User login
Interleukin-6 is an effective biomarker for poor HIV outcomes
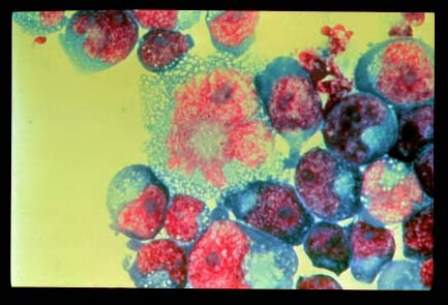
Interleukin-6 may have the strongest predictive power of the three biomarkers associated to date with adverse outcomes in patients infected with HIV, according to the results of a study published in the Journal of Infectious Diseases.
Elevated levels of the biomarkers intereukin-6 (IL-6), high-sensitivity C-reactive protein (hsCRP), and d-dimer were independently and strongly associated with a subsequent risk of death in the Strategies for Management of Anti-Retroviral Therapy trial, said first author Dr. Álvaro H. Borges of the department of infectious diseases at the center for health and infectious diseases research at the Rigshospitalet of the University of Copenhagen and colleagues.
They evaluated the relative value of IL-6, hsCRP, and d-dimer as predictors of different clinical endpoints in those infected with HIV. To accomplish this, Dr. Borges and colleagues used preserved blood samples from 4,304 patients from the control arms of two international HIV trials (SMART and ESPRIT). The investigators used the samples to measure the association of plasma levels of each biomarker with the risk of developing different clinical endpoints, including all-cause mortality, non-AIDS and nonviolent/accidental death, fatal and nonfatal progression to AIDS, fatal and nonfatal cardiovascular disease (myocardial infarction, stroke or coronary artery disease requiring a surgical procedure), and fatal and nonfatal non–AIDS-defining malignancies, excluding basal and squamous cell skin cancers (J Infect Dis. 2016 Apr 30. pii: jiw173).
IL-6 was superior to hsCRP in predicting cardiovascular and non–AIDS-defining malignancies and more strongly associated with these outcomes than d-dimer. As opposed to hsCRP and d-dimer, IL-6 showed heterogeneity as a predictor for different endpoints, suggesting that higher IL-6 level is a marker of both disease risk and disease severity.
Clinical endpoint–driven trials are needed to determine whether therapies designed to lower levels of the three assessed biomarkers can reduce morbidity and mortality in patients receiving treatment for HIV infection, the researchers said.
Funding was provided by the National Institutes of Health, the Research Council at Rigshospitalet, and the Danish National Research Foundation. Andrew N. Phillips disclosed ties to multiple industry sources. No other conflicts of interest were reported.
Interleukin-6 may have the strongest predictive power of the three biomarkers associated to date with adverse outcomes in patients infected with HIV, according to the results of a study published in the Journal of Infectious Diseases.
Elevated levels of the biomarkers intereukin-6 (IL-6), high-sensitivity C-reactive protein (hsCRP), and d-dimer were independently and strongly associated with a subsequent risk of death in the Strategies for Management of Anti-Retroviral Therapy trial, said first author Dr. Álvaro H. Borges of the department of infectious diseases at the center for health and infectious diseases research at the Rigshospitalet of the University of Copenhagen and colleagues.
They evaluated the relative value of IL-6, hsCRP, and d-dimer as predictors of different clinical endpoints in those infected with HIV. To accomplish this, Dr. Borges and colleagues used preserved blood samples from 4,304 patients from the control arms of two international HIV trials (SMART and ESPRIT). The investigators used the samples to measure the association of plasma levels of each biomarker with the risk of developing different clinical endpoints, including all-cause mortality, non-AIDS and nonviolent/accidental death, fatal and nonfatal progression to AIDS, fatal and nonfatal cardiovascular disease (myocardial infarction, stroke or coronary artery disease requiring a surgical procedure), and fatal and nonfatal non–AIDS-defining malignancies, excluding basal and squamous cell skin cancers (J Infect Dis. 2016 Apr 30. pii: jiw173).
IL-6 was superior to hsCRP in predicting cardiovascular and non–AIDS-defining malignancies and more strongly associated with these outcomes than d-dimer. As opposed to hsCRP and d-dimer, IL-6 showed heterogeneity as a predictor for different endpoints, suggesting that higher IL-6 level is a marker of both disease risk and disease severity.
Clinical endpoint–driven trials are needed to determine whether therapies designed to lower levels of the three assessed biomarkers can reduce morbidity and mortality in patients receiving treatment for HIV infection, the researchers said.
Funding was provided by the National Institutes of Health, the Research Council at Rigshospitalet, and the Danish National Research Foundation. Andrew N. Phillips disclosed ties to multiple industry sources. No other conflicts of interest were reported.
Interleukin-6 may have the strongest predictive power of the three biomarkers associated to date with adverse outcomes in patients infected with HIV, according to the results of a study published in the Journal of Infectious Diseases.
Elevated levels of the biomarkers intereukin-6 (IL-6), high-sensitivity C-reactive protein (hsCRP), and d-dimer were independently and strongly associated with a subsequent risk of death in the Strategies for Management of Anti-Retroviral Therapy trial, said first author Dr. Álvaro H. Borges of the department of infectious diseases at the center for health and infectious diseases research at the Rigshospitalet of the University of Copenhagen and colleagues.
They evaluated the relative value of IL-6, hsCRP, and d-dimer as predictors of different clinical endpoints in those infected with HIV. To accomplish this, Dr. Borges and colleagues used preserved blood samples from 4,304 patients from the control arms of two international HIV trials (SMART and ESPRIT). The investigators used the samples to measure the association of plasma levels of each biomarker with the risk of developing different clinical endpoints, including all-cause mortality, non-AIDS and nonviolent/accidental death, fatal and nonfatal progression to AIDS, fatal and nonfatal cardiovascular disease (myocardial infarction, stroke or coronary artery disease requiring a surgical procedure), and fatal and nonfatal non–AIDS-defining malignancies, excluding basal and squamous cell skin cancers (J Infect Dis. 2016 Apr 30. pii: jiw173).
IL-6 was superior to hsCRP in predicting cardiovascular and non–AIDS-defining malignancies and more strongly associated with these outcomes than d-dimer. As opposed to hsCRP and d-dimer, IL-6 showed heterogeneity as a predictor for different endpoints, suggesting that higher IL-6 level is a marker of both disease risk and disease severity.
Clinical endpoint–driven trials are needed to determine whether therapies designed to lower levels of the three assessed biomarkers can reduce morbidity and mortality in patients receiving treatment for HIV infection, the researchers said.
Funding was provided by the National Institutes of Health, the Research Council at Rigshospitalet, and the Danish National Research Foundation. Andrew N. Phillips disclosed ties to multiple industry sources. No other conflicts of interest were reported.
Key clinical point: Compared with high-sensitivity C-reactive protein and d-dimer levels, IL-6 is a stronger predictor of poor outcomes for those infected with HIV.
Major finding: Interleukin-6 was superior to high-sensitivity C-reactive protein in predicting cardiovascular and non–AIDS-defining malignancies and more strongly associated with these outcomes than was d-dimer.
Data sources: A cohort of 4,304 patients from the control arms of two international HIV trials.
Disclosures: The National Institutes of Health, the Research Council at Rigshospitalet, and the Danish National Research Foundation funded the study. Andrew N. Phillips disclosed ties to multiple industry sources. No other conflicts of interest were reported.
Ultrasound improves early diagnosis of ventilator-associated pneumonia
The use of lung ultrasound, both alone and in combination with clinical and microbiologic data, can improve the early diagnosis of ventilator-associated pneumonia (VAP), according to the results of a study published in Chest.
The early diagnosis of VAP is challenging, and leaves intensivists with two options. The first is waiting for positive results from patients’ specimens, which delays treatment and increases mortality risk. The other is to administer antibiotics to all patients suspected of having VAP, which may be inappropriate and can lead to the development of multiresistant bacteria. “A pressing need therefore exists for reliable diagnostic tools to diagnose VAP early so that antibiotics can be promptly initiated, avoiding two extreme approaches,” wrote Dr. Silvia Mongodi of the Fondazione IRCCS Policlinico San Matteo in Pavia, Italy, and her colleagues.
Based on the results of previous research, the investigators hypothesized that lung ultrasound (LUS) could be used to diagnose VAP early and help to avoid treatment delays or mistakes. To test this hypothesis, the diagnostic performance of LUS alone and in combination with clinical and microbiologic data was evaluated prospectively in 99 patients with suspected VAP in ICUs at Saint Joseph Hospital (Paris), Fondazione IRCCS Policlinico San Matteo, and Centre Hospitalier de l’Université de Montréal (Chest. 2016 Apr;149[4]:969-80. doi: 10.1016/j.chest.2015.12.012).
