User login
Research and Reviews for the Practicing Oncologist
Massive liver metastasis from colon adenocarcinoma causing cardiac tamponade
Colorectal cancer is the third most commonly diagnosed cancer in the United States.1 About 5% of Americans will be diagnosed with colorectal cancer in their lifetime, of which 20% will present with distant metastasis.2 The most common sites of metastasis are regional lymph nodes, liver, lung and peritoneum, and patients may present with signs or symptoms related to disease burden at any of these organs.
Case presentation and summary
A 55-year-old man had presented to an outside hospital in August of 2014 with 6 months of hematochezia and a 40-lb weight loss. He was found to be severely anemic on admission (hemoglobin, 4.9 g/dL [normal, 13-17 g/dL], hematocrit, 16% [normal, 35%-45%]). A computed-tomography (CT) scan of the abdomen and pelvis with contrast revealed a mass of 6.9 x 4.7 x 6.3 cm in the rectosigmoid colon and a mass of 10.0 x 12.0 x 10.7 cm in the right hepatic lobe consistent with metastatic disease. The patient was taken to the operating room where the rectosigmoid mass was resected completely. The liver mass was deemed unresectable because of its large size, and surgically directed therapy could not be performed. Pathology was consistent with a T3N1 moderately differentiated adenocarcinoma 11 cm from the anal verge. Further molecular tumor studies revealed wild type KRAS and NRAS, as well as a BRAF mutation.
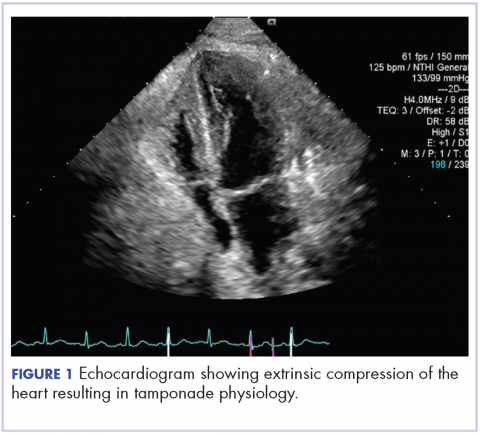
About 4 weeks after the surgery, the patient was seen at our institution for an initial consultation and was noted to have significant anasarca, including 4+ pitting lower extremity edema and scrotal edema. He complained of dyspnea on exertion, which he attributed to deconditioning. His resting heart rate was found to be 123 beats per minute (normal, 60-100 bpm). Jugular venous distention was present. The patient was sent for an urgent echocardiogram, which showed external compression of the right atrium and ventricle by his liver metastasis resulting in tamponade physiology without the presence of any pericardial effusion (Figure 1).
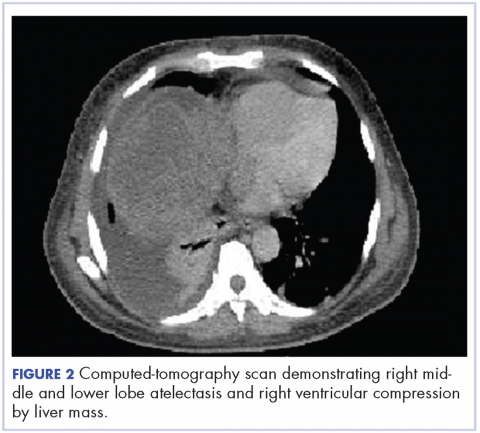
A CT of the abdomen and pelvis at that time showed that the liver mass had increased to 17.6 x 12.1 x 16.1 cm, exerting pressure on the heart and causing atelectasis of the right middle and lower lung lobes (Figure 2).
Treatment plan
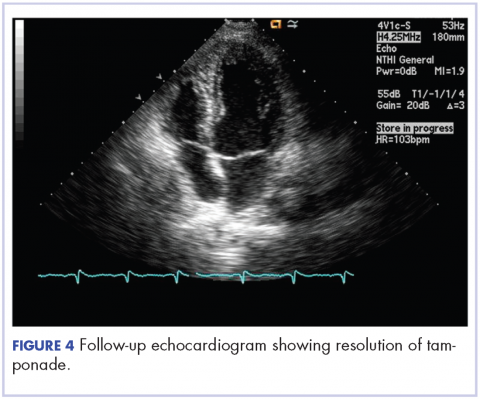
The patient was evaluated by surgical oncology for resection, but his cardiovascular status placed him at high risk for perioperative complications, so such surgery was not pursued. Radioembolization was considered but not pursued because the process needed to evaluate, plan, and treat was not considered sufficiently timely. We consulted with our radiation oncology colleagues about external beam radiotherapy (EBRT) for rapid palliation. They evaluated the patient and recommended the EBRT, and the patient signed consent for treatment. We performed a CT-based simulation and generated an external beam, linear-accelerator–based treatment plan. The plan consisted of three 15-megavoltage photon fields delivering 3,000 cGy in 10 fractions to the whole liver, with appropriate multileaf collimation blocking to minimize dose to adjacent heart, right lung, and bilateral kidneys (Figure 3).
Before initiation of the EBRT, the patient received systemic chemotherapy with a dose-adjusted FOLFOX regimen (5-FU bolus 200 mg/m2, leucovorin 200 mg/m2, oxaliplatin 85 mg/m2, with infusional 5-FU 2,400 mg/m2 over 46 hours). After completing 1 dose of modified FOLFOX, he completed 10 fractions of whole liver radiotherapy with the aforementioned plan. He tolerated the initial treatment well and his subjective symptoms improved. The patient then proceeded to further systemic therapy. After recent data demonstrated improved median progression-free survival and response rates with FOLFOXIRI plus bevacizumab (infusional 5-FU 3200 mg/m2, leucovorin 200 mg/m2, irinotecan 165 mg/m2, and oxaliplatin 85 mg/m2, bevacizumab 5 mg/kg) versus FOLFIRI plus bevacizumab,3 we decided to modify his systemic therapy to FOLFOXIRI with bevacizumab to induce a better response.
Treatment response
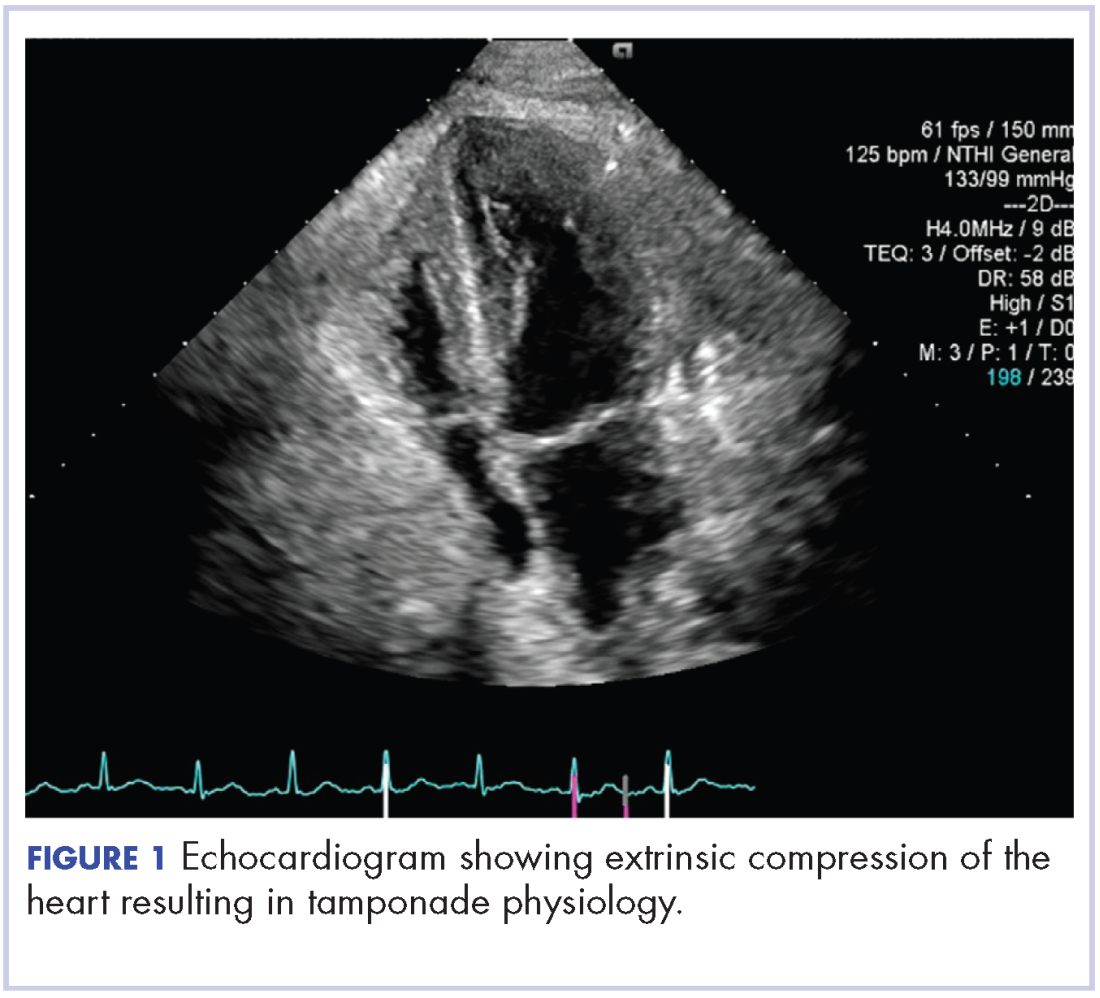
After 2 doses of chemotherapy and completion of radiotherapy, the edema and shortness of breath improved. A follow-up echocardiogram performed a month after completion of EBRT, 1 dose of FOLFOX, and 1 dose of FOLFOXIRI showed resolution of the cardiac compression (Figure 4).
A CT scan of the abdomen and pelvis obtained after 3 cycles of FOLFOXIRI showed marked decrease in the size of the right lobe hepatic mass from 17.6 x 12.1 cm to 12.0 x 8.0 cm. Given the survival benefit of VEGF inhibition in colon cancer, bevacizumab (5 mg/kg) was added to the FOLFOXIRI regimen with cycle 4. Unfortunately, after the 5th cycle, a CT scan of the abdomen showed an increase in size of the hepatic lesions. At this time, FOLFOXIRI and bevacizumab were stopped, and given the tumor’s KRAS/NRAS wild type status, systemic therapy was changed to panitumumab (6 mg/kg). The patient initially tolerated treatment well, but after 9 cycles, the total bilirubin started to increase. CT abdomen at this point was consistent with progression of disease. The patient was not eligible for a clinical trial targeting BRAF mutation given the elevated bilirubin. Regorafanib (80 mg daily for 3 weeks on and 1 week off) was started. After the first cycle, the total bilirubin increased further and the regorafanib was dose reduced to 40 mg daily. Unfortunately, a repeat CT scan of the abdomen demonstrated progression of disease, and given that he developed a progressive transaminitis and hyperbilirubinemia, hospice care was recommended. The patient died shortly thereafter, about 15 months after his initial diagnosis.
Discussion
Massive liver metastasis in the setting of disseminated cancer is not an uncommon manifestation of advanced cancer that can have life-threatening consequences. In te present case, a bulky liver metastasis caused extrinsic compression of the right atrium, resulting in obvious clinical and echocardiogram-proven cardiac tamponade physiology. To our knowledge, this is the first reported case of the treatment of a bulky hepatic metastasis causing cardiac tamponade. In this patient’s case, both radiotherapy and chemotherapy were given safely in rapid sequence resulting in quick resolution of the patient’s symptoms and echocardiogram findings. The presence of a BRAF mutation conferred a poor prognosis and poor response to systemic chemotherapy. Nevertheless, the patient showed good response to a FOLFOXIRI regimen, chosen in this emergent situation given its significantly higher response rates compared with the standard FOLFIRI regimen, which was tolerated well with minimal adverse effects.
Findings from randomized controlled trials examining the role of palliative radiotherapy for metastatic liver disease have suggested that dose escalation above 30 Gy to the whole liver may lead to unacceptably high rates of radiation-induced liver disease, which typically leads to mortality.4-8 Two prospective trials comparing twice daily with daily fractionation have shown no benefit to hyperfractionation, with possibly increased rates of acute toxicity in the setting of hepatocellular carcinoma.9,10 There is emerging evidence that partial liver irradiation, in the appropriate setting in the form of boost after whole-liver RT or stereotactic body radiotherapy, may allow for further dose escalation while avoiding clinical hepatitis.11 Although there is no clear consensus about optimal RT dose and fractionation, the aforementioned studies show that dose and fractionation schemes ranging between 21 Gy and 30 Gy in 1.5 Gy to 3 Gy daily fractions likely provide the best therapeutic ratio for whole-liver irradiation.
In conclusion, this case demonstrates the resolution of cardiac tamponade from a massive liver colorectal metastasis after chemoradiation and illustrates the potential utility of adding radiotherapy to chemotherapy in an urgent scenario where the former might not typically be considered.
1. American Cancer Society. Cancer Facts & Figures 2015. https://www.cancer.org/research/cancer-facts-statistics/all-cancer-facts-figures/cancer-facts-figures-2015.html. Published 2015. Accessed October 10, 2017.
2. Siegel R, Desantis C, Jemal A. Colorectal cancer statistics, 2014. CA Cancer J Clin. 2014;64(2):104-117.
3. Loupakis F, Cremolini C, Masi G, et al. Initial therapy with FOLFOXIRI and bevacizumab for metastatic colorectal cancer. N Engl J Med. 2014;371:1609-1618.
4. Russell AH, Clyde C, Wasserman TH, Turner SS, Rotman M. Accelerated hyperfractionated hepatic irradiation in the management of patients with liver metastases: results of the RTOG dose escalating protocol. Int J Radiat Oncol Biol Phys. 1993;27(1):117-123.
5. Turek-Maischeider M, Kazem I. Palliative irradiation for liver metastases. JAMA. 1975;232(6):625-628.
6. Sherman DM, Weichselbaum R, Order SE, Cloud L, Trey C, Piro AJ. Palliation of hepatic metastasis. Cancer. 1978;41(5):2013-2017.
7. Prasad B, Lee MS, Hendrickson FR. Irradiation of hepatic metastases. Int J Radiat Oncol Biol Phys. 1977;2:129-132.
8. Borgelt BB, Gelber R, Brady LW, Griffin T, Hendrickson FR. The palliation of hepatic metastases: results of the Radiation Therapy Oncology Group pilot study. Int J Radiat Oncol Biol Phys. 1981;7(5):587-591.
9. Raju PI, Maruyama Y, DeSimone P, MacDonald J. Treatment of liver metastases with a combination of chemotherapy and hyperfractionated external radiation therapy. Am J Clin Oncol. 1987;10(1):41-43.
10. Stillwagon GB, Order SE, Guse C, et al. 194 hepatocellular cancers treated by radiation and chemotherapy combinations: toxicity and response: a Radiation Therapy Oncology Group Study. Int J Radiat Oncol Biol Phys. 1989;17(6):1223-1229.
11. Mohiuddin M, Chen E, Ahmad N. Combined liver radiation and chemotherapy for palliation of hepatic metastases from colorectal cancer. J Clin Oncol. 1996;14(3):722-728.
Colorectal cancer is the third most commonly diagnosed cancer in the United States.1 About 5% of Americans will be diagnosed with colorectal cancer in their lifetime, of which 20% will present with distant metastasis.2 The most common sites of metastasis are regional lymph nodes, liver, lung and peritoneum, and patients may present with signs or symptoms related to disease burden at any of these organs.
Case presentation and summary
A 55-year-old man had presented to an outside hospital in August of 2014 with 6 months of hematochezia and a 40-lb weight loss. He was found to be severely anemic on admission (hemoglobin, 4.9 g/dL [normal, 13-17 g/dL], hematocrit, 16% [normal, 35%-45%]). A computed-tomography (CT) scan of the abdomen and pelvis with contrast revealed a mass of 6.9 x 4.7 x 6.3 cm in the rectosigmoid colon and a mass of 10.0 x 12.0 x 10.7 cm in the right hepatic lobe consistent with metastatic disease. The patient was taken to the operating room where the rectosigmoid mass was resected completely. The liver mass was deemed unresectable because of its large size, and surgically directed therapy could not be performed. Pathology was consistent with a T3N1 moderately differentiated adenocarcinoma 11 cm from the anal verge. Further molecular tumor studies revealed wild type KRAS and NRAS, as well as a BRAF mutation.
About 4 weeks after the surgery, the patient was seen at our institution for an initial consultation and was noted to have significant anasarca, including 4+ pitting lower extremity edema and scrotal edema. He complained of dyspnea on exertion, which he attributed to deconditioning. His resting heart rate was found to be 123 beats per minute (normal, 60-100 bpm). Jugular venous distention was present. The patient was sent for an urgent echocardiogram, which showed external compression of the right atrium and ventricle by his liver metastasis resulting in tamponade physiology without the presence of any pericardial effusion (Figure 1).
A CT of the abdomen and pelvis at that time showed that the liver mass had increased to 17.6 x 12.1 x 16.1 cm, exerting pressure on the heart and causing atelectasis of the right middle and lower lung lobes (Figure 2).
Treatment plan
The patient was evaluated by surgical oncology for resection, but his cardiovascular status placed him at high risk for perioperative complications, so such surgery was not pursued. Radioembolization was considered but not pursued because the process needed to evaluate, plan, and treat was not considered sufficiently timely. We consulted with our radiation oncology colleagues about external beam radiotherapy (EBRT) for rapid palliation. They evaluated the patient and recommended the EBRT, and the patient signed consent for treatment. We performed a CT-based simulation and generated an external beam, linear-accelerator–based treatment plan. The plan consisted of three 15-megavoltage photon fields delivering 3,000 cGy in 10 fractions to the whole liver, with appropriate multileaf collimation blocking to minimize dose to adjacent heart, right lung, and bilateral kidneys (Figure 3).
Before initiation of the EBRT, the patient received systemic chemotherapy with a dose-adjusted FOLFOX regimen (5-FU bolus 200 mg/m2, leucovorin 200 mg/m2, oxaliplatin 85 mg/m2, with infusional 5-FU 2,400 mg/m2 over 46 hours). After completing 1 dose of modified FOLFOX, he completed 10 fractions of whole liver radiotherapy with the aforementioned plan. He tolerated the initial treatment well and his subjective symptoms improved. The patient then proceeded to further systemic therapy. After recent data demonstrated improved median progression-free survival and response rates with FOLFOXIRI plus bevacizumab (infusional 5-FU 3200 mg/m2, leucovorin 200 mg/m2, irinotecan 165 mg/m2, and oxaliplatin 85 mg/m2, bevacizumab 5 mg/kg) versus FOLFIRI plus bevacizumab,3 we decided to modify his systemic therapy to FOLFOXIRI with bevacizumab to induce a better response.
Treatment response
After 2 doses of chemotherapy and completion of radiotherapy, the edema and shortness of breath improved. A follow-up echocardiogram performed a month after completion of EBRT, 1 dose of FOLFOX, and 1 dose of FOLFOXIRI showed resolution of the cardiac compression (Figure 4).
A CT scan of the abdomen and pelvis obtained after 3 cycles of FOLFOXIRI showed marked decrease in the size of the right lobe hepatic mass from 17.6 x 12.1 cm to 12.0 x 8.0 cm. Given the survival benefit of VEGF inhibition in colon cancer, bevacizumab (5 mg/kg) was added to the FOLFOXIRI regimen with cycle 4. Unfortunately, after the 5th cycle, a CT scan of the abdomen showed an increase in size of the hepatic lesions. At this time, FOLFOXIRI and bevacizumab were stopped, and given the tumor’s KRAS/NRAS wild type status, systemic therapy was changed to panitumumab (6 mg/kg). The patient initially tolerated treatment well, but after 9 cycles, the total bilirubin started to increase. CT abdomen at this point was consistent with progression of disease. The patient was not eligible for a clinical trial targeting BRAF mutation given the elevated bilirubin. Regorafanib (80 mg daily for 3 weeks on and 1 week off) was started. After the first cycle, the total bilirubin increased further and the regorafanib was dose reduced to 40 mg daily. Unfortunately, a repeat CT scan of the abdomen demonstrated progression of disease, and given that he developed a progressive transaminitis and hyperbilirubinemia, hospice care was recommended. The patient died shortly thereafter, about 15 months after his initial diagnosis.
Discussion
Massive liver metastasis in the setting of disseminated cancer is not an uncommon manifestation of advanced cancer that can have life-threatening consequences. In te present case, a bulky liver metastasis caused extrinsic compression of the right atrium, resulting in obvious clinical and echocardiogram-proven cardiac tamponade physiology. To our knowledge, this is the first reported case of the treatment of a bulky hepatic metastasis causing cardiac tamponade. In this patient’s case, both radiotherapy and chemotherapy were given safely in rapid sequence resulting in quick resolution of the patient’s symptoms and echocardiogram findings. The presence of a BRAF mutation conferred a poor prognosis and poor response to systemic chemotherapy. Nevertheless, the patient showed good response to a FOLFOXIRI regimen, chosen in this emergent situation given its significantly higher response rates compared with the standard FOLFIRI regimen, which was tolerated well with minimal adverse effects.
Findings from randomized controlled trials examining the role of palliative radiotherapy for metastatic liver disease have suggested that dose escalation above 30 Gy to the whole liver may lead to unacceptably high rates of radiation-induced liver disease, which typically leads to mortality.4-8 Two prospective trials comparing twice daily with daily fractionation have shown no benefit to hyperfractionation, with possibly increased rates of acute toxicity in the setting of hepatocellular carcinoma.9,10 There is emerging evidence that partial liver irradiation, in the appropriate setting in the form of boost after whole-liver RT or stereotactic body radiotherapy, may allow for further dose escalation while avoiding clinical hepatitis.11 Although there is no clear consensus about optimal RT dose and fractionation, the aforementioned studies show that dose and fractionation schemes ranging between 21 Gy and 30 Gy in 1.5 Gy to 3 Gy daily fractions likely provide the best therapeutic ratio for whole-liver irradiation.
In conclusion, this case demonstrates the resolution of cardiac tamponade from a massive liver colorectal metastasis after chemoradiation and illustrates the potential utility of adding radiotherapy to chemotherapy in an urgent scenario where the former might not typically be considered.
Colorectal cancer is the third most commonly diagnosed cancer in the United States.1 About 5% of Americans will be diagnosed with colorectal cancer in their lifetime, of which 20% will present with distant metastasis.2 The most common sites of metastasis are regional lymph nodes, liver, lung and peritoneum, and patients may present with signs or symptoms related to disease burden at any of these organs.
Case presentation and summary
A 55-year-old man had presented to an outside hospital in August of 2014 with 6 months of hematochezia and a 40-lb weight loss. He was found to be severely anemic on admission (hemoglobin, 4.9 g/dL [normal, 13-17 g/dL], hematocrit, 16% [normal, 35%-45%]). A computed-tomography (CT) scan of the abdomen and pelvis with contrast revealed a mass of 6.9 x 4.7 x 6.3 cm in the rectosigmoid colon and a mass of 10.0 x 12.0 x 10.7 cm in the right hepatic lobe consistent with metastatic disease. The patient was taken to the operating room where the rectosigmoid mass was resected completely. The liver mass was deemed unresectable because of its large size, and surgically directed therapy could not be performed. Pathology was consistent with a T3N1 moderately differentiated adenocarcinoma 11 cm from the anal verge. Further molecular tumor studies revealed wild type KRAS and NRAS, as well as a BRAF mutation.
About 4 weeks after the surgery, the patient was seen at our institution for an initial consultation and was noted to have significant anasarca, including 4+ pitting lower extremity edema and scrotal edema. He complained of dyspnea on exertion, which he attributed to deconditioning. His resting heart rate was found to be 123 beats per minute (normal, 60-100 bpm). Jugular venous distention was present. The patient was sent for an urgent echocardiogram, which showed external compression of the right atrium and ventricle by his liver metastasis resulting in tamponade physiology without the presence of any pericardial effusion (Figure 1).
A CT of the abdomen and pelvis at that time showed that the liver mass had increased to 17.6 x 12.1 x 16.1 cm, exerting pressure on the heart and causing atelectasis of the right middle and lower lung lobes (Figure 2).
Treatment plan
The patient was evaluated by surgical oncology for resection, but his cardiovascular status placed him at high risk for perioperative complications, so such surgery was not pursued. Radioembolization was considered but not pursued because the process needed to evaluate, plan, and treat was not considered sufficiently timely. We consulted with our radiation oncology colleagues about external beam radiotherapy (EBRT) for rapid palliation. They evaluated the patient and recommended the EBRT, and the patient signed consent for treatment. We performed a CT-based simulation and generated an external beam, linear-accelerator–based treatment plan. The plan consisted of three 15-megavoltage photon fields delivering 3,000 cGy in 10 fractions to the whole liver, with appropriate multileaf collimation blocking to minimize dose to adjacent heart, right lung, and bilateral kidneys (Figure 3).
Before initiation of the EBRT, the patient received systemic chemotherapy with a dose-adjusted FOLFOX regimen (5-FU bolus 200 mg/m2, leucovorin 200 mg/m2, oxaliplatin 85 mg/m2, with infusional 5-FU 2,400 mg/m2 over 46 hours). After completing 1 dose of modified FOLFOX, he completed 10 fractions of whole liver radiotherapy with the aforementioned plan. He tolerated the initial treatment well and his subjective symptoms improved. The patient then proceeded to further systemic therapy. After recent data demonstrated improved median progression-free survival and response rates with FOLFOXIRI plus bevacizumab (infusional 5-FU 3200 mg/m2, leucovorin 200 mg/m2, irinotecan 165 mg/m2, and oxaliplatin 85 mg/m2, bevacizumab 5 mg/kg) versus FOLFIRI plus bevacizumab,3 we decided to modify his systemic therapy to FOLFOXIRI with bevacizumab to induce a better response.
Treatment response
After 2 doses of chemotherapy and completion of radiotherapy, the edema and shortness of breath improved. A follow-up echocardiogram performed a month after completion of EBRT, 1 dose of FOLFOX, and 1 dose of FOLFOXIRI showed resolution of the cardiac compression (Figure 4).
A CT scan of the abdomen and pelvis obtained after 3 cycles of FOLFOXIRI showed marked decrease in the size of the right lobe hepatic mass from 17.6 x 12.1 cm to 12.0 x 8.0 cm. Given the survival benefit of VEGF inhibition in colon cancer, bevacizumab (5 mg/kg) was added to the FOLFOXIRI regimen with cycle 4. Unfortunately, after the 5th cycle, a CT scan of the abdomen showed an increase in size of the hepatic lesions. At this time, FOLFOXIRI and bevacizumab were stopped, and given the tumor’s KRAS/NRAS wild type status, systemic therapy was changed to panitumumab (6 mg/kg). The patient initially tolerated treatment well, but after 9 cycles, the total bilirubin started to increase. CT abdomen at this point was consistent with progression of disease. The patient was not eligible for a clinical trial targeting BRAF mutation given the elevated bilirubin. Regorafanib (80 mg daily for 3 weeks on and 1 week off) was started. After the first cycle, the total bilirubin increased further and the regorafanib was dose reduced to 40 mg daily. Unfortunately, a repeat CT scan of the abdomen demonstrated progression of disease, and given that he developed a progressive transaminitis and hyperbilirubinemia, hospice care was recommended. The patient died shortly thereafter, about 15 months after his initial diagnosis.
Discussion
Massive liver metastasis in the setting of disseminated cancer is not an uncommon manifestation of advanced cancer that can have life-threatening consequences. In te present case, a bulky liver metastasis caused extrinsic compression of the right atrium, resulting in obvious clinical and echocardiogram-proven cardiac tamponade physiology. To our knowledge, this is the first reported case of the treatment of a bulky hepatic metastasis causing cardiac tamponade. In this patient’s case, both radiotherapy and chemotherapy were given safely in rapid sequence resulting in quick resolution of the patient’s symptoms and echocardiogram findings. The presence of a BRAF mutation conferred a poor prognosis and poor response to systemic chemotherapy. Nevertheless, the patient showed good response to a FOLFOXIRI regimen, chosen in this emergent situation given its significantly higher response rates compared with the standard FOLFIRI regimen, which was tolerated well with minimal adverse effects.
Findings from randomized controlled trials examining the role of palliative radiotherapy for metastatic liver disease have suggested that dose escalation above 30 Gy to the whole liver may lead to unacceptably high rates of radiation-induced liver disease, which typically leads to mortality.4-8 Two prospective trials comparing twice daily with daily fractionation have shown no benefit to hyperfractionation, with possibly increased rates of acute toxicity in the setting of hepatocellular carcinoma.9,10 There is emerging evidence that partial liver irradiation, in the appropriate setting in the form of boost after whole-liver RT or stereotactic body radiotherapy, may allow for further dose escalation while avoiding clinical hepatitis.11 Although there is no clear consensus about optimal RT dose and fractionation, the aforementioned studies show that dose and fractionation schemes ranging between 21 Gy and 30 Gy in 1.5 Gy to 3 Gy daily fractions likely provide the best therapeutic ratio for whole-liver irradiation.
In conclusion, this case demonstrates the resolution of cardiac tamponade from a massive liver colorectal metastasis after chemoradiation and illustrates the potential utility of adding radiotherapy to chemotherapy in an urgent scenario where the former might not typically be considered.
1. American Cancer Society. Cancer Facts & Figures 2015. https://www.cancer.org/research/cancer-facts-statistics/all-cancer-facts-figures/cancer-facts-figures-2015.html. Published 2015. Accessed October 10, 2017.
2. Siegel R, Desantis C, Jemal A. Colorectal cancer statistics, 2014. CA Cancer J Clin. 2014;64(2):104-117.
3. Loupakis F, Cremolini C, Masi G, et al. Initial therapy with FOLFOXIRI and bevacizumab for metastatic colorectal cancer. N Engl J Med. 2014;371:1609-1618.
4. Russell AH, Clyde C, Wasserman TH, Turner SS, Rotman M. Accelerated hyperfractionated hepatic irradiation in the management of patients with liver metastases: results of the RTOG dose escalating protocol. Int J Radiat Oncol Biol Phys. 1993;27(1):117-123.
5. Turek-Maischeider M, Kazem I. Palliative irradiation for liver metastases. JAMA. 1975;232(6):625-628.
6. Sherman DM, Weichselbaum R, Order SE, Cloud L, Trey C, Piro AJ. Palliation of hepatic metastasis. Cancer. 1978;41(5):2013-2017.
7. Prasad B, Lee MS, Hendrickson FR. Irradiation of hepatic metastases. Int J Radiat Oncol Biol Phys. 1977;2:129-132.
8. Borgelt BB, Gelber R, Brady LW, Griffin T, Hendrickson FR. The palliation of hepatic metastases: results of the Radiation Therapy Oncology Group pilot study. Int J Radiat Oncol Biol Phys. 1981;7(5):587-591.
9. Raju PI, Maruyama Y, DeSimone P, MacDonald J. Treatment of liver metastases with a combination of chemotherapy and hyperfractionated external radiation therapy. Am J Clin Oncol. 1987;10(1):41-43.
10. Stillwagon GB, Order SE, Guse C, et al. 194 hepatocellular cancers treated by radiation and chemotherapy combinations: toxicity and response: a Radiation Therapy Oncology Group Study. Int J Radiat Oncol Biol Phys. 1989;17(6):1223-1229.
11. Mohiuddin M, Chen E, Ahmad N. Combined liver radiation and chemotherapy for palliation of hepatic metastases from colorectal cancer. J Clin Oncol. 1996;14(3):722-728.
1. American Cancer Society. Cancer Facts & Figures 2015. https://www.cancer.org/research/cancer-facts-statistics/all-cancer-facts-figures/cancer-facts-figures-2015.html. Published 2015. Accessed October 10, 2017.
2. Siegel R, Desantis C, Jemal A. Colorectal cancer statistics, 2014. CA Cancer J Clin. 2014;64(2):104-117.
3. Loupakis F, Cremolini C, Masi G, et al. Initial therapy with FOLFOXIRI and bevacizumab for metastatic colorectal cancer. N Engl J Med. 2014;371:1609-1618.
4. Russell AH, Clyde C, Wasserman TH, Turner SS, Rotman M. Accelerated hyperfractionated hepatic irradiation in the management of patients with liver metastases: results of the RTOG dose escalating protocol. Int J Radiat Oncol Biol Phys. 1993;27(1):117-123.
5. Turek-Maischeider M, Kazem I. Palliative irradiation for liver metastases. JAMA. 1975;232(6):625-628.
6. Sherman DM, Weichselbaum R, Order SE, Cloud L, Trey C, Piro AJ. Palliation of hepatic metastasis. Cancer. 1978;41(5):2013-2017.
7. Prasad B, Lee MS, Hendrickson FR. Irradiation of hepatic metastases. Int J Radiat Oncol Biol Phys. 1977;2:129-132.
8. Borgelt BB, Gelber R, Brady LW, Griffin T, Hendrickson FR. The palliation of hepatic metastases: results of the Radiation Therapy Oncology Group pilot study. Int J Radiat Oncol Biol Phys. 1981;7(5):587-591.
9. Raju PI, Maruyama Y, DeSimone P, MacDonald J. Treatment of liver metastases with a combination of chemotherapy and hyperfractionated external radiation therapy. Am J Clin Oncol. 1987;10(1):41-43.
10. Stillwagon GB, Order SE, Guse C, et al. 194 hepatocellular cancers treated by radiation and chemotherapy combinations: toxicity and response: a Radiation Therapy Oncology Group Study. Int J Radiat Oncol Biol Phys. 1989;17(6):1223-1229.
11. Mohiuddin M, Chen E, Ahmad N. Combined liver radiation and chemotherapy for palliation of hepatic metastases from colorectal cancer. J Clin Oncol. 1996;14(3):722-728.
Cardiac pleomorphic sarcoma after placement of Dacron graft
Primary cardiac tumors, either benign or malignant, are very rare. The combined incidence is 0.002% on pooled autopsy series.1 The benign tumors account for 63% of primary cardiac tumors and include myxoma, the most common, and followed by papillary fibroelastoma, fibroma, and hemangioma. The remaining 37% are malignant tumors, essentially predominated by sarcomas.1
Although myxoma is the most common tumor arising in the left atrium, we present a case that shows that sarcoma can also arise from the same chamber. In fact, sarcomas could mimic cardiac myxoma.2 The cardiac sarcomas can have similar clinical presentation and more importantly can share similar histopathological features. Sarcomas may have myxoid features.2 Cases diagnosed as cardiac myxomas should be diligently worked up to rule out the presence of sarcomas with myxoid features. In addition, foreign bodies have been found to induce sarcomas in experimental animals.3,4 In particular, 2 case reports have described sarcomas arising in association with Dacron vascular prostheses in humans.5,6 We present here the case of a patient who was diagnosed with cardiac pleomorphic sarcoma 8 years after the placement of a Dacron graft.
Case presentation and summary
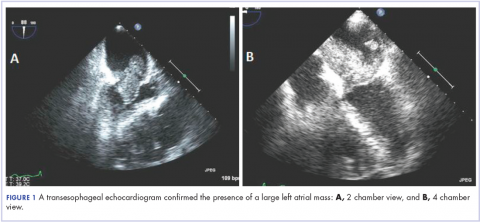
A 56-year-old woman with history of left atrial myxoma status after resection in 2005 and placement of a Dacron graft, morbid obesity, hypertension, and asthma presented to the emergency department with progressively worsening shortness of breath and blurry vision over period of 2 months. Acute coronary syndrome was ruled out by electrocardiogram and serial biomarkers. A computed-tomography angiogram was pursued because of her history of left atrial myxoma, and the results suggested the presence of a left atrial tumor. She underwent a transesophageal echocardiogram, which confirmed the presence of a large left atrial mass that likely was attached to the interatrial septum prolapsing across the mitral valve and was suggestive for recurrent left atrial myxoma (Figure 1). The results of a cardiac catheterization showed normal coronaries.
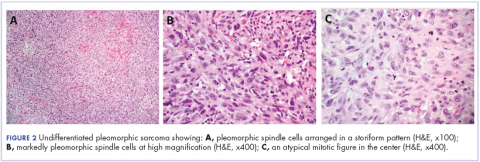
The patient subsequently underwent an excision of the left atrial tumor with profound internal and external myocardial cooling using antegrade blood cardioplegia under mildly hypothermic cardiopulmonary bypass. Frozen sections showed high-grade malignancy in favor of sarcoma. The hematoxylin and eosin stained permanent sections showed sheets of malignant pleomorphic spindle cells focally arranged in a storiform pattern. There were areas of necrosis and abundant mitotic activity. By immunohistochemical (IHC) stains, the tumor cells were diffusely positive for vimentin, and negative for pan-cytokeratin antibody (AE1/AE3), S-100 protein, Melan-A antibody, HMB45, CD34, CD31, myogenin, and MYOD1. IHC stains for CK-OSCAR, desmin, and smooth muscle actin were focally positive, and a ki-67 stain showed a proliferation index of about 80%. The histologic and IHC findings were consistent with a final diagnosis of high-grade undifferentiated pleomorphic sarcoma (Figure 2).
A positron emission tomography scan performed November 2013 did not show any other activity. The patient was scheduled for chemotherapy with adriamycin and ifosfamide with a plan for total of 6 cycles. Before her admission for the chemotherapy, the patient was admitted to the hospital for atrial fibrillation with rapid ventricular response and had multiple complications requiring prolonged hospitalization and rehabilitation. Repeat imaging 2 months later showed diffuse metastatic disease. However, her performance status had declined and she was not eligible for chemotherapy. She was placed under hospice care.
Discussion
This case demonstrates development of a cardiac pleomorphic sarcoma, a rare tumor, after placement of a Dacron graft. Given that foreign bodies have been found to induce sarcomas in experimental animals,3,4 and a few case reports have described sarcomas arising in association with Dacron vascular prostheses, 5-10 it seems that an exuberant host response around the foreign body might represent an important intermediate step in the development of the sarcoma.
There is no clearly defined pathogenesis that explains the link between a Dacron graft and sarcomas. In 1950s, Oppenheimer and colleagues described the formation of malignant tumors by various types of plastics, including Dacron, that were embedded in rats. 3,4 Most of the tumors were some form of sarcomas. It was inferred that physical properties of the plastics may have some role in tumor development. Plastics in sheet form or film that remained in situ for more than 6 months induced significant number of tumors compared with other forms such as sponges, films with holes, or powders.3,4 The 3-dimensional polymeric structure of the Dacron graft seems to play a role in induction of sarcoma as well. A pore diameter of less than 0.4 mm may increase tumorigenicity.11 The removal of the material before the 6-months mark does not lead to malignant tumors, which further supports the link between Dacron graft and formation of tumor. A pocket is formed around the foreign material after a certain period, as has been shown in histologic studies as the site of tumor origin.9,10
At the molecular level, the MDM-2/p53 pathway has been cited as possible mechanism for pathogenesis of intimal sarcoma.12,13 It has been suggested that endothelial dysplasia occurs as a precursor lesion in these sarcomas.14 The Dacron graft may cause a dysplastic effect on the endothelium leading to this precursor lesion and in certain cases transforming into sarcoma. Further definitive studies are required.
The primary treatment for cardiac sarcoma is surgical removal, although it is not always feasible. Findings in a Mayo clinic study showed that the median survival was 17 months for patients who underwent complete surgical excision, compared with 6 months for those who complete resection was not possible.15 In addition, a 10% survival rate at 1 year has been reported in primary cardiac sarcomas that are treated without any type of surgery.16
There is no clear-cut evidence supporting or refuting adjuvant chemotherapy for cardiac sarcoma. Some have inferred a potential benefit of adjuvant chemotherapy although definitive conclusions cannot be drawn. The median survival was 16.5 months in a case series of patients who received adjuvant chemotherapy, compared with 9 months and 11 months in 2 other case series.17,18,19 Multiple chemotherapy regimens have been used in the past for treatment. A retrospective s
Radiation showed some benefit in progression-free survival in a French retrospective study.21 Radiation therapies have been tried in other cases, as well in addition to chemotherapy. However, there is not enough data to support or refute it at this time.15,17,20 Several sporadic cases reported show benefit of cardiac transplantation.21,22
Conclusion
In consideration of the placement of the Dacron graft 8 years before the tumor occurrence, the anatomic proximity of the tumor to the Dacron graft, and the association between sarcoma with Dacron in medical literature, it seems logical to infer that this unusual malignancy in our patient is associated with the Dacron prosthesis.
1. Patil HR, Singh D, Hajdu M. Cardiac sarcoma presenting as heart failure and diagnosed as recurrent myxoma by echocardiogram. Eur J Echocardiogr. 2010;11(4):E12.
2. Awamleh P, Alberca MT, Gamallo C, Enrech S, Sarraj A. Left atrium myxosarcoma: an exceptional cardiac malignant primary tumor. Clin Cardiol. 2007;30(6):306-308.
3. Oppenheimer BS, Oppenheimer ET, Stout AP, Danishefsky I. Malignant tumors resulting from embedding plastics in rodents. Science. 1953;118:305-306.
4. Oppenheimer BS, Oppenheimer ET, Stout AP, Willhite M, Danishefski, I. The latent period in carcinogenesis by plastics in rats and its relation to the presarcomatous stage. Cancer. 1958;11(1):204-213.
5. Almeida NJ, Hoang P, Biddle P, Arouni A, Esterbrooks D. Primary cardiac angiosarcoma: in a patient with a Dacron aortic prosthesis. Tex Heart Inst J. 2011;38(1):61-65; discussion 65.
6. Stewart B, Manglik N, Zhao B, et al. Aortic intimal sarcoma: report of two cases with immunohistochemical analysis for pathogenesis. Cardiovasc Pathol. 2013;22(5):351-356.
7. Umscheid TW, Rouhani G, Morlang T, et al. Hemangiosarcoma after endovascular aortic aneurysm repair. J Endovasc Ther. 2007;14(1):101-105.
8. Ben-Izhak O, Vlodavsky E, Ofer A, Engel A, Nitecky S, Hoffman A. Epithelioid angiosarcoma associated with a Dacron vascular graft. Am J Surg Pathol. 1999;23(11):1418-1422.
9. Fyfe BS, Quintana CS, Kaneko M, Griepp RB. Aortic sarcoma four years after Dacron graft insertion. Ann Thorac Surg. 1994;58(6):1752-1754.
10. O’Connell TX, Fee HJ, Golding A. Sarcoma associated with Dacron prosthetic material: case report and review of the literature. J Thorac Cardiovasc Surg. 1976;72(1):94-96.
11. Karp RD, Johnson KH, Buoen LC, et al. Tumorogenesis by millipore filters in mice: histology and ultastructure of tissue reactions, as related to pore size. J Natl Cancer Inst. 1973;51:1275-1285.
12. Bode-Lesniewska B, Zhao J, Speel EJ, et al. Gains of 12q13-14 and overexpression of mdm2 are frequent findings in intimal sarcomas of the pulmonary artery. Virchows Arch. 2001;438:57-65.
13. Zeitz C, Rossle M, Haas C, et al. MDM-2 oncoprotein overexpression, p53 gene mutation, and VEGF up-regulation in angiosarcomas. Am J Surg Pathol. 1998;153:1425-1433.
14. Haber LM, Truong L. Immunohistochemical demonstration of the endothelialnature of aortic intimal sarcoma. Am J Surg Pathol. 1988 Oct;12(10):798-802. PubMed PMID: 3138923.
15. Simpson L, Kumar SK, Okuno SH, et al. Malignant primary cardiac tumors: review of a single institution experience. Cancer. 2008;112(11):2440-2446.
16. Leja MJ, Shah DJ, Reardon MJ. Primary cardiac tumors. Tex Heart Inst J. 2011;38(3):261-262.
17. Donsbeck AV, Ranchere D, Coindre JM, Le Gall F, Cordier JF, Loire R. Primary cardiac sarcomas: an immunohistochemical and grading study with long-term follow-up of 24 cases. Histopathology. 1999;34(4):295-304.
18. Putnam JB, Sweeney MS, Colon R, Lanza LA, Frazier OH, Cooley DC. Primary cardiac sarcomas. Ann Thorac Surg. 1990; 51; 906-910.
19. Murphy WR, Sweeney MS, Putnam JB et al. Surgical treatment of cardiac tumors: a 25-year experience. Ann Thorac Surg. 1990;49;612-618.
20. Llombart-Cussac A, Pivot X, Contesso G, et al. Adjuvant chemotherapy for primary cardiac sarcomas: the IGR experience. Br J Cancer. 1998;78(12):1624-1628.
21. Isambert N, Ray-Coquard I, Italiano A, et al. Primary cardiac sarcomas: a retrospective study of the French Sarcoma Group. Eur J Cancer. 2014;50(1):128-136.
22. Agaimy A, Rösch J, Weyand M, Strecker T. Primary and metastatic cardiac sarcomas: a 12-year experience at a German heart center. Int J Clin Exp Pathol. 2012;5(9):928-938.
Primary cardiac tumors, either benign or malignant, are very rare. The combined incidence is 0.002% on pooled autopsy series.1 The benign tumors account for 63% of primary cardiac tumors and include myxoma, the most common, and followed by papillary fibroelastoma, fibroma, and hemangioma. The remaining 37% are malignant tumors, essentially predominated by sarcomas.1
Although myxoma is the most common tumor arising in the left atrium, we present a case that shows that sarcoma can also arise from the same chamber. In fact, sarcomas could mimic cardiac myxoma.2 The cardiac sarcomas can have similar clinical presentation and more importantly can share similar histopathological features. Sarcomas may have myxoid features.2 Cases diagnosed as cardiac myxomas should be diligently worked up to rule out the presence of sarcomas with myxoid features. In addition, foreign bodies have been found to induce sarcomas in experimental animals.3,4 In particular, 2 case reports have described sarcomas arising in association with Dacron vascular prostheses in humans.5,6 We present here the case of a patient who was diagnosed with cardiac pleomorphic sarcoma 8 years after the placement of a Dacron graft.
Case presentation and summary
A 56-year-old woman with history of left atrial myxoma status after resection in 2005 and placement of a Dacron graft, morbid obesity, hypertension, and asthma presented to the emergency department with progressively worsening shortness of breath and blurry vision over period of 2 months. Acute coronary syndrome was ruled out by electrocardiogram and serial biomarkers. A computed-tomography angiogram was pursued because of her history of left atrial myxoma, and the results suggested the presence of a left atrial tumor. She underwent a transesophageal echocardiogram, which confirmed the presence of a large left atrial mass that likely was attached to the interatrial septum prolapsing across the mitral valve and was suggestive for recurrent left atrial myxoma (Figure 1). The results of a cardiac catheterization showed normal coronaries.
The patient subsequently underwent an excision of the left atrial tumor with profound internal and external myocardial cooling using antegrade blood cardioplegia under mildly hypothermic cardiopulmonary bypass. Frozen sections showed high-grade malignancy in favor of sarcoma. The hematoxylin and eosin stained permanent sections showed sheets of malignant pleomorphic spindle cells focally arranged in a storiform pattern. There were areas of necrosis and abundant mitotic activity. By immunohistochemical (IHC) stains, the tumor cells were diffusely positive for vimentin, and negative for pan-cytokeratin antibody (AE1/AE3), S-100 protein, Melan-A antibody, HMB45, CD34, CD31, myogenin, and MYOD1. IHC stains for CK-OSCAR, desmin, and smooth muscle actin were focally positive, and a ki-67 stain showed a proliferation index of about 80%. The histologic and IHC findings were consistent with a final diagnosis of high-grade undifferentiated pleomorphic sarcoma (Figure 2).
A positron emission tomography scan performed November 2013 did not show any other activity. The patient was scheduled for chemotherapy with adriamycin and ifosfamide with a plan for total of 6 cycles. Before her admission for the chemotherapy, the patient was admitted to the hospital for atrial fibrillation with rapid ventricular response and had multiple complications requiring prolonged hospitalization and rehabilitation. Repeat imaging 2 months later showed diffuse metastatic disease. However, her performance status had declined and she was not eligible for chemotherapy. She was placed under hospice care.
Discussion
This case demonstrates development of a cardiac pleomorphic sarcoma, a rare tumor, after placement of a Dacron graft. Given that foreign bodies have been found to induce sarcomas in experimental animals,3,4 and a few case reports have described sarcomas arising in association with Dacron vascular prostheses, 5-10 it seems that an exuberant host response around the foreign body might represent an important intermediate step in the development of the sarcoma.
There is no clearly defined pathogenesis that explains the link between a Dacron graft and sarcomas. In 1950s, Oppenheimer and colleagues described the formation of malignant tumors by various types of plastics, including Dacron, that were embedded in rats. 3,4 Most of the tumors were some form of sarcomas. It was inferred that physical properties of the plastics may have some role in tumor development. Plastics in sheet form or film that remained in situ for more than 6 months induced significant number of tumors compared with other forms such as sponges, films with holes, or powders.3,4 The 3-dimensional polymeric structure of the Dacron graft seems to play a role in induction of sarcoma as well. A pore diameter of less than 0.4 mm may increase tumorigenicity.11 The removal of the material before the 6-months mark does not lead to malignant tumors, which further supports the link between Dacron graft and formation of tumor. A pocket is formed around the foreign material after a certain period, as has been shown in histologic studies as the site of tumor origin.9,10
At the molecular level, the MDM-2/p53 pathway has been cited as possible mechanism for pathogenesis of intimal sarcoma.12,13 It has been suggested that endothelial dysplasia occurs as a precursor lesion in these sarcomas.14 The Dacron graft may cause a dysplastic effect on the endothelium leading to this precursor lesion and in certain cases transforming into sarcoma. Further definitive studies are required.
The primary treatment for cardiac sarcoma is surgical removal, although it is not always feasible. Findings in a Mayo clinic study showed that the median survival was 17 months for patients who underwent complete surgical excision, compared with 6 months for those who complete resection was not possible.15 In addition, a 10% survival rate at 1 year has been reported in primary cardiac sarcomas that are treated without any type of surgery.16
There is no clear-cut evidence supporting or refuting adjuvant chemotherapy for cardiac sarcoma. Some have inferred a potential benefit of adjuvant chemotherapy although definitive conclusions cannot be drawn. The median survival was 16.5 months in a case series of patients who received adjuvant chemotherapy, compared with 9 months and 11 months in 2 other case series.17,18,19 Multiple chemotherapy regimens have been used in the past for treatment. A retrospective s
Radiation showed some benefit in progression-free survival in a French retrospective study.21 Radiation therapies have been tried in other cases, as well in addition to chemotherapy. However, there is not enough data to support or refute it at this time.15,17,20 Several sporadic cases reported show benefit of cardiac transplantation.21,22
Conclusion
In consideration of the placement of the Dacron graft 8 years before the tumor occurrence, the anatomic proximity of the tumor to the Dacron graft, and the association between sarcoma with Dacron in medical literature, it seems logical to infer that this unusual malignancy in our patient is associated with the Dacron prosthesis.
Primary cardiac tumors, either benign or malignant, are very rare. The combined incidence is 0.002% on pooled autopsy series.1 The benign tumors account for 63% of primary cardiac tumors and include myxoma, the most common, and followed by papillary fibroelastoma, fibroma, and hemangioma. The remaining 37% are malignant tumors, essentially predominated by sarcomas.1
Although myxoma is the most common tumor arising in the left atrium, we present a case that shows that sarcoma can also arise from the same chamber. In fact, sarcomas could mimic cardiac myxoma.2 The cardiac sarcomas can have similar clinical presentation and more importantly can share similar histopathological features. Sarcomas may have myxoid features.2 Cases diagnosed as cardiac myxomas should be diligently worked up to rule out the presence of sarcomas with myxoid features. In addition, foreign bodies have been found to induce sarcomas in experimental animals.3,4 In particular, 2 case reports have described sarcomas arising in association with Dacron vascular prostheses in humans.5,6 We present here the case of a patient who was diagnosed with cardiac pleomorphic sarcoma 8 years after the placement of a Dacron graft.
