User login
The Hospitalist only
About one in five clinicians considers quitting because of pandemic
a new survey of more than 5,000 clinicians at an academic medical center illustrates.
About one in five people reported considering leaving the workforce because of the challenges of working during the COVID-19 pandemic. In addition, 30% reported they are considering cutting back work hours.
“There are a substantial number of employees and trainees who are experiencing major stress and work disruptions because of the pandemic,” lead author Rebecca K. Delaney, PhD, said in an interview. “It is particularly alarming that people who have spent 5 or more years in training for their specialty are struggling with their work, so much so that they have even considered leaving the workforce or reducing their hours.”
“Being a caregiver adds another layer of difficulty for faculty, staff, and trainees who are trying to manage work and child care,” added Dr. Delaney, a researcher in the department of population health sciences, University of Utah, Salt Lake City.
The study was published online April 2 in JAMA Network Open.
“This looks like an excellent survey,” Carol A Bernstein, MD, said in an interview when asked to comment. “I do not think it provides particularly new information as these challenges in the workplace, especially for women during COVID, have been well documented in the media and the medical literature to date.”
“That said, to the extent that data helps drive solutions, I would hope that information such as this would be considered as strong further evidence that health care systems must pay close attention to the wellbeing of the workforce,” added Dr. Bernstein, professor and vice chair of faculty development and well-being, departments of psychiatry and behavioral sciences and obstetrics and gynecology and women’s health, Montefiore Medical Center/Albert Einstein College of Medicine, New York.
When the pandemic hits home
A total of 42% of the American workforce rapidly transitioned to working from home at the onset of the COVID-19 pandemic. At the same time, many employees had to provide child care and assistance with schoolwork. This placed a burden on many individuals at academic medical centers, and women in particular.
“Women comprise 74.9% of hospital employees, many of whom are essential clinical workers,” the researchers noted. “The extent of the needs and difficulties for these workers during the pandemic remain largely unknown.”
To learn more, Dr. Delaney, senior author Angie Fagerlin, PhD, and their colleagues emailed a Qualtrics survey to 27,700 faculty, staff, and trainees at University of Utah Health. The survey was conducted Aug. 5-20, 2020 as part of a quality improvement initiative. All responses were anonymous.
Survey questions included if, because of the pandemic, people had considered leaving the workforce, considered reducing their hours, or experienced reduced productivity. The researchers also asked about career impacts and potential solutions in terms of “work culture adaptations.”
Respondents with children aged under 18 years also were asked about child care options. Dr. Delaney and colleagues also inquired about race and ethnicity because they hypothesized that employees from underrepresented groups would likely experience the pandemic differently.
The mean age of the 5,951 (21%) faculty, staff, and trainees who completed the survey was 40 years. A majority of respondents were women, reflecting the higher proportion of women within the health system.
A majority (86%) identified as White or European American. About two-thirds of respondents (66%) were staff, 16% were faculty, and 13% were trainees.
COVID-19 career concerns
Overall, 1,061 respondents (21%) “moderately or very seriously” considered leaving the workforce and 1,505 (30%) considered reducing hours. Respondents who were younger, married, a member of an underrepresented racial/ethnic group, and worked in a clinical setting were more likely to consider leaving the workforce.
The survey showed 27% felt their productivity increased whereas 39% believed their productivity decreased.
Of the 2,412 survey participants with children aged 18 years or younger, 66% reported that they did not have child care fully available.
“Failure to address and provide for child care has long been one of the many significant deficits in U.S. health care systems,” said Dr. Bernstein, lead author of a March 2021 report evaluating staff emotional support at Montefiore Medical Center during the pandemic in The Joint Commission Journal on Quality and Patient Safety.
Furthermore, 47% were “moderately or very seriously worried” about COVID-19 impacting their career development.
Women trainees were significantly more likely than male counterparts to consider leaving the workforce and reducing their work hours. Women in a faculty or trainee role were also more likely to worry about COVID-19’s impact on their career, compared with men, and compared with women in staff positions.
“It was disheartening to have our data support the gender and racial/ethnic disparity that has been highlighted in the media during the pandemic,” Dr. Delaney said. “Women and in some cases racial/ethnic groups that are underrepresented in medicine were most likely to consider leaving the workforce, reducing hours, and were worried about their career development.
“It is critical that we strategically address these important disparities,” she said.
Women also are disproportionately affected by burnout, particularly during the pandemic, according to an analysis of Medscape’s Physician Burnout and Suicide Report.
Furthermore, the COVID-19 pandemic has shifted the medical specialties now considered highest risk for burnout: critical care physicians ranked first in the report, followed by rheumatologists and infectious disease specialists.
Potential solutions
“Given the disproportionate impact COVID-19 has on employees of health systems, institutions must find ways to support their employees, both in terms of workplace cultural adaptations and assistance with familial responsibilities,” the researchers noted.
Telecommuting policies, scheduling flexibility, and expanding employee support programs are potential solutions. Institutional policies also could address the educational and direct care needs of employee children.
Limitations of the study include its generalizability beyond employees of University of Utah Health. Also, respondents included a lower proportion of racial and ethnic groups, compared with national figures, “although this is mostly accounted for by the overall low population of such groups in the state of Utah,” the researchers added.
“Our results suggest that respondents were struggling during the COVID-19 pandemic,” the researchers noted. “As a result, even after investing substantial amounts of time in years of training, many were considering leaving the workforce because of stress and caregiving responsibilities related to the pandemic.”
The Jon M. Huntsman Presidential Endowed Chair supported the work with a financial award to Dr. Fagerlin. Dr. Delaney and Dr. Bernstein disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
a new survey of more than 5,000 clinicians at an academic medical center illustrates.
About one in five people reported considering leaving the workforce because of the challenges of working during the COVID-19 pandemic. In addition, 30% reported they are considering cutting back work hours.
“There are a substantial number of employees and trainees who are experiencing major stress and work disruptions because of the pandemic,” lead author Rebecca K. Delaney, PhD, said in an interview. “It is particularly alarming that people who have spent 5 or more years in training for their specialty are struggling with their work, so much so that they have even considered leaving the workforce or reducing their hours.”
“Being a caregiver adds another layer of difficulty for faculty, staff, and trainees who are trying to manage work and child care,” added Dr. Delaney, a researcher in the department of population health sciences, University of Utah, Salt Lake City.
The study was published online April 2 in JAMA Network Open.
“This looks like an excellent survey,” Carol A Bernstein, MD, said in an interview when asked to comment. “I do not think it provides particularly new information as these challenges in the workplace, especially for women during COVID, have been well documented in the media and the medical literature to date.”
“That said, to the extent that data helps drive solutions, I would hope that information such as this would be considered as strong further evidence that health care systems must pay close attention to the wellbeing of the workforce,” added Dr. Bernstein, professor and vice chair of faculty development and well-being, departments of psychiatry and behavioral sciences and obstetrics and gynecology and women’s health, Montefiore Medical Center/Albert Einstein College of Medicine, New York.
When the pandemic hits home
A total of 42% of the American workforce rapidly transitioned to working from home at the onset of the COVID-19 pandemic. At the same time, many employees had to provide child care and assistance with schoolwork. This placed a burden on many individuals at academic medical centers, and women in particular.
“Women comprise 74.9% of hospital employees, many of whom are essential clinical workers,” the researchers noted. “The extent of the needs and difficulties for these workers during the pandemic remain largely unknown.”
To learn more, Dr. Delaney, senior author Angie Fagerlin, PhD, and their colleagues emailed a Qualtrics survey to 27,700 faculty, staff, and trainees at University of Utah Health. The survey was conducted Aug. 5-20, 2020 as part of a quality improvement initiative. All responses were anonymous.
Survey questions included if, because of the pandemic, people had considered leaving the workforce, considered reducing their hours, or experienced reduced productivity. The researchers also asked about career impacts and potential solutions in terms of “work culture adaptations.”
Respondents with children aged under 18 years also were asked about child care options. Dr. Delaney and colleagues also inquired about race and ethnicity because they hypothesized that employees from underrepresented groups would likely experience the pandemic differently.
The mean age of the 5,951 (21%) faculty, staff, and trainees who completed the survey was 40 years. A majority of respondents were women, reflecting the higher proportion of women within the health system.
A majority (86%) identified as White or European American. About two-thirds of respondents (66%) were staff, 16% were faculty, and 13% were trainees.
COVID-19 career concerns
Overall, 1,061 respondents (21%) “moderately or very seriously” considered leaving the workforce and 1,505 (30%) considered reducing hours. Respondents who were younger, married, a member of an underrepresented racial/ethnic group, and worked in a clinical setting were more likely to consider leaving the workforce.
The survey showed 27% felt their productivity increased whereas 39% believed their productivity decreased.
Of the 2,412 survey participants with children aged 18 years or younger, 66% reported that they did not have child care fully available.
“Failure to address and provide for child care has long been one of the many significant deficits in U.S. health care systems,” said Dr. Bernstein, lead author of a March 2021 report evaluating staff emotional support at Montefiore Medical Center during the pandemic in The Joint Commission Journal on Quality and Patient Safety.
Furthermore, 47% were “moderately or very seriously worried” about COVID-19 impacting their career development.
Women trainees were significantly more likely than male counterparts to consider leaving the workforce and reducing their work hours. Women in a faculty or trainee role were also more likely to worry about COVID-19’s impact on their career, compared with men, and compared with women in staff positions.
“It was disheartening to have our data support the gender and racial/ethnic disparity that has been highlighted in the media during the pandemic,” Dr. Delaney said. “Women and in some cases racial/ethnic groups that are underrepresented in medicine were most likely to consider leaving the workforce, reducing hours, and were worried about their career development.
“It is critical that we strategically address these important disparities,” she said.
Women also are disproportionately affected by burnout, particularly during the pandemic, according to an analysis of Medscape’s Physician Burnout and Suicide Report.
Furthermore, the COVID-19 pandemic has shifted the medical specialties now considered highest risk for burnout: critical care physicians ranked first in the report, followed by rheumatologists and infectious disease specialists.
Potential solutions
“Given the disproportionate impact COVID-19 has on employees of health systems, institutions must find ways to support their employees, both in terms of workplace cultural adaptations and assistance with familial responsibilities,” the researchers noted.
Telecommuting policies, scheduling flexibility, and expanding employee support programs are potential solutions. Institutional policies also could address the educational and direct care needs of employee children.
Limitations of the study include its generalizability beyond employees of University of Utah Health. Also, respondents included a lower proportion of racial and ethnic groups, compared with national figures, “although this is mostly accounted for by the overall low population of such groups in the state of Utah,” the researchers added.
“Our results suggest that respondents were struggling during the COVID-19 pandemic,” the researchers noted. “As a result, even after investing substantial amounts of time in years of training, many were considering leaving the workforce because of stress and caregiving responsibilities related to the pandemic.”
The Jon M. Huntsman Presidential Endowed Chair supported the work with a financial award to Dr. Fagerlin. Dr. Delaney and Dr. Bernstein disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
a new survey of more than 5,000 clinicians at an academic medical center illustrates.
About one in five people reported considering leaving the workforce because of the challenges of working during the COVID-19 pandemic. In addition, 30% reported they are considering cutting back work hours.
“There are a substantial number of employees and trainees who are experiencing major stress and work disruptions because of the pandemic,” lead author Rebecca K. Delaney, PhD, said in an interview. “It is particularly alarming that people who have spent 5 or more years in training for their specialty are struggling with their work, so much so that they have even considered leaving the workforce or reducing their hours.”
“Being a caregiver adds another layer of difficulty for faculty, staff, and trainees who are trying to manage work and child care,” added Dr. Delaney, a researcher in the department of population health sciences, University of Utah, Salt Lake City.
The study was published online April 2 in JAMA Network Open.
“This looks like an excellent survey,” Carol A Bernstein, MD, said in an interview when asked to comment. “I do not think it provides particularly new information as these challenges in the workplace, especially for women during COVID, have been well documented in the media and the medical literature to date.”
“That said, to the extent that data helps drive solutions, I would hope that information such as this would be considered as strong further evidence that health care systems must pay close attention to the wellbeing of the workforce,” added Dr. Bernstein, professor and vice chair of faculty development and well-being, departments of psychiatry and behavioral sciences and obstetrics and gynecology and women’s health, Montefiore Medical Center/Albert Einstein College of Medicine, New York.
When the pandemic hits home
A total of 42% of the American workforce rapidly transitioned to working from home at the onset of the COVID-19 pandemic. At the same time, many employees had to provide child care and assistance with schoolwork. This placed a burden on many individuals at academic medical centers, and women in particular.
“Women comprise 74.9% of hospital employees, many of whom are essential clinical workers,” the researchers noted. “The extent of the needs and difficulties for these workers during the pandemic remain largely unknown.”
To learn more, Dr. Delaney, senior author Angie Fagerlin, PhD, and their colleagues emailed a Qualtrics survey to 27,700 faculty, staff, and trainees at University of Utah Health. The survey was conducted Aug. 5-20, 2020 as part of a quality improvement initiative. All responses were anonymous.
Survey questions included if, because of the pandemic, people had considered leaving the workforce, considered reducing their hours, or experienced reduced productivity. The researchers also asked about career impacts and potential solutions in terms of “work culture adaptations.”
Respondents with children aged under 18 years also were asked about child care options. Dr. Delaney and colleagues also inquired about race and ethnicity because they hypothesized that employees from underrepresented groups would likely experience the pandemic differently.
The mean age of the 5,951 (21%) faculty, staff, and trainees who completed the survey was 40 years. A majority of respondents were women, reflecting the higher proportion of women within the health system.
A majority (86%) identified as White or European American. About two-thirds of respondents (66%) were staff, 16% were faculty, and 13% were trainees.
COVID-19 career concerns
Overall, 1,061 respondents (21%) “moderately or very seriously” considered leaving the workforce and 1,505 (30%) considered reducing hours. Respondents who were younger, married, a member of an underrepresented racial/ethnic group, and worked in a clinical setting were more likely to consider leaving the workforce.
The survey showed 27% felt their productivity increased whereas 39% believed their productivity decreased.
Of the 2,412 survey participants with children aged 18 years or younger, 66% reported that they did not have child care fully available.
“Failure to address and provide for child care has long been one of the many significant deficits in U.S. health care systems,” said Dr. Bernstein, lead author of a March 2021 report evaluating staff emotional support at Montefiore Medical Center during the pandemic in The Joint Commission Journal on Quality and Patient Safety.
Furthermore, 47% were “moderately or very seriously worried” about COVID-19 impacting their career development.
Women trainees were significantly more likely than male counterparts to consider leaving the workforce and reducing their work hours. Women in a faculty or trainee role were also more likely to worry about COVID-19’s impact on their career, compared with men, and compared with women in staff positions.
“It was disheartening to have our data support the gender and racial/ethnic disparity that has been highlighted in the media during the pandemic,” Dr. Delaney said. “Women and in some cases racial/ethnic groups that are underrepresented in medicine were most likely to consider leaving the workforce, reducing hours, and were worried about their career development.
“It is critical that we strategically address these important disparities,” she said.
Women also are disproportionately affected by burnout, particularly during the pandemic, according to an analysis of Medscape’s Physician Burnout and Suicide Report.
Furthermore, the COVID-19 pandemic has shifted the medical specialties now considered highest risk for burnout: critical care physicians ranked first in the report, followed by rheumatologists and infectious disease specialists.
Potential solutions
“Given the disproportionate impact COVID-19 has on employees of health systems, institutions must find ways to support their employees, both in terms of workplace cultural adaptations and assistance with familial responsibilities,” the researchers noted.
Telecommuting policies, scheduling flexibility, and expanding employee support programs are potential solutions. Institutional policies also could address the educational and direct care needs of employee children.
Limitations of the study include its generalizability beyond employees of University of Utah Health. Also, respondents included a lower proportion of racial and ethnic groups, compared with national figures, “although this is mostly accounted for by the overall low population of such groups in the state of Utah,” the researchers added.
“Our results suggest that respondents were struggling during the COVID-19 pandemic,” the researchers noted. “As a result, even after investing substantial amounts of time in years of training, many were considering leaving the workforce because of stress and caregiving responsibilities related to the pandemic.”
The Jon M. Huntsman Presidential Endowed Chair supported the work with a financial award to Dr. Fagerlin. Dr. Delaney and Dr. Bernstein disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The COVID-19 push to evolve
Has anyone else noticed how slow it has been on your pediatric floors? Well, you are not alone.
The COVID pandemic has had a significant impact on health care volumes, with pediatric volumes decreasing across the nation. A Children’s Hospital Association CEO survey, currently unpublished, noted a 10%-20% decline in inpatient admissions and a 30%-50% decline in pediatric ED visits this past year. Even our usual respiratory surge has been disrupted. The rate of influenza tracked by the CDC is around 1%, compared with the usual seasonal flu baseline national rate of 2.6%. These COVID-related declines have occurred amidst the backdrop of already-decreasing inpatient admissions because of the great work of the pediatric hospital medicine (PHM) community in reducing unnecessary admissions and lengths of stay.
For many hospitals, several factors related to the pandemic have raised significant financial concerns. According to Becker Hospital Review, as of August 2020 over 500 hospitals had furloughed workers. While 26 of those hospitals had brought back workers by December 2020, many did not. Similar financial concerns were noted in a Kaufmann Hall report from January 2021, which showed a median drop of 55% in operating margins. The CARES Act helped reduce some of the detrimental impact on operating margins, but it did not diminish the added burden of personal protective equipment expenses, longer length of stay for COVID patients, and a reimbursement shift to more government payors and uninsured caused by pandemic-forced job losses.
COVID’s impact specific to pediatric hospital medicine has been substantial. A recent unpublished survey by the PHM Economics Research Collaborative (PERC) demonstrated how COVID has affected pediatric hospital medicine programs. Forty-five unique PHM programs from over 21 states responded, with 98% reporting a decrease in pediatric inpatient admissions as well as ED visits. About 11% reported temporary unit closures, while 51% of all programs reported staffing restrictions ranging from hiring freezes to downsizing the number of hospitalists in the group. Salaries decreased in 26% of reporting programs, and 20%-56% described reduced benefits, ranging from less CME/vacation time and stipends to retirement benefits. The three most frequent benefit losses included annual salary increases, educational stipends, and bonuses.
Community hospitals felt the palpable, financial strain of decreasing pediatric admissions well before the pandemic. Hospitals like MedStar Franklin Square Hospital in Baltimore and Harrington Hospital in Southbridge, Mass., had decided to close their pediatrics units before COVID hit. In a 2014 unpublished survey of 349 community PHM (CPHM) programs, 57% of respondents felt that finances and justification for a pediatric program were primary concerns.
Responding to financial stressors is not a novel challenge for CPHM programs. To keep these vital pediatric programs in place despite lower inpatient volumes, those of us in CPHM have learned many lessons over the years on how to adapt. Such adaptations have included diversification in procedures and multifloor coverage in the hospital. Voiding cystourethrogram catheterizations and circumcisions are now more commonly performed by CPHM providers, who may also cover multiple areas of the hospital, including the ED, NICU, and well-newborn nursery. Comanagement of subspecialty or surgical patients is yet another example of such diversification.
Furthermore, the PERC survey showed that some PHM programs temporarily covered pediatric ICUs and step-down units and began doing ED and urgent care coverage as primary providers Most programs reported no change in newborn visits while 16% reported an increase in newborn volume and 14% reported a decrease in newborn volume. My own health system was one of the groups that had an increase in newborn volume. This was caused by community pediatricians who had stopped coming in to see their own newborns. This coverage adjustment has yet to return to baseline and will likely become permanent.
There was a 11% increase from prepandemic baselines (from 9% to 20%) in programs doing telemedicine. Most respondents stated that they will continue to offer telemedicine with an additional 25% of programs considering starting. There was also a slight increase during the pandemic of coverage of mental health units (from 11% to 13%), which may have led 11% of respondents to consider the addition of this service. The survey also noted that about 28% of PHM programs performed circumcisions, frenectomies, and sedation prepandemic, and 14%-18% are considering adding these services.
Overall, the financial stressors are improving, but our need to adapt in PHM is more pressing than ever. The pandemic has given us the push for evolution and some opportunities that did not exist before. One is the use of telemedicine to expand our subspecialty support to community hospitals, as well as to children’s hospitals in areas where subspecialists are in short supply. These telemedicine consults are being reimbursed for the first time, which allows more access to these services.
With the pandemic, many hospitals are moving to single room occupancy models. Construction to add more beds is costly, and unnecessary if we can utilize community hospitals to keep appropriate patients in their home communities. The opportunity to partner with community hospital programs to provide telemedicine support should not be overlooked. This is also an opportunity for academic referral centers to have more open beds for critical care and highly specialized patients.
Another opportunity is to expand scope by changing age limits, as 18% of respondents to the PERC survey reported that they had started to care for adults since the pandemic. The Pediatric Overflow Planning Contingency Response Network (POPCoRN) has been a valuable resource for education on caring for adults, guidance on which patient populations are appropriate, and the resources needed to do this. While caring for older adults, even in their 90s, was a pandemic-related phenomenon, there is an opportunity to see if the age limit we care for should be raised to 21, or even 25, as some CPHM programs had been doing prepandemic.
Along with the expansion of age limits, there are many other areas of opportunity highlighted within the PERC survey. These include expanding coverage within pediatric ICUs, EDs, and urgent care areas, along with coverage of well newborns that were previously covered by community pediatricians. Also, the increase of mental health admissions is another area where PHM programs might expand their services.
