User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
Clinical trials: Top priority for long COVID
The Centers for Disease Control and Prevention and the U.S. Census Bureau estimate that 6.1% of the U.S. adult population is living with long COVID, with millions more debilitated worldwide. The demand for substantial treatment is enormous, but the urgency to fund and begin the necessary range of clinical trials has not met the severity of the problem.
While trials are slowly beginning to happen, the treatment choices and trial design require crucial nuances and understanding of viral-onset illnesses, and few research groups are creating strong trials that fully reflect the complexities of this landscape.
These recommendations recognize that roughly half of long COVID patients have new-onset myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) and dysautonomia from COVID, which must be at the forefront of how trials are designed and conducted, and are additionally based on the current hypotheses about long COVID’s pathophysiologies.
1: Drugs proposed by experts in postviral fields should be prioritized
Upward of 50 drugs for viral-onset conditions like ME/CFS, dysautonomia, AIDS, and others have been waiting for years to go to trial, but have not had the funding to do so.
Treatments proposed by experts in viral-onset illnesses (such as ME/CFS and dysautonomia) should be prioritized (PM R. 2022 Oct;14[10]:1270-91), as outside researchers are not familiar with these fields and their potential treatment options.
2: Drugs targeting a wide range of mechanisms should be trialed
Treatments that should be trialed include anticoagulants/antiplatelets for clotting and vascular functioning, immunomodulators including JAK-STAT inhibitors, COVID-specific antivirals and antivirals against reactivated herpesviruses (Valcyte, Valacyclovir, EBV vaccine).
Other options include prescription mast cell stabilizers (ketotifen, cromolyn sodium), drugs that regulate microglial activation (low-dose naltrexone, low-dose aripiprazole), anti-CGRP medications, beta-blockers, and intravenous immunoglobulin.
Others include medications that target mitochondrial dysfunction; ivabradine; pyridostigmine;, DRP1 inhibitors; supplements showing success in patient communities including lactoferrin, ubiquinone, and nattokinase; and therapies targeting glymphatic/lymphatic dysfunction, microbiome therapies, and therapeutic peptides.
3: Use appropriate long COVID subtypes
Long COVID is an umbrella term that encompasses multiple new-onset and worsened conditions and symptoms after COVID. Roughly half of long COVID patients likely meet the criteria for ME/CFS and/or dysautonomia. Others may have new-onset diabetes, major clotting events, lung damage, neurological disorders, loss of smell or taste, and other manifestations.
Patients in different categories likely have different responses to treatments. It’s critical to identify appropriate subtypes for each trial, ideally performing detailed analyses to identify the treatments that work best, and don’t, for each subtype.
4: Behavioral treatments, especially those that have harmed similar populations, should not be trialed
Behavioral treatments including exercise, graded exercise therapy (GET), and cognitive-behavioral therapy (CBT) should not be trialed, let alone prioritized, for long COVID.
In patients with postexertional malaise (PEM), one of the most common long COVID symptoms, exercise is actively harmful and causes dysfunctional metabolic patterns, cardiac preload failure, impaired systemic oxygen extraction, and more. GET and CBT have failed similar populations , and exercise is explicitly contraindicated by the World Health Organization, the British National Institute for Health and Care Excellence, the CDC, and other organizations.
Resources should instead be put toward the wide range of medications that have not yet adequately undergone clinical trials.
5: PCR and antibody tests should not be used as inclusion criteria for trial participants
Only an estimated 1%-3% of cases in the first wave of COVID were documented, and the CDC estimates that only 25% of cases through September 2021 were documented. Similarly, antibody tests are unreliable to determine past infection, as roughly a third of patients don’t seroconvert, and a similar proportion serorevert within a few months. Using polymerase chain reaction (PCR) and antibody testing to determine who should be included in clinical trials limits who is eligible to participate in research, particularly those who have been ill for longer. Additionally, the majority of those who serorevert are women, so using antibody tests for inclusion introduces a selection bias and may miss mechanisms of immune system functioning that are part of long COVID.
PCR tests also have high false-negative rates and requiring them in research excludes people with lower viral loads with long COVID, which would confound findings.
These issues with testing also lead to COVID-infected people accidentally being included in control groups, which ruins the credibility of the research findings completely.
6: Include comparator groups
There are several common diagnoses that occur in people with long COVID, including ME/CFS, postural orthostatic tachycardia syndrome, small-fiber neuropathy, mast cell activation syndrome, and Ehlers-Danlos syndrome.
Identifying people with these conditions within the trial cohort improves research across all fields, benefiting all groups, and helps clarify what types of patients benefit most from certain medications.
7: Identify the right endpoints; avoid the wrong ones
Even though our understanding of the pathophysiology of long COVID is still evolving, it’s still possible to do clinical trials by identifying strong endpoints and outcome measures.
Several tools have been designed for viral-onset conditions and should be used alongside other endpoints. Postexertional malaise and autonomic symptoms, which are some of the most common symptoms of long COVID, can be measured with the validated DSQ-PEM and COMPASS-31, respectively. Tools for cognitive dysfunction trials should capture specific and common types of impairment, like processing speed.
Endpoints should be high-impact and aim for large improvements that have clinical significance over small improvements that do not have clinical significance.
Objective tests should be incorporated where possible; some to consider include natural killer cell functioning, cerebral blood flow, T-cell functioning, levels of reactivated herpesviruses, blood lactate levels, and microclots, as testing becomes available.
Mental health outcomes shouldn’t be primary endpoints, except where a trial is targeting a specific mental health condition because of COVID (for example, premenstrual dysphoric disorder).
If mental health conditions are tracked secondarily, it’s vital not to use questionnaires that include physical symptoms like fatigue, difficulty concentrating, difficulty sleeping, or palpitations, as these artificially increase depression and anxiety scores in chronically ill respondents. Tools that include physical symptoms (Patient Health Questionnaire–9, Beck Anxiety Inventory, Beck Depression Inventory) can be replaced with scales like the PHQ-2, General Anxiety Disorder–7, Hospital Anxiety and Depression Scale, or PROMIS-29 subscales.
Because certain cytokines and other inflammatory markers may naturally decrease over time without corresponding improvement in the ME/CFS subtype, caution should be taken when using cytokines as endpoints.
8: Consider enrollment and objectives carefully
A proportion of people with long COVID will recover in the early months after infection. Ideally, clinical trials will primarily study treatments in patients who have been ill 6 months or longer, as some natural recovery will happen before that can bias studies.
But where resources are abundant, it is ideal for trials to additionally look at whether the treatments can help patients in the early months recover and prevent progression to the later stage.
9: Tracking illness duration is crucial
Research from ME/CFS shows that there may be an immune change in the first few years of the illness, where cytokines decrease without any corresponding change in symptom improvement.
Because of this and the possibility that other markers follow the same pattern, disease duration should be a core feature of all analyses and trial designs. Trial outcomes should be designed to answer the question of whether the medication helps patients at different durations of illness.
10: Prioritize patient populations less likely to recover without intervention
Some long COVID phenotypes seem less likely to recover without intervention. Trials should take care to focus on these patient populations, which include those with neurologic symptoms and those meeting ME/CFS criteria.
11: Account for the relapsing/remitting nature
Outcome measures need to be assessed in a way that can distinguish a temporary remission, which is part of the natural course of the disease, from a permanent cure.
Factors that can contribute to the relapsing/remitting nature include physical and cognitive postexertional malaise, menstrual cycle changes, and seasonal changes.
12: Trial participants should reflect the diversity of the long COVID population
Certain demographics are more likely to be affected by acute and long COVID and need to be appropriately recruited and reflected in research, including in patient engagement.
Trials must include high numbers of Hispanic/Latinx, Black, and indigenous communities, queer and transgender populations, and women. Trial materials and design need to incorporate linguistic diversity in addition to racial/ethnic diversity.
Upward of 75% of long COVID cases happen after mild acute cases; clinical researchers should ensure that nonhospitalized patients make up the bulk of trial participants.
13: Utilize meaningful engagement of patients, especially in treatment selection and study design
Meaningful patient engagement means engaging multiple patients at every step of the trial process, from treatment selection to study design to analysis to communication of the results.
Patient experiences are extremely valuable and contain information that researchers may not be familiar with, including the nature and patterns of the illness, insights into possible treatments, and barriers to documentation and care that may also impact research. Tapping into those patient experiences will make trials stronger.
Overall, the landscape of long COVID clinical trials is ripe for discovery, and researchers choosing to go down this path will be deeply appreciated by the patient community.
Hannah Davis is a long COVID patient-researcher and cofounder of the Patient-Led Research Collaborative, an organization studying the long-term effects of COVID.
A version of this article first appeared on Medscape.com.
The Centers for Disease Control and Prevention and the U.S. Census Bureau estimate that 6.1% of the U.S. adult population is living with long COVID, with millions more debilitated worldwide. The demand for substantial treatment is enormous, but the urgency to fund and begin the necessary range of clinical trials has not met the severity of the problem.
While trials are slowly beginning to happen, the treatment choices and trial design require crucial nuances and understanding of viral-onset illnesses, and few research groups are creating strong trials that fully reflect the complexities of this landscape.
These recommendations recognize that roughly half of long COVID patients have new-onset myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) and dysautonomia from COVID, which must be at the forefront of how trials are designed and conducted, and are additionally based on the current hypotheses about long COVID’s pathophysiologies.
1: Drugs proposed by experts in postviral fields should be prioritized
Upward of 50 drugs for viral-onset conditions like ME/CFS, dysautonomia, AIDS, and others have been waiting for years to go to trial, but have not had the funding to do so.
Treatments proposed by experts in viral-onset illnesses (such as ME/CFS and dysautonomia) should be prioritized (PM R. 2022 Oct;14[10]:1270-91), as outside researchers are not familiar with these fields and their potential treatment options.
2: Drugs targeting a wide range of mechanisms should be trialed
Treatments that should be trialed include anticoagulants/antiplatelets for clotting and vascular functioning, immunomodulators including JAK-STAT inhibitors, COVID-specific antivirals and antivirals against reactivated herpesviruses (Valcyte, Valacyclovir, EBV vaccine).
Other options include prescription mast cell stabilizers (ketotifen, cromolyn sodium), drugs that regulate microglial activation (low-dose naltrexone, low-dose aripiprazole), anti-CGRP medications, beta-blockers, and intravenous immunoglobulin.
Others include medications that target mitochondrial dysfunction; ivabradine; pyridostigmine;, DRP1 inhibitors; supplements showing success in patient communities including lactoferrin, ubiquinone, and nattokinase; and therapies targeting glymphatic/lymphatic dysfunction, microbiome therapies, and therapeutic peptides.
3: Use appropriate long COVID subtypes
Long COVID is an umbrella term that encompasses multiple new-onset and worsened conditions and symptoms after COVID. Roughly half of long COVID patients likely meet the criteria for ME/CFS and/or dysautonomia. Others may have new-onset diabetes, major clotting events, lung damage, neurological disorders, loss of smell or taste, and other manifestations.
Patients in different categories likely have different responses to treatments. It’s critical to identify appropriate subtypes for each trial, ideally performing detailed analyses to identify the treatments that work best, and don’t, for each subtype.
4: Behavioral treatments, especially those that have harmed similar populations, should not be trialed
Behavioral treatments including exercise, graded exercise therapy (GET), and cognitive-behavioral therapy (CBT) should not be trialed, let alone prioritized, for long COVID.
In patients with postexertional malaise (PEM), one of the most common long COVID symptoms, exercise is actively harmful and causes dysfunctional metabolic patterns, cardiac preload failure, impaired systemic oxygen extraction, and more. GET and CBT have failed similar populations , and exercise is explicitly contraindicated by the World Health Organization, the British National Institute for Health and Care Excellence, the CDC, and other organizations.
Resources should instead be put toward the wide range of medications that have not yet adequately undergone clinical trials.
5: PCR and antibody tests should not be used as inclusion criteria for trial participants
Only an estimated 1%-3% of cases in the first wave of COVID were documented, and the CDC estimates that only 25% of cases through September 2021 were documented. Similarly, antibody tests are unreliable to determine past infection, as roughly a third of patients don’t seroconvert, and a similar proportion serorevert within a few months. Using polymerase chain reaction (PCR) and antibody testing to determine who should be included in clinical trials limits who is eligible to participate in research, particularly those who have been ill for longer. Additionally, the majority of those who serorevert are women, so using antibody tests for inclusion introduces a selection bias and may miss mechanisms of immune system functioning that are part of long COVID.
PCR tests also have high false-negative rates and requiring them in research excludes people with lower viral loads with long COVID, which would confound findings.
These issues with testing also lead to COVID-infected people accidentally being included in control groups, which ruins the credibility of the research findings completely.
6: Include comparator groups
There are several common diagnoses that occur in people with long COVID, including ME/CFS, postural orthostatic tachycardia syndrome, small-fiber neuropathy, mast cell activation syndrome, and Ehlers-Danlos syndrome.
Identifying people with these conditions within the trial cohort improves research across all fields, benefiting all groups, and helps clarify what types of patients benefit most from certain medications.
7: Identify the right endpoints; avoid the wrong ones
Even though our understanding of the pathophysiology of long COVID is still evolving, it’s still possible to do clinical trials by identifying strong endpoints and outcome measures.
Several tools have been designed for viral-onset conditions and should be used alongside other endpoints. Postexertional malaise and autonomic symptoms, which are some of the most common symptoms of long COVID, can be measured with the validated DSQ-PEM and COMPASS-31, respectively. Tools for cognitive dysfunction trials should capture specific and common types of impairment, like processing speed.
Endpoints should be high-impact and aim for large improvements that have clinical significance over small improvements that do not have clinical significance.
Objective tests should be incorporated where possible; some to consider include natural killer cell functioning, cerebral blood flow, T-cell functioning, levels of reactivated herpesviruses, blood lactate levels, and microclots, as testing becomes available.
Mental health outcomes shouldn’t be primary endpoints, except where a trial is targeting a specific mental health condition because of COVID (for example, premenstrual dysphoric disorder).
If mental health conditions are tracked secondarily, it’s vital not to use questionnaires that include physical symptoms like fatigue, difficulty concentrating, difficulty sleeping, or palpitations, as these artificially increase depression and anxiety scores in chronically ill respondents. Tools that include physical symptoms (Patient Health Questionnaire–9, Beck Anxiety Inventory, Beck Depression Inventory) can be replaced with scales like the PHQ-2, General Anxiety Disorder–7, Hospital Anxiety and Depression Scale, or PROMIS-29 subscales.
Because certain cytokines and other inflammatory markers may naturally decrease over time without corresponding improvement in the ME/CFS subtype, caution should be taken when using cytokines as endpoints.
8: Consider enrollment and objectives carefully
A proportion of people with long COVID will recover in the early months after infection. Ideally, clinical trials will primarily study treatments in patients who have been ill 6 months or longer, as some natural recovery will happen before that can bias studies.
But where resources are abundant, it is ideal for trials to additionally look at whether the treatments can help patients in the early months recover and prevent progression to the later stage.
9: Tracking illness duration is crucial
Research from ME/CFS shows that there may be an immune change in the first few years of the illness, where cytokines decrease without any corresponding change in symptom improvement.
Because of this and the possibility that other markers follow the same pattern, disease duration should be a core feature of all analyses and trial designs. Trial outcomes should be designed to answer the question of whether the medication helps patients at different durations of illness.
10: Prioritize patient populations less likely to recover without intervention
Some long COVID phenotypes seem less likely to recover without intervention. Trials should take care to focus on these patient populations, which include those with neurologic symptoms and those meeting ME/CFS criteria.
11: Account for the relapsing/remitting nature
Outcome measures need to be assessed in a way that can distinguish a temporary remission, which is part of the natural course of the disease, from a permanent cure.
Factors that can contribute to the relapsing/remitting nature include physical and cognitive postexertional malaise, menstrual cycle changes, and seasonal changes.
12: Trial participants should reflect the diversity of the long COVID population
Certain demographics are more likely to be affected by acute and long COVID and need to be appropriately recruited and reflected in research, including in patient engagement.
Trials must include high numbers of Hispanic/Latinx, Black, and indigenous communities, queer and transgender populations, and women. Trial materials and design need to incorporate linguistic diversity in addition to racial/ethnic diversity.
Upward of 75% of long COVID cases happen after mild acute cases; clinical researchers should ensure that nonhospitalized patients make up the bulk of trial participants.
13: Utilize meaningful engagement of patients, especially in treatment selection and study design
Meaningful patient engagement means engaging multiple patients at every step of the trial process, from treatment selection to study design to analysis to communication of the results.
Patient experiences are extremely valuable and contain information that researchers may not be familiar with, including the nature and patterns of the illness, insights into possible treatments, and barriers to documentation and care that may also impact research. Tapping into those patient experiences will make trials stronger.
Overall, the landscape of long COVID clinical trials is ripe for discovery, and researchers choosing to go down this path will be deeply appreciated by the patient community.
Hannah Davis is a long COVID patient-researcher and cofounder of the Patient-Led Research Collaborative, an organization studying the long-term effects of COVID.
A version of this article first appeared on Medscape.com.
The Centers for Disease Control and Prevention and the U.S. Census Bureau estimate that 6.1% of the U.S. adult population is living with long COVID, with millions more debilitated worldwide. The demand for substantial treatment is enormous, but the urgency to fund and begin the necessary range of clinical trials has not met the severity of the problem.
While trials are slowly beginning to happen, the treatment choices and trial design require crucial nuances and understanding of viral-onset illnesses, and few research groups are creating strong trials that fully reflect the complexities of this landscape.
These recommendations recognize that roughly half of long COVID patients have new-onset myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) and dysautonomia from COVID, which must be at the forefront of how trials are designed and conducted, and are additionally based on the current hypotheses about long COVID’s pathophysiologies.
1: Drugs proposed by experts in postviral fields should be prioritized
Upward of 50 drugs for viral-onset conditions like ME/CFS, dysautonomia, AIDS, and others have been waiting for years to go to trial, but have not had the funding to do so.
Treatments proposed by experts in viral-onset illnesses (such as ME/CFS and dysautonomia) should be prioritized (PM R. 2022 Oct;14[10]:1270-91), as outside researchers are not familiar with these fields and their potential treatment options.