The study results showed that subpleural consolidations and dynamic linear/arborescent air bronchograms were the principal LUS signs of VAP, and that the presence of both in the same individual made the diagnosis highly specific (88%), with a high positive predictive value (86%) and a positive likelihood ratio of 2.9. Furthermore, the addition of data from either of two different endotracheal aspirate assessment techniques (EAgram [direct Gram stain examination] or EAquant [direct Gram stain culture]) to the data from the principal LUS signs showed 97% specificity with each technique and positive likelihood ratios of 6.6 and 7.1, respectively, Dr. Mongodi and her associates reported.
Dr. Mongodi and her colleagues said that their results were encouraging but would need to be validated in larger clinical trials.
No funding was received for this study. The authors reported no conflicts of interest.
Dr. Daniel Ouellette, FCCP comments: Ultrasound techniques are increasingly being used in the intensive care unit to direct physician decisions. A report by Mongodi and colleagues suggests that ultrasound may be employed to diagnose ventilator-associated pneumonia in critically ill patients. While promising, this study is limited by small patient numbers and by the fact that reliable criteria to diagnose VAP are lacking. Further research is needed before this technique can be used reliably in the ICU.
Dr. Daniel Ouellette, FCCP comments: Ultrasound techniques are increasingly being used in the intensive care unit to direct physician decisions. A report by Mongodi and colleagues suggests that ultrasound may be employed to diagnose ventilator-associated pneumonia in critically ill patients. While promising, this study is limited by small patient numbers and by the fact that reliable criteria to diagnose VAP are lacking. Further research is needed before this technique can be used reliably in the ICU.
Dr. Daniel Ouellette, FCCP comments: Ultrasound techniques are increasingly being used in the intensive care unit to direct physician decisions. A report by Mongodi and colleagues suggests that ultrasound may be employed to diagnose ventilator-associated pneumonia in critically ill patients. While promising, this study is limited by small patient numbers and by the fact that reliable criteria to diagnose VAP are lacking. Further research is needed before this technique can be used reliably in the ICU.
The use of lung ultrasound, both alone and in combination with clinical and microbiologic data, can improve the early diagnosis of ventilator-associated pneumonia (VAP), according to the results of a study published in Chest.
The early diagnosis of VAP is challenging, and leaves intensivists with two options. The first is waiting for positive results from patients’ specimens, which delays treatment and increases mortality risk. The other is to administer antibiotics to all patients suspected of having VAP, which may be inappropriate and can lead to the development of multiresistant bacteria. “A pressing need therefore exists for reliable diagnostic tools to diagnose VAP early so that antibiotics can be promptly initiated, avoiding two extreme approaches,” wrote Dr. Silvia Mongodi of the Fondazione IRCCS Policlinico San Matteo in Pavia, Italy, and her colleagues.
Based on the results of previous research, the investigators hypothesized that lung ultrasound (LUS) could be used to diagnose VAP early and help to avoid treatment delays or mistakes. To test this hypothesis, the diagnostic performance of LUS alone and in combination with clinical and microbiologic data was evaluated prospectively in 99 patients with suspected VAP in ICUs at Saint Joseph Hospital (Paris), Fondazione IRCCS Policlinico San Matteo, and Centre Hospitalier de l’Université de Montréal (Chest. 2016 Apr;149[4]:969-80. doi: 10.1016/j.chest.2015.12.012).
The study results showed that subpleural consolidations and dynamic linear/arborescent air bronchograms were the principal LUS signs of VAP, and that the presence of both in the same individual made the diagnosis highly specific (88%), with a high positive predictive value (86%) and a positive likelihood ratio of 2.9. Furthermore, the addition of data from either of two different endotracheal aspirate assessment techniques (EAgram [direct Gram stain examination] or EAquant [direct Gram stain culture]) to the data from the principal LUS signs showed 97% specificity with each technique and positive likelihood ratios of 6.6 and 7.1, respectively, Dr. Mongodi and her associates reported.
Dr. Mongodi and her colleagues said that their results were encouraging but would need to be validated in larger clinical trials.
No funding was received for this study. The authors reported no conflicts of interest.
The use of lung ultrasound, both alone and in combination with clinical and microbiologic data, can improve the early diagnosis of ventilator-associated pneumonia (VAP), according to the results of a study published in Chest.
The early diagnosis of VAP is challenging, and leaves intensivists with two options. The first is waiting for positive results from patients’ specimens, which delays treatment and increases mortality risk. The other is to administer antibiotics to all patients suspected of having VAP, which may be inappropriate and can lead to the development of multiresistant bacteria. “A pressing need therefore exists for reliable diagnostic tools to diagnose VAP early so that antibiotics can be promptly initiated, avoiding two extreme approaches,” wrote Dr. Silvia Mongodi of the Fondazione IRCCS Policlinico San Matteo in Pavia, Italy, and her colleagues.
Based on the results of previous research, the investigators hypothesized that lung ultrasound (LUS) could be used to diagnose VAP early and help to avoid treatment delays or mistakes. To test this hypothesis, the diagnostic performance of LUS alone and in combination with clinical and microbiologic data was evaluated prospectively in 99 patients with suspected VAP in ICUs at Saint Joseph Hospital (Paris), Fondazione IRCCS Policlinico San Matteo, and Centre Hospitalier de l’Université de Montréal (Chest. 2016 Apr;149[4]:969-80. doi: 10.1016/j.chest.2015.12.012).
The study results showed that subpleural consolidations and dynamic linear/arborescent air bronchograms were the principal LUS signs of VAP, and that the presence of both in the same individual made the diagnosis highly specific (88%), with a high positive predictive value (86%) and a positive likelihood ratio of 2.9. Furthermore, the addition of data from either of two different endotracheal aspirate assessment techniques (EAgram [direct Gram stain examination] or EAquant [direct Gram stain culture]) to the data from the principal LUS signs showed 97% specificity with each technique and positive likelihood ratios of 6.6 and 7.1, respectively, Dr. Mongodi and her associates reported.
Dr. Mongodi and her colleagues said that their results were encouraging but would need to be validated in larger clinical trials.
No funding was received for this study. The authors reported no conflicts of interest.
Key clinical point: The specificity of the examination for ventilator-associated pneumonia diagnosis could be increased with daily lung-ultrasound monitoring of ICU patients.
Major finding: Lung ultrasound reliably improved the diagnosis of ventilator-associated pneumonia with high specificity (88%), high positive predictive value (86%), and a positive likelihood ratio of 2.9.
Data sources: Patients with suspected ventilator-associated pneumonia in ICUs in France, Italy, and Canada.
Disclosures: No funding was received for this study. The authors reported no conflicts of interest.
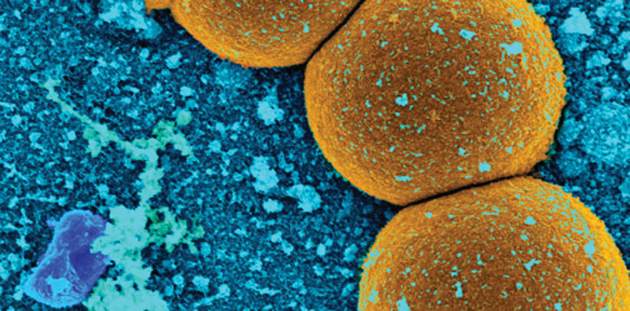
Study: Number of MRSA cases in Japan may be underestimated
In Japan, sentinel disease surveillance systems may underestimate the actual number of patients with methicillin-resistant Staphylococcus aureus (MRSA) infection because they do not include information about patients who visit nonsentinel medical facilities, according to a study published in Epidemiology and Infection.
Dr. Shinichi Tanihara of the department of public health and preventive medicine in the School of Medicine at Fukuoka University and Dr. Satowa Suzuki of the department of bacteriology II at the National Institute of Infectious Diseases in Tokyo assessed and compared the incidences of MRSA patients based on health insurance claims data and data reported to the Japan Nosocomial Infections Surveillance system (Epidemiol Infect. 2016 April 8. doi: 10.1017/S0950268816000674).
The study results suggested that health insurance claims data for MRSA cases were more useful for determining the incidence of MRSA cases in Japan from 2011 to 2012. For example, of the 2,052 eligible hospitals with 200 or more beds in 2011, roughly one-quarter (495, 23.8%) participated in the Japan Nosocomial Infections Surveillance system. Data from this relatively low percentage of eligible facilities most likely underestimated the true number of MRSA patients in Japan, the authors said.
Based on their findings, the investigators noted three major advantages of using health insurance claims data for infection surveillance. Firstly, information from health insurance claims data is not affected by health care providers’ notifications to surveillance systems. Secondly, data on patients with MRSA can be collected at low cost because of Japan’s uniform and computerized health insurance system, and the data are easy to access. Lastly, health insurance claims data prevent the duplication of patient information, as insurers can determine if a patient was treated at multiple medical facilities for the same disease.