Case presentation and summary
A 56-year-old woman with history of left atrial myxoma status after resection in 2005 and placement of a Dacron graft, morbid obesity, hypertension, and asthma presented to the emergency department with progressively worsening shortness of breath and blurry vision over period of 2 months. Acute coronary syndrome was ruled out by electrocardiogram and serial biomarkers. A computed-tomography angiogram was pursued because of her history of left atrial myxoma, and the results suggested the presence of a left atrial tumor. She underwent a transesophageal echocardiogram, which confirmed the presence of a large left atrial mass that likely was attached to the interatrial septum prolapsing across the mitral valve and was suggestive for recurrent left atrial myxoma (Figure 1). The results of a cardiac catheterization showed normal coronaries.
The patient subsequently underwent an excision of the left atrial tumor with profound internal and external myocardial cooling using antegrade blood cardioplegia under mildly hypothermic cardiopulmonary bypass. Frozen sections showed high-grade malignancy in favor of sarcoma. The hematoxylin and eosin stained permanent sections showed sheets of malignant pleomorphic spindle cells focally arranged in a storiform pattern. There were areas of necrosis and abundant mitotic activity. By immunohistochemical (IHC) stains, the tumor cells were diffusely positive for vimentin, and negative for pan-cytokeratin antibody (AE1/AE3), S-100 protein, Melan-A antibody, HMB45, CD34, CD31, myogenin, and MYOD1. IHC stains for CK-OSCAR, desmin, and smooth muscle actin were focally positive, and a ki-67 stain showed a proliferation index of about 80%. The histologic and IHC findings were consistent with a final diagnosis of high-grade undifferentiated pleomorphic sarcoma (Figure 2).
A positron emission tomography scan performed November 2013 did not show any other activity. The patient was scheduled for chemotherapy with adriamycin and ifosfamide with a plan for total of 6 cycles. Before her admission for the chemotherapy, the patient was admitted to the hospital for atrial fibrillation with rapid ventricular response and had multiple complications requiring prolonged hospitalization and rehabilitation. Repeat imaging 2 months later showed diffuse metastatic disease. However, her performance status had declined and she was not eligible for chemotherapy. She was placed under hospice care.
Discussion
This case demonstrates development of a cardiac pleomorphic sarcoma, a rare tumor, after placement of a Dacron graft. Given that foreign bodies have been found to induce sarcomas in experimental animals,3,4 and a few case reports have described sarcomas arising in association with Dacron vascular prostheses, 5-10 it seems that an exuberant host response around the foreign body might represent an important intermediate step in the development of the sarcoma.
There is no clearly defined pathogenesis that explains the link between a Dacron graft and sarcomas. In 1950s, Oppenheimer and colleagues described the formation of malignant tumors by various types of plastics, including Dacron, that were embedded in rats. 3,4 Most of the tumors were some form of sarcomas. It was inferred that physical properties of the plastics may have some role in tumor development. Plastics in sheet form or film that remained in situ for more than 6 months induced significant number of tumors compared with other forms such as sponges, films with holes, or powders.3,4 The 3-dimensional polymeric structure of the Dacron graft seems to play a role in induction of sarcoma as well. A pore diameter of less than 0.4 mm may increase tumorigenicity.11 The removal of the material before the 6-months mark does not lead to malignant tumors, which further supports the link between Dacron graft and formation of tumor. A pocket is formed around the foreign material after a certain period, as has been shown in histologic studies as the site of tumor origin.9,10
At the molecular level, the MDM-2/p53 pathway has been cited as possible mechanism for pathogenesis of intimal sarcoma.12,13 It has been suggested that endothelial dysplasia occurs as a precursor lesion in these sarcomas.14 The Dacron graft may cause a dysplastic effect on the endothelium leading to this precursor lesion and in certain cases transforming into sarcoma. Further definitive studies are required.
The primary treatment for cardiac sarcoma is surgical removal, although it is not always feasible. Findings in a Mayo clinic study showed that the median survival was 17 months for patients who underwent complete surgical excision, compared with 6 months for those who complete resection was not possible.15 In addition, a 10% survival rate at 1 year has been reported in primary cardiac sarcomas that are treated without any type of surgery.16
There is no clear-cut evidence supporting or refuting adjuvant chemotherapy for cardiac sarcoma. Some have inferred a potential benefit of adjuvant chemotherapy although definitive conclusions cannot be drawn. The median survival was 16.5 months in a case series of patients who received adjuvant chemotherapy, compared with 9 months and 11 months in 2 other case series.17,18,19 Multiple chemotherapy regimens have been used in the past for treatment. A retrospective s
Radiation showed some benefit in progression-free survival in a French retrospective study.21 Radiation therapies have been tried in other cases, as well in addition to chemotherapy. However, there is not enough data to support or refute it at this time.15,17,20 Several sporadic cases reported show benefit of cardiac transplantation.21,22
Conclusion
In consideration of the placement of the Dacron graft 8 years before the tumor occurrence, the anatomic proximity of the tumor to the Dacron graft, and the association between sarcoma with Dacron in medical literature, it seems logical to infer that this unusual malignancy in our patient is associated with the Dacron prosthesis.
1. Patil HR, Singh D, Hajdu M. Cardiac sarcoma presenting as heart failure and diagnosed as recurrent myxoma by echocardiogram. Eur J Echocardiogr. 2010;11(4):E12.
2. Awamleh P, Alberca MT, Gamallo C, Enrech S, Sarraj A. Left atrium myxosarcoma: an exceptional cardiac malignant primary tumor. Clin Cardiol. 2007;30(6):306-308.
3. Oppenheimer BS, Oppenheimer ET, Stout AP, Danishefsky I. Malignant tumors resulting from embedding plastics in rodents. Science. 1953;118:305-306.
4. Oppenheimer BS, Oppenheimer ET, Stout AP, Willhite M, Danishefski, I. The latent period in carcinogenesis by plastics in rats and its relation to the presarcomatous stage. Cancer. 1958;11(1):204-213.
5. Almeida NJ, Hoang P, Biddle P, Arouni A, Esterbrooks D. Primary cardiac angiosarcoma: in a patient with a Dacron aortic prosthesis. Tex Heart Inst J. 2011;38(1):61-65; discussion 65.
6. Stewart B, Manglik N, Zhao B, et al. Aortic intimal sarcoma: report of two cases with immunohistochemical analysis for pathogenesis. Cardiovasc Pathol. 2013;22(5):351-356.
7. Umscheid TW, Rouhani G, Morlang T, et al. Hemangiosarcoma after endovascular aortic aneurysm repair. J Endovasc Ther. 2007;14(1):101-105.
8. Ben-Izhak O, Vlodavsky E, Ofer A, Engel A, Nitecky S, Hoffman A. Epithelioid angiosarcoma associated with a Dacron vascular graft. Am J Surg Pathol. 1999;23(11):1418-1422.
9. Fyfe BS, Quintana CS, Kaneko M, Griepp RB. Aortic sarcoma four years after Dacron graft insertion. Ann Thorac Surg. 1994;58(6):1752-1754.
10. O’Connell TX, Fee HJ, Golding A. Sarcoma associated with Dacron prosthetic material: case report and review of the literature. J Thorac Cardiovasc Surg. 1976;72(1):94-96.
11. Karp RD, Johnson KH, Buoen LC, et al. Tumorogenesis by millipore filters in mice: histology and ultastructure of tissue reactions, as related to pore size. J Natl Cancer Inst. 1973;51:1275-1285.
12. Bode-Lesniewska B, Zhao J, Speel EJ, et al. Gains of 12q13-14 and overexpression of mdm2 are frequent findings in intimal sarcomas of the pulmonary artery. Virchows Arch. 2001;438:57-65.
13. Zeitz C, Rossle M, Haas C, et al. MDM-2 oncoprotein overexpression, p53 gene mutation, and VEGF up-regulation in angiosarcomas. Am J Surg Pathol. 1998;153:1425-1433.
14. Haber LM, Truong L. Immunohistochemical demonstration of the endothelialnature of aortic intimal sarcoma. Am J Surg Pathol. 1988 Oct;12(10):798-802. PubMed PMID: 3138923.
15. Simpson L, Kumar SK, Okuno SH, et al. Malignant primary cardiac tumors: review of a single institution experience. Cancer. 2008;112(11):2440-2446.
16. Leja MJ, Shah DJ, Reardon MJ. Primary cardiac tumors. Tex Heart Inst J. 2011;38(3):261-262.
17. Donsbeck AV, Ranchere D, Coindre JM, Le Gall F, Cordier JF, Loire R. Primary cardiac sarcomas: an immunohistochemical and grading study with long-term follow-up of 24 cases. Histopathology. 1999;34(4):295-304.
18. Putnam JB, Sweeney MS, Colon R, Lanza LA, Frazier OH, Cooley DC. Primary cardiac sarcomas. Ann Thorac Surg. 1990; 51; 906-910.
19. Murphy WR, Sweeney MS, Putnam JB et al. Surgical treatment of cardiac tumors: a 25-year experience. Ann Thorac Surg. 1990;49;612-618.
20. Llombart-Cussac A, Pivot X, Contesso G, et al. Adjuvant chemotherapy for primary cardiac sarcomas: the IGR experience. Br J Cancer. 1998;78(12):1624-1628.
21. Isambert N, Ray-Coquard I, Italiano A, et al. Primary cardiac sarcomas: a retrospective study of the French Sarcoma Group. Eur J Cancer. 2014;50(1):128-136.
22. Agaimy A, Rösch J, Weyand M, Strecker T. Primary and metastatic cardiac sarcomas: a 12-year experience at a German heart center. Int J Clin Exp Pathol. 2012;5(9):928-938.
1. Patil HR, Singh D, Hajdu M. Cardiac sarcoma presenting as heart failure and diagnosed as recurrent myxoma by echocardiogram. Eur J Echocardiogr. 2010;11(4):E12.
2. Awamleh P, Alberca MT, Gamallo C, Enrech S, Sarraj A. Left atrium myxosarcoma: an exceptional cardiac malignant primary tumor. Clin Cardiol. 2007;30(6):306-308.
3. Oppenheimer BS, Oppenheimer ET, Stout AP, Danishefsky I. Malignant tumors resulting from embedding plastics in rodents. Science. 1953;118:305-306.
4. Oppenheimer BS, Oppenheimer ET, Stout AP, Willhite M, Danishefski, I. The latent period in carcinogenesis by plastics in rats and its relation to the presarcomatous stage. Cancer. 1958;11(1):204-213.
5. Almeida NJ, Hoang P, Biddle P, Arouni A, Esterbrooks D. Primary cardiac angiosarcoma: in a patient with a Dacron aortic prosthesis. Tex Heart Inst J. 2011;38(1):61-65; discussion 65.
6. Stewart B, Manglik N, Zhao B, et al. Aortic intimal sarcoma: report of two cases with immunohistochemical analysis for pathogenesis. Cardiovasc Pathol. 2013;22(5):351-356.
7. Umscheid TW, Rouhani G, Morlang T, et al. Hemangiosarcoma after endovascular aortic aneurysm repair. J Endovasc Ther. 2007;14(1):101-105.
8. Ben-Izhak O, Vlodavsky E, Ofer A, Engel A, Nitecky S, Hoffman A. Epithelioid angiosarcoma associated with a Dacron vascular graft. Am J Surg Pathol. 1999;23(11):1418-1422.
9. Fyfe BS, Quintana CS, Kaneko M, Griepp RB. Aortic sarcoma four years after Dacron graft insertion. Ann Thorac Surg. 1994;58(6):1752-1754.
10. O’Connell TX, Fee HJ, Golding A. Sarcoma associated with Dacron prosthetic material: case report and review of the literature. J Thorac Cardiovasc Surg. 1976;72(1):94-96.
11. Karp RD, Johnson KH, Buoen LC, et al. Tumorogenesis by millipore filters in mice: histology and ultastructure of tissue reactions, as related to pore size. J Natl Cancer Inst. 1973;51:1275-1285.
12. Bode-Lesniewska B, Zhao J, Speel EJ, et al. Gains of 12q13-14 and overexpression of mdm2 are frequent findings in intimal sarcomas of the pulmonary artery. Virchows Arch. 2001;438:57-65.
13. Zeitz C, Rossle M, Haas C, et al. MDM-2 oncoprotein overexpression, p53 gene mutation, and VEGF up-regulation in angiosarcomas. Am J Surg Pathol. 1998;153:1425-1433.
14. Haber LM, Truong L. Immunohistochemical demonstration of the endothelialnature of aortic intimal sarcoma. Am J Surg Pathol. 1988 Oct;12(10):798-802. PubMed PMID: 3138923.
15. Simpson L, Kumar SK, Okuno SH, et al. Malignant primary cardiac tumors: review of a single institution experience. Cancer. 2008;112(11):2440-2446.
16. Leja MJ, Shah DJ, Reardon MJ. Primary cardiac tumors. Tex Heart Inst J. 2011;38(3):261-262.
17. Donsbeck AV, Ranchere D, Coindre JM, Le Gall F, Cordier JF, Loire R. Primary cardiac sarcomas: an immunohistochemical and grading study with long-term follow-up of 24 cases. Histopathology. 1999;34(4):295-304.
18. Putnam JB, Sweeney MS, Colon R, Lanza LA, Frazier OH, Cooley DC. Primary cardiac sarcomas. Ann Thorac Surg. 1990; 51; 906-910.
19. Murphy WR, Sweeney MS, Putnam JB et al. Surgical treatment of cardiac tumors: a 25-year experience. Ann Thorac Surg. 1990;49;612-618.
20. Llombart-Cussac A, Pivot X, Contesso G, et al. Adjuvant chemotherapy for primary cardiac sarcomas: the IGR experience. Br J Cancer. 1998;78(12):1624-1628.
21. Isambert N, Ray-Coquard I, Italiano A, et al. Primary cardiac sarcomas: a retrospective study of the French Sarcoma Group. Eur J Cancer. 2014;50(1):128-136.
22. Agaimy A, Rösch J, Weyand M, Strecker T. Primary and metastatic cardiac sarcomas: a 12-year experience at a German heart center. Int J Clin Exp Pathol. 2012;5(9):928-938.
Patient navigators’ personal experiences with cancer: does it have an impact on treatment?
Patient navigation has emerged in the past decade as a strategy to decrease cancer disparities among low-income, minority populations. Patient navigators help individuals who face personal and systemtic barriers to gaining access to care.1 Their role is to help patients find their way through a complex health care system,2,3 including logistic support of rescheduling appointments, assistance with transportation, and child care needs. They provide personal support, including coaching patients on their clinical visits, educating them about the cancer treatment process, and addressing their fears of diagnosis and treatment. Patient navigation has shown improvement in cancer screening rates, time to diagnostic resolution for those patients who have abnormal cancer screening tests, and quality of cancer care.4,5
In hiring patient navigators, it is not clear which professional training and skill sets and what personal experiences are most useful to becoming an effective navigator. Personal cancer experience can include a personal diagnosis, the experience of serving as a primary caregiver for a patient during treatment, or having a family member or close friend with cancer. Several current support programs specifically recruit cancer survivors on the assumption that their cancer treatment experience can provide helpful insights to a current patient for both emotional and logistical support.6 In this paper, we sought to address whether patient navigation promotes more timely diagnostic care if the navigator has experience with cancer.
Methods
This is a secondary analysis of the patients with abnormal cancer screening in the navigation arm of the national Patient Navigation Research Program (PNRP) study,1, 5 a collaborative effort across 10 centers to investigate the efficacy of patient navigation on improving patient-level outcomes for those who have abnormal results from a breast, cervical, colorectal, or prostate cancer screening test. The study demonstrated that patient navigation was effective in reducing delays in diagnosis and treatment5 and resulting in a higher quality of care,4 especially among vulnerable populations.7 The Institutional Review Board of each respective institution approved the research.
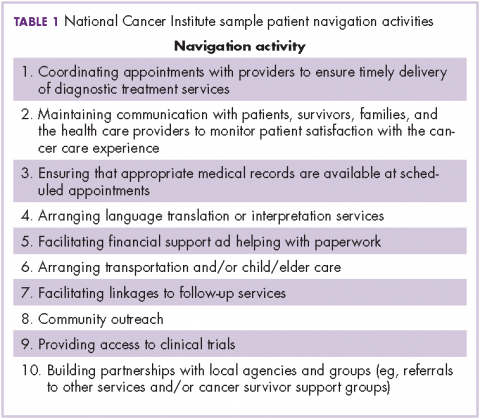
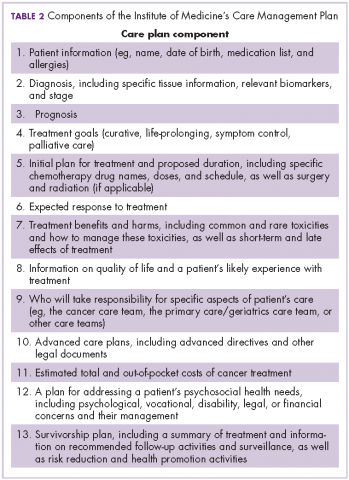
All of the patient navigators were paid employees with a minimum high-school diploma or equivalent. Navigators’ activities were standardized across centers through a national training program.8 Navigators used the care management model to identify and address barriers to care and to track participants throughout the course of their diagnostic evaluation,9 with the primary aim of timely diagnostic resolution. Most navigation programs were embedded within the clinical care system and interacted with patients through mail, by phone, and face-to-face contact.1
Data collection
Each center used agreed-upon inclusion and exclusion criteria and collected and coded the same patient-level data. Medical records were abstracted for pertinent clinical data on patients. Demographic data were collected through a patient survey or extracted from medical record registration. The central data coordinating center collected navigator information including demographic characteristics and experience with cancer.
We created a new variable, Personal experience with cancer. Personal experience with cancer was based on three questions asked of navigators: whether they were a cancer survivor; whether they were the primary caregiver to a family member or close friend with cancer; and whether they had a family member with cancer. Because of the small sample size, responses from navigators who were cancer survivors (n = 6) or primary caregivers to a family member with cancer (n = 4) were collapsed into a single category, referred to as personal experience with cancer, to compare with navigators who had no personal experience with cancer, which included those who reported a family member with cancer but who were not serving as a primary caregiver.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Each clinical center received approved from their institution’s human subjects review board. Informed consent was obtained from all patient navigator participants included in the study. Participating patients completed informed consent at some centers. At other centers where the study design was an implementation of a system intervention, a waiver of informed consent was approved by the Institutional Review Board.
Data analysis
The primary outcome variable was time to diagnostic resolution. We included only participants supported by a single navigator. A Fisher exact test by cancer type was used to compare the two groups (personal experience vs none) in the proportion of patients who achieved diagnostic resolution by 365 days. We reviewed the percentage of patients resolved for the total population as well as stratified by cancer site (breast, cervical, prostate, and colorectal), owing to the known mean differences in time to diagnostic resolution by type of cancer.
Cox proportional hazard models and adjusted hazard ratios were developed and calculated to examine the impact of navigator’s personal experience with cancer on time to resolution, controlling for patient gender, race, age, and cancer type in the models. The analysis controlled for the individual effect of navigators through clustering. We used P < .05 as the cut-off for significance, and used Stata 10.1 (StataCorp, College Station Texas 77845) for all analyses.
Results
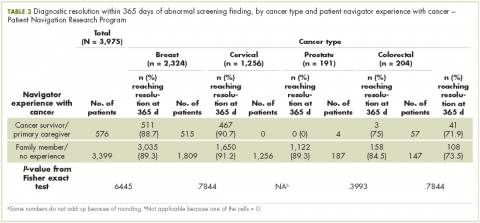
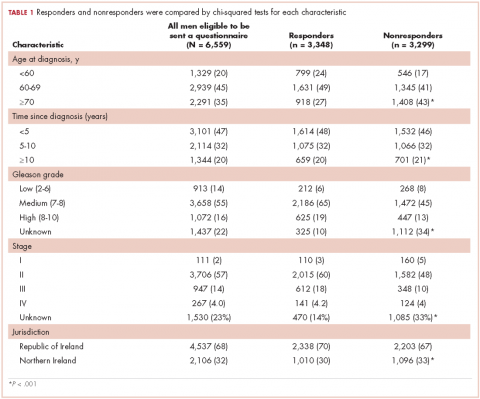
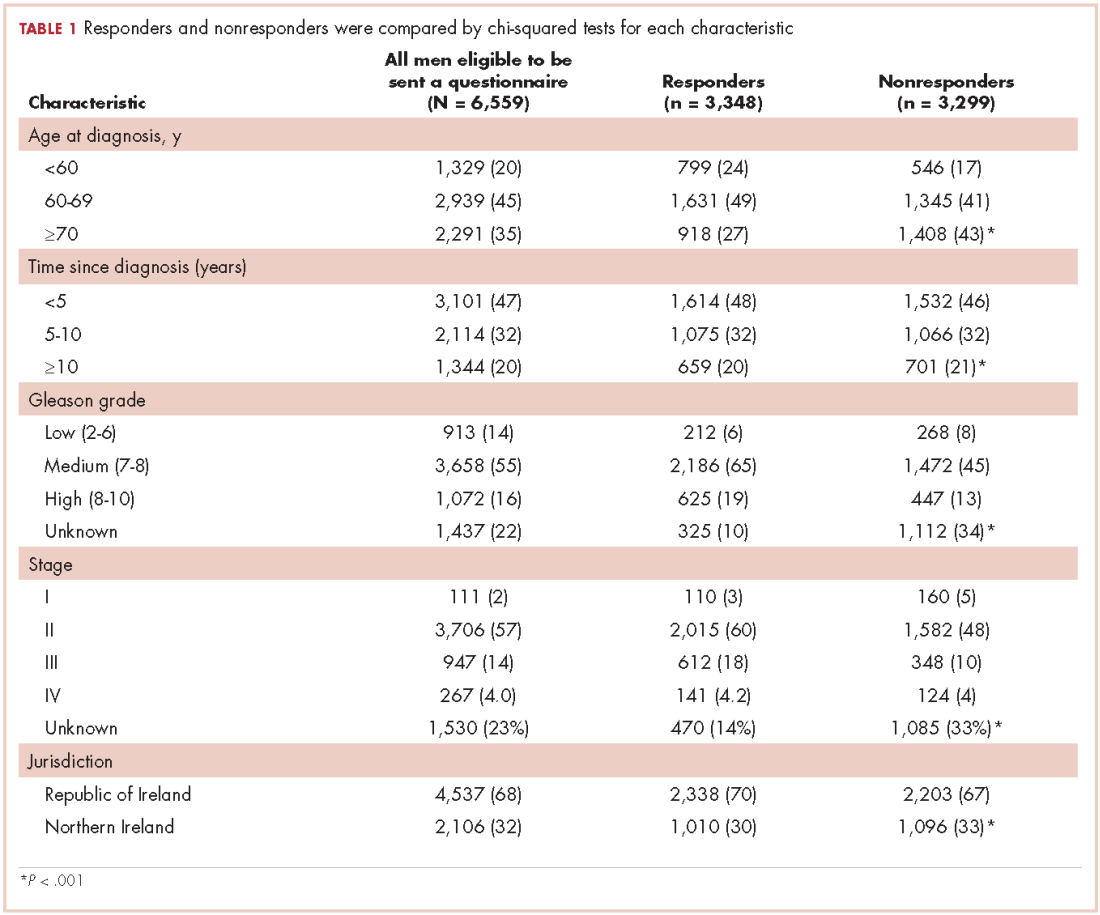
Our analytic sample included the 3,975 patients with only 1 navigator over the course of the study, 79% of the navigation (n = 5,063) arm. Most of the patients were women (93%), and most were from racial and ethnic minority communities. Most patients spoke English (60%), with Spanish (33%) as the next most common language. Most patients were publically insured (38%) or uninsured (40%) (Table 1).
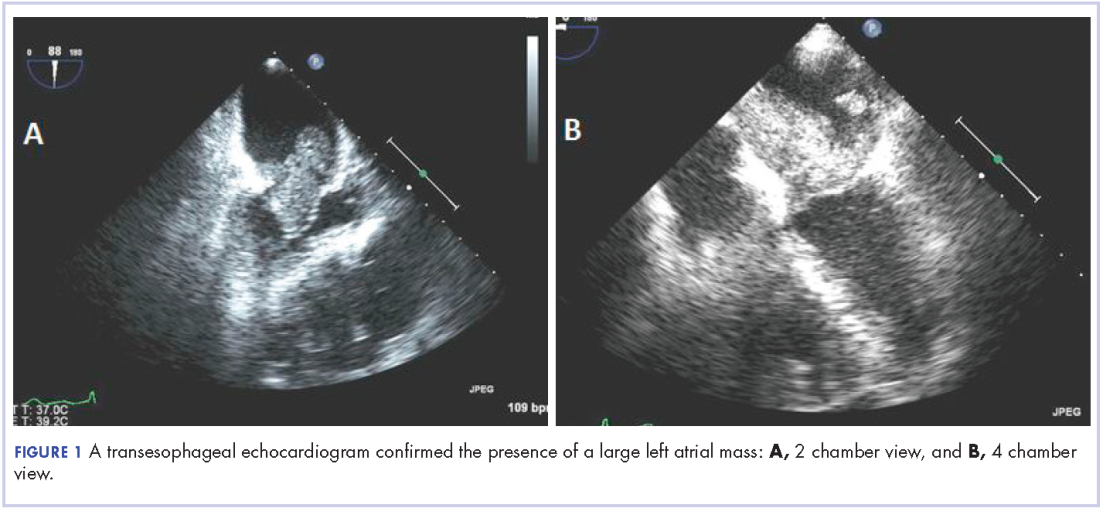
Of the total 49 navigators, 6 were cancer survivors and 4 were primary caregivers to a family member with cancer; an additional 19 reported that they had family members with cancer (Table 2). Most of the navigators were women. The racial/ethnic distribution mirrored the populations they served: white (29%); black or African American (31%); and Hispanic (37%). English was the only spoken language of 67% of the navigators; 27% spoke Spanish, and 6% reported speaking another language. Most had a college degree (63%).
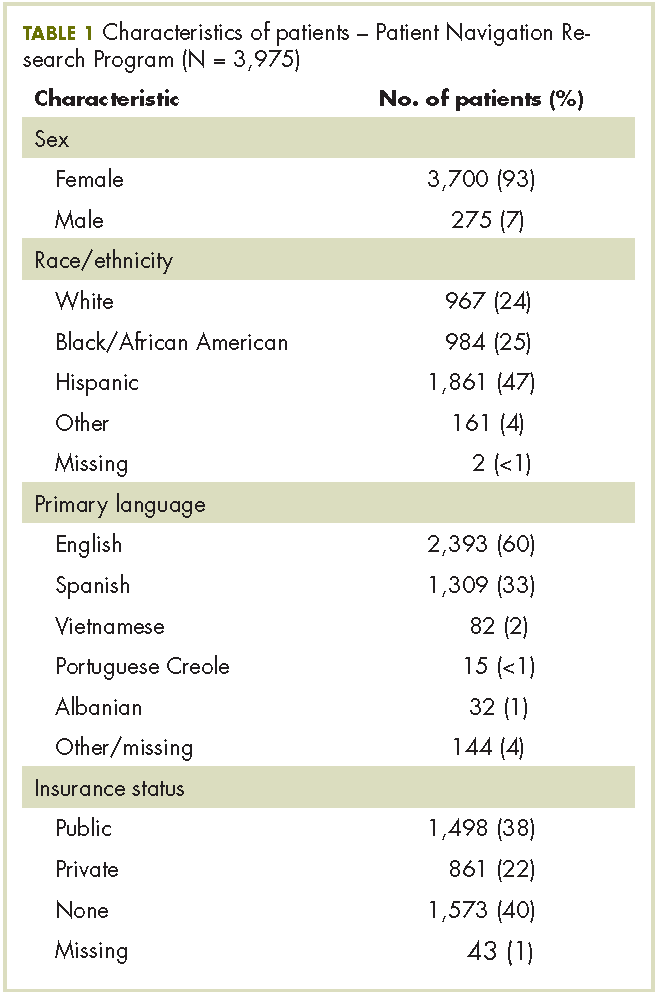
The unadjusted bivariate comparison of patients who achieved diagnostic resolution within 365 days, by navigator experience with cancer, are shown in Table 3. We found no difference in time to diagnostic resolution for those patients for whom navigators had personal experience with cancer compared with those whose navigators had no experience. When stratified by type of cancer screening abnormality (breast, cervical, prostate, or colorectal), the results also did not reveal a significant difference in the proportion of patients achieving diagnostic resolution by 365 days by navigator experience with cancer.
In the Cox proportional hazard model adjusting for patient gender, age, race/ethnicity, cancer type, and adjusting for navigator using clustering, there was no difference between patients whose navigators had experience with cancer care, and those who did not (adjusted hazard ratio, 1.03; 95% confidence interval, .83-1.3). The level of education of navigators was not significantly associated with time to diagnostic resolution for patients.
Discussion
Although several cancer support programs have explicitly used cancer survivors as patient navigators or other supports for patients in active cancer care, there are scant data on whether this expertise improves care. Our study was not able to identify that navigators with previous experience with cancer care, either as a patient or as the primary caregiver, was associated with improved time to diagnostic resolution.
As patient navigation has become the standard of cancer diagnostic and treatment practices, there is a need to develop competencies and standards for hiring and training navigators. Part of this hiring process is to determine what past experience and training are relevant for effective navigation. There is little previous research on relevant skills of navigators, with only one study having demonstrated that language and racial/ ethnic concordance between patients and navigators was associated with more timely care. The national PNRP program hired mostly lay navigators with minimal medical experience, but with affiliations to the communities of the patients receiving care. Our program has demonstrated that lay individuals can be trained in the logistic aspects of navigation.5 Although it may seem intuitive that the experience of being a cancer survivor may make a navigator more empathetic, it is also possible that being too close to the experience of survivorship can also pose challenges to a navigator. Alternatively, navigation may be equally effective with proper training regardless of previous experience with cancer.
Our study is limited to addressing the outcome of timely resolution in the diagnostic phase of care after abnormal cancer screening. It is possible that past experience with cancer care will be beneficial when providing navigation for cancer care. While this study represents one of the largest groups of navigators who have been studied, the small sample may have limited our ability to detect differences. Our study has the benefit of a diverse group of navigators from a nationally representative, multi-site study. We suggest that prior experience with cancer care is not a prerequisite to supporting diagnostic care after abnormal cancer screening. Providing appropriate training to navigators may be sufficient to ensure effective and appropriate care is provided by patient navigators.
Acknowledgments
The authors acknowledge the contributions of the following members of the Patient Navigation Research Program:Clinical centers Boston Medical Center and Boston University: Karen M Freund (principal investigator [PI]), Tracy A Battaglia (co-PI); Denver Health and Hospital Authority: Peter Raich (PI), Elizabeth Whitley (co-PI); George Washington University Cancer Institute: Steven R Patierno (PI), Lisa M Alexander, Paul H Levine, Heather A Young, Heather J Hoffman, Nancy L LaVerda; H Lee Moffitt Cancer Center and Research Institute: Richard G Roetzheim (PI), Cathy Meade, Kristen J Wells; Northwest Portland Area Indian Health Board: Victoria Warren-Mears (PI); Northwestern University Robert H Lurie Comprehensive Cancer Center: Steven Rosen (PI), Melissa Simon; The Ohio State University Comprehensive Cancer Center: Electra Paskett (PI); University of Illinois at Chicago and Access Community Health Center: Elizabeth Calhoun (PI), Julie Darnell. University of Rochester: Kevin Fiscella (PI), Samantha Hendren; University of Texas Health Science Center at San Antonio Cancer Therapy and Research Center: Donald Dudley (PI), Kevin Hall, Anand Karnard, Amelie Ramirez. Program office National Cancer Institute, Center to Reduce Cancer Health Disparities: Martha Hare, Mollie Howerton, Ken Chu, Emmanuel Taylor, Mary Ann Van Dyun. Evaluation contractor NOVA Research Company: Paul Young, Frederick Snyder
6. Macvean ML, White VM, Sanson-Fisher R. One-to-one volunteer support programs for people with cancer: a review of the literature. Patient Educ Couns. 2008;70:10-24.
7. Rodday AM, Parsons SK, Snyder F, et al. The impact of patient navigation in eliminating economic disparities in cancer care. Cancer. 2015;121(22):4025-4034.
10. Charlot M, Santana MC, Chen CA, et al. Impact of patient and navigator race and language concordance on care after cancer screening abnormalities. Cancer. 2015;121(9):1477-1483.
Patient navigation has emerged in the past decade as a strategy to decrease cancer disparities among low-income, minority populations. Patient navigators help individuals who face personal and systemtic barriers to gaining access to care.1 Their role is to help patients find their way through a complex health care system,2,3 including logistic support of rescheduling appointments, assistance with transportation, and child care needs. They provide personal support, including coaching patients on their clinical visits, educating them about the cancer treatment process, and addressing their fears of diagnosis and treatment. Patient navigation has shown improvement in cancer screening rates, time to diagnostic resolution for those patients who have abnormal cancer screening tests, and quality of cancer care.4,5
In hiring patient navigators, it is not clear which professional training and skill sets and what personal experiences are most useful to becoming an effective navigator. Personal cancer experience can include a personal diagnosis, the experience of serving as a primary caregiver for a patient during treatment, or having a family member or close friend with cancer. Several current support programs specifically recruit cancer survivors on the assumption that their cancer treatment experience can provide helpful insights to a current patient for both emotional and logistical support.6 In this paper, we sought to address whether patient navigation promotes more timely diagnostic care if the navigator has experience with cancer.
Methods
This is a secondary analysis of the patients with abnormal cancer screening in the navigation arm of the national Patient Navigation Research Program (PNRP) study,1, 5 a collaborative effort across 10 centers to investigate the efficacy of patient navigation on improving patient-level outcomes for those who have abnormal results from a breast, cervical, colorectal, or prostate cancer screening test. The study demonstrated that patient navigation was effective in reducing delays in diagnosis and treatment5 and resulting in a higher quality of care,4 especially among vulnerable populations.7 The Institutional Review Board of each respective institution approved the research.
All of the patient navigators were paid employees with a minimum high-school diploma or equivalent. Navigators’ activities were standardized across centers through a national training program.8 Navigators used the care management model to identify and address barriers to care and to track participants throughout the course of their diagnostic evaluation,9 with the primary aim of timely diagnostic resolution. Most navigation programs were embedded within the clinical care system and interacted with patients through mail, by phone, and face-to-face contact.1
Data collection
Each center used agreed-upon inclusion and exclusion criteria and collected and coded the same patient-level data. Medical records were abstracted for pertinent clinical data on patients. Demographic data were collected through a patient survey or extracted from medical record registration. The central data coordinating center collected navigator information including demographic characteristics and experience with cancer.
We created a new variable, Personal experience with cancer. Personal experience with cancer was based on three questions asked of navigators: whether they were a cancer survivor; whether they were the primary caregiver to a family member or close friend with cancer; and whether they had a family member with cancer. Because of the small sample size, responses from navigators who were cancer survivors (n = 6) or primary caregivers to a family member with cancer (n = 4) were collapsed into a single category, referred to as personal experience with cancer, to compare with navigators who had no personal experience with cancer, which included those who reported a family member with cancer but who were not serving as a primary caregiver.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Each clinical center received approved from their institution’s human subjects review board. Informed consent was obtained from all patient navigator participants included in the study. Participating patients completed informed consent at some centers. At other centers where the study design was an implementation of a system intervention, a waiver of informed consent was approved by the Institutional Review Board.
Data analysis
The primary outcome variable was time to diagnostic resolution. We included only participants supported by a single navigator. A Fisher exact test by cancer type was used to compare the two groups (personal experience vs none) in the proportion of patients who achieved diagnostic resolution by 365 days. We reviewed the percentage of patients resolved for the total population as well as stratified by cancer site (breast, cervical, prostate, and colorectal), owing to the known mean differences in time to diagnostic resolution by type of cancer.
Cox proportional hazard models and adjusted hazard ratios were developed and calculated to examine the impact of navigator’s personal experience with cancer on time to resolution, controlling for patient gender, race, age, and cancer type in the models. The analysis controlled for the individual effect of navigators through clustering. We used P < .05 as the cut-off for significance, and used Stata 10.1 (StataCorp, College Station Texas 77845) for all analyses.
Results
Our analytic sample included the 3,975 patients with only 1 navigator over the course of the study, 79% of the navigation (n = 5,063) arm. Most of the patients were women (93%), and most were from racial and ethnic minority communities. Most patients spoke English (60%), with Spanish (33%) as the next most common language. Most patients were publically insured (38%) or uninsured (40%) (Table 1).
Of the total 49 navigators, 6 were cancer survivors and 4 were primary caregivers to a family member with cancer; an additional 19 reported that they had family members with cancer (Table 2). Most of the navigators were women. The racial/ethnic distribution mirrored the populations they served: white (29%); black or African American (31%); and Hispanic (37%). English was the only spoken language of 67% of the navigators; 27% spoke Spanish, and 6% reported speaking another language. Most had a college degree (63%).
The unadjusted bivariate comparison of patients who achieved diagnostic resolution within 365 days, by navigator experience with cancer, are shown in Table 3. We found no difference in time to diagnostic resolution for those patients for whom navigators had personal experience with cancer compared with those whose navigators had no experience. When stratified by type of cancer screening abnormality (breast, cervical, prostate, or colorectal), the results also did not reveal a significant difference in the proportion of patients achieving diagnostic resolution by 365 days by navigator experience with cancer.
In the Cox proportional hazard model adjusting for patient gender, age, race/ethnicity, cancer type, and adjusting for navigator using clustering, there was no difference between patients whose navigators had experience with cancer care, and those who did not (adjusted hazard ratio, 1.03; 95% confidence interval, .83-1.3). The level of education of navigators was not significantly associated with time to diagnostic resolution for patients.
Discussion
Although several cancer support programs have explicitly used cancer survivors as patient navigators or other supports for patients in active cancer care, there are scant data on whether this expertise improves care. Our study was not able to identify that navigators with previous experience with cancer care, either as a patient or as the primary caregiver, was associated with improved time to diagnostic resolution.
As patient navigation has become the standard of cancer diagnostic and treatment practices, there is a need to develop competencies and standards for hiring and training navigators. Part of this hiring process is to determine what past experience and training are relevant for effective navigation. There is little previous research on relevant skills of navigators, with only one study having demonstrated that language and racial/ ethnic concordance between patients and navigators was associated with more timely care. The national PNRP program hired mostly lay navigators with minimal medical experience, but with affiliations to the communities of the patients receiving care. Our program has demonstrated that lay individuals can be trained in the logistic aspects of navigation.5 Although it may seem intuitive that the experience of being a cancer survivor may make a navigator more empathetic, it is also possible that being too close to the experience of survivorship can also pose challenges to a navigator. Alternatively, navigation may be equally effective with proper training regardless of previous experience with cancer.
Our study is limited to addressing the outcome of timely resolution in the diagnostic phase of care after abnormal cancer screening. It is possible that past experience with cancer care will be beneficial when providing navigation for cancer care. While this study represents one of the largest groups of navigators who have been studied, the small sample may have limited our ability to detect differences. Our study has the benefit of a diverse group of navigators from a nationally representative, multi-site study. We suggest that prior experience with cancer care is not a prerequisite to supporting diagnostic care after abnormal cancer screening. Providing appropriate training to navigators may be sufficient to ensure effective and appropriate care is provided by patient navigators.
Acknowledgments
The authors acknowledge the contributions of the following members of the Patient Navigation Research Program:Clinical centers Boston Medical Center and Boston University: Karen M Freund (principal investigator [PI]), Tracy A Battaglia (co-PI); Denver Health and Hospital Authority: Peter Raich (PI), Elizabeth Whitley (co-PI); George Washington University Cancer Institute: Steven R Patierno (PI), Lisa M Alexander, Paul H Levine, Heather A Young, Heather J Hoffman, Nancy L LaVerda; H Lee Moffitt Cancer Center and Research Institute: Richard G Roetzheim (PI), Cathy Meade, Kristen J Wells; Northwest Portland Area Indian Health Board: Victoria Warren-Mears (PI); Northwestern University Robert H Lurie Comprehensive Cancer Center: Steven Rosen (PI), Melissa Simon; The Ohio State University Comprehensive Cancer Center: Electra Paskett (PI); University of Illinois at Chicago and Access Community Health Center: Elizabeth Calhoun (PI), Julie Darnell. University of Rochester: Kevin Fiscella (PI), Samantha Hendren; University of Texas Health Science Center at San Antonio Cancer Therapy and Research Center: Donald Dudley (PI), Kevin Hall, Anand Karnard, Amelie Ramirez. Program office National Cancer Institute, Center to Reduce Cancer Health Disparities: Martha Hare, Mollie Howerton, Ken Chu, Emmanuel Taylor, Mary Ann Van Dyun. Evaluation contractor NOVA Research Company: Paul Young, Frederick Snyder
Patient navigation has emerged in the past decade as a strategy to decrease cancer disparities among low-income, minority populations. Patient navigators help individuals who face personal and systemtic barriers to gaining access to care.1 Their role is to help patients find their way through a complex health care system,2,3 including logistic support of rescheduling appointments, assistance with transportation, and child care needs. They provide personal support, including coaching patients on their clinical visits, educating them about the cancer treatment process, and addressing their fears of diagnosis and treatment. Patient navigation has shown improvement in cancer screening rates, time to diagnostic resolution for those patients who have abnormal cancer screening tests, and quality of cancer care.4,5
In hiring patient navigators, it is not clear which professional training and skill sets and what personal experiences are most useful to becoming an effective navigator. Personal cancer experience can include a personal diagnosis, the experience of serving as a primary caregiver for a patient during treatment, or having a family member or close friend with cancer. Several current support programs specifically recruit cancer survivors on the assumption that their cancer treatment experience can provide helpful insights to a current patient for both emotional and logistical support.6 In this paper, we sought to address whether patient navigation promotes more timely diagnostic care if the navigator has experience with cancer.
Methods
This is a secondary analysis of the patients with abnormal cancer screening in the navigation arm of the national Patient Navigation Research Program (PNRP) study,1, 5 a collaborative effort across 10 centers to investigate the efficacy of patient navigation on improving patient-level outcomes for those who have abnormal results from a breast, cervical, colorectal, or prostate cancer screening test. The study demonstrated that patient navigation was effective in reducing delays in diagnosis and treatment5 and resulting in a higher quality of care,4 especially among vulnerable populations.7 The Institutional Review Board of each respective institution approved the research.
All of the patient navigators were paid employees with a minimum high-school diploma or equivalent. Navigators’ activities were standardized across centers through a national training program.8 Navigators used the care management model to identify and address barriers to care and to track participants throughout the course of their diagnostic evaluation,9 with the primary aim of timely diagnostic resolution. Most navigation programs were embedded within the clinical care system and interacted with patients through mail, by phone, and face-to-face contact.1
Data collection
Each center used agreed-upon inclusion and exclusion criteria and collected and coded the same patient-level data. Medical records were abstracted for pertinent clinical data on patients. Demographic data were collected through a patient survey or extracted from medical record registration. The central data coordinating center collected navigator information including demographic characteristics and experience with cancer.
We created a new variable, Personal experience with cancer. Personal experience with cancer was based on three questions asked of navigators: whether they were a cancer survivor; whether they were the primary caregiver to a family member or close friend with cancer; and whether they had a family member with cancer. Because of the small sample size, responses from navigators who were cancer survivors (n = 6) or primary caregivers to a family member with cancer (n = 4) were collapsed into a single category, referred to as personal experience with cancer, to compare with navigators who had no personal experience with cancer, which included those who reported a family member with cancer but who were not serving as a primary caregiver.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Each clinical center received approved from their institution’s human subjects review board. Informed consent was obtained from all patient navigator participants included in the study. Participating patients completed informed consent at some centers. At other centers where the study design was an implementation of a system intervention, a waiver of informed consent was approved by the Institutional Review Board.
Data analysis
The primary outcome variable was time to diagnostic resolution. We included only participants supported by a single navigator. A Fisher exact test by cancer type was used to compare the two groups (personal experience vs none) in the proportion of patients who achieved diagnostic resolution by 365 days. We reviewed the percentage of patients resolved for the total population as well as stratified by cancer site (breast, cervical, prostate, and colorectal), owing to the known mean differences in time to diagnostic resolution by type of cancer.
Cox proportional hazard models and adjusted hazard ratios were developed and calculated to examine the impact of navigator’s personal experience with cancer on time to resolution, controlling for patient gender, race, age, and cancer type in the models. The analysis controlled for the individual effect of navigators through clustering. We used P < .05 as the cut-off for significance, and used Stata 10.1 (StataCorp, College Station Texas 77845) for all analyses.
Results
Our analytic sample included the 3,975 patients with only 1 navigator over the course of the study, 79% of the navigation (n = 5,063) arm. Most of the patients were women (93%), and most were from racial and ethnic minority communities. Most patients spoke English (60%), with Spanish (33%) as the next most common language. Most patients were publically insured (38%) or uninsured (40%) (Table 1).
Of the total 49 navigators, 6 were cancer survivors and 4 were primary caregivers to a family member with cancer; an additional 19 reported that they had family members with cancer (Table 2). Most of the navigators were women. The racial/ethnic distribution mirrored the populations they served: white (29%); black or African American (31%); and Hispanic (37%). English was the only spoken language of 67% of the navigators; 27% spoke Spanish, and 6% reported speaking another language. Most had a college degree (63%).
The unadjusted bivariate comparison of patients who achieved diagnostic resolution within 365 days, by navigator experience with cancer, are shown in Table 3. We found no difference in time to diagnostic resolution for those patients for whom navigators had personal experience with cancer compared with those whose navigators had no experience. When stratified by type of cancer screening abnormality (breast, cervical, prostate, or colorectal), the results also did not reveal a significant difference in the proportion of patients achieving diagnostic resolution by 365 days by navigator experience with cancer.
In the Cox proportional hazard model adjusting for patient gender, age, race/ethnicity, cancer type, and adjusting for navigator using clustering, there was no difference between patients whose navigators had experience with cancer care, and those who did not (adjusted hazard ratio, 1.03; 95% confidence interval, .83-1.3). The level of education of navigators was not significantly associated with time to diagnostic resolution for patients.
Discussion
Although several cancer support programs have explicitly used cancer survivors as patient navigators or other supports for patients in active cancer care, there are scant data on whether this expertise improves care. Our study was not able to identify that navigators with previous experience with cancer care, either as a patient or as the primary caregiver, was associated with improved time to diagnostic resolution.
As patient navigation has become the standard of cancer diagnostic and treatment practices, there is a need to develop competencies and standards for hiring and training navigators. Part of this hiring process is to determine what past experience and training are relevant for effective navigation. There is little previous research on relevant skills of navigators, with only one study having demonstrated that language and racial/ ethnic concordance between patients and navigators was associated with more timely care. The national PNRP program hired mostly lay navigators with minimal medical experience, but with affiliations to the communities of the patients receiving care. Our program has demonstrated that lay individuals can be trained in the logistic aspects of navigation.5 Although it may seem intuitive that the experience of being a cancer survivor may make a navigator more empathetic, it is also possible that being too close to the experience of survivorship can also pose challenges to a navigator. Alternatively, navigation may be equally effective with proper training regardless of previous experience with cancer.
Our study is limited to addressing the outcome of timely resolution in the diagnostic phase of care after abnormal cancer screening. It is possible that past experience with cancer care will be beneficial when providing navigation for cancer care. While this study represents one of the largest groups of navigators who have been studied, the small sample may have limited our ability to detect differences. Our study has the benefit of a diverse group of navigators from a nationally representative, multi-site study. We suggest that prior experience with cancer care is not a prerequisite to supporting diagnostic care after abnormal cancer screening. Providing appropriate training to navigators may be sufficient to ensure effective and appropriate care is provided by patient navigators.
Acknowledgments
The authors acknowledge the contributions of the following members of the Patient Navigation Research Program:Clinical centers Boston Medical Center and Boston University: Karen M Freund (principal investigator [PI]), Tracy A Battaglia (co-PI); Denver Health and Hospital Authority: Peter Raich (PI), Elizabeth Whitley (co-PI); George Washington University Cancer Institute: Steven R Patierno (PI), Lisa M Alexander, Paul H Levine, Heather A Young, Heather J Hoffman, Nancy L LaVerda; H Lee Moffitt Cancer Center and Research Institute: Richard G Roetzheim (PI), Cathy Meade, Kristen J Wells; Northwest Portland Area Indian Health Board: Victoria Warren-Mears (PI); Northwestern University Robert H Lurie Comprehensive Cancer Center: Steven Rosen (PI), Melissa Simon; The Ohio State University Comprehensive Cancer Center: Electra Paskett (PI); University of Illinois at Chicago and Access Community Health Center: Elizabeth Calhoun (PI), Julie Darnell. University of Rochester: Kevin Fiscella (PI), Samantha Hendren; University of Texas Health Science Center at San Antonio Cancer Therapy and Research Center: Donald Dudley (PI), Kevin Hall, Anand Karnard, Amelie Ramirez. Program office National Cancer Institute, Center to Reduce Cancer Health Disparities: Martha Hare, Mollie Howerton, Ken Chu, Emmanuel Taylor, Mary Ann Van Dyun. Evaluation contractor NOVA Research Company: Paul Young, Frederick Snyder
6. Macvean ML, White VM, Sanson-Fisher R. One-to-one volunteer support programs for people with cancer: a review of the literature. Patient Educ Couns. 2008;70:10-24.
7. Rodday AM, Parsons SK, Snyder F, et al. The impact of patient navigation in eliminating economic disparities in cancer care. Cancer. 2015;121(22):4025-4034.
10. Charlot M, Santana MC, Chen CA, et al. Impact of patient and navigator race and language concordance on care after cancer screening abnormalities. Cancer. 2015;121(9):1477-1483.
6. Macvean ML, White VM, Sanson-Fisher R. One-to-one volunteer support programs for people with cancer: a review of the literature. Patient Educ Couns. 2008;70:10-24.
7. Rodday AM, Parsons SK, Snyder F, et al. The impact of patient navigation in eliminating economic disparities in cancer care. Cancer. 2015;121(22):4025-4034.
10. Charlot M, Santana MC, Chen CA, et al. Impact of patient and navigator race and language concordance on care after cancer screening abnormalities. Cancer. 2015;121(9):1477-1483.
From angst to analytics: lessons learned from an oncology care model internal pilot
In March 2016, 13 practices affiliated with the US Oncology Network (USON) were invited to participate in the Oncology Care Model (OCM) proposed by the Center for Medicare and Medicaid Services (CMS) and Center for Medicare and Medicaid Innovation (CMMI). The OCM, a novel value-based care model, was designed to provide higher-quality and better-coordinated oncology care at a lower cost to CMS.1 Of the 13 practices, 12 agreed to participate with a start date for the program of July 1, 2016. At least 40% of the practices’ patients were insured by Medicare, and any eligible patients with active cancer were offered an opportunity to enter the program. USON practices treat more than 25,000 patients with a qualifying episode per year and the overall OCM program sees more than 150,000 beneficiaries per year,2 so we anticipated that the OCM would have a substantial impact on each of the 12 practices on USON.
Faced with the scenario of having only 3 months between notification of approval and launch of the OCM, it was imperative that all the practices be proactive in planning and preparing to launch the OCM. With this goal in mind, representatives from all OCM candidate practices convened to anticipate the needs of the OCM and chart out a program to meet those needs. In this article, we discuss the requirements and scope of the OCM, the development of an internal pilot project, the anticipated gains from the pilot, and the results and findings from the pilot, both expected and unexpected.
