User login
US 911 System Is Nearing Its Own Emergency
Just after lunchtime on June 18, Massachusetts’ leaders discovered that the statewide 911 system was down.
A scramble to handle the crisis was on.
Police texted out administrative numbers that callers could use, Boston Mayor Michelle Wu gave outage updates at a press conference outlining plans for the Celtics’ championship parade, and local officials urged people to summon help by pulling red fire alarm boxes.
About 7 million people went roughly 2 hours with no 911 service. Such crashes have become more of a feature than a bug in the nation’s fragmented emergency response system.
While some states, cities, and counties have already modernized their systems or have made plans to upgrade, many others are lagging.
911 is typically supported by fees tacked on to phone bills, but state and local governments also tap general funds or other resources.
“Now there are haves and have-nots,” said Jonathan Gilad, vice president of government affairs at the National Emergency Number Association (NENA), which represents 911 first responders. “Next-generation 911 shouldn’t be for people who happen to have an emergency in a good location.”
Meanwhile, federal legislation that could steer billions of dollars into modernizing the patchwork 911 system remains waylaid in Congress.
“This is a national security imperative,” said George Kelemen, executive director of the Industry Council for Emergency Response Technologies, a trade association that represents companies that provide hardware and software to the emergency response industry.
“In a crisis — a school shooting or a house fire or, God forbid, a terrorist attack — people call 911 first,” he said. “The system can’t go down.”
The United States debuted a single, universal 911 emergency number in February 1968 to simplify crisis response. But instead of a seamless national program, the 911 response network has evolved into a massive puzzle of many interlocking pieces. There are more than 6,000 911 call centers to handle an estimated 240 million emergency calls each year, according to federal data. More than three-quarters of call centers experienced outages in the prior 12 months, according to a survey in February by NENA, which sets standards and advocates for 911, and Carbyne, a provider of public safety technology solutions.
In April, widespread 911 outages affected millions in Nebraska, Nevada, South Dakota, and Texas. The shutdown was blamed on workers’ severing a fiber line while installing a light pole.
In February, tens of thousands of people in areas of California, Georgia, Illinois, Texas, and other states lost cellphone service, including some 911 services, from an outage.
And in June, Verizon agreed to pay a $1.05 million fine to settle a Federal Communications Commission (FCC) probe into a December 2022 outage that affected 911 calls in Alabama, Florida, Georgia, North Carolina, South Carolina, and Tennessee.
The fires that raced across the Hawaiian island of Maui in August 2023 highlighted the critical importance of 911 systems. Dispatchers there fielded more than 4,500 contacts, meaning calls and texts, on Aug. 8, the day the fires broke out, compared with about 400 on a typical day, said Davlynn Racadio, emergency services dispatch coordinator in Maui County.
“We’re dying out here,” one caller told 911 operators.
But some cell towers faltered because of widespread service outages, according to county officials. Maui County in May filed a lawsuit against four telecommunications companies, saying they failed to inform dispatchers about the outages.
“If 911 calls came in with no voice, we would send text messages,” Ms. Racadio said. “The state is looking at upgrading our system. Next-generation 911 would take us even further into the future.”
Florida, Illinois, Montana, and Oklahoma passed legislation in 2023 to advance or fund modernized 911 systems, according to the National Conference of State Legislatures. The upgrades include replacing analog 911 infrastructure with digital, Internet-based systems.
Instead of just fielding calls, next-generation systems can pinpoint a caller’s location, accept texts, and enable residents in a crisis to send videos and images to dispatchers. While outages can still occur, modernized systems often include more redundancy to minimize the odds of a shutdown, Mr. Gilad said.
Lawmakers have looked at modernizing 911 systems by tapping revenue the FCC gets from auctioning off the rights to transmit signals over specific bands of the electromagnetic spectrum.
But the U.S. Senate, in March 2023, for the first time allowed a lapse of the FCC’s authority to auction spectrum bands.
Legislation that would allocate almost $15 billion in grants from auction proceeds to speed deployment of next-generation 911 in every state unanimously passed the House Energy and Commerce Committee in May 2023. The bill, HR 3565, sponsored by Rep. Cathy McMorris Rodgers (R-Wash.), would also extend the FCC’s auction authority.
Other bills have been introduced by various lawmakers, including one in March from Sen. Ted Cruz (R-Texas) and legislation from Sen. Maria Cantwell (D-Wash.) to extend the auction authority. For now, neither effort has advanced. Nine former FCC chairs wrote lawmakers in February, urging them to make 911 upgrades a national priority. They suggested Congress tap unspent federal COVID-19 money.
“Whatever the funding source, the need is urgent and the time to act is now,” they wrote.
Ajit Pai, who served as chair of the FCC from 2017 to 2021, said outages often occur in older, legacy systems.
“The fact that the FCC doesn’t have authority to auction spectrum is a real hindrance now,” Mr. Pai said in an interview. “You may never need to call 911, but it can make the difference between life and death. We need more of an organized effort at the federal level because 911 is so decentralized.”
Meanwhile, some safety leaders are making backup plans for 911 outages or conducting investigations into their causes. In Massachusetts, a firewall designed to prevent hacking led to the recent 2-hour outage, according to the state 911 department.
“Outages bring to everyone’s attention that we rely on 911 and we don’t think about how we really rely on it until something happens,” said April Heinze, chief of 911 operations at NENA.
Mass General Brigham, a health system in the Boston area, sent out emergency alerts when the outage happened letting clinics and smaller practices know how to find their 10-digit emergency numbers. In the wake of the outage, it plans to keep the backup numbers next to phones at those facilities.
“Two hours can be a long time,” said Paul Biddinger, chief preparedness and continuity officer at the health system.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Just after lunchtime on June 18, Massachusetts’ leaders discovered that the statewide 911 system was down.
A scramble to handle the crisis was on.
Police texted out administrative numbers that callers could use, Boston Mayor Michelle Wu gave outage updates at a press conference outlining plans for the Celtics’ championship parade, and local officials urged people to summon help by pulling red fire alarm boxes.
About 7 million people went roughly 2 hours with no 911 service. Such crashes have become more of a feature than a bug in the nation’s fragmented emergency response system.
While some states, cities, and counties have already modernized their systems or have made plans to upgrade, many others are lagging.
911 is typically supported by fees tacked on to phone bills, but state and local governments also tap general funds or other resources.
“Now there are haves and have-nots,” said Jonathan Gilad, vice president of government affairs at the National Emergency Number Association (NENA), which represents 911 first responders. “Next-generation 911 shouldn’t be for people who happen to have an emergency in a good location.”
Meanwhile, federal legislation that could steer billions of dollars into modernizing the patchwork 911 system remains waylaid in Congress.
“This is a national security imperative,” said George Kelemen, executive director of the Industry Council for Emergency Response Technologies, a trade association that represents companies that provide hardware and software to the emergency response industry.
“In a crisis — a school shooting or a house fire or, God forbid, a terrorist attack — people call 911 first,” he said. “The system can’t go down.”
The United States debuted a single, universal 911 emergency number in February 1968 to simplify crisis response. But instead of a seamless national program, the 911 response network has evolved into a massive puzzle of many interlocking pieces. There are more than 6,000 911 call centers to handle an estimated 240 million emergency calls each year, according to federal data. More than three-quarters of call centers experienced outages in the prior 12 months, according to a survey in February by NENA, which sets standards and advocates for 911, and Carbyne, a provider of public safety technology solutions.
In April, widespread 911 outages affected millions in Nebraska, Nevada, South Dakota, and Texas. The shutdown was blamed on workers’ severing a fiber line while installing a light pole.
In February, tens of thousands of people in areas of California, Georgia, Illinois, Texas, and other states lost cellphone service, including some 911 services, from an outage.
And in June, Verizon agreed to pay a $1.05 million fine to settle a Federal Communications Commission (FCC) probe into a December 2022 outage that affected 911 calls in Alabama, Florida, Georgia, North Carolina, South Carolina, and Tennessee.
The fires that raced across the Hawaiian island of Maui in August 2023 highlighted the critical importance of 911 systems. Dispatchers there fielded more than 4,500 contacts, meaning calls and texts, on Aug. 8, the day the fires broke out, compared with about 400 on a typical day, said Davlynn Racadio, emergency services dispatch coordinator in Maui County.
“We’re dying out here,” one caller told 911 operators.
But some cell towers faltered because of widespread service outages, according to county officials. Maui County in May filed a lawsuit against four telecommunications companies, saying they failed to inform dispatchers about the outages.
“If 911 calls came in with no voice, we would send text messages,” Ms. Racadio said. “The state is looking at upgrading our system. Next-generation 911 would take us even further into the future.”
Florida, Illinois, Montana, and Oklahoma passed legislation in 2023 to advance or fund modernized 911 systems, according to the National Conference of State Legislatures. The upgrades include replacing analog 911 infrastructure with digital, Internet-based systems.
Instead of just fielding calls, next-generation systems can pinpoint a caller’s location, accept texts, and enable residents in a crisis to send videos and images to dispatchers. While outages can still occur, modernized systems often include more redundancy to minimize the odds of a shutdown, Mr. Gilad said.
Lawmakers have looked at modernizing 911 systems by tapping revenue the FCC gets from auctioning off the rights to transmit signals over specific bands of the electromagnetic spectrum.
But the U.S. Senate, in March 2023, for the first time allowed a lapse of the FCC’s authority to auction spectrum bands.
Legislation that would allocate almost $15 billion in grants from auction proceeds to speed deployment of next-generation 911 in every state unanimously passed the House Energy and Commerce Committee in May 2023. The bill, HR 3565, sponsored by Rep. Cathy McMorris Rodgers (R-Wash.), would also extend the FCC’s auction authority.
Other bills have been introduced by various lawmakers, including one in March from Sen. Ted Cruz (R-Texas) and legislation from Sen. Maria Cantwell (D-Wash.) to extend the auction authority. For now, neither effort has advanced. Nine former FCC chairs wrote lawmakers in February, urging them to make 911 upgrades a national priority. They suggested Congress tap unspent federal COVID-19 money.
“Whatever the funding source, the need is urgent and the time to act is now,” they wrote.
Ajit Pai, who served as chair of the FCC from 2017 to 2021, said outages often occur in older, legacy systems.
“The fact that the FCC doesn’t have authority to auction spectrum is a real hindrance now,” Mr. Pai said in an interview. “You may never need to call 911, but it can make the difference between life and death. We need more of an organized effort at the federal level because 911 is so decentralized.”
Meanwhile, some safety leaders are making backup plans for 911 outages or conducting investigations into their causes. In Massachusetts, a firewall designed to prevent hacking led to the recent 2-hour outage, according to the state 911 department.
“Outages bring to everyone’s attention that we rely on 911 and we don’t think about how we really rely on it until something happens,” said April Heinze, chief of 911 operations at NENA.
Mass General Brigham, a health system in the Boston area, sent out emergency alerts when the outage happened letting clinics and smaller practices know how to find their 10-digit emergency numbers. In the wake of the outage, it plans to keep the backup numbers next to phones at those facilities.
“Two hours can be a long time,” said Paul Biddinger, chief preparedness and continuity officer at the health system.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Just after lunchtime on June 18, Massachusetts’ leaders discovered that the statewide 911 system was down.
A scramble to handle the crisis was on.
Police texted out administrative numbers that callers could use, Boston Mayor Michelle Wu gave outage updates at a press conference outlining plans for the Celtics’ championship parade, and local officials urged people to summon help by pulling red fire alarm boxes.
About 7 million people went roughly 2 hours with no 911 service. Such crashes have become more of a feature than a bug in the nation’s fragmented emergency response system.
While some states, cities, and counties have already modernized their systems or have made plans to upgrade, many others are lagging.
911 is typically supported by fees tacked on to phone bills, but state and local governments also tap general funds or other resources.
“Now there are haves and have-nots,” said Jonathan Gilad, vice president of government affairs at the National Emergency Number Association (NENA), which represents 911 first responders. “Next-generation 911 shouldn’t be for people who happen to have an emergency in a good location.”
Meanwhile, federal legislation that could steer billions of dollars into modernizing the patchwork 911 system remains waylaid in Congress.
“This is a national security imperative,” said George Kelemen, executive director of the Industry Council for Emergency Response Technologies, a trade association that represents companies that provide hardware and software to the emergency response industry.
“In a crisis — a school shooting or a house fire or, God forbid, a terrorist attack — people call 911 first,” he said. “The system can’t go down.”
The United States debuted a single, universal 911 emergency number in February 1968 to simplify crisis response. But instead of a seamless national program, the 911 response network has evolved into a massive puzzle of many interlocking pieces. There are more than 6,000 911 call centers to handle an estimated 240 million emergency calls each year, according to federal data. More than three-quarters of call centers experienced outages in the prior 12 months, according to a survey in February by NENA, which sets standards and advocates for 911, and Carbyne, a provider of public safety technology solutions.
In April, widespread 911 outages affected millions in Nebraska, Nevada, South Dakota, and Texas. The shutdown was blamed on workers’ severing a fiber line while installing a light pole.
In February, tens of thousands of people in areas of California, Georgia, Illinois, Texas, and other states lost cellphone service, including some 911 services, from an outage.
And in June, Verizon agreed to pay a $1.05 million fine to settle a Federal Communications Commission (FCC) probe into a December 2022 outage that affected 911 calls in Alabama, Florida, Georgia, North Carolina, South Carolina, and Tennessee.
The fires that raced across the Hawaiian island of Maui in August 2023 highlighted the critical importance of 911 systems. Dispatchers there fielded more than 4,500 contacts, meaning calls and texts, on Aug. 8, the day the fires broke out, compared with about 400 on a typical day, said Davlynn Racadio, emergency services dispatch coordinator in Maui County.
“We’re dying out here,” one caller told 911 operators.
But some cell towers faltered because of widespread service outages, according to county officials. Maui County in May filed a lawsuit against four telecommunications companies, saying they failed to inform dispatchers about the outages.
“If 911 calls came in with no voice, we would send text messages,” Ms. Racadio said. “The state is looking at upgrading our system. Next-generation 911 would take us even further into the future.”
Florida, Illinois, Montana, and Oklahoma passed legislation in 2023 to advance or fund modernized 911 systems, according to the National Conference of State Legislatures. The upgrades include replacing analog 911 infrastructure with digital, Internet-based systems.
Instead of just fielding calls, next-generation systems can pinpoint a caller’s location, accept texts, and enable residents in a crisis to send videos and images to dispatchers. While outages can still occur, modernized systems often include more redundancy to minimize the odds of a shutdown, Mr. Gilad said.
Lawmakers have looked at modernizing 911 systems by tapping revenue the FCC gets from auctioning off the rights to transmit signals over specific bands of the electromagnetic spectrum.
But the U.S. Senate, in March 2023, for the first time allowed a lapse of the FCC’s authority to auction spectrum bands.
Legislation that would allocate almost $15 billion in grants from auction proceeds to speed deployment of next-generation 911 in every state unanimously passed the House Energy and Commerce Committee in May 2023. The bill, HR 3565, sponsored by Rep. Cathy McMorris Rodgers (R-Wash.), would also extend the FCC’s auction authority.
Other bills have been introduced by various lawmakers, including one in March from Sen. Ted Cruz (R-Texas) and legislation from Sen. Maria Cantwell (D-Wash.) to extend the auction authority. For now, neither effort has advanced. Nine former FCC chairs wrote lawmakers in February, urging them to make 911 upgrades a national priority. They suggested Congress tap unspent federal COVID-19 money.
“Whatever the funding source, the need is urgent and the time to act is now,” they wrote.
Ajit Pai, who served as chair of the FCC from 2017 to 2021, said outages often occur in older, legacy systems.
“The fact that the FCC doesn’t have authority to auction spectrum is a real hindrance now,” Mr. Pai said in an interview. “You may never need to call 911, but it can make the difference between life and death. We need more of an organized effort at the federal level because 911 is so decentralized.”
Meanwhile, some safety leaders are making backup plans for 911 outages or conducting investigations into their causes. In Massachusetts, a firewall designed to prevent hacking led to the recent 2-hour outage, according to the state 911 department.
“Outages bring to everyone’s attention that we rely on 911 and we don’t think about how we really rely on it until something happens,” said April Heinze, chief of 911 operations at NENA.
Mass General Brigham, a health system in the Boston area, sent out emergency alerts when the outage happened letting clinics and smaller practices know how to find their 10-digit emergency numbers. In the wake of the outage, it plans to keep the backup numbers next to phones at those facilities.
“Two hours can be a long time,” said Paul Biddinger, chief preparedness and continuity officer at the health system.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Primary Care Internal Medicine Is Dead
Editor’s Note: This piece was originally published in Dr. Glasser’s bimonthly column in The Jolt, a nonprofit online news organization based in Olympia, Washington. She was inspired to write her story after meeting Christine Laine, MD, one of three female physician presenters at the Sommer Lectures in Portland, Oregon, in May 2024. The article has been edited lightly from the original.
Primary care internal medicine — the medical field I chose, loved, and practiced for four decades — is dead.
The grief and shock I feel about this is personal and transpersonal. The loss of internists (internal medicine physicians) practicing primary care is a major loss to us all.
From the 1970s to roughly 2020, there were three groups of primary care physicians: family practice, pediatricians, and internists. In their 3-year residencies (after 4 years of medical school), pediatricians trained to care for children and adolescents; internists for adults; and FPs for children, adults, and women and pregnancy. Family practitioners are the most general of the generalists, whereas the others’ training involves comprehensive care of complex patients in their age groups.
How and when the field of primary care internal medicine flourished is my story.
I was one of those kids who was hyperfocused on science, math, and the human body. By the end of high school, I was considering medicine for my career.
To learn more, I volunteered at the local hospital. In my typical style, I requested not to be one of those candy stripers serving drinks on the wards. Instead, they put me in the emergency department, where I would transport patients and clean the stretchers. There I was free to watch whatever was going on if I did not interfere with the staff. On my first shift, a 20-year-old drowning victim arrived by ambulance. I watched the entire unsuccessful resuscitation and as shocked and saddened as I was, I knew (in the way only a headstrong 18-year-old can) that medicine was for me.
It was a fortuitous time to graduate as a female pre-med student.
In 1975, our country was in the midst of the women’s movement and a national effort to train primary care physicians. I was accepted to my state medical school. The University of Massachusetts Medical School had been established a few years earlier, with its main purpose to train primary care physicians and spread them around the state (especially out of the Boston metropolitan area). The curriculum was designed to expose students to primary care from year one. I was assigned to shadow a general practice physician in inner-city Springfield who saw over 50 patients a day! The patients knew they could see and afford him, so they crammed into his waiting room until their name was called in order of their arrival. No appointments necessary. His chart notes were a few scribbled sentences. I didn’t see myself in that practice exactly, but his work ethic and dedication inspired me.
Over half of our graduating class chose to train in primary care specialties, and most stayed in-state. It turned out to be a good bet on the part of the government of Massachusetts.
When I applied for residency in 1980, several internal medicine programs had a focus on primary care, which was my goal. I matched at Providence St. Vincent Hospital in Portland, Oregon, and moved across the country to the Pacific Northwest, never to look back. There, my attendings were doctors like I wanted to be: primary care internists in the community, not in academia. It was the perfect choice and an excellent training program.
In 1984, I hung out my private practice internal medicine shingle in Hillsboro, Oregon, across the street from the community hospital. My primary care internal medicine colleagues and I shared weekend calls and admitted and cared for our patients in the hospital, and when they were discharged. That is now called “continuity of care.” It was a time when we ate in the doctors’ lounge together, met in hallways, and informally consulted each other about our patients. These were called “curbside consults.” They were invaluable to our ability to provide comprehensive care to our patients in primary care, led to fewer specialty referrals, and were free. That would now be called interprofessional communication and collegiality.
“Burnout” was not a word you heard. We were busy and happy doing what we had spent 12 years of our precious youth to prepare for.
What did internists offer to primary care? That also is part of my story.
When I moved to Olympia, I took a position in the women’s health clinic at the American Lake Veterans Administration Medical Center.
We were a small group: two family practice doctors, three nurse practitioners, and me, the only internist. Many of our patients were sick and complex. Two of the nurse practitioners (NPs) asked me to take their most complicated patients. Being comfortable with complexity as an internist, I said yes.
One of the NPs was inappropriately hired, as she had experience in women’s health. She came to me freaked out: “Oh my God, I have no idea how to manage COPD!” The other wanted simpler patients. I don’t blame them for the patient transfers. NPs typically have 3 years of training before they practice, in contrast to primary care physicians’ 8.
Guess who made friends with the custodian, staying until 8 p.m. most evenings, and who left by 5:30 p.m.
What was I doing in those extra hours? I was trudging through clerical, yet important, tasks my medical assistant and transcriptionist used to do in private practice. In the 30 minutes allotted for the patient, I needed to focus entirely on them and their multiple complex medical problems.
What is lost with the death of primary care internal medicine?
At the recent Sommer Memorial Lectures in Portland, Steven D. Freer, MD, the current director of the residency program where I trained, has not had a single of his eight annual internal medicine graduates choose primary care in several years. Half (two of four) of those in my year did: One went to Tillamook, an underserved area on the Oregon coast, and I to Hillsboro.
Why are they not choosing primary care? As when the University of Massachusetts Medical School was established, a shortage of primary care physicians persists and probably is more severe than it was in the 1970s. Massachusetts was proactive. We are already years behind catching up. The shortage is no longer in rural areas alone.
Christine Laine, MD, who is editor in chief of Annals of Internal Medicine and spoke at the Sommer Memorial Lectures, lives in Philadelphia. Even there, she has lost her own primary care internal medicine physician and cannot find another primary care physician (much less an internist) for herself.
Washington State, where I live, scores a D grade for our primary care staffing statewide.
Is there hope for the future of primary care in general? Or for the restoration of primary care internal medicine?
Maybe. I was relieved to hear from Dr. Freer and Dr. Laine that efforts are beginning to revive the field.
Just like internists’ patients, the potential restoration of the field will be complex and multilayered. It will require new laws, policies, residency programs, and incentives for students, including debt reduction. Administrative burdens will need to be reduced; de-corporatization and restoring healthcare leadership to those with in-depth medical training will need to be a part of the solution as well.
Let’s all hope the new resuscitation efforts will be successful for the field of primary care in general and primary care internal medicine specifically. It will be good for healthcare and for your patients!
Many work for large systems in which they feel powerless to effect change.
Dr. Glasser is a retired internal medicine physician in Olympia, Washington. She can be reached at drdebra@theJOLTnews.com.
A version of this article appeared on Medscape.com.
Editor’s Note: This piece was originally published in Dr. Glasser’s bimonthly column in The Jolt, a nonprofit online news organization based in Olympia, Washington. She was inspired to write her story after meeting Christine Laine, MD, one of three female physician presenters at the Sommer Lectures in Portland, Oregon, in May 2024. The article has been edited lightly from the original.
Primary care internal medicine — the medical field I chose, loved, and practiced for four decades — is dead.
The grief and shock I feel about this is personal and transpersonal. The loss of internists (internal medicine physicians) practicing primary care is a major loss to us all.
From the 1970s to roughly 2020, there were three groups of primary care physicians: family practice, pediatricians, and internists. In their 3-year residencies (after 4 years of medical school), pediatricians trained to care for children and adolescents; internists for adults; and FPs for children, adults, and women and pregnancy. Family practitioners are the most general of the generalists, whereas the others’ training involves comprehensive care of complex patients in their age groups.
How and when the field of primary care internal medicine flourished is my story.
I was one of those kids who was hyperfocused on science, math, and the human body. By the end of high school, I was considering medicine for my career.
