosures.
The study by Johansson et al. indicates a significant risk of overdiagnosis associated with routine screening for abdominal aortic aneurysm: Those risks may not be as clinically harmful as might be assumed, Stefan Acosta, MD, wrote in an accompanying editorial (Lancet 2018; 391: 2394-95).
“Although I agree that having a small AAA that needs long-term follow-up might be associated with negative psychological consequences, there could also be a window of opportunity [eg. with statins, antiplatelet therapy, and blood pressure reduction], for individuals with increased burden of cardiovascular disease. Indeed, screening for AAA, peripheral artery disease, and hypertension, with the initiation of relevant pharmacotherapy, if positive, reduces all-cause mortality and some evidence suggests that this approach of multifaceted vascular screening instead of isolated AAA screening should be considered.”
When performed according to the established criteria for elective AAA surgery, the procedure is associated with less than 1% postoperative mortality, “mainly because of wide implementation of endovascular aneurysm repair, a minimally invasive method.”
The 6-year follow-up time, as the authors noted, is relatively short. A 2016 review of the Swedish Nationwide Abdominal Aortic Aneurysm Screening Program determined that significant mortality benefit could take 10 years to materialize(Circ 2016;134:1141-8).
The full impact of Sweden’s remarkable decrease in smoking is almost certainly making itself known in these outcomes – smoking is implicated in 75% of AAA cases.
“The decreased prevalence of smoking in Sweden, from 44% of the population in 1970 to 15% in 2010, should be viewed as the main cause of the decreasing incidence and mortality of AAA. Every percent drop in the prevalence of smoking will have a huge effect on smoking-related diseases, such as cancer and AAA.”
Dr. Stefan is a vascular disease researcher at Lund (Sweden) University. He had no financial disclosures.
The study by Johansson et al. indicates a significant risk of overdiagnosis associated with routine screening for abdominal aortic aneurysm: Those risks may not be as clinically harmful as might be assumed, Stefan Acosta, MD, wrote in an accompanying editorial (Lancet 2018; 391: 2394-95).
“Although I agree that having a small AAA that needs long-term follow-up might be associated with negative psychological consequences, there could also be a window of opportunity [eg. with statins, antiplatelet therapy, and blood pressure reduction], for individuals with increased burden of cardiovascular disease. Indeed, screening for AAA, peripheral artery disease, and hypertension, with the initiation of relevant pharmacotherapy, if positive, reduces all-cause mortality and some evidence suggests that this approach of multifaceted vascular screening instead of isolated AAA screening should be considered.”
When performed according to the established criteria for elective AAA surgery, the procedure is associated with less than 1% postoperative mortality, “mainly because of wide implementation of endovascular aneurysm repair, a minimally invasive method.”
The 6-year follow-up time, as the authors noted, is relatively short. A 2016 review of the Swedish Nationwide Abdominal Aortic Aneurysm Screening Program determined that significant mortality benefit could take 10 years to materialize(Circ 2016;134:1141-8).
The full impact of Sweden’s remarkable decrease in smoking is almost certainly making itself known in these outcomes – smoking is implicated in 75% of AAA cases.
“The decreased prevalence of smoking in Sweden, from 44% of the population in 1970 to 15% in 2010, should be viewed as the main cause of the decreasing incidence and mortality of AAA. Every percent drop in the prevalence of smoking will have a huge effect on smoking-related diseases, such as cancer and AAA.”
Dr. Stefan is a vascular disease researcher at Lund (Sweden) University. He had no financial disclosures.
The study by Johansson et al. indicates a significant risk of overdiagnosis associated with routine screening for abdominal aortic aneurysm: Those risks may not be as clinically harmful as might be assumed, Stefan Acosta, MD, wrote in an accompanying editorial (Lancet 2018; 391: 2394-95).
“Although I agree that having a small AAA that needs long-term follow-up might be associated with negative psychological consequences, there could also be a window of opportunity [eg. with statins, antiplatelet therapy, and blood pressure reduction], for individuals with increased burden of cardiovascular disease. Indeed, screening for AAA, peripheral artery disease, and hypertension, with the initiation of relevant pharmacotherapy, if positive, reduces all-cause mortality and some evidence suggests that this approach of multifaceted vascular screening instead of isolated AAA screening should be considered.”
When performed according to the established criteria for elective AAA surgery, the procedure is associated with less than 1% postoperative mortality, “mainly because of wide implementation of endovascular aneurysm repair, a minimally invasive method.”
The 6-year follow-up time, as the authors noted, is relatively short. A 2016 review of the Swedish Nationwide Abdominal Aortic Aneurysm Screening Program determined that significant mortality benefit could take 10 years to materialize(Circ 2016;134:1141-8).
The full impact of Sweden’s remarkable decrease in smoking is almost certainly making itself known in these outcomes – smoking is implicated in 75% of AAA cases.
“The decreased prevalence of smoking in Sweden, from 44% of the population in 1970 to 15% in 2010, should be viewed as the main cause of the decreasing incidence and mortality of AAA. Every percent drop in the prevalence of smoking will have a huge effect on smoking-related diseases, such as cancer and AAA.”
Dr. Stefan is a vascular disease researcher at Lund (Sweden) University. He had no financial disclosures.
Deaths from abdominal aortic aneurysm among Swedish men are going down – but not because they’re being screened for the potentially fatal condition.
Although the death rate has decreased by 70% since the early 2000s, screening only saved 2 lives per 10,000 men screened. It did, however, increase by 59% the risk of unnecessary surgery, Minna Johansson, MD, and colleagues wrote in the June 16 issue of the Lancet.
“Screening had only a minor effect on AAA mortality,” wrote Dr. Johansson of the University of Gothenburg (Sweden). “In absolute numbers, only 7% of the benefit estimated in the largest trial of AAA screening was observed. The observed large reductions in AAA mortality were present in both the screened and nonscreened cohorts and were thus mainly caused by other factors – probably reduced smoking. … Our results call the continued justification of AAA screening into question.”
In Sweden, all men aged 65 years are invited to a one-time ultrasound abdominal aorta screening. Most participate. Anyone with an aneurysm is followed up at a vascular surgery clinic, with surgery considered if the aortic diameter is 55 mm or larger.
Dr. Johansson and her colleagues plumbed national health records to estimate the risks and benefits of this routine screening. The study comprised 25,265 men invited to join the AAA screening program in Sweden from 2006 to 2009. Mortality data were compared with those from a contemporaneous cohort of 106,087 men of similar age who were not invited to screen. Finally, the mortality data were compared with national trends in AAA mortality in all Swedish men aged 40-99 years from 1987 to 2015.
A multivariate analysis adjusted for cohort year, marital status, educational level, income, and whether the patient already had an AAA diagnosis at baseline.
From the early 2000s to 2015, AAA mortality among men aged 65-74 years declined from 36 to10 deaths per 100,000. This 70% reduction was similar in both screened and unscreened populations; in fact, the decline began about a decade before population-based screening was introduced and continued to decrease at a steady rate afterward.
After 6 years of screening, there was a 30% reduction of AAA mortality in the screened population, compared with the unscreened, translating to an absolute mortality reduction of two deaths per 10,000 men offered screening.
Screening increased by 52% the number of AAAs detected. The absolute difference in incidence after 6 years of screening translated to an additional 49 overdiagnoses per 10,000 screened men.
Looking back into the mid-1990s, the investigators saw the numbers of elective AAA surgeries rise steadily. In the adjusted model, screened men were 59% more likely to have this procedure than unscreened. The increased risk didn’t come with an equally increased benefit, though. There was a 10% decrease in AAA ruptures, “rendering a risk of overtreatment of 19%, or 19 potentially avoidable elective surgeries per 10,000 men,” the team noted. “Sixty-three percent of all additional elective surgeries for AAA might therefore have constituted overtreat.”
