User login
Is This Journal Legit? Predatory Publishers
This transcript has been edited for clarity.
Andrew N. Wilner, MD: My guest today is Dr. Jose Merino, editor in chief of the Neurology family of journals and professor of neurology and co-vice chair of education at Georgetown University in Washington, DC.
Our program today is a follow-up of Dr. Merino’s presentation at the recent American Academy of Neurology meeting in Denver, Colorado. Along with two other panelists, Dr. Merino discussed the role of open-access publication and the dangers of predatory journals.
Jose G. Merino, MD, MPhil: Thank you for having me here. It’s a pleasure.
Open Access Defined
Dr. Wilner: I remember when publication in neurology was pretty straightforward. It was either the green journal or the blue journal, but things have certainly changed. I think one topic that is not clear to everyone is this concept of open access. Could you define that for us?
Dr. Merino: Sure. Open access is a mode of publication that fosters more open or accessible science. The idea of open access is that it combines two main elements. One is that the papers that are published become immediately available to anybody with an internet connection anywhere in the world without any restrictions.
The second important element from open access, which makes it different from other models we can talk about, is the fact that the authors retain the copyright of their work, but they give the journal and readers a license to use, reproduce, and modify the content.
This is different, for example, from instances where we have funder mandates. For example, NIH papers have to become available 6 months after publication, so they’re available to everybody but not immediately.
Dr. Wilner: I remember that when a journal article was published, say, in Neurology, if you didn’t have a subscription to Neurology, you went to the library that hopefully had a subscription.
If they didn’t have it, you would write to the author and say, “Hey, I heard you have this great paper because the abstract was out there. Could you send me a reprint?” Has that whole universe evaporated?
Dr. Merino: It depends on how the paper is published. For example, in Neurology, some of the research we publish is open access. Basically, if you have an internet connection, you can access the paper.
That’s the case for papers published in our wholly open-access journals in the Neurology family like Neurology Neuroimmunology & Neuroinflammation, Neurology Genetics, or Neurology Education.
For other papers that are published in Neurology, not under open access, there is a paywall. For some of them, the paywall comes down after a few months based on funder mandates and so on. As I was mentioning, the NIH-funded papers are available 6 months later.
In the first 6 months, you may have to go to your library, and if your library has a subscription, you can download it directly. [This is also true for] those that always stay behind the paywall, where you have to have a subscription or your library has to have a subscription.
Is Pay to Publish a Red Flag?
Dr. Wilner: I’m a professional writer. With any luck, when I write something, I get paid to write it. There’s been a long tradition in academic medicine that when you submit an article to, say, Neurology, you don’t get paid as an author for the publication. Your reward is the honor of it being published.
Neurology supports itself in various ways, including advertising and so on. That’s been the contract: free publication for work that merits it, and the journal survives on its own.
With open access, one of the things that’s happened is that — and I’ve published open access myself — is that I get a notification that I need to pay to have my article that I’ve slaved over published. Explain that, please.
Dr. Merino: This is the issue with open access. As I mentioned, the paper gets published. You’re giving the journal a license to publish it. You’re retaining the copyright of your work. That means that the journal cannot make money or support itself by just publishing open access because they belong to you.
Typically, open-access journals are not in print and don’t have much in terms of advertising. The contract is you’re giving me a license to publish it, but it’s your journal, so you’re paying a fee for the journal expenses to basically produce your paper. That’s what’s happening with open access.
That’s been recognized with many funders, for example, with NIH funding or many of the European funders, they’re including open-access fees as part of their funding for research. Now, of course, this doesn’t help if you’re not a funded researcher or if you’re a fellow who’s doing work and so on.
Typically, most journals will have waived fees or lower fees for these situations. The reason for the open-access fee is the fact that you’re retaining the copyright. You’re not giving it to the journal who can then use it to generate its revenue for supporting itself, the editorial staff, and so on.
Dr. Wilner: This idea of charging for publication has created a satellite business of what are called predatory journals. How does one know if the open-access journal that I’m submitting to is really just in the business of wanting my $300 or my $900 to get published? How do I know if that’s a reasonable place to publish?
Predatory Journals
Dr. Merino: That’s a big challenge that has come with this whole idea of open access and the fact that now, many journals are online only, so you’re no longer seeing a physical copy. That has given rise to the predatory journals.
The predatory journal, by definition, is a journal that claims to be open access. They’ll take your paper and publish it, but they don’t provide all the other services that you would typically expect from the fact that you’re paying an open-access fee. This includes getting appropriate peer review, production of the manuscript, and long-term curation and storage of the manuscript.
Many predatory journals will take your open-access fee, accept any paper that you submit, regardless of the quality, because they’re charging the fees for that. They don’t send it to real peer review, and then in a few months, the journal disappears so there’s no way for anybody to actually find your paper anymore.
There are certain checklists. Dr. David Moher at the University of Toronto has produced some work trying to help us identify predatory journals.
One thing I typically suggest to people who ask me this question is: Have you ever heard of this journal before? Does the journal have a track record? How far back does the story of the journal go? Is it supported by a publisher that you know? Do you know anybody who has published there? Is it something you can easily access?
If in doubt, always ask your friendly medical librarian. There used to be lists that were kept in terms of predatory journals that were being constantly updated, but those had to be shut down. As far as I understand, there were legal issues in terms of how things got on that list.
I think that overall, if you’ve heard of it, if it’s relevant, if it’s known in your field, and if your librarian knows it, it’s probably a good legitimate open-access journal. There are many very good legitimate open-access journals.
I mentioned the two that we have in our family, but all the other major journals have their own open-access journal within their family. There are some, like BMC or PLOS, that are completely open-access and legitimate journals.
Impact Factor
Dr. Wilner: What about impact factor? Many journals boast about their impact factor. I’m not sure how to interpret that number.
Dr. Merino: Impact factor is very interesting. The impact factor was developed by medical librarians to try to identify the journals they should be subscribing to. It’s a measure of the average citations to an average paper in the journal.
It doesn’t tell you about specific papers. It tells you, on average, how many of the papers in this journal get cited so many times. It’s calculated by the number of articles that were cited divided by the number of articles that were published. Journals that publish many papers, like Neurology, have a hard time bringing up their impact factor beyond a certain level.
Similarly, very small journals with one or two very highly cited papers have a very high impact factor. It’s being used as a measure, perhaps inappropriately, of how good or how reputable a journal is. We all say we don’t care about journal impact factors, but we all know our journal impact factor and we used to know it to three decimals. Now, they changed the system, and there’s only one decimal point, which makes more sense.
This is more important, for example, for authors when deciding where to submit papers. I know that in some countries, particularly in Europe, the impact factor of the journal where you publish has an impact on your promotion decisions.
I would say what’s even more important than the impact factor, is to say, “Well, is this the journal that fits the scope of my paper? Is this the journal that reaches the audience that I want to reach when I write my paper?”
There are some papers, for example, that are very influential. The impact factor just captures citations. There are some papers that are very influential that may not get cited very often. There may be papers that change clinical practice.
If you read a paper that tells you that you should be changing how you treat your patients with myasthenia based on this paper, that may not get cited. It’s a very clinically focused paper, but it’s probably more impactful than one that gets cited very much in some respect, or they make it to public policy decisions, and so on.
I think it’s important to look more at the audience and the journal scope when you submit your papers.
Dr. Wilner: One other technical question. The journals also say they’re indexed in PubMed or Google Scholar. If I want to publish my paper and I want it indexed where the right people are going to find it, where does it need to be indexed?
Dr. Merino: I grew up using Index Medicus, MedlinePlus, and the Library of Science. I still do. If I need to find something, I go to PubMed. Ideally, papers are listed in MedlinePlus or can be found in PubMed. They’re not the same thing, but you can find them through them.
That would be an important thing. Nowadays, a lot more people are using Google Scholar or Google just to identify papers. It may be a little bit less relevant, but it’s still a measure of the quality of the journal before they get indexed in some of these. For example, if you get listed in MedlinePlus, it has gone through certain quality checks by the index itself to see whether they would accept the journal or not. That’s something you want to check.
Typically, most of the large journals or the journals you and I know about are listed in more than one place, right? They’re listed in Scopus and Web of Science. They’re listed in MedlinePlus and so on. Again, if you’re submitting your paper, go somewhere where you know the journal and you’ve heard about it.
Dr. Wilner: I’m not going to ask you about artificial intelligence. We can do that another time. I want to ask something closer to me, which is this question of publish or perish.
There seems to be, in academics, more emphasis on the number of papers that one has published rather than their quality. How does a younger academician or one who really needs to publish cope with that?
Dr. Merino: Many people are writing up research that may not be relevant or that may not be high quality just because you need to have a long list of papers to get promoted, for example, if you’re an academician.
Doug Altman, who was a very influential person in the field quality of not only medical statistics but also medical publishing, had the idea that we need less research, but we need better research.
We often receive papers where you say, well, what’s the rationale behind the question in this paper? It’s like they had a large amount of data and were trying to squeeze as much as they could out of that. I think, as a young academician, the important thing to think about is whether it is an important question that matters to you and to the field, from whatever perspective, whether it’s going to advance research, advance clinical care, or have public policy implications.
Is this one where the answer will be important no matter what the answer is? If you’re thinking of that, your work will be well recognized, people will know you, and you’ll get invited to collaborate. I think that’s the most important thing rather than just churning out a large number of papers.
The productivity will come from the fact that you start by saying, let me ask something that’s really meaningful to me and to the field, with a good question and using strong research methodology.
Dr. Wilner: Thanks for that, Dr. Merino. I think that’s very valuable for all of us. This has been a great discussion. Do you have any final comments before we wrap up?
Dr. Merino: I want to encourage people to continue reading medical journals all the time and submitting to us, again, good research and important questions with robust methodology. That’s what we’re looking for in Neurology and most serious medical journals.
Dr. Wilner is an associate professor of neurology at the University of Tennessee Health Science Center, Memphis. Dr. Merino is a professor in the department of neurology at Georgetown University Medical Center, Washington, DC. Dr. Wilner reported conflicts of interest with Accordant Health Services and Lulu Publishing. Dr. Merino reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Andrew N. Wilner, MD: My guest today is Dr. Jose Merino, editor in chief of the Neurology family of journals and professor of neurology and co-vice chair of education at Georgetown University in Washington, DC.
Our program today is a follow-up of Dr. Merino’s presentation at the recent American Academy of Neurology meeting in Denver, Colorado. Along with two other panelists, Dr. Merino discussed the role of open-access publication and the dangers of predatory journals.
Jose G. Merino, MD, MPhil: Thank you for having me here. It’s a pleasure.
Open Access Defined
Dr. Wilner: I remember when publication in neurology was pretty straightforward. It was either the green journal or the blue journal, but things have certainly changed. I think one topic that is not clear to everyone is this concept of open access. Could you define that for us?
Dr. Merino: Sure. Open access is a mode of publication that fosters more open or accessible science. The idea of open access is that it combines two main elements. One is that the papers that are published become immediately available to anybody with an internet connection anywhere in the world without any restrictions.
The second important element from open access, which makes it different from other models we can talk about, is the fact that the authors retain the copyright of their work, but they give the journal and readers a license to use, reproduce, and modify the content.
This is different, for example, from instances where we have funder mandates. For example, NIH papers have to become available 6 months after publication, so they’re available to everybody but not immediately.
Dr. Wilner: I remember that when a journal article was published, say, in Neurology, if you didn’t have a subscription to Neurology, you went to the library that hopefully had a subscription.
If they didn’t have it, you would write to the author and say, “Hey, I heard you have this great paper because the abstract was out there. Could you send me a reprint?” Has that whole universe evaporated?
Dr. Merino: It depends on how the paper is published. For example, in Neurology, some of the research we publish is open access. Basically, if you have an internet connection, you can access the paper.
That’s the case for papers published in our wholly open-access journals in the Neurology family like Neurology Neuroimmunology & Neuroinflammation, Neurology Genetics, or Neurology Education.
For other papers that are published in Neurology, not under open access, there is a paywall. For some of them, the paywall comes down after a few months based on funder mandates and so on. As I was mentioning, the NIH-funded papers are available 6 months later.
In the first 6 months, you may have to go to your library, and if your library has a subscription, you can download it directly. [This is also true for] those that always stay behind the paywall, where you have to have a subscription or your library has to have a subscription.
Is Pay to Publish a Red Flag?
Dr. Wilner: I’m a professional writer. With any luck, when I write something, I get paid to write it. There’s been a long tradition in academic medicine that when you submit an article to, say, Neurology, you don’t get paid as an author for the publication. Your reward is the honor of it being published.
Neurology supports itself in various ways, including advertising and so on. That’s been the contract: free publication for work that merits it, and the journal survives on its own.
With open access, one of the things that’s happened is that — and I’ve published open access myself — is that I get a notification that I need to pay to have my article that I’ve slaved over published. Explain that, please.
Dr. Merino: This is the issue with open access. As I mentioned, the paper gets published. You’re giving the journal a license to publish it. You’re retaining the copyright of your work. That means that the journal cannot make money or support itself by just publishing open access because they belong to you.
Typically, open-access journals are not in print and don’t have much in terms of advertising. The contract is you’re giving me a license to publish it, but it’s your journal, so you’re paying a fee for the journal expenses to basically produce your paper. That’s what’s happening with open access.
That’s been recognized with many funders, for example, with NIH funding or many of the European funders, they’re including open-access fees as part of their funding for research. Now, of course, this doesn’t help if you’re not a funded researcher or if you’re a fellow who’s doing work and so on.
Typically, most journals will have waived fees or lower fees for these situations. The reason for the open-access fee is the fact that you’re retaining the copyright. You’re not giving it to the journal who can then use it to generate its revenue for supporting itself, the editorial staff, and so on.
Dr. Wilner: This idea of charging for publication has created a satellite business of what are called predatory journals. How does one know if the open-access journal that I’m submitting to is really just in the business of wanting my $300 or my $900 to get published? How do I know if that’s a reasonable place to publish?
Predatory Journals
Dr. Merino: That’s a big challenge that has come with this whole idea of open access and the fact that now, many journals are online only, so you’re no longer seeing a physical copy. That has given rise to the predatory journals.
The predatory journal, by definition, is a journal that claims to be open access. They’ll take your paper and publish it, but they don’t provide all the other services that you would typically expect from the fact that you’re paying an open-access fee. This includes getting appropriate peer review, production of the manuscript, and long-term curation and storage of the manuscript.
Many predatory journals will take your open-access fee, accept any paper that you submit, regardless of the quality, because they’re charging the fees for that. They don’t send it to real peer review, and then in a few months, the journal disappears so there’s no way for anybody to actually find your paper anymore.
There are certain checklists. Dr. David Moher at the University of Toronto has produced some work trying to help us identify predatory journals.
One thing I typically suggest to people who ask me this question is: Have you ever heard of this journal before? Does the journal have a track record? How far back does the story of the journal go? Is it supported by a publisher that you know? Do you know anybody who has published there? Is it something you can easily access?
If in doubt, always ask your friendly medical librarian. There used to be lists that were kept in terms of predatory journals that were being constantly updated, but those had to be shut down. As far as I understand, there were legal issues in terms of how things got on that list.
I think that overall, if you’ve heard of it, if it’s relevant, if it’s known in your field, and if your librarian knows it, it’s probably a good legitimate open-access journal. There are many very good legitimate open-access journals.
I mentioned the two that we have in our family, but all the other major journals have their own open-access journal within their family. There are some, like BMC or PLOS, that are completely open-access and legitimate journals.
Impact Factor
Dr. Wilner: What about impact factor? Many journals boast about their impact factor. I’m not sure how to interpret that number.
Dr. Merino: Impact factor is very interesting. The impact factor was developed by medical librarians to try to identify the journals they should be subscribing to. It’s a measure of the average citations to an average paper in the journal.
It doesn’t tell you about specific papers. It tells you, on average, how many of the papers in this journal get cited so many times. It’s calculated by the number of articles that were cited divided by the number of articles that were published. Journals that publish many papers, like Neurology, have a hard time bringing up their impact factor beyond a certain level.
Similarly, very small journals with one or two very highly cited papers have a very high impact factor. It’s being used as a measure, perhaps inappropriately, of how good or how reputable a journal is. We all say we don’t care about journal impact factors, but we all know our journal impact factor and we used to know it to three decimals. Now, they changed the system, and there’s only one decimal point, which makes more sense.
This is more important, for example, for authors when deciding where to submit papers. I know that in some countries, particularly in Europe, the impact factor of the journal where you publish has an impact on your promotion decisions.
I would say what’s even more important than the impact factor, is to say, “Well, is this the journal that fits the scope of my paper? Is this the journal that reaches the audience that I want to reach when I write my paper?”
There are some papers, for example, that are very influential. The impact factor just captures citations. There are some papers that are very influential that may not get cited very often. There may be papers that change clinical practice.
If you read a paper that tells you that you should be changing how you treat your patients with myasthenia based on this paper, that may not get cited. It’s a very clinically focused paper, but it’s probably more impactful than one that gets cited very much in some respect, or they make it to public policy decisions, and so on.
I think it’s important to look more at the audience and the journal scope when you submit your papers.
Dr. Wilner: One other technical question. The journals also say they’re indexed in PubMed or Google Scholar. If I want to publish my paper and I want it indexed where the right people are going to find it, where does it need to be indexed?
Dr. Merino: I grew up using Index Medicus, MedlinePlus, and the Library of Science. I still do. If I need to find something, I go to PubMed. Ideally, papers are listed in MedlinePlus or can be found in PubMed. They’re not the same thing, but you can find them through them.
That would be an important thing. Nowadays, a lot more people are using Google Scholar or Google just to identify papers. It may be a little bit less relevant, but it’s still a measure of the quality of the journal before they get indexed in some of these. For example, if you get listed in MedlinePlus, it has gone through certain quality checks by the index itself to see whether they would accept the journal or not. That’s something you want to check.
Typically, most of the large journals or the journals you and I know about are listed in more than one place, right? They’re listed in Scopus and Web of Science. They’re listed in MedlinePlus and so on. Again, if you’re submitting your paper, go somewhere where you know the journal and you’ve heard about it.
Dr. Wilner: I’m not going to ask you about artificial intelligence. We can do that another time. I want to ask something closer to me, which is this question of publish or perish.
There seems to be, in academics, more emphasis on the number of papers that one has published rather than their quality. How does a younger academician or one who really needs to publish cope with that?
Dr. Merino: Many people are writing up research that may not be relevant or that may not be high quality just because you need to have a long list of papers to get promoted, for example, if you’re an academician.
Doug Altman, who was a very influential person in the field quality of not only medical statistics but also medical publishing, had the idea that we need less research, but we need better research.
We often receive papers where you say, well, what’s the rationale behind the question in this paper? It’s like they had a large amount of data and were trying to squeeze as much as they could out of that. I think, as a young academician, the important thing to think about is whether it is an important question that matters to you and to the field, from whatever perspective, whether it’s going to advance research, advance clinical care, or have public policy implications.
Is this one where the answer will be important no matter what the answer is? If you’re thinking of that, your work will be well recognized, people will know you, and you’ll get invited to collaborate. I think that’s the most important thing rather than just churning out a large number of papers.
The productivity will come from the fact that you start by saying, let me ask something that’s really meaningful to me and to the field, with a good question and using strong research methodology.
Dr. Wilner: Thanks for that, Dr. Merino. I think that’s very valuable for all of us. This has been a great discussion. Do you have any final comments before we wrap up?
Dr. Merino: I want to encourage people to continue reading medical journals all the time and submitting to us, again, good research and important questions with robust methodology. That’s what we’re looking for in Neurology and most serious medical journals.
