User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
Has the time come to bury BMI in favor of other screening measures?
In 1832, Belgian statistician Adolphe Quetelet introduced the concept of body mass index (BMI) – one’s weight (in kilograms) divided by the square of one’s height (in meters) as a measurement of ideal body weight. Approximately 140 years later, nutritional epidemiologist Ancel Keys proposed the use of BMI as a surrogate marker for evaluating body fat percentage within a population.
For the past 50 years, the scientific and medical communities have relied on BMI as a research and study tool to categorize patients’ weight (that is, severely underweight, underweight, normal weight, overweight, and obesity). The World Health Organization, National Institutes of Health, and U.S. Centers for Disease Control and Prevention use the following BMI weight classifications for adult patients:
- Underweight: BMI < 18.5
- Normal weight: BMI ≥ 18.5 to 24.9
- Overweight: BMI ≥ 25 to 29.9
- Obesity: BMI ≥ 30
Of note, BMI categories for children and adolescents (aged 2-19 years) are based on sex- and age-specific percentiles and will not be addressed in this article.
BMI appears to be a straightforward, easy, and cost-effective way to identify “healthy” weight and assess a patient’s risk for related conditions. For example, studies show that a BMI ≥ 35 kg/m2 correlates to higher prevalence of type 2 diabetes, hypertension, dyslipidemia, and decreased lifespan. At least 13 types of cancer have been linked to obesity, regardless of dietary or physical activity behaviors. While the health dangers associated with BMI ≥ 35 are substantial and difficult to dispute, concerns arise when BMI alone is used to determine healthy weight and disease risk in patients with a BMI of 25-35.
BMI limitations
There are troubling limitations to using BMI alone to assess a patient’s weight and health status. BMI only takes into account a patient’s height and weight, neither of which are sole determinants of health. Moreover, BMI measurements do not distinguish between fat mass and fat-free mass, each of which has very distinct effects on health. High fat mass is associated with an increased risk for disease and mortality, while higher lean body mass correlates with increased physical fitness and longevity. BMI also does not consider age, sex, race, ethnicity, or types of adipose tissue, all of which tremendously influence disease risk across all BMI categories.
Body composition and adipose tissue
Body composition and type of excess adipose tissue better correlate disease risk than does BMI. The World Health Organization defines obesity as having a body fat percentage > 25% for men and > 35% for women. Body composition can be measured by skin-fold thickness, bioelectrical impedance, dual-energy x-ray absorptiometry (DXA), CT, or MRI.
A cross-sectional study by Shah and colleagues) comparing BMI and DXA found that BMI underestimated obesity prevalence. In the study, BMI characterized 26% of participants as obese while DXA (a direct measurement of fat) characterized 64%. Further, 39% of patients categorized as nonobese based on BMI were found to be obese on DXA. Also, BMI misclassified 25% of men and 48% of women in the study. These findings and those of other studies suggest that BMI has a high specificity but low sensitivity for diagnosing obesity, questioning its reliability as a clinical screening tool.
Current guideline recommendations on pharmacologic and surgical treatment options for patients with overweight or obesity, including those of the American Association of Clinical Endocrinology and American College of Endocrinology (AACE/ACE) and the American College of Cardiology/American Heart Association and The Obesity Society (ACC/AHA/TOS), rely on BMI, diminishing their utilization. For example, a recent literature search by Li and associates found that Asian American patients with lower BMIs and BMIs of 25 or 27 are at increased risk for metabolic disease. On the basis of study findings, some organizations recommend considering pharmacotherapy at a lower BMI cutoff of ≥ 25.0 or ≥ 27.5 for Asian people to ensure early treatment intervention in this patient population because guidelines do not recommend pharmacologic treatment unless the BMI is 27 with weight-related complications or 30. Under the current guidelines, a patient of Asian descent has greater disease severity with potentially more complications by the time pharmacotherapy is initiated.
As previously noted, body composition, which requires the use of special equipment (skinfold calipers, DXA, CT, MRI, body impedance scale), best captures the ratio of fat mass to fat-free mass. DXA is frequently used in research studies looking at body composition because of its lower cost, faster time to obtain the study, and ability to measure bone density. MRI has been found to be as accurate as CT for assessing visceral adipose tissue (VAT), skeletal muscle mass, and organ mass, and does not expose patients to ionizing radiation like CT does. MRI clinical use, however, is limited because of its high cost, and it may be problematic for patients with claustrophobia or who are unable to remain immobile for an extended period.
Patients with a high VAT mass, compared with subcutaneous adipose tissue (SAT), are at increased risk for metabolic syndrome, nonalcoholic fatty liver disease, and cardiovascular disease regardless of BMI, underscoring the clinical usefulness of measuring visceral adiposity over BMI.
One of the barriers to implementing VAT assessment in clinical practice is the cost of imaging studies. Fortunately, data suggest that waist circumference and/or waist-to-hip ratio measurements can be a valuable surrogate for VAT measurement. A waist circumference greater than 35 inches (88 cm) or a waist-to-hip ratio greater than 0.8 for women, and greater than 40 inches (102 cm) or a waist-to-hip ratio greater than 0.95 for men, increases metabolic disease risk. Obtaining these measurements requires a tape measure and a few extra minutes and offers more potent data than BMI alone. For example, a large cardiometabolic study found that within each BMI category, increasing gender-specific waist circumferences were associated with significantly higher VAT, liver fat, and a more harmful cardiometabolic risk profile. Men and women with a lower or normal BMI and a high waist circumference are at greatest relative health risk, compared with those with low waist circumference values. Yet, using the BMI alone in these patients would not raise any clinical concern, which is a missed opportunity for cardiometabolic risk reduction.
Biomarkers
Specific biomarkers are closely related to obesity. Leptin and resistin protein levels increase with adipose mass, while adiponectin decreases, probably contributing to insulin resistance. The higher levels of tumor necrosis factor–alpha and interleukin-6 from obesity contribute to chronic inflammation. The combined effect of chronic inflammation and insulin resistance allows greater bioavailability of insulinlike growth factor-1 (IGF-1), which has a role in initiating type 2 diabetes, cardiovascular disease, and cancer. Ideally, measuring these biomarkers could provide more advantageous information than BMI. Unfortunately, for now, the lack of standardized assays and imperfect knowledge of exactly how these biomarkers elicit disease prevents clinical use.
Obesity is a common, highly complex, chronic, and relapsing disease. Thankfully, a number of effective treatments and interventions are available. Although an accurate diagnosis of obesity is essential, underdiagnosed cases and missed opportunities for metabolic disease risk reduction persist. Overdiagnosing obesity, however, has the potential to incur unnecessary health care costs and result in weight bias and stigma.
While BMI is a quick and inexpensive means to assess obesity, by itself it lacks the necessary components for an accurate diagnosis. Particularly for individuals with a normal BMI or less severe overweight/obesity (BMI 27-34.9), other factors must be accounted for, including age, gender, and race. At a minimum, waist circumference should be measured to best risk-stratify and determine treatment intensity. Body composition analysis with BMI calculation refines the diagnosis of obesity.
Finally, clinicians may find best practices by using BMI delta change models. As with so many other clinical measurements, the trajectory tells the most astute story. For example, a patient whose BMI decreased from 45 to 35 may warrant less intensive treatment than a patient whose BMI increased from 26 to 31. Any change in BMI warrants clinical attention. A rapidly or consistently increasing BMI, even within normal range, should prompt clinicians to assess other factors related to obesity and metabolic disease risk (for example, lifestyle factors, waist circumference, blood pressure, cholesterol, diabetes screening) and initiate a conversation about weight management. Similarly, a consistently or rapidly decreasing BMI – even in elevated ranges and particularly with unintentional weight loss – should prompt evaluation.
Although BMI continues to be useful in clinical practice, epidemiology, and research, it should be used in combination with other clinical factors to provide the utmost quality of care.
Dr. Bartfield is assistant professor, obesity medicine specialist, Wake Forest Baptists Medical Center/Atrium Health Weight Management Center, Greensboro, N.C. She has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
In 1832, Belgian statistician Adolphe Quetelet introduced the concept of body mass index (BMI) – one’s weight (in kilograms) divided by the square of one’s height (in meters) as a measurement of ideal body weight. Approximately 140 years later, nutritional epidemiologist Ancel Keys proposed the use of BMI as a surrogate marker for evaluating body fat percentage within a population.
For the past 50 years, the scientific and medical communities have relied on BMI as a research and study tool to categorize patients’ weight (that is, severely underweight, underweight, normal weight, overweight, and obesity). The World Health Organization, National Institutes of Health, and U.S. Centers for Disease Control and Prevention use the following BMI weight classifications for adult patients:
- Underweight: BMI < 18.5
- Normal weight: BMI ≥ 18.5 to 24.9
- Overweight: BMI ≥ 25 to 29.9
- Obesity: BMI ≥ 30
Of note, BMI categories for children and adolescents (aged 2-19 years) are based on sex- and age-specific percentiles and will not be addressed in this article.
BMI appears to be a straightforward, easy, and cost-effective way to identify “healthy” weight and assess a patient’s risk for related conditions. For example, studies show that a BMI ≥ 35 kg/m2 correlates to higher prevalence of type 2 diabetes, hypertension, dyslipidemia, and decreased lifespan. At least 13 types of cancer have been linked to obesity, regardless of dietary or physical activity behaviors. While the health dangers associated with BMI ≥ 35 are substantial and difficult to dispute, concerns arise when BMI alone is used to determine healthy weight and disease risk in patients with a BMI of 25-35.
BMI limitations
There are troubling limitations to using BMI alone to assess a patient’s weight and health status. BMI only takes into account a patient’s height and weight, neither of which are sole determinants of health. Moreover, BMI measurements do not distinguish between fat mass and fat-free mass, each of which has very distinct effects on health. High fat mass is associated with an increased risk for disease and mortality, while higher lean body mass correlates with increased physical fitness and longevity. BMI also does not consider age, sex, race, ethnicity, or types of adipose tissue, all of which tremendously influence disease risk across all BMI categories.
Body composition and adipose tissue
Body composition and type of excess adipose tissue better correlate disease risk than does BMI. The World Health Organization defines obesity as having a body fat percentage > 25% for men and > 35% for women. Body composition can be measured by skin-fold thickness, bioelectrical impedance, dual-energy x-ray absorptiometry (DXA), CT, or MRI.
A cross-sectional study by Shah and colleagues) comparing BMI and DXA found that BMI underestimated obesity prevalence. In the study, BMI characterized 26% of participants as obese while DXA (a direct measurement of fat) characterized 64%. Further, 39% of patients categorized as nonobese based on BMI were found to be obese on DXA. Also, BMI misclassified 25% of men and 48% of women in the study. These findings and those of other studies suggest that BMI has a high specificity but low sensitivity for diagnosing obesity, questioning its reliability as a clinical screening tool.
Current guideline recommendations on pharmacologic and surgical treatment options for patients with overweight or obesity, including those of the American Association of Clinical Endocrinology and American College of Endocrinology (AACE/ACE) and the American College of Cardiology/American Heart Association and The Obesity Society (ACC/AHA/TOS), rely on BMI, diminishing their utilization. For example, a recent literature search by Li and associates found that Asian American patients with lower BMIs and BMIs of 25 or 27 are at increased risk for metabolic disease. On the basis of study findings, some organizations recommend considering pharmacotherapy at a lower BMI cutoff of ≥ 25.0 or ≥ 27.5 for Asian people to ensure early treatment intervention in this patient population because guidelines do not recommend pharmacologic treatment unless the BMI is 27 with weight-related complications or 30. Under the current guidelines, a patient of Asian descent has greater disease severity with potentially more complications by the time pharmacotherapy is initiated.
As previously noted, body composition, which requires the use of special equipment (skinfold calipers, DXA, CT, MRI, body impedance scale), best captures the ratio of fat mass to fat-free mass. DXA is frequently used in research studies looking at body composition because of its lower cost, faster time to obtain the study, and ability to measure bone density. MRI has been found to be as accurate as CT for assessing visceral adipose tissue (VAT), skeletal muscle mass, and organ mass, and does not expose patients to ionizing radiation like CT does. MRI clinical use, however, is limited because of its high cost, and it may be problematic for patients with claustrophobia or who are unable to remain immobile for an extended period.
Patients with a high VAT mass, compared with subcutaneous adipose tissue (SAT), are at increased risk for metabolic syndrome, nonalcoholic fatty liver disease, and cardiovascular disease regardless of BMI, underscoring the clinical usefulness of measuring visceral adiposity over BMI.
One of the barriers to implementing VAT assessment in clinical practice is the cost of imaging studies. Fortunately, data suggest that waist circumference and/or waist-to-hip ratio measurements can be a valuable surrogate for VAT measurement. A waist circumference greater than 35 inches (88 cm) or a waist-to-hip ratio greater than 0.8 for women, and greater than 40 inches (102 cm) or a waist-to-hip ratio greater than 0.95 for men, increases metabolic disease risk. Obtaining these measurements requires a tape measure and a few extra minutes and offers more potent data than BMI alone. For example, a large cardiometabolic study found that within each BMI category, increasing gender-specific waist circumferences were associated with significantly higher VAT, liver fat, and a more harmful cardiometabolic risk profile. Men and women with a lower or normal BMI and a high waist circumference are at greatest relative health risk, compared with those with low waist circumference values. Yet, using the BMI alone in these patients would not raise any clinical concern, which is a missed opportunity for cardiometabolic risk reduction.
Biomarkers
Specific biomarkers are closely related to obesity. Leptin and resistin protein levels increase with adipose mass, while adiponectin decreases, probably contributing to insulin resistance. The higher levels of tumor necrosis factor–alpha and interleukin-6 from obesity contribute to chronic inflammation. The combined effect of chronic inflammation and insulin resistance allows greater bioavailability of insulinlike growth factor-1 (IGF-1), which has a role in initiating type 2 diabetes, cardiovascular disease, and cancer. Ideally, measuring these biomarkers could provide more advantageous information than BMI. Unfortunately, for now, the lack of standardized assays and imperfect knowledge of exactly how these biomarkers elicit disease prevents clinical use.
Obesity is a common, highly complex, chronic, and relapsing disease. Thankfully, a number of effective treatments and interventions are available. Although an accurate diagnosis of obesity is essential, underdiagnosed cases and missed opportunities for metabolic disease risk reduction persist. Overdiagnosing obesity, however, has the potential to incur unnecessary health care costs and result in weight bias and stigma.
While BMI is a quick and inexpensive means to assess obesity, by itself it lacks the necessary components for an accurate diagnosis. Particularly for individuals with a normal BMI or less severe overweight/obesity (BMI 27-34.9), other factors must be accounted for, including age, gender, and race. At a minimum, waist circumference should be measured to best risk-stratify and determine treatment intensity. Body composition analysis with BMI calculation refines the diagnosis of obesity.
Finally, clinicians may find best practices by using BMI delta change models. As with so many other clinical measurements, the trajectory tells the most astute story. For example, a patient whose BMI decreased from 45 to 35 may warrant less intensive treatment than a patient whose BMI increased from 26 to 31. Any change in BMI warrants clinical attention. A rapidly or consistently increasing BMI, even within normal range, should prompt clinicians to assess other factors related to obesity and metabolic disease risk (for example, lifestyle factors, waist circumference, blood pressure, cholesterol, diabetes screening) and initiate a conversation about weight management. Similarly, a consistently or rapidly decreasing BMI – even in elevated ranges and particularly with unintentional weight loss – should prompt evaluation.
Although BMI continues to be useful in clinical practice, epidemiology, and research, it should be used in combination with other clinical factors to provide the utmost quality of care.
Dr. Bartfield is assistant professor, obesity medicine specialist, Wake Forest Baptists Medical Center/Atrium Health Weight Management Center, Greensboro, N.C. She has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
In 1832, Belgian statistician Adolphe Quetelet introduced the concept of body mass index (BMI) – one’s weight (in kilograms) divided by the square of one’s height (in meters) as a measurement of ideal body weight. Approximately 140 years later, nutritional epidemiologist Ancel Keys proposed the use of BMI as a surrogate marker for evaluating body fat percentage within a population.
For the past 50 years, the scientific and medical communities have relied on BMI as a research and study tool to categorize patients’ weight (that is, severely underweight, underweight, normal weight, overweight, and obesity). The World Health Organization, National Institutes of Health, and U.S. Centers for Disease Control and Prevention use the following BMI weight classifications for adult patients:
- Underweight: BMI < 18.5
- Normal weight: BMI ≥ 18.5 to 24.9
- Overweight: BMI ≥ 25 to 29.9
- Obesity: BMI ≥ 30
Of note, BMI categories for children and adolescents (aged 2-19 years) are based on sex- and age-specific percentiles and will not be addressed in this article.
BMI appears to be a straightforward, easy, and cost-effective way to identify “healthy” weight and assess a patient’s risk for related conditions. For example, studies show that a BMI ≥ 35 kg/m2 correlates to higher prevalence of type 2 diabetes, hypertension, dyslipidemia, and decreased lifespan. At least 13 types of cancer have been linked to obesity, regardless of dietary or physical activity behaviors. While the health dangers associated with BMI ≥ 35 are substantial and difficult to dispute, concerns arise when BMI alone is used to determine healthy weight and disease risk in patients with a BMI of 25-35.
BMI limitations
There are troubling limitations to using BMI alone to assess a patient’s weight and health status. BMI only takes into account a patient’s height and weight, neither of which are sole determinants of health. Moreover, BMI measurements do not distinguish between fat mass and fat-free mass, each of which has very distinct effects on health. High fat mass is associated with an increased risk for disease and mortality, while higher lean body mass correlates with increased physical fitness and longevity. BMI also does not consider age, sex, race, ethnicity, or types of adipose tissue, all of which tremendously influence disease risk across all BMI categories.
Body composition and adipose tissue
Body composition and type of excess adipose tissue better correlate disease risk than does BMI. The World Health Organization defines obesity as having a body fat percentage > 25% for men and > 35% for women. Body composition can be measured by skin-fold thickness, bioelectrical impedance, dual-energy x-ray absorptiometry (DXA), CT, or MRI.
A cross-sectional study by Shah and colleagues) comparing BMI and DXA found that BMI underestimated obesity prevalence. In the study, BMI characterized 26% of participants as obese while DXA (a direct measurement of fat) characterized 64%. Further, 39% of patients categorized as nonobese based on BMI were found to be obese on DXA. Also, BMI misclassified 25% of men and 48% of women in the study. These findings and those of other studies suggest that BMI has a high specificity but low sensitivity for diagnosing obesity, questioning its reliability as a clinical screening tool.
Current guideline recommendations on pharmacologic and surgical treatment options for patients with overweight or obesity, including those of the American Association of Clinical Endocrinology and American College of Endocrinology (AACE/ACE) and the American College of Cardiology/American Heart Association and The Obesity Society (ACC/AHA/TOS), rely on BMI, diminishing their utilization. For example, a recent literature search by Li and associates found that Asian American patients with lower BMIs and BMIs of 25 or 27 are at increased risk for metabolic disease. On the basis of study findings, some organizations recommend considering pharmacotherapy at a lower BMI cutoff of ≥ 25.0 or ≥ 27.5 for Asian people to ensure early treatment intervention in this patient population because guidelines do not recommend pharmacologic treatment unless the BMI is 27 with weight-related complications or 30. Under the current guidelines, a patient of Asian descent has greater disease severity with potentially more complications by the time pharmacotherapy is initiated.