The findings are at odds with large published studies that found a consistent benefit to screening.
“Compared with results at 7-year follow-up of the largest trial of screening for abdominal aortic aneurysm [Multicentre Aneurysm Screening Study (MASS)], we found about half of the benefit in terms of a relative effect and 7% of the estimated benefit in terms of absolute numbers [2 vs. 27 avoided deaths from AAA per 10,000 invited men]. Compared with previous estimates of overdiagnosis and overtreatment, we found a lower absolute number of over-diagnosed cases [49 vs.176 per 10,000 invited men] and fewer overtreated cases [19 vs. 37 per 10,000 invited men]. However, since the harms of screening decreased less than the benefit, the balance between benefits and harms seems much less appealing in today’s setting.”
None of the authors had any financial disclosures.
Deaths from abdominal aortic aneurysm among Swedish men are going down – but not because they’re being screened for the potentially fatal condition.
Although the death rate has decreased by 70% since the early 2000s, screening only saved 2 lives per 10,000 men screened. It did, however, increase by 59% the risk of unnecessary surgery, Minna Johansson, MD, and colleagues wrote in the June 16 issue of the Lancet.
“Screening had only a minor effect on AAA mortality,” wrote Dr. Johansson of the University of Gothenburg (Sweden). “In absolute numbers, only 7% of the benefit estimated in the largest trial of AAA screening was observed. The observed large reductions in AAA mortality were present in both the screened and nonscreened cohorts and were thus mainly caused by other factors – probably reduced smoking. … Our results call the continued justification of AAA screening into question.”
In Sweden, all men aged 65 years are invited to a one-time ultrasound abdominal aorta screening. Most participate. Anyone with an aneurysm is followed up at a vascular surgery clinic, with surgery considered if the aortic diameter is 55 mm or larger.
Dr. Johansson and her colleagues plumbed national health records to estimate the risks and benefits of this routine screening. The study comprised 25,265 men invited to join the AAA screening program in Sweden from 2006 to 2009. Mortality data were compared with those from a contemporaneous cohort of 106,087 men of similar age who were not invited to screen. Finally, the mortality data were compared with national trends in AAA mortality in all Swedish men aged 40-99 years from 1987 to 2015.
A multivariate analysis adjusted for cohort year, marital status, educational level, income, and whether the patient already had an AAA diagnosis at baseline.
From the early 2000s to 2015, AAA mortality among men aged 65-74 years declined from 36 to10 deaths per 100,000. This 70% reduction was similar in both screened and unscreened populations; in fact, the decline began about a decade before population-based screening was introduced and continued to decrease at a steady rate afterward.
After 6 years of screening, there was a 30% reduction of AAA mortality in the screened population, compared with the unscreened, translating to an absolute mortality reduction of two deaths per 10,000 men offered screening.
Screening increased by 52% the number of AAAs detected. The absolute difference in incidence after 6 years of screening translated to an additional 49 overdiagnoses per 10,000 screened men.
Looking back into the mid-1990s, the investigators saw the numbers of elective AAA surgeries rise steadily. In the adjusted model, screened men were 59% more likely to have this procedure than unscreened. The increased risk didn’t come with an equally increased benefit, though. There was a 10% decrease in AAA ruptures, “rendering a risk of overtreatment of 19%, or 19 potentially avoidable elective surgeries per 10,000 men,” the team noted. “Sixty-three percent of all additional elective surgeries for AAA might therefore have constituted overtreat.”
The findings are at odds with large published studies that found a consistent benefit to screening.
“Compared with results at 7-year follow-up of the largest trial of screening for abdominal aortic aneurysm [Multicentre Aneurysm Screening Study (MASS)], we found about half of the benefit in terms of a relative effect and 7% of the estimated benefit in terms of absolute numbers [2 vs. 27 avoided deaths from AAA per 10,000 invited men]. Compared with previous estimates of overdiagnosis and overtreatment, we found a lower absolute number of over-diagnosed cases [49 vs.176 per 10,000 invited men] and fewer overtreated cases [19 vs. 37 per 10,000 invited men]. However, since the harms of screening decreased less than the benefit, the balance between benefits and harms seems much less appealing in today’s setting.”
None of the authors had any financial disclosures.
FROM THE LANCET
Key clinical point: Screening for abdominal aortic aneurysms in men saved few lives, but significantly increased the risk of overdiagnosis and unnecessary surgery.
Major finding: Screening saved two lives per 10,000 men, but showed an increased risk of overtreatment of 19%.
Study details: The population-based longitudinal cohort study comprised 131,352 men.
Disclosures: The authors had no financial disclosures.
Source: Johansson et al. Lancet 2018;391:2441-7.
Ruptured abdominal aortic aneurysm repair: Preop measures that predict death
Four preoperative variables – age over 76 years, creatinine concentration greater than 2.0 mg/dL, pH less than 7.2, and lowest ever systolic blood pressure less than 70 mm Hg – predicted 30-day mortality following repair of ruptured abdominal aortic aneurysms (rAAAs), in a retrospective study of 303 patients treated at Harborview Medical Center at the University of Washington, Seattle.
Brandon T. Garland, MD, and his colleagues at Harborview, reviewed the data set of patients, noting 50% were aged older than 76 years and 80% were male. Many patients had typical vascular risk factors: 65% had hypertension, 39% had coronary artery disease, and 22% had chronic obstructive vascular disease. Patients who were treated for rAAA after 2007 and had preoperative computed tomography scans were assessed for endovascular aneurysm repair (rEVAR) based on infrarenal neck length and diameter and access vessel size. Noneligible patients and all patients treated prior to 2007 had open repair (rOR) surgery.
A primary screen of selected preoperative variables included age, hematocrit, systolic blood pressure values, use of cardiopulmonary resuscitation, pH, international normalized ratio, creatinine concentration, temperature, partial thromboplastin time, weight, history of coronary artery disease, and loss of consciousness at any time.
The four statistically significant associations were age over 76 years (odds ratio, 2.11; P less than 0.11), creatinine concentration over 2.0 mg/dL (OR, 3.66; P less than .001), pH less than 7.2 (OR 2.58; P less than .009) and lowest ever systolic blood pressure less than 70 mm Hg (OR, 2.70; P less than .002) Each of the four predictive preoperative rAAA variables was assigned a value of 1 point. Individualized scores are simply calculated by totaling the number of preoperative risk predictors.
Of the original 303 patients, 154 were alive at 30 days following rAAA repair, and there was a significant benefit from using rEVAR. Overall, patients with 1-, 2-, 3-, and 4-point mortality scores had 30-day mortality risks of 22%, 69%, 80%, and 100%, respectively. rEVAR mortalities dropped to 7% for a 1-point score and to 70% for a 3-point score. There were no 30-day survivors with 4-point risk scores regardless of whether they had rEVAR or rOR procedures.
The predictive risk scores for rAAA mortality outcomes provide helpful guides for patient care recommendations, and can be used to supplement the rOR-validated Glasgow Aneurysm Score, Hardman index, and Vascular Study Group of New England risk-predicting algorithms to “aid in clinical decision-making in the endovascular era,” the researchers wrote. The scores also add “prognostic information to the decision to transfer patients to tertiary care centers and aid in preoperative discussions with patients and their families.”
The authors reported that they had no conflicts of interest.
SOURCE: Garland BT et al. J Vasc Surg. 2018 May 9. doi: 10.1016/j.jvs.2017.12.075.