Dr. Wilner is an associate professor of neurology at the University of Tennessee Health Science Center, Memphis. Dr. Merino is a professor in the department of neurology at Georgetown University Medical Center, Washington, DC. Dr. Wilner reported conflicts of interest with Accordant Health Services and Lulu Publishing. Dr. Merino reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Andrew N. Wilner, MD: My guest today is Dr. Jose Merino, editor in chief of the Neurology family of journals and professor of neurology and co-vice chair of education at Georgetown University in Washington, DC.
Our program today is a follow-up of Dr. Merino’s presentation at the recent American Academy of Neurology meeting in Denver, Colorado. Along with two other panelists, Dr. Merino discussed the role of open-access publication and the dangers of predatory journals.
Jose G. Merino, MD, MPhil: Thank you for having me here. It’s a pleasure.
Open Access Defined
Dr. Wilner: I remember when publication in neurology was pretty straightforward. It was either the green journal or the blue journal, but things have certainly changed. I think one topic that is not clear to everyone is this concept of open access. Could you define that for us?
Dr. Merino: Sure. Open access is a mode of publication that fosters more open or accessible science. The idea of open access is that it combines two main elements. One is that the papers that are published become immediately available to anybody with an internet connection anywhere in the world without any restrictions.
The second important element from open access, which makes it different from other models we can talk about, is the fact that the authors retain the copyright of their work, but they give the journal and readers a license to use, reproduce, and modify the content.
This is different, for example, from instances where we have funder mandates. For example, NIH papers have to become available 6 months after publication, so they’re available to everybody but not immediately.
Dr. Wilner: I remember that when a journal article was published, say, in Neurology, if you didn’t have a subscription to Neurology, you went to the library that hopefully had a subscription.
If they didn’t have it, you would write to the author and say, “Hey, I heard you have this great paper because the abstract was out there. Could you send me a reprint?” Has that whole universe evaporated?
Dr. Merino: It depends on how the paper is published. For example, in Neurology, some of the research we publish is open access. Basically, if you have an internet connection, you can access the paper.
That’s the case for papers published in our wholly open-access journals in the Neurology family like Neurology Neuroimmunology & Neuroinflammation, Neurology Genetics, or Neurology Education.
For other papers that are published in Neurology, not under open access, there is a paywall. For some of them, the paywall comes down after a few months based on funder mandates and so on. As I was mentioning, the NIH-funded papers are available 6 months later.
In the first 6 months, you may have to go to your library, and if your library has a subscription, you can download it directly. [This is also true for] those that always stay behind the paywall, where you have to have a subscription or your library has to have a subscription.
Is Pay to Publish a Red Flag?
Dr. Wilner: I’m a professional writer. With any luck, when I write something, I get paid to write it. There’s been a long tradition in academic medicine that when you submit an article to, say, Neurology, you don’t get paid as an author for the publication. Your reward is the honor of it being published.
Neurology supports itself in various ways, including advertising and so on. That’s been the contract: free publication for work that merits it, and the journal survives on its own.
With open access, one of the things that’s happened is that — and I’ve published open access myself — is that I get a notification that I need to pay to have my article that I’ve slaved over published. Explain that, please.
Dr. Merino: This is the issue with open access. As I mentioned, the paper gets published. You’re giving the journal a license to publish it. You’re retaining the copyright of your work. That means that the journal cannot make money or support itself by just publishing open access because they belong to you.
Typically, open-access journals are not in print and don’t have much in terms of advertising. The contract is you’re giving me a license to publish it, but it’s your journal, so you’re paying a fee for the journal expenses to basically produce your paper. That’s what’s happening with open access.
That’s been recognized with many funders, for example, with NIH funding or many of the European funders, they’re including open-access fees as part of their funding for research. Now, of course, this doesn’t help if you’re not a funded researcher or if you’re a fellow who’s doing work and so on.
Typically, most journals will have waived fees or lower fees for these situations. The reason for the open-access fee is the fact that you’re retaining the copyright. You’re not giving it to the journal who can then use it to generate its revenue for supporting itself, the editorial staff, and so on.
Dr. Wilner: This idea of charging for publication has created a satellite business of what are called predatory journals. How does one know if the open-access journal that I’m submitting to is really just in the business of wanting my $300 or my $900 to get published? How do I know if that’s a reasonable place to publish?
Predatory Journals
Dr. Merino: That’s a big challenge that has come with this whole idea of open access and the fact that now, many journals are online only, so you’re no longer seeing a physical copy. That has given rise to the predatory journals.
The predatory journal, by definition, is a journal that claims to be open access. They’ll take your paper and publish it, but they don’t provide all the other services that you would typically expect from the fact that you’re paying an open-access fee. This includes getting appropriate peer review, production of the manuscript, and long-term curation and storage of the manuscript.
Many predatory journals will take your open-access fee, accept any paper that you submit, regardless of the quality, because they’re charging the fees for that. They don’t send it to real peer review, and then in a few months, the journal disappears so there’s no way for anybody to actually find your paper anymore.
There are certain checklists. Dr. David Moher at the University of Toronto has produced some work trying to help us identify predatory journals.
One thing I typically suggest to people who ask me this question is: Have you ever heard of this journal before? Does the journal have a track record? How far back does the story of the journal go? Is it supported by a publisher that you know? Do you know anybody who has published there? Is it something you can easily access?
If in doubt, always ask your friendly medical librarian. There used to be lists that were kept in terms of predatory journals that were being constantly updated, but those had to be shut down. As far as I understand, there were legal issues in terms of how things got on that list.
I think that overall, if you’ve heard of it, if it’s relevant, if it’s known in your field, and if your librarian knows it, it’s probably a good legitimate open-access journal. There are many very good legitimate open-access journals.
I mentioned the two that we have in our family, but all the other major journals have their own open-access journal within their family. There are some, like BMC or PLOS, that are completely open-access and legitimate journals.
Impact Factor
Dr. Wilner: What about impact factor? Many journals boast about their impact factor. I’m not sure how to interpret that number.
Dr. Merino: Impact factor is very interesting. The impact factor was developed by medical librarians to try to identify the journals they should be subscribing to. It’s a measure of the average citations to an average paper in the journal.
It doesn’t tell you about specific papers. It tells you, on average, how many of the papers in this journal get cited so many times. It’s calculated by the number of articles that were cited divided by the number of articles that were published. Journals that publish many papers, like Neurology, have a hard time bringing up their impact factor beyond a certain level.
Similarly, very small journals with one or two very highly cited papers have a very high impact factor. It’s being used as a measure, perhaps inappropriately, of how good or how reputable a journal is. We all say we don’t care about journal impact factors, but we all know our journal impact factor and we used to know it to three decimals. Now, they changed the system, and there’s only one decimal point, which makes more sense.
This is more important, for example, for authors when deciding where to submit papers. I know that in some countries, particularly in Europe, the impact factor of the journal where you publish has an impact on your promotion decisions.
I would say what’s even more important than the impact factor, is to say, “Well, is this the journal that fits the scope of my paper? Is this the journal that reaches the audience that I want to reach when I write my paper?”
There are some papers, for example, that are very influential. The impact factor just captures citations. There are some papers that are very influential that may not get cited very often. There may be papers that change clinical practice.
If you read a paper that tells you that you should be changing how you treat your patients with myasthenia based on this paper, that may not get cited. It’s a very clinically focused paper, but it’s probably more impactful than one that gets cited very much in some respect, or they make it to public policy decisions, and so on.
I think it’s important to look more at the audience and the journal scope when you submit your papers.
Dr. Wilner: One other technical question. The journals also say they’re indexed in PubMed or Google Scholar. If I want to publish my paper and I want it indexed where the right people are going to find it, where does it need to be indexed?
Dr. Merino: I grew up using Index Medicus, MedlinePlus, and the Library of Science. I still do. If I need to find something, I go to PubMed. Ideally, papers are listed in MedlinePlus or can be found in PubMed. They’re not the same thing, but you can find them through them.
That would be an important thing. Nowadays, a lot more people are using Google Scholar or Google just to identify papers. It may be a little bit less relevant, but it’s still a measure of the quality of the journal before they get indexed in some of these. For example, if you get listed in MedlinePlus, it has gone through certain quality checks by the index itself to see whether they would accept the journal or not. That’s something you want to check.
Typically, most of the large journals or the journals you and I know about are listed in more than one place, right? They’re listed in Scopus and Web of Science. They’re listed in MedlinePlus and so on. Again, if you’re submitting your paper, go somewhere where you know the journal and you’ve heard about it.
Dr. Wilner: I’m not going to ask you about artificial intelligence. We can do that another time. I want to ask something closer to me, which is this question of publish or perish.
There seems to be, in academics, more emphasis on the number of papers that one has published rather than their quality. How does a younger academician or one who really needs to publish cope with that?
Dr. Merino: Many people are writing up research that may not be relevant or that may not be high quality just because you need to have a long list of papers to get promoted, for example, if you’re an academician.
Doug Altman, who was a very influential person in the field quality of not only medical statistics but also medical publishing, had the idea that we need less research, but we need better research.
We often receive papers where you say, well, what’s the rationale behind the question in this paper? It’s like they had a large amount of data and were trying to squeeze as much as they could out of that. I think, as a young academician, the important thing to think about is whether it is an important question that matters to you and to the field, from whatever perspective, whether it’s going to advance research, advance clinical care, or have public policy implications.
Is this one where the answer will be important no matter what the answer is? If you’re thinking of that, your work will be well recognized, people will know you, and you’ll get invited to collaborate. I think that’s the most important thing rather than just churning out a large number of papers.
The productivity will come from the fact that you start by saying, let me ask something that’s really meaningful to me and to the field, with a good question and using strong research methodology.
Dr. Wilner: Thanks for that, Dr. Merino. I think that’s very valuable for all of us. This has been a great discussion. Do you have any final comments before we wrap up?
Dr. Merino: I want to encourage people to continue reading medical journals all the time and submitting to us, again, good research and important questions with robust methodology. That’s what we’re looking for in Neurology and most serious medical journals.
Dr. Wilner is an associate professor of neurology at the University of Tennessee Health Science Center, Memphis. Dr. Merino is a professor in the department of neurology at Georgetown University Medical Center, Washington, DC. Dr. Wilner reported conflicts of interest with Accordant Health Services and Lulu Publishing. Dr. Merino reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Hyperbaric oxygen therapy for traumatic brain injury: Promising or wishful thinking?
A recent review by Hadanny and colleagues recommends hyperbaric oxygen therapy (HBOT) for acute moderate to severe traumatic brain injury (TBI) and selected patients with prolonged postconcussive syndrome.
This article piqued my curiosity because I trained in HBOT more than 20 years ago. As a passionate scuba diver, my motivation was to master treatment for air embolism and decompression illness. Thankfully, these diving accidents are rare. However, I used HBOT for nonhealing wounds, and its efficacy was sometimes remarkable.
Paradoxical results with oxygen therapy
Although it may seem self-evident that “more oxygen is better” for medical illness, this is not necessarily true. I recently interviewed Ola Didrik Saugstad, MD, who demonstrated that the traditional practice of resuscitating newborns with 100% oxygen was more toxic than resuscitation with air (which contains 21% oxygen). His counterintuitive discovery led to a lifesaving change in the international newborn resuscitation guidelines.
The Food and Drug Administration has approved HBOT for a wide variety of conditions, but some practitioners enthusiastically promote it for off-label indications. These include antiaging, autism, multiple sclerosis, and the aforementioned TBI.
More than 50 years ago, HBOT was proposed for stroke, another disorder where the brain has been deprived of oxygen. Despite obvious logic, clinical trials have been unconvincing. The FDA has not approved HBOT for stroke.
HBOT in practice
During HBOT, the patient breathes 100% oxygen while the whole body is pressurized within a hyperbaric chamber. The chamber’s construction allows pressures above normal sea level of 1.0 atmosphere absolute (ATA). For example, The U.S. Navy Treatment Table for decompression sickness recommends 100% oxygen at 2.8 ATA. Chambers may hold one or more patients at a time.
The frequency of therapy varies but often consists of 20-60 sessions lasting 90-120 minutes. For off-label use like TBI, patients usually pay out of pocket. Given the multiple treatments, costs can add up.
Inconsistent evidence and sham controls
The unwieldy 33-page evidence review by Hadanny and colleagues cites multiple studies supporting HBOT for TBI. However, many, if not all, suffer from methodological flaws. These include vague inclusion criteria, lack of a control group, small patient numbers, treatment at different times since injury, poorly defined or varying HBOT protocols, varying outcome measures, and superficial results analysis.
A sham or control arm is essential for HBOT research trials, given the potential placebo effect of placing a human being inside a large, high-tech, sealed tube for an hour or more. In some sham-controlled studies, which consisted of low-pressure oxygen (that is, 1.3 ATA as sham vs. 2.4 ATA as treatment), all groups experienced symptom improvement. The review authors argue that the low-dose HBOT sham arms were biologically active and that the improvements seen mean that both high- and low-dose HBOT is therapeutic. The alternative explanation is that the placebo effect accounted for improvement in both groups.
The late Michael Bennett, a world authority on hyperbaric and underwater medicine, doubted that conventional HBOT sham controls could genuinely have a therapeutic effect, and I agree. The upcoming HOT-POCS trial (discussed below) should answer the question more definitively.
Mechanisms of action and safety
Mechanisms of benefit for HBOT include increased oxygen availability and angiogenesis. Animal research suggests that it may reduce secondary cell death from TBI, through stabilization of the blood-brain barrier and inflammation reduction.
HBOT is generally safe and well tolerated. A retrospective analysis of 1.5 million outpatient hyperbaric treatments revealed that less than 1% were associated with adverse events. The most common were ear and sinus barotrauma. Because HBOT uses increased air pressure, patients must equalize their ears and sinuses. Those who cannot because of altered consciousness, anatomical defects, or congestion must undergo myringotomy or terminate therapy. Claustrophobia was the second most common adverse effect. Convulsions and tension pneumocephalus were rare.
Perhaps the most concerning risk of HBOT for patients with TBI is the potential waste of human and financial resources.
Desperate physicians and patients
As a neurologist who regularly treats patients with TBI, I share the review authors’ frustration regarding the limited efficacy of available treatments. However, the suboptimal efficacy of currently available therapy is insufficient justification to recommend HBOT.
With respect to chronic TBI, it is difficult to imagine how HBOT could reverse brain injury that has been present for months or years. No other therapy exists that reliably encourages neuronal regeneration or prevents the development of posttraumatic epilepsy.
Frank Conidi, MD, a board-certified sports neurologist and headache specialist, shared his thoughts via email. He agrees that HBOT may have a role in TBI, but after reviewing Hadanny and colleagues’ paper, he concluded that there is insufficient evidence for the use of HBOT in all forms of TBI. He would like to see large multicenter, well-designed studies with standardized pressures and duration and a standard definition of the various types of head injury.
Ongoing research
There are at least five ongoing trials on HBOT for TBI or postconcussive syndrome, including the well-designed placebo-controlled HOT-POCS study. The latter has a novel placebo gas system that addresses Hadanny and colleagues’ contention that even low-dose HBOT might be effective.
The placebo arm in HOT-POCS mimics the HBO environment but provides only 0.21 ATA of oxygen, the same as room air. The active arm provides 100% oxygen at 2.0 ATA. If patients in both arms improve, the benefit will be caused by a placebo response, not HBOT.
Conflict of interest
Another concern with the review is that all three authors are affiliated with Aviv Scientific. This company has an exclusive partnership with the world’s largest hyperbaric medicine and research facility, the Sagol Center at Shamir Medical Center in Be’er Ya’akov, Israel.
This conflict of interest does not a priori invalidate their conclusions. However, official HBOT guidelines from a leading organization like the Undersea and Hyperbaric Medicine Society or the American Academy of Neurology would be preferable.
Conclusion
There is an urgent unmet need for more effective treatments for postconcussive syndrome and chronic TBI.
The review authors’ recommendations for HBOT seem premature. They are arguably a disservice to the many desperate patients and their families who will be tempted to expend valuable resources of time and money for an appealing but unproven therapy. Appropriately designed placebo-controlled studies such as HOT-POCS will help separate fact from wishful thinking.
Dr. Wilner is associate professor of neurology at University of Tennessee Health Science Center, Memphis. He reported a conflict of interest with Accordant Health Services.
A version of this article first appeared on Medscape.com.
A recent review by Hadanny and colleagues recommends hyperbaric oxygen therapy (HBOT) for acute moderate to severe traumatic brain injury (TBI) and selected patients with prolonged postconcussive syndrome.
This article piqued my curiosity because I trained in HBOT more than 20 years ago. As a passionate scuba diver, my motivation was to master treatment for air embolism and decompression illness. Thankfully, these diving accidents are rare. However, I used HBOT for nonhealing wounds, and its efficacy was sometimes remarkable.
Paradoxical results with oxygen therapy
Although it may seem self-evident that “more oxygen is better” for medical illness, this is not necessarily true. I recently interviewed Ola Didrik Saugstad, MD, who demonstrated that the traditional practice of resuscitating newborns with 100% oxygen was more toxic than resuscitation with air (which contains 21% oxygen). His counterintuitive discovery led to a lifesaving change in the international newborn resuscitation guidelines.
The Food and Drug Administration has approved HBOT for a wide variety of conditions, but some practitioners enthusiastically promote it for off-label indications. These include antiaging, autism, multiple sclerosis, and the aforementioned TBI.
More than 50 years ago, HBOT was proposed for stroke, another disorder where the brain has been deprived of oxygen. Despite obvious logic, clinical trials have been unconvincing. The FDA has not approved HBOT for stroke.
HBOT in practice
During HBOT, the patient breathes 100% oxygen while the whole body is pressurized within a hyperbaric chamber. The chamber’s construction allows pressures above normal sea level of 1.0 atmosphere absolute (ATA). For example, The U.S. Navy Treatment Table for decompression sickness recommends 100% oxygen at 2.8 ATA. Chambers may hold one or more patients at a time.
The frequency of therapy varies but often consists of 20-60 sessions lasting 90-120 minutes. For off-label use like TBI, patients usually pay out of pocket. Given the multiple treatments, costs can add up.
Inconsistent evidence and sham controls
The unwieldy 33-page evidence review by Hadanny and colleagues cites multiple studies supporting HBOT for TBI. However, many, if not all, suffer from methodological flaws. These include vague inclusion criteria, lack of a control group, small patient numbers, treatment at different times since injury, poorly defined or varying HBOT protocols, varying outcome measures, and superficial results analysis.
A sham or control arm is essential for HBOT research trials, given the potential placebo effect of placing a human being inside a large, high-tech, sealed tube for an hour or more. In some sham-controlled studies, which consisted of low-pressure oxygen (that is, 1.3 ATA as sham vs. 2.4 ATA as treatment), all groups experienced symptom improvement. The review authors argue that the low-dose HBOT sham arms were biologically active and that the improvements seen mean that both high- and low-dose HBOT is therapeutic. The alternative explanation is that the placebo effect accounted for improvement in both groups.
The late Michael Bennett, a world authority on hyperbaric and underwater medicine, doubted that conventional HBOT sham controls could genuinely have a therapeutic effect, and I agree. The upcoming HOT-POCS trial (discussed below) should answer the question more definitively.
Mechanisms of action and safety
Mechanisms of benefit for HBOT include increased oxygen availability and angiogenesis. Animal research suggests that it may reduce secondary cell death from TBI, through stabilization of the blood-brain barrier and inflammation reduction.
HBOT is generally safe and well tolerated. A retrospective analysis of 1.5 million outpatient hyperbaric treatments revealed that less than 1% were associated with adverse events. The most common were ear and sinus barotrauma. Because HBOT uses increased air pressure, patients must equalize their ears and sinuses. Those who cannot because of altered consciousness, anatomical defects, or congestion must undergo myringotomy or terminate therapy. Claustrophobia was the second most common adverse effect. Convulsions and tension pneumocephalus were rare.
