User login
Research and Reviews for the Practicing Oncologist
Practice-changing endocrine trials shed light on breast cancer treatment, management
At the 2016 San Antonio Breast Cancer Symposium, investigators presented findings on PFS benefits of adding an mTOR inhibitor to anti-hormonal therapy in advanced disease in postmenopausal women; the lack of clarity on the optimal duration of extended AI therapy, also in postmenopausal women; and using CTCs in helping predict breast cancer outcomes in the neoadjuvant setting.
Fulvestrant plus everolimus improves PFS in HR+, HER2- advanced breast cancer
Key clinical point This study provides further evidence of the benefits of adding an mTOR inhibitor to anti-hormonal therapy in postmenopausal women with advanced breast cancer resistant to aromatase inhibitors. Major finding Fulvestrant plus everolimus was associated with a PFS of 10.4 months, vs 5.1 months for fulvestrant alone. Data source Randomized phase 2 trial of 131 women with HR-positive, HER2-negative locally advanced of metastatic breast cancer resistant to aromatase inhibitors. Disclosures Sponsored by PrECOG with financial support from Novartis. Dr Kornblum reported having no conflicts of interest.
Adding everolimus to fulvestrant doubled median progression-free survival (PFS) among postmenopausal women with hormone receptor-positive (HR-positive), human epidermal growth factor receptor 2-negative (HER2-negative) metastatic breast cancer resistant to therapy with an aromatase inhibitor (AI), Noah S Kornblum, MD, reported during his presentation at the meeting of the PrECOG 0102 trial findings.
In the randomized phase 2 trial, the combination of the mammalian target of rapamycin (mTOR) inhibitor everolimus with the selective estrogen receptor down-regulator (SERD) fulvestrant was associated with a median PFS of 10.4 months, compared with 5.1 months for fulvestrant plus placebo, said Dr Kornblum, of Montefiore Einstein Center for Cancer Care, New York. The findings provide additional evidence that adding everolimus to anti-estrogen therapy in AI-resistant disease improves clinical outcomes,” he added.
Most women with HR-positive breast cancer who are treated with an AI will eventually develop resistance to those agents. Strategies for overcoming resistance include the addition of everolimus to a steroid AI, exemestane, as has been demonstrated in the BOLERO-2 trial. “Another strategy for overcoming AI resistance is by more completely blocking estrogen-receptor signaling through the use of a selective estrogen receptor down-regulator, which may result in more complete blockade of the ER signaling pathway than a steroidal AI such as exemestane,” Dr Kornblum said.
To test this hypothesis, the investigators enrolled 131 postmenopausal women with inoperable locally advanced or metastatic HR-positive, HER2-negative breast cancer resistant to AIs. AI resistance was defined as relapse while receiving adjuvant AI therapy, and/or progression after one or more AIs for metastatic disease. The patients could have had no more than one prior chemotherapy regimen for metastatic disease.
The patients were stratified by Eastern Cooperative Oncology Group performance status, presence of measurable disease, and previous chemotherapy status, and were then randomized to receive either high-dose fulvestrant (500 mg on day 1 and 15 of cycle 1, and then on day 1 of cycles 2-12) plus oral everolimus 10 mg/day, or fulvestrant and placebo. The trial had an induction phase, in which patients were treated until evidence of progressive disease or unacceptable toxicity for a maximum of 12 28-day cycles, and a continuation phase in which patients who had neither disease progression nor experienced unacceptable toxicities could have their data unblinded and could continue on the fulvestrant-everolimus combination.
The trial did not include the use of corticosteroid-containing mouthwash for prevention of treatment-associated stomatitis, because it was designed before the evidence of the benefit of such prophylaxis became public, Dr Kornblum said.
The primary endpoint of PFS by investigator assessment was significantly better with the fulvestrant-everolimus group at 10.4 months, compared with 5.1 months for the fulvestrant-placebo group. The hazard ratio was 0.60 (P = .02). There was no difference in overall survival (OS), however. Median OS in the combination group was 24.8 months, compared with not yet reached in the placebo arm (not statistically significant).
The combination therapy was associated with more grade 3 adverse events than the fulvestrant-placebo combination (48% vs 14%, respectively). The most common grade 3 adverse events occurring in more than 5% of patients were stomatitis, pneumonitis, fatigue, and hyperglycemia. Overall, the safety profile of the combination was consistent with that seen in BOLERO-2, Dr Kornblum said. In all, 10% of patients assigned to the combination and 12% assigned to placebo withdrew from the study because of adverse events; these patients were included in the analysis, which was by intention to treat.
— Neil Osterweil
Still no clarity on duration of extended AI therapy
Key clinical point The optimal duration of aromatase inhibitor (AI) therapy following 5 years of endocrine therapy in postmenopausal women is still unknown. Major finding There were no significant differences in disease-free or overall survival in three studies investigating extended AI therapy. Data source Randomized phase 2 NSABP B-42 with 3996 patients; randomized phase 3 DATA study with 1912 patients; randomized phase 3 IDEAL trial with 1824 patients. Disclosures NSABP B-42 was sponsored by PrECOG with financial support from Novartis. Dr Mamounas reported having no conflicts of interest. The DATA trial was sponsored by the Dutch Breast Cancer Research Group and Novartis. Dr Tjan-Heijnen reported nothing to disclose. IDEAL was supported by the Dutch Breast Cancer Research Group and Novartis. Dr Blok reported nothing to disclose.
When does adjuvant therapy with an aromatase inhibitor become too much of a good thing? Or, put another way, what’s the optimal duration of extended aromatase inhibitor therapy? That’s the question that three clinical trials have tried – but largely failed – to answer.
For example, the randomized, double-blinded NSABP B-42 trial, comparing extended therapy with letrozole in postmenopausal women with hormone receptor-positive (HR-positive) breast cancer who have completed previous adjuvant therapy with an aromatase inhibitor (AI) showed no difference in disease-free survival (DFS) after 7 years of follow-up between women treated with extended letrozole or placebo.
“Our findings suggest that careful assessment of potential risks and benefits is required before recommending extended letrozole therapy to patients with early-stage breast cancer, including patient and tumor characteristics such as age and nodal status, existing comorbidities, information on bone mineral density, and tolerance of the aromatase inhibitor in the initial years,” Eleftherios P Mamounas, MD, of NRG Oncology/NSABP, said at the symposium.
DATA data
In the DATA study, also presented at the meeting, investigators from the Netherlands compared 6 years of anastrozole with 3 years of anastrozole after 2 or 3 years of adjuvant tamoxifen for postmenopausal women with estrogen receptor-positive (ER-positive), and/or progesterone receptor-positive (PR-positive) breast cancer. They found that “adapted” DFS (DFS starting 3 years after randomization) and adapted overall survival (OS) were similar between the two groups. “The findings of the DATA study do not support extended adjuvant AI use after 5 years of sequential endocrine therapy for all postmenopausal hormone receptor-positive breast cancer patients,” said Vivianne Tjan-Heijnen, MD, of Maastricht University Medical Center in the Netherlands.
Less than IDEAL
In the optimistically named IDEAL trial, a separate team of investigators, also from the Netherlands, looked at the relative merits of continuing adjuvant therapy with letrozole for 2.5 or 5 years after 5 years of adjuvant therapy with tamoxifen, an AI, or a combination in postmenopausal women with HR-positive breast cancer. They found no differences in either DFS or OS between patients treated for 5 years or those treated for only half that long. “We conclude that there is no benefit of extending AI-based therapy longer than two-and-a-half years,” said Erik Blok, MD, of Leiden University Medical Center in the Netherlands.
Give what, to whom, for how long?
Results of the trials raise more questions than they answer, said Michael Gnant, MD, of the Medical University of Vienna, the invited discussant. “Essentially, these three trials did not reach the necessary statistical significance levels to demonstrate a clear benefit for the respective AI extension,” he said, adding that he does not think that other agents used in luminal breast cancer would help. “Based on their tolerability profile, and in part also on financial toxicity, I don’t think that the promising agents we explore in many situations for the treatment of hormone receptor-positive breast cancer will realistically be used in the extended adjuvant setting,” he said.
New strategies are needed for targeting the chronic part of luminal breast cancer recurrence risk, Dr Gnant noted. Using endocrine therapies in that setting would likely be ineffective. Instead, agents that could directly target dormant cancer stem cells would “eliminate the source of late metastases for good.”
The best evidence to date clearly points to individualized treatment plans for patients, Dr Gnant said. For example, for a patient who has had 2-5 years of tamoxifen, an AI for 2.5-5 additional years can help prevent recurrences, provided the patient has risk factors for recurrence and excellent bone health. “Based on the trial results, it is more complex for a patient who comes off initial or sequential AI. There are factors favoring the extension of AI treatment, and other factors to speak against such extension. I suggest to start with patient features at this time,” he said.
Currently, the main factor driving the choice of extended AI therapy will be how well the patient has tolerated AIs in the first years of therapy and whether she is at increased risk for fractures, suggesting younger age as a factor favoring extended AI use. Patients with higher clinicopathologic risk factors such as node positivity or more luminal type tumors, as well as higher risk according to genomic studies, might also benefit from extended AI therapy, he said.
Biomarkers needed
“What the data from these and other trials tell us is that endocrine therapy is not for everyone. We need biomarkers that can tell us who should be getting extended endocrine therapy, be it 10 years or even a longer duration of time, versus a subgroup that might do very well with 5 five years of AI,” Aditya Bardia, MBBS, MPH, of the breast cancer division at Massachusetts General Hospital Cancer Center in Boston, said in an interview.
There are several such biomarkers under investigation, but they need validation and testing in large scale clinical trials before they find their way into day-to-practice, said Dr Bardia, who was not involved in the studies.
— Neil Osterweil
CTCs help predict breast cancer outcomes in neoadjuvant setting
Key clinical point CTCs are a useful prognostic biomarker in early breast cancer patients treated with neoadjuvant chemotherapy. Major finding OS was associated with the presence of at least 2 CTCs at baseline (HR, 2.6 for 2 CTCs; 3.84 for 3-4 CTCs; and 6.25 for 5 or more CTCs). Data source Meta-analysis of data for 2156 patients. Disclosures Supported by a research grant from Janssen Diagnostics. Dr Bidard reported having no disclosures.
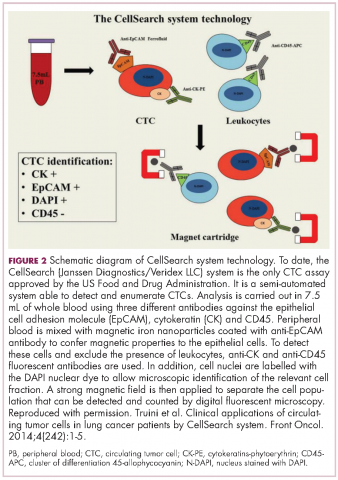
Circulating tumor cells (CTCs) are a useful prognostic biomarker in early breast cancer patients treated with neoadjuvant chemotherapy, according to findings from an international meta-analysis of individual patient data. The cells, which can be measured using a Food and Drug Administration-approved assay, are known to seed distant metastases and to be prognostic before and during therapy for patients with metastatic breast cancer, and prognostic before adjuvant therapy for patients with nonmetastatic breast cancer.
However, findings in the neoadjuvant setting have been varied, Francois-Clement Bidard, MD, of Institut Curie, Paris, reported at the symposium.
In the IMENEO study, CTCs were useful, independent of pathologic complete response, for predicting overall survival and distant disease-free survival in the neoadjuvant setting. In addition, the findings showed for the first time that CTCs also predict locoregional relapse-free survival. Based on an analysis of data from 2156 patients from 21 studies at 16 centers in 10 countries, the CTC positivity rates using thresholds of one or more, two or more, and five or more, respectively, were 25%, 13%, and 6% in 1574 patients tested at baseline; 17%, 6%, and 3% in 290 tested after neoadjuvant chemotherapy; 15%, 5%, and 1% in 1,200 tested before surgery; and 11%, 4%, and 1% in 285 tested after surgery, Dr Bidard said.
Prior to neoadjuvant chemotherapy, at least one CTC was found in 19%, 22%, 24%, 29%, and 41% of cT1, T2, T3, T4a-c, and T4d breast cancers, respectively, and this was marginally associated with hormone receptor negativity, he said, noting that later CTC detection rates were not associated with any patient baseline characteristics. Nearly one in four patients (24%) achieved pathologic complete response, but this was not associated at any time point with CTC count.
For the primary study endpoint of overall survival, a significant association was found with the presence of at least two CTCs at baseline (hazard ratio, 2.6 for two CTCs; 3.84 for three to four CTCs; and 6.25 for five or more CTCs). Similar associations were found for distant disease-free survival (hazard ratios, 2.4, 3.4, and 5.0, respectively) and for locoregional relapse-free interval with two CTCs and five or more CTCs (hazard ratios, 2.4 and 4.2, respectively).
Similar results were found using later time points, such as after the start of neoadjuvant chemotherapy or before surgery, he said.
On multivariate analysis, baseline CTC detection using any of the thresholds remained an independent predictor of overall and distant disease-free survival and locoregional relapse-free interval when considered together with pathologic complete response, cT, cN, and tumor subtype, suggesting that CTC measurement adds value to comprehensive prognostic models. That is, they complement rather than duplicate usual prognostic factors and pathologic complete response rates to better predict outcomes in patients with early breast cancer in the neoadjuvant setting, Dr Bidard said.
— Sharon Worcester
PIK3 inhibitor gives slight PFS edge at high cost for advanced breast cancer
Key clinical point The PI3K inhibitor buparlisib plus fulvestrant slightly prolonged progression-free survival of HR+/HER2- breast cancer pretreated with an aromatase inhibitor and mTOR inhibitor. Major finding The combination met its primary endpoint of better PFS than fulvestrant/placebo, but with high liver toxicity and mood disorders. Data source Randomized phase 3 trial of 432 women with HR-positive, HER2-negative, AI-pretreated breast cancer that progressed on or after mTOR inhibitor therapy. Disclosures Novartis sponsored the study. Dr Di Leo disclosed consulting and lecture fees from the company, and Dr O’Regan disclosed contracted research support. Dr Arteaga reported no disclosures relevant to the study.
A combination of a PI3K inhibitor and selective estrogen receptor down-regulator (SERD) met its primary endpoint of 2.1 months better progression-free survival (PFS) in postmenopausal women with locally advanced or metastatic breast cancer who were quickly running out of other treatment options, but the small gain in PFS came at a very high price in terms of toxicities, including mood disorders that may have led to patient suicide attempts, according to investigators.
The BELLE-3 trial looked at the combination of the SERD fulvestrant and an experimental inhibitor of the PI3 kinase, buparlisib, in postmenopausal women with hormone receptor-positive (HR-positive), human epidermal growth factor receptor 2-negative (HER2-negative) breast cancer treated with an aromatase inhibitor (AI) who experienced disease progression either on or after receiving therapy with an inhibitor of the mammalian target of rapamycin complex 1 (mTORC1).
The combination of fulvestrant and buparlisib was associated with a median PFS of 3.9 months, compared with 1.8 months for fulvestrant and placebo (P less than .001), Angelo Di Leo, MD, of Ospedale Misericordia e Dolce in Prato, Italy, reported at the symposium. Objective response rates (ORR) were low, at 7.8% in the combination arm, and 2.1% in the fulvestrant-plus-placebo arm. Although the PFS difference was statistically significant, “the higher rate of toxicity in patients receiving buparlisib and fulvestrant, including transaminase elevations and mood disorders, may represent a clinically relevant challenge for future development of this compound in this particular group of patients,” Dr Di Leo said.
Blocks AKT pathway
The preclinical rationale for the use of a P13K inhibitor after disease progression on mTORC1 inhibitor is that current mTOR inhibitors such as everolimus have a feedback mechanism that activates the AKT pathway, and that the use of P13K inhibitors can “abrogate or attenuate this activation, potentially blocking that pathway,” explained coinvestigator Ruth O’Regan, MD, head of the division of hematology and oncology at the University of Wisconsin-Madison School of Medicine and Public Health. Dr O’Regan discussed the BELLE-3 findings in a briefing before Dr Di Leo’s presentation of the data in general session.
In BELLE-3, 432 postmenopausal women with HR-positive, HER2-negative, AI-pretreated, locally advanced or metastatic breast cancer that had progressed on or after treatment with an mTOR inhibitor as the last line of therapy were enrolled. The patients were stratified by the presence or absence of visceral disease and then randomized on a 2:1 basis to fulvestrant 500 mg daily plus either buparlisib 100 mg/day (289 patients) or placebo (143). The primary endpoint of investigator-assessed PFS favored the addition of buparlisib, with a hazard ratio for progression of 0.67 (P less than .001). PFS results by independent central review were similar (HR 0.57, P less than .001).
The ORR for the buparlisib-fulvestrant combination, 7.6%, consisted of 0.3% complete responses and 7.3% partial responses. The ORR for the placebo-fulvestrant combination, 2.1%, was composed entirely of partial responses. The respective clinical benefit rates, defined as a combination of complete and partial responses and stable disease, were 24.6% and 15.4, respectively.
The benefit of buparlisib was evidently entirely among patients with visceral disease, with a PFS of 3.1 months, compared with 1.5 months. In contrast, PFS among patients with no visceral disease was 4.2 months, compared with 4.1 months, respectively, and was not significant. In addition, the P13K inhibitor seemed to benefit patients with PIK3CA mutations detected in either the primary tumor or in circulating DNA samples, but not patients with wild-type PIK3CA.
Depression, anxiety with combination
Patients assigned to buparlisib-fulvestrant group had substantially higher proportions of alanine aminotransferase and aspartate aminotransferase elevations compared with patients in the placebo-fulvestrant group, as well as more reported depression and anxiety. Three patients in the buparlisib arm attempted suicide. There were no reported suicide attempts in the placebo arm.
Dr O’Regan said at the briefing that mood disorders are known adverse events associated with buparlisib, and that patients with psychiatric disorders were excluded from the trial.
— Neil Osterweil
At the 2016 San Antonio Breast Cancer Symposium, investigators presented findings on PFS benefits of adding an mTOR inhibitor to anti-hormonal therapy in advanced disease in postmenopausal women; the lack of clarity on the optimal duration of extended AI therapy, also in postmenopausal women; and using CTCs in helping predict breast cancer outcomes in the neoadjuvant setting.
Fulvestrant plus everolimus improves PFS in HR+, HER2- advanced breast cancer
Key clinical point This study provides further evidence of the benefits of adding an mTOR inhibitor to anti-hormonal therapy in postmenopausal women with advanced breast cancer resistant to aromatase inhibitors. Major finding Fulvestrant plus everolimus was associated with a PFS of 10.4 months, vs 5.1 months for fulvestrant alone. Data source Randomized phase 2 trial of 131 women with HR-positive, HER2-negative locally advanced of metastatic breast cancer resistant to aromatase inhibitors. Disclosures Sponsored by PrECOG with financial support from Novartis. Dr Kornblum reported having no conflicts of interest.
Adding everolimus to fulvestrant doubled median progression-free survival (PFS) among postmenopausal women with hormone receptor-positive (HR-positive), human epidermal growth factor receptor 2-negative (HER2-negative) metastatic breast cancer resistant to therapy with an aromatase inhibitor (AI), Noah S Kornblum, MD, reported during his presentation at the meeting of the PrECOG 0102 trial findings.
In the randomized phase 2 trial, the combination of the mammalian target of rapamycin (mTOR) inhibitor everolimus with the selective estrogen receptor down-regulator (SERD) fulvestrant was associated with a median PFS of 10.4 months, compared with 5.1 months for fulvestrant plus placebo, said Dr Kornblum, of Montefiore Einstein Center for Cancer Care, New York. The findings provide additional evidence that adding everolimus to anti-estrogen therapy in AI-resistant disease improves clinical outcomes,” he added.
Most women with HR-positive breast cancer who are treated with an AI will eventually develop resistance to those agents. Strategies for overcoming resistance include the addition of everolimus to a steroid AI, exemestane, as has been demonstrated in the BOLERO-2 trial. “Another strategy for overcoming AI resistance is by more completely blocking estrogen-receptor signaling through the use of a selective estrogen receptor down-regulator, which may result in more complete blockade of the ER signaling pathway than a steroidal AI such as exemestane,” Dr Kornblum said.
To test this hypothesis, the investigators enrolled 131 postmenopausal women with inoperable locally advanced or metastatic HR-positive, HER2-negative breast cancer resistant to AIs. AI resistance was defined as relapse while receiving adjuvant AI therapy, and/or progression after one or more AIs for metastatic disease. The patients could have had no more than one prior chemotherapy regimen for metastatic disease.
The patients were stratified by Eastern Cooperative Oncology Group performance status, presence of measurable disease, and previous chemotherapy status, and were then randomized to receive either high-dose fulvestrant (500 mg on day 1 and 15 of cycle 1, and then on day 1 of cycles 2-12) plus oral everolimus 10 mg/day, or fulvestrant and placebo. The trial had an induction phase, in which patients were treated until evidence of progressive disease or unacceptable toxicity for a maximum of 12 28-day cycles, and a continuation phase in which patients who had neither disease progression nor experienced unacceptable toxicities could have their data unblinded and could continue on the fulvestrant-everolimus combination.
The trial did not include the use of corticosteroid-containing mouthwash for prevention of treatment-associated stomatitis, because it was designed before the evidence of the benefit of such prophylaxis became public, Dr Kornblum said.
The primary endpoint of PFS by investigator assessment was significantly better with the fulvestrant-everolimus group at 10.4 months, compared with 5.1 months for the fulvestrant-placebo group. The hazard ratio was 0.60 (P = .02). There was no difference in overall survival (OS), however. Median OS in the combination group was 24.8 months, compared with not yet reached in the placebo arm (not statistically significant).
The combination therapy was associated with more grade 3 adverse events than the fulvestrant-placebo combination (48% vs 14%, respectively). The most common grade 3 adverse events occurring in more than 5% of patients were stomatitis, pneumonitis, fatigue, and hyperglycemia. Overall, the safety profile of the combination was consistent with that seen in BOLERO-2, Dr Kornblum said. In all, 10% of patients assigned to the combination and 12% assigned to placebo withdrew from the study because of adverse events; these patients were included in the analysis, which was by intention to treat.
— Neil Osterweil
Still no clarity on duration of extended AI therapy
Key clinical point The optimal duration of aromatase inhibitor (AI) therapy following 5 years of endocrine therapy in postmenopausal women is still unknown. Major finding There were no significant differences in disease-free or overall survival in three studies investigating extended AI therapy. Data source Randomized phase 2 NSABP B-42 with 3996 patients; randomized phase 3 DATA study with 1912 patients; randomized phase 3 IDEAL trial with 1824 patients. Disclosures NSABP B-42 was sponsored by PrECOG with financial support from Novartis. Dr Mamounas reported having no conflicts of interest. The DATA trial was sponsored by the Dutch Breast Cancer Research Group and Novartis. Dr Tjan-Heijnen reported nothing to disclose. IDEAL was supported by the Dutch Breast Cancer Research Group and Novartis. Dr Blok reported nothing to disclose.
When does adjuvant therapy with an aromatase inhibitor become too much of a good thing? Or, put another way, what’s the optimal duration of extended aromatase inhibitor therapy? That’s the question that three clinical trials have tried – but largely failed – to answer.
For example, the randomized, double-blinded NSABP B-42 trial, comparing extended therapy with letrozole in postmenopausal women with hormone receptor-positive (HR-positive) breast cancer who have completed previous adjuvant therapy with an aromatase inhibitor (AI) showed no difference in disease-free survival (DFS) after 7 years of follow-up between women treated with extended letrozole or placebo.
“Our findings suggest that careful assessment of potential risks and benefits is required before recommending extended letrozole therapy to patients with early-stage breast cancer, including patient and tumor characteristics such as age and nodal status, existing comorbidities, information on bone mineral density, and tolerance of the aromatase inhibitor in the initial years,” Eleftherios P Mamounas, MD, of NRG Oncology/NSABP, said at the symposium.
DATA data
In the DATA study, also presented at the meeting, investigators from the Netherlands compared 6 years of anastrozole with 3 years of anastrozole after 2 or 3 years of adjuvant tamoxifen for postmenopausal women with estrogen receptor-positive (ER-positive), and/or progesterone receptor-positive (PR-positive) breast cancer. They found that “adapted” DFS (DFS starting 3 years after randomization) and adapted overall survival (OS) were similar between the two groups. “The findings of the DATA study do not support extended adjuvant AI use after 5 years of sequential endocrine therapy for all postmenopausal hormone receptor-positive breast cancer patients,” said Vivianne Tjan-Heijnen, MD, of Maastricht University Medical Center in the Netherlands.
Less than IDEAL
In the optimistically named IDEAL trial, a separate team of investigators, also from the Netherlands, looked at the relative merits of continuing adjuvant therapy with letrozole for 2.5 or 5 years after 5 years of adjuvant therapy with tamoxifen, an AI, or a combination in postmenopausal women with HR-positive breast cancer. They found no differences in either DFS or OS between patients treated for 5 years or those treated for only half that long. “We conclude that there is no benefit of extending AI-based therapy longer than two-and-a-half years,” said Erik Blok, MD, of Leiden University Medical Center in the Netherlands.
Give what, to whom, for how long?
Results of the trials raise more questions than they answer, said Michael Gnant, MD, of the Medical University of Vienna, the invited discussant. “Essentially, these three trials did not reach the necessary statistical significance levels to demonstrate a clear benefit for the respective AI extension,” he said, adding that he does not think that other agents used in luminal breast cancer would help. “Based on their tolerability profile, and in part also on financial toxicity, I don’t think that the promising agents we explore in many situations for the treatment of hormone receptor-positive breast cancer will realistically be used in the extended adjuvant setting,” he said.
New strategies are needed for targeting the chronic part of luminal breast cancer recurrence risk, Dr Gnant noted. Using endocrine therapies in that setting would likely be ineffective. Instead, agents that could directly target dormant cancer stem cells would “eliminate the source of late metastases for good.”
The best evidence to date clearly points to individualized treatment plans for patients, Dr Gnant said. For example, for a patient who has had 2-5 years of tamoxifen, an AI for 2.5-5 additional years can help prevent recurrences, provided the patient has risk factors for recurrence and excellent bone health. “Based on the trial results, it is more complex for a patient who comes off initial or sequential AI. There are factors favoring the extension of AI treatment, and other factors to speak against such extension. I suggest to start with patient features at this time,” he said.
Currently, the main factor driving the choice of extended AI therapy will be how well the patient has tolerated AIs in the first years of therapy and whether she is at increased risk for fractures, suggesting younger age as a factor favoring extended AI use. Patients with higher clinicopathologic risk factors such as node positivity or more luminal type tumors, as well as higher risk according to genomic studies, might also benefit from extended AI therapy, he said.
Biomarkers needed
“What the data from these and other trials tell us is that endocrine therapy is not for everyone. We need biomarkers that can tell us who should be getting extended endocrine therapy, be it 10 years or even a longer duration of time, versus a subgroup that might do very well with 5 five years of AI,” Aditya Bardia, MBBS, MPH, of the breast cancer division at Massachusetts General Hospital Cancer Center in Boston, said in an interview.
There are several such biomarkers under investigation, but they need validation and testing in large scale clinical trials before they find their way into day-to-practice, said Dr Bardia, who was not involved in the studies.
— Neil Osterweil
CTCs help predict breast cancer outcomes in neoadjuvant setting
Key clinical point CTCs are a useful prognostic biomarker in early breast cancer patients treated with neoadjuvant chemotherapy. Major finding OS was associated with the presence of at least 2 CTCs at baseline (HR, 2.6 for 2 CTCs; 3.84 for 3-4 CTCs; and 6.25 for 5 or more CTCs). Data source Meta-analysis of data for 2156 patients. Disclosures Supported by a research grant from Janssen Diagnostics. Dr Bidard reported having no disclosures.
Circulating tumor cells (CTCs) are a useful prognostic biomarker in early breast cancer patients treated with neoadjuvant chemotherapy, according to findings from an international meta-analysis of individual patient data. The cells, which can be measured using a Food and Drug Administration-approved assay, are known to seed distant metastases and to be prognostic before and during therapy for patients with metastatic breast cancer, and prognostic before adjuvant therapy for patients with nonmetastatic breast cancer.
However, findings in the neoadjuvant setting have been varied, Francois-Clement Bidard, MD, of Institut Curie, Paris, reported at the symposium.
In the IMENEO study, CTCs were useful, independent of pathologic complete response, for predicting overall survival and distant disease-free survival in the neoadjuvant setting. In addition, the findings showed for the first time that CTCs also predict locoregional relapse-free survival. Based on an analysis of data from 2156 patients from 21 studies at 16 centers in 10 countries, the CTC positivity rates using thresholds of one or more, two or more, and five or more, respectively, were 25%, 13%, and 6% in 1574 patients tested at baseline; 17%, 6%, and 3% in 290 tested after neoadjuvant chemotherapy; 15%, 5%, and 1% in 1,200 tested before surgery; and 11%, 4%, and 1% in 285 tested after surgery, Dr Bidard said.
Prior to neoadjuvant chemotherapy, at least one CTC was found in 19%, 22%, 24%, 29%, and 41% of cT1, T2, T3, T4a-c, and T4d breast cancers, respectively, and this was marginally associated with hormone receptor negativity, he said, noting that later CTC detection rates were not associated with any patient baseline characteristics. Nearly one in four patients (24%) achieved pathologic complete response, but this was not associated at any time point with CTC count.
For the primary study endpoint of overall survival, a significant association was found with the presence of at least two CTCs at baseline (hazard ratio, 2.6 for two CTCs; 3.84 for three to four CTCs; and 6.25 for five or more CTCs). Similar associations were found for distant disease-free survival (hazard ratios, 2.4, 3.4, and 5.0, respectively) and for locoregional relapse-free interval with two CTCs and five or more CTCs (hazard ratios, 2.4 and 4.2, respectively).
Similar results were found using later time points, such as after the start of neoadjuvant chemotherapy or before surgery, he said.
On multivariate analysis, baseline CTC detection using any of the thresholds remained an independent predictor of overall and distant disease-free survival and locoregional relapse-free interval when considered together with pathologic complete response, cT, cN, and tumor subtype, suggesting that CTC measurement adds value to comprehensive prognostic models. That is, they complement rather than duplicate usual prognostic factors and pathologic complete response rates to better predict outcomes in patients with early breast cancer in the neoadjuvant setting, Dr Bidard said.
— Sharon Worcester
PIK3 inhibitor gives slight PFS edge at high cost for advanced breast cancer
Key clinical point The PI3K inhibitor buparlisib plus fulvestrant slightly prolonged progression-free survival of HR+/HER2- breast cancer pretreated with an aromatase inhibitor and mTOR inhibitor. Major finding The combination met its primary endpoint of better PFS than fulvestrant/placebo, but with high liver toxicity and mood disorders. Data source Randomized phase 3 trial of 432 women with HR-positive, HER2-negative, AI-pretreated breast cancer that progressed on or after mTOR inhibitor therapy. Disclosures Novartis sponsored the study. Dr Di Leo disclosed consulting and lecture fees from the company, and Dr O’Regan disclosed contracted research support. Dr Arteaga reported no disclosures relevant to the study.
A combination of a PI3K inhibitor and selective estrogen receptor down-regulator (SERD) met its primary endpoint of 2.1 months better progression-free survival (PFS) in postmenopausal women with locally advanced or metastatic breast cancer who were quickly running out of other treatment options, but the small gain in PFS came at a very high price in terms of toxicities, including mood disorders that may have led to patient suicide attempts, according to investigators.
The BELLE-3 trial looked at the combination of the SERD fulvestrant and an experimental inhibitor of the PI3 kinase, buparlisib, in postmenopausal women with hormone receptor-positive (HR-positive), human epidermal growth factor receptor 2-negative (HER2-negative) breast cancer treated with an aromatase inhibitor (AI) who experienced disease progression either on or after receiving therapy with an inhibitor of the mammalian target of rapamycin complex 1 (mTORC1).
The combination of fulvestrant and buparlisib was associated with a median PFS of 3.9 months, compared with 1.8 months for fulvestrant and placebo (P less than .001), Angelo Di Leo, MD, of Ospedale Misericordia e Dolce in Prato, Italy, reported at the symposium. Objective response rates (ORR) were low, at 7.8% in the combination arm, and 2.1% in the fulvestrant-plus-placebo arm. Although the PFS difference was statistically significant, “the higher rate of toxicity in patients receiving buparlisib and fulvestrant, including transaminase elevations and mood disorders, may represent a clinically relevant challenge for future development of this compound in this particular group of patients,” Dr Di Leo said.
Blocks AKT pathway
The preclinical rationale for the use of a P13K inhibitor after disease progression on mTORC1 inhibitor is that current mTOR inhibitors such as everolimus have a feedback mechanism that activates the AKT pathway, and that the use of P13K inhibitors can “abrogate or attenuate this activation, potentially blocking that pathway,” explained coinvestigator Ruth O’Regan, MD, head of the division of hematology and oncology at the University of Wisconsin-Madison School of Medicine and Public Health. Dr O’Regan discussed the BELLE-3 findings in a briefing before Dr Di Leo’s presentation of the data in general session.
In BELLE-3, 432 postmenopausal women with HR-positive, HER2-negative, AI-pretreated, locally advanced or metastatic breast cancer that had progressed on or after treatment with an mTOR inhibitor as the last line of therapy were enrolled. The patients were stratified by the presence or absence of visceral disease and then randomized on a 2:1 basis to fulvestrant 500 mg daily plus either buparlisib 100 mg/day (289 patients) or placebo (143). The primary endpoint of investigator-assessed PFS favored the addition of buparlisib, with a hazard ratio for progression of 0.67 (P less than .001). PFS results by independent central review were similar (HR 0.57, P less than .001).
The ORR for the buparlisib-fulvestrant combination, 7.6%, consisted of 0.3% complete responses and 7.3% partial responses. The ORR for the placebo-fulvestrant combination, 2.1%, was composed entirely of partial responses. The respective clinical benefit rates, defined as a combination of complete and partial responses and stable disease, were 24.6% and 15.4, respectively.
The benefit of buparlisib was evidently entirely among patients with visceral disease, with a PFS of 3.1 months, compared with 1.5 months. In contrast, PFS among patients with no visceral disease was 4.2 months, compared with 4.1 months, respectively, and was not significant. In addition, the P13K inhibitor seemed to benefit patients with PIK3CA mutations detected in either the primary tumor or in circulating DNA samples, but not patients with wild-type PIK3CA.
Depression, anxiety with combination
Patients assigned to buparlisib-fulvestrant group had substantially higher proportions of alanine aminotransferase and aspartate aminotransferase elevations compared with patients in the placebo-fulvestrant group, as well as more reported depression and anxiety. Three patients in the buparlisib arm attempted suicide. There were no reported suicide attempts in the placebo arm.
Dr O’Regan said at the briefing that mood disorders are known adverse events associated with buparlisib, and that patients with psychiatric disorders were excluded from the trial.
— Neil Osterweil
At the 2016 San Antonio Breast Cancer Symposium, investigators presented findings on PFS benefits of adding an mTOR inhibitor to anti-hormonal therapy in advanced disease in postmenopausal women; the lack of clarity on the optimal duration of extended AI therapy, also in postmenopausal women; and using CTCs in helping predict breast cancer outcomes in the neoadjuvant setting.
Fulvestrant plus everolimus improves PFS in HR+, HER2- advanced breast cancer
Key clinical point This study provides further evidence of the benefits of adding an mTOR inhibitor to anti-hormonal therapy in postmenopausal women with advanced breast cancer resistant to aromatase inhibitors. Major finding Fulvestrant plus everolimus was associated with a PFS of 10.4 months, vs 5.1 months for fulvestrant alone. Data source Randomized phase 2 trial of 131 women with HR-positive, HER2-negative locally advanced of metastatic breast cancer resistant to aromatase inhibitors. Disclosures Sponsored by PrECOG with financial support from Novartis. Dr Kornblum reported having no conflicts of interest.
Adding everolimus to fulvestrant doubled median progression-free survival (PFS) among postmenopausal women with hormone receptor-positive (HR-positive), human epidermal growth factor receptor 2-negative (HER2-negative) metastatic breast cancer resistant to therapy with an aromatase inhibitor (AI), Noah S Kornblum, MD, reported during his presentation at the meeting of the PrECOG 0102 trial findings.
