User login
Supercharge your medical practice with ChatGPT: Here’s why you should upgrade
Artificial intelligence (AI) has already demonstrated its potential in various areas of healthcare, from early disease detection and drug discovery to genomics and personalized care. OpenAI’s ChatGPT, a large language model, is one AI tool that has been transforming practices across the globe, including mine.
Let me walk you through it.
ChatGPT is essentially an AI-fueled assistant, capable of interpreting and generating human-like text in response to user inputs. Imagine a well-informed and competent trainee working with you, ready to tackle tasks from handling patient inquiries to summarizing intricate medical literature.
Currently, ChatGPT works on the “freemium” pricing model; there is a free version built upon GPT-3.5 as well as a subscription “ChatGPT Plus” version based on GPT-4 which offers additional features such as the use of third-party plug-ins.
Now, you may ask, “Isn’t the free version enough?” The free version is indeed impressive, but upgrading to the paid version for $20 per month unlocks the full potential of this tool, particularly if we add plug-ins.
Here are some of the best ways to incorporate ChatGPT Plus into your practice.
Time saver and efficiency multiplier. The paid version of ChatGPT is an extraordinary time-saving tool. It can help you sort through vast amounts of medical literature in a fraction of the time it would normally take. Imagine having to sift through hundreds of articles to find the latest research relevant to a patient’s case. With the paid version of ChatGPT, you can simply ask it to provide summaries of the most recent and relevant studies, all in seconds.
Did you forget about that PowerPoint you need to make but know the potential papers you would use? No problem. ChatGPT can create slides in a few minutes. It becomes your on-demand research assistant.
Of course, you need to provide the source you find most relevant to you. Using plug-ins such as ScholarAI and Link Reader are great.
Improved patient communication. Explaining complex medical terminology and procedures to patients can sometimes be a challenge. ChatGPT can generate simplified and personalized explanations for your patients, fostering their understanding and involvement in their care process.
Epic is currently collaborating with Nuance Communications, Microsoft’s speech recognition subsidiary, to use generative AI tools for medical note-taking in the electronic health record. However, you do not need to wait for it; it just takes a prompt in ChatGPT and then copying/pasting the results into the chart.
Smoother administrative management. The premium version of ChatGPT can automate administrative tasks such as creating letters of medical necessity, clearance to other physicians for services, or even communications to staff on specific topics. This frees you to focus more on your core work: providing patient care.
Precision medicine aid. ChatGPT can be a powerful ally in the field of precision medicine. Its capabilities for analyzing large datasets and unearthing valuable insights can help deliver more personalized and potentially effective treatment plans. For example, one can prompt ChatGPT to query the reported frequency of certain genomic variants and their implications; with the upgraded version and plug-ins, the results will have fewer hallucinations — inaccurate results — and key data references.
Unlimited accessibility. Uninterrupted access is a compelling reason to upgrade. While the free version may have usage limitations, the premium version provides unrestricted, round-the-clock access. Be it a late-night research quest or an early-morning patient query, your AI assistant will always be available.
Strengthened privacy and security. The premium version of ChatGPT includes heightened privacy and security measures. Just make sure to follow HIPAA and not include identifiers when making queries.
Embracing AI tools like ChatGPT in your practice can help you stay at the cutting edge of medical care, saving you time, enhancing patient communication, and supporting you in providing personalized care.
While the free version can serve as a good starting point (there are apps for both iOS and Android), upgrading to the paid version opens up a world of possibilities that can truly supercharge your practice.
I would love to hear your comments on this column or on future topics. Contact me at Arturo.AI.MedTech@gmail.com.
Arturo Loaiza-Bonilla, MD, MSEd, is the cofounder and chief medical officer at Massive Bio, a company connecting patients to clinical trials using artificial intelligence. His research and professional interests focus on precision medicine, clinical trial design, digital health, entrepreneurship, and patient advocacy. Dr. Loaiza-Bonilla is Assistant Professor of Medicine, Drexel University School of Medicine, Philadelphia, Pennsylvania, and serves as medical director of oncology research at Capital Health in New Jersey, where he maintains a connection to patient care by attending to patients 2 days a week. He has financial relationships with Verify, PSI CRO, Bayer, AstraZeneca, Cardinal Health, BrightInsight, The Lynx Group, Fresenius, Pfizer, Ipsen, Guardant, Amgen, Eisai, Natera, Merck, and Bristol Myers Squibb.
A version of this article appeared on Medscape.com.
Artificial intelligence (AI) has already demonstrated its potential in various areas of healthcare, from early disease detection and drug discovery to genomics and personalized care. OpenAI’s ChatGPT, a large language model, is one AI tool that has been transforming practices across the globe, including mine.
Let me walk you through it.
ChatGPT is essentially an AI-fueled assistant, capable of interpreting and generating human-like text in response to user inputs. Imagine a well-informed and competent trainee working with you, ready to tackle tasks from handling patient inquiries to summarizing intricate medical literature.
Currently, ChatGPT works on the “freemium” pricing model; there is a free version built upon GPT-3.5 as well as a subscription “ChatGPT Plus” version based on GPT-4 which offers additional features such as the use of third-party plug-ins.
Now, you may ask, “Isn’t the free version enough?” The free version is indeed impressive, but upgrading to the paid version for $20 per month unlocks the full potential of this tool, particularly if we add plug-ins.
Here are some of the best ways to incorporate ChatGPT Plus into your practice.
Time saver and efficiency multiplier. The paid version of ChatGPT is an extraordinary time-saving tool. It can help you sort through vast amounts of medical literature in a fraction of the time it would normally take. Imagine having to sift through hundreds of articles to find the latest research relevant to a patient’s case. With the paid version of ChatGPT, you can simply ask it to provide summaries of the most recent and relevant studies, all in seconds.
Did you forget about that PowerPoint you need to make but know the potential papers you would use? No problem. ChatGPT can create slides in a few minutes. It becomes your on-demand research assistant.
Of course, you need to provide the source you find most relevant to you. Using plug-ins such as ScholarAI and Link Reader are great.
Improved patient communication. Explaining complex medical terminology and procedures to patients can sometimes be a challenge. ChatGPT can generate simplified and personalized explanations for your patients, fostering their understanding and involvement in their care process.
Epic is currently collaborating with Nuance Communications, Microsoft’s speech recognition subsidiary, to use generative AI tools for medical note-taking in the electronic health record. However, you do not need to wait for it; it just takes a prompt in ChatGPT and then copying/pasting the results into the chart.
Smoother administrative management. The premium version of ChatGPT can automate administrative tasks such as creating letters of medical necessity, clearance to other physicians for services, or even communications to staff on specific topics. This frees you to focus more on your core work: providing patient care.
Precision medicine aid. ChatGPT can be a powerful ally in the field of precision medicine. Its capabilities for analyzing large datasets and unearthing valuable insights can help deliver more personalized and potentially effective treatment plans. For example, one can prompt ChatGPT to query the reported frequency of certain genomic variants and their implications; with the upgraded version and plug-ins, the results will have fewer hallucinations — inaccurate results — and key data references.
Unlimited accessibility. Uninterrupted access is a compelling reason to upgrade. While the free version may have usage limitations, the premium version provides unrestricted, round-the-clock access. Be it a late-night research quest or an early-morning patient query, your AI assistant will always be available.
Strengthened privacy and security. The premium version of ChatGPT includes heightened privacy and security measures. Just make sure to follow HIPAA and not include identifiers when making queries.
Embracing AI tools like ChatGPT in your practice can help you stay at the cutting edge of medical care, saving you time, enhancing patient communication, and supporting you in providing personalized care.
While the free version can serve as a good starting point (there are apps for both iOS and Android), upgrading to the paid version opens up a world of possibilities that can truly supercharge your practice.
I would love to hear your comments on this column or on future topics. Contact me at Arturo.AI.MedTech@gmail.com.
Arturo Loaiza-Bonilla, MD, MSEd, is the cofounder and chief medical officer at Massive Bio, a company connecting patients to clinical trials using artificial intelligence. His research and professional interests focus on precision medicine, clinical trial design, digital health, entrepreneurship, and patient advocacy. Dr. Loaiza-Bonilla is Assistant Professor of Medicine, Drexel University School of Medicine, Philadelphia, Pennsylvania, and serves as medical director of oncology research at Capital Health in New Jersey, where he maintains a connection to patient care by attending to patients 2 days a week. He has financial relationships with Verify, PSI CRO, Bayer, AstraZeneca, Cardinal Health, BrightInsight, The Lynx Group, Fresenius, Pfizer, Ipsen, Guardant, Amgen, Eisai, Natera, Merck, and Bristol Myers Squibb.
A version of this article appeared on Medscape.com.
Artificial intelligence (AI) has already demonstrated its potential in various areas of healthcare, from early disease detection and drug discovery to genomics and personalized care. OpenAI’s ChatGPT, a large language model, is one AI tool that has been transforming practices across the globe, including mine.
Let me walk you through it.
ChatGPT is essentially an AI-fueled assistant, capable of interpreting and generating human-like text in response to user inputs. Imagine a well-informed and competent trainee working with you, ready to tackle tasks from handling patient inquiries to summarizing intricate medical literature.
Currently, ChatGPT works on the “freemium” pricing model; there is a free version built upon GPT-3.5 as well as a subscription “ChatGPT Plus” version based on GPT-4 which offers additional features such as the use of third-party plug-ins.
Now, you may ask, “Isn’t the free version enough?” The free version is indeed impressive, but upgrading to the paid version for $20 per month unlocks the full potential of this tool, particularly if we add plug-ins.
Here are some of the best ways to incorporate ChatGPT Plus into your practice.
Time saver and efficiency multiplier. The paid version of ChatGPT is an extraordinary time-saving tool. It can help you sort through vast amounts of medical literature in a fraction of the time it would normally take. Imagine having to sift through hundreds of articles to find the latest research relevant to a patient’s case. With the paid version of ChatGPT, you can simply ask it to provide summaries of the most recent and relevant studies, all in seconds.
Did you forget about that PowerPoint you need to make but know the potential papers you would use? No problem. ChatGPT can create slides in a few minutes. It becomes your on-demand research assistant.
Of course, you need to provide the source you find most relevant to you. Using plug-ins such as ScholarAI and Link Reader are great.
Improved patient communication. Explaining complex medical terminology and procedures to patients can sometimes be a challenge. ChatGPT can generate simplified and personalized explanations for your patients, fostering their understanding and involvement in their care process.
Epic is currently collaborating with Nuance Communications, Microsoft’s speech recognition subsidiary, to use generative AI tools for medical note-taking in the electronic health record. However, you do not need to wait for it; it just takes a prompt in ChatGPT and then copying/pasting the results into the chart.
Smoother administrative management. The premium version of ChatGPT can automate administrative tasks such as creating letters of medical necessity, clearance to other physicians for services, or even communications to staff on specific topics. This frees you to focus more on your core work: providing patient care.
Precision medicine aid. ChatGPT can be a powerful ally in the field of precision medicine. Its capabilities for analyzing large datasets and unearthing valuable insights can help deliver more personalized and potentially effective treatment plans. For example, one can prompt ChatGPT to query the reported frequency of certain genomic variants and their implications; with the upgraded version and plug-ins, the results will have fewer hallucinations — inaccurate results — and key data references.
Unlimited accessibility. Uninterrupted access is a compelling reason to upgrade. While the free version may have usage limitations, the premium version provides unrestricted, round-the-clock access. Be it a late-night research quest or an early-morning patient query, your AI assistant will always be available.
Strengthened privacy and security. The premium version of ChatGPT includes heightened privacy and security measures. Just make sure to follow HIPAA and not include identifiers when making queries.
Embracing AI tools like ChatGPT in your practice can help you stay at the cutting edge of medical care, saving you time, enhancing patient communication, and supporting you in providing personalized care.
While the free version can serve as a good starting point (there are apps for both iOS and Android), upgrading to the paid version opens up a world of possibilities that can truly supercharge your practice.
I would love to hear your comments on this column or on future topics. Contact me at Arturo.AI.MedTech@gmail.com.
Arturo Loaiza-Bonilla, MD, MSEd, is the cofounder and chief medical officer at Massive Bio, a company connecting patients to clinical trials using artificial intelligence. His research and professional interests focus on precision medicine, clinical trial design, digital health, entrepreneurship, and patient advocacy. Dr. Loaiza-Bonilla is Assistant Professor of Medicine, Drexel University School of Medicine, Philadelphia, Pennsylvania, and serves as medical director of oncology research at Capital Health in New Jersey, where he maintains a connection to patient care by attending to patients 2 days a week. He has financial relationships with Verify, PSI CRO, Bayer, AstraZeneca, Cardinal Health, BrightInsight, The Lynx Group, Fresenius, Pfizer, Ipsen, Guardant, Amgen, Eisai, Natera, Merck, and Bristol Myers Squibb.
A version of this article appeared on Medscape.com.
Few with inflammatory breast cancer get guideline-based care
SAN ANTONIO — Yet, a retrospective study of patients with inflammatory breast carcinoma shows that the majority of patients don’t receive it.
The study also showed that overall survival was lowest for Black women who didn’t receive guideline-concordant care, said Brian Diskin, MD, with the Division of Breast Surgery, Memorial Sloan Kettering Cancer Center, New York City, here at the San Antonio Breast Cancer Symposium.
The results highlight the importance of adhering to guidelines in inflammatory breast carcinoma and suggest that improving the rates among Black patients “may help to mitigate racial disparities and survival,” Dr.Diskin told the conference.
Inflammatory breast carcinoma is an aggressive form of breast cancer associated with worse survival outcomes compared with other subtypes of breast cancer. Yet, it’s unclear how often and consistently guideline-concordant care — defined as treatment with neoadjuvant chemotherapy followed by modified radical mastectomy without immediate reconstruction, and postmastectomy radiotherapy — is received and what factors play a role in receiving recommended care.
To investigate, Dr. Diskin and colleagues identified 6945 women from the National Cancer Database with nonmetastatic inflammatory breast cancer treated from 2010-2018. Guideline-concordant care was defined as trimodality treatment administered in the correct sequence, with neoadjuvant chemotherapy started within 60 days of diagnosis.
Most patients (88%) did not start neoadjuvant chemotherapy within 60 days of diagnosis.
Black and Asian patients were less likely than were White patients to start chemotherapy within 60 days (odds ratio [OR] 0.54 and 0.51, respectively; P < .001), while patients with Medicare or private insurance were more likely to receive chemotherapy within 60 days of diagnosis than uninsured patients (OR 1.37 and 1.87, respectively; P < .001).
Roughly half of all patients didn’t receive appropriate surgical treatment (modified radical mastectomy without immediate reconstruction and postmastectomy radiotherapy).
Overall, only about one third of the cohort received guideline-concordant treatment, Dr. Diskin reported.
Patients aged 60-69 were more likely than were patients aged 40-49 to receive guideline-concordant treatment (odds ratio [OR], 1.24; P < .001), as were patients with a higher clinical nodal burden (OR, 1.34 for N1; OR, 1.28 for N2; OR, 1.15 for N3 vs N0; P < .001 for N1 and N2).
Patients treated between 2014 and 2018 were less likely to receive guideline-concordant treatment than patients treated between 2010 and 2013 (OR, 0.63; P <.001).
Receiving guideline-concordant care and being privately insured were both positively associated with improved overall survival (OR, 0.75 and 0.62, respectively; P < .001). Conversely, triple-negative subtype and Black race were associated with worse overall survival (HR, 1.6 and 1.4, respectively; P < .001).
However, timely receipt of guideline-concordant care for Black patients with triple-negative disease did lead to improved overall survival. Among recipients of guideline-based care with triple-negative disease, there was no racial disparity in overall survival.
Study discussant Kathryn Hudson, MD, director of survivorship and medical oncologist at Texas Oncology, Austin, said it’s important to note that Black women have a 4% lower incidence of breast cancer than do White women but a 40% higher breast cancer death rate.
“This study is important because it confirms that those who receive guideline-based care have better outcomes and that Black women have worse survival in [inflammatory breast cancer],” Dr. Hudson said.
The finding that Black and Asian women in the study were less likely to have timely neoadjuvant chemotherapy, “likely reflects worse access to care, and this may play a role in why Black women had worse outcomes,” she added.
