User login
Metformin improves most outcomes for T2D during pregnancy
including reduced weight gain, reduced insulin doses, and fewer large-for-gestational-age babies, suggest the results of a randomized controlled trial.
However, the drug was associated with an increased risk of small-for-gestational-age babies, which poses the question as to risk versus benefit of metformin on the health of offspring.
“Better understanding of the short- and long-term implications of these effects on infants will be important to properly advise patients with type 2 diabetes contemplating use of metformin during pregnancy,” said lead author Denice S. Feig, MD, Mount Sinai Hospital, Toronto.
The research was presented at the Diabetes UK Professional Conference: Online Series on Nov. 17 and recently published in The Lancet Diabetes & Endocrinology.
Summing up, Dr. Feig said that, on balance, she would be inclined to give metformin to most pregnant women with type 2 diabetes, perhaps with the exception of those who may have risk factors for small-for-gestational-age babies; for example, women who’ve had intrauterine growth restriction, who are smokers, and have significant renal disease, or have a lower body mass index.
Increased prevalence of type 2 diabetes in pregnancy
Dr. Feig said that across the developed world there have been huge increases in the prevalence of type 2 diabetes in pregnancy in recent years.
Insulin is the standard treatment for the management of type 2 diabetes in pregnancy, but these women have marked insulin resistance that worsens in pregnancy, which means their insulin requirements increase, leading to weight gain, painful injections, high cost, and noncompliance.
So despite treatment with insulin, these women continue to face increased rates of adverse maternal and fetal outcomes.
And although metformin is increasingly being used in women with type 2 diabetes during pregnancy, there is a scarcity of data on the benefits and harms of metformin use on pregnancy outcomes in these women.
The MiTy trial was therefore undertaken to determine whether metformin could improve outcomes.
The team recruited 502 women from 29 sites in Canada and Australia who had type 2 diabetes prior to pregnancy or were diagnosed during pregnancy, before 20 weeks’ gestation. The women were randomized to metformin 1 g twice daily or placebo, in addition to their usual insulin regimen, at between 6 and 28 weeks’ gestation.
Type 2 diabetes was diagnosed prior to pregnancy in 83% of women in the metformin group and in 90% of those assigned to placebo. The mean hemoglobin A1c level at randomization was 47 mmol/mol (6.5%) in both groups.
The average maternal age at baseline was approximately 35 years and mean gestational age at randomization was 16 weeks. Mean prepregnancy BMI was approximately 34 kg/m2.
Of note, only 30% were of European ethnicity.
Less weight gain, lower A1c, less insulin needed with metformin
Dr. Feig reported that there was no significant difference between the treatment groups in terms of the proportion of women with the composite primary outcome of pregnancy loss, preterm birth, birth injury, respiratory distress, neonatal hypoglycemia, or admission to neonatal intensive care lasting more than 24 hours (P = 0.86).
However, women in the metformin group had significantly less overall weight gain during pregnancy than did those in the placebo group, at –1.8 kg (P < .0001).
They also had a significantly lower last A1c level in pregnancy, at 41 mmol/mol (5.9%) versus 43.2 mmol/mol (6.1%) in those given placebo (P = .015), and required fewer insulin doses, at 1.1 versus 1.5 units/kg/day (P < .0001), which translated to a reduction of almost 44 units/day.
Women given metformin were also less likely to require Cesarean section delivery, at 53.4% versus 62.7% in the placebo group (P = .03), although there was no difference between groups in terms of gestational hypertension or preeclampsia.
The most common adverse events were gastrointestinal complications, which occurred in 27.3% of women in the metformin group and 22.3% of those given placebo.
There were no significant differences between the metformin and placebo groups in rates of pregnancy loss (P = .81), preterm birth (P = .16), birth injury (P = .37), respiratory distress (P = .49), and congenital anomalies (P = .16).
Average birth weight lower with metformin
However, Dr. Feig showed that the average birth weight was lower for offspring of women given metformin than those assigned to placebo, at 3.2 kg (7.05 lb) versus 3.4 kg (7.4 lb) (P = .002).
Women given metformin were also less likely to have a baby with a birth weight of 4 kg (8.8 lb) or more, at 12.1% versus 19.2%, or a relative risk of 0.65 (P = .046), and a baby that was extremely large for gestational age, at 8.6% versus 14.8%, or a relative risk of 0.58 (P = .046).
But of concern, metformin was associated with an increased risk of small-for-gestational-age babies, at 12.9% versus 6.6% with placebo, or a relative risk of 1.96 (P = .03).
Dr. Feig suggested that this may be due to a direct effect of metformin “because as we know metformin inhibits the mTOR pathway,” which is a “primary nutrient sensor in the placenta” and could “attenuate nutrient flux and fetal growth.”
She said it is not clear whether the small-for-gestational-age babies were “healthy or unhealthy.”
To investigate further, the team has launched the MiTy Kids study, which will follow the offspring in the MiTy trial to determine whether metformin during pregnancy is associated with a reduction in adiposity and improvement in insulin resistance in the babies at 2 years of age.
Who should be given metformin?
During the discussion, Helen R. Murphy, MD, PhD, Norwich Medical School, University of East Anglia, England, asked whether Dr. Feig would recommend continuing metformin in pregnancy if it was started preconception for fertility issues rather than diabetes.
She replied: “If they don’t have diabetes and it’s simply for PCOS [polycystic ovary syndrome], then I have either stopped it as soon as they got pregnant or sometimes continued it through the first trimester, and then stopped.
“If the person has diabetes, however, I think given this work, for most people I would continue it,” she said.
The study was funded by the Canadian Institutes of Health Research, Lunenfeld-Tanenbaum Research Institute, and the University of Toronto. The authors have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
including reduced weight gain, reduced insulin doses, and fewer large-for-gestational-age babies, suggest the results of a randomized controlled trial.
However, the drug was associated with an increased risk of small-for-gestational-age babies, which poses the question as to risk versus benefit of metformin on the health of offspring.
“Better understanding of the short- and long-term implications of these effects on infants will be important to properly advise patients with type 2 diabetes contemplating use of metformin during pregnancy,” said lead author Denice S. Feig, MD, Mount Sinai Hospital, Toronto.
The research was presented at the Diabetes UK Professional Conference: Online Series on Nov. 17 and recently published in The Lancet Diabetes & Endocrinology.
Summing up, Dr. Feig said that, on balance, she would be inclined to give metformin to most pregnant women with type 2 diabetes, perhaps with the exception of those who may have risk factors for small-for-gestational-age babies; for example, women who’ve had intrauterine growth restriction, who are smokers, and have significant renal disease, or have a lower body mass index.
Increased prevalence of type 2 diabetes in pregnancy
Dr. Feig said that across the developed world there have been huge increases in the prevalence of type 2 diabetes in pregnancy in recent years.
Insulin is the standard treatment for the management of type 2 diabetes in pregnancy, but these women have marked insulin resistance that worsens in pregnancy, which means their insulin requirements increase, leading to weight gain, painful injections, high cost, and noncompliance.
So despite treatment with insulin, these women continue to face increased rates of adverse maternal and fetal outcomes.
And although metformin is increasingly being used in women with type 2 diabetes during pregnancy, there is a scarcity of data on the benefits and harms of metformin use on pregnancy outcomes in these women.
The MiTy trial was therefore undertaken to determine whether metformin could improve outcomes.
The team recruited 502 women from 29 sites in Canada and Australia who had type 2 diabetes prior to pregnancy or were diagnosed during pregnancy, before 20 weeks’ gestation. The women were randomized to metformin 1 g twice daily or placebo, in addition to their usual insulin regimen, at between 6 and 28 weeks’ gestation.
Type 2 diabetes was diagnosed prior to pregnancy in 83% of women in the metformin group and in 90% of those assigned to placebo. The mean hemoglobin A1c level at randomization was 47 mmol/mol (6.5%) in both groups.
The average maternal age at baseline was approximately 35 years and mean gestational age at randomization was 16 weeks. Mean prepregnancy BMI was approximately 34 kg/m2.
Of note, only 30% were of European ethnicity.
Less weight gain, lower A1c, less insulin needed with metformin
Dr. Feig reported that there was no significant difference between the treatment groups in terms of the proportion of women with the composite primary outcome of pregnancy loss, preterm birth, birth injury, respiratory distress, neonatal hypoglycemia, or admission to neonatal intensive care lasting more than 24 hours (P = 0.86).
However, women in the metformin group had significantly less overall weight gain during pregnancy than did those in the placebo group, at –1.8 kg (P < .0001).
They also had a significantly lower last A1c level in pregnancy, at 41 mmol/mol (5.9%) versus 43.2 mmol/mol (6.1%) in those given placebo (P = .015), and required fewer insulin doses, at 1.1 versus 1.5 units/kg/day (P < .0001), which translated to a reduction of almost 44 units/day.
Women given metformin were also less likely to require Cesarean section delivery, at 53.4% versus 62.7% in the placebo group (P = .03), although there was no difference between groups in terms of gestational hypertension or preeclampsia.
The most common adverse events were gastrointestinal complications, which occurred in 27.3% of women in the metformin group and 22.3% of those given placebo.
There were no significant differences between the metformin and placebo groups in rates of pregnancy loss (P = .81), preterm birth (P = .16), birth injury (P = .37), respiratory distress (P = .49), and congenital anomalies (P = .16).
Average birth weight lower with metformin
However, Dr. Feig showed that the average birth weight was lower for offspring of women given metformin than those assigned to placebo, at 3.2 kg (7.05 lb) versus 3.4 kg (7.4 lb) (P = .002).
Women given metformin were also less likely to have a baby with a birth weight of 4 kg (8.8 lb) or more, at 12.1% versus 19.2%, or a relative risk of 0.65 (P = .046), and a baby that was extremely large for gestational age, at 8.6% versus 14.8%, or a relative risk of 0.58 (P = .046).
But of concern, metformin was associated with an increased risk of small-for-gestational-age babies, at 12.9% versus 6.6% with placebo, or a relative risk of 1.96 (P = .03).
Dr. Feig suggested that this may be due to a direct effect of metformin “because as we know metformin inhibits the mTOR pathway,” which is a “primary nutrient sensor in the placenta” and could “attenuate nutrient flux and fetal growth.”
She said it is not clear whether the small-for-gestational-age babies were “healthy or unhealthy.”
To investigate further, the team has launched the MiTy Kids study, which will follow the offspring in the MiTy trial to determine whether metformin during pregnancy is associated with a reduction in adiposity and improvement in insulin resistance in the babies at 2 years of age.
Who should be given metformin?
During the discussion, Helen R. Murphy, MD, PhD, Norwich Medical School, University of East Anglia, England, asked whether Dr. Feig would recommend continuing metformin in pregnancy if it was started preconception for fertility issues rather than diabetes.
She replied: “If they don’t have diabetes and it’s simply for PCOS [polycystic ovary syndrome], then I have either stopped it as soon as they got pregnant or sometimes continued it through the first trimester, and then stopped.
“If the person has diabetes, however, I think given this work, for most people I would continue it,” she said.
The study was funded by the Canadian Institutes of Health Research, Lunenfeld-Tanenbaum Research Institute, and the University of Toronto. The authors have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
including reduced weight gain, reduced insulin doses, and fewer large-for-gestational-age babies, suggest the results of a randomized controlled trial.
However, the drug was associated with an increased risk of small-for-gestational-age babies, which poses the question as to risk versus benefit of metformin on the health of offspring.
“Better understanding of the short- and long-term implications of these effects on infants will be important to properly advise patients with type 2 diabetes contemplating use of metformin during pregnancy,” said lead author Denice S. Feig, MD, Mount Sinai Hospital, Toronto.
The research was presented at the Diabetes UK Professional Conference: Online Series on Nov. 17 and recently published in The Lancet Diabetes & Endocrinology.
Summing up, Dr. Feig said that, on balance, she would be inclined to give metformin to most pregnant women with type 2 diabetes, perhaps with the exception of those who may have risk factors for small-for-gestational-age babies; for example, women who’ve had intrauterine growth restriction, who are smokers, and have significant renal disease, or have a lower body mass index.
Increased prevalence of type 2 diabetes in pregnancy
Dr. Feig said that across the developed world there have been huge increases in the prevalence of type 2 diabetes in pregnancy in recent years.
Insulin is the standard treatment for the management of type 2 diabetes in pregnancy, but these women have marked insulin resistance that worsens in pregnancy, which means their insulin requirements increase, leading to weight gain, painful injections, high cost, and noncompliance.
So despite treatment with insulin, these women continue to face increased rates of adverse maternal and fetal outcomes.
And although metformin is increasingly being used in women with type 2 diabetes during pregnancy, there is a scarcity of data on the benefits and harms of metformin use on pregnancy outcomes in these women.
The MiTy trial was therefore undertaken to determine whether metformin could improve outcomes.
The team recruited 502 women from 29 sites in Canada and Australia who had type 2 diabetes prior to pregnancy or were diagnosed during pregnancy, before 20 weeks’ gestation. The women were randomized to metformin 1 g twice daily or placebo, in addition to their usual insulin regimen, at between 6 and 28 weeks’ gestation.
Type 2 diabetes was diagnosed prior to pregnancy in 83% of women in the metformin group and in 90% of those assigned to placebo. The mean hemoglobin A1c level at randomization was 47 mmol/mol (6.5%) in both groups.
The average maternal age at baseline was approximately 35 years and mean gestational age at randomization was 16 weeks. Mean prepregnancy BMI was approximately 34 kg/m2.
Of note, only 30% were of European ethnicity.
Less weight gain, lower A1c, less insulin needed with metformin
Dr. Feig reported that there was no significant difference between the treatment groups in terms of the proportion of women with the composite primary outcome of pregnancy loss, preterm birth, birth injury, respiratory distress, neonatal hypoglycemia, or admission to neonatal intensive care lasting more than 24 hours (P = 0.86).
However, women in the metformin group had significantly less overall weight gain during pregnancy than did those in the placebo group, at –1.8 kg (P < .0001).
They also had a significantly lower last A1c level in pregnancy, at 41 mmol/mol (5.9%) versus 43.2 mmol/mol (6.1%) in those given placebo (P = .015), and required fewer insulin doses, at 1.1 versus 1.5 units/kg/day (P < .0001), which translated to a reduction of almost 44 units/day.
Women given metformin were also less likely to require Cesarean section delivery, at 53.4% versus 62.7% in the placebo group (P = .03), although there was no difference between groups in terms of gestational hypertension or preeclampsia.
The most common adverse events were gastrointestinal complications, which occurred in 27.3% of women in the metformin group and 22.3% of those given placebo.
There were no significant differences between the metformin and placebo groups in rates of pregnancy loss (P = .81), preterm birth (P = .16), birth injury (P = .37), respiratory distress (P = .49), and congenital anomalies (P = .16).
Average birth weight lower with metformin
However, Dr. Feig showed that the average birth weight was lower for offspring of women given metformin than those assigned to placebo, at 3.2 kg (7.05 lb) versus 3.4 kg (7.4 lb) (P = .002).
Women given metformin were also less likely to have a baby with a birth weight of 4 kg (8.8 lb) or more, at 12.1% versus 19.2%, or a relative risk of 0.65 (P = .046), and a baby that was extremely large for gestational age, at 8.6% versus 14.8%, or a relative risk of 0.58 (P = .046).
But of concern, metformin was associated with an increased risk of small-for-gestational-age babies, at 12.9% versus 6.6% with placebo, or a relative risk of 1.96 (P = .03).
Dr. Feig suggested that this may be due to a direct effect of metformin “because as we know metformin inhibits the mTOR pathway,” which is a “primary nutrient sensor in the placenta” and could “attenuate nutrient flux and fetal growth.”
She said it is not clear whether the small-for-gestational-age babies were “healthy or unhealthy.”
To investigate further, the team has launched the MiTy Kids study, which will follow the offspring in the MiTy trial to determine whether metformin during pregnancy is associated with a reduction in adiposity and improvement in insulin resistance in the babies at 2 years of age.
Who should be given metformin?
During the discussion, Helen R. Murphy, MD, PhD, Norwich Medical School, University of East Anglia, England, asked whether Dr. Feig would recommend continuing metformin in pregnancy if it was started preconception for fertility issues rather than diabetes.
She replied: “If they don’t have diabetes and it’s simply for PCOS [polycystic ovary syndrome], then I have either stopped it as soon as they got pregnant or sometimes continued it through the first trimester, and then stopped.
“If the person has diabetes, however, I think given this work, for most people I would continue it,” she said.
The study was funded by the Canadian Institutes of Health Research, Lunenfeld-Tanenbaum Research Institute, and the University of Toronto. The authors have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Common newborn hearing test promising for early detection of autism
new research shows.
Results from one of the largest studies of its kind show the auditory brainstem response (ABR) test, which is carried out on most newborns, represents “a huge untapped potential” to detect autism, lead author Oren Miron, research associate, department of biomedical informatics, Harvard Medical School, Boston, and a PhD candidate at Ben Gurion University in Beersheba, Israel, said in an interview.
“The findings further reinforce our understanding that autism, in many cases, has a sensorial and auditory aspect to it,” said Mr. Miron, adding that an adverse response to sound is one of the earliest behavioral signs of autism.
The research was published online Oct. 31 in Autism Research.
Early intervention critical
Autism spectrum disorder (ASD), which involves problems in social communication and interaction, affects an estimated 1 in 59 children. Early identification and intervention are critical for improving outcomes and decreasing the economic burden associated with ASD.
The ABR test, which is used for Universal Newborn Hearing Screening (UNHS), uses surface electrodes to measure auditory nerve and brainstem responses to sound.
Previous studies identified abnormal ABR amplitude in children with ASD. However, it’s unclear whether healthy newborns who later develop autism also show ABR differences vs those who don’t develop the disorder.
Researchers used UNHS data, which allowed them to examine a larger, younger, and healthier sample compared with previous studies. The study included 321 newborns later diagnosed with ASD and 138,844 controls without a subsequent ASD diagnosis.
