User login
The Hospitalist only
Inpatient telemedicine can help address hospitalist pain points
COVID-19 has increased confidence in the technology
Since the advent of COVID-19, health care has seen an unprecedented rise in virtual health. Telemedicine has come to the forefront of our conversations, and there are many speculations around its future state. One such discussion is around the sustainability and expansion of inpatient telemedicine programs post COVID, and if – and how – it is going to be helpful for health care.
Consider the following scenarios:
Scenario 1
A patient presents to an emergency department of a small community hospital. He needs to be seen by a specialist, but (s)he is not available, so patient gets transferred out to the ED of a different hospital several miles away from his hometown.
He is evaluated in the second ED by the specialist, has repeat testing done – some of those tests were already completed at the first hospital. After evaluating him, the specialist recommends that he does not need to be admitted to the hospital and can be safely followed up as an outpatient. The patient does not require any further intervention and is discharged from the ED.
Scenario 2
Dr. N is a hospitalist in a rural hospital that does not have intensivist support at night. She works 7 on/7 off and is on call 24/7 during her “on” week. Dr. N cannot be physically present in the hospital 24/7. She receives messages from the hospital around the clock and feels that this call schedule is no longer sustainable. She doesn’t feel comfortable admitting patients in the ICU who come to the hospital at night without physically seeing them and without ICU backup. Therefore, some of the patients who are sick enough to be admitted in ICU for closer monitoring but can be potentially handled in this rural hospital get transferred out to a different hospital.
Dr. N has been asking the hospital to provide her intensivist back up at night and to give her some flexibility in the call schedule. However, from hospital’s perspective, the volume isn’t high enough to hire a dedicated nocturnist, and because the hospital is in the small rural area, it is having a hard time attracting more intensivists. After multiple conversations between both parties, Dr. N finally resigns.
Scenario 3
Dr. A is a specialist who is on call covering different hospitals and seeing patients in clinic. His call is getting busier. He has received many new consults and also has to follow up on his other patients in hospital who he saw a day prior.
Dr. A started receiving many pages from the hospitals – some of his patients and their families are anxiously waiting on him so that he can let them go home once he sees them, while some are waiting to know what the next steps and plan of action are. He ends up canceling some of his clinic patients who had scheduled an appointment with him 3, 4, or even 5 months ago. It’s already afternoon.
Dr. A now drives to one hospital, sees his new consults, orders tests which may or may not get results the same day, follows up on other patients, reviews their test results, modifies treatment plans for some while clearing other patients for discharge. He then drives to the other hospital and follows the same process. Some of the patients aren’t happy because of the long wait, a few couldn’t arrange for the ride to go home and ended up staying in hospital 1 extra night, while the ER is getting backlogged waiting on discharges.
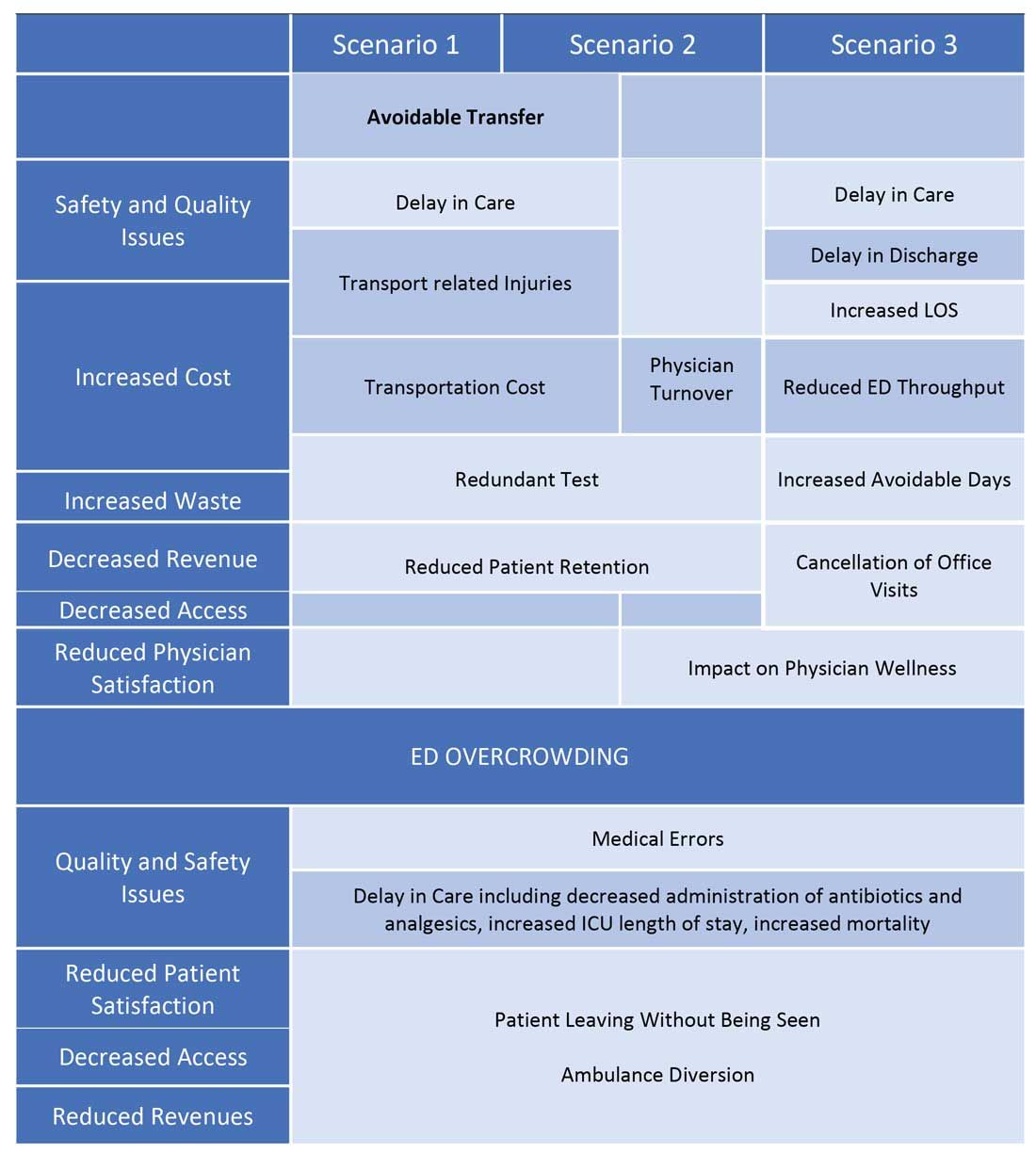
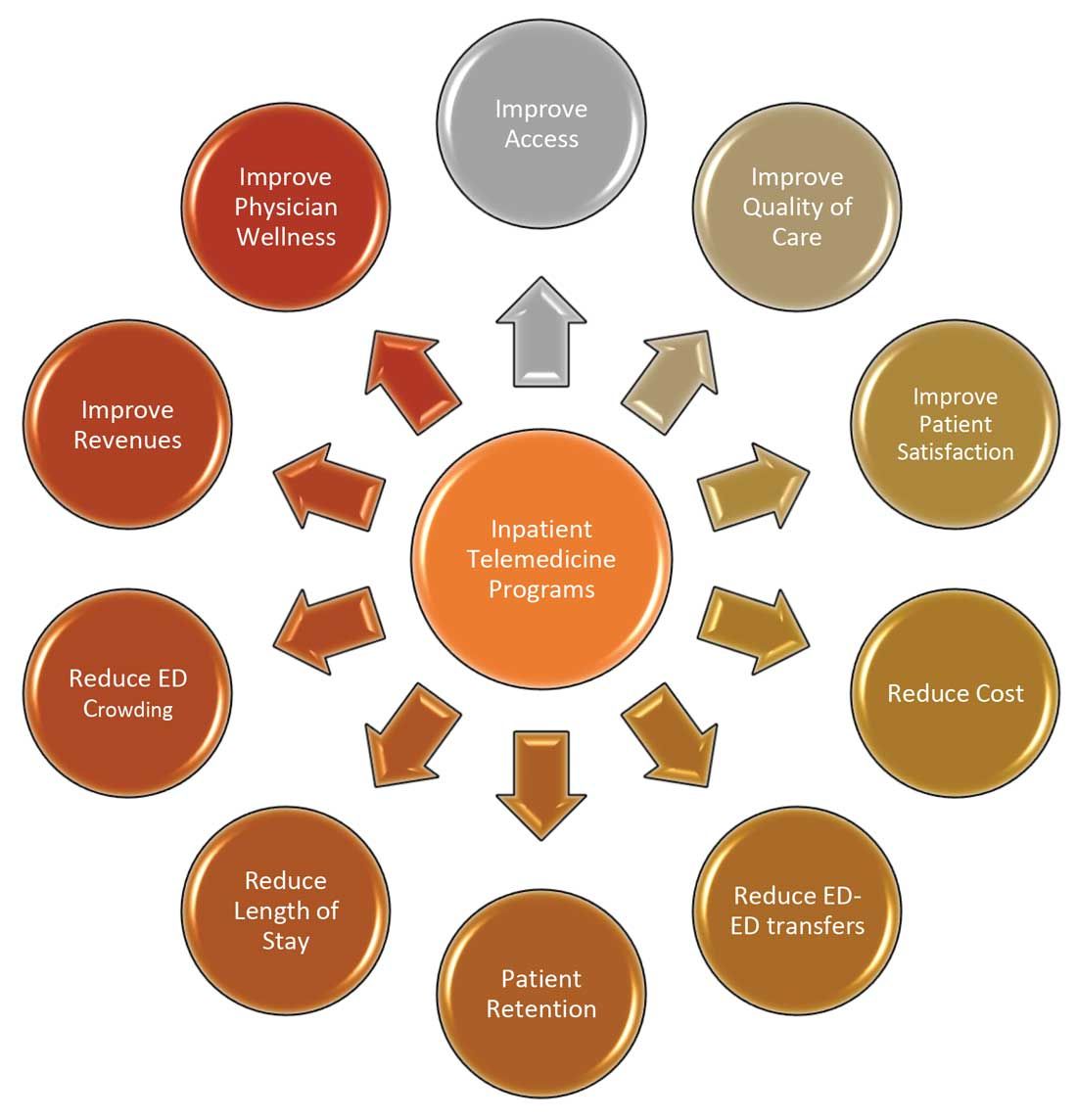
These scenarios highlight some of the important and prevalent pain points in health care as shown in Figure 1.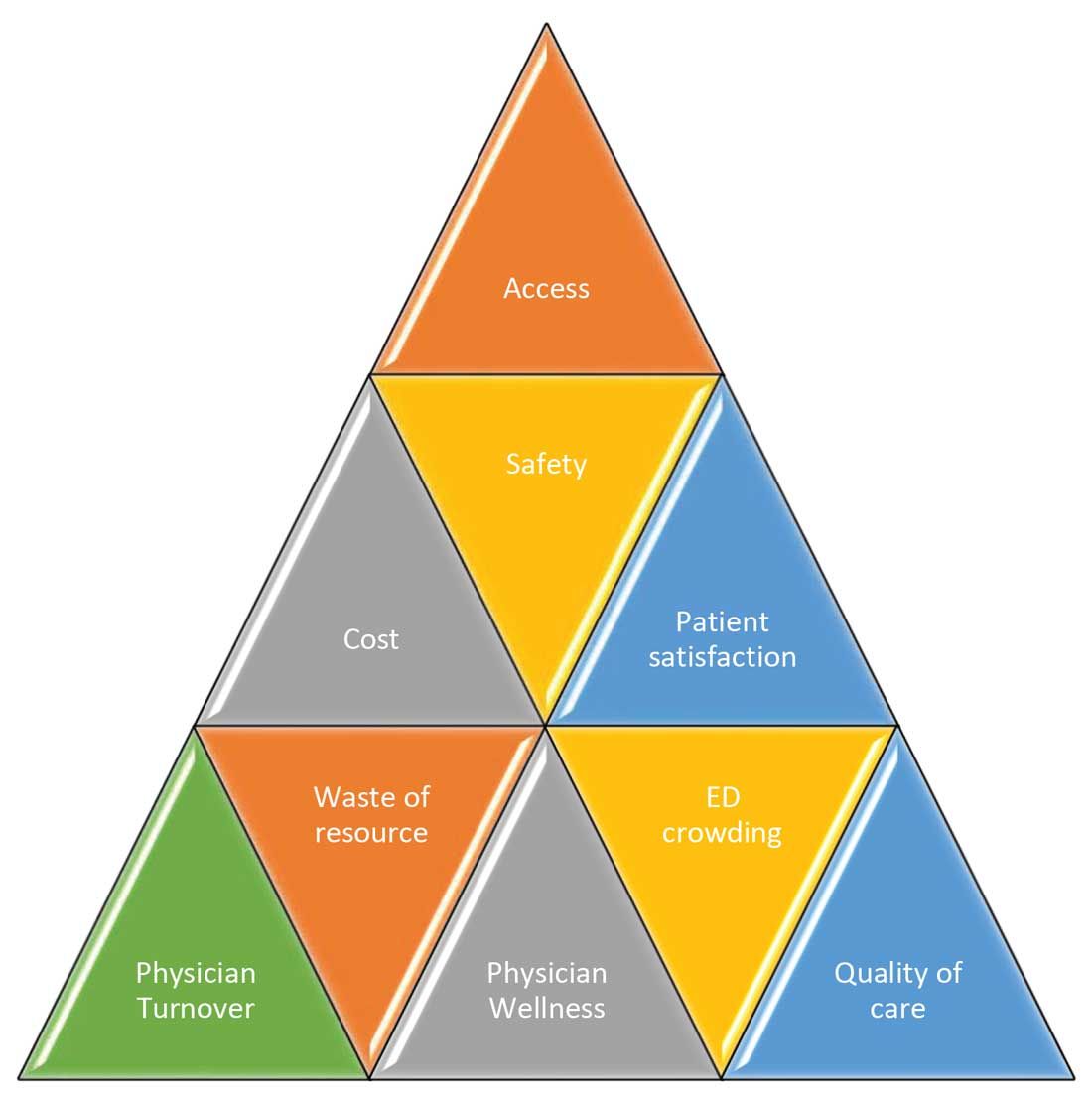
Scenario 1 and part of scenario 2 describe what is called potentially avoidable interfacility transfers. One study showed that around 8% of transferred patients (transferred from one ED to another) were discharged after ED evaluation in the second hospital, meaning they could have been retained locally without necessarily getting transferred if they could have been evaluated by the specialist.1
Transferring a patient from one hospital to another isn’t as simple as picking up a person from point A and dropping him off at point B. Rather it’s a very complicated, high-risk, capital-intensive, and time-consuming process that leads not only to excessive cost involved around transfer but also adds additional stress and burden on the patient and family. In these scenarios, having a specialist available via teleconsult could have eliminated much of this hassle and cost, allowing the patient to stay locally close to family and get access to necessary medical expertise from any part of the country in a timely manner.
Scenario 2 talks about the recruitment and retention challenges in low-volume, low-resourced locations because of call schedule and the lack of specialty support. It is reported in one study that 19% of common hospitalist admissions happen between 7:00 p.m. and 7:00 a.m. Eighty percent of admissions occurred prior to midnight. Nonrural facilities averaged 6.69 hospitalist admissions per night in that study, whereas rural facilities averaged 1.35 admissions.2 It’s like a double-edged sword for such facilities. While having a dedicated nocturnist is not a sustainable model for these hospitals, not having adequate support at night impacts physician wellness, which is already costing hospitals billions of dollars as well as leading to physician turnover: It could cost a hospital somewhere between $500,000 and $1 million to replace just one physician.3 Hence, the potential exists for a telehospitalist program in these settings to address this dilemma.
Scenario 3 sheds light on the operational issues resulting in reduced patient satisfaction and lost revenues, both on the outpatient and inpatient sides by cancellation of office visits and ED backlog. Telemedicine use in these situations can improve the turnaround time of physicians who can see some of those patients while staying at one location as they wait on other patients to show up in the clinic or wait on the operation room crew, or the procedure kit etcetera, hence improving the length of stay, ED throughput, patient satisfaction, and quality of care. This also can improve overall workflow and the wellness of physicians.
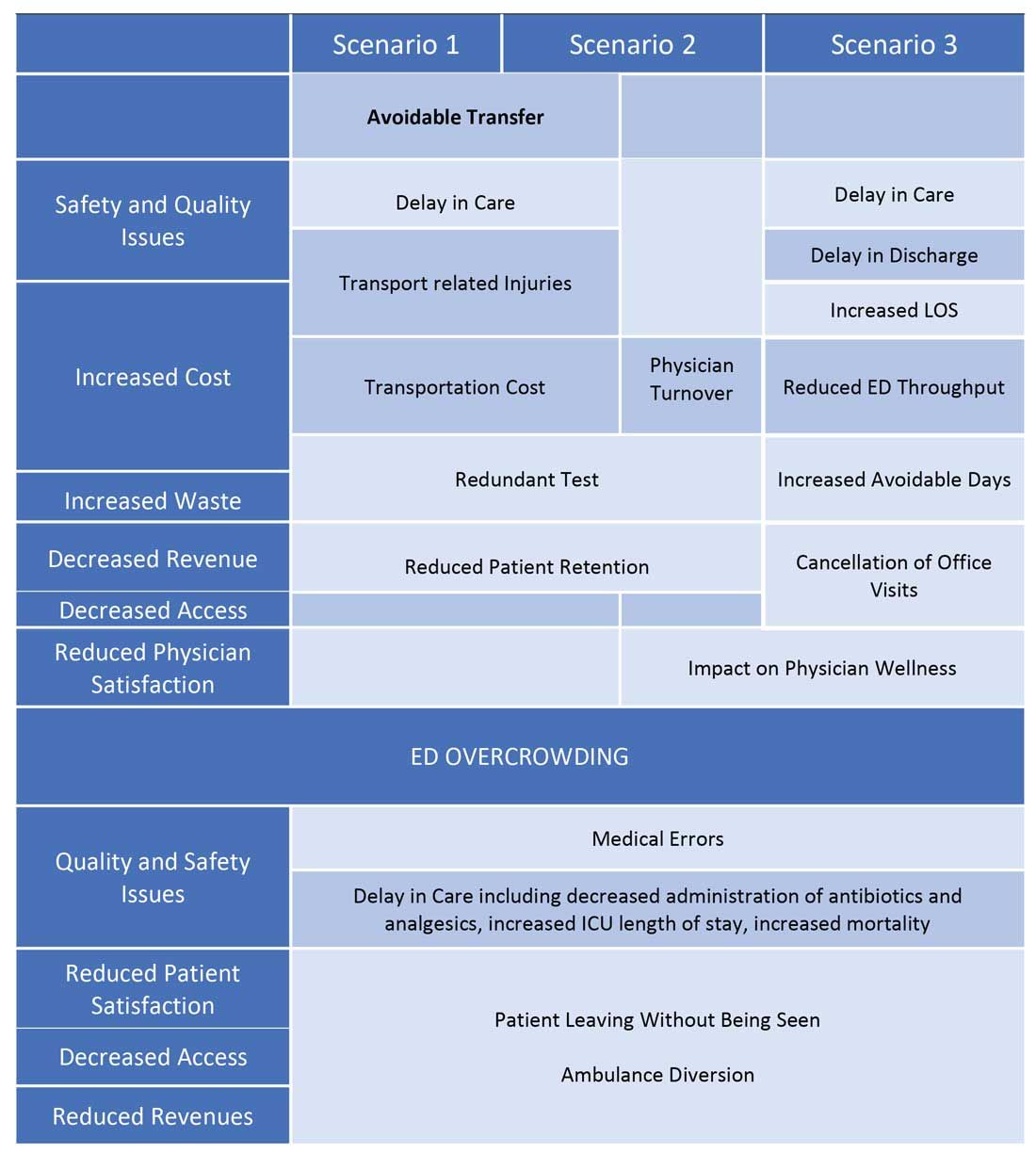
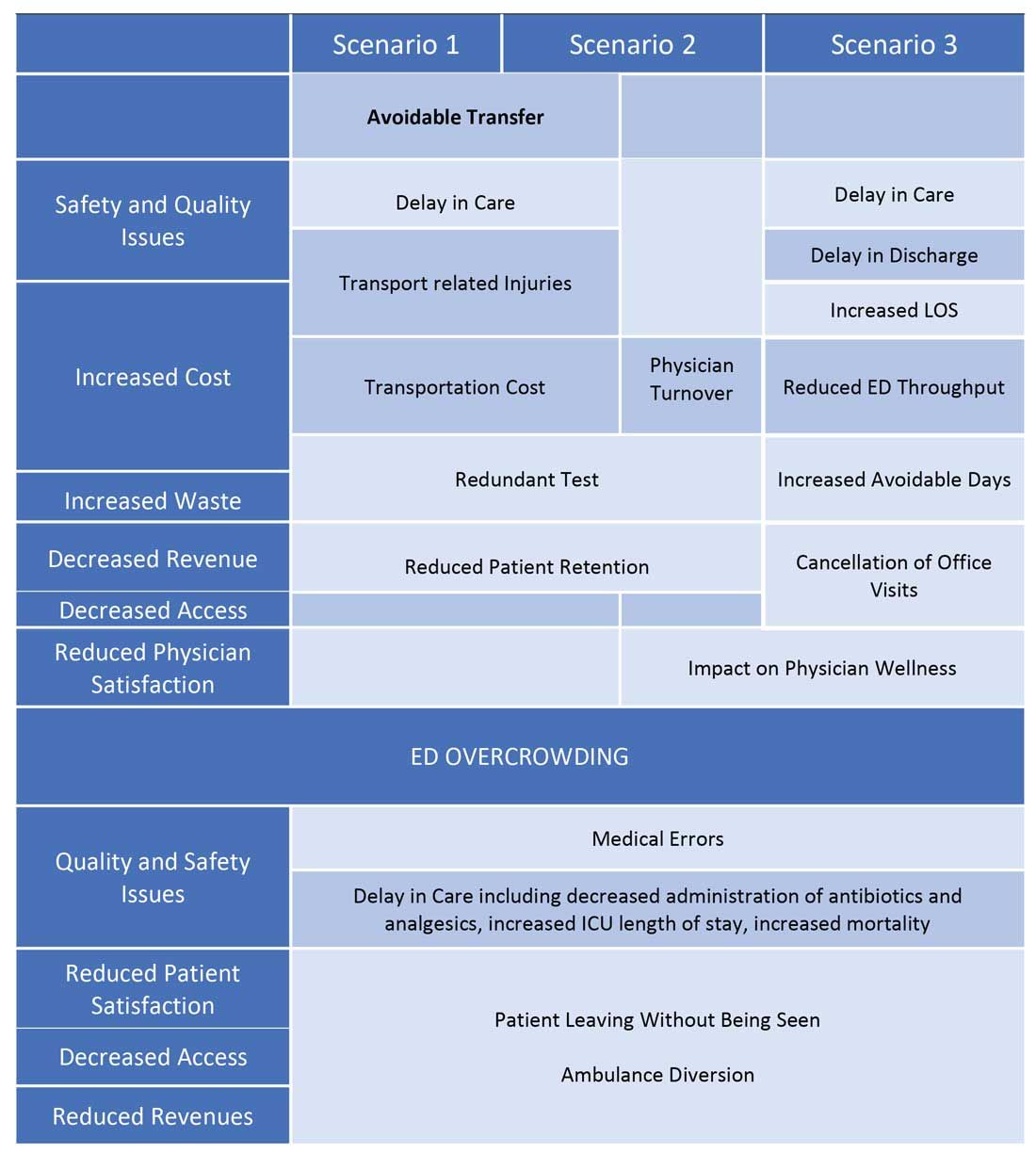
One common outcome in all these scenarios is emergency department overcrowding. There have been multiple studies that suggest that ED overcrowding can result in increased costs, lost revenues, and poor clinical outcomes, including delayed administration of antibiotics, delayed administration of analgesics to suffering patients, increased hospital length of stay, and even increased mortality.4-6 A crowded ED limits the ability of an institution to accept referrals and increases medicolegal risks. (See Figure 2.)
Another study showed that a 1-hour reduction in ED boarding time would result in over $9,000 of additional revenue by reducing ambulance diversion and the number of patients who left without being seen.7 Another found that using tele-emergency services can potentially result in net savings of $3,823 per avoided transfer, while accounting for the costs related to tele-emergency technology, hospital revenues, and patient-associated savings.8
There are other instances where gaps in staffing and cracks in workflow can have a negative impact on hospital operations. For example, the busier hospitals that do have a dedicated nocturnist also struggle with physician retention, since such hospitals have higher volumes and higher cross-coverage needs, and are therefore hard to manage by just one single physician at night. Since these are temporary surges, hiring another full-time nocturnist is not a viable option for the hospitals and is considered an expense in many places.
Similarly, during day shift, if a physician goes on vacation or there are surges in patient volumes, hiring a locum tenens hospitalist can be an expensive option, since the cost also includes travel and lodging. In many instances, hiring locum tenens in a given time frame is also not possible, and it leaves the physicians short staffed, fueling both physicians’ and patients’ dissatisfaction and leading to other operational and safety challenges, which I highlighted above.
Telemedicine services in these situations can provide cross-coverage while nocturnists can focus on admissions and other acute issues. Also, when physicians are on vacation or there is surge capacity (that can be forecast by using various predictive analytics models), hospitals can make plans accordingly and make use of telemedicine services. For example, Providence St. Joseph Health reported improvement in timeliness and efficiency of care after implementation of a telehospitalist program. Their 2-year study at a partner site showed a 59% improvement in patients admitted prior to midnight, about $547,000 improvement in first-day revenue capture, an increase in total revenue days and comparable patient experience scores, and a substantial increase in inpatient census and case mix index.9
Other institutions have successfully implemented some inpatient telemedicine programs – such as telepsych, telestroke, and tele-ICU – and some have also reported positive outcomes in terms of patient satisfaction, improved access, reduced length of stay in the ED, and improved quality metrics. Emory Healthcare in Atlanta reported $4.6 million savings in Medicare costs over a 15-month period from adopting a telemedicine model in the ICU, and a reduction in 60-day readmissions by 2.1%.10 Similarly, another study showed that one large health care center improved its direct contribution margins by 376% (from $7.9 million to $37.7 million) because of increased case volume, shorter lengths of stay, and higher case revenue relative to direct costs. When combined with a logistics center, they reported improved contribution margins by 665% (from $7.9 million to $60.6 million).11
There are barriers to the integration and implementation of inpatient telemedicine, including regulations, reimbursement, physician licensing, adoption of technology, and trust among staff and patients. However, I am cautiously optimistic that increased use of telehealth during the COVID-19 pandemic has allowed patients, physicians, nurses, and health care workers and leaders to gain experience with this technology, which will help them gain confidence and reduce hesitation in adapting to this new digital platform. Ultimately, the extent to which telemedicine is able to positively impact patient care will revolve around overcoming these barriers, likely through an evolution of both the technology itself and the attitudes and regulations surrounding it.
