User login
OTHER PEDIATRIC LITERATURE OF INTEREST
Enter text here
Enter text here
Enter text here
Calcitonin Precursors and IL-8 as a Screening Panel for Bacterial Sepsis
Enter text here
Enter text here
Enter text here
Practice Guidelines for the Management of Bacterial Meningitis
Enter text here
Enter text here
Enter text here
Issues in Determining Appropriate Levels of Hospitalist Staffing
Introduction
A major challenge for leaders of hospital medicine programs is determining appropriate staffing levels. Specifically, every hospitalist leader must answer the following question:
- What is the correct number of physician staff needed to meet the requirements of the work environment?
The Board of Directors of the Society of Hospital Medicine (SHM) asked the Benchmarks Committee to prepare a “white paper” on this subject. The Committee discussed hospitalist staffing and agreed that there is no simple formula or process for answering the question cited above. Instead, the Committee decided to prepare a paper that outlines the issues and suggests best practices for determining appropriate hospitalist staffing levels. A member of the Benchmarks Committee, Gale Ashbrener, Sr., Performance Consultant, Kaiser Permanente-Hawaii, has prepared a model for hospitalist staffing in her organization, and her work is the basis of this document.
NOTE: Most of the examples used in this document are from Kaiser-Hawaii. As such, the numbers cited are reflective of that particular organizational environment (i.e., a group model HMO). Readers should focus on the concepts and processes that are presented, recognizing that the numbers may be different for their environment.
Overview of the Issues
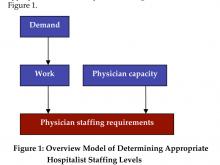
A process or simplistic model for determining the appropriate level of hospitalist staffing is summarized in Figure 1.
Staffing
Staffing is driven by demand: how many and what types of patients will the program expect to see in the upcoming year? Demand can then be converted to work: the tasks that the hospital medicine program must perform in order to treat these patients (the model must also quantify non-patient work). Once the total amount of work is described and quantified, the capacity of a hospitalist must be defined (e.g., in annual work hours). Then the number of hospitalists required to complete the projected work load can be computed.
Demand
The best practices for projecting patient demand are summarized in Box 1.
Hospitalist leaders should involve key stakeholders in the information gathering process. This helps establish the foundation for buy-in of the model down the road. You may want to pull together members of the hospitalist team and/or hospital administration to brainstorm on factors that may affect patient demand for inpatient services. At this point, keep an open mind for all considerations.
It is also critical to perform a comprehensive analysis of historical inpatient data. The analysis should examine all medical admissions at the hospital and specifically, in detail, those admissions cared for by the hospital medicine program. This analysis must look beyond the number of admissions and average length of stay (LOS). Several key characteristics of the hospitalized patients should be evaluated: age, diagnosis/severity, payer, and referring physician.
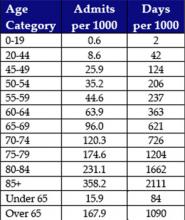
- Age: There are significant differences in inpatient utilization by age categories. It is important to further segment the “senior” Medicare (over age 65) population into several subgroups. Figure 2 (page 49) is based on data from Kaiser Permanente-Hawaii. As expected, there is a major difference in hospital utilization between the under age 65 population (15.9 admissions and 84 days per 1000) and the over age 65 population (167.9 admissions and 1,090 days per 1000). However, the differences within the Medicare subgroups are also substantial. For example, compare utilization by the population that is 65-69 years old (96.0 admissions and 621 days per 1000) with the population that is over age 85 (358.2 admissions and 2,111 days per 1000):
- Diagnoses/severity: There are acknowledged differences in LOS based on the patient’s reason for admission and many ways to characterize the reason of admission, including diagnosis and diagnostics-related groups (DRGs). Furthermore, patients with co-morbidities clearly require more coordination and patient management. There are several proprietary grouping methodologies that characterize the severity and intensity of an inpatient case, which include an assessment of co-morbidities. In analyzing historical data, the hospitalist leader should select a scheme that is used within the institution while minimizing the number of categories.
- Payer: In analyzing inpatient demand, it is also important to have an understanding of historical differences by payer (including uninsured patients). Health plans (or Medicaid programs) that are increasing or decreasing in size could affect the number of patients seen by a hospital medicine program.
- Referring physician: Community physicians (primary care, specialists, and surgeons) are a major source of inpatient cases for hospital medicine programs. It is important to analyze the historical impact of specific physicians or group practices on the patient load of the hospital medicine program.
The best way to project inpatient demand for hospitalist services is to identify and quantify what may change in the next year: what trends could increase or decrease the number of cases that will need to be treated? These change factors include the following:
- Population trends: Is the community growing? It there an influx of new residents? Is the community aging? Is it likely that there will be more seniors requiring inpatient services? Health plans and medical groups often can more easily assess population trends because they treat an enrolled population.
- Local health care factors: Will a hospital in the region be closing, resulting in additional inpatient demand? Is there a shortage of nursing home beds in the community that may affect the need for inpatient care? Is Medicaid reducing the number of covered recipients, potentially increasing the demand from uninsured patients?
- Changing referral patterns from community physicians: Do you expect additional community physicians to stop/start referring patients to the hospital medicine program? Are referring medical groups increasing or decreasing in size?
- Institution-specific factors: Does the hospital medicine program expect to assume new responsibilities in the next year – e.g., in the emergency department (ED), in the intensive care unit (ICU), providing night coverage, doing surgical co‑management, etc.?
Work
The best practices for measuring hospitalist output (work) are summarized in Box 2.
Determining how to quantify the labor of hospitalists can be the most controversial component of developing a staffing model. To ensure buy-in of these modeling decisions, participation by hospitalists and other key players (e.g., other physicians, physician leadership, and hospital/medical group administration) is crucial. Hospitalists and other key individuals must understand and agree on the quantification of time and labor.
It is critical that the analysis include ALL elements of work. Brainstorming with hospitalists can be helpful in this process. To build physician acceptance of and trust in the model, it is important to acknowledge the full set of hospitalist responsibilities in the initial stages of model development.
The services provided by a hospitalist team can vary from program to program and hospital to hospital. For example, at Kaiser Permanente-Hawaii, the dedicated hospitalist triage physician may direct patients coming from the clinic or ED to the ambulatory treatment center. A hospitalist then sees the patient in the center and an admission is often avoided. This physician labor must be captured in the model even though an admission did not occur. If your program includes a day team and a night team, you may want to handle these two teams as separate models.
Based on an analysis performed at Kaiser Permanente-Hawaii, some examples of hospitalist labor components are noted in Box 3 (page 50).
To measure the work performed by hospitalists, the model needs to recognize that there are differences in the labor components that have been identified (i.e., they are “weighted” differently). “Conventional wisdom” describes the work that hospitalists perform in terms of the number of patients seen per day (e.g., 15 patients per day). However, the work involved in a hospitalist seeing the following categories of patients is very different:
- Admitting a patient
- Rounding on a patient already admitted
- Discharging a patient
- Performing a consultation
Kaiser Permanente Hawaii developed the example in Box 4 to illustrate differences in the work required for admissions, rounding, and discharges, and how reductions in LOS do not lead to corresponding reductions in physician staffing levels.
There are basically two options in weighting the different elements of work performed by a hospitalist: time or relative value units (RVUs). Although the amount of time it takes to do a task seems to be the most sensible measurement of labor, it can be fraught with obstacles. The amount of time it takes a physician to round on a patient, for example, is not straightforward:
- Are all the patients located on one floor?
- Does the physician have to chase down test results routinely?
- Are all physicians the same, taking the same average amount of time to see a patient?
- Are all patients the same? Do older patients take more time due to social and medical complexity?
These are all factors that affect time. Furthermore, individuals are limited by their own experiences and frame of reference. Acceptance of a specific time allocation (e.g., a discharge takes 45 minutes) by those not doing the work is subjective. Despite these obstacles, it is valuable for hospitalist leaders to attempt to quantify the amount of time required to do inpatient work. Figure 3 shows example times used by a Kaiser Permanente-Hawaii medical group.
A hospital medicine program leader can use RVUs as a compliment to or as an alternative to time as the basis of weighting the work components performed by hospitalists. RVUs may account for patient acuity in a way that is hard to measure using time as the basis of measurement. Figure 4 illustrates RVUs by CPT-IV code.
Physician Capacity
The best practices for determining physician capacity are summarized in Box 5.
When determining the work capacity for a hospitalist (typically defined by the number of hours worked per year), it is critical to clearly define the unique aspects of the hospital medicine program that affect work capacity. These factors include:
- Staffing model: shift vs. call
- Scheduling approach: number of days on/off
- Non-patient care responsibilities: teaching, research, committees, etc.
- Staffing philosophy: part-time vs. full-time preference
Benchmark information is extremely helpful in determining physician capacity for a hospital medicine program. These benchmarks provide a point of comparison for hospitalist leaders developing staffing models. Medians for inpatient, non-patient, and on-call hours from the 2004 SHM Productivity and Compensation Survey are documented in Figure 5 (page 52).
The simplified example in Box 6, based on Kaiser time estimates, illustrates how demand, work, and physician capacity can be used to determine the number of hospitalists required to support a program.
As an alternative methodology or for comparative purposes, RVUs can be used rather than time. Box 7 uses RVUs from Figure 4 (initial hospital care: 1.28 RVUs; subsequent hospital care: .64 RVUs; hospital discharge < 30 minutes: 1.28 RVUs). The lowest level RVU values are used because they are consistent with the Kaiser example. Also, the median RVUs per year from Figure 5 are used (2961 for a hospital-based program).
Understand Your Work Environment
When a hospitalist program leader begins the process of developing a staffing model, it is important that he or she understands how the unique goals and characteristics of the program affects staffing. For example:
- Hospitalist-only groups are often driven by revenue. It is likely that these programs will expect hospitalists to do more billable work (i.e., see more patients)
- Academic programs typically have a broad range of other, non-patient care responsibilities, including teaching, research, and committee work. The hospitalists in these programs may see fewer patients.
The data from the 2004 SHM Productivity and Compensation Survey (Figure 5) confirms these differences. For inpatient hours worked, the national medians for these two different employment models differ by 23% (1700 vs. 2210). For RVUs worked, the national medians for the two different employment models differ by 17% (3000 vs. 3600).
Summary
Determining the right level of hospitalist staffing is important because it can positively or negatively affect the hospital medicine program and the hospital. Understaffing can lead to physician burn-out and adversely affect physician performance and hospital utilization. Overstaffing can affect the program’s financial performance and undercut the credibility of the program. The right staffing models and formulas, however, can help create a successful hospitalist work environment.
Summary of Recommendations
- There is no industry standard for a hospitalist staffing model. The analysis can be time-based or RVU-based, census driven, or based on any combination of output measures.
- Inpatient utilization drives the requirements for hospitalist staffing. A thorough analysis of historical inpatient utilization data is critical to developing a staffing model.
- In addition to understanding past utilization, projecting future inpatient demand is also important. Critical change factors include trends in: 1) the age and severity of patients; 2) population growth or decline; 3) payer sources; and 4) referral patterns.
- The services (work) performed by the hospital medicine program should be clearly identified and factored into the staffing formula. Brainstorming with the hospitalist group can be an effective technique for ensuring that the analysis is credible.
- Stakeholders should be involved early and often in developing a staffing model and in making staffing decisions.
- In developing a staffing model, particularly in the beginning stages, focus on the process and the methodology and not on the outcome (i.e., “my program needs 6 physicians”).
- Understand how the unique goals and characteristics of your hospital medicine program affect your staffing model.
Introduction
A major challenge for leaders of hospital medicine programs is determining appropriate staffing levels. Specifically, every hospitalist leader must answer the following question:
- What is the correct number of physician staff needed to meet the requirements of the work environment?
The Board of Directors of the Society of Hospital Medicine (SHM) asked the Benchmarks Committee to prepare a “white paper” on this subject. The Committee discussed hospitalist staffing and agreed that there is no simple formula or process for answering the question cited above. Instead, the Committee decided to prepare a paper that outlines the issues and suggests best practices for determining appropriate hospitalist staffing levels. A member of the Benchmarks Committee, Gale Ashbrener, Sr., Performance Consultant, Kaiser Permanente-Hawaii, has prepared a model for hospitalist staffing in her organization, and her work is the basis of this document.
NOTE: Most of the examples used in this document are from Kaiser-Hawaii. As such, the numbers cited are reflective of that particular organizational environment (i.e., a group model HMO). Readers should focus on the concepts and processes that are presented, recognizing that the numbers may be different for their environment.
Overview of the Issues
A process or simplistic model for determining the appropriate level of hospitalist staffing is summarized in Figure 1.
Staffing
Staffing is driven by demand: how many and what types of patients will the program expect to see in the upcoming year? Demand can then be converted to work: the tasks that the hospital medicine program must perform in order to treat these patients (the model must also quantify non-patient work). Once the total amount of work is described and quantified, the capacity of a hospitalist must be defined (e.g., in annual work hours). Then the number of hospitalists required to complete the projected work load can be computed.
Demand
The best practices for projecting patient demand are summarized in Box 1.
Hospitalist leaders should involve key stakeholders in the information gathering process. This helps establish the foundation for buy-in of the model down the road. You may want to pull together members of the hospitalist team and/or hospital administration to brainstorm on factors that may affect patient demand for inpatient services. At this point, keep an open mind for all considerations.
It is also critical to perform a comprehensive analysis of historical inpatient data. The analysis should examine all medical admissions at the hospital and specifically, in detail, those admissions cared for by the hospital medicine program. This analysis must look beyond the number of admissions and average length of stay (LOS). Several key characteristics of the hospitalized patients should be evaluated: age, diagnosis/severity, payer, and referring physician.
- Age: There are significant differences in inpatient utilization by age categories. It is important to further segment the “senior” Medicare (over age 65) population into several subgroups. Figure 2 (page 49) is based on data from Kaiser Permanente-Hawaii. As expected, there is a major difference in hospital utilization between the under age 65 population (15.9 admissions and 84 days per 1000) and the over age 65 population (167.9 admissions and 1,090 days per 1000). However, the differences within the Medicare subgroups are also substantial. For example, compare utilization by the population that is 65-69 years old (96.0 admissions and 621 days per 1000) with the population that is over age 85 (358.2 admissions and 2,111 days per 1000):
- Diagnoses/severity: There are acknowledged differences in LOS based on the patient’s reason for admission and many ways to characterize the reason of admission, including diagnosis and diagnostics-related groups (DRGs). Furthermore, patients with co-morbidities clearly require more coordination and patient management. There are several proprietary grouping methodologies that characterize the severity and intensity of an inpatient case, which include an assessment of co-morbidities. In analyzing historical data, the hospitalist leader should select a scheme that is used within the institution while minimizing the number of categories.
- Payer: In analyzing inpatient demand, it is also important to have an understanding of historical differences by payer (including uninsured patients). Health plans (or Medicaid programs) that are increasing or decreasing in size could affect the number of patients seen by a hospital medicine program.
- Referring physician: Community physicians (primary care, specialists, and surgeons) are a major source of inpatient cases for hospital medicine programs. It is important to analyze the historical impact of specific physicians or group practices on the patient load of the hospital medicine program.
The best way to project inpatient demand for hospitalist services is to identify and quantify what may change in the next year: what trends could increase or decrease the number of cases that will need to be treated? These change factors include the following:
- Population trends: Is the community growing? It there an influx of new residents? Is the community aging? Is it likely that there will be more seniors requiring inpatient services? Health plans and medical groups often can more easily assess population trends because they treat an enrolled population.
- Local health care factors: Will a hospital in the region be closing, resulting in additional inpatient demand? Is there a shortage of nursing home beds in the community that may affect the need for inpatient care? Is Medicaid reducing the number of covered recipients, potentially increasing the demand from uninsured patients?
- Changing referral patterns from community physicians: Do you expect additional community physicians to stop/start referring patients to the hospital medicine program? Are referring medical groups increasing or decreasing in size?
- Institution-specific factors: Does the hospital medicine program expect to assume new responsibilities in the next year – e.g., in the emergency department (ED), in the intensive care unit (ICU), providing night coverage, doing surgical co‑management, etc.?
Work
The best practices for measuring hospitalist output (work) are summarized in Box 2.
Determining how to quantify the labor of hospitalists can be the most controversial component of developing a staffing model. To ensure buy-in of these modeling decisions, participation by hospitalists and other key players (e.g., other physicians, physician leadership, and hospital/medical group administration) is crucial. Hospitalists and other key individuals must understand and agree on the quantification of time and labor.
It is critical that the analysis include ALL elements of work. Brainstorming with hospitalists can be helpful in this process. To build physician acceptance of and trust in the model, it is important to acknowledge the full set of hospitalist responsibilities in the initial stages of model development.
The services provided by a hospitalist team can vary from program to program and hospital to hospital. For example, at Kaiser Permanente-Hawaii, the dedicated hospitalist triage physician may direct patients coming from the clinic or ED to the ambulatory treatment center. A hospitalist then sees the patient in the center and an admission is often avoided. This physician labor must be captured in the model even though an admission did not occur. If your program includes a day team and a night team, you may want to handle these two teams as separate models.
Based on an analysis performed at Kaiser Permanente-Hawaii, some examples of hospitalist labor components are noted in Box 3 (page 50).
To measure the work performed by hospitalists, the model needs to recognize that there are differences in the labor components that have been identified (i.e., they are “weighted” differently). “Conventional wisdom” describes the work that hospitalists perform in terms of the number of patients seen per day (e.g., 15 patients per day). However, the work involved in a hospitalist seeing the following categories of patients is very different:
- Admitting a patient
- Rounding on a patient already admitted
- Discharging a patient
- Performing a consultation
Kaiser Permanente Hawaii developed the example in Box 4 to illustrate differences in the work required for admissions, rounding, and discharges, and how reductions in LOS do not lead to corresponding reductions in physician staffing levels.
There are basically two options in weighting the different elements of work performed by a hospitalist: time or relative value units (RVUs). Although the amount of time it takes to do a task seems to be the most sensible measurement of labor, it can be fraught with obstacles. The amount of time it takes a physician to round on a patient, for example, is not straightforward:
- Are all the patients located on one floor?
- Does the physician have to chase down test results routinely?
- Are all physicians the same, taking the same average amount of time to see a patient?
- Are all patients the same? Do older patients take more time due to social and medical complexity?
These are all factors that affect time. Furthermore, individuals are limited by their own experiences and frame of reference. Acceptance of a specific time allocation (e.g., a discharge takes 45 minutes) by those not doing the work is subjective. Despite these obstacles, it is valuable for hospitalist leaders to attempt to quantify the amount of time required to do inpatient work. Figure 3 shows example times used by a Kaiser Permanente-Hawaii medical group.
A hospital medicine program leader can use RVUs as a compliment to or as an alternative to time as the basis of weighting the work components performed by hospitalists. RVUs may account for patient acuity in a way that is hard to measure using time as the basis of measurement. Figure 4 illustrates RVUs by CPT-IV code.
Physician Capacity
The best practices for determining physician capacity are summarized in Box 5.
When determining the work capacity for a hospitalist (typically defined by the number of hours worked per year), it is critical to clearly define the unique aspects of the hospital medicine program that affect work capacity. These factors include:
- Staffing model: shift vs. call
- Scheduling approach: number of days on/off
- Non-patient care responsibilities: teaching, research, committees, etc.
- Staffing philosophy: part-time vs. full-time preference
Benchmark information is extremely helpful in determining physician capacity for a hospital medicine program. These benchmarks provide a point of comparison for hospitalist leaders developing staffing models. Medians for inpatient, non-patient, and on-call hours from the 2004 SHM Productivity and Compensation Survey are documented in Figure 5 (page 52).
The simplified example in Box 6, based on Kaiser time estimates, illustrates how demand, work, and physician capacity can be used to determine the number of hospitalists required to support a program.
As an alternative methodology or for comparative purposes, RVUs can be used rather than time. Box 7 uses RVUs from Figure 4 (initial hospital care: 1.28 RVUs; subsequent hospital care: .64 RVUs; hospital discharge < 30 minutes: 1.28 RVUs). The lowest level RVU values are used because they are consistent with the Kaiser example. Also, the median RVUs per year from Figure 5 are used (2961 for a hospital-based program).
Understand Your Work Environment
When a hospitalist program leader begins the process of developing a staffing model, it is important that he or she understands how the unique goals and characteristics of the program affects staffing. For example:
- Hospitalist-only groups are often driven by revenue. It is likely that these programs will expect hospitalists to do more billable work (i.e., see more patients)
- Academic programs typically have a broad range of other, non-patient care responsibilities, including teaching, research, and committee work. The hospitalists in these programs may see fewer patients.
The data from the 2004 SHM Productivity and Compensation Survey (Figure 5) confirms these differences. For inpatient hours worked, the national medians for these two different employment models differ by 23% (1700 vs. 2210). For RVUs worked, the national medians for the two different employment models differ by 17% (3000 vs. 3600).
Summary
Determining the right level of hospitalist staffing is important because it can positively or negatively affect the hospital medicine program and the hospital. Understaffing can lead to physician burn-out and adversely affect physician performance and hospital utilization. Overstaffing can affect the program’s financial performance and undercut the credibility of the program. The right staffing models and formulas, however, can help create a successful hospitalist work environment.
Summary of Recommendations
- There is no industry standard for a hospitalist staffing model. The analysis can be time-based or RVU-based, census driven, or based on any combination of output measures.
- Inpatient utilization drives the requirements for hospitalist staffing. A thorough analysis of historical inpatient utilization data is critical to developing a staffing model.
- In addition to understanding past utilization, projecting future inpatient demand is also important. Critical change factors include trends in: 1) the age and severity of patients; 2) population growth or decline; 3) payer sources; and 4) referral patterns.