The mean ABR testing age was 1.76 days for newborns later diagnosed with ASD and 1.86 for those in the non-ASD group.
The ASD group was 77% male and the non-ASD group was 51% male. The rate of neonatal intensive care unit admission was 8% in the ASD group and 10% in the non-ASD group.
The hearing test involves placing an earpiece in the baby’s ear and delivering a click sound at 35 dB above normal hearing level (nHL) at a rate of 77 clicks per second in the right ear and 79 clicks per second in the left ear.
Brainstem abnormalities?
The clicks create electrical activity, which is recorded by a surface electrode and used to extract the ABR waveform. When a sound reaches the brain stem, it creates five consecutive waveforms – waves I, II, III, IV, and V.
Previous studies focused on wave V, which is easiest to detect. The current study used low intensity sound that resulted in a weaker signal.
To overcome this low intensity issue, researchers focused on the negative drop (latency) after the wave V (Vn), which is easier to detect, and on the ABR phase, or entire waveform. They illustrated the differences between the ASD and non-ASD groups in a series of graphs.
Results showed that the ABR phase in the right ear was significantly prolonged in the ASD vs non-ASD group (P < .001). ABR phase in the left ear was also significantly prolonged in the ASD group (P = .021)
Vn latency in the right ear was significantly prolonged in the ASD group compared with the non-ASD group (P = .048); however, this was not the case in the left ear.
The prolongation could mean that the V-negative wave might appear after 8 ms in normally developing children compared with 8.5 or 9 ms in children with autism, said Mr. Miron.
The new study is the first to show V-negative and phase abnormalities are associated with ASD, the authors note. The brainstem prolongation could be due to anatomical abnormalities in the brainstem in individuals with ASD, the researchers added.
Present before birth?
The presence of ABR biomarkers of ASD in the first weeks after birth suggests the disorder is likely present before birth in a large group of these individuals, the researchers note.
It’s possible the ABR test could be modified to use lower intensities not only to detect hearing impairment but autism risk, said Mr. Miron. “The test has been optimized to detect hearing impairment, and it does so brilliantly and helps thousands of children. We want to do the same kind of optimization for autism.”
This could lead to earlier behavioral diagnoses, which, in turn, could lead to earlier treatment and better outcomes for children with ASD, said Mr. Miron.
At this time, the level of prolongation to detect ASD is unclear. “I would think a lot of people would want to make it one standard deviation, but it depends on a lot of factors, including for example, whether a baby is preterm,” said Mr. Miron.
More research and better accuracy and specificity are needed before the newborn hearing test is clinically useful.
He noted that the hearing test is only one marker of autism and that it could potentially be combined with other behavioral signs and genetic markers to facilitate earlier diagnosis and treatment and improve outcomes for patients with ASD.
Future research by his group will investigate whether the degree of auditory prolongation relates to autism severity. They also plan to research ASD subgroups including children with comorbid epilepsy.
Terrific, clever research
Jeremy Veenstra-VanderWeele, MD, professor, child and adolescent psychiatry, Columbia University, New York, said in an interview that the study is “terrific” and a “clever use” of an existing dataset.
“They showed a difference between a large group of kids with autism and a large group of kids without.”
However, he added, more research is needed before the test can be used as an autism screening tool.
“In order for this to be a screening test that could be broadly applied you would need to identify a cutoff where you’d think a child was at risk for autism, and if you look at the graphs in the article, there are no clear cutoffs,” said Dr. Veenstra-VanderWeele.
To turn this into a useful test, “you would have to establish sensitivity and specificity, you would have to look not just at the comparison of kids with autism and kids without but apply it in a predictive way in a second population.”
The study authors and Dr. Veenstra-VanderWeele have reported no relevant financial relationships. Veenstra-VanderWeele is an associate editor at Autism Research, which published the article, but he did not handle or view it before being interviewed.
A version of this article originally appeared on Medscape.com.
new research shows.
Results from one of the largest studies of its kind show the auditory brainstem response (ABR) test, which is carried out on most newborns, represents “a huge untapped potential” to detect autism, lead author Oren Miron, research associate, department of biomedical informatics, Harvard Medical School, Boston, and a PhD candidate at Ben Gurion University in Beersheba, Israel, said in an interview.
“The findings further reinforce our understanding that autism, in many cases, has a sensorial and auditory aspect to it,” said Mr. Miron, adding that an adverse response to sound is one of the earliest behavioral signs of autism.
The research was published online Oct. 31 in Autism Research.
Early intervention critical
Autism spectrum disorder (ASD), which involves problems in social communication and interaction, affects an estimated 1 in 59 children. Early identification and intervention are critical for improving outcomes and decreasing the economic burden associated with ASD.
The ABR test, which is used for Universal Newborn Hearing Screening (UNHS), uses surface electrodes to measure auditory nerve and brainstem responses to sound.
Previous studies identified abnormal ABR amplitude in children with ASD. However, it’s unclear whether healthy newborns who later develop autism also show ABR differences vs those who don’t develop the disorder.
Researchers used UNHS data, which allowed them to examine a larger, younger, and healthier sample compared with previous studies. The study included 321 newborns later diagnosed with ASD and 138,844 controls without a subsequent ASD diagnosis.
The mean ABR testing age was 1.76 days for newborns later diagnosed with ASD and 1.86 for those in the non-ASD group.
The ASD group was 77% male and the non-ASD group was 51% male. The rate of neonatal intensive care unit admission was 8% in the ASD group and 10% in the non-ASD group.
The hearing test involves placing an earpiece in the baby’s ear and delivering a click sound at 35 dB above normal hearing level (nHL) at a rate of 77 clicks per second in the right ear and 79 clicks per second in the left ear.
Brainstem abnormalities?
The clicks create electrical activity, which is recorded by a surface electrode and used to extract the ABR waveform. When a sound reaches the brain stem, it creates five consecutive waveforms – waves I, II, III, IV, and V.
Previous studies focused on wave V, which is easiest to detect. The current study used low intensity sound that resulted in a weaker signal.
To overcome this low intensity issue, researchers focused on the negative drop (latency) after the wave V (Vn), which is easier to detect, and on the ABR phase, or entire waveform. They illustrated the differences between the ASD and non-ASD groups in a series of graphs.
Results showed that the ABR phase in the right ear was significantly prolonged in the ASD vs non-ASD group (P < .001). ABR phase in the left ear was also significantly prolonged in the ASD group (P = .021)
Vn latency in the right ear was significantly prolonged in the ASD group compared with the non-ASD group (P = .048); however, this was not the case in the left ear.
The prolongation could mean that the V-negative wave might appear after 8 ms in normally developing children compared with 8.5 or 9 ms in children with autism, said Mr. Miron.
The new study is the first to show V-negative and phase abnormalities are associated with ASD, the authors note. The brainstem prolongation could be due to anatomical abnormalities in the brainstem in individuals with ASD, the researchers added.
Present before birth?
The presence of ABR biomarkers of ASD in the first weeks after birth suggests the disorder is likely present before birth in a large group of these individuals, the researchers note.
It’s possible the ABR test could be modified to use lower intensities not only to detect hearing impairment but autism risk, said Mr. Miron. “The test has been optimized to detect hearing impairment, and it does so brilliantly and helps thousands of children. We want to do the same kind of optimization for autism.”
This could lead to earlier behavioral diagnoses, which, in turn, could lead to earlier treatment and better outcomes for children with ASD, said Mr. Miron.
At this time, the level of prolongation to detect ASD is unclear. “I would think a lot of people would want to make it one standard deviation, but it depends on a lot of factors, including for example, whether a baby is preterm,” said Mr. Miron.
More research and better accuracy and specificity are needed before the newborn hearing test is clinically useful.
He noted that the hearing test is only one marker of autism and that it could potentially be combined with other behavioral signs and genetic markers to facilitate earlier diagnosis and treatment and improve outcomes for patients with ASD.
Future research by his group will investigate whether the degree of auditory prolongation relates to autism severity. They also plan to research ASD subgroups including children with comorbid epilepsy.
Terrific, clever research
Jeremy Veenstra-VanderWeele, MD, professor, child and adolescent psychiatry, Columbia University, New York, said in an interview that the study is “terrific” and a “clever use” of an existing dataset.
“They showed a difference between a large group of kids with autism and a large group of kids without.”
However, he added, more research is needed before the test can be used as an autism screening tool.
“In order for this to be a screening test that could be broadly applied you would need to identify a cutoff where you’d think a child was at risk for autism, and if you look at the graphs in the article, there are no clear cutoffs,” said Dr. Veenstra-VanderWeele.
To turn this into a useful test, “you would have to establish sensitivity and specificity, you would have to look not just at the comparison of kids with autism and kids without but apply it in a predictive way in a second population.”
The study authors and Dr. Veenstra-VanderWeele have reported no relevant financial relationships. Veenstra-VanderWeele is an associate editor at Autism Research, which published the article, but he did not handle or view it before being interviewed.
A version of this article originally appeared on Medscape.com.
new research shows.
Results from one of the largest studies of its kind show the auditory brainstem response (ABR) test, which is carried out on most newborns, represents “a huge untapped potential” to detect autism, lead author Oren Miron, research associate, department of biomedical informatics, Harvard Medical School, Boston, and a PhD candidate at Ben Gurion University in Beersheba, Israel, said in an interview.
“The findings further reinforce our understanding that autism, in many cases, has a sensorial and auditory aspect to it,” said Mr. Miron, adding that an adverse response to sound is one of the earliest behavioral signs of autism.
The research was published online Oct. 31 in Autism Research.
Early intervention critical
Autism spectrum disorder (ASD), which involves problems in social communication and interaction, affects an estimated 1 in 59 children. Early identification and intervention are critical for improving outcomes and decreasing the economic burden associated with ASD.
The ABR test, which is used for Universal Newborn Hearing Screening (UNHS), uses surface electrodes to measure auditory nerve and brainstem responses to sound.
Previous studies identified abnormal ABR amplitude in children with ASD. However, it’s unclear whether healthy newborns who later develop autism also show ABR differences vs those who don’t develop the disorder.
Researchers used UNHS data, which allowed them to examine a larger, younger, and healthier sample compared with previous studies. The study included 321 newborns later diagnosed with ASD and 138,844 controls without a subsequent ASD diagnosis.
The mean ABR testing age was 1.76 days for newborns later diagnosed with ASD and 1.86 for those in the non-ASD group.
The ASD group was 77% male and the non-ASD group was 51% male. The rate of neonatal intensive care unit admission was 8% in the ASD group and 10% in the non-ASD group.
The hearing test involves placing an earpiece in the baby’s ear and delivering a click sound at 35 dB above normal hearing level (nHL) at a rate of 77 clicks per second in the right ear and 79 clicks per second in the left ear.
Brainstem abnormalities?
The clicks create electrical activity, which is recorded by a surface electrode and used to extract the ABR waveform. When a sound reaches the brain stem, it creates five consecutive waveforms – waves I, II, III, IV, and V.
Previous studies focused on wave V, which is easiest to detect. The current study used low intensity sound that resulted in a weaker signal.
To overcome this low intensity issue, researchers focused on the negative drop (latency) after the wave V (Vn), which is easier to detect, and on the ABR phase, or entire waveform. They illustrated the differences between the ASD and non-ASD groups in a series of graphs.
Results showed that the ABR phase in the right ear was significantly prolonged in the ASD vs non-ASD group (P < .001). ABR phase in the left ear was also significantly prolonged in the ASD group (P = .021)
Vn latency in the right ear was significantly prolonged in the ASD group compared with the non-ASD group (P = .048); however, this was not the case in the left ear.
The prolongation could mean that the V-negative wave might appear after 8 ms in normally developing children compared with 8.5 or 9 ms in children with autism, said Mr. Miron.
The new study is the first to show V-negative and phase abnormalities are associated with ASD, the authors note. The brainstem prolongation could be due to anatomical abnormalities in the brainstem in individuals with ASD, the researchers added.
Present before birth?
The presence of ABR biomarkers of ASD in the first weeks after birth suggests the disorder is likely present before birth in a large group of these individuals, the researchers note.
It’s possible the ABR test could be modified to use lower intensities not only to detect hearing impairment but autism risk, said Mr. Miron. “The test has been optimized to detect hearing impairment, and it does so brilliantly and helps thousands of children. We want to do the same kind of optimization for autism.”
This could lead to earlier behavioral diagnoses, which, in turn, could lead to earlier treatment and better outcomes for children with ASD, said Mr. Miron.
At this time, the level of prolongation to detect ASD is unclear. “I would think a lot of people would want to make it one standard deviation, but it depends on a lot of factors, including for example, whether a baby is preterm,” said Mr. Miron.
More research and better accuracy and specificity are needed before the newborn hearing test is clinically useful.
He noted that the hearing test is only one marker of autism and that it could potentially be combined with other behavioral signs and genetic markers to facilitate earlier diagnosis and treatment and improve outcomes for patients with ASD.
Future research by his group will investigate whether the degree of auditory prolongation relates to autism severity. They also plan to research ASD subgroups including children with comorbid epilepsy.
Terrific, clever research
Jeremy Veenstra-VanderWeele, MD, professor, child and adolescent psychiatry, Columbia University, New York, said in an interview that the study is “terrific” and a “clever use” of an existing dataset.
“They showed a difference between a large group of kids with autism and a large group of kids without.”
However, he added, more research is needed before the test can be used as an autism screening tool.
“In order for this to be a screening test that could be broadly applied you would need to identify a cutoff where you’d think a child was at risk for autism, and if you look at the graphs in the article, there are no clear cutoffs,” said Dr. Veenstra-VanderWeele.
To turn this into a useful test, “you would have to establish sensitivity and specificity, you would have to look not just at the comparison of kids with autism and kids without but apply it in a predictive way in a second population.”
The study authors and Dr. Veenstra-VanderWeele have reported no relevant financial relationships. Veenstra-VanderWeele is an associate editor at Autism Research, which published the article, but he did not handle or view it before being interviewed.
A version of this article originally appeared on Medscape.com.
Nebulized surfactant shows promise in large cohort
Nebulized delivery of surfactant reduced the need for intubation and liquid surfactant administration by half among newborns with signs of respiratory distress syndrome, according to results from a large randomized, multicenter trial.
Neonatologists have long sought alternatives to intubation for administering surfactant to newborns with respiratory distress syndrome (RDS). An effective noninvasive aerosolized treatment has remained elusive, with small clinical trials that have produced mixed results.
In research published in Pediatrics, James J. Cummings, MD, of Albany (N.Y.) Medical Center, and colleagues, randomized 457 infants (mean 33 weeks’ gestational age) with signs of RDS to either usual care or a nebulized bovine surfactant. Infants were recruited at 22 neonatal ICUs in the United States. Investigators were not blinded to treatment allocation and the decision to intubate was left up to the individual treating physician, because to do so, the authors wrote, would add “pragmatic strength” to the study, and “be ethically compliant with the infant’s best interest.”
Infants in the study received usual care or up to three treatments 4 or more hours apart of 35 mg/mL calfactant suspension, 210 mg phospholipid/kg body weight delivered into the mouth through a nebulizer modified with a pacifier. Dr. Cummings and colleagues found that intubation and liquid surfactant administration within the first 4 days after birth was 26% in the intervention group and 50% in the usual care group (P < .001).
The results remained significant after investigators adjusted for gestational age, birth weight, age when randomized, sex, delivery mode, and antenatal steroids. Rates of intubation for surfactant administration were lower for infants in the intervention group in all gestational age brackets except the youngest (23-24 weeks); all of these infants needed intubation. Respiratory support at days 3, 7, and 28 did not differ between study groups.
“Our study is the first to reveal the efficacy of an aerosolized surfactant delivery system that does not require a respiratory circuit interface,” the investigators wrote.
In previous trials of aerosolized surfactants, they noted, treatment was delivered with nasal continuous positive airway pressure. “By using a separate, pacifier interface, both the aerosol delivery and [nasal continuous positive airway pressure] flow can be managed independently, which should allow for safer patient care.”
Dr. Cummings and colleagues also acknowledged several important limitations of their study, including its nonmasked, nonblinded design, and that it enrolled few infants with less than 28 weeks’ gestation. It takes 1-2 hours to deliver aerosolized calfactant, and “we did not want to delay definitive treatment.”
In an editorial comment accompanying the study, Kirsten Glaser, MD, of the University of Leipzig (Germany), and Clyde Wright, MD of the University of Colorado at Denver, Aurora, called the results promising. “Importantly, application of surfactant aerosols was well tolerated by using a modified nebulizer with a pacifier interface.”
“Clinicians were aware that every infant randomly assigned to the nebulized surfactant arm received the intervention,” they wrote. “It is possible that clinicians delayed intubation and endotracheal surfactant instillation in this group, being biased by aerosolization and the hypothesis of lower risk of air leak and lung injury.”
Dr. Glaser and Dr. Wright further lamented that there were no formal criteria for administering surfactant therapy, and that the infants in the study might not be representative of those most in need of treatment. Today, bronchopulmonary dysplasia “primarily affects infants born at less than 28 weeks’ gestational age,” a minority of the infants recruited for this study, they wrote, urging further investigation in this patient group.
In an interview, neonatologist Roger F. Soll, MD, the H. Wallace Professor of Neonatology at the Larner College of Medicine at University of Vermont in Burlington, echoed the editorialists’ concerns that the study’s pragmatic design left a number of key questions unanswered. “It’s a promising study that laudably recruited on an order of magnitude more infants than any like it in the past,” Dr. Soll said. “And the kids who got the therapy seemed to do better, which is exciting. But with the broad entry criteria, the lack of formal diagnosis of RDS, and the outcome measures ultimately potentially biased by lack of blinding, it doesn’t give us the answers we need yet to consider aerosolized treatment.”
ONY Biotech, manufacturer of the study drug Infasurf, sponsored the trial. Dr. Cummings and one coauthor disclosed consulting arrangements with the sponsor, and another coauthor is an employee of the sponsor. The remaining investigators had no relevant financial disclosures. Dr. Glaser and Dr. Wright disclosed no conflicts of interest related to their editorial; Dr. Wright’s work was supported by the National Institutes of Health. Dr. Soll is president of the Vermont Oxford Network and coordinating editor of Cochrane Neonatal.
