User login
CGRP inhibitors receive reassuring real-world safety report
Stephen D. Silberstein, MD, reported online as part of the 2020 American Academy of Neurology Science Highlights.
He presented a retrospective analysis of spontaneous postmarketing reports to the Food and Drug Administration Adverse Events Reporting System (FAERS) for Aimovig (erenumab-aooe), Ajovy (fremanezumab-vfrm), and Emgality (galcanezumab-gnlm).
The top-10 lists of adverse events for all three monoclonal antibodies targeting CGRP were skewed heavily towards injection-site reactions, such as injection-site pain, itching, swelling, and erythema. The rates were relatively low. For example, injection-site pain was reported at a rate of 2.94 cases per 1,000 patients exposed to erenumab, 0.8/1,000 for fremanezumab, and 4.9/1,000 for galcanezumab, according to Dr. Silberstein, professor of neurology and director of the headache center at Sidney Kimmel Medical College, Philadelphia.
Migraine, headache, and drug ineffectiveness were in the top 10 for all three medications, as is typical in FAERS reports, since no drug is effective in everyone. These events were reported at rates of 1-5/1,000 exposed patients. Constipation was reported in association with the use of erenumab at a rate of 4.9 cases/1,000 patients, but did not reach the top-10 lists for the other two CGRP antagonists.
Notably, cardiovascular events were not among the top-10 adverse events reported for any of the novel preventive agents.
“These results will be practice changing, since some physicians have been holding back from prescribing these drugs pending the results of this sort of longer-term safety data,” Dr. Silberstein predicted in an interview.
Asked to comment on the FAERS study, neurologist Holly Yancy, DO, said that she found the findings unsurprising because the adverse effects were essentially as expected based upon the earlier favorable clinical trials experience.
“These medications are living up to the expectations for good tolerability that were in place when they were initially approved by the FDA just under 2 years ago,” said Dr. Yancy, a headache specialist at the Banner–University Medicine Neuroscience Institute in Phoenix.
“Injection-site reactions were anticipated. Clinically, I’ve found that if the medications reduce migraine days and severity, patients find the risk of temporary pain, redness, or itching at the injection site is an easy trade off,” she added.
CGRP is a vasoactive peptide. There has been a theoretic concern that its pharmacologic inhibition for prevention of migraine could lead to an increased risk of adverse cardiovascular events, especially in individuals with coronary disease or a history of stroke. The absence of any such signal during the first 6 months of widespread clinical use of the CGRP inhibitors is highly encouraging, although this is an issue that warrants longer-term study, Dr. Yancy continued.
These drugs, which were expressly designed for migraine prevention, are a considerable advance over what was previously available in her view. They’re equally or more effective and considerably better tolerated than the preventive medications physicians had long been using off label, including antidepressants, antiepileptics, and cardiac drugs.
Dr. Silberstein reported financial relationships with close to two dozen pharmaceutical companies. Dr. Yancy reported serving on speakers’ bureaus for Amgen and Novartis.
SOURCE: Silverstein SD et al. AAN 2020, Abstract S58.008.
Stephen D. Silberstein, MD, reported online as part of the 2020 American Academy of Neurology Science Highlights.
He presented a retrospective analysis of spontaneous postmarketing reports to the Food and Drug Administration Adverse Events Reporting System (FAERS) for Aimovig (erenumab-aooe), Ajovy (fremanezumab-vfrm), and Emgality (galcanezumab-gnlm).
The top-10 lists of adverse events for all three monoclonal antibodies targeting CGRP were skewed heavily towards injection-site reactions, such as injection-site pain, itching, swelling, and erythema. The rates were relatively low. For example, injection-site pain was reported at a rate of 2.94 cases per 1,000 patients exposed to erenumab, 0.8/1,000 for fremanezumab, and 4.9/1,000 for galcanezumab, according to Dr. Silberstein, professor of neurology and director of the headache center at Sidney Kimmel Medical College, Philadelphia.
Migraine, headache, and drug ineffectiveness were in the top 10 for all three medications, as is typical in FAERS reports, since no drug is effective in everyone. These events were reported at rates of 1-5/1,000 exposed patients. Constipation was reported in association with the use of erenumab at a rate of 4.9 cases/1,000 patients, but did not reach the top-10 lists for the other two CGRP antagonists.
Notably, cardiovascular events were not among the top-10 adverse events reported for any of the novel preventive agents.
“These results will be practice changing, since some physicians have been holding back from prescribing these drugs pending the results of this sort of longer-term safety data,” Dr. Silberstein predicted in an interview.
Asked to comment on the FAERS study, neurologist Holly Yancy, DO, said that she found the findings unsurprising because the adverse effects were essentially as expected based upon the earlier favorable clinical trials experience.
“These medications are living up to the expectations for good tolerability that were in place when they were initially approved by the FDA just under 2 years ago,” said Dr. Yancy, a headache specialist at the Banner–University Medicine Neuroscience Institute in Phoenix.
“Injection-site reactions were anticipated. Clinically, I’ve found that if the medications reduce migraine days and severity, patients find the risk of temporary pain, redness, or itching at the injection site is an easy trade off,” she added.
CGRP is a vasoactive peptide. There has been a theoretic concern that its pharmacologic inhibition for prevention of migraine could lead to an increased risk of adverse cardiovascular events, especially in individuals with coronary disease or a history of stroke. The absence of any such signal during the first 6 months of widespread clinical use of the CGRP inhibitors is highly encouraging, although this is an issue that warrants longer-term study, Dr. Yancy continued.
These drugs, which were expressly designed for migraine prevention, are a considerable advance over what was previously available in her view. They’re equally or more effective and considerably better tolerated than the preventive medications physicians had long been using off label, including antidepressants, antiepileptics, and cardiac drugs.
Dr. Silberstein reported financial relationships with close to two dozen pharmaceutical companies. Dr. Yancy reported serving on speakers’ bureaus for Amgen and Novartis.
SOURCE: Silverstein SD et al. AAN 2020, Abstract S58.008.
Stephen D. Silberstein, MD, reported online as part of the 2020 American Academy of Neurology Science Highlights.
He presented a retrospective analysis of spontaneous postmarketing reports to the Food and Drug Administration Adverse Events Reporting System (FAERS) for Aimovig (erenumab-aooe), Ajovy (fremanezumab-vfrm), and Emgality (galcanezumab-gnlm).
The top-10 lists of adverse events for all three monoclonal antibodies targeting CGRP were skewed heavily towards injection-site reactions, such as injection-site pain, itching, swelling, and erythema. The rates were relatively low. For example, injection-site pain was reported at a rate of 2.94 cases per 1,000 patients exposed to erenumab, 0.8/1,000 for fremanezumab, and 4.9/1,000 for galcanezumab, according to Dr. Silberstein, professor of neurology and director of the headache center at Sidney Kimmel Medical College, Philadelphia.
Migraine, headache, and drug ineffectiveness were in the top 10 for all three medications, as is typical in FAERS reports, since no drug is effective in everyone. These events were reported at rates of 1-5/1,000 exposed patients. Constipation was reported in association with the use of erenumab at a rate of 4.9 cases/1,000 patients, but did not reach the top-10 lists for the other two CGRP antagonists.
Notably, cardiovascular events were not among the top-10 adverse events reported for any of the novel preventive agents.
“These results will be practice changing, since some physicians have been holding back from prescribing these drugs pending the results of this sort of longer-term safety data,” Dr. Silberstein predicted in an interview.
Asked to comment on the FAERS study, neurologist Holly Yancy, DO, said that she found the findings unsurprising because the adverse effects were essentially as expected based upon the earlier favorable clinical trials experience.
“These medications are living up to the expectations for good tolerability that were in place when they were initially approved by the FDA just under 2 years ago,” said Dr. Yancy, a headache specialist at the Banner–University Medicine Neuroscience Institute in Phoenix.
“Injection-site reactions were anticipated. Clinically, I’ve found that if the medications reduce migraine days and severity, patients find the risk of temporary pain, redness, or itching at the injection site is an easy trade off,” she added.
CGRP is a vasoactive peptide. There has been a theoretic concern that its pharmacologic inhibition for prevention of migraine could lead to an increased risk of adverse cardiovascular events, especially in individuals with coronary disease or a history of stroke. The absence of any such signal during the first 6 months of widespread clinical use of the CGRP inhibitors is highly encouraging, although this is an issue that warrants longer-term study, Dr. Yancy continued.
These drugs, which were expressly designed for migraine prevention, are a considerable advance over what was previously available in her view. They’re equally or more effective and considerably better tolerated than the preventive medications physicians had long been using off label, including antidepressants, antiepileptics, and cardiac drugs.
Dr. Silberstein reported financial relationships with close to two dozen pharmaceutical companies. Dr. Yancy reported serving on speakers’ bureaus for Amgen and Novartis.
SOURCE: Silverstein SD et al. AAN 2020, Abstract S58.008.
FROM AAN 2020
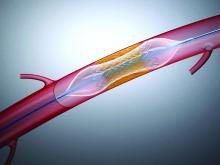
Substantial very late MACE risk after PCI for SIHD
Patients with stable ischemic heart disease remain at substantial risk for major adverse cardiovascular events 1-5 years after percutaneous coronary intervention, even with contemporary second-generation drug-eluting stents, according to a pooled analysis of long-term follow-up data on 10,987 patients in 19 prospective, randomized, head-to-head metallic stent trials.
The analysis showed that, although most major adverse cardiovascular events (MACE) occurred during the first year after stenting, no plateau in MACE was reached between years 1 and 5, Mahesh V. Madhavan, MD, reported at the joint scientific sessions of the American College of Cardiology and the World Heart Federation. The meeting was conducted online after its cancellation because of the COVID-19 pandemic.
“Further studies are required to understand the mechanisms of late events and whether improvements in stent technology, revascularization technique, and adjunctive therapies may improve outcomes in patients with SIHD [stable ischemic heart disease],” said Dr. Madhavan, a cardiology fellow at Columbia University Irving Medical Center and New York–Presbyterian Hospital.
This post hoc analysis of pooled individual patient-level data from 19 randomized trials included 10,987 metallic stent recipients with SIHD. Sixty-one percent got second-generation drug-eluting stents (DES), 25% received first-generation DES, and 15% got bare metal stents (BMS). The largest prospective head-to-head RCT was SPIRIT IV, with 2,130 patients. All five TAXUS trials were also included.
The 5-year rate of the primary composite MACE endpoint composed of cardiac death, MI, or ischemia-driven target lesion revascularization was 24.1% in patients with BMS stents, 17.9% with first-gen DES, and 13.4% with second-gen DES, reflecting the advances in stent technology over time. Most of these MACE events occurred during the first year after PCI, with rates of 18%, 8.6%, and 5.3%, respectively, in the three groups. However, the MACE rate beyond the first year out through year 5 remained substantial: 10.2% with first-gen DES, 8.5% with second-gen DES, and 7.4% in the BMS group.
The cardiac death rate from PCI through year 5 was 3.8% with second-gen DES, 3.6% with first-gen DES, and 3.3% with BMS. The MI rate was 7.7% with first-gen DES, 6.1% with BMS, and 5% with second-gen DES.
Stent thrombosis occurred during the first year in 0.9% of first-gen DES and BMS recipients and in 0.7% of patients with second-gen DES. During years 1-5, the rates were 1.6% with first-gen DES, 0.9% with second-gen devices, and 0.2% with BMS.
Second-gen DES provided a big advantage in terms of lessened need for ischemia-driven target lesion revascularization through the first 5 years, with a rate of 7.3%, compared to 18.7% in patients with first-gen DES and 10.5% with BMS.
In a multivariate regression analysis, independent predictors of MACE in the first 5 years post PCI included indicators of greater lesion and/or procedural complexity, such as left main or left anterior descending disease, greater lesion length, and more than one treated lesion, as well as standard cardiovascular risk factors, including recent smoking, hypertension, and diabetes.
In contrast, hyperlipidemia was associated with a significant 15% reduction in MACE risk, which in an interview Dr. Madhavan said may have been due to aggressive lipid-lowering therapy, although he added that this is conjecture because he and his coinvestigators didn’t have access to data on the use of guideline-directed medical therapy or antiplatelet regimens.
Asked about future prospects for reducing the substantial very late risk of MACE highlighted in his study, Dr. Madhavan cited the use of adjunctive imaging during PCI as promising.
“The currently enrolling ILUMEN IV trial, among other studies, will help determine whether imaging-guided intervention can help improve intermediate and long-term rates of MACE,” he observed.
Promising medical therapies that could potentially confer benefit in terms of reducing long-term MACE in patients who’ve undergone PCI for SIHD include novel lipid-lowering drugs, tailored antithrombotic strategies, new anti-inflammatory agents, and the SGLT2 inhibitors, Dr. Madhavan continued.
In terms of advances in stent design, he cited recent evidence that ultrathin-strut stents featuring bioresorbable polymer, such as the Orsiro stent, may reduce late stent-related MACE through 3 years.
“We’ll have to see if these benefits extend to longer-term follow-up up to 5 years,” he said.
He deemed his study results “fairly consistent” with those of the ISCHEMIA trial, where ischemic events in the patients with SIHD assigned to an initial invasive strategy continued to occur in the latter years of follow-up without any clear plateau effect (N Engl J Med. 2020 Apr 9;382[15]:1395-407).
Dr. Madhavan reported no financial conflicts regarding his study, funded by an institutional research grant from the National Heart, Lung, and Blood Institute.
Shortly following Dr. Madhavan’s presentation at ACC 2020, the study results were published online (Circ Cardiovasc Interv. 2020 Apr;13[4[:e008565. doi: 10.1161/CIRCINTERVENTIONS.119.008565).
SOURCE: Madhavan MV. ACC 2020, Abstract 909-10.
Patients with stable ischemic heart disease remain at substantial risk for major adverse cardiovascular events 1-5 years after percutaneous coronary intervention, even with contemporary second-generation drug-eluting stents, according to a pooled analysis of long-term follow-up data on 10,987 patients in 19 prospective, randomized, head-to-head metallic stent trials.
The analysis showed that, although most major adverse cardiovascular events (MACE) occurred during the first year after stenting, no plateau in MACE was reached between years 1 and 5, Mahesh V. Madhavan, MD, reported at the joint scientific sessions of the American College of Cardiology and the World Heart Federation. The meeting was conducted online after its cancellation because of the COVID-19 pandemic.
“Further studies are required to understand the mechanisms of late events and whether improvements in stent technology, revascularization technique, and adjunctive therapies may improve outcomes in patients with SIHD [stable ischemic heart disease],” said Dr. Madhavan, a cardiology fellow at Columbia University Irving Medical Center and New York–Presbyterian Hospital.
This post hoc analysis of pooled individual patient-level data from 19 randomized trials included 10,987 metallic stent recipients with SIHD. Sixty-one percent got second-generation drug-eluting stents (DES), 25% received first-generation DES, and 15% got bare metal stents (BMS). The largest prospective head-to-head RCT was SPIRIT IV, with 2,130 patients. All five TAXUS trials were also included.
The 5-year rate of the primary composite MACE endpoint composed of cardiac death, MI, or ischemia-driven target lesion revascularization was 24.1% in patients with BMS stents, 17.9% with first-gen DES, and 13.4% with second-gen DES, reflecting the advances in stent technology over time. Most of these MACE events occurred during the first year after PCI, with rates of 18%, 8.6%, and 5.3%, respectively, in the three groups. However, the MACE rate beyond the first year out through year 5 remained substantial: 10.2% with first-gen DES, 8.5% with second-gen DES, and 7.4% in the BMS group.
The cardiac death rate from PCI through year 5 was 3.8% with second-gen DES, 3.6% with first-gen DES, and 3.3% with BMS. The MI rate was 7.7% with first-gen DES, 6.1% with BMS, and 5% with second-gen DES.
Stent thrombosis occurred during the first year in 0.9% of first-gen DES and BMS recipients and in 0.7% of patients with second-gen DES. During years 1-5, the rates were 1.6% with first-gen DES, 0.9% with second-gen devices, and 0.2% with BMS.
Second-gen DES provided a big advantage in terms of lessened need for ischemia-driven target lesion revascularization through the first 5 years, with a rate of 7.3%, compared to 18.7% in patients with first-gen DES and 10.5% with BMS.
In a multivariate regression analysis, independent predictors of MACE in the first 5 years post PCI included indicators of greater lesion and/or procedural complexity, such as left main or left anterior descending disease, greater lesion length, and more than one treated lesion, as well as standard cardiovascular risk factors, including recent smoking, hypertension, and diabetes.
In contrast, hyperlipidemia was associated with a significant 15% reduction in MACE risk, which in an interview Dr. Madhavan said may have been due to aggressive lipid-lowering therapy, although he added that this is conjecture because he and his coinvestigators didn’t have access to data on the use of guideline-directed medical therapy or antiplatelet regimens.
Asked about future prospects for reducing the substantial very late risk of MACE highlighted in his study, Dr. Madhavan cited the use of adjunctive imaging during PCI as promising.
“The currently enrolling ILUMEN IV trial, among other studies, will help determine whether imaging-guided intervention can help improve intermediate and long-term rates of MACE,” he observed.
Promising medical therapies that could potentially confer benefit in terms of reducing long-term MACE in patients who’ve undergone PCI for SIHD include novel lipid-lowering drugs, tailored antithrombotic strategies, new anti-inflammatory agents, and the SGLT2 inhibitors, Dr. Madhavan continued.
In terms of advances in stent design, he cited recent evidence that ultrathin-strut stents featuring bioresorbable polymer, such as the Orsiro stent, may reduce late stent-related MACE through 3 years.
“We’ll have to see if these benefits extend to longer-term follow-up up to 5 years,” he said.
He deemed his study results “fairly consistent” with those of the ISCHEMIA trial, where ischemic events in the patients with SIHD assigned to an initial invasive strategy continued to occur in the latter years of follow-up without any clear plateau effect (N Engl J Med. 2020 Apr 9;382[15]:1395-407).
Dr. Madhavan reported no financial conflicts regarding his study, funded by an institutional research grant from the National Heart, Lung, and Blood Institute.
Shortly following Dr. Madhavan’s presentation at ACC 2020, the study results were published online (Circ Cardiovasc Interv. 2020 Apr;13[4[:e008565. doi: 10.1161/CIRCINTERVENTIONS.119.008565).
SOURCE: Madhavan MV. ACC 2020, Abstract 909-10.
Patients with stable ischemic heart disease remain at substantial risk for major adverse cardiovascular events 1-5 years after percutaneous coronary intervention, even with contemporary second-generation drug-eluting stents, according to a pooled analysis of long-term follow-up data on 10,987 patients in 19 prospective, randomized, head-to-head metallic stent trials.
The analysis showed that, although most major adverse cardiovascular events (MACE) occurred during the first year after stenting, no plateau in MACE was reached between years 1 and 5, Mahesh V. Madhavan, MD, reported at the joint scientific sessions of the American College of Cardiology and the World Heart Federation. The meeting was conducted online after its cancellation because of the COVID-19 pandemic.
“Further studies are required to understand the mechanisms of late events and whether improvements in stent technology, revascularization technique, and adjunctive therapies may improve outcomes in patients with SIHD [stable ischemic heart disease],” said Dr. Madhavan, a cardiology fellow at Columbia University Irving Medical Center and New York–Presbyterian Hospital.