- The services (work) performed by the hospital medicine program should be clearly identified and factored into the staffing formula. Brainstorming with the hospitalist group can be an effective technique for ensuring that the analysis is credible.
- Stakeholders should be involved early and often in developing a staffing model and in making staffing decisions.
- In developing a staffing model, particularly in the beginning stages, focus on the process and the methodology and not on the outcome (i.e., “my program needs 6 physicians”).
- Understand how the unique goals and characteristics of your hospital medicine program affect your staffing model.
Introduction
A major challenge for leaders of hospital medicine programs is determining appropriate staffing levels. Specifically, every hospitalist leader must answer the following question:
- What is the correct number of physician staff needed to meet the requirements of the work environment?
The Board of Directors of the Society of Hospital Medicine (SHM) asked the Benchmarks Committee to prepare a “white paper” on this subject. The Committee discussed hospitalist staffing and agreed that there is no simple formula or process for answering the question cited above. Instead, the Committee decided to prepare a paper that outlines the issues and suggests best practices for determining appropriate hospitalist staffing levels. A member of the Benchmarks Committee, Gale Ashbrener, Sr., Performance Consultant, Kaiser Permanente-Hawaii, has prepared a model for hospitalist staffing in her organization, and her work is the basis of this document.
NOTE: Most of the examples used in this document are from Kaiser-Hawaii. As such, the numbers cited are reflective of that particular organizational environment (i.e., a group model HMO). Readers should focus on the concepts and processes that are presented, recognizing that the numbers may be different for their environment.
Overview of the Issues
A process or simplistic model for determining the appropriate level of hospitalist staffing is summarized in Figure 1.
Staffing
Staffing is driven by demand: how many and what types of patients will the program expect to see in the upcoming year? Demand can then be converted to work: the tasks that the hospital medicine program must perform in order to treat these patients (the model must also quantify non-patient work). Once the total amount of work is described and quantified, the capacity of a hospitalist must be defined (e.g., in annual work hours). Then the number of hospitalists required to complete the projected work load can be computed.
Demand
The best practices for projecting patient demand are summarized in Box 1.
Hospitalist leaders should involve key stakeholders in the information gathering process. This helps establish the foundation for buy-in of the model down the road. You may want to pull together members of the hospitalist team and/or hospital administration to brainstorm on factors that may affect patient demand for inpatient services. At this point, keep an open mind for all considerations.
It is also critical to perform a comprehensive analysis of historical inpatient data. The analysis should examine all medical admissions at the hospital and specifically, in detail, those admissions cared for by the hospital medicine program. This analysis must look beyond the number of admissions and average length of stay (LOS). Several key characteristics of the hospitalized patients should be evaluated: age, diagnosis/severity, payer, and referring physician.
- Age: There are significant differences in inpatient utilization by age categories. It is important to further segment the “senior” Medicare (over age 65) population into several subgroups. Figure 2 (page 49) is based on data from Kaiser Permanente-Hawaii. As expected, there is a major difference in hospital utilization between the under age 65 population (15.9 admissions and 84 days per 1000) and the over age 65 population (167.9 admissions and 1,090 days per 1000). However, the differences within the Medicare subgroups are also substantial. For example, compare utilization by the population that is 65-69 years old (96.0 admissions and 621 days per 1000) with the population that is over age 85 (358.2 admissions and 2,111 days per 1000):
- Diagnoses/severity: There are acknowledged differences in LOS based on the patient’s reason for admission and many ways to characterize the reason of admission, including diagnosis and diagnostics-related groups (DRGs). Furthermore, patients with co-morbidities clearly require more coordination and patient management. There are several proprietary grouping methodologies that characterize the severity and intensity of an inpatient case, which include an assessment of co-morbidities. In analyzing historical data, the hospitalist leader should select a scheme that is used within the institution while minimizing the number of categories.
- Payer: In analyzing inpatient demand, it is also important to have an understanding of historical differences by payer (including uninsured patients). Health plans (or Medicaid programs) that are increasing or decreasing in size could affect the number of patients seen by a hospital medicine program.
- Referring physician: Community physicians (primary care, specialists, and surgeons) are a major source of inpatient cases for hospital medicine programs. It is important to analyze the historical impact of specific physicians or group practices on the patient load of the hospital medicine program.
The best way to project inpatient demand for hospitalist services is to identify and quantify what may change in the next year: what trends could increase or decrease the number of cases that will need to be treated? These change factors include the following:
- Population trends: Is the community growing? It there an influx of new residents? Is the community aging? Is it likely that there will be more seniors requiring inpatient services? Health plans and medical groups often can more easily assess population trends because they treat an enrolled population.
- Local health care factors: Will a hospital in the region be closing, resulting in additional inpatient demand? Is there a shortage of nursing home beds in the community that may affect the need for inpatient care? Is Medicaid reducing the number of covered recipients, potentially increasing the demand from uninsured patients?
- Changing referral patterns from community physicians: Do you expect additional community physicians to stop/start referring patients to the hospital medicine program? Are referring medical groups increasing or decreasing in size?
- Institution-specific factors: Does the hospital medicine program expect to assume new responsibilities in the next year – e.g., in the emergency department (ED), in the intensive care unit (ICU), providing night coverage, doing surgical co‑management, etc.?
Work
The best practices for measuring hospitalist output (work) are summarized in Box 2.
Determining how to quantify the labor of hospitalists can be the most controversial component of developing a staffing model. To ensure buy-in of these modeling decisions, participation by hospitalists and other key players (e.g., other physicians, physician leadership, and hospital/medical group administration) is crucial. Hospitalists and other key individuals must understand and agree on the quantification of time and labor.
It is critical that the analysis include ALL elements of work. Brainstorming with hospitalists can be helpful in this process. To build physician acceptance of and trust in the model, it is important to acknowledge the full set of hospitalist responsibilities in the initial stages of model development.
The services provided by a hospitalist team can vary from program to program and hospital to hospital. For example, at Kaiser Permanente-Hawaii, the dedicated hospitalist triage physician may direct patients coming from the clinic or ED to the ambulatory treatment center. A hospitalist then sees the patient in the center and an admission is often avoided. This physician labor must be captured in the model even though an admission did not occur. If your program includes a day team and a night team, you may want to handle these two teams as separate models.
Based on an analysis performed at Kaiser Permanente-Hawaii, some examples of hospitalist labor components are noted in Box 3 (page 50).
To measure the work performed by hospitalists, the model needs to recognize that there are differences in the labor components that have been identified (i.e., they are “weighted” differently). “Conventional wisdom” describes the work that hospitalists perform in terms of the number of patients seen per day (e.g., 15 patients per day). However, the work involved in a hospitalist seeing the following categories of patients is very different:
- Admitting a patient
- Rounding on a patient already admitted
- Discharging a patient
- Performing a consultation
Kaiser Permanente Hawaii developed the example in Box 4 to illustrate differences in the work required for admissions, rounding, and discharges, and how reductions in LOS do not lead to corresponding reductions in physician staffing levels.
There are basically two options in weighting the different elements of work performed by a hospitalist: time or relative value units (RVUs). Although the amount of time it takes to do a task seems to be the most sensible measurement of labor, it can be fraught with obstacles. The amount of time it takes a physician to round on a patient, for example, is not straightforward:
- Are all the patients located on one floor?
- Does the physician have to chase down test results routinely?
- Are all physicians the same, taking the same average amount of time to see a patient?
- Are all patients the same? Do older patients take more time due to social and medical complexity?
These are all factors that affect time. Furthermore, individuals are limited by their own experiences and frame of reference. Acceptance of a specific time allocation (e.g., a discharge takes 45 minutes) by those not doing the work is subjective. Despite these obstacles, it is valuable for hospitalist leaders to attempt to quantify the amount of time required to do inpatient work. Figure 3 shows example times used by a Kaiser Permanente-Hawaii medical group.
A hospital medicine program leader can use RVUs as a compliment to or as an alternative to time as the basis of weighting the work components performed by hospitalists. RVUs may account for patient acuity in a way that is hard to measure using time as the basis of measurement. Figure 4 illustrates RVUs by CPT-IV code.
Physician Capacity
The best practices for determining physician capacity are summarized in Box 5.
When determining the work capacity for a hospitalist (typically defined by the number of hours worked per year), it is critical to clearly define the unique aspects of the hospital medicine program that affect work capacity. These factors include:
- Staffing model: shift vs. call
- Scheduling approach: number of days on/off
- Non-patient care responsibilities: teaching, research, committees, etc.
- Staffing philosophy: part-time vs. full-time preference
Benchmark information is extremely helpful in determining physician capacity for a hospital medicine program. These benchmarks provide a point of comparison for hospitalist leaders developing staffing models. Medians for inpatient, non-patient, and on-call hours from the 2004 SHM Productivity and Compensation Survey are documented in Figure 5 (page 52).
The simplified example in Box 6, based on Kaiser time estimates, illustrates how demand, work, and physician capacity can be used to determine the number of hospitalists required to support a program.
As an alternative methodology or for comparative purposes, RVUs can be used rather than time. Box 7 uses RVUs from Figure 4 (initial hospital care: 1.28 RVUs; subsequent hospital care: .64 RVUs; hospital discharge < 30 minutes: 1.28 RVUs). The lowest level RVU values are used because they are consistent with the Kaiser example. Also, the median RVUs per year from Figure 5 are used (2961 for a hospital-based program).
Understand Your Work Environment
When a hospitalist program leader begins the process of developing a staffing model, it is important that he or she understands how the unique goals and characteristics of the program affects staffing. For example:
- Hospitalist-only groups are often driven by revenue. It is likely that these programs will expect hospitalists to do more billable work (i.e., see more patients)
- Academic programs typically have a broad range of other, non-patient care responsibilities, including teaching, research, and committee work. The hospitalists in these programs may see fewer patients.
The data from the 2004 SHM Productivity and Compensation Survey (Figure 5) confirms these differences. For inpatient hours worked, the national medians for these two different employment models differ by 23% (1700 vs. 2210). For RVUs worked, the national medians for the two different employment models differ by 17% (3000 vs. 3600).
Summary
Determining the right level of hospitalist staffing is important because it can positively or negatively affect the hospital medicine program and the hospital. Understaffing can lead to physician burn-out and adversely affect physician performance and hospital utilization. Overstaffing can affect the program’s financial performance and undercut the credibility of the program. The right staffing models and formulas, however, can help create a successful hospitalist work environment.
Summary of Recommendations
- There is no industry standard for a hospitalist staffing model. The analysis can be time-based or RVU-based, census driven, or based on any combination of output measures.
- Inpatient utilization drives the requirements for hospitalist staffing. A thorough analysis of historical inpatient utilization data is critical to developing a staffing model.
- In addition to understanding past utilization, projecting future inpatient demand is also important. Critical change factors include trends in: 1) the age and severity of patients; 2) population growth or decline; 3) payer sources; and 4) referral patterns.
- The services (work) performed by the hospital medicine program should be clearly identified and factored into the staffing formula. Brainstorming with the hospitalist group can be an effective technique for ensuring that the analysis is credible.
- Stakeholders should be involved early and often in developing a staffing model and in making staffing decisions.
- In developing a staffing model, particularly in the beginning stages, focus on the process and the methodology and not on the outcome (i.e., “my program needs 6 physicians”).
- Understand how the unique goals and characteristics of your hospital medicine program affect your staffing model.
Resident Work Hours, Hospitalist Programs, and Academic Medical Centers
In July of 2003, the Accreditation Council for Graduate Medical Education (ACGME) implemented new rules that restricted resident work hours to no more than 80 per week and restricted continuous duty to no more than 30 hours (24 hours plus 6 hours for transfer of care, the “24+6” rule). As a result, many major academic medical centers face the problem of handling increasing inpatient volume and ensuring compliance with these new work-hours regulations. The problem has become more pressing as several major academic centers have been cited for work-hours violations by the ACGME, and significant public attention has focused on the impact of excessive work hours on patient safety (1, 2).
Given the success of hospitalists in efficiently managing patents in many non-academic environments, one proposed solution has been the creation of hospitalist services to care for patients independent of residents. These services reduce the volume on resident-based services and therefore reduce resident work hours. We have recently implemented our own non-housestaff service at the University of Michigan and in this article describe the challenges and lessons learned.
Planning a Program
The first step for any institution contemplating the creation of a non-resident service is to establish clear goals. Frequently, decisions on the level and scope of uncovered services are made without any rigorous analysis of the data or without a clear idea of what it is that your program should be doing.
Goals for Resident-Service Census and Volume
The first task for any program is to understand what patient volume must be removed to ensure work-hours compliance without impeding the educational experience of the housestaff . Unfortunately, there is little published opinion on optimal resident workload, and the ACGME is surprisingly silent on this vital issue. While the ACGME does proscribe exceeding theoretical maximum workloads for internal medicine, they cite no minimum or ideal patient census (3). In the absence of firm guidelines, it is important to gather data on both the day-to-day variation of inpatient admissions and volume along with peak admission times (usually early evening). The residency program is likely to offer monthly data or a rough guess at what they think is needed. This can be misleading and does not appreciate the variability of patient flow. It is the “peaks’ that are often remembered, whereas the “troughs” are easily forgotten. Vital data elements that should be obtained include the daily admission volume for each resident-service over the course of the past year. We used this data to calculate average per-intern admission volumes and to project what future volume would be under a variety of possible scenarios, including removing a fixed number of patients per day, creating intern-admissions caps or alternating admissions between residents and hospitalists. We then discussed these models and their projected impact on the residents with residency leadership before settling upon our final model.
Structural Reform of the Resident Services
Besides the question of volume, there is also the issue of whether the new service will also be used to create other structural changes in the resident services. Some areas that programs may consider include modification of the existing call rotation such as reducing or eliminating short-call, changing the frequency of long-call, or implementing limitations on night-time admissions to the housestaff.
Each of these possibilities comes with its own structural needs, so it is vital to decide whether any of these changes are to be attempted.
Patient Complexity
There is significant temptation to use established hospitalist workload standards and apply them to non-resident services in academia. To do so is to invite disaster. The complexity of patients on most academic internal medicine services is quite different from the average community service. One big variable to address here is whether or not the new hospitalist service will have a selected patient population (such as low-complexity or “non-teaching” cases). Without specifically selected low-complexity cases, most hospitalist programs will realize that established community work standards do not apply.
Academic Inefficiencies and Workload
Much of what residents do on a day-to-day basis involves pushing their patients through the inefficient and complex maze of an academic medical center. It seems ridiculous to think that one faculty member can replace the work that was previously performed by an attending, a senior resident, and two interns, yet this is what many programs are actually proposing when they suggest that the “established” work load of 15 patients per day per hospitalist could work in academia.
What is an ideal workload in academia? Our answer is based both on our experience and on work-flow analysis of residents, which suggests that less than 20% of their time is actually spent in direct educational activities (4). We suggest that the acceptable workload for a hospitalist in a major academic center managing patients of equivalent complexity as the residents is slightly higher than what a senior resident alone can reasonably handle. In our institution we have had a service without interns, staffed with senior residents and one attending for several years. In institutions without this structure, one could look at what senior residents do on their intern’s days off. In our experience approximately 8-10 patients/day seems to be an acceptable workload that allowed the residents to provide quality care within the confines of a 10 to 12 hour day. This translates into an attending workload of 9-11 patients/day. We acknowledge that with time, an attending may develop more efficient practices than a senior resident but do not think a workload much higher than this is reasonable during the start-up phase.
The Role of Physician Extenders
Many hospitalists rely on physician extenders such as physician assistants and nurse practitioners. In academia, physician extenders have traditionally worked only in specialty areas of inpatient care such as orthopedics, oncology, or cardiology. The great unknown, however, is how extenders perform in an environment where they are asked to work with both complex and varied patients. We have seen that the training of many extenders is often not enough for them to take on the role envisioned for them in this kind of service. Over time they may develop the skill set, but there is much on-the-job learning that requires dedicated physician time. A realistic census for a physician assistant (PA) taking care of complex academic medical patients is likely to be 4 to 6. The incremental impact of extenders on a service’s total work capacity is not entirely additive, given the need for physician oversight and the need to maximize revenue by using shared visit billing. Despite these limitations, however, we believe that extenders are helpful, especially given the inefficiencies of day-to-day patient care in academic centers.
The University of Michigan
Medicine Faculty Hospitalist Service
Our own program was designed around an original goal of moving 2000 patients from the resident services. This figure was derived from a per-intern workload target of 25 to 30 admissions per month. Based on our modeling of various ways to share admissions, we ultimately settled on a system that alternates admissions with the resident services after each service admits a “baseline” number of patients. This allowed us to variably offload patients based on day-to-day variation in admission volumes. Our service is staffed 24 hours a day with a total of eight full-time physicians and four physician assistants. We have three physicians and two‑three physician assistants during the day (7 a.m. to 7 p.m.) to coincide with the bulk of the workload. There is one doctor at night (7 p.m. to 7 a.m.) for our entire service, and our hospitalists work an average of 50-55 hours a week during 18 shifts a month. Each hospitalist (working with a PA) averages from 8 to 12 billable encounters a day. We maintain a maximum daily census of 30-35 patients and admit up to 10 patients a day. Given these workloads, we do not come close to financial self-sufficiency, but this is not unique to our program.
Funding and Finances
For most institutions a non-resident service represents incremental faculty members without any significant incremental professional fee revenue. The billings on the new service really are just a shift in revenue from the resident services. In addition, given the high clinical workload and current market conditions, the salaries of hospitalists hired for such services tend to be on average $15,000 to $20,000 above that of hospitalists hired onto a traditional resident-based service. There is some opportunity for increased revenue capture because of 24-hour attending presence, but the incremental gain is unlikely to be enough to create financial self-sufficiency. In our program there has been an increase in department-wide consultative revenue as specialized patients are now placed on our general medical service where they were previously cared for by residents and a specialty attending. In addition, we have improved our charge capture by a small margin. This extra revenue will not, however, come close to offsetting our overall cost. Many programs therefore require hospital support to be viable. Given the strong incentives for hospitals to ensure compliance with ACGME rules and maintain maximal inpatient occupancy, many hospitals can be convinced to provide funding.
We argue strongly that the creation of programs developed primarily to deal with residency work hours should be viewed separately from the funding of existing or new resident-based hospitalist programs. Similar to how resident salaries are paid for by the hospital (via federal graduate medical education funding), the cost of a new hospitalist service that is created to replace residents should come from the hospital. Programs should exercise caution in using existing paradigms such as reduction in LOS or decrease in cost as a basis for funding. There is little data comparing resident-based care to non-resident-based hospital care in a tertiary center, and what little that exists does not necessarily suggest a cost benefit (5). In addition, there is a significant future risk if such proposed benefits do not become a reality
New Roles and Responsibilities
Once established, many programs will be asked to take on additional tasks that were previously performed by trainees or other faculty. This is especially true of nighttime tasks. Many programs are asked to run code-blue teams, supervise procedures at night, supervise sedation in radiology, triage patients in the ER, provide emergent patient coverage for other services: the list can go on and on. The challenge is accepting some and rejecting others without being seen as non-cooperative.
We strongly believe that taking on some of these tasks provides significant added value for non-resident programs, something that becomes vital in the long-run once the urgency of work-hours compliance has passed. Programs should pick wisely and move slowly when adding additional roles. Whatever roles are added, it is vital that ample consideration is given to the impact on workload and faculty satisfaction. Many of these roles may also present an opportunity to garner additional revenue, whether through billing or direct payment from the hospital.
The Challenges of Academia: Separate and Unequal
The greatest challenge that all major academic hospitalist programs will face will be how to create satisfying long-term faculty positions that involve providing direct inpatient care without the assistance of housestaff (6). There is already a growing problem of physician dissatisfaction among clinical-track faculty in many academic centers where the emphasis on clinical productivity has usurped the missions of teaching and research. The challenges faced by academic hospitalists working without residents are even greater than those faced by existing clinical faculty.
The first consideration for academic programs is whether to create two classes of hospitalists within the same program: those that work primarily with residents and those that do not. In our program we had an already established group of classic hospitalist-educators who worked only on resident-staffed services when we were asked to create a non-resident service. Our easiest option, therefore, was to hire new faculty whose sole responsibility is staffing a non-resident service. With this has come a significant struggle on how to ensure faculty satisfaction and avoid creating a split within the hospitalist program. We also struggle with how to administer such a program and whether leadership should have clinical roles on both services (we currently do not).
For many new programs, it may be easier to create one uniform faculty role that mixes non-resident-based and resident-based service duties and avoids the appearance of two classes of hospitalists. For many mature programs, however, the only option may be to hire new faculty who predominantly work on non-resident services. For these groups, we believe that differences in the positions must be addressed. One solution to this problem is creating viable teaching roles for these new faculty. Options that we are examing include medical student teaching, training allied-health professionals, and some involvement in resident education during the night and at regularly scheduled daytime lectures. Each of these roles requires time and will come at the expense of efficiency or work capacity. We also have struggled to create program-level rapport. We have encouraged weekly meetings and have found that clinically oriented collaboration such as case conferences and quality-improvement initiatives seem to provide the best way for the entire faculty to interact. Another solution that has been offered is to create a vigorous inpatient research agenda that uses the non-resident services as the laboratory; we encourage this approach but feel that it may not be a realistic near-term goal for many programs.
In the end, however, while creating these roles will add to faculty satisfaction and long-term viability, there will be ongoing problems similar to those faced by academic primary care faculty who have limited interactions with residents. Our program relies on junior-level faculty who are in transition between residency and further training or faculty who aspire to eventually grow into more traditional academic teaching roles and take on a more hybridized role. There is likely to be value in this variety, and we imagine that large academic programs will have faculty that run the gamut from those who are primarily research focused to those who spend most of their time in direct front-line patient care.