SOURCE: Cummings JJ et al. Pediatrics. 2020;146(5):e2020021576.
Nebulized delivery of surfactant reduced the need for intubation and liquid surfactant administration by half among newborns with signs of respiratory distress syndrome, according to results from a large randomized, multicenter trial.
Neonatologists have long sought alternatives to intubation for administering surfactant to newborns with respiratory distress syndrome (RDS). An effective noninvasive aerosolized treatment has remained elusive, with small clinical trials that have produced mixed results.
In research published in Pediatrics, James J. Cummings, MD, of Albany (N.Y.) Medical Center, and colleagues, randomized 457 infants (mean 33 weeks’ gestational age) with signs of RDS to either usual care or a nebulized bovine surfactant. Infants were recruited at 22 neonatal ICUs in the United States. Investigators were not blinded to treatment allocation and the decision to intubate was left up to the individual treating physician, because to do so, the authors wrote, would add “pragmatic strength” to the study, and “be ethically compliant with the infant’s best interest.”
Infants in the study received usual care or up to three treatments 4 or more hours apart of 35 mg/mL calfactant suspension, 210 mg phospholipid/kg body weight delivered into the mouth through a nebulizer modified with a pacifier. Dr. Cummings and colleagues found that intubation and liquid surfactant administration within the first 4 days after birth was 26% in the intervention group and 50% in the usual care group (P < .001).
The results remained significant after investigators adjusted for gestational age, birth weight, age when randomized, sex, delivery mode, and antenatal steroids. Rates of intubation for surfactant administration were lower for infants in the intervention group in all gestational age brackets except the youngest (23-24 weeks); all of these infants needed intubation. Respiratory support at days 3, 7, and 28 did not differ between study groups.
“Our study is the first to reveal the efficacy of an aerosolized surfactant delivery system that does not require a respiratory circuit interface,” the investigators wrote.
In previous trials of aerosolized surfactants, they noted, treatment was delivered with nasal continuous positive airway pressure. “By using a separate, pacifier interface, both the aerosol delivery and [nasal continuous positive airway pressure] flow can be managed independently, which should allow for safer patient care.”
Dr. Cummings and colleagues also acknowledged several important limitations of their study, including its nonmasked, nonblinded design, and that it enrolled few infants with less than 28 weeks’ gestation. It takes 1-2 hours to deliver aerosolized calfactant, and “we did not want to delay definitive treatment.”
In an editorial comment accompanying the study, Kirsten Glaser, MD, of the University of Leipzig (Germany), and Clyde Wright, MD of the University of Colorado at Denver, Aurora, called the results promising. “Importantly, application of surfactant aerosols was well tolerated by using a modified nebulizer with a pacifier interface.”
“Clinicians were aware that every infant randomly assigned to the nebulized surfactant arm received the intervention,” they wrote. “It is possible that clinicians delayed intubation and endotracheal surfactant instillation in this group, being biased by aerosolization and the hypothesis of lower risk of air leak and lung injury.”
Dr. Glaser and Dr. Wright further lamented that there were no formal criteria for administering surfactant therapy, and that the infants in the study might not be representative of those most in need of treatment. Today, bronchopulmonary dysplasia “primarily affects infants born at less than 28 weeks’ gestational age,” a minority of the infants recruited for this study, they wrote, urging further investigation in this patient group.
In an interview, neonatologist Roger F. Soll, MD, the H. Wallace Professor of Neonatology at the Larner College of Medicine at University of Vermont in Burlington, echoed the editorialists’ concerns that the study’s pragmatic design left a number of key questions unanswered. “It’s a promising study that laudably recruited on an order of magnitude more infants than any like it in the past,” Dr. Soll said. “And the kids who got the therapy seemed to do better, which is exciting. But with the broad entry criteria, the lack of formal diagnosis of RDS, and the outcome measures ultimately potentially biased by lack of blinding, it doesn’t give us the answers we need yet to consider aerosolized treatment.”
ONY Biotech, manufacturer of the study drug Infasurf, sponsored the trial. Dr. Cummings and one coauthor disclosed consulting arrangements with the sponsor, and another coauthor is an employee of the sponsor. The remaining investigators had no relevant financial disclosures. Dr. Glaser and Dr. Wright disclosed no conflicts of interest related to their editorial; Dr. Wright’s work was supported by the National Institutes of Health. Dr. Soll is president of the Vermont Oxford Network and coordinating editor of Cochrane Neonatal.
SOURCE: Cummings JJ et al. Pediatrics. 2020;146(5):e2020021576.
Nebulized delivery of surfactant reduced the need for intubation and liquid surfactant administration by half among newborns with signs of respiratory distress syndrome, according to results from a large randomized, multicenter trial.
Neonatologists have long sought alternatives to intubation for administering surfactant to newborns with respiratory distress syndrome (RDS). An effective noninvasive aerosolized treatment has remained elusive, with small clinical trials that have produced mixed results.
In research published in Pediatrics, James J. Cummings, MD, of Albany (N.Y.) Medical Center, and colleagues, randomized 457 infants (mean 33 weeks’ gestational age) with signs of RDS to either usual care or a nebulized bovine surfactant. Infants were recruited at 22 neonatal ICUs in the United States. Investigators were not blinded to treatment allocation and the decision to intubate was left up to the individual treating physician, because to do so, the authors wrote, would add “pragmatic strength” to the study, and “be ethically compliant with the infant’s best interest.”
Infants in the study received usual care or up to three treatments 4 or more hours apart of 35 mg/mL calfactant suspension, 210 mg phospholipid/kg body weight delivered into the mouth through a nebulizer modified with a pacifier. Dr. Cummings and colleagues found that intubation and liquid surfactant administration within the first 4 days after birth was 26% in the intervention group and 50% in the usual care group (P < .001).
The results remained significant after investigators adjusted for gestational age, birth weight, age when randomized, sex, delivery mode, and antenatal steroids. Rates of intubation for surfactant administration were lower for infants in the intervention group in all gestational age brackets except the youngest (23-24 weeks); all of these infants needed intubation. Respiratory support at days 3, 7, and 28 did not differ between study groups.
“Our study is the first to reveal the efficacy of an aerosolized surfactant delivery system that does not require a respiratory circuit interface,” the investigators wrote.
In previous trials of aerosolized surfactants, they noted, treatment was delivered with nasal continuous positive airway pressure. “By using a separate, pacifier interface, both the aerosol delivery and [nasal continuous positive airway pressure] flow can be managed independently, which should allow for safer patient care.”
Dr. Cummings and colleagues also acknowledged several important limitations of their study, including its nonmasked, nonblinded design, and that it enrolled few infants with less than 28 weeks’ gestation. It takes 1-2 hours to deliver aerosolized calfactant, and “we did not want to delay definitive treatment.”
In an editorial comment accompanying the study, Kirsten Glaser, MD, of the University of Leipzig (Germany), and Clyde Wright, MD of the University of Colorado at Denver, Aurora, called the results promising. “Importantly, application of surfactant aerosols was well tolerated by using a modified nebulizer with a pacifier interface.”
“Clinicians were aware that every infant randomly assigned to the nebulized surfactant arm received the intervention,” they wrote. “It is possible that clinicians delayed intubation and endotracheal surfactant instillation in this group, being biased by aerosolization and the hypothesis of lower risk of air leak and lung injury.”
Dr. Glaser and Dr. Wright further lamented that there were no formal criteria for administering surfactant therapy, and that the infants in the study might not be representative of those most in need of treatment. Today, bronchopulmonary dysplasia “primarily affects infants born at less than 28 weeks’ gestational age,” a minority of the infants recruited for this study, they wrote, urging further investigation in this patient group.
In an interview, neonatologist Roger F. Soll, MD, the H. Wallace Professor of Neonatology at the Larner College of Medicine at University of Vermont in Burlington, echoed the editorialists’ concerns that the study’s pragmatic design left a number of key questions unanswered. “It’s a promising study that laudably recruited on an order of magnitude more infants than any like it in the past,” Dr. Soll said. “And the kids who got the therapy seemed to do better, which is exciting. But with the broad entry criteria, the lack of formal diagnosis of RDS, and the outcome measures ultimately potentially biased by lack of blinding, it doesn’t give us the answers we need yet to consider aerosolized treatment.”
ONY Biotech, manufacturer of the study drug Infasurf, sponsored the trial. Dr. Cummings and one coauthor disclosed consulting arrangements with the sponsor, and another coauthor is an employee of the sponsor. The remaining investigators had no relevant financial disclosures. Dr. Glaser and Dr. Wright disclosed no conflicts of interest related to their editorial; Dr. Wright’s work was supported by the National Institutes of Health. Dr. Soll is president of the Vermont Oxford Network and coordinating editor of Cochrane Neonatal.
SOURCE: Cummings JJ et al. Pediatrics. 2020;146(5):e2020021576.
FROM PEDIATRICS
Social factors predicted peripartum depressive symptoms in Black women with HIV
Women with high-risk pregnancies because of chronic conditions are at increased risk for developing postpartum depression, and HIV may be one such risk. However, risk factors for women living with HIV, particularly Black women, have not been well studied, wrote Emmanuela Nneamaka Ojukwu of the University of Miami School of Nursing, and colleagues.
Data suggest that as many as half of cases of postpartum depression (PPD) begin before delivery, the researchers noted. “Therefore, for this study, the symptoms of both PND (prenatal depression) and PPD have been classified in what we have termed peripartum depressive symptoms (PDS),” and defined as depressive symptoms during pregnancy and within 1 year postpartum, they said.
In a study published in the Archives of Psychiatric Nursing, the researchers conducted a secondary analysis of 143 Black women living with HIV seen at specialty prenatal and women’s health clinics in Miami.
Overall, 81 women (57%) reported either perinatal or postpartum depressive symptoms, or both. “Some of the symptoms prevalent among women in our study included restlessness, depressed mood, apathy, guilt, hopelessness, and social isolation,” the researchers said.
Social factors show significant impact
In a multivariate analysis, low income, intimate partner violence, and childcare burden were significant predictors of PDS (P less than .05). Women who reported intimate partner violence or abuse were 6.5 times more likely to experience PDS than were women who did not report abuse, and women with a childcare burden involving two children were 4.6 times more likely to experience PDS than were women with no childcare burden or only one child needing child care.
The average age of the women studied was 29 years, and 59% were above the federal poverty level. Nearly two-thirds (62%) were Black and 38% were Haitian; 63% were unemployed, 62% had a high school diploma or less, and 59% received care through Medicaid.
The researchers assessed four categories of health: HIV-related, gynecologic, obstetric, and psychosocial. The average viral load among the patients was 22,359 copies/mL at baseline, and they averaged 2.5 medical comorbidities. The most common comorbid conditions were other sexually transmitted infections and blood disorders, followed by cardiovascular and metabolic conditions.
Quantitative studies needed
Larger quantitative studies of Black pregnant women living with HIV are needed to analyze social factors at multiple levels, the researchers said. “To address depression among Black women living with HIV, local and federal governments should enact measures that increase the family income and diminish the prevalence of [intimate partner violence] among these women,” they said.
The study findings were limited by several factors including retrospective design and use of self-reports, as well as the small sample size and lack of generalizability to women living with HIV of other races or from other regions, the researchers noted. However, the results reflect data from previous studies and support the value of early screening and referral to improve well being for Black women living with HIV, as well as the importance of comprehensive medical care, they said.
“Women should be counseled that postpartum physical and psychological changes (and the stresses and demands of caring for a new baby) may make [antiretroviral] adherence more difficult and that additional support may be needed during this period,” the researchers wrote.
The study received no outside funding. The researchers had no financial conflicts to disclose.
SOURCE: Ojukwu EN et al. Arch Psychiatr Nurs. 2020 May 22. doi: 10.1016/j.apnu.2020.05.004.
Women with high-risk pregnancies because of chronic conditions are at increased risk for developing postpartum depression, and HIV may be one such risk. However, risk factors for women living with HIV, particularly Black women, have not been well studied, wrote Emmanuela Nneamaka Ojukwu of the University of Miami School of Nursing, and colleagues.
Data suggest that as many as half of cases of postpartum depression (PPD) begin before delivery, the researchers noted. “Therefore, for this study, the symptoms of both PND (prenatal depression) and PPD have been classified in what we have termed peripartum depressive symptoms (PDS),” and defined as depressive symptoms during pregnancy and within 1 year postpartum, they said.
In a study published in the Archives of Psychiatric Nursing, the researchers conducted a secondary analysis of 143 Black women living with HIV seen at specialty prenatal and women’s health clinics in Miami.
Overall, 81 women (57%) reported either perinatal or postpartum depressive symptoms, or both. “Some of the symptoms prevalent among women in our study included restlessness, depressed mood, apathy, guilt, hopelessness, and social isolation,” the researchers said.
Social factors show significant impact
In a multivariate analysis, low income, intimate partner violence, and childcare burden were significant predictors of PDS (P less than .05). Women who reported intimate partner violence or abuse were 6.5 times more likely to experience PDS than were women who did not report abuse, and women with a childcare burden involving two children were 4.6 times more likely to experience PDS than were women with no childcare burden or only one child needing child care.
The average age of the women studied was 29 years, and 59% were above the federal poverty level. Nearly two-thirds (62%) were Black and 38% were Haitian; 63% were unemployed, 62% had a high school diploma or less, and 59% received care through Medicaid.
The researchers assessed four categories of health: HIV-related, gynecologic, obstetric, and psychosocial. The average viral load among the patients was 22,359 copies/mL at baseline, and they averaged 2.5 medical comorbidities. The most common comorbid conditions were other sexually transmitted infections and blood disorders, followed by cardiovascular and metabolic conditions.
Quantitative studies needed
Larger quantitative studies of Black pregnant women living with HIV are needed to analyze social factors at multiple levels, the researchers said. “To address depression among Black women living with HIV, local and federal governments should enact measures that increase the family income and diminish the prevalence of [intimate partner violence] among these women,” they said.
The study findings were limited by several factors including retrospective design and use of self-reports, as well as the small sample size and lack of generalizability to women living with HIV of other races or from other regions, the researchers noted. However, the results reflect data from previous studies and support the value of early screening and referral to improve well being for Black women living with HIV, as well as the importance of comprehensive medical care, they said.
“Women should be counseled that postpartum physical and psychological changes (and the stresses and demands of caring for a new baby) may make [antiretroviral] adherence more difficult and that additional support may be needed during this period,” the researchers wrote.
The study received no outside funding. The researchers had no financial conflicts to disclose.
SOURCE: Ojukwu EN et al. Arch Psychiatr Nurs. 2020 May 22. doi: 10.1016/j.apnu.2020.05.004.
Women with high-risk pregnancies because of chronic conditions are at increased risk for developing postpartum depression, and HIV may be one such risk. However, risk factors for women living with HIV, particularly Black women, have not been well studied, wrote Emmanuela Nneamaka Ojukwu of the University of Miami School of Nursing, and colleagues.
Data suggest that as many as half of cases of postpartum depression (PPD) begin before delivery, the researchers noted. “Therefore, for this study, the symptoms of both PND (prenatal depression) and PPD have been classified in what we have termed peripartum depressive symptoms (PDS),” and defined as depressive symptoms during pregnancy and within 1 year postpartum, they said.
In a study published in the Archives of Psychiatric Nursing, the researchers conducted a secondary analysis of 143 Black women living with HIV seen at specialty prenatal and women’s health clinics in Miami.
Overall, 81 women (57%) reported either perinatal or postpartum depressive symptoms, or both. “Some of the symptoms prevalent among women in our study included restlessness, depressed mood, apathy, guilt, hopelessness, and social isolation,” the researchers said.
Social factors show significant impact
In a multivariate analysis, low income, intimate partner violence, and childcare burden were significant predictors of PDS (P less than .05). Women who reported intimate partner violence or abuse were 6.5 times more likely to experience PDS than were women who did not report abuse, and women with a childcare burden involving two children were 4.6 times more likely to experience PDS than were women with no childcare burden or only one child needing child care.
The average age of the women studied was 29 years, and 59% were above the federal poverty level. Nearly two-thirds (62%) were Black and 38% were Haitian; 63% were unemployed, 62% had a high school diploma or less, and 59% received care through Medicaid.
The researchers assessed four categories of health: HIV-related, gynecologic, obstetric, and psychosocial. The average viral load among the patients was 22,359 copies/mL at baseline, and they averaged 2.5 medical comorbidities. The most common comorbid conditions were other sexually transmitted infections and blood disorders, followed by cardiovascular and metabolic conditions.
Quantitative studies needed
Larger quantitative studies of Black pregnant women living with HIV are needed to analyze social factors at multiple levels, the researchers said. “To address depression among Black women living with HIV, local and federal governments should enact measures that increase the family income and diminish the prevalence of [intimate partner violence] among these women,” they said.
The study findings were limited by several factors including retrospective design and use of self-reports, as well as the small sample size and lack of generalizability to women living with HIV of other races or from other regions, the researchers noted. However, the results reflect data from previous studies and support the value of early screening and referral to improve well being for Black women living with HIV, as well as the importance of comprehensive medical care, they said.
“Women should be counseled that postpartum physical and psychological changes (and the stresses and demands of caring for a new baby) may make [antiretroviral] adherence more difficult and that additional support may be needed during this period,” the researchers wrote.
The study received no outside funding. The researchers had no financial conflicts to disclose.
SOURCE: Ojukwu EN et al. Arch Psychiatr Nurs. 2020 May 22. doi: 10.1016/j.apnu.2020.05.004.
FROM ARCHIVES OF PSYCHIATRIC NURSING
Rural areas with local obstetrical care have better perinatal outcomes
according to a retrospective study using county-level data from the Alabama Department of Public Health.