The only noted drawback involving the use of health insurance claims data for infection surveillance pertained to its timeliness, the researchers wrote. This issue arises because these data are submitted monthly rather than immediately, which may limit their use in surveillance systems.
According to Dr. Tanihara and Dr. Suzuki, strengths of the study include its evaluation of sentinel surveillance quality through the use of data that were not based on physician reports, as well as the calculation of MRSA incidence by use of a standardized definition in a specific population. Reported limitations included the assessment of anti-MRSA medicine use and patients’ age only, and the lack of information on the degree of drug resistance from health insurance claims data.
Funding was provided by the Ministry of Health, Labour, and Welfare of Japan, and by the Research Programme on Emerging and Re-emerging Infectious Diseases from the Japan Agency for Medical Research and Development. Neither author reported any conflicts of interest.
In Japan, sentinel disease surveillance systems may underestimate the actual number of patients with methicillin-resistant Staphylococcus aureus (MRSA) infection because they do not include information about patients who visit nonsentinel medical facilities, according to a study published in Epidemiology and Infection.
Dr. Shinichi Tanihara of the department of public health and preventive medicine in the School of Medicine at Fukuoka University and Dr. Satowa Suzuki of the department of bacteriology II at the National Institute of Infectious Diseases in Tokyo assessed and compared the incidences of MRSA patients based on health insurance claims data and data reported to the Japan Nosocomial Infections Surveillance system (Epidemiol Infect. 2016 April 8. doi: 10.1017/S0950268816000674).
The study results suggested that health insurance claims data for MRSA cases were more useful for determining the incidence of MRSA cases in Japan from 2011 to 2012. For example, of the 2,052 eligible hospitals with 200 or more beds in 2011, roughly one-quarter (495, 23.8%) participated in the Japan Nosocomial Infections Surveillance system. Data from this relatively low percentage of eligible facilities most likely underestimated the true number of MRSA patients in Japan, the authors said.
Based on their findings, the investigators noted three major advantages of using health insurance claims data for infection surveillance. Firstly, information from health insurance claims data is not affected by health care providers’ notifications to surveillance systems. Secondly, data on patients with MRSA can be collected at low cost because of Japan’s uniform and computerized health insurance system, and the data are easy to access. Lastly, health insurance claims data prevent the duplication of patient information, as insurers can determine if a patient was treated at multiple medical facilities for the same disease.
The only noted drawback involving the use of health insurance claims data for infection surveillance pertained to its timeliness, the researchers wrote. This issue arises because these data are submitted monthly rather than immediately, which may limit their use in surveillance systems.
According to Dr. Tanihara and Dr. Suzuki, strengths of the study include its evaluation of sentinel surveillance quality through the use of data that were not based on physician reports, as well as the calculation of MRSA incidence by use of a standardized definition in a specific population. Reported limitations included the assessment of anti-MRSA medicine use and patients’ age only, and the lack of information on the degree of drug resistance from health insurance claims data.
Funding was provided by the Ministry of Health, Labour, and Welfare of Japan, and by the Research Programme on Emerging and Re-emerging Infectious Diseases from the Japan Agency for Medical Research and Development. Neither author reported any conflicts of interest.
In Japan, sentinel disease surveillance systems may underestimate the actual number of patients with methicillin-resistant Staphylococcus aureus (MRSA) infection because they do not include information about patients who visit nonsentinel medical facilities, according to a study published in Epidemiology and Infection.
Dr. Shinichi Tanihara of the department of public health and preventive medicine in the School of Medicine at Fukuoka University and Dr. Satowa Suzuki of the department of bacteriology II at the National Institute of Infectious Diseases in Tokyo assessed and compared the incidences of MRSA patients based on health insurance claims data and data reported to the Japan Nosocomial Infections Surveillance system (Epidemiol Infect. 2016 April 8. doi: 10.1017/S0950268816000674).
The study results suggested that health insurance claims data for MRSA cases were more useful for determining the incidence of MRSA cases in Japan from 2011 to 2012. For example, of the 2,052 eligible hospitals with 200 or more beds in 2011, roughly one-quarter (495, 23.8%) participated in the Japan Nosocomial Infections Surveillance system. Data from this relatively low percentage of eligible facilities most likely underestimated the true number of MRSA patients in Japan, the authors said.
Based on their findings, the investigators noted three major advantages of using health insurance claims data for infection surveillance. Firstly, information from health insurance claims data is not affected by health care providers’ notifications to surveillance systems. Secondly, data on patients with MRSA can be collected at low cost because of Japan’s uniform and computerized health insurance system, and the data are easy to access. Lastly, health insurance claims data prevent the duplication of patient information, as insurers can determine if a patient was treated at multiple medical facilities for the same disease.
The only noted drawback involving the use of health insurance claims data for infection surveillance pertained to its timeliness, the researchers wrote. This issue arises because these data are submitted monthly rather than immediately, which may limit their use in surveillance systems.
According to Dr. Tanihara and Dr. Suzuki, strengths of the study include its evaluation of sentinel surveillance quality through the use of data that were not based on physician reports, as well as the calculation of MRSA incidence by use of a standardized definition in a specific population. Reported limitations included the assessment of anti-MRSA medicine use and patients’ age only, and the lack of information on the degree of drug resistance from health insurance claims data.
Funding was provided by the Ministry of Health, Labour, and Welfare of Japan, and by the Research Programme on Emerging and Re-emerging Infectious Diseases from the Japan Agency for Medical Research and Development. Neither author reported any conflicts of interest.
Key clinical point: Sentinel surveillance systems may substantially underestimate the number of methicillin-resistant Staphylococcus aureus cases in Japan.
Major finding: Direct notification to the Japan Nosocomial Infections Surveillance system regarding methicillin-resistant Staphylococcus aureus patients was not affected by patients’ age, and information from health insurance claims was useful for evaluation of the sentinel infection surveillance system.
Data sources: The Japan Nosocomial Infections Surveillance system and the National Health Insurance Organization.
Disclosures: Funding was provided by the Ministry of Health, Labour, and Welfare of Japan, and by the Research Programme on Emerging and Re-emerging Infectious Diseases from the Japan Agency for Medical Research and Development. Neither author reported any conflicts of interest.
Atopic Dermatitis Increases Risk for ADHD, Comorbidities Add to It
Atopic dermatitis (AD) is associated with an increased risk for attention-deficit/hyperactivity disorder (ADHD) in children and adults, and a host of factors and comorbid conditions increase this risk, according to a study published in the British Journal of Dermatology.
Mark A. Strom and his associates at Northwestern University in Chicago examined data from 19 U.S. population-based surveys on 354,416 children ages 2-17 years and 34,613 adults over the age of 18 to determine if childhood and adult AD and the severity of AD were associated with ADHD. Additionally, the investigators sought to identify factors contributing to this association (Br J Dermatol. 2016 Apr 23. doi: 10.1111/bjd.14697).
The prevalence of ADHD was 9.4% in children with AD and 7.1% in children without AD. For children, the study results obtained from multivariate models adjusting for age, sex, sociodemographic variables, allergic disease, and health care utilization confirmed the previously established increase in risk for ADHD in those with AD for an adjusted odds ratio of 1.14. Severe AD and sleep disturbance were found to independently and synergistically contribute to the increased risk of ADHD. Also, the presence of AD in the absence of other allergic disease was associated with an increased risk for ADHD. Obesity, headaches, and anemia were found to further increase the risk for ADHD in those with AD.
Results from the adjusted multivariate models also established an increased risk for ADHD among adults with AD, for an adjusted odds ratio of 1.61. The presence of asthma, headaches, and insomnia increased this risk. The analysis additionally revealed that a body mass index indicative of underweight status in adults with AD was protective against the risk for developing ADHD.
Mr. Strom and his associates found a significant decrease in their initial odds ratios when they added outpatient health care visitation to their multivariate models, which resulted in an overall pooled odds ratio for the relationship between AD and ADHD just above statistical significance. They speculated that children with AD or ADHD would be more likely to visit health care providers, which could increase the likelihood for diagnosis of comorbid conditions.
Funding was provided by the Agency for Healthcare Research and Quality and the Dermatology Foundation. The authors reported no conflicts of interest.
Atopic dermatitis (AD) is associated with an increased risk for attention-deficit/hyperactivity disorder (ADHD) in children and adults, and a host of factors and comorbid conditions increase this risk, according to a study published in the British Journal of Dermatology.
Mark A. Strom and his associates at Northwestern University in Chicago examined data from 19 U.S. population-based surveys on 354,416 children ages 2-17 years and 34,613 adults over the age of 18 to determine if childhood and adult AD and the severity of AD were associated with ADHD. Additionally, the investigators sought to identify factors contributing to this association (Br J Dermatol. 2016 Apr 23. doi: 10.1111/bjd.14697).