2: Drugs targeting a wide range of mechanisms should be trialed
Treatments that should be trialed include anticoagulants/antiplatelets for clotting and vascular functioning, immunomodulators including JAK-STAT inhibitors, COVID-specific antivirals and antivirals against reactivated herpesviruses (Valcyte, Valacyclovir, EBV vaccine).
Other options include prescription mast cell stabilizers (ketotifen, cromolyn sodium), drugs that regulate microglial activation (low-dose naltrexone, low-dose aripiprazole), anti-CGRP medications, beta-blockers, and intravenous immunoglobulin.
Others include medications that target mitochondrial dysfunction; ivabradine; pyridostigmine;, DRP1 inhibitors; supplements showing success in patient communities including lactoferrin, ubiquinone, and nattokinase; and therapies targeting glymphatic/lymphatic dysfunction, microbiome therapies, and therapeutic peptides.
3: Use appropriate long COVID subtypes
Long COVID is an umbrella term that encompasses multiple new-onset and worsened conditions and symptoms after COVID. Roughly half of long COVID patients likely meet the criteria for ME/CFS and/or dysautonomia. Others may have new-onset diabetes, major clotting events, lung damage, neurological disorders, loss of smell or taste, and other manifestations.
Patients in different categories likely have different responses to treatments. It’s critical to identify appropriate subtypes for each trial, ideally performing detailed analyses to identify the treatments that work best, and don’t, for each subtype.
4: Behavioral treatments, especially those that have harmed similar populations, should not be trialed
Behavioral treatments including exercise, graded exercise therapy (GET), and cognitive-behavioral therapy (CBT) should not be trialed, let alone prioritized, for long COVID.
In patients with postexertional malaise (PEM), one of the most common long COVID symptoms, exercise is actively harmful and causes dysfunctional metabolic patterns, cardiac preload failure, impaired systemic oxygen extraction, and more. GET and CBT have failed similar populations , and exercise is explicitly contraindicated by the World Health Organization, the British National Institute for Health and Care Excellence, the CDC, and other organizations.
Resources should instead be put toward the wide range of medications that have not yet adequately undergone clinical trials.
5: PCR and antibody tests should not be used as inclusion criteria for trial participants
Only an estimated 1%-3% of cases in the first wave of COVID were documented, and the CDC estimates that only 25% of cases through September 2021 were documented. Similarly, antibody tests are unreliable to determine past infection, as roughly a third of patients don’t seroconvert, and a similar proportion serorevert within a few months. Using polymerase chain reaction (PCR) and antibody testing to determine who should be included in clinical trials limits who is eligible to participate in research, particularly those who have been ill for longer. Additionally, the majority of those who serorevert are women, so using antibody tests for inclusion introduces a selection bias and may miss mechanisms of immune system functioning that are part of long COVID.
PCR tests also have high false-negative rates and requiring them in research excludes people with lower viral loads with long COVID, which would confound findings.
These issues with testing also lead to COVID-infected people accidentally being included in control groups, which ruins the credibility of the research findings completely.
6: Include comparator groups
There are several common diagnoses that occur in people with long COVID, including ME/CFS, postural orthostatic tachycardia syndrome, small-fiber neuropathy, mast cell activation syndrome, and Ehlers-Danlos syndrome.
Identifying people with these conditions within the trial cohort improves research across all fields, benefiting all groups, and helps clarify what types of patients benefit most from certain medications.
7: Identify the right endpoints; avoid the wrong ones
Even though our understanding of the pathophysiology of long COVID is still evolving, it’s still possible to do clinical trials by identifying strong endpoints and outcome measures.
Several tools have been designed for viral-onset conditions and should be used alongside other endpoints. Postexertional malaise and autonomic symptoms, which are some of the most common symptoms of long COVID, can be measured with the validated DSQ-PEM and COMPASS-31, respectively. Tools for cognitive dysfunction trials should capture specific and common types of impairment, like processing speed.
Endpoints should be high-impact and aim for large improvements that have clinical significance over small improvements that do not have clinical significance.
Objective tests should be incorporated where possible; some to consider include natural killer cell functioning, cerebral blood flow, T-cell functioning, levels of reactivated herpesviruses, blood lactate levels, and microclots, as testing becomes available.
Mental health outcomes shouldn’t be primary endpoints, except where a trial is targeting a specific mental health condition because of COVID (for example, premenstrual dysphoric disorder).
If mental health conditions are tracked secondarily, it’s vital not to use questionnaires that include physical symptoms like fatigue, difficulty concentrating, difficulty sleeping, or palpitations, as these artificially increase depression and anxiety scores in chronically ill respondents. Tools that include physical symptoms (Patient Health Questionnaire–9, Beck Anxiety Inventory, Beck Depression Inventory) can be replaced with scales like the PHQ-2, General Anxiety Disorder–7, Hospital Anxiety and Depression Scale, or PROMIS-29 subscales.
Because certain cytokines and other inflammatory markers may naturally decrease over time without corresponding improvement in the ME/CFS subtype, caution should be taken when using cytokines as endpoints.
8: Consider enrollment and objectives carefully
A proportion of people with long COVID will recover in the early months after infection. Ideally, clinical trials will primarily study treatments in patients who have been ill 6 months or longer, as some natural recovery will happen before that can bias studies.
But where resources are abundant, it is ideal for trials to additionally look at whether the treatments can help patients in the early months recover and prevent progression to the later stage.
9: Tracking illness duration is crucial
Research from ME/CFS shows that there may be an immune change in the first few years of the illness, where cytokines decrease without any corresponding change in symptom improvement.
Because of this and the possibility that other markers follow the same pattern, disease duration should be a core feature of all analyses and trial designs. Trial outcomes should be designed to answer the question of whether the medication helps patients at different durations of illness.
10: Prioritize patient populations less likely to recover without intervention
Some long COVID phenotypes seem less likely to recover without intervention. Trials should take care to focus on these patient populations, which include those with neurologic symptoms and those meeting ME/CFS criteria.
11: Account for the relapsing/remitting nature
Outcome measures need to be assessed in a way that can distinguish a temporary remission, which is part of the natural course of the disease, from a permanent cure.
Factors that can contribute to the relapsing/remitting nature include physical and cognitive postexertional malaise, menstrual cycle changes, and seasonal changes.
12: Trial participants should reflect the diversity of the long COVID population
Certain demographics are more likely to be affected by acute and long COVID and need to be appropriately recruited and reflected in research, including in patient engagement.
Trials must include high numbers of Hispanic/Latinx, Black, and indigenous communities, queer and transgender populations, and women. Trial materials and design need to incorporate linguistic diversity in addition to racial/ethnic diversity.
Upward of 75% of long COVID cases happen after mild acute cases; clinical researchers should ensure that nonhospitalized patients make up the bulk of trial participants.
13: Utilize meaningful engagement of patients, especially in treatment selection and study design
Meaningful patient engagement means engaging multiple patients at every step of the trial process, from treatment selection to study design to analysis to communication of the results.
Patient experiences are extremely valuable and contain information that researchers may not be familiar with, including the nature and patterns of the illness, insights into possible treatments, and barriers to documentation and care that may also impact research. Tapping into those patient experiences will make trials stronger.
Overall, the landscape of long COVID clinical trials is ripe for discovery, and researchers choosing to go down this path will be deeply appreciated by the patient community.
Hannah Davis is a long COVID patient-researcher and cofounder of the Patient-Led Research Collaborative, an organization studying the long-term effects of COVID.
A version of this article first appeared on Medscape.com.
Colchicine’s 2010 price spike had major impact on gout care
A large price increase for colchicine in 2010 led to a significant falloff in its use for gout that persisted for the next decade while emergency and rheumatology visits for gout rose, suggesting poorer disease control, a retrospective cohort study reported.
The price of colchicine, commonly prescribed for acute gout attacks, climbed from $11.25 per prescription in 2009 to $190.49 in 2011, with the average out-of-pocket cost more than quadrupling, from $7.37 to $29.42, the study noted. Colchicine prescriptions for gout declined 27% over the next decade, according to adjusted analyses that the study authors performed.
“A roughly 16-fold increase in colchicine prices appeared to have lowered colchicine use over the next decade,” senior author Zirui Song, MD, PhD, an associate professor of health care policy and medicine at Harvard Medical School and an internist at Massachusetts General Hospital in Boston, told this news organization in written comments. “Over the same period, patients with gout used more of other medications that could treat gout. They also had more emergency department visits for gout and rheumatologist visits for gout, which potentially signals poorer disease control.”
The study, published online in JAMA Internal Medicine, examined MarketScan data from a longitudinal cohort of patients who had employer-sponsored health insurance and a diagnosis of gout from 2007 to 2019. MarketScan is an IBM database of medical and drug data from employers and health plans. The study examined more than 2.7 million patient-year observations over the 13-year period.
How the price increase happened
After 2011, a large percentage of patients shifted to less effective but more affordable drugs to treat gout. Prescriptions for allopurinol increased 32% (P < .001) and oral corticosteroids 8.3% over the decade. “These are imperfect substitutes,” Dr. Song said. “Allopurinol is used to prevent gout, while oral corticosteroids can be used to treat a gout flare.”
At the same time, visits for gout-related complaints to emergency departments and rheumatology offices increased through the ensuing years: 39.8% and 10.5% on an adjusted analysis, respectively (P < .001 for both).
Colchicine is actually a drug that predates the creation of the U.S. Food and Drug Administration in 1938 and had been grandfathered under its Unapproved Drug Initiative. Then in 2009, the FDA determined that colchicine was effective for treating arthritis-related gout flares after the manufacturer, URL Pharma, presented results of a randomized, controlled trial of 185 patients with gout.
The next year, the FDA granted URL Pharma 3 years of market exclusivity for the drug under the brand name Colcrys, now trademarked by Takeda Pharmaceuticals.
The latest study noted that longer-term analysis of the impact of the FDA’s decision had been lacking. The goal, said Dr. Song, was “to better understand the long-run implications of large drug price increases in the U.S. by studying the case of colchicine.”
He added, “For drugs that lack competition, large price increases can have large economic and clinical consequences over many years.”
Absorbing the cost
Lead author Dan P. Ly, MD, PhD, MPP, assistant professor at the University of California, Los Angeles, added, “Our study has large implications [for] when generic medications or other medications experience large price increases. Use of the medication in question drops or patients have to pay more out of pocket, and patient health can suffer as a result.”
The dropoff in colchicine use in this patient population could have been worse, Dr. Song said. “Despite colchicine use decreasing by 27% over nearly a decade, the fact that it did not decline more suggests that for patients with gout, the large price increase was mostly absorbed by their insurers, employers, or themselves – e.g., passed through to higher premiums, lower wages, or higher cost-sharing.”
Aaron Kesselheim, MD, JD, MPH, a professor at Harvard Medical School, Boston, reported previously on the price consequences of colchicine early on after the FDA granted the manufacturer market exclusivity.
“In our past research, we looked at how the massive increase in the price of colchicine increased spending on the drug and reduced use in a relatively short time period after the price hike,” said Dr. Kesselheim, who was not involved in this current study by Dr. Ly, Dr. Song, and Mia Giuriato, BBA, MA, from Harvard Medical School. “This study evaluated the experiences of patients with gout over multiple years and showed that the reductions in use persisted and were associated with increases in ED and rheumatology visits, suggesting worsening control of gout due to the relative inaccessibility of the drug at the new high price.”
The latest findings have public policy implications, Dr. Kesselheim said. “In the case of colchicine, the FDA made a bad pitch, leading to a home run for the manufacturer and a shutout for patients.”
“The FDA needs to make sure to take into account the quite predictable patient effects that can result from disruptions to competition when it considers taking steps like it did in the colchicine case to disrupt the market and create an artificial monopoly, even if the FDA acted in the best of intentions in this case,” Dr. Kesselheim added.
Dr. Song received funding for the study from the National Institutes of Health and Arnold Ventures. He also disclosed receiving personal fees from the Research Triangle Institute, Google Ventures, VBID Health, and the International Foundation of Employee Benefit Plans. Dr. Ly, Ms. Giuriato, and Dr. Kesselheim report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A large price increase for colchicine in 2010 led to a significant falloff in its use for gout that persisted for the next decade while emergency and rheumatology visits for gout rose, suggesting poorer disease control, a retrospective cohort study reported.
The price of colchicine, commonly prescribed for acute gout attacks, climbed from $11.25 per prescription in 2009 to $190.49 in 2011, with the average out-of-pocket cost more than quadrupling, from $7.37 to $29.42, the study noted. Colchicine prescriptions for gout declined 27% over the next decade, according to adjusted analyses that the study authors performed.
“A roughly 16-fold increase in colchicine prices appeared to have lowered colchicine use over the next decade,” senior author Zirui Song, MD, PhD, an associate professor of health care policy and medicine at Harvard Medical School and an internist at Massachusetts General Hospital in Boston, told this news organization in written comments. “Over the same period, patients with gout used more of other medications that could treat gout. They also had more emergency department visits for gout and rheumatologist visits for gout, which potentially signals poorer disease control.”
The study, published online in JAMA Internal Medicine, examined MarketScan data from a longitudinal cohort of patients who had employer-sponsored health insurance and a diagnosis of gout from 2007 to 2019. MarketScan is an IBM database of medical and drug data from employers and health plans. The study examined more than 2.7 million patient-year observations over the 13-year period.
How the price increase happened
After 2011, a large percentage of patients shifted to less effective but more affordable drugs to treat gout. Prescriptions for allopurinol increased 32% (P < .001) and oral corticosteroids 8.3% over the decade. “These are imperfect substitutes,” Dr. Song said. “Allopurinol is used to prevent gout, while oral corticosteroids can be used to treat a gout flare.”
At the same time, visits for gout-related complaints to emergency departments and rheumatology offices increased through the ensuing years: 39.8% and 10.5% on an adjusted analysis, respectively (P < .001 for both).
Colchicine is actually a drug that predates the creation of the U.S. Food and Drug Administration in 1938 and had been grandfathered under its Unapproved Drug Initiative. Then in 2009, the FDA determined that colchicine was effective for treating arthritis-related gout flares after the manufacturer, URL Pharma, presented results of a randomized, controlled trial of 185 patients with gout.
The next year, the FDA granted URL Pharma 3 years of market exclusivity for the drug under the brand name Colcrys, now trademarked by Takeda Pharmaceuticals.
The latest study noted that longer-term analysis of the impact of the FDA’s decision had been lacking. The goal, said Dr. Song, was “to better understand the long-run implications of large drug price increases in the U.S. by studying the case of colchicine.”
He added, “For drugs that lack competition, large price increases can have large economic and clinical consequences over many years.”
Absorbing the cost
Lead author Dan P. Ly, MD, PhD, MPP, assistant professor at the University of California, Los Angeles, added, “Our study has large implications [for] when generic medications or other medications experience large price increases. Use of the medication in question drops or patients have to pay more out of pocket, and patient health can suffer as a result.”
The dropoff in colchicine use in this patient population could have been worse, Dr. Song said. “Despite colchicine use decreasing by 27% over nearly a decade, the fact that it did not decline more suggests that for patients with gout, the large price increase was mostly absorbed by their insurers, employers, or themselves – e.g., passed through to higher premiums, lower wages, or higher cost-sharing.”
Aaron Kesselheim, MD, JD, MPH, a professor at Harvard Medical School, Boston, reported previously on the price consequences of colchicine early on after the FDA granted the manufacturer market exclusivity.
“In our past research, we looked at how the massive increase in the price of colchicine increased spending on the drug and reduced use in a relatively short time period after the price hike,” said Dr. Kesselheim, who was not involved in this current study by Dr. Ly, Dr. Song, and Mia Giuriato, BBA, MA, from Harvard Medical School. “This study evaluated the experiences of patients with gout over multiple years and showed that the reductions in use persisted and were associated with increases in ED and rheumatology visits, suggesting worsening control of gout due to the relative inaccessibility of the drug at the new high price.”
The latest findings have public policy implications, Dr. Kesselheim said. “In the case of colchicine, the FDA made a bad pitch, leading to a home run for the manufacturer and a shutout for patients.”
“The FDA needs to make sure to take into account the quite predictable patient effects that can result from disruptions to competition when it considers taking steps like it did in the colchicine case to disrupt the market and create an artificial monopoly, even if the FDA acted in the best of intentions in this case,” Dr. Kesselheim added.
Dr. Song received funding for the study from the National Institutes of Health and Arnold Ventures. He also disclosed receiving personal fees from the Research Triangle Institute, Google Ventures, VBID Health, and the International Foundation of Employee Benefit Plans. Dr. Ly, Ms. Giuriato, and Dr. Kesselheim report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A large price increase for colchicine in 2010 led to a significant falloff in its use for gout that persisted for the next decade while emergency and rheumatology visits for gout rose, suggesting poorer disease control, a retrospective cohort study reported.
The price of colchicine, commonly prescribed for acute gout attacks, climbed from $11.25 per prescription in 2009 to $190.49 in 2011, with the average out-of-pocket cost more than quadrupling, from $7.37 to $29.42, the study noted. Colchicine prescriptions for gout declined 27% over the next decade, according to adjusted analyses that the study authors performed.
“A roughly 16-fold increase in colchicine prices appeared to have lowered colchicine use over the next decade,” senior author Zirui Song, MD, PhD, an associate professor of health care policy and medicine at Harvard Medical School and an internist at Massachusetts General Hospital in Boston, told this news organization in written comments. “Over the same period, patients with gout used more of other medications that could treat gout. They also had more emergency department visits for gout and rheumatologist visits for gout, which potentially signals poorer disease control.”
The study, published online in JAMA Internal Medicine, examined MarketScan data from a longitudinal cohort of patients who had employer-sponsored health insurance and a diagnosis of gout from 2007 to 2019. MarketScan is an IBM database of medical and drug data from employers and health plans. The study examined more than 2.7 million patient-year observations over the 13-year period.
How the price increase happened
After 2011, a large percentage of patients shifted to less effective but more affordable drugs to treat gout. Prescriptions for allopurinol increased 32% (P < .001) and oral corticosteroids 8.3% over the decade. “These are imperfect substitutes,” Dr. Song said. “Allopurinol is used to prevent gout, while oral corticosteroids can be used to treat a gout flare.”
