User login
Start ART in first 3 months in infants with perinatal HIV
MADRID – Infants with perinatal HIV infection are significantly more likely to achieve viral suppression by age 12 months if they start antiretroviral therapy (ART) before age 3 months than if physicians wait until 3-6 months of age, Paolo Palma, MD, reported at the annual meeting of the European Society for Paediatric Infectious Diseases.
He presented a study of the factors associated with time to virologic sup
The purpose of this study was to identify the key factors involved in attaining early virologic control of perinatally acquired HIV. This information is necessary to lay the groundwork for planned future investigations of immunotherapeutic strategies designed to achieve sustained ART-free remission. Such strategies are most likely to be successful in very young children who have not yet built up a massive viral load, explained Dr. Palma of Bambino Gesù Children’s Hospital in Rome.
“A major obstacle to curing HIV infection is persistence of virus as integrated proviral DNA in long-lived cells even after many years on ART. ART-free HIV remission is more likely to occur if viral suppression is achieved very early in infection,” he said.
The median age of the 420 subjects at the time ART was initiated was 2.9 months. Their CD4 cell percentage was 34%, with a median CD4 cell count of 1,780 and an average viral load at baseline of 316,228 copies/mL.
At 12 months of age, 84% of patients had achieved viral suppression. In multivariate analyses adjusted for initial ART regimen and geographic location, three factors were associated with this outcome: younger age at ART onset, a lower baseline viral load, and a higher per
Indeed, for each 1-month increase in age at onset of ART, the likelihood of virologic response at age 12 months decreased by 16%. Similarly, the rate of virologic response at 1 year of age decreased by 15% for each 10 copies/mL increase in viral load at the start of ART. In contrast, the likelihood of virologic suppression at age 12 months increased by 10% for each 10% increase in CD4 cell percentage at the start of treatment.
Among the variables that proved unrelated to virologic suppression at 1 year of age were gender, AIDS status, feeding style (breastfed versus bottle-fed), and ethnicity.
Dr. Palma reported having no relevant financial disclosures.
MADRID – Infants with perinatal HIV infection are significantly more likely to achieve viral suppression by age 12 months if they start antiretroviral therapy (ART) before age 3 months than if physicians wait until 3-6 months of age, Paolo Palma, MD, reported at the annual meeting of the European Society for Paediatric Infectious Diseases.
He presented a study of the factors associated with time to virologic sup
The purpose of this study was to identify the key factors involved in attaining early virologic control of perinatally acquired HIV. This information is necessary to lay the groundwork for planned future investigations of immunotherapeutic strategies designed to achieve sustained ART-free remission. Such strategies are most likely to be successful in very young children who have not yet built up a massive viral load, explained Dr. Palma of Bambino Gesù Children’s Hospital in Rome.
“A major obstacle to curing HIV infection is persistence of virus as integrated proviral DNA in long-lived cells even after many years on ART. ART-free HIV remission is more likely to occur if viral suppression is achieved very early in infection,” he said.
The median age of the 420 subjects at the time ART was initiated was 2.9 months. Their CD4 cell percentage was 34%, with a median CD4 cell count of 1,780 and an average viral load at baseline of 316,228 copies/mL.
At 12 months of age, 84% of patients had achieved viral suppression. In multivariate analyses adjusted for initial ART regimen and geographic location, three factors were associated with this outcome: younger age at ART onset, a lower baseline viral load, and a higher per
Indeed, for each 1-month increase in age at onset of ART, the likelihood of virologic response at age 12 months decreased by 16%. Similarly, the rate of virologic response at 1 year of age decreased by 15% for each 10 copies/mL increase in viral load at the start of ART. In contrast, the likelihood of virologic suppression at age 12 months increased by 10% for each 10% increase in CD4 cell percentage at the start of treatment.
Among the variables that proved unrelated to virologic suppression at 1 year of age were gender, AIDS status, feeding style (breastfed versus bottle-fed), and ethnicity.
Dr. Palma reported having no relevant financial disclosures.
MADRID – Infants with perinatal HIV infection are significantly more likely to achieve viral suppression by age 12 months if they start antiretroviral therapy (ART) before age 3 months than if physicians wait until 3-6 months of age, Paolo Palma, MD, reported at the annual meeting of the European Society for Paediatric Infectious Diseases.
He presented a study of the factors associated with time to virologic sup
The purpose of this study was to identify the key factors involved in attaining early virologic control of perinatally acquired HIV. This information is necessary to lay the groundwork for planned future investigations of immunotherapeutic strategies designed to achieve sustained ART-free remission. Such strategies are most likely to be successful in very young children who have not yet built up a massive viral load, explained Dr. Palma of Bambino Gesù Children’s Hospital in Rome.
“A major obstacle to curing HIV infection is persistence of virus as integrated proviral DNA in long-lived cells even after many years on ART. ART-free HIV remission is more likely to occur if viral suppression is achieved very early in infection,” he said.
The median age of the 420 subjects at the time ART was initiated was 2.9 months. Their CD4 cell percentage was 34%, with a median CD4 cell count of 1,780 and an average viral load at baseline of 316,228 copies/mL.
At 12 months of age, 84% of patients had achieved viral suppression. In multivariate analyses adjusted for initial ART regimen and geographic location, three factors were associated with this outcome: younger age at ART onset, a lower baseline viral load, and a higher per
Indeed, for each 1-month increase in age at onset of ART, the likelihood of virologic response at age 12 months decreased by 16%. Similarly, the rate of virologic response at 1 year of age decreased by 15% for each 10 copies/mL increase in viral load at the start of ART. In contrast, the likelihood of virologic suppression at age 12 months increased by 10% for each 10% increase in CD4 cell percentage at the start of treatment.
Among the variables that proved unrelated to virologic suppression at 1 year of age were gender, AIDS status, feeding style (breastfed versus bottle-fed), and ethnicity.
Dr. Palma reported having no relevant financial disclosures.
AT ESPID 2017
Key clinical point:
Major finding: With each 1-month delay in starting antiretroviral therapy, the likelihood of attaining viral suppression by age 12 months drops by 16%.
Data source: This observational study included 420 infants with perinatally acquired HIV infection who began antiretroviral therapy prior to age 6 months.
Disclosures: Dr. Palma reported having no relevant financial disclosures.
Privacy and maternal records
At the undergraduate level, classes on medical ethics tend to focus on the big ticket items like abortion, euthanasia, and social justice. Personally, I find the more interesting clinical cases involve relatively minor issues that accumulate to create problems. Privacy is one example.
A large amount of information in the mother’s prenatal records potentially impacts a newborn’s care. Ideally, the EHR is transferring data to the newborn’s chart, but not everything automatically populates in the newborn record, so there will be times when a pediatrician needs to review the mother’s chart.
- The criteria for selecting which mothers’ charts to review involve racial profiling.
- Access to mental health records involving addiction treatment requires special authorization. State laws and hospital policies will vary.
- Mom is a Hollywood celebrity and, while reviewing her chart, prurient curiosity extends the search to records of her cosmetic surgeries.
In my opinion, most of what is and isn’t permissible is determined by medical custom and not by statutes. The judiciary reserves the power to intervene, so medical custom should be informed by laws and by legal principles. But, the primary basis for these decisions should be a commitment to patient advocacy and to common sense, which in this situation means, “Would the typical reasonable person be upset if she learned I had done something without telling her?” If the answer to that question is yes, or in any way equivocal, I think ethics would dictate obtaining consent or at least assent.
Opiate addiction has quadrupled in the past 15 years. Almost all states now have prescription registries to help detect doctor shopping, multiple prescribers, and misdirection. If you are prescribing an opiate, it is ethically reasonable (and now the law) for you to make writing the prescription contingent on your patient agreeing to your consulting the registry. No consent, no prescription.
I think the facts of that case (writing a prescription) can be distinguished (a legal term) from the case of a neonatologist accessing the narcotic registry of the mother while on a fishing expedition to find evidence that might help the baby. Perhaps it is okay with the mother’s uncoerced consent, but otherwise I think that practice reeks as an unreasonable search. Ethically and legally, it has parallels to Ferguson v. City of Charleston (SCOTUS 2001).
That was a 6-3 Supreme Court decision, so, while I agree with the majority, you may find hospital lawyers who disagree. Overall, I assert that consent and privacy are best considered ethically as advocacy for the patient and not as legalistic forms that the physician must complete.
The reverse situation also occurs. Sometimes maternal health information is placed into the newborn’s chart that doesn’t need to be there. For example, common practice has been to designate mom, after delivery, as G4P2022. This contains the information that mother has had two therapeutic abortions. Does that information belong in a newborn’s chart? Especially in the era of the EHR where this information will hang around forever and will be easily obtained by the baby 16 years later when she can access all her medical information online. Will the mother be upset for her teenage daughter to learn that mom has had two abortions? Is that private information, belonging to the mother, that was given in confidence to her obstetrician? I advocate respecting privacy.
I have similar concerns about STD information being transferred from maternal charts to the newborn’s EHR. A maternal history of gonorrhea treated 8 years previously is unlikely to be relevant and should not populate the newborn’s EHR. I can make an argument that chlamydia detected and treated during the pregnancy might be useful to the baby’s pediatrician because neither treatment nor tests of cure are perfect. Perhaps, it could exist as a Snapchat-type record and disappear from the newborn’s record in a year if no respiratory symptoms occur.
I’m aware of efforts to destigmatize abortion and STDs, but, until that occurs, sensitive information should be handled delicately to preserve privacy. That is a major component of the Hippocratic Oath.
Dr. Powell is a pediatric hospitalist and clinical ethics consultant living in St. Louis.
At the undergraduate level, classes on medical ethics tend to focus on the big ticket items like abortion, euthanasia, and social justice. Personally, I find the more interesting clinical cases involve relatively minor issues that accumulate to create problems. Privacy is one example.
A large amount of information in the mother’s prenatal records potentially impacts a newborn’s care. Ideally, the EHR is transferring data to the newborn’s chart, but not everything automatically populates in the newborn record, so there will be times when a pediatrician needs to review the mother’s chart.
- The criteria for selecting which mothers’ charts to review involve racial profiling.
- Access to mental health records involving addiction treatment requires special authorization. State laws and hospital policies will vary.
- Mom is a Hollywood celebrity and, while reviewing her chart, prurient curiosity extends the search to records of her cosmetic surgeries.
In my opinion, most of what is and isn’t permissible is determined by medical custom and not by statutes. The judiciary reserves the power to intervene, so medical custom should be informed by laws and by legal principles. But, the primary basis for these decisions should be a commitment to patient advocacy and to common sense, which in this situation means, “Would the typical reasonable person be upset if she learned I had done something without telling her?” If the answer to that question is yes, or in any way equivocal, I think ethics would dictate obtaining consent or at least assent.
Opiate addiction has quadrupled in the past 15 years. Almost all states now have prescription registries to help detect doctor shopping, multiple prescribers, and misdirection. If you are prescribing an opiate, it is ethically reasonable (and now the law) for you to make writing the prescription contingent on your patient agreeing to your consulting the registry. No consent, no prescription.