The road to the Oncology Care Model
The government and oncology practices have been on separate trajectories to the OCM. In the last 15 years, the major intersections of these trajectories had to do with price and not patient outcomes. In 2003, the Medicare Prescription Drug Improvement and Modernization Act (MMA) focused on drug price reductions from an average wholesale price–based schedule to an average sales price–based schedule.3 There was the sequester in 2013,4 and more recently a proposal to restructure the payment for Part B drugs. In the background, recurrent negotiations to fix the calculation for the sustainable growth rate allowed for periodic draconian cuts to the prices of services. The cumulative effect of these price reductions has been to put economic pressure on community oncologists such that many have moved to a hospital environment.5
This contentious relationship with community oncology began to change with the passage of the Affordable Care Act (ACA) in 2010.6 Section 3022 of the ACA established the Medicare Shared Savings Program (MSSP) with the charge to create a new type of health care entity that was responsible for achieving the triple aim of improving population health, improving individual patient care, and bending the cost curve.7 Additional programs, such as the Pioneer Accountable Care Organization (ACO) program and the Comprehensive Primary Care Initiative were established to test alternative payment models.8-10
The ACA also funded the CMMI with a mandate to “test innovative payment and service delivery models” to achieve the triple aim; US$10 billion were appropriated for the years 2011-2019 for this purpose. The CMMI funded a pilot project for cancer care, the COME HOME [Community Oncology MEdical HOME] initiative, to test whether some aspects of care could be transformed or augmented to reduce overall costs or at least reduce the rate of increase. Findings from COME HOME have helped inform the OCM program.11
Over the same period, practices belonging to the USON were paving a path toward value. An electronic health record (EHR) for the entire network was adopted in 2005. A pathways program in which chemotherapy regimens were assessed on cost as well as benefits and toxicity, was started in 2006. Higher-cost regimens with no additional benefits comparable with other evidence-based regimens were deselected for initial treatment choices at the time of initial decision support. This process was streamlined using web-based technology that improved pathways compliance and tracking of off-pathways exceptions.12 Retrospective studies indicated that pathways had the potential to bend the cost curve by reducing drug spending.13,14 USON and its practices also tested a nurse call system (Innovent Oncology) funded by a monthly management fee. This program guided patients through chemotherapy with regular telephonic symptom assessment and discussion of patient-centered values and advance care planning. Results of these programs indicated relative reductions in both drug and hospital expenses.15
Additional experience has come from participation in the United Healthcare Episodes of Care (EOC) initiative, which eliminated the chemotherapy drug incentives, compensating physicians on a per-episode basis instead. This study showed a significant reduction in the total cost of cancer therapy after modifying the fee-for-service system and incorporating feedback data and financial incentives to reward improved outcomes and cost efficiency.16
The Oncology Care Model represents a convergence of purchaser demand and provider readiness. The purchaser holds providers accountable for cost and quality. The data on outcomes and costs will provide an extensive database that can be analyzed by the participating practices to address variations and reduce unnecessary care and preventable costs. Best practices are rewarded.17
The OCM and practice readiness
As a part of the CMS proposal process, practices were required to submit implementation plans by June 30, 2015. The purpose of the implementation plan was to define how a practice could transform over 6 broad domains: 24/7 coverage; EHR certification; navigation and care coordination; continuous quality improvement; incorporation of the Institute of Medicine’s (IOM’s) Care Management Plan; and adherence to nationally recognized guidelines. The periods of patient eligibility for the program were 6-month treatment episodes triggered by a cancer diagnosis, a provider encounter claim, and a Part B or D drug claim specifically identified as a cancer treatment. The episodes could be repeated if the 3 criteria continued to be met. All charges continued to be billed as fee-for-service as before, but in addition, participating practices could bill a monthly enhanced oncology services (MEOS) payment for the duration of an episode. Reducing the total cost of care while meeting performance metrics thresholds would also qualify a practice for performance-based payments.
Of the primary components, EHR certification and adherence to guidelines had been addressed previously, but the other domains represented significant challenges. Although 24/7 physician coverage with access to an EHR is standard for all practices, most practice sites do not have an insight into the frequency of hospital admissions, the ability to efficiently add sick patients to the daily schedule, or a routine call system to assess chemotherapy toxicity.
The OCM proposes 10 potential navigation/care coordination functions (Table 1) and does not consider those functions to be the role of one person, but rather a team responsibility. Most of our practices perform at least some of these functions, but they are not formally designated, coordinated, or recorded. A similar condition exists for the IOM care plan, which includes recommendations for treatment and adverse event management (Table 2). The prognosis, toxicity, quality-of-life, and goals-of-care requirements are often found in the physician notes, but not systematically documented or searchable.
Similar challenges have been observed for continuous quality improvement programs. Although the data are available, they are often not easy to search and, therefore, are difficult to retrieve and report. The OCM, as with any transformational program, must always weigh the benefit of information with the burden of consumption of physician and staff time to collect and input these data.18
Prepilot project work
In October 2015, lead physicians and managers from the 12 participating practices were brought together with analytic, technical, process management, and business experts from USON and McKesson Specialty Health. The objective of the meeting was to define the areas of greatest need for day 1 of the OCM and to be prepared. The challenges were to identify the changes needed to meet the requirements of the OCM while improving the patient experience, sustaining the viability of the community oncology practices, creating teams to deliver more effective care, and using data to bend the cost curve. Accordingly, 4 work streams were created: Care and Support; Content; Technology; and Communications, Revenue Cycle and Incentives.
Care and Support
The key tasks of the Care and Support team were to define the workflows for navigation and the IOM care plan. As a patient’s journey through the clinic was mapped out, it became clear that although multiple personnel could participate in the navigation and care plans, there was no systematic way to organize and record the components of successful navigation. The goals for the pilot were to test various options for navigation and to identify best practices that could be translated into standard operating procedures.
Content
The Content team was charged with identifying available programs that would fit into the OCM requirements. These included advance care planning, survivorship, chemotherapy teaching, risk assessment, pathways, and symptom assessment. A longer-term goal was the development of care paths, a more comprehensive map of the patient’s journey that would include consultations, coordinated care, imaging, labs, and other services.
Technology
The task for the Technology work stream was to identify processes of care that required documentation and to evaluate current and future technology solutions to improve efficiencies. The electronic medical record satisfied for the input of data with relevant clinical details, demographics, disease types, and staging. A web-based pathways tool supported clinical decision-making, as well as compliance to pathways. The Medicare quality metric programs set the stage for development of capture and reporting tools for data from many sources. The pilot would indicate the adequacy of these tools and the need for expansion or development of new functions or programs. Of particular importance was recording the IOM care plan and navigation functions in a searchable format. As care paths are developed, risk prediction, palliative care, and other services need to be encompassed. Finally, technology will support the identification and enrollment of eligible patients, and billing activities.
Communications, Revenue Cycle, and Incentives
The final work stream was Communications, Revenue Cycle, and Incentives. For the pilot, the focus was on revenue cycle. A new category of patient needed to be identified, enrolled, and billed to CMS for services. At the outset, the technology did not address the identification of patients receiving only oral drugs. The office visit, the diagnosis, and the drug claim all had to be aligned for enrollment and billing. It was critical to understand the workload by patient and total volume to estimate the technology and personnel needs to meet the initial number of new OCM patients. Communication refers to both internal and external parties. Education of the entire practice staff regarding transformation will be critical for success.
Of the 12 participating practices, 3 practice sites were selected for the pilot program. Each had fewer than 10 medical oncologists and at least 1 radiation oncologist. Each site had a physician champion and an administrative lead. All of the sites were part of a larger regional oncology practice. A fourth site had independently started a pilot and that experience was shared with the larger group as well. The sites were distributed across the country in 4 different time zones.
The pilot experience
The pilot experience yielded important findings, some expected and some unexpected. The challenges of navigation, the treatment plan, and team building were anticipated. We were surprised at the sheer number of potential candidates and the difficulty in finding eligible candidates. Not to be overlooked was a need for continued and possibly increased emphasis on adherence to pathways and process changes to reduce hospitalizations and emergency department (ED) visits.
Navigation
At the outset, none of the pilot practices had formal navigation processes as outlined in Table 1. Many of the processes, such as coordinating appointments and facilitating follow-up services and financial support, were provided by the practice, but were not identified or coordinated as navigation. The practices, as a first step, defined who was responsible for those services and identified 1 person who would be responsible for their completion. It was agreed that navigation was a process shared by a team and not an individual responsibility, yet the person who would monitor the completion of the tasks was not identified. It soon became apparent that true navigation included more tasks than initially outlined.
Additional tasks included appropriate patient education regarding treatment toxicities, follow-up after chemotherapy or a hospitalization, and coordination of other aspects of the IOM care plan, such as survivorship and advance care planning. Each of the practices recruited staff internally to assume the navigator role, and standard operating procedures were developed for completing and documenting this expanded responsibility. True navigation, however, depends on building the team character while still having 1 or 2 members of the team identified as being responsible for following and documenting the patient’s journey through an episode. To meet those needs, navigators developed ad hoc methods, such as spreadsheets, to track patients. The technology team developed drop-down check lists within the EHR, but the burden of documentation continued. Lastly, an ongoing challenge is how best to designate responsibility and assess how many additional staffers are needed.
IOM Care Management Plan
Before initiation of the pilot project, no practice was providing patients with a comprehensive, written treatment plan. Considerably more than half of the members of the work-stream teams believed that would be difficult to implement. However, the members of the Care and Support work stream made some fundamental assumptions to make the care plan workable: first, all aspects of the plan did not occur at the same time, and were not completed by the same person; second, and critically, items 2-9 of Table 2 could be completed at one time during the early conversations between the physician and patient about the goals of treatment. Diagnosis, prognosis, treatment intent, response rate, quality of life, and toxicities were included in the treatment plan, and the remaining IOM care plan could be discussed, or at least identified, as issues for further discussion with other team members. These components were incorporated into a 1-page document that was either typed into the record and printed out or handwritten and copied for the patient. This became the treatment plan and was ready for use at the start of the pilot.
The physician response to the treatment plan was mixed. One site adopted it enthusiastically and quickly moved to use the plan for all patients. Other sites had variable uptake. One hurdle was defining response rate to therapy and prognosis. Data were provided but they often did not match the conditions of individual patients. Some physicians were uncomfortable with the process. Documentation was difficult because the plans had to be scanned into the EHR. Patients generally responded favorably to the plans and would bring them to teaching or chemotherapy sessions.
As with navigation, the treatment plan challenges pointed the technology team toward the development and implementation of an electronic version of the plan. The pilot allowed members of the technology team to visit the clinics, to evaluate workflows and make assumptions on how to structure a treatment plan electronically.
Team-based care
None of the pilot sites had a formalized structure for team-based care. Team huddles were developed and weekly and daily huddles were encouraged. The weekly huddles took about 15-30 minutes, during which patients scheduled for the coming week were reviewed. All personnel who saw patients were invited – benefit counselors, advanced practice providers, schedulers, lab technicians, medical assistants, office and infusion nurses, social workers, pharmacists, physicians, and lead administrative staff. The daily huddle was smaller and generally included a nurse, a medical assistant, and a physician, at a minimum, to review the patients in the hospital, those to be seen in the clinic that day, and any follow-up information based on scheduled contact following recent treatments or events. In some sites, these huddles were uniformly endorsed, in others, not at all. Although many physicians felt that the functions were being handled informally and the additional time commitment would not improve the process, once they began to attend the meetings, they appreciated the value of the huddles and continued attending them. As the complexity of delivery and documentation becomes more apparent, these will prove indispensable to coordinated care.
24/7 access
Hospitalization is one of the chief drivers of the total cost of care, so the pilot sites were concerned that more needed to be done to reduce unnecessary hospitalizations. One site surveyed the patients coming into the clinic about their previous ED visits. Many of the visits had been for noncancer-related events and the clinic was not aware of many of the many of the visits. These findings prompted a number of changes. Open slots were created daily for patients who needed to be worked in for any areas of concern. The on-call physician, triage nurse, or navigation lead could fill these slots. All patients discharged from the hospital were called within 48 hours after discharge and scheduled for a clinic visit within 1 week. Night and weekend call logs were scrutinized each morning and patients’ calls were returned for any issues related to symptom or toxicity management. At one site, patients were given wallet cards with the clinic number, the treatment regimen, and, on the reverse, all symptoms that would justify calling the clinic. The patients were encouraged to call the clinic earlier rather than later in the day. On the back end, the clinics were to have processes in place so that patient calls would be answered quickly to facilitate same-day evaluations in the clinic.
Enrollment and revenue cycle
The most intractable problem was the identification and enrollment of OCM patients. As already noted, 3 components were necessary for enrollment: a drug charge for Part B or D Medicare, a provider visit, and an approved cancer diagnosis. To identify those patients, the claims system would churn out a weekly list of all eligible patients. However, the claims system had no mechanism to pick up Part D claims for oral medications. This meant that any patient with a provider visit and an appropriate diagnosis was potentially eligible for enrollment. At one site, the list of potential patients was 2-3 times the number of actual candidates. It took 6 weeks of manual chart review to resolving the list. Collectively, the 12 practices could have as many as 20,000 patients eligible for the July 1 enrollment. The pilot allowed the practices to get an early start on recruitment of business office staff and plans to address the backlog of potentially eligible patients. The process of identifying eligible patients for the OCM still needs a better solution because finding the appropriate patients is a critical first step in this model.
Underlying all of these initiatives is communication, both internal and external. We have to select and celebrate best practices. We have to educate our staffs. We will have to demonstrate that we are giving better care to our patients by using patient and provider testimonials and data.
From angst to analytics
The challenges of practice transformation can be daunting. It will be difficult to formalize processes and document data in ways that were untested before the pilot program was set up. However, the pilot accomplished 2 things: it identified additional areas that needed improvement and it demonstrated that the most challenging aspects of the OCM were feasible. Navigation and the IOM care plan were broken down into parts; each component was separately addressed, and programs were put in place to make the pieces manageable and part of an overall movement toward team-based care. The addition of a technology platform has been a key factor for the success of the value-based care initiative. Additional technology support has been enlisted to facilitate the processes, and an electronic version of the treatment plan is being tested. More difficult will be efforts to address the cultural resistance to change, which we hope to do by using data and outcomes from the CMS claims data files. The OCM represents an unprecedented opportunity for measurement of the quality of care we deliver.
We are now well und
Acknowledgment
The authors thank Supriya Srinivasan, PhD, for editorial support.
1. Oncology Care Model. Centers for Medicare and Medicaid Services 2016. https://innovation.cms.gov/initiatives/oncology-care/. Last updated November 14, 2017. Accessed November 16 2016.
2. Mortimer L, Strawbridge L, Lukens E, et al. CMS’ Oncology Care Model: delivering higher value cancer care. Clin Pharmacol Ther. 2017.
3. Medicare Prescription Drug, Improvement and Modernization Act of 2003, Pub Law No. 108-173; 2003.
4. Mathews D. The sequester: absolutely everything you could possibly need to know, in one FAQ. https://www.washingtonpost.com/news/wonk/wp/2013/02/20/the-sequester-absolutely-everything-you-could-possibly-need-to-know-in-one-faq/?utm_term=.a0f3a768399b. Published February 20, 2013. Accessed December 4, 2017.
5. Community Oncology Alliance. 2016 community oncology practice impact report: tracking the changing landscape of cancer care. https://www.communityoncology.org/wp-content/uploads/2016/09/PracticeImpactReport-2016-Report.pdf. Issued October 4, 2016. Accessed April 10, 2017.
6. The Patient Protection and Affordable Care Act, Pub Law No. 111-148; 2010.
7. Centers for Medicare and Medicaid Services. Shared Savings Program 2016. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/index.html?redirect=/sharedsavingsprogram/. Last modified October 12, 2017. Accessed November 16 2016.
8. Dale SB, Ghosh A, Peikes DN, et al. Two-year costs and quality in the comprehensive primary care initiative. N Engl J Med. 2016;374:2345-2356.
9. McWilliams JM, Chernew ME, Landon BE, Schwartz AL. Performance differences in year 1 of pioneer accountable care organizations. N Engl J Med. 2015;372:1927-1936.
10. Rajkumar R, Press MJ, Conway PH. The CMS Innovation Center – a five-year self-assessment. N Engl J Med. 2015;372:1981-1983.
11. Waters TM, Webster JA, Stevens LA, et al. Community oncology medical homes: physician-driven change to improve patient care and reduce costs. J Oncol Pract. 2015;11(6):462-467.
12. Wilfong LS, Hoverman JR, Gosse N, Neubauer MA, Torres V. Changing physician compensation and implementing new technology to enhance pathways compliance. J Clin Oncol. 2016;34(Suppl 7S):Abstr 187.
13. Hoverman JR, Cartwright TH, Patt DA, et al. Pathways, outcomes, and costs in colon cancer: retrospective evaluations in two distinct databases. J Oncol Pract. 2011;7(3 Suppl):52s-59s.
14. Neubauer MA, Hoverman JR, Kolodziej M, et al. Cost effectiveness of evidence-based treatment guidelines for the treatment of non-small-cell lung cancer in the community setting. J Oncol Pract. 2010;6(1):12-18.
15. Hoverman JR, Klein I, Harrison DW, et al. Opening the black box: the impact of an oncology management program consisting of level I pathways and an outbound nurse call system. J Oncol Pract. 2014;10(1):63-67.
16. Newcomer LN, Gould B, Page RD, Donelan SA, Perkins M. Changing physician incentives for affordable, quality cancer care: results of an episode payment model. J Oncol Pract. 2014;10(5):322-326.
17. Meyer JA, Rybowski L, Eichler R. Theory and reality of value-based purchasing: lessons from the pioneers. Rockville, MD.: Agency for Health Care Policy and Research; 1997.
18. Stein CM. Academic clinical research: death by a thousand clicks. Sci Transl Med. 2015;7:318fs349.
19. Churchill W. The end of the beginning. 1st ed. Boston, MA: Little Brown & Co; 1943.
In March 2016, 13 practices affiliated with the US Oncology Network (USON) were invited to participate in the Oncology Care Model (OCM) proposed by the Center for Medicare and Medicaid Services (CMS) and Center for Medicare and Medicaid Innovation (CMMI). The OCM, a novel value-based care model, was designed to provide higher-quality and better-coordinated oncology care at a lower cost to CMS.1 Of the 13 practices, 12 agreed to participate with a start date for the program of July 1, 2016. At least 40% of the practices’ patients were insured by Medicare, and any eligible patients with active cancer were offered an opportunity to enter the program. USON practices treat more than 25,000 patients with a qualifying episode per year and the overall OCM program sees more than 150,000 beneficiaries per year,2 so we anticipated that the OCM would have a substantial impact on each of the 12 practices on USON.
Faced with the scenario of having only 3 months between notification of approval and launch of the OCM, it was imperative that all the practices be proactive in planning and preparing to launch the OCM. With this goal in mind, representatives from all OCM candidate practices convened to anticipate the needs of the OCM and chart out a program to meet those needs. In this article, we discuss the requirements and scope of the OCM, the development of an internal pilot project, the anticipated gains from the pilot, and the results and findings from the pilot, both expected and unexpected.
The road to the Oncology Care Model
The government and oncology practices have been on separate trajectories to the OCM. In the last 15 years, the major intersections of these trajectories had to do with price and not patient outcomes. In 2003, the Medicare Prescription Drug Improvement and Modernization Act (MMA) focused on drug price reductions from an average wholesale price–based schedule to an average sales price–based schedule.3 There was the sequester in 2013,4 and more recently a proposal to restructure the payment for Part B drugs. In the background, recurrent negotiations to fix the calculation for the sustainable growth rate allowed for periodic draconian cuts to the prices of services. The cumulative effect of these price reductions has been to put economic pressure on community oncologists such that many have moved to a hospital environment.5
This contentious relationship with community oncology began to change with the passage of the Affordable Care Act (ACA) in 2010.6 Section 3022 of the ACA established the Medicare Shared Savings Program (MSSP) with the charge to create a new type of health care entity that was responsible for achieving the triple aim of improving population health, improving individual patient care, and bending the cost curve.7 Additional programs, such as the Pioneer Accountable Care Organization (ACO) program and the Comprehensive Primary Care Initiative were established to test alternative payment models.8-10
The ACA also funded the CMMI with a mandate to “test innovative payment and service delivery models” to achieve the triple aim; US$10 billion were appropriated for the years 2011-2019 for this purpose. The CMMI funded a pilot project for cancer care, the COME HOME [Community Oncology MEdical HOME] initiative, to test whether some aspects of care could be transformed or augmented to reduce overall costs or at least reduce the rate of increase. Findings from COME HOME have helped inform the OCM program.11
Over the same period, practices belonging to the USON were paving a path toward value. An electronic health record (EHR) for the entire network was adopted in 2005. A pathways program in which chemotherapy regimens were assessed on cost as well as benefits and toxicity, was started in 2006. Higher-cost regimens with no additional benefits comparable with other evidence-based regimens were deselected for initial treatment choices at the time of initial decision support. This process was streamlined using web-based technology that improved pathways compliance and tracking of off-pathways exceptions.12 Retrospective studies indicated that pathways had the potential to bend the cost curve by reducing drug spending.13,14 USON and its practices also tested a nurse call system (Innovent Oncology) funded by a monthly management fee. This program guided patients through chemotherapy with regular telephonic symptom assessment and discussion of patient-centered values and advance care planning. Results of these programs indicated relative reductions in both drug and hospital expenses.15
Additional experience has come from participation in the United Healthcare Episodes of Care (EOC) initiative, which eliminated the chemotherapy drug incentives, compensating physicians on a per-episode basis instead. This study showed a significant reduction in the total cost of cancer therapy after modifying the fee-for-service system and incorporating feedback data and financial incentives to reward improved outcomes and cost efficiency.16
The Oncology Care Model represents a convergence of purchaser demand and provider readiness. The purchaser holds providers accountable for cost and quality. The data on outcomes and costs will provide an extensive database that can be analyzed by the participating practices to address variations and reduce unnecessary care and preventable costs. Best practices are rewarded.17
The OCM and practice readiness
As a part of the CMS proposal process, practices were required to submit implementation plans by June 30, 2015. The purpose of the implementation plan was to define how a practice could transform over 6 broad domains: 24/7 coverage; EHR certification; navigation and care coordination; continuous quality improvement; incorporation of the Institute of Medicine’s (IOM’s) Care Management Plan; and adherence to nationally recognized guidelines. The periods of patient eligibility for the program were 6-month treatment episodes triggered by a cancer diagnosis, a provider encounter claim, and a Part B or D drug claim specifically identified as a cancer treatment. The episodes could be repeated if the 3 criteria continued to be met. All charges continued to be billed as fee-for-service as before, but in addition, participating practices could bill a monthly enhanced oncology services (MEOS) payment for the duration of an episode. Reducing the total cost of care while meeting performance metrics thresholds would also qualify a practice for performance-based payments.
Of the primary components, EHR certification and adherence to guidelines had been addressed previously, but the other domains represented significant challenges. Although 24/7 physician coverage with access to an EHR is standard for all practices, most practice sites do not have an insight into the frequency of hospital admissions, the ability to efficiently add sick patients to the daily schedule, or a routine call system to assess chemotherapy toxicity.
The OCM proposes 10 potential navigation/care coordination functions (Table 1) and does not consider those functions to be the role of one person, but rather a team responsibility. Most of our practices perform at least some of these functions, but they are not formally designated, coordinated, or recorded. A similar condition exists for the IOM care plan, which includes recommendations for treatment and adverse event management (Table 2). The prognosis, toxicity, quality-of-life, and goals-of-care requirements are often found in the physician notes, but not systematically documented or searchable.
Similar challenges have been observed for continuous quality improvement programs. Although the data are available, they are often not easy to search and, therefore, are difficult to retrieve and report. The OCM, as with any transformational program, must always weigh the benefit of information with the burden of consumption of physician and staff time to collect and input these data.18
Prepilot project work
In October 2015, lead physicians and managers from the 12 participating practices were brought together with analytic, technical, process management, and business experts from USON and McKesson Specialty Health. The objective of the meeting was to define the areas of greatest need for day 1 of the OCM and to be prepared. The challenges were to identify the changes needed to meet the requirements of the OCM while improving the patient experience, sustaining the viability of the community oncology practices, creating teams to deliver more effective care, and using data to bend the cost curve. Accordingly, 4 work streams were created: Care and Support; Content; Technology; and Communications, Revenue Cycle and Incentives.
Care and Support
The key tasks of the Care and Support team were to define the workflows for navigation and the IOM care plan. As a patient’s journey through the clinic was mapped out, it became clear that although multiple personnel could participate in the navigation and care plans, there was no systematic way to organize and record the components of successful navigation. The goals for the pilot were to test various options for navigation and to identify best practices that could be translated into standard operating procedures.
Content
The Content team was charged with identifying available programs that would fit into the OCM requirements. These included advance care planning, survivorship, chemotherapy teaching, risk assessment, pathways, and symptom assessment. A longer-term goal was the development of care paths, a more comprehensive map of the patient’s journey that would include consultations, coordinated care, imaging, labs, and other services.
Technology
The task for the Technology work stream was to identify processes of care that required documentation and to evaluate current and future technology solutions to improve efficiencies. The electronic medical record satisfied for the input of data with relevant clinical details, demographics, disease types, and staging. A web-based pathways tool supported clinical decision-making, as well as compliance to pathways. The Medicare quality metric programs set the stage for development of capture and reporting tools for data from many sources. The pilot would indicate the adequacy of these tools and the need for expansion or development of new functions or programs. Of particular importance was recording the IOM care plan and navigation functions in a searchable format. As care paths are developed, risk prediction, palliative care, and other services need to be encompassed. Finally, technology will support the identification and enrollment of eligible patients, and billing activities.
Communications, Revenue Cycle, and Incentives
The final work stream was Communications, Revenue Cycle, and Incentives. For the pilot, the focus was on revenue cycle. A new category of patient needed to be identified, enrolled, and billed to CMS for services. At the outset, the technology did not address the identification of patients receiving only oral drugs. The office visit, the diagnosis, and the drug claim all had to be aligned for enrollment and billing. It was critical to understand the workload by patient and total volume to estimate the technology and personnel needs to meet the initial number of new OCM patients. Communication refers to both internal and external parties. Education of the entire practice staff regarding transformation will be critical for success.
Of the 12 participating practices, 3 practice sites were selected for the pilot program. Each had fewer than 10 medical oncologists and at least 1 radiation oncologist. Each site had a physician champion and an administrative lead. All of the sites were part of a larger regional oncology practice. A fourth site had independently started a pilot and that experience was shared with the larger group as well. The sites were distributed across the country in 4 different time zones.
The pilot experience
The pilot experience yielded important findings, some expected and some unexpected. The challenges of navigation, the treatment plan, and team building were anticipated. We were surprised at the sheer number of potential candidates and the difficulty in finding eligible candidates. Not to be overlooked was a need for continued and possibly increased emphasis on adherence to pathways and process changes to reduce hospitalizations and emergency department (ED) visits.
Navigation
At the outset, none of the pilot practices had formal navigation processes as outlined in Table 1. Many of the processes, such as coordinating appointments and facilitating follow-up services and financial support, were provided by the practice, but were not identified or coordinated as navigation. The practices, as a first step, defined who was responsible for those services and identified 1 person who would be responsible for their completion. It was agreed that navigation was a process shared by a team and not an individual responsibility, yet the person who would monitor the completion of the tasks was not identified. It soon became apparent that true navigation included more tasks than initially outlined.
Additional tasks included appropriate patient education regarding treatment toxicities, follow-up after chemotherapy or a hospitalization, and coordination of other aspects of the IOM care plan, such as survivorship and advance care planning. Each of the practices recruited staff internally to assume the navigator role, and standard operating procedures were developed for completing and documenting this expanded responsibility. True navigation, however, depends on building the team character while still having 1 or 2 members of the team identified as being responsible for following and documenting the patient’s journey through an episode. To meet those needs, navigators developed ad hoc methods, such as spreadsheets, to track patients. The technology team developed drop-down check lists within the EHR, but the burden of documentation continued. Lastly, an ongoing challenge is how best to designate responsibility and assess how many additional staffers are needed.
IOM Care Management Plan
Before initiation of the pilot project, no practice was providing patients with a comprehensive, written treatment plan. Considerably more than half of the members of the work-stream teams believed that would be difficult to implement. However, the members of the Care and Support work stream made some fundamental assumptions to make the care plan workable: first, all aspects of the plan did not occur at the same time, and were not completed by the same person; second, and critically, items 2-9 of Table 2 could be completed at one time during the early conversations between the physician and patient about the goals of treatment. Diagnosis, prognosis, treatment intent, response rate, quality of life, and toxicities were included in the treatment plan, and the remaining IOM care plan could be discussed, or at least identified, as issues for further discussion with other team members. These components were incorporated into a 1-page document that was either typed into the record and printed out or handwritten and copied for the patient. This became the treatment plan and was ready for use at the start of the pilot.
The physician response to the treatment plan was mixed. One site adopted it enthusiastically and quickly moved to use the plan for all patients. Other sites had variable uptake. One hurdle was defining response rate to therapy and prognosis. Data were provided but they often did not match the conditions of individual patients. Some physicians were uncomfortable with the process. Documentation was difficult because the plans had to be scanned into the EHR. Patients generally responded favorably to the plans and would bring them to teaching or chemotherapy sessions.
As with navigation, the treatment plan challenges pointed the technology team toward the development and implementation of an electronic version of the plan. The pilot allowed members of the technology team to visit the clinics, to evaluate workflows and make assumptions on how to structure a treatment plan electronically.
Team-based care
None of the pilot sites had a formalized structure for team-based care. Team huddles were developed and weekly and daily huddles were encouraged. The weekly huddles took about 15-30 minutes, during which patients scheduled for the coming week were reviewed. All personnel who saw patients were invited – benefit counselors, advanced practice providers, schedulers, lab technicians, medical assistants, office and infusion nurses, social workers, pharmacists, physicians, and lead administrative staff. The daily huddle was smaller and generally included a nurse, a medical assistant, and a physician, at a minimum, to review the patients in the hospital, those to be seen in the clinic that day, and any follow-up information based on scheduled contact following recent treatments or events. In some sites, these huddles were uniformly endorsed, in others, not at all. Although many physicians felt that the functions were being handled informally and the additional time commitment would not improve the process, once they began to attend the meetings, they appreciated the value of the huddles and continued attending them. As the complexity of delivery and documentation becomes more apparent, these will prove indispensable to coordinated care.
24/7 access
Hospitalization is one of the chief drivers of the total cost of care, so the pilot sites were concerned that more needed to be done to reduce unnecessary hospitalizations. One site surveyed the patients coming into the clinic about their previous ED visits. Many of the visits had been for noncancer-related events and the clinic was not aware of many of the many of the visits. These findings prompted a number of changes. Open slots were created daily for patients who needed to be worked in for any areas of concern. The on-call physician, triage nurse, or navigation lead could fill these slots. All patients discharged from the hospital were called within 48 hours after discharge and scheduled for a clinic visit within 1 week. Night and weekend call logs were scrutinized each morning and patients’ calls were returned for any issues related to symptom or toxicity management. At one site, patients were given wallet cards with the clinic number, the treatment regimen, and, on the reverse, all symptoms that would justify calling the clinic. The patients were encouraged to call the clinic earlier rather than later in the day. On the back end, the clinics were to have processes in place so that patient calls would be answered quickly to facilitate same-day evaluations in the clinic.
Enrollment and revenue cycle
The most intractable problem was the identification and enrollment of OCM patients. As already noted, 3 components were necessary for enrollment: a drug charge for Part B or D Medicare, a provider visit, and an approved cancer diagnosis. To identify those patients, the claims system would churn out a weekly list of all eligible patients. However, the claims system had no mechanism to pick up Part D claims for oral medications. This meant that any patient with a provider visit and an appropriate diagnosis was potentially eligible for enrollment. At one site, the list of potential patients was 2-3 times the number of actual candidates. It took 6 weeks of manual chart review to resolving the list. Collectively, the 12 practices could have as many as 20,000 patients eligible for the July 1 enrollment. The pilot allowed the practices to get an early start on recruitment of business office staff and plans to address the backlog of potentially eligible patients. The process of identifying eligible patients for the OCM still needs a better solution because finding the appropriate patients is a critical first step in this model.
Underlying all of these initiatives is communication, both internal and external. We have to select and celebrate best practices. We have to educate our staffs. We will have to demonstrate that we are giving better care to our patients by using patient and provider testimonials and data.
From angst to analytics
The challenges of practice transformation can be daunting. It will be difficult to formalize processes and document data in ways that were untested before the pilot program was set up. However, the pilot accomplished 2 things: it identified additional areas that needed improvement and it demonstrated that the most challenging aspects of the OCM were feasible. Navigation and the IOM care plan were broken down into parts; each component was separately addressed, and programs were put in place to make the pieces manageable and part of an overall movement toward team-based care. The addition of a technology platform has been a key factor for the success of the value-based care initiative. Additional technology support has been enlisted to facilitate the processes, and an electronic version of the treatment plan is being tested. More difficult will be efforts to address the cultural resistance to change, which we hope to do by using data and outcomes from the CMS claims data files. The OCM represents an unprecedented opportunity for measurement of the quality of care we deliver.
We are now well und
Acknowledgment
The authors thank Supriya Srinivasan, PhD, for editorial support.
In March 2016, 13 practices affiliated with the US Oncology Network (USON) were invited to participate in the Oncology Care Model (OCM) proposed by the Center for Medicare and Medicaid Services (CMS) and Center for Medicare and Medicaid Innovation (CMMI). The OCM, a novel value-based care model, was designed to provide higher-quality and better-coordinated oncology care at a lower cost to CMS.1 Of the 13 practices, 12 agreed to participate with a start date for the program of July 1, 2016. At least 40% of the practices’ patients were insured by Medicare, and any eligible patients with active cancer were offered an opportunity to enter the program. USON practices treat more than 25,000 patients with a qualifying episode per year and the overall OCM program sees more than 150,000 beneficiaries per year,2 so we anticipated that the OCM would have a substantial impact on each of the 12 practices on USON.
Faced with the scenario of having only 3 months between notification of approval and launch of the OCM, it was imperative that all the practices be proactive in planning and preparing to launch the OCM. With this goal in mind, representatives from all OCM candidate practices convened to anticipate the needs of the OCM and chart out a program to meet those needs. In this article, we discuss the requirements and scope of the OCM, the development of an internal pilot project, the anticipated gains from the pilot, and the results and findings from the pilot, both expected and unexpected.
The road to the Oncology Care Model
The government and oncology practices have been on separate trajectories to the OCM. In the last 15 years, the major intersections of these trajectories had to do with price and not patient outcomes. In 2003, the Medicare Prescription Drug Improvement and Modernization Act (MMA) focused on drug price reductions from an average wholesale price–based schedule to an average sales price–based schedule.3 There was the sequester in 2013,4 and more recently a proposal to restructure the payment for Part B drugs. In the background, recurrent negotiations to fix the calculation for the sustainable growth rate allowed for periodic draconian cuts to the prices of services. The cumulative effect of these price reductions has been to put economic pressure on community oncologists such that many have moved to a hospital environment.5
This contentious relationship with community oncology began to change with the passage of the Affordable Care Act (ACA) in 2010.6 Section 3022 of the ACA established the Medicare Shared Savings Program (MSSP) with the charge to create a new type of health care entity that was responsible for achieving the triple aim of improving population health, improving individual patient care, and bending the cost curve.7 Additional programs, such as the Pioneer Accountable Care Organization (ACO) program and the Comprehensive Primary Care Initiative were established to test alternative payment models.8-10
The ACA also funded the CMMI with a mandate to “test innovative payment and service delivery models” to achieve the triple aim; US$10 billion were appropriated for the years 2011-2019 for this purpose. The CMMI funded a pilot project for cancer care, the COME HOME [Community Oncology MEdical HOME] initiative, to test whether some aspects of care could be transformed or augmented to reduce overall costs or at least reduce the rate of increase. Findings from COME HOME have helped inform the OCM program.11
Over the same period, practices belonging to the USON were paving a path toward value. An electronic health record (EHR) for the entire network was adopted in 2005. A pathways program in which chemotherapy regimens were assessed on cost as well as benefits and toxicity, was started in 2006. Higher-cost regimens with no additional benefits comparable with other evidence-based regimens were deselected for initial treatment choices at the time of initial decision support. This process was streamlined using web-based technology that improved pathways compliance and tracking of off-pathways exceptions.12 Retrospective studies indicated that pathways had the potential to bend the cost curve by reducing drug spending.13,14 USON and its practices also tested a nurse call system (Innovent Oncology) funded by a monthly management fee. This program guided patients through chemotherapy with regular telephonic symptom assessment and discussion of patient-centered values and advance care planning. Results of these programs indicated relative reductions in both drug and hospital expenses.15
Additional experience has come from participation in the United Healthcare Episodes of Care (EOC) initiative, which eliminated the chemotherapy drug incentives, compensating physicians on a per-episode basis instead. This study showed a significant reduction in the total cost of cancer therapy after modifying the fee-for-service system and incorporating feedback data and financial incentives to reward improved outcomes and cost efficiency.16
The Oncology Care Model represents a convergence of purchaser demand and provider readiness. The purchaser holds providers accountable for cost and quality. The data on outcomes and costs will provide an extensive database that can be analyzed by the participating practices to address variations and reduce unnecessary care and preventable costs. Best practices are rewarded.17
The OCM and practice readiness
As a part of the CMS proposal process, practices were required to submit implementation plans by June 30, 2015. The purpose of the implementation plan was to define how a practice could transform over 6 broad domains: 24/7 coverage; EHR certification; navigation and care coordination; continuous quality improvement; incorporation of the Institute of Medicine’s (IOM’s) Care Management Plan; and adherence to nationally recognized guidelines. The periods of patient eligibility for the program were 6-month treatment episodes triggered by a cancer diagnosis, a provider encounter claim, and a Part B or D drug claim specifically identified as a cancer treatment. The episodes could be repeated if the 3 criteria continued to be met. All charges continued to be billed as fee-for-service as before, but in addition, participating practices could bill a monthly enhanced oncology services (MEOS) payment for the duration of an episode. Reducing the total cost of care while meeting performance metrics thresholds would also qualify a practice for performance-based payments.
Of the primary components, EHR certification and adherence to guidelines had been addressed previously, but the other domains represented significant challenges. Although 24/7 physician coverage with access to an EHR is standard for all practices, most practice sites do not have an insight into the frequency of hospital admissions, the ability to efficiently add sick patients to the daily schedule, or a routine call system to assess chemotherapy toxicity.
The OCM proposes 10 potential navigation/care coordination functions (Table 1) and does not consider those functions to be the role of one person, but rather a team responsibility. Most of our practices perform at least some of these functions, but they are not formally designated, coordinated, or recorded. A similar condition exists for the IOM care plan, which includes recommendations for treatment and adverse event management (Table 2). The prognosis, toxicity, quality-of-life, and goals-of-care requirements are often found in the physician notes, but not systematically documented or searchable.
Similar challenges have been observed for continuous quality improvement programs. Although the data are available, they are often not easy to search and, therefore, are difficult to retrieve and report. The OCM, as with any transformational program, must always weigh the benefit of information with the burden of consumption of physician and staff time to collect and input these data.18
Prepilot project work
In October 2015, lead physicians and managers from the 12 participating practices were brought together with analytic, technical, process management, and business experts from USON and McKesson Specialty Health. The objective of the meeting was to define the areas of greatest need for day 1 of the OCM and to be prepared. The challenges were to identify the changes needed to meet the requirements of the OCM while improving the patient experience, sustaining the viability of the community oncology practices, creating teams to deliver more effective care, and using data to bend the cost curve. Accordingly, 4 work streams were created: Care and Support; Content; Technology; and Communications, Revenue Cycle and Incentives.
Care and Support
The key tasks of the Care and Support team were to define the workflows for navigation and the IOM care plan. As a patient’s journey through the clinic was mapped out, it became clear that although multiple personnel could participate in the navigation and care plans, there was no systematic way to organize and record the components of successful navigation. The goals for the pilot were to test various options for navigation and to identify best practices that could be translated into standard operating procedures.
Content
The Content team was charged with identifying available programs that would fit into the OCM requirements. These included advance care planning, survivorship, chemotherapy teaching, risk assessment, pathways, and symptom assessment. A longer-term goal was the development of care paths, a more comprehensive map of the patient’s journey that would include consultations, coordinated care, imaging, labs, and other services.
Technology
The task for the Technology work stream was to identify processes of care that required documentation and to evaluate current and future technology solutions to improve efficiencies. The electronic medical record satisfied for the input of data with relevant clinical details, demographics, disease types, and staging. A web-based pathways tool supported clinical decision-making, as well as compliance to pathways. The Medicare quality metric programs set the stage for development of capture and reporting tools for data from many sources. The pilot would indicate the adequacy of these tools and the need for expansion or development of new functions or programs. Of particular importance was recording the IOM care plan and navigation functions in a searchable format. As care paths are developed, risk prediction, palliative care, and other services need to be encompassed. Finally, technology will support the identification and enrollment of eligible patients, and billing activities.
Communications, Revenue Cycle, and Incentives
The final work stream was Communications, Revenue Cycle, and Incentives. For the pilot, the focus was on revenue cycle. A new category of patient needed to be identified, enrolled, and billed to CMS for services. At the outset, the technology did not address the identification of patients receiving only oral drugs. The office visit, the diagnosis, and the drug claim all had to be aligned for enrollment and billing. It was critical to understand the workload by patient and total volume to estimate the technology and personnel needs to meet the initial number of new OCM patients. Communication refers to both internal and external parties. Education of the entire practice staff regarding transformation will be critical for success.
Of the 12 participating practices, 3 practice sites were selected for the pilot program. Each had fewer than 10 medical oncologists and at least 1 radiation oncologist. Each site had a physician champion and an administrative lead. All of the sites were part of a larger regional oncology practice. A fourth site had independently started a pilot and that experience was shared with the larger group as well. The sites were distributed across the country in 4 different time zones.
The pilot experience
The pilot experience yielded important findings, some expected and some unexpected. The challenges of navigation, the treatment plan, and team building were anticipated. We were surprised at the sheer number of potential candidates and the difficulty in finding eligible candidates. Not to be overlooked was a need for continued and possibly increased emphasis on adherence to pathways and process changes to reduce hospitalizations and emergency department (ED) visits.
Navigation
At the outset, none of the pilot practices had formal navigation processes as outlined in Table 1. Many of the processes, such as coordinating appointments and facilitating follow-up services and financial support, were provided by the practice, but were not identified or coordinated as navigation. The practices, as a first step, defined who was responsible for those services and identified 1 person who would be responsible for their completion. It was agreed that navigation was a process shared by a team and not an individual responsibility, yet the person who would monitor the completion of the tasks was not identified. It soon became apparent that true navigation included more tasks than initially outlined.
Additional tasks included appropriate patient education regarding treatment toxicities, follow-up after chemotherapy or a hospitalization, and coordination of other aspects of the IOM care plan, such as survivorship and advance care planning. Each of the practices recruited staff internally to assume the navigator role, and standard operating procedures were developed for completing and documenting this expanded responsibility. True navigation, however, depends on building the team character while still having 1 or 2 members of the team identified as being responsible for following and documenting the patient’s journey through an episode. To meet those needs, navigators developed ad hoc methods, such as spreadsheets, to track patients. The technology team developed drop-down check lists within the EHR, but the burden of documentation continued. Lastly, an ongoing challenge is how best to designate responsibility and assess how many additional staffers are needed.
IOM Care Management Plan
Before initiation of the pilot project, no practice was providing patients with a comprehensive, written treatment plan. Considerably more than half of the members of the work-stream teams believed that would be difficult to implement. However, the members of the Care and Support work stream made some fundamental assumptions to make the care plan workable: first, all aspects of the plan did not occur at the same time, and were not completed by the same person; second, and critically, items 2-9 of Table 2 could be completed at one time during the early conversations between the physician and patient about the goals of treatment. Diagnosis, prognosis, treatment intent, response rate, quality of life, and toxicities were included in the treatment plan, and the remaining IOM care plan could be discussed, or at least identified, as issues for further discussion with other team members. These components were incorporated into a 1-page document that was either typed into the record and printed out or handwritten and copied for the patient. This became the treatment plan and was ready for use at the start of the pilot.
The physician response to the treatment plan was mixed. One site adopted it enthusiastically and quickly moved to use the plan for all patients. Other sites had variable uptake. One hurdle was defining response rate to therapy and prognosis. Data were provided but they often did not match the conditions of individual patients. Some physicians were uncomfortable with the process. Documentation was difficult because the plans had to be scanned into the EHR. Patients generally responded favorably to the plans and would bring them to teaching or chemotherapy sessions.
As with navigation, the treatment plan challenges pointed the technology team toward the development and implementation of an electronic version of the plan. The pilot allowed members of the technology team to visit the clinics, to evaluate workflows and make assumptions on how to structure a treatment plan electronically.
Team-based care
None of the pilot sites had a formalized structure for team-based care. Team huddles were developed and weekly and daily huddles were encouraged. The weekly huddles took about 15-30 minutes, during which patients scheduled for the coming week were reviewed. All personnel who saw patients were invited – benefit counselors, advanced practice providers, schedulers, lab technicians, medical assistants, office and infusion nurses, social workers, pharmacists, physicians, and lead administrative staff. The daily huddle was smaller and generally included a nurse, a medical assistant, and a physician, at a minimum, to review the patients in the hospital, those to be seen in the clinic that day, and any follow-up information based on scheduled contact following recent treatments or events. In some sites, these huddles were uniformly endorsed, in others, not at all. Although many physicians felt that the functions were being handled informally and the additional time commitment would not improve the process, once they began to attend the meetings, they appreciated the value of the huddles and continued attending them. As the complexity of delivery and documentation becomes more apparent, these will prove indispensable to coordinated care.
24/7 access
Hospitalization is one of the chief drivers of the total cost of care, so the pilot sites were concerned that more needed to be done to reduce unnecessary hospitalizations. One site surveyed the patients coming into the clinic about their previous ED visits. Many of the visits had been for noncancer-related events and the clinic was not aware of many of the many of the visits. These findings prompted a number of changes. Open slots were created daily for patients who needed to be worked in for any areas of concern. The on-call physician, triage nurse, or navigation lead could fill these slots. All patients discharged from the hospital were called within 48 hours after discharge and scheduled for a clinic visit within 1 week. Night and weekend call logs were scrutinized each morning and patients’ calls were returned for any issues related to symptom or toxicity management. At one site, patients were given wallet cards with the clinic number, the treatment regimen, and, on the reverse, all symptoms that would justify calling the clinic. The patients were encouraged to call the clinic earlier rather than later in the day. On the back end, the clinics were to have processes in place so that patient calls would be answered quickly to facilitate same-day evaluations in the clinic.
Enrollment and revenue cycle
The most intractable problem was the identification and enrollment of OCM patients. As already noted, 3 components were necessary for enrollment: a drug charge for Part B or D Medicare, a provider visit, and an approved cancer diagnosis. To identify those patients, the claims system would churn out a weekly list of all eligible patients. However, the claims system had no mechanism to pick up Part D claims for oral medications. This meant that any patient with a provider visit and an appropriate diagnosis was potentially eligible for enrollment. At one site, the list of potential patients was 2-3 times the number of actual candidates. It took 6 weeks of manual chart review to resolving the list. Collectively, the 12 practices could have as many as 20,000 patients eligible for the July 1 enrollment. The pilot allowed the practices to get an early start on recruitment of business office staff and plans to address the backlog of potentially eligible patients. The process of identifying eligible patients for the OCM still needs a better solution because finding the appropriate patients is a critical first step in this model.
Underlying all of these initiatives is communication, both internal and external. We have to select and celebrate best practices. We have to educate our staffs. We will have to demonstrate that we are giving better care to our patients by using patient and provider testimonials and data.
From angst to analytics
The challenges of practice transformation can be daunting. It will be difficult to formalize processes and document data in ways that were untested before the pilot program was set up. However, the pilot accomplished 2 things: it identified additional areas that needed improvement and it demonstrated that the most challenging aspects of the OCM were feasible. Navigation and the IOM care plan were broken down into parts; each component was separately addressed, and programs were put in place to make the pieces manageable and part of an overall movement toward team-based care. The addition of a technology platform has been a key factor for the success of the value-based care initiative. Additional technology support has been enlisted to facilitate the processes, and an electronic version of the treatment plan is being tested. More difficult will be efforts to address the cultural resistance to change, which we hope to do by using data and outcomes from the CMS claims data files. The OCM represents an unprecedented opportunity for measurement of the quality of care we deliver.
We are now well und
Acknowledgment
The authors thank Supriya Srinivasan, PhD, for editorial support.
1. Oncology Care Model. Centers for Medicare and Medicaid Services 2016. https://innovation.cms.gov/initiatives/oncology-care/. Last updated November 14, 2017. Accessed November 16 2016.
2. Mortimer L, Strawbridge L, Lukens E, et al. CMS’ Oncology Care Model: delivering higher value cancer care. Clin Pharmacol Ther. 2017.
3. Medicare Prescription Drug, Improvement and Modernization Act of 2003, Pub Law No. 108-173; 2003.
4. Mathews D. The sequester: absolutely everything you could possibly need to know, in one FAQ. https://www.washingtonpost.com/news/wonk/wp/2013/02/20/the-sequester-absolutely-everything-you-could-possibly-need-to-know-in-one-faq/?utm_term=.a0f3a768399b. Published February 20, 2013. Accessed December 4, 2017.
5. Community Oncology Alliance. 2016 community oncology practice impact report: tracking the changing landscape of cancer care. https://www.communityoncology.org/wp-content/uploads/2016/09/PracticeImpactReport-2016-Report.pdf. Issued October 4, 2016. Accessed April 10, 2017.
6. The Patient Protection and Affordable Care Act, Pub Law No. 111-148; 2010.
7. Centers for Medicare and Medicaid Services. Shared Savings Program 2016. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/index.html?redirect=/sharedsavingsprogram/. Last modified October 12, 2017. Accessed November 16 2016.
8. Dale SB, Ghosh A, Peikes DN, et al. Two-year costs and quality in the comprehensive primary care initiative. N Engl J Med. 2016;374:2345-2356.
9. McWilliams JM, Chernew ME, Landon BE, Schwartz AL. Performance differences in year 1 of pioneer accountable care organizations. N Engl J Med. 2015;372:1927-1936.
10. Rajkumar R, Press MJ, Conway PH. The CMS Innovation Center – a five-year self-assessment. N Engl J Med. 2015;372:1981-1983.
11. Waters TM, Webster JA, Stevens LA, et al. Community oncology medical homes: physician-driven change to improve patient care and reduce costs. J Oncol Pract. 2015;11(6):462-467.
12. Wilfong LS, Hoverman JR, Gosse N, Neubauer MA, Torres V. Changing physician compensation and implementing new technology to enhance pathways compliance. J Clin Oncol. 2016;34(Suppl 7S):Abstr 187.
13. Hoverman JR, Cartwright TH, Patt DA, et al. Pathways, outcomes, and costs in colon cancer: retrospective evaluations in two distinct databases. J Oncol Pract. 2011;7(3 Suppl):52s-59s.
14. Neubauer MA, Hoverman JR, Kolodziej M, et al. Cost effectiveness of evidence-based treatment guidelines for the treatment of non-small-cell lung cancer in the community setting. J Oncol Pract. 2010;6(1):12-18.
15. Hoverman JR, Klein I, Harrison DW, et al. Opening the black box: the impact of an oncology management program consisting of level I pathways and an outbound nurse call system. J Oncol Pract. 2014;10(1):63-67.
16. Newcomer LN, Gould B, Page RD, Donelan SA, Perkins M. Changing physician incentives for affordable, quality cancer care: results of an episode payment model. J Oncol Pract. 2014;10(5):322-326.
17. Meyer JA, Rybowski L, Eichler R. Theory and reality of value-based purchasing: lessons from the pioneers. Rockville, MD.: Agency for Health Care Policy and Research; 1997.
18. Stein CM. Academic clinical research: death by a thousand clicks. Sci Transl Med. 2015;7:318fs349.
19. Churchill W. The end of the beginning. 1st ed. Boston, MA: Little Brown & Co; 1943.
1. Oncology Care Model. Centers for Medicare and Medicaid Services 2016. https://innovation.cms.gov/initiatives/oncology-care/. Last updated November 14, 2017. Accessed November 16 2016.
