User login
Roth Spots—More than Meets the Eye
A 50‐year‐old female patient with a past medical history of Sjogren's syndrome and polymyositis presented with fever, rash, swelling, and pain in her extremities. Skin biopsy confirmed vasculitis. She was treated with steroids and azathioprine. However, she developed sudden‐onset central visual blurring in her right eye on the fifth day of hospitalization. Fundoscopic exam showed multiple central white‐centered retinal hemorrhages (Roth spots, Figures 1, 2) and vascular sheathing, consistent with retinal vasculitis. Blood cultures were negative. Transthoracic and transesophageal echocardiograms were normal. She was treated with high‐dose intravenous steroids and cyclophosphamide, with visual improvement and a marked reduction in the number of Roth spots.

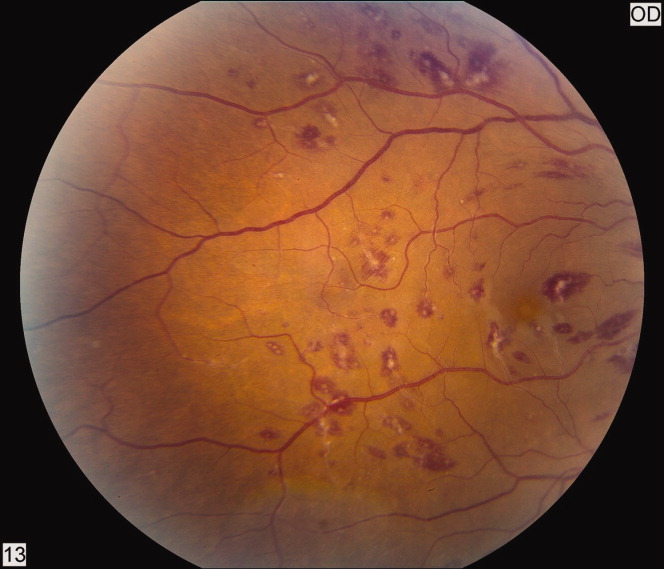
Roth spots 1 are nonspecific intraretinal hemorrhagic lesions with a white center due to fibrin deposition. Although historically associated with infective endocarditis, they can also occur in other systemic diseases such as connective tissue disorders, vasculitis, leukemia, diabetes, hypertension, anemia, trauma, as well as disseminated bacterial and fungal infections.
- , , .White centered hemorrhages: their significance.Ophthalmology.1980;87:66–69.
A 50‐year‐old female patient with a past medical history of Sjogren's syndrome and polymyositis presented with fever, rash, swelling, and pain in her extremities. Skin biopsy confirmed vasculitis. She was treated with steroids and azathioprine. However, she developed sudden‐onset central visual blurring in her right eye on the fifth day of hospitalization. Fundoscopic exam showed multiple central white‐centered retinal hemorrhages (Roth spots, Figures 1, 2) and vascular sheathing, consistent with retinal vasculitis. Blood cultures were negative. Transthoracic and transesophageal echocardiograms were normal. She was treated with high‐dose intravenous steroids and cyclophosphamide, with visual improvement and a marked reduction in the number of Roth spots.

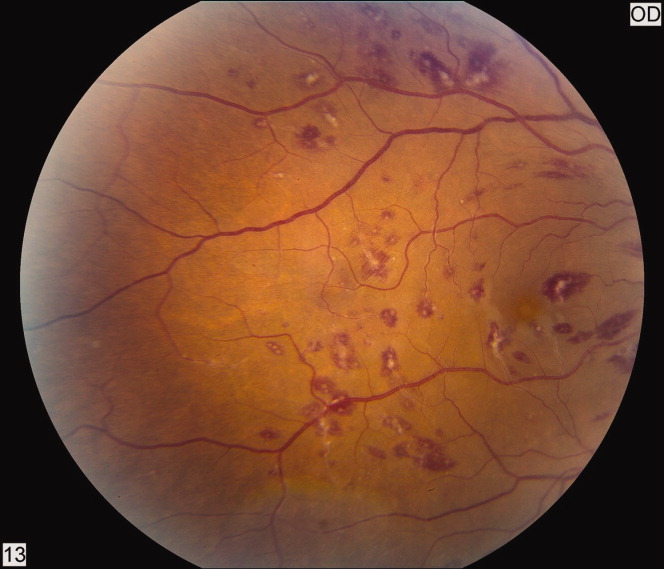
Roth spots 1 are nonspecific intraretinal hemorrhagic lesions with a white center due to fibrin deposition. Although historically associated with infective endocarditis, they can also occur in other systemic diseases such as connective tissue disorders, vasculitis, leukemia, diabetes, hypertension, anemia, trauma, as well as disseminated bacterial and fungal infections.
A 50‐year‐old female patient with a past medical history of Sjogren's syndrome and polymyositis presented with fever, rash, swelling, and pain in her extremities. Skin biopsy confirmed vasculitis. She was treated with steroids and azathioprine. However, she developed sudden‐onset central visual blurring in her right eye on the fifth day of hospitalization. Fundoscopic exam showed multiple central white‐centered retinal hemorrhages (Roth spots, Figures 1, 2) and vascular sheathing, consistent with retinal vasculitis. Blood cultures were negative. Transthoracic and transesophageal echocardiograms were normal. She was treated with high‐dose intravenous steroids and cyclophosphamide, with visual improvement and a marked reduction in the number of Roth spots.

Roth spots 1 are nonspecific intraretinal hemorrhagic lesions with a white center due to fibrin deposition. Although historically associated with infective endocarditis, they can also occur in other systemic diseases such as connective tissue disorders, vasculitis, leukemia, diabetes, hypertension, anemia, trauma, as well as disseminated bacterial and fungal infections.
- , , .White centered hemorrhages: their significance.Ophthalmology.1980;87:66–69.
- , , .White centered hemorrhages: their significance.Ophthalmology.1980;87:66–69.
“Better Late than Never”
A 59‐year‐old man presented to the emergency department with the acute onset of right‐sided abdominal and flank pain. The pain had begun the previous night, was constant and progressively worsening, and radiated to his right groin. He denied fever, nausea, emesis, or change in his bowel habits, but he did notice mild right lower quadrant discomfort with micturition. Upon further questioning, he also complained of mild dyspnea on climbing stairs and an unspecified recent weight loss.
The most common cause of acute severe right‐sided flank and abdominal pain radiating to the groin and associated with dysuria in a middle‐aged man is ureteral colic. Other etiologies important to consider include retrocecal appendicitis, pyelonephritis, and, rarely, a dissecting abdominal aortic aneurysm. This patient's seemingly recent onset exertional dyspnea and weight loss do not neatly fit any of the above, however.
His past medical history was significant for diabetes mellitus and pemphigus vulgaris diagnosed 7 months previously. He had been treated with prednisone, and the dose decreased from 100 to 60 mg daily, 1 month previously, due to poor glycemic control as well as steroid‐induced neuropathy and myopathy. His other medications included naproxen sodium and ibuprofen for back pain, azathioprine, insulin, pioglitazone, and glimiperide. He had no past surgical history. He had lived in the United States since his emigration from Thailand in 1971. His last trip to Thailand was 5 years previously. He was a taxi cab driver. He had a ten‐pack year history of tobacco use, but had quit 20 years prior. He denied history of alcohol or intravenous drug use.
Pemphigus vulgaris is unlikely to be directly related to this patient's presentation, but in light of his poorly controlled diabetes, his azathioprine use, and particularly his high‐dose corticosteroids, he is certainly immunocompromised. Accordingly, a disseminated infection, either newly acquired or reactivated, merits consideration. His history of residence in, and subsequent travel to, Southeast Asia raises the possibility of several diseases, each of which may be protean in their manifestations; these include tuberculosis, melioidosis, and penicilliosis (infection with Penicillium marneffei). The first two may reactivate long after initial exposure, particularly with insults to the immune system. The same is probably true of penicilliosis, although I am not certain of this. On a slightly less exotic note, domestically acquired infection with histoplasmosis or other endemic fungi is possible.
On examination he was afebrile, had a pulse of 130 beats per minute and a blood pressure of 65/46 mmHg. His oxygen saturation was 92%. He appeared markedly cushingoid, and had mild pallor and generalized weakness. Cardiopulmonary examination was unremarkable. His abdominal exam was notable for distention and hypoactive bowel sounds, with tenderness and firmness to palpation on the right side. Peripheral pulses were normal. Examination of the skin demonstrated ecchymoses over the bilateral forearms, and several healed pemphigus lesions on the abdomen and upper extremities.
The patient's severely deranged hemodynamic parameters indicate either current or impending shock, and resuscitative measures should proceed in tandem with diagnostic efforts. The cause of his shock seems most likely to be either hypovolemic (abdominal wall or intra‐abdominal hemorrhage, or conceivably massive third spacing from an intra‐abdominal catastrophe), or distributive (sepsis, or acute adrenal insufficiency if he has missed recent steroid doses). His ecchymoses may simply reflect chronic glucocorticoid use, but also raise suspicion for a coagulopathy. Provided the patient can be stabilized to allow this, I would urgently obtain a computed tomography (CT) scan of the abdomen and pelvis.
Initial laboratory studies demonstrated a hemoglobin of 9.1 g/dL, white blood cell count 8000/L with 33% bands, 48% segmented neutrophils, 18% lymphocytes, and 0.7% eosinophils, platelet count 356,000/L, sodium 128 mmol/L, BUN 52 mg/dL, creatinine 2.3 mg/dL, and glucose of 232 mg/dL. Coagulation studies were normal, and lactic acid was 1.8 mmol/L (normal range, 0.7‐2.1). Fibrinogen was normal at 591 and LDH was mildly elevated at 654 (normal range, 313‐618 U/L). Total protein and albumin were 3.6 and 1.9 g/dL, respectively. Total bilirubin was 0.6 mg/dL. Random serum cortisol was 20.2 g/dL. Liver enzymes, amylase, lipase, iron stores, B12, folate, and stool for occult blood were normal. Initial cardiac biomarkers were negative, but subsequent troponin‐I was 3.81 ng/mL (elevated, >1.00). Urinalysis showed 0‐4 white blood cells per high powered field.
The laboratory studies provide a variety of useful, albeit nonspecific, information. The high percentage of band forms on white blood cell differential further raises concern for an infectious process, although severe noninfectious stress can also cause this. While we do not know whether the patient's renal failure is acute, I suspect that it is, and may result from a variety of insults including sepsis, hypotension, and volume depletion. His moderately elevated troponin‐I likely reflects supplydemand mismatch or sepsis. I would like to see an electrocardiogram, and I remain very interested in obtaining abdominal imaging.
Chest radiography showed pulmonary vascular congestion without evidence of pneumothorax. Computed tomography scan of the abdomen and pelvis showed retroperitoneal fluid bilaterally (Figure 1). This was described as suspicious for ascites versus hemorrhage, but no obvious source of bleeding was identified. There was also a small amount of right perinephric fluid, but no evidence of a renal mass. The abdominal aorta was normal; there was no lymphadenopathy.

The CT image appears to speak against simple ascites, and seems most consistent with either blood or an infectious process. Consequently, the loculated right retroperitoneal collection should be aspirated, and fluid sent for fungal, acid‐fast, and modified acid‐fast (i.e., for Nocardia) stains and culture, in addition to Gram stain and routine aerobic and anaerobic cultures.
The patient was admitted to the intensive care unit. Stress‐dose steroids were administered, and he improved after resuscitation with fluid and blood. His renal function normalized. Urine and blood cultures returned negative. His hematocrit and multiple repeat CT scans of the abdomen remained stable. A retroperitoneal hemorrhage was diagnosed, and surgical intervention was deemed unnecessary. Both adenosine thallium stress test and echocardiogram were normal. He was continued on 60 mg prednisone daily and discharged home with outpatient follow‐up.
This degree of improvement with volume expansion (and steroids) suggests the patient was markedly volume depleted upon presentation. Although a formal adrenocorticotropic hormone (ACTH) stimulation test was apparently not performed, the random cortisol level suggests adrenal insufficiency was unlikely to have been primarily responsible. While retroperitoneal hemorrhage is possible, the loculated appearance of the collection suggests infection is more likely.
Three weeks later, he was readmitted with recurrent right‐sided abdominal and flank pain. His temperature was 101.3F, and he was tachycardic and hypotensive. His examination was similar to that at the time of his previous presentation. Laboratory data revealed white blood cell count of 13,100/L with 43% bands, hemoglobin of 9.2 g/dL, glucose of 343 mg/dL, bicarbonate 25 mmol/L, normal anion gap and renal function, and lactic acid of 4.5 mmol/L. Liver function tests were normal except for an albumin of 3.0 g/dL. CT scan of the abdomen revealed loculated retroperitoneal fluid collections, increased in size since the prior scan.
The patient is once again evidencing at least early shock, manifested in his deranged hemodynamics and elevated lactate level. I remain puzzled by the fact that he appeared to respond to fluids alone at the time of his initial hospital stay, unless adrenal insufficiency played a greater role than I suspected. Of note, acute adrenal insufficiency could explain much of the current picture, including fever, and bland (uninfected) hematomas are an underappreciated cause of both fever and leukocytosis. Having said this, I remain concerned that his retroperitoneal fluid collections represent abscesses. The most accessible of these should be sampled.
Aspiration of the retroperitoneal fluid yielded purulent material which grew Klebsiella pneumoniae. The cultures were negative for mycobacteria and fungus. Blood and urine cultures were negative. Drains were placed, and he was followed as an outpatient. His fever and leukocytosis subsided, and he completed a 6‐week course of trimethoprim‐sulfamethoxazole. CT imaging confirmed complete evacuation of the fluid.
Retroperitoneal abscesses frequently present in smoldering fashion, although patients may be quite ill by the time of presentation. Most of these are secondary, i.e., they arise from another abnormality in the retroperitoneum. Most commonly this is in the large bowel, kidney, pancreas, or spine. I would carefully scour his follow‐up imaging for additional clues and, if unrevealing, proceed to colonoscopy.
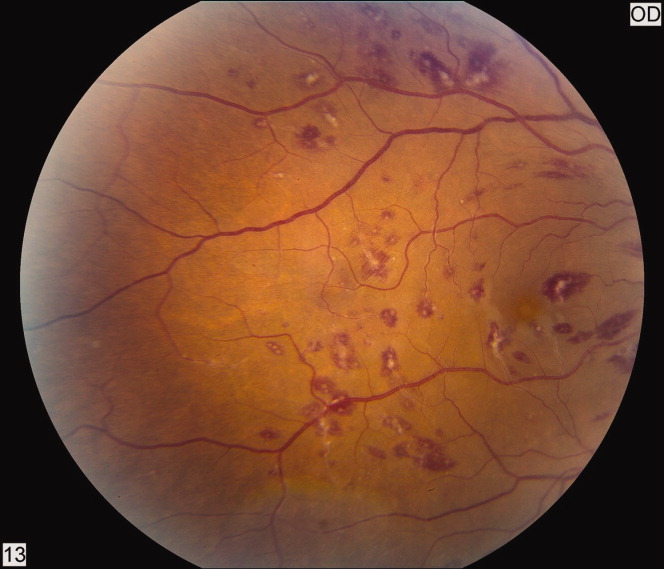
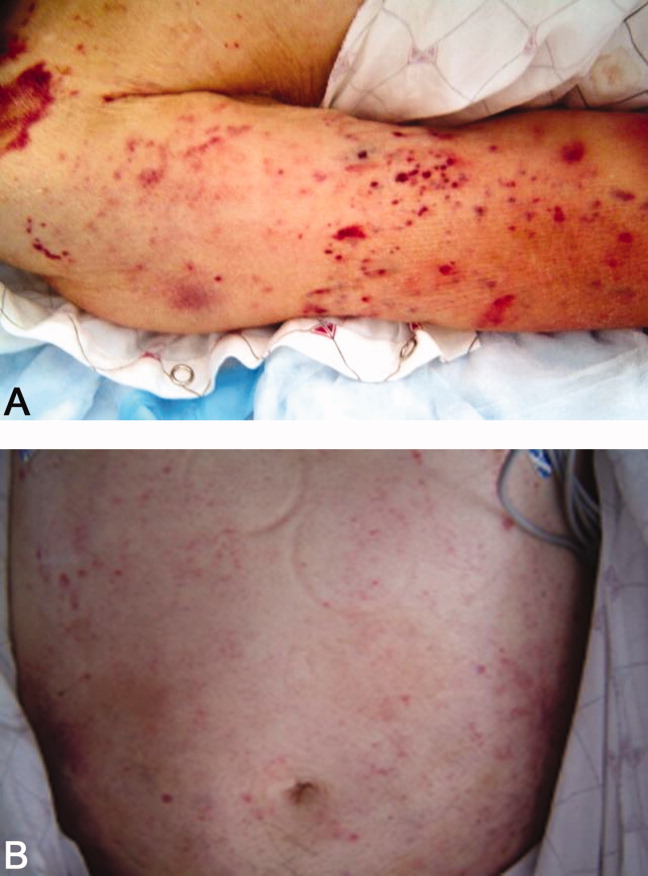
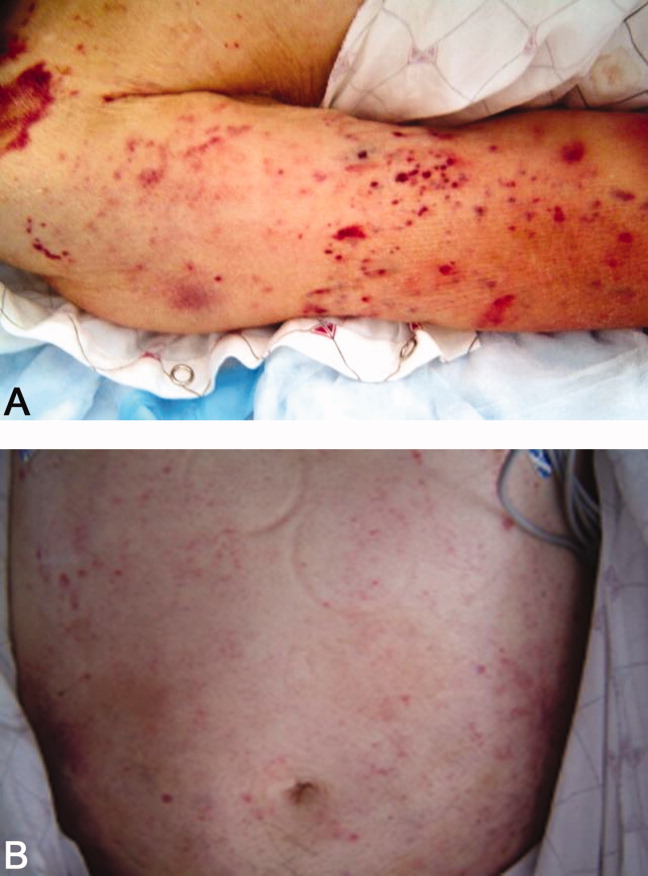
He returned 1 month after drain removal, with 2‐3 days of nausea and abdominal pain. His abdomen was moderately distended but nontender, and multiple persistent petechial and purpuric lesions were present on the upper back, chest, torso, and arms. Abdominal CT scan revealed small bowel obstruction and a collection of fluid in the left paracolic gutter extending into the left retrorenal space.
The patient does not appear to have obvious risk factors for developing a small bowel obstruction. No mention is made of the presence or absence of a transition point on the CT scan, and this should be ascertained. His left‐sided abdominal fluid collection is probably infectious in nature, and I continue to be suspicious of a large bowel (or distal small bowel) source, via either gut perforation or bacterial translocation. The collection needs to be percutaneously drained for both diagnostic and therapeutic reasons, and broadly cultured. Finally, we need to account for the described dermatologic manifestations. The purpuric/petechial lesions sound vasculitic rather than thrombocytopenic in origin based on location; conversely, they may simply reflect a corticosteroid‐related adverse effect. I would like to know whether the purpura was palpable, and to repeat a complete blood count with peripheral smear.
Laboratory data showed hemoglobin of 9.3 g/dL, a platelet count of 444,000/L, and normal coagulation studies. The purpura was nonpalpable (Figure 2). The patient had a nasogastric tube placed for decompression, with bilious drainage. His left retroperitoneal fluid was drained, with cultures yielding Enterococcus faecalis and Enterobacter cloacae. The patient was treated with a course of broad‐spectrum antibiotics. His obstruction improved and the retroperitoneal collection resolved on follow‐up imaging. However, 2 days later, he had recurrent pain; abdominal CT showed a recurrence of small bowel obstruction with an unequivocal transition point in the distal jejunum. A small fluid collection was noted in the left retroperitoneum with a trace of gas in it. He improved with nasogastric suction, his prednisone was tapered to 30 mg daily, and he was discharged home.
The isolation of both Enterococcus and Enterobacter species from his fluid collection, along with the previous isolation of Klebsiella, strongly suggest a bowel source for his recurrent abscesses. Based on this CT report, the patient has clear evidence of at least partial small bowel obstruction. He lacks a history of prior abdominal surgery or other more typical reasons for obstruction caused by extrinsic compression, such as hernia, although it is possible his recurrent abdominal infections may have led to obstruction due to scarring and adhesions. An intraluminal cause of obstruction also needs to be considered, with causes including malignancy (lymphoma, carcinoid, and adenocarcinoma), Crohn's disease, and infections including tuberculosis as well as parasites such as Taenia and Strongyloides. While the purpura is concerning, given the nonpalpable character along with a normal platelet count and coagulation studies, it may be reasonable to provisionally attribute it to high‐dose corticosteroid use.
He was admitted a fourth time a week after being discharged, with nausea, generalized weakness, and weight loss. At presentation, he had a blood pressure of 95/65 mmHg. His white blood cell count was 5,900/L, with 79% neutrophils and 20% bands. An AM cortisol was 18.8 /dL. He was thought to have adrenal insufficiency from steroid withdrawal, was treated with intravenous fluids and steroids, and discharged on a higher dose of prednisone at 60 mg daily. One week later, he again returned to the hospital with watery diarrhea, emesis, and generalized weakness. His blood pressure was 82/50 mmHg, and his abdomen appeared benign. He also had an erythematous rash over his mid‐abdomen. Laboratory data was significant for a sodium of 127 mmol/L, potassium of 3.0 mmol/L, chloride of 98 mmol/L, bicarbonate of 26 mmol/L, glucose of 40 mg/dL, lactate of 14 mmol/L, and albumin of 1.0 g/dL. Stool assay for Clostridium difficile was negative. A CT scan of the abdomen and pelvis showed small bilateral pleural effusions and small bowel fluid consistent with gastroenteritis, but without signs of obstruction. Esophagogastroduodenoscopy (EGD) showed bile backwash into the stomach, as well as inflammatory changes in the proximal and mid‐stomach, and inflammatory reaction and edema in the proximal duodenum. Colonoscopy showed normal appearing ileum and colon.
