User login
The Rise of the Scribes
“We really aren’t taking care of records — we’re taking care of people.” — Dr. Lawrence Weed
What is the purpose of a progress note? Anyone? Yes, you there. “Insurance billing?” Yes, that’s a good one. Anyone else? “To remember what you did?” Excellent. Another? Yes, that’s right, for others to follow along in your care. These are all good reasons for a progress note to exist. But they aren’t the whole story. Let’s start at the beginning.
Charts were once a collection of paper sheets with handwritten notes. Sometimes illegible, sometimes beautiful, always efficient. A progress note back then could be just 10 characters, AK, LN2, X,X,X,X,X (with X’s marking nitrogen sprays). Then came the healthcare K-Pg event: the conversion to EMRs. Those doctors who survived evolved into computer programmers, creating blocks of text from a few keystrokes. But like toddler-sized Legos, the blocks made it impossible to build a note that is nuanced or precise. Worse yet, many notes consisting of blocks from one note added awkwardly to a new note, creating grotesque structures unrecognizable as anything that should exist in nature. Words and numbers, but no information.
Thanks to the eternity of EMR, these creations live on, hideous and useless. They waste not only the server’s energy but also our time. Few things are more maddening than scrolling to reach the bottom of another physician’s note only to find there is nothing there.
Whose fault is this? Anyone? Yes, that’s right, insurers. As there are probably no payers in this audience, let’s blame them. I agree, the crushing burden of documentation-to-get-reimbursed has forced us to create “notes” that add no value to us but add up points for us to get paid for them. CMS, payers, prior authorizations, and now even patients, it seems we are documenting for lots of people except for us. There isn’t time to satisfy all and this significant burden for every encounter is a proximate cause for doctors despair. Until now.
A fully formed, comprehensive, sometimes pretty note that satisfies all audiences. Dr. Larry Weed must be dancing in heaven. It was Dr. Weed who led us from the nicotine-stained logs of the 1950s to the powerful problem-based notes we use today, an innovation that rivals the stethoscope in its impact.
Professor Weed also predicted that computers would be important to capture and make sense of patient data, helping us make accurate diagnoses and efficient plans. Again, he was right. He would surely be advocating to take advantage of AI scribes’ marvelous ability to capture salient data and present it in the form of a problem-oriented medical record.
AI scribes will be ubiquitous soon; I’m fast and even for me they save time. They also allow, for the first time in a decade, to turn from the glow of a screen to actually face the patient – we no longer have to scribe and care simultaneously. Hallelujah. And yet, lest I disappoint you without a twist, it seems with AI scribes, like EMRs we lose a little something too.
Like self-driving cars or ChatGPT-generated letters, they remove cognitive loads. They are lovely when you have to multitask or are trying to recall a visit from hours (days) ago. Using them, you’ll feel faster, lighter, freer, happier. But what’s missing is the thinking. At the end, you have an exquisite note, but you didn’t write it. It has the salient points, but none of the mental work to create it. AI scribes subvert the valuable work of synthesis. That was the critical part of Dr. Weed’s discovery: writing problem-oriented notes helped us think better.
Writing allows for the friction that helps us process what is going on with a patient. It allows for the discovery of diagnoses and prompts plans. When I was an intern, one of my attendings would hand write notes, succinctly showing what he had observed and was thinking. He’d sketch diagrams in the chart, for example, to help illustrate how we’d work though the toxic, metabolic, and infectious etiologies of acute liver failure. Sublime.
The act of writing also helps remind us there is a person attached to these words. Like a handwritten sympathy card, it is intimate, human. Even using our EMR, I’d still often type sentences that help tell the patient’s story. “Her sister just died. Utterly devastated. I’ll forward chart to Bob (her PCP) to check in on her.” Or: “Scratch golfer wants to know why he is getting so many SCCs now. ‘Like bankruptcy, gradually then suddenly,’ I explained. I think I broke through.”
Since we’ve concluded the purpose of a note is mostly to capture data, AI scribes are a godsend. They do so with remarkable quality and efficiency. We’ll just have to remember if the diagnosis is unclear, then it might help to write the note out yourself. And even when done by the AI machine, we might add human touches now and again lest there be no art left in what we do.
“For sale. Sun hat. Never worn.”
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on X. Write to him at dermnews@mdedge.com.
“We really aren’t taking care of records — we’re taking care of people.” — Dr. Lawrence Weed
What is the purpose of a progress note? Anyone? Yes, you there. “Insurance billing?” Yes, that’s a good one. Anyone else? “To remember what you did?” Excellent. Another? Yes, that’s right, for others to follow along in your care. These are all good reasons for a progress note to exist. But they aren’t the whole story. Let’s start at the beginning.
Charts were once a collection of paper sheets with handwritten notes. Sometimes illegible, sometimes beautiful, always efficient. A progress note back then could be just 10 characters, AK, LN2, X,X,X,X,X (with X’s marking nitrogen sprays). Then came the healthcare K-Pg event: the conversion to EMRs. Those doctors who survived evolved into computer programmers, creating blocks of text from a few keystrokes. But like toddler-sized Legos, the blocks made it impossible to build a note that is nuanced or precise. Worse yet, many notes consisting of blocks from one note added awkwardly to a new note, creating grotesque structures unrecognizable as anything that should exist in nature. Words and numbers, but no information.
Thanks to the eternity of EMR, these creations live on, hideous and useless. They waste not only the server’s energy but also our time. Few things are more maddening than scrolling to reach the bottom of another physician’s note only to find there is nothing there.
Whose fault is this? Anyone? Yes, that’s right, insurers. As there are probably no payers in this audience, let’s blame them. I agree, the crushing burden of documentation-to-get-reimbursed has forced us to create “notes” that add no value to us but add up points for us to get paid for them. CMS, payers, prior authorizations, and now even patients, it seems we are documenting for lots of people except for us. There isn’t time to satisfy all and this significant burden for every encounter is a proximate cause for doctors despair. Until now.
A fully formed, comprehensive, sometimes pretty note that satisfies all audiences. Dr. Larry Weed must be dancing in heaven. It was Dr. Weed who led us from the nicotine-stained logs of the 1950s to the powerful problem-based notes we use today, an innovation that rivals the stethoscope in its impact.
Professor Weed also predicted that computers would be important to capture and make sense of patient data, helping us make accurate diagnoses and efficient plans. Again, he was right. He would surely be advocating to take advantage of AI scribes’ marvelous ability to capture salient data and present it in the form of a problem-oriented medical record.
AI scribes will be ubiquitous soon; I’m fast and even for me they save time. They also allow, for the first time in a decade, to turn from the glow of a screen to actually face the patient – we no longer have to scribe and care simultaneously. Hallelujah. And yet, lest I disappoint you without a twist, it seems with AI scribes, like EMRs we lose a little something too.
Like self-driving cars or ChatGPT-generated letters, they remove cognitive loads. They are lovely when you have to multitask or are trying to recall a visit from hours (days) ago. Using them, you’ll feel faster, lighter, freer, happier. But what’s missing is the thinking. At the end, you have an exquisite note, but you didn’t write it. It has the salient points, but none of the mental work to create it. AI scribes subvert the valuable work of synthesis. That was the critical part of Dr. Weed’s discovery: writing problem-oriented notes helped us think better.
Writing allows for the friction that helps us process what is going on with a patient. It allows for the discovery of diagnoses and prompts plans. When I was an intern, one of my attendings would hand write notes, succinctly showing what he had observed and was thinking. He’d sketch diagrams in the chart, for example, to help illustrate how we’d work though the toxic, metabolic, and infectious etiologies of acute liver failure. Sublime.
The act of writing also helps remind us there is a person attached to these words. Like a handwritten sympathy card, it is intimate, human. Even using our EMR, I’d still often type sentences that help tell the patient’s story. “Her sister just died. Utterly devastated. I’ll forward chart to Bob (her PCP) to check in on her.” Or: “Scratch golfer wants to know why he is getting so many SCCs now. ‘Like bankruptcy, gradually then suddenly,’ I explained. I think I broke through.”
Since we’ve concluded the purpose of a note is mostly to capture data, AI scribes are a godsend. They do so with remarkable quality and efficiency. We’ll just have to remember if the diagnosis is unclear, then it might help to write the note out yourself. And even when done by the AI machine, we might add human touches now and again lest there be no art left in what we do.
“For sale. Sun hat. Never worn.”
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on X. Write to him at dermnews@mdedge.com.
“We really aren’t taking care of records — we’re taking care of people.” — Dr. Lawrence Weed
What is the purpose of a progress note? Anyone? Yes, you there. “Insurance billing?” Yes, that’s a good one. Anyone else? “To remember what you did?” Excellent. Another? Yes, that’s right, for others to follow along in your care. These are all good reasons for a progress note to exist. But they aren’t the whole story. Let’s start at the beginning.
Charts were once a collection of paper sheets with handwritten notes. Sometimes illegible, sometimes beautiful, always efficient. A progress note back then could be just 10 characters, AK, LN2, X,X,X,X,X (with X’s marking nitrogen sprays). Then came the healthcare K-Pg event: the conversion to EMRs. Those doctors who survived evolved into computer programmers, creating blocks of text from a few keystrokes. But like toddler-sized Legos, the blocks made it impossible to build a note that is nuanced or precise. Worse yet, many notes consisting of blocks from one note added awkwardly to a new note, creating grotesque structures unrecognizable as anything that should exist in nature. Words and numbers, but no information.
Thanks to the eternity of EMR, these creations live on, hideous and useless. They waste not only the server’s energy but also our time. Few things are more maddening than scrolling to reach the bottom of another physician’s note only to find there is nothing there.
Whose fault is this? Anyone? Yes, that’s right, insurers. As there are probably no payers in this audience, let’s blame them. I agree, the crushing burden of documentation-to-get-reimbursed has forced us to create “notes” that add no value to us but add up points for us to get paid for them. CMS, payers, prior authorizations, and now even patients, it seems we are documenting for lots of people except for us. There isn’t time to satisfy all and this significant burden for every encounter is a proximate cause for doctors despair. Until now.
A fully formed, comprehensive, sometimes pretty note that satisfies all audiences. Dr. Larry Weed must be dancing in heaven. It was Dr. Weed who led us from the nicotine-stained logs of the 1950s to the powerful problem-based notes we use today, an innovation that rivals the stethoscope in its impact.
Professor Weed also predicted that computers would be important to capture and make sense of patient data, helping us make accurate diagnoses and efficient plans. Again, he was right. He would surely be advocating to take advantage of AI scribes’ marvelous ability to capture salient data and present it in the form of a problem-oriented medical record.
AI scribes will be ubiquitous soon; I’m fast and even for me they save time. They also allow, for the first time in a decade, to turn from the glow of a screen to actually face the patient – we no longer have to scribe and care simultaneously. Hallelujah. And yet, lest I disappoint you without a twist, it seems with AI scribes, like EMRs we lose a little something too.
Like self-driving cars or ChatGPT-generated letters, they remove cognitive loads. They are lovely when you have to multitask or are trying to recall a visit from hours (days) ago. Using them, you’ll feel faster, lighter, freer, happier. But what’s missing is the thinking. At the end, you have an exquisite note, but you didn’t write it. It has the salient points, but none of the mental work to create it. AI scribes subvert the valuable work of synthesis. That was the critical part of Dr. Weed’s discovery: writing problem-oriented notes helped us think better.
Writing allows for the friction that helps us process what is going on with a patient. It allows for the discovery of diagnoses and prompts plans. When I was an intern, one of my attendings would hand write notes, succinctly showing what he had observed and was thinking. He’d sketch diagrams in the chart, for example, to help illustrate how we’d work though the toxic, metabolic, and infectious etiologies of acute liver failure. Sublime.
The act of writing also helps remind us there is a person attached to these words. Like a handwritten sympathy card, it is intimate, human. Even using our EMR, I’d still often type sentences that help tell the patient’s story. “Her sister just died. Utterly devastated. I’ll forward chart to Bob (her PCP) to check in on her.” Or: “Scratch golfer wants to know why he is getting so many SCCs now. ‘Like bankruptcy, gradually then suddenly,’ I explained. I think I broke through.”
Since we’ve concluded the purpose of a note is mostly to capture data, AI scribes are a godsend. They do so with remarkable quality and efficiency. We’ll just have to remember if the diagnosis is unclear, then it might help to write the note out yourself. And even when done by the AI machine, we might add human touches now and again lest there be no art left in what we do.
“For sale. Sun hat. Never worn.”
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on X. Write to him at dermnews@mdedge.com.
Will Artificial Intelligence Replace Some Primary Care?
Within the next few years, patients will go to their primary care facility for a medical problem. They’ll be greeted by a nonhuman who speaks in the language of their choice. Based upon the initial interview, which will be taken in note form, the patient will be diagnosed, and a prescription called into the pharmacy. They’ll pay the robot at a reception kiosk, and their meds will be delivered via driverless car.
Or so suggests Allan Stewart, MD, medical director and chief of cardiothoracic surgery at HCA Florida Mercy Hospital in Miami.
The writing is on the wall. , he said.
If that sounds far too futuristic, buckle up. AI is already here and being used by most medical specialties. However, it’s primary care that stands to gain the most from this technology — right now — thanks to its ability to radically streamline patient care.
Seeing the Doctor and His or Her AI Assistant
AI is making doctors’ work lives easier, whether the technology helps with risk prevention and intervention or closing care gaps. It can also triage patient complaints, monitor patients remotely, or even perform digital health coaching to keep patients on track with their lifestyle regimens or monitor their health conditions.
Each of these AI components enables primary care physicians to reduce some of the paperwork requirements of their jobs and do what they were trained to do — listen and assess patients. Doctors currently spend 12 hours on average each week submitting prior authorization requests, according to an American Medical Association survey.
“Primary care can be overwhelming, especially today, with the advent of electronic records and data,” said Davin Lundquist, MD, a family medicine physician and chief medical officer at Augmedix, an automated medical documentation company that provides tools to reduce clinician burnout. “The amount of data we have to go through to try to get a complete and clear picture of our patients can be overwhelming on top of the referrals, administrative burdens, and regulatory requirements, which seem to be focused on the primary care space,” Dr. Lundquist said.
With an AI assist, primary care physicians can reduce their prep and pre-charting time, lessen the time needed for paperwork outside of clinic hours, and streamline information, including access to lab results, radiology reports, and consults.
“AI is already helping doctors manage their practices, make differential diagnoses, and input progress notes or histories,” said Dr. Stewart.
In Seattle, Ford Parsons, MD, chief of operational analytics at Providence Hospitals in Seattle, has been leading a generative AI project that recently developed a tool called Provaria to prioritize incoming messages from patients. The tool ensures that those with more urgent needs get immediate attention, and it supports the personnel who lead the responses.
The process begins with Provaria reviewing patient messages to ensure those with more urgent needs, such as a mental health crisis, get immediate attention instead of answering messages in the order they were received.
Provaria also provides resources to help responding staff craft a reply. If a patient’s message cites back pain, for example, the system might suggest a referral to a physical therapist, include a link to that department, and prompt the staff to ask about red flags that indicate a more urgent situation.
After an initial rollout, Providence recently deployed Provaria to manage the messages for all 4000 of its primary care, family medicine, and internal medicine providers. The system has reviewed and categorized more than 500,000 messages so far.
“This is another example where AI can increase the human connection in healthcare,” Dr. Parsons said. “That’s the opposite of what others are saying, but by using AI, you can automate the stuff that isn’t critical that doctors have wound up doing.”
AI Helps Foster Better Person-to-Person Communication
In recent years, the first thing most doctors do when they enter the exam room with a patient is log into the in-room computer and start to take notes — which can be off-putting to patients.
Now devices can ease this process, such as PLAUD, an AI voice recognition device that attaches to a cell phone. Just the size of a credit card, the device enables conversations to be easily recorded. It not only streamlines note-taking but also enables a physician to listen intently to a patient’s concerns instead of furiously jotting down notes.
“That device is already helping transcribe conversations into notes and then into a patient’s electronic medical record,” Dr. Stewart said. “This helps save doctors the work of having to input patient information.”
AI Can’t Be a Compassionate Human
The one thing AI can’t do is show compassion, at least not yet. The someday “vision” when a robot will gather intel about a patient’s symptoms and even offer a diagnosis does have some downsides. There is no replacement for human interaction, especially in the case of dire health news.
“If you have signs of a metastatic cancer and a nonhuman is delivering this news, there’s no way AI can share this news with compassion,” said Dr. Stewart.
For now, AI is becoming instrumental in helping reduce the number of extra demands on primary care doctors, as well as physicians in other specialties, so that they can continue focusing on what matters — healing patients.
A version of this article first appeared on Medscape.com.
Within the next few years, patients will go to their primary care facility for a medical problem. They’ll be greeted by a nonhuman who speaks in the language of their choice. Based upon the initial interview, which will be taken in note form, the patient will be diagnosed, and a prescription called into the pharmacy. They’ll pay the robot at a reception kiosk, and their meds will be delivered via driverless car.
Or so suggests Allan Stewart, MD, medical director and chief of cardiothoracic surgery at HCA Florida Mercy Hospital in Miami.
The writing is on the wall. , he said.
If that sounds far too futuristic, buckle up. AI is already here and being used by most medical specialties. However, it’s primary care that stands to gain the most from this technology — right now — thanks to its ability to radically streamline patient care.
Seeing the Doctor and His or Her AI Assistant
AI is making doctors’ work lives easier, whether the technology helps with risk prevention and intervention or closing care gaps. It can also triage patient complaints, monitor patients remotely, or even perform digital health coaching to keep patients on track with their lifestyle regimens or monitor their health conditions.
Each of these AI components enables primary care physicians to reduce some of the paperwork requirements of their jobs and do what they were trained to do — listen and assess patients. Doctors currently spend 12 hours on average each week submitting prior authorization requests, according to an American Medical Association survey.
“Primary care can be overwhelming, especially today, with the advent of electronic records and data,” said Davin Lundquist, MD, a family medicine physician and chief medical officer at Augmedix, an automated medical documentation company that provides tools to reduce clinician burnout. “The amount of data we have to go through to try to get a complete and clear picture of our patients can be overwhelming on top of the referrals, administrative burdens, and regulatory requirements, which seem to be focused on the primary care space,” Dr. Lundquist said.
With an AI assist, primary care physicians can reduce their prep and pre-charting time, lessen the time needed for paperwork outside of clinic hours, and streamline information, including access to lab results, radiology reports, and consults.
“AI is already helping doctors manage their practices, make differential diagnoses, and input progress notes or histories,” said Dr. Stewart.
In Seattle, Ford Parsons, MD, chief of operational analytics at Providence Hospitals in Seattle, has been leading a generative AI project that recently developed a tool called Provaria to prioritize incoming messages from patients. The tool ensures that those with more urgent needs get immediate attention, and it supports the personnel who lead the responses.
The process begins with Provaria reviewing patient messages to ensure those with more urgent needs, such as a mental health crisis, get immediate attention instead of answering messages in the order they were received.
Provaria also provides resources to help responding staff craft a reply. If a patient’s message cites back pain, for example, the system might suggest a referral to a physical therapist, include a link to that department, and prompt the staff to ask about red flags that indicate a more urgent situation.
After an initial rollout, Providence recently deployed Provaria to manage the messages for all 4000 of its primary care, family medicine, and internal medicine providers. The system has reviewed and categorized more than 500,000 messages so far.
“This is another example where AI can increase the human connection in healthcare,” Dr. Parsons said. “That’s the opposite of what others are saying, but by using AI, you can automate the stuff that isn’t critical that doctors have wound up doing.”
AI Helps Foster Better Person-to-Person Communication
In recent years, the first thing most doctors do when they enter the exam room with a patient is log into the in-room computer and start to take notes — which can be off-putting to patients.
Now devices can ease this process, such as PLAUD, an AI voice recognition device that attaches to a cell phone. Just the size of a credit card, the device enables conversations to be easily recorded. It not only streamlines note-taking but also enables a physician to listen intently to a patient’s concerns instead of furiously jotting down notes.
“That device is already helping transcribe conversations into notes and then into a patient’s electronic medical record,” Dr. Stewart said. “This helps save doctors the work of having to input patient information.”
AI Can’t Be a Compassionate Human
The one thing AI can’t do is show compassion, at least not yet. The someday “vision” when a robot will gather intel about a patient’s symptoms and even offer a diagnosis does have some downsides. There is no replacement for human interaction, especially in the case of dire health news.
“If you have signs of a metastatic cancer and a nonhuman is delivering this news, there’s no way AI can share this news with compassion,” said Dr. Stewart.
For now, AI is becoming instrumental in helping reduce the number of extra demands on primary care doctors, as well as physicians in other specialties, so that they can continue focusing on what matters — healing patients.
A version of this article first appeared on Medscape.com.
Within the next few years, patients will go to their primary care facility for a medical problem. They’ll be greeted by a nonhuman who speaks in the language of their choice. Based upon the initial interview, which will be taken in note form, the patient will be diagnosed, and a prescription called into the pharmacy. They’ll pay the robot at a reception kiosk, and their meds will be delivered via driverless car.
Or so suggests Allan Stewart, MD, medical director and chief of cardiothoracic surgery at HCA Florida Mercy Hospital in Miami.
The writing is on the wall. , he said.
If that sounds far too futuristic, buckle up. AI is already here and being used by most medical specialties. However, it’s primary care that stands to gain the most from this technology — right now — thanks to its ability to radically streamline patient care.
Seeing the Doctor and His or Her AI Assistant
AI is making doctors’ work lives easier, whether the technology helps with risk prevention and intervention or closing care gaps. It can also triage patient complaints, monitor patients remotely, or even perform digital health coaching to keep patients on track with their lifestyle regimens or monitor their health conditions.
Each of these AI components enables primary care physicians to reduce some of the paperwork requirements of their jobs and do what they were trained to do — listen and assess patients. Doctors currently spend 12 hours on average each week submitting prior authorization requests, according to an American Medical Association survey.
“Primary care can be overwhelming, especially today, with the advent of electronic records and data,” said Davin Lundquist, MD, a family medicine physician and chief medical officer at Augmedix, an automated medical documentation company that provides tools to reduce clinician burnout. “The amount of data we have to go through to try to get a complete and clear picture of our patients can be overwhelming on top of the referrals, administrative burdens, and regulatory requirements, which seem to be focused on the primary care space,” Dr. Lundquist said.
With an AI assist, primary care physicians can reduce their prep and pre-charting time, lessen the time needed for paperwork outside of clinic hours, and streamline information, including access to lab results, radiology reports, and consults.
“AI is already helping doctors manage their practices, make differential diagnoses, and input progress notes or histories,” said Dr. Stewart.
In Seattle, Ford Parsons, MD, chief of operational analytics at Providence Hospitals in Seattle, has been leading a generative AI project that recently developed a tool called Provaria to prioritize incoming messages from patients. The tool ensures that those with more urgent needs get immediate attention, and it supports the personnel who lead the responses.
The process begins with Provaria reviewing patient messages to ensure those with more urgent needs, such as a mental health crisis, get immediate attention instead of answering messages in the order they were received.
Provaria also provides resources to help responding staff craft a reply. If a patient’s message cites back pain, for example, the system might suggest a referral to a physical therapist, include a link to that department, and prompt the staff to ask about red flags that indicate a more urgent situation.
After an initial rollout, Providence recently deployed Provaria to manage the messages for all 4000 of its primary care, family medicine, and internal medicine providers. The system has reviewed and categorized more than 500,000 messages so far.
“This is another example where AI can increase the human connection in healthcare,” Dr. Parsons said. “That’s the opposite of what others are saying, but by using AI, you can automate the stuff that isn’t critical that doctors have wound up doing.”
AI Helps Foster Better Person-to-Person Communication
In recent years, the first thing most doctors do when they enter the exam room with a patient is log into the in-room computer and start to take notes — which can be off-putting to patients.
Now devices can ease this process, such as PLAUD, an AI voice recognition device that attaches to a cell phone. Just the size of a credit card, the device enables conversations to be easily recorded. It not only streamlines note-taking but also enables a physician to listen intently to a patient’s concerns instead of furiously jotting down notes.
“That device is already helping transcribe conversations into notes and then into a patient’s electronic medical record,” Dr. Stewart said. “This helps save doctors the work of having to input patient information.”
AI Can’t Be a Compassionate Human
The one thing AI can’t do is show compassion, at least not yet. The someday “vision” when a robot will gather intel about a patient’s symptoms and even offer a diagnosis does have some downsides. There is no replacement for human interaction, especially in the case of dire health news.
“If you have signs of a metastatic cancer and a nonhuman is delivering this news, there’s no way AI can share this news with compassion,” said Dr. Stewart.
For now, AI is becoming instrumental in helping reduce the number of extra demands on primary care doctors, as well as physicians in other specialties, so that they can continue focusing on what matters — healing patients.
A version of this article first appeared on Medscape.com.
Giving Cash to Improve Health
This transcript has been edited for clarity.
It doesn’t really matter what disease you are looking at — cancer, heart disease, dementia, drug abuse, psychiatric disorders. In every case, poverty is associated with worse disease.
But the word “associated” is doing a lot of work there. Many of us feel that poverty itself is causally linked to worse disease outcomes through things like poor access to care and poor access to medicines.