Four preoperative variables – age over 76 years, creatinine concentration greater than 2.0 mg/dL, pH less than 7.2, and lowest ever systolic blood pressure less than 70 mm Hg – predicted 30-day mortality following repair of ruptured abdominal aortic aneurysms (rAAAs), in a retrospective study of 303 patients treated at Harborview Medical Center at the University of Washington, Seattle.
Brandon T. Garland, MD, and his colleagues at Harborview, reviewed the data set of patients, noting 50% were aged older than 76 years and 80% were male. Many patients had typical vascular risk factors: 65% had hypertension, 39% had coronary artery disease, and 22% had chronic obstructive vascular disease. Patients who were treated for rAAA after 2007 and had preoperative computed tomography scans were assessed for endovascular aneurysm repair (rEVAR) based on infrarenal neck length and diameter and access vessel size. Noneligible patients and all patients treated prior to 2007 had open repair (rOR) surgery.
A primary screen of selected preoperative variables included age, hematocrit, systolic blood pressure values, use of cardiopulmonary resuscitation, pH, international normalized ratio, creatinine concentration, temperature, partial thromboplastin time, weight, history of coronary artery disease, and loss of consciousness at any time.
The four statistically significant associations were age over 76 years (odds ratio, 2.11; P less than 0.11), creatinine concentration over 2.0 mg/dL (OR, 3.66; P less than .001), pH less than 7.2 (OR 2.58; P less than .009) and lowest ever systolic blood pressure less than 70 mm Hg (OR, 2.70; P less than .002) Each of the four predictive preoperative rAAA variables was assigned a value of 1 point. Individualized scores are simply calculated by totaling the number of preoperative risk predictors.
Of the original 303 patients, 154 were alive at 30 days following rAAA repair, and there was a significant benefit from using rEVAR. Overall, patients with 1-, 2-, 3-, and 4-point mortality scores had 30-day mortality risks of 22%, 69%, 80%, and 100%, respectively. rEVAR mortalities dropped to 7% for a 1-point score and to 70% for a 3-point score. There were no 30-day survivors with 4-point risk scores regardless of whether they had rEVAR or rOR procedures.
The predictive risk scores for rAAA mortality outcomes provide helpful guides for patient care recommendations, and can be used to supplement the rOR-validated Glasgow Aneurysm Score, Hardman index, and Vascular Study Group of New England risk-predicting algorithms to “aid in clinical decision-making in the endovascular era,” the researchers wrote. The scores also add “prognostic information to the decision to transfer patients to tertiary care centers and aid in preoperative discussions with patients and their families.”
The authors reported that they had no conflicts of interest.
SOURCE: Garland BT et al. J Vasc Surg. 2018 May 9. doi: 10.1016/j.jvs.2017.12.075.
Four preoperative variables – age over 76 years, creatinine concentration greater than 2.0 mg/dL, pH less than 7.2, and lowest ever systolic blood pressure less than 70 mm Hg – predicted 30-day mortality following repair of ruptured abdominal aortic aneurysms (rAAAs), in a retrospective study of 303 patients treated at Harborview Medical Center at the University of Washington, Seattle.
Brandon T. Garland, MD, and his colleagues at Harborview, reviewed the data set of patients, noting 50% were aged older than 76 years and 80% were male. Many patients had typical vascular risk factors: 65% had hypertension, 39% had coronary artery disease, and 22% had chronic obstructive vascular disease. Patients who were treated for rAAA after 2007 and had preoperative computed tomography scans were assessed for endovascular aneurysm repair (rEVAR) based on infrarenal neck length and diameter and access vessel size. Noneligible patients and all patients treated prior to 2007 had open repair (rOR) surgery.
A primary screen of selected preoperative variables included age, hematocrit, systolic blood pressure values, use of cardiopulmonary resuscitation, pH, international normalized ratio, creatinine concentration, temperature, partial thromboplastin time, weight, history of coronary artery disease, and loss of consciousness at any time.
The four statistically significant associations were age over 76 years (odds ratio, 2.11; P less than 0.11), creatinine concentration over 2.0 mg/dL (OR, 3.66; P less than .001), pH less than 7.2 (OR 2.58; P less than .009) and lowest ever systolic blood pressure less than 70 mm Hg (OR, 2.70; P less than .002) Each of the four predictive preoperative rAAA variables was assigned a value of 1 point. Individualized scores are simply calculated by totaling the number of preoperative risk predictors.
Of the original 303 patients, 154 were alive at 30 days following rAAA repair, and there was a significant benefit from using rEVAR. Overall, patients with 1-, 2-, 3-, and 4-point mortality scores had 30-day mortality risks of 22%, 69%, 80%, and 100%, respectively. rEVAR mortalities dropped to 7% for a 1-point score and to 70% for a 3-point score. There were no 30-day survivors with 4-point risk scores regardless of whether they had rEVAR or rOR procedures.
The predictive risk scores for rAAA mortality outcomes provide helpful guides for patient care recommendations, and can be used to supplement the rOR-validated Glasgow Aneurysm Score, Hardman index, and Vascular Study Group of New England risk-predicting algorithms to “aid in clinical decision-making in the endovascular era,” the researchers wrote. The scores also add “prognostic information to the decision to transfer patients to tertiary care centers and aid in preoperative discussions with patients and their families.”
The authors reported that they had no conflicts of interest.
SOURCE: Garland BT et al. J Vasc Surg. 2018 May 9. doi: 10.1016/j.jvs.2017.12.075.
FROM THE JOURNAL OF VASCULAR SURGERY
Key clinical point: Age, creatinine concentration, pH, and systolic blood pressure measures can be used to determine a 30-day mortality risk score for patients undergoing repair of ruptured abdominal aortic aneurysms (rAAAs).
Major finding: The Harborview Medical Center risk scores range from 0 to 4 points with 1-, 2-, and 3-point scores corresponding respectively to 22%, 69%, and 80% risks of 30-day mortality following rAAA repair.
Study details: A single-location retrospective study of 303 patients presenting with ruptured rAAAs.
Disclosures: The authors reported that they had no conflicts of interest.
Source: Garland BT et al. J Vasc Surg. 2018 May 9. doi: 10.1016/j.jvs.2017.12.075.
Large-vessel vasculitis: More severe in HIV-infected patients
Large-vessel vasculitis (LVV) associated with HIV-infected patients occurs more frequently in men and is significantly more severe, compared with the disease in their noninfected counterparts, according to a retrospective analysis of medical records during 2000-2015.
The study was conducted at Pitié-Salpêtrière Hospital in Paris to investigate the occurrence, characteristics, and treatment outcomes of LVV of patients infected with HIV, reported in the Journal of Vascular Surgery. Yasmina Ferfar, MD, and her colleagues diagnosed LVV using available imaging (computed tomography, positron emission tomography, and magnetic resonance angiography), histology, and Ishikawa or American College of Rheumatology (ACR) criteria of Takayasu arteritis (TA). All 93 patients selected for the study had LVV.
Vascular lesions were located in three areas; aorta (n = 7), supra-aortic trunks (7), and in digestive arteries (3). The Ishikawa or ACR criteria for TA diagnosis were met by 7 of the 11 (64%) patients.
Highly active antiretroviral therapy was prescribed for six patients at the time of vasculitis diagnosis and for four after diagnosis; HAART was delayed for the remaining patient whose HIV infection was under control.
Steroids, immunosuppressive, statins, and antiplatelet agents were provided in custom combinations to nine patients. Open surgical or endovascular repair was performed on 8 (73%) of the 11 patients with a mean follow-up at 95 months. As recorded at the last follow-up, 6 of the 11 patients had obtained stabilization of the vasculitis, improvement of vascular lesions had occurred in 4 of the 11 patients, and 1 patient had died from complications related to vascular surgery.