At the same time, visits for gout-related complaints to emergency departments and rheumatology offices increased through the ensuing years: 39.8% and 10.5% on an adjusted analysis, respectively (P < .001 for both).
Colchicine is actually a drug that predates the creation of the U.S. Food and Drug Administration in 1938 and had been grandfathered under its Unapproved Drug Initiative. Then in 2009, the FDA determined that colchicine was effective for treating arthritis-related gout flares after the manufacturer, URL Pharma, presented results of a randomized, controlled trial of 185 patients with gout.
The next year, the FDA granted URL Pharma 3 years of market exclusivity for the drug under the brand name Colcrys, now trademarked by Takeda Pharmaceuticals.
The latest study noted that longer-term analysis of the impact of the FDA’s decision had been lacking. The goal, said Dr. Song, was “to better understand the long-run implications of large drug price increases in the U.S. by studying the case of colchicine.”
He added, “For drugs that lack competition, large price increases can have large economic and clinical consequences over many years.”
Absorbing the cost
Lead author Dan P. Ly, MD, PhD, MPP, assistant professor at the University of California, Los Angeles, added, “Our study has large implications [for] when generic medications or other medications experience large price increases. Use of the medication in question drops or patients have to pay more out of pocket, and patient health can suffer as a result.”
The dropoff in colchicine use in this patient population could have been worse, Dr. Song said. “Despite colchicine use decreasing by 27% over nearly a decade, the fact that it did not decline more suggests that for patients with gout, the large price increase was mostly absorbed by their insurers, employers, or themselves – e.g., passed through to higher premiums, lower wages, or higher cost-sharing.”
Aaron Kesselheim, MD, JD, MPH, a professor at Harvard Medical School, Boston, reported previously on the price consequences of colchicine early on after the FDA granted the manufacturer market exclusivity.
“In our past research, we looked at how the massive increase in the price of colchicine increased spending on the drug and reduced use in a relatively short time period after the price hike,” said Dr. Kesselheim, who was not involved in this current study by Dr. Ly, Dr. Song, and Mia Giuriato, BBA, MA, from Harvard Medical School. “This study evaluated the experiences of patients with gout over multiple years and showed that the reductions in use persisted and were associated with increases in ED and rheumatology visits, suggesting worsening control of gout due to the relative inaccessibility of the drug at the new high price.”
The latest findings have public policy implications, Dr. Kesselheim said. “In the case of colchicine, the FDA made a bad pitch, leading to a home run for the manufacturer and a shutout for patients.”
“The FDA needs to make sure to take into account the quite predictable patient effects that can result from disruptions to competition when it considers taking steps like it did in the colchicine case to disrupt the market and create an artificial monopoly, even if the FDA acted in the best of intentions in this case,” Dr. Kesselheim added.
Dr. Song received funding for the study from the National Institutes of Health and Arnold Ventures. He also disclosed receiving personal fees from the Research Triangle Institute, Google Ventures, VBID Health, and the International Foundation of Employee Benefit Plans. Dr. Ly, Ms. Giuriato, and Dr. Kesselheim report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Study of hospitalizations in Canada quantifies benefit of COVID-19 vaccine to reduce death, ICU admissions
A cohort study of more than 1.5 million hospital admissions in Canada through the first 2 years of the COVID-19 pandemic has quantified the benefit of vaccinations. Unvaccinated patients were found to be up to 15 times more likely to die from COVID-19 than fully vaccinated patients.
Investigators analyzed 1.513 million admissions at 155 hospitals across Canada from March 15, 2020, to May 28, 2022. The study included 51,679 adult admissions and 4,035 pediatric admissions for COVID-19. Although the share of COVID-19 admissions increased in the fifth and sixth waves, from Dec. 26, 2021, to March 19, 2022 – after the full vaccine rollout – to 7.73% from 2.47% in the previous four waves, the proportion of adults admitted to the intensive care unit was significantly lower, at 8.7% versus 21.8% (odds ratio, 0.35; 95% confidence interval, 0.32-0.36).
“The good thing about waves five and six was we were able to show the COVID cases tended to be less severe, but on the other hand, because the disease in the community was so much higher, the demands on the health care system were much higher than the previous waves,” study author Charles Frenette, MD, director of infection prevention and control at McGill University, Montreal, and chair of the study’s adult subgroup, said in an interview. “But here we were able to show the benefit of vaccinations, particularly the boosting dose, in protecting against those severe outcomes.”
The study, published in JAMA Network Open, used the Canadian Nosocomial Infection Surveillance Program database, which collects hospital data across Canada. It was activated in March 2020 to collect details on all COVID-19 admissions, co-author Nisha Thampi, MD, chair of the study’s pediatric subgroup, told this news organization.
“We’re now over 3 years into the pandemic, and CNISP continues to monitor COVID-19 as well as other pathogens in near real time,” said Dr. Thampi, an associate professor and infectious disease specialist at Children’s Hospital of Eastern Ontario.
“That’s a particular strength of this surveillance program as well. We would see this data on a biweekly basis, and that allows for [us] to implement timely protection and action.”
Tracing trends over six waves
The study tracked COVID-19 hospitalizations during six waves. The first lasted from March 15 to August 31, 2020, and the second lasted from Sept. 1, 2020, to Feb. 28, 2021. The wild-type variant was dominant during both waves. The third wave lasted from March 1 to June 30, 2021, and was marked by the mixed Alpha, Beta, and Gamma variants. The fourth wave lasted from July 1 to Dec. 25, 2021, when the Alpha variant was dominant. The Omicron variant dominated during waves five (Dec. 26, 2021, to March 19, 2022) and six (March 20 to May 28, 2022).
Hospitalizations reached a peak of 14,461 in wave five. ICU admissions, however, peaked at 2,164 during wave four, and all-cause deaths peaked at 1,663 during wave two.
The investigators also analyzed how unvaccinated patients fared, compared with the fully vaccinated and the fully vaccinated-plus (that is, patients with one or more additional doses). During waves five and six, unvaccinated patients were 4.3 times more likely to end up in the ICU than fully vaccinated patients and were 12.2 times more likely than fully vaccinated-plus patients. Likewise, the rate for all-cause in-hospital death for unvaccinated patients was 3.9 times greater than that for fully vaccinated patients and 15.1 times greater than that for fully vaccinated-plus patients.
The effect of vaccines emerged in waves three and four, said Dr. Frenette. “We started to see really, really significant protection and benefit from the vaccine, not only in incidence of admission but also in the incidence of complications of ICU care, ventilation, and mortality.”
Results for pediatric patients were similar to those for adults, Dr. Thampi noted. During waves five and six, overall admissions peaked, but the share of ICU admissions decreased to 9.4% from 18.1%, which was the rate during the previous four waves (OR, 0.47).
“What’s important is how pediatric hospitalizations changed over the course of the various waves,” said Dr. Thampi.
“Where we saw the highest admissions during the early Omicron dominance, we actually had the lowest numbers of hospitalizations with death and admissions into ICUs.”
Doing more with the data
David Fisman, MD, MPH, a professor of epidemiology at the University of Toronto, said, “This is a study that shows us how tremendously dramatic the effects of the COVID-19 vaccine were in terms of saving lives during the pandemic.” Dr. Fisman was not involved in the study.
But CNISP, which receives funding from Public Health Agency of Canada, could do more with the data it collects to better protect the public from COVID-19 and other nosocomial infections, Dr. Fisman said.
“The first problematic thing about this paper is that Canadians are paying for a surveillance system that looks at risks of acquiring infections, including COVID-19 infections, in the hospital, but that data is not fed back to the people paying for its production,” he said.
“So, Canadians don’t have the ability to really understand in real time how much risk they’re experiencing via going to the hospital for some other reason.”
The study was independently supported. Dr. Frenette and Dr. Thampi report no relevant financial relationships. Dr. Fisman has disclosed financial relationships with Pfizer, AstraZeneca, Sanofi, Seqirus, Merck, the Ontario Nurses Association, and the Elementary Teachers’ Federation of Ontario.
A version of this article first appeared on Medscape.com.
A cohort study of more than 1.5 million hospital admissions in Canada through the first 2 years of the COVID-19 pandemic has quantified the benefit of vaccinations. Unvaccinated patients were found to be up to 15 times more likely to die from COVID-19 than fully vaccinated patients.
Investigators analyzed 1.513 million admissions at 155 hospitals across Canada from March 15, 2020, to May 28, 2022. The study included 51,679 adult admissions and 4,035 pediatric admissions for COVID-19. Although the share of COVID-19 admissions increased in the fifth and sixth waves, from Dec. 26, 2021, to March 19, 2022 – after the full vaccine rollout – to 7.73% from 2.47% in the previous four waves, the proportion of adults admitted to the intensive care unit was significantly lower, at 8.7% versus 21.8% (odds ratio, 0.35; 95% confidence interval, 0.32-0.36).
“The good thing about waves five and six was we were able to show the COVID cases tended to be less severe, but on the other hand, because the disease in the community was so much higher, the demands on the health care system were much higher than the previous waves,” study author Charles Frenette, MD, director of infection prevention and control at McGill University, Montreal, and chair of the study’s adult subgroup, said in an interview. “But here we were able to show the benefit of vaccinations, particularly the boosting dose, in protecting against those severe outcomes.”
The study, published in JAMA Network Open, used the Canadian Nosocomial Infection Surveillance Program database, which collects hospital data across Canada. It was activated in March 2020 to collect details on all COVID-19 admissions, co-author Nisha Thampi, MD, chair of the study’s pediatric subgroup, told this news organization.
“We’re now over 3 years into the pandemic, and CNISP continues to monitor COVID-19 as well as other pathogens in near real time,” said Dr. Thampi, an associate professor and infectious disease specialist at Children’s Hospital of Eastern Ontario.
“That’s a particular strength of this surveillance program as well. We would see this data on a biweekly basis, and that allows for [us] to implement timely protection and action.”
Tracing trends over six waves
The study tracked COVID-19 hospitalizations during six waves. The first lasted from March 15 to August 31, 2020, and the second lasted from Sept. 1, 2020, to Feb. 28, 2021. The wild-type variant was dominant during both waves. The third wave lasted from March 1 to June 30, 2021, and was marked by the mixed Alpha, Beta, and Gamma variants. The fourth wave lasted from July 1 to Dec. 25, 2021, when the Alpha variant was dominant. The Omicron variant dominated during waves five (Dec. 26, 2021, to March 19, 2022) and six (March 20 to May 28, 2022).
Hospitalizations reached a peak of 14,461 in wave five. ICU admissions, however, peaked at 2,164 during wave four, and all-cause deaths peaked at 1,663 during wave two.
The investigators also analyzed how unvaccinated patients fared, compared with the fully vaccinated and the fully vaccinated-plus (that is, patients with one or more additional doses). During waves five and six, unvaccinated patients were 4.3 times more likely to end up in the ICU than fully vaccinated patients and were 12.2 times more likely than fully vaccinated-plus patients. Likewise, the rate for all-cause in-hospital death for unvaccinated patients was 3.9 times greater than that for fully vaccinated patients and 15.1 times greater than that for fully vaccinated-plus patients.
The effect of vaccines emerged in waves three and four, said Dr. Frenette. “We started to see really, really significant protection and benefit from the vaccine, not only in incidence of admission but also in the incidence of complications of ICU care, ventilation, and mortality.”
Results for pediatric patients were similar to those for adults, Dr. Thampi noted. During waves five and six, overall admissions peaked, but the share of ICU admissions decreased to 9.4% from 18.1%, which was the rate during the previous four waves (OR, 0.47).
“What’s important is how pediatric hospitalizations changed over the course of the various waves,” said Dr. Thampi.
“Where we saw the highest admissions during the early Omicron dominance, we actually had the lowest numbers of hospitalizations with death and admissions into ICUs.”
Doing more with the data
David Fisman, MD, MPH, a professor of epidemiology at the University of Toronto, said, “This is a study that shows us how tremendously dramatic the effects of the COVID-19 vaccine were in terms of saving lives during the pandemic.” Dr. Fisman was not involved in the study.
But CNISP, which receives funding from Public Health Agency of Canada, could do more with the data it collects to better protect the public from COVID-19 and other nosocomial infections, Dr. Fisman said.
“The first problematic thing about this paper is that Canadians are paying for a surveillance system that looks at risks of acquiring infections, including COVID-19 infections, in the hospital, but that data is not fed back to the people paying for its production,” he said.
“So, Canadians don’t have the ability to really understand in real time how much risk they’re experiencing via going to the hospital for some other reason.”
The study was independently supported. Dr. Frenette and Dr. Thampi report no relevant financial relationships. Dr. Fisman has disclosed financial relationships with Pfizer, AstraZeneca, Sanofi, Seqirus, Merck, the Ontario Nurses Association, and the Elementary Teachers’ Federation of Ontario.
A version of this article first appeared on Medscape.com.
A cohort study of more than 1.5 million hospital admissions in Canada through the first 2 years of the COVID-19 pandemic has quantified the benefit of vaccinations. Unvaccinated patients were found to be up to 15 times more likely to die from COVID-19 than fully vaccinated patients.
Investigators analyzed 1.513 million admissions at 155 hospitals across Canada from March 15, 2020, to May 28, 2022. The study included 51,679 adult admissions and 4,035 pediatric admissions for COVID-19. Although the share of COVID-19 admissions increased in the fifth and sixth waves, from Dec. 26, 2021, to March 19, 2022 – after the full vaccine rollout – to 7.73% from 2.47% in the previous four waves, the proportion of adults admitted to the intensive care unit was significantly lower, at 8.7% versus 21.8% (odds ratio, 0.35; 95% confidence interval, 0.32-0.36).
“The good thing about waves five and six was we were able to show the COVID cases tended to be less severe, but on the other hand, because the disease in the community was so much higher, the demands on the health care system were much higher than the previous waves,” study author Charles Frenette, MD, director of infection prevention and control at McGill University, Montreal, and chair of the study’s adult subgroup, said in an interview. “But here we were able to show the benefit of vaccinations, particularly the boosting dose, in protecting against those severe outcomes.”
The study, published in JAMA Network Open, used the Canadian Nosocomial Infection Surveillance Program database, which collects hospital data across Canada. It was activated in March 2020 to collect details on all COVID-19 admissions, co-author Nisha Thampi, MD, chair of the study’s pediatric subgroup, told this news organization.
“We’re now over 3 years into the pandemic, and CNISP continues to monitor COVID-19 as well as other pathogens in near real time,” said Dr. Thampi, an associate professor and infectious disease specialist at Children’s Hospital of Eastern Ontario.
“That’s a particular strength of this surveillance program as well. We would see this data on a biweekly basis, and that allows for [us] to implement timely protection and action.”
Tracing trends over six waves
The study tracked COVID-19 hospitalizations during six waves. The first lasted from March 15 to August 31, 2020, and the second lasted from Sept. 1, 2020, to Feb. 28, 2021. The wild-type variant was dominant during both waves. The third wave lasted from March 1 to June 30, 2021, and was marked by the mixed Alpha, Beta, and Gamma variants. The fourth wave lasted from July 1 to Dec. 25, 2021, when the Alpha variant was dominant. The Omicron variant dominated during waves five (Dec. 26, 2021, to March 19, 2022) and six (March 20 to May 28, 2022).
Hospitalizations reached a peak of 14,461 in wave five. ICU admissions, however, peaked at 2,164 during wave four, and all-cause deaths peaked at 1,663 during wave two.
The investigators also analyzed how unvaccinated patients fared, compared with the fully vaccinated and the fully vaccinated-plus (that is, patients with one or more additional doses). During waves five and six, unvaccinated patients were 4.3 times more likely to end up in the ICU than fully vaccinated patients and were 12.2 times more likely than fully vaccinated-plus patients. Likewise, the rate for all-cause in-hospital death for unvaccinated patients was 3.9 times greater than that for fully vaccinated patients and 15.1 times greater than that for fully vaccinated-plus patients.
The effect of vaccines emerged in waves three and four, said Dr. Frenette. “We started to see really, really significant protection and benefit from the vaccine, not only in incidence of admission but also in the incidence of complications of ICU care, ventilation, and mortality.”
Results for pediatric patients were similar to those for adults, Dr. Thampi noted. During waves five and six, overall admissions peaked, but the share of ICU admissions decreased to 9.4% from 18.1%, which was the rate during the previous four waves (OR, 0.47).
“What’s important is how pediatric hospitalizations changed over the course of the various waves,” said Dr. Thampi.
“Where we saw the highest admissions during the early Omicron dominance, we actually had the lowest numbers of hospitalizations with death and admissions into ICUs.”
Doing more with the data
David Fisman, MD, MPH, a professor of epidemiology at the University of Toronto, said, “This is a study that shows us how tremendously dramatic the effects of the COVID-19 vaccine were in terms of saving lives during the pandemic.” Dr. Fisman was not involved in the study.
But CNISP, which receives funding from Public Health Agency of Canada, could do more with the data it collects to better protect the public from COVID-19 and other nosocomial infections, Dr. Fisman said.
“The first problematic thing about this paper is that Canadians are paying for a surveillance system that looks at risks of acquiring infections, including COVID-19 infections, in the hospital, but that data is not fed back to the people paying for its production,” he said.
“So, Canadians don’t have the ability to really understand in real time how much risk they’re experiencing via going to the hospital for some other reason.”
The study was independently supported. Dr. Frenette and Dr. Thampi report no relevant financial relationships. Dr. Fisman has disclosed financial relationships with Pfizer, AstraZeneca, Sanofi, Seqirus, Merck, the Ontario Nurses Association, and the Elementary Teachers’ Federation of Ontario.
A version of this article first appeared on Medscape.com.
FDA expands use of dapagliflozin to broader range of HF
– including HF with mildly reduced ejection fraction (HFmrEF) and with preserved ejection fraction (HFpEF).
The sodium-glucose cotransporter 2 (SGLT2) inhibitor was previously approved in the United States for adults with heart failure with reduced ejection fraction (HFrEF).
The expanded indication is based on data from the phase 3 DELIVER trial, which showed clear clinical benefits of the SGLT2 inhibitor for patients with HF regardless of left ventricular function.