Dr. Hudson said she found it “surprising” that only about one third of patients received guideline-concordant care.
In her view, “the take-home message is that improving guideline-concordant will improve outcomes for all patients with inflammatory breast cancer. And it’s really important, as a next step, to examine the barriers to guideline-concordant care in inflammatory breast cancer and continue to understand the reasons for worse [rates of] survival of Black women.”
Dr. Diskin has disclosed no relevant financial relationships. Dr. Hudson has received honoraria from the Menarini Group and Gilead.
A version of this article appeared on Medscape.com.
SAN ANTONIO — Yet, a retrospective study of patients with inflammatory breast carcinoma shows that the majority of patients don’t receive it.
The study also showed that overall survival was lowest for Black women who didn’t receive guideline-concordant care, said Brian Diskin, MD, with the Division of Breast Surgery, Memorial Sloan Kettering Cancer Center, New York City, here at the San Antonio Breast Cancer Symposium.
The results highlight the importance of adhering to guidelines in inflammatory breast carcinoma and suggest that improving the rates among Black patients “may help to mitigate racial disparities and survival,” Dr.Diskin told the conference.
Inflammatory breast carcinoma is an aggressive form of breast cancer associated with worse survival outcomes compared with other subtypes of breast cancer. Yet, it’s unclear how often and consistently guideline-concordant care — defined as treatment with neoadjuvant chemotherapy followed by modified radical mastectomy without immediate reconstruction, and postmastectomy radiotherapy — is received and what factors play a role in receiving recommended care.
To investigate, Dr. Diskin and colleagues identified 6945 women from the National Cancer Database with nonmetastatic inflammatory breast cancer treated from 2010-2018. Guideline-concordant care was defined as trimodality treatment administered in the correct sequence, with neoadjuvant chemotherapy started within 60 days of diagnosis.
Most patients (88%) did not start neoadjuvant chemotherapy within 60 days of diagnosis.
Black and Asian patients were less likely than were White patients to start chemotherapy within 60 days (odds ratio [OR] 0.54 and 0.51, respectively; P < .001), while patients with Medicare or private insurance were more likely to receive chemotherapy within 60 days of diagnosis than uninsured patients (OR 1.37 and 1.87, respectively; P < .001).
Roughly half of all patients didn’t receive appropriate surgical treatment (modified radical mastectomy without immediate reconstruction and postmastectomy radiotherapy).
Overall, only about one third of the cohort received guideline-concordant treatment, Dr. Diskin reported.
Patients aged 60-69 were more likely than were patients aged 40-49 to receive guideline-concordant treatment (odds ratio [OR], 1.24; P < .001), as were patients with a higher clinical nodal burden (OR, 1.34 for N1; OR, 1.28 for N2; OR, 1.15 for N3 vs N0; P < .001 for N1 and N2).
Patients treated between 2014 and 2018 were less likely to receive guideline-concordant treatment than patients treated between 2010 and 2013 (OR, 0.63; P <.001).
Receiving guideline-concordant care and being privately insured were both positively associated with improved overall survival (OR, 0.75 and 0.62, respectively; P < .001). Conversely, triple-negative subtype and Black race were associated with worse overall survival (HR, 1.6 and 1.4, respectively; P < .001).
However, timely receipt of guideline-concordant care for Black patients with triple-negative disease did lead to improved overall survival. Among recipients of guideline-based care with triple-negative disease, there was no racial disparity in overall survival.
Study discussant Kathryn Hudson, MD, director of survivorship and medical oncologist at Texas Oncology, Austin, said it’s important to note that Black women have a 4% lower incidence of breast cancer than do White women but a 40% higher breast cancer death rate.
“This study is important because it confirms that those who receive guideline-based care have better outcomes and that Black women have worse survival in [inflammatory breast cancer],” Dr. Hudson said.
The finding that Black and Asian women in the study were less likely to have timely neoadjuvant chemotherapy, “likely reflects worse access to care, and this may play a role in why Black women had worse outcomes,” she added.
Dr. Hudson said she found it “surprising” that only about one third of patients received guideline-concordant care.
In her view, “the take-home message is that improving guideline-concordant will improve outcomes for all patients with inflammatory breast cancer. And it’s really important, as a next step, to examine the barriers to guideline-concordant care in inflammatory breast cancer and continue to understand the reasons for worse [rates of] survival of Black women.”
Dr. Diskin has disclosed no relevant financial relationships. Dr. Hudson has received honoraria from the Menarini Group and Gilead.
A version of this article appeared on Medscape.com.
SAN ANTONIO — Yet, a retrospective study of patients with inflammatory breast carcinoma shows that the majority of patients don’t receive it.
The study also showed that overall survival was lowest for Black women who didn’t receive guideline-concordant care, said Brian Diskin, MD, with the Division of Breast Surgery, Memorial Sloan Kettering Cancer Center, New York City, here at the San Antonio Breast Cancer Symposium.
The results highlight the importance of adhering to guidelines in inflammatory breast carcinoma and suggest that improving the rates among Black patients “may help to mitigate racial disparities and survival,” Dr.Diskin told the conference.
Inflammatory breast carcinoma is an aggressive form of breast cancer associated with worse survival outcomes compared with other subtypes of breast cancer. Yet, it’s unclear how often and consistently guideline-concordant care — defined as treatment with neoadjuvant chemotherapy followed by modified radical mastectomy without immediate reconstruction, and postmastectomy radiotherapy — is received and what factors play a role in receiving recommended care.
To investigate, Dr. Diskin and colleagues identified 6945 women from the National Cancer Database with nonmetastatic inflammatory breast cancer treated from 2010-2018. Guideline-concordant care was defined as trimodality treatment administered in the correct sequence, with neoadjuvant chemotherapy started within 60 days of diagnosis.
Most patients (88%) did not start neoadjuvant chemotherapy within 60 days of diagnosis.
Black and Asian patients were less likely than were White patients to start chemotherapy within 60 days (odds ratio [OR] 0.54 and 0.51, respectively; P < .001), while patients with Medicare or private insurance were more likely to receive chemotherapy within 60 days of diagnosis than uninsured patients (OR 1.37 and 1.87, respectively; P < .001).
Roughly half of all patients didn’t receive appropriate surgical treatment (modified radical mastectomy without immediate reconstruction and postmastectomy radiotherapy).
Overall, only about one third of the cohort received guideline-concordant treatment, Dr. Diskin reported.
Patients aged 60-69 were more likely than were patients aged 40-49 to receive guideline-concordant treatment (odds ratio [OR], 1.24; P < .001), as were patients with a higher clinical nodal burden (OR, 1.34 for N1; OR, 1.28 for N2; OR, 1.15 for N3 vs N0; P < .001 for N1 and N2).
Patients treated between 2014 and 2018 were less likely to receive guideline-concordant treatment than patients treated between 2010 and 2013 (OR, 0.63; P <.001).
Receiving guideline-concordant care and being privately insured were both positively associated with improved overall survival (OR, 0.75 and 0.62, respectively; P < .001). Conversely, triple-negative subtype and Black race were associated with worse overall survival (HR, 1.6 and 1.4, respectively; P < .001).
However, timely receipt of guideline-concordant care for Black patients with triple-negative disease did lead to improved overall survival. Among recipients of guideline-based care with triple-negative disease, there was no racial disparity in overall survival.
Study discussant Kathryn Hudson, MD, director of survivorship and medical oncologist at Texas Oncology, Austin, said it’s important to note that Black women have a 4% lower incidence of breast cancer than do White women but a 40% higher breast cancer death rate.
“This study is important because it confirms that those who receive guideline-based care have better outcomes and that Black women have worse survival in [inflammatory breast cancer],” Dr. Hudson said.
The finding that Black and Asian women in the study were less likely to have timely neoadjuvant chemotherapy, “likely reflects worse access to care, and this may play a role in why Black women had worse outcomes,” she added.
Dr. Hudson said she found it “surprising” that only about one third of patients received guideline-concordant care.
In her view, “the take-home message is that improving guideline-concordant will improve outcomes for all patients with inflammatory breast cancer. And it’s really important, as a next step, to examine the barriers to guideline-concordant care in inflammatory breast cancer and continue to understand the reasons for worse [rates of] survival of Black women.”
Dr. Diskin has disclosed no relevant financial relationships. Dr. Hudson has received honoraria from the Menarini Group and Gilead.
A version of this article appeared on Medscape.com.
AT SABCS 2023
‘Baby TAM’ effective, tolerable for breast cancer prevention
SAN ANTONIO — The drug can reduce incidence of breast cancer in high-risk individuals, but side effects that mimic menopause have led to low rates of uptake. Lower-dose tamoxifen aims to reduce those side effects, but there remains some uncertainty about the minimum dose required to maintain efficacy.
The TAM-01 study, first published in 2019, demonstrated that a 5-mg dose of tamoxifen led to a reduction in recurrence of invasive breast cancer or ductal carcinoma in situ (DCIS). At the San Antonio Breast Cancer Symposium, two studies were presented that provided insight into dose efficacy and likelihood of medication adherence in women taking baby TAM.
“We all know that women who are at increased risk for breast cancer may benefit from the use of tamoxifen to help lower their risk, although historical uptake to tamoxifen in the prevention setting has been quite low,” said Lauren Cornell, MD, during a presentation. Her team investigated the impact of patient counseling on how well they understood their risk, as well as their likelihood of adherence to the medication.
The study included 41 women, and 31 completed follow-up at 1 year. “We saw that 90% of our patients reported good or complete understanding of their breast cancer risk after the consultation, emphasizing the benefit of that consult, and 73% reported that the availability of baby tamoxifen helped in their decision to consider a preventative medication,” said Dr. Cornell during her presentation. After 1 year of follow-up, 74% said that they had initiated baby tamoxifen, and 78% of those who started taking the drug were still taking it at 1 year.
Participants who continued to take baby TAM at 1 year had a higher estimated breast cancer risk (IBIS 10-year risk, 12.7% vs 7.6%; P = .027) than those who discontinued. “We saw that uptake to baby TAM after informed discussion in patients who qualify is high, especially in those patients with high risk and intraepithelial lesions or DCIS, and adherence and tolerability at 1 year follow up is improved, compared to what we would expect with traditional dosing of tamoxifen. It’s important to note that the NCCN guidelines and the ASCO clinical practice update now include low-dose tamoxifen as an option for select women, and future randomized control trials on de-escalation of tamoxifen and high-risk patients based on their risk model assessment still need to be done. Future study should also focus on markers to identify candidates best suited for low versus standard dose of tamoxifen,” said Dr. Cornell, who is an assistant professor of medicine at Mayo Clinic Florida in Jacksonville.
At another SABCS session, Per Hall, MD, PhD, discussed findings from the previously published KARISMA-2 study, which examined efficacy of various doses of tamoxifen. A total of 1440 participants, 240 in each arm, received tamoxifen doses of 20 mg, 10 mg, 5 mg, 2.5 mg, 1 mg, or placebo. During his talk, Dr. Hall pointed out that measuring outcomes would take a very large number of participants to identify small differences in breast cancer rates. Therefore, the researchers examined breast density changes as a proxy. As a noninferiority outcome, the researchers used the proportion of women in each arm who achieved the median decrease in breast density seen at 20 mg of tamoxifen, which is 10.1%.
The women underwent mammograms at baseline and again at 6 months to determine change in breast density. Among all women in the study, the proportion of patients who had a similar breast density reduction as the 20-mg dose were very similar in the 10 mg (50.0%; P = .002), 5 mg (49.3%; P < .001), and 2.5 mg (52.5%; P < .001) groups. The 1 mg group had a proportion of 39.5% (P = .138), while the placebo group had 38.9% (P = .161). However, the results were driven by premenopausal women, where the values were 63.3%, 70.7%, 74.4%, and 69.7% in the 20-mg, 10-mg, 5-mg, and 2.5-mg groups, respectively, and 32.9% at 1 mg and 29.7% on placebo. In postmenopausal women, the values were 41.9%, 36.7%, 33.3%, and 41.9% in the 20-mg, 10-mg, 5-mg, and 2.5-mg groups, with values of 44.2% in the 1-mg group and 43.8% in the placebo group.
The median density change was 18.5% in premenopausal women and 4.0% in postmenopausal women.
“We didn’t see anything in the postmenopausal women. The decrease for those on 20 milligrams and those on placebo were exactly the same. Why this is, we still don’t know because we do know that tamoxifen in the adjuvant setting could be used for postmenopausal women. It could be that 6 months is too short of a time [to see a benefit]. We don’t know,” said Dr. Hall, who is a medical epidemiologist and biostatistician at Karolinska Institutet, Stockholm, Sweden.
Severe vasomotor side effects like hot flashes, cold flashes, and night sweats were reduced by about 50% in the lower tamoxifen doses, compared with 20 mg.
Dr. Hall also pointed out that tamoxifen is a prodrug. The CYP2D6 enzyme produces a range of metabolites, with endoxifen having the strongest affinity to the estrogen receptor and being present at the highest plasma concentration. He showed a table of endoxifen plasma levels at various tamoxifen doses in women of various metabolizer status, ranging from poor to ultrafast. Among intermediate, normal, and ultrarapid metabolizers, 5- and 10-mg doses produced plasma endoxifen levels ranging from 2.4 to 6.2 ng/mL, which represents a good therapeutic window. “For intermediate and normal metabolizers, it could be that 5 mg [of tamoxifen] is enough, but I want to underline that we didn’t use breast cancer incidence or recurrence in this study, we used density change, so we should be careful when we use these results,” said Dr. Hall. His group is now conducting the KARISMA Endoxifen trial, which will test endoxifen directly at doses of 1 and 2 mg.
Dr. Cornell has no relevant financial disclosures. Dr. Hall is a member of the scientific advisory board for Atossa Therapeutics.
SAN ANTONIO — The drug can reduce incidence of breast cancer in high-risk individuals, but side effects that mimic menopause have led to low rates of uptake. Lower-dose tamoxifen aims to reduce those side effects, but there remains some uncertainty about the minimum dose required to maintain efficacy.
The TAM-01 study, first published in 2019, demonstrated that a 5-mg dose of tamoxifen led to a reduction in recurrence of invasive breast cancer or ductal carcinoma in situ (DCIS). At the San Antonio Breast Cancer Symposium, two studies were presented that provided insight into dose efficacy and likelihood of medication adherence in women taking baby TAM.
“We all know that women who are at increased risk for breast cancer may benefit from the use of tamoxifen to help lower their risk, although historical uptake to tamoxifen in the prevention setting has been quite low,” said Lauren Cornell, MD, during a presentation. Her team investigated the impact of patient counseling on how well they understood their risk, as well as their likelihood of adherence to the medication.
The study included 41 women, and 31 completed follow-up at 1 year. “We saw that 90% of our patients reported good or complete understanding of their breast cancer risk after the consultation, emphasizing the benefit of that consult, and 73% reported that the availability of baby tamoxifen helped in their decision to consider a preventative medication,” said Dr. Cornell during her presentation. After 1 year of follow-up, 74% said that they had initiated baby tamoxifen, and 78% of those who started taking the drug were still taking it at 1 year.
Participants who continued to take baby TAM at 1 year had a higher estimated breast cancer risk (IBIS 10-year risk, 12.7% vs 7.6%; P = .027) than those who discontinued. “We saw that uptake to baby TAM after informed discussion in patients who qualify is high, especially in those patients with high risk and intraepithelial lesions or DCIS, and adherence and tolerability at 1 year follow up is improved, compared to what we would expect with traditional dosing of tamoxifen. It’s important to note that the NCCN guidelines and the ASCO clinical practice update now include low-dose tamoxifen as an option for select women, and future randomized control trials on de-escalation of tamoxifen and high-risk patients based on their risk model assessment still need to be done. Future study should also focus on markers to identify candidates best suited for low versus standard dose of tamoxifen,” said Dr. Cornell, who is an assistant professor of medicine at Mayo Clinic Florida in Jacksonville.