I think the facts of that case (writing a prescription) can be distinguished (a legal term) from the case of a neonatologist accessing the narcotic registry of the mother while on a fishing expedition to find evidence that might help the baby. Perhaps it is okay with the mother’s uncoerced consent, but otherwise I think that practice reeks as an unreasonable search. Ethically and legally, it has parallels to Ferguson v. City of Charleston (SCOTUS 2001).
That was a 6-3 Supreme Court decision, so, while I agree with the majority, you may find hospital lawyers who disagree. Overall, I assert that consent and privacy are best considered ethically as advocacy for the patient and not as legalistic forms that the physician must complete.
The reverse situation also occurs. Sometimes maternal health information is placed into the newborn’s chart that doesn’t need to be there. For example, common practice has been to designate mom, after delivery, as G4P2022. This contains the information that mother has had two therapeutic abortions. Does that information belong in a newborn’s chart? Especially in the era of the EHR where this information will hang around forever and will be easily obtained by the baby 16 years later when she can access all her medical information online. Will the mother be upset for her teenage daughter to learn that mom has had two abortions? Is that private information, belonging to the mother, that was given in confidence to her obstetrician? I advocate respecting privacy.
I have similar concerns about STD information being transferred from maternal charts to the newborn’s EHR. A maternal history of gonorrhea treated 8 years previously is unlikely to be relevant and should not populate the newborn’s EHR. I can make an argument that chlamydia detected and treated during the pregnancy might be useful to the baby’s pediatrician because neither treatment nor tests of cure are perfect. Perhaps, it could exist as a Snapchat-type record and disappear from the newborn’s record in a year if no respiratory symptoms occur.
I’m aware of efforts to destigmatize abortion and STDs, but, until that occurs, sensitive information should be handled delicately to preserve privacy. That is a major component of the Hippocratic Oath.
Dr. Powell is a pediatric hospitalist and clinical ethics consultant living in St. Louis.
At the undergraduate level, classes on medical ethics tend to focus on the big ticket items like abortion, euthanasia, and social justice. Personally, I find the more interesting clinical cases involve relatively minor issues that accumulate to create problems. Privacy is one example.
A large amount of information in the mother’s prenatal records potentially impacts a newborn’s care. Ideally, the EHR is transferring data to the newborn’s chart, but not everything automatically populates in the newborn record, so there will be times when a pediatrician needs to review the mother’s chart.
- The criteria for selecting which mothers’ charts to review involve racial profiling.
- Access to mental health records involving addiction treatment requires special authorization. State laws and hospital policies will vary.
- Mom is a Hollywood celebrity and, while reviewing her chart, prurient curiosity extends the search to records of her cosmetic surgeries.
In my opinion, most of what is and isn’t permissible is determined by medical custom and not by statutes. The judiciary reserves the power to intervene, so medical custom should be informed by laws and by legal principles. But, the primary basis for these decisions should be a commitment to patient advocacy and to common sense, which in this situation means, “Would the typical reasonable person be upset if she learned I had done something without telling her?” If the answer to that question is yes, or in any way equivocal, I think ethics would dictate obtaining consent or at least assent.
Opiate addiction has quadrupled in the past 15 years. Almost all states now have prescription registries to help detect doctor shopping, multiple prescribers, and misdirection. If you are prescribing an opiate, it is ethically reasonable (and now the law) for you to make writing the prescription contingent on your patient agreeing to your consulting the registry. No consent, no prescription.
I think the facts of that case (writing a prescription) can be distinguished (a legal term) from the case of a neonatologist accessing the narcotic registry of the mother while on a fishing expedition to find evidence that might help the baby. Perhaps it is okay with the mother’s uncoerced consent, but otherwise I think that practice reeks as an unreasonable search. Ethically and legally, it has parallels to Ferguson v. City of Charleston (SCOTUS 2001).
That was a 6-3 Supreme Court decision, so, while I agree with the majority, you may find hospital lawyers who disagree. Overall, I assert that consent and privacy are best considered ethically as advocacy for the patient and not as legalistic forms that the physician must complete.
The reverse situation also occurs. Sometimes maternal health information is placed into the newborn’s chart that doesn’t need to be there. For example, common practice has been to designate mom, after delivery, as G4P2022. This contains the information that mother has had two therapeutic abortions. Does that information belong in a newborn’s chart? Especially in the era of the EHR where this information will hang around forever and will be easily obtained by the baby 16 years later when she can access all her medical information online. Will the mother be upset for her teenage daughter to learn that mom has had two abortions? Is that private information, belonging to the mother, that was given in confidence to her obstetrician? I advocate respecting privacy.
I have similar concerns about STD information being transferred from maternal charts to the newborn’s EHR. A maternal history of gonorrhea treated 8 years previously is unlikely to be relevant and should not populate the newborn’s EHR. I can make an argument that chlamydia detected and treated during the pregnancy might be useful to the baby’s pediatrician because neither treatment nor tests of cure are perfect. Perhaps, it could exist as a Snapchat-type record and disappear from the newborn’s record in a year if no respiratory symptoms occur.
I’m aware of efforts to destigmatize abortion and STDs, but, until that occurs, sensitive information should be handled delicately to preserve privacy. That is a major component of the Hippocratic Oath.
Dr. Powell is a pediatric hospitalist and clinical ethics consultant living in St. Louis.
Fifty-year retrospective by Dr. William G. Wilkoff
When the first issue of Pediatric News was published 50 years ago, I was starting the second half of my first year in medical school. Over the ensuing 50 years, I have lived through and witnessed some dramatic changes in pediatrics. Here are just a few of the transitions that I’ve observed and Pediatric News has covered:
The birth of interventional neonatology
When I was an intern at Duke University Medical Center in Durham, N.C., a paper appeared in the New England Journal of Medicine describing the use of a simple continuous positive pressure apparatus for the treatment of respiratory distress syndrome entitled, “Treatment of idiopathic respiratory-distress syndrome with continuous positive airway pressure,” (1971 Jun 17;284[24]:1333-40). After seeing the paper, George Brumley, MD, the head of nursery, immediately had the hospital engineers build us our own setup, and we became part of what could arguably be called the revolution that turned neonatology into an interventional specialty.
From meningitis to mental health
Although it came gradually, one of the most significant changes over the last 50 years has been the shift in the mix of pathology presenting to the general pediatrician. In the 1970s and 1980s, the threat of invasive bacterial disease, usually from Haemophilus influenzae, was always hanging over us. It was not unusual for a single community pediatrician to see four or five cases of meningitis in a year. The introduction of effective vaccines and more potent antibiotics lessened the threat of serious bacterial infection, and in its place came a flood of mental health complaints, including anxiety (25% prevalence among 13- to 18-year-olds, depression (13% prevalence among 12- to 17-year-olds) and attention-deficit/hyperactivity disorder (ADHD) (9% prevalence among 13- to 18-year-olds). The result is the impression that, at times, being a general pediatrician today feels like being a more than part-time psychiatrist/psychologist.
Mental retardation and autism
In the 1970s and 1980s, the diagnosis of autism was usually reserved for children with serious communication difficulties. Many physicians and the lay public expected that a child who was diagnosed with autism would have no speech at all. The prevalence of the condition in the last quarter of the century was felt to be about 1 in 2,000.
The more common diagnosis during that period was mental retardation. However, as the result of insensitive stereotyping, “mental retardation” has become an offensive term and has vanished from the pediatric lexicon.
Autism, however, has flourished, and a recent estimate cited by the CDC pegs its prevalence at 1 in 68. Based on my observations, I expect that much, if not most, of this increase is the result of expanded diagnostic criteria and relabeling.
Chicken scratches to mouse clicks
In keeping with a long tradition in medicine, my office notes when I began in practice were unreadable by anyone except a very few my long-term coworkers. My scribbles were brief and often included sketches of wounds and body parts. Their primary purpose was to remind me what had transpired at that office visit and to record the biometrics. Unfortunately, as the cloud of malpractice crept over the landscape, with it came the nonsensical mantra, “if it wasn’t documented, it didn’t happen.”
With the introduction of computers, medical records became inflated and often inaccurate, documents to be used primarily for data collection and risk management. The physician now is tasked with being the data entry clerk who must keep her eyes on the computer screen at the expense of a meaningful interaction with the patient. Sadly, the physician-unfriendliness of electronic medical records has driven many older and experienced pediatricians into premature retirement, robbing general pediatrics of their accumulated wisdom.
A part-time job
In 1975, there were 22,730 practicing pediatricians, of whom 23% were women. In 2011, there were 80,992 pediatricians, of whom 56.6% were women. The percentage of women practicing pediatrics continues to climb, with the most recent figure being 58%. From the patient perspective, this shift in gender dominance has been well received.
At the same time, there has been a trend toward more pediatricians of both genders pursuing part-time employment. The model of the physician being the owner/operator of a medical practice that was flourishing when I began in practice has been replaced by one in which the physician is an employee of a much larger entity, which is pressured from all sides to cut costs. To make matters worse, the Medical Home model that currently is in vogue is proving to be a more expensive vehicle for delivering health care. The patient now is asked to view his physician as the director of a team and may see him or her only infrequently, at the expense of the therapeutic benefits of familiarity.
When I was in medical school, the tuition was around $2,500/year, and I graduated with a debt of about $3,000 – with an interest rate so low that I was in no rush to pay it off. Now a student entering medical school can expect to pay around $60,000/year – an amount that has far outstripped inflation.
These realities combine to create a potentially unsustainable economic climate for pediatricians. I have had a wonderful 50 years being a pediatrician. But I can’t promise the same level of enjoyment to the next generation of pediatricians, unless someone can figure how to cut the expense of medical school and/or make part-time employment fit into a health care delivery system that must contain costs to survive.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics including “How to Say No to Your Toddler.” Email him at pdnews@frontlinemedcom.com.
When the first issue of Pediatric News was published 50 years ago, I was starting the second half of my first year in medical school. Over the ensuing 50 years, I have lived through and witnessed some dramatic changes in pediatrics. Here are just a few of the transitions that I’ve observed and Pediatric News has covered:
The birth of interventional neonatology
When I was an intern at Duke University Medical Center in Durham, N.C., a paper appeared in the New England Journal of Medicine describing the use of a simple continuous positive pressure apparatus for the treatment of respiratory distress syndrome entitled, “Treatment of idiopathic respiratory-distress syndrome with continuous positive airway pressure,” (1971 Jun 17;284[24]:1333-40). After seeing the paper, George Brumley, MD, the head of nursery, immediately had the hospital engineers build us our own setup, and we became part of what could arguably be called the revolution that turned neonatology into an interventional specialty.