The patient's latest laboratory values appear to reflect his chronic illness and superimposed diarrhea. I am perplexed by his markedly elevated serum lactate value in association with a normal bicarbonate and low anion gap, and would repeat the lactate level to ensure this is not spurious. His hypoglycemia probably reflects a failure to adjust or discontinue his diabetic medications, although both hypoglycemia and type B lactic acidosis are occasionally manifestations of a paraneoplastic syndrome. The normal colonoscopy findings are helpful in exonerating the colon, provided the preparation was adequate. Presumably, the abnormal areas of the stomach and duodenum were biopsied; I remain suspicious that the answer may lie in the jejunum.
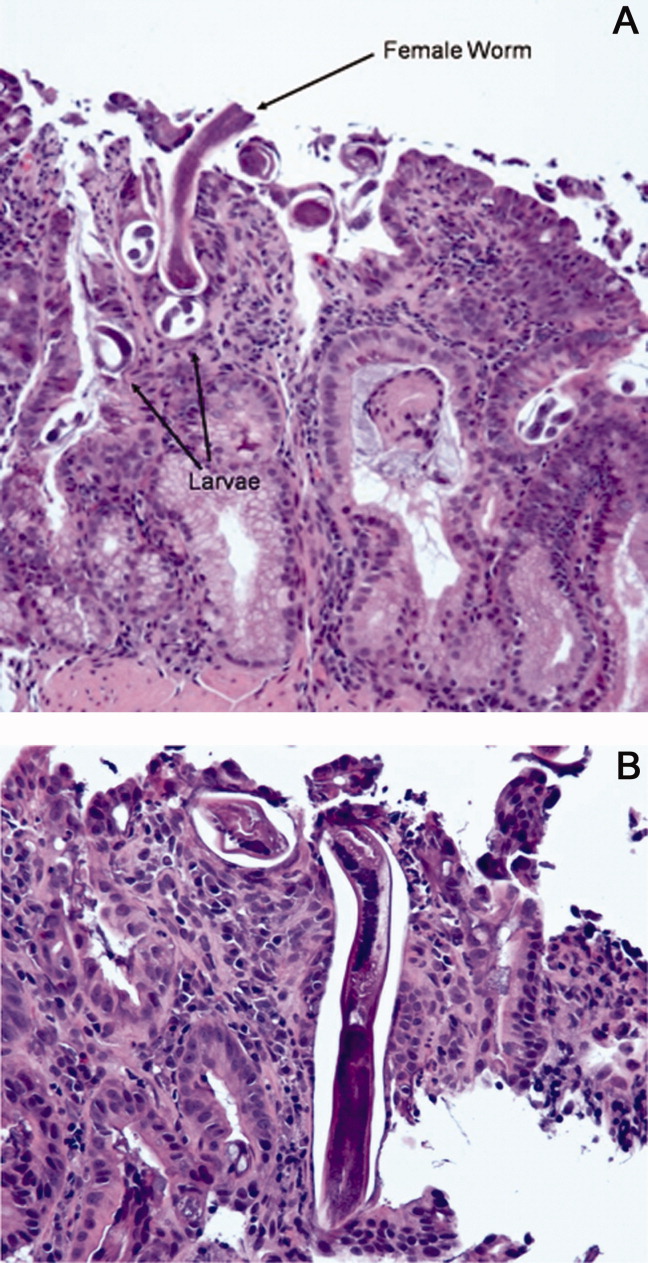
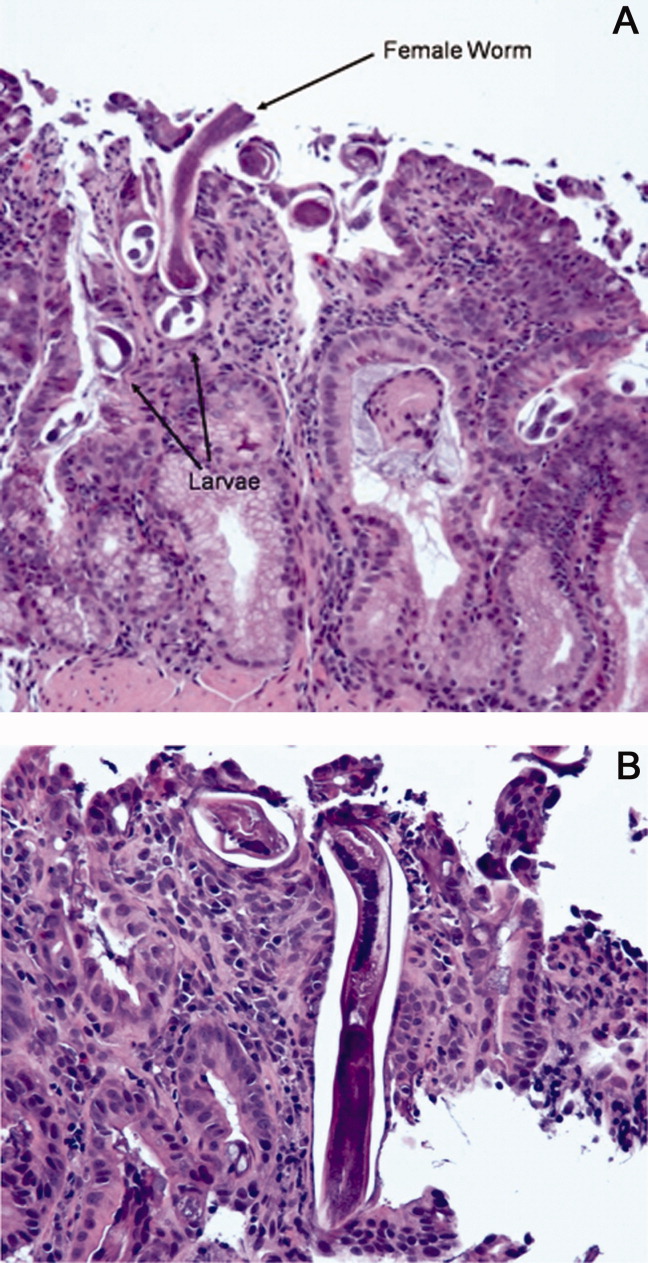
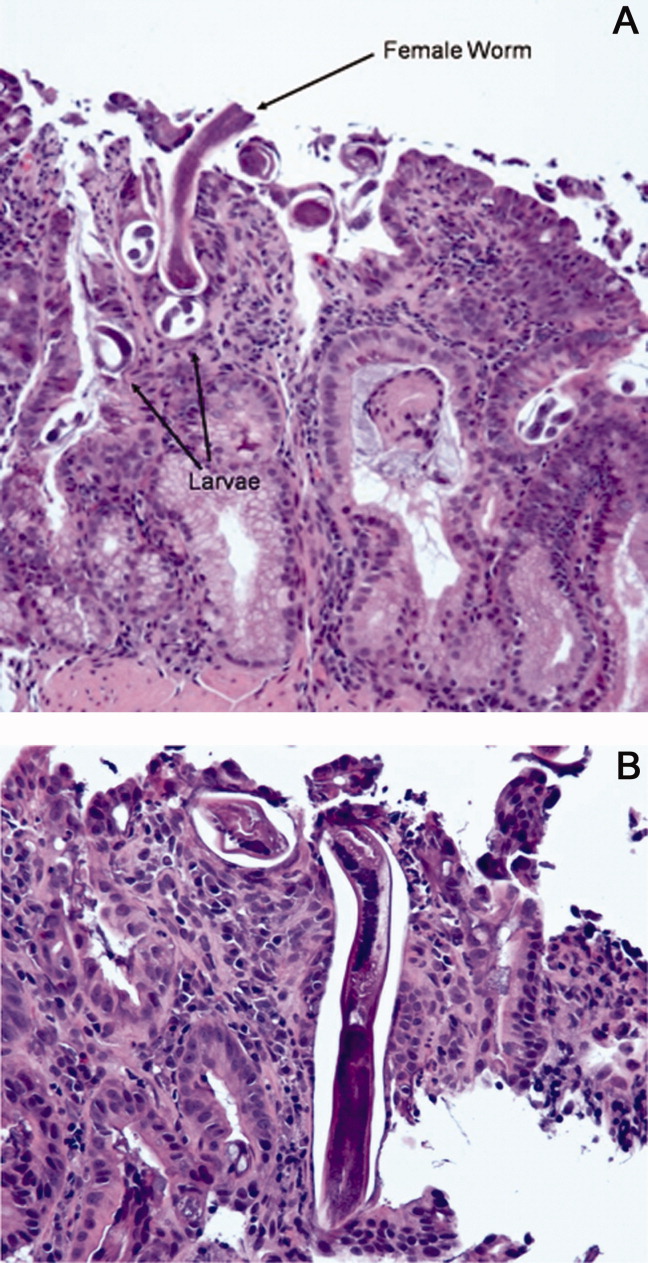
The patient was treated with intravenous fluids and stress‐dose steroids, and electrolyte abnormalities were corrected. Biopsies from the EGD and colonoscopy demonstrated numerous larvae within the mucosa of the body and antrum of the stomach, as well as duodenum. There were also rare detached larvae seen in the esophagus, and a few larvae within the ileal mucosa.
The patient appears to have Strongyloides hyperinfection, something he is at clear risk for, given his country of origin and his high‐dose corticosteroids. In retrospect, I was dissuaded from seriously considering a diagnosis of parasitic infection in large part because of the absence of peripheral eosinophilia, but this may not be seen in cases of hyperinfection. Additional clues, again in retrospect, were the repeated abscesses with bowel flora and the seemingly nonspecific abdominal rash. I would treat with a course of ivermectin, and carefully monitor his response.
The characteristics of the larvae were suggestive of Strongyloides species (Figure 3). A subsequent stool test for ova and parasites was positive for Strongyloides larvae. The patient was given a single dose of ivermectin. An endocrinology consultant felt that he did not have adrenal insufficiency, and it was recommended that his steroids be tapered off. He was discharged home once he clinically improved.
Although one or two doses of ivermectin typically suffices for uncomplicated strongyloidiasis, the risk of failure in hyperinfection mandates a longer treatment course. I don't believe this patient has been adequately treated, although the removal of his steroids will be helpful.
He was readmitted 3 days later with recrudescent symptoms, and his stool remained positive for Strongyloides. He received 2 weeks of ivermectin and albendazole, and was ultimately discharged to a rehabilitation facility after a complicated hospital stay. Nine months later, the patient was reported to be doing well.
COMMENTARY
This patient's immigration status from the developing world, high‐dose corticosteroid use, and complex clinical course all suggested the possibility of an underlying chronic infectious process. Although the discussant recognized this early on and later briefly mentioned strongyloidiasis as a potential cause of intestinal obstruction, the diagnosis of Strongyloides hyperinfection was not suspected until incontrovertible evidence for it was obtained on EGD. Failure to make the diagnosis earlier by both the involved clinicians and the discussant probably stemmed largely from two factors: the absence of eosinophilia; and lack of recognition that purpura may be seen in cases of hyperinfection, presumably reflecting larval infiltration of the dermis.1 Although eosinophilia accompanies most cases of stronglyloidiasis and may be very pronounced, patients with hyperinfection syndrome frequently fail to mount an eosinophilic response due to underlying immunosuppression, with eosinophilia absent in 70% of such patients in a study from Taiwan.2
Strongyloides stercoralis is an intestinal nematode that causes strongyloidiasis. It affects as many as 100 million people globally,3 mainly in tropical and subtropical areas, but is also endemic in the Southeastern United States, Europe, and Japan. Risk factors include male sex, White race, alcoholism, working in contact with soil (farmers, coal mine workers, etc.), chronic care institutionalization, and low socioeconomic status. In nonendemic regions, it more commonly affects travelers, immigrants, or military personnel.4, 5
The life cycle of S. stercoralis is complex. Infective larvae penetrate the skin through contact with contaminated soil, enter the venous system via lymphatics, and travel to the lung.4, 6 Here, they ascend the tracheobronchial tree and migrate to the gut. In the intestine, larvae develop into adult female worms that burrow into the intestinal mucosa. These worms lay eggs that develop into noninfective rhabditiform larvae, which are then expelled in the stool. Some of the rhabditiform larvae, however, develop into infective filariform larvae, which may penetrate colonic mucosa or perianal skin, enter the bloodstream, and lead to the cycle of autoinfection and chronic strongyloidiasis (carrier state). Autoinfection typically involves a low parasite burden, and is controlled by both host immune factors as well as parasitic factors.7 The mechanism of autoinfection can lead to the persistence of strongyloidiasis for decades after the initial infection, as has been documented in former World War II prisoners of war.8
Factors leading to the impairment of cell‐mediated immunity predispose chronically infected individuals to hyperinfection, as occurred in this patient. The most important of these are corticosteroid administration and Human T‐lymphotropic virus Type‐1 (HTLV‐1) infection, both of which cause significant derangement in TH1/TH2 immune system balance.5, 9 In the hyperinfection syndrome, the burden of parasites increases dramatically, leading to a variety of clinical manifestations. Gastrointestinal phenomena frequently predominate, including watery diarrhea, anorexia, weight loss, nausea/vomiting, gastrointestinal bleeding, and occasionally small bowel obstruction. Pulmonary manifestations are likewise common, and include cough, dyspnea, and wheezing. Cutaneous findings are not uncommon, classically pruritic linear lesions of the abdomen, buttocks, and lower extremities which may be rapidly migratory (larva currens), although purpura and petechiae as displayed by our patient appear to be under‐recognized findings in hyperinfection.2, 5 Gram‐negative bacillary meningitis has been well reported as a complication of migrating larvae, and a wide variety of other organs may rarely be involved.5, 10
The presence of chronic strongyloidiasis should be suspected in patients with ongoing gastrointestinal and/or pulmonary symptoms, or unexplained eosinophilia with a potential exposure history, such as immigrants from Southeast Asia. Diagnosis in these individuals is currently most often made serologically, although stool exam provides a somewhat higher specificity for active infection, at the expense of lower sensitivity.3, 11 In the setting of hyperinfection, stool studies are almost uniformly positive for S. stercoralis, and sputum may be diagnostic as well. Consequently, failure to reach the diagnosis usually reflects a lack of clinical suspicion.5
The therapy of choice for strongyloidiasis is currently ivermectin, with a single dose repeated once, 2 weeks later, highly efficacious in eradicating chronic infection. Treatment of hyperinfection is more challenging and less well studied, but clearly necessitates a more prolonged course of treatment. Many experts advocate treating until worms are no longer present in the stool; some have suggested the combination of ivermectin and albendazole as this patient received, although this has not been examined in controlled fashion.
The diagnosis of Strongyloides hyperinfection is typically delayed or missed because of the failure to consider it, with reported mortality rates as high as 50% in hyperinfection and 87% in disseminated disease.3, 12, 13 This patient fortunately was diagnosed, albeit in delayed fashion, proving the maxim better late than never. His case highlights the need for increased clinical awareness of strongyloidiasis, and specifically the need to consider the possibility of chronic Strongyloides infection prior to administering immunosuppressive medications. In particular, serologic screening of individuals from highly endemic areas for strongyloidiasis, when initiating extended courses of corticosteroids, seems prudent.13
Teaching Points
-
Chronic strongyloidiasis is common in the developing world (particularly Southeast Asia), and places infected individuals at significant risk of life‐threatening hyperinfection if not recognized and treated prior to the initiation of immunosuppressive medication, especially corticosteroids.
-
Strongyloides hyperinfection syndrome may be protean in its manifestations, but most commonly includes gastrointestinal, pulmonary, and cutaneous signs and symptoms.
- ,,, et al.Disseminated strongyloidiasis in immunocompromised patients—report of three cases.Int J Dermatol.2009;48(9):975–978.
- ,,, et al.Clinical manifestations of strongyloidiasis in southern Taiwan.J Microbiol Immunol Infect.2002;35(1):29–36.
- ,.Diagnosis of Strongyloides stercoralis infection.Clin Infect Dis.2001;33(7):1040–1047.
- ,,.Intestinal strongyloidiasis and hyperinfection syndrome.Clin Mol Allergy.2006;4:8.
- ,.Strongyloides stercoralis in the immunocompromised population.Clin Microbiol Rev.2004;17(1):208–217.
- ,,.Intestinal strongyloidiasis: recognition, management and determinants of outcome.J Clin Gastroenterol2005;39(3):203–211.
- .Dysregulation of strongyloidiasis: a new hypothesis.Clin Microbiol Rev.1992;5(4):345–355.
- ,,,.Consequences of captivity: health effects of Far East imprisonment in World War II.Q J Med.2009;102:87–96.
- ,,,.Strongyloides hyperinfection syndrome: an emerging global infectious disease.Trans R Soc Trop Med Hyg.2008;102(4):314–318.
- ,,,,,.Strongyloides hyperinfection presenting as acute respiratory failure and Gram‐negative sepsis.Chest.2005;128(5):3681–3684.
- ,,, et al.Use of enzyme‐linked immunosorbent assay and dipstick assay for detection of Strongyloides stercoralis infection in humans.J Clin Microbiol.2007;45:438–442.
- ,,,,,.Complicated and fatal Strongyloides infection in Canadians: risk factors, diagnosis and management.Can Med Assoc J.2004;171:479–484.
- ,,, et al.Maltreatment of Strongyloides infection: case series and worldwide physicians‐in‐training survey.Am J Med.2007;120(6):545.e1–545.e8.
A 59‐year‐old man presented to the emergency department with the acute onset of right‐sided abdominal and flank pain. The pain had begun the previous night, was constant and progressively worsening, and radiated to his right groin. He denied fever, nausea, emesis, or change in his bowel habits, but he did notice mild right lower quadrant discomfort with micturition. Upon further questioning, he also complained of mild dyspnea on climbing stairs and an unspecified recent weight loss.
The most common cause of acute severe right‐sided flank and abdominal pain radiating to the groin and associated with dysuria in a middle‐aged man is ureteral colic. Other etiologies important to consider include retrocecal appendicitis, pyelonephritis, and, rarely, a dissecting abdominal aortic aneurysm. This patient's seemingly recent onset exertional dyspnea and weight loss do not neatly fit any of the above, however.
His past medical history was significant for diabetes mellitus and pemphigus vulgaris diagnosed 7 months previously. He had been treated with prednisone, and the dose decreased from 100 to 60 mg daily, 1 month previously, due to poor glycemic control as well as steroid‐induced neuropathy and myopathy. His other medications included naproxen sodium and ibuprofen for back pain, azathioprine, insulin, pioglitazone, and glimiperide. He had no past surgical history. He had lived in the United States since his emigration from Thailand in 1971. His last trip to Thailand was 5 years previously. He was a taxi cab driver. He had a ten‐pack year history of tobacco use, but had quit 20 years prior. He denied history of alcohol or intravenous drug use.
Pemphigus vulgaris is unlikely to be directly related to this patient's presentation, but in light of his poorly controlled diabetes, his azathioprine use, and particularly his high‐dose corticosteroids, he is certainly immunocompromised. Accordingly, a disseminated infection, either newly acquired or reactivated, merits consideration. His history of residence in, and subsequent travel to, Southeast Asia raises the possibility of several diseases, each of which may be protean in their manifestations; these include tuberculosis, melioidosis, and penicilliosis (infection with Penicillium marneffei). The first two may reactivate long after initial exposure, particularly with insults to the immune system. The same is probably true of penicilliosis, although I am not certain of this. On a slightly less exotic note, domestically acquired infection with histoplasmosis or other endemic fungi is possible.
On examination he was afebrile, had a pulse of 130 beats per minute and a blood pressure of 65/46 mmHg. His oxygen saturation was 92%. He appeared markedly cushingoid, and had mild pallor and generalized weakness. Cardiopulmonary examination was unremarkable. His abdominal exam was notable for distention and hypoactive bowel sounds, with tenderness and firmness to palpation on the right side. Peripheral pulses were normal. Examination of the skin demonstrated ecchymoses over the bilateral forearms, and several healed pemphigus lesions on the abdomen and upper extremities.
The patient's severely deranged hemodynamic parameters indicate either current or impending shock, and resuscitative measures should proceed in tandem with diagnostic efforts. The cause of his shock seems most likely to be either hypovolemic (abdominal wall or intra‐abdominal hemorrhage, or conceivably massive third spacing from an intra‐abdominal catastrophe), or distributive (sepsis, or acute adrenal insufficiency if he has missed recent steroid doses). His ecchymoses may simply reflect chronic glucocorticoid use, but also raise suspicion for a coagulopathy. Provided the patient can be stabilized to allow this, I would urgently obtain a computed tomography (CT) scan of the abdomen and pelvis.
Initial laboratory studies demonstrated a hemoglobin of 9.1 g/dL, white blood cell count 8000/L with 33% bands, 48% segmented neutrophils, 18% lymphocytes, and 0.7% eosinophils, platelet count 356,000/L, sodium 128 mmol/L, BUN 52 mg/dL, creatinine 2.3 mg/dL, and glucose of 232 mg/dL. Coagulation studies were normal, and lactic acid was 1.8 mmol/L (normal range, 0.7‐2.1). Fibrinogen was normal at 591 and LDH was mildly elevated at 654 (normal range, 313‐618 U/L). Total protein and albumin were 3.6 and 1.9 g/dL, respectively. Total bilirubin was 0.6 mg/dL. Random serum cortisol was 20.2 g/dL. Liver enzymes, amylase, lipase, iron stores, B12, folate, and stool for occult blood were normal. Initial cardiac biomarkers were negative, but subsequent troponin‐I was 3.81 ng/mL (elevated, >1.00). Urinalysis showed 0‐4 white blood cells per high powered field.
The laboratory studies provide a variety of useful, albeit nonspecific, information. The high percentage of band forms on white blood cell differential further raises concern for an infectious process, although severe noninfectious stress can also cause this. While we do not know whether the patient's renal failure is acute, I suspect that it is, and may result from a variety of insults including sepsis, hypotension, and volume depletion. His moderately elevated troponin‐I likely reflects supplydemand mismatch or sepsis. I would like to see an electrocardiogram, and I remain very interested in obtaining abdominal imaging.