In the trial, which included more than 6,200 patients, dapagliflozin led to a statistically significant and clinically meaningful early reduction in the primary composite endpoint of cardiovascular (CV) death or worsening HF for patients with HFmrEF or HFpEFF.
In addition, results of a pooled analysis of the DAPA-HF and DELIVER phase 3 trials showed a consistent benefit from dapagliflozin treatment in significantly reducing the combined endpoint of CV death or HF hospitalization across the range of LVEF.
The European Commission expanded the indication for dapagliflozin (Forxiga) to include HF across the full spectrum of LVEF in February.
The SGLT2 inhibitor is also approved for use by patients with chronic kidney disease. It was first approved in 2014 to improve glycemic control for patients with diabetes mellitus.
A version of this article first appeared on Medscape.com.
– including HF with mildly reduced ejection fraction (HFmrEF) and with preserved ejection fraction (HFpEF).
The sodium-glucose cotransporter 2 (SGLT2) inhibitor was previously approved in the United States for adults with heart failure with reduced ejection fraction (HFrEF).
The expanded indication is based on data from the phase 3 DELIVER trial, which showed clear clinical benefits of the SGLT2 inhibitor for patients with HF regardless of left ventricular function.
In the trial, which included more than 6,200 patients, dapagliflozin led to a statistically significant and clinically meaningful early reduction in the primary composite endpoint of cardiovascular (CV) death or worsening HF for patients with HFmrEF or HFpEFF.
In addition, results of a pooled analysis of the DAPA-HF and DELIVER phase 3 trials showed a consistent benefit from dapagliflozin treatment in significantly reducing the combined endpoint of CV death or HF hospitalization across the range of LVEF.
The European Commission expanded the indication for dapagliflozin (Forxiga) to include HF across the full spectrum of LVEF in February.
The SGLT2 inhibitor is also approved for use by patients with chronic kidney disease. It was first approved in 2014 to improve glycemic control for patients with diabetes mellitus.
A version of this article first appeared on Medscape.com.
– including HF with mildly reduced ejection fraction (HFmrEF) and with preserved ejection fraction (HFpEF).
The sodium-glucose cotransporter 2 (SGLT2) inhibitor was previously approved in the United States for adults with heart failure with reduced ejection fraction (HFrEF).
The expanded indication is based on data from the phase 3 DELIVER trial, which showed clear clinical benefits of the SGLT2 inhibitor for patients with HF regardless of left ventricular function.
In the trial, which included more than 6,200 patients, dapagliflozin led to a statistically significant and clinically meaningful early reduction in the primary composite endpoint of cardiovascular (CV) death or worsening HF for patients with HFmrEF or HFpEFF.
In addition, results of a pooled analysis of the DAPA-HF and DELIVER phase 3 trials showed a consistent benefit from dapagliflozin treatment in significantly reducing the combined endpoint of CV death or HF hospitalization across the range of LVEF.
The European Commission expanded the indication for dapagliflozin (Forxiga) to include HF across the full spectrum of LVEF in February.
The SGLT2 inhibitor is also approved for use by patients with chronic kidney disease. It was first approved in 2014 to improve glycemic control for patients with diabetes mellitus.
A version of this article first appeared on Medscape.com.
The 30th-birthday gift that could save a life
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr F. Perry Wilson of the Yale School of Medicine.
Milestone birthdays are always memorable – those ages when your life seems to fundamentally change somehow. Age 16: A license to drive. Age 18: You can vote to determine your own future and serve in the military. At 21, 3 years after adulthood, you are finally allowed to drink alcohol, for some reason. And then ... nothing much happens. At least until you turn 65 and become eligible for Medicare.
But imagine a future when turning 30 might be the biggest milestone birthday of all. Imagine a future when, at 30, you get your genome sequenced and doctors tell you what needs to be done to save your life.
That future may not be far off, as a new study shows us that
Getting your genome sequenced is a double-edged sword. Of course, there is the potential for substantial benefit; finding certain mutations allows for definitive therapy before it’s too late. That said, there are genetic diseases without a cure and without a treatment. Knowing about that destiny may do more harm than good.
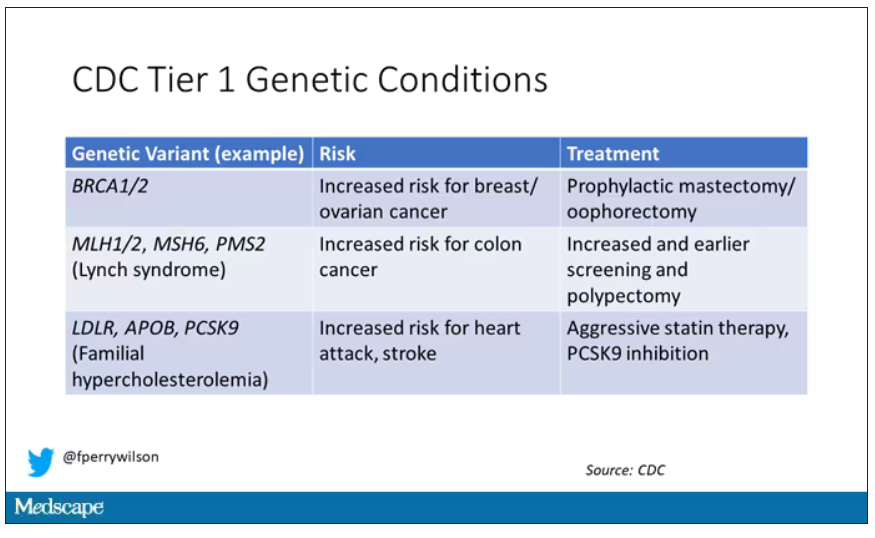
Three conditions are described by the CDC as “Tier 1” conditions, genetic syndromes with a significant impact on life expectancy that also have definitive, effective therapies.
These include mutations like BRCA1/2, associated with a high risk for breast and ovarian cancer; mutations associated with Lynch syndrome, which confer an elevated risk for colon cancer; and mutations associated with familial hypercholesterolemia, which confer elevated risk for cardiovascular events.
In each of these cases, there is clear evidence that early intervention can save lives. Individuals at high risk for breast and ovarian cancer can get prophylactic mastectomy and salpingo-oophorectomy. Those with Lynch syndrome can get more frequent screening for colon cancer and polypectomy, and those with familial hypercholesterolemia can get aggressive lipid-lowering therapy.
I think most of us would probably want to know if we had one of these conditions. Most of us would use that information to take concrete steps to decrease our risk. But just because a rational person would choose to do something doesn’t mean it’s feasible. After all, we’re talking about tests and treatments that have significant costs.
In a recent issue of Annals of Internal Medicine, Josh Peterson and David Veenstra present a detailed accounting of the cost and benefit of a hypothetical nationwide, universal screening program for Tier 1 conditions. And in the end, it may actually be worth it.
Cost-benefit analyses work by comparing two independent policy choices: the status quo – in this case, a world in which some people get tested for these conditions, but generally only if they are at high risk based on strong family history; and an alternative policy – in this case, universal screening for these conditions starting at some age.
After that, it’s time to play the assumption game. Using the best available data, the authors estimated the percentage of the population that will have each condition, the percentage of those individuals who will definitively act on the information, and how effective those actions would be if taken.
The authors provide an example. First, they assume that the prevalence of mutations leading to a high risk for breast and ovarian cancer is around 0.7%, and that up to 40% of people who learn that they have one of these mutations would undergo prophylactic mastectomy, which would reduce the risk for breast cancer by around 94%. (I ran these numbers past my wife, a breast surgical oncologist, who agreed that they seem reasonable.)
Assumptions in place, it’s time to consider costs. The cost of the screening test itself: The authors use $250 as their average per-person cost. But we also have the cost of treatment – around $22,000 per person for a bilateral prophylactic mastectomy; the cost of statin therapy for those with familial hypercholesterolemia; or the cost of all of those colonoscopies for those with Lynch syndrome.
Finally, we assess quality of life. Obviously, living longer is generally considered better than living shorter, but marginal increases in life expectancy at the cost of quality of life might not be a rational choice.
You then churn these assumptions through a computer and see what comes out. How many dollars does it take to save one quality-adjusted life-year (QALY)? I’ll tell you right now that $50,000 per QALY used to be the unofficial standard for a “cost-effective” intervention in the United States. Researchers have more recently used $100,000 as that threshold.
Let’s look at some hard numbers.
If you screened 100,000 people at age 30 years, 1,500 would get news that something in their genetics was, more or less, a ticking time bomb. Some would choose to get definitive treatment and the authors estimate that the strategy would prevent 85 cases of cancer. You’d prevent nine heart attacks and five strokes by lowering cholesterol levels among those with familial hypercholesterolemia. Obviously, these aren’t huge numbers, but of course most people don’t have these hereditary risk factors. For your average 30-year-old, the genetic screening test will be completely uneventful, but for those 1,500 it will be life-changing, and potentially life-saving.
But is it worth it? The authors estimate that, at the midpoint of all their assumptions, the cost of this program would be $68,000 per QALY saved.
Of course, that depends on all those assumptions we talked about. Interestingly, the single factor that changes the cost-effectiveness the most in this analysis is the cost of the genetic test itself, which I guess makes sense, considering we’d be talking about testing a huge segment of the population. If the test cost $100 instead of $250, the cost per QALY would be $39,700 – well within the range that most policymakers would support. And given the rate at which the cost of genetic testing is decreasing, and the obvious economies of scale here, I think $100 per test is totally feasible.
The future will bring other changes as well. Right now, there are only three hereditary conditions designated as Tier 1 by the CDC. If conditions are added, that might also swing the calculation more heavily toward benefit.
This will represent a stark change from how we think about genetic testing currently, focusing on those whose pretest probability of an abnormal result is high due to family history or other risk factors. But for the 20-year-olds out there, I wouldn’t be surprised if your 30th birthday is a bit more significant than you have been anticipating.
Dr. Wilson is an associate professor of medicine and director of Yale’s Clinical and Translational Research Accelerator in New Haven, Conn. He disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr F. Perry Wilson of the Yale School of Medicine.
Milestone birthdays are always memorable – those ages when your life seems to fundamentally change somehow. Age 16: A license to drive. Age 18: You can vote to determine your own future and serve in the military. At 21, 3 years after adulthood, you are finally allowed to drink alcohol, for some reason. And then ... nothing much happens. At least until you turn 65 and become eligible for Medicare.
But imagine a future when turning 30 might be the biggest milestone birthday of all. Imagine a future when, at 30, you get your genome sequenced and doctors tell you what needs to be done to save your life.
That future may not be far off, as a new study shows us that
Getting your genome sequenced is a double-edged sword. Of course, there is the potential for substantial benefit; finding certain mutations allows for definitive therapy before it’s too late. That said, there are genetic diseases without a cure and without a treatment. Knowing about that destiny may do more harm than good.
Three conditions are described by the CDC as “Tier 1” conditions, genetic syndromes with a significant impact on life expectancy that also have definitive, effective therapies.
These include mutations like BRCA1/2, associated with a high risk for breast and ovarian cancer; mutations associated with Lynch syndrome, which confer an elevated risk for colon cancer; and mutations associated with familial hypercholesterolemia, which confer elevated risk for cardiovascular events.
In each of these cases, there is clear evidence that early intervention can save lives. Individuals at high risk for breast and ovarian cancer can get prophylactic mastectomy and salpingo-oophorectomy. Those with Lynch syndrome can get more frequent screening for colon cancer and polypectomy, and those with familial hypercholesterolemia can get aggressive lipid-lowering therapy.
I think most of us would probably want to know if we had one of these conditions. Most of us would use that information to take concrete steps to decrease our risk. But just because a rational person would choose to do something doesn’t mean it’s feasible. After all, we’re talking about tests and treatments that have significant costs.
In a recent issue of Annals of Internal Medicine, Josh Peterson and David Veenstra present a detailed accounting of the cost and benefit of a hypothetical nationwide, universal screening program for Tier 1 conditions. And in the end, it may actually be worth it.
Cost-benefit analyses work by comparing two independent policy choices: the status quo – in this case, a world in which some people get tested for these conditions, but generally only if they are at high risk based on strong family history; and an alternative policy – in this case, universal screening for these conditions starting at some age.
After that, it’s time to play the assumption game. Using the best available data, the authors estimated the percentage of the population that will have each condition, the percentage of those individuals who will definitively act on the information, and how effective those actions would be if taken.
The authors provide an example. First, they assume that the prevalence of mutations leading to a high risk for breast and ovarian cancer is around 0.7%, and that up to 40% of people who learn that they have one of these mutations would undergo prophylactic mastectomy, which would reduce the risk for breast cancer by around 94%. (I ran these numbers past my wife, a breast surgical oncologist, who agreed that they seem reasonable.)
Assumptions in place, it’s time to consider costs. The cost of the screening test itself: The authors use $250 as their average per-person cost. But we also have the cost of treatment – around $22,000 per person for a bilateral prophylactic mastectomy; the cost of statin therapy for those with familial hypercholesterolemia; or the cost of all of those colonoscopies for those with Lynch syndrome.
Finally, we assess quality of life. Obviously, living longer is generally considered better than living shorter, but marginal increases in life expectancy at the cost of quality of life might not be a rational choice.
You then churn these assumptions through a computer and see what comes out. How many dollars does it take to save one quality-adjusted life-year (QALY)? I’ll tell you right now that $50,000 per QALY used to be the unofficial standard for a “cost-effective” intervention in the United States. Researchers have more recently used $100,000 as that threshold.
Let’s look at some hard numbers.
If you screened 100,000 people at age 30 years, 1,500 would get news that something in their genetics was, more or less, a ticking time bomb. Some would choose to get definitive treatment and the authors estimate that the strategy would prevent 85 cases of cancer. You’d prevent nine heart attacks and five strokes by lowering cholesterol levels among those with familial hypercholesterolemia. Obviously, these aren’t huge numbers, but of course most people don’t have these hereditary risk factors. For your average 30-year-old, the genetic screening test will be completely uneventful, but for those 1,500 it will be life-changing, and potentially life-saving.
But is it worth it? The authors estimate that, at the midpoint of all their assumptions, the cost of this program would be $68,000 per QALY saved.
Of course, that depends on all those assumptions we talked about. Interestingly, the single factor that changes the cost-effectiveness the most in this analysis is the cost of the genetic test itself, which I guess makes sense, considering we’d be talking about testing a huge segment of the population. If the test cost $100 instead of $250, the cost per QALY would be $39,700 – well within the range that most policymakers would support. And given the rate at which the cost of genetic testing is decreasing, and the obvious economies of scale here, I think $100 per test is totally feasible.
The future will bring other changes as well. Right now, there are only three hereditary conditions designated as Tier 1 by the CDC. If conditions are added, that might also swing the calculation more heavily toward benefit.
This will represent a stark change from how we think about genetic testing currently, focusing on those whose pretest probability of an abnormal result is high due to family history or other risk factors. But for the 20-year-olds out there, I wouldn’t be surprised if your 30th birthday is a bit more significant than you have been anticipating.
Dr. Wilson is an associate professor of medicine and director of Yale’s Clinical and Translational Research Accelerator in New Haven, Conn. He disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr F. Perry Wilson of the Yale School of Medicine.
Milestone birthdays are always memorable – those ages when your life seems to fundamentally change somehow. Age 16: A license to drive. Age 18: You can vote to determine your own future and serve in the military. At 21, 3 years after adulthood, you are finally allowed to drink alcohol, for some reason. And then ... nothing much happens. At least until you turn 65 and become eligible for Medicare.
But imagine a future when turning 30 might be the biggest milestone birthday of all. Imagine a future when, at 30, you get your genome sequenced and doctors tell you what needs to be done to save your life.
That future may not be far off, as a new study shows us that
Getting your genome sequenced is a double-edged sword. Of course, there is the potential for substantial benefit; finding certain mutations allows for definitive therapy before it’s too late. That said, there are genetic diseases without a cure and without a treatment. Knowing about that destiny may do more harm than good.
Three conditions are described by the CDC as “Tier 1” conditions, genetic syndromes with a significant impact on life expectancy that also have definitive, effective therapies.
These include mutations like BRCA1/2, associated with a high risk for breast and ovarian cancer; mutations associated with Lynch syndrome, which confer an elevated risk for colon cancer; and mutations associated with familial hypercholesterolemia, which confer elevated risk for cardiovascular events.
In each of these cases, there is clear evidence that early intervention can save lives. Individuals at high risk for breast and ovarian cancer can get prophylactic mastectomy and salpingo-oophorectomy. Those with Lynch syndrome can get more frequent screening for colon cancer and polypectomy, and those with familial hypercholesterolemia can get aggressive lipid-lowering therapy.
I think most of us would probably want to know if we had one of these conditions. Most of us would use that information to take concrete steps to decrease our risk. But just because a rational person would choose to do something doesn’t mean it’s feasible. After all, we’re talking about tests and treatments that have significant costs.
In a recent issue of Annals of Internal Medicine, Josh Peterson and David Veenstra present a detailed accounting of the cost and benefit of a hypothetical nationwide, universal screening program for Tier 1 conditions. And in the end, it may actually be worth it.
Cost-benefit analyses work by comparing two independent policy choices: the status quo – in this case, a world in which some people get tested for these conditions, but generally only if they are at high risk based on strong family history; and an alternative policy – in this case, universal screening for these conditions starting at some age.
After that, it’s time to play the assumption game. Using the best available data, the authors estimated the percentage of the population that will have each condition, the percentage of those individuals who will definitively act on the information, and how effective those actions would be if taken.
The authors provide an example. First, they assume that the prevalence of mutations leading to a high risk for breast and ovarian cancer is around 0.7%, and that up to 40% of people who learn that they have one of these mutations would undergo prophylactic mastectomy, which would reduce the risk for breast cancer by around 94%. (I ran these numbers past my wife, a breast surgical oncologist, who agreed that they seem reasonable.)
Assumptions in place, it’s time to consider costs. The cost of the screening test itself: The authors use $250 as their average per-person cost. But we also have the cost of treatment – around $22,000 per person for a bilateral prophylactic mastectomy; the cost of statin therapy for those with familial hypercholesterolemia; or the cost of all of those colonoscopies for those with Lynch syndrome.