From meningitis to mental health
Although it came gradually, one of the most significant changes over the last 50 years has been the shift in the mix of pathology presenting to the general pediatrician. In the 1970s and 1980s, the threat of invasive bacterial disease, usually from Haemophilus influenzae, was always hanging over us. It was not unusual for a single community pediatrician to see four or five cases of meningitis in a year. The introduction of effective vaccines and more potent antibiotics lessened the threat of serious bacterial infection, and in its place came a flood of mental health complaints, including anxiety (25% prevalence among 13- to 18-year-olds, depression (13% prevalence among 12- to 17-year-olds) and attention-deficit/hyperactivity disorder (ADHD) (9% prevalence among 13- to 18-year-olds). The result is the impression that, at times, being a general pediatrician today feels like being a more than part-time psychiatrist/psychologist.
Mental retardation and autism
In the 1970s and 1980s, the diagnosis of autism was usually reserved for children with serious communication difficulties. Many physicians and the lay public expected that a child who was diagnosed with autism would have no speech at all. The prevalence of the condition in the last quarter of the century was felt to be about 1 in 2,000.
The more common diagnosis during that period was mental retardation. However, as the result of insensitive stereotyping, “mental retardation” has become an offensive term and has vanished from the pediatric lexicon.
Autism, however, has flourished, and a recent estimate cited by the CDC pegs its prevalence at 1 in 68. Based on my observations, I expect that much, if not most, of this increase is the result of expanded diagnostic criteria and relabeling.
Chicken scratches to mouse clicks
In keeping with a long tradition in medicine, my office notes when I began in practice were unreadable by anyone except a very few my long-term coworkers. My scribbles were brief and often included sketches of wounds and body parts. Their primary purpose was to remind me what had transpired at that office visit and to record the biometrics. Unfortunately, as the cloud of malpractice crept over the landscape, with it came the nonsensical mantra, “if it wasn’t documented, it didn’t happen.”
With the introduction of computers, medical records became inflated and often inaccurate, documents to be used primarily for data collection and risk management. The physician now is tasked with being the data entry clerk who must keep her eyes on the computer screen at the expense of a meaningful interaction with the patient. Sadly, the physician-unfriendliness of electronic medical records has driven many older and experienced pediatricians into premature retirement, robbing general pediatrics of their accumulated wisdom.
A part-time job
In 1975, there were 22,730 practicing pediatricians, of whom 23% were women. In 2011, there were 80,992 pediatricians, of whom 56.6% were women. The percentage of women practicing pediatrics continues to climb, with the most recent figure being 58%. From the patient perspective, this shift in gender dominance has been well received.
At the same time, there has been a trend toward more pediatricians of both genders pursuing part-time employment. The model of the physician being the owner/operator of a medical practice that was flourishing when I began in practice has been replaced by one in which the physician is an employee of a much larger entity, which is pressured from all sides to cut costs. To make matters worse, the Medical Home model that currently is in vogue is proving to be a more expensive vehicle for delivering health care. The patient now is asked to view his physician as the director of a team and may see him or her only infrequently, at the expense of the therapeutic benefits of familiarity.
When I was in medical school, the tuition was around $2,500/year, and I graduated with a debt of about $3,000 – with an interest rate so low that I was in no rush to pay it off. Now a student entering medical school can expect to pay around $60,000/year – an amount that has far outstripped inflation.
These realities combine to create a potentially unsustainable economic climate for pediatricians. I have had a wonderful 50 years being a pediatrician. But I can’t promise the same level of enjoyment to the next generation of pediatricians, unless someone can figure how to cut the expense of medical school and/or make part-time employment fit into a health care delivery system that must contain costs to survive.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics including “How to Say No to Your Toddler.” Email him at pdnews@frontlinemedcom.com.
When the first issue of Pediatric News was published 50 years ago, I was starting the second half of my first year in medical school. Over the ensuing 50 years, I have lived through and witnessed some dramatic changes in pediatrics. Here are just a few of the transitions that I’ve observed and Pediatric News has covered:
The birth of interventional neonatology
When I was an intern at Duke University Medical Center in Durham, N.C., a paper appeared in the New England Journal of Medicine describing the use of a simple continuous positive pressure apparatus for the treatment of respiratory distress syndrome entitled, “Treatment of idiopathic respiratory-distress syndrome with continuous positive airway pressure,” (1971 Jun 17;284[24]:1333-40). After seeing the paper, George Brumley, MD, the head of nursery, immediately had the hospital engineers build us our own setup, and we became part of what could arguably be called the revolution that turned neonatology into an interventional specialty.
From meningitis to mental health
Although it came gradually, one of the most significant changes over the last 50 years has been the shift in the mix of pathology presenting to the general pediatrician. In the 1970s and 1980s, the threat of invasive bacterial disease, usually from Haemophilus influenzae, was always hanging over us. It was not unusual for a single community pediatrician to see four or five cases of meningitis in a year. The introduction of effective vaccines and more potent antibiotics lessened the threat of serious bacterial infection, and in its place came a flood of mental health complaints, including anxiety (25% prevalence among 13- to 18-year-olds, depression (13% prevalence among 12- to 17-year-olds) and attention-deficit/hyperactivity disorder (ADHD) (9% prevalence among 13- to 18-year-olds). The result is the impression that, at times, being a general pediatrician today feels like being a more than part-time psychiatrist/psychologist.
Mental retardation and autism
In the 1970s and 1980s, the diagnosis of autism was usually reserved for children with serious communication difficulties. Many physicians and the lay public expected that a child who was diagnosed with autism would have no speech at all. The prevalence of the condition in the last quarter of the century was felt to be about 1 in 2,000.
The more common diagnosis during that period was mental retardation. However, as the result of insensitive stereotyping, “mental retardation” has become an offensive term and has vanished from the pediatric lexicon.
Autism, however, has flourished, and a recent estimate cited by the CDC pegs its prevalence at 1 in 68. Based on my observations, I expect that much, if not most, of this increase is the result of expanded diagnostic criteria and relabeling.
Chicken scratches to mouse clicks
In keeping with a long tradition in medicine, my office notes when I began in practice were unreadable by anyone except a very few my long-term coworkers. My scribbles were brief and often included sketches of wounds and body parts. Their primary purpose was to remind me what had transpired at that office visit and to record the biometrics. Unfortunately, as the cloud of malpractice crept over the landscape, with it came the nonsensical mantra, “if it wasn’t documented, it didn’t happen.”
With the introduction of computers, medical records became inflated and often inaccurate, documents to be used primarily for data collection and risk management. The physician now is tasked with being the data entry clerk who must keep her eyes on the computer screen at the expense of a meaningful interaction with the patient. Sadly, the physician-unfriendliness of electronic medical records has driven many older and experienced pediatricians into premature retirement, robbing general pediatrics of their accumulated wisdom.
A part-time job
In 1975, there were 22,730 practicing pediatricians, of whom 23% were women. In 2011, there were 80,992 pediatricians, of whom 56.6% were women. The percentage of women practicing pediatrics continues to climb, with the most recent figure being 58%. From the patient perspective, this shift in gender dominance has been well received.
At the same time, there has been a trend toward more pediatricians of both genders pursuing part-time employment. The model of the physician being the owner/operator of a medical practice that was flourishing when I began in practice has been replaced by one in which the physician is an employee of a much larger entity, which is pressured from all sides to cut costs. To make matters worse, the Medical Home model that currently is in vogue is proving to be a more expensive vehicle for delivering health care. The patient now is asked to view his physician as the director of a team and may see him or her only infrequently, at the expense of the therapeutic benefits of familiarity.
When I was in medical school, the tuition was around $2,500/year, and I graduated with a debt of about $3,000 – with an interest rate so low that I was in no rush to pay it off. Now a student entering medical school can expect to pay around $60,000/year – an amount that has far outstripped inflation.
These realities combine to create a potentially unsustainable economic climate for pediatricians. I have had a wonderful 50 years being a pediatrician. But I can’t promise the same level of enjoyment to the next generation of pediatricians, unless someone can figure how to cut the expense of medical school and/or make part-time employment fit into a health care delivery system that must contain costs to survive.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics including “How to Say No to Your Toddler.” Email him at pdnews@frontlinemedcom.com.
All isn’t well with HIV-exposed uninfected infants
MADRID – Children who were HIV-exposed antenatally but not infected are at double the risk of hospitalization for infectious diseases during their first year of life, compared with HIV-unexposed controls, according to what’s believed to be the first prospective study examining the issue in a Western industrialized country.
That’s one key take-away message from the study conducted in Brussels. Another key finding was that the sharply increased risk of hospitalization for infection during infancy was erased if HIV-infected mothers started antiretroviral therapy prior to, rather than during, pregnancy, Catherine Adler, MD, reported at the annual meeting of the European Society for Paediatric Infectious Diseases.
She presented a prospective study of 125 HIV-positive and 119 HIV-negative pregnant Belgian women of comparable ethnic and sociodemographic backgrounds. All of the HIV-positive mothers were on antiretroviral therapy, which they started either prior to or during pregnancy.
The two groups of women gave birth to 132 HEU and 123 HIV-unexposed babies, all born after 35 weeks’ gestation. The babies didn’t differ in terms of gender, prematurity rate, mode of delivery, or the use of antibiotics at delivery. However, 17% of the HEU babies had a birth weight below 2,500 g, compared with just 3% of the HIV-unexposed controls. Also, as a matter of policy, none of the HEU babies were breastfed, while 95% of the controls were, Dr. Adler explained.
The primary outcome in the study was the rate of hospitalization for infection during the first 12 months of life. The rate was 21% in the HEU babies, significantly greater than the 11% rate in HIV-unexposed babies. In a multivariate analysis adjusted for preterm birth, low birth weight, literacy, and maternal age, HEU status was associated with twofold increased risk of hospitalization for infection in infancy.
“The increased susceptibility of HEU infants to infectious disease is not restricted to children born in developing countries,” she declared.
The disparity in hospitalization rates was driven by hospitalization for viral infections, which occurred at a rate of 20% in the HEU group, versus 9% in controls. Particularly notable were the 10 hospitalizations for respiratory syncytial virus infection in the HEU patients, compared with just 1 in the controls.
Dr. Adler and her coinvestigators will continue following the children out to about 3 years of age. After age 12 months, the two groups no longer differed significantly in their risk of hospitalization for infection.
“The first year is a vulnerable period. Our data highlight the importance of a close follow-up of these infants,” she said.
The biggest risk factor for hospitalization for infectious illness in the HEU group was initiation of antiretroviral therapy during pregnancy. The hospitalization rate in HEU infants whose mothers began therapy prior to pregnancy was the same as in HIV-unexposed infants. The inference is that it’s not in utero exposure to antiretroviral drugs that is responsible for the increased risk of hospitalization during infancy.
“This observation supports the notion that it’s the activity of the maternal HIV infection – the exposure to a strongly proinflammatory state in the mother – that contributes to the risk of severe infection in HEU infants, probably by causing changes in innate immunity cells,” according to Dr. Adler.
Even though the increased risk of hospitalization for infectious illnesses in HEU children falls off after age 12 months, she continued, her group is following them out to about age 3 years because “we have the impression that they are at risk for neurodevelopmental problems, including language delay.”
Other researchers in the audience confirmed this risk, reporting that, as they follow HEU children through adolescence, they see an increased rate of attention deficits and associated comorbidities.