At another SABCS session, Per Hall, MD, PhD, discussed findings from the previously published KARISMA-2 study, which examined efficacy of various doses of tamoxifen. A total of 1440 participants, 240 in each arm, received tamoxifen doses of 20 mg, 10 mg, 5 mg, 2.5 mg, 1 mg, or placebo. During his talk, Dr. Hall pointed out that measuring outcomes would take a very large number of participants to identify small differences in breast cancer rates. Therefore, the researchers examined breast density changes as a proxy. As a noninferiority outcome, the researchers used the proportion of women in each arm who achieved the median decrease in breast density seen at 20 mg of tamoxifen, which is 10.1%.
The women underwent mammograms at baseline and again at 6 months to determine change in breast density. Among all women in the study, the proportion of patients who had a similar breast density reduction as the 20-mg dose were very similar in the 10 mg (50.0%; P = .002), 5 mg (49.3%; P < .001), and 2.5 mg (52.5%; P < .001) groups. The 1 mg group had a proportion of 39.5% (P = .138), while the placebo group had 38.9% (P = .161). However, the results were driven by premenopausal women, where the values were 63.3%, 70.7%, 74.4%, and 69.7% in the 20-mg, 10-mg, 5-mg, and 2.5-mg groups, respectively, and 32.9% at 1 mg and 29.7% on placebo. In postmenopausal women, the values were 41.9%, 36.7%, 33.3%, and 41.9% in the 20-mg, 10-mg, 5-mg, and 2.5-mg groups, with values of 44.2% in the 1-mg group and 43.8% in the placebo group.
The median density change was 18.5% in premenopausal women and 4.0% in postmenopausal women.
“We didn’t see anything in the postmenopausal women. The decrease for those on 20 milligrams and those on placebo were exactly the same. Why this is, we still don’t know because we do know that tamoxifen in the adjuvant setting could be used for postmenopausal women. It could be that 6 months is too short of a time [to see a benefit]. We don’t know,” said Dr. Hall, who is a medical epidemiologist and biostatistician at Karolinska Institutet, Stockholm, Sweden.
Severe vasomotor side effects like hot flashes, cold flashes, and night sweats were reduced by about 50% in the lower tamoxifen doses, compared with 20 mg.
Dr. Hall also pointed out that tamoxifen is a prodrug. The CYP2D6 enzyme produces a range of metabolites, with endoxifen having the strongest affinity to the estrogen receptor and being present at the highest plasma concentration. He showed a table of endoxifen plasma levels at various tamoxifen doses in women of various metabolizer status, ranging from poor to ultrafast. Among intermediate, normal, and ultrarapid metabolizers, 5- and 10-mg doses produced plasma endoxifen levels ranging from 2.4 to 6.2 ng/mL, which represents a good therapeutic window. “For intermediate and normal metabolizers, it could be that 5 mg [of tamoxifen] is enough, but I want to underline that we didn’t use breast cancer incidence or recurrence in this study, we used density change, so we should be careful when we use these results,” said Dr. Hall. His group is now conducting the KARISMA Endoxifen trial, which will test endoxifen directly at doses of 1 and 2 mg.
Dr. Cornell has no relevant financial disclosures. Dr. Hall is a member of the scientific advisory board for Atossa Therapeutics.
SAN ANTONIO — The drug can reduce incidence of breast cancer in high-risk individuals, but side effects that mimic menopause have led to low rates of uptake. Lower-dose tamoxifen aims to reduce those side effects, but there remains some uncertainty about the minimum dose required to maintain efficacy.
The TAM-01 study, first published in 2019, demonstrated that a 5-mg dose of tamoxifen led to a reduction in recurrence of invasive breast cancer or ductal carcinoma in situ (DCIS). At the San Antonio Breast Cancer Symposium, two studies were presented that provided insight into dose efficacy and likelihood of medication adherence in women taking baby TAM.
“We all know that women who are at increased risk for breast cancer may benefit from the use of tamoxifen to help lower their risk, although historical uptake to tamoxifen in the prevention setting has been quite low,” said Lauren Cornell, MD, during a presentation. Her team investigated the impact of patient counseling on how well they understood their risk, as well as their likelihood of adherence to the medication.
The study included 41 women, and 31 completed follow-up at 1 year. “We saw that 90% of our patients reported good or complete understanding of their breast cancer risk after the consultation, emphasizing the benefit of that consult, and 73% reported that the availability of baby tamoxifen helped in their decision to consider a preventative medication,” said Dr. Cornell during her presentation. After 1 year of follow-up, 74% said that they had initiated baby tamoxifen, and 78% of those who started taking the drug were still taking it at 1 year.
Participants who continued to take baby TAM at 1 year had a higher estimated breast cancer risk (IBIS 10-year risk, 12.7% vs 7.6%; P = .027) than those who discontinued. “We saw that uptake to baby TAM after informed discussion in patients who qualify is high, especially in those patients with high risk and intraepithelial lesions or DCIS, and adherence and tolerability at 1 year follow up is improved, compared to what we would expect with traditional dosing of tamoxifen. It’s important to note that the NCCN guidelines and the ASCO clinical practice update now include low-dose tamoxifen as an option for select women, and future randomized control trials on de-escalation of tamoxifen and high-risk patients based on their risk model assessment still need to be done. Future study should also focus on markers to identify candidates best suited for low versus standard dose of tamoxifen,” said Dr. Cornell, who is an assistant professor of medicine at Mayo Clinic Florida in Jacksonville.
At another SABCS session, Per Hall, MD, PhD, discussed findings from the previously published KARISMA-2 study, which examined efficacy of various doses of tamoxifen. A total of 1440 participants, 240 in each arm, received tamoxifen doses of 20 mg, 10 mg, 5 mg, 2.5 mg, 1 mg, or placebo. During his talk, Dr. Hall pointed out that measuring outcomes would take a very large number of participants to identify small differences in breast cancer rates. Therefore, the researchers examined breast density changes as a proxy. As a noninferiority outcome, the researchers used the proportion of women in each arm who achieved the median decrease in breast density seen at 20 mg of tamoxifen, which is 10.1%.
The women underwent mammograms at baseline and again at 6 months to determine change in breast density. Among all women in the study, the proportion of patients who had a similar breast density reduction as the 20-mg dose were very similar in the 10 mg (50.0%; P = .002), 5 mg (49.3%; P < .001), and 2.5 mg (52.5%; P < .001) groups. The 1 mg group had a proportion of 39.5% (P = .138), while the placebo group had 38.9% (P = .161). However, the results were driven by premenopausal women, where the values were 63.3%, 70.7%, 74.4%, and 69.7% in the 20-mg, 10-mg, 5-mg, and 2.5-mg groups, respectively, and 32.9% at 1 mg and 29.7% on placebo. In postmenopausal women, the values were 41.9%, 36.7%, 33.3%, and 41.9% in the 20-mg, 10-mg, 5-mg, and 2.5-mg groups, with values of 44.2% in the 1-mg group and 43.8% in the placebo group.
The median density change was 18.5% in premenopausal women and 4.0% in postmenopausal women.
“We didn’t see anything in the postmenopausal women. The decrease for those on 20 milligrams and those on placebo were exactly the same. Why this is, we still don’t know because we do know that tamoxifen in the adjuvant setting could be used for postmenopausal women. It could be that 6 months is too short of a time [to see a benefit]. We don’t know,” said Dr. Hall, who is a medical epidemiologist and biostatistician at Karolinska Institutet, Stockholm, Sweden.
Severe vasomotor side effects like hot flashes, cold flashes, and night sweats were reduced by about 50% in the lower tamoxifen doses, compared with 20 mg.
Dr. Hall also pointed out that tamoxifen is a prodrug. The CYP2D6 enzyme produces a range of metabolites, with endoxifen having the strongest affinity to the estrogen receptor and being present at the highest plasma concentration. He showed a table of endoxifen plasma levels at various tamoxifen doses in women of various metabolizer status, ranging from poor to ultrafast. Among intermediate, normal, and ultrarapid metabolizers, 5- and 10-mg doses produced plasma endoxifen levels ranging from 2.4 to 6.2 ng/mL, which represents a good therapeutic window. “For intermediate and normal metabolizers, it could be that 5 mg [of tamoxifen] is enough, but I want to underline that we didn’t use breast cancer incidence or recurrence in this study, we used density change, so we should be careful when we use these results,” said Dr. Hall. His group is now conducting the KARISMA Endoxifen trial, which will test endoxifen directly at doses of 1 and 2 mg.
Dr. Cornell has no relevant financial disclosures. Dr. Hall is a member of the scientific advisory board for Atossa Therapeutics.
FROM SABCS 2023
Oncotype Score Helps Avoid Unnecessary Radiation in DCIS
SAN ANTONIO — There’s a long-standing concern among oncologists that many women with ductal carcinoma in situ (DCIS), a potential precursor to invasive breast cancer, receive more treatment than they need. The potential for overtreatment largely revolves around the extent of surgery and the use of radiation.
Using the Oncotype DX Breast DCIS Score test, a laboratory test that estimates DCIS recurrence risk, may help identify patients with low-risk DCIS who can safely avoid adjuvant radiation after surgery, according to new research (abstract GS03-01) presented at the San Antonio Breast Cancer Symposium.
Low-risk patients who skipped adjuvant radiotherapy after breast-conserving surgery demonstrated similar 5-year recurrence rates compared with high-risk patients who received adjuvant radiotherapy.
This is the first prospective study to evaluate radiation decisions among patients with DCIS.
Lead author Seema A. Khan, MD, who presented the research, called the findings “reassuring.”
However, “we need larger and better trials” as well as longer follow-up to confirm this less-is-more approach, said Dr. Khan, a breast cancer surgeon and researcher at Northwestern University, Chicago.
Virginia Kaklamani, MD, who moderated the presentation, noted that it is good to finally have prospective data on this topic. And although they are not definitive, “I personally think these results should be used” for counseling, said Dr. Kaklamani, leader of the breast cancer program at UT Health San Antonio.
To reduce the risk for DCIS recurrence or progression to invasive breast cancer, most patients with DCIS undergo breast-conserving surgery followed by adjuvant radiotherapy, Dr. Khan explained. Instead of breast-conserving surgery, about one in four patients opt for mastectomy.
Earlier results from this trial revealed that MRI helped identify patients who can safely receive breast-conserving surgery instead of mastectomy.
The current results assessed whether the Oncotype DX score can guide radiation treatment decisions.
The study included 171 patients with DCIS who had wide local excisions after MRI confirmed that they could forgo more extensive surgery.
Surgical specimens were then sent for testing to determine the DCIS score using the 12-gene Oncotype DX test.
Women who scored < 39 points on the 100-point Oncotype DX scale were considered to be at low risk for recurrence and were advised to skip radiation. Women who scored > 39 were advised to undergo radiation. Overall, 93% of the patients followed the radiation recommendations: 75 of 82 patients (91.4%) deemed as low risk skipped adjuvant radiotherapy and 84 of 89 patients (94.4%) deemed as high risk had radiotherapy.
At a median follow-up of 5 years, 5.1% (4 of 82) of low-risk patients experienced a recurrence vs. 4.5% (4 of 89) of higher-risk patients.
Recurrence rates among patients who followed the radiation recommendations mirrored these overall findings: 5.5% of 75 patients with low-risk DCIS who skipped radiotherapy experienced disease recurrence vs. 4.8% of 84 patients with high-risk DCIS who received radiotherapy.
Age did not appear to affect the outcomes. Among the 33 women younger than 50 years, two experienced a recurrence (4%), both invasive. One occurred in the low-risk group and the other in the higher-risk group. Among the 138 older women, six had recurrences, three in each group, and one recurrence in each was invasive.
In short, “women who skipped radiation based on this score did not experience an excess risk of” ipsilateral recurrence over 5 years, said Dr. Khan.
Overall, the study offers “strong evidence” that the DCIS score might help “prevent excessive treatment for some patients,” she concluded, adding that 10-year outcomes will be reported.
The work was funded by the National Cancer Institute. Dr. Khan has no conflicts of interest. Dr. Kaklamani has extensive industry ties, including being a speaker for Pfizer, Genentech, Novartis, and AstraZeneca.
A version in the article appeared on Medscape.com.
SAN ANTONIO — There’s a long-standing concern among oncologists that many women with ductal carcinoma in situ (DCIS), a potential precursor to invasive breast cancer, receive more treatment than they need. The potential for overtreatment largely revolves around the extent of surgery and the use of radiation.
Using the Oncotype DX Breast DCIS Score test, a laboratory test that estimates DCIS recurrence risk, may help identify patients with low-risk DCIS who can safely avoid adjuvant radiation after surgery, according to new research (abstract GS03-01) presented at the San Antonio Breast Cancer Symposium.
Low-risk patients who skipped adjuvant radiotherapy after breast-conserving surgery demonstrated similar 5-year recurrence rates compared with high-risk patients who received adjuvant radiotherapy.
This is the first prospective study to evaluate radiation decisions among patients with DCIS.
Lead author Seema A. Khan, MD, who presented the research, called the findings “reassuring.”
However, “we need larger and better trials” as well as longer follow-up to confirm this less-is-more approach, said Dr. Khan, a breast cancer surgeon and researcher at Northwestern University, Chicago.
Virginia Kaklamani, MD, who moderated the presentation, noted that it is good to finally have prospective data on this topic. And although they are not definitive, “I personally think these results should be used” for counseling, said Dr. Kaklamani, leader of the breast cancer program at UT Health San Antonio.
To reduce the risk for DCIS recurrence or progression to invasive breast cancer, most patients with DCIS undergo breast-conserving surgery followed by adjuvant radiotherapy, Dr. Khan explained. Instead of breast-conserving surgery, about one in four patients opt for mastectomy.
Earlier results from this trial revealed that MRI helped identify patients who can safely receive breast-conserving surgery instead of mastectomy.
The current results assessed whether the Oncotype DX score can guide radiation treatment decisions.
The study included 171 patients with DCIS who had wide local excisions after MRI confirmed that they could forgo more extensive surgery.
Surgical specimens were then sent for testing to determine the DCIS score using the 12-gene Oncotype DX test.
Women who scored < 39 points on the 100-point Oncotype DX scale were considered to be at low risk for recurrence and were advised to skip radiation. Women who scored > 39 were advised to undergo radiation. Overall, 93% of the patients followed the radiation recommendations: 75 of 82 patients (91.4%) deemed as low risk skipped adjuvant radiotherapy and 84 of 89 patients (94.4%) deemed as high risk had radiotherapy.
At a median follow-up of 5 years, 5.1% (4 of 82) of low-risk patients experienced a recurrence vs. 4.5% (4 of 89) of higher-risk patients.
Recurrence rates among patients who followed the radiation recommendations mirrored these overall findings: 5.5% of 75 patients with low-risk DCIS who skipped radiotherapy experienced disease recurrence vs. 4.8% of 84 patients with high-risk DCIS who received radiotherapy.
Age did not appear to affect the outcomes. Among the 33 women younger than 50 years, two experienced a recurrence (4%), both invasive. One occurred in the low-risk group and the other in the higher-risk group. Among the 138 older women, six had recurrences, three in each group, and one recurrence in each was invasive.
In short, “women who skipped radiation based on this score did not experience an excess risk of” ipsilateral recurrence over 5 years, said Dr. Khan.
Overall, the study offers “strong evidence” that the DCIS score might help “prevent excessive treatment for some patients,” she concluded, adding that 10-year outcomes will be reported.
The work was funded by the National Cancer Institute. Dr. Khan has no conflicts of interest. Dr. Kaklamani has extensive industry ties, including being a speaker for Pfizer, Genentech, Novartis, and AstraZeneca.
A version in the article appeared on Medscape.com.
SAN ANTONIO — There’s a long-standing concern among oncologists that many women with ductal carcinoma in situ (DCIS), a potential precursor to invasive breast cancer, receive more treatment than they need. The potential for overtreatment largely revolves around the extent of surgery and the use of radiation.
Using the Oncotype DX Breast DCIS Score test, a laboratory test that estimates DCIS recurrence risk, may help identify patients with low-risk DCIS who can safely avoid adjuvant radiation after surgery, according to new research (abstract GS03-01) presented at the San Antonio Breast Cancer Symposium.
Low-risk patients who skipped adjuvant radiotherapy after breast-conserving surgery demonstrated similar 5-year recurrence rates compared with high-risk patients who received adjuvant radiotherapy.