While I hope the financial stressors improve, hope is not a plan and therefore we need to think and prepare for what the post-COVID future may look like. Some have predicted a rebound pediatric respiratory surge next year as the masks come off and children return to in-person learning and daycare. This may be true, but we would be foolish not to use lessons from the pandemic as well as the past to consider options in our toolkit to become more financially stable. POPCoRN, as well as the American Academy of Pediatrics’ listserv and subcommittees, have been a source of collaboration and shared knowledge during a time when we have needed to quickly respond to ever-changing information. These networks and information sharing should be leveraged once the dust settles for us to prepare for future challenges.
New innovations may arise as we look at how we address the growing need for mental health services and incorporate new procedures, like point of care ultrasound. As Charles Darwin said: “It is not the strongest of the species that survives nor the most intelligent that survives. It is the one that is most adaptable to change.” It is time for us to evolve.
Dr. Dias is a clinical associate professor of pediatrics at Yale University, New Haven, Conn., in the division of pediatric hospital medicine. She has practiced community pediatric hospital medicine for over 21 years in New Jersey, Pennsylvania, and Connecticut. She is the chair of the Education Working Group for the AAP’s section on hospital medicine’s subcommittee on community hospitalists as well as the cochair of the Community Hospital Operations Group of the POPCoRN network.
Has anyone else noticed how slow it has been on your pediatric floors? Well, you are not alone.
The COVID pandemic has had a significant impact on health care volumes, with pediatric volumes decreasing across the nation. A Children’s Hospital Association CEO survey, currently unpublished, noted a 10%-20% decline in inpatient admissions and a 30%-50% decline in pediatric ED visits this past year. Even our usual respiratory surge has been disrupted. The rate of influenza tracked by the CDC is around 1%, compared with the usual seasonal flu baseline national rate of 2.6%. These COVID-related declines have occurred amidst the backdrop of already-decreasing inpatient admissions because of the great work of the pediatric hospital medicine (PHM) community in reducing unnecessary admissions and lengths of stay.
For many hospitals, several factors related to the pandemic have raised significant financial concerns. According to Becker Hospital Review, as of August 2020 over 500 hospitals had furloughed workers. While 26 of those hospitals had brought back workers by December 2020, many did not. Similar financial concerns were noted in a Kaufmann Hall report from January 2021, which showed a median drop of 55% in operating margins. The CARES Act helped reduce some of the detrimental impact on operating margins, but it did not diminish the added burden of personal protective equipment expenses, longer length of stay for COVID patients, and a reimbursement shift to more government payors and uninsured caused by pandemic-forced job losses.
COVID’s impact specific to pediatric hospital medicine has been substantial. A recent unpublished survey by the PHM Economics Research Collaborative (PERC) demonstrated how COVID has affected pediatric hospital medicine programs. Forty-five unique PHM programs from over 21 states responded, with 98% reporting a decrease in pediatric inpatient admissions as well as ED visits. About 11% reported temporary unit closures, while 51% of all programs reported staffing restrictions ranging from hiring freezes to downsizing the number of hospitalists in the group. Salaries decreased in 26% of reporting programs, and 20%-56% described reduced benefits, ranging from less CME/vacation time and stipends to retirement benefits. The three most frequent benefit losses included annual salary increases, educational stipends, and bonuses.
Community hospitals felt the palpable, financial strain of decreasing pediatric admissions well before the pandemic. Hospitals like MedStar Franklin Square Hospital in Baltimore and Harrington Hospital in Southbridge, Mass., had decided to close their pediatrics units before COVID hit. In a 2014 unpublished survey of 349 community PHM (CPHM) programs, 57% of respondents felt that finances and justification for a pediatric program were primary concerns.
Responding to financial stressors is not a novel challenge for CPHM programs. To keep these vital pediatric programs in place despite lower inpatient volumes, those of us in CPHM have learned many lessons over the years on how to adapt. Such adaptations have included diversification in procedures and multifloor coverage in the hospital. Voiding cystourethrogram catheterizations and circumcisions are now more commonly performed by CPHM providers, who may also cover multiple areas of the hospital, including the ED, NICU, and well-newborn nursery. Comanagement of subspecialty or surgical patients is yet another example of such diversification.
Furthermore, the PERC survey showed that some PHM programs temporarily covered pediatric ICUs and step-down units and began doing ED and urgent care coverage as primary providers Most programs reported no change in newborn visits while 16% reported an increase in newborn volume and 14% reported a decrease in newborn volume. My own health system was one of the groups that had an increase in newborn volume. This was caused by community pediatricians who had stopped coming in to see their own newborns. This coverage adjustment has yet to return to baseline and will likely become permanent.
There was a 11% increase from prepandemic baselines (from 9% to 20%) in programs doing telemedicine. Most respondents stated that they will continue to offer telemedicine with an additional 25% of programs considering starting. There was also a slight increase during the pandemic of coverage of mental health units (from 11% to 13%), which may have led 11% of respondents to consider the addition of this service. The survey also noted that about 28% of PHM programs performed circumcisions, frenectomies, and sedation prepandemic, and 14%-18% are considering adding these services.
Overall, the financial stressors are improving, but our need to adapt in PHM is more pressing than ever. The pandemic has given us the push for evolution and some opportunities that did not exist before. One is the use of telemedicine to expand our subspecialty support to community hospitals, as well as to children’s hospitals in areas where subspecialists are in short supply. These telemedicine consults are being reimbursed for the first time, which allows more access to these services.
With the pandemic, many hospitals are moving to single room occupancy models. Construction to add more beds is costly, and unnecessary if we can utilize community hospitals to keep appropriate patients in their home communities. The opportunity to partner with community hospital programs to provide telemedicine support should not be overlooked. This is also an opportunity for academic referral centers to have more open beds for critical care and highly specialized patients.
Another opportunity is to expand scope by changing age limits, as 18% of respondents to the PERC survey reported that they had started to care for adults since the pandemic. The Pediatric Overflow Planning Contingency Response Network (POPCoRN) has been a valuable resource for education on caring for adults, guidance on which patient populations are appropriate, and the resources needed to do this. While caring for older adults, even in their 90s, was a pandemic-related phenomenon, there is an opportunity to see if the age limit we care for should be raised to 21, or even 25, as some CPHM programs had been doing prepandemic.
Along with the expansion of age limits, there are many other areas of opportunity highlighted within the PERC survey. These include expanding coverage within pediatric ICUs, EDs, and urgent care areas, along with coverage of well newborns that were previously covered by community pediatricians. Also, the increase of mental health admissions is another area where PHM programs might expand their services.
While I hope the financial stressors improve, hope is not a plan and therefore we need to think and prepare for what the post-COVID future may look like. Some have predicted a rebound pediatric respiratory surge next year as the masks come off and children return to in-person learning and daycare. This may be true, but we would be foolish not to use lessons from the pandemic as well as the past to consider options in our toolkit to become more financially stable. POPCoRN, as well as the American Academy of Pediatrics’ listserv and subcommittees, have been a source of collaboration and shared knowledge during a time when we have needed to quickly respond to ever-changing information. These networks and information sharing should be leveraged once the dust settles for us to prepare for future challenges.
New innovations may arise as we look at how we address the growing need for mental health services and incorporate new procedures, like point of care ultrasound. As Charles Darwin said: “It is not the strongest of the species that survives nor the most intelligent that survives. It is the one that is most adaptable to change.” It is time for us to evolve.
Dr. Dias is a clinical associate professor of pediatrics at Yale University, New Haven, Conn., in the division of pediatric hospital medicine. She has practiced community pediatric hospital medicine for over 21 years in New Jersey, Pennsylvania, and Connecticut. She is the chair of the Education Working Group for the AAP’s section on hospital medicine’s subcommittee on community hospitalists as well as the cochair of the Community Hospital Operations Group of the POPCoRN network.
Has anyone else noticed how slow it has been on your pediatric floors? Well, you are not alone.
The COVID pandemic has had a significant impact on health care volumes, with pediatric volumes decreasing across the nation. A Children’s Hospital Association CEO survey, currently unpublished, noted a 10%-20% decline in inpatient admissions and a 30%-50% decline in pediatric ED visits this past year. Even our usual respiratory surge has been disrupted. The rate of influenza tracked by the CDC is around 1%, compared with the usual seasonal flu baseline national rate of 2.6%. These COVID-related declines have occurred amidst the backdrop of already-decreasing inpatient admissions because of the great work of the pediatric hospital medicine (PHM) community in reducing unnecessary admissions and lengths of stay.
For many hospitals, several factors related to the pandemic have raised significant financial concerns. According to Becker Hospital Review, as of August 2020 over 500 hospitals had furloughed workers. While 26 of those hospitals had brought back workers by December 2020, many did not. Similar financial concerns were noted in a Kaufmann Hall report from January 2021, which showed a median drop of 55% in operating margins. The CARES Act helped reduce some of the detrimental impact on operating margins, but it did not diminish the added burden of personal protective equipment expenses, longer length of stay for COVID patients, and a reimbursement shift to more government payors and uninsured caused by pandemic-forced job losses.
COVID’s impact specific to pediatric hospital medicine has been substantial. A recent unpublished survey by the PHM Economics Research Collaborative (PERC) demonstrated how COVID has affected pediatric hospital medicine programs. Forty-five unique PHM programs from over 21 states responded, with 98% reporting a decrease in pediatric inpatient admissions as well as ED visits. About 11% reported temporary unit closures, while 51% of all programs reported staffing restrictions ranging from hiring freezes to downsizing the number of hospitalists in the group. Salaries decreased in 26% of reporting programs, and 20%-56% described reduced benefits, ranging from less CME/vacation time and stipends to retirement benefits. The three most frequent benefit losses included annual salary increases, educational stipends, and bonuses.
Community hospitals felt the palpable, financial strain of decreasing pediatric admissions well before the pandemic. Hospitals like MedStar Franklin Square Hospital in Baltimore and Harrington Hospital in Southbridge, Mass., had decided to close their pediatrics units before COVID hit. In a 2014 unpublished survey of 349 community PHM (CPHM) programs, 57% of respondents felt that finances and justification for a pediatric program were primary concerns.
Responding to financial stressors is not a novel challenge for CPHM programs. To keep these vital pediatric programs in place despite lower inpatient volumes, those of us in CPHM have learned many lessons over the years on how to adapt. Such adaptations have included diversification in procedures and multifloor coverage in the hospital. Voiding cystourethrogram catheterizations and circumcisions are now more commonly performed by CPHM providers, who may also cover multiple areas of the hospital, including the ED, NICU, and well-newborn nursery. Comanagement of subspecialty or surgical patients is yet another example of such diversification.
Furthermore, the PERC survey showed that some PHM programs temporarily covered pediatric ICUs and step-down units and began doing ED and urgent care coverage as primary providers Most programs reported no change in newborn visits while 16% reported an increase in newborn volume and 14% reported a decrease in newborn volume. My own health system was one of the groups that had an increase in newborn volume. This was caused by community pediatricians who had stopped coming in to see their own newborns. This coverage adjustment has yet to return to baseline and will likely become permanent.
There was a 11% increase from prepandemic baselines (from 9% to 20%) in programs doing telemedicine. Most respondents stated that they will continue to offer telemedicine with an additional 25% of programs considering starting. There was also a slight increase during the pandemic of coverage of mental health units (from 11% to 13%), which may have led 11% of respondents to consider the addition of this service. The survey also noted that about 28% of PHM programs performed circumcisions, frenectomies, and sedation prepandemic, and 14%-18% are considering adding these services.
Overall, the financial stressors are improving, but our need to adapt in PHM is more pressing than ever. The pandemic has given us the push for evolution and some opportunities that did not exist before. One is the use of telemedicine to expand our subspecialty support to community hospitals, as well as to children’s hospitals in areas where subspecialists are in short supply. These telemedicine consults are being reimbursed for the first time, which allows more access to these services.
With the pandemic, many hospitals are moving to single room occupancy models. Construction to add more beds is costly, and unnecessary if we can utilize community hospitals to keep appropriate patients in their home communities. The opportunity to partner with community hospital programs to provide telemedicine support should not be overlooked. This is also an opportunity for academic referral centers to have more open beds for critical care and highly specialized patients.
Another opportunity is to expand scope by changing age limits, as 18% of respondents to the PERC survey reported that they had started to care for adults since the pandemic. The Pediatric Overflow Planning Contingency Response Network (POPCoRN) has been a valuable resource for education on caring for adults, guidance on which patient populations are appropriate, and the resources needed to do this. While caring for older adults, even in their 90s, was a pandemic-related phenomenon, there is an opportunity to see if the age limit we care for should be raised to 21, or even 25, as some CPHM programs had been doing prepandemic.
Along with the expansion of age limits, there are many other areas of opportunity highlighted within the PERC survey. These include expanding coverage within pediatric ICUs, EDs, and urgent care areas, along with coverage of well newborns that were previously covered by community pediatricians. Also, the increase of mental health admissions is another area where PHM programs might expand their services.
While I hope the financial stressors improve, hope is not a plan and therefore we need to think and prepare for what the post-COVID future may look like. Some have predicted a rebound pediatric respiratory surge next year as the masks come off and children return to in-person learning and daycare. This may be true, but we would be foolish not to use lessons from the pandemic as well as the past to consider options in our toolkit to become more financially stable. POPCoRN, as well as the American Academy of Pediatrics’ listserv and subcommittees, have been a source of collaboration and shared knowledge during a time when we have needed to quickly respond to ever-changing information. These networks and information sharing should be leveraged once the dust settles for us to prepare for future challenges.
New innovations may arise as we look at how we address the growing need for mental health services and incorporate new procedures, like point of care ultrasound. As Charles Darwin said: “It is not the strongest of the species that survives nor the most intelligent that survives. It is the one that is most adaptable to change.” It is time for us to evolve.
Dr. Dias is a clinical associate professor of pediatrics at Yale University, New Haven, Conn., in the division of pediatric hospital medicine. She has practiced community pediatric hospital medicine for over 21 years in New Jersey, Pennsylvania, and Connecticut. She is the chair of the Education Working Group for the AAP’s section on hospital medicine’s subcommittee on community hospitalists as well as the cochair of the Community Hospital Operations Group of the POPCoRN network.
Hospital medicine around the world
Similar needs, local adaptations
Hospital medicine has evolved rapidly and spread widely across the United States in the past 25 years in response to the health care system’s needs for patient safety, quality, efficiency, and effective coordination of care in the ever-more complex environment of the acute care hospital.
But hospital care can be just as complex in other countries, so it’s not surprising that there’s a lot of interest around the world in the U.S. model of hospital medicine. But adaptations of that model vary across – and within – countries, reflecting local culture, health care systems, payment models, and approaches to medical education.
Other countries have looked to U.S. experts for consultations, to U.S.-trained doctors who might be willing to relocate, and to the Society of Hospital Medicine as an internationally focused source of networking and other resources. Some U.S.-based institutions, led by the Cleveland Clinic, Johns Hopkins Medicine, and Weill-Cornell Medical School, have established teaching outposts in other countries, with opportunities for resident training that prepares future hospitalists on the ground.
SHM CEO Eric E. Howell, MD, MHM, said that he personally has interacted with developing hospital medicine programs in six countries, who called upon him in part because of his past research on managing length of hospital stays. Dr. Howell counts himself among a few dozen U.S. hospitalists who are regularly invited to come and consult or to give talks to established or developing hospitalist programs in other countries. Because of the COVID-19 epidemic, in-person visits to other countries have largely been curtailed, but that has introduced a more virtual world of online meetings.
“I think the interesting thing about the ‘international consultants’ for hospital medicine is that while they come from professionally diverse backgrounds, they are all working to solve remarkably similar problems: How to make health care more affordable and higher quality while staying abreast of up-to-date best practice for physicians,” he said.
“Hospital care is costly no matter where you go. Other countries are also trying to limit expense in ways that don’t compromise the quality of that care,” Dr. Howell said. Also, hospitalized patients are more complex than ever, with increasing severity of illness and comorbidities, which makes having a hospitalist available on site more important.
Dr. Howell hopes to encourage more dialogue with international colleagues. SHM has established collaborations with medical societies in other countries and makes time at its conferences for international hospitalist participants to meet and share their experiences. Hospitalists from 33 countries were represented at SHM’s 2017 conference, and the upcoming virtual SHM Converge, May 3-7, 2021, includes a dedicated international session. SHM chapters have formed in a number of other countries.
Flora Kisuule, MD, MPH, SFHM, director of the Division of Hospital Medicine at Johns Hopkins Bayview Medical Center in Baltimore, said her international hospital medicine work1 started 7 years ago when she was invited to the Middle East to help Aramco, the Saudi Arabian Oil Company, develop a hospital medicine program based on the U.S. model for its employees. This was a joint venture with Johns Hopkins Medicine. “We went there and looked at their processes and made recommendations such as duration of hospitalist shifts and how to expand the footprint of hospital medicine in the hospital,” she said.
Then Dr. Kisuule was asked to help develop a hospital medicine program in Panama, where the drivers for developing hospital medicine were improving quality of care and ensuring patient safety. The biggest barrier has been remuneration and how to pay salaries that will allow doctors to work at only one hospital. In Panama, doctors typically work at multiple hospitals or clinics so they can earn enough to make ends meet.
The need for professional identity
Arpana Vidyarthi, MD, “grew up” professionally in hospital medicine at the University of California, San Francisco, a pioneering institution for hospital medicine, and in SHM. “We used to say: If you’ve seen one hospital medicine group, you’ve seen one hospital medicine group,” she said.
Dr. Vidyarthi went to Singapore in 2011, taking a job as a hospitalist at Singapore General Hospital and the affiliated Duke–National University Medical School, eventually directing the Division of Advanced Internal Medicine (general and hospital medicine) at the National University Health System, before moving back to UCSF in 2020.
“Professional identity is one of the biggest benefits hospital medicine can bestow in Singapore and across Asia, where general medicine is underdeveloped. Just as it did 20 years ago in the U.S., that professional identity offers a road map to achieving competency in practicing medicine in the hospital setting,” Dr. Vidyarthi said.
At UCSF, the professional identity of a hospitalist is broad but defined. The research agenda, quality, safety, and educational competencies are specific, seen through a system lens, she added. “We take pride in that professional identify. This is an opportunity for countries where general medicine is underdeveloped and undervalued.”
But the term hospital medicine – or the American model – isn’t always welcomed by health care systems in other countries, Dr Vidyarthi said. “The label of 'hospital medicine' brings people together in professional identify, and that professional identity opens doors. But for it to have legs in other countries, those skills need to be of value to the local system. It needs to make sense, as it did in the United States, and to add value for the identified gaps that need to be filled.”
In Singapore, the health care system turned to the model of acute medical units (AMUs) and the acute medicine physician specialty developed in the United Kingdom, which created a new way of delivering care, a new geography of care, and new set of competencies around which to build training and certification.
AMUs manage the majority of acute medical patients who present to the emergency department and get admitted, with initial treatment for a maximum of 72 hours. Acute physicians, trained in the specialty of assessment, diagnosis, and treatment of adult patients with urgent medical needs, work in a unit situated between the emergency department entrance and the specialty care units. This specialty has been recognized since 2009.2
“Acute medicine is the standard care model in the UK and is now found in all government hospitals in Singapore. This model is being adapted across Europe, Asia, and the Pacific Islands,” Dr. Vidyarthi said. “Advantages include the specific geography of the unit, and outcomes that are value-added to these systems such as decreased use of hospital beds in areas with very high bed occupancy rates.”
In many locales, a variety of titles are used to describe doctors who are not hospitalists as we understand them but whose work is based in the hospital, including house officer, duty officer, junior officer, registrar, or general practitioner. Often these hospital-based doctors, who may in fact be residents or nongraduated trainees, lack the training and the scope of practice of a hospitalist. Because they typically need to consult the supervising physician before making inpatient management decisions, they aren’t able to provide the timely response to the patient’s changing medical condition that is needed to manage today’s acute patients.
Defining the fee schedule
In South Korea, a hospitalist model has emerged since 2015 in response to the insufficient number of hospital-based physicians needed to cover all admitted patients and to address related issues of patient safety, health care quality, and limitations on total hours per week medical residents are allowed to work.
South Korea in 1989 adopted a universal National Health Insurance System (NHIS), which took 12 years to implement. But inadequate coverage for medical work in the hospital has deterred physicians from choosing to work there. South Korea had longer lengths of hospital stay, fewer practicing physicians per 1,000 patients, and a much higher number of hospital patients per practicing physician than other countries in the Organization for Economic Cooperation and Development, according to a new study in the Journal of Hospital Medicine detailing hospitalist development in South Korea.3
A council representing leading medical associations was formed to develop a South Korean hospitalist system and charged by the Ministry of Health with designing an official proposal for implementing it. A pilot study focused on quality and on defining a fee schedule for hospital work was tested in four hospitals, and then a second phase in 31 of South Korea’s 344 general hospitals tested the proposed fee schedule, said Wonjeong Chae, MPH, the first named author on the study, based in the Department of Public Health in the College of Medicine at Yonsei University in Seoul. “But we’re still working on making the fee schedule better,” she said.
Ms. Chae estimates that there are about 250 working hospitalists in South Korea today, which leaves a lot of gaps in practice. “We did learn from America, but we have a different system, so the American concept had to be adapted. Hospital medicine is still growing in Korea despite the impact of the pandemic. We are at the beginning stages of development, but we expect it will grow more with government support.”
In Brazil, a handful of hospital medicine pioneers such as Guilherme Barcellos, MD, SFHM, in Porto Alegre have tried to grow the hospitalist model, networking with colleagues across Latin America through the Pan American Society of Hospitalists and the Brazilian chapter of SHM.
Individual hospitals have developed hospitalist programs, but there is no national model to lead the way. Frequent turnover for the Minister of Health position has made it harder to develop consistent national policy, and the country is largely still in the early stages of developing hospital medicine, depending on isolated initiatives, as Dr. Barcellos described it in a November 2015 article in The Hospitalist.4 Growth is slow but continuing, with new programs such as the one led by Reginaldo Filho, MD at Hospital São Vicente in Curitiba standing out in the confrontation against COVID-19, Dr. Barcellos said.