Results: Work Hours Success
Since the implementation of our non-housestaff service, we have seen dramatic improvements in resident work-hours compliance. Prior to our service, 40% of residents were in violation of the 80-hour week and the “24+6” hour shift limit. After successfully removing 15% of the total inpatient (non-ICU) census from resident-coverage, there have been only sporadic violations during the first 3 months of operation. Therefore, violations of the 80-hour work week rules have been virtually eliminated. Our residents have widely praised the new service and overall morale in the residency program has improved. Yet despite what has been perceived as a significant reduction in resident patient load, there are continued violations of the “24+6”-hour shift rule. In fact many have suggested that violation of the “24+6”-hour rule is a reflection of the competing tension between compliance with external regulation and our residents’ professionalism and dedication to patients. While further reductions in volume might help (although even our residents say that this might jeopardize their education), the more likely solution to this problem is both culture change over time and some re-engineering of the timing of resident shifts.
Conclusions
We envision that in the next few years, non-resident services will exist in almost every major medical center. As our experience highlights, these services can be an effective solution to the resident work-hours problem. We caution, however, that implementation is not an easy task. To be successful, programs should invest significant time in the planning stages and have clear goals in mind. Staffing and finances are likely to remain challenging as is the creation of academically viable roles. Eventually, however, we believe these services will succeed. Their growth will add to the future standing of hospital medicine in academic centers by creating a more diverse group of hospitalist faculty who focus on research, education, and, increasingly, quality patient care.
References
- Croasdale, M. “Johns Hopkins penalized for resident hour violations.” AMNews. Sept. 15, 2003.
- Mehes, A. “Med school could forfeit residency accreditation.” Yale Daily News. Oct. 25, 2002.
- Accreditation Council on Graduate Medical Education: Program Requirements for Residency Education in Internal Medicine. July, 2004. http://www.acgme.org/acWebsite/RRC_140/140_prIndex.asp. Last accessed November 17, 2004.
- Boex JR, Leahy PJ. Understanding residents’ work: moving beyond counting hours to assessing educational value. Acad Med. 2003;78:939-944.
- Halasyamani L, Valenstein P, Friedlander M, Cowen M. A comparison of two hospitalist models with traditional care in a community teaching hospital. Society of Hospital Medicine Annual Meeting (Abstract), April 2004.
- Saint S, Flanders SA. Hospitalists in teaching hospitals: opportunities but not without danger. J Gen Intern Med. 2004;Apr;19(4):392-3.
Dr. Parekh can be contacted at viparekh@umich.edu.
Dr. Flanders can be contacted at flanders@umich.edu.
In July of 2003, the Accreditation Council for Graduate Medical Education (ACGME) implemented new rules that restricted resident work hours to no more than 80 per week and restricted continuous duty to no more than 30 hours (24 hours plus 6 hours for transfer of care, the “24+6” rule). As a result, many major academic medical centers face the problem of handling increasing inpatient volume and ensuring compliance with these new work-hours regulations. The problem has become more pressing as several major academic centers have been cited for work-hours violations by the ACGME, and significant public attention has focused on the impact of excessive work hours on patient safety (1, 2).
Given the success of hospitalists in efficiently managing patents in many non-academic environments, one proposed solution has been the creation of hospitalist services to care for patients independent of residents. These services reduce the volume on resident-based services and therefore reduce resident work hours. We have recently implemented our own non-housestaff service at the University of Michigan and in this article describe the challenges and lessons learned.
Planning a Program
The first step for any institution contemplating the creation of a non-resident service is to establish clear goals. Frequently, decisions on the level and scope of uncovered services are made without any rigorous analysis of the data or without a clear idea of what it is that your program should be doing.
Goals for Resident-Service Census and Volume
The first task for any program is to understand what patient volume must be removed to ensure work-hours compliance without impeding the educational experience of the housestaff . Unfortunately, there is little published opinion on optimal resident workload, and the ACGME is surprisingly silent on this vital issue. While the ACGME does proscribe exceeding theoretical maximum workloads for internal medicine, they cite no minimum or ideal patient census (3). In the absence of firm guidelines, it is important to gather data on both the day-to-day variation of inpatient admissions and volume along with peak admission times (usually early evening). The residency program is likely to offer monthly data or a rough guess at what they think is needed. This can be misleading and does not appreciate the variability of patient flow. It is the “peaks’ that are often remembered, whereas the “troughs” are easily forgotten. Vital data elements that should be obtained include the daily admission volume for each resident-service over the course of the past year. We used this data to calculate average per-intern admission volumes and to project what future volume would be under a variety of possible scenarios, including removing a fixed number of patients per day, creating intern-admissions caps or alternating admissions between residents and hospitalists. We then discussed these models and their projected impact on the residents with residency leadership before settling upon our final model.
Structural Reform of the Resident Services
Besides the question of volume, there is also the issue of whether the new service will also be used to create other structural changes in the resident services. Some areas that programs may consider include modification of the existing call rotation such as reducing or eliminating short-call, changing the frequency of long-call, or implementing limitations on night-time admissions to the housestaff.
Each of these possibilities comes with its own structural needs, so it is vital to decide whether any of these changes are to be attempted.
Patient Complexity
There is significant temptation to use established hospitalist workload standards and apply them to non-resident services in academia. To do so is to invite disaster. The complexity of patients on most academic internal medicine services is quite different from the average community service. One big variable to address here is whether or not the new hospitalist service will have a selected patient population (such as low-complexity or “non-teaching” cases). Without specifically selected low-complexity cases, most hospitalist programs will realize that established community work standards do not apply.
Academic Inefficiencies and Workload
Much of what residents do on a day-to-day basis involves pushing their patients through the inefficient and complex maze of an academic medical center. It seems ridiculous to think that one faculty member can replace the work that was previously performed by an attending, a senior resident, and two interns, yet this is what many programs are actually proposing when they suggest that the “established” work load of 15 patients per day per hospitalist could work in academia.
What is an ideal workload in academia? Our answer is based both on our experience and on work-flow analysis of residents, which suggests that less than 20% of their time is actually spent in direct educational activities (4). We suggest that the acceptable workload for a hospitalist in a major academic center managing patients of equivalent complexity as the residents is slightly higher than what a senior resident alone can reasonably handle. In our institution we have had a service without interns, staffed with senior residents and one attending for several years. In institutions without this structure, one could look at what senior residents do on their intern’s days off. In our experience approximately 8-10 patients/day seems to be an acceptable workload that allowed the residents to provide quality care within the confines of a 10 to 12 hour day. This translates into an attending workload of 9-11 patients/day. We acknowledge that with time, an attending may develop more efficient practices than a senior resident but do not think a workload much higher than this is reasonable during the start-up phase.
The Role of Physician Extenders
Many hospitalists rely on physician extenders such as physician assistants and nurse practitioners. In academia, physician extenders have traditionally worked only in specialty areas of inpatient care such as orthopedics, oncology, or cardiology. The great unknown, however, is how extenders perform in an environment where they are asked to work with both complex and varied patients. We have seen that the training of many extenders is often not enough for them to take on the role envisioned for them in this kind of service. Over time they may develop the skill set, but there is much on-the-job learning that requires dedicated physician time. A realistic census for a physician assistant (PA) taking care of complex academic medical patients is likely to be 4 to 6. The incremental impact of extenders on a service’s total work capacity is not entirely additive, given the need for physician oversight and the need to maximize revenue by using shared visit billing. Despite these limitations, however, we believe that extenders are helpful, especially given the inefficiencies of day-to-day patient care in academic centers.
The University of Michigan
Medicine Faculty Hospitalist Service
Our own program was designed around an original goal of moving 2000 patients from the resident services. This figure was derived from a per-intern workload target of 25 to 30 admissions per month. Based on our modeling of various ways to share admissions, we ultimately settled on a system that alternates admissions with the resident services after each service admits a “baseline” number of patients. This allowed us to variably offload patients based on day-to-day variation in admission volumes. Our service is staffed 24 hours a day with a total of eight full-time physicians and four physician assistants. We have three physicians and two‑three physician assistants during the day (7 a.m. to 7 p.m.) to coincide with the bulk of the workload. There is one doctor at night (7 p.m. to 7 a.m.) for our entire service, and our hospitalists work an average of 50-55 hours a week during 18 shifts a month. Each hospitalist (working with a PA) averages from 8 to 12 billable encounters a day. We maintain a maximum daily census of 30-35 patients and admit up to 10 patients a day. Given these workloads, we do not come close to financial self-sufficiency, but this is not unique to our program.
Funding and Finances
For most institutions a non-resident service represents incremental faculty members without any significant incremental professional fee revenue. The billings on the new service really are just a shift in revenue from the resident services. In addition, given the high clinical workload and current market conditions, the salaries of hospitalists hired for such services tend to be on average $15,000 to $20,000 above that of hospitalists hired onto a traditional resident-based service. There is some opportunity for increased revenue capture because of 24-hour attending presence, but the incremental gain is unlikely to be enough to create financial self-sufficiency. In our program there has been an increase in department-wide consultative revenue as specialized patients are now placed on our general medical service where they were previously cared for by residents and a specialty attending. In addition, we have improved our charge capture by a small margin. This extra revenue will not, however, come close to offsetting our overall cost. Many programs therefore require hospital support to be viable. Given the strong incentives for hospitals to ensure compliance with ACGME rules and maintain maximal inpatient occupancy, many hospitals can be convinced to provide funding.
We argue strongly that the creation of programs developed primarily to deal with residency work hours should be viewed separately from the funding of existing or new resident-based hospitalist programs. Similar to how resident salaries are paid for by the hospital (via federal graduate medical education funding), the cost of a new hospitalist service that is created to replace residents should come from the hospital. Programs should exercise caution in using existing paradigms such as reduction in LOS or decrease in cost as a basis for funding. There is little data comparing resident-based care to non-resident-based hospital care in a tertiary center, and what little that exists does not necessarily suggest a cost benefit (5). In addition, there is a significant future risk if such proposed benefits do not become a reality
New Roles and Responsibilities
Once established, many programs will be asked to take on additional tasks that were previously performed by trainees or other faculty. This is especially true of nighttime tasks. Many programs are asked to run code-blue teams, supervise procedures at night, supervise sedation in radiology, triage patients in the ER, provide emergent patient coverage for other services: the list can go on and on. The challenge is accepting some and rejecting others without being seen as non-cooperative.
We strongly believe that taking on some of these tasks provides significant added value for non-resident programs, something that becomes vital in the long-run once the urgency of work-hours compliance has passed. Programs should pick wisely and move slowly when adding additional roles. Whatever roles are added, it is vital that ample consideration is given to the impact on workload and faculty satisfaction. Many of these roles may also present an opportunity to garner additional revenue, whether through billing or direct payment from the hospital.
The Challenges of Academia: Separate and Unequal
The greatest challenge that all major academic hospitalist programs will face will be how to create satisfying long-term faculty positions that involve providing direct inpatient care without the assistance of housestaff (6). There is already a growing problem of physician dissatisfaction among clinical-track faculty in many academic centers where the emphasis on clinical productivity has usurped the missions of teaching and research. The challenges faced by academic hospitalists working without residents are even greater than those faced by existing clinical faculty.
The first consideration for academic programs is whether to create two classes of hospitalists within the same program: those that work primarily with residents and those that do not. In our program we had an already established group of classic hospitalist-educators who worked only on resident-staffed services when we were asked to create a non-resident service. Our easiest option, therefore, was to hire new faculty whose sole responsibility is staffing a non-resident service. With this has come a significant struggle on how to ensure faculty satisfaction and avoid creating a split within the hospitalist program. We also struggle with how to administer such a program and whether leadership should have clinical roles on both services (we currently do not).
For many new programs, it may be easier to create one uniform faculty role that mixes non-resident-based and resident-based service duties and avoids the appearance of two classes of hospitalists. For many mature programs, however, the only option may be to hire new faculty who predominantly work on non-resident services. For these groups, we believe that differences in the positions must be addressed. One solution to this problem is creating viable teaching roles for these new faculty. Options that we are examing include medical student teaching, training allied-health professionals, and some involvement in resident education during the night and at regularly scheduled daytime lectures. Each of these roles requires time and will come at the expense of efficiency or work capacity. We also have struggled to create program-level rapport. We have encouraged weekly meetings and have found that clinically oriented collaboration such as case conferences and quality-improvement initiatives seem to provide the best way for the entire faculty to interact. Another solution that has been offered is to create a vigorous inpatient research agenda that uses the non-resident services as the laboratory; we encourage this approach but feel that it may not be a realistic near-term goal for many programs.
In the end, however, while creating these roles will add to faculty satisfaction and long-term viability, there will be ongoing problems similar to those faced by academic primary care faculty who have limited interactions with residents. Our program relies on junior-level faculty who are in transition between residency and further training or faculty who aspire to eventually grow into more traditional academic teaching roles and take on a more hybridized role. There is likely to be value in this variety, and we imagine that large academic programs will have faculty that run the gamut from those who are primarily research focused to those who spend most of their time in direct front-line patient care.
Results: Work Hours Success
Since the implementation of our non-housestaff service, we have seen dramatic improvements in resident work-hours compliance. Prior to our service, 40% of residents were in violation of the 80-hour week and the “24+6” hour shift limit. After successfully removing 15% of the total inpatient (non-ICU) census from resident-coverage, there have been only sporadic violations during the first 3 months of operation. Therefore, violations of the 80-hour work week rules have been virtually eliminated. Our residents have widely praised the new service and overall morale in the residency program has improved. Yet despite what has been perceived as a significant reduction in resident patient load, there are continued violations of the “24+6”-hour shift rule. In fact many have suggested that violation of the “24+6”-hour rule is a reflection of the competing tension between compliance with external regulation and our residents’ professionalism and dedication to patients. While further reductions in volume might help (although even our residents say that this might jeopardize their education), the more likely solution to this problem is both culture change over time and some re-engineering of the timing of resident shifts.
Conclusions
We envision that in the next few years, non-resident services will exist in almost every major medical center. As our experience highlights, these services can be an effective solution to the resident work-hours problem. We caution, however, that implementation is not an easy task. To be successful, programs should invest significant time in the planning stages and have clear goals in mind. Staffing and finances are likely to remain challenging as is the creation of academically viable roles. Eventually, however, we believe these services will succeed. Their growth will add to the future standing of hospital medicine in academic centers by creating a more diverse group of hospitalist faculty who focus on research, education, and, increasingly, quality patient care.
References
- Croasdale, M. “Johns Hopkins penalized for resident hour violations.” AMNews. Sept. 15, 2003.
- Mehes, A. “Med school could forfeit residency accreditation.” Yale Daily News. Oct. 25, 2002.
- Accreditation Council on Graduate Medical Education: Program Requirements for Residency Education in Internal Medicine. July, 2004. http://www.acgme.org/acWebsite/RRC_140/140_prIndex.asp. Last accessed November 17, 2004.
- Boex JR, Leahy PJ. Understanding residents’ work: moving beyond counting hours to assessing educational value. Acad Med. 2003;78:939-944.
- Halasyamani L, Valenstein P, Friedlander M, Cowen M. A comparison of two hospitalist models with traditional care in a community teaching hospital. Society of Hospital Medicine Annual Meeting (Abstract), April 2004.
- Saint S, Flanders SA. Hospitalists in teaching hospitals: opportunities but not without danger. J Gen Intern Med. 2004;Apr;19(4):392-3.
Dr. Parekh can be contacted at viparekh@umich.edu.
Dr. Flanders can be contacted at flanders@umich.edu.
In July of 2003, the Accreditation Council for Graduate Medical Education (ACGME) implemented new rules that restricted resident work hours to no more than 80 per week and restricted continuous duty to no more than 30 hours (24 hours plus 6 hours for transfer of care, the “24+6” rule). As a result, many major academic medical centers face the problem of handling increasing inpatient volume and ensuring compliance with these new work-hours regulations. The problem has become more pressing as several major academic centers have been cited for work-hours violations by the ACGME, and significant public attention has focused on the impact of excessive work hours on patient safety (1, 2).
Given the success of hospitalists in efficiently managing patents in many non-academic environments, one proposed solution has been the creation of hospitalist services to care for patients independent of residents. These services reduce the volume on resident-based services and therefore reduce resident work hours. We have recently implemented our own non-housestaff service at the University of Michigan and in this article describe the challenges and lessons learned.
Planning a Program
The first step for any institution contemplating the creation of a non-resident service is to establish clear goals. Frequently, decisions on the level and scope of uncovered services are made without any rigorous analysis of the data or without a clear idea of what it is that your program should be doing.
Goals for Resident-Service Census and Volume
The first task for any program is to understand what patient volume must be removed to ensure work-hours compliance without impeding the educational experience of the housestaff . Unfortunately, there is little published opinion on optimal resident workload, and the ACGME is surprisingly silent on this vital issue. While the ACGME does proscribe exceeding theoretical maximum workloads for internal medicine, they cite no minimum or ideal patient census (3). In the absence of firm guidelines, it is important to gather data on both the day-to-day variation of inpatient admissions and volume along with peak admission times (usually early evening). The residency program is likely to offer monthly data or a rough guess at what they think is needed. This can be misleading and does not appreciate the variability of patient flow. It is the “peaks’ that are often remembered, whereas the “troughs” are easily forgotten. Vital data elements that should be obtained include the daily admission volume for each resident-service over the course of the past year. We used this data to calculate average per-intern admission volumes and to project what future volume would be under a variety of possible scenarios, including removing a fixed number of patients per day, creating intern-admissions caps or alternating admissions between residents and hospitalists. We then discussed these models and their projected impact on the residents with residency leadership before settling upon our final model.
Structural Reform of the Resident Services
Besides the question of volume, there is also the issue of whether the new service will also be used to create other structural changes in the resident services. Some areas that programs may consider include modification of the existing call rotation such as reducing or eliminating short-call, changing the frequency of long-call, or implementing limitations on night-time admissions to the housestaff.
Each of these possibilities comes with its own structural needs, so it is vital to decide whether any of these changes are to be attempted.
Patient Complexity
There is significant temptation to use established hospitalist workload standards and apply them to non-resident services in academia. To do so is to invite disaster. The complexity of patients on most academic internal medicine services is quite different from the average community service. One big variable to address here is whether or not the new hospitalist service will have a selected patient population (such as low-complexity or “non-teaching” cases). Without specifically selected low-complexity cases, most hospitalist programs will realize that established community work standards do not apply.
Academic Inefficiencies and Workload
Much of what residents do on a day-to-day basis involves pushing their patients through the inefficient and complex maze of an academic medical center. It seems ridiculous to think that one faculty member can replace the work that was previously performed by an attending, a senior resident, and two interns, yet this is what many programs are actually proposing when they suggest that the “established” work load of 15 patients per day per hospitalist could work in academia.
What is an ideal workload in academia? Our answer is based both on our experience and on work-flow analysis of residents, which suggests that less than 20% of their time is actually spent in direct educational activities (4). We suggest that the acceptable workload for a hospitalist in a major academic center managing patients of equivalent complexity as the residents is slightly higher than what a senior resident alone can reasonably handle. In our institution we have had a service without interns, staffed with senior residents and one attending for several years. In institutions without this structure, one could look at what senior residents do on their intern’s days off. In our experience approximately 8-10 patients/day seems to be an acceptable workload that allowed the residents to provide quality care within the confines of a 10 to 12 hour day. This translates into an attending workload of 9-11 patients/day. We acknowledge that with time, an attending may develop more efficient practices than a senior resident but do not think a workload much higher than this is reasonable during the start-up phase.
The Role of Physician Extenders
Many hospitalists rely on physician extenders such as physician assistants and nurse practitioners. In academia, physician extenders have traditionally worked only in specialty areas of inpatient care such as orthopedics, oncology, or cardiology. The great unknown, however, is how extenders perform in an environment where they are asked to work with both complex and varied patients. We have seen that the training of many extenders is often not enough for them to take on the role envisioned for them in this kind of service. Over time they may develop the skill set, but there is much on-the-job learning that requires dedicated physician time. A realistic census for a physician assistant (PA) taking care of complex academic medical patients is likely to be 4 to 6. The incremental impact of extenders on a service’s total work capacity is not entirely additive, given the need for physician oversight and the need to maximize revenue by using shared visit billing. Despite these limitations, however, we believe that extenders are helpful, especially given the inefficiencies of day-to-day patient care in academic centers.
The University of Michigan
Medicine Faculty Hospitalist Service
Our own program was designed around an original goal of moving 2000 patients from the resident services. This figure was derived from a per-intern workload target of 25 to 30 admissions per month. Based on our modeling of various ways to share admissions, we ultimately settled on a system that alternates admissions with the resident services after each service admits a “baseline” number of patients. This allowed us to variably offload patients based on day-to-day variation in admission volumes. Our service is staffed 24 hours a day with a total of eight full-time physicians and four physician assistants. We have three physicians and two‑three physician assistants during the day (7 a.m. to 7 p.m.) to coincide with the bulk of the workload. There is one doctor at night (7 p.m. to 7 a.m.) for our entire service, and our hospitalists work an average of 50-55 hours a week during 18 shifts a month. Each hospitalist (working with a PA) averages from 8 to 12 billable encounters a day. We maintain a maximum daily census of 30-35 patients and admit up to 10 patients a day. Given these workloads, we do not come close to financial self-sufficiency, but this is not unique to our program.