In the randomized phase 2 trial, the combination of the mammalian target of rapamycin (mTOR) inhibitor everolimus with the selective estrogen receptor down-regulator (SERD) fulvestrant was associated with a median PFS of 10.4 months, compared with 5.1 months for fulvestrant plus placebo, said Dr Kornblum, of Montefiore Einstein Center for Cancer Care, New York. The findings provide additional evidence that adding everolimus to anti-estrogen therapy in AI-resistant disease improves clinical outcomes,” he added.
Most women with HR-positive breast cancer who are treated with an AI will eventually develop resistance to those agents. Strategies for overcoming resistance include the addition of everolimus to a steroid AI, exemestane, as has been demonstrated in the BOLERO-2 trial. “Another strategy for overcoming AI resistance is by more completely blocking estrogen-receptor signaling through the use of a selective estrogen receptor down-regulator, which may result in more complete blockade of the ER signaling pathway than a steroidal AI such as exemestane,” Dr Kornblum said.
To test this hypothesis, the investigators enrolled 131 postmenopausal women with inoperable locally advanced or metastatic HR-positive, HER2-negative breast cancer resistant to AIs. AI resistance was defined as relapse while receiving adjuvant AI therapy, and/or progression after one or more AIs for metastatic disease. The patients could have had no more than one prior chemotherapy regimen for metastatic disease.
The patients were stratified by Eastern Cooperative Oncology Group performance status, presence of measurable disease, and previous chemotherapy status, and were then randomized to receive either high-dose fulvestrant (500 mg on day 1 and 15 of cycle 1, and then on day 1 of cycles 2-12) plus oral everolimus 10 mg/day, or fulvestrant and placebo. The trial had an induction phase, in which patients were treated until evidence of progressive disease or unacceptable toxicity for a maximum of 12 28-day cycles, and a continuation phase in which patients who had neither disease progression nor experienced unacceptable toxicities could have their data unblinded and could continue on the fulvestrant-everolimus combination.
The trial did not include the use of corticosteroid-containing mouthwash for prevention of treatment-associated stomatitis, because it was designed before the evidence of the benefit of such prophylaxis became public, Dr Kornblum said.
The primary endpoint of PFS by investigator assessment was significantly better with the fulvestrant-everolimus group at 10.4 months, compared with 5.1 months for the fulvestrant-placebo group. The hazard ratio was 0.60 (P = .02). There was no difference in overall survival (OS), however. Median OS in the combination group was 24.8 months, compared with not yet reached in the placebo arm (not statistically significant).
The combination therapy was associated with more grade 3 adverse events than the fulvestrant-placebo combination (48% vs 14%, respectively). The most common grade 3 adverse events occurring in more than 5% of patients were stomatitis, pneumonitis, fatigue, and hyperglycemia. Overall, the safety profile of the combination was consistent with that seen in BOLERO-2, Dr Kornblum said. In all, 10% of patients assigned to the combination and 12% assigned to placebo withdrew from the study because of adverse events; these patients were included in the analysis, which was by intention to treat.
— Neil Osterweil
Still no clarity on duration of extended AI therapy
Key clinical point The optimal duration of aromatase inhibitor (AI) therapy following 5 years of endocrine therapy in postmenopausal women is still unknown. Major finding There were no significant differences in disease-free or overall survival in three studies investigating extended AI therapy. Data source Randomized phase 2 NSABP B-42 with 3996 patients; randomized phase 3 DATA study with 1912 patients; randomized phase 3 IDEAL trial with 1824 patients. Disclosures NSABP B-42 was sponsored by PrECOG with financial support from Novartis. Dr Mamounas reported having no conflicts of interest. The DATA trial was sponsored by the Dutch Breast Cancer Research Group and Novartis. Dr Tjan-Heijnen reported nothing to disclose. IDEAL was supported by the Dutch Breast Cancer Research Group and Novartis. Dr Blok reported nothing to disclose.
When does adjuvant therapy with an aromatase inhibitor become too much of a good thing? Or, put another way, what’s the optimal duration of extended aromatase inhibitor therapy? That’s the question that three clinical trials have tried – but largely failed – to answer.
For example, the randomized, double-blinded NSABP B-42 trial, comparing extended therapy with letrozole in postmenopausal women with hormone receptor-positive (HR-positive) breast cancer who have completed previous adjuvant therapy with an aromatase inhibitor (AI) showed no difference in disease-free survival (DFS) after 7 years of follow-up between women treated with extended letrozole or placebo.
“Our findings suggest that careful assessment of potential risks and benefits is required before recommending extended letrozole therapy to patients with early-stage breast cancer, including patient and tumor characteristics such as age and nodal status, existing comorbidities, information on bone mineral density, and tolerance of the aromatase inhibitor in the initial years,” Eleftherios P Mamounas, MD, of NRG Oncology/NSABP, said at the symposium.
DATA data
In the DATA study, also presented at the meeting, investigators from the Netherlands compared 6 years of anastrozole with 3 years of anastrozole after 2 or 3 years of adjuvant tamoxifen for postmenopausal women with estrogen receptor-positive (ER-positive), and/or progesterone receptor-positive (PR-positive) breast cancer. They found that “adapted” DFS (DFS starting 3 years after randomization) and adapted overall survival (OS) were similar between the two groups. “The findings of the DATA study do not support extended adjuvant AI use after 5 years of sequential endocrine therapy for all postmenopausal hormone receptor-positive breast cancer patients,” said Vivianne Tjan-Heijnen, MD, of Maastricht University Medical Center in the Netherlands.
Less than IDEAL
In the optimistically named IDEAL trial, a separate team of investigators, also from the Netherlands, looked at the relative merits of continuing adjuvant therapy with letrozole for 2.5 or 5 years after 5 years of adjuvant therapy with tamoxifen, an AI, or a combination in postmenopausal women with HR-positive breast cancer. They found no differences in either DFS or OS between patients treated for 5 years or those treated for only half that long. “We conclude that there is no benefit of extending AI-based therapy longer than two-and-a-half years,” said Erik Blok, MD, of Leiden University Medical Center in the Netherlands.
Give what, to whom, for how long?
Results of the trials raise more questions than they answer, said Michael Gnant, MD, of the Medical University of Vienna, the invited discussant. “Essentially, these three trials did not reach the necessary statistical significance levels to demonstrate a clear benefit for the respective AI extension,” he said, adding that he does not think that other agents used in luminal breast cancer would help. “Based on their tolerability profile, and in part also on financial toxicity, I don’t think that the promising agents we explore in many situations for the treatment of hormone receptor-positive breast cancer will realistically be used in the extended adjuvant setting,” he said.
New strategies are needed for targeting the chronic part of luminal breast cancer recurrence risk, Dr Gnant noted. Using endocrine therapies in that setting would likely be ineffective. Instead, agents that could directly target dormant cancer stem cells would “eliminate the source of late metastases for good.”
The best evidence to date clearly points to individualized treatment plans for patients, Dr Gnant said. For example, for a patient who has had 2-5 years of tamoxifen, an AI for 2.5-5 additional years can help prevent recurrences, provided the patient has risk factors for recurrence and excellent bone health. “Based on the trial results, it is more complex for a patient who comes off initial or sequential AI. There are factors favoring the extension of AI treatment, and other factors to speak against such extension. I suggest to start with patient features at this time,” he said.
Currently, the main factor driving the choice of extended AI therapy will be how well the patient has tolerated AIs in the first years of therapy and whether she is at increased risk for fractures, suggesting younger age as a factor favoring extended AI use. Patients with higher clinicopathologic risk factors such as node positivity or more luminal type tumors, as well as higher risk according to genomic studies, might also benefit from extended AI therapy, he said.
Biomarkers needed
“What the data from these and other trials tell us is that endocrine therapy is not for everyone. We need biomarkers that can tell us who should be getting extended endocrine therapy, be it 10 years or even a longer duration of time, versus a subgroup that might do very well with 5 five years of AI,” Aditya Bardia, MBBS, MPH, of the breast cancer division at Massachusetts General Hospital Cancer Center in Boston, said in an interview.
There are several such biomarkers under investigation, but they need validation and testing in large scale clinical trials before they find their way into day-to-practice, said Dr Bardia, who was not involved in the studies.
— Neil Osterweil
CTCs help predict breast cancer outcomes in neoadjuvant setting
Key clinical point CTCs are a useful prognostic biomarker in early breast cancer patients treated with neoadjuvant chemotherapy. Major finding OS was associated with the presence of at least 2 CTCs at baseline (HR, 2.6 for 2 CTCs; 3.84 for 3-4 CTCs; and 6.25 for 5 or more CTCs). Data source Meta-analysis of data for 2156 patients. Disclosures Supported by a research grant from Janssen Diagnostics. Dr Bidard reported having no disclosures.
Circulating tumor cells (CTCs) are a useful prognostic biomarker in early breast cancer patients treated with neoadjuvant chemotherapy, according to findings from an international meta-analysis of individual patient data. The cells, which can be measured using a Food and Drug Administration-approved assay, are known to seed distant metastases and to be prognostic before and during therapy for patients with metastatic breast cancer, and prognostic before adjuvant therapy for patients with nonmetastatic breast cancer.
However, findings in the neoadjuvant setting have been varied, Francois-Clement Bidard, MD, of Institut Curie, Paris, reported at the symposium.
In the IMENEO study, CTCs were useful, independent of pathologic complete response, for predicting overall survival and distant disease-free survival in the neoadjuvant setting. In addition, the findings showed for the first time that CTCs also predict locoregional relapse-free survival. Based on an analysis of data from 2156 patients from 21 studies at 16 centers in 10 countries, the CTC positivity rates using thresholds of one or more, two or more, and five or more, respectively, were 25%, 13%, and 6% in 1574 patients tested at baseline; 17%, 6%, and 3% in 290 tested after neoadjuvant chemotherapy; 15%, 5%, and 1% in 1,200 tested before surgery; and 11%, 4%, and 1% in 285 tested after surgery, Dr Bidard said.
Prior to neoadjuvant chemotherapy, at least one CTC was found in 19%, 22%, 24%, 29%, and 41% of cT1, T2, T3, T4a-c, and T4d breast cancers, respectively, and this was marginally associated with hormone receptor negativity, he said, noting that later CTC detection rates were not associated with any patient baseline characteristics. Nearly one in four patients (24%) achieved pathologic complete response, but this was not associated at any time point with CTC count.
For the primary study endpoint of overall survival, a significant association was found with the presence of at least two CTCs at baseline (hazard ratio, 2.6 for two CTCs; 3.84 for three to four CTCs; and 6.25 for five or more CTCs). Similar associations were found for distant disease-free survival (hazard ratios, 2.4, 3.4, and 5.0, respectively) and for locoregional relapse-free interval with two CTCs and five or more CTCs (hazard ratios, 2.4 and 4.2, respectively).
Similar results were found using later time points, such as after the start of neoadjuvant chemotherapy or before surgery, he said.
On multivariate analysis, baseline CTC detection using any of the thresholds remained an independent predictor of overall and distant disease-free survival and locoregional relapse-free interval when considered together with pathologic complete response, cT, cN, and tumor subtype, suggesting that CTC measurement adds value to comprehensive prognostic models. That is, they complement rather than duplicate usual prognostic factors and pathologic complete response rates to better predict outcomes in patients with early breast cancer in the neoadjuvant setting, Dr Bidard said.
— Sharon Worcester
PIK3 inhibitor gives slight PFS edge at high cost for advanced breast cancer
Key clinical point The PI3K inhibitor buparlisib plus fulvestrant slightly prolonged progression-free survival of HR+/HER2- breast cancer pretreated with an aromatase inhibitor and mTOR inhibitor. Major finding The combination met its primary endpoint of better PFS than fulvestrant/placebo, but with high liver toxicity and mood disorders. Data source Randomized phase 3 trial of 432 women with HR-positive, HER2-negative, AI-pretreated breast cancer that progressed on or after mTOR inhibitor therapy. Disclosures Novartis sponsored the study. Dr Di Leo disclosed consulting and lecture fees from the company, and Dr O’Regan disclosed contracted research support. Dr Arteaga reported no disclosures relevant to the study.
A combination of a PI3K inhibitor and selective estrogen receptor down-regulator (SERD) met its primary endpoint of 2.1 months better progression-free survival (PFS) in postmenopausal women with locally advanced or metastatic breast cancer who were quickly running out of other treatment options, but the small gain in PFS came at a very high price in terms of toxicities, including mood disorders that may have led to patient suicide attempts, according to investigators.
The BELLE-3 trial looked at the combination of the SERD fulvestrant and an experimental inhibitor of the PI3 kinase, buparlisib, in postmenopausal women with hormone receptor-positive (HR-positive), human epidermal growth factor receptor 2-negative (HER2-negative) breast cancer treated with an aromatase inhibitor (AI) who experienced disease progression either on or after receiving therapy with an inhibitor of the mammalian target of rapamycin complex 1 (mTORC1).
The combination of fulvestrant and buparlisib was associated with a median PFS of 3.9 months, compared with 1.8 months for fulvestrant and placebo (P less than .001), Angelo Di Leo, MD, of Ospedale Misericordia e Dolce in Prato, Italy, reported at the symposium. Objective response rates (ORR) were low, at 7.8% in the combination arm, and 2.1% in the fulvestrant-plus-placebo arm. Although the PFS difference was statistically significant, “the higher rate of toxicity in patients receiving buparlisib and fulvestrant, including transaminase elevations and mood disorders, may represent a clinically relevant challenge for future development of this compound in this particular group of patients,” Dr Di Leo said.
Blocks AKT pathway
The preclinical rationale for the use of a P13K inhibitor after disease progression on mTORC1 inhibitor is that current mTOR inhibitors such as everolimus have a feedback mechanism that activates the AKT pathway, and that the use of P13K inhibitors can “abrogate or attenuate this activation, potentially blocking that pathway,” explained coinvestigator Ruth O’Regan, MD, head of the division of hematology and oncology at the University of Wisconsin-Madison School of Medicine and Public Health. Dr O’Regan discussed the BELLE-3 findings in a briefing before Dr Di Leo’s presentation of the data in general session.
In BELLE-3, 432 postmenopausal women with HR-positive, HER2-negative, AI-pretreated, locally advanced or metastatic breast cancer that had progressed on or after treatment with an mTOR inhibitor as the last line of therapy were enrolled. The patients were stratified by the presence or absence of visceral disease and then randomized on a 2:1 basis to fulvestrant 500 mg daily plus either buparlisib 100 mg/day (289 patients) or placebo (143). The primary endpoint of investigator-assessed PFS favored the addition of buparlisib, with a hazard ratio for progression of 0.67 (P less than .001). PFS results by independent central review were similar (HR 0.57, P less than .001).
The ORR for the buparlisib-fulvestrant combination, 7.6%, consisted of 0.3% complete responses and 7.3% partial responses. The ORR for the placebo-fulvestrant combination, 2.1%, was composed entirely of partial responses. The respective clinical benefit rates, defined as a combination of complete and partial responses and stable disease, were 24.6% and 15.4, respectively.
The benefit of buparlisib was evidently entirely among patients with visceral disease, with a PFS of 3.1 months, compared with 1.5 months. In contrast, PFS among patients with no visceral disease was 4.2 months, compared with 4.1 months, respectively, and was not significant. In addition, the P13K inhibitor seemed to benefit patients with PIK3CA mutations detected in either the primary tumor or in circulating DNA samples, but not patients with wild-type PIK3CA.
Depression, anxiety with combination
Patients assigned to buparlisib-fulvestrant group had substantially higher proportions of alanine aminotransferase and aspartate aminotransferase elevations compared with patients in the placebo-fulvestrant group, as well as more reported depression and anxiety. Three patients in the buparlisib arm attempted suicide. There were no reported suicide attempts in the placebo arm.
Dr O’Regan said at the briefing that mood disorders are known adverse events associated with buparlisib, and that patients with psychiatric disorders were excluded from the trial.
— Neil Osterweil
Lenvatinib expands its reach into renal cell carcinoma
The US Food and Drug Administration (FDA) expanded the approval of the multitargeted tyrosine kinase inhibitor lenvatinib to a second indication in 2016. In addition to thyroid cancer, the drug is now approved in combination with the mammalian target of rapamycin (mTOR) inhibitor everolimus for the treatment of advanced renal cell carcinoma (RCC) after one prior anti-angiogenic therapy.
The current approval was based on the demonstration of synergistic efficacy and a manageable toxicity profile for the combination in a randomized, open-label, phase 2 clinical trial performed at 37 centers in 5 countries. Patients were eligible for the study if they were aged 18 years or older and had histologically verified clear cell RCC, measurable disease as assessed by RECIST (Response Evaluation Criteria in Solid Tumors) version 1.1, radiographic evidence of progression or metastasis
From March 16, 2012 to June 19, 2013, 153 patients were randomly assigned in a 1:1:1 ratio to 3 treatment arms; lenvatinib 18 mg plus everolimus 5 mg, lenvatinib 24 mg monotherapy, or everolimus 10 mg monotherapy, all administered once daily. Randomization was stratified according to hemoglobin (men ≤130 g/L and >130 g/L; women ≤115 g/L and >115 g/L) and corrected serum calcium (≥2.5 mmol/L and <2.5 mmol/L).
Radiographic tumor response assessments were performed every 8 weeks from randomization until disease progression or the start of another anticancer treatment. To enable pharmacokinetic analyses, 6 blood samples were obtained on day 1 of the first 3 treatment cycles for all patients. In addition, 9 samples were obtained over a 24-hour period for 9-12 patients in each treatment group to provide intensive samples.
The primary endpoint of the study was progression-free survival (PFS), which was significantly improved with a combination of lenvatinib and everolimus, compared with single-agent everolimus. Median PFS was 14.6 months, compared with 5.5 months, respectively (hazard ratio [HR], 0.40; P = .0005), translating into a 63% reduction in the risk of disease progression or death. In the lenvatinib monotherapy group, median PFS was 7.4 months.
Over a median follow-up of 24.2 months there was also a significant difference in overall survival (OS) between the combination arm and single-agent everolimus (24.2 months vs 15.4 months, respectively). Objective responses were seen in 43% of patients in the combination arm and 6% and 27% of patients in the everolimus and lenvatinib monotherapy arms, respectively. The median duration of response was 13 months, 8.5 months, and 7.5 months in the 3 treatment arms, respectively.
All patients had at least 1 treatment-related adverse event (AE), almost all considered to be related to the study drug. Among patients treated with lenvatinib and everolimus, 24% discontinued therapy because of AEs, whereas the rate of discontinuation was 12% and 25% among patients treated with everolimus or lenvatinib monotherapy, respectively. There was 1 instance of a trans-arterial embolization leading to death that was judged to be probably treatment related in the combination arm, compared with 2 in the everolimus arm, neither judged treatment-related, and 3 in the lenvatinib arm, 1 of which was considered to be possibly treatment related.
The rates of grade 3/4 AEs were 71% for combination therapy, compared with 50% and 79%, respectively, among patients treated with everolimus or lenvatinib alone. Most commonly, in the combination arm, these included renal failure (11%), dehydration (10%), anemia (6%), thrombocytopenia (5%), diarrhea (5%), vomiting (5%), and dyspnea (5%).
The prescribing information carries warnings and precautions about hypertension, cardiac dysfunction, arterial thromboembolic events, hepatotoxicity, proteinuria, diarrhea, renal failure and impairment, gastrointestinal perforation, and fistula formation, QT interval prolongation, hypocalcemia, reversible posterior leukoencephalopathy syndrome, hemorrhagic events, and impairment of thyroid stimulating hormone suppression or thyroid dysfunction, all of which have been reported in clinical trials of lenvatinib and everolimus. Patients should also be warned about the risk of fetal harm.
Blood pressure should be closely monitored prior to treatment, after 1 week and then every 2 weeks for the first 2 months, then at least monthly thereafter during treatment. Patients should be monitored for signs of cardiac decompensation and proteinuria. Liver function should be monitored before initiating therapy, every 2 weeks for the first 2 months and then at least monthly while treatment continues. Electrolyte abnormalities should be monitored and corrected, blood calcium levels should be monitored at least monthly, and thyroid function should be evaluated before and at least monthly during treatment.
The prescribing information details dose reductions and modifications for AEs. Treatment should be withheld for grade 3 hypertension, grade 3 cardiac dysfunction, grade 3 or greater hepatotoxicity, proteinuria >2 g/24 hours, grade 3 diarrhea, grade 3/4 renal failure or impairment, corrected QT interval prolongation >500 ms, hypocalcemia as necessary, reversible posterior leukoencephalopathy syndrome confirmed by magnetic resonance imaging, and grade 3 hemorrhagic events.
Treatment discontinuation should occur in the event of life-threatening hypertension, grade 4 cardiac dysfunction, arterial thromboembolic events, hepatic failure, grade 3 diarrhea that persists despite medical management, severe or persistent renal impairment, gastrointestinal perforation or life-threatening fistula formation, severe and persistent neurologic symptoms, and grade 4 hemorrhage. The recommended dose for lenvatinib, which is marketed as Lenvima by Eisai Inc, is 18 mg (1 x 10 mg capsule and 2 x 4 mg capsules) in combination with 5 mg everolimus orally taken daily, with or without food, until disease progression or unacceptable toxicity.
1. Lenvima (lenvatinib) capsules, for oral use. Prescribing information. Woodcliff Lake, NJ: Eisai Inc: 2016. http://www.lenvima.com/pdfs/prescribing-information.pdf. Accessed November 17, 2016.
2. Motzer RJ, Hutson TE, Glen H, et al. Lenvatinib, everolimus, and the combination in patients with metastatic renal cell carcinoma: a randomised, phase 2, open-label, multicentre trial. Lancet Oncol. 2015;16:1473-1482.
3. US Food and Drug Administration. Lenvatinib in combination with everolimus. http://www.fda.gov/Drugs/InformationOnDrugs/ApprovedDrugs/ucm501070.htm. Last updated May 16, 2016. Accessed November 17, 2016.
The US Food and Drug Administration (FDA) expanded the approval of the multitargeted tyrosine kinase inhibitor lenvatinib to a second indication in 2016. In addition to thyroid cancer, the drug is now approved in combination with the mammalian target of rapamycin (mTOR) inhibitor everolimus for the treatment of advanced renal cell carcinoma (RCC) after one prior anti-angiogenic therapy.
The current approval was based on the demonstration of synergistic efficacy and a manageable toxicity profile for the combination in a randomized, open-label, phase 2 clinical trial performed at 37 centers in 5 countries. Patients were eligible for the study if they were aged 18 years or older and had histologically verified clear cell RCC, measurable disease as assessed by RECIST (Response Evaluation Criteria in Solid Tumors) version 1.1, radiographic evidence of progression or metastasis
From March 16, 2012 to June 19, 2013, 153 patients were randomly assigned in a 1:1:1 ratio to 3 treatment arms; lenvatinib 18 mg plus everolimus 5 mg, lenvatinib 24 mg monotherapy, or everolimus 10 mg monotherapy, all administered once daily. Randomization was stratified according to hemoglobin (men ≤130 g/L and >130 g/L; women ≤115 g/L and >115 g/L) and corrected serum calcium (≥2.5 mmol/L and <2.5 mmol/L).
Radiographic tumor response assessments were performed every 8 weeks from randomization until disease progression or the start of another anticancer treatment. To enable pharmacokinetic analyses, 6 blood samples were obtained on day 1 of the first 3 treatment cycles for all patients. In addition, 9 samples were obtained over a 24-hour period for 9-12 patients in each treatment group to provide intensive samples.
The primary endpoint of the study was progression-free survival (PFS), which was significantly improved with a combination of lenvatinib and everolimus, compared with single-agent everolimus. Median PFS was 14.6 months, compared with 5.5 months, respectively (hazard ratio [HR], 0.40; P = .0005), translating into a 63% reduction in the risk of disease progression or death. In the lenvatinib monotherapy group, median PFS was 7.4 months.
Over a median follow-up of 24.2 months there was also a significant difference in overall survival (OS) between the combination arm and single-agent everolimus (24.2 months vs 15.4 months, respectively). Objective responses were seen in 43% of patients in the combination arm and 6% and 27% of patients in the everolimus and lenvatinib monotherapy arms, respectively. The median duration of response was 13 months, 8.5 months, and 7.5 months in the 3 treatment arms, respectively.
All patients had at least 1 treatment-related adverse event (AE), almost all considered to be related to the study drug. Among patients treated with lenvatinib and everolimus, 24% discontinued therapy because of AEs, whereas the rate of discontinuation was 12% and 25% among patients treated with everolimus or lenvatinib monotherapy, respectively. There was 1 instance of a trans-arterial embolization leading to death that was judged to be probably treatment related in the combination arm, compared with 2 in the everolimus arm, neither judged treatment-related, and 3 in the lenvatinib arm, 1 of which was considered to be possibly treatment related.
The rates of grade 3/4 AEs were 71% for combination therapy, compared with 50% and 79%, respectively, among patients treated with everolimus or lenvatinib alone. Most commonly, in the combination arm, these included renal failure (11%), dehydration (10%), anemia (6%), thrombocytopenia (5%), diarrhea (5%), vomiting (5%), and dyspnea (5%).
The prescribing information carries warnings and precautions about hypertension, cardiac dysfunction, arterial thromboembolic events, hepatotoxicity, proteinuria, diarrhea, renal failure and impairment, gastrointestinal perforation, and fistula formation, QT interval prolongation, hypocalcemia, reversible posterior leukoencephalopathy syndrome, hemorrhagic events, and impairment of thyroid stimulating hormone suppression or thyroid dysfunction, all of which have been reported in clinical trials of lenvatinib and everolimus. Patients should also be warned about the risk of fetal harm.
Blood pressure should be closely monitored prior to treatment, after 1 week and then every 2 weeks for the first 2 months, then at least monthly thereafter during treatment. Patients should be monitored for signs of cardiac decompensation and proteinuria. Liver function should be monitored before initiating therapy, every 2 weeks for the first 2 months and then at least monthly while treatment continues. Electrolyte abnormalities should be monitored and corrected, blood calcium levels should be monitored at least monthly, and thyroid function should be evaluated before and at least monthly during treatment.
The prescribing information details dose reductions and modifications for AEs. Treatment should be withheld for grade 3 hypertension, grade 3 cardiac dysfunction, grade 3 or greater hepatotoxicity, proteinuria >2 g/24 hours, grade 3 diarrhea, grade 3/4 renal failure or impairment, corrected QT interval prolongation >500 ms, hypocalcemia as necessary, reversible posterior leukoencephalopathy syndrome confirmed by magnetic resonance imaging, and grade 3 hemorrhagic events.
Treatment discontinuation should occur in the event of life-threatening hypertension, grade 4 cardiac dysfunction, arterial thromboembolic events, hepatic failure, grade 3 diarrhea that persists despite medical management, severe or persistent renal impairment, gastrointestinal perforation or life-threatening fistula formation, severe and persistent neurologic symptoms, and grade 4 hemorrhage. The recommended dose for lenvatinib, which is marketed as Lenvima by Eisai Inc, is 18 mg (1 x 10 mg capsule and 2 x 4 mg capsules) in combination with 5 mg everolimus orally taken daily, with or without food, until disease progression or unacceptable toxicity.
The US Food and Drug Administration (FDA) expanded the approval of the multitargeted tyrosine kinase inhibitor lenvatinib to a second indication in 2016. In addition to thyroid cancer, the drug is now approved in combination with the mammalian target of rapamycin (mTOR) inhibitor everolimus for the treatment of advanced renal cell carcinoma (RCC) after one prior anti-angiogenic therapy.
The current approval was based on the demonstration of synergistic efficacy and a manageable toxicity profile for the combination in a randomized, open-label, phase 2 clinical trial performed at 37 centers in 5 countries. Patients were eligible for the study if they were aged 18 years or older and had histologically verified clear cell RCC, measurable disease as assessed by RECIST (Response Evaluation Criteria in Solid Tumors) version 1.1, radiographic evidence of progression or metastasis
From March 16, 2012 to June 19, 2013, 153 patients were randomly assigned in a 1:1:1 ratio to 3 treatment arms; lenvatinib 18 mg plus everolimus 5 mg, lenvatinib 24 mg monotherapy, or everolimus 10 mg monotherapy, all administered once daily. Randomization was stratified according to hemoglobin (men ≤130 g/L and >130 g/L; women ≤115 g/L and >115 g/L) and corrected serum calcium (≥2.5 mmol/L and <2.5 mmol/L).
Radiographic tumor response assessments were performed every 8 weeks from randomization until disease progression or the start of another anticancer treatment. To enable pharmacokinetic analyses, 6 blood samples were obtained on day 1 of the first 3 treatment cycles for all patients. In addition, 9 samples were obtained over a 24-hour period for 9-12 patients in each treatment group to provide intensive samples.
The primary endpoint of the study was progression-free survival (PFS), which was significantly improved with a combination of lenvatinib and everolimus, compared with single-agent everolimus. Median PFS was 14.6 months, compared with 5.5 months, respectively (hazard ratio [HR], 0.40; P = .0005), translating into a 63% reduction in the risk of disease progression or death. In the lenvatinib monotherapy group, median PFS was 7.4 months.
Over a median follow-up of 24.2 months there was also a significant difference in overall survival (OS) between the combination arm and single-agent everolimus (24.2 months vs 15.4 months, respectively). Objective responses were seen in 43% of patients in the combination arm and 6% and 27% of patients in the everolimus and lenvatinib monotherapy arms, respectively. The median duration of response was 13 months, 8.5 months, and 7.5 months in the 3 treatment arms, respectively.
All patients had at least 1 treatment-related adverse event (AE), almost all considered to be related to the study drug. Among patients treated with lenvatinib and everolimus, 24% discontinued therapy because of AEs, whereas the rate of discontinuation was 12% and 25% among patients treated with everolimus or lenvatinib monotherapy, respectively. There was 1 instance of a trans-arterial embolization leading to death that was judged to be probably treatment related in the combination arm, compared with 2 in the everolimus arm, neither judged treatment-related, and 3 in the lenvatinib arm, 1 of which was considered to be possibly treatment related.
The rates of grade 3/4 AEs were 71% for combination therapy, compared with 50% and 79%, respectively, among patients treated with everolimus or lenvatinib alone. Most commonly, in the combination arm, these included renal failure (11%), dehydration (10%), anemia (6%), thrombocytopenia (5%), diarrhea (5%), vomiting (5%), and dyspnea (5%).
The prescribing information carries warnings and precautions about hypertension, cardiac dysfunction, arterial thromboembolic events, hepatotoxicity, proteinuria, diarrhea, renal failure and impairment, gastrointestinal perforation, and fistula formation, QT interval prolongation, hypocalcemia, reversible posterior leukoencephalopathy syndrome, hemorrhagic events, and impairment of thyroid stimulating hormone suppression or thyroid dysfunction, all of which have been reported in clinical trials of lenvatinib and everolimus. Patients should also be warned about the risk of fetal harm.
Blood pressure should be closely monitored prior to treatment, after 1 week and then every 2 weeks for the first 2 months, then at least monthly thereafter during treatment. Patients should be monitored for signs of cardiac decompensation and proteinuria. Liver function should be monitored before initiating therapy, every 2 weeks for the first 2 months and then at least monthly while treatment continues. Electrolyte abnormalities should be monitored and corrected, blood calcium levels should be monitored at least monthly, and thyroid function should be evaluated before and at least monthly during treatment.
The prescribing information details dose reductions and modifications for AEs. Treatment should be withheld for grade 3 hypertension, grade 3 cardiac dysfunction, grade 3 or greater hepatotoxicity, proteinuria >2 g/24 hours, grade 3 diarrhea, grade 3/4 renal failure or impairment, corrected QT interval prolongation >500 ms, hypocalcemia as necessary, reversible posterior leukoencephalopathy syndrome confirmed by magnetic resonance imaging, and grade 3 hemorrhagic events.
Treatment discontinuation should occur in the event of life-threatening hypertension, grade 4 cardiac dysfunction, arterial thromboembolic events, hepatic failure, grade 3 diarrhea that persists despite medical management, severe or persistent renal impairment, gastrointestinal perforation or life-threatening fistula formation, severe and persistent neurologic symptoms, and grade 4 hemorrhage. The recommended dose for lenvatinib, which is marketed as Lenvima by Eisai Inc, is 18 mg (1 x 10 mg capsule and 2 x 4 mg capsules) in combination with 5 mg everolimus orally taken daily, with or without food, until disease progression or unacceptable toxicity.
1. Lenvima (lenvatinib) capsules, for oral use. Prescribing information. Woodcliff Lake, NJ: Eisai Inc: 2016. http://www.lenvima.com/pdfs/prescribing-information.pdf. Accessed November 17, 2016.
2. Motzer RJ, Hutson TE, Glen H, et al. Lenvatinib, everolimus, and the combination in patients with metastatic renal cell carcinoma: a randomised, phase 2, open-label, multicentre trial. Lancet Oncol. 2015;16:1473-1482.
3. US Food and Drug Administration. Lenvatinib in combination with everolimus. http://www.fda.gov/Drugs/InformationOnDrugs/ApprovedDrugs/ucm501070.htm. Last updated May 16, 2016. Accessed November 17, 2016.
1. Lenvima (lenvatinib) capsules, for oral use. Prescribing information. Woodcliff Lake, NJ: Eisai Inc: 2016. http://www.lenvima.com/pdfs/prescribing-information.pdf. Accessed November 17, 2016.
2. Motzer RJ, Hutson TE, Glen H, et al. Lenvatinib, everolimus, and the combination in patients with metastatic renal cell carcinoma: a randomised, phase 2, open-label, multicentre trial. Lancet Oncol. 2015;16:1473-1482.
3. US Food and Drug Administration. Lenvatinib in combination with everolimus. http://www.fda.gov/Drugs/InformationOnDrugs/ApprovedDrugs/ucm501070.htm. Last updated May 16, 2016. Accessed November 17, 2016.
Single-, low-dose cyclophosphamide-associated severe hyponatremia with seizures in a patient with breast cancer
Cyclophosphamide, an agent used to treat various malignant and autoimmune disorders, can cause severe hyponatremia with seizures in rare cases. The exact mechanism of cyclophosphamide-induced hyponatremia is poorly understood, but is thought to occur from a drug- associated antidiuretic hormone (ADH) release leading to free water retention.1 This unusual phenomenon of cyclophosphamide-associated syndrome of inappropriate antidiuretic hormone secretion (SIADH) has been described only in case reports, most of which reported the development of severe hyponatremia within a week after administration of cyclophosphamide.2-5 We report a unique case of a patient who developed severe, symptomatic hyponatremia with seizures, with her serum sodium decreasing from 137 mEq to 112 mEq within 30 hours after her first dose of low-dose cyclophosphamide (600 mg/m2).
Case presentation and summary
A 68-year-old white woman with a history of bilateral invasive ductal carcinoma of the breast (status-post bilateral mastectomy) presented to the emergency department (ED) at our facility with new onset seizure. The patient had been diagnosed 8 months earlier with stage I (T1c, N0, M0) poorly differentiated infiltrating ductal carcinoma (triple negative) of the left breast for which she underwent left segmental mastectomy about 1 month after diagnosis. She was subsequently found to have progressive disease with stage IIIC (T2, N3, and M0) infiltrating ductal carcinoma with lobular features (ER/PR+, Her2) of the right breast. She underwent a right modified radical mastectomy 5 months after her stage IIIC breast cancer diagnosis. She received her first cycle of adjuvant chemotherapy with intravenous doxorubicin (60 mg/m2) and cyclophosphamide (600 mg/m2), which included pre-hydration, a day before presenting to our facility.
According to the patient’s family who provided the initial history, the patient reported tightness in her left arm while sitting at the dinner table. She was confused and subsequently had jerking movement of her right upper extremity with left facial twitching which lasted about 40 seconds. There was no loss of consciousness, or bowel or bladder control. She became unresponsive after the episode. Review of systems was negative except for a report of nausea a few hours before the onset of seizures, which resolved with ondansetron. Her past medical history was significant for breast cancer as already mentioned, seasonal allergic rhinitis, and hypertension. Home medications included hydrochlorothiazide 12.5 mg oral daily, aspirin 81 mg oral daily, and fexofenadine and loratadine oral daily as needed for allergies. There were no other significant surgical history other than already stated. The patient lived at home with her family and was independent with her instrumental activities of daily living. She is a former smoker of tobacco and quit smoking 30 years ago.