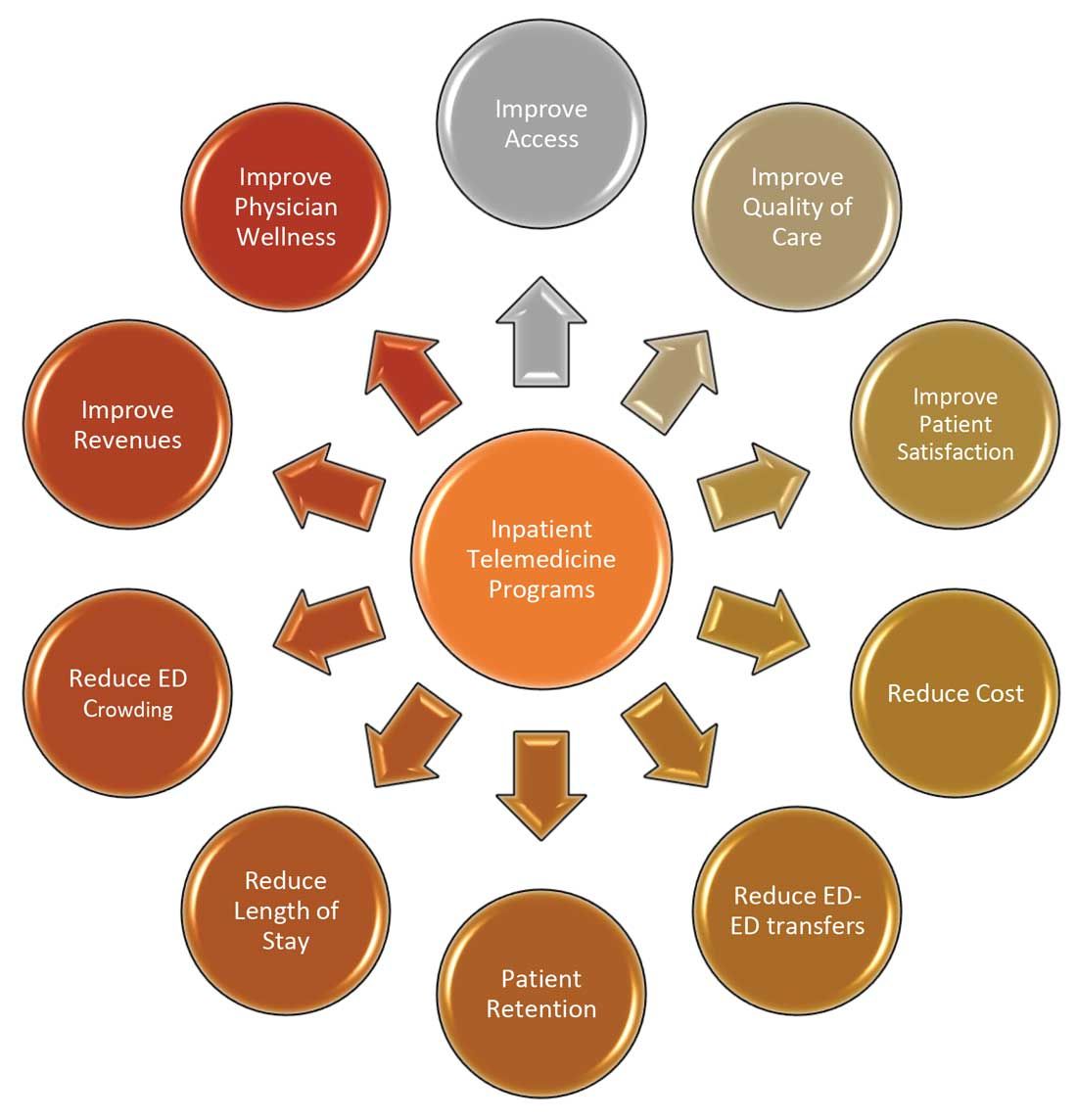
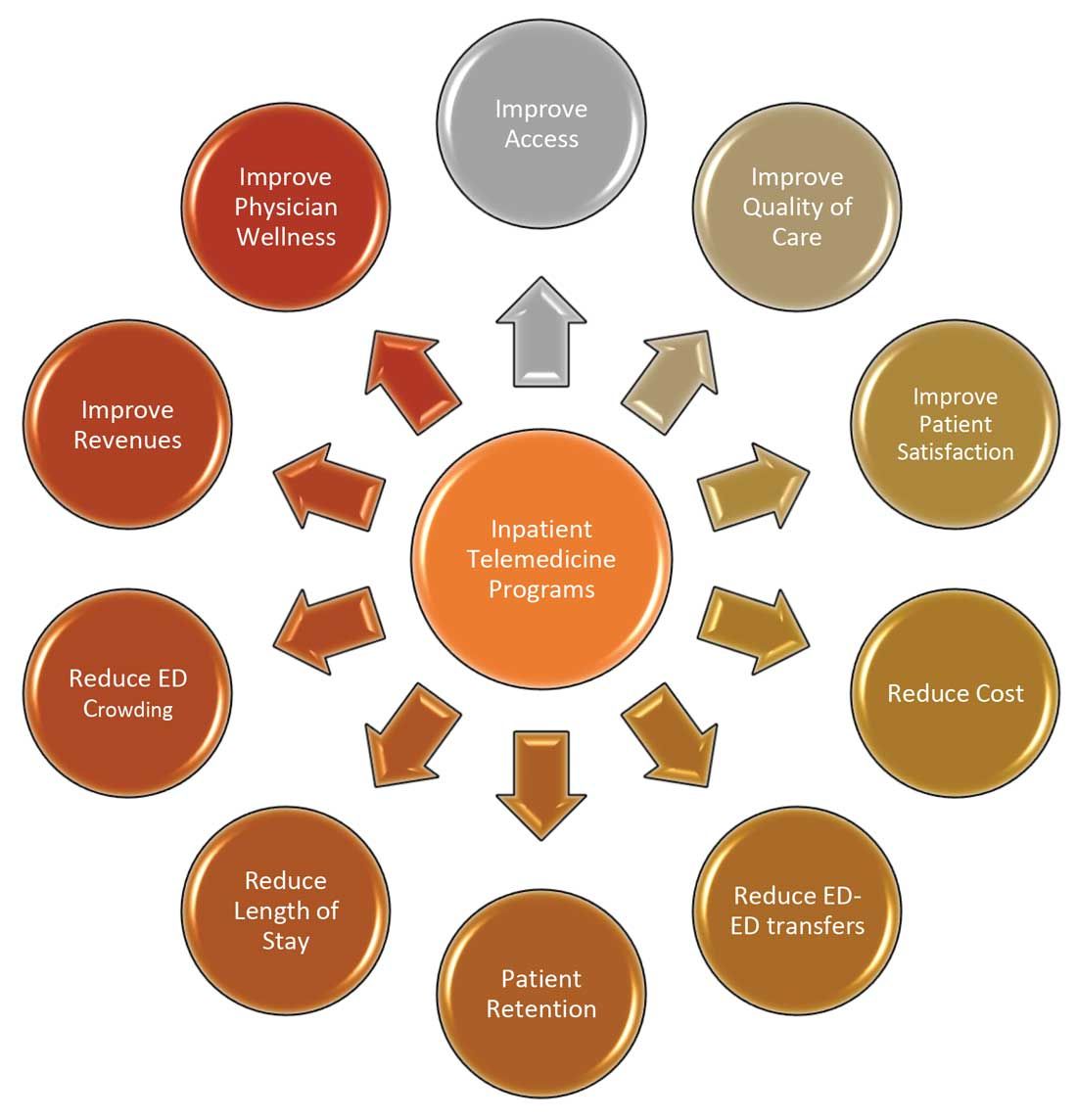
I do not suggest that telemedicine should replace the in-person encounter, but it can be implemented and used successfully in addressing the pain points in U.S. health care. (See Figure 3.)
To that end, the purpose of this article is to spark discussion around different ways of implementing telemedicine in inpatient settings to solve many of the challenges that health care faces today.
Dr. Zia is an internal medicine board-certified physician, serving as a hospitalist and physician adviser in a medically underserved area. She has also served as interim medical director of the department of hospital medicine, and medical staff president, at SIH Herrin Hospital, in Herrin, Ill., part of Southern Illinois Healthcare. She has a special interest in improving access to health care in physician shortage areas.
References
1. Kindermann DR et al. Emergency department transfers and transfer relationships in United States hospitals. Acad Emerg Med. 2015 Feb;22(2):157-65.
2. Sanders RB et al. New hospital telemedicine services: Potential market for a nighttime hospitalist service. Telemed J E Health. 2014 Oct 1;20(10):902-8.
3. Shanafelt T et al. The business case for investing in physician well-being. JAMA Intern Med. 2017;177(12):1826-32.
4. Pines JM et al. The impact of emergency department crowding measures on time to antibiotics for patients with community-acquired pneumonia. Ann Emerg Med. 2007 Nov;50(5):510-6.
5. Pines JM and Hollander JE. Emergency department crowding is associated with poor care for patients with severe pain. Ann Emerg Med. 2008 Jan;51(1):1-5.
6. Chalfin DB et al. Impact of delayed transfer of critically ill patients from the emergency department to the intensive care unit. Crit Care Med. 2007 Jun;35(6):1477-83.
7. Pines JM et al. The financial consequences of lost demand and reducing boarding in hospital emergency departments. Ann Emerg Med. 2011 Oct;58(4):331-40.
8. Natafgi N et al. Using tele-emergency to avoid patient transfers in rural emergency. J Telemed Telecare. 2018 Apri;24(3):193-201.
9. Providence.org/telehealthhospitalistcasestudy.
10. Woodruff Health Sciences Center. CMS report: eICU program reduced hospital stays, saved millions, eased provider shortage. 2017 Apr 5.
11. Lilly CM et al. ICU telemedicine program financial outcomes. Chest. 2017 Feb;151(2):286-97.
COVID-19 has increased confidence in the technology
COVID-19 has increased confidence in the technology
Since the advent of COVID-19, health care has seen an unprecedented rise in virtual health. Telemedicine has come to the forefront of our conversations, and there are many speculations around its future state. One such discussion is around the sustainability and expansion of inpatient telemedicine programs post COVID, and if – and how – it is going to be helpful for health care.
Consider the following scenarios:
Scenario 1
A patient presents to an emergency department of a small community hospital. He needs to be seen by a specialist, but (s)he is not available, so patient gets transferred out to the ED of a different hospital several miles away from his hometown.
He is evaluated in the second ED by the specialist, has repeat testing done – some of those tests were already completed at the first hospital. After evaluating him, the specialist recommends that he does not need to be admitted to the hospital and can be safely followed up as an outpatient. The patient does not require any further intervention and is discharged from the ED.
Scenario 2
Dr. N is a hospitalist in a rural hospital that does not have intensivist support at night. She works 7 on/7 off and is on call 24/7 during her “on” week. Dr. N cannot be physically present in the hospital 24/7. She receives messages from the hospital around the clock and feels that this call schedule is no longer sustainable. She doesn’t feel comfortable admitting patients in the ICU who come to the hospital at night without physically seeing them and without ICU backup. Therefore, some of the patients who are sick enough to be admitted in ICU for closer monitoring but can be potentially handled in this rural hospital get transferred out to a different hospital.
Dr. N has been asking the hospital to provide her intensivist back up at night and to give her some flexibility in the call schedule. However, from hospital’s perspective, the volume isn’t high enough to hire a dedicated nocturnist, and because the hospital is in the small rural area, it is having a hard time attracting more intensivists. After multiple conversations between both parties, Dr. N finally resigns.
Scenario 3
Dr. A is a specialist who is on call covering different hospitals and seeing patients in clinic. His call is getting busier. He has received many new consults and also has to follow up on his other patients in hospital who he saw a day prior.
Dr. A started receiving many pages from the hospitals – some of his patients and their families are anxiously waiting on him so that he can let them go home once he sees them, while some are waiting to know what the next steps and plan of action are. He ends up canceling some of his clinic patients who had scheduled an appointment with him 3, 4, or even 5 months ago. It’s already afternoon.
Dr. A now drives to one hospital, sees his new consults, orders tests which may or may not get results the same day, follows up on other patients, reviews their test results, modifies treatment plans for some while clearing other patients for discharge. He then drives to the other hospital and follows the same process. Some of the patients aren’t happy because of the long wait, a few couldn’t arrange for the ride to go home and ended up staying in hospital 1 extra night, while the ER is getting backlogged waiting on discharges.
These scenarios highlight some of the important and prevalent pain points in health care as shown in Figure 1.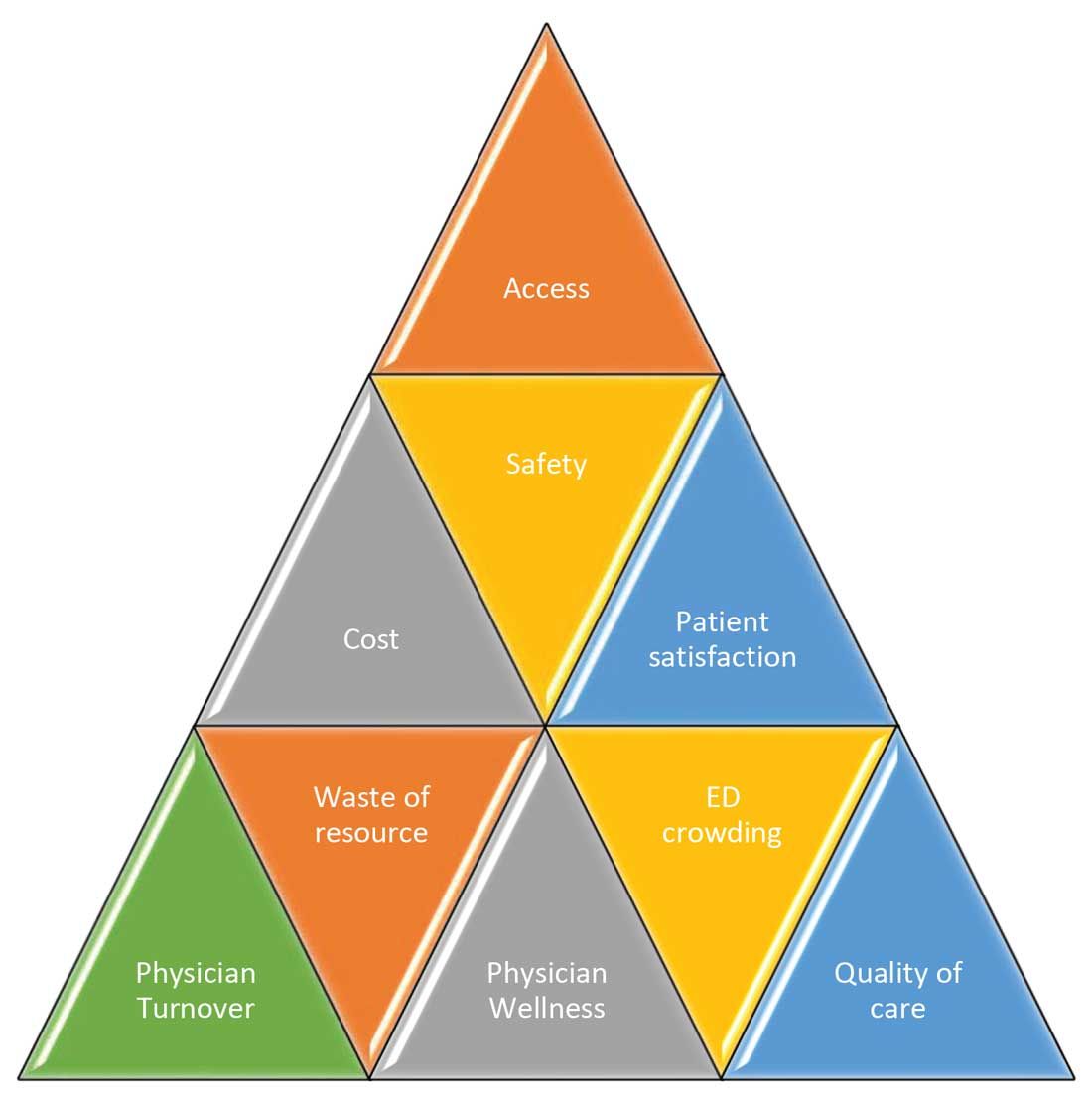
Scenario 1 and part of scenario 2 describe what is called potentially avoidable interfacility transfers. One study showed that around 8% of transferred patients (transferred from one ED to another) were discharged after ED evaluation in the second hospital, meaning they could have been retained locally without necessarily getting transferred if they could have been evaluated by the specialist.1
Transferring a patient from one hospital to another isn’t as simple as picking up a person from point A and dropping him off at point B. Rather it’s a very complicated, high-risk, capital-intensive, and time-consuming process that leads not only to excessive cost involved around transfer but also adds additional stress and burden on the patient and family. In these scenarios, having a specialist available via teleconsult could have eliminated much of this hassle and cost, allowing the patient to stay locally close to family and get access to necessary medical expertise from any part of the country in a timely manner.
Scenario 2 talks about the recruitment and retention challenges in low-volume, low-resourced locations because of call schedule and the lack of specialty support. It is reported in one study that 19% of common hospitalist admissions happen between 7:00 p.m. and 7:00 a.m. Eighty percent of admissions occurred prior to midnight. Nonrural facilities averaged 6.69 hospitalist admissions per night in that study, whereas rural facilities averaged 1.35 admissions.2 It’s like a double-edged sword for such facilities. While having a dedicated nocturnist is not a sustainable model for these hospitals, not having adequate support at night impacts physician wellness, which is already costing hospitals billions of dollars as well as leading to physician turnover: It could cost a hospital somewhere between $500,000 and $1 million to replace just one physician.3 Hence, the potential exists for a telehospitalist program in these settings to address this dilemma.
Scenario 3 sheds light on the operational issues resulting in reduced patient satisfaction and lost revenues, both on the outpatient and inpatient sides by cancellation of office visits and ED backlog. Telemedicine use in these situations can improve the turnaround time of physicians who can see some of those patients while staying at one location as they wait on other patients to show up in the clinic or wait on the operation room crew, or the procedure kit etcetera, hence improving the length of stay, ED throughput, patient satisfaction, and quality of care. This also can improve overall workflow and the wellness of physicians.
One common outcome in all these scenarios is emergency department overcrowding. There have been multiple studies that suggest that ED overcrowding can result in increased costs, lost revenues, and poor clinical outcomes, including delayed administration of antibiotics, delayed administration of analgesics to suffering patients, increased hospital length of stay, and even increased mortality.4-6 A crowded ED limits the ability of an institution to accept referrals and increases medicolegal risks. (See Figure 2.)
Another study showed that a 1-hour reduction in ED boarding time would result in over $9,000 of additional revenue by reducing ambulance diversion and the number of patients who left without being seen.7 Another found that using tele-emergency services can potentially result in net savings of $3,823 per avoided transfer, while accounting for the costs related to tele-emergency technology, hospital revenues, and patient-associated savings.8
There are other instances where gaps in staffing and cracks in workflow can have a negative impact on hospital operations. For example, the busier hospitals that do have a dedicated nocturnist also struggle with physician retention, since such hospitals have higher volumes and higher cross-coverage needs, and are therefore hard to manage by just one single physician at night. Since these are temporary surges, hiring another full-time nocturnist is not a viable option for the hospitals and is considered an expense in many places.
Similarly, during day shift, if a physician goes on vacation or there are surges in patient volumes, hiring a locum tenens hospitalist can be an expensive option, since the cost also includes travel and lodging. In many instances, hiring locum tenens in a given time frame is also not possible, and it leaves the physicians short staffed, fueling both physicians’ and patients’ dissatisfaction and leading to other operational and safety challenges, which I highlighted above.
Telemedicine services in these situations can provide cross-coverage while nocturnists can focus on admissions and other acute issues. Also, when physicians are on vacation or there is surge capacity (that can be forecast by using various predictive analytics models), hospitals can make plans accordingly and make use of telemedicine services. For example, Providence St. Joseph Health reported improvement in timeliness and efficiency of care after implementation of a telehospitalist program. Their 2-year study at a partner site showed a 59% improvement in patients admitted prior to midnight, about $547,000 improvement in first-day revenue capture, an increase in total revenue days and comparable patient experience scores, and a substantial increase in inpatient census and case mix index.9
Other institutions have successfully implemented some inpatient telemedicine programs – such as telepsych, telestroke, and tele-ICU – and some have also reported positive outcomes in terms of patient satisfaction, improved access, reduced length of stay in the ED, and improved quality metrics. Emory Healthcare in Atlanta reported $4.6 million savings in Medicare costs over a 15-month period from adopting a telemedicine model in the ICU, and a reduction in 60-day readmissions by 2.1%.10 Similarly, another study showed that one large health care center improved its direct contribution margins by 376% (from $7.9 million to $37.7 million) because of increased case volume, shorter lengths of stay, and higher case revenue relative to direct costs. When combined with a logistics center, they reported improved contribution margins by 665% (from $7.9 million to $60.6 million).11
There are barriers to the integration and implementation of inpatient telemedicine, including regulations, reimbursement, physician licensing, adoption of technology, and trust among staff and patients. However, I am cautiously optimistic that increased use of telehealth during the COVID-19 pandemic has allowed patients, physicians, nurses, and health care workers and leaders to gain experience with this technology, which will help them gain confidence and reduce hesitation in adapting to this new digital platform. Ultimately, the extent to which telemedicine is able to positively impact patient care will revolve around overcoming these barriers, likely through an evolution of both the technology itself and the attitudes and regulations surrounding it.
I do not suggest that telemedicine should replace the in-person encounter, but it can be implemented and used successfully in addressing the pain points in U.S. health care. (See Figure 3.)
To that end, the purpose of this article is to spark discussion around different ways of implementing telemedicine in inpatient settings to solve many of the challenges that health care faces today.
Dr. Zia is an internal medicine board-certified physician, serving as a hospitalist and physician adviser in a medically underserved area. She has also served as interim medical director of the department of hospital medicine, and medical staff president, at SIH Herrin Hospital, in Herrin, Ill., part of Southern Illinois Healthcare. She has a special interest in improving access to health care in physician shortage areas.
References
1. Kindermann DR et al. Emergency department transfers and transfer relationships in United States hospitals. Acad Emerg Med. 2015 Feb;22(2):157-65.
2. Sanders RB et al. New hospital telemedicine services: Potential market for a nighttime hospitalist service. Telemed J E Health. 2014 Oct 1;20(10):902-8.
3. Shanafelt T et al. The business case for investing in physician well-being. JAMA Intern Med. 2017;177(12):1826-32.
4. Pines JM et al. The impact of emergency department crowding measures on time to antibiotics for patients with community-acquired pneumonia. Ann Emerg Med. 2007 Nov;50(5):510-6.
5. Pines JM and Hollander JE. Emergency department crowding is associated with poor care for patients with severe pain. Ann Emerg Med. 2008 Jan;51(1):1-5.
6. Chalfin DB et al. Impact of delayed transfer of critically ill patients from the emergency department to the intensive care unit. Crit Care Med. 2007 Jun;35(6):1477-83.
7. Pines JM et al. The financial consequences of lost demand and reducing boarding in hospital emergency departments. Ann Emerg Med. 2011 Oct;58(4):331-40.
8. Natafgi N et al. Using tele-emergency to avoid patient transfers in rural emergency. J Telemed Telecare. 2018 Apri;24(3):193-201.
9. Providence.org/telehealthhospitalistcasestudy.
10. Woodruff Health Sciences Center. CMS report: eICU program reduced hospital stays, saved millions, eased provider shortage. 2017 Apr 5.
11. Lilly CM et al. ICU telemedicine program financial outcomes. Chest. 2017 Feb;151(2):286-97.
Since the advent of COVID-19, health care has seen an unprecedented rise in virtual health. Telemedicine has come to the forefront of our conversations, and there are many speculations around its future state. One such discussion is around the sustainability and expansion of inpatient telemedicine programs post COVID, and if – and how – it is going to be helpful for health care.
Consider the following scenarios:
Scenario 1
A patient presents to an emergency department of a small community hospital. He needs to be seen by a specialist, but (s)he is not available, so patient gets transferred out to the ED of a different hospital several miles away from his hometown.
He is evaluated in the second ED by the specialist, has repeat testing done – some of those tests were already completed at the first hospital. After evaluating him, the specialist recommends that he does not need to be admitted to the hospital and can be safely followed up as an outpatient. The patient does not require any further intervention and is discharged from the ED.
Scenario 2
Dr. N is a hospitalist in a rural hospital that does not have intensivist support at night. She works 7 on/7 off and is on call 24/7 during her “on” week. Dr. N cannot be physically present in the hospital 24/7. She receives messages from the hospital around the clock and feels that this call schedule is no longer sustainable. She doesn’t feel comfortable admitting patients in the ICU who come to the hospital at night without physically seeing them and without ICU backup. Therefore, some of the patients who are sick enough to be admitted in ICU for closer monitoring but can be potentially handled in this rural hospital get transferred out to a different hospital.
Dr. N has been asking the hospital to provide her intensivist back up at night and to give her some flexibility in the call schedule. However, from hospital’s perspective, the volume isn’t high enough to hire a dedicated nocturnist, and because the hospital is in the small rural area, it is having a hard time attracting more intensivists. After multiple conversations between both parties, Dr. N finally resigns.
Scenario 3
Dr. A is a specialist who is on call covering different hospitals and seeing patients in clinic. His call is getting busier. He has received many new consults and also has to follow up on his other patients in hospital who he saw a day prior.
Dr. A started receiving many pages from the hospitals – some of his patients and their families are anxiously waiting on him so that he can let them go home once he sees them, while some are waiting to know what the next steps and plan of action are. He ends up canceling some of his clinic patients who had scheduled an appointment with him 3, 4, or even 5 months ago. It’s already afternoon.
Dr. A now drives to one hospital, sees his new consults, orders tests which may or may not get results the same day, follows up on other patients, reviews their test results, modifies treatment plans for some while clearing other patients for discharge. He then drives to the other hospital and follows the same process. Some of the patients aren’t happy because of the long wait, a few couldn’t arrange for the ride to go home and ended up staying in hospital 1 extra night, while the ER is getting backlogged waiting on discharges.
These scenarios highlight some of the important and prevalent pain points in health care as shown in Figure 1.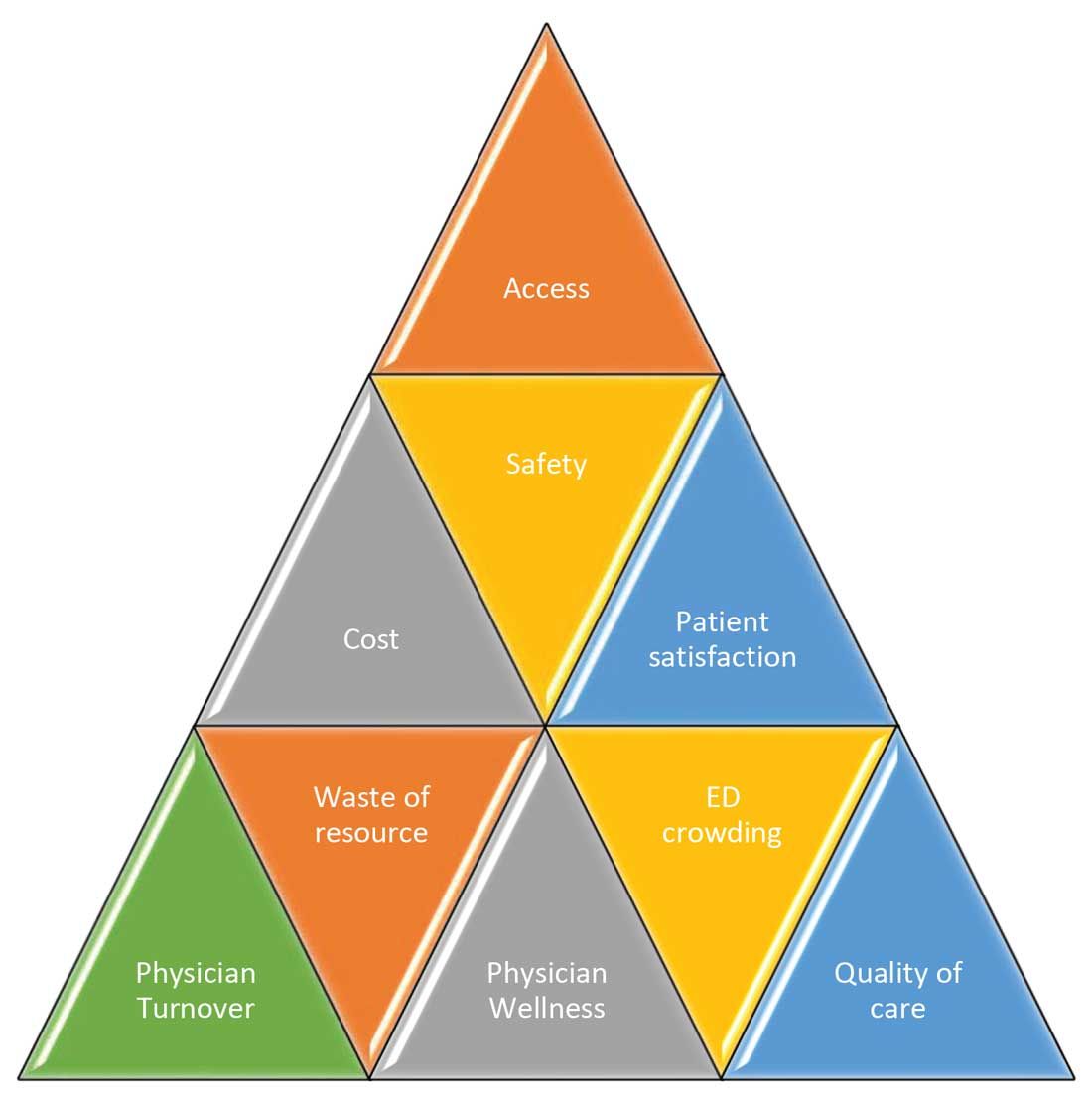
Scenario 1 and part of scenario 2 describe what is called potentially avoidable interfacility transfers. One study showed that around 8% of transferred patients (transferred from one ED to another) were discharged after ED evaluation in the second hospital, meaning they could have been retained locally without necessarily getting transferred if they could have been evaluated by the specialist.1
Transferring a patient from one hospital to another isn’t as simple as picking up a person from point A and dropping him off at point B. Rather it’s a very complicated, high-risk, capital-intensive, and time-consuming process that leads not only to excessive cost involved around transfer but also adds additional stress and burden on the patient and family. In these scenarios, having a specialist available via teleconsult could have eliminated much of this hassle and cost, allowing the patient to stay locally close to family and get access to necessary medical expertise from any part of the country in a timely manner.
