User login
FDA evaluating the use of oral fluconazole in pregnancy
The Food and Drug Administration is reviewing the results of a Danish study that concludes there is a possible increased risk of miscarriage with the use of oral fluconazole (Diflucan) in pregnancy, according to a safety alert issued April 26.
The current drug label for oral fluconazole states that data from studies in women does not suggest an increased risk of problems during pregnancy or abnormalities in developing babies when women used a single 150-mg dose to treat vaginal yeast infections. However, reports of abnormalities at birth have resulted from high doses (400-800 mg/day) taken during pregnancy for much longer than a single dose. The Danish study had most pregnant women use one or two doses of 150 mg.
Oral fluconazole is used to treat yeast infections of the vaginal area, mouth, and esophagus. It can also be used to treat a fungal infection of the brain and spinal cord.
The FDA is also evaluating additional data and will make recommendations when the review is complete.
“Until FDA’s review is complete and more is understood about this study and other available data, FDA advises cautious prescribing of oral fluconazole in pregnancy,” the safety alert states.
The FDA also noted that the Centers for Disease Control and Prevention recommends using topical antifungal products only when treating pregnant women with vulvovaginal yeast infections.
Read more about the investigation on the FDA website.
The Food and Drug Administration is reviewing the results of a Danish study that concludes there is a possible increased risk of miscarriage with the use of oral fluconazole (Diflucan) in pregnancy, according to a safety alert issued April 26.
The current drug label for oral fluconazole states that data from studies in women does not suggest an increased risk of problems during pregnancy or abnormalities in developing babies when women used a single 150-mg dose to treat vaginal yeast infections. However, reports of abnormalities at birth have resulted from high doses (400-800 mg/day) taken during pregnancy for much longer than a single dose. The Danish study had most pregnant women use one or two doses of 150 mg.
Oral fluconazole is used to treat yeast infections of the vaginal area, mouth, and esophagus. It can also be used to treat a fungal infection of the brain and spinal cord.
The FDA is also evaluating additional data and will make recommendations when the review is complete.
“Until FDA’s review is complete and more is understood about this study and other available data, FDA advises cautious prescribing of oral fluconazole in pregnancy,” the safety alert states.
The FDA also noted that the Centers for Disease Control and Prevention recommends using topical antifungal products only when treating pregnant women with vulvovaginal yeast infections.
Read more about the investigation on the FDA website.
The Food and Drug Administration is reviewing the results of a Danish study that concludes there is a possible increased risk of miscarriage with the use of oral fluconazole (Diflucan) in pregnancy, according to a safety alert issued April 26.
The current drug label for oral fluconazole states that data from studies in women does not suggest an increased risk of problems during pregnancy or abnormalities in developing babies when women used a single 150-mg dose to treat vaginal yeast infections. However, reports of abnormalities at birth have resulted from high doses (400-800 mg/day) taken during pregnancy for much longer than a single dose. The Danish study had most pregnant women use one or two doses of 150 mg.
Oral fluconazole is used to treat yeast infections of the vaginal area, mouth, and esophagus. It can also be used to treat a fungal infection of the brain and spinal cord.
The FDA is also evaluating additional data and will make recommendations when the review is complete.
“Until FDA’s review is complete and more is understood about this study and other available data, FDA advises cautious prescribing of oral fluconazole in pregnancy,” the safety alert states.
The FDA also noted that the Centers for Disease Control and Prevention recommends using topical antifungal products only when treating pregnant women with vulvovaginal yeast infections.
Read more about the investigation on the FDA website.
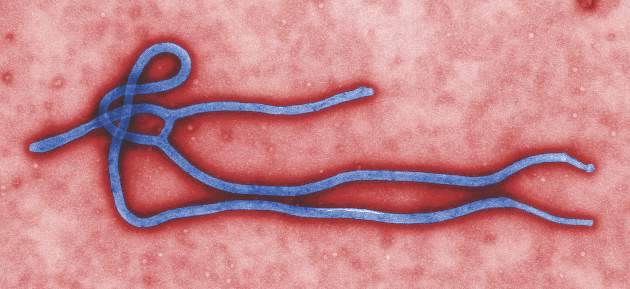
Rapid diagnostic tests used to detect Ebola
A new rapid diagnostic test for Ebola (RDT-Ebola) has been used to diagnose patients in Forécariah, Guinea. The National Ebola Coordination Cell implemented the test to enhance efforts to detect new Ebola cases and to ensure that such cases are not clinically misdiagnosed as malaria.
Jennifer Y. Huang and her associates found that among 13 sentinel sites during Oct. 1–Nov. 23, 2015, 1,544 (73%) of 2,115 consultations were for evaluation of febrile illness. Of those 1,544 consultations, 1,553 RDT-Malaria tests were reported to have been conducted and 1,000 RDT-Ebola tests were conducted. A total of 1,112 patients tested positive for malaria by RDT (the range of percentage of positive malaria tests among 13 sentinel sites was 52.3%-85.7%); none tested positive for Ebola by RDT-Ebola.
The ratio of RDT-Ebola to RDT-Malaria tests used was 0.64 overall and ranged from 0.27 to 1.00, according to the researchers.
Reported barriers to RDT-Ebola use – inadequate stock of RDT-Ebola kits, lack of understanding of the Centers for Disease Control and Prevention RDT-Ebola testing protocol, and patient refusal of RDT-Ebola testing – may have contributed to the differences in the numbers of malaria and Ebola tests conducted, the researchers wrote.
“Ongoing data collection from the sentinel sites can help to monitor the success of RDT-Ebola implementation, inform supply chain management, and identify and address barriers to RDT-Ebola use. RDT-Ebola implementation at the sentinel sites can also aid in screening for undetected Ebola cases to prevent establishment of new transmission chains,” the researchers concluded.
Find the study in Morbidity and Mortality Weekly Report (doi: 10.15585/mmwr.mm6512a4).