On arrival at our facility, the patient had normal vital signs. Significant findings on physical examination were an elderly female who seemed somnolent; not able to follow commands with a documented Glasgow Coma Scale of 10 with eyes opening spontaneously, incomprehensible sounds, and flexion withdrawal from pain as her best responses. She had an increased tone in her left upper extremity and had a brisk, deep tendon reflexes without clonus or 3+ (range, 0-5+, with 2+ being normal). The remainder of her physical exam was unremarkable. Laboratory testing revealed a glucose level of 120 mg/dL (normal, 65-110 mg/dL), sodium of 112 mEq/L (normal, 135-145 mmol/L), and chloride of 78 mEq/L (normal, 95-105 mmol/L). Serum osmolality and urine osmolality were 242 mOsm/kg (normal, 282-295 mOsm/kg) and 449 mOsm/kg (normal, 500-800 mOsm/kg) respectively, indicative of suboptimally dilute urine despite relatively low serum osmolality or SIADH. Urine electrolytes were not obtained.
Imaging studies including computed-tomography scans of the head and chest x-ray performed in the ED were unremarkable. After a phenytoin load, an electroencephalogram was obtained which showed diffuse encephalopathy without active seizure foci. A non-contrast magnetic-resonance imaging (MRI) of the brain was performed but it failed to show acute infarct, mass, mass effect, or brain herniation. There was nonspecific white matter abnormality with compromise of the bilateral cerebral hemispheres, calloseptal junction, left posterior pillar, and bilateral anterior pillars of the fornix, possibly representative of chronic white matter microvascular ischemic changes or less likely vasculitis or demyelination. Correction of her hyponatremia with normal saline was started in the ED with a change in serum sodium from 112 mEq/L to 115 mEq/L within 2 hours. She was admitted to the intensive care unit (ICU) where her sodium correction with normal saline and free water restriction was continued with a goal correction rate of 8-12 mEq/L in 24 hours. The patient’s serum sodium as well as level of consciousness improved gradually over the course of her ICU stay. After 64 hours in the hospital, her sodium had corrected to 137 mEq/L (normal, 135-145 mmol/L; Figure). She was then alert and oriented to person, place, and time. All motor findings noted on presentation had resolved. Her saline infusion was discontinued and serum sodium remained within normal range. She was discharged to a rehabilitation facility. Her hydrochlorothiazide was also discontinued.
Discussion
Hyponatremia is a common finding in cancer patients caused usually by paraneoplastic syndrome, chemotherapy, immunotherapy, or other associated treatment.6 SIADH is a frequent cause of hyponatremia in cancer patients and should be suspected in patients with hyponatremia, hypo-osmolality, and a urine osmolality above 100 mOsmol/kg.7
Our patient’s presentation and laboratory findings suggested SIADH as the likely cause of hyponatremia with a low sodium, a serum osmolality 242 mOsm/kg and urine osmolality of 449 mOsm/kg.8-10 She had no known underlying contributory comorbid condition relating to her serum lipids, thyroid, adrenal, kidney, or heart to date. Her use of a thiazide diuretic was the only confounding factor. The most plausible cause of hyponatremia/SIADH in our patient was likely cyclophosphamide based on her history, timeline of symptoms, and the absence of other possible causes. Though the mechanism for many of the previously mentioned etiologies are known, the mechanism of cyclophosphamide-induced SIADH is difficult to elucidate since the imminent complication of hemorrhagic cystitis means patients receiving this drug are often aggressively hydrated to prevent this complication.11,12 The result is that there is marked retention of water leading to potentially fatal hyponatremia in selected cases.11 This phenomenon has been fairly well described in patients receiving doses of 6 g/m2 as given in the STAMP protocol for stem cell mobilization or at doses of 30-50 mg/kg used to treat malignancy.12 Our patient clearly falls in this category given that she received a dose of 600 mg/m2. We found no evidence in her history to suggest post-operative, genetic or other cause for her hyponatremia. Our case mirrors a report by Koo and colleagues who described severe hyponatremia occurring within 24 hours following a single dose of intravenous cyclophosphamide 700 mg followed by saline infusion.13 In the case reported by Jayachandra and colleagues in which suspected cyclophosphamide-induced hyponatremia led to seizures, the patient received 500 mg IV of cyclophosphamide and had serum sodium as low as 106 mEq/L within a 24-hour period,2 similar to our patient.
There is a paucity of data on cyclophosphamide-induced SIADH. The mechanism by which cyclophosphamide causes SIADH is currently unknown. In addition, there are currently no set criteria that help identify at-risk patients who may develop such an event, including the dosage of cyclophosphamide that may trigger the SIADH, because lower doses of the drug have been associated with this complication.14
In a retrospective analysis by Lee and colleagues, cyclophosphamide-induced hyponatremia was found to be associated with male sex on a univariate analysis, but no risk factors were found in a multivariate analysis.15 It is likely that the concomitant use of diuretics, hydration, and high-dose cyclophosphamide contributed to hyponatremia/SIADH in our patient, though it is not clear through what mechanism. Harlow and colleagues proposed a mechanism for this phenomenon in 1979 based on the autopsy of a patient who had received high-dose cyclophosphamide involving degranulation of hypothalamic neurosecretory organelles and loss of Herring’s bodies. They inferred that metabolites of cyclophosphamide indirectly triggered inappropriate secretion of antidiuretic hormone as seen with a use of the structurally related analogue ifosfamide,16 but to our knowledge, this has yet to be replicated. Cyclophosphamide metabolite may have a direct tubular effect on the collecting duct epithelium leading to water retention15 as established by Campbell and colleagues. In one case, an established diabetes insipidus patient developed cyclophosphamide-induced antidiuresis without vasopressin secretion.17 It is imperative that the scientific community conduct research into the risk factors, underlying mechanisms, and methods of prevention to reduce and/or eliminate SIADH associated with use of cyclophosphamide.
1. Gilbar PJ, Richmond J, Wood J, Sullivan A. Syndrome of inappropriate antidiuretic hormone secretion induced by a single dose of oral cyclophosphamide. Ann Pharmacother. 2012.46(9):e23.
2. Jayachandran NV, Chandrasekhara PK, Thomas J, Agrawal S, Narsimulu G. Cyclophosphamide-associated complications: we need to be aware of SIADH and central pontine myelinolysis. Rheumatology (Oxford). 2009;48(1):89-90.
3. Baker M, Markman M, Niu J. Cyclophosphamide-induced severe acute hyponatremic encephalopathy in patients with breast cancer: report of two cases. Case Rep Oncol. 2014;7(2):550-554.
4. Lazarevic V, Hägg E, Wahlin A. Hiccups and severe hyponatremia associated with high-dose cyclophosphamide in conditioning regimen for allogeneic stem cell transplantation. Am J Hematol. 2007;82(1):88.
5. Geng C, Tang P, Zhang Y, Gao W. Hyponatremia induced by low-dose cyclophosphamide in two patients with breast cancer. Breast J. 2014; 20(4):442-443.
6. Kamoi K, Ebe T, Hasegawa A, et al. Hyponatremia in small cell lung cancer. Mechanisms not involving inappropriate ADH secretion. Cancer. 1987;60(5):1089-1093.
7. Matwiejczuk S, Püsküllüoğlu M, Zygulska AL. Oncological emergencies: syndrome of inappropriate antidiuretic hormone secretion (SIADH). Przegl Lek. 2014;71(10):541-543.
8. Robertson GL. Regulation of arginine vasopressin in the syndrome of inappropriate antidiuresis. Am J Med. 2006;119(7 Suppl 1):S36-42.
9. Robertson GL, Shelton RL, Athar S. The osmoregulation of vasopressin. Kidney Int. 1976;10(1):25-37.
10. Decaux G, Musch W. Clinical laboratory evaluation of the syndrome of inappropriate secretion of antidiuretic hormone. Clin J Am Soc Nephrol. 2008;3(4):1175-1184.
11. Bressler RB, Huston DP. Water intoxication following moderate-dose intravenous cyclophosphamide. Arch Intern Med. 1985;145(3):548-549.
12. Salido M, Macarron P, Hernández-García C, D’Cruz DP, Khamashta MA, Hughes GR. Water intoxication induced by low-dose cyclophosphamide in two patients with systemic lupus erythematosus. Lupus. 2003;12(8):636-639.
13. Koo TY, Bae SC, Park JS, et al. Water intoxication following low-dose intravenous cyclophosphamide. Electrolyte Blood Press. 2007;5(1):50-54.
14. [No authors listed]. Nausea and vasopressin. Lancet. 1991;337(8750):1133-1134.
15 Lee YC1, Park JS, Lee CH, et al. Hyponatraemia induced by low-dose intravenous pulse cyclophosphamide. Nephrol Dial Transplant. 2010;25(5):1520-1524.
16. Harlow PJ, DeClerck YA, Shore NA, Ortega JA, Carranza A, Heuser E. A fatal case of inappropriate ADH secretion induced by cyclophosphamide therapy. Cancer. 1979;44(3):896-898.
17. Campbell DM, Atkinson A, Gillis D, Sochett EB. Cyclophosphamide and water retention: mechanism revisited. J Pediatr Endocrinol Metab. 2000;13(6):673-675.
Cyclophosphamide, an agent used to treat various malignant and autoimmune disorders, can cause severe hyponatremia with seizures in rare cases. The exact mechanism of cyclophosphamide-induced hyponatremia is poorly understood, but is thought to occur from a drug- associated antidiuretic hormone (ADH) release leading to free water retention.1 This unusual phenomenon of cyclophosphamide-associated syndrome of inappropriate antidiuretic hormone secretion (SIADH) has been described only in case reports, most of which reported the development of severe hyponatremia within a week after administration of cyclophosphamide.2-5 We report a unique case of a patient who developed severe, symptomatic hyponatremia with seizures, with her serum sodium decreasing from 137 mEq to 112 mEq within 30 hours after her first dose of low-dose cyclophosphamide (600 mg/m2).
Case presentation and summary
A 68-year-old white woman with a history of bilateral invasive ductal carcinoma of the breast (status-post bilateral mastectomy) presented to the emergency department (ED) at our facility with new onset seizure. The patient had been diagnosed 8 months earlier with stage I (T1c, N0, M0) poorly differentiated infiltrating ductal carcinoma (triple negative) of the left breast for which she underwent left segmental mastectomy about 1 month after diagnosis. She was subsequently found to have progressive disease with stage IIIC (T2, N3, and M0) infiltrating ductal carcinoma with lobular features (ER/PR+, Her2) of the right breast. She underwent a right modified radical mastectomy 5 months after her stage IIIC breast cancer diagnosis. She received her first cycle of adjuvant chemotherapy with intravenous doxorubicin (60 mg/m2) and cyclophosphamide (600 mg/m2), which included pre-hydration, a day before presenting to our facility.
According to the patient’s family who provided the initial history, the patient reported tightness in her left arm while sitting at the dinner table. She was confused and subsequently had jerking movement of her right upper extremity with left facial twitching which lasted about 40 seconds. There was no loss of consciousness, or bowel or bladder control. She became unresponsive after the episode. Review of systems was negative except for a report of nausea a few hours before the onset of seizures, which resolved with ondansetron. Her past medical history was significant for breast cancer as already mentioned, seasonal allergic rhinitis, and hypertension. Home medications included hydrochlorothiazide 12.5 mg oral daily, aspirin 81 mg oral daily, and fexofenadine and loratadine oral daily as needed for allergies. There were no other significant surgical history other than already stated. The patient lived at home with her family and was independent with her instrumental activities of daily living. She is a former smoker of tobacco and quit smoking 30 years ago.
On arrival at our facility, the patient had normal vital signs. Significant findings on physical examination were an elderly female who seemed somnolent; not able to follow commands with a documented Glasgow Coma Scale of 10 with eyes opening spontaneously, incomprehensible sounds, and flexion withdrawal from pain as her best responses. She had an increased tone in her left upper extremity and had a brisk, deep tendon reflexes without clonus or 3+ (range, 0-5+, with 2+ being normal). The remainder of her physical exam was unremarkable. Laboratory testing revealed a glucose level of 120 mg/dL (normal, 65-110 mg/dL), sodium of 112 mEq/L (normal, 135-145 mmol/L), and chloride of 78 mEq/L (normal, 95-105 mmol/L). Serum osmolality and urine osmolality were 242 mOsm/kg (normal, 282-295 mOsm/kg) and 449 mOsm/kg (normal, 500-800 mOsm/kg) respectively, indicative of suboptimally dilute urine despite relatively low serum osmolality or SIADH. Urine electrolytes were not obtained.
Imaging studies including computed-tomography scans of the head and chest x-ray performed in the ED were unremarkable. After a phenytoin load, an electroencephalogram was obtained which showed diffuse encephalopathy without active seizure foci. A non-contrast magnetic-resonance imaging (MRI) of the brain was performed but it failed to show acute infarct, mass, mass effect, or brain herniation. There was nonspecific white matter abnormality with compromise of the bilateral cerebral hemispheres, calloseptal junction, left posterior pillar, and bilateral anterior pillars of the fornix, possibly representative of chronic white matter microvascular ischemic changes or less likely vasculitis or demyelination. Correction of her hyponatremia with normal saline was started in the ED with a change in serum sodium from 112 mEq/L to 115 mEq/L within 2 hours. She was admitted to the intensive care unit (ICU) where her sodium correction with normal saline and free water restriction was continued with a goal correction rate of 8-12 mEq/L in 24 hours. The patient’s serum sodium as well as level of consciousness improved gradually over the course of her ICU stay. After 64 hours in the hospital, her sodium had corrected to 137 mEq/L (normal, 135-145 mmol/L; Figure). She was then alert and oriented to person, place, and time. All motor findings noted on presentation had resolved. Her saline infusion was discontinued and serum sodium remained within normal range. She was discharged to a rehabilitation facility. Her hydrochlorothiazide was also discontinued.
Discussion
Hyponatremia is a common finding in cancer patients caused usually by paraneoplastic syndrome, chemotherapy, immunotherapy, or other associated treatment.6 SIADH is a frequent cause of hyponatremia in cancer patients and should be suspected in patients with hyponatremia, hypo-osmolality, and a urine osmolality above 100 mOsmol/kg.7
Our patient’s presentation and laboratory findings suggested SIADH as the likely cause of hyponatremia with a low sodium, a serum osmolality 242 mOsm/kg and urine osmolality of 449 mOsm/kg.8-10 She had no known underlying contributory comorbid condition relating to her serum lipids, thyroid, adrenal, kidney, or heart to date. Her use of a thiazide diuretic was the only confounding factor. The most plausible cause of hyponatremia/SIADH in our patient was likely cyclophosphamide based on her history, timeline of symptoms, and the absence of other possible causes. Though the mechanism for many of the previously mentioned etiologies are known, the mechanism of cyclophosphamide-induced SIADH is difficult to elucidate since the imminent complication of hemorrhagic cystitis means patients receiving this drug are often aggressively hydrated to prevent this complication.11,12 The result is that there is marked retention of water leading to potentially fatal hyponatremia in selected cases.11 This phenomenon has been fairly well described in patients receiving doses of 6 g/m2 as given in the STAMP protocol for stem cell mobilization or at doses of 30-50 mg/kg used to treat malignancy.12 Our patient clearly falls in this category given that she received a dose of 600 mg/m2. We found no evidence in her history to suggest post-operative, genetic or other cause for her hyponatremia. Our case mirrors a report by Koo and colleagues who described severe hyponatremia occurring within 24 hours following a single dose of intravenous cyclophosphamide 700 mg followed by saline infusion.13 In the case reported by Jayachandra and colleagues in which suspected cyclophosphamide-induced hyponatremia led to seizures, the patient received 500 mg IV of cyclophosphamide and had serum sodium as low as 106 mEq/L within a 24-hour period,2 similar to our patient.
There is a paucity of data on cyclophosphamide-induced SIADH. The mechanism by which cyclophosphamide causes SIADH is currently unknown. In addition, there are currently no set criteria that help identify at-risk patients who may develop such an event, including the dosage of cyclophosphamide that may trigger the SIADH, because lower doses of the drug have been associated with this complication.14
In a retrospective analysis by Lee and colleagues, cyclophosphamide-induced hyponatremia was found to be associated with male sex on a univariate analysis, but no risk factors were found in a multivariate analysis.15 It is likely that the concomitant use of diuretics, hydration, and high-dose cyclophosphamide contributed to hyponatremia/SIADH in our patient, though it is not clear through what mechanism. Harlow and colleagues proposed a mechanism for this phenomenon in 1979 based on the autopsy of a patient who had received high-dose cyclophosphamide involving degranulation of hypothalamic neurosecretory organelles and loss of Herring’s bodies. They inferred that metabolites of cyclophosphamide indirectly triggered inappropriate secretion of antidiuretic hormone as seen with a use of the structurally related analogue ifosfamide,16 but to our knowledge, this has yet to be replicated. Cyclophosphamide metabolite may have a direct tubular effect on the collecting duct epithelium leading to water retention15 as established by Campbell and colleagues. In one case, an established diabetes insipidus patient developed cyclophosphamide-induced antidiuresis without vasopressin secretion.17 It is imperative that the scientific community conduct research into the risk factors, underlying mechanisms, and methods of prevention to reduce and/or eliminate SIADH associated with use of cyclophosphamide.
Cyclophosphamide, an agent used to treat various malignant and autoimmune disorders, can cause severe hyponatremia with seizures in rare cases. The exact mechanism of cyclophosphamide-induced hyponatremia is poorly understood, but is thought to occur from a drug- associated antidiuretic hormone (ADH) release leading to free water retention.1 This unusual phenomenon of cyclophosphamide-associated syndrome of inappropriate antidiuretic hormone secretion (SIADH) has been described only in case reports, most of which reported the development of severe hyponatremia within a week after administration of cyclophosphamide.2-5 We report a unique case of a patient who developed severe, symptomatic hyponatremia with seizures, with her serum sodium decreasing from 137 mEq to 112 mEq within 30 hours after her first dose of low-dose cyclophosphamide (600 mg/m2).
Case presentation and summary
A 68-year-old white woman with a history of bilateral invasive ductal carcinoma of the breast (status-post bilateral mastectomy) presented to the emergency department (ED) at our facility with new onset seizure. The patient had been diagnosed 8 months earlier with stage I (T1c, N0, M0) poorly differentiated infiltrating ductal carcinoma (triple negative) of the left breast for which she underwent left segmental mastectomy about 1 month after diagnosis. She was subsequently found to have progressive disease with stage IIIC (T2, N3, and M0) infiltrating ductal carcinoma with lobular features (ER/PR+, Her2) of the right breast. She underwent a right modified radical mastectomy 5 months after her stage IIIC breast cancer diagnosis. She received her first cycle of adjuvant chemotherapy with intravenous doxorubicin (60 mg/m2) and cyclophosphamide (600 mg/m2), which included pre-hydration, a day before presenting to our facility.
According to the patient’s family who provided the initial history, the patient reported tightness in her left arm while sitting at the dinner table. She was confused and subsequently had jerking movement of her right upper extremity with left facial twitching which lasted about 40 seconds. There was no loss of consciousness, or bowel or bladder control. She became unresponsive after the episode. Review of systems was negative except for a report of nausea a few hours before the onset of seizures, which resolved with ondansetron. Her past medical history was significant for breast cancer as already mentioned, seasonal allergic rhinitis, and hypertension. Home medications included hydrochlorothiazide 12.5 mg oral daily, aspirin 81 mg oral daily, and fexofenadine and loratadine oral daily as needed for allergies. There were no other significant surgical history other than already stated. The patient lived at home with her family and was independent with her instrumental activities of daily living. She is a former smoker of tobacco and quit smoking 30 years ago.
On arrival at our facility, the patient had normal vital signs. Significant findings on physical examination were an elderly female who seemed somnolent; not able to follow commands with a documented Glasgow Coma Scale of 10 with eyes opening spontaneously, incomprehensible sounds, and flexion withdrawal from pain as her best responses. She had an increased tone in her left upper extremity and had a brisk, deep tendon reflexes without clonus or 3+ (range, 0-5+, with 2+ being normal). The remainder of her physical exam was unremarkable. Laboratory testing revealed a glucose level of 120 mg/dL (normal, 65-110 mg/dL), sodium of 112 mEq/L (normal, 135-145 mmol/L), and chloride of 78 mEq/L (normal, 95-105 mmol/L). Serum osmolality and urine osmolality were 242 mOsm/kg (normal, 282-295 mOsm/kg) and 449 mOsm/kg (normal, 500-800 mOsm/kg) respectively, indicative of suboptimally dilute urine despite relatively low serum osmolality or SIADH. Urine electrolytes were not obtained.
Imaging studies including computed-tomography scans of the head and chest x-ray performed in the ED were unremarkable. After a phenytoin load, an electroencephalogram was obtained which showed diffuse encephalopathy without active seizure foci. A non-contrast magnetic-resonance imaging (MRI) of the brain was performed but it failed to show acute infarct, mass, mass effect, or brain herniation. There was nonspecific white matter abnormality with compromise of the bilateral cerebral hemispheres, calloseptal junction, left posterior pillar, and bilateral anterior pillars of the fornix, possibly representative of chronic white matter microvascular ischemic changes or less likely vasculitis or demyelination. Correction of her hyponatremia with normal saline was started in the ED with a change in serum sodium from 112 mEq/L to 115 mEq/L within 2 hours. She was admitted to the intensive care unit (ICU) where her sodium correction with normal saline and free water restriction was continued with a goal correction rate of 8-12 mEq/L in 24 hours. The patient’s serum sodium as well as level of consciousness improved gradually over the course of her ICU stay. After 64 hours in the hospital, her sodium had corrected to 137 mEq/L (normal, 135-145 mmol/L; Figure). She was then alert and oriented to person, place, and time. All motor findings noted on presentation had resolved. Her saline infusion was discontinued and serum sodium remained within normal range. She was discharged to a rehabilitation facility. Her hydrochlorothiazide was also discontinued.
Discussion
Hyponatremia is a common finding in cancer patients caused usually by paraneoplastic syndrome, chemotherapy, immunotherapy, or other associated treatment.6 SIADH is a frequent cause of hyponatremia in cancer patients and should be suspected in patients with hyponatremia, hypo-osmolality, and a urine osmolality above 100 mOsmol/kg.7
Our patient’s presentation and laboratory findings suggested SIADH as the likely cause of hyponatremia with a low sodium, a serum osmolality 242 mOsm/kg and urine osmolality of 449 mOsm/kg.8-10 She had no known underlying contributory comorbid condition relating to her serum lipids, thyroid, adrenal, kidney, or heart to date. Her use of a thiazide diuretic was the only confounding factor. The most plausible cause of hyponatremia/SIADH in our patient was likely cyclophosphamide based on her history, timeline of symptoms, and the absence of other possible causes. Though the mechanism for many of the previously mentioned etiologies are known, the mechanism of cyclophosphamide-induced SIADH is difficult to elucidate since the imminent complication of hemorrhagic cystitis means patients receiving this drug are often aggressively hydrated to prevent this complication.11,12 The result is that there is marked retention of water leading to potentially fatal hyponatremia in selected cases.11 This phenomenon has been fairly well described in patients receiving doses of 6 g/m2 as given in the STAMP protocol for stem cell mobilization or at doses of 30-50 mg/kg used to treat malignancy.12 Our patient clearly falls in this category given that she received a dose of 600 mg/m2. We found no evidence in her history to suggest post-operative, genetic or other cause for her hyponatremia. Our case mirrors a report by Koo and colleagues who described severe hyponatremia occurring within 24 hours following a single dose of intravenous cyclophosphamide 700 mg followed by saline infusion.13 In the case reported by Jayachandra and colleagues in which suspected cyclophosphamide-induced hyponatremia led to seizures, the patient received 500 mg IV of cyclophosphamide and had serum sodium as low as 106 mEq/L within a 24-hour period,2 similar to our patient.
There is a paucity of data on cyclophosphamide-induced SIADH. The mechanism by which cyclophosphamide causes SIADH is currently unknown. In addition, there are currently no set criteria that help identify at-risk patients who may develop such an event, including the dosage of cyclophosphamide that may trigger the SIADH, because lower doses of the drug have been associated with this complication.14
In a retrospective analysis by Lee and colleagues, cyclophosphamide-induced hyponatremia was found to be associated with male sex on a univariate analysis, but no risk factors were found in a multivariate analysis.15 It is likely that the concomitant use of diuretics, hydration, and high-dose cyclophosphamide contributed to hyponatremia/SIADH in our patient, though it is not clear through what mechanism. Harlow and colleagues proposed a mechanism for this phenomenon in 1979 based on the autopsy of a patient who had received high-dose cyclophosphamide involving degranulation of hypothalamic neurosecretory organelles and loss of Herring’s bodies. They inferred that metabolites of cyclophosphamide indirectly triggered inappropriate secretion of antidiuretic hormone as seen with a use of the structurally related analogue ifosfamide,16 but to our knowledge, this has yet to be replicated. Cyclophosphamide metabolite may have a direct tubular effect on the collecting duct epithelium leading to water retention15 as established by Campbell and colleagues. In one case, an established diabetes insipidus patient developed cyclophosphamide-induced antidiuresis without vasopressin secretion.17 It is imperative that the scientific community conduct research into the risk factors, underlying mechanisms, and methods of prevention to reduce and/or eliminate SIADH associated with use of cyclophosphamide.
1. Gilbar PJ, Richmond J, Wood J, Sullivan A. Syndrome of inappropriate antidiuretic hormone secretion induced by a single dose of oral cyclophosphamide. Ann Pharmacother. 2012.46(9):e23.
2. Jayachandran NV, Chandrasekhara PK, Thomas J, Agrawal S, Narsimulu G. Cyclophosphamide-associated complications: we need to be aware of SIADH and central pontine myelinolysis. Rheumatology (Oxford). 2009;48(1):89-90.
3. Baker M, Markman M, Niu J. Cyclophosphamide-induced severe acute hyponatremic encephalopathy in patients with breast cancer: report of two cases. Case Rep Oncol. 2014;7(2):550-554.
4. Lazarevic V, Hägg E, Wahlin A. Hiccups and severe hyponatremia associated with high-dose cyclophosphamide in conditioning regimen for allogeneic stem cell transplantation. Am J Hematol. 2007;82(1):88.
5. Geng C, Tang P, Zhang Y, Gao W. Hyponatremia induced by low-dose cyclophosphamide in two patients with breast cancer. Breast J. 2014; 20(4):442-443.
6. Kamoi K, Ebe T, Hasegawa A, et al. Hyponatremia in small cell lung cancer. Mechanisms not involving inappropriate ADH secretion. Cancer. 1987;60(5):1089-1093.
7. Matwiejczuk S, Püsküllüoğlu M, Zygulska AL. Oncological emergencies: syndrome of inappropriate antidiuretic hormone secretion (SIADH). Przegl Lek. 2014;71(10):541-543.
8. Robertson GL. Regulation of arginine vasopressin in the syndrome of inappropriate antidiuresis. Am J Med. 2006;119(7 Suppl 1):S36-42.
9. Robertson GL, Shelton RL, Athar S. The osmoregulation of vasopressin. Kidney Int. 1976;10(1):25-37.
10. Decaux G, Musch W. Clinical laboratory evaluation of the syndrome of inappropriate secretion of antidiuretic hormone. Clin J Am Soc Nephrol. 2008;3(4):1175-1184.
11. Bressler RB, Huston DP. Water intoxication following moderate-dose intravenous cyclophosphamide. Arch Intern Med. 1985;145(3):548-549.
12. Salido M, Macarron P, Hernández-García C, D’Cruz DP, Khamashta MA, Hughes GR. Water intoxication induced by low-dose cyclophosphamide in two patients with systemic lupus erythematosus. Lupus. 2003;12(8):636-639.
13. Koo TY, Bae SC, Park JS, et al. Water intoxication following low-dose intravenous cyclophosphamide. Electrolyte Blood Press. 2007;5(1):50-54.
14. [No authors listed]. Nausea and vasopressin. Lancet. 1991;337(8750):1133-1134.
15 Lee YC1, Park JS, Lee CH, et al. Hyponatraemia induced by low-dose intravenous pulse cyclophosphamide. Nephrol Dial Transplant. 2010;25(5):1520-1524.
16. Harlow PJ, DeClerck YA, Shore NA, Ortega JA, Carranza A, Heuser E. A fatal case of inappropriate ADH secretion induced by cyclophosphamide therapy. Cancer. 1979;44(3):896-898.
17. Campbell DM, Atkinson A, Gillis D, Sochett EB. Cyclophosphamide and water retention: mechanism revisited. J Pediatr Endocrinol Metab. 2000;13(6):673-675.
1. Gilbar PJ, Richmond J, Wood J, Sullivan A. Syndrome of inappropriate antidiuretic hormone secretion induced by a single dose of oral cyclophosphamide. Ann Pharmacother. 2012.46(9):e23.
2. Jayachandran NV, Chandrasekhara PK, Thomas J, Agrawal S, Narsimulu G. Cyclophosphamide-associated complications: we need to be aware of SIADH and central pontine myelinolysis. Rheumatology (Oxford). 2009;48(1):89-90.
3. Baker M, Markman M, Niu J. Cyclophosphamide-induced severe acute hyponatremic encephalopathy in patients with breast cancer: report of two cases. Case Rep Oncol. 2014;7(2):550-554.
4. Lazarevic V, Hägg E, Wahlin A. Hiccups and severe hyponatremia associated with high-dose cyclophosphamide in conditioning regimen for allogeneic stem cell transplantation. Am J Hematol. 2007;82(1):88.
5. Geng C, Tang P, Zhang Y, Gao W. Hyponatremia induced by low-dose cyclophosphamide in two patients with breast cancer. Breast J. 2014; 20(4):442-443.
6. Kamoi K, Ebe T, Hasegawa A, et al. Hyponatremia in small cell lung cancer. Mechanisms not involving inappropriate ADH secretion. Cancer. 1987;60(5):1089-1093.
7. Matwiejczuk S, Püsküllüoğlu M, Zygulska AL. Oncological emergencies: syndrome of inappropriate antidiuretic hormone secretion (SIADH). Przegl Lek. 2014;71(10):541-543.
8. Robertson GL. Regulation of arginine vasopressin in the syndrome of inappropriate antidiuresis. Am J Med. 2006;119(7 Suppl 1):S36-42.
9. Robertson GL, Shelton RL, Athar S. The osmoregulation of vasopressin. Kidney Int. 1976;10(1):25-37.
10. Decaux G, Musch W. Clinical laboratory evaluation of the syndrome of inappropriate secretion of antidiuretic hormone. Clin J Am Soc Nephrol. 2008;3(4):1175-1184.
11. Bressler RB, Huston DP. Water intoxication following moderate-dose intravenous cyclophosphamide. Arch Intern Med. 1985;145(3):548-549.
12. Salido M, Macarron P, Hernández-García C, D’Cruz DP, Khamashta MA, Hughes GR. Water intoxication induced by low-dose cyclophosphamide in two patients with systemic lupus erythematosus. Lupus. 2003;12(8):636-639.
13. Koo TY, Bae SC, Park JS, et al. Water intoxication following low-dose intravenous cyclophosphamide. Electrolyte Blood Press. 2007;5(1):50-54.
14. [No authors listed]. Nausea and vasopressin. Lancet. 1991;337(8750):1133-1134.
15 Lee YC1, Park JS, Lee CH, et al. Hyponatraemia induced by low-dose intravenous pulse cyclophosphamide. Nephrol Dial Transplant. 2010;25(5):1520-1524.
16. Harlow PJ, DeClerck YA, Shore NA, Ortega JA, Carranza A, Heuser E. A fatal case of inappropriate ADH secretion induced by cyclophosphamide therapy. Cancer. 1979;44(3):896-898.
17. Campbell DM, Atkinson A, Gillis D, Sochett EB. Cyclophosphamide and water retention: mechanism revisited. J Pediatr Endocrinol Metab. 2000;13(6):673-675.
Paraneoplastic leukemoid reaction – poor prognostic marker in urothelial bladder carcinoma
Certain cancers have been observed to cause symptoms called paraneoplastic syndromes that are not directly attributed to tumor invasion or compression. This phenomenon is believed to be secondary to a tumor’s secretion of functional hormones, peptides, cytokines, or its immune cross-reactivity. One such variant is a paraneoplastic leukemoid reaction (PLR), defined as a leukocytosis level of >50 x 103 cells/mm³, where the white blood cell (WBC) count differential exhibits a neutrophilia or left-shift, in which a predominance of early neutrophil precursors is observed. A PLR is believed to be incited by the tumor cell’s production of its own growth factors such as granulocyte-colony stimulating factor (G-CSF) and a number of different cytokines. These reactions may at first be mistaken for infectious processes, and it is only after an infection has been ruled out or when a leukocytosis is disproportionately high in the setting of a treated infection, that a paraneoplastic leukemoid reaction (PLR) is considered and an oncologic work-up pursued.
PLR has been previously described in a variety of malignancies including lung, esophageal, nasopharyngeal and laryngeal, gastric, cholangiocarcinoma, melanoma, multiple myeloma, renal, prostate, and hepatocellular carcinoma, but has rarely been described in urothelial carcinoma.1 Leukemoid reactions and autocrine growth induced by paraneoplastic production of G-CSF have rarely been associated with urothelial carcinoma of the bladder,2 as in the case we present here of a 67-year-old white man with invasive high-grade urothelial carcinoma of the bladder. The case highlights PLR as a negative prognostic marker, secondary to urothelial bladder cancer cells’ presumed production of G-CSF, rarely reported as in the literature previously.
Case presentation and summary
A 67-year-old white man was diagnosed with clinical stage III (T3N0M0), invasive high-grade urothelial carcinoma of the bladder (Figure 1). He received neoadjuvant chemotherapy with the standard gemcitabine-cisplatin combination (1,000 mg/m2 of gemcitabine on days 1, 8, and 15 with 70 mg/m2 of cisplatin on day 1 of a 28-day cycle for 3 cycles), and had less than partial response at the end of a 3-month course. A computed tomography scan of his pelvis obtained at treatment completion revealed persistent disease with noted enhancement of the right distal ureter and a right posterior bladder mass at the ureterovesical junction measuring 1.7 x 2.6 x 2.6 cm (0.6 x 1 x 1 in), for which, a cystoprostatectomy was recommended to remove remaining disease. The patient was seen in routine follow-up 3 weeks after his last chemotherapy treatment, when his WBC count was noted to be within normal limits at a value of 8.4 x 103 cells/mm³ (normal range, 4.5-11 x 103 cells/mm³).
One week later (a month after treatment completion), the patient presented to the emergency department with complaints of dysuria, urinary frequency, and suprapubic pain. He was found to have leukocytosis, with a WBC count of 47 x 103 cells/mm³, (normal range, 4.5-11 x 103 cells/mm³), with an elevated neutrophil count of 82.7% (normal range 40%-60%), without clinical signs of systemic infection (fevers, chills, or rigors). A urinalysis revealed pyuria with 25-50 WBC/high power field, negative nitrite, positive leukocyte esterase, and moderate bacteria, consistent with what was presumed to be a urinary tract infection. The patient was discharged home with a 1-week course of the antibiotic levofloxacin and the alpha-blocker tamsulosin to make urination easier. Of note, the final results of the urine culture, which returned 48 hours after discharge, showed no growth.
One week prior to surgery, the patient underwent a cystoscopy for ureteral stent exchange, which revealed a necrotic tumor at the right bladder base surrounding the ureteral orifice and stent. Renal pelvis urine, sampled during stent exchange, revealed >100,000 CFU/ml (colony forming units; normal value, <10³) Candida albicans, for which the patient was started on intravenous fluconazole for fungal infection. We consulted with our colleagues in the infectious disease department and continued to follow the patient throughout his hospital course, which included several antibiotic regimens, a comprehensive hematological work-up and eventual urologic surgery. Work-ups for myeloproliferative disorders, leukemia, JAK-2, and BCR-ABL were all negative. A peripheral blood smear analysis showed mostly neutrophils, no immature cells, and occasional hypersegmented neutrophils, but was overall inconsistent with myeloproliferative disease. Despite the patient’s persistent leukocytosis, he remained completely asymptomatic and his neutrophilia was attributed to his malignancy.
The patient subsequently underwent a cystoprostatectomy with ileal conduit. The surgical pathologic analysis showed a high-grade, invasive urothelial (transitional cell) carcinoma measuring 5.2 x 5.0 x 4.5 cm (2 x 1.9 x 1.8 in) with squamous differentiation, extensive tumor necrosis, lymphovascular invasion, invasion into the adjacent seminal vesicle and prostatic stroma, and negative margins (pT4a pN0 pMX; Figure 2). On the day of surgical resection, the patient’s leukocytosis was 70 x 103 cells/mm³.
Despite a transient improvement in his leukocytosis to 37.7 x 103 cells/mm³ on postoperative day 1, the patient remained in the medical intensive care unit for uncontrolled pain and management of his leukocytosis. It is worth noting that the patient remained afebrile throughout his entire 45-day hospitalization, with negative culture data, and despite receiving an extensive broad spectrum antibiotic regimen (levofloxacin, piperacillin-tazobactam, cefazolin, metronidazole, ceftriaxone and fluconazole), his leukocytosis continued to progress, peaking at 161.5 x 103 cells/mm³ less than a month after his surgery (Figure 3).