Perhaps the most concerning risk of HBOT for patients with TBI is the potential waste of human and financial resources.
Desperate physicians and patients
As a neurologist who regularly treats patients with TBI, I share the review authors’ frustration regarding the limited efficacy of available treatments. However, the suboptimal efficacy of currently available therapy is insufficient justification to recommend HBOT.
With respect to chronic TBI, it is difficult to imagine how HBOT could reverse brain injury that has been present for months or years. No other therapy exists that reliably encourages neuronal regeneration or prevents the development of posttraumatic epilepsy.
Frank Conidi, MD, a board-certified sports neurologist and headache specialist, shared his thoughts via email. He agrees that HBOT may have a role in TBI, but after reviewing Hadanny and colleagues’ paper, he concluded that there is insufficient evidence for the use of HBOT in all forms of TBI. He would like to see large multicenter, well-designed studies with standardized pressures and duration and a standard definition of the various types of head injury.
Ongoing research
There are at least five ongoing trials on HBOT for TBI or postconcussive syndrome, including the well-designed placebo-controlled HOT-POCS study. The latter has a novel placebo gas system that addresses Hadanny and colleagues’ contention that even low-dose HBOT might be effective.
The placebo arm in HOT-POCS mimics the HBO environment but provides only 0.21 ATA of oxygen, the same as room air. The active arm provides 100% oxygen at 2.0 ATA. If patients in both arms improve, the benefit will be caused by a placebo response, not HBOT.
Conflict of interest
Another concern with the review is that all three authors are affiliated with Aviv Scientific. This company has an exclusive partnership with the world’s largest hyperbaric medicine and research facility, the Sagol Center at Shamir Medical Center in Be’er Ya’akov, Israel.
This conflict of interest does not a priori invalidate their conclusions. However, official HBOT guidelines from a leading organization like the Undersea and Hyperbaric Medicine Society or the American Academy of Neurology would be preferable.
Conclusion
There is an urgent unmet need for more effective treatments for postconcussive syndrome and chronic TBI.
The review authors’ recommendations for HBOT seem premature. They are arguably a disservice to the many desperate patients and their families who will be tempted to expend valuable resources of time and money for an appealing but unproven therapy. Appropriately designed placebo-controlled studies such as HOT-POCS will help separate fact from wishful thinking.
Dr. Wilner is associate professor of neurology at University of Tennessee Health Science Center, Memphis. He reported a conflict of interest with Accordant Health Services.
A version of this article first appeared on Medscape.com.
A recent review by Hadanny and colleagues recommends hyperbaric oxygen therapy (HBOT) for acute moderate to severe traumatic brain injury (TBI) and selected patients with prolonged postconcussive syndrome.
This article piqued my curiosity because I trained in HBOT more than 20 years ago. As a passionate scuba diver, my motivation was to master treatment for air embolism and decompression illness. Thankfully, these diving accidents are rare. However, I used HBOT for nonhealing wounds, and its efficacy was sometimes remarkable.
Paradoxical results with oxygen therapy
Although it may seem self-evident that “more oxygen is better” for medical illness, this is not necessarily true. I recently interviewed Ola Didrik Saugstad, MD, who demonstrated that the traditional practice of resuscitating newborns with 100% oxygen was more toxic than resuscitation with air (which contains 21% oxygen). His counterintuitive discovery led to a lifesaving change in the international newborn resuscitation guidelines.
The Food and Drug Administration has approved HBOT for a wide variety of conditions, but some practitioners enthusiastically promote it for off-label indications. These include antiaging, autism, multiple sclerosis, and the aforementioned TBI.
More than 50 years ago, HBOT was proposed for stroke, another disorder where the brain has been deprived of oxygen. Despite obvious logic, clinical trials have been unconvincing. The FDA has not approved HBOT for stroke.
HBOT in practice
During HBOT, the patient breathes 100% oxygen while the whole body is pressurized within a hyperbaric chamber. The chamber’s construction allows pressures above normal sea level of 1.0 atmosphere absolute (ATA). For example, The U.S. Navy Treatment Table for decompression sickness recommends 100% oxygen at 2.8 ATA. Chambers may hold one or more patients at a time.
The frequency of therapy varies but often consists of 20-60 sessions lasting 90-120 minutes. For off-label use like TBI, patients usually pay out of pocket. Given the multiple treatments, costs can add up.
Inconsistent evidence and sham controls
The unwieldy 33-page evidence review by Hadanny and colleagues cites multiple studies supporting HBOT for TBI. However, many, if not all, suffer from methodological flaws. These include vague inclusion criteria, lack of a control group, small patient numbers, treatment at different times since injury, poorly defined or varying HBOT protocols, varying outcome measures, and superficial results analysis.
A sham or control arm is essential for HBOT research trials, given the potential placebo effect of placing a human being inside a large, high-tech, sealed tube for an hour or more. In some sham-controlled studies, which consisted of low-pressure oxygen (that is, 1.3 ATA as sham vs. 2.4 ATA as treatment), all groups experienced symptom improvement. The review authors argue that the low-dose HBOT sham arms were biologically active and that the improvements seen mean that both high- and low-dose HBOT is therapeutic. The alternative explanation is that the placebo effect accounted for improvement in both groups.
The late Michael Bennett, a world authority on hyperbaric and underwater medicine, doubted that conventional HBOT sham controls could genuinely have a therapeutic effect, and I agree. The upcoming HOT-POCS trial (discussed below) should answer the question more definitively.
Mechanisms of action and safety
Mechanisms of benefit for HBOT include increased oxygen availability and angiogenesis. Animal research suggests that it may reduce secondary cell death from TBI, through stabilization of the blood-brain barrier and inflammation reduction.
HBOT is generally safe and well tolerated. A retrospective analysis of 1.5 million outpatient hyperbaric treatments revealed that less than 1% were associated with adverse events. The most common were ear and sinus barotrauma. Because HBOT uses increased air pressure, patients must equalize their ears and sinuses. Those who cannot because of altered consciousness, anatomical defects, or congestion must undergo myringotomy or terminate therapy. Claustrophobia was the second most common adverse effect. Convulsions and tension pneumocephalus were rare.
Perhaps the most concerning risk of HBOT for patients with TBI is the potential waste of human and financial resources.
Desperate physicians and patients
As a neurologist who regularly treats patients with TBI, I share the review authors’ frustration regarding the limited efficacy of available treatments. However, the suboptimal efficacy of currently available therapy is insufficient justification to recommend HBOT.
With respect to chronic TBI, it is difficult to imagine how HBOT could reverse brain injury that has been present for months or years. No other therapy exists that reliably encourages neuronal regeneration or prevents the development of posttraumatic epilepsy.
Frank Conidi, MD, a board-certified sports neurologist and headache specialist, shared his thoughts via email. He agrees that HBOT may have a role in TBI, but after reviewing Hadanny and colleagues’ paper, he concluded that there is insufficient evidence for the use of HBOT in all forms of TBI. He would like to see large multicenter, well-designed studies with standardized pressures and duration and a standard definition of the various types of head injury.
Ongoing research
There are at least five ongoing trials on HBOT for TBI or postconcussive syndrome, including the well-designed placebo-controlled HOT-POCS study. The latter has a novel placebo gas system that addresses Hadanny and colleagues’ contention that even low-dose HBOT might be effective.
The placebo arm in HOT-POCS mimics the HBO environment but provides only 0.21 ATA of oxygen, the same as room air. The active arm provides 100% oxygen at 2.0 ATA. If patients in both arms improve, the benefit will be caused by a placebo response, not HBOT.
Conflict of interest
Another concern with the review is that all three authors are affiliated with Aviv Scientific. This company has an exclusive partnership with the world’s largest hyperbaric medicine and research facility, the Sagol Center at Shamir Medical Center in Be’er Ya’akov, Israel.
This conflict of interest does not a priori invalidate their conclusions. However, official HBOT guidelines from a leading organization like the Undersea and Hyperbaric Medicine Society or the American Academy of Neurology would be preferable.
Conclusion
There is an urgent unmet need for more effective treatments for postconcussive syndrome and chronic TBI.
The review authors’ recommendations for HBOT seem premature. They are arguably a disservice to the many desperate patients and their families who will be tempted to expend valuable resources of time and money for an appealing but unproven therapy. Appropriately designed placebo-controlled studies such as HOT-POCS will help separate fact from wishful thinking.
Dr. Wilner is associate professor of neurology at University of Tennessee Health Science Center, Memphis. He reported a conflict of interest with Accordant Health Services.
A version of this article first appeared on Medscape.com.
New DEA CME mandate affects 2 million prescribers
The Consolidated Appropriations Act of 2023 mandates that all Drug Enforcement Administration–registered physicians and health care providers complete a one-time, 8-hour CME training on managing and treating opioid and other substance abuse disorders. This requirement goes into effect on June 27, 2023. New DEA registrants must also comply. Veterinarians are exempt.
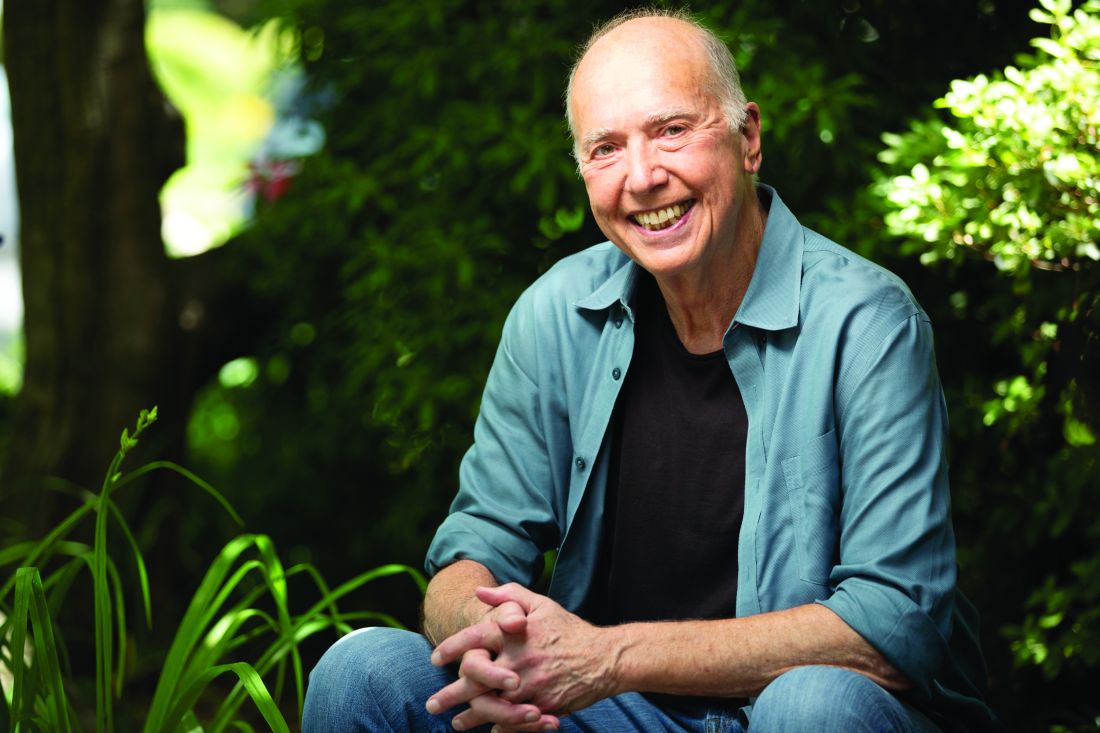
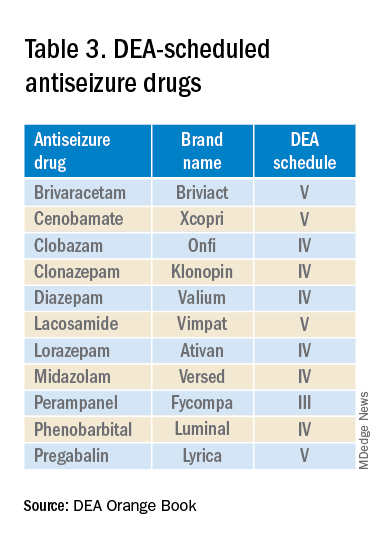
A DEA registration is required to prescribe any controlled substance. The DEA categorizes these as Schedule I-V, with V being the least likely to be abused (Table 1). For example, opioids like fentanyl, oxycodone, and morphine are Schedule II. Medications without abuse potential are not scheduled.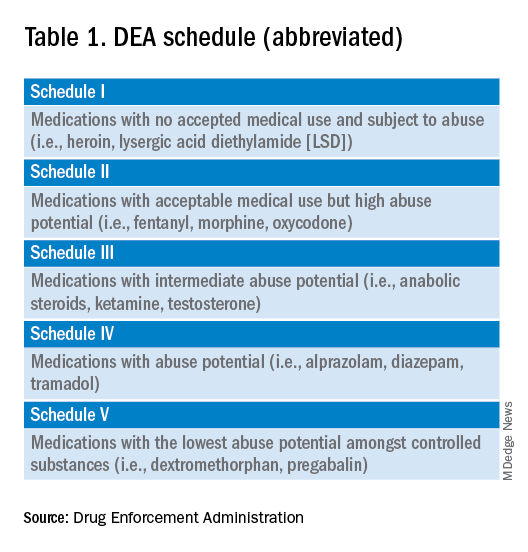
Will 16 million hours of opioid education save lives?
One should not underestimate the sweeping scope of this new federal requirement. DEA registrants include physicians and other health care providers such as nurse practitioners, physician assistants, and dentists. That is 8 hours per provider x 2 million providers: 16 million hours of CME!
Many states already require 1 or more hours of opioid training and pain management as part of their relicensure requirements (Table 2). To avoid redundancy, the DEA-mandated 8-hour training satisfies the various states’ requirements. 
An uncompensated mandate
Physicians are no strangers to lifelong learning and most eagerly pursue educational opportunities. Though some physicians may have CME time and stipends allocated by their employers, many others, such as the approximately 50,000 locum tenens doctors, do not. However, as enthusiastic as these physicians may be about this new CME course, they will likely lose a day of seeing patients (and income) to comply with this new obligation.
Not just pain doctors
The mandate’s broad brush includes many health care providers who hold DEA certificates but do not prescribe opioids. For example, as a general neurologist and epileptologist, I do not treat patients with chronic pain and cannot remember the last time I wrote an opioid prescription. However, I frequently prescribe lacosamide, a Schedule V drug. A surprisingly large number of antiseizure drugs are Schedule III, IV, or V drugs (Table 3).
Real-world abuse?
How often scheduled antiseizure drugs are diverted or abused in an epilepsy population is unknown but appears to be infrequent. For example, perampanel abuse has not been reported despite its classification as a Schedule III drug. Anecdotally, in more than 40 years of clinical practice, I have never known a patient with epilepsy to abuse their antiseizure medications.
Take the course
Many organizations are happy to charge for the new 8-hour course. For example, the Tennessee Medical Association offers the training for $299 online or $400 in person. Materials from Elite Learning satisfy the 8-hour requirement for $80. However, NEJM Knowledge+ provides a complimentary 10-hour DEA-compliant course.
I recently completed the NEJM course. The information was thorough and took the whole 10 hours to finish. As excellent as it was, the content was only tangentially relevant to my clinical practice.
Conclusions
To obtain or renew a DEA certificate, neurologists, epilepsy specialists, and many other health care providers must comply with the new 8-hour CME opioid training mandate. Because the course requires 1 day to complete, health care providers would be prudent to obtain their CME well before their DEA certificate expires.
Though efforts to control the morbidity and mortality of the opioid epidemic are laudatory, perhaps the training should be more targeted to physicians who actually prescribe opioids rather than every DEA registrant. In the meantime, whether 16 million CME hours will save lives remains to be seen.
Dr. Wilner is professor of neurology at the University of Tennessee Health Science Center, Memphis. He reported a conflict of interest with Accordant Health Services.
A version of this article first appeared on Medscape.com.
The Consolidated Appropriations Act of 2023 mandates that all Drug Enforcement Administration–registered physicians and health care providers complete a one-time, 8-hour CME training on managing and treating opioid and other substance abuse disorders. This requirement goes into effect on June 27, 2023. New DEA registrants must also comply. Veterinarians are exempt.
A DEA registration is required to prescribe any controlled substance. The DEA categorizes these as Schedule I-V, with V being the least likely to be abused (Table 1). For example, opioids like fentanyl, oxycodone, and morphine are Schedule II. Medications without abuse potential are not scheduled.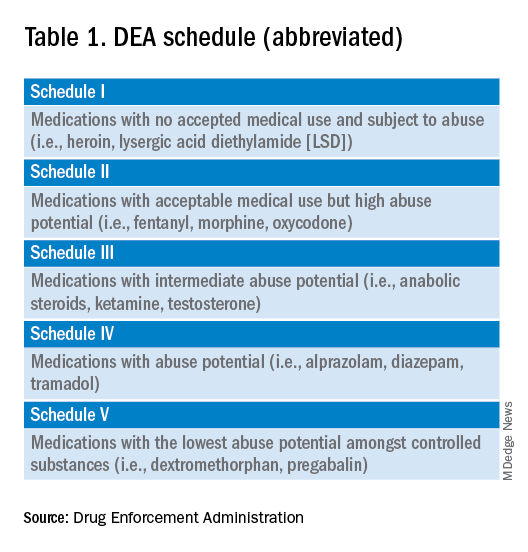
Will 16 million hours of opioid education save lives?
One should not underestimate the sweeping scope of this new federal requirement. DEA registrants include physicians and other health care providers such as nurse practitioners, physician assistants, and dentists. That is 8 hours per provider x 2 million providers: 16 million hours of CME!
Many states already require 1 or more hours of opioid training and pain management as part of their relicensure requirements (Table 2). To avoid redundancy, the DEA-mandated 8-hour training satisfies the various states’ requirements. 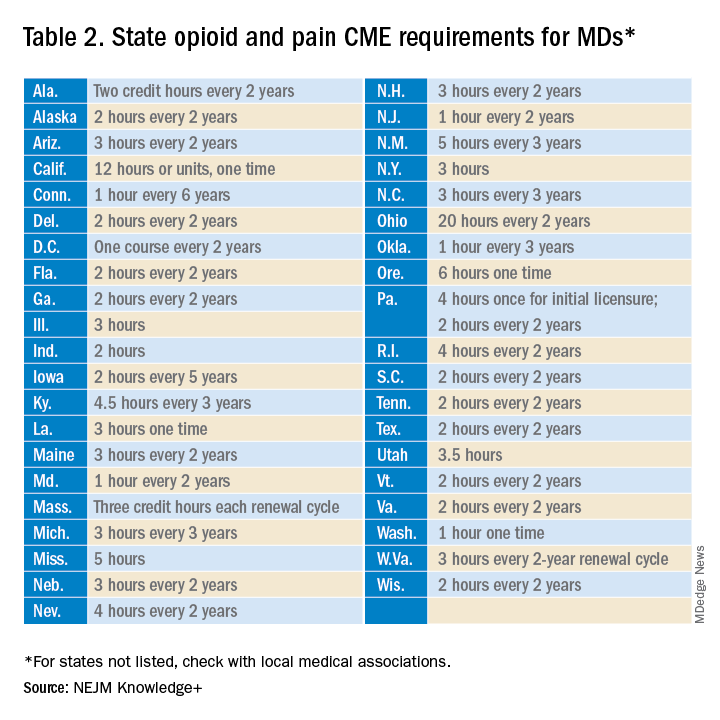
An uncompensated mandate
Physicians are no strangers to lifelong learning and most eagerly pursue educational opportunities. Though some physicians may have CME time and stipends allocated by their employers, many others, such as the approximately 50,000 locum tenens doctors, do not. However, as enthusiastic as these physicians may be about this new CME course, they will likely lose a day of seeing patients (and income) to comply with this new obligation.