A new rapid diagnostic test for Ebola (RDT-Ebola) has been used to diagnose patients in Forécariah, Guinea. The National Ebola Coordination Cell implemented the test to enhance efforts to detect new Ebola cases and to ensure that such cases are not clinically misdiagnosed as malaria.
Jennifer Y. Huang and her associates found that among 13 sentinel sites during Oct. 1–Nov. 23, 2015, 1,544 (73%) of 2,115 consultations were for evaluation of febrile illness. Of those 1,544 consultations, 1,553 RDT-Malaria tests were reported to have been conducted and 1,000 RDT-Ebola tests were conducted. A total of 1,112 patients tested positive for malaria by RDT (the range of percentage of positive malaria tests among 13 sentinel sites was 52.3%-85.7%); none tested positive for Ebola by RDT-Ebola.
The ratio of RDT-Ebola to RDT-Malaria tests used was 0.64 overall and ranged from 0.27 to 1.00, according to the researchers.
Reported barriers to RDT-Ebola use – inadequate stock of RDT-Ebola kits, lack of understanding of the Centers for Disease Control and Prevention RDT-Ebola testing protocol, and patient refusal of RDT-Ebola testing – may have contributed to the differences in the numbers of malaria and Ebola tests conducted, the researchers wrote.
“Ongoing data collection from the sentinel sites can help to monitor the success of RDT-Ebola implementation, inform supply chain management, and identify and address barriers to RDT-Ebola use. RDT-Ebola implementation at the sentinel sites can also aid in screening for undetected Ebola cases to prevent establishment of new transmission chains,” the researchers concluded.
Find the study in Morbidity and Mortality Weekly Report (doi: 10.15585/mmwr.mm6512a4).
A new rapid diagnostic test for Ebola (RDT-Ebola) has been used to diagnose patients in Forécariah, Guinea. The National Ebola Coordination Cell implemented the test to enhance efforts to detect new Ebola cases and to ensure that such cases are not clinically misdiagnosed as malaria.
Jennifer Y. Huang and her associates found that among 13 sentinel sites during Oct. 1–Nov. 23, 2015, 1,544 (73%) of 2,115 consultations were for evaluation of febrile illness. Of those 1,544 consultations, 1,553 RDT-Malaria tests were reported to have been conducted and 1,000 RDT-Ebola tests were conducted. A total of 1,112 patients tested positive for malaria by RDT (the range of percentage of positive malaria tests among 13 sentinel sites was 52.3%-85.7%); none tested positive for Ebola by RDT-Ebola.
The ratio of RDT-Ebola to RDT-Malaria tests used was 0.64 overall and ranged from 0.27 to 1.00, according to the researchers.
Reported barriers to RDT-Ebola use – inadequate stock of RDT-Ebola kits, lack of understanding of the Centers for Disease Control and Prevention RDT-Ebola testing protocol, and patient refusal of RDT-Ebola testing – may have contributed to the differences in the numbers of malaria and Ebola tests conducted, the researchers wrote.
“Ongoing data collection from the sentinel sites can help to monitor the success of RDT-Ebola implementation, inform supply chain management, and identify and address barriers to RDT-Ebola use. RDT-Ebola implementation at the sentinel sites can also aid in screening for undetected Ebola cases to prevent establishment of new transmission chains,” the researchers concluded.
Find the study in Morbidity and Mortality Weekly Report (doi: 10.15585/mmwr.mm6512a4).
FROM MMWR
Severe sepsis and septic shock syndrome linked to chikungunya
Severe sepsis and septic shock syndrome may be rare complications of chikungunya virus infection, according to a recent study in Guadeloupe.
Dr. Bruno Hoen, of the department of infectious diseases, dermatology, and internal medicine at the University Medical Center of Guadeloupe, and his associates studied 110 nonpregnant adults hospitalized at the University Hospital of Pointe-à-Pitre, Guadeloupe, with chikungunya (CHIKV) after a November 2013 outbreak in Guadeloupe. Of all patients who had a positive CHIKV reverse transcription–polymerase chain reaction (RT-PCR) test result, 34 had a common form, 34 had an atypical form, and 42 had a severe form. Among the 42 patients with severe forms, 25 patients had illness consistent with the case definition for severe sepsis and had no other identified cause for this syndrome, and 12 died.
The 25 patients identified as having severe sepsis had significantly higher occurrences of cardiac, respiratory, and renal manifestations upon admission to hospital. They also had significantly higher leukocyte counts and levels of serum lactate dehydrogenase, aspartate aminotransferase, and creatinine – all clinical and laboratory indicators of sepsis – than patients without severe sepsis or septic shock. In addition, the mortality rate for the patients with severe sepsis was significantly higher than that in patients without severe sepsis or septic shock (48% vs. 3%; P less than .001).
As none of the 25 patients with severe sepsis or septic shock in the early stages of CHIKV had another organism that could be identified as a potential cause of sepsis, the researchers concluded that this finding strongly suggests that CHIKV can, in rare cases, cause severe sepsis and septic shock syndromes, an observation that had not been reported until very recently.
Dr. Hoen and his colleagues said additional studies are needed to identify any background characteristics that might be associated with the onset of severe sepsis or septic shock. The authors reported no conflicts of interest.
Read the full study in Emerging Infectious Diseases (2016 May. doi: 10.3201/eid2205.151449).
Severe sepsis and septic shock syndrome may be rare complications of chikungunya virus infection, according to a recent study in Guadeloupe.
Dr. Bruno Hoen, of the department of infectious diseases, dermatology, and internal medicine at the University Medical Center of Guadeloupe, and his associates studied 110 nonpregnant adults hospitalized at the University Hospital of Pointe-à-Pitre, Guadeloupe, with chikungunya (CHIKV) after a November 2013 outbreak in Guadeloupe. Of all patients who had a positive CHIKV reverse transcription–polymerase chain reaction (RT-PCR) test result, 34 had a common form, 34 had an atypical form, and 42 had a severe form. Among the 42 patients with severe forms, 25 patients had illness consistent with the case definition for severe sepsis and had no other identified cause for this syndrome, and 12 died.