The patient continued to deteriorate rapidly, with a progressive leukocytosis, and developing metastases to the lung, perineum, and penis. He died a month after surgery (2 months after completion of neoadjuvant chemotherapy). The leukocytosis exhibited in this patient and the aggressive tumor cell growth are believed to have been secondary to a paraneoplastic leukemoid reaction incited by the urothelial bladder cancer cells’ presumed production of G-CSF, which has been rarely reported in the literature previously.
Discussion
We report here on the rare occurrence of PLR in a urothelial bladder cancer. Several mechanisms have been proposed to explain the pathophysiology of PLR. The levels of IL-1[alpha and beta], IL-3, G-CSF, GM-CSF, IL-6, and TNF-[alpha] have all been reported to be elevated in various solid tumors and suggested to contribute to an elevated leukocyte count.3 With previous reports that receptors for G-CSF have been found on cell surfaces of several nonhematopoietic cell types, Tachibana and Murai have proposed the mechanism of a cancer cell’s simultaneous acquisition of the ligand promotion and its receptor expression conferring an autocrine growth advantage.4 They have also reported on the capability of bladder cancer cells to induce a leukemoid reaction in their host through the stimulation of leukocyte production, which has been associated with aggressive tumor cell growth and a poor clinical outcome. In addition, He and colleagues have also described the correlation between PLR and high degree of malignancy, high probability of metastasis, recurrence, and poor prognosis.5
We observed the leukocytosis of 70 x 103 cells/mm³ on the day of resection with a slight drop postoperatively, peaking at 161.5 x 103 cells/mm³ less than a month after resection of the tumor. There is no clear understanding of the cause of the persistent and rapid progression of leukocytosis seen in this patient postoperatively. There is also a dearth of literature describing similar occurrences, with even fewer attempting to explain the pathophysiology of this occurrence.
When faced with similar occurrences in patients, clinicians usually treat for occult infection. Once infections and myeloproliferative diseases have been ruled out, clinicians may consider obtaining a patient’s serum G-CSF level or performing an immunohistochemistry analysis of urothelial cells for overexpression of G-CSF, when available.5 However, despite any efforts to diagnose earlier, there is little clinicians currently have to offer these patients as treatment.
As presented in this report, PLR portends a worse prognosis for patients because of its ability to not only masquerade as an infection leading to a delay in the proper treatment, but also because of its association with a more aggressive tumor cell behavior and growth, making it critically important for clinicians to be able to identify these patients early on. With further investigation into immune regulation and G-CSF receptor signaling, there may be future discoveries of novel methods to diagnose this condition and also advancements in the treatment options made available to these patients.
1. Chakraborty S, Keenportz B, Woodward S, Anderson J, Colan D. Paraneoplastic leukemoid reaction in solid tumors. Am J Clin Oncol. 2015;38(3):326-330.
2. Kumar AK, Satyan MT, Holzbeierlein J, Mirza M, Van Veldhuizen P. Leukemoid reaction and autocrine growth of bladder cancer induced by paraneoplastic production of granulocyte colony-stimulating factor-a potential neoplastic marker: a case report and review of the literature. J Med Case Rep. 2014;8(1):147.
3. Azuma T, Sakai I, Matsumoto T, et al. Leukemoid reaction in association with bone marrow necrosis due to metastatic prostate cancer. Intern Med. 2005;44(10):1093-1096.
4. Tachibana M, Murai M. G-CSF production in human bladder cancer and its ability to promote autocrine growth: a review. Cytokines Cell Mol Ther. 1998;4(2):113-120.
5. He H, Zhang Z, Ge J, Zhou W. Leukemoid reaction associated with transitional cell carcinoma: a case report and literature review. Niger J Clin Pract. 2014;17(3):391-394.
Certain cancers have been observed to cause symptoms called paraneoplastic syndromes that are not directly attributed to tumor invasion or compression. This phenomenon is believed to be secondary to a tumor’s secretion of functional hormones, peptides, cytokines, or its immune cross-reactivity. One such variant is a paraneoplastic leukemoid reaction (PLR), defined as a leukocytosis level of >50 x 103 cells/mm³, where the white blood cell (WBC) count differential exhibits a neutrophilia or left-shift, in which a predominance of early neutrophil precursors is observed. A PLR is believed to be incited by the tumor cell’s production of its own growth factors such as granulocyte-colony stimulating factor (G-CSF) and a number of different cytokines. These reactions may at first be mistaken for infectious processes, and it is only after an infection has been ruled out or when a leukocytosis is disproportionately high in the setting of a treated infection, that a paraneoplastic leukemoid reaction (PLR) is considered and an oncologic work-up pursued.
PLR has been previously described in a variety of malignancies including lung, esophageal, nasopharyngeal and laryngeal, gastric, cholangiocarcinoma, melanoma, multiple myeloma, renal, prostate, and hepatocellular carcinoma, but has rarely been described in urothelial carcinoma.1 Leukemoid reactions and autocrine growth induced by paraneoplastic production of G-CSF have rarely been associated with urothelial carcinoma of the bladder,2 as in the case we present here of a 67-year-old white man with invasive high-grade urothelial carcinoma of the bladder. The case highlights PLR as a negative prognostic marker, secondary to urothelial bladder cancer cells’ presumed production of G-CSF, rarely reported as in the literature previously.
Case presentation and summary
A 67-year-old white man was diagnosed with clinical stage III (T3N0M0), invasive high-grade urothelial carcinoma of the bladder (Figure 1). He received neoadjuvant chemotherapy with the standard gemcitabine-cisplatin combination (1,000 mg/m2 of gemcitabine on days 1, 8, and 15 with 70 mg/m2 of cisplatin on day 1 of a 28-day cycle for 3 cycles), and had less than partial response at the end of a 3-month course. A computed tomography scan of his pelvis obtained at treatment completion revealed persistent disease with noted enhancement of the right distal ureter and a right posterior bladder mass at the ureterovesical junction measuring 1.7 x 2.6 x 2.6 cm (0.6 x 1 x 1 in), for which, a cystoprostatectomy was recommended to remove remaining disease. The patient was seen in routine follow-up 3 weeks after his last chemotherapy treatment, when his WBC count was noted to be within normal limits at a value of 8.4 x 103 cells/mm³ (normal range, 4.5-11 x 103 cells/mm³).
One week later (a month after treatment completion), the patient presented to the emergency department with complaints of dysuria, urinary frequency, and suprapubic pain. He was found to have leukocytosis, with a WBC count of 47 x 103 cells/mm³, (normal range, 4.5-11 x 103 cells/mm³), with an elevated neutrophil count of 82.7% (normal range 40%-60%), without clinical signs of systemic infection (fevers, chills, or rigors). A urinalysis revealed pyuria with 25-50 WBC/high power field, negative nitrite, positive leukocyte esterase, and moderate bacteria, consistent with what was presumed to be a urinary tract infection. The patient was discharged home with a 1-week course of the antibiotic levofloxacin and the alpha-blocker tamsulosin to make urination easier. Of note, the final results of the urine culture, which returned 48 hours after discharge, showed no growth.
One week prior to surgery, the patient underwent a cystoscopy for ureteral stent exchange, which revealed a necrotic tumor at the right bladder base surrounding the ureteral orifice and stent. Renal pelvis urine, sampled during stent exchange, revealed >100,000 CFU/ml (colony forming units; normal value, <10³) Candida albicans, for which the patient was started on intravenous fluconazole for fungal infection. We consulted with our colleagues in the infectious disease department and continued to follow the patient throughout his hospital course, which included several antibiotic regimens, a comprehensive hematological work-up and eventual urologic surgery. Work-ups for myeloproliferative disorders, leukemia, JAK-2, and BCR-ABL were all negative. A peripheral blood smear analysis showed mostly neutrophils, no immature cells, and occasional hypersegmented neutrophils, but was overall inconsistent with myeloproliferative disease. Despite the patient’s persistent leukocytosis, he remained completely asymptomatic and his neutrophilia was attributed to his malignancy.
The patient subsequently underwent a cystoprostatectomy with ileal conduit. The surgical pathologic analysis showed a high-grade, invasive urothelial (transitional cell) carcinoma measuring 5.2 x 5.0 x 4.5 cm (2 x 1.9 x 1.8 in) with squamous differentiation, extensive tumor necrosis, lymphovascular invasion, invasion into the adjacent seminal vesicle and prostatic stroma, and negative margins (pT4a pN0 pMX; Figure 2). On the day of surgical resection, the patient’s leukocytosis was 70 x 103 cells/mm³.
Despite a transient improvement in his leukocytosis to 37.7 x 103 cells/mm³ on postoperative day 1, the patient remained in the medical intensive care unit for uncontrolled pain and management of his leukocytosis. It is worth noting that the patient remained afebrile throughout his entire 45-day hospitalization, with negative culture data, and despite receiving an extensive broad spectrum antibiotic regimen (levofloxacin, piperacillin-tazobactam, cefazolin, metronidazole, ceftriaxone and fluconazole), his leukocytosis continued to progress, peaking at 161.5 x 103 cells/mm³ less than a month after his surgery (Figure 3).
The patient continued to deteriorate rapidly, with a progressive leukocytosis, and developing metastases to the lung, perineum, and penis. He died a month after surgery (2 months after completion of neoadjuvant chemotherapy). The leukocytosis exhibited in this patient and the aggressive tumor cell growth are believed to have been secondary to a paraneoplastic leukemoid reaction incited by the urothelial bladder cancer cells’ presumed production of G-CSF, which has been rarely reported in the literature previously.
Discussion
We report here on the rare occurrence of PLR in a urothelial bladder cancer. Several mechanisms have been proposed to explain the pathophysiology of PLR. The levels of IL-1[alpha and beta], IL-3, G-CSF, GM-CSF, IL-6, and TNF-[alpha] have all been reported to be elevated in various solid tumors and suggested to contribute to an elevated leukocyte count.3 With previous reports that receptors for G-CSF have been found on cell surfaces of several nonhematopoietic cell types, Tachibana and Murai have proposed the mechanism of a cancer cell’s simultaneous acquisition of the ligand promotion and its receptor expression conferring an autocrine growth advantage.4 They have also reported on the capability of bladder cancer cells to induce a leukemoid reaction in their host through the stimulation of leukocyte production, which has been associated with aggressive tumor cell growth and a poor clinical outcome. In addition, He and colleagues have also described the correlation between PLR and high degree of malignancy, high probability of metastasis, recurrence, and poor prognosis.5
We observed the leukocytosis of 70 x 103 cells/mm³ on the day of resection with a slight drop postoperatively, peaking at 161.5 x 103 cells/mm³ less than a month after resection of the tumor. There is no clear understanding of the cause of the persistent and rapid progression of leukocytosis seen in this patient postoperatively. There is also a dearth of literature describing similar occurrences, with even fewer attempting to explain the pathophysiology of this occurrence.
When faced with similar occurrences in patients, clinicians usually treat for occult infection. Once infections and myeloproliferative diseases have been ruled out, clinicians may consider obtaining a patient’s serum G-CSF level or performing an immunohistochemistry analysis of urothelial cells for overexpression of G-CSF, when available.5 However, despite any efforts to diagnose earlier, there is little clinicians currently have to offer these patients as treatment.
As presented in this report, PLR portends a worse prognosis for patients because of its ability to not only masquerade as an infection leading to a delay in the proper treatment, but also because of its association with a more aggressive tumor cell behavior and growth, making it critically important for clinicians to be able to identify these patients early on. With further investigation into immune regulation and G-CSF receptor signaling, there may be future discoveries of novel methods to diagnose this condition and also advancements in the treatment options made available to these patients.
Certain cancers have been observed to cause symptoms called paraneoplastic syndromes that are not directly attributed to tumor invasion or compression. This phenomenon is believed to be secondary to a tumor’s secretion of functional hormones, peptides, cytokines, or its immune cross-reactivity. One such variant is a paraneoplastic leukemoid reaction (PLR), defined as a leukocytosis level of >50 x 103 cells/mm³, where the white blood cell (WBC) count differential exhibits a neutrophilia or left-shift, in which a predominance of early neutrophil precursors is observed. A PLR is believed to be incited by the tumor cell’s production of its own growth factors such as granulocyte-colony stimulating factor (G-CSF) and a number of different cytokines. These reactions may at first be mistaken for infectious processes, and it is only after an infection has been ruled out or when a leukocytosis is disproportionately high in the setting of a treated infection, that a paraneoplastic leukemoid reaction (PLR) is considered and an oncologic work-up pursued.
PLR has been previously described in a variety of malignancies including lung, esophageal, nasopharyngeal and laryngeal, gastric, cholangiocarcinoma, melanoma, multiple myeloma, renal, prostate, and hepatocellular carcinoma, but has rarely been described in urothelial carcinoma.1 Leukemoid reactions and autocrine growth induced by paraneoplastic production of G-CSF have rarely been associated with urothelial carcinoma of the bladder,2 as in the case we present here of a 67-year-old white man with invasive high-grade urothelial carcinoma of the bladder. The case highlights PLR as a negative prognostic marker, secondary to urothelial bladder cancer cells’ presumed production of G-CSF, rarely reported as in the literature previously.
Case presentation and summary
A 67-year-old white man was diagnosed with clinical stage III (T3N0M0), invasive high-grade urothelial carcinoma of the bladder (Figure 1). He received neoadjuvant chemotherapy with the standard gemcitabine-cisplatin combination (1,000 mg/m2 of gemcitabine on days 1, 8, and 15 with 70 mg/m2 of cisplatin on day 1 of a 28-day cycle for 3 cycles), and had less than partial response at the end of a 3-month course. A computed tomography scan of his pelvis obtained at treatment completion revealed persistent disease with noted enhancement of the right distal ureter and a right posterior bladder mass at the ureterovesical junction measuring 1.7 x 2.6 x 2.6 cm (0.6 x 1 x 1 in), for which, a cystoprostatectomy was recommended to remove remaining disease. The patient was seen in routine follow-up 3 weeks after his last chemotherapy treatment, when his WBC count was noted to be within normal limits at a value of 8.4 x 103 cells/mm³ (normal range, 4.5-11 x 103 cells/mm³).
One week later (a month after treatment completion), the patient presented to the emergency department with complaints of dysuria, urinary frequency, and suprapubic pain. He was found to have leukocytosis, with a WBC count of 47 x 103 cells/mm³, (normal range, 4.5-11 x 103 cells/mm³), with an elevated neutrophil count of 82.7% (normal range 40%-60%), without clinical signs of systemic infection (fevers, chills, or rigors). A urinalysis revealed pyuria with 25-50 WBC/high power field, negative nitrite, positive leukocyte esterase, and moderate bacteria, consistent with what was presumed to be a urinary tract infection. The patient was discharged home with a 1-week course of the antibiotic levofloxacin and the alpha-blocker tamsulosin to make urination easier. Of note, the final results of the urine culture, which returned 48 hours after discharge, showed no growth.
One week prior to surgery, the patient underwent a cystoscopy for ureteral stent exchange, which revealed a necrotic tumor at the right bladder base surrounding the ureteral orifice and stent. Renal pelvis urine, sampled during stent exchange, revealed >100,000 CFU/ml (colony forming units; normal value, <10³) Candida albicans, for which the patient was started on intravenous fluconazole for fungal infection. We consulted with our colleagues in the infectious disease department and continued to follow the patient throughout his hospital course, which included several antibiotic regimens, a comprehensive hematological work-up and eventual urologic surgery. Work-ups for myeloproliferative disorders, leukemia, JAK-2, and BCR-ABL were all negative. A peripheral blood smear analysis showed mostly neutrophils, no immature cells, and occasional hypersegmented neutrophils, but was overall inconsistent with myeloproliferative disease. Despite the patient’s persistent leukocytosis, he remained completely asymptomatic and his neutrophilia was attributed to his malignancy.
The patient subsequently underwent a cystoprostatectomy with ileal conduit. The surgical pathologic analysis showed a high-grade, invasive urothelial (transitional cell) carcinoma measuring 5.2 x 5.0 x 4.5 cm (2 x 1.9 x 1.8 in) with squamous differentiation, extensive tumor necrosis, lymphovascular invasion, invasion into the adjacent seminal vesicle and prostatic stroma, and negative margins (pT4a pN0 pMX; Figure 2). On the day of surgical resection, the patient’s leukocytosis was 70 x 103 cells/mm³.
Despite a transient improvement in his leukocytosis to 37.7 x 103 cells/mm³ on postoperative day 1, the patient remained in the medical intensive care unit for uncontrolled pain and management of his leukocytosis. It is worth noting that the patient remained afebrile throughout his entire 45-day hospitalization, with negative culture data, and despite receiving an extensive broad spectrum antibiotic regimen (levofloxacin, piperacillin-tazobactam, cefazolin, metronidazole, ceftriaxone and fluconazole), his leukocytosis continued to progress, peaking at 161.5 x 103 cells/mm³ less than a month after his surgery (Figure 3).
The patient continued to deteriorate rapidly, with a progressive leukocytosis, and developing metastases to the lung, perineum, and penis. He died a month after surgery (2 months after completion of neoadjuvant chemotherapy). The leukocytosis exhibited in this patient and the aggressive tumor cell growth are believed to have been secondary to a paraneoplastic leukemoid reaction incited by the urothelial bladder cancer cells’ presumed production of G-CSF, which has been rarely reported in the literature previously.
Discussion
We report here on the rare occurrence of PLR in a urothelial bladder cancer. Several mechanisms have been proposed to explain the pathophysiology of PLR. The levels of IL-1[alpha and beta], IL-3, G-CSF, GM-CSF, IL-6, and TNF-[alpha] have all been reported to be elevated in various solid tumors and suggested to contribute to an elevated leukocyte count.3 With previous reports that receptors for G-CSF have been found on cell surfaces of several nonhematopoietic cell types, Tachibana and Murai have proposed the mechanism of a cancer cell’s simultaneous acquisition of the ligand promotion and its receptor expression conferring an autocrine growth advantage.4 They have also reported on the capability of bladder cancer cells to induce a leukemoid reaction in their host through the stimulation of leukocyte production, which has been associated with aggressive tumor cell growth and a poor clinical outcome. In addition, He and colleagues have also described the correlation between PLR and high degree of malignancy, high probability of metastasis, recurrence, and poor prognosis.5
We observed the leukocytosis of 70 x 103 cells/mm³ on the day of resection with a slight drop postoperatively, peaking at 161.5 x 103 cells/mm³ less than a month after resection of the tumor. There is no clear understanding of the cause of the persistent and rapid progression of leukocytosis seen in this patient postoperatively. There is also a dearth of literature describing similar occurrences, with even fewer attempting to explain the pathophysiology of this occurrence.
When faced with similar occurrences in patients, clinicians usually treat for occult infection. Once infections and myeloproliferative diseases have been ruled out, clinicians may consider obtaining a patient’s serum G-CSF level or performing an immunohistochemistry analysis of urothelial cells for overexpression of G-CSF, when available.5 However, despite any efforts to diagnose earlier, there is little clinicians currently have to offer these patients as treatment.
As presented in this report, PLR portends a worse prognosis for patients because of its ability to not only masquerade as an infection leading to a delay in the proper treatment, but also because of its association with a more aggressive tumor cell behavior and growth, making it critically important for clinicians to be able to identify these patients early on. With further investigation into immune regulation and G-CSF receptor signaling, there may be future discoveries of novel methods to diagnose this condition and also advancements in the treatment options made available to these patients.
1. Chakraborty S, Keenportz B, Woodward S, Anderson J, Colan D. Paraneoplastic leukemoid reaction in solid tumors. Am J Clin Oncol. 2015;38(3):326-330.
2. Kumar AK, Satyan MT, Holzbeierlein J, Mirza M, Van Veldhuizen P. Leukemoid reaction and autocrine growth of bladder cancer induced by paraneoplastic production of granulocyte colony-stimulating factor-a potential neoplastic marker: a case report and review of the literature. J Med Case Rep. 2014;8(1):147.
3. Azuma T, Sakai I, Matsumoto T, et al. Leukemoid reaction in association with bone marrow necrosis due to metastatic prostate cancer. Intern Med. 2005;44(10):1093-1096.
4. Tachibana M, Murai M. G-CSF production in human bladder cancer and its ability to promote autocrine growth: a review. Cytokines Cell Mol Ther. 1998;4(2):113-120.
5. He H, Zhang Z, Ge J, Zhou W. Leukemoid reaction associated with transitional cell carcinoma: a case report and literature review. Niger J Clin Pract. 2014;17(3):391-394.
1. Chakraborty S, Keenportz B, Woodward S, Anderson J, Colan D. Paraneoplastic leukemoid reaction in solid tumors. Am J Clin Oncol. 2015;38(3):326-330.
2. Kumar AK, Satyan MT, Holzbeierlein J, Mirza M, Van Veldhuizen P. Leukemoid reaction and autocrine growth of bladder cancer induced by paraneoplastic production of granulocyte colony-stimulating factor-a potential neoplastic marker: a case report and review of the literature. J Med Case Rep. 2014;8(1):147.
3. Azuma T, Sakai I, Matsumoto T, et al. Leukemoid reaction in association with bone marrow necrosis due to metastatic prostate cancer. Intern Med. 2005;44(10):1093-1096.
4. Tachibana M, Murai M. G-CSF production in human bladder cancer and its ability to promote autocrine growth: a review. Cytokines Cell Mol Ther. 1998;4(2):113-120.
5. He H, Zhang Z, Ge J, Zhou W. Leukemoid reaction associated with transitional cell carcinoma: a case report and literature review. Niger J Clin Pract. 2014;17(3):391-394.
Demystifying the diagnosis and classification of lymphoma: a guide to the hematopathologist’s galaxy
Lymphomas constitute a very heterogeneous group of neoplasms with diverse clinical presentations, prognoses, and responses to therapy. Approximately 80,500 new cases of lymphoma are expected to be diagnosed in the United States in 2017, of which about one quarter will lead to the death of the patient.1 Perhaps more so than any other group of neoplasms, the diagnosis of lymphoma involves the integration of a multiplicity of clinical, histologic and immunophenotypic findings and, on occasion, cytogenetic and molecular results as well. An accurate diagnosis of lymphoma, usually rendered by hematopathologists, allows hematologists/oncologists to treat patients appropriately. Herein we will describe a simplified approach to the diagnosis and classification of lymphomas (Figure 1).
Lymphoma classification
Lymphomas are clonal neoplasms characterized by the expansion of abnormal lymphoid cells that may develop in any organ but commonly involve lymph nodes. The fourth edition of the World Health Organization (WHO) Classification of Tumours of Haematopoietic and Lymphoid tissues, published in 2008, is the official and most current guideline used for diagnosis of lymphoid neoplasms.2 The WHO scheme classifies lymphomas according to the type of cell from which they are derived (mature and immature B cells, T cells, or natural killer (NK) cells, findings determined by their morphology and immunophenotype) and their clinical, cytogenetic, and/or molecular features. This official classification is currently being updated3 and is expected to be published in full in 2017, at which time it is anticipated to include definitions for more than 70 distinct neoplasms.
Lymphomas are broadly and informally classified as Hodgkin lymphomas (HLs) and non-Hodgkin lymphomas (NHLs), based on the differences these two groups show in their clinical presentation, treatment, prognosis, and proportion of neoplastic cells, among others. NHLs are by far the most common type of lymphomas, accounting for approximately 90% of all new cases of lymphoma in the United States and 70% worldwide.1,2 NHLs are a very heterogeneous group of B-, T-, or NK-cell neoplasms that, in turn, can also be informally subclassified as low-grade (or indolent) or high-grade (or aggressive) according to their predicted clinical behavior. HLs are comparatively rare, less heterogeneous, uniformly of B-cell origin and, in the case of classical Hodgkin lymphoma, highly curable.1,2 It is beyond the scope of this manuscript to outline the features of each of the >70 specific entities, but the reader is referred elsewhere for more detail and encouraged to become familiarized with the complexity, challenges, and beauty of lymphoma diagnosis.2,3
Biopsy procedure
A correct diagnosis begins with an adequate biopsy procedure. It is essential that biopsy specimens for lymphoma evaluation be submitted fresh and unfixed, because some crucial analyses such as flow cytometry or conventional cytogenetics can only be performed on fresh tissue. Indeed, it is important for the hematologist/oncologist and/or surgeon and/or interventional radiologist to converse with the hematopathologist prior to and even during some procedures to ensure the correct processing of the specimen. Also, it is important to limit the compression of the specimen and the excessive use of cauterization during the biopsy procedure, both of which cause artifacts that may render impossible the interpretation of the histopathologic findings.
Given that the diagnosis of lymphoma is based not only on the cytologic details of the lymphoma cells but also on the architectural pattern with which they infiltrate an organ, the larger the biopsy specimen, the easier it will be for a hematopathologist to identify the pattern. In addition, excisional biopsies frequently contain more diagnostic tissue than needle core biopsies and this provides pathologists with the option to submit tissue fragments for ancillary tests that require unfixed tissue as noted above. Needle core biopsies of lymph nodes are increasingly being used because of their association with fewer complications and lower cost than excisional biopsies. However, needle core biopsies provide only a glimpse of the pattern of infiltration and may not be completely representative of the architecture. Therefore, excisional lymph node biopsies of lymph nodes are preferred over needle core biopsies, recognizing that in the setting of deeply seated lymph nodes, needle core biopsies may be the only or the best surgical option.
Clinical presentation
Accurate diagnosis of lymphoma cannot take place in a vacuum. The hematopathologist’s initial approach to the diagnosis of lymphoid processes in tissue biopsies should begin with a thorough review of the clinical history, although some pathology laboratories may not have immediate access to this information. The hematopathologist should evaluate factors such as age, gender, location of the tumor, symptomatology, medications, serology, and prior history of malignancy, immunosuppression or immunodeficiency in every case. Other important but frequently omitted parts of the clinical history are the patient’s occupation, history of exposure to animals, and the presence of tattoos, which may be associated with certain reactive lymphadenopathies.
Histomorphologic evaluation
Despite the plethora of new and increasingly sophisticated tools, histologic and morphologic analysis still remains the cornerstone of diagnosis in hematopathology. However, for the characterization of an increasing number of reactive and neoplastic lymphoid processes, hematopathologists may also require immunophenotypic, molecular, and cytogenetic tests for an accurate diagnosis. Upon review of the clinical information, a microscopic evaluation of the tissue submitted for processing by the histology laboratory will be performed. The results of concurrent flow cytometric evaluation (performed on fresh unfixed material) should also be available in most if not all cases before the H&E-stained slides are available for review. Upon receipt of H&E-stained slides, the hematopathologist will evaluate the quality of the submitted specimen, since many diagnostic difficulties stem from suboptimal techniques related to the biopsy procedure, fixation, processing, cutting, or staining (Figure 1). If deemed suitable for accurate diagnosis, a search for signs of preservation or disruption of the organ that was biopsied will follow. The identification of certain morphologic patterns aids the hematopathologist in answering the first question: “what organ is this and is this consistent with what is indicated on the requisition?” This is usually immediately followed by “is this sufficient and adequate material for a diagnosis?” and “is there any normal architecture?” If the architecture is not normal, “is this alteration due to a reactive or a neoplastic process?” If neoplastic, “is it lymphoma or a non-hematolymphoid neoplasm?”
Both reactive and neoplastic processes have variably unique morphologic features that if properly recognized, guide the subsequent testing. However, some reactive and neoplastic processes can present with overlapping features, and even after extensive immunophenotypic evaluation and the performance of ancillary studies, it may not be possible to conclusively determine its nature. If the lymph node architecture is altered or effaced, the predominant pattern of infiltration (eg, nodular, diffuse, interfollicular, intrasinusoidal) and the degree of alteration of the normal architecture is evaluated, usually at low magnification. When the presence of an infiltrate is recognized, its components must be characterized. If the infiltrate is composed of a homogeneous expansion of lymphoid cells that disrupts or replaces the normal lymphoid architecture, a lymphoma will be suspected or diagnosed. The pattern of distribution of the cells along with their individual morphologic characteristics (ie, size, nuclear shape, chromatin configuration, nucleoli, amount and hue of cytoplasm) are key factors for the diagnosis and classification of the lymphoma that will guide subsequent testing. The immunophenotypic analysis (by immunohistochemistry, flow cytometry or a combination of both) may confirm the reactive or neoplastic nature of the process, and its subclassification. B-cell lymphomas, in particular have variable and distinctive histologic features: as a diffuse infiltrate of large mature lymphoid cells (eg, diffuse large B-cell lymphoma), an expansion of immature lymphoid cells (lymphoblastic lymphoma), and a nodular infiltrate of small, intermediate and/or mature large B cells (eg, follicular lymphoma).
Mature T-cell lymphomas may display similar histologic, features but they can be quite heterogeneous with an infiltrate composed of one predominant cell type or a mixture of small, medium-sized, and large atypical lymphoid cells (on occasion with abundant clear cytoplasm) and a variable number of eosinophils, plasma cells, macrophages (including granulomas), and B cells. HLs most commonly efface the lymph node architecture with a nodular or diffuse infiltrate variably composed of reactive lymphocytes, granulocytes, macrophages, and plasma cells and usually a minority of large neoplastic cells (Hodgkin/Reed-Sternberg cells and/or lymphocyte predominant cells).
Once the H&E-stained slides are evaluated and a diagnosis of lymphoma is suspected or established, the hematopathologist will attempt to determine whether it has mature or immature features, and whether low- or high-grade morphologic characteristics are present. The maturity of lymphoid cells is generally determined by the nature of the chromatin, which if “fine” and homogeneous (with or without a conspicuous nucleolus) will usually, but not always, be considered immature, whereas clumped, vesicular or hyperchromatic chromatin is generally, but not always, associated with maturity. If the chromatin displays immature features, the differential diagnosis will mainly include B- and T-lymphoblastic lymphomas, but also blastoid variants of mature neoplasm such as mantle cell lymphoma, and follicular lymphoma, as well as high-grade B-cell lymphomas. Features associated with low-grade lymphomas (eg, follicular lymphoma, small lymphocytic lymphoma/chronic lymphocytic leukemia, marginal zone lymphoma, lymphoplasmacytic lymphoma) include small cell morphology, mature chromatin, absence of a significant number of mitoses or apoptotic cells, and a low proliferation index as shown by immunohistochemistry for Ki67. High-grade lymphomas, such as lymphoblastic lymphoma, Burkitt lymphoma, or certain large B-cell lymphomas tend to show opposite features, and some of the mature entities are frequently associated with MYC rearrangements. Of note, immature lymphomas tend to be clinically high grade, but not all clinically high-grade lymphomas are immature. Conversely, the majority of low-grade lymphomas are usually mature.
Immunophenotypic evaluation
Immunophenotypic evaluation is essential because the lineage of lymphoma cells cannot be determined by morphology alone. The immunophenotype is the combination of proteins/markers (eg, CD20, CD3, TdT) expressed by cells. Usually, it is evaluated by immunohistochemistry and/or flow cytometry, which help determine the proportion of lymphoid cells that express a certain marker and its location and intensity within the cells. While immunohistochemistry is normally performed on formalin-fixed and paraffin-embedded tissue, flow cytometry can be evaluated only on fresh unfixed tissue. Flow cytometry has the advantage over immunohistochemistry of being faster and better at simultaneously identifying coexpression of multiple markers on multiple cell populations. However, certain markers can only be evaluated by immunohistochemistry.
The immunophenotypic analysis will in most cases reveal whether the lymphomas is of B-, T- or NK-cell origin, and whether a lymphoma subtype associated immunophenotype is present. Typical pan B-cell antigens include PAX5, CD19, and CD79a (CD20 is less broadly expressed throughout B-cell differentiation, although it is usually evident in most mature B-cell lymphomas), and typical pan T-cell antigens include CD2, CD5, and CD7. The immature or mature nature of a lymphoma can also be confirmed by evaluation of the immunophenotype. Immature lymphomas commonly express one or more of TdT, CD10, or CD34; T-lymphoblastic lymphoma cells may also coexpress CD1a. The majority of NHLs and all HLs are derived from (or reflect) B cells at different stages of maturation. Mature B-cell lymphomas are the most common type of lymphoma and typically, but not always, express pan B-cell markers as well as surface membrane immunoglobulin, with the latter also most useful in assessing clonality via a determination of light chain restriction. Some mature B-cell lymphomas tend to acquire markers that are either never physiologically expressed by normal mature B cells (eg, cyclin D1 in mantle cell lymphoma, or BCL2 in germinal center B cells in follicular lymphoma) or only expressed in a minor fraction (eg, CD5 that is characteristically expressed in small lymphocytic and mantle cell lymphoma). The most common mature B-cell lymphomas include diffuse large B-cell lymphoma, follicular lymphoma, small lymphocytic lymphoma, mantle cell lymphoma, marginal zone lymphoma, Burkitt lymphoma, and lymphoplasmacytic lymphoma (Figures 2 and 3). Classical HLs are also lymphomas of B-cell origin that demonstrate diminished preservation of their B-cell immunophenotype (as evidenced by the dim expression of PAX5 but absence of most other pan B-cell antigens), expression of CD30, variable expression of CD15, and loss of CD45 (Figure 1). In contrast, nodular lymphocyte predominant HL shows a preserved B-cell immunophenotypic program and expression of CD45, typically without CD30 and CD15. Of note, the evaluation of the immunophenotype of the neoplastic cells in HL is routinely assessed by immunohistochemistry because most flow cytometry laboratories cannot reliably detect and characterize the low numbers of these cells.
Mature T-cell lymphomas generally express one or more T-cell markers, and tend to display a T-helper (CD4-positive) or cytotoxic (CD8-positive) immunophenotype and may show loss of markers expressed by most normal T-cells (eg, CD5, CD7; Figure 4). However, a subset of them may express markers not commonly detected in normal T cells, such as ALK. NK-cell lymphomas lack surface CD3 (expressing only cytoplasmic CD3) and CD5 but express some pan T-cell antigens (such as CD2 and CD7) as well as CD16 and/or CD56.
Patients with primary or acquired immune dysfunction are at risk for development of lymphoma and other less clearly defined lymphoproliferative disorders, the majority of which are associated with infection of the lymphoid cells with Epstein-Barr virus (EBV). Therefore, evaluation with chromogenic in situ hybridization for an EBV-encoded early RNA (EBER1) is routinely performed in these cases; it is thus essential that the hematopathologist be informed of the altered immune system of the patient. If lymphoma develops, they may be morphologically similar to those that appear in immunocompetent patients, which specifically in the post-transplant setting are known as monomorphic post-transplant lymphoproliferative disorders (PTLD). If the PTLD does not meet the criteria for any of the recognized types of lymphoma, it may be best characterized as a polymorphic PTLD.
Once the lineage (B-, T-, or NK-cell) of the mature lymphoma has been established, the sum (and on occasion the gestalt) of the clinical, morphologic, immunophenotypic and other findings will be considered for the subclassification of the neoplasm.
Cytogenetic and molecular evaluation
If the morphologic and immunophenotypic analysis is inconclusive or nondiagnostic, then molecular and/or cytogenetic testing may further aid in the characterization of the process. Some of available molecular tests include analyses for the rearrangements of the variable region of the immunoglobulin (IG) or T-cell receptor (TCR) genes and for mutations on specific genes. The identification of specific mutations not only confirms the clonal nature of the process but, on occasion, it may also help subclassify the lymphoma, whereas IG or TCR rearrangement studies are used to establish whether a lymphoid expansion is polyclonal or monoclonal. The molecular findings should not be evaluated in isolation, because not all monoclonal rearrangements are diagnostic of lymphoma, and not all lymphomas will show a monoclonal rearrangement. Other methodologies that can aid in the identification of a clonal process or specific genetic abnormalities include metaphase cytogenetics (karyotyping) and fluorescence in situ hybridization (FISH). If any cytogenetic abnormalities are found in sufficient numbers (and constitutional abnormalities are excluded), their identification indicates the presence of a clonal process. Also, some cytogenetic abnormalities are characteristic of certain lymphomas. However, they may be neither 100% diagnostically sensitive nor diagnostically specific, for example, the hallmark t(14;18)/IGH-BCL2 is not present in all follicular lymphomas and not all lymphomas with this translocation are follicular lymphomas. Whereas FISH is generally performed on a minimum of 200 cells, compared with typically 20 metaphase by “conventional” karyotyping, and is therefore considered to have higher analytical sensitivity, it evaluates only for the presence or absence of the abnormality being investigated with a given set of probes, and therefore other abnormalities, if present, will not be identified. The value of FISH cytogenetic studies is perhaps best illustrated in the need to diagnose double hit lymphomas, amongst other scenarios. The detection of certain mutations can aid in the diagnosis of certain lymphomas, such as MYD88 in lymphoplasmacytic lymphoma, prognosis of others, such as in follicular lymphoma and identify pathways that may be precisely therapeutically targeted.