Not just pain doctors
The mandate’s broad brush includes many health care providers who hold DEA certificates but do not prescribe opioids. For example, as a general neurologist and epileptologist, I do not treat patients with chronic pain and cannot remember the last time I wrote an opioid prescription. However, I frequently prescribe lacosamide, a Schedule V drug. A surprisingly large number of antiseizure drugs are Schedule III, IV, or V drugs (Table 3).
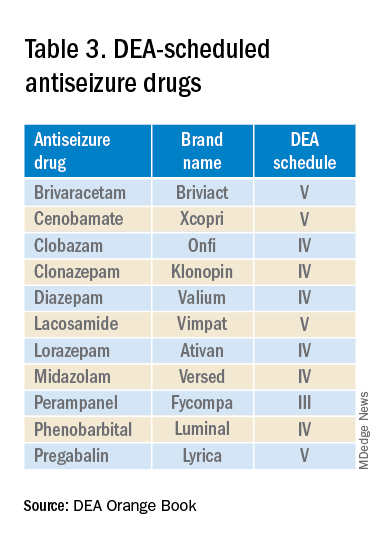
Real-world abuse?
How often scheduled antiseizure drugs are diverted or abused in an epilepsy population is unknown but appears to be infrequent. For example, perampanel abuse has not been reported despite its classification as a Schedule III drug. Anecdotally, in more than 40 years of clinical practice, I have never known a patient with epilepsy to abuse their antiseizure medications.
Take the course
Many organizations are happy to charge for the new 8-hour course. For example, the Tennessee Medical Association offers the training for $299 online or $400 in person. Materials from Elite Learning satisfy the 8-hour requirement for $80. However, NEJM Knowledge+ provides a complimentary 10-hour DEA-compliant course.
I recently completed the NEJM course. The information was thorough and took the whole 10 hours to finish. As excellent as it was, the content was only tangentially relevant to my clinical practice.
Conclusions
To obtain or renew a DEA certificate, neurologists, epilepsy specialists, and many other health care providers must comply with the new 8-hour CME opioid training mandate. Because the course requires 1 day to complete, health care providers would be prudent to obtain their CME well before their DEA certificate expires.
Though efforts to control the morbidity and mortality of the opioid epidemic are laudatory, perhaps the training should be more targeted to physicians who actually prescribe opioids rather than every DEA registrant. In the meantime, whether 16 million CME hours will save lives remains to be seen.
Dr. Wilner is professor of neurology at the University of Tennessee Health Science Center, Memphis. He reported a conflict of interest with Accordant Health Services.
A version of this article first appeared on Medscape.com.
The Consolidated Appropriations Act of 2023 mandates that all Drug Enforcement Administration–registered physicians and health care providers complete a one-time, 8-hour CME training on managing and treating opioid and other substance abuse disorders. This requirement goes into effect on June 27, 2023. New DEA registrants must also comply. Veterinarians are exempt.
A DEA registration is required to prescribe any controlled substance. The DEA categorizes these as Schedule I-V, with V being the least likely to be abused (Table 1). For example, opioids like fentanyl, oxycodone, and morphine are Schedule II. Medications without abuse potential are not scheduled.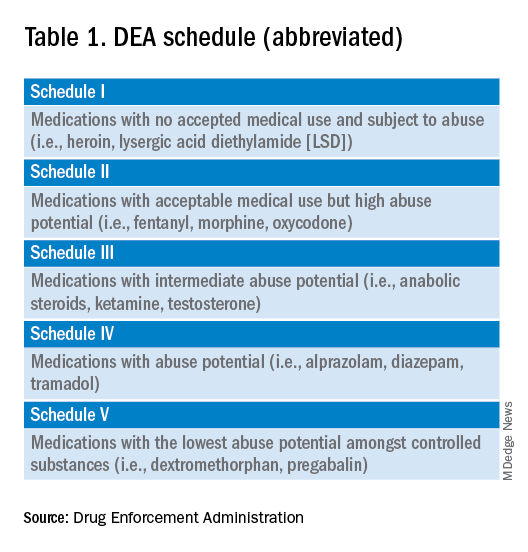
Will 16 million hours of opioid education save lives?
One should not underestimate the sweeping scope of this new federal requirement. DEA registrants include physicians and other health care providers such as nurse practitioners, physician assistants, and dentists. That is 8 hours per provider x 2 million providers: 16 million hours of CME!
Many states already require 1 or more hours of opioid training and pain management as part of their relicensure requirements (Table 2). To avoid redundancy, the DEA-mandated 8-hour training satisfies the various states’ requirements. 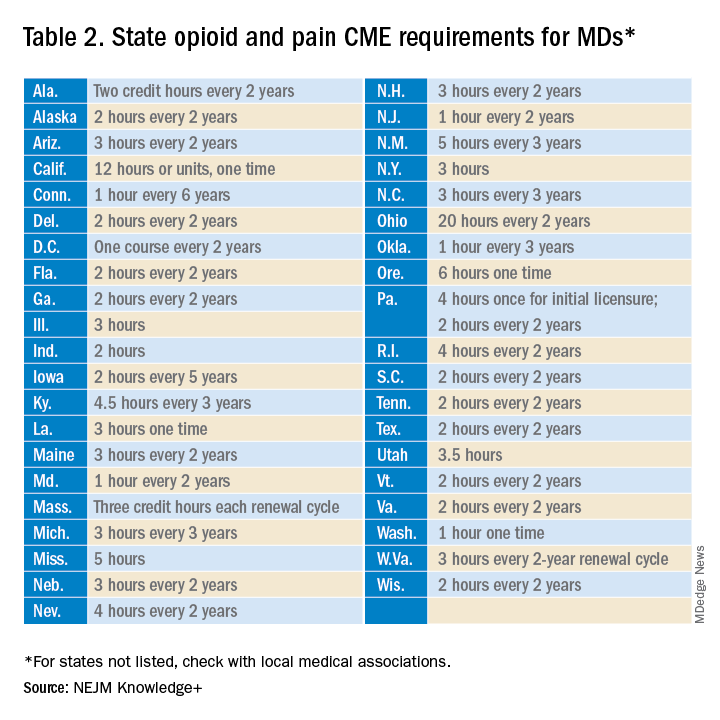
An uncompensated mandate
Physicians are no strangers to lifelong learning and most eagerly pursue educational opportunities. Though some physicians may have CME time and stipends allocated by their employers, many others, such as the approximately 50,000 locum tenens doctors, do not. However, as enthusiastic as these physicians may be about this new CME course, they will likely lose a day of seeing patients (and income) to comply with this new obligation.
Not just pain doctors
The mandate’s broad brush includes many health care providers who hold DEA certificates but do not prescribe opioids. For example, as a general neurologist and epileptologist, I do not treat patients with chronic pain and cannot remember the last time I wrote an opioid prescription. However, I frequently prescribe lacosamide, a Schedule V drug. A surprisingly large number of antiseizure drugs are Schedule III, IV, or V drugs (Table 3).
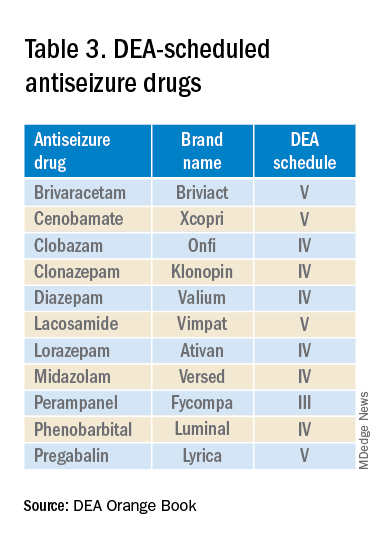
Real-world abuse?
How often scheduled antiseizure drugs are diverted or abused in an epilepsy population is unknown but appears to be infrequent. For example, perampanel abuse has not been reported despite its classification as a Schedule III drug. Anecdotally, in more than 40 years of clinical practice, I have never known a patient with epilepsy to abuse their antiseizure medications.
Take the course
Many organizations are happy to charge for the new 8-hour course. For example, the Tennessee Medical Association offers the training for $299 online or $400 in person. Materials from Elite Learning satisfy the 8-hour requirement for $80. However, NEJM Knowledge+ provides a complimentary 10-hour DEA-compliant course.
I recently completed the NEJM course. The information was thorough and took the whole 10 hours to finish. As excellent as it was, the content was only tangentially relevant to my clinical practice.
Conclusions
To obtain or renew a DEA certificate, neurologists, epilepsy specialists, and many other health care providers must comply with the new 8-hour CME opioid training mandate. Because the course requires 1 day to complete, health care providers would be prudent to obtain their CME well before their DEA certificate expires.
Though efforts to control the morbidity and mortality of the opioid epidemic are laudatory, perhaps the training should be more targeted to physicians who actually prescribe opioids rather than every DEA registrant. In the meantime, whether 16 million CME hours will save lives remains to be seen.
Dr. Wilner is professor of neurology at the University of Tennessee Health Science Center, Memphis. He reported a conflict of interest with Accordant Health Services.
A version of this article first appeared on Medscape.com.
What to expect in the new concussion guidelines
This transcript has been edited for clarity.
Andrew N. Wilner, MD: I’m your host, Dr. Andrew Wilner, reporting virtually from the 2023 American Academy of Neurology meeting in Boston. It’s my pleasure today to speak with Dr. Shae Datta, codirector of the NYU Langone Concussion Center.
She’s also a clinical assistant professor of neurology at NYU School of Medicine. Dr. Datta is chair of the AAN Sports Neurology Section, and she’s leading a panel on concussion at this year’s meeting. She’s going to give us an update. Welcome, Dr. Datta.
Shae Datta, MD: Thank you so much, Andrew. I really love the fact that I’m here speaking to you about all of the new, exciting developments in the field.
Dr. Wilner: Before we get too deep, tell us how you got interested in this topic.
Dr. Datta: I initially thought, when I was in training as a resident, that I wanted to do something like neurocritical care or EEG. It also puzzled me why these seemingly smaller head injuries that didn’t end up in the hospital or ICU were bounced from neurology headache clinic to neuro-ophthalmology headache clinic to neurovestibular headache clinic, and nobody seemed to be able to put together the dots about why they’re having so many different issues — but at the same time, nobody could help them.
At that time, this field was very new. I was on a plane to Paris to a neurocritical care conference as a resident, and I saw the movie Concussion with Will Smith.
It featured one of my current mentors who taught at the fellowship that I graduated from, and it was a fascinating field. I just started looking deeply into it, and I saw that there was a new training fellowship for sports neurology and concussion management, and this is basically why we’re here today.
New concussion consensus guidelines coming
Dr. Wilner: I think this field has really exploded. It used to be that you banged your head, you did a CT scan – remember, I trained about 45 years ago – and if there was nothing on the CT scan, you were done. If you had headaches, you took Tylenol until they went away.
Now, we do MRI, and we realized that it’s really a syndrome. I understand that there are going to be some formal guidelines that have been put together. Is that correct?
Dr. Datta: That’s correct. The 6th International Consensus Conference on Concussion in Sport, in Amsterdam, where I attended and presented a poster, was really a meeting of all the best minds – clinicians and researchers in brain injury – to form a consensus on the newest guidelines that are going to direct our treatment going forward.
Dr. Wilner: I’m going to ask you a trick question because the last time I looked it up I did not get a satisfying answer. What is a concussion?
Dr. Datta: That’s a very good question, and everyone always asks. A concussion is an external force that is emitted upon the head or the neck, or the body, in general, that may cause temporary loss of function. It’s a functional problem.
We don’t see much on CT. We can do MRI. We can do SPECT or we can do these very fancy images, sometimes, of high-velocity head injuries and see small microhemorrhages.
Often, we don’t see anything, but still the patient is loopy. They can’t see straight. They are double-visioned. They have vertigo. Why is that happening? On the cellular level, we have an energy deficit in the sodium-potassium-ATPase pump of the neurons themselves.
Dr. Wilner: Suppose you do see diffuse axonal injury; does that take it out of concussion, or can you have a concussion with visible injury?
Dr. Datta: I think you can have overlap in the symptoms. The diffuse axonal injury would put it into a higher grade of head injury as opposed to a mild traumatic brain injury. Definitely, we would need to work together with our trauma doctors to ensure that patients are not on blood thinners or anything until they heal well enough. Obviously, I would pick them up as an outpatient and follow them until we resolve or rehab them as best as possible.
Concussion assessment tools
Dr. Wilner: There are many sports out there where concussions are fairly frequent, like American football and hockey, for example. Are there any statements in the new guidelines?
Dr. Datta: There are no statements for or against a particular sport because that would really make too much of a bold statement about cause and effect. There is a cause and effect in long-term, repetitive exposure, I would say, in terms of someone being able to play or sustain injury.
Right now, at least at the concussion conference I went to and in the upcoming consensus statement, they will not comment on a specific sport. Obviously, we know that the higher-impact sports are a little more dangerous.
Let’s be honest. At the high school, middle school, or even younger level, some kids are not necessarily the most athletic, right? They play because their friends are playing. If they’re repeatedly getting injured, it’s time for an astute clinician, or a coach, and a whole team to assess them to see if maybe this person is just going to continue to get hurt if they’re not taken out of the game and perhaps they should go to a lower-impact sport.
Dr. Wilner: In schools, often there’s a big size and weight difference. There are 14-year-olds who are 6 fett 2 inches and 200 pounds, and there are 14-year-olds who are 5 feet 2 inches and 110 pounds. Obviously, they’re mismatched on the football field.
You mentioned coaches. Is there anything in the guidelines about training coaches?
Dr. Datta: Specifically, there was nothing in the guidelines about that. There’s a tool for coaches at every level to use, which is called the Sports Concussion Assessment Tool, or SCAT, which is going to be updated to the SCAT6. At the NCAA level, they must receive annual training on concussion management and be given an NCAA concussion handout for coaches.
Obviously, there are more rigorous protocols for national-level coaching. As it stands now, it is not mandatory, but they are given tools to assess someone once they’ve gotten a hit to take them out of the game.
Dr. Wilner: I’ve been following the concussion research through the years. They did some neuropsychological testing on athletes who’ve had this many concussions or that many concussions, and they would find deficits here or subtle deficits there, but they had no baseline.
Then, there was a movement to start testing athletes before the season starts so that they could do a repeat test after concussion and see if there is any difference. Is that something we’re recommending?
Dr. Datta: Most of the time, NCAA-level – certainly where I trained – and national-level sports do testing, but it’s not everywhere. Prior guidelines have indicated that preseason testing is not required. That is largely because there has been no standardized neuropsychological testing established.
There are computerized testing options where the validity and reliability are questionable. Also, let’s say it’s a college student; they didn’t sleep all night and then they took this computer test. They would probably do worse than they would if they had received a head hit.
Just to be on the safe side, most places that have collegiate-level sports that are at a high level do preseason testing. If I were to speak personally, aside from the guidelines, I would say that it’s been helpful for me to look at the before and after, in general, overall, to make a decision about my treatment protocol.
Dr. Wilner: Let’s talk about the patient. You have a 20-year-old guy. He’s playing football. There’s a big play. Bonk, he gets hit on the head. He’s on the ground. He’s dazed, staggers a little bit, gets up, and you ask how he is feeling. He says he’s fine and then he wobbles off to the sideline. What do you do with that kid?
Dr. Datta: Obviously, the first thing is to remove him from the play environment to a quiet space. Second, either an athletic trainer or a coach would administer basic screening neurologic tests, such as “where are you, what’s today’s date, what is your name?” and other orientation questions.
They’ll also go through the SCAT – that’ll be SCAT6 starting in July – the SCAT5 symptom questionnaire to see what symptoms they have. Often, they’re using sideline testing software.
There are two things that can be used on a card to test eye movements, to see if they’re slower. They come out of NYU, coincidentally – the Memory Image Completion (MIC) and the Mobile Universal Lexicon Evaluation System (MULES) – and are used to determine whether eye movements are slower. That way, you can tell whether someone is, compared with before they got their head hit, slower than before.
Based on this composite information, usually the teammates and the head people on the team will know if a player looks different.
They need to be taken out, obviously, if there is nausea or vomiting, any neurologic signs and symptoms, or a neck injury that needs to be stabilized. ABCs first, right? If there’s any vomiting or seizures, they should be taken to the ER right away.
The first thing is to take them out, then do a sideline assessment. Third, see if they need to immediately go to the ED versus follow-up outpatient with me within a day or two.
Dr. Wilner: I think it’s the subtle injuries that are the tough ones. Back to our 20-year-old. He says: “Oh, I’m fine. I want to go back in the game.” Everybody can tell he’s not quite right, even though he passed all the tests. What do you do then?
Dr. Datta: You have to make a judgment call for the safety of the player. They always want to go back, right? This is also an issue when they’re competing for college scholarships and things of that nature. Sometimes they’re sandbagging, where they memorize the answers.
Everything’s on the Internet nowadays, right? We have to make a judgment call as members of the healthcare community and the sports community to keep that player safe.
Just keep them out. Don’t bring them back in the game. Keep them out for a reasonable amount of time. There’s a test called the Buffalo Concussion Treadmill Test; Dr. John Leddy from University of Buffalo has developed a way for us to put athletes through a screening protocol.
This can be part of their vestibular and ocular rehabilitation, where if they don’t have symptoms when we bring their heart rate to certain levels, then we can slowly clear them for return to play as long as they’re nonsymptomatic.
Dr. Wilner: I spoke with your colleague, Dr. Riggins, who is also on your panel, and we were talking about when they can go back. She said they can go back when they don’t have any symptoms. No more headache, no more dizziness, no more lightheadedness, no more trouble concentrating or with memory – all those things have gone away.
Sometimes these symptoms are stubborn. If you have, say, 100 patients like our 20-year-old who got bonked on the head, has some headaches, and doesn’t feel quite right, what usually happens? How many are back to play the next day, the next week, or the next month? How many are out for the season? How does that play out?
Dr. Datta: It depends on a couple of different factors. One, have they had previous head injuries? Two, do they have preexisting symptoms or signs, or diagnoses like migraines, which are likely to get worse after a head injury? Anything that’s preexisting, like a mood disorder, anxiety, depression, or trouble sleeping, is going to get worse.
If they were compensating for untreated ADD or borderline personality or bipolar, I’ve seen many people who’ve developed them. These are not the norm, but I’m saying that you have to be very careful.
Getting back to the question, you treat them. Reasonably, if they’re healthy and they don’t have preexisting signs and symptoms, I would say more than half are back in about 2 weeks.. I would say 60%-70%. It all depends. If they have preexisting issues, then it’s going to take much longer.
From SCAT to SCOAT
Dr. Wilner: This has been very informative. Before we wrap up, tell us what to expect from these guidelines in July. How are they really going to help?
Dr. Datta: We’ve been using the SCAT, which was meant for more sideline assessment because that’s all we had, and it’s worked perfectly well.
This will be better because we often see them within 24-48 hours, when the symptoms are sometimes a little bit better.
We also will see the sport and concussion group come up with added athlete perspectives, ethics discussion, power-sport athlete considerations, and development of this new SCOAT.
Dr. Wilner: Dr. Datta, this is very exciting. I look forward to reading these guidelines in July. I want to thank you for your hard work. I also look forward to talking to you at next year’s meeting. Thank you very much for giving us this update.
Dr. Datta: No problem. It’s my pleasure.
A version of this article originally appeared on Medscape.com.
This transcript has been edited for clarity.