The 25 patients identified as having severe sepsis had significantly higher occurrences of cardiac, respiratory, and renal manifestations upon admission to hospital. They also had significantly higher leukocyte counts and levels of serum lactate dehydrogenase, aspartate aminotransferase, and creatinine – all clinical and laboratory indicators of sepsis – than patients without severe sepsis or septic shock. In addition, the mortality rate for the patients with severe sepsis was significantly higher than that in patients without severe sepsis or septic shock (48% vs. 3%; P less than .001).
As none of the 25 patients with severe sepsis or septic shock in the early stages of CHIKV had another organism that could be identified as a potential cause of sepsis, the researchers concluded that this finding strongly suggests that CHIKV can, in rare cases, cause severe sepsis and septic shock syndromes, an observation that had not been reported until very recently.
Dr. Hoen and his colleagues said additional studies are needed to identify any background characteristics that might be associated with the onset of severe sepsis or septic shock. The authors reported no conflicts of interest.
Read the full study in Emerging Infectious Diseases (2016 May. doi: 10.3201/eid2205.151449).
Severe sepsis and septic shock syndrome may be rare complications of chikungunya virus infection, according to a recent study in Guadeloupe.
Dr. Bruno Hoen, of the department of infectious diseases, dermatology, and internal medicine at the University Medical Center of Guadeloupe, and his associates studied 110 nonpregnant adults hospitalized at the University Hospital of Pointe-à-Pitre, Guadeloupe, with chikungunya (CHIKV) after a November 2013 outbreak in Guadeloupe. Of all patients who had a positive CHIKV reverse transcription–polymerase chain reaction (RT-PCR) test result, 34 had a common form, 34 had an atypical form, and 42 had a severe form. Among the 42 patients with severe forms, 25 patients had illness consistent with the case definition for severe sepsis and had no other identified cause for this syndrome, and 12 died.
The 25 patients identified as having severe sepsis had significantly higher occurrences of cardiac, respiratory, and renal manifestations upon admission to hospital. They also had significantly higher leukocyte counts and levels of serum lactate dehydrogenase, aspartate aminotransferase, and creatinine – all clinical and laboratory indicators of sepsis – than patients without severe sepsis or septic shock. In addition, the mortality rate for the patients with severe sepsis was significantly higher than that in patients without severe sepsis or septic shock (48% vs. 3%; P less than .001).
As none of the 25 patients with severe sepsis or septic shock in the early stages of CHIKV had another organism that could be identified as a potential cause of sepsis, the researchers concluded that this finding strongly suggests that CHIKV can, in rare cases, cause severe sepsis and septic shock syndromes, an observation that had not been reported until very recently.
Dr. Hoen and his colleagues said additional studies are needed to identify any background characteristics that might be associated with the onset of severe sepsis or septic shock. The authors reported no conflicts of interest.
Read the full study in Emerging Infectious Diseases (2016 May. doi: 10.3201/eid2205.151449).
FROM EMERGING INFECTIOUS DISEASES
Postvaccination anaphylaxis still possible with certain vaccines
New findings confirm that although it is rare, postvaccination anaphylaxis can still occur with certain vaccines.
Dr. Michael M. McNeil of the Centers for Disease Control and Prevention, Atlanta, and his associates identified 17,606,500 vaccination visits from Jan. 1, 2009, through Dec. 31, 2011, at which 25,173,965 vaccine doses were administered. The researchers identified 76 cases of chart-confirmed anaphylaxis; 33 anaphylaxis cases were associated with vaccination, and 43 were attributed to other causes.
Inactivated trivalent influenza vaccine (TIV) was the major contributor to vaccine-triggered anaphylaxis cases in the population, although the rate (1.35 cases per 1 million vaccine doses of TIV given alone) was similar to the rate for all vaccines. The postvaccination anaphylaxis case rate not involving TIV was 1.32 per million vaccine doses.
The study factored in race, age, gender, symptoms, and history of the patients. There were no deaths, and only 1 patient (3%) was hospitalized. A total of 28 of the 33 vaccine-triggered anaphylaxis cases involved patients with a history of atopy.
“Although anaphylaxis after immunization is rare, its immediate onset (usually within minutes) and life-threatening nature require that all personnel and facilities providing vaccinations have procedures in place for anaphylaxis management,” the investigators noted. “Additional provider education concerning current recommendations for treatment and follow-up appears to be warranted.”
Find the full story in the Journal of Allergy and Clinical Immunology (2016 Mar;137[3]:868-78).
New findings confirm that although it is rare, postvaccination anaphylaxis can still occur with certain vaccines.
Dr. Michael M. McNeil of the Centers for Disease Control and Prevention, Atlanta, and his associates identified 17,606,500 vaccination visits from Jan. 1, 2009, through Dec. 31, 2011, at which 25,173,965 vaccine doses were administered. The researchers identified 76 cases of chart-confirmed anaphylaxis; 33 anaphylaxis cases were associated with vaccination, and 43 were attributed to other causes.
Inactivated trivalent influenza vaccine (TIV) was the major contributor to vaccine-triggered anaphylaxis cases in the population, although the rate (1.35 cases per 1 million vaccine doses of TIV given alone) was similar to the rate for all vaccines. The postvaccination anaphylaxis case rate not involving TIV was 1.32 per million vaccine doses.
The study factored in race, age, gender, symptoms, and history of the patients. There were no deaths, and only 1 patient (3%) was hospitalized. A total of 28 of the 33 vaccine-triggered anaphylaxis cases involved patients with a history of atopy.
“Although anaphylaxis after immunization is rare, its immediate onset (usually within minutes) and life-threatening nature require that all personnel and facilities providing vaccinations have procedures in place for anaphylaxis management,” the investigators noted. “Additional provider education concerning current recommendations for treatment and follow-up appears to be warranted.”
Find the full story in the Journal of Allergy and Clinical Immunology (2016 Mar;137[3]:868-78).
New findings confirm that although it is rare, postvaccination anaphylaxis can still occur with certain vaccines.