Finally, we assess quality of life. Obviously, living longer is generally considered better than living shorter, but marginal increases in life expectancy at the cost of quality of life might not be a rational choice.
You then churn these assumptions through a computer and see what comes out. How many dollars does it take to save one quality-adjusted life-year (QALY)? I’ll tell you right now that $50,000 per QALY used to be the unofficial standard for a “cost-effective” intervention in the United States. Researchers have more recently used $100,000 as that threshold.
Let’s look at some hard numbers.
If you screened 100,000 people at age 30 years, 1,500 would get news that something in their genetics was, more or less, a ticking time bomb. Some would choose to get definitive treatment and the authors estimate that the strategy would prevent 85 cases of cancer. You’d prevent nine heart attacks and five strokes by lowering cholesterol levels among those with familial hypercholesterolemia. Obviously, these aren’t huge numbers, but of course most people don’t have these hereditary risk factors. For your average 30-year-old, the genetic screening test will be completely uneventful, but for those 1,500 it will be life-changing, and potentially life-saving.
But is it worth it? The authors estimate that, at the midpoint of all their assumptions, the cost of this program would be $68,000 per QALY saved.
Of course, that depends on all those assumptions we talked about. Interestingly, the single factor that changes the cost-effectiveness the most in this analysis is the cost of the genetic test itself, which I guess makes sense, considering we’d be talking about testing a huge segment of the population. If the test cost $100 instead of $250, the cost per QALY would be $39,700 – well within the range that most policymakers would support. And given the rate at which the cost of genetic testing is decreasing, and the obvious economies of scale here, I think $100 per test is totally feasible.
The future will bring other changes as well. Right now, there are only three hereditary conditions designated as Tier 1 by the CDC. If conditions are added, that might also swing the calculation more heavily toward benefit.
This will represent a stark change from how we think about genetic testing currently, focusing on those whose pretest probability of an abnormal result is high due to family history or other risk factors. But for the 20-year-olds out there, I wouldn’t be surprised if your 30th birthday is a bit more significant than you have been anticipating.
Dr. Wilson is an associate professor of medicine and director of Yale’s Clinical and Translational Research Accelerator in New Haven, Conn. He disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
AHA flags differing CVD risk in Asian American subgroups
Asian Americans have significant differences in genetics, socioeconomic factors, culture, diet, lifestyle, and acculturation levels based on the Asian region of their ancestry that likely have unique effects on their risk for type 2 diabetes and heart disease, the statement noted.
“Examining Asian subgroups separately is crucial to better understand the distinctions among them, how these differences translate into their risk of type 2 diabetes and atherosclerotic disease, and how health care professionals may provide care and support in a culturally appropriate manner,” writing group chair Tak W. Kwan, MD, chief of cardiology, Lenox Health Greenwich Village, and clinical professor of medicine, Northwell Health, New York City, said in a news release.
The statement was published online in the journal Circulation.
Impact on health outcomes
Asian American subgroups are broadly categorized by the geographic region of Asian descent and include South Asia (India, Pakistan, Sri Lanka, Bangladesh, Nepal, or Bhutan); East Asia (Japan, China, or Korea); Southeast Asia (Philippines, Vietnam, Thailand, Cambodia, Laos, Indonesia, Malaysia, Singapore, Hmong); and Native Hawaiian/Pacific Islander (Hawaii, Guam, Samoa, or other Pacific islands).
Asian Americans make up the fastest growing racial and ethnic group in the United States. Together, type 2 diabetes (T2D) and atherosclerotic cardiovascular disease (ASCVD) are the leading causes of illness and death among Asian American adults.
Yet, there is significant variability in prevalence and risk factors within the different subgroups, the writing group pointed out.
For example, based on available data, rates of coronary artery disease (CAD) among Asian Americans indicate an overall prevalence of 8% in men and about 3% in women.
However, available data for subgroups suggest higher CAD rates among Asian Indian Americans (13% for men and 4.4% for women) and Filipino Americans (about 9% and 4%, respectively).
Available data on T2D among Asian American subgroups also show varied prevalence and risk.
A study from California found overall, Asian American adults had higher rates of T2D (range of 15.6%-34.5%) compared with non-Hispanic White adults (12.8%). Among Chinese Americans, the rate was 15.8%. Among Korean and Japanese Americans, rates were about 18% and among Americans with Filipino ancestry, the rate was nearly 32%.
Yet most studies to date aggregate Asian Americans in a single group and do not examine the subgroups individually, which is a challenge to providing evidence-based recommendations, the writing group said.
“Particular attention should focus on the T2D and ASCVD risk differences among the different Asian American subgroups because they may affect the precision in clinical and health outcomes,” the group suggested.
“Culturally specific recommendations and interventions across the different Asian American subgroups related to T2D and ASCVD will help improve primary and secondary prevention and health outcomes in this population,” they added.
The writing group noted that existing CVD risk calculators, which are based on data validated in non-Hispanic Black adults and non-Hispanic White adults and less extensively studied in Asian Americans, may underestimate the risk of T2D and heart disease in South Asian adults, those of lower socioeconomic status, or those with chronic inflammatory diseases.
On the other hand, these tools may overestimate CVD risk among East Asians, those with higher socioeconomic status or those who are already participating in preventive healthcare services.
Advances in epidemiology and data analysis and the availability of larger, representative cohorts will allow for refinement of pooled cohort equations to better gauge ASCVD risk in Asian American subgroups, the group said.
Filling in the gaps
The writing group outlined several key areas to consider for strengthening the data about Asian American adults. Chief among them is the need to include disaggregated data on Asian American subgroups in clinical trials and government-sponsored studies.
Another is to standardize ways of collecting ethnic and subgroup data for Asian Americans for national health systems, surveys, and registries. National surveillance surveys should consider oversampling Asian Americans to increase representation for the various subgroups, the writing group suggested.
“All of us – health care professionals, policymakers, community leaders and patients – must advocate for more health research funding for Asian Americans and demand inclusion of Asian American subgroup information in clinical trials and government-sponsored research,” Dr. Kwan said.
“Having a platform to share and disseminate data on Asian Americans for the scientific and research community would also be an asset for the health care professionals who care for this population,” Dr. Kwan added.
The new scientific statement is a follow-up to a 2010 AHA “call to action” to seek data on health disparities among Asian American subgroups and a 2018 scientific statement addressing CVD risk in South Asians (Asian Indian, Pakistani, Sri Lankan, Bangladeshi, Nepali, or Bhutanese).
This scientific statement was prepared by the volunteer writing group on behalf of the AHA Council on Epidemiology and Prevention; the Council on Lifestyle and Cardiometabolic Health; the Council on Arteriosclerosis, Thrombosis and Vascular Biology; the Council on Clinical Cardiology; the Council on Cardiovascular and Stroke Nursing; and the Council on Genomic and Precision Medicine.
A version of this article first appeared on Medscape.com.
Asian Americans have significant differences in genetics, socioeconomic factors, culture, diet, lifestyle, and acculturation levels based on the Asian region of their ancestry that likely have unique effects on their risk for type 2 diabetes and heart disease, the statement noted.
“Examining Asian subgroups separately is crucial to better understand the distinctions among them, how these differences translate into their risk of type 2 diabetes and atherosclerotic disease, and how health care professionals may provide care and support in a culturally appropriate manner,” writing group chair Tak W. Kwan, MD, chief of cardiology, Lenox Health Greenwich Village, and clinical professor of medicine, Northwell Health, New York City, said in a news release.
The statement was published online in the journal Circulation.
Impact on health outcomes
Asian American subgroups are broadly categorized by the geographic region of Asian descent and include South Asia (India, Pakistan, Sri Lanka, Bangladesh, Nepal, or Bhutan); East Asia (Japan, China, or Korea); Southeast Asia (Philippines, Vietnam, Thailand, Cambodia, Laos, Indonesia, Malaysia, Singapore, Hmong); and Native Hawaiian/Pacific Islander (Hawaii, Guam, Samoa, or other Pacific islands).
Asian Americans make up the fastest growing racial and ethnic group in the United States. Together, type 2 diabetes (T2D) and atherosclerotic cardiovascular disease (ASCVD) are the leading causes of illness and death among Asian American adults.
Yet, there is significant variability in prevalence and risk factors within the different subgroups, the writing group pointed out.
For example, based on available data, rates of coronary artery disease (CAD) among Asian Americans indicate an overall prevalence of 8% in men and about 3% in women.
However, available data for subgroups suggest higher CAD rates among Asian Indian Americans (13% for men and 4.4% for women) and Filipino Americans (about 9% and 4%, respectively).
Available data on T2D among Asian American subgroups also show varied prevalence and risk.
A study from California found overall, Asian American adults had higher rates of T2D (range of 15.6%-34.5%) compared with non-Hispanic White adults (12.8%). Among Chinese Americans, the rate was 15.8%. Among Korean and Japanese Americans, rates were about 18% and among Americans with Filipino ancestry, the rate was nearly 32%.
Yet most studies to date aggregate Asian Americans in a single group and do not examine the subgroups individually, which is a challenge to providing evidence-based recommendations, the writing group said.
“Particular attention should focus on the T2D and ASCVD risk differences among the different Asian American subgroups because they may affect the precision in clinical and health outcomes,” the group suggested.
“Culturally specific recommendations and interventions across the different Asian American subgroups related to T2D and ASCVD will help improve primary and secondary prevention and health outcomes in this population,” they added.
The writing group noted that existing CVD risk calculators, which are based on data validated in non-Hispanic Black adults and non-Hispanic White adults and less extensively studied in Asian Americans, may underestimate the risk of T2D and heart disease in South Asian adults, those of lower socioeconomic status, or those with chronic inflammatory diseases.
On the other hand, these tools may overestimate CVD risk among East Asians, those with higher socioeconomic status or those who are already participating in preventive healthcare services.
Advances in epidemiology and data analysis and the availability of larger, representative cohorts will allow for refinement of pooled cohort equations to better gauge ASCVD risk in Asian American subgroups, the group said.
Filling in the gaps
The writing group outlined several key areas to consider for strengthening the data about Asian American adults. Chief among them is the need to include disaggregated data on Asian American subgroups in clinical trials and government-sponsored studies.
Another is to standardize ways of collecting ethnic and subgroup data for Asian Americans for national health systems, surveys, and registries. National surveillance surveys should consider oversampling Asian Americans to increase representation for the various subgroups, the writing group suggested.
“All of us – health care professionals, policymakers, community leaders and patients – must advocate for more health research funding for Asian Americans and demand inclusion of Asian American subgroup information in clinical trials and government-sponsored research,” Dr. Kwan said.
“Having a platform to share and disseminate data on Asian Americans for the scientific and research community would also be an asset for the health care professionals who care for this population,” Dr. Kwan added.
The new scientific statement is a follow-up to a 2010 AHA “call to action” to seek data on health disparities among Asian American subgroups and a 2018 scientific statement addressing CVD risk in South Asians (Asian Indian, Pakistani, Sri Lankan, Bangladeshi, Nepali, or Bhutanese).
This scientific statement was prepared by the volunteer writing group on behalf of the AHA Council on Epidemiology and Prevention; the Council on Lifestyle and Cardiometabolic Health; the Council on Arteriosclerosis, Thrombosis and Vascular Biology; the Council on Clinical Cardiology; the Council on Cardiovascular and Stroke Nursing; and the Council on Genomic and Precision Medicine.
A version of this article first appeared on Medscape.com.
Asian Americans have significant differences in genetics, socioeconomic factors, culture, diet, lifestyle, and acculturation levels based on the Asian region of their ancestry that likely have unique effects on their risk for type 2 diabetes and heart disease, the statement noted.
“Examining Asian subgroups separately is crucial to better understand the distinctions among them, how these differences translate into their risk of type 2 diabetes and atherosclerotic disease, and how health care professionals may provide care and support in a culturally appropriate manner,” writing group chair Tak W. Kwan, MD, chief of cardiology, Lenox Health Greenwich Village, and clinical professor of medicine, Northwell Health, New York City, said in a news release.
The statement was published online in the journal Circulation.
Impact on health outcomes
Asian American subgroups are broadly categorized by the geographic region of Asian descent and include South Asia (India, Pakistan, Sri Lanka, Bangladesh, Nepal, or Bhutan); East Asia (Japan, China, or Korea); Southeast Asia (Philippines, Vietnam, Thailand, Cambodia, Laos, Indonesia, Malaysia, Singapore, Hmong); and Native Hawaiian/Pacific Islander (Hawaii, Guam, Samoa, or other Pacific islands).
Asian Americans make up the fastest growing racial and ethnic group in the United States. Together, type 2 diabetes (T2D) and atherosclerotic cardiovascular disease (ASCVD) are the leading causes of illness and death among Asian American adults.
Yet, there is significant variability in prevalence and risk factors within the different subgroups, the writing group pointed out.
For example, based on available data, rates of coronary artery disease (CAD) among Asian Americans indicate an overall prevalence of 8% in men and about 3% in women.
However, available data for subgroups suggest higher CAD rates among Asian Indian Americans (13% for men and 4.4% for women) and Filipino Americans (about 9% and 4%, respectively).
Available data on T2D among Asian American subgroups also show varied prevalence and risk.
A study from California found overall, Asian American adults had higher rates of T2D (range of 15.6%-34.5%) compared with non-Hispanic White adults (12.8%). Among Chinese Americans, the rate was 15.8%. Among Korean and Japanese Americans, rates were about 18% and among Americans with Filipino ancestry, the rate was nearly 32%.
Yet most studies to date aggregate Asian Americans in a single group and do not examine the subgroups individually, which is a challenge to providing evidence-based recommendations, the writing group said.
“Particular attention should focus on the T2D and ASCVD risk differences among the different Asian American subgroups because they may affect the precision in clinical and health outcomes,” the group suggested.
“Culturally specific recommendations and interventions across the different Asian American subgroups related to T2D and ASCVD will help improve primary and secondary prevention and health outcomes in this population,” they added.
The writing group noted that existing CVD risk calculators, which are based on data validated in non-Hispanic Black adults and non-Hispanic White adults and less extensively studied in Asian Americans, may underestimate the risk of T2D and heart disease in South Asian adults, those of lower socioeconomic status, or those with chronic inflammatory diseases.
On the other hand, these tools may overestimate CVD risk among East Asians, those with higher socioeconomic status or those who are already participating in preventive healthcare services.
Advances in epidemiology and data analysis and the availability of larger, representative cohorts will allow for refinement of pooled cohort equations to better gauge ASCVD risk in Asian American subgroups, the group said.
Filling in the gaps
The writing group outlined several key areas to consider for strengthening the data about Asian American adults. Chief among them is the need to include disaggregated data on Asian American subgroups in clinical trials and government-sponsored studies.
Another is to standardize ways of collecting ethnic and subgroup data for Asian Americans for national health systems, surveys, and registries. National surveillance surveys should consider oversampling Asian Americans to increase representation for the various subgroups, the writing group suggested.
“All of us – health care professionals, policymakers, community leaders and patients – must advocate for more health research funding for Asian Americans and demand inclusion of Asian American subgroup information in clinical trials and government-sponsored research,” Dr. Kwan said.
“Having a platform to share and disseminate data on Asian Americans for the scientific and research community would also be an asset for the health care professionals who care for this population,” Dr. Kwan added.
The new scientific statement is a follow-up to a 2010 AHA “call to action” to seek data on health disparities among Asian American subgroups and a 2018 scientific statement addressing CVD risk in South Asians (Asian Indian, Pakistani, Sri Lankan, Bangladeshi, Nepali, or Bhutanese).
This scientific statement was prepared by the volunteer writing group on behalf of the AHA Council on Epidemiology and Prevention; the Council on Lifestyle and Cardiometabolic Health; the Council on Arteriosclerosis, Thrombosis and Vascular Biology; the Council on Clinical Cardiology; the Council on Cardiovascular and Stroke Nursing; and the Council on Genomic and Precision Medicine.
A version of this article first appeared on Medscape.com.
FROM CIRCULATION
Medications that scare me
An 85-year-old woman is brought to the emergency department after a syncopal episode. Her caregivers report a similar episode 2 weeks ago, but she recovered so quickly they did not seek evaluation for her.
Medications: Omeprazole 20 mg, pravastatin 40 mg, citalopram 10 mg, albuterol, donepezil 10 mg, isosorbide mononitrate 60 mg, and calcium. On exam, blood pressure is 100/60 mm Hg, pulse 55. ECG indicates bradycardia with normal intervals. What drug most likely caused her syncope?
A. Citalopram
B. Pravastatin
C. Donepezil
D. Isosorbide
E. Calcium
This woman’s syncope is likely caused by donepezil. Citalopram can lengthen the QT interval, especially in elderly patients, but the normal intervals on ECG eliminate this possibility. Donepezil can cause bradycardia, which can contribute to syncope.
Hernandez and colleagues evaluated a cohort of veterans with dementia over an 8-year period.1 They found that there was a 1.4-fold increased risk of bradycardia in patients with dementia treated with an acetylcholine inhibitor (compared with that in patients who were not taking these medications) and that there was a dose-dependent increase in risk for patients on donepezil.
Park-Wyllie et al. found in a study of 1.4 million older adults a greater than twofold risk of hospitalization for bradycardia in patients treated with a cholinesterase inhibitor.2 Gill and colleagues performed a population-based cohort study of 19,803 elderly patients with dementia who were prescribed cholinesterase inhibitors, and compared them to age-matched controls.3 They found increased hospital visits for syncope in people receiving cholinesterase inhibitors (hazard ratio, 1.76; 95% confidence interval, 1.57-1.98). Other syncope-related events were also more common in people receiving cholinesterase inhibitors, compared with controls: hospital visits for bradycardia (HR, 1.69; 95% CI, 1.32-2.15), permanent pacemaker insertion (HR, 1.49; 95% CI, 1.12-2.00), and hip fracture (HR, 1.18; (95% CI, 1.04-1.34).