Andrew N. Wilner, MD: I’m your host, Dr. Andrew Wilner, reporting virtually from the 2023 American Academy of Neurology meeting in Boston. It’s my pleasure today to speak with Dr. Shae Datta, codirector of the NYU Langone Concussion Center.
She’s also a clinical assistant professor of neurology at NYU School of Medicine. Dr. Datta is chair of the AAN Sports Neurology Section, and she’s leading a panel on concussion at this year’s meeting. She’s going to give us an update. Welcome, Dr. Datta.
Shae Datta, MD: Thank you so much, Andrew. I really love the fact that I’m here speaking to you about all of the new, exciting developments in the field.
Dr. Wilner: Before we get too deep, tell us how you got interested in this topic.
Dr. Datta: I initially thought, when I was in training as a resident, that I wanted to do something like neurocritical care or EEG. It also puzzled me why these seemingly smaller head injuries that didn’t end up in the hospital or ICU were bounced from neurology headache clinic to neuro-ophthalmology headache clinic to neurovestibular headache clinic, and nobody seemed to be able to put together the dots about why they’re having so many different issues — but at the same time, nobody could help them.
At that time, this field was very new. I was on a plane to Paris to a neurocritical care conference as a resident, and I saw the movie Concussion with Will Smith.
It featured one of my current mentors who taught at the fellowship that I graduated from, and it was a fascinating field. I just started looking deeply into it, and I saw that there was a new training fellowship for sports neurology and concussion management, and this is basically why we’re here today.
New concussion consensus guidelines coming
Dr. Wilner: I think this field has really exploded. It used to be that you banged your head, you did a CT scan – remember, I trained about 45 years ago – and if there was nothing on the CT scan, you were done. If you had headaches, you took Tylenol until they went away.
Now, we do MRI, and we realized that it’s really a syndrome. I understand that there are going to be some formal guidelines that have been put together. Is that correct?
Dr. Datta: That’s correct. The 6th International Consensus Conference on Concussion in Sport, in Amsterdam, where I attended and presented a poster, was really a meeting of all the best minds – clinicians and researchers in brain injury – to form a consensus on the newest guidelines that are going to direct our treatment going forward.
Dr. Wilner: I’m going to ask you a trick question because the last time I looked it up I did not get a satisfying answer. What is a concussion?
Dr. Datta: That’s a very good question, and everyone always asks. A concussion is an external force that is emitted upon the head or the neck, or the body, in general, that may cause temporary loss of function. It’s a functional problem.
We don’t see much on CT. We can do MRI. We can do SPECT or we can do these very fancy images, sometimes, of high-velocity head injuries and see small microhemorrhages.
Often, we don’t see anything, but still the patient is loopy. They can’t see straight. They are double-visioned. They have vertigo. Why is that happening? On the cellular level, we have an energy deficit in the sodium-potassium-ATPase pump of the neurons themselves.
Dr. Wilner: Suppose you do see diffuse axonal injury; does that take it out of concussion, or can you have a concussion with visible injury?
Dr. Datta: I think you can have overlap in the symptoms. The diffuse axonal injury would put it into a higher grade of head injury as opposed to a mild traumatic brain injury. Definitely, we would need to work together with our trauma doctors to ensure that patients are not on blood thinners or anything until they heal well enough. Obviously, I would pick them up as an outpatient and follow them until we resolve or rehab them as best as possible.
Concussion assessment tools
Dr. Wilner: There are many sports out there where concussions are fairly frequent, like American football and hockey, for example. Are there any statements in the new guidelines?
Dr. Datta: There are no statements for or against a particular sport because that would really make too much of a bold statement about cause and effect. There is a cause and effect in long-term, repetitive exposure, I would say, in terms of someone being able to play or sustain injury.
Right now, at least at the concussion conference I went to and in the upcoming consensus statement, they will not comment on a specific sport. Obviously, we know that the higher-impact sports are a little more dangerous.
Let’s be honest. At the high school, middle school, or even younger level, some kids are not necessarily the most athletic, right? They play because their friends are playing. If they’re repeatedly getting injured, it’s time for an astute clinician, or a coach, and a whole team to assess them to see if maybe this person is just going to continue to get hurt if they’re not taken out of the game and perhaps they should go to a lower-impact sport.
Dr. Wilner: In schools, often there’s a big size and weight difference. There are 14-year-olds who are 6 fett 2 inches and 200 pounds, and there are 14-year-olds who are 5 feet 2 inches and 110 pounds. Obviously, they’re mismatched on the football field.
You mentioned coaches. Is there anything in the guidelines about training coaches?
Dr. Datta: Specifically, there was nothing in the guidelines about that. There’s a tool for coaches at every level to use, which is called the Sports Concussion Assessment Tool, or SCAT, which is going to be updated to the SCAT6. At the NCAA level, they must receive annual training on concussion management and be given an NCAA concussion handout for coaches.
Obviously, there are more rigorous protocols for national-level coaching. As it stands now, it is not mandatory, but they are given tools to assess someone once they’ve gotten a hit to take them out of the game.
Dr. Wilner: I’ve been following the concussion research through the years. They did some neuropsychological testing on athletes who’ve had this many concussions or that many concussions, and they would find deficits here or subtle deficits there, but they had no baseline.
Then, there was a movement to start testing athletes before the season starts so that they could do a repeat test after concussion and see if there is any difference. Is that something we’re recommending?
Dr. Datta: Most of the time, NCAA-level – certainly where I trained – and national-level sports do testing, but it’s not everywhere. Prior guidelines have indicated that preseason testing is not required. That is largely because there has been no standardized neuropsychological testing established.
There are computerized testing options where the validity and reliability are questionable. Also, let’s say it’s a college student; they didn’t sleep all night and then they took this computer test. They would probably do worse than they would if they had received a head hit.
Just to be on the safe side, most places that have collegiate-level sports that are at a high level do preseason testing. If I were to speak personally, aside from the guidelines, I would say that it’s been helpful for me to look at the before and after, in general, overall, to make a decision about my treatment protocol.
Dr. Wilner: Let’s talk about the patient. You have a 20-year-old guy. He’s playing football. There’s a big play. Bonk, he gets hit on the head. He’s on the ground. He’s dazed, staggers a little bit, gets up, and you ask how he is feeling. He says he’s fine and then he wobbles off to the sideline. What do you do with that kid?
Dr. Datta: Obviously, the first thing is to remove him from the play environment to a quiet space. Second, either an athletic trainer or a coach would administer basic screening neurologic tests, such as “where are you, what’s today’s date, what is your name?” and other orientation questions.
They’ll also go through the SCAT – that’ll be SCAT6 starting in July – the SCAT5 symptom questionnaire to see what symptoms they have. Often, they’re using sideline testing software.
There are two things that can be used on a card to test eye movements, to see if they’re slower. They come out of NYU, coincidentally – the Memory Image Completion (MIC) and the Mobile Universal Lexicon Evaluation System (MULES) – and are used to determine whether eye movements are slower. That way, you can tell whether someone is, compared with before they got their head hit, slower than before.
Based on this composite information, usually the teammates and the head people on the team will know if a player looks different.
They need to be taken out, obviously, if there is nausea or vomiting, any neurologic signs and symptoms, or a neck injury that needs to be stabilized. ABCs first, right? If there’s any vomiting or seizures, they should be taken to the ER right away.
The first thing is to take them out, then do a sideline assessment. Third, see if they need to immediately go to the ED versus follow-up outpatient with me within a day or two.
Dr. Wilner: I think it’s the subtle injuries that are the tough ones. Back to our 20-year-old. He says: “Oh, I’m fine. I want to go back in the game.” Everybody can tell he’s not quite right, even though he passed all the tests. What do you do then?
Dr. Datta: You have to make a judgment call for the safety of the player. They always want to go back, right? This is also an issue when they’re competing for college scholarships and things of that nature. Sometimes they’re sandbagging, where they memorize the answers.
Everything’s on the Internet nowadays, right? We have to make a judgment call as members of the healthcare community and the sports community to keep that player safe.
Just keep them out. Don’t bring them back in the game. Keep them out for a reasonable amount of time. There’s a test called the Buffalo Concussion Treadmill Test; Dr. John Leddy from University of Buffalo has developed a way for us to put athletes through a screening protocol.
This can be part of their vestibular and ocular rehabilitation, where if they don’t have symptoms when we bring their heart rate to certain levels, then we can slowly clear them for return to play as long as they’re nonsymptomatic.
Dr. Wilner: I spoke with your colleague, Dr. Riggins, who is also on your panel, and we were talking about when they can go back. She said they can go back when they don’t have any symptoms. No more headache, no more dizziness, no more lightheadedness, no more trouble concentrating or with memory – all those things have gone away.
Sometimes these symptoms are stubborn. If you have, say, 100 patients like our 20-year-old who got bonked on the head, has some headaches, and doesn’t feel quite right, what usually happens? How many are back to play the next day, the next week, or the next month? How many are out for the season? How does that play out?
Dr. Datta: It depends on a couple of different factors. One, have they had previous head injuries? Two, do they have preexisting symptoms or signs, or diagnoses like migraines, which are likely to get worse after a head injury? Anything that’s preexisting, like a mood disorder, anxiety, depression, or trouble sleeping, is going to get worse.
If they were compensating for untreated ADD or borderline personality or bipolar, I’ve seen many people who’ve developed them. These are not the norm, but I’m saying that you have to be very careful.
Getting back to the question, you treat them. Reasonably, if they’re healthy and they don’t have preexisting signs and symptoms, I would say more than half are back in about 2 weeks.. I would say 60%-70%. It all depends. If they have preexisting issues, then it’s going to take much longer.
From SCAT to SCOAT
Dr. Wilner: This has been very informative. Before we wrap up, tell us what to expect from these guidelines in July. How are they really going to help?
Dr. Datta: We’ve been using the SCAT, which was meant for more sideline assessment because that’s all we had, and it’s worked perfectly well.
This will be better because we often see them within 24-48 hours, when the symptoms are sometimes a little bit better.
We also will see the sport and concussion group come up with added athlete perspectives, ethics discussion, power-sport athlete considerations, and development of this new SCOAT.
Dr. Wilner: Dr. Datta, this is very exciting. I look forward to reading these guidelines in July. I want to thank you for your hard work. I also look forward to talking to you at next year’s meeting. Thank you very much for giving us this update.
Dr. Datta: No problem. It’s my pleasure.
A version of this article originally appeared on Medscape.com.
This transcript has been edited for clarity.
Andrew N. Wilner, MD: I’m your host, Dr. Andrew Wilner, reporting virtually from the 2023 American Academy of Neurology meeting in Boston. It’s my pleasure today to speak with Dr. Shae Datta, codirector of the NYU Langone Concussion Center.
She’s also a clinical assistant professor of neurology at NYU School of Medicine. Dr. Datta is chair of the AAN Sports Neurology Section, and she’s leading a panel on concussion at this year’s meeting. She’s going to give us an update. Welcome, Dr. Datta.
Shae Datta, MD: Thank you so much, Andrew. I really love the fact that I’m here speaking to you about all of the new, exciting developments in the field.
Dr. Wilner: Before we get too deep, tell us how you got interested in this topic.
Dr. Datta: I initially thought, when I was in training as a resident, that I wanted to do something like neurocritical care or EEG. It also puzzled me why these seemingly smaller head injuries that didn’t end up in the hospital or ICU were bounced from neurology headache clinic to neuro-ophthalmology headache clinic to neurovestibular headache clinic, and nobody seemed to be able to put together the dots about why they’re having so many different issues — but at the same time, nobody could help them.
At that time, this field was very new. I was on a plane to Paris to a neurocritical care conference as a resident, and I saw the movie Concussion with Will Smith.
It featured one of my current mentors who taught at the fellowship that I graduated from, and it was a fascinating field. I just started looking deeply into it, and I saw that there was a new training fellowship for sports neurology and concussion management, and this is basically why we’re here today.
New concussion consensus guidelines coming
Dr. Wilner: I think this field has really exploded. It used to be that you banged your head, you did a CT scan – remember, I trained about 45 years ago – and if there was nothing on the CT scan, you were done. If you had headaches, you took Tylenol until they went away.
Now, we do MRI, and we realized that it’s really a syndrome. I understand that there are going to be some formal guidelines that have been put together. Is that correct?
Dr. Datta: That’s correct. The 6th International Consensus Conference on Concussion in Sport, in Amsterdam, where I attended and presented a poster, was really a meeting of all the best minds – clinicians and researchers in brain injury – to form a consensus on the newest guidelines that are going to direct our treatment going forward.
Dr. Wilner: I’m going to ask you a trick question because the last time I looked it up I did not get a satisfying answer. What is a concussion?
Dr. Datta: That’s a very good question, and everyone always asks. A concussion is an external force that is emitted upon the head or the neck, or the body, in general, that may cause temporary loss of function. It’s a functional problem.
We don’t see much on CT. We can do MRI. We can do SPECT or we can do these very fancy images, sometimes, of high-velocity head injuries and see small microhemorrhages.
Often, we don’t see anything, but still the patient is loopy. They can’t see straight. They are double-visioned. They have vertigo. Why is that happening? On the cellular level, we have an energy deficit in the sodium-potassium-ATPase pump of the neurons themselves.
Dr. Wilner: Suppose you do see diffuse axonal injury; does that take it out of concussion, or can you have a concussion with visible injury?
Dr. Datta: I think you can have overlap in the symptoms. The diffuse axonal injury would put it into a higher grade of head injury as opposed to a mild traumatic brain injury. Definitely, we would need to work together with our trauma doctors to ensure that patients are not on blood thinners or anything until they heal well enough. Obviously, I would pick them up as an outpatient and follow them until we resolve or rehab them as best as possible.
Concussion assessment tools
Dr. Wilner: There are many sports out there where concussions are fairly frequent, like American football and hockey, for example. Are there any statements in the new guidelines?
Dr. Datta: There are no statements for or against a particular sport because that would really make too much of a bold statement about cause and effect. There is a cause and effect in long-term, repetitive exposure, I would say, in terms of someone being able to play or sustain injury.
Right now, at least at the concussion conference I went to and in the upcoming consensus statement, they will not comment on a specific sport. Obviously, we know that the higher-impact sports are a little more dangerous.
Let’s be honest. At the high school, middle school, or even younger level, some kids are not necessarily the most athletic, right? They play because their friends are playing. If they’re repeatedly getting injured, it’s time for an astute clinician, or a coach, and a whole team to assess them to see if maybe this person is just going to continue to get hurt if they’re not taken out of the game and perhaps they should go to a lower-impact sport.
Dr. Wilner: In schools, often there’s a big size and weight difference. There are 14-year-olds who are 6 fett 2 inches and 200 pounds, and there are 14-year-olds who are 5 feet 2 inches and 110 pounds. Obviously, they’re mismatched on the football field.
You mentioned coaches. Is there anything in the guidelines about training coaches?
Dr. Datta: Specifically, there was nothing in the guidelines about that. There’s a tool for coaches at every level to use, which is called the Sports Concussion Assessment Tool, or SCAT, which is going to be updated to the SCAT6. At the NCAA level, they must receive annual training on concussion management and be given an NCAA concussion handout for coaches.
Obviously, there are more rigorous protocols for national-level coaching. As it stands now, it is not mandatory, but they are given tools to assess someone once they’ve gotten a hit to take them out of the game.
Dr. Wilner: I’ve been following the concussion research through the years. They did some neuropsychological testing on athletes who’ve had this many concussions or that many concussions, and they would find deficits here or subtle deficits there, but they had no baseline.
Then, there was a movement to start testing athletes before the season starts so that they could do a repeat test after concussion and see if there is any difference. Is that something we’re recommending?
Dr. Datta: Most of the time, NCAA-level – certainly where I trained – and national-level sports do testing, but it’s not everywhere. Prior guidelines have indicated that preseason testing is not required. That is largely because there has been no standardized neuropsychological testing established.
There are computerized testing options where the validity and reliability are questionable. Also, let’s say it’s a college student; they didn’t sleep all night and then they took this computer test. They would probably do worse than they would if they had received a head hit.
Just to be on the safe side, most places that have collegiate-level sports that are at a high level do preseason testing. If I were to speak personally, aside from the guidelines, I would say that it’s been helpful for me to look at the before and after, in general, overall, to make a decision about my treatment protocol.
Dr. Wilner: Let’s talk about the patient. You have a 20-year-old guy. He’s playing football. There’s a big play. Bonk, he gets hit on the head. He’s on the ground. He’s dazed, staggers a little bit, gets up, and you ask how he is feeling. He says he’s fine and then he wobbles off to the sideline. What do you do with that kid?
Dr. Datta: Obviously, the first thing is to remove him from the play environment to a quiet space. Second, either an athletic trainer or a coach would administer basic screening neurologic tests, such as “where are you, what’s today’s date, what is your name?” and other orientation questions.
They’ll also go through the SCAT – that’ll be SCAT6 starting in July – the SCAT5 symptom questionnaire to see what symptoms they have. Often, they’re using sideline testing software.
There are two things that can be used on a card to test eye movements, to see if they’re slower. They come out of NYU, coincidentally – the Memory Image Completion (MIC) and the Mobile Universal Lexicon Evaluation System (MULES) – and are used to determine whether eye movements are slower. That way, you can tell whether someone is, compared with before they got their head hit, slower than before.
Based on this composite information, usually the teammates and the head people on the team will know if a player looks different.
They need to be taken out, obviously, if there is nausea or vomiting, any neurologic signs and symptoms, or a neck injury that needs to be stabilized. ABCs first, right? If there’s any vomiting or seizures, they should be taken to the ER right away.
The first thing is to take them out, then do a sideline assessment. Third, see if they need to immediately go to the ED versus follow-up outpatient with me within a day or two.
Dr. Wilner: I think it’s the subtle injuries that are the tough ones. Back to our 20-year-old. He says: “Oh, I’m fine. I want to go back in the game.” Everybody can tell he’s not quite right, even though he passed all the tests. What do you do then?
Dr. Datta: You have to make a judgment call for the safety of the player. They always want to go back, right? This is also an issue when they’re competing for college scholarships and things of that nature. Sometimes they’re sandbagging, where they memorize the answers.
Everything’s on the Internet nowadays, right? We have to make a judgment call as members of the healthcare community and the sports community to keep that player safe.
Just keep them out. Don’t bring them back in the game. Keep them out for a reasonable amount of time. There’s a test called the Buffalo Concussion Treadmill Test; Dr. John Leddy from University of Buffalo has developed a way for us to put athletes through a screening protocol.
This can be part of their vestibular and ocular rehabilitation, where if they don’t have symptoms when we bring their heart rate to certain levels, then we can slowly clear them for return to play as long as they’re nonsymptomatic.
Dr. Wilner: I spoke with your colleague, Dr. Riggins, who is also on your panel, and we were talking about when they can go back. She said they can go back when they don’t have any symptoms. No more headache, no more dizziness, no more lightheadedness, no more trouble concentrating or with memory – all those things have gone away.
Sometimes these symptoms are stubborn. If you have, say, 100 patients like our 20-year-old who got bonked on the head, has some headaches, and doesn’t feel quite right, what usually happens? How many are back to play the next day, the next week, or the next month? How many are out for the season? How does that play out?
Dr. Datta: It depends on a couple of different factors. One, have they had previous head injuries? Two, do they have preexisting symptoms or signs, or diagnoses like migraines, which are likely to get worse after a head injury? Anything that’s preexisting, like a mood disorder, anxiety, depression, or trouble sleeping, is going to get worse.
If they were compensating for untreated ADD or borderline personality or bipolar, I’ve seen many people who’ve developed them. These are not the norm, but I’m saying that you have to be very careful.
Getting back to the question, you treat them. Reasonably, if they’re healthy and they don’t have preexisting signs and symptoms, I would say more than half are back in about 2 weeks.. I would say 60%-70%. It all depends. If they have preexisting issues, then it’s going to take much longer.