To learn more, I volunteered at the local hospital. In my typical style, I requested not to be one of those candy stripers serving drinks on the wards. Instead, they put me in the emergency department, where I would transport patients and clean the stretchers. There I was free to watch whatever was going on if I did not interfere with the staff. On my first shift, a 20-year-old drowning victim arrived by ambulance. I watched the entire unsuccessful resuscitation and as shocked and saddened as I was, I knew (in the way only a headstrong 18-year-old can) that medicine was for me.
It was a fortuitous time to graduate as a female pre-med student.
In 1975, our country was in the midst of the women’s movement and a national effort to train primary care physicians. I was accepted to my state medical school. The University of Massachusetts Medical School had been established a few years earlier, with its main purpose to train primary care physicians and spread them around the state (especially out of the Boston metropolitan area). The curriculum was designed to expose students to primary care from year one. I was assigned to shadow a general practice physician in inner-city Springfield who saw over 50 patients a day! The patients knew they could see and afford him, so they crammed into his waiting room until their name was called in order of their arrival. No appointments necessary. His chart notes were a few scribbled sentences. I didn’t see myself in that practice exactly, but his work ethic and dedication inspired me.
Over half of our graduating class chose to train in primary care specialties, and most stayed in-state. It turned out to be a good bet on the part of the government of Massachusetts.
When I applied for residency in 1980, several internal medicine programs had a focus on primary care, which was my goal. I matched at Providence St. Vincent Hospital in Portland, Oregon, and moved across the country to the Pacific Northwest, never to look back. There, my attendings were doctors like I wanted to be: primary care internists in the community, not in academia. It was the perfect choice and an excellent training program.
In 1984, I hung out my private practice internal medicine shingle in Hillsboro, Oregon, across the street from the community hospital. My primary care internal medicine colleagues and I shared weekend calls and admitted and cared for our patients in the hospital, and when they were discharged. That is now called “continuity of care.” It was a time when we ate in the doctors’ lounge together, met in hallways, and informally consulted each other about our patients. These were called “curbside consults.” They were invaluable to our ability to provide comprehensive care to our patients in primary care, led to fewer specialty referrals, and were free. That would now be called interprofessional communication and collegiality.
“Burnout” was not a word you heard. We were busy and happy doing what we had spent 12 years of our precious youth to prepare for.
What did internists offer to primary care? That also is part of my story.
When I moved to Olympia, I took a position in the women’s health clinic at the American Lake Veterans Administration Medical Center.
We were a small group: two family practice doctors, three nurse practitioners, and me, the only internist. Many of our patients were sick and complex. Two of the nurse practitioners (NPs) asked me to take their most complicated patients. Being comfortable with complexity as an internist, I said yes.
One of the NPs was inappropriately hired, as she had experience in women’s health. She came to me freaked out: “Oh my God, I have no idea how to manage COPD!” The other wanted simpler patients. I don’t blame them for the patient transfers. NPs typically have 3 years of training before they practice, in contrast to primary care physicians’ 8.
Guess who made friends with the custodian, staying until 8 p.m. most evenings, and who left by 5:30 p.m.
What was I doing in those extra hours? I was trudging through clerical, yet important, tasks my medical assistant and transcriptionist used to do in private practice. In the 30 minutes allotted for the patient, I needed to focus entirely on them and their multiple complex medical problems.
What is lost with the death of primary care internal medicine?
At the recent Sommer Memorial Lectures in Portland, Steven D. Freer, MD, the current director of the residency program where I trained, has not had a single of his eight annual internal medicine graduates choose primary care in several years. Half (two of four) of those in my year did: One went to Tillamook, an underserved area on the Oregon coast, and I to Hillsboro.
Why are they not choosing primary care? As when the University of Massachusetts Medical School was established, a shortage of primary care physicians persists and probably is more severe than it was in the 1970s. Massachusetts was proactive. We are already years behind catching up. The shortage is no longer in rural areas alone.
Christine Laine, MD, who is editor in chief of Annals of Internal Medicine and spoke at the Sommer Memorial Lectures, lives in Philadelphia. Even there, she has lost her own primary care internal medicine physician and cannot find another primary care physician (much less an internist) for herself.
Washington State, where I live, scores a D grade for our primary care staffing statewide.
Is there hope for the future of primary care in general? Or for the restoration of primary care internal medicine?
Maybe. I was relieved to hear from Dr. Freer and Dr. Laine that efforts are beginning to revive the field.
Just like internists’ patients, the potential restoration of the field will be complex and multilayered. It will require new laws, policies, residency programs, and incentives for students, including debt reduction. Administrative burdens will need to be reduced; de-corporatization and restoring healthcare leadership to those with in-depth medical training will need to be a part of the solution as well.
Let’s all hope the new resuscitation efforts will be successful for the field of primary care in general and primary care internal medicine specifically. It will be good for healthcare and for your patients!
Many work for large systems in which they feel powerless to effect change.
Dr. Glasser is a retired internal medicine physician in Olympia, Washington. She can be reached at drdebra@theJOLTnews.com.
A version of this article appeared on Medscape.com.
Editor’s Note: This piece was originally published in Dr. Glasser’s bimonthly column in The Jolt, a nonprofit online news organization based in Olympia, Washington. She was inspired to write her story after meeting Christine Laine, MD, one of three female physician presenters at the Sommer Lectures in Portland, Oregon, in May 2024. The article has been edited lightly from the original.
Primary care internal medicine — the medical field I chose, loved, and practiced for four decades — is dead.
The grief and shock I feel about this is personal and transpersonal. The loss of internists (internal medicine physicians) practicing primary care is a major loss to us all.
From the 1970s to roughly 2020, there were three groups of primary care physicians: family practice, pediatricians, and internists. In their 3-year residencies (after 4 years of medical school), pediatricians trained to care for children and adolescents; internists for adults; and FPs for children, adults, and women and pregnancy. Family practitioners are the most general of the generalists, whereas the others’ training involves comprehensive care of complex patients in their age groups.
How and when the field of primary care internal medicine flourished is my story.
I was one of those kids who was hyperfocused on science, math, and the human body. By the end of high school, I was considering medicine for my career.
To learn more, I volunteered at the local hospital. In my typical style, I requested not to be one of those candy stripers serving drinks on the wards. Instead, they put me in the emergency department, where I would transport patients and clean the stretchers. There I was free to watch whatever was going on if I did not interfere with the staff. On my first shift, a 20-year-old drowning victim arrived by ambulance. I watched the entire unsuccessful resuscitation and as shocked and saddened as I was, I knew (in the way only a headstrong 18-year-old can) that medicine was for me.
It was a fortuitous time to graduate as a female pre-med student.
In 1975, our country was in the midst of the women’s movement and a national effort to train primary care physicians. I was accepted to my state medical school. The University of Massachusetts Medical School had been established a few years earlier, with its main purpose to train primary care physicians and spread them around the state (especially out of the Boston metropolitan area). The curriculum was designed to expose students to primary care from year one. I was assigned to shadow a general practice physician in inner-city Springfield who saw over 50 patients a day! The patients knew they could see and afford him, so they crammed into his waiting room until their name was called in order of their arrival. No appointments necessary. His chart notes were a few scribbled sentences. I didn’t see myself in that practice exactly, but his work ethic and dedication inspired me.
Over half of our graduating class chose to train in primary care specialties, and most stayed in-state. It turned out to be a good bet on the part of the government of Massachusetts.
When I applied for residency in 1980, several internal medicine programs had a focus on primary care, which was my goal. I matched at Providence St. Vincent Hospital in Portland, Oregon, and moved across the country to the Pacific Northwest, never to look back. There, my attendings were doctors like I wanted to be: primary care internists in the community, not in academia. It was the perfect choice and an excellent training program.
In 1984, I hung out my private practice internal medicine shingle in Hillsboro, Oregon, across the street from the community hospital. My primary care internal medicine colleagues and I shared weekend calls and admitted and cared for our patients in the hospital, and when they were discharged. That is now called “continuity of care.” It was a time when we ate in the doctors’ lounge together, met in hallways, and informally consulted each other about our patients. These were called “curbside consults.” They were invaluable to our ability to provide comprehensive care to our patients in primary care, led to fewer specialty referrals, and were free. That would now be called interprofessional communication and collegiality.
“Burnout” was not a word you heard. We were busy and happy doing what we had spent 12 years of our precious youth to prepare for.
What did internists offer to primary care? That also is part of my story.
When I moved to Olympia, I took a position in the women’s health clinic at the American Lake Veterans Administration Medical Center.
We were a small group: two family practice doctors, three nurse practitioners, and me, the only internist. Many of our patients were sick and complex. Two of the nurse practitioners (NPs) asked me to take their most complicated patients. Being comfortable with complexity as an internist, I said yes.
One of the NPs was inappropriately hired, as she had experience in women’s health. She came to me freaked out: “Oh my God, I have no idea how to manage COPD!” The other wanted simpler patients. I don’t blame them for the patient transfers. NPs typically have 3 years of training before they practice, in contrast to primary care physicians’ 8.
Guess who made friends with the custodian, staying until 8 p.m. most evenings, and who left by 5:30 p.m.
What was I doing in those extra hours? I was trudging through clerical, yet important, tasks my medical assistant and transcriptionist used to do in private practice. In the 30 minutes allotted for the patient, I needed to focus entirely on them and their multiple complex medical problems.
What is lost with the death of primary care internal medicine?
At the recent Sommer Memorial Lectures in Portland, Steven D. Freer, MD, the current director of the residency program where I trained, has not had a single of his eight annual internal medicine graduates choose primary care in several years. Half (two of four) of those in my year did: One went to Tillamook, an underserved area on the Oregon coast, and I to Hillsboro.
Why are they not choosing primary care? As when the University of Massachusetts Medical School was established, a shortage of primary care physicians persists and probably is more severe than it was in the 1970s. Massachusetts was proactive. We are already years behind catching up. The shortage is no longer in rural areas alone.
Christine Laine, MD, who is editor in chief of Annals of Internal Medicine and spoke at the Sommer Memorial Lectures, lives in Philadelphia. Even there, she has lost her own primary care internal medicine physician and cannot find another primary care physician (much less an internist) for herself.
Washington State, where I live, scores a D grade for our primary care staffing statewide.
Is there hope for the future of primary care in general? Or for the restoration of primary care internal medicine?
Maybe. I was relieved to hear from Dr. Freer and Dr. Laine that efforts are beginning to revive the field.
Just like internists’ patients, the potential restoration of the field will be complex and multilayered. It will require new laws, policies, residency programs, and incentives for students, including debt reduction. Administrative burdens will need to be reduced; de-corporatization and restoring healthcare leadership to those with in-depth medical training will need to be a part of the solution as well.
Let’s all hope the new resuscitation efforts will be successful for the field of primary care in general and primary care internal medicine specifically. It will be good for healthcare and for your patients!
Many work for large systems in which they feel powerless to effect change.
Dr. Glasser is a retired internal medicine physician in Olympia, Washington. She can be reached at drdebra@theJOLTnews.com.
A version of this article appeared on Medscape.com.
Intervention Helps Transition From Postpartum Care to PCP Engagement
, according to study results published in JAMA Network Open. The intervention bundle includes default scheduling of postpartum primary care appointments and tailored reminders and messaging.
Researchers, led by Mark A. Clapp, MD, MPH, with Massachusetts General Hospital in Boston, highlighted a care transition gap common after a woman gives birth. More than 30% of pregnant people have at least one chronic condition and nearly 20% develop gestational diabetes or pregnancy-related hypertension, which increases the risk of future chronic disease, the authors write. They are closely monitored for these conditions during pregnancy, but many face barriers in transitioning to engagement with primary care.
Scheduling appointments, difficulty in finding information, and insurance or billing issues can impede access to care. In this study, the primary outcome measure was whether women completed a primary care visit for routine or chronic condition care within 4 months of delivery.
Intervention vs Control Group
The intervention included an introduction message talking about the importance of a primary care visit and notification that a staff member would be scheduling an appointment on the patients’ behalf within a 4-month window of the estimated due date (EDD). Patients could opt out or ask for specific scheduling. If a patient had already seen their primary care physician (PCP) for an annual visit within the year, they were scheduled for an annual visit when they were next eligible, even if outside the 4-month study follow-up.
For those who did not opt out and had appointments scheduled for them, reminders were sent about 1 month after the EDD and 1 week before the scheduled appointment through the EHR patient portal. Salient labeling of the message was used to describe the visit. For those for whom an appointment could not be scheduled, similar reminders were sent on the importance of primary care follow-up, urging patients to contact their primary care office directly to schedule. Reminders included evidence-based, best-practice wording including that “the appointment had been reserved for them.”
Patients in the control group received one message within 2 weeks of the EDD with a generic recommendation for primary care follow-up after delivery.
Researchers found that 40% of the intervention group (95% confidence interval (CI), 33.1%-47.4%) and 22% of the control group (95% CI, 6.4%-28.8%), completed a primary care visit within 4 months. “[T]he intervention increased PCP visit completion by 18.7 percentage points (95% CI, 9.1-28.2 percentage points),” they write. Those who received the intervention also had fewer postpartum readmissions (1.7% vs 5.8%) and were more likely to have had these services from a PCP: blood pressure screening (42.8% vs 28.3%); weight assessment (42.8% vs 27.7%); and depression screening (32.8% vs 16.8%).
Meghan Bellerose, MPH, with the Department of Health Services, Policy, and Practice at Brown University School of Public Health in Providence, Rhode Island, described in an accompanying editorial the “postpartum cliff.”
“Health system engagement plummets soon after childbirth in the US,” she writes. “Under current care practices, obstetric clinicians deliver a single postpartum visit within 12 weeks of delivery, after which patients are responsible for navigating the transition to primary care on their own.”
The intervention Dr. Clapp and colleagues propose could help increase the benefit of state and federal policies aimed at increasing care continuity after delivery, she writes. She pointed to the American Rescue Plan Act of 2021, in which states were given the option to provide 12 months of continuous Medicaid coverage to low-income postpartum women, up from the previous 2 months of coverage. By early May of 2024, 46 states had chosen the longer coverage.
Without a better bridge between postpartum and primary care, she notes, “we will not see the full value of extended Medicaid coverage.”
“The findings of Clapp et al. suggest that a relatively low-resource, scalable intervention including default scheduling of postpartum-to-primary care appointments and salient messaging could increase the use of primary care in the postpartum year to extend the effects of this policy.”
Still, Only 40% Used Primary Care
She noted, however, that despite the finding that the intervention in this study nearly doubled the percentage of primary care visits in 4 months, primary care use still was only 40%. Study staff were not able to schedule an appointment for 24% of the intervention group within a year, even though participants identified a PCP at enrollment. Reasons for that included the patient already having used their yearly primary care visit; patients needing to restart care with their primary care clinician or choose a new clinician; and study staff being unable to reach primary care offices for scheduling.
Clearly, “there is more work to be done to remove administrative barriers to care after delivery,” she writes.
Dr. Clapp reports holding equity from the Delfina Care Scientific Advisory Board outside the submitted work. Coauthor Dr. Ganguli reports grants from the National Institute on Aging, Commonwealth Fund, and Arnold Ventures, and personal fees from FPrime outside the submitted work. Dr. Cohen reports grants from the National Academy of Medicine and the National Academy on Aging during the conduct of the study. The study was funded by the National Institute on Aging via the Massachusetts Institute of Technology Roybal Center for Translational Research to Improve Health Care for the Aging and the National Bureau of Economic Research Roybal Center for Behavior Change in Health. Editorialist Meghan Bellerose reported no relevant financial disclosures.
, according to study results published in JAMA Network Open. The intervention bundle includes default scheduling of postpartum primary care appointments and tailored reminders and messaging.
Researchers, led by Mark A. Clapp, MD, MPH, with Massachusetts General Hospital in Boston, highlighted a care transition gap common after a woman gives birth. More than 30% of pregnant people have at least one chronic condition and nearly 20% develop gestational diabetes or pregnancy-related hypertension, which increases the risk of future chronic disease, the authors write. They are closely monitored for these conditions during pregnancy, but many face barriers in transitioning to engagement with primary care.
Scheduling appointments, difficulty in finding information, and insurance or billing issues can impede access to care. In this study, the primary outcome measure was whether women completed a primary care visit for routine or chronic condition care within 4 months of delivery.
Intervention vs Control Group
The intervention included an introduction message talking about the importance of a primary care visit and notification that a staff member would be scheduling an appointment on the patients’ behalf within a 4-month window of the estimated due date (EDD). Patients could opt out or ask for specific scheduling. If a patient had already seen their primary care physician (PCP) for an annual visit within the year, they were scheduled for an annual visit when they were next eligible, even if outside the 4-month study follow-up.
For those who did not opt out and had appointments scheduled for them, reminders were sent about 1 month after the EDD and 1 week before the scheduled appointment through the EHR patient portal. Salient labeling of the message was used to describe the visit. For those for whom an appointment could not be scheduled, similar reminders were sent on the importance of primary care follow-up, urging patients to contact their primary care office directly to schedule. Reminders included evidence-based, best-practice wording including that “the appointment had been reserved for them.”
Patients in the control group received one message within 2 weeks of the EDD with a generic recommendation for primary care follow-up after delivery.
Researchers found that 40% of the intervention group (95% confidence interval (CI), 33.1%-47.4%) and 22% of the control group (95% CI, 6.4%-28.8%), completed a primary care visit within 4 months. “[T]he intervention increased PCP visit completion by 18.7 percentage points (95% CI, 9.1-28.2 percentage points),” they write. Those who received the intervention also had fewer postpartum readmissions (1.7% vs 5.8%) and were more likely to have had these services from a PCP: blood pressure screening (42.8% vs 28.3%); weight assessment (42.8% vs 27.7%); and depression screening (32.8% vs 16.8%).
Meghan Bellerose, MPH, with the Department of Health Services, Policy, and Practice at Brown University School of Public Health in Providence, Rhode Island, described in an accompanying editorial the “postpartum cliff.”
“Health system engagement plummets soon after childbirth in the US,” she writes. “Under current care practices, obstetric clinicians deliver a single postpartum visit within 12 weeks of delivery, after which patients are responsible for navigating the transition to primary care on their own.”
The intervention Dr. Clapp and colleagues propose could help increase the benefit of state and federal policies aimed at increasing care continuity after delivery, she writes. She pointed to the American Rescue Plan Act of 2021, in which states were given the option to provide 12 months of continuous Medicaid coverage to low-income postpartum women, up from the previous 2 months of coverage. By early May of 2024, 46 states had chosen the longer coverage.
Without a better bridge between postpartum and primary care, she notes, “we will not see the full value of extended Medicaid coverage.”
“The findings of Clapp et al. suggest that a relatively low-resource, scalable intervention including default scheduling of postpartum-to-primary care appointments and salient messaging could increase the use of primary care in the postpartum year to extend the effects of this policy.”
Still, Only 40% Used Primary Care
She noted, however, that despite the finding that the intervention in this study nearly doubled the percentage of primary care visits in 4 months, primary care use still was only 40%. Study staff were not able to schedule an appointment for 24% of the intervention group within a year, even though participants identified a PCP at enrollment. Reasons for that included the patient already having used their yearly primary care visit; patients needing to restart care with their primary care clinician or choose a new clinician; and study staff being unable to reach primary care offices for scheduling.
Clearly, “there is more work to be done to remove administrative barriers to care after delivery,” she writes.
Dr. Clapp reports holding equity from the Delfina Care Scientific Advisory Board outside the submitted work. Coauthor Dr. Ganguli reports grants from the National Institute on Aging, Commonwealth Fund, and Arnold Ventures, and personal fees from FPrime outside the submitted work. Dr. Cohen reports grants from the National Academy of Medicine and the National Academy on Aging during the conduct of the study. The study was funded by the National Institute on Aging via the Massachusetts Institute of Technology Roybal Center for Translational Research to Improve Health Care for the Aging and the National Bureau of Economic Research Roybal Center for Behavior Change in Health. Editorialist Meghan Bellerose reported no relevant financial disclosures.
, according to study results published in JAMA Network Open. The intervention bundle includes default scheduling of postpartum primary care appointments and tailored reminders and messaging.
Researchers, led by Mark A. Clapp, MD, MPH, with Massachusetts General Hospital in Boston, highlighted a care transition gap common after a woman gives birth. More than 30% of pregnant people have at least one chronic condition and nearly 20% develop gestational diabetes or pregnancy-related hypertension, which increases the risk of future chronic disease, the authors write. They are closely monitored for these conditions during pregnancy, but many face barriers in transitioning to engagement with primary care.
Scheduling appointments, difficulty in finding information, and insurance or billing issues can impede access to care. In this study, the primary outcome measure was whether women completed a primary care visit for routine or chronic condition care within 4 months of delivery.
Intervention vs Control Group
The intervention included an introduction message talking about the importance of a primary care visit and notification that a staff member would be scheduling an appointment on the patients’ behalf within a 4-month window of the estimated due date (EDD). Patients could opt out or ask for specific scheduling. If a patient had already seen their primary care physician (PCP) for an annual visit within the year, they were scheduled for an annual visit when they were next eligible, even if outside the 4-month study follow-up.
For those who did not opt out and had appointments scheduled for them, reminders were sent about 1 month after the EDD and 1 week before the scheduled appointment through the EHR patient portal. Salient labeling of the message was used to describe the visit. For those for whom an appointment could not be scheduled, similar reminders were sent on the importance of primary care follow-up, urging patients to contact their primary care office directly to schedule. Reminders included evidence-based, best-practice wording including that “the appointment had been reserved for them.”
Patients in the control group received one message within 2 weeks of the EDD with a generic recommendation for primary care follow-up after delivery.
Researchers found that 40% of the intervention group (95% confidence interval (CI), 33.1%-47.4%) and 22% of the control group (95% CI, 6.4%-28.8%), completed a primary care visit within 4 months. “[T]he intervention increased PCP visit completion by 18.7 percentage points (95% CI, 9.1-28.2 percentage points),” they write. Those who received the intervention also had fewer postpartum readmissions (1.7% vs 5.8%) and were more likely to have had these services from a PCP: blood pressure screening (42.8% vs 28.3%); weight assessment (42.8% vs 27.7%); and depression screening (32.8% vs 16.8%).
Meghan Bellerose, MPH, with the Department of Health Services, Policy, and Practice at Brown University School of Public Health in Providence, Rhode Island, described in an accompanying editorial the “postpartum cliff.”
“Health system engagement plummets soon after childbirth in the US,” she writes. “Under current care practices, obstetric clinicians deliver a single postpartum visit within 12 weeks of delivery, after which patients are responsible for navigating the transition to primary care on their own.”
The intervention Dr. Clapp and colleagues propose could help increase the benefit of state and federal policies aimed at increasing care continuity after delivery, she writes. She pointed to the American Rescue Plan Act of 2021, in which states were given the option to provide 12 months of continuous Medicaid coverage to low-income postpartum women, up from the previous 2 months of coverage. By early May of 2024, 46 states had chosen the longer coverage.
Without a better bridge between postpartum and primary care, she notes, “we will not see the full value of extended Medicaid coverage.”
“The findings of Clapp et al. suggest that a relatively low-resource, scalable intervention including default scheduling of postpartum-to-primary care appointments and salient messaging could increase the use of primary care in the postpartum year to extend the effects of this policy.”
Still, Only 40% Used Primary Care
She noted, however, that despite the finding that the intervention in this study nearly doubled the percentage of primary care visits in 4 months, primary care use still was only 40%. Study staff were not able to schedule an appointment for 24% of the intervention group within a year, even though participants identified a PCP at enrollment. Reasons for that included the patient already having used their yearly primary care visit; patients needing to restart care with their primary care clinician or choose a new clinician; and study staff being unable to reach primary care offices for scheduling.
Clearly, “there is more work to be done to remove administrative barriers to care after delivery,” she writes.