The prevalence of ADHD was 9.4% in children with AD and 7.1% in children without AD. For children, the study results obtained from multivariate models adjusting for age, sex, sociodemographic variables, allergic disease, and health care utilization confirmed the previously established increase in risk for ADHD in those with AD for an adjusted odds ratio of 1.14. Severe AD and sleep disturbance were found to independently and synergistically contribute to the increased risk of ADHD. Also, the presence of AD in the absence of other allergic disease was associated with an increased risk for ADHD. Obesity, headaches, and anemia were found to further increase the risk for ADHD in those with AD.
Results from the adjusted multivariate models also established an increased risk for ADHD among adults with AD, for an adjusted odds ratio of 1.61. The presence of asthma, headaches, and insomnia increased this risk. The analysis additionally revealed that a body mass index indicative of underweight status in adults with AD was protective against the risk for developing ADHD.
Mr. Strom and his associates found a significant decrease in their initial odds ratios when they added outpatient health care visitation to their multivariate models, which resulted in an overall pooled odds ratio for the relationship between AD and ADHD just above statistical significance. They speculated that children with AD or ADHD would be more likely to visit health care providers, which could increase the likelihood for diagnosis of comorbid conditions.
Funding was provided by the Agency for Healthcare Research and Quality and the Dermatology Foundation. The authors reported no conflicts of interest.
Atopic dermatitis (AD) is associated with an increased risk for attention-deficit/hyperactivity disorder (ADHD) in children and adults, and a host of factors and comorbid conditions increase this risk, according to a study published in the British Journal of Dermatology.
Mark A. Strom and his associates at Northwestern University in Chicago examined data from 19 U.S. population-based surveys on 354,416 children ages 2-17 years and 34,613 adults over the age of 18 to determine if childhood and adult AD and the severity of AD were associated with ADHD. Additionally, the investigators sought to identify factors contributing to this association (Br J Dermatol. 2016 Apr 23. doi: 10.1111/bjd.14697).
The prevalence of ADHD was 9.4% in children with AD and 7.1% in children without AD. For children, the study results obtained from multivariate models adjusting for age, sex, sociodemographic variables, allergic disease, and health care utilization confirmed the previously established increase in risk for ADHD in those with AD for an adjusted odds ratio of 1.14. Severe AD and sleep disturbance were found to independently and synergistically contribute to the increased risk of ADHD. Also, the presence of AD in the absence of other allergic disease was associated with an increased risk for ADHD. Obesity, headaches, and anemia were found to further increase the risk for ADHD in those with AD.
Results from the adjusted multivariate models also established an increased risk for ADHD among adults with AD, for an adjusted odds ratio of 1.61. The presence of asthma, headaches, and insomnia increased this risk. The analysis additionally revealed that a body mass index indicative of underweight status in adults with AD was protective against the risk for developing ADHD.
Mr. Strom and his associates found a significant decrease in their initial odds ratios when they added outpatient health care visitation to their multivariate models, which resulted in an overall pooled odds ratio for the relationship between AD and ADHD just above statistical significance. They speculated that children with AD or ADHD would be more likely to visit health care providers, which could increase the likelihood for diagnosis of comorbid conditions.
Funding was provided by the Agency for Healthcare Research and Quality and the Dermatology Foundation. The authors reported no conflicts of interest.
FROM THE BRITISH JOURNAL OF DERMATOLOGY
Atopic dermatitis increases risk of ADHD, comorbidities add to it
Atopic dermatitis (AD) is associated with an increased risk for attention-deficit/hyperactivity disorder (ADHD) in children and adults, and a host of factors and comorbid conditions increase this risk, according to a study published in the British Journal of Dermatology.
Mark A. Strom and his associates at Northwestern University in Chicago examined data from 19 U.S. population-based surveys on 354,416 children ages 2-17 years and 34,613 adults over the age of 18 to determine if childhood and adult AD and the severity of AD were associated with ADHD. Additionally, the investigators sought to identify factors contributing to this association (Br J Dermatol. 2016 Apr 23. doi: 10.1111/bjd.14697).
The prevalence of ADHD was 9.4% in children with AD and 7.1% in children without AD. For children, the study results obtained from multivariate models adjusting for age, sex, sociodemographic variables, allergic disease, and health care utilization confirmed the previously established increase in risk for ADHD in those with AD for an adjusted odds ratio of 1.14. Severe AD and sleep disturbance were found to independently and synergistically contribute to the increased risk of ADHD. Also, the presence of AD in the absence of other allergic disease was associated with an increased risk for ADHD. Obesity, headaches, and anemia were found to further increase the risk for ADHD in those with AD.
Results from the adjusted multivariate models also established an increased risk for ADHD among adults with AD, for an adjusted odds ratio of 1.61. The presence of asthma, headaches, and insomnia increased this risk. The analysis additionally revealed that a body mass index indicative of underweight status in adults with AD was protective against the risk for developing ADHD.
Mr. Strom and his associates found a significant decrease in their initial odds ratios when they added outpatient health care visitation to their multivariate models, which resulted in an overall pooled odds ratio for the relationship between AD and ADHD just above statistical significance. They speculated that children with AD or ADHD would be more likely to visit health care providers, which could increase the likelihood for diagnosis of comorbid conditions.
Funding was provided by the Agency for Healthcare Research and Quality and the Dermatology Foundation. The authors reported no conflicts of interest.
Atopic dermatitis (AD) is associated with an increased risk for attention-deficit/hyperactivity disorder (ADHD) in children and adults, and a host of factors and comorbid conditions increase this risk, according to a study published in the British Journal of Dermatology.
Mark A. Strom and his associates at Northwestern University in Chicago examined data from 19 U.S. population-based surveys on 354,416 children ages 2-17 years and 34,613 adults over the age of 18 to determine if childhood and adult AD and the severity of AD were associated with ADHD. Additionally, the investigators sought to identify factors contributing to this association (Br J Dermatol. 2016 Apr 23. doi: 10.1111/bjd.14697).
The prevalence of ADHD was 9.4% in children with AD and 7.1% in children without AD. For children, the study results obtained from multivariate models adjusting for age, sex, sociodemographic variables, allergic disease, and health care utilization confirmed the previously established increase in risk for ADHD in those with AD for an adjusted odds ratio of 1.14. Severe AD and sleep disturbance were found to independently and synergistically contribute to the increased risk of ADHD. Also, the presence of AD in the absence of other allergic disease was associated with an increased risk for ADHD. Obesity, headaches, and anemia were found to further increase the risk for ADHD in those with AD.
Results from the adjusted multivariate models also established an increased risk for ADHD among adults with AD, for an adjusted odds ratio of 1.61. The presence of asthma, headaches, and insomnia increased this risk. The analysis additionally revealed that a body mass index indicative of underweight status in adults with AD was protective against the risk for developing ADHD.
Mr. Strom and his associates found a significant decrease in their initial odds ratios when they added outpatient health care visitation to their multivariate models, which resulted in an overall pooled odds ratio for the relationship between AD and ADHD just above statistical significance. They speculated that children with AD or ADHD would be more likely to visit health care providers, which could increase the likelihood for diagnosis of comorbid conditions.
Funding was provided by the Agency for Healthcare Research and Quality and the Dermatology Foundation. The authors reported no conflicts of interest.
Atopic dermatitis (AD) is associated with an increased risk for attention-deficit/hyperactivity disorder (ADHD) in children and adults, and a host of factors and comorbid conditions increase this risk, according to a study published in the British Journal of Dermatology.
Mark A. Strom and his associates at Northwestern University in Chicago examined data from 19 U.S. population-based surveys on 354,416 children ages 2-17 years and 34,613 adults over the age of 18 to determine if childhood and adult AD and the severity of AD were associated with ADHD. Additionally, the investigators sought to identify factors contributing to this association (Br J Dermatol. 2016 Apr 23. doi: 10.1111/bjd.14697).
The prevalence of ADHD was 9.4% in children with AD and 7.1% in children without AD. For children, the study results obtained from multivariate models adjusting for age, sex, sociodemographic variables, allergic disease, and health care utilization confirmed the previously established increase in risk for ADHD in those with AD for an adjusted odds ratio of 1.14. Severe AD and sleep disturbance were found to independently and synergistically contribute to the increased risk of ADHD. Also, the presence of AD in the absence of other allergic disease was associated with an increased risk for ADHD. Obesity, headaches, and anemia were found to further increase the risk for ADHD in those with AD.
Results from the adjusted multivariate models also established an increased risk for ADHD among adults with AD, for an adjusted odds ratio of 1.61. The presence of asthma, headaches, and insomnia increased this risk. The analysis additionally revealed that a body mass index indicative of underweight status in adults with AD was protective against the risk for developing ADHD.
Mr. Strom and his associates found a significant decrease in their initial odds ratios when they added outpatient health care visitation to their multivariate models, which resulted in an overall pooled odds ratio for the relationship between AD and ADHD just above statistical significance. They speculated that children with AD or ADHD would be more likely to visit health care providers, which could increase the likelihood for diagnosis of comorbid conditions.