This post hoc analysis of pooled individual patient-level data from 19 randomized trials included 10,987 metallic stent recipients with SIHD. Sixty-one percent got second-generation drug-eluting stents (DES), 25% received first-generation DES, and 15% got bare metal stents (BMS). The largest prospective head-to-head RCT was SPIRIT IV, with 2,130 patients. All five TAXUS trials were also included.
The 5-year rate of the primary composite MACE endpoint composed of cardiac death, MI, or ischemia-driven target lesion revascularization was 24.1% in patients with BMS stents, 17.9% with first-gen DES, and 13.4% with second-gen DES, reflecting the advances in stent technology over time. Most of these MACE events occurred during the first year after PCI, with rates of 18%, 8.6%, and 5.3%, respectively, in the three groups. However, the MACE rate beyond the first year out through year 5 remained substantial: 10.2% with first-gen DES, 8.5% with second-gen DES, and 7.4% in the BMS group.
The cardiac death rate from PCI through year 5 was 3.8% with second-gen DES, 3.6% with first-gen DES, and 3.3% with BMS. The MI rate was 7.7% with first-gen DES, 6.1% with BMS, and 5% with second-gen DES.
Stent thrombosis occurred during the first year in 0.9% of first-gen DES and BMS recipients and in 0.7% of patients with second-gen DES. During years 1-5, the rates were 1.6% with first-gen DES, 0.9% with second-gen devices, and 0.2% with BMS.
Second-gen DES provided a big advantage in terms of lessened need for ischemia-driven target lesion revascularization through the first 5 years, with a rate of 7.3%, compared to 18.7% in patients with first-gen DES and 10.5% with BMS.
In a multivariate regression analysis, independent predictors of MACE in the first 5 years post PCI included indicators of greater lesion and/or procedural complexity, such as left main or left anterior descending disease, greater lesion length, and more than one treated lesion, as well as standard cardiovascular risk factors, including recent smoking, hypertension, and diabetes.
In contrast, hyperlipidemia was associated with a significant 15% reduction in MACE risk, which in an interview Dr. Madhavan said may have been due to aggressive lipid-lowering therapy, although he added that this is conjecture because he and his coinvestigators didn’t have access to data on the use of guideline-directed medical therapy or antiplatelet regimens.
Asked about future prospects for reducing the substantial very late risk of MACE highlighted in his study, Dr. Madhavan cited the use of adjunctive imaging during PCI as promising.
“The currently enrolling ILUMEN IV trial, among other studies, will help determine whether imaging-guided intervention can help improve intermediate and long-term rates of MACE,” he observed.
Promising medical therapies that could potentially confer benefit in terms of reducing long-term MACE in patients who’ve undergone PCI for SIHD include novel lipid-lowering drugs, tailored antithrombotic strategies, new anti-inflammatory agents, and the SGLT2 inhibitors, Dr. Madhavan continued.
In terms of advances in stent design, he cited recent evidence that ultrathin-strut stents featuring bioresorbable polymer, such as the Orsiro stent, may reduce late stent-related MACE through 3 years.
“We’ll have to see if these benefits extend to longer-term follow-up up to 5 years,” he said.
He deemed his study results “fairly consistent” with those of the ISCHEMIA trial, where ischemic events in the patients with SIHD assigned to an initial invasive strategy continued to occur in the latter years of follow-up without any clear plateau effect (N Engl J Med. 2020 Apr 9;382[15]:1395-407).
Dr. Madhavan reported no financial conflicts regarding his study, funded by an institutional research grant from the National Heart, Lung, and Blood Institute.
Shortly following Dr. Madhavan’s presentation at ACC 2020, the study results were published online (Circ Cardiovasc Interv. 2020 Apr;13[4[:e008565. doi: 10.1161/CIRCINTERVENTIONS.119.008565).
SOURCE: Madhavan MV. ACC 2020, Abstract 909-10.
FROM ACC 20
COVID-19: No U.S. spike expected in pandemic-related suicidal ideation
Americans are not feeling more suicidal even in the depths of the COVID-19 pandemic of spring 2020, according to analysis of real-time national data accrued through the Crisis Text Line.
But that’s not to say Americans are feeling less distressed. Quite the contrary, Nancy Lublin, CEO and cofounder of Crisis Text Line, noted at the virtual annual meeting of the American Association of Suicidology.
“We’ve seen a 40% increase in volume since early March. Seventy-eight percent of our conversations are now including words like ‘freaked out,’ ‘panicked,’ ‘scared.’ People are worried about COVID-19. They’re nervous about symptoms; they’re concerned for family on the front lines,” she said.
And yet, from mid-March through mid-April, only 22% of texters to the crisis line expressed suicidal ideation, down from a usual background rate of 28%. Moreover, just 13% of texters who mentioned ‘COVID,’ ‘quarantine,’ or ‘virus’ expressed suicidal ideation, compared with 25% of other texters.
Ms. Lublin and her data crunchers are tracking not only the impact of the disease, but they’re also monitoring the mental health effects of the quarantine and social distancing.
“People are away from their routines, and perhaps [are] quarantined with abusive people. We’ve seen a 48% increase in texts involving sexual abuse and a 74% increase in domestic violence,” she said.
Texts focused on eating disorders or body image issues have jumped by 45%. And roughly two-thirds of texters now describe feelings of depression.
One of the biggest mental health impacts she and colleagues have seen stem from the economic recession triggered by the pandemic.
“We’ve seen more people reach out with fears of bankruptcy, fears of homelessness, fears of financial ruin. Thirty-two percent of our texters now report household incomes under $20,000 per year. That’s up from 19% before,” according to Ms. Lublin.
The Crisis Text Line (text HOME to 741741) uses machine-learning algorithms that sift through incoming text messages from people in crisis for key words, then ranks the messages by severity. Since its launch in 2013, this service, available 24/7, has processed roughly 150 million text messages. The high-risk texters – for example, someone who’s swallowed a bottle of pills or is texting from the San Francisco’s Golden Gate Bridge, as has occurred some 500 times – are connected in an average of 24 seconds with a thoroughly trained volunteer crisis counselor. And there is a third party in these texting conversations: a paid staff supervisor with a master’s degree in a relevant discipline who follows the encounter in real time and can step in if needed.
“Active rescues are involved in less than 1% of our conversations, but still we do them on average 26 times per day. Over the years, we’ve completed more than 32,000 active rescues,” she said.
The Crisis Text Line is not exclusively a suicide prevention hotline. The top five issues people text about involve relationship concerns, depression, anxiety, self-harm, and suicidal ideation. Over time, Ms. Lublin and staff have used Big Data to tweak the screening algorithm as they’ve identified even higher red flag texting words than “suicide.”
“The word ‘military’ makes it twice as likely that we’ll have to call 9-1-1 than the word ‘suicide.’ ‘Gun,’ ‘rope’ – four times as likely. In the [United KIngdom], where we’re also operating, we see the word ‘cliff’ is a more lethal word than the word ‘suicide.’ But the most dangerous words that we see are any named pill,” she said.
The Crisis Text Line was recently awarded a 2020 TED Audacious Project grant to expand their services from English to also be offered in Spanish, French, Portuguese, and Arabic worldwide within the next two and a half years. This will provide coverage to one-third of the world’s population, including people with cell phones living in countries with very limited mental health services.
Will COVID-19 trigger a spike in deaths by suicide?
Whether the COVID-19 pandemic will result in a bump in suicide rates is unclear and will remain so for quite a while, according to David Gunnell, MD, PhD, a suicidologist and professor of epidemiology at the University of Bristol (England).
In the United Kingdom, investigation of a suspicious death typically takes more than 6 months before an official declaration of suicide is recorded by the medical examiner. The lag time is even longer in the United States: The latest national suicide rate data are for 2018 because state-by-state reporting practices vary widely, he noted at a National Press Foundation briefing on COVID-19 and mental health.
Although suicide is consistently the 10th-leading cause of death in the United States, it’s important to put it in perspective, he added. In 2018, there were an average of 4,000 deaths by suicide per month nationally, whereas in March and April of 2020, there were 28,400 deaths per month attributable to COVID-19.
A classic study of the Spanish influenza pandemic in the United States during 1918-1919 concluded that there was “a slight upturn” in the rate of suicide in the months following the pandemic’s peak. More recently, a study of the 2003 SARS (severe acute respiratory syndrome) epidemic in Hong Kong found roughly a 30% increase in the rate of suicide among the elderly during that time frame, Dr. Gunnell noted.
“What limited evidence there is provides an indication of a small rise in suicides, but the number of deaths is far outweighed by the number of deaths associated with these big pandemics,” according to the epidemiologist.
Pandemics aside, there is far more compelling evidence that periods of economic recession are associated with an increase in the suicide rate, he added.
Another speaker, Holly C. Wilcox, PhD, a psychiatric epidemiologist at Johns Hopkins University, Baltimore, commented: “It’s not surprising that, during times of disaster the suicide rates decrease a bit. It could be because of people coming toghether. It could be one silver lining of COVID-19. But if there’s prolonged stress economically and socially and we can’t work towards reducing stress for people, we could see an increase. I don’t know if we will.”
In a recent article, Dr. Gunnell and coauthors offered a series of recommendations aimed at blunting the mental health consequences of COVID-19 and the related economic fallout (Lancet Psychiatry. 2020 Apr 21. doi: 10.1016/S2215-0366[20]30171-1).
The authors highlighted the need for interventions aimed at defusing the adverse impact of self-isolation, social distancing, fear, an anticipated rise in alcohol misuse, joblessness, interrupted education, bereavement, and complicated grief. Governments can blunt the well-established effect of financial distress as a risk factor for suicide by providing safety nets in the form of supports for housing, food, and unemployment benefits. And it will be important that those mental health services that develop expertise in performing psychiatric assessments and interventions remotely via telemedicine share their insights, Dr. Gunnell said.
Americans are not feeling more suicidal even in the depths of the COVID-19 pandemic of spring 2020, according to analysis of real-time national data accrued through the Crisis Text Line.
But that’s not to say Americans are feeling less distressed. Quite the contrary, Nancy Lublin, CEO and cofounder of Crisis Text Line, noted at the virtual annual meeting of the American Association of Suicidology.
“We’ve seen a 40% increase in volume since early March. Seventy-eight percent of our conversations are now including words like ‘freaked out,’ ‘panicked,’ ‘scared.’ People are worried about COVID-19. They’re nervous about symptoms; they’re concerned for family on the front lines,” she said.
And yet, from mid-March through mid-April, only 22% of texters to the crisis line expressed suicidal ideation, down from a usual background rate of 28%. Moreover, just 13% of texters who mentioned ‘COVID,’ ‘quarantine,’ or ‘virus’ expressed suicidal ideation, compared with 25% of other texters.
Ms. Lublin and her data crunchers are tracking not only the impact of the disease, but they’re also monitoring the mental health effects of the quarantine and social distancing.
“People are away from their routines, and perhaps [are] quarantined with abusive people. We’ve seen a 48% increase in texts involving sexual abuse and a 74% increase in domestic violence,” she said.
Texts focused on eating disorders or body image issues have jumped by 45%. And roughly two-thirds of texters now describe feelings of depression.
One of the biggest mental health impacts she and colleagues have seen stem from the economic recession triggered by the pandemic.
“We’ve seen more people reach out with fears of bankruptcy, fears of homelessness, fears of financial ruin. Thirty-two percent of our texters now report household incomes under $20,000 per year. That’s up from 19% before,” according to Ms. Lublin.
The Crisis Text Line (text HOME to 741741) uses machine-learning algorithms that sift through incoming text messages from people in crisis for key words, then ranks the messages by severity. Since its launch in 2013, this service, available 24/7, has processed roughly 150 million text messages. The high-risk texters – for example, someone who’s swallowed a bottle of pills or is texting from the San Francisco’s Golden Gate Bridge, as has occurred some 500 times – are connected in an average of 24 seconds with a thoroughly trained volunteer crisis counselor. And there is a third party in these texting conversations: a paid staff supervisor with a master’s degree in a relevant discipline who follows the encounter in real time and can step in if needed.
“Active rescues are involved in less than 1% of our conversations, but still we do them on average 26 times per day. Over the years, we’ve completed more than 32,000 active rescues,” she said.
The Crisis Text Line is not exclusively a suicide prevention hotline. The top five issues people text about involve relationship concerns, depression, anxiety, self-harm, and suicidal ideation. Over time, Ms. Lublin and staff have used Big Data to tweak the screening algorithm as they’ve identified even higher red flag texting words than “suicide.”
“The word ‘military’ makes it twice as likely that we’ll have to call 9-1-1 than the word ‘suicide.’ ‘Gun,’ ‘rope’ – four times as likely. In the [United KIngdom], where we’re also operating, we see the word ‘cliff’ is a more lethal word than the word ‘suicide.’ But the most dangerous words that we see are any named pill,” she said.
The Crisis Text Line was recently awarded a 2020 TED Audacious Project grant to expand their services from English to also be offered in Spanish, French, Portuguese, and Arabic worldwide within the next two and a half years. This will provide coverage to one-third of the world’s population, including people with cell phones living in countries with very limited mental health services.
Will COVID-19 trigger a spike in deaths by suicide?
Whether the COVID-19 pandemic will result in a bump in suicide rates is unclear and will remain so for quite a while, according to David Gunnell, MD, PhD, a suicidologist and professor of epidemiology at the University of Bristol (England).
In the United Kingdom, investigation of a suspicious death typically takes more than 6 months before an official declaration of suicide is recorded by the medical examiner. The lag time is even longer in the United States: The latest national suicide rate data are for 2018 because state-by-state reporting practices vary widely, he noted at a National Press Foundation briefing on COVID-19 and mental health.
Although suicide is consistently the 10th-leading cause of death in the United States, it’s important to put it in perspective, he added. In 2018, there were an average of 4,000 deaths by suicide per month nationally, whereas in March and April of 2020, there were 28,400 deaths per month attributable to COVID-19.
A classic study of the Spanish influenza pandemic in the United States during 1918-1919 concluded that there was “a slight upturn” in the rate of suicide in the months following the pandemic’s peak. More recently, a study of the 2003 SARS (severe acute respiratory syndrome) epidemic in Hong Kong found roughly a 30% increase in the rate of suicide among the elderly during that time frame, Dr. Gunnell noted.
“What limited evidence there is provides an indication of a small rise in suicides, but the number of deaths is far outweighed by the number of deaths associated with these big pandemics,” according to the epidemiologist.
Pandemics aside, there is far more compelling evidence that periods of economic recession are associated with an increase in the suicide rate, he added.
Another speaker, Holly C. Wilcox, PhD, a psychiatric epidemiologist at Johns Hopkins University, Baltimore, commented: “It’s not surprising that, during times of disaster the suicide rates decrease a bit. It could be because of people coming toghether. It could be one silver lining of COVID-19. But if there’s prolonged stress economically and socially and we can’t work towards reducing stress for people, we could see an increase. I don’t know if we will.”
In a recent article, Dr. Gunnell and coauthors offered a series of recommendations aimed at blunting the mental health consequences of COVID-19 and the related economic fallout (Lancet Psychiatry. 2020 Apr 21. doi: 10.1016/S2215-0366[20]30171-1).
The authors highlighted the need for interventions aimed at defusing the adverse impact of self-isolation, social distancing, fear, an anticipated rise in alcohol misuse, joblessness, interrupted education, bereavement, and complicated grief. Governments can blunt the well-established effect of financial distress as a risk factor for suicide by providing safety nets in the form of supports for housing, food, and unemployment benefits. And it will be important that those mental health services that develop expertise in performing psychiatric assessments and interventions remotely via telemedicine share their insights, Dr. Gunnell said.
Americans are not feeling more suicidal even in the depths of the COVID-19 pandemic of spring 2020, according to analysis of real-time national data accrued through the Crisis Text Line.
But that’s not to say Americans are feeling less distressed. Quite the contrary, Nancy Lublin, CEO and cofounder of Crisis Text Line, noted at the virtual annual meeting of the American Association of Suicidology.
“We’ve seen a 40% increase in volume since early March. Seventy-eight percent of our conversations are now including words like ‘freaked out,’ ‘panicked,’ ‘scared.’ People are worried about COVID-19. They’re nervous about symptoms; they’re concerned for family on the front lines,” she said.
And yet, from mid-March through mid-April, only 22% of texters to the crisis line expressed suicidal ideation, down from a usual background rate of 28%. Moreover, just 13% of texters who mentioned ‘COVID,’ ‘quarantine,’ or ‘virus’ expressed suicidal ideation, compared with 25% of other texters.
Ms. Lublin and her data crunchers are tracking not only the impact of the disease, but they’re also monitoring the mental health effects of the quarantine and social distancing.
“People are away from their routines, and perhaps [are] quarantined with abusive people. We’ve seen a 48% increase in texts involving sexual abuse and a 74% increase in domestic violence,” she said.
Texts focused on eating disorders or body image issues have jumped by 45%. And roughly two-thirds of texters now describe feelings of depression.
One of the biggest mental health impacts she and colleagues have seen stem from the economic recession triggered by the pandemic.
“We’ve seen more people reach out with fears of bankruptcy, fears of homelessness, fears of financial ruin. Thirty-two percent of our texters now report household incomes under $20,000 per year. That’s up from 19% before,” according to Ms. Lublin.
The Crisis Text Line (text HOME to 741741) uses machine-learning algorithms that sift through incoming text messages from people in crisis for key words, then ranks the messages by severity. Since its launch in 2013, this service, available 24/7, has processed roughly 150 million text messages. The high-risk texters – for example, someone who’s swallowed a bottle of pills or is texting from the San Francisco’s Golden Gate Bridge, as has occurred some 500 times – are connected in an average of 24 seconds with a thoroughly trained volunteer crisis counselor. And there is a third party in these texting conversations: a paid staff supervisor with a master’s degree in a relevant discipline who follows the encounter in real time and can step in if needed.
“Active rescues are involved in less than 1% of our conversations, but still we do them on average 26 times per day. Over the years, we’ve completed more than 32,000 active rescues,” she said.
The Crisis Text Line is not exclusively a suicide prevention hotline. The top five issues people text about involve relationship concerns, depression, anxiety, self-harm, and suicidal ideation. Over time, Ms. Lublin and staff have used Big Data to tweak the screening algorithm as they’ve identified even higher red flag texting words than “suicide.”
“The word ‘military’ makes it twice as likely that we’ll have to call 9-1-1 than the word ‘suicide.’ ‘Gun,’ ‘rope’ – four times as likely. In the [United KIngdom], where we’re also operating, we see the word ‘cliff’ is a more lethal word than the word ‘suicide.’ But the most dangerous words that we see are any named pill,” she said.
The Crisis Text Line was recently awarded a 2020 TED Audacious Project grant to expand their services from English to also be offered in Spanish, French, Portuguese, and Arabic worldwide within the next two and a half years. This will provide coverage to one-third of the world’s population, including people with cell phones living in countries with very limited mental health services.
Will COVID-19 trigger a spike in deaths by suicide?
Whether the COVID-19 pandemic will result in a bump in suicide rates is unclear and will remain so for quite a while, according to David Gunnell, MD, PhD, a suicidologist and professor of epidemiology at the University of Bristol (England).
In the United Kingdom, investigation of a suspicious death typically takes more than 6 months before an official declaration of suicide is recorded by the medical examiner. The lag time is even longer in the United States: The latest national suicide rate data are for 2018 because state-by-state reporting practices vary widely, he noted at a National Press Foundation briefing on COVID-19 and mental health.