Dr. Clapp reports holding equity from the Delfina Care Scientific Advisory Board outside the submitted work. Coauthor Dr. Ganguli reports grants from the National Institute on Aging, Commonwealth Fund, and Arnold Ventures, and personal fees from FPrime outside the submitted work. Dr. Cohen reports grants from the National Academy of Medicine and the National Academy on Aging during the conduct of the study. The study was funded by the National Institute on Aging via the Massachusetts Institute of Technology Roybal Center for Translational Research to Improve Health Care for the Aging and the National Bureau of Economic Research Roybal Center for Behavior Change in Health. Editorialist Meghan Bellerose reported no relevant financial disclosures.
FROM JAMA NETWORK OPEN
Could an EHR Nudge Reduce Unnecessary Biopsies?
Participating surgeons noted that the reminder system added minimal friction to their workflow, as it did not require additional clicks or actions on the day of the patient visit, reported lead author Neil Carleton, PhD, of UPMC Hillman Cancer Center, Pittsburgh, and colleagues in JAMA Surgery (JAMA Surg. 2024 Jul 17. doi: 10.1001/jamasurg.2024.2407).
This effort to reduce the rate of SLNB stems from the Choosing Wisely campaign, which recommends against axillary staging in women 70 years and older with early-stage, clinically node-negative (cN0), hormone receptor–positive (HR+) breast cancer, the investigators said.
“These recommendations were developed because axillary staging did not impact survival, and rates of SLN positivity were low because of the tumor’s biological phenotype,” they wrote. “Even in older patients with tumors that exhibit concerning clinicopathologic features, limited nodal involvement does not often alter receipt of chemotherapy independently from genomic testing. Despite these recommendations, most women still receive axillary surgery.”
How Did the Nudge System Aim to Reduce the Rate of SLNB?
The nudge intervention involved adding a new column to the Epic schedule view, which flagged eligible patients during their first outpatient surgical consultation. The flag appeared as a caution sign or red clipboard icon. When surgeons hovered over the icon, a text box appeared, reminding them to consider omitting SLNB after a detailed review of core biopsy pathology and ultrasonographic imaging.
The intervention was evaluated at eight outpatient clinics within an integrated healthcare system that included seven breast surgical oncologists.
The study began with a 12-month preintervention period to serve as a control, during which time SLNB rate was determined via 194 patients in the target demographic. SLNB rate was again collected during the 12-month intervention period, which involved 193 patients meeting enrollment criteria. Between these periods, the investigators conducted a brief session lasting less than 30 minutes to introduce the surgeons to the rationale and design of the nudge column.
How Effective Was the Nudge System?
The intervention reduced the SLNB rate from 46.9% to 23.8%, representing a 49.3% decrease in use of SLNB. Efficacy was further supported by a significant reduction in SLNB according to an interrupted time series model (adjusted odds ratio, 0.26; 95% confidence interval, 0.07 to 0.90; P = .03). Extended follow-up showed that this effect was durable beyond the intervention period, with a 6-month mean reduction in SLNB of 15.6%.
Omission of SLNB led to higher rates of pathological node positivity during the intervention period (15.2% vs 8.8%), with all positive cases staged as pN1. Adjuvant therapy recommendations were similar between groups and driven by genomic testing, not nodal status. The intervention period also saw a decrease in referrals for lymphedema evaluation (3.6% vs. 6.2%).
How Might the Nudge System Be Implemented in Other Practices?
Although the SLNB nudge system was effective in the present study, likelihood of uptake among practices could vary widely, according to Anne M. Wallace, MD, professor of clinical surgery at UC San Diego Health and director of the Moores Comprehensive Breast Health Program.
On a fundamental level, not all centers use Epic software, which could present issues with compatibility, Dr. Wallace said in an interview. More importantly, she added, many institutions already have EHR-based alerts and reminders in place, so it is not always feasible to add a new nudge for every possible clinical scenario.
“Already there are so many little icons that we have to go through now when we close a note,” she said. “That’s why electronic medical records are becoming one of the leading stressors in medicine.”
This presents a more complex challenge, Dr. Wallace said, particularly as potentially practice-changing data are becoming available, and physicians may not have time to learn about them and integrate them into routine practice. She suggested that the present system may be most appropriate for oncologists in solo practice, or in small group practices where it is more challenging to have routine conversations about changing standards of care.
What Are the Risks of Using the Nudge System?
One of those conversations may surround the validity of the recommendation implemented in the present study.
Although the Society of Surgical Oncology recommends against SLNB in the described demographic, other experts, including Dr. Wallace, take a more nuanced view of the decision.
She noted that some patients with a chronological age of 70 may have a lower biological age, casting doubt on the legitimacy of the age threshold, and those near the threshold may wish to make the decision about staging for themselves.
Beyond these concerns, Dr. Wallace described two potential risks involved in forgoing SLNB.
First, there’s the potential for underestimating the tumor’s severity, she said, as this could mean a trip back to the operating room. A tumor initially thought to be low-grade might later be found to be high-grade, necessitating further surgery. Some patients might refuse additional surgery, leaving the more aggressive tumor untreated.
Second, the nudge system could complicate radiation treatment decisions, Dr. Wallace said. Without full nodal status, some radiation oncologists might push for additional radiation therapy, which incurs a greater treatment burden than SNLB.
What Are Some Alternatives to the Nudge System?
After discussing the strengths and weaknesses of the present EHR-based nudge system, and others like it, Dr. Wallace returned to the importance of ongoing communication among colleagues managing complex cases.
At UC San Diego Health, where oncologists meet weekly for a 2-hour breast cancer conference, “we nudge each other,” she said.
This study was supported by the Shear Family Foundation, UPMC eRecord Ambulatory Decision Support and Analytics, UPMC Hillman Cancer Center Biostatistics Facility, and National Institutes of Health. The investigators disclosed relationships with Pfizer, Amgen, the Lewin Group, and Milestone Pennsylvania, and others.
Participating surgeons noted that the reminder system added minimal friction to their workflow, as it did not require additional clicks or actions on the day of the patient visit, reported lead author Neil Carleton, PhD, of UPMC Hillman Cancer Center, Pittsburgh, and colleagues in JAMA Surgery (JAMA Surg. 2024 Jul 17. doi: 10.1001/jamasurg.2024.2407).
This effort to reduce the rate of SLNB stems from the Choosing Wisely campaign, which recommends against axillary staging in women 70 years and older with early-stage, clinically node-negative (cN0), hormone receptor–positive (HR+) breast cancer, the investigators said.
“These recommendations were developed because axillary staging did not impact survival, and rates of SLN positivity were low because of the tumor’s biological phenotype,” they wrote. “Even in older patients with tumors that exhibit concerning clinicopathologic features, limited nodal involvement does not often alter receipt of chemotherapy independently from genomic testing. Despite these recommendations, most women still receive axillary surgery.”
How Did the Nudge System Aim to Reduce the Rate of SLNB?
The nudge intervention involved adding a new column to the Epic schedule view, which flagged eligible patients during their first outpatient surgical consultation. The flag appeared as a caution sign or red clipboard icon. When surgeons hovered over the icon, a text box appeared, reminding them to consider omitting SLNB after a detailed review of core biopsy pathology and ultrasonographic imaging.
The intervention was evaluated at eight outpatient clinics within an integrated healthcare system that included seven breast surgical oncologists.
The study began with a 12-month preintervention period to serve as a control, during which time SLNB rate was determined via 194 patients in the target demographic. SLNB rate was again collected during the 12-month intervention period, which involved 193 patients meeting enrollment criteria. Between these periods, the investigators conducted a brief session lasting less than 30 minutes to introduce the surgeons to the rationale and design of the nudge column.
How Effective Was the Nudge System?
The intervention reduced the SLNB rate from 46.9% to 23.8%, representing a 49.3% decrease in use of SLNB. Efficacy was further supported by a significant reduction in SLNB according to an interrupted time series model (adjusted odds ratio, 0.26; 95% confidence interval, 0.07 to 0.90; P = .03). Extended follow-up showed that this effect was durable beyond the intervention period, with a 6-month mean reduction in SLNB of 15.6%.
Omission of SLNB led to higher rates of pathological node positivity during the intervention period (15.2% vs 8.8%), with all positive cases staged as pN1. Adjuvant therapy recommendations were similar between groups and driven by genomic testing, not nodal status. The intervention period also saw a decrease in referrals for lymphedema evaluation (3.6% vs. 6.2%).
How Might the Nudge System Be Implemented in Other Practices?
Although the SLNB nudge system was effective in the present study, likelihood of uptake among practices could vary widely, according to Anne M. Wallace, MD, professor of clinical surgery at UC San Diego Health and director of the Moores Comprehensive Breast Health Program.
On a fundamental level, not all centers use Epic software, which could present issues with compatibility, Dr. Wallace said in an interview. More importantly, she added, many institutions already have EHR-based alerts and reminders in place, so it is not always feasible to add a new nudge for every possible clinical scenario.
“Already there are so many little icons that we have to go through now when we close a note,” she said. “That’s why electronic medical records are becoming one of the leading stressors in medicine.”
This presents a more complex challenge, Dr. Wallace said, particularly as potentially practice-changing data are becoming available, and physicians may not have time to learn about them and integrate them into routine practice. She suggested that the present system may be most appropriate for oncologists in solo practice, or in small group practices where it is more challenging to have routine conversations about changing standards of care.
What Are the Risks of Using the Nudge System?
One of those conversations may surround the validity of the recommendation implemented in the present study.
Although the Society of Surgical Oncology recommends against SLNB in the described demographic, other experts, including Dr. Wallace, take a more nuanced view of the decision.
She noted that some patients with a chronological age of 70 may have a lower biological age, casting doubt on the legitimacy of the age threshold, and those near the threshold may wish to make the decision about staging for themselves.
Beyond these concerns, Dr. Wallace described two potential risks involved in forgoing SLNB.
First, there’s the potential for underestimating the tumor’s severity, she said, as this could mean a trip back to the operating room. A tumor initially thought to be low-grade might later be found to be high-grade, necessitating further surgery. Some patients might refuse additional surgery, leaving the more aggressive tumor untreated.
Second, the nudge system could complicate radiation treatment decisions, Dr. Wallace said. Without full nodal status, some radiation oncologists might push for additional radiation therapy, which incurs a greater treatment burden than SNLB.
What Are Some Alternatives to the Nudge System?
After discussing the strengths and weaknesses of the present EHR-based nudge system, and others like it, Dr. Wallace returned to the importance of ongoing communication among colleagues managing complex cases.
At UC San Diego Health, where oncologists meet weekly for a 2-hour breast cancer conference, “we nudge each other,” she said.
This study was supported by the Shear Family Foundation, UPMC eRecord Ambulatory Decision Support and Analytics, UPMC Hillman Cancer Center Biostatistics Facility, and National Institutes of Health. The investigators disclosed relationships with Pfizer, Amgen, the Lewin Group, and Milestone Pennsylvania, and others.
Participating surgeons noted that the reminder system added minimal friction to their workflow, as it did not require additional clicks or actions on the day of the patient visit, reported lead author Neil Carleton, PhD, of UPMC Hillman Cancer Center, Pittsburgh, and colleagues in JAMA Surgery (JAMA Surg. 2024 Jul 17. doi: 10.1001/jamasurg.2024.2407).
This effort to reduce the rate of SLNB stems from the Choosing Wisely campaign, which recommends against axillary staging in women 70 years and older with early-stage, clinically node-negative (cN0), hormone receptor–positive (HR+) breast cancer, the investigators said.
“These recommendations were developed because axillary staging did not impact survival, and rates of SLN positivity were low because of the tumor’s biological phenotype,” they wrote. “Even in older patients with tumors that exhibit concerning clinicopathologic features, limited nodal involvement does not often alter receipt of chemotherapy independently from genomic testing. Despite these recommendations, most women still receive axillary surgery.”
How Did the Nudge System Aim to Reduce the Rate of SLNB?
The nudge intervention involved adding a new column to the Epic schedule view, which flagged eligible patients during their first outpatient surgical consultation. The flag appeared as a caution sign or red clipboard icon. When surgeons hovered over the icon, a text box appeared, reminding them to consider omitting SLNB after a detailed review of core biopsy pathology and ultrasonographic imaging.
The intervention was evaluated at eight outpatient clinics within an integrated healthcare system that included seven breast surgical oncologists.
The study began with a 12-month preintervention period to serve as a control, during which time SLNB rate was determined via 194 patients in the target demographic. SLNB rate was again collected during the 12-month intervention period, which involved 193 patients meeting enrollment criteria. Between these periods, the investigators conducted a brief session lasting less than 30 minutes to introduce the surgeons to the rationale and design of the nudge column.
How Effective Was the Nudge System?
The intervention reduced the SLNB rate from 46.9% to 23.8%, representing a 49.3% decrease in use of SLNB. Efficacy was further supported by a significant reduction in SLNB according to an interrupted time series model (adjusted odds ratio, 0.26; 95% confidence interval, 0.07 to 0.90; P = .03). Extended follow-up showed that this effect was durable beyond the intervention period, with a 6-month mean reduction in SLNB of 15.6%.
Omission of SLNB led to higher rates of pathological node positivity during the intervention period (15.2% vs 8.8%), with all positive cases staged as pN1. Adjuvant therapy recommendations were similar between groups and driven by genomic testing, not nodal status. The intervention period also saw a decrease in referrals for lymphedema evaluation (3.6% vs. 6.2%).
How Might the Nudge System Be Implemented in Other Practices?
Although the SLNB nudge system was effective in the present study, likelihood of uptake among practices could vary widely, according to Anne M. Wallace, MD, professor of clinical surgery at UC San Diego Health and director of the Moores Comprehensive Breast Health Program.
On a fundamental level, not all centers use Epic software, which could present issues with compatibility, Dr. Wallace said in an interview. More importantly, she added, many institutions already have EHR-based alerts and reminders in place, so it is not always feasible to add a new nudge for every possible clinical scenario.
“Already there are so many little icons that we have to go through now when we close a note,” she said. “That’s why electronic medical records are becoming one of the leading stressors in medicine.”
This presents a more complex challenge, Dr. Wallace said, particularly as potentially practice-changing data are becoming available, and physicians may not have time to learn about them and integrate them into routine practice. She suggested that the present system may be most appropriate for oncologists in solo practice, or in small group practices where it is more challenging to have routine conversations about changing standards of care.
What Are the Risks of Using the Nudge System?
One of those conversations may surround the validity of the recommendation implemented in the present study.
Although the Society of Surgical Oncology recommends against SLNB in the described demographic, other experts, including Dr. Wallace, take a more nuanced view of the decision.
She noted that some patients with a chronological age of 70 may have a lower biological age, casting doubt on the legitimacy of the age threshold, and those near the threshold may wish to make the decision about staging for themselves.
Beyond these concerns, Dr. Wallace described two potential risks involved in forgoing SLNB.
First, there’s the potential for underestimating the tumor’s severity, she said, as this could mean a trip back to the operating room. A tumor initially thought to be low-grade might later be found to be high-grade, necessitating further surgery. Some patients might refuse additional surgery, leaving the more aggressive tumor untreated.
Second, the nudge system could complicate radiation treatment decisions, Dr. Wallace said. Without full nodal status, some radiation oncologists might push for additional radiation therapy, which incurs a greater treatment burden than SNLB.
What Are Some Alternatives to the Nudge System?
After discussing the strengths and weaknesses of the present EHR-based nudge system, and others like it, Dr. Wallace returned to the importance of ongoing communication among colleagues managing complex cases.
At UC San Diego Health, where oncologists meet weekly for a 2-hour breast cancer conference, “we nudge each other,” she said.
This study was supported by the Shear Family Foundation, UPMC eRecord Ambulatory Decision Support and Analytics, UPMC Hillman Cancer Center Biostatistics Facility, and National Institutes of Health. The investigators disclosed relationships with Pfizer, Amgen, the Lewin Group, and Milestone Pennsylvania, and others.
FROM JAMA SURGERY
Revamping Resident Schedules to Reduce Burnout
It’s the difference between running a marathon and taking a leisurely stroll. That’s how recent pediatrics resident Joey Whelihan, MD, compared an 11-hour inpatient hospital day with an 8-hour outpatient shift where residents see patients in a clinic.
With inpatient training, “you are lucky if you have time to cook dinner, go to bed, and get ready for the next day,” said Dr. Whelihan, who recently started his adolescent medicine fellowship at Children’s Hospital of Philadelphia after 3 years of residency there. Some residents have call every fourth day during inpatient rotations, working 24-28 hours at a time. They come in one morning and go home the next, he told this news organization.
“Outpatient blocks give you more time to catch your breath and feel somewhat refreshed and ready to take care of patients.”
Longer stretches of inpatient rotations are not sustainable, Dr. Whelihan added, and residents are likely to become exhausted. Fatigue is a leading cause of burnout, a mental, physical, and emotional challenge that residency programs and national medical organizations have been struggling to address.
In recent years, there has been a movement to reduce the maximum consecutive duration of resident duty hours in residency programs across the country. Fueled by resident health and patient safety concerns, the movement is a shift from the previous 24- to 36-hour call duty schedules.
Improved Call Systems = Better Residents
The connection between burnout, well-being, and work schedules appears regularly in national program standards. “Residents and faculty members are at risk for burnout and depression,” according to the current Accreditation Council for Graduate Medical Education’s standard residency program requirements.
“Programs, in partnership with their sponsoring institutions, have the same responsibility to address well-being as other aspects of resident competence,” the guidelines state. That charge includes “attention to scheduling, work intensity, and work compression that impacts resident well-being.”
In Medscape’s Residents Lifestyle & Happiness Report 2023, a third of residents surveyed rarely or never paid attention to their well-being, which closely mirrors the 31% who rarely or never had time for a social life. Slightly more residents (37%) said their work-life balance was “somewhat worse” or “much worse” than they expected.
“I think everyone has burnout as a resident, regardless of the type of program they are in,” Dr. Whelihan said. He described the experience as when you lack fulfillment and empathy and feel exhausted, callous, and removed from interactions with colleagues and patients.
The American Medical Association’s recently released report on the state of residency well-being in 2023 also found that about 43% of residents and fellows had at least one symptom of burnout, about a 2% increase from 2022.
Efforts to Combat Burnout
One residency program found a way to reduce burnout by changing its block scheduling from 4 inpatient weeks followed by 1 outpatient week (4 + 1) to 4 inpatient call-based weeks and 4 outpatient ambulatory, non-call weeks (4 + 4), according to a survey study published recently in JAMA Network Open. The initiative drew praise from some residents and a med school professor who studies wellness issues.
In the survey of postgraduate year (PGY) 1 and PGY-2 hospitalist and primary care residents from the University of Colorado’s Internal Medicine Residency Program, Aurora, between June 2019 and June 2021, the schedule change resulted in improved burnout scores and self-reported professional, educational, and health benefits.
As part of the survey, residents rated symptoms on a 7-point scale on the basis of how frequently they experienced emotional exhaustion, depersonalization, and personal accomplishment.
Investigators also used a questionnaire to evaluate how participants perceived the rotation structure with various outcomes, including the ability to acquire clinical skills, access educational and scholarly opportunities, job satisfaction, and health.
The study concluded that the schedule change improved burnout, health, wellness, and professional development without weakening residents perceived clinical skills or standardized exam scores.
Still, the study authors acknowledged that several factors, including the pandemic, may have limited the findings. During that time, the study transitioned from in-person to electronic submissions, resulting in reduced response rates because of changes in staffing needs and fewer research and scholarly activities.
“One of the things we worried about was that the pandemic would make [burnout findings] look worse,” said lead author Dan Heppe, MD, a hospitalist and associate director of the CU Internal Medicine Residency Program. “Anecdotally, residents may have had more support in our program than perhaps some other programs. Though they had long hours with very sick patients, we tried to keep going in a positive direction.”
Dr. Heppe said in an interview that the purpose of the schedule change was to space out more intense rotations and build in more time for research, leadership, teaching, and professional development. He suggested the new schedule could help with other aspects of residents’ careers, exposing them to alternate avenues earlier in their training and in a more structured way.
Like most of the study authors, Dr. Heppe is a graduate of the residency program. He recalled how the program changed from multiple inpatient months in a row with clinic half days during those rotations to a 4 + 1 schedule. But the 1 week between inpatient rotations wasn’t enough time to recover or catch up on clinical work, said Dr. Heppe, who is also an associate professor of medicine at CU.
“It was too erratic,” he said of his former residency schedule. “There was a month of research here or there and clinic and then right back to the ICU for a couple of months without a break, and it was less predictable.”
Dr. Heppe said other residency programs have expressed interest in duplicating CU’s schedule change. He admits it may be difficult because of intensive schedule coordination, and some hospitals may not want to reduce clinical services.
The Yale Internal Medicine Traditional Residency Program also recently ended its 28-hour call, during which residents worked 24 hours with an additional 4 hours to transfer the patient to the incoming team. The move was made in response to residents’ requests, saying that the grueling call rotation’s time had come. The reaction has been overwhelmingly positive.
Proponents of alternate scheduling blocks [4 + 4 or 6 + 2] say that they improve residents’ educational experience, patient care, and continuity of care, reduce burnout, and guarantee residents time off.
Advancing Resident Well-Being
“The premise of looking at scheduling in a more intentional way is a sound one in the process of trying to support and advance resident well-being,” said Mark Greenawald, MD, vice chair of academic affairs, well-being, and professional development for the Virginia Tech Carilion School of Medicine’s Department of Family and Community Medicine in Roanoke.
He said it’s up to residency program directors or graduate medical education departments within a specialty to determine whether such scheduling changes fit their requirements for inpatient and outpatient care and training electives. Requirements may limit some scheduling changes, but within the specialty, there’s some flexibility to be creative with rotations. The CU study considered how to create a residency rhythm without stacking inpatient rotations so there’s recovery time.
“Human beings need a break. If residents work 80 hours continually, they will start to experience greater distress, which for many leads to burnout,” he said
Still, the study includes design flaws because it doesn’t explain how call times and hours differ between inpatient and outpatient rotations. “My own [family medicine] program also does outpatient clinics when we have inpatient service. We have half days in the clinic, which ensures better continuity care with the patient.”
Dr. Greenawald has yet to see much research published about the impact of resident schedule changes. By taking an experimental approach, the CU study showed that their particular change positively affected burnout. If the study leads to improvements in rotation schedules or encourages other programs to experiment with their schedules, it will be a step in the right direction.
How Residents Respond
Haidn Foster, MD, a third-year internal medicine resident at Penn State Health Milton S. Hershey Medical Center, Hershey, remembered experiencing burnout as an intern. At that time, he occasionally dealt with poor patient outcomes and sick patients while working long hours with only 1 day off each week. During a particularly challenging rotation, he felt overwhelmed and numb, which was exacerbated if a patient’s condition worsened or they passed away, he said.
His program follows a schedule of 6 weeks of inpatient training and 2 weeks of outpatient rotations (6 + 2). He said that restructuring residents’ schedules may be more effective than commonly used individual wellness modules, referring to the CU study. “The authors tried out a novel systematic way to tackle the epidemic of physician burnout overwhelming people in the medical community.”
Although the study found that schedule changes don’t affect standardized exam scores, Dr. Foster wondered about preceptor ratings, another marker for clinical competency.
He said future studies should attempt to change the structure of medical training delivery by evaluating models that best reduce burnout, are consistent with residents’ career goals, and produce competent physicians. “Burnout plagues our medical system and leads to too many physicians and physicians-in-training leaving the field or taking their lives. I’m not sure this particular mechanism gets us there, but it’s a step, and so that’s very important.”
Like Dr. Foster, Dr. Whelihan follows a 6 + 2 schedule. He said he would have welcomed a schedule that included more outpatient and less inpatient training and can see how changes in scheduling could reduce burnout. “More outpatient time gives you an opportunity to breathe. You get a little more time off working in clinic with less sick people at a slower pace.”