What can we learn from others?
India-born, U.S.-trained hospitalist Anand Kartha, MD, MS, SFHM, currently heads the Hospital Medicine Program at Hamad General Hospital in Doha, Qatar. He moved from Boston to this small nation on the Arabian Peninsula in 2014. Under the leadership of the hospital’s Department of Medicine, this program was developed to address difficulties such as scheduling, transitions of care, and networking with home care and other providers – the same issues seen in hospitals around the world.
These are not novel problems, Dr. Kartha said, but all of them have a common solution in evidence-based practice. “As hospitalists, our key is to collaborate with everyone in the hospital, using the multidisciplinary approach that is a unique feature of hospital medicine.”
The model has continued to spread across hospitals in Qatar, including academic and community programs. “We now have a full-fledged academic hospitalist system, which collaborates with community hospitals and community programs including a women’s hospital and an oncologic hospital,” he said. “Now the focus is on expanding resource capacity and the internal pipeline for hospitalists. I am getting graduates from Weill Cornell Medicine in Qatar.” Another key collaborator has been the Boston-based Institute for Healthcare Improvement, helping to develop best practices in Qatar and sponsoring the annual Middle East Forum on Quality and Safety in Health Care.
The residency training program at Hamad General is accredited by ACGME, with the same expected competencies as in the U.S. “We don’t use the term ‘hospitalist,’ ” Dr. Kartha said. “It’s better to focus on the model of care – which clearly was American. That model has encountered some resistance in some countries – on many of the same grounds U.S. hospitalists faced 20 years ago. You have to be sensitive to local culture. For hospitalists to succeed internationally, they have to possess a high degree of cultural intelligence.” There’s no shortage of issues such as language barriers, he said. “But that’s no different than at Boston Medical Center.”
SHM’s Middle East Chapter was off to a great start and then was slowed down by regional politics and COVID-19, but is looking forward to a great reboot in 2021, Dr. Kartha said. The pandemic also has been an opportunity to show how hospital medicine is the backbone of the hospital’s ability to respond, although of course many other professionals also pitched in.
Other countries around the world have learned a lot from the American model of hospital medicine. But sources for this article wonder if U.S. hospitalists, in turn, could learn from their adaptations and innovations.
“We can all learn better how to practice our field of medicine in the hospital with less resource utilization,” Dr. Vidyarthi concluded. “So many innovations are happening around us. If we open our eyes to our global colleagues and infuse some of their ideas, it could be wonderful for hospital professionals in the United States.”
References
1. Kisuule F, Howell E. Hospital medicine beyond the United States. Int J Gen Med. 2018;11:65-71. doi: 10.2147/IJGM.S151275.
2. Stosic J et al. The acute physician: The future of acute hospital care in the UK. Clin Med (Lond). 2010 Apr; 10(2):145-7. doi: 10.7861/clinmedicine.10-2-145.
3. Yan Y et al. Adoption of Hospitalist Care in Asia: Experiences From Singapore, Taiwan, Korea, and Japan. J Hosp Med. Published Online First 2021 June 11. doi: 10.12788/jhm.3621.
4. Beresford L. Hospital medicine flourishing around the world. The Hospitalist. Nov 2015.
Similar needs, local adaptations
Similar needs, local adaptations
Hospital medicine has evolved rapidly and spread widely across the United States in the past 25 years in response to the health care system’s needs for patient safety, quality, efficiency, and effective coordination of care in the ever-more complex environment of the acute care hospital.
But hospital care can be just as complex in other countries, so it’s not surprising that there’s a lot of interest around the world in the U.S. model of hospital medicine. But adaptations of that model vary across – and within – countries, reflecting local culture, health care systems, payment models, and approaches to medical education.
Other countries have looked to U.S. experts for consultations, to U.S.-trained doctors who might be willing to relocate, and to the Society of Hospital Medicine as an internationally focused source of networking and other resources. Some U.S.-based institutions, led by the Cleveland Clinic, Johns Hopkins Medicine, and Weill-Cornell Medical School, have established teaching outposts in other countries, with opportunities for resident training that prepares future hospitalists on the ground.
SHM CEO Eric E. Howell, MD, MHM, said that he personally has interacted with developing hospital medicine programs in six countries, who called upon him in part because of his past research on managing length of hospital stays. Dr. Howell counts himself among a few dozen U.S. hospitalists who are regularly invited to come and consult or to give talks to established or developing hospitalist programs in other countries. Because of the COVID-19 epidemic, in-person visits to other countries have largely been curtailed, but that has introduced a more virtual world of online meetings.
“I think the interesting thing about the ‘international consultants’ for hospital medicine is that while they come from professionally diverse backgrounds, they are all working to solve remarkably similar problems: How to make health care more affordable and higher quality while staying abreast of up-to-date best practice for physicians,” he said.
“Hospital care is costly no matter where you go. Other countries are also trying to limit expense in ways that don’t compromise the quality of that care,” Dr. Howell said. Also, hospitalized patients are more complex than ever, with increasing severity of illness and comorbidities, which makes having a hospitalist available on site more important.
Dr. Howell hopes to encourage more dialogue with international colleagues. SHM has established collaborations with medical societies in other countries and makes time at its conferences for international hospitalist participants to meet and share their experiences. Hospitalists from 33 countries were represented at SHM’s 2017 conference, and the upcoming virtual SHM Converge, May 3-7, 2021, includes a dedicated international session. SHM chapters have formed in a number of other countries.
Flora Kisuule, MD, MPH, SFHM, director of the Division of Hospital Medicine at Johns Hopkins Bayview Medical Center in Baltimore, said her international hospital medicine work1 started 7 years ago when she was invited to the Middle East to help Aramco, the Saudi Arabian Oil Company, develop a hospital medicine program based on the U.S. model for its employees. This was a joint venture with Johns Hopkins Medicine. “We went there and looked at their processes and made recommendations such as duration of hospitalist shifts and how to expand the footprint of hospital medicine in the hospital,” she said.
Then Dr. Kisuule was asked to help develop a hospital medicine program in Panama, where the drivers for developing hospital medicine were improving quality of care and ensuring patient safety. The biggest barrier has been remuneration and how to pay salaries that will allow doctors to work at only one hospital. In Panama, doctors typically work at multiple hospitals or clinics so they can earn enough to make ends meet.
The need for professional identity
Arpana Vidyarthi, MD, “grew up” professionally in hospital medicine at the University of California, San Francisco, a pioneering institution for hospital medicine, and in SHM. “We used to say: If you’ve seen one hospital medicine group, you’ve seen one hospital medicine group,” she said.
Dr. Vidyarthi went to Singapore in 2011, taking a job as a hospitalist at Singapore General Hospital and the affiliated Duke–National University Medical School, eventually directing the Division of Advanced Internal Medicine (general and hospital medicine) at the National University Health System, before moving back to UCSF in 2020.
“Professional identity is one of the biggest benefits hospital medicine can bestow in Singapore and across Asia, where general medicine is underdeveloped. Just as it did 20 years ago in the U.S., that professional identity offers a road map to achieving competency in practicing medicine in the hospital setting,” Dr. Vidyarthi said.
At UCSF, the professional identity of a hospitalist is broad but defined. The research agenda, quality, safety, and educational competencies are specific, seen through a system lens, she added. “We take pride in that professional identify. This is an opportunity for countries where general medicine is underdeveloped and undervalued.”
But the term hospital medicine – or the American model – isn’t always welcomed by health care systems in other countries, Dr Vidyarthi said. “The label of 'hospital medicine' brings people together in professional identify, and that professional identity opens doors. But for it to have legs in other countries, those skills need to be of value to the local system. It needs to make sense, as it did in the United States, and to add value for the identified gaps that need to be filled.”
In Singapore, the health care system turned to the model of acute medical units (AMUs) and the acute medicine physician specialty developed in the United Kingdom, which created a new way of delivering care, a new geography of care, and new set of competencies around which to build training and certification.
AMUs manage the majority of acute medical patients who present to the emergency department and get admitted, with initial treatment for a maximum of 72 hours. Acute physicians, trained in the specialty of assessment, diagnosis, and treatment of adult patients with urgent medical needs, work in a unit situated between the emergency department entrance and the specialty care units. This specialty has been recognized since 2009.2
“Acute medicine is the standard care model in the UK and is now found in all government hospitals in Singapore. This model is being adapted across Europe, Asia, and the Pacific Islands,” Dr. Vidyarthi said. “Advantages include the specific geography of the unit, and outcomes that are value-added to these systems such as decreased use of hospital beds in areas with very high bed occupancy rates.”
In many locales, a variety of titles are used to describe doctors who are not hospitalists as we understand them but whose work is based in the hospital, including house officer, duty officer, junior officer, registrar, or general practitioner. Often these hospital-based doctors, who may in fact be residents or nongraduated trainees, lack the training and the scope of practice of a hospitalist. Because they typically need to consult the supervising physician before making inpatient management decisions, they aren’t able to provide the timely response to the patient’s changing medical condition that is needed to manage today’s acute patients.
Defining the fee schedule
In South Korea, a hospitalist model has emerged since 2015 in response to the insufficient number of hospital-based physicians needed to cover all admitted patients and to address related issues of patient safety, health care quality, and limitations on total hours per week medical residents are allowed to work.
South Korea in 1989 adopted a universal National Health Insurance System (NHIS), which took 12 years to implement. But inadequate coverage for medical work in the hospital has deterred physicians from choosing to work there. South Korea had longer lengths of hospital stay, fewer practicing physicians per 1,000 patients, and a much higher number of hospital patients per practicing physician than other countries in the Organization for Economic Cooperation and Development, according to a new study in the Journal of Hospital Medicine detailing hospitalist development in South Korea.3
A council representing leading medical associations was formed to develop a South Korean hospitalist system and charged by the Ministry of Health with designing an official proposal for implementing it. A pilot study focused on quality and on defining a fee schedule for hospital work was tested in four hospitals, and then a second phase in 31 of South Korea’s 344 general hospitals tested the proposed fee schedule, said Wonjeong Chae, MPH, the first named author on the study, based in the Department of Public Health in the College of Medicine at Yonsei University in Seoul. “But we’re still working on making the fee schedule better,” she said.
Ms. Chae estimates that there are about 250 working hospitalists in South Korea today, which leaves a lot of gaps in practice. “We did learn from America, but we have a different system, so the American concept had to be adapted. Hospital medicine is still growing in Korea despite the impact of the pandemic. We are at the beginning stages of development, but we expect it will grow more with government support.”
In Brazil, a handful of hospital medicine pioneers such as Guilherme Barcellos, MD, SFHM, in Porto Alegre have tried to grow the hospitalist model, networking with colleagues across Latin America through the Pan American Society of Hospitalists and the Brazilian chapter of SHM.
Individual hospitals have developed hospitalist programs, but there is no national model to lead the way. Frequent turnover for the Minister of Health position has made it harder to develop consistent national policy, and the country is largely still in the early stages of developing hospital medicine, depending on isolated initiatives, as Dr. Barcellos described it in a November 2015 article in The Hospitalist.4 Growth is slow but continuing, with new programs such as the one led by Reginaldo Filho, MD at Hospital São Vicente in Curitiba standing out in the confrontation against COVID-19, Dr. Barcellos said.
What can we learn from others?
India-born, U.S.-trained hospitalist Anand Kartha, MD, MS, SFHM, currently heads the Hospital Medicine Program at Hamad General Hospital in Doha, Qatar. He moved from Boston to this small nation on the Arabian Peninsula in 2014. Under the leadership of the hospital’s Department of Medicine, this program was developed to address difficulties such as scheduling, transitions of care, and networking with home care and other providers – the same issues seen in hospitals around the world.
These are not novel problems, Dr. Kartha said, but all of them have a common solution in evidence-based practice. “As hospitalists, our key is to collaborate with everyone in the hospital, using the multidisciplinary approach that is a unique feature of hospital medicine.”
The model has continued to spread across hospitals in Qatar, including academic and community programs. “We now have a full-fledged academic hospitalist system, which collaborates with community hospitals and community programs including a women’s hospital and an oncologic hospital,” he said. “Now the focus is on expanding resource capacity and the internal pipeline for hospitalists. I am getting graduates from Weill Cornell Medicine in Qatar.” Another key collaborator has been the Boston-based Institute for Healthcare Improvement, helping to develop best practices in Qatar and sponsoring the annual Middle East Forum on Quality and Safety in Health Care.
The residency training program at Hamad General is accredited by ACGME, with the same expected competencies as in the U.S. “We don’t use the term ‘hospitalist,’ ” Dr. Kartha said. “It’s better to focus on the model of care – which clearly was American. That model has encountered some resistance in some countries – on many of the same grounds U.S. hospitalists faced 20 years ago. You have to be sensitive to local culture. For hospitalists to succeed internationally, they have to possess a high degree of cultural intelligence.” There’s no shortage of issues such as language barriers, he said. “But that’s no different than at Boston Medical Center.”
SHM’s Middle East Chapter was off to a great start and then was slowed down by regional politics and COVID-19, but is looking forward to a great reboot in 2021, Dr. Kartha said. The pandemic also has been an opportunity to show how hospital medicine is the backbone of the hospital’s ability to respond, although of course many other professionals also pitched in.
Other countries around the world have learned a lot from the American model of hospital medicine. But sources for this article wonder if U.S. hospitalists, in turn, could learn from their adaptations and innovations.
“We can all learn better how to practice our field of medicine in the hospital with less resource utilization,” Dr. Vidyarthi concluded. “So many innovations are happening around us. If we open our eyes to our global colleagues and infuse some of their ideas, it could be wonderful for hospital professionals in the United States.”
References
1. Kisuule F, Howell E. Hospital medicine beyond the United States. Int J Gen Med. 2018;11:65-71. doi: 10.2147/IJGM.S151275.
2. Stosic J et al. The acute physician: The future of acute hospital care in the UK. Clin Med (Lond). 2010 Apr; 10(2):145-7. doi: 10.7861/clinmedicine.10-2-145.
3. Yan Y et al. Adoption of Hospitalist Care in Asia: Experiences From Singapore, Taiwan, Korea, and Japan. J Hosp Med. Published Online First 2021 June 11. doi: 10.12788/jhm.3621.
4. Beresford L. Hospital medicine flourishing around the world. The Hospitalist. Nov 2015.
Hospital medicine has evolved rapidly and spread widely across the United States in the past 25 years in response to the health care system’s needs for patient safety, quality, efficiency, and effective coordination of care in the ever-more complex environment of the acute care hospital.
But hospital care can be just as complex in other countries, so it’s not surprising that there’s a lot of interest around the world in the U.S. model of hospital medicine. But adaptations of that model vary across – and within – countries, reflecting local culture, health care systems, payment models, and approaches to medical education.
Other countries have looked to U.S. experts for consultations, to U.S.-trained doctors who might be willing to relocate, and to the Society of Hospital Medicine as an internationally focused source of networking and other resources. Some U.S.-based institutions, led by the Cleveland Clinic, Johns Hopkins Medicine, and Weill-Cornell Medical School, have established teaching outposts in other countries, with opportunities for resident training that prepares future hospitalists on the ground.
SHM CEO Eric E. Howell, MD, MHM, said that he personally has interacted with developing hospital medicine programs in six countries, who called upon him in part because of his past research on managing length of hospital stays. Dr. Howell counts himself among a few dozen U.S. hospitalists who are regularly invited to come and consult or to give talks to established or developing hospitalist programs in other countries. Because of the COVID-19 epidemic, in-person visits to other countries have largely been curtailed, but that has introduced a more virtual world of online meetings.
“I think the interesting thing about the ‘international consultants’ for hospital medicine is that while they come from professionally diverse backgrounds, they are all working to solve remarkably similar problems: How to make health care more affordable and higher quality while staying abreast of up-to-date best practice for physicians,” he said.
“Hospital care is costly no matter where you go. Other countries are also trying to limit expense in ways that don’t compromise the quality of that care,” Dr. Howell said. Also, hospitalized patients are more complex than ever, with increasing severity of illness and comorbidities, which makes having a hospitalist available on site more important.
Dr. Howell hopes to encourage more dialogue with international colleagues. SHM has established collaborations with medical societies in other countries and makes time at its conferences for international hospitalist participants to meet and share their experiences. Hospitalists from 33 countries were represented at SHM’s 2017 conference, and the upcoming virtual SHM Converge, May 3-7, 2021, includes a dedicated international session. SHM chapters have formed in a number of other countries.
Flora Kisuule, MD, MPH, SFHM, director of the Division of Hospital Medicine at Johns Hopkins Bayview Medical Center in Baltimore, said her international hospital medicine work1 started 7 years ago when she was invited to the Middle East to help Aramco, the Saudi Arabian Oil Company, develop a hospital medicine program based on the U.S. model for its employees. This was a joint venture with Johns Hopkins Medicine. “We went there and looked at their processes and made recommendations such as duration of hospitalist shifts and how to expand the footprint of hospital medicine in the hospital,” she said.
Then Dr. Kisuule was asked to help develop a hospital medicine program in Panama, where the drivers for developing hospital medicine were improving quality of care and ensuring patient safety. The biggest barrier has been remuneration and how to pay salaries that will allow doctors to work at only one hospital. In Panama, doctors typically work at multiple hospitals or clinics so they can earn enough to make ends meet.
The need for professional identity
Arpana Vidyarthi, MD, “grew up” professionally in hospital medicine at the University of California, San Francisco, a pioneering institution for hospital medicine, and in SHM. “We used to say: If you’ve seen one hospital medicine group, you’ve seen one hospital medicine group,” she said.
Dr. Vidyarthi went to Singapore in 2011, taking a job as a hospitalist at Singapore General Hospital and the affiliated Duke–National University Medical School, eventually directing the Division of Advanced Internal Medicine (general and hospital medicine) at the National University Health System, before moving back to UCSF in 2020.
“Professional identity is one of the biggest benefits hospital medicine can bestow in Singapore and across Asia, where general medicine is underdeveloped. Just as it did 20 years ago in the U.S., that professional identity offers a road map to achieving competency in practicing medicine in the hospital setting,” Dr. Vidyarthi said.
At UCSF, the professional identity of a hospitalist is broad but defined. The research agenda, quality, safety, and educational competencies are specific, seen through a system lens, she added. “We take pride in that professional identify. This is an opportunity for countries where general medicine is underdeveloped and undervalued.”
But the term hospital medicine – or the American model – isn’t always welcomed by health care systems in other countries, Dr Vidyarthi said. “The label of 'hospital medicine' brings people together in professional identify, and that professional identity opens doors. But for it to have legs in other countries, those skills need to be of value to the local system. It needs to make sense, as it did in the United States, and to add value for the identified gaps that need to be filled.”
In Singapore, the health care system turned to the model of acute medical units (AMUs) and the acute medicine physician specialty developed in the United Kingdom, which created a new way of delivering care, a new geography of care, and new set of competencies around which to build training and certification.
AMUs manage the majority of acute medical patients who present to the emergency department and get admitted, with initial treatment for a maximum of 72 hours. Acute physicians, trained in the specialty of assessment, diagnosis, and treatment of adult patients with urgent medical needs, work in a unit situated between the emergency department entrance and the specialty care units. This specialty has been recognized since 2009.2
“Acute medicine is the standard care model in the UK and is now found in all government hospitals in Singapore. This model is being adapted across Europe, Asia, and the Pacific Islands,” Dr. Vidyarthi said. “Advantages include the specific geography of the unit, and outcomes that are value-added to these systems such as decreased use of hospital beds in areas with very high bed occupancy rates.”
In many locales, a variety of titles are used to describe doctors who are not hospitalists as we understand them but whose work is based in the hospital, including house officer, duty officer, junior officer, registrar, or general practitioner. Often these hospital-based doctors, who may in fact be residents or nongraduated trainees, lack the training and the scope of practice of a hospitalist. Because they typically need to consult the supervising physician before making inpatient management decisions, they aren’t able to provide the timely response to the patient’s changing medical condition that is needed to manage today’s acute patients.
Defining the fee schedule
In South Korea, a hospitalist model has emerged since 2015 in response to the insufficient number of hospital-based physicians needed to cover all admitted patients and to address related issues of patient safety, health care quality, and limitations on total hours per week medical residents are allowed to work.
South Korea in 1989 adopted a universal National Health Insurance System (NHIS), which took 12 years to implement. But inadequate coverage for medical work in the hospital has deterred physicians from choosing to work there. South Korea had longer lengths of hospital stay, fewer practicing physicians per 1,000 patients, and a much higher number of hospital patients per practicing physician than other countries in the Organization for Economic Cooperation and Development, according to a new study in the Journal of Hospital Medicine detailing hospitalist development in South Korea.3
A council representing leading medical associations was formed to develop a South Korean hospitalist system and charged by the Ministry of Health with designing an official proposal for implementing it. A pilot study focused on quality and on defining a fee schedule for hospital work was tested in four hospitals, and then a second phase in 31 of South Korea’s 344 general hospitals tested the proposed fee schedule, said Wonjeong Chae, MPH, the first named author on the study, based in the Department of Public Health in the College of Medicine at Yonsei University in Seoul. “But we’re still working on making the fee schedule better,” she said.
Ms. Chae estimates that there are about 250 working hospitalists in South Korea today, which leaves a lot of gaps in practice. “We did learn from America, but we have a different system, so the American concept had to be adapted. Hospital medicine is still growing in Korea despite the impact of the pandemic. We are at the beginning stages of development, but we expect it will grow more with government support.”
In Brazil, a handful of hospital medicine pioneers such as Guilherme Barcellos, MD, SFHM, in Porto Alegre have tried to grow the hospitalist model, networking with colleagues across Latin America through the Pan American Society of Hospitalists and the Brazilian chapter of SHM.