2. Mortimer L, Strawbridge L, Lukens E, et al. CMS’ Oncology Care Model: delivering higher value cancer care. Clin Pharmacol Ther. 2017.
3. Medicare Prescription Drug, Improvement and Modernization Act of 2003, Pub Law No. 108-173; 2003.
4. Mathews D. The sequester: absolutely everything you could possibly need to know, in one FAQ. https://www.washingtonpost.com/news/wonk/wp/2013/02/20/the-sequester-absolutely-everything-you-could-possibly-need-to-know-in-one-faq/?utm_term=.a0f3a768399b. Published February 20, 2013. Accessed December 4, 2017.
5. Community Oncology Alliance. 2016 community oncology practice impact report: tracking the changing landscape of cancer care. https://www.communityoncology.org/wp-content/uploads/2016/09/PracticeImpactReport-2016-Report.pdf. Issued October 4, 2016. Accessed April 10, 2017.
6. The Patient Protection and Affordable Care Act, Pub Law No. 111-148; 2010.
7. Centers for Medicare and Medicaid Services. Shared Savings Program 2016. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/index.html?redirect=/sharedsavingsprogram/. Last modified October 12, 2017. Accessed November 16 2016.
8. Dale SB, Ghosh A, Peikes DN, et al. Two-year costs and quality in the comprehensive primary care initiative. N Engl J Med. 2016;374:2345-2356.
9. McWilliams JM, Chernew ME, Landon BE, Schwartz AL. Performance differences in year 1 of pioneer accountable care organizations. N Engl J Med. 2015;372:1927-1936.
10. Rajkumar R, Press MJ, Conway PH. The CMS Innovation Center – a five-year self-assessment. N Engl J Med. 2015;372:1981-1983.
11. Waters TM, Webster JA, Stevens LA, et al. Community oncology medical homes: physician-driven change to improve patient care and reduce costs. J Oncol Pract. 2015;11(6):462-467.
12. Wilfong LS, Hoverman JR, Gosse N, Neubauer MA, Torres V. Changing physician compensation and implementing new technology to enhance pathways compliance. J Clin Oncol. 2016;34(Suppl 7S):Abstr 187.
13. Hoverman JR, Cartwright TH, Patt DA, et al. Pathways, outcomes, and costs in colon cancer: retrospective evaluations in two distinct databases. J Oncol Pract. 2011;7(3 Suppl):52s-59s.
14. Neubauer MA, Hoverman JR, Kolodziej M, et al. Cost effectiveness of evidence-based treatment guidelines for the treatment of non-small-cell lung cancer in the community setting. J Oncol Pract. 2010;6(1):12-18.
15. Hoverman JR, Klein I, Harrison DW, et al. Opening the black box: the impact of an oncology management program consisting of level I pathways and an outbound nurse call system. J Oncol Pract. 2014;10(1):63-67.
16. Newcomer LN, Gould B, Page RD, Donelan SA, Perkins M. Changing physician incentives for affordable, quality cancer care: results of an episode payment model. J Oncol Pract. 2014;10(5):322-326.
17. Meyer JA, Rybowski L, Eichler R. Theory and reality of value-based purchasing: lessons from the pioneers. Rockville, MD.: Agency for Health Care Policy and Research; 1997.
18. Stein CM. Academic clinical research: death by a thousand clicks. Sci Transl Med. 2015;7:318fs349.
19. Churchill W. The end of the beginning. 1st ed. Boston, MA: Little Brown & Co; 1943.
David Henry's JCSO podcast, January-February 2018
In this podcast, Dr Henry discusses research articles on analgesic management in radiation oncology for painful bone metastases, hospitalizations for fracture in patients with metastatic disease, measurement of physical activity and sedentary behavior in breast cancer survivors, and patient navigators’ personal experiences with cancer and their impact on treatment. He also highlights a New Therapies review article on hallmark tumor metabolism becoming a validated therapeutic target, as well as The JCSO Interview, in which Kenneth Anderson, MD, talks about new myeloma drugs and their associated improved response rates and extended survival. Comments on the approvals of abemaciclib for breast cancer and avelumab and durvalumab for metastatic bladder cancer, and Case Reports on concurrent ipilimumab and CMV colitis refractory to oral steroids, recurrent head and neck cancer presenting as a large retroperitoneal mass, massive liver metastasis from colon adenocarcinoma causing cardiac tamponade, and cardiac pleomorphic sarcoma after placement of Dacron graft round out the line-up of articles.
Listen to the podcast below.
In this podcast, Dr Henry discusses research articles on analgesic management in radiation oncology for painful bone metastases, hospitalizations for fracture in patients with metastatic disease, measurement of physical activity and sedentary behavior in breast cancer survivors, and patient navigators’ personal experiences with cancer and their impact on treatment. He also highlights a New Therapies review article on hallmark tumor metabolism becoming a validated therapeutic target, as well as The JCSO Interview, in which Kenneth Anderson, MD, talks about new myeloma drugs and their associated improved response rates and extended survival. Comments on the approvals of abemaciclib for breast cancer and avelumab and durvalumab for metastatic bladder cancer, and Case Reports on concurrent ipilimumab and CMV colitis refractory to oral steroids, recurrent head and neck cancer presenting as a large retroperitoneal mass, massive liver metastasis from colon adenocarcinoma causing cardiac tamponade, and cardiac pleomorphic sarcoma after placement of Dacron graft round out the line-up of articles.
Listen to the podcast below.
In this podcast, Dr Henry discusses research articles on analgesic management in radiation oncology for painful bone metastases, hospitalizations for fracture in patients with metastatic disease, measurement of physical activity and sedentary behavior in breast cancer survivors, and patient navigators’ personal experiences with cancer and their impact on treatment. He also highlights a New Therapies review article on hallmark tumor metabolism becoming a validated therapeutic target, as well as The JCSO Interview, in which Kenneth Anderson, MD, talks about new myeloma drugs and their associated improved response rates and extended survival. Comments on the approvals of abemaciclib for breast cancer and avelumab and durvalumab for metastatic bladder cancer, and Case Reports on concurrent ipilimumab and CMV colitis refractory to oral steroids, recurrent head and neck cancer presenting as a large retroperitoneal mass, massive liver metastasis from colon adenocarcinoma causing cardiac tamponade, and cardiac pleomorphic sarcoma after placement of Dacron graft round out the line-up of articles.
Listen to the podcast below.
Clinical presentation, diagnosis, and management of typical and atypical bronchopulmonary carcinoid
Carcinoid lung tumors represent the most indolent form of a spectrum of bronchopulmonary neuroendocrine tumors (NETs) that includes small-cell carcinoma as its most malignant member, as well as several other forms of intermediately aggressive tumors, such as atypical carcinoid.1 Carcinoids represent 1.2% of all primary lung malignancies. Their incidence in the United States has increased rapidly over the last 30 years and is currently about 6% a year. Lung carcinoids are more prevalent in whites compared with blacks, and in Asians compared with non-Asians. They are less common in Hispanics compared with non-Hispanics.1 Typical carcinoids represent 80%-90% of all lung carcinoids and occur more frequently in the fifth and sixth decades of life. They can, however, occur at any age, and are the most common lung tumor in childhood.1
Etiology and risk factors
Unlike carcinoma of the lung, no external environmental toxin or other stimulus has been identified as a causative agent for the development of pulmonary carcinoid tumors. It is not clear if there is an association between bronchial NETs and smoking.1 Nearly all bronchial NETs are sporadic; however, they can rarely occur in the setting of multiple endocrine neoplasia type 1.1
Presentation
About 60% of the patients with bronchial carcinoids are symptomatic at presentation. The most common clinical findings are those associated with bronchial obstruction, such as persistent cough, hemoptysis, and recurrent or obstructive pneumonitis. Wheezing, chest pain, and dyspnea also may be noted.2 Various endocrine or neuroendocrine syndromes can be initial clinical manifestations of either typical or atypical pulmonary carcinoid tumors, but that is not common Cushing syndrome (ectopic production and secretion of adrenocorticotropic hormone [ACTH]) may occur in about 2% of lung carcinoid.3 In cases of malignancy, the presence of metastatic disease can produce weight loss, weakness, and a general feeling of ill health.
Diagnostic work-up
Biochemical test
There is no biochemical study that can be used as a screening test to determine the presence of a carcinoid tumor or to diagnose a known pulmonary mass as a carcinoid tumor. Neuroendocrine cells produce biologically active amines and peptides that can be detected in serum and urine. Although the syndromes associated with lung carcinoids are seen in about 1%-2% of the patients, assays of specific hormones or other circulating neuroendocrine substances, such as ACTH, melanocyte-stimulating hormone, or growth hormone may establish the existence of a clinically suspected syndrome.
Chest radiography
An abnormal finding on chest radiography is present in about 75% of patients with a pulmonary carcinoid tumor.1 Findings include either the presence of the tumor mass itself or indirect evidence of its presence observed as parenchymal changes associated with bronchial obstruction from the mass.
Computed-tomography imaging
High-resolution computed-tomography (CT) imaging is the one of the best types of CT examination for evaluation of a pulmonary carcinoid tumor.4 A CT scan provides excellent resolution of tumor extent, location, and the presence or absence of mediastinal adenopathy. It also aids in morphologic characterization of peripheral (Figure 1) and especially centrally located carcinoids, which may be purely intraluminal (polypoid configuration), exclusively extra luminal, or more frequently, a mixture of intraluminal and extraluminal components.
CT scans may also be helpful for differentiating tumor from postobstructive atelectasis or bronchial obstruction-related mucoid impaction. Intravenous contrast in CT imaging can be useful in differentiating malignant from benign lesions. Because carcinoid tumors are highly vascular, they show greater enhancement on contrast CT than do benign lesions. The sensitivity of CT for detecting metastatic hilar or mediastinal nodes is high, but specificity is as low as 45%.4
Typical carcinoid is rarely metastatic so most patients do not need CT or MRI imaging to evaluate for liver involvement. Liver imaging is appropriate in patients with evidence of mediastinal involvement, relatively high mitotic rate, or clinical evidence of the carcinoid syndrome.8 To evaluate for metastatic spread to the liver, multiphase contrast-enhanced liver CT scans should be performed with arterial and portal-venous phases because carcinoid liver metastases are often hypervascular and appear isodense relative to the liver parenchyma after contrast administration.4 An MRI is often preferred the modality to evaluate for metastatic spread to the liver because of its higher sensitivity.5
Positron-emission tomography
Although carcinoid tumors of the lung are highly vascular, they do not show increased metabolic activity on positron-emission tomography (PET) and would be incorrectly designated as benign lesions on the basis of findings from a PET scan. Fludeoxyglucose F-18 PET has shown utility as a radiologic marker for atypical carcinoids, particularly for those with a higher proliferation index with Ki-67 index of 10%-20%.6
Radionucleotide studies
Somatostatin receptors (SSRs) are present in many tumors of neuroendocrine origin, including carcinoid tumors. These receptors interact with each other and undergo dimerization and internalization. SSTR subtypes (SSTRs) overexpressed in NETs are related to the type, origin, and grade of differentiation of tumor. The overexpression of an SSTR is a characteristic feature of bronchial NETs, which can be used to localize the primary tumor and its metastases by imaging with the radiolabeled SST analogues. Radionucleotide imaging modalities commonly used include single-photon–emission tomography and positron-emission tomography.
With regard to SSR scintigraphy testing, PET using Ga–DOTATATE/TOC is preferable to Octreoscan if it is available, because offers better spatial resolution and has a shorter scanning time. It has sensitivity of 97% and specificity of 92% and hence is preferable over Octreoscan in highly aggressive, atypical bronchial NETs. It also provides an estimate of receptor density and evidence of the functionality of receptors, which helps with selection of suitable treatments that act on these receptors.7
Tumor markers
Serum levels of chromogranin A in bronchial NETs are expressed at a lower rate than are other sites of carcinoid tumors, so its measurement is of limited utility in following disease activity in bronchial NETs.4,8
Bronchoscopy
About 75% of pulmonary carcinoids are visible on bronchoscopy. The bronchoscopic appearance may be characteristic but it is preferable that brushings or biopsy be performed to confirm the diagnosis. For central tumors endobronchial; and for peripheral tumors, CT-guided percutaneous biopsy is the accepted diagnostic approach. Cytologic study of bronchial brushings is more sensitive than sputum cytology, but the diagnostic yield of brushing is low overall (about 40%) and hence fine-needle biopsy is preferred. 8
A negative finding on biopsy should not produce a false sense of confidence. If a suspicion of malignancy exists despite a negative finding on transthoracic biopsy, surgical excision of the nodule and pathologic analysis should be undertaken.
Histological findings
In typical carcinoid tumors, cells tend to group in nests, cords, or broad sheets. Arrangement is orderly, with groups of cells separated by highly vascular septa of connective tissue.9Individual cell features include small and polygonal cells with finely granular eosinophilic cytoplasm (Figure 2). Nuclei are small and round. Mitoses are infrequent (Figure 3).
On electron microscopy, well-formed desmosomes and abundant neurosecretory granules are seen. Many pulmonary carcinoid tumors stain positive for a variety of neuroendocrine markers. Electron microscopy is of historical interest but is not used for tissue diagnosis for bronchial carcinoid patients.
Typical vs atypical tumors
In all, 10% of the carcinoid tumors are atypical in nature. They are generally larger than typical carcinoids and are located in the periphery of the lung in about 50% of cases. They have more aggressive behavior and tend to metastasize more commonly.2 Neither location nor size are distinguishing features. The distinction is based on histology and includes one or all of the following features:8,9
n Increased mitotic activity in a tumor with an identifiable carcinoid cellular arrangement with 2-10 mitotic figures per high-power field.9
n Pleomorphism and irregular nuclei with hyperchromatism and prominent nucleoli.
n Areas of increased cellularity with loss of the regular, organized architecture observed in typical carcinoid.
n Areas of necrosis within the tumor.
Ki-67 cell proliferation labeling index can be used to distinguish between high-grade lung NETs (>40%) and carcinoids (<20%), particularly in crushed biopsy specimens in which carcinoids may be mistaken for small-cell lung cancers. However, given overlap in the distribution of Ki-67 labeling index between typical carcinoids (≤5%) and atypical carcinoids (≤20%), Ki-67 expression does not reliably distinguish between well-differentiated lung carcinoids. The utility of Ki-67 to differentiate between typical and atypical carcinoids has yet to be established, and it is not presently recommended.9 Hence, the number of mitotic figures per high-power field of viable tumor area and presence or absence of necrosis continue to be the salient features distinguishing typical and atypical bronchial NETs.
Staging10
Lung NETs are staged using the same tumor, node, metastasis (TNM) classification from the American Joint Committee on Cancer (AJCC) that is used for bronchogenic lung carcinomas (Table).
Typical bronchial NETs most commonly present as stage I tumors, whereas more than one-half of atypical tumors are stage II (bronchopulmonary nodal involvement) or III (mediastinal nodal involvement) at presentation.
Treatment
Localized or nonmetastatic and rescetable disease
Surgical treatment. As with other non–small-cell lung cancers (NSCLCs), surgical resection is the treatment of choice for early-stage carcinoid. The long-term prognosis is typically excellent, with a 10-year disease-free survival of 77%-94%.11, 12 The extent of resection is determined by the tumor size, histology, and location. For NSCLC, the standard surgical approach is the minimal anatomic resection (lobectomy, sleeve lobectomy, bilobectomy, or pneumonectomy) needed to get microscopically negative margins, with an associated mediastinal and hilar lymph node dissection for staging.13
Given the indolent nature of typical carcinoids, there has been extensive research to evaluate whether a sublobar resection is oncologically appropriate for these tumors. Although there are no comprehensive randomized studies comparing sublobar resection with lobectomy for typical carcinoids, findings from numerous database reviews and single-center studies suggest that sublobar resections are noninferior.14-17 Due to the higher nodal metastatic rate and the overall poorer prognosis associated with atypical carcinoids, formal anatomic resection is still recommended with atypical histology.18
An adaptive approach must be taken for patients who undergo wedge resection of pulmonary lesions without a known diagnosis. If intraoperative frozen section is consistent with carcinoid and the margins are negative, mediastinal lymph node dissection should be performed. If the patient is node negative, then completion lobectomy is not required. In node-positive patients with adequate pulmonary reserve, lobectomy should be performed regardless of histology. If atypical features are found during pathologic evaluation, then interval completion lobectomy may be patients with adequate pulmonary reserve.19,20
As with other pulmonary malignancies, clinical or radiographic suspicion of mediastinal lymph node involvement requires invasive staging before pulmonary resection is considered. If the patient is proven to have mediastinal metastatic disease, then multimodality treatment should be considered.20
Adjuvant therapy. Postoperative adjuvant therapy for most resected bronchial NETs, even in the setting of positive lymph nodes, is generally not recommended.7 In clinical practice, adjuvant platinum-based chemotherapy with or without radiation therapy (RT) is a reasonable option for patients with histologically aggressive-appearing or poorly differentiated stage III atypical bronchial NETs, although there is only limited evidence to support this. RT is a reasonable option for atypical bronchial NETs if gross residual disease remains after surgery, although it has not been proven that this improves outcomes.7
Nonmetastatic and unresectable disease
For inoperable patients and for those with surgically unresectable but nonmetastatic disease, options for local control of tumor growth include RT with or without concurrent chemotherapy and palliative endobronchial resection of obstructing tumor.21
Metastatic and unresectable disease
Everolimus. In February 2016, everolimus was approved by the US Food and Drug Administration (FDA) as first-line therapy for progressive, well-differentiated, nonfunctional NETs of lung origin that are unresectable, locally advanced, or metastatic. The aApproval was based on the RADIANT-4 trial, in which median progression-free survival was 11 months in the 205 patients allocated to receive everolimus (10 mg/day) and 3.9 months in the 97 patients who received placebo. Everolimus was associated with a 52% reduction in the estimated risk of progression or death.22
Somastatin analogues (SSA). There is lack of comprehensive data on the role of SSA compared with everolimus in lung carcinoid. The National Comprehensive Cancer Network (NCCN) guidelines on NETs and SCLCs recommend the consideration of octreotide or lanreotide as first-line therapies for select patients with symptoms of carcinoid syndrome or octreotide-positive scans.21 Guidelines from the European Neuroendocrine Tumor Society (ENETS)19 also recommend the use of SSAs as a first-line option in patients with: lung carcinoids exhibiting hormone-related symptoms or slowly progressive typical or atypical carcinoid with a low proliferative index (preferably Ki-67 <10%), provided there is a strongly positive SSTR status.
In cases in which metastatic lung NETs are associated with the carcinoid syndrome, initiation of long-acting SSA therapy in combination with everolimus is recommended.
Cytotoxic chemotherapy. According to the NCCN guidelines, cisplatin-etoposide or other cytotoxic regimens (eg, those that are temozolomide based) are recommended for advanced typical and atypical carcinoids, with cisplatin-etoposide being the preferred first-line systemic regimen in stage IV atypical carcinoid.22 ENETS guidelines stipulate that systemic chemotherapy is generally restricted to atypical carcinoid after failure of first-line therapies and only under certain conditions (Ki-67 >15%, rapidly progressive disease, and SSTR-negative disease).19 Based on a summary of NCCN and ENET guidelines:
n For patients with highly aggressive atypical bronchial NETs, a combination of platinum- and etoposide-based regimens such as those used for small-cell lung cancer has shown better response rate and overall survival data.
n For patients with typical or atypical bronchial NETs, temozolomide can be used as monotherapy or combination with capecitabine, although there are no findings from large randomized controlled trials to support this. Capecitabine-temozolomide has recently shown moderate activity in a small, single-institution study of patients with advanced lung carcinoids (N = 19), with 11 of 17 assessable patients (65%) demonstrating stable disease or partial response.23
n The following regimens can also be used for advanced disease after failure of somastatin analogues, although there are limited data for objective responses:24,25fluorouracil plus dacarbazine; epirubicin, capecitabine plus oxaliplatin; and capecitabine plus liposomal doxorubicin.
Participation in a clinical trial should be encouraged for patients with progressive bronchial NETs during any line of therapy. For patients who have a limited, potentially resectable liver-isolated metastatic NET, surgical resection should be pursued. For more extensive unresectable liver-dominant metastatic disease, treatment options include embolization, radiofrequency ablation, and cryoablation.20,22
Posttreatment surveillance
Posttreatment surveillance after resection of node-positive typical bronchial NETs and for all atypical tumors.26 Patients with lymph-node–negative typical bronchial NETs are very unlikely to benefit from postoperative surveillance because of the very low risk of recurrence. CT imaging (including the thorax and abdomen) every 6 months for 2 years, followed by annual scans for a total of 5-10 years are a reasonable surveillance schedule.
Prognosis 18,27
Typical bronchial NETs have an excellent prognosis after surgical resection. Reported 5-year survival rates are 87%-100%; the corresponding rates at 10 years are 82%-87%. Features associated with negative prognostic significance include lymph-node involvement and incomplete resection.
Atypical bronchial NETs have a worse prognosis than do typical tumors. Five-year survival rates range widely, from 30%-95%; the corresponding rates at 10 years are 35%-56%. Atypical tumors have a greater tendency to metastasize (16%-23%) and recur locally (3%-25%). Distant metastases to the liver or bone are more common than local recurrence. Adverse influence of nodal metastases on prognosis is more profound than for typical tumors. Survival rates by stage for patients who underwent surgical resection (including typical and atypical carcinoid27) are: stage I, 93%; stage II, 85%; stage III, 75%; and stage IV, 57%.
1. Hauso O, Gustafsson BI, Kidd M, et al. Neuroendocrine tumor epidemiology: contrasting Norway and North America. Cancer. 2008;113(10):2655-2664.
2. Fink G, Krelbaum T, Yellin A, et al. Pulmonary carcinoid: presentation, diagnosis, and outcome in 142 cases in Israel and review of 640 cases from the literature. Chest. 2001;119(6):1647-1651.
3. Limper AH, Carpenter PC, Scheithauer B, Staats BA. The Cushing syndrome induced by bronchial carcinoid tumors. Ann Intern Med. 1992;117(3):209-214.
4. Meisinger QC, Klein JS, Butnor KJ, Gentchos G, Leavitt BJ. CT features of peripheral pulmonary carcinoid tumors. AJR Am J Roentgenol. 2011;197(5):1073-1080.
5. Guckel C, Schnabel K, Deimling M, Steinbrich W. Solitary pulmonary nodules: MR evaluation of enhancement patterns with contrast-enhanced dynamic snapshot gradient-echo imaging. Radiology. 1996;200(3):681-686.
6. Jindal T, Kumar A, Venkitaraman B, et al. Evaluation of the role of [18F]FDG-PET/CT and [68Ga]DOTATOC-PET/CT in differentiating typical and atypical pulmonary carcinoids. Cancer Imaging. 2011;11:70-75.
7. Caplin ME, Baudin E, Ferolla P, et al. Pulmonary neuroendocrine (carcinoid) tumors: European Neuroendocrine Tumor Society expert consensus and recommendations for best practice for typical and atypical pulmonary carcinoids. Ann Oncol. 2015;26(8):1604-1620.
8. Travis WD. Pathology and diagnosis of neuroendocrine tumors: lung neuroendocrine. Thorac Surg Clin. 2014;24(3):257-266.
9. Warren WH, Memoli VA, Gould VE. Immunohistochemical and ultrastructural analysis of bronchopulmonary neuroendocrine neoplasms. II. Well-differentiated neuroendocrine carcinomas. Ultrastruct Pathol. 1984;7(2-3):185-199.
10. Goldstraw P, Chansky K, Crowley J, et al. The IASLC Lung Cancer Staging Project: Proposals for revision of the TNM stage groupings in the forthcoming (eighth) edition of the TNM classification for lung cancer. J Thorac Oncol. 2016;11(1):39-51.
11. McCaughan BC, Martini N, Bains MS. Bronchial carcinoids. Review of 124 cases. J Thorac Cardiovasc Surg. 1985;89(1):8-17.
12. Hurt R, Bates M. Carcinoid tumours of the bronchus: a 33-year experience. Thorax. 1984;39(8):617-623.
13. Ettinger DS, Wood DE, Akerley W, et al. Non-small cell lung cancer, version 1.2015. J Natl Compr Cancer Netw. 2014;12(12):1738-1761.
14. Ferguson MK, Landreneau RJ, Hazelrigg SR, et al. Long-term outcome after resection for bronchial carcinoid tumors. Eur J Cardiothorac Surg. 2000;18(2):156-161.
15. Lucchi M, Melfi F, Ribechini A, et al. Sleeve and wedge parenchyma-sparing bronchial resections in low-grade neoplasms of the bronchial airway. J Thorac Cardiovasc Surg. 2007;134(2):373-377.
16. Yendamuri S, Gold D, Jayaprakash V, Dexter E, Nwogu C, Demmy T. Is sublobar resection sufficient for carcinoid tumors? Ann Thorac Surg. 2011;92(5):1774-1778; discussion 8-9.
17. Fox M, Van Berkel V, Bousamra M II, Sloan S, Martin RC II. Surgical management of pulmonary carcinoid tumors: sublobar resection versus lobectomy. Am J Surg. 2013;205(2):200-208.
18. Cardillo G, Sera F, Di Martino M, et al. Bronchial carcinoid tumors: nodal status and long-term survival after resection. Ann Thorac Surg. 2004;77(5):1781-1785.
19. Oberg K, Hellman P, Ferolla P, Papotti M; ESMO Guidelines Working Group. Neuroendocrine bronchial and thymic tumors: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2012;23(suppl 7:vii120-3).
20. Filosso PL, Ferolla P, Guerrera F, et al. Multidisciplinary management of advanced lung neuroendocrine tumors. J Thorac Dis. 2015;7(Suppl 2):S163-171.
21. Kulke MH, Shah MH, Benson AB III, et al. Neuroendocrine tumors, version 1.2015. J Natl Compr Cancer Netw. 2015;13(1):78-108.
22. Yao JC, Fazio N, Singh S, et al. Everolimus for the treatment of advanced, non-functional neuroendocrine tumours of the lung or gastrointestinal tract (RADIANT-4): a randomised, placebo-controlled, phase 3 study. Lancet. 2016;387(10022):968-977.
23. Ramirez RA, Beyer DT, Chauhan A, Boudreaux JP, Wang YZ, Woltering EA. The role of capecitabine/temozolomide in metastatic neuroendocrine tumors. Oncologist. 2016;21(6):671-675.
24. Bajetta E, Rimassa L, Carnaghi C, et al. 5-Fluorouracil, dacarbazine, and epirubicin in the treatment of patients with neuroendocrine tumors. Cancer. 1998;83(2):372-378.
25. Masi G, Fornaro L, Cupini S, et al. Refractory neuroendocrine tumor-response to liposomal doxorubicin and capecitabine. Nat Rev Clin Oncol. 2009;6(11):670-674.
26. Lou F, Sarkaria I, Pietanza C, et al. Recurrence of pulmonary carcinoid tumors after resection: implications for postoperative surveillance. Ann Thorac Surg. 2013;96(4):1156-1162.
27. Beasley MB, Thunnissen FB, Brambilla E, et al. Pulmonary atypical carcinoid: predictors of survival in 106 cases. Human Pathol. 2000;31(10):1255-1265.
Carcinoid lung tumors represent the most indolent form of a spectrum of bronchopulmonary neuroendocrine tumors (NETs) that includes small-cell carcinoma as its most malignant member, as well as several other forms of intermediately aggressive tumors, such as atypical carcinoid.1 Carcinoids represent 1.2% of all primary lung malignancies. Their incidence in the United States has increased rapidly over the last 30 years and is currently about 6% a year. Lung carcinoids are more prevalent in whites compared with blacks, and in Asians compared with non-Asians. They are less common in Hispanics compared with non-Hispanics.1 Typical carcinoids represent 80%-90% of all lung carcinoids and occur more frequently in the fifth and sixth decades of life. They can, however, occur at any age, and are the most common lung tumor in childhood.1
Etiology and risk factors
Unlike carcinoma of the lung, no external environmental toxin or other stimulus has been identified as a causative agent for the development of pulmonary carcinoid tumors. It is not clear if there is an association between bronchial NETs and smoking.1 Nearly all bronchial NETs are sporadic; however, they can rarely occur in the setting of multiple endocrine neoplasia type 1.1
Presentation
About 60% of the patients with bronchial carcinoids are symptomatic at presentation. The most common clinical findings are those associated with bronchial obstruction, such as persistent cough, hemoptysis, and recurrent or obstructive pneumonitis. Wheezing, chest pain, and dyspnea also may be noted.2 Various endocrine or neuroendocrine syndromes can be initial clinical manifestations of either typical or atypical pulmonary carcinoid tumors, but that is not common Cushing syndrome (ectopic production and secretion of adrenocorticotropic hormone [ACTH]) may occur in about 2% of lung carcinoid.3 In cases of malignancy, the presence of metastatic disease can produce weight loss, weakness, and a general feeling of ill health.
Diagnostic work-up
Biochemical test
There is no biochemical study that can be used as a screening test to determine the presence of a carcinoid tumor or to diagnose a known pulmonary mass as a carcinoid tumor. Neuroendocrine cells produce biologically active amines and peptides that can be detected in serum and urine. Although the syndromes associated with lung carcinoids are seen in about 1%-2% of the patients, assays of specific hormones or other circulating neuroendocrine substances, such as ACTH, melanocyte-stimulating hormone, or growth hormone may establish the existence of a clinically suspected syndrome.
Chest radiography
An abnormal finding on chest radiography is present in about 75% of patients with a pulmonary carcinoid tumor.1 Findings include either the presence of the tumor mass itself or indirect evidence of its presence observed as parenchymal changes associated with bronchial obstruction from the mass.
Computed-tomography imaging
High-resolution computed-tomography (CT) imaging is the one of the best types of CT examination for evaluation of a pulmonary carcinoid tumor.4 A CT scan provides excellent resolution of tumor extent, location, and the presence or absence of mediastinal adenopathy. It also aids in morphologic characterization of peripheral (Figure 1) and especially centrally located carcinoids, which may be purely intraluminal (polypoid configuration), exclusively extra luminal, or more frequently, a mixture of intraluminal and extraluminal components.
CT scans may also be helpful for differentiating tumor from postobstructive atelectasis or bronchial obstruction-related mucoid impaction. Intravenous contrast in CT imaging can be useful in differentiating malignant from benign lesions. Because carcinoid tumors are highly vascular, they show greater enhancement on contrast CT than do benign lesions. The sensitivity of CT for detecting metastatic hilar or mediastinal nodes is high, but specificity is as low as 45%.4
Typical carcinoid is rarely metastatic so most patients do not need CT or MRI imaging to evaluate for liver involvement. Liver imaging is appropriate in patients with evidence of mediastinal involvement, relatively high mitotic rate, or clinical evidence of the carcinoid syndrome.8 To evaluate for metastatic spread to the liver, multiphase contrast-enhanced liver CT scans should be performed with arterial and portal-venous phases because carcinoid liver metastases are often hypervascular and appear isodense relative to the liver parenchyma after contrast administration.4 An MRI is often preferred the modality to evaluate for metastatic spread to the liver because of its higher sensitivity.5
Positron-emission tomography
Although carcinoid tumors of the lung are highly vascular, they do not show increased metabolic activity on positron-emission tomography (PET) and would be incorrectly designated as benign lesions on the basis of findings from a PET scan. Fludeoxyglucose F-18 PET has shown utility as a radiologic marker for atypical carcinoids, particularly for those with a higher proliferation index with Ki-67 index of 10%-20%.6
Radionucleotide studies
Somatostatin receptors (SSRs) are present in many tumors of neuroendocrine origin, including carcinoid tumors. These receptors interact with each other and undergo dimerization and internalization. SSTR subtypes (SSTRs) overexpressed in NETs are related to the type, origin, and grade of differentiation of tumor. The overexpression of an SSTR is a characteristic feature of bronchial NETs, which can be used to localize the primary tumor and its metastases by imaging with the radiolabeled SST analogues. Radionucleotide imaging modalities commonly used include single-photon–emission tomography and positron-emission tomography.
With regard to SSR scintigraphy testing, PET using Ga–DOTATATE/TOC is preferable to Octreoscan if it is available, because offers better spatial resolution and has a shorter scanning time. It has sensitivity of 97% and specificity of 92% and hence is preferable over Octreoscan in highly aggressive, atypical bronchial NETs. It also provides an estimate of receptor density and evidence of the functionality of receptors, which helps with selection of suitable treatments that act on these receptors.7
Tumor markers
Serum levels of chromogranin A in bronchial NETs are expressed at a lower rate than are other sites of carcinoid tumors, so its measurement is of limited utility in following disease activity in bronchial NETs.4,8
Bronchoscopy
About 75% of pulmonary carcinoids are visible on bronchoscopy. The bronchoscopic appearance may be characteristic but it is preferable that brushings or biopsy be performed to confirm the diagnosis. For central tumors endobronchial; and for peripheral tumors, CT-guided percutaneous biopsy is the accepted diagnostic approach. Cytologic study of bronchial brushings is more sensitive than sputum cytology, but the diagnostic yield of brushing is low overall (about 40%) and hence fine-needle biopsy is preferred. 8
A negative finding on biopsy should not produce a false sense of confidence. If a suspicion of malignancy exists despite a negative finding on transthoracic biopsy, surgical excision of the nodule and pathologic analysis should be undertaken.
Histological findings
In typical carcinoid tumors, cells tend to group in nests, cords, or broad sheets. Arrangement is orderly, with groups of cells separated by highly vascular septa of connective tissue.9Individual cell features include small and polygonal cells with finely granular eosinophilic cytoplasm (Figure 2). Nuclei are small and round. Mitoses are infrequent (Figure 3).
On electron microscopy, well-formed desmosomes and abundant neurosecretory granules are seen. Many pulmonary carcinoid tumors stain positive for a variety of neuroendocrine markers. Electron microscopy is of historical interest but is not used for tissue diagnosis for bronchial carcinoid patients.
Typical vs atypical tumors
In all, 10% of the carcinoid tumors are atypical in nature. They are generally larger than typical carcinoids and are located in the periphery of the lung in about 50% of cases. They have more aggressive behavior and tend to metastasize more commonly.2 Neither location nor size are distinguishing features. The distinction is based on histology and includes one or all of the following features:8,9
n Increased mitotic activity in a tumor with an identifiable carcinoid cellular arrangement with 2-10 mitotic figures per high-power field.9
n Pleomorphism and irregular nuclei with hyperchromatism and prominent nucleoli.
n Areas of increased cellularity with loss of the regular, organized architecture observed in typical carcinoid.
n Areas of necrosis within the tumor.
Ki-67 cell proliferation labeling index can be used to distinguish between high-grade lung NETs (>40%) and carcinoids (<20%), particularly in crushed biopsy specimens in which carcinoids may be mistaken for small-cell lung cancers. However, given overlap in the distribution of Ki-67 labeling index between typical carcinoids (≤5%) and atypical carcinoids (≤20%), Ki-67 expression does not reliably distinguish between well-differentiated lung carcinoids. The utility of Ki-67 to differentiate between typical and atypical carcinoids has yet to be established, and it is not presently recommended.9 Hence, the number of mitotic figures per high-power field of viable tumor area and presence or absence of necrosis continue to be the salient features distinguishing typical and atypical bronchial NETs.
Staging10
Lung NETs are staged using the same tumor, node, metastasis (TNM) classification from the American Joint Committee on Cancer (AJCC) that is used for bronchogenic lung carcinomas (Table).
Typical bronchial NETs most commonly present as stage I tumors, whereas more than one-half of atypical tumors are stage II (bronchopulmonary nodal involvement) or III (mediastinal nodal involvement) at presentation.
Treatment
Localized or nonmetastatic and rescetable disease
Surgical treatment. As with other non–small-cell lung cancers (NSCLCs), surgical resection is the treatment of choice for early-stage carcinoid. The long-term prognosis is typically excellent, with a 10-year disease-free survival of 77%-94%.11, 12 The extent of resection is determined by the tumor size, histology, and location. For NSCLC, the standard surgical approach is the minimal anatomic resection (lobectomy, sleeve lobectomy, bilobectomy, or pneumonectomy) needed to get microscopically negative margins, with an associated mediastinal and hilar lymph node dissection for staging.13
Given the indolent nature of typical carcinoids, there has been extensive research to evaluate whether a sublobar resection is oncologically appropriate for these tumors. Although there are no comprehensive randomized studies comparing sublobar resection with lobectomy for typical carcinoids, findings from numerous database reviews and single-center studies suggest that sublobar resections are noninferior.14-17 Due to the higher nodal metastatic rate and the overall poorer prognosis associated with atypical carcinoids, formal anatomic resection is still recommended with atypical histology.18
An adaptive approach must be taken for patients who undergo wedge resection of pulmonary lesions without a known diagnosis. If intraoperative frozen section is consistent with carcinoid and the margins are negative, mediastinal lymph node dissection should be performed. If the patient is node negative, then completion lobectomy is not required. In node-positive patients with adequate pulmonary reserve, lobectomy should be performed regardless of histology. If atypical features are found during pathologic evaluation, then interval completion lobectomy may be patients with adequate pulmonary reserve.19,20
As with other pulmonary malignancies, clinical or radiographic suspicion of mediastinal lymph node involvement requires invasive staging before pulmonary resection is considered. If the patient is proven to have mediastinal metastatic disease, then multimodality treatment should be considered.20
Adjuvant therapy. Postoperative adjuvant therapy for most resected bronchial NETs, even in the setting of positive lymph nodes, is generally not recommended.7 In clinical practice, adjuvant platinum-based chemotherapy with or without radiation therapy (RT) is a reasonable option for patients with histologically aggressive-appearing or poorly differentiated stage III atypical bronchial NETs, although there is only limited evidence to support this. RT is a reasonable option for atypical bronchial NETs if gross residual disease remains after surgery, although it has not been proven that this improves outcomes.7
Nonmetastatic and unresectable disease
For inoperable patients and for those with surgically unresectable but nonmetastatic disease, options for local control of tumor growth include RT with or without concurrent chemotherapy and palliative endobronchial resection of obstructing tumor.21
Metastatic and unresectable disease
Everolimus. In February 2016, everolimus was approved by the US Food and Drug Administration (FDA) as first-line therapy for progressive, well-differentiated, nonfunctional NETs of lung origin that are unresectable, locally advanced, or metastatic. The aApproval was based on the RADIANT-4 trial, in which median progression-free survival was 11 months in the 205 patients allocated to receive everolimus (10 mg/day) and 3.9 months in the 97 patients who received placebo. Everolimus was associated with a 52% reduction in the estimated risk of progression or death.22
Somastatin analogues (SSA). There is lack of comprehensive data on the role of SSA compared with everolimus in lung carcinoid. The National Comprehensive Cancer Network (NCCN) guidelines on NETs and SCLCs recommend the consideration of octreotide or lanreotide as first-line therapies for select patients with symptoms of carcinoid syndrome or octreotide-positive scans.21 Guidelines from the European Neuroendocrine Tumor Society (ENETS)19 also recommend the use of SSAs as a first-line option in patients with: lung carcinoids exhibiting hormone-related symptoms or slowly progressive typical or atypical carcinoid with a low proliferative index (preferably Ki-67 <10%), provided there is a strongly positive SSTR status.
In cases in which metastatic lung NETs are associated with the carcinoid syndrome, initiation of long-acting SSA therapy in combination with everolimus is recommended.
Cytotoxic chemotherapy. According to the NCCN guidelines, cisplatin-etoposide or other cytotoxic regimens (eg, those that are temozolomide based) are recommended for advanced typical and atypical carcinoids, with cisplatin-etoposide being the preferred first-line systemic regimen in stage IV atypical carcinoid.22 ENETS guidelines stipulate that systemic chemotherapy is generally restricted to atypical carcinoid after failure of first-line therapies and only under certain conditions (Ki-67 >15%, rapidly progressive disease, and SSTR-negative disease).19 Based on a summary of NCCN and ENET guidelines:
n For patients with highly aggressive atypical bronchial NETs, a combination of platinum- and etoposide-based regimens such as those used for small-cell lung cancer has shown better response rate and overall survival data.
n For patients with typical or atypical bronchial NETs, temozolomide can be used as monotherapy or combination with capecitabine, although there are no findings from large randomized controlled trials to support this. Capecitabine-temozolomide has recently shown moderate activity in a small, single-institution study of patients with advanced lung carcinoids (N = 19), with 11 of 17 assessable patients (65%) demonstrating stable disease or partial response.23
n The following regimens can also be used for advanced disease after failure of somastatin analogues, although there are limited data for objective responses:24,25fluorouracil plus dacarbazine; epirubicin, capecitabine plus oxaliplatin; and capecitabine plus liposomal doxorubicin.
Participation in a clinical trial should be encouraged for patients with progressive bronchial NETs during any line of therapy. For patients who have a limited, potentially resectable liver-isolated metastatic NET, surgical resection should be pursued. For more extensive unresectable liver-dominant metastatic disease, treatment options include embolization, radiofrequency ablation, and cryoablation.20,22
Posttreatment surveillance
Posttreatment surveillance after resection of node-positive typical bronchial NETs and for all atypical tumors.26 Patients with lymph-node–negative typical bronchial NETs are very unlikely to benefit from postoperative surveillance because of the very low risk of recurrence. CT imaging (including the thorax and abdomen) every 6 months for 2 years, followed by annual scans for a total of 5-10 years are a reasonable surveillance schedule.
Prognosis 18,27
Typical bronchial NETs have an excellent prognosis after surgical resection. Reported 5-year survival rates are 87%-100%; the corresponding rates at 10 years are 82%-87%. Features associated with negative prognostic significance include lymph-node involvement and incomplete resection.
Atypical bronchial NETs have a worse prognosis than do typical tumors. Five-year survival rates range widely, from 30%-95%; the corresponding rates at 10 years are 35%-56%. Atypical tumors have a greater tendency to metastasize (16%-23%) and recur locally (3%-25%). Distant metastases to the liver or bone are more common than local recurrence. Adverse influence of nodal metastases on prognosis is more profound than for typical tumors. Survival rates by stage for patients who underwent surgical resection (including typical and atypical carcinoid27) are: stage I, 93%; stage II, 85%; stage III, 75%; and stage IV, 57%.
Carcinoid lung tumors represent the most indolent form of a spectrum of bronchopulmonary neuroendocrine tumors (NETs) that includes small-cell carcinoma as its most malignant member, as well as several other forms of intermediately aggressive tumors, such as atypical carcinoid.1 Carcinoids represent 1.2% of all primary lung malignancies. Their incidence in the United States has increased rapidly over the last 30 years and is currently about 6% a year. Lung carcinoids are more prevalent in whites compared with blacks, and in Asians compared with non-Asians. They are less common in Hispanics compared with non-Hispanics.1 Typical carcinoids represent 80%-90% of all lung carcinoids and occur more frequently in the fifth and sixth decades of life. They can, however, occur at any age, and are the most common lung tumor in childhood.1
Etiology and risk factors
Unlike carcinoma of the lung, no external environmental toxin or other stimulus has been identified as a causative agent for the development of pulmonary carcinoid tumors. It is not clear if there is an association between bronchial NETs and smoking.1 Nearly all bronchial NETs are sporadic; however, they can rarely occur in the setting of multiple endocrine neoplasia type 1.1
Presentation
About 60% of the patients with bronchial carcinoids are symptomatic at presentation. The most common clinical findings are those associated with bronchial obstruction, such as persistent cough, hemoptysis, and recurrent or obstructive pneumonitis. Wheezing, chest pain, and dyspnea also may be noted.2 Various endocrine or neuroendocrine syndromes can be initial clinical manifestations of either typical or atypical pulmonary carcinoid tumors, but that is not common Cushing syndrome (ectopic production and secretion of adrenocorticotropic hormone [ACTH]) may occur in about 2% of lung carcinoid.3 In cases of malignancy, the presence of metastatic disease can produce weight loss, weakness, and a general feeling of ill health.
Diagnostic work-up
Biochemical test
There is no biochemical study that can be used as a screening test to determine the presence of a carcinoid tumor or to diagnose a known pulmonary mass as a carcinoid tumor. Neuroendocrine cells produce biologically active amines and peptides that can be detected in serum and urine. Although the syndromes associated with lung carcinoids are seen in about 1%-2% of the patients, assays of specific hormones or other circulating neuroendocrine substances, such as ACTH, melanocyte-stimulating hormone, or growth hormone may establish the existence of a clinically suspected syndrome.
Chest radiography
An abnormal finding on chest radiography is present in about 75% of patients with a pulmonary carcinoid tumor.1 Findings include either the presence of the tumor mass itself or indirect evidence of its presence observed as parenchymal changes associated with bronchial obstruction from the mass.
Computed-tomography imaging
High-resolution computed-tomography (CT) imaging is the one of the best types of CT examination for evaluation of a pulmonary carcinoid tumor.4 A CT scan provides excellent resolution of tumor extent, location, and the presence or absence of mediastinal adenopathy. It also aids in morphologic characterization of peripheral (Figure 1) and especially centrally located carcinoids, which may be purely intraluminal (polypoid configuration), exclusively extra luminal, or more frequently, a mixture of intraluminal and extraluminal components.
CT scans may also be helpful for differentiating tumor from postobstructive atelectasis or bronchial obstruction-related mucoid impaction. Intravenous contrast in CT imaging can be useful in differentiating malignant from benign lesions. Because carcinoid tumors are highly vascular, they show greater enhancement on contrast CT than do benign lesions. The sensitivity of CT for detecting metastatic hilar or mediastinal nodes is high, but specificity is as low as 45%.4
Typical carcinoid is rarely metastatic so most patients do not need CT or MRI imaging to evaluate for liver involvement. Liver imaging is appropriate in patients with evidence of mediastinal involvement, relatively high mitotic rate, or clinical evidence of the carcinoid syndrome.8 To evaluate for metastatic spread to the liver, multiphase contrast-enhanced liver CT scans should be performed with arterial and portal-venous phases because carcinoid liver metastases are often hypervascular and appear isodense relative to the liver parenchyma after contrast administration.4 An MRI is often preferred the modality to evaluate for metastatic spread to the liver because of its higher sensitivity.5
Positron-emission tomography
Although carcinoid tumors of the lung are highly vascular, they do not show increased metabolic activity on positron-emission tomography (PET) and would be incorrectly designated as benign lesions on the basis of findings from a PET scan. Fludeoxyglucose F-18 PET has shown utility as a radiologic marker for atypical carcinoids, particularly for those with a higher proliferation index with Ki-67 index of 10%-20%.6
Radionucleotide studies
Somatostatin receptors (SSRs) are present in many tumors of neuroendocrine origin, including carcinoid tumors. These receptors interact with each other and undergo dimerization and internalization. SSTR subtypes (SSTRs) overexpressed in NETs are related to the type, origin, and grade of differentiation of tumor. The overexpression of an SSTR is a characteristic feature of bronchial NETs, which can be used to localize the primary tumor and its metastases by imaging with the radiolabeled SST analogues. Radionucleotide imaging modalities commonly used include single-photon–emission tomography and positron-emission tomography.
With regard to SSR scintigraphy testing, PET using Ga–DOTATATE/TOC is preferable to Octreoscan if it is available, because offers better spatial resolution and has a shorter scanning time. It has sensitivity of 97% and specificity of 92% and hence is preferable over Octreoscan in highly aggressive, atypical bronchial NETs. It also provides an estimate of receptor density and evidence of the functionality of receptors, which helps with selection of suitable treatments that act on these receptors.7
Tumor markers
Serum levels of chromogranin A in bronchial NETs are expressed at a lower rate than are other sites of carcinoid tumors, so its measurement is of limited utility in following disease activity in bronchial NETs.4,8
Bronchoscopy
About 75% of pulmonary carcinoids are visible on bronchoscopy. The bronchoscopic appearance may be characteristic but it is preferable that brushings or biopsy be performed to confirm the diagnosis. For central tumors endobronchial; and for peripheral tumors, CT-guided percutaneous biopsy is the accepted diagnostic approach. Cytologic study of bronchial brushings is more sensitive than sputum cytology, but the diagnostic yield of brushing is low overall (about 40%) and hence fine-needle biopsy is preferred. 8
A negative finding on biopsy should not produce a false sense of confidence. If a suspicion of malignancy exists despite a negative finding on transthoracic biopsy, surgical excision of the nodule and pathologic analysis should be undertaken.
Histological findings
In typical carcinoid tumors, cells tend to group in nests, cords, or broad sheets. Arrangement is orderly, with groups of cells separated by highly vascular septa of connective tissue.9Individual cell features include small and polygonal cells with finely granular eosinophilic cytoplasm (Figure 2). Nuclei are small and round. Mitoses are infrequent (Figure 3).
On electron microscopy, well-formed desmosomes and abundant neurosecretory granules are seen. Many pulmonary carcinoid tumors stain positive for a variety of neuroendocrine markers. Electron microscopy is of historical interest but is not used for tissue diagnosis for bronchial carcinoid patients.
Typical vs atypical tumors
In all, 10% of the carcinoid tumors are atypical in nature. They are generally larger than typical carcinoids and are located in the periphery of the lung in about 50% of cases. They have more aggressive behavior and tend to metastasize more commonly.2 Neither location nor size are distinguishing features. The distinction is based on histology and includes one or all of the following features:8,9
n Increased mitotic activity in a tumor with an identifiable carcinoid cellular arrangement with 2-10 mitotic figures per high-power field.9
n Pleomorphism and irregular nuclei with hyperchromatism and prominent nucleoli.
n Areas of increased cellularity with loss of the regular, organized architecture observed in typical carcinoid.
n Areas of necrosis within the tumor.
Ki-67 cell proliferation labeling index can be used to distinguish between high-grade lung NETs (>40%) and carcinoids (<20%), particularly in crushed biopsy specimens in which carcinoids may be mistaken for small-cell lung cancers. However, given overlap in the distribution of Ki-67 labeling index between typical carcinoids (≤5%) and atypical carcinoids (≤20%), Ki-67 expression does not reliably distinguish between well-differentiated lung carcinoids. The utility of Ki-67 to differentiate between typical and atypical carcinoids has yet to be established, and it is not presently recommended.9 Hence, the number of mitotic figures per high-power field of viable tumor area and presence or absence of necrosis continue to be the salient features distinguishing typical and atypical bronchial NETs.
Staging10
Lung NETs are staged using the same tumor, node, metastasis (TNM) classification from the American Joint Committee on Cancer (AJCC) that is used for bronchogenic lung carcinomas (Table).
Typical bronchial NETs most commonly present as stage I tumors, whereas more than one-half of atypical tumors are stage II (bronchopulmonary nodal involvement) or III (mediastinal nodal involvement) at presentation.