As previously noted, body composition, which requires the use of special equipment (skinfold calipers, DXA, CT, MRI, body impedance scale), best captures the ratio of fat mass to fat-free mass. DXA is frequently used in research studies looking at body composition because of its lower cost, faster time to obtain the study, and ability to measure bone density. MRI has been found to be as accurate as CT for assessing visceral adipose tissue (VAT), skeletal muscle mass, and organ mass, and does not expose patients to ionizing radiation like CT does. MRI clinical use, however, is limited because of its high cost, and it may be problematic for patients with claustrophobia or who are unable to remain immobile for an extended period.
Patients with a high VAT mass, compared with subcutaneous adipose tissue (SAT), are at increased risk for metabolic syndrome, nonalcoholic fatty liver disease, and cardiovascular disease regardless of BMI, underscoring the clinical usefulness of measuring visceral adiposity over BMI.
One of the barriers to implementing VAT assessment in clinical practice is the cost of imaging studies. Fortunately, data suggest that waist circumference and/or waist-to-hip ratio measurements can be a valuable surrogate for VAT measurement. A waist circumference greater than 35 inches (88 cm) or a waist-to-hip ratio greater than 0.8 for women, and greater than 40 inches (102 cm) or a waist-to-hip ratio greater than 0.95 for men, increases metabolic disease risk. Obtaining these measurements requires a tape measure and a few extra minutes and offers more potent data than BMI alone. For example, a large cardiometabolic study found that within each BMI category, increasing gender-specific waist circumferences were associated with significantly higher VAT, liver fat, and a more harmful cardiometabolic risk profile. Men and women with a lower or normal BMI and a high waist circumference are at greatest relative health risk, compared with those with low waist circumference values. Yet, using the BMI alone in these patients would not raise any clinical concern, which is a missed opportunity for cardiometabolic risk reduction.
Biomarkers
Specific biomarkers are closely related to obesity. Leptin and resistin protein levels increase with adipose mass, while adiponectin decreases, probably contributing to insulin resistance. The higher levels of tumor necrosis factor–alpha and interleukin-6 from obesity contribute to chronic inflammation. The combined effect of chronic inflammation and insulin resistance allows greater bioavailability of insulinlike growth factor-1 (IGF-1), which has a role in initiating type 2 diabetes, cardiovascular disease, and cancer. Ideally, measuring these biomarkers could provide more advantageous information than BMI. Unfortunately, for now, the lack of standardized assays and imperfect knowledge of exactly how these biomarkers elicit disease prevents clinical use.
Obesity is a common, highly complex, chronic, and relapsing disease. Thankfully, a number of effective treatments and interventions are available. Although an accurate diagnosis of obesity is essential, underdiagnosed cases and missed opportunities for metabolic disease risk reduction persist. Overdiagnosing obesity, however, has the potential to incur unnecessary health care costs and result in weight bias and stigma.
While BMI is a quick and inexpensive means to assess obesity, by itself it lacks the necessary components for an accurate diagnosis. Particularly for individuals with a normal BMI or less severe overweight/obesity (BMI 27-34.9), other factors must be accounted for, including age, gender, and race. At a minimum, waist circumference should be measured to best risk-stratify and determine treatment intensity. Body composition analysis with BMI calculation refines the diagnosis of obesity.
Finally, clinicians may find best practices by using BMI delta change models. As with so many other clinical measurements, the trajectory tells the most astute story. For example, a patient whose BMI decreased from 45 to 35 may warrant less intensive treatment than a patient whose BMI increased from 26 to 31. Any change in BMI warrants clinical attention. A rapidly or consistently increasing BMI, even within normal range, should prompt clinicians to assess other factors related to obesity and metabolic disease risk (for example, lifestyle factors, waist circumference, blood pressure, cholesterol, diabetes screening) and initiate a conversation about weight management. Similarly, a consistently or rapidly decreasing BMI – even in elevated ranges and particularly with unintentional weight loss – should prompt evaluation.
Although BMI continues to be useful in clinical practice, epidemiology, and research, it should be used in combination with other clinical factors to provide the utmost quality of care.
Dr. Bartfield is assistant professor, obesity medicine specialist, Wake Forest Baptists Medical Center/Atrium Health Weight Management Center, Greensboro, N.C. She has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Debate: Initial combination therapy for type 2 diabetes?
SAN DIEGO –
This question was debated by two well-known clinician-researchers in the diabetes world at the recent annual scientific sessions of the American Diabetes Association.
Ralph A. DeFronzo, MD, argued for combination therapy at the time of diagnosis, and David M. Nathan, MD, countered that sequential therapy is a better way to go.
‘The ominous octet’: Addressing multiple underlying defects
Of course, Dr. DeFronzo said, the right agents must be selected. “The drugs we’re going to use as combination at a minimum have to correct the underlying insulin resistance and beta-cell failure, or we are not going to be successful.”
In addition, he said, these drugs should also provide protection against cardiovascular, kidney, and fatty liver disease, because “[managing] diabetes is more than just controlling the glucose.”
Recent U.S. data suggest that half of people with diabetes have a hemoglobin A1c above 7%, and a quarter remain above 8%. “We’re not really doing a very good job in terms of glycemic control,” said Dr. DeFronzo, chief of the diabetes division at University of Texas, San Antonio.
One reason for this failure, he said, is the complex pathophysiology of type 2 diabetes represented by eight major defects, what he called the “ominous octet”: decreased pancreatic insulin secretion, gut incretin effects, glucose uptake in the muscle, increased lipolysis, glucose reabsorption in the kidney, hepatic glucose production, increased glucagon secretion, and neurotransmitter dysfunction.
“There are eight problems, so you’re going to need multiple drugs in combination ... not ones that just lower the A1c.”
And, Dr. DeFronzo said, these drugs “must be started early in the natural history of type 2 diabetes if progressive beta-cell failure is to be prevented.”
He pointed to the United Kingdom Prospective Diabetes Study (UKPDS), in which the sulfonylurea glyburide was used first, followed by metformin. With each drug, the A1c decreased initially but then rose within 3 years. By 15 years, 65% of participants were taking insulin.
More recently, the GRADE study examined the effects of adding four different glucose-lowering agents (glimepiride, sitagliptin, liraglutide, or insulin glargine) in people who hadn’t achieved target A1c with metformin.
“So, by definition, drug number one failed,” he observed.
During the study, all participants showed an initial A1c drop, followed by progressive failure, “again ... showing that stepwise therapy doesn’t work.”
All patients with type 2 diabetes at his center are treated using the “DeFronzo algorithm” consisting of three drug classes: a glucagon-like peptide-1 (GLP-1) agonist, a sodium-glucose cotransporter-2 (SGLT2) inhibitor, and pioglitazone, as each of them targets more than one of the “ominous octet” defects.
“The drugs that clearly do not work on a long-term basis are metformin and sulfonylureas,” he emphasized.
Several studies demonstrate the efficacy of combination therapy, he said. In one, DURATION 8, the combination of exenatide and dapagliflozin was superior to either agent individually in lowering A1c, cardiovascular events, and all-cause mortality over 2 years.
And in the 5-year VERIFY study, early combination therapy with vildagliptin plus metformin proved superior in A1c-lowering to starting patients on metformin and adding vildagliptin later.
Dr. DeFronzo’s own “knock-out punch” study, EDICT, in people with new-onset type 2 diabetes, compared the initial combination of metformin, pioglitazone, and exenatide with conventional sequential add-on therapy with metformin, glipizide, and insulin glargine.
The primary endpoint – the difference in the proportion of patients with A1c less than 6.5% – was 70% versus 29% with combination compared with sequential therapy, a difference “as robust as you can be going against the stepwise approach” at P < .00001, he said.
The combination therapy virtually normalized both insulin sensitivity and beta-cell function, whereas the conventional therapy did neither.
Also from Dr. DeFronzo’s group, in the Qatar study, which compared exenatide plus pioglitazone with basal-bolus insulin in people with about 10 years’ duration of type 2 diabetes and A1c above 7.5% taking sulfonylurea plus metformin, the combination therapy produced an A1c of 6.2% versus 7.1% with insulin.
Dr. DeFronzo pointed to new language added to the ADA Standards of Medical Care in Diabetes in 2022.
While still endorsing stepwise therapy, the document also says that “there are data to support initial combination therapy for more rapid attainment of glycemic targets and longer durability of glycemic effect.” The two references cited are EDICT and VERIFY.
“Finally, the American Diabetes Association has gotten the message,” he concluded.
Sequential therapy: Far more data, lower cost
Dr. Nathan began by pointing out that the ADA Standards of Care continue to advise use of metformin as first-line therapy for type 2 diabetes “because of its high efficacy in lowering A1c, minimal hypoglycemia risk when used as monotherapy, weight neutrality with the potential for modest weight loss, good safety profile, and low cost.”
He emphasized that he was not arguing “against the use of early or even initial combination therapy when there are co-existent morbidities [such as cardiovascular or chronic kidney disease] that merit use of demonstrably effective medications.” But Dr. Nathan pointed out, those patients are not the majority with type 2 diabetes.
He laid out four main arguments for choosing traditional sequential therapy over initial combination therapy. For one, it “enables determination of efficacy of adding individual medications, while initial combination precludes determining benefits of individual drugs.”
Second, traditional sequential therapy allows for assessment of side effects from individual drugs.
“With Dr. DeFronzo’s algorithm you throw everything at them, and if they get nausea, vomiting, or diarrhea, you won’t know which drug it is ... If they get an allergic reaction, you won’t know which medication it is,” observed Dr. Nathan, who is director of the clinical research center and the diabetes center at Massachusetts General Hospital, Boston.
Moreover, he said, traditional sequential therapy “promotes individualization, with selection of drugs, which is something we’re laboring to achieve. Initial combination obviously limits that.”
Further, sequential therapy is “parsimonious and cost-effective, whereas initial combination therapy is expensive, with modest advantages at most.”
And, there are “lots of data” supporting traditional sequential therapy and relatively little for initial combination therapy.
Dr. Nathan added that when he searched the literature for relevant randomized clinical trials, he found 16 investigating initial combination therapy versus monotherapy, but only three that examined combination versus sequential therapy.
“Very few of them, except for EDICT and VERIFY, actually include the sequential therapy that we would use in practice,” he said.
Moreover, he observed, except for the VERIFY study, most are less than half a year in duration. And in VERIFY, there was an initial 20% difference in the proportions of patients with A1c below 7.0%, but by 12 months, that difference had shrunk to just 5%-6%.
“So, looking over time is very important,” Dr. Nathan cautioned. “We really have to be careful ... Six months is barely enough time to see A1c equilibrate ... You really need to study a long-term, chronic, progressive disease like type 2 diabetes over a long enough period of time to be clinically meaningful.”
Dr. Nathan acknowledged to Dr. DeFronzo that the latter’s EDICT study was “well conducted” and “long enough,” and that the researchers did examine monotherapy versus sequential therapy. However, he pointed out that it was a small study with 249 patients and the dropout rate was high, with 58% of patients remaining in the study with triple therapy versus 68% for conventional treatment. “That’s a bit problematic,” Dr. Nathan noted.
At 2 years, the “trivial” difference in A1c was 6.5% with conventional therapy versus 6.0% with triple therapy. “This is all on the very flat complications curve with regard to A1c,” he observed.
Patients treated with sequential therapy with sulfonylurea and insulin had higher rates of hypoglycemia and weight gain, whereas the combination triple therapy group had more gastrointestinal side effects and edema.
However, the most dramatic difference was cost: the average wholesale price for sequential therapy totaled about $85 per month, compared with $1,310 for initial combination therapy. For the approximately 1.5 million patients with new-onset type 2 diabetes in the United States, that difference comes to an additional cost per year of about $22 billion, Dr. Nathan calculated.
“Although current sequential therapy leaves much to be desired ... initial combination therapy has generally only been tested for brief, clinically insufficient periods.
“And therefore, I think sequential therapy is still what is called for,” he concluded. “Well-powered, acceptable-duration studies need to be performed before we can adopt initial/early combination therapy as the standard of care.”
Dr. DeFronzo has reported receiving research support from Boehringer Ingelheim, AstraZeneca, and Merck; payment or honoraria for lectures, presentations, speakers bureaus, manuscript writing, or educational events from AstraZeneca; and participation on a data safety monitoring board or advisory board for AstraZeneca, Intarcia, Novo Nordisk, and Boehringer Ingelheim. Dr. Nathan has reported no relevant financial relationships.
A version of this article appeared on Medscape.com.
SAN DIEGO –
This question was debated by two well-known clinician-researchers in the diabetes world at the recent annual scientific sessions of the American Diabetes Association.
Ralph A. DeFronzo, MD, argued for combination therapy at the time of diagnosis, and David M. Nathan, MD, countered that sequential therapy is a better way to go.
‘The ominous octet’: Addressing multiple underlying defects
Of course, Dr. DeFronzo said, the right agents must be selected. “The drugs we’re going to use as combination at a minimum have to correct the underlying insulin resistance and beta-cell failure, or we are not going to be successful.”
In addition, he said, these drugs should also provide protection against cardiovascular, kidney, and fatty liver disease, because “[managing] diabetes is more than just controlling the glucose.”
Recent U.S. data suggest that half of people with diabetes have a hemoglobin A1c above 7%, and a quarter remain above 8%. “We’re not really doing a very good job in terms of glycemic control,” said Dr. DeFronzo, chief of the diabetes division at University of Texas, San Antonio.
One reason for this failure, he said, is the complex pathophysiology of type 2 diabetes represented by eight major defects, what he called the “ominous octet”: decreased pancreatic insulin secretion, gut incretin effects, glucose uptake in the muscle, increased lipolysis, glucose reabsorption in the kidney, hepatic glucose production, increased glucagon secretion, and neurotransmitter dysfunction.
“There are eight problems, so you’re going to need multiple drugs in combination ... not ones that just lower the A1c.”
And, Dr. DeFronzo said, these drugs “must be started early in the natural history of type 2 diabetes if progressive beta-cell failure is to be prevented.”
He pointed to the United Kingdom Prospective Diabetes Study (UKPDS), in which the sulfonylurea glyburide was used first, followed by metformin. With each drug, the A1c decreased initially but then rose within 3 years. By 15 years, 65% of participants were taking insulin.
More recently, the GRADE study examined the effects of adding four different glucose-lowering agents (glimepiride, sitagliptin, liraglutide, or insulin glargine) in people who hadn’t achieved target A1c with metformin.
“So, by definition, drug number one failed,” he observed.
During the study, all participants showed an initial A1c drop, followed by progressive failure, “again ... showing that stepwise therapy doesn’t work.”
All patients with type 2 diabetes at his center are treated using the “DeFronzo algorithm” consisting of three drug classes: a glucagon-like peptide-1 (GLP-1) agonist, a sodium-glucose cotransporter-2 (SGLT2) inhibitor, and pioglitazone, as each of them targets more than one of the “ominous octet” defects.
“The drugs that clearly do not work on a long-term basis are metformin and sulfonylureas,” he emphasized.
Several studies demonstrate the efficacy of combination therapy, he said. In one, DURATION 8, the combination of exenatide and dapagliflozin was superior to either agent individually in lowering A1c, cardiovascular events, and all-cause mortality over 2 years.
And in the 5-year VERIFY study, early combination therapy with vildagliptin plus metformin proved superior in A1c-lowering to starting patients on metformin and adding vildagliptin later.
Dr. DeFronzo’s own “knock-out punch” study, EDICT, in people with new-onset type 2 diabetes, compared the initial combination of metformin, pioglitazone, and exenatide with conventional sequential add-on therapy with metformin, glipizide, and insulin glargine.
The primary endpoint – the difference in the proportion of patients with A1c less than 6.5% – was 70% versus 29% with combination compared with sequential therapy, a difference “as robust as you can be going against the stepwise approach” at P < .00001, he said.
The combination therapy virtually normalized both insulin sensitivity and beta-cell function, whereas the conventional therapy did neither.
Also from Dr. DeFronzo’s group, in the Qatar study, which compared exenatide plus pioglitazone with basal-bolus insulin in people with about 10 years’ duration of type 2 diabetes and A1c above 7.5% taking sulfonylurea plus metformin, the combination therapy produced an A1c of 6.2% versus 7.1% with insulin.
Dr. DeFronzo pointed to new language added to the ADA Standards of Medical Care in Diabetes in 2022.
While still endorsing stepwise therapy, the document also says that “there are data to support initial combination therapy for more rapid attainment of glycemic targets and longer durability of glycemic effect.” The two references cited are EDICT and VERIFY.
“Finally, the American Diabetes Association has gotten the message,” he concluded.
Sequential therapy: Far more data, lower cost
Dr. Nathan began by pointing out that the ADA Standards of Care continue to advise use of metformin as first-line therapy for type 2 diabetes “because of its high efficacy in lowering A1c, minimal hypoglycemia risk when used as monotherapy, weight neutrality with the potential for modest weight loss, good safety profile, and low cost.”
He emphasized that he was not arguing “against the use of early or even initial combination therapy when there are co-existent morbidities [such as cardiovascular or chronic kidney disease] that merit use of demonstrably effective medications.” But Dr. Nathan pointed out, those patients are not the majority with type 2 diabetes.
He laid out four main arguments for choosing traditional sequential therapy over initial combination therapy. For one, it “enables determination of efficacy of adding individual medications, while initial combination precludes determining benefits of individual drugs.”
Second, traditional sequential therapy allows for assessment of side effects from individual drugs.
“With Dr. DeFronzo’s algorithm you throw everything at them, and if they get nausea, vomiting, or diarrhea, you won’t know which drug it is ... If they get an allergic reaction, you won’t know which medication it is,” observed Dr. Nathan, who is director of the clinical research center and the diabetes center at Massachusetts General Hospital, Boston.
Moreover, he said, traditional sequential therapy “promotes individualization, with selection of drugs, which is something we’re laboring to achieve. Initial combination obviously limits that.”
Further, sequential therapy is “parsimonious and cost-effective, whereas initial combination therapy is expensive, with modest advantages at most.”
And, there are “lots of data” supporting traditional sequential therapy and relatively little for initial combination therapy.
Dr. Nathan added that when he searched the literature for relevant randomized clinical trials, he found 16 investigating initial combination therapy versus monotherapy, but only three that examined combination versus sequential therapy.
“Very few of them, except for EDICT and VERIFY, actually include the sequential therapy that we would use in practice,” he said.
Moreover, he observed, except for the VERIFY study, most are less than half a year in duration. And in VERIFY, there was an initial 20% difference in the proportions of patients with A1c below 7.0%, but by 12 months, that difference had shrunk to just 5%-6%.
“So, looking over time is very important,” Dr. Nathan cautioned. “We really have to be careful ... Six months is barely enough time to see A1c equilibrate ... You really need to study a long-term, chronic, progressive disease like type 2 diabetes over a long enough period of time to be clinically meaningful.”
Dr. Nathan acknowledged to Dr. DeFronzo that the latter’s EDICT study was “well conducted” and “long enough,” and that the researchers did examine monotherapy versus sequential therapy. However, he pointed out that it was a small study with 249 patients and the dropout rate was high, with 58% of patients remaining in the study with triple therapy versus 68% for conventional treatment. “That’s a bit problematic,” Dr. Nathan noted.