Individual hospitals have developed hospitalist programs, but there is no national model to lead the way. Frequent turnover for the Minister of Health position has made it harder to develop consistent national policy, and the country is largely still in the early stages of developing hospital medicine, depending on isolated initiatives, as Dr. Barcellos described it in a November 2015 article in The Hospitalist.4 Growth is slow but continuing, with new programs such as the one led by Reginaldo Filho, MD at Hospital São Vicente in Curitiba standing out in the confrontation against COVID-19, Dr. Barcellos said.
What can we learn from others?
India-born, U.S.-trained hospitalist Anand Kartha, MD, MS, SFHM, currently heads the Hospital Medicine Program at Hamad General Hospital in Doha, Qatar. He moved from Boston to this small nation on the Arabian Peninsula in 2014. Under the leadership of the hospital’s Department of Medicine, this program was developed to address difficulties such as scheduling, transitions of care, and networking with home care and other providers – the same issues seen in hospitals around the world.
These are not novel problems, Dr. Kartha said, but all of them have a common solution in evidence-based practice. “As hospitalists, our key is to collaborate with everyone in the hospital, using the multidisciplinary approach that is a unique feature of hospital medicine.”
The model has continued to spread across hospitals in Qatar, including academic and community programs. “We now have a full-fledged academic hospitalist system, which collaborates with community hospitals and community programs including a women’s hospital and an oncologic hospital,” he said. “Now the focus is on expanding resource capacity and the internal pipeline for hospitalists. I am getting graduates from Weill Cornell Medicine in Qatar.” Another key collaborator has been the Boston-based Institute for Healthcare Improvement, helping to develop best practices in Qatar and sponsoring the annual Middle East Forum on Quality and Safety in Health Care.
The residency training program at Hamad General is accredited by ACGME, with the same expected competencies as in the U.S. “We don’t use the term ‘hospitalist,’ ” Dr. Kartha said. “It’s better to focus on the model of care – which clearly was American. That model has encountered some resistance in some countries – on many of the same grounds U.S. hospitalists faced 20 years ago. You have to be sensitive to local culture. For hospitalists to succeed internationally, they have to possess a high degree of cultural intelligence.” There’s no shortage of issues such as language barriers, he said. “But that’s no different than at Boston Medical Center.”
SHM’s Middle East Chapter was off to a great start and then was slowed down by regional politics and COVID-19, but is looking forward to a great reboot in 2021, Dr. Kartha said. The pandemic also has been an opportunity to show how hospital medicine is the backbone of the hospital’s ability to respond, although of course many other professionals also pitched in.
Other countries around the world have learned a lot from the American model of hospital medicine. But sources for this article wonder if U.S. hospitalists, in turn, could learn from their adaptations and innovations.
“We can all learn better how to practice our field of medicine in the hospital with less resource utilization,” Dr. Vidyarthi concluded. “So many innovations are happening around us. If we open our eyes to our global colleagues and infuse some of their ideas, it could be wonderful for hospital professionals in the United States.”
References
1. Kisuule F, Howell E. Hospital medicine beyond the United States. Int J Gen Med. 2018;11:65-71. doi: 10.2147/IJGM.S151275.
2. Stosic J et al. The acute physician: The future of acute hospital care in the UK. Clin Med (Lond). 2010 Apr; 10(2):145-7. doi: 10.7861/clinmedicine.10-2-145.
3. Yan Y et al. Adoption of Hospitalist Care in Asia: Experiences From Singapore, Taiwan, Korea, and Japan. J Hosp Med. Published Online First 2021 June 11. doi: 10.12788/jhm.3621.
4. Beresford L. Hospital medicine flourishing around the world. The Hospitalist. Nov 2015.
Longitudinal associations between income changes and incident CVD
Background: Low income is associated with CVD, although causality remains debated because low income is also associated with depression and negative health behaviors, which can be associated with CVD. For more robust causal inference, changes in income and their association with CVD must be observed.
Study design: Prospective observational cohort study.
Setting: Four U.S. urban centers – Jackson, Miss.; suburbs of Minneapolis; Washington County, Md.; and Forsyth County, N.C.
Synopsis: Among a large cohort of community-dwelling middle-aged adults, this study showed that negative income changes are associated with an increased incidence of CVD. Among 8,989 patients recruited from the four urban centers above, 10% experienced an income drop, 70% did not have a change in income, and 20% experienced an income increase over the first 6 years of the study. Patients were followed for a mean of 17 years, and those who experienced an income drop were found to have a 17% higher risk of incident CVD, whereas those who experienced an income increase had a 14% lower risk of CVD.
The study was limited by difficulties classifying income and its changes; the complicated nature of income, its relationship with other socioeconomic factors, and causation inferences; and the relatively short span over which income was monitored.
Bottom line: Income decrease is associated with an increased risk of incident CVD.
Citation: Wang S et al. Longitudinal associations between income changes and incident cardiovascular disease, the atherosclerosis risk in communities study. JAMA Cardiol. 2019 Oct 9;4(12):1203-12.
Dr. Rupp is a hospitalist and clinical instructor of medicine at the University of Utah, Salt Lake City.
Background: Low income is associated with CVD, although causality remains debated because low income is also associated with depression and negative health behaviors, which can be associated with CVD. For more robust causal inference, changes in income and their association with CVD must be observed.
Study design: Prospective observational cohort study.
Setting: Four U.S. urban centers – Jackson, Miss.; suburbs of Minneapolis; Washington County, Md.; and Forsyth County, N.C.
Synopsis: Among a large cohort of community-dwelling middle-aged adults, this study showed that negative income changes are associated with an increased incidence of CVD. Among 8,989 patients recruited from the four urban centers above, 10% experienced an income drop, 70% did not have a change in income, and 20% experienced an income increase over the first 6 years of the study. Patients were followed for a mean of 17 years, and those who experienced an income drop were found to have a 17% higher risk of incident CVD, whereas those who experienced an income increase had a 14% lower risk of CVD.
The study was limited by difficulties classifying income and its changes; the complicated nature of income, its relationship with other socioeconomic factors, and causation inferences; and the relatively short span over which income was monitored.
Bottom line: Income decrease is associated with an increased risk of incident CVD.
Citation: Wang S et al. Longitudinal associations between income changes and incident cardiovascular disease, the atherosclerosis risk in communities study. JAMA Cardiol. 2019 Oct 9;4(12):1203-12.
Dr. Rupp is a hospitalist and clinical instructor of medicine at the University of Utah, Salt Lake City.
Background: Low income is associated with CVD, although causality remains debated because low income is also associated with depression and negative health behaviors, which can be associated with CVD. For more robust causal inference, changes in income and their association with CVD must be observed.
Study design: Prospective observational cohort study.
Setting: Four U.S. urban centers – Jackson, Miss.; suburbs of Minneapolis; Washington County, Md.; and Forsyth County, N.C.
Synopsis: Among a large cohort of community-dwelling middle-aged adults, this study showed that negative income changes are associated with an increased incidence of CVD. Among 8,989 patients recruited from the four urban centers above, 10% experienced an income drop, 70% did not have a change in income, and 20% experienced an income increase over the first 6 years of the study. Patients were followed for a mean of 17 years, and those who experienced an income drop were found to have a 17% higher risk of incident CVD, whereas those who experienced an income increase had a 14% lower risk of CVD.
The study was limited by difficulties classifying income and its changes; the complicated nature of income, its relationship with other socioeconomic factors, and causation inferences; and the relatively short span over which income was monitored.
Bottom line: Income decrease is associated with an increased risk of incident CVD.
Citation: Wang S et al. Longitudinal associations between income changes and incident cardiovascular disease, the atherosclerosis risk in communities study. JAMA Cardiol. 2019 Oct 9;4(12):1203-12.
Dr. Rupp is a hospitalist and clinical instructor of medicine at the University of Utah, Salt Lake City.
Senate confirms Murthy as Surgeon General
Seven Republicans – Bill Cassidy (La.), Susan Collins (Maine), Roger Marshall (Kan.), Susan Murkowski (Alaska), Rob Portman (Ohio), Mitt Romney (Utah), and Dan Sullivan (Alaska) – joined all the Democrats and independents in the 57-43 vote approving Dr. Murthy’s nomination.
Dr. Murthy, 43, previously served as the 19th Surgeon General, from December 2014 to April 2017, when he was asked to step down by President Donald J. Trump.
Surgeons General serve 4-year terms.
During his first tenure, Dr. Murthy issued the first-ever Surgeon General’s report on the crisis of addiction and issued a call to action to doctors to help battle the opioid crisis.
When Dr. Murthy was nominated by President-elect Joseph R. Biden Jr. in December, he was acting as cochair of the incoming administration’s COVID-19 transition advisory board.
Early in 2020, before the COVID-19 pandemic hit, Dr. Murthy published a timely book: “Together: The Healing Power of Human Connection in a Sometimes Lonely World”.
He earned his bachelor’s degree from Harvard and his MD and MBA degrees from Yale. He completed his internal medicine residency at Brigham and Women’s Hospital in Boston, where he also served as a hospitalist, and later joined Harvard Medical School as a faculty member in internal medicine.
He is married to Alice Chen, MD. The couple have two children.
A version of this article first appeared on WebMD.com.
Seven Republicans – Bill Cassidy (La.), Susan Collins (Maine), Roger Marshall (Kan.), Susan Murkowski (Alaska), Rob Portman (Ohio), Mitt Romney (Utah), and Dan Sullivan (Alaska) – joined all the Democrats and independents in the 57-43 vote approving Dr. Murthy’s nomination.
Dr. Murthy, 43, previously served as the 19th Surgeon General, from December 2014 to April 2017, when he was asked to step down by President Donald J. Trump.
Surgeons General serve 4-year terms.
During his first tenure, Dr. Murthy issued the first-ever Surgeon General’s report on the crisis of addiction and issued a call to action to doctors to help battle the opioid crisis.
When Dr. Murthy was nominated by President-elect Joseph R. Biden Jr. in December, he was acting as cochair of the incoming administration’s COVID-19 transition advisory board.
Early in 2020, before the COVID-19 pandemic hit, Dr. Murthy published a timely book: “Together: The Healing Power of Human Connection in a Sometimes Lonely World”.
He earned his bachelor’s degree from Harvard and his MD and MBA degrees from Yale. He completed his internal medicine residency at Brigham and Women’s Hospital in Boston, where he also served as a hospitalist, and later joined Harvard Medical School as a faculty member in internal medicine.
He is married to Alice Chen, MD. The couple have two children.
A version of this article first appeared on WebMD.com.
Seven Republicans – Bill Cassidy (La.), Susan Collins (Maine), Roger Marshall (Kan.), Susan Murkowski (Alaska), Rob Portman (Ohio), Mitt Romney (Utah), and Dan Sullivan (Alaska) – joined all the Democrats and independents in the 57-43 vote approving Dr. Murthy’s nomination.
Dr. Murthy, 43, previously served as the 19th Surgeon General, from December 2014 to April 2017, when he was asked to step down by President Donald J. Trump.
Surgeons General serve 4-year terms.
During his first tenure, Dr. Murthy issued the first-ever Surgeon General’s report on the crisis of addiction and issued a call to action to doctors to help battle the opioid crisis.
When Dr. Murthy was nominated by President-elect Joseph R. Biden Jr. in December, he was acting as cochair of the incoming administration’s COVID-19 transition advisory board.
Early in 2020, before the COVID-19 pandemic hit, Dr. Murthy published a timely book: “Together: The Healing Power of Human Connection in a Sometimes Lonely World”.
He earned his bachelor’s degree from Harvard and his MD and MBA degrees from Yale. He completed his internal medicine residency at Brigham and Women’s Hospital in Boston, where he also served as a hospitalist, and later joined Harvard Medical School as a faculty member in internal medicine.
He is married to Alice Chen, MD. The couple have two children.
A version of this article first appeared on WebMD.com.
Do you want to become a hospitalist leader?
Learn how or even whether you should
Have you ever thought you could be a leader, in your hospitalist group, in hospital administration, or at another institution? The reasons to seek a leadership role as a hospitalist are many, but there are also many drawbacks. According to hospitalists who have reached high rungs on the leadership ladder, you will need a blend of desire, enthusiasm, education, and experience if you want to succeed in leadership.
The right reasons
“People who make good leaders have a sense of purpose and want to make a difference,” said Eric Howell, MD, MHM, CEO of the Society of Hospital Medicine, and former chief of medical units at Johns Hopkins Bayview in Baltimore. “I think most hospitalists have that sense of wanting to help patients and society, so that’s a strong mission in itself. Just by training and the very design of our health care system, hospitalists are often natural leaders, and in leadership roles, because they run teams of clinicians and train medical students.”
Danielle Scheurer, MD, SFHM, chief quality officer and professor of medicine at the Medical University of South Carolina, and current president of SHM, said some hospitalists end up in leadership roles almost by accident – because there is a leadership “void” in the health system where they work, and no one else wants to step up. Others disconnect from the leadership track and are happy to simply be part of a team.
“If you are yearning to make a difference and that’s your motivation then you will find leadership is more fulfilling than difficult,” she said. “But if you take a leadership role to fill a void or think you just want to take some nonclinical time, it’s probably not a good idea. Some people think administrative leadership is easier than being a hospitalist, but it is not. Leadership should not be about getting away from something else. It should be a thoughtful career move, and if it is, being a leader can be meaningful and fulfilling.”
Nancy Spector, MD, the vice dean for faculty and executive director of the Executive Leadership in Academic Medicine program at Drexel University College of Medicine in Philadelphia, said a willingness to fail is vital for a leader. “You have to be open to successes, yes, but also to making mistakes,” she said. “It’s about honing the skills that leadership requires and be open to development and change.”
Kierstin Cates Kennedy, MD, SFHM, chief of hospital medicine at the University of Alabama at Birmingham, said that a hospitalist fresh out of residency will gain insight into whether leadership is the right path by acquiring a deeper understanding of how health care institutions work.
“When you are new to the hospital, you see how things work, how people interact with each other, and learn the politics,” she said. “One of the easiest ways to do it is get involved in a committee and be a part of meetings. You can have some input and get exposure to other leaders and they can learn more about you. Once you get an organizational understanding under your belt, then you can start taking on projects to gain even more understanding.”
Still up for it?
If you think you have the commitment and desire for leadership as an early career hospitalist, how would you continue down the leadership path?
“A great way is to find a person you want to be like, who could be a mentor. Find a successful leader that you admire, and one who is willing to guide you,” Dr. Howell said. “Books are helpful as well, and I still find I’m learning today – I have a list that includes Drive by Daniel Pink and Good to Great by Jim Collins. There are Malcolm Gladwell books that also have terrific knowledge to impart.”
Mark W. Shen, MD, SFHM, associate professor at Dell Medical School at the University of Texas at Austin and former president of St. Louis Children’s Hospital, said potential hospitalist leaders must be aware of their fellow clinicians.
“Pay attention to the needs of the hospitalist group as they are articulated by the lead hospitalist, the administration, and the patients,” he said. “There are so many activities that come up on a day-in, day-out basis. You should jump in and volunteer to take the lead on some of those activities. Leading your peers is often one of the most challenging parts of leadership. I think taking on even just a small activity like, say, working on a clinical pathway for the group, will result in a lot of preparation for future leadership roles.”
An example of an early career activity that Dr. Shen felt was valuable to future leaders was helping in the development of a hospitalist core curriculum. “We would use the core curriculum to educate students and residents coming through our rotation and have some degree of commonality or standardization,” he said. “So even though I wasn’t an explicit leader of the hospitalist group at the time, I’d say that helping develop the core curriculum aided me in understanding what leadership was all about.”
Getting started in a leadership role, Dr. Spector said, can be helped by embracing a knowledge of the business of medicine. “Business and finance are a reality you shouldn’t avoid,” she said. “Another way to learn is to partner with your local administrators or whoever is running your division or your department. There are business managers and business partners in every institution, and you can learn a great deal from them. It’s important to network and get to know people because we’re a people business, and opportunity comes when people know who you are.”
Dr. Howell noted that advocating for yourself is sometimes hard, and it can be a red flag in some circumstances, but you should tell your bosses where you want to go professionally.
“You can say that you want to grow professionally, and let’s face it, there are naturally-inclined leaders. We all need to be transparent in goal paths,” he said. “But if you want a leadership role for power, money, and prestige then you’re not applying the right thinking. If you want to help others and you have a mission you believe in, then communicate that to your bosses.”
Dr. Scheurer believes choosing between clinical and administrative leadership is not so clear cut, because in the health care setting they tend to morph into each other. “Many times clinicians will end up taking on a leadership role that has a significant administrative component to it,” she said. “I do think if clinicians make a career move and get the right training then they can be exemplary leaders in health care, but I do worry a little about clinicians going into leadership roles without any formal training. They are usually well-intentioned but that’s not enough. It’s not any different than medical training. If you want to be a good leader you need training to develop your skills, and a lot of those skills do not come naturally or easily. We thrust good clinicians into leadership roles because they are good clinicians, but if they don’t have the right skills, being a leader can be a problem.”
How do leaders improve?
If you have made it to a leadership position, and have been in that role for a while, you might start to feel you are stuck in your growth trajectory. If so, how do you continue to improve?
According to Dr. Kennedy, whether you are looking to get into leadership or want to improve, focusing on emotional intelligence is important. “A book like Emotional Intelligence 2.0 by Travis Bradbury is a great introduction,” she said. “With my leadership team, we did a book club where we read Primal Leadership, which is focused on emotional intelligence and on aspects like setting a culture.”
Dr. Howell said that to grow as a leader, be careful what you say no to. “I used to talk about having a tag line that was ‘just say yes,’” he said. “At least try to say yes most of the time because it opens up opportunities and shows you are looking to do more, not less.”
Also, Dr. Howell recommends that leaders look for tools that minimize blind spots and get information from staff through survey assessments. “Get the input of others on your strengths and weaknesses,” he said. “Nurses, doctors, and sometimes patients can give you good information that will help you grow as a leader. Don’t be afraid of feedback.”
Never stop learning
Dr. Scheurer said it is important to recognize that you are never finished learning when you are a leader.
“See leadership as a continuous learning journey. You can never be too good of a leader in medicine,” she said. “Never stop learning, because the field keeps changing and you have to constantly learn and find pleasure in that learning. You should look at leadership the same way. A lot of leadership theories change with the times and you should always try to get good advice. You don’t take every piece of advice – just like in medicine when you read an article and you try to apply it to patients in your practice. Take some advice, leave some advice, and develop a leadership style that is genuine and authentic.”
Dr. Kennedy believes that a hospitalist’s leadership potential may be limited if you see continued learning as a chore, rather than an opportunity.
“If you resent it learning about leadership, then is it really for you?” she asked. “I find myself reading on the topic or talking about it, and it’s fun. How do you make an environment work better, how do you inspire people, how do you help them grow? These are some of the most important questions leaders face. Isn’t it fun if you can find some answers?”
Learn how or even whether you should
Learn how or even whether you should
Have you ever thought you could be a leader, in your hospitalist group, in hospital administration, or at another institution? The reasons to seek a leadership role as a hospitalist are many, but there are also many drawbacks. According to hospitalists who have reached high rungs on the leadership ladder, you will need a blend of desire, enthusiasm, education, and experience if you want to succeed in leadership.
The right reasons
“People who make good leaders have a sense of purpose and want to make a difference,” said Eric Howell, MD, MHM, CEO of the Society of Hospital Medicine, and former chief of medical units at Johns Hopkins Bayview in Baltimore. “I think most hospitalists have that sense of wanting to help patients and society, so that’s a strong mission in itself. Just by training and the very design of our health care system, hospitalists are often natural leaders, and in leadership roles, because they run teams of clinicians and train medical students.”
Danielle Scheurer, MD, SFHM, chief quality officer and professor of medicine at the Medical University of South Carolina, and current president of SHM, said some hospitalists end up in leadership roles almost by accident – because there is a leadership “void” in the health system where they work, and no one else wants to step up. Others disconnect from the leadership track and are happy to simply be part of a team.
“If you are yearning to make a difference and that’s your motivation then you will find leadership is more fulfilling than difficult,” she said. “But if you take a leadership role to fill a void or think you just want to take some nonclinical time, it’s probably not a good idea. Some people think administrative leadership is easier than being a hospitalist, but it is not. Leadership should not be about getting away from something else. It should be a thoughtful career move, and if it is, being a leader can be meaningful and fulfilling.”
Nancy Spector, MD, the vice dean for faculty and executive director of the Executive Leadership in Academic Medicine program at Drexel University College of Medicine in Philadelphia, said a willingness to fail is vital for a leader. “You have to be open to successes, yes, but also to making mistakes,” she said. “It’s about honing the skills that leadership requires and be open to development and change.”
Kierstin Cates Kennedy, MD, SFHM, chief of hospital medicine at the University of Alabama at Birmingham, said that a hospitalist fresh out of residency will gain insight into whether leadership is the right path by acquiring a deeper understanding of how health care institutions work.
“When you are new to the hospital, you see how things work, how people interact with each other, and learn the politics,” she said. “One of the easiest ways to do it is get involved in a committee and be a part of meetings. You can have some input and get exposure to other leaders and they can learn more about you. Once you get an organizational understanding under your belt, then you can start taking on projects to gain even more understanding.”
Still up for it?
If you think you have the commitment and desire for leadership as an early career hospitalist, how would you continue down the leadership path?
“A great way is to find a person you want to be like, who could be a mentor. Find a successful leader that you admire, and one who is willing to guide you,” Dr. Howell said. “Books are helpful as well, and I still find I’m learning today – I have a list that includes Drive by Daniel Pink and Good to Great by Jim Collins. There are Malcolm Gladwell books that also have terrific knowledge to impart.”