Dr. Adler called the administration of antiretroviral therapy to pregnant HIV-infected women in order to prevent maternal-to-child transmission of the disease “one of the major successes of the 21st century.”
“The number of new HIV infections among children has collapsed, leading to an increasing number of HIV-exposed but uninfected children. One million of them are born each year,” she said.
Dr. Adler reported having no financial conflicts of interest regarding her study.
*The article was updated 6/15/17.
MADRID – Children who were HIV-exposed antenatally but not infected are at double the risk of hospitalization for infectious diseases during their first year of life, compared with HIV-unexposed controls, according to what’s believed to be the first prospective study examining the issue in a Western industrialized country.
That’s one key take-away message from the study conducted in Brussels. Another key finding was that the sharply increased risk of hospitalization for infection during infancy was erased if HIV-infected mothers started antiretroviral therapy prior to, rather than during, pregnancy, Catherine Adler, MD, reported at the annual meeting of the European Society for Paediatric Infectious Diseases.
She presented a prospective study of 125 HIV-positive and 119 HIV-negative pregnant Belgian women of comparable ethnic and sociodemographic backgrounds. All of the HIV-positive mothers were on antiretroviral therapy, which they started either prior to or during pregnancy.
The two groups of women gave birth to 132 HEU and 123 HIV-unexposed babies, all born after 35 weeks’ gestation. The babies didn’t differ in terms of gender, prematurity rate, mode of delivery, or the use of antibiotics at delivery. However, 17% of the HEU babies had a birth weight below 2,500 g, compared with just 3% of the HIV-unexposed controls. Also, as a matter of policy, none of the HEU babies were breastfed, while 95% of the controls were, Dr. Adler explained.
The primary outcome in the study was the rate of hospitalization for infection during the first 12 months of life. The rate was 21% in the HEU babies, significantly greater than the 11% rate in HIV-unexposed babies. In a multivariate analysis adjusted for preterm birth, low birth weight, literacy, and maternal age, HEU status was associated with twofold increased risk of hospitalization for infection in infancy.
“The increased susceptibility of HEU infants to infectious disease is not restricted to children born in developing countries,” she declared.
The disparity in hospitalization rates was driven by hospitalization for viral infections, which occurred at a rate of 20% in the HEU group, versus 9% in controls. Particularly notable were the 10 hospitalizations for respiratory syncytial virus infection in the HEU patients, compared with just 1 in the controls.
Dr. Adler and her coinvestigators will continue following the children out to about 3 years of age. After age 12 months, the two groups no longer differed significantly in their risk of hospitalization for infection.
“The first year is a vulnerable period. Our data highlight the importance of a close follow-up of these infants,” she said.
The biggest risk factor for hospitalization for infectious illness in the HEU group was initiation of antiretroviral therapy during pregnancy. The hospitalization rate in HEU infants whose mothers began therapy prior to pregnancy was the same as in HIV-unexposed infants. The inference is that it’s not in utero exposure to antiretroviral drugs that is responsible for the increased risk of hospitalization during infancy.
“This observation supports the notion that it’s the activity of the maternal HIV infection – the exposure to a strongly proinflammatory state in the mother – that contributes to the risk of severe infection in HEU infants, probably by causing changes in innate immunity cells,” according to Dr. Adler.
Even though the increased risk of hospitalization for infectious illnesses in HEU children falls off after age 12 months, she continued, her group is following them out to about age 3 years because “we have the impression that they are at risk for neurodevelopmental problems, including language delay.”
Other researchers in the audience confirmed this risk, reporting that, as they follow HEU children through adolescence, they see an increased rate of attention deficits and associated comorbidities.
Dr. Adler called the administration of antiretroviral therapy to pregnant HIV-infected women in order to prevent maternal-to-child transmission of the disease “one of the major successes of the 21st century.”
“The number of new HIV infections among children has collapsed, leading to an increasing number of HIV-exposed but uninfected children. One million of them are born each year,” she said.
Dr. Adler reported having no financial conflicts of interest regarding her study.
*The article was updated 6/15/17.
MADRID – Children who were HIV-exposed antenatally but not infected are at double the risk of hospitalization for infectious diseases during their first year of life, compared with HIV-unexposed controls, according to what’s believed to be the first prospective study examining the issue in a Western industrialized country.
That’s one key take-away message from the study conducted in Brussels. Another key finding was that the sharply increased risk of hospitalization for infection during infancy was erased if HIV-infected mothers started antiretroviral therapy prior to, rather than during, pregnancy, Catherine Adler, MD, reported at the annual meeting of the European Society for Paediatric Infectious Diseases.
She presented a prospective study of 125 HIV-positive and 119 HIV-negative pregnant Belgian women of comparable ethnic and sociodemographic backgrounds. All of the HIV-positive mothers were on antiretroviral therapy, which they started either prior to or during pregnancy.
The two groups of women gave birth to 132 HEU and 123 HIV-unexposed babies, all born after 35 weeks’ gestation. The babies didn’t differ in terms of gender, prematurity rate, mode of delivery, or the use of antibiotics at delivery. However, 17% of the HEU babies had a birth weight below 2,500 g, compared with just 3% of the HIV-unexposed controls. Also, as a matter of policy, none of the HEU babies were breastfed, while 95% of the controls were, Dr. Adler explained.
The primary outcome in the study was the rate of hospitalization for infection during the first 12 months of life. The rate was 21% in the HEU babies, significantly greater than the 11% rate in HIV-unexposed babies. In a multivariate analysis adjusted for preterm birth, low birth weight, literacy, and maternal age, HEU status was associated with twofold increased risk of hospitalization for infection in infancy.
“The increased susceptibility of HEU infants to infectious disease is not restricted to children born in developing countries,” she declared.
The disparity in hospitalization rates was driven by hospitalization for viral infections, which occurred at a rate of 20% in the HEU group, versus 9% in controls. Particularly notable were the 10 hospitalizations for respiratory syncytial virus infection in the HEU patients, compared with just 1 in the controls.
Dr. Adler and her coinvestigators will continue following the children out to about 3 years of age. After age 12 months, the two groups no longer differed significantly in their risk of hospitalization for infection.
“The first year is a vulnerable period. Our data highlight the importance of a close follow-up of these infants,” she said.
The biggest risk factor for hospitalization for infectious illness in the HEU group was initiation of antiretroviral therapy during pregnancy. The hospitalization rate in HEU infants whose mothers began therapy prior to pregnancy was the same as in HIV-unexposed infants. The inference is that it’s not in utero exposure to antiretroviral drugs that is responsible for the increased risk of hospitalization during infancy.
“This observation supports the notion that it’s the activity of the maternal HIV infection – the exposure to a strongly proinflammatory state in the mother – that contributes to the risk of severe infection in HEU infants, probably by causing changes in innate immunity cells,” according to Dr. Adler.
Even though the increased risk of hospitalization for infectious illnesses in HEU children falls off after age 12 months, she continued, her group is following them out to about age 3 years because “we have the impression that they are at risk for neurodevelopmental problems, including language delay.”
Other researchers in the audience confirmed this risk, reporting that, as they follow HEU children through adolescence, they see an increased rate of attention deficits and associated comorbidities.
Dr. Adler called the administration of antiretroviral therapy to pregnant HIV-infected women in order to prevent maternal-to-child transmission of the disease “one of the major successes of the 21st century.”
“The number of new HIV infections among children has collapsed, leading to an increasing number of HIV-exposed but uninfected children. One million of them are born each year,” she said.
Dr. Adler reported having no financial conflicts of interest regarding her study.
*The article was updated 6/15/17.
AT ESPID 2017
Key clinical point:
Major finding: The rate of hospitalization for a serious infectious illness during the first 12 months of life was 21% in HIV-exposed uninfected children, significantly greater than the 11% rate in HIV-unexposed babies.
Data source: This prospective observational study included 125 HIV-positive and 119 HIV-negative pregnant Belgian women of comparable ethnic and sociodemographic backgrounds and their offspring, followed to date through the infants’ first birthday.
Disclosures: Dr. Adler reported having no financial conflicts of interest.
OSA in pregnancy linked to congenital anomalies
BOSTON – Newborns exposed to obstructive sleep apnea (OSA) in utero are at a higher risk of being diagnosed with congenital anomalies, according to a new study presented at the annual meeting of the Associated Professional Sleep Societies.
The researchers’ analysis covered data from more than 1.4 million births during 2010-2014. Circulatory, musculoskeletal, and central nervous systems were among the types of anomalies they saw in the 17.3% of babies born to mothers who had OSA during pregnancy. These babies were also more likely to require intensive care at birth, compared with those born to mothers who had not been diagnosed with OSA.
Additionally, the investigators found that the 0.1% of women who had a diagnosis of OSA were 2.76 times more likely to have babies that required some kind of resuscitative effort at birth. Specifically, 0.5% of the newborns of the mothers with OSA required resuscitation, compared with 0.1% of the other group’s babies. The newborns of women with OSA were also 2.25 times more likely to have a longer hospital stay.
Mothers with OSA were older and more likely to be non-Hispanic black and have a diagnosis of obesity, tobacco use, and drug use but not alcohol use.
“We can’t say for sure that sleep apnea is causing these outcomes,” said abstract presenter and principal investigator Ghada Bourjeily, MD, of Brown University and Miriam Hospital, both in Providence, R.I., in an interview.
“We know that women who have sleep apnea also often have other morbidities, so we don’t know what might have contributed to the congenital outcomes,” said Dr. Bourjeily. “We also don’t know if treating sleep apnea can reverse or prevent birth complications or even maternal complications, like preeclampsia or gestational diabetes.”
Ongoing studies are looking at maternal continuous positive airway pressure therapy use and neonatal outcomes, but “they are nothing to write home about yet,” she said.
“This is an underdiagnosed condition and it’s probably undercoded too, but we know from another study that the prevalence of OSA in the first trimester in an all-comers population that was screened for the condition is 4%,” said Dr. Bourjeily. “If another 3% of [the study participants] actually had OSA, then all of these findings are potentially underestimated.”
The majority of OSA in pregnant women that has been identified in prospective studies is mild and not necessarily something that most physicians would treat, she noted. “In our study, the ones who were diagnosed were those who probably went to their doctors and complained of sleepiness or loud snoring.”
The researchers also determined that the newborns of mothers with sleep apnea were more likely to be admitted to an intensive care unit (25.3% vs. 8.1%) or a special care nursery (34.9% vs. 13.6%).
A diagnosis of OSA was established when a diagnosis code for OSA was present on the delivery discharge record. Maternal and infant outcomes were collected for ICD-9 and procedural codes.
Dr. Bourjeily received research equipment support from Respironics.
BOSTON – Newborns exposed to obstructive sleep apnea (OSA) in utero are at a higher risk of being diagnosed with congenital anomalies, according to a new study presented at the annual meeting of the Associated Professional Sleep Societies.
The researchers’ analysis covered data from more than 1.4 million births during 2010-2014. Circulatory, musculoskeletal, and central nervous systems were among the types of anomalies they saw in the 17.3% of babies born to mothers who had OSA during pregnancy. These babies were also more likely to require intensive care at birth, compared with those born to mothers who had not been diagnosed with OSA.