Although suicide is consistently the 10th-leading cause of death in the United States, it’s important to put it in perspective, he added. In 2018, there were an average of 4,000 deaths by suicide per month nationally, whereas in March and April of 2020, there were 28,400 deaths per month attributable to COVID-19.
A classic study of the Spanish influenza pandemic in the United States during 1918-1919 concluded that there was “a slight upturn” in the rate of suicide in the months following the pandemic’s peak. More recently, a study of the 2003 SARS (severe acute respiratory syndrome) epidemic in Hong Kong found roughly a 30% increase in the rate of suicide among the elderly during that time frame, Dr. Gunnell noted.
“What limited evidence there is provides an indication of a small rise in suicides, but the number of deaths is far outweighed by the number of deaths associated with these big pandemics,” according to the epidemiologist.
Pandemics aside, there is far more compelling evidence that periods of economic recession are associated with an increase in the suicide rate, he added.
Another speaker, Holly C. Wilcox, PhD, a psychiatric epidemiologist at Johns Hopkins University, Baltimore, commented: “It’s not surprising that, during times of disaster the suicide rates decrease a bit. It could be because of people coming toghether. It could be one silver lining of COVID-19. But if there’s prolonged stress economically and socially and we can’t work towards reducing stress for people, we could see an increase. I don’t know if we will.”
In a recent article, Dr. Gunnell and coauthors offered a series of recommendations aimed at blunting the mental health consequences of COVID-19 and the related economic fallout (Lancet Psychiatry. 2020 Apr 21. doi: 10.1016/S2215-0366[20]30171-1).
The authors highlighted the need for interventions aimed at defusing the adverse impact of self-isolation, social distancing, fear, an anticipated rise in alcohol misuse, joblessness, interrupted education, bereavement, and complicated grief. Governments can blunt the well-established effect of financial distress as a risk factor for suicide by providing safety nets in the form of supports for housing, food, and unemployment benefits. And it will be important that those mental health services that develop expertise in performing psychiatric assessments and interventions remotely via telemedicine share their insights, Dr. Gunnell said.
FROM AAS 2020
European COVID-19 insights: Try helmet CPAP
Noninvasive ventilation with helmet continuous positive air pressure (CPAP) deserves to be embraced as an effective strategy in preventing self-induced lung injury, often a key factor in progression from the early milder expression of COVID-19 disease to classic severe acute respiratory distress syndrome, according to European physicians who have been through what they hope are the worst days of the pandemic in the Lombardy region of Northern Italy.
Helmet CPAP is a relatively inexpensive, convenient, well-tolerated intervention. It allows patients to remain conscious and responsive to commands such as “Time to roll over,” which in turn frees up nursing staff. The purpose of helmet CPAP is to curb the huge inspiratory drive that’s a defining feature of this disease and which, unchecked, can lead to self-induced lung injury (SILI), Luciano Gattinoni, MD, explained at a webinar hosted by the European Society of Anaesthesiology.
“Paranoid attention to inspiratory effort – checking it and correcting it – is something where we can make the difference between death and life. It’s extremely important,” said Dr. Gattinoni, guest professor of anesthesiology and intensive care at the University of Gottingen (Germany).
He and his fellow panelists were in accord regarding the merits of helmet CPAP as the premier method of noninvasive ventilatory assistance. They also addressed the importance of monitoring for hypercoagulation, as well as what they’ve come to see as the essential role of pronation in what they define as Type H disease, and the need to have detailed respiratory physiotherapy protocols in place.
“COVID-19 doesn’t like physiotherapy,” explained Paolo Pelosi, MD, professor of anesthesiology and intensive care medicine at the University of Genoa (Italy).
Dr. Gattinoni is credited for identification of two polar phenotypes of what he considers to be a single COVID-19 disease. Early on, many patients present with an atypical form of acute respiratory distress syndrome (ARDS), distinguished by an often-unexpected degree of hypoxia accompanied by high pulmonary compliance and surprisingly little shortness of breath. Dr. Gattinoni and colleagues call this Type L disease, which stands for low elastane, low ventilation to perfusion ratio, low lung weight on CT, and low lung recruitability, which means the patient has a high proportion of aerated lung tissue. Over time, because of either the natural history of the disease or SILI, this may shift to Type H disease, marked by high elastane, high right-to-left shunt, high lung weight, and high recruitability.
“If the pulmonary compliance is above 60 [mL/cm H2O], I’m pretty sure it’s Type L. If it’s 30 [mL/cm H2O] or less, I’m pretty sure it’s Type H. Don’t ask me about 45-55 [mL/cm H2O]; it’s a grey zone,” Dr. Gattinoni said.
Giuseppe Foti, MD, said helmet CPAP in patients with COVID-19 should be free flow, not attached to a ventilator, and the gas flow should be set high – at least 50 L/min – in order to prevent CO2 rebreathing. Although noninvasive ventilation is well accepted for patients with chronic obstructive pulmonary disease or acute cardiogenic pulmonary edema, it hasn’t been extensively studied in the setting of ARDS. A notable exception is a single-center randomized trial in which 83 patients with ARDS at the University of Chicago were assigned to noninvasive ventilation delivered by helmet or face mask (JAMA. 2016 Jun 14;315[22]:2435-41). The endotracheal intubation rate was just 18% in the helmet group, compared with 62% in the face mask group. The 90-day mortality rate was significantly lower in the helmet group as well, noted Dr. Foti, director of the department of anesthesia and intensive care at Monza University Hospital in Milan.
Christian Putensen, MD, said he views intubation for mechanical ventilation as wise in moderate or severe ARDS with an arterial oxygen partial pressure/fraction of inspired oxygen (PaO2/FiO2) ratio below 150. But in milder, Type L COVID-19 disease, he also likes helmet CPAP. It spares the patient from the traumatic compressive stress to the lung induced by mechanical ventilation, which may cause alveolar edema and SILI.
There is, however, a caveat: “Watch carefully and do not delay intubation if you see helmet CPAP is not working; that is, if the blood gas analysis doesn’t improve, the respiratory rate increases, tidal volume increases, and there is still increased respiratory drive,” advised Dr. Putensen, an anesthesiologist at the University of Bonn (Germany).
There is no agreed-upon practical quantitative measure of respiratory drive. A clinical evaluation of the patient’s depth of inspiration is the best guide, he added.
Dr. Gattinoni said that, when helmet CPAP can’t control respiratory drive in a patient with early-stage disease, he feels the only way to interrupt this destructive process is through early intubation and what he termed “gentle mechanical ventilation,” not with a positive end expiratory pressure of 20 cm H2O, but more like 4-5.
Watch for hypercoagulation
Thromboembolic complications are a common feature in COVID-19 disease.
“I’ve had occasion to see the autopsy results in more than 100 patients. It’s devastating to see the number of thromboses and microthromboses in the lungs, the liver, the kidney, and in the brain,” Dr. Gattinoni said.
“COVID-19 is a serial killer, no doubt,” Dr. Pelosi agreed. “He has no mercy for anyone. And he has two bullets: The first one is for the lung, the second is on the vascular side.”
Dr. Putensen is aggressive in utilizing prophylactic high-dose anticoagulation with heparin. He carefully monitors levels of fibrinogen, Factors V and VIII, and d-dimers. In the setting of COVID-19, he has found thromboelastography to be more reliable than partial thromboplastin time in guiding heparin titration.
Pronation
Panelists agreed that pronation is an especially valuable means of enhancing oxygenation in patients with Type H disease. Dr. Putensen tries for more than 16 hours per day. Dr. Foti is preparing a study of the impact of pronation in 50 awake, nonintubated patients, most of whom were on helmet CPAP. Seven of them couldn’t tolerate pronation for even an hour at a time; for the others, the median duration was 3.5 hours at a time.
“We saw a dramatic improvement, a nearly doubling in the PaO2/FiO2 ratio,” Dr. Foti said.
The helmet CPAP study was done outside of the ICU because, in March 2020, the Milan hospital was utterly overwhelmed by COVID-19. The university hospital ordinarily has 25 ICU beds. This was expanded to 100 ICU beds in an effort to meet the emergency, but that still wasn’t sufficient. Indeed, COVID-19 patients occupied 600 of the hospital’s 650 beds. Physicians were forced to do something formerly unthinkable: triage patients for intubation and mechanical ventilation based upon age, comorbidities, and survival prospects.
“We felt schizophrenic. I completely agree with Luciano’s idea to intubate early when we cannot control the respiratory drive that’s due to the disease. But we couldn’t do it because we had too many patients. So we had to triage,” Dr. Foti recalled, breaking off with a sob as other panelists wiped away their own tears during the webcast.
Respiratory physical therapy
Dr. Pelosi said he believes that optimal care of patients with COVID-19 disease requires a major commitment to physical therapy. He strongly recommends having thoughtfully designed separate written protocols in place for respiratory physiotherapy during mechanical ventilation, weaning, and postextubation. COVID-19 patients typically require 7-10 days of assisted ventilation before weaning, and weaning is a protracted process as well.
“I like to say COVID-19 always requires patience. You have to be very, very patient with this disease,” he emphasized. “These patients have a long and difficult weaning. If the patient isn’t improving during weaning, look at two issues: superinfection and thrombembolism, macro and micro.” The physical therapy measures routinely utilized at his hospital during mechanical ventilation include elevation of the bed head greater than 30 degrees, neuromuscular electrical stimulation, subglottic secretion suctioning, tracheal and oral aspiration, and cough assistance. Separate physical therapy menus are used during before and after extubation.
Dr. Gattinoni offered a final word: “We can do almost nothing with this disease. We try our best to keep the patient alive. What we can do is avoid excessive ventilation of the patient. Applying the typical treatment of ARDS in atypical [Type L] ARDS does not make sense and may be extremely harmful.”
Noninvasive ventilation with helmet continuous positive air pressure (CPAP) deserves to be embraced as an effective strategy in preventing self-induced lung injury, often a key factor in progression from the early milder expression of COVID-19 disease to classic severe acute respiratory distress syndrome, according to European physicians who have been through what they hope are the worst days of the pandemic in the Lombardy region of Northern Italy.
Helmet CPAP is a relatively inexpensive, convenient, well-tolerated intervention. It allows patients to remain conscious and responsive to commands such as “Time to roll over,” which in turn frees up nursing staff. The purpose of helmet CPAP is to curb the huge inspiratory drive that’s a defining feature of this disease and which, unchecked, can lead to self-induced lung injury (SILI), Luciano Gattinoni, MD, explained at a webinar hosted by the European Society of Anaesthesiology.
“Paranoid attention to inspiratory effort – checking it and correcting it – is something where we can make the difference between death and life. It’s extremely important,” said Dr. Gattinoni, guest professor of anesthesiology and intensive care at the University of Gottingen (Germany).
He and his fellow panelists were in accord regarding the merits of helmet CPAP as the premier method of noninvasive ventilatory assistance. They also addressed the importance of monitoring for hypercoagulation, as well as what they’ve come to see as the essential role of pronation in what they define as Type H disease, and the need to have detailed respiratory physiotherapy protocols in place.
“COVID-19 doesn’t like physiotherapy,” explained Paolo Pelosi, MD, professor of anesthesiology and intensive care medicine at the University of Genoa (Italy).
Dr. Gattinoni is credited for identification of two polar phenotypes of what he considers to be a single COVID-19 disease. Early on, many patients present with an atypical form of acute respiratory distress syndrome (ARDS), distinguished by an often-unexpected degree of hypoxia accompanied by high pulmonary compliance and surprisingly little shortness of breath. Dr. Gattinoni and colleagues call this Type L disease, which stands for low elastane, low ventilation to perfusion ratio, low lung weight on CT, and low lung recruitability, which means the patient has a high proportion of aerated lung tissue. Over time, because of either the natural history of the disease or SILI, this may shift to Type H disease, marked by high elastane, high right-to-left shunt, high lung weight, and high recruitability.
“If the pulmonary compliance is above 60 [mL/cm H2O], I’m pretty sure it’s Type L. If it’s 30 [mL/cm H2O] or less, I’m pretty sure it’s Type H. Don’t ask me about 45-55 [mL/cm H2O]; it’s a grey zone,” Dr. Gattinoni said.
Giuseppe Foti, MD, said helmet CPAP in patients with COVID-19 should be free flow, not attached to a ventilator, and the gas flow should be set high – at least 50 L/min – in order to prevent CO2 rebreathing. Although noninvasive ventilation is well accepted for patients with chronic obstructive pulmonary disease or acute cardiogenic pulmonary edema, it hasn’t been extensively studied in the setting of ARDS. A notable exception is a single-center randomized trial in which 83 patients with ARDS at the University of Chicago were assigned to noninvasive ventilation delivered by helmet or face mask (JAMA. 2016 Jun 14;315[22]:2435-41). The endotracheal intubation rate was just 18% in the helmet group, compared with 62% in the face mask group. The 90-day mortality rate was significantly lower in the helmet group as well, noted Dr. Foti, director of the department of anesthesia and intensive care at Monza University Hospital in Milan.
Christian Putensen, MD, said he views intubation for mechanical ventilation as wise in moderate or severe ARDS with an arterial oxygen partial pressure/fraction of inspired oxygen (PaO2/FiO2) ratio below 150. But in milder, Type L COVID-19 disease, he also likes helmet CPAP. It spares the patient from the traumatic compressive stress to the lung induced by mechanical ventilation, which may cause alveolar edema and SILI.
There is, however, a caveat: “Watch carefully and do not delay intubation if you see helmet CPAP is not working; that is, if the blood gas analysis doesn’t improve, the respiratory rate increases, tidal volume increases, and there is still increased respiratory drive,” advised Dr. Putensen, an anesthesiologist at the University of Bonn (Germany).
There is no agreed-upon practical quantitative measure of respiratory drive. A clinical evaluation of the patient’s depth of inspiration is the best guide, he added.
Dr. Gattinoni said that, when helmet CPAP can’t control respiratory drive in a patient with early-stage disease, he feels the only way to interrupt this destructive process is through early intubation and what he termed “gentle mechanical ventilation,” not with a positive end expiratory pressure of 20 cm H2O, but more like 4-5.
Watch for hypercoagulation
Thromboembolic complications are a common feature in COVID-19 disease.
“I’ve had occasion to see the autopsy results in more than 100 patients. It’s devastating to see the number of thromboses and microthromboses in the lungs, the liver, the kidney, and in the brain,” Dr. Gattinoni said.
“COVID-19 is a serial killer, no doubt,” Dr. Pelosi agreed. “He has no mercy for anyone. And he has two bullets: The first one is for the lung, the second is on the vascular side.”
Dr. Putensen is aggressive in utilizing prophylactic high-dose anticoagulation with heparin. He carefully monitors levels of fibrinogen, Factors V and VIII, and d-dimers. In the setting of COVID-19, he has found thromboelastography to be more reliable than partial thromboplastin time in guiding heparin titration.
Pronation
Panelists agreed that pronation is an especially valuable means of enhancing oxygenation in patients with Type H disease. Dr. Putensen tries for more than 16 hours per day. Dr. Foti is preparing a study of the impact of pronation in 50 awake, nonintubated patients, most of whom were on helmet CPAP. Seven of them couldn’t tolerate pronation for even an hour at a time; for the others, the median duration was 3.5 hours at a time.
“We saw a dramatic improvement, a nearly doubling in the PaO2/FiO2 ratio,” Dr. Foti said.
The helmet CPAP study was done outside of the ICU because, in March 2020, the Milan hospital was utterly overwhelmed by COVID-19. The university hospital ordinarily has 25 ICU beds. This was expanded to 100 ICU beds in an effort to meet the emergency, but that still wasn’t sufficient. Indeed, COVID-19 patients occupied 600 of the hospital’s 650 beds. Physicians were forced to do something formerly unthinkable: triage patients for intubation and mechanical ventilation based upon age, comorbidities, and survival prospects.
“We felt schizophrenic. I completely agree with Luciano’s idea to intubate early when we cannot control the respiratory drive that’s due to the disease. But we couldn’t do it because we had too many patients. So we had to triage,” Dr. Foti recalled, breaking off with a sob as other panelists wiped away their own tears during the webcast.
Respiratory physical therapy
Dr. Pelosi said he believes that optimal care of patients with COVID-19 disease requires a major commitment to physical therapy. He strongly recommends having thoughtfully designed separate written protocols in place for respiratory physiotherapy during mechanical ventilation, weaning, and postextubation. COVID-19 patients typically require 7-10 days of assisted ventilation before weaning, and weaning is a protracted process as well.
“I like to say COVID-19 always requires patience. You have to be very, very patient with this disease,” he emphasized. “These patients have a long and difficult weaning. If the patient isn’t improving during weaning, look at two issues: superinfection and thrombembolism, macro and micro.” The physical therapy measures routinely utilized at his hospital during mechanical ventilation include elevation of the bed head greater than 30 degrees, neuromuscular electrical stimulation, subglottic secretion suctioning, tracheal and oral aspiration, and cough assistance. Separate physical therapy menus are used during before and after extubation.
Dr. Gattinoni offered a final word: “We can do almost nothing with this disease. We try our best to keep the patient alive. What we can do is avoid excessive ventilation of the patient. Applying the typical treatment of ARDS in atypical [Type L] ARDS does not make sense and may be extremely harmful.”
Noninvasive ventilation with helmet continuous positive air pressure (CPAP) deserves to be embraced as an effective strategy in preventing self-induced lung injury, often a key factor in progression from the early milder expression of COVID-19 disease to classic severe acute respiratory distress syndrome, according to European physicians who have been through what they hope are the worst days of the pandemic in the Lombardy region of Northern Italy.
Helmet CPAP is a relatively inexpensive, convenient, well-tolerated intervention. It allows patients to remain conscious and responsive to commands such as “Time to roll over,” which in turn frees up nursing staff. The purpose of helmet CPAP is to curb the huge inspiratory drive that’s a defining feature of this disease and which, unchecked, can lead to self-induced lung injury (SILI), Luciano Gattinoni, MD, explained at a webinar hosted by the European Society of Anaesthesiology.
“Paranoid attention to inspiratory effort – checking it and correcting it – is something where we can make the difference between death and life. It’s extremely important,” said Dr. Gattinoni, guest professor of anesthesiology and intensive care at the University of Gottingen (Germany).
He and his fellow panelists were in accord regarding the merits of helmet CPAP as the premier method of noninvasive ventilatory assistance. They also addressed the importance of monitoring for hypercoagulation, as well as what they’ve come to see as the essential role of pronation in what they define as Type H disease, and the need to have detailed respiratory physiotherapy protocols in place.
“COVID-19 doesn’t like physiotherapy,” explained Paolo Pelosi, MD, professor of anesthesiology and intensive care medicine at the University of Genoa (Italy).
Dr. Gattinoni is credited for identification of two polar phenotypes of what he considers to be a single COVID-19 disease. Early on, many patients present with an atypical form of acute respiratory distress syndrome (ARDS), distinguished by an often-unexpected degree of hypoxia accompanied by high pulmonary compliance and surprisingly little shortness of breath. Dr. Gattinoni and colleagues call this Type L disease, which stands for low elastane, low ventilation to perfusion ratio, low lung weight on CT, and low lung recruitability, which means the patient has a high proportion of aerated lung tissue. Over time, because of either the natural history of the disease or SILI, this may shift to Type H disease, marked by high elastane, high right-to-left shunt, high lung weight, and high recruitability.