And there is an argument that the arrow goes the other way; perhaps people with worse illness are more likely to be poor because, in this country at least, being sick is incredibly expensive.
Causality is what all medical research is fundamentally about. We want to know if A causes B, because if A causes B, then changing A changes B. If poverty causes bad health outcomes, then alleviating poverty should alleviate bad health outcomes.
But that’s a hard proposition to test. You can’t exactly randomize some people to get extra money and some not to, right? Actually, you can. And in Massachusetts, they did.
What happened in Chelsea, Massachusetts, wasn’t exactly a randomized trial of cash supplementation to avoid bad health outcomes. It was actually a government program instituted during the pandemic. Chelsea has a large immigrant population, many of whom are living in poverty. From April to August 2020, the city ran a food distribution program to aid those in need. But the decision was then made to convert the money spent on that program to cash distributions — free of obligations. Chelsea residents making less than 30% of the median income for the Boston metro area — around $30,000 per family — were invited to enter a lottery. Only one member of any given family could enter. If selected, an individual would receive $200 a month, or $300 for a family of two, or $400 for a family of three or more. These payments went on for about 9 months.
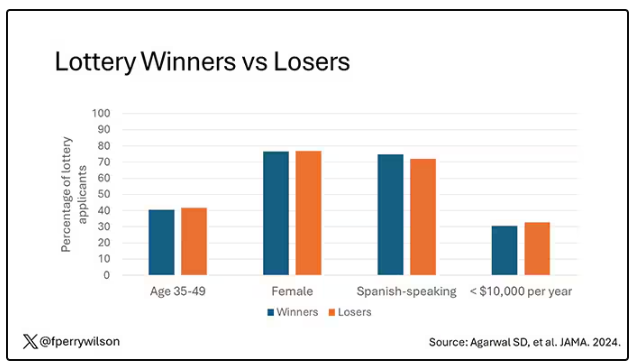
The key thing here is that not everyone won the lottery. The lottery picked winners randomly; 1746 individuals were selected to receive the benefits in the form of a reloadable gift card, and 1134 applied but did not receive any assistance.
This is a perfect natural experiment. As you can see here — and as expected, given that the lottery winners were chosen randomly — winners and losers were similar in terms of age, sex, race, language, income, and more.
Researchers, led by Sumit Agarwal at the Brigham, leveraged that randomization to ask how these cash benefits would affect healthcare utilization. Their results appeared this week in JAMA.
I know what you’re thinking: Is $400 a month really enough to make a difference? Does $400 a month, less than $5000 a year, really fix poverty? We’ll get to that. But I will point out that the average family income of individuals in this study was about $1400 a month. An extra $400 might not change someone’s life, but it may really make a difference.
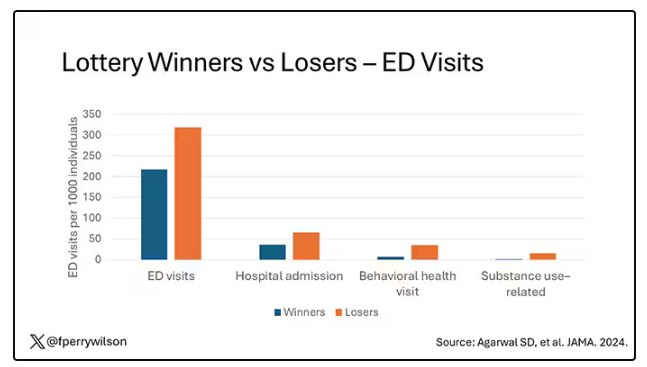
The primary outcome of this study was ED visits. There are a few ways this could go. Perhaps the money would lead to improved health and thus fewer ED visits. Or perhaps it would help people get transportation to primary care or other services that would offload the ED. Or maybe it would make things worse. Some folks have suggested that cash payments could increase the use of drugs and alcohol, and lead to more ED visits associated with the complications of using those substances.
Here are the actual data. Per 1000 individuals, there were 217 ED visits in the cash-benefit group, 318 in the no-benefit group. That was a statistically significant finding.
Breaking those ED visits down, you can see that fewer visits resulted in hospital admission, with fewer behavioral health–related visits and — a key finding — fewer visits for substance use disorder. This puts the lie to the idea that cash benefits increase drug use.
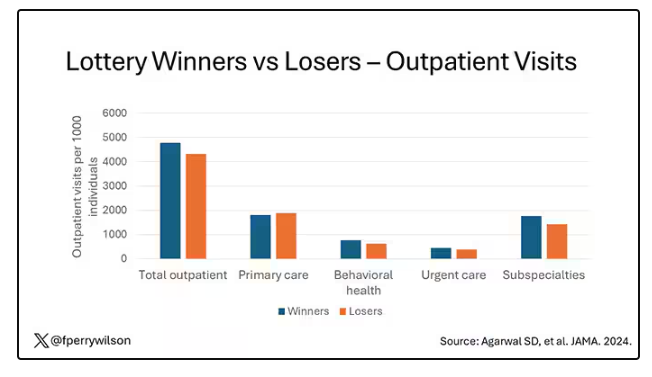
But the authors also looked at other causes of healthcare utilization. Outpatient visits were slightly higher in the cash-benefit group, driven largely by an increase in specialty care visits. The authors note that this is likely due to the fact that reaching a specialist often requires more travel, which can be costly. Indeed, this effect was most pronounced among the people living furthest from a specialty center.
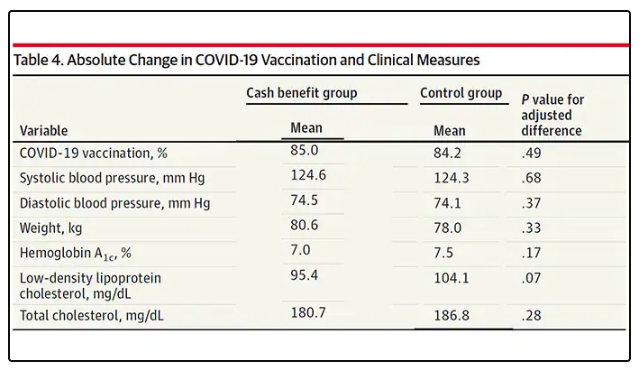
Outside of utilization, the researchers examined a variety of individual health markers — things like blood pressure — to see if the cash benefit had any effect. A bit of caution here because these data were available only among those who interacted with the healthcare system, which may bias the results a bit. Regardless, no major differences were seen in blood pressure, weight, hemoglobin A1c, cholesterol, or COVID vaccination.
So, it seems that $400 a month doesn’t move the needle too much on risk factors for cardiovascular disease, but the effect on ED visits on their own is fairly impressive.
Is it worth it? The authors did their best to calculate the net effect of this program, accounting for the reduced ED visits and hospitalizations (that’s a big one), but also for the increased number of specialty visits. All told, the program saves about $450 per person in healthcare costs over 9 months. That’s about one seventh of the cost of the overall program.
But remember that they only looked at outcomes for the individual who got the gift cards; it’s likely that there were benefits to their family members as well. And, of course, programs like this can recoup costs indirectly though increases in economic activity, a phenomenon known as the multiplier effect.
I’m not here to tell you whether this program was a good idea; people tend to have quite strong feelings about this sort of thing. But I can tell you what it tells me about healthcare in America. It may not be surprising, but it confirms that access is far from fairly distributed.
I started this story asking about the arrow of causality between poverty and poor health. The truth is, you probably have causality in both directions.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
It doesn’t really matter what disease you are looking at — cancer, heart disease, dementia, drug abuse, psychiatric disorders. In every case, poverty is associated with worse disease.
But the word “associated” is doing a lot of work there. Many of us feel that poverty itself is causally linked to worse disease outcomes through things like poor access to care and poor access to medicines.
And there is an argument that the arrow goes the other way; perhaps people with worse illness are more likely to be poor because, in this country at least, being sick is incredibly expensive.
Causality is what all medical research is fundamentally about. We want to know if A causes B, because if A causes B, then changing A changes B. If poverty causes bad health outcomes, then alleviating poverty should alleviate bad health outcomes.
But that’s a hard proposition to test. You can’t exactly randomize some people to get extra money and some not to, right? Actually, you can. And in Massachusetts, they did.
What happened in Chelsea, Massachusetts, wasn’t exactly a randomized trial of cash supplementation to avoid bad health outcomes. It was actually a government program instituted during the pandemic. Chelsea has a large immigrant population, many of whom are living in poverty. From April to August 2020, the city ran a food distribution program to aid those in need. But the decision was then made to convert the money spent on that program to cash distributions — free of obligations. Chelsea residents making less than 30% of the median income for the Boston metro area — around $30,000 per family — were invited to enter a lottery. Only one member of any given family could enter. If selected, an individual would receive $200 a month, or $300 for a family of two, or $400 for a family of three or more. These payments went on for about 9 months.
The key thing here is that not everyone won the lottery. The lottery picked winners randomly; 1746 individuals were selected to receive the benefits in the form of a reloadable gift card, and 1134 applied but did not receive any assistance.
This is a perfect natural experiment. As you can see here — and as expected, given that the lottery winners were chosen randomly — winners and losers were similar in terms of age, sex, race, language, income, and more.
Researchers, led by Sumit Agarwal at the Brigham, leveraged that randomization to ask how these cash benefits would affect healthcare utilization. Their results appeared this week in JAMA.
I know what you’re thinking: Is $400 a month really enough to make a difference? Does $400 a month, less than $5000 a year, really fix poverty? We’ll get to that. But I will point out that the average family income of individuals in this study was about $1400 a month. An extra $400 might not change someone’s life, but it may really make a difference.
The primary outcome of this study was ED visits. There are a few ways this could go. Perhaps the money would lead to improved health and thus fewer ED visits. Or perhaps it would help people get transportation to primary care or other services that would offload the ED. Or maybe it would make things worse. Some folks have suggested that cash payments could increase the use of drugs and alcohol, and lead to more ED visits associated with the complications of using those substances.
Here are the actual data. Per 1000 individuals, there were 217 ED visits in the cash-benefit group, 318 in the no-benefit group. That was a statistically significant finding.
Breaking those ED visits down, you can see that fewer visits resulted in hospital admission, with fewer behavioral health–related visits and — a key finding — fewer visits for substance use disorder. This puts the lie to the idea that cash benefits increase drug use.
But the authors also looked at other causes of healthcare utilization. Outpatient visits were slightly higher in the cash-benefit group, driven largely by an increase in specialty care visits. The authors note that this is likely due to the fact that reaching a specialist often requires more travel, which can be costly. Indeed, this effect was most pronounced among the people living furthest from a specialty center.
Outside of utilization, the researchers examined a variety of individual health markers — things like blood pressure — to see if the cash benefit had any effect. A bit of caution here because these data were available only among those who interacted with the healthcare system, which may bias the results a bit. Regardless, no major differences were seen in blood pressure, weight, hemoglobin A1c, cholesterol, or COVID vaccination.
So, it seems that $400 a month doesn’t move the needle too much on risk factors for cardiovascular disease, but the effect on ED visits on their own is fairly impressive.
Is it worth it? The authors did their best to calculate the net effect of this program, accounting for the reduced ED visits and hospitalizations (that’s a big one), but also for the increased number of specialty visits. All told, the program saves about $450 per person in healthcare costs over 9 months. That’s about one seventh of the cost of the overall program.
But remember that they only looked at outcomes for the individual who got the gift cards; it’s likely that there were benefits to their family members as well. And, of course, programs like this can recoup costs indirectly though increases in economic activity, a phenomenon known as the multiplier effect.
I’m not here to tell you whether this program was a good idea; people tend to have quite strong feelings about this sort of thing. But I can tell you what it tells me about healthcare in America. It may not be surprising, but it confirms that access is far from fairly distributed.
I started this story asking about the arrow of causality between poverty and poor health. The truth is, you probably have causality in both directions.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
It doesn’t really matter what disease you are looking at — cancer, heart disease, dementia, drug abuse, psychiatric disorders. In every case, poverty is associated with worse disease.
But the word “associated” is doing a lot of work there. Many of us feel that poverty itself is causally linked to worse disease outcomes through things like poor access to care and poor access to medicines.
And there is an argument that the arrow goes the other way; perhaps people with worse illness are more likely to be poor because, in this country at least, being sick is incredibly expensive.
Causality is what all medical research is fundamentally about. We want to know if A causes B, because if A causes B, then changing A changes B. If poverty causes bad health outcomes, then alleviating poverty should alleviate bad health outcomes.
But that’s a hard proposition to test. You can’t exactly randomize some people to get extra money and some not to, right? Actually, you can. And in Massachusetts, they did.
What happened in Chelsea, Massachusetts, wasn’t exactly a randomized trial of cash supplementation to avoid bad health outcomes. It was actually a government program instituted during the pandemic. Chelsea has a large immigrant population, many of whom are living in poverty. From April to August 2020, the city ran a food distribution program to aid those in need. But the decision was then made to convert the money spent on that program to cash distributions — free of obligations. Chelsea residents making less than 30% of the median income for the Boston metro area — around $30,000 per family — were invited to enter a lottery. Only one member of any given family could enter. If selected, an individual would receive $200 a month, or $300 for a family of two, or $400 for a family of three or more. These payments went on for about 9 months.
The key thing here is that not everyone won the lottery. The lottery picked winners randomly; 1746 individuals were selected to receive the benefits in the form of a reloadable gift card, and 1134 applied but did not receive any assistance.
This is a perfect natural experiment. As you can see here — and as expected, given that the lottery winners were chosen randomly — winners and losers were similar in terms of age, sex, race, language, income, and more.
Researchers, led by Sumit Agarwal at the Brigham, leveraged that randomization to ask how these cash benefits would affect healthcare utilization. Their results appeared this week in JAMA.
I know what you’re thinking: Is $400 a month really enough to make a difference? Does $400 a month, less than $5000 a year, really fix poverty? We’ll get to that. But I will point out that the average family income of individuals in this study was about $1400 a month. An extra $400 might not change someone’s life, but it may really make a difference.
The primary outcome of this study was ED visits. There are a few ways this could go. Perhaps the money would lead to improved health and thus fewer ED visits. Or perhaps it would help people get transportation to primary care or other services that would offload the ED. Or maybe it would make things worse. Some folks have suggested that cash payments could increase the use of drugs and alcohol, and lead to more ED visits associated with the complications of using those substances.
Here are the actual data. Per 1000 individuals, there were 217 ED visits in the cash-benefit group, 318 in the no-benefit group. That was a statistically significant finding.
Breaking those ED visits down, you can see that fewer visits resulted in hospital admission, with fewer behavioral health–related visits and — a key finding — fewer visits for substance use disorder. This puts the lie to the idea that cash benefits increase drug use.
But the authors also looked at other causes of healthcare utilization. Outpatient visits were slightly higher in the cash-benefit group, driven largely by an increase in specialty care visits. The authors note that this is likely due to the fact that reaching a specialist often requires more travel, which can be costly. Indeed, this effect was most pronounced among the people living furthest from a specialty center.
Outside of utilization, the researchers examined a variety of individual health markers — things like blood pressure — to see if the cash benefit had any effect. A bit of caution here because these data were available only among those who interacted with the healthcare system, which may bias the results a bit. Regardless, no major differences were seen in blood pressure, weight, hemoglobin A1c, cholesterol, or COVID vaccination.
So, it seems that $400 a month doesn’t move the needle too much on risk factors for cardiovascular disease, but the effect on ED visits on their own is fairly impressive.
Is it worth it? The authors did their best to calculate the net effect of this program, accounting for the reduced ED visits and hospitalizations (that’s a big one), but also for the increased number of specialty visits. All told, the program saves about $450 per person in healthcare costs over 9 months. That’s about one seventh of the cost of the overall program.
But remember that they only looked at outcomes for the individual who got the gift cards; it’s likely that there were benefits to their family members as well. And, of course, programs like this can recoup costs indirectly though increases in economic activity, a phenomenon known as the multiplier effect.
I’m not here to tell you whether this program was a good idea; people tend to have quite strong feelings about this sort of thing. But I can tell you what it tells me about healthcare in America. It may not be surprising, but it confirms that access is far from fairly distributed.
I started this story asking about the arrow of causality between poverty and poor health. The truth is, you probably have causality in both directions.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Doctor on Death Row: Ahmad Reza Djalali Begins Hunger Strike
Ahmad Reza Djalali, an Iranian-Swedish physician specializing in disaster medicine, has begun a hunger strike after being sentenced to death in 2017.
Last year, Iran set a grim record, leading the world in executions. The country carried out at least 853 executions, which accounted for three quarters of the officially recorded executions worldwide. The Iranian government uses the death penalty to intimidate political opponents, especially since the women’s uprising in 2022, and to exert pressure on Western states in diplomatic standoffs.
He emigrated to Sweden in 2009 and joined the Karolinska Institutet in Stockholm, Sweden. Over the years, he became one of Europe’s leading experts in disaster medicine. His work has been cited more than 700 times in medical literature, and he played a key role in establishing the emergency and disaster research center at the University of Piedmont.
In Italy, Denmark, and Sweden, Dr. Djalali helped hospitals and healthcare professionals in preparing for earthquakes, nuclear accidents, and terrorist attacks and designed several disaster medicine training programs.
‘Spreading Corruption’
Despite settling in Sweden with his family, Dr. Djalali never forgot his Iranian roots. His doctoral thesis was dedicated to the victims of the 2003 Bam earthquake in Iran, which killed 23,000 people. He expressed a desire to share his knowledge with his Iranian colleagues to help people. So when he was invited to participate in a 2016 conference at the University of Tehran, he accepted without hesitation.
Unfortunately, this decision had severe consequences. On April 25, 2016, as he was concluding his trip to Iran, the researcher was arrested by intelligence agents. After being held incommunicado for several days, he was officially accused of passing confidential information to Israeli intelligence services. According to his family, this accusation was baseless. They believed he was targeted for refusing to work for Iranian intelligence services in Europe.
On October 21, 2017, Dr. Djalali was sentenced to death for “spreading corruption on Earth,” a vague charge often used by Islamic courts against those who allegedly have challenged the regime. A few days later, a video of his “confessions” was broadcast on Iranian television. These confessions were coerced; Dr. Djalali later revealed that Iranian police had threatened to harm his mother in Iran and his family in Sweden.
Since then, Dr. Djalali and his loved ones have anxiously awaited the moment when the regime might carry out the sentence. Several times over the years, he has seemed on the verge of execution, only to receive a last-minute reprieve each time.
His imprisonment has taken a severe toll on his physical and mental health. He has reportedly lost 24 kg since his incarceration, and his family, who receive sporadic updates, suspect he has leukemia. Despite his deteriorating condition, the authorities have refused him access to a hematologist.
‘Forgotten’ in Exchange
The international medical community has rallied to secure Dr. Djalali’s release, but their efforts have so far been fruitless. The United Nations, the European Union, Amnesty International, several universities, and the World Medical Association have called for his release. In 2018, Sweden granted him citizenship in an attempt to increase pressure on Tehran, but Iranian law does not recognize dual citizenship.
On June 16, after nearly 7 years on death row, Dr. Djalali informed his family that he had begun a hunger strike. “It’s the only way to make my voice heard in the world,” he explained. “As a doctor, Ahmad Reza knows all too well that his fragile physical state makes a hunger strike potentially fatal, but he sees no other option. He suffers from cardiac arrhythmia, bradycardia, hypotension, chronic gastritis, anemia, and extreme weight loss following his two previous hunger strikes,” his wife told the press.
Aside from a potential (and unlikely) act of clemency by the Iranian authorities, Dr. Djalali’s best hope lies in a prisoner exchange. The Iranian government often imprisons foreign nationals to exchange them for Iranians detained in Western countries.
On June 15, Sweden agreed to release an Iranian dignitary serving a life sentence in exchange for the release of Swedish nationals detained in Iran. For a long time, Dr. Djalali’s family had hoped he would be included in this exchange.
However, to avoid jeopardizing the deal, the Swedish prime minister chose to accept the release of only two other Swedish nationals, leaving Dr. Djalali to his grim fate. “Mr Prime Minister, you have decided to abandon me at the enormous risk of being executed,” Dr. Djalali responded bitterly, knowing he could be hanged at any moment.
This story was translated from JIM using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Ahmad Reza Djalali, an Iranian-Swedish physician specializing in disaster medicine, has begun a hunger strike after being sentenced to death in 2017.
Last year, Iran set a grim record, leading the world in executions. The country carried out at least 853 executions, which accounted for three quarters of the officially recorded executions worldwide. The Iranian government uses the death penalty to intimidate political opponents, especially since the women’s uprising in 2022, and to exert pressure on Western states in diplomatic standoffs.
He emigrated to Sweden in 2009 and joined the Karolinska Institutet in Stockholm, Sweden. Over the years, he became one of Europe’s leading experts in disaster medicine. His work has been cited more than 700 times in medical literature, and he played a key role in establishing the emergency and disaster research center at the University of Piedmont.
In Italy, Denmark, and Sweden, Dr. Djalali helped hospitals and healthcare professionals in preparing for earthquakes, nuclear accidents, and terrorist attacks and designed several disaster medicine training programs.
‘Spreading Corruption’
Despite settling in Sweden with his family, Dr. Djalali never forgot his Iranian roots. His doctoral thesis was dedicated to the victims of the 2003 Bam earthquake in Iran, which killed 23,000 people. He expressed a desire to share his knowledge with his Iranian colleagues to help people. So when he was invited to participate in a 2016 conference at the University of Tehran, he accepted without hesitation.
Unfortunately, this decision had severe consequences. On April 25, 2016, as he was concluding his trip to Iran, the researcher was arrested by intelligence agents. After being held incommunicado for several days, he was officially accused of passing confidential information to Israeli intelligence services. According to his family, this accusation was baseless. They believed he was targeted for refusing to work for Iranian intelligence services in Europe.
On October 21, 2017, Dr. Djalali was sentenced to death for “spreading corruption on Earth,” a vague charge often used by Islamic courts against those who allegedly have challenged the regime. A few days later, a video of his “confessions” was broadcast on Iranian television. These confessions were coerced; Dr. Djalali later revealed that Iranian police had threatened to harm his mother in Iran and his family in Sweden.
Since then, Dr. Djalali and his loved ones have anxiously awaited the moment when the regime might carry out the sentence. Several times over the years, he has seemed on the verge of execution, only to receive a last-minute reprieve each time.
His imprisonment has taken a severe toll on his physical and mental health. He has reportedly lost 24 kg since his incarceration, and his family, who receive sporadic updates, suspect he has leukemia. Despite his deteriorating condition, the authorities have refused him access to a hematologist.
‘Forgotten’ in Exchange
The international medical community has rallied to secure Dr. Djalali’s release, but their efforts have so far been fruitless. The United Nations, the European Union, Amnesty International, several universities, and the World Medical Association have called for his release. In 2018, Sweden granted him citizenship in an attempt to increase pressure on Tehran, but Iranian law does not recognize dual citizenship.
On June 16, after nearly 7 years on death row, Dr. Djalali informed his family that he had begun a hunger strike. “It’s the only way to make my voice heard in the world,” he explained. “As a doctor, Ahmad Reza knows all too well that his fragile physical state makes a hunger strike potentially fatal, but he sees no other option. He suffers from cardiac arrhythmia, bradycardia, hypotension, chronic gastritis, anemia, and extreme weight loss following his two previous hunger strikes,” his wife told the press.
Aside from a potential (and unlikely) act of clemency by the Iranian authorities, Dr. Djalali’s best hope lies in a prisoner exchange. The Iranian government often imprisons foreign nationals to exchange them for Iranians detained in Western countries.
On June 15, Sweden agreed to release an Iranian dignitary serving a life sentence in exchange for the release of Swedish nationals detained in Iran. For a long time, Dr. Djalali’s family had hoped he would be included in this exchange.
However, to avoid jeopardizing the deal, the Swedish prime minister chose to accept the release of only two other Swedish nationals, leaving Dr. Djalali to his grim fate. “Mr Prime Minister, you have decided to abandon me at the enormous risk of being executed,” Dr. Djalali responded bitterly, knowing he could be hanged at any moment.
This story was translated from JIM using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Ahmad Reza Djalali, an Iranian-Swedish physician specializing in disaster medicine, has begun a hunger strike after being sentenced to death in 2017.
Last year, Iran set a grim record, leading the world in executions. The country carried out at least 853 executions, which accounted for three quarters of the officially recorded executions worldwide. The Iranian government uses the death penalty to intimidate political opponents, especially since the women’s uprising in 2022, and to exert pressure on Western states in diplomatic standoffs.
He emigrated to Sweden in 2009 and joined the Karolinska Institutet in Stockholm, Sweden. Over the years, he became one of Europe’s leading experts in disaster medicine. His work has been cited more than 700 times in medical literature, and he played a key role in establishing the emergency and disaster research center at the University of Piedmont.
In Italy, Denmark, and Sweden, Dr. Djalali helped hospitals and healthcare professionals in preparing for earthquakes, nuclear accidents, and terrorist attacks and designed several disaster medicine training programs.
‘Spreading Corruption’
Despite settling in Sweden with his family, Dr. Djalali never forgot his Iranian roots. His doctoral thesis was dedicated to the victims of the 2003 Bam earthquake in Iran, which killed 23,000 people. He expressed a desire to share his knowledge with his Iranian colleagues to help people. So when he was invited to participate in a 2016 conference at the University of Tehran, he accepted without hesitation.