Additionally, the investigators found that the 0.1% of women who had a diagnosis of OSA were 2.76 times more likely to have babies that required some kind of resuscitative effort at birth. Specifically, 0.5% of the newborns of the mothers with OSA required resuscitation, compared with 0.1% of the other group’s babies. The newborns of women with OSA were also 2.25 times more likely to have a longer hospital stay.
Mothers with OSA were older and more likely to be non-Hispanic black and have a diagnosis of obesity, tobacco use, and drug use but not alcohol use.
“We can’t say for sure that sleep apnea is causing these outcomes,” said abstract presenter and principal investigator Ghada Bourjeily, MD, of Brown University and Miriam Hospital, both in Providence, R.I., in an interview.
“We know that women who have sleep apnea also often have other morbidities, so we don’t know what might have contributed to the congenital outcomes,” said Dr. Bourjeily. “We also don’t know if treating sleep apnea can reverse or prevent birth complications or even maternal complications, like preeclampsia or gestational diabetes.”
Ongoing studies are looking at maternal continuous positive airway pressure therapy use and neonatal outcomes, but “they are nothing to write home about yet,” she said.
“This is an underdiagnosed condition and it’s probably undercoded too, but we know from another study that the prevalence of OSA in the first trimester in an all-comers population that was screened for the condition is 4%,” said Dr. Bourjeily. “If another 3% of [the study participants] actually had OSA, then all of these findings are potentially underestimated.”
The majority of OSA in pregnant women that has been identified in prospective studies is mild and not necessarily something that most physicians would treat, she noted. “In our study, the ones who were diagnosed were those who probably went to their doctors and complained of sleepiness or loud snoring.”
The researchers also determined that the newborns of mothers with sleep apnea were more likely to be admitted to an intensive care unit (25.3% vs. 8.1%) or a special care nursery (34.9% vs. 13.6%).
A diagnosis of OSA was established when a diagnosis code for OSA was present on the delivery discharge record. Maternal and infant outcomes were collected for ICD-9 and procedural codes.
Dr. Bourjeily received research equipment support from Respironics.
BOSTON – Newborns exposed to obstructive sleep apnea (OSA) in utero are at a higher risk of being diagnosed with congenital anomalies, according to a new study presented at the annual meeting of the Associated Professional Sleep Societies.
The researchers’ analysis covered data from more than 1.4 million births during 2010-2014. Circulatory, musculoskeletal, and central nervous systems were among the types of anomalies they saw in the 17.3% of babies born to mothers who had OSA during pregnancy. These babies were also more likely to require intensive care at birth, compared with those born to mothers who had not been diagnosed with OSA.
Additionally, the investigators found that the 0.1% of women who had a diagnosis of OSA were 2.76 times more likely to have babies that required some kind of resuscitative effort at birth. Specifically, 0.5% of the newborns of the mothers with OSA required resuscitation, compared with 0.1% of the other group’s babies. The newborns of women with OSA were also 2.25 times more likely to have a longer hospital stay.
Mothers with OSA were older and more likely to be non-Hispanic black and have a diagnosis of obesity, tobacco use, and drug use but not alcohol use.
“We can’t say for sure that sleep apnea is causing these outcomes,” said abstract presenter and principal investigator Ghada Bourjeily, MD, of Brown University and Miriam Hospital, both in Providence, R.I., in an interview.
“We know that women who have sleep apnea also often have other morbidities, so we don’t know what might have contributed to the congenital outcomes,” said Dr. Bourjeily. “We also don’t know if treating sleep apnea can reverse or prevent birth complications or even maternal complications, like preeclampsia or gestational diabetes.”
Ongoing studies are looking at maternal continuous positive airway pressure therapy use and neonatal outcomes, but “they are nothing to write home about yet,” she said.
“This is an underdiagnosed condition and it’s probably undercoded too, but we know from another study that the prevalence of OSA in the first trimester in an all-comers population that was screened for the condition is 4%,” said Dr. Bourjeily. “If another 3% of [the study participants] actually had OSA, then all of these findings are potentially underestimated.”
The majority of OSA in pregnant women that has been identified in prospective studies is mild and not necessarily something that most physicians would treat, she noted. “In our study, the ones who were diagnosed were those who probably went to their doctors and complained of sleepiness or loud snoring.”
The researchers also determined that the newborns of mothers with sleep apnea were more likely to be admitted to an intensive care unit (25.3% vs. 8.1%) or a special care nursery (34.9% vs. 13.6%).
A diagnosis of OSA was established when a diagnosis code for OSA was present on the delivery discharge record. Maternal and infant outcomes were collected for ICD-9 and procedural codes.
Dr. Bourjeily received research equipment support from Respironics.
AT SLEEP 2017
Key clinical point: This large cohort study is the first study to show an increased risk of congenital anomalies and resuscitation at birth in newborns born to mothers with diagnosed obstructive sleep apnea (OSA).
Major finding: Of babies born to a mother with OSA, 17.3% had a congenital anomaly, compared with 10.6% of those born to mothers without OSA (P less than .001). This difference remained significant after adjusting for potential confounders.
Data source: A national cohort study including more than 1.4 million linked maternal and newborn records with a delivery hospitalization during 2010-2014.
Disclosures: Dr. Bourjeily received research equipment support from Respironics.
Telemedicine visits after NICU discharge improved care, processes
SAN FRANCISCO – Using telemedicine for a follow-up appointment 1 week after discharge of medically complex infants reduced extra visits or calls to a clinic or emergency department, a recent study found.
The telemedicine visits also helped providers identify ways to improve the neonatal ICU (NICU) discharge process while assessing infants’ home care and answering parents’ questions.
The researchers assessed whether telemedicine visits could ease the transition from neonatal intensive care to home care, respond adequately to caregivers’ needs during that transition, reduce emergency department visits and readmissions, and detect and address any potential problems. The visits also provided an opportunity for feedback on caregivers’ experiences during discharge.
The 92 patients all were medically complex infants who went home with respiratory or feeding equipment, surgical sites and/or complex medication administration. For example, 28 infants had been sent home with a nasogastric tube, 13 had a gastrostomy tube, and 13 had an apnea monitor. Overall, participants had been discharged with an average 2.3 medications and 4.8 scheduled subspecialty follow-up appointments.
The most common conditions among the participants were gastrointestinal disease, neurologic disease, and congenital diaphragmatic hernia or lung lesions. Other conditions included omphalocele, genetic disorders, tracheoesophageal fistula or esophageal atresia and chronic lung disease, or another respiratory disease, Dr. Brant reported at the Pediatric Academic Societies meeting.
Families could enroll in the study only if they had a smart device (such as a tablet) and wireless Internet access at home. One week after the infant’s discharge from the NICU, the caregivers received one telemedicine visit with a team that included neonatologists, neonatal fellows, nurse practitioners, and a telemedicine coordinator or support staffer. During the visit, the providers observed the infant and the home environment, and evaluated care practices, including tube feedings, respiratory support, management of surgical wound sites, and administration of medications.
The providers also reviewed how to use the medical equipment, gathered follow-up information about the child’s health, and answered caregivers’ questions. The providers did not bill for telemedicine visits since it was part of a pilot study, but the participants did need to reside in Pennsylvania or New Jersey to meet provider licensing regulations.
Among the 93 telemedicine visits, half (50%) prevented the family from calling or visiting a provider, and 12% of them led to an earlier follow-up appointment for the child. During the video observations, providers addressed 14 issues related to the child’s sleep environment, respiratory status, surgical sites, or dermatological issues. Among 78 total concerns identified in the visits, 35% related to the surgical site, 33% related to feeding, 19% related to respiratory concerns, and 13% related to medication administration.
The provider team also asked families during the visit about their experiences during discharge. A quarter of the families (26%) said they needed more parental education during discharge. In addition, 14% mentioned problems with scheduling follow-up appointments, and 12% had problems related to case management and insurance. Other issues raised by parents related to home equipment, early intervention, home feeding or medications, and diagnostic logistics.
In subsequent satisfaction surveys filled out by caregivers about the telemedicine visit itself, the median rating was 94.5 on a scale of 0 (not at all satisfied) to 100 (extremely satisfied). The overall intervention was 92% successful in its completion. The only follow-up telemedicine visits that did not occur resulted from malfunctioning wireless connection or a mobile app problem. On a scale of 1 to 100 (best), caregivers rated the video quality as an average 78, the Internet reliability as 79, and the ease of using the camera as 91. One of the biggest benefits of the intervention, Dr. Brant pointed out, is that using telemedicine bypasses some of the geographic and time-related obstacles that can occur with follow-ups.
Dr. Brant had no relevant financial disclosures and did not report using any external funding.
SAN FRANCISCO – Using telemedicine for a follow-up appointment 1 week after discharge of medically complex infants reduced extra visits or calls to a clinic or emergency department, a recent study found.
The telemedicine visits also helped providers identify ways to improve the neonatal ICU (NICU) discharge process while assessing infants’ home care and answering parents’ questions.
The researchers assessed whether telemedicine visits could ease the transition from neonatal intensive care to home care, respond adequately to caregivers’ needs during that transition, reduce emergency department visits and readmissions, and detect and address any potential problems. The visits also provided an opportunity for feedback on caregivers’ experiences during discharge.
The 92 patients all were medically complex infants who went home with respiratory or feeding equipment, surgical sites and/or complex medication administration. For example, 28 infants had been sent home with a nasogastric tube, 13 had a gastrostomy tube, and 13 had an apnea monitor. Overall, participants had been discharged with an average 2.3 medications and 4.8 scheduled subspecialty follow-up appointments.
The most common conditions among the participants were gastrointestinal disease, neurologic disease, and congenital diaphragmatic hernia or lung lesions. Other conditions included omphalocele, genetic disorders, tracheoesophageal fistula or esophageal atresia and chronic lung disease, or another respiratory disease, Dr. Brant reported at the Pediatric Academic Societies meeting.
Families could enroll in the study only if they had a smart device (such as a tablet) and wireless Internet access at home. One week after the infant’s discharge from the NICU, the caregivers received one telemedicine visit with a team that included neonatologists, neonatal fellows, nurse practitioners, and a telemedicine coordinator or support staffer. During the visit, the providers observed the infant and the home environment, and evaluated care practices, including tube feedings, respiratory support, management of surgical wound sites, and administration of medications.
The providers also reviewed how to use the medical equipment, gathered follow-up information about the child’s health, and answered caregivers’ questions. The providers did not bill for telemedicine visits since it was part of a pilot study, but the participants did need to reside in Pennsylvania or New Jersey to meet provider licensing regulations.
Among the 93 telemedicine visits, half (50%) prevented the family from calling or visiting a provider, and 12% of them led to an earlier follow-up appointment for the child. During the video observations, providers addressed 14 issues related to the child’s sleep environment, respiratory status, surgical sites, or dermatological issues. Among 78 total concerns identified in the visits, 35% related to the surgical site, 33% related to feeding, 19% related to respiratory concerns, and 13% related to medication administration.