Although association does not establish causation, these data raise concern “for the current trend of diminishing L&D units that is occurring in many rural settings,” according to the authors of the study, led by John B. Waits, MD, of Cahaba Medical Care, Centreville, Ala., in Annals of Family Medicine.
When mortality per 1,000 live births was compared over a 15-year period (2003-2017) between 15 counties with and 21 counties without local L&D units, those with the units had lower overall infant mortality (9.23 vs. 7.89; P = .0011), perinatal mortality (8.89 vs. 10.82; P < .001), and neonatal mortality (4.74 vs. 5.67; P = .0034). The percentages of low-birth-weight babies born between 2003 and 2014 were 9.86% versus 10.61% (P < .001) for counties with and without L&D units, respectively.
The relative increased risks (RR) for these adverse outcomes in counties without L&D units were statistically significant and substantial, ranging from about 8% for a pregnancy resulting in a low-birth-weight infant to slightly more than 21% for perinatal mortality.
Over the study period, there were 165,525 live births in the 15 counties with L&D units and 72,177 births in the 21 counties with no such units. In counties without L&D units, the average proportion of White people was higher (73.47% vs. 60.86%), and that of African Americans was lower (22.76% vs. 36.23%). Median income ($40,759 vs. $35,604) and per capita income ($22,474 vs. $20,641) was slightly higher.
Of the 67 counties in Alabama, this study did not include those considered urbanized by the Alabama Office of Management and Budget even if classified rural by other statewide offices, such as the Alabama Rural Health Association. Any county with at least one L&D unit was considered to have a local unit. Three counties with L&D units that closed before the observation period was completed were excluded from the analysis.
The Alabama data appear to identify a major problem in need of an urgent solution, according to John S. Cullen, MD, a family physician in Valdez, Alaska, and chair of the American Academy of Family Physicians Board of Directors.
“Almost 20% of U.S. women of reproductive age live in rural communities,” he said in an interview. The data from this study provides compelling evidence “that the loss of rural maternity care in this country has contributed to the increase in newborn mortality in rural communities.”
There are many limitations for this study, according to the authors. They acknowledged that they could not control for many potentially important variables, such as travel time to hospitals for those in counties with L&D units when compared with those without. They also acknowledged the lack of data regarding availability of prenatal care in places with or without L&D units.
If lack of L&D services in rural areas is a source of adverse outcomes, data suggesting that the ongoing decline in L&D units are worrisome, according to the authors. Of studies they cited, one showed nearly a 10% loss in rural L&D services in a recent 10-year period.
The authors also noted that about half of the 3,143 counties in the United States do not have a practicing obstetrician, and that fewer than 7% of obstetricians-gynecologists practice in rural settings.
In many rural counties, including the county where the lead author practices, family practitioners provide 100% of local obstetric care, but access to these clinicians also appears to be declining, according to the paper. The ratio of primary care physicians to patients is already lower in non-metropolitan than metropolitan areas (39.8 vs. 53.3). The American Board of Family Medicine has reported that fewer than 10% of family physicians now provide maternity care, the authors wrote.
“If a causal relationship does exist [between lack of L&D units and adverse perinatal outcomes], then rural populations would definitively benefit from having local access to a L&D unit,” the authors stated.
The lead author, Dr. Waits, said in an interview that there are two obstacles to an increase in rural L&D units: malpractice premiums and reimbursement for indigent deliveries. The large malpractice premiums required to cover OB care are hurdles for caregivers, such as family physicians, as well as the hospitals where they practice.
Reforms from the legislative or regulatory perspective are needed to permit malpractice insurance to be issued at a reasonable cost, according to Dr. Waits. Such reforms are a “moral imperative” so that the malpractice issue is not allowed to “shipwreck infant and maternal mortality,” he said.
Of the many potential solutions, such as increased use of telemedicine, legislative initiatives to reduce the malpractice burden, or new support and incentives for family physicians to deliver OB care, each is burdened with obstacles to overcome, according to Dr. Waits. This does not mean these solutions should not be pursued alone or together, but he made it clear that the no solution is easy. In the meantime, Dr. Waits indicated a need to consider practical and immediate strategies to fix the problem.
“There should be incentives for rural emergency departments and ambulance systems to train in the [American Academy of Family Physicians’] Basic Life Support in Obstetrics (BLSO) certification courses each year. I am not aware of any specific evidence around this, but it is a known fact that, when L&Ds close, institutional memory of OB emergencies recede, and preparedness suffers,” he said.
Dr. Cullen agreed that if the closing of L&D units explains the higher rate of perinatal mortality in rural areas, both short-term and long-term solutions are needed.
“Every community must have a plan for obstetric and newborn emergencies. The decision to not offer maternity care means that rural providers will still provide maternity care but not be ready for emergencies,” he said, echoing a point made by Dr. Waits.
The study authors disclosed no conflicts. Dr. Cullen reported having no disclosures.
SOURCE: Waits JB et al. Ann Fam Med. 2020;18:446-51.
according to a retrospective study using county-level data from the Alabama Department of Public Health.
Although association does not establish causation, these data raise concern “for the current trend of diminishing L&D units that is occurring in many rural settings,” according to the authors of the study, led by John B. Waits, MD, of Cahaba Medical Care, Centreville, Ala., in Annals of Family Medicine.
When mortality per 1,000 live births was compared over a 15-year period (2003-2017) between 15 counties with and 21 counties without local L&D units, those with the units had lower overall infant mortality (9.23 vs. 7.89; P = .0011), perinatal mortality (8.89 vs. 10.82; P < .001), and neonatal mortality (4.74 vs. 5.67; P = .0034). The percentages of low-birth-weight babies born between 2003 and 2014 were 9.86% versus 10.61% (P < .001) for counties with and without L&D units, respectively.
The relative increased risks (RR) for these adverse outcomes in counties without L&D units were statistically significant and substantial, ranging from about 8% for a pregnancy resulting in a low-birth-weight infant to slightly more than 21% for perinatal mortality.
Over the study period, there were 165,525 live births in the 15 counties with L&D units and 72,177 births in the 21 counties with no such units. In counties without L&D units, the average proportion of White people was higher (73.47% vs. 60.86%), and that of African Americans was lower (22.76% vs. 36.23%). Median income ($40,759 vs. $35,604) and per capita income ($22,474 vs. $20,641) was slightly higher.
Of the 67 counties in Alabama, this study did not include those considered urbanized by the Alabama Office of Management and Budget even if classified rural by other statewide offices, such as the Alabama Rural Health Association. Any county with at least one L&D unit was considered to have a local unit. Three counties with L&D units that closed before the observation period was completed were excluded from the analysis.
The Alabama data appear to identify a major problem in need of an urgent solution, according to John S. Cullen, MD, a family physician in Valdez, Alaska, and chair of the American Academy of Family Physicians Board of Directors.
“Almost 20% of U.S. women of reproductive age live in rural communities,” he said in an interview. The data from this study provides compelling evidence “that the loss of rural maternity care in this country has contributed to the increase in newborn mortality in rural communities.”
There are many limitations for this study, according to the authors. They acknowledged that they could not control for many potentially important variables, such as travel time to hospitals for those in counties with L&D units when compared with those without. They also acknowledged the lack of data regarding availability of prenatal care in places with or without L&D units.
If lack of L&D services in rural areas is a source of adverse outcomes, data suggesting that the ongoing decline in L&D units are worrisome, according to the authors. Of studies they cited, one showed nearly a 10% loss in rural L&D services in a recent 10-year period.
The authors also noted that about half of the 3,143 counties in the United States do not have a practicing obstetrician, and that fewer than 7% of obstetricians-gynecologists practice in rural settings.
In many rural counties, including the county where the lead author practices, family practitioners provide 100% of local obstetric care, but access to these clinicians also appears to be declining, according to the paper. The ratio of primary care physicians to patients is already lower in non-metropolitan than metropolitan areas (39.8 vs. 53.3). The American Board of Family Medicine has reported that fewer than 10% of family physicians now provide maternity care, the authors wrote.
“If a causal relationship does exist [between lack of L&D units and adverse perinatal outcomes], then rural populations would definitively benefit from having local access to a L&D unit,” the authors stated.
The lead author, Dr. Waits, said in an interview that there are two obstacles to an increase in rural L&D units: malpractice premiums and reimbursement for indigent deliveries. The large malpractice premiums required to cover OB care are hurdles for caregivers, such as family physicians, as well as the hospitals where they practice.
Reforms from the legislative or regulatory perspective are needed to permit malpractice insurance to be issued at a reasonable cost, according to Dr. Waits. Such reforms are a “moral imperative” so that the malpractice issue is not allowed to “shipwreck infant and maternal mortality,” he said.
Of the many potential solutions, such as increased use of telemedicine, legislative initiatives to reduce the malpractice burden, or new support and incentives for family physicians to deliver OB care, each is burdened with obstacles to overcome, according to Dr. Waits. This does not mean these solutions should not be pursued alone or together, but he made it clear that the no solution is easy. In the meantime, Dr. Waits indicated a need to consider practical and immediate strategies to fix the problem.
“There should be incentives for rural emergency departments and ambulance systems to train in the [American Academy of Family Physicians’] Basic Life Support in Obstetrics (BLSO) certification courses each year. I am not aware of any specific evidence around this, but it is a known fact that, when L&Ds close, institutional memory of OB emergencies recede, and preparedness suffers,” he said.
Dr. Cullen agreed that if the closing of L&D units explains the higher rate of perinatal mortality in rural areas, both short-term and long-term solutions are needed.
“Every community must have a plan for obstetric and newborn emergencies. The decision to not offer maternity care means that rural providers will still provide maternity care but not be ready for emergencies,” he said, echoing a point made by Dr. Waits.
The study authors disclosed no conflicts. Dr. Cullen reported having no disclosures.
SOURCE: Waits JB et al. Ann Fam Med. 2020;18:446-51.
according to a retrospective study using county-level data from the Alabama Department of Public Health.
Although association does not establish causation, these data raise concern “for the current trend of diminishing L&D units that is occurring in many rural settings,” according to the authors of the study, led by John B. Waits, MD, of Cahaba Medical Care, Centreville, Ala., in Annals of Family Medicine.
When mortality per 1,000 live births was compared over a 15-year period (2003-2017) between 15 counties with and 21 counties without local L&D units, those with the units had lower overall infant mortality (9.23 vs. 7.89; P = .0011), perinatal mortality (8.89 vs. 10.82; P < .001), and neonatal mortality (4.74 vs. 5.67; P = .0034). The percentages of low-birth-weight babies born between 2003 and 2014 were 9.86% versus 10.61% (P < .001) for counties with and without L&D units, respectively.
The relative increased risks (RR) for these adverse outcomes in counties without L&D units were statistically significant and substantial, ranging from about 8% for a pregnancy resulting in a low-birth-weight infant to slightly more than 21% for perinatal mortality.
Over the study period, there were 165,525 live births in the 15 counties with L&D units and 72,177 births in the 21 counties with no such units. In counties without L&D units, the average proportion of White people was higher (73.47% vs. 60.86%), and that of African Americans was lower (22.76% vs. 36.23%). Median income ($40,759 vs. $35,604) and per capita income ($22,474 vs. $20,641) was slightly higher.
Of the 67 counties in Alabama, this study did not include those considered urbanized by the Alabama Office of Management and Budget even if classified rural by other statewide offices, such as the Alabama Rural Health Association. Any county with at least one L&D unit was considered to have a local unit. Three counties with L&D units that closed before the observation period was completed were excluded from the analysis.
The Alabama data appear to identify a major problem in need of an urgent solution, according to John S. Cullen, MD, a family physician in Valdez, Alaska, and chair of the American Academy of Family Physicians Board of Directors.
“Almost 20% of U.S. women of reproductive age live in rural communities,” he said in an interview. The data from this study provides compelling evidence “that the loss of rural maternity care in this country has contributed to the increase in newborn mortality in rural communities.”
There are many limitations for this study, according to the authors. They acknowledged that they could not control for many potentially important variables, such as travel time to hospitals for those in counties with L&D units when compared with those without. They also acknowledged the lack of data regarding availability of prenatal care in places with or without L&D units.
If lack of L&D services in rural areas is a source of adverse outcomes, data suggesting that the ongoing decline in L&D units are worrisome, according to the authors. Of studies they cited, one showed nearly a 10% loss in rural L&D services in a recent 10-year period.
The authors also noted that about half of the 3,143 counties in the United States do not have a practicing obstetrician, and that fewer than 7% of obstetricians-gynecologists practice in rural settings.
In many rural counties, including the county where the lead author practices, family practitioners provide 100% of local obstetric care, but access to these clinicians also appears to be declining, according to the paper. The ratio of primary care physicians to patients is already lower in non-metropolitan than metropolitan areas (39.8 vs. 53.3). The American Board of Family Medicine has reported that fewer than 10% of family physicians now provide maternity care, the authors wrote.
“If a causal relationship does exist [between lack of L&D units and adverse perinatal outcomes], then rural populations would definitively benefit from having local access to a L&D unit,” the authors stated.
The lead author, Dr. Waits, said in an interview that there are two obstacles to an increase in rural L&D units: malpractice premiums and reimbursement for indigent deliveries. The large malpractice premiums required to cover OB care are hurdles for caregivers, such as family physicians, as well as the hospitals where they practice.
Reforms from the legislative or regulatory perspective are needed to permit malpractice insurance to be issued at a reasonable cost, according to Dr. Waits. Such reforms are a “moral imperative” so that the malpractice issue is not allowed to “shipwreck infant and maternal mortality,” he said.
Of the many potential solutions, such as increased use of telemedicine, legislative initiatives to reduce the malpractice burden, or new support and incentives for family physicians to deliver OB care, each is burdened with obstacles to overcome, according to Dr. Waits. This does not mean these solutions should not be pursued alone or together, but he made it clear that the no solution is easy. In the meantime, Dr. Waits indicated a need to consider practical and immediate strategies to fix the problem.
“There should be incentives for rural emergency departments and ambulance systems to train in the [American Academy of Family Physicians’] Basic Life Support in Obstetrics (BLSO) certification courses each year. I am not aware of any specific evidence around this, but it is a known fact that, when L&Ds close, institutional memory of OB emergencies recede, and preparedness suffers,” he said.
Dr. Cullen agreed that if the closing of L&D units explains the higher rate of perinatal mortality in rural areas, both short-term and long-term solutions are needed.
“Every community must have a plan for obstetric and newborn emergencies. The decision to not offer maternity care means that rural providers will still provide maternity care but not be ready for emergencies,” he said, echoing a point made by Dr. Waits.
The study authors disclosed no conflicts. Dr. Cullen reported having no disclosures.
SOURCE: Waits JB et al. Ann Fam Med. 2020;18:446-51.
FROM ANNALS OF FAMILY MEDICINE
Key clinical point: The absence of labor and delivery (L&D) services in rural counties predicts adverse outcomes, including higher child mortality.
Major finding: In the absence of L&D units, the risk of perinatal mortality per 1,000 live births is 19% higher (5.67 vs. 4.74; P = .0034).
Data Source: Retrospective cohort study.
Disclosures: Potential conflicts of interest involving this topic were not reported.
Source: Waits JB et al. Ann Fam Med. 2020;18:446-51.
More research needed on how fetal exposure affects later development
The number of genes in humans seems inadequate to account for the diversity seen in people. While maternal and paternal factors do play a role in the development of offspring, increased attention is being paid to the forces that express these genes and the impact they have on the health of a person, including development of psychiatric conditions, according to Dolores Malaspina, MD.
Epigenetics, or changes that occur in a fetal phenotype that do not involve changes to the genotype, involve factors such as DNA methylation to control gene expression, histone modification or the wrapping of genes, or the silencing and activation of certain genes with noncoding RNA-associated factors, said Dr. Malaspina of the Icahn School of Medicine at Mount Sinai, New York.
When this occurs during pregnancy, “the fetus does not simply develop from a genetic blueprint of the genes from its father and mother. Instead, signals are received throughout the pregnancy as to the health of the mother and signals about the environment,” she said in a virtual meeting presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
There is an evolutionary advantage to this so-called survival phenotype. “If, during the pregnancy, there’s a deficit of available nutrition, that may be a signal to the fetus that food will be scarce. In the setting of food scarcity, certain physiological adaptations during development can make the fetus more likely to survive to adulthood,” Dr. Malaspina said at the meeting, presented by Global Academy for Medical Education. But a fetus programmed to adapt to scarcity of food may also develop cardiovascular disease, metabolic disease, or mortality later in life if the prediction of scarce nutrition proved incorrect.
This approach to thinking about the developmental origins of health and disease, which examines how prenatal and perinatal exposure to environmental factors affect disease in adulthood, has also found a link between some exposures and psychiatric disorders. The most famous example, the Dutch Hunger Winter Families Study, found an increased risk of schizophrenia among children born during the height of the famine (Int J Epidemiol. 2007 Dec;36[6]:1196-204). During the Arab-Israeli war of 1967 (the Six-Day War), which took place in June, the fetuses of mothers who were pregnant during that month had a higher risk of schizophrenia if the fetus was in the second month (relative risk, 2.3; 95% confidence interval, 1.1-4.7) or third month (RR, 2.5; 95% CI, 1.2-5.2) of fetal life during June 1967, Dr. Malaspina and associates wrote (BMC Psychiatry. 2008 Aug 21;8:71).
“The key aspect is the ascertainment of individuals during a circumscribed period, the assessment and then the longitudinal follow-up,” she said. “Obviously, these are not easy studies to do, but enough of them have been done such that for the last decade at least, the general population should be aware of the developmental origins of health and disease.”
Maternal depression is another psychiatric condition that can serve as a prenatal exposure to adversity. A recent review found that children of women with untreated depression were 56% more likely to be born preterm and 96% more likely to have a low birth weight (Pediatr Res. 2019 Jan;85[2]:134-45). “Preterm birth and early birth along with low birth weight, these have ramifying effects throughout life, not only on neonatal and infant mortality, but on developmental disorders and lifetime morbidity,” she said. “These effects of maternal depression withstand all sorts of accounting for other correlated exposures, including maternal age and her medical complications or substance use.”