Final remarks
The diagnosis of lymphoma can be complex and usually requires the hematopathologist to integrate multiple parameters. The classification of lymphomas is not static, and new entities or variants are continuously described, and the facets of well-known ones refined. While such changes are often to the chagrin of hematologists/oncologists and hematopathologists alike, we should embrace the incorporation of nascent and typically cool data into our practice, as more therapeutically relevant entities are molded.
1. Siegel RL, Miller KD, Jemal A. Cancer Statistics, 2017. CA Cancer J Clin. 2017 ;67(1):7-30.
2. Swerdlow SH, Campo E, Harris NL, et al, eds. WHO classification of tumours of haematopoietic and lymphoid tissues. In: Bosman FT, Jaffe ES, Lakhani SR, Ohgaki H, eds. World Health Organization Classification of Tumours. Lyon, France: IARC; 2008.
3. Swerdlow SH, Campo E, Pileri SA, et al. The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood. 2016 ;127(20):2375-2390.
Lymphomas constitute a very heterogeneous group of neoplasms with diverse clinical presentations, prognoses, and responses to therapy. Approximately 80,500 new cases of lymphoma are expected to be diagnosed in the United States in 2017, of which about one quarter will lead to the death of the patient.1 Perhaps more so than any other group of neoplasms, the diagnosis of lymphoma involves the integration of a multiplicity of clinical, histologic and immunophenotypic findings and, on occasion, cytogenetic and molecular results as well. An accurate diagnosis of lymphoma, usually rendered by hematopathologists, allows hematologists/oncologists to treat patients appropriately. Herein we will describe a simplified approach to the diagnosis and classification of lymphomas (Figure 1).
Lymphoma classification
Lymphomas are clonal neoplasms characterized by the expansion of abnormal lymphoid cells that may develop in any organ but commonly involve lymph nodes. The fourth edition of the World Health Organization (WHO) Classification of Tumours of Haematopoietic and Lymphoid tissues, published in 2008, is the official and most current guideline used for diagnosis of lymphoid neoplasms.2 The WHO scheme classifies lymphomas according to the type of cell from which they are derived (mature and immature B cells, T cells, or natural killer (NK) cells, findings determined by their morphology and immunophenotype) and their clinical, cytogenetic, and/or molecular features. This official classification is currently being updated3 and is expected to be published in full in 2017, at which time it is anticipated to include definitions for more than 70 distinct neoplasms.
Lymphomas are broadly and informally classified as Hodgkin lymphomas (HLs) and non-Hodgkin lymphomas (NHLs), based on the differences these two groups show in their clinical presentation, treatment, prognosis, and proportion of neoplastic cells, among others. NHLs are by far the most common type of lymphomas, accounting for approximately 90% of all new cases of lymphoma in the United States and 70% worldwide.1,2 NHLs are a very heterogeneous group of B-, T-, or NK-cell neoplasms that, in turn, can also be informally subclassified as low-grade (or indolent) or high-grade (or aggressive) according to their predicted clinical behavior. HLs are comparatively rare, less heterogeneous, uniformly of B-cell origin and, in the case of classical Hodgkin lymphoma, highly curable.1,2 It is beyond the scope of this manuscript to outline the features of each of the >70 specific entities, but the reader is referred elsewhere for more detail and encouraged to become familiarized with the complexity, challenges, and beauty of lymphoma diagnosis.2,3
Biopsy procedure
A correct diagnosis begins with an adequate biopsy procedure. It is essential that biopsy specimens for lymphoma evaluation be submitted fresh and unfixed, because some crucial analyses such as flow cytometry or conventional cytogenetics can only be performed on fresh tissue. Indeed, it is important for the hematologist/oncologist and/or surgeon and/or interventional radiologist to converse with the hematopathologist prior to and even during some procedures to ensure the correct processing of the specimen. Also, it is important to limit the compression of the specimen and the excessive use of cauterization during the biopsy procedure, both of which cause artifacts that may render impossible the interpretation of the histopathologic findings.
Given that the diagnosis of lymphoma is based not only on the cytologic details of the lymphoma cells but also on the architectural pattern with which they infiltrate an organ, the larger the biopsy specimen, the easier it will be for a hematopathologist to identify the pattern. In addition, excisional biopsies frequently contain more diagnostic tissue than needle core biopsies and this provides pathologists with the option to submit tissue fragments for ancillary tests that require unfixed tissue as noted above. Needle core biopsies of lymph nodes are increasingly being used because of their association with fewer complications and lower cost than excisional biopsies. However, needle core biopsies provide only a glimpse of the pattern of infiltration and may not be completely representative of the architecture. Therefore, excisional lymph node biopsies of lymph nodes are preferred over needle core biopsies, recognizing that in the setting of deeply seated lymph nodes, needle core biopsies may be the only or the best surgical option.
Clinical presentation
Accurate diagnosis of lymphoma cannot take place in a vacuum. The hematopathologist’s initial approach to the diagnosis of lymphoid processes in tissue biopsies should begin with a thorough review of the clinical history, although some pathology laboratories may not have immediate access to this information. The hematopathologist should evaluate factors such as age, gender, location of the tumor, symptomatology, medications, serology, and prior history of malignancy, immunosuppression or immunodeficiency in every case. Other important but frequently omitted parts of the clinical history are the patient’s occupation, history of exposure to animals, and the presence of tattoos, which may be associated with certain reactive lymphadenopathies.
Histomorphologic evaluation
Despite the plethora of new and increasingly sophisticated tools, histologic and morphologic analysis still remains the cornerstone of diagnosis in hematopathology. However, for the characterization of an increasing number of reactive and neoplastic lymphoid processes, hematopathologists may also require immunophenotypic, molecular, and cytogenetic tests for an accurate diagnosis. Upon review of the clinical information, a microscopic evaluation of the tissue submitted for processing by the histology laboratory will be performed. The results of concurrent flow cytometric evaluation (performed on fresh unfixed material) should also be available in most if not all cases before the H&E-stained slides are available for review. Upon receipt of H&E-stained slides, the hematopathologist will evaluate the quality of the submitted specimen, since many diagnostic difficulties stem from suboptimal techniques related to the biopsy procedure, fixation, processing, cutting, or staining (Figure 1). If deemed suitable for accurate diagnosis, a search for signs of preservation or disruption of the organ that was biopsied will follow. The identification of certain morphologic patterns aids the hematopathologist in answering the first question: “what organ is this and is this consistent with what is indicated on the requisition?” This is usually immediately followed by “is this sufficient and adequate material for a diagnosis?” and “is there any normal architecture?” If the architecture is not normal, “is this alteration due to a reactive or a neoplastic process?” If neoplastic, “is it lymphoma or a non-hematolymphoid neoplasm?”
Both reactive and neoplastic processes have variably unique morphologic features that if properly recognized, guide the subsequent testing. However, some reactive and neoplastic processes can present with overlapping features, and even after extensive immunophenotypic evaluation and the performance of ancillary studies, it may not be possible to conclusively determine its nature. If the lymph node architecture is altered or effaced, the predominant pattern of infiltration (eg, nodular, diffuse, interfollicular, intrasinusoidal) and the degree of alteration of the normal architecture is evaluated, usually at low magnification. When the presence of an infiltrate is recognized, its components must be characterized. If the infiltrate is composed of a homogeneous expansion of lymphoid cells that disrupts or replaces the normal lymphoid architecture, a lymphoma will be suspected or diagnosed. The pattern of distribution of the cells along with their individual morphologic characteristics (ie, size, nuclear shape, chromatin configuration, nucleoli, amount and hue of cytoplasm) are key factors for the diagnosis and classification of the lymphoma that will guide subsequent testing. The immunophenotypic analysis (by immunohistochemistry, flow cytometry or a combination of both) may confirm the reactive or neoplastic nature of the process, and its subclassification. B-cell lymphomas, in particular have variable and distinctive histologic features: as a diffuse infiltrate of large mature lymphoid cells (eg, diffuse large B-cell lymphoma), an expansion of immature lymphoid cells (lymphoblastic lymphoma), and a nodular infiltrate of small, intermediate and/or mature large B cells (eg, follicular lymphoma).
Mature T-cell lymphomas may display similar histologic, features but they can be quite heterogeneous with an infiltrate composed of one predominant cell type or a mixture of small, medium-sized, and large atypical lymphoid cells (on occasion with abundant clear cytoplasm) and a variable number of eosinophils, plasma cells, macrophages (including granulomas), and B cells. HLs most commonly efface the lymph node architecture with a nodular or diffuse infiltrate variably composed of reactive lymphocytes, granulocytes, macrophages, and plasma cells and usually a minority of large neoplastic cells (Hodgkin/Reed-Sternberg cells and/or lymphocyte predominant cells).
Once the H&E-stained slides are evaluated and a diagnosis of lymphoma is suspected or established, the hematopathologist will attempt to determine whether it has mature or immature features, and whether low- or high-grade morphologic characteristics are present. The maturity of lymphoid cells is generally determined by the nature of the chromatin, which if “fine” and homogeneous (with or without a conspicuous nucleolus) will usually, but not always, be considered immature, whereas clumped, vesicular or hyperchromatic chromatin is generally, but not always, associated with maturity. If the chromatin displays immature features, the differential diagnosis will mainly include B- and T-lymphoblastic lymphomas, but also blastoid variants of mature neoplasm such as mantle cell lymphoma, and follicular lymphoma, as well as high-grade B-cell lymphomas. Features associated with low-grade lymphomas (eg, follicular lymphoma, small lymphocytic lymphoma/chronic lymphocytic leukemia, marginal zone lymphoma, lymphoplasmacytic lymphoma) include small cell morphology, mature chromatin, absence of a significant number of mitoses or apoptotic cells, and a low proliferation index as shown by immunohistochemistry for Ki67. High-grade lymphomas, such as lymphoblastic lymphoma, Burkitt lymphoma, or certain large B-cell lymphomas tend to show opposite features, and some of the mature entities are frequently associated with MYC rearrangements. Of note, immature lymphomas tend to be clinically high grade, but not all clinically high-grade lymphomas are immature. Conversely, the majority of low-grade lymphomas are usually mature.
Immunophenotypic evaluation
Immunophenotypic evaluation is essential because the lineage of lymphoma cells cannot be determined by morphology alone. The immunophenotype is the combination of proteins/markers (eg, CD20, CD3, TdT) expressed by cells. Usually, it is evaluated by immunohistochemistry and/or flow cytometry, which help determine the proportion of lymphoid cells that express a certain marker and its location and intensity within the cells. While immunohistochemistry is normally performed on formalin-fixed and paraffin-embedded tissue, flow cytometry can be evaluated only on fresh unfixed tissue. Flow cytometry has the advantage over immunohistochemistry of being faster and better at simultaneously identifying coexpression of multiple markers on multiple cell populations. However, certain markers can only be evaluated by immunohistochemistry.
The immunophenotypic analysis will in most cases reveal whether the lymphomas is of B-, T- or NK-cell origin, and whether a lymphoma subtype associated immunophenotype is present. Typical pan B-cell antigens include PAX5, CD19, and CD79a (CD20 is less broadly expressed throughout B-cell differentiation, although it is usually evident in most mature B-cell lymphomas), and typical pan T-cell antigens include CD2, CD5, and CD7. The immature or mature nature of a lymphoma can also be confirmed by evaluation of the immunophenotype. Immature lymphomas commonly express one or more of TdT, CD10, or CD34; T-lymphoblastic lymphoma cells may also coexpress CD1a. The majority of NHLs and all HLs are derived from (or reflect) B cells at different stages of maturation. Mature B-cell lymphomas are the most common type of lymphoma and typically, but not always, express pan B-cell markers as well as surface membrane immunoglobulin, with the latter also most useful in assessing clonality via a determination of light chain restriction. Some mature B-cell lymphomas tend to acquire markers that are either never physiologically expressed by normal mature B cells (eg, cyclin D1 in mantle cell lymphoma, or BCL2 in germinal center B cells in follicular lymphoma) or only expressed in a minor fraction (eg, CD5 that is characteristically expressed in small lymphocytic and mantle cell lymphoma). The most common mature B-cell lymphomas include diffuse large B-cell lymphoma, follicular lymphoma, small lymphocytic lymphoma, mantle cell lymphoma, marginal zone lymphoma, Burkitt lymphoma, and lymphoplasmacytic lymphoma (Figures 2 and 3). Classical HLs are also lymphomas of B-cell origin that demonstrate diminished preservation of their B-cell immunophenotype (as evidenced by the dim expression of PAX5 but absence of most other pan B-cell antigens), expression of CD30, variable expression of CD15, and loss of CD45 (Figure 1). In contrast, nodular lymphocyte predominant HL shows a preserved B-cell immunophenotypic program and expression of CD45, typically without CD30 and CD15. Of note, the evaluation of the immunophenotype of the neoplastic cells in HL is routinely assessed by immunohistochemistry because most flow cytometry laboratories cannot reliably detect and characterize the low numbers of these cells.
Mature T-cell lymphomas generally express one or more T-cell markers, and tend to display a T-helper (CD4-positive) or cytotoxic (CD8-positive) immunophenotype and may show loss of markers expressed by most normal T-cells (eg, CD5, CD7; Figure 4). However, a subset of them may express markers not commonly detected in normal T cells, such as ALK. NK-cell lymphomas lack surface CD3 (expressing only cytoplasmic CD3) and CD5 but express some pan T-cell antigens (such as CD2 and CD7) as well as CD16 and/or CD56.
Patients with primary or acquired immune dysfunction are at risk for development of lymphoma and other less clearly defined lymphoproliferative disorders, the majority of which are associated with infection of the lymphoid cells with Epstein-Barr virus (EBV). Therefore, evaluation with chromogenic in situ hybridization for an EBV-encoded early RNA (EBER1) is routinely performed in these cases; it is thus essential that the hematopathologist be informed of the altered immune system of the patient. If lymphoma develops, they may be morphologically similar to those that appear in immunocompetent patients, which specifically in the post-transplant setting are known as monomorphic post-transplant lymphoproliferative disorders (PTLD). If the PTLD does not meet the criteria for any of the recognized types of lymphoma, it may be best characterized as a polymorphic PTLD.
Once the lineage (B-, T-, or NK-cell) of the mature lymphoma has been established, the sum (and on occasion the gestalt) of the clinical, morphologic, immunophenotypic and other findings will be considered for the subclassification of the neoplasm.
Cytogenetic and molecular evaluation
If the morphologic and immunophenotypic analysis is inconclusive or nondiagnostic, then molecular and/or cytogenetic testing may further aid in the characterization of the process. Some of available molecular tests include analyses for the rearrangements of the variable region of the immunoglobulin (IG) or T-cell receptor (TCR) genes and for mutations on specific genes. The identification of specific mutations not only confirms the clonal nature of the process but, on occasion, it may also help subclassify the lymphoma, whereas IG or TCR rearrangement studies are used to establish whether a lymphoid expansion is polyclonal or monoclonal. The molecular findings should not be evaluated in isolation, because not all monoclonal rearrangements are diagnostic of lymphoma, and not all lymphomas will show a monoclonal rearrangement. Other methodologies that can aid in the identification of a clonal process or specific genetic abnormalities include metaphase cytogenetics (karyotyping) and fluorescence in situ hybridization (FISH). If any cytogenetic abnormalities are found in sufficient numbers (and constitutional abnormalities are excluded), their identification indicates the presence of a clonal process. Also, some cytogenetic abnormalities are characteristic of certain lymphomas. However, they may be neither 100% diagnostically sensitive nor diagnostically specific, for example, the hallmark t(14;18)/IGH-BCL2 is not present in all follicular lymphomas and not all lymphomas with this translocation are follicular lymphomas. Whereas FISH is generally performed on a minimum of 200 cells, compared with typically 20 metaphase by “conventional” karyotyping, and is therefore considered to have higher analytical sensitivity, it evaluates only for the presence or absence of the abnormality being investigated with a given set of probes, and therefore other abnormalities, if present, will not be identified. The value of FISH cytogenetic studies is perhaps best illustrated in the need to diagnose double hit lymphomas, amongst other scenarios. The detection of certain mutations can aid in the diagnosis of certain lymphomas, such as MYD88 in lymphoplasmacytic lymphoma, prognosis of others, such as in follicular lymphoma and identify pathways that may be precisely therapeutically targeted.
Final remarks
The diagnosis of lymphoma can be complex and usually requires the hematopathologist to integrate multiple parameters. The classification of lymphomas is not static, and new entities or variants are continuously described, and the facets of well-known ones refined. While such changes are often to the chagrin of hematologists/oncologists and hematopathologists alike, we should embrace the incorporation of nascent and typically cool data into our practice, as more therapeutically relevant entities are molded.
Lymphomas constitute a very heterogeneous group of neoplasms with diverse clinical presentations, prognoses, and responses to therapy. Approximately 80,500 new cases of lymphoma are expected to be diagnosed in the United States in 2017, of which about one quarter will lead to the death of the patient.1 Perhaps more so than any other group of neoplasms, the diagnosis of lymphoma involves the integration of a multiplicity of clinical, histologic and immunophenotypic findings and, on occasion, cytogenetic and molecular results as well. An accurate diagnosis of lymphoma, usually rendered by hematopathologists, allows hematologists/oncologists to treat patients appropriately. Herein we will describe a simplified approach to the diagnosis and classification of lymphomas (Figure 1).
Lymphoma classification
Lymphomas are clonal neoplasms characterized by the expansion of abnormal lymphoid cells that may develop in any organ but commonly involve lymph nodes. The fourth edition of the World Health Organization (WHO) Classification of Tumours of Haematopoietic and Lymphoid tissues, published in 2008, is the official and most current guideline used for diagnosis of lymphoid neoplasms.2 The WHO scheme classifies lymphomas according to the type of cell from which they are derived (mature and immature B cells, T cells, or natural killer (NK) cells, findings determined by their morphology and immunophenotype) and their clinical, cytogenetic, and/or molecular features. This official classification is currently being updated3 and is expected to be published in full in 2017, at which time it is anticipated to include definitions for more than 70 distinct neoplasms.
Lymphomas are broadly and informally classified as Hodgkin lymphomas (HLs) and non-Hodgkin lymphomas (NHLs), based on the differences these two groups show in their clinical presentation, treatment, prognosis, and proportion of neoplastic cells, among others. NHLs are by far the most common type of lymphomas, accounting for approximately 90% of all new cases of lymphoma in the United States and 70% worldwide.1,2 NHLs are a very heterogeneous group of B-, T-, or NK-cell neoplasms that, in turn, can also be informally subclassified as low-grade (or indolent) or high-grade (or aggressive) according to their predicted clinical behavior. HLs are comparatively rare, less heterogeneous, uniformly of B-cell origin and, in the case of classical Hodgkin lymphoma, highly curable.1,2 It is beyond the scope of this manuscript to outline the features of each of the >70 specific entities, but the reader is referred elsewhere for more detail and encouraged to become familiarized with the complexity, challenges, and beauty of lymphoma diagnosis.2,3
Biopsy procedure
A correct diagnosis begins with an adequate biopsy procedure. It is essential that biopsy specimens for lymphoma evaluation be submitted fresh and unfixed, because some crucial analyses such as flow cytometry or conventional cytogenetics can only be performed on fresh tissue. Indeed, it is important for the hematologist/oncologist and/or surgeon and/or interventional radiologist to converse with the hematopathologist prior to and even during some procedures to ensure the correct processing of the specimen. Also, it is important to limit the compression of the specimen and the excessive use of cauterization during the biopsy procedure, both of which cause artifacts that may render impossible the interpretation of the histopathologic findings.
Given that the diagnosis of lymphoma is based not only on the cytologic details of the lymphoma cells but also on the architectural pattern with which they infiltrate an organ, the larger the biopsy specimen, the easier it will be for a hematopathologist to identify the pattern. In addition, excisional biopsies frequently contain more diagnostic tissue than needle core biopsies and this provides pathologists with the option to submit tissue fragments for ancillary tests that require unfixed tissue as noted above. Needle core biopsies of lymph nodes are increasingly being used because of their association with fewer complications and lower cost than excisional biopsies. However, needle core biopsies provide only a glimpse of the pattern of infiltration and may not be completely representative of the architecture. Therefore, excisional lymph node biopsies of lymph nodes are preferred over needle core biopsies, recognizing that in the setting of deeply seated lymph nodes, needle core biopsies may be the only or the best surgical option.
Clinical presentation
Accurate diagnosis of lymphoma cannot take place in a vacuum. The hematopathologist’s initial approach to the diagnosis of lymphoid processes in tissue biopsies should begin with a thorough review of the clinical history, although some pathology laboratories may not have immediate access to this information. The hematopathologist should evaluate factors such as age, gender, location of the tumor, symptomatology, medications, serology, and prior history of malignancy, immunosuppression or immunodeficiency in every case. Other important but frequently omitted parts of the clinical history are the patient’s occupation, history of exposure to animals, and the presence of tattoos, which may be associated with certain reactive lymphadenopathies.
Histomorphologic evaluation
Despite the plethora of new and increasingly sophisticated tools, histologic and morphologic analysis still remains the cornerstone of diagnosis in hematopathology. However, for the characterization of an increasing number of reactive and neoplastic lymphoid processes, hematopathologists may also require immunophenotypic, molecular, and cytogenetic tests for an accurate diagnosis. Upon review of the clinical information, a microscopic evaluation of the tissue submitted for processing by the histology laboratory will be performed. The results of concurrent flow cytometric evaluation (performed on fresh unfixed material) should also be available in most if not all cases before the H&E-stained slides are available for review. Upon receipt of H&E-stained slides, the hematopathologist will evaluate the quality of the submitted specimen, since many diagnostic difficulties stem from suboptimal techniques related to the biopsy procedure, fixation, processing, cutting, or staining (Figure 1). If deemed suitable for accurate diagnosis, a search for signs of preservation or disruption of the organ that was biopsied will follow. The identification of certain morphologic patterns aids the hematopathologist in answering the first question: “what organ is this and is this consistent with what is indicated on the requisition?” This is usually immediately followed by “is this sufficient and adequate material for a diagnosis?” and “is there any normal architecture?” If the architecture is not normal, “is this alteration due to a reactive or a neoplastic process?” If neoplastic, “is it lymphoma or a non-hematolymphoid neoplasm?”
Both reactive and neoplastic processes have variably unique morphologic features that if properly recognized, guide the subsequent testing. However, some reactive and neoplastic processes can present with overlapping features, and even after extensive immunophenotypic evaluation and the performance of ancillary studies, it may not be possible to conclusively determine its nature. If the lymph node architecture is altered or effaced, the predominant pattern of infiltration (eg, nodular, diffuse, interfollicular, intrasinusoidal) and the degree of alteration of the normal architecture is evaluated, usually at low magnification. When the presence of an infiltrate is recognized, its components must be characterized. If the infiltrate is composed of a homogeneous expansion of lymphoid cells that disrupts or replaces the normal lymphoid architecture, a lymphoma will be suspected or diagnosed. The pattern of distribution of the cells along with their individual morphologic characteristics (ie, size, nuclear shape, chromatin configuration, nucleoli, amount and hue of cytoplasm) are key factors for the diagnosis and classification of the lymphoma that will guide subsequent testing. The immunophenotypic analysis (by immunohistochemistry, flow cytometry or a combination of both) may confirm the reactive or neoplastic nature of the process, and its subclassification. B-cell lymphomas, in particular have variable and distinctive histologic features: as a diffuse infiltrate of large mature lymphoid cells (eg, diffuse large B-cell lymphoma), an expansion of immature lymphoid cells (lymphoblastic lymphoma), and a nodular infiltrate of small, intermediate and/or mature large B cells (eg, follicular lymphoma).
Mature T-cell lymphomas may display similar histologic, features but they can be quite heterogeneous with an infiltrate composed of one predominant cell type or a mixture of small, medium-sized, and large atypical lymphoid cells (on occasion with abundant clear cytoplasm) and a variable number of eosinophils, plasma cells, macrophages (including granulomas), and B cells. HLs most commonly efface the lymph node architecture with a nodular or diffuse infiltrate variably composed of reactive lymphocytes, granulocytes, macrophages, and plasma cells and usually a minority of large neoplastic cells (Hodgkin/Reed-Sternberg cells and/or lymphocyte predominant cells).
Once the H&E-stained slides are evaluated and a diagnosis of lymphoma is suspected or established, the hematopathologist will attempt to determine whether it has mature or immature features, and whether low- or high-grade morphologic characteristics are present. The maturity of lymphoid cells is generally determined by the nature of the chromatin, which if “fine” and homogeneous (with or without a conspicuous nucleolus) will usually, but not always, be considered immature, whereas clumped, vesicular or hyperchromatic chromatin is generally, but not always, associated with maturity. If the chromatin displays immature features, the differential diagnosis will mainly include B- and T-lymphoblastic lymphomas, but also blastoid variants of mature neoplasm such as mantle cell lymphoma, and follicular lymphoma, as well as high-grade B-cell lymphomas. Features associated with low-grade lymphomas (eg, follicular lymphoma, small lymphocytic lymphoma/chronic lymphocytic leukemia, marginal zone lymphoma, lymphoplasmacytic lymphoma) include small cell morphology, mature chromatin, absence of a significant number of mitoses or apoptotic cells, and a low proliferation index as shown by immunohistochemistry for Ki67. High-grade lymphomas, such as lymphoblastic lymphoma, Burkitt lymphoma, or certain large B-cell lymphomas tend to show opposite features, and some of the mature entities are frequently associated with MYC rearrangements. Of note, immature lymphomas tend to be clinically high grade, but not all clinically high-grade lymphomas are immature. Conversely, the majority of low-grade lymphomas are usually mature.
Immunophenotypic evaluation
Immunophenotypic evaluation is essential because the lineage of lymphoma cells cannot be determined by morphology alone. The immunophenotype is the combination of proteins/markers (eg, CD20, CD3, TdT) expressed by cells. Usually, it is evaluated by immunohistochemistry and/or flow cytometry, which help determine the proportion of lymphoid cells that express a certain marker and its location and intensity within the cells. While immunohistochemistry is normally performed on formalin-fixed and paraffin-embedded tissue, flow cytometry can be evaluated only on fresh unfixed tissue. Flow cytometry has the advantage over immunohistochemistry of being faster and better at simultaneously identifying coexpression of multiple markers on multiple cell populations. However, certain markers can only be evaluated by immunohistochemistry.
The immunophenotypic analysis will in most cases reveal whether the lymphomas is of B-, T- or NK-cell origin, and whether a lymphoma subtype associated immunophenotype is present. Typical pan B-cell antigens include PAX5, CD19, and CD79a (CD20 is less broadly expressed throughout B-cell differentiation, although it is usually evident in most mature B-cell lymphomas), and typical pan T-cell antigens include CD2, CD5, and CD7. The immature or mature nature of a lymphoma can also be confirmed by evaluation of the immunophenotype. Immature lymphomas commonly express one or more of TdT, CD10, or CD34; T-lymphoblastic lymphoma cells may also coexpress CD1a. The majority of NHLs and all HLs are derived from (or reflect) B cells at different stages of maturation. Mature B-cell lymphomas are the most common type of lymphoma and typically, but not always, express pan B-cell markers as well as surface membrane immunoglobulin, with the latter also most useful in assessing clonality via a determination of light chain restriction. Some mature B-cell lymphomas tend to acquire markers that are either never physiologically expressed by normal mature B cells (eg, cyclin D1 in mantle cell lymphoma, or BCL2 in germinal center B cells in follicular lymphoma) or only expressed in a minor fraction (eg, CD5 that is characteristically expressed in small lymphocytic and mantle cell lymphoma). The most common mature B-cell lymphomas include diffuse large B-cell lymphoma, follicular lymphoma, small lymphocytic lymphoma, mantle cell lymphoma, marginal zone lymphoma, Burkitt lymphoma, and lymphoplasmacytic lymphoma (Figures 2 and 3). Classical HLs are also lymphomas of B-cell origin that demonstrate diminished preservation of their B-cell immunophenotype (as evidenced by the dim expression of PAX5 but absence of most other pan B-cell antigens), expression of CD30, variable expression of CD15, and loss of CD45 (Figure 1). In contrast, nodular lymphocyte predominant HL shows a preserved B-cell immunophenotypic program and expression of CD45, typically without CD30 and CD15. Of note, the evaluation of the immunophenotype of the neoplastic cells in HL is routinely assessed by immunohistochemistry because most flow cytometry laboratories cannot reliably detect and characterize the low numbers of these cells.
Mature T-cell lymphomas generally express one or more T-cell markers, and tend to display a T-helper (CD4-positive) or cytotoxic (CD8-positive) immunophenotype and may show loss of markers expressed by most normal T-cells (eg, CD5, CD7; Figure 4). However, a subset of them may express markers not commonly detected in normal T cells, such as ALK. NK-cell lymphomas lack surface CD3 (expressing only cytoplasmic CD3) and CD5 but express some pan T-cell antigens (such as CD2 and CD7) as well as CD16 and/or CD56.
Patients with primary or acquired immune dysfunction are at risk for development of lymphoma and other less clearly defined lymphoproliferative disorders, the majority of which are associated with infection of the lymphoid cells with Epstein-Barr virus (EBV). Therefore, evaluation with chromogenic in situ hybridization for an EBV-encoded early RNA (EBER1) is routinely performed in these cases; it is thus essential that the hematopathologist be informed of the altered immune system of the patient. If lymphoma develops, they may be morphologically similar to those that appear in immunocompetent patients, which specifically in the post-transplant setting are known as monomorphic post-transplant lymphoproliferative disorders (PTLD). If the PTLD does not meet the criteria for any of the recognized types of lymphoma, it may be best characterized as a polymorphic PTLD.
Once the lineage (B-, T-, or NK-cell) of the mature lymphoma has been established, the sum (and on occasion the gestalt) of the clinical, morphologic, immunophenotypic and other findings will be considered for the subclassification of the neoplasm.
Cytogenetic and molecular evaluation
If the morphologic and immunophenotypic analysis is inconclusive or nondiagnostic, then molecular and/or cytogenetic testing may further aid in the characterization of the process. Some of available molecular tests include analyses for the rearrangements of the variable region of the immunoglobulin (IG) or T-cell receptor (TCR) genes and for mutations on specific genes. The identification of specific mutations not only confirms the clonal nature of the process but, on occasion, it may also help subclassify the lymphoma, whereas IG or TCR rearrangement studies are used to establish whether a lymphoid expansion is polyclonal or monoclonal. The molecular findings should not be evaluated in isolation, because not all monoclonal rearrangements are diagnostic of lymphoma, and not all lymphomas will show a monoclonal rearrangement. Other methodologies that can aid in the identification of a clonal process or specific genetic abnormalities include metaphase cytogenetics (karyotyping) and fluorescence in situ hybridization (FISH). If any cytogenetic abnormalities are found in sufficient numbers (and constitutional abnormalities are excluded), their identification indicates the presence of a clonal process. Also, some cytogenetic abnormalities are characteristic of certain lymphomas. However, they may be neither 100% diagnostically sensitive nor diagnostically specific, for example, the hallmark t(14;18)/IGH-BCL2 is not present in all follicular lymphomas and not all lymphomas with this translocation are follicular lymphomas. Whereas FISH is generally performed on a minimum of 200 cells, compared with typically 20 metaphase by “conventional” karyotyping, and is therefore considered to have higher analytical sensitivity, it evaluates only for the presence or absence of the abnormality being investigated with a given set of probes, and therefore other abnormalities, if present, will not be identified. The value of FISH cytogenetic studies is perhaps best illustrated in the need to diagnose double hit lymphomas, amongst other scenarios. The detection of certain mutations can aid in the diagnosis of certain lymphomas, such as MYD88 in lymphoplasmacytic lymphoma, prognosis of others, such as in follicular lymphoma and identify pathways that may be precisely therapeutically targeted.
Final remarks
The diagnosis of lymphoma can be complex and usually requires the hematopathologist to integrate multiple parameters. The classification of lymphomas is not static, and new entities or variants are continuously described, and the facets of well-known ones refined. While such changes are often to the chagrin of hematologists/oncologists and hematopathologists alike, we should embrace the incorporation of nascent and typically cool data into our practice, as more therapeutically relevant entities are molded.
1. Siegel RL, Miller KD, Jemal A. Cancer Statistics, 2017. CA Cancer J Clin. 2017 ;67(1):7-30.
2. Swerdlow SH, Campo E, Harris NL, et al, eds. WHO classification of tumours of haematopoietic and lymphoid tissues. In: Bosman FT, Jaffe ES, Lakhani SR, Ohgaki H, eds. World Health Organization Classification of Tumours. Lyon, France: IARC; 2008.
3. Swerdlow SH, Campo E, Pileri SA, et al. The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood. 2016 ;127(20):2375-2390.
1. Siegel RL, Miller KD, Jemal A. Cancer Statistics, 2017. CA Cancer J Clin. 2017 ;67(1):7-30.
2. Swerdlow SH, Campo E, Harris NL, et al, eds. WHO classification of tumours of haematopoietic and lymphoid tissues. In: Bosman FT, Jaffe ES, Lakhani SR, Ohgaki H, eds. World Health Organization Classification of Tumours. Lyon, France: IARC; 2008.
3. Swerdlow SH, Campo E, Pileri SA, et al. The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood. 2016 ;127(20):2375-2390.
Liquid gold: blood-based biopsies make headway
Pathologic and, increasingly, molecular analysis of tumor tissue biopsies is the gold standard in initial diagnosis of cancer, but liquid biopsies, which analyze tumor-derived material circulating in the bloodstream are gaining traction. Here, we discuss the current state of development of this complementary and potentially alternative approach to tumor analysis.
Liquid biopsy gaining traction
Biopsies enable oncologists to gather information about a potential or established tumor, including confirmation of the presence of cancerous tissue and determination of its histological characteristics, such as tumor grade and stage, as well as its molecular features, such as the presence of certain gene mutations. Ultimately, this information can be put to use in determining the most appropriate course of treatment.
The current gold standard is a tissue biopsy that typically involves an invasive procedure to permit the collection of a piece of tumor tissue. Yet, tissue biopsies are not always feasible because of the location of the tumor or the poor performance status of many patients with advanced disease. They also provide only a snapshot of the disease at the time at which they were taken and don’t necessarily reflect the genetic heterogeneity or evolution of a tumor over time.