Treatment
Localized or nonmetastatic and rescetable disease
Surgical treatment. As with other non–small-cell lung cancers (NSCLCs), surgical resection is the treatment of choice for early-stage carcinoid. The long-term prognosis is typically excellent, with a 10-year disease-free survival of 77%-94%.11, 12 The extent of resection is determined by the tumor size, histology, and location. For NSCLC, the standard surgical approach is the minimal anatomic resection (lobectomy, sleeve lobectomy, bilobectomy, or pneumonectomy) needed to get microscopically negative margins, with an associated mediastinal and hilar lymph node dissection for staging.13
Given the indolent nature of typical carcinoids, there has been extensive research to evaluate whether a sublobar resection is oncologically appropriate for these tumors. Although there are no comprehensive randomized studies comparing sublobar resection with lobectomy for typical carcinoids, findings from numerous database reviews and single-center studies suggest that sublobar resections are noninferior.14-17 Due to the higher nodal metastatic rate and the overall poorer prognosis associated with atypical carcinoids, formal anatomic resection is still recommended with atypical histology.18
An adaptive approach must be taken for patients who undergo wedge resection of pulmonary lesions without a known diagnosis. If intraoperative frozen section is consistent with carcinoid and the margins are negative, mediastinal lymph node dissection should be performed. If the patient is node negative, then completion lobectomy is not required. In node-positive patients with adequate pulmonary reserve, lobectomy should be performed regardless of histology. If atypical features are found during pathologic evaluation, then interval completion lobectomy may be patients with adequate pulmonary reserve.19,20
As with other pulmonary malignancies, clinical or radiographic suspicion of mediastinal lymph node involvement requires invasive staging before pulmonary resection is considered. If the patient is proven to have mediastinal metastatic disease, then multimodality treatment should be considered.20
Adjuvant therapy. Postoperative adjuvant therapy for most resected bronchial NETs, even in the setting of positive lymph nodes, is generally not recommended.7 In clinical practice, adjuvant platinum-based chemotherapy with or without radiation therapy (RT) is a reasonable option for patients with histologically aggressive-appearing or poorly differentiated stage III atypical bronchial NETs, although there is only limited evidence to support this. RT is a reasonable option for atypical bronchial NETs if gross residual disease remains after surgery, although it has not been proven that this improves outcomes.7
Nonmetastatic and unresectable disease
For inoperable patients and for those with surgically unresectable but nonmetastatic disease, options for local control of tumor growth include RT with or without concurrent chemotherapy and palliative endobronchial resection of obstructing tumor.21
Metastatic and unresectable disease
Everolimus. In February 2016, everolimus was approved by the US Food and Drug Administration (FDA) as first-line therapy for progressive, well-differentiated, nonfunctional NETs of lung origin that are unresectable, locally advanced, or metastatic. The aApproval was based on the RADIANT-4 trial, in which median progression-free survival was 11 months in the 205 patients allocated to receive everolimus (10 mg/day) and 3.9 months in the 97 patients who received placebo. Everolimus was associated with a 52% reduction in the estimated risk of progression or death.22
Somastatin analogues (SSA). There is lack of comprehensive data on the role of SSA compared with everolimus in lung carcinoid. The National Comprehensive Cancer Network (NCCN) guidelines on NETs and SCLCs recommend the consideration of octreotide or lanreotide as first-line therapies for select patients with symptoms of carcinoid syndrome or octreotide-positive scans.21 Guidelines from the European Neuroendocrine Tumor Society (ENETS)19 also recommend the use of SSAs as a first-line option in patients with: lung carcinoids exhibiting hormone-related symptoms or slowly progressive typical or atypical carcinoid with a low proliferative index (preferably Ki-67 <10%), provided there is a strongly positive SSTR status.
In cases in which metastatic lung NETs are associated with the carcinoid syndrome, initiation of long-acting SSA therapy in combination with everolimus is recommended.
Cytotoxic chemotherapy. According to the NCCN guidelines, cisplatin-etoposide or other cytotoxic regimens (eg, those that are temozolomide based) are recommended for advanced typical and atypical carcinoids, with cisplatin-etoposide being the preferred first-line systemic regimen in stage IV atypical carcinoid.22 ENETS guidelines stipulate that systemic chemotherapy is generally restricted to atypical carcinoid after failure of first-line therapies and only under certain conditions (Ki-67 >15%, rapidly progressive disease, and SSTR-negative disease).19 Based on a summary of NCCN and ENET guidelines:
n For patients with highly aggressive atypical bronchial NETs, a combination of platinum- and etoposide-based regimens such as those used for small-cell lung cancer has shown better response rate and overall survival data.
n For patients with typical or atypical bronchial NETs, temozolomide can be used as monotherapy or combination with capecitabine, although there are no findings from large randomized controlled trials to support this. Capecitabine-temozolomide has recently shown moderate activity in a small, single-institution study of patients with advanced lung carcinoids (N = 19), with 11 of 17 assessable patients (65%) demonstrating stable disease or partial response.23
n The following regimens can also be used for advanced disease after failure of somastatin analogues, although there are limited data for objective responses:24,25fluorouracil plus dacarbazine; epirubicin, capecitabine plus oxaliplatin; and capecitabine plus liposomal doxorubicin.
Participation in a clinical trial should be encouraged for patients with progressive bronchial NETs during any line of therapy. For patients who have a limited, potentially resectable liver-isolated metastatic NET, surgical resection should be pursued. For more extensive unresectable liver-dominant metastatic disease, treatment options include embolization, radiofrequency ablation, and cryoablation.20,22
Posttreatment surveillance
Posttreatment surveillance after resection of node-positive typical bronchial NETs and for all atypical tumors.26 Patients with lymph-node–negative typical bronchial NETs are very unlikely to benefit from postoperative surveillance because of the very low risk of recurrence. CT imaging (including the thorax and abdomen) every 6 months for 2 years, followed by annual scans for a total of 5-10 years are a reasonable surveillance schedule.
Prognosis 18,27
Typical bronchial NETs have an excellent prognosis after surgical resection. Reported 5-year survival rates are 87%-100%; the corresponding rates at 10 years are 82%-87%. Features associated with negative prognostic significance include lymph-node involvement and incomplete resection.
Atypical bronchial NETs have a worse prognosis than do typical tumors. Five-year survival rates range widely, from 30%-95%; the corresponding rates at 10 years are 35%-56%. Atypical tumors have a greater tendency to metastasize (16%-23%) and recur locally (3%-25%). Distant metastases to the liver or bone are more common than local recurrence. Adverse influence of nodal metastases on prognosis is more profound than for typical tumors. Survival rates by stage for patients who underwent surgical resection (including typical and atypical carcinoid27) are: stage I, 93%; stage II, 85%; stage III, 75%; and stage IV, 57%.
1. Hauso O, Gustafsson BI, Kidd M, et al. Neuroendocrine tumor epidemiology: contrasting Norway and North America. Cancer. 2008;113(10):2655-2664.
2. Fink G, Krelbaum T, Yellin A, et al. Pulmonary carcinoid: presentation, diagnosis, and outcome in 142 cases in Israel and review of 640 cases from the literature. Chest. 2001;119(6):1647-1651.
3. Limper AH, Carpenter PC, Scheithauer B, Staats BA. The Cushing syndrome induced by bronchial carcinoid tumors. Ann Intern Med. 1992;117(3):209-214.
4. Meisinger QC, Klein JS, Butnor KJ, Gentchos G, Leavitt BJ. CT features of peripheral pulmonary carcinoid tumors. AJR Am J Roentgenol. 2011;197(5):1073-1080.
5. Guckel C, Schnabel K, Deimling M, Steinbrich W. Solitary pulmonary nodules: MR evaluation of enhancement patterns with contrast-enhanced dynamic snapshot gradient-echo imaging. Radiology. 1996;200(3):681-686.
6. Jindal T, Kumar A, Venkitaraman B, et al. Evaluation of the role of [18F]FDG-PET/CT and [68Ga]DOTATOC-PET/CT in differentiating typical and atypical pulmonary carcinoids. Cancer Imaging. 2011;11:70-75.
7. Caplin ME, Baudin E, Ferolla P, et al. Pulmonary neuroendocrine (carcinoid) tumors: European Neuroendocrine Tumor Society expert consensus and recommendations for best practice for typical and atypical pulmonary carcinoids. Ann Oncol. 2015;26(8):1604-1620.
8. Travis WD. Pathology and diagnosis of neuroendocrine tumors: lung neuroendocrine. Thorac Surg Clin. 2014;24(3):257-266.
9. Warren WH, Memoli VA, Gould VE. Immunohistochemical and ultrastructural analysis of bronchopulmonary neuroendocrine neoplasms. II. Well-differentiated neuroendocrine carcinomas. Ultrastruct Pathol. 1984;7(2-3):185-199.
10. Goldstraw P, Chansky K, Crowley J, et al. The IASLC Lung Cancer Staging Project: Proposals for revision of the TNM stage groupings in the forthcoming (eighth) edition of the TNM classification for lung cancer. J Thorac Oncol. 2016;11(1):39-51.
11. McCaughan BC, Martini N, Bains MS. Bronchial carcinoids. Review of 124 cases. J Thorac Cardiovasc Surg. 1985;89(1):8-17.
12. Hurt R, Bates M. Carcinoid tumours of the bronchus: a 33-year experience. Thorax. 1984;39(8):617-623.
13. Ettinger DS, Wood DE, Akerley W, et al. Non-small cell lung cancer, version 1.2015. J Natl Compr Cancer Netw. 2014;12(12):1738-1761.
14. Ferguson MK, Landreneau RJ, Hazelrigg SR, et al. Long-term outcome after resection for bronchial carcinoid tumors. Eur J Cardiothorac Surg. 2000;18(2):156-161.
15. Lucchi M, Melfi F, Ribechini A, et al. Sleeve and wedge parenchyma-sparing bronchial resections in low-grade neoplasms of the bronchial airway. J Thorac Cardiovasc Surg. 2007;134(2):373-377.
16. Yendamuri S, Gold D, Jayaprakash V, Dexter E, Nwogu C, Demmy T. Is sublobar resection sufficient for carcinoid tumors? Ann Thorac Surg. 2011;92(5):1774-1778; discussion 8-9.
17. Fox M, Van Berkel V, Bousamra M II, Sloan S, Martin RC II. Surgical management of pulmonary carcinoid tumors: sublobar resection versus lobectomy. Am J Surg. 2013;205(2):200-208.
18. Cardillo G, Sera F, Di Martino M, et al. Bronchial carcinoid tumors: nodal status and long-term survival after resection. Ann Thorac Surg. 2004;77(5):1781-1785.
19. Oberg K, Hellman P, Ferolla P, Papotti M; ESMO Guidelines Working Group. Neuroendocrine bronchial and thymic tumors: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2012;23(suppl 7:vii120-3).
20. Filosso PL, Ferolla P, Guerrera F, et al. Multidisciplinary management of advanced lung neuroendocrine tumors. J Thorac Dis. 2015;7(Suppl 2):S163-171.
21. Kulke MH, Shah MH, Benson AB III, et al. Neuroendocrine tumors, version 1.2015. J Natl Compr Cancer Netw. 2015;13(1):78-108.
22. Yao JC, Fazio N, Singh S, et al. Everolimus for the treatment of advanced, non-functional neuroendocrine tumours of the lung or gastrointestinal tract (RADIANT-4): a randomised, placebo-controlled, phase 3 study. Lancet. 2016;387(10022):968-977.
23. Ramirez RA, Beyer DT, Chauhan A, Boudreaux JP, Wang YZ, Woltering EA. The role of capecitabine/temozolomide in metastatic neuroendocrine tumors. Oncologist. 2016;21(6):671-675.
24. Bajetta E, Rimassa L, Carnaghi C, et al. 5-Fluorouracil, dacarbazine, and epirubicin in the treatment of patients with neuroendocrine tumors. Cancer. 1998;83(2):372-378.
25. Masi G, Fornaro L, Cupini S, et al. Refractory neuroendocrine tumor-response to liposomal doxorubicin and capecitabine. Nat Rev Clin Oncol. 2009;6(11):670-674.
26. Lou F, Sarkaria I, Pietanza C, et al. Recurrence of pulmonary carcinoid tumors after resection: implications for postoperative surveillance. Ann Thorac Surg. 2013;96(4):1156-1162.
27. Beasley MB, Thunnissen FB, Brambilla E, et al. Pulmonary atypical carcinoid: predictors of survival in 106 cases. Human Pathol. 2000;31(10):1255-1265.
1. Hauso O, Gustafsson BI, Kidd M, et al. Neuroendocrine tumor epidemiology: contrasting Norway and North America. Cancer. 2008;113(10):2655-2664.
2. Fink G, Krelbaum T, Yellin A, et al. Pulmonary carcinoid: presentation, diagnosis, and outcome in 142 cases in Israel and review of 640 cases from the literature. Chest. 2001;119(6):1647-1651.
3. Limper AH, Carpenter PC, Scheithauer B, Staats BA. The Cushing syndrome induced by bronchial carcinoid tumors. Ann Intern Med. 1992;117(3):209-214.
4. Meisinger QC, Klein JS, Butnor KJ, Gentchos G, Leavitt BJ. CT features of peripheral pulmonary carcinoid tumors. AJR Am J Roentgenol. 2011;197(5):1073-1080.
5. Guckel C, Schnabel K, Deimling M, Steinbrich W. Solitary pulmonary nodules: MR evaluation of enhancement patterns with contrast-enhanced dynamic snapshot gradient-echo imaging. Radiology. 1996;200(3):681-686.
6. Jindal T, Kumar A, Venkitaraman B, et al. Evaluation of the role of [18F]FDG-PET/CT and [68Ga]DOTATOC-PET/CT in differentiating typical and atypical pulmonary carcinoids. Cancer Imaging. 2011;11:70-75.
7. Caplin ME, Baudin E, Ferolla P, et al. Pulmonary neuroendocrine (carcinoid) tumors: European Neuroendocrine Tumor Society expert consensus and recommendations for best practice for typical and atypical pulmonary carcinoids. Ann Oncol. 2015;26(8):1604-1620.
8. Travis WD. Pathology and diagnosis of neuroendocrine tumors: lung neuroendocrine. Thorac Surg Clin. 2014;24(3):257-266.
9. Warren WH, Memoli VA, Gould VE. Immunohistochemical and ultrastructural analysis of bronchopulmonary neuroendocrine neoplasms. II. Well-differentiated neuroendocrine carcinomas. Ultrastruct Pathol. 1984;7(2-3):185-199.
10. Goldstraw P, Chansky K, Crowley J, et al. The IASLC Lung Cancer Staging Project: Proposals for revision of the TNM stage groupings in the forthcoming (eighth) edition of the TNM classification for lung cancer. J Thorac Oncol. 2016;11(1):39-51.
11. McCaughan BC, Martini N, Bains MS. Bronchial carcinoids. Review of 124 cases. J Thorac Cardiovasc Surg. 1985;89(1):8-17.
12. Hurt R, Bates M. Carcinoid tumours of the bronchus: a 33-year experience. Thorax. 1984;39(8):617-623.
13. Ettinger DS, Wood DE, Akerley W, et al. Non-small cell lung cancer, version 1.2015. J Natl Compr Cancer Netw. 2014;12(12):1738-1761.
14. Ferguson MK, Landreneau RJ, Hazelrigg SR, et al. Long-term outcome after resection for bronchial carcinoid tumors. Eur J Cardiothorac Surg. 2000;18(2):156-161.
15. Lucchi M, Melfi F, Ribechini A, et al. Sleeve and wedge parenchyma-sparing bronchial resections in low-grade neoplasms of the bronchial airway. J Thorac Cardiovasc Surg. 2007;134(2):373-377.
16. Yendamuri S, Gold D, Jayaprakash V, Dexter E, Nwogu C, Demmy T. Is sublobar resection sufficient for carcinoid tumors? Ann Thorac Surg. 2011;92(5):1774-1778; discussion 8-9.
17. Fox M, Van Berkel V, Bousamra M II, Sloan S, Martin RC II. Surgical management of pulmonary carcinoid tumors: sublobar resection versus lobectomy. Am J Surg. 2013;205(2):200-208.
18. Cardillo G, Sera F, Di Martino M, et al. Bronchial carcinoid tumors: nodal status and long-term survival after resection. Ann Thorac Surg. 2004;77(5):1781-1785.
19. Oberg K, Hellman P, Ferolla P, Papotti M; ESMO Guidelines Working Group. Neuroendocrine bronchial and thymic tumors: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2012;23(suppl 7:vii120-3).
20. Filosso PL, Ferolla P, Guerrera F, et al. Multidisciplinary management of advanced lung neuroendocrine tumors. J Thorac Dis. 2015;7(Suppl 2):S163-171.
21. Kulke MH, Shah MH, Benson AB III, et al. Neuroendocrine tumors, version 1.2015. J Natl Compr Cancer Netw. 2015;13(1):78-108.
22. Yao JC, Fazio N, Singh S, et al. Everolimus for the treatment of advanced, non-functional neuroendocrine tumours of the lung or gastrointestinal tract (RADIANT-4): a randomised, placebo-controlled, phase 3 study. Lancet. 2016;387(10022):968-977.
23. Ramirez RA, Beyer DT, Chauhan A, Boudreaux JP, Wang YZ, Woltering EA. The role of capecitabine/temozolomide in metastatic neuroendocrine tumors. Oncologist. 2016;21(6):671-675.
24. Bajetta E, Rimassa L, Carnaghi C, et al. 5-Fluorouracil, dacarbazine, and epirubicin in the treatment of patients with neuroendocrine tumors. Cancer. 1998;83(2):372-378.
25. Masi G, Fornaro L, Cupini S, et al. Refractory neuroendocrine tumor-response to liposomal doxorubicin and capecitabine. Nat Rev Clin Oncol. 2009;6(11):670-674.
26. Lou F, Sarkaria I, Pietanza C, et al. Recurrence of pulmonary carcinoid tumors after resection: implications for postoperative surveillance. Ann Thorac Surg. 2013;96(4):1156-1162.
27. Beasley MB, Thunnissen FB, Brambilla E, et al. Pulmonary atypical carcinoid: predictors of survival in 106 cases. Human Pathol. 2000;31(10):1255-1265.
Cancer care in 2017: the promise of more cures with the challenges of an unstable health care system
This past year will likely be remembered as one of breakthrough advances in reducing the burden of cancer, with some landmark “firsts” coming out of the US Food and Drug Admini
Our excitement has also been tempered by the rapid rise in the cost of effective biologic, immunologic, and targeted therapies. With the approval of trastuzumab-dkst (Ogivri), the first targeted biosimilar for HER2-positive breast and gastrointestinal cancers, we can look forward to price decreases possibly in the 20%-30% range over time from a targeted therapy with remarkable clinical efficacy. We know that approved biosimilars have demonstrated clinical efficacy along with similar minor biologic diversity that is also seen in the reference biologic.1 We can also hope that increasing competition among biosimilar and reference compounds will lead to improvements in production methodologies that can allow further price reductions so that even more patients can gain access to these highly effective therapies.
In addition, the first FDA approval for the next-generation sequencing (NGS) FoundationOne profiling test and the rapid announcement by the Centers for Medicare & Medicaid Services (CMS) that it will cover the cost of that testing brings us a step closer to knowing which patients most likely will or won’t benefit from costly and toxic targeted therapies. Along with the many clinical trials studying which mutations predict which efficacies of individual or combinations of targeted agents, the approval and CMS coverage policy will help us improve value to our patients; when we can recommend the most beneficial therapies and avoid futile ones.
Finally, the approval for the DigniCap Scalp Cooling System for patients on chemotherapy for all solid tumors is of great importance. Pending coverage availability, it may influence some patients to get chemotherapy they might otherwise have forgone to avoid hair loss (see related article).
More consolidation: the best of all worlds?
In my 27 years in private practice, during which practice revenues grew with the favorable profit margins on novel therapies, forward-thinking physician leaders piloted innovations in oncology electronic medical records (EMRs), the delivery of team-based care, clinical research partnerships, and more comprehensive care services to better serve diverse communities, including those in rural areas. At my previous practice, that included adding clinicians to our group to serve patients at hospital clinics in 2 counties in southern California, each county with populations larger than 15 states. Our private practice worked with these public entities to bring state-of-the art care and private practice efficiencies to the uninsured and underserved in our region.
Unfortunately, revenues plummeted with changes in reimbursement after passage of the Medicare Modernization Act in 2003 and they continue to destabilize and reduce the number of community practices across the country. Many oncologists and oncology practices, including mine, chose to join larger academic or hospital systems or larger oncology networks at a time they are also facing growing pressures to contain costs, focus on out-patient care, complex clinical trials, and expanded access to care.
Although we may lament the shrinking landscape of private oncology practices, we can also be inspired by the physicians who have joined ranks with the better-funded, better-resourced, more traditional hospital and academic systems. These larger systems have more resources, more clincial trial offerings, staffing, technology, and analytics to expand value-based care initiatives to larger numbers of patients.
The hub-and-spoke models of oncology care with integrated networks linked by technology, and networked into larger analytic and decision support systems such as CancerLinQ, the health information technology program of the American Society of Clinical Oncology (ASCO),2 could facilitate documentable delivery of comprehensive, evidence-based care, moving us closer to meeting the Quadruple Aim of optimal health care: improving the patient experience of care (including quality and satisfaction); improving the health of populations; reducing the per capita cost of health care; and improving the work life of those who deliver care.3,4
Payment reform: working to align incentives
Everyone seems to agree that the fee-for-service payment models do not align incentives for improving total health outcomes at the lowest costs, but at the moment, there seems to be no best way of aligning them. Robinson has reported on the oncology payment initiatives at four major health insurance plans – Medicare (public) and Anthem, Aetna, and UnitedHealthcare (all private), noting that:5
- Medicare is testing its Oncology Care Model at more than 200 sites in the United States, and early data are expected to be released in 2018.
- Anthem continues with its Cancer Care Quality Program that includes adherence to 2 key requirements: that participants are compliant with Anthem-approved drug pathways, and that they register their patients at the insurer’s oncology website and enter their clinical data. Anthem is also considering expanding the management fee for certain high priority clinical trials.
- Aetna’s Oncology Solutions takes a different approach by providing increased payments for generic chemotherapies.
- United has eliminated the mark-up for new drugs and continues to mark up the prices of the older and generic therapies. Its episode-based pricing gives practices upfront payments based on expected drug margins so that practices can fund more comprehensive evidence-based care. In a presentation at a Washington State Medical Oncology Society meeting recently, United’s Lee Newcomer, reported that the insurer continues to see improved clinical and financial outcomes as well as encouraging early data showing that patients might do better in the real-world setting on some therapies that have not been fully compared in head-to-head randomized clinical trials.6,7
ASCO is pulling these ideas together at the national level with its Patient-Centered Oncology Payment (PCOP) model, which is similar to Medicare’s alternative payment model. The PCOP model focuses on high-value, quality care. Higher upfront payments would cover the additional diagnostic services, care planning, and management to improve compliance and adherence as well as clinical trial evaluations. The model was developed and vetted by the ASCO Clinical Practice Committee and practicing oncologists, and is supported by staff and consultants. It is currently in its second year of operation with a commercial payer and will be submitted for review to the Physician-Focused Payment Model Technical Advisory Committee of the Health and Human Services. The results of the review are expected in 2018. If the model is approved, it could provide a uniform approach for payers that would align incentives for high-quality cancer care and allow for better predictive modeling for practices, irrespective of size, to invest in infrastructure and staffing to meet the growing demand for high-quality, value-based cancer care.
Better science: the promise of more cures
The FDA approved a record number drugs and biologics in 2017 for various cancers,8 including the landmark approval of the first CART therapy for cancer, tisagenlecleucel, which targets CD19 on B cells in the treatment of acute leukemia. That approval was rapidly followed by a second anti-CD19 CART therapy, axicabtagene ciloluecel, for refractory, aggressive B-cell non-Hodgkin lymphoma.9,10 Although these therapies can achieve remarkable response and even complete response rates in otherwise refractory patients, only some achieve a long-term remission, and the costs are an order of magnitude above most other cancer therapies. That raises the question of what duration of benefit we should expect for treatments that cost in the range of $500,000 for the therapy alone, along with the additional costs for care, hospitalization, monitoring, expensive biologics (eg, tocilizumab, for the severe and potentially life-threatening cytokine-release syndrome associated with CART therapies), and significant neurologic and other therapy-related toxicities.
Novel arrangements between pharmaceutical companies and payers are currently being discussed so that only patients who meet specific response criteria would be charged for the therapy. In addition, we await findings from ongoing research to see if new approaches can find specific targetable sites on solid tumors that could spare the healthy organ tissues while eliminating highly resistant or heterogeneous populations of mutations in patients with advanced solid tumors. Such development of highly specific targets for CART therapies would improve their efficacy and safety, and with defined protocols in place to address toxicities and efforts to reduce the costs of the therapies, we can hopefully ensure broader access for patients to this potentially transformative therapeutic tool.
In addition to the excitement around the CART therapies, many of the years other new approvals will bring incremental but meaningful improvement in outcomes for patients with common cancers. The approval of neratinib, the first agent approved as extended adjuvant therapy for women with early-stage HER2/neu-positive breast cancer, is welcome, given the current 30% recurrence risk that extends past 10 years for women in that disease population who have completed standard adjuvant HER2-directed therapies. The 34% reduction in recurrence risk with a year of extended oral adjuvant therapy, as reported by Martin and colleagues,11 with benefits sustained out to 5 years and with controllable diarrhea as the major toxicity, are encouraging. This oral therapy may be especially beneficial for hormone-receptor–positive women in whom blocking the HER2/neu pathway may enhance cell signaling through the hormone pathways, which can be blocked with oral agents at the same time to provide significant reduction of recurrence risk.
Diagnostics
The concept of personalized medicine is based on identifying biomarkers that are predictive of a patient’s response to treatment. There has been much progress toward applying NGS of tumors for use in the clinic, but we are still awaiting evidence from randomized clinical trials that such approaches prolong overall or progression-free survival.12 Dr Julie Lange, an associate professor of clinical surgery and director of the Breast Cancer Program at the Keck School of Medicine at the University of Southern California, Los Angeles, provided me with the references to key studies in this field in which she is a leading researcher.13 However, she pointed out that in the absence of effective therapies, advanced biomarker testing may be less helpful, as is the case in heavily pretreated patients,14 unless a molecular test can pinpoint a potentially clinically actionable mutation. With the plethora of available assays and the high costs of molecular testing, clinicians are challenged in knowing what testing is best for which patients. Findings from a number of key ongoing national trials may eventually help us understand which tumor mutations in which tumor types can be most effectively targeted when multiple targetable mutations are found (TAPUR,15 MATCH,16 and QUILT17 and other basket trials18). The complexity of molecular testing has led to the development of institutional, trial-based, or co-operative group molecular tumor boards to provide guidance on specific targeted therapies for specific tumor mutations.
ASCO has launched a monthly series called Molecular Oncology Tumor Boards19 to expand the knowledge base in this field. It is presented as user-driven discussions designed to help providers integrate the use of the new genetic and genomic tests and their results into the day-to-day clinical care of patients with cancer.20
Liquid biopsies
As busy clinicians, we need to understand the differences in liquid biopsy tests and their correlation with actionable targets, especially given the rapid progress in this field. Again, Dr Lange offered clarity on those differences. Liquid biopsy, refers to using a blood draw to isolate circulating tumor cells (CTCs) or circulating tumor DNA (ctDNA) to assess tumor biomarkers.21 Both CTCs and ctDNA tests have been shown to be prognostic of worse survival.22-24 Liquid biopsies are currently supplemental to direct tumor biopsies, not replacements for them. The theoretical advantage of liquid biopsies is that they may reflect tumor heterogeneity by examining the repertoire of mutations contributed by diverse metastatic sites that shed CTCs or ctDNA into the circulation. The question is which type of testing can best inform therapy decisions.
Assays for ctDNA using droplet digital PCR [polymerase chain reaction], a digital PCR method based on water-oil emulsion droplet technology, require a priori knowledge of the specific mutation associated with response or lack of response to a specific therapy.25,26 Technical issues related to the detection of rare alleles present within a mixed population of leukocytes, and ctDNA remains a challenge for many ctDNA assays. However, there is evidence to suggest that whole-exome sequencing of ctDNA is concordant with mutations in metastases,27 however benchmarking ctDNA against tissue biopsies of metastases was not possible in all studies because tumor blocks were not available or because of the failure of tumor NGS assays. 28,29
Newer generations of CTC assays take advantage of the circulating tumor cell as a functional assay for mutational status, gene expression, proteomics, epigenetics, and/or chemosensitivity of cultured cells. The relationship between CTCs and ctDNA remains uncertain as to whether CTCs are the cell of origin for ctDNA or if ctDNA may reflect responding or resistant tumor populations. The use of NGS on tumor specimens, ctDNA, and CTCs as a discovery tool is advancing the field by improving the understanding of disease heterogeneity and potential treatment targets. These results require correlation with patterns of response to therapy, and ultimately require validation in randomized clinical trials to provide strong evidence justifying their use outside of clinical trials. We can look forward to a time in the not distant future when specific liquid biopsy assays will reflect the array of mutations in different metastatic sites with validation that they correlate with efficacy of targeting those mutations that have targetable therapies.
From the FDA
New approvals
- Trastuzumab-dkst (Ogivri, Mylan; Dec 1) was approved as a biosimilar to trastuzumab (Herceptin, Genentech) for the treatment of patients with HER2-overexpressing breast or metastatic stomach cancer (gastric or gastroesophageal junction adenocarcinoma).
- Sunitinib malate (Sutent, Pfizer; Nov 16) was approved for the adjuvant treatment of adult patients at high risk of recurrent renal cell carcinoma after nephrectomy.
- Obinutuzumab (Gazyva, Genentech; Nov 16) received regular approval in combination with chemotherapy, followed by obinutuzumab monotherapy in patients achieving partial remission, for adult patients with previously untreated stage II bulky, III, or IV follicular lymphoma.
- Emicizumab-kxwh (Hemlibra, Genentech; Nov 16) was approved for routine prophylaxis to prevent or reduce the frequency of bleeding episodes in adult and pediatric patients with hemophilia A with factor VIII inhibitors.
- Dasatinib (Sprycel, Bristol-Myers Squibb; Nov 9) was approved for the treatment of pediatric patients with Philadelphia chromosome-positive chronic myeloid leukemia (CML) in the chronic phase.
- Brentuximab vedotin (Adcetris, Seattle Genetics; Nov 9) for the treatment of previously treated adult patients with primary cutaneous anaplastic large cell lymphoma (pcALCL) or CD30-expressing mycosis fungoides.
- Alectinib (Alecensa, Hoffmann-La Roche/Genentech; Nov 6) was approved for treatment of patients with anaplastic lymphoma kinase–positive metastatic non-small cell lung cancer (NSCLC), as detected by an FDA-approved test.
- Vemurafenib (Zelboraf, Hoffmann-La Roche; Nov 6) received approval for the treatment of Acalabrutinib (Calquence, AstraZeneca/Acerta; Oct 31) was granted accelerated approval for treatment of adult patients with mantle cell lymphoma (MCL) who have received at least one previous therapy.
- Axicabtagene ciloleucel (Yescarta, Kite; Oct 18), a CART therapy, was approved for treatment of adult patients with relapsed or refractory large B-cell lymphoma after two or more lines of systemic therapy, including diffuse large B-cell lymphoma (DLBCL) not otherwise specified, primary mediastinal large B-cell lymphoma, high-grade B-cell lymphoma, and DLBCL arising from follicular lymphoma. The complete remission rate reviewed by the FDA for trial patients was 51%.30 It was the second CART therapy this year to receive approval (see tisagenlecleucel; Aug 30). The agency granted orphan drug designation and priority review to therapy for this indication.
- Abemaciclib (Verzenio, Eli Lilly; Sep 28) was approved in combination with fulvestrant for women with hormone receptor-positive, HER2-negative advanced or metastatic breast cancer with disease progression following endocrine therapy.
- Copanlisib (Aliqopa, Bayer; Sep 14) got accelerated approval for the treatment of adult patients with relapsed follicular lymphoma who have received at least two prior systemic therapies.
- Bevacizumab-awwb (Mvasi, Amgen; Sep 14) was approved as a biosimilar to bevacizumab (Avastin, Genentech) for treating multiple types of cancer. It was the first biosimilar approved in the US for the treatment of cancer.
- Gemtuzumab ozogamicin (Mylotarg, Pfizer; Sep 1) was approved for the treatment of newly diagnosed CD33-positive acute myeloid leukemia (AML) in adults and of relapsed/refractory CD33-positive AML in adults and pediatric patients aged 2 or older. It can be used in combination with daunorubicin and cytarabine for adults with newly diagnosed AML, or as a standalone treatment for certain adult and pediatric patients. The drug was originally approved in 2000 as a standalone treatment for CD33-positive AML in patients older than 60 years, but was withdrawn in 2010 because of safety concerns and postmarketing trials could not confirm benefit. The current approval is for a lower recommended dose and schedule.31
- Tisagenlecleucel (Kymriah, Novartis; Aug 30) was approved for the treatment of patients up to age 25 years with B-cell precursor acute lymphoblastic leukemia (ALL) that is refractory or in second or later relapse. It is the first CART immunotherapy approved by the agency.
- Inotuzumab ozogamicin (Besponsa, Wyeth; Aug 17) was approved for the treatment of adults with relapsed or refractory B-cell precursor ALL.
- A liposome-encapsulated combination of daunorubicin and cytarabine (Vyxeos, Jazz; Aug 3) was approved for the treatment of adults with newly diagnosed therapy-related AML (t-AML) or AML with myelodysplasia-related changes (AML-MRC), two types of AML having a poor prognosis.
- Enasidenib (Idhifa, Celgene; Aug 1) was approved for the treatment of adult patients with relapsed or refractory AML with an isocitrate dehydrogenase-2 mutation as detected by an FDA-approved test.
- Neratinib (Nerlynx, Puma; Jul 17) was approved as the first extended adjuvant therapy for adult patients with early stage HER2-overexpressed/amplified breast cancer, to follow adjuvant trastuzumab-based therapy.
- Blinatumomab (Blincyto, Amgen; Jul 11) was approved for the treatment of relapsed or refractory B-cell precursor acute lymphoblastic leukemia in adults and children.
- L-glutamine oral powder (Endari, Emmaus; Jul 7) was approved for oral administration to reduce the acute complications of sickle cell disease in adult and pediatric patients 5 years and older.
- Betrixaban (Bevyxxa, Portola; Jun 23) was approved for the prophylaxis of venous thromboembolism (VTE) in adult patients hospitalized for an acute medical illness who are at risk for thromboembolic complications because of moderate or severe restricted mobility and other risk factors for VTE.
- The combination of rituximab and hyaluronidase human (Rituxan Hycela, Genentech; Jun 22) was approved for adult patients with follicular lymphoma, DLBCL, and chronic lymphocytic leukemia. Hyaluronidase human is an enzyme that helps deliver the rituximab. This formulation allows subcutaneous administration of the combination, which will shorten patient visit times and potentially even allow at-home therapy delivery.
- Ceritinib (Zykadia, Novartis; May 26) was approved for patients with metastatic NSCLC whose tumors are anaplastic lymphoma kinase (ALK)-positive as detected by an FDA-approved test.
- Avelumab (Bavencio, EMD Serono; May 9) got accelerated approval for patients with locally advanced or metastatic urothelial carcinoma whose disease progressed during or following platinum-containing chemotherapy or within 12 months of neoadjuvant or adjuvant platinum-containing chemotherapy.
- Durvalumab (ImfinzI, AstraZeneca; May 1) got accelerated approval for the treatment of patients with locally advanced or metastatic urothelial carcinoma who have disease progression during or following platinum-containing chemotherapy or who have disease progression within 12 months of neoadjuvant or adjuvant treatment with platinum-containing chemotherapy.
- Brigatinib (Alunbrig tablets, Takeda through Ariad; Apr 28) got accelerated approval for the treatment of patients with metastatic anaplastic lymphoma kinase (ALK)-positive NSCLC who have progressed on or are intolerant to crizotinib.
- Midostaurin (Rydapt, Novartis; Apr 28) was approved for the treatment of adult patients with newly diagnosed AML who are FLT3 mutation-positive, as detected by an FDA-approved test, in combination with standard cytarabine and daunorubicin induction and cytarabine consolidation.
- Osimertinib (Tagrisso, AstraZeneca; Mar 30) got regular approval for the treatment of patients with metastatic epidermal growth factor receptor (EGFR) T790M mutation-positive NSCLC, as detected by an FDA-approved test, whose disease has progressed on or after EGFR tyrosine-kinase inhibitor therapy.
- Niraparib (Zejula, Tesaro; Mar 27), a poly ADP-ribose polymerase (PARP) inhibitor, was approved for the maintenance treatment of adult patients with recurrent epithelial ovarian, fallopian tube, or primary peritoneal cancer who are in complete or partial response to platinum-based chemotherapy.
- Avelumab (Mar 23), a PD-L1–blocking human IgG1 lambda monoclonal antibody, got accelerated approval for the treatment of patients 12 years and older with metastatic Merkel cell carcinoma. It is the first FDA-approved product to treat this type of cancer.
- Ribociclib (Kisqali, Novartis; Mar 13), a CDK4/6 inhibitor, was approved as a breakthrough therapy after priority review for use in combination with an aromatase inhibitor as initial endocrine-based therapy for the treatment of postmenopausal women with HR-positive, HER2-negative advanced or metastatic breast cancer.
Expanded/additional indications
- Nivolumab (Opdivo, Bristol-Myers Squibb; Sep 22) got accelerated expanded indication approval for treatment of hepatocellular carcinoma (HCC) in patients previously treated with sorafenib.
- Pembrolizumab (Keytruda, Merck; Sep 22) got accelerated expanded indication approval for recurrent locally advanced or metastatic gastric or gastroesophageal junction adenocarcinoma in patients whose tumors express PD-L1 as determined by an FDA-approved test.
- DigniCap Scalp Cooling System (Dignitana Inc; Jul 3) was cleared for expanded use for reducing hair loss during chemotherapy for all solid tumors. Marketing authorization for the cooling cap had been granted in 2015 for patients with breast cancer.
- Olaparib tablets (Lynparza, AstraZeneca; Aug 17) got approval for an expanded indication as maintenance treatment of adult patients with recurrent epithelial ovarian, fallopian tube, or primary peritoneal cancer, who are in a complete or partial response to platinum-based chemotherapy.
- Ibrutinib (Imbruvica, Pharmacyclics; Aug 2) got expanded indication approval for the treatment of adult patients with chronic graft-versus-host disease (cGVHD) after failure of one or more lines of systemic therapy. It was the first FDA-approved therapy for the treatment of cGVHD. (Ibrutinib was previously approved for chronic lymphocytic leukemia/small lymphocytic lymphoma, chronic lymphocytic leukemia/small lymphocytic lymphoma with 17p deletion, Waldenström’s macroglobulinemia, marginal zone lymphoma, and mantle cell lymphoma).
- Nivolumab (Aug 2) got an accelerated expanded indication for the treatment of patients 12 years and older with mismatch repair deficient (dMMR) and microsatellite instability-high (MSI-H) metastatic colorectal cancer that has progressed after treatment with a fluoropyrimidine, oxaliplatin, and irinotecan.
- Dabrafenib and trametinib (Tafinlar and Mekinist, Novartis; Jun 22) were approved for the expanded indication in combination for patients with metastatic NSCLC with BRAF V600E mutation as detected by an FDA-approved test. The combination demonstrated superior efficacy compared with dabrafenib alone (overall response rate: 61% and 27%, respectively).32
- Pembrolizumab (May 23) got approved for expanded indication for adult and pediatric patients with unresectable or metastatic, MSI-H or dMMR solid tumors that have progressed after treatment and who have no satisfactory alternative treatment options or with MSI-H or dMMR colorectal cancer that has progressed after treatment with a fluoropyrimidine, oxaliplatin, and irinotecan.
- Pembrolizumab (May 18) got approval for expanded indication for patients with locally advanced or metastatic urothelial carcinoma who have disease progression during or following platinum-containing chemotherapy or within 12 months of neoadjuvant or adjuvant treatment with platinum-containing chemotherapy.
- Pembrolizumab (May 10) got accelerated expanded indication for use combination with pemetrexed and carboplatin for the treatment of patients with previously untreated metastatic NSCLC.
- Regorafenib (Stivarga, Bayer; Apr 27) got an additional indication for the treatment of patients with HCC who have been previously treated with sorafenib.
- Palbociclib (Ibrance, Pfizer; Mar 31) got an expanded indication that includes first-line therapy for the treatment of hormone receptor–positive, HER2-negative advanced or metastatic breast cancer in combination with an aromatase inhibitor as initial endocrine based therapy in postmenopausal women.
- Pembrolizumab (Mar 15) got an accelerated additional indication approval for treatment of adult and pediatric patients with refractory classical Hodgkin lymphoma, or those who have relapsed after three or more previous lines of therapy.
- Lenalidomide (Revlimid, Celgene; Feb 22) got an additional indication as maintenance therapy for patients with multiple myeloma following autologous stem cell transplant.
- Nivolumab (Feb 2) got an accelerated expanded indication for treatment of patients with locally advanced or metastatic urothelial carcinoma who have disease progression during or following platinum-containing chemotherapy or have disease progression within 12 months of neoadjuvant or adjuvant treatment with a platinum-containing chemotherapy.
Modified use
- Cabazitaxel (Jevtana, Sanofi-Aventis; Sep 14) in combination with prednisone was approved at a lower dose of 20 mg/m2 every 3 weeks for the treatment of patients with metastatic castration-resistant prostate cancer previously treated with a docetaxel-containing treatment regimen. It had been approved at 25 mg/m2 every 3 weeks for this indication in 2010.
Tests/diagnostics
- Marketing approval was given to the FoundationOne CDx (Foundation Medicine; Nov 30), an NGS-based in vitro diagnostic to detect genetic mutations in 324 genes and 2 genomic signatures in any solid tumor type.
- Marketing approval was given to the Praxis Extended RAS Panel (Illumina; Jun 29), a next generation sequencing test to detect certain genetic mutations in RAS genes in tumor samples of patients with metastatic colorectal cancer. The test is used to aid in the identification of patients who may be eligible for treatment with panitumumab (Vectibix, Amgen).
- Marketing was approved for ipsogen JAK2 RGQ PCR Kit (Qiagen ; Mar 27) to detect mutations affecting the Janus tyrosine kinase 2 gene. This is the first FDA-authorized test intended to help physicians in evaluating patients for suspected polycythemia vera.
Imaging and pathology aids
- Aminolevulinic acid hydrochloride, known as ALA HCl (Gleolan, NX; Jun 6) was approved as an optical imaging agent indicated in patients with gliomas (suspected World Health Organization grades III or IV on preoperative imaging) as an adjunct for the visualization of malignant tissue during surgery.
- Marketing was approved for the Philips IntelliSite Pathology Solution (PIPS, Philips Medical Systems Nederland; Apr 17), as an aid to the pathologist to review and interpret digital images of surgical pathology slides prepared from formalin-fixed paraffin embedded tissue.
Challenges and uncertainties
The current administration’s initiatives to reduce administrative burdens is underway with the Patients Over Paperwork initiative. Eliminating and streamlining regulations to increase efficiency and improve beneficiary experience could be helpful to both oncologists and patients. For now, the Medicare Access and CHIP Reauthorization Act (MACRA) program, allows you to “pick your pace” in the 2017 performance year and report on at least one measure to avoid a payment reduction penalty on your Medicare payments in 2019. In the final rule for 2018, the CMS finalized a proposal to apply the MIPS [Merit-based Incentive Payment System] adjustment to all Part B items and services, which will include Part B drugs. This would be unfair to oncologists who treat on the basis of evidence-based guidelines and pathways and have no control over the costs of the drugs they prescribe.
In addition, more requirements will be imposed in 2018 in a move toward full MACRA implementation. All four composite categories (Quality – 60% for 2017; Advancing Care Information (ACI, renamed from Meaningful Use) – 25% for 2017; Improvement Activities (IA) – 15% for 2017; and Cost – 0% for 2017, but weighted in the future) will be scored, including resource use (cost) at 10%. CMS will collect data to assess the total cost of care and the Medicare Spend per Beneficiary to assess use. Full program implementation, with cost being assessed at 30% of your score is expected in the 2019 performance year. ASCO’s clinical affairs and policy experts have studied the implications of Part B chemotherapy drugs being included in the cost component of the MIPS scoring and will continue advocating for policies that hold clinicians responsible only for the aspects of care they can control, such as providing high-quality care based on the patient’s disease, biomarkers, comorbidities, and preferences, and not the costs of the evidence-based therapies needed by patients.
Toward a better 2018 for ourselves and our patients
As an eternal optimist, I remain enthusiastic that despite the many challenges, we will find effective ways to bring standard as well as newer, cell-based and targeted therapies to our patients and cover the costs of highly effective therapies. I also remain hopeful that improving technological capabilities and payment reforms will be used by innovative clinical and administrative care teams to give clinicians more time to improve the care and health of patients while validating the methodologies so that real world data can help us further craft therapies to improve the health of each individual who needs our care. As we close this 15th year of our journal, we hope our presentations of practical science and implementation content has helped support your work while freeing some time for you to enjoy the journey. Our best wishes for a joyful holiday season celebrated with friends and family and the patients who entrust us to help them face and live beyond their cancer diagnoses.
1. US Food & Drug Administration. Biosimilar and interchangeable
products. https://www.fda.gov/Drugs/DevelopmentApprovalProcess/
HowDrugsareDevelopedandApproved/ApprovalApplications/
¬erapeuticBiologicApplications/Biosimilars/ucm580419.htm. Last
updated October 23, 2017. Accessed December 11, 2017.
2. ASCO CancerLinQ website. https://cancerlinq.org/. Publishing/
update information not available. Accessed November 3, 2017.
3. Bodenheimer T, Sinsky C. From triple to quadruple aim: care of the
patient requires care of the provider. https://www.ncbi.nlm.nih.gov/
pmc/articles/PMC4226781/. Published November 2014. Accessed
November 7.
4. Institute for Healthcare Improvement. http://www.ihi.org/Engage/
Initiatives/TripleAim/Pages/default.aspx. No update information
given. Accessed November 3, 2017.
5. Robinson JC. Value-based physician payment in oncology: public and
private insurer initiatives. Milbank Q. 2017;95(1);184-203.
6. Newcomer L. Oral communication: Washington State Medical
Oncology Society meeting, August 19, 2017.
7. Newcomer LN, Gould B, Page RD, Donelan SA, Perkins M.
Changing physician incentives for aordable, quality cancer
care: results of an episode payment model. J Oncol Pract.
2014;10(5):322-326.
8. US Department of Health and Human Services website. Hematology/
oncology (cancer) approvals & safety notications. https://www.fda.
gov/Drugs/InformationOnDrugs/ApprovedDrugs/ucm279174.htm.
Last updated December 1, 2017. Accessed December 3, 2017.
9. Hem-Onc Today website. CAR T-cell therapy approval huge
step for oncology, but only ‘beginning of story’. https://www.
healio.com/hematology-oncology/leukemia/news/print/hemonctoday/%
7B33119631-5996-45cf-9be6-8e36466ded9e%7D/car-tcell-
therapy-approval-huge-step-for-oncology-but-only-beginningof-
story. Published September 25, 2017. Accessed November 9, 2017.
10. Gauthier J, Yakoub-Agha I. Chimeric antigen-receptor T-cell therapy
for hematological malignancies and solid tumors: Clinical data
to date, current limitations and perspectives. Curr Res in Transl Med.
2017;65(3):93-102.
11. Martin M, Holmes FA, Ejlertsen B, et al. Neratinib after trastuzumab-
based adjuvant therapy in early-stage HER2+ breast cancer:
5-year analysis of the phase III ExteNET trial [ESMO oral presentation].
Ann Oncol. 2017;28(suppl 5):v43-v67.
12. Le Tourneau C, Delord JP, Goncalves A, et al. Molecularly targeted
therapy based on tumour molecular proling versus conventional
therapy for advanced cancer SHIVA): a multicentre, openlabel,
proof-of-concept, randomised, controlled phase 2 trial. Lancet
Oncol. 2015;16(13):1324-1334.
13. Forte V, Barrak DK, Elhodaky M, Tung L, Snow A, Lang JE. ¬e
potential for liquid biopsies in the precision medical treatment of
breast cancer. Cancer Biol Med. 2016;13(1):19-40.
14. Smerage JB, Barlow WE, Hortobagyi GN, et al. Circulating tumor
cells and response to chemotherapy in metastatic breast cancer:
SWOG S0500. J Clin Oncol. 2014;32(31):3483-3489.
15. US National Library of Medicine. TAPUR: testing the use of food
and drug administration (FDA) approved drugs that target a specific
abnormality in a tumor gene in people with advanced stage cancer
(TAPUR). https://clinicaltrials.gov/ct2/show/NCT02693535.
First posted February 26, 2016; last updated September 18, 2017.
Accessed November 10, 2017.
16. US National Library of Medicine. NCI-MATCH: Targeted therapy
directed by genetic testing in treating patients with advanced refractory
solid tumors, lymphomas, or multiple myeloma. https://clinicaltrials.
gov/ct2/show/NCT02465060. First posted June 8, 2015; last
updated November 9, 2017. Accessed November 10, 2017.
17. US National Library of Medicine. QUILT-3.039: NANT Pancreatic
cancer vaccine: combination immunotherapy in subjects with pancreatic
cancer who have progressed on or after standard-of-care therapy.
https://clinicaltrials.gov/ct2/show/NCT03136406. First posted May
2, 2017; last updated October 30, 2017. Accessed November 10,
2017.
18. Cunanan KM, Gonen M, Shen R, et al. Basket trials in oncology:
A trade-o between complexity and eciency. J Clin Oncol.
2017;35(3):271-273.
19. ASCO website. https://university.asco.org/motb. Last update
November 2017. Accessed November 10, 2017.
20. ASCO website. Molecular oncology tumor boards invite discussion
of growing eld in cancer care. http://www.ascopost.com/issues/
february-25-2015/molecular-oncology-tumor-boards-invite-discussion-
of-growing-eld-in-cancer-care/. Published February 25, 2017.
Accessed November 10, 2017.
21. de Lartigue J. Liquid gold: blood-based biopsies make headway.
JCSO 2017;15(1):49-54.
22. Cristofanilli M, Budd GT, Ellis MJ, et al. Circulating tumor cells,
disease progression, and survival in metastatic breast cancer. N Engl J
Med. 2004;351(8):781-791.
23. Lucci A, Hall CS, Lodhi AK, et al. Circulating tumour cells in
non-metastatic breast cancer: a prospective study. Lancet Oncol.
2012;13(7):688-695.
24. Dawson SJ, Tsui DW, Murtaza M, et al. Analysis of circulating
tumor DNA to monitor metastatic breast cancer. N Engl J Med.
2013;368(13):1199-1209.
25. Chandarlapaty S, Chen D, He W, et al. Prevalence of ESR1 mutations
in cell-free DNA and outcomes in metastatic breast cancer: a
secondary analysis of the BOLERO-2 clinical trial. JAMA Oncol.
2016;2(10):1310-1315.
26. Kim SB, Dent R, Wongchenko WJ, et al. Concordance between
plasma-based and tissue-based next-generation sequencing in
LOTUS [Correspondence]. http://www.thelancet.com/journals/
lanonc/article/PIIS1470-2045(17)30785-4/fulltext. Published
November 2017. Accessed December 3, 2017.
27. Adalsteinsson VA, Ha G, Freeman SS, et al. Scalable whole-exome
sequencing of cell-free DNA reveals high concordance with metastatic
tumors. https://www.nature.com/articles/s41467-017-00965-y.
Published online November 6, 2017. Accessed November 19, 2017.
28. Parsons DW, Roy A, Yang Y, et al. Clinical genomics for children
with solid tumors: current realities and future opportunities
[Abstract]. Clin Cancer Res. 2016;22(1 Suppl):abstract IA16.
29. ¬ompson JC, Yee SS, Troxel AB, et al. Detection of therapeutically
targetable driver and resistance mutations in lung cancer patients by
next-generation sequencing of cell-free circulating tumor DNA. Clin
Cancer Res. 2016;22(23):5772-5782.
30. Press release, FDA. FDA approves axicabtagene ciloleucel
for large B-cell lymphoma. https://www.fda.gov/Drugs/
InformationOnDrugs/ApprovedDrugs/ucm581296.htm. Last
updated October 25, 2017. Accessed November 6, 2017.
31. Press release, FDA. FDA Approves gemtuzumab ozogamicin
for CD33-positive AML. https://www.fda.gov/Drugs/
InformationOnDrugs/ApprovedDrugs/ucm574518.htm. Last
updated September 1, 2017. Accessed November 6, 2017.
32. Press release, FDA. FDA grants regular approval to dabrafenib and
trametinib combination for metastatic NSCLC with BRAF V600E
mutation. https://www.fda.gov/Drugs/InformationOnDrugs/
ApprovedDrugs/ucm564331.htm. Last updated June 22, 2017.
Accessed November 6, 2017.