At 2 years, the “trivial” difference in A1c was 6.5% with conventional therapy versus 6.0% with triple therapy. “This is all on the very flat complications curve with regard to A1c,” he observed.
Patients treated with sequential therapy with sulfonylurea and insulin had higher rates of hypoglycemia and weight gain, whereas the combination triple therapy group had more gastrointestinal side effects and edema.
However, the most dramatic difference was cost: the average wholesale price for sequential therapy totaled about $85 per month, compared with $1,310 for initial combination therapy. For the approximately 1.5 million patients with new-onset type 2 diabetes in the United States, that difference comes to an additional cost per year of about $22 billion, Dr. Nathan calculated.
“Although current sequential therapy leaves much to be desired ... initial combination therapy has generally only been tested for brief, clinically insufficient periods.
“And therefore, I think sequential therapy is still what is called for,” he concluded. “Well-powered, acceptable-duration studies need to be performed before we can adopt initial/early combination therapy as the standard of care.”
Dr. DeFronzo has reported receiving research support from Boehringer Ingelheim, AstraZeneca, and Merck; payment or honoraria for lectures, presentations, speakers bureaus, manuscript writing, or educational events from AstraZeneca; and participation on a data safety monitoring board or advisory board for AstraZeneca, Intarcia, Novo Nordisk, and Boehringer Ingelheim. Dr. Nathan has reported no relevant financial relationships.
A version of this article appeared on Medscape.com.
SAN DIEGO –
This question was debated by two well-known clinician-researchers in the diabetes world at the recent annual scientific sessions of the American Diabetes Association.
Ralph A. DeFronzo, MD, argued for combination therapy at the time of diagnosis, and David M. Nathan, MD, countered that sequential therapy is a better way to go.
‘The ominous octet’: Addressing multiple underlying defects
Of course, Dr. DeFronzo said, the right agents must be selected. “The drugs we’re going to use as combination at a minimum have to correct the underlying insulin resistance and beta-cell failure, or we are not going to be successful.”
In addition, he said, these drugs should also provide protection against cardiovascular, kidney, and fatty liver disease, because “[managing] diabetes is more than just controlling the glucose.”
Recent U.S. data suggest that half of people with diabetes have a hemoglobin A1c above 7%, and a quarter remain above 8%. “We’re not really doing a very good job in terms of glycemic control,” said Dr. DeFronzo, chief of the diabetes division at University of Texas, San Antonio.
One reason for this failure, he said, is the complex pathophysiology of type 2 diabetes represented by eight major defects, what he called the “ominous octet”: decreased pancreatic insulin secretion, gut incretin effects, glucose uptake in the muscle, increased lipolysis, glucose reabsorption in the kidney, hepatic glucose production, increased glucagon secretion, and neurotransmitter dysfunction.
“There are eight problems, so you’re going to need multiple drugs in combination ... not ones that just lower the A1c.”
And, Dr. DeFronzo said, these drugs “must be started early in the natural history of type 2 diabetes if progressive beta-cell failure is to be prevented.”
He pointed to the United Kingdom Prospective Diabetes Study (UKPDS), in which the sulfonylurea glyburide was used first, followed by metformin. With each drug, the A1c decreased initially but then rose within 3 years. By 15 years, 65% of participants were taking insulin.
More recently, the GRADE study examined the effects of adding four different glucose-lowering agents (glimepiride, sitagliptin, liraglutide, or insulin glargine) in people who hadn’t achieved target A1c with metformin.
“So, by definition, drug number one failed,” he observed.
During the study, all participants showed an initial A1c drop, followed by progressive failure, “again ... showing that stepwise therapy doesn’t work.”
All patients with type 2 diabetes at his center are treated using the “DeFronzo algorithm” consisting of three drug classes: a glucagon-like peptide-1 (GLP-1) agonist, a sodium-glucose cotransporter-2 (SGLT2) inhibitor, and pioglitazone, as each of them targets more than one of the “ominous octet” defects.
“The drugs that clearly do not work on a long-term basis are metformin and sulfonylureas,” he emphasized.
Several studies demonstrate the efficacy of combination therapy, he said. In one, DURATION 8, the combination of exenatide and dapagliflozin was superior to either agent individually in lowering A1c, cardiovascular events, and all-cause mortality over 2 years.
And in the 5-year VERIFY study, early combination therapy with vildagliptin plus metformin proved superior in A1c-lowering to starting patients on metformin and adding vildagliptin later.
Dr. DeFronzo’s own “knock-out punch” study, EDICT, in people with new-onset type 2 diabetes, compared the initial combination of metformin, pioglitazone, and exenatide with conventional sequential add-on therapy with metformin, glipizide, and insulin glargine.
The primary endpoint – the difference in the proportion of patients with A1c less than 6.5% – was 70% versus 29% with combination compared with sequential therapy, a difference “as robust as you can be going against the stepwise approach” at P < .00001, he said.
The combination therapy virtually normalized both insulin sensitivity and beta-cell function, whereas the conventional therapy did neither.
Also from Dr. DeFronzo’s group, in the Qatar study, which compared exenatide plus pioglitazone with basal-bolus insulin in people with about 10 years’ duration of type 2 diabetes and A1c above 7.5% taking sulfonylurea plus metformin, the combination therapy produced an A1c of 6.2% versus 7.1% with insulin.
Dr. DeFronzo pointed to new language added to the ADA Standards of Medical Care in Diabetes in 2022.
While still endorsing stepwise therapy, the document also says that “there are data to support initial combination therapy for more rapid attainment of glycemic targets and longer durability of glycemic effect.” The two references cited are EDICT and VERIFY.
“Finally, the American Diabetes Association has gotten the message,” he concluded.
Sequential therapy: Far more data, lower cost
Dr. Nathan began by pointing out that the ADA Standards of Care continue to advise use of metformin as first-line therapy for type 2 diabetes “because of its high efficacy in lowering A1c, minimal hypoglycemia risk when used as monotherapy, weight neutrality with the potential for modest weight loss, good safety profile, and low cost.”
He emphasized that he was not arguing “against the use of early or even initial combination therapy when there are co-existent morbidities [such as cardiovascular or chronic kidney disease] that merit use of demonstrably effective medications.” But Dr. Nathan pointed out, those patients are not the majority with type 2 diabetes.
He laid out four main arguments for choosing traditional sequential therapy over initial combination therapy. For one, it “enables determination of efficacy of adding individual medications, while initial combination precludes determining benefits of individual drugs.”
Second, traditional sequential therapy allows for assessment of side effects from individual drugs.
“With Dr. DeFronzo’s algorithm you throw everything at them, and if they get nausea, vomiting, or diarrhea, you won’t know which drug it is ... If they get an allergic reaction, you won’t know which medication it is,” observed Dr. Nathan, who is director of the clinical research center and the diabetes center at Massachusetts General Hospital, Boston.
Moreover, he said, traditional sequential therapy “promotes individualization, with selection of drugs, which is something we’re laboring to achieve. Initial combination obviously limits that.”
Further, sequential therapy is “parsimonious and cost-effective, whereas initial combination therapy is expensive, with modest advantages at most.”
And, there are “lots of data” supporting traditional sequential therapy and relatively little for initial combination therapy.
Dr. Nathan added that when he searched the literature for relevant randomized clinical trials, he found 16 investigating initial combination therapy versus monotherapy, but only three that examined combination versus sequential therapy.
“Very few of them, except for EDICT and VERIFY, actually include the sequential therapy that we would use in practice,” he said.
Moreover, he observed, except for the VERIFY study, most are less than half a year in duration. And in VERIFY, there was an initial 20% difference in the proportions of patients with A1c below 7.0%, but by 12 months, that difference had shrunk to just 5%-6%.
“So, looking over time is very important,” Dr. Nathan cautioned. “We really have to be careful ... Six months is barely enough time to see A1c equilibrate ... You really need to study a long-term, chronic, progressive disease like type 2 diabetes over a long enough period of time to be clinically meaningful.”
Dr. Nathan acknowledged to Dr. DeFronzo that the latter’s EDICT study was “well conducted” and “long enough,” and that the researchers did examine monotherapy versus sequential therapy. However, he pointed out that it was a small study with 249 patients and the dropout rate was high, with 58% of patients remaining in the study with triple therapy versus 68% for conventional treatment. “That’s a bit problematic,” Dr. Nathan noted.
At 2 years, the “trivial” difference in A1c was 6.5% with conventional therapy versus 6.0% with triple therapy. “This is all on the very flat complications curve with regard to A1c,” he observed.
Patients treated with sequential therapy with sulfonylurea and insulin had higher rates of hypoglycemia and weight gain, whereas the combination triple therapy group had more gastrointestinal side effects and edema.
However, the most dramatic difference was cost: the average wholesale price for sequential therapy totaled about $85 per month, compared with $1,310 for initial combination therapy. For the approximately 1.5 million patients with new-onset type 2 diabetes in the United States, that difference comes to an additional cost per year of about $22 billion, Dr. Nathan calculated.
“Although current sequential therapy leaves much to be desired ... initial combination therapy has generally only been tested for brief, clinically insufficient periods.
“And therefore, I think sequential therapy is still what is called for,” he concluded. “Well-powered, acceptable-duration studies need to be performed before we can adopt initial/early combination therapy as the standard of care.”
Dr. DeFronzo has reported receiving research support from Boehringer Ingelheim, AstraZeneca, and Merck; payment or honoraria for lectures, presentations, speakers bureaus, manuscript writing, or educational events from AstraZeneca; and participation on a data safety monitoring board or advisory board for AstraZeneca, Intarcia, Novo Nordisk, and Boehringer Ingelheim. Dr. Nathan has reported no relevant financial relationships.
A version of this article appeared on Medscape.com.
LAMA-LABA surpasses corticosteroid combination as COPD therapy
Use of inhalers with long-acting muscarinic antagonists and long-acting beta-agonists reduced COPD exacerbations and pneumonia hospitalizations compared with inhalers with corticosteroids and long-acting beta-agonists, based on data from more than 30,000 individuals.
Current clinical guidelines for chronic obstructive pulmonary disease (COPD) patients recommend inhalers with long-acting muscarinic antagonists (LAMAs) and long-acting beta-agonists (LABAs) over those with inhaled corticosteroids (ICSs) and LABAs, but data comparing the two formulations have been inconsistent, and concerns about generalizability persist, wrote William B. Feldman, MD, of Brigham and Women’s Hospital, Boston, and colleagues.
In a study published in JAMA Internal Medicine, the researchers reviewed data from a commercial insurance claims database of individuals diagnosed with COPD who filled a new prescription for a LAMA-LABA inhaler or ICS-LABA inhaler between Jan. 1, 2014, and Dec. 31, 2019. Patients with asthma and those younger than 40 years were excluded. The study population included 137,833 individuals with a mean age of 70.2 years; 50.4% were female. Of the 107,004 ICS-LABA users and 30,829 LAMA-LABA users, 30,216 matched pairs were included in a 1:1 propensity score matched study. The primary outcomes were effectiveness, based on the rate of first moderate or severe COPD exacerbation, and safety, based on the rate of first pneumonia hospitalization.
Use of LAMA-LABA inhalers was associated with an 8% reduction in the rate of first moderate or severe COPD exacerbation and a 20% reduction in the rate of first pneumonia hospitalization compared with use of ICS-LABA (hazard ratios 0.92 and 0.80, respectively). The absolute rate reductions with LAMA-LABA inhalers for first moderate or severe COPD exacerbations and for first pneumonia hospitalizations were was 43.0 events per 1,000 person-years and 91.8 events per person-years, respectively.
The overall rates of total moderate to severe COPD and pneumonia hospitalizations were 5% and 17% lower, respectively, among patients who used LAMA-LABA than those treated with ICS-LABA. The results were consistently robust in subgroup and sensitivity analyses, the researchers wrote in their discussion. However, the results must be interpreted cautiously in comparison to other large studies because of the significant differences in the cohorts of patients studied, notably that most patients in the current study had no received previous inhaler therapy.
The study findings were limited by several factors including the relatively short follow-up time and reliance on prescription fills as an indicator of medication use, the researchers noted. Other limitations included notable differences between the LAMA-LABA patients and ICS-LABA patients, such as more severe COPD and less access to respiratory care, they wrote.
Although the current study is not the definitive answer to conflicting results from previous trials, it is the largest know to date to compare LAMA-LABA with ICS-LABA, and the results support LAMA-LABA as the preferred therapy for COPD patients, the researchers concluded.
Findings clarify clinical practice guidelines
“This study was required to provide clarity regarding the optimal choice of treatment for COPD given conflicting data from other recent trials,” Suman Pal, MBBS, of the University of New Mexico, Albuquerque, said in an interview.
“The study findings reinforce the benefits of combined LAMA-LABA in improving clinical outcomes in COPD in a real-world setting,” and the data provide further support for choosing LAMA-LABA over ICS-LABA in COPD patients, said Dr. Pal, who was not involved in the study.
However, availability and affordability of LAMA-LABA inhalers may be barriers to expanding their use in clinical practice, he noted.
“Additional research is needed to accurately define which patient populations would benefit most from the therapy and whether patients who have previously been stabilized on ICS-LABA would derive additional benefit from a change in therapy,” Dr. Pal said.
The study was supported by the National Heart, Lung, and Blood Institute and funding from the Commonwealth Fund and Arnold Ventures.
Dr. Feldman disclosed receiving personal fees from Alosa Health and Aetion, serving as an expert witness in litigation against inhaler manufacturers, and receiving an honorarium for a presentation to Blue Cross Blue Shield of Massachusetts unrelated to the current study. Dr. Pal had no financial conflicts to disclose.
Use of inhalers with long-acting muscarinic antagonists and long-acting beta-agonists reduced COPD exacerbations and pneumonia hospitalizations compared with inhalers with corticosteroids and long-acting beta-agonists, based on data from more than 30,000 individuals.
Current clinical guidelines for chronic obstructive pulmonary disease (COPD) patients recommend inhalers with long-acting muscarinic antagonists (LAMAs) and long-acting beta-agonists (LABAs) over those with inhaled corticosteroids (ICSs) and LABAs, but data comparing the two formulations have been inconsistent, and concerns about generalizability persist, wrote William B. Feldman, MD, of Brigham and Women’s Hospital, Boston, and colleagues.
In a study published in JAMA Internal Medicine, the researchers reviewed data from a commercial insurance claims database of individuals diagnosed with COPD who filled a new prescription for a LAMA-LABA inhaler or ICS-LABA inhaler between Jan. 1, 2014, and Dec. 31, 2019. Patients with asthma and those younger than 40 years were excluded. The study population included 137,833 individuals with a mean age of 70.2 years; 50.4% were female. Of the 107,004 ICS-LABA users and 30,829 LAMA-LABA users, 30,216 matched pairs were included in a 1:1 propensity score matched study. The primary outcomes were effectiveness, based on the rate of first moderate or severe COPD exacerbation, and safety, based on the rate of first pneumonia hospitalization.
Use of LAMA-LABA inhalers was associated with an 8% reduction in the rate of first moderate or severe COPD exacerbation and a 20% reduction in the rate of first pneumonia hospitalization compared with use of ICS-LABA (hazard ratios 0.92 and 0.80, respectively). The absolute rate reductions with LAMA-LABA inhalers for first moderate or severe COPD exacerbations and for first pneumonia hospitalizations were was 43.0 events per 1,000 person-years and 91.8 events per person-years, respectively.
The overall rates of total moderate to severe COPD and pneumonia hospitalizations were 5% and 17% lower, respectively, among patients who used LAMA-LABA than those treated with ICS-LABA. The results were consistently robust in subgroup and sensitivity analyses, the researchers wrote in their discussion. However, the results must be interpreted cautiously in comparison to other large studies because of the significant differences in the cohorts of patients studied, notably that most patients in the current study had no received previous inhaler therapy.
The study findings were limited by several factors including the relatively short follow-up time and reliance on prescription fills as an indicator of medication use, the researchers noted. Other limitations included notable differences between the LAMA-LABA patients and ICS-LABA patients, such as more severe COPD and less access to respiratory care, they wrote.
Although the current study is not the definitive answer to conflicting results from previous trials, it is the largest know to date to compare LAMA-LABA with ICS-LABA, and the results support LAMA-LABA as the preferred therapy for COPD patients, the researchers concluded.
Findings clarify clinical practice guidelines
“This study was required to provide clarity regarding the optimal choice of treatment for COPD given conflicting data from other recent trials,” Suman Pal, MBBS, of the University of New Mexico, Albuquerque, said in an interview.
“The study findings reinforce the benefits of combined LAMA-LABA in improving clinical outcomes in COPD in a real-world setting,” and the data provide further support for choosing LAMA-LABA over ICS-LABA in COPD patients, said Dr. Pal, who was not involved in the study.
However, availability and affordability of LAMA-LABA inhalers may be barriers to expanding their use in clinical practice, he noted.
“Additional research is needed to accurately define which patient populations would benefit most from the therapy and whether patients who have previously been stabilized on ICS-LABA would derive additional benefit from a change in therapy,” Dr. Pal said.
The study was supported by the National Heart, Lung, and Blood Institute and funding from the Commonwealth Fund and Arnold Ventures.
Dr. Feldman disclosed receiving personal fees from Alosa Health and Aetion, serving as an expert witness in litigation against inhaler manufacturers, and receiving an honorarium for a presentation to Blue Cross Blue Shield of Massachusetts unrelated to the current study. Dr. Pal had no financial conflicts to disclose.
Use of inhalers with long-acting muscarinic antagonists and long-acting beta-agonists reduced COPD exacerbations and pneumonia hospitalizations compared with inhalers with corticosteroids and long-acting beta-agonists, based on data from more than 30,000 individuals.
Current clinical guidelines for chronic obstructive pulmonary disease (COPD) patients recommend inhalers with long-acting muscarinic antagonists (LAMAs) and long-acting beta-agonists (LABAs) over those with inhaled corticosteroids (ICSs) and LABAs, but data comparing the two formulations have been inconsistent, and concerns about generalizability persist, wrote William B. Feldman, MD, of Brigham and Women’s Hospital, Boston, and colleagues.
In a study published in JAMA Internal Medicine, the researchers reviewed data from a commercial insurance claims database of individuals diagnosed with COPD who filled a new prescription for a LAMA-LABA inhaler or ICS-LABA inhaler between Jan. 1, 2014, and Dec. 31, 2019. Patients with asthma and those younger than 40 years were excluded. The study population included 137,833 individuals with a mean age of 70.2 years; 50.4% were female. Of the 107,004 ICS-LABA users and 30,829 LAMA-LABA users, 30,216 matched pairs were included in a 1:1 propensity score matched study. The primary outcomes were effectiveness, based on the rate of first moderate or severe COPD exacerbation, and safety, based on the rate of first pneumonia hospitalization.
Use of LAMA-LABA inhalers was associated with an 8% reduction in the rate of first moderate or severe COPD exacerbation and a 20% reduction in the rate of first pneumonia hospitalization compared with use of ICS-LABA (hazard ratios 0.92 and 0.80, respectively). The absolute rate reductions with LAMA-LABA inhalers for first moderate or severe COPD exacerbations and for first pneumonia hospitalizations were was 43.0 events per 1,000 person-years and 91.8 events per person-years, respectively.