Funding was provided by the Agency for Healthcare Research and Quality and the Dermatology Foundation. The authors reported no conflicts of interest.
FROM THE BRITISH JOURNAL OF DERMATOLOGY
Key clinical point: Several factors contribute to the increased risk for ADHD in children and adults with atopic dermatitis.
Major finding: Children and adults with atopic dermatitis had increased odds of having ADHD of 1.14, which were further increased by the presence of certain comorbidities.
Data sources: Nineteen U.S. population-based surveys on 354,416 children aged 2-17 and 34,613 adults over the age of 18.
Disclosures: Funding was provided by the Agency for Healthcare Research and Quality and the Dermatology Foundation. The authors reported no conflicts of interest.
Predictors of abnormal longitudinal patterns of lung-function growth and decline
When it comes to predictive demographic and clinical factors associated with abnormal patterns of lung growth and decline in those with persistent, mild-to-moderate asthma in childhood, male sex and childhood levels of lung function as assessed by the forced expiratory volume in 1 second (FEV1) make all the difference, according to the results of a study published in the New England Journal of Medicine.
“Determinants of abnormal patterns of FEV1 growth and decline are multifactorial and complex, and identification of factors associated with the timing of a decline from the maximal level requires longitudinal data,” said author Michael McGeachie, Ph.D., of Brigham and Women’s Hospital, Boston, and his colleagues.
To identify these determinants, particularly in those with asthma, Dr. McGeachie and colleagues analyzed longitudinal data from a subset of participants from the Childhood Asthma Management Program (CAMP) cohort who were followed from enrollment at the age of 5 to 12 years, into the third decade of life. The trajectory of lung growth and the decline from maximum growth in this large cohort of persons who had persistent, mild-to-moderate asthma in childhood were compared against those from persons without asthma who were participants in the third National Health and Nutrition Examination Survey. (N Engl J Med. 2016;374:1842-52).
Data from 684 participants from the CAMP cohort were assessed and 25% had normal lung-function growth without an early decline, 26% had normal growth and an early decline, 23% had reduced growth without an early decline, and 26% had reduced growth and an early decline. Results of the multinomial logistic-regression analysis of risk factors for abnormal patterns of lung growth and decline showed that the 26% of participants with reduced growth and an early decline had lower FEV1 lung function at enrollment and were more likely to be male, compared with those who had normal growth.
Additional study results indicated that 18% of the participants who had reduced lung-function growth, with or without an early decline, met the case definition for chronic obstructive pulmonary disease (COPD) based on the postbronchodilator spirometric criteria at an age of less than 30 years.
Based on their data, Dr. McGeachie and his colleagues said that detection of an abnormal trajectory by means of early and ongoing serial FEV1 monitoring may help identify children and young adults at risk for abnormal lung-function growth that could lead to chronic airflow obstruction in adulthood.
Funding for this project was provided by grants from the Parker B. Francis Foundation, the National Institutes of Health, the National Human Genome Research Institute, and the Human Frontier Science Program Organization. Dr. McGeachie reported grant support from one of the funding sources during the conduct of the study. Nineteen coauthors reported they had nothing to disclose and the remainder either reported grant support or ties to industry sources.
When it comes to predictive demographic and clinical factors associated with abnormal patterns of lung growth and decline in those with persistent, mild-to-moderate asthma in childhood, male sex and childhood levels of lung function as assessed by the forced expiratory volume in 1 second (FEV1) make all the difference, according to the results of a study published in the New England Journal of Medicine.
“Determinants of abnormal patterns of FEV1 growth and decline are multifactorial and complex, and identification of factors associated with the timing of a decline from the maximal level requires longitudinal data,” said author Michael McGeachie, Ph.D., of Brigham and Women’s Hospital, Boston, and his colleagues.
To identify these determinants, particularly in those with asthma, Dr. McGeachie and colleagues analyzed longitudinal data from a subset of participants from the Childhood Asthma Management Program (CAMP) cohort who were followed from enrollment at the age of 5 to 12 years, into the third decade of life. The trajectory of lung growth and the decline from maximum growth in this large cohort of persons who had persistent, mild-to-moderate asthma in childhood were compared against those from persons without asthma who were participants in the third National Health and Nutrition Examination Survey. (N Engl J Med. 2016;374:1842-52).
Data from 684 participants from the CAMP cohort were assessed and 25% had normal lung-function growth without an early decline, 26% had normal growth and an early decline, 23% had reduced growth without an early decline, and 26% had reduced growth and an early decline. Results of the multinomial logistic-regression analysis of risk factors for abnormal patterns of lung growth and decline showed that the 26% of participants with reduced growth and an early decline had lower FEV1 lung function at enrollment and were more likely to be male, compared with those who had normal growth.
Additional study results indicated that 18% of the participants who had reduced lung-function growth, with or without an early decline, met the case definition for chronic obstructive pulmonary disease (COPD) based on the postbronchodilator spirometric criteria at an age of less than 30 years.
Based on their data, Dr. McGeachie and his colleagues said that detection of an abnormal trajectory by means of early and ongoing serial FEV1 monitoring may help identify children and young adults at risk for abnormal lung-function growth that could lead to chronic airflow obstruction in adulthood.
Funding for this project was provided by grants from the Parker B. Francis Foundation, the National Institutes of Health, the National Human Genome Research Institute, and the Human Frontier Science Program Organization. Dr. McGeachie reported grant support from one of the funding sources during the conduct of the study. Nineteen coauthors reported they had nothing to disclose and the remainder either reported grant support or ties to industry sources.
When it comes to predictive demographic and clinical factors associated with abnormal patterns of lung growth and decline in those with persistent, mild-to-moderate asthma in childhood, male sex and childhood levels of lung function as assessed by the forced expiratory volume in 1 second (FEV1) make all the difference, according to the results of a study published in the New England Journal of Medicine.
“Determinants of abnormal patterns of FEV1 growth and decline are multifactorial and complex, and identification of factors associated with the timing of a decline from the maximal level requires longitudinal data,” said author Michael McGeachie, Ph.D., of Brigham and Women’s Hospital, Boston, and his colleagues.
To identify these determinants, particularly in those with asthma, Dr. McGeachie and colleagues analyzed longitudinal data from a subset of participants from the Childhood Asthma Management Program (CAMP) cohort who were followed from enrollment at the age of 5 to 12 years, into the third decade of life. The trajectory of lung growth and the decline from maximum growth in this large cohort of persons who had persistent, mild-to-moderate asthma in childhood were compared against those from persons without asthma who were participants in the third National Health and Nutrition Examination Survey. (N Engl J Med. 2016;374:1842-52).
Data from 684 participants from the CAMP cohort were assessed and 25% had normal lung-function growth without an early decline, 26% had normal growth and an early decline, 23% had reduced growth without an early decline, and 26% had reduced growth and an early decline. Results of the multinomial logistic-regression analysis of risk factors for abnormal patterns of lung growth and decline showed that the 26% of participants with reduced growth and an early decline had lower FEV1 lung function at enrollment and were more likely to be male, compared with those who had normal growth.
Additional study results indicated that 18% of the participants who had reduced lung-function growth, with or without an early decline, met the case definition for chronic obstructive pulmonary disease (COPD) based on the postbronchodilator spirometric criteria at an age of less than 30 years.
Based on their data, Dr. McGeachie and his colleagues said that detection of an abnormal trajectory by means of early and ongoing serial FEV1 monitoring may help identify children and young adults at risk for abnormal lung-function growth that could lead to chronic airflow obstruction in adulthood.
Funding for this project was provided by grants from the Parker B. Francis Foundation, the National Institutes of Health, the National Human Genome Research Institute, and the Human Frontier Science Program Organization. Dr. McGeachie reported grant support from one of the funding sources during the conduct of the study. Nineteen coauthors reported they had nothing to disclose and the remainder either reported grant support or ties to industry sources.
Key clinical point: Abnormal longitudinal patterns of lung-function growth in young asthma patients are associated with specific risk factors and may be related to development of COPD.
Major finding: Those with reduced lung growth and an early decline had a lower forced expiratory volume in 1 second lung function in childhood and were more likely to be male.
Data sources: A subset of participants from the Childhood Asthma Management Program cohort.
Disclosures: Funding for this project was provided by grants from the Parker B. Francis Foundation, the National Institutes of Health, the National Human Genome Research Institute, and the Human Frontier Science Program Organization. Dr. McGeachie reported grant support from one of the funding sources during the conduct of the study. Nineteen coauthors reported they had nothing to disclose and the remainder either reported grant support or ties to industry sources.
Azithromycin Fails to Ameliorate Treatment-resistant Cough
Azithromycin does not appear to be an effective agent for those with treatment-resistant cough, but may be useful in treating those with comorbid asthma, according to the results of a study published in Chest.