Scenario 2 talks about the recruitment and retention challenges in low-volume, low-resourced locations because of call schedule and the lack of specialty support. It is reported in one study that 19% of common hospitalist admissions happen between 7:00 p.m. and 7:00 a.m. Eighty percent of admissions occurred prior to midnight. Nonrural facilities averaged 6.69 hospitalist admissions per night in that study, whereas rural facilities averaged 1.35 admissions.2 It’s like a double-edged sword for such facilities. While having a dedicated nocturnist is not a sustainable model for these hospitals, not having adequate support at night impacts physician wellness, which is already costing hospitals billions of dollars as well as leading to physician turnover: It could cost a hospital somewhere between $500,000 and $1 million to replace just one physician.3 Hence, the potential exists for a telehospitalist program in these settings to address this dilemma.
Scenario 3 sheds light on the operational issues resulting in reduced patient satisfaction and lost revenues, both on the outpatient and inpatient sides by cancellation of office visits and ED backlog. Telemedicine use in these situations can improve the turnaround time of physicians who can see some of those patients while staying at one location as they wait on other patients to show up in the clinic or wait on the operation room crew, or the procedure kit etcetera, hence improving the length of stay, ED throughput, patient satisfaction, and quality of care. This also can improve overall workflow and the wellness of physicians.
One common outcome in all these scenarios is emergency department overcrowding. There have been multiple studies that suggest that ED overcrowding can result in increased costs, lost revenues, and poor clinical outcomes, including delayed administration of antibiotics, delayed administration of analgesics to suffering patients, increased hospital length of stay, and even increased mortality.4-6 A crowded ED limits the ability of an institution to accept referrals and increases medicolegal risks. (See Figure 2.)
Another study showed that a 1-hour reduction in ED boarding time would result in over $9,000 of additional revenue by reducing ambulance diversion and the number of patients who left without being seen.7 Another found that using tele-emergency services can potentially result in net savings of $3,823 per avoided transfer, while accounting for the costs related to tele-emergency technology, hospital revenues, and patient-associated savings.8
There are other instances where gaps in staffing and cracks in workflow can have a negative impact on hospital operations. For example, the busier hospitals that do have a dedicated nocturnist also struggle with physician retention, since such hospitals have higher volumes and higher cross-coverage needs, and are therefore hard to manage by just one single physician at night. Since these are temporary surges, hiring another full-time nocturnist is not a viable option for the hospitals and is considered an expense in many places.
Similarly, during day shift, if a physician goes on vacation or there are surges in patient volumes, hiring a locum tenens hospitalist can be an expensive option, since the cost also includes travel and lodging. In many instances, hiring locum tenens in a given time frame is also not possible, and it leaves the physicians short staffed, fueling both physicians’ and patients’ dissatisfaction and leading to other operational and safety challenges, which I highlighted above.
Telemedicine services in these situations can provide cross-coverage while nocturnists can focus on admissions and other acute issues. Also, when physicians are on vacation or there is surge capacity (that can be forecast by using various predictive analytics models), hospitals can make plans accordingly and make use of telemedicine services. For example, Providence St. Joseph Health reported improvement in timeliness and efficiency of care after implementation of a telehospitalist program. Their 2-year study at a partner site showed a 59% improvement in patients admitted prior to midnight, about $547,000 improvement in first-day revenue capture, an increase in total revenue days and comparable patient experience scores, and a substantial increase in inpatient census and case mix index.9
Other institutions have successfully implemented some inpatient telemedicine programs – such as telepsych, telestroke, and tele-ICU – and some have also reported positive outcomes in terms of patient satisfaction, improved access, reduced length of stay in the ED, and improved quality metrics. Emory Healthcare in Atlanta reported $4.6 million savings in Medicare costs over a 15-month period from adopting a telemedicine model in the ICU, and a reduction in 60-day readmissions by 2.1%.10 Similarly, another study showed that one large health care center improved its direct contribution margins by 376% (from $7.9 million to $37.7 million) because of increased case volume, shorter lengths of stay, and higher case revenue relative to direct costs. When combined with a logistics center, they reported improved contribution margins by 665% (from $7.9 million to $60.6 million).11
There are barriers to the integration and implementation of inpatient telemedicine, including regulations, reimbursement, physician licensing, adoption of technology, and trust among staff and patients. However, I am cautiously optimistic that increased use of telehealth during the COVID-19 pandemic has allowed patients, physicians, nurses, and health care workers and leaders to gain experience with this technology, which will help them gain confidence and reduce hesitation in adapting to this new digital platform. Ultimately, the extent to which telemedicine is able to positively impact patient care will revolve around overcoming these barriers, likely through an evolution of both the technology itself and the attitudes and regulations surrounding it.
I do not suggest that telemedicine should replace the in-person encounter, but it can be implemented and used successfully in addressing the pain points in U.S. health care. (See Figure 3.)
To that end, the purpose of this article is to spark discussion around different ways of implementing telemedicine in inpatient settings to solve many of the challenges that health care faces today.
Dr. Zia is an internal medicine board-certified physician, serving as a hospitalist and physician adviser in a medically underserved area. She has also served as interim medical director of the department of hospital medicine, and medical staff president, at SIH Herrin Hospital, in Herrin, Ill., part of Southern Illinois Healthcare. She has a special interest in improving access to health care in physician shortage areas.
References
1. Kindermann DR et al. Emergency department transfers and transfer relationships in United States hospitals. Acad Emerg Med. 2015 Feb;22(2):157-65.
2. Sanders RB et al. New hospital telemedicine services: Potential market for a nighttime hospitalist service. Telemed J E Health. 2014 Oct 1;20(10):902-8.
3. Shanafelt T et al. The business case for investing in physician well-being. JAMA Intern Med. 2017;177(12):1826-32.
4. Pines JM et al. The impact of emergency department crowding measures on time to antibiotics for patients with community-acquired pneumonia. Ann Emerg Med. 2007 Nov;50(5):510-6.
5. Pines JM and Hollander JE. Emergency department crowding is associated with poor care for patients with severe pain. Ann Emerg Med. 2008 Jan;51(1):1-5.
6. Chalfin DB et al. Impact of delayed transfer of critically ill patients from the emergency department to the intensive care unit. Crit Care Med. 2007 Jun;35(6):1477-83.
7. Pines JM et al. The financial consequences of lost demand and reducing boarding in hospital emergency departments. Ann Emerg Med. 2011 Oct;58(4):331-40.
8. Natafgi N et al. Using tele-emergency to avoid patient transfers in rural emergency. J Telemed Telecare. 2018 Apri;24(3):193-201.
9. Providence.org/telehealthhospitalistcasestudy.
10. Woodruff Health Sciences Center. CMS report: eICU program reduced hospital stays, saved millions, eased provider shortage. 2017 Apr 5.
11. Lilly CM et al. ICU telemedicine program financial outcomes. Chest. 2017 Feb;151(2):286-97.
Accessing data during EHR downtime
Reducing loss of efficiency
Electronic health record (EHR) implementations involve long downtimes, which are an under-recognized patient safety risk, as clinicians are forced to switch to completely manual, paper-based, and important unfamiliar workflows to care for their acutely ill patients, said Subha Airan-Javia, MD, FAMIA, a hospitalist at the University of Pennsylvania, Philadelphia.
“In this setting, we discovered an unanticipated benefit of our tool [Carelign, initially built to digitize the handoff process] as a clinical resource during EHR downtime, giving clinicians access to critical data as well as an electronic platform to collaborate as a team around the care of their patients,” she said.
There are two important takeaways from their study on this issue. “The first is that Carelign was able to give clinicians access to clinical data that would otherwise have been unavailable, including vitals, labs, medications, care plans and care team assignments,” Dr. Airan-Javia said. “This undoubtedly mitigated patient safety risks during the EHR downtime.”
The second: “As many clinicians know, any change in workflow, even for a few hours, can make providing a high level of patient care very difficult,” she added. “During a downtime without a tool like Carelign, clinicians have to rely on paper and bedside charts, writing notes on paper and then re-typing them into the EHR when it is back up. This adds to the already excessive amount of administrative work that is burning clinicians out.” Using a tool like Carelign means no such loss in efficiency.
“A tool like Carelign, particularly because it is something that can be used without having to integrate it with the EHR, can put some control back into a hospitalist’s hands, to have a say in their workflow,” Dr. Airan-Javia said. “In a world where EHRs are designed to optimize billing, it can be game-changer to have a tool like Carelign that was created by a practicing clinician, for clinicians. Anyone interested in this area is welcome to reach out to me at subhaairan@gmail.com for collaboration or more information.”
Reference
1. Airan-Javia SL, et al. Mind the gap: Revolutionizing the EHR downtime experience with an interoperable workflow tool. Abstract published at Hospital Medicine 2019, March 24-27, National Harbor, Md. Abstract 380. https://www.shmabstracts.com/abstract/mind-the-gap-revolutionizing-the-ehr-downtime-experience-with-an-interoperable-workflow-tool/. Accessed Dec 11, 2019.
Reducing loss of efficiency
Reducing loss of efficiency
Electronic health record (EHR) implementations involve long downtimes, which are an under-recognized patient safety risk, as clinicians are forced to switch to completely manual, paper-based, and important unfamiliar workflows to care for their acutely ill patients, said Subha Airan-Javia, MD, FAMIA, a hospitalist at the University of Pennsylvania, Philadelphia.
“In this setting, we discovered an unanticipated benefit of our tool [Carelign, initially built to digitize the handoff process] as a clinical resource during EHR downtime, giving clinicians access to critical data as well as an electronic platform to collaborate as a team around the care of their patients,” she said.
There are two important takeaways from their study on this issue. “The first is that Carelign was able to give clinicians access to clinical data that would otherwise have been unavailable, including vitals, labs, medications, care plans and care team assignments,” Dr. Airan-Javia said. “This undoubtedly mitigated patient safety risks during the EHR downtime.”
The second: “As many clinicians know, any change in workflow, even for a few hours, can make providing a high level of patient care very difficult,” she added. “During a downtime without a tool like Carelign, clinicians have to rely on paper and bedside charts, writing notes on paper and then re-typing them into the EHR when it is back up. This adds to the already excessive amount of administrative work that is burning clinicians out.” Using a tool like Carelign means no such loss in efficiency.
“A tool like Carelign, particularly because it is something that can be used without having to integrate it with the EHR, can put some control back into a hospitalist’s hands, to have a say in their workflow,” Dr. Airan-Javia said. “In a world where EHRs are designed to optimize billing, it can be game-changer to have a tool like Carelign that was created by a practicing clinician, for clinicians. Anyone interested in this area is welcome to reach out to me at subhaairan@gmail.com for collaboration or more information.”
Reference
1. Airan-Javia SL, et al. Mind the gap: Revolutionizing the EHR downtime experience with an interoperable workflow tool. Abstract published at Hospital Medicine 2019, March 24-27, National Harbor, Md. Abstract 380. https://www.shmabstracts.com/abstract/mind-the-gap-revolutionizing-the-ehr-downtime-experience-with-an-interoperable-workflow-tool/. Accessed Dec 11, 2019.
Electronic health record (EHR) implementations involve long downtimes, which are an under-recognized patient safety risk, as clinicians are forced to switch to completely manual, paper-based, and important unfamiliar workflows to care for their acutely ill patients, said Subha Airan-Javia, MD, FAMIA, a hospitalist at the University of Pennsylvania, Philadelphia.
“In this setting, we discovered an unanticipated benefit of our tool [Carelign, initially built to digitize the handoff process] as a clinical resource during EHR downtime, giving clinicians access to critical data as well as an electronic platform to collaborate as a team around the care of their patients,” she said.
There are two important takeaways from their study on this issue. “The first is that Carelign was able to give clinicians access to clinical data that would otherwise have been unavailable, including vitals, labs, medications, care plans and care team assignments,” Dr. Airan-Javia said. “This undoubtedly mitigated patient safety risks during the EHR downtime.”
The second: “As many clinicians know, any change in workflow, even for a few hours, can make providing a high level of patient care very difficult,” she added. “During a downtime without a tool like Carelign, clinicians have to rely on paper and bedside charts, writing notes on paper and then re-typing them into the EHR when it is back up. This adds to the already excessive amount of administrative work that is burning clinicians out.” Using a tool like Carelign means no such loss in efficiency.
“A tool like Carelign, particularly because it is something that can be used without having to integrate it with the EHR, can put some control back into a hospitalist’s hands, to have a say in their workflow,” Dr. Airan-Javia said. “In a world where EHRs are designed to optimize billing, it can be game-changer to have a tool like Carelign that was created by a practicing clinician, for clinicians. Anyone interested in this area is welcome to reach out to me at subhaairan@gmail.com for collaboration or more information.”
Reference
1. Airan-Javia SL, et al. Mind the gap: Revolutionizing the EHR downtime experience with an interoperable workflow tool. Abstract published at Hospital Medicine 2019, March 24-27, National Harbor, Md. Abstract 380. https://www.shmabstracts.com/abstract/mind-the-gap-revolutionizing-the-ehr-downtime-experience-with-an-interoperable-workflow-tool/. Accessed Dec 11, 2019.
Roots of physician burnout: It’s the work load
Work load, not personal vulnerability, may be at the root of the current physician burnout crisis, a recent study has concluded.
The cutting-edge research utilized cognitive theory and work load analysis to get at the source of burnout among practitioners. The findings indicate that, although some institutions continue to emphasize personal responsibility of physicians to address the issue, it may be the amount and structure of the work itself that triggers burnout in doctors.
“We evaluated the cognitive load of a clinical workday in a national sample of U.S. physicians and its relationship with burnout and professional satisfaction,” wrote Elizabeth Harry, MD, SFHM, a hospitalist at the University of Colorado at Denver, Aurora and coauthors. The results were reported in the Joint Commission Journal on Quality and Patient Safety.
The researchers investigated whether task load correlated with burnout scores in a large national study of U.S. physicians from October 2017 to March 2018.
As the delivery of health care becomes more complex, physicians are charged with ever-increasing amount of administrative and cognitive tasks. Recent evidence indicates that this growing complexity of work is tied to a greater risk of burnout in physicians, compared with workers in other fields. Cognitive load theory, pioneered by psychologist Jonathan Sweller, identified limitations in working memory that humans depend on to carry out cognitive tasks. Cognitive load refers to the amount of working memory used, which can be reduced in the presence of external emotional or physiological stressors. While a potential link between cognitive load and burnout may seem self-evident, the correlation between the cognitive load of physicians and burnout has not been evaluated in a large-scale study until recently.
Physician task load (PTL) was measured using the National Aeronautics and Space Administration Task Load Index (NASA-TLX), a validated questionnaire frequently used to evaluate the cognitive load of work environments, including health care environments. Four domains (perception of effort and mental, physical, and temporal demands) were used to calculate the total PTL score.
Burnout was evaluated using the Emotional Exhaustion and Depersonalization scales of the Maslach Burnout Inventory, a validated tool considered the gold standard for measurement.
The survey sample consisted of physicians of all specialties and was assembled using the American Medical Association Physician Masterfile, an almost complete record of all U.S. physicians independent of AMA membership. All responses were anonymous and participation was voluntary.
Results
Among 30,456 physicians who received the survey, 5,197 (17.1%) responded. In total, 5,276 physicians were included in the analysis.
The median age of respondents was 53 years, and 61.8% self-identified as male. Twenty-four specialties were identified: 23.8% were from a primary care discipline and internal medicine represented the largest respondent group (12.1%).
Almost half of respondents (49.7%) worked in private practice, and 44.8% had been in practice for 21 years or longer.
Overall, 44.0% had at least one symptom of burnout, 38.8% of participants scored in the high range for emotional exhaustion, and 27.4% scored in the high range for depersonalization. The mean score in task load dimension varied by specialty.
The mean PTL score was 260.9 (standard deviation, 71.4). The specialties with the highest PTL score were emergency medicine (369.8), urology (353.7), general surgery subspecialties (343.9), internal medicine subspecialties (342.2), and radiology (341.6).
Aside from specialty, PTL scores also varied by practice setting, gender, age, number of hours worked per week, number of nights on call per week, and years in practice.
The researchers observed a dose response relationship between PTL and risk of burnout. For every 40-point (10%) reduction in PTL, there was 33% lower odds of experiencing burnout (odds ratio, 0.67; 95% confidence interval, 0.65-0.70; P < .0001). Multivariable analyses also indicated that PTL was a significant predictor of burnout, independent of practice setting, specialty, age, gender, and hours worked.
Organizational strategies to reduce physician burnout
Coauthors of the study, Tait D. Shanafelt, MD, professor of medicine at Stanford (Calif.) University and Colin P. West, MD, PhD, of the Mayo Clinic in Rochester, Minn., are both experts on physician well-being and are passionate about finding new ways to reduce physician distress and improving health care delivery.
“Authentic efforts to address this problem must move beyond personal resilience,” Dr. Shanafelt said in an interview. “Organizations that fail to get serious about this issue are going to be left behind and struggle in the war for talent.
“Much like our efforts to improve quality, advancing clinician well-being requires organizations to make it a priority and establish the structure, process, and leadership to promote the desired outcomes,” said Dr. Shanafelt.
One potential strategy for improvement is appointing a chief wellness officer, a dedicated individual within the health care system that leads the organizational effort, explained Dr. Shanafelt. “Over 30 vanguard institutions across the United States have already taken this step.”
Dr. West, a coauthor of the study, explained that conducting an analysis of PTL is fairly straightforward for hospitals and individual institutions. “The NASA-TLX tool is widely available, free to use, and not overly complex, and it could be used to provide insight into physician effort and mental, physical, and temporal demand levels,” he said in an interview.
“Deeper evaluations could follow to identify specific potential solutions, particularly system-level approaches to alleviate PTL,” Dr. West explained. “In the short term, such analyses and solutions would have costs, but helping physicians work more optimally and with less chronic strain from excessive task load would save far more than these costs overall.”
Dr. West also noted that physician burnout is very expensive to a health care system, and strategies to promote physician well-being would be a prudent financial decision long term for health care organizations.
Dr. Harry, lead author of the study, agreed with Dr. West, noting that “quality improvement literature has demonstrated that improvements in inefficiencies that lead to increased demand in the workplace often has the benefit of reduced cost.
“Many studies have demonstrated the risk of turnover due to burnout and the significant cost of physician turn over,” she said in an interview. “This cost avoidance is well worth the investment in improved operations to minimize unnecessary task load.”
Dr. Harry also recommended the NASA-TLX tool as a free resource for health systems and organizations. She noted that future studies will further validate the reliability of the tool.
“At the core, we need to focus on system redesign at both the micro and the macro level,” Dr. Harry said. “Each health system will need to assess inefficiencies in their work flow, while regulatory bodies need to consider the downstream task load of mandates and reporting requirements, all of which contribute to more cognitive load.”
The study was supported by funding from the Stanford Medicine WellMD Center, the American Medical Association, and the Mayo Clinic department of medicine program on physician well-being. Coauthors Lotte N. Dyrbye, MD, and Dr. Shanafelt are coinventors of the Physician Well-being Index, Medical Student Well-Being Index, Nurse Well-Being, and Well-Being Index. Mayo Clinic holds the copyright to these instruments and has licensed them for external use. Dr. Dyrbye and Dr. Shanafelt receive a portion of any royalties paid to Mayo Clinic. All other authors reported no conflicts of interest.
Work load, not personal vulnerability, may be at the root of the current physician burnout crisis, a recent study has concluded.
The cutting-edge research utilized cognitive theory and work load analysis to get at the source of burnout among practitioners. The findings indicate that, although some institutions continue to emphasize personal responsibility of physicians to address the issue, it may be the amount and structure of the work itself that triggers burnout in doctors.
“We evaluated the cognitive load of a clinical workday in a national sample of U.S. physicians and its relationship with burnout and professional satisfaction,” wrote Elizabeth Harry, MD, SFHM, a hospitalist at the University of Colorado at Denver, Aurora and coauthors. The results were reported in the Joint Commission Journal on Quality and Patient Safety.
The researchers investigated whether task load correlated with burnout scores in a large national study of U.S. physicians from October 2017 to March 2018.
As the delivery of health care becomes more complex, physicians are charged with ever-increasing amount of administrative and cognitive tasks. Recent evidence indicates that this growing complexity of work is tied to a greater risk of burnout in physicians, compared with workers in other fields. Cognitive load theory, pioneered by psychologist Jonathan Sweller, identified limitations in working memory that humans depend on to carry out cognitive tasks. Cognitive load refers to the amount of working memory used, which can be reduced in the presence of external emotional or physiological stressors. While a potential link between cognitive load and burnout may seem self-evident, the correlation between the cognitive load of physicians and burnout has not been evaluated in a large-scale study until recently.
Physician task load (PTL) was measured using the National Aeronautics and Space Administration Task Load Index (NASA-TLX), a validated questionnaire frequently used to evaluate the cognitive load of work environments, including health care environments. Four domains (perception of effort and mental, physical, and temporal demands) were used to calculate the total PTL score.
Burnout was evaluated using the Emotional Exhaustion and Depersonalization scales of the Maslach Burnout Inventory, a validated tool considered the gold standard for measurement.
The survey sample consisted of physicians of all specialties and was assembled using the American Medical Association Physician Masterfile, an almost complete record of all U.S. physicians independent of AMA membership. All responses were anonymous and participation was voluntary.
Results
Among 30,456 physicians who received the survey, 5,197 (17.1%) responded. In total, 5,276 physicians were included in the analysis.
The median age of respondents was 53 years, and 61.8% self-identified as male. Twenty-four specialties were identified: 23.8% were from a primary care discipline and internal medicine represented the largest respondent group (12.1%).
Almost half of respondents (49.7%) worked in private practice, and 44.8% had been in practice for 21 years or longer.
Overall, 44.0% had at least one symptom of burnout, 38.8% of participants scored in the high range for emotional exhaustion, and 27.4% scored in the high range for depersonalization. The mean score in task load dimension varied by specialty.
The mean PTL score was 260.9 (standard deviation, 71.4). The specialties with the highest PTL score were emergency medicine (369.8), urology (353.7), general surgery subspecialties (343.9), internal medicine subspecialties (342.2), and radiology (341.6).
Aside from specialty, PTL scores also varied by practice setting, gender, age, number of hours worked per week, number of nights on call per week, and years in practice.
The researchers observed a dose response relationship between PTL and risk of burnout. For every 40-point (10%) reduction in PTL, there was 33% lower odds of experiencing burnout (odds ratio, 0.67; 95% confidence interval, 0.65-0.70; P < .0001). Multivariable analyses also indicated that PTL was a significant predictor of burnout, independent of practice setting, specialty, age, gender, and hours worked.
Organizational strategies to reduce physician burnout
Coauthors of the study, Tait D. Shanafelt, MD, professor of medicine at Stanford (Calif.) University and Colin P. West, MD, PhD, of the Mayo Clinic in Rochester, Minn., are both experts on physician well-being and are passionate about finding new ways to reduce physician distress and improving health care delivery.
“Authentic efforts to address this problem must move beyond personal resilience,” Dr. Shanafelt said in an interview. “Organizations that fail to get serious about this issue are going to be left behind and struggle in the war for talent.
“Much like our efforts to improve quality, advancing clinician well-being requires organizations to make it a priority and establish the structure, process, and leadership to promote the desired outcomes,” said Dr. Shanafelt.
One potential strategy for improvement is appointing a chief wellness officer, a dedicated individual within the health care system that leads the organizational effort, explained Dr. Shanafelt. “Over 30 vanguard institutions across the United States have already taken this step.”
Dr. West, a coauthor of the study, explained that conducting an analysis of PTL is fairly straightforward for hospitals and individual institutions. “The NASA-TLX tool is widely available, free to use, and not overly complex, and it could be used to provide insight into physician effort and mental, physical, and temporal demand levels,” he said in an interview.
“Deeper evaluations could follow to identify specific potential solutions, particularly system-level approaches to alleviate PTL,” Dr. West explained. “In the short term, such analyses and solutions would have costs, but helping physicians work more optimally and with less chronic strain from excessive task load would save far more than these costs overall.”
Dr. West also noted that physician burnout is very expensive to a health care system, and strategies to promote physician well-being would be a prudent financial decision long term for health care organizations.
Dr. Harry, lead author of the study, agreed with Dr. West, noting that “quality improvement literature has demonstrated that improvements in inefficiencies that lead to increased demand in the workplace often has the benefit of reduced cost.
“Many studies have demonstrated the risk of turnover due to burnout and the significant cost of physician turn over,” she said in an interview. “This cost avoidance is well worth the investment in improved operations to minimize unnecessary task load.”
Dr. Harry also recommended the NASA-TLX tool as a free resource for health systems and organizations. She noted that future studies will further validate the reliability of the tool.
“At the core, we need to focus on system redesign at both the micro and the macro level,” Dr. Harry said. “Each health system will need to assess inefficiencies in their work flow, while regulatory bodies need to consider the downstream task load of mandates and reporting requirements, all of which contribute to more cognitive load.”
The study was supported by funding from the Stanford Medicine WellMD Center, the American Medical Association, and the Mayo Clinic department of medicine program on physician well-being. Coauthors Lotte N. Dyrbye, MD, and Dr. Shanafelt are coinventors of the Physician Well-being Index, Medical Student Well-Being Index, Nurse Well-Being, and Well-Being Index. Mayo Clinic holds the copyright to these instruments and has licensed them for external use. Dr. Dyrbye and Dr. Shanafelt receive a portion of any royalties paid to Mayo Clinic. All other authors reported no conflicts of interest.
Work load, not personal vulnerability, may be at the root of the current physician burnout crisis, a recent study has concluded.
The cutting-edge research utilized cognitive theory and work load analysis to get at the source of burnout among practitioners. The findings indicate that, although some institutions continue to emphasize personal responsibility of physicians to address the issue, it may be the amount and structure of the work itself that triggers burnout in doctors.
“We evaluated the cognitive load of a clinical workday in a national sample of U.S. physicians and its relationship with burnout and professional satisfaction,” wrote Elizabeth Harry, MD, SFHM, a hospitalist at the University of Colorado at Denver, Aurora and coauthors. The results were reported in the Joint Commission Journal on Quality and Patient Safety.
The researchers investigated whether task load correlated with burnout scores in a large national study of U.S. physicians from October 2017 to March 2018.
As the delivery of health care becomes more complex, physicians are charged with ever-increasing amount of administrative and cognitive tasks. Recent evidence indicates that this growing complexity of work is tied to a greater risk of burnout in physicians, compared with workers in other fields. Cognitive load theory, pioneered by psychologist Jonathan Sweller, identified limitations in working memory that humans depend on to carry out cognitive tasks. Cognitive load refers to the amount of working memory used, which can be reduced in the presence of external emotional or physiological stressors. While a potential link between cognitive load and burnout may seem self-evident, the correlation between the cognitive load of physicians and burnout has not been evaluated in a large-scale study until recently.
Physician task load (PTL) was measured using the National Aeronautics and Space Administration Task Load Index (NASA-TLX), a validated questionnaire frequently used to evaluate the cognitive load of work environments, including health care environments. Four domains (perception of effort and mental, physical, and temporal demands) were used to calculate the total PTL score.
Burnout was evaluated using the Emotional Exhaustion and Depersonalization scales of the Maslach Burnout Inventory, a validated tool considered the gold standard for measurement.
The survey sample consisted of physicians of all specialties and was assembled using the American Medical Association Physician Masterfile, an almost complete record of all U.S. physicians independent of AMA membership. All responses were anonymous and participation was voluntary.
Results
Among 30,456 physicians who received the survey, 5,197 (17.1%) responded. In total, 5,276 physicians were included in the analysis.