Ally Fuher, MD, said she chose CU’s Internal Medicine Residency Program 4 years ago largely because of its innovative schedule. Now the program’s chief medical resident, she knew the structure would give her more time to pursue other nonclinical interests including research and medical education, meet regularly with mentors, visit family in another state, and attend important life events.
She acknowledged that the alternative would have meant a more irregular schedule with the possibility of working as many as 80 hours a week on back-to-back inpatient rotations with only 1 day off a week, leaving minimal time to plan other activities, let alone rest and recover.
Dr. Fuher said a balanced schedule made her a more well-rounded person excited to engage in her profession. While she hasn’t personally experienced burnout, she realizes a schedule change may not completely solve the issue for others. However, it shows what progress programs can make when they create systemic structural change.
A version of this article first appeared on Medscape.com.
It’s the difference between running a marathon and taking a leisurely stroll. That’s how recent pediatrics resident Joey Whelihan, MD, compared an 11-hour inpatient hospital day with an 8-hour outpatient shift where residents see patients in a clinic.
With inpatient training, “you are lucky if you have time to cook dinner, go to bed, and get ready for the next day,” said Dr. Whelihan, who recently started his adolescent medicine fellowship at Children’s Hospital of Philadelphia after 3 years of residency there. Some residents have call every fourth day during inpatient rotations, working 24-28 hours at a time. They come in one morning and go home the next, he told this news organization.
“Outpatient blocks give you more time to catch your breath and feel somewhat refreshed and ready to take care of patients.”
Longer stretches of inpatient rotations are not sustainable, Dr. Whelihan added, and residents are likely to become exhausted. Fatigue is a leading cause of burnout, a mental, physical, and emotional challenge that residency programs and national medical organizations have been struggling to address.
In recent years, there has been a movement to reduce the maximum consecutive duration of resident duty hours in residency programs across the country. Fueled by resident health and patient safety concerns, the movement is a shift from the previous 24- to 36-hour call duty schedules.
Improved Call Systems = Better Residents
The connection between burnout, well-being, and work schedules appears regularly in national program standards. “Residents and faculty members are at risk for burnout and depression,” according to the current Accreditation Council for Graduate Medical Education’s standard residency program requirements.
“Programs, in partnership with their sponsoring institutions, have the same responsibility to address well-being as other aspects of resident competence,” the guidelines state. That charge includes “attention to scheduling, work intensity, and work compression that impacts resident well-being.”
In Medscape’s Residents Lifestyle & Happiness Report 2023, a third of residents surveyed rarely or never paid attention to their well-being, which closely mirrors the 31% who rarely or never had time for a social life. Slightly more residents (37%) said their work-life balance was “somewhat worse” or “much worse” than they expected.
“I think everyone has burnout as a resident, regardless of the type of program they are in,” Dr. Whelihan said. He described the experience as when you lack fulfillment and empathy and feel exhausted, callous, and removed from interactions with colleagues and patients.
The American Medical Association’s recently released report on the state of residency well-being in 2023 also found that about 43% of residents and fellows had at least one symptom of burnout, about a 2% increase from 2022.
Efforts to Combat Burnout
One residency program found a way to reduce burnout by changing its block scheduling from 4 inpatient weeks followed by 1 outpatient week (4 + 1) to 4 inpatient call-based weeks and 4 outpatient ambulatory, non-call weeks (4 + 4), according to a survey study published recently in JAMA Network Open. The initiative drew praise from some residents and a med school professor who studies wellness issues.
In the survey of postgraduate year (PGY) 1 and PGY-2 hospitalist and primary care residents from the University of Colorado’s Internal Medicine Residency Program, Aurora, between June 2019 and June 2021, the schedule change resulted in improved burnout scores and self-reported professional, educational, and health benefits.
As part of the survey, residents rated symptoms on a 7-point scale on the basis of how frequently they experienced emotional exhaustion, depersonalization, and personal accomplishment.
Investigators also used a questionnaire to evaluate how participants perceived the rotation structure with various outcomes, including the ability to acquire clinical skills, access educational and scholarly opportunities, job satisfaction, and health.
The study concluded that the schedule change improved burnout, health, wellness, and professional development without weakening residents perceived clinical skills or standardized exam scores.
Still, the study authors acknowledged that several factors, including the pandemic, may have limited the findings. During that time, the study transitioned from in-person to electronic submissions, resulting in reduced response rates because of changes in staffing needs and fewer research and scholarly activities.
“One of the things we worried about was that the pandemic would make [burnout findings] look worse,” said lead author Dan Heppe, MD, a hospitalist and associate director of the CU Internal Medicine Residency Program. “Anecdotally, residents may have had more support in our program than perhaps some other programs. Though they had long hours with very sick patients, we tried to keep going in a positive direction.”
Dr. Heppe said in an interview that the purpose of the schedule change was to space out more intense rotations and build in more time for research, leadership, teaching, and professional development. He suggested the new schedule could help with other aspects of residents’ careers, exposing them to alternate avenues earlier in their training and in a more structured way.
Like most of the study authors, Dr. Heppe is a graduate of the residency program. He recalled how the program changed from multiple inpatient months in a row with clinic half days during those rotations to a 4 + 1 schedule. But the 1 week between inpatient rotations wasn’t enough time to recover or catch up on clinical work, said Dr. Heppe, who is also an associate professor of medicine at CU.
“It was too erratic,” he said of his former residency schedule. “There was a month of research here or there and clinic and then right back to the ICU for a couple of months without a break, and it was less predictable.”
Dr. Heppe said other residency programs have expressed interest in duplicating CU’s schedule change. He admits it may be difficult because of intensive schedule coordination, and some hospitals may not want to reduce clinical services.
The Yale Internal Medicine Traditional Residency Program also recently ended its 28-hour call, during which residents worked 24 hours with an additional 4 hours to transfer the patient to the incoming team. The move was made in response to residents’ requests, saying that the grueling call rotation’s time had come. The reaction has been overwhelmingly positive.
Proponents of alternate scheduling blocks [4 + 4 or 6 + 2] say that they improve residents’ educational experience, patient care, and continuity of care, reduce burnout, and guarantee residents time off.
Advancing Resident Well-Being
“The premise of looking at scheduling in a more intentional way is a sound one in the process of trying to support and advance resident well-being,” said Mark Greenawald, MD, vice chair of academic affairs, well-being, and professional development for the Virginia Tech Carilion School of Medicine’s Department of Family and Community Medicine in Roanoke.
He said it’s up to residency program directors or graduate medical education departments within a specialty to determine whether such scheduling changes fit their requirements for inpatient and outpatient care and training electives. Requirements may limit some scheduling changes, but within the specialty, there’s some flexibility to be creative with rotations. The CU study considered how to create a residency rhythm without stacking inpatient rotations so there’s recovery time.
“Human beings need a break. If residents work 80 hours continually, they will start to experience greater distress, which for many leads to burnout,” he said
Still, the study includes design flaws because it doesn’t explain how call times and hours differ between inpatient and outpatient rotations. “My own [family medicine] program also does outpatient clinics when we have inpatient service. We have half days in the clinic, which ensures better continuity care with the patient.”
Dr. Greenawald has yet to see much research published about the impact of resident schedule changes. By taking an experimental approach, the CU study showed that their particular change positively affected burnout. If the study leads to improvements in rotation schedules or encourages other programs to experiment with their schedules, it will be a step in the right direction.
How Residents Respond
Haidn Foster, MD, a third-year internal medicine resident at Penn State Health Milton S. Hershey Medical Center, Hershey, remembered experiencing burnout as an intern. At that time, he occasionally dealt with poor patient outcomes and sick patients while working long hours with only 1 day off each week. During a particularly challenging rotation, he felt overwhelmed and numb, which was exacerbated if a patient’s condition worsened or they passed away, he said.
His program follows a schedule of 6 weeks of inpatient training and 2 weeks of outpatient rotations (6 + 2). He said that restructuring residents’ schedules may be more effective than commonly used individual wellness modules, referring to the CU study. “The authors tried out a novel systematic way to tackle the epidemic of physician burnout overwhelming people in the medical community.”
Although the study found that schedule changes don’t affect standardized exam scores, Dr. Foster wondered about preceptor ratings, another marker for clinical competency.
He said future studies should attempt to change the structure of medical training delivery by evaluating models that best reduce burnout, are consistent with residents’ career goals, and produce competent physicians. “Burnout plagues our medical system and leads to too many physicians and physicians-in-training leaving the field or taking their lives. I’m not sure this particular mechanism gets us there, but it’s a step, and so that’s very important.”
Like Dr. Foster, Dr. Whelihan follows a 6 + 2 schedule. He said he would have welcomed a schedule that included more outpatient and less inpatient training and can see how changes in scheduling could reduce burnout. “More outpatient time gives you an opportunity to breathe. You get a little more time off working in clinic with less sick people at a slower pace.”
Ally Fuher, MD, said she chose CU’s Internal Medicine Residency Program 4 years ago largely because of its innovative schedule. Now the program’s chief medical resident, she knew the structure would give her more time to pursue other nonclinical interests including research and medical education, meet regularly with mentors, visit family in another state, and attend important life events.
She acknowledged that the alternative would have meant a more irregular schedule with the possibility of working as many as 80 hours a week on back-to-back inpatient rotations with only 1 day off a week, leaving minimal time to plan other activities, let alone rest and recover.
Dr. Fuher said a balanced schedule made her a more well-rounded person excited to engage in her profession. While she hasn’t personally experienced burnout, she realizes a schedule change may not completely solve the issue for others. However, it shows what progress programs can make when they create systemic structural change.
A version of this article first appeared on Medscape.com.
It’s the difference between running a marathon and taking a leisurely stroll. That’s how recent pediatrics resident Joey Whelihan, MD, compared an 11-hour inpatient hospital day with an 8-hour outpatient shift where residents see patients in a clinic.
With inpatient training, “you are lucky if you have time to cook dinner, go to bed, and get ready for the next day,” said Dr. Whelihan, who recently started his adolescent medicine fellowship at Children’s Hospital of Philadelphia after 3 years of residency there. Some residents have call every fourth day during inpatient rotations, working 24-28 hours at a time. They come in one morning and go home the next, he told this news organization.
“Outpatient blocks give you more time to catch your breath and feel somewhat refreshed and ready to take care of patients.”
Longer stretches of inpatient rotations are not sustainable, Dr. Whelihan added, and residents are likely to become exhausted. Fatigue is a leading cause of burnout, a mental, physical, and emotional challenge that residency programs and national medical organizations have been struggling to address.
In recent years, there has been a movement to reduce the maximum consecutive duration of resident duty hours in residency programs across the country. Fueled by resident health and patient safety concerns, the movement is a shift from the previous 24- to 36-hour call duty schedules.
Improved Call Systems = Better Residents
The connection between burnout, well-being, and work schedules appears regularly in national program standards. “Residents and faculty members are at risk for burnout and depression,” according to the current Accreditation Council for Graduate Medical Education’s standard residency program requirements.
“Programs, in partnership with their sponsoring institutions, have the same responsibility to address well-being as other aspects of resident competence,” the guidelines state. That charge includes “attention to scheduling, work intensity, and work compression that impacts resident well-being.”
In Medscape’s Residents Lifestyle & Happiness Report 2023, a third of residents surveyed rarely or never paid attention to their well-being, which closely mirrors the 31% who rarely or never had time for a social life. Slightly more residents (37%) said their work-life balance was “somewhat worse” or “much worse” than they expected.
“I think everyone has burnout as a resident, regardless of the type of program they are in,” Dr. Whelihan said. He described the experience as when you lack fulfillment and empathy and feel exhausted, callous, and removed from interactions with colleagues and patients.
The American Medical Association’s recently released report on the state of residency well-being in 2023 also found that about 43% of residents and fellows had at least one symptom of burnout, about a 2% increase from 2022.
Efforts to Combat Burnout
One residency program found a way to reduce burnout by changing its block scheduling from 4 inpatient weeks followed by 1 outpatient week (4 + 1) to 4 inpatient call-based weeks and 4 outpatient ambulatory, non-call weeks (4 + 4), according to a survey study published recently in JAMA Network Open. The initiative drew praise from some residents and a med school professor who studies wellness issues.
In the survey of postgraduate year (PGY) 1 and PGY-2 hospitalist and primary care residents from the University of Colorado’s Internal Medicine Residency Program, Aurora, between June 2019 and June 2021, the schedule change resulted in improved burnout scores and self-reported professional, educational, and health benefits.
As part of the survey, residents rated symptoms on a 7-point scale on the basis of how frequently they experienced emotional exhaustion, depersonalization, and personal accomplishment.
Investigators also used a questionnaire to evaluate how participants perceived the rotation structure with various outcomes, including the ability to acquire clinical skills, access educational and scholarly opportunities, job satisfaction, and health.
The study concluded that the schedule change improved burnout, health, wellness, and professional development without weakening residents perceived clinical skills or standardized exam scores.
Still, the study authors acknowledged that several factors, including the pandemic, may have limited the findings. During that time, the study transitioned from in-person to electronic submissions, resulting in reduced response rates because of changes in staffing needs and fewer research and scholarly activities.
“One of the things we worried about was that the pandemic would make [burnout findings] look worse,” said lead author Dan Heppe, MD, a hospitalist and associate director of the CU Internal Medicine Residency Program. “Anecdotally, residents may have had more support in our program than perhaps some other programs. Though they had long hours with very sick patients, we tried to keep going in a positive direction.”
Dr. Heppe said in an interview that the purpose of the schedule change was to space out more intense rotations and build in more time for research, leadership, teaching, and professional development. He suggested the new schedule could help with other aspects of residents’ careers, exposing them to alternate avenues earlier in their training and in a more structured way.
Like most of the study authors, Dr. Heppe is a graduate of the residency program. He recalled how the program changed from multiple inpatient months in a row with clinic half days during those rotations to a 4 + 1 schedule. But the 1 week between inpatient rotations wasn’t enough time to recover or catch up on clinical work, said Dr. Heppe, who is also an associate professor of medicine at CU.
“It was too erratic,” he said of his former residency schedule. “There was a month of research here or there and clinic and then right back to the ICU for a couple of months without a break, and it was less predictable.”
Dr. Heppe said other residency programs have expressed interest in duplicating CU’s schedule change. He admits it may be difficult because of intensive schedule coordination, and some hospitals may not want to reduce clinical services.
The Yale Internal Medicine Traditional Residency Program also recently ended its 28-hour call, during which residents worked 24 hours with an additional 4 hours to transfer the patient to the incoming team. The move was made in response to residents’ requests, saying that the grueling call rotation’s time had come. The reaction has been overwhelmingly positive.
Proponents of alternate scheduling blocks [4 + 4 or 6 + 2] say that they improve residents’ educational experience, patient care, and continuity of care, reduce burnout, and guarantee residents time off.
Advancing Resident Well-Being
“The premise of looking at scheduling in a more intentional way is a sound one in the process of trying to support and advance resident well-being,” said Mark Greenawald, MD, vice chair of academic affairs, well-being, and professional development for the Virginia Tech Carilion School of Medicine’s Department of Family and Community Medicine in Roanoke.
He said it’s up to residency program directors or graduate medical education departments within a specialty to determine whether such scheduling changes fit their requirements for inpatient and outpatient care and training electives. Requirements may limit some scheduling changes, but within the specialty, there’s some flexibility to be creative with rotations. The CU study considered how to create a residency rhythm without stacking inpatient rotations so there’s recovery time.
“Human beings need a break. If residents work 80 hours continually, they will start to experience greater distress, which for many leads to burnout,” he said
Still, the study includes design flaws because it doesn’t explain how call times and hours differ between inpatient and outpatient rotations. “My own [family medicine] program also does outpatient clinics when we have inpatient service. We have half days in the clinic, which ensures better continuity care with the patient.”
Dr. Greenawald has yet to see much research published about the impact of resident schedule changes. By taking an experimental approach, the CU study showed that their particular change positively affected burnout. If the study leads to improvements in rotation schedules or encourages other programs to experiment with their schedules, it will be a step in the right direction.
How Residents Respond
Haidn Foster, MD, a third-year internal medicine resident at Penn State Health Milton S. Hershey Medical Center, Hershey, remembered experiencing burnout as an intern. At that time, he occasionally dealt with poor patient outcomes and sick patients while working long hours with only 1 day off each week. During a particularly challenging rotation, he felt overwhelmed and numb, which was exacerbated if a patient’s condition worsened or they passed away, he said.
His program follows a schedule of 6 weeks of inpatient training and 2 weeks of outpatient rotations (6 + 2). He said that restructuring residents’ schedules may be more effective than commonly used individual wellness modules, referring to the CU study. “The authors tried out a novel systematic way to tackle the epidemic of physician burnout overwhelming people in the medical community.”
Although the study found that schedule changes don’t affect standardized exam scores, Dr. Foster wondered about preceptor ratings, another marker for clinical competency.
He said future studies should attempt to change the structure of medical training delivery by evaluating models that best reduce burnout, are consistent with residents’ career goals, and produce competent physicians. “Burnout plagues our medical system and leads to too many physicians and physicians-in-training leaving the field or taking their lives. I’m not sure this particular mechanism gets us there, but it’s a step, and so that’s very important.”
Like Dr. Foster, Dr. Whelihan follows a 6 + 2 schedule. He said he would have welcomed a schedule that included more outpatient and less inpatient training and can see how changes in scheduling could reduce burnout. “More outpatient time gives you an opportunity to breathe. You get a little more time off working in clinic with less sick people at a slower pace.”
Ally Fuher, MD, said she chose CU’s Internal Medicine Residency Program 4 years ago largely because of its innovative schedule. Now the program’s chief medical resident, she knew the structure would give her more time to pursue other nonclinical interests including research and medical education, meet regularly with mentors, visit family in another state, and attend important life events.
She acknowledged that the alternative would have meant a more irregular schedule with the possibility of working as many as 80 hours a week on back-to-back inpatient rotations with only 1 day off a week, leaving minimal time to plan other activities, let alone rest and recover.
Dr. Fuher said a balanced schedule made her a more well-rounded person excited to engage in her profession. While she hasn’t personally experienced burnout, she realizes a schedule change may not completely solve the issue for others. However, it shows what progress programs can make when they create systemic structural change.
A version of this article first appeared on Medscape.com.
Rural Hospitals Built During Baby Boom Now Face Baby Bust
Rural regions like the one surrounding a southern Iowa town used to have a lot more babies and many more places to give birth to them.
At least 41 Iowa hospitals have shuttered their labor and delivery units since 2000. Those facilities, representing about a third of all Iowa hospitals, are located mostly in rural areas where birth numbers have plummeted. In some Iowa counties, annual numbers of births have fallen by three quarters since the height of the baby boom in the 1950s and 1960s, when many rural hospitals were built or expanded, state and federal records show.
Similar trends are playing out nationwide, as hospitals struggle to maintain staff and facilities to safely handle dwindling numbers of births. More than half of rural US hospitals now lack the service.
“People just aren’t having as many kids,” said Addie Comegys, who lives in southern Iowa and has regularly traveled 45 minutes each way for prenatal checkups at Oskaloosa’s hospital this summer. Her mother had six children, starting in the 1980s, when big families didn’t seem so rare.
“Now, if you have three kids, people are like, ‘Oh my gosh, are you ever going to stop?’ ” said Ms. Comegys, 29, who is expecting her second child in late August.
These days, many Americans choose to have small families or no children at all. Modern birth control methods help make such decisions stick. The trend is amplified in small towns when young adults move away, taking any childbearing potential with them.
Hospital leaders who close obstetrics units often cite declining birth numbers, along with staffing challenges and financial losses. The closures can be a particular challenge for pregnant women who lack the reliable transportation and flexible schedules needed to travel long distances for prenatal care and birthing services.
The baby boom peaked in 1957, when about 4.3 million children were born in the United States. The annual number of births dropped below 3.7 million by 2022, even though the overall US population nearly doubled over that same period.
West Virginia has seen the steepest decline in births, a 62% drop in those 65 years, according to federal data. Iowa’s births dropped 43% over that period. Of the state’s 99 counties, just four — all urban or suburban — recorded more births.
Births have increased in only 13 states since 1957. Most of them, such as Arizona, California, Florida, and Nevada, are places that have attracted waves of newcomers from other states and countries. But even those states have had obstetrics units close in rural areas.
In Iowa, Oskaloosa’s hospital has bucked the trend and kept its labor and delivery unit open, partly by pulling in patients from 14 other counties. Last year, the hospital even managed the rare feat of recruiting two obstetrician-gynecologists to expand its services.
The publicly owned hospital, called Mahaska Health, expects to deliver 250 babies this year, up from about 160 in previous years, CEO Kevin DeRonde said.
“It’s an essential service, and we needed to keep it going and grow it,” Mr. DeRonde said.
Many of the US hospitals that are now dropping obstetrics units were built or expanded in the mid-1900s, when America went on a rural-hospital building spree, thanks to federal funding from the Hill-Burton Act.
“It was an amazing program,” said Brock Slabach, chief operations officer for the National Rural Health Association. “Basically, if you were a county that wanted a hospital, they gave you the money.”
Mr. Slabach said that in addition to declining birth numbers, obstetrics units are experiencing a drop in occupancy because most patients go home after a night or two. In the past, patients typically spent several days in the hospital after giving birth.
Dwindling caseloads can raise safety concerns for obstetrics units.
A study published in JAMA in 2023 found that women were more likely to suffer serious complications if they gave birth in rural hospitals that handled 110 or fewer births a year. The authors said they didn’t support closing low-volume units because that could lead more women to have complications related to traveling for care. Instead, they recommended improving training and coordination among rural health providers.
Stephanie Radke, MD, a University of Iowa obstetrics and gynecology professor who studies access to birthing services, said it is almost inevitable that when rural birth numbers plunge, some obstetrics units will close. “We talk about that as a bad event, but we don’t really talk about why it happens,” she said.
Dr. Radke said maintaining a set number of obstetrics units is less important than ensuring good care for pregnant women and their babies. It’s difficult to maintain quality of care when the staff doesn’t consistently practice deliveries, she said, but it is hard to define that line. “What is realistic?” she said. “I don’t think a unit should be open that only delivers 50 babies a year.”
In some cases, she said, hospitals near each other have consolidated obstetrics units, pooling their resources into one program that has enough staffers and handles sufficient cases. “You’re not always really creating a care desert when that happens,” she said.
The decline in births has accelerated in many areas in recent years. Kenneth Johnson, a sociology professor and demographer at the University of New Hampshire, said it is understandable that many rural hospitals have closed obstetrics units. “I’m actually surprised some of them have lasted as long as they have,” he said.
Dr. Johnson said rural areas that have seen the steepest population declines tend to be far from cities and lack recreational attractions, such as mountains or large bodies of water. Some have avoided population losses by attracting immigrant workers, who tend to have larger families in the first generation or two after they move to the United States, he said.
Katy B. Kozhimannil, a University of Minnesota health policy professor who studies rural issues, said declining birth numbers and obstetric unit closures can create a vicious cycle. Fewer babies being born in a region can lead a birthing unit to shutter. Then the loss of such a unit can discourage young people from moving to the area, driving birth numbers even lower.
In many regions, people with private insurance, flexible schedules, and reliable transportation choose to travel to larger hospitals for their prenatal care and to give birth, Dr. Kozhimannil said. That leaves rural hospitals with a larger proportion of patients on Medicaid, a public program that pays about half what private insurance pays for the same services, she said.
Iowa ranks near the bottom of all states for obstetrician-gynecologists per capita. But Oskaloosa’s hospital hit the jackpot last year, when it recruited Taylar Swartz Summers, DO, and Garth Summers, DO, a married couple who both recently finished their obstetrics training. Dr. Swartz Summers grew up in the area, and she wanted to return to serve women there.