David Hodgson, Ph.D., from the Nottingham Respiratory Research Unit at the University of Nottingham (England), and colleagues conducted an 8-week randomized, double-blind, placebo-controlled parallel group trial with follow-up visits at 4, 8, and 12 weeks to determine whether treatment with low-dose azithromycin would affect the Leicester Cough Questionnaire (LCQ) score, cough severity on a visual analog scale, and fraction of exhaled nitric oxide (FENO) in patients with treatment-resistant chronic cough. (Chest. 2016 Apr;149[4]:1052-60. doi: 10.1016/j.chest.2015.12.036).
The study included 40 nonsmoking patients who were being investigated for chronic cough in respiratory clinics at Nottingham University Hospitals National Health Service Trust in the United Kingdom. Twenty patients were randomized to receive azithromycin capsules 500 mg daily for 3 days, followed by 250 mg three times a week for 8 weeks, and 20 received lactose-containing placebo capsules taken according to the same dosing schedule. The primary outcome measure was change from baseline in LCQ score at week 8.
The study results suggested differences in the primary endpoint in response to treatment with azithromycin; however, statistical significance was not detected after adjusting for baseline values. Ancillary analyses suggested that study subjects with asthma treated with azithromycin exhibited a large and statistically significant improvement in LCQ score when compared with those treated with placebo. This difference was detected at 4 weeks and was statistically significant at the end of the 8-week trial and at all follow-ups. There were no significant changes in FENO levels between any groups in this study, and treatment was considered to be well tolerated.
Based on their data, Dr. Hodgson and colleagues said that their results were not supportive of the routine use of low-dose macrolides in patients with treatment-resistant chronic cough. They also noted that data from their ancillary analyses were suggestive of an association between azithromycin treatment and improvement in LCQ in those with chronic cough and coexisting asthma that could be a focus of additional research.
Funding for this project was provided by a National Institute for Health Research Biomedical Research Fellowship. The authors reported no conflicts of interest.
Azithromycin does not appear to be an effective agent for those with treatment-resistant cough, but may be useful in treating those with comorbid asthma, according to the results of a study published in Chest.
David Hodgson, Ph.D., from the Nottingham Respiratory Research Unit at the University of Nottingham (England), and colleagues conducted an 8-week randomized, double-blind, placebo-controlled parallel group trial with follow-up visits at 4, 8, and 12 weeks to determine whether treatment with low-dose azithromycin would affect the Leicester Cough Questionnaire (LCQ) score, cough severity on a visual analog scale, and fraction of exhaled nitric oxide (FENO) in patients with treatment-resistant chronic cough. (Chest. 2016 Apr;149[4]:1052-60. doi: 10.1016/j.chest.2015.12.036).
The study included 40 nonsmoking patients who were being investigated for chronic cough in respiratory clinics at Nottingham University Hospitals National Health Service Trust in the United Kingdom. Twenty patients were randomized to receive azithromycin capsules 500 mg daily for 3 days, followed by 250 mg three times a week for 8 weeks, and 20 received lactose-containing placebo capsules taken according to the same dosing schedule. The primary outcome measure was change from baseline in LCQ score at week 8.
The study results suggested differences in the primary endpoint in response to treatment with azithromycin; however, statistical significance was not detected after adjusting for baseline values. Ancillary analyses suggested that study subjects with asthma treated with azithromycin exhibited a large and statistically significant improvement in LCQ score when compared with those treated with placebo. This difference was detected at 4 weeks and was statistically significant at the end of the 8-week trial and at all follow-ups. There were no significant changes in FENO levels between any groups in this study, and treatment was considered to be well tolerated.
Based on their data, Dr. Hodgson and colleagues said that their results were not supportive of the routine use of low-dose macrolides in patients with treatment-resistant chronic cough. They also noted that data from their ancillary analyses were suggestive of an association between azithromycin treatment and improvement in LCQ in those with chronic cough and coexisting asthma that could be a focus of additional research.
Funding for this project was provided by a National Institute for Health Research Biomedical Research Fellowship. The authors reported no conflicts of interest.
Azithromycin does not appear to be an effective agent for those with treatment-resistant cough, but may be useful in treating those with comorbid asthma, according to the results of a study published in Chest.
David Hodgson, Ph.D., from the Nottingham Respiratory Research Unit at the University of Nottingham (England), and colleagues conducted an 8-week randomized, double-blind, placebo-controlled parallel group trial with follow-up visits at 4, 8, and 12 weeks to determine whether treatment with low-dose azithromycin would affect the Leicester Cough Questionnaire (LCQ) score, cough severity on a visual analog scale, and fraction of exhaled nitric oxide (FENO) in patients with treatment-resistant chronic cough. (Chest. 2016 Apr;149[4]:1052-60. doi: 10.1016/j.chest.2015.12.036).
The study included 40 nonsmoking patients who were being investigated for chronic cough in respiratory clinics at Nottingham University Hospitals National Health Service Trust in the United Kingdom. Twenty patients were randomized to receive azithromycin capsules 500 mg daily for 3 days, followed by 250 mg three times a week for 8 weeks, and 20 received lactose-containing placebo capsules taken according to the same dosing schedule. The primary outcome measure was change from baseline in LCQ score at week 8.
The study results suggested differences in the primary endpoint in response to treatment with azithromycin; however, statistical significance was not detected after adjusting for baseline values. Ancillary analyses suggested that study subjects with asthma treated with azithromycin exhibited a large and statistically significant improvement in LCQ score when compared with those treated with placebo. This difference was detected at 4 weeks and was statistically significant at the end of the 8-week trial and at all follow-ups. There were no significant changes in FENO levels between any groups in this study, and treatment was considered to be well tolerated.
Based on their data, Dr. Hodgson and colleagues said that their results were not supportive of the routine use of low-dose macrolides in patients with treatment-resistant chronic cough. They also noted that data from their ancillary analyses were suggestive of an association between azithromycin treatment and improvement in LCQ in those with chronic cough and coexisting asthma that could be a focus of additional research.
Funding for this project was provided by a National Institute for Health Research Biomedical Research Fellowship. The authors reported no conflicts of interest.
FROM CHEST
Azithromycin fails to ameliorate treatment-resistant cough
Azithromycin does not appear to be an effective agent for those with treatment-resistant cough, but may be useful in treating those with comorbid asthma, according to the results of a study published in Chest.
David Hodgson, Ph.D., from the Nottingham Respiratory Research Unit at the University of Nottingham (England), and colleagues conducted an 8-week randomized, double-blind, placebo-controlled parallel group trial with follow-up visits at 4, 8, and 12 weeks to determine whether treatment with low-dose azithromycin would affect the Leicester Cough Questionnaire (LCQ) score, cough severity on a visual analog scale, and fraction of exhaled nitric oxide (FENO) in patients with treatment-resistant chronic cough. (Chest. 2016 Apr;149[4]:1052-60. doi: 10.1016/j.chest.2015.12.036).
The study included 40 nonsmoking patients who were being investigated for chronic cough in respiratory clinics at Nottingham University Hospitals National Health Service Trust in the United Kingdom. Twenty patients were randomized to receive azithromycin capsules 500 mg daily for 3 days, followed by 250 mg three times a week for 8 weeks, and 20 received lactose-containing placebo capsules taken according to the same dosing schedule. The primary outcome measure was change from baseline in LCQ score at week 8.
The study results suggested differences in the primary endpoint in response to treatment with azithromycin; however, statistical significance was not detected after adjusting for baseline values. Ancillary analyses suggested that study subjects with asthma treated with azithromycin exhibited a large and statistically significant improvement in LCQ score when compared with those treated with placebo. This difference was detected at 4 weeks and was statistically significant at the end of the 8-week trial and at all follow-ups. There were no significant changes in FENO levels between any groups in this study, and treatment was considered to be well tolerated.
Based on their data, Dr. Hodgson and colleagues said that their results were not supportive of the routine use of low-dose macrolides in patients with treatment-resistant chronic cough. They also noted that data from their ancillary analyses were suggestive of an association between azithromycin treatment and improvement in LCQ in those with chronic cough and coexisting asthma that could be a focus of additional research.
Funding for this project was provided by a National Institute for Health Research Biomedical Research Fellowship. The authors reported no conflicts of interest.
Azithromycin does not appear to be an effective agent for those with treatment-resistant cough, but may be useful in treating those with comorbid asthma, according to the results of a study published in Chest.
David Hodgson, Ph.D., from the Nottingham Respiratory Research Unit at the University of Nottingham (England), and colleagues conducted an 8-week randomized, double-blind, placebo-controlled parallel group trial with follow-up visits at 4, 8, and 12 weeks to determine whether treatment with low-dose azithromycin would affect the Leicester Cough Questionnaire (LCQ) score, cough severity on a visual analog scale, and fraction of exhaled nitric oxide (FENO) in patients with treatment-resistant chronic cough. (Chest. 2016 Apr;149[4]:1052-60. doi: 10.1016/j.chest.2015.12.036).