Dr. Michael M. McNeil of the Centers for Disease Control and Prevention, Atlanta, and his associates identified 17,606,500 vaccination visits from Jan. 1, 2009, through Dec. 31, 2011, at which 25,173,965 vaccine doses were administered. The researchers identified 76 cases of chart-confirmed anaphylaxis; 33 anaphylaxis cases were associated with vaccination, and 43 were attributed to other causes.
Inactivated trivalent influenza vaccine (TIV) was the major contributor to vaccine-triggered anaphylaxis cases in the population, although the rate (1.35 cases per 1 million vaccine doses of TIV given alone) was similar to the rate for all vaccines. The postvaccination anaphylaxis case rate not involving TIV was 1.32 per million vaccine doses.
The study factored in race, age, gender, symptoms, and history of the patients. There were no deaths, and only 1 patient (3%) was hospitalized. A total of 28 of the 33 vaccine-triggered anaphylaxis cases involved patients with a history of atopy.
“Although anaphylaxis after immunization is rare, its immediate onset (usually within minutes) and life-threatening nature require that all personnel and facilities providing vaccinations have procedures in place for anaphylaxis management,” the investigators noted. “Additional provider education concerning current recommendations for treatment and follow-up appears to be warranted.”
Find the full story in the Journal of Allergy and Clinical Immunology (2016 Mar;137[3]:868-78).
FROM THE JOURNAL OF ALLERGY AND CLINICAL IMMUNOLOGY
Risk factors identified for thrombosis in pediatric SLE
Pediatric patients with systemic lupus erythematosus may have greater odds for developing thrombosis if they have a history of vasculitis, antiphospholipid antibody positivity (aPL), and/or avascular necrosis (AVN), according to Dr. Kyla Driest and her associates.
Among 974 pediatric systemic lupus erythematosus (pSLE) patients in the CARRA (Childhood Arthritis & Rheumatology Research Alliance) registry cohort who had available data on thrombosis history, 24 (2.5%) had a history of arterial thrombosis and 35 (3.6%) had a history of venous thrombosis. The researchers conducted a multivariable analysis that found statistically higher odds of thrombosis (P less than .10) among patients with histories of AVN (odds ratio, 4.24; 95% confidence interval, 1.53-11.74), aPL (OR, 2.95; 95% CI, 1.38-6.28), and vasculitis (OR, 2.19; 95% CI, 1.03-4.77), whereas significantly lower odds occurred in patients with a history of renal disease (OR, 0.47; 95% CI, 0.24-0.92). Gender and body-mass index were not statistically significant.
“This study adds to our understanding of which pSLE patients are at the most risk for thrombosis,” the researchers concluded. “These results may prompt discussion concerning potential measures to prevent thrombosis in high-risk patients.”
Find the full study in Lupus (doi: 10.1177/0961203316638164).
Pediatric patients with systemic lupus erythematosus may have greater odds for developing thrombosis if they have a history of vasculitis, antiphospholipid antibody positivity (aPL), and/or avascular necrosis (AVN), according to Dr. Kyla Driest and her associates.
Among 974 pediatric systemic lupus erythematosus (pSLE) patients in the CARRA (Childhood Arthritis & Rheumatology Research Alliance) registry cohort who had available data on thrombosis history, 24 (2.5%) had a history of arterial thrombosis and 35 (3.6%) had a history of venous thrombosis. The researchers conducted a multivariable analysis that found statistically higher odds of thrombosis (P less than .10) among patients with histories of AVN (odds ratio, 4.24; 95% confidence interval, 1.53-11.74), aPL (OR, 2.95; 95% CI, 1.38-6.28), and vasculitis (OR, 2.19; 95% CI, 1.03-4.77), whereas significantly lower odds occurred in patients with a history of renal disease (OR, 0.47; 95% CI, 0.24-0.92). Gender and body-mass index were not statistically significant.
“This study adds to our understanding of which pSLE patients are at the most risk for thrombosis,” the researchers concluded. “These results may prompt discussion concerning potential measures to prevent thrombosis in high-risk patients.”
Find the full study in Lupus (doi: 10.1177/0961203316638164).
Pediatric patients with systemic lupus erythematosus may have greater odds for developing thrombosis if they have a history of vasculitis, antiphospholipid antibody positivity (aPL), and/or avascular necrosis (AVN), according to Dr. Kyla Driest and her associates.
Among 974 pediatric systemic lupus erythematosus (pSLE) patients in the CARRA (Childhood Arthritis & Rheumatology Research Alliance) registry cohort who had available data on thrombosis history, 24 (2.5%) had a history of arterial thrombosis and 35 (3.6%) had a history of venous thrombosis. The researchers conducted a multivariable analysis that found statistically higher odds of thrombosis (P less than .10) among patients with histories of AVN (odds ratio, 4.24; 95% confidence interval, 1.53-11.74), aPL (OR, 2.95; 95% CI, 1.38-6.28), and vasculitis (OR, 2.19; 95% CI, 1.03-4.77), whereas significantly lower odds occurred in patients with a history of renal disease (OR, 0.47; 95% CI, 0.24-0.92). Gender and body-mass index were not statistically significant.
“This study adds to our understanding of which pSLE patients are at the most risk for thrombosis,” the researchers concluded. “These results may prompt discussion concerning potential measures to prevent thrombosis in high-risk patients.”
Find the full study in Lupus (doi: 10.1177/0961203316638164).
FROM LUPUS
No Evidence Supports Hydrolyzed Formula Over Cows’ Milk for Allergy Prevention
Findings on the use of hydrolyzed formula in place of standard cows’ milk formula to prevent allergy in high-risk infants do not support current guidelines, according to Dr. Robert J Boyle of Imperial College London and his associates.
A review and meta-analysis were performed on 28 randomized control trials, 6 quasirandomized trials, and 3 controlled clinical trials describing allergic or autoimmune outcomes, with more than 19,000 participants. Among 13 studies reporting on the risk of food allergy, no significant difference was found in the risk of any food allergy with partially hydrolyzed formula (risk ratio, 1.73; 95% confidence interval, 0.79-3.80) and extensively hydrolyzed formula (RR, 0.86; CI, 0.26-2.82), compared with standard formula at age 0-4 years, and for extensively hydrolyzed formula at age 5-14 years.