She hopes the number of obstetrics units will level off after the wave of closures. “It’s not even just for delivery, but we need access just to women’s healthcare in general,” she said. “I would love to see women’s healthcare be at the forefront of our government’s mind.”
Dr. Swartz Summers noted that the state has only one obstetrics training program, which is at the University of Iowa. She said she and her husband plan to help spark interest in rural obstetrics by hosting University of Iowa residency rotations at the Oskaloosa hospital.
Ms. Comegys, a patient of Dr. Swartz Summer’s, could have chosen a hospital birthing center closer to her home, but she wasn’t confident in its quality. Other hospitals in her region had shuttered their obstetrics units. She is grateful to have a flexible job, a reliable car, and a supportive family, so she can travel to Oskaloosa for checkups and to give birth there. She knows many other women are not so lucky, and she worries other obstetrics units are at risk.
“It’s sad, but I could see more closing,” she said.
A version of this article first appeared on Medscape.com.
Rural regions like the one surrounding a southern Iowa town used to have a lot more babies and many more places to give birth to them.
At least 41 Iowa hospitals have shuttered their labor and delivery units since 2000. Those facilities, representing about a third of all Iowa hospitals, are located mostly in rural areas where birth numbers have plummeted. In some Iowa counties, annual numbers of births have fallen by three quarters since the height of the baby boom in the 1950s and 1960s, when many rural hospitals were built or expanded, state and federal records show.
Similar trends are playing out nationwide, as hospitals struggle to maintain staff and facilities to safely handle dwindling numbers of births. More than half of rural US hospitals now lack the service.
“People just aren’t having as many kids,” said Addie Comegys, who lives in southern Iowa and has regularly traveled 45 minutes each way for prenatal checkups at Oskaloosa’s hospital this summer. Her mother had six children, starting in the 1980s, when big families didn’t seem so rare.
“Now, if you have three kids, people are like, ‘Oh my gosh, are you ever going to stop?’ ” said Ms. Comegys, 29, who is expecting her second child in late August.
These days, many Americans choose to have small families or no children at all. Modern birth control methods help make such decisions stick. The trend is amplified in small towns when young adults move away, taking any childbearing potential with them.
Hospital leaders who close obstetrics units often cite declining birth numbers, along with staffing challenges and financial losses. The closures can be a particular challenge for pregnant women who lack the reliable transportation and flexible schedules needed to travel long distances for prenatal care and birthing services.
The baby boom peaked in 1957, when about 4.3 million children were born in the United States. The annual number of births dropped below 3.7 million by 2022, even though the overall US population nearly doubled over that same period.
West Virginia has seen the steepest decline in births, a 62% drop in those 65 years, according to federal data. Iowa’s births dropped 43% over that period. Of the state’s 99 counties, just four — all urban or suburban — recorded more births.
Births have increased in only 13 states since 1957. Most of them, such as Arizona, California, Florida, and Nevada, are places that have attracted waves of newcomers from other states and countries. But even those states have had obstetrics units close in rural areas.
In Iowa, Oskaloosa’s hospital has bucked the trend and kept its labor and delivery unit open, partly by pulling in patients from 14 other counties. Last year, the hospital even managed the rare feat of recruiting two obstetrician-gynecologists to expand its services.
The publicly owned hospital, called Mahaska Health, expects to deliver 250 babies this year, up from about 160 in previous years, CEO Kevin DeRonde said.
“It’s an essential service, and we needed to keep it going and grow it,” Mr. DeRonde said.
Many of the US hospitals that are now dropping obstetrics units were built or expanded in the mid-1900s, when America went on a rural-hospital building spree, thanks to federal funding from the Hill-Burton Act.
“It was an amazing program,” said Brock Slabach, chief operations officer for the National Rural Health Association. “Basically, if you were a county that wanted a hospital, they gave you the money.”
Mr. Slabach said that in addition to declining birth numbers, obstetrics units are experiencing a drop in occupancy because most patients go home after a night or two. In the past, patients typically spent several days in the hospital after giving birth.
Dwindling caseloads can raise safety concerns for obstetrics units.
A study published in JAMA in 2023 found that women were more likely to suffer serious complications if they gave birth in rural hospitals that handled 110 or fewer births a year. The authors said they didn’t support closing low-volume units because that could lead more women to have complications related to traveling for care. Instead, they recommended improving training and coordination among rural health providers.
Stephanie Radke, MD, a University of Iowa obstetrics and gynecology professor who studies access to birthing services, said it is almost inevitable that when rural birth numbers plunge, some obstetrics units will close. “We talk about that as a bad event, but we don’t really talk about why it happens,” she said.
Dr. Radke said maintaining a set number of obstetrics units is less important than ensuring good care for pregnant women and their babies. It’s difficult to maintain quality of care when the staff doesn’t consistently practice deliveries, she said, but it is hard to define that line. “What is realistic?” she said. “I don’t think a unit should be open that only delivers 50 babies a year.”
In some cases, she said, hospitals near each other have consolidated obstetrics units, pooling their resources into one program that has enough staffers and handles sufficient cases. “You’re not always really creating a care desert when that happens,” she said.
The decline in births has accelerated in many areas in recent years. Kenneth Johnson, a sociology professor and demographer at the University of New Hampshire, said it is understandable that many rural hospitals have closed obstetrics units. “I’m actually surprised some of them have lasted as long as they have,” he said.
Dr. Johnson said rural areas that have seen the steepest population declines tend to be far from cities and lack recreational attractions, such as mountains or large bodies of water. Some have avoided population losses by attracting immigrant workers, who tend to have larger families in the first generation or two after they move to the United States, he said.
Katy B. Kozhimannil, a University of Minnesota health policy professor who studies rural issues, said declining birth numbers and obstetric unit closures can create a vicious cycle. Fewer babies being born in a region can lead a birthing unit to shutter. Then the loss of such a unit can discourage young people from moving to the area, driving birth numbers even lower.
In many regions, people with private insurance, flexible schedules, and reliable transportation choose to travel to larger hospitals for their prenatal care and to give birth, Dr. Kozhimannil said. That leaves rural hospitals with a larger proportion of patients on Medicaid, a public program that pays about half what private insurance pays for the same services, she said.
Iowa ranks near the bottom of all states for obstetrician-gynecologists per capita. But Oskaloosa’s hospital hit the jackpot last year, when it recruited Taylar Swartz Summers, DO, and Garth Summers, DO, a married couple who both recently finished their obstetrics training. Dr. Swartz Summers grew up in the area, and she wanted to return to serve women there.
She hopes the number of obstetrics units will level off after the wave of closures. “It’s not even just for delivery, but we need access just to women’s healthcare in general,” she said. “I would love to see women’s healthcare be at the forefront of our government’s mind.”
Dr. Swartz Summers noted that the state has only one obstetrics training program, which is at the University of Iowa. She said she and her husband plan to help spark interest in rural obstetrics by hosting University of Iowa residency rotations at the Oskaloosa hospital.
Ms. Comegys, a patient of Dr. Swartz Summer’s, could have chosen a hospital birthing center closer to her home, but she wasn’t confident in its quality. Other hospitals in her region had shuttered their obstetrics units. She is grateful to have a flexible job, a reliable car, and a supportive family, so she can travel to Oskaloosa for checkups and to give birth there. She knows many other women are not so lucky, and she worries other obstetrics units are at risk.
“It’s sad, but I could see more closing,” she said.
A version of this article first appeared on Medscape.com.
Rural regions like the one surrounding a southern Iowa town used to have a lot more babies and many more places to give birth to them.
At least 41 Iowa hospitals have shuttered their labor and delivery units since 2000. Those facilities, representing about a third of all Iowa hospitals, are located mostly in rural areas where birth numbers have plummeted. In some Iowa counties, annual numbers of births have fallen by three quarters since the height of the baby boom in the 1950s and 1960s, when many rural hospitals were built or expanded, state and federal records show.
Similar trends are playing out nationwide, as hospitals struggle to maintain staff and facilities to safely handle dwindling numbers of births. More than half of rural US hospitals now lack the service.
“People just aren’t having as many kids,” said Addie Comegys, who lives in southern Iowa and has regularly traveled 45 minutes each way for prenatal checkups at Oskaloosa’s hospital this summer. Her mother had six children, starting in the 1980s, when big families didn’t seem so rare.
“Now, if you have three kids, people are like, ‘Oh my gosh, are you ever going to stop?’ ” said Ms. Comegys, 29, who is expecting her second child in late August.
These days, many Americans choose to have small families or no children at all. Modern birth control methods help make such decisions stick. The trend is amplified in small towns when young adults move away, taking any childbearing potential with them.
Hospital leaders who close obstetrics units often cite declining birth numbers, along with staffing challenges and financial losses. The closures can be a particular challenge for pregnant women who lack the reliable transportation and flexible schedules needed to travel long distances for prenatal care and birthing services.
The baby boom peaked in 1957, when about 4.3 million children were born in the United States. The annual number of births dropped below 3.7 million by 2022, even though the overall US population nearly doubled over that same period.
West Virginia has seen the steepest decline in births, a 62% drop in those 65 years, according to federal data. Iowa’s births dropped 43% over that period. Of the state’s 99 counties, just four — all urban or suburban — recorded more births.
Births have increased in only 13 states since 1957. Most of them, such as Arizona, California, Florida, and Nevada, are places that have attracted waves of newcomers from other states and countries. But even those states have had obstetrics units close in rural areas.
In Iowa, Oskaloosa’s hospital has bucked the trend and kept its labor and delivery unit open, partly by pulling in patients from 14 other counties. Last year, the hospital even managed the rare feat of recruiting two obstetrician-gynecologists to expand its services.
The publicly owned hospital, called Mahaska Health, expects to deliver 250 babies this year, up from about 160 in previous years, CEO Kevin DeRonde said.
“It’s an essential service, and we needed to keep it going and grow it,” Mr. DeRonde said.
Many of the US hospitals that are now dropping obstetrics units were built or expanded in the mid-1900s, when America went on a rural-hospital building spree, thanks to federal funding from the Hill-Burton Act.
“It was an amazing program,” said Brock Slabach, chief operations officer for the National Rural Health Association. “Basically, if you were a county that wanted a hospital, they gave you the money.”
Mr. Slabach said that in addition to declining birth numbers, obstetrics units are experiencing a drop in occupancy because most patients go home after a night or two. In the past, patients typically spent several days in the hospital after giving birth.
Dwindling caseloads can raise safety concerns for obstetrics units.
A study published in JAMA in 2023 found that women were more likely to suffer serious complications if they gave birth in rural hospitals that handled 110 or fewer births a year. The authors said they didn’t support closing low-volume units because that could lead more women to have complications related to traveling for care. Instead, they recommended improving training and coordination among rural health providers.
Stephanie Radke, MD, a University of Iowa obstetrics and gynecology professor who studies access to birthing services, said it is almost inevitable that when rural birth numbers plunge, some obstetrics units will close. “We talk about that as a bad event, but we don’t really talk about why it happens,” she said.
Dr. Radke said maintaining a set number of obstetrics units is less important than ensuring good care for pregnant women and their babies. It’s difficult to maintain quality of care when the staff doesn’t consistently practice deliveries, she said, but it is hard to define that line. “What is realistic?” she said. “I don’t think a unit should be open that only delivers 50 babies a year.”
In some cases, she said, hospitals near each other have consolidated obstetrics units, pooling their resources into one program that has enough staffers and handles sufficient cases. “You’re not always really creating a care desert when that happens,” she said.
The decline in births has accelerated in many areas in recent years. Kenneth Johnson, a sociology professor and demographer at the University of New Hampshire, said it is understandable that many rural hospitals have closed obstetrics units. “I’m actually surprised some of them have lasted as long as they have,” he said.
Dr. Johnson said rural areas that have seen the steepest population declines tend to be far from cities and lack recreational attractions, such as mountains or large bodies of water. Some have avoided population losses by attracting immigrant workers, who tend to have larger families in the first generation or two after they move to the United States, he said.
Katy B. Kozhimannil, a University of Minnesota health policy professor who studies rural issues, said declining birth numbers and obstetric unit closures can create a vicious cycle. Fewer babies being born in a region can lead a birthing unit to shutter. Then the loss of such a unit can discourage young people from moving to the area, driving birth numbers even lower.
In many regions, people with private insurance, flexible schedules, and reliable transportation choose to travel to larger hospitals for their prenatal care and to give birth, Dr. Kozhimannil said. That leaves rural hospitals with a larger proportion of patients on Medicaid, a public program that pays about half what private insurance pays for the same services, she said.
Iowa ranks near the bottom of all states for obstetrician-gynecologists per capita. But Oskaloosa’s hospital hit the jackpot last year, when it recruited Taylar Swartz Summers, DO, and Garth Summers, DO, a married couple who both recently finished their obstetrics training. Dr. Swartz Summers grew up in the area, and she wanted to return to serve women there.
She hopes the number of obstetrics units will level off after the wave of closures. “It’s not even just for delivery, but we need access just to women’s healthcare in general,” she said. “I would love to see women’s healthcare be at the forefront of our government’s mind.”
Dr. Swartz Summers noted that the state has only one obstetrics training program, which is at the University of Iowa. She said she and her husband plan to help spark interest in rural obstetrics by hosting University of Iowa residency rotations at the Oskaloosa hospital.
Ms. Comegys, a patient of Dr. Swartz Summer’s, could have chosen a hospital birthing center closer to her home, but she wasn’t confident in its quality. Other hospitals in her region had shuttered their obstetrics units. She is grateful to have a flexible job, a reliable car, and a supportive family, so she can travel to Oskaloosa for checkups and to give birth there. She knows many other women are not so lucky, and she worries other obstetrics units are at risk.
“It’s sad, but I could see more closing,” she said.
A version of this article first appeared on Medscape.com.
Penalty for No-Shows?
Earlier in 2024 the French government proposed fining patients €5 ($5.36 at the time of writing) for no-show doctor appointments.
The rationale is that there are 27 million missed medical appointments annually in France (just based on population size, I’d guess it’s higher in the United States) and that they not only waste time, but also keep people who need to be seen sooner from getting in.
The penalty wouldn’t be automatic, and it’s up to the physician to decide if a patient’s excuse is valid. As I understand it, the €5 is paid as a fine to the national healthcare service, and not to the physician (I may be wrong on that).
In many ways I agree with this. Given the patchwork of regulations and insurance rules we face in the United States, it’s almost impossible to penalize patients for missed visits unless you don’t take insurance at all.
Some people have legitimate reasons for no-showing. Cars break, family emergencies happen, storms roll in. Even the most punctual of us sometimes just space on something. If someone calls in at the last minute to say “I can’t make it” I’m more forgiving than if we never hear from them at all. That’s why it’s good to have the doctors, who know the people they’re dealing with, make the final call.
Of course, there are those who will just lie and make up an excuse, and sometimes it’s tricky to know who is or isn’t worth penalizing. Some people just don’t care, or are dishonest, or both.
$5.36 isn’t a huge amount for most. But it’s still symbolic. It forces people to, as they say, “have skin in the game.” Yes, they may still have a copay, but that’s only paid if they show up. This puts them in the position of being penalized for thoughtlessness.
Is it a great idea? Not really. I suspect most of us would dismiss it rather than fight with the patient.
But there aren’t any easy answers, and I’d like to see how, if they go ahead with the proposal, it plays out. If it works, I hope we won’t be too far behind.
Dr. Block has a solo neurology practice in Scottsdale, Arizona.
Earlier in 2024 the French government proposed fining patients €5 ($5.36 at the time of writing) for no-show doctor appointments.
The rationale is that there are 27 million missed medical appointments annually in France (just based on population size, I’d guess it’s higher in the United States) and that they not only waste time, but also keep people who need to be seen sooner from getting in.
The penalty wouldn’t be automatic, and it’s up to the physician to decide if a patient’s excuse is valid. As I understand it, the €5 is paid as a fine to the national healthcare service, and not to the physician (I may be wrong on that).
In many ways I agree with this. Given the patchwork of regulations and insurance rules we face in the United States, it’s almost impossible to penalize patients for missed visits unless you don’t take insurance at all.
Some people have legitimate reasons for no-showing. Cars break, family emergencies happen, storms roll in. Even the most punctual of us sometimes just space on something. If someone calls in at the last minute to say “I can’t make it” I’m more forgiving than if we never hear from them at all. That’s why it’s good to have the doctors, who know the people they’re dealing with, make the final call.
Of course, there are those who will just lie and make up an excuse, and sometimes it’s tricky to know who is or isn’t worth penalizing. Some people just don’t care, or are dishonest, or both.
$5.36 isn’t a huge amount for most. But it’s still symbolic. It forces people to, as they say, “have skin in the game.” Yes, they may still have a copay, but that’s only paid if they show up. This puts them in the position of being penalized for thoughtlessness.
Is it a great idea? Not really. I suspect most of us would dismiss it rather than fight with the patient.
But there aren’t any easy answers, and I’d like to see how, if they go ahead with the proposal, it plays out. If it works, I hope we won’t be too far behind.
Dr. Block has a solo neurology practice in Scottsdale, Arizona.
Earlier in 2024 the French government proposed fining patients €5 ($5.36 at the time of writing) for no-show doctor appointments.
The rationale is that there are 27 million missed medical appointments annually in France (just based on population size, I’d guess it’s higher in the United States) and that they not only waste time, but also keep people who need to be seen sooner from getting in.
The penalty wouldn’t be automatic, and it’s up to the physician to decide if a patient’s excuse is valid. As I understand it, the €5 is paid as a fine to the national healthcare service, and not to the physician (I may be wrong on that).
In many ways I agree with this. Given the patchwork of regulations and insurance rules we face in the United States, it’s almost impossible to penalize patients for missed visits unless you don’t take insurance at all.
Some people have legitimate reasons for no-showing. Cars break, family emergencies happen, storms roll in. Even the most punctual of us sometimes just space on something. If someone calls in at the last minute to say “I can’t make it” I’m more forgiving than if we never hear from them at all. That’s why it’s good to have the doctors, who know the people they’re dealing with, make the final call.
Of course, there are those who will just lie and make up an excuse, and sometimes it’s tricky to know who is or isn’t worth penalizing. Some people just don’t care, or are dishonest, or both.
$5.36 isn’t a huge amount for most. But it’s still symbolic. It forces people to, as they say, “have skin in the game.” Yes, they may still have a copay, but that’s only paid if they show up. This puts them in the position of being penalized for thoughtlessness.
Is it a great idea? Not really. I suspect most of us would dismiss it rather than fight with the patient.
But there aren’t any easy answers, and I’d like to see how, if they go ahead with the proposal, it plays out. If it works, I hope we won’t be too far behind.
Dr. Block has a solo neurology practice in Scottsdale, Arizona.
Expanding Use of GLP-1 RAs for Weight Management
To discuss issues related to counseling patients about weight loss with glucagon-like peptide 1 receptor agonists (GLP-1 RAs), I recently posted a case from my own practice. This was a 44-year-old woman with hyperlipidemia, hypertension, and obesity who wanted to try to lose weight with a GLP-1 RA, having been unsuccessful in maintaining a normal weight with lifestyle change alone.
I am very happy to see a high number of favorable responses to this article, and I also recognize that it was very focused on GLP-1 RA therapy while not addressing the multivariate treatment of obesity.
A healthy lifestyle remains foundational for the management of obesity, and clinicians should guide patients to make constructive choices regarding their diet, physical activity, mental health, and sleep. However, like for our patient introduced in that article, lifestyle changes are rarely sufficient to obtain a goal of sustained weight loss that promotes better health outcomes. A meta-analysis of clinical trials testing lifestyle interventions to lose weight among adults with overweight and obesity found that the relative reduction in body weight in the intervention vs control cohorts was −3.63 kg at 1 year and −2.45 kg at 3 years. More intensive programs with at least 28 interventions per year were associated with slightly more weight loss than less intensive programs.
That is why clinicians and patients have been reaching for effective pharmacotherapy to create better outcomes among adults with obesity. In a national survey of 1479 US adults, 12% reported having used a GLP-1 RA. Diabetes was the most common indication (43%), followed by heart disease (26%) and overweight/obesity (22%).
The high cost of GLP-1 RA therapy was a major barrier to even wider use. Some 54% of participants said that it was difficult to afford GLP-1 RA therapy, and an additional 22% found it very difficult to pay for the drugs. Having health insurance did not alter these figures substantially.
While cost and access remain some of the greatest challenges with the use of GLP-1 RAs, there is hope for change there. In March 2024, the US Food and Drug Administration approved semaglutide to reduce the risk for cardiovascular events among patients with overweight and obesity and existing cardiovascular disease. It appears that Medicare will cover semaglutide for that indication, which bucks a trend of more than 20 years during which Medicare Part D would not cover pharmacotherapy for weight loss.
There is bipartisan support in the US Congress to further increase coverage of GLP-1 RAs for obesity, which makes sense. GLP-1 RAs are associated with greater average weight loss than either lifestyle interventions alone or that associated with previous anti-obesity medications. While there are no safety data for these drugs stretching back for 50 or 100 years, clinicians should bear in mind that exenatide was approved for the management of type 2 diabetes in 2005. So, we are approaching two decades of practical experience with these drugs, and it appears clear that the benefits of GLP-1 RAs outweigh any known harms. For the right patient, and with the right kind of guidance by clinicians, GLP-1 RA therapy can have a profound effect on individual and public health.
Dr. Vega, health sciences clinical professor, Family Medicine, University of California, Irvine, disclosed ties with McNeil Pharmaceuticals.
A version of this article first appeared on Medscape.com.
To discuss issues related to counseling patients about weight loss with glucagon-like peptide 1 receptor agonists (GLP-1 RAs), I recently posted a case from my own practice. This was a 44-year-old woman with hyperlipidemia, hypertension, and obesity who wanted to try to lose weight with a GLP-1 RA, having been unsuccessful in maintaining a normal weight with lifestyle change alone.
I am very happy to see a high number of favorable responses to this article, and I also recognize that it was very focused on GLP-1 RA therapy while not addressing the multivariate treatment of obesity.
A healthy lifestyle remains foundational for the management of obesity, and clinicians should guide patients to make constructive choices regarding their diet, physical activity, mental health, and sleep. However, like for our patient introduced in that article, lifestyle changes are rarely sufficient to obtain a goal of sustained weight loss that promotes better health outcomes. A meta-analysis of clinical trials testing lifestyle interventions to lose weight among adults with overweight and obesity found that the relative reduction in body weight in the intervention vs control cohorts was −3.63 kg at 1 year and −2.45 kg at 3 years. More intensive programs with at least 28 interventions per year were associated with slightly more weight loss than less intensive programs.
That is why clinicians and patients have been reaching for effective pharmacotherapy to create better outcomes among adults with obesity. In a national survey of 1479 US adults, 12% reported having used a GLP-1 RA. Diabetes was the most common indication (43%), followed by heart disease (26%) and overweight/obesity (22%).
The high cost of GLP-1 RA therapy was a major barrier to even wider use. Some 54% of participants said that it was difficult to afford GLP-1 RA therapy, and an additional 22% found it very difficult to pay for the drugs. Having health insurance did not alter these figures substantially.
While cost and access remain some of the greatest challenges with the use of GLP-1 RAs, there is hope for change there. In March 2024, the US Food and Drug Administration approved semaglutide to reduce the risk for cardiovascular events among patients with overweight and obesity and existing cardiovascular disease. It appears that Medicare will cover semaglutide for that indication, which bucks a trend of more than 20 years during which Medicare Part D would not cover pharmacotherapy for weight loss.