Mark W. Shen, MD, SFHM, associate professor at Dell Medical School at the University of Texas at Austin and former president of St. Louis Children’s Hospital, said potential hospitalist leaders must be aware of their fellow clinicians.
“Pay attention to the needs of the hospitalist group as they are articulated by the lead hospitalist, the administration, and the patients,” he said. “There are so many activities that come up on a day-in, day-out basis. You should jump in and volunteer to take the lead on some of those activities. Leading your peers is often one of the most challenging parts of leadership. I think taking on even just a small activity like, say, working on a clinical pathway for the group, will result in a lot of preparation for future leadership roles.”
An example of an early career activity that Dr. Shen felt was valuable to future leaders was helping in the development of a hospitalist core curriculum. “We would use the core curriculum to educate students and residents coming through our rotation and have some degree of commonality or standardization,” he said. “So even though I wasn’t an explicit leader of the hospitalist group at the time, I’d say that helping develop the core curriculum aided me in understanding what leadership was all about.”
Getting started in a leadership role, Dr. Spector said, can be helped by embracing a knowledge of the business of medicine. “Business and finance are a reality you shouldn’t avoid,” she said. “Another way to learn is to partner with your local administrators or whoever is running your division or your department. There are business managers and business partners in every institution, and you can learn a great deal from them. It’s important to network and get to know people because we’re a people business, and opportunity comes when people know who you are.”
Dr. Howell noted that advocating for yourself is sometimes hard, and it can be a red flag in some circumstances, but you should tell your bosses where you want to go professionally.
“You can say that you want to grow professionally, and let’s face it, there are naturally-inclined leaders. We all need to be transparent in goal paths,” he said. “But if you want a leadership role for power, money, and prestige then you’re not applying the right thinking. If you want to help others and you have a mission you believe in, then communicate that to your bosses.”
Dr. Scheurer believes choosing between clinical and administrative leadership is not so clear cut, because in the health care setting they tend to morph into each other. “Many times clinicians will end up taking on a leadership role that has a significant administrative component to it,” she said. “I do think if clinicians make a career move and get the right training then they can be exemplary leaders in health care, but I do worry a little about clinicians going into leadership roles without any formal training. They are usually well-intentioned but that’s not enough. It’s not any different than medical training. If you want to be a good leader you need training to develop your skills, and a lot of those skills do not come naturally or easily. We thrust good clinicians into leadership roles because they are good clinicians, but if they don’t have the right skills, being a leader can be a problem.”
How do leaders improve?
If you have made it to a leadership position, and have been in that role for a while, you might start to feel you are stuck in your growth trajectory. If so, how do you continue to improve?
According to Dr. Kennedy, whether you are looking to get into leadership or want to improve, focusing on emotional intelligence is important. “A book like Emotional Intelligence 2.0 by Travis Bradbury is a great introduction,” she said. “With my leadership team, we did a book club where we read Primal Leadership, which is focused on emotional intelligence and on aspects like setting a culture.”
Dr. Howell said that to grow as a leader, be careful what you say no to. “I used to talk about having a tag line that was ‘just say yes,’” he said. “At least try to say yes most of the time because it opens up opportunities and shows you are looking to do more, not less.”
Also, Dr. Howell recommends that leaders look for tools that minimize blind spots and get information from staff through survey assessments. “Get the input of others on your strengths and weaknesses,” he said. “Nurses, doctors, and sometimes patients can give you good information that will help you grow as a leader. Don’t be afraid of feedback.”
Never stop learning
Dr. Scheurer said it is important to recognize that you are never finished learning when you are a leader.
“See leadership as a continuous learning journey. You can never be too good of a leader in medicine,” she said. “Never stop learning, because the field keeps changing and you have to constantly learn and find pleasure in that learning. You should look at leadership the same way. A lot of leadership theories change with the times and you should always try to get good advice. You don’t take every piece of advice – just like in medicine when you read an article and you try to apply it to patients in your practice. Take some advice, leave some advice, and develop a leadership style that is genuine and authentic.”
Dr. Kennedy believes that a hospitalist’s leadership potential may be limited if you see continued learning as a chore, rather than an opportunity.
“If you resent it learning about leadership, then is it really for you?” she asked. “I find myself reading on the topic or talking about it, and it’s fun. How do you make an environment work better, how do you inspire people, how do you help them grow? These are some of the most important questions leaders face. Isn’t it fun if you can find some answers?”
Have you ever thought you could be a leader, in your hospitalist group, in hospital administration, or at another institution? The reasons to seek a leadership role as a hospitalist are many, but there are also many drawbacks. According to hospitalists who have reached high rungs on the leadership ladder, you will need a blend of desire, enthusiasm, education, and experience if you want to succeed in leadership.
The right reasons
“People who make good leaders have a sense of purpose and want to make a difference,” said Eric Howell, MD, MHM, CEO of the Society of Hospital Medicine, and former chief of medical units at Johns Hopkins Bayview in Baltimore. “I think most hospitalists have that sense of wanting to help patients and society, so that’s a strong mission in itself. Just by training and the very design of our health care system, hospitalists are often natural leaders, and in leadership roles, because they run teams of clinicians and train medical students.”
Danielle Scheurer, MD, SFHM, chief quality officer and professor of medicine at the Medical University of South Carolina, and current president of SHM, said some hospitalists end up in leadership roles almost by accident – because there is a leadership “void” in the health system where they work, and no one else wants to step up. Others disconnect from the leadership track and are happy to simply be part of a team.
“If you are yearning to make a difference and that’s your motivation then you will find leadership is more fulfilling than difficult,” she said. “But if you take a leadership role to fill a void or think you just want to take some nonclinical time, it’s probably not a good idea. Some people think administrative leadership is easier than being a hospitalist, but it is not. Leadership should not be about getting away from something else. It should be a thoughtful career move, and if it is, being a leader can be meaningful and fulfilling.”
Nancy Spector, MD, the vice dean for faculty and executive director of the Executive Leadership in Academic Medicine program at Drexel University College of Medicine in Philadelphia, said a willingness to fail is vital for a leader. “You have to be open to successes, yes, but also to making mistakes,” she said. “It’s about honing the skills that leadership requires and be open to development and change.”
Kierstin Cates Kennedy, MD, SFHM, chief of hospital medicine at the University of Alabama at Birmingham, said that a hospitalist fresh out of residency will gain insight into whether leadership is the right path by acquiring a deeper understanding of how health care institutions work.
“When you are new to the hospital, you see how things work, how people interact with each other, and learn the politics,” she said. “One of the easiest ways to do it is get involved in a committee and be a part of meetings. You can have some input and get exposure to other leaders and they can learn more about you. Once you get an organizational understanding under your belt, then you can start taking on projects to gain even more understanding.”
Still up for it?
If you think you have the commitment and desire for leadership as an early career hospitalist, how would you continue down the leadership path?
“A great way is to find a person you want to be like, who could be a mentor. Find a successful leader that you admire, and one who is willing to guide you,” Dr. Howell said. “Books are helpful as well, and I still find I’m learning today – I have a list that includes Drive by Daniel Pink and Good to Great by Jim Collins. There are Malcolm Gladwell books that also have terrific knowledge to impart.”
Mark W. Shen, MD, SFHM, associate professor at Dell Medical School at the University of Texas at Austin and former president of St. Louis Children’s Hospital, said potential hospitalist leaders must be aware of their fellow clinicians.
“Pay attention to the needs of the hospitalist group as they are articulated by the lead hospitalist, the administration, and the patients,” he said. “There are so many activities that come up on a day-in, day-out basis. You should jump in and volunteer to take the lead on some of those activities. Leading your peers is often one of the most challenging parts of leadership. I think taking on even just a small activity like, say, working on a clinical pathway for the group, will result in a lot of preparation for future leadership roles.”
An example of an early career activity that Dr. Shen felt was valuable to future leaders was helping in the development of a hospitalist core curriculum. “We would use the core curriculum to educate students and residents coming through our rotation and have some degree of commonality or standardization,” he said. “So even though I wasn’t an explicit leader of the hospitalist group at the time, I’d say that helping develop the core curriculum aided me in understanding what leadership was all about.”
Getting started in a leadership role, Dr. Spector said, can be helped by embracing a knowledge of the business of medicine. “Business and finance are a reality you shouldn’t avoid,” she said. “Another way to learn is to partner with your local administrators or whoever is running your division or your department. There are business managers and business partners in every institution, and you can learn a great deal from them. It’s important to network and get to know people because we’re a people business, and opportunity comes when people know who you are.”
Dr. Howell noted that advocating for yourself is sometimes hard, and it can be a red flag in some circumstances, but you should tell your bosses where you want to go professionally.
“You can say that you want to grow professionally, and let’s face it, there are naturally-inclined leaders. We all need to be transparent in goal paths,” he said. “But if you want a leadership role for power, money, and prestige then you’re not applying the right thinking. If you want to help others and you have a mission you believe in, then communicate that to your bosses.”
Dr. Scheurer believes choosing between clinical and administrative leadership is not so clear cut, because in the health care setting they tend to morph into each other. “Many times clinicians will end up taking on a leadership role that has a significant administrative component to it,” she said. “I do think if clinicians make a career move and get the right training then they can be exemplary leaders in health care, but I do worry a little about clinicians going into leadership roles without any formal training. They are usually well-intentioned but that’s not enough. It’s not any different than medical training. If you want to be a good leader you need training to develop your skills, and a lot of those skills do not come naturally or easily. We thrust good clinicians into leadership roles because they are good clinicians, but if they don’t have the right skills, being a leader can be a problem.”
How do leaders improve?
If you have made it to a leadership position, and have been in that role for a while, you might start to feel you are stuck in your growth trajectory. If so, how do you continue to improve?
According to Dr. Kennedy, whether you are looking to get into leadership or want to improve, focusing on emotional intelligence is important. “A book like Emotional Intelligence 2.0 by Travis Bradbury is a great introduction,” she said. “With my leadership team, we did a book club where we read Primal Leadership, which is focused on emotional intelligence and on aspects like setting a culture.”
Dr. Howell said that to grow as a leader, be careful what you say no to. “I used to talk about having a tag line that was ‘just say yes,’” he said. “At least try to say yes most of the time because it opens up opportunities and shows you are looking to do more, not less.”
Also, Dr. Howell recommends that leaders look for tools that minimize blind spots and get information from staff through survey assessments. “Get the input of others on your strengths and weaknesses,” he said. “Nurses, doctors, and sometimes patients can give you good information that will help you grow as a leader. Don’t be afraid of feedback.”
Never stop learning
Dr. Scheurer said it is important to recognize that you are never finished learning when you are a leader.
“See leadership as a continuous learning journey. You can never be too good of a leader in medicine,” she said. “Never stop learning, because the field keeps changing and you have to constantly learn and find pleasure in that learning. You should look at leadership the same way. A lot of leadership theories change with the times and you should always try to get good advice. You don’t take every piece of advice – just like in medicine when you read an article and you try to apply it to patients in your practice. Take some advice, leave some advice, and develop a leadership style that is genuine and authentic.”
Dr. Kennedy believes that a hospitalist’s leadership potential may be limited if you see continued learning as a chore, rather than an opportunity.
“If you resent it learning about leadership, then is it really for you?” she asked. “I find myself reading on the topic or talking about it, and it’s fun. How do you make an environment work better, how do you inspire people, how do you help them grow? These are some of the most important questions leaders face. Isn’t it fun if you can find some answers?”
The skill set of the ‘pluripotent’ hospitalist
Editor’s note: National Hospitalist Day occurs the first Thursday in March annually, and serves to celebrate the fastest growing specialty in modern medicine and hospitalists’ enduring contributions to the evolving health care landscape. On National Hospitalist Day in 2021, SHM convened a virtual roundtable with a diverse group of hospitalists to discuss skill set, wellness, and other key issues for hospitalists. To listen to the entire roundtable discussion, visit this Explore The Space podcast episode.
A hospitalist isn’t just a physician who happens to work in a hospital. They are medical professionals with a robust skill set that they use both inside and outside the hospital setting. But what skill sets do hospitalists need to become successful in their careers? And what skill sets does a “pluripotent” hospitalist need in their armamentarium?
These were the issues discussed by participants of a virtual roundtable discussion on National Hospitalist Day – March 4, 2021 – as part of a joint effort of the Society of Hospital Medicine and the Explore the Space podcast.
Maylyn S. Martinez, MD, clinician-researcher and clinical associate at the University of Chicago, sees her hospitalist and research skill sets as two “buckets” of skills she can sort through, with diagnostic, knowledge-based care coordination, and interpersonal skills as lanes where she can focus and improve. “I’m always trying to work in, and sharpen, and find ways to get better at something in each of those every day,” she said.
For Anika Kumar, MD, FHM, pediatric editor of the Hospitalist and clinical assistant professor of pediatrics at the Cleveland Clinic Lerner College of Medicine, much of her work is focused on problem solving. “I approach that as: ‘How do I come up with my differential diagnosis, and how do I diagnose the patient?’ I think that the lanes are a little bit different, but there is some overlap.”
Adaptability is another important part of the skill set for the hospitalist, Ndidi Unaka, MD, MEd, associate professor in the division of hospital medicine at Cincinnati Children’s Hospital Medical Center, said during the discussion. “I think we all really value teamwork, and we take on the role of being the coordinator and making sure things are getting done in a seamless and thoughtful manner. Communicating with families, communicating with our research team, communicating with primary care physicians. I think that is something we’re very used to doing, and I think we do it well. I think we don’t shy away from difficult conversations with consultants. And I think that’s what makes being a hospitalist so amazing.”
Achieving wellness as a hospitalist
Another topic discussed during the roundtable was “comprehensive care for the hospitalist” and how they can achieve a sense of wellness for themselves. Gurpreet Dhaliwal, MD, clinician-educator and professor of medicine at the University of California, San Francisco, said long-term satisfaction in one’s career is less about compensation and more about autonomy, mastery, and purpose.
“Autonomy is shrinking a little bit in health care. But if we connect to our purpose – ‘what are we doing here and how do we connect?’ – it’s either learning about patients and their stories, being with a team of people that you work with, that really builds that purpose,” he said.
Regarding mastery, there’s “tremendous joy if you’re in an environment where people value your mastery, whether it is working in a team or communicating or diagnosing or doing a procedure. If you think of setting up the work environment and those things are in place, I think a lot of wellness can actually happen at work, even though another component, of course, is balancing your life outside of work,” Dr. Dhaliwal said.
This may seem out of reach during COVID-19, but wellness is still achievable during the pandemic, Dr. Martinez said. Her time is spent 75% as a researcher and 25% as a clinician, which is her ideal balance. “I enjoy doing my research, doing my own statistics and writing grants and just learning about this problem that I’ve developed an interest in,” she said. “I just think that’s an important piece for people to focus on as far as health care for the hospitalist, is that there’s no no-one-size-fits-all, that’s for sure.”
Dr. Kumar noted that her clinical time gives her energy for nonclinical work. “I love my clinical time. It’s one of my favorite things that I do,” she said. Although she is tired at the end of the week, “I feel like I am not only giving back to my patients and my team, but I’m also giving back to myself and reminding myself why it is I do what I do every day,” she said.
Wellness for Dr. Unaka meant remembering what drew her to medicine. “It was definitely the opportunity to build strong relationships with patients and families,” she said. While these encounters can sometimes be heavy and stay with a hospitalist, “the fact that we’re in it with them is something that gives a lot of us purpose. I think that when I reflect on all of those things, I’m so happy that I’m in the role that I am.”
Unique skills during COVID-19
Mark Shapiro, MD, hospitalist and host of the roundtable and the Explore the Space podcast, also asked the panelists what skills they unexpectedly leveraged during the pandemic. Communication – with colleagues and with the community they serve – was a universal answer among the panelists.
“I learned – really from seeing some of our senior leaders here do it so well – the importance of being visible, particularly at a time when people were not together and more isolated,” Dr. Unaka said. “I think being able to be visible when you can, in order to deliver really complicated or tough news or communicate about uncertainty, for instance. Being here for our residents – many of our interns moved here sight unseen. I think they needed to feel like they had some sense of normalcy and a sense of community. I really learned how important it was to be visible, and available, and how important the little things mattered.”
Dr. Martinez said that worrying about her patients with COVID-19 in the hospital and the uncertainty around the disease kept her up at night. “I think we always have a hard time leaving work at work and getting a good night’s sleep. I just could not let go of worrying about these patients and having terrible insomnia, trying to leave work at work and I couldn’t – even after they were discharged.”
Dr. Shapiro said the skill he most needed to work on during the pandemic was his courage. “I remember the first time I took care of COVID patients. I was scared. I have no problems saying that out loud. That was a scary experience.”
The demeanor of the nurses on his unit, who had already seen patients with COVID-19, helped ground him during those moments and gave him the courage to move forward. “They’d already been doing it and they were the same. Same affect, same jokes, same everything,” he said. “That actually really helped, and I’ve leaned on that every time I’ve been back on our COVID service.”
Importance of mental health
The COVID-19 pandemic has also shined a light on the importance of mental health. “I think it is important to acknowledge that as hospitalists who have been out on the bleeding edge for a year, mental health is critically important, and we know that we face shortages in that space for the public at large and also for our profession,” Dr. Shapiro said.
When asked about what mental health and self-care looks like for her, Dr. Kumar referenced the need for exercise, meditation, and yoga. “My mental health was better knowing that the people closest to me – whether they be colleagues or friends or family – their mental health was also in a good place and they were also in a good place. And that helped to build me up,” she said.
Dr. Unaka called attention to the stigma around mental health, particularly among physicians, and the lack of resources to address the issue. “It’s a real problem,” she said. “I think it’s at a point where we as a profession need to advocate on behalf of each other and on behalf of our trainees. And honestly, I think we need to view mental health as just ‘health’ and stop separating it out in order for us to move to a place where people feel like they can access what they need without feeling shame about it.”
Editor’s note: National Hospitalist Day occurs the first Thursday in March annually, and serves to celebrate the fastest growing specialty in modern medicine and hospitalists’ enduring contributions to the evolving health care landscape. On National Hospitalist Day in 2021, SHM convened a virtual roundtable with a diverse group of hospitalists to discuss skill set, wellness, and other key issues for hospitalists. To listen to the entire roundtable discussion, visit this Explore The Space podcast episode.
A hospitalist isn’t just a physician who happens to work in a hospital. They are medical professionals with a robust skill set that they use both inside and outside the hospital setting. But what skill sets do hospitalists need to become successful in their careers? And what skill sets does a “pluripotent” hospitalist need in their armamentarium?
These were the issues discussed by participants of a virtual roundtable discussion on National Hospitalist Day – March 4, 2021 – as part of a joint effort of the Society of Hospital Medicine and the Explore the Space podcast.
Maylyn S. Martinez, MD, clinician-researcher and clinical associate at the University of Chicago, sees her hospitalist and research skill sets as two “buckets” of skills she can sort through, with diagnostic, knowledge-based care coordination, and interpersonal skills as lanes where she can focus and improve. “I’m always trying to work in, and sharpen, and find ways to get better at something in each of those every day,” she said.
For Anika Kumar, MD, FHM, pediatric editor of the Hospitalist and clinical assistant professor of pediatrics at the Cleveland Clinic Lerner College of Medicine, much of her work is focused on problem solving. “I approach that as: ‘How do I come up with my differential diagnosis, and how do I diagnose the patient?’ I think that the lanes are a little bit different, but there is some overlap.”
Adaptability is another important part of the skill set for the hospitalist, Ndidi Unaka, MD, MEd, associate professor in the division of hospital medicine at Cincinnati Children’s Hospital Medical Center, said during the discussion. “I think we all really value teamwork, and we take on the role of being the coordinator and making sure things are getting done in a seamless and thoughtful manner. Communicating with families, communicating with our research team, communicating with primary care physicians. I think that is something we’re very used to doing, and I think we do it well. I think we don’t shy away from difficult conversations with consultants. And I think that’s what makes being a hospitalist so amazing.”
Achieving wellness as a hospitalist
Another topic discussed during the roundtable was “comprehensive care for the hospitalist” and how they can achieve a sense of wellness for themselves. Gurpreet Dhaliwal, MD, clinician-educator and professor of medicine at the University of California, San Francisco, said long-term satisfaction in one’s career is less about compensation and more about autonomy, mastery, and purpose.
“Autonomy is shrinking a little bit in health care. But if we connect to our purpose – ‘what are we doing here and how do we connect?’ – it’s either learning about patients and their stories, being with a team of people that you work with, that really builds that purpose,” he said.
Regarding mastery, there’s “tremendous joy if you’re in an environment where people value your mastery, whether it is working in a team or communicating or diagnosing or doing a procedure. If you think of setting up the work environment and those things are in place, I think a lot of wellness can actually happen at work, even though another component, of course, is balancing your life outside of work,” Dr. Dhaliwal said.
This may seem out of reach during COVID-19, but wellness is still achievable during the pandemic, Dr. Martinez said. Her time is spent 75% as a researcher and 25% as a clinician, which is her ideal balance. “I enjoy doing my research, doing my own statistics and writing grants and just learning about this problem that I’ve developed an interest in,” she said. “I just think that’s an important piece for people to focus on as far as health care for the hospitalist, is that there’s no no-one-size-fits-all, that’s for sure.”
Dr. Kumar noted that her clinical time gives her energy for nonclinical work. “I love my clinical time. It’s one of my favorite things that I do,” she said. Although she is tired at the end of the week, “I feel like I am not only giving back to my patients and my team, but I’m also giving back to myself and reminding myself why it is I do what I do every day,” she said.
Wellness for Dr. Unaka meant remembering what drew her to medicine. “It was definitely the opportunity to build strong relationships with patients and families,” she said. While these encounters can sometimes be heavy and stay with a hospitalist, “the fact that we’re in it with them is something that gives a lot of us purpose. I think that when I reflect on all of those things, I’m so happy that I’m in the role that I am.”