This is the first prospective study to evaluate radiation decisions among patients with DCIS.
Lead author Seema A. Khan, MD, who presented the research, called the findings “reassuring.”
However, “we need larger and better trials” as well as longer follow-up to confirm this less-is-more approach, said Dr. Khan, a breast cancer surgeon and researcher at Northwestern University, Chicago.
Virginia Kaklamani, MD, who moderated the presentation, noted that it is good to finally have prospective data on this topic. And although they are not definitive, “I personally think these results should be used” for counseling, said Dr. Kaklamani, leader of the breast cancer program at UT Health San Antonio.
To reduce the risk for DCIS recurrence or progression to invasive breast cancer, most patients with DCIS undergo breast-conserving surgery followed by adjuvant radiotherapy, Dr. Khan explained. Instead of breast-conserving surgery, about one in four patients opt for mastectomy.
Earlier results from this trial revealed that MRI helped identify patients who can safely receive breast-conserving surgery instead of mastectomy.
The current results assessed whether the Oncotype DX score can guide radiation treatment decisions.
The study included 171 patients with DCIS who had wide local excisions after MRI confirmed that they could forgo more extensive surgery.
Surgical specimens were then sent for testing to determine the DCIS score using the 12-gene Oncotype DX test.
Women who scored < 39 points on the 100-point Oncotype DX scale were considered to be at low risk for recurrence and were advised to skip radiation. Women who scored > 39 were advised to undergo radiation. Overall, 93% of the patients followed the radiation recommendations: 75 of 82 patients (91.4%) deemed as low risk skipped adjuvant radiotherapy and 84 of 89 patients (94.4%) deemed as high risk had radiotherapy.
At a median follow-up of 5 years, 5.1% (4 of 82) of low-risk patients experienced a recurrence vs. 4.5% (4 of 89) of higher-risk patients.
Recurrence rates among patients who followed the radiation recommendations mirrored these overall findings: 5.5% of 75 patients with low-risk DCIS who skipped radiotherapy experienced disease recurrence vs. 4.8% of 84 patients with high-risk DCIS who received radiotherapy.
Age did not appear to affect the outcomes. Among the 33 women younger than 50 years, two experienced a recurrence (4%), both invasive. One occurred in the low-risk group and the other in the higher-risk group. Among the 138 older women, six had recurrences, three in each group, and one recurrence in each was invasive.
In short, “women who skipped radiation based on this score did not experience an excess risk of” ipsilateral recurrence over 5 years, said Dr. Khan.
Overall, the study offers “strong evidence” that the DCIS score might help “prevent excessive treatment for some patients,” she concluded, adding that 10-year outcomes will be reported.
The work was funded by the National Cancer Institute. Dr. Khan has no conflicts of interest. Dr. Kaklamani has extensive industry ties, including being a speaker for Pfizer, Genentech, Novartis, and AstraZeneca.
A version in the article appeared on Medscape.com.
FROM SABCS 2023
What will help ease the financial toll of breast cancer?
SAN ANTONIO — , new survey findings show.
Almost half of patients surveyed reported a “significant” or “catastrophic” financial burden related to their breast cancer care. But patients also found a range of resources helpful for minimizing this burden, including direct assistance programs that reduce the cost of medications, grants from nonprofits that can cover cancer-related expenses, as well as programs that offer free or low-cost transportation to medical appointments.
Financial toxicity remains a “pervasive problem in the breast cancer community and we really need to go to the next step, which is designing patient-centered, patient-facing interventions to make improvements,” Fumiko Chino, MD, with Memorial Sloan Kettering Cancer Center in New York City, said when presenting the survey results at the San Antonio Breast Cancer Symposium.
A growing body of evidence shows that cancer care, especially for breast cancer, can take a heavy financial toll on patients. However, routine screening for financial toxicity is not necessarily a routine part of clinical care, and providers may not know the types of financial assistance patients value most, Dr. Chino explained.
Dr. Chino and colleagues surveyed 1437 women with breast cancer about their level of financial distress as well as the specific interventions or education initiatives they found most helpful.
Most patients (60%) were White, 27% were Hispanic, and 8% Black. Three quarters of patients were on active treatments, 89% had nonmetastatic disease, and 11% had metastatic disease.
Overall, 47% of patients reported a significant or catastrophic financial burden related to their breast cancer diagnosis and care. This burden was higher for those with metastatic disease (61% vs 45%).
Patients assessed 10 strategies for coping with the financial burdens of care. The top-rated interventions included patient assistance programs offered by pharmaceutical or medical test companies, rated highly by 32% of respondents, and grants from nonprofits, rated highly by 31% of respondents. Patients also found financial assistance departments at cancer centers or hospitals helpful (29%); coupons and savings cards to reduce the cost of prescription drugs (28%); and programs that provide free or low-cost transportation to medical appointments (28%).
In terms of education, respondents said having a checklist of questions to ask their oncology team as well as a list of breast cancer-specific financial grants to apply for would be especially helpful when navigating the financial burdens of breast cancer care.
These preferences, however, did vary by race/ethnicity and disease status. Hispanic patients, for instance, found patient assistance programs offered by companies and cancer centers as well as transportation assistance more helpful than other groups.
Patients with metastatic disease found patient assistance programs offered by medical companies particularly helpful compared with patients with nonmetastatic disease. And compared with patients with metastatic disease, those with nonmetastatic breast cancer found assistance through clinical trials and professional medical billing advocates helpful.
This study confirms the high rates of financial burden in women with breast cancer and clearly demonstrates that intervention preferences vary by sociodemographic and clinical characteristics, study discussant Claire C. Conley, PhD, from Georgetown University, Washington, DC, commented.
“This highlights that one size really doesn’t fit all when it comes to those financial burden interventions,” Dr. Conley said. “We need to think about factors at the patient level, the organizational level, and the environment level.”
The study had no commercial funding. Dr. Chino and Dr. Conley have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
SAN ANTONIO — , new survey findings show.
Almost half of patients surveyed reported a “significant” or “catastrophic” financial burden related to their breast cancer care. But patients also found a range of resources helpful for minimizing this burden, including direct assistance programs that reduce the cost of medications, grants from nonprofits that can cover cancer-related expenses, as well as programs that offer free or low-cost transportation to medical appointments.
Financial toxicity remains a “pervasive problem in the breast cancer community and we really need to go to the next step, which is designing patient-centered, patient-facing interventions to make improvements,” Fumiko Chino, MD, with Memorial Sloan Kettering Cancer Center in New York City, said when presenting the survey results at the San Antonio Breast Cancer Symposium.
A growing body of evidence shows that cancer care, especially for breast cancer, can take a heavy financial toll on patients. However, routine screening for financial toxicity is not necessarily a routine part of clinical care, and providers may not know the types of financial assistance patients value most, Dr. Chino explained.
Dr. Chino and colleagues surveyed 1437 women with breast cancer about their level of financial distress as well as the specific interventions or education initiatives they found most helpful.
Most patients (60%) were White, 27% were Hispanic, and 8% Black. Three quarters of patients were on active treatments, 89% had nonmetastatic disease, and 11% had metastatic disease.
Overall, 47% of patients reported a significant or catastrophic financial burden related to their breast cancer diagnosis and care. This burden was higher for those with metastatic disease (61% vs 45%).
Patients assessed 10 strategies for coping with the financial burdens of care. The top-rated interventions included patient assistance programs offered by pharmaceutical or medical test companies, rated highly by 32% of respondents, and grants from nonprofits, rated highly by 31% of respondents. Patients also found financial assistance departments at cancer centers or hospitals helpful (29%); coupons and savings cards to reduce the cost of prescription drugs (28%); and programs that provide free or low-cost transportation to medical appointments (28%).
In terms of education, respondents said having a checklist of questions to ask their oncology team as well as a list of breast cancer-specific financial grants to apply for would be especially helpful when navigating the financial burdens of breast cancer care.
These preferences, however, did vary by race/ethnicity and disease status. Hispanic patients, for instance, found patient assistance programs offered by companies and cancer centers as well as transportation assistance more helpful than other groups.
Patients with metastatic disease found patient assistance programs offered by medical companies particularly helpful compared with patients with nonmetastatic disease. And compared with patients with metastatic disease, those with nonmetastatic breast cancer found assistance through clinical trials and professional medical billing advocates helpful.
This study confirms the high rates of financial burden in women with breast cancer and clearly demonstrates that intervention preferences vary by sociodemographic and clinical characteristics, study discussant Claire C. Conley, PhD, from Georgetown University, Washington, DC, commented.
“This highlights that one size really doesn’t fit all when it comes to those financial burden interventions,” Dr. Conley said. “We need to think about factors at the patient level, the organizational level, and the environment level.”
The study had no commercial funding. Dr. Chino and Dr. Conley have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
SAN ANTONIO — , new survey findings show.
Almost half of patients surveyed reported a “significant” or “catastrophic” financial burden related to their breast cancer care. But patients also found a range of resources helpful for minimizing this burden, including direct assistance programs that reduce the cost of medications, grants from nonprofits that can cover cancer-related expenses, as well as programs that offer free or low-cost transportation to medical appointments.
Financial toxicity remains a “pervasive problem in the breast cancer community and we really need to go to the next step, which is designing patient-centered, patient-facing interventions to make improvements,” Fumiko Chino, MD, with Memorial Sloan Kettering Cancer Center in New York City, said when presenting the survey results at the San Antonio Breast Cancer Symposium.
A growing body of evidence shows that cancer care, especially for breast cancer, can take a heavy financial toll on patients. However, routine screening for financial toxicity is not necessarily a routine part of clinical care, and providers may not know the types of financial assistance patients value most, Dr. Chino explained.
Dr. Chino and colleagues surveyed 1437 women with breast cancer about their level of financial distress as well as the specific interventions or education initiatives they found most helpful.
Most patients (60%) were White, 27% were Hispanic, and 8% Black. Three quarters of patients were on active treatments, 89% had nonmetastatic disease, and 11% had metastatic disease.
Overall, 47% of patients reported a significant or catastrophic financial burden related to their breast cancer diagnosis and care. This burden was higher for those with metastatic disease (61% vs 45%).
Patients assessed 10 strategies for coping with the financial burdens of care. The top-rated interventions included patient assistance programs offered by pharmaceutical or medical test companies, rated highly by 32% of respondents, and grants from nonprofits, rated highly by 31% of respondents. Patients also found financial assistance departments at cancer centers or hospitals helpful (29%); coupons and savings cards to reduce the cost of prescription drugs (28%); and programs that provide free or low-cost transportation to medical appointments (28%).
In terms of education, respondents said having a checklist of questions to ask their oncology team as well as a list of breast cancer-specific financial grants to apply for would be especially helpful when navigating the financial burdens of breast cancer care.
These preferences, however, did vary by race/ethnicity and disease status. Hispanic patients, for instance, found patient assistance programs offered by companies and cancer centers as well as transportation assistance more helpful than other groups.
Patients with metastatic disease found patient assistance programs offered by medical companies particularly helpful compared with patients with nonmetastatic disease. And compared with patients with metastatic disease, those with nonmetastatic breast cancer found assistance through clinical trials and professional medical billing advocates helpful.
This study confirms the high rates of financial burden in women with breast cancer and clearly demonstrates that intervention preferences vary by sociodemographic and clinical characteristics, study discussant Claire C. Conley, PhD, from Georgetown University, Washington, DC, commented.
“This highlights that one size really doesn’t fit all when it comes to those financial burden interventions,” Dr. Conley said. “We need to think about factors at the patient level, the organizational level, and the environment level.”
The study had no commercial funding. Dr. Chino and Dr. Conley have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM SABCS 2023
Are you sure your patient is alive?
This transcript has been edited for clarity.
Much of my research focuses on what is known as clinical decision support — prompts and messages to providers to help them make good decisions for their patients. I know that these things can be annoying, which is exactly why I study them — to figure out which ones actually help.
When I got started on this about 10 years ago, we were learning a lot about how best to message providers about their patients. My team had developed a simple alert for acute kidney injury (AKI). We knew that providers often missed the diagnosis, so maybe letting them know would improve patient outcomes.
As we tested the alert, we got feedback, and I have kept an email from an ICU doctor from those early days. It read:
Dear Dr. Wilson: Thank you for the automated alert informing me that my patient had AKI. Regrettably, the alert fired about an hour after the patient had died. I feel that the information is less than actionable at this time.
Our early system had neglected to add a conditional flag ensuring that the patient was still alive at the time it sent the alert message. A small oversight, but one that had very large implications. Future studies would show that “false positive” alerts like this seriously degrade physician confidence in the system. And why wouldn’t they?
Not knowing the vital status of a patient can have major consequences.
Health systems send messages to their patients all the time: reminders of appointments, reminders for preventive care, reminders for vaccinations, and so on.
But what if the patient being reminded has died? It’s a waste of resources, of course, but more than that, it can be painful for their families and reflects poorly on the health care system. Of all the people who should know whether someone is alive or dead, shouldn’t their doctor be at the top of the list?
A new study in JAMA Internal Medicine quantifies this very phenomenon.
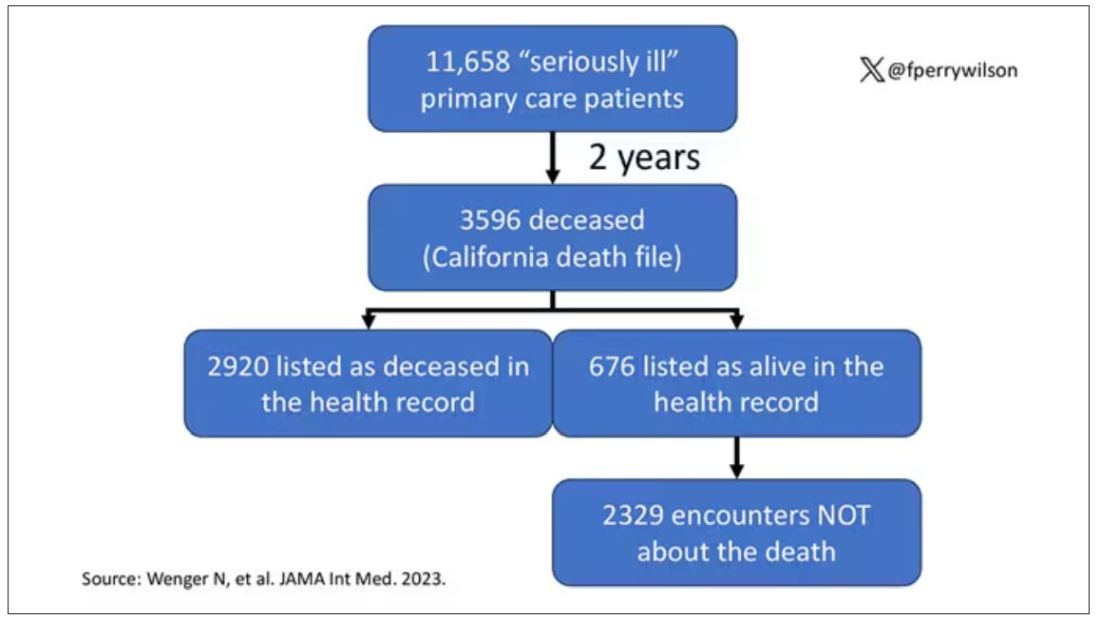
Researchers examined 11,658 primary care patients in their health system who met the criteria of being “seriously ill” and followed them for 2 years. During that period of time, 25% were recorded as deceased in the electronic health record. But 30.8% had died. That left 676 patients who had died, but were not known to have died, left in the system.