There is bipartisan support in the US Congress to further increase coverage of GLP-1 RAs for obesity, which makes sense. GLP-1 RAs are associated with greater average weight loss than either lifestyle interventions alone or that associated with previous anti-obesity medications. While there are no safety data for these drugs stretching back for 50 or 100 years, clinicians should bear in mind that exenatide was approved for the management of type 2 diabetes in 2005. So, we are approaching two decades of practical experience with these drugs, and it appears clear that the benefits of GLP-1 RAs outweigh any known harms. For the right patient, and with the right kind of guidance by clinicians, GLP-1 RA therapy can have a profound effect on individual and public health.
Dr. Vega, health sciences clinical professor, Family Medicine, University of California, Irvine, disclosed ties with McNeil Pharmaceuticals.
A version of this article first appeared on Medscape.com.
To discuss issues related to counseling patients about weight loss with glucagon-like peptide 1 receptor agonists (GLP-1 RAs), I recently posted a case from my own practice. This was a 44-year-old woman with hyperlipidemia, hypertension, and obesity who wanted to try to lose weight with a GLP-1 RA, having been unsuccessful in maintaining a normal weight with lifestyle change alone.
I am very happy to see a high number of favorable responses to this article, and I also recognize that it was very focused on GLP-1 RA therapy while not addressing the multivariate treatment of obesity.
A healthy lifestyle remains foundational for the management of obesity, and clinicians should guide patients to make constructive choices regarding their diet, physical activity, mental health, and sleep. However, like for our patient introduced in that article, lifestyle changes are rarely sufficient to obtain a goal of sustained weight loss that promotes better health outcomes. A meta-analysis of clinical trials testing lifestyle interventions to lose weight among adults with overweight and obesity found that the relative reduction in body weight in the intervention vs control cohorts was −3.63 kg at 1 year and −2.45 kg at 3 years. More intensive programs with at least 28 interventions per year were associated with slightly more weight loss than less intensive programs.
That is why clinicians and patients have been reaching for effective pharmacotherapy to create better outcomes among adults with obesity. In a national survey of 1479 US adults, 12% reported having used a GLP-1 RA. Diabetes was the most common indication (43%), followed by heart disease (26%) and overweight/obesity (22%).
The high cost of GLP-1 RA therapy was a major barrier to even wider use. Some 54% of participants said that it was difficult to afford GLP-1 RA therapy, and an additional 22% found it very difficult to pay for the drugs. Having health insurance did not alter these figures substantially.
While cost and access remain some of the greatest challenges with the use of GLP-1 RAs, there is hope for change there. In March 2024, the US Food and Drug Administration approved semaglutide to reduce the risk for cardiovascular events among patients with overweight and obesity and existing cardiovascular disease. It appears that Medicare will cover semaglutide for that indication, which bucks a trend of more than 20 years during which Medicare Part D would not cover pharmacotherapy for weight loss.
There is bipartisan support in the US Congress to further increase coverage of GLP-1 RAs for obesity, which makes sense. GLP-1 RAs are associated with greater average weight loss than either lifestyle interventions alone or that associated with previous anti-obesity medications. While there are no safety data for these drugs stretching back for 50 or 100 years, clinicians should bear in mind that exenatide was approved for the management of type 2 diabetes in 2005. So, we are approaching two decades of practical experience with these drugs, and it appears clear that the benefits of GLP-1 RAs outweigh any known harms. For the right patient, and with the right kind of guidance by clinicians, GLP-1 RA therapy can have a profound effect on individual and public health.
Dr. Vega, health sciences clinical professor, Family Medicine, University of California, Irvine, disclosed ties with McNeil Pharmaceuticals.
A version of this article first appeared on Medscape.com.
Mounjaro Beats Ozempic, So Why Isn’t It More Popular?
This transcript has been edited for clarity.
It’s July, which means our hospital is filled with new interns, residents, and fellows all eager to embark on a new stage of their career. It’s an exciting time — a bit of a scary time — but it’s also the time when the medical strategies I’ve been taking for granted get called into question. At this point in the year, I tend to get a lot of “why” questions. Why did you order that test? Why did you suspect that diagnosis? Why did you choose that medication?
Meds are the hardest, I find. Sure, I can explain that I prescribed a glucagon-like peptide 1 (GLP-1) receptor agonist because the patient had diabetes and was overweight, and multiple studies show that this class of drug leads to weight loss and reduced mortality risk. But then I get the follow-up: Sure, but why THAT GLP-1 drug? Why did you pick semaglutide (Ozempic) over tirzepatide (Mounjaro)?
Here’s where I run out of good answers. Sometimes I choose a drug because that’s what the patient’s insurance has on their formulary. Sometimes it’s because it’s cheaper in general. Sometimes, it’s just force of habit. I know the correct dose, I have experience with the side effects — it’s comfortable.
What I can’t say is that I have solid evidence that one drug is superior to another, say from a randomized trial of semaglutide vs tirzepatide. I don’t have that evidence because that trial has never happened and, as I’ll explain in a minute, may never happen at all.
But we might have the next best thing. And the results may surprise you.
Why don’t we see more head-to-head trials of competitor drugs? The answer is pretty simple, honestly: risk management. For drugs that are on patent, like the GLP-1s, conducting a trial without the buy-in of the pharmaceutical company is simply too expensive — we can’t run a trial unless someone provides the drug for free. That gives the companies a lot of say in what trials get done, and it seems that most pharma companies have reached the same conclusion: A head-to-head trial is too risky. Be happy with the market share you have, and try to nibble away at the edges through good old-fashioned marketing.
But if you look at the data that are out there, you might wonder why Ozempic is the market leader. I mean, sure, it’s a heck of a weight loss drug. But the weight loss in the trials of Mounjaro was actually a bit higher. It’s worth noting here that tirzepatide (Mounjaro) is not just a GLP-1 receptor agonist; it is also a gastric inhibitory polypeptide agonist. 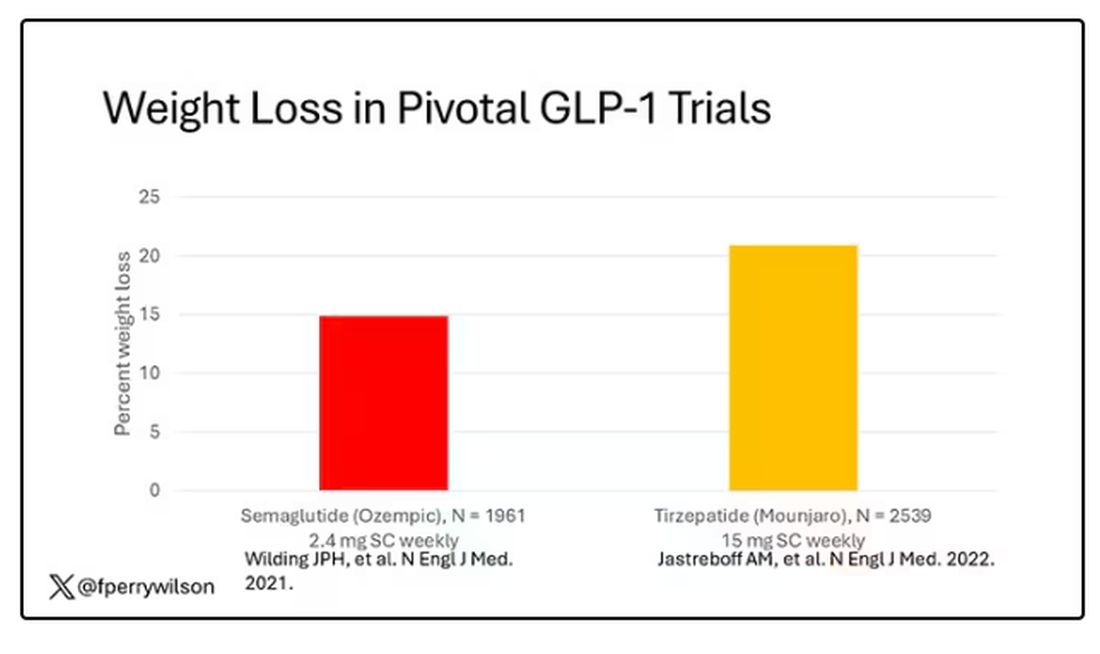
But it’s very hard to compare the results of a trial pitting Ozempic against placebo with a totally different trial pitting Mounjaro against placebo. You can always argue that the patients studied were just too different at baseline — an apples and oranges situation.
Newly published, a study appearing in JAMA Internal Medicine uses real-world data and propensity-score matching to turn oranges back into apples. I’ll walk you through it.
The data and analysis here come from Truveta, a collective of various US healthcare systems that share a broad swath of electronic health record data. Researchers identified 41,222 adults with overweight or obesity who were prescribed semaglutide or tirzepatide between May 2022 and September 2023.
You’d be tempted to just see which group lost more weight over time, but that is the apples and oranges problem. People prescribed Mounjaro were different from people who were prescribed Ozempic. There are a variety of factors to look at here, but the vibe is that the Mounjaro group seems healthier at baseline. They were younger and had less kidney disease, less hypertension, and less hyperlipidemia. They had higher incomes and were more likely to be White. They were also dramatically less likely to have diabetes. 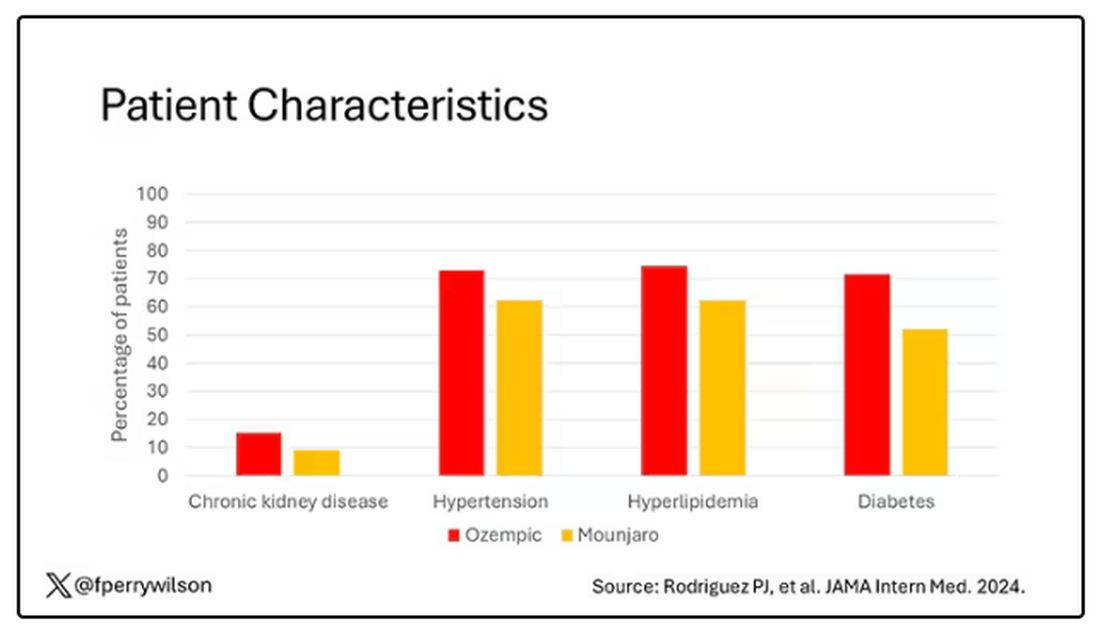
To account for this, the researchers used a statistical technique called propensity-score matching. Briefly, you create a model based on a variety of patient factors to predict who would be prescribed Ozempic and who would be prescribed Mounjaro. You then identify pairs of patients with similar probability (or propensity) of receiving, say, Ozempic, where one member of the pair got Ozempic and one got Mounjaro. Any unmatched individuals simply get dropped from the analysis.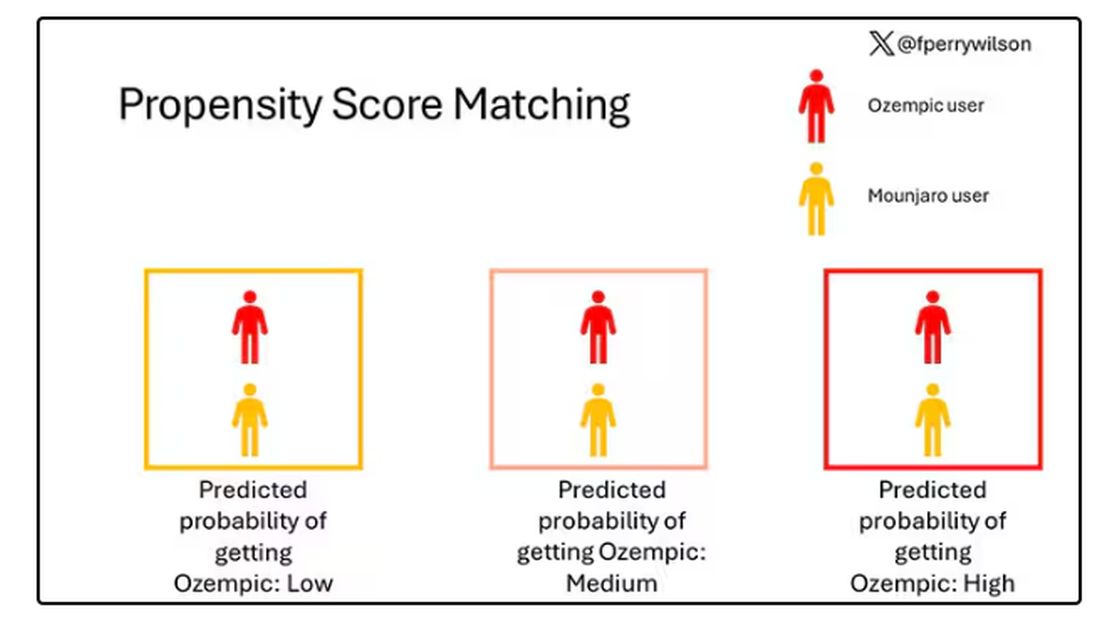
Thus, the researchers took the 41,222 individuals who started the analysis, of whom 9193 received Mounjaro, and identified the 9193 patients who got Ozempic that most closely matched the Mounjaro crowd. I know, it sounds confusing. But as an example, in the original dataset, 51.9% of those who got Mounjaro had diabetes compared with 71.5% of those who got Ozempic. Among the 9193 individuals who remained in the Ozempic group after matching, 52.1% had diabetes. By matching in this way, you balance your baseline characteristics. Turning apples into oranges. Or, maybe the better metaphor would be plucking the oranges out of a big pile of mostly apples.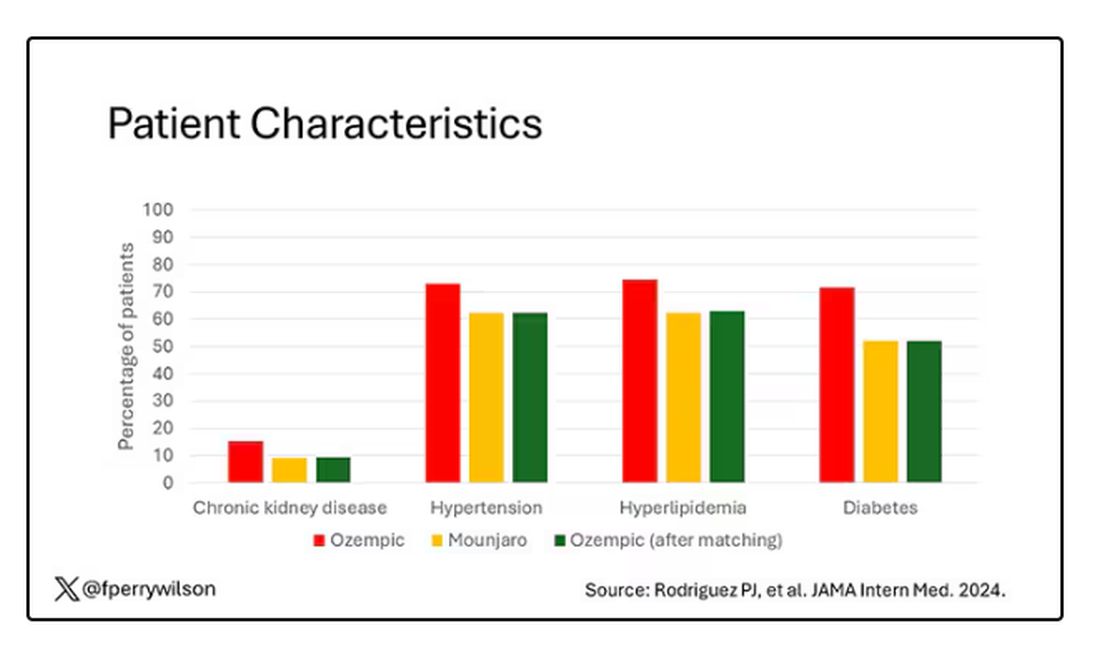
Once that’s done, we can go back to do what we wanted to do in the beginning, which is to look at the weight loss between the groups.
What I’m showing you here is the average percent change in body weight at 3, 6, and 12 months across the two drugs in the matched cohort. By a year out, you have basically 15% weight loss in the Mounjaro group compared with 8% or so in the Ozempic group. 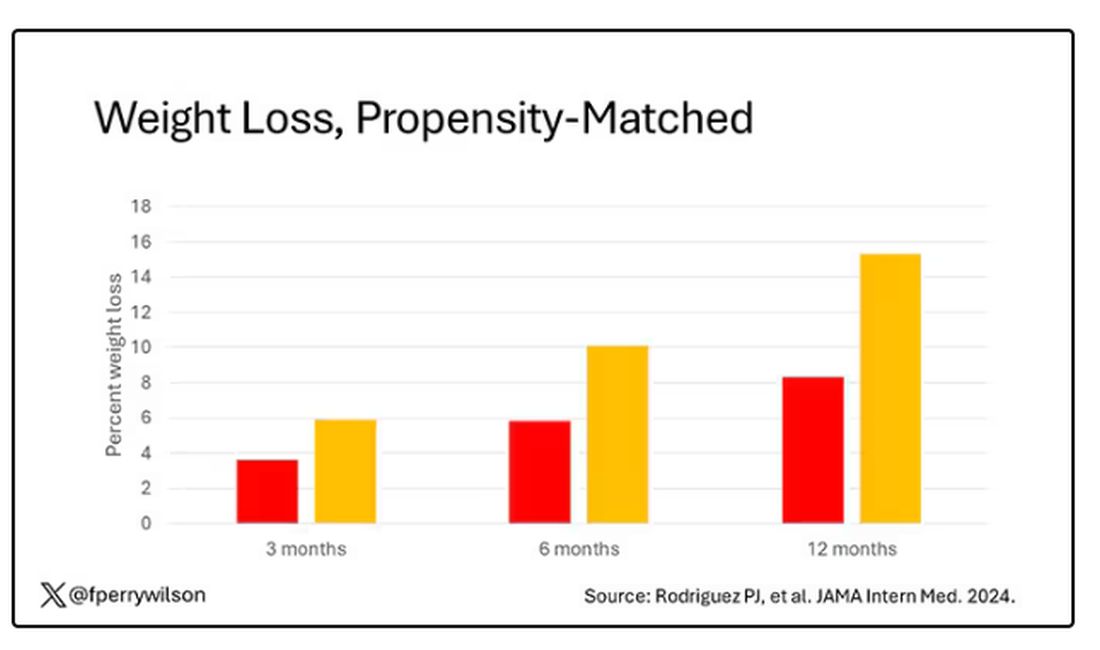
We can slice this a different way as well — asking what percent of people in each group achieve, say, 10% weight loss? This graph examines the percentage of each treatment group who hit that weight loss target over time. Mounjaro gets there faster.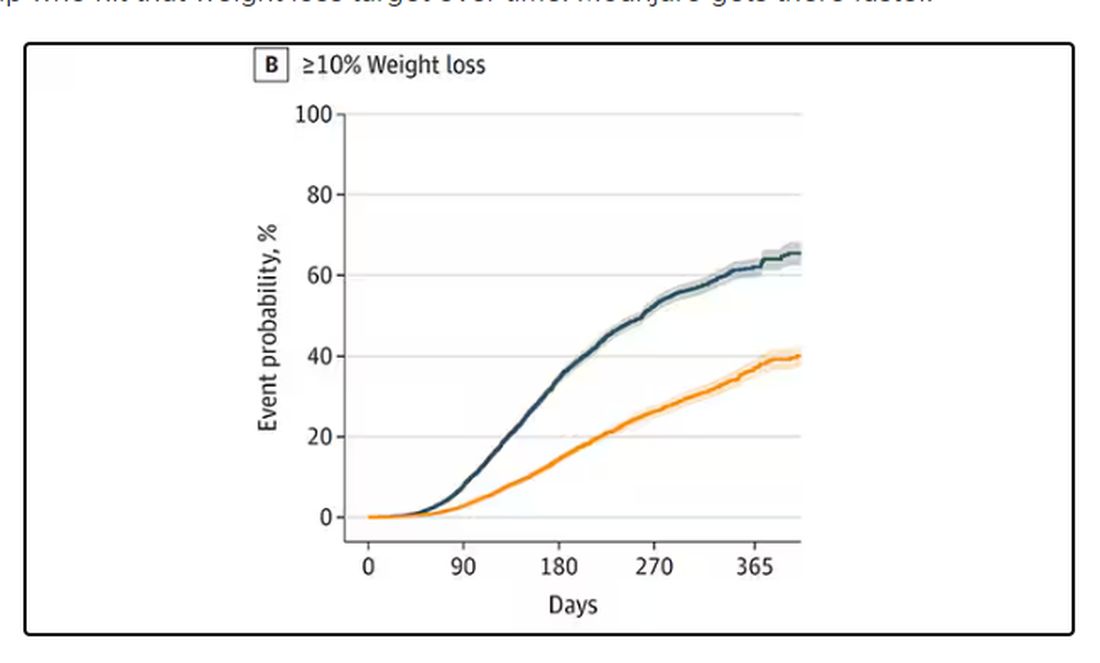
I should point out that this was a so-called “on treatment” analysis: If people stopped taking either of the drugs, they were no longer included in the study. That tends to make drugs like this appear better than they are because as time goes on, you may weed out the people who stop the drug owing to lack of efficacy or to side effects. But in a sensitivity analysis, the authors see what happens if they just treat people as if they were taking the drug for the entire year once they had it prescribed, and the results, while not as dramatic, were broadly similar. Mounjaro still came out on top.
Adverse events— stuff like gastroparesis and pancreatitis — were rare, but rates were similar between the two groups.
It’s great to see studies like this that leverage real world data and a solid statistical underpinning to give us providers actionable information. Is it 100% definitive? No. But, especially considering the clinical trial data, I don’t think I’m going out on a limb to say that Mounjaro seems to be the more effective weight loss agent. That said, we don’t actually live in a world where we can prescribe medications based on a silly little thing like which is the most effective. Especially given the cost of these agents — the patient’s insurance status is going to guide our prescription pen more than this study ever could. And of course, given the demand for this class of agents and the fact that both are actually quite effective, you may be best off prescribing whatever you can get your hands on.
But I’d like to see more of this. When I do have a choice of a medication, when costs and availability are similar, I’d like to be able to answer that question of “why did you choose that one?” with an evidence-based answer: “It’s better.”
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Connecticut. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
It’s July, which means our hospital is filled with new interns, residents, and fellows all eager to embark on a new stage of their career. It’s an exciting time — a bit of a scary time — but it’s also the time when the medical strategies I’ve been taking for granted get called into question. At this point in the year, I tend to get a lot of “why” questions. Why did you order that test? Why did you suspect that diagnosis? Why did you choose that medication?
Meds are the hardest, I find. Sure, I can explain that I prescribed a glucagon-like peptide 1 (GLP-1) receptor agonist because the patient had diabetes and was overweight, and multiple studies show that this class of drug leads to weight loss and reduced mortality risk. But then I get the follow-up: Sure, but why THAT GLP-1 drug? Why did you pick semaglutide (Ozempic) over tirzepatide (Mounjaro)?