The review also examined and found no significant evidence favoring the use of hydrolyzed formula in place of standard cows’ milk formula to avert the risk of eczema, wheeze, allergic rhinitis, or type 1 diabetes mellitus.
The researchers suggest that guidelines be updated and revised to reflect these new findings.
“We found no consistent evidence to support the current recommendations and found evidence of publication bias, methodological biases, and conflict of interest in those studies reporting allergic outcomes,” Dr. Boyle and his associates concluded. “We suggest that any future trials on hydrolyzed formula should be prospectively registered, independently funded, and include adequate oversight to ensure that they do not negatively impact on breastfeeding in study participants”.
Read the full study at the British Medical Journal (doi: 10.1136/bmj.i974)
Findings on the use of hydrolyzed formula in place of standard cows’ milk formula to prevent allergy in high-risk infants do not support current guidelines, according to Dr. Robert J Boyle of Imperial College London and his associates.
A review and meta-analysis were performed on 28 randomized control trials, 6 quasirandomized trials, and 3 controlled clinical trials describing allergic or autoimmune outcomes, with more than 19,000 participants. Among 13 studies reporting on the risk of food allergy, no significant difference was found in the risk of any food allergy with partially hydrolyzed formula (risk ratio, 1.73; 95% confidence interval, 0.79-3.80) and extensively hydrolyzed formula (RR, 0.86; CI, 0.26-2.82), compared with standard formula at age 0-4 years, and for extensively hydrolyzed formula at age 5-14 years.
The review also examined and found no significant evidence favoring the use of hydrolyzed formula in place of standard cows’ milk formula to avert the risk of eczema, wheeze, allergic rhinitis, or type 1 diabetes mellitus.
The researchers suggest that guidelines be updated and revised to reflect these new findings.
“We found no consistent evidence to support the current recommendations and found evidence of publication bias, methodological biases, and conflict of interest in those studies reporting allergic outcomes,” Dr. Boyle and his associates concluded. “We suggest that any future trials on hydrolyzed formula should be prospectively registered, independently funded, and include adequate oversight to ensure that they do not negatively impact on breastfeeding in study participants”.
Read the full study at the British Medical Journal (doi: 10.1136/bmj.i974)
Findings on the use of hydrolyzed formula in place of standard cows’ milk formula to prevent allergy in high-risk infants do not support current guidelines, according to Dr. Robert J Boyle of Imperial College London and his associates.
A review and meta-analysis were performed on 28 randomized control trials, 6 quasirandomized trials, and 3 controlled clinical trials describing allergic or autoimmune outcomes, with more than 19,000 participants. Among 13 studies reporting on the risk of food allergy, no significant difference was found in the risk of any food allergy with partially hydrolyzed formula (risk ratio, 1.73; 95% confidence interval, 0.79-3.80) and extensively hydrolyzed formula (RR, 0.86; CI, 0.26-2.82), compared with standard formula at age 0-4 years, and for extensively hydrolyzed formula at age 5-14 years.
The review also examined and found no significant evidence favoring the use of hydrolyzed formula in place of standard cows’ milk formula to avert the risk of eczema, wheeze, allergic rhinitis, or type 1 diabetes mellitus.
The researchers suggest that guidelines be updated and revised to reflect these new findings.
“We found no consistent evidence to support the current recommendations and found evidence of publication bias, methodological biases, and conflict of interest in those studies reporting allergic outcomes,” Dr. Boyle and his associates concluded. “We suggest that any future trials on hydrolyzed formula should be prospectively registered, independently funded, and include adequate oversight to ensure that they do not negatively impact on breastfeeding in study participants”.
Read the full study at the British Medical Journal (doi: 10.1136/bmj.i974)
FROM BRITISH MEDICAL JOURNAL
No evidence supports hydrolyzed formula over cows’ milk for allergy prevention
Findings on the use of hydrolyzed formula in place of standard cows’ milk formula to prevent allergy in high-risk infants do not support current guidelines, according to Dr. Robert J Boyle of Imperial College London and his associates.
A review and meta-analysis were performed on 28 randomized control trials, 6 quasirandomized trials, and 3 controlled clinical trials describing allergic or autoimmune outcomes, with more than 19,000 participants. Among 13 studies reporting on the risk of food allergy, no significant difference was found in the risk of any food allergy with partially hydrolyzed formula (risk ratio, 1.73; 95% confidence interval, 0.79-3.80) and extensively hydrolyzed formula (RR, 0.86; CI, 0.26-2.82), compared with standard formula at age 0-4 years, and for extensively hydrolyzed formula at age 5-14 years.
The review also examined and found no significant evidence favoring the use of hydrolyzed formula in place of standard cows’ milk formula to avert the risk of eczema, wheeze, allergic rhinitis, or type 1 diabetes mellitus.
The researchers suggest that guidelines be updated and revised to reflect these new findings.
“We found no consistent evidence to support the current recommendations and found evidence of publication bias, methodological biases, and conflict of interest in those studies reporting allergic outcomes,” Dr. Boyle and his associates concluded. “We suggest that any future trials on hydrolyzed formula should be prospectively registered, independently funded, and include adequate oversight to ensure that they do not negatively impact on breastfeeding in study participants”.
Read the full study at the British Medical Journal (doi: 10.1136/bmj.i974)
Findings on the use of hydrolyzed formula in place of standard cows’ milk formula to prevent allergy in high-risk infants do not support current guidelines, according to Dr. Robert J Boyle of Imperial College London and his associates.
A review and meta-analysis were performed on 28 randomized control trials, 6 quasirandomized trials, and 3 controlled clinical trials describing allergic or autoimmune outcomes, with more than 19,000 participants. Among 13 studies reporting on the risk of food allergy, no significant difference was found in the risk of any food allergy with partially hydrolyzed formula (risk ratio, 1.73; 95% confidence interval, 0.79-3.80) and extensively hydrolyzed formula (RR, 0.86; CI, 0.26-2.82), compared with standard formula at age 0-4 years, and for extensively hydrolyzed formula at age 5-14 years.