Chest radiography showed pulmonary vascular congestion without evidence of pneumothorax. Computed tomography scan of the abdomen and pelvis showed retroperitoneal fluid bilaterally (Figure 1). This was described as suspicious for ascites versus hemorrhage, but no obvious source of bleeding was identified. There was also a small amount of right perinephric fluid, but no evidence of a renal mass. The abdominal aorta was normal; there was no lymphadenopathy.

The CT image appears to speak against simple ascites, and seems most consistent with either blood or an infectious process. Consequently, the loculated right retroperitoneal collection should be aspirated, and fluid sent for fungal, acid‐fast, and modified acid‐fast (i.e., for Nocardia) stains and culture, in addition to Gram stain and routine aerobic and anaerobic cultures.
The patient was admitted to the intensive care unit. Stress‐dose steroids were administered, and he improved after resuscitation with fluid and blood. His renal function normalized. Urine and blood cultures returned negative. His hematocrit and multiple repeat CT scans of the abdomen remained stable. A retroperitoneal hemorrhage was diagnosed, and surgical intervention was deemed unnecessary. Both adenosine thallium stress test and echocardiogram were normal. He was continued on 60 mg prednisone daily and discharged home with outpatient follow‐up.
This degree of improvement with volume expansion (and steroids) suggests the patient was markedly volume depleted upon presentation. Although a formal adrenocorticotropic hormone (ACTH) stimulation test was apparently not performed, the random cortisol level suggests adrenal insufficiency was unlikely to have been primarily responsible. While retroperitoneal hemorrhage is possible, the loculated appearance of the collection suggests infection is more likely.
Three weeks later, he was readmitted with recurrent right‐sided abdominal and flank pain. His temperature was 101.3F, and he was tachycardic and hypotensive. His examination was similar to that at the time of his previous presentation. Laboratory data revealed white blood cell count of 13,100/L with 43% bands, hemoglobin of 9.2 g/dL, glucose of 343 mg/dL, bicarbonate 25 mmol/L, normal anion gap and renal function, and lactic acid of 4.5 mmol/L. Liver function tests were normal except for an albumin of 3.0 g/dL. CT scan of the abdomen revealed loculated retroperitoneal fluid collections, increased in size since the prior scan.
The patient is once again evidencing at least early shock, manifested in his deranged hemodynamics and elevated lactate level. I remain puzzled by the fact that he appeared to respond to fluids alone at the time of his initial hospital stay, unless adrenal insufficiency played a greater role than I suspected. Of note, acute adrenal insufficiency could explain much of the current picture, including fever, and bland (uninfected) hematomas are an underappreciated cause of both fever and leukocytosis. Having said this, I remain concerned that his retroperitoneal fluid collections represent abscesses. The most accessible of these should be sampled.
Aspiration of the retroperitoneal fluid yielded purulent material which grew Klebsiella pneumoniae. The cultures were negative for mycobacteria and fungus. Blood and urine cultures were negative. Drains were placed, and he was followed as an outpatient. His fever and leukocytosis subsided, and he completed a 6‐week course of trimethoprim‐sulfamethoxazole. CT imaging confirmed complete evacuation of the fluid.
Retroperitoneal abscesses frequently present in smoldering fashion, although patients may be quite ill by the time of presentation. Most of these are secondary, i.e., they arise from another abnormality in the retroperitoneum. Most commonly this is in the large bowel, kidney, pancreas, or spine. I would carefully scour his follow‐up imaging for additional clues and, if unrevealing, proceed to colonoscopy.
He returned 1 month after drain removal, with 2‐3 days of nausea and abdominal pain. His abdomen was moderately distended but nontender, and multiple persistent petechial and purpuric lesions were present on the upper back, chest, torso, and arms. Abdominal CT scan revealed small bowel obstruction and a collection of fluid in the left paracolic gutter extending into the left retrorenal space.
The patient does not appear to have obvious risk factors for developing a small bowel obstruction. No mention is made of the presence or absence of a transition point on the CT scan, and this should be ascertained. His left‐sided abdominal fluid collection is probably infectious in nature, and I continue to be suspicious of a large bowel (or distal small bowel) source, via either gut perforation or bacterial translocation. The collection needs to be percutaneously drained for both diagnostic and therapeutic reasons, and broadly cultured. Finally, we need to account for the described dermatologic manifestations. The purpuric/petechial lesions sound vasculitic rather than thrombocytopenic in origin based on location; conversely, they may simply reflect a corticosteroid‐related adverse effect. I would like to know whether the purpura was palpable, and to repeat a complete blood count with peripheral smear.
Laboratory data showed hemoglobin of 9.3 g/dL, a platelet count of 444,000/L, and normal coagulation studies. The purpura was nonpalpable (Figure 2). The patient had a nasogastric tube placed for decompression, with bilious drainage. His left retroperitoneal fluid was drained, with cultures yielding Enterococcus faecalis and Enterobacter cloacae. The patient was treated with a course of broad‐spectrum antibiotics. His obstruction improved and the retroperitoneal collection resolved on follow‐up imaging. However, 2 days later, he had recurrent pain; abdominal CT showed a recurrence of small bowel obstruction with an unequivocal transition point in the distal jejunum. A small fluid collection was noted in the left retroperitoneum with a trace of gas in it. He improved with nasogastric suction, his prednisone was tapered to 30 mg daily, and he was discharged home.
The isolation of both Enterococcus and Enterobacter species from his fluid collection, along with the previous isolation of Klebsiella, strongly suggest a bowel source for his recurrent abscesses. Based on this CT report, the patient has clear evidence of at least partial small bowel obstruction. He lacks a history of prior abdominal surgery or other more typical reasons for obstruction caused by extrinsic compression, such as hernia, although it is possible his recurrent abdominal infections may have led to obstruction due to scarring and adhesions. An intraluminal cause of obstruction also needs to be considered, with causes including malignancy (lymphoma, carcinoid, and adenocarcinoma), Crohn's disease, and infections including tuberculosis as well as parasites such as Taenia and Strongyloides. While the purpura is concerning, given the nonpalpable character along with a normal platelet count and coagulation studies, it may be reasonable to provisionally attribute it to high‐dose corticosteroid use.
He was admitted a fourth time a week after being discharged, with nausea, generalized weakness, and weight loss. At presentation, he had a blood pressure of 95/65 mmHg. His white blood cell count was 5,900/L, with 79% neutrophils and 20% bands. An AM cortisol was 18.8 /dL. He was thought to have adrenal insufficiency from steroid withdrawal, was treated with intravenous fluids and steroids, and discharged on a higher dose of prednisone at 60 mg daily. One week later, he again returned to the hospital with watery diarrhea, emesis, and generalized weakness. His blood pressure was 82/50 mmHg, and his abdomen appeared benign. He also had an erythematous rash over his mid‐abdomen. Laboratory data was significant for a sodium of 127 mmol/L, potassium of 3.0 mmol/L, chloride of 98 mmol/L, bicarbonate of 26 mmol/L, glucose of 40 mg/dL, lactate of 14 mmol/L, and albumin of 1.0 g/dL. Stool assay for Clostridium difficile was negative. A CT scan of the abdomen and pelvis showed small bilateral pleural effusions and small bowel fluid consistent with gastroenteritis, but without signs of obstruction. Esophagogastroduodenoscopy (EGD) showed bile backwash into the stomach, as well as inflammatory changes in the proximal and mid‐stomach, and inflammatory reaction and edema in the proximal duodenum. Colonoscopy showed normal appearing ileum and colon.
The patient's latest laboratory values appear to reflect his chronic illness and superimposed diarrhea. I am perplexed by his markedly elevated serum lactate value in association with a normal bicarbonate and low anion gap, and would repeat the lactate level to ensure this is not spurious. His hypoglycemia probably reflects a failure to adjust or discontinue his diabetic medications, although both hypoglycemia and type B lactic acidosis are occasionally manifestations of a paraneoplastic syndrome. The normal colonoscopy findings are helpful in exonerating the colon, provided the preparation was adequate. Presumably, the abnormal areas of the stomach and duodenum were biopsied; I remain suspicious that the answer may lie in the jejunum.
The patient was treated with intravenous fluids and stress‐dose steroids, and electrolyte abnormalities were corrected. Biopsies from the EGD and colonoscopy demonstrated numerous larvae within the mucosa of the body and antrum of the stomach, as well as duodenum. There were also rare detached larvae seen in the esophagus, and a few larvae within the ileal mucosa.
The patient appears to have Strongyloides hyperinfection, something he is at clear risk for, given his country of origin and his high‐dose corticosteroids. In retrospect, I was dissuaded from seriously considering a diagnosis of parasitic infection in large part because of the absence of peripheral eosinophilia, but this may not be seen in cases of hyperinfection. Additional clues, again in retrospect, were the repeated abscesses with bowel flora and the seemingly nonspecific abdominal rash. I would treat with a course of ivermectin, and carefully monitor his response.
The characteristics of the larvae were suggestive of Strongyloides species (Figure 3). A subsequent stool test for ova and parasites was positive for Strongyloides larvae. The patient was given a single dose of ivermectin. An endocrinology consultant felt that he did not have adrenal insufficiency, and it was recommended that his steroids be tapered off. He was discharged home once he clinically improved.
Although one or two doses of ivermectin typically suffices for uncomplicated strongyloidiasis, the risk of failure in hyperinfection mandates a longer treatment course. I don't believe this patient has been adequately treated, although the removal of his steroids will be helpful.
He was readmitted 3 days later with recrudescent symptoms, and his stool remained positive for Strongyloides. He received 2 weeks of ivermectin and albendazole, and was ultimately discharged to a rehabilitation facility after a complicated hospital stay. Nine months later, the patient was reported to be doing well.
COMMENTARY
This patient's immigration status from the developing world, high‐dose corticosteroid use, and complex clinical course all suggested the possibility of an underlying chronic infectious process. Although the discussant recognized this early on and later briefly mentioned strongyloidiasis as a potential cause of intestinal obstruction, the diagnosis of Strongyloides hyperinfection was not suspected until incontrovertible evidence for it was obtained on EGD. Failure to make the diagnosis earlier by both the involved clinicians and the discussant probably stemmed largely from two factors: the absence of eosinophilia; and lack of recognition that purpura may be seen in cases of hyperinfection, presumably reflecting larval infiltration of the dermis.1 Although eosinophilia accompanies most cases of stronglyloidiasis and may be very pronounced, patients with hyperinfection syndrome frequently fail to mount an eosinophilic response due to underlying immunosuppression, with eosinophilia absent in 70% of such patients in a study from Taiwan.2
Strongyloides stercoralis is an intestinal nematode that causes strongyloidiasis. It affects as many as 100 million people globally,3 mainly in tropical and subtropical areas, but is also endemic in the Southeastern United States, Europe, and Japan. Risk factors include male sex, White race, alcoholism, working in contact with soil (farmers, coal mine workers, etc.), chronic care institutionalization, and low socioeconomic status. In nonendemic regions, it more commonly affects travelers, immigrants, or military personnel.4, 5
The life cycle of S. stercoralis is complex. Infective larvae penetrate the skin through contact with contaminated soil, enter the venous system via lymphatics, and travel to the lung.4, 6 Here, they ascend the tracheobronchial tree and migrate to the gut. In the intestine, larvae develop into adult female worms that burrow into the intestinal mucosa. These worms lay eggs that develop into noninfective rhabditiform larvae, which are then expelled in the stool. Some of the rhabditiform larvae, however, develop into infective filariform larvae, which may penetrate colonic mucosa or perianal skin, enter the bloodstream, and lead to the cycle of autoinfection and chronic strongyloidiasis (carrier state). Autoinfection typically involves a low parasite burden, and is controlled by both host immune factors as well as parasitic factors.7 The mechanism of autoinfection can lead to the persistence of strongyloidiasis for decades after the initial infection, as has been documented in former World War II prisoners of war.8
Factors leading to the impairment of cell‐mediated immunity predispose chronically infected individuals to hyperinfection, as occurred in this patient. The most important of these are corticosteroid administration and Human T‐lymphotropic virus Type‐1 (HTLV‐1) infection, both of which cause significant derangement in TH1/TH2 immune system balance.5, 9 In the hyperinfection syndrome, the burden of parasites increases dramatically, leading to a variety of clinical manifestations. Gastrointestinal phenomena frequently predominate, including watery diarrhea, anorexia, weight loss, nausea/vomiting, gastrointestinal bleeding, and occasionally small bowel obstruction. Pulmonary manifestations are likewise common, and include cough, dyspnea, and wheezing. Cutaneous findings are not uncommon, classically pruritic linear lesions of the abdomen, buttocks, and lower extremities which may be rapidly migratory (larva currens), although purpura and petechiae as displayed by our patient appear to be under‐recognized findings in hyperinfection.2, 5 Gram‐negative bacillary meningitis has been well reported as a complication of migrating larvae, and a wide variety of other organs may rarely be involved.5, 10
The presence of chronic strongyloidiasis should be suspected in patients with ongoing gastrointestinal and/or pulmonary symptoms, or unexplained eosinophilia with a potential exposure history, such as immigrants from Southeast Asia. Diagnosis in these individuals is currently most often made serologically, although stool exam provides a somewhat higher specificity for active infection, at the expense of lower sensitivity.3, 11 In the setting of hyperinfection, stool studies are almost uniformly positive for S. stercoralis, and sputum may be diagnostic as well. Consequently, failure to reach the diagnosis usually reflects a lack of clinical suspicion.5
The therapy of choice for strongyloidiasis is currently ivermectin, with a single dose repeated once, 2 weeks later, highly efficacious in eradicating chronic infection. Treatment of hyperinfection is more challenging and less well studied, but clearly necessitates a more prolonged course of treatment. Many experts advocate treating until worms are no longer present in the stool; some have suggested the combination of ivermectin and albendazole as this patient received, although this has not been examined in controlled fashion.
The diagnosis of Strongyloides hyperinfection is typically delayed or missed because of the failure to consider it, with reported mortality rates as high as 50% in hyperinfection and 87% in disseminated disease.3, 12, 13 This patient fortunately was diagnosed, albeit in delayed fashion, proving the maxim better late than never. His case highlights the need for increased clinical awareness of strongyloidiasis, and specifically the need to consider the possibility of chronic Strongyloides infection prior to administering immunosuppressive medications. In particular, serologic screening of individuals from highly endemic areas for strongyloidiasis, when initiating extended courses of corticosteroids, seems prudent.13
Teaching Points
-
Chronic strongyloidiasis is common in the developing world (particularly Southeast Asia), and places infected individuals at significant risk of life‐threatening hyperinfection if not recognized and treated prior to the initiation of immunosuppressive medication, especially corticosteroids.
-
Strongyloides hyperinfection syndrome may be protean in its manifestations, but most commonly includes gastrointestinal, pulmonary, and cutaneous signs and symptoms.
A 59‐year‐old man presented to the emergency department with the acute onset of right‐sided abdominal and flank pain. The pain had begun the previous night, was constant and progressively worsening, and radiated to his right groin. He denied fever, nausea, emesis, or change in his bowel habits, but he did notice mild right lower quadrant discomfort with micturition. Upon further questioning, he also complained of mild dyspnea on climbing stairs and an unspecified recent weight loss.
The most common cause of acute severe right‐sided flank and abdominal pain radiating to the groin and associated with dysuria in a middle‐aged man is ureteral colic. Other etiologies important to consider include retrocecal appendicitis, pyelonephritis, and, rarely, a dissecting abdominal aortic aneurysm. This patient's seemingly recent onset exertional dyspnea and weight loss do not neatly fit any of the above, however.
His past medical history was significant for diabetes mellitus and pemphigus vulgaris diagnosed 7 months previously. He had been treated with prednisone, and the dose decreased from 100 to 60 mg daily, 1 month previously, due to poor glycemic control as well as steroid‐induced neuropathy and myopathy. His other medications included naproxen sodium and ibuprofen for back pain, azathioprine, insulin, pioglitazone, and glimiperide. He had no past surgical history. He had lived in the United States since his emigration from Thailand in 1971. His last trip to Thailand was 5 years previously. He was a taxi cab driver. He had a ten‐pack year history of tobacco use, but had quit 20 years prior. He denied history of alcohol or intravenous drug use.
Pemphigus vulgaris is unlikely to be directly related to this patient's presentation, but in light of his poorly controlled diabetes, his azathioprine use, and particularly his high‐dose corticosteroids, he is certainly immunocompromised. Accordingly, a disseminated infection, either newly acquired or reactivated, merits consideration. His history of residence in, and subsequent travel to, Southeast Asia raises the possibility of several diseases, each of which may be protean in their manifestations; these include tuberculosis, melioidosis, and penicilliosis (infection with Penicillium marneffei). The first two may reactivate long after initial exposure, particularly with insults to the immune system. The same is probably true of penicilliosis, although I am not certain of this. On a slightly less exotic note, domestically acquired infection with histoplasmosis or other endemic fungi is possible.
On examination he was afebrile, had a pulse of 130 beats per minute and a blood pressure of 65/46 mmHg. His oxygen saturation was 92%. He appeared markedly cushingoid, and had mild pallor and generalized weakness. Cardiopulmonary examination was unremarkable. His abdominal exam was notable for distention and hypoactive bowel sounds, with tenderness and firmness to palpation on the right side. Peripheral pulses were normal. Examination of the skin demonstrated ecchymoses over the bilateral forearms, and several healed pemphigus lesions on the abdomen and upper extremities.
The patient's severely deranged hemodynamic parameters indicate either current or impending shock, and resuscitative measures should proceed in tandem with diagnostic efforts. The cause of his shock seems most likely to be either hypovolemic (abdominal wall or intra‐abdominal hemorrhage, or conceivably massive third spacing from an intra‐abdominal catastrophe), or distributive (sepsis, or acute adrenal insufficiency if he has missed recent steroid doses). His ecchymoses may simply reflect chronic glucocorticoid use, but also raise suspicion for a coagulopathy. Provided the patient can be stabilized to allow this, I would urgently obtain a computed tomography (CT) scan of the abdomen and pelvis.
Initial laboratory studies demonstrated a hemoglobin of 9.1 g/dL, white blood cell count 8000/L with 33% bands, 48% segmented neutrophils, 18% lymphocytes, and 0.7% eosinophils, platelet count 356,000/L, sodium 128 mmol/L, BUN 52 mg/dL, creatinine 2.3 mg/dL, and glucose of 232 mg/dL. Coagulation studies were normal, and lactic acid was 1.8 mmol/L (normal range, 0.7‐2.1). Fibrinogen was normal at 591 and LDH was mildly elevated at 654 (normal range, 313‐618 U/L). Total protein and albumin were 3.6 and 1.9 g/dL, respectively. Total bilirubin was 0.6 mg/dL. Random serum cortisol was 20.2 g/dL. Liver enzymes, amylase, lipase, iron stores, B12, folate, and stool for occult blood were normal. Initial cardiac biomarkers were negative, but subsequent troponin‐I was 3.81 ng/mL (elevated, >1.00). Urinalysis showed 0‐4 white blood cells per high powered field.
The laboratory studies provide a variety of useful, albeit nonspecific, information. The high percentage of band forms on white blood cell differential further raises concern for an infectious process, although severe noninfectious stress can also cause this. While we do not know whether the patient's renal failure is acute, I suspect that it is, and may result from a variety of insults including sepsis, hypotension, and volume depletion. His moderately elevated troponin‐I likely reflects supplydemand mismatch or sepsis. I would like to see an electrocardiogram, and I remain very interested in obtaining abdominal imaging.
Chest radiography showed pulmonary vascular congestion without evidence of pneumothorax. Computed tomography scan of the abdomen and pelvis showed retroperitoneal fluid bilaterally (Figure 1). This was described as suspicious for ascites versus hemorrhage, but no obvious source of bleeding was identified. There was also a small amount of right perinephric fluid, but no evidence of a renal mass. The abdominal aorta was normal; there was no lymphadenopathy.

The CT image appears to speak against simple ascites, and seems most consistent with either blood or an infectious process. Consequently, the loculated right retroperitoneal collection should be aspirated, and fluid sent for fungal, acid‐fast, and modified acid‐fast (i.e., for Nocardia) stains and culture, in addition to Gram stain and routine aerobic and anaerobic cultures.
The patient was admitted to the intensive care unit. Stress‐dose steroids were administered, and he improved after resuscitation with fluid and blood. His renal function normalized. Urine and blood cultures returned negative. His hematocrit and multiple repeat CT scans of the abdomen remained stable. A retroperitoneal hemorrhage was diagnosed, and surgical intervention was deemed unnecessary. Both adenosine thallium stress test and echocardiogram were normal. He was continued on 60 mg prednisone daily and discharged home with outpatient follow‐up.
This degree of improvement with volume expansion (and steroids) suggests the patient was markedly volume depleted upon presentation. Although a formal adrenocorticotropic hormone (ACTH) stimulation test was apparently not performed, the random cortisol level suggests adrenal insufficiency was unlikely to have been primarily responsible. While retroperitoneal hemorrhage is possible, the loculated appearance of the collection suggests infection is more likely.
Three weeks later, he was readmitted with recurrent right‐sided abdominal and flank pain. His temperature was 101.3F, and he was tachycardic and hypotensive. His examination was similar to that at the time of his previous presentation. Laboratory data revealed white blood cell count of 13,100/L with 43% bands, hemoglobin of 9.2 g/dL, glucose of 343 mg/dL, bicarbonate 25 mmol/L, normal anion gap and renal function, and lactic acid of 4.5 mmol/L. Liver function tests were normal except for an albumin of 3.0 g/dL. CT scan of the abdomen revealed loculated retroperitoneal fluid collections, increased in size since the prior scan.
The patient is once again evidencing at least early shock, manifested in his deranged hemodynamics and elevated lactate level. I remain puzzled by the fact that he appeared to respond to fluids alone at the time of his initial hospital stay, unless adrenal insufficiency played a greater role than I suspected. Of note, acute adrenal insufficiency could explain much of the current picture, including fever, and bland (uninfected) hematomas are an underappreciated cause of both fever and leukocytosis. Having said this, I remain concerned that his retroperitoneal fluid collections represent abscesses. The most accessible of these should be sampled.