The overall rates of total moderate to severe COPD and pneumonia hospitalizations were 5% and 17% lower, respectively, among patients who used LAMA-LABA than those treated with ICS-LABA. The results were consistently robust in subgroup and sensitivity analyses, the researchers wrote in their discussion. However, the results must be interpreted cautiously in comparison to other large studies because of the significant differences in the cohorts of patients studied, notably that most patients in the current study had no received previous inhaler therapy.
The study findings were limited by several factors including the relatively short follow-up time and reliance on prescription fills as an indicator of medication use, the researchers noted. Other limitations included notable differences between the LAMA-LABA patients and ICS-LABA patients, such as more severe COPD and less access to respiratory care, they wrote.
Although the current study is not the definitive answer to conflicting results from previous trials, it is the largest know to date to compare LAMA-LABA with ICS-LABA, and the results support LAMA-LABA as the preferred therapy for COPD patients, the researchers concluded.
Findings clarify clinical practice guidelines
“This study was required to provide clarity regarding the optimal choice of treatment for COPD given conflicting data from other recent trials,” Suman Pal, MBBS, of the University of New Mexico, Albuquerque, said in an interview.
“The study findings reinforce the benefits of combined LAMA-LABA in improving clinical outcomes in COPD in a real-world setting,” and the data provide further support for choosing LAMA-LABA over ICS-LABA in COPD patients, said Dr. Pal, who was not involved in the study.
However, availability and affordability of LAMA-LABA inhalers may be barriers to expanding their use in clinical practice, he noted.
“Additional research is needed to accurately define which patient populations would benefit most from the therapy and whether patients who have previously been stabilized on ICS-LABA would derive additional benefit from a change in therapy,” Dr. Pal said.
The study was supported by the National Heart, Lung, and Blood Institute and funding from the Commonwealth Fund and Arnold Ventures.
Dr. Feldman disclosed receiving personal fees from Alosa Health and Aetion, serving as an expert witness in litigation against inhaler manufacturers, and receiving an honorarium for a presentation to Blue Cross Blue Shield of Massachusetts unrelated to the current study. Dr. Pal had no financial conflicts to disclose.
FROM JAMA INTERNAL MEDICINE
Conflicting blood pressure targets: Déjà vu all over again
Stop me if you’ve heard this before. There’s a controversy over blood pressure targets. Some argue for 140/90 mm Hg, others for 130/80 mm Hg, and some super ambitious folks think that we should aim for 120/80 mm Hg. If this sounds familiar, it should. We did it in 2017. It’s unclear what, if anything, we learned from the experience. On the upside, it’s not as bad as it was 100 years ago.
When high blood pressure was a ‘good’ thing
Back then, many believed that you needed higher blood pressure as you got older to push the blood through your progressively stiffened and hardened arteries. Hence the name “essential” hypertension. The concern was that lowering blood pressure would hypoperfuse your organs and be dangerous. In the 1930s, John Hay told an audience at a British Medical Association lecture: “The greatest danger to a man with high blood pressure lies in its discovery, because then some fool is certain to try and reduce it.”
The 1900s were a simpler time when people had fatal strokes in their 50s, and their families were consoled by the knowledge that they had lived a good life.
If our thinking around blood pressure had evolved slightly faster, perhaps President Roosevelt wouldn’t have died of a stroke during World War II as his doctors watched his systolic blood pressure climb above 200 mm Hg and suggested massages and barbiturates to take the edge off.
The current controversy
Not that long ago, 180 mm Hg was considered mild hypertension. Now, we are arguing about a systolic blood pressure of 140 versus 130 mm Hg.
The American Academy of Family Physicians takes the view that 140/90 mm Hg is good enough for most people. Their most recent clinical practice guideline, based primarily on two 2020 Cochrane Reviews of blood pressure targets in patients with and without cardiovascular disease, did not find any mortality benefit for a lower blood pressure threshold.
This puts the AAFP guideline in conflict with the 2017 guideline issued jointly by the American College of Cardiology, American Heart Association, and nine other groups, which recommended a target of 130/80 mm Hg for pretty much everyone. Though they say greater than 140/90 mm Hg should be the threshold for low-risk patients or for starting therapy post stroke, we often forget those nuances. The main point of contention is that the AAFP guideline was looking for a mortality benefit, whereas the ACC/AHA/everyone else guideline was looking at preventing cardiovascular events. The latter guideline was driven mainly by the results of the SPRINT trial. ACC/AHA argue for more aggressive targets to prevent the things that cardiologists care about, namely heart attacks.
The AAFP guideline conceded that more aggressive control will result in fewer myocardial infarctions but warn that it comes with more adverse events. Treating 1,000 patients to this lower target would theoretically prevent four MIs, possibly prevent three strokes, but result in 30 adverse events.
In the end, what we are seeing here is not so much a debate over the evidence as a debate over priorities. Interventions that don’t improve mortality can be questioned in terms of their cost effectiveness. But you probably don’t want to have a heart attack (even a nonfatal one). And you certainly don’t want to have a stroke. However, lower blood pressure targets inevitably require more medications. Notwithstanding the economic costs, the dangers of polypharmacy, medication interactions, side effects, and syncope leading to falls cannot be ignored. Falls are not benign adverse events, especially in older adults.
The counter argument is that physicians are human and often let things slide. Set the target at 140/90 mm Hg, and many physicians won’t jump on a systolic blood pressure of 144 mm Hg. Set the target at 130 mm Hg, and maybe they’ll be more likely to react. There’s a fine line between permissiveness and complacency.
If you zoom out and look at the multitude of blood pressure guidelines, you start to notice an important fact. There is not much daylight between them. There are subtle differences in what constitutes high risk and different definitions of older (older should be defined as 10 years older than the reader’s current age). But otherwise, the blood pressure targets are not that different.
Does that final 10 mm Hg really matter when barriers to care mean that tens of millions in the United States are unaware they have hypertension? Even among those diagnosed, many are either untreated or inadequately treated.
With this context, perhaps the most insightful thing that can be said about the blood pressure guideline controversy is that it’s not all that controversial. We can likely all agree that we need to be better at treating hypertension and that creative solutions to reach underserved communities are necessary.
Arguing about 140/90 mm Hg or 130/80 mm Hg is less important than acknowledging that we should be aggressive in screening for and treating hypertension. We should acknowledge that beyond a certain point any cardiovascular benefit comes at the cost of hypotension and side effects. That tipping point will be different for different groups, and probably at a higher set point in older patients.
Individualizing care isn’t difficult. We do it all the time. We just shouldn’t be letting people walk around with untreated hypertension. It’s not the 1900s anymore.
Dr. Labos is a cardiologist at Hôpital Notre-Dame, Montreal. He reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
Stop me if you’ve heard this before. There’s a controversy over blood pressure targets. Some argue for 140/90 mm Hg, others for 130/80 mm Hg, and some super ambitious folks think that we should aim for 120/80 mm Hg. If this sounds familiar, it should. We did it in 2017. It’s unclear what, if anything, we learned from the experience. On the upside, it’s not as bad as it was 100 years ago.
When high blood pressure was a ‘good’ thing
Back then, many believed that you needed higher blood pressure as you got older to push the blood through your progressively stiffened and hardened arteries. Hence the name “essential” hypertension. The concern was that lowering blood pressure would hypoperfuse your organs and be dangerous. In the 1930s, John Hay told an audience at a British Medical Association lecture: “The greatest danger to a man with high blood pressure lies in its discovery, because then some fool is certain to try and reduce it.”
The 1900s were a simpler time when people had fatal strokes in their 50s, and their families were consoled by the knowledge that they had lived a good life.
If our thinking around blood pressure had evolved slightly faster, perhaps President Roosevelt wouldn’t have died of a stroke during World War II as his doctors watched his systolic blood pressure climb above 200 mm Hg and suggested massages and barbiturates to take the edge off.
The current controversy
Not that long ago, 180 mm Hg was considered mild hypertension. Now, we are arguing about a systolic blood pressure of 140 versus 130 mm Hg.
The American Academy of Family Physicians takes the view that 140/90 mm Hg is good enough for most people. Their most recent clinical practice guideline, based primarily on two 2020 Cochrane Reviews of blood pressure targets in patients with and without cardiovascular disease, did not find any mortality benefit for a lower blood pressure threshold.
This puts the AAFP guideline in conflict with the 2017 guideline issued jointly by the American College of Cardiology, American Heart Association, and nine other groups, which recommended a target of 130/80 mm Hg for pretty much everyone. Though they say greater than 140/90 mm Hg should be the threshold for low-risk patients or for starting therapy post stroke, we often forget those nuances. The main point of contention is that the AAFP guideline was looking for a mortality benefit, whereas the ACC/AHA/everyone else guideline was looking at preventing cardiovascular events. The latter guideline was driven mainly by the results of the SPRINT trial. ACC/AHA argue for more aggressive targets to prevent the things that cardiologists care about, namely heart attacks.
The AAFP guideline conceded that more aggressive control will result in fewer myocardial infarctions but warn that it comes with more adverse events. Treating 1,000 patients to this lower target would theoretically prevent four MIs, possibly prevent three strokes, but result in 30 adverse events.
In the end, what we are seeing here is not so much a debate over the evidence as a debate over priorities. Interventions that don’t improve mortality can be questioned in terms of their cost effectiveness. But you probably don’t want to have a heart attack (even a nonfatal one). And you certainly don’t want to have a stroke. However, lower blood pressure targets inevitably require more medications. Notwithstanding the economic costs, the dangers of polypharmacy, medication interactions, side effects, and syncope leading to falls cannot be ignored. Falls are not benign adverse events, especially in older adults.
The counter argument is that physicians are human and often let things slide. Set the target at 140/90 mm Hg, and many physicians won’t jump on a systolic blood pressure of 144 mm Hg. Set the target at 130 mm Hg, and maybe they’ll be more likely to react. There’s a fine line between permissiveness and complacency.
If you zoom out and look at the multitude of blood pressure guidelines, you start to notice an important fact. There is not much daylight between them. There are subtle differences in what constitutes high risk and different definitions of older (older should be defined as 10 years older than the reader’s current age). But otherwise, the blood pressure targets are not that different.
Does that final 10 mm Hg really matter when barriers to care mean that tens of millions in the United States are unaware they have hypertension? Even among those diagnosed, many are either untreated or inadequately treated.
With this context, perhaps the most insightful thing that can be said about the blood pressure guideline controversy is that it’s not all that controversial. We can likely all agree that we need to be better at treating hypertension and that creative solutions to reach underserved communities are necessary.
Arguing about 140/90 mm Hg or 130/80 mm Hg is less important than acknowledging that we should be aggressive in screening for and treating hypertension. We should acknowledge that beyond a certain point any cardiovascular benefit comes at the cost of hypotension and side effects. That tipping point will be different for different groups, and probably at a higher set point in older patients.
Individualizing care isn’t difficult. We do it all the time. We just shouldn’t be letting people walk around with untreated hypertension. It’s not the 1900s anymore.
Dr. Labos is a cardiologist at Hôpital Notre-Dame, Montreal. He reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
Stop me if you’ve heard this before. There’s a controversy over blood pressure targets. Some argue for 140/90 mm Hg, others for 130/80 mm Hg, and some super ambitious folks think that we should aim for 120/80 mm Hg. If this sounds familiar, it should. We did it in 2017. It’s unclear what, if anything, we learned from the experience. On the upside, it’s not as bad as it was 100 years ago.
When high blood pressure was a ‘good’ thing
Back then, many believed that you needed higher blood pressure as you got older to push the blood through your progressively stiffened and hardened arteries. Hence the name “essential” hypertension. The concern was that lowering blood pressure would hypoperfuse your organs and be dangerous. In the 1930s, John Hay told an audience at a British Medical Association lecture: “The greatest danger to a man with high blood pressure lies in its discovery, because then some fool is certain to try and reduce it.”
The 1900s were a simpler time when people had fatal strokes in their 50s, and their families were consoled by the knowledge that they had lived a good life.
If our thinking around blood pressure had evolved slightly faster, perhaps President Roosevelt wouldn’t have died of a stroke during World War II as his doctors watched his systolic blood pressure climb above 200 mm Hg and suggested massages and barbiturates to take the edge off.
The current controversy
Not that long ago, 180 mm Hg was considered mild hypertension. Now, we are arguing about a systolic blood pressure of 140 versus 130 mm Hg.
The American Academy of Family Physicians takes the view that 140/90 mm Hg is good enough for most people. Their most recent clinical practice guideline, based primarily on two 2020 Cochrane Reviews of blood pressure targets in patients with and without cardiovascular disease, did not find any mortality benefit for a lower blood pressure threshold.
This puts the AAFP guideline in conflict with the 2017 guideline issued jointly by the American College of Cardiology, American Heart Association, and nine other groups, which recommended a target of 130/80 mm Hg for pretty much everyone. Though they say greater than 140/90 mm Hg should be the threshold for low-risk patients or for starting therapy post stroke, we often forget those nuances. The main point of contention is that the AAFP guideline was looking for a mortality benefit, whereas the ACC/AHA/everyone else guideline was looking at preventing cardiovascular events. The latter guideline was driven mainly by the results of the SPRINT trial. ACC/AHA argue for more aggressive targets to prevent the things that cardiologists care about, namely heart attacks.
The AAFP guideline conceded that more aggressive control will result in fewer myocardial infarctions but warn that it comes with more adverse events. Treating 1,000 patients to this lower target would theoretically prevent four MIs, possibly prevent three strokes, but result in 30 adverse events.
In the end, what we are seeing here is not so much a debate over the evidence as a debate over priorities. Interventions that don’t improve mortality can be questioned in terms of their cost effectiveness. But you probably don’t want to have a heart attack (even a nonfatal one). And you certainly don’t want to have a stroke. However, lower blood pressure targets inevitably require more medications. Notwithstanding the economic costs, the dangers of polypharmacy, medication interactions, side effects, and syncope leading to falls cannot be ignored. Falls are not benign adverse events, especially in older adults.
The counter argument is that physicians are human and often let things slide. Set the target at 140/90 mm Hg, and many physicians won’t jump on a systolic blood pressure of 144 mm Hg. Set the target at 130 mm Hg, and maybe they’ll be more likely to react. There’s a fine line between permissiveness and complacency.
If you zoom out and look at the multitude of blood pressure guidelines, you start to notice an important fact. There is not much daylight between them. There are subtle differences in what constitutes high risk and different definitions of older (older should be defined as 10 years older than the reader’s current age). But otherwise, the blood pressure targets are not that different.
Does that final 10 mm Hg really matter when barriers to care mean that tens of millions in the United States are unaware they have hypertension? Even among those diagnosed, many are either untreated or inadequately treated.
With this context, perhaps the most insightful thing that can be said about the blood pressure guideline controversy is that it’s not all that controversial. We can likely all agree that we need to be better at treating hypertension and that creative solutions to reach underserved communities are necessary.
Arguing about 140/90 mm Hg or 130/80 mm Hg is less important than acknowledging that we should be aggressive in screening for and treating hypertension. We should acknowledge that beyond a certain point any cardiovascular benefit comes at the cost of hypotension and side effects. That tipping point will be different for different groups, and probably at a higher set point in older patients.
Individualizing care isn’t difficult. We do it all the time. We just shouldn’t be letting people walk around with untreated hypertension. It’s not the 1900s anymore.
Dr. Labos is a cardiologist at Hôpital Notre-Dame, Montreal. He reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
Can berberine live up to the claim that it’s ‘nature’s Ozempic’?
Berberine, a plant-derived compound historically used in traditional Chinese medicine, is experiencing increased popularity thanks to social media, especially TikTok, where the hashtag #berberine has more than 75 million views at the time of this writing.
Off-the-shelf berberine comes as a yellow-orange powder usually encased in a capsule or mixed into tablet form. It’s extracted from the roots, stems, and leaves of various plants, including goldenseal and barberry.
Its use is additionally promoted for insulin resistance, polycystic ovary syndrome, and even cancer, but medical experts are warning potential users that it lacks robust evidence to support its use.
“There’s not that much data on it,” says Reshmi Srinath, MD, director of the Mount Sinai weight and metabolism management program, New York. “It’s sort of shocking now that it’s popped up into the media, to be frank.”
In response to berberine’s online popularity, the National Center for Complementary and Integrative Health issued a warning, stating that “there isn’t enough rigorous scientific evidence to determine whether it is effective.”
Overstated claims, lack of scientific research?
Other endocrinologists and weight management experts agree. “The claims are pretty overstated when it comes to the impact on weight loss, based on the evidence in the literature that’s currently available,” says Jaime Almandoz, MD, medical director of the UT Southwestern Medical Center, Dallas, weight wellness program.
A review of 12 randomized controlled trials evaluating berberine’s effects on obesity concluded that the treatment moderately decreased body weight. The trials included were conducted over only a few months and had small numbers of participants, and weight loss was not the primary outcome measure.
“There are few randomized controlled trials,” says Ivania Rizo, MD, an endocrinologist at Boston University. “It appears that they all have some low quality of methods which essentially can lead to an increased risk of bias.”
Another review, of 35 studies – most of them on animals and human cells and similarly underpowered – concluded that berberine showed promise for reducing blood glucose. A separate study found that berberine treatment actually increased the body weight and appetite of rats.
How exactly berberine elicits these effects is not entirely clear. Several studies point to its activation of AMP-activated protein kinase, which improves glucose tolerance in rats, as the mechanism for weight loss. Metformin, a drug used to improve glycemic control in people with type 2 diabetes, works in a similar way. Other researchers have hypothesized a link between berberine and the gut microbiome to explain its effect on type 2 diabetes and weight loss, though the clinical data to substantiate this link are shaky.
“I caution my patients about dietary supplements for weight management because we do not have high-quality data demonstrating efficacy,” Katherine Saunders, MD, DABOM, an obesity expert and cofounder of Intellihealth, a platform for obesity management, said in an email.
Experimenting with berberine
Despite the lack of substantial evidence supporting berberine’s use for weight management and obesity, interest in the supplement seems to be increasing. One reason could be that lifestyle interventions aren’t sufficient for most people with obesity to lose a significant amount of weight, with many requiring medical intervention, according to Dr. Saunders.
But access to treatment providers is limited. “As a result, it is not uncommon for individuals with obesity to experiment with dietary supplements like berberine,” she observed.
Dr. Srinath, the Mount Sinai doctor, says many patients have asked for her thoughts on berberine as a weight loss supplement. “I say, you know, it’s something you’re welcome to try, but we don’t have enough data at this time to recommend it.”
The hype surrounding the supplement isn’t all that surprising. About 42% of adults in the United States have obesity, according to 2019-2023 National Health and Nutrition Examination Survey data, pointing to a serious need for accessible drugs to address the condition. Berberine is available over the counter and is far cheaper than most of the newer U.S. Food and Drug Administration–approved drugs for weight loss.
Wegovy, semaglutide approved to treat obesity, can cost as much as $1,300 per package; and Ozempic, semaglutide approved to treat type 2 diabetes, can cost more than $1,000 per month. “That’s a very steep price to pay,” says Dr. Srinath.