Funding and Finances
For most institutions a non-resident service represents incremental faculty members without any significant incremental professional fee revenue. The billings on the new service really are just a shift in revenue from the resident services. In addition, given the high clinical workload and current market conditions, the salaries of hospitalists hired for such services tend to be on average $15,000 to $20,000 above that of hospitalists hired onto a traditional resident-based service. There is some opportunity for increased revenue capture because of 24-hour attending presence, but the incremental gain is unlikely to be enough to create financial self-sufficiency. In our program there has been an increase in department-wide consultative revenue as specialized patients are now placed on our general medical service where they were previously cared for by residents and a specialty attending. In addition, we have improved our charge capture by a small margin. This extra revenue will not, however, come close to offsetting our overall cost. Many programs therefore require hospital support to be viable. Given the strong incentives for hospitals to ensure compliance with ACGME rules and maintain maximal inpatient occupancy, many hospitals can be convinced to provide funding.
We argue strongly that the creation of programs developed primarily to deal with residency work hours should be viewed separately from the funding of existing or new resident-based hospitalist programs. Similar to how resident salaries are paid for by the hospital (via federal graduate medical education funding), the cost of a new hospitalist service that is created to replace residents should come from the hospital. Programs should exercise caution in using existing paradigms such as reduction in LOS or decrease in cost as a basis for funding. There is little data comparing resident-based care to non-resident-based hospital care in a tertiary center, and what little that exists does not necessarily suggest a cost benefit (5). In addition, there is a significant future risk if such proposed benefits do not become a reality
New Roles and Responsibilities
Once established, many programs will be asked to take on additional tasks that were previously performed by trainees or other faculty. This is especially true of nighttime tasks. Many programs are asked to run code-blue teams, supervise procedures at night, supervise sedation in radiology, triage patients in the ER, provide emergent patient coverage for other services: the list can go on and on. The challenge is accepting some and rejecting others without being seen as non-cooperative.
We strongly believe that taking on some of these tasks provides significant added value for non-resident programs, something that becomes vital in the long-run once the urgency of work-hours compliance has passed. Programs should pick wisely and move slowly when adding additional roles. Whatever roles are added, it is vital that ample consideration is given to the impact on workload and faculty satisfaction. Many of these roles may also present an opportunity to garner additional revenue, whether through billing or direct payment from the hospital.
The Challenges of Academia: Separate and Unequal
The greatest challenge that all major academic hospitalist programs will face will be how to create satisfying long-term faculty positions that involve providing direct inpatient care without the assistance of housestaff (6). There is already a growing problem of physician dissatisfaction among clinical-track faculty in many academic centers where the emphasis on clinical productivity has usurped the missions of teaching and research. The challenges faced by academic hospitalists working without residents are even greater than those faced by existing clinical faculty.
The first consideration for academic programs is whether to create two classes of hospitalists within the same program: those that work primarily with residents and those that do not. In our program we had an already established group of classic hospitalist-educators who worked only on resident-staffed services when we were asked to create a non-resident service. Our easiest option, therefore, was to hire new faculty whose sole responsibility is staffing a non-resident service. With this has come a significant struggle on how to ensure faculty satisfaction and avoid creating a split within the hospitalist program. We also struggle with how to administer such a program and whether leadership should have clinical roles on both services (we currently do not).
For many new programs, it may be easier to create one uniform faculty role that mixes non-resident-based and resident-based service duties and avoids the appearance of two classes of hospitalists. For many mature programs, however, the only option may be to hire new faculty who predominantly work on non-resident services. For these groups, we believe that differences in the positions must be addressed. One solution to this problem is creating viable teaching roles for these new faculty. Options that we are examing include medical student teaching, training allied-health professionals, and some involvement in resident education during the night and at regularly scheduled daytime lectures. Each of these roles requires time and will come at the expense of efficiency or work capacity. We also have struggled to create program-level rapport. We have encouraged weekly meetings and have found that clinically oriented collaboration such as case conferences and quality-improvement initiatives seem to provide the best way for the entire faculty to interact. Another solution that has been offered is to create a vigorous inpatient research agenda that uses the non-resident services as the laboratory; we encourage this approach but feel that it may not be a realistic near-term goal for many programs.
In the end, however, while creating these roles will add to faculty satisfaction and long-term viability, there will be ongoing problems similar to those faced by academic primary care faculty who have limited interactions with residents. Our program relies on junior-level faculty who are in transition between residency and further training or faculty who aspire to eventually grow into more traditional academic teaching roles and take on a more hybridized role. There is likely to be value in this variety, and we imagine that large academic programs will have faculty that run the gamut from those who are primarily research focused to those who spend most of their time in direct front-line patient care.
Results: Work Hours Success
Since the implementation of our non-housestaff service, we have seen dramatic improvements in resident work-hours compliance. Prior to our service, 40% of residents were in violation of the 80-hour week and the “24+6” hour shift limit. After successfully removing 15% of the total inpatient (non-ICU) census from resident-coverage, there have been only sporadic violations during the first 3 months of operation. Therefore, violations of the 80-hour work week rules have been virtually eliminated. Our residents have widely praised the new service and overall morale in the residency program has improved. Yet despite what has been perceived as a significant reduction in resident patient load, there are continued violations of the “24+6”-hour shift rule. In fact many have suggested that violation of the “24+6”-hour rule is a reflection of the competing tension between compliance with external regulation and our residents’ professionalism and dedication to patients. While further reductions in volume might help (although even our residents say that this might jeopardize their education), the more likely solution to this problem is both culture change over time and some re-engineering of the timing of resident shifts.
Conclusions
We envision that in the next few years, non-resident services will exist in almost every major medical center. As our experience highlights, these services can be an effective solution to the resident work-hours problem. We caution, however, that implementation is not an easy task. To be successful, programs should invest significant time in the planning stages and have clear goals in mind. Staffing and finances are likely to remain challenging as is the creation of academically viable roles. Eventually, however, we believe these services will succeed. Their growth will add to the future standing of hospital medicine in academic centers by creating a more diverse group of hospitalist faculty who focus on research, education, and, increasingly, quality patient care.
References
- Croasdale, M. “Johns Hopkins penalized for resident hour violations.” AMNews. Sept. 15, 2003.
- Mehes, A. “Med school could forfeit residency accreditation.” Yale Daily News. Oct. 25, 2002.
- Accreditation Council on Graduate Medical Education: Program Requirements for Residency Education in Internal Medicine. July, 2004. http://www.acgme.org/acWebsite/RRC_140/140_prIndex.asp. Last accessed November 17, 2004.
- Boex JR, Leahy PJ. Understanding residents’ work: moving beyond counting hours to assessing educational value. Acad Med. 2003;78:939-944.
- Halasyamani L, Valenstein P, Friedlander M, Cowen M. A comparison of two hospitalist models with traditional care in a community teaching hospital. Society of Hospital Medicine Annual Meeting (Abstract), April 2004.
- Saint S, Flanders SA. Hospitalists in teaching hospitals: opportunities but not without danger. J Gen Intern Med. 2004;Apr;19(4):392-3.
Dr. Parekh can be contacted at viparekh@umich.edu.
Dr. Flanders can be contacted at flanders@umich.edu.
Taking Your Best Shot at the Flu
In a year when the United States has been riddled with bad news, confusion, and even threats of fines and incarceration (1) surrounding the use of influenza vaccines, the last thing you may be interested in thinking about is instituting a comprehensive inpatient influenza vaccination initiative. Despite the chaos, it is important to remember that, on average, 36,000 (2) people die and 226,000 (3) people are hospitalized annually from influenza, or “the flu,” and its complications. Additionally, a significant proportion of patients hospitalized will have co-morbid illness or be old enough to be considered in the highest risk category for complications of flu (4). Hospitalists are poised to act centrally in improving vaccination rates given the intensity of their patient contact and their expertise in developing best-practices-based systems.
What follows is a step-wise plan to help you begin an inpatient influenza vaccination initiative at your institution. Clearly, elements of this plan will need to be modified based on institutional structure and preference.
1. Define the problem locally. It is important to identify if any inpatient vaccination systems are already in place for any other vaccination (e.g., pneumococcal vaccination for splenectomy patients; tetanus for trauma patients, etc). If such a system already exists, review its successes and see if any of them may be borrowed for the influenza plan. Also determine if influenza vaccines have ever (even in a random, sptty fashion) been given out on your institution’s inpatient service. Understanding this history will help you address the issues of the “culture” of the institution.
2. Talk with your administration about making influenza vaccination a quality goal. One of the barriers ahead may be the mindset that vaccinations should only live in the world of outpatient physicians. By obtaining “buyin” from administration (e.g., the Chief Medical Officer), you may have some additional resources made available to you, and you may also be able to leverage the weight of the administration in recruiting help for the program. Remember, the 2005 Disease-Specific Patient Safety Goals from the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) state that it is important to “develop and implement a protocol for administration and documentation of the flu vaccine.” (5)
3. Identify key players and meet with them. This plan cannot be sustained successfully as a one-person show. Ideally, you should create an influenza vaccination committee that has representatives of all the inpatient services (medicine, family medicine, surgery, obstetrics and gynecology, and pediatrics), as well as nursing leadership, infection control, pharmacy, information technology (for computerized order entry systems), and quality assurance. In academic institutions, you might also consider including a house officer and/or medical student. The initial meeting should review your findings with #1 and #2 above, as well as assessing this committee’s concerns about implementing an inpatient vaccination scheme. You should plan to initiate committee activities at least two to three months in advance of the anticipated availability of the vaccine.
4. Create a culture of vaccination. Vaccines are often not on the radar screen of most inpatient physicians as they deal with the more acute reasons for hospitalization. It is therefore important to begin introducing a culture change, demonstrating the importance of vaccinations to your staff, and shifting the prevalent mindset towards active engagement with your vaccination program. Identifying foreseeable problems and developing action plans will assist this process. Some issues may include:
- Physician and nurse attitudes and education about influenza and the vaccine (e.g., dispelling flu shot rumors, educating staff on the low risk of re-vaccinating a patient already vaccinated previously this season, explaining the lack of requirements for written informed consent for flu vaccination, encouraging health care workers to get flu shots themselves (6), etc.)
- Reminder systems for physicians to reinforce the need to vaccinate (posters, screen savers, emails, buttons)
- Communication with primary care physicians about patients who have been vaccinated
- Patient misconceptions about the vaccine’s side effects
5. Set a goal. It may be helpful to assess your inpatient service’s demographics for the past few years to identify the approximate denominator of eligible candidates for the vaccine based on age and key diagnoses. However, if your institution does not already have a history of active influenza vaccination on the inpatient service, start with a humble goal. It is attractive to assume that every patient who qualifies will be vaccinated. It is just not so. Have your influenza committee pick an achievable goal for your first flu season and stretch it in subsequent seasons. To achieve the goal, make sure each clinical area has an identifiable “champion” who can gently remind clinicians about the importance of vaccination. The higher the profile of the local champion the better, assuming the champion has the time and can offer the effort required to do the periodic reminders. Also make sure your pharmacy tracking and distributions systems are prepared to handle the increase in requests for the vaccines. Of note, many patients who are candidates for flu shots are also candidates for pneumococcal vaccines and both may be given together. Consider adding the pneumococcal vaccine to your efforts in appropriate patients.
6. Develop an “Opt Out” system. The CDC’s Advisory Committee on Immunization Practices recommends developing standing orders for both influenza and pneumococcal vaccinations (7). In computerized order entry, this suggestion may lead to a pre-selected order-set being built into the discharge orders that requires the physician to actively opt-out of the order. Paper-based systems may include standing printed orders, again, which require a physician to decline the order specifically. Such opt out systems have been shown to improve rates of vaccination significantly (8). Opt-out programs, however, still require that the clinician ordering the vaccine discusses the vaccine with the patient before it is administered.
7. Roll it out with a bang. Make sure the commencement of your flu shot program gets some press. Announce it at departmental meetings, on system-wide emails, and in hospital publications. Remember, this program is a demonstrable way of improving your patients’ health and an excellent way for hospitalists to show their systems-oriented approaches. Begin your roll-out as early as recommended by the local Department of Public Health so that your patients, many of whom will be at very high risk for complications of the flu, get early vaccination.
8. Give frequent feedback. Obtain vaccine distribution and utilization data at least twice monthly during the first two or three months. This period corresponds to the most critical period of the program as it is when flu shots must be delivered to ensure their efficacy come December-February when flu season typically peaks (9). Some groups may find that a bit of healthy competition (e.g., between services or between nursing units) may offer that edge to keep people vaccinating. Nonetheless, it is critical to keep your clinical areas updated with their performance, with public appreciation being expressed for the top notable clinical areas and low performers receiving extra encouragement and assistance. After the first few months, monthly reports and feedback will suffice, with the program running through the end of March.
9. Remain aware of the local and national flu scene. With the vaccine production problems of the current flu season and with the panic about the high mortality rates of the Fujian strain that was not included in the vaccine last season, it is clear that the flu news scene can be volatile and controversial. It is important to remain up to date on the current facts and be able to dispel any misinformation that may circulate. The following resources may prove helpful:
- The CDC’s influenza home page: http://www.cdc.gov/flu/
- The WHO’s influenza site: http://www.who.int/csr/disease/influenza/en/
- The state Department of Public Health
10. Plan for next season. At the end of flu season, reconvene the influenza committee and debrief. It is important to keep a log of the successes and failures of the season’s flu vaccine initiative to permit growth in subsequent seasons.
The CDC’s program, Healthy People 2010, has set a goal for influenza and pneumococcal vaccination of appropriate non-institutionalized individuals of 90% (10). This goal is achievable if all available resources for reaching out to such patients are utilized. The Massachusetts Hospital Association reports:
“Inpatient hospital stays are among the many missed opportunities for flu and pneumonia vaccination across health care settings. Up to 46% of subsequent influenza-related hospitalizations and 2/3 of influenza-related deaths occur among the elderly who have been previously hospitalized during the flu season. Up to 2/3 of patients hospitalized with serious pneumococcal infections have been hospitalized at least once within the previous 3-5 years (8).”
Hospitalists must take advantage of the opportunity that hospitalization affords our patients to receive the vaccines they need to stay healthy. Appropriate vaccine delivery is no longer solely the purview of the primary care physician – hospitalists must share this goal as well.
References
- The Commonwealth of Massachusetts Executive Office of Health and Human Services Department of Public Health. Revised order to establish rules and priorities for the distribution and use of influenza vaccine. Available at: http://www.mass.gov/dph/cdc/epii/flu/flu_order.htm. Accessed November 3, 2004.
- Thompson WW, Shay DK, Weintraub E, et al. Mortality associated with influenza and respiratory syncytial virus in the United States. JAMA.2003;289:179-86.
- Thompson WW, Shay DK, Weintraub E, et al. Influenza-associated hospitalizations in the United States. JAMA. 2004;292:1333-40.
- CDC. Interim Influenza Vaccination Recommendations – 2004-2005 Season. Available at: http://www.cdc.gov/flu/protect/whoshouldget.htm. Accessed November 3, 2004.
- JCAHO. 2005 Disease-specific care national patient safety goals. Available at: http://www.jcaho.org/accredited+organizations/patient+safety/05+npsg/05_npsg_dsc.htm. Accessed November 3, 2004.
- Martinello RA, Jones L, Topal JE. Correlation between healthcare workers’ knowledge of influenza vaccine and vaccine receipt. Infect Control Hosp Epidemiol. 2003.Nov;24(11):799-800.
- CDC. Prevention and Control of Influenza Recommendations of the Advisory Committee on Immunization Practices (ACIP). Available at: http://www.cdc.gov/mmwr/preview/mmwrhtml/ rr5306a1.htm. Accessed November 8, 2004.
- Massachusetts Hospital Association. Opt-Out Standing Orders for Pneumonia and Influenza Vaccination for Hospital Inpatients: Best Practice Adoption Proposal to Improve Massachusetts Hospital Performance and Public Health. Available at: http://www.masspro.org/publications/pubs/misc/PNEUMHA2.pdf.
- CDC. Influenza: the disease. Available at: http://www.cdc.gov/flu/about/disease.htm. Accessed November 8, 2004.
- CDC. Healthy People 2010. Immunization and Infectious Diseases. Section 14-29a. Available at: http://www.healthypeople.gov/document/html/volume1/14immunization.htm. Accessed November 8, 2004.
In a year when the United States has been riddled with bad news, confusion, and even threats of fines and incarceration (1) surrounding the use of influenza vaccines, the last thing you may be interested in thinking about is instituting a comprehensive inpatient influenza vaccination initiative. Despite the chaos, it is important to remember that, on average, 36,000 (2) people die and 226,000 (3) people are hospitalized annually from influenza, or “the flu,” and its complications. Additionally, a significant proportion of patients hospitalized will have co-morbid illness or be old enough to be considered in the highest risk category for complications of flu (4). Hospitalists are poised to act centrally in improving vaccination rates given the intensity of their patient contact and their expertise in developing best-practices-based systems.
What follows is a step-wise plan to help you begin an inpatient influenza vaccination initiative at your institution. Clearly, elements of this plan will need to be modified based on institutional structure and preference.
1. Define the problem locally. It is important to identify if any inpatient vaccination systems are already in place for any other vaccination (e.g., pneumococcal vaccination for splenectomy patients; tetanus for trauma patients, etc). If such a system already exists, review its successes and see if any of them may be borrowed for the influenza plan. Also determine if influenza vaccines have ever (even in a random, sptty fashion) been given out on your institution’s inpatient service. Understanding this history will help you address the issues of the “culture” of the institution.
2. Talk with your administration about making influenza vaccination a quality goal. One of the barriers ahead may be the mindset that vaccinations should only live in the world of outpatient physicians. By obtaining “buyin” from administration (e.g., the Chief Medical Officer), you may have some additional resources made available to you, and you may also be able to leverage the weight of the administration in recruiting help for the program. Remember, the 2005 Disease-Specific Patient Safety Goals from the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) state that it is important to “develop and implement a protocol for administration and documentation of the flu vaccine.” (5)
3. Identify key players and meet with them. This plan cannot be sustained successfully as a one-person show. Ideally, you should create an influenza vaccination committee that has representatives of all the inpatient services (medicine, family medicine, surgery, obstetrics and gynecology, and pediatrics), as well as nursing leadership, infection control, pharmacy, information technology (for computerized order entry systems), and quality assurance. In academic institutions, you might also consider including a house officer and/or medical student. The initial meeting should review your findings with #1 and #2 above, as well as assessing this committee’s concerns about implementing an inpatient vaccination scheme. You should plan to initiate committee activities at least two to three months in advance of the anticipated availability of the vaccine.
4. Create a culture of vaccination. Vaccines are often not on the radar screen of most inpatient physicians as they deal with the more acute reasons for hospitalization. It is therefore important to begin introducing a culture change, demonstrating the importance of vaccinations to your staff, and shifting the prevalent mindset towards active engagement with your vaccination program. Identifying foreseeable problems and developing action plans will assist this process. Some issues may include:
- Physician and nurse attitudes and education about influenza and the vaccine (e.g., dispelling flu shot rumors, educating staff on the low risk of re-vaccinating a patient already vaccinated previously this season, explaining the lack of requirements for written informed consent for flu vaccination, encouraging health care workers to get flu shots themselves (6), etc.)
- Reminder systems for physicians to reinforce the need to vaccinate (posters, screen savers, emails, buttons)
- Communication with primary care physicians about patients who have been vaccinated
- Patient misconceptions about the vaccine’s side effects
5. Set a goal. It may be helpful to assess your inpatient service’s demographics for the past few years to identify the approximate denominator of eligible candidates for the vaccine based on age and key diagnoses. However, if your institution does not already have a history of active influenza vaccination on the inpatient service, start with a humble goal. It is attractive to assume that every patient who qualifies will be vaccinated. It is just not so. Have your influenza committee pick an achievable goal for your first flu season and stretch it in subsequent seasons. To achieve the goal, make sure each clinical area has an identifiable “champion” who can gently remind clinicians about the importance of vaccination. The higher the profile of the local champion the better, assuming the champion has the time and can offer the effort required to do the periodic reminders. Also make sure your pharmacy tracking and distributions systems are prepared to handle the increase in requests for the vaccines. Of note, many patients who are candidates for flu shots are also candidates for pneumococcal vaccines and both may be given together. Consider adding the pneumococcal vaccine to your efforts in appropriate patients.
6. Develop an “Opt Out” system. The CDC’s Advisory Committee on Immunization Practices recommends developing standing orders for both influenza and pneumococcal vaccinations (7). In computerized order entry, this suggestion may lead to a pre-selected order-set being built into the discharge orders that requires the physician to actively opt-out of the order. Paper-based systems may include standing printed orders, again, which require a physician to decline the order specifically. Such opt out systems have been shown to improve rates of vaccination significantly (8). Opt-out programs, however, still require that the clinician ordering the vaccine discusses the vaccine with the patient before it is administered.
7. Roll it out with a bang. Make sure the commencement of your flu shot program gets some press. Announce it at departmental meetings, on system-wide emails, and in hospital publications. Remember, this program is a demonstrable way of improving your patients’ health and an excellent way for hospitalists to show their systems-oriented approaches. Begin your roll-out as early as recommended by the local Department of Public Health so that your patients, many of whom will be at very high risk for complications of the flu, get early vaccination.
8. Give frequent feedback. Obtain vaccine distribution and utilization data at least twice monthly during the first two or three months. This period corresponds to the most critical period of the program as it is when flu shots must be delivered to ensure their efficacy come December-February when flu season typically peaks (9). Some groups may find that a bit of healthy competition (e.g., between services or between nursing units) may offer that edge to keep people vaccinating. Nonetheless, it is critical to keep your clinical areas updated with their performance, with public appreciation being expressed for the top notable clinical areas and low performers receiving extra encouragement and assistance. After the first few months, monthly reports and feedback will suffice, with the program running through the end of March.