An age-matched control test comparison was performed between HIV-infected patients with large-vessel vasculitis and the HIV-negative patients with Takayasu arteritis that were identified in this study. The 82 patients in the LVV HIV-negative group had a median age of 42 years and 72 (88%) were women. Inflammatory syndrome was reported for 30 patients. Glucocorticosteroid treatments were given to 70 patients and immunosuppressive treatments were given to 57 patients.
Comparing LVV between the HIV-infected and their HIV-negative counterparts showed that vascular disease was significantly more severe for HIV-infected patients, according to the Ishikawa score (P = .017) and there was significantly greater use of vascular procedures (P = .047). LVV in association with HIV-infection also occurred more frequently with men (P = .014).
Dr. Ferfar and colleagues suggested that “HIV infection might be an accelerant for vasculitis,” based upon the increased severity of the disease they noted. They also indicated that glucocorticosteroids and immunosuppressive treatments were less often prescribed in HIV-positive patients (P = .001).
The effectiveness of steroids and immunosuppressant drugs seen with 7 of the 11 HIV-positive patients that met the Ishikawa or ACR criteria of TA suggests an overlap between HIV-associated LVV and TA, according to the researchers. Therefore, “HIV-infected patients with LVV should be treated with corticosteroids to avoid complications. Studies with a greater number of HIV-infected patients with LVV are required to confirm this hypothesis”.
The authors reported that they had no conflicts of interest.
SOURCE: Ferfar Y. et al. J Vasc Surg. 2018 Dec 11. doi. org/10.1016/j.jvs.2017.08.099.
Large-vessel vasculitis (LVV) associated with HIV-infected patients occurs more frequently in men and is significantly more severe, compared with the disease in their noninfected counterparts, according to a retrospective analysis of medical records during 2000-2015.
The study was conducted at Pitié-Salpêtrière Hospital in Paris to investigate the occurrence, characteristics, and treatment outcomes of LVV of patients infected with HIV, reported in the Journal of Vascular Surgery. Yasmina Ferfar, MD, and her colleagues diagnosed LVV using available imaging (computed tomography, positron emission tomography, and magnetic resonance angiography), histology, and Ishikawa or American College of Rheumatology (ACR) criteria of Takayasu arteritis (TA). All 93 patients selected for the study had LVV.
Vascular lesions were located in three areas; aorta (n = 7), supra-aortic trunks (7), and in digestive arteries (3). The Ishikawa or ACR criteria for TA diagnosis were met by 7 of the 11 (64%) patients.
Highly active antiretroviral therapy was prescribed for six patients at the time of vasculitis diagnosis and for four after diagnosis; HAART was delayed for the remaining patient whose HIV infection was under control.
Steroids, immunosuppressive, statins, and antiplatelet agents were provided in custom combinations to nine patients. Open surgical or endovascular repair was performed on 8 (73%) of the 11 patients with a mean follow-up at 95 months. As recorded at the last follow-up, 6 of the 11 patients had obtained stabilization of the vasculitis, improvement of vascular lesions had occurred in 4 of the 11 patients, and 1 patient had died from complications related to vascular surgery.
An age-matched control test comparison was performed between HIV-infected patients with large-vessel vasculitis and the HIV-negative patients with Takayasu arteritis that were identified in this study. The 82 patients in the LVV HIV-negative group had a median age of 42 years and 72 (88%) were women. Inflammatory syndrome was reported for 30 patients. Glucocorticosteroid treatments were given to 70 patients and immunosuppressive treatments were given to 57 patients.
Comparing LVV between the HIV-infected and their HIV-negative counterparts showed that vascular disease was significantly more severe for HIV-infected patients, according to the Ishikawa score (P = .017) and there was significantly greater use of vascular procedures (P = .047). LVV in association with HIV-infection also occurred more frequently with men (P = .014).
Dr. Ferfar and colleagues suggested that “HIV infection might be an accelerant for vasculitis,” based upon the increased severity of the disease they noted. They also indicated that glucocorticosteroids and immunosuppressive treatments were less often prescribed in HIV-positive patients (P = .001).
The effectiveness of steroids and immunosuppressant drugs seen with 7 of the 11 HIV-positive patients that met the Ishikawa or ACR criteria of TA suggests an overlap between HIV-associated LVV and TA, according to the researchers. Therefore, “HIV-infected patients with LVV should be treated with corticosteroids to avoid complications. Studies with a greater number of HIV-infected patients with LVV are required to confirm this hypothesis”.
The authors reported that they had no conflicts of interest.
SOURCE: Ferfar Y. et al. J Vasc Surg. 2018 Dec 11. doi. org/10.1016/j.jvs.2017.08.099.
Large-vessel vasculitis (LVV) associated with HIV-infected patients occurs more frequently in men and is significantly more severe, compared with the disease in their noninfected counterparts, according to a retrospective analysis of medical records during 2000-2015.
The study was conducted at Pitié-Salpêtrière Hospital in Paris to investigate the occurrence, characteristics, and treatment outcomes of LVV of patients infected with HIV, reported in the Journal of Vascular Surgery. Yasmina Ferfar, MD, and her colleagues diagnosed LVV using available imaging (computed tomography, positron emission tomography, and magnetic resonance angiography), histology, and Ishikawa or American College of Rheumatology (ACR) criteria of Takayasu arteritis (TA). All 93 patients selected for the study had LVV.
Vascular lesions were located in three areas; aorta (n = 7), supra-aortic trunks (7), and in digestive arteries (3). The Ishikawa or ACR criteria for TA diagnosis were met by 7 of the 11 (64%) patients.
Highly active antiretroviral therapy was prescribed for six patients at the time of vasculitis diagnosis and for four after diagnosis; HAART was delayed for the remaining patient whose HIV infection was under control.
Steroids, immunosuppressive, statins, and antiplatelet agents were provided in custom combinations to nine patients. Open surgical or endovascular repair was performed on 8 (73%) of the 11 patients with a mean follow-up at 95 months. As recorded at the last follow-up, 6 of the 11 patients had obtained stabilization of the vasculitis, improvement of vascular lesions had occurred in 4 of the 11 patients, and 1 patient had died from complications related to vascular surgery.
An age-matched control test comparison was performed between HIV-infected patients with large-vessel vasculitis and the HIV-negative patients with Takayasu arteritis that were identified in this study. The 82 patients in the LVV HIV-negative group had a median age of 42 years and 72 (88%) were women. Inflammatory syndrome was reported for 30 patients. Glucocorticosteroid treatments were given to 70 patients and immunosuppressive treatments were given to 57 patients.
Comparing LVV between the HIV-infected and their HIV-negative counterparts showed that vascular disease was significantly more severe for HIV-infected patients, according to the Ishikawa score (P = .017) and there was significantly greater use of vascular procedures (P = .047). LVV in association with HIV-infection also occurred more frequently with men (P = .014).
Dr. Ferfar and colleagues suggested that “HIV infection might be an accelerant for vasculitis,” based upon the increased severity of the disease they noted. They also indicated that glucocorticosteroids and immunosuppressive treatments were less often prescribed in HIV-positive patients (P = .001).
The effectiveness of steroids and immunosuppressant drugs seen with 7 of the 11 HIV-positive patients that met the Ishikawa or ACR criteria of TA suggests an overlap between HIV-associated LVV and TA, according to the researchers. Therefore, “HIV-infected patients with LVV should be treated with corticosteroids to avoid complications. Studies with a greater number of HIV-infected patients with LVV are required to confirm this hypothesis”.