“If the pulmonary compliance is above 60 [mL/cm H2O], I’m pretty sure it’s Type L. If it’s 30 [mL/cm H2O] or less, I’m pretty sure it’s Type H. Don’t ask me about 45-55 [mL/cm H2O]; it’s a grey zone,” Dr. Gattinoni said.
Giuseppe Foti, MD, said helmet CPAP in patients with COVID-19 should be free flow, not attached to a ventilator, and the gas flow should be set high – at least 50 L/min – in order to prevent CO2 rebreathing. Although noninvasive ventilation is well accepted for patients with chronic obstructive pulmonary disease or acute cardiogenic pulmonary edema, it hasn’t been extensively studied in the setting of ARDS. A notable exception is a single-center randomized trial in which 83 patients with ARDS at the University of Chicago were assigned to noninvasive ventilation delivered by helmet or face mask (JAMA. 2016 Jun 14;315[22]:2435-41). The endotracheal intubation rate was just 18% in the helmet group, compared with 62% in the face mask group. The 90-day mortality rate was significantly lower in the helmet group as well, noted Dr. Foti, director of the department of anesthesia and intensive care at Monza University Hospital in Milan.
Christian Putensen, MD, said he views intubation for mechanical ventilation as wise in moderate or severe ARDS with an arterial oxygen partial pressure/fraction of inspired oxygen (PaO2/FiO2) ratio below 150. But in milder, Type L COVID-19 disease, he also likes helmet CPAP. It spares the patient from the traumatic compressive stress to the lung induced by mechanical ventilation, which may cause alveolar edema and SILI.
There is, however, a caveat: “Watch carefully and do not delay intubation if you see helmet CPAP is not working; that is, if the blood gas analysis doesn’t improve, the respiratory rate increases, tidal volume increases, and there is still increased respiratory drive,” advised Dr. Putensen, an anesthesiologist at the University of Bonn (Germany).
There is no agreed-upon practical quantitative measure of respiratory drive. A clinical evaluation of the patient’s depth of inspiration is the best guide, he added.
Dr. Gattinoni said that, when helmet CPAP can’t control respiratory drive in a patient with early-stage disease, he feels the only way to interrupt this destructive process is through early intubation and what he termed “gentle mechanical ventilation,” not with a positive end expiratory pressure of 20 cm H2O, but more like 4-5.
Watch for hypercoagulation
Thromboembolic complications are a common feature in COVID-19 disease.
“I’ve had occasion to see the autopsy results in more than 100 patients. It’s devastating to see the number of thromboses and microthromboses in the lungs, the liver, the kidney, and in the brain,” Dr. Gattinoni said.
“COVID-19 is a serial killer, no doubt,” Dr. Pelosi agreed. “He has no mercy for anyone. And he has two bullets: The first one is for the lung, the second is on the vascular side.”
Dr. Putensen is aggressive in utilizing prophylactic high-dose anticoagulation with heparin. He carefully monitors levels of fibrinogen, Factors V and VIII, and d-dimers. In the setting of COVID-19, he has found thromboelastography to be more reliable than partial thromboplastin time in guiding heparin titration.
Pronation
Panelists agreed that pronation is an especially valuable means of enhancing oxygenation in patients with Type H disease. Dr. Putensen tries for more than 16 hours per day. Dr. Foti is preparing a study of the impact of pronation in 50 awake, nonintubated patients, most of whom were on helmet CPAP. Seven of them couldn’t tolerate pronation for even an hour at a time; for the others, the median duration was 3.5 hours at a time.
“We saw a dramatic improvement, a nearly doubling in the PaO2/FiO2 ratio,” Dr. Foti said.
The helmet CPAP study was done outside of the ICU because, in March 2020, the Milan hospital was utterly overwhelmed by COVID-19. The university hospital ordinarily has 25 ICU beds. This was expanded to 100 ICU beds in an effort to meet the emergency, but that still wasn’t sufficient. Indeed, COVID-19 patients occupied 600 of the hospital’s 650 beds. Physicians were forced to do something formerly unthinkable: triage patients for intubation and mechanical ventilation based upon age, comorbidities, and survival prospects.
“We felt schizophrenic. I completely agree with Luciano’s idea to intubate early when we cannot control the respiratory drive that’s due to the disease. But we couldn’t do it because we had too many patients. So we had to triage,” Dr. Foti recalled, breaking off with a sob as other panelists wiped away their own tears during the webcast.
Respiratory physical therapy
Dr. Pelosi said he believes that optimal care of patients with COVID-19 disease requires a major commitment to physical therapy. He strongly recommends having thoughtfully designed separate written protocols in place for respiratory physiotherapy during mechanical ventilation, weaning, and postextubation. COVID-19 patients typically require 7-10 days of assisted ventilation before weaning, and weaning is a protracted process as well.
“I like to say COVID-19 always requires patience. You have to be very, very patient with this disease,” he emphasized. “These patients have a long and difficult weaning. If the patient isn’t improving during weaning, look at two issues: superinfection and thrombembolism, macro and micro.” The physical therapy measures routinely utilized at his hospital during mechanical ventilation include elevation of the bed head greater than 30 degrees, neuromuscular electrical stimulation, subglottic secretion suctioning, tracheal and oral aspiration, and cough assistance. Separate physical therapy menus are used during before and after extubation.
Dr. Gattinoni offered a final word: “We can do almost nothing with this disease. We try our best to keep the patient alive. What we can do is avoid excessive ventilation of the patient. Applying the typical treatment of ARDS in atypical [Type L] ARDS does not make sense and may be extremely harmful.”
Methotrexate adherence: It’s worse than you think
MAUI, HAWAII – Results of a carefully conducted real-world study of adherence to oral methotrexate in patients with RA were “kind of scary,” Arthur Kavanaugh, MD, said at the 2020 Rheumatology Winter Clinical Symposium.
“At 24 weeks, adherence was only 75%. And these were people who knew they were being monitored, so this is the best of the best. And yet less than 20% took the drug perfectly, meaning they took every dose as it was supposed to be,” noted Dr. Kavanaugh, professor of medicine at the University of California, San Diego, and RWCS program director.
“Adherence to methotrexate is really not very good. This is our cornerstone drug – methotrexate – and I think it certainly applies to other medications that we’re using,” he added.
He and his fellow panelist John J. Cush, MD, discussed the implications of this recent study, led by Kaleb Michaud, PhD, of the University of Nebraska Medical Center, Omaha.
The methotrexate adherence study included 60 patients with RA whose use of the disease-modifying antirheumatic drug (DMARD) over 24 weeks was monitored via the electronic Medication Event Monitoring System. These were motivated patients seen in routine clinical practice: They were participants in Forward, the National Databank for Rheumatic Diseases, and they understood that their use of methotrexate was being monitored.
Among the key findings: Patients on average took their weekly dose as directed for a total of 18 of the 24 weeks, although adherence decreased over time. Overall, 13% of participants missed 1 week, and 68% skipped 2 or more weeks. There was no significant difference in methotrexate adherence between biologic-naive and -experienced patients, nor between those on methotrexate monotherapy versus those on additional medication. Patient demographics and RA severity were similar between patients who missed taking their methotrexate for 2 weeks or more and those who missed fewer or no doses.
Higher Patient Global Assessment of Disease Activity scores were associated with correct dosing. So was being unemployed, having no prior conventional DMARD experience, and having less disability. A higher baseline score on the Beliefs about Medicines Questionnaire Specific-Necessity subscale, which indicates stronger belief in the necessity of the medication, were associated with greater likelihood of appropriate dosing, while lower scores were linked with more weeks of early dosing. However, the other elements of the Beliefs about Medicines Questionnaire weren’t significantly associated with adherence.
“This is a big problem. A lot of factors go into medication nonadherence. The solution has to begin with your relationship with the patient. If you want people to trust you, you’re going to have to work at that,” observed Dr. Cush, who is professor of medicine and rheumatology at Baylor University Medical Center, Dallas, and director of clinical rheumatology at the Baylor Research Institute.
Roy Fleischmann, MD, a rheumatologist and medical director of the Metroplex Clinical Research Center, Dallas, said that widespread suboptimal adherence to oral methotrexate has important implications for clinical trials. Often the placebo response rate in a randomized trial where the control group is on background methotrexate is so unexpectedly high that the potential efficacy of the active drug is masked; in such situations, it’s quite possible that patients who previously weren’t taking their methotrexate consistently start doing so when they join a closely supervised study, with a resultant inflated placebo response rate, he said.
One audience member who sees lots of medication adherence issues in his practice suggested that it might be time to become more aggressive in using intravenous infusion therapy instead of subcutaneously administered agents in patients with active RA and adherence problems.
“Maybe that’s why rituximab does so well in the clinical trials,” he said.
Dr. Cush and Dr. Kavanaugh reported receiving research funding from and/or serving as consultants to numerous pharmaceutical companies.
MAUI, HAWAII – Results of a carefully conducted real-world study of adherence to oral methotrexate in patients with RA were “kind of scary,” Arthur Kavanaugh, MD, said at the 2020 Rheumatology Winter Clinical Symposium.
“At 24 weeks, adherence was only 75%. And these were people who knew they were being monitored, so this is the best of the best. And yet less than 20% took the drug perfectly, meaning they took every dose as it was supposed to be,” noted Dr. Kavanaugh, professor of medicine at the University of California, San Diego, and RWCS program director.
“Adherence to methotrexate is really not very good. This is our cornerstone drug – methotrexate – and I think it certainly applies to other medications that we’re using,” he added.
He and his fellow panelist John J. Cush, MD, discussed the implications of this recent study, led by Kaleb Michaud, PhD, of the University of Nebraska Medical Center, Omaha.
The methotrexate adherence study included 60 patients with RA whose use of the disease-modifying antirheumatic drug (DMARD) over 24 weeks was monitored via the electronic Medication Event Monitoring System. These were motivated patients seen in routine clinical practice: They were participants in Forward, the National Databank for Rheumatic Diseases, and they understood that their use of methotrexate was being monitored.
Among the key findings: Patients on average took their weekly dose as directed for a total of 18 of the 24 weeks, although adherence decreased over time. Overall, 13% of participants missed 1 week, and 68% skipped 2 or more weeks. There was no significant difference in methotrexate adherence between biologic-naive and -experienced patients, nor between those on methotrexate monotherapy versus those on additional medication. Patient demographics and RA severity were similar between patients who missed taking their methotrexate for 2 weeks or more and those who missed fewer or no doses.
Higher Patient Global Assessment of Disease Activity scores were associated with correct dosing. So was being unemployed, having no prior conventional DMARD experience, and having less disability. A higher baseline score on the Beliefs about Medicines Questionnaire Specific-Necessity subscale, which indicates stronger belief in the necessity of the medication, were associated with greater likelihood of appropriate dosing, while lower scores were linked with more weeks of early dosing. However, the other elements of the Beliefs about Medicines Questionnaire weren’t significantly associated with adherence.
“This is a big problem. A lot of factors go into medication nonadherence. The solution has to begin with your relationship with the patient. If you want people to trust you, you’re going to have to work at that,” observed Dr. Cush, who is professor of medicine and rheumatology at Baylor University Medical Center, Dallas, and director of clinical rheumatology at the Baylor Research Institute.
Roy Fleischmann, MD, a rheumatologist and medical director of the Metroplex Clinical Research Center, Dallas, said that widespread suboptimal adherence to oral methotrexate has important implications for clinical trials. Often the placebo response rate in a randomized trial where the control group is on background methotrexate is so unexpectedly high that the potential efficacy of the active drug is masked; in such situations, it’s quite possible that patients who previously weren’t taking their methotrexate consistently start doing so when they join a closely supervised study, with a resultant inflated placebo response rate, he said.
One audience member who sees lots of medication adherence issues in his practice suggested that it might be time to become more aggressive in using intravenous infusion therapy instead of subcutaneously administered agents in patients with active RA and adherence problems.
“Maybe that’s why rituximab does so well in the clinical trials,” he said.
Dr. Cush and Dr. Kavanaugh reported receiving research funding from and/or serving as consultants to numerous pharmaceutical companies.
MAUI, HAWAII – Results of a carefully conducted real-world study of adherence to oral methotrexate in patients with RA were “kind of scary,” Arthur Kavanaugh, MD, said at the 2020 Rheumatology Winter Clinical Symposium.
“At 24 weeks, adherence was only 75%. And these were people who knew they were being monitored, so this is the best of the best. And yet less than 20% took the drug perfectly, meaning they took every dose as it was supposed to be,” noted Dr. Kavanaugh, professor of medicine at the University of California, San Diego, and RWCS program director.
“Adherence to methotrexate is really not very good. This is our cornerstone drug – methotrexate – and I think it certainly applies to other medications that we’re using,” he added.
He and his fellow panelist John J. Cush, MD, discussed the implications of this recent study, led by Kaleb Michaud, PhD, of the University of Nebraska Medical Center, Omaha.
The methotrexate adherence study included 60 patients with RA whose use of the disease-modifying antirheumatic drug (DMARD) over 24 weeks was monitored via the electronic Medication Event Monitoring System. These were motivated patients seen in routine clinical practice: They were participants in Forward, the National Databank for Rheumatic Diseases, and they understood that their use of methotrexate was being monitored.
Among the key findings: Patients on average took their weekly dose as directed for a total of 18 of the 24 weeks, although adherence decreased over time. Overall, 13% of participants missed 1 week, and 68% skipped 2 or more weeks. There was no significant difference in methotrexate adherence between biologic-naive and -experienced patients, nor between those on methotrexate monotherapy versus those on additional medication. Patient demographics and RA severity were similar between patients who missed taking their methotrexate for 2 weeks or more and those who missed fewer or no doses.
Higher Patient Global Assessment of Disease Activity scores were associated with correct dosing. So was being unemployed, having no prior conventional DMARD experience, and having less disability. A higher baseline score on the Beliefs about Medicines Questionnaire Specific-Necessity subscale, which indicates stronger belief in the necessity of the medication, were associated with greater likelihood of appropriate dosing, while lower scores were linked with more weeks of early dosing. However, the other elements of the Beliefs about Medicines Questionnaire weren’t significantly associated with adherence.
“This is a big problem. A lot of factors go into medication nonadherence. The solution has to begin with your relationship with the patient. If you want people to trust you, you’re going to have to work at that,” observed Dr. Cush, who is professor of medicine and rheumatology at Baylor University Medical Center, Dallas, and director of clinical rheumatology at the Baylor Research Institute.
Roy Fleischmann, MD, a rheumatologist and medical director of the Metroplex Clinical Research Center, Dallas, said that widespread suboptimal adherence to oral methotrexate has important implications for clinical trials. Often the placebo response rate in a randomized trial where the control group is on background methotrexate is so unexpectedly high that the potential efficacy of the active drug is masked; in such situations, it’s quite possible that patients who previously weren’t taking their methotrexate consistently start doing so when they join a closely supervised study, with a resultant inflated placebo response rate, he said.
One audience member who sees lots of medication adherence issues in his practice suggested that it might be time to become more aggressive in using intravenous infusion therapy instead of subcutaneously administered agents in patients with active RA and adherence problems.
“Maybe that’s why rituximab does so well in the clinical trials,” he said.
Dr. Cush and Dr. Kavanaugh reported receiving research funding from and/or serving as consultants to numerous pharmaceutical companies.
REPORTING FROM RWCS 2020
Differentiating hypersensitivity reactions to monoclonal antibodies
MAUI, HAWAII – Desensitization is a powerful and effective tool in patients with certain types of hypersensitivity reactions to therapeutic monoclonal antibodies, but it’s best considered a last resort reserved for individuals with no options left other than the offending biologic, Anna Postolova, MD, said at the 2020 Rheumatology Winter Clinical Symposium.
Why so selective? Desensitization is considered a high-risk intervention. It’s typically done as an inpatient procedure involving an overnight hospital stay followed by an elaborate 12-step protocol involving administration of small quantities of the culprit biologic in ascending concentrations over a 5- to 6-hour period.
Moreover, for an intravenous agent, such as infliximab (Remicade), desensitization has to be repeated prior to giving every dose of the biologic. So it makes sense to skip desensitization and simply switch to an alternative tumor necrosis factor inhibitor or a different class of biologic unless experience has shown that the culprit monoclonal antibody is the only one that works for that patient. It’s known, for example, that infliximab has no crossreactivity with adalimumab (Humira), explained Dr. Postolova, a dual rheumatologist and allergist/immunologist at Stanford (Calif.) University.
Defining type and severity of the hypersensitivity reaction
Dr. Postolova favors the hypersensitivity reaction classification system developed by Mariana Castells, MD, PhD, and coworkers at Brigham and Women’s Hospital, Boston.
They divide the field into immediate and delayed hypersensitivity reactions. Immediate hypersensitivity reactions arise rapidly, between minutes and a few hours. They can be categorized as infusion reactions, cytokine-release reactions, and IgE-mediated reactions. Phenotypically, infusion reactions and cytokine-release reactions are typically characterized by various combinations of chills, fever, flushing, hypertension, tachycardia, nausea, vomiting, syncope, and shortness of breath.
IgE-mediated reactions can also involve flushing and shortness of breath, and in addition itch, urticaria, and hypotension. These are anaphylactic reactions. Neither hypertension nor fever is part of the anaphylactic picture; those findings point instead to an infusion reaction or cytokine-release reaction.
Most allergists grade reaction severity on a 1-3 scale. Grade 1 reactions are considered mild and involve symptoms limited to the skin, such as flushing, or a single other organ system.
“That being said, if my patient is having a reaction with bronchospasm, I consider that a moderate, grade 2 reaction, and I stop the infusion. There’s only so much you can do for bronchospasm. It’s a very serious reaction,” Dr. Postolova observed.
Grade 2 reactions ordinarily involve two or more organ systems, but without hypotension or cyanosis. Grade 3 reactions are severe anaphylactic reactions with cardiovascular and/or neurologic compromise.
Delayed hypersensitivity reactions are of two types: serum sickness–like reactions and type IV cell-mediated mucocutaneous reactions.
Type IV reactions can range from a mild maculopapular rash to erythema multiforme, Stevens-Johnson syndrome, toxic epidermal necrolysis, and DRESS (drug reaction with eosinophilia and systemic symptoms). Onset of type IV reactions can occur after 12 hours up to several weeks after exposure.
Serum sickness–like reactions typically begin 5-7 days after the infusion. These reactions are marked by evidence of immune overactivation: fever, arthralgia, arthritis, malaise, purpura, skin rash, and even renal failure.
Management of reactions
A patient with a grade 3 reaction who needs to continue using the culprit monoclonal antibody should be referred to an allergist for skin testing in an effort to identify an IgE-mediated reaction.
The timing of the referral for skin testing is important: The allergist wants to test roughly 4-6 weeks after the hypersensitivity reaction. Test too early and the results will be uninformative because the patient will still be anergic. On the other hand, after 7-8 weeks the patient will have lost the allergy. So there is a sweet spot.
If the patient is skin test positive – with the caveat that skin testing in this setting is not well validated – then the allergist will suggest desensitization, usually as an inpatient.
In contrast, infusion reactions can be handled in the rheumatologist’s infusion center. They are self-limited upon repeat exposure with premedication using antihistamines, NSAIDs, oral or injectable steroids, and perhaps montelukast (Singulair).