“The modulation of mood and affect can affect temperament and affect mental health. Studies exist linking maternal depression to autism, attention-deficit disorder, developmental delay, behavioral problems, sleep problems, externalizing behavior and depression, showing a very large effect of maternal depression on offspring well-being.”
To complicate matters, at least 15% of women will experience major depression during pregnancy, but of these, major depression is not being addressed in about half. Nonpharmacologic interventions can include cognitive-behavioral therapy and relaxation practices, but medication should be considered as well. “There’s an ongoing debate about whether antidepressant medications are harmful for the offspring,” she said. However, reviews conducted by Dr. Malaspina’s group have found low evidence of serious harm.
“My summary would be the depression itself holds much more evidence for disrupting offspring health and development than medications,” Dr. Malaspina said. “Most studies find no adverse birth effects when they properly controlled accounting for maternal age and the other conditions and other medications.”
Global Academy and this news organization are owned by the same parent company. Dr. Malaspina reported no relevant conflicts of interest.
The number of genes in humans seems inadequate to account for the diversity seen in people. While maternal and paternal factors do play a role in the development of offspring, increased attention is being paid to the forces that express these genes and the impact they have on the health of a person, including development of psychiatric conditions, according to Dolores Malaspina, MD.
Epigenetics, or changes that occur in a fetal phenotype that do not involve changes to the genotype, involve factors such as DNA methylation to control gene expression, histone modification or the wrapping of genes, or the silencing and activation of certain genes with noncoding RNA-associated factors, said Dr. Malaspina of the Icahn School of Medicine at Mount Sinai, New York.
When this occurs during pregnancy, “the fetus does not simply develop from a genetic blueprint of the genes from its father and mother. Instead, signals are received throughout the pregnancy as to the health of the mother and signals about the environment,” she said in a virtual meeting presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
There is an evolutionary advantage to this so-called survival phenotype. “If, during the pregnancy, there’s a deficit of available nutrition, that may be a signal to the fetus that food will be scarce. In the setting of food scarcity, certain physiological adaptations during development can make the fetus more likely to survive to adulthood,” Dr. Malaspina said at the meeting, presented by Global Academy for Medical Education. But a fetus programmed to adapt to scarcity of food may also develop cardiovascular disease, metabolic disease, or mortality later in life if the prediction of scarce nutrition proved incorrect.
This approach to thinking about the developmental origins of health and disease, which examines how prenatal and perinatal exposure to environmental factors affect disease in adulthood, has also found a link between some exposures and psychiatric disorders. The most famous example, the Dutch Hunger Winter Families Study, found an increased risk of schizophrenia among children born during the height of the famine (Int J Epidemiol. 2007 Dec;36[6]:1196-204). During the Arab-Israeli war of 1967 (the Six-Day War), which took place in June, the fetuses of mothers who were pregnant during that month had a higher risk of schizophrenia if the fetus was in the second month (relative risk, 2.3; 95% confidence interval, 1.1-4.7) or third month (RR, 2.5; 95% CI, 1.2-5.2) of fetal life during June 1967, Dr. Malaspina and associates wrote (BMC Psychiatry. 2008 Aug 21;8:71).
“The key aspect is the ascertainment of individuals during a circumscribed period, the assessment and then the longitudinal follow-up,” she said. “Obviously, these are not easy studies to do, but enough of them have been done such that for the last decade at least, the general population should be aware of the developmental origins of health and disease.”
Maternal depression is another psychiatric condition that can serve as a prenatal exposure to adversity. A recent review found that children of women with untreated depression were 56% more likely to be born preterm and 96% more likely to have a low birth weight (Pediatr Res. 2019 Jan;85[2]:134-45). “Preterm birth and early birth along with low birth weight, these have ramifying effects throughout life, not only on neonatal and infant mortality, but on developmental disorders and lifetime morbidity,” she said. “These effects of maternal depression withstand all sorts of accounting for other correlated exposures, including maternal age and her medical complications or substance use.”
“The modulation of mood and affect can affect temperament and affect mental health. Studies exist linking maternal depression to autism, attention-deficit disorder, developmental delay, behavioral problems, sleep problems, externalizing behavior and depression, showing a very large effect of maternal depression on offspring well-being.”
To complicate matters, at least 15% of women will experience major depression during pregnancy, but of these, major depression is not being addressed in about half. Nonpharmacologic interventions can include cognitive-behavioral therapy and relaxation practices, but medication should be considered as well. “There’s an ongoing debate about whether antidepressant medications are harmful for the offspring,” she said. However, reviews conducted by Dr. Malaspina’s group have found low evidence of serious harm.
“My summary would be the depression itself holds much more evidence for disrupting offspring health and development than medications,” Dr. Malaspina said. “Most studies find no adverse birth effects when they properly controlled accounting for maternal age and the other conditions and other medications.”
Global Academy and this news organization are owned by the same parent company. Dr. Malaspina reported no relevant conflicts of interest.
The number of genes in humans seems inadequate to account for the diversity seen in people. While maternal and paternal factors do play a role in the development of offspring, increased attention is being paid to the forces that express these genes and the impact they have on the health of a person, including development of psychiatric conditions, according to Dolores Malaspina, MD.
Epigenetics, or changes that occur in a fetal phenotype that do not involve changes to the genotype, involve factors such as DNA methylation to control gene expression, histone modification or the wrapping of genes, or the silencing and activation of certain genes with noncoding RNA-associated factors, said Dr. Malaspina of the Icahn School of Medicine at Mount Sinai, New York.
When this occurs during pregnancy, “the fetus does not simply develop from a genetic blueprint of the genes from its father and mother. Instead, signals are received throughout the pregnancy as to the health of the mother and signals about the environment,” she said in a virtual meeting presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
There is an evolutionary advantage to this so-called survival phenotype. “If, during the pregnancy, there’s a deficit of available nutrition, that may be a signal to the fetus that food will be scarce. In the setting of food scarcity, certain physiological adaptations during development can make the fetus more likely to survive to adulthood,” Dr. Malaspina said at the meeting, presented by Global Academy for Medical Education. But a fetus programmed to adapt to scarcity of food may also develop cardiovascular disease, metabolic disease, or mortality later in life if the prediction of scarce nutrition proved incorrect.
This approach to thinking about the developmental origins of health and disease, which examines how prenatal and perinatal exposure to environmental factors affect disease in adulthood, has also found a link between some exposures and psychiatric disorders. The most famous example, the Dutch Hunger Winter Families Study, found an increased risk of schizophrenia among children born during the height of the famine (Int J Epidemiol. 2007 Dec;36[6]:1196-204). During the Arab-Israeli war of 1967 (the Six-Day War), which took place in June, the fetuses of mothers who were pregnant during that month had a higher risk of schizophrenia if the fetus was in the second month (relative risk, 2.3; 95% confidence interval, 1.1-4.7) or third month (RR, 2.5; 95% CI, 1.2-5.2) of fetal life during June 1967, Dr. Malaspina and associates wrote (BMC Psychiatry. 2008 Aug 21;8:71).
“The key aspect is the ascertainment of individuals during a circumscribed period, the assessment and then the longitudinal follow-up,” she said. “Obviously, these are not easy studies to do, but enough of them have been done such that for the last decade at least, the general population should be aware of the developmental origins of health and disease.”
Maternal depression is another psychiatric condition that can serve as a prenatal exposure to adversity. A recent review found that children of women with untreated depression were 56% more likely to be born preterm and 96% more likely to have a low birth weight (Pediatr Res. 2019 Jan;85[2]:134-45). “Preterm birth and early birth along with low birth weight, these have ramifying effects throughout life, not only on neonatal and infant mortality, but on developmental disorders and lifetime morbidity,” she said. “These effects of maternal depression withstand all sorts of accounting for other correlated exposures, including maternal age and her medical complications or substance use.”
“The modulation of mood and affect can affect temperament and affect mental health. Studies exist linking maternal depression to autism, attention-deficit disorder, developmental delay, behavioral problems, sleep problems, externalizing behavior and depression, showing a very large effect of maternal depression on offspring well-being.”
To complicate matters, at least 15% of women will experience major depression during pregnancy, but of these, major depression is not being addressed in about half. Nonpharmacologic interventions can include cognitive-behavioral therapy and relaxation practices, but medication should be considered as well. “There’s an ongoing debate about whether antidepressant medications are harmful for the offspring,” she said. However, reviews conducted by Dr. Malaspina’s group have found low evidence of serious harm.
“My summary would be the depression itself holds much more evidence for disrupting offspring health and development than medications,” Dr. Malaspina said. “Most studies find no adverse birth effects when they properly controlled accounting for maternal age and the other conditions and other medications.”
Global Academy and this news organization are owned by the same parent company. Dr. Malaspina reported no relevant conflicts of interest.
FROM FOCUS ON NEUROPSYCHIATRY 2020
Health disparity: Race, mortality, and infants of teenage mothers
according to a new analysis from the National Center for Health Statistics.
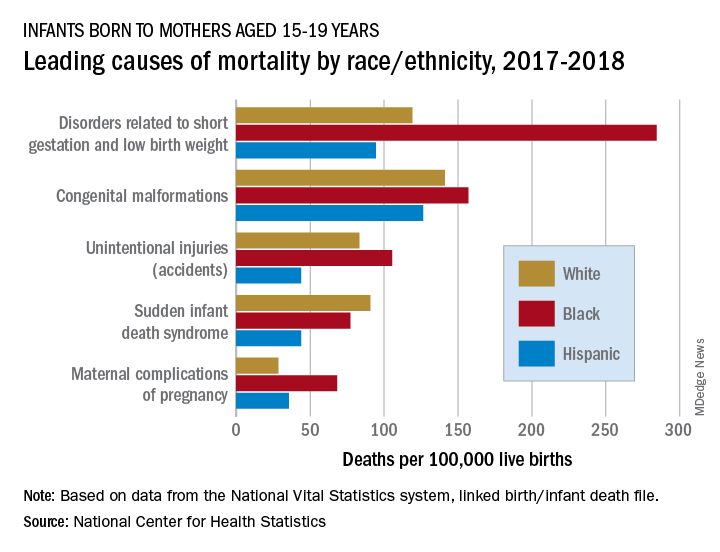
In 2017-2018, overall mortality rates were 12.5 per 100,000 live births for infants born to Black mothers aged 15-19 years, 8.4 per 100,000 for infants born to White teenagers, and 6.5 per 100,000 for those born to Hispanic teens, Ashley M. Woodall, MPH, and Anne K. Driscoll, PhD, of the NCHS said in a data brief.
Looking at the five leading causes of those deaths shows that deaths of Black infants were the highest by significant margins in four, although, when it comes to “disorders related to short gestation and low birth weight,” significant may be an understatement.
The rate of preterm/low-birth-weight deaths for white infants in 2017-2018 was 119 per 100,000 live births; for Hispanic infants it was 94 per 100,000. Among infants born to Black teenagers, however, it was 284 deaths per 100,000, they reported based on data from the National Vital Statistics System’s linked birth/infant death file.
The numbers for congenital malformations and accidents were closer but still significantly different, and with each of the three most common causes, the rates for infants of Hispanic mothers also were significantly lower than those of White infants, the researchers said.
The situation changes for mortality-cause No. 4, sudden infant death syndrome, which was significantly more common among infants born to White teenagers, with a rate of 91 deaths per 100,000 live births, compared with either black (77) or Hispanic (44) infants, Ms. Woodall and Dr. Driscoll said.
Infants born to Black teens had the highest death rate again (68 per 100,000) for maternal complications of pregnancy, the fifth-leading cause of mortality, but for the first time Hispanic infants had a higher rate (36) than did those of White teenagers (29), they reported.
according to a new analysis from the National Center for Health Statistics.
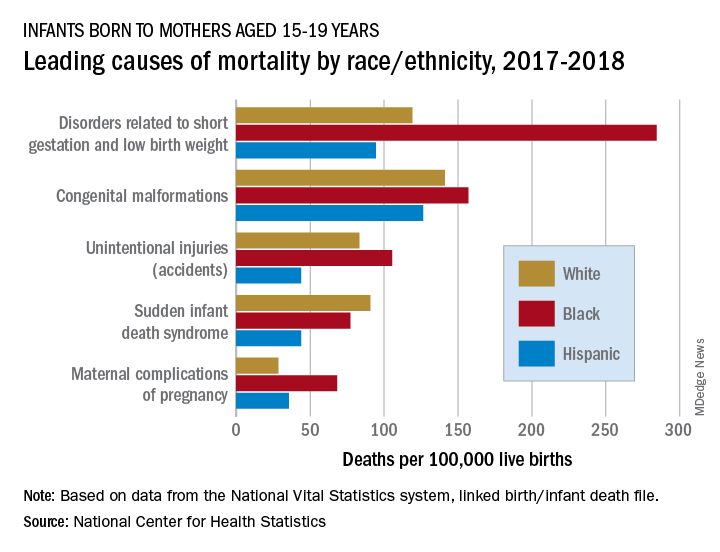
In 2017-2018, overall mortality rates were 12.5 per 100,000 live births for infants born to Black mothers aged 15-19 years, 8.4 per 100,000 for infants born to White teenagers, and 6.5 per 100,000 for those born to Hispanic teens, Ashley M. Woodall, MPH, and Anne K. Driscoll, PhD, of the NCHS said in a data brief.
Looking at the five leading causes of those deaths shows that deaths of Black infants were the highest by significant margins in four, although, when it comes to “disorders related to short gestation and low birth weight,” significant may be an understatement.
The rate of preterm/low-birth-weight deaths for white infants in 2017-2018 was 119 per 100,000 live births; for Hispanic infants it was 94 per 100,000. Among infants born to Black teenagers, however, it was 284 deaths per 100,000, they reported based on data from the National Vital Statistics System’s linked birth/infant death file.
The numbers for congenital malformations and accidents were closer but still significantly different, and with each of the three most common causes, the rates for infants of Hispanic mothers also were significantly lower than those of White infants, the researchers said.
The situation changes for mortality-cause No. 4, sudden infant death syndrome, which was significantly more common among infants born to White teenagers, with a rate of 91 deaths per 100,000 live births, compared with either black (77) or Hispanic (44) infants, Ms. Woodall and Dr. Driscoll said.
Infants born to Black teens had the highest death rate again (68 per 100,000) for maternal complications of pregnancy, the fifth-leading cause of mortality, but for the first time Hispanic infants had a higher rate (36) than did those of White teenagers (29), they reported.
according to a new analysis from the National Center for Health Statistics.
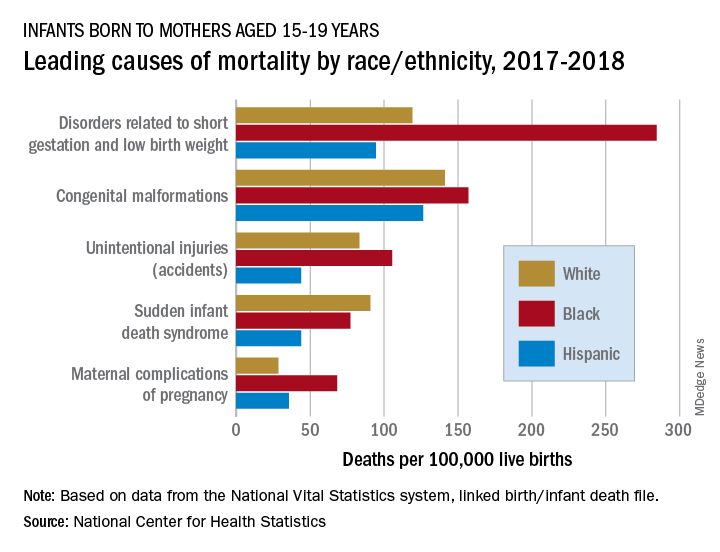
In 2017-2018, overall mortality rates were 12.5 per 100,000 live births for infants born to Black mothers aged 15-19 years, 8.4 per 100,000 for infants born to White teenagers, and 6.5 per 100,000 for those born to Hispanic teens, Ashley M. Woodall, MPH, and Anne K. Driscoll, PhD, of the NCHS said in a data brief.
Looking at the five leading causes of those deaths shows that deaths of Black infants were the highest by significant margins in four, although, when it comes to “disorders related to short gestation and low birth weight,” significant may be an understatement.
The rate of preterm/low-birth-weight deaths for white infants in 2017-2018 was 119 per 100,000 live births; for Hispanic infants it was 94 per 100,000. Among infants born to Black teenagers, however, it was 284 deaths per 100,000, they reported based on data from the National Vital Statistics System’s linked birth/infant death file.
The numbers for congenital malformations and accidents were closer but still significantly different, and with each of the three most common causes, the rates for infants of Hispanic mothers also were significantly lower than those of White infants, the researchers said.
The situation changes for mortality-cause No. 4, sudden infant death syndrome, which was significantly more common among infants born to White teenagers, with a rate of 91 deaths per 100,000 live births, compared with either black (77) or Hispanic (44) infants, Ms. Woodall and Dr. Driscoll said.
Infants born to Black teens had the highest death rate again (68 per 100,000) for maternal complications of pregnancy, the fifth-leading cause of mortality, but for the first time Hispanic infants had a higher rate (36) than did those of White teenagers (29), they reported.
Parental refusal of neonatal therapy a growing problem
according to an update at the virtual Pediatric Hospital Medicine virtual. This finding indicates the value of preparing policies and strategies to guide parents to appropriate medical decisions in advance.
“Elimination of nonmedical exceptions to vaccinations and intramuscular vitamin K made it into two of the AAP [American Academy of Pediatrics] top 10 public health resolutions, most likely because refusal rates are going up,” reported Ha N. Nguyen, MD, of the division of pediatric hospital medicine at Stanford (Calif.) University.
Importantly, state laws differ. For example, erythromycin ointment is mandated in neonates for prevention of gonococcal ophthalmia neonatorum in many states, including New York, where it can be administered without consent, according to Dr. Nguyen. Conversely, California does not mandate this preventive therapy even though the law does not offer medico-legal protection to providers if it is not given.