The authors reported that they had no conflicts of interest.
SOURCE: Ferfar Y. et al. J Vasc Surg. 2018 Dec 11. doi. org/10.1016/j.jvs.2017.08.099.
FROM THE JOURNAL OF VASCULAR SURGERY
Key clinical point: Corticosteroid treatments may reduce severity and avoid some complications of LVV in HIV-infected patients.
Major finding: LVV is significantly more severe in HIV-infected patients and is associated more frequently with men.
Study details: A Pitié-Salpêtrière Hospital retrospective study of 11 HIV-infected patients with LVV, compared with 82 uninfected age-matched patients with LVV.
Disclosures: The authors reported that they had no conflicts of interest.
Source: Ferfar Y et al. J Vasc Surg. 2018. doi. org/10.1016/j.jvs.2017.08.099.
Know risk factors for ischemic colitis after AAA repair
EXPERT ANALYSIS FROM THE NORTHWESTERN VASCULAR SYMPOSIUM
CHICAGO – Postoperative ischemic colitis after abdominal aortic aneurysm (AAA) repair is a feared, potentially devastating complication with a mortality approaching 50%, but early diagnosis can mitigate that risk, Roy M. Fujitani, MD, said at a symposium on vascular surgery sponsored by Northwestern University in Chicago.
The most common etiology of ischemic colitis following AAA repair is hypoperfusion of the mesenteric vasculature leading to nonocclusive ischemia. Caught early – in the initial hyperactive phase of colonic ischemia – the complication is typically transient and can be managed medically without further sequelae. Improvement is generally noted within a day or 2, with complete resolution within 1-2 weeks.
The earliest indicator that a patient is in the hyperactive phase of ischemic colitis following completion of an AAA repair can be defecation while still on the operating table.
“When you’ve just completed an operation and the patient has a bowel movement right on the operating table, that always makes me very, very concerned because of the likelihood of an associated ischemic colitis,” the surgeon noted.
A conscious patient in the first phase of ischemic colitis will describe an urgent desire to defecate, along with crampy pain and loose bowel movements with or without blood in the stool.
In the second, paralytic phase of ischemic colitis, the pain diminishes in intensity but becomes more continuous and diffuse, usually in the lateral borders of the abdomen. The abdomen becomes distended and much more tender, and there are no bowel sounds.
In patients whose ischemic colitis has been misdiagnosed or undiagnosed, the shock phase comes next. This is marked by massive fluid, protein, and electrolyte loss through the gangrenous mucosa. The result is severe dehydration, metabolic acidosis, and hypovolemic shock.
Nonocclusive colonic ischemia most often affects the watershed areas of the colon, such as the Sudeck point at the rectosigmoid junction.
The two other etiologies of ischemic colitis occurring as a complication of AAA repair are acute arterial occlusion, typically caused by iatrogenic embolization from a proximal source, often during endovascular aneurysm repair (EVAR), or rarely, venous thrombosis.
Making the diagnosis
When a patient is suspected of having ischemic colitis, one of the easiest ways of advancing toward a diagnosis is to obtain an abdominal plain x-ray, which classically shows thumb printing indicative of submucosal edema. CT with IV contrast typically shows bowel wall thickening, pericolonic fat stranding, and – most significantly – there may be free air within the colonic wall, an indicator of more advanced ischemia that occurs shortly before transmural gangrenous changes.
Colonoscopy is, however, the mainstay of diagnosis. It should be performed in any patient where postoperative ischemic colitis is suspected.
Ischemic colitis risk factors and outcomes
Dr. Fujitani was senior author of the largest ever study of risk factors for and outcomes of postoperative ischemic colitis in patients undergoing contemporary methods of open and endovascular AAA repair. This retrospective analysis of the American College of Surgeons National Surgical Quality Improvement Program (NSQIP) database included 3,486 patients who underwent AAA repair in U.S. hospitals during 2011-2012. Twelve percent had an open repair, while the other 88% underwent EVAR.
The incidence of postoperative ischemic colitis was 2.2%. The median time of diagnosis was on postoperative day 2. The rate was nearly threefold higher in the open repair group: 5.2% versus 1.8%. However, the open-repair group had a higher rate of emergency admission, ruptured aneurysm before surgery, and other high-risk features. Upon multivariate analysis, the adjusted risk of postoperative ischemic colitis was no longer significantly different in the open-repair and EVAR groups.
The mean hospital length of stay in patients with postoperative ischemic colitis was 20 days, compared with 5 days in those without the complication. The unadjusted in-hospital mortality rate in patients with ischemic colitis was 39% versus 4% in those without ischemic colitis.
Of the 75 patients who developed postoperative ischemic colitis, 37 were managed medically, 38 surgically.
“What was quite surprising was that there was a 56.8% in-hospital mortality in the surgically treated patients. The point being that if you end up having ischemic colitis, there’s a 50% chance you’ll end up requiring an operation, and if you do undergo an operation you have more than a 50% chance of succumbing from the process,” Dr. Fujitani observed.
Dr. Fujitani and his coinvestigators scrutinized a plethora of potential risk factors for postoperative ischemic colitis. Six emerged as significant upon multivariate analysis: ruptured aneurysm before surgery, with an associated adjusted 4.1-fold increased risk; need for intra- or postoperative transfusion, with a 6-fold increased risk; renal failure requiring dialysis, with a 3.9-fold risk; proximal extension of the aneurysm, with a 2.2-fold elevation in risk; diabetes, with a 1.9-fold risk; and female sex, with an adjusted 1.75-fold increased risk (J Vasc Surg. 2016 Apr;63[4]:866-72).
Of note, these risk factors are largely unmodifiable, which underscores the importance of vigorous surveillance for possible signs of ischemic colitis during the first 4 days after AAA repair, especially in patients with multiple risk factors, Dr. Fujitani said.
Also, careful intraoperative assessment of the collateral mesenteric vascular anatomy is important in assessing a patient’s risk for postoperative ischemic colitis. This assessment should include the superior and inferior mesenteric arteries, as well as the celiac and internal iliac arteries. It’s worth bearing in mind that, even though collateral flow may appear adequate, it can be affected by hypovolemia, hypotension, or low cardiac output, the surgeon continued.
In the NSQIP data analysis, no patients who underwent reimplantation of the inferior mesenteric artery during open repair developed postoperative ischemic colitis. While this is an encouraging finding, the numbers were too small to draw definitive conclusions as to whether reimplantation of the artery is protective. It’s an important issue for further study, though, since so few of the recognized risk factors for the complication are modifiable, Dr. Fujitani noted.
He reported having no financial conflicts regarding his presentation.
EXPERT ANALYSIS FROM THE NORTHWESTERN VASCULAR SYMPOSIUM
CHICAGO – Postoperative ischemic colitis after abdominal aortic aneurysm (AAA) repair is a feared, potentially devastating complication with a mortality approaching 50%, but early diagnosis can mitigate that risk, Roy M. Fujitani, MD, said at a symposium on vascular surgery sponsored by Northwestern University in Chicago.
The most common etiology of ischemic colitis following AAA repair is hypoperfusion of the mesenteric vasculature leading to nonocclusive ischemia. Caught early – in the initial hyperactive phase of colonic ischemia – the complication is typically transient and can be managed medically without further sequelae. Improvement is generally noted within a day or 2, with complete resolution within 1-2 weeks.
The earliest indicator that a patient is in the hyperactive phase of ischemic colitis following completion of an AAA repair can be defecation while still on the operating table.
“When you’ve just completed an operation and the patient has a bowel movement right on the operating table, that always makes me very, very concerned because of the likelihood of an associated ischemic colitis,” the surgeon noted.