The review also examined and found no significant evidence favoring the use of hydrolyzed formula in place of standard cows’ milk formula to avert the risk of eczema, wheeze, allergic rhinitis, or type 1 diabetes mellitus.
The researchers suggest that guidelines be updated and revised to reflect these new findings.
“We found no consistent evidence to support the current recommendations and found evidence of publication bias, methodological biases, and conflict of interest in those studies reporting allergic outcomes,” Dr. Boyle and his associates concluded. “We suggest that any future trials on hydrolyzed formula should be prospectively registered, independently funded, and include adequate oversight to ensure that they do not negatively impact on breastfeeding in study participants”.
Read the full study at the British Medical Journal (doi: 10.1136/bmj.i974)
Findings on the use of hydrolyzed formula in place of standard cows’ milk formula to prevent allergy in high-risk infants do not support current guidelines, according to Dr. Robert J Boyle of Imperial College London and his associates.
A review and meta-analysis were performed on 28 randomized control trials, 6 quasirandomized trials, and 3 controlled clinical trials describing allergic or autoimmune outcomes, with more than 19,000 participants. Among 13 studies reporting on the risk of food allergy, no significant difference was found in the risk of any food allergy with partially hydrolyzed formula (risk ratio, 1.73; 95% confidence interval, 0.79-3.80) and extensively hydrolyzed formula (RR, 0.86; CI, 0.26-2.82), compared with standard formula at age 0-4 years, and for extensively hydrolyzed formula at age 5-14 years.
The review also examined and found no significant evidence favoring the use of hydrolyzed formula in place of standard cows’ milk formula to avert the risk of eczema, wheeze, allergic rhinitis, or type 1 diabetes mellitus.
The researchers suggest that guidelines be updated and revised to reflect these new findings.
“We found no consistent evidence to support the current recommendations and found evidence of publication bias, methodological biases, and conflict of interest in those studies reporting allergic outcomes,” Dr. Boyle and his associates concluded. “We suggest that any future trials on hydrolyzed formula should be prospectively registered, independently funded, and include adequate oversight to ensure that they do not negatively impact on breastfeeding in study participants”.
Read the full study at the British Medical Journal (doi: 10.1136/bmj.i974)
FROM BRITISH MEDICAL JOURNAL
High coffee consumption linked to decreased risk for MS
High coffee consumption decreased the odds of developing multiple sclerosis (MS) in two separate case-control studies conducted by Dr. Anna K. Hedström of the Karolinska Institute, Stockholm, and her associates.
The investigators analyzed coffee consumption across certain ages among 1,620 cases and 2,788 controls in the Swedish Epidemiological Investigation of Multiple Sclerosis (EIMS) and 1,159 cases and 1,172 controls in the Kaiser Permanente Medical Care Plan, Northern California Region (KPNC).
In EIMS, the adjusted odds ratio (OR) was 0.70 (95% confidence interval, 0.49-0.99; P = .04) among participants who drank six or more cups of coffee (greater than 900 mL) daily at the index year, which was defined as the year of the initial appearance of symptoms indicative of MS. The corresponding OR for those who reported high coffee consumption at 5 and 10 years before the study was 0.72 and 0.71, respectively, but neither comparison reached statistical significance.
In KPNC, those who consumed four or more cups of coffee (more than 948 mL in this study) daily were significantly less likely to develop MS than were those who never drank coffee (OR, 0.69; 95% CI, 0.50-0.96; P = .05). And the cohorts who drank four or more cups of coffee daily at least 5 years prior to the study were associated with significantly reduced odds of MS (OR, 0.64).
The combined results of the two studies in a meta-analysis found a significant, 29% reduction in the likelihood of developing MS among the highest drinkers of coffee (greater than 900 mL daily in EIMS and greater than 948 mL in KPNC). The investigators adjusted all the analyses for many demographic and environmental risk factors for MS, including age, gender, residential area, ancestry, smoking habits, exposure to passive smoking, sun exposure habits, and body mass index at age 20 years.
No evidence was found for associations between increased amounts of tea or soda intake and MS.
“Further studies are required to establish if it is in fact caffeine, or if there is another molecule in coffee underlying the findings, to longitudinally assess the association between consumption of coffee and disease activity in MS, and to evaluate the mechanisms by which coffee may be acting, which could thus lead to new therapeutic targets,” the researchers concluded.
Find the full study in the Journal of Neurology, Neurosurgery & Psychiatry (doi: 10.1136/jnnp-2015-312176).
High coffee consumption decreased the odds of developing multiple sclerosis (MS) in two separate case-control studies conducted by Dr. Anna K. Hedström of the Karolinska Institute, Stockholm, and her associates.
The investigators analyzed coffee consumption across certain ages among 1,620 cases and 2,788 controls in the Swedish Epidemiological Investigation of Multiple Sclerosis (EIMS) and 1,159 cases and 1,172 controls in the Kaiser Permanente Medical Care Plan, Northern California Region (KPNC).
In EIMS, the adjusted odds ratio (OR) was 0.70 (95% confidence interval, 0.49-0.99; P = .04) among participants who drank six or more cups of coffee (greater than 900 mL) daily at the index year, which was defined as the year of the initial appearance of symptoms indicative of MS. The corresponding OR for those who reported high coffee consumption at 5 and 10 years before the study was 0.72 and 0.71, respectively, but neither comparison reached statistical significance.
In KPNC, those who consumed four or more cups of coffee (more than 948 mL in this study) daily were significantly less likely to develop MS than were those who never drank coffee (OR, 0.69; 95% CI, 0.50-0.96; P = .05). And the cohorts who drank four or more cups of coffee daily at least 5 years prior to the study were associated with significantly reduced odds of MS (OR, 0.64).