From SCAT to SCOAT
Dr. Wilner: This has been very informative. Before we wrap up, tell us what to expect from these guidelines in July. How are they really going to help?
Dr. Datta: We’ve been using the SCAT, which was meant for more sideline assessment because that’s all we had, and it’s worked perfectly well.
This will be better because we often see them within 24-48 hours, when the symptoms are sometimes a little bit better.
We also will see the sport and concussion group come up with added athlete perspectives, ethics discussion, power-sport athlete considerations, and development of this new SCOAT.
Dr. Wilner: Dr. Datta, this is very exciting. I look forward to reading these guidelines in July. I want to thank you for your hard work. I also look forward to talking to you at next year’s meeting. Thank you very much for giving us this update.
Dr. Datta: No problem. It’s my pleasure.
A version of this article originally appeared on Medscape.com.
Smartphone diagnosis in infant seizures could be highly effective
This video transcript has been edited for clarity.
Andrew N. Wilner, MD: Welcome to Medscape. I’m Dr Andrew Wilner, reporting from the American Epilepsy Society meeting.
Today, I have the pleasure of speaking with Dr. Chethan Rao, a child and adolescent neurology resident from the Mayo Clinic in Jacksonville, Fla. Dr. Rao has a particular interest in pediatric epilepsy. Welcome, Dr. Rao.
Chethan Rao, DO: Thank you, Dr. Wilner. It’s a pleasure to be here, and thanks for taking the time to highlight our work.
Dr. Wilner: You had a very interesting paper at the meeting that I wanted to talk about, focused on infantile spasms and smartphone video. Before we dive into the paper, tell us: What are infantile spasms, and why is it important to diagnose them early?
Dr. Rao: Infantile spasms, also known as epileptic spasms, are 1- to 2-second seizures, and they typically consist of sudden stiffening of the body with brief bending forward or backward of the arms, legs, and head. They usually happen around age 3-8 months, and they typically occur in clusters, most often after awakening from sleep.
The incidence is about 1 in 2,000-3,000 children. Many kids with spasms go on to develop seizures that are very difficult to treat, like Lennox-Gastaut epilepsy, and many go on to have developmental delays as well.
Dr. Wilner: Are these subtle? In other words, could a parent have a child like that and not really recognize that this is something abnormal? Or are they so dramatic that parents say: “We’re going to the emergency room?”
Dr. Rao: One of the problems that we encounter often is that in this age group of infants, they have benign sleep myoclonus; they have Sandifer syndrome related to reflux. Those can be very difficult mimics of spasms. They’re not the most clear-cut, but they look usually different enough from normal baby movements that they get parents to seek medical attention.
Dr. Wilner: You mentioned that the infantile spasms really are a type of epilepsy and symptomatic, usually, of some underlying neurologic condition. Why is it so important to diagnose them early?
Dr. Rao: Great question. Many studies have looked at developmental outcomes based on when spasms were diagnosed and treated, and all of them have replicated time over time that the earlier you get to treatment for the spasms, the better the outcomes are for seizure control and for development.
For this reason, infantile spasm is considered a neurologic urgency in our world. Like I said, accurate diagnosis is often complicated by these potential mimics. Prompt EEG is one of the most important things for confirmation of diagnosis.
Dr. Wilner: But to get that EEG, it has to get all the way to the neurologist, right? It’s not something they’re going to do in the ER. I saw a statistic: There are millions, if not billions, of smartphones out there. Where does the smartphone come in?
Dr. Rao: Absolutely. One of the things that we have on our side these days is that almost everyone has a smartphone at their disposal. One of the recent polls in 2021 showed that more than 95% of adults of childbearing age have smartphones with video access. As some other studies have shown in the adult world, we all really have an epilepsy monitoring unit minus the EEG in our own pockets.
It’s definitely a useful tool, as that first screening video can be used in adjunct to history and physical. There have been many of studies on the adult epilepsy side showing the predictive value of smartphone video for differentiating things like epileptic seizures and nonepileptic spells. What we wanted to do is use smartphone video to pin the diagnosis early of infantile spasms and get it treated as quickly as possible.
Dr. Wilner: I’m a fan. Every now and then, I do have a patient who brings in a video of some spell. I’m an adult neurologist. The patient had a spell, and you ask them – of course they don’t remember – and you ask the witness, who usually is not a trained observer. There have been one or two occasions where I thought: “Well, I don’t know if that was really a seizure.” Then they show me the video and it’s like, “Wow, that is definitely a convulsion.” A picture definitely can be worth a thousand words.
You studied this systematically for your poster. Tell me about what you did.
Dr. Rao: Since the poster, we’ve actually expanded the study, so I’ll give you the updated version. We looked at 101 infants retrospectively at two large children’s health care centers: Nemours Children’s, associated with Mayo Clinic in Jacksonville, Fla., and Texas Children’s Hospital in Houston. We narrowed it down to 80 patients whom we included. Of these, 43 had smartphone video capture when they first presented and 37 had no video when they first presented.
We found a 17-day difference by median in the time to diagnosis and treatment. In other words, the video group was diagnosed and treated 17 days by median, compared with the no-video group. Although 17 days may not sound like a big number, in this context it can make a huge difference. That’s been shown by one of these key studies in our field called the UK Infantile Spasms Study. The 2-week difference made about a 10-point difference on the developmental scale that they use – so pretty significant.
Dr. Wilner: Let me think about this for a minute. Was that because the parents brought the child in with their video and the doctor said, “Hey, that’s infantile spasms. Here’s your shot of ACTH [or whatever they’re using these days].” Or was it because the parents who were attentive enough to use video brought their kids in sooner?
Or was this the time from when they brought the child in to treatment? Is that the time you looked at? So it wasn’t just that these were more attentive parents and more likely to use the video – you’re looking at the time from presentation with or without video until treatment, is that right?
Dr. Rao: We looked to the time from the start of the spasms, as reported by the parents, to the time of diagnosis and then the start of spasms to the time of treatment. What you asked was a fantastic question. We wanted to know who these parents are who are taking videos versus the ones that are not.
We looked at the race/ethnicity data and socioeconomic status data. There were no significant differences between the video and nonvideo group. That would not explain the difference in our results here.
Dr. Wilner: Do you have plans to follow these approximately 40 children 5 years from now and see who’s riding a bicycle and who’s still stuck in the stroller? Is there going to be a difference?
Dr. Rao: Because time to diagnosis and time to treatment were our primary outcomes, long-term follow-up may not really help as much in this study. We did have a couple of other ideas for future studies. One that we wanted to look at was kids who have risk factors for developing spasms, such as trisomy 21, tuberous sclerosis, and congenital cortical malformations; those kids are at a much higher risk for developing spasms around 3-8 months of life.
In giving targeted counseling to those families about how they can use smartphone video to minimize the time to diagnosis and treatment, we think we may be able to learn more and maybe do that prospectively.
The other interesting idea is using artificial intelligence technology for spasm detection in some of these smartphone videos. They’re already using it for different seizure types. It could be an efficient first pass when we get a whole bunch of smartphone videos to determine which ones we need to pursue further steps – to see whether we need to get long-term EEG monitoring or not.
Dr. Wilner: As an epileptologist, I was going to say that we have smartphone EKG. All we need now is smartphone EEG, and then you’ll have all the information you need on day one. It may be a ways away.
As a bottom line, would it be fair to say that parents should not hesitate to take a video of any suspiciously abnormal behavior and bring it to their family doctor or pediatric neurologist?
Dr. Rao: Yes. I was happy to see the Tuberous Sclerosis Alliance put out a promotional video that had some steps for when parents see things that are suspicious for spasms, and they do recommend using smartphone video and promptly showing it to their doctors. I think the difference that we hope to provide in this study is that we can now quantify the effect of having that smartphone video when they first present.
My takeaway from this study that I would like to show is encouraging the use of smartphone video as an adjunct tool and for providers to ask for the videos, but also for these pediatric centers to develop an infrastructure – either a secure, monitored email address like we have at our center or a patient portal – where parents can submit video concerning for spasms.
Dr. Wilner: Save the trip to the doctor. Get that video out there first.
Dr. Rao: Especially in the pandemic world, right?
Dr. Wilner: Yes. I understand that you are a neurology resident. To wrap up, what’s the next step for you?
Dr. Rao: I’m finishing up my child neurology residency this year, and I’m moving out to Stanford for pediatric epilepsy fellowship. We’re preparing this project we’re talking about for submission soon, and we’re working on another project, which is a systematic review of genetic testing and the presurgical workup for pediatric drug-resistant focal epilepsy.
Dr. Wilner: Excellent. That’s pretty exciting. Good luck to you. I want to thank you very much for telling us about your research.
Dr. Rao: It was a pleasure speaking with you, and I look forward to the next time.
Dr. Wilner: I’m Dr Andrew Wilner, reporting for Medscape. Thanks for watching.
A version of this article first appeared on Medscape.com.
This video transcript has been edited for clarity.
Andrew N. Wilner, MD: Welcome to Medscape. I’m Dr Andrew Wilner, reporting from the American Epilepsy Society meeting.
Today, I have the pleasure of speaking with Dr. Chethan Rao, a child and adolescent neurology resident from the Mayo Clinic in Jacksonville, Fla. Dr. Rao has a particular interest in pediatric epilepsy. Welcome, Dr. Rao.
Chethan Rao, DO: Thank you, Dr. Wilner. It’s a pleasure to be here, and thanks for taking the time to highlight our work.
Dr. Wilner: You had a very interesting paper at the meeting that I wanted to talk about, focused on infantile spasms and smartphone video. Before we dive into the paper, tell us: What are infantile spasms, and why is it important to diagnose them early?
Dr. Rao: Infantile spasms, also known as epileptic spasms, are 1- to 2-second seizures, and they typically consist of sudden stiffening of the body with brief bending forward or backward of the arms, legs, and head. They usually happen around age 3-8 months, and they typically occur in clusters, most often after awakening from sleep.
The incidence is about 1 in 2,000-3,000 children. Many kids with spasms go on to develop seizures that are very difficult to treat, like Lennox-Gastaut epilepsy, and many go on to have developmental delays as well.
Dr. Wilner: Are these subtle? In other words, could a parent have a child like that and not really recognize that this is something abnormal? Or are they so dramatic that parents say: “We’re going to the emergency room?”
Dr. Rao: One of the problems that we encounter often is that in this age group of infants, they have benign sleep myoclonus; they have Sandifer syndrome related to reflux. Those can be very difficult mimics of spasms. They’re not the most clear-cut, but they look usually different enough from normal baby movements that they get parents to seek medical attention.
Dr. Wilner: You mentioned that the infantile spasms really are a type of epilepsy and symptomatic, usually, of some underlying neurologic condition. Why is it so important to diagnose them early?
Dr. Rao: Great question. Many studies have looked at developmental outcomes based on when spasms were diagnosed and treated, and all of them have replicated time over time that the earlier you get to treatment for the spasms, the better the outcomes are for seizure control and for development.
For this reason, infantile spasm is considered a neurologic urgency in our world. Like I said, accurate diagnosis is often complicated by these potential mimics. Prompt EEG is one of the most important things for confirmation of diagnosis.
Dr. Wilner: But to get that EEG, it has to get all the way to the neurologist, right? It’s not something they’re going to do in the ER. I saw a statistic: There are millions, if not billions, of smartphones out there. Where does the smartphone come in?
Dr. Rao: Absolutely. One of the things that we have on our side these days is that almost everyone has a smartphone at their disposal. One of the recent polls in 2021 showed that more than 95% of adults of childbearing age have smartphones with video access. As some other studies have shown in the adult world, we all really have an epilepsy monitoring unit minus the EEG in our own pockets.
It’s definitely a useful tool, as that first screening video can be used in adjunct to history and physical. There have been many of studies on the adult epilepsy side showing the predictive value of smartphone video for differentiating things like epileptic seizures and nonepileptic spells. What we wanted to do is use smartphone video to pin the diagnosis early of infantile spasms and get it treated as quickly as possible.
Dr. Wilner: I’m a fan. Every now and then, I do have a patient who brings in a video of some spell. I’m an adult neurologist. The patient had a spell, and you ask them – of course they don’t remember – and you ask the witness, who usually is not a trained observer. There have been one or two occasions where I thought: “Well, I don’t know if that was really a seizure.” Then they show me the video and it’s like, “Wow, that is definitely a convulsion.” A picture definitely can be worth a thousand words.
You studied this systematically for your poster. Tell me about what you did.
Dr. Rao: Since the poster, we’ve actually expanded the study, so I’ll give you the updated version. We looked at 101 infants retrospectively at two large children’s health care centers: Nemours Children’s, associated with Mayo Clinic in Jacksonville, Fla., and Texas Children’s Hospital in Houston. We narrowed it down to 80 patients whom we included. Of these, 43 had smartphone video capture when they first presented and 37 had no video when they first presented.
We found a 17-day difference by median in the time to diagnosis and treatment. In other words, the video group was diagnosed and treated 17 days by median, compared with the no-video group. Although 17 days may not sound like a big number, in this context it can make a huge difference. That’s been shown by one of these key studies in our field called the UK Infantile Spasms Study. The 2-week difference made about a 10-point difference on the developmental scale that they use – so pretty significant.
Dr. Wilner: Let me think about this for a minute. Was that because the parents brought the child in with their video and the doctor said, “Hey, that’s infantile spasms. Here’s your shot of ACTH [or whatever they’re using these days].” Or was it because the parents who were attentive enough to use video brought their kids in sooner?
Or was this the time from when they brought the child in to treatment? Is that the time you looked at? So it wasn’t just that these were more attentive parents and more likely to use the video – you’re looking at the time from presentation with or without video until treatment, is that right?
Dr. Rao: We looked to the time from the start of the spasms, as reported by the parents, to the time of diagnosis and then the start of spasms to the time of treatment. What you asked was a fantastic question. We wanted to know who these parents are who are taking videos versus the ones that are not.
We looked at the race/ethnicity data and socioeconomic status data. There were no significant differences between the video and nonvideo group. That would not explain the difference in our results here.
Dr. Wilner: Do you have plans to follow these approximately 40 children 5 years from now and see who’s riding a bicycle and who’s still stuck in the stroller? Is there going to be a difference?
Dr. Rao: Because time to diagnosis and time to treatment were our primary outcomes, long-term follow-up may not really help as much in this study. We did have a couple of other ideas for future studies. One that we wanted to look at was kids who have risk factors for developing spasms, such as trisomy 21, tuberous sclerosis, and congenital cortical malformations; those kids are at a much higher risk for developing spasms around 3-8 months of life.
In giving targeted counseling to those families about how they can use smartphone video to minimize the time to diagnosis and treatment, we think we may be able to learn more and maybe do that prospectively.
The other interesting idea is using artificial intelligence technology for spasm detection in some of these smartphone videos. They’re already using it for different seizure types. It could be an efficient first pass when we get a whole bunch of smartphone videos to determine which ones we need to pursue further steps – to see whether we need to get long-term EEG monitoring or not.
Dr. Wilner: As an epileptologist, I was going to say that we have smartphone EKG. All we need now is smartphone EEG, and then you’ll have all the information you need on day one. It may be a ways away.
As a bottom line, would it be fair to say that parents should not hesitate to take a video of any suspiciously abnormal behavior and bring it to their family doctor or pediatric neurologist?
Dr. Rao: Yes. I was happy to see the Tuberous Sclerosis Alliance put out a promotional video that had some steps for when parents see things that are suspicious for spasms, and they do recommend using smartphone video and promptly showing it to their doctors. I think the difference that we hope to provide in this study is that we can now quantify the effect of having that smartphone video when they first present.
My takeaway from this study that I would like to show is encouraging the use of smartphone video as an adjunct tool and for providers to ask for the videos, but also for these pediatric centers to develop an infrastructure – either a secure, monitored email address like we have at our center or a patient portal – where parents can submit video concerning for spasms.
Dr. Wilner: Save the trip to the doctor. Get that video out there first.
Dr. Rao: Especially in the pandemic world, right?
Dr. Wilner: Yes. I understand that you are a neurology resident. To wrap up, what’s the next step for you?
Dr. Rao: I’m finishing up my child neurology residency this year, and I’m moving out to Stanford for pediatric epilepsy fellowship. We’re preparing this project we’re talking about for submission soon, and we’re working on another project, which is a systematic review of genetic testing and the presurgical workup for pediatric drug-resistant focal epilepsy.
Dr. Wilner: Excellent. That’s pretty exciting. Good luck to you. I want to thank you very much for telling us about your research.
Dr. Rao: It was a pleasure speaking with you, and I look forward to the next time.
Dr. Wilner: I’m Dr Andrew Wilner, reporting for Medscape. Thanks for watching.
A version of this article first appeared on Medscape.com.
This video transcript has been edited for clarity.
Andrew N. Wilner, MD: Welcome to Medscape. I’m Dr Andrew Wilner, reporting from the American Epilepsy Society meeting.
Today, I have the pleasure of speaking with Dr. Chethan Rao, a child and adolescent neurology resident from the Mayo Clinic in Jacksonville, Fla. Dr. Rao has a particular interest in pediatric epilepsy. Welcome, Dr. Rao.
Chethan Rao, DO: Thank you, Dr. Wilner. It’s a pleasure to be here, and thanks for taking the time to highlight our work.
Dr. Wilner: You had a very interesting paper at the meeting that I wanted to talk about, focused on infantile spasms and smartphone video. Before we dive into the paper, tell us: What are infantile spasms, and why is it important to diagnose them early?
Dr. Rao: Infantile spasms, also known as epileptic spasms, are 1- to 2-second seizures, and they typically consist of sudden stiffening of the body with brief bending forward or backward of the arms, legs, and head. They usually happen around age 3-8 months, and they typically occur in clusters, most often after awakening from sleep.
The incidence is about 1 in 2,000-3,000 children. Many kids with spasms go on to develop seizures that are very difficult to treat, like Lennox-Gastaut epilepsy, and many go on to have developmental delays as well.
Dr. Wilner: Are these subtle? In other words, could a parent have a child like that and not really recognize that this is something abnormal? Or are they so dramatic that parents say: “We’re going to the emergency room?”
Dr. Rao: One of the problems that we encounter often is that in this age group of infants, they have benign sleep myoclonus; they have Sandifer syndrome related to reflux. Those can be very difficult mimics of spasms. They’re not the most clear-cut, but they look usually different enough from normal baby movements that they get parents to seek medical attention.
Dr. Wilner: You mentioned that the infantile spasms really are a type of epilepsy and symptomatic, usually, of some underlying neurologic condition. Why is it so important to diagnose them early?
Dr. Rao: Great question. Many studies have looked at developmental outcomes based on when spasms were diagnosed and treated, and all of them have replicated time over time that the earlier you get to treatment for the spasms, the better the outcomes are for seizure control and for development.
For this reason, infantile spasm is considered a neurologic urgency in our world. Like I said, accurate diagnosis is often complicated by these potential mimics. Prompt EEG is one of the most important things for confirmation of diagnosis.
Dr. Wilner: But to get that EEG, it has to get all the way to the neurologist, right? It’s not something they’re going to do in the ER. I saw a statistic: There are millions, if not billions, of smartphones out there. Where does the smartphone come in?
Dr. Rao: Absolutely. One of the things that we have on our side these days is that almost everyone has a smartphone at their disposal. One of the recent polls in 2021 showed that more than 95% of adults of childbearing age have smartphones with video access. As some other studies have shown in the adult world, we all really have an epilepsy monitoring unit minus the EEG in our own pockets.
It’s definitely a useful tool, as that first screening video can be used in adjunct to history and physical. There have been many of studies on the adult epilepsy side showing the predictive value of smartphone video for differentiating things like epileptic seizures and nonepileptic spells. What we wanted to do is use smartphone video to pin the diagnosis early of infantile spasms and get it treated as quickly as possible.