Unique skills during COVID-19
Mark Shapiro, MD, hospitalist and host of the roundtable and the Explore the Space podcast, also asked the panelists what skills they unexpectedly leveraged during the pandemic. Communication – with colleagues and with the community they serve – was a universal answer among the panelists.
“I learned – really from seeing some of our senior leaders here do it so well – the importance of being visible, particularly at a time when people were not together and more isolated,” Dr. Unaka said. “I think being able to be visible when you can, in order to deliver really complicated or tough news or communicate about uncertainty, for instance. Being here for our residents – many of our interns moved here sight unseen. I think they needed to feel like they had some sense of normalcy and a sense of community. I really learned how important it was to be visible, and available, and how important the little things mattered.”
Dr. Martinez said that worrying about her patients with COVID-19 in the hospital and the uncertainty around the disease kept her up at night. “I think we always have a hard time leaving work at work and getting a good night’s sleep. I just could not let go of worrying about these patients and having terrible insomnia, trying to leave work at work and I couldn’t – even after they were discharged.”
Dr. Shapiro said the skill he most needed to work on during the pandemic was his courage. “I remember the first time I took care of COVID patients. I was scared. I have no problems saying that out loud. That was a scary experience.”
The demeanor of the nurses on his unit, who had already seen patients with COVID-19, helped ground him during those moments and gave him the courage to move forward. “They’d already been doing it and they were the same. Same affect, same jokes, same everything,” he said. “That actually really helped, and I’ve leaned on that every time I’ve been back on our COVID service.”
Importance of mental health
The COVID-19 pandemic has also shined a light on the importance of mental health. “I think it is important to acknowledge that as hospitalists who have been out on the bleeding edge for a year, mental health is critically important, and we know that we face shortages in that space for the public at large and also for our profession,” Dr. Shapiro said.
When asked about what mental health and self-care looks like for her, Dr. Kumar referenced the need for exercise, meditation, and yoga. “My mental health was better knowing that the people closest to me – whether they be colleagues or friends or family – their mental health was also in a good place and they were also in a good place. And that helped to build me up,” she said.
Dr. Unaka called attention to the stigma around mental health, particularly among physicians, and the lack of resources to address the issue. “It’s a real problem,” she said. “I think it’s at a point where we as a profession need to advocate on behalf of each other and on behalf of our trainees. And honestly, I think we need to view mental health as just ‘health’ and stop separating it out in order for us to move to a place where people feel like they can access what they need without feeling shame about it.”
Editor’s note: National Hospitalist Day occurs the first Thursday in March annually, and serves to celebrate the fastest growing specialty in modern medicine and hospitalists’ enduring contributions to the evolving health care landscape. On National Hospitalist Day in 2021, SHM convened a virtual roundtable with a diverse group of hospitalists to discuss skill set, wellness, and other key issues for hospitalists. To listen to the entire roundtable discussion, visit this Explore The Space podcast episode.
A hospitalist isn’t just a physician who happens to work in a hospital. They are medical professionals with a robust skill set that they use both inside and outside the hospital setting. But what skill sets do hospitalists need to become successful in their careers? And what skill sets does a “pluripotent” hospitalist need in their armamentarium?
These were the issues discussed by participants of a virtual roundtable discussion on National Hospitalist Day – March 4, 2021 – as part of a joint effort of the Society of Hospital Medicine and the Explore the Space podcast.
Maylyn S. Martinez, MD, clinician-researcher and clinical associate at the University of Chicago, sees her hospitalist and research skill sets as two “buckets” of skills she can sort through, with diagnostic, knowledge-based care coordination, and interpersonal skills as lanes where she can focus and improve. “I’m always trying to work in, and sharpen, and find ways to get better at something in each of those every day,” she said.
For Anika Kumar, MD, FHM, pediatric editor of the Hospitalist and clinical assistant professor of pediatrics at the Cleveland Clinic Lerner College of Medicine, much of her work is focused on problem solving. “I approach that as: ‘How do I come up with my differential diagnosis, and how do I diagnose the patient?’ I think that the lanes are a little bit different, but there is some overlap.”
Adaptability is another important part of the skill set for the hospitalist, Ndidi Unaka, MD, MEd, associate professor in the division of hospital medicine at Cincinnati Children’s Hospital Medical Center, said during the discussion. “I think we all really value teamwork, and we take on the role of being the coordinator and making sure things are getting done in a seamless and thoughtful manner. Communicating with families, communicating with our research team, communicating with primary care physicians. I think that is something we’re very used to doing, and I think we do it well. I think we don’t shy away from difficult conversations with consultants. And I think that’s what makes being a hospitalist so amazing.”
Achieving wellness as a hospitalist
Another topic discussed during the roundtable was “comprehensive care for the hospitalist” and how they can achieve a sense of wellness for themselves. Gurpreet Dhaliwal, MD, clinician-educator and professor of medicine at the University of California, San Francisco, said long-term satisfaction in one’s career is less about compensation and more about autonomy, mastery, and purpose.
“Autonomy is shrinking a little bit in health care. But if we connect to our purpose – ‘what are we doing here and how do we connect?’ – it’s either learning about patients and their stories, being with a team of people that you work with, that really builds that purpose,” he said.
Regarding mastery, there’s “tremendous joy if you’re in an environment where people value your mastery, whether it is working in a team or communicating or diagnosing or doing a procedure. If you think of setting up the work environment and those things are in place, I think a lot of wellness can actually happen at work, even though another component, of course, is balancing your life outside of work,” Dr. Dhaliwal said.
This may seem out of reach during COVID-19, but wellness is still achievable during the pandemic, Dr. Martinez said. Her time is spent 75% as a researcher and 25% as a clinician, which is her ideal balance. “I enjoy doing my research, doing my own statistics and writing grants and just learning about this problem that I’ve developed an interest in,” she said. “I just think that’s an important piece for people to focus on as far as health care for the hospitalist, is that there’s no no-one-size-fits-all, that’s for sure.”
Dr. Kumar noted that her clinical time gives her energy for nonclinical work. “I love my clinical time. It’s one of my favorite things that I do,” she said. Although she is tired at the end of the week, “I feel like I am not only giving back to my patients and my team, but I’m also giving back to myself and reminding myself why it is I do what I do every day,” she said.
Wellness for Dr. Unaka meant remembering what drew her to medicine. “It was definitely the opportunity to build strong relationships with patients and families,” she said. While these encounters can sometimes be heavy and stay with a hospitalist, “the fact that we’re in it with them is something that gives a lot of us purpose. I think that when I reflect on all of those things, I’m so happy that I’m in the role that I am.”
Unique skills during COVID-19
Mark Shapiro, MD, hospitalist and host of the roundtable and the Explore the Space podcast, also asked the panelists what skills they unexpectedly leveraged during the pandemic. Communication – with colleagues and with the community they serve – was a universal answer among the panelists.
“I learned – really from seeing some of our senior leaders here do it so well – the importance of being visible, particularly at a time when people were not together and more isolated,” Dr. Unaka said. “I think being able to be visible when you can, in order to deliver really complicated or tough news or communicate about uncertainty, for instance. Being here for our residents – many of our interns moved here sight unseen. I think they needed to feel like they had some sense of normalcy and a sense of community. I really learned how important it was to be visible, and available, and how important the little things mattered.”
Dr. Martinez said that worrying about her patients with COVID-19 in the hospital and the uncertainty around the disease kept her up at night. “I think we always have a hard time leaving work at work and getting a good night’s sleep. I just could not let go of worrying about these patients and having terrible insomnia, trying to leave work at work and I couldn’t – even after they were discharged.”
Dr. Shapiro said the skill he most needed to work on during the pandemic was his courage. “I remember the first time I took care of COVID patients. I was scared. I have no problems saying that out loud. That was a scary experience.”
The demeanor of the nurses on his unit, who had already seen patients with COVID-19, helped ground him during those moments and gave him the courage to move forward. “They’d already been doing it and they were the same. Same affect, same jokes, same everything,” he said. “That actually really helped, and I’ve leaned on that every time I’ve been back on our COVID service.”
Importance of mental health
The COVID-19 pandemic has also shined a light on the importance of mental health. “I think it is important to acknowledge that as hospitalists who have been out on the bleeding edge for a year, mental health is critically important, and we know that we face shortages in that space for the public at large and also for our profession,” Dr. Shapiro said.
When asked about what mental health and self-care looks like for her, Dr. Kumar referenced the need for exercise, meditation, and yoga. “My mental health was better knowing that the people closest to me – whether they be colleagues or friends or family – their mental health was also in a good place and they were also in a good place. And that helped to build me up,” she said.
Dr. Unaka called attention to the stigma around mental health, particularly among physicians, and the lack of resources to address the issue. “It’s a real problem,” she said. “I think it’s at a point where we as a profession need to advocate on behalf of each other and on behalf of our trainees. And honestly, I think we need to view mental health as just ‘health’ and stop separating it out in order for us to move to a place where people feel like they can access what they need without feeling shame about it.”
Virtual is the new real
Why did we fall short on maximizing telehealth’s value in the COVID-19 pandemic?
The COVID-19 pandemic catalyzed the transformation of Internet-based, remotely accessible innovative technologies. Internet-based customer service delivery technology was rapidly adopted and utilized by several services industries, but health care systems in most of the countries across the world faced unique challenges in adopting the technology for the delivery of health care services. The health care ecosystem of the United States was not immune to such challenges, and several significant barriers surfaced while the pandemic was underway.
Complexly structured, fragmented, unprepared, and overly burnt-out health systems in the United States arguably have fallen short of maximizing the value of telehealth in delivering safe, easily accessible, comprehensive, and cost-effective health care services. In this essay, we examine the reasons for such a suboptimal performance and discuss a few important strategies that may be useful in maximizing the value of telehealth value in several, appropriate health care services.
Hospitals and telehealth
Are hospitalists preparing ourselves “not to see” patients in a hospital-based health care delivery setting? If you have not yet started yet, now may be the right time! Yes, a certain percentage of doctor-patient encounters in hospital settings will remain virtual forever.
A well-established telehealth infrastructure is rarely found in most U.S. hospitals, although the COVID-19 pandemic has unexpectedly boosted the rapid growth of telehealth in the country.1 Public health emergency declarations in the United States in the face of the COVID-19 crisis have facilitated two important initiatives to restore health care delivery amidst formal and informal lockdowns that brought states to a grinding halt. These extend from expansion of virtual services, including telehealth, virtual check-ins, and e-visits, to the decision by the Department of Health & Human Services Office of Civil Rights to exercise enforcement discretion and waive penalties for the use of relatively inexpensive, non–public-facing mobile and other audiovisual technology tools.2
Hospital-based care in the United States taps nearly 33% of national health expenditure. An additional 30% of national health expenditure that is related to physicians, prescriptions, and other facilities is indirectly influenced by care delivered at health care facilities.3 Studies show that about 20% of ED visits could potentially be avoided via virtual urgent care offerings.4 A rapidly changing health care ecosystem is proving formidable for most hospital systems, and a test for their resilience and agility. Not just the implementation of telehealth is challenging, but getting it right is the key success factor.
Hospital-based telehealth
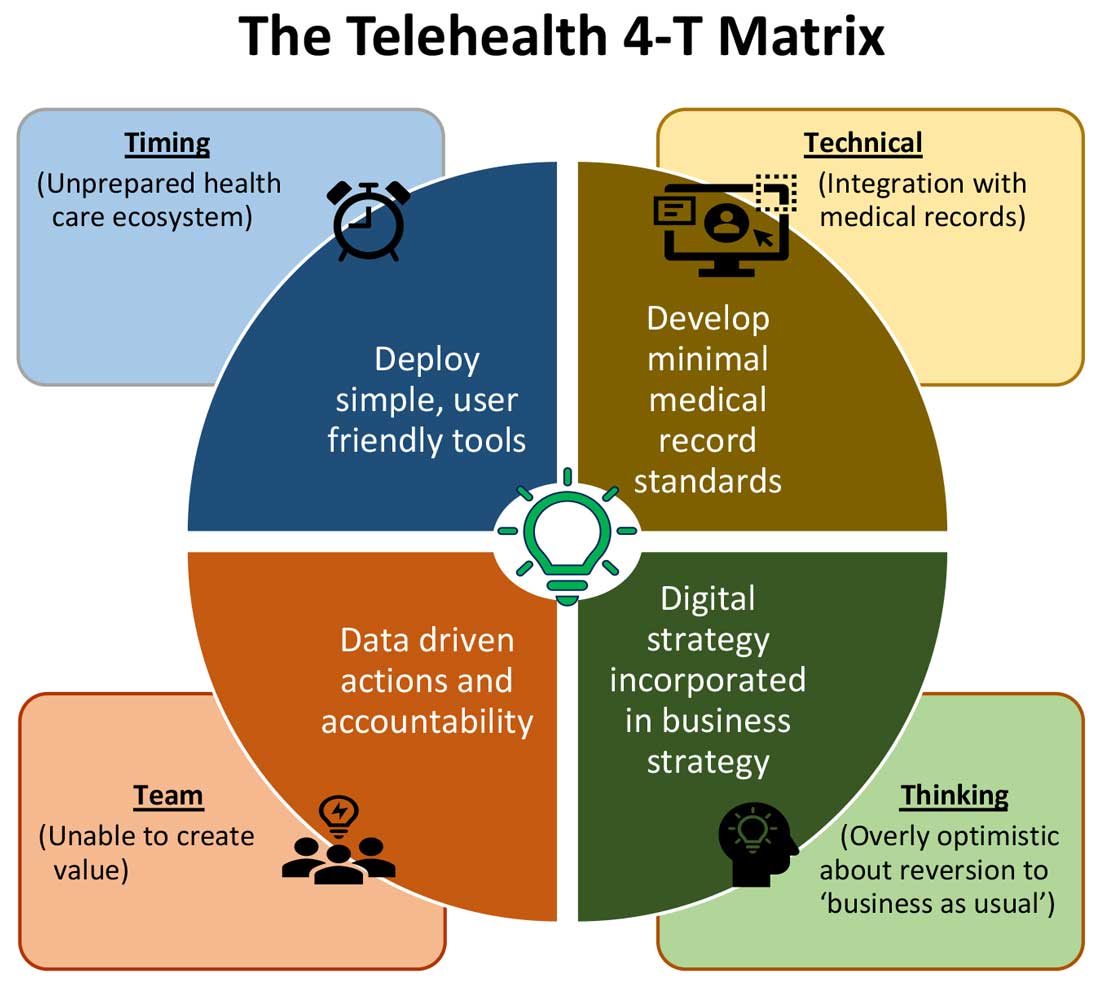
Expansion of telehealth coverage by the Centers for Medicare & Medicaid Services and most commercial payers did not quite ride the pandemic-induced momentum across the care continuum. Hospitals are lagging far behind ambulatory care in implementing telehealth. As illustrated in the “4-T Matrix” (see graphic) we would like to examine four key reasons for such a sluggish initial uptake and try to propose four important strategies that may help us to maximize the value created by telehealth technologies.
1. Timing
The health care system has always lagged far behind other service industries in terms of technology adaptation. Because of the unique nature of health care services, face-to-face interaction supersedes all other forms of communication. A rapidly evolving pandemic was not matched by simultaneous technology education for patients and providers. The enormous choice of hard-to-navigate telehealth tools; time and labor-intensive implementation; and uncertainty around payer, policy, and regulatory expectations might have precluded providers from the rapid adoption of telehealth in the hospital setting. Patients’ specific characteristics, such as the absence of technology-centered education, information, age, comorbidities, lack of technical literacy, and dependency on caregivers contributed to the suboptimal response from patients and families.
Deploying simple, ubiquitous, user-friendly, and technologically less challenging telehealth solutions may be a better approach to increase the adoption of such solutions by providers and patients. Hospitals need to develop and distribute telehealth user guides in all possible modes of communication. Provider-centric in-service sessions, workshops, and live support by “superuser teams” often work well in reducing end-user resistance.
2. Technical
Current electronic medical records vary widely in their features and offerings, and their ability to interact with third-party software and platforms. Dissatisfaction of end users with EMRs is well known, as is their likely relationship to burnout. Recent research continues to show a strong relationship between EMR usability and the odds of burnout among physicians.5 In the current climate, administrators and health informaticists have the responsibility to avoid adding increased burdens to end users.
Another issue is the limited connectivity in many remote/rural areas that would impact implementation of telehealth platforms. Studies indicate that 33% of rural Americans lack access to high-speed broadband Internet to support video visits.6 The recent successful implementation of telehealth across 530 providers in 75 ambulatory practices operated by Munson Healthcare, a rural health system in northern Michigan, sheds light on the technology’s enormous potential in providing safe access to rural populations.6,7
Privacy and safety of patient data is of paramount importance. According to a national poll on healthy aging by the University of Michigan in May 2019, targeting older adults, 47% of survey responders expressed difficulty using technology and 49% of survey responders were concerned about privacy.8 Use of certification and other tools offered by the Office of the National Coordinator for Health Information Technology would help reassure users, and the ability to capture and share images between providers would be of immense benefit in facilitating e-consults.
The need of the hour is redesigned work flow, to help providers adopt and use virtual care/telehealth efficiently. Work flow redesign must be coupled with technological advances to allow seamless integration of third-party telehealth platforms into existing EMR systems or built directly into EMRs. Use of quality metrics and analytical tools specific to telehealth would help measure the technology’s impact on patient care, outcomes, and end-user/provider experience.
3. Teams and training
Outcomes of health care interventions are often determined by the effectiveness of teams. Irrespective of how robust health care systems may have been initially, rapidly spreading infectious diseases like COVID-19 can quickly derail the system, bringing the workforce and patients to a breaking point.5 Decentralized, uncoordinated, and siloed efforts by individual teams across the care continuum were contributing factors for the partial success of telehealth care delivery pathways. The hospital systems with telehealth-ready teams at the start of the COVID-19 pandemic were so rare that the knowledge and technical training opportunities for innovators grew severalfold during the pandemic.
As per the American Medical Association, telehealth success is massively dependent on building the right team. Core, leadership, advisory, and implementation teams comprised of clinical representatives, end users, administrative personnel, executive members of the organization, technical experts, and payment/policy experts should be put together before implementing a telehealth strategy.9 Seamless integration of hospital-based care with ambulatory care via a telehealth platform is only complete when care managers are trained and deployed to fulfill the needs of a diverse group of patients. Deriving overall value from telehealth is only possible when there is a skill development, training and mentoring team put in place.
4. Thinking
In most U.S. hospitals, inpatient health care is equally distributed between nonprocedure and procedure-based services. Hospitals resorted to suspension of nonemergent procedures to mitigate the risk of spreading COVID-19. This was further compounded by many patients’ self-selection to defer care, an abrupt reduction in the influx of patients from the referral base because of suboptimally operating ambulatory care services, leading to low hospital occupancy.
Hospitals across the nation have gone through a massive short-term financial crunch and unfavorable cash-flow forecast, which prompted a paradoxical work-force reduction. While some argue that it may be akin to strategic myopia, the authors believed that such a response is strategically imperative to keep the hospital afloat. It is reasonable to attribute the paucity of innovation to constrained resources, and health systems are simply staying overly optimistic about “weathering the storm” and reverting soon to “business as usual.” The technological framework necessary for deploying a telehealth solution often comes with a price. Financially challenged hospital systems rarely exercise any capital-intensive activities. By contrast, telehealth adoption by ambulatory care can result in quicker resumption of patient care in community settings. A lack of operational and infrastructure synchrony between ambulatory and in-hospital systems has failed to capture telehealth-driven inpatient volume. For example, direct admissions from ambulatory telehealth referrals was a missed opportunity in several places. Referrals for labs, diagnostic tests, and other allied services could have helped hospitals offset their fixed costs. Similarly, work flows related to discharge and postdischarge follow up rarely embrace telehealth tools or telehealth care pathways. A brisk change in the health care ecosystem is partly responsible for this.
Digital strategy needs to be incorporated into business strategy. For the reasons already discussed, telehealth technology is not a “nice to have” anymore, but a “must have.” At present, providers are of the opinion that about 20% of their patient services can be delivered via a telehealth platform. Similar trends are observed among patients, as a new modality of access to care is increasingly beneficial to them. Telehealth must be incorporated in standardized hospital work flows. Use of telehealth for preoperative clearance will greatly minimize same-day surgery cancellations. Given the potential shortage in resources, telehealth adoption for inpatient consultations will help systems conserve personal protective equipment, minimize the risk of staff exposure to COVID-19, and improve efficiency.
Digital strategy also prompts the reengineering of care delivery.10 Excessive and unused physical capacity can be converted into digital care hubs. Health maintenance, prevention, health promotion, health education, and chronic disease management not only can serve a variety of patient groups but can also help address the “last-mile problem” in health care. A successful digital strategy usually has three important components – Commitment: Hospital leadership is committed to include digital transformation as a strategic objective; Cost: Digital strategy is added as a line item in the budget; and Control: Measurable metrics are put in place to monitor the performance, impact, and influence of the digital strategy.
Conclusion
For decades, most U.S. health systems occupied the periphery of technological transformation when compared to the rest of the service industry. While most health systems took a heroic approach to the adoption of telehealth during COVID-19, despite being unprepared, the need for a systematic telehealth deployment is far from being adequately fulfilled. The COVID-19 pandemic brought permanent changes to several business disciplines globally. Given the impact of the pandemic on the health and overall wellbeing of American society, the U.S. health care industry must leave no stone unturned in its quest for transformation.