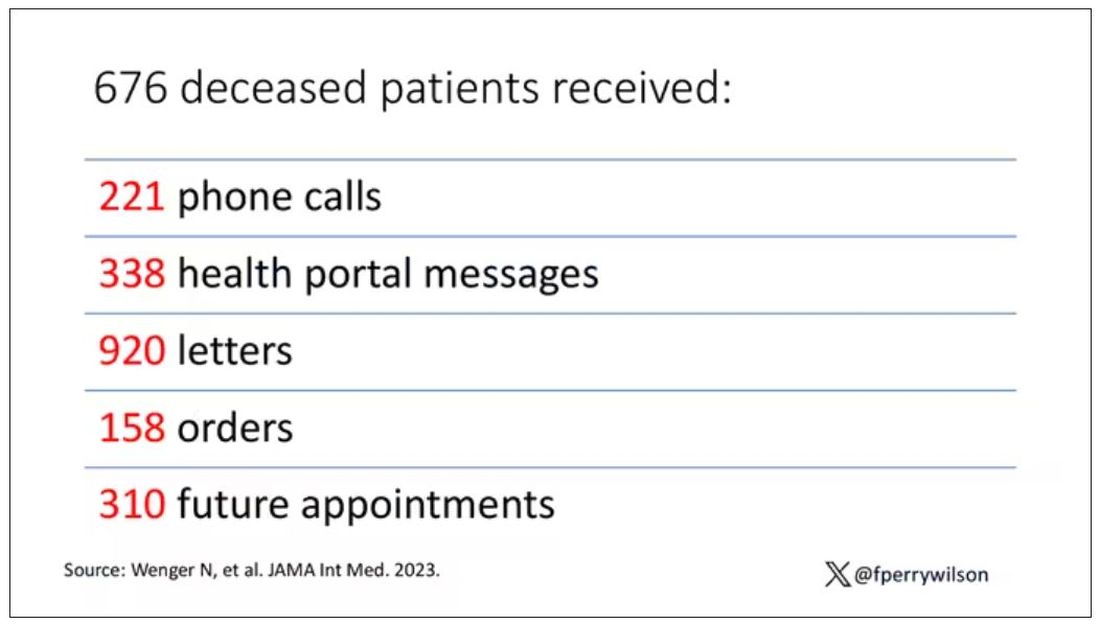
And those 676 were not left to rest in peace. They received 221 telephone and 338 health portal messages not related to death, and 920 letters reminding them about unmet primary care metrics like flu shots and cancer screening. Orders were entered into the health record for things like vaccines and routine screenings for 158 patients, and 310 future appointments — destined to be no-shows — were still on the books. One can only imagine the frustration of families checking their mail and finding yet another letter reminding their deceased loved one to get a mammogram.
How did the researchers figure out who had died? It turns out it’s not that hard. California keeps a record of all deaths in the state; they simply had to search it. Like all state death records, they tend to lag a bit so it’s not clinically terribly useful, but it works. California and most other states also have a very accurate and up-to-date death file which can only be used by law enforcement to investigate criminal activity and fraud; health care is left in the lurch.
Nationwide, there is the real-time fact of death service, supported by the National Association for Public Health Statistics and Information Systems. This allows employers to verify, in real time, whether the person applying for a job is alive. Healthcare systems are not allowed to use it.
Let’s also remember that very few people die in this country without some health care agency knowing about it and recording it. But sharing of medical information is so poor in the United States that your patient could die in a hospital one city away from you and you might not find out until you’re calling them to see why they missed a scheduled follow-up appointment.
These events — the embarrassing lack of knowledge about the very vital status of our patients — highlight a huge problem with health care in our country. The fragmented health care system is terrible at data sharing, in part because of poor protocols, in part because of unfounded concerns about patient privacy, and in part because of a tendency to hoard data that might be valuable in the future. It has to stop. We need to know how our patients are doing even when they are not sitting in front of us. When it comes to life and death, the knowledge is out there; we just can’t access it. Seems like a pretty easy fix.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Connecticut. He has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com .
This transcript has been edited for clarity.
Much of my research focuses on what is known as clinical decision support — prompts and messages to providers to help them make good decisions for their patients. I know that these things can be annoying, which is exactly why I study them — to figure out which ones actually help.
When I got started on this about 10 years ago, we were learning a lot about how best to message providers about their patients. My team had developed a simple alert for acute kidney injury (AKI). We knew that providers often missed the diagnosis, so maybe letting them know would improve patient outcomes.
As we tested the alert, we got feedback, and I have kept an email from an ICU doctor from those early days. It read:
Dear Dr. Wilson: Thank you for the automated alert informing me that my patient had AKI. Regrettably, the alert fired about an hour after the patient had died. I feel that the information is less than actionable at this time.
Our early system had neglected to add a conditional flag ensuring that the patient was still alive at the time it sent the alert message. A small oversight, but one that had very large implications. Future studies would show that “false positive” alerts like this seriously degrade physician confidence in the system. And why wouldn’t they?
Not knowing the vital status of a patient can have major consequences.
Health systems send messages to their patients all the time: reminders of appointments, reminders for preventive care, reminders for vaccinations, and so on.
But what if the patient being reminded has died? It’s a waste of resources, of course, but more than that, it can be painful for their families and reflects poorly on the health care system. Of all the people who should know whether someone is alive or dead, shouldn’t their doctor be at the top of the list?
A new study in JAMA Internal Medicine quantifies this very phenomenon.
Researchers examined 11,658 primary care patients in their health system who met the criteria of being “seriously ill” and followed them for 2 years. During that period of time, 25% were recorded as deceased in the electronic health record. But 30.8% had died. That left 676 patients who had died, but were not known to have died, left in the system.
And those 676 were not left to rest in peace. They received 221 telephone and 338 health portal messages not related to death, and 920 letters reminding them about unmet primary care metrics like flu shots and cancer screening. Orders were entered into the health record for things like vaccines and routine screenings for 158 patients, and 310 future appointments — destined to be no-shows — were still on the books. One can only imagine the frustration of families checking their mail and finding yet another letter reminding their deceased loved one to get a mammogram.
How did the researchers figure out who had died? It turns out it’s not that hard. California keeps a record of all deaths in the state; they simply had to search it. Like all state death records, they tend to lag a bit so it’s not clinically terribly useful, but it works. California and most other states also have a very accurate and up-to-date death file which can only be used by law enforcement to investigate criminal activity and fraud; health care is left in the lurch.
Nationwide, there is the real-time fact of death service, supported by the National Association for Public Health Statistics and Information Systems. This allows employers to verify, in real time, whether the person applying for a job is alive. Healthcare systems are not allowed to use it.
Let’s also remember that very few people die in this country without some health care agency knowing about it and recording it. But sharing of medical information is so poor in the United States that your patient could die in a hospital one city away from you and you might not find out until you’re calling them to see why they missed a scheduled follow-up appointment.
These events — the embarrassing lack of knowledge about the very vital status of our patients — highlight a huge problem with health care in our country. The fragmented health care system is terrible at data sharing, in part because of poor protocols, in part because of unfounded concerns about patient privacy, and in part because of a tendency to hoard data that might be valuable in the future. It has to stop. We need to know how our patients are doing even when they are not sitting in front of us. When it comes to life and death, the knowledge is out there; we just can’t access it. Seems like a pretty easy fix.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Connecticut. He has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com .
This transcript has been edited for clarity.
Much of my research focuses on what is known as clinical decision support — prompts and messages to providers to help them make good decisions for their patients. I know that these things can be annoying, which is exactly why I study them — to figure out which ones actually help.
When I got started on this about 10 years ago, we were learning a lot about how best to message providers about their patients. My team had developed a simple alert for acute kidney injury (AKI). We knew that providers often missed the diagnosis, so maybe letting them know would improve patient outcomes.
As we tested the alert, we got feedback, and I have kept an email from an ICU doctor from those early days. It read:
Dear Dr. Wilson: Thank you for the automated alert informing me that my patient had AKI. Regrettably, the alert fired about an hour after the patient had died. I feel that the information is less than actionable at this time.
Our early system had neglected to add a conditional flag ensuring that the patient was still alive at the time it sent the alert message. A small oversight, but one that had very large implications. Future studies would show that “false positive” alerts like this seriously degrade physician confidence in the system. And why wouldn’t they?
Not knowing the vital status of a patient can have major consequences.
Health systems send messages to their patients all the time: reminders of appointments, reminders for preventive care, reminders for vaccinations, and so on.
But what if the patient being reminded has died? It’s a waste of resources, of course, but more than that, it can be painful for their families and reflects poorly on the health care system. Of all the people who should know whether someone is alive or dead, shouldn’t their doctor be at the top of the list?
A new study in JAMA Internal Medicine quantifies this very phenomenon.
Researchers examined 11,658 primary care patients in their health system who met the criteria of being “seriously ill” and followed them for 2 years. During that period of time, 25% were recorded as deceased in the electronic health record. But 30.8% had died. That left 676 patients who had died, but were not known to have died, left in the system.
And those 676 were not left to rest in peace. They received 221 telephone and 338 health portal messages not related to death, and 920 letters reminding them about unmet primary care metrics like flu shots and cancer screening. Orders were entered into the health record for things like vaccines and routine screenings for 158 patients, and 310 future appointments — destined to be no-shows — were still on the books. One can only imagine the frustration of families checking their mail and finding yet another letter reminding their deceased loved one to get a mammogram.
How did the researchers figure out who had died? It turns out it’s not that hard. California keeps a record of all deaths in the state; they simply had to search it. Like all state death records, they tend to lag a bit so it’s not clinically terribly useful, but it works. California and most other states also have a very accurate and up-to-date death file which can only be used by law enforcement to investigate criminal activity and fraud; health care is left in the lurch.
Nationwide, there is the real-time fact of death service, supported by the National Association for Public Health Statistics and Information Systems. This allows employers to verify, in real time, whether the person applying for a job is alive. Healthcare systems are not allowed to use it.
Let’s also remember that very few people die in this country without some health care agency knowing about it and recording it. But sharing of medical information is so poor in the United States that your patient could die in a hospital one city away from you and you might not find out until you’re calling them to see why they missed a scheduled follow-up appointment.
These events — the embarrassing lack of knowledge about the very vital status of our patients — highlight a huge problem with health care in our country. The fragmented health care system is terrible at data sharing, in part because of poor protocols, in part because of unfounded concerns about patient privacy, and in part because of a tendency to hoard data that might be valuable in the future. It has to stop. We need to know how our patients are doing even when they are not sitting in front of us. When it comes to life and death, the knowledge is out there; we just can’t access it. Seems like a pretty easy fix.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Connecticut. He has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com .
Even with insurance, cancer out-of-pocket costs can be punishing
TOPLINE:
METHODOLOGY:
- Out-of-pocket costs contribute to financial toxicity in cancer, but little is known about how they vary across various tumor types and stages over time.
- To find out, investigators reviewed claims data for 7494 US patients diagnosed with stage I-IV breast, cervical, colorectal, lung, ovarian, or prostate cancer from 2016 to 2020.
- They assessed cumulative out-of-pocket (OOP) costs — defined as copayments, deductibles, and coinsurance — in the first 3 years following diagnosis.
- Subjects had private, commercial health insurance through United Healthcare.
TAKEAWAY:
- By the end of 3 years, average cumulative OOP costs ranged from $16,673 for stage I prostate cancer to $35,253 for stage IV lung cancer.
- Across all cancer types, average OOP costs in the first year ranged from $2,754 for stage I anal cancer to $25,876 for stage IV vaginal cancer.
- However, the upper limits of OOP costs exceeded $100,000 across many tumors and stages in the first year, reaching a high of $450,374 for stage I breast cancer and far exceeding $200,000 for stage II-IV colorectal and lung cancer.
- OOP costs were generally highest during the first year of treatment and for cancers diagnosed at later stages.
IN PRACTICE:
“OOP costs may present an extreme economic stressor on patients diagnosed with cancer,” leading to emotional distress, reduced treatment adherence, and poor outcomes. “Even cancer patients with insurance coverage [are] not protected.” Future research is “needed to help clarify the type of patient most burdened by OOP costs” as well as ways to reduce them, including promoting “diagnosis at an earlier stage and increas[ing] access to health plans that minimize patient cost sharing.”
SOURCE:
The work was led by November McGarvey of BluePath Solutions, Los Angeles, and published in the Journal of Medical Economics.
LIMITATIONS:
The study did not include additional OOP costs, such as transportation. It also did not assess the long-term impacts of cancer-related out-of-pocket spending. Details on health plan types and features were limited, and the results are limited to patients with commercial health insurance.
DISCLOSURES:
The work was funded by Grail. The investigators are employees of Grail or BluePath Solutions.
TOPLINE:
METHODOLOGY:
- Out-of-pocket costs contribute to financial toxicity in cancer, but little is known about how they vary across various tumor types and stages over time.
- To find out, investigators reviewed claims data for 7494 US patients diagnosed with stage I-IV breast, cervical, colorectal, lung, ovarian, or prostate cancer from 2016 to 2020.
- They assessed cumulative out-of-pocket (OOP) costs — defined as copayments, deductibles, and coinsurance — in the first 3 years following diagnosis.
- Subjects had private, commercial health insurance through United Healthcare.
TAKEAWAY:
- By the end of 3 years, average cumulative OOP costs ranged from $16,673 for stage I prostate cancer to $35,253 for stage IV lung cancer.
- Across all cancer types, average OOP costs in the first year ranged from $2,754 for stage I anal cancer to $25,876 for stage IV vaginal cancer.
- However, the upper limits of OOP costs exceeded $100,000 across many tumors and stages in the first year, reaching a high of $450,374 for stage I breast cancer and far exceeding $200,000 for stage II-IV colorectal and lung cancer.
- OOP costs were generally highest during the first year of treatment and for cancers diagnosed at later stages.
IN PRACTICE:
“OOP costs may present an extreme economic stressor on patients diagnosed with cancer,” leading to emotional distress, reduced treatment adherence, and poor outcomes. “Even cancer patients with insurance coverage [are] not protected.” Future research is “needed to help clarify the type of patient most burdened by OOP costs” as well as ways to reduce them, including promoting “diagnosis at an earlier stage and increas[ing] access to health plans that minimize patient cost sharing.”
SOURCE:
The work was led by November McGarvey of BluePath Solutions, Los Angeles, and published in the Journal of Medical Economics.
LIMITATIONS:
The study did not include additional OOP costs, such as transportation. It also did not assess the long-term impacts of cancer-related out-of-pocket spending. Details on health plan types and features were limited, and the results are limited to patients with commercial health insurance.
DISCLOSURES:
The work was funded by Grail. The investigators are employees of Grail or BluePath Solutions.
TOPLINE:
METHODOLOGY:
- Out-of-pocket costs contribute to financial toxicity in cancer, but little is known about how they vary across various tumor types and stages over time.
- To find out, investigators reviewed claims data for 7494 US patients diagnosed with stage I-IV breast, cervical, colorectal, lung, ovarian, or prostate cancer from 2016 to 2020.
- They assessed cumulative out-of-pocket (OOP) costs — defined as copayments, deductibles, and coinsurance — in the first 3 years following diagnosis.
- Subjects had private, commercial health insurance through United Healthcare.
TAKEAWAY:
- By the end of 3 years, average cumulative OOP costs ranged from $16,673 for stage I prostate cancer to $35,253 for stage IV lung cancer.
- Across all cancer types, average OOP costs in the first year ranged from $2,754 for stage I anal cancer to $25,876 for stage IV vaginal cancer.
- However, the upper limits of OOP costs exceeded $100,000 across many tumors and stages in the first year, reaching a high of $450,374 for stage I breast cancer and far exceeding $200,000 for stage II-IV colorectal and lung cancer.
- OOP costs were generally highest during the first year of treatment and for cancers diagnosed at later stages.
IN PRACTICE:
“OOP costs may present an extreme economic stressor on patients diagnosed with cancer,” leading to emotional distress, reduced treatment adherence, and poor outcomes. “Even cancer patients with insurance coverage [are] not protected.” Future research is “needed to help clarify the type of patient most burdened by OOP costs” as well as ways to reduce them, including promoting “diagnosis at an earlier stage and increas[ing] access to health plans that minimize patient cost sharing.”
SOURCE:
The work was led by November McGarvey of BluePath Solutions, Los Angeles, and published in the Journal of Medical Economics.
LIMITATIONS:
The study did not include additional OOP costs, such as transportation. It also did not assess the long-term impacts of cancer-related out-of-pocket spending. Details on health plan types and features were limited, and the results are limited to patients with commercial health insurance.
DISCLOSURES:
The work was funded by Grail. The investigators are employees of Grail or BluePath Solutions.