Aspiration of the retroperitoneal fluid yielded purulent material which grew Klebsiella pneumoniae. The cultures were negative for mycobacteria and fungus. Blood and urine cultures were negative. Drains were placed, and he was followed as an outpatient. His fever and leukocytosis subsided, and he completed a 6‐week course of trimethoprim‐sulfamethoxazole. CT imaging confirmed complete evacuation of the fluid.
Retroperitoneal abscesses frequently present in smoldering fashion, although patients may be quite ill by the time of presentation. Most of these are secondary, i.e., they arise from another abnormality in the retroperitoneum. Most commonly this is in the large bowel, kidney, pancreas, or spine. I would carefully scour his follow‐up imaging for additional clues and, if unrevealing, proceed to colonoscopy.
He returned 1 month after drain removal, with 2‐3 days of nausea and abdominal pain. His abdomen was moderately distended but nontender, and multiple persistent petechial and purpuric lesions were present on the upper back, chest, torso, and arms. Abdominal CT scan revealed small bowel obstruction and a collection of fluid in the left paracolic gutter extending into the left retrorenal space.
The patient does not appear to have obvious risk factors for developing a small bowel obstruction. No mention is made of the presence or absence of a transition point on the CT scan, and this should be ascertained. His left‐sided abdominal fluid collection is probably infectious in nature, and I continue to be suspicious of a large bowel (or distal small bowel) source, via either gut perforation or bacterial translocation. The collection needs to be percutaneously drained for both diagnostic and therapeutic reasons, and broadly cultured. Finally, we need to account for the described dermatologic manifestations. The purpuric/petechial lesions sound vasculitic rather than thrombocytopenic in origin based on location; conversely, they may simply reflect a corticosteroid‐related adverse effect. I would like to know whether the purpura was palpable, and to repeat a complete blood count with peripheral smear.
Laboratory data showed hemoglobin of 9.3 g/dL, a platelet count of 444,000/L, and normal coagulation studies. The purpura was nonpalpable (Figure 2). The patient had a nasogastric tube placed for decompression, with bilious drainage. His left retroperitoneal fluid was drained, with cultures yielding Enterococcus faecalis and Enterobacter cloacae. The patient was treated with a course of broad‐spectrum antibiotics. His obstruction improved and the retroperitoneal collection resolved on follow‐up imaging. However, 2 days later, he had recurrent pain; abdominal CT showed a recurrence of small bowel obstruction with an unequivocal transition point in the distal jejunum. A small fluid collection was noted in the left retroperitoneum with a trace of gas in it. He improved with nasogastric suction, his prednisone was tapered to 30 mg daily, and he was discharged home.
The isolation of both Enterococcus and Enterobacter species from his fluid collection, along with the previous isolation of Klebsiella, strongly suggest a bowel source for his recurrent abscesses. Based on this CT report, the patient has clear evidence of at least partial small bowel obstruction. He lacks a history of prior abdominal surgery or other more typical reasons for obstruction caused by extrinsic compression, such as hernia, although it is possible his recurrent abdominal infections may have led to obstruction due to scarring and adhesions. An intraluminal cause of obstruction also needs to be considered, with causes including malignancy (lymphoma, carcinoid, and adenocarcinoma), Crohn's disease, and infections including tuberculosis as well as parasites such as Taenia and Strongyloides. While the purpura is concerning, given the nonpalpable character along with a normal platelet count and coagulation studies, it may be reasonable to provisionally attribute it to high‐dose corticosteroid use.
He was admitted a fourth time a week after being discharged, with nausea, generalized weakness, and weight loss. At presentation, he had a blood pressure of 95/65 mmHg. His white blood cell count was 5,900/L, with 79% neutrophils and 20% bands. An AM cortisol was 18.8 /dL. He was thought to have adrenal insufficiency from steroid withdrawal, was treated with intravenous fluids and steroids, and discharged on a higher dose of prednisone at 60 mg daily. One week later, he again returned to the hospital with watery diarrhea, emesis, and generalized weakness. His blood pressure was 82/50 mmHg, and his abdomen appeared benign. He also had an erythematous rash over his mid‐abdomen. Laboratory data was significant for a sodium of 127 mmol/L, potassium of 3.0 mmol/L, chloride of 98 mmol/L, bicarbonate of 26 mmol/L, glucose of 40 mg/dL, lactate of 14 mmol/L, and albumin of 1.0 g/dL. Stool assay for Clostridium difficile was negative. A CT scan of the abdomen and pelvis showed small bilateral pleural effusions and small bowel fluid consistent with gastroenteritis, but without signs of obstruction. Esophagogastroduodenoscopy (EGD) showed bile backwash into the stomach, as well as inflammatory changes in the proximal and mid‐stomach, and inflammatory reaction and edema in the proximal duodenum. Colonoscopy showed normal appearing ileum and colon.
The patient's latest laboratory values appear to reflect his chronic illness and superimposed diarrhea. I am perplexed by his markedly elevated serum lactate value in association with a normal bicarbonate and low anion gap, and would repeat the lactate level to ensure this is not spurious. His hypoglycemia probably reflects a failure to adjust or discontinue his diabetic medications, although both hypoglycemia and type B lactic acidosis are occasionally manifestations of a paraneoplastic syndrome. The normal colonoscopy findings are helpful in exonerating the colon, provided the preparation was adequate. Presumably, the abnormal areas of the stomach and duodenum were biopsied; I remain suspicious that the answer may lie in the jejunum.
The patient was treated with intravenous fluids and stress‐dose steroids, and electrolyte abnormalities were corrected. Biopsies from the EGD and colonoscopy demonstrated numerous larvae within the mucosa of the body and antrum of the stomach, as well as duodenum. There were also rare detached larvae seen in the esophagus, and a few larvae within the ileal mucosa.
The patient appears to have Strongyloides hyperinfection, something he is at clear risk for, given his country of origin and his high‐dose corticosteroids. In retrospect, I was dissuaded from seriously considering a diagnosis of parasitic infection in large part because of the absence of peripheral eosinophilia, but this may not be seen in cases of hyperinfection. Additional clues, again in retrospect, were the repeated abscesses with bowel flora and the seemingly nonspecific abdominal rash. I would treat with a course of ivermectin, and carefully monitor his response.
The characteristics of the larvae were suggestive of Strongyloides species (Figure 3). A subsequent stool test for ova and parasites was positive for Strongyloides larvae. The patient was given a single dose of ivermectin. An endocrinology consultant felt that he did not have adrenal insufficiency, and it was recommended that his steroids be tapered off. He was discharged home once he clinically improved.
Although one or two doses of ivermectin typically suffices for uncomplicated strongyloidiasis, the risk of failure in hyperinfection mandates a longer treatment course. I don't believe this patient has been adequately treated, although the removal of his steroids will be helpful.
He was readmitted 3 days later with recrudescent symptoms, and his stool remained positive for Strongyloides. He received 2 weeks of ivermectin and albendazole, and was ultimately discharged to a rehabilitation facility after a complicated hospital stay. Nine months later, the patient was reported to be doing well.
COMMENTARY
This patient's immigration status from the developing world, high‐dose corticosteroid use, and complex clinical course all suggested the possibility of an underlying chronic infectious process. Although the discussant recognized this early on and later briefly mentioned strongyloidiasis as a potential cause of intestinal obstruction, the diagnosis of Strongyloides hyperinfection was not suspected until incontrovertible evidence for it was obtained on EGD. Failure to make the diagnosis earlier by both the involved clinicians and the discussant probably stemmed largely from two factors: the absence of eosinophilia; and lack of recognition that purpura may be seen in cases of hyperinfection, presumably reflecting larval infiltration of the dermis.1 Although eosinophilia accompanies most cases of stronglyloidiasis and may be very pronounced, patients with hyperinfection syndrome frequently fail to mount an eosinophilic response due to underlying immunosuppression, with eosinophilia absent in 70% of such patients in a study from Taiwan.2
Strongyloides stercoralis is an intestinal nematode that causes strongyloidiasis. It affects as many as 100 million people globally,3 mainly in tropical and subtropical areas, but is also endemic in the Southeastern United States, Europe, and Japan. Risk factors include male sex, White race, alcoholism, working in contact with soil (farmers, coal mine workers, etc.), chronic care institutionalization, and low socioeconomic status. In nonendemic regions, it more commonly affects travelers, immigrants, or military personnel.4, 5
The life cycle of S. stercoralis is complex. Infective larvae penetrate the skin through contact with contaminated soil, enter the venous system via lymphatics, and travel to the lung.4, 6 Here, they ascend the tracheobronchial tree and migrate to the gut. In the intestine, larvae develop into adult female worms that burrow into the intestinal mucosa. These worms lay eggs that develop into noninfective rhabditiform larvae, which are then expelled in the stool. Some of the rhabditiform larvae, however, develop into infective filariform larvae, which may penetrate colonic mucosa or perianal skin, enter the bloodstream, and lead to the cycle of autoinfection and chronic strongyloidiasis (carrier state). Autoinfection typically involves a low parasite burden, and is controlled by both host immune factors as well as parasitic factors.7 The mechanism of autoinfection can lead to the persistence of strongyloidiasis for decades after the initial infection, as has been documented in former World War II prisoners of war.8
Factors leading to the impairment of cell‐mediated immunity predispose chronically infected individuals to hyperinfection, as occurred in this patient. The most important of these are corticosteroid administration and Human T‐lymphotropic virus Type‐1 (HTLV‐1) infection, both of which cause significant derangement in TH1/TH2 immune system balance.5, 9 In the hyperinfection syndrome, the burden of parasites increases dramatically, leading to a variety of clinical manifestations. Gastrointestinal phenomena frequently predominate, including watery diarrhea, anorexia, weight loss, nausea/vomiting, gastrointestinal bleeding, and occasionally small bowel obstruction. Pulmonary manifestations are likewise common, and include cough, dyspnea, and wheezing. Cutaneous findings are not uncommon, classically pruritic linear lesions of the abdomen, buttocks, and lower extremities which may be rapidly migratory (larva currens), although purpura and petechiae as displayed by our patient appear to be under‐recognized findings in hyperinfection.2, 5 Gram‐negative bacillary meningitis has been well reported as a complication of migrating larvae, and a wide variety of other organs may rarely be involved.5, 10
The presence of chronic strongyloidiasis should be suspected in patients with ongoing gastrointestinal and/or pulmonary symptoms, or unexplained eosinophilia with a potential exposure history, such as immigrants from Southeast Asia. Diagnosis in these individuals is currently most often made serologically, although stool exam provides a somewhat higher specificity for active infection, at the expense of lower sensitivity.3, 11 In the setting of hyperinfection, stool studies are almost uniformly positive for S. stercoralis, and sputum may be diagnostic as well. Consequently, failure to reach the diagnosis usually reflects a lack of clinical suspicion.5
The therapy of choice for strongyloidiasis is currently ivermectin, with a single dose repeated once, 2 weeks later, highly efficacious in eradicating chronic infection. Treatment of hyperinfection is more challenging and less well studied, but clearly necessitates a more prolonged course of treatment. Many experts advocate treating until worms are no longer present in the stool; some have suggested the combination of ivermectin and albendazole as this patient received, although this has not been examined in controlled fashion.
The diagnosis of Strongyloides hyperinfection is typically delayed or missed because of the failure to consider it, with reported mortality rates as high as 50% in hyperinfection and 87% in disseminated disease.3, 12, 13 This patient fortunately was diagnosed, albeit in delayed fashion, proving the maxim better late than never. His case highlights the need for increased clinical awareness of strongyloidiasis, and specifically the need to consider the possibility of chronic Strongyloides infection prior to administering immunosuppressive medications. In particular, serologic screening of individuals from highly endemic areas for strongyloidiasis, when initiating extended courses of corticosteroids, seems prudent.13
Teaching Points
-
Chronic strongyloidiasis is common in the developing world (particularly Southeast Asia), and places infected individuals at significant risk of life‐threatening hyperinfection if not recognized and treated prior to the initiation of immunosuppressive medication, especially corticosteroids.
-
Strongyloides hyperinfection syndrome may be protean in its manifestations, but most commonly includes gastrointestinal, pulmonary, and cutaneous signs and symptoms.
- ,,, et al.Disseminated strongyloidiasis in immunocompromised patients—report of three cases.Int J Dermatol.2009;48(9):975–978.
- ,,, et al.Clinical manifestations of strongyloidiasis in southern Taiwan.J Microbiol Immunol Infect.2002;35(1):29–36.
- ,.Diagnosis of Strongyloides stercoralis infection.Clin Infect Dis.2001;33(7):1040–1047.
- ,,.Intestinal strongyloidiasis and hyperinfection syndrome.Clin Mol Allergy.2006;4:8.
- ,.Strongyloides stercoralis in the immunocompromised population.Clin Microbiol Rev.2004;17(1):208–217.
- ,,.Intestinal strongyloidiasis: recognition, management and determinants of outcome.J Clin Gastroenterol2005;39(3):203–211.
- .Dysregulation of strongyloidiasis: a new hypothesis.Clin Microbiol Rev.1992;5(4):345–355.
- ,,,.Consequences of captivity: health effects of Far East imprisonment in World War II.Q J Med.2009;102:87–96.
- ,,,.Strongyloides hyperinfection syndrome: an emerging global infectious disease.Trans R Soc Trop Med Hyg.2008;102(4):314–318.
- ,,,,,.Strongyloides hyperinfection presenting as acute respiratory failure and Gram‐negative sepsis.Chest.2005;128(5):3681–3684.
- ,,, et al.Use of enzyme‐linked immunosorbent assay and dipstick assay for detection of Strongyloides stercoralis infection in humans.J Clin Microbiol.2007;45:438–442.
- ,,,,,.Complicated and fatal Strongyloides infection in Canadians: risk factors, diagnosis and management.Can Med Assoc J.2004;171:479–484.
- ,,, et al.Maltreatment of Strongyloides infection: case series and worldwide physicians‐in‐training survey.Am J Med.2007;120(6):545.e1–545.e8.
- ,,, et al.Disseminated strongyloidiasis in immunocompromised patients—report of three cases.Int J Dermatol.2009;48(9):975–978.
- ,,, et al.Clinical manifestations of strongyloidiasis in southern Taiwan.J Microbiol Immunol Infect.2002;35(1):29–36.
- ,.Diagnosis of Strongyloides stercoralis infection.Clin Infect Dis.2001;33(7):1040–1047.
- ,,.Intestinal strongyloidiasis and hyperinfection syndrome.Clin Mol Allergy.2006;4:8.
- ,.Strongyloides stercoralis in the immunocompromised population.Clin Microbiol Rev.2004;17(1):208–217.
- ,,.Intestinal strongyloidiasis: recognition, management and determinants of outcome.J Clin Gastroenterol2005;39(3):203–211.
- .Dysregulation of strongyloidiasis: a new hypothesis.Clin Microbiol Rev.1992;5(4):345–355.
- ,,,.Consequences of captivity: health effects of Far East imprisonment in World War II.Q J Med.2009;102:87–96.
- ,,,.Strongyloides hyperinfection syndrome: an emerging global infectious disease.Trans R Soc Trop Med Hyg.2008;102(4):314–318.
- ,,,,,.Strongyloides hyperinfection presenting as acute respiratory failure and Gram‐negative sepsis.Chest.2005;128(5):3681–3684.
- ,,, et al.Use of enzyme‐linked immunosorbent assay and dipstick assay for detection of Strongyloides stercoralis infection in humans.J Clin Microbiol.2007;45:438–442.
- ,,,,,.Complicated and fatal Strongyloides infection in Canadians: risk factors, diagnosis and management.Can Med Assoc J.2004;171:479–484.
- ,,, et al.Maltreatment of Strongyloides infection: case series and worldwide physicians‐in‐training survey.Am J Med.2007;120(6):545.e1–545.e8.
In the Literature
In This Edition
Literature at a Glance
A guide to this month’s studies
- Effect of restrictive antibiotic policies on dosing timeliness
- Desired consultation format and content
- Risk of cancer associated with CT imaging
- Bleeding, mortality with aspirin after peptic ulcer bleed
- Diagnosis of lung cancer after pneumonia
- Outcomes associated with hyponatremia
- Patient awareness, interest in inpatient medication list
- Monoclonal antibodies in C. difficile
Restrictive Antimicrobial Policy Delays Administration
Clinical question: Does the approval process for restricted on-formulary antimicrobials cause a significant delay in their administration?
Background: Widespread and often unwarranted, antimicrobial use in the hospital lends itself to the development of microbial resistance and increases overall costs. To curb such practices, many hospitals require subspecialty approval prior to dispensing select broad-spectrum antimicrobials. Though shown to improve outcomes, the impact of the approval process on the timeliness of antimicrobial administration remains to be seen.
Study design: Retrospective cohort study.
Setting: Tertiary-care university hospital.
Synopsis: The study included 3,251 inpatients with computerized orders for a “stat” first dose of any of 24 pre-selected, parenteral antimicrobials. Time lag (more than one hour, and more than two hours) to nursing documentation of drug administration was separately analyzed for restricted and unrestricted antimicrobials.
Delay of more than one hour was significantly higher for restricted antimicrobials with an odds ratio of 1.49 (95% CI; 1.23-1.82), while the odds ratio for a delay of more than two hours was 1.78 (95% CI, 1.39-2.21). Also, for restricted antimicrobials, the percentage of orders delayed for more than one hour was significantly different between daytime and nighttime (when the first dose was exempt from pre-approval) orders: 46.1% versus 38.8% (P<0.001). For unrestricted drugs, delay was uniform irrespective of time of day (36.4% of daytime and 36.6% of nighttime orders were delayed more than one hour). The effect of delay in drug administration on patient outcomes was not evaluated.
Though the approval process aims in part to affect resistance patterns and overall costs, this research highlights the need to minimize the delay in administration and probably skip the approval for the first dose in critically ill patients.
Bottom line: Antibiotic approval processes can delay their administration in hospitalized patients, but the effect of this delay on patient outcomes is not yet known.
Citation: Winters BD, Thiemann DR, Brotman DJ. Impact of a restrictive antimicrobial policy on the process and timing of antimicrobial administration. J Hosp Med. 2010;5(1):E41-45.
Physicians Uphold Tenets of Effective Consultation while Highlighting Some Newer Viewpoints
Clinical question: What key features of a consultation are most desirable for physicians?
Background: With new changes in healthcare delivery, the standardization offered by the electronic health record (EHR) system will undoubtedly be confronted by the heterogeneity of clinical consultations. Determination of the various characteristics considered essential for a consultation can help standardize the processes and improve the quality of communication.
Study design: Opinion surveys with a 16-question, Web-based questionnaire about inpatient consultations.
Setting: Four Minnesota teaching hospitals affiliated with the University of Minnesota.
Synopsis: This study surveyed 651 physicians, mostly from general medicine and pediatrics (30% in-training; 54% were more than five years out of training). The response rate to the survey was 50% (323). Responses were analyzed separately for physicians predominantly requesting consultations (requesters) and those predominantly providing them (consultants).
Regarding the consultation request, the majority of consultants preferred a precise consult question (94%), contact information of the ordering provider (68%), and the urgency of consultation (66%), with telephonic communication for emergent consults (75%). Responses were similar regardless of practice site, specialty, or experience.
Regarding the consultation, more requesters desired verbal communication over written advice alone: Sixty-six percent preferred to have the rationale of the recommendations explained. They also preferred a separate recommendations section (48%) with bulleted suggestions (69%) at the top or bottom of the note (74%). Emphasis was placed on specificity of drug names, dose, and duration of therapy (80%), along with alternative options (76%). Most requesters desired a clear “signoff” note when appropriate, with a follow-up plan (74%) or scheduled appointments (44%).
Bottom line: For consultations, the majority of physicians prefer an explanation of medical decision-making, a crisp recommendation section, and specific directions for follow-up.
Citation: Boulware DR, Dekarske AS, Filice GA. Physician preferences for elements of effective consultations. J Gen Intern Med. 2010;25(1):25-30.
CT Scanning Could Be Related to a Future Risk of Cancer at a Population Level
Clinical question: Does the accelerated use of CT scans increase the future risk for radiation-related cancer?
Background: Computed tomography (CT) has come through as a powerful diagnostic and interventional imaging modality at the cost of higher radiation exposures. The potential cancer risk is minimal at an individual level; however, CT technology is used in more than 70 million scans annually. This volume can translate into a significant number of future cancers in the population.
Study design: Indirect risk modeling based on CT scan frequencies and radiation risk models.
Synopsis: Annual frequencies of CT scans (age- and sex-specific) were extracted from insurance claims. The study included 57 million scans, of which 30% were performed in adults 35 to 54 years old. The majority of scans were in females (60%).
Age-specific cancer risk for each CT scan type was estimated through published radiation risk models and national surveys. The projected number of incident cancers per 10,000 scans was highest for chest or abdominal CT angiography (CTA) and whole-body CT. Incidence was higher for females.
The CT scan frequencies were combined with the cancer risk, and it was estimated that approximately 29,000 (95% UL, 15,000-45,000) future cancers could be related to the exposure from CT scans. Uncertainty limits (UL), an estimation of the total error of measurement, accounted for statistical and subjective uncertainties. The risk was dependent on the radiation dose (chest CTA) and frequency of use (abdomen/pelvis followed by chest and head). The most common cancers were lung, colon, and leukemia.
Two-thirds of the projected cancers were in females and attributable to the higher frequency of scans in women coupled with their dual risk of breast and lung cancer with chest radiation. The results provide potential study targets for risk-reduction efforts.
Bottom line: CTA of the chest, abdomen, or pelvis could be related to risk of future cancers, especially in middle-aged females.
Citation: Berrington de González A, Mahesh M, Kim KP, et al. Projected cancer risks from computed tomographic scans performed in the United States in 2007. Arch Intern Med. 2009;169(22):2071-2077.
Early Resumption of Low-Dose Aspirin after Peptic Ulcer Bleeding Might Be Beneficial
Clinical question: Is it safe to restart aspirin after acute gastrointestinal (GI) bleeding in patients with cardiovascular or cerebrovascular disease?
Background: The increasing cardiovascular burden in the aging population has indirectly increased aspirin-related peptic ulcer bleeding. Proton-pump inhibitors (PPI) have shown promise in reducing recurrent GI bleeding in non-aspirin-related cases. It is unclear if this protective effect applies to patients on aspirin and, if so, if aspirin resumption after endoscopic treatment is safe.
Study design: Parallel, randomized, placebo-controlled, noninferiority trial.