Dr. Lingisetty is a hospitalist and physician executive at Baptist Health System, Little Rock, Ark, and is cofounder/president of SHM’s Arkansas chapter. Dr. Prasad is medical director of care management and a hospitalist at Advocate Aurora Health in Milwaukee. He is cochair of SHM’s IT Special Interest Group, sits on the HQPS committee, and is president of SHM’s Wisconsin chapter. Dr. Palabindala is the medical director, utilization management, and physician advisory services at the University of Mississippi Medical Center and an associate professor of medicine and academic hospitalist at the University of Mississippi, both in Jackson.
References
1. Finnegan M. “Telehealth booms amid COVID-19 crisis.” Computerworld. 2020 Apr 27. www.computerworld.com/article/3540315/telehealth-booms-amid-covid-19-crisis-virtual-care-is-here-to-stay.html. Accessed 2020 Sep 12.
2. Department of Health & Human Services. “OCR Announces Notification of Enforcement Discretion for Telehealth Remote Communications During the COVID-19 Nationwide Public Health Emergency.” 2020 Mar 17. www.hhs.gov/about/news/2020/03/17/ocr-announces-notification-of-enforcement-discretion-for-telehealth-remote-communications-during-the-covid-19.html. Accessed 2020 Sep 12.
3. National Center for Health Statistics. “Health Expenditures.” www.cdc.gov/nchs/fastats/health-expenditures.htm. Accessed 2020 Sep 12.
4. Bestsennyy O et al. “Telehealth: A post–COVID-19 reality?” McKinsey & Company. 2020 May 29. www.mckinsey.com/industries/healthcare-systems-and-services/our-insights/telehealth-a-quarter-trillion-dollar-post-covid-19-reality. Accessed 2020 Sep 12.
5. Melnick ER et al. The Association Between Perceived Electronic Health Record Usability and Professional Burnout Among U.S. Physicians. Mayo Clin Proc. 2020 March;95(3):476-87.
6. Hirko KA et al. Telehealth in response to the COVID-19 pandemic: Implications for rural health disparities. J Am Med Inform Assoc. 2020 Nov;27(11):1816-8. .
7. American Academy of Family Physicians. “Study Examines Telehealth, Rural Disparities in Pandemic.” 2020 July 30. www.aafp.org/news/practice-professional-issues/20200730ruraltelehealth.html. Accessed 2020 Dec 15.
8. Kurlander J et al. “Virtual Visits: Telehealth and Older Adults.” National Poll on Healthy Aging. 2019 Oct. hdl.handle.net/2027.42/151376.
9. American Medical Association. Telehealth Implementation Playbook. 2019. www.ama-assn.org/system/files/2020-04/ama-telehealth-implementation-playbook.pdf.
10. Smith AC et al. Telehealth for global emergencies: Implications for coronavirus disease 2019 (COVID-19). J Telemed Telecare. 2020 Jun;26(5):309-13.
Why did we fall short on maximizing telehealth’s value in the COVID-19 pandemic?
Why did we fall short on maximizing telehealth’s value in the COVID-19 pandemic?
The COVID-19 pandemic catalyzed the transformation of Internet-based, remotely accessible innovative technologies. Internet-based customer service delivery technology was rapidly adopted and utilized by several services industries, but health care systems in most of the countries across the world faced unique challenges in adopting the technology for the delivery of health care services. The health care ecosystem of the United States was not immune to such challenges, and several significant barriers surfaced while the pandemic was underway.
Complexly structured, fragmented, unprepared, and overly burnt-out health systems in the United States arguably have fallen short of maximizing the value of telehealth in delivering safe, easily accessible, comprehensive, and cost-effective health care services. In this essay, we examine the reasons for such a suboptimal performance and discuss a few important strategies that may be useful in maximizing the value of telehealth value in several, appropriate health care services.
Hospitals and telehealth
Are hospitalists preparing ourselves “not to see” patients in a hospital-based health care delivery setting? If you have not yet started yet, now may be the right time! Yes, a certain percentage of doctor-patient encounters in hospital settings will remain virtual forever.
A well-established telehealth infrastructure is rarely found in most U.S. hospitals, although the COVID-19 pandemic has unexpectedly boosted the rapid growth of telehealth in the country.1 Public health emergency declarations in the United States in the face of the COVID-19 crisis have facilitated two important initiatives to restore health care delivery amidst formal and informal lockdowns that brought states to a grinding halt. These extend from expansion of virtual services, including telehealth, virtual check-ins, and e-visits, to the decision by the Department of Health & Human Services Office of Civil Rights to exercise enforcement discretion and waive penalties for the use of relatively inexpensive, non–public-facing mobile and other audiovisual technology tools.2
Hospital-based care in the United States taps nearly 33% of national health expenditure. An additional 30% of national health expenditure that is related to physicians, prescriptions, and other facilities is indirectly influenced by care delivered at health care facilities.3 Studies show that about 20% of ED visits could potentially be avoided via virtual urgent care offerings.4 A rapidly changing health care ecosystem is proving formidable for most hospital systems, and a test for their resilience and agility. Not just the implementation of telehealth is challenging, but getting it right is the key success factor.
Hospital-based telehealth
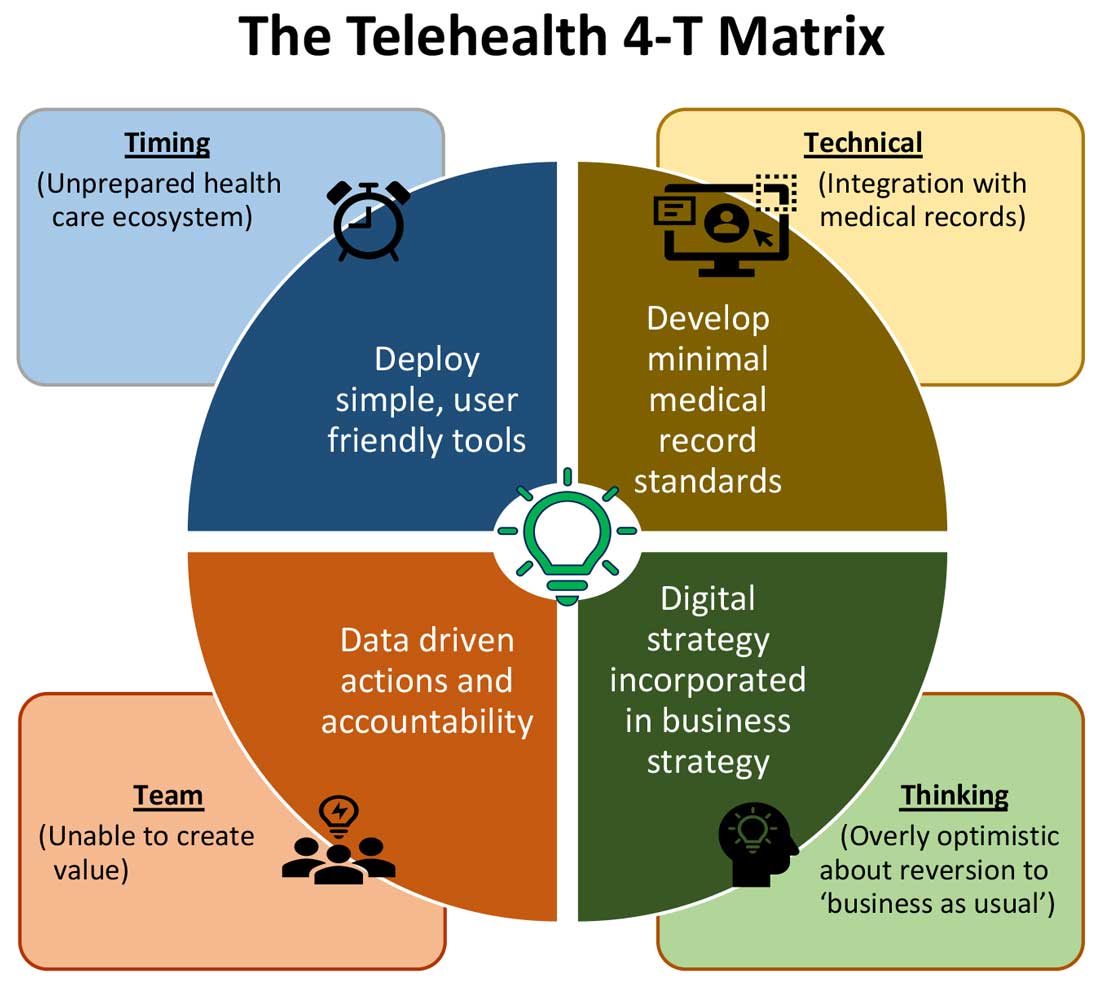
Expansion of telehealth coverage by the Centers for Medicare & Medicaid Services and most commercial payers did not quite ride the pandemic-induced momentum across the care continuum. Hospitals are lagging far behind ambulatory care in implementing telehealth. As illustrated in the “4-T Matrix” (see graphic) we would like to examine four key reasons for such a sluggish initial uptake and try to propose four important strategies that may help us to maximize the value created by telehealth technologies.
1. Timing
The health care system has always lagged far behind other service industries in terms of technology adaptation. Because of the unique nature of health care services, face-to-face interaction supersedes all other forms of communication. A rapidly evolving pandemic was not matched by simultaneous technology education for patients and providers. The enormous choice of hard-to-navigate telehealth tools; time and labor-intensive implementation; and uncertainty around payer, policy, and regulatory expectations might have precluded providers from the rapid adoption of telehealth in the hospital setting. Patients’ specific characteristics, such as the absence of technology-centered education, information, age, comorbidities, lack of technical literacy, and dependency on caregivers contributed to the suboptimal response from patients and families.
Deploying simple, ubiquitous, user-friendly, and technologically less challenging telehealth solutions may be a better approach to increase the adoption of such solutions by providers and patients. Hospitals need to develop and distribute telehealth user guides in all possible modes of communication. Provider-centric in-service sessions, workshops, and live support by “superuser teams” often work well in reducing end-user resistance.
2. Technical
Current electronic medical records vary widely in their features and offerings, and their ability to interact with third-party software and platforms. Dissatisfaction of end users with EMRs is well known, as is their likely relationship to burnout. Recent research continues to show a strong relationship between EMR usability and the odds of burnout among physicians.5 In the current climate, administrators and health informaticists have the responsibility to avoid adding increased burdens to end users.
Another issue is the limited connectivity in many remote/rural areas that would impact implementation of telehealth platforms. Studies indicate that 33% of rural Americans lack access to high-speed broadband Internet to support video visits.6 The recent successful implementation of telehealth across 530 providers in 75 ambulatory practices operated by Munson Healthcare, a rural health system in northern Michigan, sheds light on the technology’s enormous potential in providing safe access to rural populations.6,7
Privacy and safety of patient data is of paramount importance. According to a national poll on healthy aging by the University of Michigan in May 2019, targeting older adults, 47% of survey responders expressed difficulty using technology and 49% of survey responders were concerned about privacy.8 Use of certification and other tools offered by the Office of the National Coordinator for Health Information Technology would help reassure users, and the ability to capture and share images between providers would be of immense benefit in facilitating e-consults.
The need of the hour is redesigned work flow, to help providers adopt and use virtual care/telehealth efficiently. Work flow redesign must be coupled with technological advances to allow seamless integration of third-party telehealth platforms into existing EMR systems or built directly into EMRs. Use of quality metrics and analytical tools specific to telehealth would help measure the technology’s impact on patient care, outcomes, and end-user/provider experience.
3. Teams and training
Outcomes of health care interventions are often determined by the effectiveness of teams. Irrespective of how robust health care systems may have been initially, rapidly spreading infectious diseases like COVID-19 can quickly derail the system, bringing the workforce and patients to a breaking point.5 Decentralized, uncoordinated, and siloed efforts by individual teams across the care continuum were contributing factors for the partial success of telehealth care delivery pathways. The hospital systems with telehealth-ready teams at the start of the COVID-19 pandemic were so rare that the knowledge and technical training opportunities for innovators grew severalfold during the pandemic.
As per the American Medical Association, telehealth success is massively dependent on building the right team. Core, leadership, advisory, and implementation teams comprised of clinical representatives, end users, administrative personnel, executive members of the organization, technical experts, and payment/policy experts should be put together before implementing a telehealth strategy.9 Seamless integration of hospital-based care with ambulatory care via a telehealth platform is only complete when care managers are trained and deployed to fulfill the needs of a diverse group of patients. Deriving overall value from telehealth is only possible when there is a skill development, training and mentoring team put in place.
4. Thinking
In most U.S. hospitals, inpatient health care is equally distributed between nonprocedure and procedure-based services. Hospitals resorted to suspension of nonemergent procedures to mitigate the risk of spreading COVID-19. This was further compounded by many patients’ self-selection to defer care, an abrupt reduction in the influx of patients from the referral base because of suboptimally operating ambulatory care services, leading to low hospital occupancy.
Hospitals across the nation have gone through a massive short-term financial crunch and unfavorable cash-flow forecast, which prompted a paradoxical work-force reduction. While some argue that it may be akin to strategic myopia, the authors believed that such a response is strategically imperative to keep the hospital afloat. It is reasonable to attribute the paucity of innovation to constrained resources, and health systems are simply staying overly optimistic about “weathering the storm” and reverting soon to “business as usual.” The technological framework necessary for deploying a telehealth solution often comes with a price. Financially challenged hospital systems rarely exercise any capital-intensive activities. By contrast, telehealth adoption by ambulatory care can result in quicker resumption of patient care in community settings. A lack of operational and infrastructure synchrony between ambulatory and in-hospital systems has failed to capture telehealth-driven inpatient volume. For example, direct admissions from ambulatory telehealth referrals was a missed opportunity in several places. Referrals for labs, diagnostic tests, and other allied services could have helped hospitals offset their fixed costs. Similarly, work flows related to discharge and postdischarge follow up rarely embrace telehealth tools or telehealth care pathways. A brisk change in the health care ecosystem is partly responsible for this.
Digital strategy needs to be incorporated into business strategy. For the reasons already discussed, telehealth technology is not a “nice to have” anymore, but a “must have.” At present, providers are of the opinion that about 20% of their patient services can be delivered via a telehealth platform. Similar trends are observed among patients, as a new modality of access to care is increasingly beneficial to them. Telehealth must be incorporated in standardized hospital work flows. Use of telehealth for preoperative clearance will greatly minimize same-day surgery cancellations. Given the potential shortage in resources, telehealth adoption for inpatient consultations will help systems conserve personal protective equipment, minimize the risk of staff exposure to COVID-19, and improve efficiency.
Digital strategy also prompts the reengineering of care delivery.10 Excessive and unused physical capacity can be converted into digital care hubs. Health maintenance, prevention, health promotion, health education, and chronic disease management not only can serve a variety of patient groups but can also help address the “last-mile problem” in health care. A successful digital strategy usually has three important components – Commitment: Hospital leadership is committed to include digital transformation as a strategic objective; Cost: Digital strategy is added as a line item in the budget; and Control: Measurable metrics are put in place to monitor the performance, impact, and influence of the digital strategy.
Conclusion
For decades, most U.S. health systems occupied the periphery of technological transformation when compared to the rest of the service industry. While most health systems took a heroic approach to the adoption of telehealth during COVID-19, despite being unprepared, the need for a systematic telehealth deployment is far from being adequately fulfilled. The COVID-19 pandemic brought permanent changes to several business disciplines globally. Given the impact of the pandemic on the health and overall wellbeing of American society, the U.S. health care industry must leave no stone unturned in its quest for transformation.
Dr. Lingisetty is a hospitalist and physician executive at Baptist Health System, Little Rock, Ark, and is cofounder/president of SHM’s Arkansas chapter. Dr. Prasad is medical director of care management and a hospitalist at Advocate Aurora Health in Milwaukee. He is cochair of SHM’s IT Special Interest Group, sits on the HQPS committee, and is president of SHM’s Wisconsin chapter. Dr. Palabindala is the medical director, utilization management, and physician advisory services at the University of Mississippi Medical Center and an associate professor of medicine and academic hospitalist at the University of Mississippi, both in Jackson.
References
1. Finnegan M. “Telehealth booms amid COVID-19 crisis.” Computerworld. 2020 Apr 27. www.computerworld.com/article/3540315/telehealth-booms-amid-covid-19-crisis-virtual-care-is-here-to-stay.html. Accessed 2020 Sep 12.
2. Department of Health & Human Services. “OCR Announces Notification of Enforcement Discretion for Telehealth Remote Communications During the COVID-19 Nationwide Public Health Emergency.” 2020 Mar 17. www.hhs.gov/about/news/2020/03/17/ocr-announces-notification-of-enforcement-discretion-for-telehealth-remote-communications-during-the-covid-19.html. Accessed 2020 Sep 12.
3. National Center for Health Statistics. “Health Expenditures.” www.cdc.gov/nchs/fastats/health-expenditures.htm. Accessed 2020 Sep 12.
4. Bestsennyy O et al. “Telehealth: A post–COVID-19 reality?” McKinsey & Company. 2020 May 29. www.mckinsey.com/industries/healthcare-systems-and-services/our-insights/telehealth-a-quarter-trillion-dollar-post-covid-19-reality. Accessed 2020 Sep 12.
5. Melnick ER et al. The Association Between Perceived Electronic Health Record Usability and Professional Burnout Among U.S. Physicians. Mayo Clin Proc. 2020 March;95(3):476-87.
6. Hirko KA et al. Telehealth in response to the COVID-19 pandemic: Implications for rural health disparities. J Am Med Inform Assoc. 2020 Nov;27(11):1816-8. .
7. American Academy of Family Physicians. “Study Examines Telehealth, Rural Disparities in Pandemic.” 2020 July 30. www.aafp.org/news/practice-professional-issues/20200730ruraltelehealth.html. Accessed 2020 Dec 15.
8. Kurlander J et al. “Virtual Visits: Telehealth and Older Adults.” National Poll on Healthy Aging. 2019 Oct. hdl.handle.net/2027.42/151376.
9. American Medical Association. Telehealth Implementation Playbook. 2019. www.ama-assn.org/system/files/2020-04/ama-telehealth-implementation-playbook.pdf.
10. Smith AC et al. Telehealth for global emergencies: Implications for coronavirus disease 2019 (COVID-19). J Telemed Telecare. 2020 Jun;26(5):309-13.
The COVID-19 pandemic catalyzed the transformation of Internet-based, remotely accessible innovative technologies. Internet-based customer service delivery technology was rapidly adopted and utilized by several services industries, but health care systems in most of the countries across the world faced unique challenges in adopting the technology for the delivery of health care services. The health care ecosystem of the United States was not immune to such challenges, and several significant barriers surfaced while the pandemic was underway.
Complexly structured, fragmented, unprepared, and overly burnt-out health systems in the United States arguably have fallen short of maximizing the value of telehealth in delivering safe, easily accessible, comprehensive, and cost-effective health care services. In this essay, we examine the reasons for such a suboptimal performance and discuss a few important strategies that may be useful in maximizing the value of telehealth value in several, appropriate health care services.
Hospitals and telehealth
Are hospitalists preparing ourselves “not to see” patients in a hospital-based health care delivery setting? If you have not yet started yet, now may be the right time! Yes, a certain percentage of doctor-patient encounters in hospital settings will remain virtual forever.
A well-established telehealth infrastructure is rarely found in most U.S. hospitals, although the COVID-19 pandemic has unexpectedly boosted the rapid growth of telehealth in the country.1 Public health emergency declarations in the United States in the face of the COVID-19 crisis have facilitated two important initiatives to restore health care delivery amidst formal and informal lockdowns that brought states to a grinding halt. These extend from expansion of virtual services, including telehealth, virtual check-ins, and e-visits, to the decision by the Department of Health & Human Services Office of Civil Rights to exercise enforcement discretion and waive penalties for the use of relatively inexpensive, non–public-facing mobile and other audiovisual technology tools.2
Hospital-based care in the United States taps nearly 33% of national health expenditure. An additional 30% of national health expenditure that is related to physicians, prescriptions, and other facilities is indirectly influenced by care delivered at health care facilities.3 Studies show that about 20% of ED visits could potentially be avoided via virtual urgent care offerings.4 A rapidly changing health care ecosystem is proving formidable for most hospital systems, and a test for their resilience and agility. Not just the implementation of telehealth is challenging, but getting it right is the key success factor.