The median age of respondents was 53 years, and 61.8% self-identified as male. Twenty-four specialties were identified: 23.8% were from a primary care discipline and internal medicine represented the largest respondent group (12.1%).
Almost half of respondents (49.7%) worked in private practice, and 44.8% had been in practice for 21 years or longer.
Overall, 44.0% had at least one symptom of burnout, 38.8% of participants scored in the high range for emotional exhaustion, and 27.4% scored in the high range for depersonalization. The mean score in task load dimension varied by specialty.
The mean PTL score was 260.9 (standard deviation, 71.4). The specialties with the highest PTL score were emergency medicine (369.8), urology (353.7), general surgery subspecialties (343.9), internal medicine subspecialties (342.2), and radiology (341.6).
Aside from specialty, PTL scores also varied by practice setting, gender, age, number of hours worked per week, number of nights on call per week, and years in practice.
The researchers observed a dose response relationship between PTL and risk of burnout. For every 40-point (10%) reduction in PTL, there was 33% lower odds of experiencing burnout (odds ratio, 0.67; 95% confidence interval, 0.65-0.70; P < .0001). Multivariable analyses also indicated that PTL was a significant predictor of burnout, independent of practice setting, specialty, age, gender, and hours worked.
Organizational strategies to reduce physician burnout
Coauthors of the study, Tait D. Shanafelt, MD, professor of medicine at Stanford (Calif.) University and Colin P. West, MD, PhD, of the Mayo Clinic in Rochester, Minn., are both experts on physician well-being and are passionate about finding new ways to reduce physician distress and improving health care delivery.
“Authentic efforts to address this problem must move beyond personal resilience,” Dr. Shanafelt said in an interview. “Organizations that fail to get serious about this issue are going to be left behind and struggle in the war for talent.
“Much like our efforts to improve quality, advancing clinician well-being requires organizations to make it a priority and establish the structure, process, and leadership to promote the desired outcomes,” said Dr. Shanafelt.
One potential strategy for improvement is appointing a chief wellness officer, a dedicated individual within the health care system that leads the organizational effort, explained Dr. Shanafelt. “Over 30 vanguard institutions across the United States have already taken this step.”
Dr. West, a coauthor of the study, explained that conducting an analysis of PTL is fairly straightforward for hospitals and individual institutions. “The NASA-TLX tool is widely available, free to use, and not overly complex, and it could be used to provide insight into physician effort and mental, physical, and temporal demand levels,” he said in an interview.
“Deeper evaluations could follow to identify specific potential solutions, particularly system-level approaches to alleviate PTL,” Dr. West explained. “In the short term, such analyses and solutions would have costs, but helping physicians work more optimally and with less chronic strain from excessive task load would save far more than these costs overall.”
Dr. West also noted that physician burnout is very expensive to a health care system, and strategies to promote physician well-being would be a prudent financial decision long term for health care organizations.
Dr. Harry, lead author of the study, agreed with Dr. West, noting that “quality improvement literature has demonstrated that improvements in inefficiencies that lead to increased demand in the workplace often has the benefit of reduced cost.
“Many studies have demonstrated the risk of turnover due to burnout and the significant cost of physician turn over,” she said in an interview. “This cost avoidance is well worth the investment in improved operations to minimize unnecessary task load.”
Dr. Harry also recommended the NASA-TLX tool as a free resource for health systems and organizations. She noted that future studies will further validate the reliability of the tool.
“At the core, we need to focus on system redesign at both the micro and the macro level,” Dr. Harry said. “Each health system will need to assess inefficiencies in their work flow, while regulatory bodies need to consider the downstream task load of mandates and reporting requirements, all of which contribute to more cognitive load.”
The study was supported by funding from the Stanford Medicine WellMD Center, the American Medical Association, and the Mayo Clinic department of medicine program on physician well-being. Coauthors Lotte N. Dyrbye, MD, and Dr. Shanafelt are coinventors of the Physician Well-being Index, Medical Student Well-Being Index, Nurse Well-Being, and Well-Being Index. Mayo Clinic holds the copyright to these instruments and has licensed them for external use. Dr. Dyrbye and Dr. Shanafelt receive a portion of any royalties paid to Mayo Clinic. All other authors reported no conflicts of interest.
FROM THE JOINT COMMISSION JOURNAL ON QUALITY AND PATIENT SAFETY
Key trends in hospitalist compensation from the 2020 SoHM Report
In a time of tremendous uncertainty, there is one trend that seems consistent year over year – the undisputed value of hospitalists. In the 2020 State of Hospital Medicine (SoHM) Report, the Society of Hospital Medicine partnered with the Medical Group Management Association (MGMA) to provide data on hospitalist compensation and productivity. The Report provides resounding evidence that hospitalists continue to be compensated at rising rates. This may be driven by both the continued demand-supply mismatch and a recognition of the overall value they generate rather than strictly the volume of their productivity.
In 2020, the median total compensation nationally for adult hospitalists (internal medicine and family medicine) was $307,633, representing an increase of over 6% from the 2018 Survey (see Figure 1). 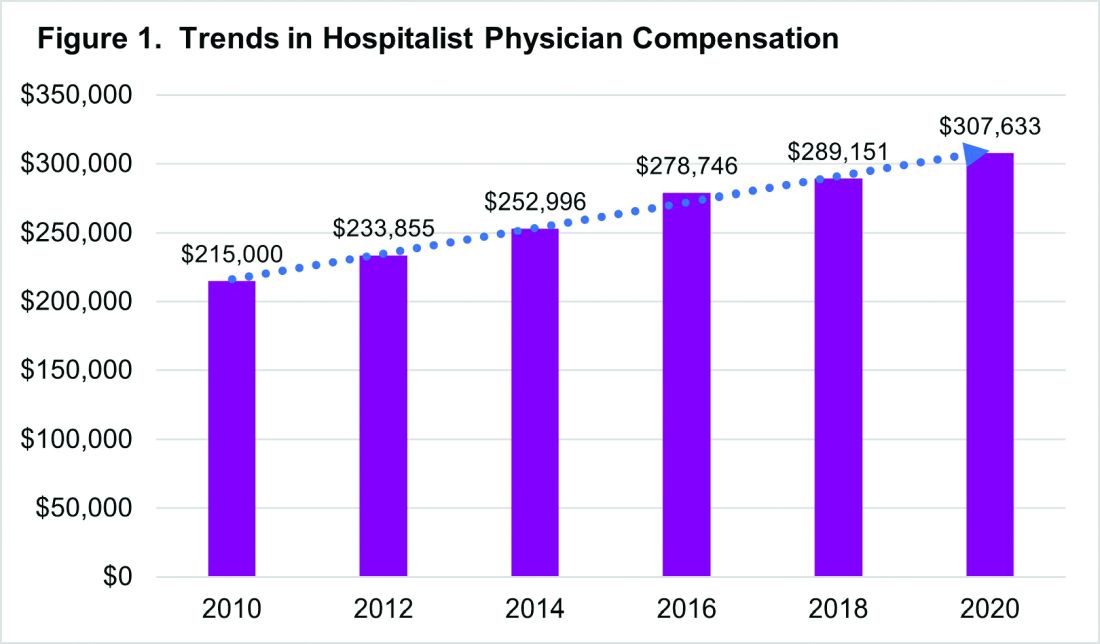
With significant regional variability in compensation across the country, hospitalists in the South continue to earn more than their colleagues in the East – a median compensation difference of about $33,000. However, absolute wage comparisons can be misleading without also considering regional variations in productivity as well.
Reviewing compensation per work relative value unit (wRVU) and per encounter offer additional insight for a more comprehensive assessment. When comparing regional compensation per wRVU, the 2020 Survey continues to show a trend toward hospitalists in the Midwest and West earning more per wRVU than their colleagues in other parts of the country ($78.13 per RVU in the Midwest, $78.95 per RVU in the West). More striking is how hospital medicine groups (HMGs) in the South garner lower compensation per RVU ($57.77) than those in the East ($67.54), even though their total compensation was much higher. This could reflect the gradual decline in compensation per wRVU that’s observed at higher productivity levels. While it’s typical for compensation to increase as productivity does, the rate of increase is generally to a lesser degree.
Like past SoHM Surveys, the 2020 Report revealed that academic and non-academic hospitalists are compensated similarly per wRVU (see Figure 2). 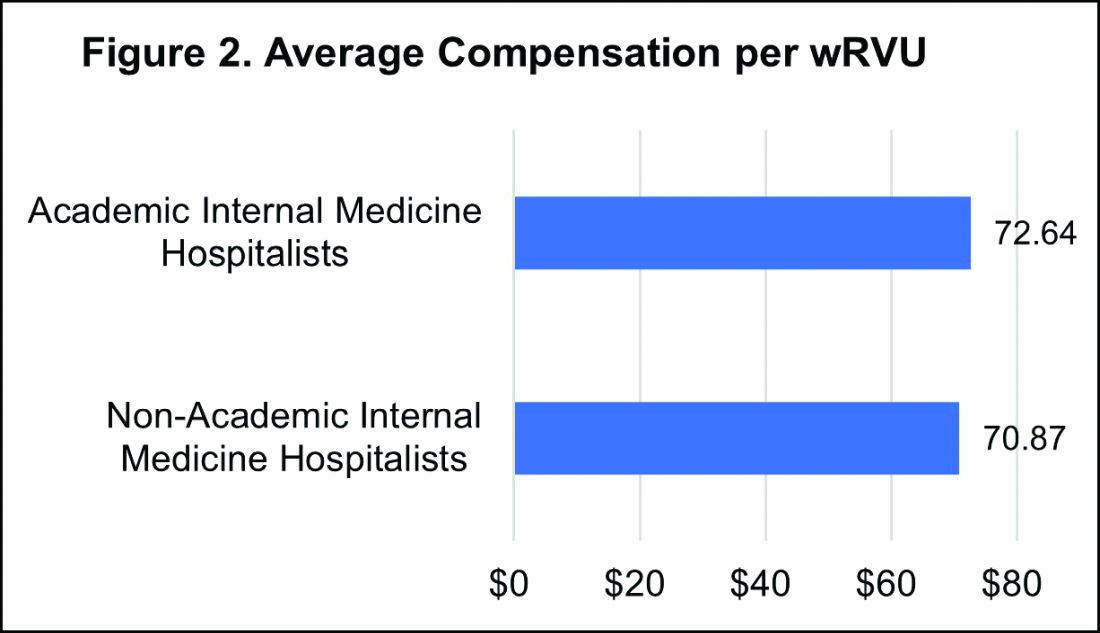
However, the total compensation continues to be lower for academic hospitalists, with a median compensation difference of approximately $70,000 compared to their non-academic colleagues. Some of this sizable variance is offset by the fact that academic HMGs receive more in employee benefits packages than non-academic groups – a difference in median value of $10,500. Ideally, academic hospitalist compensation models should appropriately reflect and value their work efforts toward the tripartite academic mission of clinical care, education, and research. It would be valuable for future surveys to define and measure academic production in order to develop national standards for compensation models that recognize these non-billable forms of productivity.
While it’s important to review compensation benchmarks to remain competitive, it’s difficult to put a price on some factors that many may consider more valuable – group culture, opportunities for professional growth, and schedules that afford better work-life integration. Indirect measures of such benefits include paid time off, paid sick days, CME allowances and time, and retirement benefits programs. In 2020, the median employer contribution to retirement plans was reported to be $13,955, with respondents in the Midwest receiving the highest retirement benefit of $33,771.
It’s encouraging to see that hospitalist compensation continues to rise compared to previous years, despite relatively flat trends in wRVUs and total patient encounters. Another continued trend over the past years is the rising amount of financial support per physician that hospitals or other organizations provide HMGs (see Figure 3). 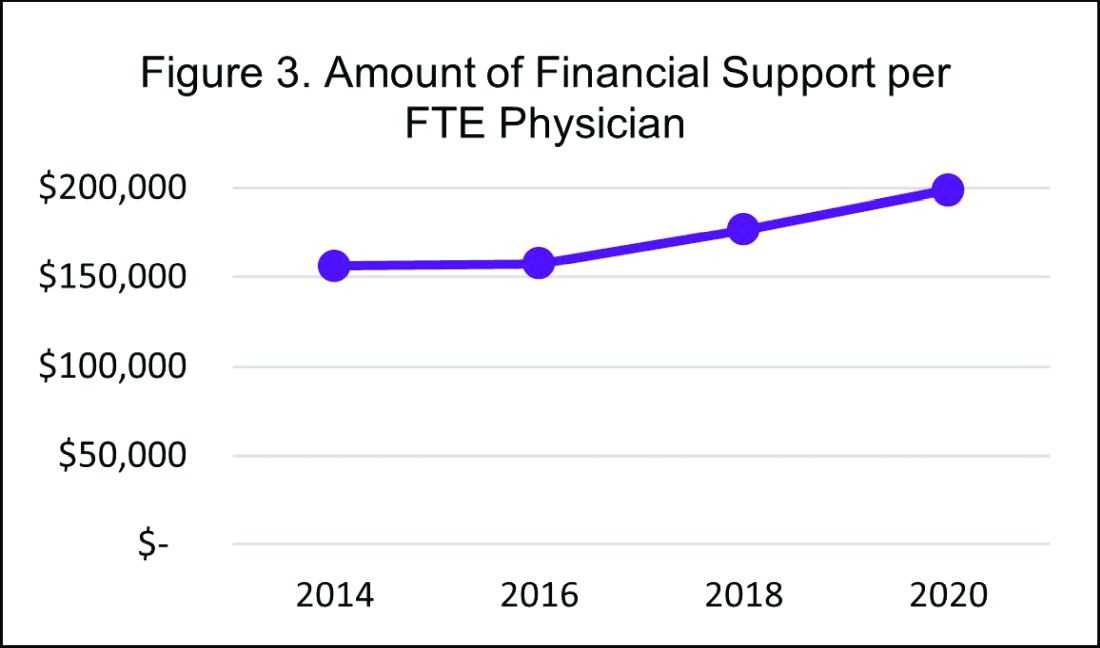
In 2020, the median financial support per FTE (full time equivalent) physician serving adult patients increased by 12% over 2018, to $198,750. Collectively these trends indicate hospitals are willing to compensate hospitalists for more than just their clinical volume.
There’s no doubt that the COVID-19 pandemic had some financial impact on hospital medicine groups in 2020. To assess this impact, SHM conducted a follow-up survey and compiled a COVID-19 Addendum to the SoHM Report. While 20.5% of HMG group respondents from the East reported providing hazard pay to clinicians caring for COVID-19 patients, nationally only 9.8% of groups said they offered this benefit. Of the 121 HMGs responding from across the country, 42% reported reductions in compensation, which included measures such as reductions in pay level and elimination or delays to bonus payments. The degree of reductions was not quantified, but fortunately the vast majority of these groups reported that these changes were likely to be temporary. To access all data in the 2020 SoHM Report and COVID-19 Addendum, visit hospitalmedicine.org/sohm to purchase your copy.
It’s certainly unclear what the future holds, but despite any transient changes observed during the COVID-19 pandemic, I believe that historical trends in hospitalist compensation will continue. If 2020 has taught us anything, it’s that hospitalists are essential, not only during an acute care crisis but for daily operations of any hospital.
Dr. Kurian is chief of the Division of Hospital Medicine at Northwell Health in New York. She is a member of SHM’s Practice Analysis Committee.
In a time of tremendous uncertainty, there is one trend that seems consistent year over year – the undisputed value of hospitalists. In the 2020 State of Hospital Medicine (SoHM) Report, the Society of Hospital Medicine partnered with the Medical Group Management Association (MGMA) to provide data on hospitalist compensation and productivity. The Report provides resounding evidence that hospitalists continue to be compensated at rising rates. This may be driven by both the continued demand-supply mismatch and a recognition of the overall value they generate rather than strictly the volume of their productivity.
In 2020, the median total compensation nationally for adult hospitalists (internal medicine and family medicine) was $307,633, representing an increase of over 6% from the 2018 Survey (see Figure 1). 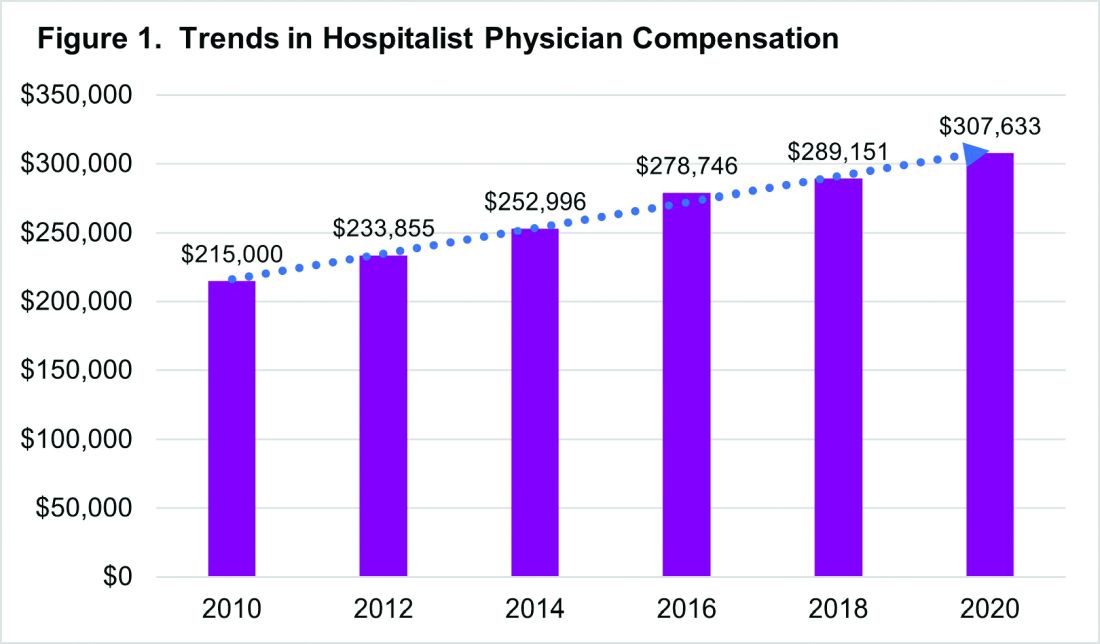
With significant regional variability in compensation across the country, hospitalists in the South continue to earn more than their colleagues in the East – a median compensation difference of about $33,000. However, absolute wage comparisons can be misleading without also considering regional variations in productivity as well.
Reviewing compensation per work relative value unit (wRVU) and per encounter offer additional insight for a more comprehensive assessment. When comparing regional compensation per wRVU, the 2020 Survey continues to show a trend toward hospitalists in the Midwest and West earning more per wRVU than their colleagues in other parts of the country ($78.13 per RVU in the Midwest, $78.95 per RVU in the West). More striking is how hospital medicine groups (HMGs) in the South garner lower compensation per RVU ($57.77) than those in the East ($67.54), even though their total compensation was much higher. This could reflect the gradual decline in compensation per wRVU that’s observed at higher productivity levels. While it’s typical for compensation to increase as productivity does, the rate of increase is generally to a lesser degree.
Like past SoHM Surveys, the 2020 Report revealed that academic and non-academic hospitalists are compensated similarly per wRVU (see Figure 2). 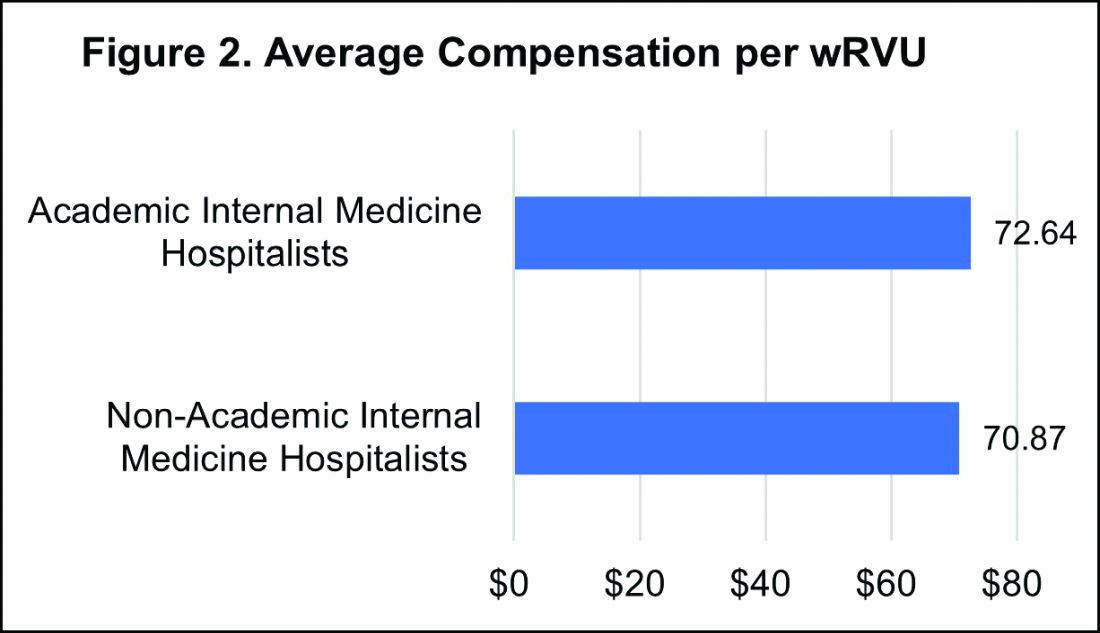
However, the total compensation continues to be lower for academic hospitalists, with a median compensation difference of approximately $70,000 compared to their non-academic colleagues. Some of this sizable variance is offset by the fact that academic HMGs receive more in employee benefits packages than non-academic groups – a difference in median value of $10,500. Ideally, academic hospitalist compensation models should appropriately reflect and value their work efforts toward the tripartite academic mission of clinical care, education, and research. It would be valuable for future surveys to define and measure academic production in order to develop national standards for compensation models that recognize these non-billable forms of productivity.
While it’s important to review compensation benchmarks to remain competitive, it’s difficult to put a price on some factors that many may consider more valuable – group culture, opportunities for professional growth, and schedules that afford better work-life integration. Indirect measures of such benefits include paid time off, paid sick days, CME allowances and time, and retirement benefits programs. In 2020, the median employer contribution to retirement plans was reported to be $13,955, with respondents in the Midwest receiving the highest retirement benefit of $33,771.
It’s encouraging to see that hospitalist compensation continues to rise compared to previous years, despite relatively flat trends in wRVUs and total patient encounters. Another continued trend over the past years is the rising amount of financial support per physician that hospitals or other organizations provide HMGs (see Figure 3). 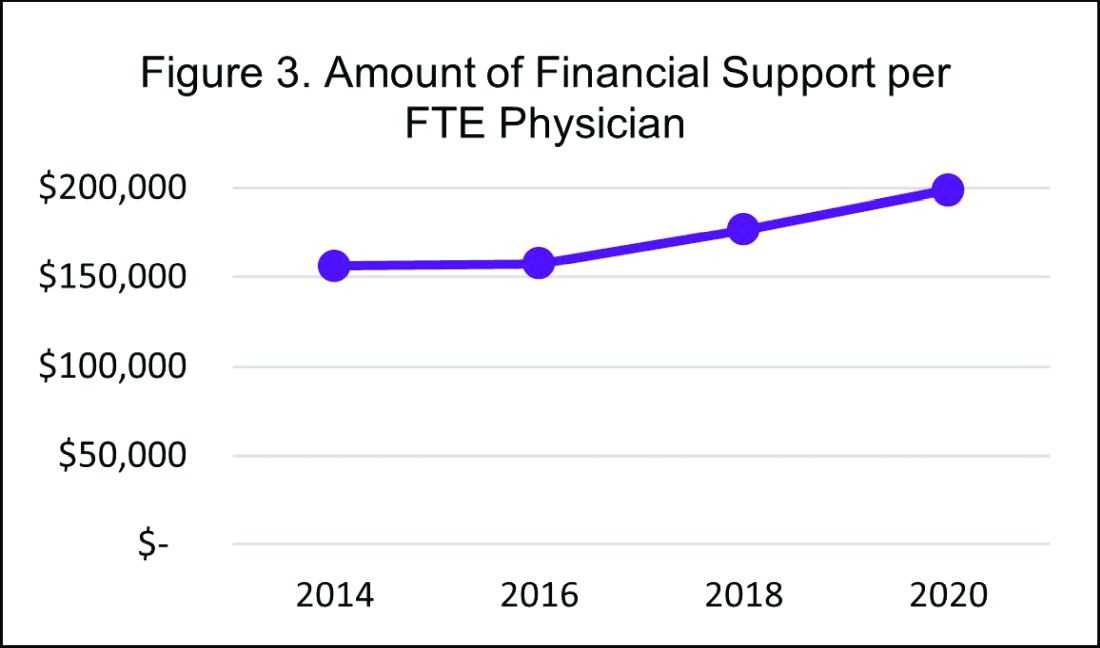
In 2020, the median financial support per FTE (full time equivalent) physician serving adult patients increased by 12% over 2018, to $198,750. Collectively these trends indicate hospitals are willing to compensate hospitalists for more than just their clinical volume.
There’s no doubt that the COVID-19 pandemic had some financial impact on hospital medicine groups in 2020. To assess this impact, SHM conducted a follow-up survey and compiled a COVID-19 Addendum to the SoHM Report. While 20.5% of HMG group respondents from the East reported providing hazard pay to clinicians caring for COVID-19 patients, nationally only 9.8% of groups said they offered this benefit. Of the 121 HMGs responding from across the country, 42% reported reductions in compensation, which included measures such as reductions in pay level and elimination or delays to bonus payments. The degree of reductions was not quantified, but fortunately the vast majority of these groups reported that these changes were likely to be temporary. To access all data in the 2020 SoHM Report and COVID-19 Addendum, visit hospitalmedicine.org/sohm to purchase your copy.
It’s certainly unclear what the future holds, but despite any transient changes observed during the COVID-19 pandemic, I believe that historical trends in hospitalist compensation will continue. If 2020 has taught us anything, it’s that hospitalists are essential, not only during an acute care crisis but for daily operations of any hospital.
Dr. Kurian is chief of the Division of Hospital Medicine at Northwell Health in New York. She is a member of SHM’s Practice Analysis Committee.
In a time of tremendous uncertainty, there is one trend that seems consistent year over year – the undisputed value of hospitalists. In the 2020 State of Hospital Medicine (SoHM) Report, the Society of Hospital Medicine partnered with the Medical Group Management Association (MGMA) to provide data on hospitalist compensation and productivity. The Report provides resounding evidence that hospitalists continue to be compensated at rising rates. This may be driven by both the continued demand-supply mismatch and a recognition of the overall value they generate rather than strictly the volume of their productivity.
In 2020, the median total compensation nationally for adult hospitalists (internal medicine and family medicine) was $307,633, representing an increase of over 6% from the 2018 Survey (see Figure 1). 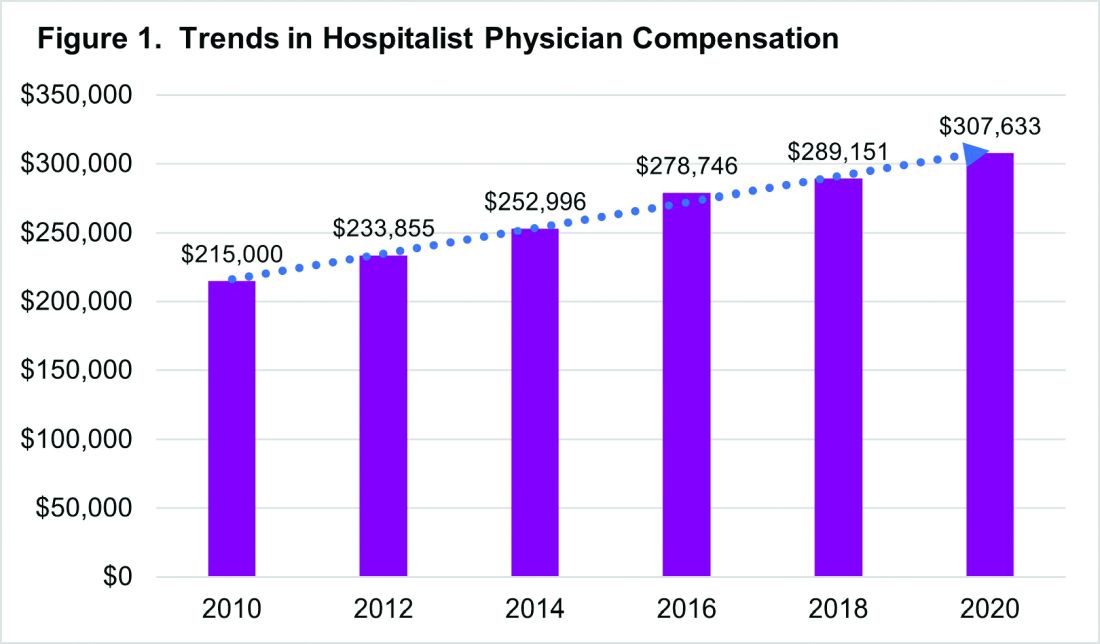
With significant regional variability in compensation across the country, hospitalists in the South continue to earn more than their colleagues in the East – a median compensation difference of about $33,000. However, absolute wage comparisons can be misleading without also considering regional variations in productivity as well.