Many insurance companies won’t cover the drugs, curbing access to Americans who need them, says Dr. Almandoz. Federally sponsored programs such as Medicare and Medicaid also don’t cover the drugs, which are approved for obesity and weight management. “That’s been a huge hole in our health care system,” says Dr. Srinath. “That’s sort of what’s been driving interest in supplements and things like that.”
Among adults trying to lose weight, only about 3% said they took prescription medication for weight loss, according to a report from the U.S. Government Accountability Office. This report includes 2013-2016 data, predating Wegovy’s approval for chronic weight management.
“These classes are notorious for being quite pricey and not well covered by insurance,” says Dr. Almandoz. “It’s easy to see why someone would promote something that someone may have more access to.”
Comparing Ozempic or Wegovy with berberine can be misleading. Those drugs work by mimicking the effect of the hormone GLP-1 to help reduce appetite.
A clinical trial assessing the efficacy of semaglutide found that adults with obesity who took the drug for 68 weeks lost approximately 15% of their body weight in combination with lifestyle changes. The FDA approval was based on this trial and three others that showed similarly substantial reductions in weight.
The trials also document the many side effects of taking the drugs, primarily gastrointestinal in nature. The short- and long-term effects of berberine, on the other hand, are less clear. Some of the clinical trials reported diarrhea and stomach upset as the most common adverse effects.
Its perception as a naturally derived option for weight loss, though, might encourage people to overlook the potential interactions that berberine could have with other drugs, according to Dr. Almandoz.
He says clinicians considering natural products or nutraceuticals for patients should check for potential side effects and find reliable database sources to determine any potential medication interactions for patients. But the unregulated nature of berberine makes this challenging, Dr. Almandoz adds.
The dosage, formulations, and quality of berberine vary in each study and each product because supplements don’t need to pass through the checks and balances of the FDA to land on shelves.
The lack of regulation could incentivize some companies to add stimulants to enhance any weight loss effect that the supplement may have. Those additives might interact with other health conditions or cause side effects like anxiety, says Dr. Almandoz.
Berberine should also not be taken during pregnancy or while breastfeeding, and it is unsafe for young children; in newborns and children, the supplement can cause higher levels of bilirubin in the blood, worsening any jaundice at birth and posing a greater risk for kernicterus.
Dr. Rizo urges patients, before they ask for berberine, to first ask for safe and effective interventions they can access. “I don’t want to have people not use effective interventions that are currently available to them, and instead use something that needs to be better studied and needs to be better regulated,” she says.
While the “nature’s Ozempic” catchphrase could be drawing in potential users with its dubious comparison, berberine’s escalating popularity might also be a symptom of people seeking a quick fix, the experts worry.
“That’s my fear,” says Dr. Srinath. “ ‘Let me get this medicine, let me lose the weight fast,’ but at the end of the day, weight management is a long-term journey. It takes time, it takes effort, it is not easy, and there is no quick fix.”
This is another concern for doctors; for people who’ve struggled with losing weight for years, not seeing results from berberine could feel like another failure.
“It will give them another opportunity to feel like they are being unsuccessful or that they are failing at weight loss again,” says Dr. Almandoz. “It feeds into the hopelessness that many people with obesity have around their weight management.”
A version of this article first appeared on Medscape.com.
Berberine, a plant-derived compound historically used in traditional Chinese medicine, is experiencing increased popularity thanks to social media, especially TikTok, where the hashtag #berberine has more than 75 million views at the time of this writing.
Off-the-shelf berberine comes as a yellow-orange powder usually encased in a capsule or mixed into tablet form. It’s extracted from the roots, stems, and leaves of various plants, including goldenseal and barberry.
Its use is additionally promoted for insulin resistance, polycystic ovary syndrome, and even cancer, but medical experts are warning potential users that it lacks robust evidence to support its use.
“There’s not that much data on it,” says Reshmi Srinath, MD, director of the Mount Sinai weight and metabolism management program, New York. “It’s sort of shocking now that it’s popped up into the media, to be frank.”
In response to berberine’s online popularity, the National Center for Complementary and Integrative Health issued a warning, stating that “there isn’t enough rigorous scientific evidence to determine whether it is effective.”
Overstated claims, lack of scientific research?
Other endocrinologists and weight management experts agree. “The claims are pretty overstated when it comes to the impact on weight loss, based on the evidence in the literature that’s currently available,” says Jaime Almandoz, MD, medical director of the UT Southwestern Medical Center, Dallas, weight wellness program.
A review of 12 randomized controlled trials evaluating berberine’s effects on obesity concluded that the treatment moderately decreased body weight. The trials included were conducted over only a few months and had small numbers of participants, and weight loss was not the primary outcome measure.
“There are few randomized controlled trials,” says Ivania Rizo, MD, an endocrinologist at Boston University. “It appears that they all have some low quality of methods which essentially can lead to an increased risk of bias.”
Another review, of 35 studies – most of them on animals and human cells and similarly underpowered – concluded that berberine showed promise for reducing blood glucose. A separate study found that berberine treatment actually increased the body weight and appetite of rats.
How exactly berberine elicits these effects is not entirely clear. Several studies point to its activation of AMP-activated protein kinase, which improves glucose tolerance in rats, as the mechanism for weight loss. Metformin, a drug used to improve glycemic control in people with type 2 diabetes, works in a similar way. Other researchers have hypothesized a link between berberine and the gut microbiome to explain its effect on type 2 diabetes and weight loss, though the clinical data to substantiate this link are shaky.
“I caution my patients about dietary supplements for weight management because we do not have high-quality data demonstrating efficacy,” Katherine Saunders, MD, DABOM, an obesity expert and cofounder of Intellihealth, a platform for obesity management, said in an email.
Experimenting with berberine
Despite the lack of substantial evidence supporting berberine’s use for weight management and obesity, interest in the supplement seems to be increasing. One reason could be that lifestyle interventions aren’t sufficient for most people with obesity to lose a significant amount of weight, with many requiring medical intervention, according to Dr. Saunders.
But access to treatment providers is limited. “As a result, it is not uncommon for individuals with obesity to experiment with dietary supplements like berberine,” she observed.
Dr. Srinath, the Mount Sinai doctor, says many patients have asked for her thoughts on berberine as a weight loss supplement. “I say, you know, it’s something you’re welcome to try, but we don’t have enough data at this time to recommend it.”
The hype surrounding the supplement isn’t all that surprising. About 42% of adults in the United States have obesity, according to 2019-2023 National Health and Nutrition Examination Survey data, pointing to a serious need for accessible drugs to address the condition. Berberine is available over the counter and is far cheaper than most of the newer U.S. Food and Drug Administration–approved drugs for weight loss.
Wegovy, semaglutide approved to treat obesity, can cost as much as $1,300 per package; and Ozempic, semaglutide approved to treat type 2 diabetes, can cost more than $1,000 per month. “That’s a very steep price to pay,” says Dr. Srinath.
Many insurance companies won’t cover the drugs, curbing access to Americans who need them, says Dr. Almandoz. Federally sponsored programs such as Medicare and Medicaid also don’t cover the drugs, which are approved for obesity and weight management. “That’s been a huge hole in our health care system,” says Dr. Srinath. “That’s sort of what’s been driving interest in supplements and things like that.”
Among adults trying to lose weight, only about 3% said they took prescription medication for weight loss, according to a report from the U.S. Government Accountability Office. This report includes 2013-2016 data, predating Wegovy’s approval for chronic weight management.
“These classes are notorious for being quite pricey and not well covered by insurance,” says Dr. Almandoz. “It’s easy to see why someone would promote something that someone may have more access to.”
Comparing Ozempic or Wegovy with berberine can be misleading. Those drugs work by mimicking the effect of the hormone GLP-1 to help reduce appetite.
A clinical trial assessing the efficacy of semaglutide found that adults with obesity who took the drug for 68 weeks lost approximately 15% of their body weight in combination with lifestyle changes. The FDA approval was based on this trial and three others that showed similarly substantial reductions in weight.
The trials also document the many side effects of taking the drugs, primarily gastrointestinal in nature. The short- and long-term effects of berberine, on the other hand, are less clear. Some of the clinical trials reported diarrhea and stomach upset as the most common adverse effects.
Its perception as a naturally derived option for weight loss, though, might encourage people to overlook the potential interactions that berberine could have with other drugs, according to Dr. Almandoz.
He says clinicians considering natural products or nutraceuticals for patients should check for potential side effects and find reliable database sources to determine any potential medication interactions for patients. But the unregulated nature of berberine makes this challenging, Dr. Almandoz adds.
The dosage, formulations, and quality of berberine vary in each study and each product because supplements don’t need to pass through the checks and balances of the FDA to land on shelves.
The lack of regulation could incentivize some companies to add stimulants to enhance any weight loss effect that the supplement may have. Those additives might interact with other health conditions or cause side effects like anxiety, says Dr. Almandoz.
Berberine should also not be taken during pregnancy or while breastfeeding, and it is unsafe for young children; in newborns and children, the supplement can cause higher levels of bilirubin in the blood, worsening any jaundice at birth and posing a greater risk for kernicterus.
Dr. Rizo urges patients, before they ask for berberine, to first ask for safe and effective interventions they can access. “I don’t want to have people not use effective interventions that are currently available to them, and instead use something that needs to be better studied and needs to be better regulated,” she says.
While the “nature’s Ozempic” catchphrase could be drawing in potential users with its dubious comparison, berberine’s escalating popularity might also be a symptom of people seeking a quick fix, the experts worry.
“That’s my fear,” says Dr. Srinath. “ ‘Let me get this medicine, let me lose the weight fast,’ but at the end of the day, weight management is a long-term journey. It takes time, it takes effort, it is not easy, and there is no quick fix.”
This is another concern for doctors; for people who’ve struggled with losing weight for years, not seeing results from berberine could feel like another failure.
“It will give them another opportunity to feel like they are being unsuccessful or that they are failing at weight loss again,” says Dr. Almandoz. “It feeds into the hopelessness that many people with obesity have around their weight management.”
A version of this article first appeared on Medscape.com.
Berberine, a plant-derived compound historically used in traditional Chinese medicine, is experiencing increased popularity thanks to social media, especially TikTok, where the hashtag #berberine has more than 75 million views at the time of this writing.
Off-the-shelf berberine comes as a yellow-orange powder usually encased in a capsule or mixed into tablet form. It’s extracted from the roots, stems, and leaves of various plants, including goldenseal and barberry.
Its use is additionally promoted for insulin resistance, polycystic ovary syndrome, and even cancer, but medical experts are warning potential users that it lacks robust evidence to support its use.
“There’s not that much data on it,” says Reshmi Srinath, MD, director of the Mount Sinai weight and metabolism management program, New York. “It’s sort of shocking now that it’s popped up into the media, to be frank.”
In response to berberine’s online popularity, the National Center for Complementary and Integrative Health issued a warning, stating that “there isn’t enough rigorous scientific evidence to determine whether it is effective.”
Overstated claims, lack of scientific research?
Other endocrinologists and weight management experts agree. “The claims are pretty overstated when it comes to the impact on weight loss, based on the evidence in the literature that’s currently available,” says Jaime Almandoz, MD, medical director of the UT Southwestern Medical Center, Dallas, weight wellness program.
A review of 12 randomized controlled trials evaluating berberine’s effects on obesity concluded that the treatment moderately decreased body weight. The trials included were conducted over only a few months and had small numbers of participants, and weight loss was not the primary outcome measure.
“There are few randomized controlled trials,” says Ivania Rizo, MD, an endocrinologist at Boston University. “It appears that they all have some low quality of methods which essentially can lead to an increased risk of bias.”
Another review, of 35 studies – most of them on animals and human cells and similarly underpowered – concluded that berberine showed promise for reducing blood glucose. A separate study found that berberine treatment actually increased the body weight and appetite of rats.
How exactly berberine elicits these effects is not entirely clear. Several studies point to its activation of AMP-activated protein kinase, which improves glucose tolerance in rats, as the mechanism for weight loss. Metformin, a drug used to improve glycemic control in people with type 2 diabetes, works in a similar way. Other researchers have hypothesized a link between berberine and the gut microbiome to explain its effect on type 2 diabetes and weight loss, though the clinical data to substantiate this link are shaky.
“I caution my patients about dietary supplements for weight management because we do not have high-quality data demonstrating efficacy,” Katherine Saunders, MD, DABOM, an obesity expert and cofounder of Intellihealth, a platform for obesity management, said in an email.
Experimenting with berberine
Despite the lack of substantial evidence supporting berberine’s use for weight management and obesity, interest in the supplement seems to be increasing. One reason could be that lifestyle interventions aren’t sufficient for most people with obesity to lose a significant amount of weight, with many requiring medical intervention, according to Dr. Saunders.
But access to treatment providers is limited. “As a result, it is not uncommon for individuals with obesity to experiment with dietary supplements like berberine,” she observed.
Dr. Srinath, the Mount Sinai doctor, says many patients have asked for her thoughts on berberine as a weight loss supplement. “I say, you know, it’s something you’re welcome to try, but we don’t have enough data at this time to recommend it.”
The hype surrounding the supplement isn’t all that surprising. About 42% of adults in the United States have obesity, according to 2019-2023 National Health and Nutrition Examination Survey data, pointing to a serious need for accessible drugs to address the condition. Berberine is available over the counter and is far cheaper than most of the newer U.S. Food and Drug Administration–approved drugs for weight loss.
Wegovy, semaglutide approved to treat obesity, can cost as much as $1,300 per package; and Ozempic, semaglutide approved to treat type 2 diabetes, can cost more than $1,000 per month. “That’s a very steep price to pay,” says Dr. Srinath.
Many insurance companies won’t cover the drugs, curbing access to Americans who need them, says Dr. Almandoz. Federally sponsored programs such as Medicare and Medicaid also don’t cover the drugs, which are approved for obesity and weight management. “That’s been a huge hole in our health care system,” says Dr. Srinath. “That’s sort of what’s been driving interest in supplements and things like that.”
Among adults trying to lose weight, only about 3% said they took prescription medication for weight loss, according to a report from the U.S. Government Accountability Office. This report includes 2013-2016 data, predating Wegovy’s approval for chronic weight management.
“These classes are notorious for being quite pricey and not well covered by insurance,” says Dr. Almandoz. “It’s easy to see why someone would promote something that someone may have more access to.”
Comparing Ozempic or Wegovy with berberine can be misleading. Those drugs work by mimicking the effect of the hormone GLP-1 to help reduce appetite.
A clinical trial assessing the efficacy of semaglutide found that adults with obesity who took the drug for 68 weeks lost approximately 15% of their body weight in combination with lifestyle changes. The FDA approval was based on this trial and three others that showed similarly substantial reductions in weight.
The trials also document the many side effects of taking the drugs, primarily gastrointestinal in nature. The short- and long-term effects of berberine, on the other hand, are less clear. Some of the clinical trials reported diarrhea and stomach upset as the most common adverse effects.
Its perception as a naturally derived option for weight loss, though, might encourage people to overlook the potential interactions that berberine could have with other drugs, according to Dr. Almandoz.
He says clinicians considering natural products or nutraceuticals for patients should check for potential side effects and find reliable database sources to determine any potential medication interactions for patients. But the unregulated nature of berberine makes this challenging, Dr. Almandoz adds.
The dosage, formulations, and quality of berberine vary in each study and each product because supplements don’t need to pass through the checks and balances of the FDA to land on shelves.
The lack of regulation could incentivize some companies to add stimulants to enhance any weight loss effect that the supplement may have. Those additives might interact with other health conditions or cause side effects like anxiety, says Dr. Almandoz.
Berberine should also not be taken during pregnancy or while breastfeeding, and it is unsafe for young children; in newborns and children, the supplement can cause higher levels of bilirubin in the blood, worsening any jaundice at birth and posing a greater risk for kernicterus.
Dr. Rizo urges patients, before they ask for berberine, to first ask for safe and effective interventions they can access. “I don’t want to have people not use effective interventions that are currently available to them, and instead use something that needs to be better studied and needs to be better regulated,” she says.
While the “nature’s Ozempic” catchphrase could be drawing in potential users with its dubious comparison, berberine’s escalating popularity might also be a symptom of people seeking a quick fix, the experts worry.
“That’s my fear,” says Dr. Srinath. “ ‘Let me get this medicine, let me lose the weight fast,’ but at the end of the day, weight management is a long-term journey. It takes time, it takes effort, it is not easy, and there is no quick fix.”
This is another concern for doctors; for people who’ve struggled with losing weight for years, not seeing results from berberine could feel like another failure.
“It will give them another opportunity to feel like they are being unsuccessful or that they are failing at weight loss again,” says Dr. Almandoz. “It feeds into the hopelessness that many people with obesity have around their weight management.”
A version of this article first appeared on Medscape.com.
FDA approves first over-the-counter birth control pill
The Food and Drug Administration’s approval today of the first birth control pill for women to be available without a prescription is being hailed by many as a long-needed development, but there remain questions to be resolved, including how much the drug will cost and how it will be used.
The drug, Opill, is expected to be available early next year, and its maker has yet to reveal a retail price. It is the same birth control pill that has been available by prescription for 50 years. But for the first time, women will be able to buy the contraception at a local pharmacy, other retail locations, or online without having to see a doctor first.
Likely to drive debate
Contraception in the United States is not without controversy. The FDA’s approval spurred reactions both for and against making hormonal birth control for women available without a prescription.
“It’s an exciting time, especially right now when reproductive rights are being curtailed in a lot of states. Giving people an additional option for contraception will change people’s lives,” said Beverly Gray, MD, division director of Women’s Community and Population Health at Duke University Medical Center in Durham, N.C.
“It’s a huge win for patients who need better access to contraception,” said Dr. Gray, who is also a spokesperson for the American College of Obstetricians and Gynecologists.
Women who want hormonal birth control but live in areas without convenient access to a doctor, women who cannot easily take time off of work to see a doctor and get a prescription filled, and women without insurance are examples of people who will benefit, she said.
The Catholic Medical Association, in contrast, expressed “deep concern and disappointment” after an FDA advisory committee’s unanimous vote on May 11 recommending the drug be available over the counter. In a statement after the vote, the group cited “extensive medical studies demonstrating the risks and adverse effects of hormonal contraceptives,” adding that “the social impact of [full approval] would be dramatic.”
But doctors largely disagreed.
“It is definitely a huge win for reproductive autonomy. I’m glad that the FDA is prioritizing patient safety and well-being over politics,” said Catherine Cansino, MD, MPH, an ob.gyn. and clinical professor in the University of California Davis department of obstetrics and gynecology. She said the FDA approved the over-the-counter version because the medication is safe.
While opponents like the Catholic Medical Association cite safety concerns and believe doctors should screen all women before prescribing hormonal contraception, Dr. Gray disagreed. “There’s a lot of evidence that patients can figure out if a progestin-only pill is right for them and safe for them. Medical professionals don’t have to be the gatekeepers for contraception,” she said.
Pricing unknown
Whether insurance companies will pay for Opill now that it will be available without a prescription remains unknown. For some medications, paying a copay through insurance can be less expensive than buying at a retail price.
“Although pricing issues will be relevant, the FDA’s decision will enhance women’s access to hormonal birth control,” said Andrew M. Kaunitz, MD, a professor and associate chairman in the department of obstetrics and gynecology at the University of Florida College of Medicine in Jacksonville.