Unfortunately, this decision had severe consequences. On April 25, 2016, as he was concluding his trip to Iran, the researcher was arrested by intelligence agents. After being held incommunicado for several days, he was officially accused of passing confidential information to Israeli intelligence services. According to his family, this accusation was baseless. They believed he was targeted for refusing to work for Iranian intelligence services in Europe.
On October 21, 2017, Dr. Djalali was sentenced to death for “spreading corruption on Earth,” a vague charge often used by Islamic courts against those who allegedly have challenged the regime. A few days later, a video of his “confessions” was broadcast on Iranian television. These confessions were coerced; Dr. Djalali later revealed that Iranian police had threatened to harm his mother in Iran and his family in Sweden.
Since then, Dr. Djalali and his loved ones have anxiously awaited the moment when the regime might carry out the sentence. Several times over the years, he has seemed on the verge of execution, only to receive a last-minute reprieve each time.
His imprisonment has taken a severe toll on his physical and mental health. He has reportedly lost 24 kg since his incarceration, and his family, who receive sporadic updates, suspect he has leukemia. Despite his deteriorating condition, the authorities have refused him access to a hematologist.
‘Forgotten’ in Exchange
The international medical community has rallied to secure Dr. Djalali’s release, but their efforts have so far been fruitless. The United Nations, the European Union, Amnesty International, several universities, and the World Medical Association have called for his release. In 2018, Sweden granted him citizenship in an attempt to increase pressure on Tehran, but Iranian law does not recognize dual citizenship.
On June 16, after nearly 7 years on death row, Dr. Djalali informed his family that he had begun a hunger strike. “It’s the only way to make my voice heard in the world,” he explained. “As a doctor, Ahmad Reza knows all too well that his fragile physical state makes a hunger strike potentially fatal, but he sees no other option. He suffers from cardiac arrhythmia, bradycardia, hypotension, chronic gastritis, anemia, and extreme weight loss following his two previous hunger strikes,” his wife told the press.
Aside from a potential (and unlikely) act of clemency by the Iranian authorities, Dr. Djalali’s best hope lies in a prisoner exchange. The Iranian government often imprisons foreign nationals to exchange them for Iranians detained in Western countries.
On June 15, Sweden agreed to release an Iranian dignitary serving a life sentence in exchange for the release of Swedish nationals detained in Iran. For a long time, Dr. Djalali’s family had hoped he would be included in this exchange.
However, to avoid jeopardizing the deal, the Swedish prime minister chose to accept the release of only two other Swedish nationals, leaving Dr. Djalali to his grim fate. “Mr Prime Minister, you have decided to abandon me at the enormous risk of being executed,” Dr. Djalali responded bitterly, knowing he could be hanged at any moment.
This story was translated from JIM using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Greater Transparency of Oncologists’ Pharma Relationships Needed
The findings reflect limited awareness in low-income countries about what scenarios constitute a conflict of interest, first author, Khalid El Bairi, MD, said during an interview. “There is a lack of training in ethics and integrity in medical schools [in countries in Africa], so people are not informed about conflicts of interest,” continued Dr. El Bairi, who presented the new research at the annual meeting of the American Society of Clinical Oncology. “There is also a lack of policies in universities and hospitals to guide clinicians about conflict of interest reporting.”
Overall, 58.5% of survey participants categorized honoraria as a conflict of interest that required disclosure, while 50% said the same of gifts from pharmaceutical representatives, and 44.5% identified travel grants for attending conferences as conflicts of interests. The report was published in JCO Global Oncology. Less often considered conflicts of interest were personal and institutional research funding, trips to conferences, consulting or advisory roles, food and beverages, expert testimony, and sample drugs provided by the pharmaceutical industry.
Just 24% of participants indicated that all of the listed items were deemed conflicts of interest. The survey — called Oncology Transparency Under Scrutiny and Tracking, or ONCOTRUST-1 — considered the perceptions of 200 oncologists, about 70% of whom practice in low- and middle-income countries.
What’s more, 37.5% of respondents identified fear of losing financial support as a reason not to report a conflict of interest. Still, 75% indicated that industry-sponsored speaking does not affect treatment decisions, and 60% said conflicts of interest do not impair objective appraisal of clinical trials.
Dr. El Bairi, a research associate in the department of medical oncology at Mohammed VI University Hospital, Oujda, Morocco, and his colleagues undertook the study in part because of an editorial published in The Lancet Oncology last year. First author Fidel Rubagumya, MD, a consultant oncologist and director of research at Rwanda Military Hospital, Kigali, and colleagues called for more research on the ties between oncologists and industry in Africa. The ONCOTRUST-1 findings set the stage for a planned follow-up study, which aims to compare views surrounding conflicts of interests between oncologists in different economic settings.
Open Payments Houses US Physicians’ Conflicts of Interest
To be sure, many authors of research published in major US journals are based outside of the United States. According to JAMA Network Open, 69% of submissions to the journal are from international authors. However, Dr. El Bairi also raised other potential signs of industry influence that he said need global discussion, such as the role of pharmaceutical companies in presentations of clinical trial findings at large cancer societies’ conferences, a shift toward progression-free survival as the endpoint in clinical cancer trials, and the rise of third-party writing assistance.
“There are two sides of the story,” Dr. El Bairi said. “The good side is that unfortunately, sometimes [industry money is] the only way for African oncologists to go abroad for training, to conferences for their continuous medical education. The bad is now we may harm patients, we might harm science by having conflicts of interest not reported.”
Unlike other countries, the United States has plentiful data on the scale of physicians’ financial conflicts of interest in the form of the Open Payments platform. Championed by Sen. Chuck Grassley (R-Iowa), the federal repository of payments to doctors and teaching hospitals by drug and medical device companies was established as part of the Affordable Care Act (ACA).
The health care reform law, which passed in 2010, requires pharmaceutical companies and medical device makers to report this information.
From 2013 to 2021, the pharmaceutical and medical device industry paid physicians $12.1 billion, according to a research letter published in JAMA in March of 2024 that reviewed Open Payments data.
Ranked by specialty, hematologists and oncologists received the fourth-largest amount of money in aggregate, the study shows. Their total of $825.8 million trailed only physicians in orthopedics ($1.36 billion), neurology and psychiatry ($1.32 billion) and cardiology ($1.29 billion). What’s more, this specialty had the biggest share of physicians taking industry money, with 74.2% of hematologists and oncologists receiving payments.
The payments from industry include fees for consulting services and speaking, as well as food and beverages, travel and lodging, education, gifts, grants, and honoraria.
Joseph S. Ross, MD, MHS, one of the JAMA study’s coauthors, said in an interview that the continued prevalence of such funding runs counter to the expectation behind the measure, which was that transparency would lead to physicians’ becoming less likely to accept a payment.
“We as a profession need to take a cold hard look in the mirror,” he said, referring to physicians in general.
Dr. Ross, professor of medicine at Yale University School of Medicine, New Haven, Connecticut, said he hopes that the profession will self-police, and that patients will make a bigger deal of the issue. Still, he acknowledged that “the vast majority” of patient advocacy groups, too, are funded by the pharmaceutical industry.
Exposing Industry Payments May Have Perverse Effect
A growing body of research explores the effect that physicians’ financial relationships with pharmaceutical companies can have on their prescribing practices. Indeed, oncologists taking industry payments seem to be more likely to prescribe nonrecommended and low-value drugs in some clinical settings, according to a study published in The BMJ last year.
That study’s first author, Aaron P. Mitchell, MD, a medical oncologist and assistant attending physician at Memorial Sloan Kettering Cancer Center, New York City, suggested in an interview that exposing industry payments to the sunlight may have had a perverse effect on physicians.
“There’s this idea of having license to do something,” Dr. Mitchell said, speaking broadly about human psychology rather than drawing on empirical data. “You might feel a little less bad about then prescribing more of that company’s drug, because the disclosure has already been done.”
The influence of pharmaceutical industry money on oncologists goes beyond what’s prescribed to which treatments get studied, approved, and recommended by guidelines, Dr. Mitchell said. He was also first author of a 2016 paper published in JAMA Oncology that found 86% of authors of the National Comprehensive Cancer Network guidelines had at least one conflict of interest reported on Open Systems in 2014.
Meanwhile, the fact that physicians’ payments from industry are a matter of public record on Open Systems has not guaranteed that doctors will disclose their conflicts of interest in other forums. A study published in JAMA earlier this year, for which Dr. Mitchell served as first author, found that almost one in three physicians endorsing drugs and devices on the social media platform X failed to disclose that the manufacturer paid them.
The lack of disclosure seems to extend beyond social media. A 2018 study published in JAMA Oncology found that 32% of oncologist authors of clinical drug trials for drugs approved over a 20-month period from 2016 to 2017 did not fully disclose payments from the trial sponsor when checked against the Open Payments database.
A lion’s share of industry payments within oncology appears to be going to a small group of high-profile physicians, suggested a 2022 study published in JCO Oncology Practice. It found that just 1% of all US oncologists accounted for 37% of industry payments, with each receiving more than $100,000 a year.
Experts: Professional Societies Should Further Limit Industry Payments
While partnerships between drug companies and physicians are necessary and have often been positive, more than disclosure is needed to minimize the risk of patient harm, according to an editorial published in March in JCO Oncology Practice. In it, Nina Niu Sanford, MD, a radiation oncologist UT Southwestern Medical Center, Dallas, and Bishal Gyawali, MD, PhD, a medical oncologist at Queen’s University, Kingston, Ontario, Canada, argue that following a specific blueprint could help mitigate financial conflicts of interest.
For starters, Dr. Sanford and Dr. Gyawali contend in the editorial that the maximum general payment NCCN members are allowed to receive from industry should be $0, compared with a current bar of $20,000 from a single entity or $50,000 from all external entities combined. They also urge professional societies to follow the current policy of the American Society of Clinical Oncology and ban members serving in their leadership from receiving any general payments from the industry.
The authors further suggest that investigators of clinical trials should be barred from holding stock for the drug or product while it is under study and that editorialists should not have conflicts of interest with the company whose drug or product they are discussing.
Pharmaceutical money can harm patients in ways that are not always obvious, Dr. Gyawali said in an interview.
“It can dominate the conversation by removing critical viewpoints from these top people about certain drugs,” he said. “It’s not always about saying good things about the drug.”
For instance, he suggested, a doctor receiving payments from Pfizer might openly criticize perceived flaws in drugs from other companies but refrain from weighing in negatively on a Pfizer drug.
From 2016 to 2018, industry made general payments to more than 52,000 physicians for 137 unique cancer drugs, according to a separate 2021 study published in the Journal of Cancer Policy, for which Dr. Gyawali served as one of the coauthors.
The results suggest that pharmaceutical money affects the entire cancer system, not relatively few oncology leaders. The amounts and dollar values grew each year covered by the study, to nearly 466,000 payments totaling $98.5 million in 2018.
Adriane Fugh-Berman, MD, professor of pharmacology and physiology at Georgetown University, Washington, DC, and director of PharmedOut, a Georgetown-based project that advances evidence-based prescribing and educates healthcare professionals about pharmaceutical marketing practices, has called for a ban on industry gifts to physicians.
When a publication asks physicians to disclose relevant conflicts of interest, physicians may choose not to disclose, because they don’t feel that their conflicts are relevant, Dr. Fugh-Berman said. Drug and device makers have also grown sophisticated about how they work with physicians, she suggested. “It’s illegal to market a drug before it comes on the market, but it’s not illegal to market the disease,” said Dr. Fugh-Berman, noting that drugmakers often work on long timelines.
“The doctor is going around saying we don’t have good therapies. They’re not pushing a drug. And so they feel totally fine about it.”
Anecdotally, Dr. Fugh-Berman noted that, if anything, speaking fees and similar payments only improve doctors’ reputations. She said that’s especially true if the physicians are paid by multiple companies, on the supposed theory that their conflicts of interest cancel each other out.
“I’m not defending this,” added Dr. Fugh-Berman, observing that, at the end of the day, such conflicts may go against the interests of patients.
“Sometimes the best drugs are older, generic, cheap drugs, and if oncologists or other specialists are only choosing among the most promoted drugs, they’re not necessarily choosing the best drugs.”
Beyond any prestige, doctors have other possible nonfinancial incentives for receiving industry payments. “It’s the relationships,” Dr. Fugh-Berman said. “Companies are very good at offering friendship.”
Dr. El Bairi reported NCODA leadership and honoraria along with expert testimony through techspert.io. Dr. Ross reported that he is a deputy editor of JAMA but was not involved in decisions regarding acceptance of or the review of the manuscript he authored and discussed in this article. Dr. Ross also reported receiving grants from the Food and Drug Administration, Johnson & Johnson, the Medical Device Innovation Consortium, the Agency for Healthcare Research and Quality, and the National Heart, Lung, and Blood Institute. He was an expert witness in a qui tam suit alleging violations of the False Claims Act and Anti-Kickback Statute against Biogen that was settled in 2022. Dr. Mitchell reported no relevant financial relationships. Dr. Gyawali reported a consulting or advisory role with Vivio Health. Dr. Fugh-Berman reported being an expert witness for plaintiffs in complaints about drug and device marketing practices.
The findings reflect limited awareness in low-income countries about what scenarios constitute a conflict of interest, first author, Khalid El Bairi, MD, said during an interview. “There is a lack of training in ethics and integrity in medical schools [in countries in Africa], so people are not informed about conflicts of interest,” continued Dr. El Bairi, who presented the new research at the annual meeting of the American Society of Clinical Oncology. “There is also a lack of policies in universities and hospitals to guide clinicians about conflict of interest reporting.”
Overall, 58.5% of survey participants categorized honoraria as a conflict of interest that required disclosure, while 50% said the same of gifts from pharmaceutical representatives, and 44.5% identified travel grants for attending conferences as conflicts of interests. The report was published in JCO Global Oncology. Less often considered conflicts of interest were personal and institutional research funding, trips to conferences, consulting or advisory roles, food and beverages, expert testimony, and sample drugs provided by the pharmaceutical industry.
Just 24% of participants indicated that all of the listed items were deemed conflicts of interest. The survey — called Oncology Transparency Under Scrutiny and Tracking, or ONCOTRUST-1 — considered the perceptions of 200 oncologists, about 70% of whom practice in low- and middle-income countries.
What’s more, 37.5% of respondents identified fear of losing financial support as a reason not to report a conflict of interest. Still, 75% indicated that industry-sponsored speaking does not affect treatment decisions, and 60% said conflicts of interest do not impair objective appraisal of clinical trials.
Dr. El Bairi, a research associate in the department of medical oncology at Mohammed VI University Hospital, Oujda, Morocco, and his colleagues undertook the study in part because of an editorial published in The Lancet Oncology last year. First author Fidel Rubagumya, MD, a consultant oncologist and director of research at Rwanda Military Hospital, Kigali, and colleagues called for more research on the ties between oncologists and industry in Africa. The ONCOTRUST-1 findings set the stage for a planned follow-up study, which aims to compare views surrounding conflicts of interests between oncologists in different economic settings.
Open Payments Houses US Physicians’ Conflicts of Interest
To be sure, many authors of research published in major US journals are based outside of the United States. According to JAMA Network Open, 69% of submissions to the journal are from international authors. However, Dr. El Bairi also raised other potential signs of industry influence that he said need global discussion, such as the role of pharmaceutical companies in presentations of clinical trial findings at large cancer societies’ conferences, a shift toward progression-free survival as the endpoint in clinical cancer trials, and the rise of third-party writing assistance.
“There are two sides of the story,” Dr. El Bairi said. “The good side is that unfortunately, sometimes [industry money is] the only way for African oncologists to go abroad for training, to conferences for their continuous medical education. The bad is now we may harm patients, we might harm science by having conflicts of interest not reported.”
Unlike other countries, the United States has plentiful data on the scale of physicians’ financial conflicts of interest in the form of the Open Payments platform. Championed by Sen. Chuck Grassley (R-Iowa), the federal repository of payments to doctors and teaching hospitals by drug and medical device companies was established as part of the Affordable Care Act (ACA).
The health care reform law, which passed in 2010, requires pharmaceutical companies and medical device makers to report this information.
From 2013 to 2021, the pharmaceutical and medical device industry paid physicians $12.1 billion, according to a research letter published in JAMA in March of 2024 that reviewed Open Payments data.
Ranked by specialty, hematologists and oncologists received the fourth-largest amount of money in aggregate, the study shows. Their total of $825.8 million trailed only physicians in orthopedics ($1.36 billion), neurology and psychiatry ($1.32 billion) and cardiology ($1.29 billion). What’s more, this specialty had the biggest share of physicians taking industry money, with 74.2% of hematologists and oncologists receiving payments.
The payments from industry include fees for consulting services and speaking, as well as food and beverages, travel and lodging, education, gifts, grants, and honoraria.
Joseph S. Ross, MD, MHS, one of the JAMA study’s coauthors, said in an interview that the continued prevalence of such funding runs counter to the expectation behind the measure, which was that transparency would lead to physicians’ becoming less likely to accept a payment.
“We as a profession need to take a cold hard look in the mirror,” he said, referring to physicians in general.
Dr. Ross, professor of medicine at Yale University School of Medicine, New Haven, Connecticut, said he hopes that the profession will self-police, and that patients will make a bigger deal of the issue. Still, he acknowledged that “the vast majority” of patient advocacy groups, too, are funded by the pharmaceutical industry.
Exposing Industry Payments May Have Perverse Effect
A growing body of research explores the effect that physicians’ financial relationships with pharmaceutical companies can have on their prescribing practices. Indeed, oncologists taking industry payments seem to be more likely to prescribe nonrecommended and low-value drugs in some clinical settings, according to a study published in The BMJ last year.
That study’s first author, Aaron P. Mitchell, MD, a medical oncologist and assistant attending physician at Memorial Sloan Kettering Cancer Center, New York City, suggested in an interview that exposing industry payments to the sunlight may have had a perverse effect on physicians.
“There’s this idea of having license to do something,” Dr. Mitchell said, speaking broadly about human psychology rather than drawing on empirical data. “You might feel a little less bad about then prescribing more of that company’s drug, because the disclosure has already been done.”
The influence of pharmaceutical industry money on oncologists goes beyond what’s prescribed to which treatments get studied, approved, and recommended by guidelines, Dr. Mitchell said. He was also first author of a 2016 paper published in JAMA Oncology that found 86% of authors of the National Comprehensive Cancer Network guidelines had at least one conflict of interest reported on Open Systems in 2014.
Meanwhile, the fact that physicians’ payments from industry are a matter of public record on Open Systems has not guaranteed that doctors will disclose their conflicts of interest in other forums. A study published in JAMA earlier this year, for which Dr. Mitchell served as first author, found that almost one in three physicians endorsing drugs and devices on the social media platform X failed to disclose that the manufacturer paid them.
The lack of disclosure seems to extend beyond social media. A 2018 study published in JAMA Oncology found that 32% of oncologist authors of clinical drug trials for drugs approved over a 20-month period from 2016 to 2017 did not fully disclose payments from the trial sponsor when checked against the Open Payments database.
A lion’s share of industry payments within oncology appears to be going to a small group of high-profile physicians, suggested a 2022 study published in JCO Oncology Practice. It found that just 1% of all US oncologists accounted for 37% of industry payments, with each receiving more than $100,000 a year.
Experts: Professional Societies Should Further Limit Industry Payments
While partnerships between drug companies and physicians are necessary and have often been positive, more than disclosure is needed to minimize the risk of patient harm, according to an editorial published in March in JCO Oncology Practice. In it, Nina Niu Sanford, MD, a radiation oncologist UT Southwestern Medical Center, Dallas, and Bishal Gyawali, MD, PhD, a medical oncologist at Queen’s University, Kingston, Ontario, Canada, argue that following a specific blueprint could help mitigate financial conflicts of interest.
For starters, Dr. Sanford and Dr. Gyawali contend in the editorial that the maximum general payment NCCN members are allowed to receive from industry should be $0, compared with a current bar of $20,000 from a single entity or $50,000 from all external entities combined. They also urge professional societies to follow the current policy of the American Society of Clinical Oncology and ban members serving in their leadership from receiving any general payments from the industry.
The authors further suggest that investigators of clinical trials should be barred from holding stock for the drug or product while it is under study and that editorialists should not have conflicts of interest with the company whose drug or product they are discussing.
Pharmaceutical money can harm patients in ways that are not always obvious, Dr. Gyawali said in an interview.
“It can dominate the conversation by removing critical viewpoints from these top people about certain drugs,” he said. “It’s not always about saying good things about the drug.”
For instance, he suggested, a doctor receiving payments from Pfizer might openly criticize perceived flaws in drugs from other companies but refrain from weighing in negatively on a Pfizer drug.
From 2016 to 2018, industry made general payments to more than 52,000 physicians for 137 unique cancer drugs, according to a separate 2021 study published in the Journal of Cancer Policy, for which Dr. Gyawali served as one of the coauthors.
The results suggest that pharmaceutical money affects the entire cancer system, not relatively few oncology leaders. The amounts and dollar values grew each year covered by the study, to nearly 466,000 payments totaling $98.5 million in 2018.
Adriane Fugh-Berman, MD, professor of pharmacology and physiology at Georgetown University, Washington, DC, and director of PharmedOut, a Georgetown-based project that advances evidence-based prescribing and educates healthcare professionals about pharmaceutical marketing practices, has called for a ban on industry gifts to physicians.
When a publication asks physicians to disclose relevant conflicts of interest, physicians may choose not to disclose, because they don’t feel that their conflicts are relevant, Dr. Fugh-Berman said. Drug and device makers have also grown sophisticated about how they work with physicians, she suggested. “It’s illegal to market a drug before it comes on the market, but it’s not illegal to market the disease,” said Dr. Fugh-Berman, noting that drugmakers often work on long timelines.
“The doctor is going around saying we don’t have good therapies. They’re not pushing a drug. And so they feel totally fine about it.”
Anecdotally, Dr. Fugh-Berman noted that, if anything, speaking fees and similar payments only improve doctors’ reputations. She said that’s especially true if the physicians are paid by multiple companies, on the supposed theory that their conflicts of interest cancel each other out.
“I’m not defending this,” added Dr. Fugh-Berman, observing that, at the end of the day, such conflicts may go against the interests of patients.
“Sometimes the best drugs are older, generic, cheap drugs, and if oncologists or other specialists are only choosing among the most promoted drugs, they’re not necessarily choosing the best drugs.”
Beyond any prestige, doctors have other possible nonfinancial incentives for receiving industry payments. “It’s the relationships,” Dr. Fugh-Berman said. “Companies are very good at offering friendship.”
Dr. El Bairi reported NCODA leadership and honoraria along with expert testimony through techspert.io. Dr. Ross reported that he is a deputy editor of JAMA but was not involved in decisions regarding acceptance of or the review of the manuscript he authored and discussed in this article. Dr. Ross also reported receiving grants from the Food and Drug Administration, Johnson & Johnson, the Medical Device Innovation Consortium, the Agency for Healthcare Research and Quality, and the National Heart, Lung, and Blood Institute. He was an expert witness in a qui tam suit alleging violations of the False Claims Act and Anti-Kickback Statute against Biogen that was settled in 2022. Dr. Mitchell reported no relevant financial relationships. Dr. Gyawali reported a consulting or advisory role with Vivio Health. Dr. Fugh-Berman reported being an expert witness for plaintiffs in complaints about drug and device marketing practices.
The findings reflect limited awareness in low-income countries about what scenarios constitute a conflict of interest, first author, Khalid El Bairi, MD, said during an interview. “There is a lack of training in ethics and integrity in medical schools [in countries in Africa], so people are not informed about conflicts of interest,” continued Dr. El Bairi, who presented the new research at the annual meeting of the American Society of Clinical Oncology. “There is also a lack of policies in universities and hospitals to guide clinicians about conflict of interest reporting.”
Overall, 58.5% of survey participants categorized honoraria as a conflict of interest that required disclosure, while 50% said the same of gifts from pharmaceutical representatives, and 44.5% identified travel grants for attending conferences as conflicts of interests. The report was published in JCO Global Oncology. Less often considered conflicts of interest were personal and institutional research funding, trips to conferences, consulting or advisory roles, food and beverages, expert testimony, and sample drugs provided by the pharmaceutical industry.
Just 24% of participants indicated that all of the listed items were deemed conflicts of interest. The survey — called Oncology Transparency Under Scrutiny and Tracking, or ONCOTRUST-1 — considered the perceptions of 200 oncologists, about 70% of whom practice in low- and middle-income countries.
What’s more, 37.5% of respondents identified fear of losing financial support as a reason not to report a conflict of interest. Still, 75% indicated that industry-sponsored speaking does not affect treatment decisions, and 60% said conflicts of interest do not impair objective appraisal of clinical trials.
Dr. El Bairi, a research associate in the department of medical oncology at Mohammed VI University Hospital, Oujda, Morocco, and his colleagues undertook the study in part because of an editorial published in The Lancet Oncology last year. First author Fidel Rubagumya, MD, a consultant oncologist and director of research at Rwanda Military Hospital, Kigali, and colleagues called for more research on the ties between oncologists and industry in Africa. The ONCOTRUST-1 findings set the stage for a planned follow-up study, which aims to compare views surrounding conflicts of interests between oncologists in different economic settings.