“There is a glaring gap in the way the [California] law was written,” said Dr. Nguyen, who used this as an example of why protocols and strategies to reduce risk of parental refusal of neonatal therapies should be informed by, and consistent with, state laws.
Because of the low levels of vitamin K in infants, the rate of bleeding within the first few months of life is nearly 2%, according to figures cited by Dr. Nguyen. It falls to less than 0.001% with administration of intramuscular vitamin K.
Families who refuse intramuscular vitamin K often state that they understand the risks, but data from a survey Dr. Nguyen cited found this is not necessarily true. In this survey, about two-thirds knew that bleeding was the risk, but less than 20% understood bleeding risks included intracranial hemorrhage, and less than 10% were aware that there was potential for a fatal outcome.
“This is a huge piece of the puzzle for counseling,” Dr. Nguyen said. “The discussion with parents should explicitly involve the explanation that the risks include brain bleeds and death.”
Although most infant bleeds attributed to low vitamin K stores are mucocutaneous or gastrointestinal, intracranial hemorrhage does occur, and these outcomes can be devastating. Up to 25% of infants who experience an intracranial hemorrhage die, while 60% of those who survive have some degree of neurodevelopmental impairment, according to Dr. Nguyen.
Oral vitamin K, which requires multiple doses, is not an appropriate substitute for the recommended single injection of the intramuscular formulation. The one study that compared intramuscular and oral vitamin K did not prove equivalence, and no oral vitamin K products have been approved by the Food and Drug Administration, Dr. Nguyen reported.
“We do know confidently that oral vitamin K does often result in poor adherence,” she said,
In a recent review article of parental vitamin K refusal, one of the most significant predictors of refusal of any recommended neonatal preventive treatment was refusal of another. According to data in that article, summarized by Dr. Nguyen, 68% of the parents who declined intramuscular vitamin K also declined erythromycin ointment, and more than 90% declined hepatitis B vaccine.
“One reason that many parents refuse the hepatitis B vaccine is that they do not think their child is at risk,” explained Kimberly Horstman, MD, from Stanford University and John Muir Medical Center in Walnut Creek, Calif.
Yet hepatitis B virus (HBV) infection, which is asymptomatic, can be acquired from many sources, including nonfamily contacts, according to Dr. Horstman.
“The AAP supports universal hepatitis B vaccine within 24 hours of birth for all infants over 2,000 g at birth,” Dr. Horstman said. In those weighing less, the vaccine is recommended within the first month of life.
The risk of parental refusal for recommended neonatal preventive medicines is higher among those with more education and higher income relative to those with less, Dr. Nguyen said. Other predictors include older maternal age, private insurance, and delivery by a midwife or at a birthing center.
Many parents who refuse preventive neonatal medications do not fully grasp what risks they are accepting by avoiding a recommended medication, according to both Dr. Nguyen and Dr. Horstman. In some cases, the goal is to protect their child from the pain of a needlestick, even when the health consequences might include far more invasive and painful therapies if the child develops the disease the medication would have prevented.
In the case of intramuscular vitamin K, “we encourage a presumptive approach,” Dr. Nguyen said. Concerns can then be addressed only if the parents refuse.
For another strategy, Dr. Nguyen recommended counseling parents about the need and value of preventive therapies during pregnancy. She cited data suggesting that it is more difficult to change the minds of parents after delivery.
Echoing this approach in regard to HBV vaccine, Dr. Horstman suggested encouraging colleagues, including obstetricians and community pediatricians, to raise and address this topic during prenatal counseling. By preparing parents for the recommended medications in the prenatal period, concerns can be addressed in advance.
The health risks posed by parents who refuse recommended medications is recognized by the Centers for Disease Control and Prevention. Both Dr. Horstman and Dr. Nguyen said there are handouts from the CDC and the AAP to inform parents of the purpose and benefit of recommended preventive therapies, as well as to equip caregivers with facts for effective counseling.
according to an update at the virtual Pediatric Hospital Medicine virtual. This finding indicates the value of preparing policies and strategies to guide parents to appropriate medical decisions in advance.
“Elimination of nonmedical exceptions to vaccinations and intramuscular vitamin K made it into two of the AAP [American Academy of Pediatrics] top 10 public health resolutions, most likely because refusal rates are going up,” reported Ha N. Nguyen, MD, of the division of pediatric hospital medicine at Stanford (Calif.) University.
Importantly, state laws differ. For example, erythromycin ointment is mandated in neonates for prevention of gonococcal ophthalmia neonatorum in many states, including New York, where it can be administered without consent, according to Dr. Nguyen. Conversely, California does not mandate this preventive therapy even though the law does not offer medico-legal protection to providers if it is not given.
“There is a glaring gap in the way the [California] law was written,” said Dr. Nguyen, who used this as an example of why protocols and strategies to reduce risk of parental refusal of neonatal therapies should be informed by, and consistent with, state laws.
Because of the low levels of vitamin K in infants, the rate of bleeding within the first few months of life is nearly 2%, according to figures cited by Dr. Nguyen. It falls to less than 0.001% with administration of intramuscular vitamin K.
Families who refuse intramuscular vitamin K often state that they understand the risks, but data from a survey Dr. Nguyen cited found this is not necessarily true. In this survey, about two-thirds knew that bleeding was the risk, but less than 20% understood bleeding risks included intracranial hemorrhage, and less than 10% were aware that there was potential for a fatal outcome.
“This is a huge piece of the puzzle for counseling,” Dr. Nguyen said. “The discussion with parents should explicitly involve the explanation that the risks include brain bleeds and death.”
Although most infant bleeds attributed to low vitamin K stores are mucocutaneous or gastrointestinal, intracranial hemorrhage does occur, and these outcomes can be devastating. Up to 25% of infants who experience an intracranial hemorrhage die, while 60% of those who survive have some degree of neurodevelopmental impairment, according to Dr. Nguyen.
Oral vitamin K, which requires multiple doses, is not an appropriate substitute for the recommended single injection of the intramuscular formulation. The one study that compared intramuscular and oral vitamin K did not prove equivalence, and no oral vitamin K products have been approved by the Food and Drug Administration, Dr. Nguyen reported.
“We do know confidently that oral vitamin K does often result in poor adherence,” she said,
In a recent review article of parental vitamin K refusal, one of the most significant predictors of refusal of any recommended neonatal preventive treatment was refusal of another. According to data in that article, summarized by Dr. Nguyen, 68% of the parents who declined intramuscular vitamin K also declined erythromycin ointment, and more than 90% declined hepatitis B vaccine.
“One reason that many parents refuse the hepatitis B vaccine is that they do not think their child is at risk,” explained Kimberly Horstman, MD, from Stanford University and John Muir Medical Center in Walnut Creek, Calif.
Yet hepatitis B virus (HBV) infection, which is asymptomatic, can be acquired from many sources, including nonfamily contacts, according to Dr. Horstman.
“The AAP supports universal hepatitis B vaccine within 24 hours of birth for all infants over 2,000 g at birth,” Dr. Horstman said. In those weighing less, the vaccine is recommended within the first month of life.
The risk of parental refusal for recommended neonatal preventive medicines is higher among those with more education and higher income relative to those with less, Dr. Nguyen said. Other predictors include older maternal age, private insurance, and delivery by a midwife or at a birthing center.
Many parents who refuse preventive neonatal medications do not fully grasp what risks they are accepting by avoiding a recommended medication, according to both Dr. Nguyen and Dr. Horstman. In some cases, the goal is to protect their child from the pain of a needlestick, even when the health consequences might include far more invasive and painful therapies if the child develops the disease the medication would have prevented.
In the case of intramuscular vitamin K, “we encourage a presumptive approach,” Dr. Nguyen said. Concerns can then be addressed only if the parents refuse.
For another strategy, Dr. Nguyen recommended counseling parents about the need and value of preventive therapies during pregnancy. She cited data suggesting that it is more difficult to change the minds of parents after delivery.
Echoing this approach in regard to HBV vaccine, Dr. Horstman suggested encouraging colleagues, including obstetricians and community pediatricians, to raise and address this topic during prenatal counseling. By preparing parents for the recommended medications in the prenatal period, concerns can be addressed in advance.
The health risks posed by parents who refuse recommended medications is recognized by the Centers for Disease Control and Prevention. Both Dr. Horstman and Dr. Nguyen said there are handouts from the CDC and the AAP to inform parents of the purpose and benefit of recommended preventive therapies, as well as to equip caregivers with facts for effective counseling.
according to an update at the virtual Pediatric Hospital Medicine virtual. This finding indicates the value of preparing policies and strategies to guide parents to appropriate medical decisions in advance.
“Elimination of nonmedical exceptions to vaccinations and intramuscular vitamin K made it into two of the AAP [American Academy of Pediatrics] top 10 public health resolutions, most likely because refusal rates are going up,” reported Ha N. Nguyen, MD, of the division of pediatric hospital medicine at Stanford (Calif.) University.
Importantly, state laws differ. For example, erythromycin ointment is mandated in neonates for prevention of gonococcal ophthalmia neonatorum in many states, including New York, where it can be administered without consent, according to Dr. Nguyen. Conversely, California does not mandate this preventive therapy even though the law does not offer medico-legal protection to providers if it is not given.
“There is a glaring gap in the way the [California] law was written,” said Dr. Nguyen, who used this as an example of why protocols and strategies to reduce risk of parental refusal of neonatal therapies should be informed by, and consistent with, state laws.
Because of the low levels of vitamin K in infants, the rate of bleeding within the first few months of life is nearly 2%, according to figures cited by Dr. Nguyen. It falls to less than 0.001% with administration of intramuscular vitamin K.
Families who refuse intramuscular vitamin K often state that they understand the risks, but data from a survey Dr. Nguyen cited found this is not necessarily true. In this survey, about two-thirds knew that bleeding was the risk, but less than 20% understood bleeding risks included intracranial hemorrhage, and less than 10% were aware that there was potential for a fatal outcome.
“This is a huge piece of the puzzle for counseling,” Dr. Nguyen said. “The discussion with parents should explicitly involve the explanation that the risks include brain bleeds and death.”
Although most infant bleeds attributed to low vitamin K stores are mucocutaneous or gastrointestinal, intracranial hemorrhage does occur, and these outcomes can be devastating. Up to 25% of infants who experience an intracranial hemorrhage die, while 60% of those who survive have some degree of neurodevelopmental impairment, according to Dr. Nguyen.
Oral vitamin K, which requires multiple doses, is not an appropriate substitute for the recommended single injection of the intramuscular formulation. The one study that compared intramuscular and oral vitamin K did not prove equivalence, and no oral vitamin K products have been approved by the Food and Drug Administration, Dr. Nguyen reported.
“We do know confidently that oral vitamin K does often result in poor adherence,” she said,
In a recent review article of parental vitamin K refusal, one of the most significant predictors of refusal of any recommended neonatal preventive treatment was refusal of another. According to data in that article, summarized by Dr. Nguyen, 68% of the parents who declined intramuscular vitamin K also declined erythromycin ointment, and more than 90% declined hepatitis B vaccine.
“One reason that many parents refuse the hepatitis B vaccine is that they do not think their child is at risk,” explained Kimberly Horstman, MD, from Stanford University and John Muir Medical Center in Walnut Creek, Calif.
Yet hepatitis B virus (HBV) infection, which is asymptomatic, can be acquired from many sources, including nonfamily contacts, according to Dr. Horstman.
“The AAP supports universal hepatitis B vaccine within 24 hours of birth for all infants over 2,000 g at birth,” Dr. Horstman said. In those weighing less, the vaccine is recommended within the first month of life.
The risk of parental refusal for recommended neonatal preventive medicines is higher among those with more education and higher income relative to those with less, Dr. Nguyen said. Other predictors include older maternal age, private insurance, and delivery by a midwife or at a birthing center.
Many parents who refuse preventive neonatal medications do not fully grasp what risks they are accepting by avoiding a recommended medication, according to both Dr. Nguyen and Dr. Horstman. In some cases, the goal is to protect their child from the pain of a needlestick, even when the health consequences might include far more invasive and painful therapies if the child develops the disease the medication would have prevented.
In the case of intramuscular vitamin K, “we encourage a presumptive approach,” Dr. Nguyen said. Concerns can then be addressed only if the parents refuse.
For another strategy, Dr. Nguyen recommended counseling parents about the need and value of preventive therapies during pregnancy. She cited data suggesting that it is more difficult to change the minds of parents after delivery.
Echoing this approach in regard to HBV vaccine, Dr. Horstman suggested encouraging colleagues, including obstetricians and community pediatricians, to raise and address this topic during prenatal counseling. By preparing parents for the recommended medications in the prenatal period, concerns can be addressed in advance.
The health risks posed by parents who refuse recommended medications is recognized by the Centers for Disease Control and Prevention. Both Dr. Horstman and Dr. Nguyen said there are handouts from the CDC and the AAP to inform parents of the purpose and benefit of recommended preventive therapies, as well as to equip caregivers with facts for effective counseling.
FROM PHM 2020
Small NY study: Mother-baby transmission of COVID-19 not seen
according to a study out of New York-Presbyterian Hospital.
“It is suggested in the cumulative data that the virus does not confer additional risk to the fetus during labor or during the early postnatal period in both preterm and term infants,” concluded Jeffrey Perlman, MB ChB, and colleagues in Pediatrics.
But other experts suggest substantial gaps remain in our understanding of maternal transmission of SARS-CoV-2.
“Much more needs to be known,” Munish Gupta, MD, and colleagues from Beth Israel Deaconess Medical Center and Harvard Medical School, Boston, said in an accompanying editorial.
The prospective study is the first to describe a cohort of U.S. COVID-19–related deliveries, with the prior neonatal impact of COVID-19 “almost exclusively” reported from China, noted the authors. They included a cohort of 326 women who were tested for SARS-CoV-2 on admission to labor and delivery at New York-Presbyterian Hospital between March 22 and April 15th, 2020. Of the 31 (10%) mothers who tested positive, 15 (48%) were asymptomatic and 16 (52%) were symptomatic.
Two babies were born prematurely (one by Cesarean) and were isolated in negative pressure rooms with continuous positive airway pressure. Both were moved out of isolation after two negative test results and “have exhibited an unremarkable clinical course,” the authors reported.
The other 29 term babies were cared for in their mothers’ rooms, with breastfeeding allowed, if desired. These babies and their mothers were discharged from the hospital between 24 and 48 hours after delivery.
“Visitor restriction for mothers who were positive for COVID-19 included 14 days of no visitation from the start of symptoms,” noted the team.
They added “since the prepublication release there have been a total of 47 mothers positive for COVID-19, resulting in 47 infants; 4 have been admitted to neonatal intensive care. In addition, 32 other infants have been tested for a variety of indications within the unit. All infants test results have been negative.”
The brief report outlined the institution’s checklist for delivery preparedness in either the operating room or labor delivery room, including personal protective equipment, resuscitation, transportation to the neonatal intensive care unit, and early postresuscitation care. “Suspected or confirmed COVID-19 alone in an otherwise uncomplicated pregnancy is not an indication for the resuscitation team or the neonatal fellow,” they noted, adding delivery room preparation and management should include contact precautions. “With scrupulous attention to infectious precautions, horizontal viral transmission should be minimized,” they advised.
Dr. Perlman and associates emphasized that rapid turnaround SARSCoV-2 testing is “crucial to minimize the likelihood of a provider becoming infected and/or infecting the infant.”
Although the findings are “clearly reassuring,” Dr. Gupta and colleagues have reservations. “To what extent does this report address concerns for infection risk with a rooming-in approach to care?” they asked in their accompanying editorial. “The answer is likely some, but not much.”
Many questions remain, they said, including: “What precautions were used to minimize infection risk during the postbirth hospital course? What was the approach to skin-to-skin care and direct mother-newborn contact? Were restrictions placed on family members? Were changes made to routine interventions such as hearing screens or circumcisions? What practices were in place around environmental cleaning? Most important, how did the newborns do after discharge?”
The current uncertainty around neonatal COVID-19 infection risk has led to “disparate” variations in care recommendations, they pointed out. Whereas China’s consensus guidelines recommend a 14-day separation of COVID-19–positive mothers from their healthy infants, a practice supported by the American Academy of Pediatrics “when possible,” the Italian Society of Neonatology, the Royal College of Paediatrics and Child Health, and the Canadian Paediatric Society advise “rooming-in and breastfeeding with appropriate infection prevention measures.”
Dr. Gupta and colleagues pointed to the following as at least three “critical and time-sensitive needs for research around neonatal care and outcomes related to COVID-19”:
- Studies need to have much larger sample sizes and include diverse populations. This will allow for reliable measurement of outcomes.
- Descriptions of care practices must be in detail, especially about infection prevention; these should be presented in a way to compare the efficacy of different approaches.
- There needs to be follow-up information on outcomes of both the mother and the neonate after the birth hospitalization.
Asked to comment, Lillian Beard, MD, of George Washington University in Washington welcomed the data as “good news.”
“Although small, the study was done during a 3-week peak period at the hottest spot of the pandemic in the United States during that period. It illustrates how delivery room preparedness, adequate personal protective equipment, and carefully planned infection control precautions can positively impact outcomes even during a seemingly impossible period,” she said.
“Although there are many uncertainties about maternal COVID-19 transmission and neonatal infection risks ... in my opinion, during the after birth hospitalization, the inherent benefits of rooming in for breast feeding and the opportunities for the demonstration and teaching of infection prevention practices for the family home, far outweigh the risks of disease transmission,” said Dr. Beard, who was not involved with the study.
The study and the commentary emphasize the likely low risk of vertical transmission of the virus, with horizontal transmission being the greater risk. However, cases of transplacental transmission have been reported, and the lead investigator of one recent placental study cautions against complacency.
“Neonates can get infected in both ways. The majority of cases seem to be horizontal, but those who have been infected or highly suspected to be vertically infected are not a small percentage either,” said Daniele de Luca, MD, PhD, president-elect of the European Society for Pediatric and Neonatal Intensive Care (ESPNIC) and a neonatologist at Antoine Béclère Hospital in Clamart, France.