9. Remain aware of the local and national flu scene. With the vaccine production problems of the current flu season and with the panic about the high mortality rates of the Fujian strain that was not included in the vaccine last season, it is clear that the flu news scene can be volatile and controversial. It is important to remain up to date on the current facts and be able to dispel any misinformation that may circulate. The following resources may prove helpful:
- The CDC’s influenza home page: http://www.cdc.gov/flu/
- The WHO’s influenza site: http://www.who.int/csr/disease/influenza/en/
- The state Department of Public Health
10. Plan for next season. At the end of flu season, reconvene the influenza committee and debrief. It is important to keep a log of the successes and failures of the season’s flu vaccine initiative to permit growth in subsequent seasons.
The CDC’s program, Healthy People 2010, has set a goal for influenza and pneumococcal vaccination of appropriate non-institutionalized individuals of 90% (10). This goal is achievable if all available resources for reaching out to such patients are utilized. The Massachusetts Hospital Association reports:
“Inpatient hospital stays are among the many missed opportunities for flu and pneumonia vaccination across health care settings. Up to 46% of subsequent influenza-related hospitalizations and 2/3 of influenza-related deaths occur among the elderly who have been previously hospitalized during the flu season. Up to 2/3 of patients hospitalized with serious pneumococcal infections have been hospitalized at least once within the previous 3-5 years (8).”
Hospitalists must take advantage of the opportunity that hospitalization affords our patients to receive the vaccines they need to stay healthy. Appropriate vaccine delivery is no longer solely the purview of the primary care physician – hospitalists must share this goal as well.
References
- The Commonwealth of Massachusetts Executive Office of Health and Human Services Department of Public Health. Revised order to establish rules and priorities for the distribution and use of influenza vaccine. Available at: http://www.mass.gov/dph/cdc/epii/flu/flu_order.htm. Accessed November 3, 2004.
- Thompson WW, Shay DK, Weintraub E, et al. Mortality associated with influenza and respiratory syncytial virus in the United States. JAMA.2003;289:179-86.
- Thompson WW, Shay DK, Weintraub E, et al. Influenza-associated hospitalizations in the United States. JAMA. 2004;292:1333-40.
- CDC. Interim Influenza Vaccination Recommendations – 2004-2005 Season. Available at: http://www.cdc.gov/flu/protect/whoshouldget.htm. Accessed November 3, 2004.
- JCAHO. 2005 Disease-specific care national patient safety goals. Available at: http://www.jcaho.org/accredited+organizations/patient+safety/05+npsg/05_npsg_dsc.htm. Accessed November 3, 2004.
- Martinello RA, Jones L, Topal JE. Correlation between healthcare workers’ knowledge of influenza vaccine and vaccine receipt. Infect Control Hosp Epidemiol. 2003.Nov;24(11):799-800.
- CDC. Prevention and Control of Influenza Recommendations of the Advisory Committee on Immunization Practices (ACIP). Available at: http://www.cdc.gov/mmwr/preview/mmwrhtml/ rr5306a1.htm. Accessed November 8, 2004.
- Massachusetts Hospital Association. Opt-Out Standing Orders for Pneumonia and Influenza Vaccination for Hospital Inpatients: Best Practice Adoption Proposal to Improve Massachusetts Hospital Performance and Public Health. Available at: http://www.masspro.org/publications/pubs/misc/PNEUMHA2.pdf.
- CDC. Influenza: the disease. Available at: http://www.cdc.gov/flu/about/disease.htm. Accessed November 8, 2004.
- CDC. Healthy People 2010. Immunization and Infectious Diseases. Section 14-29a. Available at: http://www.healthypeople.gov/document/html/volume1/14immunization.htm. Accessed November 8, 2004.
In a year when the United States has been riddled with bad news, confusion, and even threats of fines and incarceration (1) surrounding the use of influenza vaccines, the last thing you may be interested in thinking about is instituting a comprehensive inpatient influenza vaccination initiative. Despite the chaos, it is important to remember that, on average, 36,000 (2) people die and 226,000 (3) people are hospitalized annually from influenza, or “the flu,” and its complications. Additionally, a significant proportion of patients hospitalized will have co-morbid illness or be old enough to be considered in the highest risk category for complications of flu (4). Hospitalists are poised to act centrally in improving vaccination rates given the intensity of their patient contact and their expertise in developing best-practices-based systems.
What follows is a step-wise plan to help you begin an inpatient influenza vaccination initiative at your institution. Clearly, elements of this plan will need to be modified based on institutional structure and preference.
1. Define the problem locally. It is important to identify if any inpatient vaccination systems are already in place for any other vaccination (e.g., pneumococcal vaccination for splenectomy patients; tetanus for trauma patients, etc). If such a system already exists, review its successes and see if any of them may be borrowed for the influenza plan. Also determine if influenza vaccines have ever (even in a random, sptty fashion) been given out on your institution’s inpatient service. Understanding this history will help you address the issues of the “culture” of the institution.
2. Talk with your administration about making influenza vaccination a quality goal. One of the barriers ahead may be the mindset that vaccinations should only live in the world of outpatient physicians. By obtaining “buyin” from administration (e.g., the Chief Medical Officer), you may have some additional resources made available to you, and you may also be able to leverage the weight of the administration in recruiting help for the program. Remember, the 2005 Disease-Specific Patient Safety Goals from the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) state that it is important to “develop and implement a protocol for administration and documentation of the flu vaccine.” (5)
3. Identify key players and meet with them. This plan cannot be sustained successfully as a one-person show. Ideally, you should create an influenza vaccination committee that has representatives of all the inpatient services (medicine, family medicine, surgery, obstetrics and gynecology, and pediatrics), as well as nursing leadership, infection control, pharmacy, information technology (for computerized order entry systems), and quality assurance. In academic institutions, you might also consider including a house officer and/or medical student. The initial meeting should review your findings with #1 and #2 above, as well as assessing this committee’s concerns about implementing an inpatient vaccination scheme. You should plan to initiate committee activities at least two to three months in advance of the anticipated availability of the vaccine.
4. Create a culture of vaccination. Vaccines are often not on the radar screen of most inpatient physicians as they deal with the more acute reasons for hospitalization. It is therefore important to begin introducing a culture change, demonstrating the importance of vaccinations to your staff, and shifting the prevalent mindset towards active engagement with your vaccination program. Identifying foreseeable problems and developing action plans will assist this process. Some issues may include:
- Physician and nurse attitudes and education about influenza and the vaccine (e.g., dispelling flu shot rumors, educating staff on the low risk of re-vaccinating a patient already vaccinated previously this season, explaining the lack of requirements for written informed consent for flu vaccination, encouraging health care workers to get flu shots themselves (6), etc.)
- Reminder systems for physicians to reinforce the need to vaccinate (posters, screen savers, emails, buttons)
- Communication with primary care physicians about patients who have been vaccinated
- Patient misconceptions about the vaccine’s side effects
5. Set a goal. It may be helpful to assess your inpatient service’s demographics for the past few years to identify the approximate denominator of eligible candidates for the vaccine based on age and key diagnoses. However, if your institution does not already have a history of active influenza vaccination on the inpatient service, start with a humble goal. It is attractive to assume that every patient who qualifies will be vaccinated. It is just not so. Have your influenza committee pick an achievable goal for your first flu season and stretch it in subsequent seasons. To achieve the goal, make sure each clinical area has an identifiable “champion” who can gently remind clinicians about the importance of vaccination. The higher the profile of the local champion the better, assuming the champion has the time and can offer the effort required to do the periodic reminders. Also make sure your pharmacy tracking and distributions systems are prepared to handle the increase in requests for the vaccines. Of note, many patients who are candidates for flu shots are also candidates for pneumococcal vaccines and both may be given together. Consider adding the pneumococcal vaccine to your efforts in appropriate patients.
6. Develop an “Opt Out” system. The CDC’s Advisory Committee on Immunization Practices recommends developing standing orders for both influenza and pneumococcal vaccinations (7). In computerized order entry, this suggestion may lead to a pre-selected order-set being built into the discharge orders that requires the physician to actively opt-out of the order. Paper-based systems may include standing printed orders, again, which require a physician to decline the order specifically. Such opt out systems have been shown to improve rates of vaccination significantly (8). Opt-out programs, however, still require that the clinician ordering the vaccine discusses the vaccine with the patient before it is administered.
7. Roll it out with a bang. Make sure the commencement of your flu shot program gets some press. Announce it at departmental meetings, on system-wide emails, and in hospital publications. Remember, this program is a demonstrable way of improving your patients’ health and an excellent way for hospitalists to show their systems-oriented approaches. Begin your roll-out as early as recommended by the local Department of Public Health so that your patients, many of whom will be at very high risk for complications of the flu, get early vaccination.
8. Give frequent feedback. Obtain vaccine distribution and utilization data at least twice monthly during the first two or three months. This period corresponds to the most critical period of the program as it is when flu shots must be delivered to ensure their efficacy come December-February when flu season typically peaks (9). Some groups may find that a bit of healthy competition (e.g., between services or between nursing units) may offer that edge to keep people vaccinating. Nonetheless, it is critical to keep your clinical areas updated with their performance, with public appreciation being expressed for the top notable clinical areas and low performers receiving extra encouragement and assistance. After the first few months, monthly reports and feedback will suffice, with the program running through the end of March.
9. Remain aware of the local and national flu scene. With the vaccine production problems of the current flu season and with the panic about the high mortality rates of the Fujian strain that was not included in the vaccine last season, it is clear that the flu news scene can be volatile and controversial. It is important to remain up to date on the current facts and be able to dispel any misinformation that may circulate. The following resources may prove helpful:
- The CDC’s influenza home page: http://www.cdc.gov/flu/
- The WHO’s influenza site: http://www.who.int/csr/disease/influenza/en/
- The state Department of Public Health
10. Plan for next season. At the end of flu season, reconvene the influenza committee and debrief. It is important to keep a log of the successes and failures of the season’s flu vaccine initiative to permit growth in subsequent seasons.
The CDC’s program, Healthy People 2010, has set a goal for influenza and pneumococcal vaccination of appropriate non-institutionalized individuals of 90% (10). This goal is achievable if all available resources for reaching out to such patients are utilized. The Massachusetts Hospital Association reports:
“Inpatient hospital stays are among the many missed opportunities for flu and pneumonia vaccination across health care settings. Up to 46% of subsequent influenza-related hospitalizations and 2/3 of influenza-related deaths occur among the elderly who have been previously hospitalized during the flu season. Up to 2/3 of patients hospitalized with serious pneumococcal infections have been hospitalized at least once within the previous 3-5 years (8).”
Hospitalists must take advantage of the opportunity that hospitalization affords our patients to receive the vaccines they need to stay healthy. Appropriate vaccine delivery is no longer solely the purview of the primary care physician – hospitalists must share this goal as well.
References
- The Commonwealth of Massachusetts Executive Office of Health and Human Services Department of Public Health. Revised order to establish rules and priorities for the distribution and use of influenza vaccine. Available at: http://www.mass.gov/dph/cdc/epii/flu/flu_order.htm. Accessed November 3, 2004.
- Thompson WW, Shay DK, Weintraub E, et al. Mortality associated with influenza and respiratory syncytial virus in the United States. JAMA.2003;289:179-86.
- Thompson WW, Shay DK, Weintraub E, et al. Influenza-associated hospitalizations in the United States. JAMA. 2004;292:1333-40.
- CDC. Interim Influenza Vaccination Recommendations – 2004-2005 Season. Available at: http://www.cdc.gov/flu/protect/whoshouldget.htm. Accessed November 3, 2004.
- JCAHO. 2005 Disease-specific care national patient safety goals. Available at: http://www.jcaho.org/accredited+organizations/patient+safety/05+npsg/05_npsg_dsc.htm. Accessed November 3, 2004.
- Martinello RA, Jones L, Topal JE. Correlation between healthcare workers’ knowledge of influenza vaccine and vaccine receipt. Infect Control Hosp Epidemiol. 2003.Nov;24(11):799-800.
- CDC. Prevention and Control of Influenza Recommendations of the Advisory Committee on Immunization Practices (ACIP). Available at: http://www.cdc.gov/mmwr/preview/mmwrhtml/ rr5306a1.htm. Accessed November 8, 2004.
- Massachusetts Hospital Association. Opt-Out Standing Orders for Pneumonia and Influenza Vaccination for Hospital Inpatients: Best Practice Adoption Proposal to Improve Massachusetts Hospital Performance and Public Health. Available at: http://www.masspro.org/publications/pubs/misc/PNEUMHA2.pdf.
- CDC. Influenza: the disease. Available at: http://www.cdc.gov/flu/about/disease.htm. Accessed November 8, 2004.
- CDC. Healthy People 2010. Immunization and Infectious Diseases. Section 14-29a. Available at: http://www.healthypeople.gov/document/html/volume1/14immunization.htm. Accessed November 8, 2004.
A State-of-the-Art Report on Hospital Medicine Education
The Society of Hospital Medicine (SHM) is committed to improving the quality of in-patient care through the provision of educational programs, tools, and resources to its membership. In 2002, the SHM Education Committee and leadership met to develop its first strategic plan for education. Long-range and short-term goals were determined, establishing a strategic vision and direction for education for the organization. Long-range goals included defining and developing a core curriculum in hospital medicine; developing a variety of modalities to deliver education; promoting collaborative efforts with other organizations; promoting original research in hospital medicine; and establishing a recognition program for completion of the core curriculum.
To help achieve its short-term goals, the Education Committee formed three task forces: the Core Curriculum Task Force, Leadership Task Force, and Geriatrics Task Force. As a result of the work of committees, task forces, and members, an impressive array of educational programs and products has been developed for membership, and much progress has been made in reaching SHM’s long-term educational goals. SHM would like to acknowledge and thank all of the members who have contributed countless hours and tireless effort to the educational initiatives of the organization.
The Education Committee formed two Core Curriculum Task Forces, an Adult and a Pediatric task force. Each task force has been defining and developing the core curriculum, which will identify the expected proficiencies of members and establish the distinctive differences between hospital medicine and other related medical specialties. The Adult Core Curriculum Task Force executive committee includes Mike Pistoria, Alpesh Amin, Tina Budnitz, Dan Dressler, and Sylvia McKean. An Adult Core Curriculum Guide is expected to be published and released in the spring of 2005. The Guide will contain three sections, each with multiple chapters: Clinical Conditions, Systems, and Procedures. Each chapter begins with an introduction articulating its importance to the practice of hospital medicine, followed by competencies categorized into four areas: knowledge, skills, attitudes, and systems organization and improvement. The core curriculum will be the basis for all future SHM educational activities. It is anticipated that the Core Curriculum Guide will standardize efforts to educate hospitalists across the continuum of medical education. The guide will be provided to internal medicine clerkship and residency program directors and hospitalist fellowship directors. Educators responsible for developing continuing medical education activities for physicians will find the guide to be a valuable resource.
The Pediatric Core Curriculum Guide will be similar in structure to the Adult Guide and is a work in progress. The Pediatric Core Curriculum Task Force executive committee includes Tim Cornell, Dan Rauch, and Alpesh Amin.
The Society of Hospital Medicine’s annual meeting has become the premier meeting for health care professionals who specialize in hospital medicine. The annual meeting provides a wide range of opportunities for learning. Participants can select from a variety of tracks, which include adult and pediatric clinical topics, operational and organizational issues, and challenges for academic hospitalists. The diversity of the annual meeting allows for more personal and individualized learning and tremendous opportunities for networking with colleagues. Preetha Basaviah is the course director of the 2005 annual meeting, which will be held April 28-30, in Chicago, Illinois. The theme for this 8th annual meeting is, “Hospital Medicine in 2005: Strategies for Success.”
In 2004, Regional meetings were held in the Northeast, Western, and Southern regions with much success. Forty-three chapters across the country are also developing educational sessions for their local meetings. Several courses focusing on specific topics of interest to hospitalists have been developed and are offered the day prior to the annual or regional meetings. Pre-courses include Practice Management, Leadership Survival, Perioperative and Consultative Medicine, and Critical Care for the Hospitalist, offering additional opportunities for members to enhance their skills and knowledge.
The Society of Hospital Medicine continues to develop educational tools and resources for the Web site (www.hospitalmedicine.org). The first resource room, addressing the prevention of antimicrobial resistance, was created. Resource rooms provide links to guidelines and relevant CME on-line courses, reviews of pertinent literature, methods to create quality-improvement programs, fact sheets, slide sets and other important information to assist hospitalists in their daily practice. Several unrestricted educational grants have been secured through pharmaceutical companies to support the creation of additional resource rooms to be launched in the near future on topics such as DVT awareness, stroke, and geriatric inpatient care.
The Centers for Disease Control and Prevention (CDC) has extended their Cooperative Agreement with SHM for an additional year. As a part of this agreement, SHM will evaluate and revise the applied learning workshop, “Implementing Quality Improvement Programs to Reduce Antimicrobial Resistance,” by Dan Dressler. This revised workshop will be conducted at three different chapter or other local meetings. If you are interested in bringing this great workshop to your chapter meeting, contact Tina Budnitz at TBudnitz@hospitalmedicine.org.
SHM has also received a substantial grant from the John A. Hartford Foundation to assist in the creation of educational symposia and enduring materials related to improving outcomes in older adults. The grant also supports the development of a discharge planning tool for hospitalists, and a demonstration project at three sites to implement quality improvement programs to educate members about important issues affecting outcomes in older patients. Members interested in participating in the creation of a discharge planning tool and supporting guidelines should plan to attend the discharge planning workshop at the 2005 Annual Meeting.
An outgrowth of the Hartford grant has been the establishment of the Leadership Academy. A Leadership pre-course for 100 hospitalist leaders was successfully included in the 2004 Annual Meeting. The next intensive workshop is scheduled for January 2005 under the direction of course directors Mark Williams and Russ Holman in Arizona, with a subsequent session scheduled for September 2005 in Vail, CO. The Leadership Academy was developed to provide the skills and resources required to successfully lead and manage a hospital medicine program now and in the future. In-depth training is provided on strategic planning, conflict resolution and negotiation, understanding critical hospital performance metrics, and leading and managing change.
SHM’s vision for hospital medicine education is forwarded through the development of strategic collaboration with organizations such as the American Board of Internal Medicine, Society of General Internal Medicine, JCAHO, the American Hospital Association, and other specialty societies such as the American College of Chest Physicians and the American Academy of Pediatrics. SHM continues its strong affiliation and relationship with the American College of Physicians. Relationships with these key organizations will enable SHM to refine its recognition program for members completing the core curriculum and further the recognition of hospital medicine as a distinct specialty.
In 2006, the Society of Hospital Medicine will launch its official journal, The Journal of Hospital Medicine. The journal will provide a vehicle for the dissemination of research and innovations in hospital medicine.
To further signify its commitment to education, SHM hired a Director of Education, Jane Mihelic, to establish a Division of Education in July of 2004. As the development phase of the core curriculum concludes, SHM will hold the second education summit meeting early in 2005 to develop the next phase of the strategic plan for education and establish new goals and objectives. Future plans will include implementing the core curriculum, becoming an accredited provider of continuing medical education, and developing additional interactive self-directed learning materials.
Care of the hospitalized patient necessitates mastery and continued maintenance of sophisticated knowledge, skills, attitudes, and systems organization. The Society of Hospital Medicine is poised to foster, promote, and support hospitalists in meeting their life-long learning needs.
Please feel free to contact Alpesh Amin, MD, (anamin@uci.edu) Chair, SHM Education Committee, or Jane Mihelic (jmihelic@hospitalmedicine.org), SHM Director of Education, regarding thoughts or ideas on hospital medicine education.
The Society of Hospital Medicine (SHM) is committed to improving the quality of in-patient care through the provision of educational programs, tools, and resources to its membership. In 2002, the SHM Education Committee and leadership met to develop its first strategic plan for education. Long-range and short-term goals were determined, establishing a strategic vision and direction for education for the organization. Long-range goals included defining and developing a core curriculum in hospital medicine; developing a variety of modalities to deliver education; promoting collaborative efforts with other organizations; promoting original research in hospital medicine; and establishing a recognition program for completion of the core curriculum.
To help achieve its short-term goals, the Education Committee formed three task forces: the Core Curriculum Task Force, Leadership Task Force, and Geriatrics Task Force. As a result of the work of committees, task forces, and members, an impressive array of educational programs and products has been developed for membership, and much progress has been made in reaching SHM’s long-term educational goals. SHM would like to acknowledge and thank all of the members who have contributed countless hours and tireless effort to the educational initiatives of the organization.
The Education Committee formed two Core Curriculum Task Forces, an Adult and a Pediatric task force. Each task force has been defining and developing the core curriculum, which will identify the expected proficiencies of members and establish the distinctive differences between hospital medicine and other related medical specialties. The Adult Core Curriculum Task Force executive committee includes Mike Pistoria, Alpesh Amin, Tina Budnitz, Dan Dressler, and Sylvia McKean. An Adult Core Curriculum Guide is expected to be published and released in the spring of 2005. The Guide will contain three sections, each with multiple chapters: Clinical Conditions, Systems, and Procedures. Each chapter begins with an introduction articulating its importance to the practice of hospital medicine, followed by competencies categorized into four areas: knowledge, skills, attitudes, and systems organization and improvement. The core curriculum will be the basis for all future SHM educational activities. It is anticipated that the Core Curriculum Guide will standardize efforts to educate hospitalists across the continuum of medical education. The guide will be provided to internal medicine clerkship and residency program directors and hospitalist fellowship directors. Educators responsible for developing continuing medical education activities for physicians will find the guide to be a valuable resource.
The Pediatric Core Curriculum Guide will be similar in structure to the Adult Guide and is a work in progress. The Pediatric Core Curriculum Task Force executive committee includes Tim Cornell, Dan Rauch, and Alpesh Amin.