Open Payments Houses US Physicians’ Conflicts of Interest
To be sure, many authors of research published in major US journals are based outside of the United States. According to JAMA Network Open, 69% of submissions to the journal are from international authors. However, Dr. El Bairi also raised other potential signs of industry influence that he said need global discussion, such as the role of pharmaceutical companies in presentations of clinical trial findings at large cancer societies’ conferences, a shift toward progression-free survival as the endpoint in clinical cancer trials, and the rise of third-party writing assistance.
“There are two sides of the story,” Dr. El Bairi said. “The good side is that unfortunately, sometimes [industry money is] the only way for African oncologists to go abroad for training, to conferences for their continuous medical education. The bad is now we may harm patients, we might harm science by having conflicts of interest not reported.”
Unlike other countries, the United States has plentiful data on the scale of physicians’ financial conflicts of interest in the form of the Open Payments platform. Championed by Sen. Chuck Grassley (R-Iowa), the federal repository of payments to doctors and teaching hospitals by drug and medical device companies was established as part of the Affordable Care Act (ACA).
The health care reform law, which passed in 2010, requires pharmaceutical companies and medical device makers to report this information.
From 2013 to 2021, the pharmaceutical and medical device industry paid physicians $12.1 billion, according to a research letter published in JAMA in March of 2024 that reviewed Open Payments data.
Ranked by specialty, hematologists and oncologists received the fourth-largest amount of money in aggregate, the study shows. Their total of $825.8 million trailed only physicians in orthopedics ($1.36 billion), neurology and psychiatry ($1.32 billion) and cardiology ($1.29 billion). What’s more, this specialty had the biggest share of physicians taking industry money, with 74.2% of hematologists and oncologists receiving payments.
The payments from industry include fees for consulting services and speaking, as well as food and beverages, travel and lodging, education, gifts, grants, and honoraria.
Joseph S. Ross, MD, MHS, one of the JAMA study’s coauthors, said in an interview that the continued prevalence of such funding runs counter to the expectation behind the measure, which was that transparency would lead to physicians’ becoming less likely to accept a payment.
“We as a profession need to take a cold hard look in the mirror,” he said, referring to physicians in general.
Dr. Ross, professor of medicine at Yale University School of Medicine, New Haven, Connecticut, said he hopes that the profession will self-police, and that patients will make a bigger deal of the issue. Still, he acknowledged that “the vast majority” of patient advocacy groups, too, are funded by the pharmaceutical industry.
Exposing Industry Payments May Have Perverse Effect
A growing body of research explores the effect that physicians’ financial relationships with pharmaceutical companies can have on their prescribing practices. Indeed, oncologists taking industry payments seem to be more likely to prescribe nonrecommended and low-value drugs in some clinical settings, according to a study published in The BMJ last year.
That study’s first author, Aaron P. Mitchell, MD, a medical oncologist and assistant attending physician at Memorial Sloan Kettering Cancer Center, New York City, suggested in an interview that exposing industry payments to the sunlight may have had a perverse effect on physicians.
“There’s this idea of having license to do something,” Dr. Mitchell said, speaking broadly about human psychology rather than drawing on empirical data. “You might feel a little less bad about then prescribing more of that company’s drug, because the disclosure has already been done.”
The influence of pharmaceutical industry money on oncologists goes beyond what’s prescribed to which treatments get studied, approved, and recommended by guidelines, Dr. Mitchell said. He was also first author of a 2016 paper published in JAMA Oncology that found 86% of authors of the National Comprehensive Cancer Network guidelines had at least one conflict of interest reported on Open Systems in 2014.
Meanwhile, the fact that physicians’ payments from industry are a matter of public record on Open Systems has not guaranteed that doctors will disclose their conflicts of interest in other forums. A study published in JAMA earlier this year, for which Dr. Mitchell served as first author, found that almost one in three physicians endorsing drugs and devices on the social media platform X failed to disclose that the manufacturer paid them.
The lack of disclosure seems to extend beyond social media. A 2018 study published in JAMA Oncology found that 32% of oncologist authors of clinical drug trials for drugs approved over a 20-month period from 2016 to 2017 did not fully disclose payments from the trial sponsor when checked against the Open Payments database.
A lion’s share of industry payments within oncology appears to be going to a small group of high-profile physicians, suggested a 2022 study published in JCO Oncology Practice. It found that just 1% of all US oncologists accounted for 37% of industry payments, with each receiving more than $100,000 a year.
Experts: Professional Societies Should Further Limit Industry Payments
While partnerships between drug companies and physicians are necessary and have often been positive, more than disclosure is needed to minimize the risk of patient harm, according to an editorial published in March in JCO Oncology Practice. In it, Nina Niu Sanford, MD, a radiation oncologist UT Southwestern Medical Center, Dallas, and Bishal Gyawali, MD, PhD, a medical oncologist at Queen’s University, Kingston, Ontario, Canada, argue that following a specific blueprint could help mitigate financial conflicts of interest.
For starters, Dr. Sanford and Dr. Gyawali contend in the editorial that the maximum general payment NCCN members are allowed to receive from industry should be $0, compared with a current bar of $20,000 from a single entity or $50,000 from all external entities combined. They also urge professional societies to follow the current policy of the American Society of Clinical Oncology and ban members serving in their leadership from receiving any general payments from the industry.
The authors further suggest that investigators of clinical trials should be barred from holding stock for the drug or product while it is under study and that editorialists should not have conflicts of interest with the company whose drug or product they are discussing.
Pharmaceutical money can harm patients in ways that are not always obvious, Dr. Gyawali said in an interview.
“It can dominate the conversation by removing critical viewpoints from these top people about certain drugs,” he said. “It’s not always about saying good things about the drug.”
For instance, he suggested, a doctor receiving payments from Pfizer might openly criticize perceived flaws in drugs from other companies but refrain from weighing in negatively on a Pfizer drug.
From 2016 to 2018, industry made general payments to more than 52,000 physicians for 137 unique cancer drugs, according to a separate 2021 study published in the Journal of Cancer Policy, for which Dr. Gyawali served as one of the coauthors.
The results suggest that pharmaceutical money affects the entire cancer system, not relatively few oncology leaders. The amounts and dollar values grew each year covered by the study, to nearly 466,000 payments totaling $98.5 million in 2018.
Adriane Fugh-Berman, MD, professor of pharmacology and physiology at Georgetown University, Washington, DC, and director of PharmedOut, a Georgetown-based project that advances evidence-based prescribing and educates healthcare professionals about pharmaceutical marketing practices, has called for a ban on industry gifts to physicians.
When a publication asks physicians to disclose relevant conflicts of interest, physicians may choose not to disclose, because they don’t feel that their conflicts are relevant, Dr. Fugh-Berman said. Drug and device makers have also grown sophisticated about how they work with physicians, she suggested. “It’s illegal to market a drug before it comes on the market, but it’s not illegal to market the disease,” said Dr. Fugh-Berman, noting that drugmakers often work on long timelines.
“The doctor is going around saying we don’t have good therapies. They’re not pushing a drug. And so they feel totally fine about it.”
Anecdotally, Dr. Fugh-Berman noted that, if anything, speaking fees and similar payments only improve doctors’ reputations. She said that’s especially true if the physicians are paid by multiple companies, on the supposed theory that their conflicts of interest cancel each other out.
“I’m not defending this,” added Dr. Fugh-Berman, observing that, at the end of the day, such conflicts may go against the interests of patients.
“Sometimes the best drugs are older, generic, cheap drugs, and if oncologists or other specialists are only choosing among the most promoted drugs, they’re not necessarily choosing the best drugs.”
Beyond any prestige, doctors have other possible nonfinancial incentives for receiving industry payments. “It’s the relationships,” Dr. Fugh-Berman said. “Companies are very good at offering friendship.”
Dr. El Bairi reported NCODA leadership and honoraria along with expert testimony through techspert.io. Dr. Ross reported that he is a deputy editor of JAMA but was not involved in decisions regarding acceptance of or the review of the manuscript he authored and discussed in this article. Dr. Ross also reported receiving grants from the Food and Drug Administration, Johnson & Johnson, the Medical Device Innovation Consortium, the Agency for Healthcare Research and Quality, and the National Heart, Lung, and Blood Institute. He was an expert witness in a qui tam suit alleging violations of the False Claims Act and Anti-Kickback Statute against Biogen that was settled in 2022. Dr. Mitchell reported no relevant financial relationships. Dr. Gyawali reported a consulting or advisory role with Vivio Health. Dr. Fugh-Berman reported being an expert witness for plaintiffs in complaints about drug and device marketing practices.
FROM ASCO 2024
Push, Fail, Push Harder: Olympic Athletes Who Became MDs
Your odds are 1 in 562,400.
Or, as Bill Mallon, the past president and cofounder of the International Society of Olympic Historians, has said, aspiring athletes have a 0.00000178% chance of making the Games.
Now imagine the odds of making the Olympics and then going on to become a physician. And maybe it’s not surprising that those who have done it credit the training they received as Olympic athletes as key to their success in medicine.
“Dealing with poor outcomes and having to get back up and try again,” said Olympian-turned-physician Ogonna Nnamani Silva, MD, “that reiterative process of trying to obtain perfection in your craft — that’s athletics 101.”
This connection isn’t just anecdotal. It has been discussed in medical journals and examined in surveys. The consensus is that, yes, there are specific characteristics elite athletes develop that physicians — regardless of their athletic background — can learn to apply to their work in medicine.
Maybe it’s something else, too: Certain mindsets don’t worry about long odds. They seek out crucibles again and again without concern for the heat involved. Because the outcome is worth it.
Here are four athletes who became high-performing physicians and how they did it.
The Gymnast/The Pediatric Surgeon
“Gymnastics helped me build a skill set for my career,” said Canadian Olympic gymnast-turned-pediatric orthopedic surgeon Lise Leveille, MD. “It led me to be successful as a medical student and ultimately obtain the job that I want in the area that I want working with the people that I want.”
The skills Dr. Leveille prizes include time management, teamwork, goal setting, and a strong work ethic, all of which propel an athlete to the crucial moment of “performance.”
“I miss performing,” said Dr. Leveille. “It defines who I was at that time. I miss being able to work toward something and then deliver when it counted” — like when she qualified for the 1998 Commonwealth games in Kuala Lumpur at 16.
The Canadian national team came third at that event, and Dr. Leveille built on that success at the Pan American Games, taking gold on the balance beam and as a team, and then qualifying for the Olympics at the 1999 World Championships. She competed in the team and five individual events at the 2000 Olympic Games in Sydney.
Though Dr. Leveille started gymnastics at age 3, her parents, both teachers, instilled in her the importance of education. Gymnastics opened academic doors for her, like being recruited to Stanford where she completed her undergraduate degree in biomedical engineering and human biology in 2004 before entering medical school at the University of British Columbia in Vancouver.
Now 41, Dr. Leveille accepts that she’ll never nail another gymnastics routine, but she channels that love of sticking the landing into the operating room at British Columbia Children’s Hospital, also in Vancouver.
“Some of the unknown variables within the operating room and how you deal with those unknown variables is exactly like showing up for a competition,” Dr. Leveille said. “When I have one of those cases where I have to perform under pressure and everything comes together, that’s exactly like nailing your routine when it counts most.”
The Pole Vaulter/The Emergency Medicine Physician
Tunisian American pole vaulter Leila Ben-Youssef, MD, had what could be considered a disappointing showing at the 2008 Olympic Games in Beijing. She collapsed from severe abdominal pain during the opening ceremony and had to be carried out. On the day of competition, she was still suffering. “I could barely run down the runway,” she recalled. “I cleared one bar. I was just happy to have been able to do that.”
When Dr. Ben-Youssef, who grew up in Montana, returned home, she underwent emergency surgery to remove the source of the pain: A large, benign tumor.
While some might be devastated by such bad luck, Dr. Ben-Youssef focuses on the success of her journey — the fact that she qualified and competed at the Olympics in the first place. The ability to accept setbacks is something she said comes with the territory.
“As an athlete, you’re always facing injury, and someone told me early in my career that the best athletes are the ones that know how to manage their expectations because it’s bound to happen,” she said. “So, there is disappointment. But recognizing that I did qualify for the Olympics despite being uncomfortable and having issues, I was still able to meet my goal.”
Prior to the games, Dr. Ben-Youssef had been accepted into medical school at the University of Washington School of Medicine at Montana State University in Bozeman, Montana. Thankfully, the school was supportive of Dr. Ben-Youssef’s Olympic dreams and allowed her to begin her studies a month behind her class. Upon her return from Beijing, she spent the rest of her medical school training with her head down, grinding.
“Medicine is hard,” said Dr. Ben-Youssef. “It’s grueling both physically and emotionally, and I think that’s similar to any elite sport. You’re going to deal with challenges and disappointment. I think having gone through that as an athlete really prepares you for the medical education system, for residency, and even for day-to-day work.”
Now a physician working in emergency medicine in Hawaii, Dr. Ben-Youssef feels the setbacks she experienced as an athlete help her connect with her patients as they deal with health challenges.
And as a volunteer pole vaulting coach for a local high school, Dr. Ben-Youssef has been able to surround herself with the positive, joyful energy of athletes. “Emergency medicine is often a sad place,” she said. “But in a sports environment, if people don’t succeed or are injured, there is still that energy there that strives for something, and it’s so fun to be around.”
The Rower/The Sports Medicine Specialist
Three-time US Olympic rower Genevra “Gevvie” Stone, MD, wanted to be a doctor even before she gave a thought to rowing. She was in eighth grade when she dislocated her knee for the third time. Her parents took her to a pediatric orthopedist, and Dr. Stone, according to her mom, declared: “That’s what I want to do when I grow up.”
“I’m a very stubborn person, and when I make a decision like that, I usually don’t veer from it,” Dr. Stone said.
That laser focus combined with a deep love of both sports and medicine has served Dr. Stone well. “Becoming a doctor and becoming an Olympian require you to dedicate not just your time and your energy but also your passion to that focus,” she said. “In both, you aren’t going to be successful if you don’t love what you’re doing. Finding the reward in it is what makes it achievable.”
Dr. Stone actually resisted rowing until she was 16 because both of her parents were Olympians in the sport and met on the US team. “It was their thing, and I didn’t want it to be my thing,” she recalled.
Nonetheless, Dr. Stone easily fell into the sport in her late teens and was recruited by Princeton University. “I had grown up around Olympians and kind of took it for granted that if you worked hard enough and were decent at rowing, then you could be one of the best in the world, without really realizing how difficult it would be to achieve that,” she said.
Dr. Stone’s team won the NCAA Championship in 2006 and was invited to try out for the 2008 Olympic team at the US training center after she graduated from college. But she didn’t make it.
Instead, Dr. Stone entered medical school at Tufts University School of Medicine, Boston, thinking her competitive rowing career had come to end. But her love for the sport was still strong, and she realized she wasn’t finished.
After 2 years of medical school, Dr. Stone requested 2 years off so she might have another shot at making the Olympic team. The timing was right. She went to the London Olympics in 2012, graduated from medical school in 2014, and then took 2 more years off to train full time for the 2016 Olympics in Rio where she won silver.
At the 2020 Olympic Games in Tokyo, Dr. Stone took fifth place in the double sculls. While she continues to race the master’s circuit, she’s primarily dedicated to completing her sports medicine fellowship at University of Utah Health.
Fortunately, Dr. Stone’s parents, coaches, and teachers always supported her goals. “No one turned to me and told me I was crazy, just choose medicine or rowing,” she said. “Everyone said that if this is what you want to do, we’re here to support you, and I wouldn’t have been able to do it without that support.”
The Volleyball Player/The Plastic Surgeon
Dr. Nnamani Silva’s journey to the Olympics was also paved with an extensive list of supporters, beginning with her parents. And she has taken that sense of collaboration, coordination, and teamwork into her medical career.
The daughter of Nigerian immigrants who came to the United States to escape civil war, Dr. Nnamani Silva said her parents embraced the American dream. “To see what they were able to do with hard work, dedication, and sacrifice, I had no choice but to work hard because I saw their example. And that love for and belief in America was so strong in my house growing up,” she said.
Dreams of practicing medicine came first. A severe asthmatic growing up, Dr. Nnamani Silva recalled having wonderful doctors. “I had so many emergency room visits and hospitalizations,” she said. “But the doctors always gave me hope, and they literally transformed my life. I thought if I could pass that on to my future patients, that would be the greatest honor of my life.”
Volleyball gave Dr. Nnamani Silva the opportunity to attend Stanford, and she took time off during her junior year to train and compete in the 2004 Olympic Games in Athens. She also played for the United States at the 2008 Olympic Games in Beijing where the team took silver. Afterward, she continued to play overseas for several years.
At 33, and with a newborn daughter, Dr. Nnamani Silva returned to her original goal of becoming a doctor. She attended the University of California, San Francisco, and is currently a resident in the Harvard Plastic Surgery Program. She includes her husband, parents, and in-laws in this achievement, whom she said “saved” her. “There is no chance I would have finished medical school and survived residency without them.”
As a volleyball player, Dr. Nnamani Silva said she “believes in teams wholeheartedly,” valuing the exchange of energy and skill that she feels brings out the best in people. As a medical student, she initially didn’t realize how her previous life would apply to teamwork in the operating room. But it soon became clear.
“In surgery, when you harness the talents of everyone around you and you create that synergy, it’s an amazing feeling,” she said. And the stakes are often high. “It requires a lot of focus, discipline, determination, and resilience because you’re going to be humbled all the time.” Something athletes know a little bit about.
A version of this article first appeared on Medscape.com.
Your odds are 1 in 562,400.
Or, as Bill Mallon, the past president and cofounder of the International Society of Olympic Historians, has said, aspiring athletes have a 0.00000178% chance of making the Games.
Now imagine the odds of making the Olympics and then going on to become a physician. And maybe it’s not surprising that those who have done it credit the training they received as Olympic athletes as key to their success in medicine.
“Dealing with poor outcomes and having to get back up and try again,” said Olympian-turned-physician Ogonna Nnamani Silva, MD, “that reiterative process of trying to obtain perfection in your craft — that’s athletics 101.”
This connection isn’t just anecdotal. It has been discussed in medical journals and examined in surveys. The consensus is that, yes, there are specific characteristics elite athletes develop that physicians — regardless of their athletic background — can learn to apply to their work in medicine.
Maybe it’s something else, too: Certain mindsets don’t worry about long odds. They seek out crucibles again and again without concern for the heat involved. Because the outcome is worth it.
Here are four athletes who became high-performing physicians and how they did it.
The Gymnast/The Pediatric Surgeon
“Gymnastics helped me build a skill set for my career,” said Canadian Olympic gymnast-turned-pediatric orthopedic surgeon Lise Leveille, MD. “It led me to be successful as a medical student and ultimately obtain the job that I want in the area that I want working with the people that I want.”
The skills Dr. Leveille prizes include time management, teamwork, goal setting, and a strong work ethic, all of which propel an athlete to the crucial moment of “performance.”
“I miss performing,” said Dr. Leveille. “It defines who I was at that time. I miss being able to work toward something and then deliver when it counted” — like when she qualified for the 1998 Commonwealth games in Kuala Lumpur at 16.
The Canadian national team came third at that event, and Dr. Leveille built on that success at the Pan American Games, taking gold on the balance beam and as a team, and then qualifying for the Olympics at the 1999 World Championships. She competed in the team and five individual events at the 2000 Olympic Games in Sydney.
Though Dr. Leveille started gymnastics at age 3, her parents, both teachers, instilled in her the importance of education. Gymnastics opened academic doors for her, like being recruited to Stanford where she completed her undergraduate degree in biomedical engineering and human biology in 2004 before entering medical school at the University of British Columbia in Vancouver.
Now 41, Dr. Leveille accepts that she’ll never nail another gymnastics routine, but she channels that love of sticking the landing into the operating room at British Columbia Children’s Hospital, also in Vancouver.
“Some of the unknown variables within the operating room and how you deal with those unknown variables is exactly like showing up for a competition,” Dr. Leveille said. “When I have one of those cases where I have to perform under pressure and everything comes together, that’s exactly like nailing your routine when it counts most.”
The Pole Vaulter/The Emergency Medicine Physician
Tunisian American pole vaulter Leila Ben-Youssef, MD, had what could be considered a disappointing showing at the 2008 Olympic Games in Beijing. She collapsed from severe abdominal pain during the opening ceremony and had to be carried out. On the day of competition, she was still suffering. “I could barely run down the runway,” she recalled. “I cleared one bar. I was just happy to have been able to do that.”
When Dr. Ben-Youssef, who grew up in Montana, returned home, she underwent emergency surgery to remove the source of the pain: A large, benign tumor.
While some might be devastated by such bad luck, Dr. Ben-Youssef focuses on the success of her journey — the fact that she qualified and competed at the Olympics in the first place. The ability to accept setbacks is something she said comes with the territory.
“As an athlete, you’re always facing injury, and someone told me early in my career that the best athletes are the ones that know how to manage their expectations because it’s bound to happen,” she said. “So, there is disappointment. But recognizing that I did qualify for the Olympics despite being uncomfortable and having issues, I was still able to meet my goal.”
Prior to the games, Dr. Ben-Youssef had been accepted into medical school at the University of Washington School of Medicine at Montana State University in Bozeman, Montana. Thankfully, the school was supportive of Dr. Ben-Youssef’s Olympic dreams and allowed her to begin her studies a month behind her class. Upon her return from Beijing, she spent the rest of her medical school training with her head down, grinding.
“Medicine is hard,” said Dr. Ben-Youssef. “It’s grueling both physically and emotionally, and I think that’s similar to any elite sport. You’re going to deal with challenges and disappointment. I think having gone through that as an athlete really prepares you for the medical education system, for residency, and even for day-to-day work.”
Now a physician working in emergency medicine in Hawaii, Dr. Ben-Youssef feels the setbacks she experienced as an athlete help her connect with her patients as they deal with health challenges.
And as a volunteer pole vaulting coach for a local high school, Dr. Ben-Youssef has been able to surround herself with the positive, joyful energy of athletes. “Emergency medicine is often a sad place,” she said. “But in a sports environment, if people don’t succeed or are injured, there is still that energy there that strives for something, and it’s so fun to be around.”
The Rower/The Sports Medicine Specialist
Three-time US Olympic rower Genevra “Gevvie” Stone, MD, wanted to be a doctor even before she gave a thought to rowing. She was in eighth grade when she dislocated her knee for the third time. Her parents took her to a pediatric orthopedist, and Dr. Stone, according to her mom, declared: “That’s what I want to do when I grow up.”
“I’m a very stubborn person, and when I make a decision like that, I usually don’t veer from it,” Dr. Stone said.
That laser focus combined with a deep love of both sports and medicine has served Dr. Stone well. “Becoming a doctor and becoming an Olympian require you to dedicate not just your time and your energy but also your passion to that focus,” she said. “In both, you aren’t going to be successful if you don’t love what you’re doing. Finding the reward in it is what makes it achievable.”
Dr. Stone actually resisted rowing until she was 16 because both of her parents were Olympians in the sport and met on the US team. “It was their thing, and I didn’t want it to be my thing,” she recalled.
Nonetheless, Dr. Stone easily fell into the sport in her late teens and was recruited by Princeton University. “I had grown up around Olympians and kind of took it for granted that if you worked hard enough and were decent at rowing, then you could be one of the best in the world, without really realizing how difficult it would be to achieve that,” she said.
Dr. Stone’s team won the NCAA Championship in 2006 and was invited to try out for the 2008 Olympic team at the US training center after she graduated from college. But she didn’t make it.
Instead, Dr. Stone entered medical school at Tufts University School of Medicine, Boston, thinking her competitive rowing career had come to end. But her love for the sport was still strong, and she realized she wasn’t finished.
After 2 years of medical school, Dr. Stone requested 2 years off so she might have another shot at making the Olympic team. The timing was right. She went to the London Olympics in 2012, graduated from medical school in 2014, and then took 2 more years off to train full time for the 2016 Olympics in Rio where she won silver.
At the 2020 Olympic Games in Tokyo, Dr. Stone took fifth place in the double sculls. While she continues to race the master’s circuit, she’s primarily dedicated to completing her sports medicine fellowship at University of Utah Health.
Fortunately, Dr. Stone’s parents, coaches, and teachers always supported her goals. “No one turned to me and told me I was crazy, just choose medicine or rowing,” she said. “Everyone said that if this is what you want to do, we’re here to support you, and I wouldn’t have been able to do it without that support.”
The Volleyball Player/The Plastic Surgeon
Dr. Nnamani Silva’s journey to the Olympics was also paved with an extensive list of supporters, beginning with her parents. And she has taken that sense of collaboration, coordination, and teamwork into her medical career.
The daughter of Nigerian immigrants who came to the United States to escape civil war, Dr. Nnamani Silva said her parents embraced the American dream. “To see what they were able to do with hard work, dedication, and sacrifice, I had no choice but to work hard because I saw their example. And that love for and belief in America was so strong in my house growing up,” she said.