Nausea, vomiting, and weight loss are much more common than the rarer side effects of bradycardia and syncope. The frequency of gastroenterological side effects is up to 25%. Cholinesterase inhibitors have modest effects on cognitive function with a high number needed to treat (NNT) of 10, and an NNT as high as 100 for global function. The number needed to harm (NNH) is 4, when gastrointestinal symptoms are added in.4 Another important, problematic side effect of cholinesterase inhibitors is urinary incontinence. This often leads to patients receiving medications, to combat this side effect, that may worsen cognitive function.
Another commonly used medication that scares me in certain circumstances is trimethoprim-sulfamethoxazole. My main concern is when it is used in patients who are elderly, have chronic kidney disease, or are taking other medications that can cause hyperkalemia (ACEIs, ARBs, potassium-sparing diuretics including spironolactone). Hyperkalemia is a real concern in these patient populations. Trimethoprim reduces renal potassium excretion through the competitive inhibition of sodium channels in the distal nephron, in a manner similar to the potassium-sparing diuretic amiloride. Hospitalizations for hyperkalemia are more common in patients who take ACEIs and ARBs and are prescribed trimethoprim-sulfamethoxazole, compared with other antibiotics.5
Sudden cardiac death is also more common in patients who are taking ACEIs or ARBs and receive trimethoprim-sulfamethoxazole.6 Trimethoprim-sulfamethoxazole also has a powerful interaction with warfarin, both displacing warfarin from albumin and inhibiting its metabolism. It raises the INR (international normalized ratio) in warfarin-treated patients much greater than do other antibiotics.7
Pearls
- Think carefully about the use of cholinesterase inhibitors because of the unfavorable NNH vs. NNT.
- Use caution prescribing trimethoprim for patients who are elderly, especially if they are on an ACEI, an ARB, or spironolactone, and in patients with chronic kidney disease.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at dpaauw@uw.edu.
References
1. Hernandez RK et al. J Am Geriatr Soc. 2009;57:1997-2003.
2. Park-Wyllie LY et al. PLoS Med. 2009;6:e1000157.
3. Gill SS et al. Arch Intern Med 2009;169:867-73.
4. Peters KR. J Am Geriatr Soc. 2013 Jul;61(7):1170-4.
5. Antoniou TN et al. Arch Intern Med. 2010;170(12):1045-9.
6. Fralick M et al. BMJ. 2014 Oct 30;349:g6196.
7. Glasheen JJ et al. J Gen Intern Med. 2005 Jul;20(7):653-6.
An 85-year-old woman is brought to the emergency department after a syncopal episode. Her caregivers report a similar episode 2 weeks ago, but she recovered so quickly they did not seek evaluation for her.
Medications: Omeprazole 20 mg, pravastatin 40 mg, citalopram 10 mg, albuterol, donepezil 10 mg, isosorbide mononitrate 60 mg, and calcium. On exam, blood pressure is 100/60 mm Hg, pulse 55. ECG indicates bradycardia with normal intervals. What drug most likely caused her syncope?
A. Citalopram
B. Pravastatin
C. Donepezil
D. Isosorbide
E. Calcium
This woman’s syncope is likely caused by donepezil. Citalopram can lengthen the QT interval, especially in elderly patients, but the normal intervals on ECG eliminate this possibility. Donepezil can cause bradycardia, which can contribute to syncope.
Hernandez and colleagues evaluated a cohort of veterans with dementia over an 8-year period.1 They found that there was a 1.4-fold increased risk of bradycardia in patients with dementia treated with an acetylcholine inhibitor (compared with that in patients who were not taking these medications) and that there was a dose-dependent increase in risk for patients on donepezil.
Park-Wyllie et al. found in a study of 1.4 million older adults a greater than twofold risk of hospitalization for bradycardia in patients treated with a cholinesterase inhibitor.2 Gill and colleagues performed a population-based cohort study of 19,803 elderly patients with dementia who were prescribed cholinesterase inhibitors, and compared them to age-matched controls.3 They found increased hospital visits for syncope in people receiving cholinesterase inhibitors (hazard ratio, 1.76; 95% confidence interval, 1.57-1.98). Other syncope-related events were also more common in people receiving cholinesterase inhibitors, compared with controls: hospital visits for bradycardia (HR, 1.69; 95% CI, 1.32-2.15), permanent pacemaker insertion (HR, 1.49; 95% CI, 1.12-2.00), and hip fracture (HR, 1.18; (95% CI, 1.04-1.34).
Nausea, vomiting, and weight loss are much more common than the rarer side effects of bradycardia and syncope. The frequency of gastroenterological side effects is up to 25%. Cholinesterase inhibitors have modest effects on cognitive function with a high number needed to treat (NNT) of 10, and an NNT as high as 100 for global function. The number needed to harm (NNH) is 4, when gastrointestinal symptoms are added in.4 Another important, problematic side effect of cholinesterase inhibitors is urinary incontinence. This often leads to patients receiving medications, to combat this side effect, that may worsen cognitive function.
Another commonly used medication that scares me in certain circumstances is trimethoprim-sulfamethoxazole. My main concern is when it is used in patients who are elderly, have chronic kidney disease, or are taking other medications that can cause hyperkalemia (ACEIs, ARBs, potassium-sparing diuretics including spironolactone). Hyperkalemia is a real concern in these patient populations. Trimethoprim reduces renal potassium excretion through the competitive inhibition of sodium channels in the distal nephron, in a manner similar to the potassium-sparing diuretic amiloride. Hospitalizations for hyperkalemia are more common in patients who take ACEIs and ARBs and are prescribed trimethoprim-sulfamethoxazole, compared with other antibiotics.5
Sudden cardiac death is also more common in patients who are taking ACEIs or ARBs and receive trimethoprim-sulfamethoxazole.6 Trimethoprim-sulfamethoxazole also has a powerful interaction with warfarin, both displacing warfarin from albumin and inhibiting its metabolism. It raises the INR (international normalized ratio) in warfarin-treated patients much greater than do other antibiotics.7
Pearls
- Think carefully about the use of cholinesterase inhibitors because of the unfavorable NNH vs. NNT.
- Use caution prescribing trimethoprim for patients who are elderly, especially if they are on an ACEI, an ARB, or spironolactone, and in patients with chronic kidney disease.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at dpaauw@uw.edu.
References
1. Hernandez RK et al. J Am Geriatr Soc. 2009;57:1997-2003.
2. Park-Wyllie LY et al. PLoS Med. 2009;6:e1000157.
3. Gill SS et al. Arch Intern Med 2009;169:867-73.
4. Peters KR. J Am Geriatr Soc. 2013 Jul;61(7):1170-4.
5. Antoniou TN et al. Arch Intern Med. 2010;170(12):1045-9.
6. Fralick M et al. BMJ. 2014 Oct 30;349:g6196.
7. Glasheen JJ et al. J Gen Intern Med. 2005 Jul;20(7):653-6.
An 85-year-old woman is brought to the emergency department after a syncopal episode. Her caregivers report a similar episode 2 weeks ago, but she recovered so quickly they did not seek evaluation for her.
Medications: Omeprazole 20 mg, pravastatin 40 mg, citalopram 10 mg, albuterol, donepezil 10 mg, isosorbide mononitrate 60 mg, and calcium. On exam, blood pressure is 100/60 mm Hg, pulse 55. ECG indicates bradycardia with normal intervals. What drug most likely caused her syncope?
A. Citalopram
B. Pravastatin
C. Donepezil
D. Isosorbide
E. Calcium
This woman’s syncope is likely caused by donepezil. Citalopram can lengthen the QT interval, especially in elderly patients, but the normal intervals on ECG eliminate this possibility. Donepezil can cause bradycardia, which can contribute to syncope.
Hernandez and colleagues evaluated a cohort of veterans with dementia over an 8-year period.1 They found that there was a 1.4-fold increased risk of bradycardia in patients with dementia treated with an acetylcholine inhibitor (compared with that in patients who were not taking these medications) and that there was a dose-dependent increase in risk for patients on donepezil.
Park-Wyllie et al. found in a study of 1.4 million older adults a greater than twofold risk of hospitalization for bradycardia in patients treated with a cholinesterase inhibitor.2 Gill and colleagues performed a population-based cohort study of 19,803 elderly patients with dementia who were prescribed cholinesterase inhibitors, and compared them to age-matched controls.3 They found increased hospital visits for syncope in people receiving cholinesterase inhibitors (hazard ratio, 1.76; 95% confidence interval, 1.57-1.98). Other syncope-related events were also more common in people receiving cholinesterase inhibitors, compared with controls: hospital visits for bradycardia (HR, 1.69; 95% CI, 1.32-2.15), permanent pacemaker insertion (HR, 1.49; 95% CI, 1.12-2.00), and hip fracture (HR, 1.18; (95% CI, 1.04-1.34).
Nausea, vomiting, and weight loss are much more common than the rarer side effects of bradycardia and syncope. The frequency of gastroenterological side effects is up to 25%. Cholinesterase inhibitors have modest effects on cognitive function with a high number needed to treat (NNT) of 10, and an NNT as high as 100 for global function. The number needed to harm (NNH) is 4, when gastrointestinal symptoms are added in.4 Another important, problematic side effect of cholinesterase inhibitors is urinary incontinence. This often leads to patients receiving medications, to combat this side effect, that may worsen cognitive function.
Another commonly used medication that scares me in certain circumstances is trimethoprim-sulfamethoxazole. My main concern is when it is used in patients who are elderly, have chronic kidney disease, or are taking other medications that can cause hyperkalemia (ACEIs, ARBs, potassium-sparing diuretics including spironolactone). Hyperkalemia is a real concern in these patient populations. Trimethoprim reduces renal potassium excretion through the competitive inhibition of sodium channels in the distal nephron, in a manner similar to the potassium-sparing diuretic amiloride. Hospitalizations for hyperkalemia are more common in patients who take ACEIs and ARBs and are prescribed trimethoprim-sulfamethoxazole, compared with other antibiotics.5
Sudden cardiac death is also more common in patients who are taking ACEIs or ARBs and receive trimethoprim-sulfamethoxazole.6 Trimethoprim-sulfamethoxazole also has a powerful interaction with warfarin, both displacing warfarin from albumin and inhibiting its metabolism. It raises the INR (international normalized ratio) in warfarin-treated patients much greater than do other antibiotics.7
Pearls
- Think carefully about the use of cholinesterase inhibitors because of the unfavorable NNH vs. NNT.
- Use caution prescribing trimethoprim for patients who are elderly, especially if they are on an ACEI, an ARB, or spironolactone, and in patients with chronic kidney disease.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at dpaauw@uw.edu.
References
1. Hernandez RK et al. J Am Geriatr Soc. 2009;57:1997-2003.
2. Park-Wyllie LY et al. PLoS Med. 2009;6:e1000157.
3. Gill SS et al. Arch Intern Med 2009;169:867-73.
4. Peters KR. J Am Geriatr Soc. 2013 Jul;61(7):1170-4.
5. Antoniou TN et al. Arch Intern Med. 2010;170(12):1045-9.
6. Fralick M et al. BMJ. 2014 Oct 30;349:g6196.
7. Glasheen JJ et al. J Gen Intern Med. 2005 Jul;20(7):653-6.
New AACE type 2 diabetes algorithm individualizes care
SEATTLE – The latest American Association of Clinical Endocrinology type 2 diabetes management algorithm uses graphics to focus on individualized care while adding newly compiled information about medication access and affordability, vaccinations, and weight loss drugs.
The clinical guidance document was presented at the annual scientific & clinical congress of the American Association of Clinical Endocrinology and simultaneously published in Endocrine Practice.
Using text and colorful graphics, the document summarizes information from last year’s update and other recent AACE documents, including those addressing dyslipidemia and use of diabetes technology.
lead author Susan L. Samson, MD, PhD, chair of endocrinology, diabetes & metabolism at the Mayo Clinic Florida, Jacksonville, said in an interview.
Asked to comment, Anne L. Peters, MD, professor of clinical medicine at the University of Southern California, Los Angeles, said: “I like their simple graphics. For the Department of Health Services in Los Angeles County, we have been painstakingly trying to create our own flow diagrams. ... These will help.”
Eleven separate algorithms with text and graphics
Included are 11 visual management algorithms, with accompanying text for each one. The first lists 10 overall management principles, including “lifestyle modification underlies all therapy,” “maintain or achieve optimal weight,” “choice of therapy includes ease of use and access,” “individualize all glucose targets,” “avoid hypoglycemia,” and “comorbidities must be managed for comprehensive care.”
Three more algorithms cover the diabetes-adjacent topics of adiposity-based chronic disease, prediabetes, dyslipidemia, and hypertension.
Four separate graphics address glucose-lowering. Two are “complications-centric” and “glucose-centric” algorithms, another covers insulin initiation and titration, and a table summarizes the benefits and risks of currently available glucose-lowering medications, as well as cost.
Splitting the glucose-lowering algorithms into “complications-centric” and “glucose-centric” graphics is new, Dr. Samson said. “The complications one comes first, deliberately. You need to think about: Does my patient have a history of or high risk for cardiovascular disease, heart failure, stroke, or diabetic kidney disease? And, you want to prioritize those medications that have evidence to improve outcomes with those different diabetes complications versus a one-size-fits-all approach.”
And for patients without those complications, the glucose-centric algorithm considers obesity, hypoglycemia risk, and access/cost issues. “So, overall the diabetes medication algorithm has been split in order to emphasize that personalized approach to decision-making,” Dr. Samson explained.
Also new is a table listing the benefits and risks of weight-loss medications, and another covering immunization guidance for people with diabetes based on recommendations from the U.S. Centers for Disease Control and Prevention. “Coming out of the pandemic, we’re thinking about how can we protect our patients from infectious disease and all the comorbidities. In some cases, people with diabetes can have a much higher risk for adverse events,” Dr. Samson noted.
Regarding the weight-loss medications table, she pointed out that the task force couldn’t include the blockbuster twincretin tirzepatide because it’s not yet approved for weight loss by the U.S. Food and Drug Administration. However, it is included in the glucose-lowering drug table with weight loss listed among its benefits.
“We want this to be a living document that should be updated in a timely fashion, and so, as these new indications are approved and we see more evidence supporting their different uses, this should be updated in a really timely fashion to reflect that,” Dr. Samson said.
The end of the document includes a full page of each graphic, meant for wall posting.
Dr. Peters noted that for the most part, the AACE guidelines and algorithm align with joint guidance by the American Diabetes Association and European Association for the Study of Diabetes.
“For many years there seemed to be big differences between the AACE and ADA guidelines for the management of type 2 diabetes. Although small differences still exist ... the ADA and AACE guidelines have become quite similar,” she said.
Dr. Peters also praised the AACE algorithm for providing “a pathway for people who have issues with access and cost.”
“I am incredibly proud that in the County of Los Angeles you can get a [glucagon-like peptide-1 receptor agonist] and/or a [sodium-glucose cotransporter-2 inhibitor] even with the most restricted MediCal insurance if indications are met. But there remain many people in many places where access and cost limit options, and I am grateful that AACE includes this in their algorithms,” she said.
Dr. Samson has reported receiving research support to the Mayo Clinic from Corcept, serving on a steering committee and being a national or overall principal investigator for Chiasma and Novartis, and being a committee chair for the American Board of Internal Medicine. Dr. Peters has reported relationships with Blue Circle Health, Vertex, and Abbott Diabetes Care, receiving research grants from Abbott Diabetes Care and Insulet, and holding stock options in Teladoc and Omada Health.
A version of this article originally appeared on Medscape.com.
SEATTLE – The latest American Association of Clinical Endocrinology type 2 diabetes management algorithm uses graphics to focus on individualized care while adding newly compiled information about medication access and affordability, vaccinations, and weight loss drugs.
The clinical guidance document was presented at the annual scientific & clinical congress of the American Association of Clinical Endocrinology and simultaneously published in Endocrine Practice.
Using text and colorful graphics, the document summarizes information from last year’s update and other recent AACE documents, including those addressing dyslipidemia and use of diabetes technology.
lead author Susan L. Samson, MD, PhD, chair of endocrinology, diabetes & metabolism at the Mayo Clinic Florida, Jacksonville, said in an interview.
Asked to comment, Anne L. Peters, MD, professor of clinical medicine at the University of Southern California, Los Angeles, said: “I like their simple graphics. For the Department of Health Services in Los Angeles County, we have been painstakingly trying to create our own flow diagrams. ... These will help.”
Eleven separate algorithms with text and graphics
Included are 11 visual management algorithms, with accompanying text for each one. The first lists 10 overall management principles, including “lifestyle modification underlies all therapy,” “maintain or achieve optimal weight,” “choice of therapy includes ease of use and access,” “individualize all glucose targets,” “avoid hypoglycemia,” and “comorbidities must be managed for comprehensive care.”
Three more algorithms cover the diabetes-adjacent topics of adiposity-based chronic disease, prediabetes, dyslipidemia, and hypertension.
Four separate graphics address glucose-lowering. Two are “complications-centric” and “glucose-centric” algorithms, another covers insulin initiation and titration, and a table summarizes the benefits and risks of currently available glucose-lowering medications, as well as cost.
Splitting the glucose-lowering algorithms into “complications-centric” and “glucose-centric” graphics is new, Dr. Samson said. “The complications one comes first, deliberately. You need to think about: Does my patient have a history of or high risk for cardiovascular disease, heart failure, stroke, or diabetic kidney disease? And, you want to prioritize those medications that have evidence to improve outcomes with those different diabetes complications versus a one-size-fits-all approach.”
And for patients without those complications, the glucose-centric algorithm considers obesity, hypoglycemia risk, and access/cost issues. “So, overall the diabetes medication algorithm has been split in order to emphasize that personalized approach to decision-making,” Dr. Samson explained.
Also new is a table listing the benefits and risks of weight-loss medications, and another covering immunization guidance for people with diabetes based on recommendations from the U.S. Centers for Disease Control and Prevention. “Coming out of the pandemic, we’re thinking about how can we protect our patients from infectious disease and all the comorbidities. In some cases, people with diabetes can have a much higher risk for adverse events,” Dr. Samson noted.
Regarding the weight-loss medications table, she pointed out that the task force couldn’t include the blockbuster twincretin tirzepatide because it’s not yet approved for weight loss by the U.S. Food and Drug Administration. However, it is included in the glucose-lowering drug table with weight loss listed among its benefits.