If a patient initially thought to have an infusion reaction continues to experience reactions even after the biologic is being delivered more slowly and under the protection of premedication, it’s time to consider the possibility that what’s really going on is a cytokine-release reaction or an IgE-mediated reaction. Diagnostic skin testing is in order.
For a skin test–negative patient with a suspected cytokine-release reaction, the allergist may propose a therapeutic challenge. This is reserved for patients who the allergist believe will not experience an immediate reaction, and unlike desensitization it’s not an intervention intended to induce drug tolerance. The challenge involves giving 10% of a full dose of the biologic, waiting in the allergist’s office for 30-60 minutes, then giving the other 90% of the medication, followed by an hour of in-office observation.
The solution to severe type IV delayed hypersensitivity reactions is strict medication avoidance, not desensitization, according to Dr. Postolova.
Top offending monoclonal antibodies
Infliximab and rituximab (Rituxan) are the most common culprits when it comes to immediate hypersensitivity reactions. About 10% of infliximab-treated patients develop these reactions. Although the reaction can occur with the first dose, the peak incidence is with the seventh infusion. Patients with anti-infliximab IgG antibodies are at 140%-300% increased risk; however, concomitant disease-modifying antirheumatic drug therapy lessens that risk.
Infusion reactions or cytokine-release reactions occur upon the first infusion of rituximab in about 25% of treated rheumatology patients and in a higher proportion of cancer patients. Most of these reactions are mild and don’t recur when the biologic is administered more slowly and with premedication. Severe recurrent reactions upon subsequent exposure are much more likely to be an IgE-mediated hypersensitivity reaction.
“Stop the medication, send the patient to your local allergist for skin testing, and they’ll use a desensitization protocol if rituximab is the best drug for your patient,” Dr. Postolova advised.
She reported having no financial conflicts regarding her presentation.
MAUI, HAWAII – Desensitization is a powerful and effective tool in patients with certain types of hypersensitivity reactions to therapeutic monoclonal antibodies, but it’s best considered a last resort reserved for individuals with no options left other than the offending biologic, Anna Postolova, MD, said at the 2020 Rheumatology Winter Clinical Symposium.
Why so selective? Desensitization is considered a high-risk intervention. It’s typically done as an inpatient procedure involving an overnight hospital stay followed by an elaborate 12-step protocol involving administration of small quantities of the culprit biologic in ascending concentrations over a 5- to 6-hour period.
Moreover, for an intravenous agent, such as infliximab (Remicade), desensitization has to be repeated prior to giving every dose of the biologic. So it makes sense to skip desensitization and simply switch to an alternative tumor necrosis factor inhibitor or a different class of biologic unless experience has shown that the culprit monoclonal antibody is the only one that works for that patient. It’s known, for example, that infliximab has no crossreactivity with adalimumab (Humira), explained Dr. Postolova, a dual rheumatologist and allergist/immunologist at Stanford (Calif.) University.
Defining type and severity of the hypersensitivity reaction
Dr. Postolova favors the hypersensitivity reaction classification system developed by Mariana Castells, MD, PhD, and coworkers at Brigham and Women’s Hospital, Boston.
They divide the field into immediate and delayed hypersensitivity reactions. Immediate hypersensitivity reactions arise rapidly, between minutes and a few hours. They can be categorized as infusion reactions, cytokine-release reactions, and IgE-mediated reactions. Phenotypically, infusion reactions and cytokine-release reactions are typically characterized by various combinations of chills, fever, flushing, hypertension, tachycardia, nausea, vomiting, syncope, and shortness of breath.
IgE-mediated reactions can also involve flushing and shortness of breath, and in addition itch, urticaria, and hypotension. These are anaphylactic reactions. Neither hypertension nor fever is part of the anaphylactic picture; those findings point instead to an infusion reaction or cytokine-release reaction.
Most allergists grade reaction severity on a 1-3 scale. Grade 1 reactions are considered mild and involve symptoms limited to the skin, such as flushing, or a single other organ system.
“That being said, if my patient is having a reaction with bronchospasm, I consider that a moderate, grade 2 reaction, and I stop the infusion. There’s only so much you can do for bronchospasm. It’s a very serious reaction,” Dr. Postolova observed.
Grade 2 reactions ordinarily involve two or more organ systems, but without hypotension or cyanosis. Grade 3 reactions are severe anaphylactic reactions with cardiovascular and/or neurologic compromise.
Delayed hypersensitivity reactions are of two types: serum sickness–like reactions and type IV cell-mediated mucocutaneous reactions.
Type IV reactions can range from a mild maculopapular rash to erythema multiforme, Stevens-Johnson syndrome, toxic epidermal necrolysis, and DRESS (drug reaction with eosinophilia and systemic symptoms). Onset of type IV reactions can occur after 12 hours up to several weeks after exposure.
Serum sickness–like reactions typically begin 5-7 days after the infusion. These reactions are marked by evidence of immune overactivation: fever, arthralgia, arthritis, malaise, purpura, skin rash, and even renal failure.
Management of reactions
A patient with a grade 3 reaction who needs to continue using the culprit monoclonal antibody should be referred to an allergist for skin testing in an effort to identify an IgE-mediated reaction.
The timing of the referral for skin testing is important: The allergist wants to test roughly 4-6 weeks after the hypersensitivity reaction. Test too early and the results will be uninformative because the patient will still be anergic. On the other hand, after 7-8 weeks the patient will have lost the allergy. So there is a sweet spot.
If the patient is skin test positive – with the caveat that skin testing in this setting is not well validated – then the allergist will suggest desensitization, usually as an inpatient.
In contrast, infusion reactions can be handled in the rheumatologist’s infusion center. They are self-limited upon repeat exposure with premedication using antihistamines, NSAIDs, oral or injectable steroids, and perhaps montelukast (Singulair).
If a patient initially thought to have an infusion reaction continues to experience reactions even after the biologic is being delivered more slowly and under the protection of premedication, it’s time to consider the possibility that what’s really going on is a cytokine-release reaction or an IgE-mediated reaction. Diagnostic skin testing is in order.
For a skin test–negative patient with a suspected cytokine-release reaction, the allergist may propose a therapeutic challenge. This is reserved for patients who the allergist believe will not experience an immediate reaction, and unlike desensitization it’s not an intervention intended to induce drug tolerance. The challenge involves giving 10% of a full dose of the biologic, waiting in the allergist’s office for 30-60 minutes, then giving the other 90% of the medication, followed by an hour of in-office observation.
The solution to severe type IV delayed hypersensitivity reactions is strict medication avoidance, not desensitization, according to Dr. Postolova.
Top offending monoclonal antibodies
Infliximab and rituximab (Rituxan) are the most common culprits when it comes to immediate hypersensitivity reactions. About 10% of infliximab-treated patients develop these reactions. Although the reaction can occur with the first dose, the peak incidence is with the seventh infusion. Patients with anti-infliximab IgG antibodies are at 140%-300% increased risk; however, concomitant disease-modifying antirheumatic drug therapy lessens that risk.
Infusion reactions or cytokine-release reactions occur upon the first infusion of rituximab in about 25% of treated rheumatology patients and in a higher proportion of cancer patients. Most of these reactions are mild and don’t recur when the biologic is administered more slowly and with premedication. Severe recurrent reactions upon subsequent exposure are much more likely to be an IgE-mediated hypersensitivity reaction.
“Stop the medication, send the patient to your local allergist for skin testing, and they’ll use a desensitization protocol if rituximab is the best drug for your patient,” Dr. Postolova advised.
She reported having no financial conflicts regarding her presentation.
MAUI, HAWAII – Desensitization is a powerful and effective tool in patients with certain types of hypersensitivity reactions to therapeutic monoclonal antibodies, but it’s best considered a last resort reserved for individuals with no options left other than the offending biologic, Anna Postolova, MD, said at the 2020 Rheumatology Winter Clinical Symposium.
Why so selective? Desensitization is considered a high-risk intervention. It’s typically done as an inpatient procedure involving an overnight hospital stay followed by an elaborate 12-step protocol involving administration of small quantities of the culprit biologic in ascending concentrations over a 5- to 6-hour period.
Moreover, for an intravenous agent, such as infliximab (Remicade), desensitization has to be repeated prior to giving every dose of the biologic. So it makes sense to skip desensitization and simply switch to an alternative tumor necrosis factor inhibitor or a different class of biologic unless experience has shown that the culprit monoclonal antibody is the only one that works for that patient. It’s known, for example, that infliximab has no crossreactivity with adalimumab (Humira), explained Dr. Postolova, a dual rheumatologist and allergist/immunologist at Stanford (Calif.) University.
Defining type and severity of the hypersensitivity reaction
Dr. Postolova favors the hypersensitivity reaction classification system developed by Mariana Castells, MD, PhD, and coworkers at Brigham and Women’s Hospital, Boston.
They divide the field into immediate and delayed hypersensitivity reactions. Immediate hypersensitivity reactions arise rapidly, between minutes and a few hours. They can be categorized as infusion reactions, cytokine-release reactions, and IgE-mediated reactions. Phenotypically, infusion reactions and cytokine-release reactions are typically characterized by various combinations of chills, fever, flushing, hypertension, tachycardia, nausea, vomiting, syncope, and shortness of breath.
IgE-mediated reactions can also involve flushing and shortness of breath, and in addition itch, urticaria, and hypotension. These are anaphylactic reactions. Neither hypertension nor fever is part of the anaphylactic picture; those findings point instead to an infusion reaction or cytokine-release reaction.
Most allergists grade reaction severity on a 1-3 scale. Grade 1 reactions are considered mild and involve symptoms limited to the skin, such as flushing, or a single other organ system.
“That being said, if my patient is having a reaction with bronchospasm, I consider that a moderate, grade 2 reaction, and I stop the infusion. There’s only so much you can do for bronchospasm. It’s a very serious reaction,” Dr. Postolova observed.
Grade 2 reactions ordinarily involve two or more organ systems, but without hypotension or cyanosis. Grade 3 reactions are severe anaphylactic reactions with cardiovascular and/or neurologic compromise.
Delayed hypersensitivity reactions are of two types: serum sickness–like reactions and type IV cell-mediated mucocutaneous reactions.
Type IV reactions can range from a mild maculopapular rash to erythema multiforme, Stevens-Johnson syndrome, toxic epidermal necrolysis, and DRESS (drug reaction with eosinophilia and systemic symptoms). Onset of type IV reactions can occur after 12 hours up to several weeks after exposure.
Serum sickness–like reactions typically begin 5-7 days after the infusion. These reactions are marked by evidence of immune overactivation: fever, arthralgia, arthritis, malaise, purpura, skin rash, and even renal failure.
Management of reactions
A patient with a grade 3 reaction who needs to continue using the culprit monoclonal antibody should be referred to an allergist for skin testing in an effort to identify an IgE-mediated reaction.
The timing of the referral for skin testing is important: The allergist wants to test roughly 4-6 weeks after the hypersensitivity reaction. Test too early and the results will be uninformative because the patient will still be anergic. On the other hand, after 7-8 weeks the patient will have lost the allergy. So there is a sweet spot.
If the patient is skin test positive – with the caveat that skin testing in this setting is not well validated – then the allergist will suggest desensitization, usually as an inpatient.
In contrast, infusion reactions can be handled in the rheumatologist’s infusion center. They are self-limited upon repeat exposure with premedication using antihistamines, NSAIDs, oral or injectable steroids, and perhaps montelukast (Singulair).
If a patient initially thought to have an infusion reaction continues to experience reactions even after the biologic is being delivered more slowly and under the protection of premedication, it’s time to consider the possibility that what’s really going on is a cytokine-release reaction or an IgE-mediated reaction. Diagnostic skin testing is in order.
For a skin test–negative patient with a suspected cytokine-release reaction, the allergist may propose a therapeutic challenge. This is reserved for patients who the allergist believe will not experience an immediate reaction, and unlike desensitization it’s not an intervention intended to induce drug tolerance. The challenge involves giving 10% of a full dose of the biologic, waiting in the allergist’s office for 30-60 minutes, then giving the other 90% of the medication, followed by an hour of in-office observation.
The solution to severe type IV delayed hypersensitivity reactions is strict medication avoidance, not desensitization, according to Dr. Postolova.
Top offending monoclonal antibodies
Infliximab and rituximab (Rituxan) are the most common culprits when it comes to immediate hypersensitivity reactions. About 10% of infliximab-treated patients develop these reactions. Although the reaction can occur with the first dose, the peak incidence is with the seventh infusion. Patients with anti-infliximab IgG antibodies are at 140%-300% increased risk; however, concomitant disease-modifying antirheumatic drug therapy lessens that risk.
Infusion reactions or cytokine-release reactions occur upon the first infusion of rituximab in about 25% of treated rheumatology patients and in a higher proportion of cancer patients. Most of these reactions are mild and don’t recur when the biologic is administered more slowly and with premedication. Severe recurrent reactions upon subsequent exposure are much more likely to be an IgE-mediated hypersensitivity reaction.
“Stop the medication, send the patient to your local allergist for skin testing, and they’ll use a desensitization protocol if rituximab is the best drug for your patient,” Dr. Postolova advised.
She reported having no financial conflicts regarding her presentation.
REPORTING FROM RWCS 2020
HFpEF: Gender difference in sacubitril/valsartan response remains mystery
The explanation for the impressive clinical benefits of sacubitril/valsartan in women with heart failure with preserved ejection fraction in the PARAGON-HF trial – but not in the men – remains elusive, Jonathan W. Cunningham, MD, said at the joint scientific sessions of the American College of Cardiology and the World Heart Federation. The meeting was conducted online after its cancellation because of the COVID-19 pandemic.
“We’ve all been trying to unravel the explanation for the differential effects between men and women in the primary trial. I don’t know that this NT-proBNP substudy gives a clear answer because we did see similar reduction in NT-proBNP in the men and women,” said Dr. Cunningham of Brigham and Women’s Hospital, Boston.
“Unfortunately, I think we’re still looking for the underlying physiological explanation for that very interesting interaction,” he added.
The PARAGON-HF trial included 4,796 patients with heart failure with preserved ejection fraction (HFpEF) who were randomized double-blind to sacubitril/valsartan (Entresto) or valsartan on top of background guideline-directed medical therapy and followed for a median of 34 months (N Engl J Med. 2019 Oct 24;381[17]:1609-20). The sacubitril/valsartan group’s 13% relative risk reduction in the primary composite endpoint of cardiovascular death and total heart failure hospitalizations fell tantalizingly short of statistical significance (P = 0.058).
In women, however, who comprised more than half of the study population, the benefit of sacubitril/valsartan was larger: a 27% relative risk reduction compared to valsartan alone. That’s a statistically significant difference in a prespecified subgroup analysis, but according to the rules of clinical trials and statistics it must be considered hypothesis-generating and nondefinitive, since the overall trial was negative. Men randomized to sacubitril/valsartan had a modest 3% increased risk of the primary endpoint compared to men on valsartan.
Because of the enormous unmet need for effective therapy for HFpEF, and the fact that HFpEF is more common in women than men, the search is on for an explanation that would account for the striking gender difference in outcome in PARAGON-HF. At ACC 2020, Dr. Cunningham presented a secondary analysis of the trial focusing on the relationships between baseline and on-treatment N-terminal pro-B-type natriuretic peptide (NT-proBNP) levels and clinical outcomes.
Among the key findings was that the higher the baseline NT-proBNP, the greater the likelihood of the primary endpoint. Also, sacubitril/valsartan reduced NT-proBNP to a similar extent in men and women: For example, by 20% compared to valsartan in men and by 18% in women when measured 16 weeks after randomization. And reduction in NT-proBNP was associated with reduced risk of cardiovascular death and heart failure hospitalizations; indeed, 60% of participants in PARAGON-HF experienced a decrease in NT-proBNP, and they had a 23% lower event rate compared to patients whose NT-proBNP increased during the course of the study.
Another intriguing finding in the parent PARAGON-HF trial was that HFpEF patients with an LVEF of 45%-57% had a 22% lower rate of the primary endpoint than those with an LVEF of 58% or more. But as with the gender difference in clinical outcomes in response to sacubitril/valsartan, the difference in outcomes based on ejection fraction was not mediated by the drug’s impact on NT-proBNP, since sacubitril/valsartan reduced NT-proBNP to a similar degree in HFpEF patients with an LVEF above or below 57%.
The difference in outcomes by ejection fraction wasn’t entirely surprising, because those low-normal–range ejection fractions where sacubitril/valsartan had a favorable impact approach those characteristic of heart failure with reduced ejection fraction (HFrEF), and guidelines give sacubitril/valsartan a class I recommendation in patients with HFrEF on the strength of the medication’s demonstrated reduction in morbidity and mortality in the PARADIGM-HF trial.
Discussant Lee R. Goldberg, MD, predicted this analysis will have an impact on the design of future clinical trials in HFpEF, which up until now have required certain minimum NT-proBNP levels for participation.
“Maybe this is why so many of our trials in HFpEF have been unsuccessful. It’s a very heterogeneous population and perhaps NT-proBNP cutoffs are leading to a lot of mischief or heterogeneity that causes us some difficulty,” said Dr. Goldberg, professor of medicine and chief of the section of advanced heart failure and cardiac transplantation at the University of Pennsylvania, Philadelphia.
Dr. Cunningham reported having no financial conflicts regarding his study. The PARAGON-HF trial was funded by Novartis.
Simultaneously with Dr. Cunningham’s presentation at ACC 2020, the study results were published online (JACC Heart Fail. 2020 Mar 26; doi: 10.1016/j.jchf.2020.03.002.
SOURCE: Cunningham JW. ACC 2020, Abstract 412-08.
The explanation for the impressive clinical benefits of sacubitril/valsartan in women with heart failure with preserved ejection fraction in the PARAGON-HF trial – but not in the men – remains elusive, Jonathan W. Cunningham, MD, said at the joint scientific sessions of the American College of Cardiology and the World Heart Federation. The meeting was conducted online after its cancellation because of the COVID-19 pandemic.
“We’ve all been trying to unravel the explanation for the differential effects between men and women in the primary trial. I don’t know that this NT-proBNP substudy gives a clear answer because we did see similar reduction in NT-proBNP in the men and women,” said Dr. Cunningham of Brigham and Women’s Hospital, Boston.
“Unfortunately, I think we’re still looking for the underlying physiological explanation for that very interesting interaction,” he added.
The PARAGON-HF trial included 4,796 patients with heart failure with preserved ejection fraction (HFpEF) who were randomized double-blind to sacubitril/valsartan (Entresto) or valsartan on top of background guideline-directed medical therapy and followed for a median of 34 months (N Engl J Med. 2019 Oct 24;381[17]:1609-20). The sacubitril/valsartan group’s 13% relative risk reduction in the primary composite endpoint of cardiovascular death and total heart failure hospitalizations fell tantalizingly short of statistical significance (P = 0.058).
In women, however, who comprised more than half of the study population, the benefit of sacubitril/valsartan was larger: a 27% relative risk reduction compared to valsartan alone. That’s a statistically significant difference in a prespecified subgroup analysis, but according to the rules of clinical trials and statistics it must be considered hypothesis-generating and nondefinitive, since the overall trial was negative. Men randomized to sacubitril/valsartan had a modest 3% increased risk of the primary endpoint compared to men on valsartan.