Dr. Wilner: I’m a fan. Every now and then, I do have a patient who brings in a video of some spell. I’m an adult neurologist. The patient had a spell, and you ask them – of course they don’t remember – and you ask the witness, who usually is not a trained observer. There have been one or two occasions where I thought: “Well, I don’t know if that was really a seizure.” Then they show me the video and it’s like, “Wow, that is definitely a convulsion.” A picture definitely can be worth a thousand words.
You studied this systematically for your poster. Tell me about what you did.
Dr. Rao: Since the poster, we’ve actually expanded the study, so I’ll give you the updated version. We looked at 101 infants retrospectively at two large children’s health care centers: Nemours Children’s, associated with Mayo Clinic in Jacksonville, Fla., and Texas Children’s Hospital in Houston. We narrowed it down to 80 patients whom we included. Of these, 43 had smartphone video capture when they first presented and 37 had no video when they first presented.
We found a 17-day difference by median in the time to diagnosis and treatment. In other words, the video group was diagnosed and treated 17 days by median, compared with the no-video group. Although 17 days may not sound like a big number, in this context it can make a huge difference. That’s been shown by one of these key studies in our field called the UK Infantile Spasms Study. The 2-week difference made about a 10-point difference on the developmental scale that they use – so pretty significant.
Dr. Wilner: Let me think about this for a minute. Was that because the parents brought the child in with their video and the doctor said, “Hey, that’s infantile spasms. Here’s your shot of ACTH [or whatever they’re using these days].” Or was it because the parents who were attentive enough to use video brought their kids in sooner?
Or was this the time from when they brought the child in to treatment? Is that the time you looked at? So it wasn’t just that these were more attentive parents and more likely to use the video – you’re looking at the time from presentation with or without video until treatment, is that right?
Dr. Rao: We looked to the time from the start of the spasms, as reported by the parents, to the time of diagnosis and then the start of spasms to the time of treatment. What you asked was a fantastic question. We wanted to know who these parents are who are taking videos versus the ones that are not.
We looked at the race/ethnicity data and socioeconomic status data. There were no significant differences between the video and nonvideo group. That would not explain the difference in our results here.
Dr. Wilner: Do you have plans to follow these approximately 40 children 5 years from now and see who’s riding a bicycle and who’s still stuck in the stroller? Is there going to be a difference?
Dr. Rao: Because time to diagnosis and time to treatment were our primary outcomes, long-term follow-up may not really help as much in this study. We did have a couple of other ideas for future studies. One that we wanted to look at was kids who have risk factors for developing spasms, such as trisomy 21, tuberous sclerosis, and congenital cortical malformations; those kids are at a much higher risk for developing spasms around 3-8 months of life.
In giving targeted counseling to those families about how they can use smartphone video to minimize the time to diagnosis and treatment, we think we may be able to learn more and maybe do that prospectively.
The other interesting idea is using artificial intelligence technology for spasm detection in some of these smartphone videos. They’re already using it for different seizure types. It could be an efficient first pass when we get a whole bunch of smartphone videos to determine which ones we need to pursue further steps – to see whether we need to get long-term EEG monitoring or not.
Dr. Wilner: As an epileptologist, I was going to say that we have smartphone EKG. All we need now is smartphone EEG, and then you’ll have all the information you need on day one. It may be a ways away.
As a bottom line, would it be fair to say that parents should not hesitate to take a video of any suspiciously abnormal behavior and bring it to their family doctor or pediatric neurologist?
Dr. Rao: Yes. I was happy to see the Tuberous Sclerosis Alliance put out a promotional video that had some steps for when parents see things that are suspicious for spasms, and they do recommend using smartphone video and promptly showing it to their doctors. I think the difference that we hope to provide in this study is that we can now quantify the effect of having that smartphone video when they first present.
My takeaway from this study that I would like to show is encouraging the use of smartphone video as an adjunct tool and for providers to ask for the videos, but also for these pediatric centers to develop an infrastructure – either a secure, monitored email address like we have at our center or a patient portal – where parents can submit video concerning for spasms.
Dr. Wilner: Save the trip to the doctor. Get that video out there first.
Dr. Rao: Especially in the pandemic world, right?
Dr. Wilner: Yes. I understand that you are a neurology resident. To wrap up, what’s the next step for you?
Dr. Rao: I’m finishing up my child neurology residency this year, and I’m moving out to Stanford for pediatric epilepsy fellowship. We’re preparing this project we’re talking about for submission soon, and we’re working on another project, which is a systematic review of genetic testing and the presurgical workup for pediatric drug-resistant focal epilepsy.
Dr. Wilner: Excellent. That’s pretty exciting. Good luck to you. I want to thank you very much for telling us about your research.
Dr. Rao: It was a pleasure speaking with you, and I look forward to the next time.
Dr. Wilner: I’m Dr Andrew Wilner, reporting for Medscape. Thanks for watching.
A version of this article first appeared on Medscape.com.
Meditations in an emergency: Talking through pandemic anxiety with a pioneer of mind-body medicine
Andrew N. Wilner, MD: Welcome to Medscape. I’m Dr Andrew Wilner. Today I have a special guest, Dr James Gordon, founder and executive director of the Center for Mind-Body Medicine. Welcome, Dr Gordon.
James S. Gordon, MD: Thank you very much. It’s good to be with you.
Dr. Wilner: Thanks for joining us. We are recording this in late May 2020, in the midst of the coronavirus pandemic. Millions of people have been infected. Hundreds of thousands have died. Millions have lost their jobs. I think it’s fair to say that people are under a greater degree of stress than they’re normally accustomed to. Would you agree with that?
Dr. Gordon: I think it’s more than fair to say that everybody in the United States, and actually pretty much everyone in the world, is under extreme stress. And that compounds any stresses that they’ve experienced before in their lives. Everyone is affected.
Dr. Wilner: The mind-body medicine concept is one that you’ve pursued for decades. Tell us a little bit about the Center for Mind-Body Medicine and how that’s led to the program that you have to help us deal with the coronavirus.
Dr. Gordon: I started the Center for Mind-Body Medicine about 30 years ago. I’d been a researcher at the National Institute of Mental Health for a number of years, in private practice, and a professor at Georgetown Medical School. But I wanted to really focus on how to change and enrich medicine by making self-care, self-awareness, and group support central to all healthcare.
Western medicine is enormously powerful in certain situations, such as physical trauma, high levels of infection, congenital anomalies. But we’re not so good at working with chronic physical or psychological problems. Those are much more complex.
We’ve been discovering that what is going to make the long-term difference in conditions like type 2 diabetes, pain syndromes, hypertension, depression, and anxiety are those approaches that we can learn to do for ourselves. These are changes we can make in how we deal with stress, eat, exercise, relate to other people, and whether we find meaning and purpose in our lives.
by wars, climate-related disasters, the opioid epidemic, chronic poverty, historical trauma. We do a lot of work with indigenous people here in North America. We’ve worked in a number of communities where school shootings have traumatized everyone.
What we’ve learned over these past 25 years, and what interested me professionally as well as personally over the past 50 years, is what we’re now bringing out on an even larger scale. The kind of approaches that we’ve developed, studied, and published research on are exactly what everyone needs to include and incorporate in their daily life, as well as in their medical and health care, from now on.
Dr. Wilner: Do you have a program that’s specifically for health care providers?
Dr. Gordon: Yes. The Center for Mind-Body Medicine is primarily an educational organization rather than a service organization. Since the beginning, I’ve been focused on training health professionals. My first passion was for training physicians – I’m a physician, so there’s a feeling of fellowship there – but also health care workers and mental health professionals of every kind.
We teach health professionals a whole system, a comprehensive program of techniques of self-awareness and self-care. We teach them so that they can practice on themselves and study the underlying science, so they can then teach what they’ve learned to the patients or clients they work with. They integrate it into what they’re already doing, regardless of their specialty. At times we also offer some of the same kinds of mind-body skills groups that are the fundamental part of our training as a stand-alone intervention. You can’t really teach other people how to take care of themselves unless you’re also doing it yourself. Otherwise, it’s just a theory.
Dr. Wilner: As a neurologist, I’m interested in the mind-body system. You are a psychiatrist and understand that it’s a lot more difficult to objectify certain things. What is stress? What is happiness? What is sadness? It’s very hard to measure. You can have scales, but it requires insight on the part of the individual. So I think it’s certainly an ambitious project.
Dr. Gordon: You’re absolutely right. It requires insight. And one of the shortcomings of our medical education is that it doesn’t encourage us to look inside ourselves enough. There’s so much focus on objectivity and on data, that we’ve lost some of the subjective art of medicine.
My experience with myself, as well as with the thousands of people we’ve trained here in the United States and around the world and the many hundreds of thousands with whom they’ve worked, is that all of us have a greater capacity to understand and help ourselves than we ordinarily think or than most of us learn about in our medical education.
This work is saying to people to take a little bit of time and relax a little in order to allow yourself to come into a meditative state. And I don’t mean anything fancy by that. Meditation is just being relaxed. Moment-to-moment awareness doesn’t have to do with any particular religion or spiritual practice. It’s part of all of them. If you can get into that state, then you can begin to say, “Oh, that’s what’s going on with me. That’s why my pain is worse.”
For example, you often wonder in people with peripheral neuropathy why it becomes worse or better at certain points. I would encourage neurologists and other physicians to ask your patients, “Why do you think it’s worse?” They may say, “I don’t know, doc; that’s why I’m here.” But I would ask them to take a couple of minutes to let me know. They could think it has something to do with the fact that they had a big fight with their wife that morning, they don’t want to go to work, or whatever it is. This is part of the lost art that we need to bring back into medicine for ourselves and especially for our patients.
Dr. Wilner: Can you give me an example of some of the exercises you’d do in a class?
Dr. Gordon: All of the exercises and our entire program that we teach at the Center for Mind-Body Medicine is in this new book of mine, “The Transformation: Discovering Wholeness and Healing After Trauma.” It’s really the distillation of not just the past 25 or 30 years, but really 50 years of work.
The techniques are all pretty simple and, as we say, evidence based. There is evidence that shows how they work on us physiologically, as well as psychologically. And they’re all pretty easy to teach to anyone.
Myself and about 60 or 70 of our faculty at the Center for Mind-Body Medicine are currently leading online groups. Then several hundred of the other people we’ve trained are also leading these groups. We’re still counting it up, but we probably have between 700 and 1,000 groups going around the world, led by our faculty and by people we’ve trained.
We teach a different technique every week in these online groups. Last week, after getting people energized and focused, we did a written dialogue with an emotion. You put down the initial of your name – in my case, “J” for Jim – and create a dialogue with an emotion, such as sadness. I would write it as fast as I can.
I would say, “OK, Sadness. Why are you here? What are you doing? I don’t enjoy having you around.” And Sadness writes back to me, “But you need me.” And J says, “What do you mean I need you?” And Sadness says, “Well, your brother died 7 weeks ago, didn’t he?” And I say, “Yes, he did.” And Sadness says, “Aren’t you sad?” I say, “Yes. I’m terribly sad and grieving all the time. But I wasn’t thinking about him at this moment.” And Sadness says, “But he’s there with you all the time and that sadness is in you.” And I say, “You mean it’s in me even here, now, as I’m talking with Andrew in this interview?” And Sadness says, “Yes. You can talk about your work. But in between the words, as you take a breath, don’t you feel it in your chest?” That’s the way the dialogue goes.
Dr. Wilner: What about specifically with the coronavirus? Fear is certainly an emotion. Nobody wants to get sick and die. Nobody wants to bring this disease home to their family. People are reluctant to even go outside and you can’t shake someone’s hand. Are there precedents for this?
Dr. Gordon: There are precedents, but only relatively small groups were affected before by, for example, severe acute respiratory syndrome or H1N1, at least in the United States. But we haven’t seen a global pandemic like this since 1918. None of us was around then – or I certainly wasn’t around. So for most everyone, not only has it not happened before, but we’ve never been so globally aware of everything that’s going on and how different groups are reacting.
I’ve been reading Daniel Defoe’s book, “A Journal of the Plague Year.” It’s really very interesting. It’s about the bubonic plague in 1665 London, although he wrote it in the 1720s. Some of the same things were going on then: the enormous fear, the isolation; rich people being able to escape, poor people having nowhere to go; conspiracy theories of one kind or another, about where the plague came from or blaming a group of people for it; magical thinking that it’s just going to go away. All of those things that happened several hundred years ago are going on now.
And we’re all simultaneously aware of all those things. There’s not only the fear, which should be universal because it’s a reasonable response to this situation, but also the terrible confusion about what to do. The President is saying one thing, governors something else; Anthony Fauci is saying something else, and Deborah Birx is saying something a little bit different. There’s this tremendous confusion that overlays the fear, and I think everybody is more or less feeling these things.
So yes, a dialogue with fear is a good thing to do because it can be clarifying. What we need here is a sense of, what is it that makes sense for me to do? What precautions should I take? What precautions shouldn’t I take?
I have a 17-year-old son who lives with his mom in California. He and I were on the phone the other day. He’s a basketball player and very serious about it. He said, “I don’t want to put my life on hold.” And my response was, “If you go outside too soon, your life may be on hold for a hell of a lot longer than if you stay inside because, if you get sick, it’s serious. But you also need to start looking at the evidence and asking yourself the right questions because I can’t be there all the time and neither can your mom.”
Everybody really needs to use these kinds of tools to help themselves. The tools we teach are extremely good at bringing us back into a state of psychological and physiological balance — slow, deep breathing being a very basic one. Because it’s only in that state that we’re going to be able to make the most intelligent decisions about what to do. It’s only in that state that we’re going to be able to really look our fear in the face and find out what we should be afraid of and what we shouldn’t be afraid of.
It’s a process that’s very much integrated. We’re talking now about how to deal with the emotions. But the first part of what we do in our groups and our online trainings and webinars is teach people to just take a few deep breaths. Just take a few deep breaths in through the nose, out through the mouth, with your belly soft and relaxed. You can keep breathing this way while talking. That’s the antidote to the fight-or-flight response. We all learn about fight-or-flight in first-year physiology. We need to deal with it. We need to bring ourselves into balance. That’s the way we’re going to make the wisest decisions for ourselves and be best able to help our patients.
Dr. Wilner: As you mentioned, part of modern culture is that we now have access to all of this information worldwide. There’s a continual stream of newsfeeds, people flipping on their phones, receiving constant updates, 24/7. That’s a new phenomenon. Does that steal from us the time we had before for just breathing and synthesizing data as opposed to just acquiring it all the time?
Dr. Gordon: You’re absolutely right. It does and it’s a challenge. It can’t steal from us unless we’re letting our emotional, psychological, and physiological pockets be picked!
What we need to do is to make it our priority to come into balance. I don’t watch news all day long – a little tiny bit in the morning and in the evening, just to get a sense of what’s happening. That’s enough. And I think everybody needs to take a step back, ask if this is really what they want to be doing, and to come into balance.
The other thing that’s really important is physical activity, especially during this time. In addition to using slow, deep breathing to come into balance, physical exercise and movement of any kind is extremely good as an antidote to fight-or-flight and that shut-down, freeze-up response that we get into when we feel completely overwhelmed.
We’ve got to take it into our own hands. The media just want to sell us things. Let’s face it: They’re not here for our good. Our job as physicians and health care professionals is to really reinforce for people not only what we can do for them but what they can do for themselves.
Dr. Wilner: I’m certainly interested in learning more about mind-body medicine. For those who feel the same, where do you recommend they go to learn more?
Dr. Gordon: We have a website, cmbm.org, which features a number of webinars. I do a free webinar there every week. We have mind-body skills groups that meet once a week for 8 weeks. There are six physicians in my group and all kinds of health professionals in other groups. We have a training program that we’re bringing online. We’ve trained well over 6,000 people around the world and would love to train more. You can read about that on the website.
We’re starting to do more and more consulting with health care organizations. We’re working with the largest division of Veterans Affairs, which is in Florida, as well as in south Georgia and the Caribbean. We’re working with a large health system in Indiana and others elsewhere. In addition, we’re working with groups of physicians and mental health professionals, helping them to integrate what we have to offer into what they’re already doing.
That’s our job – to help you do your job.
Dr. Wilner: Dr Gordon, I feel more relaxed just speaking with you. Thank you for talking with me and sharing your experiences with Medscape. I look forward to learning more.
Dr. Gordon: Thank you. My pleasure.
A version of this article originally appeared on Medscape.com.
Andrew N. Wilner, MD: Welcome to Medscape. I’m Dr Andrew Wilner. Today I have a special guest, Dr James Gordon, founder and executive director of the Center for Mind-Body Medicine. Welcome, Dr Gordon.
James S. Gordon, MD: Thank you very much. It’s good to be with you.
Dr. Wilner: Thanks for joining us. We are recording this in late May 2020, in the midst of the coronavirus pandemic. Millions of people have been infected. Hundreds of thousands have died. Millions have lost their jobs. I think it’s fair to say that people are under a greater degree of stress than they’re normally accustomed to. Would you agree with that?
Dr. Gordon: I think it’s more than fair to say that everybody in the United States, and actually pretty much everyone in the world, is under extreme stress. And that compounds any stresses that they’ve experienced before in their lives. Everyone is affected.
Dr. Wilner: The mind-body medicine concept is one that you’ve pursued for decades. Tell us a little bit about the Center for Mind-Body Medicine and how that’s led to the program that you have to help us deal with the coronavirus.
Dr. Gordon: I started the Center for Mind-Body Medicine about 30 years ago. I’d been a researcher at the National Institute of Mental Health for a number of years, in private practice, and a professor at Georgetown Medical School. But I wanted to really focus on how to change and enrich medicine by making self-care, self-awareness, and group support central to all healthcare.
Western medicine is enormously powerful in certain situations, such as physical trauma, high levels of infection, congenital anomalies. But we’re not so good at working with chronic physical or psychological problems. Those are much more complex.
We’ve been discovering that what is going to make the long-term difference in conditions like type 2 diabetes, pain syndromes, hypertension, depression, and anxiety are those approaches that we can learn to do for ourselves. These are changes we can make in how we deal with stress, eat, exercise, relate to other people, and whether we find meaning and purpose in our lives.
by wars, climate-related disasters, the opioid epidemic, chronic poverty, historical trauma. We do a lot of work with indigenous people here in North America. We’ve worked in a number of communities where school shootings have traumatized everyone.
What we’ve learned over these past 25 years, and what interested me professionally as well as personally over the past 50 years, is what we’re now bringing out on an even larger scale. The kind of approaches that we’ve developed, studied, and published research on are exactly what everyone needs to include and incorporate in their daily life, as well as in their medical and health care, from now on.
Dr. Wilner: Do you have a program that’s specifically for health care providers?
Dr. Gordon: Yes. The Center for Mind-Body Medicine is primarily an educational organization rather than a service organization. Since the beginning, I’ve been focused on training health professionals. My first passion was for training physicians – I’m a physician, so there’s a feeling of fellowship there – but also health care workers and mental health professionals of every kind.
We teach health professionals a whole system, a comprehensive program of techniques of self-awareness and self-care. We teach them so that they can practice on themselves and study the underlying science, so they can then teach what they’ve learned to the patients or clients they work with. They integrate it into what they’re already doing, regardless of their specialty. At times we also offer some of the same kinds of mind-body skills groups that are the fundamental part of our training as a stand-alone intervention. You can’t really teach other people how to take care of themselves unless you’re also doing it yourself. Otherwise, it’s just a theory.
Dr. Wilner: As a neurologist, I’m interested in the mind-body system. You are a psychiatrist and understand that it’s a lot more difficult to objectify certain things. What is stress? What is happiness? What is sadness? It’s very hard to measure. You can have scales, but it requires insight on the part of the individual. So I think it’s certainly an ambitious project.