The Society of Hospital Medicine’s annual meeting has become the premier meeting for health care professionals who specialize in hospital medicine. The annual meeting provides a wide range of opportunities for learning. Participants can select from a variety of tracks, which include adult and pediatric clinical topics, operational and organizational issues, and challenges for academic hospitalists. The diversity of the annual meeting allows for more personal and individualized learning and tremendous opportunities for networking with colleagues. Preetha Basaviah is the course director of the 2005 annual meeting, which will be held April 28-30, in Chicago, Illinois. The theme for this 8th annual meeting is, “Hospital Medicine in 2005: Strategies for Success.”
In 2004, Regional meetings were held in the Northeast, Western, and Southern regions with much success. Forty-three chapters across the country are also developing educational sessions for their local meetings. Several courses focusing on specific topics of interest to hospitalists have been developed and are offered the day prior to the annual or regional meetings. Pre-courses include Practice Management, Leadership Survival, Perioperative and Consultative Medicine, and Critical Care for the Hospitalist, offering additional opportunities for members to enhance their skills and knowledge.
The Society of Hospital Medicine continues to develop educational tools and resources for the Web site (www.hospitalmedicine.org). The first resource room, addressing the prevention of antimicrobial resistance, was created. Resource rooms provide links to guidelines and relevant CME on-line courses, reviews of pertinent literature, methods to create quality-improvement programs, fact sheets, slide sets and other important information to assist hospitalists in their daily practice. Several unrestricted educational grants have been secured through pharmaceutical companies to support the creation of additional resource rooms to be launched in the near future on topics such as DVT awareness, stroke, and geriatric inpatient care.
The Centers for Disease Control and Prevention (CDC) has extended their Cooperative Agreement with SHM for an additional year. As a part of this agreement, SHM will evaluate and revise the applied learning workshop, “Implementing Quality Improvement Programs to Reduce Antimicrobial Resistance,” by Dan Dressler. This revised workshop will be conducted at three different chapter or other local meetings. If you are interested in bringing this great workshop to your chapter meeting, contact Tina Budnitz at TBudnitz@hospitalmedicine.org.
SHM has also received a substantial grant from the John A. Hartford Foundation to assist in the creation of educational symposia and enduring materials related to improving outcomes in older adults. The grant also supports the development of a discharge planning tool for hospitalists, and a demonstration project at three sites to implement quality improvement programs to educate members about important issues affecting outcomes in older patients. Members interested in participating in the creation of a discharge planning tool and supporting guidelines should plan to attend the discharge planning workshop at the 2005 Annual Meeting.
An outgrowth of the Hartford grant has been the establishment of the Leadership Academy. A Leadership pre-course for 100 hospitalist leaders was successfully included in the 2004 Annual Meeting. The next intensive workshop is scheduled for January 2005 under the direction of course directors Mark Williams and Russ Holman in Arizona, with a subsequent session scheduled for September 2005 in Vail, CO. The Leadership Academy was developed to provide the skills and resources required to successfully lead and manage a hospital medicine program now and in the future. In-depth training is provided on strategic planning, conflict resolution and negotiation, understanding critical hospital performance metrics, and leading and managing change.
SHM’s vision for hospital medicine education is forwarded through the development of strategic collaboration with organizations such as the American Board of Internal Medicine, Society of General Internal Medicine, JCAHO, the American Hospital Association, and other specialty societies such as the American College of Chest Physicians and the American Academy of Pediatrics. SHM continues its strong affiliation and relationship with the American College of Physicians. Relationships with these key organizations will enable SHM to refine its recognition program for members completing the core curriculum and further the recognition of hospital medicine as a distinct specialty.
In 2006, the Society of Hospital Medicine will launch its official journal, The Journal of Hospital Medicine. The journal will provide a vehicle for the dissemination of research and innovations in hospital medicine.
To further signify its commitment to education, SHM hired a Director of Education, Jane Mihelic, to establish a Division of Education in July of 2004. As the development phase of the core curriculum concludes, SHM will hold the second education summit meeting early in 2005 to develop the next phase of the strategic plan for education and establish new goals and objectives. Future plans will include implementing the core curriculum, becoming an accredited provider of continuing medical education, and developing additional interactive self-directed learning materials.
Care of the hospitalized patient necessitates mastery and continued maintenance of sophisticated knowledge, skills, attitudes, and systems organization. The Society of Hospital Medicine is poised to foster, promote, and support hospitalists in meeting their life-long learning needs.
Please feel free to contact Alpesh Amin, MD, (anamin@uci.edu) Chair, SHM Education Committee, or Jane Mihelic (jmihelic@hospitalmedicine.org), SHM Director of Education, regarding thoughts or ideas on hospital medicine education.
The Society of Hospital Medicine (SHM) is committed to improving the quality of in-patient care through the provision of educational programs, tools, and resources to its membership. In 2002, the SHM Education Committee and leadership met to develop its first strategic plan for education. Long-range and short-term goals were determined, establishing a strategic vision and direction for education for the organization. Long-range goals included defining and developing a core curriculum in hospital medicine; developing a variety of modalities to deliver education; promoting collaborative efforts with other organizations; promoting original research in hospital medicine; and establishing a recognition program for completion of the core curriculum.
To help achieve its short-term goals, the Education Committee formed three task forces: the Core Curriculum Task Force, Leadership Task Force, and Geriatrics Task Force. As a result of the work of committees, task forces, and members, an impressive array of educational programs and products has been developed for membership, and much progress has been made in reaching SHM’s long-term educational goals. SHM would like to acknowledge and thank all of the members who have contributed countless hours and tireless effort to the educational initiatives of the organization.
The Education Committee formed two Core Curriculum Task Forces, an Adult and a Pediatric task force. Each task force has been defining and developing the core curriculum, which will identify the expected proficiencies of members and establish the distinctive differences between hospital medicine and other related medical specialties. The Adult Core Curriculum Task Force executive committee includes Mike Pistoria, Alpesh Amin, Tina Budnitz, Dan Dressler, and Sylvia McKean. An Adult Core Curriculum Guide is expected to be published and released in the spring of 2005. The Guide will contain three sections, each with multiple chapters: Clinical Conditions, Systems, and Procedures. Each chapter begins with an introduction articulating its importance to the practice of hospital medicine, followed by competencies categorized into four areas: knowledge, skills, attitudes, and systems organization and improvement. The core curriculum will be the basis for all future SHM educational activities. It is anticipated that the Core Curriculum Guide will standardize efforts to educate hospitalists across the continuum of medical education. The guide will be provided to internal medicine clerkship and residency program directors and hospitalist fellowship directors. Educators responsible for developing continuing medical education activities for physicians will find the guide to be a valuable resource.
The Pediatric Core Curriculum Guide will be similar in structure to the Adult Guide and is a work in progress. The Pediatric Core Curriculum Task Force executive committee includes Tim Cornell, Dan Rauch, and Alpesh Amin.
The Society of Hospital Medicine’s annual meeting has become the premier meeting for health care professionals who specialize in hospital medicine. The annual meeting provides a wide range of opportunities for learning. Participants can select from a variety of tracks, which include adult and pediatric clinical topics, operational and organizational issues, and challenges for academic hospitalists. The diversity of the annual meeting allows for more personal and individualized learning and tremendous opportunities for networking with colleagues. Preetha Basaviah is the course director of the 2005 annual meeting, which will be held April 28-30, in Chicago, Illinois. The theme for this 8th annual meeting is, “Hospital Medicine in 2005: Strategies for Success.”
In 2004, Regional meetings were held in the Northeast, Western, and Southern regions with much success. Forty-three chapters across the country are also developing educational sessions for their local meetings. Several courses focusing on specific topics of interest to hospitalists have been developed and are offered the day prior to the annual or regional meetings. Pre-courses include Practice Management, Leadership Survival, Perioperative and Consultative Medicine, and Critical Care for the Hospitalist, offering additional opportunities for members to enhance their skills and knowledge.
The Society of Hospital Medicine continues to develop educational tools and resources for the Web site (www.hospitalmedicine.org). The first resource room, addressing the prevention of antimicrobial resistance, was created. Resource rooms provide links to guidelines and relevant CME on-line courses, reviews of pertinent literature, methods to create quality-improvement programs, fact sheets, slide sets and other important information to assist hospitalists in their daily practice. Several unrestricted educational grants have been secured through pharmaceutical companies to support the creation of additional resource rooms to be launched in the near future on topics such as DVT awareness, stroke, and geriatric inpatient care.
The Centers for Disease Control and Prevention (CDC) has extended their Cooperative Agreement with SHM for an additional year. As a part of this agreement, SHM will evaluate and revise the applied learning workshop, “Implementing Quality Improvement Programs to Reduce Antimicrobial Resistance,” by Dan Dressler. This revised workshop will be conducted at three different chapter or other local meetings. If you are interested in bringing this great workshop to your chapter meeting, contact Tina Budnitz at TBudnitz@hospitalmedicine.org.
SHM has also received a substantial grant from the John A. Hartford Foundation to assist in the creation of educational symposia and enduring materials related to improving outcomes in older adults. The grant also supports the development of a discharge planning tool for hospitalists, and a demonstration project at three sites to implement quality improvement programs to educate members about important issues affecting outcomes in older patients. Members interested in participating in the creation of a discharge planning tool and supporting guidelines should plan to attend the discharge planning workshop at the 2005 Annual Meeting.
An outgrowth of the Hartford grant has been the establishment of the Leadership Academy. A Leadership pre-course for 100 hospitalist leaders was successfully included in the 2004 Annual Meeting. The next intensive workshop is scheduled for January 2005 under the direction of course directors Mark Williams and Russ Holman in Arizona, with a subsequent session scheduled for September 2005 in Vail, CO. The Leadership Academy was developed to provide the skills and resources required to successfully lead and manage a hospital medicine program now and in the future. In-depth training is provided on strategic planning, conflict resolution and negotiation, understanding critical hospital performance metrics, and leading and managing change.
SHM’s vision for hospital medicine education is forwarded through the development of strategic collaboration with organizations such as the American Board of Internal Medicine, Society of General Internal Medicine, JCAHO, the American Hospital Association, and other specialty societies such as the American College of Chest Physicians and the American Academy of Pediatrics. SHM continues its strong affiliation and relationship with the American College of Physicians. Relationships with these key organizations will enable SHM to refine its recognition program for members completing the core curriculum and further the recognition of hospital medicine as a distinct specialty.
In 2006, the Society of Hospital Medicine will launch its official journal, The Journal of Hospital Medicine. The journal will provide a vehicle for the dissemination of research and innovations in hospital medicine.
To further signify its commitment to education, SHM hired a Director of Education, Jane Mihelic, to establish a Division of Education in July of 2004. As the development phase of the core curriculum concludes, SHM will hold the second education summit meeting early in 2005 to develop the next phase of the strategic plan for education and establish new goals and objectives. Future plans will include implementing the core curriculum, becoming an accredited provider of continuing medical education, and developing additional interactive self-directed learning materials.
Care of the hospitalized patient necessitates mastery and continued maintenance of sophisticated knowledge, skills, attitudes, and systems organization. The Society of Hospital Medicine is poised to foster, promote, and support hospitalists in meeting their life-long learning needs.
Please feel free to contact Alpesh Amin, MD, (anamin@uci.edu) Chair, SHM Education Committee, or Jane Mihelic (jmihelic@hospitalmedicine.org), SHM Director of Education, regarding thoughts or ideas on hospital medicine education.
Rates, Predictors, and Outcomes of Major Hemorrhage in Patients with Atrial Fibrillation
Background: Although warfarin is extremely effective in reducing the risk of ischemic stroke from atrial fibrillation (AF), it also increases the risk for significant hemorrhage. We assessed rates, predictors, and short-term mortality after hospitalization for major hemorrhage in a cohort of AF patients on and off warfarin.
Methods: We prospectively studied 13,559 adults with AF. Patients hospitalized for hemorrhage were identified from clinical databases and confirmed using chart review. Major hemorrhage was defined as fatal, transfusion of ≥ 2 units packed blood cells, or into a critical anatomic site; separate analyses were performed for intracranial hemorrhage (ICH) and extracranial hemorrhage. We used multivariable log-linear regression to assess for predictors of hemorrhage, adjusting for demographic and clinical characteristics.
Results: Out of 30,994 person-years of follow-up, we identified 78 ICHs in patients on warfarin and 51 off warfarin. Out of 30,830 person-years, there were 98 major extracranial hemorrhages on warfarin and 116 off warfarin. Although rates of hemorrhage increased with age, absolute rates of hemorrhage in anticoagulated patients were similar to those in non-anticoagulated patients. In patients aged 80 and older, the annual rate of ICH was 0.8% on warfarin and 0.7% off warfarin; for extracranial hemorrhage, the rate was 0.7% on warfarin and 1.0% off warfarin. In patients who developed ICH while taking warfarin, independent risk factors included age ≥ 80 (OR 2.8 [1.1-7.2] compared to age <60) and hypertension (OR 1.7 [1.0-2.8]).
Predictors of ICH off warfarin were age ≥ 80 (OR 6.2 [1.7-23]) and prior stroke (OR 2.4 [1.1-5.0]). Independent predictors of extracranial hemorrhage were age ≥ 80 (OR 3.8 [1.1-13] on warfarin and 3.8 [1.7-8.6] off warfarin) and prior gastrointestinal hemorrhage (OR 5.3 [2.9-9.8] on warfarin and 2.0 [1.1-3.6] off warfarin). INR ≥ 4.0 (compared to INR<4.0) was the strongest predictor of hemorrhage in patients taking warfarin: OR 15 [8.1-29] for ICH and OR 18 [10-30] for extracranial hemorrhage. Of the 48 deaths, 81% were from ICH, with a 30-day mortality rate of 50% after ICH on warfarin and 28% off warfarin. In contrast, 30-day mortality after major extracranial hemorrhage was relatively low (5% for patients on warfarin and 10% off warfarin).
Conclusions: In this largest prospective study to date of individuals with AF, absolute rates of major hemorrhage were low and similar in patients on and off warfarin, even in the most elderly. Hemorrhage contributed to few short-term deaths and the majority of deaths resulted from ICH, not extracranial hemorrhage. The benefits of warfarin in reducing ischemic stroke continue to outweigh the risk of hemorrhage, especially in older patients.
Background: Although warfarin is extremely effective in reducing the risk of ischemic stroke from atrial fibrillation (AF), it also increases the risk for significant hemorrhage. We assessed rates, predictors, and short-term mortality after hospitalization for major hemorrhage in a cohort of AF patients on and off warfarin.
Methods: We prospectively studied 13,559 adults with AF. Patients hospitalized for hemorrhage were identified from clinical databases and confirmed using chart review. Major hemorrhage was defined as fatal, transfusion of ≥ 2 units packed blood cells, or into a critical anatomic site; separate analyses were performed for intracranial hemorrhage (ICH) and extracranial hemorrhage. We used multivariable log-linear regression to assess for predictors of hemorrhage, adjusting for demographic and clinical characteristics.
Results: Out of 30,994 person-years of follow-up, we identified 78 ICHs in patients on warfarin and 51 off warfarin. Out of 30,830 person-years, there were 98 major extracranial hemorrhages on warfarin and 116 off warfarin. Although rates of hemorrhage increased with age, absolute rates of hemorrhage in anticoagulated patients were similar to those in non-anticoagulated patients. In patients aged 80 and older, the annual rate of ICH was 0.8% on warfarin and 0.7% off warfarin; for extracranial hemorrhage, the rate was 0.7% on warfarin and 1.0% off warfarin. In patients who developed ICH while taking warfarin, independent risk factors included age ≥ 80 (OR 2.8 [1.1-7.2] compared to age <60) and hypertension (OR 1.7 [1.0-2.8]).
Predictors of ICH off warfarin were age ≥ 80 (OR 6.2 [1.7-23]) and prior stroke (OR 2.4 [1.1-5.0]). Independent predictors of extracranial hemorrhage were age ≥ 80 (OR 3.8 [1.1-13] on warfarin and 3.8 [1.7-8.6] off warfarin) and prior gastrointestinal hemorrhage (OR 5.3 [2.9-9.8] on warfarin and 2.0 [1.1-3.6] off warfarin). INR ≥ 4.0 (compared to INR<4.0) was the strongest predictor of hemorrhage in patients taking warfarin: OR 15 [8.1-29] for ICH and OR 18 [10-30] for extracranial hemorrhage. Of the 48 deaths, 81% were from ICH, with a 30-day mortality rate of 50% after ICH on warfarin and 28% off warfarin. In contrast, 30-day mortality after major extracranial hemorrhage was relatively low (5% for patients on warfarin and 10% off warfarin).
Conclusions: In this largest prospective study to date of individuals with AF, absolute rates of major hemorrhage were low and similar in patients on and off warfarin, even in the most elderly. Hemorrhage contributed to few short-term deaths and the majority of deaths resulted from ICH, not extracranial hemorrhage. The benefits of warfarin in reducing ischemic stroke continue to outweigh the risk of hemorrhage, especially in older patients.
Background: Although warfarin is extremely effective in reducing the risk of ischemic stroke from atrial fibrillation (AF), it also increases the risk for significant hemorrhage. We assessed rates, predictors, and short-term mortality after hospitalization for major hemorrhage in a cohort of AF patients on and off warfarin.
Methods: We prospectively studied 13,559 adults with AF. Patients hospitalized for hemorrhage were identified from clinical databases and confirmed using chart review. Major hemorrhage was defined as fatal, transfusion of ≥ 2 units packed blood cells, or into a critical anatomic site; separate analyses were performed for intracranial hemorrhage (ICH) and extracranial hemorrhage. We used multivariable log-linear regression to assess for predictors of hemorrhage, adjusting for demographic and clinical characteristics.
Results: Out of 30,994 person-years of follow-up, we identified 78 ICHs in patients on warfarin and 51 off warfarin. Out of 30,830 person-years, there were 98 major extracranial hemorrhages on warfarin and 116 off warfarin. Although rates of hemorrhage increased with age, absolute rates of hemorrhage in anticoagulated patients were similar to those in non-anticoagulated patients. In patients aged 80 and older, the annual rate of ICH was 0.8% on warfarin and 0.7% off warfarin; for extracranial hemorrhage, the rate was 0.7% on warfarin and 1.0% off warfarin. In patients who developed ICH while taking warfarin, independent risk factors included age ≥ 80 (OR 2.8 [1.1-7.2] compared to age <60) and hypertension (OR 1.7 [1.0-2.8]).
Predictors of ICH off warfarin were age ≥ 80 (OR 6.2 [1.7-23]) and prior stroke (OR 2.4 [1.1-5.0]). Independent predictors of extracranial hemorrhage were age ≥ 80 (OR 3.8 [1.1-13] on warfarin and 3.8 [1.7-8.6] off warfarin) and prior gastrointestinal hemorrhage (OR 5.3 [2.9-9.8] on warfarin and 2.0 [1.1-3.6] off warfarin). INR ≥ 4.0 (compared to INR<4.0) was the strongest predictor of hemorrhage in patients taking warfarin: OR 15 [8.1-29] for ICH and OR 18 [10-30] for extracranial hemorrhage. Of the 48 deaths, 81% were from ICH, with a 30-day mortality rate of 50% after ICH on warfarin and 28% off warfarin. In contrast, 30-day mortality after major extracranial hemorrhage was relatively low (5% for patients on warfarin and 10% off warfarin).
Conclusions: In this largest prospective study to date of individuals with AF, absolute rates of major hemorrhage were low and similar in patients on and off warfarin, even in the most elderly. Hemorrhage contributed to few short-term deaths and the majority of deaths resulted from ICH, not extracranial hemorrhage. The benefits of warfarin in reducing ischemic stroke continue to outweigh the risk of hemorrhage, especially in older patients.
The Fountain of Youth
Photo Quiz:
What is the etiology of the dermatologic and nail abnormalities in this 53‑year‑old man with cirrhosis due to chronic hepatitis B infection?
Diagnosis: Argyria
Discussion
This patient had progressive liver failure and was hospitalized for possible liver transplantation. During the initial history, he disclosed that he had noticed progressive discoloration of his skin, hair, and nails for the past several months. Our clinical suspicion of argyria was confirmed when the patient’s serum silver level returned at 54 ug/ml (normal range 0.0-14 ug/ml). Serum levels of arsenic, mercury, and lead were within normal limits.
Despite treatment of encephalopathy, esophageal varices, and peritonitis, this patient’s liver disease deteriorated and he underwent orthotopic liver transplantation. Unfortunately, he died 24 days post-transplantation from progressive multi-organ failure.
At autopsy, gross silver discoloration was noted in many organs, including the bowel, bladder, pancreas, and renal papillae.
Microscopically, fine black pigments were noted in almost all basement membranes, including the skin, glomeruli (see Figure), choroid plexus, and myocardial connective tissue.
Similar fine granules were seen in the basement membranes of the patient’s native liver but not within the newly transplanted liver.
The patient admitted to drinking one pint of colloid silver almost daily for 15 years. This homeopathic remedy has been purported to cure many illnesses, including the common cold, cancer, diabetes, and HIV. Equipment and recipes are readily available on the internet, and as a “food supplement” silver remedies bypass strict regulatory controls. Colloid silver can be made easily by connecting a 9-volt battery to two silver wires placed in a tub of water. The electric reaction draws silver off the wire and into the water, producing the liquid silver elixir.
After ingestion, silver deposits permanently in the skin, producing the characteristic color changes of argyria, especially pronounced in sun-exposed areas where sunlight reduces the metal to an inert salt, analogous to processes used in photography. Although ingested silver is known to alter skin color irreversibly and deposit widely in the body, permanent extracutaneous organ damage from silver ingestion has not been firmly established. Thus, argyria remains a cosmetically altering disease and is not a contraindication to liver transplant.