This past year will likely be remembered as one of breakthrough advances in reducing the burden of cancer, with some landmark “firsts” coming out of the US Food and Drug Admini
Our excitement has also been tempered by the rapid rise in the cost of effective biologic, immunologic, and targeted therapies. With the approval of trastuzumab-dkst (Ogivri), the first targeted biosimilar for HER2-positive breast and gastrointestinal cancers, we can look forward to price decreases possibly in the 20%-30% range over time from a targeted therapy with remarkable clinical efficacy. We know that approved biosimilars have demonstrated clinical efficacy along with similar minor biologic diversity that is also seen in the reference biologic.1 We can also hope that increasing competition among biosimilar and reference compounds will lead to improvements in production methodologies that can allow further price reductions so that even more patients can gain access to these highly effective therapies.
In addition, the first FDA approval for the next-generation sequencing (NGS) FoundationOne profiling test and the rapid announcement by the Centers for Medicare & Medicaid Services (CMS) that it will cover the cost of that testing brings us a step closer to knowing which patients most likely will or won’t benefit from costly and toxic targeted therapies. Along with the many clinical trials studying which mutations predict which efficacies of individual or combinations of targeted agents, the approval and CMS coverage policy will help us improve value to our patients; when we can recommend the most beneficial therapies and avoid futile ones.
Finally, the approval for the DigniCap Scalp Cooling System for patients on chemotherapy for all solid tumors is of great importance. Pending coverage availability, it may influence some patients to get chemotherapy they might otherwise have forgone to avoid hair loss (see related article).
More consolidation: the best of all worlds?
In my 27 years in private practice, during which practice revenues grew with the favorable profit margins on novel therapies, forward-thinking physician leaders piloted innovations in oncology electronic medical records (EMRs), the delivery of team-based care, clinical research partnerships, and more comprehensive care services to better serve diverse communities, including those in rural areas. At my previous practice, that included adding clinicians to our group to serve patients at hospital clinics in 2 counties in southern California, each county with populations larger than 15 states. Our private practice worked with these public entities to bring state-of-the art care and private practice efficiencies to the uninsured and underserved in our region.
Unfortunately, revenues plummeted with changes in reimbursement after passage of the Medicare Modernization Act in 2003 and they continue to destabilize and reduce the number of community practices across the country. Many oncologists and oncology practices, including mine, chose to join larger academic or hospital systems or larger oncology networks at a time they are also facing growing pressures to contain costs, focus on out-patient care, complex clinical trials, and expanded access to care.
Although we may lament the shrinking landscape of private oncology practices, we can also be inspired by the physicians who have joined ranks with the better-funded, better-resourced, more traditional hospital and academic systems. These larger systems have more resources, more clincial trial offerings, staffing, technology, and analytics to expand value-based care initiatives to larger numbers of patients.
The hub-and-spoke models of oncology care with integrated networks linked by technology, and networked into larger analytic and decision support systems such as CancerLinQ, the health information technology program of the American Society of Clinical Oncology (ASCO),2 could facilitate documentable delivery of comprehensive, evidence-based care, moving us closer to meeting the Quadruple Aim of optimal health care: improving the patient experience of care (including quality and satisfaction); improving the health of populations; reducing the per capita cost of health care; and improving the work life of those who deliver care.3,4
Payment reform: working to align incentives
Everyone seems to agree that the fee-for-service payment models do not align incentives for improving total health outcomes at the lowest costs, but at the moment, there seems to be no best way of aligning them. Robinson has reported on the oncology payment initiatives at four major health insurance plans – Medicare (public) and Anthem, Aetna, and UnitedHealthcare (all private), noting that:5
- Medicare is testing its Oncology Care Model at more than 200 sites in the United States, and early data are expected to be released in 2018.
- Anthem continues with its Cancer Care Quality Program that includes adherence to 2 key requirements: that participants are compliant with Anthem-approved drug pathways, and that they register their patients at the insurer’s oncology website and enter their clinical data. Anthem is also considering expanding the management fee for certain high priority clinical trials.
- Aetna’s Oncology Solutions takes a different approach by providing increased payments for generic chemotherapies.
- United has eliminated the mark-up for new drugs and continues to mark up the prices of the older and generic therapies. Its episode-based pricing gives practices upfront payments based on expected drug margins so that practices can fund more comprehensive evidence-based care. In a presentation at a Washington State Medical Oncology Society meeting recently, United’s Lee Newcomer, reported that the insurer continues to see improved clinical and financial outcomes as well as encouraging early data showing that patients might do better in the real-world setting on some therapies that have not been fully compared in head-to-head randomized clinical trials.6,7
ASCO is pulling these ideas together at the national level with its Patient-Centered Oncology Payment (PCOP) model, which is similar to Medicare’s alternative payment model. The PCOP model focuses on high-value, quality care. Higher upfront payments would cover the additional diagnostic services, care planning, and management to improve compliance and adherence as well as clinical trial evaluations. The model was developed and vetted by the ASCO Clinical Practice Committee and practicing oncologists, and is supported by staff and consultants. It is currently in its second year of operation with a commercial payer and will be submitted for review to the Physician-Focused Payment Model Technical Advisory Committee of the Health and Human Services. The results of the review are expected in 2018. If the model is approved, it could provide a uniform approach for payers that would align incentives for high-quality cancer care and allow for better predictive modeling for practices, irrespective of size, to invest in infrastructure and staffing to meet the growing demand for high-quality, value-based cancer care.
Better science: the promise of more cures
The FDA approved a record number drugs and biologics in 2017 for various cancers,8 including the landmark approval of the first CART therapy for cancer, tisagenlecleucel, which targets CD19 on B cells in the treatment of acute leukemia. That approval was rapidly followed by a second anti-CD19 CART therapy, axicabtagene ciloluecel, for refractory, aggressive B-cell non-Hodgkin lymphoma.9,10 Although these therapies can achieve remarkable response and even complete response rates in otherwise refractory patients, only some achieve a long-term remission, and the costs are an order of magnitude above most other cancer therapies. That raises the question of what duration of benefit we should expect for treatments that cost in the range of $500,000 for the therapy alone, along with the additional costs for care, hospitalization, monitoring, expensive biologics (eg, tocilizumab, for the severe and potentially life-threatening cytokine-release syndrome associated with CART therapies), and significant neurologic and other therapy-related toxicities.
Novel arrangements between pharmaceutical companies and payers are currently being discussed so that only patients who meet specific response criteria would be charged for the therapy. In addition, we await findings from ongoing research to see if new approaches can find specific targetable sites on solid tumors that could spare the healthy organ tissues while eliminating highly resistant or heterogeneous populations of mutations in patients with advanced solid tumors. Such development of highly specific targets for CART therapies would improve their efficacy and safety, and with defined protocols in place to address toxicities and efforts to reduce the costs of the therapies, we can hopefully ensure broader access for patients to this potentially transformative therapeutic tool.
In addition to the excitement around the CART therapies, many of the years other new approvals will bring incremental but meaningful improvement in outcomes for patients with common cancers. The approval of neratinib, the first agent approved as extended adjuvant therapy for women with early-stage HER2/neu-positive breast cancer, is welcome, given the current 30% recurrence risk that extends past 10 years for women in that disease population who have completed standard adjuvant HER2-directed therapies. The 34% reduction in recurrence risk with a year of extended oral adjuvant therapy, as reported by Martin and colleagues,11 with benefits sustained out to 5 years and with controllable diarrhea as the major toxicity, are encouraging. This oral therapy may be especially beneficial for hormone-receptor–positive women in whom blocking the HER2/neu pathway may enhance cell signaling through the hormone pathways, which can be blocked with oral agents at the same time to provide significant reduction of recurrence risk.
Diagnostics
The concept of personalized medicine is based on identifying biomarkers that are predictive of a patient’s response to treatment. There has been much progress toward applying NGS of tumors for use in the clinic, but we are still awaiting evidence from randomized clinical trials that such approaches prolong overall or progression-free survival.12 Dr Julie Lange, an associate professor of clinical surgery and director of the Breast Cancer Program at the Keck School of Medicine at the University of Southern California, Los Angeles, provided me with the references to key studies in this field in which she is a leading researcher.13 However, she pointed out that in the absence of effective therapies, advanced biomarker testing may be less helpful, as is the case in heavily pretreated patients,14 unless a molecular test can pinpoint a potentially clinically actionable mutation. With the plethora of available assays and the high costs of molecular testing, clinicians are challenged in knowing what testing is best for which patients. Findings from a number of key ongoing national trials may eventually help us understand which tumor mutations in which tumor types can be most effectively targeted when multiple targetable mutations are found (TAPUR,15 MATCH,16 and QUILT17 and other basket trials18). The complexity of molecular testing has led to the development of institutional, trial-based, or co-operative group molecular tumor boards to provide guidance on specific targeted therapies for specific tumor mutations.
ASCO has launched a monthly series called Molecular Oncology Tumor Boards19 to expand the knowledge base in this field. It is presented as user-driven discussions designed to help providers integrate the use of the new genetic and genomic tests and their results into the day-to-day clinical care of patients with cancer.20
Liquid biopsies
As busy clinicians, we need to understand the differences in liquid biopsy tests and their correlation with actionable targets, especially given the rapid progress in this field. Again, Dr Lange offered clarity on those differences. Liquid biopsy, refers to using a blood draw to isolate circulating tumor cells (CTCs) or circulating tumor DNA (ctDNA) to assess tumor biomarkers.21 Both CTCs and ctDNA tests have been shown to be prognostic of worse survival.22-24 Liquid biopsies are currently supplemental to direct tumor biopsies, not replacements for them. The theoretical advantage of liquid biopsies is that they may reflect tumor heterogeneity by examining the repertoire of mutations contributed by diverse metastatic sites that shed CTCs or ctDNA into the circulation. The question is which type of testing can best inform therapy decisions.
Assays for ctDNA using droplet digital PCR [polymerase chain reaction], a digital PCR method based on water-oil emulsion droplet technology, require a priori knowledge of the specific mutation associated with response or lack of response to a specific therapy.25,26 Technical issues related to the detection of rare alleles present within a mixed population of leukocytes, and ctDNA remains a challenge for many ctDNA assays. However, there is evidence to suggest that whole-exome sequencing of ctDNA is concordant with mutations in metastases,27 however benchmarking ctDNA against tissue biopsies of metastases was not possible in all studies because tumor blocks were not available or because of the failure of tumor NGS assays. 28,29
Newer generations of CTC assays take advantage of the circulating tumor cell as a functional assay for mutational status, gene expression, proteomics, epigenetics, and/or chemosensitivity of cultured cells. The relationship between CTCs and ctDNA remains uncertain as to whether CTCs are the cell of origin for ctDNA or if ctDNA may reflect responding or resistant tumor populations. The use of NGS on tumor specimens, ctDNA, and CTCs as a discovery tool is advancing the field by improving the understanding of disease heterogeneity and potential treatment targets. These results require correlation with patterns of response to therapy, and ultimately require validation in randomized clinical trials to provide strong evidence justifying their use outside of clinical trials. We can look forward to a time in the not distant future when specific liquid biopsy assays will reflect the array of mutations in different metastatic sites with validation that they correlate with efficacy of targeting those mutations that have targetable therapies.
From the FDA
New approvals
- Trastuzumab-dkst (Ogivri, Mylan; Dec 1) was approved as a biosimilar to trastuzumab (Herceptin, Genentech) for the treatment of patients with HER2-overexpressing breast or metastatic stomach cancer (gastric or gastroesophageal junction adenocarcinoma).
- Sunitinib malate (Sutent, Pfizer; Nov 16) was approved for the adjuvant treatment of adult patients at high risk of recurrent renal cell carcinoma after nephrectomy.
- Obinutuzumab (Gazyva, Genentech; Nov 16) received regular approval in combination with chemotherapy, followed by obinutuzumab monotherapy in patients achieving partial remission, for adult patients with previously untreated stage II bulky, III, or IV follicular lymphoma.
- Emicizumab-kxwh (Hemlibra, Genentech; Nov 16) was approved for routine prophylaxis to prevent or reduce the frequency of bleeding episodes in adult and pediatric patients with hemophilia A with factor VIII inhibitors.
- Dasatinib (Sprycel, Bristol-Myers Squibb; Nov 9) was approved for the treatment of pediatric patients with Philadelphia chromosome-positive chronic myeloid leukemia (CML) in the chronic phase.
- Brentuximab vedotin (Adcetris, Seattle Genetics; Nov 9) for the treatment of previously treated adult patients with primary cutaneous anaplastic large cell lymphoma (pcALCL) or CD30-expressing mycosis fungoides.
- Alectinib (Alecensa, Hoffmann-La Roche/Genentech; Nov 6) was approved for treatment of patients with anaplastic lymphoma kinase–positive metastatic non-small cell lung cancer (NSCLC), as detected by an FDA-approved test.
- Vemurafenib (Zelboraf, Hoffmann-La Roche; Nov 6) received approval for the treatment of Acalabrutinib (Calquence, AstraZeneca/Acerta; Oct 31) was granted accelerated approval for treatment of adult patients with mantle cell lymphoma (MCL) who have received at least one previous therapy.
- Axicabtagene ciloleucel (Yescarta, Kite; Oct 18), a CART therapy, was approved for treatment of adult patients with relapsed or refractory large B-cell lymphoma after two or more lines of systemic therapy, including diffuse large B-cell lymphoma (DLBCL) not otherwise specified, primary mediastinal large B-cell lymphoma, high-grade B-cell lymphoma, and DLBCL arising from follicular lymphoma. The complete remission rate reviewed by the FDA for trial patients was 51%.30 It was the second CART therapy this year to receive approval (see tisagenlecleucel; Aug 30). The agency granted orphan drug designation and priority review to therapy for this indication.
- Abemaciclib (Verzenio, Eli Lilly; Sep 28) was approved in combination with fulvestrant for women with hormone receptor-positive, HER2-negative advanced or metastatic breast cancer with disease progression following endocrine therapy.
- Copanlisib (Aliqopa, Bayer; Sep 14) got accelerated approval for the treatment of adult patients with relapsed follicular lymphoma who have received at least two prior systemic therapies.
- Bevacizumab-awwb (Mvasi, Amgen; Sep 14) was approved as a biosimilar to bevacizumab (Avastin, Genentech) for treating multiple types of cancer. It was the first biosimilar approved in the US for the treatment of cancer.
- Gemtuzumab ozogamicin (Mylotarg, Pfizer; Sep 1) was approved for the treatment of newly diagnosed CD33-positive acute myeloid leukemia (AML) in adults and of relapsed/refractory CD33-positive AML in adults and pediatric patients aged 2 or older. It can be used in combination with daunorubicin and cytarabine for adults with newly diagnosed AML, or as a standalone treatment for certain adult and pediatric patients. The drug was originally approved in 2000 as a standalone treatment for CD33-positive AML in patients older than 60 years, but was withdrawn in 2010 because of safety concerns and postmarketing trials could not confirm benefit. The current approval is for a lower recommended dose and schedule.31
- Tisagenlecleucel (Kymriah, Novartis; Aug 30) was approved for the treatment of patients up to age 25 years with B-cell precursor acute lymphoblastic leukemia (ALL) that is refractory or in second or later relapse. It is the first CART immunotherapy approved by the agency.
- Inotuzumab ozogamicin (Besponsa, Wyeth; Aug 17) was approved for the treatment of adults with relapsed or refractory B-cell precursor ALL.
- A liposome-encapsulated combination of daunorubicin and cytarabine (Vyxeos, Jazz; Aug 3) was approved for the treatment of adults with newly diagnosed therapy-related AML (t-AML) or AML with myelodysplasia-related changes (AML-MRC), two types of AML having a poor prognosis.
- Enasidenib (Idhifa, Celgene; Aug 1) was approved for the treatment of adult patients with relapsed or refractory AML with an isocitrate dehydrogenase-2 mutation as detected by an FDA-approved test.
- Neratinib (Nerlynx, Puma; Jul 17) was approved as the first extended adjuvant therapy for adult patients with early stage HER2-overexpressed/amplified breast cancer, to follow adjuvant trastuzumab-based therapy.
- Blinatumomab (Blincyto, Amgen; Jul 11) was approved for the treatment of relapsed or refractory B-cell precursor acute lymphoblastic leukemia in adults and children.
- L-glutamine oral powder (Endari, Emmaus; Jul 7) was approved for oral administration to reduce the acute complications of sickle cell disease in adult and pediatric patients 5 years and older.
- Betrixaban (Bevyxxa, Portola; Jun 23) was approved for the prophylaxis of venous thromboembolism (VTE) in adult patients hospitalized for an acute medical illness who are at risk for thromboembolic complications because of moderate or severe restricted mobility and other risk factors for VTE.
- The combination of rituximab and hyaluronidase human (Rituxan Hycela, Genentech; Jun 22) was approved for adult patients with follicular lymphoma, DLBCL, and chronic lymphocytic leukemia. Hyaluronidase human is an enzyme that helps deliver the rituximab. This formulation allows subcutaneous administration of the combination, which will shorten patient visit times and potentially even allow at-home therapy delivery.
- Ceritinib (Zykadia, Novartis; May 26) was approved for patients with metastatic NSCLC whose tumors are anaplastic lymphoma kinase (ALK)-positive as detected by an FDA-approved test.
- Avelumab (Bavencio, EMD Serono; May 9) got accelerated approval for patients with locally advanced or metastatic urothelial carcinoma whose disease progressed during or following platinum-containing chemotherapy or within 12 months of neoadjuvant or adjuvant platinum-containing chemotherapy.
- Durvalumab (ImfinzI, AstraZeneca; May 1) got accelerated approval for the treatment of patients with locally advanced or metastatic urothelial carcinoma who have disease progression during or following platinum-containing chemotherapy or who have disease progression within 12 months of neoadjuvant or adjuvant treatment with platinum-containing chemotherapy.
- Brigatinib (Alunbrig tablets, Takeda through Ariad; Apr 28) got accelerated approval for the treatment of patients with metastatic anaplastic lymphoma kinase (ALK)-positive NSCLC who have progressed on or are intolerant to crizotinib.
- Midostaurin (Rydapt, Novartis; Apr 28) was approved for the treatment of adult patients with newly diagnosed AML who are FLT3 mutation-positive, as detected by an FDA-approved test, in combination with standard cytarabine and daunorubicin induction and cytarabine consolidation.
- Osimertinib (Tagrisso, AstraZeneca; Mar 30) got regular approval for the treatment of patients with metastatic epidermal growth factor receptor (EGFR) T790M mutation-positive NSCLC, as detected by an FDA-approved test, whose disease has progressed on or after EGFR tyrosine-kinase inhibitor therapy.
- Niraparib (Zejula, Tesaro; Mar 27), a poly ADP-ribose polymerase (PARP) inhibitor, was approved for the maintenance treatment of adult patients with recurrent epithelial ovarian, fallopian tube, or primary peritoneal cancer who are in complete or partial response to platinum-based chemotherapy.
- Avelumab (Mar 23), a PD-L1–blocking human IgG1 lambda monoclonal antibody, got accelerated approval for the treatment of patients 12 years and older with metastatic Merkel cell carcinoma. It is the first FDA-approved product to treat this type of cancer.
- Ribociclib (Kisqali, Novartis; Mar 13), a CDK4/6 inhibitor, was approved as a breakthrough therapy after priority review for use in combination with an aromatase inhibitor as initial endocrine-based therapy for the treatment of postmenopausal women with HR-positive, HER2-negative advanced or metastatic breast cancer.
Expanded/additional indications
- Nivolumab (Opdivo, Bristol-Myers Squibb; Sep 22) got accelerated expanded indication approval for treatment of hepatocellular carcinoma (HCC) in patients previously treated with sorafenib.
- Pembrolizumab (Keytruda, Merck; Sep 22) got accelerated expanded indication approval for recurrent locally advanced or metastatic gastric or gastroesophageal junction adenocarcinoma in patients whose tumors express PD-L1 as determined by an FDA-approved test.
- DigniCap Scalp Cooling System (Dignitana Inc; Jul 3) was cleared for expanded use for reducing hair loss during chemotherapy for all solid tumors. Marketing authorization for the cooling cap had been granted in 2015 for patients with breast cancer.
- Olaparib tablets (Lynparza, AstraZeneca; Aug 17) got approval for an expanded indication as maintenance treatment of adult patients with recurrent epithelial ovarian, fallopian tube, or primary peritoneal cancer, who are in a complete or partial response to platinum-based chemotherapy.
- Ibrutinib (Imbruvica, Pharmacyclics; Aug 2) got expanded indication approval for the treatment of adult patients with chronic graft-versus-host disease (cGVHD) after failure of one or more lines of systemic therapy. It was the first FDA-approved therapy for the treatment of cGVHD. (Ibrutinib was previously approved for chronic lymphocytic leukemia/small lymphocytic lymphoma, chronic lymphocytic leukemia/small lymphocytic lymphoma with 17p deletion, Waldenström’s macroglobulinemia, marginal zone lymphoma, and mantle cell lymphoma).
- Nivolumab (Aug 2) got an accelerated expanded indication for the treatment of patients 12 years and older with mismatch repair deficient (dMMR) and microsatellite instability-high (MSI-H) metastatic colorectal cancer that has progressed after treatment with a fluoropyrimidine, oxaliplatin, and irinotecan.
- Dabrafenib and trametinib (Tafinlar and Mekinist, Novartis; Jun 22) were approved for the expanded indication in combination for patients with metastatic NSCLC with BRAF V600E mutation as detected by an FDA-approved test. The combination demonstrated superior efficacy compared with dabrafenib alone (overall response rate: 61% and 27%, respectively).32
- Pembrolizumab (May 23) got approved for expanded indication for adult and pediatric patients with unresectable or metastatic, MSI-H or dMMR solid tumors that have progressed after treatment and who have no satisfactory alternative treatment options or with MSI-H or dMMR colorectal cancer that has progressed after treatment with a fluoropyrimidine, oxaliplatin, and irinotecan.
- Pembrolizumab (May 18) got approval for expanded indication for patients with locally advanced or metastatic urothelial carcinoma who have disease progression during or following platinum-containing chemotherapy or within 12 months of neoadjuvant or adjuvant treatment with platinum-containing chemotherapy.
- Pembrolizumab (May 10) got accelerated expanded indication for use combination with pemetrexed and carboplatin for the treatment of patients with previously untreated metastatic NSCLC.
- Regorafenib (Stivarga, Bayer; Apr 27) got an additional indication for the treatment of patients with HCC who have been previously treated with sorafenib.
- Palbociclib (Ibrance, Pfizer; Mar 31) got an expanded indication that includes first-line therapy for the treatment of hormone receptor–positive, HER2-negative advanced or metastatic breast cancer in combination with an aromatase inhibitor as initial endocrine based therapy in postmenopausal women.
- Pembrolizumab (Mar 15) got an accelerated additional indication approval for treatment of adult and pediatric patients with refractory classical Hodgkin lymphoma, or those who have relapsed after three or more previous lines of therapy.
- Lenalidomide (Revlimid, Celgene; Feb 22) got an additional indication as maintenance therapy for patients with multiple myeloma following autologous stem cell transplant.
- Nivolumab (Feb 2) got an accelerated expanded indication for treatment of patients with locally advanced or metastatic urothelial carcinoma who have disease progression during or following platinum-containing chemotherapy or have disease progression within 12 months of neoadjuvant or adjuvant treatment with a platinum-containing chemotherapy.
Modified use
- Cabazitaxel (Jevtana, Sanofi-Aventis; Sep 14) in combination with prednisone was approved at a lower dose of 20 mg/m2 every 3 weeks for the treatment of patients with metastatic castration-resistant prostate cancer previously treated with a docetaxel-containing treatment regimen. It had been approved at 25 mg/m2 every 3 weeks for this indication in 2010.
Tests/diagnostics
- Marketing approval was given to the FoundationOne CDx (Foundation Medicine; Nov 30), an NGS-based in vitro diagnostic to detect genetic mutations in 324 genes and 2 genomic signatures in any solid tumor type.
- Marketing approval was given to the Praxis Extended RAS Panel (Illumina; Jun 29), a next generation sequencing test to detect certain genetic mutations in RAS genes in tumor samples of patients with metastatic colorectal cancer. The test is used to aid in the identification of patients who may be eligible for treatment with panitumumab (Vectibix, Amgen).
- Marketing was approved for ipsogen JAK2 RGQ PCR Kit (Qiagen ; Mar 27) to detect mutations affecting the Janus tyrosine kinase 2 gene. This is the first FDA-authorized test intended to help physicians in evaluating patients for suspected polycythemia vera.
Imaging and pathology aids
- Aminolevulinic acid hydrochloride, known as ALA HCl (Gleolan, NX; Jun 6) was approved as an optical imaging agent indicated in patients with gliomas (suspected World Health Organization grades III or IV on preoperative imaging) as an adjunct for the visualization of malignant tissue during surgery.
- Marketing was approved for the Philips IntelliSite Pathology Solution (PIPS, Philips Medical Systems Nederland; Apr 17), as an aid to the pathologist to review and interpret digital images of surgical pathology slides prepared from formalin-fixed paraffin embedded tissue.
Challenges and uncertainties
The current administration’s initiatives to reduce administrative burdens is underway with the Patients Over Paperwork initiative. Eliminating and streamlining regulations to increase efficiency and improve beneficiary experience could be helpful to both oncologists and patients. For now, the Medicare Access and CHIP Reauthorization Act (MACRA) program, allows you to “pick your pace” in the 2017 performance year and report on at least one measure to avoid a payment reduction penalty on your Medicare payments in 2019. In the final rule for 2018, the CMS finalized a proposal to apply the MIPS [Merit-based Incentive Payment System] adjustment to all Part B items and services, which will include Part B drugs. This would be unfair to oncologists who treat on the basis of evidence-based guidelines and pathways and have no control over the costs of the drugs they prescribe.
In addition, more requirements will be imposed in 2018 in a move toward full MACRA implementation. All four composite categories (Quality – 60% for 2017; Advancing Care Information (ACI, renamed from Meaningful Use) – 25% for 2017; Improvement Activities (IA) – 15% for 2017; and Cost – 0% for 2017, but weighted in the future) will be scored, including resource use (cost) at 10%. CMS will collect data to assess the total cost of care and the Medicare Spend per Beneficiary to assess use. Full program implementation, with cost being assessed at 30% of your score is expected in the 2019 performance year. ASCO’s clinical affairs and policy experts have studied the implications of Part B chemotherapy drugs being included in the cost component of the MIPS scoring and will continue advocating for policies that hold clinicians responsible only for the aspects of care they can control, such as providing high-quality care based on the patient’s disease, biomarkers, comorbidities, and preferences, and not the costs of the evidence-based therapies needed by patients.
Toward a better 2018 for ourselves and our patients
As an eternal optimist, I remain enthusiastic that despite the many challenges, we will find effective ways to bring standard as well as newer, cell-based and targeted therapies to our patients and cover the costs of highly effective therapies. I also remain hopeful that improving technological capabilities and payment reforms will be used by innovative clinical and administrative care teams to give clinicians more time to improve the care and health of patients while validating the methodologies so that real world data can help us further craft therapies to improve the health of each individual who needs our care. As we close this 15th year of our journal, we hope our presentations of practical science and implementation content has helped support your work while freeing some time for you to enjoy the journey. Our best wishes for a joyful holiday season celebrated with friends and family and the patients who entrust us to help them face and live beyond their cancer diagnoses.
This past year will likely be remembered as one of breakthrough advances in reducing the burden of cancer, with some landmark “firsts” coming out of the US Food and Drug Admini
Our excitement has also been tempered by the rapid rise in the cost of effective biologic, immunologic, and targeted therapies. With the approval of trastuzumab-dkst (Ogivri), the first targeted biosimilar for HER2-positive breast and gastrointestinal cancers, we can look forward to price decreases possibly in the 20%-30% range over time from a targeted therapy with remarkable clinical efficacy. We know that approved biosimilars have demonstrated clinical efficacy along with similar minor biologic diversity that is also seen in the reference biologic.1 We can also hope that increasing competition among biosimilar and reference compounds will lead to improvements in production methodologies that can allow further price reductions so that even more patients can gain access to these highly effective therapies.
In addition, the first FDA approval for the next-generation sequencing (NGS) FoundationOne profiling test and the rapid announcement by the Centers for Medicare & Medicaid Services (CMS) that it will cover the cost of that testing brings us a step closer to knowing which patients most likely will or won’t benefit from costly and toxic targeted therapies. Along with the many clinical trials studying which mutations predict which efficacies of individual or combinations of targeted agents, the approval and CMS coverage policy will help us improve value to our patients; when we can recommend the most beneficial therapies and avoid futile ones.
Finally, the approval for the DigniCap Scalp Cooling System for patients on chemotherapy for all solid tumors is of great importance. Pending coverage availability, it may influence some patients to get chemotherapy they might otherwise have forgone to avoid hair loss (see related article).
More consolidation: the best of all worlds?
In my 27 years in private practice, during which practice revenues grew with the favorable profit margins on novel therapies, forward-thinking physician leaders piloted innovations in oncology electronic medical records (EMRs), the delivery of team-based care, clinical research partnerships, and more comprehensive care services to better serve diverse communities, including those in rural areas. At my previous practice, that included adding clinicians to our group to serve patients at hospital clinics in 2 counties in southern California, each county with populations larger than 15 states. Our private practice worked with these public entities to bring state-of-the art care and private practice efficiencies to the uninsured and underserved in our region.
Unfortunately, revenues plummeted with changes in reimbursement after passage of the Medicare Modernization Act in 2003 and they continue to destabilize and reduce the number of community practices across the country. Many oncologists and oncology practices, including mine, chose to join larger academic or hospital systems or larger oncology networks at a time they are also facing growing pressures to contain costs, focus on out-patient care, complex clinical trials, and expanded access to care.
Although we may lament the shrinking landscape of private oncology practices, we can also be inspired by the physicians who have joined ranks with the better-funded, better-resourced, more traditional hospital and academic systems. These larger systems have more resources, more clincial trial offerings, staffing, technology, and analytics to expand value-based care initiatives to larger numbers of patients.
The hub-and-spoke models of oncology care with integrated networks linked by technology, and networked into larger analytic and decision support systems such as CancerLinQ, the health information technology program of the American Society of Clinical Oncology (ASCO),2 could facilitate documentable delivery of comprehensive, evidence-based care, moving us closer to meeting the Quadruple Aim of optimal health care: improving the patient experience of care (including quality and satisfaction); improving the health of populations; reducing the per capita cost of health care; and improving the work life of those who deliver care.3,4
Payment reform: working to align incentives
Everyone seems to agree that the fee-for-service payment models do not align incentives for improving total health outcomes at the lowest costs, but at the moment, there seems to be no best way of aligning them. Robinson has reported on the oncology payment initiatives at four major health insurance plans – Medicare (public) and Anthem, Aetna, and UnitedHealthcare (all private), noting that:5
- Medicare is testing its Oncology Care Model at more than 200 sites in the United States, and early data are expected to be released in 2018.
- Anthem continues with its Cancer Care Quality Program that includes adherence to 2 key requirements: that participants are compliant with Anthem-approved drug pathways, and that they register their patients at the insurer’s oncology website and enter their clinical data. Anthem is also considering expanding the management fee for certain high priority clinical trials.
- Aetna’s Oncology Solutions takes a different approach by providing increased payments for generic chemotherapies.
- United has eliminated the mark-up for new drugs and continues to mark up the prices of the older and generic therapies. Its episode-based pricing gives practices upfront payments based on expected drug margins so that practices can fund more comprehensive evidence-based care. In a presentation at a Washington State Medical Oncology Society meeting recently, United’s Lee Newcomer, reported that the insurer continues to see improved clinical and financial outcomes as well as encouraging early data showing that patients might do better in the real-world setting on some therapies that have not been fully compared in head-to-head randomized clinical trials.6,7
ASCO is pulling these ideas together at the national level with its Patient-Centered Oncology Payment (PCOP) model, which is similar to Medicare’s alternative payment model. The PCOP model focuses on high-value, quality care. Higher upfront payments would cover the additional diagnostic services, care planning, and management to improve compliance and adherence as well as clinical trial evaluations. The model was developed and vetted by the ASCO Clinical Practice Committee and practicing oncologists, and is supported by staff and consultants. It is currently in its second year of operation with a commercial payer and will be submitted for review to the Physician-Focused Payment Model Technical Advisory Committee of the Health and Human Services. The results of the review are expected in 2018. If the model is approved, it could provide a uniform approach for payers that would align incentives for high-quality cancer care and allow for better predictive modeling for practices, irrespective of size, to invest in infrastructure and staffing to meet the growing demand for high-quality, value-based cancer care.
Better science: the promise of more cures
The FDA approved a record number drugs and biologics in 2017 for various cancers,8 including the landmark approval of the first CART therapy for cancer, tisagenlecleucel, which targets CD19 on B cells in the treatment of acute leukemia. That approval was rapidly followed by a second anti-CD19 CART therapy, axicabtagene ciloluecel, for refractory, aggressive B-cell non-Hodgkin lymphoma.9,10 Although these therapies can achieve remarkable response and even complete response rates in otherwise refractory patients, only some achieve a long-term remission, and the costs are an order of magnitude above most other cancer therapies. That raises the question of what duration of benefit we should expect for treatments that cost in the range of $500,000 for the therapy alone, along with the additional costs for care, hospitalization, monitoring, expensive biologics (eg, tocilizumab, for the severe and potentially life-threatening cytokine-release syndrome associated with CART therapies), and significant neurologic and other therapy-related toxicities.
Novel arrangements between pharmaceutical companies and payers are currently being discussed so that only patients who meet specific response criteria would be charged for the therapy. In addition, we await findings from ongoing research to see if new approaches can find specific targetable sites on solid tumors that could spare the healthy organ tissues while eliminating highly resistant or heterogeneous populations of mutations in patients with advanced solid tumors. Such development of highly specific targets for CART therapies would improve their efficacy and safety, and with defined protocols in place to address toxicities and efforts to reduce the costs of the therapies, we can hopefully ensure broader access for patients to this potentially transformative therapeutic tool.
In addition to the excitement around the CART therapies, many of the years other new approvals will bring incremental but meaningful improvement in outcomes for patients with common cancers. The approval of neratinib, the first agent approved as extended adjuvant therapy for women with early-stage HER2/neu-positive breast cancer, is welcome, given the current 30% recurrence risk that extends past 10 years for women in that disease population who have completed standard adjuvant HER2-directed therapies. The 34% reduction in recurrence risk with a year of extended oral adjuvant therapy, as reported by Martin and colleagues,11 with benefits sustained out to 5 years and with controllable diarrhea as the major toxicity, are encouraging. This oral therapy may be especially beneficial for hormone-receptor–positive women in whom blocking the HER2/neu pathway may enhance cell signaling through the hormone pathways, which can be blocked with oral agents at the same time to provide significant reduction of recurrence risk.
Diagnostics
The concept of personalized medicine is based on identifying biomarkers that are predictive of a patient’s response to treatment. There has been much progress toward applying NGS of tumors for use in the clinic, but we are still awaiting evidence from randomized clinical trials that such approaches prolong overall or progression-free survival.12 Dr Julie Lange, an associate professor of clinical surgery and director of the Breast Cancer Program at the Keck School of Medicine at the University of Southern California, Los Angeles, provided me with the references to key studies in this field in which she is a leading researcher.13 However, she pointed out that in the absence of effective therapies, advanced biomarker testing may be less helpful, as is the case in heavily pretreated patients,14 unless a molecular test can pinpoint a potentially clinically actionable mutation. With the plethora of available assays and the high costs of molecular testing, clinicians are challenged in knowing what testing is best for which patients. Findings from a number of key ongoing national trials may eventually help us understand which tumor mutations in which tumor types can be most effectively targeted when multiple targetable mutations are found (TAPUR,15 MATCH,16 and QUILT17 and other basket trials18). The complexity of molecular testing has led to the development of institutional, trial-based, or co-operative group molecular tumor boards to provide guidance on specific targeted therapies for specific tumor mutations.
ASCO has launched a monthly series called Molecular Oncology Tumor Boards19 to expand the knowledge base in this field. It is presented as user-driven discussions designed to help providers integrate the use of the new genetic and genomic tests and their results into the day-to-day clinical care of patients with cancer.20
Liquid biopsies
As busy clinicians, we need to understand the differences in liquid biopsy tests and their correlation with actionable targets, especially given the rapid progress in this field. Again, Dr Lange offered clarity on those differences. Liquid biopsy, refers to using a blood draw to isolate circulating tumor cells (CTCs) or circulating tumor DNA (ctDNA) to assess tumor biomarkers.21 Both CTCs and ctDNA tests have been shown to be prognostic of worse survival.22-24 Liquid biopsies are currently supplemental to direct tumor biopsies, not replacements for them. The theoretical advantage of liquid biopsies is that they may reflect tumor heterogeneity by examining the repertoire of mutations contributed by diverse metastatic sites that shed CTCs or ctDNA into the circulation. The question is which type of testing can best inform therapy decisions.
Assays for ctDNA using droplet digital PCR [polymerase chain reaction], a digital PCR method based on water-oil emulsion droplet technology, require a priori knowledge of the specific mutation associated with response or lack of response to a specific therapy.25,26 Technical issues related to the detection of rare alleles present within a mixed population of leukocytes, and ctDNA remains a challenge for many ctDNA assays. However, there is evidence to suggest that whole-exome sequencing of ctDNA is concordant with mutations in metastases,27 however benchmarking ctDNA against tissue biopsies of metastases was not possible in all studies because tumor blocks were not available or because of the failure of tumor NGS assays. 28,29
Newer generations of CTC assays take advantage of the circulating tumor cell as a functional assay for mutational status, gene expression, proteomics, epigenetics, and/or chemosensitivity of cultured cells. The relationship between CTCs and ctDNA remains uncertain as to whether CTCs are the cell of origin for ctDNA or if ctDNA may reflect responding or resistant tumor populations. The use of NGS on tumor specimens, ctDNA, and CTCs as a discovery tool is advancing the field by improving the understanding of disease heterogeneity and potential treatment targets. These results require correlation with patterns of response to therapy, and ultimately require validation in randomized clinical trials to provide strong evidence justifying their use outside of clinical trials. We can look forward to a time in the not distant future when specific liquid biopsy assays will reflect the array of mutations in different metastatic sites with validation that they correlate with efficacy of targeting those mutations that have targetable therapies.
From the FDA
New approvals
- Trastuzumab-dkst (Ogivri, Mylan; Dec 1) was approved as a biosimilar to trastuzumab (Herceptin, Genentech) for the treatment of patients with HER2-overexpressing breast or metastatic stomach cancer (gastric or gastroesophageal junction adenocarcinoma).
- Sunitinib malate (Sutent, Pfizer; Nov 16) was approved for the adjuvant treatment of adult patients at high risk of recurrent renal cell carcinoma after nephrectomy.
- Obinutuzumab (Gazyva, Genentech; Nov 16) received regular approval in combination with chemotherapy, followed by obinutuzumab monotherapy in patients achieving partial remission, for adult patients with previously untreated stage II bulky, III, or IV follicular lymphoma.
- Emicizumab-kxwh (Hemlibra, Genentech; Nov 16) was approved for routine prophylaxis to prevent or reduce the frequency of bleeding episodes in adult and pediatric patients with hemophilia A with factor VIII inhibitors.
- Dasatinib (Sprycel, Bristol-Myers Squibb; Nov 9) was approved for the treatment of pediatric patients with Philadelphia chromosome-positive chronic myeloid leukemia (CML) in the chronic phase.
- Brentuximab vedotin (Adcetris, Seattle Genetics; Nov 9) for the treatment of previously treated adult patients with primary cutaneous anaplastic large cell lymphoma (pcALCL) or CD30-expressing mycosis fungoides.
- Alectinib (Alecensa, Hoffmann-La Roche/Genentech; Nov 6) was approved for treatment of patients with anaplastic lymphoma kinase–positive metastatic non-small cell lung cancer (NSCLC), as detected by an FDA-approved test.
- Vemurafenib (Zelboraf, Hoffmann-La Roche; Nov 6) received approval for the treatment of Acalabrutinib (Calquence, AstraZeneca/Acerta; Oct 31) was granted accelerated approval for treatment of adult patients with mantle cell lymphoma (MCL) who have received at least one previous therapy.
- Axicabtagene ciloleucel (Yescarta, Kite; Oct 18), a CART therapy, was approved for treatment of adult patients with relapsed or refractory large B-cell lymphoma after two or more lines of systemic therapy, including diffuse large B-cell lymphoma (DLBCL) not otherwise specified, primary mediastinal large B-cell lymphoma, high-grade B-cell lymphoma, and DLBCL arising from follicular lymphoma. The complete remission rate reviewed by the FDA for trial patients was 51%.30 It was the second CART therapy this year to receive approval (see tisagenlecleucel; Aug 30). The agency granted orphan drug designation and priority review to therapy for this indication.
- Abemaciclib (Verzenio, Eli Lilly; Sep 28) was approved in combination with fulvestrant for women with hormone receptor-positive, HER2-negative advanced or metastatic breast cancer with disease progression following endocrine therapy.
- Copanlisib (Aliqopa, Bayer; Sep 14) got accelerated approval for the treatment of adult patients with relapsed follicular lymphoma who have received at least two prior systemic therapies.
- Bevacizumab-awwb (Mvasi, Amgen; Sep 14) was approved as a biosimilar to bevacizumab (Avastin, Genentech) for treating multiple types of cancer. It was the first biosimilar approved in the US for the treatment of cancer.
- Gemtuzumab ozogamicin (Mylotarg, Pfizer; Sep 1) was approved for the treatment of newly diagnosed CD33-positive acute myeloid leukemia (AML) in adults and of relapsed/refractory CD33-positive AML in adults and pediatric patients aged 2 or older. It can be used in combination with daunorubicin and cytarabine for adults with newly diagnosed AML, or as a standalone treatment for certain adult and pediatric patients. The drug was originally approved in 2000 as a standalone treatment for CD33-positive AML in patients older than 60 years, but was withdrawn in 2010 because of safety concerns and postmarketing trials could not confirm benefit. The current approval is for a lower recommended dose and schedule.31
- Tisagenlecleucel (Kymriah, Novartis; Aug 30) was approved for the treatment of patients up to age 25 years with B-cell precursor acute lymphoblastic leukemia (ALL) that is refractory or in second or later relapse. It is the first CART immunotherapy approved by the agency.
- Inotuzumab ozogamicin (Besponsa, Wyeth; Aug 17) was approved for the treatment of adults with relapsed or refractory B-cell precursor ALL.
- A liposome-encapsulated combination of daunorubicin and cytarabine (Vyxeos, Jazz; Aug 3) was approved for the treatment of adults with newly diagnosed therapy-related AML (t-AML) or AML with myelodysplasia-related changes (AML-MRC), two types of AML having a poor prognosis.
- Enasidenib (Idhifa, Celgene; Aug 1) was approved for the treatment of adult patients with relapsed or refractory AML with an isocitrate dehydrogenase-2 mutation as detected by an FDA-approved test.
- Neratinib (Nerlynx, Puma; Jul 17) was approved as the first extended adjuvant therapy for adult patients with early stage HER2-overexpressed/amplified breast cancer, to follow adjuvant trastuzumab-based therapy.
- Blinatumomab (Blincyto, Amgen; Jul 11) was approved for the treatment of relapsed or refractory B-cell precursor acute lymphoblastic leukemia in adults and children.
- L-glutamine oral powder (Endari, Emmaus; Jul 7) was approved for oral administration to reduce the acute complications of sickle cell disease in adult and pediatric patients 5 years and older.
- Betrixaban (Bevyxxa, Portola; Jun 23) was approved for the prophylaxis of venous thromboembolism (VTE) in adult patients hospitalized for an acute medical illness who are at risk for thromboembolic complications because of moderate or severe restricted mobility and other risk factors for VTE.
- The combination of rituximab and hyaluronidase human (Rituxan Hycela, Genentech; Jun 22) was approved for adult patients with follicular lymphoma, DLBCL, and chronic lymphocytic leukemia. Hyaluronidase human is an enzyme that helps deliver the rituximab. This formulation allows subcutaneous administration of the combination, which will shorten patient visit times and potentially even allow at-home therapy delivery.
- Ceritinib (Zykadia, Novartis; May 26) was approved for patients with metastatic NSCLC whose tumors are anaplastic lymphoma kinase (ALK)-positive as detected by an FDA-approved test.
- Avelumab (Bavencio, EMD Serono; May 9) got accelerated approval for patients with locally advanced or metastatic urothelial carcinoma whose disease progressed during or following platinum-containing chemotherapy or within 12 months of neoadjuvant or adjuvant platinum-containing chemotherapy.
- Durvalumab (ImfinzI, AstraZeneca; May 1) got accelerated approval for the treatment of patients with locally advanced or metastatic urothelial carcinoma who have disease progression during or following platinum-containing chemotherapy or who have disease progression within 12 months of neoadjuvant or adjuvant treatment with platinum-containing chemotherapy.
- Brigatinib (Alunbrig tablets, Takeda through Ariad; Apr 28) got accelerated approval for the treatment of patients with metastatic anaplastic lymphoma kinase (ALK)-positive NSCLC who have progressed on or are intolerant to crizotinib.
- Midostaurin (Rydapt, Novartis; Apr 28) was approved for the treatment of adult patients with newly diagnosed AML who are FLT3 mutation-positive, as detected by an FDA-approved test, in combination with standard cytarabine and daunorubicin induction and cytarabine consolidation.
- Osimertinib (Tagrisso, AstraZeneca; Mar 30) got regular approval for the treatment of patients with metastatic epidermal growth factor receptor (EGFR) T790M mutation-positive NSCLC, as detected by an FDA-approved test, whose disease has progressed on or after EGFR tyrosine-kinase inhibitor therapy.
- Niraparib (Zejula, Tesaro; Mar 27), a poly ADP-ribose polymerase (PARP) inhibitor, was approved for the maintenance treatment of adult patients with recurrent epithelial ovarian, fallopian tube, or primary peritoneal cancer who are in complete or partial response to platinum-based chemotherapy.
- Avelumab (Mar 23), a PD-L1–blocking human IgG1 lambda monoclonal antibody, got accelerated approval for the treatment of patients 12 years and older with metastatic Merkel cell carcinoma. It is the first FDA-approved product to treat this type of cancer.
- Ribociclib (Kisqali, Novartis; Mar 13), a CDK4/6 inhibitor, was approved as a breakthrough therapy after priority review for use in combination with an aromatase inhibitor as initial endocrine-based therapy for the treatment of postmenopausal women with HR-positive, HER2-negative advanced or metastatic breast cancer.
Expanded/additional indications
- Nivolumab (Opdivo, Bristol-Myers Squibb; Sep 22) got accelerated expanded indication approval for treatment of hepatocellular carcinoma (HCC) in patients previously treated with sorafenib.
- Pembrolizumab (Keytruda, Merck; Sep 22) got accelerated expanded indication approval for recurrent locally advanced or metastatic gastric or gastroesophageal junction adenocarcinoma in patients whose tumors express PD-L1 as determined by an FDA-approved test.
- DigniCap Scalp Cooling System (Dignitana Inc; Jul 3) was cleared for expanded use for reducing hair loss during chemotherapy for all solid tumors. Marketing authorization for the cooling cap had been granted in 2015 for patients with breast cancer.
- Olaparib tablets (Lynparza, AstraZeneca; Aug 17) got approval for an expanded indication as maintenance treatment of adult patients with recurrent epithelial ovarian, fallopian tube, or primary peritoneal cancer, who are in a complete or partial response to platinum-based chemotherapy.
- Ibrutinib (Imbruvica, Pharmacyclics; Aug 2) got expanded indication approval for the treatment of adult patients with chronic graft-versus-host disease (cGVHD) after failure of one or more lines of systemic therapy. It was the first FDA-approved therapy for the treatment of cGVHD. (Ibrutinib was previously approved for chronic lymphocytic leukemia/small lymphocytic lymphoma, chronic lymphocytic leukemia/small lymphocytic lymphoma with 17p deletion, Waldenström’s macroglobulinemia, marginal zone lymphoma, and mantle cell lymphoma).
- Nivolumab (Aug 2) got an accelerated expanded indication for the treatment of patients 12 years and older with mismatch repair deficient (dMMR) and microsatellite instability-high (MSI-H) metastatic colorectal cancer that has progressed after treatment with a fluoropyrimidine, oxaliplatin, and irinotecan.
- Dabrafenib and trametinib (Tafinlar and Mekinist, Novartis; Jun 22) were approved for the expanded indication in combination for patients with metastatic NSCLC with BRAF V600E mutation as detected by an FDA-approved test. The combination demonstrated superior efficacy compared with dabrafenib alone (overall response rate: 61% and 27%, respectively).32
- Pembrolizumab (May 23) got approved for expanded indication for adult and pediatric patients with unresectable or metastatic, MSI-H or dMMR solid tumors that have progressed after treatment and who have no satisfactory alternative treatment options or with MSI-H or dMMR colorectal cancer that has progressed after treatment with a fluoropyrimidine, oxaliplatin, and irinotecan.
- Pembrolizumab (May 18) got approval for expanded indication for patients with locally advanced or metastatic urothelial carcinoma who have disease progression during or following platinum-containing chemotherapy or within 12 months of neoadjuvant or adjuvant treatment with platinum-containing chemotherapy.
- Pembrolizumab (May 10) got accelerated expanded indication for use combination with pemetrexed and carboplatin for the treatment of patients with previously untreated metastatic NSCLC.
- Regorafenib (Stivarga, Bayer; Apr 27) got an additional indication for the treatment of patients with HCC who have been previously treated with sorafenib.
- Palbociclib (Ibrance, Pfizer; Mar 31) got an expanded indication that includes first-line therapy for the treatment of hormone receptor–positive, HER2-negative advanced or metastatic breast cancer in combination with an aromatase inhibitor as initial endocrine based therapy in postmenopausal women.
- Pembrolizumab (Mar 15) got an accelerated additional indication approval for treatment of adult and pediatric patients with refractory classical Hodgkin lymphoma, or those who have relapsed after three or more previous lines of therapy.
- Lenalidomide (Revlimid, Celgene; Feb 22) got an additional indication as maintenance therapy for patients with multiple myeloma following autologous stem cell transplant.
- Nivolumab (Feb 2) got an accelerated expanded indication for treatment of patients with locally advanced or metastatic urothelial carcinoma who have disease progression during or following platinum-containing chemotherapy or have disease progression within 12 months of neoadjuvant or adjuvant treatment with a platinum-containing chemotherapy.
Modified use
- Cabazitaxel (Jevtana, Sanofi-Aventis; Sep 14) in combination with prednisone was approved at a lower dose of 20 mg/m2 every 3 weeks for the treatment of patients with metastatic castration-resistant prostate cancer previously treated with a docetaxel-containing treatment regimen. It had been approved at 25 mg/m2 every 3 weeks for this indication in 2010.
Tests/diagnostics
- Marketing approval was given to the FoundationOne CDx (Foundation Medicine; Nov 30), an NGS-based in vitro diagnostic to detect genetic mutations in 324 genes and 2 genomic signatures in any solid tumor type.
- Marketing approval was given to the Praxis Extended RAS Panel (Illumina; Jun 29), a next generation sequencing test to detect certain genetic mutations in RAS genes in tumor samples of patients with metastatic colorectal cancer. The test is used to aid in the identification of patients who may be eligible for treatment with panitumumab (Vectibix, Amgen).
- Marketing was approved for ipsogen JAK2 RGQ PCR Kit (Qiagen ; Mar 27) to detect mutations affecting the Janus tyrosine kinase 2 gene. This is the first FDA-authorized test intended to help physicians in evaluating patients for suspected polycythemia vera.
Imaging and pathology aids
- Aminolevulinic acid hydrochloride, known as ALA HCl (Gleolan, NX; Jun 6) was approved as an optical imaging agent indicated in patients with gliomas (suspected World Health Organization grades III or IV on preoperative imaging) as an adjunct for the visualization of malignant tissue during surgery.