The detection of components that are derived from the tumor circulating in the blood of cancer patients had fueled the idea of blood-based diagnostics in oncology – so-called liquid biopsies. These have rapidly gained traction in the past several decades as a less expensive (the cost of performing genomic analyses on blood samples is at least an order of magnitude less than on tissue samples), less invasive (requiring only a simple blood draw) alternative source of information about tumors.1
As researchers have refined the ability to exploit liquid biopsies, commercial interest has been piqued. More than 35 companies within the United States alone are developing liquid biopsies, and it’s easy to see why with a market projected to be in the many billions of dollars.2
Seeking out tumor clues in the blood
Liquid biopsies consist of a 10-15 mL blood sample drawn into a tube that contains an anticoagulant and it can contain several different types of tumor-associated material. Thus far, two components – circulating tumor cells (CTCs) and circulating tumor DNA (ctDNA) – have formed the cornerstone of liquid biopsies. At present, it is not clear whether these components are released randomly, as a by-product of tumor cell death or if they are released as part of a specific biologic process, such as for the colonization of metastatic sites. It reality, it may be a little of both, and active dissemination may be particularly relevant for CTCs, among which are postulated to be a population of cancer stem cells that can initiate distant metastases.3,4
The discovery of CTCs dates back to the 1860s, when cells that were morphologically identical to the tumor were identified in the blood of a patient with metastatic cancer. Their potential significance was not fully realized until a few decades ago, when they were found to exist from early on in the course of disease.3,4
CTCs, which can be either single cells or clusters of cells known as microemboli, have a short half-life in the bloodstream – less than 2 ½ hours – and are also extremely rare (1 mL of blood contains 1-10 CTCs) against a background of many millions of normal cells. Thus the detection and isolation of CTCs presents a significant challenge. More than 40 different platforms are being developed for the isolation and enrichment of CTCs. For the most part, these use a method called positive selection to pick out CTCs.1,3,4
Positive selection exploits the biological or physical properties that are specific to CTCs and absent in normal cells, for example, the presence of a specific tumor-associated antigen on their surface or differences in size, density or electric charge. The limitations of this method are that, not only do you need to know something about CTCs to begin to understand what makes them truly unique and ensure only isolation of CTCs, but their phenotype is also thought to be continually changing.1,3,4
In recent years, the focus has shifted toward technologies that use negative depletion, meaning that they target the other types of cells in the blood sample and filter those away until only the CTCs are left behind. The most advanced are devices that use microfluidic technology to sort the cells, such as the CTC-iChip system being developed by researchers at Massachusetts General Hospital in Boston.5
ctDNA consists of small fragments of nucleic acids that are not contained within a cell or associated with cell fragments and is thought to be present in 50%-90% of patients, depending on the type of cancer they have. ctDNA has a similarly short half-life in the circulation to CTCs and, like CTCs, ctDNA is present at very low levels in the bloodstream. Although levels of ctDNA have been shown to increase with increasing tumor burden, it is still often obscured by the presence of other cell-free DNA derived from non-tumor cells.
ctDNA can be distinguished from other cell-free DNA by the presence of somatic mutations and a number of highly sensitive methods have been developed to detect them, including the amplification-refractory mutation system (ARMS); digital polymerase chain reaction; and the beads, emulsification, amplification, and magnetics (BEAMing) system. Next-generation sequencing technologies, including tagged-amplicon deep sequencing (TAm-Seq), the Safe-Sequencing System (Safe-SeqS), and cancer personalized profiling by deep sequencing (CAPP-seq), can also be used and the race for ever more sensitive analytical tools is ongoing.1,3,4,6
Applying liquid biopsies now and in the future
There are a plethora of potential applications for liquid biopsies3,7 (Figure 1), and probably the most exciting among them is the potential for screening for and early detection of cancer. The fact that ctDNA and CTCs have both been shown to be present from the earliest stages of disease has sparked interest in the possibility of developing simple blood tests to identify tumors before they become detectable by other methods and at a point at which they may be curable.
Given that both are present at such low levels within the circulation and are particularly sparse at earlier stages of disease, current technologies may lack the specificity and sensitivity for this application at present. However, numerous clinical trials are ongoing.
For CTCs, simple enumeration has been the most extensively investigated application to date. Numerous studies have shown that the number of CTCs in the bloodstream has prognostic significance in various different tumor types. Three such studies led to the first regulatory approval for a CTC detection system (Table 1 and Table 2).8-10
One area in which liquid biopsies could really come into their own is in providing more real-time analysis of tumors. This is something that has proven particularly challenging with tissue biopsies because repeating these invasive procedures is problematic. But the ease of repeat blood draws means that serial liquid biopsies could be performed and might offer the possibility of monitoring disease progression and evolution over the course of disease and particularly in response to treatment.
Indeed, studies have shown that in addition to baseline CTC counts, changes in CTC number during treatment are also prognostic. There was improved survival among patients whose CTC counts decreased below a threshold value during treatment and vice versa. This is also an approved use for CellSearch though at present it is not widely clinically implemented.12
Clinical utility remains elusive
The ultimate goal would be for liquid biopsies to have an impact on treatment decisions, allowing oncologists to change management strategy based on predicted sensitivity or resistance to therapy, so-called clinical utility. Thus far, clinical utility has proved elusive, though liquid biopsies using ctDNA to evaluate tumor genotype have come closest.
The Cobas EGFR Mutation Test v2 recently became the first ctDNA-based liquid biopsy to receive regulatory approval. It was approved as a companion diagnostic to identify patients with advanced non–small-cell lung cancer (NSCLC) who have specific mutations in the epidermal growth factor receptor (EGFR) gene and are therefore eligible for treatment with the EGFR inhibitor erlotinib.13
Approval was based on comparison of EGFR mutation identification rates using plasma ctDNA samples and tumor tissue samples from patients enrolled in the phase 3 ENSURE trial, which compared the efficacy of erlotinib with chemotherapy as first-line therapy in patients with advanced NSCLC. Of the 217 patients enrolled in the trial, 98.6% of patients had both tumor biopsy and plasma ctDNA samples available for testing. Concordance between the two types of biopsy in identifying patients with EGFR mutations was high and patients with EGFR positivity according to liquid biopsy results demonstrated improved progression-free survival when treated with erlotinib.14
The results of a large-scale genomic analysis of various different types of tumors using ctDNA were also recently presented at the 2016 American Society of Clinical Oncology meeting. Blood samples from more than 15,000 patients with 50 different tumor types, including advanced lung cancer (37%), breast cancer (14%), and CRC (10%), were collected and compared with either available tumor biopsy samples from the same cases (n = 398) or, in the majority of cases, with The Cancer Genome Atlas database, which uses tumor biopsies to perform genome-wide sequencing studies. Both types of biopsy revealed very similar mutation patterns when the Guardant360 next-generation sequencing test, which targets 70 genes, was applied. In particular, when EGFR, BRAF, KRAS, ALK, RET, and ROS1 mutations were identified by tumor tissue biopsy, the same mutations were reported in 94%-100% of plasma samples.15
Studies of the clinical utility of ctDNA and CTCs are among ongoing clinical trials of liquid biopsies (Tables 2 and 3). The potential for using CTCs to guide treatment decisions has become particularly relevant in breast cancer in light of results showing that patients with primary tumors that are negative for human epidermal growth factor receptor 2 (HER2) amplification, an important biomarker in breast cancer, may have CTCs that are HER2-positive, in up to 30% of cases. These patients may therefore still benefit from HER2-targeted therapy.16
The DETECT studies are the first phase 3 trials in which treatment decisions are being based on the phenotypic characteristics of CTCs. DETECT III (NCT01619111) is comparing lapatinib in combination with standard therapy with standard therapy alone in patients with HER2-negative metastatic breast cancer who have HER2-positive CTCs, whereas DETECT IV (NCT02035813) is enrolling patients with HER2-negative, hormone receptor-positive metastatic breast cancer and persistent HER2-negative CTCs to receive standard endocrine therapy and the mammalian target of rapamycin inhibitor everolimus.
Other targets and sources for liquid biopsy
Another approach to liquid biopsies that is also beginning to take off is to collect tumor-derived exosomes from the bloodstream. Exosomes are tiny, fluid-filled, membrane-bound sacks that bud off from the surface of a cell to expel waste or to transport cargo from one cell to another. DNA, RNA, and protein can be extracted from tumor-derived exosomes and could also serve as molecular biomarkers relating to the cancer cells from which they came.6,7
Exosome Diagnostics is bringing the first exosome-based diagnostic tests to the market and recently teamed up with Amgen for the development of these liquid biopsies.17 In January 2016, they launched ExoDx Lung (ALK), for detection of EML4-ALK gene fusions in patients with NSCLC, using a proprietary platform for the isolation of RNA from exosomes. Data that was presented at several different conferences in 2015 demonstrated a sensitivity of 88% and specificity of 100% for this diagnostic when compared with tissue ALK status in NSCLC patients receiving a second-generation ALK inhibitor following progression on prior ALK inhibitor therapy.18
In September, they subsequently announced the launch of a test that analyses genetic information from exosomes collected from a urine sample taken from prostate cancer patients. Using a 3-gene signature, in combination with a proprietary algorithm, this diagnostic generates a score assessing a prostate cancer patient’s risk for higher grade, more aggressive disease. It is designed to complement the prostate-specific antigen score and has demonstrated accuracy in ruling out the presence of high-grade cancer before an initial biopsy in more than 1,
1. Lennon NK, Adalsteinsson VA, Gabriel SB. Technological considerations for genome-guided diagnosis and management of cancer. Genome Med. 2016;8:112.
2. MIT Technology Review website. Liquid biopsy: fast DNA-sequencing machines are leading to simple blood tests for cancer. https://www.technologyreview.com/s/534991/liquid-biopsy/. Published 2015. Accessed December 19, 2016.
3. Alix-Panabières C and Pantel K. Clinical applications of circulating tumor cells and circulating tumor DNA as liquid biopsy. Cancer Discov. 2016;6(5):479-491.
4. Calabuig-Farinãs S, Jantus-Lewintre E, Herreros-Pomares A, Camps C. Circulating tumor cells versus circulating tumor DNA in lung cancer – which one will win? Transl Lung Cancer Res. 2016;5(5):466-482.
5. Karabacak, NM, Spuhler PS, Fachin F, et al. Microfluidic, marker-free isolation of circulating tumor cells from blood samples. Nat Protoc. 2014;9:694-710.
6. Buder A, Tomuta C, and Filipits M. The potential of liquid biopsies. Curr Opin Oncol. 2016;28:130-134.
7. Hofman P, Popper HH. Pathologists and liquid biopsies: to be or not to be? Virchows Arch. 2016;469:601-609.
8. Bidard FC, Peeters DJ, Fehm T, et al. Clinical validity of circulating tumor cells in patients with metastatic breast cancer: a pooled analysis of individual patient data. Lancet Oncol. 2014;15(4):406-414.
9. de Bono JS, Scher HI, Montgomery RB, et al. Circulating tumor cells predict survival benefit from treatment in metastatic castration-resistant prostate cancer. Clin Cancer Res. 2008;14(19):6302-6309.
10. Cohen SJ, Punt CJ, Iannotti N, et al. Relationship of circulating tumor cells to tumor response, progression-free survival, and overall survival in patients with metastatic colorectal cancer. J Clin Oncol. 2008;26(19):3213-3221.
11. CellSearch Web site. What is the CELLSEARCH® System? https://www.cellsearchctc.com/product-systems-overview/cellsearch-system-overview. Last updated December 5th, 2016. Accessed online December 19th, 2016.
12. CellSearch Web site [advertisement]. https://www.cellsearchctc.com/clinical-applications/clinical-applications-overview. Last updated December 5, 2016. Accessed December 19, 2016.
13. US Food and Drug Administration. cobas EGFR Mutation Test v2 – P150047. http://www.fda.gov/MedicalDevices/ProductsandMedicalProcedures/DeviceApprovalsandClearances/Recently-ApprovedDevices/ucm519922.htm. Last updated September 9, 2016. Accessed December 19, 2016.
14. Wu YL, Zhou C, Liam CK, et al. First-line erlotinib versus gemcitabine/cisplatin in patients with advanced EGFR mutation-positive non-small cell lung cancer: analyses from the phase III, randomized, open-label, ENSURE study. Ann Oncol. 2015;26(9):1883-1889.
15. Zill OA, Mortimer S, Banks KC, et al. Somatic genomic landscape of over 15,000 patients with advanced-stage cancer from clinical next-generation sequencing analysis of circulating tumor DNA. J Clin Oncol. 2016;34(suppl;abstr LBA11501).
16. Jordan NV, Bardia A, Wittner BS, et al. HER2 expression identifies dynamic functional states within circulating breast cancer cells. Nature. 2016;537:102-106.
17. Exosome Diagnostics. Exosome diagnostics enters agreement with Amgen. http://www.exosomedx.com/news-events/press-releases/exosome-diagnostics-enters-agreement-amgen. Published October 3, 2016. Accessed December 19, 2016.
18. Brinkman K, Emenegger J, Tannous B, et al. Exosomal RNA-based liquid biopsy detection of EML4-ALK in plasma from NSCLC patients [2015 World Conference on Lung Cancer, Denver, CO; abstract 2591]. http://library.iaslc.org/search-speaker?search_speaker=30493. Accessed January 6, 2017.
19. Exosome Diagnostics website. Prostate cancer. http://www.exosomedx.com/prostate-cancer-0. Last updated 2017. Accessed online December 19, 2016.
Pathologic and, increasingly, molecular analysis of tumor tissue biopsies is the gold standard in initial diagnosis of cancer, but liquid biopsies, which analyze tumor-derived material circulating in the bloodstream are gaining traction. Here, we discuss the current state of development of this complementary and potentially alternative approach to tumor analysis.
Liquid biopsy gaining traction
Biopsies enable oncologists to gather information about a potential or established tumor, including confirmation of the presence of cancerous tissue and determination of its histological characteristics, such as tumor grade and stage, as well as its molecular features, such as the presence of certain gene mutations. Ultimately, this information can be put to use in determining the most appropriate course of treatment.
The current gold standard is a tissue biopsy that typically involves an invasive procedure to permit the collection of a piece of tumor tissue. Yet, tissue biopsies are not always feasible because of the location of the tumor or the poor performance status of many patients with advanced disease. They also provide only a snapshot of the disease at the time at which they were taken and don’t necessarily reflect the genetic heterogeneity or evolution of a tumor over time.
The detection of components that are derived from the tumor circulating in the blood of cancer patients had fueled the idea of blood-based diagnostics in oncology – so-called liquid biopsies. These have rapidly gained traction in the past several decades as a less expensive (the cost of performing genomic analyses on blood samples is at least an order of magnitude less than on tissue samples), less invasive (requiring only a simple blood draw) alternative source of information about tumors.1
As researchers have refined the ability to exploit liquid biopsies, commercial interest has been piqued. More than 35 companies within the United States alone are developing liquid biopsies, and it’s easy to see why with a market projected to be in the many billions of dollars.2
Seeking out tumor clues in the blood
Liquid biopsies consist of a 10-15 mL blood sample drawn into a tube that contains an anticoagulant and it can contain several different types of tumor-associated material. Thus far, two components – circulating tumor cells (CTCs) and circulating tumor DNA (ctDNA) – have formed the cornerstone of liquid biopsies. At present, it is not clear whether these components are released randomly, as a by-product of tumor cell death or if they are released as part of a specific biologic process, such as for the colonization of metastatic sites. It reality, it may be a little of both, and active dissemination may be particularly relevant for CTCs, among which are postulated to be a population of cancer stem cells that can initiate distant metastases.3,4
The discovery of CTCs dates back to the 1860s, when cells that were morphologically identical to the tumor were identified in the blood of a patient with metastatic cancer. Their potential significance was not fully realized until a few decades ago, when they were found to exist from early on in the course of disease.3,4
CTCs, which can be either single cells or clusters of cells known as microemboli, have a short half-life in the bloodstream – less than 2 ½ hours – and are also extremely rare (1 mL of blood contains 1-10 CTCs) against a background of many millions of normal cells. Thus the detection and isolation of CTCs presents a significant challenge. More than 40 different platforms are being developed for the isolation and enrichment of CTCs. For the most part, these use a method called positive selection to pick out CTCs.1,3,4
Positive selection exploits the biological or physical properties that are specific to CTCs and absent in normal cells, for example, the presence of a specific tumor-associated antigen on their surface or differences in size, density or electric charge. The limitations of this method are that, not only do you need to know something about CTCs to begin to understand what makes them truly unique and ensure only isolation of CTCs, but their phenotype is also thought to be continually changing.1,3,4
In recent years, the focus has shifted toward technologies that use negative depletion, meaning that they target the other types of cells in the blood sample and filter those away until only the CTCs are left behind. The most advanced are devices that use microfluidic technology to sort the cells, such as the CTC-iChip system being developed by researchers at Massachusetts General Hospital in Boston.5
ctDNA consists of small fragments of nucleic acids that are not contained within a cell or associated with cell fragments and is thought to be present in 50%-90% of patients, depending on the type of cancer they have. ctDNA has a similarly short half-life in the circulation to CTCs and, like CTCs, ctDNA is present at very low levels in the bloodstream. Although levels of ctDNA have been shown to increase with increasing tumor burden, it is still often obscured by the presence of other cell-free DNA derived from non-tumor cells.
ctDNA can be distinguished from other cell-free DNA by the presence of somatic mutations and a number of highly sensitive methods have been developed to detect them, including the amplification-refractory mutation system (ARMS); digital polymerase chain reaction; and the beads, emulsification, amplification, and magnetics (BEAMing) system. Next-generation sequencing technologies, including tagged-amplicon deep sequencing (TAm-Seq), the Safe-Sequencing System (Safe-SeqS), and cancer personalized profiling by deep sequencing (CAPP-seq), can also be used and the race for ever more sensitive analytical tools is ongoing.1,3,4,6
Applying liquid biopsies now and in the future
There are a plethora of potential applications for liquid biopsies3,7 (Figure 1), and probably the most exciting among them is the potential for screening for and early detection of cancer. The fact that ctDNA and CTCs have both been shown to be present from the earliest stages of disease has sparked interest in the possibility of developing simple blood tests to identify tumors before they become detectable by other methods and at a point at which they may be curable.
Given that both are present at such low levels within the circulation and are particularly sparse at earlier stages of disease, current technologies may lack the specificity and sensitivity for this application at present. However, numerous clinical trials are ongoing.
For CTCs, simple enumeration has been the most extensively investigated application to date. Numerous studies have shown that the number of CTCs in the bloodstream has prognostic significance in various different tumor types. Three such studies led to the first regulatory approval for a CTC detection system (Table 1 and Table 2).8-10
One area in which liquid biopsies could really come into their own is in providing more real-time analysis of tumors. This is something that has proven particularly challenging with tissue biopsies because repeating these invasive procedures is problematic. But the ease of repeat blood draws means that serial liquid biopsies could be performed and might offer the possibility of monitoring disease progression and evolution over the course of disease and particularly in response to treatment.
Indeed, studies have shown that in addition to baseline CTC counts, changes in CTC number during treatment are also prognostic. There was improved survival among patients whose CTC counts decreased below a threshold value during treatment and vice versa. This is also an approved use for CellSearch though at present it is not widely clinically implemented.12
Clinical utility remains elusive
The ultimate goal would be for liquid biopsies to have an impact on treatment decisions, allowing oncologists to change management strategy based on predicted sensitivity or resistance to therapy, so-called clinical utility. Thus far, clinical utility has proved elusive, though liquid biopsies using ctDNA to evaluate tumor genotype have come closest.
The Cobas EGFR Mutation Test v2 recently became the first ctDNA-based liquid biopsy to receive regulatory approval. It was approved as a companion diagnostic to identify patients with advanced non–small-cell lung cancer (NSCLC) who have specific mutations in the epidermal growth factor receptor (EGFR) gene and are therefore eligible for treatment with the EGFR inhibitor erlotinib.13
Approval was based on comparison of EGFR mutation identification rates using plasma ctDNA samples and tumor tissue samples from patients enrolled in the phase 3 ENSURE trial, which compared the efficacy of erlotinib with chemotherapy as first-line therapy in patients with advanced NSCLC. Of the 217 patients enrolled in the trial, 98.6% of patients had both tumor biopsy and plasma ctDNA samples available for testing. Concordance between the two types of biopsy in identifying patients with EGFR mutations was high and patients with EGFR positivity according to liquid biopsy results demonstrated improved progression-free survival when treated with erlotinib.14
The results of a large-scale genomic analysis of various different types of tumors using ctDNA were also recently presented at the 2016 American Society of Clinical Oncology meeting. Blood samples from more than 15,000 patients with 50 different tumor types, including advanced lung cancer (37%), breast cancer (14%), and CRC (10%), were collected and compared with either available tumor biopsy samples from the same cases (n = 398) or, in the majority of cases, with The Cancer Genome Atlas database, which uses tumor biopsies to perform genome-wide sequencing studies. Both types of biopsy revealed very similar mutation patterns when the Guardant360 next-generation sequencing test, which targets 70 genes, was applied. In particular, when EGFR, BRAF, KRAS, ALK, RET, and ROS1 mutations were identified by tumor tissue biopsy, the same mutations were reported in 94%-100% of plasma samples.15
Studies of the clinical utility of ctDNA and CTCs are among ongoing clinical trials of liquid biopsies (Tables 2 and 3). The potential for using CTCs to guide treatment decisions has become particularly relevant in breast cancer in light of results showing that patients with primary tumors that are negative for human epidermal growth factor receptor 2 (HER2) amplification, an important biomarker in breast cancer, may have CTCs that are HER2-positive, in up to 30% of cases. These patients may therefore still benefit from HER2-targeted therapy.16
The DETECT studies are the first phase 3 trials in which treatment decisions are being based on the phenotypic characteristics of CTCs. DETECT III (NCT01619111) is comparing lapatinib in combination with standard therapy with standard therapy alone in patients with HER2-negative metastatic breast cancer who have HER2-positive CTCs, whereas DETECT IV (NCT02035813) is enrolling patients with HER2-negative, hormone receptor-positive metastatic breast cancer and persistent HER2-negative CTCs to receive standard endocrine therapy and the mammalian target of rapamycin inhibitor everolimus.
Other targets and sources for liquid biopsy
Another approach to liquid biopsies that is also beginning to take off is to collect tumor-derived exosomes from the bloodstream. Exosomes are tiny, fluid-filled, membrane-bound sacks that bud off from the surface of a cell to expel waste or to transport cargo from one cell to another. DNA, RNA, and protein can be extracted from tumor-derived exosomes and could also serve as molecular biomarkers relating to the cancer cells from which they came.6,7
Exosome Diagnostics is bringing the first exosome-based diagnostic tests to the market and recently teamed up with Amgen for the development of these liquid biopsies.17 In January 2016, they launched ExoDx Lung (ALK), for detection of EML4-ALK gene fusions in patients with NSCLC, using a proprietary platform for the isolation of RNA from exosomes. Data that was presented at several different conferences in 2015 demonstrated a sensitivity of 88% and specificity of 100% for this diagnostic when compared with tissue ALK status in NSCLC patients receiving a second-generation ALK inhibitor following progression on prior ALK inhibitor therapy.18
In September, they subsequently announced the launch of a test that analyses genetic information from exosomes collected from a urine sample taken from prostate cancer patients. Using a 3-gene signature, in combination with a proprietary algorithm, this diagnostic generates a score assessing a prostate cancer patient’s risk for higher grade, more aggressive disease. It is designed to complement the prostate-specific antigen score and has demonstrated accuracy in ruling out the presence of high-grade cancer before an initial biopsy in more than 1,
Pathologic and, increasingly, molecular analysis of tumor tissue biopsies is the gold standard in initial diagnosis of cancer, but liquid biopsies, which analyze tumor-derived material circulating in the bloodstream are gaining traction. Here, we discuss the current state of development of this complementary and potentially alternative approach to tumor analysis.
Liquid biopsy gaining traction
Biopsies enable oncologists to gather information about a potential or established tumor, including confirmation of the presence of cancerous tissue and determination of its histological characteristics, such as tumor grade and stage, as well as its molecular features, such as the presence of certain gene mutations. Ultimately, this information can be put to use in determining the most appropriate course of treatment.
The current gold standard is a tissue biopsy that typically involves an invasive procedure to permit the collection of a piece of tumor tissue. Yet, tissue biopsies are not always feasible because of the location of the tumor or the poor performance status of many patients with advanced disease. They also provide only a snapshot of the disease at the time at which they were taken and don’t necessarily reflect the genetic heterogeneity or evolution of a tumor over time.
The detection of components that are derived from the tumor circulating in the blood of cancer patients had fueled the idea of blood-based diagnostics in oncology – so-called liquid biopsies. These have rapidly gained traction in the past several decades as a less expensive (the cost of performing genomic analyses on blood samples is at least an order of magnitude less than on tissue samples), less invasive (requiring only a simple blood draw) alternative source of information about tumors.1
As researchers have refined the ability to exploit liquid biopsies, commercial interest has been piqued. More than 35 companies within the United States alone are developing liquid biopsies, and it’s easy to see why with a market projected to be in the many billions of dollars.2
Seeking out tumor clues in the blood
Liquid biopsies consist of a 10-15 mL blood sample drawn into a tube that contains an anticoagulant and it can contain several different types of tumor-associated material. Thus far, two components – circulating tumor cells (CTCs) and circulating tumor DNA (ctDNA) – have formed the cornerstone of liquid biopsies. At present, it is not clear whether these components are released randomly, as a by-product of tumor cell death or if they are released as part of a specific biologic process, such as for the colonization of metastatic sites. It reality, it may be a little of both, and active dissemination may be particularly relevant for CTCs, among which are postulated to be a population of cancer stem cells that can initiate distant metastases.3,4
The discovery of CTCs dates back to the 1860s, when cells that were morphologically identical to the tumor were identified in the blood of a patient with metastatic cancer. Their potential significance was not fully realized until a few decades ago, when they were found to exist from early on in the course of disease.3,4
CTCs, which can be either single cells or clusters of cells known as microemboli, have a short half-life in the bloodstream – less than 2 ½ hours – and are also extremely rare (1 mL of blood contains 1-10 CTCs) against a background of many millions of normal cells. Thus the detection and isolation of CTCs presents a significant challenge. More than 40 different platforms are being developed for the isolation and enrichment of CTCs. For the most part, these use a method called positive selection to pick out CTCs.1,3,4
Positive selection exploits the biological or physical properties that are specific to CTCs and absent in normal cells, for example, the presence of a specific tumor-associated antigen on their surface or differences in size, density or electric charge. The limitations of this method are that, not only do you need to know something about CTCs to begin to understand what makes them truly unique and ensure only isolation of CTCs, but their phenotype is also thought to be continually changing.1,3,4
In recent years, the focus has shifted toward technologies that use negative depletion, meaning that they target the other types of cells in the blood sample and filter those away until only the CTCs are left behind. The most advanced are devices that use microfluidic technology to sort the cells, such as the CTC-iChip system being developed by researchers at Massachusetts General Hospital in Boston.5
ctDNA consists of small fragments of nucleic acids that are not contained within a cell or associated with cell fragments and is thought to be present in 50%-90% of patients, depending on the type of cancer they have. ctDNA has a similarly short half-life in the circulation to CTCs and, like CTCs, ctDNA is present at very low levels in the bloodstream. Although levels of ctDNA have been shown to increase with increasing tumor burden, it is still often obscured by the presence of other cell-free DNA derived from non-tumor cells.
ctDNA can be distinguished from other cell-free DNA by the presence of somatic mutations and a number of highly sensitive methods have been developed to detect them, including the amplification-refractory mutation system (ARMS); digital polymerase chain reaction; and the beads, emulsification, amplification, and magnetics (BEAMing) system. Next-generation sequencing technologies, including tagged-amplicon deep sequencing (TAm-Seq), the Safe-Sequencing System (Safe-SeqS), and cancer personalized profiling by deep sequencing (CAPP-seq), can also be used and the race for ever more sensitive analytical tools is ongoing.1,3,4,6
Applying liquid biopsies now and in the future
There are a plethora of potential applications for liquid biopsies3,7 (Figure 1), and probably the most exciting among them is the potential for screening for and early detection of cancer. The fact that ctDNA and CTCs have both been shown to be present from the earliest stages of disease has sparked interest in the possibility of developing simple blood tests to identify tumors before they become detectable by other methods and at a point at which they may be curable.
Given that both are present at such low levels within the circulation and are particularly sparse at earlier stages of disease, current technologies may lack the specificity and sensitivity for this application at present. However, numerous clinical trials are ongoing.
For CTCs, simple enumeration has been the most extensively investigated application to date. Numerous studies have shown that the number of CTCs in the bloodstream has prognostic significance in various different tumor types. Three such studies led to the first regulatory approval for a CTC detection system (Table 1 and Table 2).8-10
One area in which liquid biopsies could really come into their own is in providing more real-time analysis of tumors. This is something that has proven particularly challenging with tissue biopsies because repeating these invasive procedures is problematic. But the ease of repeat blood draws means that serial liquid biopsies could be performed and might offer the possibility of monitoring disease progression and evolution over the course of disease and particularly in response to treatment.
Indeed, studies have shown that in addition to baseline CTC counts, changes in CTC number during treatment are also prognostic. There was improved survival among patients whose CTC counts decreased below a threshold value during treatment and vice versa. This is also an approved use for CellSearch though at present it is not widely clinically implemented.12
Clinical utility remains elusive
The ultimate goal would be for liquid biopsies to have an impact on treatment decisions, allowing oncologists to change management strategy based on predicted sensitivity or resistance to therapy, so-called clinical utility. Thus far, clinical utility has proved elusive, though liquid biopsies using ctDNA to evaluate tumor genotype have come closest.
The Cobas EGFR Mutation Test v2 recently became the first ctDNA-based liquid biopsy to receive regulatory approval. It was approved as a companion diagnostic to identify patients with advanced non–small-cell lung cancer (NSCLC) who have specific mutations in the epidermal growth factor receptor (EGFR) gene and are therefore eligible for treatment with the EGFR inhibitor erlotinib.13
Approval was based on comparison of EGFR mutation identification rates using plasma ctDNA samples and tumor tissue samples from patients enrolled in the phase 3 ENSURE trial, which compared the efficacy of erlotinib with chemotherapy as first-line therapy in patients with advanced NSCLC. Of the 217 patients enrolled in the trial, 98.6% of patients had both tumor biopsy and plasma ctDNA samples available for testing. Concordance between the two types of biopsy in identifying patients with EGFR mutations was high and patients with EGFR positivity according to liquid biopsy results demonstrated improved progression-free survival when treated with erlotinib.14
The results of a large-scale genomic analysis of various different types of tumors using ctDNA were also recently presented at the 2016 American Society of Clinical Oncology meeting. Blood samples from more than 15,000 patients with 50 different tumor types, including advanced lung cancer (37%), breast cancer (14%), and CRC (10%), were collected and compared with either available tumor biopsy samples from the same cases (n = 398) or, in the majority of cases, with The Cancer Genome Atlas database, which uses tumor biopsies to perform genome-wide sequencing studies. Both types of biopsy revealed very similar mutation patterns when the Guardant360 next-generation sequencing test, which targets 70 genes, was applied. In particular, when EGFR, BRAF, KRAS, ALK, RET, and ROS1 mutations were identified by tumor tissue biopsy, the same mutations were reported in 94%-100% of plasma samples.15
Studies of the clinical utility of ctDNA and CTCs are among ongoing clinical trials of liquid biopsies (Tables 2 and 3). The potential for using CTCs to guide treatment decisions has become particularly relevant in breast cancer in light of results showing that patients with primary tumors that are negative for human epidermal growth factor receptor 2 (HER2) amplification, an important biomarker in breast cancer, may have CTCs that are HER2-positive, in up to 30% of cases. These patients may therefore still benefit from HER2-targeted therapy.16
The DETECT studies are the first phase 3 trials in which treatment decisions are being based on the phenotypic characteristics of CTCs. DETECT III (NCT01619111) is comparing lapatinib in combination with standard therapy with standard therapy alone in patients with HER2-negative metastatic breast cancer who have HER2-positive CTCs, whereas DETECT IV (NCT02035813) is enrolling patients with HER2-negative, hormone receptor-positive metastatic breast cancer and persistent HER2-negative CTCs to receive standard endocrine therapy and the mammalian target of rapamycin inhibitor everolimus.
Other targets and sources for liquid biopsy
Another approach to liquid biopsies that is also beginning to take off is to collect tumor-derived exosomes from the bloodstream. Exosomes are tiny, fluid-filled, membrane-bound sacks that bud off from the surface of a cell to expel waste or to transport cargo from one cell to another. DNA, RNA, and protein can be extracted from tumor-derived exosomes and could also serve as molecular biomarkers relating to the cancer cells from which they came.6,7
Exosome Diagnostics is bringing the first exosome-based diagnostic tests to the market and recently teamed up with Amgen for the development of these liquid biopsies.17 In January 2016, they launched ExoDx Lung (ALK), for detection of EML4-ALK gene fusions in patients with NSCLC, using a proprietary platform for the isolation of RNA from exosomes. Data that was presented at several different conferences in 2015 demonstrated a sensitivity of 88% and specificity of 100% for this diagnostic when compared with tissue ALK status in NSCLC patients receiving a second-generation ALK inhibitor following progression on prior ALK inhibitor therapy.18
In September, they subsequently announced the launch of a test that analyses genetic information from exosomes collected from a urine sample taken from prostate cancer patients. Using a 3-gene signature, in combination with a proprietary algorithm, this diagnostic generates a score assessing a prostate cancer patient’s risk for higher grade, more aggressive disease. It is designed to complement the prostate-specific antigen score and has demonstrated accuracy in ruling out the presence of high-grade cancer before an initial biopsy in more than 1,
1. Lennon NK, Adalsteinsson VA, Gabriel SB. Technological considerations for genome-guided diagnosis and management of cancer. Genome Med. 2016;8:112.
2. MIT Technology Review website. Liquid biopsy: fast DNA-sequencing machines are leading to simple blood tests for cancer. https://www.technologyreview.com/s/534991/liquid-biopsy/. Published 2015. Accessed December 19, 2016.
3. Alix-Panabières C and Pantel K. Clinical applications of circulating tumor cells and circulating tumor DNA as liquid biopsy. Cancer Discov. 2016;6(5):479-491.
4. Calabuig-Farinãs S, Jantus-Lewintre E, Herreros-Pomares A, Camps C. Circulating tumor cells versus circulating tumor DNA in lung cancer – which one will win? Transl Lung Cancer Res. 2016;5(5):466-482.
5. Karabacak, NM, Spuhler PS, Fachin F, et al. Microfluidic, marker-free isolation of circulating tumor cells from blood samples. Nat Protoc. 2014;9:694-710.
6. Buder A, Tomuta C, and Filipits M. The potential of liquid biopsies. Curr Opin Oncol. 2016;28:130-134.
7. Hofman P, Popper HH. Pathologists and liquid biopsies: to be or not to be? Virchows Arch. 2016;469:601-609.
8. Bidard FC, Peeters DJ, Fehm T, et al. Clinical validity of circulating tumor cells in patients with metastatic breast cancer: a pooled analysis of individual patient data. Lancet Oncol. 2014;15(4):406-414.
9. de Bono JS, Scher HI, Montgomery RB, et al. Circulating tumor cells predict survival benefit from treatment in metastatic castration-resistant prostate cancer. Clin Cancer Res. 2008;14(19):6302-6309.
10. Cohen SJ, Punt CJ, Iannotti N, et al. Relationship of circulating tumor cells to tumor response, progression-free survival, and overall survival in patients with metastatic colorectal cancer. J Clin Oncol. 2008;26(19):3213-3221.
11. CellSearch Web site. What is the CELLSEARCH® System? https://www.cellsearchctc.com/product-systems-overview/cellsearch-system-overview. Last updated December 5th, 2016. Accessed online December 19th, 2016.
12. CellSearch Web site [advertisement]. https://www.cellsearchctc.com/clinical-applications/clinical-applications-overview. Last updated December 5, 2016. Accessed December 19, 2016.
13. US Food and Drug Administration. cobas EGFR Mutation Test v2 – P150047. http://www.fda.gov/MedicalDevices/ProductsandMedicalProcedures/DeviceApprovalsandClearances/Recently-ApprovedDevices/ucm519922.htm. Last updated September 9, 2016. Accessed December 19, 2016.
14. Wu YL, Zhou C, Liam CK, et al. First-line erlotinib versus gemcitabine/cisplatin in patients with advanced EGFR mutation-positive non-small cell lung cancer: analyses from the phase III, randomized, open-label, ENSURE study. Ann Oncol. 2015;26(9):1883-1889.
15. Zill OA, Mortimer S, Banks KC, et al. Somatic genomic landscape of over 15,000 patients with advanced-stage cancer from clinical next-generation sequencing analysis of circulating tumor DNA. J Clin Oncol. 2016;34(suppl;abstr LBA11501).
16. Jordan NV, Bardia A, Wittner BS, et al. HER2 expression identifies dynamic functional states within circulating breast cancer cells. Nature. 2016;537:102-106.
17. Exosome Diagnostics. Exosome diagnostics enters agreement with Amgen. http://www.exosomedx.com/news-events/press-releases/exosome-diagnostics-enters-agreement-amgen. Published October 3, 2016. Accessed December 19, 2016.
18. Brinkman K, Emenegger J, Tannous B, et al. Exosomal RNA-based liquid biopsy detection of EML4-ALK in plasma from NSCLC patients [2015 World Conference on Lung Cancer, Denver, CO; abstract 2591]. http://library.iaslc.org/search-speaker?search_speaker=30493. Accessed January 6, 2017.
19. Exosome Diagnostics website. Prostate cancer. http://www.exosomedx.com/prostate-cancer-0. Last updated 2017. Accessed online December 19, 2016.
1. Lennon NK, Adalsteinsson VA, Gabriel SB. Technological considerations for genome-guided diagnosis and management of cancer. Genome Med. 2016;8:112.
2. MIT Technology Review website. Liquid biopsy: fast DNA-sequencing machines are leading to simple blood tests for cancer. https://www.technologyreview.com/s/534991/liquid-biopsy/. Published 2015. Accessed December 19, 2016.
3. Alix-Panabières C and Pantel K. Clinical applications of circulating tumor cells and circulating tumor DNA as liquid biopsy. Cancer Discov. 2016;6(5):479-491.