Eight wealth tips just for doctors
The average physician makes $352,000, and some earn well into the $500,000s. So, doctors don’t have to worry about money, right?
You know the answer to that.
One thing all physicians have in common about money, says James M. Dahle, MD, FACEP, founder of The White Coat Investor, is that they don’t receive any training in business, personal finance, or investing throughout their schooling or careers unless they seek it out. This leaves many unprepared to make the best investing and money-saving decisions, while others get too frustrated about their lack of knowledge to even dip their toe into the investing pool.
Exhibit A: Four out of 10 physicians have a net worth below $1 million, according to the Medscape Physician Wealth & Debt Report 2023. Elizabeth Chiang, MD, PhD, an oculoplastic surgeon and a physician money coach at Grow Your Wealthy Mindset, notes that many of those doctors are over age 65, “which means they essentially can’t retire.”
And that’s just one pain point.
Physicians have money concerns specific to their profession and background. Luckily, some fellow doctors also serve as financial and wealth advisors just for other doctors.
Blind Spot #1
The early lean years skew doctors’ money outlook. “We have an extended training period, which commonly consists of taking on a large amount of debt, followed by 3 to 8 years of being paid a modest salary, and then finally a large boost in income,” explains Dr. Chiang. This can lay a shaky foundation for the earning years to come, and as a result, a lot of doctors just don’t think about money in healthy ways. Once their incomes increase, physicians may be surprised, for example, that making a multiple six-figure salary means paying six figures in taxes.
The Fix
Treat financial health like physical health. That means money cannot be a taboo subject. “The misguided mindset is that we didn’t become physicians to make money, we did it to help people,” explains Jordan Frey, MD, creator of the blog, The Prudent Plastic Surgeon.
Dr. Frey acknowledges that the desire to help is certainly true. But the result is a false idea that “to think about our personal finances makes us a worse doctor.”
Blind Spot #2
Because doctors know a lot about one thing (medicine), they might assume they know a lot about everything (such as investing). “Totally different fields with a different language and different way to think about it,” Dahle explains. This overconfidence could lead to some negligent or risky financial decisions.
The Fix
Educate yourself. There are several books on personal finance and investing written by physicians for physicians. Dr. Chiang recommends The Physician Philosopher’s Guide to Personal Finance, by James Turner, MD; Financial Freedom Rx, by Chirag Shah, MD, and Jayanth Sridhar, MD; and The Physician’s Guide to Finance, by Nicholas Christian and Amanda Christian, MD. There are also podcasts, blogs, and courses to help educate doctors on finance, such as the Fire Your Financial Advisor course by The White Coat Investor.
Blind Spot #3
Undersaving. Retirement saving is one thing, but 24% of doctors say they don’t even put money away in a taxable savings account, according to the Wealth & Debt Report.
Cobin Soelberg, MD, JD, a board-certified anesthesiologist and founder and principal advisor with Greeley Wealth Management, is the treasurer of his anesthesiology group. “I get to see every month how much people are saving, and even on an anesthesiologist salary, where everyone’s making about $400,000 a year, a lot of people are not saving anything, which is crazy.”
Undersaving can be both a time issue and a mindset one.
Time: Doctors often start investing in their retirement accounts later than the average professional, says Dr. Chiang. “A lot of physicians will max out their 401k or 403b,” she explains. “But if you’re putting in $20,000 a year and only starting when you’re in your early 30s, that’s not enough to get you to retirement.”
Mindset: Doctors also see people of all ages who are sick, dying, and injured. “They all know someone who worked hard and saved and then dropped dead at 55,” explains Dr. Dahle. This, he says, can lead to a bit of a “you only live once” attitude that prioritizes spending over saving.
The Fix
Shoot for 20%. If you can’t save 20% of your gross now, strive to get to that point. Think of it as telling a patient they have to change their behavior or trouble will come - not if, but when. “Develop a written investing plan and then stick with it through thick and thin,” says Dr. Dahle. “Once you have a reasonable plan, all you have to do is fund it adequately by saving 20% of your gross income, and a doctor will easily retire as a multimillionaire.”
Blind Spot #4
Bad investment strategies. Thirty-six percent of doctors experience their largest financial losses from lousy investments, according to the Wealth & Debt Report. Meanwhile, 17% of PCPs and 12% of specialists say they haven’t made any investments at all. That’s a terrible mix of doing the wrong thing and doing a worse thing.
The Fix
Don’t overthink investing, but don’t underthink it either. “As high-income earners, doctors just don’t need to take this high level of risk to reach their financial goals,” Dr. Frey says. A good investment plan doesn’t require you to time the stock market or predict individual stock winners. Consider what Vanguard founder Jack Bogle once said about investing: “Be bored by the process but elated by the outcome.”
Dr. Frey suggests going super-simple: index funds. Ignore investing strategies with actively managed mutual funds or individual stocks, as well as risky alternative investments such as cryptocurrency and angel investments. Everyone assumes doctors have money to burn, and they will push sketchy investment ideas at them. Avoid.
Blind Spot #5
Not taking debt seriously enough. The average medical student debt is $250,000 and can exceed $500,000, says Dr. Soelberg. Many doctors spend the first 10 to 20 years of their careers paying this off. Today’s graduates are paying more than 7% on their loans.
And it’s not just student debt: 39% of physicians carry five or more credit cards, and 34% have mortgages larger than $300,000 (with half of those are more than than $500K), per the Wealth & Debt Report.
The Fix
Treat debt like cancer. It’s a lethal enemy you can’t get rid of right away, but a steady, aggressive, long-term attack will have the best results. Dr. Soelberg suggests allocating the most you can afford per month, whether that’s $1000 or $5000, toward debt. Raise the amount as your income grows. Do the same with your 401k or retirement plan. Whatever is left, you can spend. Five to 10 years later, you will realize, “Wow. I’m debt free.”
Blind Spot #6
Not putting in the work to improve your situation. Seventy-one percent of doctors admit they haven’t done anything to reduce major expenses, according to the Wealth & Debt Report. Are you leaving major money on the table?
The Fix
Audit yourself in major areas like housing and taxes. While the average professional may need to put 10% to 20% down on a home, physicians can qualify for physician mortgage loans and can often put down 3% or less, says Dr. Chiang. If you can afford the higher mortgage payment, excess savings earmarked for a larger down payment can be put toward debt or invested.
Another trick, if you’re able, is to seek an area that is less in demand at a higher salary. “Physicians in places like New York City or San Francisco tend to make less than physicians in the Midwest or the South,” Dr. Chiang explains. A colleague of hers moved to rural Pennsylvania, where he made a high salary and had a low cost of living for 3½ years, paid off his student debt, and then relocated to an area where he wanted to live long term.
As for taxes, become familiar with tax law. Research things like, “What is considered a business expense for doctors?” says Brett Mollard, MD, a diagnostic radiologist who provides financial advice to younger physicians. “What will your estimated total tax burden be at the end of the year? Will you need to make extra payments to prevent owing a large sum of money from underpaying or to avoid tax penalties?”
Blind Spot #7
Living like a rock star on a doctor’s income. Getting caught up in trying to live the same lifestyle as your colleagues is a classic bear trap. “Sitting in the doctor’s lounge, it’s so crazy,” Dr. Soelberg says. He describes conversations like, “‘Where did you go on your trip?’ ‘What new toys are you buying?’” There’s pressure to live up to an image of what a doctor’s life is supposed to look like before you’ve sorted the basic things like paying off debt.
The Fix
Live like a resident even if you haven’t been one for years, at least until you’re in a better financial position. “You’re already used to living a life of lower means, and you’re an expert when it comes to delaying gratification,” says Dr. Mollard. “Do it a little longer.” Live frugally and spend only on things that bring you joy. “A lot of physicians are trying to be really rich in all areas of their life instead of the ones that actually matter to them,” Dr. Soelberg says. Identify what’s important to you and only splurge on that.
Blind Spot #8
Never asking for help. The right financial planner can provide expert help. Emphasis on right. “Doctors can be very trusting of other professionals, even when they should not be,” says Dr. Dahle. He notes that in financial services, many people masquerade as knowledgeable advisors who are really just salespeople. While legitimate financial advisors strive to make their clients money, they are also ultimately out to line their pockets and love to work with physician salaries. Thus, doctors can end up working with financial planners that don’t specifically understand their situations or end up taking too much from their clients.
The Fix
Find a planner who specializes in, or at least understands, physicians. Ask them how they make money, says Dr. Chiang. If someone hesitates to tell you about their fee structure or if it sounds like a lot, shop around and ask colleagues for recommendations.
“Ultimately, the path to wealth is to create and grow the margin between what you make and what you spend,” says Dr. Frey. Throw some investing into the mix and physicians can set themselves up on a path for a stress-free financial life.
A version of this article appeared on Medscape.com.
The average physician makes $352,000, and some earn well into the $500,000s. So, doctors don’t have to worry about money, right?
You know the answer to that.
One thing all physicians have in common about money, says James M. Dahle, MD, FACEP, founder of The White Coat Investor, is that they don’t receive any training in business, personal finance, or investing throughout their schooling or careers unless they seek it out. This leaves many unprepared to make the best investing and money-saving decisions, while others get too frustrated about their lack of knowledge to even dip their toe into the investing pool.
Exhibit A: Four out of 10 physicians have a net worth below $1 million, according to the Medscape Physician Wealth & Debt Report 2023. Elizabeth Chiang, MD, PhD, an oculoplastic surgeon and a physician money coach at Grow Your Wealthy Mindset, notes that many of those doctors are over age 65, “which means they essentially can’t retire.”
And that’s just one pain point.
Physicians have money concerns specific to their profession and background. Luckily, some fellow doctors also serve as financial and wealth advisors just for other doctors.
Blind Spot #1
The early lean years skew doctors’ money outlook. “We have an extended training period, which commonly consists of taking on a large amount of debt, followed by 3 to 8 years of being paid a modest salary, and then finally a large boost in income,” explains Dr. Chiang. This can lay a shaky foundation for the earning years to come, and as a result, a lot of doctors just don’t think about money in healthy ways. Once their incomes increase, physicians may be surprised, for example, that making a multiple six-figure salary means paying six figures in taxes.
The Fix
Treat financial health like physical health. That means money cannot be a taboo subject. “The misguided mindset is that we didn’t become physicians to make money, we did it to help people,” explains Jordan Frey, MD, creator of the blog, The Prudent Plastic Surgeon.
Dr. Frey acknowledges that the desire to help is certainly true. But the result is a false idea that “to think about our personal finances makes us a worse doctor.”
Blind Spot #2
Because doctors know a lot about one thing (medicine), they might assume they know a lot about everything (such as investing). “Totally different fields with a different language and different way to think about it,” Dahle explains. This overconfidence could lead to some negligent or risky financial decisions.
The Fix
Educate yourself. There are several books on personal finance and investing written by physicians for physicians. Dr. Chiang recommends The Physician Philosopher’s Guide to Personal Finance, by James Turner, MD; Financial Freedom Rx, by Chirag Shah, MD, and Jayanth Sridhar, MD; and The Physician’s Guide to Finance, by Nicholas Christian and Amanda Christian, MD. There are also podcasts, blogs, and courses to help educate doctors on finance, such as the Fire Your Financial Advisor course by The White Coat Investor.
Blind Spot #3
Undersaving. Retirement saving is one thing, but 24% of doctors say they don’t even put money away in a taxable savings account, according to the Wealth & Debt Report.
Cobin Soelberg, MD, JD, a board-certified anesthesiologist and founder and principal advisor with Greeley Wealth Management, is the treasurer of his anesthesiology group. “I get to see every month how much people are saving, and even on an anesthesiologist salary, where everyone’s making about $400,000 a year, a lot of people are not saving anything, which is crazy.”
Undersaving can be both a time issue and a mindset one.
Time: Doctors often start investing in their retirement accounts later than the average professional, says Dr. Chiang. “A lot of physicians will max out their 401k or 403b,” she explains. “But if you’re putting in $20,000 a year and only starting when you’re in your early 30s, that’s not enough to get you to retirement.”
Mindset: Doctors also see people of all ages who are sick, dying, and injured. “They all know someone who worked hard and saved and then dropped dead at 55,” explains Dr. Dahle. This, he says, can lead to a bit of a “you only live once” attitude that prioritizes spending over saving.
The Fix
Shoot for 20%. If you can’t save 20% of your gross now, strive to get to that point. Think of it as telling a patient they have to change their behavior or trouble will come - not if, but when. “Develop a written investing plan and then stick with it through thick and thin,” says Dr. Dahle. “Once you have a reasonable plan, all you have to do is fund it adequately by saving 20% of your gross income, and a doctor will easily retire as a multimillionaire.”
Blind Spot #4
Bad investment strategies. Thirty-six percent of doctors experience their largest financial losses from lousy investments, according to the Wealth & Debt Report. Meanwhile, 17% of PCPs and 12% of specialists say they haven’t made any investments at all. That’s a terrible mix of doing the wrong thing and doing a worse thing.
The Fix
Don’t overthink investing, but don’t underthink it either. “As high-income earners, doctors just don’t need to take this high level of risk to reach their financial goals,” Dr. Frey says. A good investment plan doesn’t require you to time the stock market or predict individual stock winners. Consider what Vanguard founder Jack Bogle once said about investing: “Be bored by the process but elated by the outcome.”
Dr. Frey suggests going super-simple: index funds. Ignore investing strategies with actively managed mutual funds or individual stocks, as well as risky alternative investments such as cryptocurrency and angel investments. Everyone assumes doctors have money to burn, and they will push sketchy investment ideas at them. Avoid.
Blind Spot #5
Not taking debt seriously enough. The average medical student debt is $250,000 and can exceed $500,000, says Dr. Soelberg. Many doctors spend the first 10 to 20 years of their careers paying this off. Today’s graduates are paying more than 7% on their loans.
And it’s not just student debt: 39% of physicians carry five or more credit cards, and 34% have mortgages larger than $300,000 (with half of those are more than than $500K), per the Wealth & Debt Report.
The Fix
Treat debt like cancer. It’s a lethal enemy you can’t get rid of right away, but a steady, aggressive, long-term attack will have the best results. Dr. Soelberg suggests allocating the most you can afford per month, whether that’s $1000 or $5000, toward debt. Raise the amount as your income grows. Do the same with your 401k or retirement plan. Whatever is left, you can spend. Five to 10 years later, you will realize, “Wow. I’m debt free.”
Blind Spot #6
Not putting in the work to improve your situation. Seventy-one percent of doctors admit they haven’t done anything to reduce major expenses, according to the Wealth & Debt Report. Are you leaving major money on the table?
The Fix
Audit yourself in major areas like housing and taxes. While the average professional may need to put 10% to 20% down on a home, physicians can qualify for physician mortgage loans and can often put down 3% or less, says Dr. Chiang. If you can afford the higher mortgage payment, excess savings earmarked for a larger down payment can be put toward debt or invested.
Another trick, if you’re able, is to seek an area that is less in demand at a higher salary. “Physicians in places like New York City or San Francisco tend to make less than physicians in the Midwest or the South,” Dr. Chiang explains. A colleague of hers moved to rural Pennsylvania, where he made a high salary and had a low cost of living for 3½ years, paid off his student debt, and then relocated to an area where he wanted to live long term.
As for taxes, become familiar with tax law. Research things like, “What is considered a business expense for doctors?” says Brett Mollard, MD, a diagnostic radiologist who provides financial advice to younger physicians. “What will your estimated total tax burden be at the end of the year? Will you need to make extra payments to prevent owing a large sum of money from underpaying or to avoid tax penalties?”
Blind Spot #7
Living like a rock star on a doctor’s income. Getting caught up in trying to live the same lifestyle as your colleagues is a classic bear trap. “Sitting in the doctor’s lounge, it’s so crazy,” Dr. Soelberg says. He describes conversations like, “‘Where did you go on your trip?’ ‘What new toys are you buying?’” There’s pressure to live up to an image of what a doctor’s life is supposed to look like before you’ve sorted the basic things like paying off debt.
The Fix
Live like a resident even if you haven’t been one for years, at least until you’re in a better financial position. “You’re already used to living a life of lower means, and you’re an expert when it comes to delaying gratification,” says Dr. Mollard. “Do it a little longer.” Live frugally and spend only on things that bring you joy. “A lot of physicians are trying to be really rich in all areas of their life instead of the ones that actually matter to them,” Dr. Soelberg says. Identify what’s important to you and only splurge on that.