The study included 40 nonsmoking patients who were being investigated for chronic cough in respiratory clinics at Nottingham University Hospitals National Health Service Trust in the United Kingdom. Twenty patients were randomized to receive azithromycin capsules 500 mg daily for 3 days, followed by 250 mg three times a week for 8 weeks, and 20 received lactose-containing placebo capsules taken according to the same dosing schedule. The primary outcome measure was change from baseline in LCQ score at week 8.
The study results suggested differences in the primary endpoint in response to treatment with azithromycin; however, statistical significance was not detected after adjusting for baseline values. Ancillary analyses suggested that study subjects with asthma treated with azithromycin exhibited a large and statistically significant improvement in LCQ score when compared with those treated with placebo. This difference was detected at 4 weeks and was statistically significant at the end of the 8-week trial and at all follow-ups. There were no significant changes in FENO levels between any groups in this study, and treatment was considered to be well tolerated.
Based on their data, Dr. Hodgson and colleagues said that their results were not supportive of the routine use of low-dose macrolides in patients with treatment-resistant chronic cough. They also noted that data from their ancillary analyses were suggestive of an association between azithromycin treatment and improvement in LCQ in those with chronic cough and coexisting asthma that could be a focus of additional research.
Funding for this project was provided by a National Institute for Health Research Biomedical Research Fellowship. The authors reported no conflicts of interest.
Azithromycin does not appear to be an effective agent for those with treatment-resistant cough, but may be useful in treating those with comorbid asthma, according to the results of a study published in Chest.
David Hodgson, Ph.D., from the Nottingham Respiratory Research Unit at the University of Nottingham (England), and colleagues conducted an 8-week randomized, double-blind, placebo-controlled parallel group trial with follow-up visits at 4, 8, and 12 weeks to determine whether treatment with low-dose azithromycin would affect the Leicester Cough Questionnaire (LCQ) score, cough severity on a visual analog scale, and fraction of exhaled nitric oxide (FENO) in patients with treatment-resistant chronic cough. (Chest. 2016 Apr;149[4]:1052-60. doi: 10.1016/j.chest.2015.12.036).
The study included 40 nonsmoking patients who were being investigated for chronic cough in respiratory clinics at Nottingham University Hospitals National Health Service Trust in the United Kingdom. Twenty patients were randomized to receive azithromycin capsules 500 mg daily for 3 days, followed by 250 mg three times a week for 8 weeks, and 20 received lactose-containing placebo capsules taken according to the same dosing schedule. The primary outcome measure was change from baseline in LCQ score at week 8.
The study results suggested differences in the primary endpoint in response to treatment with azithromycin; however, statistical significance was not detected after adjusting for baseline values. Ancillary analyses suggested that study subjects with asthma treated with azithromycin exhibited a large and statistically significant improvement in LCQ score when compared with those treated with placebo. This difference was detected at 4 weeks and was statistically significant at the end of the 8-week trial and at all follow-ups. There were no significant changes in FENO levels between any groups in this study, and treatment was considered to be well tolerated.
Based on their data, Dr. Hodgson and colleagues said that their results were not supportive of the routine use of low-dose macrolides in patients with treatment-resistant chronic cough. They also noted that data from their ancillary analyses were suggestive of an association between azithromycin treatment and improvement in LCQ in those with chronic cough and coexisting asthma that could be a focus of additional research.
Funding for this project was provided by a National Institute for Health Research Biomedical Research Fellowship. The authors reported no conflicts of interest.
FROM CHEST
Key clinical point: This study did not support the clinical efficacy of low-dose macrolides for patients with treatment-resistant chronic cough.
Major finding: Leicester Cough Questionnaire scores did not differ significantly between the azithromycin and placebo groups after 8 weeks of treatment.
Data sources: Patients being investigated for chronic cough identified from respiratory clinics at Nottingham University Hospitals National Health Service Trust in the United Kingdom between July 2009 and August 2012.
Disclosures: Funding for this project was provided by a National Institute for Health Research Biomedical Research Fellowship. The authors reported no conflicts of interest.
Brodalumab effective for rare, severe types of psoriasis
The investigational interleukin-17 inhibitor brodalumab was safe and effective in a small phase III Japanese study of adults with two rare and severe types of psoriasis, generalized pustular psoriasis (GPP) and psoriatic erythroderma (PsE). The results were published in the British Journal of Dermatology.
The 52-week open label studyevaluated the safety and efficacy of brodalumab in 30 Japanese adults (mean age 48 years) with GPP (12 patients) and PsE (18 patients). Brodalumab, a human monoclonal antibody against human IL-17RA that blocks the biologic activities of IL-17, was administered by subcutaneous injection. Efficacy was assessed via Clinical Global Impression of Improvement (CGI) scores, the primary endpoint (Br J Dermatol. 2016 April 23. doi: 10.1111/bjd.14702).
A high proportion of patients with either disease achieved “improved” or “remission” CGI scores at weeks 2, 12, and 52, reported Dr. Kenshi Yamasaki, of the department of dermatology at Tohoku University, Miyagi, Japan, and his associates
At week 52, almost 92% of those with GPP and 100% of those with PsE had achieved “improved” or “remission” scores. The most common adverse event was nasopharyngitis, which occurred in one-third of patients. Infection-related adverse events were grade 1 or 2, no adverse events were fatal, and none of the five serious adverse events noted were considered to be attributable to treatment, they added. Although anti-brodalumab neutralizing antibodies were not detected, one patient tested positive for anti-brodalumab binding antibodies.
Noting that treatment with brodalumab has been associated with significant improvements in patients with plaque psoriasis and psoriatic arthritis in phase II and III studies, “results from this study confirm that brodalumab can improve patient symptoms not long after treatment is initiated,” in patients with GPP and PsE, the authors concluded. While acknowledging the study limitations, including the open label design and a small sample size, they added, “IL-17RA blocking will be a promising therapeutic target in patients with GPP and PsE.”
The safety profile and low expression of anti-brodalumab antibodies indicated that brodalumab was suitable for long-term use, they said.
The study was funded by Kyowa Hakko Kirin. All authors disclosed ties to pharmaceutical companies, including the funding source; one author is an employee of the company.
The investigational interleukin-17 inhibitor brodalumab was safe and effective in a small phase III Japanese study of adults with two rare and severe types of psoriasis, generalized pustular psoriasis (GPP) and psoriatic erythroderma (PsE). The results were published in the British Journal of Dermatology.
The 52-week open label studyevaluated the safety and efficacy of brodalumab in 30 Japanese adults (mean age 48 years) with GPP (12 patients) and PsE (18 patients). Brodalumab, a human monoclonal antibody against human IL-17RA that blocks the biologic activities of IL-17, was administered by subcutaneous injection. Efficacy was assessed via Clinical Global Impression of Improvement (CGI) scores, the primary endpoint (Br J Dermatol. 2016 April 23. doi: 10.1111/bjd.14702).
A high proportion of patients with either disease achieved “improved” or “remission” CGI scores at weeks 2, 12, and 52, reported Dr. Kenshi Yamasaki, of the department of dermatology at Tohoku University, Miyagi, Japan, and his associates
At week 52, almost 92% of those with GPP and 100% of those with PsE had achieved “improved” or “remission” scores. The most common adverse event was nasopharyngitis, which occurred in one-third of patients. Infection-related adverse events were grade 1 or 2, no adverse events were fatal, and none of the five serious adverse events noted were considered to be attributable to treatment, they added. Although anti-brodalumab neutralizing antibodies were not detected, one patient tested positive for anti-brodalumab binding antibodies.
Noting that treatment with brodalumab has been associated with significant improvements in patients with plaque psoriasis and psoriatic arthritis in phase II and III studies, “results from this study confirm that brodalumab can improve patient symptoms not long after treatment is initiated,” in patients with GPP and PsE, the authors concluded. While acknowledging the study limitations, including the open label design and a small sample size, they added, “IL-17RA blocking will be a promising therapeutic target in patients with GPP and PsE.”
The safety profile and low expression of anti-brodalumab antibodies indicated that brodalumab was suitable for long-term use, they said.
The study was funded by Kyowa Hakko Kirin. All authors disclosed ties to pharmaceutical companies, including the funding source; one author is an employee of the company.
The investigational interleukin-17 inhibitor brodalumab was safe and effective in a small phase III Japanese study of adults with two rare and severe types of psoriasis, generalized pustular psoriasis (GPP) and psoriatic erythroderma (PsE). The results were published in the British Journal of Dermatology.
The 52-week open label studyevaluated the safety and efficacy of brodalumab in 30 Japanese adults (mean age 48 years) with GPP (12 patients) and PsE (18 patients). Brodalumab, a human monoclonal antibody against human IL-17RA that blocks the biologic activities of IL-17, was administered by subcutaneous injection. Efficacy was assessed via Clinical Global Impression of Improvement (CGI) scores, the primary endpoint (Br J Dermatol. 2016 April 23. doi: 10.1111/bjd.14702).