4. Calabuig-Farinãs S, Jantus-Lewintre E, Herreros-Pomares A, Camps C. Circulating tumor cells versus circulating tumor DNA in lung cancer – which one will win? Transl Lung Cancer Res. 2016;5(5):466-482.
5. Karabacak, NM, Spuhler PS, Fachin F, et al. Microfluidic, marker-free isolation of circulating tumor cells from blood samples. Nat Protoc. 2014;9:694-710.
6. Buder A, Tomuta C, and Filipits M. The potential of liquid biopsies. Curr Opin Oncol. 2016;28:130-134.
7. Hofman P, Popper HH. Pathologists and liquid biopsies: to be or not to be? Virchows Arch. 2016;469:601-609.
8. Bidard FC, Peeters DJ, Fehm T, et al. Clinical validity of circulating tumor cells in patients with metastatic breast cancer: a pooled analysis of individual patient data. Lancet Oncol. 2014;15(4):406-414.
9. de Bono JS, Scher HI, Montgomery RB, et al. Circulating tumor cells predict survival benefit from treatment in metastatic castration-resistant prostate cancer. Clin Cancer Res. 2008;14(19):6302-6309.
10. Cohen SJ, Punt CJ, Iannotti N, et al. Relationship of circulating tumor cells to tumor response, progression-free survival, and overall survival in patients with metastatic colorectal cancer. J Clin Oncol. 2008;26(19):3213-3221.
11. CellSearch Web site. What is the CELLSEARCH® System? https://www.cellsearchctc.com/product-systems-overview/cellsearch-system-overview. Last updated December 5th, 2016. Accessed online December 19th, 2016.
12. CellSearch Web site [advertisement]. https://www.cellsearchctc.com/clinical-applications/clinical-applications-overview. Last updated December 5, 2016. Accessed December 19, 2016.
13. US Food and Drug Administration. cobas EGFR Mutation Test v2 – P150047. http://www.fda.gov/MedicalDevices/ProductsandMedicalProcedures/DeviceApprovalsandClearances/Recently-ApprovedDevices/ucm519922.htm. Last updated September 9, 2016. Accessed December 19, 2016.
14. Wu YL, Zhou C, Liam CK, et al. First-line erlotinib versus gemcitabine/cisplatin in patients with advanced EGFR mutation-positive non-small cell lung cancer: analyses from the phase III, randomized, open-label, ENSURE study. Ann Oncol. 2015;26(9):1883-1889.
15. Zill OA, Mortimer S, Banks KC, et al. Somatic genomic landscape of over 15,000 patients with advanced-stage cancer from clinical next-generation sequencing analysis of circulating tumor DNA. J Clin Oncol. 2016;34(suppl;abstr LBA11501).
16. Jordan NV, Bardia A, Wittner BS, et al. HER2 expression identifies dynamic functional states within circulating breast cancer cells. Nature. 2016;537:102-106.
17. Exosome Diagnostics. Exosome diagnostics enters agreement with Amgen. http://www.exosomedx.com/news-events/press-releases/exosome-diagnostics-enters-agreement-amgen. Published October 3, 2016. Accessed December 19, 2016.
18. Brinkman K, Emenegger J, Tannous B, et al. Exosomal RNA-based liquid biopsy detection of EML4-ALK in plasma from NSCLC patients [2015 World Conference on Lung Cancer, Denver, CO; abstract 2591]. http://library.iaslc.org/search-speaker?search_speaker=30493. Accessed January 6, 2017.
19. Exosome Diagnostics website. Prostate cancer. http://www.exosomedx.com/prostate-cancer-0. Last updated 2017. Accessed online December 19, 2016.
Point of prostate cancer diagnosis experiences and needs of black men: the Florida CaPCaS study
As of 2016, Florida ranks second among all states in the United States in estimated new cases of prostate cancer and second in estimated deaths from prostate cancer.1 Disparities in diagnosis, mortality rates, and access to cancer care also continue to be a major problem in Florida, especially for black men. For example, black men were the only racial/ethnic group that did not meet the Healthy People (HP) 2010 objective to reduce the prostate cancer death rate to 28.2 per 100,000 men and that has not met the HP 2020 objective to reduce the prostate cancer death rate to 21.2 per 100,000 men (Table 1). Based on the 2013 prostate cancer mortality rates for Florida,2 the death rate for black men is almost twice the HP 2020 goal (37.49 per 100,000).
A diagnosis of prostate cancer is a life changing event for a man. In particular, there is limited research on the experiences and coping mechanisms of black men at diagnosis. This limited body of research indicates that black men’s reactions to their initial diagnoses varied, from being shocked when notified of their initial diagnosis of prostate cancer,3 to perceiving that they had received a “death sentence”.4 In regard to having to make decisions about their treatment options, some black men indicated that the information about treatment that they received from physicians decreased their anxiety,5 whereas others noted that they had not been given adequate information by a physician to make a decision.6 Patients have also reported that they felt as though they were not knowledgeable enough to ask questions concerning treatment options and preferred for the physician to make the treatment choice for them.6 Decisional regret is now a common observation among men who are not involved in making decisions about their treatment.3
According to the American Cancer Society, about 30,000 black men were diagnosed with prostate cancer in 2016.7 It is important to understand these men’s needs and help them cope effectively as they navigate the survivorship continuum. In line with our research program’s goal of ensuring quality cancer care for black men, the primary objective of this study was to explore the experiences and needs of black men at the point of prostate cancer diagnosis (PPCD). Specifically, we developed an interpretative framework for black men’s experiences at the PPCD, focusing on United States or native-born black men (NBBM) and Caribbean-born black men (CBBM). African-born black men were not included in this study because of the low sample size for that ethnicity. This study is part of a large-scale study that focuses on developing a model of prostate cancer care and survivorship (CaPCaS model) using grounded theory to study black, ethnically diverse prostate cancer survivors.
Methods
The study aims to close the prostate health disparity gap for black men in Florida through community engaged research in partnership with survivors of prostate cancer and their advocates. The current study was a prospective, grounded theory study that involved one-on-one, in-depth interviews with 31 prostate cancer patients about their care and survivorship experiences. Specifically, 17 NBBM and 14 CBBM were enrolled in the project. Appropriate human subjects review and approval were obtained from the University of Florida, the Florida Department of Health, and the Department of Defense.
Research design
This is a qualitative research study. Based on the principles of community engaged research and using a rigorous qualitative research methodology, we recruited NBBM and CBBM with a personal history of prostate cancer. Guided by open-ended questions developed by the team, one-on-one in-depth interviews were conducted with each participant in their home or at a convenient location in the community. Our primary focus was on the participants’ care and survivorship experiences, with primary focus on their prostate cancer diagnosis. Qualitative research was our methodology of choice because little is known about the PPCD experiences of black men.8 With qualitative research, we were able to get our participants to “relive” their experiences in the presence of a culturally competent, well-trained interviewer and elicit the information about their care and survivorship experiences based on their interpretation. In addition, we were able to capture the dynamic processes associated with their experiences, documenting sequential patterns and change through both verbal and nonverbal communications, because the participants were interviewed twice.
Research population and recruitment
The study setting was Florida. The inclusion criteria were: black men, personal history of prostate cancer, ability to complete two separate interviews with each one expected to last 2-3 hours, and flexibility to meet interviewers at a convenient community site for the interviews. Participants were identified through the Florida Cancer Data System (FCDS)9 database. At the time of the study, the most recent FCDS database was for 2010. The FCDS has collected the number of new cancer cancers diagnosed in the state of Florida annually since 1981. It is a comprehensive incidence-only registry and does not extract data on patients with a death certificate. All investigators are bounded by the confidential pledge required for the use of the FCDS data.
We used the Florida Department of Health’s (DoH’s) Bureau of Epidemiology standard procedure for the FCDS9 to recruit participants. Our recruitment strategies included: initial patient contact by written correspondence; second mailing that included a telephone opt-out card after 3 weeks for nonrespondents (the telephone opt-out card explained to the patient that if no response was received, the study investigator would attempt a telephone call to introduce the study); and a telephone call by a study staff to introduce the study for nonrespondents. As per the Florida DoH standard procedure, we did not disclose on the cover of the study mailings that the patient was being contacted for a study specific to cancer. Efforts to recruit a patient stopped immediately if a patient indicated that he did not wish to participate. All of the study staff making participant contact were extensively trained to provide a clear and accurate description of cancer registration in Florida. In addition, to assist the study staff in providing clear and accurate responses, responses to frequently asked questions were made available to the study staff. During the participant recruitment phase, anyone who seemed to be upset when contacted was reported immediately (within 24 hours) to the DoH cancer epidemiologist. In addition, the name of anyone who stated that he did not wish to be contacted again was given to the DoH so that the person would not be re-contacted.
Prescreening of participants for eligibility
All eligible participants who agreed to participate in the study comprised the pool of potential study participants. For those who agreed to participate, the following information was obtained by telephone interview using REDCap software:10 name and contact information, country of birth, age, marital status, and education level. The demographic information facilitated a purposeful systematic selection of black men of diverse age groups (younger than 50 years or older than 50 years), marital status (single, including divorced or separated, or married/in a relationship), and educational level (college degree or not college educated). An incentive of a $5 gift card was provided to all the men who participated in the screening phase. Using systematic sampling to ensure demographically diverse participants, 40 participants (20 NBBM, 20 CBBM) were selected from the initial pool of participants to participate in the study.
Data collection
The data collection was conducted by a trained Community Health Worker (CHW) using semi-structured interview process. The interview guide was constructed by the research team and the study community advisory board members to ensure language appropriateness, understanding and cultural sensitivity. For this study, the interview questions focused on participants’ background information and diagnosis history, including: participants’ personal story of diagnosis, feelings, emotions, reactions, regrets and level of personal/family/physician involvement in diagnosis. For the CBBM, we also obtained information on the age at which they immigrated to the United States. The CHW interviewer was trained to question participants and encourage them to elaborate on areas of importance to their experience.
A total time of about 5-6 hours was scheduled for the data collection per participant, which is sufficient for gathering in-depth perspectives. We scheduled two interviews lasting not more than 3 hours at a time so as not to create burden for study participants. Participants had the choice to have the interviews completed in a single session or spread out over 2 days. The interviews were audio-recorded to provide ease of transcription and back-up of data. At the end of the interviews, participants were compensated for participating in the study.
Data management and analyses
The study dataset included interview transcripts and field notes of the CHW interviewer describing his insights about the interviews. The data analyses included preparing and verifying the narrative data, coding data, and developing an interpretative framework for black men’s experiences at the PPCD. Interviews were transcribed verbatim by a professional transcription service that has policies in place for protected health information. Each transcript was then verified for accuracy by the CHW interviewer. The interview transcripts were imported directly into NVivo 11, a computer-assisted data analysis software that allows coding and modeling of complex narrative data. The data coding was conducted by our interdisciplinary team of clinicians, behavioral scientists, and social scientists. It is important to note that the NVivo 11 software was not used to analyze the data per se. However, it provided a sophisticated and systematic way to manage the following tasks for the analyses: organizing large quantities of narrative data, coding text, retrieving text by codes, querying the data, comparing sets of data interpretation between NBBM and CBBM; and developing analytic models. The study team members coded the data in weekly team meetings. The coding consisted of reading the data and identifying major themes, then assigning labels to and defining emerging categories.
Two levels of coding were used. The first, open coding, refers to an approach to data with no preconceived ideas about what will be found; and the second, focused or axial coding, refers to reviewing data for the purpose of more richly coding on a particular theme.11 We used dimensional analysis to ensure that each emerging concept was carefully defined. The study team went back and forth between the data and the emerging analytic framework, using constant comparison of new data with already coded data and new categories with previously analyzed text.12
To ensure trustworthiness and credibility,13 the study team maintained an audit trail that documented how and when analytic decisions were made. In addition, peer debriefing was conducted to ensure credibility, including the presentation of findings to the study community advisory board members as part of the community engaged research approach.
Results
Description of participants
The FCDS provided a database of 1,813 participants identified as black men diagnosed with prostate cancer in 2010. Because the FCDS does not extract data on patients with a death certificate, we found out during the pre-screening phase that a few of the men were deceased. In addition, there were a significant number of incorrect addresses. We obtained a total of 212 completed responses by phone during the prescreening phase. The majority of the participants were aged 60-69 years (48.2%), had a high school diploma only (26.1%), and were currently married (65.3%). Relative to ethnicity, 67% of participants classified themselves NBBM, 24% as CBBM, 3.5% as black men born in Africa, and 5.5% as Other/Don’t know/Refused. For the CBBM, the most common countries of birth were Jamaica, Haiti, and Guyana, respectively.
In all, 40 participants (20 NBBM and 20 CBBM) were selected from the 212 participants to participate in the study. Selection was conducted systematically to ensure representation in terms of age, marital status, education, and geographical location. Data saturation was achieved with 17 NBBM and 14 CBBM, after which we ended data collection (Table 2). Data saturation is the standard for deciding that we are not finding anything different from the interviews first coded and last coded. Although we were specifically looking for differences between the two groups (NBBM and CBBM), no between-group differences emerged. Each man’s experience was unique to him with some common themes emerging described hereinafter (Figure).
Moderating factors and experiences at PPCD
Some of the moderating factors that the study participants identified as affecting their reactions to the PPCD included health literacy, insurance status, spirituality, mistrust, prior experience with cancer, perceived susceptibility to cancer, and delay in diagnosis (Table 3). Health literacy, defined as personal, cognitive, and social skills that determine the ability of individuals to gain access to, understand, and use information to promote and maintain good health, was one of the moderating factors found in this study.13 Some of the black men came to the PPCD with a low level of health literacy, which had an impact on their understanding of the treatment options. For example, in the interview, participant 798 (NBBM) was confused about what tests had been done and was not able to accurately describe the treatments offered to him. Participant 1263 (CBBM) struggled to express the purpose and procedures associated with diagnostic biopsy. However, there were participants with a high level of health literacy (eg, participant 449 [NBBM]), who decided to research the disease.
Another factor to consider is the insurance status of participants at the PPCD. The majority of the participants had good insurance coverage, but some were affected by poor insurance coverage. Participant 1881(NBBM) made his treatment decision primarily on the basis of the pending lapse of his insurance coverage rather than the best clinical option for him. Participant 1979 (CBBM) described both his confusion on the screening tests and the impact of not having insurance coverage. Upon obtaining insurance coverage, he sought treatment for his prostate cancer with an urgency that he did not experience when he was first diagnosed when uninsured.
The spirituality of black men was another moderating factor at the PPCD. Participant 827 (NBBM) noted that he was unaffected when he received his diagnosis because he was a true believer. Some of the black men also came to the PPCD with lack of trust in the physician and/or the health care system and perceived a sense of contempt from the physician. Participant 1594 (NBBM) described mistrust based on the history of medical exploitation of black men as well as a perception of current discriminatory practices.
Another important PPCD status to note for black men is prior experience with cancer, including prior personal cancer history and/or prior cancer history of a family member. Participant 2024 (CBBM) described the meaning of cancer to him, while participant 798 (NBBM) echoed the despair of the cancer diagnosis based on experience with other cancers in the family. Sometimes there were multiple cancers in the family or even among the significant others of the participant, as was the case with Participant 1936 (CBBM).
Of greatest concern were men who delayed their diagnosis or treatment, perhaps resulting in their cancer being at a more advanced stage when they eventually did return for care. Finally, some of the men came to the PPCD appointment with a low expectation of receiving a diagnosis of prostate cancer, whereas others came to the PPCD fearful of the results of their testing.
In describing their experiences, participants expressed both positive and negative experiences: on the positive side, they found the information provided by the physician to be helpful; but on the negative side, the sterile or medically focused encounter was perceived as a lack empathy on the part of the physician.
Cognitive, emotional, and behavioral coping experiences
As expected, there were ranges of emotions, including shock, disbelief and denial (Table 4). Some of the men questioned why this (the cancer) was happening to them when they had done “nothing” to deserve it. Doing nothing in this case meant that they had lived a healthy lifestyle with no obvious apparent cause to have the cancer. Fear and cancer fatalism were experienced by a significant number of the men, with their thoughts immediately turning to death and dying. This was especially the case for men who had lost a loved one to cancer. Conversely, some of the men wanted immediate resolution, focusing instead on ways to beat the cancer and with a strong will to live.
Reliance on faith was a big part of coping at the PPCD. Some of the men drew strength from their faith to get them through their cancer journey. Others found a way to accept the diagnosis – one participant accepted the diagnosis and the fact that this could mean dying (after living a good life), whereas another participant accepted the diagnosis with the hope that he would find a cure. Hope was more realistic with the knowledge that other men had survived prostate cancer.
Reflecting back on their experiences, the men also identified clear needs at the PPCD. One of the needs they identified was having a physician they were comfortable with to discuss their diagnosis. Another need was for a second opinion. Participant 1594 (NBBM) advised that it was important for black men to take control by requesting a second opinion. Participant 2039 (NBBM) described a feeling of navigating blindly and trying to find answers that would be helpful to him in his cancer journey. However, his experience with a second opinion was not helpful because the second physician was at the same clinic as his primary physician. His recommendation was to get a second opinion at a different clinic or center. Another important need was emotional support at the PPCD. Participant 2024 (CBBM) made a strong case for emotional support, especially for men who are not accompanied during diagnosis. In addition, Participant 2024’s (CBBM) reflections underscore the fact that the PPCD may not be an ideal place or time to discuss treatment options. With the range of emotions that the men go through at the PPCD, it is difficult to comprehend any follow-up discussions after hearing the words “you have prostate cancer.” Participant 2024 (CBBM) also strongly expressed that men need time to deal with the diagnosis at the PPCD.
Discussion
The primary goal of this study was to develop an interpretative framework of black men’s experiences at the PPCD. The Figure provides a pictorial summary of the framework. Study results indicated that black men come to the PPCD with different emotions and different experiences. Although the majority of the men were NBBM, there is a significantly increasing number of foreign-born black men receiving a diagnosis of prostate cancer in the United States. Given that black men carry a disproportionate burden of the disease, with a significantly higher incidence compared with any other racial group, it is important that tailored services are provided to black men at the PPCD.
We also found that black men came to the PPCD diverse in terms of their ethnicity, health literacy, spirituality, trust in health care system/physician, prior experience with cancer, perceived susceptibility to cancer, delayed time for diagnosis, and fear of diagnosis. Of importance for physicians is that the black race is not homogeneous. There is a significant number of foreign-born blacks at the PPCD, and they often have different cultural beliefs and values compared with NBBM. In addition, some of the foreign-born black men may not have English proficiency and may need a medical interpreter during the PPCD consultation. In addition, a patient’s pre-existing lack of trust in the health care system may have a negative impact on the PPCD consultation. It is thus important that the physician takes the time to instill trust and make the men comfortable during the PPCD consultation.
For some of the men who had fear of a prostate cancer diagnosis and/or prior experience with cancer, cancer fatalism was experienced at the PPCD. Cancer fatalism, defined as an individual’s belief that death is bound to happen when diagnosed with cancer, has been documented as a major barrier to cancer detection and control.15 For example, fatalistic perspectives have been reported to affect cervical cancer,16 breast cancer,17,18 colorectal cancer,19 and prostate cancer20,21 among blacks. It is thus important to effectively address fatalistic beliefs when a man is diagnosed with prostate cancer.
Other emotions at the PPCD that may affect effective treatment decision making also need to be addressed immediately. For example, the emotions of fear, denial, and feeling overwhelmed are potential barriers to timely treatment decision making. Psycho-oncology interventions to appropriately deal with these emotions at PPCD or right after the diagnosis may be crucial for the men. In particular, a group-based psychosocial intervention focusing on: provision of education about treatment options for prostate cancer and their acute and late effects; negotiating treatment and treatment side effects; enhancing communication with treatment providers; managing distress; and engaging positive family- and community-based social support to optimize emotional, behavioral, social, and physical outcomes in black men with prostate cancer.
In addition to having physicians make them comfortable at PPCD, the PPCD needs expressed by participants included having time to come to terms with the diagnosis and receiving psycho-oncology/emotional support. Anyone who has just received a diagnosis of cancer cannot be expected to immediately continue to function as he did before the PPCD. This is especially difficult for men who are alone at the PPCD. Nevertheless, it is expected that they will listen attentively and understand subsequent consultation by the physician, then leave the consultation room almost immediately, and be able drive home or back to work right after the diagnosis. There seems to be a support gap that needs to be closed at the PPCD. Providing the men with immediate support to cope with the diagnosis may make a significant difference in effective treatment choices and eliminating treatment decisional regrets.
Methodological rigor was established through purposeful sampling, extended time with participants, standardized procedures for data collection, management and analysis, multidisciplinary interpretation, and validation of results with the community advisory board. Because the research participants were purposefully selected from a statewide database of black men diagnosed with CaP, generalizability of findings to the two target groups of NBBM and CBBM can be assumed, with the caveat that men with different experiences may have chosen not to respond to recruitment efforts or refused participation. Black men who were not sufficiently fluent in English to be interviewed were also excluded and are not represented in these findings. Black men of other nativity (including African-born black men) and residing outside of Florida were also not represented.
In conclusion, the PPCD interpretative framework developed in this study, describes the status of black men at the PPCD, their experiences during the PPCD, and their needs at the PPCD. The framework provides information that can be used by physicians to prepare for their PPCD consultation with black men as well as develop a support system for black men at the PPCD.
Acknowledgments
The authors thank the men who participated in the CaPCaS study. They also thank the CaPCaS project community advisory board chairs (Mr Jim West, Dr Angela Adams, and Prince Oladapo Odedina) and all the CaPCaS project community advisory board members for their effort throughout the project. Finally, they rxecognize the effort of additional CaPCaS scientific team, especially the primary interviewer, Mr Kenneth Stokes. Weekly meeting support for this study was provided by the University of Florida MiCaRT Center, which is funded by the NIH-National Cancer Institute Award # 1P20CA192990-02. REDCaP software was supported by the UF Clinical and Translational Science Institute, which is funded in part by the NIH Clinical and Translational Science Award program (grants UL1TR001427, KL2TR001429 and TL1TR001428).
1. American Cancer Society. Cancer facts & figures 2016. http://www.cancer.org/research/cancerfactsstatistics/cancerfactsfigures2016/. Published 2016. Accessed January 10, 2017.
2. Florida Cancer Data System. Florida Statewide Population-Based Cancer Registry. https://fcds.med.miami.edu/scripts/fcdspubrates/production/doSelection.aspx?election=map. Processed February 16, 2016.
3. Sinfield P, Baker R, Camosso-Stefinovic J, et al. Men’s and carers’ experiences of care for prostate cancer: a narrative literature review. Health Expect. 2009;12:301-312.
4. Maliski SL, Connor SE, Williams L, Litwin MS. Faith among low-income, African American/ black men treated for prostate cancer. Cancer Nurs. 2010;33(6):470-478.
5. Jones RA, Wenzel J, Hinton I, et el. Exploring cancer support needs for older African-American men with prostate cancer. Support Care Cancer. 2011;19(9):1411-1419.
6. Sinfield P, Baker R, Agarwal S, Tarrant C. Patient-centred care: what are the experiences of prostate cancer patients and their partners? Patient Educ Couns. 2008;73(1):91-96.
7. American Cancer Society. Cancer facts & figures for African Americans 2016-2018. http://www.cancer.org/research/cancerfactsstatistics/cancer-facts-figures-for-african-americans. Published 2016. Accessed January 10, 2017.
8. Patton MQ. Qualitative research & evaluation methods. 4th ed. Thousand Oaks, CA: Sage Publications; 2001.
9. Florida Department of Health, Bureau of Epidemiology. Procedure guide for studies that utilize patient identifiable data from the Florida Cancer Data System. http://www.fcds.med.miami.edu/downloads/datarequest/Procedure%20Guide_Revised%20
October%202007.pdf. Accessed July 24, 2010.
10. Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap) – a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377-381.
11. Strauss A. Qualitative analysis for social scientists. New York, NY: Cambridge University Press; 1987.
12. Glaser BG, Strauss AL. The discovery of grounded theory: strategies for qualitative research. Chicago, IL: Aldine; 1967.
13. Miles MB, Huberman AM. Qualitative data analysis: an expanded sourcebook. 2nd ed. Thousand Oaks, CA: Sage Publications; 1994.
14. Nutbeam, D. Health literacy as a public health goal: a challenge for contemporary health education and communication strategies into the 21st century. Health Promot Int. 2000;15(3):259-267.
15. Powe BD, Finnie R. Cancer fatalism: the state of the science. Cancer Nurs. 2003;26:454-467.
16. Powe BD. Fatalism among elderly African Americans: effects on colorectal cancer screening. Cancer Nurs. 1995;18:285-392.
17. Powe BD. Cancer fatalism among elderly Caucasians and African Americans. Oncol Nurs Forum. 1995;22(9):1355-1359.
18. Thoresen CE. Spirituality, health, and science: the coming revival? In: Roth RS, Kurpius SR, eds. The emerging role of counseling psychology in health care. New York, NY: WW Norton; 1998.
19. Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies: a theoretically based approach. J Pers Soc Psychol. 1989;56:267-283.
21. Odedina FT, Yu D, Akinremi TO, Reams RR, Freedman ML, Kumar N. Prostate cancer cognitive-behavioral factors in a West African population. J Immigr Minor Health. 2009;11(4):258-267.
22. Odedina FT, Scrivens JJ Jr, Larose-Pierre M, et al. Modifiable prostate cancer risk reduction and early detection behaviors in black men. Am J Health Behav. 2011;35(4):470-484.
As of 2016, Florida ranks second among all states in the United States in estimated new cases of prostate cancer and second in estimated deaths from prostate cancer.1 Disparities in diagnosis, mortality rates, and access to cancer care also continue to be a major problem in Florida, especially for black men. For example, black men were the only racial/ethnic group that did not meet the Healthy People (HP) 2010 objective to reduce the prostate cancer death rate to 28.2 per 100,000 men and that has not met the HP 2020 objective to reduce the prostate cancer death rate to 21.2 per 100,000 men (Table 1). Based on the 2013 prostate cancer mortality rates for Florida,2 the death rate for black men is almost twice the HP 2020 goal (37.49 per 100,000).
A diagnosis of prostate cancer is a life changing event for a man. In particular, there is limited research on the experiences and coping mechanisms of black men at diagnosis. This limited body of research indicates that black men’s reactions to their initial diagnoses varied, from being shocked when notified of their initial diagnosis of prostate cancer,3 to perceiving that they had received a “death sentence”.4 In regard to having to make decisions about their treatment options, some black men indicated that the information about treatment that they received from physicians decreased their anxiety,5 whereas others noted that they had not been given adequate information by a physician to make a decision.6 Patients have also reported that they felt as though they were not knowledgeable enough to ask questions concerning treatment options and preferred for the physician to make the treatment choice for them.6 Decisional regret is now a common observation among men who are not involved in making decisions about their treatment.3
According to the American Cancer Society, about 30,000 black men were diagnosed with prostate cancer in 2016.7 It is important to understand these men’s needs and help them cope effectively as they navigate the survivorship continuum. In line with our research program’s goal of ensuring quality cancer care for black men, the primary objective of this study was to explore the experiences and needs of black men at the point of prostate cancer diagnosis (PPCD). Specifically, we developed an interpretative framework for black men’s experiences at the PPCD, focusing on United States or native-born black men (NBBM) and Caribbean-born black men (CBBM). African-born black men were not included in this study because of the low sample size for that ethnicity. This study is part of a large-scale study that focuses on developing a model of prostate cancer care and survivorship (CaPCaS model) using grounded theory to study black, ethnically diverse prostate cancer survivors.
Methods
The study aims to close the prostate health disparity gap for black men in Florida through community engaged research in partnership with survivors of prostate cancer and their advocates. The current study was a prospective, grounded theory study that involved one-on-one, in-depth interviews with 31 prostate cancer patients about their care and survivorship experiences. Specifically, 17 NBBM and 14 CBBM were enrolled in the project. Appropriate human subjects review and approval were obtained from the University of Florida, the Florida Department of Health, and the Department of Defense.
Research design
This is a qualitative research study. Based on the principles of community engaged research and using a rigorous qualitative research methodology, we recruited NBBM and CBBM with a personal history of prostate cancer. Guided by open-ended questions developed by the team, one-on-one in-depth interviews were conducted with each participant in their home or at a convenient location in the community. Our primary focus was on the participants’ care and survivorship experiences, with primary focus on their prostate cancer diagnosis. Qualitative research was our methodology of choice because little is known about the PPCD experiences of black men.8 With qualitative research, we were able to get our participants to “relive” their experiences in the presence of a culturally competent, well-trained interviewer and elicit the information about their care and survivorship experiences based on their interpretation. In addition, we were able to capture the dynamic processes associated with their experiences, documenting sequential patterns and change through both verbal and nonverbal communications, because the participants were interviewed twice.
Research population and recruitment
The study setting was Florida. The inclusion criteria were: black men, personal history of prostate cancer, ability to complete two separate interviews with each one expected to last 2-3 hours, and flexibility to meet interviewers at a convenient community site for the interviews. Participants were identified through the Florida Cancer Data System (FCDS)9 database. At the time of the study, the most recent FCDS database was for 2010. The FCDS has collected the number of new cancer cancers diagnosed in the state of Florida annually since 1981. It is a comprehensive incidence-only registry and does not extract data on patients with a death certificate. All investigators are bounded by the confidential pledge required for the use of the FCDS data.
We used the Florida Department of Health’s (DoH’s) Bureau of Epidemiology standard procedure for the FCDS9 to recruit participants. Our recruitment strategies included: initial patient contact by written correspondence; second mailing that included a telephone opt-out card after 3 weeks for nonrespondents (the telephone opt-out card explained to the patient that if no response was received, the study investigator would attempt a telephone call to introduce the study); and a telephone call by a study staff to introduce the study for nonrespondents. As per the Florida DoH standard procedure, we did not disclose on the cover of the study mailings that the patient was being contacted for a study specific to cancer. Efforts to recruit a patient stopped immediately if a patient indicated that he did not wish to participate. All of the study staff making participant contact were extensively trained to provide a clear and accurate description of cancer registration in Florida. In addition, to assist the study staff in providing clear and accurate responses, responses to frequently asked questions were made available to the study staff. During the participant recruitment phase, anyone who seemed to be upset when contacted was reported immediately (within 24 hours) to the DoH cancer epidemiologist. In addition, the name of anyone who stated that he did not wish to be contacted again was given to the DoH so that the person would not be re-contacted.
Prescreening of participants for eligibility
All eligible participants who agreed to participate in the study comprised the pool of potential study participants. For those who agreed to participate, the following information was obtained by telephone interview using REDCap software:10 name and contact information, country of birth, age, marital status, and education level. The demographic information facilitated a purposeful systematic selection of black men of diverse age groups (younger than 50 years or older than 50 years), marital status (single, including divorced or separated, or married/in a relationship), and educational level (college degree or not college educated). An incentive of a $5 gift card was provided to all the men who participated in the screening phase. Using systematic sampling to ensure demographically diverse participants, 40 participants (20 NBBM, 20 CBBM) were selected from the initial pool of participants to participate in the study.
Data collection
The data collection was conducted by a trained Community Health Worker (CHW) using semi-structured interview process. The interview guide was constructed by the research team and the study community advisory board members to ensure language appropriateness, understanding and cultural sensitivity. For this study, the interview questions focused on participants’ background information and diagnosis history, including: participants’ personal story of diagnosis, feelings, emotions, reactions, regrets and level of personal/family/physician involvement in diagnosis. For the CBBM, we also obtained information on the age at which they immigrated to the United States. The CHW interviewer was trained to question participants and encourage them to elaborate on areas of importance to their experience.
A total time of about 5-6 hours was scheduled for the data collection per participant, which is sufficient for gathering in-depth perspectives. We scheduled two interviews lasting not more than 3 hours at a time so as not to create burden for study participants. Participants had the choice to have the interviews completed in a single session or spread out over 2 days. The interviews were audio-recorded to provide ease of transcription and back-up of data. At the end of the interviews, participants were compensated for participating in the study.
Data management and analyses
The study dataset included interview transcripts and field notes of the CHW interviewer describing his insights about the interviews. The data analyses included preparing and verifying the narrative data, coding data, and developing an interpretative framework for black men’s experiences at the PPCD. Interviews were transcribed verbatim by a professional transcription service that has policies in place for protected health information. Each transcript was then verified for accuracy by the CHW interviewer. The interview transcripts were imported directly into NVivo 11, a computer-assisted data analysis software that allows coding and modeling of complex narrative data. The data coding was conducted by our interdisciplinary team of clinicians, behavioral scientists, and social scientists. It is important to note that the NVivo 11 software was not used to analyze the data per se. However, it provided a sophisticated and systematic way to manage the following tasks for the analyses: organizing large quantities of narrative data, coding text, retrieving text by codes, querying the data, comparing sets of data interpretation between NBBM and CBBM; and developing analytic models. The study team members coded the data in weekly team meetings. The coding consisted of reading the data and identifying major themes, then assigning labels to and defining emerging categories.
Two levels of coding were used. The first, open coding, refers to an approach to data with no preconceived ideas about what will be found; and the second, focused or axial coding, refers to reviewing data for the purpose of more richly coding on a particular theme.11 We used dimensional analysis to ensure that each emerging concept was carefully defined. The study team went back and forth between the data and the emerging analytic framework, using constant comparison of new data with already coded data and new categories with previously analyzed text.12
To ensure trustworthiness and credibility,13 the study team maintained an audit trail that documented how and when analytic decisions were made. In addition, peer debriefing was conducted to ensure credibility, including the presentation of findings to the study community advisory board members as part of the community engaged research approach.
Results
Description of participants
The FCDS provided a database of 1,813 participants identified as black men diagnosed with prostate cancer in 2010. Because the FCDS does not extract data on patients with a death certificate, we found out during the pre-screening phase that a few of the men were deceased. In addition, there were a significant number of incorrect addresses. We obtained a total of 212 completed responses by phone during the prescreening phase. The majority of the participants were aged 60-69 years (48.2%), had a high school diploma only (26.1%), and were currently married (65.3%). Relative to ethnicity, 67% of participants classified themselves NBBM, 24% as CBBM, 3.5% as black men born in Africa, and 5.5% as Other/Don’t know/Refused. For the CBBM, the most common countries of birth were Jamaica, Haiti, and Guyana, respectively.
In all, 40 participants (20 NBBM and 20 CBBM) were selected from the 212 participants to participate in the study. Selection was conducted systematically to ensure representation in terms of age, marital status, education, and geographical location. Data saturation was achieved with 17 NBBM and 14 CBBM, after which we ended data collection (Table 2). Data saturation is the standard for deciding that we are not finding anything different from the interviews first coded and last coded. Although we were specifically looking for differences between the two groups (NBBM and CBBM), no between-group differences emerged. Each man’s experience was unique to him with some common themes emerging described hereinafter (Figure).
Moderating factors and experiences at PPCD
Some of the moderating factors that the study participants identified as affecting their reactions to the PPCD included health literacy, insurance status, spirituality, mistrust, prior experience with cancer, perceived susceptibility to cancer, and delay in diagnosis (Table 3). Health literacy, defined as personal, cognitive, and social skills that determine the ability of individuals to gain access to, understand, and use information to promote and maintain good health, was one of the moderating factors found in this study.13 Some of the black men came to the PPCD with a low level of health literacy, which had an impact on their understanding of the treatment options. For example, in the interview, participant 798 (NBBM) was confused about what tests had been done and was not able to accurately describe the treatments offered to him. Participant 1263 (CBBM) struggled to express the purpose and procedures associated with diagnostic biopsy. However, there were participants with a high level of health literacy (eg, participant 449 [NBBM]), who decided to research the disease.
Another factor to consider is the insurance status of participants at the PPCD. The majority of the participants had good insurance coverage, but some were affected by poor insurance coverage. Participant 1881(NBBM) made his treatment decision primarily on the basis of the pending lapse of his insurance coverage rather than the best clinical option for him. Participant 1979 (CBBM) described both his confusion on the screening tests and the impact of not having insurance coverage. Upon obtaining insurance coverage, he sought treatment for his prostate cancer with an urgency that he did not experience when he was first diagnosed when uninsured.
The spirituality of black men was another moderating factor at the PPCD. Participant 827 (NBBM) noted that he was unaffected when he received his diagnosis because he was a true believer. Some of the black men also came to the PPCD with lack of trust in the physician and/or the health care system and perceived a sense of contempt from the physician. Participant 1594 (NBBM) described mistrust based on the history of medical exploitation of black men as well as a perception of current discriminatory practices.