Dreams of practicing medicine came first. A severe asthmatic growing up, Dr. Nnamani Silva recalled having wonderful doctors. “I had so many emergency room visits and hospitalizations,” she said. “But the doctors always gave me hope, and they literally transformed my life. I thought if I could pass that on to my future patients, that would be the greatest honor of my life.”
Volleyball gave Dr. Nnamani Silva the opportunity to attend Stanford, and she took time off during her junior year to train and compete in the 2004 Olympic Games in Athens. She also played for the United States at the 2008 Olympic Games in Beijing where the team took silver. Afterward, she continued to play overseas for several years.
At 33, and with a newborn daughter, Dr. Nnamani Silva returned to her original goal of becoming a doctor. She attended the University of California, San Francisco, and is currently a resident in the Harvard Plastic Surgery Program. She includes her husband, parents, and in-laws in this achievement, whom she said “saved” her. “There is no chance I would have finished medical school and survived residency without them.”
As a volleyball player, Dr. Nnamani Silva said she “believes in teams wholeheartedly,” valuing the exchange of energy and skill that she feels brings out the best in people. As a medical student, she initially didn’t realize how her previous life would apply to teamwork in the operating room. But it soon became clear.
“In surgery, when you harness the talents of everyone around you and you create that synergy, it’s an amazing feeling,” she said. And the stakes are often high. “It requires a lot of focus, discipline, determination, and resilience because you’re going to be humbled all the time.” Something athletes know a little bit about.
A version of this article first appeared on Medscape.com.
Your odds are 1 in 562,400.
Or, as Bill Mallon, the past president and cofounder of the International Society of Olympic Historians, has said, aspiring athletes have a 0.00000178% chance of making the Games.
Now imagine the odds of making the Olympics and then going on to become a physician. And maybe it’s not surprising that those who have done it credit the training they received as Olympic athletes as key to their success in medicine.
“Dealing with poor outcomes and having to get back up and try again,” said Olympian-turned-physician Ogonna Nnamani Silva, MD, “that reiterative process of trying to obtain perfection in your craft — that’s athletics 101.”
This connection isn’t just anecdotal. It has been discussed in medical journals and examined in surveys. The consensus is that, yes, there are specific characteristics elite athletes develop that physicians — regardless of their athletic background — can learn to apply to their work in medicine.
Maybe it’s something else, too: Certain mindsets don’t worry about long odds. They seek out crucibles again and again without concern for the heat involved. Because the outcome is worth it.
Here are four athletes who became high-performing physicians and how they did it.
The Gymnast/The Pediatric Surgeon
“Gymnastics helped me build a skill set for my career,” said Canadian Olympic gymnast-turned-pediatric orthopedic surgeon Lise Leveille, MD. “It led me to be successful as a medical student and ultimately obtain the job that I want in the area that I want working with the people that I want.”
The skills Dr. Leveille prizes include time management, teamwork, goal setting, and a strong work ethic, all of which propel an athlete to the crucial moment of “performance.”
“I miss performing,” said Dr. Leveille. “It defines who I was at that time. I miss being able to work toward something and then deliver when it counted” — like when she qualified for the 1998 Commonwealth games in Kuala Lumpur at 16.
The Canadian national team came third at that event, and Dr. Leveille built on that success at the Pan American Games, taking gold on the balance beam and as a team, and then qualifying for the Olympics at the 1999 World Championships. She competed in the team and five individual events at the 2000 Olympic Games in Sydney.
Though Dr. Leveille started gymnastics at age 3, her parents, both teachers, instilled in her the importance of education. Gymnastics opened academic doors for her, like being recruited to Stanford where she completed her undergraduate degree in biomedical engineering and human biology in 2004 before entering medical school at the University of British Columbia in Vancouver.
Now 41, Dr. Leveille accepts that she’ll never nail another gymnastics routine, but she channels that love of sticking the landing into the operating room at British Columbia Children’s Hospital, also in Vancouver.
“Some of the unknown variables within the operating room and how you deal with those unknown variables is exactly like showing up for a competition,” Dr. Leveille said. “When I have one of those cases where I have to perform under pressure and everything comes together, that’s exactly like nailing your routine when it counts most.”
The Pole Vaulter/The Emergency Medicine Physician
Tunisian American pole vaulter Leila Ben-Youssef, MD, had what could be considered a disappointing showing at the 2008 Olympic Games in Beijing. She collapsed from severe abdominal pain during the opening ceremony and had to be carried out. On the day of competition, she was still suffering. “I could barely run down the runway,” she recalled. “I cleared one bar. I was just happy to have been able to do that.”
When Dr. Ben-Youssef, who grew up in Montana, returned home, she underwent emergency surgery to remove the source of the pain: A large, benign tumor.
While some might be devastated by such bad luck, Dr. Ben-Youssef focuses on the success of her journey — the fact that she qualified and competed at the Olympics in the first place. The ability to accept setbacks is something she said comes with the territory.
“As an athlete, you’re always facing injury, and someone told me early in my career that the best athletes are the ones that know how to manage their expectations because it’s bound to happen,” she said. “So, there is disappointment. But recognizing that I did qualify for the Olympics despite being uncomfortable and having issues, I was still able to meet my goal.”
Prior to the games, Dr. Ben-Youssef had been accepted into medical school at the University of Washington School of Medicine at Montana State University in Bozeman, Montana. Thankfully, the school was supportive of Dr. Ben-Youssef’s Olympic dreams and allowed her to begin her studies a month behind her class. Upon her return from Beijing, she spent the rest of her medical school training with her head down, grinding.
“Medicine is hard,” said Dr. Ben-Youssef. “It’s grueling both physically and emotionally, and I think that’s similar to any elite sport. You’re going to deal with challenges and disappointment. I think having gone through that as an athlete really prepares you for the medical education system, for residency, and even for day-to-day work.”
Now a physician working in emergency medicine in Hawaii, Dr. Ben-Youssef feels the setbacks she experienced as an athlete help her connect with her patients as they deal with health challenges.
And as a volunteer pole vaulting coach for a local high school, Dr. Ben-Youssef has been able to surround herself with the positive, joyful energy of athletes. “Emergency medicine is often a sad place,” she said. “But in a sports environment, if people don’t succeed or are injured, there is still that energy there that strives for something, and it’s so fun to be around.”
The Rower/The Sports Medicine Specialist
Three-time US Olympic rower Genevra “Gevvie” Stone, MD, wanted to be a doctor even before she gave a thought to rowing. She was in eighth grade when she dislocated her knee for the third time. Her parents took her to a pediatric orthopedist, and Dr. Stone, according to her mom, declared: “That’s what I want to do when I grow up.”
“I’m a very stubborn person, and when I make a decision like that, I usually don’t veer from it,” Dr. Stone said.
That laser focus combined with a deep love of both sports and medicine has served Dr. Stone well. “Becoming a doctor and becoming an Olympian require you to dedicate not just your time and your energy but also your passion to that focus,” she said. “In both, you aren’t going to be successful if you don’t love what you’re doing. Finding the reward in it is what makes it achievable.”
Dr. Stone actually resisted rowing until she was 16 because both of her parents were Olympians in the sport and met on the US team. “It was their thing, and I didn’t want it to be my thing,” she recalled.
Nonetheless, Dr. Stone easily fell into the sport in her late teens and was recruited by Princeton University. “I had grown up around Olympians and kind of took it for granted that if you worked hard enough and were decent at rowing, then you could be one of the best in the world, without really realizing how difficult it would be to achieve that,” she said.
Dr. Stone’s team won the NCAA Championship in 2006 and was invited to try out for the 2008 Olympic team at the US training center after she graduated from college. But she didn’t make it.
Instead, Dr. Stone entered medical school at Tufts University School of Medicine, Boston, thinking her competitive rowing career had come to end. But her love for the sport was still strong, and she realized she wasn’t finished.
After 2 years of medical school, Dr. Stone requested 2 years off so she might have another shot at making the Olympic team. The timing was right. She went to the London Olympics in 2012, graduated from medical school in 2014, and then took 2 more years off to train full time for the 2016 Olympics in Rio where she won silver.
At the 2020 Olympic Games in Tokyo, Dr. Stone took fifth place in the double sculls. While she continues to race the master’s circuit, she’s primarily dedicated to completing her sports medicine fellowship at University of Utah Health.
Fortunately, Dr. Stone’s parents, coaches, and teachers always supported her goals. “No one turned to me and told me I was crazy, just choose medicine or rowing,” she said. “Everyone said that if this is what you want to do, we’re here to support you, and I wouldn’t have been able to do it without that support.”
The Volleyball Player/The Plastic Surgeon
Dr. Nnamani Silva’s journey to the Olympics was also paved with an extensive list of supporters, beginning with her parents. And she has taken that sense of collaboration, coordination, and teamwork into her medical career.
The daughter of Nigerian immigrants who came to the United States to escape civil war, Dr. Nnamani Silva said her parents embraced the American dream. “To see what they were able to do with hard work, dedication, and sacrifice, I had no choice but to work hard because I saw their example. And that love for and belief in America was so strong in my house growing up,” she said.
Dreams of practicing medicine came first. A severe asthmatic growing up, Dr. Nnamani Silva recalled having wonderful doctors. “I had so many emergency room visits and hospitalizations,” she said. “But the doctors always gave me hope, and they literally transformed my life. I thought if I could pass that on to my future patients, that would be the greatest honor of my life.”
Volleyball gave Dr. Nnamani Silva the opportunity to attend Stanford, and she took time off during her junior year to train and compete in the 2004 Olympic Games in Athens. She also played for the United States at the 2008 Olympic Games in Beijing where the team took silver. Afterward, she continued to play overseas for several years.
At 33, and with a newborn daughter, Dr. Nnamani Silva returned to her original goal of becoming a doctor. She attended the University of California, San Francisco, and is currently a resident in the Harvard Plastic Surgery Program. She includes her husband, parents, and in-laws in this achievement, whom she said “saved” her. “There is no chance I would have finished medical school and survived residency without them.”
As a volleyball player, Dr. Nnamani Silva said she “believes in teams wholeheartedly,” valuing the exchange of energy and skill that she feels brings out the best in people. As a medical student, she initially didn’t realize how her previous life would apply to teamwork in the operating room. But it soon became clear.
“In surgery, when you harness the talents of everyone around you and you create that synergy, it’s an amazing feeling,” she said. And the stakes are often high. “It requires a lot of focus, discipline, determination, and resilience because you’re going to be humbled all the time.” Something athletes know a little bit about.
A version of this article first appeared on Medscape.com.
Healthcare Workers Face Gender-Based Violence
Across the world, healthcare workers experience workplace violence, which can differ by gender, seniority, and the type of workplace, according to a recent study.
An analysis found that men were more likely to report physical violence, while women were more likely to face nonphysical violence, such as verbal abuse, sexual harassment, and bullying.
“Our study was sparked by the increasing research on workplace violence in healthcare settings. Yet, there’s less empirical data about workplace violence based on gender, its effects on individuals and the collective workforce, and its subsequent impact on patient care and healthcare organizations,” study author Basnama Ayaz, a PhD candidate in nursing at the University of Toronto, told this news organization.
“Workplace violence in healthcare settings is a critical issue that requires attention and action from all stakeholders, including individual providers, healthcare and other institutions, policymakers, and the community,” she said. “By recognizing the problem and implementing evidence-based solutions, we can create safer work environments that protect healthcare workers and improve quality care for patients and organizational effectiveness.”
The study was published online in PLOS Global Public Health.
Widespread and Severe
Although women represent most of the healthcare workforce worldwide, hierarchical structures tend to reflect traditional gender norms, where men hold leadership positions and women serve in front-line care roles, said Ms. Ayaz. Women are often marginalized, and their concerns dismissed, which can exacerbate their vulnerability to gender-based workplace violence, she added.
To better understand these imbalances on a global scale, the investigators conducted a scoping review of the prevalence of and risk factors for gender-based workplace violence in healthcare settings. Participants included physicians, nurses, and midwives, between 2010 and 2024. Although the authors acknowledged that gender-based workplace violence affects the full gender spectrum, only a handful of studies included information about nonbinary personnel, so the review focused on men and women.
Among 226 studies, half focused on physicians, 22% focused on nurses, and 28% included physicians, nurses, midwives, and other medical workers. About 64% of studies reported a higher prevalence of all forms of workplace violence for women, including sexual violence, verbal abuse, discrimination, bullying, and physical violence, while 17% reported a higher prevalence for men.
Overall, across most countries, men experienced more physical violence than did women, and women experienced more verbal abuse, sexual harassment, and bullying. Female nurses were particularly likely to experience violence.
Healthcare workers were also more likely to experience violence if they were younger, less experienced, had a lower professional status, or were part of a minority group based on ethnicity, nationality, culture, or language. These factors were sensitive to gender, “reflecting women’s structural disadvantages in the workplace,” wrote the authors.
As a result of workplace violence, women were more likely to report changes in mental health and social behaviors, as well as dissatisfaction, burnout, and changes in their career goals.
The research team identified various factors linked to violent episodes. In clinical settings where most perpetrators were patients and their relatives, abuse and violence could be related to overcrowding, waiting time, and heavy workloads for healthcare providers. When supervisors or colleagues were the perpetrators, workplace violence appeared to be more likely with long hours, night shifts, and certain clinical settings, such as emergency departments, psychiatric settings, operating rooms, and maternity wards, said Ms. Ayaz. Sexual or gender harassment toward women was more prevalent in male-dominated surgical specialties.
“We were surprised by the extent and severity of workplace violence that healthcare workers face around the globe based on gender,” she said. “One aspect that stood out was the significant role that organizational culture and support systems play either in mitigating or exacerbating these incidents, particularly the power structures between and within professions.”
For instance, trainees in lower hierarchical positions often face a higher risk for violence, especially gender-based harassment, she said. Many times, they feel they can’t report these incidents to trainers or managers, who may also be the perpetrators, she added.
Addressing Systemic Issues
In 2002, the World Health Organization, International Council of Nurses, and other major medical and labor groups worldwide launched a program focused on ways to eliminate workplace violence in healthcare settings. Since 2020, the call for a solution has grown louder as clinicians, nurses, and other health professionals faced more physical and verbal violence during the COVID-19 pandemic, often leading to burnout.
“Workplace violence is very important because it is more prevalent in healthcare workers than in many other settings and is on the rise,” said Karen Abrams, MD, assistant professor of psychiatry at the University of Toronto. Dr. Abrams, who wasn’t involved with this study, has researched physicians’ experiences of stalking by patients.
Workplace violence “can affect physical and mental health and lead to burnout, depression, anxiety, and symptoms of PTSD,” said Dr. Abrams. “It can affect one’s sleep and concentration and, therefore, ability to perform one’s job.”
Dr. Ayaz and colleagues suggested recommendations to improve gender-based workplace violence, noting the complex and multifaceted aspects of enhancing current policies, fortifying institutional capacities to respond, and implementing tailored interventions. Changes are needed at various levels, including at the healthcare system and provincial, territorial, and national levels, she said.
In Canada, for instance, lawmakers passed a bill in 2021 that amended the national criminal code to make intimidation or bullying a healthcare worker punishable by as many as 10 years in prison. The changes also required courts to consider more serious penalties for offenders who target healthcare workers aggressively.
But more needs to be done, medical professional groups say. The Canadian Nurses Association and Canadian Federation of Nurses Unions, as well as provincial groups, have called for a pan-Canadian violence-prevention framework, targeted funding for violence prevention infrastructure, and an update to the nation’s health human resources strategy to address severe staffing shortages across the country.
“Canada needs a bold vision for the future of our healthcare. Amid an ongoing staffing crisis, the cracks in our public healthcare systems have only grown deeper and wider, with too many going without the care they need when they need it,” Linda Silas, president of the Canadian Federation of Nurses Unions, told this news organization.
“Access to care relies on safe staffing. Years of unsafe working conditions and insufficient staffing are pushing nurses out of our public healthcare system,” she said. “Working collaboratively, we can make healthcare jobs the best jobs in our communities.”
The authors received no specific funding for the study. Ms. Ayaz, Dr. Abrams, and Ms. Silas reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Across the world, healthcare workers experience workplace violence, which can differ by gender, seniority, and the type of workplace, according to a recent study.
An analysis found that men were more likely to report physical violence, while women were more likely to face nonphysical violence, such as verbal abuse, sexual harassment, and bullying.
“Our study was sparked by the increasing research on workplace violence in healthcare settings. Yet, there’s less empirical data about workplace violence based on gender, its effects on individuals and the collective workforce, and its subsequent impact on patient care and healthcare organizations,” study author Basnama Ayaz, a PhD candidate in nursing at the University of Toronto, told this news organization.
“Workplace violence in healthcare settings is a critical issue that requires attention and action from all stakeholders, including individual providers, healthcare and other institutions, policymakers, and the community,” she said. “By recognizing the problem and implementing evidence-based solutions, we can create safer work environments that protect healthcare workers and improve quality care for patients and organizational effectiveness.”
The study was published online in PLOS Global Public Health.
Widespread and Severe
Although women represent most of the healthcare workforce worldwide, hierarchical structures tend to reflect traditional gender norms, where men hold leadership positions and women serve in front-line care roles, said Ms. Ayaz. Women are often marginalized, and their concerns dismissed, which can exacerbate their vulnerability to gender-based workplace violence, she added.
To better understand these imbalances on a global scale, the investigators conducted a scoping review of the prevalence of and risk factors for gender-based workplace violence in healthcare settings. Participants included physicians, nurses, and midwives, between 2010 and 2024. Although the authors acknowledged that gender-based workplace violence affects the full gender spectrum, only a handful of studies included information about nonbinary personnel, so the review focused on men and women.
Among 226 studies, half focused on physicians, 22% focused on nurses, and 28% included physicians, nurses, midwives, and other medical workers. About 64% of studies reported a higher prevalence of all forms of workplace violence for women, including sexual violence, verbal abuse, discrimination, bullying, and physical violence, while 17% reported a higher prevalence for men.
Overall, across most countries, men experienced more physical violence than did women, and women experienced more verbal abuse, sexual harassment, and bullying. Female nurses were particularly likely to experience violence.
Healthcare workers were also more likely to experience violence if they were younger, less experienced, had a lower professional status, or were part of a minority group based on ethnicity, nationality, culture, or language. These factors were sensitive to gender, “reflecting women’s structural disadvantages in the workplace,” wrote the authors.
As a result of workplace violence, women were more likely to report changes in mental health and social behaviors, as well as dissatisfaction, burnout, and changes in their career goals.
The research team identified various factors linked to violent episodes. In clinical settings where most perpetrators were patients and their relatives, abuse and violence could be related to overcrowding, waiting time, and heavy workloads for healthcare providers. When supervisors or colleagues were the perpetrators, workplace violence appeared to be more likely with long hours, night shifts, and certain clinical settings, such as emergency departments, psychiatric settings, operating rooms, and maternity wards, said Ms. Ayaz. Sexual or gender harassment toward women was more prevalent in male-dominated surgical specialties.
“We were surprised by the extent and severity of workplace violence that healthcare workers face around the globe based on gender,” she said. “One aspect that stood out was the significant role that organizational culture and support systems play either in mitigating or exacerbating these incidents, particularly the power structures between and within professions.”
For instance, trainees in lower hierarchical positions often face a higher risk for violence, especially gender-based harassment, she said. Many times, they feel they can’t report these incidents to trainers or managers, who may also be the perpetrators, she added.
Addressing Systemic Issues
In 2002, the World Health Organization, International Council of Nurses, and other major medical and labor groups worldwide launched a program focused on ways to eliminate workplace violence in healthcare settings. Since 2020, the call for a solution has grown louder as clinicians, nurses, and other health professionals faced more physical and verbal violence during the COVID-19 pandemic, often leading to burnout.
“Workplace violence is very important because it is more prevalent in healthcare workers than in many other settings and is on the rise,” said Karen Abrams, MD, assistant professor of psychiatry at the University of Toronto. Dr. Abrams, who wasn’t involved with this study, has researched physicians’ experiences of stalking by patients.
Workplace violence “can affect physical and mental health and lead to burnout, depression, anxiety, and symptoms of PTSD,” said Dr. Abrams. “It can affect one’s sleep and concentration and, therefore, ability to perform one’s job.”
Dr. Ayaz and colleagues suggested recommendations to improve gender-based workplace violence, noting the complex and multifaceted aspects of enhancing current policies, fortifying institutional capacities to respond, and implementing tailored interventions. Changes are needed at various levels, including at the healthcare system and provincial, territorial, and national levels, she said.
In Canada, for instance, lawmakers passed a bill in 2021 that amended the national criminal code to make intimidation or bullying a healthcare worker punishable by as many as 10 years in prison. The changes also required courts to consider more serious penalties for offenders who target healthcare workers aggressively.
But more needs to be done, medical professional groups say. The Canadian Nurses Association and Canadian Federation of Nurses Unions, as well as provincial groups, have called for a pan-Canadian violence-prevention framework, targeted funding for violence prevention infrastructure, and an update to the nation’s health human resources strategy to address severe staffing shortages across the country.
“Canada needs a bold vision for the future of our healthcare. Amid an ongoing staffing crisis, the cracks in our public healthcare systems have only grown deeper and wider, with too many going without the care they need when they need it,” Linda Silas, president of the Canadian Federation of Nurses Unions, told this news organization.
“Access to care relies on safe staffing. Years of unsafe working conditions and insufficient staffing are pushing nurses out of our public healthcare system,” she said. “Working collaboratively, we can make healthcare jobs the best jobs in our communities.”
The authors received no specific funding for the study. Ms. Ayaz, Dr. Abrams, and Ms. Silas reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Across the world, healthcare workers experience workplace violence, which can differ by gender, seniority, and the type of workplace, according to a recent study.
An analysis found that men were more likely to report physical violence, while women were more likely to face nonphysical violence, such as verbal abuse, sexual harassment, and bullying.
“Our study was sparked by the increasing research on workplace violence in healthcare settings. Yet, there’s less empirical data about workplace violence based on gender, its effects on individuals and the collective workforce, and its subsequent impact on patient care and healthcare organizations,” study author Basnama Ayaz, a PhD candidate in nursing at the University of Toronto, told this news organization.
“Workplace violence in healthcare settings is a critical issue that requires attention and action from all stakeholders, including individual providers, healthcare and other institutions, policymakers, and the community,” she said. “By recognizing the problem and implementing evidence-based solutions, we can create safer work environments that protect healthcare workers and improve quality care for patients and organizational effectiveness.”
The study was published online in PLOS Global Public Health.
Widespread and Severe
Although women represent most of the healthcare workforce worldwide, hierarchical structures tend to reflect traditional gender norms, where men hold leadership positions and women serve in front-line care roles, said Ms. Ayaz. Women are often marginalized, and their concerns dismissed, which can exacerbate their vulnerability to gender-based workplace violence, she added.
To better understand these imbalances on a global scale, the investigators conducted a scoping review of the prevalence of and risk factors for gender-based workplace violence in healthcare settings. Participants included physicians, nurses, and midwives, between 2010 and 2024. Although the authors acknowledged that gender-based workplace violence affects the full gender spectrum, only a handful of studies included information about nonbinary personnel, so the review focused on men and women.
Among 226 studies, half focused on physicians, 22% focused on nurses, and 28% included physicians, nurses, midwives, and other medical workers. About 64% of studies reported a higher prevalence of all forms of workplace violence for women, including sexual violence, verbal abuse, discrimination, bullying, and physical violence, while 17% reported a higher prevalence for men.
Overall, across most countries, men experienced more physical violence than did women, and women experienced more verbal abuse, sexual harassment, and bullying. Female nurses were particularly likely to experience violence.
Healthcare workers were also more likely to experience violence if they were younger, less experienced, had a lower professional status, or were part of a minority group based on ethnicity, nationality, culture, or language. These factors were sensitive to gender, “reflecting women’s structural disadvantages in the workplace,” wrote the authors.
As a result of workplace violence, women were more likely to report changes in mental health and social behaviors, as well as dissatisfaction, burnout, and changes in their career goals.
The research team identified various factors linked to violent episodes. In clinical settings where most perpetrators were patients and their relatives, abuse and violence could be related to overcrowding, waiting time, and heavy workloads for healthcare providers. When supervisors or colleagues were the perpetrators, workplace violence appeared to be more likely with long hours, night shifts, and certain clinical settings, such as emergency departments, psychiatric settings, operating rooms, and maternity wards, said Ms. Ayaz. Sexual or gender harassment toward women was more prevalent in male-dominated surgical specialties.
“We were surprised by the extent and severity of workplace violence that healthcare workers face around the globe based on gender,” she said. “One aspect that stood out was the significant role that organizational culture and support systems play either in mitigating or exacerbating these incidents, particularly the power structures between and within professions.”
For instance, trainees in lower hierarchical positions often face a higher risk for violence, especially gender-based harassment, she said. Many times, they feel they can’t report these incidents to trainers or managers, who may also be the perpetrators, she added.
Addressing Systemic Issues
In 2002, the World Health Organization, International Council of Nurses, and other major medical and labor groups worldwide launched a program focused on ways to eliminate workplace violence in healthcare settings. Since 2020, the call for a solution has grown louder as clinicians, nurses, and other health professionals faced more physical and verbal violence during the COVID-19 pandemic, often leading to burnout.