The provider team also asked families during the visit about their experiences during discharge. A quarter of the families (26%) said they needed more parental education during discharge. In addition, 14% mentioned problems with scheduling follow-up appointments, and 12% had problems related to case management and insurance. Other issues raised by parents related to home equipment, early intervention, home feeding or medications, and diagnostic logistics.
In subsequent satisfaction surveys filled out by caregivers about the telemedicine visit itself, the median rating was 94.5 on a scale of 0 (not at all satisfied) to 100 (extremely satisfied). The overall intervention was 92% successful in its completion. The only follow-up telemedicine visits that did not occur resulted from malfunctioning wireless connection or a mobile app problem. On a scale of 1 to 100 (best), caregivers rated the video quality as an average 78, the Internet reliability as 79, and the ease of using the camera as 91. One of the biggest benefits of the intervention, Dr. Brant pointed out, is that using telemedicine bypasses some of the geographic and time-related obstacles that can occur with follow-ups.
Dr. Brant had no relevant financial disclosures and did not report using any external funding.
SAN FRANCISCO – Using telemedicine for a follow-up appointment 1 week after discharge of medically complex infants reduced extra visits or calls to a clinic or emergency department, a recent study found.
The telemedicine visits also helped providers identify ways to improve the neonatal ICU (NICU) discharge process while assessing infants’ home care and answering parents’ questions.
The researchers assessed whether telemedicine visits could ease the transition from neonatal intensive care to home care, respond adequately to caregivers’ needs during that transition, reduce emergency department visits and readmissions, and detect and address any potential problems. The visits also provided an opportunity for feedback on caregivers’ experiences during discharge.
The 92 patients all were medically complex infants who went home with respiratory or feeding equipment, surgical sites and/or complex medication administration. For example, 28 infants had been sent home with a nasogastric tube, 13 had a gastrostomy tube, and 13 had an apnea monitor. Overall, participants had been discharged with an average 2.3 medications and 4.8 scheduled subspecialty follow-up appointments.
The most common conditions among the participants were gastrointestinal disease, neurologic disease, and congenital diaphragmatic hernia or lung lesions. Other conditions included omphalocele, genetic disorders, tracheoesophageal fistula or esophageal atresia and chronic lung disease, or another respiratory disease, Dr. Brant reported at the Pediatric Academic Societies meeting.
Families could enroll in the study only if they had a smart device (such as a tablet) and wireless Internet access at home. One week after the infant’s discharge from the NICU, the caregivers received one telemedicine visit with a team that included neonatologists, neonatal fellows, nurse practitioners, and a telemedicine coordinator or support staffer. During the visit, the providers observed the infant and the home environment, and evaluated care practices, including tube feedings, respiratory support, management of surgical wound sites, and administration of medications.
The providers also reviewed how to use the medical equipment, gathered follow-up information about the child’s health, and answered caregivers’ questions. The providers did not bill for telemedicine visits since it was part of a pilot study, but the participants did need to reside in Pennsylvania or New Jersey to meet provider licensing regulations.
Among the 93 telemedicine visits, half (50%) prevented the family from calling or visiting a provider, and 12% of them led to an earlier follow-up appointment for the child. During the video observations, providers addressed 14 issues related to the child’s sleep environment, respiratory status, surgical sites, or dermatological issues. Among 78 total concerns identified in the visits, 35% related to the surgical site, 33% related to feeding, 19% related to respiratory concerns, and 13% related to medication administration.
The provider team also asked families during the visit about their experiences during discharge. A quarter of the families (26%) said they needed more parental education during discharge. In addition, 14% mentioned problems with scheduling follow-up appointments, and 12% had problems related to case management and insurance. Other issues raised by parents related to home equipment, early intervention, home feeding or medications, and diagnostic logistics.
In subsequent satisfaction surveys filled out by caregivers about the telemedicine visit itself, the median rating was 94.5 on a scale of 0 (not at all satisfied) to 100 (extremely satisfied). The overall intervention was 92% successful in its completion. The only follow-up telemedicine visits that did not occur resulted from malfunctioning wireless connection or a mobile app problem. On a scale of 1 to 100 (best), caregivers rated the video quality as an average 78, the Internet reliability as 79, and the ease of using the camera as 91. One of the biggest benefits of the intervention, Dr. Brant pointed out, is that using telemedicine bypasses some of the geographic and time-related obstacles that can occur with follow-ups.
Dr. Brant had no relevant financial disclosures and did not report using any external funding.
FROM PAS 17
Key clinical point:
Major finding: Telemedicine visits prevented 50% of participants from calling or visiting a provider and led 12% of families to bring infants in sooner than originally scheduled.
Data source: The findings are based on a pilot project at the Children’s Hospital of Philadelphia involving 93 medically complex infants discharged from the NICU with medical equipment, surgical sites, and/or complex medication administration.
Disclosures: Dr. Brant had no relevant financial disclosures and did not report external funding.
‘How could he?’
The headline in a Portland, Maine, newspaper read, “Standish man sentenced to serve 15 years in prison for death of his 3-month-old son” (Edward Murphy, May 23, 2017). I suspect that many of the folks who read the story under the headline feel that the sentence was too light. Others are asking themselves how a 21-year-old man could beat a fragile 5-pound infant to death. What kind of evil monster is this guy?
However, even with the snatches of information provided in the 500-word newspaper story, the unfortunate scenario makes sense, and the child’s death is a tragic culmination of a series of events that shouldn’t surprise any pediatrician. It turns out the infant was a twin who, with his sister, had been born at 30 weeks’ gestation. He had spent a month or more in the hospital, and his sister was still in neonatal ICU at the time of his death. While it is unclear from the newspaper article whether the twins’ parents were married, they were living in a house with eight other adults and some other children. The mother was out of the home working while the father was left to care for his son.
I am sure that the neonatologists and social workers at the hospital where the twins were born were aware of at least some of the red flags that waved over this unfortunate family. I also am confident that they did what they could to assure this infant a safe home environment when it was time for his discharge from the NICU. However, risks factors may have been missed that now seem obvious in retrospect. We should all realize by now from our experience with domestic terrorism that simply appearing on someone’s radar doesn’t mean that preemptive action can or will be taken. Short of keeping the parents of high-risk neonates under constant surveillance for a year or 2, there are few other workable options to prevent every tragedy like this one.
This case is another example of the erosive power of a baby’s cry. Most pediatricians have developed a filtering mechanism that allows us to function in a cacophonous environment dominated by a screaming infant. However, even adults without this young father’s deprived background crack under the stress when they are confined in a space with a crying child. The risk of decompensation is compounded when the adult also feels some responsibility for the child’s welfare. I don’t think we can condone what the father did in this tragic scenario, but we can certainly understand how the dominoes fell.
We are all potential child abusers. When faced with the right, or I guess the wrong, set of circumstances we might lash out to stop the crying. Luckily, most of us are several body lengths from the end of that rope.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at pdnews@frontlinemedcom.com.
The headline in a Portland, Maine, newspaper read, “Standish man sentenced to serve 15 years in prison for death of his 3-month-old son” (Edward Murphy, May 23, 2017). I suspect that many of the folks who read the story under the headline feel that the sentence was too light. Others are asking themselves how a 21-year-old man could beat a fragile 5-pound infant to death. What kind of evil monster is this guy?
However, even with the snatches of information provided in the 500-word newspaper story, the unfortunate scenario makes sense, and the child’s death is a tragic culmination of a series of events that shouldn’t surprise any pediatrician. It turns out the infant was a twin who, with his sister, had been born at 30 weeks’ gestation. He had spent a month or more in the hospital, and his sister was still in neonatal ICU at the time of his death. While it is unclear from the newspaper article whether the twins’ parents were married, they were living in a house with eight other adults and some other children. The mother was out of the home working while the father was left to care for his son.
I am sure that the neonatologists and social workers at the hospital where the twins were born were aware of at least some of the red flags that waved over this unfortunate family. I also am confident that they did what they could to assure this infant a safe home environment when it was time for his discharge from the NICU. However, risks factors may have been missed that now seem obvious in retrospect. We should all realize by now from our experience with domestic terrorism that simply appearing on someone’s radar doesn’t mean that preemptive action can or will be taken. Short of keeping the parents of high-risk neonates under constant surveillance for a year or 2, there are few other workable options to prevent every tragedy like this one.
This case is another example of the erosive power of a baby’s cry. Most pediatricians have developed a filtering mechanism that allows us to function in a cacophonous environment dominated by a screaming infant. However, even adults without this young father’s deprived background crack under the stress when they are confined in a space with a crying child. The risk of decompensation is compounded when the adult also feels some responsibility for the child’s welfare. I don’t think we can condone what the father did in this tragic scenario, but we can certainly understand how the dominoes fell.
We are all potential child abusers. When faced with the right, or I guess the wrong, set of circumstances we might lash out to stop the crying. Luckily, most of us are several body lengths from the end of that rope.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at pdnews@frontlinemedcom.com.
The headline in a Portland, Maine, newspaper read, “Standish man sentenced to serve 15 years in prison for death of his 3-month-old son” (Edward Murphy, May 23, 2017). I suspect that many of the folks who read the story under the headline feel that the sentence was too light. Others are asking themselves how a 21-year-old man could beat a fragile 5-pound infant to death. What kind of evil monster is this guy?
However, even with the snatches of information provided in the 500-word newspaper story, the unfortunate scenario makes sense, and the child’s death is a tragic culmination of a series of events that shouldn’t surprise any pediatrician. It turns out the infant was a twin who, with his sister, had been born at 30 weeks’ gestation. He had spent a month or more in the hospital, and his sister was still in neonatal ICU at the time of his death. While it is unclear from the newspaper article whether the twins’ parents were married, they were living in a house with eight other adults and some other children. The mother was out of the home working while the father was left to care for his son.
I am sure that the neonatologists and social workers at the hospital where the twins were born were aware of at least some of the red flags that waved over this unfortunate family. I also am confident that they did what they could to assure this infant a safe home environment when it was time for his discharge from the NICU. However, risks factors may have been missed that now seem obvious in retrospect. We should all realize by now from our experience with domestic terrorism that simply appearing on someone’s radar doesn’t mean that preemptive action can or will be taken. Short of keeping the parents of high-risk neonates under constant surveillance for a year or 2, there are few other workable options to prevent every tragedy like this one.
This case is another example of the erosive power of a baby’s cry. Most pediatricians have developed a filtering mechanism that allows us to function in a cacophonous environment dominated by a screaming infant. However, even adults without this young father’s deprived background crack under the stress when they are confined in a space with a crying child. The risk of decompensation is compounded when the adult also feels some responsibility for the child’s welfare. I don’t think we can condone what the father did in this tragic scenario, but we can certainly understand how the dominoes fell.
We are all potential child abusers. When faced with the right, or I guess the wrong, set of circumstances we might lash out to stop the crying. Luckily, most of us are several body lengths from the end of that rope.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at pdnews@frontlinemedcom.com.