Setting: Single tertiary endoscopy center in Hong Kong.
Synopsis: One hundred fifty-six patients with aspirin-related peptic ulcer bleeding were selected for the study. After successful endoscopic treatment and 72 hours on pantoprazole infusion, the patients were started on oral pantoprazole for the duration of the study (eight weeks). Patients were equally randomized to receive low-dose aspirin (80 mg/d) or placebo. Primary outcome was recurrent bleeding within 30 days. Secondary outcomes included eight-week all-cause mortality, cause-specific mortality, and recurrence of cardiovascular events.
The aspirin group had a 50% higher risk of recurrent bleeding within 30 days compared with placebo (10.3% vs. 5.4%). However, for the secondary endpoints, aspirin had lower all-cause mortality (1.3% vs. 12.9%), which was not related to increased GI bleeding. On the other hand, discontinuation of aspirin and use of PPI in the placebo group did not prevent mortality related to GI complications.
The small numbers restrict interpretation of the mortality rates but offer support to the fact that the cardioprotective effects of aspirin outweigh its potential for GI bleeding. It is to be noted that these results cannot be extrapolated to higher doses of aspirin.
Bottom line: Early resumption of aspirin after successful treatment of peptic ulcer bleeding might increase the risk of rebleeding but potentially decreases overall mortality.
Citation: Sung JJ, Lau JY, Ching JY, et al. Continuation of low-dose aspirin therapy in peptic ulcer bleeding: a randomized trial. Ann Intern Med. 2010;152(1):1-9.
A Substantial Number of Elderly Patients with Pneumonia Have Pulmonary Malignancy
Clinical question: What is the incidence of, and risk factors for, diagnosis of lung cancer after discharge for pneumonia?
Background: Pneumonia-related admissions in elderly individuals have increased by nearly 20% during the past two decades. Based on the risk profile of this age group, many physicians recommend follow-up chest imaging after pneumonia to ensure resolution and exclude underlying malignancy. However, this practice is not backed by substantial evidence.
Study design: Retrospective cohort study from administrative databases of the VA system.
Setting: Veteran Affairs (VA) Health Care System.
Synopsis: More than 40,000 patients (older than 65, 98.1% male) hospitalized for pneumonia were included in the study. These patients had no pneumonia in the preceding year and did not carry a diagnosis of lung cancer. During the follow-up period of up to five years, a significant proportion (9.2%) of these patients were diagnosed with pulmonary malignancy.
Pertinent factors associated with increased risk of diagnosis included active tobacco use, COPD, and prior nonpulmonary malignancy. Interestingly, stroke, diabetes, dementia, and heart failure were associated with a lower risk of diagnosis, likely due to early mortality from these diseases prior to diagnosis of lung cancer.
Mean time to diagnosis was 297 days, with just 27% diagnosed within 30 days. On mortality analysis, 12.9% (n=5270) of the patients died within 30 days and 20.7% (n=8451) within 90 days. Thus, a period of surveillance of 30 to 90 days following pneumonia, especially in patients with risk factors, could be beneficial.
This study was limited due to the shortcomings of database analyses. Also, the predominantly male, elderly, veteran population restricts extrapolation to the general population.
Bottom line: Patients with risk factors for lung cancer might benefit from surveillance chest imaging after hospitalization for pneumonia to rule out an underlying malignancy.
Citation: Mortensen EM, Copeland LA, Pugh MJ, et al. Diagnosis of pulmonary malignancy after hospitalization for pneumonia. Am J Med. 2010:123(1):66-71.
Hospital-Associated Hyponatremia of Any Severity Adversely Impacts Mortality and Financial Metrics
Clinical question: Does hyponatremia during a hospitalization prophesize a worse outcome?
Study design: Retrospective cohort study from 2002-2007.
Setting: Urban academic medical center.
Synopsis: This study included 53,236 adults based on the presence of admission or subsequent hyponatremia (defined as [Na+] <138 mEq/L). The patients were classified as community-acquired (CAH=37.9%), hospital-aggravated (5.7%), or hospital-acquired hyponatremia (HAH=38.2%).
Across all subgroups, all types of hyponatremia were independently associated with worse primary outcomes, including an increase in hospital mortality (CAH 52%, HAH 66%), prolongation of hospital stay, and discharge to a facility. Also, for the same [Na+], HAH had significantly increased mortality compared with CAH. Though the elderly were more prone to develop hyponatremia, patients younger than 65 had worse outcomes.
The severity of hyponatremia prognosticated adverse outcomes. The liberal definition of hyponatremia, as opposed to the current standard of <135 mEq/L, explains the large numbers in prevalence. However, even mild hyponatremia (133 mEq/L to 137) was linked to poor outcomes (adjusted OR 1.34; CI 1.18-1.51).
The study weaknesses include the use of administrative codes to identify comorbidities, less applicability to outpatient setting, and lack of evaluation of outcomes postdischarge. However, the robust numbers do establish inpatient hyponatremia as a marker of worse outcomes.
Bottom line: Inpatient hyponatremia of any severity is a marker of increased mortality and excessive financial burden.
Citation: Wald R, Jaber BL, Price LL, Upadhyay A, Madias NE. Impact of hospital-associated hyponatremia on selected outcomes. Arch Intern Med. 2010;170(3):294-302.
Patients Lack Awareness and Prefer to Be Updated Regarding Their Inpatient Medications
Clinical question: Is patient knowledge of their medications deficient, and does this reflect a lack of desire to be involved in the medication reconciliation process?
Background: Medication errors remain a significant healthcare problem due to their potential to increase morbidity. For medication administration errors, apart from the dispensing pharmacist and the nurses, patients could be the final checkpoint to ensure medication safety. However, their awareness and enthusiasm to participate has not been adequately assessed in the literature.
Study design: A cross-sectional study using individual surveys to assess awareness and attitudes regarding inpatient medications.
Setting: Single tertiary-care academic teaching hospital.
Synopsis: Fifty cognitively intact adult patients were consented for the study. Of these, 54% provided an accurate recollection of their outpatient medications. When they were surveyed regarding inpatient medications, 96% omitted at least one medication, with the average of 6.8 medication omissions. This was noted to correlate with age >65 years. Also, 44% erroneously presumed they were on a medication while they were in the hospital, even though they weren’t.
When attitudes were surveyed, most of the patients would have preferred to get an inpatient medication list (78%) with the goal of improving their satisfaction (81%) and reducing errors (94%). Also, no association was found between patients’ errors of omission and their reported desire to be involved in the medication safety process.
This small study was limited to cognitively intact patients only. Also, the relatively younger age might cause an overestimation of patient interest in participation. However, the results highlight key medication reconciliation issues. Although patient involvement is desirable, a systematic program of educating them about their medications would be required to make their feedback effective and useful.
Bottom line: Healthy patients might be unaware of their exact hospital medications but prefer to be kept in the loop.
Citation: Cumbler E, Wald H, Kutner J. Lack of patient knowledge regarding hospital medications. J Hosp Med. 2010;5(2):83-86.
Monoclonal Antibodies against Clostridium difficile Toxins Prevent Recurrence
Clinical question: Are human monoclonal antibodies against C. difficile toxin A (CDA1) and B (CDB1) effective in preventing recurrence of C. diff infection (CDI)?
Background: Widespread use of antibiotics, coupled with the emergence of the hypervirulent (B1/NAP1/027) strain of C. diff, has altered the epidemiology of CDI. Even with effective treatment regimens, there is an escalation in severity, treatment failures, and recurrences. Antibodies against the C. diff toxins are being evaluated as the next frontier in treatment of CDI.
Study design: Phase 2 randomized, double-blind, placebo-controlled trial.
Setting: Thirty study centers in Canada and the U.S.
Synopsis: Two hundred patients with laboratory documented CDI on standard therapy with either metronidazole or vancomycin were randomized to receive a single IV infusion of combined monoclonal antibodies against CDA1 and CDB1 (n=101) or a normal saline placebo infusion (n=99). Patients were followed for 84 days with daily stool counts and intermittent blood samples for immunogenicity analysis.
The primary endpoint of recurrence of laboratory-proven C. diff diarrhea was significantly lower in the monoclonal antibody group (7% vs. 25% in placebo. 95% CI, 7-29; P <0.001). In a subgroup analysis of the epidemic BI/NAP1/027 strain, this favorable association persisted (8% vs. 32%). Recurrence in the antibody group was seen more in elderly patients hospitalized with a higher severity of underlying disease.
Secondary endpoints relating to the initial episode of CDI including treatment failure, severity of diarrhea, and duration to resolution were not significantly different between the two groups. Fewer accounts of serious adverse events were documented in the antibody group (18 patients vs. 28 patients in placebo, P=0.09), and immunogenicity was not detected in any patient.
Bottom line: Monoclonal antibody infusion against C. diff toxins reduces recurrence of infection, even with a hypervirulent (B1/NAP1/027) strain, without any significant adverse events.
Citation: Lowy I, Molrine DC, Leav BA, et al. Treatment with monoclonal antibodies against Clostridium difficile toxins. N Engl J Med. 2010; 362(3):197-205. TH
In This Edition
Literature at a Glance
A guide to this month’s studies
- Effect of restrictive antibiotic policies on dosing timeliness
- Desired consultation format and content
- Risk of cancer associated with CT imaging
- Bleeding, mortality with aspirin after peptic ulcer bleed
- Diagnosis of lung cancer after pneumonia
- Outcomes associated with hyponatremia
- Patient awareness, interest in inpatient medication list
- Monoclonal antibodies in C. difficile
Restrictive Antimicrobial Policy Delays Administration
Clinical question: Does the approval process for restricted on-formulary antimicrobials cause a significant delay in their administration?
Background: Widespread and often unwarranted, antimicrobial use in the hospital lends itself to the development of microbial resistance and increases overall costs. To curb such practices, many hospitals require subspecialty approval prior to dispensing select broad-spectrum antimicrobials. Though shown to improve outcomes, the impact of the approval process on the timeliness of antimicrobial administration remains to be seen.
Study design: Retrospective cohort study.
Setting: Tertiary-care university hospital.
Synopsis: The study included 3,251 inpatients with computerized orders for a “stat” first dose of any of 24 pre-selected, parenteral antimicrobials. Time lag (more than one hour, and more than two hours) to nursing documentation of drug administration was separately analyzed for restricted and unrestricted antimicrobials.
Delay of more than one hour was significantly higher for restricted antimicrobials with an odds ratio of 1.49 (95% CI; 1.23-1.82), while the odds ratio for a delay of more than two hours was 1.78 (95% CI, 1.39-2.21). Also, for restricted antimicrobials, the percentage of orders delayed for more than one hour was significantly different between daytime and nighttime (when the first dose was exempt from pre-approval) orders: 46.1% versus 38.8% (P<0.001). For unrestricted drugs, delay was uniform irrespective of time of day (36.4% of daytime and 36.6% of nighttime orders were delayed more than one hour). The effect of delay in drug administration on patient outcomes was not evaluated.
Though the approval process aims in part to affect resistance patterns and overall costs, this research highlights the need to minimize the delay in administration and probably skip the approval for the first dose in critically ill patients.
Bottom line: Antibiotic approval processes can delay their administration in hospitalized patients, but the effect of this delay on patient outcomes is not yet known.
Citation: Winters BD, Thiemann DR, Brotman DJ. Impact of a restrictive antimicrobial policy on the process and timing of antimicrobial administration. J Hosp Med. 2010;5(1):E41-45.
Physicians Uphold Tenets of Effective Consultation while Highlighting Some Newer Viewpoints
Clinical question: What key features of a consultation are most desirable for physicians?
Background: With new changes in healthcare delivery, the standardization offered by the electronic health record (EHR) system will undoubtedly be confronted by the heterogeneity of clinical consultations. Determination of the various characteristics considered essential for a consultation can help standardize the processes and improve the quality of communication.
Study design: Opinion surveys with a 16-question, Web-based questionnaire about inpatient consultations.
Setting: Four Minnesota teaching hospitals affiliated with the University of Minnesota.
Synopsis: This study surveyed 651 physicians, mostly from general medicine and pediatrics (30% in-training; 54% were more than five years out of training). The response rate to the survey was 50% (323). Responses were analyzed separately for physicians predominantly requesting consultations (requesters) and those predominantly providing them (consultants).
Regarding the consultation request, the majority of consultants preferred a precise consult question (94%), contact information of the ordering provider (68%), and the urgency of consultation (66%), with telephonic communication for emergent consults (75%). Responses were similar regardless of practice site, specialty, or experience.
Regarding the consultation, more requesters desired verbal communication over written advice alone: Sixty-six percent preferred to have the rationale of the recommendations explained. They also preferred a separate recommendations section (48%) with bulleted suggestions (69%) at the top or bottom of the note (74%). Emphasis was placed on specificity of drug names, dose, and duration of therapy (80%), along with alternative options (76%). Most requesters desired a clear “signoff” note when appropriate, with a follow-up plan (74%) or scheduled appointments (44%).
Bottom line: For consultations, the majority of physicians prefer an explanation of medical decision-making, a crisp recommendation section, and specific directions for follow-up.
Citation: Boulware DR, Dekarske AS, Filice GA. Physician preferences for elements of effective consultations. J Gen Intern Med. 2010;25(1):25-30.
CT Scanning Could Be Related to a Future Risk of Cancer at a Population Level
Clinical question: Does the accelerated use of CT scans increase the future risk for radiation-related cancer?
Background: Computed tomography (CT) has come through as a powerful diagnostic and interventional imaging modality at the cost of higher radiation exposures. The potential cancer risk is minimal at an individual level; however, CT technology is used in more than 70 million scans annually. This volume can translate into a significant number of future cancers in the population.
Study design: Indirect risk modeling based on CT scan frequencies and radiation risk models.
Synopsis: Annual frequencies of CT scans (age- and sex-specific) were extracted from insurance claims. The study included 57 million scans, of which 30% were performed in adults 35 to 54 years old. The majority of scans were in females (60%).
Age-specific cancer risk for each CT scan type was estimated through published radiation risk models and national surveys. The projected number of incident cancers per 10,000 scans was highest for chest or abdominal CT angiography (CTA) and whole-body CT. Incidence was higher for females.
The CT scan frequencies were combined with the cancer risk, and it was estimated that approximately 29,000 (95% UL, 15,000-45,000) future cancers could be related to the exposure from CT scans. Uncertainty limits (UL), an estimation of the total error of measurement, accounted for statistical and subjective uncertainties. The risk was dependent on the radiation dose (chest CTA) and frequency of use (abdomen/pelvis followed by chest and head). The most common cancers were lung, colon, and leukemia.
Two-thirds of the projected cancers were in females and attributable to the higher frequency of scans in women coupled with their dual risk of breast and lung cancer with chest radiation. The results provide potential study targets for risk-reduction efforts.
Bottom line: CTA of the chest, abdomen, or pelvis could be related to risk of future cancers, especially in middle-aged females.
Citation: Berrington de González A, Mahesh M, Kim KP, et al. Projected cancer risks from computed tomographic scans performed in the United States in 2007. Arch Intern Med. 2009;169(22):2071-2077.
Early Resumption of Low-Dose Aspirin after Peptic Ulcer Bleeding Might Be Beneficial
Clinical question: Is it safe to restart aspirin after acute gastrointestinal (GI) bleeding in patients with cardiovascular or cerebrovascular disease?
Background: The increasing cardiovascular burden in the aging population has indirectly increased aspirin-related peptic ulcer bleeding. Proton-pump inhibitors (PPI) have shown promise in reducing recurrent GI bleeding in non-aspirin-related cases. It is unclear if this protective effect applies to patients on aspirin and, if so, if aspirin resumption after endoscopic treatment is safe.
Study design: Parallel, randomized, placebo-controlled, noninferiority trial.
Setting: Single tertiary endoscopy center in Hong Kong.
Synopsis: One hundred fifty-six patients with aspirin-related peptic ulcer bleeding were selected for the study. After successful endoscopic treatment and 72 hours on pantoprazole infusion, the patients were started on oral pantoprazole for the duration of the study (eight weeks). Patients were equally randomized to receive low-dose aspirin (80 mg/d) or placebo. Primary outcome was recurrent bleeding within 30 days. Secondary outcomes included eight-week all-cause mortality, cause-specific mortality, and recurrence of cardiovascular events.
The aspirin group had a 50% higher risk of recurrent bleeding within 30 days compared with placebo (10.3% vs. 5.4%). However, for the secondary endpoints, aspirin had lower all-cause mortality (1.3% vs. 12.9%), which was not related to increased GI bleeding. On the other hand, discontinuation of aspirin and use of PPI in the placebo group did not prevent mortality related to GI complications.
The small numbers restrict interpretation of the mortality rates but offer support to the fact that the cardioprotective effects of aspirin outweigh its potential for GI bleeding. It is to be noted that these results cannot be extrapolated to higher doses of aspirin.
Bottom line: Early resumption of aspirin after successful treatment of peptic ulcer bleeding might increase the risk of rebleeding but potentially decreases overall mortality.
Citation: Sung JJ, Lau JY, Ching JY, et al. Continuation of low-dose aspirin therapy in peptic ulcer bleeding: a randomized trial. Ann Intern Med. 2010;152(1):1-9.
A Substantial Number of Elderly Patients with Pneumonia Have Pulmonary Malignancy
Clinical question: What is the incidence of, and risk factors for, diagnosis of lung cancer after discharge for pneumonia?
Background: Pneumonia-related admissions in elderly individuals have increased by nearly 20% during the past two decades. Based on the risk profile of this age group, many physicians recommend follow-up chest imaging after pneumonia to ensure resolution and exclude underlying malignancy. However, this practice is not backed by substantial evidence.
Study design: Retrospective cohort study from administrative databases of the VA system.
Setting: Veteran Affairs (VA) Health Care System.
Synopsis: More than 40,000 patients (older than 65, 98.1% male) hospitalized for pneumonia were included in the study. These patients had no pneumonia in the preceding year and did not carry a diagnosis of lung cancer. During the follow-up period of up to five years, a significant proportion (9.2%) of these patients were diagnosed with pulmonary malignancy.
Pertinent factors associated with increased risk of diagnosis included active tobacco use, COPD, and prior nonpulmonary malignancy. Interestingly, stroke, diabetes, dementia, and heart failure were associated with a lower risk of diagnosis, likely due to early mortality from these diseases prior to diagnosis of lung cancer.
Mean time to diagnosis was 297 days, with just 27% diagnosed within 30 days. On mortality analysis, 12.9% (n=5270) of the patients died within 30 days and 20.7% (n=8451) within 90 days. Thus, a period of surveillance of 30 to 90 days following pneumonia, especially in patients with risk factors, could be beneficial.
This study was limited due to the shortcomings of database analyses. Also, the predominantly male, elderly, veteran population restricts extrapolation to the general population.
Bottom line: Patients with risk factors for lung cancer might benefit from surveillance chest imaging after hospitalization for pneumonia to rule out an underlying malignancy.
Citation: Mortensen EM, Copeland LA, Pugh MJ, et al. Diagnosis of pulmonary malignancy after hospitalization for pneumonia. Am J Med. 2010:123(1):66-71.
Hospital-Associated Hyponatremia of Any Severity Adversely Impacts Mortality and Financial Metrics
Clinical question: Does hyponatremia during a hospitalization prophesize a worse outcome?
Study design: Retrospective cohort study from 2002-2007.
Setting: Urban academic medical center.
Synopsis: This study included 53,236 adults based on the presence of admission or subsequent hyponatremia (defined as [Na+] <138 mEq/L). The patients were classified as community-acquired (CAH=37.9%), hospital-aggravated (5.7%), or hospital-acquired hyponatremia (HAH=38.2%).
Across all subgroups, all types of hyponatremia were independently associated with worse primary outcomes, including an increase in hospital mortality (CAH 52%, HAH 66%), prolongation of hospital stay, and discharge to a facility. Also, for the same [Na+], HAH had significantly increased mortality compared with CAH. Though the elderly were more prone to develop hyponatremia, patients younger than 65 had worse outcomes.
The severity of hyponatremia prognosticated adverse outcomes. The liberal definition of hyponatremia, as opposed to the current standard of <135 mEq/L, explains the large numbers in prevalence. However, even mild hyponatremia (133 mEq/L to 137) was linked to poor outcomes (adjusted OR 1.34; CI 1.18-1.51).
The study weaknesses include the use of administrative codes to identify comorbidities, less applicability to outpatient setting, and lack of evaluation of outcomes postdischarge. However, the robust numbers do establish inpatient hyponatremia as a marker of worse outcomes.
Bottom line: Inpatient hyponatremia of any severity is a marker of increased mortality and excessive financial burden.
Citation: Wald R, Jaber BL, Price LL, Upadhyay A, Madias NE. Impact of hospital-associated hyponatremia on selected outcomes. Arch Intern Med. 2010;170(3):294-302.
Patients Lack Awareness and Prefer to Be Updated Regarding Their Inpatient Medications
Clinical question: Is patient knowledge of their medications deficient, and does this reflect a lack of desire to be involved in the medication reconciliation process?
Background: Medication errors remain a significant healthcare problem due to their potential to increase morbidity. For medication administration errors, apart from the dispensing pharmacist and the nurses, patients could be the final checkpoint to ensure medication safety. However, their awareness and enthusiasm to participate has not been adequately assessed in the literature.
Study design: A cross-sectional study using individual surveys to assess awareness and attitudes regarding inpatient medications.
Setting: Single tertiary-care academic teaching hospital.
Synopsis: Fifty cognitively intact adult patients were consented for the study. Of these, 54% provided an accurate recollection of their outpatient medications. When they were surveyed regarding inpatient medications, 96% omitted at least one medication, with the average of 6.8 medication omissions. This was noted to correlate with age >65 years. Also, 44% erroneously presumed they were on a medication while they were in the hospital, even though they weren’t.
When attitudes were surveyed, most of the patients would have preferred to get an inpatient medication list (78%) with the goal of improving their satisfaction (81%) and reducing errors (94%). Also, no association was found between patients’ errors of omission and their reported desire to be involved in the medication safety process.
This small study was limited to cognitively intact patients only. Also, the relatively younger age might cause an overestimation of patient interest in participation. However, the results highlight key medication reconciliation issues. Although patient involvement is desirable, a systematic program of educating them about their medications would be required to make their feedback effective and useful.
Bottom line: Healthy patients might be unaware of their exact hospital medications but prefer to be kept in the loop.