“Perlman’s data are interesting and consistent with other reports around the world. However, two things must be remembered,” he said in an interview. “First, newborn infants are at relatively low risk from SARS-CoV-2 infections, but this is very far from zero risk. Neonatal SARS-CoV-2 infections do exist and have been described around the world. While they have a mild course in the majority of cases, neonatologists should not forget them and should be prepared to offer the best care to these babies.”
“Second, how this can be balanced with the need to promote breastfeeding and avoid overtreatment or separation from the mother is a question far from being answered. Gupta et al. in their commentary are right in saying that we have more questions than answers. While waiting for the results of large initiatives (such as the ESPNIC EPICENTRE Registry that they cite) to answer these open points, the best we can do is to provide a personalised case by case approach, transparent information to parents, and an open counselling informing clinical decisions.”
The study received no external funding. Dr. Perlman and associates had no financial disclosures. Dr. Gupta and colleagues had no relevant financial disclosures. Neither Dr. Beard nor Dr. de Luca had any relevant financial disclosures.
SOURCE: Perlman J et al. Pediatrics. 2020;146(2):e20201567.
according to a study out of New York-Presbyterian Hospital.
“It is suggested in the cumulative data that the virus does not confer additional risk to the fetus during labor or during the early postnatal period in both preterm and term infants,” concluded Jeffrey Perlman, MB ChB, and colleagues in Pediatrics.
But other experts suggest substantial gaps remain in our understanding of maternal transmission of SARS-CoV-2.
“Much more needs to be known,” Munish Gupta, MD, and colleagues from Beth Israel Deaconess Medical Center and Harvard Medical School, Boston, said in an accompanying editorial.
The prospective study is the first to describe a cohort of U.S. COVID-19–related deliveries, with the prior neonatal impact of COVID-19 “almost exclusively” reported from China, noted the authors. They included a cohort of 326 women who were tested for SARS-CoV-2 on admission to labor and delivery at New York-Presbyterian Hospital between March 22 and April 15th, 2020. Of the 31 (10%) mothers who tested positive, 15 (48%) were asymptomatic and 16 (52%) were symptomatic.
Two babies were born prematurely (one by Cesarean) and were isolated in negative pressure rooms with continuous positive airway pressure. Both were moved out of isolation after two negative test results and “have exhibited an unremarkable clinical course,” the authors reported.
The other 29 term babies were cared for in their mothers’ rooms, with breastfeeding allowed, if desired. These babies and their mothers were discharged from the hospital between 24 and 48 hours after delivery.
“Visitor restriction for mothers who were positive for COVID-19 included 14 days of no visitation from the start of symptoms,” noted the team.
They added “since the prepublication release there have been a total of 47 mothers positive for COVID-19, resulting in 47 infants; 4 have been admitted to neonatal intensive care. In addition, 32 other infants have been tested for a variety of indications within the unit. All infants test results have been negative.”
The brief report outlined the institution’s checklist for delivery preparedness in either the operating room or labor delivery room, including personal protective equipment, resuscitation, transportation to the neonatal intensive care unit, and early postresuscitation care. “Suspected or confirmed COVID-19 alone in an otherwise uncomplicated pregnancy is not an indication for the resuscitation team or the neonatal fellow,” they noted, adding delivery room preparation and management should include contact precautions. “With scrupulous attention to infectious precautions, horizontal viral transmission should be minimized,” they advised.
Dr. Perlman and associates emphasized that rapid turnaround SARSCoV-2 testing is “crucial to minimize the likelihood of a provider becoming infected and/or infecting the infant.”
Although the findings are “clearly reassuring,” Dr. Gupta and colleagues have reservations. “To what extent does this report address concerns for infection risk with a rooming-in approach to care?” they asked in their accompanying editorial. “The answer is likely some, but not much.”
Many questions remain, they said, including: “What precautions were used to minimize infection risk during the postbirth hospital course? What was the approach to skin-to-skin care and direct mother-newborn contact? Were restrictions placed on family members? Were changes made to routine interventions such as hearing screens or circumcisions? What practices were in place around environmental cleaning? Most important, how did the newborns do after discharge?”
The current uncertainty around neonatal COVID-19 infection risk has led to “disparate” variations in care recommendations, they pointed out. Whereas China’s consensus guidelines recommend a 14-day separation of COVID-19–positive mothers from their healthy infants, a practice supported by the American Academy of Pediatrics “when possible,” the Italian Society of Neonatology, the Royal College of Paediatrics and Child Health, and the Canadian Paediatric Society advise “rooming-in and breastfeeding with appropriate infection prevention measures.”
Dr. Gupta and colleagues pointed to the following as at least three “critical and time-sensitive needs for research around neonatal care and outcomes related to COVID-19”:
- Studies need to have much larger sample sizes and include diverse populations. This will allow for reliable measurement of outcomes.
- Descriptions of care practices must be in detail, especially about infection prevention; these should be presented in a way to compare the efficacy of different approaches.
- There needs to be follow-up information on outcomes of both the mother and the neonate after the birth hospitalization.
Asked to comment, Lillian Beard, MD, of George Washington University in Washington welcomed the data as “good news.”
“Although small, the study was done during a 3-week peak period at the hottest spot of the pandemic in the United States during that period. It illustrates how delivery room preparedness, adequate personal protective equipment, and carefully planned infection control precautions can positively impact outcomes even during a seemingly impossible period,” she said.
“Although there are many uncertainties about maternal COVID-19 transmission and neonatal infection risks ... in my opinion, during the after birth hospitalization, the inherent benefits of rooming in for breast feeding and the opportunities for the demonstration and teaching of infection prevention practices for the family home, far outweigh the risks of disease transmission,” said Dr. Beard, who was not involved with the study.
The study and the commentary emphasize the likely low risk of vertical transmission of the virus, with horizontal transmission being the greater risk. However, cases of transplacental transmission have been reported, and the lead investigator of one recent placental study cautions against complacency.
“Neonates can get infected in both ways. The majority of cases seem to be horizontal, but those who have been infected or highly suspected to be vertically infected are not a small percentage either,” said Daniele de Luca, MD, PhD, president-elect of the European Society for Pediatric and Neonatal Intensive Care (ESPNIC) and a neonatologist at Antoine Béclère Hospital in Clamart, France.
“Perlman’s data are interesting and consistent with other reports around the world. However, two things must be remembered,” he said in an interview. “First, newborn infants are at relatively low risk from SARS-CoV-2 infections, but this is very far from zero risk. Neonatal SARS-CoV-2 infections do exist and have been described around the world. While they have a mild course in the majority of cases, neonatologists should not forget them and should be prepared to offer the best care to these babies.”
“Second, how this can be balanced with the need to promote breastfeeding and avoid overtreatment or separation from the mother is a question far from being answered. Gupta et al. in their commentary are right in saying that we have more questions than answers. While waiting for the results of large initiatives (such as the ESPNIC EPICENTRE Registry that they cite) to answer these open points, the best we can do is to provide a personalised case by case approach, transparent information to parents, and an open counselling informing clinical decisions.”
The study received no external funding. Dr. Perlman and associates had no financial disclosures. Dr. Gupta and colleagues had no relevant financial disclosures. Neither Dr. Beard nor Dr. de Luca had any relevant financial disclosures.
SOURCE: Perlman J et al. Pediatrics. 2020;146(2):e20201567.
according to a study out of New York-Presbyterian Hospital.
“It is suggested in the cumulative data that the virus does not confer additional risk to the fetus during labor or during the early postnatal period in both preterm and term infants,” concluded Jeffrey Perlman, MB ChB, and colleagues in Pediatrics.
But other experts suggest substantial gaps remain in our understanding of maternal transmission of SARS-CoV-2.
“Much more needs to be known,” Munish Gupta, MD, and colleagues from Beth Israel Deaconess Medical Center and Harvard Medical School, Boston, said in an accompanying editorial.
The prospective study is the first to describe a cohort of U.S. COVID-19–related deliveries, with the prior neonatal impact of COVID-19 “almost exclusively” reported from China, noted the authors. They included a cohort of 326 women who were tested for SARS-CoV-2 on admission to labor and delivery at New York-Presbyterian Hospital between March 22 and April 15th, 2020. Of the 31 (10%) mothers who tested positive, 15 (48%) were asymptomatic and 16 (52%) were symptomatic.
Two babies were born prematurely (one by Cesarean) and were isolated in negative pressure rooms with continuous positive airway pressure. Both were moved out of isolation after two negative test results and “have exhibited an unremarkable clinical course,” the authors reported.
The other 29 term babies were cared for in their mothers’ rooms, with breastfeeding allowed, if desired. These babies and their mothers were discharged from the hospital between 24 and 48 hours after delivery.
“Visitor restriction for mothers who were positive for COVID-19 included 14 days of no visitation from the start of symptoms,” noted the team.
They added “since the prepublication release there have been a total of 47 mothers positive for COVID-19, resulting in 47 infants; 4 have been admitted to neonatal intensive care. In addition, 32 other infants have been tested for a variety of indications within the unit. All infants test results have been negative.”
The brief report outlined the institution’s checklist for delivery preparedness in either the operating room or labor delivery room, including personal protective equipment, resuscitation, transportation to the neonatal intensive care unit, and early postresuscitation care. “Suspected or confirmed COVID-19 alone in an otherwise uncomplicated pregnancy is not an indication for the resuscitation team or the neonatal fellow,” they noted, adding delivery room preparation and management should include contact precautions. “With scrupulous attention to infectious precautions, horizontal viral transmission should be minimized,” they advised.
Dr. Perlman and associates emphasized that rapid turnaround SARSCoV-2 testing is “crucial to minimize the likelihood of a provider becoming infected and/or infecting the infant.”
Although the findings are “clearly reassuring,” Dr. Gupta and colleagues have reservations. “To what extent does this report address concerns for infection risk with a rooming-in approach to care?” they asked in their accompanying editorial. “The answer is likely some, but not much.”
Many questions remain, they said, including: “What precautions were used to minimize infection risk during the postbirth hospital course? What was the approach to skin-to-skin care and direct mother-newborn contact? Were restrictions placed on family members? Were changes made to routine interventions such as hearing screens or circumcisions? What practices were in place around environmental cleaning? Most important, how did the newborns do after discharge?”
The current uncertainty around neonatal COVID-19 infection risk has led to “disparate” variations in care recommendations, they pointed out. Whereas China’s consensus guidelines recommend a 14-day separation of COVID-19–positive mothers from their healthy infants, a practice supported by the American Academy of Pediatrics “when possible,” the Italian Society of Neonatology, the Royal College of Paediatrics and Child Health, and the Canadian Paediatric Society advise “rooming-in and breastfeeding with appropriate infection prevention measures.”
Dr. Gupta and colleagues pointed to the following as at least three “critical and time-sensitive needs for research around neonatal care and outcomes related to COVID-19”:
- Studies need to have much larger sample sizes and include diverse populations. This will allow for reliable measurement of outcomes.
- Descriptions of care practices must be in detail, especially about infection prevention; these should be presented in a way to compare the efficacy of different approaches.
- There needs to be follow-up information on outcomes of both the mother and the neonate after the birth hospitalization.
Asked to comment, Lillian Beard, MD, of George Washington University in Washington welcomed the data as “good news.”
“Although small, the study was done during a 3-week peak period at the hottest spot of the pandemic in the United States during that period. It illustrates how delivery room preparedness, adequate personal protective equipment, and carefully planned infection control precautions can positively impact outcomes even during a seemingly impossible period,” she said.
“Although there are many uncertainties about maternal COVID-19 transmission and neonatal infection risks ... in my opinion, during the after birth hospitalization, the inherent benefits of rooming in for breast feeding and the opportunities for the demonstration and teaching of infection prevention practices for the family home, far outweigh the risks of disease transmission,” said Dr. Beard, who was not involved with the study.
The study and the commentary emphasize the likely low risk of vertical transmission of the virus, with horizontal transmission being the greater risk. However, cases of transplacental transmission have been reported, and the lead investigator of one recent placental study cautions against complacency.
“Neonates can get infected in both ways. The majority of cases seem to be horizontal, but those who have been infected or highly suspected to be vertically infected are not a small percentage either,” said Daniele de Luca, MD, PhD, president-elect of the European Society for Pediatric and Neonatal Intensive Care (ESPNIC) and a neonatologist at Antoine Béclère Hospital in Clamart, France.
“Perlman’s data are interesting and consistent with other reports around the world. However, two things must be remembered,” he said in an interview. “First, newborn infants are at relatively low risk from SARS-CoV-2 infections, but this is very far from zero risk. Neonatal SARS-CoV-2 infections do exist and have been described around the world. While they have a mild course in the majority of cases, neonatologists should not forget them and should be prepared to offer the best care to these babies.”
“Second, how this can be balanced with the need to promote breastfeeding and avoid overtreatment or separation from the mother is a question far from being answered. Gupta et al. in their commentary are right in saying that we have more questions than answers. While waiting for the results of large initiatives (such as the ESPNIC EPICENTRE Registry that they cite) to answer these open points, the best we can do is to provide a personalised case by case approach, transparent information to parents, and an open counselling informing clinical decisions.”
The study received no external funding. Dr. Perlman and associates had no financial disclosures. Dr. Gupta and colleagues had no relevant financial disclosures. Neither Dr. Beard nor Dr. de Luca had any relevant financial disclosures.
SOURCE: Perlman J et al. Pediatrics. 2020;146(2):e20201567.
FROM PEDIATRICS
Ob.gyns. struggle to keep pace with changing COVID-19 knowledge
In early April, Maura Quinlan, MD, was working nights on the labor and delivery unit at Northwestern Medicine Prentice Women’s Hospital in Chicago. At the time, hospital policy was to test only patients with known COVID-19 symptoms for SARS-CoV-2. Women in labor wore N95 masks, but only while pushing – and practitioners didn’t always don proper protection in time.
Babies came and families rejoiced. But Dr. Quinlan looks back on those weeks with a degree of horror. “We were laboring a bunch of patients that probably had COVID,” she said, and they were doing so without proper protection.
She’s probably right. According to one study in the New England Journal of Medicine, 13.7% of 211 women who came into the labor and delivery unit at one New York City hospital between March 22 and April 2 were asymptomatic but infected, potentially putting staff and doctors at risk.
Dr. Quinlan already knew she and her fellow ob.gyns. had been walking a thin line and, upon seeing that research, her heart sank. In the middle of a pandemic, they had been racing to keep up with the reality of delivering babies. But despite their efforts to protect both practitioners and patients, some aspects slipped through the cracks. Today, every laboring patient admitted to Northwestern is now tested for the novel coronavirus.
Across the country, hospital labor and delivery wards have been working to find a careful and informed balance among multiple competing interests: the safety of their health care workers, the health of tiny and vulnerable new humans, and the stability of a birthing mother. Each hospital has been making the best decisions it can based on available data. The result is a patchwork of policies, but all of them center around rapid testing and appropriate protection.
Shifting recommendations
One case study of women in a New York City hospital during the height of the city’s surge found that, of seven confirmed COVID-19–positive patients, two were asymptomatic upon admission to the obstetrical service, and these same two patients ultimately required unplanned ICU admission. The women’s care prior to their positive diagnosis had exposed multiple health care workers, all of whom lacked appropriate personal protective equipment (PPE), the study authors wrote. “Further, five of seven confirmed COVID-19–positive women were afebrile on initial screen, and four did not first report a cough. In some locations where testing availability remains limited, the minimal symptoms reported for some of these cases might have been insufficient to prompt COVID-19 testing.”
As studies like this pour in, societies continue to update their recommendations accordingly. The latest guidance from the American College of Obstetricians and Gynecologists came on July 1. The group suggests testing all labor and delivery patients, particularly in high-prevalence areas. If tests are in short supply, it recommends prioritizing testing pregnant women with suspected COVID-19 and those who develop symptoms during admission.
At Northwestern, the hospital requests patients stay home and quarantine for the weeks leading up to their delivery date. Then, they rapidly test every patient who comes in for delivery and aim to have results available within a few hours.
The hospital’s 30-room labor and delivery wing remains reserved for patients who test negative. Those with positive COVID-19 results are sent to a 6-bed COVID labor and delivery unit elsewhere in the hospital. “We were lucky we had the space to do that, because smaller community hospitals wouldn’t have a separate unused unit where they could put these women,” Dr. Quinlan said.
In the COVID unit, women deliver without a support person – no partner, doula, or family member can join. Doctors and nurses wear full PPE and work only in that ward. And because some research shows that pregnant women who are asymptomatic or presymptomatic may develop symptoms quickly after starting labor with no measurable illness, Dr. Quinlan must decide on a case-by-case basis what to do, if anything at all.
Delaying an induction could allow the infection to resolve or it could result in her patient moving from presymptomatic disease to full-blown pneumonia. Accelerating labor could bring on symptoms or it could allow a mother to deliver safely and get out of the hospital as quickly as possible. “There is an advantage to having the baby now if you feel okay – even if it’s alone – and getting home,” Dr. Quinlan said.
The hospital also tests the partners of women who are COVID-19 positive. Those with negative results can take the newborn home and try to maintain distance until the mother is no longer symptomatic.
In different parts of the country, hospitals have developed different approaches. Southern California is experiencing its own surge, but at the Ronald Reagan University of California, Los Angeles, Medical Center there still haven’t been enough COVID-19 patients to warrant a separate labor and delivery unit.
At UCLA, staff swab patients when they enter the labor and delivery ward — those who test positive have specific room designations. For both COVID-19–positive patients and women who progress faster than test results can be returned, the goals are the same, said Rashmi Rao, MD, an ob.gyn. at UCLA: Deliver in the safest way possible for both mother and baby.
All women, positive or negative, must wear masks during labor – as much as they can tolerate, at least. For patients who are only mildly ill or asymptomatic, the only difference is that everyone wears protective gear. But if a patient’s oxygen levels dip, or her baby is in distress, the team moves more quickly to a cesarean delivery than they’d do with a healthy patient.