The drugmaker, Perrigo, based in Ireland, has not yet announced how much the pill will cost. The price tag could affect how widely available this form of birth control is. The drug has been shown to be as much as 93% effective for pregnancy prevention. Perrigo says it plans to make the pill available at low or no cost to some women.
Caveats to consider
There are some women for whom hormonal contraceptives have always carried greater risks. For example, women who have breast cancer or a history of breast cancer should not use hormonal contraceptives, the FDA said in a news release announcing the approval. Women with other types of cancer should check with their doctors first, the agency noted.
Women who smoke, who take some medications to lower blood pressure, or who have migraines should also take caution, Dr. Cansino said. “People with migraines may not be suitable for over-the-counter oral contraceptives. But a simple screening through a provider can identify whether you are truly eligible or not.”
Irregular bleeding, headaches, dizziness, nausea, increased appetite, belly pain, cramps, or bloating are the most common side effects of Opill, the FDA said.
The Opill is a progestin-only birth control pill. Similar pills have been available in the United Kingdiom for about 2 years, often referred to as “mini pills” because they contain a single hormone. In contrast, prescription birth control pills in the United States and elsewhere contain more than one hormone, estrogen and progestin, to prevent pregnancy.
Prescription pill packs for combination contraception often feature a week of placebo pills without an active ingredient. While skipping a placebo pill might not make a difference in pregnancy prevention, Opill is different. Every pill in the packet will contain medication, Gray said. “So it’s important to take the pill the same time every day for it to be most effective.”
Even though this may mean one less visit to your doctor, Dr. Kaunitz hopes women will stay up to date on their other medical checkups. “One of our challenges as providers of care to women will be to encourage them to continue to receive important services, including cancer screening and vaccinations, even while they can initiate and continue hormonal contraception without contact with a provider.”
Just the beginning?
The American Medical Association hopes this approval signals more to come.
“While we applaud this move, the AMA continues to urge the FDA and HHS to consider a variety of oral contraceptive options for over-the-counter use,” the association, which has more than 250,000 doctor members, said in a statement. “It is important patients have options when choosing which type of birth control works best for them,”
The American College of Obstetricians and Gynecologists said the FDA’s decision will help many women. “We are glad that more patients will now be empowered to choose when and where they obtain a safe method of contraception without having to wait for a medical appointment or for a prescription to be filled,” Verda J. Hicks, MD, the group’s president, and Christopher M. Zahn, MD, interim chief executive officer, said in a statement.
“Allowing individuals to access birth control at their local pharmacy or drug store will eliminate some barriers,” they said.
A version of this article first appeared on WebMD.com.
This article was updated 7/13/23.
The Food and Drug Administration’s approval today of the first birth control pill for women to be available without a prescription is being hailed by many as a long-needed development, but there remain questions to be resolved, including how much the drug will cost and how it will be used.
The drug, Opill, is expected to be available early next year, and its maker has yet to reveal a retail price. It is the same birth control pill that has been available by prescription for 50 years. But for the first time, women will be able to buy the contraception at a local pharmacy, other retail locations, or online without having to see a doctor first.
Likely to drive debate
Contraception in the United States is not without controversy. The FDA’s approval spurred reactions both for and against making hormonal birth control for women available without a prescription.
“It’s an exciting time, especially right now when reproductive rights are being curtailed in a lot of states. Giving people an additional option for contraception will change people’s lives,” said Beverly Gray, MD, division director of Women’s Community and Population Health at Duke University Medical Center in Durham, N.C.
“It’s a huge win for patients who need better access to contraception,” said Dr. Gray, who is also a spokesperson for the American College of Obstetricians and Gynecologists.
Women who want hormonal birth control but live in areas without convenient access to a doctor, women who cannot easily take time off of work to see a doctor and get a prescription filled, and women without insurance are examples of people who will benefit, she said.
The Catholic Medical Association, in contrast, expressed “deep concern and disappointment” after an FDA advisory committee’s unanimous vote on May 11 recommending the drug be available over the counter. In a statement after the vote, the group cited “extensive medical studies demonstrating the risks and adverse effects of hormonal contraceptives,” adding that “the social impact of [full approval] would be dramatic.”
But doctors largely disagreed.
“It is definitely a huge win for reproductive autonomy. I’m glad that the FDA is prioritizing patient safety and well-being over politics,” said Catherine Cansino, MD, MPH, an ob.gyn. and clinical professor in the University of California Davis department of obstetrics and gynecology. She said the FDA approved the over-the-counter version because the medication is safe.
While opponents like the Catholic Medical Association cite safety concerns and believe doctors should screen all women before prescribing hormonal contraception, Dr. Gray disagreed. “There’s a lot of evidence that patients can figure out if a progestin-only pill is right for them and safe for them. Medical professionals don’t have to be the gatekeepers for contraception,” she said.
Pricing unknown
Whether insurance companies will pay for Opill now that it will be available without a prescription remains unknown. For some medications, paying a copay through insurance can be less expensive than buying at a retail price.
“Although pricing issues will be relevant, the FDA’s decision will enhance women’s access to hormonal birth control,” said Andrew M. Kaunitz, MD, a professor and associate chairman in the department of obstetrics and gynecology at the University of Florida College of Medicine in Jacksonville.
The drugmaker, Perrigo, based in Ireland, has not yet announced how much the pill will cost. The price tag could affect how widely available this form of birth control is. The drug has been shown to be as much as 93% effective for pregnancy prevention. Perrigo says it plans to make the pill available at low or no cost to some women.
Caveats to consider
There are some women for whom hormonal contraceptives have always carried greater risks. For example, women who have breast cancer or a history of breast cancer should not use hormonal contraceptives, the FDA said in a news release announcing the approval. Women with other types of cancer should check with their doctors first, the agency noted.
Women who smoke, who take some medications to lower blood pressure, or who have migraines should also take caution, Dr. Cansino said. “People with migraines may not be suitable for over-the-counter oral contraceptives. But a simple screening through a provider can identify whether you are truly eligible or not.”
Irregular bleeding, headaches, dizziness, nausea, increased appetite, belly pain, cramps, or bloating are the most common side effects of Opill, the FDA said.
The Opill is a progestin-only birth control pill. Similar pills have been available in the United Kingdiom for about 2 years, often referred to as “mini pills” because they contain a single hormone. In contrast, prescription birth control pills in the United States and elsewhere contain more than one hormone, estrogen and progestin, to prevent pregnancy.
Prescription pill packs for combination contraception often feature a week of placebo pills without an active ingredient. While skipping a placebo pill might not make a difference in pregnancy prevention, Opill is different. Every pill in the packet will contain medication, Gray said. “So it’s important to take the pill the same time every day for it to be most effective.”
Even though this may mean one less visit to your doctor, Dr. Kaunitz hopes women will stay up to date on their other medical checkups. “One of our challenges as providers of care to women will be to encourage them to continue to receive important services, including cancer screening and vaccinations, even while they can initiate and continue hormonal contraception without contact with a provider.”
Just the beginning?
The American Medical Association hopes this approval signals more to come.
“While we applaud this move, the AMA continues to urge the FDA and HHS to consider a variety of oral contraceptive options for over-the-counter use,” the association, which has more than 250,000 doctor members, said in a statement. “It is important patients have options when choosing which type of birth control works best for them,”
The American College of Obstetricians and Gynecologists said the FDA’s decision will help many women. “We are glad that more patients will now be empowered to choose when and where they obtain a safe method of contraception without having to wait for a medical appointment or for a prescription to be filled,” Verda J. Hicks, MD, the group’s president, and Christopher M. Zahn, MD, interim chief executive officer, said in a statement.
“Allowing individuals to access birth control at their local pharmacy or drug store will eliminate some barriers,” they said.
A version of this article first appeared on WebMD.com.
This article was updated 7/13/23.
The Food and Drug Administration’s approval today of the first birth control pill for women to be available without a prescription is being hailed by many as a long-needed development, but there remain questions to be resolved, including how much the drug will cost and how it will be used.
The drug, Opill, is expected to be available early next year, and its maker has yet to reveal a retail price. It is the same birth control pill that has been available by prescription for 50 years. But for the first time, women will be able to buy the contraception at a local pharmacy, other retail locations, or online without having to see a doctor first.
Likely to drive debate
Contraception in the United States is not without controversy. The FDA’s approval spurred reactions both for and against making hormonal birth control for women available without a prescription.
“It’s an exciting time, especially right now when reproductive rights are being curtailed in a lot of states. Giving people an additional option for contraception will change people’s lives,” said Beverly Gray, MD, division director of Women’s Community and Population Health at Duke University Medical Center in Durham, N.C.
“It’s a huge win for patients who need better access to contraception,” said Dr. Gray, who is also a spokesperson for the American College of Obstetricians and Gynecologists.
Women who want hormonal birth control but live in areas without convenient access to a doctor, women who cannot easily take time off of work to see a doctor and get a prescription filled, and women without insurance are examples of people who will benefit, she said.
The Catholic Medical Association, in contrast, expressed “deep concern and disappointment” after an FDA advisory committee’s unanimous vote on May 11 recommending the drug be available over the counter. In a statement after the vote, the group cited “extensive medical studies demonstrating the risks and adverse effects of hormonal contraceptives,” adding that “the social impact of [full approval] would be dramatic.”
But doctors largely disagreed.
“It is definitely a huge win for reproductive autonomy. I’m glad that the FDA is prioritizing patient safety and well-being over politics,” said Catherine Cansino, MD, MPH, an ob.gyn. and clinical professor in the University of California Davis department of obstetrics and gynecology. She said the FDA approved the over-the-counter version because the medication is safe.
While opponents like the Catholic Medical Association cite safety concerns and believe doctors should screen all women before prescribing hormonal contraception, Dr. Gray disagreed. “There’s a lot of evidence that patients can figure out if a progestin-only pill is right for them and safe for them. Medical professionals don’t have to be the gatekeepers for contraception,” she said.
Pricing unknown
Whether insurance companies will pay for Opill now that it will be available without a prescription remains unknown. For some medications, paying a copay through insurance can be less expensive than buying at a retail price.
“Although pricing issues will be relevant, the FDA’s decision will enhance women’s access to hormonal birth control,” said Andrew M. Kaunitz, MD, a professor and associate chairman in the department of obstetrics and gynecology at the University of Florida College of Medicine in Jacksonville.
The drugmaker, Perrigo, based in Ireland, has not yet announced how much the pill will cost. The price tag could affect how widely available this form of birth control is. The drug has been shown to be as much as 93% effective for pregnancy prevention. Perrigo says it plans to make the pill available at low or no cost to some women.
Caveats to consider
There are some women for whom hormonal contraceptives have always carried greater risks. For example, women who have breast cancer or a history of breast cancer should not use hormonal contraceptives, the FDA said in a news release announcing the approval. Women with other types of cancer should check with their doctors first, the agency noted.
Women who smoke, who take some medications to lower blood pressure, or who have migraines should also take caution, Dr. Cansino said. “People with migraines may not be suitable for over-the-counter oral contraceptives. But a simple screening through a provider can identify whether you are truly eligible or not.”
Irregular bleeding, headaches, dizziness, nausea, increased appetite, belly pain, cramps, or bloating are the most common side effects of Opill, the FDA said.
The Opill is a progestin-only birth control pill. Similar pills have been available in the United Kingdiom for about 2 years, often referred to as “mini pills” because they contain a single hormone. In contrast, prescription birth control pills in the United States and elsewhere contain more than one hormone, estrogen and progestin, to prevent pregnancy.
Prescription pill packs for combination contraception often feature a week of placebo pills without an active ingredient. While skipping a placebo pill might not make a difference in pregnancy prevention, Opill is different. Every pill in the packet will contain medication, Gray said. “So it’s important to take the pill the same time every day for it to be most effective.”
Even though this may mean one less visit to your doctor, Dr. Kaunitz hopes women will stay up to date on their other medical checkups. “One of our challenges as providers of care to women will be to encourage them to continue to receive important services, including cancer screening and vaccinations, even while they can initiate and continue hormonal contraception without contact with a provider.”
Just the beginning?
The American Medical Association hopes this approval signals more to come.
“While we applaud this move, the AMA continues to urge the FDA and HHS to consider a variety of oral contraceptive options for over-the-counter use,” the association, which has more than 250,000 doctor members, said in a statement. “It is important patients have options when choosing which type of birth control works best for them,”
The American College of Obstetricians and Gynecologists said the FDA’s decision will help many women. “We are glad that more patients will now be empowered to choose when and where they obtain a safe method of contraception without having to wait for a medical appointment or for a prescription to be filled,” Verda J. Hicks, MD, the group’s president, and Christopher M. Zahn, MD, interim chief executive officer, said in a statement.
“Allowing individuals to access birth control at their local pharmacy or drug store will eliminate some barriers,” they said.
A version of this article first appeared on WebMD.com.
This article was updated 7/13/23.
Spirometry predicts mortality in type 2 diabetes
Among adults with type 2 diabetes, the presence of preserved ratio impaired spirometry (PRISm) was significantly associated with increased risk of mortality and both macro- and microvascular complications, as well as increased mortality, based on data from more than 20,000 individuals.
Guochen Li, MD, of the Medical College of Soochow University, Suzhou, China, and colleagues wrote.
“A growing number of studies have demonstrated that impaired lung function and type 2 diabetes could trigger shared pathophysiological injuries, such as microangiopathy and chronic inflammation,” they said, but the potential role of PRISm as an early predictor of adverse outcomes in patients with type 2 diabetes has not been fully examined.
In a study published in the journal Chest, the researchers reviewed data from 20,047 individuals with type 2 diabetes in the UK Biobank, a population-based cohort of adults aged 37-73 years recruited between 2006 and 2010.
The main exposure was lung function based on spirometry. PRISm was defined as predicted forced expiratory volume per second (FEV1) less than 80%, with an FEV1/ forced vital capacity (FVC) ratio of at least 0.70. Individuals with normal spirometry (defined as predicted FEV1 ≥ 80% with an FEV1/FVC ratio ≥ 0.70) served as controls.
The primary outcomes were major complications of type 2 diabetes including macrovascular events (myocardial infarction, unstable angina, coronary heart disease [CHD], ischemic stroke, and any type of stroke), microvascular events (diabetic retinopathy and diabetic kidney disease) and mortality (all-cause, cardiovascular, and respiratory).
Overall, 16.9% of study participants (3385 patients) had obstructive spirometry and 22.6% (4521 patients) had PRISm. Compared with individuals with normal spirometry, those with PRISm were more likely to be current smokers, obese, and living in economically disadvantaged areas. Individuals with PRISm also were significantly more likely to be long-term patients with diabetes who were taking glucose-lowering or lipid-lowering drugs (P < .001 for all).
The median follow-up for each of the type 2 diabetes complications and mortality was approximately 12 years. Over this time, 5.0% of patients developed incident MI, 1.3% developed unstable angina, 15.6% had CHD, 3.5% had an ischemic stroke, and 4.7% had any type of stroke. As for microvascular events, 7.8% developed diabetic retinopathy and 6.7% developed diabetic kidney disease. A total of 2588 patients died during the study period (15.1%), including 544 from cardiovascular disease and 319 from respiratory disease.
PRISm was significantly associated with increased risk of each of the complications and mortality types. These associations persisted after adjusting for lifestyle and other factors. The fully adjusted hazard ratios for PRISm versus normal spirometry were 1.23 for MI, 1.23 for unstable angina, 1.21 for CHD, 1.38 for ischemic stroke, 1.41 for any type of stroke, 1.31 for diabetic retinopathy, and 1.38 for diabetic kidney disease. Adjusted HRs for mortality were 1.34, 1.60, and 1.56 for all-cause, cardiovascular, and respiratory mortality, respectively.
The researchers also found that adding PRISm to an office-based risk score significantly improved the risk classification and predictive power for type 2 diabetes complications with the exception of unstable angina and mortality. They found little evidence for an association with sex, smoking, or PRISm duration and any mortality types. However, in subgroup analyses by age, sex, and duration of diabetes, PRISm remained associated with increased risk of macrovascular and microvascular complications, as well as mortality.
Potential mechanisms for the association between PRISm and diabetes complications include the role of insulin resistance in the exacerbation of lung damage in patients with type 2 diabetes, the increased rate of supplemental oxygen use among individuals with PRISm, and the increased prevalence of pulmonary artery enlargement in the PRISm subjects, the researchers wrote.
The findings were limited by several factors including the prospective design, the homogeneous population of individuals primarily of British or Irish ancestry, and the exclusion of diabetic neuropathy from the analysis, the researchers noted.
However, the results were strengthened by the large cohort, use of professional spirometry, and relatively long follow-up. “The findings underscore the relevance of PRISm for prognostic classification in type 2 diabetes and its potential for optimizing prevention strategies in this condition,” they concluded.
The study was supported by the National Natural Science Foundation of China, Natural Science Foundation of Jiangsu Province, and the Priority Academic Program Development of Jiangsu Higher Education Institutions. The researchers reported no relevant financial relationships.
A version of this article first appeared on Medscape.com
Among adults with type 2 diabetes, the presence of preserved ratio impaired spirometry (PRISm) was significantly associated with increased risk of mortality and both macro- and microvascular complications, as well as increased mortality, based on data from more than 20,000 individuals.
Guochen Li, MD, of the Medical College of Soochow University, Suzhou, China, and colleagues wrote.
“A growing number of studies have demonstrated that impaired lung function and type 2 diabetes could trigger shared pathophysiological injuries, such as microangiopathy and chronic inflammation,” they said, but the potential role of PRISm as an early predictor of adverse outcomes in patients with type 2 diabetes has not been fully examined.
In a study published in the journal Chest, the researchers reviewed data from 20,047 individuals with type 2 diabetes in the UK Biobank, a population-based cohort of adults aged 37-73 years recruited between 2006 and 2010.
The main exposure was lung function based on spirometry. PRISm was defined as predicted forced expiratory volume per second (FEV1) less than 80%, with an FEV1/ forced vital capacity (FVC) ratio of at least 0.70. Individuals with normal spirometry (defined as predicted FEV1 ≥ 80% with an FEV1/FVC ratio ≥ 0.70) served as controls.
The primary outcomes were major complications of type 2 diabetes including macrovascular events (myocardial infarction, unstable angina, coronary heart disease [CHD], ischemic stroke, and any type of stroke), microvascular events (diabetic retinopathy and diabetic kidney disease) and mortality (all-cause, cardiovascular, and respiratory).
Overall, 16.9% of study participants (3385 patients) had obstructive spirometry and 22.6% (4521 patients) had PRISm. Compared with individuals with normal spirometry, those with PRISm were more likely to be current smokers, obese, and living in economically disadvantaged areas. Individuals with PRISm also were significantly more likely to be long-term patients with diabetes who were taking glucose-lowering or lipid-lowering drugs (P < .001 for all).
The median follow-up for each of the type 2 diabetes complications and mortality was approximately 12 years. Over this time, 5.0% of patients developed incident MI, 1.3% developed unstable angina, 15.6% had CHD, 3.5% had an ischemic stroke, and 4.7% had any type of stroke. As for microvascular events, 7.8% developed diabetic retinopathy and 6.7% developed diabetic kidney disease. A total of 2588 patients died during the study period (15.1%), including 544 from cardiovascular disease and 319 from respiratory disease.