Dr. Gordon: You’re absolutely right. It requires insight. And one of the shortcomings of our medical education is that it doesn’t encourage us to look inside ourselves enough. There’s so much focus on objectivity and on data, that we’ve lost some of the subjective art of medicine.
My experience with myself, as well as with the thousands of people we’ve trained here in the United States and around the world and the many hundreds of thousands with whom they’ve worked, is that all of us have a greater capacity to understand and help ourselves than we ordinarily think or than most of us learn about in our medical education.
This work is saying to people to take a little bit of time and relax a little in order to allow yourself to come into a meditative state. And I don’t mean anything fancy by that. Meditation is just being relaxed. Moment-to-moment awareness doesn’t have to do with any particular religion or spiritual practice. It’s part of all of them. If you can get into that state, then you can begin to say, “Oh, that’s what’s going on with me. That’s why my pain is worse.”
For example, you often wonder in people with peripheral neuropathy why it becomes worse or better at certain points. I would encourage neurologists and other physicians to ask your patients, “Why do you think it’s worse?” They may say, “I don’t know, doc; that’s why I’m here.” But I would ask them to take a couple of minutes to let me know. They could think it has something to do with the fact that they had a big fight with their wife that morning, they don’t want to go to work, or whatever it is. This is part of the lost art that we need to bring back into medicine for ourselves and especially for our patients.
Dr. Wilner: Can you give me an example of some of the exercises you’d do in a class?
Dr. Gordon: All of the exercises and our entire program that we teach at the Center for Mind-Body Medicine is in this new book of mine, “The Transformation: Discovering Wholeness and Healing After Trauma.” It’s really the distillation of not just the past 25 or 30 years, but really 50 years of work.
The techniques are all pretty simple and, as we say, evidence based. There is evidence that shows how they work on us physiologically, as well as psychologically. And they’re all pretty easy to teach to anyone.
Myself and about 60 or 70 of our faculty at the Center for Mind-Body Medicine are currently leading online groups. Then several hundred of the other people we’ve trained are also leading these groups. We’re still counting it up, but we probably have between 700 and 1,000 groups going around the world, led by our faculty and by people we’ve trained.
We teach a different technique every week in these online groups. Last week, after getting people energized and focused, we did a written dialogue with an emotion. You put down the initial of your name – in my case, “J” for Jim – and create a dialogue with an emotion, such as sadness. I would write it as fast as I can.
I would say, “OK, Sadness. Why are you here? What are you doing? I don’t enjoy having you around.” And Sadness writes back to me, “But you need me.” And J says, “What do you mean I need you?” And Sadness says, “Well, your brother died 7 weeks ago, didn’t he?” And I say, “Yes, he did.” And Sadness says, “Aren’t you sad?” I say, “Yes. I’m terribly sad and grieving all the time. But I wasn’t thinking about him at this moment.” And Sadness says, “But he’s there with you all the time and that sadness is in you.” And I say, “You mean it’s in me even here, now, as I’m talking with Andrew in this interview?” And Sadness says, “Yes. You can talk about your work. But in between the words, as you take a breath, don’t you feel it in your chest?” That’s the way the dialogue goes.
Dr. Wilner: What about specifically with the coronavirus? Fear is certainly an emotion. Nobody wants to get sick and die. Nobody wants to bring this disease home to their family. People are reluctant to even go outside and you can’t shake someone’s hand. Are there precedents for this?
Dr. Gordon: There are precedents, but only relatively small groups were affected before by, for example, severe acute respiratory syndrome or H1N1, at least in the United States. But we haven’t seen a global pandemic like this since 1918. None of us was around then – or I certainly wasn’t around. So for most everyone, not only has it not happened before, but we’ve never been so globally aware of everything that’s going on and how different groups are reacting.
I’ve been reading Daniel Defoe’s book, “A Journal of the Plague Year.” It’s really very interesting. It’s about the bubonic plague in 1665 London, although he wrote it in the 1720s. Some of the same things were going on then: the enormous fear, the isolation; rich people being able to escape, poor people having nowhere to go; conspiracy theories of one kind or another, about where the plague came from or blaming a group of people for it; magical thinking that it’s just going to go away. All of those things that happened several hundred years ago are going on now.
And we’re all simultaneously aware of all those things. There’s not only the fear, which should be universal because it’s a reasonable response to this situation, but also the terrible confusion about what to do. The President is saying one thing, governors something else; Anthony Fauci is saying something else, and Deborah Birx is saying something a little bit different. There’s this tremendous confusion that overlays the fear, and I think everybody is more or less feeling these things.
So yes, a dialogue with fear is a good thing to do because it can be clarifying. What we need here is a sense of, what is it that makes sense for me to do? What precautions should I take? What precautions shouldn’t I take?
I have a 17-year-old son who lives with his mom in California. He and I were on the phone the other day. He’s a basketball player and very serious about it. He said, “I don’t want to put my life on hold.” And my response was, “If you go outside too soon, your life may be on hold for a hell of a lot longer than if you stay inside because, if you get sick, it’s serious. But you also need to start looking at the evidence and asking yourself the right questions because I can’t be there all the time and neither can your mom.”
Everybody really needs to use these kinds of tools to help themselves. The tools we teach are extremely good at bringing us back into a state of psychological and physiological balance — slow, deep breathing being a very basic one. Because it’s only in that state that we’re going to be able to make the most intelligent decisions about what to do. It’s only in that state that we’re going to be able to really look our fear in the face and find out what we should be afraid of and what we shouldn’t be afraid of.
It’s a process that’s very much integrated. We’re talking now about how to deal with the emotions. But the first part of what we do in our groups and our online trainings and webinars is teach people to just take a few deep breaths. Just take a few deep breaths in through the nose, out through the mouth, with your belly soft and relaxed. You can keep breathing this way while talking. That’s the antidote to the fight-or-flight response. We all learn about fight-or-flight in first-year physiology. We need to deal with it. We need to bring ourselves into balance. That’s the way we’re going to make the wisest decisions for ourselves and be best able to help our patients.
Dr. Wilner: As you mentioned, part of modern culture is that we now have access to all of this information worldwide. There’s a continual stream of newsfeeds, people flipping on their phones, receiving constant updates, 24/7. That’s a new phenomenon. Does that steal from us the time we had before for just breathing and synthesizing data as opposed to just acquiring it all the time?
Dr. Gordon: You’re absolutely right. It does and it’s a challenge. It can’t steal from us unless we’re letting our emotional, psychological, and physiological pockets be picked!
What we need to do is to make it our priority to come into balance. I don’t watch news all day long – a little tiny bit in the morning and in the evening, just to get a sense of what’s happening. That’s enough. And I think everybody needs to take a step back, ask if this is really what they want to be doing, and to come into balance.
The other thing that’s really important is physical activity, especially during this time. In addition to using slow, deep breathing to come into balance, physical exercise and movement of any kind is extremely good as an antidote to fight-or-flight and that shut-down, freeze-up response that we get into when we feel completely overwhelmed.
We’ve got to take it into our own hands. The media just want to sell us things. Let’s face it: They’re not here for our good. Our job as physicians and health care professionals is to really reinforce for people not only what we can do for them but what they can do for themselves.
Dr. Wilner: I’m certainly interested in learning more about mind-body medicine. For those who feel the same, where do you recommend they go to learn more?
Dr. Gordon: We have a website, cmbm.org, which features a number of webinars. I do a free webinar there every week. We have mind-body skills groups that meet once a week for 8 weeks. There are six physicians in my group and all kinds of health professionals in other groups. We have a training program that we’re bringing online. We’ve trained well over 6,000 people around the world and would love to train more. You can read about that on the website.
We’re starting to do more and more consulting with health care organizations. We’re working with the largest division of Veterans Affairs, which is in Florida, as well as in south Georgia and the Caribbean. We’re working with a large health system in Indiana and others elsewhere. In addition, we’re working with groups of physicians and mental health professionals, helping them to integrate what we have to offer into what they’re already doing.
That’s our job – to help you do your job.
Dr. Wilner: Dr Gordon, I feel more relaxed just speaking with you. Thank you for talking with me and sharing your experiences with Medscape. I look forward to learning more.
Dr. Gordon: Thank you. My pleasure.
A version of this article originally appeared on Medscape.com.
Andrew N. Wilner, MD: Welcome to Medscape. I’m Dr Andrew Wilner. Today I have a special guest, Dr James Gordon, founder and executive director of the Center for Mind-Body Medicine. Welcome, Dr Gordon.
James S. Gordon, MD: Thank you very much. It’s good to be with you.
Dr. Wilner: Thanks for joining us. We are recording this in late May 2020, in the midst of the coronavirus pandemic. Millions of people have been infected. Hundreds of thousands have died. Millions have lost their jobs. I think it’s fair to say that people are under a greater degree of stress than they’re normally accustomed to. Would you agree with that?
Dr. Gordon: I think it’s more than fair to say that everybody in the United States, and actually pretty much everyone in the world, is under extreme stress. And that compounds any stresses that they’ve experienced before in their lives. Everyone is affected.
Dr. Wilner: The mind-body medicine concept is one that you’ve pursued for decades. Tell us a little bit about the Center for Mind-Body Medicine and how that’s led to the program that you have to help us deal with the coronavirus.
Dr. Gordon: I started the Center for Mind-Body Medicine about 30 years ago. I’d been a researcher at the National Institute of Mental Health for a number of years, in private practice, and a professor at Georgetown Medical School. But I wanted to really focus on how to change and enrich medicine by making self-care, self-awareness, and group support central to all healthcare.
Western medicine is enormously powerful in certain situations, such as physical trauma, high levels of infection, congenital anomalies. But we’re not so good at working with chronic physical or psychological problems. Those are much more complex.
We’ve been discovering that what is going to make the long-term difference in conditions like type 2 diabetes, pain syndromes, hypertension, depression, and anxiety are those approaches that we can learn to do for ourselves. These are changes we can make in how we deal with stress, eat, exercise, relate to other people, and whether we find meaning and purpose in our lives.
by wars, climate-related disasters, the opioid epidemic, chronic poverty, historical trauma. We do a lot of work with indigenous people here in North America. We’ve worked in a number of communities where school shootings have traumatized everyone.
What we’ve learned over these past 25 years, and what interested me professionally as well as personally over the past 50 years, is what we’re now bringing out on an even larger scale. The kind of approaches that we’ve developed, studied, and published research on are exactly what everyone needs to include and incorporate in their daily life, as well as in their medical and health care, from now on.
Dr. Wilner: Do you have a program that’s specifically for health care providers?
Dr. Gordon: Yes. The Center for Mind-Body Medicine is primarily an educational organization rather than a service organization. Since the beginning, I’ve been focused on training health professionals. My first passion was for training physicians – I’m a physician, so there’s a feeling of fellowship there – but also health care workers and mental health professionals of every kind.
We teach health professionals a whole system, a comprehensive program of techniques of self-awareness and self-care. We teach them so that they can practice on themselves and study the underlying science, so they can then teach what they’ve learned to the patients or clients they work with. They integrate it into what they’re already doing, regardless of their specialty. At times we also offer some of the same kinds of mind-body skills groups that are the fundamental part of our training as a stand-alone intervention. You can’t really teach other people how to take care of themselves unless you’re also doing it yourself. Otherwise, it’s just a theory.
Dr. Wilner: As a neurologist, I’m interested in the mind-body system. You are a psychiatrist and understand that it’s a lot more difficult to objectify certain things. What is stress? What is happiness? What is sadness? It’s very hard to measure. You can have scales, but it requires insight on the part of the individual. So I think it’s certainly an ambitious project.
Dr. Gordon: You’re absolutely right. It requires insight. And one of the shortcomings of our medical education is that it doesn’t encourage us to look inside ourselves enough. There’s so much focus on objectivity and on data, that we’ve lost some of the subjective art of medicine.
My experience with myself, as well as with the thousands of people we’ve trained here in the United States and around the world and the many hundreds of thousands with whom they’ve worked, is that all of us have a greater capacity to understand and help ourselves than we ordinarily think or than most of us learn about in our medical education.
This work is saying to people to take a little bit of time and relax a little in order to allow yourself to come into a meditative state. And I don’t mean anything fancy by that. Meditation is just being relaxed. Moment-to-moment awareness doesn’t have to do with any particular religion or spiritual practice. It’s part of all of them. If you can get into that state, then you can begin to say, “Oh, that’s what’s going on with me. That’s why my pain is worse.”
For example, you often wonder in people with peripheral neuropathy why it becomes worse or better at certain points. I would encourage neurologists and other physicians to ask your patients, “Why do you think it’s worse?” They may say, “I don’t know, doc; that’s why I’m here.” But I would ask them to take a couple of minutes to let me know. They could think it has something to do with the fact that they had a big fight with their wife that morning, they don’t want to go to work, or whatever it is. This is part of the lost art that we need to bring back into medicine for ourselves and especially for our patients.
Dr. Wilner: Can you give me an example of some of the exercises you’d do in a class?
Dr. Gordon: All of the exercises and our entire program that we teach at the Center for Mind-Body Medicine is in this new book of mine, “The Transformation: Discovering Wholeness and Healing After Trauma.” It’s really the distillation of not just the past 25 or 30 years, but really 50 years of work.
The techniques are all pretty simple and, as we say, evidence based. There is evidence that shows how they work on us physiologically, as well as psychologically. And they’re all pretty easy to teach to anyone.
Myself and about 60 or 70 of our faculty at the Center for Mind-Body Medicine are currently leading online groups. Then several hundred of the other people we’ve trained are also leading these groups. We’re still counting it up, but we probably have between 700 and 1,000 groups going around the world, led by our faculty and by people we’ve trained.
We teach a different technique every week in these online groups. Last week, after getting people energized and focused, we did a written dialogue with an emotion. You put down the initial of your name – in my case, “J” for Jim – and create a dialogue with an emotion, such as sadness. I would write it as fast as I can.
I would say, “OK, Sadness. Why are you here? What are you doing? I don’t enjoy having you around.” And Sadness writes back to me, “But you need me.” And J says, “What do you mean I need you?” And Sadness says, “Well, your brother died 7 weeks ago, didn’t he?” And I say, “Yes, he did.” And Sadness says, “Aren’t you sad?” I say, “Yes. I’m terribly sad and grieving all the time. But I wasn’t thinking about him at this moment.” And Sadness says, “But he’s there with you all the time and that sadness is in you.” And I say, “You mean it’s in me even here, now, as I’m talking with Andrew in this interview?” And Sadness says, “Yes. You can talk about your work. But in between the words, as you take a breath, don’t you feel it in your chest?” That’s the way the dialogue goes.
Dr. Wilner: What about specifically with the coronavirus? Fear is certainly an emotion. Nobody wants to get sick and die. Nobody wants to bring this disease home to their family. People are reluctant to even go outside and you can’t shake someone’s hand. Are there precedents for this?
Dr. Gordon: There are precedents, but only relatively small groups were affected before by, for example, severe acute respiratory syndrome or H1N1, at least in the United States. But we haven’t seen a global pandemic like this since 1918. None of us was around then – or I certainly wasn’t around. So for most everyone, not only has it not happened before, but we’ve never been so globally aware of everything that’s going on and how different groups are reacting.
I’ve been reading Daniel Defoe’s book, “A Journal of the Plague Year.” It’s really very interesting. It’s about the bubonic plague in 1665 London, although he wrote it in the 1720s. Some of the same things were going on then: the enormous fear, the isolation; rich people being able to escape, poor people having nowhere to go; conspiracy theories of one kind or another, about where the plague came from or blaming a group of people for it; magical thinking that it’s just going to go away. All of those things that happened several hundred years ago are going on now.
And we’re all simultaneously aware of all those things. There’s not only the fear, which should be universal because it’s a reasonable response to this situation, but also the terrible confusion about what to do. The President is saying one thing, governors something else; Anthony Fauci is saying something else, and Deborah Birx is saying something a little bit different. There’s this tremendous confusion that overlays the fear, and I think everybody is more or less feeling these things.
So yes, a dialogue with fear is a good thing to do because it can be clarifying. What we need here is a sense of, what is it that makes sense for me to do? What precautions should I take? What precautions shouldn’t I take?
I have a 17-year-old son who lives with his mom in California. He and I were on the phone the other day. He’s a basketball player and very serious about it. He said, “I don’t want to put my life on hold.” And my response was, “If you go outside too soon, your life may be on hold for a hell of a lot longer than if you stay inside because, if you get sick, it’s serious. But you also need to start looking at the evidence and asking yourself the right questions because I can’t be there all the time and neither can your mom.”
Everybody really needs to use these kinds of tools to help themselves. The tools we teach are extremely good at bringing us back into a state of psychological and physiological balance — slow, deep breathing being a very basic one. Because it’s only in that state that we’re going to be able to make the most intelligent decisions about what to do. It’s only in that state that we’re going to be able to really look our fear in the face and find out what we should be afraid of and what we shouldn’t be afraid of.
It’s a process that’s very much integrated. We’re talking now about how to deal with the emotions. But the first part of what we do in our groups and our online trainings and webinars is teach people to just take a few deep breaths. Just take a few deep breaths in through the nose, out through the mouth, with your belly soft and relaxed. You can keep breathing this way while talking. That’s the antidote to the fight-or-flight response. We all learn about fight-or-flight in first-year physiology. We need to deal with it. We need to bring ourselves into balance. That’s the way we’re going to make the wisest decisions for ourselves and be best able to help our patients.
Dr. Wilner: As you mentioned, part of modern culture is that we now have access to all of this information worldwide. There’s a continual stream of newsfeeds, people flipping on their phones, receiving constant updates, 24/7. That’s a new phenomenon. Does that steal from us the time we had before for just breathing and synthesizing data as opposed to just acquiring it all the time?
Dr. Gordon: You’re absolutely right. It does and it’s a challenge. It can’t steal from us unless we’re letting our emotional, psychological, and physiological pockets be picked!
What we need to do is to make it our priority to come into balance. I don’t watch news all day long – a little tiny bit in the morning and in the evening, just to get a sense of what’s happening. That’s enough. And I think everybody needs to take a step back, ask if this is really what they want to be doing, and to come into balance.
The other thing that’s really important is physical activity, especially during this time. In addition to using slow, deep breathing to come into balance, physical exercise and movement of any kind is extremely good as an antidote to fight-or-flight and that shut-down, freeze-up response that we get into when we feel completely overwhelmed.
We’ve got to take it into our own hands. The media just want to sell us things. Let’s face it: They’re not here for our good. Our job as physicians and health care professionals is to really reinforce for people not only what we can do for them but what they can do for themselves.
Dr. Wilner: I’m certainly interested in learning more about mind-body medicine. For those who feel the same, where do you recommend they go to learn more?
Dr. Gordon: We have a website, cmbm.org, which features a number of webinars. I do a free webinar there every week. We have mind-body skills groups that meet once a week for 8 weeks. There are six physicians in my group and all kinds of health professionals in other groups. We have a training program that we’re bringing online. We’ve trained well over 6,000 people around the world and would love to train more. You can read about that on the website.
We’re starting to do more and more consulting with health care organizations. We’re working with the largest division of Veterans Affairs, which is in Florida, as well as in south Georgia and the Caribbean. We’re working with a large health system in Indiana and others elsewhere. In addition, we’re working with groups of physicians and mental health professionals, helping them to integrate what we have to offer into what they’re already doing.
That’s our job – to help you do your job.
Dr. Wilner: Dr Gordon, I feel more relaxed just speaking with you. Thank you for talking with me and sharing your experiences with Medscape. I look forward to learning more.
Dr. Gordon: Thank you. My pleasure.
A version of this article originally appeared on Medscape.com.