“Workplace violence is very important because it is more prevalent in healthcare workers than in many other settings and is on the rise,” said Karen Abrams, MD, assistant professor of psychiatry at the University of Toronto. Dr. Abrams, who wasn’t involved with this study, has researched physicians’ experiences of stalking by patients.
Workplace violence “can affect physical and mental health and lead to burnout, depression, anxiety, and symptoms of PTSD,” said Dr. Abrams. “It can affect one’s sleep and concentration and, therefore, ability to perform one’s job.”
Dr. Ayaz and colleagues suggested recommendations to improve gender-based workplace violence, noting the complex and multifaceted aspects of enhancing current policies, fortifying institutional capacities to respond, and implementing tailored interventions. Changes are needed at various levels, including at the healthcare system and provincial, territorial, and national levels, she said.
In Canada, for instance, lawmakers passed a bill in 2021 that amended the national criminal code to make intimidation or bullying a healthcare worker punishable by as many as 10 years in prison. The changes also required courts to consider more serious penalties for offenders who target healthcare workers aggressively.
But more needs to be done, medical professional groups say. The Canadian Nurses Association and Canadian Federation of Nurses Unions, as well as provincial groups, have called for a pan-Canadian violence-prevention framework, targeted funding for violence prevention infrastructure, and an update to the nation’s health human resources strategy to address severe staffing shortages across the country.
“Canada needs a bold vision for the future of our healthcare. Amid an ongoing staffing crisis, the cracks in our public healthcare systems have only grown deeper and wider, with too many going without the care they need when they need it,” Linda Silas, president of the Canadian Federation of Nurses Unions, told this news organization.
“Access to care relies on safe staffing. Years of unsafe working conditions and insufficient staffing are pushing nurses out of our public healthcare system,” she said. “Working collaboratively, we can make healthcare jobs the best jobs in our communities.”
The authors received no specific funding for the study. Ms. Ayaz, Dr. Abrams, and Ms. Silas reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
For Richer, for Poorer: Low-Carb Diets Work for All Incomes
For 3 years, Ajala Efem’s type 2 diabetes was so poorly controlled that her blood sugar often soared northward of 500 mg/dL despite insulin shots three to five times a day. She would experience dizziness, vomiting, severe headaches, and the neuropathy in her feet made walking painful. She was also — literally — frothing at the mouth. The 47-year-old single mother of two adult children with mental disabilities feared that she would die.
Ms. Efem lives in the South Bronx, which is among the poorest areas of New York City, where the combined rate of prediabetes and diabetes is close to 30%, the highest rate of any borough in the city.
She had to wait 8 months for an appointment with an endocrinologist, but that visit proved to be life-changing. She lost 28 pounds and got off 15 medications in a single month. She did not join a gym or count calories; she simply changed the food she ate and adopted a low-carb diet.
“I went from being sick to feeling so great,” she told her endocrinologist recently: “My feet aren’t hurting; I’m not in pain; I’m eating as much as I want, and I really enjoy my food so much.”
Ms. Efem’s life-changing visit was with Mariela Glandt, MD, at the offices of Essen Health Care. One month earlier, Dr. Glandt’s company, OwnaHealth, was contracted by Essen to conduct a 100-person pilot program for endocrinology patients. Essen is the largest Medicaid provider in New York City, and “they were desperate for an endocrinologist,” said Dr. Glandt, who trained at Columbia University in New York. So she came — all the way from Madrid, Spain. She commutes monthly, staying for a week each visit.
Dr. Glandt keeps up this punishing schedule because, as she explains, “it’s such a high for me to see these incredible transformations.” Her mostly Black and Hispanic patients are poor and lack resources, yet they lose significant amounts of weight, and their health issues resolve.
“Food is medicine” is an idea very much in vogue. The concept was central to the landmark White House Conference on Hunger, Nutrition, and Health in 2022 and is now the focus of a number of a wide range of government programs. Recently, the Senate held a hearing aimed at further expanding food as medicine programs.
Still, only a single randomized controlled clinical trial has been conducted on this nutritional approach, with unexpectedly disappointing results. In the mid-Atlantic region, 456 food-insecure adults with type 2 diabetes were randomly assigned to usual care or the provision of weekly groceries for their entire families for about 1 year. Provisions for a Mediterranean-style diet included whole grains, fruits and vegetables, lean protein, low-fat dairy products, cereal, brown rice, and bread. In addition, participants received dietary consultations. Yet, those who got free food and coaching did not see improvements in their average blood sugar (the study’s primary outcome), and their low-density lipoprotein (LDL) cholesterol and high-density lipoprotein (HDL) cholesterol levels appeared to have worsened.
“To be honest, I was surprised,” the study’s lead author, Joseph Doyle, PhD, professor at the Sloan School of Management at MIT in Cambridge, Massachusetts, told me. “I was hoping we would show improved outcomes, but the way to make progress is to do well-randomized trials to find out what works.”
I was not surprised by these results because a recent rigorous systematic review and meta-analysis in The BMJ did not show a Mediterranean-style diet to be the most effective for glycemic control. And Ms. Efem was not in fact following a Mediterranean-style diet.
Ms. Efem’s low-carb success story is anecdotal, but Dr. Glandt has an established track record from her 9 years’ experience as the medical director of the eponymous diabetes center she founded in Tel Aviv. A recent audit of 344 patients from the center found that after 6 months of following a very low–carbohydrate diet, 96.3% of those with diabetes saw their A1c fall from a median 7.6% to 6.3%. Weight loss was significant, with a median drop of 6.5 kg (14 pounds) for patients with diabetes and 5.7 kg for those with prediabetes. The diet comprises 5%-10% of calories from carbs, but Dr. Glandt does not use numeric targets with her patients.
Blood pressure, triglycerides, and liver enzymes also improved. And though LDL cholesterol went up by 8%, this result may have been offset by an accompanying 13% rise in HDL cholesterol. Of the 78 patients initially on insulin, 62 were able to stop this medication entirely.
Although these results aren’t from a clinical trial, they’re still highly meaningful because the current dietary standard of care for type 2 diabetes can only slow the progression of the disease, not cause remission. Indeed, the idea that type 2 diabetes could be put into remission was not seriously considered by the American Diabetes Association (ADA) until 2009. By 2019, an ADA report concluded that “[r]educing overall carbohydrate intake for individuals with diabetes has demonstrated the most evidence for improving glycemia.” In other words, the best way to improve the key factor in diabetes is to reduce total carbohydrates. Yet, the ADA still advocates filling one quarter of one’s plate with carbohydrate-based foods, an amount that will prevent remission. Given that the ADA’s vision statement is “a life free of diabetes,” it seems negligent not to tell people with a deadly condition that they can reverse this diagnosis.
A 2023 meta-analysis of 42 controlled clinical trials on 4809 patients showed that a very low–carbohydrate ketogenic diet (keto) was “superior” to alternatives for glycemic control. A more recent review of 11 clinical trials found that this diet was equal but not superior to other nutritional approaches in terms of blood sugar control, but this review also concluded that keto led to greater increases in HDL cholesterol and lower triglycerides.
Dr. Glandt’s patients in the Bronx might not seem like obvious low-carb candidates. The diet is considered expensive and difficult to sustain. My interviews with a half dozen patients revealed some of these difficulties, but even for a woman living in a homeless shelter, the obstacles are not insurmountable.
Jerrilyn, who preferred that I use only her first name, lives in a shelter in Queens. While we strolled through a nearby park, she told me about her desire to lose weight and recover from polycystic ovary syndrome, which terrified her because it had caused dramatic hair loss. When she landed in Dr. Glandt’s office at age 28, she weighed 180 pounds.
Less than 5 months later, Jerrilyn had lost 25 pounds, and her period had returned with some regularity. She said she used “food stamps,” known as the Supplemental Nutrition Assistance Program (SNAP), to buy most of her food at local delis because the meals served at the shelter were too heavy in starches. She starts her day with eggs, turkey bacon, and avocado.
“It was hard to give up carbohydrates because in my culture [Latina], we have nothing but carbs: rice, potatoes, yuca,” Jerrilyn shared. She noticed that carbs make her hungrier, but after 3 days of going low-carb, her cravings diminished. “It was like getting over an addiction,” she said.
Jerrilyn told me she’d seen many doctors but none as involved as Dr. Glandt. “It feels awesome to know that I have a lot of really useful information coming from her all the time.” The OwnaHealth app tracks weight, blood pressure, blood sugar, ketones, meals, mood, and cravings. Patients wear continuous glucose monitors and enter other information manually. Ketone bodies are used to measure dietary adherence and are obtained through finger pricks and test strips provided by OwnaHealth. Dr. Glandt gives patients her own food plan, along with free visual guides to low-carbohydrate foods by dietdoctor.com.
Dr. Glandt also sends her patients for regular blood work. She says she does not frequently see a rise in LDL cholesterol, which can sometimes occur on a low-carbohydrate diet. This effect is most common among people who are lean and fit. She says she doesn’t discontinue statins unless cholesterol levels improve significantly.
Samuel Gonzalez, age 56, weighed 275 pounds when he walked into Dr. Glandt’s office this past November. His A1c was 9.2%, but none of his previous doctors had diagnosed him with diabetes. “I was like a walking bag of sugar!” he joked.
A low-carbohydrate diet seemed absurd to a Puerto Rican like himself: “Having coffee without sugar? That’s like sacrilegious in my culture!” exclaimed Mr. Gonzalez. Still, he managed, with SNAP, to cook eggs and bacon for breakfast and some kind of protein for dinner. He keeps lunch light, “like tuna fish,” and finds checking in with the OwnaHealth app to be very helpful. “Every day, I’m on it,” he said. In the past 7 months, he’s lost 50 pounds, normalized his cholesterol and blood pressure levels, and lowered his A1c to 5.5%.
Mr. Gonzalez gets disability payments due to a back injury, and Ms. Efem receives government payments because her husband died serving in the military. Ms. Efem says her new diet challenges her budget, but Mr. Gonzalez says he manages easily.
Mélissa Cruz, a 28-year-old studying to be a nail technician while also doing back office work at a physical therapy practice, says she’s stretched thin. “I end up sad because I can’t put energy into looking up recipes and cooking for me and my boyfriend,” she told me. She’ll often cook rice and plantains for him and meat for herself, but “it’s frustrating when I’m low on funds and can’t figure out what to eat.”
Low-carbohydrate diets have a reputation for being expensive because people often start eating pricier foods, like meat and cheese, to replace cheaper starchy foods such as pasta and rice.
A 2019 cost analysis published in Nutrition & Dietetics compared a low-carbohydrate dietary pattern with the New Zealand government’s recommended guidelines (which are almost identical to those in the United States) and found that it cost only an extra $1.27 in US dollars per person per day. One explanation is that protein and fat are more satiating than carbohydrates, so people who mostly consume these macronutrients often cut back on snacks like packaged chips, crackers, and even fruits. Also, those on a ketogenic diet usually cut down on medications, so the additional $1.27 daily is likely offset by reduced spending at the pharmacy.
It’s not just Bronx residents with low socioeconomic status (SES) who adapt well to low-carbohydrate diets. Among Alabama state employees with diabetes enrolled in a low-carbohydrate dietary program provided by a company called Virta, the low SES population had the best outcomes. Virta also published survey data in 2023 showing that participants in a program with the Veteran’s Administration did not find additional costs to be an obstacle to dietary adherence. In fact, some participants saw cost reductions due to decreased spending on processed snacks and fast foods.
Ms. Cruz told me she struggles financially, yet she’s still lost nearly 30 pounds in 5 months, and her A1c went from 7.1% down to 5.9%, putting her diabetes into remission. Equally motivating for her are the improvements she’s seen in other hormonal issues. Since childhood, she’s had acanthosis, a condition that causes the skin to darken in velvety patches, and more recently, she developed severe hirsutism to the point of growing sideburns. “I had tried going vegan and fasting, but these just weren’t sustainable for me, and I was so overwhelmed with counting calories all the time.” Now, on a low-carbohydrate diet, which doesn’t require calorie counting, she’s finally seeing both these conditions improve significantly.
When I last checked in with Ms. Cruz, she said she had “kind of ghosted” Dr. Glandt due to her work and school constraints, but she hadn’t abandoned the diet. She appreciated, too, that Dr. Glandt had not given up on her and kept calling and messaging. “She’s not at all like a typical doctor who would just tell me to lose weight and shake their head at me,” Ms. Cruz said.
Because Dr. Glandt’s approach is time-intensive and high-touch, it might seem impractical to scale up, but Dr. Glandt’s app uses artificial intelligence to help with communications thus allowing her, with help from part-time health coaches, to care for patients.
This early success in one of the United States’ poorest and sickest neighborhoods should give us hope that type 2 diabetes need not to be a progressive irreversible disease, even among the disadvantaged.
OwnaHealth’s track record, along with that of Virta and other similar low-carbohydrate medical practices also give hope to the food-is-medicine idea. Diabetes can go into remission, and people can be healed, provided that health practitioners prescribe the right foods. And in truth, it’s not a diet. It’s a way of eating that must be maintained. The sustainability of low-carbohydrate diets has been a point of contention, but the Virta trial, with 38% of patients sustaining remission at 2 years, showed that it’s possible. (OwnaHealth, for its part, offers long-term maintenance plans to help patients stay very low-carb permanently.)
Given the tremendous costs and health burden of diabetes, this approach should no doubt be the first line of treatment for doctors and the ADA. The past two decades of clinical trial research have demonstrated that remission of type 2 diabetes is possible through diet alone. It turns out that for metabolic diseases, only certain foods are truly medicine.
Tools and Tips for Clinicians:
- Free two-page keto starter’s guide by OwnaHealth; Dr. Glandt uses this guide with her patients.
- Illustrated low-carb guides by dietdoctor.com
- Free low-carbohydrate starter guide by the Michigan Collaborative for Type 2 Diabetes
- Low-Carb for Any Budget, a free digital booklet by Mark Cucuzzella, MD, and Kristie Sullivan, PhD
- Recipe and meal ideas from Ruled.me, Keto-Mojo.com, and
Dr. Teicholz is the founder of Nutrition Coalition, an independent nonprofit dedicated to ensuring that US dietary guidelines align with current science. She disclosed receiving book royalties from The Big Fat Surprise, and received honorarium not exceeding $2000 for speeches from various sources.
A version of this article appeared on Medscape.com.
For 3 years, Ajala Efem’s type 2 diabetes was so poorly controlled that her blood sugar often soared northward of 500 mg/dL despite insulin shots three to five times a day. She would experience dizziness, vomiting, severe headaches, and the neuropathy in her feet made walking painful. She was also — literally — frothing at the mouth. The 47-year-old single mother of two adult children with mental disabilities feared that she would die.
Ms. Efem lives in the South Bronx, which is among the poorest areas of New York City, where the combined rate of prediabetes and diabetes is close to 30%, the highest rate of any borough in the city.
She had to wait 8 months for an appointment with an endocrinologist, but that visit proved to be life-changing. She lost 28 pounds and got off 15 medications in a single month. She did not join a gym or count calories; she simply changed the food she ate and adopted a low-carb diet.
“I went from being sick to feeling so great,” she told her endocrinologist recently: “My feet aren’t hurting; I’m not in pain; I’m eating as much as I want, and I really enjoy my food so much.”
Ms. Efem’s life-changing visit was with Mariela Glandt, MD, at the offices of Essen Health Care. One month earlier, Dr. Glandt’s company, OwnaHealth, was contracted by Essen to conduct a 100-person pilot program for endocrinology patients. Essen is the largest Medicaid provider in New York City, and “they were desperate for an endocrinologist,” said Dr. Glandt, who trained at Columbia University in New York. So she came — all the way from Madrid, Spain. She commutes monthly, staying for a week each visit.
Dr. Glandt keeps up this punishing schedule because, as she explains, “it’s such a high for me to see these incredible transformations.” Her mostly Black and Hispanic patients are poor and lack resources, yet they lose significant amounts of weight, and their health issues resolve.
“Food is medicine” is an idea very much in vogue. The concept was central to the landmark White House Conference on Hunger, Nutrition, and Health in 2022 and is now the focus of a number of a wide range of government programs. Recently, the Senate held a hearing aimed at further expanding food as medicine programs.
Still, only a single randomized controlled clinical trial has been conducted on this nutritional approach, with unexpectedly disappointing results. In the mid-Atlantic region, 456 food-insecure adults with type 2 diabetes were randomly assigned to usual care or the provision of weekly groceries for their entire families for about 1 year. Provisions for a Mediterranean-style diet included whole grains, fruits and vegetables, lean protein, low-fat dairy products, cereal, brown rice, and bread. In addition, participants received dietary consultations. Yet, those who got free food and coaching did not see improvements in their average blood sugar (the study’s primary outcome), and their low-density lipoprotein (LDL) cholesterol and high-density lipoprotein (HDL) cholesterol levels appeared to have worsened.
“To be honest, I was surprised,” the study’s lead author, Joseph Doyle, PhD, professor at the Sloan School of Management at MIT in Cambridge, Massachusetts, told me. “I was hoping we would show improved outcomes, but the way to make progress is to do well-randomized trials to find out what works.”
I was not surprised by these results because a recent rigorous systematic review and meta-analysis in The BMJ did not show a Mediterranean-style diet to be the most effective for glycemic control. And Ms. Efem was not in fact following a Mediterranean-style diet.
Ms. Efem’s low-carb success story is anecdotal, but Dr. Glandt has an established track record from her 9 years’ experience as the medical director of the eponymous diabetes center she founded in Tel Aviv. A recent audit of 344 patients from the center found that after 6 months of following a very low–carbohydrate diet, 96.3% of those with diabetes saw their A1c fall from a median 7.6% to 6.3%. Weight loss was significant, with a median drop of 6.5 kg (14 pounds) for patients with diabetes and 5.7 kg for those with prediabetes. The diet comprises 5%-10% of calories from carbs, but Dr. Glandt does not use numeric targets with her patients.
Blood pressure, triglycerides, and liver enzymes also improved. And though LDL cholesterol went up by 8%, this result may have been offset by an accompanying 13% rise in HDL cholesterol. Of the 78 patients initially on insulin, 62 were able to stop this medication entirely.
Although these results aren’t from a clinical trial, they’re still highly meaningful because the current dietary standard of care for type 2 diabetes can only slow the progression of the disease, not cause remission. Indeed, the idea that type 2 diabetes could be put into remission was not seriously considered by the American Diabetes Association (ADA) until 2009. By 2019, an ADA report concluded that “[r]educing overall carbohydrate intake for individuals with diabetes has demonstrated the most evidence for improving glycemia.” In other words, the best way to improve the key factor in diabetes is to reduce total carbohydrates. Yet, the ADA still advocates filling one quarter of one’s plate with carbohydrate-based foods, an amount that will prevent remission. Given that the ADA’s vision statement is “a life free of diabetes,” it seems negligent not to tell people with a deadly condition that they can reverse this diagnosis.
A 2023 meta-analysis of 42 controlled clinical trials on 4809 patients showed that a very low–carbohydrate ketogenic diet (keto) was “superior” to alternatives for glycemic control. A more recent review of 11 clinical trials found that this diet was equal but not superior to other nutritional approaches in terms of blood sugar control, but this review also concluded that keto led to greater increases in HDL cholesterol and lower triglycerides.
Dr. Glandt’s patients in the Bronx might not seem like obvious low-carb candidates. The diet is considered expensive and difficult to sustain. My interviews with a half dozen patients revealed some of these difficulties, but even for a woman living in a homeless shelter, the obstacles are not insurmountable.
Jerrilyn, who preferred that I use only her first name, lives in a shelter in Queens. While we strolled through a nearby park, she told me about her desire to lose weight and recover from polycystic ovary syndrome, which terrified her because it had caused dramatic hair loss. When she landed in Dr. Glandt’s office at age 28, she weighed 180 pounds.
Less than 5 months later, Jerrilyn had lost 25 pounds, and her period had returned with some regularity. She said she used “food stamps,” known as the Supplemental Nutrition Assistance Program (SNAP), to buy most of her food at local delis because the meals served at the shelter were too heavy in starches. She starts her day with eggs, turkey bacon, and avocado.
“It was hard to give up carbohydrates because in my culture [Latina], we have nothing but carbs: rice, potatoes, yuca,” Jerrilyn shared. She noticed that carbs make her hungrier, but after 3 days of going low-carb, her cravings diminished. “It was like getting over an addiction,” she said.
Jerrilyn told me she’d seen many doctors but none as involved as Dr. Glandt. “It feels awesome to know that I have a lot of really useful information coming from her all the time.” The OwnaHealth app tracks weight, blood pressure, blood sugar, ketones, meals, mood, and cravings. Patients wear continuous glucose monitors and enter other information manually. Ketone bodies are used to measure dietary adherence and are obtained through finger pricks and test strips provided by OwnaHealth. Dr. Glandt gives patients her own food plan, along with free visual guides to low-carbohydrate foods by dietdoctor.com.
Dr. Glandt also sends her patients for regular blood work. She says she does not frequently see a rise in LDL cholesterol, which can sometimes occur on a low-carbohydrate diet. This effect is most common among people who are lean and fit. She says she doesn’t discontinue statins unless cholesterol levels improve significantly.
Samuel Gonzalez, age 56, weighed 275 pounds when he walked into Dr. Glandt’s office this past November. His A1c was 9.2%, but none of his previous doctors had diagnosed him with diabetes. “I was like a walking bag of sugar!” he joked.
A low-carbohydrate diet seemed absurd to a Puerto Rican like himself: “Having coffee without sugar? That’s like sacrilegious in my culture!” exclaimed Mr. Gonzalez. Still, he managed, with SNAP, to cook eggs and bacon for breakfast and some kind of protein for dinner. He keeps lunch light, “like tuna fish,” and finds checking in with the OwnaHealth app to be very helpful. “Every day, I’m on it,” he said. In the past 7 months, he’s lost 50 pounds, normalized his cholesterol and blood pressure levels, and lowered his A1c to 5.5%.
Mr. Gonzalez gets disability payments due to a back injury, and Ms. Efem receives government payments because her husband died serving in the military. Ms. Efem says her new diet challenges her budget, but Mr. Gonzalez says he manages easily.
Mélissa Cruz, a 28-year-old studying to be a nail technician while also doing back office work at a physical therapy practice, says she’s stretched thin. “I end up sad because I can’t put energy into looking up recipes and cooking for me and my boyfriend,” she told me. She’ll often cook rice and plantains for him and meat for herself, but “it’s frustrating when I’m low on funds and can’t figure out what to eat.”
Low-carbohydrate diets have a reputation for being expensive because people often start eating pricier foods, like meat and cheese, to replace cheaper starchy foods such as pasta and rice.
A 2019 cost analysis published in Nutrition & Dietetics compared a low-carbohydrate dietary pattern with the New Zealand government’s recommended guidelines (which are almost identical to those in the United States) and found that it cost only an extra $1.27 in US dollars per person per day. One explanation is that protein and fat are more satiating than carbohydrates, so people who mostly consume these macronutrients often cut back on snacks like packaged chips, crackers, and even fruits. Also, those on a ketogenic diet usually cut down on medications, so the additional $1.27 daily is likely offset by reduced spending at the pharmacy.
It’s not just Bronx residents with low socioeconomic status (SES) who adapt well to low-carbohydrate diets. Among Alabama state employees with diabetes enrolled in a low-carbohydrate dietary program provided by a company called Virta, the low SES population had the best outcomes. Virta also published survey data in 2023 showing that participants in a program with the Veteran’s Administration did not find additional costs to be an obstacle to dietary adherence. In fact, some participants saw cost reductions due to decreased spending on processed snacks and fast foods.
Ms. Cruz told me she struggles financially, yet she’s still lost nearly 30 pounds in 5 months, and her A1c went from 7.1% down to 5.9%, putting her diabetes into remission. Equally motivating for her are the improvements she’s seen in other hormonal issues. Since childhood, she’s had acanthosis, a condition that causes the skin to darken in velvety patches, and more recently, she developed severe hirsutism to the point of growing sideburns. “I had tried going vegan and fasting, but these just weren’t sustainable for me, and I was so overwhelmed with counting calories all the time.” Now, on a low-carbohydrate diet, which doesn’t require calorie counting, she’s finally seeing both these conditions improve significantly.
When I last checked in with Ms. Cruz, she said she had “kind of ghosted” Dr. Glandt due to her work and school constraints, but she hadn’t abandoned the diet. She appreciated, too, that Dr. Glandt had not given up on her and kept calling and messaging. “She’s not at all like a typical doctor who would just tell me to lose weight and shake their head at me,” Ms. Cruz said.
Because Dr. Glandt’s approach is time-intensive and high-touch, it might seem impractical to scale up, but Dr. Glandt’s app uses artificial intelligence to help with communications thus allowing her, with help from part-time health coaches, to care for patients.
This early success in one of the United States’ poorest and sickest neighborhoods should give us hope that type 2 diabetes need not to be a progressive irreversible disease, even among the disadvantaged.
OwnaHealth’s track record, along with that of Virta and other similar low-carbohydrate medical practices also give hope to the food-is-medicine idea. Diabetes can go into remission, and people can be healed, provided that health practitioners prescribe the right foods. And in truth, it’s not a diet. It’s a way of eating that must be maintained. The sustainability of low-carbohydrate diets has been a point of contention, but the Virta trial, with 38% of patients sustaining remission at 2 years, showed that it’s possible. (OwnaHealth, for its part, offers long-term maintenance plans to help patients stay very low-carb permanently.)