Citation: Cumbler E, Wald H, Kutner J. Lack of patient knowledge regarding hospital medications. J Hosp Med. 2010;5(2):83-86.
Monoclonal Antibodies against Clostridium difficile Toxins Prevent Recurrence
Clinical question: Are human monoclonal antibodies against C. difficile toxin A (CDA1) and B (CDB1) effective in preventing recurrence of C. diff infection (CDI)?
Background: Widespread use of antibiotics, coupled with the emergence of the hypervirulent (B1/NAP1/027) strain of C. diff, has altered the epidemiology of CDI. Even with effective treatment regimens, there is an escalation in severity, treatment failures, and recurrences. Antibodies against the C. diff toxins are being evaluated as the next frontier in treatment of CDI.
Study design: Phase 2 randomized, double-blind, placebo-controlled trial.
Setting: Thirty study centers in Canada and the U.S.
Synopsis: Two hundred patients with laboratory documented CDI on standard therapy with either metronidazole or vancomycin were randomized to receive a single IV infusion of combined monoclonal antibodies against CDA1 and CDB1 (n=101) or a normal saline placebo infusion (n=99). Patients were followed for 84 days with daily stool counts and intermittent blood samples for immunogenicity analysis.
The primary endpoint of recurrence of laboratory-proven C. diff diarrhea was significantly lower in the monoclonal antibody group (7% vs. 25% in placebo. 95% CI, 7-29; P <0.001). In a subgroup analysis of the epidemic BI/NAP1/027 strain, this favorable association persisted (8% vs. 32%). Recurrence in the antibody group was seen more in elderly patients hospitalized with a higher severity of underlying disease.
Secondary endpoints relating to the initial episode of CDI including treatment failure, severity of diarrhea, and duration to resolution were not significantly different between the two groups. Fewer accounts of serious adverse events were documented in the antibody group (18 patients vs. 28 patients in placebo, P=0.09), and immunogenicity was not detected in any patient.
Bottom line: Monoclonal antibody infusion against C. diff toxins reduces recurrence of infection, even with a hypervirulent (B1/NAP1/027) strain, without any significant adverse events.
Citation: Lowy I, Molrine DC, Leav BA, et al. Treatment with monoclonal antibodies against Clostridium difficile toxins. N Engl J Med. 2010; 362(3):197-205. TH
In This Edition
Literature at a Glance
A guide to this month’s studies
- Effect of restrictive antibiotic policies on dosing timeliness
- Desired consultation format and content
- Risk of cancer associated with CT imaging
- Bleeding, mortality with aspirin after peptic ulcer bleed
- Diagnosis of lung cancer after pneumonia
- Outcomes associated with hyponatremia
- Patient awareness, interest in inpatient medication list
- Monoclonal antibodies in C. difficile
Restrictive Antimicrobial Policy Delays Administration
Clinical question: Does the approval process for restricted on-formulary antimicrobials cause a significant delay in their administration?
Background: Widespread and often unwarranted, antimicrobial use in the hospital lends itself to the development of microbial resistance and increases overall costs. To curb such practices, many hospitals require subspecialty approval prior to dispensing select broad-spectrum antimicrobials. Though shown to improve outcomes, the impact of the approval process on the timeliness of antimicrobial administration remains to be seen.
Study design: Retrospective cohort study.
Setting: Tertiary-care university hospital.
Synopsis: The study included 3,251 inpatients with computerized orders for a “stat” first dose of any of 24 pre-selected, parenteral antimicrobials. Time lag (more than one hour, and more than two hours) to nursing documentation of drug administration was separately analyzed for restricted and unrestricted antimicrobials.
Delay of more than one hour was significantly higher for restricted antimicrobials with an odds ratio of 1.49 (95% CI; 1.23-1.82), while the odds ratio for a delay of more than two hours was 1.78 (95% CI, 1.39-2.21). Also, for restricted antimicrobials, the percentage of orders delayed for more than one hour was significantly different between daytime and nighttime (when the first dose was exempt from pre-approval) orders: 46.1% versus 38.8% (P<0.001). For unrestricted drugs, delay was uniform irrespective of time of day (36.4% of daytime and 36.6% of nighttime orders were delayed more than one hour). The effect of delay in drug administration on patient outcomes was not evaluated.
Though the approval process aims in part to affect resistance patterns and overall costs, this research highlights the need to minimize the delay in administration and probably skip the approval for the first dose in critically ill patients.
Bottom line: Antibiotic approval processes can delay their administration in hospitalized patients, but the effect of this delay on patient outcomes is not yet known.
Citation: Winters BD, Thiemann DR, Brotman DJ. Impact of a restrictive antimicrobial policy on the process and timing of antimicrobial administration. J Hosp Med. 2010;5(1):E41-45.
Physicians Uphold Tenets of Effective Consultation while Highlighting Some Newer Viewpoints
Clinical question: What key features of a consultation are most desirable for physicians?
Background: With new changes in healthcare delivery, the standardization offered by the electronic health record (EHR) system will undoubtedly be confronted by the heterogeneity of clinical consultations. Determination of the various characteristics considered essential for a consultation can help standardize the processes and improve the quality of communication.
Study design: Opinion surveys with a 16-question, Web-based questionnaire about inpatient consultations.
Setting: Four Minnesota teaching hospitals affiliated with the University of Minnesota.
Synopsis: This study surveyed 651 physicians, mostly from general medicine and pediatrics (30% in-training; 54% were more than five years out of training). The response rate to the survey was 50% (323). Responses were analyzed separately for physicians predominantly requesting consultations (requesters) and those predominantly providing them (consultants).
Regarding the consultation request, the majority of consultants preferred a precise consult question (94%), contact information of the ordering provider (68%), and the urgency of consultation (66%), with telephonic communication for emergent consults (75%). Responses were similar regardless of practice site, specialty, or experience.
Regarding the consultation, more requesters desired verbal communication over written advice alone: Sixty-six percent preferred to have the rationale of the recommendations explained. They also preferred a separate recommendations section (48%) with bulleted suggestions (69%) at the top or bottom of the note (74%). Emphasis was placed on specificity of drug names, dose, and duration of therapy (80%), along with alternative options (76%). Most requesters desired a clear “signoff” note when appropriate, with a follow-up plan (74%) or scheduled appointments (44%).
Bottom line: For consultations, the majority of physicians prefer an explanation of medical decision-making, a crisp recommendation section, and specific directions for follow-up.
Citation: Boulware DR, Dekarske AS, Filice GA. Physician preferences for elements of effective consultations. J Gen Intern Med. 2010;25(1):25-30.
CT Scanning Could Be Related to a Future Risk of Cancer at a Population Level
Clinical question: Does the accelerated use of CT scans increase the future risk for radiation-related cancer?
Background: Computed tomography (CT) has come through as a powerful diagnostic and interventional imaging modality at the cost of higher radiation exposures. The potential cancer risk is minimal at an individual level; however, CT technology is used in more than 70 million scans annually. This volume can translate into a significant number of future cancers in the population.
Study design: Indirect risk modeling based on CT scan frequencies and radiation risk models.
Synopsis: Annual frequencies of CT scans (age- and sex-specific) were extracted from insurance claims. The study included 57 million scans, of which 30% were performed in adults 35 to 54 years old. The majority of scans were in females (60%).
Age-specific cancer risk for each CT scan type was estimated through published radiation risk models and national surveys. The projected number of incident cancers per 10,000 scans was highest for chest or abdominal CT angiography (CTA) and whole-body CT. Incidence was higher for females.
The CT scan frequencies were combined with the cancer risk, and it was estimated that approximately 29,000 (95% UL, 15,000-45,000) future cancers could be related to the exposure from CT scans. Uncertainty limits (UL), an estimation of the total error of measurement, accounted for statistical and subjective uncertainties. The risk was dependent on the radiation dose (chest CTA) and frequency of use (abdomen/pelvis followed by chest and head). The most common cancers were lung, colon, and leukemia.
Two-thirds of the projected cancers were in females and attributable to the higher frequency of scans in women coupled with their dual risk of breast and lung cancer with chest radiation. The results provide potential study targets for risk-reduction efforts.
Bottom line: CTA of the chest, abdomen, or pelvis could be related to risk of future cancers, especially in middle-aged females.
Citation: Berrington de González A, Mahesh M, Kim KP, et al. Projected cancer risks from computed tomographic scans performed in the United States in 2007. Arch Intern Med. 2009;169(22):2071-2077.
Early Resumption of Low-Dose Aspirin after Peptic Ulcer Bleeding Might Be Beneficial
Clinical question: Is it safe to restart aspirin after acute gastrointestinal (GI) bleeding in patients with cardiovascular or cerebrovascular disease?
Background: The increasing cardiovascular burden in the aging population has indirectly increased aspirin-related peptic ulcer bleeding. Proton-pump inhibitors (PPI) have shown promise in reducing recurrent GI bleeding in non-aspirin-related cases. It is unclear if this protective effect applies to patients on aspirin and, if so, if aspirin resumption after endoscopic treatment is safe.
Study design: Parallel, randomized, placebo-controlled, noninferiority trial.
Setting: Single tertiary endoscopy center in Hong Kong.
Synopsis: One hundred fifty-six patients with aspirin-related peptic ulcer bleeding were selected for the study. After successful endoscopic treatment and 72 hours on pantoprazole infusion, the patients were started on oral pantoprazole for the duration of the study (eight weeks). Patients were equally randomized to receive low-dose aspirin (80 mg/d) or placebo. Primary outcome was recurrent bleeding within 30 days. Secondary outcomes included eight-week all-cause mortality, cause-specific mortality, and recurrence of cardiovascular events.
The aspirin group had a 50% higher risk of recurrent bleeding within 30 days compared with placebo (10.3% vs. 5.4%). However, for the secondary endpoints, aspirin had lower all-cause mortality (1.3% vs. 12.9%), which was not related to increased GI bleeding. On the other hand, discontinuation of aspirin and use of PPI in the placebo group did not prevent mortality related to GI complications.
The small numbers restrict interpretation of the mortality rates but offer support to the fact that the cardioprotective effects of aspirin outweigh its potential for GI bleeding. It is to be noted that these results cannot be extrapolated to higher doses of aspirin.
Bottom line: Early resumption of aspirin after successful treatment of peptic ulcer bleeding might increase the risk of rebleeding but potentially decreases overall mortality.
Citation: Sung JJ, Lau JY, Ching JY, et al. Continuation of low-dose aspirin therapy in peptic ulcer bleeding: a randomized trial. Ann Intern Med. 2010;152(1):1-9.
A Substantial Number of Elderly Patients with Pneumonia Have Pulmonary Malignancy
Clinical question: What is the incidence of, and risk factors for, diagnosis of lung cancer after discharge for pneumonia?
Background: Pneumonia-related admissions in elderly individuals have increased by nearly 20% during the past two decades. Based on the risk profile of this age group, many physicians recommend follow-up chest imaging after pneumonia to ensure resolution and exclude underlying malignancy. However, this practice is not backed by substantial evidence.
Study design: Retrospective cohort study from administrative databases of the VA system.
Setting: Veteran Affairs (VA) Health Care System.
Synopsis: More than 40,000 patients (older than 65, 98.1% male) hospitalized for pneumonia were included in the study. These patients had no pneumonia in the preceding year and did not carry a diagnosis of lung cancer. During the follow-up period of up to five years, a significant proportion (9.2%) of these patients were diagnosed with pulmonary malignancy.
Pertinent factors associated with increased risk of diagnosis included active tobacco use, COPD, and prior nonpulmonary malignancy. Interestingly, stroke, diabetes, dementia, and heart failure were associated with a lower risk of diagnosis, likely due to early mortality from these diseases prior to diagnosis of lung cancer.
Mean time to diagnosis was 297 days, with just 27% diagnosed within 30 days. On mortality analysis, 12.9% (n=5270) of the patients died within 30 days and 20.7% (n=8451) within 90 days. Thus, a period of surveillance of 30 to 90 days following pneumonia, especially in patients with risk factors, could be beneficial.
This study was limited due to the shortcomings of database analyses. Also, the predominantly male, elderly, veteran population restricts extrapolation to the general population.
Bottom line: Patients with risk factors for lung cancer might benefit from surveillance chest imaging after hospitalization for pneumonia to rule out an underlying malignancy.
Citation: Mortensen EM, Copeland LA, Pugh MJ, et al. Diagnosis of pulmonary malignancy after hospitalization for pneumonia. Am J Med. 2010:123(1):66-71.
Hospital-Associated Hyponatremia of Any Severity Adversely Impacts Mortality and Financial Metrics
Clinical question: Does hyponatremia during a hospitalization prophesize a worse outcome?
Study design: Retrospective cohort study from 2002-2007.
Setting: Urban academic medical center.
Synopsis: This study included 53,236 adults based on the presence of admission or subsequent hyponatremia (defined as [Na+] <138 mEq/L). The patients were classified as community-acquired (CAH=37.9%), hospital-aggravated (5.7%), or hospital-acquired hyponatremia (HAH=38.2%).
Across all subgroups, all types of hyponatremia were independently associated with worse primary outcomes, including an increase in hospital mortality (CAH 52%, HAH 66%), prolongation of hospital stay, and discharge to a facility. Also, for the same [Na+], HAH had significantly increased mortality compared with CAH. Though the elderly were more prone to develop hyponatremia, patients younger than 65 had worse outcomes.
The severity of hyponatremia prognosticated adverse outcomes. The liberal definition of hyponatremia, as opposed to the current standard of <135 mEq/L, explains the large numbers in prevalence. However, even mild hyponatremia (133 mEq/L to 137) was linked to poor outcomes (adjusted OR 1.34; CI 1.18-1.51).
The study weaknesses include the use of administrative codes to identify comorbidities, less applicability to outpatient setting, and lack of evaluation of outcomes postdischarge. However, the robust numbers do establish inpatient hyponatremia as a marker of worse outcomes.
Bottom line: Inpatient hyponatremia of any severity is a marker of increased mortality and excessive financial burden.
Citation: Wald R, Jaber BL, Price LL, Upadhyay A, Madias NE. Impact of hospital-associated hyponatremia on selected outcomes. Arch Intern Med. 2010;170(3):294-302.
Patients Lack Awareness and Prefer to Be Updated Regarding Their Inpatient Medications
Clinical question: Is patient knowledge of their medications deficient, and does this reflect a lack of desire to be involved in the medication reconciliation process?
Background: Medication errors remain a significant healthcare problem due to their potential to increase morbidity. For medication administration errors, apart from the dispensing pharmacist and the nurses, patients could be the final checkpoint to ensure medication safety. However, their awareness and enthusiasm to participate has not been adequately assessed in the literature.
Study design: A cross-sectional study using individual surveys to assess awareness and attitudes regarding inpatient medications.
Setting: Single tertiary-care academic teaching hospital.
Synopsis: Fifty cognitively intact adult patients were consented for the study. Of these, 54% provided an accurate recollection of their outpatient medications. When they were surveyed regarding inpatient medications, 96% omitted at least one medication, with the average of 6.8 medication omissions. This was noted to correlate with age >65 years. Also, 44% erroneously presumed they were on a medication while they were in the hospital, even though they weren’t.
When attitudes were surveyed, most of the patients would have preferred to get an inpatient medication list (78%) with the goal of improving their satisfaction (81%) and reducing errors (94%). Also, no association was found between patients’ errors of omission and their reported desire to be involved in the medication safety process.
This small study was limited to cognitively intact patients only. Also, the relatively younger age might cause an overestimation of patient interest in participation. However, the results highlight key medication reconciliation issues. Although patient involvement is desirable, a systematic program of educating them about their medications would be required to make their feedback effective and useful.
Bottom line: Healthy patients might be unaware of their exact hospital medications but prefer to be kept in the loop.
Citation: Cumbler E, Wald H, Kutner J. Lack of patient knowledge regarding hospital medications. J Hosp Med. 2010;5(2):83-86.
Monoclonal Antibodies against Clostridium difficile Toxins Prevent Recurrence
Clinical question: Are human monoclonal antibodies against C. difficile toxin A (CDA1) and B (CDB1) effective in preventing recurrence of C. diff infection (CDI)?
Background: Widespread use of antibiotics, coupled with the emergence of the hypervirulent (B1/NAP1/027) strain of C. diff, has altered the epidemiology of CDI. Even with effective treatment regimens, there is an escalation in severity, treatment failures, and recurrences. Antibodies against the C. diff toxins are being evaluated as the next frontier in treatment of CDI.
Study design: Phase 2 randomized, double-blind, placebo-controlled trial.
Setting: Thirty study centers in Canada and the U.S.
Synopsis: Two hundred patients with laboratory documented CDI on standard therapy with either metronidazole or vancomycin were randomized to receive a single IV infusion of combined monoclonal antibodies against CDA1 and CDB1 (n=101) or a normal saline placebo infusion (n=99). Patients were followed for 84 days with daily stool counts and intermittent blood samples for immunogenicity analysis.
The primary endpoint of recurrence of laboratory-proven C. diff diarrhea was significantly lower in the monoclonal antibody group (7% vs. 25% in placebo. 95% CI, 7-29; P <0.001). In a subgroup analysis of the epidemic BI/NAP1/027 strain, this favorable association persisted (8% vs. 32%). Recurrence in the antibody group was seen more in elderly patients hospitalized with a higher severity of underlying disease.
Secondary endpoints relating to the initial episode of CDI including treatment failure, severity of diarrhea, and duration to resolution were not significantly different between the two groups. Fewer accounts of serious adverse events were documented in the antibody group (18 patients vs. 28 patients in placebo, P=0.09), and immunogenicity was not detected in any patient.
Bottom line: Monoclonal antibody infusion against C. diff toxins reduces recurrence of infection, even with a hypervirulent (B1/NAP1/027) strain, without any significant adverse events.
Citation: Lowy I, Molrine DC, Leav BA, et al. Treatment with monoclonal antibodies against Clostridium difficile toxins. N Engl J Med. 2010; 362(3):197-205. TH
Incidence and nature of postoperative complications in patients with obstructive sleep apnea undergoing noncardiac surgery
‘High’-pertension
In the Literature
Literature at a Glance
A guide to this month’s studies
- Inhaled steroids and COPD.
- Communication about dietary supplement use.
- Glycemic control in stroke.
- Hospitalist-PCP communication and outcomes.
- Gentamicin nephrotoxicity in endocarditis.
- Outcomes after osteoporotic fractures.
- Predictors of readmission after pulmonary embolism.
- Provider awareness of hospital readmission.
Inhaled Corticosteroid Use in COPD Associated with Increased Pneumonia Risk
Clinical question: Does long-term use of inhaled corticosteroids in chronic obstructive pulmonary disease (COPD) increase the risk of developing pneumonia?
Background: Guidelines recommend a combination of inhaled corticosteroids and long-acting bronchodilators in patients with severe COPD. However, recent evidence has raised concerns about the increased risk of pneumonia in patients on inhaled steroids. The exact nature of this association and its specificity to the inhaled corticosteroid component is unclear.
Study design: Meta-analysis and systematic review of 18 randomized controlled trials (RCTs) evaluating inhaled corticosteroid use in COPD.
Setting: Medline, EMBASE, the Cochrane Database of Systematic Reviews, regulatory documents, and trial registries.
Synopsis: This study, which totaled 16,996 case reviews, focused on inhaled corticosteroid use in COPD (excluding asthma) with at least 24 weeks of followup. The study authors evaluated inhaled corticosteroid use—alone or in combination with long-acting beta-agonists (LABA)—against a control (placebo or LABA alone). Primary outcomes were any pneumonia and serious pneumonia leading to increased morbidity and mortality. Secondary outcomes included pneumonia-related mortality and all-cause mortality.
Inhaled corticosteroids—irrespective of associated LABA use—significantly increased the risk of pneumonia (7.4% vs. 4.7%) with a relative risk (RR) of 1.60; 95% CI, 1.33-1.92, P<0.001. Inhaled corticosteroids were strongly associated with an increase in serious pneumonia (RR 1.71; 95% CI, 1.46-1.99, P<0.001). However, inhaled corticosteroid use did not translate to significantly increased pneumonia-related or overall mortality, possibly due to the inadequate power of most of the individual trials.
The findings reflect those from other database studies, but lend specificity to the inhaled corticosteroid component. This can be cause for concern as studies of long-term inhaled corticosteroid use in patients with COPD have failed to show a benefit in mortality or decreased exacerbations.
Bottom line: Risk-benefit analysis for inhaled corticosteroid use in COPD patients should consider the increased risk of pneumonia, possibly related to local immunosuppression.
Citation: Singh S, Amin AV, Loke YK. Long-term use of inhaled corticosteroids and the risk of pneumonia in chronic obstructive pulmonary disease: a meta-analysis. Arch Intern Med. 2009;169(3):219-229.
Inadequate Physician Communication Regarding Dietary Supplement Usage
Clinical question: How frequently do hospital physicians communicate about the use of dietary supplements?
Background: About 20% of the U.S. population uses dietary supplements, products that have potential interactions with other prescription medications. Dietary supplement usage patterns, disclosure, and discussion with physicians have been studied in the outpatient setting. However, these metrics have not been evaluated in the inpatient setting.
Study design: A cross-sectional, observational pilot study.
Setting: Inpatients on a general medicine and geriatrics service at the University of North Carolina Medical Center.
Synopsis: Sixty inpatients were questioned regarding their use of dietary supplements in the past year. Patients were asked about their communication with the admitting resident physician regarding dietary supplements and their beliefs regarding continued use during hospitalization. Patient responses revealed prevalent dietary supplement use, with about 80% of patients using supplements and 52% using nonvitamin/nonmineral supplements.
The study revealed poor communication between residents and their patients. Only 20% of residents inquired about dietary supplement use during the admission process, while 74% of patients neglected to disclose their use of dietary supplements. Furthermore, 56% of patients thought communication was unimportant; they assumed that it was in their medical records (18%), or they expected the physician to ask them about it (20%). Though most patients agreed to stop using dietary supplements as inpatients, 13% did not think dietary supplement use was a problem, even if it went against medical advice.
Study limitations include the small sample size and recall bias inherent to the design. It also is likely that more patients using dietary supplements consented for the study, as evidenced by higher prevalence of use.
Bottom line: Use of dietary supplements in hospitalized patients is common, and communication about their use between patients and physicians is limited.
Citation: Young LA, Faurot KR, Gaylord SA. Use of and communication about dietary supplements among hospitalized patients. J Gen Intern Med. 2009;24(3):366-369.