Hospital-based telehealth
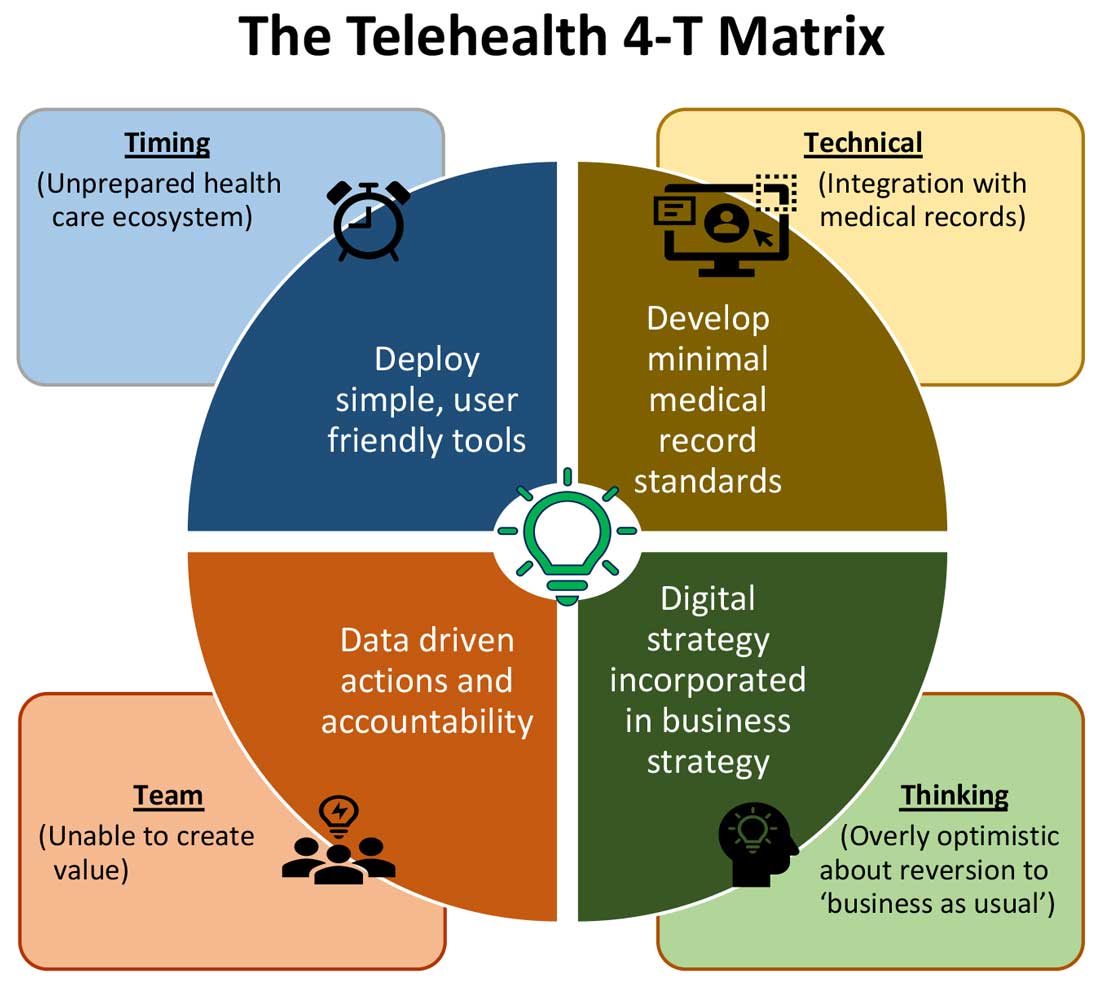
Expansion of telehealth coverage by the Centers for Medicare & Medicaid Services and most commercial payers did not quite ride the pandemic-induced momentum across the care continuum. Hospitals are lagging far behind ambulatory care in implementing telehealth. As illustrated in the “4-T Matrix” (see graphic) we would like to examine four key reasons for such a sluggish initial uptake and try to propose four important strategies that may help us to maximize the value created by telehealth technologies.
1. Timing
The health care system has always lagged far behind other service industries in terms of technology adaptation. Because of the unique nature of health care services, face-to-face interaction supersedes all other forms of communication. A rapidly evolving pandemic was not matched by simultaneous technology education for patients and providers. The enormous choice of hard-to-navigate telehealth tools; time and labor-intensive implementation; and uncertainty around payer, policy, and regulatory expectations might have precluded providers from the rapid adoption of telehealth in the hospital setting. Patients’ specific characteristics, such as the absence of technology-centered education, information, age, comorbidities, lack of technical literacy, and dependency on caregivers contributed to the suboptimal response from patients and families.
Deploying simple, ubiquitous, user-friendly, and technologically less challenging telehealth solutions may be a better approach to increase the adoption of such solutions by providers and patients. Hospitals need to develop and distribute telehealth user guides in all possible modes of communication. Provider-centric in-service sessions, workshops, and live support by “superuser teams” often work well in reducing end-user resistance.
2. Technical
Current electronic medical records vary widely in their features and offerings, and their ability to interact with third-party software and platforms. Dissatisfaction of end users with EMRs is well known, as is their likely relationship to burnout. Recent research continues to show a strong relationship between EMR usability and the odds of burnout among physicians.5 In the current climate, administrators and health informaticists have the responsibility to avoid adding increased burdens to end users.
Another issue is the limited connectivity in many remote/rural areas that would impact implementation of telehealth platforms. Studies indicate that 33% of rural Americans lack access to high-speed broadband Internet to support video visits.6 The recent successful implementation of telehealth across 530 providers in 75 ambulatory practices operated by Munson Healthcare, a rural health system in northern Michigan, sheds light on the technology’s enormous potential in providing safe access to rural populations.6,7
Privacy and safety of patient data is of paramount importance. According to a national poll on healthy aging by the University of Michigan in May 2019, targeting older adults, 47% of survey responders expressed difficulty using technology and 49% of survey responders were concerned about privacy.8 Use of certification and other tools offered by the Office of the National Coordinator for Health Information Technology would help reassure users, and the ability to capture and share images between providers would be of immense benefit in facilitating e-consults.
The need of the hour is redesigned work flow, to help providers adopt and use virtual care/telehealth efficiently. Work flow redesign must be coupled with technological advances to allow seamless integration of third-party telehealth platforms into existing EMR systems or built directly into EMRs. Use of quality metrics and analytical tools specific to telehealth would help measure the technology’s impact on patient care, outcomes, and end-user/provider experience.
3. Teams and training
Outcomes of health care interventions are often determined by the effectiveness of teams. Irrespective of how robust health care systems may have been initially, rapidly spreading infectious diseases like COVID-19 can quickly derail the system, bringing the workforce and patients to a breaking point.5 Decentralized, uncoordinated, and siloed efforts by individual teams across the care continuum were contributing factors for the partial success of telehealth care delivery pathways. The hospital systems with telehealth-ready teams at the start of the COVID-19 pandemic were so rare that the knowledge and technical training opportunities for innovators grew severalfold during the pandemic.
As per the American Medical Association, telehealth success is massively dependent on building the right team. Core, leadership, advisory, and implementation teams comprised of clinical representatives, end users, administrative personnel, executive members of the organization, technical experts, and payment/policy experts should be put together before implementing a telehealth strategy.9 Seamless integration of hospital-based care with ambulatory care via a telehealth platform is only complete when care managers are trained and deployed to fulfill the needs of a diverse group of patients. Deriving overall value from telehealth is only possible when there is a skill development, training and mentoring team put in place.
4. Thinking
In most U.S. hospitals, inpatient health care is equally distributed between nonprocedure and procedure-based services. Hospitals resorted to suspension of nonemergent procedures to mitigate the risk of spreading COVID-19. This was further compounded by many patients’ self-selection to defer care, an abrupt reduction in the influx of patients from the referral base because of suboptimally operating ambulatory care services, leading to low hospital occupancy.
Hospitals across the nation have gone through a massive short-term financial crunch and unfavorable cash-flow forecast, which prompted a paradoxical work-force reduction. While some argue that it may be akin to strategic myopia, the authors believed that such a response is strategically imperative to keep the hospital afloat. It is reasonable to attribute the paucity of innovation to constrained resources, and health systems are simply staying overly optimistic about “weathering the storm” and reverting soon to “business as usual.” The technological framework necessary for deploying a telehealth solution often comes with a price. Financially challenged hospital systems rarely exercise any capital-intensive activities. By contrast, telehealth adoption by ambulatory care can result in quicker resumption of patient care in community settings. A lack of operational and infrastructure synchrony between ambulatory and in-hospital systems has failed to capture telehealth-driven inpatient volume. For example, direct admissions from ambulatory telehealth referrals was a missed opportunity in several places. Referrals for labs, diagnostic tests, and other allied services could have helped hospitals offset their fixed costs. Similarly, work flows related to discharge and postdischarge follow up rarely embrace telehealth tools or telehealth care pathways. A brisk change in the health care ecosystem is partly responsible for this.
Digital strategy needs to be incorporated into business strategy. For the reasons already discussed, telehealth technology is not a “nice to have” anymore, but a “must have.” At present, providers are of the opinion that about 20% of their patient services can be delivered via a telehealth platform. Similar trends are observed among patients, as a new modality of access to care is increasingly beneficial to them. Telehealth must be incorporated in standardized hospital work flows. Use of telehealth for preoperative clearance will greatly minimize same-day surgery cancellations. Given the potential shortage in resources, telehealth adoption for inpatient consultations will help systems conserve personal protective equipment, minimize the risk of staff exposure to COVID-19, and improve efficiency.
Digital strategy also prompts the reengineering of care delivery.10 Excessive and unused physical capacity can be converted into digital care hubs. Health maintenance, prevention, health promotion, health education, and chronic disease management not only can serve a variety of patient groups but can also help address the “last-mile problem” in health care. A successful digital strategy usually has three important components – Commitment: Hospital leadership is committed to include digital transformation as a strategic objective; Cost: Digital strategy is added as a line item in the budget; and Control: Measurable metrics are put in place to monitor the performance, impact, and influence of the digital strategy.
Conclusion
For decades, most U.S. health systems occupied the periphery of technological transformation when compared to the rest of the service industry. While most health systems took a heroic approach to the adoption of telehealth during COVID-19, despite being unprepared, the need for a systematic telehealth deployment is far from being adequately fulfilled. The COVID-19 pandemic brought permanent changes to several business disciplines globally. Given the impact of the pandemic on the health and overall wellbeing of American society, the U.S. health care industry must leave no stone unturned in its quest for transformation.
Dr. Lingisetty is a hospitalist and physician executive at Baptist Health System, Little Rock, Ark, and is cofounder/president of SHM’s Arkansas chapter. Dr. Prasad is medical director of care management and a hospitalist at Advocate Aurora Health in Milwaukee. He is cochair of SHM’s IT Special Interest Group, sits on the HQPS committee, and is president of SHM’s Wisconsin chapter. Dr. Palabindala is the medical director, utilization management, and physician advisory services at the University of Mississippi Medical Center and an associate professor of medicine and academic hospitalist at the University of Mississippi, both in Jackson.
References
1. Finnegan M. “Telehealth booms amid COVID-19 crisis.” Computerworld. 2020 Apr 27. www.computerworld.com/article/3540315/telehealth-booms-amid-covid-19-crisis-virtual-care-is-here-to-stay.html. Accessed 2020 Sep 12.
2. Department of Health & Human Services. “OCR Announces Notification of Enforcement Discretion for Telehealth Remote Communications During the COVID-19 Nationwide Public Health Emergency.” 2020 Mar 17. www.hhs.gov/about/news/2020/03/17/ocr-announces-notification-of-enforcement-discretion-for-telehealth-remote-communications-during-the-covid-19.html. Accessed 2020 Sep 12.
3. National Center for Health Statistics. “Health Expenditures.” www.cdc.gov/nchs/fastats/health-expenditures.htm. Accessed 2020 Sep 12.
4. Bestsennyy O et al. “Telehealth: A post–COVID-19 reality?” McKinsey & Company. 2020 May 29. www.mckinsey.com/industries/healthcare-systems-and-services/our-insights/telehealth-a-quarter-trillion-dollar-post-covid-19-reality. Accessed 2020 Sep 12.
5. Melnick ER et al. The Association Between Perceived Electronic Health Record Usability and Professional Burnout Among U.S. Physicians. Mayo Clin Proc. 2020 March;95(3):476-87.
6. Hirko KA et al. Telehealth in response to the COVID-19 pandemic: Implications for rural health disparities. J Am Med Inform Assoc. 2020 Nov;27(11):1816-8. .
7. American Academy of Family Physicians. “Study Examines Telehealth, Rural Disparities in Pandemic.” 2020 July 30. www.aafp.org/news/practice-professional-issues/20200730ruraltelehealth.html. Accessed 2020 Dec 15.
8. Kurlander J et al. “Virtual Visits: Telehealth and Older Adults.” National Poll on Healthy Aging. 2019 Oct. hdl.handle.net/2027.42/151376.
9. American Medical Association. Telehealth Implementation Playbook. 2019. www.ama-assn.org/system/files/2020-04/ama-telehealth-implementation-playbook.pdf.
10. Smith AC et al. Telehealth for global emergencies: Implications for coronavirus disease 2019 (COVID-19). J Telemed Telecare. 2020 Jun;26(5):309-13.
Hospital medicine groups are getting larger
What are the implications for your workplace?
Although readers will be forgiven for missing the subtle change, the tables in the 2020 State of Hospital Medicine (SoHM) Report underwent a landmark structural change that echoes the growth of our field. In the latest SoHM Report, the hospital medicine group (HMG) size categories all increased significantly to reflect the fact that hospitalist groups have grown from a median of 9 physician full time equivalents (FTE) in 2016 to a median of 15.2 employed/contracted FTE (excluding FTE provided by locum tenens providers) in 2020.
For many years, the Report considered “large” adult HMGs to be those with 30 or more FTE of physicians, and smaller groups were organized by FTE categories of <5, 5-9, 10-19, and 20-29. Now the SoHM Report describes a large HMG as 50 employed/contracted FTE or greater, a category that represents 12.7% of HMGs serving adults. The other categories expanded to <5, 5-14, 15-29, and 30-49, respectively. Overall, HMGs are growing in size, and the SoHM displays new data slices that help leaders to compare their group to modern peers.
There are some caveats to consider. First, these figures only represent physician FTE, and essentially all these large groups employ NP/PA hospitalists as well. Second, these HMGs typically employ some part-time and contracted PRN physicians in this FTE count. In combination, these two factors mean that large HMGs often employ many more than 50 individual clinicians. In fact, the average number of physicians in this cohort was 72.3 before counting NP/PAs and locums. Third, do not interpret the portion of large groups in the survey (12.7%) as insignificant. Because each one employs so many total hospitalists, large HMGs collectively represent a common work environment for many hospitalists in the US. Lastly, although pediatric HMGs have grown, far fewer (3.1%) have over 50 FTE, so this column focuses on HMGs serving adults.
Why does it matter that groups are growing in size? The SoHM Report offers extensive data to answer this question. Here are a couple of highlights but consider buying the report to dig deeper. First, large groups are far more likely to offer variable scheduling. Although the 7-on, 7-off scheduling pattern is still the norm in all group sizes, large HMGs are most likely to offer something flexible that might enhance career sustainability for hospitalists. Second, large groups are the most likely to employ a few hospitalists with extra training, whether that be geriatrics, palliative care, pediatrics, or a medicine subspecialty. Working in a large group means you can ask for curbside consults from a diverse and well-trained bunch of colleagues. Third, large groups were most likely to employ nocturnists, meaning fewer night shifts are allocated to the hospitalists who want to focus on daytime work. From an individual perspective, there is a lot to like about working in a large HMG.
There are some drawbacks to larger groups, of course. Large groups can be less socially cohesive and the costs of managing 70-100 hospitalists typically grow well past the capacity of a single group leader. My personal belief is that these downsides can be solved through economies of scale and skilled management teams. In addition, a large group can afford to dedicate leadership FTE to niche hospitalist needs, such as career development and coaching, which are difficult to fund in small practices. This also provides more opportunities for staff hospitalists to begin taking on some leadership or administrative duties or branch out into related areas such as quality improvement, case management physician advisor roles, or IT expertise.
Ultimately, large groups typically represent the maturation of an HMG within a large hospital – it signifies that the hospital relies on that group to deliver great patient outcomes in every corner of the hospital. Where you practice remains a personal choice, but the emergence of large groups hints at the clout and sophistication hospitalists can build by banding together. Learn more about the full 2020 SoHM Report at hospitalmedicine.org/sohm.
Dr. White is associate professor of medicine at the University of Washington, Seattle. He is the chair of SHM’s Practice Analysis Committee.
What are the implications for your workplace?
What are the implications for your workplace?
Although readers will be forgiven for missing the subtle change, the tables in the 2020 State of Hospital Medicine (SoHM) Report underwent a landmark structural change that echoes the growth of our field. In the latest SoHM Report, the hospital medicine group (HMG) size categories all increased significantly to reflect the fact that hospitalist groups have grown from a median of 9 physician full time equivalents (FTE) in 2016 to a median of 15.2 employed/contracted FTE (excluding FTE provided by locum tenens providers) in 2020.
For many years, the Report considered “large” adult HMGs to be those with 30 or more FTE of physicians, and smaller groups were organized by FTE categories of <5, 5-9, 10-19, and 20-29. Now the SoHM Report describes a large HMG as 50 employed/contracted FTE or greater, a category that represents 12.7% of HMGs serving adults. The other categories expanded to <5, 5-14, 15-29, and 30-49, respectively. Overall, HMGs are growing in size, and the SoHM displays new data slices that help leaders to compare their group to modern peers.
There are some caveats to consider. First, these figures only represent physician FTE, and essentially all these large groups employ NP/PA hospitalists as well. Second, these HMGs typically employ some part-time and contracted PRN physicians in this FTE count. In combination, these two factors mean that large HMGs often employ many more than 50 individual clinicians. In fact, the average number of physicians in this cohort was 72.3 before counting NP/PAs and locums. Third, do not interpret the portion of large groups in the survey (12.7%) as insignificant. Because each one employs so many total hospitalists, large HMGs collectively represent a common work environment for many hospitalists in the US. Lastly, although pediatric HMGs have grown, far fewer (3.1%) have over 50 FTE, so this column focuses on HMGs serving adults.
Why does it matter that groups are growing in size? The SoHM Report offers extensive data to answer this question. Here are a couple of highlights but consider buying the report to dig deeper. First, large groups are far more likely to offer variable scheduling. Although the 7-on, 7-off scheduling pattern is still the norm in all group sizes, large HMGs are most likely to offer something flexible that might enhance career sustainability for hospitalists. Second, large groups are the most likely to employ a few hospitalists with extra training, whether that be geriatrics, palliative care, pediatrics, or a medicine subspecialty. Working in a large group means you can ask for curbside consults from a diverse and well-trained bunch of colleagues. Third, large groups were most likely to employ nocturnists, meaning fewer night shifts are allocated to the hospitalists who want to focus on daytime work. From an individual perspective, there is a lot to like about working in a large HMG.
There are some drawbacks to larger groups, of course. Large groups can be less socially cohesive and the costs of managing 70-100 hospitalists typically grow well past the capacity of a single group leader. My personal belief is that these downsides can be solved through economies of scale and skilled management teams. In addition, a large group can afford to dedicate leadership FTE to niche hospitalist needs, such as career development and coaching, which are difficult to fund in small practices. This also provides more opportunities for staff hospitalists to begin taking on some leadership or administrative duties or branch out into related areas such as quality improvement, case management physician advisor roles, or IT expertise.
Ultimately, large groups typically represent the maturation of an HMG within a large hospital – it signifies that the hospital relies on that group to deliver great patient outcomes in every corner of the hospital. Where you practice remains a personal choice, but the emergence of large groups hints at the clout and sophistication hospitalists can build by banding together. Learn more about the full 2020 SoHM Report at hospitalmedicine.org/sohm.
Dr. White is associate professor of medicine at the University of Washington, Seattle. He is the chair of SHM’s Practice Analysis Committee.
Although readers will be forgiven for missing the subtle change, the tables in the 2020 State of Hospital Medicine (SoHM) Report underwent a landmark structural change that echoes the growth of our field. In the latest SoHM Report, the hospital medicine group (HMG) size categories all increased significantly to reflect the fact that hospitalist groups have grown from a median of 9 physician full time equivalents (FTE) in 2016 to a median of 15.2 employed/contracted FTE (excluding FTE provided by locum tenens providers) in 2020.
For many years, the Report considered “large” adult HMGs to be those with 30 or more FTE of physicians, and smaller groups were organized by FTE categories of <5, 5-9, 10-19, and 20-29. Now the SoHM Report describes a large HMG as 50 employed/contracted FTE or greater, a category that represents 12.7% of HMGs serving adults. The other categories expanded to <5, 5-14, 15-29, and 30-49, respectively. Overall, HMGs are growing in size, and the SoHM displays new data slices that help leaders to compare their group to modern peers.
There are some caveats to consider. First, these figures only represent physician FTE, and essentially all these large groups employ NP/PA hospitalists as well. Second, these HMGs typically employ some part-time and contracted PRN physicians in this FTE count. In combination, these two factors mean that large HMGs often employ many more than 50 individual clinicians. In fact, the average number of physicians in this cohort was 72.3 before counting NP/PAs and locums. Third, do not interpret the portion of large groups in the survey (12.7%) as insignificant. Because each one employs so many total hospitalists, large HMGs collectively represent a common work environment for many hospitalists in the US. Lastly, although pediatric HMGs have grown, far fewer (3.1%) have over 50 FTE, so this column focuses on HMGs serving adults.
Why does it matter that groups are growing in size? The SoHM Report offers extensive data to answer this question. Here are a couple of highlights but consider buying the report to dig deeper. First, large groups are far more likely to offer variable scheduling. Although the 7-on, 7-off scheduling pattern is still the norm in all group sizes, large HMGs are most likely to offer something flexible that might enhance career sustainability for hospitalists. Second, large groups are the most likely to employ a few hospitalists with extra training, whether that be geriatrics, palliative care, pediatrics, or a medicine subspecialty. Working in a large group means you can ask for curbside consults from a diverse and well-trained bunch of colleagues. Third, large groups were most likely to employ nocturnists, meaning fewer night shifts are allocated to the hospitalists who want to focus on daytime work. From an individual perspective, there is a lot to like about working in a large HMG.
There are some drawbacks to larger groups, of course. Large groups can be less socially cohesive and the costs of managing 70-100 hospitalists typically grow well past the capacity of a single group leader. My personal belief is that these downsides can be solved through economies of scale and skilled management teams. In addition, a large group can afford to dedicate leadership FTE to niche hospitalist needs, such as career development and coaching, which are difficult to fund in small practices. This also provides more opportunities for staff hospitalists to begin taking on some leadership or administrative duties or branch out into related areas such as quality improvement, case management physician advisor roles, or IT expertise.
Ultimately, large groups typically represent the maturation of an HMG within a large hospital – it signifies that the hospital relies on that group to deliver great patient outcomes in every corner of the hospital. Where you practice remains a personal choice, but the emergence of large groups hints at the clout and sophistication hospitalists can build by banding together. Learn more about the full 2020 SoHM Report at hospitalmedicine.org/sohm.
Dr. White is associate professor of medicine at the University of Washington, Seattle. He is the chair of SHM’s Practice Analysis Committee.