Blind Spot #8
Never asking for help. The right financial planner can provide expert help. Emphasis on right. “Doctors can be very trusting of other professionals, even when they should not be,” says Dr. Dahle. He notes that in financial services, many people masquerade as knowledgeable advisors who are really just salespeople. While legitimate financial advisors strive to make their clients money, they are also ultimately out to line their pockets and love to work with physician salaries. Thus, doctors can end up working with financial planners that don’t specifically understand their situations or end up taking too much from their clients.
The Fix
Find a planner who specializes in, or at least understands, physicians. Ask them how they make money, says Dr. Chiang. If someone hesitates to tell you about their fee structure or if it sounds like a lot, shop around and ask colleagues for recommendations.
“Ultimately, the path to wealth is to create and grow the margin between what you make and what you spend,” says Dr. Frey. Throw some investing into the mix and physicians can set themselves up on a path for a stress-free financial life.
A version of this article appeared on Medscape.com.
The average physician makes $352,000, and some earn well into the $500,000s. So, doctors don’t have to worry about money, right?
You know the answer to that.
One thing all physicians have in common about money, says James M. Dahle, MD, FACEP, founder of The White Coat Investor, is that they don’t receive any training in business, personal finance, or investing throughout their schooling or careers unless they seek it out. This leaves many unprepared to make the best investing and money-saving decisions, while others get too frustrated about their lack of knowledge to even dip their toe into the investing pool.
Exhibit A: Four out of 10 physicians have a net worth below $1 million, according to the Medscape Physician Wealth & Debt Report 2023. Elizabeth Chiang, MD, PhD, an oculoplastic surgeon and a physician money coach at Grow Your Wealthy Mindset, notes that many of those doctors are over age 65, “which means they essentially can’t retire.”
And that’s just one pain point.
Physicians have money concerns specific to their profession and background. Luckily, some fellow doctors also serve as financial and wealth advisors just for other doctors.
Blind Spot #1
The early lean years skew doctors’ money outlook. “We have an extended training period, which commonly consists of taking on a large amount of debt, followed by 3 to 8 years of being paid a modest salary, and then finally a large boost in income,” explains Dr. Chiang. This can lay a shaky foundation for the earning years to come, and as a result, a lot of doctors just don’t think about money in healthy ways. Once their incomes increase, physicians may be surprised, for example, that making a multiple six-figure salary means paying six figures in taxes.
The Fix
Treat financial health like physical health. That means money cannot be a taboo subject. “The misguided mindset is that we didn’t become physicians to make money, we did it to help people,” explains Jordan Frey, MD, creator of the blog, The Prudent Plastic Surgeon.
Dr. Frey acknowledges that the desire to help is certainly true. But the result is a false idea that “to think about our personal finances makes us a worse doctor.”
Blind Spot #2
Because doctors know a lot about one thing (medicine), they might assume they know a lot about everything (such as investing). “Totally different fields with a different language and different way to think about it,” Dahle explains. This overconfidence could lead to some negligent or risky financial decisions.
The Fix
Educate yourself. There are several books on personal finance and investing written by physicians for physicians. Dr. Chiang recommends The Physician Philosopher’s Guide to Personal Finance, by James Turner, MD; Financial Freedom Rx, by Chirag Shah, MD, and Jayanth Sridhar, MD; and The Physician’s Guide to Finance, by Nicholas Christian and Amanda Christian, MD. There are also podcasts, blogs, and courses to help educate doctors on finance, such as the Fire Your Financial Advisor course by The White Coat Investor.
Blind Spot #3
Undersaving. Retirement saving is one thing, but 24% of doctors say they don’t even put money away in a taxable savings account, according to the Wealth & Debt Report.
Cobin Soelberg, MD, JD, a board-certified anesthesiologist and founder and principal advisor with Greeley Wealth Management, is the treasurer of his anesthesiology group. “I get to see every month how much people are saving, and even on an anesthesiologist salary, where everyone’s making about $400,000 a year, a lot of people are not saving anything, which is crazy.”
Undersaving can be both a time issue and a mindset one.
Time: Doctors often start investing in their retirement accounts later than the average professional, says Dr. Chiang. “A lot of physicians will max out their 401k or 403b,” she explains. “But if you’re putting in $20,000 a year and only starting when you’re in your early 30s, that’s not enough to get you to retirement.”
Mindset: Doctors also see people of all ages who are sick, dying, and injured. “They all know someone who worked hard and saved and then dropped dead at 55,” explains Dr. Dahle. This, he says, can lead to a bit of a “you only live once” attitude that prioritizes spending over saving.
The Fix
Shoot for 20%. If you can’t save 20% of your gross now, strive to get to that point. Think of it as telling a patient they have to change their behavior or trouble will come - not if, but when. “Develop a written investing plan and then stick with it through thick and thin,” says Dr. Dahle. “Once you have a reasonable plan, all you have to do is fund it adequately by saving 20% of your gross income, and a doctor will easily retire as a multimillionaire.”
Blind Spot #4
Bad investment strategies. Thirty-six percent of doctors experience their largest financial losses from lousy investments, according to the Wealth & Debt Report. Meanwhile, 17% of PCPs and 12% of specialists say they haven’t made any investments at all. That’s a terrible mix of doing the wrong thing and doing a worse thing.
The Fix
Don’t overthink investing, but don’t underthink it either. “As high-income earners, doctors just don’t need to take this high level of risk to reach their financial goals,” Dr. Frey says. A good investment plan doesn’t require you to time the stock market or predict individual stock winners. Consider what Vanguard founder Jack Bogle once said about investing: “Be bored by the process but elated by the outcome.”
Dr. Frey suggests going super-simple: index funds. Ignore investing strategies with actively managed mutual funds or individual stocks, as well as risky alternative investments such as cryptocurrency and angel investments. Everyone assumes doctors have money to burn, and they will push sketchy investment ideas at them. Avoid.
Blind Spot #5
Not taking debt seriously enough. The average medical student debt is $250,000 and can exceed $500,000, says Dr. Soelberg. Many doctors spend the first 10 to 20 years of their careers paying this off. Today’s graduates are paying more than 7% on their loans.
And it’s not just student debt: 39% of physicians carry five or more credit cards, and 34% have mortgages larger than $300,000 (with half of those are more than than $500K), per the Wealth & Debt Report.
The Fix
Treat debt like cancer. It’s a lethal enemy you can’t get rid of right away, but a steady, aggressive, long-term attack will have the best results. Dr. Soelberg suggests allocating the most you can afford per month, whether that’s $1000 or $5000, toward debt. Raise the amount as your income grows. Do the same with your 401k or retirement plan. Whatever is left, you can spend. Five to 10 years later, you will realize, “Wow. I’m debt free.”
Blind Spot #6
Not putting in the work to improve your situation. Seventy-one percent of doctors admit they haven’t done anything to reduce major expenses, according to the Wealth & Debt Report. Are you leaving major money on the table?
The Fix
Audit yourself in major areas like housing and taxes. While the average professional may need to put 10% to 20% down on a home, physicians can qualify for physician mortgage loans and can often put down 3% or less, says Dr. Chiang. If you can afford the higher mortgage payment, excess savings earmarked for a larger down payment can be put toward debt or invested.
Another trick, if you’re able, is to seek an area that is less in demand at a higher salary. “Physicians in places like New York City or San Francisco tend to make less than physicians in the Midwest or the South,” Dr. Chiang explains. A colleague of hers moved to rural Pennsylvania, where he made a high salary and had a low cost of living for 3½ years, paid off his student debt, and then relocated to an area where he wanted to live long term.
As for taxes, become familiar with tax law. Research things like, “What is considered a business expense for doctors?” says Brett Mollard, MD, a diagnostic radiologist who provides financial advice to younger physicians. “What will your estimated total tax burden be at the end of the year? Will you need to make extra payments to prevent owing a large sum of money from underpaying or to avoid tax penalties?”
Blind Spot #7
Living like a rock star on a doctor’s income. Getting caught up in trying to live the same lifestyle as your colleagues is a classic bear trap. “Sitting in the doctor’s lounge, it’s so crazy,” Dr. Soelberg says. He describes conversations like, “‘Where did you go on your trip?’ ‘What new toys are you buying?’” There’s pressure to live up to an image of what a doctor’s life is supposed to look like before you’ve sorted the basic things like paying off debt.
The Fix
Live like a resident even if you haven’t been one for years, at least until you’re in a better financial position. “You’re already used to living a life of lower means, and you’re an expert when it comes to delaying gratification,” says Dr. Mollard. “Do it a little longer.” Live frugally and spend only on things that bring you joy. “A lot of physicians are trying to be really rich in all areas of their life instead of the ones that actually matter to them,” Dr. Soelberg says. Identify what’s important to you and only splurge on that.
Blind Spot #8
Never asking for help. The right financial planner can provide expert help. Emphasis on right. “Doctors can be very trusting of other professionals, even when they should not be,” says Dr. Dahle. He notes that in financial services, many people masquerade as knowledgeable advisors who are really just salespeople. While legitimate financial advisors strive to make their clients money, they are also ultimately out to line their pockets and love to work with physician salaries. Thus, doctors can end up working with financial planners that don’t specifically understand their situations or end up taking too much from their clients.
The Fix
Find a planner who specializes in, or at least understands, physicians. Ask them how they make money, says Dr. Chiang. If someone hesitates to tell you about their fee structure or if it sounds like a lot, shop around and ask colleagues for recommendations.
“Ultimately, the path to wealth is to create and grow the margin between what you make and what you spend,” says Dr. Frey. Throw some investing into the mix and physicians can set themselves up on a path for a stress-free financial life.
A version of this article appeared on Medscape.com.
Valedictory
All that’s bright must fade,
The brightest still the fleetest;
All that’s sweet was made
But to be lost when sweetest.
Thomas Moore
I sometimes hold it half a sin
To put in words the grief I feel;
For words, like Nature, half reveal
And half conceal the Soul within.
Alfred, Lord Tennyson, In Memoriam
Dear Readers,
I have sad news to share with you. This is the last issue of
During my travels around the country over the past 2 decades, countless psychiatrists have told me that
As the saying goes: All good things eventually come to an end. I am so grateful to have had the opportunity to collaborate with a wonderful, highly competent editorial staff, as well as with outstanding colleagues who served on the editorial board all those years. A special shout-out to Jeff Bauer, the publishing staff editor, with whom I worked so closely. I very much appreciated all the authors and peer reviewers who contributed timely clinical articles month after month and made
This has been a unique journey for all of us who strived to transform
All that’s bright must fade,
The brightest still the fleetest;
All that’s sweet was made
But to be lost when sweetest.
Thomas Moore
I sometimes hold it half a sin
To put in words the grief I feel;
For words, like Nature, half reveal
And half conceal the Soul within.
Alfred, Lord Tennyson, In Memoriam
Dear Readers,
I have sad news to share with you. This is the last issue of
During my travels around the country over the past 2 decades, countless psychiatrists have told me that
As the saying goes: All good things eventually come to an end. I am so grateful to have had the opportunity to collaborate with a wonderful, highly competent editorial staff, as well as with outstanding colleagues who served on the editorial board all those years. A special shout-out to Jeff Bauer, the publishing staff editor, with whom I worked so closely. I very much appreciated all the authors and peer reviewers who contributed timely clinical articles month after month and made
This has been a unique journey for all of us who strived to transform
All that’s bright must fade,
The brightest still the fleetest;
All that’s sweet was made
But to be lost when sweetest.
Thomas Moore
I sometimes hold it half a sin
To put in words the grief I feel;
For words, like Nature, half reveal
And half conceal the Soul within.
Alfred, Lord Tennyson, In Memoriam
Dear Readers,
I have sad news to share with you. This is the last issue of
During my travels around the country over the past 2 decades, countless psychiatrists have told me that
As the saying goes: All good things eventually come to an end. I am so grateful to have had the opportunity to collaborate with a wonderful, highly competent editorial staff, as well as with outstanding colleagues who served on the editorial board all those years. A special shout-out to Jeff Bauer, the publishing staff editor, with whom I worked so closely. I very much appreciated all the authors and peer reviewers who contributed timely clinical articles month after month and made
This has been a unique journey for all of us who strived to transform
Rx for resilience: Five prescriptions for physician burnout
Physician burnout persists even as the height of the COVID-19 crisis fades farther into the rear-view mirror. The causes for the sadness, stress, and frustration among doctors vary, but the effects are universal and often debilitating: exhaustion, emotional detachment, lethargy, feeling useless, and lacking purpose.
When surveyed, physicians pointed to many systemic solutions for burnout in Medscape’s Physician Burnout & Depression Report 2023, such as a need for greater compensation, more manageable workloads and schedules, and more support staff. But for many doctors, these fixes may be years if not decades away. Equally important are strategies for relieving burnout symptoms now, especially as we head into a busy holiday season.
Because not every stress-relief practice works for everyone, it’s crucial to try various methods until you find something that makes a difference for you, said Christine Gibson, MD, a family physician and trauma therapist in Calgary, Alta., and author of The Modern Trauma Toolkit.
“Every person should have a toolkit of the things that bring them out of the psychological and physical distress that dysregulates their nervous system,” said Dr. Gibson.
Once you learn the personal ways to alleviate your specific brand of burnout, you can start working on systemic changes that might help the culture of medicine overall.
Symptoms speak louder than words
It seems obvious, but if you aren’t aware that what you’re feeling is burnout, you probably aren’t going to find effective steps to relieve it. Jessi Gold, MD, assistant professor and director of wellness, engagement, and outreach in the department of psychiatry, Washington University in St. Louis, is a psychiatrist who treats health care professionals, including frontline workers during the height of the pandemic. But even as a burnout expert, she admits that she misses the signs in herself.
“I was fighting constant fatigue, falling asleep the minute I got home from work every day, but I thought a B12 shot would solve all my problems. I didn’t realize I was having symptoms of burnout until my own therapist told me,” said Dr. Gold. “As doctors, we spend so much time focusing on other people that we don’t necessarily notice very much in ourselves – usually once it starts to impact our job.”
Practices like meditation and mindfulness can help you delve into your feelings and emotions and notice how you’re doing. But you may also need to ask spouses, partners, and friends and family – or better yet, a mental health professional – if they notice that you seem burnt out.
Practice ‘in the moment’ relief
Sometimes, walking away at the moment of stress helps like when stepping away from a heated argument. “Step out of a frustrating staff meeting to go to the bathroom and splash your face,” said Eran Magan, PhD, a psychologist at the University of Pennsylvania, Philadelphia, and founder and CEO of the suicide prevention system EarlyAlert.me. “Tell a patient you need to check something in the next room, so you have time to take a breath.”
Dr. Magan recommended finding techniques that help lower acute stress while it’s actually happening. First, find a way to escape or excuse yourself from the event, and when possible, stop situations that are actively upsetting or triggering in their tracks.
Next, recharge by doing something that helps you feel better, like looking at a cute video of your child or grandchild or closing your eyes and taking a deep breath. You can also try to “catch” good feelings from someone else, said Dr. Magan. Ask someone about a trip, vacation, holiday, or pleasant event. “Ask a colleague about something that makes [them] happy,” he said. “Happiness can be infectious too.”
Burnout is also in the body
“Body psychotherapy” or somatic therapy is a treatment that focuses on how emotions appear within your body. Dr. Gibson said it’s a valuable tool for addressing trauma and a mainstay in many a medical career; it’s useful to help physicians learn to “befriend” their nervous system.
Somatic therapy exercises involve things like body scanning, scanning for physical sensations; conscious breathing, connecting to each inhale and exhale; grounding your weight by releasing tension through your feet, doing a total body stretch; or releasing shoulder and neck tension by consciously relaxing each of these muscle groups.
“We spend our whole day in sympathetic tone; our amygdala’s are firing, telling us that we’re in danger,” said Dr. Gibson. “We actually have to practice getting into and spending time in our parasympathetic nervous system to restore the balance in our autonomic nervous system.”