Reviewing compensation per work relative value unit (wRVU) and per encounter offer additional insight for a more comprehensive assessment. When comparing regional compensation per wRVU, the 2020 Survey continues to show a trend toward hospitalists in the Midwest and West earning more per wRVU than their colleagues in other parts of the country ($78.13 per RVU in the Midwest, $78.95 per RVU in the West). More striking is how hospital medicine groups (HMGs) in the South garner lower compensation per RVU ($57.77) than those in the East ($67.54), even though their total compensation was much higher. This could reflect the gradual decline in compensation per wRVU that’s observed at higher productivity levels. While it’s typical for compensation to increase as productivity does, the rate of increase is generally to a lesser degree.
Like past SoHM Surveys, the 2020 Report revealed that academic and non-academic hospitalists are compensated similarly per wRVU (see Figure 2). 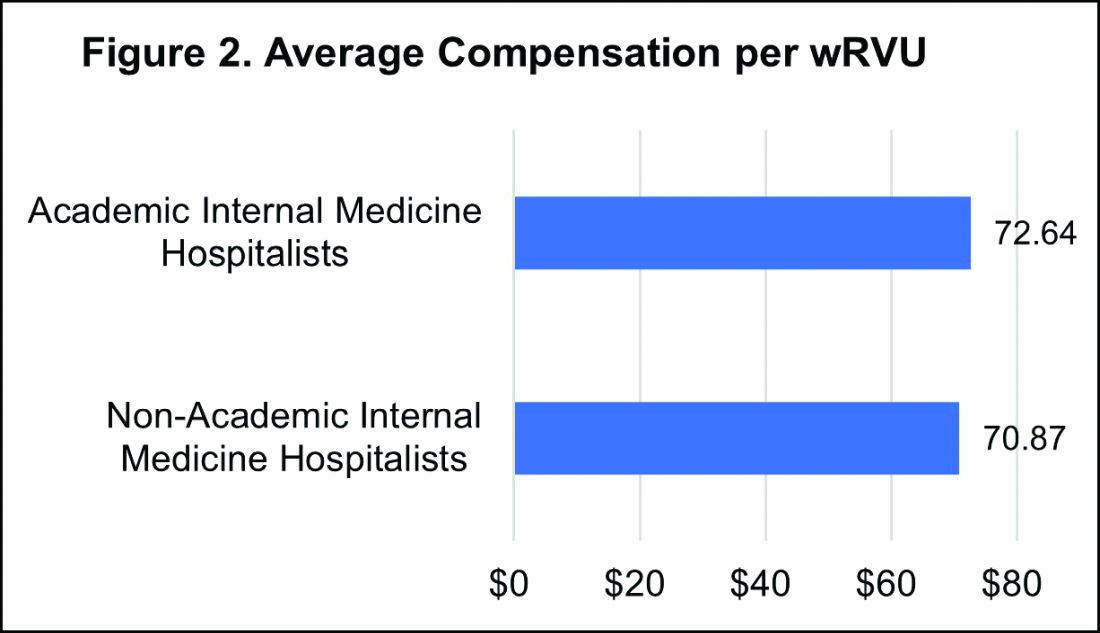
However, the total compensation continues to be lower for academic hospitalists, with a median compensation difference of approximately $70,000 compared to their non-academic colleagues. Some of this sizable variance is offset by the fact that academic HMGs receive more in employee benefits packages than non-academic groups – a difference in median value of $10,500. Ideally, academic hospitalist compensation models should appropriately reflect and value their work efforts toward the tripartite academic mission of clinical care, education, and research. It would be valuable for future surveys to define and measure academic production in order to develop national standards for compensation models that recognize these non-billable forms of productivity.
While it’s important to review compensation benchmarks to remain competitive, it’s difficult to put a price on some factors that many may consider more valuable – group culture, opportunities for professional growth, and schedules that afford better work-life integration. Indirect measures of such benefits include paid time off, paid sick days, CME allowances and time, and retirement benefits programs. In 2020, the median employer contribution to retirement plans was reported to be $13,955, with respondents in the Midwest receiving the highest retirement benefit of $33,771.
It’s encouraging to see that hospitalist compensation continues to rise compared to previous years, despite relatively flat trends in wRVUs and total patient encounters. Another continued trend over the past years is the rising amount of financial support per physician that hospitals or other organizations provide HMGs (see Figure 3). 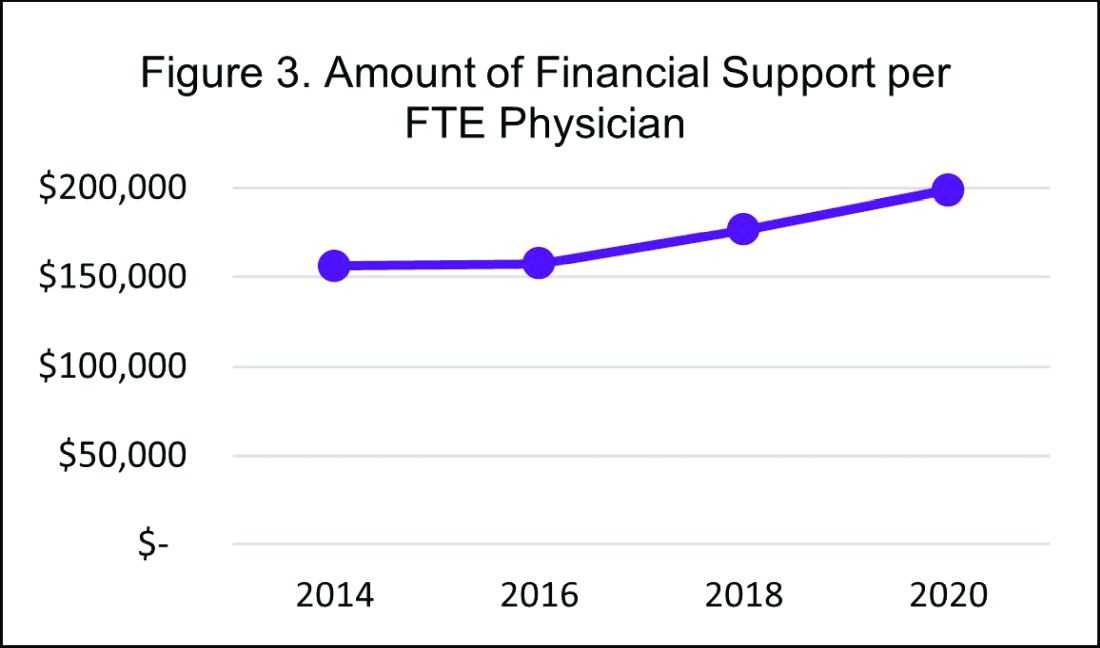
In 2020, the median financial support per FTE (full time equivalent) physician serving adult patients increased by 12% over 2018, to $198,750. Collectively these trends indicate hospitals are willing to compensate hospitalists for more than just their clinical volume.
There’s no doubt that the COVID-19 pandemic had some financial impact on hospital medicine groups in 2020. To assess this impact, SHM conducted a follow-up survey and compiled a COVID-19 Addendum to the SoHM Report. While 20.5% of HMG group respondents from the East reported providing hazard pay to clinicians caring for COVID-19 patients, nationally only 9.8% of groups said they offered this benefit. Of the 121 HMGs responding from across the country, 42% reported reductions in compensation, which included measures such as reductions in pay level and elimination or delays to bonus payments. The degree of reductions was not quantified, but fortunately the vast majority of these groups reported that these changes were likely to be temporary. To access all data in the 2020 SoHM Report and COVID-19 Addendum, visit hospitalmedicine.org/sohm to purchase your copy.
It’s certainly unclear what the future holds, but despite any transient changes observed during the COVID-19 pandemic, I believe that historical trends in hospitalist compensation will continue. If 2020 has taught us anything, it’s that hospitalists are essential, not only during an acute care crisis but for daily operations of any hospital.
Dr. Kurian is chief of the Division of Hospital Medicine at Northwell Health in New York. She is a member of SHM’s Practice Analysis Committee.
The journey from burnout to wellbeing
A check-in for you and your peers
COVID-19 did not discriminate when it came to the impact it imposed on our hospitalist community. As the nomenclature moves away from the negative connotations of ‘burnout’ to ‘wellbeing,’ the pandemic has taught us something important about being intentional about our personal health: we must secure our own oxygen masks before helping others.
In February 2020, the Society of Hospital Medicine’s Wellbeing Taskforce efforts quickly changed focus from addressing general wellbeing, to wellbeing during COVID-19. Our Taskforce was commissioned by SHM’s Board with a new charge: Address immediate and ongoing needs of well-being and resiliency support for hospitalists during the COVID-19 pandemic. In this essay, I will discuss how our SHM Wellbeing Taskforce approached the overall topic of wellbeing for hospitalists during the COVID-19 pandemic, including some of our Taskforce group experiences.
The Taskforce started with a framework to aide in cultivating open and authentic conversations within hospital medicine groups. Creating spaces for honest sharing around how providers are doing is a crucial first step to reducing stigma, building mutual support within a group, and elevating issues of wellbeing to the level where structural change can take place. The Taskforce established two objectives for normalizing and mitigating stressors we face as hospitalists during the COVID-19 pandemic:
- Provide a framework for hospitalists to take their own emotional pulse
- Provide an approach to reduce stigma of hospitalists who are suffering from pandemic stress
While a more typical approach to fix stress and burnout is using formal institutional interventions, we used the value and insight provided by SHM’s 7 Drivers of Burnout in Hospital Medicine to help guide the creation of SHM resources in addressing the severe emotional strain being felt across the country by hospitalists. The 7 Drivers support the idea that the social role peers and hospital leaders can make a crucial difference in mitigating stress and burnout. Two examples of social support come to mind from the Wellbeing Taskforce experience:
- Participate in your meetings. One example comes from a member of our group who had underestimated the “healing power” that our group meetings had provided to his psyche. The simple act of participating in our Taskforce meeting and being in the presence of our group had provided such a positive impact that he was better able to face the “death and misery” in his unit with a smile on his face.
- Share what is stressful. The second example of social support comes from an hour of Zoom-based facilitation meetings between the SHM’s Wellbeing Taskforce members and Chapter Leaders in late October. During our Taskforce debrief after the meeting, we came to realize the enormous burden of grief our peers were carrying as one hospitalist had lost a group colleague the previous week due to suicide. Our member who led this meeting was moved – as were we – at how this had impacted his small team, and he was reminded he was not alone.
To form meaningful relationships that foster support, there needs to be a space where people can safely come together at times that initially might feel awkward. After taking steps toward your peers, these conversations can become normalized and contribute to meaningful relationships, providing the opportunity for healthy exchanges on vulnerable topics like emotional and psychological wellbeing. A printable guide for this specific purpose (“HM COVID-19 Check-In Guide for Self and Peers”) was designed to help hospitalists move into safe and supportive conversations with each other. While it is difficult to place a value on the importance these types of conversations have on individual wellbeing, it is known that the quality of a positive work environment where people feel supported can moderate stress, morale, and depression. In other words, hospitalist groups can positively contribute to their social environment during stressful times by sharing meaningful and difficult experiences with one another.
Second, the Taskforce created a social media campaign to provide a public social space for sharing hospitalists’ COVID-19 experiences. We believed that sharing collective experiences with the theme of #YouAreNotAlone and a complementary social media campaign, SHM Cares, on SHM’s social media channels, would further connect the national hospitalist community and provide a different communication pathway to decrease a sense of isolation. This idea came from the second social support idea mentioned earlier to share what is stressful with others in a safe space. We understood that some hospitalists would be more comfortable sharing publicly their comments, photos, and videos in achieving a sense of hospitalist unity.
Using our shared experiences, we identified three pillars for the final structure of the HM COVID-19 Check-In Guide for Self and Peers:
- Pillar 1. Recognize your issues. Recall our oxygen mask metaphor and this is what we mean by recognizing symptoms of new stressors (e.g., sleeplessness, irritability, forgetfulness).
- Pillar 2. Know what to say. A simple open-ended question about how the other person is working through the pandemic is an easy way to start a connection. We learned from a mental health perspective that it is unlikely that you could say anything to make a situation worse by offering a listening ear.
- Pillar 3. Check in with others. Listen to others without trying to fix the person or the situation. When appropriate, offer humorous reflections without diminishing the problem. Be a partner and commit to check in regularly with the other person.
Cultivating human connections outside of your immediate peer group can be valuable and offer additional perspective to stressful situations. For instance, one of my roles as a hospitalist administrator has been offering support by regularly listening as my physicians ‘talk out’ their day confidentially for as long as they needed. Offering open conversation in a safe and confidential way can have a healing effect. As one of my former hospitalists used to say, if issues are not addressed, they will “ooze out somewhere else.”
The HM COVID-19 Check-In Guide for Self and Peers and the SHM Cares social media campaign was the result of the Taskforce’s collective observations to help others normalize the feeling that ‘it’s OK not to be OK.’ Using the pandemic as context, the 7 Drivers of Hospitalist Burnout reminded us that the increased burnout issues we face will require continued attention past the pandemic. The value in cultivating human connections has never been more important. The SHM Wellbeing Taskforce is committed to provide continued resources. Checking in with others and listening to peers are all part of a personal wellbeing and resilience strategy. On behalf of the SHM Wellbeing Taskforce, we hope the information in this article will highlight the importance of continued attention to personal wellbeing during and after the pandemic.
Dr. Robinson received her PhD in organizational learning, performance and change from Colorado State University in 2019. Her dissertation topic was exploring hospitalist burnout, engagement, and social support. She is administrative director of inpatient medicine at St. Mary’s Medical Center in Grand Junction, Colo., a part of SCL Health. She has volunteered in numerous SHM committees, and currently serves on the SHM Wellbeing Taskforce.
A check-in for you and your peers
A check-in for you and your peers
COVID-19 did not discriminate when it came to the impact it imposed on our hospitalist community. As the nomenclature moves away from the negative connotations of ‘burnout’ to ‘wellbeing,’ the pandemic has taught us something important about being intentional about our personal health: we must secure our own oxygen masks before helping others.
In February 2020, the Society of Hospital Medicine’s Wellbeing Taskforce efforts quickly changed focus from addressing general wellbeing, to wellbeing during COVID-19. Our Taskforce was commissioned by SHM’s Board with a new charge: Address immediate and ongoing needs of well-being and resiliency support for hospitalists during the COVID-19 pandemic. In this essay, I will discuss how our SHM Wellbeing Taskforce approached the overall topic of wellbeing for hospitalists during the COVID-19 pandemic, including some of our Taskforce group experiences.
The Taskforce started with a framework to aide in cultivating open and authentic conversations within hospital medicine groups. Creating spaces for honest sharing around how providers are doing is a crucial first step to reducing stigma, building mutual support within a group, and elevating issues of wellbeing to the level where structural change can take place. The Taskforce established two objectives for normalizing and mitigating stressors we face as hospitalists during the COVID-19 pandemic:
- Provide a framework for hospitalists to take their own emotional pulse
- Provide an approach to reduce stigma of hospitalists who are suffering from pandemic stress
While a more typical approach to fix stress and burnout is using formal institutional interventions, we used the value and insight provided by SHM’s 7 Drivers of Burnout in Hospital Medicine to help guide the creation of SHM resources in addressing the severe emotional strain being felt across the country by hospitalists. The 7 Drivers support the idea that the social role peers and hospital leaders can make a crucial difference in mitigating stress and burnout. Two examples of social support come to mind from the Wellbeing Taskforce experience:
- Participate in your meetings. One example comes from a member of our group who had underestimated the “healing power” that our group meetings had provided to his psyche. The simple act of participating in our Taskforce meeting and being in the presence of our group had provided such a positive impact that he was better able to face the “death and misery” in his unit with a smile on his face.
- Share what is stressful. The second example of social support comes from an hour of Zoom-based facilitation meetings between the SHM’s Wellbeing Taskforce members and Chapter Leaders in late October. During our Taskforce debrief after the meeting, we came to realize the enormous burden of grief our peers were carrying as one hospitalist had lost a group colleague the previous week due to suicide. Our member who led this meeting was moved – as were we – at how this had impacted his small team, and he was reminded he was not alone.
To form meaningful relationships that foster support, there needs to be a space where people can safely come together at times that initially might feel awkward. After taking steps toward your peers, these conversations can become normalized and contribute to meaningful relationships, providing the opportunity for healthy exchanges on vulnerable topics like emotional and psychological wellbeing. A printable guide for this specific purpose (“HM COVID-19 Check-In Guide for Self and Peers”) was designed to help hospitalists move into safe and supportive conversations with each other. While it is difficult to place a value on the importance these types of conversations have on individual wellbeing, it is known that the quality of a positive work environment where people feel supported can moderate stress, morale, and depression. In other words, hospitalist groups can positively contribute to their social environment during stressful times by sharing meaningful and difficult experiences with one another.
Second, the Taskforce created a social media campaign to provide a public social space for sharing hospitalists’ COVID-19 experiences. We believed that sharing collective experiences with the theme of #YouAreNotAlone and a complementary social media campaign, SHM Cares, on SHM’s social media channels, would further connect the national hospitalist community and provide a different communication pathway to decrease a sense of isolation. This idea came from the second social support idea mentioned earlier to share what is stressful with others in a safe space. We understood that some hospitalists would be more comfortable sharing publicly their comments, photos, and videos in achieving a sense of hospitalist unity.
Using our shared experiences, we identified three pillars for the final structure of the HM COVID-19 Check-In Guide for Self and Peers:
- Pillar 1. Recognize your issues. Recall our oxygen mask metaphor and this is what we mean by recognizing symptoms of new stressors (e.g., sleeplessness, irritability, forgetfulness).
- Pillar 2. Know what to say. A simple open-ended question about how the other person is working through the pandemic is an easy way to start a connection. We learned from a mental health perspective that it is unlikely that you could say anything to make a situation worse by offering a listening ear.
- Pillar 3. Check in with others. Listen to others without trying to fix the person or the situation. When appropriate, offer humorous reflections without diminishing the problem. Be a partner and commit to check in regularly with the other person.
Cultivating human connections outside of your immediate peer group can be valuable and offer additional perspective to stressful situations. For instance, one of my roles as a hospitalist administrator has been offering support by regularly listening as my physicians ‘talk out’ their day confidentially for as long as they needed. Offering open conversation in a safe and confidential way can have a healing effect. As one of my former hospitalists used to say, if issues are not addressed, they will “ooze out somewhere else.”
The HM COVID-19 Check-In Guide for Self and Peers and the SHM Cares social media campaign was the result of the Taskforce’s collective observations to help others normalize the feeling that ‘it’s OK not to be OK.’ Using the pandemic as context, the 7 Drivers of Hospitalist Burnout reminded us that the increased burnout issues we face will require continued attention past the pandemic. The value in cultivating human connections has never been more important. The SHM Wellbeing Taskforce is committed to provide continued resources. Checking in with others and listening to peers are all part of a personal wellbeing and resilience strategy. On behalf of the SHM Wellbeing Taskforce, we hope the information in this article will highlight the importance of continued attention to personal wellbeing during and after the pandemic.
Dr. Robinson received her PhD in organizational learning, performance and change from Colorado State University in 2019. Her dissertation topic was exploring hospitalist burnout, engagement, and social support. She is administrative director of inpatient medicine at St. Mary’s Medical Center in Grand Junction, Colo., a part of SCL Health. She has volunteered in numerous SHM committees, and currently serves on the SHM Wellbeing Taskforce.
COVID-19 did not discriminate when it came to the impact it imposed on our hospitalist community. As the nomenclature moves away from the negative connotations of ‘burnout’ to ‘wellbeing,’ the pandemic has taught us something important about being intentional about our personal health: we must secure our own oxygen masks before helping others.
In February 2020, the Society of Hospital Medicine’s Wellbeing Taskforce efforts quickly changed focus from addressing general wellbeing, to wellbeing during COVID-19. Our Taskforce was commissioned by SHM’s Board with a new charge: Address immediate and ongoing needs of well-being and resiliency support for hospitalists during the COVID-19 pandemic. In this essay, I will discuss how our SHM Wellbeing Taskforce approached the overall topic of wellbeing for hospitalists during the COVID-19 pandemic, including some of our Taskforce group experiences.
The Taskforce started with a framework to aide in cultivating open and authentic conversations within hospital medicine groups. Creating spaces for honest sharing around how providers are doing is a crucial first step to reducing stigma, building mutual support within a group, and elevating issues of wellbeing to the level where structural change can take place. The Taskforce established two objectives for normalizing and mitigating stressors we face as hospitalists during the COVID-19 pandemic:
- Provide a framework for hospitalists to take their own emotional pulse
- Provide an approach to reduce stigma of hospitalists who are suffering from pandemic stress
While a more typical approach to fix stress and burnout is using formal institutional interventions, we used the value and insight provided by SHM’s 7 Drivers of Burnout in Hospital Medicine to help guide the creation of SHM resources in addressing the severe emotional strain being felt across the country by hospitalists. The 7 Drivers support the idea that the social role peers and hospital leaders can make a crucial difference in mitigating stress and burnout. Two examples of social support come to mind from the Wellbeing Taskforce experience:
- Participate in your meetings. One example comes from a member of our group who had underestimated the “healing power” that our group meetings had provided to his psyche. The simple act of participating in our Taskforce meeting and being in the presence of our group had provided such a positive impact that he was better able to face the “death and misery” in his unit with a smile on his face.
- Share what is stressful. The second example of social support comes from an hour of Zoom-based facilitation meetings between the SHM’s Wellbeing Taskforce members and Chapter Leaders in late October. During our Taskforce debrief after the meeting, we came to realize the enormous burden of grief our peers were carrying as one hospitalist had lost a group colleague the previous week due to suicide. Our member who led this meeting was moved – as were we – at how this had impacted his small team, and he was reminded he was not alone.
To form meaningful relationships that foster support, there needs to be a space where people can safely come together at times that initially might feel awkward. After taking steps toward your peers, these conversations can become normalized and contribute to meaningful relationships, providing the opportunity for healthy exchanges on vulnerable topics like emotional and psychological wellbeing. A printable guide for this specific purpose (“HM COVID-19 Check-In Guide for Self and Peers”) was designed to help hospitalists move into safe and supportive conversations with each other. While it is difficult to place a value on the importance these types of conversations have on individual wellbeing, it is known that the quality of a positive work environment where people feel supported can moderate stress, morale, and depression. In other words, hospitalist groups can positively contribute to their social environment during stressful times by sharing meaningful and difficult experiences with one another.
Second, the Taskforce created a social media campaign to provide a public social space for sharing hospitalists’ COVID-19 experiences. We believed that sharing collective experiences with the theme of #YouAreNotAlone and a complementary social media campaign, SHM Cares, on SHM’s social media channels, would further connect the national hospitalist community and provide a different communication pathway to decrease a sense of isolation. This idea came from the second social support idea mentioned earlier to share what is stressful with others in a safe space. We understood that some hospitalists would be more comfortable sharing publicly their comments, photos, and videos in achieving a sense of hospitalist unity.
Using our shared experiences, we identified three pillars for the final structure of the HM COVID-19 Check-In Guide for Self and Peers:
- Pillar 1. Recognize your issues. Recall our oxygen mask metaphor and this is what we mean by recognizing symptoms of new stressors (e.g., sleeplessness, irritability, forgetfulness).
- Pillar 2. Know what to say. A simple open-ended question about how the other person is working through the pandemic is an easy way to start a connection. We learned from a mental health perspective that it is unlikely that you could say anything to make a situation worse by offering a listening ear.
- Pillar 3. Check in with others. Listen to others without trying to fix the person or the situation. When appropriate, offer humorous reflections without diminishing the problem. Be a partner and commit to check in regularly with the other person.
Cultivating human connections outside of your immediate peer group can be valuable and offer additional perspective to stressful situations. For instance, one of my roles as a hospitalist administrator has been offering support by regularly listening as my physicians ‘talk out’ their day confidentially for as long as they needed. Offering open conversation in a safe and confidential way can have a healing effect. As one of my former hospitalists used to say, if issues are not addressed, they will “ooze out somewhere else.”
The HM COVID-19 Check-In Guide for Self and Peers and the SHM Cares social media campaign was the result of the Taskforce’s collective observations to help others normalize the feeling that ‘it’s OK not to be OK.’ Using the pandemic as context, the 7 Drivers of Hospitalist Burnout reminded us that the increased burnout issues we face will require continued attention past the pandemic. The value in cultivating human connections has never been more important. The SHM Wellbeing Taskforce is committed to provide continued resources. Checking in with others and listening to peers are all part of a personal wellbeing and resilience strategy. On behalf of the SHM Wellbeing Taskforce, we hope the information in this article will highlight the importance of continued attention to personal wellbeing during and after the pandemic.
Dr. Robinson received her PhD in organizational learning, performance and change from Colorado State University in 2019. Her dissertation topic was exploring hospitalist burnout, engagement, and social support. She is administrative director of inpatient medicine at St. Mary’s Medical Center in Grand Junction, Colo., a part of SCL Health. She has volunteered in numerous SHM committees, and currently serves on the SHM Wellbeing Taskforce.
JHM Twitter chat sparks connections
Monthly social media event links editors, authors, and readers
Once upon a time, physicians wrote letters to peers and colleagues around the world, sharing their medical discoveries, theories, case reports, and questions; conferring on problems; and then waiting for return mail to bring a reply. And the science of medicine advanced at a glacial pace.
Today, communication in multiple mediums flows much faster, almost instantaneously, between many more physicians, regardless of distance, addressing a much greater complexity of medical topics and treatments. And one of the chief mediums for this rapid electronic conversation among doctors is Twitter, according to Charlie Wray, DO, MS, a hospitalist at the University of California, San Francisco.
Dr. Wray, associate editor and digital media editor for the Journal of Hospital Medicine, is one of the moderators of #JHMchat, a monthly get-together on Twitter for interested hospitalists to link up virtually; respond to questions posed by JHM editors and other moderators; exchange perspectives, experiences, and tips with their peers; and build professional relationships and personal friendships. Relationship building has become particularly important in the age of COVID-19, when opportunities to connect in person at events such as SHM’s annual conferences have been curtailed.
The online #JHMchat community began in 2015, shortly after Dr. Wray completed a hospitalist research fellowship at the University of Chicago. His fellowship mentor, Vineet Arora, MD, MAPP, MHM, associate chief medical officer for the clinical learning environment at University of Chicago Medicine, had noticed how other online medical communities were engaging in discussions around different topics.
“She thought it could be a great way for hospitalists to meet online and talk about the articles published in JHM,” Dr. Wray explained. “We were all getting into social media and learning how to moderate interactive discussions such as Twitter.”
The chat’s founders approached JHM’s then-editor Andrew Auerbach, MD, MHM, a hospitalist at UCSF, who agreed that it was a great idea. They asked Christopher Moriates, MD, author of a recently published paper on the advisability of nebulized bronchodilators for obstructive pulmonary symptoms and assistant dean for health care value at the University of Texas, Austin, to come on the chat and talk about his paper. Visiting Dr. Arora at the time, he joined her in her living room for the first chat on Oct. 12, 2015. Seventy-five participants posted 431 tweets, with a total of 2 million Twitter impressions, suggesting that they had tapped a latent need.
How the chat works
To participate in the JHM chats on Twitter, one needs to open an account on the platform (it’s free) and follow the Journal’s Twitter feed (@jhospmedicine). But that’s pretty much it, Dr. Wray said. The group convenes on a Monday evening each month for an hour, starting at 9 p.m. Eastern time. Upcoming chats and topics are announced on Twitter and at SHM’s website.