Like other homeopathic remedies, colloid silver recipes may be accessed by the public directly. Despite a lack of peer-reviewed scientific evidence to support its use, public testimonials touting silver as the new panacea nonetheless will remain prevalent. Physicians must educate themselves, and inform their patients, that colloid silver is not the “fountain of youth.”
Photo Quiz:
What is the etiology of the dermatologic and nail abnormalities in this 53‑year‑old man with cirrhosis due to chronic hepatitis B infection?
Diagnosis: Argyria
Discussion
This patient had progressive liver failure and was hospitalized for possible liver transplantation. During the initial history, he disclosed that he had noticed progressive discoloration of his skin, hair, and nails for the past several months. Our clinical suspicion of argyria was confirmed when the patient’s serum silver level returned at 54 ug/ml (normal range 0.0-14 ug/ml). Serum levels of arsenic, mercury, and lead were within normal limits.
Despite treatment of encephalopathy, esophageal varices, and peritonitis, this patient’s liver disease deteriorated and he underwent orthotopic liver transplantation. Unfortunately, he died 24 days post-transplantation from progressive multi-organ failure.
At autopsy, gross silver discoloration was noted in many organs, including the bowel, bladder, pancreas, and renal papillae.
Microscopically, fine black pigments were noted in almost all basement membranes, including the skin, glomeruli (see Figure), choroid plexus, and myocardial connective tissue.
Similar fine granules were seen in the basement membranes of the patient’s native liver but not within the newly transplanted liver.
The patient admitted to drinking one pint of colloid silver almost daily for 15 years. This homeopathic remedy has been purported to cure many illnesses, including the common cold, cancer, diabetes, and HIV. Equipment and recipes are readily available on the internet, and as a “food supplement” silver remedies bypass strict regulatory controls. Colloid silver can be made easily by connecting a 9-volt battery to two silver wires placed in a tub of water. The electric reaction draws silver off the wire and into the water, producing the liquid silver elixir.
After ingestion, silver deposits permanently in the skin, producing the characteristic color changes of argyria, especially pronounced in sun-exposed areas where sunlight reduces the metal to an inert salt, analogous to processes used in photography. Although ingested silver is known to alter skin color irreversibly and deposit widely in the body, permanent extracutaneous organ damage from silver ingestion has not been firmly established. Thus, argyria remains a cosmetically altering disease and is not a contraindication to liver transplant.
Like other homeopathic remedies, colloid silver recipes may be accessed by the public directly. Despite a lack of peer-reviewed scientific evidence to support its use, public testimonials touting silver as the new panacea nonetheless will remain prevalent. Physicians must educate themselves, and inform their patients, that colloid silver is not the “fountain of youth.”
Photo Quiz:
What is the etiology of the dermatologic and nail abnormalities in this 53‑year‑old man with cirrhosis due to chronic hepatitis B infection?
Diagnosis: Argyria
Discussion
This patient had progressive liver failure and was hospitalized for possible liver transplantation. During the initial history, he disclosed that he had noticed progressive discoloration of his skin, hair, and nails for the past several months. Our clinical suspicion of argyria was confirmed when the patient’s serum silver level returned at 54 ug/ml (normal range 0.0-14 ug/ml). Serum levels of arsenic, mercury, and lead were within normal limits.
Despite treatment of encephalopathy, esophageal varices, and peritonitis, this patient’s liver disease deteriorated and he underwent orthotopic liver transplantation. Unfortunately, he died 24 days post-transplantation from progressive multi-organ failure.
At autopsy, gross silver discoloration was noted in many organs, including the bowel, bladder, pancreas, and renal papillae.
Microscopically, fine black pigments were noted in almost all basement membranes, including the skin, glomeruli (see Figure), choroid plexus, and myocardial connective tissue.
Similar fine granules were seen in the basement membranes of the patient’s native liver but not within the newly transplanted liver.
The patient admitted to drinking one pint of colloid silver almost daily for 15 years. This homeopathic remedy has been purported to cure many illnesses, including the common cold, cancer, diabetes, and HIV. Equipment and recipes are readily available on the internet, and as a “food supplement” silver remedies bypass strict regulatory controls. Colloid silver can be made easily by connecting a 9-volt battery to two silver wires placed in a tub of water. The electric reaction draws silver off the wire and into the water, producing the liquid silver elixir.
After ingestion, silver deposits permanently in the skin, producing the characteristic color changes of argyria, especially pronounced in sun-exposed areas where sunlight reduces the metal to an inert salt, analogous to processes used in photography. Although ingested silver is known to alter skin color irreversibly and deposit widely in the body, permanent extracutaneous organ damage from silver ingestion has not been firmly established. Thus, argyria remains a cosmetically altering disease and is not a contraindication to liver transplant.
Like other homeopathic remedies, colloid silver recipes may be accessed by the public directly. Despite a lack of peer-reviewed scientific evidence to support its use, public testimonials touting silver as the new panacea nonetheless will remain prevalent. Physicians must educate themselves, and inform their patients, that colloid silver is not the “fountain of youth.”
Education: Hospitalists Add Value to Formal and Informal Learning Processes
Type a medical condition or term into a search engine and watch what happens. A search on the words “diabetes” yields more than 13 million Web pages, and “pneumonia” produces another 1.65 million. In 1998, the Internet hosted approximately 5000 health-related Web sites; two years later that number quadrupled (1). Between 30,000 and 45,000 medical articles on various drug therapies are published annually. The Patent and Trademark Office issued between 2000 and 4200 drug patents each year between 1979 and 1989 (2). The National Library of Medicine reports that it adds more than 2000 journal article citations to its MEDLINE database on a daily basis. In 2003, more than 460,000 citations were entered.
Deciphering and applying this myriad of changing information is a critical activity in the medical field. Without disseminating new knowledge through ongoing education, medical practices and procedures would become outdated, and uninformed medical professionals and patients would continue to operate under misinformation that might be detrimental to health or worse.
Hospitalists as Inpatient Experts
In an inpatient setting, hospitalists are uniquely qualified to play the role of educator. They analyze and interpret a wide range of medical information to treat their patients and provide updated information to patients and their families, residents, interns, nursing staff, other health care professionals, and hospital administrators. The hospitalist can be viewed as the “hub” of educational activities in the inpatient environment, absorbing, synthesizing, and disseminating information. They are “inpatient experts” in the following five spheres of knowledge:
- patient management
- clinical knowledge
- clinical skills
- health care industry issues
- research and management/leadership (3)
Hospitalists are uniquely qualified in the sphere of patient management, efficiently and effectively guiding the patient through the mazelike inpatient environment. Most hospitalists are quite familiar with critical hospital functions and activities, including treatment in the emergency department, the admissions process, bedside care on the medical floor, treatment in the intensive care unit, and the discharge process. Hospitalists, because they understand “how to get things done” by ancillary departments, including diagnostic and therapeutic services, often find themselves as conductors of inpatient care. Many hospitalists have developed unique proficiency in co-managing surgical cases due to expertise in peri-operative evaluation and care. Hospitalists are recognized as inpatient team leaders, facilitating and coordinating a range of support services needed to treat the patient, including nursing, case management, pharmacy, occupational/physical therapy, and social work. Hospitalists must also be effective in managing relationships with health care personnel external to the inpatient environment, including community physicians, homecare providers, extended care facilities, and visiting nurse services. Finally, hospitalists are oaen well informed about hospital processes, procedures, rules, regulations, and information systems.
As inpatient generalists, hospitalists continually treat the most common reasons for admission and have exceptional clinical knowledge of these conditions. These conditions include pneumonia, deep vein thrombosis (DVT), congestive heart failure (CHF), diabetes, end-of-life care, and other medical diagnoses. Since they treat many elderly patients, hospitalists are considered experts in managing patients with multiple co-morbidities. A related area of expertise is clinical guidelines/pathways, quality of care metrics, and practice standards. Since they spend nearly all of their time treating inpatients, hospitalists develop extraordinary familiarity with the clinical rules and tools supporting the patient care process.
In addition to clinical knowledge, hospitalists have the experience and expertise to teach inpatient clinical skills. These skills include diagnosis, physical examination, discharge planning, medical chart recording, family meeting coordination, and oversight. Also, most hospitalists are familiar with a range of technical procedures, including insertion of central lines and arterial lines, lumbar puncture, arthrocentesis, paracentesis, and thoracentesis.
Hospitalists often are the most knowledgeable inpatient clinicians with regard to a wide range of health care industry issues. These include comprehension of the payer/insurance regulations regarding medication formularies, utilization review requirements, and other care policies. Their expertise may extend to knowledge of state and federal regulations, public health initiatives, and recently enacted or pending health care legislation. Finally, hospitalists also are often conversant in the field of health care economics, especially regarding the financial impact on hospitals of reimbursement policies, legislative initiatives, technology, etc.
The fifth sphere of hospitalist expertise combines several knowledge domains. Individual hospitalists have specialized expertise in particular fields related to hospital medicine. Some hospitalists, mostly affiliated with academic institutions, are researchers who may develop research protocols, gather data, perform statistical analyses, and write papers that may potentially become the basis of improved patient care. Other hospitalists are exceptionally experienced in management/leadership. A hospitalist may be highly qualified to manage projects (e.g., computer-based physician order entry systems, throughput initiatives, etc.),or a hospitalist could be a strategic thinker who is viewed as a key clinical member of the hospital’s management team.
As a growing specialty, hospitalists have established a proficiency in a range of disciplines and intellectual domains. They are well positioned to assume the role of educator in the hospital environment. Given the exceptional knowledge and skills needed to be a hospitalist, the Society of Hospital Medicine (SHM) is pursing an effort to standardize education and lend greater credibility to the hospitalist profession. The “core curriculum” project is currently formalizing training that will provide a solid foundation for effective clinical practice in the field of hospital medicine.
Dual Educational Tracks
As depicted in Figure 1 below, medical education activity and the ways in which knowledge is imparted fall into two categories: formal and informal. Although some overlap may occur, there are distinct characteristics attributable to both classifications.
“Formal”
Formal education refers to the traditional “teacher-learner” roles in medicine. The learner can be a medical student, resident, or fellow. Education is typically transmitted from teacher to learner (as depicted in the diagram by a solid line), with some reciprocal feedback from the learner to the teacher (dotted line). It should be noted that as the importance and value of hospital medicine programs gain recognition, fellowship programs focusing on this specialty have been established. As of August 2004, eight active hospital medicine fellowship programs exist in the United States: three in California, two in Minnesota, and one each in Ohio, Illinois, and Texas. There are also pediatric hospital medicine fellowship programs in Boston, Washington DC, Houston, and San Diego. Each program enrolls one or two fellows annually (4).
Formal education can take place in both academic medical centers and community hospitals. By definition, academic medical centers provide supervised practical training for medical students, student nurses, and/or other health care professionals, as well as residents and fellows. In many academic medical centers throughout the country, hospitalists are emerging as core teachers of inpatient medicine. A prime example is the University of California, San Francisco. In 2002, 15 faculty hospitalists served as staff for approximately two-thirds of ward-attending months, as well as all medical consults (5).
By the same token, community hospitals that have residency programs also incorporate education to some degree into their daily operations. Today, medical education places a significant burden on residents and on the professionals charged with teaching students to absorb and understand vast amounts of science and medical information. On July 1, 2003, the Accreditation Council for Graduate Medical Education (ACGME) revised the regulations governing the number of resident duty hours. These changes have forced residency programs to find viable options for imparting the required knowledge and hands-on experience to residents in fewer hours. Many consider hospitalists, by virtue of their “superior clinical and educational skills,” as representative of “the solution to the residency work duty problem.” In addition to providing excellence in teaching, hospitalists, known for their “superior clinical and educational skills,” may lead the way in creating and leading a clinical research agenda, which presents as the ultimate pedagogical experience (6).
In 2002, ACGME required six general competencies to be incorporated into residency curriculum and evaluation: patient care, medical knowledge, practice-based learning and improvement, interpersonal and communication skills, professionalism, and systems-based practice. Hospitalists, because their practice already incorporates many aspects of these competencies, may be more effective at teaching these concepts to residents.
In the formal capacity of teacher, hospitalists can participate in attending/teaching rounds and in didactic patient-specific sessions presented in a case-based format, which provides residents with basic knowledge. As teaching supervisors, they can oversee the full range of clinical processes and procedures from the admission stage to post-discharge. Hospitalist teachers can also serve as mentors, providing a role model to residents who may be searching for direction regarding future plans. Through career counseling, hospitalists may steer learners into appropriate areas of study and training. Table 1 summarizes a series of research studies that document the positive impact hospitalists have achieved as educators in the academic environment.
Hospitalists may also have formal responsibility for developing curricula for learners in the academic environment. Whether the focus is on teaching medical students, residents, or hospitalist fellows, there is a need to determine the topics and material to be covered, incorporate them into a cogent curriculum, and update regularly to reflect the changing standards of care.
“Informal”
Informal education can be viewed as an exchange of information among stakeholders in the health care industry attempting to improve outcomes. Figure 1 depicts this as a two-way information exchange (solid arrows in both directions). As hospitalists impart knowledge to primary care physicians (PCPs), specialists/surgeons, other health care professionals (including nurses and pharmacists), patients, families, and hospital administrators, they reap benefits as well. These stakeholders stand to profit from the knowledge hospitalists can impart in daily interactions within the hospital and in less formal settings.
By working together with nurses, emergency room physicians, medical specialists, and PCPs, hospitalists can help achieve efficient and effective processes of care. The use of available software programs enables health care professionals to cooperatively exchange reliable information regarding patient management. Ongoing conversations regarding diagnoses, treatment, medications, and procedures serve to keep each member of the team educated and informed, thus ensuring more efficient delivery of care (12).
Alpesh Amin, MD, executive director of the hospitalist program at the University of California, Irvine, and chair of SHM’s Education Committee, points out that hospitalists frequently have opportunities to act as educators during case-by-case interactions with PCPs and other health care providers. “Every time you talk to a doctor about admitting or discharging a patient, it’s an opportunity to educate,” he says. In addition, “the hospitalist can apply and/or develop critical pathways and algorithms to educate others.” In the course of managing care, criteria can be developed for previously unaddressed medical issues.
This same opportunity for education extends to the hospital floor where team building serves to enlighten each member of the group providing patient care. In a reciprocal environment, both hospitalists and their medical professional “teammates” benefit from each other’s knowledge. Amin points out that specialists typically focus on one condition, while hospitalists consider the entire patient. By openly receiving the specialist’s input and advice, processing it, and then applying it to the patient, the hospitalist can develop a comprehensive approach to disease management. By considering co-morbidities and long-term care, the health care team should base decisions on “patient-centered education (13).”
Hospitalists can initiate informal in-house educational outreach, such as informational programs about medical breakthroughs, new medications, explanations of existing medical legislation, and other relevant topics. These programs can enlighten nurses, case managers, pharmacists, and other health care professionals about issues important to managing patients and/or achieving quality outcomes. The format for these programs may be one-on-one interactions (either in-person or by telephone) relating to one specific patient; formal in-service lectures; “Lunch and Learns”; pharmaceutically funded drug- or-disease-management seminars; committee or departmental meetings, and/or random written communications (sent electronically or by interoffice mail) that incorporate history and physical findings, consultations, discharge summaries, or hard-copy articles (12).
Conclusion
Because they spend so much time in the hospital, hospitalists are experts on all aspects of inpatient care: clinical, administrative, patient flow, and health care industry issues. Published research shows that academic institutions that employ hospitalists will have more satisfied and better-educated students. Common sense suggests that nurses and other stakeholders who work with hospitalists will be more informed and better-educated team members in the patient care process. Hospitalists can be the key ingredient and centerpiece in effective inpatient medical education.
References
- Yale New Haven Hospital Report, March 2004.
- Ward, Michael R. “Drug approval overregulation.” Regulation: the Review of Business and Government. Cato Institute, September 27, 2004.
- Pak, MH. Associate Professor of Medicine, Hospitalist, Director, General Medicine Consultation Service, University of Wisconsin School of Medicine, Madison, WI.
- Ranji S, Rosenman D. “Hospital medicine fellowship update.” The Hospitalist. 2004; 8 (5): 39.
- Wachter RM, Goldman L. “The hospitalist movement five years later.” JAMA.2002; 287(4): 487-94.
- Saint S, Flanders SA. “Hospitalists in teaching hospitals: opportunities but not without danger.” J Gen Intern Med. 2004; 19: 392-3.
- Chung P, Morrison J, Jin L, Levinson W, Humphrey H, Meltzer D. “Resident satisfaction on an academic hospitalist service: time to teach.” Am J Med. 2002; 112: 597-601.
- Landrigan CP, Muret-Wagstaff S, Chiang VW, Nigrin DJ, Goldmann DA, Finkelstein JA. “Effect of a pediatric hospitalist system on housestaff education and experience.” Arch Ped Adoles Med. 2002; 156 (9): 877-83.
- Hunter AJ, Desai SS, Harrison RA, Chan BK. “Medical student evaluation of the quality of hospitalist and non-hospitalist teaching faculty on inpatient medicine rotations.” Acad Med. 2004; 79:78-82.
- 10. Kulaga, ME. “The positive impact of initiation of hospitalist clinician educators.” J Gen Intern Med.2004; 19(4): 293-301.
- Hauer K, Wachter R, McCulloch C, Woo G, Auerbach A. Effects of hospitalist attending physicians on trainee satisfaction with teaching and with internal medicine rotations. Arch Intern Med. 2004; 164: 1866-71.
- Jones T, DO. Director of Medical Affairs, IPC, The Hospitalist Company, Mesa, AZ.
- Amin A, MD, MBA, FACP, executive director, Hospitalist Program, University of California, Irvine. Chair, Education Committee, Society of Hospital Medicine. Personal interview. October 7, 2004.
Type a medical condition or term into a search engine and watch what happens. A search on the words “diabetes” yields more than 13 million Web pages, and “pneumonia” produces another 1.65 million. In 1998, the Internet hosted approximately 5000 health-related Web sites; two years later that number quadrupled (1). Between 30,000 and 45,000 medical articles on various drug therapies are published annually. The Patent and Trademark Office issued between 2000 and 4200 drug patents each year between 1979 and 1989 (2). The National Library of Medicine reports that it adds more than 2000 journal article citations to its MEDLINE database on a daily basis. In 2003, more than 460,000 citations were entered.
Deciphering and applying this myriad of changing information is a critical activity in the medical field. Without disseminating new knowledge through ongoing education, medical practices and procedures would become outdated, and uninformed medical professionals and patients would continue to operate under misinformation that might be detrimental to health or worse.
Hospitalists as Inpatient Experts
In an inpatient setting, hospitalists are uniquely qualified to play the role of educator. They analyze and interpret a wide range of medical information to treat their patients and provide updated information to patients and their families, residents, interns, nursing staff, other health care professionals, and hospital administrators. The hospitalist can be viewed as the “hub” of educational activities in the inpatient environment, absorbing, synthesizing, and disseminating information. They are “inpatient experts” in the following five spheres of knowledge:
- patient management
- clinical knowledge
- clinical skills
- health care industry issues
- research and management/leadership (3)
Hospitalists are uniquely qualified in the sphere of patient management, efficiently and effectively guiding the patient through the mazelike inpatient environment. Most hospitalists are quite familiar with critical hospital functions and activities, including treatment in the emergency department, the admissions process, bedside care on the medical floor, treatment in the intensive care unit, and the discharge process. Hospitalists, because they understand “how to get things done” by ancillary departments, including diagnostic and therapeutic services, often find themselves as conductors of inpatient care. Many hospitalists have developed unique proficiency in co-managing surgical cases due to expertise in peri-operative evaluation and care. Hospitalists are recognized as inpatient team leaders, facilitating and coordinating a range of support services needed to treat the patient, including nursing, case management, pharmacy, occupational/physical therapy, and social work. Hospitalists must also be effective in managing relationships with health care personnel external to the inpatient environment, including community physicians, homecare providers, extended care facilities, and visiting nurse services. Finally, hospitalists are oaen well informed about hospital processes, procedures, rules, regulations, and information systems.
As inpatient generalists, hospitalists continually treat the most common reasons for admission and have exceptional clinical knowledge of these conditions. These conditions include pneumonia, deep vein thrombosis (DVT), congestive heart failure (CHF), diabetes, end-of-life care, and other medical diagnoses. Since they treat many elderly patients, hospitalists are considered experts in managing patients with multiple co-morbidities. A related area of expertise is clinical guidelines/pathways, quality of care metrics, and practice standards. Since they spend nearly all of their time treating inpatients, hospitalists develop extraordinary familiarity with the clinical rules and tools supporting the patient care process.
In addition to clinical knowledge, hospitalists have the experience and expertise to teach inpatient clinical skills. These skills include diagnosis, physical examination, discharge planning, medical chart recording, family meeting coordination, and oversight. Also, most hospitalists are familiar with a range of technical procedures, including insertion of central lines and arterial lines, lumbar puncture, arthrocentesis, paracentesis, and thoracentesis.
Hospitalists often are the most knowledgeable inpatient clinicians with regard to a wide range of health care industry issues. These include comprehension of the payer/insurance regulations regarding medication formularies, utilization review requirements, and other care policies. Their expertise may extend to knowledge of state and federal regulations, public health initiatives, and recently enacted or pending health care legislation. Finally, hospitalists also are often conversant in the field of health care economics, especially regarding the financial impact on hospitals of reimbursement policies, legislative initiatives, technology, etc.