“We want this to be a living document that should be updated in a timely fashion, and so, as these new indications are approved and we see more evidence supporting their different uses, this should be updated in a really timely fashion to reflect that,” Dr. Samson said.
The end of the document includes a full page of each graphic, meant for wall posting.
Dr. Peters noted that for the most part, the AACE guidelines and algorithm align with joint guidance by the American Diabetes Association and European Association for the Study of Diabetes.
“For many years there seemed to be big differences between the AACE and ADA guidelines for the management of type 2 diabetes. Although small differences still exist ... the ADA and AACE guidelines have become quite similar,” she said.
Dr. Peters also praised the AACE algorithm for providing “a pathway for people who have issues with access and cost.”
“I am incredibly proud that in the County of Los Angeles you can get a [glucagon-like peptide-1 receptor agonist] and/or a [sodium-glucose cotransporter-2 inhibitor] even with the most restricted MediCal insurance if indications are met. But there remain many people in many places where access and cost limit options, and I am grateful that AACE includes this in their algorithms,” she said.
Dr. Samson has reported receiving research support to the Mayo Clinic from Corcept, serving on a steering committee and being a national or overall principal investigator for Chiasma and Novartis, and being a committee chair for the American Board of Internal Medicine. Dr. Peters has reported relationships with Blue Circle Health, Vertex, and Abbott Diabetes Care, receiving research grants from Abbott Diabetes Care and Insulet, and holding stock options in Teladoc and Omada Health.
A version of this article originally appeared on Medscape.com.
SEATTLE – The latest American Association of Clinical Endocrinology type 2 diabetes management algorithm uses graphics to focus on individualized care while adding newly compiled information about medication access and affordability, vaccinations, and weight loss drugs.
The clinical guidance document was presented at the annual scientific & clinical congress of the American Association of Clinical Endocrinology and simultaneously published in Endocrine Practice.
Using text and colorful graphics, the document summarizes information from last year’s update and other recent AACE documents, including those addressing dyslipidemia and use of diabetes technology.
lead author Susan L. Samson, MD, PhD, chair of endocrinology, diabetes & metabolism at the Mayo Clinic Florida, Jacksonville, said in an interview.
Asked to comment, Anne L. Peters, MD, professor of clinical medicine at the University of Southern California, Los Angeles, said: “I like their simple graphics. For the Department of Health Services in Los Angeles County, we have been painstakingly trying to create our own flow diagrams. ... These will help.”
Eleven separate algorithms with text and graphics
Included are 11 visual management algorithms, with accompanying text for each one. The first lists 10 overall management principles, including “lifestyle modification underlies all therapy,” “maintain or achieve optimal weight,” “choice of therapy includes ease of use and access,” “individualize all glucose targets,” “avoid hypoglycemia,” and “comorbidities must be managed for comprehensive care.”
Three more algorithms cover the diabetes-adjacent topics of adiposity-based chronic disease, prediabetes, dyslipidemia, and hypertension.
Four separate graphics address glucose-lowering. Two are “complications-centric” and “glucose-centric” algorithms, another covers insulin initiation and titration, and a table summarizes the benefits and risks of currently available glucose-lowering medications, as well as cost.
Splitting the glucose-lowering algorithms into “complications-centric” and “glucose-centric” graphics is new, Dr. Samson said. “The complications one comes first, deliberately. You need to think about: Does my patient have a history of or high risk for cardiovascular disease, heart failure, stroke, or diabetic kidney disease? And, you want to prioritize those medications that have evidence to improve outcomes with those different diabetes complications versus a one-size-fits-all approach.”
And for patients without those complications, the glucose-centric algorithm considers obesity, hypoglycemia risk, and access/cost issues. “So, overall the diabetes medication algorithm has been split in order to emphasize that personalized approach to decision-making,” Dr. Samson explained.
Also new is a table listing the benefits and risks of weight-loss medications, and another covering immunization guidance for people with diabetes based on recommendations from the U.S. Centers for Disease Control and Prevention. “Coming out of the pandemic, we’re thinking about how can we protect our patients from infectious disease and all the comorbidities. In some cases, people with diabetes can have a much higher risk for adverse events,” Dr. Samson noted.
Regarding the weight-loss medications table, she pointed out that the task force couldn’t include the blockbuster twincretin tirzepatide because it’s not yet approved for weight loss by the U.S. Food and Drug Administration. However, it is included in the glucose-lowering drug table with weight loss listed among its benefits.
“We want this to be a living document that should be updated in a timely fashion, and so, as these new indications are approved and we see more evidence supporting their different uses, this should be updated in a really timely fashion to reflect that,” Dr. Samson said.
The end of the document includes a full page of each graphic, meant for wall posting.
Dr. Peters noted that for the most part, the AACE guidelines and algorithm align with joint guidance by the American Diabetes Association and European Association for the Study of Diabetes.
“For many years there seemed to be big differences between the AACE and ADA guidelines for the management of type 2 diabetes. Although small differences still exist ... the ADA and AACE guidelines have become quite similar,” she said.
Dr. Peters also praised the AACE algorithm for providing “a pathway for people who have issues with access and cost.”
“I am incredibly proud that in the County of Los Angeles you can get a [glucagon-like peptide-1 receptor agonist] and/or a [sodium-glucose cotransporter-2 inhibitor] even with the most restricted MediCal insurance if indications are met. But there remain many people in many places where access and cost limit options, and I am grateful that AACE includes this in their algorithms,” she said.
Dr. Samson has reported receiving research support to the Mayo Clinic from Corcept, serving on a steering committee and being a national or overall principal investigator for Chiasma and Novartis, and being a committee chair for the American Board of Internal Medicine. Dr. Peters has reported relationships with Blue Circle Health, Vertex, and Abbott Diabetes Care, receiving research grants from Abbott Diabetes Care and Insulet, and holding stock options in Teladoc and Omada Health.
A version of this article originally appeared on Medscape.com.
AT AACE 2023
New AACE statement tries to fight weight bias and stigma
SEATTLE –
Highlights from the statement, entitled “Addressing stigma and bias in the diagnosis and management of patients with obesity/adiposity-based chronic disease and assessing bias and stigmatization as determinants of disease severity,” were presented at the annual scientific & clinical congress of the American Association of Clinical Endocrinology. It will be published later this year in Endocrine Practice.
The document reiterates AACE’s previous proposal to use the term “adiposity-based chronic disease (ABCD)” to refer to the spectrum of complications of obesity beyond weight. AACE has incorporated weight bias, stigmatization, psychological health, and social determinants of health into disease staging based on the degree to which these factors impair quality of life and could negatively affect treatment. Another change is the use of a scale from 1 to 3 for ABCD staging, in contrast to the previous scale from 0 to 3, as follows.
Stage 1 (previously 0): No known physical ABCD complications (for example, cardiovascular, biomechanical) but with increased risk that might be reduced by weight loss, and/or internalized weight bias and stigmatization, psychological conditions, and social determinants of health that don’t have immediate adverse health effects but may require individualized care.
Stage 2 (previously 1): One or more mild-moderate ABCD complications plus increased risk of other complications and/or bias/stigma/social determinants that adversely affect quality of life or could impair ABCD treatment.
Stage 3 (previously 2): At least one severe ABCD complication plus increased risk for others, and/or bias/stigma/social determinants with pronounced adverse effects on quality of life or that interfere with weight loss treatment plans or render them harmful.
To accomplish this staging, clinicians are advised to use validated questionnaires to screen patients for the presence and degree of self-stigmatization and internalized weight bias and to refer patients to mental health professionals for related psychological issues. The document also advises clinicians to implement practice policies such as implicit bias training and obesity education for their staff.
“I really hope that this document will increase awareness of the vicious cycle of weight bias, stigma, and internalized weight bias for patients with obesity, both on an individual basis and a bigger chronic care model basis ... By utilizing these concepts in the document, we hope to at least take steps towards reducing the stigma and internalized weight bias and slowing down or reversing that vicious cycle to better care for people with a focus on their health ... It’s not just about a person’s weight,” Karl Nadolsky, DO, the statement’s co-lead author, said.
The new statement builds on previous AACE efforts, including the 2014 publication entitled, “Advanced framework for a new diagnosis of obesity as a chronic disease,” the 2016 management guidelines, and the 2016 position statement, which introduced the ABCD term. All are meant to advance the concept of obesity or ABCD as a medical condition, rather than a cosmetic problem or lifestyle choice.
Now, AACE is explicitly calling attention to the integral role of internal and external weight bias and stigma as both drivers and complications of the condition. The AACE writing panel adopted some of the concepts from a 2020 international consensus statement focusing on obesity stigma, Dr. Nadolsky said.
“We need to focus on health, the biopsychosocial mode. We have to think about the person as a whole. The disease of obesity is really a quintessential disease state that needs a very good holistic approach,” he said.
Asked to comment, Yoni Freedhoff, MD, associate professor, department of family medicine, University of Ottawa, and Medical Director of the Bariatric Medical Institute, said: “I do think staging/categorization are important in the context of bias and stigma and also to combat the notion that the goal is simple medicalization ... It’s good to see the consideration of internalized weight bias as part of an effort to understand the impact of obesity on an individual.”
However, Dr. Freedhoff said he would have preferred that the implicit and internalized bias concepts had been incorporated into the 2009 Edmonton Obesity Staging System, which he believes is easier to use than the AACE staging system.
Dr. Freedhoff also disagrees that it was necessary to remove “0” from the staging (still present in the Edmonton system), done by AACE out of concern that people might mistakenly think it implies zero risk. “It just means no current objective or subjective impact of weight on health or quality of life,” he said.
But, Dr. Nadolsky noted that data on people with “metabolically healthy obesity” suggest that “they might have zero complications but they’re still at high risk, from cancer to stigma and bias, which are a cause of and consequence of obesity and should be part of the ABCD staging system.”
Indeed, Dr. Freedhoff noted, “Obesity confers risk. Just like hypertension. And just like with hypertension, risk is not a guarantee of problems. But we still discuss treatment and people can be symptom- or problem-free when we start it. It can also be ‘borderline’ or mild. But no one gets upset about the idea of treating a known risk factor, or diagnosing a known risk factor, when minor, and when it’s not had any impact on a person’s health. That we don’t do same with obesity is consequent to bias.”
In addition to influencing health care providers and health care systems, the statement also concludes: “Society, including payers and policymakers, should support policies, education, research, and access to care to limit bias and stigma faced by individuals with obesity/ABCD.”
Dr. Nadolsky has reported no relevant financial relationships. Dr. Freedhoff has reported working with the Bariatric Medical Institute and Constant Health, which has received a research grant from Novo Nordisk.
A version of this article originally appeared on Medscape.com.
SEATTLE –
Highlights from the statement, entitled “Addressing stigma and bias in the diagnosis and management of patients with obesity/adiposity-based chronic disease and assessing bias and stigmatization as determinants of disease severity,” were presented at the annual scientific & clinical congress of the American Association of Clinical Endocrinology. It will be published later this year in Endocrine Practice.
The document reiterates AACE’s previous proposal to use the term “adiposity-based chronic disease (ABCD)” to refer to the spectrum of complications of obesity beyond weight. AACE has incorporated weight bias, stigmatization, psychological health, and social determinants of health into disease staging based on the degree to which these factors impair quality of life and could negatively affect treatment. Another change is the use of a scale from 1 to 3 for ABCD staging, in contrast to the previous scale from 0 to 3, as follows.
Stage 1 (previously 0): No known physical ABCD complications (for example, cardiovascular, biomechanical) but with increased risk that might be reduced by weight loss, and/or internalized weight bias and stigmatization, psychological conditions, and social determinants of health that don’t have immediate adverse health effects but may require individualized care.
Stage 2 (previously 1): One or more mild-moderate ABCD complications plus increased risk of other complications and/or bias/stigma/social determinants that adversely affect quality of life or could impair ABCD treatment.
Stage 3 (previously 2): At least one severe ABCD complication plus increased risk for others, and/or bias/stigma/social determinants with pronounced adverse effects on quality of life or that interfere with weight loss treatment plans or render them harmful.
To accomplish this staging, clinicians are advised to use validated questionnaires to screen patients for the presence and degree of self-stigmatization and internalized weight bias and to refer patients to mental health professionals for related psychological issues. The document also advises clinicians to implement practice policies such as implicit bias training and obesity education for their staff.
“I really hope that this document will increase awareness of the vicious cycle of weight bias, stigma, and internalized weight bias for patients with obesity, both on an individual basis and a bigger chronic care model basis ... By utilizing these concepts in the document, we hope to at least take steps towards reducing the stigma and internalized weight bias and slowing down or reversing that vicious cycle to better care for people with a focus on their health ... It’s not just about a person’s weight,” Karl Nadolsky, DO, the statement’s co-lead author, said.
The new statement builds on previous AACE efforts, including the 2014 publication entitled, “Advanced framework for a new diagnosis of obesity as a chronic disease,” the 2016 management guidelines, and the 2016 position statement, which introduced the ABCD term. All are meant to advance the concept of obesity or ABCD as a medical condition, rather than a cosmetic problem or lifestyle choice.
Now, AACE is explicitly calling attention to the integral role of internal and external weight bias and stigma as both drivers and complications of the condition. The AACE writing panel adopted some of the concepts from a 2020 international consensus statement focusing on obesity stigma, Dr. Nadolsky said.
“We need to focus on health, the biopsychosocial mode. We have to think about the person as a whole. The disease of obesity is really a quintessential disease state that needs a very good holistic approach,” he said.
Asked to comment, Yoni Freedhoff, MD, associate professor, department of family medicine, University of Ottawa, and Medical Director of the Bariatric Medical Institute, said: “I do think staging/categorization are important in the context of bias and stigma and also to combat the notion that the goal is simple medicalization ... It’s good to see the consideration of internalized weight bias as part of an effort to understand the impact of obesity on an individual.”
However, Dr. Freedhoff said he would have preferred that the implicit and internalized bias concepts had been incorporated into the 2009 Edmonton Obesity Staging System, which he believes is easier to use than the AACE staging system.
Dr. Freedhoff also disagrees that it was necessary to remove “0” from the staging (still present in the Edmonton system), done by AACE out of concern that people might mistakenly think it implies zero risk. “It just means no current objective or subjective impact of weight on health or quality of life,” he said.
But, Dr. Nadolsky noted that data on people with “metabolically healthy obesity” suggest that “they might have zero complications but they’re still at high risk, from cancer to stigma and bias, which are a cause of and consequence of obesity and should be part of the ABCD staging system.”
Indeed, Dr. Freedhoff noted, “Obesity confers risk. Just like hypertension. And just like with hypertension, risk is not a guarantee of problems. But we still discuss treatment and people can be symptom- or problem-free when we start it. It can also be ‘borderline’ or mild. But no one gets upset about the idea of treating a known risk factor, or diagnosing a known risk factor, when minor, and when it’s not had any impact on a person’s health. That we don’t do same with obesity is consequent to bias.”
In addition to influencing health care providers and health care systems, the statement also concludes: “Society, including payers and policymakers, should support policies, education, research, and access to care to limit bias and stigma faced by individuals with obesity/ABCD.”
Dr. Nadolsky has reported no relevant financial relationships. Dr. Freedhoff has reported working with the Bariatric Medical Institute and Constant Health, which has received a research grant from Novo Nordisk.
A version of this article originally appeared on Medscape.com.
SEATTLE –
Highlights from the statement, entitled “Addressing stigma and bias in the diagnosis and management of patients with obesity/adiposity-based chronic disease and assessing bias and stigmatization as determinants of disease severity,” were presented at the annual scientific & clinical congress of the American Association of Clinical Endocrinology. It will be published later this year in Endocrine Practice.
The document reiterates AACE’s previous proposal to use the term “adiposity-based chronic disease (ABCD)” to refer to the spectrum of complications of obesity beyond weight. AACE has incorporated weight bias, stigmatization, psychological health, and social determinants of health into disease staging based on the degree to which these factors impair quality of life and could negatively affect treatment. Another change is the use of a scale from 1 to 3 for ABCD staging, in contrast to the previous scale from 0 to 3, as follows.
Stage 1 (previously 0): No known physical ABCD complications (for example, cardiovascular, biomechanical) but with increased risk that might be reduced by weight loss, and/or internalized weight bias and stigmatization, psychological conditions, and social determinants of health that don’t have immediate adverse health effects but may require individualized care.
Stage 2 (previously 1): One or more mild-moderate ABCD complications plus increased risk of other complications and/or bias/stigma/social determinants that adversely affect quality of life or could impair ABCD treatment.
Stage 3 (previously 2): At least one severe ABCD complication plus increased risk for others, and/or bias/stigma/social determinants with pronounced adverse effects on quality of life or that interfere with weight loss treatment plans or render them harmful.
To accomplish this staging, clinicians are advised to use validated questionnaires to screen patients for the presence and degree of self-stigmatization and internalized weight bias and to refer patients to mental health professionals for related psychological issues. The document also advises clinicians to implement practice policies such as implicit bias training and obesity education for their staff.
“I really hope that this document will increase awareness of the vicious cycle of weight bias, stigma, and internalized weight bias for patients with obesity, both on an individual basis and a bigger chronic care model basis ... By utilizing these concepts in the document, we hope to at least take steps towards reducing the stigma and internalized weight bias and slowing down or reversing that vicious cycle to better care for people with a focus on their health ... It’s not just about a person’s weight,” Karl Nadolsky, DO, the statement’s co-lead author, said.
The new statement builds on previous AACE efforts, including the 2014 publication entitled, “Advanced framework for a new diagnosis of obesity as a chronic disease,” the 2016 management guidelines, and the 2016 position statement, which introduced the ABCD term. All are meant to advance the concept of obesity or ABCD as a medical condition, rather than a cosmetic problem or lifestyle choice.
Now, AACE is explicitly calling attention to the integral role of internal and external weight bias and stigma as both drivers and complications of the condition. The AACE writing panel adopted some of the concepts from a 2020 international consensus statement focusing on obesity stigma, Dr. Nadolsky said.
“We need to focus on health, the biopsychosocial mode. We have to think about the person as a whole. The disease of obesity is really a quintessential disease state that needs a very good holistic approach,” he said.