The chats have grown and evolved since 2015, shifting in focus given recent social upheavals over the pandemic and heated discussions about diversity, equity, and racial justice in medicine, he said. “When COVID hit, the journal’s editor – Dr. Samir Shah – recognized that we were in a unique moment with the pandemic. The journal took advantage of the opportunity to publish a lot more personal perspectives and viewpoints around COVID, along with a special issue devoted to social justice.”
Moderators for the chat typically choose three or four questions based on recently published articles or other relevant topics, such as racial inequities in health care or how to apply military principles to hospital medicine leadership. “We reach out to authors and tell them they can explain their articles to interested readers through the chat. I can’t think of a single one who said no. They see the opportunity to highlight their work and engage with readers who want to ask them questions,” Dr. Wray said.
The moderators’ questions are posed to stimulate participation, but another goal is to use that hour for networking. “It’s a powerful tool to allow SHM members to engage with each other,” he said. “Sometimes the chat has the feeling of trying to drink water from a fire hose – with the messages flashing past so quickly. But the key is not to try to respond to everything but rather to follow those threads that particularly interest you. We encourage you to engage, but it’s totally fine if you just sit back and observe. One thing we have done to make it a little more formal is to offer CME credits for participants.”
The chat welcomes hospitalists and nonhospitalists, nurse practitioners, physician assistants, academics, and nonacademics. “No matter how engaged you are with Twitter, if you have 10,000 followers or 10, we’ll amplify your voice,” he said. “We also have medical students participating and consider their perspectives valuable, too.”
Dr. Wray identified three main types of participants in the monthly chats. The first are regulars who come every month, rain or shine. Like the character Norm in the old television comedy “Cheers,” everybody knows their name. They become friends, sharing and reveling in each other’s accomplishments. “These are people who have multiple connections, personally and professionally, at a lot of different levels. I probably know a hundred or more people who I’ve primarily gotten to know online.”
A second and larger group might be drawn in because of an interest in a specific topic or article, but they’re also welcome to participate in the chat. And the third group may lurk in the background, following along but not commenting. The size of that third group is unknown, but metrics from SHM show a total of 796 participants posting 4,088 tweets during chats in 2020 (for an average of 132 participants and 681 tweets per chat). This adds up to a total of 34 million impressions across the platform for #JHMchat tweets for the year.
Creating community online
“Why do we do it? It’s difficult to read all of the relevant published articles and keep up to date,” said Dr. Arora, a medical educator whose job at Chicago Medicine is to improve the clinical learning environment for trainees and staff by aligning learning with the health system’s institutional quality, safety and value missions.
“Our idea was to bring together a kind of virtual journal club and have discussions around topics such as: how do you create a shared vision on rounds? How do you integrate that into clinical practice? How do we preserve work/life balance or address structural racism?” she said. Other topics have included work flow concerns, burnout, difficult conversations with patients, and career planning.
“The people we’re trying to reach are hospitalists – and they’re busy at the front lines of care. We also thought this was an interesting way to raise the journal’s profile and spark broader interest in the articles it publishes. But it’s really about creating community, with people who look forward to talking and connecting with each other each month through the chats,” Dr. Arora said. If they miss a chat, they feel they’ve missed important interactions.
“Many times when people log onto the chat, they give a status report on where they are at, such as ‘I’m home putting my kids to bed,’ or ‘I’m on call tonight,’ ” she added. “People are willing to engage with the medium because it’s easy to engage with. We can forget that physicians are like everyone else. They like to learn, but they want that learning to be fun.”
On Dec. 14, 2020, at 9 p.m. Eastern time, the first question for the monthly #JHMchat was posted: How will caring for COVID-19 patients this winter differ from caring for patients in the first wave? Given that another surge of hospitalized COVID patients is looming, participants posted that they feel familiar and more confident with effective clinical strategies for hospitalized COVID patients, having learned so much more about the virus. But they’re facing greater numbers of patients than in prior surges. “In March, we were in crisis, now we’re in complexity,” one noted.
Joining the moderators was the Pediatric Overflow Planning Contingency Response Network (POPCoRN), a group formed earlier this year to help mobilize pediatric medical capacity for COVID patients during pandemic surges (see “POPCoRN network mobilizes pediatric capacity during pandemic,” The Hospitalist, April 30, 2020). One of its questions involved the redeployment of physicians in response to COVID demands and what, for example, pediatric hospitalists need as resources and tools when they are reassigned to adult patients or to new roles in unfamiliar settings. A variety of educational resources were cited from POPCoRN, SHM, and ImproveDX, among others.
Defining medical communication
Another chat moderator is Angela Castellanos, MD, a pediatric hospitalist at Tufts Medical Center in Boston. Dr. Castellanos did a 1-year, full-time fellowship right after residency at the New England Journal of Medicine, participating hands-on as a member of the editorial team for the print and online editions of the venerable journal. She is now doing a digital media fellowship with JHM, a part-time commitment while holding down a full-time job as a hospitalist. She also puts together a Spanish language podcast covering primary care pediatric issues for parents and families.
“I’m interested in medical communication generally, as I try to figure out what that means,” she said. “I have continued to look for ways to be part of the social media community and to be more creative about it. The JHM fellowship came at a perfect time for me to learn to do more in digital media.”
COVID has created new opportunities for more immediate dialogue with colleagues – what are they seeing and what’s working in the absence of clinical trials, she explained. “That’s how we communicate, as a way to get information out fast, such as when hospitals began proning COVID patients to make it easier for them to breathe.”
Dr. Castellanos said she grew up with text messaging and social media and wants to continue to grow her skills in this area. “I think I developed some skills at NEJM, but the opportunity to see how they do things at another journal with a different mission was also valuable. I get to share the space with people in academic settings and leaders in my field. I tweet at them; they tweet at me. These two fellowships have given me unique insights and mentorships. I know I want to continue doing pediatric hospital medicine and to engage academically and learn how to do research.”
Twitter sometimes gets a bad reputation for hostile or incendiary posts, Dr. Wray noted. “If you look at social media writ large, it can sometimes seem like a dumpster fire.” But what has happened in the medical community and in most medical Twitter encounters is a more cordial approach to conversations. “People who work in medicine converse with each other, with room for respectful disagreements. We’re extra supportive of each other,” he said.
“I think if hospitalists are looking for a community of peers, to engage with them and network and to find colleagues in similar circumstances, the JHM chat is such a fantastic place,” Dr. Wray concluded. “Don’t just come once, come several times, meet people along the way. For me, one of the most beneficial ways to advance my career has been by connecting with people through the chat. It allows me to share my work and success with the hospitalist community, as well as highlighting my trainees’ and colleagues’ successes, and it has created opportunities I never would have expected for getting involved in other projects.”
Monthly social media event links editors, authors, and readers
Monthly social media event links editors, authors, and readers
Once upon a time, physicians wrote letters to peers and colleagues around the world, sharing their medical discoveries, theories, case reports, and questions; conferring on problems; and then waiting for return mail to bring a reply. And the science of medicine advanced at a glacial pace.
Today, communication in multiple mediums flows much faster, almost instantaneously, between many more physicians, regardless of distance, addressing a much greater complexity of medical topics and treatments. And one of the chief mediums for this rapid electronic conversation among doctors is Twitter, according to Charlie Wray, DO, MS, a hospitalist at the University of California, San Francisco.
Dr. Wray, associate editor and digital media editor for the Journal of Hospital Medicine, is one of the moderators of #JHMchat, a monthly get-together on Twitter for interested hospitalists to link up virtually; respond to questions posed by JHM editors and other moderators; exchange perspectives, experiences, and tips with their peers; and build professional relationships and personal friendships. Relationship building has become particularly important in the age of COVID-19, when opportunities to connect in person at events such as SHM’s annual conferences have been curtailed.
The online #JHMchat community began in 2015, shortly after Dr. Wray completed a hospitalist research fellowship at the University of Chicago. His fellowship mentor, Vineet Arora, MD, MAPP, MHM, associate chief medical officer for the clinical learning environment at University of Chicago Medicine, had noticed how other online medical communities were engaging in discussions around different topics.
“She thought it could be a great way for hospitalists to meet online and talk about the articles published in JHM,” Dr. Wray explained. “We were all getting into social media and learning how to moderate interactive discussions such as Twitter.”
The chat’s founders approached JHM’s then-editor Andrew Auerbach, MD, MHM, a hospitalist at UCSF, who agreed that it was a great idea. They asked Christopher Moriates, MD, author of a recently published paper on the advisability of nebulized bronchodilators for obstructive pulmonary symptoms and assistant dean for health care value at the University of Texas, Austin, to come on the chat and talk about his paper. Visiting Dr. Arora at the time, he joined her in her living room for the first chat on Oct. 12, 2015. Seventy-five participants posted 431 tweets, with a total of 2 million Twitter impressions, suggesting that they had tapped a latent need.
How the chat works
To participate in the JHM chats on Twitter, one needs to open an account on the platform (it’s free) and follow the Journal’s Twitter feed (@jhospmedicine). But that’s pretty much it, Dr. Wray said. The group convenes on a Monday evening each month for an hour, starting at 9 p.m. Eastern time. Upcoming chats and topics are announced on Twitter and at SHM’s website.
The chats have grown and evolved since 2015, shifting in focus given recent social upheavals over the pandemic and heated discussions about diversity, equity, and racial justice in medicine, he said. “When COVID hit, the journal’s editor – Dr. Samir Shah – recognized that we were in a unique moment with the pandemic. The journal took advantage of the opportunity to publish a lot more personal perspectives and viewpoints around COVID, along with a special issue devoted to social justice.”
Moderators for the chat typically choose three or four questions based on recently published articles or other relevant topics, such as racial inequities in health care or how to apply military principles to hospital medicine leadership. “We reach out to authors and tell them they can explain their articles to interested readers through the chat. I can’t think of a single one who said no. They see the opportunity to highlight their work and engage with readers who want to ask them questions,” Dr. Wray said.
The moderators’ questions are posed to stimulate participation, but another goal is to use that hour for networking. “It’s a powerful tool to allow SHM members to engage with each other,” he said. “Sometimes the chat has the feeling of trying to drink water from a fire hose – with the messages flashing past so quickly. But the key is not to try to respond to everything but rather to follow those threads that particularly interest you. We encourage you to engage, but it’s totally fine if you just sit back and observe. One thing we have done to make it a little more formal is to offer CME credits for participants.”
The chat welcomes hospitalists and nonhospitalists, nurse practitioners, physician assistants, academics, and nonacademics. “No matter how engaged you are with Twitter, if you have 10,000 followers or 10, we’ll amplify your voice,” he said. “We also have medical students participating and consider their perspectives valuable, too.”
Dr. Wray identified three main types of participants in the monthly chats. The first are regulars who come every month, rain or shine. Like the character Norm in the old television comedy “Cheers,” everybody knows their name. They become friends, sharing and reveling in each other’s accomplishments. “These are people who have multiple connections, personally and professionally, at a lot of different levels. I probably know a hundred or more people who I’ve primarily gotten to know online.”
A second and larger group might be drawn in because of an interest in a specific topic or article, but they’re also welcome to participate in the chat. And the third group may lurk in the background, following along but not commenting. The size of that third group is unknown, but metrics from SHM show a total of 796 participants posting 4,088 tweets during chats in 2020 (for an average of 132 participants and 681 tweets per chat). This adds up to a total of 34 million impressions across the platform for #JHMchat tweets for the year.
Creating community online
“Why do we do it? It’s difficult to read all of the relevant published articles and keep up to date,” said Dr. Arora, a medical educator whose job at Chicago Medicine is to improve the clinical learning environment for trainees and staff by aligning learning with the health system’s institutional quality, safety and value missions.
“Our idea was to bring together a kind of virtual journal club and have discussions around topics such as: how do you create a shared vision on rounds? How do you integrate that into clinical practice? How do we preserve work/life balance or address structural racism?” she said. Other topics have included work flow concerns, burnout, difficult conversations with patients, and career planning.
“The people we’re trying to reach are hospitalists – and they’re busy at the front lines of care. We also thought this was an interesting way to raise the journal’s profile and spark broader interest in the articles it publishes. But it’s really about creating community, with people who look forward to talking and connecting with each other each month through the chats,” Dr. Arora said. If they miss a chat, they feel they’ve missed important interactions.
“Many times when people log onto the chat, they give a status report on where they are at, such as ‘I’m home putting my kids to bed,’ or ‘I’m on call tonight,’ ” she added. “People are willing to engage with the medium because it’s easy to engage with. We can forget that physicians are like everyone else. They like to learn, but they want that learning to be fun.”
On Dec. 14, 2020, at 9 p.m. Eastern time, the first question for the monthly #JHMchat was posted: How will caring for COVID-19 patients this winter differ from caring for patients in the first wave? Given that another surge of hospitalized COVID patients is looming, participants posted that they feel familiar and more confident with effective clinical strategies for hospitalized COVID patients, having learned so much more about the virus. But they’re facing greater numbers of patients than in prior surges. “In March, we were in crisis, now we’re in complexity,” one noted.
Joining the moderators was the Pediatric Overflow Planning Contingency Response Network (POPCoRN), a group formed earlier this year to help mobilize pediatric medical capacity for COVID patients during pandemic surges (see “POPCoRN network mobilizes pediatric capacity during pandemic,” The Hospitalist, April 30, 2020). One of its questions involved the redeployment of physicians in response to COVID demands and what, for example, pediatric hospitalists need as resources and tools when they are reassigned to adult patients or to new roles in unfamiliar settings. A variety of educational resources were cited from POPCoRN, SHM, and ImproveDX, among others.
Defining medical communication
Another chat moderator is Angela Castellanos, MD, a pediatric hospitalist at Tufts Medical Center in Boston. Dr. Castellanos did a 1-year, full-time fellowship right after residency at the New England Journal of Medicine, participating hands-on as a member of the editorial team for the print and online editions of the venerable journal. She is now doing a digital media fellowship with JHM, a part-time commitment while holding down a full-time job as a hospitalist. She also puts together a Spanish language podcast covering primary care pediatric issues for parents and families.
“I’m interested in medical communication generally, as I try to figure out what that means,” she said. “I have continued to look for ways to be part of the social media community and to be more creative about it. The JHM fellowship came at a perfect time for me to learn to do more in digital media.”
COVID has created new opportunities for more immediate dialogue with colleagues – what are they seeing and what’s working in the absence of clinical trials, she explained. “That’s how we communicate, as a way to get information out fast, such as when hospitals began proning COVID patients to make it easier for them to breathe.”
Dr. Castellanos said she grew up with text messaging and social media and wants to continue to grow her skills in this area. “I think I developed some skills at NEJM, but the opportunity to see how they do things at another journal with a different mission was also valuable. I get to share the space with people in academic settings and leaders in my field. I tweet at them; they tweet at me. These two fellowships have given me unique insights and mentorships. I know I want to continue doing pediatric hospital medicine and to engage academically and learn how to do research.”
Twitter sometimes gets a bad reputation for hostile or incendiary posts, Dr. Wray noted. “If you look at social media writ large, it can sometimes seem like a dumpster fire.” But what has happened in the medical community and in most medical Twitter encounters is a more cordial approach to conversations. “People who work in medicine converse with each other, with room for respectful disagreements. We’re extra supportive of each other,” he said.
“I think if hospitalists are looking for a community of peers, to engage with them and network and to find colleagues in similar circumstances, the JHM chat is such a fantastic place,” Dr. Wray concluded. “Don’t just come once, come several times, meet people along the way. For me, one of the most beneficial ways to advance my career has been by connecting with people through the chat. It allows me to share my work and success with the hospitalist community, as well as highlighting my trainees’ and colleagues’ successes, and it has created opportunities I never would have expected for getting involved in other projects.”
Once upon a time, physicians wrote letters to peers and colleagues around the world, sharing their medical discoveries, theories, case reports, and questions; conferring on problems; and then waiting for return mail to bring a reply. And the science of medicine advanced at a glacial pace.
Today, communication in multiple mediums flows much faster, almost instantaneously, between many more physicians, regardless of distance, addressing a much greater complexity of medical topics and treatments. And one of the chief mediums for this rapid electronic conversation among doctors is Twitter, according to Charlie Wray, DO, MS, a hospitalist at the University of California, San Francisco.
Dr. Wray, associate editor and digital media editor for the Journal of Hospital Medicine, is one of the moderators of #JHMchat, a monthly get-together on Twitter for interested hospitalists to link up virtually; respond to questions posed by JHM editors and other moderators; exchange perspectives, experiences, and tips with their peers; and build professional relationships and personal friendships. Relationship building has become particularly important in the age of COVID-19, when opportunities to connect in person at events such as SHM’s annual conferences have been curtailed.
The online #JHMchat community began in 2015, shortly after Dr. Wray completed a hospitalist research fellowship at the University of Chicago. His fellowship mentor, Vineet Arora, MD, MAPP, MHM, associate chief medical officer for the clinical learning environment at University of Chicago Medicine, had noticed how other online medical communities were engaging in discussions around different topics.
“She thought it could be a great way for hospitalists to meet online and talk about the articles published in JHM,” Dr. Wray explained. “We were all getting into social media and learning how to moderate interactive discussions such as Twitter.”
The chat’s founders approached JHM’s then-editor Andrew Auerbach, MD, MHM, a hospitalist at UCSF, who agreed that it was a great idea. They asked Christopher Moriates, MD, author of a recently published paper on the advisability of nebulized bronchodilators for obstructive pulmonary symptoms and assistant dean for health care value at the University of Texas, Austin, to come on the chat and talk about his paper. Visiting Dr. Arora at the time, he joined her in her living room for the first chat on Oct. 12, 2015. Seventy-five participants posted 431 tweets, with a total of 2 million Twitter impressions, suggesting that they had tapped a latent need.
How the chat works
To participate in the JHM chats on Twitter, one needs to open an account on the platform (it’s free) and follow the Journal’s Twitter feed (@jhospmedicine). But that’s pretty much it, Dr. Wray said. The group convenes on a Monday evening each month for an hour, starting at 9 p.m. Eastern time. Upcoming chats and topics are announced on Twitter and at SHM’s website.
The chats have grown and evolved since 2015, shifting in focus given recent social upheavals over the pandemic and heated discussions about diversity, equity, and racial justice in medicine, he said. “When COVID hit, the journal’s editor – Dr. Samir Shah – recognized that we were in a unique moment with the pandemic. The journal took advantage of the opportunity to publish a lot more personal perspectives and viewpoints around COVID, along with a special issue devoted to social justice.”
Moderators for the chat typically choose three or four questions based on recently published articles or other relevant topics, such as racial inequities in health care or how to apply military principles to hospital medicine leadership. “We reach out to authors and tell them they can explain their articles to interested readers through the chat. I can’t think of a single one who said no. They see the opportunity to highlight their work and engage with readers who want to ask them questions,” Dr. Wray said.
The moderators’ questions are posed to stimulate participation, but another goal is to use that hour for networking. “It’s a powerful tool to allow SHM members to engage with each other,” he said. “Sometimes the chat has the feeling of trying to drink water from a fire hose – with the messages flashing past so quickly. But the key is not to try to respond to everything but rather to follow those threads that particularly interest you. We encourage you to engage, but it’s totally fine if you just sit back and observe. One thing we have done to make it a little more formal is to offer CME credits for participants.”
The chat welcomes hospitalists and nonhospitalists, nurse practitioners, physician assistants, academics, and nonacademics. “No matter how engaged you are with Twitter, if you have 10,000 followers or 10, we’ll amplify your voice,” he said. “We also have medical students participating and consider their perspectives valuable, too.”
Dr. Wray identified three main types of participants in the monthly chats. The first are regulars who come every month, rain or shine. Like the character Norm in the old television comedy “Cheers,” everybody knows their name. They become friends, sharing and reveling in each other’s accomplishments. “These are people who have multiple connections, personally and professionally, at a lot of different levels. I probably know a hundred or more people who I’ve primarily gotten to know online.”
A second and larger group might be drawn in because of an interest in a specific topic or article, but they’re also welcome to participate in the chat. And the third group may lurk in the background, following along but not commenting. The size of that third group is unknown, but metrics from SHM show a total of 796 participants posting 4,088 tweets during chats in 2020 (for an average of 132 participants and 681 tweets per chat). This adds up to a total of 34 million impressions across the platform for #JHMchat tweets for the year.
Creating community online
“Why do we do it? It’s difficult to read all of the relevant published articles and keep up to date,” said Dr. Arora, a medical educator whose job at Chicago Medicine is to improve the clinical learning environment for trainees and staff by aligning learning with the health system’s institutional quality, safety and value missions.
“Our idea was to bring together a kind of virtual journal club and have discussions around topics such as: how do you create a shared vision on rounds? How do you integrate that into clinical practice? How do we preserve work/life balance or address structural racism?” she said. Other topics have included work flow concerns, burnout, difficult conversations with patients, and career planning.
“The people we’re trying to reach are hospitalists – and they’re busy at the front lines of care. We also thought this was an interesting way to raise the journal’s profile and spark broader interest in the articles it publishes. But it’s really about creating community, with people who look forward to talking and connecting with each other each month through the chats,” Dr. Arora said. If they miss a chat, they feel they’ve missed important interactions.
“Many times when people log onto the chat, they give a status report on where they are at, such as ‘I’m home putting my kids to bed,’ or ‘I’m on call tonight,’ ” she added. “People are willing to engage with the medium because it’s easy to engage with. We can forget that physicians are like everyone else. They like to learn, but they want that learning to be fun.”
On Dec. 14, 2020, at 9 p.m. Eastern time, the first question for the monthly #JHMchat was posted: How will caring for COVID-19 patients this winter differ from caring for patients in the first wave? Given that another surge of hospitalized COVID patients is looming, participants posted that they feel familiar and more confident with effective clinical strategies for hospitalized COVID patients, having learned so much more about the virus. But they’re facing greater numbers of patients than in prior surges. “In March, we were in crisis, now we’re in complexity,” one noted.
Joining the moderators was the Pediatric Overflow Planning Contingency Response Network (POPCoRN), a group formed earlier this year to help mobilize pediatric medical capacity for COVID patients during pandemic surges (see “POPCoRN network mobilizes pediatric capacity during pandemic,” The Hospitalist, April 30, 2020). One of its questions involved the redeployment of physicians in response to COVID demands and what, for example, pediatric hospitalists need as resources and tools when they are reassigned to adult patients or to new roles in unfamiliar settings. A variety of educational resources were cited from POPCoRN, SHM, and ImproveDX, among others.
Defining medical communication
Another chat moderator is Angela Castellanos, MD, a pediatric hospitalist at Tufts Medical Center in Boston. Dr. Castellanos did a 1-year, full-time fellowship right after residency at the New England Journal of Medicine, participating hands-on as a member of the editorial team for the print and online editions of the venerable journal. She is now doing a digital media fellowship with JHM, a part-time commitment while holding down a full-time job as a hospitalist. She also puts together a Spanish language podcast covering primary care pediatric issues for parents and families.
“I’m interested in medical communication generally, as I try to figure out what that means,” she said. “I have continued to look for ways to be part of the social media community and to be more creative about it. The JHM fellowship came at a perfect time for me to learn to do more in digital media.”
COVID has created new opportunities for more immediate dialogue with colleagues – what are they seeing and what’s working in the absence of clinical trials, she explained. “That’s how we communicate, as a way to get information out fast, such as when hospitals began proning COVID patients to make it easier for them to breathe.”
Dr. Castellanos said she grew up with text messaging and social media and wants to continue to grow her skills in this area. “I think I developed some skills at NEJM, but the opportunity to see how they do things at another journal with a different mission was also valuable. I get to share the space with people in academic settings and leaders in my field. I tweet at them; they tweet at me. These two fellowships have given me unique insights and mentorships. I know I want to continue doing pediatric hospital medicine and to engage academically and learn how to do research.”
Twitter sometimes gets a bad reputation for hostile or incendiary posts, Dr. Wray noted. “If you look at social media writ large, it can sometimes seem like a dumpster fire.” But what has happened in the medical community and in most medical Twitter encounters is a more cordial approach to conversations. “People who work in medicine converse with each other, with room for respectful disagreements. We’re extra supportive of each other,” he said.
“I think if hospitalists are looking for a community of peers, to engage with them and network and to find colleagues in similar circumstances, the JHM chat is such a fantastic place,” Dr. Wray concluded. “Don’t just come once, come several times, meet people along the way. For me, one of the most beneficial ways to advance my career has been by connecting with people through the chat. It allows me to share my work and success with the hospitalist community, as well as highlighting my trainees’ and colleagues’ successes, and it has created opportunities I never would have expected for getting involved in other projects.”
Pediatric HM highlights from the 2020 State of Hospital Medicine Report
To improve the pediatric data in the State of Hospital Medicine (SoHM) Report, the Practice Analysis Committee (PAC) developed a pediatric task force to recommend content specific to pediatric practice and garner support for survey participation. The pediatric hospital medicine (PHM) community responded with its usual enthusiasm, resulting in a threefold increase in PHM participation (99 groups), making the data from 2020 SoHM Report the most meaningful ever for pediatric practices.
However, data collection for the 2020 SoHM Report concluded in February, just before the face of medical practice and hospital care changed dramatically. A recent report at the virtual Pediatric Hospital Medicine meeting stated that pre–COVID-19 hospital operating margins had already taken a significant decline (from 5% to 2%-3%), putting pressure on pediatric programs in community settings that typically do not generate much revenue. After COVID-19, hospital revenues took an even greater downturn, affecting many hospital-based pediatric programs. While the future direction of many PHM programs remains unclear, the robust nature of the pediatric data in the 2020 SoHM Report defines where we were and where we once again hope to be. In addition, the PAC conducted a supplemental survey designed to assess the impact of COVID-19 on the practice of hospital medicine. Here’s a quick review of PHM highlights from the 2020 SoHM Report, with preliminary findings from the supplemental survey.
Diversity of service and scope of practice: pediatric hospitalist programs continue to provide a wide variety of services beyond care on inpatient wards, with the most common being procedure performance (56.6%), care of healthy newborns (51.5%), and rapid response team (38.4%) coverage. In addition, most PHM programs have a role in comanagement of a wide variety of patient populations, with the greatest presence among the surgical specialties. Approximately 90% of programs report some role in the care of patients admitted to general surgery, orthopedic surgery, and other surgical subspecialties. The role for comanagement with medical specialties remains diverse, with PHM programs routinely having some role in caring for patients hospitalized for neurologic, gastroenterological, cardiac concerns, and others. With the recent decline in hospital revenues affecting PHM practices, one way to ensure program value is to continue to diversify. Based on data from the 2020 SoHM report, broadening of clinical coverage will not require a significant change in practice for most PHM programs.
PHM board certification: With the first certifying exam for PHM taking place just months before SoHM data collection, the survey sought to establish a baseline percentage of providers board certified in PHM. With 98 groups responding, an average of 26.4% of PHM practitioners per group were reported to be board certified. While no difference was seen based on academic status, practitioners in PHM programs employed by a hospital, health system, or integrated delivery system were much more likely to be board certified than those employed by a university or medical school (31% vs. 20%). Regional differences were noted as well, with the East region reporting a much higher median proportion of PHM-certified physicians. It will be interesting to watch the trend in board certification status evolve over the upcoming years.
Anticipated change of budgeted full-time equivalents in the next year/post–COVID-19 analysis: Of the PHM programs responding to the SoHM Survey, 46.5% predicted an increase in budgeted full-time equivalents in the next year, while only 5.1% anticipated a decrease. Expecting this to change in response to COVID-19, the supplemental survey sought to update this information. Of the 30 PHM respondents to the supplemental survey, 41% instituted a temporary hiring freeze because of COVID-19, while 8.3% instituted a hiring freeze felt likely to be permanent. As PHM programs gear up for the next viral season, we wait to see whether the impact of COVID-19 will continue to be reflected in the volume and variety of patients admitted. It is clear that PHM programs will need to remain nimble to stay ahead of the changing landscape of practice in the days ahead. View all data by obtaining access to the 2020 SoHM Report at hospitalmedicine.org/sohm.
Many thanks to pediatric task force members Jack Percelay, MD; Vivien Kon-Ea Sun, MD; Marcos Mestre, MD; Ann Allen, MD; Dimple Khona, MD; Jeff Grill, MD; and Michelle Marks, MD.
Dr. Gage is director of faculty development, pediatric hospital medicine, at Phoenix Children’s Hospital, and associate professor of pediatrics at the University of Arizona, Phoenix.