Here’s where I run out of good answers. Sometimes I choose a drug because that’s what the patient’s insurance has on their formulary. Sometimes it’s because it’s cheaper in general. Sometimes, it’s just force of habit. I know the correct dose, I have experience with the side effects — it’s comfortable.
What I can’t say is that I have solid evidence that one drug is superior to another, say from a randomized trial of semaglutide vs tirzepatide. I don’t have that evidence because that trial has never happened and, as I’ll explain in a minute, may never happen at all.
But we might have the next best thing. And the results may surprise you.
Why don’t we see more head-to-head trials of competitor drugs? The answer is pretty simple, honestly: risk management. For drugs that are on patent, like the GLP-1s, conducting a trial without the buy-in of the pharmaceutical company is simply too expensive — we can’t run a trial unless someone provides the drug for free. That gives the companies a lot of say in what trials get done, and it seems that most pharma companies have reached the same conclusion: A head-to-head trial is too risky. Be happy with the market share you have, and try to nibble away at the edges through good old-fashioned marketing.
But if you look at the data that are out there, you might wonder why Ozempic is the market leader. I mean, sure, it’s a heck of a weight loss drug. But the weight loss in the trials of Mounjaro was actually a bit higher. It’s worth noting here that tirzepatide (Mounjaro) is not just a GLP-1 receptor agonist; it is also a gastric inhibitory polypeptide agonist. 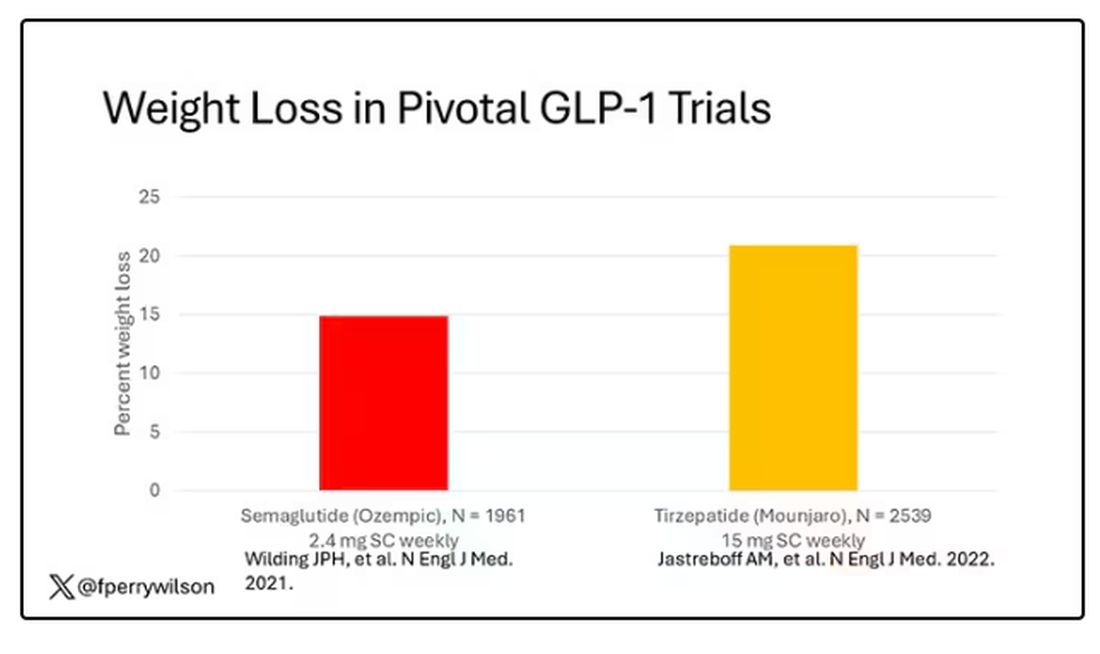
But it’s very hard to compare the results of a trial pitting Ozempic against placebo with a totally different trial pitting Mounjaro against placebo. You can always argue that the patients studied were just too different at baseline — an apples and oranges situation.
Newly published, a study appearing in JAMA Internal Medicine uses real-world data and propensity-score matching to turn oranges back into apples. I’ll walk you through it.
The data and analysis here come from Truveta, a collective of various US healthcare systems that share a broad swath of electronic health record data. Researchers identified 41,222 adults with overweight or obesity who were prescribed semaglutide or tirzepatide between May 2022 and September 2023.
You’d be tempted to just see which group lost more weight over time, but that is the apples and oranges problem. People prescribed Mounjaro were different from people who were prescribed Ozempic. There are a variety of factors to look at here, but the vibe is that the Mounjaro group seems healthier at baseline. They were younger and had less kidney disease, less hypertension, and less hyperlipidemia. They had higher incomes and were more likely to be White. They were also dramatically less likely to have diabetes. 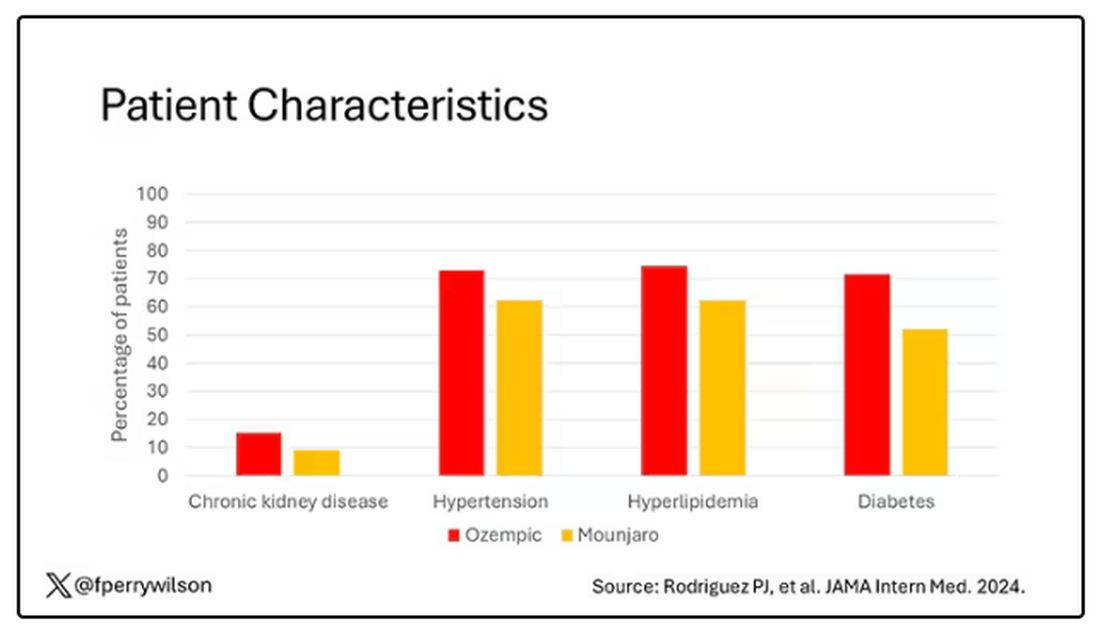
To account for this, the researchers used a statistical technique called propensity-score matching. Briefly, you create a model based on a variety of patient factors to predict who would be prescribed Ozempic and who would be prescribed Mounjaro. You then identify pairs of patients with similar probability (or propensity) of receiving, say, Ozempic, where one member of the pair got Ozempic and one got Mounjaro. Any unmatched individuals simply get dropped from the analysis.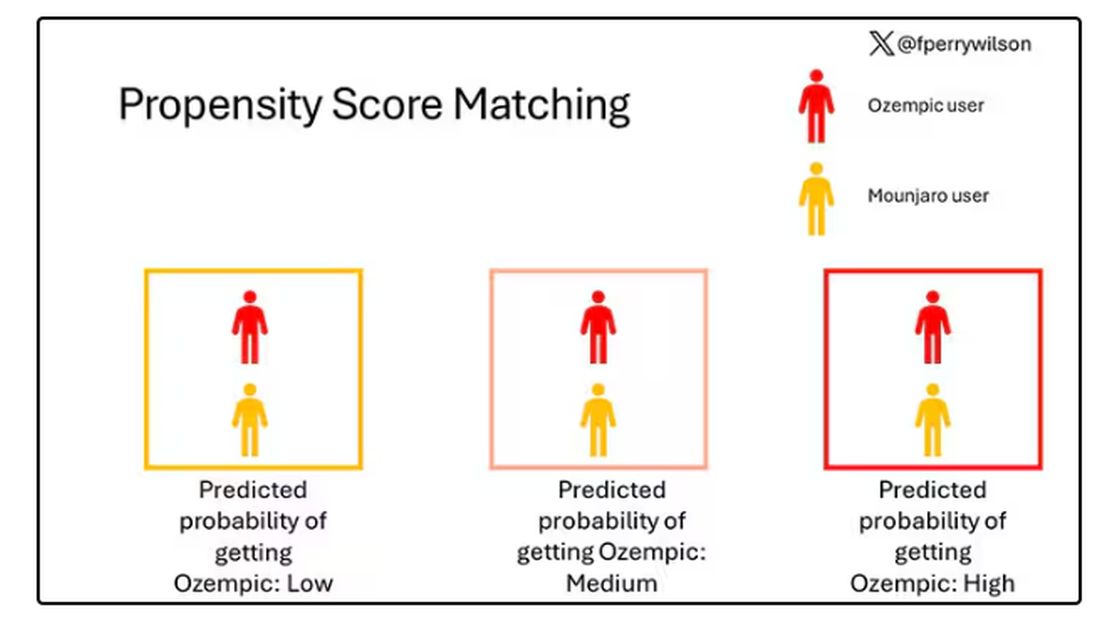
Thus, the researchers took the 41,222 individuals who started the analysis, of whom 9193 received Mounjaro, and identified the 9193 patients who got Ozempic that most closely matched the Mounjaro crowd. I know, it sounds confusing. But as an example, in the original dataset, 51.9% of those who got Mounjaro had diabetes compared with 71.5% of those who got Ozempic. Among the 9193 individuals who remained in the Ozempic group after matching, 52.1% had diabetes. By matching in this way, you balance your baseline characteristics. Turning apples into oranges. Or, maybe the better metaphor would be plucking the oranges out of a big pile of mostly apples.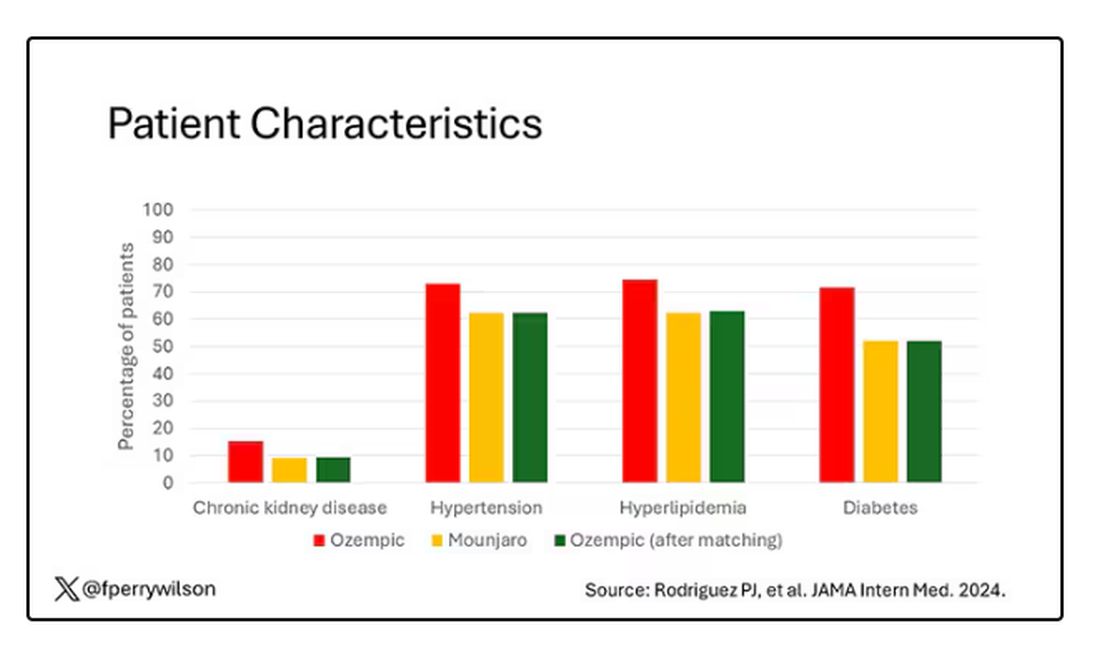
Once that’s done, we can go back to do what we wanted to do in the beginning, which is to look at the weight loss between the groups.
What I’m showing you here is the average percent change in body weight at 3, 6, and 12 months across the two drugs in the matched cohort. By a year out, you have basically 15% weight loss in the Mounjaro group compared with 8% or so in the Ozempic group. 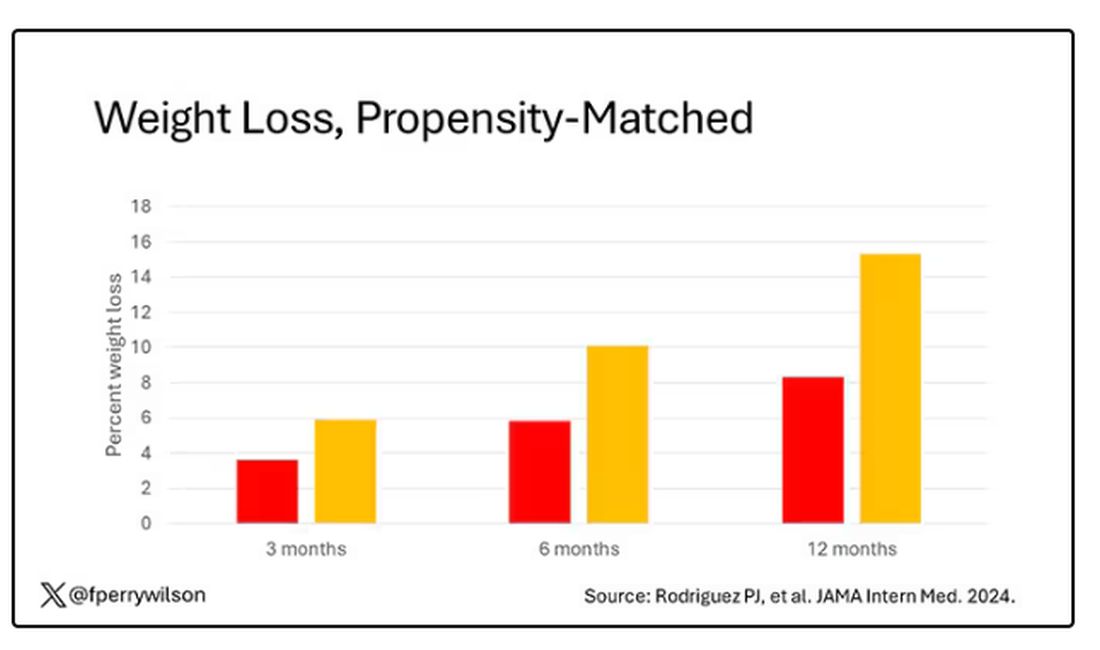
We can slice this a different way as well — asking what percent of people in each group achieve, say, 10% weight loss? This graph examines the percentage of each treatment group who hit that weight loss target over time. Mounjaro gets there faster.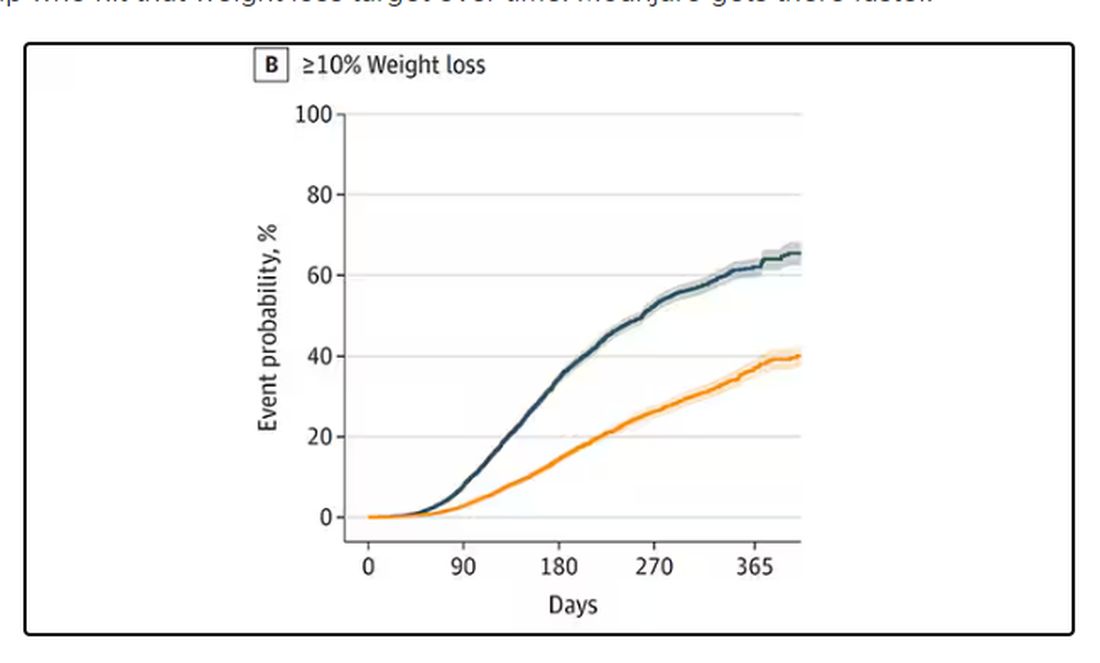
I should point out that this was a so-called “on treatment” analysis: If people stopped taking either of the drugs, they were no longer included in the study. That tends to make drugs like this appear better than they are because as time goes on, you may weed out the people who stop the drug owing to lack of efficacy or to side effects. But in a sensitivity analysis, the authors see what happens if they just treat people as if they were taking the drug for the entire year once they had it prescribed, and the results, while not as dramatic, were broadly similar. Mounjaro still came out on top.
Adverse events— stuff like gastroparesis and pancreatitis — were rare, but rates were similar between the two groups.
It’s great to see studies like this that leverage real world data and a solid statistical underpinning to give us providers actionable information. Is it 100% definitive? No. But, especially considering the clinical trial data, I don’t think I’m going out on a limb to say that Mounjaro seems to be the more effective weight loss agent. That said, we don’t actually live in a world where we can prescribe medications based on a silly little thing like which is the most effective. Especially given the cost of these agents — the patient’s insurance status is going to guide our prescription pen more than this study ever could. And of course, given the demand for this class of agents and the fact that both are actually quite effective, you may be best off prescribing whatever you can get your hands on.
But I’d like to see more of this. When I do have a choice of a medication, when costs and availability are similar, I’d like to be able to answer that question of “why did you choose that one?” with an evidence-based answer: “It’s better.”
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Connecticut. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
It’s July, which means our hospital is filled with new interns, residents, and fellows all eager to embark on a new stage of their career. It’s an exciting time — a bit of a scary time — but it’s also the time when the medical strategies I’ve been taking for granted get called into question. At this point in the year, I tend to get a lot of “why” questions. Why did you order that test? Why did you suspect that diagnosis? Why did you choose that medication?
Meds are the hardest, I find. Sure, I can explain that I prescribed a glucagon-like peptide 1 (GLP-1) receptor agonist because the patient had diabetes and was overweight, and multiple studies show that this class of drug leads to weight loss and reduced mortality risk. But then I get the follow-up: Sure, but why THAT GLP-1 drug? Why did you pick semaglutide (Ozempic) over tirzepatide (Mounjaro)?
Here’s where I run out of good answers. Sometimes I choose a drug because that’s what the patient’s insurance has on their formulary. Sometimes it’s because it’s cheaper in general. Sometimes, it’s just force of habit. I know the correct dose, I have experience with the side effects — it’s comfortable.
What I can’t say is that I have solid evidence that one drug is superior to another, say from a randomized trial of semaglutide vs tirzepatide. I don’t have that evidence because that trial has never happened and, as I’ll explain in a minute, may never happen at all.
But we might have the next best thing. And the results may surprise you.
Why don’t we see more head-to-head trials of competitor drugs? The answer is pretty simple, honestly: risk management. For drugs that are on patent, like the GLP-1s, conducting a trial without the buy-in of the pharmaceutical company is simply too expensive — we can’t run a trial unless someone provides the drug for free. That gives the companies a lot of say in what trials get done, and it seems that most pharma companies have reached the same conclusion: A head-to-head trial is too risky. Be happy with the market share you have, and try to nibble away at the edges through good old-fashioned marketing.
But if you look at the data that are out there, you might wonder why Ozempic is the market leader. I mean, sure, it’s a heck of a weight loss drug. But the weight loss in the trials of Mounjaro was actually a bit higher. It’s worth noting here that tirzepatide (Mounjaro) is not just a GLP-1 receptor agonist; it is also a gastric inhibitory polypeptide agonist. 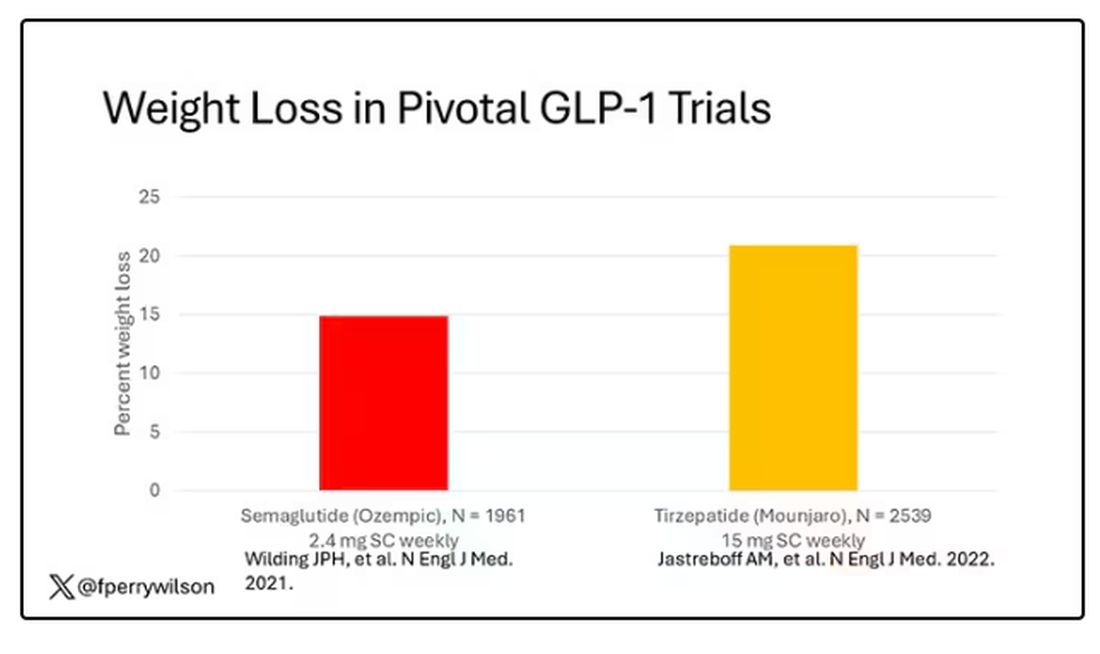
But it’s very hard to compare the results of a trial pitting Ozempic against placebo with a totally different trial pitting Mounjaro against placebo. You can always argue that the patients studied were just too different at baseline — an apples and oranges situation.
Newly published, a study appearing in JAMA Internal Medicine uses real-world data and propensity-score matching to turn oranges back into apples. I’ll walk you through it.