- Marketing was approved for the Philips IntelliSite Pathology Solution (PIPS, Philips Medical Systems Nederland; Apr 17), as an aid to the pathologist to review and interpret digital images of surgical pathology slides prepared from formalin-fixed paraffin embedded tissue.
Challenges and uncertainties
The current administration’s initiatives to reduce administrative burdens is underway with the Patients Over Paperwork initiative. Eliminating and streamlining regulations to increase efficiency and improve beneficiary experience could be helpful to both oncologists and patients. For now, the Medicare Access and CHIP Reauthorization Act (MACRA) program, allows you to “pick your pace” in the 2017 performance year and report on at least one measure to avoid a payment reduction penalty on your Medicare payments in 2019. In the final rule for 2018, the CMS finalized a proposal to apply the MIPS [Merit-based Incentive Payment System] adjustment to all Part B items and services, which will include Part B drugs. This would be unfair to oncologists who treat on the basis of evidence-based guidelines and pathways and have no control over the costs of the drugs they prescribe.
In addition, more requirements will be imposed in 2018 in a move toward full MACRA implementation. All four composite categories (Quality – 60% for 2017; Advancing Care Information (ACI, renamed from Meaningful Use) – 25% for 2017; Improvement Activities (IA) – 15% for 2017; and Cost – 0% for 2017, but weighted in the future) will be scored, including resource use (cost) at 10%. CMS will collect data to assess the total cost of care and the Medicare Spend per Beneficiary to assess use. Full program implementation, with cost being assessed at 30% of your score is expected in the 2019 performance year. ASCO’s clinical affairs and policy experts have studied the implications of Part B chemotherapy drugs being included in the cost component of the MIPS scoring and will continue advocating for policies that hold clinicians responsible only for the aspects of care they can control, such as providing high-quality care based on the patient’s disease, biomarkers, comorbidities, and preferences, and not the costs of the evidence-based therapies needed by patients.
Toward a better 2018 for ourselves and our patients
As an eternal optimist, I remain enthusiastic that despite the many challenges, we will find effective ways to bring standard as well as newer, cell-based and targeted therapies to our patients and cover the costs of highly effective therapies. I also remain hopeful that improving technological capabilities and payment reforms will be used by innovative clinical and administrative care teams to give clinicians more time to improve the care and health of patients while validating the methodologies so that real world data can help us further craft therapies to improve the health of each individual who needs our care. As we close this 15th year of our journal, we hope our presentations of practical science and implementation content has helped support your work while freeing some time for you to enjoy the journey. Our best wishes for a joyful holiday season celebrated with friends and family and the patients who entrust us to help them face and live beyond their cancer diagnoses.
1. US Food & Drug Administration. Biosimilar and interchangeable
products. https://www.fda.gov/Drugs/DevelopmentApprovalProcess/
HowDrugsareDevelopedandApproved/ApprovalApplications/
¬erapeuticBiologicApplications/Biosimilars/ucm580419.htm. Last
updated October 23, 2017. Accessed December 11, 2017.
2. ASCO CancerLinQ website. https://cancerlinq.org/. Publishing/
update information not available. Accessed November 3, 2017.
3. Bodenheimer T, Sinsky C. From triple to quadruple aim: care of the
patient requires care of the provider. https://www.ncbi.nlm.nih.gov/
pmc/articles/PMC4226781/. Published November 2014. Accessed
November 7.
4. Institute for Healthcare Improvement. http://www.ihi.org/Engage/
Initiatives/TripleAim/Pages/default.aspx. No update information
given. Accessed November 3, 2017.
5. Robinson JC. Value-based physician payment in oncology: public and
private insurer initiatives. Milbank Q. 2017;95(1);184-203.
6. Newcomer L. Oral communication: Washington State Medical
Oncology Society meeting, August 19, 2017.
7. Newcomer LN, Gould B, Page RD, Donelan SA, Perkins M.
Changing physician incentives for aordable, quality cancer
care: results of an episode payment model. J Oncol Pract.
2014;10(5):322-326.
8. US Department of Health and Human Services website. Hematology/
oncology (cancer) approvals & safety notications. https://www.fda.
gov/Drugs/InformationOnDrugs/ApprovedDrugs/ucm279174.htm.
Last updated December 1, 2017. Accessed December 3, 2017.
9. Hem-Onc Today website. CAR T-cell therapy approval huge
step for oncology, but only ‘beginning of story’. https://www.
healio.com/hematology-oncology/leukemia/news/print/hemonctoday/%
7B33119631-5996-45cf-9be6-8e36466ded9e%7D/car-tcell-
therapy-approval-huge-step-for-oncology-but-only-beginningof-
story. Published September 25, 2017. Accessed November 9, 2017.
10. Gauthier J, Yakoub-Agha I. Chimeric antigen-receptor T-cell therapy
for hematological malignancies and solid tumors: Clinical data
to date, current limitations and perspectives. Curr Res in Transl Med.
2017;65(3):93-102.
11. Martin M, Holmes FA, Ejlertsen B, et al. Neratinib after trastuzumab-
based adjuvant therapy in early-stage HER2+ breast cancer:
5-year analysis of the phase III ExteNET trial [ESMO oral presentation].
Ann Oncol. 2017;28(suppl 5):v43-v67.
12. Le Tourneau C, Delord JP, Goncalves A, et al. Molecularly targeted
therapy based on tumour molecular proling versus conventional
therapy for advanced cancer SHIVA): a multicentre, openlabel,
proof-of-concept, randomised, controlled phase 2 trial. Lancet
Oncol. 2015;16(13):1324-1334.
13. Forte V, Barrak DK, Elhodaky M, Tung L, Snow A, Lang JE. ¬e
potential for liquid biopsies in the precision medical treatment of
breast cancer. Cancer Biol Med. 2016;13(1):19-40.
14. Smerage JB, Barlow WE, Hortobagyi GN, et al. Circulating tumor
cells and response to chemotherapy in metastatic breast cancer:
SWOG S0500. J Clin Oncol. 2014;32(31):3483-3489.
15. US National Library of Medicine. TAPUR: testing the use of food
and drug administration (FDA) approved drugs that target a specific
abnormality in a tumor gene in people with advanced stage cancer
(TAPUR). https://clinicaltrials.gov/ct2/show/NCT02693535.
First posted February 26, 2016; last updated September 18, 2017.
Accessed November 10, 2017.
16. US National Library of Medicine. NCI-MATCH: Targeted therapy
directed by genetic testing in treating patients with advanced refractory
solid tumors, lymphomas, or multiple myeloma. https://clinicaltrials.
gov/ct2/show/NCT02465060. First posted June 8, 2015; last
updated November 9, 2017. Accessed November 10, 2017.
17. US National Library of Medicine. QUILT-3.039: NANT Pancreatic
cancer vaccine: combination immunotherapy in subjects with pancreatic
cancer who have progressed on or after standard-of-care therapy.
https://clinicaltrials.gov/ct2/show/NCT03136406. First posted May
2, 2017; last updated October 30, 2017. Accessed November 10,
2017.
18. Cunanan KM, Gonen M, Shen R, et al. Basket trials in oncology:
A trade-o between complexity and eciency. J Clin Oncol.
2017;35(3):271-273.
19. ASCO website. https://university.asco.org/motb. Last update
November 2017. Accessed November 10, 2017.
20. ASCO website. Molecular oncology tumor boards invite discussion
of growing eld in cancer care. http://www.ascopost.com/issues/
february-25-2015/molecular-oncology-tumor-boards-invite-discussion-
of-growing-eld-in-cancer-care/. Published February 25, 2017.
Accessed November 10, 2017.
21. de Lartigue J. Liquid gold: blood-based biopsies make headway.
JCSO 2017;15(1):49-54.
22. Cristofanilli M, Budd GT, Ellis MJ, et al. Circulating tumor cells,
disease progression, and survival in metastatic breast cancer. N Engl J
Med. 2004;351(8):781-791.
23. Lucci A, Hall CS, Lodhi AK, et al. Circulating tumour cells in
non-metastatic breast cancer: a prospective study. Lancet Oncol.
2012;13(7):688-695.
24. Dawson SJ, Tsui DW, Murtaza M, et al. Analysis of circulating
tumor DNA to monitor metastatic breast cancer. N Engl J Med.
2013;368(13):1199-1209.
25. Chandarlapaty S, Chen D, He W, et al. Prevalence of ESR1 mutations
in cell-free DNA and outcomes in metastatic breast cancer: a
secondary analysis of the BOLERO-2 clinical trial. JAMA Oncol.
2016;2(10):1310-1315.
26. Kim SB, Dent R, Wongchenko WJ, et al. Concordance between
plasma-based and tissue-based next-generation sequencing in
LOTUS [Correspondence]. http://www.thelancet.com/journals/
lanonc/article/PIIS1470-2045(17)30785-4/fulltext. Published
November 2017. Accessed December 3, 2017.
27. Adalsteinsson VA, Ha G, Freeman SS, et al. Scalable whole-exome
sequencing of cell-free DNA reveals high concordance with metastatic
tumors. https://www.nature.com/articles/s41467-017-00965-y.
Published online November 6, 2017. Accessed November 19, 2017.
28. Parsons DW, Roy A, Yang Y, et al. Clinical genomics for children
with solid tumors: current realities and future opportunities
[Abstract]. Clin Cancer Res. 2016;22(1 Suppl):abstract IA16.
29. ¬ompson JC, Yee SS, Troxel AB, et al. Detection of therapeutically
targetable driver and resistance mutations in lung cancer patients by
next-generation sequencing of cell-free circulating tumor DNA. Clin
Cancer Res. 2016;22(23):5772-5782.
30. Press release, FDA. FDA approves axicabtagene ciloleucel
for large B-cell lymphoma. https://www.fda.gov/Drugs/
InformationOnDrugs/ApprovedDrugs/ucm581296.htm. Last
updated October 25, 2017. Accessed November 6, 2017.
31. Press release, FDA. FDA Approves gemtuzumab ozogamicin
for CD33-positive AML. https://www.fda.gov/Drugs/
InformationOnDrugs/ApprovedDrugs/ucm574518.htm. Last
updated September 1, 2017. Accessed November 6, 2017.
32. Press release, FDA. FDA grants regular approval to dabrafenib and
trametinib combination for metastatic NSCLC with BRAF V600E
mutation. https://www.fda.gov/Drugs/InformationOnDrugs/
ApprovedDrugs/ucm564331.htm. Last updated June 22, 2017.
Accessed November 6, 2017.
1. US Food & Drug Administration. Biosimilar and interchangeable
products. https://www.fda.gov/Drugs/DevelopmentApprovalProcess/
HowDrugsareDevelopedandApproved/ApprovalApplications/
¬erapeuticBiologicApplications/Biosimilars/ucm580419.htm. Last
updated October 23, 2017. Accessed December 11, 2017.
2. ASCO CancerLinQ website. https://cancerlinq.org/. Publishing/
update information not available. Accessed November 3, 2017.
3. Bodenheimer T, Sinsky C. From triple to quadruple aim: care of the
patient requires care of the provider. https://www.ncbi.nlm.nih.gov/
pmc/articles/PMC4226781/. Published November 2014. Accessed
November 7.
4. Institute for Healthcare Improvement. http://www.ihi.org/Engage/
Initiatives/TripleAim/Pages/default.aspx. No update information
given. Accessed November 3, 2017.
5. Robinson JC. Value-based physician payment in oncology: public and
private insurer initiatives. Milbank Q. 2017;95(1);184-203.
6. Newcomer L. Oral communication: Washington State Medical
Oncology Society meeting, August 19, 2017.
7. Newcomer LN, Gould B, Page RD, Donelan SA, Perkins M.
Changing physician incentives for aordable, quality cancer
care: results of an episode payment model. J Oncol Pract.
2014;10(5):322-326.
8. US Department of Health and Human Services website. Hematology/
oncology (cancer) approvals & safety notications. https://www.fda.
gov/Drugs/InformationOnDrugs/ApprovedDrugs/ucm279174.htm.
Last updated December 1, 2017. Accessed December 3, 2017.
9. Hem-Onc Today website. CAR T-cell therapy approval huge
step for oncology, but only ‘beginning of story’. https://www.
healio.com/hematology-oncology/leukemia/news/print/hemonctoday/%
7B33119631-5996-45cf-9be6-8e36466ded9e%7D/car-tcell-
therapy-approval-huge-step-for-oncology-but-only-beginningof-
story. Published September 25, 2017. Accessed November 9, 2017.
10. Gauthier J, Yakoub-Agha I. Chimeric antigen-receptor T-cell therapy
for hematological malignancies and solid tumors: Clinical data
to date, current limitations and perspectives. Curr Res in Transl Med.
2017;65(3):93-102.
11. Martin M, Holmes FA, Ejlertsen B, et al. Neratinib after trastuzumab-
based adjuvant therapy in early-stage HER2+ breast cancer:
5-year analysis of the phase III ExteNET trial [ESMO oral presentation].
Ann Oncol. 2017;28(suppl 5):v43-v67.
12. Le Tourneau C, Delord JP, Goncalves A, et al. Molecularly targeted
therapy based on tumour molecular proling versus conventional
therapy for advanced cancer SHIVA): a multicentre, openlabel,
proof-of-concept, randomised, controlled phase 2 trial. Lancet
Oncol. 2015;16(13):1324-1334.
13. Forte V, Barrak DK, Elhodaky M, Tung L, Snow A, Lang JE. ¬e
potential for liquid biopsies in the precision medical treatment of
breast cancer. Cancer Biol Med. 2016;13(1):19-40.
14. Smerage JB, Barlow WE, Hortobagyi GN, et al. Circulating tumor
cells and response to chemotherapy in metastatic breast cancer:
SWOG S0500. J Clin Oncol. 2014;32(31):3483-3489.
15. US National Library of Medicine. TAPUR: testing the use of food
and drug administration (FDA) approved drugs that target a specific
abnormality in a tumor gene in people with advanced stage cancer
(TAPUR). https://clinicaltrials.gov/ct2/show/NCT02693535.
First posted February 26, 2016; last updated September 18, 2017.
Accessed November 10, 2017.
16. US National Library of Medicine. NCI-MATCH: Targeted therapy
directed by genetic testing in treating patients with advanced refractory
solid tumors, lymphomas, or multiple myeloma. https://clinicaltrials.
gov/ct2/show/NCT02465060. First posted June 8, 2015; last
updated November 9, 2017. Accessed November 10, 2017.
17. US National Library of Medicine. QUILT-3.039: NANT Pancreatic
cancer vaccine: combination immunotherapy in subjects with pancreatic
cancer who have progressed on or after standard-of-care therapy.
https://clinicaltrials.gov/ct2/show/NCT03136406. First posted May
2, 2017; last updated October 30, 2017. Accessed November 10,
2017.
18. Cunanan KM, Gonen M, Shen R, et al. Basket trials in oncology:
A trade-o between complexity and eciency. J Clin Oncol.
2017;35(3):271-273.
19. ASCO website. https://university.asco.org/motb. Last update
November 2017. Accessed November 10, 2017.
20. ASCO website. Molecular oncology tumor boards invite discussion
of growing eld in cancer care. http://www.ascopost.com/issues/
february-25-2015/molecular-oncology-tumor-boards-invite-discussion-
of-growing-eld-in-cancer-care/. Published February 25, 2017.
Accessed November 10, 2017.
21. de Lartigue J. Liquid gold: blood-based biopsies make headway.
JCSO 2017;15(1):49-54.
22. Cristofanilli M, Budd GT, Ellis MJ, et al. Circulating tumor cells,
disease progression, and survival in metastatic breast cancer. N Engl J
Med. 2004;351(8):781-791.
23. Lucci A, Hall CS, Lodhi AK, et al. Circulating tumour cells in
non-metastatic breast cancer: a prospective study. Lancet Oncol.
2012;13(7):688-695.
24. Dawson SJ, Tsui DW, Murtaza M, et al. Analysis of circulating
tumor DNA to monitor metastatic breast cancer. N Engl J Med.
2013;368(13):1199-1209.
25. Chandarlapaty S, Chen D, He W, et al. Prevalence of ESR1 mutations
in cell-free DNA and outcomes in metastatic breast cancer: a
secondary analysis of the BOLERO-2 clinical trial. JAMA Oncol.
2016;2(10):1310-1315.
26. Kim SB, Dent R, Wongchenko WJ, et al. Concordance between
plasma-based and tissue-based next-generation sequencing in
LOTUS [Correspondence]. http://www.thelancet.com/journals/
lanonc/article/PIIS1470-2045(17)30785-4/fulltext. Published
November 2017. Accessed December 3, 2017.
27. Adalsteinsson VA, Ha G, Freeman SS, et al. Scalable whole-exome
sequencing of cell-free DNA reveals high concordance with metastatic
tumors. https://www.nature.com/articles/s41467-017-00965-y.
Published online November 6, 2017. Accessed November 19, 2017.
28. Parsons DW, Roy A, Yang Y, et al. Clinical genomics for children
with solid tumors: current realities and future opportunities
[Abstract]. Clin Cancer Res. 2016;22(1 Suppl):abstract IA16.
29. ¬ompson JC, Yee SS, Troxel AB, et al. Detection of therapeutically
targetable driver and resistance mutations in lung cancer patients by
next-generation sequencing of cell-free circulating tumor DNA. Clin
Cancer Res. 2016;22(23):5772-5782.
30. Press release, FDA. FDA approves axicabtagene ciloleucel
for large B-cell lymphoma. https://www.fda.gov/Drugs/
InformationOnDrugs/ApprovedDrugs/ucm581296.htm. Last
updated October 25, 2017. Accessed November 6, 2017.
31. Press release, FDA. FDA Approves gemtuzumab ozogamicin
for CD33-positive AML. https://www.fda.gov/Drugs/
InformationOnDrugs/ApprovedDrugs/ucm574518.htm. Last
updated September 1, 2017. Accessed November 6, 2017.
32. Press release, FDA. FDA grants regular approval to dabrafenib and
trametinib combination for metastatic NSCLC with BRAF V600E
mutation. https://www.fda.gov/Drugs/InformationOnDrugs/
ApprovedDrugs/ucm564331.htm. Last updated June 22, 2017.
Accessed November 6, 2017.
Expanding treatment options for diverse neuroendocrine tumors
Neuroendocrine tumors (NETs) are an extremely diverse group of cancers that have steadily increased in incidence in recent years. They can prove challenging to treat but, as we discuss here, a steady evolution in our understanding of NETs has significantly expanded the scope of therapeutic options.
A unique tumor type
NETs arise from neuroendocrine cells – cells with features of both nerve and endocrine cells that have important physiological functions, including the production and release of hormones. These tumors were first recognized by a German pathologist in the mid-1800s and were initially referred to as carcinoids in reference to their carcinoma-like appearance but lack of other malignant features.1
Unlike other solid tumors, which are associated with a particular primary location, NETs can arise anywhere in the body where neuroendocrine cells are found. They are also unique in their ability to oversecrete bioactive substances that regulate bodily functions, which results in an associated clinical syndrome, known as carcinoid syndrome, in up to 35% of patients.2,3
Although they are considered to be a relatively rare type of tumor, the incidence of NETs has been increasing in recent years. According to data from the Surveillance, Epidemiology and End Results (SEER) program, the age-adjusted incidence of NETs increased more than two-and-a-half fold during 1973-2004 and the rise is predicted to continue at an accelerated rate.4
Historically, NETs have been thought of as relatively benign because of their slow-growing nature, but it is now widely appreciated that they often metastasize. Furthermore, many patients are not symptomatic at first, so around half of all cases are not diagnosed until they have reached this more aggressive stage.4
The challenge of NET diversity
The most common type of NETs are those that arise in the gastrointestinal tract (GI-NET), representing more than 65% of cases, and for which the “carcinoid” terminology often is still applied. GI-NETs most frequently arise in the small intestine (41.8%), rectum (27.4%), and stomach (8.7%).4,5
About a quarter of NETs originate in the bronchopulmonary system, including the lungs and the thymus. Thymic NETs are particularly aggressive and are associated with a poor prognosis. Pancreatic NETs (pNETs) make up the next largest group, although they represent less than 1% of total NETs. Compared with the most common type of pancreatic cancer, pancreatic ductal adenocarcinoma, they have a more favorable prognosis. pNETs are often grouped together with GI-NETs and referred to as gastroenteropancreatic NETs (GEP-NETs).3-5 Other rarer types of NET include Merkel cell carcinoma (a type of skin cancer) and medullary thyroid cancers.
The classification network
NETs are classified according to the anatomic site from which they originate, as well as their histology, grade, and stage. Another important consideration is their level of hormone secretion. “Functional” and “nonfunctional” NETs both produce hormones, but only the former cause related symptoms.3,4,6
Functionality plays a particularly important role in the subclassification of GEP-NETs. Functional pNETs, for instance, are further divided according to the clinical syndromes associated with the hormones they produce, as insulinomas, glucagonomas, gastrinomas, somatostatinomas, and VIPomas (producing vasoactive intestinal peptide).7,8
In 2010, the World Health Organization developed a classification system for GEP-NETs that categorized these tumors as well differentiated (grade 1 or 2, depending on their rate of proliferation) and poorly differentiated (grade 3).9 The WHO classification of bronchopulmonary NETs, published in 2015, is slightly different; broken down into 3 subgroups, typical carcinoid, atypical carcinoid (corresponding to grade 1 and 2 GEP-NETs), and large and small-cell NETs (equivalent to grade 3 GEP-NETs).10
Although NETs develop from the same cell type, they in fact comprise a spectrum of diseases that vary extensively in their underlying biology, histology, and clinical behavior. Both the diversity and unique nature of NETs have become increasingly evident in recent years with the application of next-generation sequencing technologies to this tumor type. In general, NETs seem to be more genetically stable than other tumor types from the same primary location, and have fewer somatic mutations. The classic tumor suppressors and oncogenes that drive other tumor types are not common in NETs.6,11
The diversity of NETs presents a diagnostic and therapeutic challenge and, until recently, there was a paucity of effective treatment options. In the past decade, an evolution in our understanding of the molecular mechanisms underlying these tumors has altered the treatment landscape for well-differentiated tumors as an expanding array of targeted therapies with proven efficacy have become available (Table 1).
Their poorly differentiated counterparts, on the other hand, continue to present a significant unmet need.
Somatostatin analogs lead the charge
The fact that many NETs overexpress hormone receptors presents a significant therapeutic opportunity, and among the most successful targets to date are the somatostatin receptors (SSTRs). There are 5 main SSTRs that each bind to somatostatin with different effects on cell signaling and expression that varies according to the type of NET.
More stable synthetic analogs of the somatostatin hormone (somatostatin analogs [SSAs]), which has a very short half-life in the circulation, have been developed that act as SSTR agonists. Two long-acting SSAs, octreotide (Sandostatin LAR Depot) and lanreotide (Somatuline Depot), which bind SSTR2 and SSTR5, have been approved by the United States Food and Drug Administration (FDA), but were primarily used for the alleviation of the symptoms associated with NETs resulting from carcinoid syndrome.
In recent years, evidence has begun to emerge that SSAs also have an anti-tumor effect, which is thought to be both direct and indirect in nature. Direct effects result from the interaction between the SSA and SSTRs expressed on tumor cells, blocking the protumor cellular effects of SSTR signaling that are poorly understood but thought to involve the mitogen-activated protein kinase (MAPK) pathway. Indirect effects are fortuitous side effects mediated through off-target effects, such as the suppression of other cellular activities of SSTRs and the other growth factors that they bind to, which can impact processes such as angiogenesis and immune modulation.7,12
Several clinical trials have been designed to test the anti-tumor effects of NETs, including the PROMID trial of octreotide and the CLARINET trial of lanreotide, the latter leading to the 2014 approval of lanreotide for the improvement of progression-free survival (PFS) in patients with advanced GI- and pNETs.
The randomized phase 3 study compared lanreotide 120 mg with placebo in 204 patients with locally advanced or metastatic nonfunctioning pancreatic or intestinal NETs. Lanreotide treatment resulted in a significant improvement in PFS (Not yet reached vs 18 months for placebo; hazard ratio [HR], 0.47; P < .001).13
Meanwhile, the PROMID trial compared octreotide 30 mg with placebo in 85 patients with advanced midgut NETs and demonstrated that octreotide increased time to progression (TTP; 14.3 months vs 6 months for placebo; P = .000072) with no significant difference in side effects.14
Pasireotide is a second-generation SSA with improved binding affinity to SSTR1, 3, and 5. Despite its improved specificity, pasireotide has not proved more effective than other SSAs and its development for the treatment of NETs has been discontinued.
Coupling radioisotopes to SSAs provides another promising therapeutic option for NETs, known as peptide receptor radionuclide therapy, or PRRT, which uses SSAs to deliver therapeutic radiation directly to the tumor cells. Several variations have been studied with different radioactive isotopes, but most promising is lutetium-177 (177Lu). A 177Lu-labelled octreotide (177Lu-Dotatate) recently demonstrated significant efficacy in the phase 3 NETTER-1 clinical trial in patients with advanced stage NETs of the small bowel. The trial randomly assigned 229 patients who were progressing on an SSA to either 177Lu-Dotatate or high-dose octreotide LAR (long-acting release). There was a significant increase in PFS in the 177Lu-Dotatate arm (Not yet reached vs 8.4 months; P < .0001). There was also a trend toward improved overall survival (OS), and longer follow-up is eagerly anticipated for confirmation. 177Lu-Dotatate has been granted priority review by the FDA, and a decision on its approval is expected in the next few months.11,15-17
Molecularly and immune-targeted therapies continue to take aim
The mammalian target of rapamycin, or mTOR, is a serine/threonine kinase that sits at the confluence of a number of different upstream signaling pathways and mediates key cellular processes including cell proliferation and survival (Figure 1).
Alterations in nearly all members of the mTOR pathway, including upstream activators and downstream effectors, have been observed in NETs, in both sporadic disease and the genetic syndromes associated with the development of NETs.18
The involvement of the mTOR pathway in the pathogenesis of NETs first came into focus in pNETs and the mTOR inhibitor, everolimus (Afinitor) has been extensively studied in this indication, culminating in its regulatory approval in 2011. In the pivotal trial (RADIANT-3), everolimus monotherapy was compared with placebo in 410 patients with low- and intermediate-grade pNETs. There was a statistically significant improvement in PFS from 4.6 months to 11 months (HR, 0.77; P = .026).19 The final OS analysis for this trial also revealed a benefit of more than 6 months in the everolimus arm, although this was not statistically significant, which the study authors attribute to the high rate of crossover from the placebo arm after progression.20
More recently, the results of the RADIANT-4 trial, in which everolimus was compare with placebo in patients with advanced, well-differentiated, nonfunctioning NETs of the GI tract and lung, led to a new approved indication for the mTOR inhibitor and the first approved targeted therapy for advanced lung NETs. In the overall study population (n = 285), everolimus prolonged PFS by more than 7 months (11 months vs 3.9 months for placebo; HR, 0.48; P = .000001), corresponding to a 52% reduction in the risk of disease progression or death.21,22
Everolimus continues to be evaluated, with a particular focus on combination therapy to overcome the resistance that commonly occurs after treatment with molecularly targeted drugs (Table 2). For example, preclinical studies suggested that mTOR inhibitors and SSAs may have synergistic activity owing to combined inhibition of the mTOR and insulin-like growth factor pathways. In a phase 1 study, the combination of pasireotide and everolimus was found to be safe and to have preliminary anti-tumor activity. However, the subsequent phase 2 COOPERATE-2 study failed to show improved PFS.23,24
The observation that NETs are highly vascularized and frequently express vascular endothelial growth factor (VEGF) and its receptor (VEGFR), which play a key role in coordinating angiogenesis, led to the pursuit of anti-angiogenic therapies in NETs. Both the anti-VEGF monoclonal antibody bevacizumab and small molecule tyrosine kinase inhibitors that include among their targets VEGFRs and other receptors involved in angiogenesis, such as platelet-derived growth factor receptor, have been tested.
Sunitinib was approved for the treatment of pNETs in 2011, making it a banner year for this tumor type. Approval was granted on the basis of significantly improved PFS in the sunitinib arm of a phase 3 randomized trial, but long-term follow-up suggested that sunitinib also improved OS by 10 months. Like everolimus, the OS benefit was not statistically significant, and again this was thought to be the result of extensive crossover.
Two other multikinase inhibitors have received regulatory approval for a much rarer form of NET, medullary thyroid cancer. Vandetanib and cabozantinib were approved for this indication in 2011 and 2012, respectively. Early in 2017, the results of a single-arm phase 2 trial of cabozantinib suggested that this drug may also have significant activity in other types of NET. In patients with advanced carcinoid and pNETs who received cabozantinib at 60 mg/day orally, partial responses were observed in 15% of patients and the median PFS was 21.8 months in the pNET cohort and >30 months in the carcinoid tumor cohort.25 Confirmatory phase 3 trials are planned but not currently underway.
Sulfatinib is a novel kinase inhibitor that targets the VEGFRs and fibroblast growth factor receptor 1. It has recently shown significant promise in the treatment of patients with advanced NETs. According to data presented at this year’s annual conference of the European Neuroendocrine Tumor Society in Barcelona, sulfatinib demonstrated an overall response rate of 17.1% in pancreatic NETs and 15% in extra-pancreatic NETs, with an overall disease control rate of 91.4%, and was well tolerated.26 Based on these and other promising phase 1 and 2 data, 2 phase 3 trials are ongoing.
Meanwhile, earlier this year, Mateon Therapeutics presented data from a phase 2 trial of a different kind of anti-angiogenic drug in patients with GI- or pNETs. Fosbretabulin is a vascular disrupting agent that targets the existing tumor vasculature rather than preventing the formation of new blood vessels. They do this via a number of different mechanisms, in the case of fosbretabulin it specifically targets endothelial cells and inhibits the assembly of microtubules and, hence, blocks mitosis. In 18 patients, fosbretabulin treatment resulted in 1 partial response and 7 patients who had stable disease; more than half of the patients reported improved quality of life.27 Fosbretabulin continues to be studied in NETs in combination with everolimus.
Finally, researchers are beginning to make a foray into the immunotherapy field that has revolutionized the treatment of many other tumor types. The immune checkpoint inhibitors nivolumab and pembrolizumab are being evaluated in ongoing phase 1 and 2 trials, while avelumab (Bavencio) was very recently approved by the FDA for the treatment of Merkel cell carcinoma.28,29
1. Pinchot SN, Holen K, Sippel RS, Chen H. Carcinoid tumors. Oncologist. 2008;13(12):1255-1269.
2. Rorstad O. Prognostic indicators for carcinoid neuroendocrine tumors of the gastrointestinal tract. J Surg Oncol. 2005;89(3):151-160.
3. The NET Alliance. Characterizing a challenging cancer. http://www.thenetalliance.com/hcp/facts-about-net/characterization/. Publishing date not provided. Accessed October 18, 2017.
4. Yao JC, Hassan M, Phan A, et al. One hundred years after ‘carcinoid’: epidemiology of and prognostic factors for neuroendocrine tumors in 35,825 cases in the United States. J Clin Oncol. 2008;26(18):3063-3072.
5. Modlin IM, Lye KD, Kidd M. A 5-decade analysis of 13,715 carcinoid tumors. Cancer. 2003;97(4):934-959.
6. Spada F, Valente M. Review of recent advances in medical treatment for neuroendocrine neoplasms: somatostatin analogs and chemotherapy. J Cancer Metastasis Treat. 2016;2(8):313-320.
7. Kelgiorgi D, Dervenis C. Pancreatic neuroendocrine tumors: the basics, the gray zone, and the target. F1000Research. 2017;6:663.
8. Viudez A, De Jesus-Acosta A, Carvalho FL, Vera R, Martin-Algarra S, Ramirez N. Pancreatic neuroendocrine tumors: Challenges in an underestimated disease. Crit Rev Oncol Hematol. 2016;101:193-206.
9. World Health Organization, International Agency for Research on Cancer. Bosman FT, Carneiro F, Hruban RH, Theise ND (eds). WHO classification of tumours of the digestive system. 2010, 4th ed (vol 3).
10. Travis WD, Brambilla E, Nicholson AG, et al. The 2015 World Health Organization classification of lung tumors. J Thorac Oncol. 2015;10(9):1243-1260.
11. Lee A, Chan DL, Wong MH, et al. Systematic review of the role of targeted therapy in metastatic neuroendocrine tumors. Neuroendocrinology. 2017;104(3):209-222.
12. Theodoropoulou M, Stalla GK. Somatostatin receptors: from signaling to clinical practice. Front Neuroendocrinol. 2013;34(3):228-252.
13. Caplin ME, Pavel M, Cwikła JB, et al. Lanreotide in metastatic enteropancreatic neuroendocrine tumors. N Engl J Med. 2014;371(3):224-233.
14. Rinke A, Muller HH, Schade-Brittinger C, et al. Placebo-controlled, double-blind, prospective, randomized study on the effect of octreotide LAR in the control of tumor growth in patients with metastatic neuroendocrine midgut tumors: a report from the PROMID Study Group. J Clin Oncol. 2009;27(28):4656-4663.
15. Strosberg J, El-Haddad G, Wolin E, et al. Phase 3 trial of 177Lu-Dotatate for midgut neuroendocrine tumors. N Engl J Med. 2017;376(2):125-135.
16. Falconi M, Partelli S. Neuroendocrine tumours in 2016: defining rules for increasingly personalized treatments. Nat Rev Clin Oncol. 2017;14(2):80-82.
17. Hutchinson L. Targeted therapies: widening the treatment NET. Nat Rev Clin Oncol. 2017;14(1):2-3.
18. Cingarlini S, Bonomi M, Corbo V, Scarpa A, Tortora G. Profiling mTOR pathway in neuroendocrine tumors. Target Oncol. 2012;7(3):183-188.
19. Yao JC, Shah MH, Ito T, et al. Everolimus for advanced pancreatic neuroendocrine tumors. N Engl J Med. 2011;364(6):514-523.
20. Yao JC, Pavel M, Lombard-Bohas C, et al. Everolimus for the treatment of advanced pancreatic neuroendocrine tumors: overall survival and circulating biomarkers from the randomized, phase III RADIANT-3 study. J Clin Oncol. http://ascopubs.org/ doi/abs/10.1200/JCO.2016.68.0702?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed. September 12, 2016. E-pub ahead of print.
21. Yao JC, Fazio N, Singh S, et al. Everolimus for the treatment of advanced, non-functional neuroendocrine tumours of the lung or gastrointestinal tract (RADIANT-4): a randomised, placebo-controlled, phase 3 study. Lancet. 2016;387(10022):968-977.
22. Gajate P, Martínez-Sáez O, Alonso-Gordoa T, Grande E. Emerging use of everolimus in the treatment of neuroendocrine tumors. Cancer Manage Res. 2017;9:215-224.
23. Chan JA, Ryan DP, Zhu AX, et al. Phase I study of pasireotide (SOM 230) and everolimus (RAD001) in advanced neuroendocrine tumors. Endocr Relat Cancer. 2012;19(5):615-623.
24. Kulke MH, Ruszniewski P, Van Cutsem E, et al. A randomized, open-label, phase 2 study of everolimus in combination with pasireotide LAR or everolimus alone in advanced, well-dierentiated, progressive pancreatic neuroendocrine tumors: COOPERATE-2 trial. Ann Oncol. 2017;28(6):1309-1315.
25. Chan JA, Faris JE, Murphy JE, et al. Phase II trial of cabozantinib in patients with carcinoid and pancreatic neuroendocrine tumors (pNET). J Clin Oncol. 2017;35(4 suppl):228-228.
26. Xu J, Li J, Bai CM, et al. An open-label phase Ib/II study of sulfatinib in patients with advanced neuroendocrine tumors (NCT02267967). Paper presented at the 14th Annual European Neuroendocrine Tumor Society Conference for the Diagnosis and Treatment of Neuroendocrine Tumor Disease; March 8-10, 2017, Barcelona, Spain.
27. Libutti SK, Anthony LB, Chaplin DJ, Sosa JA. A phase II study of combretastatin A4-phosphate (CA4P) in the treatment of well-differentiated, low- to intermediate-grade, unresectable, recurrent, or metastatic pancreatic, or GI neuroendocrine tumors/carcinoid (GI-NETs/PNETs) with elevated biomarkers. J Clin Oncol. 2017;35(4 suppl):432-432.
28. Cordes LM, Gulley JL. Avelumab for the treatment of metastatic Merkel cell carcinoma. Drugs Today (Barc). 2017;53(7):377-383.
29. Kaufman HL, Russell J, Hamid O, et al. Avelumab in patients with chemotherapy-refractory metastatic Merkel cell carcinoma: a multicentre, single-group, open-label, phase 2 trial. Lancet Oncol. 2016;17(10):1374-1385.
Neuroendocrine tumors (NETs) are an extremely diverse group of cancers that have steadily increased in incidence in recent years. They can prove challenging to treat but, as we discuss here, a steady evolution in our understanding of NETs has significantly expanded the scope of therapeutic options.
A unique tumor type
NETs arise from neuroendocrine cells – cells with features of both nerve and endocrine cells that have important physiological functions, including the production and release of hormones. These tumors were first recognized by a German pathologist in the mid-1800s and were initially referred to as carcinoids in reference to their carcinoma-like appearance but lack of other malignant features.1
Unlike other solid tumors, which are associated with a particular primary location, NETs can arise anywhere in the body where neuroendocrine cells are found. They are also unique in their ability to oversecrete bioactive substances that regulate bodily functions, which results in an associated clinical syndrome, known as carcinoid syndrome, in up to 35% of patients.2,3
Although they are considered to be a relatively rare type of tumor, the incidence of NETs has been increasing in recent years. According to data from the Surveillance, Epidemiology and End Results (SEER) program, the age-adjusted incidence of NETs increased more than two-and-a-half fold during 1973-2004 and the rise is predicted to continue at an accelerated rate.4
Historically, NETs have been thought of as relatively benign because of their slow-growing nature, but it is now widely appreciated that they often metastasize. Furthermore, many patients are not symptomatic at first, so around half of all cases are not diagnosed until they have reached this more aggressive stage.4
The challenge of NET diversity
The most common type of NETs are those that arise in the gastrointestinal tract (GI-NET), representing more than 65% of cases, and for which the “carcinoid” terminology often is still applied. GI-NETs most frequently arise in the small intestine (41.8%), rectum (27.4%), and stomach (8.7%).4,5
About a quarter of NETs originate in the bronchopulmonary system, including the lungs and the thymus. Thymic NETs are particularly aggressive and are associated with a poor prognosis. Pancreatic NETs (pNETs) make up the next largest group, although they represent less than 1% of total NETs. Compared with the most common type of pancreatic cancer, pancreatic ductal adenocarcinoma, they have a more favorable prognosis. pNETs are often grouped together with GI-NETs and referred to as gastroenteropancreatic NETs (GEP-NETs).3-5 Other rarer types of NET include Merkel cell carcinoma (a type of skin cancer) and medullary thyroid cancers.
The classification network
NETs are classified according to the anatomic site from which they originate, as well as their histology, grade, and stage. Another important consideration is their level of hormone secretion. “Functional” and “nonfunctional” NETs both produce hormones, but only the former cause related symptoms.3,4,6
Functionality plays a particularly important role in the subclassification of GEP-NETs. Functional pNETs, for instance, are further divided according to the clinical syndromes associated with the hormones they produce, as insulinomas, glucagonomas, gastrinomas, somatostatinomas, and VIPomas (producing vasoactive intestinal peptide).7,8
In 2010, the World Health Organization developed a classification system for GEP-NETs that categorized these tumors as well differentiated (grade 1 or 2, depending on their rate of proliferation) and poorly differentiated (grade 3).9 The WHO classification of bronchopulmonary NETs, published in 2015, is slightly different; broken down into 3 subgroups, typical carcinoid, atypical carcinoid (corresponding to grade 1 and 2 GEP-NETs), and large and small-cell NETs (equivalent to grade 3 GEP-NETs).10
Although NETs develop from the same cell type, they in fact comprise a spectrum of diseases that vary extensively in their underlying biology, histology, and clinical behavior. Both the diversity and unique nature of NETs have become increasingly evident in recent years with the application of next-generation sequencing technologies to this tumor type. In general, NETs seem to be more genetically stable than other tumor types from the same primary location, and have fewer somatic mutations. The classic tumor suppressors and oncogenes that drive other tumor types are not common in NETs.6,11
The diversity of NETs presents a diagnostic and therapeutic challenge and, until recently, there was a paucity of effective treatment options. In the past decade, an evolution in our understanding of the molecular mechanisms underlying these tumors has altered the treatment landscape for well-differentiated tumors as an expanding array of targeted therapies with proven efficacy have become available (Table 1).
Their poorly differentiated counterparts, on the other hand, continue to present a significant unmet need.
Somatostatin analogs lead the charge
The fact that many NETs overexpress hormone receptors presents a significant therapeutic opportunity, and among the most successful targets to date are the somatostatin receptors (SSTRs). There are 5 main SSTRs that each bind to somatostatin with different effects on cell signaling and expression that varies according to the type of NET.
More stable synthetic analogs of the somatostatin hormone (somatostatin analogs [SSAs]), which has a very short half-life in the circulation, have been developed that act as SSTR agonists. Two long-acting SSAs, octreotide (Sandostatin LAR Depot) and lanreotide (Somatuline Depot), which bind SSTR2 and SSTR5, have been approved by the United States Food and Drug Administration (FDA), but were primarily used for the alleviation of the symptoms associated with NETs resulting from carcinoid syndrome.
In recent years, evidence has begun to emerge that SSAs also have an anti-tumor effect, which is thought to be both direct and indirect in nature. Direct effects result from the interaction between the SSA and SSTRs expressed on tumor cells, blocking the protumor cellular effects of SSTR signaling that are poorly understood but thought to involve the mitogen-activated protein kinase (MAPK) pathway. Indirect effects are fortuitous side effects mediated through off-target effects, such as the suppression of other cellular activities of SSTRs and the other growth factors that they bind to, which can impact processes such as angiogenesis and immune modulation.7,12
Several clinical trials have been designed to test the anti-tumor effects of NETs, including the PROMID trial of octreotide and the CLARINET trial of lanreotide, the latter leading to the 2014 approval of lanreotide for the improvement of progression-free survival (PFS) in patients with advanced GI- and pNETs.
The randomized phase 3 study compared lanreotide 120 mg with placebo in 204 patients with locally advanced or metastatic nonfunctioning pancreatic or intestinal NETs. Lanreotide treatment resulted in a significant improvement in PFS (Not yet reached vs 18 months for placebo; hazard ratio [HR], 0.47; P < .001).13
Meanwhile, the PROMID trial compared octreotide 30 mg with placebo in 85 patients with advanced midgut NETs and demonstrated that octreotide increased time to progression (TTP; 14.3 months vs 6 months for placebo; P = .000072) with no significant difference in side effects.14
Pasireotide is a second-generation SSA with improved binding affinity to SSTR1, 3, and 5. Despite its improved specificity, pasireotide has not proved more effective than other SSAs and its development for the treatment of NETs has been discontinued.
Coupling radioisotopes to SSAs provides another promising therapeutic option for NETs, known as peptide receptor radionuclide therapy, or PRRT, which uses SSAs to deliver therapeutic radiation directly to the tumor cells. Several variations have been studied with different radioactive isotopes, but most promising is lutetium-177 (177Lu). A 177Lu-labelled octreotide (177Lu-Dotatate) recently demonstrated significant efficacy in the phase 3 NETTER-1 clinical trial in patients with advanced stage NETs of the small bowel. The trial randomly assigned 229 patients who were progressing on an SSA to either 177Lu-Dotatate or high-dose octreotide LAR (long-acting release). There was a significant increase in PFS in the 177Lu-Dotatate arm (Not yet reached vs 8.4 months; P < .0001). There was also a trend toward improved overall survival (OS), and longer follow-up is eagerly anticipated for confirmation. 177Lu-Dotatate has been granted priority review by the FDA, and a decision on its approval is expected in the next few months.11,15-17
Molecularly and immune-targeted therapies continue to take aim
The mammalian target of rapamycin, or mTOR, is a serine/threonine kinase that sits at the confluence of a number of different upstream signaling pathways and mediates key cellular processes including cell proliferation and survival (Figure 1).
Alterations in nearly all members of the mTOR pathway, including upstream activators and downstream effectors, have been observed in NETs, in both sporadic disease and the genetic syndromes associated with the development of NETs.18
The involvement of the mTOR pathway in the pathogenesis of NETs first came into focus in pNETs and the mTOR inhibitor, everolimus (Afinitor) has been extensively studied in this indication, culminating in its regulatory approval in 2011. In the pivotal trial (RADIANT-3), everolimus monotherapy was compared with placebo in 410 patients with low- and intermediate-grade pNETs. There was a statistically significant improvement in PFS from 4.6 months to 11 months (HR, 0.77; P = .026).19 The final OS analysis for this trial also revealed a benefit of more than 6 months in the everolimus arm, although this was not statistically significant, which the study authors attribute to the high rate of crossover from the placebo arm after progression.20
More recently, the results of the RADIANT-4 trial, in which everolimus was compare with placebo in patients with advanced, well-differentiated, nonfunctioning NETs of the GI tract and lung, led to a new approved indication for the mTOR inhibitor and the first approved targeted therapy for advanced lung NETs. In the overall study population (n = 285), everolimus prolonged PFS by more than 7 months (11 months vs 3.9 months for placebo; HR, 0.48; P = .000001), corresponding to a 52% reduction in the risk of disease progression or death.21,22
Everolimus continues to be evaluated, with a particular focus on combination therapy to overcome the resistance that commonly occurs after treatment with molecularly targeted drugs (Table 2). For example, preclinical studies suggested that mTOR inhibitors and SSAs may have synergistic activity owing to combined inhibition of the mTOR and insulin-like growth factor pathways. In a phase 1 study, the combination of pasireotide and everolimus was found to be safe and to have preliminary anti-tumor activity. However, the subsequent phase 2 COOPERATE-2 study failed to show improved PFS.23,24
The observation that NETs are highly vascularized and frequently express vascular endothelial growth factor (VEGF) and its receptor (VEGFR), which play a key role in coordinating angiogenesis, led to the pursuit of anti-angiogenic therapies in NETs. Both the anti-VEGF monoclonal antibody bevacizumab and small molecule tyrosine kinase inhibitors that include among their targets VEGFRs and other receptors involved in angiogenesis, such as platelet-derived growth factor receptor, have been tested.
Sunitinib was approved for the treatment of pNETs in 2011, making it a banner year for this tumor type. Approval was granted on the basis of significantly improved PFS in the sunitinib arm of a phase 3 randomized trial, but long-term follow-up suggested that sunitinib also improved OS by 10 months. Like everolimus, the OS benefit was not statistically significant, and again this was thought to be the result of extensive crossover.
Two other multikinase inhibitors have received regulatory approval for a much rarer form of NET, medullary thyroid cancer. Vandetanib and cabozantinib were approved for this indication in 2011 and 2012, respectively. Early in 2017, the results of a single-arm phase 2 trial of cabozantinib suggested that this drug may also have significant activity in other types of NET. In patients with advanced carcinoid and pNETs who received cabozantinib at 60 mg/day orally, partial responses were observed in 15% of patients and the median PFS was 21.8 months in the pNET cohort and >30 months in the carcinoid tumor cohort.25 Confirmatory phase 3 trials are planned but not currently underway.
Sulfatinib is a novel kinase inhibitor that targets the VEGFRs and fibroblast growth factor receptor 1. It has recently shown significant promise in the treatment of patients with advanced NETs. According to data presented at this year’s annual conference of the European Neuroendocrine Tumor Society in Barcelona, sulfatinib demonstrated an overall response rate of 17.1% in pancreatic NETs and 15% in extra-pancreatic NETs, with an overall disease control rate of 91.4%, and was well tolerated.26 Based on these and other promising phase 1 and 2 data, 2 phase 3 trials are ongoing.
Meanwhile, earlier this year, Mateon Therapeutics presented data from a phase 2 trial of a different kind of anti-angiogenic drug in patients with GI- or pNETs. Fosbretabulin is a vascular disrupting agent that targets the existing tumor vasculature rather than preventing the formation of new blood vessels. They do this via a number of different mechanisms, in the case of fosbretabulin it specifically targets endothelial cells and inhibits the assembly of microtubules and, hence, blocks mitosis. In 18 patients, fosbretabulin treatment resulted in 1 partial response and 7 patients who had stable disease; more than half of the patients reported improved quality of life.27 Fosbretabulin continues to be studied in NETs in combination with everolimus.
Finally, researchers are beginning to make a foray into the immunotherapy field that has revolutionized the treatment of many other tumor types. The immune checkpoint inhibitors nivolumab and pembrolizumab are being evaluated in ongoing phase 1 and 2 trials, while avelumab (Bavencio) was very recently approved by the FDA for the treatment of Merkel cell carcinoma.28,29
Neuroendocrine tumors (NETs) are an extremely diverse group of cancers that have steadily increased in incidence in recent years. They can prove challenging to treat but, as we discuss here, a steady evolution in our understanding of NETs has significantly expanded the scope of therapeutic options.
A unique tumor type
NETs arise from neuroendocrine cells – cells with features of both nerve and endocrine cells that have important physiological functions, including the production and release of hormones. These tumors were first recognized by a German pathologist in the mid-1800s and were initially referred to as carcinoids in reference to their carcinoma-like appearance but lack of other malignant features.1
Unlike other solid tumors, which are associated with a particular primary location, NETs can arise anywhere in the body where neuroendocrine cells are found. They are also unique in their ability to oversecrete bioactive substances that regulate bodily functions, which results in an associated clinical syndrome, known as carcinoid syndrome, in up to 35% of patients.2,3
Although they are considered to be a relatively rare type of tumor, the incidence of NETs has been increasing in recent years. According to data from the Surveillance, Epidemiology and End Results (SEER) program, the age-adjusted incidence of NETs increased more than two-and-a-half fold during 1973-2004 and the rise is predicted to continue at an accelerated rate.4
Historically, NETs have been thought of as relatively benign because of their slow-growing nature, but it is now widely appreciated that they often metastasize. Furthermore, many patients are not symptomatic at first, so around half of all cases are not diagnosed until they have reached this more aggressive stage.4
The challenge of NET diversity
The most common type of NETs are those that arise in the gastrointestinal tract (GI-NET), representing more than 65% of cases, and for which the “carcinoid” terminology often is still applied. GI-NETs most frequently arise in the small intestine (41.8%), rectum (27.4%), and stomach (8.7%).4,5
About a quarter of NETs originate in the bronchopulmonary system, including the lungs and the thymus. Thymic NETs are particularly aggressive and are associated with a poor prognosis. Pancreatic NETs (pNETs) make up the next largest group, although they represent less than 1% of total NETs. Compared with the most common type of pancreatic cancer, pancreatic ductal adenocarcinoma, they have a more favorable prognosis. pNETs are often grouped together with GI-NETs and referred to as gastroenteropancreatic NETs (GEP-NETs).3-5 Other rarer types of NET include Merkel cell carcinoma (a type of skin cancer) and medullary thyroid cancers.
The classification network
NETs are classified according to the anatomic site from which they originate, as well as their histology, grade, and stage. Another important consideration is their level of hormone secretion. “Functional” and “nonfunctional” NETs both produce hormones, but only the former cause related symptoms.3,4,6
Functionality plays a particularly important role in the subclassification of GEP-NETs. Functional pNETs, for instance, are further divided according to the clinical syndromes associated with the hormones they produce, as insulinomas, glucagonomas, gastrinomas, somatostatinomas, and VIPomas (producing vasoactive intestinal peptide).7,8
In 2010, the World Health Organization developed a classification system for GEP-NETs that categorized these tumors as well differentiated (grade 1 or 2, depending on their rate of proliferation) and poorly differentiated (grade 3).9 The WHO classification of bronchopulmonary NETs, published in 2015, is slightly different; broken down into 3 subgroups, typical carcinoid, atypical carcinoid (corresponding to grade 1 and 2 GEP-NETs), and large and small-cell NETs (equivalent to grade 3 GEP-NETs).10
Although NETs develop from the same cell type, they in fact comprise a spectrum of diseases that vary extensively in their underlying biology, histology, and clinical behavior. Both the diversity and unique nature of NETs have become increasingly evident in recent years with the application of next-generation sequencing technologies to this tumor type. In general, NETs seem to be more genetically stable than other tumor types from the same primary location, and have fewer somatic mutations. The classic tumor suppressors and oncogenes that drive other tumor types are not common in NETs.6,11
The diversity of NETs presents a diagnostic and therapeutic challenge and, until recently, there was a paucity of effective treatment options. In the past decade, an evolution in our understanding of the molecular mechanisms underlying these tumors has altered the treatment landscape for well-differentiated tumors as an expanding array of targeted therapies with proven efficacy have become available (Table 1).