Early Hyperglycemia Associated with Poor Outcomes After Acute Ischemic Stroke
Clinical question: Is there a threshold of hyperglycemia after an acute ischemic stroke (IS) that predicts a poor outcome?
Background: A growing body of evidence shows that admission hyperglycemia in an acute IS predicts a poor outcome. Current triggers to initiate glucose control measures are based on consensus data. However, capillary glucose is a continuous variable and could have a linear relationship with stroke outcomes. A particular glucose level may herald poor outcomes.
Study design: Prospective observational cohort study.
Setting: Seven university hospitals with dedicated stroke units in Spain.
Synopsis: 476 patients with acute IS had admission and maximum glucose levels recorded during the first 48 hours of admission. Stroke scales and brain imaging assessed the patients’ stroke severity. The primary endpoint of a poor outcome at three months was defined by a modified Rankin score of >2.
The primary endpoint was noted in 156 (38%) patients. Receiver operating characteristic curves for both capillary glucose at admission and maximal values within 48 hours pointed to 155mg/dL as a cutoff for the primary outcome. However, subsequent regression analysis confirmed only the maximal value as an independent predictor of poor outcome (OR 2.73; 95% CI, 1.42 to 5.24). Additionally, in contrast to patient age and infarct volume, the maximal glucose value of ≥155 mg/dL was associated with stroke severity on admission and a higher three-month mortality (HR 3.80; 95% CI, 1.79 to 8.10; P=0.001).
The observational nature of the study opens it to speculation: Does lowering the level to less than 155 mg/dl improve patient outcomes? However, it does offer a potential target for future interventional studies.
Bottom line: Hyperglycemia within the first 48 hours of an ischemic stroke offers a more robust predictor of poor outcomes compared with admission glucose levels. A glucose level less than 155 mg/dL could be a potential treatment goal in the future.
Citation: Fuentes B, Castillo J, San José B, et al. The prognostic value of capillary glucose levels in acute stroke: The GLycemia In Acute Stroke (GLIAS) study. Stroke. 2009;40(2):562-568.
Communication Between Inpatient Medical Teams and PCPs Does Not Improve Outcomes
Clinical question: Does communication between patients’ physicians in the hospital and their primary-care physicians (PCPs) improve outcomes after discharge?
Background: The increased use of the hospitalist model has resulted in concerns about discontinuity of patient care after discharge. This might hamper the quality of clinical care and increase adverse outcomes, including readmission or death. Effective communication could have the potential to improve clinical outcomes.
Study design: Survey based in a quasi-randomized cohort of medical inpatients.
Setting: Six academic medical centers throughout the U.S.
Synopsis: Of the initial 2,526 patients, only 1,078 were available for final analysis based on failure of patient followup and a 68% PCP response rate. PCP surveys were faxed two weeks after patient discharge. PCPs were asked about hospitalization awareness and communication methods. Patients were contacted post-discharge, and National Death Index data were reviewed to determine the primary composite outcomes of ED visits, hospital readmissions, or death at 30 days.
Four out of five PCPs surveyed were aware of their patients’ hospitalizations—23% via direct communication and 42% by discharge summary. The primary outcome occurred in 184 (22%) of 834 patients. In contrast, of the 244 PCPs unaware of their patients’ hospitalizations, the primary outcome occurred in 49 (20%) patients. After logistic regression, PCP awareness of hospitalization, irrespective of communication method, was not associated with risk of outcomes (adjusted OR 1.08, 95% CI, 0.73 to 1.59). Having a hospitalist as the hospital physician (34%) did not affect outcomes. These results could reflect the inclusion of patients with fewer comorbidities. Additionally, effect on adverse drug events, patient satisfaction, and quality of life were not evaluated.
Bottom line: Communication between inpatient physicians and PCPs needs improvement to affect clinical outcomes, especially in high-risk patients.
Citation: Bell CM, Schnipper JL, Auerbach AD, et al. Association of communication between hospital-based physicians and primary care providers with patient outcomes. J Gen Intern Med. 2008;24(3):381-386.
Gentamicin Use in Staphylococcal Bacteremia or Endocarditis Causes Nephrotoxicity
Clinical question: Does gentamicin synergism in Staphylococcal bacteremia and endocarditis achieve faster eradication at the cost of nephrotoxicity?
Background: Gentamicin has been used to help with sterilization of blood or cardiac vegetations in patients with Staphylococcal bacteremia or infective endocarditis (IE). However, historic data negate its role in decreasing morbidity or mortality. If its potential nephrotoxicity were better characterized, it could help assess the overall utility of this practice.
Study design: Retrospective analysis of a cohort from a published randomized control trial.
Setting: 44 hospitals in the U.S. and Europe.
Synopsis: Two hundred thirty-six patients with Staphylococcal bacteremia or native-valve IE (mostly right-sided) were randomized to receive standard therapy (vancomycin or antistaphylococcal penicillin) or daptomycin. Patients receiving standard therapy and those with left-side IE in the daptomycin arm also received low-dose gentamicin. Sequential creatinine levels were used to determine primary outcomes of renal impairment events and a decrease in creatinine clearance.
Renal impairment events, elevation of mean serum creatinine, and decrease in creatinine clearance were more prevalent with standard therapy, especially in the elderly and those with diabetes. Combination of gentamicin with penicillin caused an earlier creatinine elevation compared with that with vancomycin.
Patients on gentamicin had a modest decrease in creatinine clearance (22% vs. 8%; P= 0.005), especially if their baseline was 50 to 80 mL/min. The decrease was early and sustained with gentamicin exposure. Multivariate analysis revealed age (≥65 years) and gentamicin use (not dose and duration) to be independent predictors of renal impairment. The analysis fails to address use of gentamicin in prosthetic-valve IE and left-side IE.
Bottom line: Initial low-dose gentamicin use in Staphylococcal bacteremia or endocarditis increases nephrotoxicity with no clear mortality benefit.
Citation: Cosgrove SE, Vigliani GA, Fowler VG, et al. Initial low-dose gentamicin for Staphylococcus aureus bacteremia and endocarditis is nephrotoxic. Clin Infect Dis. 2009;48(6):713-721.
Osteoporotic Fractures Increase Five-Year Mortality, Especially in the Elderly
Clinical question: What is the effect of initial osteoporotic fractures and subsequent fractures on mortality?
Background: With an aging population, osteoporotic fractures are poised to escalate into a national healthcare problem. Studies have outlined the increase in premature and long-term mortality associated with hip or vertebral fractures. However, other appendicular fractures have not been studied, and little is known about the mortality risk with subsequent fracturing.
Study design: Prospective cohort from the Dubbo Osteoporosis Epidemiology Study, a longitudinal, population-based study.
Setting: Stable population of men and women 60 and older in Dubbo, Australia.
Synopsis: 1,300 people with at least one minimal-trauma fracture were selected. Fractures were grouped as hip, vertebral, major (long bones and ribs), and minor (any remaining). Mortality data were extracted from local media, along with state and national registries. Age- and sex-specific mortality rates in each group were compared with population mortality rates to provide standardized mortality ratios (SMRs) over five-year periods.
Osteoporotic fractures increased five-year mortality with SMRs of 1.38 to 2.53 for women and 1.64 to 3.52 for men. An exception was minor fractures in patients 60 to 75 years old with no increase in mortality. Only hip fractures influenced mortality adversely for up to 10 years.
Interestingly, the nonhip, nonvertebral group included 50% of the fractures and contributed to 29% of overall mortality. Another five-year increase in mortality was evident in 364 people with a subsequent fracture.
A subgroup analysis revealed independent predictors of mortality, including lower bone mineral density, weaker quadriceps, smoking history, and increased sway in female patients; weaker quadriceps and decreased activities were independent predictors in male patients. Apart from the limitation that most subjects were white, the study gives a robust mortality analysis on osteoporotic fractures.
Bottom line: Osteoporotic fractures, initial and subsequent, increase five-year mortality. This is true even for nonhip, nonvertebral fractures, especially in the elderly.
Citation: Bliuc D, Nguyen ND, Milch VE, Nguyen TV, Eisman JA, Center JR. Mortality risk associated with low-trauma osteoporotic fracture and subsequent fracture in men and women. JAMA. 2009;301(5): 513-521.
Early Rehospitalization After Pulmonary Embolism Dictated by Clinical Severity and Anticoagulation Practices
Clinical question: What factors portend readmission after acute pulmonary embolism (PE)?
Background: The significant clinical and economic burden of acute pulmonary embolism (PE) has fueled studies to define predictors of early mortality. However, the variables leading to readmission after PE remain uncharted. Knowledge of these factors can provide additional targets to improve the quality of care.
Study design: Prospective population-based cohort study.
Setting: 186 acute-care hospitals in Pennsylvania.
Synopsis: Using ICD-9-CM codes, 14,426 PE patients were selected for the study. Primary outcome was hospital readmission within 30 days; secondary outcomes were venous thromboembolism (VTE) and bleeding.
More than 2,000 patients (14.3%) experienced a 30-day readmission. The predominant reasons were VTE (21.9%) and bleeding (5%), with the rest related to comorbidities, such as cancer (10.8%), pneumonia (5.2%), and chest pain (5.0%).
The discrete proportional odds model showed a significant association of high PE Severity Index score (OR 2.04; 95% CI, 1.73-2.40) and previous home care provision (OR 1.40; 95% CI, 1.27-1.54) with readmission, indicating that sicker patients tend to be readmitted. Black patients and Medicaid recipients were more likely to be readmitted, especially for VTE, which reflects the possible socioeconomic bearing on outcomes. Surprisingly, the few patients leaving the hospital against medical advice (0.4%) had a high OR of 2.84 (95% CI, 1.80-4.48) for readmission. Academic centers were not associated with increased readmissions but had significantly more readmissions for bleeding.
Anticoagulation practices—initial choice of agents, intensity of treatment, and monitoring—were not evaluated, which could affect readmission after PE, especially due to VTE and bleeding.
Bottom line: Apart from severity of illness and demographics, high rates of readmission after PE, especially for bleeding and VTE, might be related to poor anticoagulation practices.
Citation: Aujesky D, Mor MK, Geng M, Stone RA, Fine MJ, Ibrahim SA. Predictors of early hospital readmission after acute pulmonary embolism. Arch Intern Med. 2009;169(3):287-293.
Need for Improved Awareness of Hospital Readmission
Clinical question: What is the frequency of readmission awareness in discharging physicians and the trends in their communications with readmitting physicians?
Background: Rotation-based schedules of inpatient physicians, especially at academic centers, increase the likelihood that patients with complex medical or psychosocial issues requiring readmission will be cared for by a different team.
Though gaps in communication between the successive teams have the potential to hamper the quality of care, these gaps have not been adequately characterized in the literature.
Study design: Prospective cohort study.
Setting: Inpatient general-medicine services at two academic medical centers.
Synopsis: Researchers selected 225 patients readmitted within two weeks. The discharge and readmission teams were surveyed by e-mail within 48 hours of readmission regarding frequency and content of communications.
On analysis, the discharging teams were aware of patient readmissions only 48.5% of the time. Most of the remaining teams acknowledged a desire to be notified.
Actual communication occurred in 43.7% of cases and included information on medical assessments (61.9%), psychosocial issues (52.9%), pending tests (34%), and discharge medications (30.9%).
As expected, physician perception of higher medical complexity increased the likelihood of communication. Surprisingly, though psychosocial issues did not predict communication, they were discussed in almost half the cases. Lapses in communication were attributed to lack of time, perceived necessity, and contact information.
The observational nature, nongeneralizable population, and effect of responder bias limit the study. Though an interventional study can better evaluate improvement in patient outcomes, communication at readmission can be used as an educational feedback tool for house staff and attendings.
Bottom line: Modest frequency of communication between discharge and readmission physicians is driven mostly by medical complexity. It bears the potential to improve patient outcomes and offer valuable feedback.
Citation: Roy CL, Kachalia A, Woolf S, Burdick E, Karson A, Gandhi TK. Hospital readmissions: physician awareness and communication practices. J Gen Intern Med. 2009;24(3):374–380. TH
Literature at a Glance
A guide to this month’s studies
- Inhaled steroids and COPD.
- Communication about dietary supplement use.
- Glycemic control in stroke.
- Hospitalist-PCP communication and outcomes.
- Gentamicin nephrotoxicity in endocarditis.
- Outcomes after osteoporotic fractures.
- Predictors of readmission after pulmonary embolism.
- Provider awareness of hospital readmission.
Inhaled Corticosteroid Use in COPD Associated with Increased Pneumonia Risk
Clinical question: Does long-term use of inhaled corticosteroids in chronic obstructive pulmonary disease (COPD) increase the risk of developing pneumonia?
Background: Guidelines recommend a combination of inhaled corticosteroids and long-acting bronchodilators in patients with severe COPD. However, recent evidence has raised concerns about the increased risk of pneumonia in patients on inhaled steroids. The exact nature of this association and its specificity to the inhaled corticosteroid component is unclear.
Study design: Meta-analysis and systematic review of 18 randomized controlled trials (RCTs) evaluating inhaled corticosteroid use in COPD.
Setting: Medline, EMBASE, the Cochrane Database of Systematic Reviews, regulatory documents, and trial registries.
Synopsis: This study, which totaled 16,996 case reviews, focused on inhaled corticosteroid use in COPD (excluding asthma) with at least 24 weeks of followup. The study authors evaluated inhaled corticosteroid use—alone or in combination with long-acting beta-agonists (LABA)—against a control (placebo or LABA alone). Primary outcomes were any pneumonia and serious pneumonia leading to increased morbidity and mortality. Secondary outcomes included pneumonia-related mortality and all-cause mortality.
Inhaled corticosteroids—irrespective of associated LABA use—significantly increased the risk of pneumonia (7.4% vs. 4.7%) with a relative risk (RR) of 1.60; 95% CI, 1.33-1.92, P<0.001. Inhaled corticosteroids were strongly associated with an increase in serious pneumonia (RR 1.71; 95% CI, 1.46-1.99, P<0.001). However, inhaled corticosteroid use did not translate to significantly increased pneumonia-related or overall mortality, possibly due to the inadequate power of most of the individual trials.
The findings reflect those from other database studies, but lend specificity to the inhaled corticosteroid component. This can be cause for concern as studies of long-term inhaled corticosteroid use in patients with COPD have failed to show a benefit in mortality or decreased exacerbations.
Bottom line: Risk-benefit analysis for inhaled corticosteroid use in COPD patients should consider the increased risk of pneumonia, possibly related to local immunosuppression.
Citation: Singh S, Amin AV, Loke YK. Long-term use of inhaled corticosteroids and the risk of pneumonia in chronic obstructive pulmonary disease: a meta-analysis. Arch Intern Med. 2009;169(3):219-229.
Inadequate Physician Communication Regarding Dietary Supplement Usage
Clinical question: How frequently do hospital physicians communicate about the use of dietary supplements?
Background: About 20% of the U.S. population uses dietary supplements, products that have potential interactions with other prescription medications. Dietary supplement usage patterns, disclosure, and discussion with physicians have been studied in the outpatient setting. However, these metrics have not been evaluated in the inpatient setting.
Study design: A cross-sectional, observational pilot study.
Setting: Inpatients on a general medicine and geriatrics service at the University of North Carolina Medical Center.
Synopsis: Sixty inpatients were questioned regarding their use of dietary supplements in the past year. Patients were asked about their communication with the admitting resident physician regarding dietary supplements and their beliefs regarding continued use during hospitalization. Patient responses revealed prevalent dietary supplement use, with about 80% of patients using supplements and 52% using nonvitamin/nonmineral supplements.
The study revealed poor communication between residents and their patients. Only 20% of residents inquired about dietary supplement use during the admission process, while 74% of patients neglected to disclose their use of dietary supplements. Furthermore, 56% of patients thought communication was unimportant; they assumed that it was in their medical records (18%), or they expected the physician to ask them about it (20%). Though most patients agreed to stop using dietary supplements as inpatients, 13% did not think dietary supplement use was a problem, even if it went against medical advice.
Study limitations include the small sample size and recall bias inherent to the design. It also is likely that more patients using dietary supplements consented for the study, as evidenced by higher prevalence of use.
Bottom line: Use of dietary supplements in hospitalized patients is common, and communication about their use between patients and physicians is limited.
Citation: Young LA, Faurot KR, Gaylord SA. Use of and communication about dietary supplements among hospitalized patients. J Gen Intern Med. 2009;24(3):366-369.
Early Hyperglycemia Associated with Poor Outcomes After Acute Ischemic Stroke
Clinical question: Is there a threshold of hyperglycemia after an acute ischemic stroke (IS) that predicts a poor outcome?
Background: A growing body of evidence shows that admission hyperglycemia in an acute IS predicts a poor outcome. Current triggers to initiate glucose control measures are based on consensus data. However, capillary glucose is a continuous variable and could have a linear relationship with stroke outcomes. A particular glucose level may herald poor outcomes.
Study design: Prospective observational cohort study.
Setting: Seven university hospitals with dedicated stroke units in Spain.
Synopsis: 476 patients with acute IS had admission and maximum glucose levels recorded during the first 48 hours of admission. Stroke scales and brain imaging assessed the patients’ stroke severity. The primary endpoint of a poor outcome at three months was defined by a modified Rankin score of >2.
The primary endpoint was noted in 156 (38%) patients. Receiver operating characteristic curves for both capillary glucose at admission and maximal values within 48 hours pointed to 155mg/dL as a cutoff for the primary outcome. However, subsequent regression analysis confirmed only the maximal value as an independent predictor of poor outcome (OR 2.73; 95% CI, 1.42 to 5.24). Additionally, in contrast to patient age and infarct volume, the maximal glucose value of ≥155 mg/dL was associated with stroke severity on admission and a higher three-month mortality (HR 3.80; 95% CI, 1.79 to 8.10; P=0.001).
The observational nature of the study opens it to speculation: Does lowering the level to less than 155 mg/dl improve patient outcomes? However, it does offer a potential target for future interventional studies.
Bottom line: Hyperglycemia within the first 48 hours of an ischemic stroke offers a more robust predictor of poor outcomes compared with admission glucose levels. A glucose level less than 155 mg/dL could be a potential treatment goal in the future.
Citation: Fuentes B, Castillo J, San José B, et al. The prognostic value of capillary glucose levels in acute stroke: The GLycemia In Acute Stroke (GLIAS) study. Stroke. 2009;40(2):562-568.
Communication Between Inpatient Medical Teams and PCPs Does Not Improve Outcomes
Clinical question: Does communication between patients’ physicians in the hospital and their primary-care physicians (PCPs) improve outcomes after discharge?
Background: The increased use of the hospitalist model has resulted in concerns about discontinuity of patient care after discharge. This might hamper the quality of clinical care and increase adverse outcomes, including readmission or death. Effective communication could have the potential to improve clinical outcomes.
Study design: Survey based in a quasi-randomized cohort of medical inpatients.
Setting: Six academic medical centers throughout the U.S.
Synopsis: Of the initial 2,526 patients, only 1,078 were available for final analysis based on failure of patient followup and a 68% PCP response rate. PCP surveys were faxed two weeks after patient discharge. PCPs were asked about hospitalization awareness and communication methods. Patients were contacted post-discharge, and National Death Index data were reviewed to determine the primary composite outcomes of ED visits, hospital readmissions, or death at 30 days.
Four out of five PCPs surveyed were aware of their patients’ hospitalizations—23% via direct communication and 42% by discharge summary. The primary outcome occurred in 184 (22%) of 834 patients. In contrast, of the 244 PCPs unaware of their patients’ hospitalizations, the primary outcome occurred in 49 (20%) patients. After logistic regression, PCP awareness of hospitalization, irrespective of communication method, was not associated with risk of outcomes (adjusted OR 1.08, 95% CI, 0.73 to 1.59). Having a hospitalist as the hospital physician (34%) did not affect outcomes. These results could reflect the inclusion of patients with fewer comorbidities. Additionally, effect on adverse drug events, patient satisfaction, and quality of life were not evaluated.
Bottom line: Communication between inpatient physicians and PCPs needs improvement to affect clinical outcomes, especially in high-risk patients.
Citation: Bell CM, Schnipper JL, Auerbach AD, et al. Association of communication between hospital-based physicians and primary care providers with patient outcomes. J Gen Intern Med. 2008;24(3):381-386.
Gentamicin Use in Staphylococcal Bacteremia or Endocarditis Causes Nephrotoxicity
Clinical question: Does gentamicin synergism in Staphylococcal bacteremia and endocarditis achieve faster eradication at the cost of nephrotoxicity?
Background: Gentamicin has been used to help with sterilization of blood or cardiac vegetations in patients with Staphylococcal bacteremia or infective endocarditis (IE). However, historic data negate its role in decreasing morbidity or mortality. If its potential nephrotoxicity were better characterized, it could help assess the overall utility of this practice.
Study design: Retrospective analysis of a cohort from a published randomized control trial.
Setting: 44 hospitals in the U.S. and Europe.
Synopsis: Two hundred thirty-six patients with Staphylococcal bacteremia or native-valve IE (mostly right-sided) were randomized to receive standard therapy (vancomycin or antistaphylococcal penicillin) or daptomycin. Patients receiving standard therapy and those with left-side IE in the daptomycin arm also received low-dose gentamicin. Sequential creatinine levels were used to determine primary outcomes of renal impairment events and a decrease in creatinine clearance.
Renal impairment events, elevation of mean serum creatinine, and decrease in creatinine clearance were more prevalent with standard therapy, especially in the elderly and those with diabetes. Combination of gentamicin with penicillin caused an earlier creatinine elevation compared with that with vancomycin.
Patients on gentamicin had a modest decrease in creatinine clearance (22% vs. 8%; P= 0.005), especially if their baseline was 50 to 80 mL/min. The decrease was early and sustained with gentamicin exposure. Multivariate analysis revealed age (≥65 years) and gentamicin use (not dose and duration) to be independent predictors of renal impairment. The analysis fails to address use of gentamicin in prosthetic-valve IE and left-side IE.
Bottom line: Initial low-dose gentamicin use in Staphylococcal bacteremia or endocarditis increases nephrotoxicity with no clear mortality benefit.
Citation: Cosgrove SE, Vigliani GA, Fowler VG, et al. Initial low-dose gentamicin for Staphylococcus aureus bacteremia and endocarditis is nephrotoxic. Clin Infect Dis. 2009;48(6):713-721.