To improve the pediatric data in the State of Hospital Medicine (SoHM) Report, the Practice Analysis Committee (PAC) developed a pediatric task force to recommend content specific to pediatric practice and garner support for survey participation. The pediatric hospital medicine (PHM) community responded with its usual enthusiasm, resulting in a threefold increase in PHM participation (99 groups), making the data from 2020 SoHM Report the most meaningful ever for pediatric practices.
However, data collection for the 2020 SoHM Report concluded in February, just before the face of medical practice and hospital care changed dramatically. A recent report at the virtual Pediatric Hospital Medicine meeting stated that pre–COVID-19 hospital operating margins had already taken a significant decline (from 5% to 2%-3%), putting pressure on pediatric programs in community settings that typically do not generate much revenue. After COVID-19, hospital revenues took an even greater downturn, affecting many hospital-based pediatric programs. While the future direction of many PHM programs remains unclear, the robust nature of the pediatric data in the 2020 SoHM Report defines where we were and where we once again hope to be. In addition, the PAC conducted a supplemental survey designed to assess the impact of COVID-19 on the practice of hospital medicine. Here’s a quick review of PHM highlights from the 2020 SoHM Report, with preliminary findings from the supplemental survey.
Diversity of service and scope of practice: pediatric hospitalist programs continue to provide a wide variety of services beyond care on inpatient wards, with the most common being procedure performance (56.6%), care of healthy newborns (51.5%), and rapid response team (38.4%) coverage. In addition, most PHM programs have a role in comanagement of a wide variety of patient populations, with the greatest presence among the surgical specialties. Approximately 90% of programs report some role in the care of patients admitted to general surgery, orthopedic surgery, and other surgical subspecialties. The role for comanagement with medical specialties remains diverse, with PHM programs routinely having some role in caring for patients hospitalized for neurologic, gastroenterological, cardiac concerns, and others. With the recent decline in hospital revenues affecting PHM practices, one way to ensure program value is to continue to diversify. Based on data from the 2020 SoHM report, broadening of clinical coverage will not require a significant change in practice for most PHM programs.
PHM board certification: With the first certifying exam for PHM taking place just months before SoHM data collection, the survey sought to establish a baseline percentage of providers board certified in PHM. With 98 groups responding, an average of 26.4% of PHM practitioners per group were reported to be board certified. While no difference was seen based on academic status, practitioners in PHM programs employed by a hospital, health system, or integrated delivery system were much more likely to be board certified than those employed by a university or medical school (31% vs. 20%). Regional differences were noted as well, with the East region reporting a much higher median proportion of PHM-certified physicians. It will be interesting to watch the trend in board certification status evolve over the upcoming years.
Anticipated change of budgeted full-time equivalents in the next year/post–COVID-19 analysis: Of the PHM programs responding to the SoHM Survey, 46.5% predicted an increase in budgeted full-time equivalents in the next year, while only 5.1% anticipated a decrease. Expecting this to change in response to COVID-19, the supplemental survey sought to update this information. Of the 30 PHM respondents to the supplemental survey, 41% instituted a temporary hiring freeze because of COVID-19, while 8.3% instituted a hiring freeze felt likely to be permanent. As PHM programs gear up for the next viral season, we wait to see whether the impact of COVID-19 will continue to be reflected in the volume and variety of patients admitted. It is clear that PHM programs will need to remain nimble to stay ahead of the changing landscape of practice in the days ahead. View all data by obtaining access to the 2020 SoHM Report at hospitalmedicine.org/sohm.
Many thanks to pediatric task force members Jack Percelay, MD; Vivien Kon-Ea Sun, MD; Marcos Mestre, MD; Ann Allen, MD; Dimple Khona, MD; Jeff Grill, MD; and Michelle Marks, MD.
Dr. Gage is director of faculty development, pediatric hospital medicine, at Phoenix Children’s Hospital, and associate professor of pediatrics at the University of Arizona, Phoenix.
To improve the pediatric data in the State of Hospital Medicine (SoHM) Report, the Practice Analysis Committee (PAC) developed a pediatric task force to recommend content specific to pediatric practice and garner support for survey participation. The pediatric hospital medicine (PHM) community responded with its usual enthusiasm, resulting in a threefold increase in PHM participation (99 groups), making the data from 2020 SoHM Report the most meaningful ever for pediatric practices.
However, data collection for the 2020 SoHM Report concluded in February, just before the face of medical practice and hospital care changed dramatically. A recent report at the virtual Pediatric Hospital Medicine meeting stated that pre–COVID-19 hospital operating margins had already taken a significant decline (from 5% to 2%-3%), putting pressure on pediatric programs in community settings that typically do not generate much revenue. After COVID-19, hospital revenues took an even greater downturn, affecting many hospital-based pediatric programs. While the future direction of many PHM programs remains unclear, the robust nature of the pediatric data in the 2020 SoHM Report defines where we were and where we once again hope to be. In addition, the PAC conducted a supplemental survey designed to assess the impact of COVID-19 on the practice of hospital medicine. Here’s a quick review of PHM highlights from the 2020 SoHM Report, with preliminary findings from the supplemental survey.
Diversity of service and scope of practice: pediatric hospitalist programs continue to provide a wide variety of services beyond care on inpatient wards, with the most common being procedure performance (56.6%), care of healthy newborns (51.5%), and rapid response team (38.4%) coverage. In addition, most PHM programs have a role in comanagement of a wide variety of patient populations, with the greatest presence among the surgical specialties. Approximately 90% of programs report some role in the care of patients admitted to general surgery, orthopedic surgery, and other surgical subspecialties. The role for comanagement with medical specialties remains diverse, with PHM programs routinely having some role in caring for patients hospitalized for neurologic, gastroenterological, cardiac concerns, and others. With the recent decline in hospital revenues affecting PHM practices, one way to ensure program value is to continue to diversify. Based on data from the 2020 SoHM report, broadening of clinical coverage will not require a significant change in practice for most PHM programs.
PHM board certification: With the first certifying exam for PHM taking place just months before SoHM data collection, the survey sought to establish a baseline percentage of providers board certified in PHM. With 98 groups responding, an average of 26.4% of PHM practitioners per group were reported to be board certified. While no difference was seen based on academic status, practitioners in PHM programs employed by a hospital, health system, or integrated delivery system were much more likely to be board certified than those employed by a university or medical school (31% vs. 20%). Regional differences were noted as well, with the East region reporting a much higher median proportion of PHM-certified physicians. It will be interesting to watch the trend in board certification status evolve over the upcoming years.
Anticipated change of budgeted full-time equivalents in the next year/post–COVID-19 analysis: Of the PHM programs responding to the SoHM Survey, 46.5% predicted an increase in budgeted full-time equivalents in the next year, while only 5.1% anticipated a decrease. Expecting this to change in response to COVID-19, the supplemental survey sought to update this information. Of the 30 PHM respondents to the supplemental survey, 41% instituted a temporary hiring freeze because of COVID-19, while 8.3% instituted a hiring freeze felt likely to be permanent. As PHM programs gear up for the next viral season, we wait to see whether the impact of COVID-19 will continue to be reflected in the volume and variety of patients admitted. It is clear that PHM programs will need to remain nimble to stay ahead of the changing landscape of practice in the days ahead. View all data by obtaining access to the 2020 SoHM Report at hospitalmedicine.org/sohm.
Many thanks to pediatric task force members Jack Percelay, MD; Vivien Kon-Ea Sun, MD; Marcos Mestre, MD; Ann Allen, MD; Dimple Khona, MD; Jeff Grill, MD; and Michelle Marks, MD.
Dr. Gage is director of faculty development, pediatric hospital medicine, at Phoenix Children’s Hospital, and associate professor of pediatrics at the University of Arizona, Phoenix.
COVID-19 drives physician burnout for some specialties
Physician burnout remains at a critical level, at 42% overall – the same percentage as last year – but COVID-19 has changed the specialties hit hardest, according to Medscape’s Death by 1,000 Cuts: Physician Burnout & Suicide Report.
Critical care physicians now top the list of those experiencing burnout, at 51%, up from 44% last year, followed by rheumatologists (50%, up from 46%) and infectious disease specialists (49%, up from 45%). Forty-nine percent of urologists reported burnout, but that was a reduction from 54% last year.
Last year, the specialties burdened most by burnout were urology, neurology, nephrology, endocrinology, and family medicine.
Women hit particularly hard
Women in medicine traditionally have experienced higher levels of burnout than men, and the pandemic seems to have widened that gap, with the divide now at 51% for women and 36% for men.
“Many women physicians are in families with children at home,” said Carol Bernstein, MD, psychiatrist at Montefiore Medical Center, New York. “It’s already known that women assume more responsibilities in the home than do men. The pressures have increased during COVID-19 – having to be their child’s teacher during home schooling, no child care, and the grandparents can’t babysit. In addition, all doctors and nurses are worried about bringing the virus home to their families.”
Data were collected from Aug. 30 through Nov. 5, 2020. More than 12,000 physicians from 29 specialties responded.
For many, (79%) burnout has been building over years, but for some (21%), it started with the pandemic. Factors cited include lack of adequate personal protective equipment, grief from losing patients, watching families suffer, long hours, and difficult working conditions.
More than 70% of those who responded feel that burnout has had at least a moderate impact on their lives.
“One-tenth consider it severe enough to consider leaving medicine,” survey authors wrote, “an unexpected outcome after having spent so many years in training to become a physician.”
Tragically, an estimated 300 physicians each year in the United States are consumed by the struggle and take their own lives.
One percent have attempted suicide
In this survey, 13% of physicians had thoughts of suicide, and 1% have attempted it; 81% said they had no thoughts of suicide; and 5% preferred not to answer.
By specialty, obstetricians/gynecologists were most likely to have thoughts of suicide (19%), followed by orthopedists (18%) and otolaryngologists and plastic surgeons (17%).
“I yell all the time, I am angry and frustrated all the time. I think about quitting all the time,” said an internist who admitted having suicidal thoughts. “No one in my organization cares about doing the right things for patients as much as I do.”
Yet, many with such thoughts tell no one. By age group, 32% of millennials, 40% of generation X physicians, and 41% of baby boomer physicians who had had thoughts of suicide said they had told no one about those thoughts.
Fear of being reported to the medical board, fear of colleagues finding out, and other factors perpetuate a cycle of burnout and depression, and most don’t seek help.
Top reasons physicians listed for not seeking help for burnout and depression include “symptoms are not severe enough” (52%); “I can deal with without help from a professional” (46%); and feeling “too busy” (40%).
Administrative tasks fuel burnout
The top driver of burnout continues to be “too many administrative tasks.” This year, 58% put it at the top. The next highest categories (named by 37%) were “spending too many hours at work” and “lack of respect from administrators/employers, colleagues or staff.” Others mentioned lack of control or insufficient compensation and government regulations.
Notably, only 8% said stress from treating COVID-19 patients was the top driver.
An internist said, “I’m working 6 days a week, nights, weekends, holidays!”
A general surgeon said, “Being forced to see four patients an hour when complicated patients and procedures are involved” was the biggest contributor to burnout.
One physician in the survey summarized it: “It’s all of these causes; it’s death by 1,000 cuts.”
Exercise tops coping list
Asked how they cope with stress and burnout, physicians put exercise at the top (48%). Next was talking with family and friends (43%), though 43% said they cope by isolating themselves.
Drinking alcohol and overeating junk food were up slightly in the past year: for alcohol, 26%, up from 24%; for junk food, 35%, up from 33%.
The action respondents said would help most to reduce burnout was “increased compensation to avoid financial stress,” chosen by 45%. Next, at 42%, was “more manageable work and schedule,” followed by greater respect from employers, colleagues, and staff (39%).
Asked whether their workplace offered programs to reduce stress and/or burnout, almost half (47%) of physicians said no; 35% said yes; and 18% didn’t know.
Participation in such programs has been low. Almost half (42%) of physicians in this survey said they would be unlikely to attend such a program. Thirty percent they would be likely to participate; 28% said they were neutral on the idea.
“Anti-stress/burnout programs focus on individual approaches to much larger problems,” Wendy K. Dean, MD, psychiatrist and president of Moral Injury of Healthcare, said in an interview. “The programs offer temporary symptomatic relief rather than lasting systemic change. Many physicians are frustrated by these approaches.”
A study last year by the Mayo Clinic found that “the most efficacious strategy to alleviate physician burnout will target organization-directed changes rather than the level of the individual.”
A version of this article first appeared on Medscape.com.
Physician burnout remains at a critical level, at 42% overall – the same percentage as last year – but COVID-19 has changed the specialties hit hardest, according to Medscape’s Death by 1,000 Cuts: Physician Burnout & Suicide Report.
Critical care physicians now top the list of those experiencing burnout, at 51%, up from 44% last year, followed by rheumatologists (50%, up from 46%) and infectious disease specialists (49%, up from 45%). Forty-nine percent of urologists reported burnout, but that was a reduction from 54% last year.
Last year, the specialties burdened most by burnout were urology, neurology, nephrology, endocrinology, and family medicine.
Women hit particularly hard
Women in medicine traditionally have experienced higher levels of burnout than men, and the pandemic seems to have widened that gap, with the divide now at 51% for women and 36% for men.
“Many women physicians are in families with children at home,” said Carol Bernstein, MD, psychiatrist at Montefiore Medical Center, New York. “It’s already known that women assume more responsibilities in the home than do men. The pressures have increased during COVID-19 – having to be their child’s teacher during home schooling, no child care, and the grandparents can’t babysit. In addition, all doctors and nurses are worried about bringing the virus home to their families.”
Data were collected from Aug. 30 through Nov. 5, 2020. More than 12,000 physicians from 29 specialties responded.
For many, (79%) burnout has been building over years, but for some (21%), it started with the pandemic. Factors cited include lack of adequate personal protective equipment, grief from losing patients, watching families suffer, long hours, and difficult working conditions.
More than 70% of those who responded feel that burnout has had at least a moderate impact on their lives.
“One-tenth consider it severe enough to consider leaving medicine,” survey authors wrote, “an unexpected outcome after having spent so many years in training to become a physician.”
Tragically, an estimated 300 physicians each year in the United States are consumed by the struggle and take their own lives.
One percent have attempted suicide
In this survey, 13% of physicians had thoughts of suicide, and 1% have attempted it; 81% said they had no thoughts of suicide; and 5% preferred not to answer.
By specialty, obstetricians/gynecologists were most likely to have thoughts of suicide (19%), followed by orthopedists (18%) and otolaryngologists and plastic surgeons (17%).
“I yell all the time, I am angry and frustrated all the time. I think about quitting all the time,” said an internist who admitted having suicidal thoughts. “No one in my organization cares about doing the right things for patients as much as I do.”
Yet, many with such thoughts tell no one. By age group, 32% of millennials, 40% of generation X physicians, and 41% of baby boomer physicians who had had thoughts of suicide said they had told no one about those thoughts.
Fear of being reported to the medical board, fear of colleagues finding out, and other factors perpetuate a cycle of burnout and depression, and most don’t seek help.
Top reasons physicians listed for not seeking help for burnout and depression include “symptoms are not severe enough” (52%); “I can deal with without help from a professional” (46%); and feeling “too busy” (40%).
Administrative tasks fuel burnout
The top driver of burnout continues to be “too many administrative tasks.” This year, 58% put it at the top. The next highest categories (named by 37%) were “spending too many hours at work” and “lack of respect from administrators/employers, colleagues or staff.” Others mentioned lack of control or insufficient compensation and government regulations.
Notably, only 8% said stress from treating COVID-19 patients was the top driver.
An internist said, “I’m working 6 days a week, nights, weekends, holidays!”
A general surgeon said, “Being forced to see four patients an hour when complicated patients and procedures are involved” was the biggest contributor to burnout.
One physician in the survey summarized it: “It’s all of these causes; it’s death by 1,000 cuts.”
Exercise tops coping list
Asked how they cope with stress and burnout, physicians put exercise at the top (48%). Next was talking with family and friends (43%), though 43% said they cope by isolating themselves.
Drinking alcohol and overeating junk food were up slightly in the past year: for alcohol, 26%, up from 24%; for junk food, 35%, up from 33%.
The action respondents said would help most to reduce burnout was “increased compensation to avoid financial stress,” chosen by 45%. Next, at 42%, was “more manageable work and schedule,” followed by greater respect from employers, colleagues, and staff (39%).
Asked whether their workplace offered programs to reduce stress and/or burnout, almost half (47%) of physicians said no; 35% said yes; and 18% didn’t know.
Participation in such programs has been low. Almost half (42%) of physicians in this survey said they would be unlikely to attend such a program. Thirty percent they would be likely to participate; 28% said they were neutral on the idea.
“Anti-stress/burnout programs focus on individual approaches to much larger problems,” Wendy K. Dean, MD, psychiatrist and president of Moral Injury of Healthcare, said in an interview. “The programs offer temporary symptomatic relief rather than lasting systemic change. Many physicians are frustrated by these approaches.”
A study last year by the Mayo Clinic found that “the most efficacious strategy to alleviate physician burnout will target organization-directed changes rather than the level of the individual.”
A version of this article first appeared on Medscape.com.
Physician burnout remains at a critical level, at 42% overall – the same percentage as last year – but COVID-19 has changed the specialties hit hardest, according to Medscape’s Death by 1,000 Cuts: Physician Burnout & Suicide Report.
Critical care physicians now top the list of those experiencing burnout, at 51%, up from 44% last year, followed by rheumatologists (50%, up from 46%) and infectious disease specialists (49%, up from 45%). Forty-nine percent of urologists reported burnout, but that was a reduction from 54% last year.
Last year, the specialties burdened most by burnout were urology, neurology, nephrology, endocrinology, and family medicine.
Women hit particularly hard
Women in medicine traditionally have experienced higher levels of burnout than men, and the pandemic seems to have widened that gap, with the divide now at 51% for women and 36% for men.
“Many women physicians are in families with children at home,” said Carol Bernstein, MD, psychiatrist at Montefiore Medical Center, New York. “It’s already known that women assume more responsibilities in the home than do men. The pressures have increased during COVID-19 – having to be their child’s teacher during home schooling, no child care, and the grandparents can’t babysit. In addition, all doctors and nurses are worried about bringing the virus home to their families.”
Data were collected from Aug. 30 through Nov. 5, 2020. More than 12,000 physicians from 29 specialties responded.
For many, (79%) burnout has been building over years, but for some (21%), it started with the pandemic. Factors cited include lack of adequate personal protective equipment, grief from losing patients, watching families suffer, long hours, and difficult working conditions.
More than 70% of those who responded feel that burnout has had at least a moderate impact on their lives.
“One-tenth consider it severe enough to consider leaving medicine,” survey authors wrote, “an unexpected outcome after having spent so many years in training to become a physician.”
Tragically, an estimated 300 physicians each year in the United States are consumed by the struggle and take their own lives.
One percent have attempted suicide
In this survey, 13% of physicians had thoughts of suicide, and 1% have attempted it; 81% said they had no thoughts of suicide; and 5% preferred not to answer.
By specialty, obstetricians/gynecologists were most likely to have thoughts of suicide (19%), followed by orthopedists (18%) and otolaryngologists and plastic surgeons (17%).
“I yell all the time, I am angry and frustrated all the time. I think about quitting all the time,” said an internist who admitted having suicidal thoughts. “No one in my organization cares about doing the right things for patients as much as I do.”
Yet, many with such thoughts tell no one. By age group, 32% of millennials, 40% of generation X physicians, and 41% of baby boomer physicians who had had thoughts of suicide said they had told no one about those thoughts.
Fear of being reported to the medical board, fear of colleagues finding out, and other factors perpetuate a cycle of burnout and depression, and most don’t seek help.
Top reasons physicians listed for not seeking help for burnout and depression include “symptoms are not severe enough” (52%); “I can deal with without help from a professional” (46%); and feeling “too busy” (40%).
Administrative tasks fuel burnout
The top driver of burnout continues to be “too many administrative tasks.” This year, 58% put it at the top. The next highest categories (named by 37%) were “spending too many hours at work” and “lack of respect from administrators/employers, colleagues or staff.” Others mentioned lack of control or insufficient compensation and government regulations.
Notably, only 8% said stress from treating COVID-19 patients was the top driver.
An internist said, “I’m working 6 days a week, nights, weekends, holidays!”
A general surgeon said, “Being forced to see four patients an hour when complicated patients and procedures are involved” was the biggest contributor to burnout.
One physician in the survey summarized it: “It’s all of these causes; it’s death by 1,000 cuts.”
Exercise tops coping list
Asked how they cope with stress and burnout, physicians put exercise at the top (48%). Next was talking with family and friends (43%), though 43% said they cope by isolating themselves.
Drinking alcohol and overeating junk food were up slightly in the past year: for alcohol, 26%, up from 24%; for junk food, 35%, up from 33%.
The action respondents said would help most to reduce burnout was “increased compensation to avoid financial stress,” chosen by 45%. Next, at 42%, was “more manageable work and schedule,” followed by greater respect from employers, colleagues, and staff (39%).
Asked whether their workplace offered programs to reduce stress and/or burnout, almost half (47%) of physicians said no; 35% said yes; and 18% didn’t know.
Participation in such programs has been low. Almost half (42%) of physicians in this survey said they would be unlikely to attend such a program. Thirty percent they would be likely to participate; 28% said they were neutral on the idea.
“Anti-stress/burnout programs focus on individual approaches to much larger problems,” Wendy K. Dean, MD, psychiatrist and president of Moral Injury of Healthcare, said in an interview. “The programs offer temporary symptomatic relief rather than lasting systemic change. Many physicians are frustrated by these approaches.”
A study last year by the Mayo Clinic found that “the most efficacious strategy to alleviate physician burnout will target organization-directed changes rather than the level of the individual.”
A version of this article first appeared on Medscape.com.
Finding meaning in ‘Lean’?
Using systems improvement strategies to support the Quadruple Aim
General background on well-being and burnout
With burnout increasingly recognized as a shared responsibility that requires addressing organizational drivers while supporting individuals to be well,1-4 practical strategies and examples of successful implementation of systems interventions to address burnout will be helpful for service directors to support their staff. The Charter on Physician Well-being, recently developed through collaborative input from multiple organizations, defines guiding principles and key commitments at the societal, organizational, interpersonal, and individual levels and may be a useful framework for organizations that are developing well-being initiatives.5
The charter advocates including physician well-being as a quality improvement metric for health systems, aligned with the concept of the Quadruple Aim of optimizing patient care by enhancing provider experience, promoting high-value care, and improving population health.6 Identifying areas of alignment between the charter’s recommendations and systems improvement strategies that seek to optimize efficiency and reduce waste, such as Lean Management, may help physician leaders to contextualize well-being initiatives more easily within ongoing systems improvement efforts. In this perspective, we provide one division’s experience using the Charter to assess successes and identify additional areas of improvement for well-being initiatives developed using Lean Management methodology.
Past and current state of affairs
In 2011, the division of hospital medicine at Zuckerberg San Francisco General Hospital was established and has seen continual expansion in terms of direct patient care, medical education, and hospital leadership.
In 2015, the division of hospital medicine experienced leadership transitions, faculty attrition, and insufficient recruitment resulting in staffing shortages, service line closure, schedule instability, and ultimately, low morale. A baseline survey conducted using the 2-Item Maslach Burnout Inventory. This survey, which uses one item in the domain of emotional exhaustion and one item in the domain of depersonalization, has shown good correlation with the full Maslach Burnout Inventory.7 At baseline, approximately one-third of the division’s physicians experienced burnout.
In response, a subsequent retreat focused on the three greatest areas of concern identified by the survey: scheduling, faculty development, and well-being.
Like many health systems, the hospital has adopted Lean as its preferred systems-improvement framework. The retreat was structured around the principles of Lean philosophy, and was designed to emulate that of a consolidated Kaizen workshop.
“Kaizen” in Japanese means “change for the better.” A typical Kaizen workshop revolves around rapid problem-solving over the course of 3-5 days, in which a team of people come together to identify and implement significant improvements for a selected process. To this end, the retreat was divided into subgroups for each area of concern. In turn, each subgroup mapped out existing workflows (“value stream”), identified areas of waste and non–value added time, and generated ideas of what an idealized process would be. Next, a root-cause analysis was performed and subsequent interventions (“countermeasures”) developed to address each problem. At the conclusion of the retreat, each subgroup shared a summary of their findings with the larger group.
Moving forward, this information served as a guiding framework for service and division leadership to run small tests of change. We enacted a series of countermeasures over the course of several years, and multiple cycles of improvement work addressed the three areas of concern. We developed an A3 report (a Lean project management tool that incorporates the plan-do-study-act cycle, organizes strategic efforts, and tracks progress on a single page) to summarize and present these initiatives to the Performance Improvement and Patient Safety Committee of the hospital executive leadership team. This structure illustrated alignment with the hospital’s core values (“true north”) of “developing people” and “care experience.”
In 2018, interval surveys demonstrated a gradual reduction of burnout to approximately one-fifth of division physicians as measured by the 2-item Maslach Burnout Inventory.
Initiatives in faculty well-being
The Charter of Physician Well-being outlines a framework to promote well-being among doctors by maximizing a sense of fulfillment and minimizing the harms of burnout. It shares this responsibility among societal, organizational, and interpersonal and individual commitments.5
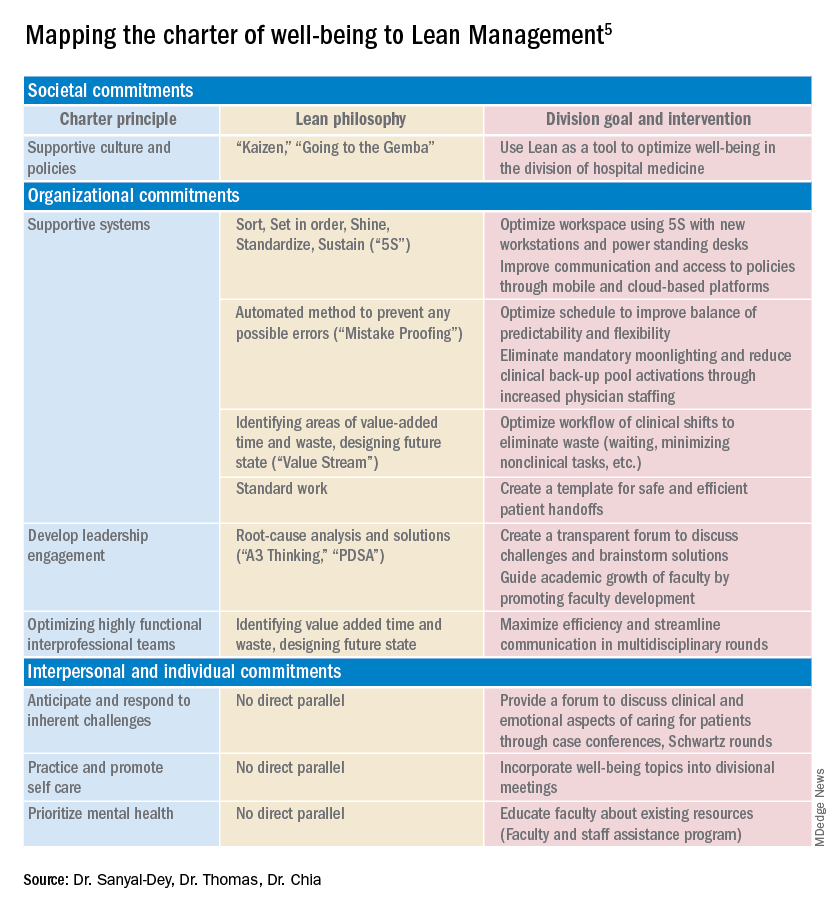
As illustrated above, we used principles of Lean Management to prospectively create initiatives to improve well-being in our division. Lean in health care is designed to optimize primarily the patient experience; its implementation has subsequently demonstrated mixed provider and staff experiences,8,9 and many providers are skeptical of Lean’s potential to improve their own well-being. If, however, Lean is aligned with best practice frameworks for well-being such as those outline in the charter, it may also help to meet the Quadruple Aim of optimizing both provider well-being and patient experience. To further test this hypothesis, we retrospectively categorized our Lean-based interventions into the commitments described by the charter to identify areas of alignment and gaps that were not initially addressed using Lean Management (Table).
Organizational commitments5Supportive systems
We optimized scheduling and enhanced physician staffing by budgeting for a physician staffing buffer each academic year in order to minimize mandatory moonlighting and jeopardy pool activations that result from operating on a thin staffing margin when expected personal leave and reductions in clinical effort occur. Furthermore, we revised scheduling principles to balance patient continuity and individual time off requests while setting limits on the maximum duration of clinical stretches and instituting mandatory minimum time off between them.