Because of the enormous unmet need for effective therapy for HFpEF, and the fact that HFpEF is more common in women than men, the search is on for an explanation that would account for the striking gender difference in outcome in PARAGON-HF. At ACC 2020, Dr. Cunningham presented a secondary analysis of the trial focusing on the relationships between baseline and on-treatment N-terminal pro-B-type natriuretic peptide (NT-proBNP) levels and clinical outcomes.
Among the key findings was that the higher the baseline NT-proBNP, the greater the likelihood of the primary endpoint. Also, sacubitril/valsartan reduced NT-proBNP to a similar extent in men and women: For example, by 20% compared to valsartan in men and by 18% in women when measured 16 weeks after randomization. And reduction in NT-proBNP was associated with reduced risk of cardiovascular death and heart failure hospitalizations; indeed, 60% of participants in PARAGON-HF experienced a decrease in NT-proBNP, and they had a 23% lower event rate compared to patients whose NT-proBNP increased during the course of the study.
Another intriguing finding in the parent PARAGON-HF trial was that HFpEF patients with an LVEF of 45%-57% had a 22% lower rate of the primary endpoint than those with an LVEF of 58% or more. But as with the gender difference in clinical outcomes in response to sacubitril/valsartan, the difference in outcomes based on ejection fraction was not mediated by the drug’s impact on NT-proBNP, since sacubitril/valsartan reduced NT-proBNP to a similar degree in HFpEF patients with an LVEF above or below 57%.
The difference in outcomes by ejection fraction wasn’t entirely surprising, because those low-normal–range ejection fractions where sacubitril/valsartan had a favorable impact approach those characteristic of heart failure with reduced ejection fraction (HFrEF), and guidelines give sacubitril/valsartan a class I recommendation in patients with HFrEF on the strength of the medication’s demonstrated reduction in morbidity and mortality in the PARADIGM-HF trial.
Discussant Lee R. Goldberg, MD, predicted this analysis will have an impact on the design of future clinical trials in HFpEF, which up until now have required certain minimum NT-proBNP levels for participation.
“Maybe this is why so many of our trials in HFpEF have been unsuccessful. It’s a very heterogeneous population and perhaps NT-proBNP cutoffs are leading to a lot of mischief or heterogeneity that causes us some difficulty,” said Dr. Goldberg, professor of medicine and chief of the section of advanced heart failure and cardiac transplantation at the University of Pennsylvania, Philadelphia.
Dr. Cunningham reported having no financial conflicts regarding his study. The PARAGON-HF trial was funded by Novartis.
Simultaneously with Dr. Cunningham’s presentation at ACC 2020, the study results were published online (JACC Heart Fail. 2020 Mar 26; doi: 10.1016/j.jchf.2020.03.002.
SOURCE: Cunningham JW. ACC 2020, Abstract 412-08.
The explanation for the impressive clinical benefits of sacubitril/valsartan in women with heart failure with preserved ejection fraction in the PARAGON-HF trial – but not in the men – remains elusive, Jonathan W. Cunningham, MD, said at the joint scientific sessions of the American College of Cardiology and the World Heart Federation. The meeting was conducted online after its cancellation because of the COVID-19 pandemic.
“We’ve all been trying to unravel the explanation for the differential effects between men and women in the primary trial. I don’t know that this NT-proBNP substudy gives a clear answer because we did see similar reduction in NT-proBNP in the men and women,” said Dr. Cunningham of Brigham and Women’s Hospital, Boston.
“Unfortunately, I think we’re still looking for the underlying physiological explanation for that very interesting interaction,” he added.
The PARAGON-HF trial included 4,796 patients with heart failure with preserved ejection fraction (HFpEF) who were randomized double-blind to sacubitril/valsartan (Entresto) or valsartan on top of background guideline-directed medical therapy and followed for a median of 34 months (N Engl J Med. 2019 Oct 24;381[17]:1609-20). The sacubitril/valsartan group’s 13% relative risk reduction in the primary composite endpoint of cardiovascular death and total heart failure hospitalizations fell tantalizingly short of statistical significance (P = 0.058).
In women, however, who comprised more than half of the study population, the benefit of sacubitril/valsartan was larger: a 27% relative risk reduction compared to valsartan alone. That’s a statistically significant difference in a prespecified subgroup analysis, but according to the rules of clinical trials and statistics it must be considered hypothesis-generating and nondefinitive, since the overall trial was negative. Men randomized to sacubitril/valsartan had a modest 3% increased risk of the primary endpoint compared to men on valsartan.
Because of the enormous unmet need for effective therapy for HFpEF, and the fact that HFpEF is more common in women than men, the search is on for an explanation that would account for the striking gender difference in outcome in PARAGON-HF. At ACC 2020, Dr. Cunningham presented a secondary analysis of the trial focusing on the relationships between baseline and on-treatment N-terminal pro-B-type natriuretic peptide (NT-proBNP) levels and clinical outcomes.
Among the key findings was that the higher the baseline NT-proBNP, the greater the likelihood of the primary endpoint. Also, sacubitril/valsartan reduced NT-proBNP to a similar extent in men and women: For example, by 20% compared to valsartan in men and by 18% in women when measured 16 weeks after randomization. And reduction in NT-proBNP was associated with reduced risk of cardiovascular death and heart failure hospitalizations; indeed, 60% of participants in PARAGON-HF experienced a decrease in NT-proBNP, and they had a 23% lower event rate compared to patients whose NT-proBNP increased during the course of the study.
Another intriguing finding in the parent PARAGON-HF trial was that HFpEF patients with an LVEF of 45%-57% had a 22% lower rate of the primary endpoint than those with an LVEF of 58% or more. But as with the gender difference in clinical outcomes in response to sacubitril/valsartan, the difference in outcomes based on ejection fraction was not mediated by the drug’s impact on NT-proBNP, since sacubitril/valsartan reduced NT-proBNP to a similar degree in HFpEF patients with an LVEF above or below 57%.
The difference in outcomes by ejection fraction wasn’t entirely surprising, because those low-normal–range ejection fractions where sacubitril/valsartan had a favorable impact approach those characteristic of heart failure with reduced ejection fraction (HFrEF), and guidelines give sacubitril/valsartan a class I recommendation in patients with HFrEF on the strength of the medication’s demonstrated reduction in morbidity and mortality in the PARADIGM-HF trial.
Discussant Lee R. Goldberg, MD, predicted this analysis will have an impact on the design of future clinical trials in HFpEF, which up until now have required certain minimum NT-proBNP levels for participation.
“Maybe this is why so many of our trials in HFpEF have been unsuccessful. It’s a very heterogeneous population and perhaps NT-proBNP cutoffs are leading to a lot of mischief or heterogeneity that causes us some difficulty,” said Dr. Goldberg, professor of medicine and chief of the section of advanced heart failure and cardiac transplantation at the University of Pennsylvania, Philadelphia.
Dr. Cunningham reported having no financial conflicts regarding his study. The PARAGON-HF trial was funded by Novartis.
Simultaneously with Dr. Cunningham’s presentation at ACC 2020, the study results were published online (JACC Heart Fail. 2020 Mar 26; doi: 10.1016/j.jchf.2020.03.002.
SOURCE: Cunningham JW. ACC 2020, Abstract 412-08.
FROM ACC 2020
Experts review recent winners and losers in the RA pipeline
MAUI, HAWAII – Filgotinib, the oral Janus kinase (JAK) inhibitor now under Food and Drug Administration review for the treatment of RA, has a better safety profile than some of the approved oral JAK inhibitors, but that’s unlikely to save it from being saddled with a black-box safety warning label, experts agreed at the 2020 Rheumatology Winter Clinical Symposium.
“There’s probably a class label out there,” according to Mark C. Genovese, MD, professor of medicine and clinical chief of the division of immunology and rheumatology at Stanford (Calif.) University.
He cited the example of upadacitinib (Rinvoq), approved last year as the third oral JAK inhibitor for RA. Even though venous thromboembolic (VTE) events weren’t seen with any significantly increased frequency, compared with placebo, in the upadacitinib development program – unlike for the earlier-approved tofacitinib (Xeljanz) and baricitinib (Olumiant) –the FDA nevertheless required that upadacitinib’s product labeling include this black-box warning: “Thrombosis, including deep vein thrombosis, pulmonary embolism, and arterial thrombosis, have occurred in patients treated with Janus kinase inhibitors used to treat inflammatory conditions.”
“I would fully expect that there’ll be a similar label in the filgotinib package insert saying that VTEs have been seen in other members of the class,” he predicted.
His copanelist Roy Fleischmann, MD, noted that filgotinib displayed a clean long-term safety profile in a pooled analysis of the 24-week results in the 2,088 filgotinib-treated participants in all phase 3 clinical trials for RA. For example, the incidence of herpes zoster in that large treated population was a mere 0.1%.
“Herpes zoster is almost nonexistent across the program,” observed Dr. Fleischmann, a rheumatologist at the University of Texas and medical director of the Metroplex Clinical Research Center, both in Dallas.
That’s consistent with what he’s heard from Japanese investigators about their experience. They tell him that in their studies the incidence of herpes zoster with filgotinib is five times less than with other JAK inhibitors.
The long-term pooled phase 3 filgotinib safety data also show less than a 0.1% incidence of adjudicated VTE/pulmonary embolism through 24 weeks. That’s a substantially lower rate than with tofacitinib or baricitinib, he noted.
The two rheumatologists, long-time observers of the FDA regulatory scene, stressed that they have no inside information regarding what the agency will do about filgotinib. It seems beyond doubt that the JAK inhibitor will be approved. But an open question of practical importance to clinicians is whether the agency will approve only the 100-mg dose or the 200-mg dose as well. The panelists agreed that having access to both would be advantageous since the clinical trials data indicate the higher dose is more effective and this greater efficacy doesn’t come at a cost of additional safety issues.
“If the 100 mg is sufficient, that’s great, but the reality is if you want to push to low disease activity or remission, the 200 mg seems to work better, particularly in patients who’ve already failed TNF [tumor necrosis factor] inhibitors or other biologics,” Dr. Genovese said. “If you’re not having additional safety concerns and you can get additional efficacy, I love the idea of having flexibility.”
Dr. Fleischmann is skeptical that the regulators will see things that way.
“There is a real risk that the FDA will do what it’s done before and say: ‘Well, the 200 works and the 100 works, so we’re going to approve the lower dose.’ But there doesn’t appear to be a big safety difference between 100 and 200. So I can see why they would approve the two doses, but I think that’d be unusual,” according to the rheumatologist.
The RA pipeline
The two speakers also highlighted several agents with novel mechanisms of action moving through the RA developmental pipeline, including olokizumab, otilimab, fenebrutinib, and a promising oral selective interleukin-1 receptor–associated kinase 4 inhibitor (IRAK4).
Olokizumab: This humanized monoclonal antibody targets IL-6. It has a different mechanism of action than the two commercially available IL-6 inhibitors approved for RA, tocilizumab (Actemra) and sarilumab (Kevzara), in that olokizumab uniquely targets the IL-6 ligand.
At the 2019 annual meeting of the American College of Rheumatology, Dr. Genovese presented the positive findings of a double-blind, placebo-controlled, randomized, phase 3 clinical trial of olokizumab in 428 RA patients with an inadequate response to methotrexate. The primary outcome, an ACR 20 response at 12 weeks, occurred in 25.9% of patients on placebo, 63.6% with 64 mg of olokizumab given subcutaneously every 2 weeks, and 70.4% with 64 mg every 4 weeks, with all participants on background methotrexate. An ACR 50 response at week 24 occurred in 7.7%, 42.7%, and 48.6%, respectively, with an acceptable side effect profile.
This was the first phase 3 trial to be presented from a large, ongoing phase 3 olokizumab developmental program for a variety of diseases.
“The results certainly support the idea that a 4-week regimen would probably be quite useful with this medication, although we’ll have to see what happens with the remaining phase 3 trials,” Dr. Genovese said.
Dr. Fleischmann posed a question: Do we really need a third IL-6 inhibitor?
That would make for a crowded field, Dr. Genovese agreed, adding that grabbing a reasonable market share for olokizumab may come down to cost, formulary access, and the convenience factor of once-monthly dosing. Whether the biologic’s unique mechanism of action in blocking the IL-6 ligand makes any practical difference in outcomes is unknown.
IRAK4 inhibitor: PF-06650833 is an oral selective reversible inhibitor of IRAK4, a key signaling kinase for IL-1 and toll-like receptors.
“This should be a really good drug for IL-1-mediated diseases,” according to Dr. Fleischmann.
In a phase 2b, double-blind, randomized, placebo-controlled, 12-week study featuring tofacitinib at 5 mg twice daily as an active comparator, the IRAK4 inhibitor exhibited dose-dependent efficacy for the primary endpoint of improvement from baseline in Simple Disease Activity Index score, compared with placebo. The same was true for the secondary endpoint, change over time in 28-joint Disease Activity Score using C-reactive protein (DAS28-CRP). The trial results were also presented at the 2019 ACR annual meeting.
“This is a drug they should probably take forward and see how far it goes in RA,” he said.
Dr. Genovese concurred.
“We’re still trying to figure out how we can put together rational combinations in RA, and this might be something that could be considered as a combination play. In fact, Pfizer has already teed up a study looking at a JAK inhibitor/IRAK4 combination. The question will be whether this is a standalone or has an opportunity to be part of a combination approach,” the rheumatologist said.
Otilimab: This monoclonal antibody is a granulocyte-macrophage colony-stimulating factor inhibitor. In a secondary analysis of the BAROQUE trial, a phase 2b, 50-week study in RA inadequately responsive to methotrexate, otilimab demonstrated an impressive effect in terms of pain reduction. This new analysis, which was first presented at the 2019 ACR annual meeting, showed that, at week 12, a minimum clinically important difference in pain was achieved in 29% of placebo-treated controls, compared with 65%-75% of patients on low to higher doses of otilimab.
“The question is: Is this pain effect unique to this molecule, this pathway, or is it a simple reflection of the treated patient population?” Dr. Genovese commented. “It’s an interesting molecule. It’s being developed in RA, and it might have unique benefits on the pain side.”
A tale of two BTK inhibitors: Bruton tyrosine kinase (BTK) is an intracellular kinase viewed as a promising target in autoimmune disease. Fenebrutinib is an oral, noncovalent, reversible, and highly selective BTK inhibitor that performed well in a phase 2, randomized, double-blind, placebo-controlled clinical trial with adalimumab as an active comparator in 480 patients with an inadequate response to methotrexate in one branch, and in 98 patients with an inadequate response to TNF inhibitor therapy in the other. All subjects were on background methotrexate. (The study results were published April 9 in Arthritis & Rheumatology.)
In the group with a prior inadequate response to TNF inhibitors, the ACR 50 response rate at 12 weeks was 25% in the group on fenebrutinib at 200 mg twice daily, significantly better than the 12% rate in placebo. And there were favorable effects on biomarkers: The reduction in erythrocyte sedimentation rate from baseline was nearly twice as great with fenebrutinib, the drop in CRP was nearly three times greater than with placebo, and there was also a significantly greater decrease over time in DAS28-CRP.
In the methotrexate-inadequate responders, the ACR50 rates were 28% and 35% with the BTK inhibitor at 150 and 200 mg once daily, respectively, compared with 15% in controls.
The safety picture was encouraging, with similarly low adverse event rates across all treatment arms.
In contrast to the fenebrutinib experience, Dr. Genovese was lead investigator in a 250-patient, phase 2 study of another oral BTK inhibitor, poseltinib, which differs from fenebrutinib in that it is an irreversible covalent inhibitor. It was a failed study, with no significant difference between poseltinib and placebo in ACR 20 response at 12 weeks. It’s unclear whether the problem was insufficient dosing or that poseltinib is a failed molecule, perhaps because of its irreversible covalent binding to BTK, he said.
Other notable failures
The spleen tyrosine kinase (Syk) inhibitor known as GS-9876 showed no clinical efficacy in a phase 2, double-blind, randomized trial in 83 RA patients with an inadequate response to methotrexate or a biologic DMARD.
“This is like the fourth Syk inhibitor that’s failed. Syk inhibition is not sick, Syk is dead,” Dr. Fleischmann declared.
Cadherin-11 is an inflammatory cytokine expressed on fibroblasts in RA joints. In a phase 2, double-blind, randomized trial in 109 patients with RA inadequately responsive to TNF inhibitors, RG6125, a humanized monoclonal antibody directed against cadherin-11, failed to outperform placebo.
“It should have worked. It didn’t. So the question is whether this pathway is not an appropriate pathway, or the molecule was not quite the right molecule. I have a feeling it was possibly not the right molecule and the pathway may be viable,” according to Dr. Fleischmann.
He reported receiving clinical trial research grants from and serving as a consultant to more than a dozen pharmaceutical companies. Dr. Genovese also reported financial relationships with more than a dozen pharmaceutical companies.
MAUI, HAWAII – Filgotinib, the oral Janus kinase (JAK) inhibitor now under Food and Drug Administration review for the treatment of RA, has a better safety profile than some of the approved oral JAK inhibitors, but that’s unlikely to save it from being saddled with a black-box safety warning label, experts agreed at the 2020 Rheumatology Winter Clinical Symposium.
“There’s probably a class label out there,” according to Mark C. Genovese, MD, professor of medicine and clinical chief of the division of immunology and rheumatology at Stanford (Calif.) University.
He cited the example of upadacitinib (Rinvoq), approved last year as the third oral JAK inhibitor for RA. Even though venous thromboembolic (VTE) events weren’t seen with any significantly increased frequency, compared with placebo, in the upadacitinib development program – unlike for the earlier-approved tofacitinib (Xeljanz) and baricitinib (Olumiant) –the FDA nevertheless required that upadacitinib’s product labeling include this black-box warning: “Thrombosis, including deep vein thrombosis, pulmonary embolism, and arterial thrombosis, have occurred in patients treated with Janus kinase inhibitors used to treat inflammatory conditions.”
“I would fully expect that there’ll be a similar label in the filgotinib package insert saying that VTEs have been seen in other members of the class,” he predicted.
His copanelist Roy Fleischmann, MD, noted that filgotinib displayed a clean long-term safety profile in a pooled analysis of the 24-week results in the 2,088 filgotinib-treated participants in all phase 3 clinical trials for RA. For example, the incidence of herpes zoster in that large treated population was a mere 0.1%.
“Herpes zoster is almost nonexistent across the program,” observed Dr. Fleischmann, a rheumatologist at the University of Texas and medical director of the Metroplex Clinical Research Center, both in Dallas.
That’s consistent with what he’s heard from Japanese investigators about their experience. They tell him that in their studies the incidence of herpes zoster with filgotinib is five times less than with other JAK inhibitors.
The long-term pooled phase 3 filgotinib safety data also show less than a 0.1% incidence of adjudicated VTE/pulmonary embolism through 24 weeks. That’s a substantially lower rate than with tofacitinib or baricitinib, he noted.
The two rheumatologists, long-time observers of the FDA regulatory scene, stressed that they have no inside information regarding what the agency will do about filgotinib. It seems beyond doubt that the JAK inhibitor will be approved. But an open question of practical importance to clinicians is whether the agency will approve only the 100-mg dose or the 200-mg dose as well. The panelists agreed that having access to both would be advantageous since the clinical trials data indicate the higher dose is more effective and this greater efficacy doesn’t come at a cost of additional safety issues.