A conscious patient in the first phase of ischemic colitis will describe an urgent desire to defecate, along with crampy pain and loose bowel movements with or without blood in the stool.
In the second, paralytic phase of ischemic colitis, the pain diminishes in intensity but becomes more continuous and diffuse, usually in the lateral borders of the abdomen. The abdomen becomes distended and much more tender, and there are no bowel sounds.
In patients whose ischemic colitis has been misdiagnosed or undiagnosed, the shock phase comes next. This is marked by massive fluid, protein, and electrolyte loss through the gangrenous mucosa. The result is severe dehydration, metabolic acidosis, and hypovolemic shock.
Nonocclusive colonic ischemia most often affects the watershed areas of the colon, such as the Sudeck point at the rectosigmoid junction.
The two other etiologies of ischemic colitis occurring as a complication of AAA repair are acute arterial occlusion, typically caused by iatrogenic embolization from a proximal source, often during endovascular aneurysm repair (EVAR), or rarely, venous thrombosis.
Making the diagnosis
When a patient is suspected of having ischemic colitis, one of the easiest ways of advancing toward a diagnosis is to obtain an abdominal plain x-ray, which classically shows thumb printing indicative of submucosal edema. CT with IV contrast typically shows bowel wall thickening, pericolonic fat stranding, and – most significantly – there may be free air within the colonic wall, an indicator of more advanced ischemia that occurs shortly before transmural gangrenous changes.
Colonoscopy is, however, the mainstay of diagnosis. It should be performed in any patient where postoperative ischemic colitis is suspected.
Ischemic colitis risk factors and outcomes
Dr. Fujitani was senior author of the largest ever study of risk factors for and outcomes of postoperative ischemic colitis in patients undergoing contemporary methods of open and endovascular AAA repair. This retrospective analysis of the American College of Surgeons National Surgical Quality Improvement Program (NSQIP) database included 3,486 patients who underwent AAA repair in U.S. hospitals during 2011-2012. Twelve percent had an open repair, while the other 88% underwent EVAR.
The incidence of postoperative ischemic colitis was 2.2%. The median time of diagnosis was on postoperative day 2. The rate was nearly threefold higher in the open repair group: 5.2% versus 1.8%. However, the open-repair group had a higher rate of emergency admission, ruptured aneurysm before surgery, and other high-risk features. Upon multivariate analysis, the adjusted risk of postoperative ischemic colitis was no longer significantly different in the open-repair and EVAR groups.
The mean hospital length of stay in patients with postoperative ischemic colitis was 20 days, compared with 5 days in those without the complication. The unadjusted in-hospital mortality rate in patients with ischemic colitis was 39% versus 4% in those without ischemic colitis.
Of the 75 patients who developed postoperative ischemic colitis, 37 were managed medically, 38 surgically.
“What was quite surprising was that there was a 56.8% in-hospital mortality in the surgically treated patients. The point being that if you end up having ischemic colitis, there’s a 50% chance you’ll end up requiring an operation, and if you do undergo an operation you have more than a 50% chance of succumbing from the process,” Dr. Fujitani observed.
Dr. Fujitani and his coinvestigators scrutinized a plethora of potential risk factors for postoperative ischemic colitis. Six emerged as significant upon multivariate analysis: ruptured aneurysm before surgery, with an associated adjusted 4.1-fold increased risk; need for intra- or postoperative transfusion, with a 6-fold increased risk; renal failure requiring dialysis, with a 3.9-fold risk; proximal extension of the aneurysm, with a 2.2-fold elevation in risk; diabetes, with a 1.9-fold risk; and female sex, with an adjusted 1.75-fold increased risk (J Vasc Surg. 2016 Apr;63[4]:866-72).
Of note, these risk factors are largely unmodifiable, which underscores the importance of vigorous surveillance for possible signs of ischemic colitis during the first 4 days after AAA repair, especially in patients with multiple risk factors, Dr. Fujitani said.
Also, careful intraoperative assessment of the collateral mesenteric vascular anatomy is important in assessing a patient’s risk for postoperative ischemic colitis. This assessment should include the superior and inferior mesenteric arteries, as well as the celiac and internal iliac arteries. It’s worth bearing in mind that, even though collateral flow may appear adequate, it can be affected by hypovolemia, hypotension, or low cardiac output, the surgeon continued.
In the NSQIP data analysis, no patients who underwent reimplantation of the inferior mesenteric artery during open repair developed postoperative ischemic colitis. While this is an encouraging finding, the numbers were too small to draw definitive conclusions as to whether reimplantation of the artery is protective. It’s an important issue for further study, though, since so few of the recognized risk factors for the complication are modifiable, Dr. Fujitani noted.
He reported having no financial conflicts regarding his presentation.
EXPERT ANALYSIS FROM THE NORTHWESTERN VASCULAR SYMPOSIUM
CHICAGO – Postoperative ischemic colitis after abdominal aortic aneurysm (AAA) repair is a feared, potentially devastating complication with a mortality approaching 50%, but early diagnosis can mitigate that risk, Roy M. Fujitani, MD, said at a symposium on vascular surgery sponsored by Northwestern University in Chicago.
The most common etiology of ischemic colitis following AAA repair is hypoperfusion of the mesenteric vasculature leading to nonocclusive ischemia. Caught early – in the initial hyperactive phase of colonic ischemia – the complication is typically transient and can be managed medically without further sequelae. Improvement is generally noted within a day or 2, with complete resolution within 1-2 weeks.
The earliest indicator that a patient is in the hyperactive phase of ischemic colitis following completion of an AAA repair can be defecation while still on the operating table.
“When you’ve just completed an operation and the patient has a bowel movement right on the operating table, that always makes me very, very concerned because of the likelihood of an associated ischemic colitis,” the surgeon noted.
A conscious patient in the first phase of ischemic colitis will describe an urgent desire to defecate, along with crampy pain and loose bowel movements with or without blood in the stool.
In the second, paralytic phase of ischemic colitis, the pain diminishes in intensity but becomes more continuous and diffuse, usually in the lateral borders of the abdomen. The abdomen becomes distended and much more tender, and there are no bowel sounds.
In patients whose ischemic colitis has been misdiagnosed or undiagnosed, the shock phase comes next. This is marked by massive fluid, protein, and electrolyte loss through the gangrenous mucosa. The result is severe dehydration, metabolic acidosis, and hypovolemic shock.
Nonocclusive colonic ischemia most often affects the watershed areas of the colon, such as the Sudeck point at the rectosigmoid junction.
The two other etiologies of ischemic colitis occurring as a complication of AAA repair are acute arterial occlusion, typically caused by iatrogenic embolization from a proximal source, often during endovascular aneurysm repair (EVAR), or rarely, venous thrombosis.
Making the diagnosis
When a patient is suspected of having ischemic colitis, one of the easiest ways of advancing toward a diagnosis is to obtain an abdominal plain x-ray, which classically shows thumb printing indicative of submucosal edema. CT with IV contrast typically shows bowel wall thickening, pericolonic fat stranding, and – most significantly – there may be free air within the colonic wall, an indicator of more advanced ischemia that occurs shortly before transmural gangrenous changes.
Colonoscopy is, however, the mainstay of diagnosis. It should be performed in any patient where postoperative ischemic colitis is suspected.
Ischemic colitis risk factors and outcomes
Dr. Fujitani was senior author of the largest ever study of risk factors for and outcomes of postoperative ischemic colitis in patients undergoing contemporary methods of open and endovascular AAA repair. This retrospective analysis of the American College of Surgeons National Surgical Quality Improvement Program (NSQIP) database included 3,486 patients who underwent AAA repair in U.S. hospitals during 2011-2012. Twelve percent had an open repair, while the other 88% underwent EVAR.