The combined results of the two studies in a meta-analysis found a significant, 29% reduction in the likelihood of developing MS among the highest drinkers of coffee (greater than 900 mL daily in EIMS and greater than 948 mL in KPNC). The investigators adjusted all the analyses for many demographic and environmental risk factors for MS, including age, gender, residential area, ancestry, smoking habits, exposure to passive smoking, sun exposure habits, and body mass index at age 20 years.
No evidence was found for associations between increased amounts of tea or soda intake and MS.
“Further studies are required to establish if it is in fact caffeine, or if there is another molecule in coffee underlying the findings, to longitudinally assess the association between consumption of coffee and disease activity in MS, and to evaluate the mechanisms by which coffee may be acting, which could thus lead to new therapeutic targets,” the researchers concluded.
Find the full study in the Journal of Neurology, Neurosurgery & Psychiatry (doi: 10.1136/jnnp-2015-312176).
High coffee consumption decreased the odds of developing multiple sclerosis (MS) in two separate case-control studies conducted by Dr. Anna K. Hedström of the Karolinska Institute, Stockholm, and her associates.
The investigators analyzed coffee consumption across certain ages among 1,620 cases and 2,788 controls in the Swedish Epidemiological Investigation of Multiple Sclerosis (EIMS) and 1,159 cases and 1,172 controls in the Kaiser Permanente Medical Care Plan, Northern California Region (KPNC).
In EIMS, the adjusted odds ratio (OR) was 0.70 (95% confidence interval, 0.49-0.99; P = .04) among participants who drank six or more cups of coffee (greater than 900 mL) daily at the index year, which was defined as the year of the initial appearance of symptoms indicative of MS. The corresponding OR for those who reported high coffee consumption at 5 and 10 years before the study was 0.72 and 0.71, respectively, but neither comparison reached statistical significance.
In KPNC, those who consumed four or more cups of coffee (more than 948 mL in this study) daily were significantly less likely to develop MS than were those who never drank coffee (OR, 0.69; 95% CI, 0.50-0.96; P = .05). And the cohorts who drank four or more cups of coffee daily at least 5 years prior to the study were associated with significantly reduced odds of MS (OR, 0.64).
The combined results of the two studies in a meta-analysis found a significant, 29% reduction in the likelihood of developing MS among the highest drinkers of coffee (greater than 900 mL daily in EIMS and greater than 948 mL in KPNC). The investigators adjusted all the analyses for many demographic and environmental risk factors for MS, including age, gender, residential area, ancestry, smoking habits, exposure to passive smoking, sun exposure habits, and body mass index at age 20 years.
No evidence was found for associations between increased amounts of tea or soda intake and MS.
“Further studies are required to establish if it is in fact caffeine, or if there is another molecule in coffee underlying the findings, to longitudinally assess the association between consumption of coffee and disease activity in MS, and to evaluate the mechanisms by which coffee may be acting, which could thus lead to new therapeutic targets,” the researchers concluded.
Find the full study in the Journal of Neurology, Neurosurgery & Psychiatry (doi: 10.1136/jnnp-2015-312176).
FROM JOURNAL OF NEUROLOGY, NEUROSURGERY & PSYCHIATRY
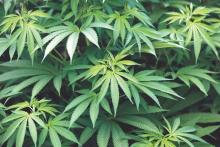
Pot tied to increased risk of substance use disorders, not depression or anxiety
Cannabis use is associated with an increased risk of later addiction to cannabis, alcohol, and other drugs, a longitudinal survey of almost 35,000 adults shows.
Dr. Carlos Blanco and his associates analyzed two waves of data from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) from 2001-2002 and 2004-2005. They found that, among respondents who used cannabis in the past 12 months, the risk of developing any substance use disorder (odds ratio, 8; 95% confidence interval, 6.9-9.2) was higher than the risk of developing any mood (OR, 2.1; 95% CI, 1.8-2.0) or anxiety disorder (OR, 1.9; CI, 1.6-2.3). Similar trends were found for the risk of alcohol use disorder (OR, 7.3; 95% CI, 6.3-8.6) and nicotine dependence (OR, 4.2; 95% CI, 3.6-4.9). The investigators also found a dose-response effect; more frequent cannabis use was tied to a greater risk of later addiction.
Together, the findings suggest caution in implementing policies tied to the legalization of cannabis for recreational use, noted Dr. Blanco of the National Institute on Drug Abuse, Bethesda, Md. Adverse outcomes such as substance use disorders “should be taken under careful consideration in clinical care and policy planning.”
Find the full study in JAMA Psychiatry: (2016 Feb 17. doi: 10.1001/jamapsychiatry.2015.3229)
Cannabis use is associated with an increased risk of later addiction to cannabis, alcohol, and other drugs, a longitudinal survey of almost 35,000 adults shows.
Dr. Carlos Blanco and his associates analyzed two waves of data from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) from 2001-2002 and 2004-2005. They found that, among respondents who used cannabis in the past 12 months, the risk of developing any substance use disorder (odds ratio, 8; 95% confidence interval, 6.9-9.2) was higher than the risk of developing any mood (OR, 2.1; 95% CI, 1.8-2.0) or anxiety disorder (OR, 1.9; CI, 1.6-2.3). Similar trends were found for the risk of alcohol use disorder (OR, 7.3; 95% CI, 6.3-8.6) and nicotine dependence (OR, 4.2; 95% CI, 3.6-4.9). The investigators also found a dose-response effect; more frequent cannabis use was tied to a greater risk of later addiction.
Together, the findings suggest caution in implementing policies tied to the legalization of cannabis for recreational use, noted Dr. Blanco of the National Institute on Drug Abuse, Bethesda, Md. Adverse outcomes such as substance use disorders “should be taken under careful consideration in clinical care and policy planning.”
Find the full study in JAMA Psychiatry: (2016 Feb 17. doi: 10.1001/jamapsychiatry.2015.3229)
Cannabis use is associated with an increased risk of later addiction to cannabis, alcohol, and other drugs, a longitudinal survey of almost 35,000 adults shows.