“If the 100 mg is sufficient, that’s great, but the reality is if you want to push to low disease activity or remission, the 200 mg seems to work better, particularly in patients who’ve already failed TNF [tumor necrosis factor] inhibitors or other biologics,” Dr. Genovese said. “If you’re not having additional safety concerns and you can get additional efficacy, I love the idea of having flexibility.”
Dr. Fleischmann is skeptical that the regulators will see things that way.
“There is a real risk that the FDA will do what it’s done before and say: ‘Well, the 200 works and the 100 works, so we’re going to approve the lower dose.’ But there doesn’t appear to be a big safety difference between 100 and 200. So I can see why they would approve the two doses, but I think that’d be unusual,” according to the rheumatologist.
The RA pipeline
The two speakers also highlighted several agents with novel mechanisms of action moving through the RA developmental pipeline, including olokizumab, otilimab, fenebrutinib, and a promising oral selective interleukin-1 receptor–associated kinase 4 inhibitor (IRAK4).
Olokizumab: This humanized monoclonal antibody targets IL-6. It has a different mechanism of action than the two commercially available IL-6 inhibitors approved for RA, tocilizumab (Actemra) and sarilumab (Kevzara), in that olokizumab uniquely targets the IL-6 ligand.
At the 2019 annual meeting of the American College of Rheumatology, Dr. Genovese presented the positive findings of a double-blind, placebo-controlled, randomized, phase 3 clinical trial of olokizumab in 428 RA patients with an inadequate response to methotrexate. The primary outcome, an ACR 20 response at 12 weeks, occurred in 25.9% of patients on placebo, 63.6% with 64 mg of olokizumab given subcutaneously every 2 weeks, and 70.4% with 64 mg every 4 weeks, with all participants on background methotrexate. An ACR 50 response at week 24 occurred in 7.7%, 42.7%, and 48.6%, respectively, with an acceptable side effect profile.
This was the first phase 3 trial to be presented from a large, ongoing phase 3 olokizumab developmental program for a variety of diseases.
“The results certainly support the idea that a 4-week regimen would probably be quite useful with this medication, although we’ll have to see what happens with the remaining phase 3 trials,” Dr. Genovese said.
Dr. Fleischmann posed a question: Do we really need a third IL-6 inhibitor?
That would make for a crowded field, Dr. Genovese agreed, adding that grabbing a reasonable market share for olokizumab may come down to cost, formulary access, and the convenience factor of once-monthly dosing. Whether the biologic’s unique mechanism of action in blocking the IL-6 ligand makes any practical difference in outcomes is unknown.
IRAK4 inhibitor: PF-06650833 is an oral selective reversible inhibitor of IRAK4, a key signaling kinase for IL-1 and toll-like receptors.
“This should be a really good drug for IL-1-mediated diseases,” according to Dr. Fleischmann.
In a phase 2b, double-blind, randomized, placebo-controlled, 12-week study featuring tofacitinib at 5 mg twice daily as an active comparator, the IRAK4 inhibitor exhibited dose-dependent efficacy for the primary endpoint of improvement from baseline in Simple Disease Activity Index score, compared with placebo. The same was true for the secondary endpoint, change over time in 28-joint Disease Activity Score using C-reactive protein (DAS28-CRP). The trial results were also presented at the 2019 ACR annual meeting.
“This is a drug they should probably take forward and see how far it goes in RA,” he said.
Dr. Genovese concurred.
“We’re still trying to figure out how we can put together rational combinations in RA, and this might be something that could be considered as a combination play. In fact, Pfizer has already teed up a study looking at a JAK inhibitor/IRAK4 combination. The question will be whether this is a standalone or has an opportunity to be part of a combination approach,” the rheumatologist said.
Otilimab: This monoclonal antibody is a granulocyte-macrophage colony-stimulating factor inhibitor. In a secondary analysis of the BAROQUE trial, a phase 2b, 50-week study in RA inadequately responsive to methotrexate, otilimab demonstrated an impressive effect in terms of pain reduction. This new analysis, which was first presented at the 2019 ACR annual meeting, showed that, at week 12, a minimum clinically important difference in pain was achieved in 29% of placebo-treated controls, compared with 65%-75% of patients on low to higher doses of otilimab.
“The question is: Is this pain effect unique to this molecule, this pathway, or is it a simple reflection of the treated patient population?” Dr. Genovese commented. “It’s an interesting molecule. It’s being developed in RA, and it might have unique benefits on the pain side.”
A tale of two BTK inhibitors: Bruton tyrosine kinase (BTK) is an intracellular kinase viewed as a promising target in autoimmune disease. Fenebrutinib is an oral, noncovalent, reversible, and highly selective BTK inhibitor that performed well in a phase 2, randomized, double-blind, placebo-controlled clinical trial with adalimumab as an active comparator in 480 patients with an inadequate response to methotrexate in one branch, and in 98 patients with an inadequate response to TNF inhibitor therapy in the other. All subjects were on background methotrexate. (The study results were published April 9 in Arthritis & Rheumatology.)
In the group with a prior inadequate response to TNF inhibitors, the ACR 50 response rate at 12 weeks was 25% in the group on fenebrutinib at 200 mg twice daily, significantly better than the 12% rate in placebo. And there were favorable effects on biomarkers: The reduction in erythrocyte sedimentation rate from baseline was nearly twice as great with fenebrutinib, the drop in CRP was nearly three times greater than with placebo, and there was also a significantly greater decrease over time in DAS28-CRP.
In the methotrexate-inadequate responders, the ACR50 rates were 28% and 35% with the BTK inhibitor at 150 and 200 mg once daily, respectively, compared with 15% in controls.
The safety picture was encouraging, with similarly low adverse event rates across all treatment arms.
In contrast to the fenebrutinib experience, Dr. Genovese was lead investigator in a 250-patient, phase 2 study of another oral BTK inhibitor, poseltinib, which differs from fenebrutinib in that it is an irreversible covalent inhibitor. It was a failed study, with no significant difference between poseltinib and placebo in ACR 20 response at 12 weeks. It’s unclear whether the problem was insufficient dosing or that poseltinib is a failed molecule, perhaps because of its irreversible covalent binding to BTK, he said.
Other notable failures
The spleen tyrosine kinase (Syk) inhibitor known as GS-9876 showed no clinical efficacy in a phase 2, double-blind, randomized trial in 83 RA patients with an inadequate response to methotrexate or a biologic DMARD.
“This is like the fourth Syk inhibitor that’s failed. Syk inhibition is not sick, Syk is dead,” Dr. Fleischmann declared.
Cadherin-11 is an inflammatory cytokine expressed on fibroblasts in RA joints. In a phase 2, double-blind, randomized trial in 109 patients with RA inadequately responsive to TNF inhibitors, RG6125, a humanized monoclonal antibody directed against cadherin-11, failed to outperform placebo.
“It should have worked. It didn’t. So the question is whether this pathway is not an appropriate pathway, or the molecule was not quite the right molecule. I have a feeling it was possibly not the right molecule and the pathway may be viable,” according to Dr. Fleischmann.
He reported receiving clinical trial research grants from and serving as a consultant to more than a dozen pharmaceutical companies. Dr. Genovese also reported financial relationships with more than a dozen pharmaceutical companies.
MAUI, HAWAII – Filgotinib, the oral Janus kinase (JAK) inhibitor now under Food and Drug Administration review for the treatment of RA, has a better safety profile than some of the approved oral JAK inhibitors, but that’s unlikely to save it from being saddled with a black-box safety warning label, experts agreed at the 2020 Rheumatology Winter Clinical Symposium.
“There’s probably a class label out there,” according to Mark C. Genovese, MD, professor of medicine and clinical chief of the division of immunology and rheumatology at Stanford (Calif.) University.
He cited the example of upadacitinib (Rinvoq), approved last year as the third oral JAK inhibitor for RA. Even though venous thromboembolic (VTE) events weren’t seen with any significantly increased frequency, compared with placebo, in the upadacitinib development program – unlike for the earlier-approved tofacitinib (Xeljanz) and baricitinib (Olumiant) –the FDA nevertheless required that upadacitinib’s product labeling include this black-box warning: “Thrombosis, including deep vein thrombosis, pulmonary embolism, and arterial thrombosis, have occurred in patients treated with Janus kinase inhibitors used to treat inflammatory conditions.”
“I would fully expect that there’ll be a similar label in the filgotinib package insert saying that VTEs have been seen in other members of the class,” he predicted.
His copanelist Roy Fleischmann, MD, noted that filgotinib displayed a clean long-term safety profile in a pooled analysis of the 24-week results in the 2,088 filgotinib-treated participants in all phase 3 clinical trials for RA. For example, the incidence of herpes zoster in that large treated population was a mere 0.1%.
“Herpes zoster is almost nonexistent across the program,” observed Dr. Fleischmann, a rheumatologist at the University of Texas and medical director of the Metroplex Clinical Research Center, both in Dallas.
That’s consistent with what he’s heard from Japanese investigators about their experience. They tell him that in their studies the incidence of herpes zoster with filgotinib is five times less than with other JAK inhibitors.
The long-term pooled phase 3 filgotinib safety data also show less than a 0.1% incidence of adjudicated VTE/pulmonary embolism through 24 weeks. That’s a substantially lower rate than with tofacitinib or baricitinib, he noted.
The two rheumatologists, long-time observers of the FDA regulatory scene, stressed that they have no inside information regarding what the agency will do about filgotinib. It seems beyond doubt that the JAK inhibitor will be approved. But an open question of practical importance to clinicians is whether the agency will approve only the 100-mg dose or the 200-mg dose as well. The panelists agreed that having access to both would be advantageous since the clinical trials data indicate the higher dose is more effective and this greater efficacy doesn’t come at a cost of additional safety issues.
“If the 100 mg is sufficient, that’s great, but the reality is if you want to push to low disease activity or remission, the 200 mg seems to work better, particularly in patients who’ve already failed TNF [tumor necrosis factor] inhibitors or other biologics,” Dr. Genovese said. “If you’re not having additional safety concerns and you can get additional efficacy, I love the idea of having flexibility.”
Dr. Fleischmann is skeptical that the regulators will see things that way.
“There is a real risk that the FDA will do what it’s done before and say: ‘Well, the 200 works and the 100 works, so we’re going to approve the lower dose.’ But there doesn’t appear to be a big safety difference between 100 and 200. So I can see why they would approve the two doses, but I think that’d be unusual,” according to the rheumatologist.
The RA pipeline
The two speakers also highlighted several agents with novel mechanisms of action moving through the RA developmental pipeline, including olokizumab, otilimab, fenebrutinib, and a promising oral selective interleukin-1 receptor–associated kinase 4 inhibitor (IRAK4).
Olokizumab: This humanized monoclonal antibody targets IL-6. It has a different mechanism of action than the two commercially available IL-6 inhibitors approved for RA, tocilizumab (Actemra) and sarilumab (Kevzara), in that olokizumab uniquely targets the IL-6 ligand.
At the 2019 annual meeting of the American College of Rheumatology, Dr. Genovese presented the positive findings of a double-blind, placebo-controlled, randomized, phase 3 clinical trial of olokizumab in 428 RA patients with an inadequate response to methotrexate. The primary outcome, an ACR 20 response at 12 weeks, occurred in 25.9% of patients on placebo, 63.6% with 64 mg of olokizumab given subcutaneously every 2 weeks, and 70.4% with 64 mg every 4 weeks, with all participants on background methotrexate. An ACR 50 response at week 24 occurred in 7.7%, 42.7%, and 48.6%, respectively, with an acceptable side effect profile.
This was the first phase 3 trial to be presented from a large, ongoing phase 3 olokizumab developmental program for a variety of diseases.
“The results certainly support the idea that a 4-week regimen would probably be quite useful with this medication, although we’ll have to see what happens with the remaining phase 3 trials,” Dr. Genovese said.
Dr. Fleischmann posed a question: Do we really need a third IL-6 inhibitor?
That would make for a crowded field, Dr. Genovese agreed, adding that grabbing a reasonable market share for olokizumab may come down to cost, formulary access, and the convenience factor of once-monthly dosing. Whether the biologic’s unique mechanism of action in blocking the IL-6 ligand makes any practical difference in outcomes is unknown.
IRAK4 inhibitor: PF-06650833 is an oral selective reversible inhibitor of IRAK4, a key signaling kinase for IL-1 and toll-like receptors.
“This should be a really good drug for IL-1-mediated diseases,” according to Dr. Fleischmann.
In a phase 2b, double-blind, randomized, placebo-controlled, 12-week study featuring tofacitinib at 5 mg twice daily as an active comparator, the IRAK4 inhibitor exhibited dose-dependent efficacy for the primary endpoint of improvement from baseline in Simple Disease Activity Index score, compared with placebo. The same was true for the secondary endpoint, change over time in 28-joint Disease Activity Score using C-reactive protein (DAS28-CRP). The trial results were also presented at the 2019 ACR annual meeting.
“This is a drug they should probably take forward and see how far it goes in RA,” he said.
Dr. Genovese concurred.
“We’re still trying to figure out how we can put together rational combinations in RA, and this might be something that could be considered as a combination play. In fact, Pfizer has already teed up a study looking at a JAK inhibitor/IRAK4 combination. The question will be whether this is a standalone or has an opportunity to be part of a combination approach,” the rheumatologist said.
Otilimab: This monoclonal antibody is a granulocyte-macrophage colony-stimulating factor inhibitor. In a secondary analysis of the BAROQUE trial, a phase 2b, 50-week study in RA inadequately responsive to methotrexate, otilimab demonstrated an impressive effect in terms of pain reduction. This new analysis, which was first presented at the 2019 ACR annual meeting, showed that, at week 12, a minimum clinically important difference in pain was achieved in 29% of placebo-treated controls, compared with 65%-75% of patients on low to higher doses of otilimab.
“The question is: Is this pain effect unique to this molecule, this pathway, or is it a simple reflection of the treated patient population?” Dr. Genovese commented. “It’s an interesting molecule. It’s being developed in RA, and it might have unique benefits on the pain side.”
A tale of two BTK inhibitors: Bruton tyrosine kinase (BTK) is an intracellular kinase viewed as a promising target in autoimmune disease. Fenebrutinib is an oral, noncovalent, reversible, and highly selective BTK inhibitor that performed well in a phase 2, randomized, double-blind, placebo-controlled clinical trial with adalimumab as an active comparator in 480 patients with an inadequate response to methotrexate in one branch, and in 98 patients with an inadequate response to TNF inhibitor therapy in the other. All subjects were on background methotrexate. (The study results were published April 9 in Arthritis & Rheumatology.)
In the group with a prior inadequate response to TNF inhibitors, the ACR 50 response rate at 12 weeks was 25% in the group on fenebrutinib at 200 mg twice daily, significantly better than the 12% rate in placebo. And there were favorable effects on biomarkers: The reduction in erythrocyte sedimentation rate from baseline was nearly twice as great with fenebrutinib, the drop in CRP was nearly three times greater than with placebo, and there was also a significantly greater decrease over time in DAS28-CRP.
In the methotrexate-inadequate responders, the ACR50 rates were 28% and 35% with the BTK inhibitor at 150 and 200 mg once daily, respectively, compared with 15% in controls.
The safety picture was encouraging, with similarly low adverse event rates across all treatment arms.
In contrast to the fenebrutinib experience, Dr. Genovese was lead investigator in a 250-patient, phase 2 study of another oral BTK inhibitor, poseltinib, which differs from fenebrutinib in that it is an irreversible covalent inhibitor. It was a failed study, with no significant difference between poseltinib and placebo in ACR 20 response at 12 weeks. It’s unclear whether the problem was insufficient dosing or that poseltinib is a failed molecule, perhaps because of its irreversible covalent binding to BTK, he said.
Other notable failures
The spleen tyrosine kinase (Syk) inhibitor known as GS-9876 showed no clinical efficacy in a phase 2, double-blind, randomized trial in 83 RA patients with an inadequate response to methotrexate or a biologic DMARD.
“This is like the fourth Syk inhibitor that’s failed. Syk inhibition is not sick, Syk is dead,” Dr. Fleischmann declared.
Cadherin-11 is an inflammatory cytokine expressed on fibroblasts in RA joints. In a phase 2, double-blind, randomized trial in 109 patients with RA inadequately responsive to TNF inhibitors, RG6125, a humanized monoclonal antibody directed against cadherin-11, failed to outperform placebo.
“It should have worked. It didn’t. So the question is whether this pathway is not an appropriate pathway, or the molecule was not quite the right molecule. I have a feeling it was possibly not the right molecule and the pathway may be viable,” according to Dr. Fleischmann.
He reported receiving clinical trial research grants from and serving as a consultant to more than a dozen pharmaceutical companies. Dr. Genovese also reported financial relationships with more than a dozen pharmaceutical companies.
REPORTING FROM RWCS 2020
A case of neutrophilic eccrine hidradenitis attributed to HIV treatment
arising in an affected patient, Jessica Kalen, MD, advised during a virtual meeting held by the George Washington University department of dermatology.
The virtual meeting included presentations that had been slated for the annual meeting of the American Academy of Dermatology, which was canceled because of the COVID-19 pandemic.
In a presentation entitled, “When HAART [highly active antiretroviral therapy] Hurts,” Dr. Kalen, a dermatology resident at the university, presented a case report involving a 65-year-old man who presented with juicy red edematous papules and plaques on his scalp and ears. He was on the three-drug combination of rilpivirine (a non-nucleoside reverse transcriptase inhibitor), and the NRTIs tenofovir, and emtricitabine (Odefsey) for treatment of HIV infection, which was well controlled, with no detectable viral load.
The patient was also on insulin detemir for diabetes; pravastatin, amlodipine, and lisinopril for hypertension; and episodic acyclovir for recurrent herpes simplex outbreaks. However, none of those drugs has been associated with NEH. In contrast, Dr. Kalen found three published case reports describing a link between NRTIs and NEH.
Lesional biopsy of her patient showed the classic features of NEH: a dermal neutrophilic infiltrate surrounding the eccrine secretory coils and ducts, with vacuolar degeneration that spared the acrosyringium.
The most common causes of NEH, a rare dermatologic disorder first described in 1982, are hematologic malignancies and some of the chemotherapeutic agents used in treating them. Particularly prominent are acute myelogenous leukemia and cytarabine, which are often prescribed for that cancer. Carbamazepine, granulocyte-colony stimulating factor, and BRAF inhibitors have also been associated with NEH.
The pathogenesis of NEH is not fully worked out; however, NRTIs are secreted via eccrine structures, and that close contact could potentially promote an environment favoring inflammation and destruction of the eccrine coils. Also, NRTIs inhibit DNA polymerase, as does cytarabine, Dr. Kalen noted.
Her patient’s NEH was treated with triamcinolone. His skin condition resolved completely while he remained on NRTI therapy, with no relapses to date.
Dr. Kalen reported having no financial conflicts regarding her presentation.
arising in an affected patient, Jessica Kalen, MD, advised during a virtual meeting held by the George Washington University department of dermatology.
The virtual meeting included presentations that had been slated for the annual meeting of the American Academy of Dermatology, which was canceled because of the COVID-19 pandemic.