The incidence of postoperative ischemic colitis was 2.2%. The median time of diagnosis was on postoperative day 2. The rate was nearly threefold higher in the open repair group: 5.2% versus 1.8%. However, the open-repair group had a higher rate of emergency admission, ruptured aneurysm before surgery, and other high-risk features. Upon multivariate analysis, the adjusted risk of postoperative ischemic colitis was no longer significantly different in the open-repair and EVAR groups.
The mean hospital length of stay in patients with postoperative ischemic colitis was 20 days, compared with 5 days in those without the complication. The unadjusted in-hospital mortality rate in patients with ischemic colitis was 39% versus 4% in those without ischemic colitis.
Of the 75 patients who developed postoperative ischemic colitis, 37 were managed medically, 38 surgically.
“What was quite surprising was that there was a 56.8% in-hospital mortality in the surgically treated patients. The point being that if you end up having ischemic colitis, there’s a 50% chance you’ll end up requiring an operation, and if you do undergo an operation you have more than a 50% chance of succumbing from the process,” Dr. Fujitani observed.
Dr. Fujitani and his coinvestigators scrutinized a plethora of potential risk factors for postoperative ischemic colitis. Six emerged as significant upon multivariate analysis: ruptured aneurysm before surgery, with an associated adjusted 4.1-fold increased risk; need for intra- or postoperative transfusion, with a 6-fold increased risk; renal failure requiring dialysis, with a 3.9-fold risk; proximal extension of the aneurysm, with a 2.2-fold elevation in risk; diabetes, with a 1.9-fold risk; and female sex, with an adjusted 1.75-fold increased risk (J Vasc Surg. 2016 Apr;63[4]:866-72).
Of note, these risk factors are largely unmodifiable, which underscores the importance of vigorous surveillance for possible signs of ischemic colitis during the first 4 days after AAA repair, especially in patients with multiple risk factors, Dr. Fujitani said.
Also, careful intraoperative assessment of the collateral mesenteric vascular anatomy is important in assessing a patient’s risk for postoperative ischemic colitis. This assessment should include the superior and inferior mesenteric arteries, as well as the celiac and internal iliac arteries. It’s worth bearing in mind that, even though collateral flow may appear adequate, it can be affected by hypovolemia, hypotension, or low cardiac output, the surgeon continued.
In the NSQIP data analysis, no patients who underwent reimplantation of the inferior mesenteric artery during open repair developed postoperative ischemic colitis. While this is an encouraging finding, the numbers were too small to draw definitive conclusions as to whether reimplantation of the artery is protective. It’s an important issue for further study, though, since so few of the recognized risk factors for the complication are modifiable, Dr. Fujitani noted.
He reported having no financial conflicts regarding his presentation.
Medicaid expansion meant earlier presentation, better surgical outcomes
The for five common surgical conditions, according to a Jan. 24 report in JAMA Surgery.
“Given current debate on the ACA [Affordable Care Act] and reforms to the Medicaid program, evidence on the effects of these policies is critical ... As policy makers weigh changes to or a potential repeal of the ACA, these findings provide important new data on the early clinical effects of the law’s coverage expansion,” said investigators led by Andrew Loehrer, MD, of the department of surgical oncology at MD Anderson Cancer Center, Houston.
For a baseline, the team used hospital administrative data from the Vizient Clinical Data Base and Resource Manager to assess outcomes for appendicitis, cholecystitis, diverticulitis, peripheral artery disease, and aortic aneurysm in 42 states during 2010-2013, before the ACA took effect in 2014. They then compared outcomes during 2014-2015 in the 27 states that expanded Medicaid programs under the ACA with 15 states that did not. The study included 225,572 hospital admissions in the Medicaid expansion states and 67,957 in the nonexpansion states at more than 200 academic medical centers and affiliated hospitals.
Medicaid expansion in the 27 states was associated with a 7.5-percentage point decreased probability of patients being uninsured (95% confidence interval, –12.2 to –2.9; P = .002) and an 8.6-percentage point increased probability of having Medicaid (95% CI, 6.1-11.1; P less than .001).
Medicaid expansion was also associated with a 1.8-percentage point increase in the probability of early, uncomplicated presentation (95% CI, 0.7-2.9; P = .001) and a 2.6-percentage point increase in the probability of receiving optimal management after admission, most likely due to the earlier presentation (95% CI, 0.8-4.4; P = .006).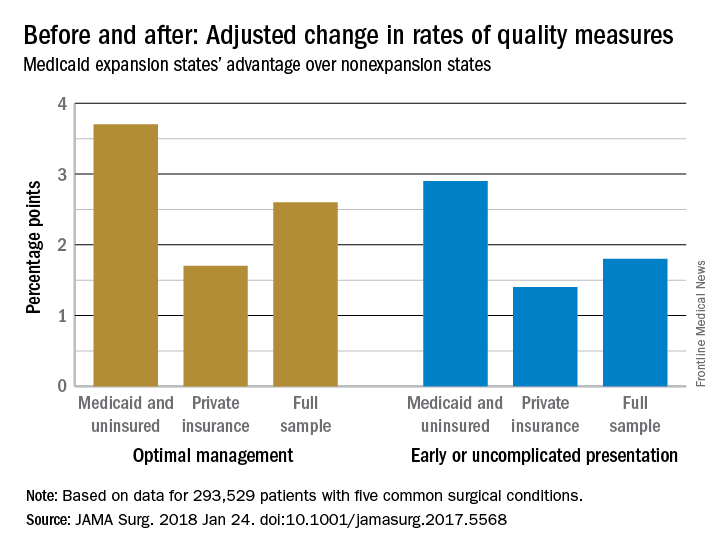
The improvements were concentrated among Medicaid and uninsured patients, who were most likely to benefit from coverage expansion, rather than those with private insurance.
The investigators acknowledged the limitations of their data for tracking changes access and quality of care for surgical patients. “We recognize that the data on improved quality of care are not as clear. Our use of composite outcomes has specific limitations,” they wrote.
“As expected for the conditions studied, our analysis found no significant change in the overall number of individuals treated but rather a change in the timeliness in which individuals received care.” Meanwhile, “our sample revealed an increase in the percentage of surgical patients who were uninsured in nonexpansion states after 2014,” which was associated with “worsening of outcomes ... whereas expansion states had stabilization or improvement,” they said. In Medicaid expansion states, the number of uninsured dropped from 14.% to 6.8%, but in the nonexpansion states, the number of uninsured actually increased slightly from 21.2% to 21.9%.
There was no funding source reported for the study. The authors had no conflicts of interest.
SOURCE: Loehrer AP et. al. JAMA Surg. 2018 Jan 24. doi: 10.1001/jamasurg.2017.5568
The for five common surgical conditions, according to a Jan. 24 report in JAMA Surgery.
“Given current debate on the ACA [Affordable Care Act] and reforms to the Medicaid program, evidence on the effects of these policies is critical ... As policy makers weigh changes to or a potential repeal of the ACA, these findings provide important new data on the early clinical effects of the law’s coverage expansion,” said investigators led by Andrew Loehrer, MD, of the department of surgical oncology at MD Anderson Cancer Center, Houston.
For a baseline, the team used hospital administrative data from the Vizient Clinical Data Base and Resource Manager to assess outcomes for appendicitis, cholecystitis, diverticulitis, peripheral artery disease, and aortic aneurysm in 42 states during 2010-2013, before the ACA took effect in 2014. They then compared outcomes during 2014-2015 in the 27 states that expanded Medicaid programs under the ACA with 15 states that did not. The study included 225,572 hospital admissions in the Medicaid expansion states and 67,957 in the nonexpansion states at more than 200 academic medical centers and affiliated hospitals.