Asked to comment, Yoni Freedhoff, MD, associate professor, department of family medicine, University of Ottawa, and Medical Director of the Bariatric Medical Institute, said: “I do think staging/categorization are important in the context of bias and stigma and also to combat the notion that the goal is simple medicalization ... It’s good to see the consideration of internalized weight bias as part of an effort to understand the impact of obesity on an individual.”
However, Dr. Freedhoff said he would have preferred that the implicit and internalized bias concepts had been incorporated into the 2009 Edmonton Obesity Staging System, which he believes is easier to use than the AACE staging system.
Dr. Freedhoff also disagrees that it was necessary to remove “0” from the staging (still present in the Edmonton system), done by AACE out of concern that people might mistakenly think it implies zero risk. “It just means no current objective or subjective impact of weight on health or quality of life,” he said.
But, Dr. Nadolsky noted that data on people with “metabolically healthy obesity” suggest that “they might have zero complications but they’re still at high risk, from cancer to stigma and bias, which are a cause of and consequence of obesity and should be part of the ABCD staging system.”
Indeed, Dr. Freedhoff noted, “Obesity confers risk. Just like hypertension. And just like with hypertension, risk is not a guarantee of problems. But we still discuss treatment and people can be symptom- or problem-free when we start it. It can also be ‘borderline’ or mild. But no one gets upset about the idea of treating a known risk factor, or diagnosing a known risk factor, when minor, and when it’s not had any impact on a person’s health. That we don’t do same with obesity is consequent to bias.”
In addition to influencing health care providers and health care systems, the statement also concludes: “Society, including payers and policymakers, should support policies, education, research, and access to care to limit bias and stigma faced by individuals with obesity/ABCD.”
Dr. Nadolsky has reported no relevant financial relationships. Dr. Freedhoff has reported working with the Bariatric Medical Institute and Constant Health, which has received a research grant from Novo Nordisk.
A version of this article originally appeared on Medscape.com.
AT AACE 2023
Contact allergens lurk in diabetes devices
in a presentation at the annual meeting of the American Contact Dermatitis Society.
Advanced technologies used for the management of diabetes fall into three main categories, said Dr. Chen, of the department of dermatology, Stanford University, Redwood City, Calif. Continuous glucose monitoring (CGM) devices, which are worn on the body, collect glucose measurements. Continuous subcutaneous insulin infusion (CSII) devices are attached to the body via an infusion set and are now available as tubing-free patch pumps that are attached directly to the skin via a catheter. Glucose-responsive insulin delivery systems combine the sensing and delivery features of the other two types of devices.
Once thought to be rare, reports of skin complications related to diabetes devices have been increasing in recent years, she said. Some reports suggest that at any given time, skin complications may affect as many as one quarter to one half of patients who use these devices, “so this is an important issue,” she emphasized. “Skin reactions are a major factor in device discontinuation, so we as clinicians need to be really proactive about treating these reactions.”
Risk factors for skin complications related to diabetes devices include sensitization to the adhesive used with the devices, as well as prolonged exposure to the device, Dr. Chen said. Younger age also appears to be a risk factor, as is a compromised skin barrier in the area where the device is used.
Unfortunately, obtaining details on the specific adhesives and the raw materials used in these devices, so as to customize patch testing, remains a challenge, she said. “Patch testing initially was often negative to commercially available allergens, even while patients were testing positive to pieces of device adhesive,” she noted.
Consider isobornyl acrylate
An article published in 2017 in Contact Dermatitis was “a major breakthrough” in that it identified isobornyl acrylate (IBOA) as an allergen in connection with the Freestyle Libre, a CGM device that was relatively new at the time. The finding was serendipitous, Dr. Chen said. A patient being treated for suspected allergic contact dermatitis in connection with use of a Freestyle Libre device was tested for IBOA accidentally, after the nurse administering the patch test thought that this was part of the standard acrylate series, she explained.
Subsequently, researchers identified 15 patients who had experienced reactions to the Freestyle Libre; 12 of 13 patients who were patch tested for IBOA tested positive. IBOA was found throughout the device, particularly where the top and bottom plastic components were connected, Dr. Chen said. This suggested that the IBOA was in the device housing and had diffused into the adhesive that attached the device to the skin.
An article published in 2018 in the Journal of Diabetes Science described three patients who developed severe allergic contact dermatitis from IBOA while using a CGM device, Dr. Chen said. The investigators confirmed that there were no reactions to the adhesive itself, again suggesting that IBOA had diffused into the adhesive from other parts of the device.
Although the authors were bound by a confidentiality agreement regarding the individual adhesive components, “the authors noted most of the acrylates in the adhesive were not present in commercially available acrylate series for patch testing,” she said.
IBOA, the ACDS’ Allergen of the Year in 2020, is common in sealants, glues, and adhesives, Dr. Chen said. Although IBOA had been reported infrequently as an allergen, it has now been identified as a “potential culprit” behind skin reactions in many diabetes devices, including CSII and CGM devices, she added.
In addition, N,N-dimethylacrylamide (DMAA) is an allergen that has been identified in several diabetes devices and often occurs with IBOA in medical-grade UV-cured adhesives, Dr. Chen noted. Other allergens identified in diabetes devices include colophony, which is present in many adhesives, as well as other acrylates and epoxy resin.
Diabetes devices are constantly evolving. IBOA is no longer found in Freestyle Libre devices. It is important that clinicians stay up to date with the medical literature and advocate for partnership with device manufacturers, she emphasized.
Patch testing
When diabetes devices are suspected as the source of allergic contact dermatitis, a minimum of a baseline series that contains colophony at a concentration of 20% in petrolatum should be carried out, Dr. Chen said. Commercialized patch test trays, which include plastics, glues, acrylates, epoxy resins/isocyanates, and colophony derivatives, should be ideal. “Personal-care products should be included if they are potentially relevant,” she added.
Dr. Chen shared tables published in Contact Dermatitis in 2021 with examples of screening test series. She said to consider including screening for other allergens more recently discovered in diabetes devices, including 2,2’-methylenebis(6-tert-butyl-4-methylphenol) monoacrylate (MBPA) 1.5% pet; dipropylene glycol diacrylate (DPGDA) 0.1% pet; and butylated hydroxytoluene (BHT) 2% pet.
Testing for monomethyl ether of hydroquinone should also be considered; this may be included in the test preparations for IBOA and DMAA.
Management strategies
For patients who experience skin reactions to their diabetes devices, consideration may given to relocating the device to another area of skin or changing sensors more frequently, according to Dr. Chen.
For some patients, the reaction can be managed with corticosteroid cream, ointment, solution, or nasal spray. Topical antibiotics or topical antihistamines can be helpful, as can barrier dressings, solutions, or sprays, she said. The best solution is to change to a device that does not have the culprit allergen, “but that is difficult, since we don’t know what is in these devices,” she added. Good alternatives include the Eversense CGM device or devices that have been demonstrated not to contain IBOA, such as the Freestyle Libre 2 or the newer version of the Omnipod, an insulin delivery system
Looking ahead, Dr. Chen said that “mandatory labeling is needed, as devices with the same name may have different compositions, depending on the date of manufacture.” Allergens relevant to people with diabetes are constantly evolving, and many are still unidentified, so clinicians and manufacturers need to work together to identify the culprit allergens and their sources, she said.
Dr. Chen has served as principal investigator or subinvestigator for Amgen, AbbVie, and Sanofi Regeneron and as a consultant for Purity Brands.
A version of this article first appeared on Medscape.com.
in a presentation at the annual meeting of the American Contact Dermatitis Society.
Advanced technologies used for the management of diabetes fall into three main categories, said Dr. Chen, of the department of dermatology, Stanford University, Redwood City, Calif. Continuous glucose monitoring (CGM) devices, which are worn on the body, collect glucose measurements. Continuous subcutaneous insulin infusion (CSII) devices are attached to the body via an infusion set and are now available as tubing-free patch pumps that are attached directly to the skin via a catheter. Glucose-responsive insulin delivery systems combine the sensing and delivery features of the other two types of devices.
Once thought to be rare, reports of skin complications related to diabetes devices have been increasing in recent years, she said. Some reports suggest that at any given time, skin complications may affect as many as one quarter to one half of patients who use these devices, “so this is an important issue,” she emphasized. “Skin reactions are a major factor in device discontinuation, so we as clinicians need to be really proactive about treating these reactions.”
Risk factors for skin complications related to diabetes devices include sensitization to the adhesive used with the devices, as well as prolonged exposure to the device, Dr. Chen said. Younger age also appears to be a risk factor, as is a compromised skin barrier in the area where the device is used.
Unfortunately, obtaining details on the specific adhesives and the raw materials used in these devices, so as to customize patch testing, remains a challenge, she said. “Patch testing initially was often negative to commercially available allergens, even while patients were testing positive to pieces of device adhesive,” she noted.
Consider isobornyl acrylate
An article published in 2017 in Contact Dermatitis was “a major breakthrough” in that it identified isobornyl acrylate (IBOA) as an allergen in connection with the Freestyle Libre, a CGM device that was relatively new at the time. The finding was serendipitous, Dr. Chen said. A patient being treated for suspected allergic contact dermatitis in connection with use of a Freestyle Libre device was tested for IBOA accidentally, after the nurse administering the patch test thought that this was part of the standard acrylate series, she explained.
Subsequently, researchers identified 15 patients who had experienced reactions to the Freestyle Libre; 12 of 13 patients who were patch tested for IBOA tested positive. IBOA was found throughout the device, particularly where the top and bottom plastic components were connected, Dr. Chen said. This suggested that the IBOA was in the device housing and had diffused into the adhesive that attached the device to the skin.
An article published in 2018 in the Journal of Diabetes Science described three patients who developed severe allergic contact dermatitis from IBOA while using a CGM device, Dr. Chen said. The investigators confirmed that there were no reactions to the adhesive itself, again suggesting that IBOA had diffused into the adhesive from other parts of the device.
Although the authors were bound by a confidentiality agreement regarding the individual adhesive components, “the authors noted most of the acrylates in the adhesive were not present in commercially available acrylate series for patch testing,” she said.
IBOA, the ACDS’ Allergen of the Year in 2020, is common in sealants, glues, and adhesives, Dr. Chen said. Although IBOA had been reported infrequently as an allergen, it has now been identified as a “potential culprit” behind skin reactions in many diabetes devices, including CSII and CGM devices, she added.
In addition, N,N-dimethylacrylamide (DMAA) is an allergen that has been identified in several diabetes devices and often occurs with IBOA in medical-grade UV-cured adhesives, Dr. Chen noted. Other allergens identified in diabetes devices include colophony, which is present in many adhesives, as well as other acrylates and epoxy resin.
Diabetes devices are constantly evolving. IBOA is no longer found in Freestyle Libre devices. It is important that clinicians stay up to date with the medical literature and advocate for partnership with device manufacturers, she emphasized.
Patch testing
When diabetes devices are suspected as the source of allergic contact dermatitis, a minimum of a baseline series that contains colophony at a concentration of 20% in petrolatum should be carried out, Dr. Chen said. Commercialized patch test trays, which include plastics, glues, acrylates, epoxy resins/isocyanates, and colophony derivatives, should be ideal. “Personal-care products should be included if they are potentially relevant,” she added.
Dr. Chen shared tables published in Contact Dermatitis in 2021 with examples of screening test series. She said to consider including screening for other allergens more recently discovered in diabetes devices, including 2,2’-methylenebis(6-tert-butyl-4-methylphenol) monoacrylate (MBPA) 1.5% pet; dipropylene glycol diacrylate (DPGDA) 0.1% pet; and butylated hydroxytoluene (BHT) 2% pet.
Testing for monomethyl ether of hydroquinone should also be considered; this may be included in the test preparations for IBOA and DMAA.
Management strategies
For patients who experience skin reactions to their diabetes devices, consideration may given to relocating the device to another area of skin or changing sensors more frequently, according to Dr. Chen.
For some patients, the reaction can be managed with corticosteroid cream, ointment, solution, or nasal spray. Topical antibiotics or topical antihistamines can be helpful, as can barrier dressings, solutions, or sprays, she said. The best solution is to change to a device that does not have the culprit allergen, “but that is difficult, since we don’t know what is in these devices,” she added. Good alternatives include the Eversense CGM device or devices that have been demonstrated not to contain IBOA, such as the Freestyle Libre 2 or the newer version of the Omnipod, an insulin delivery system
Looking ahead, Dr. Chen said that “mandatory labeling is needed, as devices with the same name may have different compositions, depending on the date of manufacture.” Allergens relevant to people with diabetes are constantly evolving, and many are still unidentified, so clinicians and manufacturers need to work together to identify the culprit allergens and their sources, she said.
Dr. Chen has served as principal investigator or subinvestigator for Amgen, AbbVie, and Sanofi Regeneron and as a consultant for Purity Brands.
A version of this article first appeared on Medscape.com.
in a presentation at the annual meeting of the American Contact Dermatitis Society.
Advanced technologies used for the management of diabetes fall into three main categories, said Dr. Chen, of the department of dermatology, Stanford University, Redwood City, Calif. Continuous glucose monitoring (CGM) devices, which are worn on the body, collect glucose measurements. Continuous subcutaneous insulin infusion (CSII) devices are attached to the body via an infusion set and are now available as tubing-free patch pumps that are attached directly to the skin via a catheter. Glucose-responsive insulin delivery systems combine the sensing and delivery features of the other two types of devices.
Once thought to be rare, reports of skin complications related to diabetes devices have been increasing in recent years, she said. Some reports suggest that at any given time, skin complications may affect as many as one quarter to one half of patients who use these devices, “so this is an important issue,” she emphasized. “Skin reactions are a major factor in device discontinuation, so we as clinicians need to be really proactive about treating these reactions.”
Risk factors for skin complications related to diabetes devices include sensitization to the adhesive used with the devices, as well as prolonged exposure to the device, Dr. Chen said. Younger age also appears to be a risk factor, as is a compromised skin barrier in the area where the device is used.
Unfortunately, obtaining details on the specific adhesives and the raw materials used in these devices, so as to customize patch testing, remains a challenge, she said. “Patch testing initially was often negative to commercially available allergens, even while patients were testing positive to pieces of device adhesive,” she noted.
Consider isobornyl acrylate
An article published in 2017 in Contact Dermatitis was “a major breakthrough” in that it identified isobornyl acrylate (IBOA) as an allergen in connection with the Freestyle Libre, a CGM device that was relatively new at the time. The finding was serendipitous, Dr. Chen said. A patient being treated for suspected allergic contact dermatitis in connection with use of a Freestyle Libre device was tested for IBOA accidentally, after the nurse administering the patch test thought that this was part of the standard acrylate series, she explained.
Subsequently, researchers identified 15 patients who had experienced reactions to the Freestyle Libre; 12 of 13 patients who were patch tested for IBOA tested positive. IBOA was found throughout the device, particularly where the top and bottom plastic components were connected, Dr. Chen said. This suggested that the IBOA was in the device housing and had diffused into the adhesive that attached the device to the skin.
An article published in 2018 in the Journal of Diabetes Science described three patients who developed severe allergic contact dermatitis from IBOA while using a CGM device, Dr. Chen said. The investigators confirmed that there were no reactions to the adhesive itself, again suggesting that IBOA had diffused into the adhesive from other parts of the device.
Although the authors were bound by a confidentiality agreement regarding the individual adhesive components, “the authors noted most of the acrylates in the adhesive were not present in commercially available acrylate series for patch testing,” she said.
IBOA, the ACDS’ Allergen of the Year in 2020, is common in sealants, glues, and adhesives, Dr. Chen said. Although IBOA had been reported infrequently as an allergen, it has now been identified as a “potential culprit” behind skin reactions in many diabetes devices, including CSII and CGM devices, she added.
In addition, N,N-dimethylacrylamide (DMAA) is an allergen that has been identified in several diabetes devices and often occurs with IBOA in medical-grade UV-cured adhesives, Dr. Chen noted. Other allergens identified in diabetes devices include colophony, which is present in many adhesives, as well as other acrylates and epoxy resin.
Diabetes devices are constantly evolving. IBOA is no longer found in Freestyle Libre devices. It is important that clinicians stay up to date with the medical literature and advocate for partnership with device manufacturers, she emphasized.
Patch testing
When diabetes devices are suspected as the source of allergic contact dermatitis, a minimum of a baseline series that contains colophony at a concentration of 20% in petrolatum should be carried out, Dr. Chen said. Commercialized patch test trays, which include plastics, glues, acrylates, epoxy resins/isocyanates, and colophony derivatives, should be ideal. “Personal-care products should be included if they are potentially relevant,” she added.
Dr. Chen shared tables published in Contact Dermatitis in 2021 with examples of screening test series. She said to consider including screening for other allergens more recently discovered in diabetes devices, including 2,2’-methylenebis(6-tert-butyl-4-methylphenol) monoacrylate (MBPA) 1.5% pet; dipropylene glycol diacrylate (DPGDA) 0.1% pet; and butylated hydroxytoluene (BHT) 2% pet.
Testing for monomethyl ether of hydroquinone should also be considered; this may be included in the test preparations for IBOA and DMAA.
Management strategies
For patients who experience skin reactions to their diabetes devices, consideration may given to relocating the device to another area of skin or changing sensors more frequently, according to Dr. Chen.
For some patients, the reaction can be managed with corticosteroid cream, ointment, solution, or nasal spray. Topical antibiotics or topical antihistamines can be helpful, as can barrier dressings, solutions, or sprays, she said. The best solution is to change to a device that does not have the culprit allergen, “but that is difficult, since we don’t know what is in these devices,” she added. Good alternatives include the Eversense CGM device or devices that have been demonstrated not to contain IBOA, such as the Freestyle Libre 2 or the newer version of the Omnipod, an insulin delivery system
Looking ahead, Dr. Chen said that “mandatory labeling is needed, as devices with the same name may have different compositions, depending on the date of manufacture.” Allergens relevant to people with diabetes are constantly evolving, and many are still unidentified, so clinicians and manufacturers need to work together to identify the culprit allergens and their sources, she said.
Dr. Chen has served as principal investigator or subinvestigator for Amgen, AbbVie, and Sanofi Regeneron and as a consultant for Purity Brands.
A version of this article first appeared on Medscape.com.
FROM ACDS 2023