Somatic therapy includes a wide array of exercises that help reconnect you to your body through calming or activation. The movements release tension, ground you, and restore balance.
Bite-sized tools for well-being
Because of the prevalence of physician burnout, there’s been a groundswell of researchers and organizations who have turned their focus toward improving the well-being in the health care workforce.
One such effort comes from the Duke Center for the Advancement of Well-being Science, which “camouflages” well-being tools as continuing education credits to make them accessible for busy, stressed, and overworked physicians.
“They’re called bite-sized tools for well-being, and they have actual evidence behind them,” said Dr. Gold. For example, she said, one tools is a text program called Three Good Things that encourages physicians to send a text listing three positive things that happened during the day. The exercise lasts 15 days, and texters have access to others’ answers as well. After 3 months, participants’ baseline depression, gratitude, and life satisfaction had all “significantly improved.”
“It feels almost ridiculous that that could work, but it does,” said Dr. Gold. “I’ve had patients push back and say: ‘Well, isn’t that toxic positivity?’ But really what it is is dialectics. It’s not saying there’s only positive; it’s just making you realize there is more than just the negative.”
These and other short interventions focus on concepts such as joy, humor, awe, engagement, and self-kindness to build resilience and help physicians recover from burnout symptoms.
Cognitive restructuring could work
Cognitive restructuring is a therapeutic process of learning new ways of interpreting and responding to people and situations. It helps you change the “filter” through which you interact with your environment. Dr. Gibson said it’s a tool to use with care after other modes of therapy that help you understand your patterns and how they developed because of how you view and understand the world.
“The message of [cognitive-behavioral therapy] or cognitive restructuring is there’s something wrong with the way you’re thinking, and we need to change it or fix it, but in a traumatic system [like health care], you’re thinking has been an adaptive process related to the harm in the environment you’re in,” said Dr. Gibson.
“So, if you [jump straight to cognitive restructuring before other types of therapy], then we just gaslight ourselves into believing that there’s something wrong with us, that we haven’t adapted sufficiently to an environment that’s actually harmful.”
Strive for a few systemic changes
Systemic changes can be small ones within your own sphere. For example, Dr. Magan said, work toward making little tweaks to the flow of your day that will increase calm and reduce frustration.
“Make a ‘bug list,’ little, regular demands that drain your energy, and discuss them with your colleagues and supervisors to see if they can be improved,” he said. Examples include everyday frustrations like having unsolicited visitors popping into your office, scheduling complex patients too late in the day, or having a computer freeze whenever you access patient charts.
Though not always financially feasible, affecting real change and finding relief from all these insidious bugs can improve your mental health and burnout symptoms.
“Physicians tend to work extremely hard in order to keep holding together a system that is often not inherently sustainable, like the fascia of a body under tremendous strain,” said Dr. Magan. “Sometimes the brave thing to do is to refuse to continue being the lynchpin and let things break, so the system will have to start improving itself, rather than demanding more and more of the people in it.”
A version of this article first appeared on Medscape.com.
Physician burnout persists even as the height of the COVID-19 crisis fades farther into the rear-view mirror. The causes for the sadness, stress, and frustration among doctors vary, but the effects are universal and often debilitating: exhaustion, emotional detachment, lethargy, feeling useless, and lacking purpose.
When surveyed, physicians pointed to many systemic solutions for burnout in Medscape’s Physician Burnout & Depression Report 2023, such as a need for greater compensation, more manageable workloads and schedules, and more support staff. But for many doctors, these fixes may be years if not decades away. Equally important are strategies for relieving burnout symptoms now, especially as we head into a busy holiday season.
Because not every stress-relief practice works for everyone, it’s crucial to try various methods until you find something that makes a difference for you, said Christine Gibson, MD, a family physician and trauma therapist in Calgary, Alta., and author of The Modern Trauma Toolkit.
“Every person should have a toolkit of the things that bring them out of the psychological and physical distress that dysregulates their nervous system,” said Dr. Gibson.
Once you learn the personal ways to alleviate your specific brand of burnout, you can start working on systemic changes that might help the culture of medicine overall.
Symptoms speak louder than words
It seems obvious, but if you aren’t aware that what you’re feeling is burnout, you probably aren’t going to find effective steps to relieve it. Jessi Gold, MD, assistant professor and director of wellness, engagement, and outreach in the department of psychiatry, Washington University in St. Louis, is a psychiatrist who treats health care professionals, including frontline workers during the height of the pandemic. But even as a burnout expert, she admits that she misses the signs in herself.
“I was fighting constant fatigue, falling asleep the minute I got home from work every day, but I thought a B12 shot would solve all my problems. I didn’t realize I was having symptoms of burnout until my own therapist told me,” said Dr. Gold. “As doctors, we spend so much time focusing on other people that we don’t necessarily notice very much in ourselves – usually once it starts to impact our job.”
Practices like meditation and mindfulness can help you delve into your feelings and emotions and notice how you’re doing. But you may also need to ask spouses, partners, and friends and family – or better yet, a mental health professional – if they notice that you seem burnt out.
Practice ‘in the moment’ relief
Sometimes, walking away at the moment of stress helps like when stepping away from a heated argument. “Step out of a frustrating staff meeting to go to the bathroom and splash your face,” said Eran Magan, PhD, a psychologist at the University of Pennsylvania, Philadelphia, and founder and CEO of the suicide prevention system EarlyAlert.me. “Tell a patient you need to check something in the next room, so you have time to take a breath.”
Dr. Magan recommended finding techniques that help lower acute stress while it’s actually happening. First, find a way to escape or excuse yourself from the event, and when possible, stop situations that are actively upsetting or triggering in their tracks.
Next, recharge by doing something that helps you feel better, like looking at a cute video of your child or grandchild or closing your eyes and taking a deep breath. You can also try to “catch” good feelings from someone else, said Dr. Magan. Ask someone about a trip, vacation, holiday, or pleasant event. “Ask a colleague about something that makes [them] happy,” he said. “Happiness can be infectious too.”
Burnout is also in the body
“Body psychotherapy” or somatic therapy is a treatment that focuses on how emotions appear within your body. Dr. Gibson said it’s a valuable tool for addressing trauma and a mainstay in many a medical career; it’s useful to help physicians learn to “befriend” their nervous system.
Somatic therapy exercises involve things like body scanning, scanning for physical sensations; conscious breathing, connecting to each inhale and exhale; grounding your weight by releasing tension through your feet, doing a total body stretch; or releasing shoulder and neck tension by consciously relaxing each of these muscle groups.
“We spend our whole day in sympathetic tone; our amygdala’s are firing, telling us that we’re in danger,” said Dr. Gibson. “We actually have to practice getting into and spending time in our parasympathetic nervous system to restore the balance in our autonomic nervous system.”
Somatic therapy includes a wide array of exercises that help reconnect you to your body through calming or activation. The movements release tension, ground you, and restore balance.
Bite-sized tools for well-being
Because of the prevalence of physician burnout, there’s been a groundswell of researchers and organizations who have turned their focus toward improving the well-being in the health care workforce.
One such effort comes from the Duke Center for the Advancement of Well-being Science, which “camouflages” well-being tools as continuing education credits to make them accessible for busy, stressed, and overworked physicians.
“They’re called bite-sized tools for well-being, and they have actual evidence behind them,” said Dr. Gold. For example, she said, one tools is a text program called Three Good Things that encourages physicians to send a text listing three positive things that happened during the day. The exercise lasts 15 days, and texters have access to others’ answers as well. After 3 months, participants’ baseline depression, gratitude, and life satisfaction had all “significantly improved.”
“It feels almost ridiculous that that could work, but it does,” said Dr. Gold. “I’ve had patients push back and say: ‘Well, isn’t that toxic positivity?’ But really what it is is dialectics. It’s not saying there’s only positive; it’s just making you realize there is more than just the negative.”
These and other short interventions focus on concepts such as joy, humor, awe, engagement, and self-kindness to build resilience and help physicians recover from burnout symptoms.
Cognitive restructuring could work
Cognitive restructuring is a therapeutic process of learning new ways of interpreting and responding to people and situations. It helps you change the “filter” through which you interact with your environment. Dr. Gibson said it’s a tool to use with care after other modes of therapy that help you understand your patterns and how they developed because of how you view and understand the world.
“The message of [cognitive-behavioral therapy] or cognitive restructuring is there’s something wrong with the way you’re thinking, and we need to change it or fix it, but in a traumatic system [like health care], you’re thinking has been an adaptive process related to the harm in the environment you’re in,” said Dr. Gibson.
“So, if you [jump straight to cognitive restructuring before other types of therapy], then we just gaslight ourselves into believing that there’s something wrong with us, that we haven’t adapted sufficiently to an environment that’s actually harmful.”
Strive for a few systemic changes
Systemic changes can be small ones within your own sphere. For example, Dr. Magan said, work toward making little tweaks to the flow of your day that will increase calm and reduce frustration.
“Make a ‘bug list,’ little, regular demands that drain your energy, and discuss them with your colleagues and supervisors to see if they can be improved,” he said. Examples include everyday frustrations like having unsolicited visitors popping into your office, scheduling complex patients too late in the day, or having a computer freeze whenever you access patient charts.
Though not always financially feasible, affecting real change and finding relief from all these insidious bugs can improve your mental health and burnout symptoms.
“Physicians tend to work extremely hard in order to keep holding together a system that is often not inherently sustainable, like the fascia of a body under tremendous strain,” said Dr. Magan. “Sometimes the brave thing to do is to refuse to continue being the lynchpin and let things break, so the system will have to start improving itself, rather than demanding more and more of the people in it.”
A version of this article first appeared on Medscape.com.
Physician burnout persists even as the height of the COVID-19 crisis fades farther into the rear-view mirror. The causes for the sadness, stress, and frustration among doctors vary, but the effects are universal and often debilitating: exhaustion, emotional detachment, lethargy, feeling useless, and lacking purpose.
When surveyed, physicians pointed to many systemic solutions for burnout in Medscape’s Physician Burnout & Depression Report 2023, such as a need for greater compensation, more manageable workloads and schedules, and more support staff. But for many doctors, these fixes may be years if not decades away. Equally important are strategies for relieving burnout symptoms now, especially as we head into a busy holiday season.
Because not every stress-relief practice works for everyone, it’s crucial to try various methods until you find something that makes a difference for you, said Christine Gibson, MD, a family physician and trauma therapist in Calgary, Alta., and author of The Modern Trauma Toolkit.
“Every person should have a toolkit of the things that bring them out of the psychological and physical distress that dysregulates their nervous system,” said Dr. Gibson.
Once you learn the personal ways to alleviate your specific brand of burnout, you can start working on systemic changes that might help the culture of medicine overall.
Symptoms speak louder than words
It seems obvious, but if you aren’t aware that what you’re feeling is burnout, you probably aren’t going to find effective steps to relieve it. Jessi Gold, MD, assistant professor and director of wellness, engagement, and outreach in the department of psychiatry, Washington University in St. Louis, is a psychiatrist who treats health care professionals, including frontline workers during the height of the pandemic. But even as a burnout expert, she admits that she misses the signs in herself.
“I was fighting constant fatigue, falling asleep the minute I got home from work every day, but I thought a B12 shot would solve all my problems. I didn’t realize I was having symptoms of burnout until my own therapist told me,” said Dr. Gold. “As doctors, we spend so much time focusing on other people that we don’t necessarily notice very much in ourselves – usually once it starts to impact our job.”
Practices like meditation and mindfulness can help you delve into your feelings and emotions and notice how you’re doing. But you may also need to ask spouses, partners, and friends and family – or better yet, a mental health professional – if they notice that you seem burnt out.
Practice ‘in the moment’ relief
Sometimes, walking away at the moment of stress helps like when stepping away from a heated argument. “Step out of a frustrating staff meeting to go to the bathroom and splash your face,” said Eran Magan, PhD, a psychologist at the University of Pennsylvania, Philadelphia, and founder and CEO of the suicide prevention system EarlyAlert.me. “Tell a patient you need to check something in the next room, so you have time to take a breath.”
Dr. Magan recommended finding techniques that help lower acute stress while it’s actually happening. First, find a way to escape or excuse yourself from the event, and when possible, stop situations that are actively upsetting or triggering in their tracks.
Next, recharge by doing something that helps you feel better, like looking at a cute video of your child or grandchild or closing your eyes and taking a deep breath. You can also try to “catch” good feelings from someone else, said Dr. Magan. Ask someone about a trip, vacation, holiday, or pleasant event. “Ask a colleague about something that makes [them] happy,” he said. “Happiness can be infectious too.”
Burnout is also in the body
“Body psychotherapy” or somatic therapy is a treatment that focuses on how emotions appear within your body. Dr. Gibson said it’s a valuable tool for addressing trauma and a mainstay in many a medical career; it’s useful to help physicians learn to “befriend” their nervous system.
Somatic therapy exercises involve things like body scanning, scanning for physical sensations; conscious breathing, connecting to each inhale and exhale; grounding your weight by releasing tension through your feet, doing a total body stretch; or releasing shoulder and neck tension by consciously relaxing each of these muscle groups.
“We spend our whole day in sympathetic tone; our amygdala’s are firing, telling us that we’re in danger,” said Dr. Gibson. “We actually have to practice getting into and spending time in our parasympathetic nervous system to restore the balance in our autonomic nervous system.”
Somatic therapy includes a wide array of exercises that help reconnect you to your body through calming or activation. The movements release tension, ground you, and restore balance.
Bite-sized tools for well-being
Because of the prevalence of physician burnout, there’s been a groundswell of researchers and organizations who have turned their focus toward improving the well-being in the health care workforce.
One such effort comes from the Duke Center for the Advancement of Well-being Science, which “camouflages” well-being tools as continuing education credits to make them accessible for busy, stressed, and overworked physicians.
“They’re called bite-sized tools for well-being, and they have actual evidence behind them,” said Dr. Gold. For example, she said, one tools is a text program called Three Good Things that encourages physicians to send a text listing three positive things that happened during the day. The exercise lasts 15 days, and texters have access to others’ answers as well. After 3 months, participants’ baseline depression, gratitude, and life satisfaction had all “significantly improved.”
“It feels almost ridiculous that that could work, but it does,” said Dr. Gold. “I’ve had patients push back and say: ‘Well, isn’t that toxic positivity?’ But really what it is is dialectics. It’s not saying there’s only positive; it’s just making you realize there is more than just the negative.”
These and other short interventions focus on concepts such as joy, humor, awe, engagement, and self-kindness to build resilience and help physicians recover from burnout symptoms.
Cognitive restructuring could work
Cognitive restructuring is a therapeutic process of learning new ways of interpreting and responding to people and situations. It helps you change the “filter” through which you interact with your environment. Dr. Gibson said it’s a tool to use with care after other modes of therapy that help you understand your patterns and how they developed because of how you view and understand the world.
“The message of [cognitive-behavioral therapy] or cognitive restructuring is there’s something wrong with the way you’re thinking, and we need to change it or fix it, but in a traumatic system [like health care], you’re thinking has been an adaptive process related to the harm in the environment you’re in,” said Dr. Gibson.
“So, if you [jump straight to cognitive restructuring before other types of therapy], then we just gaslight ourselves into believing that there’s something wrong with us, that we haven’t adapted sufficiently to an environment that’s actually harmful.”
Strive for a few systemic changes
Systemic changes can be small ones within your own sphere. For example, Dr. Magan said, work toward making little tweaks to the flow of your day that will increase calm and reduce frustration.
“Make a ‘bug list,’ little, regular demands that drain your energy, and discuss them with your colleagues and supervisors to see if they can be improved,” he said. Examples include everyday frustrations like having unsolicited visitors popping into your office, scheduling complex patients too late in the day, or having a computer freeze whenever you access patient charts.
Though not always financially feasible, affecting real change and finding relief from all these insidious bugs can improve your mental health and burnout symptoms.
“Physicians tend to work extremely hard in order to keep holding together a system that is often not inherently sustainable, like the fascia of a body under tremendous strain,” said Dr. Magan. “Sometimes the brave thing to do is to refuse to continue being the lynchpin and let things break, so the system will have to start improving itself, rather than demanding more and more of the people in it.”
A version of this article first appeared on Medscape.com.