Not better late ...
You all know the statistics or at least have a sense of the scope of the problem. While 85% of mothers in this country intend to breastfeed their infants exclusively for at least 3 months, only slightly more than 30% achieve this goal. Among the dozens of reasons for this unfortunate shortfall is what some experts view as inadequate support by primary care physicians and their offices. In the May 2017 Pediatrics, two members of the American Academy of Pediatrics Section on Breastfeeding offer a clinical report that hopes to remedy this situation (“The Breastfeeding-Friendly Pediatric Office Practice.” Pediatrics. 2017 May. 139[5]:e20170647). It is a document that begins with an excellent review of the background and epidemiology of breastfeeding in the United States and a survey of the current initiatives targeted at improving our dismal performance. What follows is an extensive set of 19 evidence-based recommendations for the pediatric outpatient practice that hopes to “meet or exceed the AAP recommendations.”
A large part of the problem is the failure of the point person in the office, usually the receptionist, to realize that a tearful call from a new mother who is struggling with breastfeeding is an emergency, one that demands a response in minutes … not hours. Even when the call is eventually routed to someone with a compassionate voice who will call back with the right answers, if that process takes just an hour or two, that is enough time for a mother with a screaming and hungry newborn to reach for a bottle of formula.
I urge you to read this exhaustive clinical report in Pediatrics because it is very likely you will come across some things that you can include in your office practice to make it more breastfeeding friendly. However, Even if you and your staff have the right advice, this is not a situation of “better late than never.”
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.”
You all know the statistics or at least have a sense of the scope of the problem. While 85% of mothers in this country intend to breastfeed their infants exclusively for at least 3 months, only slightly more than 30% achieve this goal. Among the dozens of reasons for this unfortunate shortfall is what some experts view as inadequate support by primary care physicians and their offices. In the May 2017 Pediatrics, two members of the American Academy of Pediatrics Section on Breastfeeding offer a clinical report that hopes to remedy this situation (“The Breastfeeding-Friendly Pediatric Office Practice.” Pediatrics. 2017 May. 139[5]:e20170647). It is a document that begins with an excellent review of the background and epidemiology of breastfeeding in the United States and a survey of the current initiatives targeted at improving our dismal performance. What follows is an extensive set of 19 evidence-based recommendations for the pediatric outpatient practice that hopes to “meet or exceed the AAP recommendations.”
A large part of the problem is the failure of the point person in the office, usually the receptionist, to realize that a tearful call from a new mother who is struggling with breastfeeding is an emergency, one that demands a response in minutes … not hours. Even when the call is eventually routed to someone with a compassionate voice who will call back with the right answers, if that process takes just an hour or two, that is enough time for a mother with a screaming and hungry newborn to reach for a bottle of formula.
I urge you to read this exhaustive clinical report in Pediatrics because it is very likely you will come across some things that you can include in your office practice to make it more breastfeeding friendly. However, Even if you and your staff have the right advice, this is not a situation of “better late than never.”
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.”
You all know the statistics or at least have a sense of the scope of the problem. While 85% of mothers in this country intend to breastfeed their infants exclusively for at least 3 months, only slightly more than 30% achieve this goal. Among the dozens of reasons for this unfortunate shortfall is what some experts view as inadequate support by primary care physicians and their offices. In the May 2017 Pediatrics, two members of the American Academy of Pediatrics Section on Breastfeeding offer a clinical report that hopes to remedy this situation (“The Breastfeeding-Friendly Pediatric Office Practice.” Pediatrics. 2017 May. 139[5]:e20170647). It is a document that begins with an excellent review of the background and epidemiology of breastfeeding in the United States and a survey of the current initiatives targeted at improving our dismal performance. What follows is an extensive set of 19 evidence-based recommendations for the pediatric outpatient practice that hopes to “meet or exceed the AAP recommendations.”
A large part of the problem is the failure of the point person in the office, usually the receptionist, to realize that a tearful call from a new mother who is struggling with breastfeeding is an emergency, one that demands a response in minutes … not hours. Even when the call is eventually routed to someone with a compassionate voice who will call back with the right answers, if that process takes just an hour or two, that is enough time for a mother with a screaming and hungry newborn to reach for a bottle of formula.
I urge you to read this exhaustive clinical report in Pediatrics because it is very likely you will come across some things that you can include in your office practice to make it more breastfeeding friendly. However, Even if you and your staff have the right advice, this is not a situation of “better late than never.”
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.”
Infant mortality down in most states
Infant mortality in the United States was down by 15% from 2005 to 2014, with 33 states reporting significant declines, according to the National Center for Health Statistics.
The overall rate for 2014 was 5.82 infant deaths per 1,000 live births, compared with 6.84 per 1,000 in 2005. The data for individual states were grouped into 3-year periods, so between the periods of 2005-2007 and 2012-2014, there were 33 states (and the District of Columbia) with a significant decline and 17 states with no significant change. Three states – Maine, South Dakota, and Utah – had increased infant mortality, but the changes did not reach significance, the NCHS reported, using data from the National Vital Statistics System.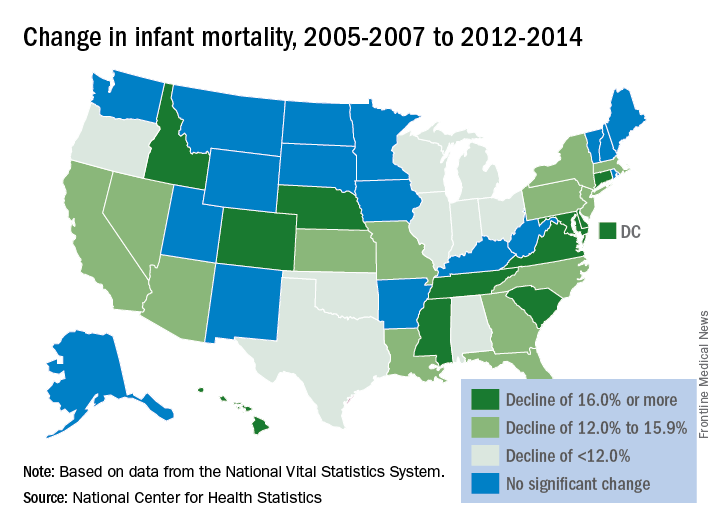
Infant mortality in the United States was down by 15% from 2005 to 2014, with 33 states reporting significant declines, according to the National Center for Health Statistics.
The overall rate for 2014 was 5.82 infant deaths per 1,000 live births, compared with 6.84 per 1,000 in 2005. The data for individual states were grouped into 3-year periods, so between the periods of 2005-2007 and 2012-2014, there were 33 states (and the District of Columbia) with a significant decline and 17 states with no significant change. Three states – Maine, South Dakota, and Utah – had increased infant mortality, but the changes did not reach significance, the NCHS reported, using data from the National Vital Statistics System.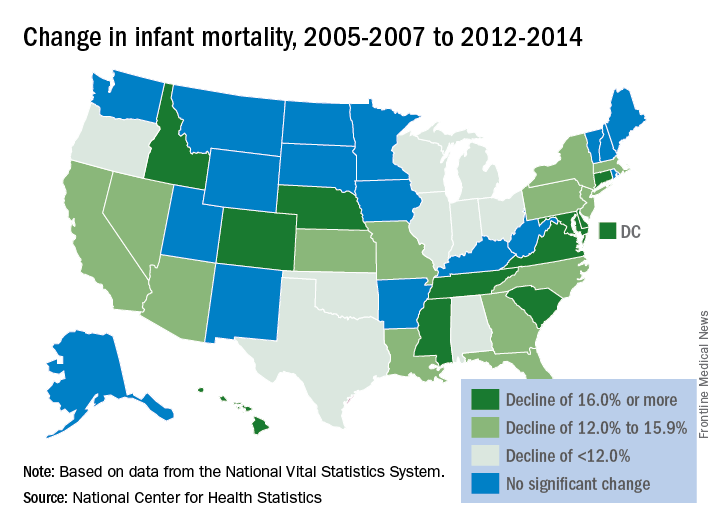
Infant mortality in the United States was down by 15% from 2005 to 2014, with 33 states reporting significant declines, according to the National Center for Health Statistics.
The overall rate for 2014 was 5.82 infant deaths per 1,000 live births, compared with 6.84 per 1,000 in 2005. The data for individual states were grouped into 3-year periods, so between the periods of 2005-2007 and 2012-2014, there were 33 states (and the District of Columbia) with a significant decline and 17 states with no significant change. Three states – Maine, South Dakota, and Utah – had increased infant mortality, but the changes did not reach significance, the NCHS reported, using data from the National Vital Statistics System.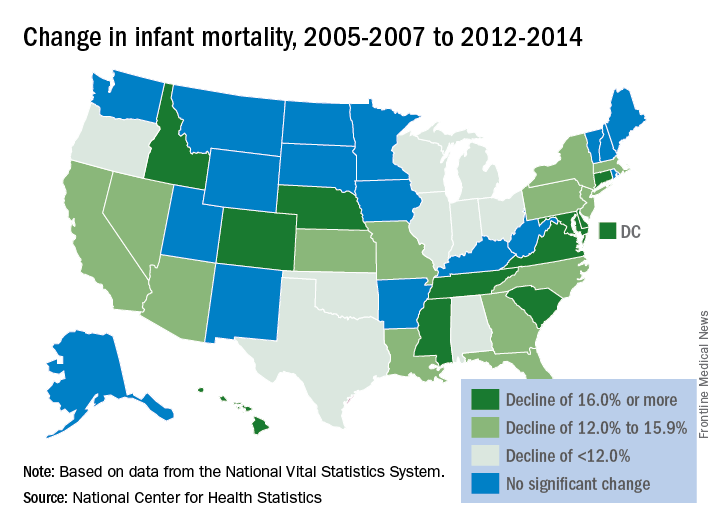
Management of asymptomatic chorioamnionitis-exposed neonates needs revamping
Clinical observation and laboratory evaluation without immediate antibiotic use in asymptomatic chorioamnionitis-exposed neonates prevented neonatal intensive care unit (NICU) admission in two-thirds of these infants, Amanda I. Jan, MD, of the University of Southern California, Los Angeles, and her associates reported in a study.
Since maternal intrapartum antibiotic prophylaxis was introduced, neonatal early-onset sepsis (EOS) rates have dropped considerably, and rates remain low even in chorioamnionitis-exposed infants. Despite these low risks, current American Academy of Pediatrics and Centers for Disease Control and Prevention recommendations still call for a limited laboratory evaluation and immediate empirical antibiotic therapy in all infants exposed to chorioamnionitis, often necessitating NICU admission for IV antibiotics, the researchers noted.
Of the 78 infants admitted to the NICU and put on antibiotics, 76% were treated with antibiotics for more than 72 hours, with a median 7 days of treatment, compared with a median 2 days for nonadmitted infants (P less than .001). Only 85% of admitted infants received any breast milk, compared with 94% of infants in the mother-infant unit (P = .032), and none of the admitted infants were exclusively breastfed.