Given the tremendous costs and health burden of diabetes, this approach should no doubt be the first line of treatment for doctors and the ADA. The past two decades of clinical trial research have demonstrated that remission of type 2 diabetes is possible through diet alone. It turns out that for metabolic diseases, only certain foods are truly medicine.
Tools and Tips for Clinicians:
- Free two-page keto starter’s guide by OwnaHealth; Dr. Glandt uses this guide with her patients.
- Illustrated low-carb guides by dietdoctor.com
- Free low-carbohydrate starter guide by the Michigan Collaborative for Type 2 Diabetes
- Low-Carb for Any Budget, a free digital booklet by Mark Cucuzzella, MD, and Kristie Sullivan, PhD
- Recipe and meal ideas from Ruled.me, Keto-Mojo.com, and
Dr. Teicholz is the founder of Nutrition Coalition, an independent nonprofit dedicated to ensuring that US dietary guidelines align with current science. She disclosed receiving book royalties from The Big Fat Surprise, and received honorarium not exceeding $2000 for speeches from various sources.
A version of this article appeared on Medscape.com.
For 3 years, Ajala Efem’s type 2 diabetes was so poorly controlled that her blood sugar often soared northward of 500 mg/dL despite insulin shots three to five times a day. She would experience dizziness, vomiting, severe headaches, and the neuropathy in her feet made walking painful. She was also — literally — frothing at the mouth. The 47-year-old single mother of two adult children with mental disabilities feared that she would die.
Ms. Efem lives in the South Bronx, which is among the poorest areas of New York City, where the combined rate of prediabetes and diabetes is close to 30%, the highest rate of any borough in the city.
She had to wait 8 months for an appointment with an endocrinologist, but that visit proved to be life-changing. She lost 28 pounds and got off 15 medications in a single month. She did not join a gym or count calories; she simply changed the food she ate and adopted a low-carb diet.
“I went from being sick to feeling so great,” she told her endocrinologist recently: “My feet aren’t hurting; I’m not in pain; I’m eating as much as I want, and I really enjoy my food so much.”
Ms. Efem’s life-changing visit was with Mariela Glandt, MD, at the offices of Essen Health Care. One month earlier, Dr. Glandt’s company, OwnaHealth, was contracted by Essen to conduct a 100-person pilot program for endocrinology patients. Essen is the largest Medicaid provider in New York City, and “they were desperate for an endocrinologist,” said Dr. Glandt, who trained at Columbia University in New York. So she came — all the way from Madrid, Spain. She commutes monthly, staying for a week each visit.
Dr. Glandt keeps up this punishing schedule because, as she explains, “it’s such a high for me to see these incredible transformations.” Her mostly Black and Hispanic patients are poor and lack resources, yet they lose significant amounts of weight, and their health issues resolve.
“Food is medicine” is an idea very much in vogue. The concept was central to the landmark White House Conference on Hunger, Nutrition, and Health in 2022 and is now the focus of a number of a wide range of government programs. Recently, the Senate held a hearing aimed at further expanding food as medicine programs.
Still, only a single randomized controlled clinical trial has been conducted on this nutritional approach, with unexpectedly disappointing results. In the mid-Atlantic region, 456 food-insecure adults with type 2 diabetes were randomly assigned to usual care or the provision of weekly groceries for their entire families for about 1 year. Provisions for a Mediterranean-style diet included whole grains, fruits and vegetables, lean protein, low-fat dairy products, cereal, brown rice, and bread. In addition, participants received dietary consultations. Yet, those who got free food and coaching did not see improvements in their average blood sugar (the study’s primary outcome), and their low-density lipoprotein (LDL) cholesterol and high-density lipoprotein (HDL) cholesterol levels appeared to have worsened.
“To be honest, I was surprised,” the study’s lead author, Joseph Doyle, PhD, professor at the Sloan School of Management at MIT in Cambridge, Massachusetts, told me. “I was hoping we would show improved outcomes, but the way to make progress is to do well-randomized trials to find out what works.”
I was not surprised by these results because a recent rigorous systematic review and meta-analysis in The BMJ did not show a Mediterranean-style diet to be the most effective for glycemic control. And Ms. Efem was not in fact following a Mediterranean-style diet.
Ms. Efem’s low-carb success story is anecdotal, but Dr. Glandt has an established track record from her 9 years’ experience as the medical director of the eponymous diabetes center she founded in Tel Aviv. A recent audit of 344 patients from the center found that after 6 months of following a very low–carbohydrate diet, 96.3% of those with diabetes saw their A1c fall from a median 7.6% to 6.3%. Weight loss was significant, with a median drop of 6.5 kg (14 pounds) for patients with diabetes and 5.7 kg for those with prediabetes. The diet comprises 5%-10% of calories from carbs, but Dr. Glandt does not use numeric targets with her patients.
Blood pressure, triglycerides, and liver enzymes also improved. And though LDL cholesterol went up by 8%, this result may have been offset by an accompanying 13% rise in HDL cholesterol. Of the 78 patients initially on insulin, 62 were able to stop this medication entirely.
Although these results aren’t from a clinical trial, they’re still highly meaningful because the current dietary standard of care for type 2 diabetes can only slow the progression of the disease, not cause remission. Indeed, the idea that type 2 diabetes could be put into remission was not seriously considered by the American Diabetes Association (ADA) until 2009. By 2019, an ADA report concluded that “[r]educing overall carbohydrate intake for individuals with diabetes has demonstrated the most evidence for improving glycemia.” In other words, the best way to improve the key factor in diabetes is to reduce total carbohydrates. Yet, the ADA still advocates filling one quarter of one’s plate with carbohydrate-based foods, an amount that will prevent remission. Given that the ADA’s vision statement is “a life free of diabetes,” it seems negligent not to tell people with a deadly condition that they can reverse this diagnosis.
A 2023 meta-analysis of 42 controlled clinical trials on 4809 patients showed that a very low–carbohydrate ketogenic diet (keto) was “superior” to alternatives for glycemic control. A more recent review of 11 clinical trials found that this diet was equal but not superior to other nutritional approaches in terms of blood sugar control, but this review also concluded that keto led to greater increases in HDL cholesterol and lower triglycerides.
Dr. Glandt’s patients in the Bronx might not seem like obvious low-carb candidates. The diet is considered expensive and difficult to sustain. My interviews with a half dozen patients revealed some of these difficulties, but even for a woman living in a homeless shelter, the obstacles are not insurmountable.
Jerrilyn, who preferred that I use only her first name, lives in a shelter in Queens. While we strolled through a nearby park, she told me about her desire to lose weight and recover from polycystic ovary syndrome, which terrified her because it had caused dramatic hair loss. When she landed in Dr. Glandt’s office at age 28, she weighed 180 pounds.
Less than 5 months later, Jerrilyn had lost 25 pounds, and her period had returned with some regularity. She said she used “food stamps,” known as the Supplemental Nutrition Assistance Program (SNAP), to buy most of her food at local delis because the meals served at the shelter were too heavy in starches. She starts her day with eggs, turkey bacon, and avocado.
“It was hard to give up carbohydrates because in my culture [Latina], we have nothing but carbs: rice, potatoes, yuca,” Jerrilyn shared. She noticed that carbs make her hungrier, but after 3 days of going low-carb, her cravings diminished. “It was like getting over an addiction,” she said.
Jerrilyn told me she’d seen many doctors but none as involved as Dr. Glandt. “It feels awesome to know that I have a lot of really useful information coming from her all the time.” The OwnaHealth app tracks weight, blood pressure, blood sugar, ketones, meals, mood, and cravings. Patients wear continuous glucose monitors and enter other information manually. Ketone bodies are used to measure dietary adherence and are obtained through finger pricks and test strips provided by OwnaHealth. Dr. Glandt gives patients her own food plan, along with free visual guides to low-carbohydrate foods by dietdoctor.com.
Dr. Glandt also sends her patients for regular blood work. She says she does not frequently see a rise in LDL cholesterol, which can sometimes occur on a low-carbohydrate diet. This effect is most common among people who are lean and fit. She says she doesn’t discontinue statins unless cholesterol levels improve significantly.
Samuel Gonzalez, age 56, weighed 275 pounds when he walked into Dr. Glandt’s office this past November. His A1c was 9.2%, but none of his previous doctors had diagnosed him with diabetes. “I was like a walking bag of sugar!” he joked.
A low-carbohydrate diet seemed absurd to a Puerto Rican like himself: “Having coffee without sugar? That’s like sacrilegious in my culture!” exclaimed Mr. Gonzalez. Still, he managed, with SNAP, to cook eggs and bacon for breakfast and some kind of protein for dinner. He keeps lunch light, “like tuna fish,” and finds checking in with the OwnaHealth app to be very helpful. “Every day, I’m on it,” he said. In the past 7 months, he’s lost 50 pounds, normalized his cholesterol and blood pressure levels, and lowered his A1c to 5.5%.
Mr. Gonzalez gets disability payments due to a back injury, and Ms. Efem receives government payments because her husband died serving in the military. Ms. Efem says her new diet challenges her budget, but Mr. Gonzalez says he manages easily.
Mélissa Cruz, a 28-year-old studying to be a nail technician while also doing back office work at a physical therapy practice, says she’s stretched thin. “I end up sad because I can’t put energy into looking up recipes and cooking for me and my boyfriend,” she told me. She’ll often cook rice and plantains for him and meat for herself, but “it’s frustrating when I’m low on funds and can’t figure out what to eat.”
Low-carbohydrate diets have a reputation for being expensive because people often start eating pricier foods, like meat and cheese, to replace cheaper starchy foods such as pasta and rice.
A 2019 cost analysis published in Nutrition & Dietetics compared a low-carbohydrate dietary pattern with the New Zealand government’s recommended guidelines (which are almost identical to those in the United States) and found that it cost only an extra $1.27 in US dollars per person per day. One explanation is that protein and fat are more satiating than carbohydrates, so people who mostly consume these macronutrients often cut back on snacks like packaged chips, crackers, and even fruits. Also, those on a ketogenic diet usually cut down on medications, so the additional $1.27 daily is likely offset by reduced spending at the pharmacy.
It’s not just Bronx residents with low socioeconomic status (SES) who adapt well to low-carbohydrate diets. Among Alabama state employees with diabetes enrolled in a low-carbohydrate dietary program provided by a company called Virta, the low SES population had the best outcomes. Virta also published survey data in 2023 showing that participants in a program with the Veteran’s Administration did not find additional costs to be an obstacle to dietary adherence. In fact, some participants saw cost reductions due to decreased spending on processed snacks and fast foods.
Ms. Cruz told me she struggles financially, yet she’s still lost nearly 30 pounds in 5 months, and her A1c went from 7.1% down to 5.9%, putting her diabetes into remission. Equally motivating for her are the improvements she’s seen in other hormonal issues. Since childhood, she’s had acanthosis, a condition that causes the skin to darken in velvety patches, and more recently, she developed severe hirsutism to the point of growing sideburns. “I had tried going vegan and fasting, but these just weren’t sustainable for me, and I was so overwhelmed with counting calories all the time.” Now, on a low-carbohydrate diet, which doesn’t require calorie counting, she’s finally seeing both these conditions improve significantly.
When I last checked in with Ms. Cruz, she said she had “kind of ghosted” Dr. Glandt due to her work and school constraints, but she hadn’t abandoned the diet. She appreciated, too, that Dr. Glandt had not given up on her and kept calling and messaging. “She’s not at all like a typical doctor who would just tell me to lose weight and shake their head at me,” Ms. Cruz said.
Because Dr. Glandt’s approach is time-intensive and high-touch, it might seem impractical to scale up, but Dr. Glandt’s app uses artificial intelligence to help with communications thus allowing her, with help from part-time health coaches, to care for patients.
This early success in one of the United States’ poorest and sickest neighborhoods should give us hope that type 2 diabetes need not to be a progressive irreversible disease, even among the disadvantaged.
OwnaHealth’s track record, along with that of Virta and other similar low-carbohydrate medical practices also give hope to the food-is-medicine idea. Diabetes can go into remission, and people can be healed, provided that health practitioners prescribe the right foods. And in truth, it’s not a diet. It’s a way of eating that must be maintained. The sustainability of low-carbohydrate diets has been a point of contention, but the Virta trial, with 38% of patients sustaining remission at 2 years, showed that it’s possible. (OwnaHealth, for its part, offers long-term maintenance plans to help patients stay very low-carb permanently.)
Given the tremendous costs and health burden of diabetes, this approach should no doubt be the first line of treatment for doctors and the ADA. The past two decades of clinical trial research have demonstrated that remission of type 2 diabetes is possible through diet alone. It turns out that for metabolic diseases, only certain foods are truly medicine.
Tools and Tips for Clinicians:
- Free two-page keto starter’s guide by OwnaHealth; Dr. Glandt uses this guide with her patients.
- Illustrated low-carb guides by dietdoctor.com
- Free low-carbohydrate starter guide by the Michigan Collaborative for Type 2 Diabetes
- Low-Carb for Any Budget, a free digital booklet by Mark Cucuzzella, MD, and Kristie Sullivan, PhD
- Recipe and meal ideas from Ruled.me, Keto-Mojo.com, and
Dr. Teicholz is the founder of Nutrition Coalition, an independent nonprofit dedicated to ensuring that US dietary guidelines align with current science. She disclosed receiving book royalties from The Big Fat Surprise, and received honorarium not exceeding $2000 for speeches from various sources.
A version of this article appeared on Medscape.com.
Pulsed Field Ablation for AF: Are US Electrophysiologists Too Easily Impressed?
It dominated 2024’s heart rhythm meetings, and it dominates my private electrophysiologist chat groups. My Google alert for “AF ablation” most often includes notices on PFA and the expansion of the atrial fibrillation ablation market.
Yet, the excitement does not match the empirical data.
Despite having strong brains, electrophysiologists adopt new things as if we were emotional shoppers. Our neighbor buys a sports car and we think we need the same car. Left atrial appendage occlusion and subcutaneous defibrillators were past examples.
The most recent example of soft thinking (especially in the United States) is the enthusiasm and early adoption of first-generation PFA systems for the treatment of AF.
Readers of cardiac news (including some of my patients) might think PFA has solved the AF puzzle. It has not.
A true breakthrough in AF would be to find its cause. PFA is simply another way to destroy (ablate) cardiac myocytes. PFA uses electrical energy (think shocks) to create pores in the cell membranes of myocytes. It’s delivered through various types of catheters.
The main theoretical advantage of PFA is cardioselectivity, which is possible because myocytes have lower thresholds for irreversible electroporation than surrounding tissues. The dose of electrical energy that ablates cardiac tissue does not affect surrounding tissues. Cardioselectivity decreases the chance of the most feared complication of standard AF ablation, thermal damage to the esophagus, which is often fatal. The esophagus lies immediately behind the posterior wall of the left atrium and can be inadvertently injured during thermal ablation.
The challenge in assessing this potential advantage is that thermal esophageal damage is, thankfully, exceedingly rare. Its incidence is in the range of 1 in 10,000 AF ablations. But it might be even lower than that in contemporary practice, because knowledge of esophageal injury has led to innovations that probably have reduced its incidence even further.
Proponents of PFA would rightly point to the fact that not having to worry about esophageal injury allows operators to add posterior wall ablation to the normal pulmonary vein isolation lesion set. This ability, they would argue, is likely to improve AF ablation outcomes. The problem is that the strongest and most recent trial of posterior wall isolation (with radiofrequency ablation) did not show better outcomes. A more recent observational analysis also showed no benefit to posterior wall isolation (using PFA) over pulmonary vein isolation alone.
What About PFA Efficacy?
I’ve long spoken and written about the lack of progress in AF ablation. In 1998, the first report on ablation of AF showed a 62% arrhythmia-free rate. Two decades later, in the carefully chosen labs treating patients in the CABANA trial, arrhythmia-free rates after AF ablation remain unchanged. We have improved our speed and ability to isolate pulmonary veins, but this has not increased our success in eliminating AF. The reason, I believe, is that we have made little to no progress in understanding the pathophysiology of AF.
The Food and Drug Administration regulatory trial called ADVENT randomly assigned more than 600 patients to thermal ablation or PFA, and the primary endpoint of ablation success was nearly identical. Single-center studies, observational registries, and single-arm studies have all shown similar efficacy of PFA and thermal ablation.
Proponents of PFA might argue that these early studies used first-generation PFA systems, and iteration will lead to better efficacy. Perhaps, but we’ve had 20 years of iteration of thermal ablation, and its efficacy has not budged.
What About PFA Safety?
In the ADVENT randomized trial, safety results were similar, though the one death, caused by cardiac perforation and tamponade, occurred in the PFA arm. In the MANIFEST-17K multinational survey of PFA ablation, safety events were in the range reported with thermal ablation. PFA still involves placing catheters in the heart, and complications such as tamponade, stroke, and vascular damage occur.
The large MANIFEST-17K survey also exposed two PFA-specific complications: coronary artery spasm, which can occur when PFA is delivered close to coronary arteries; and hemolysis-related kidney failure — severe enough to require dialysis in five patients. Supporters of PFA speculate that hemolysis occurs because electrical energy within the atrium can shred red blood cells. Their solution is to strive for good contact and use hydration. The irony of this latter fix is that one of the best advances in thermal ablation has been catheters that deliver less fluid and less need for diuresis after the procedure.
No PFA study has shown a decreased incidence of thermal damage to the esophagus with PFA ablation. Of course, this is because it is such a low-incidence event.
One of my concerns with PFA is brain safety. PFA creates substantial microbubbles in the left atrium, which can then travel north to the brain. In a small series from ADVENT, three patients had brain lesions after PFA vs none with thermal ablation. PFA proponents wrote that brain safety was important to study, but few patients have been systematically studied with brain MRI scans. Asymptomatic brain lesions have been noted after many arterial procedures. The clinical significance of these is not known. As a new technology, and one that creates substantial microbubbles in the left atrium, I agree with the PFA proponents that brain safety should be thoroughly studied — before widespread adoption.
What About Speed and Cost?
Observational studies from European labs report fast procedure times. I have seen PFA procedures in Europe; they’re fast — typically under an hour. A standard thermal ablation takes me about 60-70 minutes.
I am not sure that US operators can duplicate European procedural times. In the ADVENT regulatory trial, the mean procedure time was 105 minutes and that was in experienced US centers. While this still represents early experience with PFA, the culture of US AF ablation entails far more mapping and extra catheters than I have seen used in European labs.
Cost is a major issue. It’s hard to sort out exact costs in the United States, but a PFA catheter costs approximately threefold more than a standard ablation catheter. A recent study from Liverpool, England, found that PFA ablation was faster but more expensive than standard thermal ablation because of higher PFA equipment prices. For better or worse, US patients are not directly affected by the higher procedural costs. But the fact remains that PFA adds more costs to the healthcare system.
What Drives the Enthusiasm for First-Generation PFA?
So why all the enthusiasm? It’s surely not the empirical data. Evidence thus far shows no obvious advantage in safety or efficacy. European use of PFA does seem to reduce procedure time. But in many electrophysiology labs in the United States, the rate-limiting step for AF ablation is not time in the lab but having enough staff to turn rooms around.
The main factor driving early acceptance of PFA relates to basic human nature. It is the fear of missing out. Marketing works on consumers, and it surely works on doctors. Companies that make PFA systems sponsor key opinion leaders to discuss PFA. These companies have beautiful booths in the expo of our meetings; they host dinners and talks. When a hospital in a city does PFA, the other hospitals feel the urge to keep up. It’s hard to be a Top Person in electrophysiology and not be a PFA user.
One of my favorite comments came from a key opinion leader. He told me that he advised his administration to buy a PFA system, promote that they have it, and keep it in the closet until better systems are released.
Iteration in the medical device field is tricky. There are negatives to being too harsh on first-generation systems. Early cardiac resynchronization tools, for instance, were horrible. Now CRT is transformative in selected patients with heart failure.
It’s possible (but not certain) that electrical ablative therapy will iterate and surpass thermal ablation in the future. Maybe.
But for now, the enthusiasm for PFA far outstrips its evidence. Until better evidence emerges, I will be a slow adopter. And I hope that our field gathers evidence before widespread adoption makes it impossible to do proper studies.
Dr. Mandrola, clinical electrophysiologist, Baptist Medical Associates, Louisville, Kentucky, has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
It dominated 2024’s heart rhythm meetings, and it dominates my private electrophysiologist chat groups. My Google alert for “AF ablation” most often includes notices on PFA and the expansion of the atrial fibrillation ablation market.
Yet, the excitement does not match the empirical data.
Despite having strong brains, electrophysiologists adopt new things as if we were emotional shoppers. Our neighbor buys a sports car and we think we need the same car. Left atrial appendage occlusion and subcutaneous defibrillators were past examples.
The most recent example of soft thinking (especially in the United States) is the enthusiasm and early adoption of first-generation PFA systems for the treatment of AF.
Readers of cardiac news (including some of my patients) might think PFA has solved the AF puzzle. It has not.
A true breakthrough in AF would be to find its cause. PFA is simply another way to destroy (ablate) cardiac myocytes. PFA uses electrical energy (think shocks) to create pores in the cell membranes of myocytes. It’s delivered through various types of catheters.
The main theoretical advantage of PFA is cardioselectivity, which is possible because myocytes have lower thresholds for irreversible electroporation than surrounding tissues. The dose of electrical energy that ablates cardiac tissue does not affect surrounding tissues. Cardioselectivity decreases the chance of the most feared complication of standard AF ablation, thermal damage to the esophagus, which is often fatal. The esophagus lies immediately behind the posterior wall of the left atrium and can be inadvertently injured during thermal ablation.
The challenge in assessing this potential advantage is that thermal esophageal damage is, thankfully, exceedingly rare. Its incidence is in the range of 1 in 10,000 AF ablations. But it might be even lower than that in contemporary practice, because knowledge of esophageal injury has led to innovations that probably have reduced its incidence even further.
Proponents of PFA would rightly point to the fact that not having to worry about esophageal injury allows operators to add posterior wall ablation to the normal pulmonary vein isolation lesion set. This ability, they would argue, is likely to improve AF ablation outcomes. The problem is that the strongest and most recent trial of posterior wall isolation (with radiofrequency ablation) did not show better outcomes. A more recent observational analysis also showed no benefit to posterior wall isolation (using PFA) over pulmonary vein isolation alone.
What About PFA Efficacy?
I’ve long spoken and written about the lack of progress in AF ablation. In 1998, the first report on ablation of AF showed a 62% arrhythmia-free rate. Two decades later, in the carefully chosen labs treating patients in the CABANA trial, arrhythmia-free rates after AF ablation remain unchanged. We have improved our speed and ability to isolate pulmonary veins, but this has not increased our success in eliminating AF. The reason, I believe, is that we have made little to no progress in understanding the pathophysiology of AF.
The Food and Drug Administration regulatory trial called ADVENT randomly assigned more than 600 patients to thermal ablation or PFA, and the primary endpoint of ablation success was nearly identical. Single-center studies, observational registries, and single-arm studies have all shown similar efficacy of PFA and thermal ablation.
Proponents of PFA might argue that these early studies used first-generation PFA systems, and iteration will lead to better efficacy. Perhaps, but we’ve had 20 years of iteration of thermal ablation, and its efficacy has not budged.
What About PFA Safety?
In the ADVENT randomized trial, safety results were similar, though the one death, caused by cardiac perforation and tamponade, occurred in the PFA arm. In the MANIFEST-17K multinational survey of PFA ablation, safety events were in the range reported with thermal ablation. PFA still involves placing catheters in the heart, and complications such as tamponade, stroke, and vascular damage occur.
The large MANIFEST-17K survey also exposed two PFA-specific complications: coronary artery spasm, which can occur when PFA is delivered close to coronary arteries; and hemolysis-related kidney failure — severe enough to require dialysis in five patients. Supporters of PFA speculate that hemolysis occurs because electrical energy within the atrium can shred red blood cells. Their solution is to strive for good contact and use hydration. The irony of this latter fix is that one of the best advances in thermal ablation has been catheters that deliver less fluid and less need for diuresis after the procedure.
No PFA study has shown a decreased incidence of thermal damage to the esophagus with PFA ablation. Of course, this is because it is such a low-incidence event.
One of my concerns with PFA is brain safety. PFA creates substantial microbubbles in the left atrium, which can then travel north to the brain. In a small series from ADVENT, three patients had brain lesions after PFA vs none with thermal ablation. PFA proponents wrote that brain safety was important to study, but few patients have been systematically studied with brain MRI scans. Asymptomatic brain lesions have been noted after many arterial procedures. The clinical significance of these is not known. As a new technology, and one that creates substantial microbubbles in the left atrium, I agree with the PFA proponents that brain safety should be thoroughly studied — before widespread adoption.
What About Speed and Cost?
Observational studies from European labs report fast procedure times. I have seen PFA procedures in Europe; they’re fast — typically under an hour. A standard thermal ablation takes me about 60-70 minutes.
I am not sure that US operators can duplicate European procedural times. In the ADVENT regulatory trial, the mean procedure time was 105 minutes and that was in experienced US centers. While this still represents early experience with PFA, the culture of US AF ablation entails far more mapping and extra catheters than I have seen used in European labs.