Osteoporotic Fractures Increase Five-Year Mortality, Especially in the Elderly
Clinical question: What is the effect of initial osteoporotic fractures and subsequent fractures on mortality?
Background: With an aging population, osteoporotic fractures are poised to escalate into a national healthcare problem. Studies have outlined the increase in premature and long-term mortality associated with hip or vertebral fractures. However, other appendicular fractures have not been studied, and little is known about the mortality risk with subsequent fracturing.
Study design: Prospective cohort from the Dubbo Osteoporosis Epidemiology Study, a longitudinal, population-based study.
Setting: Stable population of men and women 60 and older in Dubbo, Australia.
Synopsis: 1,300 people with at least one minimal-trauma fracture were selected. Fractures were grouped as hip, vertebral, major (long bones and ribs), and minor (any remaining). Mortality data were extracted from local media, along with state and national registries. Age- and sex-specific mortality rates in each group were compared with population mortality rates to provide standardized mortality ratios (SMRs) over five-year periods.
Osteoporotic fractures increased five-year mortality with SMRs of 1.38 to 2.53 for women and 1.64 to 3.52 for men. An exception was minor fractures in patients 60 to 75 years old with no increase in mortality. Only hip fractures influenced mortality adversely for up to 10 years.
Interestingly, the nonhip, nonvertebral group included 50% of the fractures and contributed to 29% of overall mortality. Another five-year increase in mortality was evident in 364 people with a subsequent fracture.
A subgroup analysis revealed independent predictors of mortality, including lower bone mineral density, weaker quadriceps, smoking history, and increased sway in female patients; weaker quadriceps and decreased activities were independent predictors in male patients. Apart from the limitation that most subjects were white, the study gives a robust mortality analysis on osteoporotic fractures.
Bottom line: Osteoporotic fractures, initial and subsequent, increase five-year mortality. This is true even for nonhip, nonvertebral fractures, especially in the elderly.
Citation: Bliuc D, Nguyen ND, Milch VE, Nguyen TV, Eisman JA, Center JR. Mortality risk associated with low-trauma osteoporotic fracture and subsequent fracture in men and women. JAMA. 2009;301(5): 513-521.
Early Rehospitalization After Pulmonary Embolism Dictated by Clinical Severity and Anticoagulation Practices
Clinical question: What factors portend readmission after acute pulmonary embolism (PE)?
Background: The significant clinical and economic burden of acute pulmonary embolism (PE) has fueled studies to define predictors of early mortality. However, the variables leading to readmission after PE remain uncharted. Knowledge of these factors can provide additional targets to improve the quality of care.
Study design: Prospective population-based cohort study.
Setting: 186 acute-care hospitals in Pennsylvania.
Synopsis: Using ICD-9-CM codes, 14,426 PE patients were selected for the study. Primary outcome was hospital readmission within 30 days; secondary outcomes were venous thromboembolism (VTE) and bleeding.
More than 2,000 patients (14.3%) experienced a 30-day readmission. The predominant reasons were VTE (21.9%) and bleeding (5%), with the rest related to comorbidities, such as cancer (10.8%), pneumonia (5.2%), and chest pain (5.0%).
The discrete proportional odds model showed a significant association of high PE Severity Index score (OR 2.04; 95% CI, 1.73-2.40) and previous home care provision (OR 1.40; 95% CI, 1.27-1.54) with readmission, indicating that sicker patients tend to be readmitted. Black patients and Medicaid recipients were more likely to be readmitted, especially for VTE, which reflects the possible socioeconomic bearing on outcomes. Surprisingly, the few patients leaving the hospital against medical advice (0.4%) had a high OR of 2.84 (95% CI, 1.80-4.48) for readmission. Academic centers were not associated with increased readmissions but had significantly more readmissions for bleeding.
Anticoagulation practices—initial choice of agents, intensity of treatment, and monitoring—were not evaluated, which could affect readmission after PE, especially due to VTE and bleeding.
Bottom line: Apart from severity of illness and demographics, high rates of readmission after PE, especially for bleeding and VTE, might be related to poor anticoagulation practices.
Citation: Aujesky D, Mor MK, Geng M, Stone RA, Fine MJ, Ibrahim SA. Predictors of early hospital readmission after acute pulmonary embolism. Arch Intern Med. 2009;169(3):287-293.
Need for Improved Awareness of Hospital Readmission
Clinical question: What is the frequency of readmission awareness in discharging physicians and the trends in their communications with readmitting physicians?
Background: Rotation-based schedules of inpatient physicians, especially at academic centers, increase the likelihood that patients with complex medical or psychosocial issues requiring readmission will be cared for by a different team.
Though gaps in communication between the successive teams have the potential to hamper the quality of care, these gaps have not been adequately characterized in the literature.
Study design: Prospective cohort study.
Setting: Inpatient general-medicine services at two academic medical centers.
Synopsis: Researchers selected 225 patients readmitted within two weeks. The discharge and readmission teams were surveyed by e-mail within 48 hours of readmission regarding frequency and content of communications.
On analysis, the discharging teams were aware of patient readmissions only 48.5% of the time. Most of the remaining teams acknowledged a desire to be notified.
Actual communication occurred in 43.7% of cases and included information on medical assessments (61.9%), psychosocial issues (52.9%), pending tests (34%), and discharge medications (30.9%).
As expected, physician perception of higher medical complexity increased the likelihood of communication. Surprisingly, though psychosocial issues did not predict communication, they were discussed in almost half the cases. Lapses in communication were attributed to lack of time, perceived necessity, and contact information.
The observational nature, nongeneralizable population, and effect of responder bias limit the study. Though an interventional study can better evaluate improvement in patient outcomes, communication at readmission can be used as an educational feedback tool for house staff and attendings.
Bottom line: Modest frequency of communication between discharge and readmission physicians is driven mostly by medical complexity. It bears the potential to improve patient outcomes and offer valuable feedback.
Citation: Roy CL, Kachalia A, Woolf S, Burdick E, Karson A, Gandhi TK. Hospital readmissions: physician awareness and communication practices. J Gen Intern Med. 2009;24(3):374–380. TH
Literature at a Glance
A guide to this month’s studies
- Inhaled steroids and COPD.
- Communication about dietary supplement use.
- Glycemic control in stroke.
- Hospitalist-PCP communication and outcomes.
- Gentamicin nephrotoxicity in endocarditis.
- Outcomes after osteoporotic fractures.
- Predictors of readmission after pulmonary embolism.
- Provider awareness of hospital readmission.
Inhaled Corticosteroid Use in COPD Associated with Increased Pneumonia Risk
Clinical question: Does long-term use of inhaled corticosteroids in chronic obstructive pulmonary disease (COPD) increase the risk of developing pneumonia?
Background: Guidelines recommend a combination of inhaled corticosteroids and long-acting bronchodilators in patients with severe COPD. However, recent evidence has raised concerns about the increased risk of pneumonia in patients on inhaled steroids. The exact nature of this association and its specificity to the inhaled corticosteroid component is unclear.
Study design: Meta-analysis and systematic review of 18 randomized controlled trials (RCTs) evaluating inhaled corticosteroid use in COPD.
Setting: Medline, EMBASE, the Cochrane Database of Systematic Reviews, regulatory documents, and trial registries.
Synopsis: This study, which totaled 16,996 case reviews, focused on inhaled corticosteroid use in COPD (excluding asthma) with at least 24 weeks of followup. The study authors evaluated inhaled corticosteroid use—alone or in combination with long-acting beta-agonists (LABA)—against a control (placebo or LABA alone). Primary outcomes were any pneumonia and serious pneumonia leading to increased morbidity and mortality. Secondary outcomes included pneumonia-related mortality and all-cause mortality.
Inhaled corticosteroids—irrespective of associated LABA use—significantly increased the risk of pneumonia (7.4% vs. 4.7%) with a relative risk (RR) of 1.60; 95% CI, 1.33-1.92, P<0.001. Inhaled corticosteroids were strongly associated with an increase in serious pneumonia (RR 1.71; 95% CI, 1.46-1.99, P<0.001). However, inhaled corticosteroid use did not translate to significantly increased pneumonia-related or overall mortality, possibly due to the inadequate power of most of the individual trials.
The findings reflect those from other database studies, but lend specificity to the inhaled corticosteroid component. This can be cause for concern as studies of long-term inhaled corticosteroid use in patients with COPD have failed to show a benefit in mortality or decreased exacerbations.
Bottom line: Risk-benefit analysis for inhaled corticosteroid use in COPD patients should consider the increased risk of pneumonia, possibly related to local immunosuppression.
Citation: Singh S, Amin AV, Loke YK. Long-term use of inhaled corticosteroids and the risk of pneumonia in chronic obstructive pulmonary disease: a meta-analysis. Arch Intern Med. 2009;169(3):219-229.
Inadequate Physician Communication Regarding Dietary Supplement Usage
Clinical question: How frequently do hospital physicians communicate about the use of dietary supplements?
Background: About 20% of the U.S. population uses dietary supplements, products that have potential interactions with other prescription medications. Dietary supplement usage patterns, disclosure, and discussion with physicians have been studied in the outpatient setting. However, these metrics have not been evaluated in the inpatient setting.
Study design: A cross-sectional, observational pilot study.
Setting: Inpatients on a general medicine and geriatrics service at the University of North Carolina Medical Center.
Synopsis: Sixty inpatients were questioned regarding their use of dietary supplements in the past year. Patients were asked about their communication with the admitting resident physician regarding dietary supplements and their beliefs regarding continued use during hospitalization. Patient responses revealed prevalent dietary supplement use, with about 80% of patients using supplements and 52% using nonvitamin/nonmineral supplements.
The study revealed poor communication between residents and their patients. Only 20% of residents inquired about dietary supplement use during the admission process, while 74% of patients neglected to disclose their use of dietary supplements. Furthermore, 56% of patients thought communication was unimportant; they assumed that it was in their medical records (18%), or they expected the physician to ask them about it (20%). Though most patients agreed to stop using dietary supplements as inpatients, 13% did not think dietary supplement use was a problem, even if it went against medical advice.
Study limitations include the small sample size and recall bias inherent to the design. It also is likely that more patients using dietary supplements consented for the study, as evidenced by higher prevalence of use.
Bottom line: Use of dietary supplements in hospitalized patients is common, and communication about their use between patients and physicians is limited.
Citation: Young LA, Faurot KR, Gaylord SA. Use of and communication about dietary supplements among hospitalized patients. J Gen Intern Med. 2009;24(3):366-369.
Early Hyperglycemia Associated with Poor Outcomes After Acute Ischemic Stroke
Clinical question: Is there a threshold of hyperglycemia after an acute ischemic stroke (IS) that predicts a poor outcome?
Background: A growing body of evidence shows that admission hyperglycemia in an acute IS predicts a poor outcome. Current triggers to initiate glucose control measures are based on consensus data. However, capillary glucose is a continuous variable and could have a linear relationship with stroke outcomes. A particular glucose level may herald poor outcomes.
Study design: Prospective observational cohort study.
Setting: Seven university hospitals with dedicated stroke units in Spain.
Synopsis: 476 patients with acute IS had admission and maximum glucose levels recorded during the first 48 hours of admission. Stroke scales and brain imaging assessed the patients’ stroke severity. The primary endpoint of a poor outcome at three months was defined by a modified Rankin score of >2.
The primary endpoint was noted in 156 (38%) patients. Receiver operating characteristic curves for both capillary glucose at admission and maximal values within 48 hours pointed to 155mg/dL as a cutoff for the primary outcome. However, subsequent regression analysis confirmed only the maximal value as an independent predictor of poor outcome (OR 2.73; 95% CI, 1.42 to 5.24). Additionally, in contrast to patient age and infarct volume, the maximal glucose value of ≥155 mg/dL was associated with stroke severity on admission and a higher three-month mortality (HR 3.80; 95% CI, 1.79 to 8.10; P=0.001).
The observational nature of the study opens it to speculation: Does lowering the level to less than 155 mg/dl improve patient outcomes? However, it does offer a potential target for future interventional studies.
Bottom line: Hyperglycemia within the first 48 hours of an ischemic stroke offers a more robust predictor of poor outcomes compared with admission glucose levels. A glucose level less than 155 mg/dL could be a potential treatment goal in the future.
Citation: Fuentes B, Castillo J, San José B, et al. The prognostic value of capillary glucose levels in acute stroke: The GLycemia In Acute Stroke (GLIAS) study. Stroke. 2009;40(2):562-568.
Communication Between Inpatient Medical Teams and PCPs Does Not Improve Outcomes
Clinical question: Does communication between patients’ physicians in the hospital and their primary-care physicians (PCPs) improve outcomes after discharge?
Background: The increased use of the hospitalist model has resulted in concerns about discontinuity of patient care after discharge. This might hamper the quality of clinical care and increase adverse outcomes, including readmission or death. Effective communication could have the potential to improve clinical outcomes.
Study design: Survey based in a quasi-randomized cohort of medical inpatients.
Setting: Six academic medical centers throughout the U.S.
Synopsis: Of the initial 2,526 patients, only 1,078 were available for final analysis based on failure of patient followup and a 68% PCP response rate. PCP surveys were faxed two weeks after patient discharge. PCPs were asked about hospitalization awareness and communication methods. Patients were contacted post-discharge, and National Death Index data were reviewed to determine the primary composite outcomes of ED visits, hospital readmissions, or death at 30 days.
Four out of five PCPs surveyed were aware of their patients’ hospitalizations—23% via direct communication and 42% by discharge summary. The primary outcome occurred in 184 (22%) of 834 patients. In contrast, of the 244 PCPs unaware of their patients’ hospitalizations, the primary outcome occurred in 49 (20%) patients. After logistic regression, PCP awareness of hospitalization, irrespective of communication method, was not associated with risk of outcomes (adjusted OR 1.08, 95% CI, 0.73 to 1.59). Having a hospitalist as the hospital physician (34%) did not affect outcomes. These results could reflect the inclusion of patients with fewer comorbidities. Additionally, effect on adverse drug events, patient satisfaction, and quality of life were not evaluated.
Bottom line: Communication between inpatient physicians and PCPs needs improvement to affect clinical outcomes, especially in high-risk patients.
Citation: Bell CM, Schnipper JL, Auerbach AD, et al. Association of communication between hospital-based physicians and primary care providers with patient outcomes. J Gen Intern Med. 2008;24(3):381-386.
Gentamicin Use in Staphylococcal Bacteremia or Endocarditis Causes Nephrotoxicity
Clinical question: Does gentamicin synergism in Staphylococcal bacteremia and endocarditis achieve faster eradication at the cost of nephrotoxicity?
Background: Gentamicin has been used to help with sterilization of blood or cardiac vegetations in patients with Staphylococcal bacteremia or infective endocarditis (IE). However, historic data negate its role in decreasing morbidity or mortality. If its potential nephrotoxicity were better characterized, it could help assess the overall utility of this practice.
Study design: Retrospective analysis of a cohort from a published randomized control trial.
Setting: 44 hospitals in the U.S. and Europe.
Synopsis: Two hundred thirty-six patients with Staphylococcal bacteremia or native-valve IE (mostly right-sided) were randomized to receive standard therapy (vancomycin or antistaphylococcal penicillin) or daptomycin. Patients receiving standard therapy and those with left-side IE in the daptomycin arm also received low-dose gentamicin. Sequential creatinine levels were used to determine primary outcomes of renal impairment events and a decrease in creatinine clearance.
Renal impairment events, elevation of mean serum creatinine, and decrease in creatinine clearance were more prevalent with standard therapy, especially in the elderly and those with diabetes. Combination of gentamicin with penicillin caused an earlier creatinine elevation compared with that with vancomycin.
Patients on gentamicin had a modest decrease in creatinine clearance (22% vs. 8%; P= 0.005), especially if their baseline was 50 to 80 mL/min. The decrease was early and sustained with gentamicin exposure. Multivariate analysis revealed age (≥65 years) and gentamicin use (not dose and duration) to be independent predictors of renal impairment. The analysis fails to address use of gentamicin in prosthetic-valve IE and left-side IE.
Bottom line: Initial low-dose gentamicin use in Staphylococcal bacteremia or endocarditis increases nephrotoxicity with no clear mortality benefit.
Citation: Cosgrove SE, Vigliani GA, Fowler VG, et al. Initial low-dose gentamicin for Staphylococcus aureus bacteremia and endocarditis is nephrotoxic. Clin Infect Dis. 2009;48(6):713-721.
Osteoporotic Fractures Increase Five-Year Mortality, Especially in the Elderly
Clinical question: What is the effect of initial osteoporotic fractures and subsequent fractures on mortality?
Background: With an aging population, osteoporotic fractures are poised to escalate into a national healthcare problem. Studies have outlined the increase in premature and long-term mortality associated with hip or vertebral fractures. However, other appendicular fractures have not been studied, and little is known about the mortality risk with subsequent fracturing.
Study design: Prospective cohort from the Dubbo Osteoporosis Epidemiology Study, a longitudinal, population-based study.
Setting: Stable population of men and women 60 and older in Dubbo, Australia.
Synopsis: 1,300 people with at least one minimal-trauma fracture were selected. Fractures were grouped as hip, vertebral, major (long bones and ribs), and minor (any remaining). Mortality data were extracted from local media, along with state and national registries. Age- and sex-specific mortality rates in each group were compared with population mortality rates to provide standardized mortality ratios (SMRs) over five-year periods.
Osteoporotic fractures increased five-year mortality with SMRs of 1.38 to 2.53 for women and 1.64 to 3.52 for men. An exception was minor fractures in patients 60 to 75 years old with no increase in mortality. Only hip fractures influenced mortality adversely for up to 10 years.
Interestingly, the nonhip, nonvertebral group included 50% of the fractures and contributed to 29% of overall mortality. Another five-year increase in mortality was evident in 364 people with a subsequent fracture.
A subgroup analysis revealed independent predictors of mortality, including lower bone mineral density, weaker quadriceps, smoking history, and increased sway in female patients; weaker quadriceps and decreased activities were independent predictors in male patients. Apart from the limitation that most subjects were white, the study gives a robust mortality analysis on osteoporotic fractures.
Bottom line: Osteoporotic fractures, initial and subsequent, increase five-year mortality. This is true even for nonhip, nonvertebral fractures, especially in the elderly.
Citation: Bliuc D, Nguyen ND, Milch VE, Nguyen TV, Eisman JA, Center JR. Mortality risk associated with low-trauma osteoporotic fracture and subsequent fracture in men and women. JAMA. 2009;301(5): 513-521.
Early Rehospitalization After Pulmonary Embolism Dictated by Clinical Severity and Anticoagulation Practices
Clinical question: What factors portend readmission after acute pulmonary embolism (PE)?
Background: The significant clinical and economic burden of acute pulmonary embolism (PE) has fueled studies to define predictors of early mortality. However, the variables leading to readmission after PE remain uncharted. Knowledge of these factors can provide additional targets to improve the quality of care.
Study design: Prospective population-based cohort study.
Setting: 186 acute-care hospitals in Pennsylvania.
Synopsis: Using ICD-9-CM codes, 14,426 PE patients were selected for the study. Primary outcome was hospital readmission within 30 days; secondary outcomes were venous thromboembolism (VTE) and bleeding.
More than 2,000 patients (14.3%) experienced a 30-day readmission. The predominant reasons were VTE (21.9%) and bleeding (5%), with the rest related to comorbidities, such as cancer (10.8%), pneumonia (5.2%), and chest pain (5.0%).
The discrete proportional odds model showed a significant association of high PE Severity Index score (OR 2.04; 95% CI, 1.73-2.40) and previous home care provision (OR 1.40; 95% CI, 1.27-1.54) with readmission, indicating that sicker patients tend to be readmitted. Black patients and Medicaid recipients were more likely to be readmitted, especially for VTE, which reflects the possible socioeconomic bearing on outcomes. Surprisingly, the few patients leaving the hospital against medical advice (0.4%) had a high OR of 2.84 (95% CI, 1.80-4.48) for readmission. Academic centers were not associated with increased readmissions but had significantly more readmissions for bleeding.
Anticoagulation practices—initial choice of agents, intensity of treatment, and monitoring—were not evaluated, which could affect readmission after PE, especially due to VTE and bleeding.
Bottom line: Apart from severity of illness and demographics, high rates of readmission after PE, especially for bleeding and VTE, might be related to poor anticoagulation practices.
Citation: Aujesky D, Mor MK, Geng M, Stone RA, Fine MJ, Ibrahim SA. Predictors of early hospital readmission after acute pulmonary embolism. Arch Intern Med. 2009;169(3):287-293.
Need for Improved Awareness of Hospital Readmission
Clinical question: What is the frequency of readmission awareness in discharging physicians and the trends in their communications with readmitting physicians?
Background: Rotation-based schedules of inpatient physicians, especially at academic centers, increase the likelihood that patients with complex medical or psychosocial issues requiring readmission will be cared for by a different team.
Though gaps in communication between the successive teams have the potential to hamper the quality of care, these gaps have not been adequately characterized in the literature.
Study design: Prospective cohort study.
Setting: Inpatient general-medicine services at two academic medical centers.
Synopsis: Researchers selected 225 patients readmitted within two weeks. The discharge and readmission teams were surveyed by e-mail within 48 hours of readmission regarding frequency and content of communications.
On analysis, the discharging teams were aware of patient readmissions only 48.5% of the time. Most of the remaining teams acknowledged a desire to be notified.
Actual communication occurred in 43.7% of cases and included information on medical assessments (61.9%), psychosocial issues (52.9%), pending tests (34%), and discharge medications (30.9%).
As expected, physician perception of higher medical complexity increased the likelihood of communication. Surprisingly, though psychosocial issues did not predict communication, they were discussed in almost half the cases. Lapses in communication were attributed to lack of time, perceived necessity, and contact information.
The observational nature, nongeneralizable population, and effect of responder bias limit the study. Though an interventional study can better evaluate improvement in patient outcomes, communication at readmission can be used as an educational feedback tool for house staff and attendings.
Bottom line: Modest frequency of communication between discharge and readmission physicians is driven mostly by medical complexity. It bears the potential to improve patient outcomes and offer valuable feedback.
Citation: Roy CL, Kachalia A, Woolf S, Burdick E, Karson A, Gandhi TK. Hospital readmissions: physician awareness and communication practices. J Gen Intern Med. 2009;24(3):374–380. TH