Just as hospital policies have been evolving, rules for visitors have been constantly changing too. Initially, UCLA allowed a support person to be present during delivery but had to leave immediately following. Now, each new mother is allowed one visitor for the duration of their stay. And the hospital suggests that patients who are COVID-19 positive recover in separate rooms from their babies and encourages them to maintain distance from their infants, except when breastfeeding.
“We respect and understand that this is a joyous occasion and we’re trying to keep families together as much as possible,” Dr. Rao said.
Care conundrums
How hospitals protect their smallest charges keeps changing too. Reports have been circulating about newborns being taken away from COVID-19-positive mothers, especially in marginalized communities. The stories have led many to worry they’d be forcibly separated from their babies. Most hospitals, however, leave it up to the woman and her doctors to decide how much separation is needed. “After delivery, it depends on how someone is feeling,” Dr. Rao said.
The American Academy of Pediatrics recommends that mothers who are COVID-19–positive pump breast milk and have a healthy caregiver use that milk, or formula, to bottle-feed the baby, with the new mother remaining 6 feet away from the child as much as she can. If that’s not possible, she should wear gloves and a mask while breastfeeding until she has been naturally afebrile for 72 hours and at least 1 week removed from the first appearance of her symptoms.
“It’s tragically hard,” said Dr. Quinlan, to keep a COVID-19–positive mother even 6 feet away from her newborn baby. “If a mother declines separation, we ask the acting pediatric team to discuss the theoretical risks and paucity of data.”
Until recently, research indicated that SARS-CoV-2 wasn’t being transmitted through the uterus from mothers to their babies. And despite a recent case study reporting transplacental transmission between a mother and her fetus in France, researchers still say that the risk of transference is low. To ensure newborn risk remains as low as possible, UCLA’s policy is to swab the baby when he/she is 24 hours old and keep watch for signs of infection: increased lethargy, difficulty waking, or gastrointestinal symptoms like vomiting.
Transmission via breast milk has also, to date, proven relatively unlikely. One study in The Lancet detected the novel coronavirus in breast milk, although it’s not clear that the virus can be passed on in the fluid, says Christina Chambers, PhD, a professor of pediatrics at the University of California, San Diego. Dr. Chambers is studying breast milk to see if the virus or antibodies to it are present. She is also investigating how infection with SARS-CoV-2 impacts women at different times in pregnancy, something that’s still an open question.
“[In] pregnant women with a deteriorating infection, the decisions are the same you would make with any delivery: Save the mom and save the baby,” Dr. Chambers said. “Beyond that, I am encouraged to see that pregnant women are prioritized to being tested,” something that will help researchers understand prevalence of disease in order to better understand whether some symptoms are more dangerous than others.
The situation is evolving so quickly that hospitals and providers are simply trying to stay abreast of the flood of new research. In the absence of definitive answers, they are using the information available and adjusting on the fly. “We are cautiously waiting for more data,” said Dr. Rao. “With the information we have we are doing the best we can to keep our patients safe. And we’re just going to keep at it.”
A version of this article originally appeared on Medscape.com.
In early April, Maura Quinlan, MD, was working nights on the labor and delivery unit at Northwestern Medicine Prentice Women’s Hospital in Chicago. At the time, hospital policy was to test only patients with known COVID-19 symptoms for SARS-CoV-2. Women in labor wore N95 masks, but only while pushing – and practitioners didn’t always don proper protection in time.
Babies came and families rejoiced. But Dr. Quinlan looks back on those weeks with a degree of horror. “We were laboring a bunch of patients that probably had COVID,” she said, and they were doing so without proper protection.
She’s probably right. According to one study in the New England Journal of Medicine, 13.7% of 211 women who came into the labor and delivery unit at one New York City hospital between March 22 and April 2 were asymptomatic but infected, potentially putting staff and doctors at risk.
Dr. Quinlan already knew she and her fellow ob.gyns. had been walking a thin line and, upon seeing that research, her heart sank. In the middle of a pandemic, they had been racing to keep up with the reality of delivering babies. But despite their efforts to protect both practitioners and patients, some aspects slipped through the cracks. Today, every laboring patient admitted to Northwestern is now tested for the novel coronavirus.
Across the country, hospital labor and delivery wards have been working to find a careful and informed balance among multiple competing interests: the safety of their health care workers, the health of tiny and vulnerable new humans, and the stability of a birthing mother. Each hospital has been making the best decisions it can based on available data. The result is a patchwork of policies, but all of them center around rapid testing and appropriate protection.
Shifting recommendations
One case study of women in a New York City hospital during the height of the city’s surge found that, of seven confirmed COVID-19–positive patients, two were asymptomatic upon admission to the obstetrical service, and these same two patients ultimately required unplanned ICU admission. The women’s care prior to their positive diagnosis had exposed multiple health care workers, all of whom lacked appropriate personal protective equipment (PPE), the study authors wrote. “Further, five of seven confirmed COVID-19–positive women were afebrile on initial screen, and four did not first report a cough. In some locations where testing availability remains limited, the minimal symptoms reported for some of these cases might have been insufficient to prompt COVID-19 testing.”
As studies like this pour in, societies continue to update their recommendations accordingly. The latest guidance from the American College of Obstetricians and Gynecologists came on July 1. The group suggests testing all labor and delivery patients, particularly in high-prevalence areas. If tests are in short supply, it recommends prioritizing testing pregnant women with suspected COVID-19 and those who develop symptoms during admission.
At Northwestern, the hospital requests patients stay home and quarantine for the weeks leading up to their delivery date. Then, they rapidly test every patient who comes in for delivery and aim to have results available within a few hours.
The hospital’s 30-room labor and delivery wing remains reserved for patients who test negative. Those with positive COVID-19 results are sent to a 6-bed COVID labor and delivery unit elsewhere in the hospital. “We were lucky we had the space to do that, because smaller community hospitals wouldn’t have a separate unused unit where they could put these women,” Dr. Quinlan said.
In the COVID unit, women deliver without a support person – no partner, doula, or family member can join. Doctors and nurses wear full PPE and work only in that ward. And because some research shows that pregnant women who are asymptomatic or presymptomatic may develop symptoms quickly after starting labor with no measurable illness, Dr. Quinlan must decide on a case-by-case basis what to do, if anything at all.
Delaying an induction could allow the infection to resolve or it could result in her patient moving from presymptomatic disease to full-blown pneumonia. Accelerating labor could bring on symptoms or it could allow a mother to deliver safely and get out of the hospital as quickly as possible. “There is an advantage to having the baby now if you feel okay – even if it’s alone – and getting home,” Dr. Quinlan said.
The hospital also tests the partners of women who are COVID-19 positive. Those with negative results can take the newborn home and try to maintain distance until the mother is no longer symptomatic.
In different parts of the country, hospitals have developed different approaches. Southern California is experiencing its own surge, but at the Ronald Reagan University of California, Los Angeles, Medical Center there still haven’t been enough COVID-19 patients to warrant a separate labor and delivery unit.
At UCLA, staff swab patients when they enter the labor and delivery ward — those who test positive have specific room designations. For both COVID-19–positive patients and women who progress faster than test results can be returned, the goals are the same, said Rashmi Rao, MD, an ob.gyn. at UCLA: Deliver in the safest way possible for both mother and baby.
All women, positive or negative, must wear masks during labor – as much as they can tolerate, at least. For patients who are only mildly ill or asymptomatic, the only difference is that everyone wears protective gear. But if a patient’s oxygen levels dip, or her baby is in distress, the team moves more quickly to a cesarean delivery than they’d do with a healthy patient.
Just as hospital policies have been evolving, rules for visitors have been constantly changing too. Initially, UCLA allowed a support person to be present during delivery but had to leave immediately following. Now, each new mother is allowed one visitor for the duration of their stay. And the hospital suggests that patients who are COVID-19 positive recover in separate rooms from their babies and encourages them to maintain distance from their infants, except when breastfeeding.
“We respect and understand that this is a joyous occasion and we’re trying to keep families together as much as possible,” Dr. Rao said.
Care conundrums
How hospitals protect their smallest charges keeps changing too. Reports have been circulating about newborns being taken away from COVID-19-positive mothers, especially in marginalized communities. The stories have led many to worry they’d be forcibly separated from their babies. Most hospitals, however, leave it up to the woman and her doctors to decide how much separation is needed. “After delivery, it depends on how someone is feeling,” Dr. Rao said.
The American Academy of Pediatrics recommends that mothers who are COVID-19–positive pump breast milk and have a healthy caregiver use that milk, or formula, to bottle-feed the baby, with the new mother remaining 6 feet away from the child as much as she can. If that’s not possible, she should wear gloves and a mask while breastfeeding until she has been naturally afebrile for 72 hours and at least 1 week removed from the first appearance of her symptoms.
“It’s tragically hard,” said Dr. Quinlan, to keep a COVID-19–positive mother even 6 feet away from her newborn baby. “If a mother declines separation, we ask the acting pediatric team to discuss the theoretical risks and paucity of data.”
Until recently, research indicated that SARS-CoV-2 wasn’t being transmitted through the uterus from mothers to their babies. And despite a recent case study reporting transplacental transmission between a mother and her fetus in France, researchers still say that the risk of transference is low. To ensure newborn risk remains as low as possible, UCLA’s policy is to swab the baby when he/she is 24 hours old and keep watch for signs of infection: increased lethargy, difficulty waking, or gastrointestinal symptoms like vomiting.
Transmission via breast milk has also, to date, proven relatively unlikely. One study in The Lancet detected the novel coronavirus in breast milk, although it’s not clear that the virus can be passed on in the fluid, says Christina Chambers, PhD, a professor of pediatrics at the University of California, San Diego. Dr. Chambers is studying breast milk to see if the virus or antibodies to it are present. She is also investigating how infection with SARS-CoV-2 impacts women at different times in pregnancy, something that’s still an open question.
“[In] pregnant women with a deteriorating infection, the decisions are the same you would make with any delivery: Save the mom and save the baby,” Dr. Chambers said. “Beyond that, I am encouraged to see that pregnant women are prioritized to being tested,” something that will help researchers understand prevalence of disease in order to better understand whether some symptoms are more dangerous than others.
The situation is evolving so quickly that hospitals and providers are simply trying to stay abreast of the flood of new research. In the absence of definitive answers, they are using the information available and adjusting on the fly. “We are cautiously waiting for more data,” said Dr. Rao. “With the information we have we are doing the best we can to keep our patients safe. And we’re just going to keep at it.”
A version of this article originally appeared on Medscape.com.
In early April, Maura Quinlan, MD, was working nights on the labor and delivery unit at Northwestern Medicine Prentice Women’s Hospital in Chicago. At the time, hospital policy was to test only patients with known COVID-19 symptoms for SARS-CoV-2. Women in labor wore N95 masks, but only while pushing – and practitioners didn’t always don proper protection in time.
Babies came and families rejoiced. But Dr. Quinlan looks back on those weeks with a degree of horror. “We were laboring a bunch of patients that probably had COVID,” she said, and they were doing so without proper protection.
She’s probably right. According to one study in the New England Journal of Medicine, 13.7% of 211 women who came into the labor and delivery unit at one New York City hospital between March 22 and April 2 were asymptomatic but infected, potentially putting staff and doctors at risk.
Dr. Quinlan already knew she and her fellow ob.gyns. had been walking a thin line and, upon seeing that research, her heart sank. In the middle of a pandemic, they had been racing to keep up with the reality of delivering babies. But despite their efforts to protect both practitioners and patients, some aspects slipped through the cracks. Today, every laboring patient admitted to Northwestern is now tested for the novel coronavirus.
Across the country, hospital labor and delivery wards have been working to find a careful and informed balance among multiple competing interests: the safety of their health care workers, the health of tiny and vulnerable new humans, and the stability of a birthing mother. Each hospital has been making the best decisions it can based on available data. The result is a patchwork of policies, but all of them center around rapid testing and appropriate protection.
Shifting recommendations
One case study of women in a New York City hospital during the height of the city’s surge found that, of seven confirmed COVID-19–positive patients, two were asymptomatic upon admission to the obstetrical service, and these same two patients ultimately required unplanned ICU admission. The women’s care prior to their positive diagnosis had exposed multiple health care workers, all of whom lacked appropriate personal protective equipment (PPE), the study authors wrote. “Further, five of seven confirmed COVID-19–positive women were afebrile on initial screen, and four did not first report a cough. In some locations where testing availability remains limited, the minimal symptoms reported for some of these cases might have been insufficient to prompt COVID-19 testing.”
As studies like this pour in, societies continue to update their recommendations accordingly. The latest guidance from the American College of Obstetricians and Gynecologists came on July 1. The group suggests testing all labor and delivery patients, particularly in high-prevalence areas. If tests are in short supply, it recommends prioritizing testing pregnant women with suspected COVID-19 and those who develop symptoms during admission.
At Northwestern, the hospital requests patients stay home and quarantine for the weeks leading up to their delivery date. Then, they rapidly test every patient who comes in for delivery and aim to have results available within a few hours.
The hospital’s 30-room labor and delivery wing remains reserved for patients who test negative. Those with positive COVID-19 results are sent to a 6-bed COVID labor and delivery unit elsewhere in the hospital. “We were lucky we had the space to do that, because smaller community hospitals wouldn’t have a separate unused unit where they could put these women,” Dr. Quinlan said.
In the COVID unit, women deliver without a support person – no partner, doula, or family member can join. Doctors and nurses wear full PPE and work only in that ward. And because some research shows that pregnant women who are asymptomatic or presymptomatic may develop symptoms quickly after starting labor with no measurable illness, Dr. Quinlan must decide on a case-by-case basis what to do, if anything at all.
Delaying an induction could allow the infection to resolve or it could result in her patient moving from presymptomatic disease to full-blown pneumonia. Accelerating labor could bring on symptoms or it could allow a mother to deliver safely and get out of the hospital as quickly as possible. “There is an advantage to having the baby now if you feel okay – even if it’s alone – and getting home,” Dr. Quinlan said.
The hospital also tests the partners of women who are COVID-19 positive. Those with negative results can take the newborn home and try to maintain distance until the mother is no longer symptomatic.
In different parts of the country, hospitals have developed different approaches. Southern California is experiencing its own surge, but at the Ronald Reagan University of California, Los Angeles, Medical Center there still haven’t been enough COVID-19 patients to warrant a separate labor and delivery unit.
At UCLA, staff swab patients when they enter the labor and delivery ward — those who test positive have specific room designations. For both COVID-19–positive patients and women who progress faster than test results can be returned, the goals are the same, said Rashmi Rao, MD, an ob.gyn. at UCLA: Deliver in the safest way possible for both mother and baby.
All women, positive or negative, must wear masks during labor – as much as they can tolerate, at least. For patients who are only mildly ill or asymptomatic, the only difference is that everyone wears protective gear. But if a patient’s oxygen levels dip, or her baby is in distress, the team moves more quickly to a cesarean delivery than they’d do with a healthy patient.
Just as hospital policies have been evolving, rules for visitors have been constantly changing too. Initially, UCLA allowed a support person to be present during delivery but had to leave immediately following. Now, each new mother is allowed one visitor for the duration of their stay. And the hospital suggests that patients who are COVID-19 positive recover in separate rooms from their babies and encourages them to maintain distance from their infants, except when breastfeeding.
“We respect and understand that this is a joyous occasion and we’re trying to keep families together as much as possible,” Dr. Rao said.
Care conundrums
How hospitals protect their smallest charges keeps changing too. Reports have been circulating about newborns being taken away from COVID-19-positive mothers, especially in marginalized communities. The stories have led many to worry they’d be forcibly separated from their babies. Most hospitals, however, leave it up to the woman and her doctors to decide how much separation is needed. “After delivery, it depends on how someone is feeling,” Dr. Rao said.
The American Academy of Pediatrics recommends that mothers who are COVID-19–positive pump breast milk and have a healthy caregiver use that milk, or formula, to bottle-feed the baby, with the new mother remaining 6 feet away from the child as much as she can. If that’s not possible, she should wear gloves and a mask while breastfeeding until she has been naturally afebrile for 72 hours and at least 1 week removed from the first appearance of her symptoms.
“It’s tragically hard,” said Dr. Quinlan, to keep a COVID-19–positive mother even 6 feet away from her newborn baby. “If a mother declines separation, we ask the acting pediatric team to discuss the theoretical risks and paucity of data.”
Until recently, research indicated that SARS-CoV-2 wasn’t being transmitted through the uterus from mothers to their babies. And despite a recent case study reporting transplacental transmission between a mother and her fetus in France, researchers still say that the risk of transference is low. To ensure newborn risk remains as low as possible, UCLA’s policy is to swab the baby when he/she is 24 hours old and keep watch for signs of infection: increased lethargy, difficulty waking, or gastrointestinal symptoms like vomiting.
Transmission via breast milk has also, to date, proven relatively unlikely. One study in The Lancet detected the novel coronavirus in breast milk, although it’s not clear that the virus can be passed on in the fluid, says Christina Chambers, PhD, a professor of pediatrics at the University of California, San Diego. Dr. Chambers is studying breast milk to see if the virus or antibodies to it are present. She is also investigating how infection with SARS-CoV-2 impacts women at different times in pregnancy, something that’s still an open question.
“[In] pregnant women with a deteriorating infection, the decisions are the same you would make with any delivery: Save the mom and save the baby,” Dr. Chambers said. “Beyond that, I am encouraged to see that pregnant women are prioritized to being tested,” something that will help researchers understand prevalence of disease in order to better understand whether some symptoms are more dangerous than others.
The situation is evolving so quickly that hospitals and providers are simply trying to stay abreast of the flood of new research. In the absence of definitive answers, they are using the information available and adjusting on the fly. “We are cautiously waiting for more data,” said Dr. Rao. “With the information we have we are doing the best we can to keep our patients safe. And we’re just going to keep at it.”
A version of this article originally appeared on Medscape.com.