Cost is a major issue. It’s hard to sort out exact costs in the United States, but a PFA catheter costs approximately threefold more than a standard ablation catheter. A recent study from Liverpool, England, found that PFA ablation was faster but more expensive than standard thermal ablation because of higher PFA equipment prices. For better or worse, US patients are not directly affected by the higher procedural costs. But the fact remains that PFA adds more costs to the healthcare system.
What Drives the Enthusiasm for First-Generation PFA?
So why all the enthusiasm? It’s surely not the empirical data. Evidence thus far shows no obvious advantage in safety or efficacy. European use of PFA does seem to reduce procedure time. But in many electrophysiology labs in the United States, the rate-limiting step for AF ablation is not time in the lab but having enough staff to turn rooms around.
The main factor driving early acceptance of PFA relates to basic human nature. It is the fear of missing out. Marketing works on consumers, and it surely works on doctors. Companies that make PFA systems sponsor key opinion leaders to discuss PFA. These companies have beautiful booths in the expo of our meetings; they host dinners and talks. When a hospital in a city does PFA, the other hospitals feel the urge to keep up. It’s hard to be a Top Person in electrophysiology and not be a PFA user.
One of my favorite comments came from a key opinion leader. He told me that he advised his administration to buy a PFA system, promote that they have it, and keep it in the closet until better systems are released.
Iteration in the medical device field is tricky. There are negatives to being too harsh on first-generation systems. Early cardiac resynchronization tools, for instance, were horrible. Now CRT is transformative in selected patients with heart failure.
It’s possible (but not certain) that electrical ablative therapy will iterate and surpass thermal ablation in the future. Maybe.
But for now, the enthusiasm for PFA far outstrips its evidence. Until better evidence emerges, I will be a slow adopter. And I hope that our field gathers evidence before widespread adoption makes it impossible to do proper studies.
Dr. Mandrola, clinical electrophysiologist, Baptist Medical Associates, Louisville, Kentucky, has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
It dominated 2024’s heart rhythm meetings, and it dominates my private electrophysiologist chat groups. My Google alert for “AF ablation” most often includes notices on PFA and the expansion of the atrial fibrillation ablation market.
Yet, the excitement does not match the empirical data.
Despite having strong brains, electrophysiologists adopt new things as if we were emotional shoppers. Our neighbor buys a sports car and we think we need the same car. Left atrial appendage occlusion and subcutaneous defibrillators were past examples.
The most recent example of soft thinking (especially in the United States) is the enthusiasm and early adoption of first-generation PFA systems for the treatment of AF.
Readers of cardiac news (including some of my patients) might think PFA has solved the AF puzzle. It has not.
A true breakthrough in AF would be to find its cause. PFA is simply another way to destroy (ablate) cardiac myocytes. PFA uses electrical energy (think shocks) to create pores in the cell membranes of myocytes. It’s delivered through various types of catheters.
The main theoretical advantage of PFA is cardioselectivity, which is possible because myocytes have lower thresholds for irreversible electroporation than surrounding tissues. The dose of electrical energy that ablates cardiac tissue does not affect surrounding tissues. Cardioselectivity decreases the chance of the most feared complication of standard AF ablation, thermal damage to the esophagus, which is often fatal. The esophagus lies immediately behind the posterior wall of the left atrium and can be inadvertently injured during thermal ablation.
The challenge in assessing this potential advantage is that thermal esophageal damage is, thankfully, exceedingly rare. Its incidence is in the range of 1 in 10,000 AF ablations. But it might be even lower than that in contemporary practice, because knowledge of esophageal injury has led to innovations that probably have reduced its incidence even further.
Proponents of PFA would rightly point to the fact that not having to worry about esophageal injury allows operators to add posterior wall ablation to the normal pulmonary vein isolation lesion set. This ability, they would argue, is likely to improve AF ablation outcomes. The problem is that the strongest and most recent trial of posterior wall isolation (with radiofrequency ablation) did not show better outcomes. A more recent observational analysis also showed no benefit to posterior wall isolation (using PFA) over pulmonary vein isolation alone.
What About PFA Efficacy?
I’ve long spoken and written about the lack of progress in AF ablation. In 1998, the first report on ablation of AF showed a 62% arrhythmia-free rate. Two decades later, in the carefully chosen labs treating patients in the CABANA trial, arrhythmia-free rates after AF ablation remain unchanged. We have improved our speed and ability to isolate pulmonary veins, but this has not increased our success in eliminating AF. The reason, I believe, is that we have made little to no progress in understanding the pathophysiology of AF.
The Food and Drug Administration regulatory trial called ADVENT randomly assigned more than 600 patients to thermal ablation or PFA, and the primary endpoint of ablation success was nearly identical. Single-center studies, observational registries, and single-arm studies have all shown similar efficacy of PFA and thermal ablation.
Proponents of PFA might argue that these early studies used first-generation PFA systems, and iteration will lead to better efficacy. Perhaps, but we’ve had 20 years of iteration of thermal ablation, and its efficacy has not budged.
What About PFA Safety?
In the ADVENT randomized trial, safety results were similar, though the one death, caused by cardiac perforation and tamponade, occurred in the PFA arm. In the MANIFEST-17K multinational survey of PFA ablation, safety events were in the range reported with thermal ablation. PFA still involves placing catheters in the heart, and complications such as tamponade, stroke, and vascular damage occur.
The large MANIFEST-17K survey also exposed two PFA-specific complications: coronary artery spasm, which can occur when PFA is delivered close to coronary arteries; and hemolysis-related kidney failure — severe enough to require dialysis in five patients. Supporters of PFA speculate that hemolysis occurs because electrical energy within the atrium can shred red blood cells. Their solution is to strive for good contact and use hydration. The irony of this latter fix is that one of the best advances in thermal ablation has been catheters that deliver less fluid and less need for diuresis after the procedure.
No PFA study has shown a decreased incidence of thermal damage to the esophagus with PFA ablation. Of course, this is because it is such a low-incidence event.
One of my concerns with PFA is brain safety. PFA creates substantial microbubbles in the left atrium, which can then travel north to the brain. In a small series from ADVENT, three patients had brain lesions after PFA vs none with thermal ablation. PFA proponents wrote that brain safety was important to study, but few patients have been systematically studied with brain MRI scans. Asymptomatic brain lesions have been noted after many arterial procedures. The clinical significance of these is not known. As a new technology, and one that creates substantial microbubbles in the left atrium, I agree with the PFA proponents that brain safety should be thoroughly studied — before widespread adoption.
What About Speed and Cost?
Observational studies from European labs report fast procedure times. I have seen PFA procedures in Europe; they’re fast — typically under an hour. A standard thermal ablation takes me about 60-70 minutes.
I am not sure that US operators can duplicate European procedural times. In the ADVENT regulatory trial, the mean procedure time was 105 minutes and that was in experienced US centers. While this still represents early experience with PFA, the culture of US AF ablation entails far more mapping and extra catheters than I have seen used in European labs.
Cost is a major issue. It’s hard to sort out exact costs in the United States, but a PFA catheter costs approximately threefold more than a standard ablation catheter. A recent study from Liverpool, England, found that PFA ablation was faster but more expensive than standard thermal ablation because of higher PFA equipment prices. For better or worse, US patients are not directly affected by the higher procedural costs. But the fact remains that PFA adds more costs to the healthcare system.
What Drives the Enthusiasm for First-Generation PFA?
So why all the enthusiasm? It’s surely not the empirical data. Evidence thus far shows no obvious advantage in safety or efficacy. European use of PFA does seem to reduce procedure time. But in many electrophysiology labs in the United States, the rate-limiting step for AF ablation is not time in the lab but having enough staff to turn rooms around.
The main factor driving early acceptance of PFA relates to basic human nature. It is the fear of missing out. Marketing works on consumers, and it surely works on doctors. Companies that make PFA systems sponsor key opinion leaders to discuss PFA. These companies have beautiful booths in the expo of our meetings; they host dinners and talks. When a hospital in a city does PFA, the other hospitals feel the urge to keep up. It’s hard to be a Top Person in electrophysiology and not be a PFA user.
One of my favorite comments came from a key opinion leader. He told me that he advised his administration to buy a PFA system, promote that they have it, and keep it in the closet until better systems are released.
Iteration in the medical device field is tricky. There are negatives to being too harsh on first-generation systems. Early cardiac resynchronization tools, for instance, were horrible. Now CRT is transformative in selected patients with heart failure.
It’s possible (but not certain) that electrical ablative therapy will iterate and surpass thermal ablation in the future. Maybe.
But for now, the enthusiasm for PFA far outstrips its evidence. Until better evidence emerges, I will be a slow adopter. And I hope that our field gathers evidence before widespread adoption makes it impossible to do proper studies.
Dr. Mandrola, clinical electrophysiologist, Baptist Medical Associates, Louisville, Kentucky, has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
US 911 System Is Nearing Its Own Emergency
Just after lunchtime on June 18, Massachusetts’ leaders discovered that the statewide 911 system was down.
A scramble to handle the crisis was on.
Police texted out administrative numbers that callers could use, Boston Mayor Michelle Wu gave outage updates at a press conference outlining plans for the Celtics’ championship parade, and local officials urged people to summon help by pulling red fire alarm boxes.
About 7 million people went roughly 2 hours with no 911 service. Such crashes have become more of a feature than a bug in the nation’s fragmented emergency response system.
While some states, cities, and counties have already modernized their systems or have made plans to upgrade, many others are lagging.
911 is typically supported by fees tacked on to phone bills, but state and local governments also tap general funds or other resources.
“Now there are haves and have-nots,” said Jonathan Gilad, vice president of government affairs at the National Emergency Number Association (NENA), which represents 911 first responders. “Next-generation 911 shouldn’t be for people who happen to have an emergency in a good location.”
Meanwhile, federal legislation that could steer billions of dollars into modernizing the patchwork 911 system remains waylaid in Congress.
“This is a national security imperative,” said George Kelemen, executive director of the Industry Council for Emergency Response Technologies, a trade association that represents companies that provide hardware and software to the emergency response industry.
“In a crisis — a school shooting or a house fire or, God forbid, a terrorist attack — people call 911 first,” he said. “The system can’t go down.”
The United States debuted a single, universal 911 emergency number in February 1968 to simplify crisis response. But instead of a seamless national program, the 911 response network has evolved into a massive puzzle of many interlocking pieces. There are more than 6,000 911 call centers to handle an estimated 240 million emergency calls each year, according to federal data. More than three-quarters of call centers experienced outages in the prior 12 months, according to a survey in February by NENA, which sets standards and advocates for 911, and Carbyne, a provider of public safety technology solutions.
In April, widespread 911 outages affected millions in Nebraska, Nevada, South Dakota, and Texas. The shutdown was blamed on workers’ severing a fiber line while installing a light pole.
In February, tens of thousands of people in areas of California, Georgia, Illinois, Texas, and other states lost cellphone service, including some 911 services, from an outage.
And in June, Verizon agreed to pay a $1.05 million fine to settle a Federal Communications Commission (FCC) probe into a December 2022 outage that affected 911 calls in Alabama, Florida, Georgia, North Carolina, South Carolina, and Tennessee.
The fires that raced across the Hawaiian island of Maui in August 2023 highlighted the critical importance of 911 systems. Dispatchers there fielded more than 4,500 contacts, meaning calls and texts, on Aug. 8, the day the fires broke out, compared with about 400 on a typical day, said Davlynn Racadio, emergency services dispatch coordinator in Maui County.
“We’re dying out here,” one caller told 911 operators.
But some cell towers faltered because of widespread service outages, according to county officials. Maui County in May filed a lawsuit against four telecommunications companies, saying they failed to inform dispatchers about the outages.
“If 911 calls came in with no voice, we would send text messages,” Ms. Racadio said. “The state is looking at upgrading our system. Next-generation 911 would take us even further into the future.”
Florida, Illinois, Montana, and Oklahoma passed legislation in 2023 to advance or fund modernized 911 systems, according to the National Conference of State Legislatures. The upgrades include replacing analog 911 infrastructure with digital, Internet-based systems.
Instead of just fielding calls, next-generation systems can pinpoint a caller’s location, accept texts, and enable residents in a crisis to send videos and images to dispatchers. While outages can still occur, modernized systems often include more redundancy to minimize the odds of a shutdown, Mr. Gilad said.
Lawmakers have looked at modernizing 911 systems by tapping revenue the FCC gets from auctioning off the rights to transmit signals over specific bands of the electromagnetic spectrum.
But the U.S. Senate, in March 2023, for the first time allowed a lapse of the FCC’s authority to auction spectrum bands.
Legislation that would allocate almost $15 billion in grants from auction proceeds to speed deployment of next-generation 911 in every state unanimously passed the House Energy and Commerce Committee in May 2023. The bill, HR 3565, sponsored by Rep. Cathy McMorris Rodgers (R-Wash.), would also extend the FCC’s auction authority.
Other bills have been introduced by various lawmakers, including one in March from Sen. Ted Cruz (R-Texas) and legislation from Sen. Maria Cantwell (D-Wash.) to extend the auction authority. For now, neither effort has advanced. Nine former FCC chairs wrote lawmakers in February, urging them to make 911 upgrades a national priority. They suggested Congress tap unspent federal COVID-19 money.
“Whatever the funding source, the need is urgent and the time to act is now,” they wrote.
Ajit Pai, who served as chair of the FCC from 2017 to 2021, said outages often occur in older, legacy systems.
“The fact that the FCC doesn’t have authority to auction spectrum is a real hindrance now,” Mr. Pai said in an interview. “You may never need to call 911, but it can make the difference between life and death. We need more of an organized effort at the federal level because 911 is so decentralized.”
Meanwhile, some safety leaders are making backup plans for 911 outages or conducting investigations into their causes. In Massachusetts, a firewall designed to prevent hacking led to the recent 2-hour outage, according to the state 911 department.
“Outages bring to everyone’s attention that we rely on 911 and we don’t think about how we really rely on it until something happens,” said April Heinze, chief of 911 operations at NENA.
Mass General Brigham, a health system in the Boston area, sent out emergency alerts when the outage happened letting clinics and smaller practices know how to find their 10-digit emergency numbers. In the wake of the outage, it plans to keep the backup numbers next to phones at those facilities.
“Two hours can be a long time,” said Paul Biddinger, chief preparedness and continuity officer at the health system.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Just after lunchtime on June 18, Massachusetts’ leaders discovered that the statewide 911 system was down.
A scramble to handle the crisis was on.
Police texted out administrative numbers that callers could use, Boston Mayor Michelle Wu gave outage updates at a press conference outlining plans for the Celtics’ championship parade, and local officials urged people to summon help by pulling red fire alarm boxes.
About 7 million people went roughly 2 hours with no 911 service. Such crashes have become more of a feature than a bug in the nation’s fragmented emergency response system.
While some states, cities, and counties have already modernized their systems or have made plans to upgrade, many others are lagging.
911 is typically supported by fees tacked on to phone bills, but state and local governments also tap general funds or other resources.
“Now there are haves and have-nots,” said Jonathan Gilad, vice president of government affairs at the National Emergency Number Association (NENA), which represents 911 first responders. “Next-generation 911 shouldn’t be for people who happen to have an emergency in a good location.”
Meanwhile, federal legislation that could steer billions of dollars into modernizing the patchwork 911 system remains waylaid in Congress.
“This is a national security imperative,” said George Kelemen, executive director of the Industry Council for Emergency Response Technologies, a trade association that represents companies that provide hardware and software to the emergency response industry.
“In a crisis — a school shooting or a house fire or, God forbid, a terrorist attack — people call 911 first,” he said. “The system can’t go down.”
The United States debuted a single, universal 911 emergency number in February 1968 to simplify crisis response. But instead of a seamless national program, the 911 response network has evolved into a massive puzzle of many interlocking pieces. There are more than 6,000 911 call centers to handle an estimated 240 million emergency calls each year, according to federal data. More than three-quarters of call centers experienced outages in the prior 12 months, according to a survey in February by NENA, which sets standards and advocates for 911, and Carbyne, a provider of public safety technology solutions.
In April, widespread 911 outages affected millions in Nebraska, Nevada, South Dakota, and Texas. The shutdown was blamed on workers’ severing a fiber line while installing a light pole.
In February, tens of thousands of people in areas of California, Georgia, Illinois, Texas, and other states lost cellphone service, including some 911 services, from an outage.
And in June, Verizon agreed to pay a $1.05 million fine to settle a Federal Communications Commission (FCC) probe into a December 2022 outage that affected 911 calls in Alabama, Florida, Georgia, North Carolina, South Carolina, and Tennessee.
The fires that raced across the Hawaiian island of Maui in August 2023 highlighted the critical importance of 911 systems. Dispatchers there fielded more than 4,500 contacts, meaning calls and texts, on Aug. 8, the day the fires broke out, compared with about 400 on a typical day, said Davlynn Racadio, emergency services dispatch coordinator in Maui County.
“We’re dying out here,” one caller told 911 operators.
But some cell towers faltered because of widespread service outages, according to county officials. Maui County in May filed a lawsuit against four telecommunications companies, saying they failed to inform dispatchers about the outages.
“If 911 calls came in with no voice, we would send text messages,” Ms. Racadio said. “The state is looking at upgrading our system. Next-generation 911 would take us even further into the future.”
Florida, Illinois, Montana, and Oklahoma passed legislation in 2023 to advance or fund modernized 911 systems, according to the National Conference of State Legislatures. The upgrades include replacing analog 911 infrastructure with digital, Internet-based systems.
Instead of just fielding calls, next-generation systems can pinpoint a caller’s location, accept texts, and enable residents in a crisis to send videos and images to dispatchers. While outages can still occur, modernized systems often include more redundancy to minimize the odds of a shutdown, Mr. Gilad said.
Lawmakers have looked at modernizing 911 systems by tapping revenue the FCC gets from auctioning off the rights to transmit signals over specific bands of the electromagnetic spectrum.
But the U.S. Senate, in March 2023, for the first time allowed a lapse of the FCC’s authority to auction spectrum bands.
Legislation that would allocate almost $15 billion in grants from auction proceeds to speed deployment of next-generation 911 in every state unanimously passed the House Energy and Commerce Committee in May 2023. The bill, HR 3565, sponsored by Rep. Cathy McMorris Rodgers (R-Wash.), would also extend the FCC’s auction authority.
Other bills have been introduced by various lawmakers, including one in March from Sen. Ted Cruz (R-Texas) and legislation from Sen. Maria Cantwell (D-Wash.) to extend the auction authority. For now, neither effort has advanced. Nine former FCC chairs wrote lawmakers in February, urging them to make 911 upgrades a national priority. They suggested Congress tap unspent federal COVID-19 money.
“Whatever the funding source, the need is urgent and the time to act is now,” they wrote.
Ajit Pai, who served as chair of the FCC from 2017 to 2021, said outages often occur in older, legacy systems.
“The fact that the FCC doesn’t have authority to auction spectrum is a real hindrance now,” Mr. Pai said in an interview. “You may never need to call 911, but it can make the difference between life and death. We need more of an organized effort at the federal level because 911 is so decentralized.”
Meanwhile, some safety leaders are making backup plans for 911 outages or conducting investigations into their causes. In Massachusetts, a firewall designed to prevent hacking led to the recent 2-hour outage, according to the state 911 department.
“Outages bring to everyone’s attention that we rely on 911 and we don’t think about how we really rely on it until something happens,” said April Heinze, chief of 911 operations at NENA.
Mass General Brigham, a health system in the Boston area, sent out emergency alerts when the outage happened letting clinics and smaller practices know how to find their 10-digit emergency numbers. In the wake of the outage, it plans to keep the backup numbers next to phones at those facilities.
“Two hours can be a long time,” said Paul Biddinger, chief preparedness and continuity officer at the health system.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Just after lunchtime on June 18, Massachusetts’ leaders discovered that the statewide 911 system was down.
A scramble to handle the crisis was on.
Police texted out administrative numbers that callers could use, Boston Mayor Michelle Wu gave outage updates at a press conference outlining plans for the Celtics’ championship parade, and local officials urged people to summon help by pulling red fire alarm boxes.
About 7 million people went roughly 2 hours with no 911 service. Such crashes have become more of a feature than a bug in the nation’s fragmented emergency response system.
While some states, cities, and counties have already modernized their systems or have made plans to upgrade, many others are lagging.
911 is typically supported by fees tacked on to phone bills, but state and local governments also tap general funds or other resources.
“Now there are haves and have-nots,” said Jonathan Gilad, vice president of government affairs at the National Emergency Number Association (NENA), which represents 911 first responders. “Next-generation 911 shouldn’t be for people who happen to have an emergency in a good location.”
Meanwhile, federal legislation that could steer billions of dollars into modernizing the patchwork 911 system remains waylaid in Congress.
“This is a national security imperative,” said George Kelemen, executive director of the Industry Council for Emergency Response Technologies, a trade association that represents companies that provide hardware and software to the emergency response industry.
“In a crisis — a school shooting or a house fire or, God forbid, a terrorist attack — people call 911 first,” he said. “The system can’t go down.”
The United States debuted a single, universal 911 emergency number in February 1968 to simplify crisis response. But instead of a seamless national program, the 911 response network has evolved into a massive puzzle of many interlocking pieces. There are more than 6,000 911 call centers to handle an estimated 240 million emergency calls each year, according to federal data. More than three-quarters of call centers experienced outages in the prior 12 months, according to a survey in February by NENA, which sets standards and advocates for 911, and Carbyne, a provider of public safety technology solutions.
In April, widespread 911 outages affected millions in Nebraska, Nevada, South Dakota, and Texas. The shutdown was blamed on workers’ severing a fiber line while installing a light pole.
In February, tens of thousands of people in areas of California, Georgia, Illinois, Texas, and other states lost cellphone service, including some 911 services, from an outage.
And in June, Verizon agreed to pay a $1.05 million fine to settle a Federal Communications Commission (FCC) probe into a December 2022 outage that affected 911 calls in Alabama, Florida, Georgia, North Carolina, South Carolina, and Tennessee.
The fires that raced across the Hawaiian island of Maui in August 2023 highlighted the critical importance of 911 systems. Dispatchers there fielded more than 4,500 contacts, meaning calls and texts, on Aug. 8, the day the fires broke out, compared with about 400 on a typical day, said Davlynn Racadio, emergency services dispatch coordinator in Maui County.
“We’re dying out here,” one caller told 911 operators.
But some cell towers faltered because of widespread service outages, according to county officials. Maui County in May filed a lawsuit against four telecommunications companies, saying they failed to inform dispatchers about the outages.
“If 911 calls came in with no voice, we would send text messages,” Ms. Racadio said. “The state is looking at upgrading our system. Next-generation 911 would take us even further into the future.”
Florida, Illinois, Montana, and Oklahoma passed legislation in 2023 to advance or fund modernized 911 systems, according to the National Conference of State Legislatures. The upgrades include replacing analog 911 infrastructure with digital, Internet-based systems.
Instead of just fielding calls, next-generation systems can pinpoint a caller’s location, accept texts, and enable residents in a crisis to send videos and images to dispatchers. While outages can still occur, modernized systems often include more redundancy to minimize the odds of a shutdown, Mr. Gilad said.
Lawmakers have looked at modernizing 911 systems by tapping revenue the FCC gets from auctioning off the rights to transmit signals over specific bands of the electromagnetic spectrum.
But the U.S. Senate, in March 2023, for the first time allowed a lapse of the FCC’s authority to auction spectrum bands.
Legislation that would allocate almost $15 billion in grants from auction proceeds to speed deployment of next-generation 911 in every state unanimously passed the House Energy and Commerce Committee in May 2023. The bill, HR 3565, sponsored by Rep. Cathy McMorris Rodgers (R-Wash.), would also extend the FCC’s auction authority.
Other bills have been introduced by various lawmakers, including one in March from Sen. Ted Cruz (R-Texas) and legislation from Sen. Maria Cantwell (D-Wash.) to extend the auction authority. For now, neither effort has advanced. Nine former FCC chairs wrote lawmakers in February, urging them to make 911 upgrades a national priority. They suggested Congress tap unspent federal COVID-19 money.
“Whatever the funding source, the need is urgent and the time to act is now,” they wrote.
Ajit Pai, who served as chair of the FCC from 2017 to 2021, said outages often occur in older, legacy systems.
“The fact that the FCC doesn’t have authority to auction spectrum is a real hindrance now,” Mr. Pai said in an interview. “You may never need to call 911, but it can make the difference between life and death. We need more of an organized effort at the federal level because 911 is so decentralized.”
Meanwhile, some safety leaders are making backup plans for 911 outages or conducting investigations into their causes. In Massachusetts, a firewall designed to prevent hacking led to the recent 2-hour outage, according to the state 911 department.
“Outages bring to everyone’s attention that we rely on 911 and we don’t think about how we really rely on it until something happens,” said April Heinze, chief of 911 operations at NENA.
Mass General Brigham, a health system in the Boston area, sent out emergency alerts when the outage happened letting clinics and smaller practices know how to find their 10-digit emergency numbers. In the wake of the outage, it plans to keep the backup numbers next to phones at those facilities.
“Two hours can be a long time,” said Paul Biddinger, chief preparedness and continuity officer at the health system.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.