The data and analysis here come from Truveta, a collective of various US healthcare systems that share a broad swath of electronic health record data. Researchers identified 41,222 adults with overweight or obesity who were prescribed semaglutide or tirzepatide between May 2022 and September 2023.
You’d be tempted to just see which group lost more weight over time, but that is the apples and oranges problem. People prescribed Mounjaro were different from people who were prescribed Ozempic. There are a variety of factors to look at here, but the vibe is that the Mounjaro group seems healthier at baseline. They were younger and had less kidney disease, less hypertension, and less hyperlipidemia. They had higher incomes and were more likely to be White. They were also dramatically less likely to have diabetes. 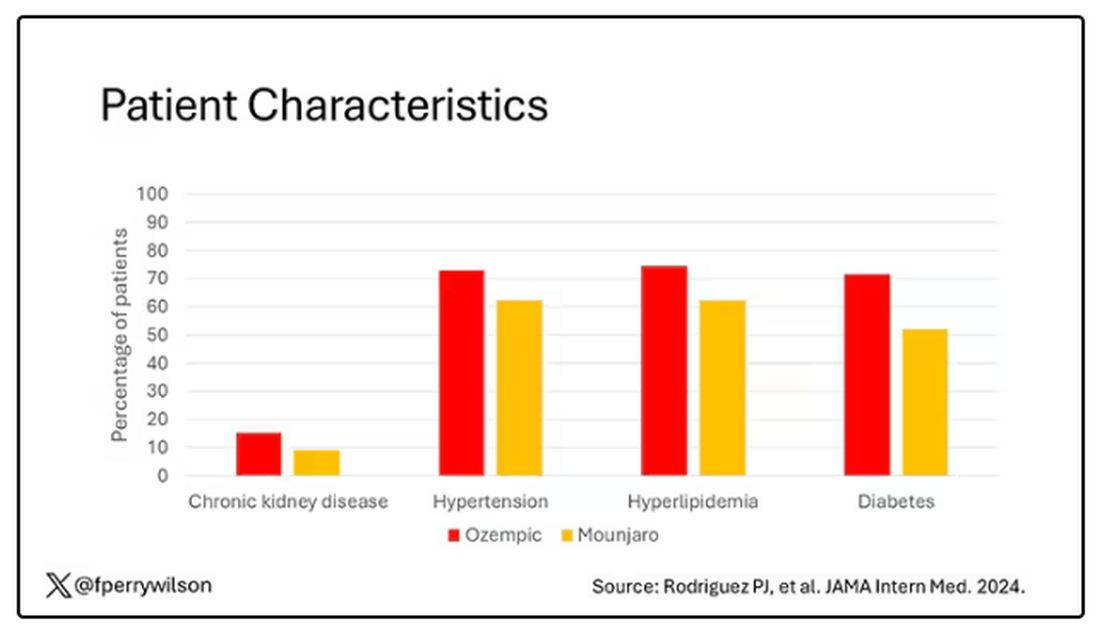
To account for this, the researchers used a statistical technique called propensity-score matching. Briefly, you create a model based on a variety of patient factors to predict who would be prescribed Ozempic and who would be prescribed Mounjaro. You then identify pairs of patients with similar probability (or propensity) of receiving, say, Ozempic, where one member of the pair got Ozempic and one got Mounjaro. Any unmatched individuals simply get dropped from the analysis.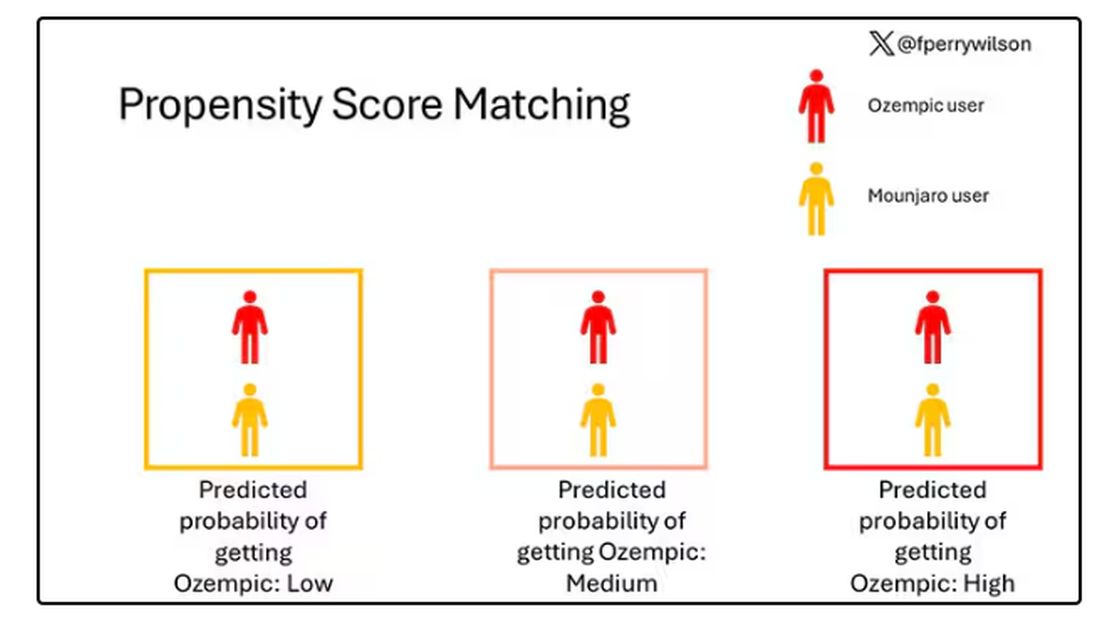
Thus, the researchers took the 41,222 individuals who started the analysis, of whom 9193 received Mounjaro, and identified the 9193 patients who got Ozempic that most closely matched the Mounjaro crowd. I know, it sounds confusing. But as an example, in the original dataset, 51.9% of those who got Mounjaro had diabetes compared with 71.5% of those who got Ozempic. Among the 9193 individuals who remained in the Ozempic group after matching, 52.1% had diabetes. By matching in this way, you balance your baseline characteristics. Turning apples into oranges. Or, maybe the better metaphor would be plucking the oranges out of a big pile of mostly apples.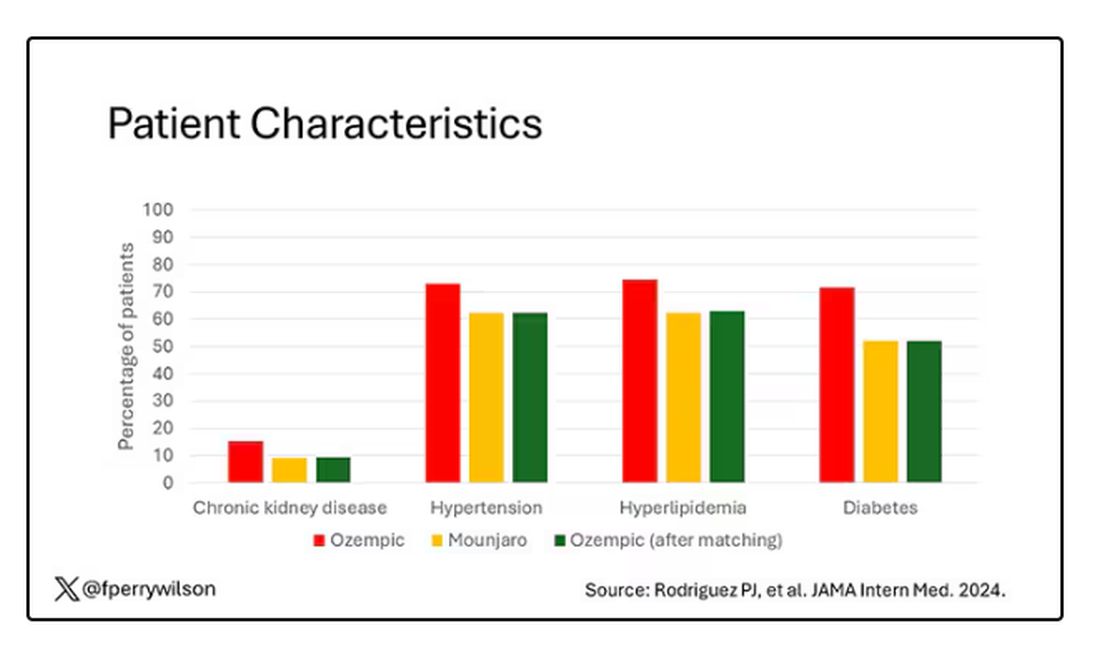
Once that’s done, we can go back to do what we wanted to do in the beginning, which is to look at the weight loss between the groups.
What I’m showing you here is the average percent change in body weight at 3, 6, and 12 months across the two drugs in the matched cohort. By a year out, you have basically 15% weight loss in the Mounjaro group compared with 8% or so in the Ozempic group. 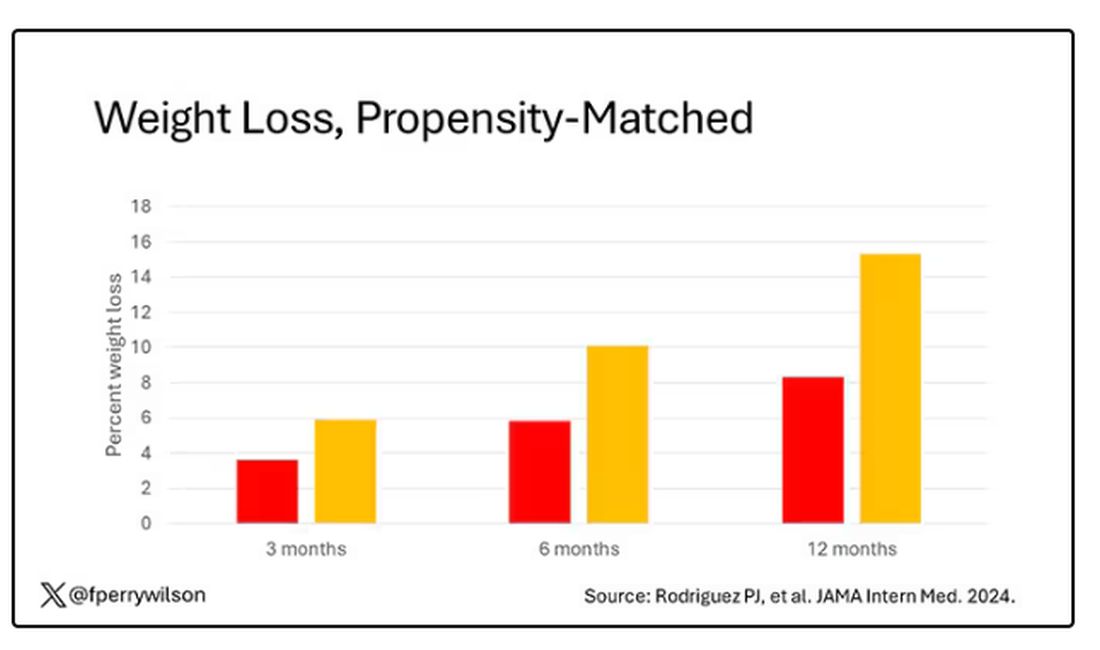
We can slice this a different way as well — asking what percent of people in each group achieve, say, 10% weight loss? This graph examines the percentage of each treatment group who hit that weight loss target over time. Mounjaro gets there faster.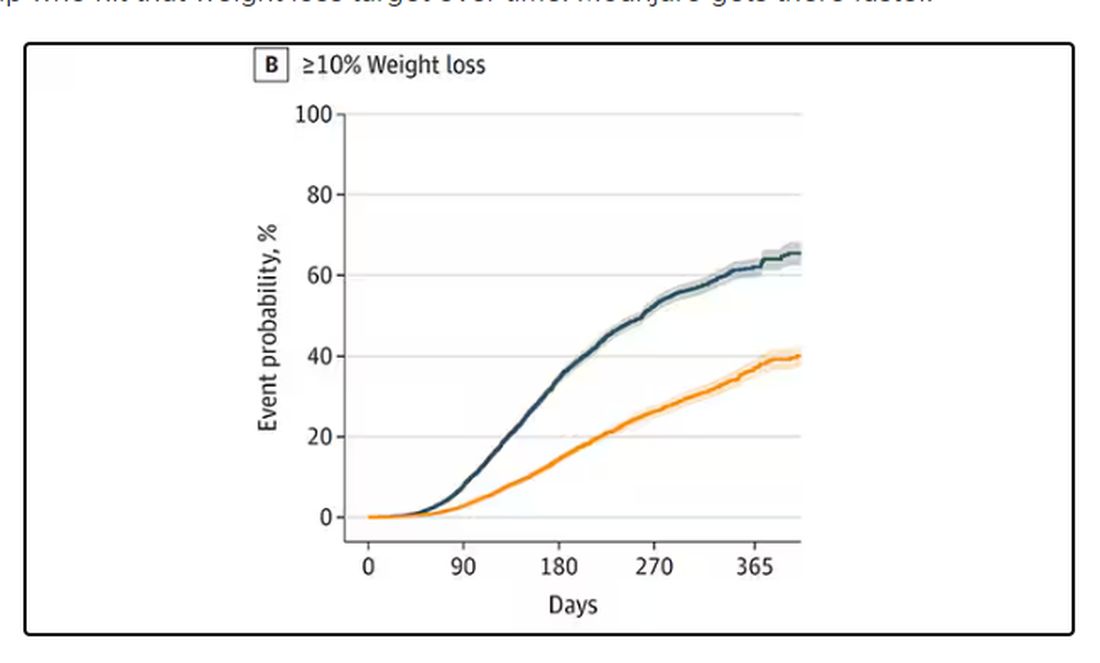
I should point out that this was a so-called “on treatment” analysis: If people stopped taking either of the drugs, they were no longer included in the study. That tends to make drugs like this appear better than they are because as time goes on, you may weed out the people who stop the drug owing to lack of efficacy or to side effects. But in a sensitivity analysis, the authors see what happens if they just treat people as if they were taking the drug for the entire year once they had it prescribed, and the results, while not as dramatic, were broadly similar. Mounjaro still came out on top.
Adverse events— stuff like gastroparesis and pancreatitis — were rare, but rates were similar between the two groups.
It’s great to see studies like this that leverage real world data and a solid statistical underpinning to give us providers actionable information. Is it 100% definitive? No. But, especially considering the clinical trial data, I don’t think I’m going out on a limb to say that Mounjaro seems to be the more effective weight loss agent. That said, we don’t actually live in a world where we can prescribe medications based on a silly little thing like which is the most effective. Especially given the cost of these agents — the patient’s insurance status is going to guide our prescription pen more than this study ever could. And of course, given the demand for this class of agents and the fact that both are actually quite effective, you may be best off prescribing whatever you can get your hands on.
But I’d like to see more of this. When I do have a choice of a medication, when costs and availability are similar, I’d like to be able to answer that question of “why did you choose that one?” with an evidence-based answer: “It’s better.”
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Connecticut. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Does Medicare Enrollment Raise Diabetes Medication Costs?
TOPLINE:
Reaching age 65 years and enrolling in Medicare is associated with a $23 increase in quarterly out-of-pocket costs for type 2 diabetes (T2D) medications. Medication usage decreased by 5.3%, with a notable shift toward more expensive insulin use.
METHODOLOGY:
- Researchers conducted a retrospective cohort study using 2012-2020 prescription drug claims data from the TriNetX Diamond Network.
- A total of 129,997 individuals diagnosed with T2D were included, with claims observed both before and after age 65 years.
- The primary outcome was patient out-of-pocket costs for T2D drugs per quarter, adjusted to 2020 dollars.
- Drugs measured included biguanides (metformin), sulfonylureas, thiazolidinediones, insulin, dipeptidyl peptidase 4 (DPP-4) inhibitors, glucagon-like peptide 1 (GLP-1) receptor agonists, sodium-glucose cotransporter 2 (SGLT-2 inhibitors), and amylin analogs, among others.
- Regression discontinuity design was used to examine the outcomes, adjusting for differential linear quarterly time trends, year fixed effects, and utilization composition and intensity.
TAKEAWAY:
- Reaching age 65 years was associated with an increase of $23.04 in mean quarterly out-of-pocket costs for T2D drugs (95% confidence interval [CI], $19.86-$26.22).
- The 95th percentile of out-of-pocket spending increased by $56.36 (95% CI, $51.48-$61.23) after utilization adjustment.
- T2D medication usage decreased by 5.3% at age 65 years, from 3.40 claims per quarter to 3.22 claims per quarter.
- Higher out-of-pockets were associated with insulin use, DPP-4 inhibitors, GLP-1s, and SGLT2 inhibitors.
IN PRACTICE:
“Our results have important implications for the provisions of the Inflation Reduction Act, many of which aim to reduce these costs. Reduced patient cost burden will improve adherence and the management of type 2 diabetes, likely leading to reductions in T2D complications,” wrote the authors of the study.
SOURCE:
The study was led by Douglas Barthold, PhD, Jing Li, MA, PhD, and Anirban Basu, MS, PhD, at the Comparative Health Outcomes, Policy, and Economics Institute, School of Pharmacy, University of Washington, Seattle. It was published online in JAMA Network Open.
LIMITATIONS:
The study’s limitations include the possibility that not all claims of an individual were observed, as TriNetX claims data may not capture individuals who leave the healthcare system or have inaccurate or changing diagnoses. Additionally, the data lack individual-level insurance characteristics. The assumption that individuals transition to Medicare at age 65 years may not be true for all participants. The study also lacks clinical information regarding the severity of T2D, which could influence medication usage and out-of-pocket costs.
DISCLOSURES:
The study was supported by grants from the National Institute on Aging (NIA) and the University of Washington’s Population Health Initiative, Student Technology Fee program, and Provost’s office. Dr. Barthold and Dr. Li received grants from the NIA. Dr. Basu reported receiving personal fees from Salutis Consulting LLC outside the submitted work. Additional disclosures are noted in the original article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Reaching age 65 years and enrolling in Medicare is associated with a $23 increase in quarterly out-of-pocket costs for type 2 diabetes (T2D) medications. Medication usage decreased by 5.3%, with a notable shift toward more expensive insulin use.
METHODOLOGY:
- Researchers conducted a retrospective cohort study using 2012-2020 prescription drug claims data from the TriNetX Diamond Network.
- A total of 129,997 individuals diagnosed with T2D were included, with claims observed both before and after age 65 years.
- The primary outcome was patient out-of-pocket costs for T2D drugs per quarter, adjusted to 2020 dollars.
- Drugs measured included biguanides (metformin), sulfonylureas, thiazolidinediones, insulin, dipeptidyl peptidase 4 (DPP-4) inhibitors, glucagon-like peptide 1 (GLP-1) receptor agonists, sodium-glucose cotransporter 2 (SGLT-2 inhibitors), and amylin analogs, among others.
- Regression discontinuity design was used to examine the outcomes, adjusting for differential linear quarterly time trends, year fixed effects, and utilization composition and intensity.
TAKEAWAY:
- Reaching age 65 years was associated with an increase of $23.04 in mean quarterly out-of-pocket costs for T2D drugs (95% confidence interval [CI], $19.86-$26.22).
- The 95th percentile of out-of-pocket spending increased by $56.36 (95% CI, $51.48-$61.23) after utilization adjustment.
- T2D medication usage decreased by 5.3% at age 65 years, from 3.40 claims per quarter to 3.22 claims per quarter.
- Higher out-of-pockets were associated with insulin use, DPP-4 inhibitors, GLP-1s, and SGLT2 inhibitors.
IN PRACTICE:
“Our results have important implications for the provisions of the Inflation Reduction Act, many of which aim to reduce these costs. Reduced patient cost burden will improve adherence and the management of type 2 diabetes, likely leading to reductions in T2D complications,” wrote the authors of the study.
SOURCE:
The study was led by Douglas Barthold, PhD, Jing Li, MA, PhD, and Anirban Basu, MS, PhD, at the Comparative Health Outcomes, Policy, and Economics Institute, School of Pharmacy, University of Washington, Seattle. It was published online in JAMA Network Open.
LIMITATIONS:
The study’s limitations include the possibility that not all claims of an individual were observed, as TriNetX claims data may not capture individuals who leave the healthcare system or have inaccurate or changing diagnoses. Additionally, the data lack individual-level insurance characteristics. The assumption that individuals transition to Medicare at age 65 years may not be true for all participants. The study also lacks clinical information regarding the severity of T2D, which could influence medication usage and out-of-pocket costs.
DISCLOSURES:
The study was supported by grants from the National Institute on Aging (NIA) and the University of Washington’s Population Health Initiative, Student Technology Fee program, and Provost’s office. Dr. Barthold and Dr. Li received grants from the NIA. Dr. Basu reported receiving personal fees from Salutis Consulting LLC outside the submitted work. Additional disclosures are noted in the original article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Reaching age 65 years and enrolling in Medicare is associated with a $23 increase in quarterly out-of-pocket costs for type 2 diabetes (T2D) medications. Medication usage decreased by 5.3%, with a notable shift toward more expensive insulin use.
METHODOLOGY:
- Researchers conducted a retrospective cohort study using 2012-2020 prescription drug claims data from the TriNetX Diamond Network.
- A total of 129,997 individuals diagnosed with T2D were included, with claims observed both before and after age 65 years.
- The primary outcome was patient out-of-pocket costs for T2D drugs per quarter, adjusted to 2020 dollars.
- Drugs measured included biguanides (metformin), sulfonylureas, thiazolidinediones, insulin, dipeptidyl peptidase 4 (DPP-4) inhibitors, glucagon-like peptide 1 (GLP-1) receptor agonists, sodium-glucose cotransporter 2 (SGLT-2 inhibitors), and amylin analogs, among others.
- Regression discontinuity design was used to examine the outcomes, adjusting for differential linear quarterly time trends, year fixed effects, and utilization composition and intensity.
TAKEAWAY:
- Reaching age 65 years was associated with an increase of $23.04 in mean quarterly out-of-pocket costs for T2D drugs (95% confidence interval [CI], $19.86-$26.22).
- The 95th percentile of out-of-pocket spending increased by $56.36 (95% CI, $51.48-$61.23) after utilization adjustment.
- T2D medication usage decreased by 5.3% at age 65 years, from 3.40 claims per quarter to 3.22 claims per quarter.
- Higher out-of-pockets were associated with insulin use, DPP-4 inhibitors, GLP-1s, and SGLT2 inhibitors.
IN PRACTICE:
“Our results have important implications for the provisions of the Inflation Reduction Act, many of which aim to reduce these costs. Reduced patient cost burden will improve adherence and the management of type 2 diabetes, likely leading to reductions in T2D complications,” wrote the authors of the study.
SOURCE:
The study was led by Douglas Barthold, PhD, Jing Li, MA, PhD, and Anirban Basu, MS, PhD, at the Comparative Health Outcomes, Policy, and Economics Institute, School of Pharmacy, University of Washington, Seattle. It was published online in JAMA Network Open.
LIMITATIONS:
The study’s limitations include the possibility that not all claims of an individual were observed, as TriNetX claims data may not capture individuals who leave the healthcare system or have inaccurate or changing diagnoses. Additionally, the data lack individual-level insurance characteristics. The assumption that individuals transition to Medicare at age 65 years may not be true for all participants. The study also lacks clinical information regarding the severity of T2D, which could influence medication usage and out-of-pocket costs.
DISCLOSURES:
The study was supported by grants from the National Institute on Aging (NIA) and the University of Washington’s Population Health Initiative, Student Technology Fee program, and Provost’s office. Dr. Barthold and Dr. Li received grants from the NIA. Dr. Basu reported receiving personal fees from Salutis Consulting LLC outside the submitted work. Additional disclosures are noted in the original article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.