A high proportion of patients with either disease achieved “improved” or “remission” CGI scores at weeks 2, 12, and 52, reported Dr. Kenshi Yamasaki, of the department of dermatology at Tohoku University, Miyagi, Japan, and his associates
At week 52, almost 92% of those with GPP and 100% of those with PsE had achieved “improved” or “remission” scores. The most common adverse event was nasopharyngitis, which occurred in one-third of patients. Infection-related adverse events were grade 1 or 2, no adverse events were fatal, and none of the five serious adverse events noted were considered to be attributable to treatment, they added. Although anti-brodalumab neutralizing antibodies were not detected, one patient tested positive for anti-brodalumab binding antibodies.
Noting that treatment with brodalumab has been associated with significant improvements in patients with plaque psoriasis and psoriatic arthritis in phase II and III studies, “results from this study confirm that brodalumab can improve patient symptoms not long after treatment is initiated,” in patients with GPP and PsE, the authors concluded. While acknowledging the study limitations, including the open label design and a small sample size, they added, “IL-17RA blocking will be a promising therapeutic target in patients with GPP and PsE.”
The safety profile and low expression of anti-brodalumab antibodies indicated that brodalumab was suitable for long-term use, they said.
The study was funded by Kyowa Hakko Kirin. All authors disclosed ties to pharmaceutical companies, including the funding source; one author is an employee of the company.
FROM THE BRITISH JOURNAL OF DERMATOLOGY
Key clinical point: The interluekin-17 inhibitor brodalumab significantly improved symptoms of generalized pustular psoriasis and psoriatic erythroderma in a small, Japanese open label study.
Major finding: Almost all brodalumab-treated patients with generalized pustular psoriasis (GPP) or psoriatic erythroderma (PsE) showed high levels of clinical improvement and low levels of adverse events.
Data sources: The phase III open-label multicenter study evaluated the safety and efficacy of brodalumab in 30 adults with GPP or PsE over 52 weeks.
Disclosures: Funding was provided by Kyowa Hakko Kirin. All authors disclosed ties to industry sources, including the funding source.
Neighborhood demographics linked with NSCLC treatment and survival
The demographic characteristics of neighborhoods are associated with the odds of receiving surgical treatment for early non–small-cell lung cancer (NSCLC), according to a study published in Cancer Epidemiology, Biomarkers & Prevention.
Living in areas with higher economic deprivation was associated with lower odds of receiving surgery for both black and white patients, in a retrospective study of 8,322 patients with early-stage NSCLC.
“The results of this study are intended to bring importance to segregation and other characteristics as determinants of lung cancer outcomes. As a result, what is learned from these epidemiologic findings can be applied to interventions and public policies to improve patient outcomes and contribute to the difficult and complex task of reducing racial health disparities,” wrote Dr. Asal M. Johnson of Stetson University and her associates (Cancer Epidemiol Biomarkers Prev; 25[5];750-8).
The early-stage NSCLC patients were identified in the Georgia Comprehensive Cancer Registry from 2000 to 2009 to determine the effects of residential segregation and other neighborhood characteristics on the odds of receiving surgical treatment and the risk of death based on 5-year survival.
Three separate multilevel models were employed: A, economic deprivation; B, segregation; and C, segregation and economic deprivation. Individual-level variables (age, sex, and tumor grade) and area-level variables (place of residence, educational attainment, and elderly concentration) were controlled for in all models.
Regarding odds of surgical intervention, model A showed that living in areas with higher economic deprivation was associated with lower odds of receiving surgery for both black and white patients. Model B demonstrated that living in highly segregated areas was associated with lower odds of receiving surgery among black patients only. For white patients, no significant associations were observed between living in areas with combined segregation-deprivation and receipt of surgery using model C; however, living in segregated areas, regardless of the level of economic deprivation, was associated with decreased odds of receiving surgery for black patients.
As for 5-year survival, all three models indicated no effects of economic deprivation, segregation, or the combination of segregation and deprivation on survival among white patients. Models A and B showed no effects of economic deprivation or segregation on survival in black patients. In model C, however, the combination of high residential segregation and high economic deprivation was associated with a 31% higher risk of death in these patients, even after surgery.
Funding was provided by Stetson University. The authors reported no conflicts of interest.
The demographic characteristics of neighborhoods are associated with the odds of receiving surgical treatment for early non–small-cell lung cancer (NSCLC), according to a study published in Cancer Epidemiology, Biomarkers & Prevention.
Living in areas with higher economic deprivation was associated with lower odds of receiving surgery for both black and white patients, in a retrospective study of 8,322 patients with early-stage NSCLC.
“The results of this study are intended to bring importance to segregation and other characteristics as determinants of lung cancer outcomes. As a result, what is learned from these epidemiologic findings can be applied to interventions and public policies to improve patient outcomes and contribute to the difficult and complex task of reducing racial health disparities,” wrote Dr. Asal M. Johnson of Stetson University and her associates (Cancer Epidemiol Biomarkers Prev; 25[5];750-8).
The early-stage NSCLC patients were identified in the Georgia Comprehensive Cancer Registry from 2000 to 2009 to determine the effects of residential segregation and other neighborhood characteristics on the odds of receiving surgical treatment and the risk of death based on 5-year survival.
Three separate multilevel models were employed: A, economic deprivation; B, segregation; and C, segregation and economic deprivation. Individual-level variables (age, sex, and tumor grade) and area-level variables (place of residence, educational attainment, and elderly concentration) were controlled for in all models.
Regarding odds of surgical intervention, model A showed that living in areas with higher economic deprivation was associated with lower odds of receiving surgery for both black and white patients. Model B demonstrated that living in highly segregated areas was associated with lower odds of receiving surgery among black patients only. For white patients, no significant associations were observed between living in areas with combined segregation-deprivation and receipt of surgery using model C; however, living in segregated areas, regardless of the level of economic deprivation, was associated with decreased odds of receiving surgery for black patients.
As for 5-year survival, all three models indicated no effects of economic deprivation, segregation, or the combination of segregation and deprivation on survival among white patients. Models A and B showed no effects of economic deprivation or segregation on survival in black patients. In model C, however, the combination of high residential segregation and high economic deprivation was associated with a 31% higher risk of death in these patients, even after surgery.
Funding was provided by Stetson University. The authors reported no conflicts of interest.
The demographic characteristics of neighborhoods are associated with the odds of receiving surgical treatment for early non–small-cell lung cancer (NSCLC), according to a study published in Cancer Epidemiology, Biomarkers & Prevention.
Living in areas with higher economic deprivation was associated with lower odds of receiving surgery for both black and white patients, in a retrospective study of 8,322 patients with early-stage NSCLC.
“The results of this study are intended to bring importance to segregation and other characteristics as determinants of lung cancer outcomes. As a result, what is learned from these epidemiologic findings can be applied to interventions and public policies to improve patient outcomes and contribute to the difficult and complex task of reducing racial health disparities,” wrote Dr. Asal M. Johnson of Stetson University and her associates (Cancer Epidemiol Biomarkers Prev; 25[5];750-8).
The early-stage NSCLC patients were identified in the Georgia Comprehensive Cancer Registry from 2000 to 2009 to determine the effects of residential segregation and other neighborhood characteristics on the odds of receiving surgical treatment and the risk of death based on 5-year survival.
Three separate multilevel models were employed: A, economic deprivation; B, segregation; and C, segregation and economic deprivation. Individual-level variables (age, sex, and tumor grade) and area-level variables (place of residence, educational attainment, and elderly concentration) were controlled for in all models.
Regarding odds of surgical intervention, model A showed that living in areas with higher economic deprivation was associated with lower odds of receiving surgery for both black and white patients. Model B demonstrated that living in highly segregated areas was associated with lower odds of receiving surgery among black patients only. For white patients, no significant associations were observed between living in areas with combined segregation-deprivation and receipt of surgery using model C; however, living in segregated areas, regardless of the level of economic deprivation, was associated with decreased odds of receiving surgery for black patients.
As for 5-year survival, all three models indicated no effects of economic deprivation, segregation, or the combination of segregation and deprivation on survival among white patients. Models A and B showed no effects of economic deprivation or segregation on survival in black patients. In model C, however, the combination of high residential segregation and high economic deprivation was associated with a 31% higher risk of death in these patients, even after surgery.
Funding was provided by Stetson University. The authors reported no conflicts of interest.
FROM CANCER EPIDEMIOLOGY, BIOMARKERS & PREVENTION
Key clinical point: Neighborhood characteristics are linked with lung cancer treatment and outcomes.
Major finding: Patients with non–small-cell lung cancer living in areas with high levels of racial segregation had decreased odds of receiving surgery.
Data sources: Patients in the Georgia Comprehensive Cancer Registry diagnosed with non–small-cell lung cancer from January 2000 to December 2009.
Disclosures: Funding was provided by Stetson University. The authors reported no conflicts of interest.