PRISm was significantly associated with increased risk of each of the complications and mortality types. These associations persisted after adjusting for lifestyle and other factors. The fully adjusted hazard ratios for PRISm versus normal spirometry were 1.23 for MI, 1.23 for unstable angina, 1.21 for CHD, 1.38 for ischemic stroke, 1.41 for any type of stroke, 1.31 for diabetic retinopathy, and 1.38 for diabetic kidney disease. Adjusted HRs for mortality were 1.34, 1.60, and 1.56 for all-cause, cardiovascular, and respiratory mortality, respectively.
The researchers also found that adding PRISm to an office-based risk score significantly improved the risk classification and predictive power for type 2 diabetes complications with the exception of unstable angina and mortality. They found little evidence for an association with sex, smoking, or PRISm duration and any mortality types. However, in subgroup analyses by age, sex, and duration of diabetes, PRISm remained associated with increased risk of macrovascular and microvascular complications, as well as mortality.
Potential mechanisms for the association between PRISm and diabetes complications include the role of insulin resistance in the exacerbation of lung damage in patients with type 2 diabetes, the increased rate of supplemental oxygen use among individuals with PRISm, and the increased prevalence of pulmonary artery enlargement in the PRISm subjects, the researchers wrote.
The findings were limited by several factors including the prospective design, the homogeneous population of individuals primarily of British or Irish ancestry, and the exclusion of diabetic neuropathy from the analysis, the researchers noted.
However, the results were strengthened by the large cohort, use of professional spirometry, and relatively long follow-up. “The findings underscore the relevance of PRISm for prognostic classification in type 2 diabetes and its potential for optimizing prevention strategies in this condition,” they concluded.
The study was supported by the National Natural Science Foundation of China, Natural Science Foundation of Jiangsu Province, and the Priority Academic Program Development of Jiangsu Higher Education Institutions. The researchers reported no relevant financial relationships.
A version of this article first appeared on Medscape.com
Among adults with type 2 diabetes, the presence of preserved ratio impaired spirometry (PRISm) was significantly associated with increased risk of mortality and both macro- and microvascular complications, as well as increased mortality, based on data from more than 20,000 individuals.
Guochen Li, MD, of the Medical College of Soochow University, Suzhou, China, and colleagues wrote.
“A growing number of studies have demonstrated that impaired lung function and type 2 diabetes could trigger shared pathophysiological injuries, such as microangiopathy and chronic inflammation,” they said, but the potential role of PRISm as an early predictor of adverse outcomes in patients with type 2 diabetes has not been fully examined.
In a study published in the journal Chest, the researchers reviewed data from 20,047 individuals with type 2 diabetes in the UK Biobank, a population-based cohort of adults aged 37-73 years recruited between 2006 and 2010.
The main exposure was lung function based on spirometry. PRISm was defined as predicted forced expiratory volume per second (FEV1) less than 80%, with an FEV1/ forced vital capacity (FVC) ratio of at least 0.70. Individuals with normal spirometry (defined as predicted FEV1 ≥ 80% with an FEV1/FVC ratio ≥ 0.70) served as controls.
The primary outcomes were major complications of type 2 diabetes including macrovascular events (myocardial infarction, unstable angina, coronary heart disease [CHD], ischemic stroke, and any type of stroke), microvascular events (diabetic retinopathy and diabetic kidney disease) and mortality (all-cause, cardiovascular, and respiratory).
Overall, 16.9% of study participants (3385 patients) had obstructive spirometry and 22.6% (4521 patients) had PRISm. Compared with individuals with normal spirometry, those with PRISm were more likely to be current smokers, obese, and living in economically disadvantaged areas. Individuals with PRISm also were significantly more likely to be long-term patients with diabetes who were taking glucose-lowering or lipid-lowering drugs (P < .001 for all).
The median follow-up for each of the type 2 diabetes complications and mortality was approximately 12 years. Over this time, 5.0% of patients developed incident MI, 1.3% developed unstable angina, 15.6% had CHD, 3.5% had an ischemic stroke, and 4.7% had any type of stroke. As for microvascular events, 7.8% developed diabetic retinopathy and 6.7% developed diabetic kidney disease. A total of 2588 patients died during the study period (15.1%), including 544 from cardiovascular disease and 319 from respiratory disease.
PRISm was significantly associated with increased risk of each of the complications and mortality types. These associations persisted after adjusting for lifestyle and other factors. The fully adjusted hazard ratios for PRISm versus normal spirometry were 1.23 for MI, 1.23 for unstable angina, 1.21 for CHD, 1.38 for ischemic stroke, 1.41 for any type of stroke, 1.31 for diabetic retinopathy, and 1.38 for diabetic kidney disease. Adjusted HRs for mortality were 1.34, 1.60, and 1.56 for all-cause, cardiovascular, and respiratory mortality, respectively.
The researchers also found that adding PRISm to an office-based risk score significantly improved the risk classification and predictive power for type 2 diabetes complications with the exception of unstable angina and mortality. They found little evidence for an association with sex, smoking, or PRISm duration and any mortality types. However, in subgroup analyses by age, sex, and duration of diabetes, PRISm remained associated with increased risk of macrovascular and microvascular complications, as well as mortality.
Potential mechanisms for the association between PRISm and diabetes complications include the role of insulin resistance in the exacerbation of lung damage in patients with type 2 diabetes, the increased rate of supplemental oxygen use among individuals with PRISm, and the increased prevalence of pulmonary artery enlargement in the PRISm subjects, the researchers wrote.
The findings were limited by several factors including the prospective design, the homogeneous population of individuals primarily of British or Irish ancestry, and the exclusion of diabetic neuropathy from the analysis, the researchers noted.
However, the results were strengthened by the large cohort, use of professional spirometry, and relatively long follow-up. “The findings underscore the relevance of PRISm for prognostic classification in type 2 diabetes and its potential for optimizing prevention strategies in this condition,” they concluded.
The study was supported by the National Natural Science Foundation of China, Natural Science Foundation of Jiangsu Province, and the Priority Academic Program Development of Jiangsu Higher Education Institutions. The researchers reported no relevant financial relationships.
A version of this article first appeared on Medscape.com
FROM THE JOURNAL CHEST
Hearing loss tied to more fatigue in middle and older age
Like many stressful chronic conditions, hearing loss appears to foster fatigue, according to an analysis of National Health and Nutrition Examination Study data published in JAMA Otolaryngology – Head & Neck Surgery.
Researchers at Johns Hopkins University, Baltimore, examined NHANES data from 2015 to 2016 and 2017 to 2018, including findings on more than 3,000 participants aged 40 and older. Based on the audiometry subset of NHANES data, hearing loss was associated with a higher frequency of fatigue – even after adjustment for demographics, comorbidities, and lifestyle variables such as smoking, alcohol, and body mass index, in a nationally representative sample of adults in middle and older age.
“We wanted to get away from small clinical data and take a look at the population level to see if hearing loss was related to fatigue and, further perhaps, to cognitive decline,” said coauthor Nicholas S. Reed, AuD, PhD, an assistant professor of epidemiology at Johns Hopkins University, Baltimore, in an interview. “We found people with hearing loss had twice the risk of reporting fatigue nearly every day versus those not reporting fatigue.” This cross-sectional study provides needed population-based evidence from a nationally representative sample, according to Dr. Reed and associates, who have been researching the possible connection between age-related hearing loss, physical activity levels, and cognitive decline.
Study details
The 3,031 age-eligible participants had a mean age of 58 years; 48% were male, and 10% were Black. Some hearing loss was reported by 24%.
They responded to the following question: “Over the last 2 weeks, how often have you been bothered by feeling tired or having little energy?” Response categories were “not at all,” “several days,” “more than half the days,” and “nearly every day.” Those with hearing loss were more likely to report fatigue for more than half the days (relative risk ratio, 2.16; 95% confidence interval, 1.27-3.67) and nearly every day (RRR, 2.05; 95% CI, 1.16-3.65), compared with not having fatigue. Additional adjustment for comorbidities and depressive symptoms showed similar results.
Hearing loss was defined as > 25 decibels hearing level (dB HL) versus normal hearing of ≤ 25 dB HL, and continuously by every 10 dB HL poorer. Each 10-dB HL of audiometric hearing loss was associated with a higher likelihood of reporting fatigue nearly every day (RRR, 1.24; 95% CI,1.04-1.47), but not for more than half the days.
The association tended to be stronger in younger, non-Hispanic White, and female participants, but statistical testing did not support differential associations by age, sex, race, or ethnicity.
While some might intuitively expect hearing loss to cause noticeably more fatigue in middle-aged people who may be straining to hear during hours in the daily workplace or at home, Dr. Reed said older people probably feel more hearing-related fatigue owing to age and comorbidities. “And higher physical activity levels of middle-aged adults can be protective.”
Dr. Reed advised primary care physicians to be sure to ask about fatigue and hearing status during wellness exams and take appropriate steps to diagnose and correct hearing problems. “Make sure hearing is part of the health equation because hearing loss can be part of the culprit. And it’s very possible that hearing loss is also contributing to cognitive decline.”
Dr. Reed’s group will soon release data on a clinical trial on hearing loss and cognitive decline.
The authors called for studies incorporating fatigue assessments in order to clarify how hearing loss might contribute to physical and mental fatigue and how it could be associated with downstream outcomes such as fatigue-related physical impairment. Dr. Reed reported grants from the National Institute on Aging during the conduct of the study and stock compensation from the Neosensory Advisory Board outside of the submitted work. Several coauthors reported academic or government research funding as well as fees and honoraria from various private-sector companies.
Like many stressful chronic conditions, hearing loss appears to foster fatigue, according to an analysis of National Health and Nutrition Examination Study data published in JAMA Otolaryngology – Head & Neck Surgery.
Researchers at Johns Hopkins University, Baltimore, examined NHANES data from 2015 to 2016 and 2017 to 2018, including findings on more than 3,000 participants aged 40 and older. Based on the audiometry subset of NHANES data, hearing loss was associated with a higher frequency of fatigue – even after adjustment for demographics, comorbidities, and lifestyle variables such as smoking, alcohol, and body mass index, in a nationally representative sample of adults in middle and older age.
“We wanted to get away from small clinical data and take a look at the population level to see if hearing loss was related to fatigue and, further perhaps, to cognitive decline,” said coauthor Nicholas S. Reed, AuD, PhD, an assistant professor of epidemiology at Johns Hopkins University, Baltimore, in an interview. “We found people with hearing loss had twice the risk of reporting fatigue nearly every day versus those not reporting fatigue.” This cross-sectional study provides needed population-based evidence from a nationally representative sample, according to Dr. Reed and associates, who have been researching the possible connection between age-related hearing loss, physical activity levels, and cognitive decline.
Study details
The 3,031 age-eligible participants had a mean age of 58 years; 48% were male, and 10% were Black. Some hearing loss was reported by 24%.
They responded to the following question: “Over the last 2 weeks, how often have you been bothered by feeling tired or having little energy?” Response categories were “not at all,” “several days,” “more than half the days,” and “nearly every day.” Those with hearing loss were more likely to report fatigue for more than half the days (relative risk ratio, 2.16; 95% confidence interval, 1.27-3.67) and nearly every day (RRR, 2.05; 95% CI, 1.16-3.65), compared with not having fatigue. Additional adjustment for comorbidities and depressive symptoms showed similar results.
Hearing loss was defined as > 25 decibels hearing level (dB HL) versus normal hearing of ≤ 25 dB HL, and continuously by every 10 dB HL poorer. Each 10-dB HL of audiometric hearing loss was associated with a higher likelihood of reporting fatigue nearly every day (RRR, 1.24; 95% CI,1.04-1.47), but not for more than half the days.
The association tended to be stronger in younger, non-Hispanic White, and female participants, but statistical testing did not support differential associations by age, sex, race, or ethnicity.
While some might intuitively expect hearing loss to cause noticeably more fatigue in middle-aged people who may be straining to hear during hours in the daily workplace or at home, Dr. Reed said older people probably feel more hearing-related fatigue owing to age and comorbidities. “And higher physical activity levels of middle-aged adults can be protective.”
Dr. Reed advised primary care physicians to be sure to ask about fatigue and hearing status during wellness exams and take appropriate steps to diagnose and correct hearing problems. “Make sure hearing is part of the health equation because hearing loss can be part of the culprit. And it’s very possible that hearing loss is also contributing to cognitive decline.”
Dr. Reed’s group will soon release data on a clinical trial on hearing loss and cognitive decline.
The authors called for studies incorporating fatigue assessments in order to clarify how hearing loss might contribute to physical and mental fatigue and how it could be associated with downstream outcomes such as fatigue-related physical impairment. Dr. Reed reported grants from the National Institute on Aging during the conduct of the study and stock compensation from the Neosensory Advisory Board outside of the submitted work. Several coauthors reported academic or government research funding as well as fees and honoraria from various private-sector companies.
Like many stressful chronic conditions, hearing loss appears to foster fatigue, according to an analysis of National Health and Nutrition Examination Study data published in JAMA Otolaryngology – Head & Neck Surgery.
Researchers at Johns Hopkins University, Baltimore, examined NHANES data from 2015 to 2016 and 2017 to 2018, including findings on more than 3,000 participants aged 40 and older. Based on the audiometry subset of NHANES data, hearing loss was associated with a higher frequency of fatigue – even after adjustment for demographics, comorbidities, and lifestyle variables such as smoking, alcohol, and body mass index, in a nationally representative sample of adults in middle and older age.
“We wanted to get away from small clinical data and take a look at the population level to see if hearing loss was related to fatigue and, further perhaps, to cognitive decline,” said coauthor Nicholas S. Reed, AuD, PhD, an assistant professor of epidemiology at Johns Hopkins University, Baltimore, in an interview. “We found people with hearing loss had twice the risk of reporting fatigue nearly every day versus those not reporting fatigue.” This cross-sectional study provides needed population-based evidence from a nationally representative sample, according to Dr. Reed and associates, who have been researching the possible connection between age-related hearing loss, physical activity levels, and cognitive decline.
Study details
The 3,031 age-eligible participants had a mean age of 58 years; 48% were male, and 10% were Black. Some hearing loss was reported by 24%.
They responded to the following question: “Over the last 2 weeks, how often have you been bothered by feeling tired or having little energy?” Response categories were “not at all,” “several days,” “more than half the days,” and “nearly every day.” Those with hearing loss were more likely to report fatigue for more than half the days (relative risk ratio, 2.16; 95% confidence interval, 1.27-3.67) and nearly every day (RRR, 2.05; 95% CI, 1.16-3.65), compared with not having fatigue. Additional adjustment for comorbidities and depressive symptoms showed similar results.
Hearing loss was defined as > 25 decibels hearing level (dB HL) versus normal hearing of ≤ 25 dB HL, and continuously by every 10 dB HL poorer. Each 10-dB HL of audiometric hearing loss was associated with a higher likelihood of reporting fatigue nearly every day (RRR, 1.24; 95% CI,1.04-1.47), but not for more than half the days.
The association tended to be stronger in younger, non-Hispanic White, and female participants, but statistical testing did not support differential associations by age, sex, race, or ethnicity.
While some might intuitively expect hearing loss to cause noticeably more fatigue in middle-aged people who may be straining to hear during hours in the daily workplace or at home, Dr. Reed said older people probably feel more hearing-related fatigue owing to age and comorbidities. “And higher physical activity levels of middle-aged adults can be protective.”
Dr. Reed advised primary care physicians to be sure to ask about fatigue and hearing status during wellness exams and take appropriate steps to diagnose and correct hearing problems. “Make sure hearing is part of the health equation because hearing loss can be part of the culprit. And it’s very possible that hearing loss is also contributing to cognitive decline.”
Dr. Reed’s group will soon release data on a clinical trial on hearing loss and cognitive decline.
The authors called for studies incorporating fatigue assessments in order to clarify how hearing loss might contribute to physical and mental fatigue and how it could be associated with downstream outcomes such as fatigue-related physical impairment. Dr. Reed reported grants from the National Institute on Aging during the conduct of the study and stock compensation from the Neosensory Advisory Board outside of the submitted work. Several coauthors reported academic or government research funding as well as fees and honoraria from various private-sector companies.
FROM JAMA OTOLARYNGOLOGY – HEAD & NECK SURGERY
Intensely itchy normal skin
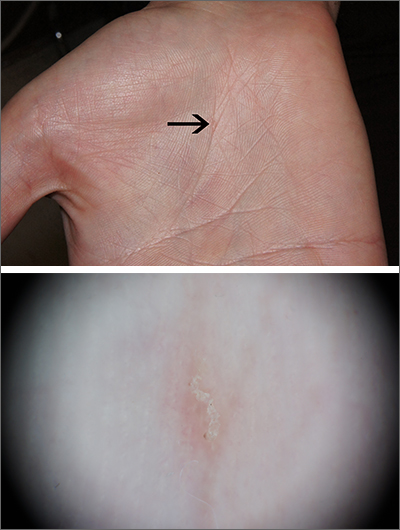
Severe itching should prompt suspicion for scabies and the hands are the highest-yield location. In this patient’s case, there weren’t findings in the web spaces and, in general, skin findings were largely absent; dermoscopy confirmed the diagnosis of scabies.
Sarcoptes scabiei, is a parasitic mite that lives and reproduces in and on human skin and is transmitted by very close contact, either skin-to-skin or by living within a household or institution with shared linens and furnishings. After infection, itching develops within days to weeks from both the physical movement and burrowing of mites within the skin and from the allergic and inflammatory response to mite bodies and their waste.1 Symptoms and infections may persist for years in the absence of treatment.
Sometimes (as in this case), burrows are few and very subtle. More often, there are widespread burrows and excoriated papules over the hands, trunk, extremities, and genitals. A burrowed mite is often adjacent to, but not directly in, an excoriation. Dermoscopy has transformed the ability to diagnose this condition quickly by enabling clinicians to visualize the triangular shape of the head and front legs of a mite (called the “delta sign”). This localization allows easy microscopic confirmation by paring the mite from the skin with a small scalpel blade. (A #11 or #15 blade works very well.)
Topical permethrin 5% cream is highly curative. The cream should be applied from the top of the neck to the tips of the patient’s toes and left on for 8 hours; the process should be repeated a week later. Very close contacts (eg, symptomatic household members or sexual partners) should be treated concurrently. A 60 g tube will treat 1 adult twice. (A 60 g tube of permethrin with a refill, therefore, will treat 2 adults twice.) Oral ivermectin 3 mg dosed at 200 mcg/kg in a single dose repeated in 1 to 2 weeks is an alternative.
Outbreaks in an institutional setting present a significant challenge and require population-based control and often the assistance of infection control specialists or local public health officials. Often this involves weekly treatment with ivermectin for all potentially affected individuals for 3 to 4 weeks and surveillance for follow-up. While there is some resistance to ivermectin, many failures relate more to reinfection from unidentified sources.
This patient received topical permethrin 5% cream dosed as noted above. Itching can be expected to persist for 3 to 4 weeks, so topical triamcinolone 0.1% cream was prescribed as needed for itching on days when permethrin wasn’t applied. At 6 weeks, this patient’s symptoms had resolved.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, ME.