Leadership engagement
We initiated monthly operations meetings as a forum to discuss challenges, brainstorm solutions, and message new initiatives with group input. For example, as a result of these meetings, we designed and implemented an additional service line to address the high census, revised the distribution of new patient admissions to level-load clinical shifts, and established a maximum number of weekends worked per month and year. This approach aligns with recommendations to use participatory leadership strategies to enhance physician well-being.10 Engaging both executive level and service level management to focus on burnout and other related well-being metrics is necessary for sustaining such work.
Interprofessional teamwork
We revised multidisciplinary rounds with social work, utilization management, and physical therapy to maximize efficiency and streamline communication by developing standard approaches for each patient presentation.
Interpersonal and individual commitments5Address emotional challenges of physician work
Although these commitments did not have a direct corollary with Lean philosophy, some of these needs were identified by our physician group at our annual retreats. As a result, we initiated a monthly faculty-led noon conference series focused on the clinical challenges of caring for vulnerable populations, a particular source of distress in our practice setting, and revised the division schedule to encourage attendance at the hospital’s Schwartz rounds.
Mental health and self-care
We organized focus groups and faculty development sessions on provider well-being and burnout and dealing with challenging patients and invited the Faculty and Staff Assistance Program, our institution’s mental health service provider, to our weekly division meeting.
Future directions
After using Lean Management as an approach to prospectively improve physician well-being, we were able to use the Charter on Physician Well-being retrospectively as a “checklist” to identify additional gaps for targeted intervention to ensure all commitments are sufficiently addressed.
Overall, we found that, not surprisingly, Lean Management aligned best with the organizational commitments in the charter. Reviewing the organizational commitments, we found our biggest remaining challenges are in building supportive systems, namely ensuring sustainable workloads, offloading and delegating nonphysician tasks, and minimizing the burden of documentation and administration.
Reviewing the societal commitments helped us to identify opportunities for future directions that we may not have otherwise considered. As a safety-net institution, we benefit from a strong sense of mission and shared values within our hospital and division. However, we recognize the need to continue to be vigilant to ensure that our physicians perceive that their own values are aligned with the division’s stated mission. Devoting a Kaizen-style retreat to well-being likely helped, and allocating divisional resources to a well-being committee indirectly helped, to foster a culture of well-being; however, we could more deliberately identify local policies that may benefit from advocacy or revision. Although our faculty identified interventions to improve interpersonal and individual drivers of well-being, these charter commitments did not have direct parallels in Lean philosophy, and organizations may need to deliberately seek to address these commitments outside of a Lean approach. Specifically, by reviewing the charter, we identified opportunities to provide additional resources for peer support and protected time for mental health care and self-care.
Conclusion
Lean Management can be an effective strategy to address many of the organizational commitments outlined in the Charter on Physician Well-being. This approach may be particularly effective for solving local challenges with systems and workflows. Those who use Lean as a primary method to approach systems improvement in support of the Quadruple Aim may need to use additional strategies to address societal and interpersonal and individual commitments outlined in the charter.
Dr. Sanyal-Dey is visiting associate clinical professor of medicine at Zuckerberg San Francisco General Hospital and director of client services, LeanTaaS. Dr. Thomas is associate clinical professor of medicine at Zuckerberg San Francisco General Hospital. Dr. Chia is associate professor of clinical medicine at Zuckerberg San Francisco General Hospital.
References
1. West CP et al. Interventions to prevent and reduce physician burnout: A systematic review and meta-analysis. Lancet. 2016;388(10057):2272-81.
2. Shanafelt TD, Noseworthy JH. Executive leadership and physician: Nine organizational strategies to promote engagement and reduce burnout. Mayo Clin Proc. 2017;92(1):129-46.
3. Shanafelt T et al. The business case for investing in physician well-being. JAMA Intern Med. 2017;177(12):1826-32.
4. Shanafelt T et al. Building a program on well-being: Key design considerations to meet the unique needs of each organization. Acad Med. 2019 Feb;94(2):156-161.
5. Thomas LR et al. Charter on physician well-being. JAMA. 2018;319(15):1541-42.
6. Bodenheimer T, Sinsky C. From triple to quadruple aim: Care of the patient requires care of the provider. Ann Fam Med. 2014;12(6):573-6.
7. West CP et al. Concurrent Validity of Single-Item Measures of Emotional Exhaustion and Depersonalization in Burnout Assessment. J Gen Intern Med. 2012;27(11):1445-52.
8. Hung DY et al. Experiences of primary care physicians and staff following lean workflow redesign. BMC Health Serv Res. 2018 Apr 10;18(1):274.
9. Zibrowski E et al. Easier and faster is not always better: Grounded theory of the impact of large-scale system transformation on the clinical work of emergency medicine nurses and physicians. JMIR Hum Factors. 2018. doi: 10.2196/11013.
10. Shanafelt TD et al. Impact of organizational leadership on physician burnout and satisfaction. Mayo Clin Proc. 2015;90(4):432-40.
Using systems improvement strategies to support the Quadruple Aim
Using systems improvement strategies to support the Quadruple Aim
General background on well-being and burnout
With burnout increasingly recognized as a shared responsibility that requires addressing organizational drivers while supporting individuals to be well,1-4 practical strategies and examples of successful implementation of systems interventions to address burnout will be helpful for service directors to support their staff. The Charter on Physician Well-being, recently developed through collaborative input from multiple organizations, defines guiding principles and key commitments at the societal, organizational, interpersonal, and individual levels and may be a useful framework for organizations that are developing well-being initiatives.5
The charter advocates including physician well-being as a quality improvement metric for health systems, aligned with the concept of the Quadruple Aim of optimizing patient care by enhancing provider experience, promoting high-value care, and improving population health.6 Identifying areas of alignment between the charter’s recommendations and systems improvement strategies that seek to optimize efficiency and reduce waste, such as Lean Management, may help physician leaders to contextualize well-being initiatives more easily within ongoing systems improvement efforts. In this perspective, we provide one division’s experience using the Charter to assess successes and identify additional areas of improvement for well-being initiatives developed using Lean Management methodology.
Past and current state of affairs
In 2011, the division of hospital medicine at Zuckerberg San Francisco General Hospital was established and has seen continual expansion in terms of direct patient care, medical education, and hospital leadership.
In 2015, the division of hospital medicine experienced leadership transitions, faculty attrition, and insufficient recruitment resulting in staffing shortages, service line closure, schedule instability, and ultimately, low morale. A baseline survey conducted using the 2-Item Maslach Burnout Inventory. This survey, which uses one item in the domain of emotional exhaustion and one item in the domain of depersonalization, has shown good correlation with the full Maslach Burnout Inventory.7 At baseline, approximately one-third of the division’s physicians experienced burnout.
In response, a subsequent retreat focused on the three greatest areas of concern identified by the survey: scheduling, faculty development, and well-being.
Like many health systems, the hospital has adopted Lean as its preferred systems-improvement framework. The retreat was structured around the principles of Lean philosophy, and was designed to emulate that of a consolidated Kaizen workshop.
“Kaizen” in Japanese means “change for the better.” A typical Kaizen workshop revolves around rapid problem-solving over the course of 3-5 days, in which a team of people come together to identify and implement significant improvements for a selected process. To this end, the retreat was divided into subgroups for each area of concern. In turn, each subgroup mapped out existing workflows (“value stream”), identified areas of waste and non–value added time, and generated ideas of what an idealized process would be. Next, a root-cause analysis was performed and subsequent interventions (“countermeasures”) developed to address each problem. At the conclusion of the retreat, each subgroup shared a summary of their findings with the larger group.
Moving forward, this information served as a guiding framework for service and division leadership to run small tests of change. We enacted a series of countermeasures over the course of several years, and multiple cycles of improvement work addressed the three areas of concern. We developed an A3 report (a Lean project management tool that incorporates the plan-do-study-act cycle, organizes strategic efforts, and tracks progress on a single page) to summarize and present these initiatives to the Performance Improvement and Patient Safety Committee of the hospital executive leadership team. This structure illustrated alignment with the hospital’s core values (“true north”) of “developing people” and “care experience.”
In 2018, interval surveys demonstrated a gradual reduction of burnout to approximately one-fifth of division physicians as measured by the 2-item Maslach Burnout Inventory.
Initiatives in faculty well-being
The Charter of Physician Well-being outlines a framework to promote well-being among doctors by maximizing a sense of fulfillment and minimizing the harms of burnout. It shares this responsibility among societal, organizational, and interpersonal and individual commitments.5
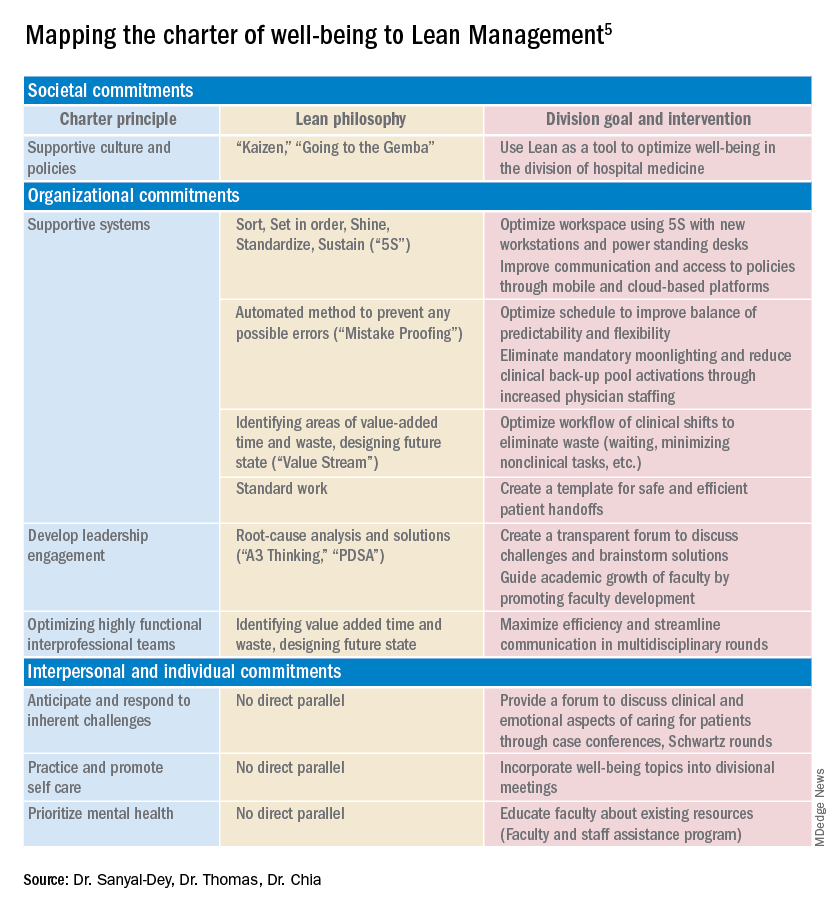
As illustrated above, we used principles of Lean Management to prospectively create initiatives to improve well-being in our division. Lean in health care is designed to optimize primarily the patient experience; its implementation has subsequently demonstrated mixed provider and staff experiences,8,9 and many providers are skeptical of Lean’s potential to improve their own well-being. If, however, Lean is aligned with best practice frameworks for well-being such as those outline in the charter, it may also help to meet the Quadruple Aim of optimizing both provider well-being and patient experience. To further test this hypothesis, we retrospectively categorized our Lean-based interventions into the commitments described by the charter to identify areas of alignment and gaps that were not initially addressed using Lean Management (Table).
Organizational commitments5Supportive systems
We optimized scheduling and enhanced physician staffing by budgeting for a physician staffing buffer each academic year in order to minimize mandatory moonlighting and jeopardy pool activations that result from operating on a thin staffing margin when expected personal leave and reductions in clinical effort occur. Furthermore, we revised scheduling principles to balance patient continuity and individual time off requests while setting limits on the maximum duration of clinical stretches and instituting mandatory minimum time off between them.
Leadership engagement
We initiated monthly operations meetings as a forum to discuss challenges, brainstorm solutions, and message new initiatives with group input. For example, as a result of these meetings, we designed and implemented an additional service line to address the high census, revised the distribution of new patient admissions to level-load clinical shifts, and established a maximum number of weekends worked per month and year. This approach aligns with recommendations to use participatory leadership strategies to enhance physician well-being.10 Engaging both executive level and service level management to focus on burnout and other related well-being metrics is necessary for sustaining such work.
Interprofessional teamwork
We revised multidisciplinary rounds with social work, utilization management, and physical therapy to maximize efficiency and streamline communication by developing standard approaches for each patient presentation.
Interpersonal and individual commitments5Address emotional challenges of physician work
Although these commitments did not have a direct corollary with Lean philosophy, some of these needs were identified by our physician group at our annual retreats. As a result, we initiated a monthly faculty-led noon conference series focused on the clinical challenges of caring for vulnerable populations, a particular source of distress in our practice setting, and revised the division schedule to encourage attendance at the hospital’s Schwartz rounds.
Mental health and self-care
We organized focus groups and faculty development sessions on provider well-being and burnout and dealing with challenging patients and invited the Faculty and Staff Assistance Program, our institution’s mental health service provider, to our weekly division meeting.
Future directions
After using Lean Management as an approach to prospectively improve physician well-being, we were able to use the Charter on Physician Well-being retrospectively as a “checklist” to identify additional gaps for targeted intervention to ensure all commitments are sufficiently addressed.
Overall, we found that, not surprisingly, Lean Management aligned best with the organizational commitments in the charter. Reviewing the organizational commitments, we found our biggest remaining challenges are in building supportive systems, namely ensuring sustainable workloads, offloading and delegating nonphysician tasks, and minimizing the burden of documentation and administration.
Reviewing the societal commitments helped us to identify opportunities for future directions that we may not have otherwise considered. As a safety-net institution, we benefit from a strong sense of mission and shared values within our hospital and division. However, we recognize the need to continue to be vigilant to ensure that our physicians perceive that their own values are aligned with the division’s stated mission. Devoting a Kaizen-style retreat to well-being likely helped, and allocating divisional resources to a well-being committee indirectly helped, to foster a culture of well-being; however, we could more deliberately identify local policies that may benefit from advocacy or revision. Although our faculty identified interventions to improve interpersonal and individual drivers of well-being, these charter commitments did not have direct parallels in Lean philosophy, and organizations may need to deliberately seek to address these commitments outside of a Lean approach. Specifically, by reviewing the charter, we identified opportunities to provide additional resources for peer support and protected time for mental health care and self-care.
Conclusion
Lean Management can be an effective strategy to address many of the organizational commitments outlined in the Charter on Physician Well-being. This approach may be particularly effective for solving local challenges with systems and workflows. Those who use Lean as a primary method to approach systems improvement in support of the Quadruple Aim may need to use additional strategies to address societal and interpersonal and individual commitments outlined in the charter.
Dr. Sanyal-Dey is visiting associate clinical professor of medicine at Zuckerberg San Francisco General Hospital and director of client services, LeanTaaS. Dr. Thomas is associate clinical professor of medicine at Zuckerberg San Francisco General Hospital. Dr. Chia is associate professor of clinical medicine at Zuckerberg San Francisco General Hospital.
References
1. West CP et al. Interventions to prevent and reduce physician burnout: A systematic review and meta-analysis. Lancet. 2016;388(10057):2272-81.
2. Shanafelt TD, Noseworthy JH. Executive leadership and physician: Nine organizational strategies to promote engagement and reduce burnout. Mayo Clin Proc. 2017;92(1):129-46.
3. Shanafelt T et al. The business case for investing in physician well-being. JAMA Intern Med. 2017;177(12):1826-32.
4. Shanafelt T et al. Building a program on well-being: Key design considerations to meet the unique needs of each organization. Acad Med. 2019 Feb;94(2):156-161.
5. Thomas LR et al. Charter on physician well-being. JAMA. 2018;319(15):1541-42.
6. Bodenheimer T, Sinsky C. From triple to quadruple aim: Care of the patient requires care of the provider. Ann Fam Med. 2014;12(6):573-6.
7. West CP et al. Concurrent Validity of Single-Item Measures of Emotional Exhaustion and Depersonalization in Burnout Assessment. J Gen Intern Med. 2012;27(11):1445-52.
8. Hung DY et al. Experiences of primary care physicians and staff following lean workflow redesign. BMC Health Serv Res. 2018 Apr 10;18(1):274.
9. Zibrowski E et al. Easier and faster is not always better: Grounded theory of the impact of large-scale system transformation on the clinical work of emergency medicine nurses and physicians. JMIR Hum Factors. 2018. doi: 10.2196/11013.
10. Shanafelt TD et al. Impact of organizational leadership on physician burnout and satisfaction. Mayo Clin Proc. 2015;90(4):432-40.
General background on well-being and burnout
With burnout increasingly recognized as a shared responsibility that requires addressing organizational drivers while supporting individuals to be well,1-4 practical strategies and examples of successful implementation of systems interventions to address burnout will be helpful for service directors to support their staff. The Charter on Physician Well-being, recently developed through collaborative input from multiple organizations, defines guiding principles and key commitments at the societal, organizational, interpersonal, and individual levels and may be a useful framework for organizations that are developing well-being initiatives.5
The charter advocates including physician well-being as a quality improvement metric for health systems, aligned with the concept of the Quadruple Aim of optimizing patient care by enhancing provider experience, promoting high-value care, and improving population health.6 Identifying areas of alignment between the charter’s recommendations and systems improvement strategies that seek to optimize efficiency and reduce waste, such as Lean Management, may help physician leaders to contextualize well-being initiatives more easily within ongoing systems improvement efforts. In this perspective, we provide one division’s experience using the Charter to assess successes and identify additional areas of improvement for well-being initiatives developed using Lean Management methodology.
Past and current state of affairs
In 2011, the division of hospital medicine at Zuckerberg San Francisco General Hospital was established and has seen continual expansion in terms of direct patient care, medical education, and hospital leadership.
In 2015, the division of hospital medicine experienced leadership transitions, faculty attrition, and insufficient recruitment resulting in staffing shortages, service line closure, schedule instability, and ultimately, low morale. A baseline survey conducted using the 2-Item Maslach Burnout Inventory. This survey, which uses one item in the domain of emotional exhaustion and one item in the domain of depersonalization, has shown good correlation with the full Maslach Burnout Inventory.7 At baseline, approximately one-third of the division’s physicians experienced burnout.
In response, a subsequent retreat focused on the three greatest areas of concern identified by the survey: scheduling, faculty development, and well-being.
Like many health systems, the hospital has adopted Lean as its preferred systems-improvement framework. The retreat was structured around the principles of Lean philosophy, and was designed to emulate that of a consolidated Kaizen workshop.
“Kaizen” in Japanese means “change for the better.” A typical Kaizen workshop revolves around rapid problem-solving over the course of 3-5 days, in which a team of people come together to identify and implement significant improvements for a selected process. To this end, the retreat was divided into subgroups for each area of concern. In turn, each subgroup mapped out existing workflows (“value stream”), identified areas of waste and non–value added time, and generated ideas of what an idealized process would be. Next, a root-cause analysis was performed and subsequent interventions (“countermeasures”) developed to address each problem. At the conclusion of the retreat, each subgroup shared a summary of their findings with the larger group.
Moving forward, this information served as a guiding framework for service and division leadership to run small tests of change. We enacted a series of countermeasures over the course of several years, and multiple cycles of improvement work addressed the three areas of concern. We developed an A3 report (a Lean project management tool that incorporates the plan-do-study-act cycle, organizes strategic efforts, and tracks progress on a single page) to summarize and present these initiatives to the Performance Improvement and Patient Safety Committee of the hospital executive leadership team. This structure illustrated alignment with the hospital’s core values (“true north”) of “developing people” and “care experience.”
In 2018, interval surveys demonstrated a gradual reduction of burnout to approximately one-fifth of division physicians as measured by the 2-item Maslach Burnout Inventory.
Initiatives in faculty well-being
The Charter of Physician Well-being outlines a framework to promote well-being among doctors by maximizing a sense of fulfillment and minimizing the harms of burnout. It shares this responsibility among societal, organizational, and interpersonal and individual commitments.5
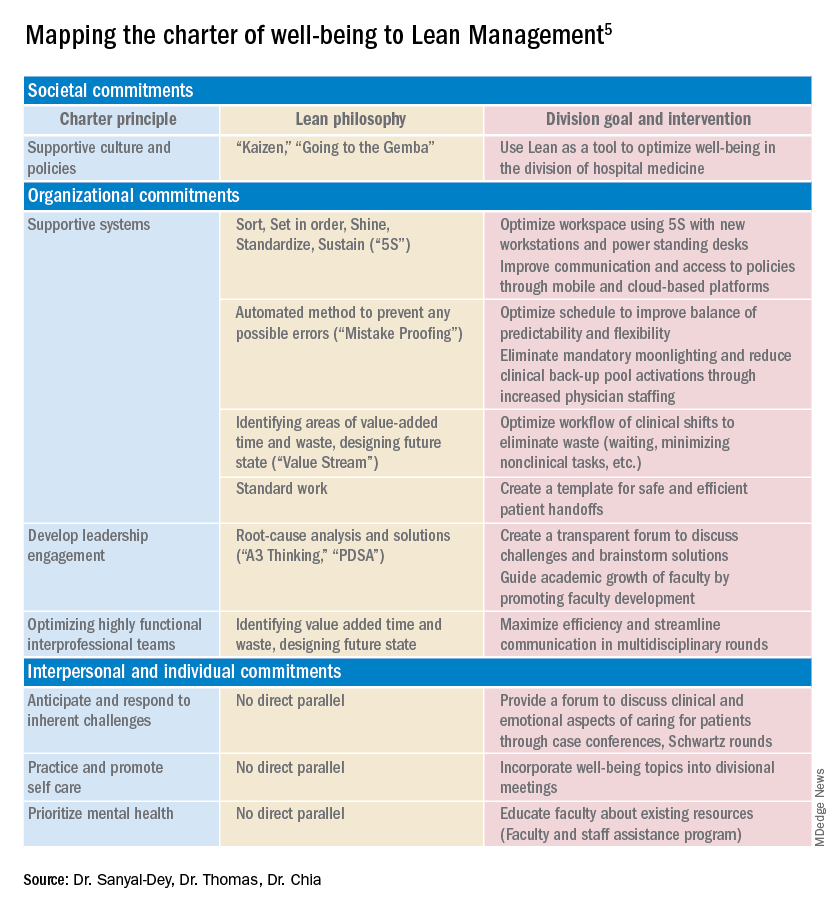
As illustrated above, we used principles of Lean Management to prospectively create initiatives to improve well-being in our division. Lean in health care is designed to optimize primarily the patient experience; its implementation has subsequently demonstrated mixed provider and staff experiences,8,9 and many providers are skeptical of Lean’s potential to improve their own well-being. If, however, Lean is aligned with best practice frameworks for well-being such as those outline in the charter, it may also help to meet the Quadruple Aim of optimizing both provider well-being and patient experience. To further test this hypothesis, we retrospectively categorized our Lean-based interventions into the commitments described by the charter to identify areas of alignment and gaps that were not initially addressed using Lean Management (Table).
Organizational commitments5Supportive systems
We optimized scheduling and enhanced physician staffing by budgeting for a physician staffing buffer each academic year in order to minimize mandatory moonlighting and jeopardy pool activations that result from operating on a thin staffing margin when expected personal leave and reductions in clinical effort occur. Furthermore, we revised scheduling principles to balance patient continuity and individual time off requests while setting limits on the maximum duration of clinical stretches and instituting mandatory minimum time off between them.
Leadership engagement
We initiated monthly operations meetings as a forum to discuss challenges, brainstorm solutions, and message new initiatives with group input. For example, as a result of these meetings, we designed and implemented an additional service line to address the high census, revised the distribution of new patient admissions to level-load clinical shifts, and established a maximum number of weekends worked per month and year. This approach aligns with recommendations to use participatory leadership strategies to enhance physician well-being.10 Engaging both executive level and service level management to focus on burnout and other related well-being metrics is necessary for sustaining such work.
Interprofessional teamwork
We revised multidisciplinary rounds with social work, utilization management, and physical therapy to maximize efficiency and streamline communication by developing standard approaches for each patient presentation.
Interpersonal and individual commitments5Address emotional challenges of physician work
Although these commitments did not have a direct corollary with Lean philosophy, some of these needs were identified by our physician group at our annual retreats. As a result, we initiated a monthly faculty-led noon conference series focused on the clinical challenges of caring for vulnerable populations, a particular source of distress in our practice setting, and revised the division schedule to encourage attendance at the hospital’s Schwartz rounds.
Mental health and self-care
We organized focus groups and faculty development sessions on provider well-being and burnout and dealing with challenging patients and invited the Faculty and Staff Assistance Program, our institution’s mental health service provider, to our weekly division meeting.
Future directions
After using Lean Management as an approach to prospectively improve physician well-being, we were able to use the Charter on Physician Well-being retrospectively as a “checklist” to identify additional gaps for targeted intervention to ensure all commitments are sufficiently addressed.
Overall, we found that, not surprisingly, Lean Management aligned best with the organizational commitments in the charter. Reviewing the organizational commitments, we found our biggest remaining challenges are in building supportive systems, namely ensuring sustainable workloads, offloading and delegating nonphysician tasks, and minimizing the burden of documentation and administration.
Reviewing the societal commitments helped us to identify opportunities for future directions that we may not have otherwise considered. As a safety-net institution, we benefit from a strong sense of mission and shared values within our hospital and division. However, we recognize the need to continue to be vigilant to ensure that our physicians perceive that their own values are aligned with the division’s stated mission. Devoting a Kaizen-style retreat to well-being likely helped, and allocating divisional resources to a well-being committee indirectly helped, to foster a culture of well-being; however, we could more deliberately identify local policies that may benefit from advocacy or revision. Although our faculty identified interventions to improve interpersonal and individual drivers of well-being, these charter commitments did not have direct parallels in Lean philosophy, and organizations may need to deliberately seek to address these commitments outside of a Lean approach. Specifically, by reviewing the charter, we identified opportunities to provide additional resources for peer support and protected time for mental health care and self-care.
Conclusion
Lean Management can be an effective strategy to address many of the organizational commitments outlined in the Charter on Physician Well-being. This approach may be particularly effective for solving local challenges with systems and workflows. Those who use Lean as a primary method to approach systems improvement in support of the Quadruple Aim may need to use additional strategies to address societal and interpersonal and individual commitments outlined in the charter.
Dr. Sanyal-Dey is visiting associate clinical professor of medicine at Zuckerberg San Francisco General Hospital and director of client services, LeanTaaS. Dr. Thomas is associate clinical professor of medicine at Zuckerberg San Francisco General Hospital. Dr. Chia is associate professor of clinical medicine at Zuckerberg San Francisco General Hospital.
References
1. West CP et al. Interventions to prevent and reduce physician burnout: A systematic review and meta-analysis. Lancet. 2016;388(10057):2272-81.
2. Shanafelt TD, Noseworthy JH. Executive leadership and physician: Nine organizational strategies to promote engagement and reduce burnout. Mayo Clin Proc. 2017;92(1):129-46.
3. Shanafelt T et al. The business case for investing in physician well-being. JAMA Intern Med. 2017;177(12):1826-32.
4. Shanafelt T et al. Building a program on well-being: Key design considerations to meet the unique needs of each organization. Acad Med. 2019 Feb;94(2):156-161.
5. Thomas LR et al. Charter on physician well-being. JAMA. 2018;319(15):1541-42.
6. Bodenheimer T, Sinsky C. From triple to quadruple aim: Care of the patient requires care of the provider. Ann Fam Med. 2014;12(6):573-6.
7. West CP et al. Concurrent Validity of Single-Item Measures of Emotional Exhaustion and Depersonalization in Burnout Assessment. J Gen Intern Med. 2012;27(11):1445-52.
8. Hung DY et al. Experiences of primary care physicians and staff following lean workflow redesign. BMC Health Serv Res. 2018 Apr 10;18(1):274.
9. Zibrowski E et al. Easier and faster is not always better: Grounded theory of the impact of large-scale system transformation on the clinical work of emergency medicine nurses and physicians. JMIR Hum Factors. 2018. doi: 10.2196/11013.
10. Shanafelt TD et al. Impact of organizational leadership on physician burnout and satisfaction. Mayo Clin Proc. 2015;90(4):432-40.





