“When the overall risks of EOS are low, exposure of large numbers of well-appearing infants to even short courses of antibiotics is no longer justified,” Dr. Jan and her associates stated. “The [difference in] cost of a stay in the mother-infant unit for 2 days, compared with a NICU stay, which averaged a week, is substantial. The charge for our NICU is $12,612 per day in contrast to $5,300 per day in the mother-infant unit. The cost savings for the 162 infants who were cared for 2 days in the mother-infant unit, compared with an EOS evaluation and antibiotic therapy in the NICU, totals $2,369,088, or $359,861 per year.
“There were no deaths or morbidities identified in any infant during the study period,” they reported. No infant was readmitted to the study hospital for sepsis after discharge.
Dr. Jan and her associates recommend their alternative management of asymptomatic chorioamnionitis-exposed neonates involving lab evaluations and close clinical observation without immediate antibiotic administration in a mother-infant unit. They believe this prevents unnecessary antibiotic exposure, unnecessarily high hospitalization costs, and disruption of maternal-neonatal bonding and breastfeeding. Additional studies are needed to determine the safety of this approach.
This study received no external funding, and Dr. Jan and her associates reported no relevant financial disclosures.
Dr. Jan and her associates have taken steps in the right direction in altering management of asymptomatic term and near-term newborns with a maternal history of chorioamnionitis to avoid administering empirical antibiotics to all these babies, which is sorely needed as the current American Academy of Pediatrics and Centers for Disease Control and Prevention guidelines are outdated.
However, their alternative plan needs some tweaking. The positive predictive value of abnormal complete blood count or C-reactive protein results is too low to be of use in diagnosing sepsis. “We believe a better approach would be to forgo routine laboratory evaluations among this population altogether and manage them using clinical signs alone.”
They said it was important to state two key caveats. “First, in the immediate postpartum period, mild respiratory distress among term or near-term newborns may be attributable to the physiologic transition, which occurs in all newborn infants. It is not necessary to draw laboratories or start antibiotics on these patients as long as their symptoms improve and resolve within the first 6 hours of life. Second, if newborns with a maternal history of chorioamnionitis are to be monitored for signs of sepsis outside the NICU setting, observations must be frequent (at least hourly for the first 6 hours of life and then every 3 hours for the next 18 hours) and performed by adequately trained medical staff. In the absence of frequent, reliable observation, there is a possibility that the early signs of sepsis will be missed and go untreated with potentially severe consequences.”
This approach, as with any other, needs additional study.
Thomas A. Hooven, MD, and Richard A. Polin, MD, pediatricians at the Columbia University, New York, discussed the study by Jan et al. in a commentary, which is summarized here (Pediatrics. 2017;140[1]:e20171155). They reported that they received no external funding and had no relevant financial disclosures.
Dr. Jan and her associates have taken steps in the right direction in altering management of asymptomatic term and near-term newborns with a maternal history of chorioamnionitis to avoid administering empirical antibiotics to all these babies, which is sorely needed as the current American Academy of Pediatrics and Centers for Disease Control and Prevention guidelines are outdated.
However, their alternative plan needs some tweaking. The positive predictive value of abnormal complete blood count or C-reactive protein results is too low to be of use in diagnosing sepsis. “We believe a better approach would be to forgo routine laboratory evaluations among this population altogether and manage them using clinical signs alone.”
They said it was important to state two key caveats. “First, in the immediate postpartum period, mild respiratory distress among term or near-term newborns may be attributable to the physiologic transition, which occurs in all newborn infants. It is not necessary to draw laboratories or start antibiotics on these patients as long as their symptoms improve and resolve within the first 6 hours of life. Second, if newborns with a maternal history of chorioamnionitis are to be monitored for signs of sepsis outside the NICU setting, observations must be frequent (at least hourly for the first 6 hours of life and then every 3 hours for the next 18 hours) and performed by adequately trained medical staff. In the absence of frequent, reliable observation, there is a possibility that the early signs of sepsis will be missed and go untreated with potentially severe consequences.”
This approach, as with any other, needs additional study.
Thomas A. Hooven, MD, and Richard A. Polin, MD, pediatricians at the Columbia University, New York, discussed the study by Jan et al. in a commentary, which is summarized here (Pediatrics. 2017;140[1]:e20171155). They reported that they received no external funding and had no relevant financial disclosures.
Dr. Jan and her associates have taken steps in the right direction in altering management of asymptomatic term and near-term newborns with a maternal history of chorioamnionitis to avoid administering empirical antibiotics to all these babies, which is sorely needed as the current American Academy of Pediatrics and Centers for Disease Control and Prevention guidelines are outdated.
However, their alternative plan needs some tweaking. The positive predictive value of abnormal complete blood count or C-reactive protein results is too low to be of use in diagnosing sepsis. “We believe a better approach would be to forgo routine laboratory evaluations among this population altogether and manage them using clinical signs alone.”
They said it was important to state two key caveats. “First, in the immediate postpartum period, mild respiratory distress among term or near-term newborns may be attributable to the physiologic transition, which occurs in all newborn infants. It is not necessary to draw laboratories or start antibiotics on these patients as long as their symptoms improve and resolve within the first 6 hours of life. Second, if newborns with a maternal history of chorioamnionitis are to be monitored for signs of sepsis outside the NICU setting, observations must be frequent (at least hourly for the first 6 hours of life and then every 3 hours for the next 18 hours) and performed by adequately trained medical staff. In the absence of frequent, reliable observation, there is a possibility that the early signs of sepsis will be missed and go untreated with potentially severe consequences.”
This approach, as with any other, needs additional study.
Thomas A. Hooven, MD, and Richard A. Polin, MD, pediatricians at the Columbia University, New York, discussed the study by Jan et al. in a commentary, which is summarized here (Pediatrics. 2017;140[1]:e20171155). They reported that they received no external funding and had no relevant financial disclosures.
Clinical observation and laboratory evaluation without immediate antibiotic use in asymptomatic chorioamnionitis-exposed neonates prevented neonatal intensive care unit (NICU) admission in two-thirds of these infants, Amanda I. Jan, MD, of the University of Southern California, Los Angeles, and her associates reported in a study.
Since maternal intrapartum antibiotic prophylaxis was introduced, neonatal early-onset sepsis (EOS) rates have dropped considerably, and rates remain low even in chorioamnionitis-exposed infants. Despite these low risks, current American Academy of Pediatrics and Centers for Disease Control and Prevention recommendations still call for a limited laboratory evaluation and immediate empirical antibiotic therapy in all infants exposed to chorioamnionitis, often necessitating NICU admission for IV antibiotics, the researchers noted.
Of the 78 infants admitted to the NICU and put on antibiotics, 76% were treated with antibiotics for more than 72 hours, with a median 7 days of treatment, compared with a median 2 days for nonadmitted infants (P less than .001). Only 85% of admitted infants received any breast milk, compared with 94% of infants in the mother-infant unit (P = .032), and none of the admitted infants were exclusively breastfed.
“When the overall risks of EOS are low, exposure of large numbers of well-appearing infants to even short courses of antibiotics is no longer justified,” Dr. Jan and her associates stated. “The [difference in] cost of a stay in the mother-infant unit for 2 days, compared with a NICU stay, which averaged a week, is substantial. The charge for our NICU is $12,612 per day in contrast to $5,300 per day in the mother-infant unit. The cost savings for the 162 infants who were cared for 2 days in the mother-infant unit, compared with an EOS evaluation and antibiotic therapy in the NICU, totals $2,369,088, or $359,861 per year.
“There were no deaths or morbidities identified in any infant during the study period,” they reported. No infant was readmitted to the study hospital for sepsis after discharge.
Dr. Jan and her associates recommend their alternative management of asymptomatic chorioamnionitis-exposed neonates involving lab evaluations and close clinical observation without immediate antibiotic administration in a mother-infant unit. They believe this prevents unnecessary antibiotic exposure, unnecessarily high hospitalization costs, and disruption of maternal-neonatal bonding and breastfeeding. Additional studies are needed to determine the safety of this approach.
This study received no external funding, and Dr. Jan and her associates reported no relevant financial disclosures.
Clinical observation and laboratory evaluation without immediate antibiotic use in asymptomatic chorioamnionitis-exposed neonates prevented neonatal intensive care unit (NICU) admission in two-thirds of these infants, Amanda I. Jan, MD, of the University of Southern California, Los Angeles, and her associates reported in a study.
Since maternal intrapartum antibiotic prophylaxis was introduced, neonatal early-onset sepsis (EOS) rates have dropped considerably, and rates remain low even in chorioamnionitis-exposed infants. Despite these low risks, current American Academy of Pediatrics and Centers for Disease Control and Prevention recommendations still call for a limited laboratory evaluation and immediate empirical antibiotic therapy in all infants exposed to chorioamnionitis, often necessitating NICU admission for IV antibiotics, the researchers noted.
Of the 78 infants admitted to the NICU and put on antibiotics, 76% were treated with antibiotics for more than 72 hours, with a median 7 days of treatment, compared with a median 2 days for nonadmitted infants (P less than .001). Only 85% of admitted infants received any breast milk, compared with 94% of infants in the mother-infant unit (P = .032), and none of the admitted infants were exclusively breastfed.
“When the overall risks of EOS are low, exposure of large numbers of well-appearing infants to even short courses of antibiotics is no longer justified,” Dr. Jan and her associates stated. “The [difference in] cost of a stay in the mother-infant unit for 2 days, compared with a NICU stay, which averaged a week, is substantial. The charge for our NICU is $12,612 per day in contrast to $5,300 per day in the mother-infant unit. The cost savings for the 162 infants who were cared for 2 days in the mother-infant unit, compared with an EOS evaluation and antibiotic therapy in the NICU, totals $2,369,088, or $359,861 per year.
“There were no deaths or morbidities identified in any infant during the study period,” they reported. No infant was readmitted to the study hospital for sepsis after discharge.
Dr. Jan and her associates recommend their alternative management of asymptomatic chorioamnionitis-exposed neonates involving lab evaluations and close clinical observation without immediate antibiotic administration in a mother-infant unit. They believe this prevents unnecessary antibiotic exposure, unnecessarily high hospitalization costs, and disruption of maternal-neonatal bonding and breastfeeding. Additional studies are needed to determine the safety of this approach.
This study received no external funding, and Dr. Jan and her associates reported no relevant financial disclosures.
FROM PEDIATRICS
Key clinical point: Alternative management of asymptomatic chorioamnionitis-exposed neonates will prevent unnecessary antibiotic exposure, unnecessarily high hospitalization costs, and disruption of maternal-neonatal bonding and breastfeeding.
Major finding: Of the 240 infants, 67.5% remained well with a routine newborn course in the mother-infant unit and 32.5% subsequently were admitted to the NICU because of abnormal laboratory data, a positive blood culture, or the onset of clinical signs of sepsis.
Data source: A retrospective cohort study of 240 asymptomatic chorioamnionitis-exposed neonates.
Disclosures: This study received no external funding, and Dr. Jan and her associates reported no relevant financial disclosures.