Medicaid expansion in the 27 states was associated with a 7.5-percentage point decreased probability of patients being uninsured (95% confidence interval, –12.2 to –2.9; P = .002) and an 8.6-percentage point increased probability of having Medicaid (95% CI, 6.1-11.1; P less than .001).
Medicaid expansion was also associated with a 1.8-percentage point increase in the probability of early, uncomplicated presentation (95% CI, 0.7-2.9; P = .001) and a 2.6-percentage point increase in the probability of receiving optimal management after admission, most likely due to the earlier presentation (95% CI, 0.8-4.4; P = .006).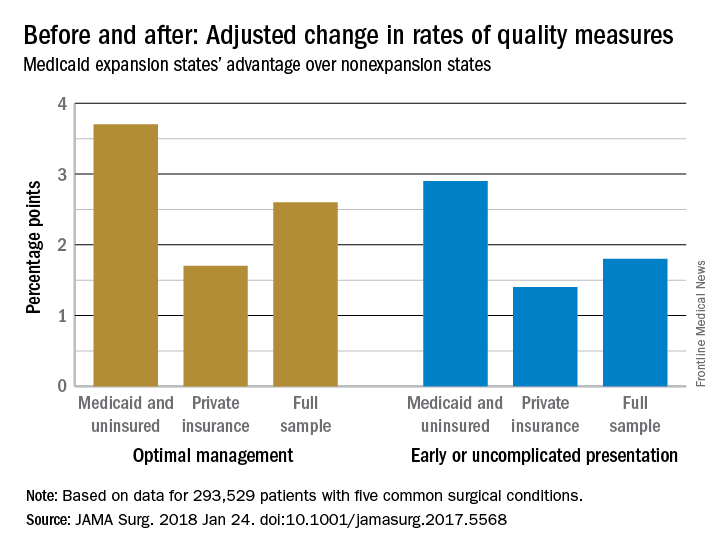
The improvements were concentrated among Medicaid and uninsured patients, who were most likely to benefit from coverage expansion, rather than those with private insurance.
The investigators acknowledged the limitations of their data for tracking changes access and quality of care for surgical patients. “We recognize that the data on improved quality of care are not as clear. Our use of composite outcomes has specific limitations,” they wrote.
“As expected for the conditions studied, our analysis found no significant change in the overall number of individuals treated but rather a change in the timeliness in which individuals received care.” Meanwhile, “our sample revealed an increase in the percentage of surgical patients who were uninsured in nonexpansion states after 2014,” which was associated with “worsening of outcomes ... whereas expansion states had stabilization or improvement,” they said. In Medicaid expansion states, the number of uninsured dropped from 14.% to 6.8%, but in the nonexpansion states, the number of uninsured actually increased slightly from 21.2% to 21.9%.
There was no funding source reported for the study. The authors had no conflicts of interest.
SOURCE: Loehrer AP et. al. JAMA Surg. 2018 Jan 24. doi: 10.1001/jamasurg.2017.5568
The for five common surgical conditions, according to a Jan. 24 report in JAMA Surgery.
“Given current debate on the ACA [Affordable Care Act] and reforms to the Medicaid program, evidence on the effects of these policies is critical ... As policy makers weigh changes to or a potential repeal of the ACA, these findings provide important new data on the early clinical effects of the law’s coverage expansion,” said investigators led by Andrew Loehrer, MD, of the department of surgical oncology at MD Anderson Cancer Center, Houston.
For a baseline, the team used hospital administrative data from the Vizient Clinical Data Base and Resource Manager to assess outcomes for appendicitis, cholecystitis, diverticulitis, peripheral artery disease, and aortic aneurysm in 42 states during 2010-2013, before the ACA took effect in 2014. They then compared outcomes during 2014-2015 in the 27 states that expanded Medicaid programs under the ACA with 15 states that did not. The study included 225,572 hospital admissions in the Medicaid expansion states and 67,957 in the nonexpansion states at more than 200 academic medical centers and affiliated hospitals.
Medicaid expansion in the 27 states was associated with a 7.5-percentage point decreased probability of patients being uninsured (95% confidence interval, –12.2 to –2.9; P = .002) and an 8.6-percentage point increased probability of having Medicaid (95% CI, 6.1-11.1; P less than .001).
Medicaid expansion was also associated with a 1.8-percentage point increase in the probability of early, uncomplicated presentation (95% CI, 0.7-2.9; P = .001) and a 2.6-percentage point increase in the probability of receiving optimal management after admission, most likely due to the earlier presentation (95% CI, 0.8-4.4; P = .006).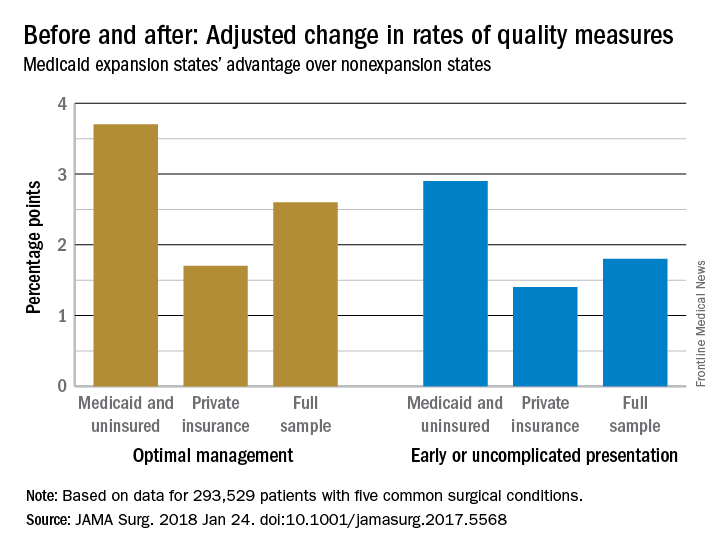
The improvements were concentrated among Medicaid and uninsured patients, who were most likely to benefit from coverage expansion, rather than those with private insurance.
The investigators acknowledged the limitations of their data for tracking changes access and quality of care for surgical patients. “We recognize that the data on improved quality of care are not as clear. Our use of composite outcomes has specific limitations,” they wrote.
“As expected for the conditions studied, our analysis found no significant change in the overall number of individuals treated but rather a change in the timeliness in which individuals received care.” Meanwhile, “our sample revealed an increase in the percentage of surgical patients who were uninsured in nonexpansion states after 2014,” which was associated with “worsening of outcomes ... whereas expansion states had stabilization or improvement,” they said. In Medicaid expansion states, the number of uninsured dropped from 14.% to 6.8%, but in the nonexpansion states, the number of uninsured actually increased slightly from 21.2% to 21.9%.
There was no funding source reported for the study. The authors had no conflicts of interest.
SOURCE: Loehrer AP et. al. JAMA Surg. 2018 Jan 24. doi: 10.1001/jamasurg.2017.5568
FROM JAMA SURGERY
Key clinical point: The Patient Protection and Affordable Care Act’s Medicaid expansion led to increased coverage of patients, earlier presentation, and improved care for five common surgical conditions.
Major finding: Medicaid expansion was associated with a 2.6 percentage-point increase in the probability of receiving optimal management after admission, most likely due to the earlier presentation.
Study details: Review of more than 200,000 patients, pre- and post-ACA
Disclosures: The authors had no disclosures.
Source: Loehrer AP et. al. JAMA Surg. 2018 Jan 24. doi: 10.1001/jamasurg.2017.5568