Dr. Carlos Blanco and his associates analyzed two waves of data from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) from 2001-2002 and 2004-2005. They found that, among respondents who used cannabis in the past 12 months, the risk of developing any substance use disorder (odds ratio, 8; 95% confidence interval, 6.9-9.2) was higher than the risk of developing any mood (OR, 2.1; 95% CI, 1.8-2.0) or anxiety disorder (OR, 1.9; CI, 1.6-2.3). Similar trends were found for the risk of alcohol use disorder (OR, 7.3; 95% CI, 6.3-8.6) and nicotine dependence (OR, 4.2; 95% CI, 3.6-4.9). The investigators also found a dose-response effect; more frequent cannabis use was tied to a greater risk of later addiction.
Together, the findings suggest caution in implementing policies tied to the legalization of cannabis for recreational use, noted Dr. Blanco of the National Institute on Drug Abuse, Bethesda, Md. Adverse outcomes such as substance use disorders “should be taken under careful consideration in clinical care and policy planning.”
Find the full study in JAMA Psychiatry: (2016 Feb 17. doi: 10.1001/jamapsychiatry.2015.3229)
FROM JAMA PSYCHIATRY
Rapid growth, childhood obesity tied to fish and pregnancy
Greater risk of rapid growth in infancy and childhood obesity appeared to be tied to an increased maternal consumption of fish while pregnant, according to Nikos Stratakis of the University of Crete, Heraklion, Greece, and his associates.
The study comprised 26,184 pregnant women from Europe and the United States, during 1996-2011. Among children of women who ate fish during their pregnancy, 31% showed rapid growth between birth and 2 years, and 34.6% of those aged 4-6 years were classified as overweight or obese.
Women who ate more fish (more than 3 times per week) gave birth to offspring with higher body mass indices (BMI) at ages 2, 4, and 6 years, compared with women who rarely ate fish (once or fewer times per week). High fish intake during pregnancy was linked with a higher risk of rapid infant growth from birth to 2 years (adjusted odds ratio [aOR], 1.22) and a higher risk of offspring overweight/obesity at 4 years (aOR, 1.14) and 6 years of age (aOR, 1.22).
The cohorts provided information on child height and weight up to a maximum follow-up of 6 years. The information was obtained from clinical examinations, medical records, or parents’ questionnaires. The permissible intervals of the nominal ages were within 3 months for the first 2 years and within 6 months onwards.
“This large, multicenter study indicates that fish intake of more than 3 times/week in pregnancy is associated with increased risk of rapid growth in infancy and increased adiposity in childhood,” the researchers concluded. The findings “are in line with the fish intake limit for pregnancy proposed by the U.S. Food and Drug Administration and Environmental Protection Agency,” they wrote.
Find the full study in JAMA Pediatrics (2016 [doi:10.1001/jamapediatrics.2015.4430]).
Greater risk of rapid growth in infancy and childhood obesity appeared to be tied to an increased maternal consumption of fish while pregnant, according to Nikos Stratakis of the University of Crete, Heraklion, Greece, and his associates.
The study comprised 26,184 pregnant women from Europe and the United States, during 1996-2011. Among children of women who ate fish during their pregnancy, 31% showed rapid growth between birth and 2 years, and 34.6% of those aged 4-6 years were classified as overweight or obese.
Women who ate more fish (more than 3 times per week) gave birth to offspring with higher body mass indices (BMI) at ages 2, 4, and 6 years, compared with women who rarely ate fish (once or fewer times per week). High fish intake during pregnancy was linked with a higher risk of rapid infant growth from birth to 2 years (adjusted odds ratio [aOR], 1.22) and a higher risk of offspring overweight/obesity at 4 years (aOR, 1.14) and 6 years of age (aOR, 1.22).
The cohorts provided information on child height and weight up to a maximum follow-up of 6 years. The information was obtained from clinical examinations, medical records, or parents’ questionnaires. The permissible intervals of the nominal ages were within 3 months for the first 2 years and within 6 months onwards.
“This large, multicenter study indicates that fish intake of more than 3 times/week in pregnancy is associated with increased risk of rapid growth in infancy and increased adiposity in childhood,” the researchers concluded. The findings “are in line with the fish intake limit for pregnancy proposed by the U.S. Food and Drug Administration and Environmental Protection Agency,” they wrote.
Find the full study in JAMA Pediatrics (2016 [doi:10.1001/jamapediatrics.2015.4430]).
Greater risk of rapid growth in infancy and childhood obesity appeared to be tied to an increased maternal consumption of fish while pregnant, according to Nikos Stratakis of the University of Crete, Heraklion, Greece, and his associates.
The study comprised 26,184 pregnant women from Europe and the United States, during 1996-2011. Among children of women who ate fish during their pregnancy, 31% showed rapid growth between birth and 2 years, and 34.6% of those aged 4-6 years were classified as overweight or obese.
Women who ate more fish (more than 3 times per week) gave birth to offspring with higher body mass indices (BMI) at ages 2, 4, and 6 years, compared with women who rarely ate fish (once or fewer times per week). High fish intake during pregnancy was linked with a higher risk of rapid infant growth from birth to 2 years (adjusted odds ratio [aOR], 1.22) and a higher risk of offspring overweight/obesity at 4 years (aOR, 1.14) and 6 years of age (aOR, 1.22).
The cohorts provided information on child height and weight up to a maximum follow-up of 6 years. The information was obtained from clinical examinations, medical records, or parents’ questionnaires. The permissible intervals of the nominal ages were within 3 months for the first 2 years and within 6 months onwards.
“This large, multicenter study indicates that fish intake of more than 3 times/week in pregnancy is associated with increased risk of rapid growth in infancy and increased adiposity in childhood,” the researchers concluded. The findings “are in line with the fish intake limit for pregnancy proposed by the U.S. Food and Drug Administration and Environmental Protection Agency,” they wrote.
Find the full study in JAMA Pediatrics (2016 [doi:10.1001/jamapediatrics.2015.4430]).
FROM JAMA PEDIATRICS