Another important PPCD status to note for black men is prior experience with cancer, including prior personal cancer history and/or prior cancer history of a family member. Participant 2024 (CBBM) described the meaning of cancer to him, while participant 798 (NBBM) echoed the despair of the cancer diagnosis based on experience with other cancers in the family. Sometimes there were multiple cancers in the family or even among the significant others of the participant, as was the case with Participant 1936 (CBBM).
Of greatest concern were men who delayed their diagnosis or treatment, perhaps resulting in their cancer being at a more advanced stage when they eventually did return for care. Finally, some of the men came to the PPCD appointment with a low expectation of receiving a diagnosis of prostate cancer, whereas others came to the PPCD fearful of the results of their testing.
In describing their experiences, participants expressed both positive and negative experiences: on the positive side, they found the information provided by the physician to be helpful; but on the negative side, the sterile or medically focused encounter was perceived as a lack empathy on the part of the physician.
Cognitive, emotional, and behavioral coping experiences
As expected, there were ranges of emotions, including shock, disbelief and denial (Table 4). Some of the men questioned why this (the cancer) was happening to them when they had done “nothing” to deserve it. Doing nothing in this case meant that they had lived a healthy lifestyle with no obvious apparent cause to have the cancer. Fear and cancer fatalism were experienced by a significant number of the men, with their thoughts immediately turning to death and dying. This was especially the case for men who had lost a loved one to cancer. Conversely, some of the men wanted immediate resolution, focusing instead on ways to beat the cancer and with a strong will to live.
Reliance on faith was a big part of coping at the PPCD. Some of the men drew strength from their faith to get them through their cancer journey. Others found a way to accept the diagnosis – one participant accepted the diagnosis and the fact that this could mean dying (after living a good life), whereas another participant accepted the diagnosis with the hope that he would find a cure. Hope was more realistic with the knowledge that other men had survived prostate cancer.
Reflecting back on their experiences, the men also identified clear needs at the PPCD. One of the needs they identified was having a physician they were comfortable with to discuss their diagnosis. Another need was for a second opinion. Participant 1594 (NBBM) advised that it was important for black men to take control by requesting a second opinion. Participant 2039 (NBBM) described a feeling of navigating blindly and trying to find answers that would be helpful to him in his cancer journey. However, his experience with a second opinion was not helpful because the second physician was at the same clinic as his primary physician. His recommendation was to get a second opinion at a different clinic or center. Another important need was emotional support at the PPCD. Participant 2024 (CBBM) made a strong case for emotional support, especially for men who are not accompanied during diagnosis. In addition, Participant 2024’s (CBBM) reflections underscore the fact that the PPCD may not be an ideal place or time to discuss treatment options. With the range of emotions that the men go through at the PPCD, it is difficult to comprehend any follow-up discussions after hearing the words “you have prostate cancer.” Participant 2024 (CBBM) also strongly expressed that men need time to deal with the diagnosis at the PPCD.
Discussion
The primary goal of this study was to develop an interpretative framework of black men’s experiences at the PPCD. The Figure provides a pictorial summary of the framework. Study results indicated that black men come to the PPCD with different emotions and different experiences. Although the majority of the men were NBBM, there is a significantly increasing number of foreign-born black men receiving a diagnosis of prostate cancer in the United States. Given that black men carry a disproportionate burden of the disease, with a significantly higher incidence compared with any other racial group, it is important that tailored services are provided to black men at the PPCD.
We also found that black men came to the PPCD diverse in terms of their ethnicity, health literacy, spirituality, trust in health care system/physician, prior experience with cancer, perceived susceptibility to cancer, delayed time for diagnosis, and fear of diagnosis. Of importance for physicians is that the black race is not homogeneous. There is a significant number of foreign-born blacks at the PPCD, and they often have different cultural beliefs and values compared with NBBM. In addition, some of the foreign-born black men may not have English proficiency and may need a medical interpreter during the PPCD consultation. In addition, a patient’s pre-existing lack of trust in the health care system may have a negative impact on the PPCD consultation. It is thus important that the physician takes the time to instill trust and make the men comfortable during the PPCD consultation.
For some of the men who had fear of a prostate cancer diagnosis and/or prior experience with cancer, cancer fatalism was experienced at the PPCD. Cancer fatalism, defined as an individual’s belief that death is bound to happen when diagnosed with cancer, has been documented as a major barrier to cancer detection and control.15 For example, fatalistic perspectives have been reported to affect cervical cancer,16 breast cancer,17,18 colorectal cancer,19 and prostate cancer20,21 among blacks. It is thus important to effectively address fatalistic beliefs when a man is diagnosed with prostate cancer.
Other emotions at the PPCD that may affect effective treatment decision making also need to be addressed immediately. For example, the emotions of fear, denial, and feeling overwhelmed are potential barriers to timely treatment decision making. Psycho-oncology interventions to appropriately deal with these emotions at PPCD or right after the diagnosis may be crucial for the men. In particular, a group-based psychosocial intervention focusing on: provision of education about treatment options for prostate cancer and their acute and late effects; negotiating treatment and treatment side effects; enhancing communication with treatment providers; managing distress; and engaging positive family- and community-based social support to optimize emotional, behavioral, social, and physical outcomes in black men with prostate cancer.
In addition to having physicians make them comfortable at PPCD, the PPCD needs expressed by participants included having time to come to terms with the diagnosis and receiving psycho-oncology/emotional support. Anyone who has just received a diagnosis of cancer cannot be expected to immediately continue to function as he did before the PPCD. This is especially difficult for men who are alone at the PPCD. Nevertheless, it is expected that they will listen attentively and understand subsequent consultation by the physician, then leave the consultation room almost immediately, and be able drive home or back to work right after the diagnosis. There seems to be a support gap that needs to be closed at the PPCD. Providing the men with immediate support to cope with the diagnosis may make a significant difference in effective treatment choices and eliminating treatment decisional regrets.
Methodological rigor was established through purposeful sampling, extended time with participants, standardized procedures for data collection, management and analysis, multidisciplinary interpretation, and validation of results with the community advisory board. Because the research participants were purposefully selected from a statewide database of black men diagnosed with CaP, generalizability of findings to the two target groups of NBBM and CBBM can be assumed, with the caveat that men with different experiences may have chosen not to respond to recruitment efforts or refused participation. Black men who were not sufficiently fluent in English to be interviewed were also excluded and are not represented in these findings. Black men of other nativity (including African-born black men) and residing outside of Florida were also not represented.
In conclusion, the PPCD interpretative framework developed in this study, describes the status of black men at the PPCD, their experiences during the PPCD, and their needs at the PPCD. The framework provides information that can be used by physicians to prepare for their PPCD consultation with black men as well as develop a support system for black men at the PPCD.
Acknowledgments
The authors thank the men who participated in the CaPCaS study. They also thank the CaPCaS project community advisory board chairs (Mr Jim West, Dr Angela Adams, and Prince Oladapo Odedina) and all the CaPCaS project community advisory board members for their effort throughout the project. Finally, they rxecognize the effort of additional CaPCaS scientific team, especially the primary interviewer, Mr Kenneth Stokes. Weekly meeting support for this study was provided by the University of Florida MiCaRT Center, which is funded by the NIH-National Cancer Institute Award # 1P20CA192990-02. REDCaP software was supported by the UF Clinical and Translational Science Institute, which is funded in part by the NIH Clinical and Translational Science Award program (grants UL1TR001427, KL2TR001429 and TL1TR001428).
As of 2016, Florida ranks second among all states in the United States in estimated new cases of prostate cancer and second in estimated deaths from prostate cancer.1 Disparities in diagnosis, mortality rates, and access to cancer care also continue to be a major problem in Florida, especially for black men. For example, black men were the only racial/ethnic group that did not meet the Healthy People (HP) 2010 objective to reduce the prostate cancer death rate to 28.2 per 100,000 men and that has not met the HP 2020 objective to reduce the prostate cancer death rate to 21.2 per 100,000 men (Table 1). Based on the 2013 prostate cancer mortality rates for Florida,2 the death rate for black men is almost twice the HP 2020 goal (37.49 per 100,000).
A diagnosis of prostate cancer is a life changing event for a man. In particular, there is limited research on the experiences and coping mechanisms of black men at diagnosis. This limited body of research indicates that black men’s reactions to their initial diagnoses varied, from being shocked when notified of their initial diagnosis of prostate cancer,3 to perceiving that they had received a “death sentence”.4 In regard to having to make decisions about their treatment options, some black men indicated that the information about treatment that they received from physicians decreased their anxiety,5 whereas others noted that they had not been given adequate information by a physician to make a decision.6 Patients have also reported that they felt as though they were not knowledgeable enough to ask questions concerning treatment options and preferred for the physician to make the treatment choice for them.6 Decisional regret is now a common observation among men who are not involved in making decisions about their treatment.3
According to the American Cancer Society, about 30,000 black men were diagnosed with prostate cancer in 2016.7 It is important to understand these men’s needs and help them cope effectively as they navigate the survivorship continuum. In line with our research program’s goal of ensuring quality cancer care for black men, the primary objective of this study was to explore the experiences and needs of black men at the point of prostate cancer diagnosis (PPCD). Specifically, we developed an interpretative framework for black men’s experiences at the PPCD, focusing on United States or native-born black men (NBBM) and Caribbean-born black men (CBBM). African-born black men were not included in this study because of the low sample size for that ethnicity. This study is part of a large-scale study that focuses on developing a model of prostate cancer care and survivorship (CaPCaS model) using grounded theory to study black, ethnically diverse prostate cancer survivors.
Methods
The study aims to close the prostate health disparity gap for black men in Florida through community engaged research in partnership with survivors of prostate cancer and their advocates. The current study was a prospective, grounded theory study that involved one-on-one, in-depth interviews with 31 prostate cancer patients about their care and survivorship experiences. Specifically, 17 NBBM and 14 CBBM were enrolled in the project. Appropriate human subjects review and approval were obtained from the University of Florida, the Florida Department of Health, and the Department of Defense.
Research design
This is a qualitative research study. Based on the principles of community engaged research and using a rigorous qualitative research methodology, we recruited NBBM and CBBM with a personal history of prostate cancer. Guided by open-ended questions developed by the team, one-on-one in-depth interviews were conducted with each participant in their home or at a convenient location in the community. Our primary focus was on the participants’ care and survivorship experiences, with primary focus on their prostate cancer diagnosis. Qualitative research was our methodology of choice because little is known about the PPCD experiences of black men.8 With qualitative research, we were able to get our participants to “relive” their experiences in the presence of a culturally competent, well-trained interviewer and elicit the information about their care and survivorship experiences based on their interpretation. In addition, we were able to capture the dynamic processes associated with their experiences, documenting sequential patterns and change through both verbal and nonverbal communications, because the participants were interviewed twice.
Research population and recruitment
The study setting was Florida. The inclusion criteria were: black men, personal history of prostate cancer, ability to complete two separate interviews with each one expected to last 2-3 hours, and flexibility to meet interviewers at a convenient community site for the interviews. Participants were identified through the Florida Cancer Data System (FCDS)9 database. At the time of the study, the most recent FCDS database was for 2010. The FCDS has collected the number of new cancer cancers diagnosed in the state of Florida annually since 1981. It is a comprehensive incidence-only registry and does not extract data on patients with a death certificate. All investigators are bounded by the confidential pledge required for the use of the FCDS data.
We used the Florida Department of Health’s (DoH’s) Bureau of Epidemiology standard procedure for the FCDS9 to recruit participants. Our recruitment strategies included: initial patient contact by written correspondence; second mailing that included a telephone opt-out card after 3 weeks for nonrespondents (the telephone opt-out card explained to the patient that if no response was received, the study investigator would attempt a telephone call to introduce the study); and a telephone call by a study staff to introduce the study for nonrespondents. As per the Florida DoH standard procedure, we did not disclose on the cover of the study mailings that the patient was being contacted for a study specific to cancer. Efforts to recruit a patient stopped immediately if a patient indicated that he did not wish to participate. All of the study staff making participant contact were extensively trained to provide a clear and accurate description of cancer registration in Florida. In addition, to assist the study staff in providing clear and accurate responses, responses to frequently asked questions were made available to the study staff. During the participant recruitment phase, anyone who seemed to be upset when contacted was reported immediately (within 24 hours) to the DoH cancer epidemiologist. In addition, the name of anyone who stated that he did not wish to be contacted again was given to the DoH so that the person would not be re-contacted.
Prescreening of participants for eligibility
All eligible participants who agreed to participate in the study comprised the pool of potential study participants. For those who agreed to participate, the following information was obtained by telephone interview using REDCap software:10 name and contact information, country of birth, age, marital status, and education level. The demographic information facilitated a purposeful systematic selection of black men of diverse age groups (younger than 50 years or older than 50 years), marital status (single, including divorced or separated, or married/in a relationship), and educational level (college degree or not college educated). An incentive of a $5 gift card was provided to all the men who participated in the screening phase. Using systematic sampling to ensure demographically diverse participants, 40 participants (20 NBBM, 20 CBBM) were selected from the initial pool of participants to participate in the study.
Data collection
The data collection was conducted by a trained Community Health Worker (CHW) using semi-structured interview process. The interview guide was constructed by the research team and the study community advisory board members to ensure language appropriateness, understanding and cultural sensitivity. For this study, the interview questions focused on participants’ background information and diagnosis history, including: participants’ personal story of diagnosis, feelings, emotions, reactions, regrets and level of personal/family/physician involvement in diagnosis. For the CBBM, we also obtained information on the age at which they immigrated to the United States. The CHW interviewer was trained to question participants and encourage them to elaborate on areas of importance to their experience.
A total time of about 5-6 hours was scheduled for the data collection per participant, which is sufficient for gathering in-depth perspectives. We scheduled two interviews lasting not more than 3 hours at a time so as not to create burden for study participants. Participants had the choice to have the interviews completed in a single session or spread out over 2 days. The interviews were audio-recorded to provide ease of transcription and back-up of data. At the end of the interviews, participants were compensated for participating in the study.
Data management and analyses
The study dataset included interview transcripts and field notes of the CHW interviewer describing his insights about the interviews. The data analyses included preparing and verifying the narrative data, coding data, and developing an interpretative framework for black men’s experiences at the PPCD. Interviews were transcribed verbatim by a professional transcription service that has policies in place for protected health information. Each transcript was then verified for accuracy by the CHW interviewer. The interview transcripts were imported directly into NVivo 11, a computer-assisted data analysis software that allows coding and modeling of complex narrative data. The data coding was conducted by our interdisciplinary team of clinicians, behavioral scientists, and social scientists. It is important to note that the NVivo 11 software was not used to analyze the data per se. However, it provided a sophisticated and systematic way to manage the following tasks for the analyses: organizing large quantities of narrative data, coding text, retrieving text by codes, querying the data, comparing sets of data interpretation between NBBM and CBBM; and developing analytic models. The study team members coded the data in weekly team meetings. The coding consisted of reading the data and identifying major themes, then assigning labels to and defining emerging categories.
Two levels of coding were used. The first, open coding, refers to an approach to data with no preconceived ideas about what will be found; and the second, focused or axial coding, refers to reviewing data for the purpose of more richly coding on a particular theme.11 We used dimensional analysis to ensure that each emerging concept was carefully defined. The study team went back and forth between the data and the emerging analytic framework, using constant comparison of new data with already coded data and new categories with previously analyzed text.12
To ensure trustworthiness and credibility,13 the study team maintained an audit trail that documented how and when analytic decisions were made. In addition, peer debriefing was conducted to ensure credibility, including the presentation of findings to the study community advisory board members as part of the community engaged research approach.
Results
Description of participants
The FCDS provided a database of 1,813 participants identified as black men diagnosed with prostate cancer in 2010. Because the FCDS does not extract data on patients with a death certificate, we found out during the pre-screening phase that a few of the men were deceased. In addition, there were a significant number of incorrect addresses. We obtained a total of 212 completed responses by phone during the prescreening phase. The majority of the participants were aged 60-69 years (48.2%), had a high school diploma only (26.1%), and were currently married (65.3%). Relative to ethnicity, 67% of participants classified themselves NBBM, 24% as CBBM, 3.5% as black men born in Africa, and 5.5% as Other/Don’t know/Refused. For the CBBM, the most common countries of birth were Jamaica, Haiti, and Guyana, respectively.
In all, 40 participants (20 NBBM and 20 CBBM) were selected from the 212 participants to participate in the study. Selection was conducted systematically to ensure representation in terms of age, marital status, education, and geographical location. Data saturation was achieved with 17 NBBM and 14 CBBM, after which we ended data collection (Table 2). Data saturation is the standard for deciding that we are not finding anything different from the interviews first coded and last coded. Although we were specifically looking for differences between the two groups (NBBM and CBBM), no between-group differences emerged. Each man’s experience was unique to him with some common themes emerging described hereinafter (Figure).
Moderating factors and experiences at PPCD
Some of the moderating factors that the study participants identified as affecting their reactions to the PPCD included health literacy, insurance status, spirituality, mistrust, prior experience with cancer, perceived susceptibility to cancer, and delay in diagnosis (Table 3). Health literacy, defined as personal, cognitive, and social skills that determine the ability of individuals to gain access to, understand, and use information to promote and maintain good health, was one of the moderating factors found in this study.13 Some of the black men came to the PPCD with a low level of health literacy, which had an impact on their understanding of the treatment options. For example, in the interview, participant 798 (NBBM) was confused about what tests had been done and was not able to accurately describe the treatments offered to him. Participant 1263 (CBBM) struggled to express the purpose and procedures associated with diagnostic biopsy. However, there were participants with a high level of health literacy (eg, participant 449 [NBBM]), who decided to research the disease.
Another factor to consider is the insurance status of participants at the PPCD. The majority of the participants had good insurance coverage, but some were affected by poor insurance coverage. Participant 1881(NBBM) made his treatment decision primarily on the basis of the pending lapse of his insurance coverage rather than the best clinical option for him. Participant 1979 (CBBM) described both his confusion on the screening tests and the impact of not having insurance coverage. Upon obtaining insurance coverage, he sought treatment for his prostate cancer with an urgency that he did not experience when he was first diagnosed when uninsured.
The spirituality of black men was another moderating factor at the PPCD. Participant 827 (NBBM) noted that he was unaffected when he received his diagnosis because he was a true believer. Some of the black men also came to the PPCD with lack of trust in the physician and/or the health care system and perceived a sense of contempt from the physician. Participant 1594 (NBBM) described mistrust based on the history of medical exploitation of black men as well as a perception of current discriminatory practices.
Another important PPCD status to note for black men is prior experience with cancer, including prior personal cancer history and/or prior cancer history of a family member. Participant 2024 (CBBM) described the meaning of cancer to him, while participant 798 (NBBM) echoed the despair of the cancer diagnosis based on experience with other cancers in the family. Sometimes there were multiple cancers in the family or even among the significant others of the participant, as was the case with Participant 1936 (CBBM).
Of greatest concern were men who delayed their diagnosis or treatment, perhaps resulting in their cancer being at a more advanced stage when they eventually did return for care. Finally, some of the men came to the PPCD appointment with a low expectation of receiving a diagnosis of prostate cancer, whereas others came to the PPCD fearful of the results of their testing.
In describing their experiences, participants expressed both positive and negative experiences: on the positive side, they found the information provided by the physician to be helpful; but on the negative side, the sterile or medically focused encounter was perceived as a lack empathy on the part of the physician.
Cognitive, emotional, and behavioral coping experiences
As expected, there were ranges of emotions, including shock, disbelief and denial (Table 4). Some of the men questioned why this (the cancer) was happening to them when they had done “nothing” to deserve it. Doing nothing in this case meant that they had lived a healthy lifestyle with no obvious apparent cause to have the cancer. Fear and cancer fatalism were experienced by a significant number of the men, with their thoughts immediately turning to death and dying. This was especially the case for men who had lost a loved one to cancer. Conversely, some of the men wanted immediate resolution, focusing instead on ways to beat the cancer and with a strong will to live.
Reliance on faith was a big part of coping at the PPCD. Some of the men drew strength from their faith to get them through their cancer journey. Others found a way to accept the diagnosis – one participant accepted the diagnosis and the fact that this could mean dying (after living a good life), whereas another participant accepted the diagnosis with the hope that he would find a cure. Hope was more realistic with the knowledge that other men had survived prostate cancer.
Reflecting back on their experiences, the men also identified clear needs at the PPCD. One of the needs they identified was having a physician they were comfortable with to discuss their diagnosis. Another need was for a second opinion. Participant 1594 (NBBM) advised that it was important for black men to take control by requesting a second opinion. Participant 2039 (NBBM) described a feeling of navigating blindly and trying to find answers that would be helpful to him in his cancer journey. However, his experience with a second opinion was not helpful because the second physician was at the same clinic as his primary physician. His recommendation was to get a second opinion at a different clinic or center. Another important need was emotional support at the PPCD. Participant 2024 (CBBM) made a strong case for emotional support, especially for men who are not accompanied during diagnosis. In addition, Participant 2024’s (CBBM) reflections underscore the fact that the PPCD may not be an ideal place or time to discuss treatment options. With the range of emotions that the men go through at the PPCD, it is difficult to comprehend any follow-up discussions after hearing the words “you have prostate cancer.” Participant 2024 (CBBM) also strongly expressed that men need time to deal with the diagnosis at the PPCD.
Discussion
The primary goal of this study was to develop an interpretative framework of black men’s experiences at the PPCD. The Figure provides a pictorial summary of the framework. Study results indicated that black men come to the PPCD with different emotions and different experiences. Although the majority of the men were NBBM, there is a significantly increasing number of foreign-born black men receiving a diagnosis of prostate cancer in the United States. Given that black men carry a disproportionate burden of the disease, with a significantly higher incidence compared with any other racial group, it is important that tailored services are provided to black men at the PPCD.
We also found that black men came to the PPCD diverse in terms of their ethnicity, health literacy, spirituality, trust in health care system/physician, prior experience with cancer, perceived susceptibility to cancer, delayed time for diagnosis, and fear of diagnosis. Of importance for physicians is that the black race is not homogeneous. There is a significant number of foreign-born blacks at the PPCD, and they often have different cultural beliefs and values compared with NBBM. In addition, some of the foreign-born black men may not have English proficiency and may need a medical interpreter during the PPCD consultation. In addition, a patient’s pre-existing lack of trust in the health care system may have a negative impact on the PPCD consultation. It is thus important that the physician takes the time to instill trust and make the men comfortable during the PPCD consultation.
For some of the men who had fear of a prostate cancer diagnosis and/or prior experience with cancer, cancer fatalism was experienced at the PPCD. Cancer fatalism, defined as an individual’s belief that death is bound to happen when diagnosed with cancer, has been documented as a major barrier to cancer detection and control.15 For example, fatalistic perspectives have been reported to affect cervical cancer,16 breast cancer,17,18 colorectal cancer,19 and prostate cancer20,21 among blacks. It is thus important to effectively address fatalistic beliefs when a man is diagnosed with prostate cancer.
Other emotions at the PPCD that may affect effective treatment decision making also need to be addressed immediately. For example, the emotions of fear, denial, and feeling overwhelmed are potential barriers to timely treatment decision making. Psycho-oncology interventions to appropriately deal with these emotions at PPCD or right after the diagnosis may be crucial for the men. In particular, a group-based psychosocial intervention focusing on: provision of education about treatment options for prostate cancer and their acute and late effects; negotiating treatment and treatment side effects; enhancing communication with treatment providers; managing distress; and engaging positive family- and community-based social support to optimize emotional, behavioral, social, and physical outcomes in black men with prostate cancer.
In addition to having physicians make them comfortable at PPCD, the PPCD needs expressed by participants included having time to come to terms with the diagnosis and receiving psycho-oncology/emotional support. Anyone who has just received a diagnosis of cancer cannot be expected to immediately continue to function as he did before the PPCD. This is especially difficult for men who are alone at the PPCD. Nevertheless, it is expected that they will listen attentively and understand subsequent consultation by the physician, then leave the consultation room almost immediately, and be able drive home or back to work right after the diagnosis. There seems to be a support gap that needs to be closed at the PPCD. Providing the men with immediate support to cope with the diagnosis may make a significant difference in effective treatment choices and eliminating treatment decisional regrets.
Methodological rigor was established through purposeful sampling, extended time with participants, standardized procedures for data collection, management and analysis, multidisciplinary interpretation, and validation of results with the community advisory board. Because the research participants were purposefully selected from a statewide database of black men diagnosed with CaP, generalizability of findings to the two target groups of NBBM and CBBM can be assumed, with the caveat that men with different experiences may have chosen not to respond to recruitment efforts or refused participation. Black men who were not sufficiently fluent in English to be interviewed were also excluded and are not represented in these findings. Black men of other nativity (including African-born black men) and residing outside of Florida were also not represented.
In conclusion, the PPCD interpretative framework developed in this study, describes the status of black men at the PPCD, their experiences during the PPCD, and their needs at the PPCD. The framework provides information that can be used by physicians to prepare for their PPCD consultation with black men as well as develop a support system for black men at the PPCD.
Acknowledgments
The authors thank the men who participated in the CaPCaS study. They also thank the CaPCaS project community advisory board chairs (Mr Jim West, Dr Angela Adams, and Prince Oladapo Odedina) and all the CaPCaS project community advisory board members for their effort throughout the project. Finally, they rxecognize the effort of additional CaPCaS scientific team, especially the primary interviewer, Mr Kenneth Stokes. Weekly meeting support for this study was provided by the University of Florida MiCaRT Center, which is funded by the NIH-National Cancer Institute Award # 1P20CA192990-02. REDCaP software was supported by the UF Clinical and Translational Science Institute, which is funded in part by the NIH Clinical and Translational Science Award program (grants UL1TR001427, KL2TR001429 and TL1TR001428).
1. American Cancer Society. Cancer facts & figures 2016. http://www.cancer.org/research/cancerfactsstatistics/cancerfactsfigures2016/. Published 2016. Accessed January 10, 2017.
2. Florida Cancer Data System. Florida Statewide Population-Based Cancer Registry. https://fcds.med.miami.edu/scripts/fcdspubrates/production/doSelection.aspx?election=map. Processed February 16, 2016.
3. Sinfield P, Baker R, Camosso-Stefinovic J, et al. Men’s and carers’ experiences of care for prostate cancer: a narrative literature review. Health Expect. 2009;12:301-312.
4. Maliski SL, Connor SE, Williams L, Litwin MS. Faith among low-income, African American/ black men treated for prostate cancer. Cancer Nurs. 2010;33(6):470-478.
5. Jones RA, Wenzel J, Hinton I, et el. Exploring cancer support needs for older African-American men with prostate cancer. Support Care Cancer. 2011;19(9):1411-1419.
6. Sinfield P, Baker R, Agarwal S, Tarrant C. Patient-centred care: what are the experiences of prostate cancer patients and their partners? Patient Educ Couns. 2008;73(1):91-96.
7. American Cancer Society. Cancer facts & figures for African Americans 2016-2018. http://www.cancer.org/research/cancerfactsstatistics/cancer-facts-figures-for-african-americans. Published 2016. Accessed January 10, 2017.
8. Patton MQ. Qualitative research & evaluation methods. 4th ed. Thousand Oaks, CA: Sage Publications; 2001.
9. Florida Department of Health, Bureau of Epidemiology. Procedure guide for studies that utilize patient identifiable data from the Florida Cancer Data System. http://www.fcds.med.miami.edu/downloads/datarequest/Procedure%20Guide_Revised%20
October%202007.pdf. Accessed July 24, 2010.
10. Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap) – a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377-381.
11. Strauss A. Qualitative analysis for social scientists. New York, NY: Cambridge University Press; 1987.
12. Glaser BG, Strauss AL. The discovery of grounded theory: strategies for qualitative research. Chicago, IL: Aldine; 1967.
13. Miles MB, Huberman AM. Qualitative data analysis: an expanded sourcebook. 2nd ed. Thousand Oaks, CA: Sage Publications; 1994.
14. Nutbeam, D. Health literacy as a public health goal: a challenge for contemporary health education and communication strategies into the 21st century. Health Promot Int. 2000;15(3):259-267.
15. Powe BD, Finnie R. Cancer fatalism: the state of the science. Cancer Nurs. 2003;26:454-467.
16. Powe BD. Fatalism among elderly African Americans: effects on colorectal cancer screening. Cancer Nurs. 1995;18:285-392.
17. Powe BD. Cancer fatalism among elderly Caucasians and African Americans. Oncol Nurs Forum. 1995;22(9):1355-1359.
18. Thoresen CE. Spirituality, health, and science: the coming revival? In: Roth RS, Kurpius SR, eds. The emerging role of counseling psychology in health care. New York, NY: WW Norton; 1998.
19. Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies: a theoretically based approach. J Pers Soc Psychol. 1989;56:267-283.
21. Odedina FT, Yu D, Akinremi TO, Reams RR, Freedman ML, Kumar N. Prostate cancer cognitive-behavioral factors in a West African population. J Immigr Minor Health. 2009;11(4):258-267.
22. Odedina FT, Scrivens JJ Jr, Larose-Pierre M, et al. Modifiable prostate cancer risk reduction and early detection behaviors in black men. Am J Health Behav. 2011;35(4):470-484.
1. American Cancer Society. Cancer facts & figures 2016. http://www.cancer.org/research/cancerfactsstatistics/cancerfactsfigures2016/. Published 2016. Accessed January 10, 2017.
2. Florida Cancer Data System. Florida Statewide Population-Based Cancer Registry. https://fcds.med.miami.edu/scripts/fcdspubrates/production/doSelection.aspx?election=map. Processed February 16, 2016.
3. Sinfield P, Baker R, Camosso-Stefinovic J, et al. Men’s and carers’ experiences of care for prostate cancer: a narrative literature review. Health Expect. 2009;12:301-312.
4. Maliski SL, Connor SE, Williams L, Litwin MS. Faith among low-income, African American/ black men treated for prostate cancer. Cancer Nurs. 2010;33(6):470-478.
5. Jones RA, Wenzel J, Hinton I, et el. Exploring cancer support needs for older African-American men with prostate cancer. Support Care Cancer. 2011;19(9):1411-1419.
6. Sinfield P, Baker R, Agarwal S, Tarrant C. Patient-centred care: what are the experiences of prostate cancer patients and their partners? Patient Educ Couns. 2008;73(1):91-96.
7. American Cancer Society. Cancer facts & figures for African Americans 2016-2018. http://www.cancer.org/research/cancerfactsstatistics/cancer-facts-figures-for-african-americans. Published 2016. Accessed January 10, 2017.
8. Patton MQ. Qualitative research & evaluation methods. 4th ed. Thousand Oaks, CA: Sage Publications; 2001.
9. Florida Department of Health, Bureau of Epidemiology. Procedure guide for studies that utilize patient identifiable data from the Florida Cancer Data System. http://www.fcds.med.miami.edu/downloads/datarequest/Procedure%20Guide_Revised%20
October%202007.pdf. Accessed July 24, 2010.
10. Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap) – a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377-381.
11. Strauss A. Qualitative analysis for social scientists. New York, NY: Cambridge University Press; 1987.
12. Glaser BG, Strauss AL. The discovery of grounded theory: strategies for qualitative research. Chicago, IL: Aldine; 1967.
13. Miles MB, Huberman AM. Qualitative data analysis: an expanded sourcebook. 2nd ed. Thousand Oaks, CA: Sage Publications; 1994.
14. Nutbeam, D. Health literacy as a public health goal: a challenge for contemporary health education and communication strategies into the 21st century. Health Promot Int. 2000;15(3):259-267.
15. Powe BD, Finnie R. Cancer fatalism: the state of the science. Cancer Nurs. 2003;26:454-467.
16. Powe BD. Fatalism among elderly African Americans: effects on colorectal cancer screening. Cancer Nurs. 1995;18:285-392.
17. Powe BD. Cancer fatalism among elderly Caucasians and African Americans. Oncol Nurs Forum. 1995;22(9):1355-1359.
18. Thoresen CE. Spirituality, health, and science: the coming revival? In: Roth RS, Kurpius SR, eds. The emerging role of counseling psychology in health care. New York, NY: WW Norton; 1998.
19. Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies: a theoretically based approach. J Pers Soc Psychol. 1989;56:267-283.
21. Odedina FT, Yu D, Akinremi TO, Reams RR, Freedman ML, Kumar N. Prostate cancer cognitive-behavioral factors in a West African population. J Immigr Minor Health. 2009;11(4):258-267.
22. Odedina FT, Scrivens JJ Jr, Larose-Pierre M, et al. Modifiable prostate cancer risk reduction and early detection behaviors in black men. Am J Health Behav. 2011;35(4):470-484.
David Henry's JCSO podcast, March-April 2017
For the March-April issue of the Journal of Community and Supportive Oncology, the Editor in Chief, Dr David Henry, discusses two informative “how-to” articles, one on the implementation of a distress management program at an oncology hospital in Puerto Rico, the other on the prevention and treatment options for mTOR inhibitor-associated stomatitis. Dr Henry also shares his preferences for addressing health care reform, and he highlights a letter to the journal in response to the January-February issue Commentary on physician-assisted dying. Immunotherapies are at the fore again, this time with an insightful essay by Jane de Lartigue who writes that combination therapy is likely to be key in expanding the scope of immunotherapy into currently unresponsive patient populations, which raises questions about the optimal combinations and the timing and sequencing of combination immunotherapy. Three Original Reports span the clinical, supportive, and quality- and value-based care components of cancer care, with their respective foci on APF530 for nausea and vomiting prevention after cisplatin; patterns of care in whole-brain radiotherapy technique and delivery; and emergency department use by newly diagnosed cancer patients. As usual, there is a line-up of rare and challenging presentations in Case Reports on pulmonary sarcomatoid carcinoma presenting as a necrotizing cavitary lung lesions, palmoplantar exacerbation of psoriasis after nivolumab for lung cancer, primary cardiac prosthetic valve-associated lymphoma; and atraumatic splenic rupture as an initial presentation of chronic myelogenous leukemia.
Listen to the podcast below.
For the March-April issue of the Journal of Community and Supportive Oncology, the Editor in Chief, Dr David Henry, discusses two informative “how-to” articles, one on the implementation of a distress management program at an oncology hospital in Puerto Rico, the other on the prevention and treatment options for mTOR inhibitor-associated stomatitis. Dr Henry also shares his preferences for addressing health care reform, and he highlights a letter to the journal in response to the January-February issue Commentary on physician-assisted dying. Immunotherapies are at the fore again, this time with an insightful essay by Jane de Lartigue who writes that combination therapy is likely to be key in expanding the scope of immunotherapy into currently unresponsive patient populations, which raises questions about the optimal combinations and the timing and sequencing of combination immunotherapy. Three Original Reports span the clinical, supportive, and quality- and value-based care components of cancer care, with their respective foci on APF530 for nausea and vomiting prevention after cisplatin; patterns of care in whole-brain radiotherapy technique and delivery; and emergency department use by newly diagnosed cancer patients. As usual, there is a line-up of rare and challenging presentations in Case Reports on pulmonary sarcomatoid carcinoma presenting as a necrotizing cavitary lung lesions, palmoplantar exacerbation of psoriasis after nivolumab for lung cancer, primary cardiac prosthetic valve-associated lymphoma; and atraumatic splenic rupture as an initial presentation of chronic myelogenous leukemia.
Listen to the podcast below.
For the March-April issue of the Journal of Community and Supportive Oncology, the Editor in Chief, Dr David Henry, discusses two informative “how-to” articles, one on the implementation of a distress management program at an oncology hospital in Puerto Rico, the other on the prevention and treatment options for mTOR inhibitor-associated stomatitis. Dr Henry also shares his preferences for addressing health care reform, and he highlights a letter to the journal in response to the January-February issue Commentary on physician-assisted dying. Immunotherapies are at the fore again, this time with an insightful essay by Jane de Lartigue who writes that combination therapy is likely to be key in expanding the scope of immunotherapy into currently unresponsive patient populations, which raises questions about the optimal combinations and the timing and sequencing of combination immunotherapy. Three Original Reports span the clinical, supportive, and quality- and value-based care components of cancer care, with their respective foci on APF530 for nausea and vomiting prevention after cisplatin; patterns of care in whole-brain radiotherapy technique and delivery; and emergency department use by newly diagnosed cancer patients. As usual, there is a line-up of rare and challenging presentations in Case Reports on pulmonary sarcomatoid carcinoma presenting as a necrotizing cavitary lung lesions, palmoplantar exacerbation of psoriasis after nivolumab for lung cancer, primary cardiac prosthetic valve-associated lymphoma; and atraumatic splenic rupture as an initial presentation of chronic myelogenous leukemia.
Listen to the podcast below.