In a presentation entitled, “When HAART [highly active antiretroviral therapy] Hurts,” Dr. Kalen, a dermatology resident at the university, presented a case report involving a 65-year-old man who presented with juicy red edematous papules and plaques on his scalp and ears. He was on the three-drug combination of rilpivirine (a non-nucleoside reverse transcriptase inhibitor), and the NRTIs tenofovir, and emtricitabine (Odefsey) for treatment of HIV infection, which was well controlled, with no detectable viral load.
The patient was also on insulin detemir for diabetes; pravastatin, amlodipine, and lisinopril for hypertension; and episodic acyclovir for recurrent herpes simplex outbreaks. However, none of those drugs has been associated with NEH. In contrast, Dr. Kalen found three published case reports describing a link between NRTIs and NEH.
Lesional biopsy of her patient showed the classic features of NEH: a dermal neutrophilic infiltrate surrounding the eccrine secretory coils and ducts, with vacuolar degeneration that spared the acrosyringium.
The most common causes of NEH, a rare dermatologic disorder first described in 1982, are hematologic malignancies and some of the chemotherapeutic agents used in treating them. Particularly prominent are acute myelogenous leukemia and cytarabine, which are often prescribed for that cancer. Carbamazepine, granulocyte-colony stimulating factor, and BRAF inhibitors have also been associated with NEH.
The pathogenesis of NEH is not fully worked out; however, NRTIs are secreted via eccrine structures, and that close contact could potentially promote an environment favoring inflammation and destruction of the eccrine coils. Also, NRTIs inhibit DNA polymerase, as does cytarabine, Dr. Kalen noted.
Her patient’s NEH was treated with triamcinolone. His skin condition resolved completely while he remained on NRTI therapy, with no relapses to date.
Dr. Kalen reported having no financial conflicts regarding her presentation.
arising in an affected patient, Jessica Kalen, MD, advised during a virtual meeting held by the George Washington University department of dermatology.
The virtual meeting included presentations that had been slated for the annual meeting of the American Academy of Dermatology, which was canceled because of the COVID-19 pandemic.
In a presentation entitled, “When HAART [highly active antiretroviral therapy] Hurts,” Dr. Kalen, a dermatology resident at the university, presented a case report involving a 65-year-old man who presented with juicy red edematous papules and plaques on his scalp and ears. He was on the three-drug combination of rilpivirine (a non-nucleoside reverse transcriptase inhibitor), and the NRTIs tenofovir, and emtricitabine (Odefsey) for treatment of HIV infection, which was well controlled, with no detectable viral load.
The patient was also on insulin detemir for diabetes; pravastatin, amlodipine, and lisinopril for hypertension; and episodic acyclovir for recurrent herpes simplex outbreaks. However, none of those drugs has been associated with NEH. In contrast, Dr. Kalen found three published case reports describing a link between NRTIs and NEH.
Lesional biopsy of her patient showed the classic features of NEH: a dermal neutrophilic infiltrate surrounding the eccrine secretory coils and ducts, with vacuolar degeneration that spared the acrosyringium.
The most common causes of NEH, a rare dermatologic disorder first described in 1982, are hematologic malignancies and some of the chemotherapeutic agents used in treating them. Particularly prominent are acute myelogenous leukemia and cytarabine, which are often prescribed for that cancer. Carbamazepine, granulocyte-colony stimulating factor, and BRAF inhibitors have also been associated with NEH.
The pathogenesis of NEH is not fully worked out; however, NRTIs are secreted via eccrine structures, and that close contact could potentially promote an environment favoring inflammation and destruction of the eccrine coils. Also, NRTIs inhibit DNA polymerase, as does cytarabine, Dr. Kalen noted.
Her patient’s NEH was treated with triamcinolone. His skin condition resolved completely while he remained on NRTI therapy, with no relapses to date.
Dr. Kalen reported having no financial conflicts regarding her presentation.
TWILIGHT-COMPLEX: Tap ticagrelor monotherapy early after complex PCI
Patients who underwent complex PCI for acute coronary syndrome followed by 3 months of dual-antiplatelet therapy (DAPT) with ticagrelor plus aspirin fared significantly better by dropping aspirin at that point in favor of long-term ticagrelor monotherapy than with continued dual-antiplatelet therapy in the TWILIGHT-COMPLEX study.
The rate of clinically relevant bleeding was significantly lower at 12 months of follow-up in the ticagrelor monotherapy group than it was in patients randomized to continued DAPT. Moreover, this major benefit came at no cost in terms of ischemic events, which were actually numerically less frequent in the ticagrelor plus placebo group, George D. Dangas, MD, reported at the joint scientific sessions of the American College of Cardiology and the World Heart Federation. ACC organizers chose to present parts of the meeting virtually after COVID-19 concerns caused them to cancel the meeting.
“We found that the aspirin just doesn’t add that much, even in complex patients – just bleeding complications, for the most part,” explained Dr. Dangas, professor of medicine and of surgery at the Icahn School of Medicine at Mount Sinai, New York.
The TWILIGHT-COMPLEX study was a secondary post hoc analysis of outcomes in 2,342 participants in the previously reported larger parent TWILIGHT randomized trial who underwent complex PCI. The main TWILIGHT trial included 7,119 patients in 11 countries who underwent PCI for acute coronary syndrome, successfully completed 3 months of DAPT with ticagrelor plus aspirin without incident, and were then randomized double blind to 12 months of ticagrelor plus placebo or to another 12 months of ticagrelor and aspirin.
In the overall TWILIGHT trial, ticagrelor alone resulted in a significantly lower clinically relevant bleeding rate than did long-term ticagrelor plus aspirin, with no increase in the risk of death, MI, or stroke (N Engl J Med 2019; 381:2032-42). But the results left many interventional cardiologists wondering if a ticagrelor monotherapy strategy was really applicable to their more challenging patients undergoing complex PCI given that the risk of ischemic events is known to climb with PCI complexity. The TWILIGHT-COMPLEX study was specifically designed to address that concern.
To be eligible for TWILIGHT-COMPLEX, patients had to meet one or more prespecified angiographic or procedural criteria for complex PCI, such as a total stent length in excess of 60 mm, three or more treated lesions, use of an atherectomy device, or PCI of a left main lesion, a chronic total occlusion, or a bifurcation lesion with two stents. These complex PCI patients accounted for one-third of the total study population in TWILIGHT; 36% of them met more than one criteria for complex PCI.
TWILIGHT-COMPLEX findings
In the 12 months after randomization, patients who received ticagrelor plus placebo had a 4.2% incidence of clinically significant Bleeding Academic Research Consortium (BARC) type 2, 3, or 5 bleeding, which was significantly lower than the 7.7% rate in the group on long-term DAPT and represented a 46% relative risk reduction. Severe or fatal bleeding – that is, BARC type 3 or 5 – occurred in 1.1% of those on ticagrelor monotherapy and 2.6% of the DAPT group, for a significant 59% relative risk reduction.
The composite ischemic endpoint comprising cardiovascular death, MI, or ischemic stroke occurred in 3.6% of the ticagrelor monotherapy group and 4.8% of patients on long-term DAPT, a trend that didn’t achieve statistical significance. The all-cause mortality rate was 0.9% in the ticagrelor monotherapy group and 1.5% with extended DAPT, again a nonsignificant difference. Similarly, the rate of definite or probable stent thrombosis was numerically lower with ticagrelor monotherapy, by a margin of 0.4% versus 0.8%, a nonsignificant difference.
The results were consistent regardless of which specific criteria for complex PCI a patient had or how many of them.
Results are ‘reassuring’
At a press conference where Dr. Dangas presented the TWILIGHT-COMPLEX results, discussant Claire S. Duvernoy, MD, said she was “very impressed” with just how complex the PCIs were in the study participants.
“Really, these are the patients that in my own practice we’ve always been the most cautious about, the most worried about thrombotic risk, and the ones where we get down on our house staff when they drop an antiplatelet agent. So this study is very reassuring,” said Dr. Duvernoy, professor of medicine at the University of Michigan, Ann Arbor.
She identified two key differences between TWILIGHT-COMPLEX and earlier studies that showed a benefit for extended DAPT in higher-risk patients. In the earlier studies, it was the P2Y12 inhibitor that was dropped; TWILIGHT was the first major randomized trial to discontinue the aspirin instead. And patients in the TWILIGHT study received second-generation drug-eluting stents.
“That makes a huge difference,” Dr. Duvernoy said. “We have stents now that are much safer than the old ones were, and that’s what allows us to gain this incredible benefit of reduced bleeding.”
Dr. Dangas cautioned that since this was a secondary post hoc analysis, the TWILIGHT-COMPLEX study must be viewed as hypothesis-generating.
The TWILIGHT trial was funded by AstraZeneca. Dr. Dangas reported receiving institutional research grants from that company as well as Bayer and Daichi-Sankyo. He also served as a paid consultant to Abbott Vascular, Boston Scientific, and Biosensors.
Simultaneous with his presentation at ACC 2020, the TWILIGHT-COMPLEX results were published online (J Am Coll Cardiol. 2020 Mar 13. doi: 10.1016/j.jacc.2020.03.011).
SOURCE: Dangas GD. ACC 20, Abstract 410-09.
Patients who underwent complex PCI for acute coronary syndrome followed by 3 months of dual-antiplatelet therapy (DAPT) with ticagrelor plus aspirin fared significantly better by dropping aspirin at that point in favor of long-term ticagrelor monotherapy than with continued dual-antiplatelet therapy in the TWILIGHT-COMPLEX study.
The rate of clinically relevant bleeding was significantly lower at 12 months of follow-up in the ticagrelor monotherapy group than it was in patients randomized to continued DAPT. Moreover, this major benefit came at no cost in terms of ischemic events, which were actually numerically less frequent in the ticagrelor plus placebo group, George D. Dangas, MD, reported at the joint scientific sessions of the American College of Cardiology and the World Heart Federation. ACC organizers chose to present parts of the meeting virtually after COVID-19 concerns caused them to cancel the meeting.
“We found that the aspirin just doesn’t add that much, even in complex patients – just bleeding complications, for the most part,” explained Dr. Dangas, professor of medicine and of surgery at the Icahn School of Medicine at Mount Sinai, New York.
The TWILIGHT-COMPLEX study was a secondary post hoc analysis of outcomes in 2,342 participants in the previously reported larger parent TWILIGHT randomized trial who underwent complex PCI. The main TWILIGHT trial included 7,119 patients in 11 countries who underwent PCI for acute coronary syndrome, successfully completed 3 months of DAPT with ticagrelor plus aspirin without incident, and were then randomized double blind to 12 months of ticagrelor plus placebo or to another 12 months of ticagrelor and aspirin.
In the overall TWILIGHT trial, ticagrelor alone resulted in a significantly lower clinically relevant bleeding rate than did long-term ticagrelor plus aspirin, with no increase in the risk of death, MI, or stroke (N Engl J Med 2019; 381:2032-42). But the results left many interventional cardiologists wondering if a ticagrelor monotherapy strategy was really applicable to their more challenging patients undergoing complex PCI given that the risk of ischemic events is known to climb with PCI complexity. The TWILIGHT-COMPLEX study was specifically designed to address that concern.
To be eligible for TWILIGHT-COMPLEX, patients had to meet one or more prespecified angiographic or procedural criteria for complex PCI, such as a total stent length in excess of 60 mm, three or more treated lesions, use of an atherectomy device, or PCI of a left main lesion, a chronic total occlusion, or a bifurcation lesion with two stents. These complex PCI patients accounted for one-third of the total study population in TWILIGHT; 36% of them met more than one criteria for complex PCI.
TWILIGHT-COMPLEX findings
In the 12 months after randomization, patients who received ticagrelor plus placebo had a 4.2% incidence of clinically significant Bleeding Academic Research Consortium (BARC) type 2, 3, or 5 bleeding, which was significantly lower than the 7.7% rate in the group on long-term DAPT and represented a 46% relative risk reduction. Severe or fatal bleeding – that is, BARC type 3 or 5 – occurred in 1.1% of those on ticagrelor monotherapy and 2.6% of the DAPT group, for a significant 59% relative risk reduction.
The composite ischemic endpoint comprising cardiovascular death, MI, or ischemic stroke occurred in 3.6% of the ticagrelor monotherapy group and 4.8% of patients on long-term DAPT, a trend that didn’t achieve statistical significance. The all-cause mortality rate was 0.9% in the ticagrelor monotherapy group and 1.5% with extended DAPT, again a nonsignificant difference. Similarly, the rate of definite or probable stent thrombosis was numerically lower with ticagrelor monotherapy, by a margin of 0.4% versus 0.8%, a nonsignificant difference.
The results were consistent regardless of which specific criteria for complex PCI a patient had or how many of them.
Results are ‘reassuring’
At a press conference where Dr. Dangas presented the TWILIGHT-COMPLEX results, discussant Claire S. Duvernoy, MD, said she was “very impressed” with just how complex the PCIs were in the study participants.
“Really, these are the patients that in my own practice we’ve always been the most cautious about, the most worried about thrombotic risk, and the ones where we get down on our house staff when they drop an antiplatelet agent. So this study is very reassuring,” said Dr. Duvernoy, professor of medicine at the University of Michigan, Ann Arbor.
She identified two key differences between TWILIGHT-COMPLEX and earlier studies that showed a benefit for extended DAPT in higher-risk patients. In the earlier studies, it was the P2Y12 inhibitor that was dropped; TWILIGHT was the first major randomized trial to discontinue the aspirin instead. And patients in the TWILIGHT study received second-generation drug-eluting stents.
“That makes a huge difference,” Dr. Duvernoy said. “We have stents now that are much safer than the old ones were, and that’s what allows us to gain this incredible benefit of reduced bleeding.”
Dr. Dangas cautioned that since this was a secondary post hoc analysis, the TWILIGHT-COMPLEX study must be viewed as hypothesis-generating.
The TWILIGHT trial was funded by AstraZeneca. Dr. Dangas reported receiving institutional research grants from that company as well as Bayer and Daichi-Sankyo. He also served as a paid consultant to Abbott Vascular, Boston Scientific, and Biosensors.
Simultaneous with his presentation at ACC 2020, the TWILIGHT-COMPLEX results were published online (J Am Coll Cardiol. 2020 Mar 13. doi: 10.1016/j.jacc.2020.03.011).
SOURCE: Dangas GD. ACC 20, Abstract 410-09.
Patients who underwent complex PCI for acute coronary syndrome followed by 3 months of dual-antiplatelet therapy (DAPT) with ticagrelor plus aspirin fared significantly better by dropping aspirin at that point in favor of long-term ticagrelor monotherapy than with continued dual-antiplatelet therapy in the TWILIGHT-COMPLEX study.
The rate of clinically relevant bleeding was significantly lower at 12 months of follow-up in the ticagrelor monotherapy group than it was in patients randomized to continued DAPT. Moreover, this major benefit came at no cost in terms of ischemic events, which were actually numerically less frequent in the ticagrelor plus placebo group, George D. Dangas, MD, reported at the joint scientific sessions of the American College of Cardiology and the World Heart Federation. ACC organizers chose to present parts of the meeting virtually after COVID-19 concerns caused them to cancel the meeting.
“We found that the aspirin just doesn’t add that much, even in complex patients – just bleeding complications, for the most part,” explained Dr. Dangas, professor of medicine and of surgery at the Icahn School of Medicine at Mount Sinai, New York.
The TWILIGHT-COMPLEX study was a secondary post hoc analysis of outcomes in 2,342 participants in the previously reported larger parent TWILIGHT randomized trial who underwent complex PCI. The main TWILIGHT trial included 7,119 patients in 11 countries who underwent PCI for acute coronary syndrome, successfully completed 3 months of DAPT with ticagrelor plus aspirin without incident, and were then randomized double blind to 12 months of ticagrelor plus placebo or to another 12 months of ticagrelor and aspirin.
In the overall TWILIGHT trial, ticagrelor alone resulted in a significantly lower clinically relevant bleeding rate than did long-term ticagrelor plus aspirin, with no increase in the risk of death, MI, or stroke (N Engl J Med 2019; 381:2032-42). But the results left many interventional cardiologists wondering if a ticagrelor monotherapy strategy was really applicable to their more challenging patients undergoing complex PCI given that the risk of ischemic events is known to climb with PCI complexity. The TWILIGHT-COMPLEX study was specifically designed to address that concern.
To be eligible for TWILIGHT-COMPLEX, patients had to meet one or more prespecified angiographic or procedural criteria for complex PCI, such as a total stent length in excess of 60 mm, three or more treated lesions, use of an atherectomy device, or PCI of a left main lesion, a chronic total occlusion, or a bifurcation lesion with two stents. These complex PCI patients accounted for one-third of the total study population in TWILIGHT; 36% of them met more than one criteria for complex PCI.
TWILIGHT-COMPLEX findings
In the 12 months after randomization, patients who received ticagrelor plus placebo had a 4.2% incidence of clinically significant Bleeding Academic Research Consortium (BARC) type 2, 3, or 5 bleeding, which was significantly lower than the 7.7% rate in the group on long-term DAPT and represented a 46% relative risk reduction. Severe or fatal bleeding – that is, BARC type 3 or 5 – occurred in 1.1% of those on ticagrelor monotherapy and 2.6% of the DAPT group, for a significant 59% relative risk reduction.
The composite ischemic endpoint comprising cardiovascular death, MI, or ischemic stroke occurred in 3.6% of the ticagrelor monotherapy group and 4.8% of patients on long-term DAPT, a trend that didn’t achieve statistical significance. The all-cause mortality rate was 0.9% in the ticagrelor monotherapy group and 1.5% with extended DAPT, again a nonsignificant difference. Similarly, the rate of definite or probable stent thrombosis was numerically lower with ticagrelor monotherapy, by a margin of 0.4% versus 0.8%, a nonsignificant difference.
The results were consistent regardless of which specific criteria for complex PCI a patient had or how many of them.
Results are ‘reassuring’
At a press conference where Dr. Dangas presented the TWILIGHT-COMPLEX results, discussant Claire S. Duvernoy, MD, said she was “very impressed” with just how complex the PCIs were in the study participants.
“Really, these are the patients that in my own practice we’ve always been the most cautious about, the most worried about thrombotic risk, and the ones where we get down on our house staff when they drop an antiplatelet agent. So this study is very reassuring,” said Dr. Duvernoy, professor of medicine at the University of Michigan, Ann Arbor.
She identified two key differences between TWILIGHT-COMPLEX and earlier studies that showed a benefit for extended DAPT in higher-risk patients. In the earlier studies, it was the P2Y12 inhibitor that was dropped; TWILIGHT was the first major randomized trial to discontinue the aspirin instead. And patients in the TWILIGHT study received second-generation drug-eluting stents.
“That makes a huge difference,” Dr. Duvernoy said. “We have stents now that are much safer than the old ones were, and that’s what allows us to gain this incredible benefit of reduced bleeding.”
Dr. Dangas cautioned that since this was a secondary post hoc analysis, the TWILIGHT-COMPLEX study must be viewed as hypothesis-generating.
The TWILIGHT trial was funded by AstraZeneca. Dr. Dangas reported receiving institutional research grants from that company as well as Bayer and Daichi-Sankyo. He also served as a paid consultant to Abbott Vascular, Boston Scientific, and Biosensors.
Simultaneous with his presentation at ACC 2020, the TWILIGHT-COMPLEX results were published online (J Am Coll Cardiol. 2020 Mar 13. doi: 10.1016/j.jacc.2020.03.011).
SOURCE: Dangas GD. ACC 20, Abstract 410-09.
FROM ACC 2020