Their poorly differentiated counterparts, on the other hand, continue to present a significant unmet need.
Somatostatin analogs lead the charge
The fact that many NETs overexpress hormone receptors presents a significant therapeutic opportunity, and among the most successful targets to date are the somatostatin receptors (SSTRs). There are 5 main SSTRs that each bind to somatostatin with different effects on cell signaling and expression that varies according to the type of NET.
More stable synthetic analogs of the somatostatin hormone (somatostatin analogs [SSAs]), which has a very short half-life in the circulation, have been developed that act as SSTR agonists. Two long-acting SSAs, octreotide (Sandostatin LAR Depot) and lanreotide (Somatuline Depot), which bind SSTR2 and SSTR5, have been approved by the United States Food and Drug Administration (FDA), but were primarily used for the alleviation of the symptoms associated with NETs resulting from carcinoid syndrome.
In recent years, evidence has begun to emerge that SSAs also have an anti-tumor effect, which is thought to be both direct and indirect in nature. Direct effects result from the interaction between the SSA and SSTRs expressed on tumor cells, blocking the protumor cellular effects of SSTR signaling that are poorly understood but thought to involve the mitogen-activated protein kinase (MAPK) pathway. Indirect effects are fortuitous side effects mediated through off-target effects, such as the suppression of other cellular activities of SSTRs and the other growth factors that they bind to, which can impact processes such as angiogenesis and immune modulation.7,12
Several clinical trials have been designed to test the anti-tumor effects of NETs, including the PROMID trial of octreotide and the CLARINET trial of lanreotide, the latter leading to the 2014 approval of lanreotide for the improvement of progression-free survival (PFS) in patients with advanced GI- and pNETs.
The randomized phase 3 study compared lanreotide 120 mg with placebo in 204 patients with locally advanced or metastatic nonfunctioning pancreatic or intestinal NETs. Lanreotide treatment resulted in a significant improvement in PFS (Not yet reached vs 18 months for placebo; hazard ratio [HR], 0.47; P < .001).13
Meanwhile, the PROMID trial compared octreotide 30 mg with placebo in 85 patients with advanced midgut NETs and demonstrated that octreotide increased time to progression (TTP; 14.3 months vs 6 months for placebo; P = .000072) with no significant difference in side effects.14
Pasireotide is a second-generation SSA with improved binding affinity to SSTR1, 3, and 5. Despite its improved specificity, pasireotide has not proved more effective than other SSAs and its development for the treatment of NETs has been discontinued.
Coupling radioisotopes to SSAs provides another promising therapeutic option for NETs, known as peptide receptor radionuclide therapy, or PRRT, which uses SSAs to deliver therapeutic radiation directly to the tumor cells. Several variations have been studied with different radioactive isotopes, but most promising is lutetium-177 (177Lu). A 177Lu-labelled octreotide (177Lu-Dotatate) recently demonstrated significant efficacy in the phase 3 NETTER-1 clinical trial in patients with advanced stage NETs of the small bowel. The trial randomly assigned 229 patients who were progressing on an SSA to either 177Lu-Dotatate or high-dose octreotide LAR (long-acting release). There was a significant increase in PFS in the 177Lu-Dotatate arm (Not yet reached vs 8.4 months; P < .0001). There was also a trend toward improved overall survival (OS), and longer follow-up is eagerly anticipated for confirmation. 177Lu-Dotatate has been granted priority review by the FDA, and a decision on its approval is expected in the next few months.11,15-17
Molecularly and immune-targeted therapies continue to take aim
The mammalian target of rapamycin, or mTOR, is a serine/threonine kinase that sits at the confluence of a number of different upstream signaling pathways and mediates key cellular processes including cell proliferation and survival (Figure 1).
Alterations in nearly all members of the mTOR pathway, including upstream activators and downstream effectors, have been observed in NETs, in both sporadic disease and the genetic syndromes associated with the development of NETs.18
The involvement of the mTOR pathway in the pathogenesis of NETs first came into focus in pNETs and the mTOR inhibitor, everolimus (Afinitor) has been extensively studied in this indication, culminating in its regulatory approval in 2011. In the pivotal trial (RADIANT-3), everolimus monotherapy was compared with placebo in 410 patients with low- and intermediate-grade pNETs. There was a statistically significant improvement in PFS from 4.6 months to 11 months (HR, 0.77; P = .026).19 The final OS analysis for this trial also revealed a benefit of more than 6 months in the everolimus arm, although this was not statistically significant, which the study authors attribute to the high rate of crossover from the placebo arm after progression.20
More recently, the results of the RADIANT-4 trial, in which everolimus was compare with placebo in patients with advanced, well-differentiated, nonfunctioning NETs of the GI tract and lung, led to a new approved indication for the mTOR inhibitor and the first approved targeted therapy for advanced lung NETs. In the overall study population (n = 285), everolimus prolonged PFS by more than 7 months (11 months vs 3.9 months for placebo; HR, 0.48; P = .000001), corresponding to a 52% reduction in the risk of disease progression or death.21,22
Everolimus continues to be evaluated, with a particular focus on combination therapy to overcome the resistance that commonly occurs after treatment with molecularly targeted drugs (Table 2). For example, preclinical studies suggested that mTOR inhibitors and SSAs may have synergistic activity owing to combined inhibition of the mTOR and insulin-like growth factor pathways. In a phase 1 study, the combination of pasireotide and everolimus was found to be safe and to have preliminary anti-tumor activity. However, the subsequent phase 2 COOPERATE-2 study failed to show improved PFS.23,24
The observation that NETs are highly vascularized and frequently express vascular endothelial growth factor (VEGF) and its receptor (VEGFR), which play a key role in coordinating angiogenesis, led to the pursuit of anti-angiogenic therapies in NETs. Both the anti-VEGF monoclonal antibody bevacizumab and small molecule tyrosine kinase inhibitors that include among their targets VEGFRs and other receptors involved in angiogenesis, such as platelet-derived growth factor receptor, have been tested.
Sunitinib was approved for the treatment of pNETs in 2011, making it a banner year for this tumor type. Approval was granted on the basis of significantly improved PFS in the sunitinib arm of a phase 3 randomized trial, but long-term follow-up suggested that sunitinib also improved OS by 10 months. Like everolimus, the OS benefit was not statistically significant, and again this was thought to be the result of extensive crossover.
Two other multikinase inhibitors have received regulatory approval for a much rarer form of NET, medullary thyroid cancer. Vandetanib and cabozantinib were approved for this indication in 2011 and 2012, respectively. Early in 2017, the results of a single-arm phase 2 trial of cabozantinib suggested that this drug may also have significant activity in other types of NET. In patients with advanced carcinoid and pNETs who received cabozantinib at 60 mg/day orally, partial responses were observed in 15% of patients and the median PFS was 21.8 months in the pNET cohort and >30 months in the carcinoid tumor cohort.25 Confirmatory phase 3 trials are planned but not currently underway.
Sulfatinib is a novel kinase inhibitor that targets the VEGFRs and fibroblast growth factor receptor 1. It has recently shown significant promise in the treatment of patients with advanced NETs. According to data presented at this year’s annual conference of the European Neuroendocrine Tumor Society in Barcelona, sulfatinib demonstrated an overall response rate of 17.1% in pancreatic NETs and 15% in extra-pancreatic NETs, with an overall disease control rate of 91.4%, and was well tolerated.26 Based on these and other promising phase 1 and 2 data, 2 phase 3 trials are ongoing.
Meanwhile, earlier this year, Mateon Therapeutics presented data from a phase 2 trial of a different kind of anti-angiogenic drug in patients with GI- or pNETs. Fosbretabulin is a vascular disrupting agent that targets the existing tumor vasculature rather than preventing the formation of new blood vessels. They do this via a number of different mechanisms, in the case of fosbretabulin it specifically targets endothelial cells and inhibits the assembly of microtubules and, hence, blocks mitosis. In 18 patients, fosbretabulin treatment resulted in 1 partial response and 7 patients who had stable disease; more than half of the patients reported improved quality of life.27 Fosbretabulin continues to be studied in NETs in combination with everolimus.
Finally, researchers are beginning to make a foray into the immunotherapy field that has revolutionized the treatment of many other tumor types. The immune checkpoint inhibitors nivolumab and pembrolizumab are being evaluated in ongoing phase 1 and 2 trials, while avelumab (Bavencio) was very recently approved by the FDA for the treatment of Merkel cell carcinoma.28,29
1. Pinchot SN, Holen K, Sippel RS, Chen H. Carcinoid tumors. Oncologist. 2008;13(12):1255-1269.
2. Rorstad O. Prognostic indicators for carcinoid neuroendocrine tumors of the gastrointestinal tract. J Surg Oncol. 2005;89(3):151-160.
3. The NET Alliance. Characterizing a challenging cancer. http://www.thenetalliance.com/hcp/facts-about-net/characterization/. Publishing date not provided. Accessed October 18, 2017.
4. Yao JC, Hassan M, Phan A, et al. One hundred years after ‘carcinoid’: epidemiology of and prognostic factors for neuroendocrine tumors in 35,825 cases in the United States. J Clin Oncol. 2008;26(18):3063-3072.
5. Modlin IM, Lye KD, Kidd M. A 5-decade analysis of 13,715 carcinoid tumors. Cancer. 2003;97(4):934-959.
6. Spada F, Valente M. Review of recent advances in medical treatment for neuroendocrine neoplasms: somatostatin analogs and chemotherapy. J Cancer Metastasis Treat. 2016;2(8):313-320.
7. Kelgiorgi D, Dervenis C. Pancreatic neuroendocrine tumors: the basics, the gray zone, and the target. F1000Research. 2017;6:663.
8. Viudez A, De Jesus-Acosta A, Carvalho FL, Vera R, Martin-Algarra S, Ramirez N. Pancreatic neuroendocrine tumors: Challenges in an underestimated disease. Crit Rev Oncol Hematol. 2016;101:193-206.
9. World Health Organization, International Agency for Research on Cancer. Bosman FT, Carneiro F, Hruban RH, Theise ND (eds). WHO classification of tumours of the digestive system. 2010, 4th ed (vol 3).
10. Travis WD, Brambilla E, Nicholson AG, et al. The 2015 World Health Organization classification of lung tumors. J Thorac Oncol. 2015;10(9):1243-1260.
11. Lee A, Chan DL, Wong MH, et al. Systematic review of the role of targeted therapy in metastatic neuroendocrine tumors. Neuroendocrinology. 2017;104(3):209-222.
12. Theodoropoulou M, Stalla GK. Somatostatin receptors: from signaling to clinical practice. Front Neuroendocrinol. 2013;34(3):228-252.
13. Caplin ME, Pavel M, Cwikła JB, et al. Lanreotide in metastatic enteropancreatic neuroendocrine tumors. N Engl J Med. 2014;371(3):224-233.
14. Rinke A, Muller HH, Schade-Brittinger C, et al. Placebo-controlled, double-blind, prospective, randomized study on the effect of octreotide LAR in the control of tumor growth in patients with metastatic neuroendocrine midgut tumors: a report from the PROMID Study Group. J Clin Oncol. 2009;27(28):4656-4663.
15. Strosberg J, El-Haddad G, Wolin E, et al. Phase 3 trial of 177Lu-Dotatate for midgut neuroendocrine tumors. N Engl J Med. 2017;376(2):125-135.
16. Falconi M, Partelli S. Neuroendocrine tumours in 2016: defining rules for increasingly personalized treatments. Nat Rev Clin Oncol. 2017;14(2):80-82.
17. Hutchinson L. Targeted therapies: widening the treatment NET. Nat Rev Clin Oncol. 2017;14(1):2-3.
18. Cingarlini S, Bonomi M, Corbo V, Scarpa A, Tortora G. Profiling mTOR pathway in neuroendocrine tumors. Target Oncol. 2012;7(3):183-188.
19. Yao JC, Shah MH, Ito T, et al. Everolimus for advanced pancreatic neuroendocrine tumors. N Engl J Med. 2011;364(6):514-523.
20. Yao JC, Pavel M, Lombard-Bohas C, et al. Everolimus for the treatment of advanced pancreatic neuroendocrine tumors: overall survival and circulating biomarkers from the randomized, phase III RADIANT-3 study. J Clin Oncol. http://ascopubs.org/ doi/abs/10.1200/JCO.2016.68.0702?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed. September 12, 2016. E-pub ahead of print.
21. Yao JC, Fazio N, Singh S, et al. Everolimus for the treatment of advanced, non-functional neuroendocrine tumours of the lung or gastrointestinal tract (RADIANT-4): a randomised, placebo-controlled, phase 3 study. Lancet. 2016;387(10022):968-977.
22. Gajate P, Martínez-Sáez O, Alonso-Gordoa T, Grande E. Emerging use of everolimus in the treatment of neuroendocrine tumors. Cancer Manage Res. 2017;9:215-224.
23. Chan JA, Ryan DP, Zhu AX, et al. Phase I study of pasireotide (SOM 230) and everolimus (RAD001) in advanced neuroendocrine tumors. Endocr Relat Cancer. 2012;19(5):615-623.
24. Kulke MH, Ruszniewski P, Van Cutsem E, et al. A randomized, open-label, phase 2 study of everolimus in combination with pasireotide LAR or everolimus alone in advanced, well-dierentiated, progressive pancreatic neuroendocrine tumors: COOPERATE-2 trial. Ann Oncol. 2017;28(6):1309-1315.
25. Chan JA, Faris JE, Murphy JE, et al. Phase II trial of cabozantinib in patients with carcinoid and pancreatic neuroendocrine tumors (pNET). J Clin Oncol. 2017;35(4 suppl):228-228.
26. Xu J, Li J, Bai CM, et al. An open-label phase Ib/II study of sulfatinib in patients with advanced neuroendocrine tumors (NCT02267967). Paper presented at the 14th Annual European Neuroendocrine Tumor Society Conference for the Diagnosis and Treatment of Neuroendocrine Tumor Disease; March 8-10, 2017, Barcelona, Spain.
27. Libutti SK, Anthony LB, Chaplin DJ, Sosa JA. A phase II study of combretastatin A4-phosphate (CA4P) in the treatment of well-differentiated, low- to intermediate-grade, unresectable, recurrent, or metastatic pancreatic, or GI neuroendocrine tumors/carcinoid (GI-NETs/PNETs) with elevated biomarkers. J Clin Oncol. 2017;35(4 suppl):432-432.
28. Cordes LM, Gulley JL. Avelumab for the treatment of metastatic Merkel cell carcinoma. Drugs Today (Barc). 2017;53(7):377-383.
29. Kaufman HL, Russell J, Hamid O, et al. Avelumab in patients with chemotherapy-refractory metastatic Merkel cell carcinoma: a multicentre, single-group, open-label, phase 2 trial. Lancet Oncol. 2016;17(10):1374-1385.
1. Pinchot SN, Holen K, Sippel RS, Chen H. Carcinoid tumors. Oncologist. 2008;13(12):1255-1269.
2. Rorstad O. Prognostic indicators for carcinoid neuroendocrine tumors of the gastrointestinal tract. J Surg Oncol. 2005;89(3):151-160.
3. The NET Alliance. Characterizing a challenging cancer. http://www.thenetalliance.com/hcp/facts-about-net/characterization/. Publishing date not provided. Accessed October 18, 2017.
4. Yao JC, Hassan M, Phan A, et al. One hundred years after ‘carcinoid’: epidemiology of and prognostic factors for neuroendocrine tumors in 35,825 cases in the United States. J Clin Oncol. 2008;26(18):3063-3072.
5. Modlin IM, Lye KD, Kidd M. A 5-decade analysis of 13,715 carcinoid tumors. Cancer. 2003;97(4):934-959.
6. Spada F, Valente M. Review of recent advances in medical treatment for neuroendocrine neoplasms: somatostatin analogs and chemotherapy. J Cancer Metastasis Treat. 2016;2(8):313-320.
7. Kelgiorgi D, Dervenis C. Pancreatic neuroendocrine tumors: the basics, the gray zone, and the target. F1000Research. 2017;6:663.
8. Viudez A, De Jesus-Acosta A, Carvalho FL, Vera R, Martin-Algarra S, Ramirez N. Pancreatic neuroendocrine tumors: Challenges in an underestimated disease. Crit Rev Oncol Hematol. 2016;101:193-206.
9. World Health Organization, International Agency for Research on Cancer. Bosman FT, Carneiro F, Hruban RH, Theise ND (eds). WHO classification of tumours of the digestive system. 2010, 4th ed (vol 3).
10. Travis WD, Brambilla E, Nicholson AG, et al. The 2015 World Health Organization classification of lung tumors. J Thorac Oncol. 2015;10(9):1243-1260.
11. Lee A, Chan DL, Wong MH, et al. Systematic review of the role of targeted therapy in metastatic neuroendocrine tumors. Neuroendocrinology. 2017;104(3):209-222.
12. Theodoropoulou M, Stalla GK. Somatostatin receptors: from signaling to clinical practice. Front Neuroendocrinol. 2013;34(3):228-252.
13. Caplin ME, Pavel M, Cwikła JB, et al. Lanreotide in metastatic enteropancreatic neuroendocrine tumors. N Engl J Med. 2014;371(3):224-233.
14. Rinke A, Muller HH, Schade-Brittinger C, et al. Placebo-controlled, double-blind, prospective, randomized study on the effect of octreotide LAR in the control of tumor growth in patients with metastatic neuroendocrine midgut tumors: a report from the PROMID Study Group. J Clin Oncol. 2009;27(28):4656-4663.
15. Strosberg J, El-Haddad G, Wolin E, et al. Phase 3 trial of 177Lu-Dotatate for midgut neuroendocrine tumors. N Engl J Med. 2017;376(2):125-135.
16. Falconi M, Partelli S. Neuroendocrine tumours in 2016: defining rules for increasingly personalized treatments. Nat Rev Clin Oncol. 2017;14(2):80-82.
17. Hutchinson L. Targeted therapies: widening the treatment NET. Nat Rev Clin Oncol. 2017;14(1):2-3.
18. Cingarlini S, Bonomi M, Corbo V, Scarpa A, Tortora G. Profiling mTOR pathway in neuroendocrine tumors. Target Oncol. 2012;7(3):183-188.
19. Yao JC, Shah MH, Ito T, et al. Everolimus for advanced pancreatic neuroendocrine tumors. N Engl J Med. 2011;364(6):514-523.
20. Yao JC, Pavel M, Lombard-Bohas C, et al. Everolimus for the treatment of advanced pancreatic neuroendocrine tumors: overall survival and circulating biomarkers from the randomized, phase III RADIANT-3 study. J Clin Oncol. http://ascopubs.org/ doi/abs/10.1200/JCO.2016.68.0702?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed. September 12, 2016. E-pub ahead of print.
21. Yao JC, Fazio N, Singh S, et al. Everolimus for the treatment of advanced, non-functional neuroendocrine tumours of the lung or gastrointestinal tract (RADIANT-4): a randomised, placebo-controlled, phase 3 study. Lancet. 2016;387(10022):968-977.
22. Gajate P, Martínez-Sáez O, Alonso-Gordoa T, Grande E. Emerging use of everolimus in the treatment of neuroendocrine tumors. Cancer Manage Res. 2017;9:215-224.
23. Chan JA, Ryan DP, Zhu AX, et al. Phase I study of pasireotide (SOM 230) and everolimus (RAD001) in advanced neuroendocrine tumors. Endocr Relat Cancer. 2012;19(5):615-623.
24. Kulke MH, Ruszniewski P, Van Cutsem E, et al. A randomized, open-label, phase 2 study of everolimus in combination with pasireotide LAR or everolimus alone in advanced, well-dierentiated, progressive pancreatic neuroendocrine tumors: COOPERATE-2 trial. Ann Oncol. 2017;28(6):1309-1315.
25. Chan JA, Faris JE, Murphy JE, et al. Phase II trial of cabozantinib in patients with carcinoid and pancreatic neuroendocrine tumors (pNET). J Clin Oncol. 2017;35(4 suppl):228-228.
26. Xu J, Li J, Bai CM, et al. An open-label phase Ib/II study of sulfatinib in patients with advanced neuroendocrine tumors (NCT02267967). Paper presented at the 14th Annual European Neuroendocrine Tumor Society Conference for the Diagnosis and Treatment of Neuroendocrine Tumor Disease; March 8-10, 2017, Barcelona, Spain.
27. Libutti SK, Anthony LB, Chaplin DJ, Sosa JA. A phase II study of combretastatin A4-phosphate (CA4P) in the treatment of well-differentiated, low- to intermediate-grade, unresectable, recurrent, or metastatic pancreatic, or GI neuroendocrine tumors/carcinoid (GI-NETs/PNETs) with elevated biomarkers. J Clin Oncol. 2017;35(4 suppl):432-432.
28. Cordes LM, Gulley JL. Avelumab for the treatment of metastatic Merkel cell carcinoma. Drugs Today (Barc). 2017;53(7):377-383.
29. Kaufman HL, Russell J, Hamid O, et al. Avelumab in patients with chemotherapy-refractory metastatic Merkel cell carcinoma: a multicentre, single-group, open-label, phase 2 trial. Lancet Oncol. 2016;17(10):1374-1385.
Supportive medications and interventions received by prostate cancer survivors: results from the PiCTure study
Prostate cancer treatments are associated with various physical after-effects, including urinary, sexual, and bowel symptoms.1 These after-effects can have an impact on survivors’ health-related quality of life (HRQoL).2 Pharmaceutical and surgical interventions are available to manage or ameliorate many of these after-effects (eg, sildenafil citrate taken during and after radiotherapy improves sexual function),3 and their receipt has a positive impact on HRQoL.4
However, studies of clinicians suggest that such interventions may not be used widely.5,6 Patient-reported data on this topic is lacking. Therefore, we investigated the use of supportive medications and interventions in this population-based study of prostate cancer survivors.
Methods
The PiCTure (Prostate Cancer Treatment, Your Experience) study methods have been described elsewhere.7 Briefly, 6,559 prostate cancer survivors 2-15 years after diagnosis (diagnosed during January 1, 1995-March 31, 2010, and alive in November 2011), identified from population-based cancer registries in the Republic of Ireland and Northern Ireland, were invited to complete a postal survey. Information was sought on after-effects (incontinence, impotence, gynaecomastia, hot flashes/sweats, bowel problems, depression) that had been experienced at any time after treatment. For each after-effect, men were asked if they had received any medication or interventions to alleviate symptoms, and, if so, what they had received; examples of common interventions were provided. Men were also asked if they had been told they may become infertile and, if so, whether they had preserved their sperm. The Decisional Regret Scale8 was used to measure survivors’ regret over their entire treatment experience. This 5-item scale, rated on a 5-point Likert scale from 1 (strongly agree) to 5 (strongly disagree) was summed and standardized to a value of 0-100, with higher scores reflecting higher levels of decisional regret. 8 This scale has good psychometric properties8 and strong reliability in our sample (Cronbach’s alpha = 0.85). Responders were categorized as having any regret (score ≥1) or no regret (score = 0).
The number of men who reported receiving an intervention was expressed as a percentage of survey responders and of men who reported ever having the relevant after-effect. Chi-square tests were used to investigate variations in receipt by: age at diagnosis (≤59, 60-69, ≥70 years); time since diagnosis (≤5, 5-10, >10 years); jurisdiction (Republic of Ireland, or Northern Ireland); and primary treatment(s) received (radical prostatectomy [RP], external beam radiotherapy [EBRT] with androgen deprivation therapy [ADT], EBRT without ADT, brachytherapy, ADT [without other therapies], and active surveillance/watchful waiting). Among survivors who ever experienced an after-effect, chi-square tests were used to investigate whether the percentage who reported decisional regret differed depending on whether or not they received the relevant supportive intervention.
Ethics approval was from the Irish College of General Practitioners (Republic of Ireland) and the Office for Research Ethics Committee Northern Ireland.
Results
In all, 3,348 survivors participated in the survey (adjusted response rate, 54%). Compared with nonresponders, responders were more often from the Republic of Ireland (P = .007), <70 years at diagnosis (P < .001), 5-10 years post diagnosis (P < .001), with low or medium Gleason grade (Gleason scores of ≤6 [good prognosis] and 7, respectively; P < .001), and clinical stage II-IV (P < .001; Table 1).
Impotence (70%) was the most commonly reported after-effect, followed by hot flashes/sweats (40%), incontinence (37%), bowel problems (23%), gynaecomastia (19%), and depression (18%; Table 2).
Of responders, 2% received an artificial sphincter, representing 6% of men who ever experienced incontinence post diagnosis (Table 2). This percentage was significantly higher in participants diagnosed longer ago, from the Republic of Ireland, and who received RP (Table 3).
Incontinence medication was received by 8% of participants (21% of those who experienced incontinence). Use varied significantly by age, jurisdiction, and treatment. For impotence, medications were more commonly used (20% of participants; 28% with impotence) than were injections (5% and 7%, respectively) or penile implants/pumps (2% and 3%, respectively). Use of all 3 types of intervention was highest in men who had RP; injections and implants/pumps were significantly more common among younger men. Of those experiencing gynaecomastia, 13% received interventions; receipt was highest in men who had EBRT with ADT, were <5 years post diagnosis and from Northern Ireland. For hot flashes/sweats, 3% of participants (8% who experienced symptoms) received mediations; this was higher in men who had EBRT. Of those who reported depression, 28% received medication; receipt was highest in younger men and in Northern Ireland. Medication for bowel problems was used by 35% of men who experienced these; use was highest in older men, those diagnosed more recently, and those who had EBRT. Sixty percent of men reported having been told they would become infertile; 11 (0.3% of participants) preserved their sperm, 7 from the Republic of Ireland and 4 from Northern Ireland.
A total of 35.6% of survivors reported any decisional regret. Among survivors who ever had an after-effect, a higher percentage of those who used a supportive intervention reported decisional regret compared with those who did not; this was only statistically significant for those using medication or alprostadil injections for impotence (Table 2).
Discussion
This study documents, for the first time, population-based data on patient-reported use of supportive medications and interventions to alleviate adverse effects of prostate cancer and its treatment. Among survivors who experienced after-effects, use was highest for bowel problems, impotence, and depression, but even for those, only 28%-35% of men took medication. Although it is possible that some survivors declined medications or other interventions, these low levels of use strongly suggest that not all survivors who might benefit from supports receive them.
There was little evidence that utilisation was higher in survivors diagnosed more recently. This suggests that, although the number of prostate cancer survivors has grown, and there is greater focus on survivorship issues in clinical practice, this has not translated into more men receiving support to manage after-effects. Care is needed to ensure that the newer models of post-cancer follow-up being considered or adopted in many settings,9 do not exacerbate this issue.
As expected, patterns of utilisation varied by treatment(s) received. Higher use of surgical and pharmaceutical interventions to alleviate incontinence among survivors in the Republic of Ireland than in Northern Ireland is likely owing to the higher rate of radical prostatectomy in the Republic of Ireland, whereas greater use of treatments for gynaecomastia in Northern Ireland reflects higher use of hormone therapy there.10 Other variations in intervention use were more surprising. Younger men were significantly more likely to report using supportive interventions for depression and impotence, the latter finding being consistent with findings in a Swedish population-based study.11 Older men were significantly more likely to report interventions for incontinence and bowel problems. Although those trends could be explained by differences in treatment receipt by age, it is possible that men of different ages may be more likely to seek, or be offered, help for certain types of after-effects. With the exception of interventions for bowel problems, a higher percentage of men who received intervention(s) for an after-effect reported decisional regret. There are a number of possible explanations: these men may have experienced more severe after-effects, which required interventions; they may have been less satisfied with their posttreatment function and/or more proactive about recovering or treating their after-effects. This requires further investigation.
This is a large, international, population-based study, the first such study to describe patient-reported use of supportive care following a range of prostate cancer treatments. Although this study is novel, there are a number of limitations. It is a cross-sectional, descriptive study. We did not ask survivors whether the supportive interventions received matched their needs and wants, and whether they were satisfied with the supportive care received. Furthermore, although the response rate is comparable with other similar studies,12,13 it is possible that the supportive care of nonresponders was different to that of responders.
Our study included men from 2 jurisdictions with separate health care systems, suggesting that low use of supportive interventions may be common across systems. There is a need for further research into patient and health care system factors associated with the receipt of supportive interventions and how satisfied men are with these, in this and other health care settings. Presently, it is clear that more needs to be done in the clinical setting to support prostate cancer survivors manage treatment after-effects; this in turn could improve survivors’ HRQoL.
1. Drummond FJ, Kinnear H, O’Leary E, Donnelly, Gavin A, Sharp L. Long-term health-related quality of life of prostate cancer survivors varies by primary treatment. Results from the PiCTure (Prostate Cancer Treatment, your experience) study. J Cancer Surviv. 2015;9(2):361-72.
2. Smith DP, King MT, Egger S, et al. Quality of life three years after diagnosis of localised prostate cancer: population based cohort study. BMJ 2009; 339:b4817.
3. Zelefsky MJ, Shasha D, Branco RD, et al. Prophylactic sildenafil citrate improves select aspects of sexual function in men treated with radiotherapy for prostate cancer. J Urol. 2014;192(3):868-874.
4. Haab F, Trockman BA, Zimmern PE, Leach GE. Quality of life and continence assessment of the artificial urinary sphincter in men with minimum 3.5 years of follow-up. J Urol. 1997;158(2):435-439.
5. Tanvetyanon T. Physician practices of bone density testing and drug prescribing to prevent or treat osteoporosis during androgen deprivation therapy. Cancer. 2005;103(2):237-241.
6. Alibhai SM, Rahman S, Warde PR, Jewett MA, Jaffer T, Cheung AM. Prevention and management of osteoporosis in men receiving androgen deprivation therapy: a survey of urologists and radiation oncologists. Urology. 2006;68(1):126-131,
7. Drummond FJ, Kinnear H, Donnelly C, et al. Establishing a population-based patient reported outcomes study (PROMs) using national cancer registries across two jurisdictions: Prostate Cancer Treatment, your experience (PiCTure) Study. BMJ Open 2015;5:e006851.
8. Brehaut JC, O’Connor AM, Wood TJ, et al. Validation of a decision regret scale. Med Decis Making. 2003;23(4):281-92.
9. Howell D, Hack TF, Oliver et al. Models of care for post-treatment follow-up of adult cancer survivors: a systematic review and quality appraisal of the evidence. J Cancer Surviv. 2012;6(4):359-371.
10. Donnelly DW, Gavin AT, Comber H. Cancer in Ireland 1994-2004. A comprehensive report. Northern Ireland Cancer Registry/National Cancer Registry, Ireland, 2009.
11. Plym A, Folkvaljon Y, Garmo H, et al. Drug prescription for erectile dysfunction before and after diagnosis of localized prostate cancer. J Sex Med. 2014;11(8):2100-2108.
12. Hervouet S, Savard J, Simard S, et al. Psychological functioning associated with prostate cancer: cross-sectional comparison of patients treated with radiotherapy, brachytherapy, or surgery. J Pain Symptom Manage. 2005;30(5):474-484.
13. Glaser AW, Fraser LK, Corner J, et al. Patient-reported outcomes of cancer survivors in England 1-5 years after diagnosis: a cross-sectional survey. BMJ Open. 2013;3(4). pii: e002317.
Prostate cancer treatments are associated with various physical after-effects, including urinary, sexual, and bowel symptoms.1 These after-effects can have an impact on survivors’ health-related quality of life (HRQoL).2 Pharmaceutical and surgical interventions are available to manage or ameliorate many of these after-effects (eg, sildenafil citrate taken during and after radiotherapy improves sexual function),3 and their receipt has a positive impact on HRQoL.4
However, studies of clinicians suggest that such interventions may not be used widely.5,6 Patient-reported data on this topic is lacking. Therefore, we investigated the use of supportive medications and interventions in this population-based study of prostate cancer survivors.
Methods
The PiCTure (Prostate Cancer Treatment, Your Experience) study methods have been described elsewhere.7 Briefly, 6,559 prostate cancer survivors 2-15 years after diagnosis (diagnosed during January 1, 1995-March 31, 2010, and alive in November 2011), identified from population-based cancer registries in the Republic of Ireland and Northern Ireland, were invited to complete a postal survey. Information was sought on after-effects (incontinence, impotence, gynaecomastia, hot flashes/sweats, bowel problems, depression) that had been experienced at any time after treatment. For each after-effect, men were asked if they had received any medication or interventions to alleviate symptoms, and, if so, what they had received; examples of common interventions were provided. Men were also asked if they had been told they may become infertile and, if so, whether they had preserved their sperm. The Decisional Regret Scale8 was used to measure survivors’ regret over their entire treatment experience. This 5-item scale, rated on a 5-point Likert scale from 1 (strongly agree) to 5 (strongly disagree) was summed and standardized to a value of 0-100, with higher scores reflecting higher levels of decisional regret. 8 This scale has good psychometric properties8 and strong reliability in our sample (Cronbach’s alpha = 0.85). Responders were categorized as having any regret (score ≥1) or no regret (score = 0).
The number of men who reported receiving an intervention was expressed as a percentage of survey responders and of men who reported ever having the relevant after-effect. Chi-square tests were used to investigate variations in receipt by: age at diagnosis (≤59, 60-69, ≥70 years); time since diagnosis (≤5, 5-10, >10 years); jurisdiction (Republic of Ireland, or Northern Ireland); and primary treatment(s) received (radical prostatectomy [RP], external beam radiotherapy [EBRT] with androgen deprivation therapy [ADT], EBRT without ADT, brachytherapy, ADT [without other therapies], and active surveillance/watchful waiting). Among survivors who ever experienced an after-effect, chi-square tests were used to investigate whether the percentage who reported decisional regret differed depending on whether or not they received the relevant supportive intervention.
Ethics approval was from the Irish College of General Practitioners (Republic of Ireland) and the Office for Research Ethics Committee Northern Ireland.
Results
In all, 3,348 survivors participated in the survey (adjusted response rate, 54%). Compared with nonresponders, responders were more often from the Republic of Ireland (P = .007), <70 years at diagnosis (P < .001), 5-10 years post diagnosis (P < .001), with low or medium Gleason grade (Gleason scores of ≤6 [good prognosis] and 7, respectively; P < .001), and clinical stage II-IV (P < .001; Table 1).
Impotence (70%) was the most commonly reported after-effect, followed by hot flashes/sweats (40%), incontinence (37%), bowel problems (23%), gynaecomastia (19%), and depression (18%; Table 2).
Of responders, 2% received an artificial sphincter, representing 6% of men who ever experienced incontinence post diagnosis (Table 2). This percentage was significantly higher in participants diagnosed longer ago, from the Republic of Ireland, and who received RP (Table 3).
Incontinence medication was received by 8% of participants (21% of those who experienced incontinence). Use varied significantly by age, jurisdiction, and treatment. For impotence, medications were more commonly used (20% of participants; 28% with impotence) than were injections (5% and 7%, respectively) or penile implants/pumps (2% and 3%, respectively). Use of all 3 types of intervention was highest in men who had RP; injections and implants/pumps were significantly more common among younger men. Of those experiencing gynaecomastia, 13% received interventions; receipt was highest in men who had EBRT with ADT, were <5 years post diagnosis and from Northern Ireland. For hot flashes/sweats, 3% of participants (8% who experienced symptoms) received mediations; this was higher in men who had EBRT. Of those who reported depression, 28% received medication; receipt was highest in younger men and in Northern Ireland. Medication for bowel problems was used by 35% of men who experienced these; use was highest in older men, those diagnosed more recently, and those who had EBRT. Sixty percent of men reported having been told they would become infertile; 11 (0.3% of participants) preserved their sperm, 7 from the Republic of Ireland and 4 from Northern Ireland.
A total of 35.6% of survivors reported any decisional regret. Among survivors who ever had an after-effect, a higher percentage of those who used a supportive intervention reported decisional regret compared with those who did not; this was only statistically significant for those using medication or alprostadil injections for impotence (Table 2).
Discussion
This study documents, for the first time, population-based data on patient-reported use of supportive medications and interventions to alleviate adverse effects of prostate cancer and its treatment. Among survivors who experienced after-effects, use was highest for bowel problems, impotence, and depression, but even for those, only 28%-35% of men took medication. Although it is possible that some survivors declined medications or other interventions, these low levels of use strongly suggest that not all survivors who might benefit from supports receive them.
There was little evidence that utilisation was higher in survivors diagnosed more recently. This suggests that, although the number of prostate cancer survivors has grown, and there is greater focus on survivorship issues in clinical practice, this has not translated into more men receiving support to manage after-effects. Care is needed to ensure that the newer models of post-cancer follow-up being considered or adopted in many settings,9 do not exacerbate this issue.
As expected, patterns of utilisation varied by treatment(s) received. Higher use of surgical and pharmaceutical interventions to alleviate incontinence among survivors in the Republic of Ireland than in Northern Ireland is likely owing to the higher rate of radical prostatectomy in the Republic of Ireland, whereas greater use of treatments for gynaecomastia in Northern Ireland reflects higher use of hormone therapy there.10 Other variations in intervention use were more surprising. Younger men were significantly more likely to report using supportive interventions for depression and impotence, the latter finding being consistent with findings in a Swedish population-based study.11 Older men were significantly more likely to report interventions for incontinence and bowel problems. Although those trends could be explained by differences in treatment receipt by age, it is possible that men of different ages may be more likely to seek, or be offered, help for certain types of after-effects. With the exception of interventions for bowel problems, a higher percentage of men who received intervention(s) for an after-effect reported decisional regret. There are a number of possible explanations: these men may have experienced more severe after-effects, which required interventions; they may have been less satisfied with their posttreatment function and/or more proactive about recovering or treating their after-effects. This requires further investigation.
This is a large, international, population-based study, the first such study to describe patient-reported use of supportive care following a range of prostate cancer treatments. Although this study is novel, there are a number of limitations. It is a cross-sectional, descriptive study. We did not ask survivors whether the supportive interventions received matched their needs and wants, and whether they were satisfied with the supportive care received. Furthermore, although the response rate is comparable with other similar studies,12,13 it is possible that the supportive care of nonresponders was different to that of responders.
Our study included men from 2 jurisdictions with separate health care systems, suggesting that low use of supportive interventions may be common across systems. There is a need for further research into patient and health care system factors associated with the receipt of supportive interventions and how satisfied men are with these, in this and other health care settings. Presently, it is clear that more needs to be done in the clinical setting to support prostate cancer survivors manage treatment after-effects; this in turn could improve survivors’ HRQoL.
Prostate cancer treatments are associated with various physical after-effects, including urinary, sexual, and bowel symptoms.1 These after-effects can have an impact on survivors’ health-related quality of life (HRQoL).2 Pharmaceutical and surgical interventions are available to manage or ameliorate many of these after-effects (eg, sildenafil citrate taken during and after radiotherapy improves sexual function),3 and their receipt has a positive impact on HRQoL.4
However, studies of clinicians suggest that such interventions may not be used widely.5,6 Patient-reported data on this topic is lacking. Therefore, we investigated the use of supportive medications and interventions in this population-based study of prostate cancer survivors.
Methods
The PiCTure (Prostate Cancer Treatment, Your Experience) study methods have been described elsewhere.7 Briefly, 6,559 prostate cancer survivors 2-15 years after diagnosis (diagnosed during January 1, 1995-March 31, 2010, and alive in November 2011), identified from population-based cancer registries in the Republic of Ireland and Northern Ireland, were invited to complete a postal survey. Information was sought on after-effects (incontinence, impotence, gynaecomastia, hot flashes/sweats, bowel problems, depression) that had been experienced at any time after treatment. For each after-effect, men were asked if they had received any medication or interventions to alleviate symptoms, and, if so, what they had received; examples of common interventions were provided. Men were also asked if they had been told they may become infertile and, if so, whether they had preserved their sperm. The Decisional Regret Scale8 was used to measure survivors’ regret over their entire treatment experience. This 5-item scale, rated on a 5-point Likert scale from 1 (strongly agree) to 5 (strongly disagree) was summed and standardized to a value of 0-100, with higher scores reflecting higher levels of decisional regret. 8 This scale has good psychometric properties8 and strong reliability in our sample (Cronbach’s alpha = 0.85). Responders were categorized as having any regret (score ≥1) or no regret (score = 0).
The number of men who reported receiving an intervention was expressed as a percentage of survey responders and of men who reported ever having the relevant after-effect. Chi-square tests were used to investigate variations in receipt by: age at diagnosis (≤59, 60-69, ≥70 years); time since diagnosis (≤5, 5-10, >10 years); jurisdiction (Republic of Ireland, or Northern Ireland); and primary treatment(s) received (radical prostatectomy [RP], external beam radiotherapy [EBRT] with androgen deprivation therapy [ADT], EBRT without ADT, brachytherapy, ADT [without other therapies], and active surveillance/watchful waiting). Among survivors who ever experienced an after-effect, chi-square tests were used to investigate whether the percentage who reported decisional regret differed depending on whether or not they received the relevant supportive intervention.
Ethics approval was from the Irish College of General Practitioners (Republic of Ireland) and the Office for Research Ethics Committee Northern Ireland.
Results
In all, 3,348 survivors participated in the survey (adjusted response rate, 54%). Compared with nonresponders, responders were more often from the Republic of Ireland (P = .007), <70 years at diagnosis (P < .001), 5-10 years post diagnosis (P < .001), with low or medium Gleason grade (Gleason scores of ≤6 [good prognosis] and 7, respectively; P < .001), and clinical stage II-IV (P < .001; Table 1).
Impotence (70%) was the most commonly reported after-effect, followed by hot flashes/sweats (40%), incontinence (37%), bowel problems (23%), gynaecomastia (19%), and depression (18%; Table 2).
Of responders, 2% received an artificial sphincter, representing 6% of men who ever experienced incontinence post diagnosis (Table 2). This percentage was significantly higher in participants diagnosed longer ago, from the Republic of Ireland, and who received RP (Table 3).
Incontinence medication was received by 8% of participants (21% of those who experienced incontinence). Use varied significantly by age, jurisdiction, and treatment. For impotence, medications were more commonly used (20% of participants; 28% with impotence) than were injections (5% and 7%, respectively) or penile implants/pumps (2% and 3%, respectively). Use of all 3 types of intervention was highest in men who had RP; injections and implants/pumps were significantly more common among younger men. Of those experiencing gynaecomastia, 13% received interventions; receipt was highest in men who had EBRT with ADT, were <5 years post diagnosis and from Northern Ireland. For hot flashes/sweats, 3% of participants (8% who experienced symptoms) received mediations; this was higher in men who had EBRT. Of those who reported depression, 28% received medication; receipt was highest in younger men and in Northern Ireland. Medication for bowel problems was used by 35% of men who experienced these; use was highest in older men, those diagnosed more recently, and those who had EBRT. Sixty percent of men reported having been told they would become infertile; 11 (0.3% of participants) preserved their sperm, 7 from the Republic of Ireland and 4 from Northern Ireland.
A total of 35.6% of survivors reported any decisional regret. Among survivors who ever had an after-effect, a higher percentage of those who used a supportive intervention reported decisional regret compared with those who did not; this was only statistically significant for those using medication or alprostadil injections for impotence (Table 2).
Discussion
This study documents, for the first time, population-based data on patient-reported use of supportive medications and interventions to alleviate adverse effects of prostate cancer and its treatment. Among survivors who experienced after-effects, use was highest for bowel problems, impotence, and depression, but even for those, only 28%-35% of men took medication. Although it is possible that some survivors declined medications or other interventions, these low levels of use strongly suggest that not all survivors who might benefit from supports receive them.
There was little evidence that utilisation was higher in survivors diagnosed more recently. This suggests that, although the number of prostate cancer survivors has grown, and there is greater focus on survivorship issues in clinical practice, this has not translated into more men receiving support to manage after-effects. Care is needed to ensure that the newer models of post-cancer follow-up being considered or adopted in many settings,9 do not exacerbate this issue.
As expected, patterns of utilisation varied by treatment(s) received. Higher use of surgical and pharmaceutical interventions to alleviate incontinence among survivors in the Republic of Ireland than in Northern Ireland is likely owing to the higher rate of radical prostatectomy in the Republic of Ireland, whereas greater use of treatments for gynaecomastia in Northern Ireland reflects higher use of hormone therapy there.10 Other variations in intervention use were more surprising. Younger men were significantly more likely to report using supportive interventions for depression and impotence, the latter finding being consistent with findings in a Swedish population-based study.11 Older men were significantly more likely to report interventions for incontinence and bowel problems. Although those trends could be explained by differences in treatment receipt by age, it is possible that men of different ages may be more likely to seek, or be offered, help for certain types of after-effects. With the exception of interventions for bowel problems, a higher percentage of men who received intervention(s) for an after-effect reported decisional regret. There are a number of possible explanations: these men may have experienced more severe after-effects, which required interventions; they may have been less satisfied with their posttreatment function and/or more proactive about recovering or treating their after-effects. This requires further investigation.
This is a large, international, population-based study, the first such study to describe patient-reported use of supportive care following a range of prostate cancer treatments. Although this study is novel, there are a number of limitations. It is a cross-sectional, descriptive study. We did not ask survivors whether the supportive interventions received matched their needs and wants, and whether they were satisfied with the supportive care received. Furthermore, although the response rate is comparable with other similar studies,12,13 it is possible that the supportive care of nonresponders was different to that of responders.
Our study included men from 2 jurisdictions with separate health care systems, suggesting that low use of supportive interventions may be common across systems. There is a need for further research into patient and health care system factors associated with the receipt of supportive interventions and how satisfied men are with these, in this and other health care settings. Presently, it is clear that more needs to be done in the clinical setting to support prostate cancer survivors manage treatment after-effects; this in turn could improve survivors’ HRQoL.
1. Drummond FJ, Kinnear H, O’Leary E, Donnelly, Gavin A, Sharp L. Long-term health-related quality of life of prostate cancer survivors varies by primary treatment. Results from the PiCTure (Prostate Cancer Treatment, your experience) study. J Cancer Surviv. 2015;9(2):361-72.
2. Smith DP, King MT, Egger S, et al. Quality of life three years after diagnosis of localised prostate cancer: population based cohort study. BMJ 2009; 339:b4817.
3. Zelefsky MJ, Shasha D, Branco RD, et al. Prophylactic sildenafil citrate improves select aspects of sexual function in men treated with radiotherapy for prostate cancer. J Urol. 2014;192(3):868-874.
4. Haab F, Trockman BA, Zimmern PE, Leach GE. Quality of life and continence assessment of the artificial urinary sphincter in men with minimum 3.5 years of follow-up. J Urol. 1997;158(2):435-439.
5. Tanvetyanon T. Physician practices of bone density testing and drug prescribing to prevent or treat osteoporosis during androgen deprivation therapy. Cancer. 2005;103(2):237-241.
6. Alibhai SM, Rahman S, Warde PR, Jewett MA, Jaffer T, Cheung AM. Prevention and management of osteoporosis in men receiving androgen deprivation therapy: a survey of urologists and radiation oncologists. Urology. 2006;68(1):126-131,
7. Drummond FJ, Kinnear H, Donnelly C, et al. Establishing a population-based patient reported outcomes study (PROMs) using national cancer registries across two jurisdictions: Prostate Cancer Treatment, your experience (PiCTure) Study. BMJ Open 2015;5:e006851.
8. Brehaut JC, O’Connor AM, Wood TJ, et al. Validation of a decision regret scale. Med Decis Making. 2003;23(4):281-92.
9. Howell D, Hack TF, Oliver et al. Models of care for post-treatment follow-up of adult cancer survivors: a systematic review and quality appraisal of the evidence. J Cancer Surviv. 2012;6(4):359-371.
10. Donnelly DW, Gavin AT, Comber H. Cancer in Ireland 1994-2004. A comprehensive report. Northern Ireland Cancer Registry/National Cancer Registry, Ireland, 2009.
11. Plym A, Folkvaljon Y, Garmo H, et al. Drug prescription for erectile dysfunction before and after diagnosis of localized prostate cancer. J Sex Med. 2014;11(8):2100-2108.
12. Hervouet S, Savard J, Simard S, et al. Psychological functioning associated with prostate cancer: cross-sectional comparison of patients treated with radiotherapy, brachytherapy, or surgery. J Pain Symptom Manage. 2005;30(5):474-484.
13. Glaser AW, Fraser LK, Corner J, et al. Patient-reported outcomes of cancer survivors in England 1-5 years after diagnosis: a cross-sectional survey. BMJ Open. 2013;3(4). pii: e002317.
1. Drummond FJ, Kinnear H, O’Leary E, Donnelly, Gavin A, Sharp L. Long-term health-related quality of life of prostate cancer survivors varies by primary treatment. Results from the PiCTure (Prostate Cancer Treatment, your experience) study. J Cancer Surviv. 2015;9(2):361-72.
2. Smith DP, King MT, Egger S, et al. Quality of life three years after diagnosis of localised prostate cancer: population based cohort study. BMJ 2009; 339:b4817.
3. Zelefsky MJ, Shasha D, Branco RD, et al. Prophylactic sildenafil citrate improves select aspects of sexual function in men treated with radiotherapy for prostate cancer. J Urol. 2014;192(3):868-874.
4. Haab F, Trockman BA, Zimmern PE, Leach GE. Quality of life and continence assessment of the artificial urinary sphincter in men with minimum 3.5 years of follow-up. J Urol. 1997;158(2):435-439.
5. Tanvetyanon T. Physician practices of bone density testing and drug prescribing to prevent or treat osteoporosis during androgen deprivation therapy. Cancer. 2005;103(2):237-241.
6. Alibhai SM, Rahman S, Warde PR, Jewett MA, Jaffer T, Cheung AM. Prevention and management of osteoporosis in men receiving androgen deprivation therapy: a survey of urologists and radiation oncologists. Urology. 2006;68(1):126-131,
7. Drummond FJ, Kinnear H, Donnelly C, et al. Establishing a population-based patient reported outcomes study (PROMs) using national cancer registries across two jurisdictions: Prostate Cancer Treatment, your experience (PiCTure) Study. BMJ Open 2015;5:e006851.
8. Brehaut JC, O’Connor AM, Wood TJ, et al. Validation of a decision regret scale. Med Decis Making. 2003;23(4):281-92.
9. Howell D, Hack TF, Oliver et al. Models of care for post-treatment follow-up of adult cancer survivors: a systematic review and quality appraisal of the evidence. J Cancer Surviv. 2012;6(4):359-371.
10. Donnelly DW, Gavin AT, Comber H. Cancer in Ireland 1994-2004. A comprehensive report. Northern Ireland Cancer Registry/National Cancer Registry, Ireland, 2009.
11. Plym A, Folkvaljon Y, Garmo H, et al. Drug prescription for erectile dysfunction before and after diagnosis of localized prostate cancer. J Sex Med. 2014;11(8):2100-2108.
12. Hervouet S, Savard J, Simard S, et al. Psychological functioning associated with prostate cancer: cross-sectional comparison of patients treated with radiotherapy, brachytherapy, or surgery. J Pain Symptom Manage. 2005;30(5):474-484.
13. Glaser AW, Fraser LK, Corner J, et al. Patient-reported outcomes of cancer survivors in England 1-5 years after diagnosis: a cross-sectional survey. BMJ Open. 2013;3(4). pii: e002317.