1. Richards RN. Scabies: diagnostic and therapeutic update. J Cutan Med Surg. 2021;25:95-101. doi: 10.1177/1203475420960446
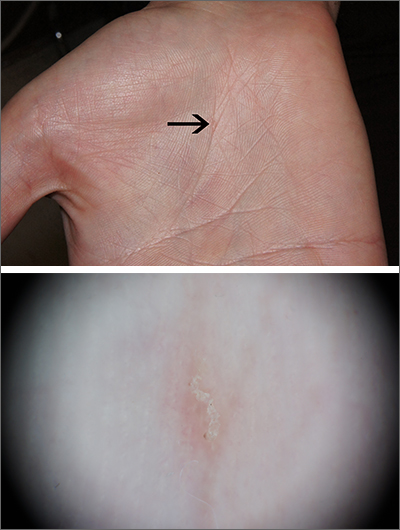
Severe itching should prompt suspicion for scabies and the hands are the highest-yield location. In this patient’s case, there weren’t findings in the web spaces and, in general, skin findings were largely absent; dermoscopy confirmed the diagnosis of scabies.
Sarcoptes scabiei, is a parasitic mite that lives and reproduces in and on human skin and is transmitted by very close contact, either skin-to-skin or by living within a household or institution with shared linens and furnishings. After infection, itching develops within days to weeks from both the physical movement and burrowing of mites within the skin and from the allergic and inflammatory response to mite bodies and their waste.1 Symptoms and infections may persist for years in the absence of treatment.
Sometimes (as in this case), burrows are few and very subtle. More often, there are widespread burrows and excoriated papules over the hands, trunk, extremities, and genitals. A burrowed mite is often adjacent to, but not directly in, an excoriation. Dermoscopy has transformed the ability to diagnose this condition quickly by enabling clinicians to visualize the triangular shape of the head and front legs of a mite (called the “delta sign”). This localization allows easy microscopic confirmation by paring the mite from the skin with a small scalpel blade. (A #11 or #15 blade works very well.)
Topical permethrin 5% cream is highly curative. The cream should be applied from the top of the neck to the tips of the patient’s toes and left on for 8 hours; the process should be repeated a week later. Very close contacts (eg, symptomatic household members or sexual partners) should be treated concurrently. A 60 g tube will treat 1 adult twice. (A 60 g tube of permethrin with a refill, therefore, will treat 2 adults twice.) Oral ivermectin 3 mg dosed at 200 mcg/kg in a single dose repeated in 1 to 2 weeks is an alternative.
Outbreaks in an institutional setting present a significant challenge and require population-based control and often the assistance of infection control specialists or local public health officials. Often this involves weekly treatment with ivermectin for all potentially affected individuals for 3 to 4 weeks and surveillance for follow-up. While there is some resistance to ivermectin, many failures relate more to reinfection from unidentified sources.
This patient received topical permethrin 5% cream dosed as noted above. Itching can be expected to persist for 3 to 4 weeks, so topical triamcinolone 0.1% cream was prescribed as needed for itching on days when permethrin wasn’t applied. At 6 weeks, this patient’s symptoms had resolved.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, ME.
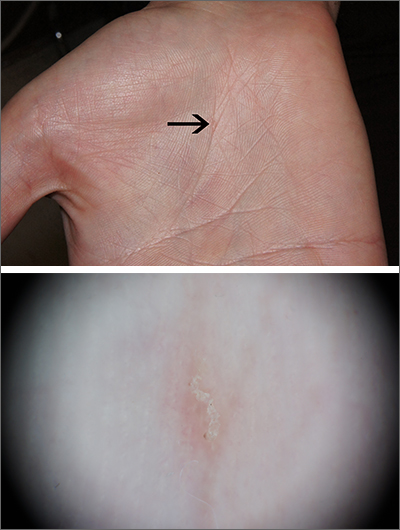
Severe itching should prompt suspicion for scabies and the hands are the highest-yield location. In this patient’s case, there weren’t findings in the web spaces and, in general, skin findings were largely absent; dermoscopy confirmed the diagnosis of scabies.
Sarcoptes scabiei, is a parasitic mite that lives and reproduces in and on human skin and is transmitted by very close contact, either skin-to-skin or by living within a household or institution with shared linens and furnishings. After infection, itching develops within days to weeks from both the physical movement and burrowing of mites within the skin and from the allergic and inflammatory response to mite bodies and their waste.1 Symptoms and infections may persist for years in the absence of treatment.
Sometimes (as in this case), burrows are few and very subtle. More often, there are widespread burrows and excoriated papules over the hands, trunk, extremities, and genitals. A burrowed mite is often adjacent to, but not directly in, an excoriation. Dermoscopy has transformed the ability to diagnose this condition quickly by enabling clinicians to visualize the triangular shape of the head and front legs of a mite (called the “delta sign”). This localization allows easy microscopic confirmation by paring the mite from the skin with a small scalpel blade. (A #11 or #15 blade works very well.)
Topical permethrin 5% cream is highly curative. The cream should be applied from the top of the neck to the tips of the patient’s toes and left on for 8 hours; the process should be repeated a week later. Very close contacts (eg, symptomatic household members or sexual partners) should be treated concurrently. A 60 g tube will treat 1 adult twice. (A 60 g tube of permethrin with a refill, therefore, will treat 2 adults twice.) Oral ivermectin 3 mg dosed at 200 mcg/kg in a single dose repeated in 1 to 2 weeks is an alternative.
Outbreaks in an institutional setting present a significant challenge and require population-based control and often the assistance of infection control specialists or local public health officials. Often this involves weekly treatment with ivermectin for all potentially affected individuals for 3 to 4 weeks and surveillance for follow-up. While there is some resistance to ivermectin, many failures relate more to reinfection from unidentified sources.
This patient received topical permethrin 5% cream dosed as noted above. Itching can be expected to persist for 3 to 4 weeks, so topical triamcinolone 0.1% cream was prescribed as needed for itching on days when permethrin wasn’t applied. At 6 weeks, this patient’s symptoms had resolved.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, ME.
1. Richards RN. Scabies: diagnostic and therapeutic update. J Cutan Med Surg. 2021;25:95-101. doi: 10.1177/1203475420960446
1. Richards RN. Scabies: diagnostic and therapeutic update. J Cutan Med Surg. 2021;25:95-101. doi: 10.1177/1203475420960446
Evidence weighed for suicide/self-harm with obesity drugs
Following reports that the European Medicines Agency is looking into instances of suicide or self-harm after patients took the weight loss drugs semaglutide or liraglutide, the manufacturer, Novo Nordisk, issued a statement to this news organization in which it says it “remains confident in the benefit risk profile of the products and remains committed to ensuring patient safety.”
U.S. experts say they haven’t personally seen this adverse effect in any patients except for one isolated case. An increase in suicidal ideation, particularly among younger people, has been reported following bariatric surgery for weight loss.
In the United States, the two drugs – both GLP-1 agonists – already come with a warning about the potential for these adverse effects on the branded versions approved for weight loss, Wegovy and Saxenda. (Years earlier, both drugs, marketed as Ozempic and Victoza, were also approved for treatment of type 2 diabetes.)
Of more than 1,200 reports of adverse reactions with semaglutide, 60 cases of suicidal ideation and 7 suicide attempts have been reported since 2018, according to the Food and Drug Administration’s Adverse Event Reporting System (FAERS) public database. For liraglutide, there were 71 cases of suicidal ideation, 28 suicide attempts, and 25 completed suicides out of more than 35,000 reports of adverse reactions.
The FAERS website cautions users that the data may be duplicated or incomplete, that rates of occurrence cannot be established using the data, that reports have not been verified, and that the existence of a report cannot establish causation.
The EMA is looking into about 150 reports of possible cases of self-injury and suicidal thoughts, according to a press release from the agency.
“It is not yet clear whether the reported cases are linked to the medicines themselves or to the patients’ underlying conditions or other factors,” it says. The medicines are widely used in the European Union, according to the press release.
The review of Ozempic, Saxenda, and Wegovy, which started on July 3, 2023, has been extended to include other GLP-1 receptor agonists, which include dulaglutide, exenatide, and lixisenatide. This review is expected to conclude in November 2023.
In a statement, Novo Nordisk did not directly dispute a potential link between the drugs and suicidal ideation.
“In the U.S., FDA requires medications for chronic weight management that work on the central nervous system, including Wegovy and Saxenda, to carry a warning about suicidal behavior and ideation,” the statement indicates. “This event had been reported in clinical trials with other weight management products.”
It adds: “Novo Nordisk is continuously performing surveillance of the data from ongoing clinical trials and real-world use of its products and collaborates closely with the authorities to ensure patient safety and adequate information to healthcare professionals.”
Important to know the denominator
“What’s important to know is the denominator,” said Holly Lofton, MD, a clinical associate professor of surgery and medicine and the director of the medical weight management program at NYU Langone, New York. “It needs a denominator with the total population on the medication so we can determine if that’s really a significant risk.”
Dr. Lofton described an isolated, anecdotal case of a patient who had no history of depression or mental health problems but developed suicidal thoughts after taking Saxenda for several months. In that case, the 25-year-old was experiencing problems in a personal relationship and with social media.
Two other weight loss specialists contacted by this news organization had not had patients who had experienced suicidal ideation with the drugs. “These are not very common in practice,” Dr. Lofton said in an interview.
The U.S. prescribing information for Saxenda, which contains liraglutide and has been approved as an adjunct to diet and exercise for chronic weight management, recommends monitoring for the emergence of depression and suicidal thoughts. In the clinical trials, 6 of the 3,384 patients who took the drug reported suicidal ideation; none of the 1,941 patients who received placebo did so, according to the FDA.
Similarly, the U.S. prescribing information for Wegovy, which contains semaglutide, recommends monitoring for the emergence of suicidal thoughts or depression, but this recommendation was based on clinical trials of other weight management products. The prescribing information for Ozempic, the brand name for semaglutide for type 2 diabetes, does not include this recommendation.
Is it the weight loss, rather than the meds? Seen with bariatric surgery too
Speculating what the link, if any, might be, Dr. Lofton suggested dopamine release could be playing a role. Small trials in humans as well as animal studies hint at a blunting of dopamine responses to usual triggers – including addictive substances and possibly food – that may also affect mood.
Young people (aged 18-34) who undergo bariatric surgery are at an increased risk of suicide during follow-up compared to their peers who don’t have surgery. And a study found an increase in events involving self-harm after bariatric surgery, especially among patients who already had a mental health disorder.
For a patient who derives comfort from food, not being able to eat in response to a stressful event may lead that patient to act out in more serious ways, according to Dr. Lofton. “That’s why, again, surgical follow-up is so important and their presurgical psychiatric evaluation is so important.”
A version of this article originally appeared on Medscape.com.
Following reports that the European Medicines Agency is looking into instances of suicide or self-harm after patients took the weight loss drugs semaglutide or liraglutide, the manufacturer, Novo Nordisk, issued a statement to this news organization in which it says it “remains confident in the benefit risk profile of the products and remains committed to ensuring patient safety.”
U.S. experts say they haven’t personally seen this adverse effect in any patients except for one isolated case. An increase in suicidal ideation, particularly among younger people, has been reported following bariatric surgery for weight loss.
In the United States, the two drugs – both GLP-1 agonists – already come with a warning about the potential for these adverse effects on the branded versions approved for weight loss, Wegovy and Saxenda. (Years earlier, both drugs, marketed as Ozempic and Victoza, were also approved for treatment of type 2 diabetes.)
Of more than 1,200 reports of adverse reactions with semaglutide, 60 cases of suicidal ideation and 7 suicide attempts have been reported since 2018, according to the Food and Drug Administration’s Adverse Event Reporting System (FAERS) public database. For liraglutide, there were 71 cases of suicidal ideation, 28 suicide attempts, and 25 completed suicides out of more than 35,000 reports of adverse reactions.
The FAERS website cautions users that the data may be duplicated or incomplete, that rates of occurrence cannot be established using the data, that reports have not been verified, and that the existence of a report cannot establish causation.
The EMA is looking into about 150 reports of possible cases of self-injury and suicidal thoughts, according to a press release from the agency.
“It is not yet clear whether the reported cases are linked to the medicines themselves or to the patients’ underlying conditions or other factors,” it says. The medicines are widely used in the European Union, according to the press release.
The review of Ozempic, Saxenda, and Wegovy, which started on July 3, 2023, has been extended to include other GLP-1 receptor agonists, which include dulaglutide, exenatide, and lixisenatide. This review is expected to conclude in November 2023.
In a statement, Novo Nordisk did not directly dispute a potential link between the drugs and suicidal ideation.
“In the U.S., FDA requires medications for chronic weight management that work on the central nervous system, including Wegovy and Saxenda, to carry a warning about suicidal behavior and ideation,” the statement indicates. “This event had been reported in clinical trials with other weight management products.”
It adds: “Novo Nordisk is continuously performing surveillance of the data from ongoing clinical trials and real-world use of its products and collaborates closely with the authorities to ensure patient safety and adequate information to healthcare professionals.”
Important to know the denominator
“What’s important to know is the denominator,” said Holly Lofton, MD, a clinical associate professor of surgery and medicine and the director of the medical weight management program at NYU Langone, New York. “It needs a denominator with the total population on the medication so we can determine if that’s really a significant risk.”
Dr. Lofton described an isolated, anecdotal case of a patient who had no history of depression or mental health problems but developed suicidal thoughts after taking Saxenda for several months. In that case, the 25-year-old was experiencing problems in a personal relationship and with social media.
Two other weight loss specialists contacted by this news organization had not had patients who had experienced suicidal ideation with the drugs. “These are not very common in practice,” Dr. Lofton said in an interview.
The U.S. prescribing information for Saxenda, which contains liraglutide and has been approved as an adjunct to diet and exercise for chronic weight management, recommends monitoring for the emergence of depression and suicidal thoughts. In the clinical trials, 6 of the 3,384 patients who took the drug reported suicidal ideation; none of the 1,941 patients who received placebo did so, according to the FDA.
Similarly, the U.S. prescribing information for Wegovy, which contains semaglutide, recommends monitoring for the emergence of suicidal thoughts or depression, but this recommendation was based on clinical trials of other weight management products. The prescribing information for Ozempic, the brand name for semaglutide for type 2 diabetes, does not include this recommendation.
Is it the weight loss, rather than the meds? Seen with bariatric surgery too
Speculating what the link, if any, might be, Dr. Lofton suggested dopamine release could be playing a role. Small trials in humans as well as animal studies hint at a blunting of dopamine responses to usual triggers – including addictive substances and possibly food – that may also affect mood.
Young people (aged 18-34) who undergo bariatric surgery are at an increased risk of suicide during follow-up compared to their peers who don’t have surgery. And a study found an increase in events involving self-harm after bariatric surgery, especially among patients who already had a mental health disorder.
For a patient who derives comfort from food, not being able to eat in response to a stressful event may lead that patient to act out in more serious ways, according to Dr. Lofton. “That’s why, again, surgical follow-up is so important and their presurgical psychiatric evaluation is so important.”
A version of this article originally appeared on Medscape.com.
Following reports that the European Medicines Agency is looking into instances of suicide or self-harm after patients took the weight loss drugs semaglutide or liraglutide, the manufacturer, Novo Nordisk, issued a statement to this news organization in which it says it “remains confident in the benefit risk profile of the products and remains committed to ensuring patient safety.”
U.S. experts say they haven’t personally seen this adverse effect in any patients except for one isolated case. An increase in suicidal ideation, particularly among younger people, has been reported following bariatric surgery for weight loss.
In the United States, the two drugs – both GLP-1 agonists – already come with a warning about the potential for these adverse effects on the branded versions approved for weight loss, Wegovy and Saxenda. (Years earlier, both drugs, marketed as Ozempic and Victoza, were also approved for treatment of type 2 diabetes.)
Of more than 1,200 reports of adverse reactions with semaglutide, 60 cases of suicidal ideation and 7 suicide attempts have been reported since 2018, according to the Food and Drug Administration’s Adverse Event Reporting System (FAERS) public database. For liraglutide, there were 71 cases of suicidal ideation, 28 suicide attempts, and 25 completed suicides out of more than 35,000 reports of adverse reactions.
The FAERS website cautions users that the data may be duplicated or incomplete, that rates of occurrence cannot be established using the data, that reports have not been verified, and that the existence of a report cannot establish causation.
The EMA is looking into about 150 reports of possible cases of self-injury and suicidal thoughts, according to a press release from the agency.
“It is not yet clear whether the reported cases are linked to the medicines themselves or to the patients’ underlying conditions or other factors,” it says. The medicines are widely used in the European Union, according to the press release.
The review of Ozempic, Saxenda, and Wegovy, which started on July 3, 2023, has been extended to include other GLP-1 receptor agonists, which include dulaglutide, exenatide, and lixisenatide. This review is expected to conclude in November 2023.
In a statement, Novo Nordisk did not directly dispute a potential link between the drugs and suicidal ideation.
“In the U.S., FDA requires medications for chronic weight management that work on the central nervous system, including Wegovy and Saxenda, to carry a warning about suicidal behavior and ideation,” the statement indicates. “This event had been reported in clinical trials with other weight management products.”
It adds: “Novo Nordisk is continuously performing surveillance of the data from ongoing clinical trials and real-world use of its products and collaborates closely with the authorities to ensure patient safety and adequate information to healthcare professionals.”
Important to know the denominator
“What’s important to know is the denominator,” said Holly Lofton, MD, a clinical associate professor of surgery and medicine and the director of the medical weight management program at NYU Langone, New York. “It needs a denominator with the total population on the medication so we can determine if that’s really a significant risk.”
Dr. Lofton described an isolated, anecdotal case of a patient who had no history of depression or mental health problems but developed suicidal thoughts after taking Saxenda for several months. In that case, the 25-year-old was experiencing problems in a personal relationship and with social media.
Two other weight loss specialists contacted by this news organization had not had patients who had experienced suicidal ideation with the drugs. “These are not very common in practice,” Dr. Lofton said in an interview.
The U.S. prescribing information for Saxenda, which contains liraglutide and has been approved as an adjunct to diet and exercise for chronic weight management, recommends monitoring for the emergence of depression and suicidal thoughts. In the clinical trials, 6 of the 3,384 patients who took the drug reported suicidal ideation; none of the 1,941 patients who received placebo did so, according to the FDA.
Similarly, the U.S. prescribing information for Wegovy, which contains semaglutide, recommends monitoring for the emergence of suicidal thoughts or depression, but this recommendation was based on clinical trials of other weight management products. The prescribing information for Ozempic, the brand name for semaglutide for type 2 diabetes, does not include this recommendation.
Is it the weight loss, rather than the meds? Seen with bariatric surgery too
Speculating what the link, if any, might be, Dr. Lofton suggested dopamine release could be playing a role. Small trials in humans as well as animal studies hint at a blunting of dopamine responses to usual triggers – including addictive substances and possibly food – that may also affect mood.
Young people (aged 18-34) who undergo bariatric surgery are at an increased risk of suicide during follow-up compared to their peers who don’t have surgery. And a study found an increase in events involving self-harm after bariatric surgery, especially among patients who already had a mental health disorder.
For a patient who derives comfort from food, not being able to eat in response to a stressful event may lead that patient to act out in more serious ways, according to Dr. Lofton. “That’s why, again, surgical follow-up is so important and their presurgical psychiatric evaluation is so important.”
A version of this article originally appeared on Medscape.com.