The fifth sphere of hospitalist expertise combines several knowledge domains. Individual hospitalists have specialized expertise in particular fields related to hospital medicine. Some hospitalists, mostly affiliated with academic institutions, are researchers who may develop research protocols, gather data, perform statistical analyses, and write papers that may potentially become the basis of improved patient care. Other hospitalists are exceptionally experienced in management/leadership. A hospitalist may be highly qualified to manage projects (e.g., computer-based physician order entry systems, throughput initiatives, etc.),or a hospitalist could be a strategic thinker who is viewed as a key clinical member of the hospital’s management team.
As a growing specialty, hospitalists have established a proficiency in a range of disciplines and intellectual domains. They are well positioned to assume the role of educator in the hospital environment. Given the exceptional knowledge and skills needed to be a hospitalist, the Society of Hospital Medicine (SHM) is pursing an effort to standardize education and lend greater credibility to the hospitalist profession. The “core curriculum” project is currently formalizing training that will provide a solid foundation for effective clinical practice in the field of hospital medicine.
Dual Educational Tracks
As depicted in Figure 1 below, medical education activity and the ways in which knowledge is imparted fall into two categories: formal and informal. Although some overlap may occur, there are distinct characteristics attributable to both classifications.
“Formal”
Formal education refers to the traditional “teacher-learner” roles in medicine. The learner can be a medical student, resident, or fellow. Education is typically transmitted from teacher to learner (as depicted in the diagram by a solid line), with some reciprocal feedback from the learner to the teacher (dotted line). It should be noted that as the importance and value of hospital medicine programs gain recognition, fellowship programs focusing on this specialty have been established. As of August 2004, eight active hospital medicine fellowship programs exist in the United States: three in California, two in Minnesota, and one each in Ohio, Illinois, and Texas. There are also pediatric hospital medicine fellowship programs in Boston, Washington DC, Houston, and San Diego. Each program enrolls one or two fellows annually (4).
Formal education can take place in both academic medical centers and community hospitals. By definition, academic medical centers provide supervised practical training for medical students, student nurses, and/or other health care professionals, as well as residents and fellows. In many academic medical centers throughout the country, hospitalists are emerging as core teachers of inpatient medicine. A prime example is the University of California, San Francisco. In 2002, 15 faculty hospitalists served as staff for approximately two-thirds of ward-attending months, as well as all medical consults (5).
By the same token, community hospitals that have residency programs also incorporate education to some degree into their daily operations. Today, medical education places a significant burden on residents and on the professionals charged with teaching students to absorb and understand vast amounts of science and medical information. On July 1, 2003, the Accreditation Council for Graduate Medical Education (ACGME) revised the regulations governing the number of resident duty hours. These changes have forced residency programs to find viable options for imparting the required knowledge and hands-on experience to residents in fewer hours. Many consider hospitalists, by virtue of their “superior clinical and educational skills,” as representative of “the solution to the residency work duty problem.” In addition to providing excellence in teaching, hospitalists, known for their “superior clinical and educational skills,” may lead the way in creating and leading a clinical research agenda, which presents as the ultimate pedagogical experience (6).
In 2002, ACGME required six general competencies to be incorporated into residency curriculum and evaluation: patient care, medical knowledge, practice-based learning and improvement, interpersonal and communication skills, professionalism, and systems-based practice. Hospitalists, because their practice already incorporates many aspects of these competencies, may be more effective at teaching these concepts to residents.
In the formal capacity of teacher, hospitalists can participate in attending/teaching rounds and in didactic patient-specific sessions presented in a case-based format, which provides residents with basic knowledge. As teaching supervisors, they can oversee the full range of clinical processes and procedures from the admission stage to post-discharge. Hospitalist teachers can also serve as mentors, providing a role model to residents who may be searching for direction regarding future plans. Through career counseling, hospitalists may steer learners into appropriate areas of study and training. Table 1 summarizes a series of research studies that document the positive impact hospitalists have achieved as educators in the academic environment.
Hospitalists may also have formal responsibility for developing curricula for learners in the academic environment. Whether the focus is on teaching medical students, residents, or hospitalist fellows, there is a need to determine the topics and material to be covered, incorporate them into a cogent curriculum, and update regularly to reflect the changing standards of care.
“Informal”
Informal education can be viewed as an exchange of information among stakeholders in the health care industry attempting to improve outcomes. Figure 1 depicts this as a two-way information exchange (solid arrows in both directions). As hospitalists impart knowledge to primary care physicians (PCPs), specialists/surgeons, other health care professionals (including nurses and pharmacists), patients, families, and hospital administrators, they reap benefits as well. These stakeholders stand to profit from the knowledge hospitalists can impart in daily interactions within the hospital and in less formal settings.
By working together with nurses, emergency room physicians, medical specialists, and PCPs, hospitalists can help achieve efficient and effective processes of care. The use of available software programs enables health care professionals to cooperatively exchange reliable information regarding patient management. Ongoing conversations regarding diagnoses, treatment, medications, and procedures serve to keep each member of the team educated and informed, thus ensuring more efficient delivery of care (12).
Alpesh Amin, MD, executive director of the hospitalist program at the University of California, Irvine, and chair of SHM’s Education Committee, points out that hospitalists frequently have opportunities to act as educators during case-by-case interactions with PCPs and other health care providers. “Every time you talk to a doctor about admitting or discharging a patient, it’s an opportunity to educate,” he says. In addition, “the hospitalist can apply and/or develop critical pathways and algorithms to educate others.” In the course of managing care, criteria can be developed for previously unaddressed medical issues.
This same opportunity for education extends to the hospital floor where team building serves to enlighten each member of the group providing patient care. In a reciprocal environment, both hospitalists and their medical professional “teammates” benefit from each other’s knowledge. Amin points out that specialists typically focus on one condition, while hospitalists consider the entire patient. By openly receiving the specialist’s input and advice, processing it, and then applying it to the patient, the hospitalist can develop a comprehensive approach to disease management. By considering co-morbidities and long-term care, the health care team should base decisions on “patient-centered education (13).”
Hospitalists can initiate informal in-house educational outreach, such as informational programs about medical breakthroughs, new medications, explanations of existing medical legislation, and other relevant topics. These programs can enlighten nurses, case managers, pharmacists, and other health care professionals about issues important to managing patients and/or achieving quality outcomes. The format for these programs may be one-on-one interactions (either in-person or by telephone) relating to one specific patient; formal in-service lectures; “Lunch and Learns”; pharmaceutically funded drug- or-disease-management seminars; committee or departmental meetings, and/or random written communications (sent electronically or by interoffice mail) that incorporate history and physical findings, consultations, discharge summaries, or hard-copy articles (12).
Conclusion
Because they spend so much time in the hospital, hospitalists are experts on all aspects of inpatient care: clinical, administrative, patient flow, and health care industry issues. Published research shows that academic institutions that employ hospitalists will have more satisfied and better-educated students. Common sense suggests that nurses and other stakeholders who work with hospitalists will be more informed and better-educated team members in the patient care process. Hospitalists can be the key ingredient and centerpiece in effective inpatient medical education.
References
- Yale New Haven Hospital Report, March 2004.
- Ward, Michael R. “Drug approval overregulation.” Regulation: the Review of Business and Government. Cato Institute, September 27, 2004.
- Pak, MH. Associate Professor of Medicine, Hospitalist, Director, General Medicine Consultation Service, University of Wisconsin School of Medicine, Madison, WI.
- Ranji S, Rosenman D. “Hospital medicine fellowship update.” The Hospitalist. 2004; 8 (5): 39.
- Wachter RM, Goldman L. “The hospitalist movement five years later.” JAMA.2002; 287(4): 487-94.
- Saint S, Flanders SA. “Hospitalists in teaching hospitals: opportunities but not without danger.” J Gen Intern Med. 2004; 19: 392-3.
- Chung P, Morrison J, Jin L, Levinson W, Humphrey H, Meltzer D. “Resident satisfaction on an academic hospitalist service: time to teach.” Am J Med. 2002; 112: 597-601.
- Landrigan CP, Muret-Wagstaff S, Chiang VW, Nigrin DJ, Goldmann DA, Finkelstein JA. “Effect of a pediatric hospitalist system on housestaff education and experience.” Arch Ped Adoles Med. 2002; 156 (9): 877-83.
- Hunter AJ, Desai SS, Harrison RA, Chan BK. “Medical student evaluation of the quality of hospitalist and non-hospitalist teaching faculty on inpatient medicine rotations.” Acad Med. 2004; 79:78-82.
- 10. Kulaga, ME. “The positive impact of initiation of hospitalist clinician educators.” J Gen Intern Med.2004; 19(4): 293-301.
- Hauer K, Wachter R, McCulloch C, Woo G, Auerbach A. Effects of hospitalist attending physicians on trainee satisfaction with teaching and with internal medicine rotations. Arch Intern Med. 2004; 164: 1866-71.
- Jones T, DO. Director of Medical Affairs, IPC, The Hospitalist Company, Mesa, AZ.
- Amin A, MD, MBA, FACP, executive director, Hospitalist Program, University of California, Irvine. Chair, Education Committee, Society of Hospital Medicine. Personal interview. October 7, 2004.
Type a medical condition or term into a search engine and watch what happens. A search on the words “diabetes” yields more than 13 million Web pages, and “pneumonia” produces another 1.65 million. In 1998, the Internet hosted approximately 5000 health-related Web sites; two years later that number quadrupled (1). Between 30,000 and 45,000 medical articles on various drug therapies are published annually. The Patent and Trademark Office issued between 2000 and 4200 drug patents each year between 1979 and 1989 (2). The National Library of Medicine reports that it adds more than 2000 journal article citations to its MEDLINE database on a daily basis. In 2003, more than 460,000 citations were entered.
Deciphering and applying this myriad of changing information is a critical activity in the medical field. Without disseminating new knowledge through ongoing education, medical practices and procedures would become outdated, and uninformed medical professionals and patients would continue to operate under misinformation that might be detrimental to health or worse.
Hospitalists as Inpatient Experts
In an inpatient setting, hospitalists are uniquely qualified to play the role of educator. They analyze and interpret a wide range of medical information to treat their patients and provide updated information to patients and their families, residents, interns, nursing staff, other health care professionals, and hospital administrators. The hospitalist can be viewed as the “hub” of educational activities in the inpatient environment, absorbing, synthesizing, and disseminating information. They are “inpatient experts” in the following five spheres of knowledge:
- patient management
- clinical knowledge
- clinical skills
- health care industry issues
- research and management/leadership (3)
Hospitalists are uniquely qualified in the sphere of patient management, efficiently and effectively guiding the patient through the mazelike inpatient environment. Most hospitalists are quite familiar with critical hospital functions and activities, including treatment in the emergency department, the admissions process, bedside care on the medical floor, treatment in the intensive care unit, and the discharge process. Hospitalists, because they understand “how to get things done” by ancillary departments, including diagnostic and therapeutic services, often find themselves as conductors of inpatient care. Many hospitalists have developed unique proficiency in co-managing surgical cases due to expertise in peri-operative evaluation and care. Hospitalists are recognized as inpatient team leaders, facilitating and coordinating a range of support services needed to treat the patient, including nursing, case management, pharmacy, occupational/physical therapy, and social work. Hospitalists must also be effective in managing relationships with health care personnel external to the inpatient environment, including community physicians, homecare providers, extended care facilities, and visiting nurse services. Finally, hospitalists are oaen well informed about hospital processes, procedures, rules, regulations, and information systems.
As inpatient generalists, hospitalists continually treat the most common reasons for admission and have exceptional clinical knowledge of these conditions. These conditions include pneumonia, deep vein thrombosis (DVT), congestive heart failure (CHF), diabetes, end-of-life care, and other medical diagnoses. Since they treat many elderly patients, hospitalists are considered experts in managing patients with multiple co-morbidities. A related area of expertise is clinical guidelines/pathways, quality of care metrics, and practice standards. Since they spend nearly all of their time treating inpatients, hospitalists develop extraordinary familiarity with the clinical rules and tools supporting the patient care process.
In addition to clinical knowledge, hospitalists have the experience and expertise to teach inpatient clinical skills. These skills include diagnosis, physical examination, discharge planning, medical chart recording, family meeting coordination, and oversight. Also, most hospitalists are familiar with a range of technical procedures, including insertion of central lines and arterial lines, lumbar puncture, arthrocentesis, paracentesis, and thoracentesis.
Hospitalists often are the most knowledgeable inpatient clinicians with regard to a wide range of health care industry issues. These include comprehension of the payer/insurance regulations regarding medication formularies, utilization review requirements, and other care policies. Their expertise may extend to knowledge of state and federal regulations, public health initiatives, and recently enacted or pending health care legislation. Finally, hospitalists also are often conversant in the field of health care economics, especially regarding the financial impact on hospitals of reimbursement policies, legislative initiatives, technology, etc.
The fifth sphere of hospitalist expertise combines several knowledge domains. Individual hospitalists have specialized expertise in particular fields related to hospital medicine. Some hospitalists, mostly affiliated with academic institutions, are researchers who may develop research protocols, gather data, perform statistical analyses, and write papers that may potentially become the basis of improved patient care. Other hospitalists are exceptionally experienced in management/leadership. A hospitalist may be highly qualified to manage projects (e.g., computer-based physician order entry systems, throughput initiatives, etc.),or a hospitalist could be a strategic thinker who is viewed as a key clinical member of the hospital’s management team.
As a growing specialty, hospitalists have established a proficiency in a range of disciplines and intellectual domains. They are well positioned to assume the role of educator in the hospital environment. Given the exceptional knowledge and skills needed to be a hospitalist, the Society of Hospital Medicine (SHM) is pursing an effort to standardize education and lend greater credibility to the hospitalist profession. The “core curriculum” project is currently formalizing training that will provide a solid foundation for effective clinical practice in the field of hospital medicine.
Dual Educational Tracks
As depicted in Figure 1 below, medical education activity and the ways in which knowledge is imparted fall into two categories: formal and informal. Although some overlap may occur, there are distinct characteristics attributable to both classifications.
“Formal”
Formal education refers to the traditional “teacher-learner” roles in medicine. The learner can be a medical student, resident, or fellow. Education is typically transmitted from teacher to learner (as depicted in the diagram by a solid line), with some reciprocal feedback from the learner to the teacher (dotted line). It should be noted that as the importance and value of hospital medicine programs gain recognition, fellowship programs focusing on this specialty have been established. As of August 2004, eight active hospital medicine fellowship programs exist in the United States: three in California, two in Minnesota, and one each in Ohio, Illinois, and Texas. There are also pediatric hospital medicine fellowship programs in Boston, Washington DC, Houston, and San Diego. Each program enrolls one or two fellows annually (4).
Formal education can take place in both academic medical centers and community hospitals. By definition, academic medical centers provide supervised practical training for medical students, student nurses, and/or other health care professionals, as well as residents and fellows. In many academic medical centers throughout the country, hospitalists are emerging as core teachers of inpatient medicine. A prime example is the University of California, San Francisco. In 2002, 15 faculty hospitalists served as staff for approximately two-thirds of ward-attending months, as well as all medical consults (5).
By the same token, community hospitals that have residency programs also incorporate education to some degree into their daily operations. Today, medical education places a significant burden on residents and on the professionals charged with teaching students to absorb and understand vast amounts of science and medical information. On July 1, 2003, the Accreditation Council for Graduate Medical Education (ACGME) revised the regulations governing the number of resident duty hours. These changes have forced residency programs to find viable options for imparting the required knowledge and hands-on experience to residents in fewer hours. Many consider hospitalists, by virtue of their “superior clinical and educational skills,” as representative of “the solution to the residency work duty problem.” In addition to providing excellence in teaching, hospitalists, known for their “superior clinical and educational skills,” may lead the way in creating and leading a clinical research agenda, which presents as the ultimate pedagogical experience (6).
In 2002, ACGME required six general competencies to be incorporated into residency curriculum and evaluation: patient care, medical knowledge, practice-based learning and improvement, interpersonal and communication skills, professionalism, and systems-based practice. Hospitalists, because their practice already incorporates many aspects of these competencies, may be more effective at teaching these concepts to residents.
In the formal capacity of teacher, hospitalists can participate in attending/teaching rounds and in didactic patient-specific sessions presented in a case-based format, which provides residents with basic knowledge. As teaching supervisors, they can oversee the full range of clinical processes and procedures from the admission stage to post-discharge. Hospitalist teachers can also serve as mentors, providing a role model to residents who may be searching for direction regarding future plans. Through career counseling, hospitalists may steer learners into appropriate areas of study and training. Table 1 summarizes a series of research studies that document the positive impact hospitalists have achieved as educators in the academic environment.
Hospitalists may also have formal responsibility for developing curricula for learners in the academic environment. Whether the focus is on teaching medical students, residents, or hospitalist fellows, there is a need to determine the topics and material to be covered, incorporate them into a cogent curriculum, and update regularly to reflect the changing standards of care.
“Informal”
Informal education can be viewed as an exchange of information among stakeholders in the health care industry attempting to improve outcomes. Figure 1 depicts this as a two-way information exchange (solid arrows in both directions). As hospitalists impart knowledge to primary care physicians (PCPs), specialists/surgeons, other health care professionals (including nurses and pharmacists), patients, families, and hospital administrators, they reap benefits as well. These stakeholders stand to profit from the knowledge hospitalists can impart in daily interactions within the hospital and in less formal settings.
By working together with nurses, emergency room physicians, medical specialists, and PCPs, hospitalists can help achieve efficient and effective processes of care. The use of available software programs enables health care professionals to cooperatively exchange reliable information regarding patient management. Ongoing conversations regarding diagnoses, treatment, medications, and procedures serve to keep each member of the team educated and informed, thus ensuring more efficient delivery of care (12).
Alpesh Amin, MD, executive director of the hospitalist program at the University of California, Irvine, and chair of SHM’s Education Committee, points out that hospitalists frequently have opportunities to act as educators during case-by-case interactions with PCPs and other health care providers. “Every time you talk to a doctor about admitting or discharging a patient, it’s an opportunity to educate,” he says. In addition, “the hospitalist can apply and/or develop critical pathways and algorithms to educate others.” In the course of managing care, criteria can be developed for previously unaddressed medical issues.
This same opportunity for education extends to the hospital floor where team building serves to enlighten each member of the group providing patient care. In a reciprocal environment, both hospitalists and their medical professional “teammates” benefit from each other’s knowledge. Amin points out that specialists typically focus on one condition, while hospitalists consider the entire patient. By openly receiving the specialist’s input and advice, processing it, and then applying it to the patient, the hospitalist can develop a comprehensive approach to disease management. By considering co-morbidities and long-term care, the health care team should base decisions on “patient-centered education (13).”
Hospitalists can initiate informal in-house educational outreach, such as informational programs about medical breakthroughs, new medications, explanations of existing medical legislation, and other relevant topics. These programs can enlighten nurses, case managers, pharmacists, and other health care professionals about issues important to managing patients and/or achieving quality outcomes. The format for these programs may be one-on-one interactions (either in-person or by telephone) relating to one specific patient; formal in-service lectures; “Lunch and Learns”; pharmaceutically funded drug- or-disease-management seminars; committee or departmental meetings, and/or random written communications (sent electronically or by interoffice mail) that incorporate history and physical findings, consultations, discharge summaries, or hard-copy articles (12).
Conclusion
Because they spend so much time in the hospital, hospitalists are experts on all aspects of inpatient care: clinical, administrative, patient flow, and health care industry issues. Published research shows that academic institutions that employ hospitalists will have more satisfied and better-educated students. Common sense suggests that nurses and other stakeholders who work with hospitalists will be more informed and better-educated team members in the patient care process. Hospitalists can be the key ingredient and centerpiece in effective inpatient medical education.
References
- Yale New Haven Hospital Report, March 2004.
- Ward, Michael R. “Drug approval overregulation.” Regulation: the Review of Business and Government. Cato Institute, September 27, 2004.
- Pak, MH. Associate Professor of Medicine, Hospitalist, Director, General Medicine Consultation Service, University of Wisconsin School of Medicine, Madison, WI.
- Ranji S, Rosenman D. “Hospital medicine fellowship update.” The Hospitalist. 2004; 8 (5): 39.
- Wachter RM, Goldman L. “The hospitalist movement five years later.” JAMA.2002; 287(4): 487-94.
- Saint S, Flanders SA. “Hospitalists in teaching hospitals: opportunities but not without danger.” J Gen Intern Med. 2004; 19: 392-3.
- Chung P, Morrison J, Jin L, Levinson W, Humphrey H, Meltzer D. “Resident satisfaction on an academic hospitalist service: time to teach.” Am J Med. 2002; 112: 597-601.
- Landrigan CP, Muret-Wagstaff S, Chiang VW, Nigrin DJ, Goldmann DA, Finkelstein JA. “Effect of a pediatric hospitalist system on housestaff education and experience.” Arch Ped Adoles Med. 2002; 156 (9): 877-83.
- Hunter AJ, Desai SS, Harrison RA, Chan BK. “Medical student evaluation of the quality of hospitalist and non-hospitalist teaching faculty on inpatient medicine rotations.” Acad Med. 2004; 79:78-82.
- 10. Kulaga, ME. “The positive impact of initiation of hospitalist clinician educators.” J Gen Intern Med.2004; 19(4): 293-301.
- Hauer K, Wachter R, McCulloch C, Woo G, Auerbach A. Effects of hospitalist attending physicians on trainee satisfaction with teaching and with internal medicine rotations. Arch Intern Med. 2004; 164: 1866-71.
- Jones T, DO. Director of Medical Affairs, IPC, The Hospitalist Company, Mesa, AZ.
- Amin A, MD, MBA, FACP, executive director, Hospitalist Program, University of California, Irvine. Chair, Education Committee, Society of Hospital Medicine. Personal interview. October 7, 2004.